User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
Free U.K. tool could help guide COVID-19 care for cancer patients
An online support tool for health care professionals that recommends whether to admit or discharge a cancer patient with COVID-19, based on their risk of a severe complication, has been developed by researchers from Manchester.
The team used machine learning on data from more than 900 cancer patients with COVID-19, conducting multiple analyses to arrive at a set of features that could accurately predict the need for admission or oxygen therapy, as well as the risk of death.
Dr. Rebecca Lee, The Christie NHS Foundation Trust, Manchester, and colleagues then developed thresholds to derive a score that recommended admission in 95% of patients who went on to need oxygen and an even greater proportion of those who later died.
The research was presented at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting on June 4.
CORONET
The resulting COVID-19 Risk in Oncology Evaluation Tool (CORONET) model “performs very well at predicting admission and severity of COVID-19 in patients with cancer,” Dr. Lee said. “We have set pragmatic and clinically relevant thresholds that focus on the safety regarding an admission versus discharge decision.”
To help health care professionals, the researchers have built a free online support tool that allows them to enter data and receive a recommendation “as to whether their patient should be considered for discharge, considered for admission, or is at high risk of having a severe outcome of coronavirus,” Dr. Lee explained.
“The health care professional can then explore the recommendation by seeing how their patient … compares with the rest of the cohort.”
The tool also includes a “diagram showing which features are most important to recommend a discharge decision versus an admission decision for each individual patient.”
Clinically intuitive
Dr. Alexi Wright, associate professor, Dana-Faber Cancer Institute, Boston, who was not involved in the study, commented that there were many things that were “really nice about the study.”
“First and foremost that they were establishing a tool to efficiently triage [patients] presenting with COVID,” she said, adding that it was “clinically intuitive” that the team made “pragmatic choices,” and the use of a random forest algorithm means the results are “very interpretable.”
However, Dr. Wright wondered whether the results can be replicated.
Alongside a lack of information on the deaths in the cohort, she pointed out that “ideally you have three data sets, with a training set, a testing set, and a validation set.”
The CORONET model was, however, trained and evaluated on the same dataset, “so it really needs external validation before it would be ready for direct clinical application.”
She continued that there is a “critical need to establish that studies can both be reproduced and replicated,” noting that a recent review showed that 85% of machine-learning studies that were used to detect COVID-19 using chest radiographs “failed fundamental reproducibility and quality checks.”
Risk factors
Dr. Lee began her presentation by reminding the audience that cancer patients are at increased risk of severe COVID-19 and death, with older age, male sex, nosocomial infection, higher ECOG performance status, and active cancer among the risk factors for mortality.
“However, outcomes are very heterogeneous, ranging from patients without symptoms at all to cases with multi-organ failure and death,” she said.
It is consequently “very important for the treating clinician to determine which patients could be safely discharged to the community versus those who need additional support in being admitted to hospital.”
To develop a tool that could distinguish between those two groups of patients, the researchers collected data on 1,743 cancer patients, which was reduced down to 920 patients after excluding those without laboratory confirmed COVID-19 and those with missing data.
Using recursive feature elimination, they selected 10 key patient features associated with prognosis, then compared a lasso regression model with a random forest model, with the latter performing the best.
The team then divided their patients into four cohorts, with the model trained on three cohorts and tested on the fourth. This resulted in the CORONET score, with the final model determined by testing it against the entire patient population.
Next, thresholds were determined for assessing patients for admission versus discharge, as well as for severity of illness, giving the final CORONET model, from which the online tool was developed.
Checking performance
The results showed that the model was able to predict admission with an area under the receiver operating characteristics curve (AUROC) of 0.82 for admission, 0.85 for oxygen requirement, and 0.79 for death.
Further analysis revealed that the most important feature at the time of presentation for determining outcome was the National Early Warning Score 2 (NEWS2), “which is a composite score of heart rate, respiratory rate, saturations and confusion level,” Dr. Lee said.
In addition, C-reactive protein levels, albumin, age, and platelet counts “were also very important features,” she continued, “and these have also been shown in a number of different studies to be important at determining the outcome from coronavirus.”
To examine the performance of the CORONET score further, they applied it to a European hospital dataset, ESMO-CoCARE registry data, and a U.S. cohort, the COVID-19 and Cancer Consortium Registry (CCC19). They found that the score discriminated between patients, but it did so with some degree of heterogeneity.
This was largely driven by higher patient age among the U.S. patients, a higher NEWS2 score, and lower albumin levels, Dr. Lee said.
To ensure the score’s applicability to clinical practice, the team set pragmatic thresholds to determine whether or not a patient required admission or whether they were at risk of dying.
For admission, they set a sensitivity of 85% and a specificity of 56%, while for mortality they set a sensitivity of 43% and a specificity of 92%.
When this was converted into a decision support tool, the model recommended hospital admission for 95% of patients who eventually required oxygen and 97% of patients who died.
The study was funded by The Christie Charitable Foundation. Dr. Lee declares relationships with AstraZeneca and Bristol-Myers Squibb (Inst). Dr. Wright declares relationships with NCCN/AstraZeneca (Inst).
A version of this article first appeared on Medscape.com.
An online support tool for health care professionals that recommends whether to admit or discharge a cancer patient with COVID-19, based on their risk of a severe complication, has been developed by researchers from Manchester.
The team used machine learning on data from more than 900 cancer patients with COVID-19, conducting multiple analyses to arrive at a set of features that could accurately predict the need for admission or oxygen therapy, as well as the risk of death.
Dr. Rebecca Lee, The Christie NHS Foundation Trust, Manchester, and colleagues then developed thresholds to derive a score that recommended admission in 95% of patients who went on to need oxygen and an even greater proportion of those who later died.
The research was presented at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting on June 4.
CORONET
The resulting COVID-19 Risk in Oncology Evaluation Tool (CORONET) model “performs very well at predicting admission and severity of COVID-19 in patients with cancer,” Dr. Lee said. “We have set pragmatic and clinically relevant thresholds that focus on the safety regarding an admission versus discharge decision.”
To help health care professionals, the researchers have built a free online support tool that allows them to enter data and receive a recommendation “as to whether their patient should be considered for discharge, considered for admission, or is at high risk of having a severe outcome of coronavirus,” Dr. Lee explained.
“The health care professional can then explore the recommendation by seeing how their patient … compares with the rest of the cohort.”
The tool also includes a “diagram showing which features are most important to recommend a discharge decision versus an admission decision for each individual patient.”
Clinically intuitive
Dr. Alexi Wright, associate professor, Dana-Faber Cancer Institute, Boston, who was not involved in the study, commented that there were many things that were “really nice about the study.”
“First and foremost that they were establishing a tool to efficiently triage [patients] presenting with COVID,” she said, adding that it was “clinically intuitive” that the team made “pragmatic choices,” and the use of a random forest algorithm means the results are “very interpretable.”
However, Dr. Wright wondered whether the results can be replicated.
Alongside a lack of information on the deaths in the cohort, she pointed out that “ideally you have three data sets, with a training set, a testing set, and a validation set.”
The CORONET model was, however, trained and evaluated on the same dataset, “so it really needs external validation before it would be ready for direct clinical application.”
She continued that there is a “critical need to establish that studies can both be reproduced and replicated,” noting that a recent review showed that 85% of machine-learning studies that were used to detect COVID-19 using chest radiographs “failed fundamental reproducibility and quality checks.”
Risk factors
Dr. Lee began her presentation by reminding the audience that cancer patients are at increased risk of severe COVID-19 and death, with older age, male sex, nosocomial infection, higher ECOG performance status, and active cancer among the risk factors for mortality.
“However, outcomes are very heterogeneous, ranging from patients without symptoms at all to cases with multi-organ failure and death,” she said.
It is consequently “very important for the treating clinician to determine which patients could be safely discharged to the community versus those who need additional support in being admitted to hospital.”
To develop a tool that could distinguish between those two groups of patients, the researchers collected data on 1,743 cancer patients, which was reduced down to 920 patients after excluding those without laboratory confirmed COVID-19 and those with missing data.
Using recursive feature elimination, they selected 10 key patient features associated with prognosis, then compared a lasso regression model with a random forest model, with the latter performing the best.
The team then divided their patients into four cohorts, with the model trained on three cohorts and tested on the fourth. This resulted in the CORONET score, with the final model determined by testing it against the entire patient population.
Next, thresholds were determined for assessing patients for admission versus discharge, as well as for severity of illness, giving the final CORONET model, from which the online tool was developed.
Checking performance
The results showed that the model was able to predict admission with an area under the receiver operating characteristics curve (AUROC) of 0.82 for admission, 0.85 for oxygen requirement, and 0.79 for death.
Further analysis revealed that the most important feature at the time of presentation for determining outcome was the National Early Warning Score 2 (NEWS2), “which is a composite score of heart rate, respiratory rate, saturations and confusion level,” Dr. Lee said.
In addition, C-reactive protein levels, albumin, age, and platelet counts “were also very important features,” she continued, “and these have also been shown in a number of different studies to be important at determining the outcome from coronavirus.”
To examine the performance of the CORONET score further, they applied it to a European hospital dataset, ESMO-CoCARE registry data, and a U.S. cohort, the COVID-19 and Cancer Consortium Registry (CCC19). They found that the score discriminated between patients, but it did so with some degree of heterogeneity.
This was largely driven by higher patient age among the U.S. patients, a higher NEWS2 score, and lower albumin levels, Dr. Lee said.
To ensure the score’s applicability to clinical practice, the team set pragmatic thresholds to determine whether or not a patient required admission or whether they were at risk of dying.
For admission, they set a sensitivity of 85% and a specificity of 56%, while for mortality they set a sensitivity of 43% and a specificity of 92%.
When this was converted into a decision support tool, the model recommended hospital admission for 95% of patients who eventually required oxygen and 97% of patients who died.
The study was funded by The Christie Charitable Foundation. Dr. Lee declares relationships with AstraZeneca and Bristol-Myers Squibb (Inst). Dr. Wright declares relationships with NCCN/AstraZeneca (Inst).
A version of this article first appeared on Medscape.com.
An online support tool for health care professionals that recommends whether to admit or discharge a cancer patient with COVID-19, based on their risk of a severe complication, has been developed by researchers from Manchester.
The team used machine learning on data from more than 900 cancer patients with COVID-19, conducting multiple analyses to arrive at a set of features that could accurately predict the need for admission or oxygen therapy, as well as the risk of death.
Dr. Rebecca Lee, The Christie NHS Foundation Trust, Manchester, and colleagues then developed thresholds to derive a score that recommended admission in 95% of patients who went on to need oxygen and an even greater proportion of those who later died.
The research was presented at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting on June 4.
CORONET
The resulting COVID-19 Risk in Oncology Evaluation Tool (CORONET) model “performs very well at predicting admission and severity of COVID-19 in patients with cancer,” Dr. Lee said. “We have set pragmatic and clinically relevant thresholds that focus on the safety regarding an admission versus discharge decision.”
To help health care professionals, the researchers have built a free online support tool that allows them to enter data and receive a recommendation “as to whether their patient should be considered for discharge, considered for admission, or is at high risk of having a severe outcome of coronavirus,” Dr. Lee explained.
“The health care professional can then explore the recommendation by seeing how their patient … compares with the rest of the cohort.”
The tool also includes a “diagram showing which features are most important to recommend a discharge decision versus an admission decision for each individual patient.”
Clinically intuitive
Dr. Alexi Wright, associate professor, Dana-Faber Cancer Institute, Boston, who was not involved in the study, commented that there were many things that were “really nice about the study.”
“First and foremost that they were establishing a tool to efficiently triage [patients] presenting with COVID,” she said, adding that it was “clinically intuitive” that the team made “pragmatic choices,” and the use of a random forest algorithm means the results are “very interpretable.”
However, Dr. Wright wondered whether the results can be replicated.
Alongside a lack of information on the deaths in the cohort, she pointed out that “ideally you have three data sets, with a training set, a testing set, and a validation set.”
The CORONET model was, however, trained and evaluated on the same dataset, “so it really needs external validation before it would be ready for direct clinical application.”
She continued that there is a “critical need to establish that studies can both be reproduced and replicated,” noting that a recent review showed that 85% of machine-learning studies that were used to detect COVID-19 using chest radiographs “failed fundamental reproducibility and quality checks.”
Risk factors
Dr. Lee began her presentation by reminding the audience that cancer patients are at increased risk of severe COVID-19 and death, with older age, male sex, nosocomial infection, higher ECOG performance status, and active cancer among the risk factors for mortality.
“However, outcomes are very heterogeneous, ranging from patients without symptoms at all to cases with multi-organ failure and death,” she said.
It is consequently “very important for the treating clinician to determine which patients could be safely discharged to the community versus those who need additional support in being admitted to hospital.”
To develop a tool that could distinguish between those two groups of patients, the researchers collected data on 1,743 cancer patients, which was reduced down to 920 patients after excluding those without laboratory confirmed COVID-19 and those with missing data.
Using recursive feature elimination, they selected 10 key patient features associated with prognosis, then compared a lasso regression model with a random forest model, with the latter performing the best.
The team then divided their patients into four cohorts, with the model trained on three cohorts and tested on the fourth. This resulted in the CORONET score, with the final model determined by testing it against the entire patient population.
Next, thresholds were determined for assessing patients for admission versus discharge, as well as for severity of illness, giving the final CORONET model, from which the online tool was developed.
Checking performance
The results showed that the model was able to predict admission with an area under the receiver operating characteristics curve (AUROC) of 0.82 for admission, 0.85 for oxygen requirement, and 0.79 for death.
Further analysis revealed that the most important feature at the time of presentation for determining outcome was the National Early Warning Score 2 (NEWS2), “which is a composite score of heart rate, respiratory rate, saturations and confusion level,” Dr. Lee said.
In addition, C-reactive protein levels, albumin, age, and platelet counts “were also very important features,” she continued, “and these have also been shown in a number of different studies to be important at determining the outcome from coronavirus.”
To examine the performance of the CORONET score further, they applied it to a European hospital dataset, ESMO-CoCARE registry data, and a U.S. cohort, the COVID-19 and Cancer Consortium Registry (CCC19). They found that the score discriminated between patients, but it did so with some degree of heterogeneity.
This was largely driven by higher patient age among the U.S. patients, a higher NEWS2 score, and lower albumin levels, Dr. Lee said.
To ensure the score’s applicability to clinical practice, the team set pragmatic thresholds to determine whether or not a patient required admission or whether they were at risk of dying.
For admission, they set a sensitivity of 85% and a specificity of 56%, while for mortality they set a sensitivity of 43% and a specificity of 92%.
When this was converted into a decision support tool, the model recommended hospital admission for 95% of patients who eventually required oxygen and 97% of patients who died.
The study was funded by The Christie Charitable Foundation. Dr. Lee declares relationships with AstraZeneca and Bristol-Myers Squibb (Inst). Dr. Wright declares relationships with NCCN/AstraZeneca (Inst).
A version of this article first appeared on Medscape.com.
By the numbers: Children and COVID-19 prevention
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
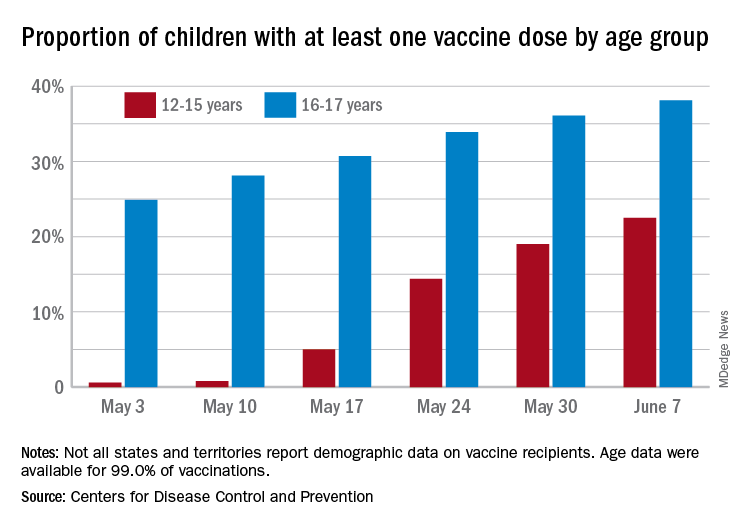
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
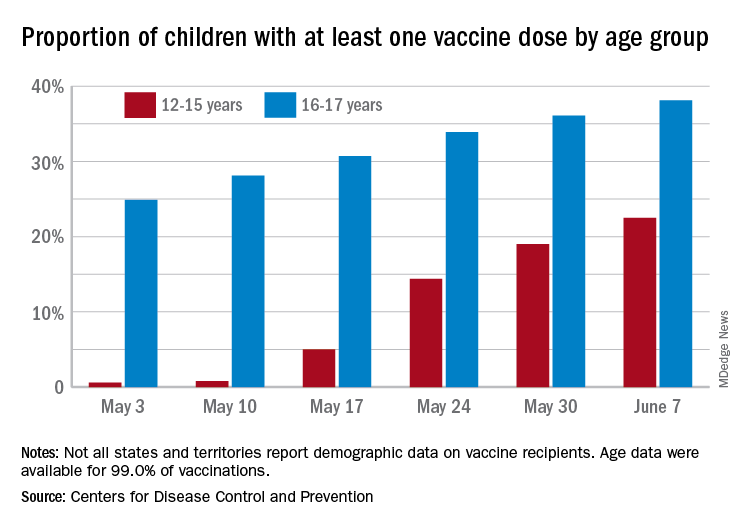
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
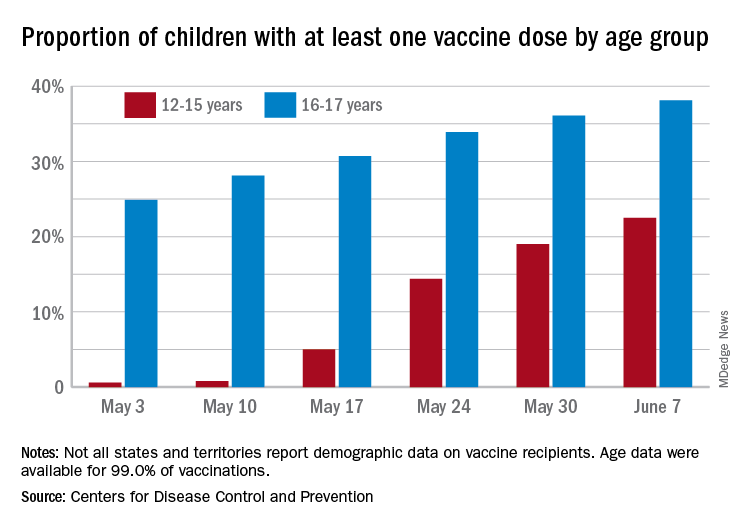
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
NIAID advances universal flu vaccine candidate into phase 1 trial
Last month, U.S. government researchers began a test of an experimental influenza vaccine that they hope will provide long-lasting immunity against multiple strains of the virus. Their project adds to the many approaches that have been tried in the decades-long quest for a universal flu shot.
For the first time, the National Institute of Allergy and Infectious Diseases (NIAID) is testing an investigational flu vaccine, known as FluMos-v1, on people. Researchers in recent years have targeted the stalk or stem of an influenza surface protein called hemagglutinin (HA) in trying to develop better flu vaccines. NIAID said FluMos-v1 is designed to spark production of antibodies against the HA protein from different virus strains, which could make it superior to vaccines now available, NIAID said.
“It could be longer lasting than the traditional flu vaccine and give us what we call super seasonal protection that might go beyond just one flu season to next year’s or the year after, or offer additional protection in a pandemic setting,” Alicia T. Widge, MD, of NIAID’s Vaccine Research Center, who is the principal investigator of the trial, said in an interview.
The phase 1 study (NCT04896086) aims to enroll 35 participants, 15 of whom will receive a single intramuscular injection of a comparator treatment, Flucelvax, which has already been approved by the U.S. Food and Drug Administration. The FluMos-v1 group will start with five participants who will receive one 20-μg dose. If no safety problems emerge at that dosage, another 15 volunteers will receive one 60-μg dose of the investigational vaccine.
The incorporation of a comparator group in the phase 1 study may help investigators get an early idea of how well FluMos-v1 compares to a marketed product, Dr. Widge said. The test will be carried out through the National Institutes of Health Clinical Center.
‘Renaissance’ of flu-vaccine research?
Currently, flu vaccines are reformulated each year in an attempt to match the dominant strain for the upcoming season, an effort that often falls notably short. The estimated vaccine effectiveness rate in the United States has ranged from a low of 19% to a high of 60% in recent years, according to the Centers for Disease Control and Prevention.
Scientists have been working for decades on a universal flu vaccine that would offer better results but haven’t yet identified the right strategy to outwit mutations in the virus. Recent setbacks include BiondVax Pharmaceuticals’ October 2020 announcement of a failed phase 3 trial of its experimental M-001 universal flu vaccine candidate.
But advances in understanding the immune system may set the stage for a “renaissance” in efforts to develop a universal flu vaccine, Michael Osterholm, PhD, MPH, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, said in an interview.
The COVID-19 pandemic has spurred greater interest in the need to develop a universal flu vaccine, he said. Dr. Osterholm said he is “more optimistic now than ever” about the chances for developing vaccines that can fend off multiple strains over longer periods, although the goal of a shot that can ward off influenza in all cases may remain elusive.
“How good can we make them? Will they ever be really universal? Will they have long periods of protection? I don’t think any of us know that yet,” Dr. Osterholm said. “But this is not the influenza vaccine world of 5 or 7 years ago.”
The mRNA technology used to develop the world’s first approved COVID-19 vaccines, for example, may be applied against influenza, Dr. Osterholm said.
In January 2021, Moderna announced plans to test three development candidates for a seasonal influenza vaccine and aims to start a phase 1 study this year. In an April interview on CNBC’s Squawk Box program, Moderna’s chief executive, Stephané Bancel, spoke about the company’s plans to eventually create a combination vaccine for SARS-Cov-2 and flu viruses.
SARS-CoV-2 “is not going away.” Like flu, this virus will persist and change forms, Ms. Bancel said. Creating a flu shot that outperforms the existing ones would boost confidence in influenza vaccines, which many people now skip, Ms. Bancel said. People might someday be able to get a combination of this more effective flu shot with a COVID-19 vaccine booster in their local pharmacies.
“You can take one dose and then have a nice winter,” Ms. Bancel said of Moderna’s goal for a combination vaccine.
A version of this article first appeared on Medscape.com.
Last month, U.S. government researchers began a test of an experimental influenza vaccine that they hope will provide long-lasting immunity against multiple strains of the virus. Their project adds to the many approaches that have been tried in the decades-long quest for a universal flu shot.
For the first time, the National Institute of Allergy and Infectious Diseases (NIAID) is testing an investigational flu vaccine, known as FluMos-v1, on people. Researchers in recent years have targeted the stalk or stem of an influenza surface protein called hemagglutinin (HA) in trying to develop better flu vaccines. NIAID said FluMos-v1 is designed to spark production of antibodies against the HA protein from different virus strains, which could make it superior to vaccines now available, NIAID said.
“It could be longer lasting than the traditional flu vaccine and give us what we call super seasonal protection that might go beyond just one flu season to next year’s or the year after, or offer additional protection in a pandemic setting,” Alicia T. Widge, MD, of NIAID’s Vaccine Research Center, who is the principal investigator of the trial, said in an interview.
The phase 1 study (NCT04896086) aims to enroll 35 participants, 15 of whom will receive a single intramuscular injection of a comparator treatment, Flucelvax, which has already been approved by the U.S. Food and Drug Administration. The FluMos-v1 group will start with five participants who will receive one 20-μg dose. If no safety problems emerge at that dosage, another 15 volunteers will receive one 60-μg dose of the investigational vaccine.
The incorporation of a comparator group in the phase 1 study may help investigators get an early idea of how well FluMos-v1 compares to a marketed product, Dr. Widge said. The test will be carried out through the National Institutes of Health Clinical Center.
‘Renaissance’ of flu-vaccine research?
Currently, flu vaccines are reformulated each year in an attempt to match the dominant strain for the upcoming season, an effort that often falls notably short. The estimated vaccine effectiveness rate in the United States has ranged from a low of 19% to a high of 60% in recent years, according to the Centers for Disease Control and Prevention.
Scientists have been working for decades on a universal flu vaccine that would offer better results but haven’t yet identified the right strategy to outwit mutations in the virus. Recent setbacks include BiondVax Pharmaceuticals’ October 2020 announcement of a failed phase 3 trial of its experimental M-001 universal flu vaccine candidate.
But advances in understanding the immune system may set the stage for a “renaissance” in efforts to develop a universal flu vaccine, Michael Osterholm, PhD, MPH, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, said in an interview.
The COVID-19 pandemic has spurred greater interest in the need to develop a universal flu vaccine, he said. Dr. Osterholm said he is “more optimistic now than ever” about the chances for developing vaccines that can fend off multiple strains over longer periods, although the goal of a shot that can ward off influenza in all cases may remain elusive.
“How good can we make them? Will they ever be really universal? Will they have long periods of protection? I don’t think any of us know that yet,” Dr. Osterholm said. “But this is not the influenza vaccine world of 5 or 7 years ago.”
The mRNA technology used to develop the world’s first approved COVID-19 vaccines, for example, may be applied against influenza, Dr. Osterholm said.
In January 2021, Moderna announced plans to test three development candidates for a seasonal influenza vaccine and aims to start a phase 1 study this year. In an April interview on CNBC’s Squawk Box program, Moderna’s chief executive, Stephané Bancel, spoke about the company’s plans to eventually create a combination vaccine for SARS-Cov-2 and flu viruses.
SARS-CoV-2 “is not going away.” Like flu, this virus will persist and change forms, Ms. Bancel said. Creating a flu shot that outperforms the existing ones would boost confidence in influenza vaccines, which many people now skip, Ms. Bancel said. People might someday be able to get a combination of this more effective flu shot with a COVID-19 vaccine booster in their local pharmacies.
“You can take one dose and then have a nice winter,” Ms. Bancel said of Moderna’s goal for a combination vaccine.
A version of this article first appeared on Medscape.com.
Last month, U.S. government researchers began a test of an experimental influenza vaccine that they hope will provide long-lasting immunity against multiple strains of the virus. Their project adds to the many approaches that have been tried in the decades-long quest for a universal flu shot.
For the first time, the National Institute of Allergy and Infectious Diseases (NIAID) is testing an investigational flu vaccine, known as FluMos-v1, on people. Researchers in recent years have targeted the stalk or stem of an influenza surface protein called hemagglutinin (HA) in trying to develop better flu vaccines. NIAID said FluMos-v1 is designed to spark production of antibodies against the HA protein from different virus strains, which could make it superior to vaccines now available, NIAID said.
“It could be longer lasting than the traditional flu vaccine and give us what we call super seasonal protection that might go beyond just one flu season to next year’s or the year after, or offer additional protection in a pandemic setting,” Alicia T. Widge, MD, of NIAID’s Vaccine Research Center, who is the principal investigator of the trial, said in an interview.
The phase 1 study (NCT04896086) aims to enroll 35 participants, 15 of whom will receive a single intramuscular injection of a comparator treatment, Flucelvax, which has already been approved by the U.S. Food and Drug Administration. The FluMos-v1 group will start with five participants who will receive one 20-μg dose. If no safety problems emerge at that dosage, another 15 volunteers will receive one 60-μg dose of the investigational vaccine.
The incorporation of a comparator group in the phase 1 study may help investigators get an early idea of how well FluMos-v1 compares to a marketed product, Dr. Widge said. The test will be carried out through the National Institutes of Health Clinical Center.
‘Renaissance’ of flu-vaccine research?
Currently, flu vaccines are reformulated each year in an attempt to match the dominant strain for the upcoming season, an effort that often falls notably short. The estimated vaccine effectiveness rate in the United States has ranged from a low of 19% to a high of 60% in recent years, according to the Centers for Disease Control and Prevention.
Scientists have been working for decades on a universal flu vaccine that would offer better results but haven’t yet identified the right strategy to outwit mutations in the virus. Recent setbacks include BiondVax Pharmaceuticals’ October 2020 announcement of a failed phase 3 trial of its experimental M-001 universal flu vaccine candidate.
But advances in understanding the immune system may set the stage for a “renaissance” in efforts to develop a universal flu vaccine, Michael Osterholm, PhD, MPH, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, said in an interview.
The COVID-19 pandemic has spurred greater interest in the need to develop a universal flu vaccine, he said. Dr. Osterholm said he is “more optimistic now than ever” about the chances for developing vaccines that can fend off multiple strains over longer periods, although the goal of a shot that can ward off influenza in all cases may remain elusive.
“How good can we make them? Will they ever be really universal? Will they have long periods of protection? I don’t think any of us know that yet,” Dr. Osterholm said. “But this is not the influenza vaccine world of 5 or 7 years ago.”
The mRNA technology used to develop the world’s first approved COVID-19 vaccines, for example, may be applied against influenza, Dr. Osterholm said.
In January 2021, Moderna announced plans to test three development candidates for a seasonal influenza vaccine and aims to start a phase 1 study this year. In an April interview on CNBC’s Squawk Box program, Moderna’s chief executive, Stephané Bancel, spoke about the company’s plans to eventually create a combination vaccine for SARS-Cov-2 and flu viruses.
SARS-CoV-2 “is not going away.” Like flu, this virus will persist and change forms, Ms. Bancel said. Creating a flu shot that outperforms the existing ones would boost confidence in influenza vaccines, which many people now skip, Ms. Bancel said. People might someday be able to get a combination of this more effective flu shot with a COVID-19 vaccine booster in their local pharmacies.
“You can take one dose and then have a nice winter,” Ms. Bancel said of Moderna’s goal for a combination vaccine.
A version of this article first appeared on Medscape.com.
CDC director cites rise in hospitalizations in urging teen vaccinations
“I am deeply concerned by the numbers of hospitalized adolescents and saddened to see the number of adolescents who required treatment in intensive care units or mechanical ventilation,” CDC Director Rochelle Walensky, MD, said in a statement.
While urging teenagers to wear masks and take precautions around others, she asked “parents, relatives, and close friends to join me and talk with teens about the importance of these prevention strategies and to encourage them to get vaccinated.”
Dr. Walensky referred to the CDC’s Morbidity and Mortality Weekly Report that showed adolescent hospitalizations peaked at 2.1 per 100,000 in early January 2021, then dropped to 0.6 per 100,000 in mid-March.
Alarmingly, hospitalizations rose to 1.3 per 100,000 in April, and a number of teens required serious interventions.
“Among hospitalized adolescents, nearly one-third required intensive care unit admission, and 5% required invasive mechanical ventilation,” the report said. No deaths occurred.
The study looked at 376 adolescents aged 12-17 who were hospitalized and tested positive for coronavirus. Of that group, 204 were hospitalized for COVID-19 and the other 172 were hospitalized for reasons not directly related to COVID-19.
Of the 204 hospitalized for COVID-19, 70.6% had an underlying medical condition such as obesity or chronic lung disease.
The study noted that children and teenagers have lower hospitalization rates and generally show less severe symptoms than do older people.
Possible causes for the rise in adolescent COVID-19 hospitalizations include the arrival of variants, the growing number of children returning to in-person education, and the changes in mask-wearing and other safety precautions, the study said.
The American Academy of Pediatrics said that as of May 27, 4 million children have tested positive for COVID-19 since the pandemic began, with about 34,500 new child cases reported for the week ending May 27.
The AAP said children have represented 14.1% of total cases since the pandemic began, but for the week ending May 27, children represented 24.3% of new reported weekly COVID-19 cases.
On May 10, the FDA granted emergency use authorization for the Pfizer coronavirus vaccine to be given to children aged 12-15 years. Previously, the FDA had authorized the Pfizer vaccine for people aged 16 years and up, whereas the Moderna and Johnson & Johnson vaccines are authorized for people aged 18 years and up.
“Vaccination is our way out of this pandemic,” Dr. Walensky said in her statement. “I continue to see promising signs in CDC data that we are nearing the end of this pandemic in this country; however, we all have to do our part and get vaccinated to cross the finish line.”
A version of this article was first published on WebMD.com.
“I am deeply concerned by the numbers of hospitalized adolescents and saddened to see the number of adolescents who required treatment in intensive care units or mechanical ventilation,” CDC Director Rochelle Walensky, MD, said in a statement.
While urging teenagers to wear masks and take precautions around others, she asked “parents, relatives, and close friends to join me and talk with teens about the importance of these prevention strategies and to encourage them to get vaccinated.”
Dr. Walensky referred to the CDC’s Morbidity and Mortality Weekly Report that showed adolescent hospitalizations peaked at 2.1 per 100,000 in early January 2021, then dropped to 0.6 per 100,000 in mid-March.
Alarmingly, hospitalizations rose to 1.3 per 100,000 in April, and a number of teens required serious interventions.
“Among hospitalized adolescents, nearly one-third required intensive care unit admission, and 5% required invasive mechanical ventilation,” the report said. No deaths occurred.
The study looked at 376 adolescents aged 12-17 who were hospitalized and tested positive for coronavirus. Of that group, 204 were hospitalized for COVID-19 and the other 172 were hospitalized for reasons not directly related to COVID-19.
Of the 204 hospitalized for COVID-19, 70.6% had an underlying medical condition such as obesity or chronic lung disease.
The study noted that children and teenagers have lower hospitalization rates and generally show less severe symptoms than do older people.
Possible causes for the rise in adolescent COVID-19 hospitalizations include the arrival of variants, the growing number of children returning to in-person education, and the changes in mask-wearing and other safety precautions, the study said.
The American Academy of Pediatrics said that as of May 27, 4 million children have tested positive for COVID-19 since the pandemic began, with about 34,500 new child cases reported for the week ending May 27.
The AAP said children have represented 14.1% of total cases since the pandemic began, but for the week ending May 27, children represented 24.3% of new reported weekly COVID-19 cases.
On May 10, the FDA granted emergency use authorization for the Pfizer coronavirus vaccine to be given to children aged 12-15 years. Previously, the FDA had authorized the Pfizer vaccine for people aged 16 years and up, whereas the Moderna and Johnson & Johnson vaccines are authorized for people aged 18 years and up.
“Vaccination is our way out of this pandemic,” Dr. Walensky said in her statement. “I continue to see promising signs in CDC data that we are nearing the end of this pandemic in this country; however, we all have to do our part and get vaccinated to cross the finish line.”
A version of this article was first published on WebMD.com.
“I am deeply concerned by the numbers of hospitalized adolescents and saddened to see the number of adolescents who required treatment in intensive care units or mechanical ventilation,” CDC Director Rochelle Walensky, MD, said in a statement.
While urging teenagers to wear masks and take precautions around others, she asked “parents, relatives, and close friends to join me and talk with teens about the importance of these prevention strategies and to encourage them to get vaccinated.”
Dr. Walensky referred to the CDC’s Morbidity and Mortality Weekly Report that showed adolescent hospitalizations peaked at 2.1 per 100,000 in early January 2021, then dropped to 0.6 per 100,000 in mid-March.
Alarmingly, hospitalizations rose to 1.3 per 100,000 in April, and a number of teens required serious interventions.
“Among hospitalized adolescents, nearly one-third required intensive care unit admission, and 5% required invasive mechanical ventilation,” the report said. No deaths occurred.
The study looked at 376 adolescents aged 12-17 who were hospitalized and tested positive for coronavirus. Of that group, 204 were hospitalized for COVID-19 and the other 172 were hospitalized for reasons not directly related to COVID-19.
Of the 204 hospitalized for COVID-19, 70.6% had an underlying medical condition such as obesity or chronic lung disease.
The study noted that children and teenagers have lower hospitalization rates and generally show less severe symptoms than do older people.
Possible causes for the rise in adolescent COVID-19 hospitalizations include the arrival of variants, the growing number of children returning to in-person education, and the changes in mask-wearing and other safety precautions, the study said.
The American Academy of Pediatrics said that as of May 27, 4 million children have tested positive for COVID-19 since the pandemic began, with about 34,500 new child cases reported for the week ending May 27.
The AAP said children have represented 14.1% of total cases since the pandemic began, but for the week ending May 27, children represented 24.3% of new reported weekly COVID-19 cases.
On May 10, the FDA granted emergency use authorization for the Pfizer coronavirus vaccine to be given to children aged 12-15 years. Previously, the FDA had authorized the Pfizer vaccine for people aged 16 years and up, whereas the Moderna and Johnson & Johnson vaccines are authorized for people aged 18 years and up.
“Vaccination is our way out of this pandemic,” Dr. Walensky said in her statement. “I continue to see promising signs in CDC data that we are nearing the end of this pandemic in this country; however, we all have to do our part and get vaccinated to cross the finish line.”
A version of this article was first published on WebMD.com.
Physician convicted in buprenorphine scheme faces up to 20 years in prison
A West Virginia physician faces up to 20 years in prison in the wake of his conviction by a federal jury for illegally distributing buprenorphine.
The jury convicted Sriramloo Kesari, MD, 78, of Charleston, for distributing buprenorphine outside the scope of medical practice, according to a U.S. Department of Justice statement.
Investigators from the Drug Enforcement Administration presented evidence at the trial that Dr. Kesari, a general practitioner, operated a cash-only business selling buprenorphine prescriptions.
Federal prosecutors said that the physician signed prescriptions, which were then distributed by an employee in exchange for cash. Dr. Kesari was often absent, at times physically located in California, according to the federal government.
Prosecutors indicted the West Virginia physician in September 2019 as part of an “opioid strikeforce takedown” in Ohio, Virginia, and West Virginia that resulted in charges against 13 individuals, including 11 physicians.
Dr. Kesari’s attorneys filed motions during the course of the lengthy case showing that psychiatric and neurological exams indicated that the physician was cognitively impaired.
Based on that evidence and the federal indictment, the West Virginia Board of Medicine suspended Dr. Kesari’s license in February 2020, stating that he is not “mentally and/or physically fit to practice medicine and surgery with reasonable skill and safety.”
Dr. Kesari was first licensed in West Virginia in 1979. In 1987, the Board of Medicine placed Dr. Kesari on a 3-year probation because of his failure to keep records for patients for whom he was prescribing controlled substances.
However, within a few months, the Board changed the probation order to allow Dr. Kesari to write prescriptions for schedule II and III substances in the Boone Hospital emergency room where he continued to work.
The physician had no other disciplinary actions until his license suspension, but the Board lists settlement of four malpractice cases and the dismissal of a fifth between 1986 and 2001.
A version of this article first appeared on Medscape.com.
A West Virginia physician faces up to 20 years in prison in the wake of his conviction by a federal jury for illegally distributing buprenorphine.
The jury convicted Sriramloo Kesari, MD, 78, of Charleston, for distributing buprenorphine outside the scope of medical practice, according to a U.S. Department of Justice statement.
Investigators from the Drug Enforcement Administration presented evidence at the trial that Dr. Kesari, a general practitioner, operated a cash-only business selling buprenorphine prescriptions.
Federal prosecutors said that the physician signed prescriptions, which were then distributed by an employee in exchange for cash. Dr. Kesari was often absent, at times physically located in California, according to the federal government.
Prosecutors indicted the West Virginia physician in September 2019 as part of an “opioid strikeforce takedown” in Ohio, Virginia, and West Virginia that resulted in charges against 13 individuals, including 11 physicians.
Dr. Kesari’s attorneys filed motions during the course of the lengthy case showing that psychiatric and neurological exams indicated that the physician was cognitively impaired.
Based on that evidence and the federal indictment, the West Virginia Board of Medicine suspended Dr. Kesari’s license in February 2020, stating that he is not “mentally and/or physically fit to practice medicine and surgery with reasonable skill and safety.”
Dr. Kesari was first licensed in West Virginia in 1979. In 1987, the Board of Medicine placed Dr. Kesari on a 3-year probation because of his failure to keep records for patients for whom he was prescribing controlled substances.
However, within a few months, the Board changed the probation order to allow Dr. Kesari to write prescriptions for schedule II and III substances in the Boone Hospital emergency room where he continued to work.
The physician had no other disciplinary actions until his license suspension, but the Board lists settlement of four malpractice cases and the dismissal of a fifth between 1986 and 2001.
A version of this article first appeared on Medscape.com.
A West Virginia physician faces up to 20 years in prison in the wake of his conviction by a federal jury for illegally distributing buprenorphine.
The jury convicted Sriramloo Kesari, MD, 78, of Charleston, for distributing buprenorphine outside the scope of medical practice, according to a U.S. Department of Justice statement.
Investigators from the Drug Enforcement Administration presented evidence at the trial that Dr. Kesari, a general practitioner, operated a cash-only business selling buprenorphine prescriptions.
Federal prosecutors said that the physician signed prescriptions, which were then distributed by an employee in exchange for cash. Dr. Kesari was often absent, at times physically located in California, according to the federal government.
Prosecutors indicted the West Virginia physician in September 2019 as part of an “opioid strikeforce takedown” in Ohio, Virginia, and West Virginia that resulted in charges against 13 individuals, including 11 physicians.
Dr. Kesari’s attorneys filed motions during the course of the lengthy case showing that psychiatric and neurological exams indicated that the physician was cognitively impaired.
Based on that evidence and the federal indictment, the West Virginia Board of Medicine suspended Dr. Kesari’s license in February 2020, stating that he is not “mentally and/or physically fit to practice medicine and surgery with reasonable skill and safety.”
Dr. Kesari was first licensed in West Virginia in 1979. In 1987, the Board of Medicine placed Dr. Kesari on a 3-year probation because of his failure to keep records for patients for whom he was prescribing controlled substances.
However, within a few months, the Board changed the probation order to allow Dr. Kesari to write prescriptions for schedule II and III substances in the Boone Hospital emergency room where he continued to work.
The physician had no other disciplinary actions until his license suspension, but the Board lists settlement of four malpractice cases and the dismissal of a fifth between 1986 and 2001.
A version of this article first appeared on Medscape.com.
Patients with RA on rituximab at risk for worse COVID-19 outcomes
Patients with rheumatoid arthritis who were using rituximab at the time of COVID-19 onset had a fourfold higher risk of being hospitalized, needing mechanical ventilation, or dying, compared with patients taking a tumor necrosis factor inhibitor (TNFi), according to a report given at the annual European Congress of Rheumatology.
The use of Janus kinase inhibitors (JAKi) also was associated with a twofold higher risk for these COVID-19 outcomes, said Jeffrey A. Sparks, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, in presenting the analysis from the COVID-19 Global Rheumatology Alliance (GRA) Physician Registry.
“The strong association of rituximab and JAK inhibitor use with poor COVID-19 outcomes highlights the prioritization of risk mitigation strategies for these patients,” Dr. Sparks said at the meeting.
The full findings have now been published in Annals of the Rheumatic Diseases.
JAKi association questioned
These findings provide “an important understanding for the risk of our patients in times before vaccination,” said Hendrik Schulze-Koops, MD, of Ludwig Maximilian University of Munich, who chaired the session in which the study was presented.
However, “recently, baricitinib was licensed to prevent particular aspects of severe COVID. What’s the explanation for this discrepancy?” he asked.
“Certainly, the JAK inhibitor finding deserves further study,” Dr. Sparks acknowledged, adding that the data were analyzed by class rather than for individual drugs.
“One possible explanation could be when JAK inhibitors are used,” he suggested. “It might be different for patients who [have been] just infected – that might have different biologic effects – as opposed to choosing to treat patients right when there’s a hyperinflammatory cascade, or there’s oxygen need.”
Regarding the JAK inhibitor finding, Ronald van Vollenhoven, MD, PhD, of the University of Amsterdam, pointed out during the online Q&A that “JAKi have a very short half-life compared to biologics.”
Dr. van Vollenhoven asked: “Could the practice of stopping these drugs upon COVID infection have a negative impact on the course?” To which Dr. Sparks responded: “The different half-life of drugs would be a promising avenue to look at, to see whether increases in disease activity might have imparted some of the effects we saw.”
Performing the analysis
As of April 12, 2021, the GRA Physician Registry contained the records of more than 15,000 patients. Dr. Sparks, collaborator Zachary Wallace, MD, of Massachusetts General Hospital, Boston, and associates limited their analysis to 2,869 patients with RA who had been treated with either a biologic or targeted synthetic disease-modifying antirheumatic drug (b/tsDMARD) at the time they were diagnosed with COVID-19.
“We wanted to limit it to a single disease and also limit it to drugs that are considered for that disease,” Dr. Sparks explained in an interview.
“Because patients with rheumatoid arthritis are often treated sequentially, we wanted to further limit the analysis to patients who were on advanced therapies so that they were at a similar disease state, and also had the opportunity to receive advanced therapies.”
This approach hopefully minimizes the possibility of confounding by indication, Dr. Sparks said.
Most of the patients included in the analysis had received a TNFi (n = 1,388), and they were used as the control arm of the analysis. Outcomes associated with treatment with the other b/tsDMARDs, which included abatacept (n = 237), rituximab (n = 364), interleukin-6 inhibitors (IL-6i; n = 317), and JAKi (n = 563), were then compared with TNFi.
Baseline characteristics of patients were broadly similar across the groups. The mean age was 56.7 years and 80.8% of the study population was female. There were a few expected differences among users of rituximab versus TNFi, notably a higher percentage of patients with interstitial lung disease (11% vs. 1.4% of TNFi users) or cancer (7.4% vs. 0.9%) among patients treated with rituximab since it is commonly used in these patients, Dr. Sparks said.
“We did perform a sensitivity analysis where we restricted the population to not having ILD or cancer and we actually found really similar findings,” he added.
Four COVID-19 outcomes assessed
The researchers used a four-point ordinal scale modeled after one set by the World Health Organization to assess four COVID-19 outcomes: not hospitalized, hospitalized without oxygenation, hospitalized with oxygenation or ventilation, and death.
Odds ratios (ORs) comparing rituximab to TNFi for these four COVID-19 outcomes were a respective 4.53, 2.87, 4.05, and 4.57. The ORs for JAKi versus TNFi were a respective 2.4, 1.55, 2.03, and 2.04.
“We found no consistent associations of abatacept or interleukin-6 inhibitors with COVID-19 severity, compared to TNF inhibitors,” which is reassuring, Dr. Sparks said.
ORs for the four COVID-19 outcomes with abatacept were a respective 1.18, 1.12, 1.41, and 1.46, and for IL-6i were 0.84, 0.72, 0.75, and 1.13.
Rituximab use in patients with RA who develop COVID-19
So, should rituximab be stopped in patients with RA if they develop COVID-19? “This is an important question and one that would be decided on a case-by-case basis,” Dr. Sparks said. “Of course, the drug has a very long half-life, so risk mitigation strategies are still of utmost importance,” he added.
“I think everyone’s a bit reticent to want to start rituximab in this environment, but it might also make me pause about starting a JAK inhibitor,” Dr. Sparks added. “Given that this is a first finding, I’m not sure I would necessarily change patients who are doing well on these medications. I think what it really makes me want to do is to try to obviously vaccinate the patients on JAK inhibitors as they do have a short half-life.”
More observational studies would be helpful, Dr. Sparks said, adding that “the most pressing need is to try to figure out how to protect our patients with rituximab.”
The COVID-19 Global Rheumatology Alliance Physician Registry is supported by the American College of Rheumatology and the European Alliance of Associations for Rheumatology. Dr. Sparks disclosed serving as a consultant for Bristol Myers Squibb, Gilead, Inova, Optum, and Pfizer for work unrelated to this study. Dr. Wallace disclosed receiving grant support from Bristol Myers Squibb and Principia/Sanofi and serving as a consultant for Viela Bio and Medpace for work unrelated to this study.
Patients with rheumatoid arthritis who were using rituximab at the time of COVID-19 onset had a fourfold higher risk of being hospitalized, needing mechanical ventilation, or dying, compared with patients taking a tumor necrosis factor inhibitor (TNFi), according to a report given at the annual European Congress of Rheumatology.
The use of Janus kinase inhibitors (JAKi) also was associated with a twofold higher risk for these COVID-19 outcomes, said Jeffrey A. Sparks, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, in presenting the analysis from the COVID-19 Global Rheumatology Alliance (GRA) Physician Registry.
“The strong association of rituximab and JAK inhibitor use with poor COVID-19 outcomes highlights the prioritization of risk mitigation strategies for these patients,” Dr. Sparks said at the meeting.
The full findings have now been published in Annals of the Rheumatic Diseases.
JAKi association questioned
These findings provide “an important understanding for the risk of our patients in times before vaccination,” said Hendrik Schulze-Koops, MD, of Ludwig Maximilian University of Munich, who chaired the session in which the study was presented.
However, “recently, baricitinib was licensed to prevent particular aspects of severe COVID. What’s the explanation for this discrepancy?” he asked.
“Certainly, the JAK inhibitor finding deserves further study,” Dr. Sparks acknowledged, adding that the data were analyzed by class rather than for individual drugs.
“One possible explanation could be when JAK inhibitors are used,” he suggested. “It might be different for patients who [have been] just infected – that might have different biologic effects – as opposed to choosing to treat patients right when there’s a hyperinflammatory cascade, or there’s oxygen need.”
Regarding the JAK inhibitor finding, Ronald van Vollenhoven, MD, PhD, of the University of Amsterdam, pointed out during the online Q&A that “JAKi have a very short half-life compared to biologics.”
Dr. van Vollenhoven asked: “Could the practice of stopping these drugs upon COVID infection have a negative impact on the course?” To which Dr. Sparks responded: “The different half-life of drugs would be a promising avenue to look at, to see whether increases in disease activity might have imparted some of the effects we saw.”
Performing the analysis
As of April 12, 2021, the GRA Physician Registry contained the records of more than 15,000 patients. Dr. Sparks, collaborator Zachary Wallace, MD, of Massachusetts General Hospital, Boston, and associates limited their analysis to 2,869 patients with RA who had been treated with either a biologic or targeted synthetic disease-modifying antirheumatic drug (b/tsDMARD) at the time they were diagnosed with COVID-19.
“We wanted to limit it to a single disease and also limit it to drugs that are considered for that disease,” Dr. Sparks explained in an interview.
“Because patients with rheumatoid arthritis are often treated sequentially, we wanted to further limit the analysis to patients who were on advanced therapies so that they were at a similar disease state, and also had the opportunity to receive advanced therapies.”
This approach hopefully minimizes the possibility of confounding by indication, Dr. Sparks said.
Most of the patients included in the analysis had received a TNFi (n = 1,388), and they were used as the control arm of the analysis. Outcomes associated with treatment with the other b/tsDMARDs, which included abatacept (n = 237), rituximab (n = 364), interleukin-6 inhibitors (IL-6i; n = 317), and JAKi (n = 563), were then compared with TNFi.
Baseline characteristics of patients were broadly similar across the groups. The mean age was 56.7 years and 80.8% of the study population was female. There were a few expected differences among users of rituximab versus TNFi, notably a higher percentage of patients with interstitial lung disease (11% vs. 1.4% of TNFi users) or cancer (7.4% vs. 0.9%) among patients treated with rituximab since it is commonly used in these patients, Dr. Sparks said.
“We did perform a sensitivity analysis where we restricted the population to not having ILD or cancer and we actually found really similar findings,” he added.
Four COVID-19 outcomes assessed
The researchers used a four-point ordinal scale modeled after one set by the World Health Organization to assess four COVID-19 outcomes: not hospitalized, hospitalized without oxygenation, hospitalized with oxygenation or ventilation, and death.
Odds ratios (ORs) comparing rituximab to TNFi for these four COVID-19 outcomes were a respective 4.53, 2.87, 4.05, and 4.57. The ORs for JAKi versus TNFi were a respective 2.4, 1.55, 2.03, and 2.04.
“We found no consistent associations of abatacept or interleukin-6 inhibitors with COVID-19 severity, compared to TNF inhibitors,” which is reassuring, Dr. Sparks said.
ORs for the four COVID-19 outcomes with abatacept were a respective 1.18, 1.12, 1.41, and 1.46, and for IL-6i were 0.84, 0.72, 0.75, and 1.13.
Rituximab use in patients with RA who develop COVID-19
So, should rituximab be stopped in patients with RA if they develop COVID-19? “This is an important question and one that would be decided on a case-by-case basis,” Dr. Sparks said. “Of course, the drug has a very long half-life, so risk mitigation strategies are still of utmost importance,” he added.
“I think everyone’s a bit reticent to want to start rituximab in this environment, but it might also make me pause about starting a JAK inhibitor,” Dr. Sparks added. “Given that this is a first finding, I’m not sure I would necessarily change patients who are doing well on these medications. I think what it really makes me want to do is to try to obviously vaccinate the patients on JAK inhibitors as they do have a short half-life.”
More observational studies would be helpful, Dr. Sparks said, adding that “the most pressing need is to try to figure out how to protect our patients with rituximab.”
The COVID-19 Global Rheumatology Alliance Physician Registry is supported by the American College of Rheumatology and the European Alliance of Associations for Rheumatology. Dr. Sparks disclosed serving as a consultant for Bristol Myers Squibb, Gilead, Inova, Optum, and Pfizer for work unrelated to this study. Dr. Wallace disclosed receiving grant support from Bristol Myers Squibb and Principia/Sanofi and serving as a consultant for Viela Bio and Medpace for work unrelated to this study.
Patients with rheumatoid arthritis who were using rituximab at the time of COVID-19 onset had a fourfold higher risk of being hospitalized, needing mechanical ventilation, or dying, compared with patients taking a tumor necrosis factor inhibitor (TNFi), according to a report given at the annual European Congress of Rheumatology.
The use of Janus kinase inhibitors (JAKi) also was associated with a twofold higher risk for these COVID-19 outcomes, said Jeffrey A. Sparks, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, in presenting the analysis from the COVID-19 Global Rheumatology Alliance (GRA) Physician Registry.
“The strong association of rituximab and JAK inhibitor use with poor COVID-19 outcomes highlights the prioritization of risk mitigation strategies for these patients,” Dr. Sparks said at the meeting.
The full findings have now been published in Annals of the Rheumatic Diseases.
JAKi association questioned
These findings provide “an important understanding for the risk of our patients in times before vaccination,” said Hendrik Schulze-Koops, MD, of Ludwig Maximilian University of Munich, who chaired the session in which the study was presented.
However, “recently, baricitinib was licensed to prevent particular aspects of severe COVID. What’s the explanation for this discrepancy?” he asked.
“Certainly, the JAK inhibitor finding deserves further study,” Dr. Sparks acknowledged, adding that the data were analyzed by class rather than for individual drugs.
“One possible explanation could be when JAK inhibitors are used,” he suggested. “It might be different for patients who [have been] just infected – that might have different biologic effects – as opposed to choosing to treat patients right when there’s a hyperinflammatory cascade, or there’s oxygen need.”
Regarding the JAK inhibitor finding, Ronald van Vollenhoven, MD, PhD, of the University of Amsterdam, pointed out during the online Q&A that “JAKi have a very short half-life compared to biologics.”
Dr. van Vollenhoven asked: “Could the practice of stopping these drugs upon COVID infection have a negative impact on the course?” To which Dr. Sparks responded: “The different half-life of drugs would be a promising avenue to look at, to see whether increases in disease activity might have imparted some of the effects we saw.”
Performing the analysis
As of April 12, 2021, the GRA Physician Registry contained the records of more than 15,000 patients. Dr. Sparks, collaborator Zachary Wallace, MD, of Massachusetts General Hospital, Boston, and associates limited their analysis to 2,869 patients with RA who had been treated with either a biologic or targeted synthetic disease-modifying antirheumatic drug (b/tsDMARD) at the time they were diagnosed with COVID-19.
“We wanted to limit it to a single disease and also limit it to drugs that are considered for that disease,” Dr. Sparks explained in an interview.
“Because patients with rheumatoid arthritis are often treated sequentially, we wanted to further limit the analysis to patients who were on advanced therapies so that they were at a similar disease state, and also had the opportunity to receive advanced therapies.”
This approach hopefully minimizes the possibility of confounding by indication, Dr. Sparks said.
Most of the patients included in the analysis had received a TNFi (n = 1,388), and they were used as the control arm of the analysis. Outcomes associated with treatment with the other b/tsDMARDs, which included abatacept (n = 237), rituximab (n = 364), interleukin-6 inhibitors (IL-6i; n = 317), and JAKi (n = 563), were then compared with TNFi.
Baseline characteristics of patients were broadly similar across the groups. The mean age was 56.7 years and 80.8% of the study population was female. There were a few expected differences among users of rituximab versus TNFi, notably a higher percentage of patients with interstitial lung disease (11% vs. 1.4% of TNFi users) or cancer (7.4% vs. 0.9%) among patients treated with rituximab since it is commonly used in these patients, Dr. Sparks said.
“We did perform a sensitivity analysis where we restricted the population to not having ILD or cancer and we actually found really similar findings,” he added.
Four COVID-19 outcomes assessed
The researchers used a four-point ordinal scale modeled after one set by the World Health Organization to assess four COVID-19 outcomes: not hospitalized, hospitalized without oxygenation, hospitalized with oxygenation or ventilation, and death.
Odds ratios (ORs) comparing rituximab to TNFi for these four COVID-19 outcomes were a respective 4.53, 2.87, 4.05, and 4.57. The ORs for JAKi versus TNFi were a respective 2.4, 1.55, 2.03, and 2.04.
“We found no consistent associations of abatacept or interleukin-6 inhibitors with COVID-19 severity, compared to TNF inhibitors,” which is reassuring, Dr. Sparks said.
ORs for the four COVID-19 outcomes with abatacept were a respective 1.18, 1.12, 1.41, and 1.46, and for IL-6i were 0.84, 0.72, 0.75, and 1.13.
Rituximab use in patients with RA who develop COVID-19
So, should rituximab be stopped in patients with RA if they develop COVID-19? “This is an important question and one that would be decided on a case-by-case basis,” Dr. Sparks said. “Of course, the drug has a very long half-life, so risk mitigation strategies are still of utmost importance,” he added.
“I think everyone’s a bit reticent to want to start rituximab in this environment, but it might also make me pause about starting a JAK inhibitor,” Dr. Sparks added. “Given that this is a first finding, I’m not sure I would necessarily change patients who are doing well on these medications. I think what it really makes me want to do is to try to obviously vaccinate the patients on JAK inhibitors as they do have a short half-life.”
More observational studies would be helpful, Dr. Sparks said, adding that “the most pressing need is to try to figure out how to protect our patients with rituximab.”
The COVID-19 Global Rheumatology Alliance Physician Registry is supported by the American College of Rheumatology and the European Alliance of Associations for Rheumatology. Dr. Sparks disclosed serving as a consultant for Bristol Myers Squibb, Gilead, Inova, Optum, and Pfizer for work unrelated to this study. Dr. Wallace disclosed receiving grant support from Bristol Myers Squibb and Principia/Sanofi and serving as a consultant for Viela Bio and Medpace for work unrelated to this study.
FROM THE EULAR 2021 CONGRESS
Texas hospital workers sue over vaccine mandates
objecting to its policy of requiring employees and contractors to be vaccinated against COVID-19 or risk losing their jobs.
Plaintiffs include Jennifer Bridges, RN, a medical-surgical nurse at the hospital who has become the public face and voice of health care workers who object to mandatory vaccination, as well as Bob Nevens, the hospital’s director of corporate risk.
Mr. Nevens said the hospital was requiring him to be vaccinated even though he doesn’t treat patients and has been working from home for most of the past year.
“My civil rights and liberties have been trampled on,” he said in comments posted on an online petition. “My right to protect myself from unknown side effects of these vaccines has been placed below the optics of ‘leading medicine,’ “ he said.
Mr. Nevens says in his comments that he was fired on April 15, although the lawsuit says he is currently employed by the hospital’s corporate office.
The Texas attorney who filed the lawsuit, Jared Woodfill, is known to champion conservative causes. In March 2020, he challenged Harris County’s stay-at-home order, charging that it violated religious liberty. He was chairman of the Harris County Republican Party for more than a decade. His website says he is a frequent guest on the local Fox News affiliate.
The lawsuit hinges on a section of the federal law that authorizes emergency use of medical products – US Code 360bbb-3.
That law says that individuals to whom the product is administered should be informed “of the option to accept or refuse administration of the product, of the consequence, if any, of refusing administration of the product, and of the alternatives to the product that are available and of their benefits and risks.”
Legal experts are split as to what the provision means for vaccination mandates. Courts have not yet weighed in with their interpretations of the law.
The petition also repeats a popular antivaccination argument that likens requiring a vaccine approved for emergency use to the kind of medical experimentation performed by Nazi doctors on Jewish prisoners in concentration camps. It says forcing people to choose between an experimental vaccine and a job is a violation of the Nuremberg Code, which says that people must voluntarily and knowingly consent to participating in research.
The vaccines have already been tested in clinical trials. People who are getting them now are not part of those studies, though vaccine manufacturers, regulators, and safety experts are still watching closely for any sign of problems tied to the new shots.
It is true, however, that the emergency use authorization granted by the U.S. Food and Drug Administraiton sped up the process of getting the vaccines onto market. Vaccine manufacturers are currently completing the process of submitting documentation required for a full biologics license application, the mechanism the FDA uses for full approval.
Houston Methodist sent an email to employees in April notifying them that they had until June 7 to start the vaccination process or apply for a medical or religious exemption. Those who decide not to will be terminated.
Marc Boom, MD, the health care system’s president and CEO, has explained that the policy is in place to protect patients and that it was the first hospital in the United States to require it. Since then, other hospitals, including the University of Pennsylvania Health System, have required COVID vaccines.
A version of this article first appeared on Medscape.com.
objecting to its policy of requiring employees and contractors to be vaccinated against COVID-19 or risk losing their jobs.
Plaintiffs include Jennifer Bridges, RN, a medical-surgical nurse at the hospital who has become the public face and voice of health care workers who object to mandatory vaccination, as well as Bob Nevens, the hospital’s director of corporate risk.
Mr. Nevens said the hospital was requiring him to be vaccinated even though he doesn’t treat patients and has been working from home for most of the past year.
“My civil rights and liberties have been trampled on,” he said in comments posted on an online petition. “My right to protect myself from unknown side effects of these vaccines has been placed below the optics of ‘leading medicine,’ “ he said.
Mr. Nevens says in his comments that he was fired on April 15, although the lawsuit says he is currently employed by the hospital’s corporate office.
The Texas attorney who filed the lawsuit, Jared Woodfill, is known to champion conservative causes. In March 2020, he challenged Harris County’s stay-at-home order, charging that it violated religious liberty. He was chairman of the Harris County Republican Party for more than a decade. His website says he is a frequent guest on the local Fox News affiliate.
The lawsuit hinges on a section of the federal law that authorizes emergency use of medical products – US Code 360bbb-3.
That law says that individuals to whom the product is administered should be informed “of the option to accept or refuse administration of the product, of the consequence, if any, of refusing administration of the product, and of the alternatives to the product that are available and of their benefits and risks.”
Legal experts are split as to what the provision means for vaccination mandates. Courts have not yet weighed in with their interpretations of the law.
The petition also repeats a popular antivaccination argument that likens requiring a vaccine approved for emergency use to the kind of medical experimentation performed by Nazi doctors on Jewish prisoners in concentration camps. It says forcing people to choose between an experimental vaccine and a job is a violation of the Nuremberg Code, which says that people must voluntarily and knowingly consent to participating in research.
The vaccines have already been tested in clinical trials. People who are getting them now are not part of those studies, though vaccine manufacturers, regulators, and safety experts are still watching closely for any sign of problems tied to the new shots.
It is true, however, that the emergency use authorization granted by the U.S. Food and Drug Administraiton sped up the process of getting the vaccines onto market. Vaccine manufacturers are currently completing the process of submitting documentation required for a full biologics license application, the mechanism the FDA uses for full approval.
Houston Methodist sent an email to employees in April notifying them that they had until June 7 to start the vaccination process or apply for a medical or religious exemption. Those who decide not to will be terminated.
Marc Boom, MD, the health care system’s president and CEO, has explained that the policy is in place to protect patients and that it was the first hospital in the United States to require it. Since then, other hospitals, including the University of Pennsylvania Health System, have required COVID vaccines.
A version of this article first appeared on Medscape.com.
objecting to its policy of requiring employees and contractors to be vaccinated against COVID-19 or risk losing their jobs.
Plaintiffs include Jennifer Bridges, RN, a medical-surgical nurse at the hospital who has become the public face and voice of health care workers who object to mandatory vaccination, as well as Bob Nevens, the hospital’s director of corporate risk.
Mr. Nevens said the hospital was requiring him to be vaccinated even though he doesn’t treat patients and has been working from home for most of the past year.
“My civil rights and liberties have been trampled on,” he said in comments posted on an online petition. “My right to protect myself from unknown side effects of these vaccines has been placed below the optics of ‘leading medicine,’ “ he said.
Mr. Nevens says in his comments that he was fired on April 15, although the lawsuit says he is currently employed by the hospital’s corporate office.
The Texas attorney who filed the lawsuit, Jared Woodfill, is known to champion conservative causes. In March 2020, he challenged Harris County’s stay-at-home order, charging that it violated religious liberty. He was chairman of the Harris County Republican Party for more than a decade. His website says he is a frequent guest on the local Fox News affiliate.
The lawsuit hinges on a section of the federal law that authorizes emergency use of medical products – US Code 360bbb-3.
That law says that individuals to whom the product is administered should be informed “of the option to accept or refuse administration of the product, of the consequence, if any, of refusing administration of the product, and of the alternatives to the product that are available and of their benefits and risks.”
Legal experts are split as to what the provision means for vaccination mandates. Courts have not yet weighed in with their interpretations of the law.
The petition also repeats a popular antivaccination argument that likens requiring a vaccine approved for emergency use to the kind of medical experimentation performed by Nazi doctors on Jewish prisoners in concentration camps. It says forcing people to choose between an experimental vaccine and a job is a violation of the Nuremberg Code, which says that people must voluntarily and knowingly consent to participating in research.
The vaccines have already been tested in clinical trials. People who are getting them now are not part of those studies, though vaccine manufacturers, regulators, and safety experts are still watching closely for any sign of problems tied to the new shots.
It is true, however, that the emergency use authorization granted by the U.S. Food and Drug Administraiton sped up the process of getting the vaccines onto market. Vaccine manufacturers are currently completing the process of submitting documentation required for a full biologics license application, the mechanism the FDA uses for full approval.
Houston Methodist sent an email to employees in April notifying them that they had until June 7 to start the vaccination process or apply for a medical or religious exemption. Those who decide not to will be terminated.
Marc Boom, MD, the health care system’s president and CEO, has explained that the policy is in place to protect patients and that it was the first hospital in the United States to require it. Since then, other hospitals, including the University of Pennsylvania Health System, have required COVID vaccines.
A version of this article first appeared on Medscape.com.
Concerts may be safe to attend with proper safety precautions: Study
Researchers in Spain have shared heartening results from the first randomized controlled trial to assess risk for COVID-19 transmission at an indoor live music concert.
The study, published May 27 in The Lancet Infectious Diseases, led by virologist Boris Revollo, MD, from the Germans Trias i Pujol University Hospital in Barcelona, included comprehensive safety measures.
It was conducted on Dec. 12, 2020, at a time when local travel restrictions were in place, indoor meetings were limited to six people, and vaccines were not yet available.
All 465 event attendees got same-day SARS-CoV-2 screening with antigen-detecting rapid diagnostic tests before they entered, wore masks throughout, and followed crowd-control measures in the well-ventilated venue, which can hold up to 900 people.
The control group consisted of 495 participants randomly assigned to go home instead of attending the concert after the screening.
None of the attendees tested positive for SARS-CoV-2 infection by polymerase chain reaction (PCR) test 8 days after the 5-hour event, but two in the control group did.
In fact, the study showed that the risk for infection was no higher among those at the concert than it was for those who lived in the same community and did not attend.
The Bayesian estimate for the incidence between the test and control groups was –0.15% (95% confidence Interval, –0.72 to 0.44).
“Our findings pave the way to reactivate cultural activities halted during COVID-19, which could have important sociocultural and economic implications,” the authors wrote.
All wore masks throughout
Among the comprehensive safety measures were that, in addition to testing, all attendees had their temperature checked before gaining access and were given an N95 face mask, which had to be worn at all times inside.
Hand sanitizer was provided in multiple locations, access doors remained open to allow fresh air to circulate, and the coat room was closed to prevent clustering.
There was no mandated distancing, people could sing and dance, and alcohol was available in a bar located in a separate room – and drinks were allowed only in that space.
Rosanna W Peeling, PhD, professor and chair of diagnostic research at the London School of Hygiene and Tropical Medicine in the United Kingdom, and David L. Heymann, MD, of the department of infectious disease epidemiology there, said in an accompanying commentary that there is a great need for studies like this one to help build evidence for a return to normal gatherings.
“So many countries don’t have any policy or any way of doing this because they don’t have the evidence,” Dr. Peeling said in an interview.
The study was well done and a strength was the testing 8 days later, which can be hard to do for similar events when people disperse to locations outside the community where the event or gathering was held, she said.
Study prompts additional questions
Dr. Peeling and Dr. Heymann wrote that the work raises questions such as whether triple-layered masks would have been sufficient. Or how does rapid antigen testing at the entrance compare with molecular screening within 72 hours of entering?
They noted that there are questions around whether existing rapid diagnostic tests are able to detect COVID-19 variants.
Dr. Peeling said that these kinds of results need to be shared and shared more quickly, “if we’re ever going to get out of this pandemic.”
Studies like this are also difficult, she noted, because they may involve non–health sector entities such as city governments and concert organizers working together with researchers.
In addition, the safety measures come at considerable expense and it’s unclear whether those could be employed routinely at such events.
“It’s not really sustainable at sports events with 20,000 people,” Dr. Peeling said.
Infectious disease expert William Schaffner, MD, of Vanderbilt University, Nashville, Tenn., told this news organization that the study results “come a little late to the party.”
If this study had been done in today’s era with authorized vaccines, “it would have been a moot issue,” he said. “The mask is a barrier to transmission, but we now have a much more solid barrier we could put in place, which is vaccination.
“That said, it does reinforce the fact that classical mask wearing does really offer protection even in a crowded venue,” Dr. Schaffner said.
He added that the study was relatively small and he’d like to see it replicated in larger concerts or group gatherings.
Dr. Peeling and Dr. Heymann report no relevant financial relationships. A coauthor is an employee and stockholder of Primavera Sound, sponsor of the study. All other authors declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers in Spain have shared heartening results from the first randomized controlled trial to assess risk for COVID-19 transmission at an indoor live music concert.
The study, published May 27 in The Lancet Infectious Diseases, led by virologist Boris Revollo, MD, from the Germans Trias i Pujol University Hospital in Barcelona, included comprehensive safety measures.
It was conducted on Dec. 12, 2020, at a time when local travel restrictions were in place, indoor meetings were limited to six people, and vaccines were not yet available.
All 465 event attendees got same-day SARS-CoV-2 screening with antigen-detecting rapid diagnostic tests before they entered, wore masks throughout, and followed crowd-control measures in the well-ventilated venue, which can hold up to 900 people.
The control group consisted of 495 participants randomly assigned to go home instead of attending the concert after the screening.
None of the attendees tested positive for SARS-CoV-2 infection by polymerase chain reaction (PCR) test 8 days after the 5-hour event, but two in the control group did.
In fact, the study showed that the risk for infection was no higher among those at the concert than it was for those who lived in the same community and did not attend.
The Bayesian estimate for the incidence between the test and control groups was –0.15% (95% confidence Interval, –0.72 to 0.44).
“Our findings pave the way to reactivate cultural activities halted during COVID-19, which could have important sociocultural and economic implications,” the authors wrote.
All wore masks throughout
Among the comprehensive safety measures were that, in addition to testing, all attendees had their temperature checked before gaining access and were given an N95 face mask, which had to be worn at all times inside.
Hand sanitizer was provided in multiple locations, access doors remained open to allow fresh air to circulate, and the coat room was closed to prevent clustering.
There was no mandated distancing, people could sing and dance, and alcohol was available in a bar located in a separate room – and drinks were allowed only in that space.
Rosanna W Peeling, PhD, professor and chair of diagnostic research at the London School of Hygiene and Tropical Medicine in the United Kingdom, and David L. Heymann, MD, of the department of infectious disease epidemiology there, said in an accompanying commentary that there is a great need for studies like this one to help build evidence for a return to normal gatherings.
“So many countries don’t have any policy or any way of doing this because they don’t have the evidence,” Dr. Peeling said in an interview.
The study was well done and a strength was the testing 8 days later, which can be hard to do for similar events when people disperse to locations outside the community where the event or gathering was held, she said.
Study prompts additional questions
Dr. Peeling and Dr. Heymann wrote that the work raises questions such as whether triple-layered masks would have been sufficient. Or how does rapid antigen testing at the entrance compare with molecular screening within 72 hours of entering?
They noted that there are questions around whether existing rapid diagnostic tests are able to detect COVID-19 variants.
Dr. Peeling said that these kinds of results need to be shared and shared more quickly, “if we’re ever going to get out of this pandemic.”
Studies like this are also difficult, she noted, because they may involve non–health sector entities such as city governments and concert organizers working together with researchers.
In addition, the safety measures come at considerable expense and it’s unclear whether those could be employed routinely at such events.
“It’s not really sustainable at sports events with 20,000 people,” Dr. Peeling said.
Infectious disease expert William Schaffner, MD, of Vanderbilt University, Nashville, Tenn., told this news organization that the study results “come a little late to the party.”
If this study had been done in today’s era with authorized vaccines, “it would have been a moot issue,” he said. “The mask is a barrier to transmission, but we now have a much more solid barrier we could put in place, which is vaccination.
“That said, it does reinforce the fact that classical mask wearing does really offer protection even in a crowded venue,” Dr. Schaffner said.
He added that the study was relatively small and he’d like to see it replicated in larger concerts or group gatherings.
Dr. Peeling and Dr. Heymann report no relevant financial relationships. A coauthor is an employee and stockholder of Primavera Sound, sponsor of the study. All other authors declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers in Spain have shared heartening results from the first randomized controlled trial to assess risk for COVID-19 transmission at an indoor live music concert.
The study, published May 27 in The Lancet Infectious Diseases, led by virologist Boris Revollo, MD, from the Germans Trias i Pujol University Hospital in Barcelona, included comprehensive safety measures.
It was conducted on Dec. 12, 2020, at a time when local travel restrictions were in place, indoor meetings were limited to six people, and vaccines were not yet available.
All 465 event attendees got same-day SARS-CoV-2 screening with antigen-detecting rapid diagnostic tests before they entered, wore masks throughout, and followed crowd-control measures in the well-ventilated venue, which can hold up to 900 people.
The control group consisted of 495 participants randomly assigned to go home instead of attending the concert after the screening.
None of the attendees tested positive for SARS-CoV-2 infection by polymerase chain reaction (PCR) test 8 days after the 5-hour event, but two in the control group did.
In fact, the study showed that the risk for infection was no higher among those at the concert than it was for those who lived in the same community and did not attend.
The Bayesian estimate for the incidence between the test and control groups was –0.15% (95% confidence Interval, –0.72 to 0.44).
“Our findings pave the way to reactivate cultural activities halted during COVID-19, which could have important sociocultural and economic implications,” the authors wrote.
All wore masks throughout
Among the comprehensive safety measures were that, in addition to testing, all attendees had their temperature checked before gaining access and were given an N95 face mask, which had to be worn at all times inside.
Hand sanitizer was provided in multiple locations, access doors remained open to allow fresh air to circulate, and the coat room was closed to prevent clustering.
There was no mandated distancing, people could sing and dance, and alcohol was available in a bar located in a separate room – and drinks were allowed only in that space.
Rosanna W Peeling, PhD, professor and chair of diagnostic research at the London School of Hygiene and Tropical Medicine in the United Kingdom, and David L. Heymann, MD, of the department of infectious disease epidemiology there, said in an accompanying commentary that there is a great need for studies like this one to help build evidence for a return to normal gatherings.
“So many countries don’t have any policy or any way of doing this because they don’t have the evidence,” Dr. Peeling said in an interview.
The study was well done and a strength was the testing 8 days later, which can be hard to do for similar events when people disperse to locations outside the community where the event or gathering was held, she said.
Study prompts additional questions
Dr. Peeling and Dr. Heymann wrote that the work raises questions such as whether triple-layered masks would have been sufficient. Or how does rapid antigen testing at the entrance compare with molecular screening within 72 hours of entering?
They noted that there are questions around whether existing rapid diagnostic tests are able to detect COVID-19 variants.
Dr. Peeling said that these kinds of results need to be shared and shared more quickly, “if we’re ever going to get out of this pandemic.”
Studies like this are also difficult, she noted, because they may involve non–health sector entities such as city governments and concert organizers working together with researchers.
In addition, the safety measures come at considerable expense and it’s unclear whether those could be employed routinely at such events.
“It’s not really sustainable at sports events with 20,000 people,” Dr. Peeling said.
Infectious disease expert William Schaffner, MD, of Vanderbilt University, Nashville, Tenn., told this news organization that the study results “come a little late to the party.”
If this study had been done in today’s era with authorized vaccines, “it would have been a moot issue,” he said. “The mask is a barrier to transmission, but we now have a much more solid barrier we could put in place, which is vaccination.
“That said, it does reinforce the fact that classical mask wearing does really offer protection even in a crowded venue,” Dr. Schaffner said.
He added that the study was relatively small and he’d like to see it replicated in larger concerts or group gatherings.
Dr. Peeling and Dr. Heymann report no relevant financial relationships. A coauthor is an employee and stockholder of Primavera Sound, sponsor of the study. All other authors declare no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Medical licensing questions continue to violate ADA
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
FROM JAMA
NCAA athletes: ECG abnormalities persist after COVID-19
College athletes who have recently recovered from COVID-19 infection show cardiac abnormalities on electrocardiography.
In a small study of ECGs on National Collegiate Athletic Association Division II athletes, those who had been infected with COVID-19 had a prolonged PR interval, compared with matched athletes who had not been infected.
The study was presented at the 2021 Virtual American College of Sports Medicine Annual Meeting & World Congresses.
“The NCAA was requiring athletes to have an ECG for return to play after noting there could be some myocardial abnormalities following COVID-19 infection,” lead author Frank Wyatt, EdD, a sports physiologist and professor at Midwestern State University in Wichita Falls, Tex., told this news organization.
“Our head athletic trainer asked me if I could do ECGs on our COVID-19–recovered athletes, and I decided to do a matched pair–design study to see how our infected and noninfected athletes compared,” Dr. Wyatt said.
Research in the general population has suggested that COVID-19 can cause damage not only to the lungs, but also to the myocardium, he said. “Recent literature suggests COVID-19 is actually infusing itself into the cells of the myocardium and killing those cells, much the way it did in the lung, and possibly kidney and liver, so it’s going after those organs as well, not just the lungs.”
Dr. Wyatt presented results of ECGs that were done in seven COVID-infected athletes and in seven controls, who were free of infection.
The athletes’ recovery from COVID-19 infection was documented after two negative tests.
All subjects were matched by sport, gender, ethnicity, and anthropometry. Investigators obtained ECG recordings 2-4 weeks after the infected athletes had their recovery documented.
Study participants engaged in football, basketball, soccer, and volleyball, and Dr. Wyatt and associates were blinded as to their infected or control status.
Participants self-reported their ethnicity. Most were White or African American.
The main abnormality found was a prolonged PR interval. In the athletes who were recovered from COVID-19, the mean PR interval was 183.6 milliseconds (± 32.4 ms), compared with 141.7 ms (± 22.7 ms) among the controls.
Baseline ECGs for all young athletes?
Dr. Wyatt said he would like to see ECGs done at baseline as part of the physical exam NCAA athletes have to undergo at the start of each season. But that would be expensive.
“It has been suggested that they all need to have ECGs for baseline information, but they don’t do it because of money. If we had that baseline data on these athletes it would really give us a better picture of whether there was damage or not,” he said. “At our small university, if I wasn’t available to do these ECGs, our athletic department would then have to go to the cardiologist to do them, and that is tremendously expensive. It has also been suggested that high school athletes get ECGs as a preliminary test when they start their season, and I think that is warranted as well as for the NCAA athletes, but because of the expense, they’re not doing it.”
Dr. Wyatt has continued to do ECGs on athletes who have survived COVID-19 and to date has ECG data on 70 athletes. He plans further comparisons between the infected and noninfected athletes.
“We want to see if we can solidify the results we presented at ACSM. We had small numbers, so our follow up is to see if we can statistically show in a more robust manner whether or not there was widespread abnormality in the athletes who got infected. They were only 2-4 weeks post infected, and I don’t know what the long-term effects are going to be,” he said.
May be an important finding
“This may be an important finding, but needs many more athletes, as there were only seven in each group,” commented Curt J. Daniels, MD, director of the sports cardiology program and professor at Ohio State University Wexner Medical Center, Columbus.
“Plus, it will need some imaging correlate and recovery ECGs to see if this effect of PR interval prolongation correlates with myocardial changes and whether it persists or resolves,” added Dr. Daniels, who was not part of the study. “But I do find this interesting. ... I agree we are looking for any ECG sign that might help tell us who needs a cardiac MRI. The Big Ten COVID-19 Cardiac Registry has 1,597 ECGs on post COVID athletes we are analyzing, but preliminarily did not see any changes.”
Dr. Wyatt and Dr. Daniels reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
College athletes who have recently recovered from COVID-19 infection show cardiac abnormalities on electrocardiography.
In a small study of ECGs on National Collegiate Athletic Association Division II athletes, those who had been infected with COVID-19 had a prolonged PR interval, compared with matched athletes who had not been infected.
The study was presented at the 2021 Virtual American College of Sports Medicine Annual Meeting & World Congresses.
“The NCAA was requiring athletes to have an ECG for return to play after noting there could be some myocardial abnormalities following COVID-19 infection,” lead author Frank Wyatt, EdD, a sports physiologist and professor at Midwestern State University in Wichita Falls, Tex., told this news organization.
“Our head athletic trainer asked me if I could do ECGs on our COVID-19–recovered athletes, and I decided to do a matched pair–design study to see how our infected and noninfected athletes compared,” Dr. Wyatt said.
Research in the general population has suggested that COVID-19 can cause damage not only to the lungs, but also to the myocardium, he said. “Recent literature suggests COVID-19 is actually infusing itself into the cells of the myocardium and killing those cells, much the way it did in the lung, and possibly kidney and liver, so it’s going after those organs as well, not just the lungs.”
Dr. Wyatt presented results of ECGs that were done in seven COVID-infected athletes and in seven controls, who were free of infection.
The athletes’ recovery from COVID-19 infection was documented after two negative tests.
All subjects were matched by sport, gender, ethnicity, and anthropometry. Investigators obtained ECG recordings 2-4 weeks after the infected athletes had their recovery documented.
Study participants engaged in football, basketball, soccer, and volleyball, and Dr. Wyatt and associates were blinded as to their infected or control status.
Participants self-reported their ethnicity. Most were White or African American.
The main abnormality found was a prolonged PR interval. In the athletes who were recovered from COVID-19, the mean PR interval was 183.6 milliseconds (± 32.4 ms), compared with 141.7 ms (± 22.7 ms) among the controls.
Baseline ECGs for all young athletes?
Dr. Wyatt said he would like to see ECGs done at baseline as part of the physical exam NCAA athletes have to undergo at the start of each season. But that would be expensive.
“It has been suggested that they all need to have ECGs for baseline information, but they don’t do it because of money. If we had that baseline data on these athletes it would really give us a better picture of whether there was damage or not,” he said. “At our small university, if I wasn’t available to do these ECGs, our athletic department would then have to go to the cardiologist to do them, and that is tremendously expensive. It has also been suggested that high school athletes get ECGs as a preliminary test when they start their season, and I think that is warranted as well as for the NCAA athletes, but because of the expense, they’re not doing it.”
Dr. Wyatt has continued to do ECGs on athletes who have survived COVID-19 and to date has ECG data on 70 athletes. He plans further comparisons between the infected and noninfected athletes.
“We want to see if we can solidify the results we presented at ACSM. We had small numbers, so our follow up is to see if we can statistically show in a more robust manner whether or not there was widespread abnormality in the athletes who got infected. They were only 2-4 weeks post infected, and I don’t know what the long-term effects are going to be,” he said.
May be an important finding
“This may be an important finding, but needs many more athletes, as there were only seven in each group,” commented Curt J. Daniels, MD, director of the sports cardiology program and professor at Ohio State University Wexner Medical Center, Columbus.
“Plus, it will need some imaging correlate and recovery ECGs to see if this effect of PR interval prolongation correlates with myocardial changes and whether it persists or resolves,” added Dr. Daniels, who was not part of the study. “But I do find this interesting. ... I agree we are looking for any ECG sign that might help tell us who needs a cardiac MRI. The Big Ten COVID-19 Cardiac Registry has 1,597 ECGs on post COVID athletes we are analyzing, but preliminarily did not see any changes.”
Dr. Wyatt and Dr. Daniels reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
College athletes who have recently recovered from COVID-19 infection show cardiac abnormalities on electrocardiography.
In a small study of ECGs on National Collegiate Athletic Association Division II athletes, those who had been infected with COVID-19 had a prolonged PR interval, compared with matched athletes who had not been infected.
The study was presented at the 2021 Virtual American College of Sports Medicine Annual Meeting & World Congresses.
“The NCAA was requiring athletes to have an ECG for return to play after noting there could be some myocardial abnormalities following COVID-19 infection,” lead author Frank Wyatt, EdD, a sports physiologist and professor at Midwestern State University in Wichita Falls, Tex., told this news organization.
“Our head athletic trainer asked me if I could do ECGs on our COVID-19–recovered athletes, and I decided to do a matched pair–design study to see how our infected and noninfected athletes compared,” Dr. Wyatt said.
Research in the general population has suggested that COVID-19 can cause damage not only to the lungs, but also to the myocardium, he said. “Recent literature suggests COVID-19 is actually infusing itself into the cells of the myocardium and killing those cells, much the way it did in the lung, and possibly kidney and liver, so it’s going after those organs as well, not just the lungs.”
Dr. Wyatt presented results of ECGs that were done in seven COVID-infected athletes and in seven controls, who were free of infection.
The athletes’ recovery from COVID-19 infection was documented after two negative tests.
All subjects were matched by sport, gender, ethnicity, and anthropometry. Investigators obtained ECG recordings 2-4 weeks after the infected athletes had their recovery documented.
Study participants engaged in football, basketball, soccer, and volleyball, and Dr. Wyatt and associates were blinded as to their infected or control status.
Participants self-reported their ethnicity. Most were White or African American.
The main abnormality found was a prolonged PR interval. In the athletes who were recovered from COVID-19, the mean PR interval was 183.6 milliseconds (± 32.4 ms), compared with 141.7 ms (± 22.7 ms) among the controls.
Baseline ECGs for all young athletes?
Dr. Wyatt said he would like to see ECGs done at baseline as part of the physical exam NCAA athletes have to undergo at the start of each season. But that would be expensive.
“It has been suggested that they all need to have ECGs for baseline information, but they don’t do it because of money. If we had that baseline data on these athletes it would really give us a better picture of whether there was damage or not,” he said. “At our small university, if I wasn’t available to do these ECGs, our athletic department would then have to go to the cardiologist to do them, and that is tremendously expensive. It has also been suggested that high school athletes get ECGs as a preliminary test when they start their season, and I think that is warranted as well as for the NCAA athletes, but because of the expense, they’re not doing it.”
Dr. Wyatt has continued to do ECGs on athletes who have survived COVID-19 and to date has ECG data on 70 athletes. He plans further comparisons between the infected and noninfected athletes.
“We want to see if we can solidify the results we presented at ACSM. We had small numbers, so our follow up is to see if we can statistically show in a more robust manner whether or not there was widespread abnormality in the athletes who got infected. They were only 2-4 weeks post infected, and I don’t know what the long-term effects are going to be,” he said.
May be an important finding
“This may be an important finding, but needs many more athletes, as there were only seven in each group,” commented Curt J. Daniels, MD, director of the sports cardiology program and professor at Ohio State University Wexner Medical Center, Columbus.
“Plus, it will need some imaging correlate and recovery ECGs to see if this effect of PR interval prolongation correlates with myocardial changes and whether it persists or resolves,” added Dr. Daniels, who was not part of the study. “But I do find this interesting. ... I agree we are looking for any ECG sign that might help tell us who needs a cardiac MRI. The Big Ten COVID-19 Cardiac Registry has 1,597 ECGs on post COVID athletes we are analyzing, but preliminarily did not see any changes.”
Dr. Wyatt and Dr. Daniels reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.






