User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
Post–COVID-19 lung injury: What we know so far
With vaccination rates increasing and new infections declining, we all hope the worst of the COVID-19 pandemic is over (fingers crossed really tight). Regardless, the post–COVID-19 syndrome pandemic has already begun. What is post–COVID-19 syndrome (or long-haulers or long-COVID)? Is it standard postviral fatigue? Prolonged deconditioning following debilitating illness? Permanent lung or vascular injury? Common sense and past experience say it’s all of these.
In theory, the burden of actual lung injury post COVID-19 should be the easiest to quantify, so let’s discuss what we think we know. I’ve heard experts break post–COVID-19 lung injury into three broad categories:
- Preexisting lung disease that is exacerbated by acute COVID-19 infection.
- Acute COVID-19 infection that causes acute respiratory distress syndrome (ARDS) or other acute lung injury (ALI).
- Non–critically ill acute COVID-19 with residual lung damage and abnormal repair.
These categories are necessarily imprecise, making it challenging to fit some patients neatly into a single definition.
For patients in the first category, management will be dictated largely by the nature of the preexisting lung disease. For those in category two, we already know a lot about what their recovery from ARDS will look like. There’s no longer reason to believe that COVID-19–related ARDS is particularly unique, and all things being equal, lung recovery should mimic that seen with non–COVID-19 ARDS.
It’s going to take patience and time, and beyond targeted rehabilitation it’s not clear that we have anything available to expedite the process.
The third category of patients is the most intriguing. Is there a group of patients who have residual lung injury but didn’t have evident ARDS/ALI during their acute COVID-19 infection? Anecdotally we think so, but we know little about prevalence and less about management. A recent study published in Annals of the American Thoracic Society addresses both issues. In an observational report on patients recovering after being hospitalized with COVID-19 infection, the authors found that 3.6% of patients had residual lung injury that improved with 3 weeks of corticosteroid treatment.
The report is timely and helpful but hardly definitive. It’s observational, and patients required extensive screening and identification by a multidisciplinary committee of experts in interstitial lung disease. Patients were diagnosed as having organizing pneumonia (OP) as their “lung injury” if certain radiographic criteria were met. There were no biopsies. Last, there was no control group. Still, this report is critically important. It tells us that at 6 weeks post discharge, about 3.6% of patients who were hospitalized for COVID-19 will have persistent symptoms, radiographic abnormalities, and a plateau in their recovery.
Beyond that, it tells us little. Did these patients really have OP? It’s impossible to know. The CT findings used to establish the diagnosis are nonspecific. Response to steroids is consistent with OP, but the treatment course was quite short. If truly OP, one would expect a high relapse rate after steroid withdrawal. Patients weren’t followed long enough to monitor recurrence rates. Also, as appropriately discussed in the accompanying editorial, there’s no control group so we can’t know whether the patients treated with steroids would have recovered without treatment. There was objective improvement in lung function for the two to three patients they followed who did not receive steroids. However, it was of lesser magnitude than in the steroid group.
Post–COVID-19 symptoms will remain a challenge for the foreseeable future. More than 30 million patients have been diagnosed with COVID-19 in the United States and close to half will experience persistent dyspnea. Putting the numbers together, I conclude that the vast majority will not have identifiable lung injury that will benefit from steroids. I wish I could prescribe patience to both physicians and patients.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He covers a wide range of topics in pulmonary, critical care, and sleep medicine.
A version of this article first appeared on Medscape.com.
With vaccination rates increasing and new infections declining, we all hope the worst of the COVID-19 pandemic is over (fingers crossed really tight). Regardless, the post–COVID-19 syndrome pandemic has already begun. What is post–COVID-19 syndrome (or long-haulers or long-COVID)? Is it standard postviral fatigue? Prolonged deconditioning following debilitating illness? Permanent lung or vascular injury? Common sense and past experience say it’s all of these.
In theory, the burden of actual lung injury post COVID-19 should be the easiest to quantify, so let’s discuss what we think we know. I’ve heard experts break post–COVID-19 lung injury into three broad categories:
- Preexisting lung disease that is exacerbated by acute COVID-19 infection.
- Acute COVID-19 infection that causes acute respiratory distress syndrome (ARDS) or other acute lung injury (ALI).
- Non–critically ill acute COVID-19 with residual lung damage and abnormal repair.
These categories are necessarily imprecise, making it challenging to fit some patients neatly into a single definition.
For patients in the first category, management will be dictated largely by the nature of the preexisting lung disease. For those in category two, we already know a lot about what their recovery from ARDS will look like. There’s no longer reason to believe that COVID-19–related ARDS is particularly unique, and all things being equal, lung recovery should mimic that seen with non–COVID-19 ARDS.
It’s going to take patience and time, and beyond targeted rehabilitation it’s not clear that we have anything available to expedite the process.
The third category of patients is the most intriguing. Is there a group of patients who have residual lung injury but didn’t have evident ARDS/ALI during their acute COVID-19 infection? Anecdotally we think so, but we know little about prevalence and less about management. A recent study published in Annals of the American Thoracic Society addresses both issues. In an observational report on patients recovering after being hospitalized with COVID-19 infection, the authors found that 3.6% of patients had residual lung injury that improved with 3 weeks of corticosteroid treatment.
The report is timely and helpful but hardly definitive. It’s observational, and patients required extensive screening and identification by a multidisciplinary committee of experts in interstitial lung disease. Patients were diagnosed as having organizing pneumonia (OP) as their “lung injury” if certain radiographic criteria were met. There were no biopsies. Last, there was no control group. Still, this report is critically important. It tells us that at 6 weeks post discharge, about 3.6% of patients who were hospitalized for COVID-19 will have persistent symptoms, radiographic abnormalities, and a plateau in their recovery.
Beyond that, it tells us little. Did these patients really have OP? It’s impossible to know. The CT findings used to establish the diagnosis are nonspecific. Response to steroids is consistent with OP, but the treatment course was quite short. If truly OP, one would expect a high relapse rate after steroid withdrawal. Patients weren’t followed long enough to monitor recurrence rates. Also, as appropriately discussed in the accompanying editorial, there’s no control group so we can’t know whether the patients treated with steroids would have recovered without treatment. There was objective improvement in lung function for the two to three patients they followed who did not receive steroids. However, it was of lesser magnitude than in the steroid group.
Post–COVID-19 symptoms will remain a challenge for the foreseeable future. More than 30 million patients have been diagnosed with COVID-19 in the United States and close to half will experience persistent dyspnea. Putting the numbers together, I conclude that the vast majority will not have identifiable lung injury that will benefit from steroids. I wish I could prescribe patience to both physicians and patients.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He covers a wide range of topics in pulmonary, critical care, and sleep medicine.
A version of this article first appeared on Medscape.com.
With vaccination rates increasing and new infections declining, we all hope the worst of the COVID-19 pandemic is over (fingers crossed really tight). Regardless, the post–COVID-19 syndrome pandemic has already begun. What is post–COVID-19 syndrome (or long-haulers or long-COVID)? Is it standard postviral fatigue? Prolonged deconditioning following debilitating illness? Permanent lung or vascular injury? Common sense and past experience say it’s all of these.
In theory, the burden of actual lung injury post COVID-19 should be the easiest to quantify, so let’s discuss what we think we know. I’ve heard experts break post–COVID-19 lung injury into three broad categories:
- Preexisting lung disease that is exacerbated by acute COVID-19 infection.
- Acute COVID-19 infection that causes acute respiratory distress syndrome (ARDS) or other acute lung injury (ALI).
- Non–critically ill acute COVID-19 with residual lung damage and abnormal repair.
These categories are necessarily imprecise, making it challenging to fit some patients neatly into a single definition.
For patients in the first category, management will be dictated largely by the nature of the preexisting lung disease. For those in category two, we already know a lot about what their recovery from ARDS will look like. There’s no longer reason to believe that COVID-19–related ARDS is particularly unique, and all things being equal, lung recovery should mimic that seen with non–COVID-19 ARDS.
It’s going to take patience and time, and beyond targeted rehabilitation it’s not clear that we have anything available to expedite the process.
The third category of patients is the most intriguing. Is there a group of patients who have residual lung injury but didn’t have evident ARDS/ALI during their acute COVID-19 infection? Anecdotally we think so, but we know little about prevalence and less about management. A recent study published in Annals of the American Thoracic Society addresses both issues. In an observational report on patients recovering after being hospitalized with COVID-19 infection, the authors found that 3.6% of patients had residual lung injury that improved with 3 weeks of corticosteroid treatment.
The report is timely and helpful but hardly definitive. It’s observational, and patients required extensive screening and identification by a multidisciplinary committee of experts in interstitial lung disease. Patients were diagnosed as having organizing pneumonia (OP) as their “lung injury” if certain radiographic criteria were met. There were no biopsies. Last, there was no control group. Still, this report is critically important. It tells us that at 6 weeks post discharge, about 3.6% of patients who were hospitalized for COVID-19 will have persistent symptoms, radiographic abnormalities, and a plateau in their recovery.
Beyond that, it tells us little. Did these patients really have OP? It’s impossible to know. The CT findings used to establish the diagnosis are nonspecific. Response to steroids is consistent with OP, but the treatment course was quite short. If truly OP, one would expect a high relapse rate after steroid withdrawal. Patients weren’t followed long enough to monitor recurrence rates. Also, as appropriately discussed in the accompanying editorial, there’s no control group so we can’t know whether the patients treated with steroids would have recovered without treatment. There was objective improvement in lung function for the two to three patients they followed who did not receive steroids. However, it was of lesser magnitude than in the steroid group.
Post–COVID-19 symptoms will remain a challenge for the foreseeable future. More than 30 million patients have been diagnosed with COVID-19 in the United States and close to half will experience persistent dyspnea. Putting the numbers together, I conclude that the vast majority will not have identifiable lung injury that will benefit from steroids. I wish I could prescribe patience to both physicians and patients.
Dr. Holley is associate professor of medicine at Uniformed Services University and program director of pulmonary and critical care medicine at Walter Reed National Military Medical Center. He covers a wide range of topics in pulmonary, critical care, and sleep medicine.
A version of this article first appeared on Medscape.com.
A pacemaker that 'just disappears' and a magnetic diet device
Ignore this pacemaker and it will go away
At some point – and now seems to be that point – we have to say enough is enough. The throwaway culture that produces phones, TVs, and computers that get tossed in the trash because they can’t be repaired has gone too far. That’s right, we’re looking at you, medical science!
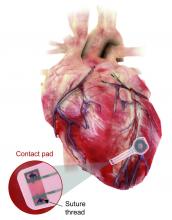
This time, it’s a pacemaker that just disappears when it’s no longer needed. Some lazy heart surgeon decided that it was way too much trouble to do another surgery to remove the leads when a temporary pacemaker was no longer needed. You know the type: “It sure would be nice if the pacemaker components were biocompatible and were naturally absorbed by the body over the course of a few weeks and wouldn’t need to be surgically extracted.” Slacker.
Well, get a load of this. Researchers at Northwestern and George Washington universities say that they have come up with a transient pacemaker that “harvests energy from an external, remote antenna using near-field communication protocols – the same technology used in smartphones for electronic payments and in RFID tags.”
That means no batteries and no wires that have to be removed and can cause infections. Because the infectious disease docs also are too lazy to do their jobs, apparently.
The lack of onboard infrastructure means that the device can be very small – it weighs less than half a gram and is only 250 microns thick. And yes, it is bioresorbable and completely harmless. It fully degrades and disappears in 5-7 weeks through the body’s natural biologic processes, “thereby avoiding the need for physical removal of the pacemaker electrodes. This is potentially a major victory for postoperative patients,” said Dr. Rishi Arora, one of the investigators.
A victory for patients, he says. Not a word about the time and effort saved by the surgeons. Typical.
It’s a mask! No, it’s a COVID-19 test!
Mask wearing has gotten more lax as people get vaccinated for COVID-19, but as wearing masks for virus prevention is becoming more normalized in western society, some saw an opportunity to make them work for diagnosis.
Researchers from the Massachusetts Institute of Technology and the Wyss Institute for Biologically Inspired Engineering at Harvard University have found a way to do just that with their wearable freeze-dried cell-free (wFDCF) technology. A single push of a button releases water from a reservoir in the mask that sequentially activates three different freeze-dried biological reactions, which detect the SARS-CoV-2 virus in the wearer’s breath.
Initially meant as a tool for the Zika outbreak in 2015, the team made a quick pivot in May 2020. But this isn’t just some run-of-the-mill, at-home test. The data prove that the wFDCF mask is comparable to polymerase chain reactions tests, the standard in COVID-19 detection. Plus there aren’t any extra factors to deal with, like room or instrument temperature to ensure accuracy. In just 90 minutes, the mask gives results on a readout in a way similar to that of a pregnancy test. Voilà! To have COVID-19 or not to have COVID-19 is an easily answered question.
At LOTME, we think this is a big improvement from having dogs, or even three-foot rats, sniffing out coronavirus.
But wait, there’s more. “In addition to face masks, our programmable biosensors can be integrated into other garments to provide on-the-go detection of dangerous substances including viruses, bacteria, toxins, and chemical agents,” said Peter Nguyen, PhD, study coauthor and research scientist at the Wyss Institute. The technology can be used on lab coats, scrubs, military uniforms, and uniforms of first responders who may come in contact with hazardous pathogens and toxins. Think of all the lives saved and possible avoidances.
If only it could diagnose bad breath.
Finally, an excuse for the all-beer diet
Weight loss is hard work. Extremely hard work, and, as evidenced by the constant inundation and advertisement of quick fixes, crash diets, and expensive gym memberships, there’s not really a solid, 100% solution to the issue. Until now, thanks to a team of doctors from New Zealand, who’ve decided that the best way to combat obesity is to leave you in constant agony.
The DentalSlim Diet Control device is certainly a radical yet comically logical attempt to combat obesity. The creators say that the biggest problem with dieting is compliance, and, well, it’s difficult to eat too much if you can’t actually open your mouth. The metal contraption is mounted onto your teeth and uses magnetic locks to prevent the user from opening their mouths more than 2 mm. That’s less than a tenth of an inch. Which is not a lot. So not a lot that essentially all you can consume is liquid.
Oh, and they’ve got results to back up their madness. In a small study, seven otherwise healthy obese women lost an average of 5.1% of their body weight after using the DentalSlim for 2 weeks, though they did complain that the device was difficult to use, caused discomfort and difficulty speaking, made them more tense, and in general made life “less satisfying.” And one participant was able to cheat the system and consume nonhealthy food like chocolate by melting it.
So, there you are, if you want a weight-loss solution that tortures you and has far bigger holes than the one it leaves for your mouth, try the DentalSlim. Or, you know, don’t eat that eighth slice of pizza and maybe go for a walk later. Your choice.
Ignore this pacemaker and it will go away
At some point – and now seems to be that point – we have to say enough is enough. The throwaway culture that produces phones, TVs, and computers that get tossed in the trash because they can’t be repaired has gone too far. That’s right, we’re looking at you, medical science!
This time, it’s a pacemaker that just disappears when it’s no longer needed. Some lazy heart surgeon decided that it was way too much trouble to do another surgery to remove the leads when a temporary pacemaker was no longer needed. You know the type: “It sure would be nice if the pacemaker components were biocompatible and were naturally absorbed by the body over the course of a few weeks and wouldn’t need to be surgically extracted.” Slacker.
Well, get a load of this. Researchers at Northwestern and George Washington universities say that they have come up with a transient pacemaker that “harvests energy from an external, remote antenna using near-field communication protocols – the same technology used in smartphones for electronic payments and in RFID tags.”
That means no batteries and no wires that have to be removed and can cause infections. Because the infectious disease docs also are too lazy to do their jobs, apparently.
The lack of onboard infrastructure means that the device can be very small – it weighs less than half a gram and is only 250 microns thick. And yes, it is bioresorbable and completely harmless. It fully degrades and disappears in 5-7 weeks through the body’s natural biologic processes, “thereby avoiding the need for physical removal of the pacemaker electrodes. This is potentially a major victory for postoperative patients,” said Dr. Rishi Arora, one of the investigators.
A victory for patients, he says. Not a word about the time and effort saved by the surgeons. Typical.
It’s a mask! No, it’s a COVID-19 test!
Mask wearing has gotten more lax as people get vaccinated for COVID-19, but as wearing masks for virus prevention is becoming more normalized in western society, some saw an opportunity to make them work for diagnosis.
Researchers from the Massachusetts Institute of Technology and the Wyss Institute for Biologically Inspired Engineering at Harvard University have found a way to do just that with their wearable freeze-dried cell-free (wFDCF) technology. A single push of a button releases water from a reservoir in the mask that sequentially activates three different freeze-dried biological reactions, which detect the SARS-CoV-2 virus in the wearer’s breath.
Initially meant as a tool for the Zika outbreak in 2015, the team made a quick pivot in May 2020. But this isn’t just some run-of-the-mill, at-home test. The data prove that the wFDCF mask is comparable to polymerase chain reactions tests, the standard in COVID-19 detection. Plus there aren’t any extra factors to deal with, like room or instrument temperature to ensure accuracy. In just 90 minutes, the mask gives results on a readout in a way similar to that of a pregnancy test. Voilà! To have COVID-19 or not to have COVID-19 is an easily answered question.
At LOTME, we think this is a big improvement from having dogs, or even three-foot rats, sniffing out coronavirus.
But wait, there’s more. “In addition to face masks, our programmable biosensors can be integrated into other garments to provide on-the-go detection of dangerous substances including viruses, bacteria, toxins, and chemical agents,” said Peter Nguyen, PhD, study coauthor and research scientist at the Wyss Institute. The technology can be used on lab coats, scrubs, military uniforms, and uniforms of first responders who may come in contact with hazardous pathogens and toxins. Think of all the lives saved and possible avoidances.
If only it could diagnose bad breath.
Finally, an excuse for the all-beer diet
Weight loss is hard work. Extremely hard work, and, as evidenced by the constant inundation and advertisement of quick fixes, crash diets, and expensive gym memberships, there’s not really a solid, 100% solution to the issue. Until now, thanks to a team of doctors from New Zealand, who’ve decided that the best way to combat obesity is to leave you in constant agony.
The DentalSlim Diet Control device is certainly a radical yet comically logical attempt to combat obesity. The creators say that the biggest problem with dieting is compliance, and, well, it’s difficult to eat too much if you can’t actually open your mouth. The metal contraption is mounted onto your teeth and uses magnetic locks to prevent the user from opening their mouths more than 2 mm. That’s less than a tenth of an inch. Which is not a lot. So not a lot that essentially all you can consume is liquid.
Oh, and they’ve got results to back up their madness. In a small study, seven otherwise healthy obese women lost an average of 5.1% of their body weight after using the DentalSlim for 2 weeks, though they did complain that the device was difficult to use, caused discomfort and difficulty speaking, made them more tense, and in general made life “less satisfying.” And one participant was able to cheat the system and consume nonhealthy food like chocolate by melting it.
So, there you are, if you want a weight-loss solution that tortures you and has far bigger holes than the one it leaves for your mouth, try the DentalSlim. Or, you know, don’t eat that eighth slice of pizza and maybe go for a walk later. Your choice.
Ignore this pacemaker and it will go away
At some point – and now seems to be that point – we have to say enough is enough. The throwaway culture that produces phones, TVs, and computers that get tossed in the trash because they can’t be repaired has gone too far. That’s right, we’re looking at you, medical science!
This time, it’s a pacemaker that just disappears when it’s no longer needed. Some lazy heart surgeon decided that it was way too much trouble to do another surgery to remove the leads when a temporary pacemaker was no longer needed. You know the type: “It sure would be nice if the pacemaker components were biocompatible and were naturally absorbed by the body over the course of a few weeks and wouldn’t need to be surgically extracted.” Slacker.
Well, get a load of this. Researchers at Northwestern and George Washington universities say that they have come up with a transient pacemaker that “harvests energy from an external, remote antenna using near-field communication protocols – the same technology used in smartphones for electronic payments and in RFID tags.”
That means no batteries and no wires that have to be removed and can cause infections. Because the infectious disease docs also are too lazy to do their jobs, apparently.
The lack of onboard infrastructure means that the device can be very small – it weighs less than half a gram and is only 250 microns thick. And yes, it is bioresorbable and completely harmless. It fully degrades and disappears in 5-7 weeks through the body’s natural biologic processes, “thereby avoiding the need for physical removal of the pacemaker electrodes. This is potentially a major victory for postoperative patients,” said Dr. Rishi Arora, one of the investigators.
A victory for patients, he says. Not a word about the time and effort saved by the surgeons. Typical.
It’s a mask! No, it’s a COVID-19 test!
Mask wearing has gotten more lax as people get vaccinated for COVID-19, but as wearing masks for virus prevention is becoming more normalized in western society, some saw an opportunity to make them work for diagnosis.
Researchers from the Massachusetts Institute of Technology and the Wyss Institute for Biologically Inspired Engineering at Harvard University have found a way to do just that with their wearable freeze-dried cell-free (wFDCF) technology. A single push of a button releases water from a reservoir in the mask that sequentially activates three different freeze-dried biological reactions, which detect the SARS-CoV-2 virus in the wearer’s breath.
Initially meant as a tool for the Zika outbreak in 2015, the team made a quick pivot in May 2020. But this isn’t just some run-of-the-mill, at-home test. The data prove that the wFDCF mask is comparable to polymerase chain reactions tests, the standard in COVID-19 detection. Plus there aren’t any extra factors to deal with, like room or instrument temperature to ensure accuracy. In just 90 minutes, the mask gives results on a readout in a way similar to that of a pregnancy test. Voilà! To have COVID-19 or not to have COVID-19 is an easily answered question.
At LOTME, we think this is a big improvement from having dogs, or even three-foot rats, sniffing out coronavirus.
But wait, there’s more. “In addition to face masks, our programmable biosensors can be integrated into other garments to provide on-the-go detection of dangerous substances including viruses, bacteria, toxins, and chemical agents,” said Peter Nguyen, PhD, study coauthor and research scientist at the Wyss Institute. The technology can be used on lab coats, scrubs, military uniforms, and uniforms of first responders who may come in contact with hazardous pathogens and toxins. Think of all the lives saved and possible avoidances.
If only it could diagnose bad breath.
Finally, an excuse for the all-beer diet
Weight loss is hard work. Extremely hard work, and, as evidenced by the constant inundation and advertisement of quick fixes, crash diets, and expensive gym memberships, there’s not really a solid, 100% solution to the issue. Until now, thanks to a team of doctors from New Zealand, who’ve decided that the best way to combat obesity is to leave you in constant agony.
The DentalSlim Diet Control device is certainly a radical yet comically logical attempt to combat obesity. The creators say that the biggest problem with dieting is compliance, and, well, it’s difficult to eat too much if you can’t actually open your mouth. The metal contraption is mounted onto your teeth and uses magnetic locks to prevent the user from opening their mouths more than 2 mm. That’s less than a tenth of an inch. Which is not a lot. So not a lot that essentially all you can consume is liquid.
Oh, and they’ve got results to back up their madness. In a small study, seven otherwise healthy obese women lost an average of 5.1% of their body weight after using the DentalSlim for 2 weeks, though they did complain that the device was difficult to use, caused discomfort and difficulty speaking, made them more tense, and in general made life “less satisfying.” And one participant was able to cheat the system and consume nonhealthy food like chocolate by melting it.
So, there you are, if you want a weight-loss solution that tortures you and has far bigger holes than the one it leaves for your mouth, try the DentalSlim. Or, you know, don’t eat that eighth slice of pizza and maybe go for a walk later. Your choice.
Two case reports identify Guillain-Barré variants after SARS-CoV-2 vaccination
Guillain-Barré syndrome, a rare peripheral nerve disorder that can occur after certain types of viral and bacterial infections, has not to date been definitively linked to infection by SARS-CoV-2 or with vaccination against the virus, despite surveillance searching for such associations.
Spikes in Guillain-Barré syndrome incidence have previously, but rarely, been associated with outbreaks of other viral diseases, including Zika, but not with vaccination, except for a 1976-1977 swine influenza vaccine campaign in the United States that was seen associated with a slight elevation in risk, and was halted when that risk became known. Since then, all sorts of vaccines in the European Union and United States have come with warnings about Guillain-Barré syndrome in their package inserts – a fact that some Guillain-Barré syndrome experts lament as perpetuating the notion that vaccines cause Guillain-Barré syndrome.
Epidemiologic studies in the United Kingdom and Singapore did not detect increases in Guillain-Barré syndrome incidence during the COVID-19 pandemic. And as mass vaccination against COVID-19 got underway early this year, experts cautioned against the temptation to attribute incident Guillain-Barré syndrome cases following vaccination to SARS-CoV-2 without careful statistical and epidemiological analysis. Until now reports of Guillain-Barré syndrome have been scant: clinical trials of a viral vector vaccine developed by Johnson & Johnson saw one in the placebo arm and another in the intervention arm, while another case was reported following administration of a Pfizer mRNA SARS-Cov-2 vaccine.
Recent case reports
None of the patients had evidence of current SARS-CoV-2 infection.
From India, Boby V. Maramattom, MD, of Aster Medcity in Kochi, India, and colleagues reported on seven severe cases of Guillain-Barré syndrome occurring between 10 and 14 days after a first dose of the AstraZeneca vaccine. All but one of the patients were women, all had bilateral facial paresis, all progressed to areflexic quadriplegia, and six required respiratory support. Patients’ ages ranged from 43 to 70. Four developed other cranial neuropathies, including abducens palsy and trigeminal sensory nerve involvement, which are rare in reports of Guillain-Barré syndrome from India, Dr. Maramattom and colleagues noted.
The authors argued that their findings “should prompt all physicians to be vigilant in recognizing Guillain-Barré syndrome in patients who have received the AstraZeneca vaccine. While the risk per patient (5.8 per million) may be relatively low, our observations suggest that this clinically distinct [Guillain-Barré syndrome] variant is more severe than usual and may require mechanical ventilation.”
The U.K. cases, reported by Christopher Martin Allen, MD, and colleagues at Nottingham (England) University Hospitals NHS Trust, describe bifacial weakness and normal facial sensation in four men between 11 and 22 days after their first doses of the Astra-Zeneca vaccine. This type of facial palsy, the authors wrote, was unusual Guillain-Barré syndrome variant that one rapid review found in 3 of 42 European patients diagnosed with Guillain-Barré syndrome following SARS-CoV-2 infection.
Dr. Allen and colleagues acknowledged that causality could not be assumed from the temporal relationship of immunization to onset of bifacial weakness in their report, but argued that their findings argued for “robust postvaccination surveillance” and that “the report of a similar syndrome in the setting of SARS-CoV-2 infection suggests an immunologic response to the spike protein.” If the link is casual, they wrote, “it could be due to a cross-reactive immune response to the SARS-CoV-2 spike protein and components of the peripheral immune system.”
‘The jury is still out’
Asked for comment, neurologist Anthony Amato, MD, of Brigham and Women’s Hospital, Boston, said that he did not see what the two new studies add to what is already known. “Guillain-Barré syndrome has already been reported temporally following COVID-19 along with accompanying editorials that such temporal occurrences do not imply causation and there is a need for surveillance and epidemiological studies.”
Robert Lisak, MD, of Wayne State University, Detroit, and a longtime adviser to the GBS-CIDP Foundation International, commented that “the relationship between vaccines and association with Guillain-Barré syndrome continues to be controversial in part because Guillain-Barré syndrome, a rare disorder, has many reported associated illnesses including infections. Many vaccines have been implicated but with the probable exception of the ‘swine flu’ vaccine in the 1970s, most have not stood up to scrutiny.”
With SARS-Cov-2 infection and vaccines, “the jury is still out,” Dr. Lisak said. “The report from the U.K. is intriguing since they report several cases of an uncommon variant, but the cases from India seem to be more of the usual forms of Guillain-Barré syndrome.”
Dr. Lisak noted that, even if an association turns out to be valid, “we are talking about a very low incidence of Guillain-Barré syndrome associated with COVID-19 vaccines,” one that would not justify avoiding them because of a possible association with Guillain-Barré syndrome.
The GBS-CIDP Foundation, which supports research into Guillain-Barré syndrome and related diseases, has likewise stressed the low risk presented by SARS-CoV-2 vaccines, noting on its website that “the risk of death or long-term complications from COVID in adults still far exceeds the risk of any possible risk of Guillain-Barré syndrome by several orders of magnitude.”
None of the study authors reported financial conflicts of interest related to their research. Dr. Amato is an adviser to the pharmaceutical firms Alexion and Argenx, while Dr. Lisak has received research support or honoraria from Alexion, Novartis, Hoffmann–La Roche, and others.
Guillain-Barré syndrome, a rare peripheral nerve disorder that can occur after certain types of viral and bacterial infections, has not to date been definitively linked to infection by SARS-CoV-2 or with vaccination against the virus, despite surveillance searching for such associations.
Spikes in Guillain-Barré syndrome incidence have previously, but rarely, been associated with outbreaks of other viral diseases, including Zika, but not with vaccination, except for a 1976-1977 swine influenza vaccine campaign in the United States that was seen associated with a slight elevation in risk, and was halted when that risk became known. Since then, all sorts of vaccines in the European Union and United States have come with warnings about Guillain-Barré syndrome in their package inserts – a fact that some Guillain-Barré syndrome experts lament as perpetuating the notion that vaccines cause Guillain-Barré syndrome.
Epidemiologic studies in the United Kingdom and Singapore did not detect increases in Guillain-Barré syndrome incidence during the COVID-19 pandemic. And as mass vaccination against COVID-19 got underway early this year, experts cautioned against the temptation to attribute incident Guillain-Barré syndrome cases following vaccination to SARS-CoV-2 without careful statistical and epidemiological analysis. Until now reports of Guillain-Barré syndrome have been scant: clinical trials of a viral vector vaccine developed by Johnson & Johnson saw one in the placebo arm and another in the intervention arm, while another case was reported following administration of a Pfizer mRNA SARS-Cov-2 vaccine.
Recent case reports
None of the patients had evidence of current SARS-CoV-2 infection.
From India, Boby V. Maramattom, MD, of Aster Medcity in Kochi, India, and colleagues reported on seven severe cases of Guillain-Barré syndrome occurring between 10 and 14 days after a first dose of the AstraZeneca vaccine. All but one of the patients were women, all had bilateral facial paresis, all progressed to areflexic quadriplegia, and six required respiratory support. Patients’ ages ranged from 43 to 70. Four developed other cranial neuropathies, including abducens palsy and trigeminal sensory nerve involvement, which are rare in reports of Guillain-Barré syndrome from India, Dr. Maramattom and colleagues noted.
The authors argued that their findings “should prompt all physicians to be vigilant in recognizing Guillain-Barré syndrome in patients who have received the AstraZeneca vaccine. While the risk per patient (5.8 per million) may be relatively low, our observations suggest that this clinically distinct [Guillain-Barré syndrome] variant is more severe than usual and may require mechanical ventilation.”
The U.K. cases, reported by Christopher Martin Allen, MD, and colleagues at Nottingham (England) University Hospitals NHS Trust, describe bifacial weakness and normal facial sensation in four men between 11 and 22 days after their first doses of the Astra-Zeneca vaccine. This type of facial palsy, the authors wrote, was unusual Guillain-Barré syndrome variant that one rapid review found in 3 of 42 European patients diagnosed with Guillain-Barré syndrome following SARS-CoV-2 infection.
Dr. Allen and colleagues acknowledged that causality could not be assumed from the temporal relationship of immunization to onset of bifacial weakness in their report, but argued that their findings argued for “robust postvaccination surveillance” and that “the report of a similar syndrome in the setting of SARS-CoV-2 infection suggests an immunologic response to the spike protein.” If the link is casual, they wrote, “it could be due to a cross-reactive immune response to the SARS-CoV-2 spike protein and components of the peripheral immune system.”
‘The jury is still out’
Asked for comment, neurologist Anthony Amato, MD, of Brigham and Women’s Hospital, Boston, said that he did not see what the two new studies add to what is already known. “Guillain-Barré syndrome has already been reported temporally following COVID-19 along with accompanying editorials that such temporal occurrences do not imply causation and there is a need for surveillance and epidemiological studies.”
Robert Lisak, MD, of Wayne State University, Detroit, and a longtime adviser to the GBS-CIDP Foundation International, commented that “the relationship between vaccines and association with Guillain-Barré syndrome continues to be controversial in part because Guillain-Barré syndrome, a rare disorder, has many reported associated illnesses including infections. Many vaccines have been implicated but with the probable exception of the ‘swine flu’ vaccine in the 1970s, most have not stood up to scrutiny.”
With SARS-Cov-2 infection and vaccines, “the jury is still out,” Dr. Lisak said. “The report from the U.K. is intriguing since they report several cases of an uncommon variant, but the cases from India seem to be more of the usual forms of Guillain-Barré syndrome.”
Dr. Lisak noted that, even if an association turns out to be valid, “we are talking about a very low incidence of Guillain-Barré syndrome associated with COVID-19 vaccines,” one that would not justify avoiding them because of a possible association with Guillain-Barré syndrome.
The GBS-CIDP Foundation, which supports research into Guillain-Barré syndrome and related diseases, has likewise stressed the low risk presented by SARS-CoV-2 vaccines, noting on its website that “the risk of death or long-term complications from COVID in adults still far exceeds the risk of any possible risk of Guillain-Barré syndrome by several orders of magnitude.”
None of the study authors reported financial conflicts of interest related to their research. Dr. Amato is an adviser to the pharmaceutical firms Alexion and Argenx, while Dr. Lisak has received research support or honoraria from Alexion, Novartis, Hoffmann–La Roche, and others.
Guillain-Barré syndrome, a rare peripheral nerve disorder that can occur after certain types of viral and bacterial infections, has not to date been definitively linked to infection by SARS-CoV-2 or with vaccination against the virus, despite surveillance searching for such associations.
Spikes in Guillain-Barré syndrome incidence have previously, but rarely, been associated with outbreaks of other viral diseases, including Zika, but not with vaccination, except for a 1976-1977 swine influenza vaccine campaign in the United States that was seen associated with a slight elevation in risk, and was halted when that risk became known. Since then, all sorts of vaccines in the European Union and United States have come with warnings about Guillain-Barré syndrome in their package inserts – a fact that some Guillain-Barré syndrome experts lament as perpetuating the notion that vaccines cause Guillain-Barré syndrome.
Epidemiologic studies in the United Kingdom and Singapore did not detect increases in Guillain-Barré syndrome incidence during the COVID-19 pandemic. And as mass vaccination against COVID-19 got underway early this year, experts cautioned against the temptation to attribute incident Guillain-Barré syndrome cases following vaccination to SARS-CoV-2 without careful statistical and epidemiological analysis. Until now reports of Guillain-Barré syndrome have been scant: clinical trials of a viral vector vaccine developed by Johnson & Johnson saw one in the placebo arm and another in the intervention arm, while another case was reported following administration of a Pfizer mRNA SARS-Cov-2 vaccine.
Recent case reports
None of the patients had evidence of current SARS-CoV-2 infection.
From India, Boby V. Maramattom, MD, of Aster Medcity in Kochi, India, and colleagues reported on seven severe cases of Guillain-Barré syndrome occurring between 10 and 14 days after a first dose of the AstraZeneca vaccine. All but one of the patients were women, all had bilateral facial paresis, all progressed to areflexic quadriplegia, and six required respiratory support. Patients’ ages ranged from 43 to 70. Four developed other cranial neuropathies, including abducens palsy and trigeminal sensory nerve involvement, which are rare in reports of Guillain-Barré syndrome from India, Dr. Maramattom and colleagues noted.
The authors argued that their findings “should prompt all physicians to be vigilant in recognizing Guillain-Barré syndrome in patients who have received the AstraZeneca vaccine. While the risk per patient (5.8 per million) may be relatively low, our observations suggest that this clinically distinct [Guillain-Barré syndrome] variant is more severe than usual and may require mechanical ventilation.”
The U.K. cases, reported by Christopher Martin Allen, MD, and colleagues at Nottingham (England) University Hospitals NHS Trust, describe bifacial weakness and normal facial sensation in four men between 11 and 22 days after their first doses of the Astra-Zeneca vaccine. This type of facial palsy, the authors wrote, was unusual Guillain-Barré syndrome variant that one rapid review found in 3 of 42 European patients diagnosed with Guillain-Barré syndrome following SARS-CoV-2 infection.
Dr. Allen and colleagues acknowledged that causality could not be assumed from the temporal relationship of immunization to onset of bifacial weakness in their report, but argued that their findings argued for “robust postvaccination surveillance” and that “the report of a similar syndrome in the setting of SARS-CoV-2 infection suggests an immunologic response to the spike protein.” If the link is casual, they wrote, “it could be due to a cross-reactive immune response to the SARS-CoV-2 spike protein and components of the peripheral immune system.”
‘The jury is still out’
Asked for comment, neurologist Anthony Amato, MD, of Brigham and Women’s Hospital, Boston, said that he did not see what the two new studies add to what is already known. “Guillain-Barré syndrome has already been reported temporally following COVID-19 along with accompanying editorials that such temporal occurrences do not imply causation and there is a need for surveillance and epidemiological studies.”
Robert Lisak, MD, of Wayne State University, Detroit, and a longtime adviser to the GBS-CIDP Foundation International, commented that “the relationship between vaccines and association with Guillain-Barré syndrome continues to be controversial in part because Guillain-Barré syndrome, a rare disorder, has many reported associated illnesses including infections. Many vaccines have been implicated but with the probable exception of the ‘swine flu’ vaccine in the 1970s, most have not stood up to scrutiny.”
With SARS-Cov-2 infection and vaccines, “the jury is still out,” Dr. Lisak said. “The report from the U.K. is intriguing since they report several cases of an uncommon variant, but the cases from India seem to be more of the usual forms of Guillain-Barré syndrome.”
Dr. Lisak noted that, even if an association turns out to be valid, “we are talking about a very low incidence of Guillain-Barré syndrome associated with COVID-19 vaccines,” one that would not justify avoiding them because of a possible association with Guillain-Barré syndrome.
The GBS-CIDP Foundation, which supports research into Guillain-Barré syndrome and related diseases, has likewise stressed the low risk presented by SARS-CoV-2 vaccines, noting on its website that “the risk of death or long-term complications from COVID in adults still far exceeds the risk of any possible risk of Guillain-Barré syndrome by several orders of magnitude.”
None of the study authors reported financial conflicts of interest related to their research. Dr. Amato is an adviser to the pharmaceutical firms Alexion and Argenx, while Dr. Lisak has received research support or honoraria from Alexion, Novartis, Hoffmann–La Roche, and others.
FROM ANNALS OF NEUROLOGY
The pandemic hurt patients with liver disease in many ways
The COVID-19 pandemic has worsened the health of patients with liver disease worldwide, researchers say.
Not only does liver disease make people more vulnerable to the virus that causes COVID-19, precautions to prevent its spread have delayed health care and worsened alcohol abuse.
At this year’s virtual International Liver Congress (ILC) 2021, experts from around the world documented this toll on their patients.
Surgeons have seen a surge in patients needing transplants because of alcoholic liver disease, the campaign to snuff out hepatitis C slowed down, and procedures such as endoscopy and ultrasound exams postponed, said Mario Mondelli, MD, PhD, a professor and consultant physician of infectious diseases at the University of Pavia, Italy.
“We were able to ensure only emergency treatments, not routine surveillance,” he said in an interview.
Of 1,994 people with chronic liver disease who responded to a survey through the Global Liver Registry, 11% reported that the pandemic had affected their liver health.
This proportion was not statistically different for the 165 patients (8.2%) who had been diagnosed with COVID-19 compared with those who had not. But many of those who had been diagnosed with COVID-19 reported that it severely affected them. They reported worse overall heath, more mental illness, and greater need for supportive service than those who evaded the virus. Thirty-three respondents (20.8%) were hospitalized.
The global effort to eradicate hepatitis C slowed as a result of the pandemic. Already in 2019, the United States was behind the World Health Organization schedule for eliminating this virus. In 2020, it slipped further, with 25% fewer patients starting treatment for hepatitis C than in 2019, according to researchers at the U.S. Centers for Disease Control and Prevention.
Similar delays in eliminating hepatitis C occurred around the world, Dr. Mondelli said, noting that the majority of countries will not be able to reach the WHO objectives.
One striking result of the pandemic was an uptick of patients needing liver transplants as a result of alcoholic liver disease, said George Cholankeril, MD, a liver transplant surgeon at Baylor College of Medicine, Houston.
Before the pandemic, he and his colleagues had noted an increase in the number of people needing liver transplants because of alcohol abuse. During the pandemic, that trend accelerated.
They defined the pre-COVID era as June 1, 2019, to Feb. 29, 2020, and the COVID era as after April 1, 2020. In the COVID era, alcoholic liver disease accounted for 40% of patients whom the hospital put on its list for liver transplant. Hepatitis C and nonalcoholic fatty liver disease combined accounted for only 36%.
The change has resulted in part from the effectiveness of hepatitis C treatments, which have reduced the number of patients with livers damaged by that virus. But the change also resulted from the increased severity of illness in the patients with alcoholic liver disease, Dr. Cholankeril said in an interview. Overall, Model for End-Stage Liver Disease scores – which are used to predict survival – worsened for patients with alcoholic liver disease but remained the same for patients with nonalcoholic liver disease.
In the pre-COVID era, patients with alcoholic liver disease had a 10% higher chance for undergoing transplant, compared with patients with nonalcoholic liver disease. In the COVID era, they had a 50% higher chance, a statistically significant change (P < .001).
The finding parallels those of other studies that have shown a spike in consults for alcohol-related gastrointestinal and liver diseases, as reported by this news organization.
“We feel that the increase in alcoholic hepatitis is possibly from binge drinking and alcoholic consumption during the pandemic,” said Dr. Cholankeril. “Anecdotally, I can’t tell you how many patients say that the video meetings for Alcoholic Anonymous just don’t work. It’s not the same as in person. They don’t feel that they’re getting the support that they need.”
In Europe, fewer of the people who need liver transplants may be receiving them, said Dr. Mondelli.
“There are several papers indicating, particularly in Italy, in France, and in the United Kingdom, that during the pandemic, the offer for organs significantly declined,” he said.
Other studies have shown increases in mortality from liver disease during the pandemic, Dr. Mondelli said. The same is true of myocardial infarction, cancer, and most other life-threatening illnesses, he pointed out.
“Because of the enormous tsunami that has affected hospital services during the peaks of the pandemic, there has been an increase in deceased patients from a variety of other diseases, not only liver disease,” he said.
But Dr. Mondelli also added that physicians had improved in their ability to safely care for their patients while protecting themselves over the course of the pandemic.
Dr. Mondelli and Dr. Cholankeril have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic has worsened the health of patients with liver disease worldwide, researchers say.
Not only does liver disease make people more vulnerable to the virus that causes COVID-19, precautions to prevent its spread have delayed health care and worsened alcohol abuse.
At this year’s virtual International Liver Congress (ILC) 2021, experts from around the world documented this toll on their patients.
Surgeons have seen a surge in patients needing transplants because of alcoholic liver disease, the campaign to snuff out hepatitis C slowed down, and procedures such as endoscopy and ultrasound exams postponed, said Mario Mondelli, MD, PhD, a professor and consultant physician of infectious diseases at the University of Pavia, Italy.
“We were able to ensure only emergency treatments, not routine surveillance,” he said in an interview.
Of 1,994 people with chronic liver disease who responded to a survey through the Global Liver Registry, 11% reported that the pandemic had affected their liver health.
This proportion was not statistically different for the 165 patients (8.2%) who had been diagnosed with COVID-19 compared with those who had not. But many of those who had been diagnosed with COVID-19 reported that it severely affected them. They reported worse overall heath, more mental illness, and greater need for supportive service than those who evaded the virus. Thirty-three respondents (20.8%) were hospitalized.
The global effort to eradicate hepatitis C slowed as a result of the pandemic. Already in 2019, the United States was behind the World Health Organization schedule for eliminating this virus. In 2020, it slipped further, with 25% fewer patients starting treatment for hepatitis C than in 2019, according to researchers at the U.S. Centers for Disease Control and Prevention.
Similar delays in eliminating hepatitis C occurred around the world, Dr. Mondelli said, noting that the majority of countries will not be able to reach the WHO objectives.
One striking result of the pandemic was an uptick of patients needing liver transplants as a result of alcoholic liver disease, said George Cholankeril, MD, a liver transplant surgeon at Baylor College of Medicine, Houston.
Before the pandemic, he and his colleagues had noted an increase in the number of people needing liver transplants because of alcohol abuse. During the pandemic, that trend accelerated.
They defined the pre-COVID era as June 1, 2019, to Feb. 29, 2020, and the COVID era as after April 1, 2020. In the COVID era, alcoholic liver disease accounted for 40% of patients whom the hospital put on its list for liver transplant. Hepatitis C and nonalcoholic fatty liver disease combined accounted for only 36%.
The change has resulted in part from the effectiveness of hepatitis C treatments, which have reduced the number of patients with livers damaged by that virus. But the change also resulted from the increased severity of illness in the patients with alcoholic liver disease, Dr. Cholankeril said in an interview. Overall, Model for End-Stage Liver Disease scores – which are used to predict survival – worsened for patients with alcoholic liver disease but remained the same for patients with nonalcoholic liver disease.
In the pre-COVID era, patients with alcoholic liver disease had a 10% higher chance for undergoing transplant, compared with patients with nonalcoholic liver disease. In the COVID era, they had a 50% higher chance, a statistically significant change (P < .001).
The finding parallels those of other studies that have shown a spike in consults for alcohol-related gastrointestinal and liver diseases, as reported by this news organization.
“We feel that the increase in alcoholic hepatitis is possibly from binge drinking and alcoholic consumption during the pandemic,” said Dr. Cholankeril. “Anecdotally, I can’t tell you how many patients say that the video meetings for Alcoholic Anonymous just don’t work. It’s not the same as in person. They don’t feel that they’re getting the support that they need.”
In Europe, fewer of the people who need liver transplants may be receiving them, said Dr. Mondelli.
“There are several papers indicating, particularly in Italy, in France, and in the United Kingdom, that during the pandemic, the offer for organs significantly declined,” he said.
Other studies have shown increases in mortality from liver disease during the pandemic, Dr. Mondelli said. The same is true of myocardial infarction, cancer, and most other life-threatening illnesses, he pointed out.
“Because of the enormous tsunami that has affected hospital services during the peaks of the pandemic, there has been an increase in deceased patients from a variety of other diseases, not only liver disease,” he said.
But Dr. Mondelli also added that physicians had improved in their ability to safely care for their patients while protecting themselves over the course of the pandemic.
Dr. Mondelli and Dr. Cholankeril have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic has worsened the health of patients with liver disease worldwide, researchers say.
Not only does liver disease make people more vulnerable to the virus that causes COVID-19, precautions to prevent its spread have delayed health care and worsened alcohol abuse.
At this year’s virtual International Liver Congress (ILC) 2021, experts from around the world documented this toll on their patients.
Surgeons have seen a surge in patients needing transplants because of alcoholic liver disease, the campaign to snuff out hepatitis C slowed down, and procedures such as endoscopy and ultrasound exams postponed, said Mario Mondelli, MD, PhD, a professor and consultant physician of infectious diseases at the University of Pavia, Italy.
“We were able to ensure only emergency treatments, not routine surveillance,” he said in an interview.
Of 1,994 people with chronic liver disease who responded to a survey through the Global Liver Registry, 11% reported that the pandemic had affected their liver health.
This proportion was not statistically different for the 165 patients (8.2%) who had been diagnosed with COVID-19 compared with those who had not. But many of those who had been diagnosed with COVID-19 reported that it severely affected them. They reported worse overall heath, more mental illness, and greater need for supportive service than those who evaded the virus. Thirty-three respondents (20.8%) were hospitalized.
The global effort to eradicate hepatitis C slowed as a result of the pandemic. Already in 2019, the United States was behind the World Health Organization schedule for eliminating this virus. In 2020, it slipped further, with 25% fewer patients starting treatment for hepatitis C than in 2019, according to researchers at the U.S. Centers for Disease Control and Prevention.
Similar delays in eliminating hepatitis C occurred around the world, Dr. Mondelli said, noting that the majority of countries will not be able to reach the WHO objectives.
One striking result of the pandemic was an uptick of patients needing liver transplants as a result of alcoholic liver disease, said George Cholankeril, MD, a liver transplant surgeon at Baylor College of Medicine, Houston.
Before the pandemic, he and his colleagues had noted an increase in the number of people needing liver transplants because of alcohol abuse. During the pandemic, that trend accelerated.
They defined the pre-COVID era as June 1, 2019, to Feb. 29, 2020, and the COVID era as after April 1, 2020. In the COVID era, alcoholic liver disease accounted for 40% of patients whom the hospital put on its list for liver transplant. Hepatitis C and nonalcoholic fatty liver disease combined accounted for only 36%.
The change has resulted in part from the effectiveness of hepatitis C treatments, which have reduced the number of patients with livers damaged by that virus. But the change also resulted from the increased severity of illness in the patients with alcoholic liver disease, Dr. Cholankeril said in an interview. Overall, Model for End-Stage Liver Disease scores – which are used to predict survival – worsened for patients with alcoholic liver disease but remained the same for patients with nonalcoholic liver disease.
In the pre-COVID era, patients with alcoholic liver disease had a 10% higher chance for undergoing transplant, compared with patients with nonalcoholic liver disease. In the COVID era, they had a 50% higher chance, a statistically significant change (P < .001).
The finding parallels those of other studies that have shown a spike in consults for alcohol-related gastrointestinal and liver diseases, as reported by this news organization.
“We feel that the increase in alcoholic hepatitis is possibly from binge drinking and alcoholic consumption during the pandemic,” said Dr. Cholankeril. “Anecdotally, I can’t tell you how many patients say that the video meetings for Alcoholic Anonymous just don’t work. It’s not the same as in person. They don’t feel that they’re getting the support that they need.”
In Europe, fewer of the people who need liver transplants may be receiving them, said Dr. Mondelli.
“There are several papers indicating, particularly in Italy, in France, and in the United Kingdom, that during the pandemic, the offer for organs significantly declined,” he said.
Other studies have shown increases in mortality from liver disease during the pandemic, Dr. Mondelli said. The same is true of myocardial infarction, cancer, and most other life-threatening illnesses, he pointed out.
“Because of the enormous tsunami that has affected hospital services during the peaks of the pandemic, there has been an increase in deceased patients from a variety of other diseases, not only liver disease,” he said.
But Dr. Mondelli also added that physicians had improved in their ability to safely care for their patients while protecting themselves over the course of the pandemic.
Dr. Mondelli and Dr. Cholankeril have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Doxycycline trumps azithromycin for asymptomatic rectal chlamydia in men who have sex with men
A 1-week course of doxycycline is more effective than single-dose azithromycin to treat rectal chlamydia in men who have sex with men (MSM), according to newly published results in the New England Journal of Medicine.
Chlamydia is the most commonly reported bacterial STI in the United States, with 4 million cases reported in 2018, and 127 million globally. Most infections are asymptomatic.
Rates of rectal chlamydia among MSM screened for infection range from 3% to 10.5%.
The most recent Centers for Disease Control and Prevention chlamydia guidelines recommend either a single dose of azithromycin (1 g) or doxycycline 100 mg twice daily for 7 days. These 2015 guidelines were based on a meta-analysis of urogenital chlamydia infections, which showed comparable efficacy of 97% or 98%, respectively.
Study coauthor Jane S. Hocking, PhD, head of the sexual health unit at the University of Melbourne, told this news organization that “observational studies had suggested that azithromycin was about 20% less effective than doxycycline,” prompting this clinical trial.
The study, conducted at five sexual health clinics in Australia, was a double-blind, randomized, controlled trial of doxycycline (100 mg twice daily for 7 days) or azithromycin (1-g single dose).
Because 85% of infected men are asymptomatic, the study’s primary outcome was a negative nucleic acid amplification test at 4 weeks, confirming a microbiologic cure.
Using a modified intention-to-treat population, the study showed a microbiologic cure in 281 of 290 men (96.9%) in the doxycycline group and 227 of 297 (76.4%) in the azithromycin group (P < .001).
Adverse events were more common in the azithromycin group. Nausea, diarrhea, and vomiting occurred in 134 (45.1%) men in that group versus 98 men (33.8%) in those receiving doxycycline (P = .006).
A similar study was reported in Clinical Infectious Diseases in February 2021 by Dombrowski and colleagues. It was also randomized, double blinded, and placebo controlled but was smaller and conducted in Seattle and Boston. A 20% difference was found, with 80/88 (91%) in the doxycycline group and 63/89 (71%) in the azithromycin group having a microbiologic cure at 4 weeks of follow-up.
Jeanne Marrazzo, MD, director of the division of infectious diseases at the University of Alabama at Birmingham, said in an interview that the researchers focused solely on asymptomatic proctitis because “other symptoms might indicate need for broader presumptive antibiotics” for coinfections. Similarly, symptomatic proctitis “could indicate LGV [lymphogranuloma venereum] chlamydia, which ... automatically mandates that 3-weeks of doxycycline be used.” Dr. Marrazzo concluded: “The fact that this was a blinded study obviously strengthens the conclusions/findings, which is great. It’s very reassuring that results overall are so consistent with the CID paper.” Dr. Marrazzo was not involved in either the New England Journal of Medicine investigation or CID study.
Ina Park, MD, associate professor in the department of family and community medicine at the University of California, San Francisco, and author of “Strange Bedfellows: Adventures in the Science, History, and Surprising Secrets of STDs,” (New York: Flatiron Books, 2021) was not involved in either study but has a long history of working with adolescents in clinics for STDs. Based on that experience, she told this news organization that, while doxycycline now clearly appears to be the drug of choice, “if compliance is an issue and rectal chlamydia is not likely, then I think azithromycin is still something we need to consider, particularly for younger patients, and folks for whom compliance is going to be an issue.” She added: “with adolescent patients, there are issues of parents possibly discovering the antibiotic and asking lots of questions. So, it’s very nice for folks to be able to get therapy, sort of a one and done approach in the clinic.”
The 2020 CDC Guidelines for Gonococcal Infections says: “CDC recommends a single 500 mg intramuscular dose of ceftriaxone for uncomplicated gonorrhea. Treatment for coinfection with Chlamydia trachomatis with oral doxycycline (100 mg twice daily for 7 days) should be administered when chlamydial infection has not been excluded.”
Hocking concluded – and Dr. Marrazzo and Dr. Park concur – that this study “provides conclusive evidence that doxycycline should be the first-line treatment for rectal chlamydia, but probably for just any chlamydia infection,” with specific exceptions.
The University of Melbourne researchers also noted that the doxycycline course requires more compliant patients, as adherence isn’t assured. The issue of compliance and need for directly observed therapy, allergy to doxycycline, and pregnancy (where doxycycline is contraindicated) will remain the primary indications for continued use of azithromycin.
A version of this article first appeared on Medscape.com.
A 1-week course of doxycycline is more effective than single-dose azithromycin to treat rectal chlamydia in men who have sex with men (MSM), according to newly published results in the New England Journal of Medicine.
Chlamydia is the most commonly reported bacterial STI in the United States, with 4 million cases reported in 2018, and 127 million globally. Most infections are asymptomatic.
Rates of rectal chlamydia among MSM screened for infection range from 3% to 10.5%.
The most recent Centers for Disease Control and Prevention chlamydia guidelines recommend either a single dose of azithromycin (1 g) or doxycycline 100 mg twice daily for 7 days. These 2015 guidelines were based on a meta-analysis of urogenital chlamydia infections, which showed comparable efficacy of 97% or 98%, respectively.
Study coauthor Jane S. Hocking, PhD, head of the sexual health unit at the University of Melbourne, told this news organization that “observational studies had suggested that azithromycin was about 20% less effective than doxycycline,” prompting this clinical trial.
The study, conducted at five sexual health clinics in Australia, was a double-blind, randomized, controlled trial of doxycycline (100 mg twice daily for 7 days) or azithromycin (1-g single dose).
Because 85% of infected men are asymptomatic, the study’s primary outcome was a negative nucleic acid amplification test at 4 weeks, confirming a microbiologic cure.
Using a modified intention-to-treat population, the study showed a microbiologic cure in 281 of 290 men (96.9%) in the doxycycline group and 227 of 297 (76.4%) in the azithromycin group (P < .001).
Adverse events were more common in the azithromycin group. Nausea, diarrhea, and vomiting occurred in 134 (45.1%) men in that group versus 98 men (33.8%) in those receiving doxycycline (P = .006).
A similar study was reported in Clinical Infectious Diseases in February 2021 by Dombrowski and colleagues. It was also randomized, double blinded, and placebo controlled but was smaller and conducted in Seattle and Boston. A 20% difference was found, with 80/88 (91%) in the doxycycline group and 63/89 (71%) in the azithromycin group having a microbiologic cure at 4 weeks of follow-up.
Jeanne Marrazzo, MD, director of the division of infectious diseases at the University of Alabama at Birmingham, said in an interview that the researchers focused solely on asymptomatic proctitis because “other symptoms might indicate need for broader presumptive antibiotics” for coinfections. Similarly, symptomatic proctitis “could indicate LGV [lymphogranuloma venereum] chlamydia, which ... automatically mandates that 3-weeks of doxycycline be used.” Dr. Marrazzo concluded: “The fact that this was a blinded study obviously strengthens the conclusions/findings, which is great. It’s very reassuring that results overall are so consistent with the CID paper.” Dr. Marrazzo was not involved in either the New England Journal of Medicine investigation or CID study.
Ina Park, MD, associate professor in the department of family and community medicine at the University of California, San Francisco, and author of “Strange Bedfellows: Adventures in the Science, History, and Surprising Secrets of STDs,” (New York: Flatiron Books, 2021) was not involved in either study but has a long history of working with adolescents in clinics for STDs. Based on that experience, she told this news organization that, while doxycycline now clearly appears to be the drug of choice, “if compliance is an issue and rectal chlamydia is not likely, then I think azithromycin is still something we need to consider, particularly for younger patients, and folks for whom compliance is going to be an issue.” She added: “with adolescent patients, there are issues of parents possibly discovering the antibiotic and asking lots of questions. So, it’s very nice for folks to be able to get therapy, sort of a one and done approach in the clinic.”
The 2020 CDC Guidelines for Gonococcal Infections says: “CDC recommends a single 500 mg intramuscular dose of ceftriaxone for uncomplicated gonorrhea. Treatment for coinfection with Chlamydia trachomatis with oral doxycycline (100 mg twice daily for 7 days) should be administered when chlamydial infection has not been excluded.”
Hocking concluded – and Dr. Marrazzo and Dr. Park concur – that this study “provides conclusive evidence that doxycycline should be the first-line treatment for rectal chlamydia, but probably for just any chlamydia infection,” with specific exceptions.
The University of Melbourne researchers also noted that the doxycycline course requires more compliant patients, as adherence isn’t assured. The issue of compliance and need for directly observed therapy, allergy to doxycycline, and pregnancy (where doxycycline is contraindicated) will remain the primary indications for continued use of azithromycin.
A version of this article first appeared on Medscape.com.
A 1-week course of doxycycline is more effective than single-dose azithromycin to treat rectal chlamydia in men who have sex with men (MSM), according to newly published results in the New England Journal of Medicine.
Chlamydia is the most commonly reported bacterial STI in the United States, with 4 million cases reported in 2018, and 127 million globally. Most infections are asymptomatic.
Rates of rectal chlamydia among MSM screened for infection range from 3% to 10.5%.
The most recent Centers for Disease Control and Prevention chlamydia guidelines recommend either a single dose of azithromycin (1 g) or doxycycline 100 mg twice daily for 7 days. These 2015 guidelines were based on a meta-analysis of urogenital chlamydia infections, which showed comparable efficacy of 97% or 98%, respectively.
Study coauthor Jane S. Hocking, PhD, head of the sexual health unit at the University of Melbourne, told this news organization that “observational studies had suggested that azithromycin was about 20% less effective than doxycycline,” prompting this clinical trial.
The study, conducted at five sexual health clinics in Australia, was a double-blind, randomized, controlled trial of doxycycline (100 mg twice daily for 7 days) or azithromycin (1-g single dose).
Because 85% of infected men are asymptomatic, the study’s primary outcome was a negative nucleic acid amplification test at 4 weeks, confirming a microbiologic cure.
Using a modified intention-to-treat population, the study showed a microbiologic cure in 281 of 290 men (96.9%) in the doxycycline group and 227 of 297 (76.4%) in the azithromycin group (P < .001).
Adverse events were more common in the azithromycin group. Nausea, diarrhea, and vomiting occurred in 134 (45.1%) men in that group versus 98 men (33.8%) in those receiving doxycycline (P = .006).
A similar study was reported in Clinical Infectious Diseases in February 2021 by Dombrowski and colleagues. It was also randomized, double blinded, and placebo controlled but was smaller and conducted in Seattle and Boston. A 20% difference was found, with 80/88 (91%) in the doxycycline group and 63/89 (71%) in the azithromycin group having a microbiologic cure at 4 weeks of follow-up.
Jeanne Marrazzo, MD, director of the division of infectious diseases at the University of Alabama at Birmingham, said in an interview that the researchers focused solely on asymptomatic proctitis because “other symptoms might indicate need for broader presumptive antibiotics” for coinfections. Similarly, symptomatic proctitis “could indicate LGV [lymphogranuloma venereum] chlamydia, which ... automatically mandates that 3-weeks of doxycycline be used.” Dr. Marrazzo concluded: “The fact that this was a blinded study obviously strengthens the conclusions/findings, which is great. It’s very reassuring that results overall are so consistent with the CID paper.” Dr. Marrazzo was not involved in either the New England Journal of Medicine investigation or CID study.
Ina Park, MD, associate professor in the department of family and community medicine at the University of California, San Francisco, and author of “Strange Bedfellows: Adventures in the Science, History, and Surprising Secrets of STDs,” (New York: Flatiron Books, 2021) was not involved in either study but has a long history of working with adolescents in clinics for STDs. Based on that experience, she told this news organization that, while doxycycline now clearly appears to be the drug of choice, “if compliance is an issue and rectal chlamydia is not likely, then I think azithromycin is still something we need to consider, particularly for younger patients, and folks for whom compliance is going to be an issue.” She added: “with adolescent patients, there are issues of parents possibly discovering the antibiotic and asking lots of questions. So, it’s very nice for folks to be able to get therapy, sort of a one and done approach in the clinic.”
The 2020 CDC Guidelines for Gonococcal Infections says: “CDC recommends a single 500 mg intramuscular dose of ceftriaxone for uncomplicated gonorrhea. Treatment for coinfection with Chlamydia trachomatis with oral doxycycline (100 mg twice daily for 7 days) should be administered when chlamydial infection has not been excluded.”
Hocking concluded – and Dr. Marrazzo and Dr. Park concur – that this study “provides conclusive evidence that doxycycline should be the first-line treatment for rectal chlamydia, but probably for just any chlamydia infection,” with specific exceptions.
The University of Melbourne researchers also noted that the doxycycline course requires more compliant patients, as adherence isn’t assured. The issue of compliance and need for directly observed therapy, allergy to doxycycline, and pregnancy (where doxycycline is contraindicated) will remain the primary indications for continued use of azithromycin.
A version of this article first appeared on Medscape.com.
Almost all U.S. COVID-19 deaths now in the unvaccinated
If you, a friend, or a loved one remain unvaccinated against COVID-19 at this point – for whatever reason – you are at higher risk of dying if you become infected.
That’s the conclusion of a new report released by the Associated Press looking at COVID-19 deaths during May 2021.
Of more than 18,000 people who died from COVID-19, for example, only about 150 were fully vaccinated. That’s less than 1%.
“Recently, I was working in the emergency room [and] I saw a 21-year-old African American who came in with shortness of breath,” said Vino K. Palli, MD, MPH, a physician specializing in emergency medicine, internal medicine, and urgent care.
The patient rapidly deteriorated and required intubation and ventilation. She was transferred to a specialized hospital for possible extracorporeal membrane oxygenation (ECMO) treatment.
“This patient was unvaccinated, along with her entire family. This would have been easily preventable,” added Dr. Palli, who is also founder and CEO of MiDoctor Urgent Care in New York City.
“Vaccine misinformation, compounded with vaccine inertia and vaccine access, have contributed to this,” he added. “Even though we have a surplus amount of vaccines at this time, we are only seeing 50% to 55% of completely vaccinated patients.”
Authors of the Associated Press report also acknowledge that some people who are fully vaccinated can get a breakthrough infection. These occurred in fewer than 1,200 of more than 853,000 people hospitalized for COVID-19 in May, or about 0.1%.
The Associated Press came up with these numbers using data from the Centers for Disease Control and Prevention. The CDC tracks the numbers of cases, hospitalizations, and deaths but does not breakdown rates by vaccination status.
Stronger argument for vaccination?
“The fact that only 0.8% of COVID-19 deaths are in the fully vaccinated should persuade those people still hesitant about vaccination,” said Hugh Cassiere, MD, medical director of Respiratory Therapy Services at North Shore University Hospital in Manhasset, New York.
Stuart C. Ray, MD, professor of medicine and oncology in the Division of Infectious Diseases at Johns Hopkins University, Baltimore, agreed. “It seems compelling, even for skeptics, that unvaccinated people represent 99% of those now dying from COVID-19 when they represent less than 50% of the adult population in the United States.”
The findings from the study could be more persuasive than previous arguments made in favor of immunization, Dr. Ray said. “These recent findings of striking reductions in risk of death in the vaccinated are more directly attributable and harder to ignore or dismiss.”
Brian Labus, PhD, MPH, of the University of Nevada Las Vegas (UNLV) is less convinced. “While this might change some peoples’ minds, it probably won’t make a major difference. People have many different reasons for not getting vaccinated, and this is only one of the things they consider.”
The study adds information that was not available before, said Dr. Labus, assistant professor in the Department of Epidemiology and Biostatistics at the UNLV School of Public Health. “We study the vaccine under tightly controlled, ideal conditions. This is the evidence that it works as well in the real world as it did in the trials, and that is what is most important in implementing a vaccination program,” added Dr. Labus.
“The scientific data has honed in on one thing: Vaccines are effective in preventing hospitalizations, ICU admissions, ventilations, and deaths,” agreed Dr. Palli.
“We now know that almost all deaths occurred in patients who were not vaccinated. We also know that all vaccines are effective against various strains that are in circulation right now, including the Delta variant, which is rapidly spreading,” Dr. Palli said.
Dr. Cassiere pointed out that the unvaccinated are not only at higher risk of developing COVID-19 but also of spreading, being hospitalized for, and dying from the infection. Avoiding “long hauler” symptoms is another argument in favor of immunization, he added.
As of June 28, the CDC reports that 63% of Americans 12 years and older have received at least one dose of a COVID-19 vaccine, and 54% are fully vaccinated.
Worldwide worry?
Although overall rates of U.S. COVID-19 hospitalizations and deaths are down, the outlook may not remain as encouraging. “I hope I’m wrong about this, but I anticipate that the coming fall and winter will bring increasingly localized versions of similar findings – severe disease and death due to SARS-CoV-2 infection in regions or groups with lower vaccination rates,” Dr. Ray said.
There could be a silver lining, he added: “If this unfortunate surge occurs, the health and economic consequences seem likely to erode much of the remaining hesitancy regarding vaccination.”
The rise of more infectious SARS-CoV-2 variants, such as the Delta variant, could also throw a wrench in controlling COVID-19. “This isn’t just a domestic issue,” Dr. Ray said. “We have learned that the world is a small place in pandemic times.”
The Associated Press investigators state that their findings support the high efficacy of the vaccine. Also, given the current widespread availability of COVID-19 vaccines in the United States, they believe many of the COVID-19 deaths now occurring are preventable.
Public health measures should have continued longer to protect unvaccinated individuals, especially Black Americans, Hispanic Americans, and other minorities, Dr. Palli said. “Only time will tell if re-opening and abandoning all public health measures by the CDC was premature.”
A version of this article first appeared on Medscape.com.
If you, a friend, or a loved one remain unvaccinated against COVID-19 at this point – for whatever reason – you are at higher risk of dying if you become infected.
That’s the conclusion of a new report released by the Associated Press looking at COVID-19 deaths during May 2021.
Of more than 18,000 people who died from COVID-19, for example, only about 150 were fully vaccinated. That’s less than 1%.
“Recently, I was working in the emergency room [and] I saw a 21-year-old African American who came in with shortness of breath,” said Vino K. Palli, MD, MPH, a physician specializing in emergency medicine, internal medicine, and urgent care.
The patient rapidly deteriorated and required intubation and ventilation. She was transferred to a specialized hospital for possible extracorporeal membrane oxygenation (ECMO) treatment.
“This patient was unvaccinated, along with her entire family. This would have been easily preventable,” added Dr. Palli, who is also founder and CEO of MiDoctor Urgent Care in New York City.
“Vaccine misinformation, compounded with vaccine inertia and vaccine access, have contributed to this,” he added. “Even though we have a surplus amount of vaccines at this time, we are only seeing 50% to 55% of completely vaccinated patients.”
Authors of the Associated Press report also acknowledge that some people who are fully vaccinated can get a breakthrough infection. These occurred in fewer than 1,200 of more than 853,000 people hospitalized for COVID-19 in May, or about 0.1%.
The Associated Press came up with these numbers using data from the Centers for Disease Control and Prevention. The CDC tracks the numbers of cases, hospitalizations, and deaths but does not breakdown rates by vaccination status.
Stronger argument for vaccination?
“The fact that only 0.8% of COVID-19 deaths are in the fully vaccinated should persuade those people still hesitant about vaccination,” said Hugh Cassiere, MD, medical director of Respiratory Therapy Services at North Shore University Hospital in Manhasset, New York.
Stuart C. Ray, MD, professor of medicine and oncology in the Division of Infectious Diseases at Johns Hopkins University, Baltimore, agreed. “It seems compelling, even for skeptics, that unvaccinated people represent 99% of those now dying from COVID-19 when they represent less than 50% of the adult population in the United States.”
The findings from the study could be more persuasive than previous arguments made in favor of immunization, Dr. Ray said. “These recent findings of striking reductions in risk of death in the vaccinated are more directly attributable and harder to ignore or dismiss.”
Brian Labus, PhD, MPH, of the University of Nevada Las Vegas (UNLV) is less convinced. “While this might change some peoples’ minds, it probably won’t make a major difference. People have many different reasons for not getting vaccinated, and this is only one of the things they consider.”
The study adds information that was not available before, said Dr. Labus, assistant professor in the Department of Epidemiology and Biostatistics at the UNLV School of Public Health. “We study the vaccine under tightly controlled, ideal conditions. This is the evidence that it works as well in the real world as it did in the trials, and that is what is most important in implementing a vaccination program,” added Dr. Labus.
“The scientific data has honed in on one thing: Vaccines are effective in preventing hospitalizations, ICU admissions, ventilations, and deaths,” agreed Dr. Palli.
“We now know that almost all deaths occurred in patients who were not vaccinated. We also know that all vaccines are effective against various strains that are in circulation right now, including the Delta variant, which is rapidly spreading,” Dr. Palli said.
Dr. Cassiere pointed out that the unvaccinated are not only at higher risk of developing COVID-19 but also of spreading, being hospitalized for, and dying from the infection. Avoiding “long hauler” symptoms is another argument in favor of immunization, he added.
As of June 28, the CDC reports that 63% of Americans 12 years and older have received at least one dose of a COVID-19 vaccine, and 54% are fully vaccinated.
Worldwide worry?
Although overall rates of U.S. COVID-19 hospitalizations and deaths are down, the outlook may not remain as encouraging. “I hope I’m wrong about this, but I anticipate that the coming fall and winter will bring increasingly localized versions of similar findings – severe disease and death due to SARS-CoV-2 infection in regions or groups with lower vaccination rates,” Dr. Ray said.
There could be a silver lining, he added: “If this unfortunate surge occurs, the health and economic consequences seem likely to erode much of the remaining hesitancy regarding vaccination.”
The rise of more infectious SARS-CoV-2 variants, such as the Delta variant, could also throw a wrench in controlling COVID-19. “This isn’t just a domestic issue,” Dr. Ray said. “We have learned that the world is a small place in pandemic times.”
The Associated Press investigators state that their findings support the high efficacy of the vaccine. Also, given the current widespread availability of COVID-19 vaccines in the United States, they believe many of the COVID-19 deaths now occurring are preventable.
Public health measures should have continued longer to protect unvaccinated individuals, especially Black Americans, Hispanic Americans, and other minorities, Dr. Palli said. “Only time will tell if re-opening and abandoning all public health measures by the CDC was premature.”
A version of this article first appeared on Medscape.com.
If you, a friend, or a loved one remain unvaccinated against COVID-19 at this point – for whatever reason – you are at higher risk of dying if you become infected.
That’s the conclusion of a new report released by the Associated Press looking at COVID-19 deaths during May 2021.
Of more than 18,000 people who died from COVID-19, for example, only about 150 were fully vaccinated. That’s less than 1%.
“Recently, I was working in the emergency room [and] I saw a 21-year-old African American who came in with shortness of breath,” said Vino K. Palli, MD, MPH, a physician specializing in emergency medicine, internal medicine, and urgent care.
The patient rapidly deteriorated and required intubation and ventilation. She was transferred to a specialized hospital for possible extracorporeal membrane oxygenation (ECMO) treatment.
“This patient was unvaccinated, along with her entire family. This would have been easily preventable,” added Dr. Palli, who is also founder and CEO of MiDoctor Urgent Care in New York City.
“Vaccine misinformation, compounded with vaccine inertia and vaccine access, have contributed to this,” he added. “Even though we have a surplus amount of vaccines at this time, we are only seeing 50% to 55% of completely vaccinated patients.”
Authors of the Associated Press report also acknowledge that some people who are fully vaccinated can get a breakthrough infection. These occurred in fewer than 1,200 of more than 853,000 people hospitalized for COVID-19 in May, or about 0.1%.
The Associated Press came up with these numbers using data from the Centers for Disease Control and Prevention. The CDC tracks the numbers of cases, hospitalizations, and deaths but does not breakdown rates by vaccination status.
Stronger argument for vaccination?
“The fact that only 0.8% of COVID-19 deaths are in the fully vaccinated should persuade those people still hesitant about vaccination,” said Hugh Cassiere, MD, medical director of Respiratory Therapy Services at North Shore University Hospital in Manhasset, New York.
Stuart C. Ray, MD, professor of medicine and oncology in the Division of Infectious Diseases at Johns Hopkins University, Baltimore, agreed. “It seems compelling, even for skeptics, that unvaccinated people represent 99% of those now dying from COVID-19 when they represent less than 50% of the adult population in the United States.”
The findings from the study could be more persuasive than previous arguments made in favor of immunization, Dr. Ray said. “These recent findings of striking reductions in risk of death in the vaccinated are more directly attributable and harder to ignore or dismiss.”
Brian Labus, PhD, MPH, of the University of Nevada Las Vegas (UNLV) is less convinced. “While this might change some peoples’ minds, it probably won’t make a major difference. People have many different reasons for not getting vaccinated, and this is only one of the things they consider.”
The study adds information that was not available before, said Dr. Labus, assistant professor in the Department of Epidemiology and Biostatistics at the UNLV School of Public Health. “We study the vaccine under tightly controlled, ideal conditions. This is the evidence that it works as well in the real world as it did in the trials, and that is what is most important in implementing a vaccination program,” added Dr. Labus.
“The scientific data has honed in on one thing: Vaccines are effective in preventing hospitalizations, ICU admissions, ventilations, and deaths,” agreed Dr. Palli.
“We now know that almost all deaths occurred in patients who were not vaccinated. We also know that all vaccines are effective against various strains that are in circulation right now, including the Delta variant, which is rapidly spreading,” Dr. Palli said.
Dr. Cassiere pointed out that the unvaccinated are not only at higher risk of developing COVID-19 but also of spreading, being hospitalized for, and dying from the infection. Avoiding “long hauler” symptoms is another argument in favor of immunization, he added.
As of June 28, the CDC reports that 63% of Americans 12 years and older have received at least one dose of a COVID-19 vaccine, and 54% are fully vaccinated.
Worldwide worry?
Although overall rates of U.S. COVID-19 hospitalizations and deaths are down, the outlook may not remain as encouraging. “I hope I’m wrong about this, but I anticipate that the coming fall and winter will bring increasingly localized versions of similar findings – severe disease and death due to SARS-CoV-2 infection in regions or groups with lower vaccination rates,” Dr. Ray said.
There could be a silver lining, he added: “If this unfortunate surge occurs, the health and economic consequences seem likely to erode much of the remaining hesitancy regarding vaccination.”
The rise of more infectious SARS-CoV-2 variants, such as the Delta variant, could also throw a wrench in controlling COVID-19. “This isn’t just a domestic issue,” Dr. Ray said. “We have learned that the world is a small place in pandemic times.”
The Associated Press investigators state that their findings support the high efficacy of the vaccine. Also, given the current widespread availability of COVID-19 vaccines in the United States, they believe many of the COVID-19 deaths now occurring are preventable.
Public health measures should have continued longer to protect unvaccinated individuals, especially Black Americans, Hispanic Americans, and other minorities, Dr. Palli said. “Only time will tell if re-opening and abandoning all public health measures by the CDC was premature.”
A version of this article first appeared on Medscape.com.
New COVID-19 vaccinations decline again in 12- to 15-year-olds
Even though less than 21% of all children aged 12-15 years are fully vaccinated against COVID-19, the number seeking first vaccinations continues to decline, according to data from the Centers for Disease Control and Prevention.

and 462,000 during the week ending June 14. Collectively, 30.2% of 12- to 15-year-olds have gotten at least one dose of vaccine so far and 20.7% are now fully vaccinated, the CDC said on its COVID Data Tracker site.
Among children aged 16-17 years, who were able to start the vaccination process earlier, 42.9% have received at least one dose and 34.0% have completed the COVID-19 vaccine regimen. Vaccine initiation – measured as the proportion of all individuals getting a first shot over the previous 2 weeks – has been consistently around 4.8% during the month of June for this age group but has dropped from 17.9% on June 7 to 14.3% on June 28 for those aged 12-15, the CDC data show.
Looking at the same measure for vaccine completion, 16.7% of all those who reached full vaccination status in the 14 days ending June 28 were 12- to 15-years-olds, down from 21.5% on June 21 and 19.6% on June 14. The numbers for those aged 15-16 were, respectively, 4.6%, 4.5%, and 4.2%, the CDC reported.
Fortunately, in the wake of recent vaccination trends, new cases of COVID-19 in children were down to their lowest level – just 8,447 for the week ending June 24 – since May of 2020, according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
New cases had been well over 15,000 the previous week (June 17), following weeks of 14,000 (June 10) and 16,000 (June 3) new cases, so the latest drop down to just four digits represents a 1-week decline of over 46% in the 49 states (excluding New York) that are reporting age distribution, along with the District of Columbia, New York City, Puerto Rico, and Guam.
The cumulative number of child COVID-19 cases in those jurisdictions is about 4.03 million since the beginning of the pandemic, which represents 14.2% of all cases in the United States. At the state level, the cumulative rate of cases in children is highest in Vermont (22.7%) and lowest in Florida (8.9%), which uses an age range of 0-14 years for children, compared with 0-17 or 0-19 for most states, the AAP and CHA said.
Severe illness has been rare in children, which is reflected in the proportion of children among all hospitalizations, 2.2% in 24 jurisdictions, and the proportion of deaths, 0.06% in 46 jurisdictions, since the start of the pandemic, the AAP and CHA said, with a total of 336 COVID-19–related deaths reported.
Even though less than 21% of all children aged 12-15 years are fully vaccinated against COVID-19, the number seeking first vaccinations continues to decline, according to data from the Centers for Disease Control and Prevention.

and 462,000 during the week ending June 14. Collectively, 30.2% of 12- to 15-year-olds have gotten at least one dose of vaccine so far and 20.7% are now fully vaccinated, the CDC said on its COVID Data Tracker site.
Among children aged 16-17 years, who were able to start the vaccination process earlier, 42.9% have received at least one dose and 34.0% have completed the COVID-19 vaccine regimen. Vaccine initiation – measured as the proportion of all individuals getting a first shot over the previous 2 weeks – has been consistently around 4.8% during the month of June for this age group but has dropped from 17.9% on June 7 to 14.3% on June 28 for those aged 12-15, the CDC data show.
Looking at the same measure for vaccine completion, 16.7% of all those who reached full vaccination status in the 14 days ending June 28 were 12- to 15-years-olds, down from 21.5% on June 21 and 19.6% on June 14. The numbers for those aged 15-16 were, respectively, 4.6%, 4.5%, and 4.2%, the CDC reported.
Fortunately, in the wake of recent vaccination trends, new cases of COVID-19 in children were down to their lowest level – just 8,447 for the week ending June 24 – since May of 2020, according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
New cases had been well over 15,000 the previous week (June 17), following weeks of 14,000 (June 10) and 16,000 (June 3) new cases, so the latest drop down to just four digits represents a 1-week decline of over 46% in the 49 states (excluding New York) that are reporting age distribution, along with the District of Columbia, New York City, Puerto Rico, and Guam.
The cumulative number of child COVID-19 cases in those jurisdictions is about 4.03 million since the beginning of the pandemic, which represents 14.2% of all cases in the United States. At the state level, the cumulative rate of cases in children is highest in Vermont (22.7%) and lowest in Florida (8.9%), which uses an age range of 0-14 years for children, compared with 0-17 or 0-19 for most states, the AAP and CHA said.
Severe illness has been rare in children, which is reflected in the proportion of children among all hospitalizations, 2.2% in 24 jurisdictions, and the proportion of deaths, 0.06% in 46 jurisdictions, since the start of the pandemic, the AAP and CHA said, with a total of 336 COVID-19–related deaths reported.
Even though less than 21% of all children aged 12-15 years are fully vaccinated against COVID-19, the number seeking first vaccinations continues to decline, according to data from the Centers for Disease Control and Prevention.

and 462,000 during the week ending June 14. Collectively, 30.2% of 12- to 15-year-olds have gotten at least one dose of vaccine so far and 20.7% are now fully vaccinated, the CDC said on its COVID Data Tracker site.
Among children aged 16-17 years, who were able to start the vaccination process earlier, 42.9% have received at least one dose and 34.0% have completed the COVID-19 vaccine regimen. Vaccine initiation – measured as the proportion of all individuals getting a first shot over the previous 2 weeks – has been consistently around 4.8% during the month of June for this age group but has dropped from 17.9% on June 7 to 14.3% on June 28 for those aged 12-15, the CDC data show.
Looking at the same measure for vaccine completion, 16.7% of all those who reached full vaccination status in the 14 days ending June 28 were 12- to 15-years-olds, down from 21.5% on June 21 and 19.6% on June 14. The numbers for those aged 15-16 were, respectively, 4.6%, 4.5%, and 4.2%, the CDC reported.
Fortunately, in the wake of recent vaccination trends, new cases of COVID-19 in children were down to their lowest level – just 8,447 for the week ending June 24 – since May of 2020, according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
New cases had been well over 15,000 the previous week (June 17), following weeks of 14,000 (June 10) and 16,000 (June 3) new cases, so the latest drop down to just four digits represents a 1-week decline of over 46% in the 49 states (excluding New York) that are reporting age distribution, along with the District of Columbia, New York City, Puerto Rico, and Guam.
The cumulative number of child COVID-19 cases in those jurisdictions is about 4.03 million since the beginning of the pandemic, which represents 14.2% of all cases in the United States. At the state level, the cumulative rate of cases in children is highest in Vermont (22.7%) and lowest in Florida (8.9%), which uses an age range of 0-14 years for children, compared with 0-17 or 0-19 for most states, the AAP and CHA said.
Severe illness has been rare in children, which is reflected in the proportion of children among all hospitalizations, 2.2% in 24 jurisdictions, and the proportion of deaths, 0.06% in 46 jurisdictions, since the start of the pandemic, the AAP and CHA said, with a total of 336 COVID-19–related deaths reported.
New! Spotlight on medical power couples: Their extraordinary lives
When people started dying from lethal anthrax spores sent through the mail in 2001, infectious disease expert Jeannette Guarner, MD, was called to Florida and Connecticut to analyze the bodies. She and her pathology team investigated how the bacteria had entered the victims and examined tissue samples from across the country to discern the scale of the attacks.

After conducting autopsies and identifying that inhalation anthrax had caused the deaths, Dr. Guarner rushed home to Atlanta just in time for Thanksgiving. Exhausted, the beloved family chef still managed to cook the big turkey that holiday, but she enlisted help with dessert.
“She returned home on Thanksgiving at like three in the morning,” recalls Carlos del Rio, MD. “She said to me, ‘In order for us to have Thanksgiving, you have to be in charge of the pies.’ When I told my daughter, she said, ‘This is going to be a disaster! If mom’s not cooking, this is not going to be good.’”
“It didn’t turn out that bad,” Dr. Guarner laughs. “There was dessert.”
As two of the top infectious disease experts in the country, Dr. Guarner and Dr. del Rio are no strangers to juggling their personal lives around disease outbreaks, last-minute travel, and pressing research.
Former director of the clinical laboratory at Mexico’s National Cancer Institute, Dr. Guarner worked for the Centers for Disease Control and Prevention for 10 years, where she played an integral part in the discovery of SARS. She and her team identified that a coronavirus was in cultures taken from a health care worker who died after working in Asia and determined through molecular testing that the virus was different from any other coronaviruses at the time.
Dr. Guarner went on to search for the novel virus in tissue samples and determine that it was SARS that had caused the damage. She is now a professor in the department of pathology and laboratory medicine at Emory University, Atlanta, medical director of the clinical laboratory at Emory University Hospital Midtown, and vice chair for faculty affairs.
Dr. Del Rio, who served as director of the National AIDS Council of Mexico, is a distinguished professor of medicine in Emory University’s division of infectious diseases and a professor of global health and epidemiology in the Rollins School of Public Health at Emory University. He is also co-director of the Emory Center for AIDS Research and co-principal investigator of the Emory-CDC HIV Clinical Trials Unit and the Emory Vaccine and Treatment Evaluation Unit.
Dr. Del Rio’s work in HIV prevention and care has made great strides, including developing the concept for the HIV Care Continuum, a public health model that outlines the stages that HIV patients go through, from diagnosis to achieving viral suppression. Dr. Del Rio, who is foreign secretary of the National Academy of Medicine, has also worked on emerging infections such as pandemic influenza and was a member of the WHO Influenza A (H1N1) Clinical Advisory Group and of the CDC Influenza A Task Force during the 2009 pandemic.
Dr. Del Rio and Dr. Guarner met during medical school in Mexico City. At first, the two carpooled to classes, but when Dr. Guarner fell ill with hepatitis A, Dr. del Rio brought Dr. Guarner the class notes so she wouldn’t fall behind. The study buddies later became a couple and married just before coming to the United States for residency.
With their expertise in infectious disease, Dr. del Rio and Dr. Guarner have worked collaboratively in the past, but the couple says they’ve always maintained separate professional identities.
“We try to create our own spaces,” Dr. del Rio said. “You try to keep your personal and professional identity independent as much as possible. You don’t want people to say, ‘Oh, you got this or you’re doing this because you are married to this other person.’ You want, to a certain degree, intellectual independence.”
This has been easier in some ways because Dr. del Rio and Dr. Guarner have different last names. Over the years they have frequently encountered people who had no idea that they are married.
“One time, we were both down in the lab and Jeanette was discussing a case, and she started teasing me or poking me, making fun,” recalls Dr. del Rio. “Some of the ID fellows were like, ‘Oh my God, who the hell is this woman?’ They didn’t realize she was my wife.”
Since the COVID-19 outbreak, both Dr. Guarner and Dr. del Rio have been involved in different ways with the pandemic. Dr. Del Rio has seen patients, conducted clinical trials, and given hundreds of local and national interviews about the virus. As a laboratory director, Dr. Guarner has validated tests for the diagnosis of COVID-19 and counseled staff on exposure concerns.
“An important aspect has also been to make sure that our laboratory technologists understand the disease and the need for the different protection elements we have had to use in the hospital,” she said. “In many ways I have had to scale down fears the techs have had when handling specimens from these patients.”
In their own words
What was one of your most surprising discoveries?
Jeannette: During the anthrax attacks, we received lots of tissues on live patients, particularly skin biopsies from different parts of the country where pathologists had concerns that there was anthrax. From New York, we received more than 50 skin biopsies and discovered that the necrotic lesions suspected of anthrax had Rickettsia in them. In other words, we discovered that rickettsialpox – a mite-borne infectious disease – was circulating in the city, which was unknown at the time.
Describe a challenge that you overcame:
Carlos: When I was appointed as director of the National AIDS Council of Mexico (CONASIDA), I was quite young, only 32 years old. I had to learn to listen to others who had expertise and institutional memory, to respect their opinions, and at the same time to push for change. A huge challenge was the role of the Catholic Church and conservative groups that were adamantly against condom promotion. Thus, I learned how to advance policies based in science without being confrontational.
Have you ever been famous for anything other than your work?
Jeannette: In 2017, a tree fell on our house during Hurricane Irma. It fell right on my husband’s office a few minutes after he left the room. Fortunately, I have always been small and flexible, and I crawled through the rubble to save our valuables before they were ruined by the rain. Later, a local Atlanta TV news crew was in the neighborhood reporting on the damage, and I told them to come to our house if they wanted to see real damage. That night, we were on the local news.
Power couple Paul and Mary Klotman
When Mary Klotman, MD, was offered an opportunity with the National Institutes of Health in 1991, Paul Klotman, MD, didn’t hesitate to resign his post at Duke University, Durham, N.C., and join his wife in Washington. Paul says he wanted to support Mary’s aspirations, even though it meant an uncertain track for his own career.

Fortunately for the Klotmans, the move proved instrumental for both of their careers and spurred one of their proudest scientific breakthroughs.
At NIH, Mary was a member of the Public Health Service and worked in the laboratory of tumor cell biology, and Paul became chief of the institute’s molecular medicine section in the laboratory of developmental biology. Together, their work led to the first animal model of HIV-associated nephropathy using transgenic techniques. The Klotmans and their team demonstrated that HIV resides in and evolves separately in kidney cells, a critical step in HIV-associated kidney disease.
“That’s where our longstanding collaboration around HIV-associated nephropathy started,” Mary says. “Paul and I have a passion for research, and we’ve had the same grant together for 25 years.”
After their successful stint at NIH, the Klotmans next climbed the ranks at the Icahn School of Medicine at Mount Sinai, where Paul started as chief of the nephrology division and became chair of medicine, and Mary became chief of infectious diseases and co-director of Mount Sinai’s Global Health and Emerging Pathogens Institute.
Today, Mary and Paul are the first – and only – married couple in the United States to lead separate medical schools. Mary is dean and vice chancellor for health affairs at Duke, and Paul is president and executive dean of Baylor College of Medicine, Houston.
Despite their 1,100-mile separation, the Klotmans manage their relationship in an unconventional way that some might balk at: Every Friday, one spouse hops on a plane and travels to the other for a date night and weekend.
“When we started this crazy lifestyle, we committed to being together every weekend,” says Mary. “And in 10 years – before COVID – we missed only one weekend together.”
The Klotmans say the scheduled time together places a hard end to each work week and enables them to truly enjoy their quality time.
“Friday at noon, I’m on the plane going to Durham, and I know that in 2 hours I’m going to have a date with my wife,” Paul said. “There are institutions that we’ve run into that think you have to be 7 days a week on site. But Duke and Baylor have been very supportive [of our situation].”
No doubt, the arrangement means a lot of time in the air for the couple. Paul says he travels about 150,000 miles every year by plane.
Having dual leadership positions in academic medicine has kept the Klotmans tightly connected, and the couple says their strong partnership has contributed to their success.
“It’s really been helpful having a deep understanding of our career paths, because we’ve been able to understand when one of us needed to be really focused on work and the other one would step back a bit with the kids and vice versa,” Mary said.
“There’s no question that we wouldn’t be in the positions we are in now if it weren’t for the fact that we’ve had each other,” Paul said.
In their own words
What is a little-known title that you have?
Paul: Purse-carrier for my wife. When she is honored at a national meeting or event, she often stands up and hands me her purse. I now make sure I have on an appropriate outfit that matches the purse.
Tell us about your children.
Mary: We had a very traumatic first pregnancy that we lost. Six years later, we adopted our first child, which was an amazing blessing. Our second son was Duke’s first successful frozen embryo transfer.
Describe a memorable moment in your relationship.
Paul: As we were leaving for our honeymoon, Mary’s dad handed me this booklet. It was the receipts for Mary’s medical school loans for the next 10 years. He said, “Congratulations, she’s all yours!”
A version of this article first appeared on Medscape.com.
When people started dying from lethal anthrax spores sent through the mail in 2001, infectious disease expert Jeannette Guarner, MD, was called to Florida and Connecticut to analyze the bodies. She and her pathology team investigated how the bacteria had entered the victims and examined tissue samples from across the country to discern the scale of the attacks.

After conducting autopsies and identifying that inhalation anthrax had caused the deaths, Dr. Guarner rushed home to Atlanta just in time for Thanksgiving. Exhausted, the beloved family chef still managed to cook the big turkey that holiday, but she enlisted help with dessert.
“She returned home on Thanksgiving at like three in the morning,” recalls Carlos del Rio, MD. “She said to me, ‘In order for us to have Thanksgiving, you have to be in charge of the pies.’ When I told my daughter, she said, ‘This is going to be a disaster! If mom’s not cooking, this is not going to be good.’”
“It didn’t turn out that bad,” Dr. Guarner laughs. “There was dessert.”
As two of the top infectious disease experts in the country, Dr. Guarner and Dr. del Rio are no strangers to juggling their personal lives around disease outbreaks, last-minute travel, and pressing research.
Former director of the clinical laboratory at Mexico’s National Cancer Institute, Dr. Guarner worked for the Centers for Disease Control and Prevention for 10 years, where she played an integral part in the discovery of SARS. She and her team identified that a coronavirus was in cultures taken from a health care worker who died after working in Asia and determined through molecular testing that the virus was different from any other coronaviruses at the time.
Dr. Guarner went on to search for the novel virus in tissue samples and determine that it was SARS that had caused the damage. She is now a professor in the department of pathology and laboratory medicine at Emory University, Atlanta, medical director of the clinical laboratory at Emory University Hospital Midtown, and vice chair for faculty affairs.
Dr. Del Rio, who served as director of the National AIDS Council of Mexico, is a distinguished professor of medicine in Emory University’s division of infectious diseases and a professor of global health and epidemiology in the Rollins School of Public Health at Emory University. He is also co-director of the Emory Center for AIDS Research and co-principal investigator of the Emory-CDC HIV Clinical Trials Unit and the Emory Vaccine and Treatment Evaluation Unit.
Dr. Del Rio’s work in HIV prevention and care has made great strides, including developing the concept for the HIV Care Continuum, a public health model that outlines the stages that HIV patients go through, from diagnosis to achieving viral suppression. Dr. Del Rio, who is foreign secretary of the National Academy of Medicine, has also worked on emerging infections such as pandemic influenza and was a member of the WHO Influenza A (H1N1) Clinical Advisory Group and of the CDC Influenza A Task Force during the 2009 pandemic.
Dr. Del Rio and Dr. Guarner met during medical school in Mexico City. At first, the two carpooled to classes, but when Dr. Guarner fell ill with hepatitis A, Dr. del Rio brought Dr. Guarner the class notes so she wouldn’t fall behind. The study buddies later became a couple and married just before coming to the United States for residency.
With their expertise in infectious disease, Dr. del Rio and Dr. Guarner have worked collaboratively in the past, but the couple says they’ve always maintained separate professional identities.
“We try to create our own spaces,” Dr. del Rio said. “You try to keep your personal and professional identity independent as much as possible. You don’t want people to say, ‘Oh, you got this or you’re doing this because you are married to this other person.’ You want, to a certain degree, intellectual independence.”
This has been easier in some ways because Dr. del Rio and Dr. Guarner have different last names. Over the years they have frequently encountered people who had no idea that they are married.
“One time, we were both down in the lab and Jeanette was discussing a case, and she started teasing me or poking me, making fun,” recalls Dr. del Rio. “Some of the ID fellows were like, ‘Oh my God, who the hell is this woman?’ They didn’t realize she was my wife.”
Since the COVID-19 outbreak, both Dr. Guarner and Dr. del Rio have been involved in different ways with the pandemic. Dr. Del Rio has seen patients, conducted clinical trials, and given hundreds of local and national interviews about the virus. As a laboratory director, Dr. Guarner has validated tests for the diagnosis of COVID-19 and counseled staff on exposure concerns.
“An important aspect has also been to make sure that our laboratory technologists understand the disease and the need for the different protection elements we have had to use in the hospital,” she said. “In many ways I have had to scale down fears the techs have had when handling specimens from these patients.”
In their own words
What was one of your most surprising discoveries?
Jeannette: During the anthrax attacks, we received lots of tissues on live patients, particularly skin biopsies from different parts of the country where pathologists had concerns that there was anthrax. From New York, we received more than 50 skin biopsies and discovered that the necrotic lesions suspected of anthrax had Rickettsia in them. In other words, we discovered that rickettsialpox – a mite-borne infectious disease – was circulating in the city, which was unknown at the time.
Describe a challenge that you overcame:
Carlos: When I was appointed as director of the National AIDS Council of Mexico (CONASIDA), I was quite young, only 32 years old. I had to learn to listen to others who had expertise and institutional memory, to respect their opinions, and at the same time to push for change. A huge challenge was the role of the Catholic Church and conservative groups that were adamantly against condom promotion. Thus, I learned how to advance policies based in science without being confrontational.
Have you ever been famous for anything other than your work?
Jeannette: In 2017, a tree fell on our house during Hurricane Irma. It fell right on my husband’s office a few minutes after he left the room. Fortunately, I have always been small and flexible, and I crawled through the rubble to save our valuables before they were ruined by the rain. Later, a local Atlanta TV news crew was in the neighborhood reporting on the damage, and I told them to come to our house if they wanted to see real damage. That night, we were on the local news.
Power couple Paul and Mary Klotman
When Mary Klotman, MD, was offered an opportunity with the National Institutes of Health in 1991, Paul Klotman, MD, didn’t hesitate to resign his post at Duke University, Durham, N.C., and join his wife in Washington. Paul says he wanted to support Mary’s aspirations, even though it meant an uncertain track for his own career.

Fortunately for the Klotmans, the move proved instrumental for both of their careers and spurred one of their proudest scientific breakthroughs.
At NIH, Mary was a member of the Public Health Service and worked in the laboratory of tumor cell biology, and Paul became chief of the institute’s molecular medicine section in the laboratory of developmental biology. Together, their work led to the first animal model of HIV-associated nephropathy using transgenic techniques. The Klotmans and their team demonstrated that HIV resides in and evolves separately in kidney cells, a critical step in HIV-associated kidney disease.
“That’s where our longstanding collaboration around HIV-associated nephropathy started,” Mary says. “Paul and I have a passion for research, and we’ve had the same grant together for 25 years.”
After their successful stint at NIH, the Klotmans next climbed the ranks at the Icahn School of Medicine at Mount Sinai, where Paul started as chief of the nephrology division and became chair of medicine, and Mary became chief of infectious diseases and co-director of Mount Sinai’s Global Health and Emerging Pathogens Institute.
Today, Mary and Paul are the first – and only – married couple in the United States to lead separate medical schools. Mary is dean and vice chancellor for health affairs at Duke, and Paul is president and executive dean of Baylor College of Medicine, Houston.
Despite their 1,100-mile separation, the Klotmans manage their relationship in an unconventional way that some might balk at: Every Friday, one spouse hops on a plane and travels to the other for a date night and weekend.
“When we started this crazy lifestyle, we committed to being together every weekend,” says Mary. “And in 10 years – before COVID – we missed only one weekend together.”
The Klotmans say the scheduled time together places a hard end to each work week and enables them to truly enjoy their quality time.
“Friday at noon, I’m on the plane going to Durham, and I know that in 2 hours I’m going to have a date with my wife,” Paul said. “There are institutions that we’ve run into that think you have to be 7 days a week on site. But Duke and Baylor have been very supportive [of our situation].”
No doubt, the arrangement means a lot of time in the air for the couple. Paul says he travels about 150,000 miles every year by plane.
Having dual leadership positions in academic medicine has kept the Klotmans tightly connected, and the couple says their strong partnership has contributed to their success.
“It’s really been helpful having a deep understanding of our career paths, because we’ve been able to understand when one of us needed to be really focused on work and the other one would step back a bit with the kids and vice versa,” Mary said.
“There’s no question that we wouldn’t be in the positions we are in now if it weren’t for the fact that we’ve had each other,” Paul said.
In their own words
What is a little-known title that you have?
Paul: Purse-carrier for my wife. When she is honored at a national meeting or event, she often stands up and hands me her purse. I now make sure I have on an appropriate outfit that matches the purse.
Tell us about your children.
Mary: We had a very traumatic first pregnancy that we lost. Six years later, we adopted our first child, which was an amazing blessing. Our second son was Duke’s first successful frozen embryo transfer.
Describe a memorable moment in your relationship.
Paul: As we were leaving for our honeymoon, Mary’s dad handed me this booklet. It was the receipts for Mary’s medical school loans for the next 10 years. He said, “Congratulations, she’s all yours!”
A version of this article first appeared on Medscape.com.
When people started dying from lethal anthrax spores sent through the mail in 2001, infectious disease expert Jeannette Guarner, MD, was called to Florida and Connecticut to analyze the bodies. She and her pathology team investigated how the bacteria had entered the victims and examined tissue samples from across the country to discern the scale of the attacks.

After conducting autopsies and identifying that inhalation anthrax had caused the deaths, Dr. Guarner rushed home to Atlanta just in time for Thanksgiving. Exhausted, the beloved family chef still managed to cook the big turkey that holiday, but she enlisted help with dessert.
“She returned home on Thanksgiving at like three in the morning,” recalls Carlos del Rio, MD. “She said to me, ‘In order for us to have Thanksgiving, you have to be in charge of the pies.’ When I told my daughter, she said, ‘This is going to be a disaster! If mom’s not cooking, this is not going to be good.’”
“It didn’t turn out that bad,” Dr. Guarner laughs. “There was dessert.”
As two of the top infectious disease experts in the country, Dr. Guarner and Dr. del Rio are no strangers to juggling their personal lives around disease outbreaks, last-minute travel, and pressing research.
Former director of the clinical laboratory at Mexico’s National Cancer Institute, Dr. Guarner worked for the Centers for Disease Control and Prevention for 10 years, where she played an integral part in the discovery of SARS. She and her team identified that a coronavirus was in cultures taken from a health care worker who died after working in Asia and determined through molecular testing that the virus was different from any other coronaviruses at the time.
Dr. Guarner went on to search for the novel virus in tissue samples and determine that it was SARS that had caused the damage. She is now a professor in the department of pathology and laboratory medicine at Emory University, Atlanta, medical director of the clinical laboratory at Emory University Hospital Midtown, and vice chair for faculty affairs.
Dr. Del Rio, who served as director of the National AIDS Council of Mexico, is a distinguished professor of medicine in Emory University’s division of infectious diseases and a professor of global health and epidemiology in the Rollins School of Public Health at Emory University. He is also co-director of the Emory Center for AIDS Research and co-principal investigator of the Emory-CDC HIV Clinical Trials Unit and the Emory Vaccine and Treatment Evaluation Unit.
Dr. Del Rio’s work in HIV prevention and care has made great strides, including developing the concept for the HIV Care Continuum, a public health model that outlines the stages that HIV patients go through, from diagnosis to achieving viral suppression. Dr. Del Rio, who is foreign secretary of the National Academy of Medicine, has also worked on emerging infections such as pandemic influenza and was a member of the WHO Influenza A (H1N1) Clinical Advisory Group and of the CDC Influenza A Task Force during the 2009 pandemic.
Dr. Del Rio and Dr. Guarner met during medical school in Mexico City. At first, the two carpooled to classes, but when Dr. Guarner fell ill with hepatitis A, Dr. del Rio brought Dr. Guarner the class notes so she wouldn’t fall behind. The study buddies later became a couple and married just before coming to the United States for residency.
With their expertise in infectious disease, Dr. del Rio and Dr. Guarner have worked collaboratively in the past, but the couple says they’ve always maintained separate professional identities.
“We try to create our own spaces,” Dr. del Rio said. “You try to keep your personal and professional identity independent as much as possible. You don’t want people to say, ‘Oh, you got this or you’re doing this because you are married to this other person.’ You want, to a certain degree, intellectual independence.”
This has been easier in some ways because Dr. del Rio and Dr. Guarner have different last names. Over the years they have frequently encountered people who had no idea that they are married.
“One time, we were both down in the lab and Jeanette was discussing a case, and she started teasing me or poking me, making fun,” recalls Dr. del Rio. “Some of the ID fellows were like, ‘Oh my God, who the hell is this woman?’ They didn’t realize she was my wife.”
Since the COVID-19 outbreak, both Dr. Guarner and Dr. del Rio have been involved in different ways with the pandemic. Dr. Del Rio has seen patients, conducted clinical trials, and given hundreds of local and national interviews about the virus. As a laboratory director, Dr. Guarner has validated tests for the diagnosis of COVID-19 and counseled staff on exposure concerns.
“An important aspect has also been to make sure that our laboratory technologists understand the disease and the need for the different protection elements we have had to use in the hospital,” she said. “In many ways I have had to scale down fears the techs have had when handling specimens from these patients.”
In their own words
What was one of your most surprising discoveries?
Jeannette: During the anthrax attacks, we received lots of tissues on live patients, particularly skin biopsies from different parts of the country where pathologists had concerns that there was anthrax. From New York, we received more than 50 skin biopsies and discovered that the necrotic lesions suspected of anthrax had Rickettsia in them. In other words, we discovered that rickettsialpox – a mite-borne infectious disease – was circulating in the city, which was unknown at the time.
Describe a challenge that you overcame:
Carlos: When I was appointed as director of the National AIDS Council of Mexico (CONASIDA), I was quite young, only 32 years old. I had to learn to listen to others who had expertise and institutional memory, to respect their opinions, and at the same time to push for change. A huge challenge was the role of the Catholic Church and conservative groups that were adamantly against condom promotion. Thus, I learned how to advance policies based in science without being confrontational.
Have you ever been famous for anything other than your work?
Jeannette: In 2017, a tree fell on our house during Hurricane Irma. It fell right on my husband’s office a few minutes after he left the room. Fortunately, I have always been small and flexible, and I crawled through the rubble to save our valuables before they were ruined by the rain. Later, a local Atlanta TV news crew was in the neighborhood reporting on the damage, and I told them to come to our house if they wanted to see real damage. That night, we were on the local news.
Power couple Paul and Mary Klotman
When Mary Klotman, MD, was offered an opportunity with the National Institutes of Health in 1991, Paul Klotman, MD, didn’t hesitate to resign his post at Duke University, Durham, N.C., and join his wife in Washington. Paul says he wanted to support Mary’s aspirations, even though it meant an uncertain track for his own career.

Fortunately for the Klotmans, the move proved instrumental for both of their careers and spurred one of their proudest scientific breakthroughs.
At NIH, Mary was a member of the Public Health Service and worked in the laboratory of tumor cell biology, and Paul became chief of the institute’s molecular medicine section in the laboratory of developmental biology. Together, their work led to the first animal model of HIV-associated nephropathy using transgenic techniques. The Klotmans and their team demonstrated that HIV resides in and evolves separately in kidney cells, a critical step in HIV-associated kidney disease.
“That’s where our longstanding collaboration around HIV-associated nephropathy started,” Mary says. “Paul and I have a passion for research, and we’ve had the same grant together for 25 years.”
After their successful stint at NIH, the Klotmans next climbed the ranks at the Icahn School of Medicine at Mount Sinai, where Paul started as chief of the nephrology division and became chair of medicine, and Mary became chief of infectious diseases and co-director of Mount Sinai’s Global Health and Emerging Pathogens Institute.
Today, Mary and Paul are the first – and only – married couple in the United States to lead separate medical schools. Mary is dean and vice chancellor for health affairs at Duke, and Paul is president and executive dean of Baylor College of Medicine, Houston.
Despite their 1,100-mile separation, the Klotmans manage their relationship in an unconventional way that some might balk at: Every Friday, one spouse hops on a plane and travels to the other for a date night and weekend.
“When we started this crazy lifestyle, we committed to being together every weekend,” says Mary. “And in 10 years – before COVID – we missed only one weekend together.”
The Klotmans say the scheduled time together places a hard end to each work week and enables them to truly enjoy their quality time.
“Friday at noon, I’m on the plane going to Durham, and I know that in 2 hours I’m going to have a date with my wife,” Paul said. “There are institutions that we’ve run into that think you have to be 7 days a week on site. But Duke and Baylor have been very supportive [of our situation].”
No doubt, the arrangement means a lot of time in the air for the couple. Paul says he travels about 150,000 miles every year by plane.
Having dual leadership positions in academic medicine has kept the Klotmans tightly connected, and the couple says their strong partnership has contributed to their success.
“It’s really been helpful having a deep understanding of our career paths, because we’ve been able to understand when one of us needed to be really focused on work and the other one would step back a bit with the kids and vice versa,” Mary said.
“There’s no question that we wouldn’t be in the positions we are in now if it weren’t for the fact that we’ve had each other,” Paul said.
In their own words
What is a little-known title that you have?
Paul: Purse-carrier for my wife. When she is honored at a national meeting or event, she often stands up and hands me her purse. I now make sure I have on an appropriate outfit that matches the purse.
Tell us about your children.
Mary: We had a very traumatic first pregnancy that we lost. Six years later, we adopted our first child, which was an amazing blessing. Our second son was Duke’s first successful frozen embryo transfer.
Describe a memorable moment in your relationship.
Paul: As we were leaving for our honeymoon, Mary’s dad handed me this booklet. It was the receipts for Mary’s medical school loans for the next 10 years. He said, “Congratulations, she’s all yours!”
A version of this article first appeared on Medscape.com.
Profound brain changes found in patients who died of COVID-19
The most comprehensive molecular study to date of brain tissue from people who died of COVID-19 provides clear evidence that SARS-CoV-2 causes profound molecular changes in the brain, despite no molecular trace of the virus in brain tissue.
“The signature the virus leaves in the brain speaks of strong inflammation and disrupted brain circuits and resembles signatures the field has observed in Alzheimer’s or other neurodegenerative diseases,” senior author Tony Wyss-Coray, PhD, professor of neurology and neurological sciences, Stanford (Calif.) University, told this news organization.
The study was published online June 21 in Nature.
Signs of distress
“We know that up to a third of SARS-CoV-2-infected people show brain symptoms including brain fog, memory problems, and fatigue, and a growing number of people have such symptoms long after they [have] seemingly recovered from virus infection,” said Dr. Wyss-Coray.
“However, we have very little understanding of how the virus causes these symptoms and what its effects are on the brain at a molecular level,” he added.
Using single-cell RNA sequencing, the researchers profiled the transcriptomes of 65,309 nuclei isolated from frontal cortex and choroid plexus samples from eight patients who died of COVID-19 and 14 controls who died of other causes.
There was no molecular evidence of SARS-CoV-2 in brain tissue samples from the patients who died of COVID-19.
Yet, “we were very surprised to learn that no matter which type of cell we studied (different types of nerve cells, immune cells, or different support cells in the brain) there were prominent changes” compared with brain tissue samples from controls who died of other causes, said Dr. Wyss-Coray.
The changes in the COVID-19 brains showed signatures of inflammation, abnormal nerve cell communication, and chronic neurodegeneration.
“Across cell types, COVID-19 perturbations overlap with those in chronic brain disorders and reside in genetic variants associated with cognition, schizophrenia, and depression,” the researchers report.
“Viral infection appears to trigger inflammatory responses throughout the body that may cause inflammatory signaling across the blood–brain barrier, which in turn could ‘trip off’ neuroinflammation in the brain,” Dr. Wyss-Coray said.
The findings may help explain the brain fog, fatigue, and other neurological and psychiatric symptoms of long COVID.
“While we studied only brains from people who died of COVID-19, we believe it is likely that similar, but hopefully weaker, signs of inflammation and chronic neurodegeneration will be found in COVID-19 survivors, especially those with chronic brain symptoms,” Dr. Wyss-Coray said.
This research was funded by the Nomis Foundation, the National Institutes of Health, Nan Fung Life Sciences, the Wu Tsai Neurosciences Institute and the Stanford Alzheimer’s Disease Research Center. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The most comprehensive molecular study to date of brain tissue from people who died of COVID-19 provides clear evidence that SARS-CoV-2 causes profound molecular changes in the brain, despite no molecular trace of the virus in brain tissue.
“The signature the virus leaves in the brain speaks of strong inflammation and disrupted brain circuits and resembles signatures the field has observed in Alzheimer’s or other neurodegenerative diseases,” senior author Tony Wyss-Coray, PhD, professor of neurology and neurological sciences, Stanford (Calif.) University, told this news organization.
The study was published online June 21 in Nature.
Signs of distress
“We know that up to a third of SARS-CoV-2-infected people show brain symptoms including brain fog, memory problems, and fatigue, and a growing number of people have such symptoms long after they [have] seemingly recovered from virus infection,” said Dr. Wyss-Coray.
“However, we have very little understanding of how the virus causes these symptoms and what its effects are on the brain at a molecular level,” he added.
Using single-cell RNA sequencing, the researchers profiled the transcriptomes of 65,309 nuclei isolated from frontal cortex and choroid plexus samples from eight patients who died of COVID-19 and 14 controls who died of other causes.
There was no molecular evidence of SARS-CoV-2 in brain tissue samples from the patients who died of COVID-19.
Yet, “we were very surprised to learn that no matter which type of cell we studied (different types of nerve cells, immune cells, or different support cells in the brain) there were prominent changes” compared with brain tissue samples from controls who died of other causes, said Dr. Wyss-Coray.
The changes in the COVID-19 brains showed signatures of inflammation, abnormal nerve cell communication, and chronic neurodegeneration.
“Across cell types, COVID-19 perturbations overlap with those in chronic brain disorders and reside in genetic variants associated with cognition, schizophrenia, and depression,” the researchers report.
“Viral infection appears to trigger inflammatory responses throughout the body that may cause inflammatory signaling across the blood–brain barrier, which in turn could ‘trip off’ neuroinflammation in the brain,” Dr. Wyss-Coray said.
The findings may help explain the brain fog, fatigue, and other neurological and psychiatric symptoms of long COVID.
“While we studied only brains from people who died of COVID-19, we believe it is likely that similar, but hopefully weaker, signs of inflammation and chronic neurodegeneration will be found in COVID-19 survivors, especially those with chronic brain symptoms,” Dr. Wyss-Coray said.
This research was funded by the Nomis Foundation, the National Institutes of Health, Nan Fung Life Sciences, the Wu Tsai Neurosciences Institute and the Stanford Alzheimer’s Disease Research Center. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The most comprehensive molecular study to date of brain tissue from people who died of COVID-19 provides clear evidence that SARS-CoV-2 causes profound molecular changes in the brain, despite no molecular trace of the virus in brain tissue.
“The signature the virus leaves in the brain speaks of strong inflammation and disrupted brain circuits and resembles signatures the field has observed in Alzheimer’s or other neurodegenerative diseases,” senior author Tony Wyss-Coray, PhD, professor of neurology and neurological sciences, Stanford (Calif.) University, told this news organization.
The study was published online June 21 in Nature.
Signs of distress
“We know that up to a third of SARS-CoV-2-infected people show brain symptoms including brain fog, memory problems, and fatigue, and a growing number of people have such symptoms long after they [have] seemingly recovered from virus infection,” said Dr. Wyss-Coray.
“However, we have very little understanding of how the virus causes these symptoms and what its effects are on the brain at a molecular level,” he added.
Using single-cell RNA sequencing, the researchers profiled the transcriptomes of 65,309 nuclei isolated from frontal cortex and choroid plexus samples from eight patients who died of COVID-19 and 14 controls who died of other causes.
There was no molecular evidence of SARS-CoV-2 in brain tissue samples from the patients who died of COVID-19.
Yet, “we were very surprised to learn that no matter which type of cell we studied (different types of nerve cells, immune cells, or different support cells in the brain) there were prominent changes” compared with brain tissue samples from controls who died of other causes, said Dr. Wyss-Coray.
The changes in the COVID-19 brains showed signatures of inflammation, abnormal nerve cell communication, and chronic neurodegeneration.
“Across cell types, COVID-19 perturbations overlap with those in chronic brain disorders and reside in genetic variants associated with cognition, schizophrenia, and depression,” the researchers report.
“Viral infection appears to trigger inflammatory responses throughout the body that may cause inflammatory signaling across the blood–brain barrier, which in turn could ‘trip off’ neuroinflammation in the brain,” Dr. Wyss-Coray said.
The findings may help explain the brain fog, fatigue, and other neurological and psychiatric symptoms of long COVID.
“While we studied only brains from people who died of COVID-19, we believe it is likely that similar, but hopefully weaker, signs of inflammation and chronic neurodegeneration will be found in COVID-19 survivors, especially those with chronic brain symptoms,” Dr. Wyss-Coray said.
This research was funded by the Nomis Foundation, the National Institutes of Health, Nan Fung Life Sciences, the Wu Tsai Neurosciences Institute and the Stanford Alzheimer’s Disease Research Center. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MD jailed for road rage, career spirals downhill
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.