User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
Mortality trends in childhood after infant bacterial meningitis
Among infants younger than 1 year of age, bacterial meningitis is associated with worse long-term mortality, even after recovery from the initial infection. Heightened mortality risk stretched out to 10 years, and was highest in the wake of infection from Streptococcus agalactiae, according to a retrospective analysis of children in the Netherlands.
“The adjusted hazard rates were high for the whole group of bacterial meningitis, especially within the first year after onset. (Staphylococcus agalactiae) meningitis has the highest mortality risk within one year of disease onset,” Linde Snoek said during her presentation of the study (abstract 913) at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. Ms. Snoek is a PhD student at Amsterdam University Medical Center.
Over longer time periods, the mortality associations were different. “The adjusted hazard rates were highest for pneumococcal meningitis compared to the other pathogens. And this was the case for 1 year, 5 years, and 10 years after disease onset,” said Ms. Snoek.
The study appears to be the first to look at extended mortality following bacterial meningitis in this age group, according to Marie Rohr, MD, who comoderated the session where the research was presented.
“In a quick review of the literature I did not find any [equivalent] study concerning short- and long-term mortality after bacterial meningitis in under 1 year of age,” said Dr. Rohr, a fellow in pediatric infectious diseases at University Hospitals of Geneva. But the message to physicians is clear. “Children with history of bacterial meningitis have a higher long-term mortality than children without a history of bacterial meningitis,” said Dr. Rohr.
The study did have a key limitation: For matched controls, it relied on anonymous data from the Municipal Personal Records Database in Statistics Netherlands. “Important information like cause of death is lacking,” said Dr. Rohr.
Bacterial meningitis is associated with significant mortality and morbidity. Pathogens behind the infections vary with age group and geographic location, as well as immunization status.
To examine long-term mortality after bacterial meningitis, the researchers collected 1,646 records from an exposed cohort, with a date range of 1995 to 2018, from the Netherlands Reference Laboratory for Bacterial Meningitis. Included patients had a positive culture diagnosis of bacterial meningitis during the first year of life. Each exposed subject was compared to 10 controls matched by birth month, birth year, and sex, who had no exposure to bacterial meningitis.
Staphylococcus pneumoniae accounted for the most cases, at 32.0% (median age of onset, 180 days), followed by Neisseria meningitidis at 29.0% (median age of onset, 203 days). Other pathogens included S. agalactiae (19.7%, 10 days), Escherichia coli (8.8%, 13 days), and Haemophilus influenzae (5.4%, 231 days).
The mortality risk within 1 year of disease onset was higher for all pathogens (6.2% vs. 0.2% unexposed). The highest mortality risk was seen for S. agalactiae (8.7%), followed by E. coli (6.4%), N. meningitidis (4.9%), and H. influenzae (3.4%).
Hazard ratios (HR) for mortality were also higher, particularly in the first year after disease onset. For all pathogens, mortality rates were higher within 1 year (HR, 39.2), 5 years (HR, 28.7), and 10 years (HR, 24.1). The consistently highest mortality rates were associated with S. pneumoniae over 1-year, 5-year, and 10-year follow-up (HR, 42.8; HR, 45.6; HR, 40.6, respectively). Within 1 year, the highest mortality rate was associated with N. meningitidis (HR, 58.4).
Ms. Snoek and Dr. Rohr have no relevant financial disclosures.
Among infants younger than 1 year of age, bacterial meningitis is associated with worse long-term mortality, even after recovery from the initial infection. Heightened mortality risk stretched out to 10 years, and was highest in the wake of infection from Streptococcus agalactiae, according to a retrospective analysis of children in the Netherlands.
“The adjusted hazard rates were high for the whole group of bacterial meningitis, especially within the first year after onset. (Staphylococcus agalactiae) meningitis has the highest mortality risk within one year of disease onset,” Linde Snoek said during her presentation of the study (abstract 913) at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. Ms. Snoek is a PhD student at Amsterdam University Medical Center.
Over longer time periods, the mortality associations were different. “The adjusted hazard rates were highest for pneumococcal meningitis compared to the other pathogens. And this was the case for 1 year, 5 years, and 10 years after disease onset,” said Ms. Snoek.
The study appears to be the first to look at extended mortality following bacterial meningitis in this age group, according to Marie Rohr, MD, who comoderated the session where the research was presented.
“In a quick review of the literature I did not find any [equivalent] study concerning short- and long-term mortality after bacterial meningitis in under 1 year of age,” said Dr. Rohr, a fellow in pediatric infectious diseases at University Hospitals of Geneva. But the message to physicians is clear. “Children with history of bacterial meningitis have a higher long-term mortality than children without a history of bacterial meningitis,” said Dr. Rohr.
The study did have a key limitation: For matched controls, it relied on anonymous data from the Municipal Personal Records Database in Statistics Netherlands. “Important information like cause of death is lacking,” said Dr. Rohr.
Bacterial meningitis is associated with significant mortality and morbidity. Pathogens behind the infections vary with age group and geographic location, as well as immunization status.
To examine long-term mortality after bacterial meningitis, the researchers collected 1,646 records from an exposed cohort, with a date range of 1995 to 2018, from the Netherlands Reference Laboratory for Bacterial Meningitis. Included patients had a positive culture diagnosis of bacterial meningitis during the first year of life. Each exposed subject was compared to 10 controls matched by birth month, birth year, and sex, who had no exposure to bacterial meningitis.
Staphylococcus pneumoniae accounted for the most cases, at 32.0% (median age of onset, 180 days), followed by Neisseria meningitidis at 29.0% (median age of onset, 203 days). Other pathogens included S. agalactiae (19.7%, 10 days), Escherichia coli (8.8%, 13 days), and Haemophilus influenzae (5.4%, 231 days).
The mortality risk within 1 year of disease onset was higher for all pathogens (6.2% vs. 0.2% unexposed). The highest mortality risk was seen for S. agalactiae (8.7%), followed by E. coli (6.4%), N. meningitidis (4.9%), and H. influenzae (3.4%).
Hazard ratios (HR) for mortality were also higher, particularly in the first year after disease onset. For all pathogens, mortality rates were higher within 1 year (HR, 39.2), 5 years (HR, 28.7), and 10 years (HR, 24.1). The consistently highest mortality rates were associated with S. pneumoniae over 1-year, 5-year, and 10-year follow-up (HR, 42.8; HR, 45.6; HR, 40.6, respectively). Within 1 year, the highest mortality rate was associated with N. meningitidis (HR, 58.4).
Ms. Snoek and Dr. Rohr have no relevant financial disclosures.
Among infants younger than 1 year of age, bacterial meningitis is associated with worse long-term mortality, even after recovery from the initial infection. Heightened mortality risk stretched out to 10 years, and was highest in the wake of infection from Streptococcus agalactiae, according to a retrospective analysis of children in the Netherlands.
“The adjusted hazard rates were high for the whole group of bacterial meningitis, especially within the first year after onset. (Staphylococcus agalactiae) meningitis has the highest mortality risk within one year of disease onset,” Linde Snoek said during her presentation of the study (abstract 913) at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. Ms. Snoek is a PhD student at Amsterdam University Medical Center.
Over longer time periods, the mortality associations were different. “The adjusted hazard rates were highest for pneumococcal meningitis compared to the other pathogens. And this was the case for 1 year, 5 years, and 10 years after disease onset,” said Ms. Snoek.
The study appears to be the first to look at extended mortality following bacterial meningitis in this age group, according to Marie Rohr, MD, who comoderated the session where the research was presented.
“In a quick review of the literature I did not find any [equivalent] study concerning short- and long-term mortality after bacterial meningitis in under 1 year of age,” said Dr. Rohr, a fellow in pediatric infectious diseases at University Hospitals of Geneva. But the message to physicians is clear. “Children with history of bacterial meningitis have a higher long-term mortality than children without a history of bacterial meningitis,” said Dr. Rohr.
The study did have a key limitation: For matched controls, it relied on anonymous data from the Municipal Personal Records Database in Statistics Netherlands. “Important information like cause of death is lacking,” said Dr. Rohr.
Bacterial meningitis is associated with significant mortality and morbidity. Pathogens behind the infections vary with age group and geographic location, as well as immunization status.
To examine long-term mortality after bacterial meningitis, the researchers collected 1,646 records from an exposed cohort, with a date range of 1995 to 2018, from the Netherlands Reference Laboratory for Bacterial Meningitis. Included patients had a positive culture diagnosis of bacterial meningitis during the first year of life. Each exposed subject was compared to 10 controls matched by birth month, birth year, and sex, who had no exposure to bacterial meningitis.
Staphylococcus pneumoniae accounted for the most cases, at 32.0% (median age of onset, 180 days), followed by Neisseria meningitidis at 29.0% (median age of onset, 203 days). Other pathogens included S. agalactiae (19.7%, 10 days), Escherichia coli (8.8%, 13 days), and Haemophilus influenzae (5.4%, 231 days).
The mortality risk within 1 year of disease onset was higher for all pathogens (6.2% vs. 0.2% unexposed). The highest mortality risk was seen for S. agalactiae (8.7%), followed by E. coli (6.4%), N. meningitidis (4.9%), and H. influenzae (3.4%).
Hazard ratios (HR) for mortality were also higher, particularly in the first year after disease onset. For all pathogens, mortality rates were higher within 1 year (HR, 39.2), 5 years (HR, 28.7), and 10 years (HR, 24.1). The consistently highest mortality rates were associated with S. pneumoniae over 1-year, 5-year, and 10-year follow-up (HR, 42.8; HR, 45.6; HR, 40.6, respectively). Within 1 year, the highest mortality rate was associated with N. meningitidis (HR, 58.4).
Ms. Snoek and Dr. Rohr have no relevant financial disclosures.
FROM ESPID 2021
Neurologists brace and prepare for long-COVID fallout
“If there’s one universal truth amongst all the patients I’ve interviewed, it’s that they’re often brushed aside, pigeonholed, or, frankly, abandoned,” said Greg Vanichkachorn, MD, MPH, a family physician and founder of Mayo Clinic’s COVID-19 Activity Rehabilitation Program (CARP).
Take a nap. Tough it out. Push through it. Dr. Vanichkachorn describes the frustration voiced by thousands of patients whose lives continue to be disrupted and thrown into upheaval.
Brain fog. Cognitive dysfunction. Headaches. These are just a few of the manifestations of what the National Institutes of Health has termed post-acute sequelae of SARS COVID-2 (PASC), more commonly known as long-COVID.
PASC is loosely defined as symptoms and/or sequelae that persist for several weeks to months after the initial infection has cleared.
A total of 33.6% (95% confidence interval, 11.17-34.07) of patients with COVID-19 experience neurologic sequelae in the first 6 months following resolution of the infection. Almost half of cases (12.8%; 95% CI, 12.36-13.33) represented first-time diagnoses.
“Anecdotally, the longer we go into this, and the more people that, in the past, have been infected with COVID-19, the more patients will be seeing neurologists with some of these complaints,” said Ralph Sacco, MD, professor and Olemberg chair of neurology at University of Miami, and past president of the American Academy of Neurology.
Neurologic detritus
Further complicating the epidemiologic picture is the broad array of clinical and functional symptoms. “What we call long-haul COVID is not a single entity,” explained Michel Toledano, MD, a neurology consultant and a member of the CARP team at the Mayo Clinic in Rochester, Minnesota. Patients present with persistent or emergent polysymptomatic and multisystemic diseases that often include neurologic symptoms, he said. In many circumstances, they had an acute infection with either very mild symptoms or no symptoms at all.
“There’s no doubt that these people are experiencing significant neurologic symptoms, but it remains unclear whether the driving factor is mainly systemic or the nervous system independently of what is happening in the body,” he said.
Like patients with SARS-CoV-1 and Middle Eastern respiratory syndrome (MERS), patients recovering from confirmed or suspected SARS-CoV-2 infections experience a variety of self-reported neurologic symptoms that vary in terms of time frame, duration, and severity.
Take Jacqueline Jolly, for example, a 50-year-old single mother and construction permit contractor living outside of Tampa, Florida. She was diagnosed with COVID-19 in January 2021. Jolly explained that she was never sick enough to be admitted to the hospital and yet is still not close to full recovery. Lingering, debilitating symptoms include executive function challenges, anosmia, headaches, and paresthesia that frequently bring her to the edge of losing consciousness. She has not returned to work, despite multiple attempts.
Vicky Nunally, a 35-year-old single mother and medical office assistant who lives in the suburbs of Atlanta, Georgia, recounted that she landed in the intensive care unit with a severe SARS-CoV-2 infection. Roughly 6 months later, she continues to experience debilitating headaches, brain fog, and cognitive delays. Her endometriosis has flared up. She says that she is depressed, anxious, and has returned to therapy. “It makes you feel crazy,” she said.
Debilitating, pervasive symptoms
Findings from an international survey of 3,762 respondents that was published on April 21 in medRXiv underscore that PASC occurs predominantly in middle-aged women (78.9% were women; 31% were aged 40-49 years; 25.0% were aged 50-59 years). For the most part, it manifests similarly among people with prior confirmed or suspected SARS-CoV-2 infections. In the study, symptoms were reported in both cohorts well past the initial infection; symptoms persisted past 90 days in 96% of patients and for at least 6 months in 65.2%.
Similarly, a recent study showed that 68% of patients who were enrolled in Mayo Clinic’s CARP as of June 2020 were women, middle aged (mean age, 45 ± 14.2 years), and presented roughly 3 months (94.4 ± 65 days) post diagnosis. Of these patients, 75% had not been previously hospitalized.
In both studies, fatigue and cognitive dysfunction were consistently cited as the most debilitating and pervasive manifestations lasting more than 6 months. Others included postexertional (physical or mental) malaise, sensorimotor symptoms, headaches, and memory problems.
Reports of even more severe neurologic first-time diagnoses are emerging. Findings from the Lancet Psychiatry study showed there was a small but clinically relevant risk for a range of conditions that included intracranial hemorrhage (0.14%; 95% CI, 0.10-0.20), ischemic stroke (0.43%; 95% CI, 0.36-0.52), parkinsonism (0.07%; 95% CI, 0.05-0.12), and nerve root/plexus disorders (2.69%; 95% CI, 2.51-2.89).
Dr. Toledano noted that he’s also seen patients who developed autonomic/small-fiber dysfunction. Preliminary data from a retrospective chart review suggest that the most likely diagnosis is orthostatic intolerance without tachycardia or hypotension.
In the study, 63% (17) of the 27 participants who met the inclusion criteria had abnormal results on function testing, but Composite Autonomic Severity Score results indicated mostly mild disease (sudomotor range, 0-3 [median, 0]; cardiovagal, 0-3 [median, 0]; cardiovascular adrenergic, 0-4 [median, 0]).
“The pattern that’s emerging is consistent with deconditioning,” Dr. Toledano said. “However, a small proportion of patients do have evidence of damage to the nervous system, which is something we’ve seen with other viruses.”
Proliferation of long-COVID clinics
A few of these patients with orthostatic intolerance developed postural tachycardia syndrome or experienced exacerbations of preexisting sensory or autonomic small-fiber neuropathies. “These post-viral, autonomic neuropathies tend to be self-limiting, but we’re starting to see different levels of involvement,” Dr. Toledano explained. At present, causality and/or underlying mechanisms are unclear.
Speaking on behalf of the American Academy of Neurology, Dr. Sacco acknowledged the challenges that lie ahead. “Like any neurological symptom that continues to affect a patient’s quality of life, you may need to seek the expertise of a neurologist. The only issue is that some may still not be sure exactly what to do; we don’t have all the data yet,” he said.
On the flip side, he pointed to the lessons of the past year and how quickly health care systems were able to pivot to deal with the pandemic and critically ill patients, then pivot again to disseminate vaccines, and how they are pivoting yet again to address PASC.
Across the nation, numerous hospitals and health care systems and even small private clinics have launched clinics that focus on long-COVID, including Mayo.
The program has a multidisciplinary, collaborative framework and offers both face-to-face and video telemedicine consultations. The latter are geared toward ensuring that under-resourced populations can access needed care and assistance.
“At Mayo, we have a centralized triage system to help target patients’ visits so that appropriate subspecialties and studies can be preordered,” explained Dr. Toledano. During these visits, patients are assessed for underlying conditions and possible signs of decompensation, as well as functional and physical needs and psychosocial challenges. Thereafter, patients enter either CARP, which offers active rehabilitation for up to 3 months after resolution of the acute infection, or the Post-COVID Care Center, which focuses on patients whose condition is not improving or who are demonstrating signs of central sensitization.
An uphill battle
Both programs incorporate individually paced occupational and physical therapy aimed at ameliorating symptoms, restoring function, developing psychosocial coping skills, and, ultimately, facilitating a return to work. “The idea is, if we can meet with these patients sooner than later and help them recover in an appropriate fashion, they will exit the program faster,” Dr. Vanichkachorn said. “We do see a group of patients who tend to get better right around the 4-month period.”
Although telemedicine provides an opportunity for clinicians outside these hospital systems to engage patients, Dr. Vanichkachorn pointed out that almost all the initial treatments can be offered in the local community by a provider who has adequate time and knowledge of the condition.
He also acknowledged the potential for an uphill battle, especially among those who cling to the belief that PASC is simply a manifestation of anxiety or depression. “This is something that we’ve seen previously with SARS and MERS, as well as in conjunction with fibromyalgia and chronic fatigue, only now with greater magnitude,” he said. “This is a real condition that has important and huge ramifications on a person’s ability to function.”
The silver lining is that last December, the NIH announced that it was allocating $1.1 billion for research through its NIH PASC Initiative. Like other institutions, Mayo is waiting to hear what it has been awarded. In the meantime, it has developed a biorepository of patient samples to better understand pathophysiologic mechanisms underlying PASC and to identify possible biomarkers that differentiate these patients.
Despite the challenges, Dr. Vanichkachorn is hopeful. “If we can get a concrete understanding of what is occurring on the chemical level and develop diagnostic tests, then the education will follow. Providers won’t be able to ignore it any longer,” he said.
The interviewees have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“If there’s one universal truth amongst all the patients I’ve interviewed, it’s that they’re often brushed aside, pigeonholed, or, frankly, abandoned,” said Greg Vanichkachorn, MD, MPH, a family physician and founder of Mayo Clinic’s COVID-19 Activity Rehabilitation Program (CARP).
Take a nap. Tough it out. Push through it. Dr. Vanichkachorn describes the frustration voiced by thousands of patients whose lives continue to be disrupted and thrown into upheaval.
Brain fog. Cognitive dysfunction. Headaches. These are just a few of the manifestations of what the National Institutes of Health has termed post-acute sequelae of SARS COVID-2 (PASC), more commonly known as long-COVID.
PASC is loosely defined as symptoms and/or sequelae that persist for several weeks to months after the initial infection has cleared.
A total of 33.6% (95% confidence interval, 11.17-34.07) of patients with COVID-19 experience neurologic sequelae in the first 6 months following resolution of the infection. Almost half of cases (12.8%; 95% CI, 12.36-13.33) represented first-time diagnoses.
“Anecdotally, the longer we go into this, and the more people that, in the past, have been infected with COVID-19, the more patients will be seeing neurologists with some of these complaints,” said Ralph Sacco, MD, professor and Olemberg chair of neurology at University of Miami, and past president of the American Academy of Neurology.
Neurologic detritus
Further complicating the epidemiologic picture is the broad array of clinical and functional symptoms. “What we call long-haul COVID is not a single entity,” explained Michel Toledano, MD, a neurology consultant and a member of the CARP team at the Mayo Clinic in Rochester, Minnesota. Patients present with persistent or emergent polysymptomatic and multisystemic diseases that often include neurologic symptoms, he said. In many circumstances, they had an acute infection with either very mild symptoms or no symptoms at all.
“There’s no doubt that these people are experiencing significant neurologic symptoms, but it remains unclear whether the driving factor is mainly systemic or the nervous system independently of what is happening in the body,” he said.
Like patients with SARS-CoV-1 and Middle Eastern respiratory syndrome (MERS), patients recovering from confirmed or suspected SARS-CoV-2 infections experience a variety of self-reported neurologic symptoms that vary in terms of time frame, duration, and severity.
Take Jacqueline Jolly, for example, a 50-year-old single mother and construction permit contractor living outside of Tampa, Florida. She was diagnosed with COVID-19 in January 2021. Jolly explained that she was never sick enough to be admitted to the hospital and yet is still not close to full recovery. Lingering, debilitating symptoms include executive function challenges, anosmia, headaches, and paresthesia that frequently bring her to the edge of losing consciousness. She has not returned to work, despite multiple attempts.
Vicky Nunally, a 35-year-old single mother and medical office assistant who lives in the suburbs of Atlanta, Georgia, recounted that she landed in the intensive care unit with a severe SARS-CoV-2 infection. Roughly 6 months later, she continues to experience debilitating headaches, brain fog, and cognitive delays. Her endometriosis has flared up. She says that she is depressed, anxious, and has returned to therapy. “It makes you feel crazy,” she said.
Debilitating, pervasive symptoms
Findings from an international survey of 3,762 respondents that was published on April 21 in medRXiv underscore that PASC occurs predominantly in middle-aged women (78.9% were women; 31% were aged 40-49 years; 25.0% were aged 50-59 years). For the most part, it manifests similarly among people with prior confirmed or suspected SARS-CoV-2 infections. In the study, symptoms were reported in both cohorts well past the initial infection; symptoms persisted past 90 days in 96% of patients and for at least 6 months in 65.2%.
Similarly, a recent study showed that 68% of patients who were enrolled in Mayo Clinic’s CARP as of June 2020 were women, middle aged (mean age, 45 ± 14.2 years), and presented roughly 3 months (94.4 ± 65 days) post diagnosis. Of these patients, 75% had not been previously hospitalized.
In both studies, fatigue and cognitive dysfunction were consistently cited as the most debilitating and pervasive manifestations lasting more than 6 months. Others included postexertional (physical or mental) malaise, sensorimotor symptoms, headaches, and memory problems.
Reports of even more severe neurologic first-time diagnoses are emerging. Findings from the Lancet Psychiatry study showed there was a small but clinically relevant risk for a range of conditions that included intracranial hemorrhage (0.14%; 95% CI, 0.10-0.20), ischemic stroke (0.43%; 95% CI, 0.36-0.52), parkinsonism (0.07%; 95% CI, 0.05-0.12), and nerve root/plexus disorders (2.69%; 95% CI, 2.51-2.89).
Dr. Toledano noted that he’s also seen patients who developed autonomic/small-fiber dysfunction. Preliminary data from a retrospective chart review suggest that the most likely diagnosis is orthostatic intolerance without tachycardia or hypotension.
In the study, 63% (17) of the 27 participants who met the inclusion criteria had abnormal results on function testing, but Composite Autonomic Severity Score results indicated mostly mild disease (sudomotor range, 0-3 [median, 0]; cardiovagal, 0-3 [median, 0]; cardiovascular adrenergic, 0-4 [median, 0]).
“The pattern that’s emerging is consistent with deconditioning,” Dr. Toledano said. “However, a small proportion of patients do have evidence of damage to the nervous system, which is something we’ve seen with other viruses.”
Proliferation of long-COVID clinics
A few of these patients with orthostatic intolerance developed postural tachycardia syndrome or experienced exacerbations of preexisting sensory or autonomic small-fiber neuropathies. “These post-viral, autonomic neuropathies tend to be self-limiting, but we’re starting to see different levels of involvement,” Dr. Toledano explained. At present, causality and/or underlying mechanisms are unclear.
Speaking on behalf of the American Academy of Neurology, Dr. Sacco acknowledged the challenges that lie ahead. “Like any neurological symptom that continues to affect a patient’s quality of life, you may need to seek the expertise of a neurologist. The only issue is that some may still not be sure exactly what to do; we don’t have all the data yet,” he said.
On the flip side, he pointed to the lessons of the past year and how quickly health care systems were able to pivot to deal with the pandemic and critically ill patients, then pivot again to disseminate vaccines, and how they are pivoting yet again to address PASC.
Across the nation, numerous hospitals and health care systems and even small private clinics have launched clinics that focus on long-COVID, including Mayo.
The program has a multidisciplinary, collaborative framework and offers both face-to-face and video telemedicine consultations. The latter are geared toward ensuring that under-resourced populations can access needed care and assistance.
“At Mayo, we have a centralized triage system to help target patients’ visits so that appropriate subspecialties and studies can be preordered,” explained Dr. Toledano. During these visits, patients are assessed for underlying conditions and possible signs of decompensation, as well as functional and physical needs and psychosocial challenges. Thereafter, patients enter either CARP, which offers active rehabilitation for up to 3 months after resolution of the acute infection, or the Post-COVID Care Center, which focuses on patients whose condition is not improving or who are demonstrating signs of central sensitization.
An uphill battle
Both programs incorporate individually paced occupational and physical therapy aimed at ameliorating symptoms, restoring function, developing psychosocial coping skills, and, ultimately, facilitating a return to work. “The idea is, if we can meet with these patients sooner than later and help them recover in an appropriate fashion, they will exit the program faster,” Dr. Vanichkachorn said. “We do see a group of patients who tend to get better right around the 4-month period.”
Although telemedicine provides an opportunity for clinicians outside these hospital systems to engage patients, Dr. Vanichkachorn pointed out that almost all the initial treatments can be offered in the local community by a provider who has adequate time and knowledge of the condition.
He also acknowledged the potential for an uphill battle, especially among those who cling to the belief that PASC is simply a manifestation of anxiety or depression. “This is something that we’ve seen previously with SARS and MERS, as well as in conjunction with fibromyalgia and chronic fatigue, only now with greater magnitude,” he said. “This is a real condition that has important and huge ramifications on a person’s ability to function.”
The silver lining is that last December, the NIH announced that it was allocating $1.1 billion for research through its NIH PASC Initiative. Like other institutions, Mayo is waiting to hear what it has been awarded. In the meantime, it has developed a biorepository of patient samples to better understand pathophysiologic mechanisms underlying PASC and to identify possible biomarkers that differentiate these patients.
Despite the challenges, Dr. Vanichkachorn is hopeful. “If we can get a concrete understanding of what is occurring on the chemical level and develop diagnostic tests, then the education will follow. Providers won’t be able to ignore it any longer,” he said.
The interviewees have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
“If there’s one universal truth amongst all the patients I’ve interviewed, it’s that they’re often brushed aside, pigeonholed, or, frankly, abandoned,” said Greg Vanichkachorn, MD, MPH, a family physician and founder of Mayo Clinic’s COVID-19 Activity Rehabilitation Program (CARP).
Take a nap. Tough it out. Push through it. Dr. Vanichkachorn describes the frustration voiced by thousands of patients whose lives continue to be disrupted and thrown into upheaval.
Brain fog. Cognitive dysfunction. Headaches. These are just a few of the manifestations of what the National Institutes of Health has termed post-acute sequelae of SARS COVID-2 (PASC), more commonly known as long-COVID.
PASC is loosely defined as symptoms and/or sequelae that persist for several weeks to months after the initial infection has cleared.
A total of 33.6% (95% confidence interval, 11.17-34.07) of patients with COVID-19 experience neurologic sequelae in the first 6 months following resolution of the infection. Almost half of cases (12.8%; 95% CI, 12.36-13.33) represented first-time diagnoses.
“Anecdotally, the longer we go into this, and the more people that, in the past, have been infected with COVID-19, the more patients will be seeing neurologists with some of these complaints,” said Ralph Sacco, MD, professor and Olemberg chair of neurology at University of Miami, and past president of the American Academy of Neurology.
Neurologic detritus
Further complicating the epidemiologic picture is the broad array of clinical and functional symptoms. “What we call long-haul COVID is not a single entity,” explained Michel Toledano, MD, a neurology consultant and a member of the CARP team at the Mayo Clinic in Rochester, Minnesota. Patients present with persistent or emergent polysymptomatic and multisystemic diseases that often include neurologic symptoms, he said. In many circumstances, they had an acute infection with either very mild symptoms or no symptoms at all.
“There’s no doubt that these people are experiencing significant neurologic symptoms, but it remains unclear whether the driving factor is mainly systemic or the nervous system independently of what is happening in the body,” he said.
Like patients with SARS-CoV-1 and Middle Eastern respiratory syndrome (MERS), patients recovering from confirmed or suspected SARS-CoV-2 infections experience a variety of self-reported neurologic symptoms that vary in terms of time frame, duration, and severity.
Take Jacqueline Jolly, for example, a 50-year-old single mother and construction permit contractor living outside of Tampa, Florida. She was diagnosed with COVID-19 in January 2021. Jolly explained that she was never sick enough to be admitted to the hospital and yet is still not close to full recovery. Lingering, debilitating symptoms include executive function challenges, anosmia, headaches, and paresthesia that frequently bring her to the edge of losing consciousness. She has not returned to work, despite multiple attempts.
Vicky Nunally, a 35-year-old single mother and medical office assistant who lives in the suburbs of Atlanta, Georgia, recounted that she landed in the intensive care unit with a severe SARS-CoV-2 infection. Roughly 6 months later, she continues to experience debilitating headaches, brain fog, and cognitive delays. Her endometriosis has flared up. She says that she is depressed, anxious, and has returned to therapy. “It makes you feel crazy,” she said.
Debilitating, pervasive symptoms
Findings from an international survey of 3,762 respondents that was published on April 21 in medRXiv underscore that PASC occurs predominantly in middle-aged women (78.9% were women; 31% were aged 40-49 years; 25.0% were aged 50-59 years). For the most part, it manifests similarly among people with prior confirmed or suspected SARS-CoV-2 infections. In the study, symptoms were reported in both cohorts well past the initial infection; symptoms persisted past 90 days in 96% of patients and for at least 6 months in 65.2%.
Similarly, a recent study showed that 68% of patients who were enrolled in Mayo Clinic’s CARP as of June 2020 were women, middle aged (mean age, 45 ± 14.2 years), and presented roughly 3 months (94.4 ± 65 days) post diagnosis. Of these patients, 75% had not been previously hospitalized.
In both studies, fatigue and cognitive dysfunction were consistently cited as the most debilitating and pervasive manifestations lasting more than 6 months. Others included postexertional (physical or mental) malaise, sensorimotor symptoms, headaches, and memory problems.
Reports of even more severe neurologic first-time diagnoses are emerging. Findings from the Lancet Psychiatry study showed there was a small but clinically relevant risk for a range of conditions that included intracranial hemorrhage (0.14%; 95% CI, 0.10-0.20), ischemic stroke (0.43%; 95% CI, 0.36-0.52), parkinsonism (0.07%; 95% CI, 0.05-0.12), and nerve root/plexus disorders (2.69%; 95% CI, 2.51-2.89).
Dr. Toledano noted that he’s also seen patients who developed autonomic/small-fiber dysfunction. Preliminary data from a retrospective chart review suggest that the most likely diagnosis is orthostatic intolerance without tachycardia or hypotension.
In the study, 63% (17) of the 27 participants who met the inclusion criteria had abnormal results on function testing, but Composite Autonomic Severity Score results indicated mostly mild disease (sudomotor range, 0-3 [median, 0]; cardiovagal, 0-3 [median, 0]; cardiovascular adrenergic, 0-4 [median, 0]).
“The pattern that’s emerging is consistent with deconditioning,” Dr. Toledano said. “However, a small proportion of patients do have evidence of damage to the nervous system, which is something we’ve seen with other viruses.”
Proliferation of long-COVID clinics
A few of these patients with orthostatic intolerance developed postural tachycardia syndrome or experienced exacerbations of preexisting sensory or autonomic small-fiber neuropathies. “These post-viral, autonomic neuropathies tend to be self-limiting, but we’re starting to see different levels of involvement,” Dr. Toledano explained. At present, causality and/or underlying mechanisms are unclear.
Speaking on behalf of the American Academy of Neurology, Dr. Sacco acknowledged the challenges that lie ahead. “Like any neurological symptom that continues to affect a patient’s quality of life, you may need to seek the expertise of a neurologist. The only issue is that some may still not be sure exactly what to do; we don’t have all the data yet,” he said.
On the flip side, he pointed to the lessons of the past year and how quickly health care systems were able to pivot to deal with the pandemic and critically ill patients, then pivot again to disseminate vaccines, and how they are pivoting yet again to address PASC.
Across the nation, numerous hospitals and health care systems and even small private clinics have launched clinics that focus on long-COVID, including Mayo.
The program has a multidisciplinary, collaborative framework and offers both face-to-face and video telemedicine consultations. The latter are geared toward ensuring that under-resourced populations can access needed care and assistance.
“At Mayo, we have a centralized triage system to help target patients’ visits so that appropriate subspecialties and studies can be preordered,” explained Dr. Toledano. During these visits, patients are assessed for underlying conditions and possible signs of decompensation, as well as functional and physical needs and psychosocial challenges. Thereafter, patients enter either CARP, which offers active rehabilitation for up to 3 months after resolution of the acute infection, or the Post-COVID Care Center, which focuses on patients whose condition is not improving or who are demonstrating signs of central sensitization.
An uphill battle
Both programs incorporate individually paced occupational and physical therapy aimed at ameliorating symptoms, restoring function, developing psychosocial coping skills, and, ultimately, facilitating a return to work. “The idea is, if we can meet with these patients sooner than later and help them recover in an appropriate fashion, they will exit the program faster,” Dr. Vanichkachorn said. “We do see a group of patients who tend to get better right around the 4-month period.”
Although telemedicine provides an opportunity for clinicians outside these hospital systems to engage patients, Dr. Vanichkachorn pointed out that almost all the initial treatments can be offered in the local community by a provider who has adequate time and knowledge of the condition.
He also acknowledged the potential for an uphill battle, especially among those who cling to the belief that PASC is simply a manifestation of anxiety or depression. “This is something that we’ve seen previously with SARS and MERS, as well as in conjunction with fibromyalgia and chronic fatigue, only now with greater magnitude,” he said. “This is a real condition that has important and huge ramifications on a person’s ability to function.”
The silver lining is that last December, the NIH announced that it was allocating $1.1 billion for research through its NIH PASC Initiative. Like other institutions, Mayo is waiting to hear what it has been awarded. In the meantime, it has developed a biorepository of patient samples to better understand pathophysiologic mechanisms underlying PASC and to identify possible biomarkers that differentiate these patients.
Despite the challenges, Dr. Vanichkachorn is hopeful. “If we can get a concrete understanding of what is occurring on the chemical level and develop diagnostic tests, then the education will follow. Providers won’t be able to ignore it any longer,” he said.
The interviewees have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA approves ibrexafungerp for vaginal yeast infection
Ibrexafungerp is the first drug approved in a new antifungal class for vulvovaginal candidiasis (VVC) in more than 20 years, the drug’s manufacturer Scynexis said in a press release. It becomes the first and only nonazole treatment for vaginal yeast infections.
The biotechnology company said approval came after positive results from two phase 3 studies in which oral ibrexafungerp demonstrated efficacy and tolerability. The most common reactions observed in clinical trials were diarrhea, nausea, abdominal pain, dizziness, and vomiting.
There are few other treatments for vaginal yeast infections, which is the second most common cause of vaginitis. Those previously approved agents include several topical azole antifungals and oral fluconazole (Diflucan), which, Scynexis said, is the only other orally administered antifungal approved for the treatment of VVC in the United States and has accounted for over more than 90% of prescriptions written for the condition each year.
However, the company noted, oral fluconazole reports a 55% therapeutic cure rate on its label, which now also includes warnings of potential fetal harm, demonstrating the need for new oral options.
The new drug may not fill that need for pregnant women, however, as the company noted that ibrexafungerp should not be used during pregnancy, and administration during pregnancy “may cause fetal harm based on animal studies.”
Because of possible teratogenic effects, the company advised clinicians to verify pregnancy status in females of reproductive potential before prescribing ibrexafungerp and advises effective contraception during treatment.
VVC can come with substantial morbidity, including genital pain, itching and burning, reduced sexual pleasure, and psychological distress.
David Angulo, MD, chief medical officer for Scynexis, said in a statement the tablets brings new benefits.
Dr. Angulo said the drug “has a differentiated fungicidal mechanism of action that kills a broad range of Candida species, including azole-resistant strains. We are working on completing our CANDLE study investigating ibrexafungerp for the prevention of recurrent VVC and expect we will be submitting a supplemental NDA [new drug application] in the first half of 2022.”
Scynexis said it partnered with Amplity Health, a Pennsylvania-based pharmaceutical company, to support U.S. marketing of the drug. The commercial launch will follow the approval.
Ibrexafungerp was granted approval through both the FDA’s Qualified Infectious Disease Product and Fast Track designations. It is expected to be marketed exclusively in the United States for 10 years.
A version of this article first appeared on Medscape.com.
Ibrexafungerp is the first drug approved in a new antifungal class for vulvovaginal candidiasis (VVC) in more than 20 years, the drug’s manufacturer Scynexis said in a press release. It becomes the first and only nonazole treatment for vaginal yeast infections.
The biotechnology company said approval came after positive results from two phase 3 studies in which oral ibrexafungerp demonstrated efficacy and tolerability. The most common reactions observed in clinical trials were diarrhea, nausea, abdominal pain, dizziness, and vomiting.
There are few other treatments for vaginal yeast infections, which is the second most common cause of vaginitis. Those previously approved agents include several topical azole antifungals and oral fluconazole (Diflucan), which, Scynexis said, is the only other orally administered antifungal approved for the treatment of VVC in the United States and has accounted for over more than 90% of prescriptions written for the condition each year.
However, the company noted, oral fluconazole reports a 55% therapeutic cure rate on its label, which now also includes warnings of potential fetal harm, demonstrating the need for new oral options.
The new drug may not fill that need for pregnant women, however, as the company noted that ibrexafungerp should not be used during pregnancy, and administration during pregnancy “may cause fetal harm based on animal studies.”
Because of possible teratogenic effects, the company advised clinicians to verify pregnancy status in females of reproductive potential before prescribing ibrexafungerp and advises effective contraception during treatment.
VVC can come with substantial morbidity, including genital pain, itching and burning, reduced sexual pleasure, and psychological distress.
David Angulo, MD, chief medical officer for Scynexis, said in a statement the tablets brings new benefits.
Dr. Angulo said the drug “has a differentiated fungicidal mechanism of action that kills a broad range of Candida species, including azole-resistant strains. We are working on completing our CANDLE study investigating ibrexafungerp for the prevention of recurrent VVC and expect we will be submitting a supplemental NDA [new drug application] in the first half of 2022.”
Scynexis said it partnered with Amplity Health, a Pennsylvania-based pharmaceutical company, to support U.S. marketing of the drug. The commercial launch will follow the approval.
Ibrexafungerp was granted approval through both the FDA’s Qualified Infectious Disease Product and Fast Track designations. It is expected to be marketed exclusively in the United States for 10 years.
A version of this article first appeared on Medscape.com.
Ibrexafungerp is the first drug approved in a new antifungal class for vulvovaginal candidiasis (VVC) in more than 20 years, the drug’s manufacturer Scynexis said in a press release. It becomes the first and only nonazole treatment for vaginal yeast infections.
The biotechnology company said approval came after positive results from two phase 3 studies in which oral ibrexafungerp demonstrated efficacy and tolerability. The most common reactions observed in clinical trials were diarrhea, nausea, abdominal pain, dizziness, and vomiting.
There are few other treatments for vaginal yeast infections, which is the second most common cause of vaginitis. Those previously approved agents include several topical azole antifungals and oral fluconazole (Diflucan), which, Scynexis said, is the only other orally administered antifungal approved for the treatment of VVC in the United States and has accounted for over more than 90% of prescriptions written for the condition each year.
However, the company noted, oral fluconazole reports a 55% therapeutic cure rate on its label, which now also includes warnings of potential fetal harm, demonstrating the need for new oral options.
The new drug may not fill that need for pregnant women, however, as the company noted that ibrexafungerp should not be used during pregnancy, and administration during pregnancy “may cause fetal harm based on animal studies.”
Because of possible teratogenic effects, the company advised clinicians to verify pregnancy status in females of reproductive potential before prescribing ibrexafungerp and advises effective contraception during treatment.
VVC can come with substantial morbidity, including genital pain, itching and burning, reduced sexual pleasure, and psychological distress.
David Angulo, MD, chief medical officer for Scynexis, said in a statement the tablets brings new benefits.
Dr. Angulo said the drug “has a differentiated fungicidal mechanism of action that kills a broad range of Candida species, including azole-resistant strains. We are working on completing our CANDLE study investigating ibrexafungerp for the prevention of recurrent VVC and expect we will be submitting a supplemental NDA [new drug application] in the first half of 2022.”
Scynexis said it partnered with Amplity Health, a Pennsylvania-based pharmaceutical company, to support U.S. marketing of the drug. The commercial launch will follow the approval.
Ibrexafungerp was granted approval through both the FDA’s Qualified Infectious Disease Product and Fast Track designations. It is expected to be marketed exclusively in the United States for 10 years.
A version of this article first appeared on Medscape.com.
CDC: New botulism guidelines focus on mass casualty events
Botulinum toxin is said to be the most lethal substance known. Inhaling just 1-3 nanograms of toxin per kilogram of body mass constitutes a lethal dose.
The CDC has been working on these guidelines since 2015, initially establishing a technical development group and steering committee to prioritize topics for review and make recommendations. Since then, the agency published 15 systematic reviews in Clinical Infectious Diseases early in 2018. The reviews addressed the recognition of botulism clinically, treatment with botulinum antitoxin, and complications from that treatment. They also looked at the epidemiology of botulism outbreaks and botulism in the special populations of vulnerable pediatric and pregnant patients.
In 2016, the CDC held two extended forums and convened a workshop with 72 experts. In addition to the more standard topics of diagnosis and treatment, attention was given to crisis standards of care, caring for multiple patients at once, and ethical considerations in management.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, said in an interview that the new guidance “was really specific [and] was meant to address the gap in guidance for mass casualty settings.”
While clinicians are used to focusing on an individual patient, in times of crises, with multiple patients from a food-borne outbreak or a bioterrorism attack, the focus must shift to the population rather than the individual. The workshop explored issues of triaging, adding beds, and caring for patients when a hospital is overwhelmed with an acute influx of severely ill patients.
Such a mass casualty event is similar to the stress encountered this past year with COVID-19 patients swamping the hospitals, which had too little oxygen, too few ventilators, and too few staff members to care for the sudden influx of critically ill patients.
Diagnosis
Leslie Edwards, MHS, BSN, a CDC epidemiologist and botulism expert, said that “botulism is rare and [so] could be difficult to diagnose.” The CDC “wanted to highlight some of those key clinical factors” to speed recognition.
Hospitals and health officials are being urged to develop crisis protocols as part of emergency preparedness plans. And clinicians should be able to recognize four major syndromes: botulism from food, wounds, and inhalation, as well as iatrogenic botulism (from exposure via injection of the neurotoxin).
Botulism has a characteristic and unusual pattern of symptoms, which begin with cranial nerve palsies. Then there is typically a descending, symmetric flaccid paralysis. Symptoms might progress to respiratory failure and death. Other critical clues that implicate botulism include a lack of sensory deficits and the absence of pain.
Symptoms are most likely to be mistaken for myasthenia gravis or Guillain-Barré syndrome, but the latter has an ascending paralysis. Cranial nerve involvement can present as blurred vision, ptosis (drooping lid), diplopia (double vision), ophthalmoplegia (weak eye muscles), or difficulty with speech and swallowing. Shortness of breath and abdominal discomfort can also occur. Respiratory failure may occur from weakness or paralysis of cranial nerves. Cranial nerve signs and symptoms in the absence of fever, along with a descending paralysis, should strongly suggest the diagnosis.
With food-borne botulism, vomiting occurs in half the patients. Improperly sterilized home-canned food is the major risk factor. While the toxin is rapidly destroyed by heat, the bacterial spores are not. Wound botulism is most commonly associated with the injection of drugs, particularly black tar heroin.
Dr. Edwards stressed that “time is of the essence when it comes to botulism diagnostics and treating. Timely administration of the botulism antitoxin early in the course of illness can arrest the progression of paralysis and possibly avert the need for intubation or ventilation.”
It’s essential to note that botulism is an urgent diagnosis that has to be made on clinical grounds. Lab assays for botulinum neurotoxins take too long and are only conducted in public health laboratories. The decision to use antitoxin must not be delayed to wait for confirmation.
Clinicians should immediately contact the local or state health department’s emergency on-call team if botulism is suspected. They will arrange for expert consultation.
Treatment
Botulinum antitoxin is the only specific therapy for this infection. If given early – preferably within 24-48 hours of symptom onset – it can stop the progression of paralysis. But antitoxin will not reverse existing paralysis. If paralysis is still progressing outside of that 24- to 48-hour window, the antitoxin should still provide benefit. The antitoxin is available only through state health departments and a request to the CDC.
Botulism antitoxin is made from horse serum and therefore may cause a variety of allergic reactions. The risk for anaphylaxis is less than 2%, far lower than the mortality from untreated botulism.
While these guidelines have an important focus on triaging and treating mass casualties from botulism, it’s important to note that food-borne outbreaks and prevention issues are covered elsewhere on the CDC site.
Dr. Edwards has disclosed no relevant financial relationships. Dr. Adalja is a consultant for Emergent BioSolutions, which makes the heptavalent botulism antitoxin.
Dr. Stone is an infectious disease specialist and author of “Resilience: One Family’s Story of Hope and Triumph Over Evil” and of “Conducting Clinical Research,” the essential guide to the topic. You can find her at drjudystone.com or on Twitter @drjudystone.
A version of this article first appeared on Medscape.com.
Botulinum toxin is said to be the most lethal substance known. Inhaling just 1-3 nanograms of toxin per kilogram of body mass constitutes a lethal dose.
The CDC has been working on these guidelines since 2015, initially establishing a technical development group and steering committee to prioritize topics for review and make recommendations. Since then, the agency published 15 systematic reviews in Clinical Infectious Diseases early in 2018. The reviews addressed the recognition of botulism clinically, treatment with botulinum antitoxin, and complications from that treatment. They also looked at the epidemiology of botulism outbreaks and botulism in the special populations of vulnerable pediatric and pregnant patients.
In 2016, the CDC held two extended forums and convened a workshop with 72 experts. In addition to the more standard topics of diagnosis and treatment, attention was given to crisis standards of care, caring for multiple patients at once, and ethical considerations in management.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, said in an interview that the new guidance “was really specific [and] was meant to address the gap in guidance for mass casualty settings.”
While clinicians are used to focusing on an individual patient, in times of crises, with multiple patients from a food-borne outbreak or a bioterrorism attack, the focus must shift to the population rather than the individual. The workshop explored issues of triaging, adding beds, and caring for patients when a hospital is overwhelmed with an acute influx of severely ill patients.
Such a mass casualty event is similar to the stress encountered this past year with COVID-19 patients swamping the hospitals, which had too little oxygen, too few ventilators, and too few staff members to care for the sudden influx of critically ill patients.
Diagnosis
Leslie Edwards, MHS, BSN, a CDC epidemiologist and botulism expert, said that “botulism is rare and [so] could be difficult to diagnose.” The CDC “wanted to highlight some of those key clinical factors” to speed recognition.
Hospitals and health officials are being urged to develop crisis protocols as part of emergency preparedness plans. And clinicians should be able to recognize four major syndromes: botulism from food, wounds, and inhalation, as well as iatrogenic botulism (from exposure via injection of the neurotoxin).
Botulism has a characteristic and unusual pattern of symptoms, which begin with cranial nerve palsies. Then there is typically a descending, symmetric flaccid paralysis. Symptoms might progress to respiratory failure and death. Other critical clues that implicate botulism include a lack of sensory deficits and the absence of pain.
Symptoms are most likely to be mistaken for myasthenia gravis or Guillain-Barré syndrome, but the latter has an ascending paralysis. Cranial nerve involvement can present as blurred vision, ptosis (drooping lid), diplopia (double vision), ophthalmoplegia (weak eye muscles), or difficulty with speech and swallowing. Shortness of breath and abdominal discomfort can also occur. Respiratory failure may occur from weakness or paralysis of cranial nerves. Cranial nerve signs and symptoms in the absence of fever, along with a descending paralysis, should strongly suggest the diagnosis.
With food-borne botulism, vomiting occurs in half the patients. Improperly sterilized home-canned food is the major risk factor. While the toxin is rapidly destroyed by heat, the bacterial spores are not. Wound botulism is most commonly associated with the injection of drugs, particularly black tar heroin.
Dr. Edwards stressed that “time is of the essence when it comes to botulism diagnostics and treating. Timely administration of the botulism antitoxin early in the course of illness can arrest the progression of paralysis and possibly avert the need for intubation or ventilation.”
It’s essential to note that botulism is an urgent diagnosis that has to be made on clinical grounds. Lab assays for botulinum neurotoxins take too long and are only conducted in public health laboratories. The decision to use antitoxin must not be delayed to wait for confirmation.
Clinicians should immediately contact the local or state health department’s emergency on-call team if botulism is suspected. They will arrange for expert consultation.
Treatment
Botulinum antitoxin is the only specific therapy for this infection. If given early – preferably within 24-48 hours of symptom onset – it can stop the progression of paralysis. But antitoxin will not reverse existing paralysis. If paralysis is still progressing outside of that 24- to 48-hour window, the antitoxin should still provide benefit. The antitoxin is available only through state health departments and a request to the CDC.
Botulism antitoxin is made from horse serum and therefore may cause a variety of allergic reactions. The risk for anaphylaxis is less than 2%, far lower than the mortality from untreated botulism.
While these guidelines have an important focus on triaging and treating mass casualties from botulism, it’s important to note that food-borne outbreaks and prevention issues are covered elsewhere on the CDC site.
Dr. Edwards has disclosed no relevant financial relationships. Dr. Adalja is a consultant for Emergent BioSolutions, which makes the heptavalent botulism antitoxin.
Dr. Stone is an infectious disease specialist and author of “Resilience: One Family’s Story of Hope and Triumph Over Evil” and of “Conducting Clinical Research,” the essential guide to the topic. You can find her at drjudystone.com or on Twitter @drjudystone.
A version of this article first appeared on Medscape.com.
Botulinum toxin is said to be the most lethal substance known. Inhaling just 1-3 nanograms of toxin per kilogram of body mass constitutes a lethal dose.
The CDC has been working on these guidelines since 2015, initially establishing a technical development group and steering committee to prioritize topics for review and make recommendations. Since then, the agency published 15 systematic reviews in Clinical Infectious Diseases early in 2018. The reviews addressed the recognition of botulism clinically, treatment with botulinum antitoxin, and complications from that treatment. They also looked at the epidemiology of botulism outbreaks and botulism in the special populations of vulnerable pediatric and pregnant patients.
In 2016, the CDC held two extended forums and convened a workshop with 72 experts. In addition to the more standard topics of diagnosis and treatment, attention was given to crisis standards of care, caring for multiple patients at once, and ethical considerations in management.
Amesh Adalja, MD, senior scholar, Johns Hopkins Center for Health Security, Baltimore, said in an interview that the new guidance “was really specific [and] was meant to address the gap in guidance for mass casualty settings.”
While clinicians are used to focusing on an individual patient, in times of crises, with multiple patients from a food-borne outbreak or a bioterrorism attack, the focus must shift to the population rather than the individual. The workshop explored issues of triaging, adding beds, and caring for patients when a hospital is overwhelmed with an acute influx of severely ill patients.
Such a mass casualty event is similar to the stress encountered this past year with COVID-19 patients swamping the hospitals, which had too little oxygen, too few ventilators, and too few staff members to care for the sudden influx of critically ill patients.
Diagnosis
Leslie Edwards, MHS, BSN, a CDC epidemiologist and botulism expert, said that “botulism is rare and [so] could be difficult to diagnose.” The CDC “wanted to highlight some of those key clinical factors” to speed recognition.
Hospitals and health officials are being urged to develop crisis protocols as part of emergency preparedness plans. And clinicians should be able to recognize four major syndromes: botulism from food, wounds, and inhalation, as well as iatrogenic botulism (from exposure via injection of the neurotoxin).
Botulism has a characteristic and unusual pattern of symptoms, which begin with cranial nerve palsies. Then there is typically a descending, symmetric flaccid paralysis. Symptoms might progress to respiratory failure and death. Other critical clues that implicate botulism include a lack of sensory deficits and the absence of pain.
Symptoms are most likely to be mistaken for myasthenia gravis or Guillain-Barré syndrome, but the latter has an ascending paralysis. Cranial nerve involvement can present as blurred vision, ptosis (drooping lid), diplopia (double vision), ophthalmoplegia (weak eye muscles), or difficulty with speech and swallowing. Shortness of breath and abdominal discomfort can also occur. Respiratory failure may occur from weakness or paralysis of cranial nerves. Cranial nerve signs and symptoms in the absence of fever, along with a descending paralysis, should strongly suggest the diagnosis.
With food-borne botulism, vomiting occurs in half the patients. Improperly sterilized home-canned food is the major risk factor. While the toxin is rapidly destroyed by heat, the bacterial spores are not. Wound botulism is most commonly associated with the injection of drugs, particularly black tar heroin.
Dr. Edwards stressed that “time is of the essence when it comes to botulism diagnostics and treating. Timely administration of the botulism antitoxin early in the course of illness can arrest the progression of paralysis and possibly avert the need for intubation or ventilation.”
It’s essential to note that botulism is an urgent diagnosis that has to be made on clinical grounds. Lab assays for botulinum neurotoxins take too long and are only conducted in public health laboratories. The decision to use antitoxin must not be delayed to wait for confirmation.
Clinicians should immediately contact the local or state health department’s emergency on-call team if botulism is suspected. They will arrange for expert consultation.
Treatment
Botulinum antitoxin is the only specific therapy for this infection. If given early – preferably within 24-48 hours of symptom onset – it can stop the progression of paralysis. But antitoxin will not reverse existing paralysis. If paralysis is still progressing outside of that 24- to 48-hour window, the antitoxin should still provide benefit. The antitoxin is available only through state health departments and a request to the CDC.
Botulism antitoxin is made from horse serum and therefore may cause a variety of allergic reactions. The risk for anaphylaxis is less than 2%, far lower than the mortality from untreated botulism.
While these guidelines have an important focus on triaging and treating mass casualties from botulism, it’s important to note that food-borne outbreaks and prevention issues are covered elsewhere on the CDC site.
Dr. Edwards has disclosed no relevant financial relationships. Dr. Adalja is a consultant for Emergent BioSolutions, which makes the heptavalent botulism antitoxin.
Dr. Stone is an infectious disease specialist and author of “Resilience: One Family’s Story of Hope and Triumph Over Evil” and of “Conducting Clinical Research,” the essential guide to the topic. You can find her at drjudystone.com or on Twitter @drjudystone.
A version of this article first appeared on Medscape.com.
DOJ charges 14 with COVID-19–related fraud nearing $150M
The U.S. Department of Justice (DOJ) on May 26 announced charges against 14 defendants across the country who allegedly engaged in health care fraud schemes that exploited the COVID-19 pandemic and resulted in over $143 million in false billings to Medicare.
Among the defendants, a DOJ news release said, were a telemedicine company executive, a physician, marketers, and medical business owners.
In addition, the Centers for Medicare and Medicaid Services separately announced that it had taken “adverse administrative actions” against more than 50 providers for their involvement in fraud schemes related to COVID-19 or the abuse of CMS programs that were designed to encourage access to medical care during the pandemic.
Several of the defendants allegedly offered COVID-19 tests to Medicare beneficiaries in senior living facilities, drive-through COVID-19 testing sites, and medical offices to induce the beneficiaries to provide their personal identifying information and a saliva or a blood sample.
The DOJ charges claim the defendants then misused the information and the samples to submit claims to Medicare for unrelated, medically unnecessary, and far more expensive lab tests, including cancer genetic testing, allergy testing, and respiratory pathogen panel tests.
In some cases, it’s alleged, the lab results were not provided to the individuals in a timely fashion or were not reliable.
Other defendants are charged with exploiting temporary changes in CMS telehealth regulations that were designed to increase access to health care during the pandemic. In these cases, which the DOJ said were the first charges related to the expansion of telehealth under the COVID-19 emergency declaration, the defendants allegedly submitted false and fraudulent claims to Medicare for sham telemedicine encounters that did not occur.
“As part of these cases, medical professionals are alleged to have [been] offered and paid bribes in exchange for the medical professionals’ referral of unnecessary testing,” the DOJ news release said. However, no physicians were identified by the department.
Commenting on this aspect of the law enforcement action, FBI Director Christopher Wray said in the release: “Medical providers have been the unsung heroes for the American public throughout the pandemic. It’s disheartening that some have abused their authorities and committed COVID-19–related fraud against trusting citizens. The FBI, along with our federal law enforcement and private sector partners, are committed to continuing to combat health care fraud and protect the American people.”
The law enforcement action includes the third set of criminal charges related to the misuse of Provider Relief Fund monies, according to the release.
More than 340 individuals were charged in September 2020 with submitting $6 billion in fraudulent claims to federal health care programs and private insurers for telehealth consultations and substance abuse treatment. About $4.5 billion of that was related to telehealth, as reported by this news organization.
The new criminal charges were brought in federal district courts in Arkansas, California, Louisiana, Florida, New Jersey, and New York.
Case summaries
The DOJ provided several case summaries. One defendant, lab owner Billy Joe Taylor of Lavaca, Ark., was charged with participating in a scheme to defraud the government of over $42 million by filing false claims that were billed in combination with COVID-19 testing claims. He also allegedly billed for tests that were not performed.
Petros Hannesyan of Burbank, Calif., the owner of a home health agency, was charged with obtaining over $229,000 from COVID-19 relief programs under false pretenses. His firm allegedly misappropriated funds from the CARES Act Provider Relief Fund and submitted false loan applications and a false loan agreement to the Economic Injury Disaster Loan Program.
Michael Stein and Leonel Palatnik of Palm Beach County, Fla., were charged in a connection with an alleged $73 million conspiracy to defraud the government and to pay and receive health care kickbacks during the pandemic.
Mr. Stein, who owned a “purported” consulting company, and Mr. Palatnik, who owned testing labs in Texas, allegedly exploited Medicare’s waiver of telehealth restrictions “by offering telehealth providers access to Medicare beneficiaries for whom they could bill consultations. In exchange, these providers agreed to refer beneficiaries to [Mr. Palatnik’s] laboratories for expensive and medically unnecessary cancer and cardiovascular genetic testing.”
A version of this article first appeared on Medscape.com.
The U.S. Department of Justice (DOJ) on May 26 announced charges against 14 defendants across the country who allegedly engaged in health care fraud schemes that exploited the COVID-19 pandemic and resulted in over $143 million in false billings to Medicare.
Among the defendants, a DOJ news release said, were a telemedicine company executive, a physician, marketers, and medical business owners.
In addition, the Centers for Medicare and Medicaid Services separately announced that it had taken “adverse administrative actions” against more than 50 providers for their involvement in fraud schemes related to COVID-19 or the abuse of CMS programs that were designed to encourage access to medical care during the pandemic.
Several of the defendants allegedly offered COVID-19 tests to Medicare beneficiaries in senior living facilities, drive-through COVID-19 testing sites, and medical offices to induce the beneficiaries to provide their personal identifying information and a saliva or a blood sample.
The DOJ charges claim the defendants then misused the information and the samples to submit claims to Medicare for unrelated, medically unnecessary, and far more expensive lab tests, including cancer genetic testing, allergy testing, and respiratory pathogen panel tests.
In some cases, it’s alleged, the lab results were not provided to the individuals in a timely fashion or were not reliable.
Other defendants are charged with exploiting temporary changes in CMS telehealth regulations that were designed to increase access to health care during the pandemic. In these cases, which the DOJ said were the first charges related to the expansion of telehealth under the COVID-19 emergency declaration, the defendants allegedly submitted false and fraudulent claims to Medicare for sham telemedicine encounters that did not occur.
“As part of these cases, medical professionals are alleged to have [been] offered and paid bribes in exchange for the medical professionals’ referral of unnecessary testing,” the DOJ news release said. However, no physicians were identified by the department.
Commenting on this aspect of the law enforcement action, FBI Director Christopher Wray said in the release: “Medical providers have been the unsung heroes for the American public throughout the pandemic. It’s disheartening that some have abused their authorities and committed COVID-19–related fraud against trusting citizens. The FBI, along with our federal law enforcement and private sector partners, are committed to continuing to combat health care fraud and protect the American people.”
The law enforcement action includes the third set of criminal charges related to the misuse of Provider Relief Fund monies, according to the release.
More than 340 individuals were charged in September 2020 with submitting $6 billion in fraudulent claims to federal health care programs and private insurers for telehealth consultations and substance abuse treatment. About $4.5 billion of that was related to telehealth, as reported by this news organization.
The new criminal charges were brought in federal district courts in Arkansas, California, Louisiana, Florida, New Jersey, and New York.
Case summaries
The DOJ provided several case summaries. One defendant, lab owner Billy Joe Taylor of Lavaca, Ark., was charged with participating in a scheme to defraud the government of over $42 million by filing false claims that were billed in combination with COVID-19 testing claims. He also allegedly billed for tests that were not performed.
Petros Hannesyan of Burbank, Calif., the owner of a home health agency, was charged with obtaining over $229,000 from COVID-19 relief programs under false pretenses. His firm allegedly misappropriated funds from the CARES Act Provider Relief Fund and submitted false loan applications and a false loan agreement to the Economic Injury Disaster Loan Program.
Michael Stein and Leonel Palatnik of Palm Beach County, Fla., were charged in a connection with an alleged $73 million conspiracy to defraud the government and to pay and receive health care kickbacks during the pandemic.
Mr. Stein, who owned a “purported” consulting company, and Mr. Palatnik, who owned testing labs in Texas, allegedly exploited Medicare’s waiver of telehealth restrictions “by offering telehealth providers access to Medicare beneficiaries for whom they could bill consultations. In exchange, these providers agreed to refer beneficiaries to [Mr. Palatnik’s] laboratories for expensive and medically unnecessary cancer and cardiovascular genetic testing.”
A version of this article first appeared on Medscape.com.
The U.S. Department of Justice (DOJ) on May 26 announced charges against 14 defendants across the country who allegedly engaged in health care fraud schemes that exploited the COVID-19 pandemic and resulted in over $143 million in false billings to Medicare.
Among the defendants, a DOJ news release said, were a telemedicine company executive, a physician, marketers, and medical business owners.
In addition, the Centers for Medicare and Medicaid Services separately announced that it had taken “adverse administrative actions” against more than 50 providers for their involvement in fraud schemes related to COVID-19 or the abuse of CMS programs that were designed to encourage access to medical care during the pandemic.
Several of the defendants allegedly offered COVID-19 tests to Medicare beneficiaries in senior living facilities, drive-through COVID-19 testing sites, and medical offices to induce the beneficiaries to provide their personal identifying information and a saliva or a blood sample.
The DOJ charges claim the defendants then misused the information and the samples to submit claims to Medicare for unrelated, medically unnecessary, and far more expensive lab tests, including cancer genetic testing, allergy testing, and respiratory pathogen panel tests.
In some cases, it’s alleged, the lab results were not provided to the individuals in a timely fashion or were not reliable.
Other defendants are charged with exploiting temporary changes in CMS telehealth regulations that were designed to increase access to health care during the pandemic. In these cases, which the DOJ said were the first charges related to the expansion of telehealth under the COVID-19 emergency declaration, the defendants allegedly submitted false and fraudulent claims to Medicare for sham telemedicine encounters that did not occur.
“As part of these cases, medical professionals are alleged to have [been] offered and paid bribes in exchange for the medical professionals’ referral of unnecessary testing,” the DOJ news release said. However, no physicians were identified by the department.
Commenting on this aspect of the law enforcement action, FBI Director Christopher Wray said in the release: “Medical providers have been the unsung heroes for the American public throughout the pandemic. It’s disheartening that some have abused their authorities and committed COVID-19–related fraud against trusting citizens. The FBI, along with our federal law enforcement and private sector partners, are committed to continuing to combat health care fraud and protect the American people.”
The law enforcement action includes the third set of criminal charges related to the misuse of Provider Relief Fund monies, according to the release.
More than 340 individuals were charged in September 2020 with submitting $6 billion in fraudulent claims to federal health care programs and private insurers for telehealth consultations and substance abuse treatment. About $4.5 billion of that was related to telehealth, as reported by this news organization.
The new criminal charges were brought in federal district courts in Arkansas, California, Louisiana, Florida, New Jersey, and New York.
Case summaries
The DOJ provided several case summaries. One defendant, lab owner Billy Joe Taylor of Lavaca, Ark., was charged with participating in a scheme to defraud the government of over $42 million by filing false claims that were billed in combination with COVID-19 testing claims. He also allegedly billed for tests that were not performed.
Petros Hannesyan of Burbank, Calif., the owner of a home health agency, was charged with obtaining over $229,000 from COVID-19 relief programs under false pretenses. His firm allegedly misappropriated funds from the CARES Act Provider Relief Fund and submitted false loan applications and a false loan agreement to the Economic Injury Disaster Loan Program.
Michael Stein and Leonel Palatnik of Palm Beach County, Fla., were charged in a connection with an alleged $73 million conspiracy to defraud the government and to pay and receive health care kickbacks during the pandemic.
Mr. Stein, who owned a “purported” consulting company, and Mr. Palatnik, who owned testing labs in Texas, allegedly exploited Medicare’s waiver of telehealth restrictions “by offering telehealth providers access to Medicare beneficiaries for whom they could bill consultations. In exchange, these providers agreed to refer beneficiaries to [Mr. Palatnik’s] laboratories for expensive and medically unnecessary cancer and cardiovascular genetic testing.”
A version of this article first appeared on Medscape.com.
In Zambia, PCR tracks pertussis
In the periurban slum of Lusaka, Zambia, asymptomatic pertussis infections were common among both mothers and infants, a surprising finding since asymptomatic infections are assumed to be rare in infants. The findings suggested that pertussis should be considered in cases of chronic cough, and that current standards of treating pertussis infections in low-resource settings may need to be reexamined.
The results come from testing of 1,320 infant-mother pairs who were first enrolled at a public health clinic, then followed over at least four visits. The researchers tracked pertussis infection using quantitative PCR (qPCR) on nasopharyngeal swabs. Over the course of the study, 8.9% tested positive, although only one infant developed clinical pertussis during the study.
The study was presented by Christian Gunning, a postdoctoral researcher at the University of Georgia, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. The group also included researchers at Boston University and the University of Zambia, where PCR tests were conducted.
“That was amazing,” said session moderator Vana Spoulou, MD, PhD, professor of pediatric infectious diseases at National and Kapodistrian University of Athens, who is associated with Aghia Sofia Children’s Hospital of Athens. She noted that the study found that many physicians misdiagnosed coughs, believing them to be caused by another agent. “It was very interesting that there was so much pertussis spreading around in that community, and that nobody knew that it was around,” said Dr. Spoulou.
It’s important that physicians provide appropriate treatment, since ampicillin, which is typically prescribed for childhood upper respiratory illnesses, is believed to be ineffective against pertussis, while macrolides are effective and can prevent transmission.
Dr. Spoulou also noted that Zambia uses a whole cell vaccine, which is contraindicated in pregnant women because of potential side effects. “The good thing, despite that there was [a lot of] infection, there were no deaths, which means that maybe because the mother was infected, maybe some antibodies of the mother had passed to the child and could help the child to develop milder symptoms. So these are the pros and cons of natural infection,” said Dr. Spoulou.
The study took place in 2015, and participants were seen at the Chawama Public Health Clinic from about age 1 week to 4 months (with a target of seven clinic visits). Researchers recorded respiratory symptoms and antibiotics use at each visit, and collected a nasopharyngeal swab that was tested retrospectively using qPCR for Bordetella pertussis.
Real-time PCR analysis of the samples yields the CT value, which represents the number of amplification cycles that the PCR test must complete before Bordetella pertussis is detectable. The fewer the cycles (and the lower the CT value), the more infectious particles must have been present in the sample. For pertussis testing, a value below 35 is considered a clinically positive result. Tests that come back with higher CT values are increasingly likely to be false positives.
The researchers plotted a value called evidence for infection (EFI), which combined a range of CT values with the number of positive tests over the seven clinic visits to group patients into none, weak, or strong EFI. Among infants with no symptoms, 77% were in the no EFI category, 16% were in the weak category, and 7% were in the strong EFI group. Of infants with minimal respiratory symptoms, 18% were in the strong group, and 20% with moderate to severe symptoms were in the strong EFI group. Among mothers, 13% with no symptoms were in the strong group. 19% in the minimal symptom group were categorized as strong EFI, as were 11% in the moderate to severe symptom group.
The study used a full range of CT, not just positive test results (for pertussis, CT ≤ 35). Beyond contributing to composite measures such as EFI, CT values can serve as leading indicators of infectious disease outbreaks in a population, according to Dr. Gunning. That’s because weaker qPCR signals (CT > 35) can provide additional information within a large sample population. Higher CT values are successively more prone to false positives, but that’s less important for disease surveillance where sensitivity is of the highest importance. The false positive “noise” tends to cancel out over time. “It may be the case that you don’t make that call (correctly) 100% of the time for 100% of the people, but if you get it right in 80 out of 100 people, that’s sufficient to say we see this pathogen circulating in the population,” said Dr. Gunning.
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Gunning and Dr. Spoulou have no relevant financial disclosures.
In the periurban slum of Lusaka, Zambia, asymptomatic pertussis infections were common among both mothers and infants, a surprising finding since asymptomatic infections are assumed to be rare in infants. The findings suggested that pertussis should be considered in cases of chronic cough, and that current standards of treating pertussis infections in low-resource settings may need to be reexamined.
The results come from testing of 1,320 infant-mother pairs who were first enrolled at a public health clinic, then followed over at least four visits. The researchers tracked pertussis infection using quantitative PCR (qPCR) on nasopharyngeal swabs. Over the course of the study, 8.9% tested positive, although only one infant developed clinical pertussis during the study.
The study was presented by Christian Gunning, a postdoctoral researcher at the University of Georgia, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. The group also included researchers at Boston University and the University of Zambia, where PCR tests were conducted.
“That was amazing,” said session moderator Vana Spoulou, MD, PhD, professor of pediatric infectious diseases at National and Kapodistrian University of Athens, who is associated with Aghia Sofia Children’s Hospital of Athens. She noted that the study found that many physicians misdiagnosed coughs, believing them to be caused by another agent. “It was very interesting that there was so much pertussis spreading around in that community, and that nobody knew that it was around,” said Dr. Spoulou.
It’s important that physicians provide appropriate treatment, since ampicillin, which is typically prescribed for childhood upper respiratory illnesses, is believed to be ineffective against pertussis, while macrolides are effective and can prevent transmission.
Dr. Spoulou also noted that Zambia uses a whole cell vaccine, which is contraindicated in pregnant women because of potential side effects. “The good thing, despite that there was [a lot of] infection, there were no deaths, which means that maybe because the mother was infected, maybe some antibodies of the mother had passed to the child and could help the child to develop milder symptoms. So these are the pros and cons of natural infection,” said Dr. Spoulou.
The study took place in 2015, and participants were seen at the Chawama Public Health Clinic from about age 1 week to 4 months (with a target of seven clinic visits). Researchers recorded respiratory symptoms and antibiotics use at each visit, and collected a nasopharyngeal swab that was tested retrospectively using qPCR for Bordetella pertussis.
Real-time PCR analysis of the samples yields the CT value, which represents the number of amplification cycles that the PCR test must complete before Bordetella pertussis is detectable. The fewer the cycles (and the lower the CT value), the more infectious particles must have been present in the sample. For pertussis testing, a value below 35 is considered a clinically positive result. Tests that come back with higher CT values are increasingly likely to be false positives.
The researchers plotted a value called evidence for infection (EFI), which combined a range of CT values with the number of positive tests over the seven clinic visits to group patients into none, weak, or strong EFI. Among infants with no symptoms, 77% were in the no EFI category, 16% were in the weak category, and 7% were in the strong EFI group. Of infants with minimal respiratory symptoms, 18% were in the strong group, and 20% with moderate to severe symptoms were in the strong EFI group. Among mothers, 13% with no symptoms were in the strong group. 19% in the minimal symptom group were categorized as strong EFI, as were 11% in the moderate to severe symptom group.
The study used a full range of CT, not just positive test results (for pertussis, CT ≤ 35). Beyond contributing to composite measures such as EFI, CT values can serve as leading indicators of infectious disease outbreaks in a population, according to Dr. Gunning. That’s because weaker qPCR signals (CT > 35) can provide additional information within a large sample population. Higher CT values are successively more prone to false positives, but that’s less important for disease surveillance where sensitivity is of the highest importance. The false positive “noise” tends to cancel out over time. “It may be the case that you don’t make that call (correctly) 100% of the time for 100% of the people, but if you get it right in 80 out of 100 people, that’s sufficient to say we see this pathogen circulating in the population,” said Dr. Gunning.
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Gunning and Dr. Spoulou have no relevant financial disclosures.
In the periurban slum of Lusaka, Zambia, asymptomatic pertussis infections were common among both mothers and infants, a surprising finding since asymptomatic infections are assumed to be rare in infants. The findings suggested that pertussis should be considered in cases of chronic cough, and that current standards of treating pertussis infections in low-resource settings may need to be reexamined.
The results come from testing of 1,320 infant-mother pairs who were first enrolled at a public health clinic, then followed over at least four visits. The researchers tracked pertussis infection using quantitative PCR (qPCR) on nasopharyngeal swabs. Over the course of the study, 8.9% tested positive, although only one infant developed clinical pertussis during the study.
The study was presented by Christian Gunning, a postdoctoral researcher at the University of Georgia, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. The group also included researchers at Boston University and the University of Zambia, where PCR tests were conducted.
“That was amazing,” said session moderator Vana Spoulou, MD, PhD, professor of pediatric infectious diseases at National and Kapodistrian University of Athens, who is associated with Aghia Sofia Children’s Hospital of Athens. She noted that the study found that many physicians misdiagnosed coughs, believing them to be caused by another agent. “It was very interesting that there was so much pertussis spreading around in that community, and that nobody knew that it was around,” said Dr. Spoulou.
It’s important that physicians provide appropriate treatment, since ampicillin, which is typically prescribed for childhood upper respiratory illnesses, is believed to be ineffective against pertussis, while macrolides are effective and can prevent transmission.
Dr. Spoulou also noted that Zambia uses a whole cell vaccine, which is contraindicated in pregnant women because of potential side effects. “The good thing, despite that there was [a lot of] infection, there were no deaths, which means that maybe because the mother was infected, maybe some antibodies of the mother had passed to the child and could help the child to develop milder symptoms. So these are the pros and cons of natural infection,” said Dr. Spoulou.
The study took place in 2015, and participants were seen at the Chawama Public Health Clinic from about age 1 week to 4 months (with a target of seven clinic visits). Researchers recorded respiratory symptoms and antibiotics use at each visit, and collected a nasopharyngeal swab that was tested retrospectively using qPCR for Bordetella pertussis.
Real-time PCR analysis of the samples yields the CT value, which represents the number of amplification cycles that the PCR test must complete before Bordetella pertussis is detectable. The fewer the cycles (and the lower the CT value), the more infectious particles must have been present in the sample. For pertussis testing, a value below 35 is considered a clinically positive result. Tests that come back with higher CT values are increasingly likely to be false positives.
The researchers plotted a value called evidence for infection (EFI), which combined a range of CT values with the number of positive tests over the seven clinic visits to group patients into none, weak, or strong EFI. Among infants with no symptoms, 77% were in the no EFI category, 16% were in the weak category, and 7% were in the strong EFI group. Of infants with minimal respiratory symptoms, 18% were in the strong group, and 20% with moderate to severe symptoms were in the strong EFI group. Among mothers, 13% with no symptoms were in the strong group. 19% in the minimal symptom group were categorized as strong EFI, as were 11% in the moderate to severe symptom group.
The study used a full range of CT, not just positive test results (for pertussis, CT ≤ 35). Beyond contributing to composite measures such as EFI, CT values can serve as leading indicators of infectious disease outbreaks in a population, according to Dr. Gunning. That’s because weaker qPCR signals (CT > 35) can provide additional information within a large sample population. Higher CT values are successively more prone to false positives, but that’s less important for disease surveillance where sensitivity is of the highest importance. The false positive “noise” tends to cancel out over time. “It may be the case that you don’t make that call (correctly) 100% of the time for 100% of the people, but if you get it right in 80 out of 100 people, that’s sufficient to say we see this pathogen circulating in the population,” said Dr. Gunning.
The study was funded by the National Institute of Allergy and Infectious Diseases. Dr. Gunning and Dr. Spoulou have no relevant financial disclosures.
FROM ESPID 2021
Children aged 12-15 years continue to close COVID-19 vaccination gap
More children aged 12-15 years already have received at least one dose of a COVID-19 vaccine than have 16- and 17-year-olds, based on data from the Centers for Disease Control and Prevention.
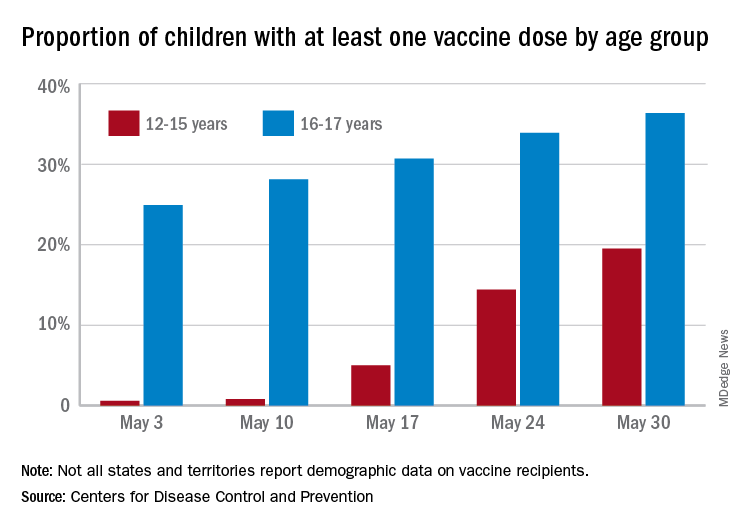
with those figures representing increases of 31.6% and 6.6% in the past week, respectively. Since the overall size of the 12-15 population is much larger, however, the proportion vaccinated is still smaller: 19.5% to 36.4%, according to the CDC’s COVID Data Tracker.
A look at full vaccination status shows that only 0.7% of those aged 12-15 years have received both doses of a two-dose vaccine or one dose of the single-shot variety, compared with 24% of those aged 16-17. For the country as a whole, 50.5% of all ages have received at least one dose and 40.7% are fully vaccinated, the CDC said.
Children aged 12-15 represent the largest share of the U.S. population (23.4%) initiating vaccination in the 14 days ending May 30, while children aged 16-17 made up just 4.5% of those getting their first dose. The younger group’s later entry into the vaccination pool shows up again when looking at completion rates, though, representing just 0.4% of all Americans who reached full vaccination during that same 14-day period, compared with 4.6% of the older children, the CDC data show.
Not all states are reporting data such as age for vaccine recipients, the CDC noted, and there are other variables that affect data collection. “Demographic data ... might differ by populations prioritized within each state or jurisdiction’s vaccination phase. Every geographic area has a different racial and ethnic composition, and not all are in the same vaccination phase,” the CDC said.
More children aged 12-15 years already have received at least one dose of a COVID-19 vaccine than have 16- and 17-year-olds, based on data from the Centers for Disease Control and Prevention.
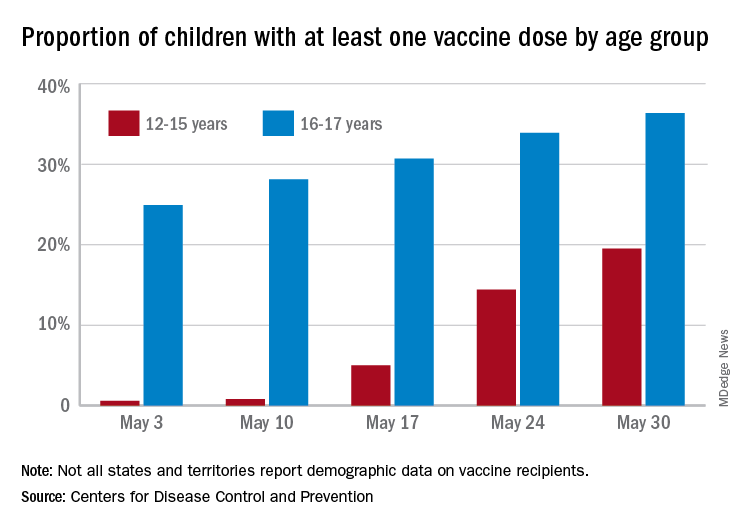
with those figures representing increases of 31.6% and 6.6% in the past week, respectively. Since the overall size of the 12-15 population is much larger, however, the proportion vaccinated is still smaller: 19.5% to 36.4%, according to the CDC’s COVID Data Tracker.
A look at full vaccination status shows that only 0.7% of those aged 12-15 years have received both doses of a two-dose vaccine or one dose of the single-shot variety, compared with 24% of those aged 16-17. For the country as a whole, 50.5% of all ages have received at least one dose and 40.7% are fully vaccinated, the CDC said.
Children aged 12-15 represent the largest share of the U.S. population (23.4%) initiating vaccination in the 14 days ending May 30, while children aged 16-17 made up just 4.5% of those getting their first dose. The younger group’s later entry into the vaccination pool shows up again when looking at completion rates, though, representing just 0.4% of all Americans who reached full vaccination during that same 14-day period, compared with 4.6% of the older children, the CDC data show.
Not all states are reporting data such as age for vaccine recipients, the CDC noted, and there are other variables that affect data collection. “Demographic data ... might differ by populations prioritized within each state or jurisdiction’s vaccination phase. Every geographic area has a different racial and ethnic composition, and not all are in the same vaccination phase,” the CDC said.
More children aged 12-15 years already have received at least one dose of a COVID-19 vaccine than have 16- and 17-year-olds, based on data from the Centers for Disease Control and Prevention.
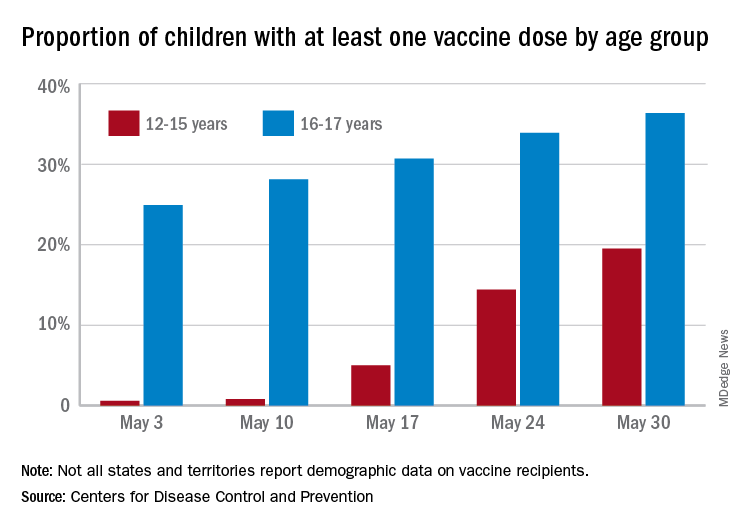
with those figures representing increases of 31.6% and 6.6% in the past week, respectively. Since the overall size of the 12-15 population is much larger, however, the proportion vaccinated is still smaller: 19.5% to 36.4%, according to the CDC’s COVID Data Tracker.
A look at full vaccination status shows that only 0.7% of those aged 12-15 years have received both doses of a two-dose vaccine or one dose of the single-shot variety, compared with 24% of those aged 16-17. For the country as a whole, 50.5% of all ages have received at least one dose and 40.7% are fully vaccinated, the CDC said.
Children aged 12-15 represent the largest share of the U.S. population (23.4%) initiating vaccination in the 14 days ending May 30, while children aged 16-17 made up just 4.5% of those getting their first dose. The younger group’s later entry into the vaccination pool shows up again when looking at completion rates, though, representing just 0.4% of all Americans who reached full vaccination during that same 14-day period, compared with 4.6% of the older children, the CDC data show.
Not all states are reporting data such as age for vaccine recipients, the CDC noted, and there are other variables that affect data collection. “Demographic data ... might differ by populations prioritized within each state or jurisdiction’s vaccination phase. Every geographic area has a different racial and ethnic composition, and not all are in the same vaccination phase,” the CDC said.
Sickle cell disease: Epidemiological change in bacterial infections
Among children with sickle cell disease who have not undergone hematopoietic stem cell transplant, Salmonella is now the leading cause of invasive bacterial infection (IBI), according to a new retrospective study (BACT-SPRING) conducted in Europe. Streptococcus pneumoniae was the second most common source of infection, marking a shift from years past, when S. pneumoniae was the most common source. The epidemiology of IBI in Europe has been altered by adoption of prophylaxis and the introduction of the pneumococcal conjugated vaccine (PCV13) in 2009.
Previous studies of IBI have been single center with small sample sizes, and few have been conducted since 2016, said Jean Gaschignard, MD, PhD, during his presentation of the study at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
Dr. Gaschignard is head of pediatrics at Groupe Hospitalier Nord Essonne in Longjumeau, France.
The study produced some unexpected results. “We were surprised,” said Dr. Gaschignard, by results indicating that not all children aged under 10 years were undergoing prophylaxis. Instead, the figures were closer to 80% or 90%. Among children over 10, the rate of prophylaxis varies between countries. “Our study is a clue to discuss again the indications for the age limit for prophylaxis against pneumococcus,” said Dr. Gauschignard, during the question-and-answer session following his talk.
The data give clinicians an updated picture of the epidemiology in this population following introduction of the PCV13 vaccine. “It was very important to have new data on microbiology after this implementation,” said Marie Rohr, MD, who is a fellow in pediatric infectious diseases at the University Hospitals of Geneva. Dr. Rohr moderated the session where the study was presented.
Dr. Rohr noted the shift from the dominant cause of IBI after the introduction of the PCV10/13 vaccine, from S. pneumoniae to Salmonella. The researchers also found a preponderance of bacteremia and osteoarticular infections. “The mortality and morbidity are still considerable despite infection preventive measures,” said Dr. Rohr.
The results should also prompt a second look at prevention strategies. “Even if the antibiotic prophylaxis is prescribed for a large [proportion of children with sickle cell disease] under 10 years old, the median age of invasive bacterial infection is 7 years old. This calls into question systematic antibiotic prophylaxis and case-control studies are needed to evaluate this and possibly modify antibiotic prophylaxis recommendations in the future,” said Dr. Rohr.
The BACT-SPRING study was conducted between Jan. 1, 2014, and Dec. 31, 2019, using online data. It included 217 IBI episodes from 26 centers in five European countries. Just over half were from France, while about a quarter occurred in Spain. Other countries included Belgium, Portugal, and Great Britain. Participants were younger than 18 and had an IBI confirmed by bacterial culture or PCR from normally sterile fluid.
Thirty-eight episodes occurred in children who had undergone hematopoietic stem cell transplantation (HSCT), and 179 in children who had not undergone HSCT. The presentation focused exclusively on the latter group.
Among episodes in children without HSCT, the mean age was 7. Forty-eight patients had a history of acute chest syndrome, 47 had a history of ICU admission, 29 had a history of IBI, and 27 had a history of acute splenic sequestration. Thirteen underwent a splenectomy. Almost half of children had none of these characteristics, while about one-fourth had two or more.
In the HSCT group, 141 children were on prophylaxis at the time of the infection; 74 were on hydroxyurea, and 36 were currently or previously on a transfusion program. Sixty-eight cases were primary bacteremia and 55 were osteoarticular. Other syndromes included pneumonia empyema (n = 18), and meningitis (n = 17), among others. In 44 cases, the isolated bacteria was Salmonella, followed by S. pneumoniae in 32 cases. Escherichia coli accounted for 22. Haemophilus influenza was identified in six episodes, and group A Streptococcus in three.
The study is the first large European epidemiologic study investigating IBI in children with sickle cell disease, and one of its strengths was the strict inclusion criteria. However, it was limited by its retrospective nature.
Dr. Gaschignard and Dr. Rohr have no relevant financial disclosures.
Among children with sickle cell disease who have not undergone hematopoietic stem cell transplant, Salmonella is now the leading cause of invasive bacterial infection (IBI), according to a new retrospective study (BACT-SPRING) conducted in Europe. Streptococcus pneumoniae was the second most common source of infection, marking a shift from years past, when S. pneumoniae was the most common source. The epidemiology of IBI in Europe has been altered by adoption of prophylaxis and the introduction of the pneumococcal conjugated vaccine (PCV13) in 2009.
Previous studies of IBI have been single center with small sample sizes, and few have been conducted since 2016, said Jean Gaschignard, MD, PhD, during his presentation of the study at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
Dr. Gaschignard is head of pediatrics at Groupe Hospitalier Nord Essonne in Longjumeau, France.
The study produced some unexpected results. “We were surprised,” said Dr. Gaschignard, by results indicating that not all children aged under 10 years were undergoing prophylaxis. Instead, the figures were closer to 80% or 90%. Among children over 10, the rate of prophylaxis varies between countries. “Our study is a clue to discuss again the indications for the age limit for prophylaxis against pneumococcus,” said Dr. Gauschignard, during the question-and-answer session following his talk.
The data give clinicians an updated picture of the epidemiology in this population following introduction of the PCV13 vaccine. “It was very important to have new data on microbiology after this implementation,” said Marie Rohr, MD, who is a fellow in pediatric infectious diseases at the University Hospitals of Geneva. Dr. Rohr moderated the session where the study was presented.
Dr. Rohr noted the shift from the dominant cause of IBI after the introduction of the PCV10/13 vaccine, from S. pneumoniae to Salmonella. The researchers also found a preponderance of bacteremia and osteoarticular infections. “The mortality and morbidity are still considerable despite infection preventive measures,” said Dr. Rohr.
The results should also prompt a second look at prevention strategies. “Even if the antibiotic prophylaxis is prescribed for a large [proportion of children with sickle cell disease] under 10 years old, the median age of invasive bacterial infection is 7 years old. This calls into question systematic antibiotic prophylaxis and case-control studies are needed to evaluate this and possibly modify antibiotic prophylaxis recommendations in the future,” said Dr. Rohr.
The BACT-SPRING study was conducted between Jan. 1, 2014, and Dec. 31, 2019, using online data. It included 217 IBI episodes from 26 centers in five European countries. Just over half were from France, while about a quarter occurred in Spain. Other countries included Belgium, Portugal, and Great Britain. Participants were younger than 18 and had an IBI confirmed by bacterial culture or PCR from normally sterile fluid.
Thirty-eight episodes occurred in children who had undergone hematopoietic stem cell transplantation (HSCT), and 179 in children who had not undergone HSCT. The presentation focused exclusively on the latter group.
Among episodes in children without HSCT, the mean age was 7. Forty-eight patients had a history of acute chest syndrome, 47 had a history of ICU admission, 29 had a history of IBI, and 27 had a history of acute splenic sequestration. Thirteen underwent a splenectomy. Almost half of children had none of these characteristics, while about one-fourth had two or more.
In the HSCT group, 141 children were on prophylaxis at the time of the infection; 74 were on hydroxyurea, and 36 were currently or previously on a transfusion program. Sixty-eight cases were primary bacteremia and 55 were osteoarticular. Other syndromes included pneumonia empyema (n = 18), and meningitis (n = 17), among others. In 44 cases, the isolated bacteria was Salmonella, followed by S. pneumoniae in 32 cases. Escherichia coli accounted for 22. Haemophilus influenza was identified in six episodes, and group A Streptococcus in three.
The study is the first large European epidemiologic study investigating IBI in children with sickle cell disease, and one of its strengths was the strict inclusion criteria. However, it was limited by its retrospective nature.
Dr. Gaschignard and Dr. Rohr have no relevant financial disclosures.
Among children with sickle cell disease who have not undergone hematopoietic stem cell transplant, Salmonella is now the leading cause of invasive bacterial infection (IBI), according to a new retrospective study (BACT-SPRING) conducted in Europe. Streptococcus pneumoniae was the second most common source of infection, marking a shift from years past, when S. pneumoniae was the most common source. The epidemiology of IBI in Europe has been altered by adoption of prophylaxis and the introduction of the pneumococcal conjugated vaccine (PCV13) in 2009.
Previous studies of IBI have been single center with small sample sizes, and few have been conducted since 2016, said Jean Gaschignard, MD, PhD, during his presentation of the study at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
Dr. Gaschignard is head of pediatrics at Groupe Hospitalier Nord Essonne in Longjumeau, France.
The study produced some unexpected results. “We were surprised,” said Dr. Gaschignard, by results indicating that not all children aged under 10 years were undergoing prophylaxis. Instead, the figures were closer to 80% or 90%. Among children over 10, the rate of prophylaxis varies between countries. “Our study is a clue to discuss again the indications for the age limit for prophylaxis against pneumococcus,” said Dr. Gauschignard, during the question-and-answer session following his talk.
The data give clinicians an updated picture of the epidemiology in this population following introduction of the PCV13 vaccine. “It was very important to have new data on microbiology after this implementation,” said Marie Rohr, MD, who is a fellow in pediatric infectious diseases at the University Hospitals of Geneva. Dr. Rohr moderated the session where the study was presented.
Dr. Rohr noted the shift from the dominant cause of IBI after the introduction of the PCV10/13 vaccine, from S. pneumoniae to Salmonella. The researchers also found a preponderance of bacteremia and osteoarticular infections. “The mortality and morbidity are still considerable despite infection preventive measures,” said Dr. Rohr.
The results should also prompt a second look at prevention strategies. “Even if the antibiotic prophylaxis is prescribed for a large [proportion of children with sickle cell disease] under 10 years old, the median age of invasive bacterial infection is 7 years old. This calls into question systematic antibiotic prophylaxis and case-control studies are needed to evaluate this and possibly modify antibiotic prophylaxis recommendations in the future,” said Dr. Rohr.
The BACT-SPRING study was conducted between Jan. 1, 2014, and Dec. 31, 2019, using online data. It included 217 IBI episodes from 26 centers in five European countries. Just over half were from France, while about a quarter occurred in Spain. Other countries included Belgium, Portugal, and Great Britain. Participants were younger than 18 and had an IBI confirmed by bacterial culture or PCR from normally sterile fluid.
Thirty-eight episodes occurred in children who had undergone hematopoietic stem cell transplantation (HSCT), and 179 in children who had not undergone HSCT. The presentation focused exclusively on the latter group.
Among episodes in children without HSCT, the mean age was 7. Forty-eight patients had a history of acute chest syndrome, 47 had a history of ICU admission, 29 had a history of IBI, and 27 had a history of acute splenic sequestration. Thirteen underwent a splenectomy. Almost half of children had none of these characteristics, while about one-fourth had two or more.
In the HSCT group, 141 children were on prophylaxis at the time of the infection; 74 were on hydroxyurea, and 36 were currently or previously on a transfusion program. Sixty-eight cases were primary bacteremia and 55 were osteoarticular. Other syndromes included pneumonia empyema (n = 18), and meningitis (n = 17), among others. In 44 cases, the isolated bacteria was Salmonella, followed by S. pneumoniae in 32 cases. Escherichia coli accounted for 22. Haemophilus influenza was identified in six episodes, and group A Streptococcus in three.
The study is the first large European epidemiologic study investigating IBI in children with sickle cell disease, and one of its strengths was the strict inclusion criteria. However, it was limited by its retrospective nature.
Dr. Gaschignard and Dr. Rohr have no relevant financial disclosures.
FROM ESPID 2021
Antiviral may improve hearing loss in congenital CMV
Infants with isolated sensorineural hearing loss as a result of congenital cytomegalovirus (cCMV) infection may benefit from treatment with valganciclovir, according to results from the CONCERT nonrandomized trial.
Subjects were found through the Newborn Hearing Screening program, using dried blood spot screening to confirm cCMV Infection. As a result of 6 weeks of therapy, more patients in the treatment group had improvements in hearing at age 20 months, and fewer had deterioration compared with untreated controls.
There is a general consensus that symptomatic cCMV should be treated with valganciclovir for 6 weeks or 6 months, but treatment of patients with only hearing loss is still under debate. The average age of participants was 8 weeks.
The study was presented by Pui Khi Chung, MD, a clinical microbiologist at the Leiden University Medical Center, the Netherlands, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
Out of 1,377 NHS-referred infants, 59 were diagnosed with cCMV (4.3%), and 35 were included in the study. Twenty-five patients received 6 weeks of valganciclovir, while 10 patients received placebo. The control group was expanded to 12 when two additional subjects were identified retrospectively and were successfully followed up at 20 months. Subjects in the treatment group were an average of 8 weeks old when treatment began. Both groups had similar neurodevelopmental outcomes at 20 months, as measured by the Bayley Scales of Infant and Toddler Development (BSID-III) and the Child Development Inventory (CDI). There were no serious adverse events associated with treatment.
To measure efficacy, the researchers used a random intercept, random slope model that accounted for repeated measurements. The differences in slopes for analyses of the best ear were significantly different between the treatment and control groups (estimated difference in slopes, –0.93; P = .0071). Further analyses of total hearing found that improvement was more common in the treatment group, and deterioration/no change was more common in the nontreatment group (P = .044). In another analysis that excluded the most profoundly impaired ears (> 70 db hearing loss), none in the control group experienced improvement and almost half deteriorated. In the treatment group, most were unchanged and a small number improved, with almost none deteriorating (P = .006).
Asked whether the treatment has any effect on the most profoundly impaired ears, Dr. Chung said she had not yet completed that analysis, but the hypothesis is that the treatment is unlikely to lead to any improvement. “When you take out the severely impaired ears, you can see a greater [treatment] effect, so it does suggest that it doesn’t do anything for those ears,” Dr. Chung said during the Q&A session following her talk.
She was also asked why the treatment period was 6 weeks, rather than 6 months – a period of treatment that has shown a better effect on long-term hearing and developmental outcomes than 6 weeks of treatment in symptomatic patients. Dr. Chung replied that she wasn’t involved in the study design, but said that at her center, the 6-month regimen is not standard.
There were two key weaknesses in the study. One was the small sample size, and the other was its nonrandomized nature, which could have led to bias in the treated versus untreated group. “Although we don’t see any baseline differences between the groups, we have to be wary in analyses. Unfortunately, an RCT proved impossible in our setting. The CONCERT Trial started as randomized but this was amended to nonrandomized, as both parents and pediatricians had a clear preference for treatment,” said Dr. Chung.
The study could provide useful information about the timing of oral antiviral medication, according to Vana Spoulou, MD, who moderated the session where the research was presented. “The earliest you can give it is best, but sometimes it’s not easy to get them diagnosed immediately after birth. What they showed us is that even giving it so late, there was some improvement,” Dr. Spoulou said in an interview.
Dr. Spoulou isn’t ready to change practice based on the results, because she noted that some other studies have shown no benefit of treatment at 3 months. “But this was a hint that maybe even in these later diagnosed cases there could be some benefit,” she said.
Dr. Chung and Dr. Spoulou have no relevant financial disclosures.
Infants with isolated sensorineural hearing loss as a result of congenital cytomegalovirus (cCMV) infection may benefit from treatment with valganciclovir, according to results from the CONCERT nonrandomized trial.
Subjects were found through the Newborn Hearing Screening program, using dried blood spot screening to confirm cCMV Infection. As a result of 6 weeks of therapy, more patients in the treatment group had improvements in hearing at age 20 months, and fewer had deterioration compared with untreated controls.
There is a general consensus that symptomatic cCMV should be treated with valganciclovir for 6 weeks or 6 months, but treatment of patients with only hearing loss is still under debate. The average age of participants was 8 weeks.
The study was presented by Pui Khi Chung, MD, a clinical microbiologist at the Leiden University Medical Center, the Netherlands, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
Out of 1,377 NHS-referred infants, 59 were diagnosed with cCMV (4.3%), and 35 were included in the study. Twenty-five patients received 6 weeks of valganciclovir, while 10 patients received placebo. The control group was expanded to 12 when two additional subjects were identified retrospectively and were successfully followed up at 20 months. Subjects in the treatment group were an average of 8 weeks old when treatment began. Both groups had similar neurodevelopmental outcomes at 20 months, as measured by the Bayley Scales of Infant and Toddler Development (BSID-III) and the Child Development Inventory (CDI). There were no serious adverse events associated with treatment.
To measure efficacy, the researchers used a random intercept, random slope model that accounted for repeated measurements. The differences in slopes for analyses of the best ear were significantly different between the treatment and control groups (estimated difference in slopes, –0.93; P = .0071). Further analyses of total hearing found that improvement was more common in the treatment group, and deterioration/no change was more common in the nontreatment group (P = .044). In another analysis that excluded the most profoundly impaired ears (> 70 db hearing loss), none in the control group experienced improvement and almost half deteriorated. In the treatment group, most were unchanged and a small number improved, with almost none deteriorating (P = .006).
Asked whether the treatment has any effect on the most profoundly impaired ears, Dr. Chung said she had not yet completed that analysis, but the hypothesis is that the treatment is unlikely to lead to any improvement. “When you take out the severely impaired ears, you can see a greater [treatment] effect, so it does suggest that it doesn’t do anything for those ears,” Dr. Chung said during the Q&A session following her talk.
She was also asked why the treatment period was 6 weeks, rather than 6 months – a period of treatment that has shown a better effect on long-term hearing and developmental outcomes than 6 weeks of treatment in symptomatic patients. Dr. Chung replied that she wasn’t involved in the study design, but said that at her center, the 6-month regimen is not standard.
There were two key weaknesses in the study. One was the small sample size, and the other was its nonrandomized nature, which could have led to bias in the treated versus untreated group. “Although we don’t see any baseline differences between the groups, we have to be wary in analyses. Unfortunately, an RCT proved impossible in our setting. The CONCERT Trial started as randomized but this was amended to nonrandomized, as both parents and pediatricians had a clear preference for treatment,” said Dr. Chung.
The study could provide useful information about the timing of oral antiviral medication, according to Vana Spoulou, MD, who moderated the session where the research was presented. “The earliest you can give it is best, but sometimes it’s not easy to get them diagnosed immediately after birth. What they showed us is that even giving it so late, there was some improvement,” Dr. Spoulou said in an interview.
Dr. Spoulou isn’t ready to change practice based on the results, because she noted that some other studies have shown no benefit of treatment at 3 months. “But this was a hint that maybe even in these later diagnosed cases there could be some benefit,” she said.
Dr. Chung and Dr. Spoulou have no relevant financial disclosures.
Infants with isolated sensorineural hearing loss as a result of congenital cytomegalovirus (cCMV) infection may benefit from treatment with valganciclovir, according to results from the CONCERT nonrandomized trial.
Subjects were found through the Newborn Hearing Screening program, using dried blood spot screening to confirm cCMV Infection. As a result of 6 weeks of therapy, more patients in the treatment group had improvements in hearing at age 20 months, and fewer had deterioration compared with untreated controls.
There is a general consensus that symptomatic cCMV should be treated with valganciclovir for 6 weeks or 6 months, but treatment of patients with only hearing loss is still under debate. The average age of participants was 8 weeks.
The study was presented by Pui Khi Chung, MD, a clinical microbiologist at the Leiden University Medical Center, the Netherlands, at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year.
Out of 1,377 NHS-referred infants, 59 were diagnosed with cCMV (4.3%), and 35 were included in the study. Twenty-five patients received 6 weeks of valganciclovir, while 10 patients received placebo. The control group was expanded to 12 when two additional subjects were identified retrospectively and were successfully followed up at 20 months. Subjects in the treatment group were an average of 8 weeks old when treatment began. Both groups had similar neurodevelopmental outcomes at 20 months, as measured by the Bayley Scales of Infant and Toddler Development (BSID-III) and the Child Development Inventory (CDI). There were no serious adverse events associated with treatment.
To measure efficacy, the researchers used a random intercept, random slope model that accounted for repeated measurements. The differences in slopes for analyses of the best ear were significantly different between the treatment and control groups (estimated difference in slopes, –0.93; P = .0071). Further analyses of total hearing found that improvement was more common in the treatment group, and deterioration/no change was more common in the nontreatment group (P = .044). In another analysis that excluded the most profoundly impaired ears (> 70 db hearing loss), none in the control group experienced improvement and almost half deteriorated. In the treatment group, most were unchanged and a small number improved, with almost none deteriorating (P = .006).
Asked whether the treatment has any effect on the most profoundly impaired ears, Dr. Chung said she had not yet completed that analysis, but the hypothesis is that the treatment is unlikely to lead to any improvement. “When you take out the severely impaired ears, you can see a greater [treatment] effect, so it does suggest that it doesn’t do anything for those ears,” Dr. Chung said during the Q&A session following her talk.
She was also asked why the treatment period was 6 weeks, rather than 6 months – a period of treatment that has shown a better effect on long-term hearing and developmental outcomes than 6 weeks of treatment in symptomatic patients. Dr. Chung replied that she wasn’t involved in the study design, but said that at her center, the 6-month regimen is not standard.
There were two key weaknesses in the study. One was the small sample size, and the other was its nonrandomized nature, which could have led to bias in the treated versus untreated group. “Although we don’t see any baseline differences between the groups, we have to be wary in analyses. Unfortunately, an RCT proved impossible in our setting. The CONCERT Trial started as randomized but this was amended to nonrandomized, as both parents and pediatricians had a clear preference for treatment,” said Dr. Chung.
The study could provide useful information about the timing of oral antiviral medication, according to Vana Spoulou, MD, who moderated the session where the research was presented. “The earliest you can give it is best, but sometimes it’s not easy to get them diagnosed immediately after birth. What they showed us is that even giving it so late, there was some improvement,” Dr. Spoulou said in an interview.
Dr. Spoulou isn’t ready to change practice based on the results, because she noted that some other studies have shown no benefit of treatment at 3 months. “But this was a hint that maybe even in these later diagnosed cases there could be some benefit,” she said.
Dr. Chung and Dr. Spoulou have no relevant financial disclosures.
FROM ESPID 2021
GI symptoms and chronic fatigue may persist months after COVID-19
Gastrointestinal symptoms and chronic fatigue may persist months after the COVID-19 virus infection resolves, results of a recent cohort-controlled study suggest.
About 5 months after SARS-CoV-2 infection, relative risks of loose stools, somatization, and chronic fatigue were increased by approximately two- to three fold, compared to individuals who had not been infected, according to study results presented at the annual Digestive Disease Week® (DDW).
These longer-term consequences of SARS-CoV-2 appeared to be more severe in patients who had experienced diarrhea during the acute infection, according to investigator Daniele Noviello, MD, a second-year resident in gastroenterology and hepatology at the University of Milan.
This is the first cohort-controlled study that specifically investigates gastrointestinal symptoms and somatoform disorders, Dr. Noviello said in a virtual presentation of the results.
“Based on our data, chronic fatigue, gastrointestinal, and somatoform symptoms may have a common postinfectious origin, and they should be investigated in the follow-up of SARS-CoV-2 patients,” he said.
Links between SARS-CoV-2 and gastrointestinal symptoms
Gastrointestinal symptoms are known to be relatively common during acute infection. According to Dr. Noviello, the most frequent gastrointestinal symptom associated with SARS-CoV-2 is diarrhea, occurring in 4% to nearly 40% of patients in case series to date.
However, data on the longer-term gastrointestinal impacts of SARS-CoV-2 remain scarce.
In one noncontrolled cohort study in China, loss of appetite, nausea, acid reflux, and diarrhea were seen in 15%-24% of patients 3 months after the infection, Dr. Noviello said. In another cohort study in China, diarrhea and vomiting were reported in 5% of patients 6 months after infection.
In any case, it is known that viral, bacterial, and protozoal infections of the gastrointestinal tract are a risk factor for development of functional disorders including irritable bowel syndrome (IBS), functional dyspepsia, and chronic fatigue, according to Dr. Noviello.
Accordingly, the results of the present study suggest that SARS-CoV-2 also “may affect the brain-gut axis in the long term,” Dr. Noviello and coauthors wrote in an abstract of the study.
It is plausible that SARS-CoV-2 infection could be a trigger for longer-term gastrointestinal symptoms, especially given the previous evidence linking infections and IBS symptoms, or postinfectious IBS, said Juan Pablo Stefanolo, MD, a physician with the neurogastroenterology and motility section, Hospital de Clínicas José de San Martín, Buenos Aires University.
“If it is demonstrated [that SARS-CoV-2 infection is a trigger], the microbiota-gut-brain axis concept in IBS pathophysiology is reinforced,” Dr. Stefanolo said in an interview.
In the meantime, practitioners may want to take into account COVID-19 infection history in the evaluation of a patient with IBS-like symptoms and, in case of a known positive COVID-19 result in an IBS patient, be aware of the possibility of symptom exacerbation, Dr. Stefanolo said.
Pandemic in Italy: Unique study opportunity
The severe outbreak in the Milan region early in the COVID-19 pandemic provided a “unique opportunity” to assess the long-term impact of infection on gastrointestinal and extraintestinal somatoform symptoms, said Dr. Noviello.
The investigators sent an online questionnaire to patients who had a molecular diagnosis of SARS-CoV-2 infection by nasal swab between February and April of 2020. To form a control group, they also sent questionnaires to hospital employees and health care providers who had tested negative over that same time period.
In all, 378 questionnaires were completed by 177 SARS-CoV-2–positive individuals and 201 controls. The SARS-CoV-2–positive patients were somewhat older (about 44 years vs. 40 years for controls), were less often female (40% vs. 61%), had a lower education level, and smoked less than did controls, according to the investigators.
A mean of 4.8 months had elapsed between the time of SARS-CoV-2 infection and when the questionnaires were compiled, said Dr. Noviello.
In the acute phase, diarrhea was the most common gastrointestinal symptom among virus-positive individuals, occurring in about 50% compared to 20% of controls (P < .001), data show. Other symptoms reported by 40% of SARS-CoV-2–infected individuals included fever, dyspnea, loss of smell or taste, weight loss, myalgia, arthralgia, and asthenia in the acute phase controls in the acute phase, Dr. Noviello said.
Persistent gastrointestinal symptoms after SARS-CoV-2
Persistent symptoms included loose stools, as measured by the Bristol Stool scale, occurring in 17.8% of SARS-CoV-2–positive individuals, but only 9.3% of the SARS-CoV-2–negative controls, according to Dr. Noviello, with an adjusted risk ratio of 1.88 (95% confidence interval, 0.99-3.54).
Chronic fatigue symptoms, as measured by the Structured Assessment of Gastrointestinal Symptoms questionnaire, were reported by about 30% of SARS-CoV-2–positive patients and about 15% of controls, for an adjusted risk ratio of 2.24 (95% CI, 1.48-3.37), according to Dr. Noviello’s presentation.
The mean t-score on the Symptom Checklist–12 for somatoform disorders was higher for the virus-positive patients compared to controls, according to Dr. Noviello. The scores were 54.6 and 50.5, respectively, with an adjusted score difference of 3.6 (95% CI, 1.0-6.2).
The longer-term sequelae of SARS-CoV-2 infection might be more severe in individuals who experienced diarrhea during acute infection, according to Dr. Noviello. In a post hoc analysis, reports of irritable bowel syndrome and loose stools were significantly higher in SARS-CoV-2–infected individuals who had diarrhea in the acute phase compared to those who did not experience diarrhea, he said.
Somatoform disorder scores were significantly higher, and reports of headache, back pain, and chronic fatigue were significantly more common, in individuals who had diarrhea at the time of SARS-CoV-2 infection, he added.
Dr. Noviello and coauthors reported no competing interests related to the study. Dr. Stefanolo had no disclosures to report.
Gastrointestinal symptoms and chronic fatigue may persist months after the COVID-19 virus infection resolves, results of a recent cohort-controlled study suggest.
About 5 months after SARS-CoV-2 infection, relative risks of loose stools, somatization, and chronic fatigue were increased by approximately two- to three fold, compared to individuals who had not been infected, according to study results presented at the annual Digestive Disease Week® (DDW).
These longer-term consequences of SARS-CoV-2 appeared to be more severe in patients who had experienced diarrhea during the acute infection, according to investigator Daniele Noviello, MD, a second-year resident in gastroenterology and hepatology at the University of Milan.
This is the first cohort-controlled study that specifically investigates gastrointestinal symptoms and somatoform disorders, Dr. Noviello said in a virtual presentation of the results.
“Based on our data, chronic fatigue, gastrointestinal, and somatoform symptoms may have a common postinfectious origin, and they should be investigated in the follow-up of SARS-CoV-2 patients,” he said.
Links between SARS-CoV-2 and gastrointestinal symptoms
Gastrointestinal symptoms are known to be relatively common during acute infection. According to Dr. Noviello, the most frequent gastrointestinal symptom associated with SARS-CoV-2 is diarrhea, occurring in 4% to nearly 40% of patients in case series to date.
However, data on the longer-term gastrointestinal impacts of SARS-CoV-2 remain scarce.
In one noncontrolled cohort study in China, loss of appetite, nausea, acid reflux, and diarrhea were seen in 15%-24% of patients 3 months after the infection, Dr. Noviello said. In another cohort study in China, diarrhea and vomiting were reported in 5% of patients 6 months after infection.
In any case, it is known that viral, bacterial, and protozoal infections of the gastrointestinal tract are a risk factor for development of functional disorders including irritable bowel syndrome (IBS), functional dyspepsia, and chronic fatigue, according to Dr. Noviello.
Accordingly, the results of the present study suggest that SARS-CoV-2 also “may affect the brain-gut axis in the long term,” Dr. Noviello and coauthors wrote in an abstract of the study.
It is plausible that SARS-CoV-2 infection could be a trigger for longer-term gastrointestinal symptoms, especially given the previous evidence linking infections and IBS symptoms, or postinfectious IBS, said Juan Pablo Stefanolo, MD, a physician with the neurogastroenterology and motility section, Hospital de Clínicas José de San Martín, Buenos Aires University.
“If it is demonstrated [that SARS-CoV-2 infection is a trigger], the microbiota-gut-brain axis concept in IBS pathophysiology is reinforced,” Dr. Stefanolo said in an interview.
In the meantime, practitioners may want to take into account COVID-19 infection history in the evaluation of a patient with IBS-like symptoms and, in case of a known positive COVID-19 result in an IBS patient, be aware of the possibility of symptom exacerbation, Dr. Stefanolo said.
Pandemic in Italy: Unique study opportunity
The severe outbreak in the Milan region early in the COVID-19 pandemic provided a “unique opportunity” to assess the long-term impact of infection on gastrointestinal and extraintestinal somatoform symptoms, said Dr. Noviello.
The investigators sent an online questionnaire to patients who had a molecular diagnosis of SARS-CoV-2 infection by nasal swab between February and April of 2020. To form a control group, they also sent questionnaires to hospital employees and health care providers who had tested negative over that same time period.
In all, 378 questionnaires were completed by 177 SARS-CoV-2–positive individuals and 201 controls. The SARS-CoV-2–positive patients were somewhat older (about 44 years vs. 40 years for controls), were less often female (40% vs. 61%), had a lower education level, and smoked less than did controls, according to the investigators.
A mean of 4.8 months had elapsed between the time of SARS-CoV-2 infection and when the questionnaires were compiled, said Dr. Noviello.
In the acute phase, diarrhea was the most common gastrointestinal symptom among virus-positive individuals, occurring in about 50% compared to 20% of controls (P < .001), data show. Other symptoms reported by 40% of SARS-CoV-2–infected individuals included fever, dyspnea, loss of smell or taste, weight loss, myalgia, arthralgia, and asthenia in the acute phase controls in the acute phase, Dr. Noviello said.
Persistent gastrointestinal symptoms after SARS-CoV-2
Persistent symptoms included loose stools, as measured by the Bristol Stool scale, occurring in 17.8% of SARS-CoV-2–positive individuals, but only 9.3% of the SARS-CoV-2–negative controls, according to Dr. Noviello, with an adjusted risk ratio of 1.88 (95% confidence interval, 0.99-3.54).
Chronic fatigue symptoms, as measured by the Structured Assessment of Gastrointestinal Symptoms questionnaire, were reported by about 30% of SARS-CoV-2–positive patients and about 15% of controls, for an adjusted risk ratio of 2.24 (95% CI, 1.48-3.37), according to Dr. Noviello’s presentation.
The mean t-score on the Symptom Checklist–12 for somatoform disorders was higher for the virus-positive patients compared to controls, according to Dr. Noviello. The scores were 54.6 and 50.5, respectively, with an adjusted score difference of 3.6 (95% CI, 1.0-6.2).
The longer-term sequelae of SARS-CoV-2 infection might be more severe in individuals who experienced diarrhea during acute infection, according to Dr. Noviello. In a post hoc analysis, reports of irritable bowel syndrome and loose stools were significantly higher in SARS-CoV-2–infected individuals who had diarrhea in the acute phase compared to those who did not experience diarrhea, he said.
Somatoform disorder scores were significantly higher, and reports of headache, back pain, and chronic fatigue were significantly more common, in individuals who had diarrhea at the time of SARS-CoV-2 infection, he added.
Dr. Noviello and coauthors reported no competing interests related to the study. Dr. Stefanolo had no disclosures to report.
Gastrointestinal symptoms and chronic fatigue may persist months after the COVID-19 virus infection resolves, results of a recent cohort-controlled study suggest.
About 5 months after SARS-CoV-2 infection, relative risks of loose stools, somatization, and chronic fatigue were increased by approximately two- to three fold, compared to individuals who had not been infected, according to study results presented at the annual Digestive Disease Week® (DDW).
These longer-term consequences of SARS-CoV-2 appeared to be more severe in patients who had experienced diarrhea during the acute infection, according to investigator Daniele Noviello, MD, a second-year resident in gastroenterology and hepatology at the University of Milan.
This is the first cohort-controlled study that specifically investigates gastrointestinal symptoms and somatoform disorders, Dr. Noviello said in a virtual presentation of the results.
“Based on our data, chronic fatigue, gastrointestinal, and somatoform symptoms may have a common postinfectious origin, and they should be investigated in the follow-up of SARS-CoV-2 patients,” he said.
Links between SARS-CoV-2 and gastrointestinal symptoms
Gastrointestinal symptoms are known to be relatively common during acute infection. According to Dr. Noviello, the most frequent gastrointestinal symptom associated with SARS-CoV-2 is diarrhea, occurring in 4% to nearly 40% of patients in case series to date.
However, data on the longer-term gastrointestinal impacts of SARS-CoV-2 remain scarce.
In one noncontrolled cohort study in China, loss of appetite, nausea, acid reflux, and diarrhea were seen in 15%-24% of patients 3 months after the infection, Dr. Noviello said. In another cohort study in China, diarrhea and vomiting were reported in 5% of patients 6 months after infection.
In any case, it is known that viral, bacterial, and protozoal infections of the gastrointestinal tract are a risk factor for development of functional disorders including irritable bowel syndrome (IBS), functional dyspepsia, and chronic fatigue, according to Dr. Noviello.
Accordingly, the results of the present study suggest that SARS-CoV-2 also “may affect the brain-gut axis in the long term,” Dr. Noviello and coauthors wrote in an abstract of the study.
It is plausible that SARS-CoV-2 infection could be a trigger for longer-term gastrointestinal symptoms, especially given the previous evidence linking infections and IBS symptoms, or postinfectious IBS, said Juan Pablo Stefanolo, MD, a physician with the neurogastroenterology and motility section, Hospital de Clínicas José de San Martín, Buenos Aires University.
“If it is demonstrated [that SARS-CoV-2 infection is a trigger], the microbiota-gut-brain axis concept in IBS pathophysiology is reinforced,” Dr. Stefanolo said in an interview.
In the meantime, practitioners may want to take into account COVID-19 infection history in the evaluation of a patient with IBS-like symptoms and, in case of a known positive COVID-19 result in an IBS patient, be aware of the possibility of symptom exacerbation, Dr. Stefanolo said.
Pandemic in Italy: Unique study opportunity
The severe outbreak in the Milan region early in the COVID-19 pandemic provided a “unique opportunity” to assess the long-term impact of infection on gastrointestinal and extraintestinal somatoform symptoms, said Dr. Noviello.
The investigators sent an online questionnaire to patients who had a molecular diagnosis of SARS-CoV-2 infection by nasal swab between February and April of 2020. To form a control group, they also sent questionnaires to hospital employees and health care providers who had tested negative over that same time period.
In all, 378 questionnaires were completed by 177 SARS-CoV-2–positive individuals and 201 controls. The SARS-CoV-2–positive patients were somewhat older (about 44 years vs. 40 years for controls), were less often female (40% vs. 61%), had a lower education level, and smoked less than did controls, according to the investigators.
A mean of 4.8 months had elapsed between the time of SARS-CoV-2 infection and when the questionnaires were compiled, said Dr. Noviello.
In the acute phase, diarrhea was the most common gastrointestinal symptom among virus-positive individuals, occurring in about 50% compared to 20% of controls (P < .001), data show. Other symptoms reported by 40% of SARS-CoV-2–infected individuals included fever, dyspnea, loss of smell or taste, weight loss, myalgia, arthralgia, and asthenia in the acute phase controls in the acute phase, Dr. Noviello said.
Persistent gastrointestinal symptoms after SARS-CoV-2
Persistent symptoms included loose stools, as measured by the Bristol Stool scale, occurring in 17.8% of SARS-CoV-2–positive individuals, but only 9.3% of the SARS-CoV-2–negative controls, according to Dr. Noviello, with an adjusted risk ratio of 1.88 (95% confidence interval, 0.99-3.54).
Chronic fatigue symptoms, as measured by the Structured Assessment of Gastrointestinal Symptoms questionnaire, were reported by about 30% of SARS-CoV-2–positive patients and about 15% of controls, for an adjusted risk ratio of 2.24 (95% CI, 1.48-3.37), according to Dr. Noviello’s presentation.
The mean t-score on the Symptom Checklist–12 for somatoform disorders was higher for the virus-positive patients compared to controls, according to Dr. Noviello. The scores were 54.6 and 50.5, respectively, with an adjusted score difference of 3.6 (95% CI, 1.0-6.2).
The longer-term sequelae of SARS-CoV-2 infection might be more severe in individuals who experienced diarrhea during acute infection, according to Dr. Noviello. In a post hoc analysis, reports of irritable bowel syndrome and loose stools were significantly higher in SARS-CoV-2–infected individuals who had diarrhea in the acute phase compared to those who did not experience diarrhea, he said.
Somatoform disorder scores were significantly higher, and reports of headache, back pain, and chronic fatigue were significantly more common, in individuals who had diarrhea at the time of SARS-CoV-2 infection, he added.
Dr. Noviello and coauthors reported no competing interests related to the study. Dr. Stefanolo had no disclosures to report.
FROM DDW 2021