User login
When to suspect a severe skin reaction to an AED
NEW ORLEANS – Most skin eruptions in patients taking antiepileptic drugs (AEDs) are relatively benign. With close supervision, some patients with epilepsy may continue treatment despite having a benign drug rash, according to a lecture at the annual meeting of the American Epilepsy Society.
“When do you know that you’re not dealing with that kind of eruption?” said Jeanne M. Young, MD, assistant professor of dermatology at the University of Virginia in Charlottesville.
Signs and symptoms that raise concerns about severe cutaneous reactions include swelling of the face; lesions that are fluid-filled, dusky, or painful; mucus membrane involvement; and signs of systemic involvement.
Associations with anticonvulsants
Diffuse swelling of the face is a hallmark symptom of DRESS. Fluid-filled lesions such as pustules, vesicles, and bullae indicate a condition other than a benign drug eruption. Signs of systemic involvement may include fever, marked eosinophilia, transaminitis, and evidence of lymphocyte activation. “In general, I want to see systemic involvement that can’t be explained by the patient’s other systemic diseases,” Dr. Young said.
A 2018 study found that AEDs are associated with SJS and TEN, and the labels for lamotrigine and carbamazepine include black box warnings about the risk of severe cutaneous adverse events. Carbamazepine’s warning, which was added in 2007, notes that SJS and TEN are significantly more common in patients of Asian ancestry with the human leukocyte antigen allele HLA-B*1502 and that physicians should screen at-risk patients before starting treatment.
Benign drug rashes
Morbilliform drug eruptions, sometimes called benign exanthems, are “by far the most common drug rash that we see” and typically are “the rashes that people refer to as drug rashes,” Dr. Young said. The mechanisms appear to be primarily immune complex mediated and cell mediated. “When the drug is stopped, these rashes tend to go away quite predictably in 2-3 weeks.”
For any class of drug, about 1% of people taking that medication may have this type of reaction, Dr. Young said. “We expect to see erythematous papules and plaques that oftentimes become confluent on the skin.” These reactions generally occur 7-10 days after the first exposure to the medication, and most patients do not have other symptoms, although the rash may itch. In addition, patients may have erythroderma with desquamation. “I think it’s important to point out the difference between desquamation, which is loss of the stratum corneum, and epidermal sloughing, which is what you see in something like [SJS] or TEN, where you’re actually losing the entire epidermis,” Dr. Young said. Recovering from desquamation is “sort of like recovering from a sun burn, and it’s not particularly dangerous.” Management of morbilliform drug eruptions is largely symptomatic.
Treat through, taper, or rechallenge
In the case a benign drug rash, “if you feel like you … need to keep a patient on a drug, you do have that option with close supervision,” Dr. Young said. “Communicate that with the dermatologist. Say, ‘I have really struggled getting this patient stabilized. Can we keep them on this drug?’ ”
The dermatologist may not fully realize the implications of stopping an effective AED in a patient with seizures that have been difficult to control. If the drug rash is benign, treating through may be an option. Patients often resolve the rash while continuing the medication, which may be because of desensitization, Dr. Young said. If a patient’s symptoms are too great to continue the drug, neurologists have the option of slowly tapering the drug and reinitiating with a new drug, Dr. Young said. Neurologists also may choose to rechallenge.
If a patient is on several medications, making it difficult to elucidate a causative agent, after stopping those drugs and allowing the rash to resolve, “there is little danger in restarting a medication,” she said.
Benign rash or DRESS?
“When I see a morbilliform eruption, usually what’s on my mind is, ‘Is this just a drug rash or is this DRESS?’ ” Dr. Young said. DRESS often starts with a morbilliform eruption that is indistinguishable from a benign drug eruption.
“Timing is a major difference,” she said. “If a patient develops a morbilliform drug eruption much later than I would expect, then my suspicion [for DRESS] goes up.” Patients with DRESS often have fever and systemic symptoms. Proposed DRESS diagnostic criteria can be useful, but clinical judgment still plays a key role. If a patient does not satisfy diagnostic criteria but has some signs and is taking a drug that is associated with DRESS, “it is going to make me more suspicious and maybe make me recommend stopping that drug sooner,” she said. Anticonvulsants such as carbamazepine, lamotrigine, and phenobarbital are among the drugs most commonly associated with DRESS.
Toxic erythemas
Patients may present with toxic erythemas, such as fixed drug reactions, erythema multiforme, SJS, and TEN. These drug reactions appear similar on biopsy but have different courses.
A patient with a fixed drug reaction often has a single lesion, and the lesion will occur in the same location every time the patient is exposed to the drug. Patients may develop additional lesions with subsequent exposures. These lesions typically are large, erythematous, well-demarcated plaques with central duskiness. “They can be bullous in the center, and they typically will heal with pigmentation, which is unique to this particular drug reaction,” said Dr. Young. “When it gets more concerning and most important to differentiate is when you get generalized bullous fixed drug eruption.” Generalized bullous fixed drug eruptions mimic and are difficult to clinically distinguish from TEN, which has a much has a much poorer prognosis.
Patients with a fixed drug eruption are not as ill as patients with TEN and tend not to slough their skin to the extent seen with TEN. Interferon gamma, perforin, and Fas ligand have been implicated as mechanisms involved in fixed drug reactions. Unlike in TEN, regulatory T cells are abundant, which may explain why TEN and fixed drug reactions progress differently even though they appear to share pathologic mechanisms, Dr. Young said.
Erythema multiforme generally presents with classic target lesions and little mucosal involvement. Infections, most commonly herpes simplex virus (HSV) 1 and 2, may trigger erythema multiforme. Dr. Young recommends evaluating patients for HSV and checking serologies, even if patients have never had a herpes outbreak. “If you have no evidence for infection, you do have to consider discontinuing a medication,” she said.
Stevens–Johnson syndrome and TEN
SJS and TEN are “the rarest of the severe cutaneous adverse drug reactions” and have “the highest morbidity and mortality,” Dr. Young said. They appear to exist on a continuum where SJS may represent early TEN.
“This is a situation where you expect to see blistering of the skin [and] always mucosal involvement. You need to stop the drug immediately when you suspect this drug reaction,” Dr. Young said.
One reason to distinguish SJS or early TEN from later TEN is that high-dose steroids may play a role in the treatment of SJS or early TEN. “Once you get past about 10% total body surface area, there is good evidence that steroids actually increase morbidity and mortality,” she said.
If the eruption has occurred before, that factor suggests that a diagnosis of erythema multiforme or fixed drug reaction may be more likely than TEN.
An apparent lack of regulatory T cells in TEN could explain why patients with HIV infection are at much higher risk of developing SJS and TEN. Understanding the role that regulatory T cells play in severe drug eruptions may lead to new therapeutic options in the future, Dr. Young said.
Dr. Young had no disclosures.
NEW ORLEANS – Most skin eruptions in patients taking antiepileptic drugs (AEDs) are relatively benign. With close supervision, some patients with epilepsy may continue treatment despite having a benign drug rash, according to a lecture at the annual meeting of the American Epilepsy Society.
“When do you know that you’re not dealing with that kind of eruption?” said Jeanne M. Young, MD, assistant professor of dermatology at the University of Virginia in Charlottesville.
Signs and symptoms that raise concerns about severe cutaneous reactions include swelling of the face; lesions that are fluid-filled, dusky, or painful; mucus membrane involvement; and signs of systemic involvement.
Associations with anticonvulsants
Diffuse swelling of the face is a hallmark symptom of DRESS. Fluid-filled lesions such as pustules, vesicles, and bullae indicate a condition other than a benign drug eruption. Signs of systemic involvement may include fever, marked eosinophilia, transaminitis, and evidence of lymphocyte activation. “In general, I want to see systemic involvement that can’t be explained by the patient’s other systemic diseases,” Dr. Young said.
A 2018 study found that AEDs are associated with SJS and TEN, and the labels for lamotrigine and carbamazepine include black box warnings about the risk of severe cutaneous adverse events. Carbamazepine’s warning, which was added in 2007, notes that SJS and TEN are significantly more common in patients of Asian ancestry with the human leukocyte antigen allele HLA-B*1502 and that physicians should screen at-risk patients before starting treatment.
Benign drug rashes
Morbilliform drug eruptions, sometimes called benign exanthems, are “by far the most common drug rash that we see” and typically are “the rashes that people refer to as drug rashes,” Dr. Young said. The mechanisms appear to be primarily immune complex mediated and cell mediated. “When the drug is stopped, these rashes tend to go away quite predictably in 2-3 weeks.”
For any class of drug, about 1% of people taking that medication may have this type of reaction, Dr. Young said. “We expect to see erythematous papules and plaques that oftentimes become confluent on the skin.” These reactions generally occur 7-10 days after the first exposure to the medication, and most patients do not have other symptoms, although the rash may itch. In addition, patients may have erythroderma with desquamation. “I think it’s important to point out the difference between desquamation, which is loss of the stratum corneum, and epidermal sloughing, which is what you see in something like [SJS] or TEN, where you’re actually losing the entire epidermis,” Dr. Young said. Recovering from desquamation is “sort of like recovering from a sun burn, and it’s not particularly dangerous.” Management of morbilliform drug eruptions is largely symptomatic.
Treat through, taper, or rechallenge
In the case a benign drug rash, “if you feel like you … need to keep a patient on a drug, you do have that option with close supervision,” Dr. Young said. “Communicate that with the dermatologist. Say, ‘I have really struggled getting this patient stabilized. Can we keep them on this drug?’ ”
The dermatologist may not fully realize the implications of stopping an effective AED in a patient with seizures that have been difficult to control. If the drug rash is benign, treating through may be an option. Patients often resolve the rash while continuing the medication, which may be because of desensitization, Dr. Young said. If a patient’s symptoms are too great to continue the drug, neurologists have the option of slowly tapering the drug and reinitiating with a new drug, Dr. Young said. Neurologists also may choose to rechallenge.
If a patient is on several medications, making it difficult to elucidate a causative agent, after stopping those drugs and allowing the rash to resolve, “there is little danger in restarting a medication,” she said.
Benign rash or DRESS?
“When I see a morbilliform eruption, usually what’s on my mind is, ‘Is this just a drug rash or is this DRESS?’ ” Dr. Young said. DRESS often starts with a morbilliform eruption that is indistinguishable from a benign drug eruption.
“Timing is a major difference,” she said. “If a patient develops a morbilliform drug eruption much later than I would expect, then my suspicion [for DRESS] goes up.” Patients with DRESS often have fever and systemic symptoms. Proposed DRESS diagnostic criteria can be useful, but clinical judgment still plays a key role. If a patient does not satisfy diagnostic criteria but has some signs and is taking a drug that is associated with DRESS, “it is going to make me more suspicious and maybe make me recommend stopping that drug sooner,” she said. Anticonvulsants such as carbamazepine, lamotrigine, and phenobarbital are among the drugs most commonly associated with DRESS.
Toxic erythemas
Patients may present with toxic erythemas, such as fixed drug reactions, erythema multiforme, SJS, and TEN. These drug reactions appear similar on biopsy but have different courses.
A patient with a fixed drug reaction often has a single lesion, and the lesion will occur in the same location every time the patient is exposed to the drug. Patients may develop additional lesions with subsequent exposures. These lesions typically are large, erythematous, well-demarcated plaques with central duskiness. “They can be bullous in the center, and they typically will heal with pigmentation, which is unique to this particular drug reaction,” said Dr. Young. “When it gets more concerning and most important to differentiate is when you get generalized bullous fixed drug eruption.” Generalized bullous fixed drug eruptions mimic and are difficult to clinically distinguish from TEN, which has a much has a much poorer prognosis.
Patients with a fixed drug eruption are not as ill as patients with TEN and tend not to slough their skin to the extent seen with TEN. Interferon gamma, perforin, and Fas ligand have been implicated as mechanisms involved in fixed drug reactions. Unlike in TEN, regulatory T cells are abundant, which may explain why TEN and fixed drug reactions progress differently even though they appear to share pathologic mechanisms, Dr. Young said.
Erythema multiforme generally presents with classic target lesions and little mucosal involvement. Infections, most commonly herpes simplex virus (HSV) 1 and 2, may trigger erythema multiforme. Dr. Young recommends evaluating patients for HSV and checking serologies, even if patients have never had a herpes outbreak. “If you have no evidence for infection, you do have to consider discontinuing a medication,” she said.
Stevens–Johnson syndrome and TEN
SJS and TEN are “the rarest of the severe cutaneous adverse drug reactions” and have “the highest morbidity and mortality,” Dr. Young said. They appear to exist on a continuum where SJS may represent early TEN.
“This is a situation where you expect to see blistering of the skin [and] always mucosal involvement. You need to stop the drug immediately when you suspect this drug reaction,” Dr. Young said.
One reason to distinguish SJS or early TEN from later TEN is that high-dose steroids may play a role in the treatment of SJS or early TEN. “Once you get past about 10% total body surface area, there is good evidence that steroids actually increase morbidity and mortality,” she said.
If the eruption has occurred before, that factor suggests that a diagnosis of erythema multiforme or fixed drug reaction may be more likely than TEN.
An apparent lack of regulatory T cells in TEN could explain why patients with HIV infection are at much higher risk of developing SJS and TEN. Understanding the role that regulatory T cells play in severe drug eruptions may lead to new therapeutic options in the future, Dr. Young said.
Dr. Young had no disclosures.
NEW ORLEANS – Most skin eruptions in patients taking antiepileptic drugs (AEDs) are relatively benign. With close supervision, some patients with epilepsy may continue treatment despite having a benign drug rash, according to a lecture at the annual meeting of the American Epilepsy Society.
“When do you know that you’re not dealing with that kind of eruption?” said Jeanne M. Young, MD, assistant professor of dermatology at the University of Virginia in Charlottesville.
Signs and symptoms that raise concerns about severe cutaneous reactions include swelling of the face; lesions that are fluid-filled, dusky, or painful; mucus membrane involvement; and signs of systemic involvement.
Associations with anticonvulsants
Diffuse swelling of the face is a hallmark symptom of DRESS. Fluid-filled lesions such as pustules, vesicles, and bullae indicate a condition other than a benign drug eruption. Signs of systemic involvement may include fever, marked eosinophilia, transaminitis, and evidence of lymphocyte activation. “In general, I want to see systemic involvement that can’t be explained by the patient’s other systemic diseases,” Dr. Young said.
A 2018 study found that AEDs are associated with SJS and TEN, and the labels for lamotrigine and carbamazepine include black box warnings about the risk of severe cutaneous adverse events. Carbamazepine’s warning, which was added in 2007, notes that SJS and TEN are significantly more common in patients of Asian ancestry with the human leukocyte antigen allele HLA-B*1502 and that physicians should screen at-risk patients before starting treatment.
Benign drug rashes
Morbilliform drug eruptions, sometimes called benign exanthems, are “by far the most common drug rash that we see” and typically are “the rashes that people refer to as drug rashes,” Dr. Young said. The mechanisms appear to be primarily immune complex mediated and cell mediated. “When the drug is stopped, these rashes tend to go away quite predictably in 2-3 weeks.”
For any class of drug, about 1% of people taking that medication may have this type of reaction, Dr. Young said. “We expect to see erythematous papules and plaques that oftentimes become confluent on the skin.” These reactions generally occur 7-10 days after the first exposure to the medication, and most patients do not have other symptoms, although the rash may itch. In addition, patients may have erythroderma with desquamation. “I think it’s important to point out the difference between desquamation, which is loss of the stratum corneum, and epidermal sloughing, which is what you see in something like [SJS] or TEN, where you’re actually losing the entire epidermis,” Dr. Young said. Recovering from desquamation is “sort of like recovering from a sun burn, and it’s not particularly dangerous.” Management of morbilliform drug eruptions is largely symptomatic.
Treat through, taper, or rechallenge
In the case a benign drug rash, “if you feel like you … need to keep a patient on a drug, you do have that option with close supervision,” Dr. Young said. “Communicate that with the dermatologist. Say, ‘I have really struggled getting this patient stabilized. Can we keep them on this drug?’ ”
The dermatologist may not fully realize the implications of stopping an effective AED in a patient with seizures that have been difficult to control. If the drug rash is benign, treating through may be an option. Patients often resolve the rash while continuing the medication, which may be because of desensitization, Dr. Young said. If a patient’s symptoms are too great to continue the drug, neurologists have the option of slowly tapering the drug and reinitiating with a new drug, Dr. Young said. Neurologists also may choose to rechallenge.
If a patient is on several medications, making it difficult to elucidate a causative agent, after stopping those drugs and allowing the rash to resolve, “there is little danger in restarting a medication,” she said.
Benign rash or DRESS?
“When I see a morbilliform eruption, usually what’s on my mind is, ‘Is this just a drug rash or is this DRESS?’ ” Dr. Young said. DRESS often starts with a morbilliform eruption that is indistinguishable from a benign drug eruption.
“Timing is a major difference,” she said. “If a patient develops a morbilliform drug eruption much later than I would expect, then my suspicion [for DRESS] goes up.” Patients with DRESS often have fever and systemic symptoms. Proposed DRESS diagnostic criteria can be useful, but clinical judgment still plays a key role. If a patient does not satisfy diagnostic criteria but has some signs and is taking a drug that is associated with DRESS, “it is going to make me more suspicious and maybe make me recommend stopping that drug sooner,” she said. Anticonvulsants such as carbamazepine, lamotrigine, and phenobarbital are among the drugs most commonly associated with DRESS.
Toxic erythemas
Patients may present with toxic erythemas, such as fixed drug reactions, erythema multiforme, SJS, and TEN. These drug reactions appear similar on biopsy but have different courses.
A patient with a fixed drug reaction often has a single lesion, and the lesion will occur in the same location every time the patient is exposed to the drug. Patients may develop additional lesions with subsequent exposures. These lesions typically are large, erythematous, well-demarcated plaques with central duskiness. “They can be bullous in the center, and they typically will heal with pigmentation, which is unique to this particular drug reaction,” said Dr. Young. “When it gets more concerning and most important to differentiate is when you get generalized bullous fixed drug eruption.” Generalized bullous fixed drug eruptions mimic and are difficult to clinically distinguish from TEN, which has a much has a much poorer prognosis.
Patients with a fixed drug eruption are not as ill as patients with TEN and tend not to slough their skin to the extent seen with TEN. Interferon gamma, perforin, and Fas ligand have been implicated as mechanisms involved in fixed drug reactions. Unlike in TEN, regulatory T cells are abundant, which may explain why TEN and fixed drug reactions progress differently even though they appear to share pathologic mechanisms, Dr. Young said.
Erythema multiforme generally presents with classic target lesions and little mucosal involvement. Infections, most commonly herpes simplex virus (HSV) 1 and 2, may trigger erythema multiforme. Dr. Young recommends evaluating patients for HSV and checking serologies, even if patients have never had a herpes outbreak. “If you have no evidence for infection, you do have to consider discontinuing a medication,” she said.
Stevens–Johnson syndrome and TEN
SJS and TEN are “the rarest of the severe cutaneous adverse drug reactions” and have “the highest morbidity and mortality,” Dr. Young said. They appear to exist on a continuum where SJS may represent early TEN.
“This is a situation where you expect to see blistering of the skin [and] always mucosal involvement. You need to stop the drug immediately when you suspect this drug reaction,” Dr. Young said.
One reason to distinguish SJS or early TEN from later TEN is that high-dose steroids may play a role in the treatment of SJS or early TEN. “Once you get past about 10% total body surface area, there is good evidence that steroids actually increase morbidity and mortality,” she said.
If the eruption has occurred before, that factor suggests that a diagnosis of erythema multiforme or fixed drug reaction may be more likely than TEN.
An apparent lack of regulatory T cells in TEN could explain why patients with HIV infection are at much higher risk of developing SJS and TEN. Understanding the role that regulatory T cells play in severe drug eruptions may lead to new therapeutic options in the future, Dr. Young said.
Dr. Young had no disclosures.
EXPERT ANALYSIS FROM AES 2018
How seizure prediction may benefit patients with epilepsy
NEW ORLEANS – For people with epilepsy, “the sudden and apparently unpredictable nature of seizures is one of the most disabling aspects of having the disorder,” said Michael Privitera, MD.
If a patient knew that “tomorrow will be a dangerous day” with a 50% chance of having a seizure, the patient could avoid hazardous activities, try to reduce stress, or increase supervision to reduce the risk of sudden, unexpected death in epilepsy, said Dr. Privitera, professor of neurology and director of the epilepsy center at the University of Cincinnati Gardner Neuroscience Institute. Physicians might be able to intervene during high-risk periods by altering antiepileptic drug regimens.
Evidence suggests that seizure prediction is possible today and that advances in wearable devices and analysis of chronic EEG recordings likely will improve the ability to predict seizures, Dr. Privitera said at the annual meeting of the American Epilepsy Society. Studies have found that some patients can predict the likelihood of seizures in the next 24 hours better than chance. In the future, algorithms that incorporate variables such as pulse, stress, mood, electrodermal activity, circadian rhythms, and EEG may further refine seizure prediction.
A complex picture
One problem with predicting seizures is that “you can have substantial changes in the seizure tendency, but not have a seizure,” Dr. Privitera said. Stress, alcohol, and missed medications, for example, may affect the seizure threshold. “They may be additive, and it may be when those things all hit at once that a seizure happens.”
Many patients report prodromal or premonitory symptoms before a seizure. “Most of us as clinicians will say, ‘Well, maybe you have some inkling, but I don’t think you’re really able to predict it,’ ” Dr. Privitera said.
Sheryl R. Haut, MD, professor of neurology at the Albert Einstein College of Medicine, New York, and her colleagues prospectively looked at patient self-prediction in 2007 (Neurology. 2007 Jan 23;68[4]:262-6). The investigators followed 74 people with epilepsy who completed a daily diary in which they predicted the likelihood of a seizure occurring in the next 24 hours. Their analysis included approximately 15,000 diary days and 1,400 seizure days.
A subset of participants, about 20%, was significantly better than chance at predicting when a seizure would happen. If a patient in this subgroup said that a seizure was extremely likely, then a seizure occurred approximately 37% of the time. If a patient predicted that a seizure was extremely unlikely, there was about a 10% chance of having a seizure.
“This was a pretty substantial difference,” Dr. Privitera said. Combining patients’ predictions with their self-reported stress levels seemed to yield the most accurate predictions.
Stress and the SMILE study
About 90% of people with epilepsy identify at least one seizure precipitant, and the most commonly cited trigger is stress. When Dr. Privitera and his colleagues surveyed patients in their clinic, 82% identified stress as a trigger (Epilepsy Behav. 2014 Dec;41:74-7). More than half of these patients had used some form of stress reduction, such as exercise, yoga, or meditation; 88% of those patients thought that stress reduction helped their seizures.
Underlying anxiety was the only difference between patients who thought that their seizures were triggered by stress and those who did not. Patients who did not think that stress triggered their seizures had significantly lower scores on the Generalized Anxiety Disorders–7.
Subsequently, Dr. Haut, Dr. Privitera, and colleagues conducted the Stress Management Intervention for Living with Epilepsy (SMILE) study, a prospective, controlled trial assessing the efficacy of a stress reduction intervention for reducing seizures, as well as measuring seizure self-prediction (Neurology. 2018 Mar 13;90[11]:e963-70). The researchers randomized patients to a progressive muscle relaxation intervention or to a control group; patients in the control group wrote down their activities for the day.
Patients posted diary entries twice daily into a smartphone, reporting stress levels and mood-related variables. As in Dr. Haut’s earlier study, patients predicted whether having a seizure was extremely unlikely, unlikely, neutral, likely, or extremely likely. Mood and stress variables (such as feeling unpleasant or pleasant, relaxed or stressed, and not worried or extremely worried) were ranked on a visual analog scale from 0 to 100.
The trial included participants who had at least two seizures per month and any seizure trigger. Medications were kept stable throughout the study. During a 2-month baseline, patients tracked their seizures and stress levels. During the 3-month treatment period, patients received the active or control intervention.
In all, 64 subjects completed the study, completing all diary entries on 94% of the days. In the active-treatment group, median seizure frequency decreased by 29%, compared with a 25% decrease in the control group. However, the difference between the groups was not statistically significant. Although the 25% reduction in the control group probably is partly attributable to the placebo effect, part of the decrease may be related to a mindfulness effect from completing the diary, Dr. Privitera said.
The active-treatment group had a statistically significant reduction in self-reported stress, compared with the control group, but this decrease did not correlate with seizure reduction. Changes in anxiety levels also did not correlate with seizures.
“It does not disprove the [stress] hypothesis, but it does tell us that there is more going on with stress and seizure triggers than just patients’ self-reported stress,” Dr. Privitera said.
Patients’ predictions
The seizure prediction findings in SMILE were similar to those of Dr. Haut’s earlier study. Among the 10 highest predictors out of the 64 participants, “when they said that a seizure was extremely likely, they were 8.36 times more likely to have a seizure than when they said a seizure was extremely unlikely,” Dr. Privitera said.
Many patients seemed to increase their predicted seizure probabilities in the days after having a seizure. In addition, feeling sad, nervous, worried, tense, or stressed significantly increased the likelihood that a patient would predict that a seizure was coming. However, these feelings were “not very accurate [for predicting] actual seizures,” he said. “Some people are better predictors, but really the basis of that prediction remains to be seen. One of my hypotheses is that some of these people may actually be responding to subclinical EEG changes.”
Together, these self-prediction studies include data from 4,500 seizures and 26,000 diary entries and show that “there is some information in patient self-report that can help us in understanding how to predict and when to predict seizures,” Dr. Privitera said.
Incorporating cardiac, EEG, and other variables
Various other factors may warrant inclusion in a seizure forecasting system. A new vagus nerve stimulation system responds to heart rate changes that occur at seizure onset. And for decades, researchers have studied the potential for EEG readings to predict seizures. A 2008 analysis of 47 reports concluded that limited progress had been made in predicting a seizure from interictal EEG (Epilepsy Behav. 2008 Jan;12[1]:128-35). Now, however, long-term intracranial recordings are providing new and important information about EEG patterns.
Whereas early studies examined EEG recordings from epilepsy monitoring units – when patients may have been sleep deprived, had medications removed, or recently undergone surgery – chronic intracranial recordings from devices such as the RNS (responsive neurostimulation) System have allowed researchers to look long term at EEG changes that are more representative of patients’ typical EEG patterns.
The RNS System detects interictal spikes and seizure discharges and then provides an electrical stimulation to stop seizures. “When you look at these recordings, there are a lot more electrographic seizures than clinical seizures that trigger these stimulations,” said Dr. Privitera. “If you look at somebody with a typical RNS, they may have 100 stimulations in a day and no clinical seizures. There are lots and lots of subclinical electrographic bursts – and not just spikes, but things that look like short electrographic seizures – that occur throughout the day.”
A handheld device
Researchers in Melbourne designed a system that uses implanted electrodes to provide chronic recordings (Lancet Neurol. 2013 Jun;12[6]:563-71). An algorithm then learned to predict the likelihood of a seizure from the patient’s data as the system recorded over time. The system could indicate when a seizure was likely by displaying a light on a handheld device. Patients were recorded for between 6 months and 3 years.
“There was a statistically significant ability to predict when seizures were happening,” Dr. Privitera said. “There is information in long-term intracranial recordings in many of these people that will help allow us to do a better prediction than what we are able to do right now, which is essentially not much.”
This research suggests that pooling data across patients may not be an effective seizure prediction strategy because different epilepsy types have different patterns. In addition, an individual’s patterns may differ from a group’s patterns. Complicating matters, individual patients may have multiple seizure types with different onset mechanisms.
“Another important lesson is that false positives in a deterministic sense may not represent false positives in a probabilistic sense,” Dr. Privitera said. “That is, when the seizure prediction program – whether it is the diary or the intracranial EEG or anything else – says the threshold changed, but you did not have a seizure, it does not mean that your prediction system was wrong. If the seizure tendency is going up … and your system says the seizure tendency went up, but all you are measuring is actual seizures, it looks like it is a false positive prediction of seizures. But in fact it is a true positive prediction of the seizure tendency changing but not necessarily reaching seizure threshold.”
Multiday patterns
Recent research shows that “we are just at the start,” Dr. Privitera said. “There are patterns underlying seizure frequency that … we are only beginning to be able to look at because of these chronic recordings.”
Baud et al. analyzed interictal epileptiform activity and seizures in patients who have had responsive neurostimulators for as long as 10 years (Nat Commun. 2018 Jan 8;9[1]:88). “What they found was that interictal spikes and rhythmic discharges oscillate with circadian and multiday periods that differ from person to person,” Dr. Privitera said. “There were multiday periodicities, most commonly in the 20- to 30-day duration, that were relatively stable over periods of time that lasted up to years.”
Researchers knew that seizures in women of childbearing age can cluster in association with the menstrual cycle, but similar cycles also were seen in men. In addition, the researchers found that seizures “occur preferentially during the rising phase of these multiday interictal rhythms,” which has implications for seizure forecasts, Dr. Privitera noted.
Stress biomarkers and wearables
Future seizure prediction methods may incorporate other biomarkers, such as stress hormones. A researcher at the University of Cincinnati, Jason Heikenfeld, PhD, is conducting research with a sensor that sticks to the wrist and measures sweat content, Dr. Privitera said. The technology originally was developed to measure sodium and potassium in sweat, but Dr. Privitera’s group has been working with him to measure cortisol, which may be a biomarker for stress and be useful for seizure prediction.
“Multivariate models are needed. We have lots of different ways that we can look at seizure prediction, and most likely the most accurate seizure prediction programs will incorporate multiple different areas,” Dr. Privitera said. “Seizure forecasting is possible. We can do it now. We can probably do it better than chance in many patients. ... It is important because changes in seizure likelihood could lead to pharmacologic or device or behavioral interventions that may help prevent seizures.”
Dr. Privitera reported conducting contracted research for Greenwich and SK Life Science and receiving consulting fees from Upsher-Smith and Astellas.
SOURCE: Privitera M. AES 2018, Judith Hoyer Lecture in Epilepsy.
NEW ORLEANS – For people with epilepsy, “the sudden and apparently unpredictable nature of seizures is one of the most disabling aspects of having the disorder,” said Michael Privitera, MD.
If a patient knew that “tomorrow will be a dangerous day” with a 50% chance of having a seizure, the patient could avoid hazardous activities, try to reduce stress, or increase supervision to reduce the risk of sudden, unexpected death in epilepsy, said Dr. Privitera, professor of neurology and director of the epilepsy center at the University of Cincinnati Gardner Neuroscience Institute. Physicians might be able to intervene during high-risk periods by altering antiepileptic drug regimens.
Evidence suggests that seizure prediction is possible today and that advances in wearable devices and analysis of chronic EEG recordings likely will improve the ability to predict seizures, Dr. Privitera said at the annual meeting of the American Epilepsy Society. Studies have found that some patients can predict the likelihood of seizures in the next 24 hours better than chance. In the future, algorithms that incorporate variables such as pulse, stress, mood, electrodermal activity, circadian rhythms, and EEG may further refine seizure prediction.
A complex picture
One problem with predicting seizures is that “you can have substantial changes in the seizure tendency, but not have a seizure,” Dr. Privitera said. Stress, alcohol, and missed medications, for example, may affect the seizure threshold. “They may be additive, and it may be when those things all hit at once that a seizure happens.”
Many patients report prodromal or premonitory symptoms before a seizure. “Most of us as clinicians will say, ‘Well, maybe you have some inkling, but I don’t think you’re really able to predict it,’ ” Dr. Privitera said.
Sheryl R. Haut, MD, professor of neurology at the Albert Einstein College of Medicine, New York, and her colleagues prospectively looked at patient self-prediction in 2007 (Neurology. 2007 Jan 23;68[4]:262-6). The investigators followed 74 people with epilepsy who completed a daily diary in which they predicted the likelihood of a seizure occurring in the next 24 hours. Their analysis included approximately 15,000 diary days and 1,400 seizure days.
A subset of participants, about 20%, was significantly better than chance at predicting when a seizure would happen. If a patient in this subgroup said that a seizure was extremely likely, then a seizure occurred approximately 37% of the time. If a patient predicted that a seizure was extremely unlikely, there was about a 10% chance of having a seizure.
“This was a pretty substantial difference,” Dr. Privitera said. Combining patients’ predictions with their self-reported stress levels seemed to yield the most accurate predictions.
Stress and the SMILE study
About 90% of people with epilepsy identify at least one seizure precipitant, and the most commonly cited trigger is stress. When Dr. Privitera and his colleagues surveyed patients in their clinic, 82% identified stress as a trigger (Epilepsy Behav. 2014 Dec;41:74-7). More than half of these patients had used some form of stress reduction, such as exercise, yoga, or meditation; 88% of those patients thought that stress reduction helped their seizures.
Underlying anxiety was the only difference between patients who thought that their seizures were triggered by stress and those who did not. Patients who did not think that stress triggered their seizures had significantly lower scores on the Generalized Anxiety Disorders–7.
Subsequently, Dr. Haut, Dr. Privitera, and colleagues conducted the Stress Management Intervention for Living with Epilepsy (SMILE) study, a prospective, controlled trial assessing the efficacy of a stress reduction intervention for reducing seizures, as well as measuring seizure self-prediction (Neurology. 2018 Mar 13;90[11]:e963-70). The researchers randomized patients to a progressive muscle relaxation intervention or to a control group; patients in the control group wrote down their activities for the day.
Patients posted diary entries twice daily into a smartphone, reporting stress levels and mood-related variables. As in Dr. Haut’s earlier study, patients predicted whether having a seizure was extremely unlikely, unlikely, neutral, likely, or extremely likely. Mood and stress variables (such as feeling unpleasant or pleasant, relaxed or stressed, and not worried or extremely worried) were ranked on a visual analog scale from 0 to 100.
The trial included participants who had at least two seizures per month and any seizure trigger. Medications were kept stable throughout the study. During a 2-month baseline, patients tracked their seizures and stress levels. During the 3-month treatment period, patients received the active or control intervention.
In all, 64 subjects completed the study, completing all diary entries on 94% of the days. In the active-treatment group, median seizure frequency decreased by 29%, compared with a 25% decrease in the control group. However, the difference between the groups was not statistically significant. Although the 25% reduction in the control group probably is partly attributable to the placebo effect, part of the decrease may be related to a mindfulness effect from completing the diary, Dr. Privitera said.
The active-treatment group had a statistically significant reduction in self-reported stress, compared with the control group, but this decrease did not correlate with seizure reduction. Changes in anxiety levels also did not correlate with seizures.
“It does not disprove the [stress] hypothesis, but it does tell us that there is more going on with stress and seizure triggers than just patients’ self-reported stress,” Dr. Privitera said.
Patients’ predictions
The seizure prediction findings in SMILE were similar to those of Dr. Haut’s earlier study. Among the 10 highest predictors out of the 64 participants, “when they said that a seizure was extremely likely, they were 8.36 times more likely to have a seizure than when they said a seizure was extremely unlikely,” Dr. Privitera said.
Many patients seemed to increase their predicted seizure probabilities in the days after having a seizure. In addition, feeling sad, nervous, worried, tense, or stressed significantly increased the likelihood that a patient would predict that a seizure was coming. However, these feelings were “not very accurate [for predicting] actual seizures,” he said. “Some people are better predictors, but really the basis of that prediction remains to be seen. One of my hypotheses is that some of these people may actually be responding to subclinical EEG changes.”
Together, these self-prediction studies include data from 4,500 seizures and 26,000 diary entries and show that “there is some information in patient self-report that can help us in understanding how to predict and when to predict seizures,” Dr. Privitera said.
Incorporating cardiac, EEG, and other variables
Various other factors may warrant inclusion in a seizure forecasting system. A new vagus nerve stimulation system responds to heart rate changes that occur at seizure onset. And for decades, researchers have studied the potential for EEG readings to predict seizures. A 2008 analysis of 47 reports concluded that limited progress had been made in predicting a seizure from interictal EEG (Epilepsy Behav. 2008 Jan;12[1]:128-35). Now, however, long-term intracranial recordings are providing new and important information about EEG patterns.
Whereas early studies examined EEG recordings from epilepsy monitoring units – when patients may have been sleep deprived, had medications removed, or recently undergone surgery – chronic intracranial recordings from devices such as the RNS (responsive neurostimulation) System have allowed researchers to look long term at EEG changes that are more representative of patients’ typical EEG patterns.
The RNS System detects interictal spikes and seizure discharges and then provides an electrical stimulation to stop seizures. “When you look at these recordings, there are a lot more electrographic seizures than clinical seizures that trigger these stimulations,” said Dr. Privitera. “If you look at somebody with a typical RNS, they may have 100 stimulations in a day and no clinical seizures. There are lots and lots of subclinical electrographic bursts – and not just spikes, but things that look like short electrographic seizures – that occur throughout the day.”
A handheld device
Researchers in Melbourne designed a system that uses implanted electrodes to provide chronic recordings (Lancet Neurol. 2013 Jun;12[6]:563-71). An algorithm then learned to predict the likelihood of a seizure from the patient’s data as the system recorded over time. The system could indicate when a seizure was likely by displaying a light on a handheld device. Patients were recorded for between 6 months and 3 years.
“There was a statistically significant ability to predict when seizures were happening,” Dr. Privitera said. “There is information in long-term intracranial recordings in many of these people that will help allow us to do a better prediction than what we are able to do right now, which is essentially not much.”
This research suggests that pooling data across patients may not be an effective seizure prediction strategy because different epilepsy types have different patterns. In addition, an individual’s patterns may differ from a group’s patterns. Complicating matters, individual patients may have multiple seizure types with different onset mechanisms.
“Another important lesson is that false positives in a deterministic sense may not represent false positives in a probabilistic sense,” Dr. Privitera said. “That is, when the seizure prediction program – whether it is the diary or the intracranial EEG or anything else – says the threshold changed, but you did not have a seizure, it does not mean that your prediction system was wrong. If the seizure tendency is going up … and your system says the seizure tendency went up, but all you are measuring is actual seizures, it looks like it is a false positive prediction of seizures. But in fact it is a true positive prediction of the seizure tendency changing but not necessarily reaching seizure threshold.”
Multiday patterns
Recent research shows that “we are just at the start,” Dr. Privitera said. “There are patterns underlying seizure frequency that … we are only beginning to be able to look at because of these chronic recordings.”
Baud et al. analyzed interictal epileptiform activity and seizures in patients who have had responsive neurostimulators for as long as 10 years (Nat Commun. 2018 Jan 8;9[1]:88). “What they found was that interictal spikes and rhythmic discharges oscillate with circadian and multiday periods that differ from person to person,” Dr. Privitera said. “There were multiday periodicities, most commonly in the 20- to 30-day duration, that were relatively stable over periods of time that lasted up to years.”
Researchers knew that seizures in women of childbearing age can cluster in association with the menstrual cycle, but similar cycles also were seen in men. In addition, the researchers found that seizures “occur preferentially during the rising phase of these multiday interictal rhythms,” which has implications for seizure forecasts, Dr. Privitera noted.
Stress biomarkers and wearables
Future seizure prediction methods may incorporate other biomarkers, such as stress hormones. A researcher at the University of Cincinnati, Jason Heikenfeld, PhD, is conducting research with a sensor that sticks to the wrist and measures sweat content, Dr. Privitera said. The technology originally was developed to measure sodium and potassium in sweat, but Dr. Privitera’s group has been working with him to measure cortisol, which may be a biomarker for stress and be useful for seizure prediction.
“Multivariate models are needed. We have lots of different ways that we can look at seizure prediction, and most likely the most accurate seizure prediction programs will incorporate multiple different areas,” Dr. Privitera said. “Seizure forecasting is possible. We can do it now. We can probably do it better than chance in many patients. ... It is important because changes in seizure likelihood could lead to pharmacologic or device or behavioral interventions that may help prevent seizures.”
Dr. Privitera reported conducting contracted research for Greenwich and SK Life Science and receiving consulting fees from Upsher-Smith and Astellas.
SOURCE: Privitera M. AES 2018, Judith Hoyer Lecture in Epilepsy.
NEW ORLEANS – For people with epilepsy, “the sudden and apparently unpredictable nature of seizures is one of the most disabling aspects of having the disorder,” said Michael Privitera, MD.
If a patient knew that “tomorrow will be a dangerous day” with a 50% chance of having a seizure, the patient could avoid hazardous activities, try to reduce stress, or increase supervision to reduce the risk of sudden, unexpected death in epilepsy, said Dr. Privitera, professor of neurology and director of the epilepsy center at the University of Cincinnati Gardner Neuroscience Institute. Physicians might be able to intervene during high-risk periods by altering antiepileptic drug regimens.
Evidence suggests that seizure prediction is possible today and that advances in wearable devices and analysis of chronic EEG recordings likely will improve the ability to predict seizures, Dr. Privitera said at the annual meeting of the American Epilepsy Society. Studies have found that some patients can predict the likelihood of seizures in the next 24 hours better than chance. In the future, algorithms that incorporate variables such as pulse, stress, mood, electrodermal activity, circadian rhythms, and EEG may further refine seizure prediction.
A complex picture
One problem with predicting seizures is that “you can have substantial changes in the seizure tendency, but not have a seizure,” Dr. Privitera said. Stress, alcohol, and missed medications, for example, may affect the seizure threshold. “They may be additive, and it may be when those things all hit at once that a seizure happens.”
Many patients report prodromal or premonitory symptoms before a seizure. “Most of us as clinicians will say, ‘Well, maybe you have some inkling, but I don’t think you’re really able to predict it,’ ” Dr. Privitera said.
Sheryl R. Haut, MD, professor of neurology at the Albert Einstein College of Medicine, New York, and her colleagues prospectively looked at patient self-prediction in 2007 (Neurology. 2007 Jan 23;68[4]:262-6). The investigators followed 74 people with epilepsy who completed a daily diary in which they predicted the likelihood of a seizure occurring in the next 24 hours. Their analysis included approximately 15,000 diary days and 1,400 seizure days.
A subset of participants, about 20%, was significantly better than chance at predicting when a seizure would happen. If a patient in this subgroup said that a seizure was extremely likely, then a seizure occurred approximately 37% of the time. If a patient predicted that a seizure was extremely unlikely, there was about a 10% chance of having a seizure.
“This was a pretty substantial difference,” Dr. Privitera said. Combining patients’ predictions with their self-reported stress levels seemed to yield the most accurate predictions.
Stress and the SMILE study
About 90% of people with epilepsy identify at least one seizure precipitant, and the most commonly cited trigger is stress. When Dr. Privitera and his colleagues surveyed patients in their clinic, 82% identified stress as a trigger (Epilepsy Behav. 2014 Dec;41:74-7). More than half of these patients had used some form of stress reduction, such as exercise, yoga, or meditation; 88% of those patients thought that stress reduction helped their seizures.
Underlying anxiety was the only difference between patients who thought that their seizures were triggered by stress and those who did not. Patients who did not think that stress triggered their seizures had significantly lower scores on the Generalized Anxiety Disorders–7.
Subsequently, Dr. Haut, Dr. Privitera, and colleagues conducted the Stress Management Intervention for Living with Epilepsy (SMILE) study, a prospective, controlled trial assessing the efficacy of a stress reduction intervention for reducing seizures, as well as measuring seizure self-prediction (Neurology. 2018 Mar 13;90[11]:e963-70). The researchers randomized patients to a progressive muscle relaxation intervention or to a control group; patients in the control group wrote down their activities for the day.
Patients posted diary entries twice daily into a smartphone, reporting stress levels and mood-related variables. As in Dr. Haut’s earlier study, patients predicted whether having a seizure was extremely unlikely, unlikely, neutral, likely, or extremely likely. Mood and stress variables (such as feeling unpleasant or pleasant, relaxed or stressed, and not worried or extremely worried) were ranked on a visual analog scale from 0 to 100.
The trial included participants who had at least two seizures per month and any seizure trigger. Medications were kept stable throughout the study. During a 2-month baseline, patients tracked their seizures and stress levels. During the 3-month treatment period, patients received the active or control intervention.
In all, 64 subjects completed the study, completing all diary entries on 94% of the days. In the active-treatment group, median seizure frequency decreased by 29%, compared with a 25% decrease in the control group. However, the difference between the groups was not statistically significant. Although the 25% reduction in the control group probably is partly attributable to the placebo effect, part of the decrease may be related to a mindfulness effect from completing the diary, Dr. Privitera said.
The active-treatment group had a statistically significant reduction in self-reported stress, compared with the control group, but this decrease did not correlate with seizure reduction. Changes in anxiety levels also did not correlate with seizures.
“It does not disprove the [stress] hypothesis, but it does tell us that there is more going on with stress and seizure triggers than just patients’ self-reported stress,” Dr. Privitera said.
Patients’ predictions
The seizure prediction findings in SMILE were similar to those of Dr. Haut’s earlier study. Among the 10 highest predictors out of the 64 participants, “when they said that a seizure was extremely likely, they were 8.36 times more likely to have a seizure than when they said a seizure was extremely unlikely,” Dr. Privitera said.
Many patients seemed to increase their predicted seizure probabilities in the days after having a seizure. In addition, feeling sad, nervous, worried, tense, or stressed significantly increased the likelihood that a patient would predict that a seizure was coming. However, these feelings were “not very accurate [for predicting] actual seizures,” he said. “Some people are better predictors, but really the basis of that prediction remains to be seen. One of my hypotheses is that some of these people may actually be responding to subclinical EEG changes.”
Together, these self-prediction studies include data from 4,500 seizures and 26,000 diary entries and show that “there is some information in patient self-report that can help us in understanding how to predict and when to predict seizures,” Dr. Privitera said.
Incorporating cardiac, EEG, and other variables
Various other factors may warrant inclusion in a seizure forecasting system. A new vagus nerve stimulation system responds to heart rate changes that occur at seizure onset. And for decades, researchers have studied the potential for EEG readings to predict seizures. A 2008 analysis of 47 reports concluded that limited progress had been made in predicting a seizure from interictal EEG (Epilepsy Behav. 2008 Jan;12[1]:128-35). Now, however, long-term intracranial recordings are providing new and important information about EEG patterns.
Whereas early studies examined EEG recordings from epilepsy monitoring units – when patients may have been sleep deprived, had medications removed, or recently undergone surgery – chronic intracranial recordings from devices such as the RNS (responsive neurostimulation) System have allowed researchers to look long term at EEG changes that are more representative of patients’ typical EEG patterns.
The RNS System detects interictal spikes and seizure discharges and then provides an electrical stimulation to stop seizures. “When you look at these recordings, there are a lot more electrographic seizures than clinical seizures that trigger these stimulations,” said Dr. Privitera. “If you look at somebody with a typical RNS, they may have 100 stimulations in a day and no clinical seizures. There are lots and lots of subclinical electrographic bursts – and not just spikes, but things that look like short electrographic seizures – that occur throughout the day.”
A handheld device
Researchers in Melbourne designed a system that uses implanted electrodes to provide chronic recordings (Lancet Neurol. 2013 Jun;12[6]:563-71). An algorithm then learned to predict the likelihood of a seizure from the patient’s data as the system recorded over time. The system could indicate when a seizure was likely by displaying a light on a handheld device. Patients were recorded for between 6 months and 3 years.
“There was a statistically significant ability to predict when seizures were happening,” Dr. Privitera said. “There is information in long-term intracranial recordings in many of these people that will help allow us to do a better prediction than what we are able to do right now, which is essentially not much.”
This research suggests that pooling data across patients may not be an effective seizure prediction strategy because different epilepsy types have different patterns. In addition, an individual’s patterns may differ from a group’s patterns. Complicating matters, individual patients may have multiple seizure types with different onset mechanisms.
“Another important lesson is that false positives in a deterministic sense may not represent false positives in a probabilistic sense,” Dr. Privitera said. “That is, when the seizure prediction program – whether it is the diary or the intracranial EEG or anything else – says the threshold changed, but you did not have a seizure, it does not mean that your prediction system was wrong. If the seizure tendency is going up … and your system says the seizure tendency went up, but all you are measuring is actual seizures, it looks like it is a false positive prediction of seizures. But in fact it is a true positive prediction of the seizure tendency changing but not necessarily reaching seizure threshold.”
Multiday patterns
Recent research shows that “we are just at the start,” Dr. Privitera said. “There are patterns underlying seizure frequency that … we are only beginning to be able to look at because of these chronic recordings.”
Baud et al. analyzed interictal epileptiform activity and seizures in patients who have had responsive neurostimulators for as long as 10 years (Nat Commun. 2018 Jan 8;9[1]:88). “What they found was that interictal spikes and rhythmic discharges oscillate with circadian and multiday periods that differ from person to person,” Dr. Privitera said. “There were multiday periodicities, most commonly in the 20- to 30-day duration, that were relatively stable over periods of time that lasted up to years.”
Researchers knew that seizures in women of childbearing age can cluster in association with the menstrual cycle, but similar cycles also were seen in men. In addition, the researchers found that seizures “occur preferentially during the rising phase of these multiday interictal rhythms,” which has implications for seizure forecasts, Dr. Privitera noted.
Stress biomarkers and wearables
Future seizure prediction methods may incorporate other biomarkers, such as stress hormones. A researcher at the University of Cincinnati, Jason Heikenfeld, PhD, is conducting research with a sensor that sticks to the wrist and measures sweat content, Dr. Privitera said. The technology originally was developed to measure sodium and potassium in sweat, but Dr. Privitera’s group has been working with him to measure cortisol, which may be a biomarker for stress and be useful for seizure prediction.
“Multivariate models are needed. We have lots of different ways that we can look at seizure prediction, and most likely the most accurate seizure prediction programs will incorporate multiple different areas,” Dr. Privitera said. “Seizure forecasting is possible. We can do it now. We can probably do it better than chance in many patients. ... It is important because changes in seizure likelihood could lead to pharmacologic or device or behavioral interventions that may help prevent seizures.”
Dr. Privitera reported conducting contracted research for Greenwich and SK Life Science and receiving consulting fees from Upsher-Smith and Astellas.
SOURCE: Privitera M. AES 2018, Judith Hoyer Lecture in Epilepsy.
REPORTING FROM AES 2018
Population-level rate of SUDEP may have decreased
NEW ORLEANS – according to data described at the annual meeting of the American Epilepsy Society. Whether this decrease resulted from an improved understanding of SUDEP risk or a focus on risk-reduction strategies is unknown, said Daniel Friedman, MD, associate professor of neurology at the New York University Langone Health.
In addition, the rates of SUDEP in various populations differ according to their socioeconomic status. Differences in access to care are a potential, but unconfirmed, explanation for this association, said Dr. Friedman. Another possible explanation is that confounders such as mental health disorders, substance abuse, and insufficient social support affect individuals’ ability to manage their disorder.
Dr. Friedman and colleagues initially examined SUDEP rates over time in a cohort of patients who received vagus nerve stimulator (VNS) implantation for drug-resistant epilepsy. They analyzed data for 40,443 patients who underwent surgery during 1988-2012. The age-adjusted SUDEP rate per 1,000 person-years of follow-up decreased significantly from 2.47 in years 1-2 to 1.68 in years 3-10. “There was no control group, so we couldn’t necessarily attribute the SUDEP rate reduction to the intervention,” said Dr. Friedman. A study by Tomson et al of patients with epilepsy who received VNS implantation had similar findings.
The literature about the mechanisms of SUDEP and reduction of SUDEP risk has increased in recent years. Neurologists have advocated for greater disclosure to patients of SUDEP risk, as well as better risk counseling. Dr. Friedman and his colleagues decided to investigate whether these factors have affected the risk of SUDEP during the past decade.
They retrospectively examined data for people whose deaths had been investigated at medical examiner’s offices in New York City, San Diego County, and Maryland. They focused on decedents for whom epilepsy or seizure was listed as a cause or contributor to death or as a comorbid condition on the death certificate. They reviewed all available reports, including investigator notes, autopsy reports, and medical records. Next, Dr. Friedman and his colleagues calculated the annual SUDEP rate as a proportion of the general population, estimated using annual Census and American Community Survey data. They used the Mann-Kendall test to analyze the trends in SUDEP rate during 2009-2015.
Of 1,466 deaths in people with epilepsy during this period, 1,124 were classified as definite SUDEP, probable SUDEP, or near SUDEP. Approximately 63% of SUDEP cases were male, and 45% were African-American. The mean age at death was 38 years.
Dr. Friedman’s group found a significant decrease in the overall incidence of SUDEP in the total population during 2009-2015. When they examined the three regions separately, they found decreases in SUDEP incidence in New York City and Maryland, but not in San Diego County. They found no difference in SUDEP rates by season or by day of the week.
In a subsequent analysis, Dr. Friedman and his colleagues adjudicated all deaths related to seizure and epilepsy in the three regions during 2009-2010 and 2014-2015 and identified all cases of definite and probable SUDEP. The estimated rate of SUDEP decreased by about 36% from the first period to the second period. SUDEP rates as a proportion of the total population in those regions also declined.
The investigators also examined differences in estimated SUDEP rates in the United States according to median household income. In New York, the zip codes with the highest SUDEP rates tended to have the lowest median household incomes. The zip codes in the lowest quartile of family household income had a SUDEP rate more than twice as high as that in the zip codes in the highest income quartile. This association held true for the period from 2009-2010 and for 2014-2015.
Dr. Friedman and colleagues received funding from Finding a Cure for Epilepsy and Seizures, which is affiliated with the NYU Comprehensive Epilepsy Center and NYU Langone Health.
SOURCE: Cihan E et al. AES 2018, Abstract 2.419.
NEW ORLEANS – according to data described at the annual meeting of the American Epilepsy Society. Whether this decrease resulted from an improved understanding of SUDEP risk or a focus on risk-reduction strategies is unknown, said Daniel Friedman, MD, associate professor of neurology at the New York University Langone Health.
In addition, the rates of SUDEP in various populations differ according to their socioeconomic status. Differences in access to care are a potential, but unconfirmed, explanation for this association, said Dr. Friedman. Another possible explanation is that confounders such as mental health disorders, substance abuse, and insufficient social support affect individuals’ ability to manage their disorder.
Dr. Friedman and colleagues initially examined SUDEP rates over time in a cohort of patients who received vagus nerve stimulator (VNS) implantation for drug-resistant epilepsy. They analyzed data for 40,443 patients who underwent surgery during 1988-2012. The age-adjusted SUDEP rate per 1,000 person-years of follow-up decreased significantly from 2.47 in years 1-2 to 1.68 in years 3-10. “There was no control group, so we couldn’t necessarily attribute the SUDEP rate reduction to the intervention,” said Dr. Friedman. A study by Tomson et al of patients with epilepsy who received VNS implantation had similar findings.
The literature about the mechanisms of SUDEP and reduction of SUDEP risk has increased in recent years. Neurologists have advocated for greater disclosure to patients of SUDEP risk, as well as better risk counseling. Dr. Friedman and his colleagues decided to investigate whether these factors have affected the risk of SUDEP during the past decade.
They retrospectively examined data for people whose deaths had been investigated at medical examiner’s offices in New York City, San Diego County, and Maryland. They focused on decedents for whom epilepsy or seizure was listed as a cause or contributor to death or as a comorbid condition on the death certificate. They reviewed all available reports, including investigator notes, autopsy reports, and medical records. Next, Dr. Friedman and his colleagues calculated the annual SUDEP rate as a proportion of the general population, estimated using annual Census and American Community Survey data. They used the Mann-Kendall test to analyze the trends in SUDEP rate during 2009-2015.
Of 1,466 deaths in people with epilepsy during this period, 1,124 were classified as definite SUDEP, probable SUDEP, or near SUDEP. Approximately 63% of SUDEP cases were male, and 45% were African-American. The mean age at death was 38 years.
Dr. Friedman’s group found a significant decrease in the overall incidence of SUDEP in the total population during 2009-2015. When they examined the three regions separately, they found decreases in SUDEP incidence in New York City and Maryland, but not in San Diego County. They found no difference in SUDEP rates by season or by day of the week.
In a subsequent analysis, Dr. Friedman and his colleagues adjudicated all deaths related to seizure and epilepsy in the three regions during 2009-2010 and 2014-2015 and identified all cases of definite and probable SUDEP. The estimated rate of SUDEP decreased by about 36% from the first period to the second period. SUDEP rates as a proportion of the total population in those regions also declined.
The investigators also examined differences in estimated SUDEP rates in the United States according to median household income. In New York, the zip codes with the highest SUDEP rates tended to have the lowest median household incomes. The zip codes in the lowest quartile of family household income had a SUDEP rate more than twice as high as that in the zip codes in the highest income quartile. This association held true for the period from 2009-2010 and for 2014-2015.
Dr. Friedman and colleagues received funding from Finding a Cure for Epilepsy and Seizures, which is affiliated with the NYU Comprehensive Epilepsy Center and NYU Langone Health.
SOURCE: Cihan E et al. AES 2018, Abstract 2.419.
NEW ORLEANS – according to data described at the annual meeting of the American Epilepsy Society. Whether this decrease resulted from an improved understanding of SUDEP risk or a focus on risk-reduction strategies is unknown, said Daniel Friedman, MD, associate professor of neurology at the New York University Langone Health.
In addition, the rates of SUDEP in various populations differ according to their socioeconomic status. Differences in access to care are a potential, but unconfirmed, explanation for this association, said Dr. Friedman. Another possible explanation is that confounders such as mental health disorders, substance abuse, and insufficient social support affect individuals’ ability to manage their disorder.
Dr. Friedman and colleagues initially examined SUDEP rates over time in a cohort of patients who received vagus nerve stimulator (VNS) implantation for drug-resistant epilepsy. They analyzed data for 40,443 patients who underwent surgery during 1988-2012. The age-adjusted SUDEP rate per 1,000 person-years of follow-up decreased significantly from 2.47 in years 1-2 to 1.68 in years 3-10. “There was no control group, so we couldn’t necessarily attribute the SUDEP rate reduction to the intervention,” said Dr. Friedman. A study by Tomson et al of patients with epilepsy who received VNS implantation had similar findings.
The literature about the mechanisms of SUDEP and reduction of SUDEP risk has increased in recent years. Neurologists have advocated for greater disclosure to patients of SUDEP risk, as well as better risk counseling. Dr. Friedman and his colleagues decided to investigate whether these factors have affected the risk of SUDEP during the past decade.
They retrospectively examined data for people whose deaths had been investigated at medical examiner’s offices in New York City, San Diego County, and Maryland. They focused on decedents for whom epilepsy or seizure was listed as a cause or contributor to death or as a comorbid condition on the death certificate. They reviewed all available reports, including investigator notes, autopsy reports, and medical records. Next, Dr. Friedman and his colleagues calculated the annual SUDEP rate as a proportion of the general population, estimated using annual Census and American Community Survey data. They used the Mann-Kendall test to analyze the trends in SUDEP rate during 2009-2015.
Of 1,466 deaths in people with epilepsy during this period, 1,124 were classified as definite SUDEP, probable SUDEP, or near SUDEP. Approximately 63% of SUDEP cases were male, and 45% were African-American. The mean age at death was 38 years.
Dr. Friedman’s group found a significant decrease in the overall incidence of SUDEP in the total population during 2009-2015. When they examined the three regions separately, they found decreases in SUDEP incidence in New York City and Maryland, but not in San Diego County. They found no difference in SUDEP rates by season or by day of the week.
In a subsequent analysis, Dr. Friedman and his colleagues adjudicated all deaths related to seizure and epilepsy in the three regions during 2009-2010 and 2014-2015 and identified all cases of definite and probable SUDEP. The estimated rate of SUDEP decreased by about 36% from the first period to the second period. SUDEP rates as a proportion of the total population in those regions also declined.
The investigators also examined differences in estimated SUDEP rates in the United States according to median household income. In New York, the zip codes with the highest SUDEP rates tended to have the lowest median household incomes. The zip codes in the lowest quartile of family household income had a SUDEP rate more than twice as high as that in the zip codes in the highest income quartile. This association held true for the period from 2009-2010 and for 2014-2015.
Dr. Friedman and colleagues received funding from Finding a Cure for Epilepsy and Seizures, which is affiliated with the NYU Comprehensive Epilepsy Center and NYU Langone Health.
SOURCE: Cihan E et al. AES 2018, Abstract 2.419.
REPORTING FROM AES 2018
Key clinical point: Data indicate a decline over time in the incidence of SUDEP.
Major finding: The incidence of SUDEP declined by 36% from 2009-2010 to 2014-2015.
Study details: A retrospective analysis of medical examiner data on 1,466 deaths in people with epilepsy.
Disclosures: Finding a Cure for Epilepsy and Seizures provided funding for the study.
Source: Cihan E et al. AES 2018, Abstract 2.419.
Onset of pediatric status epilepticus may have a circadian pattern
NEW ORLEANS – according to research presented at the annual meeting of the American Epilepsy Society. The number of episodes is greatest between 10 a.m. and 11 a.m. and smallest between 10 p.m. and 11 p.m.
“Our findings may inform the increase in preventive monitoring, such as video monitoring or seizure-tracking devices for patients,” said Justice Clark, MPH, a program coordinator at Boston Children’s Hospital. “They may also inform chronotherapeutic strategies.”
Research suggests that various types of seizures cluster at different times of the day. Data about the circadian distribution of status epilepticus, however, are limited.
Ms. Clark and colleagues conducted a prospective observational study at 25 hospitals in the United States and Canada from June 2011 to January 2018. Eligible participants were between ages 1 month and 21 years, had focal or generalized convulsive status epilepticus, and had failed to respond to one benzodiazepine and one nonbenzodiazepine antiseizure medication. For patients with more than one episode of refractory status epilepticus during the study, the researchers included only the first episode.
The investigators examined whether the temporal distribution of pediatric refractory status epilepticus onset followed a circadian pattern using a cosinor analysis with a 12-hour cycle. They used the midline-estimating statistic of rhythm (MESOR) technique to estimate the mean number of refractory status epilepticus episodes per hour if onset was evenly distributed. The amplitude in this analysis was the difference in number of episodes per hour between the MESOR and the peak or the MESOR and the trough.
Ms. Clark and her colleagues included 300 patients in their analysis, each of whom had one episode. Approximately 45% of participants were female. The population’s median age was 4.2 years, and the median duration of status epilepticus was 120 minutes.
The MESOR was 12.5 episodes per hour, and the amplitude was 2.4 episodes per hour, indicating that the distribution was not even over 24 hours. The peak number of onsets was between 10 a.m. and 11 a.m., and the trough was between 10 p.m. and 11 p.m.
A secondary analysis examined the circadian distribution of time to treatment with rescue medications. The distribution of time to treatment with the first benzodiazepine did not differ significantly from a uniform distribution. The time to treatment with the first nonbenzodiazepine antiseizure medication, however, was not uniformly distributed. The longest time to treatment occurred between 3 a.m. and 4 a.m., and the shortest time was between 3 p.m. and 4 p.m. “Although fewer refractory status epilepticus episodes occurred at night, the time to antiseizure medication administration was the longest [during that period]. Thus, nighttime refractory status epilepticus episodes may be at higher risk for delayed treatment,” said Ms. Clark. A limitation of this analysis is that it was influenced by outliers, she added.
The Pediatric Epilepsy Research Foundation and the Epilepsy Research Fund supported the study.
SOURCE: Clark J et al. AES 2018. Abstract 3.426.
NEW ORLEANS – according to research presented at the annual meeting of the American Epilepsy Society. The number of episodes is greatest between 10 a.m. and 11 a.m. and smallest between 10 p.m. and 11 p.m.
“Our findings may inform the increase in preventive monitoring, such as video monitoring or seizure-tracking devices for patients,” said Justice Clark, MPH, a program coordinator at Boston Children’s Hospital. “They may also inform chronotherapeutic strategies.”
Research suggests that various types of seizures cluster at different times of the day. Data about the circadian distribution of status epilepticus, however, are limited.
Ms. Clark and colleagues conducted a prospective observational study at 25 hospitals in the United States and Canada from June 2011 to January 2018. Eligible participants were between ages 1 month and 21 years, had focal or generalized convulsive status epilepticus, and had failed to respond to one benzodiazepine and one nonbenzodiazepine antiseizure medication. For patients with more than one episode of refractory status epilepticus during the study, the researchers included only the first episode.
The investigators examined whether the temporal distribution of pediatric refractory status epilepticus onset followed a circadian pattern using a cosinor analysis with a 12-hour cycle. They used the midline-estimating statistic of rhythm (MESOR) technique to estimate the mean number of refractory status epilepticus episodes per hour if onset was evenly distributed. The amplitude in this analysis was the difference in number of episodes per hour between the MESOR and the peak or the MESOR and the trough.
Ms. Clark and her colleagues included 300 patients in their analysis, each of whom had one episode. Approximately 45% of participants were female. The population’s median age was 4.2 years, and the median duration of status epilepticus was 120 minutes.
The MESOR was 12.5 episodes per hour, and the amplitude was 2.4 episodes per hour, indicating that the distribution was not even over 24 hours. The peak number of onsets was between 10 a.m. and 11 a.m., and the trough was between 10 p.m. and 11 p.m.
A secondary analysis examined the circadian distribution of time to treatment with rescue medications. The distribution of time to treatment with the first benzodiazepine did not differ significantly from a uniform distribution. The time to treatment with the first nonbenzodiazepine antiseizure medication, however, was not uniformly distributed. The longest time to treatment occurred between 3 a.m. and 4 a.m., and the shortest time was between 3 p.m. and 4 p.m. “Although fewer refractory status epilepticus episodes occurred at night, the time to antiseizure medication administration was the longest [during that period]. Thus, nighttime refractory status epilepticus episodes may be at higher risk for delayed treatment,” said Ms. Clark. A limitation of this analysis is that it was influenced by outliers, she added.
The Pediatric Epilepsy Research Foundation and the Epilepsy Research Fund supported the study.
SOURCE: Clark J et al. AES 2018. Abstract 3.426.
NEW ORLEANS – according to research presented at the annual meeting of the American Epilepsy Society. The number of episodes is greatest between 10 a.m. and 11 a.m. and smallest between 10 p.m. and 11 p.m.
“Our findings may inform the increase in preventive monitoring, such as video monitoring or seizure-tracking devices for patients,” said Justice Clark, MPH, a program coordinator at Boston Children’s Hospital. “They may also inform chronotherapeutic strategies.”
Research suggests that various types of seizures cluster at different times of the day. Data about the circadian distribution of status epilepticus, however, are limited.
Ms. Clark and colleagues conducted a prospective observational study at 25 hospitals in the United States and Canada from June 2011 to January 2018. Eligible participants were between ages 1 month and 21 years, had focal or generalized convulsive status epilepticus, and had failed to respond to one benzodiazepine and one nonbenzodiazepine antiseizure medication. For patients with more than one episode of refractory status epilepticus during the study, the researchers included only the first episode.
The investigators examined whether the temporal distribution of pediatric refractory status epilepticus onset followed a circadian pattern using a cosinor analysis with a 12-hour cycle. They used the midline-estimating statistic of rhythm (MESOR) technique to estimate the mean number of refractory status epilepticus episodes per hour if onset was evenly distributed. The amplitude in this analysis was the difference in number of episodes per hour between the MESOR and the peak or the MESOR and the trough.
Ms. Clark and her colleagues included 300 patients in their analysis, each of whom had one episode. Approximately 45% of participants were female. The population’s median age was 4.2 years, and the median duration of status epilepticus was 120 minutes.
The MESOR was 12.5 episodes per hour, and the amplitude was 2.4 episodes per hour, indicating that the distribution was not even over 24 hours. The peak number of onsets was between 10 a.m. and 11 a.m., and the trough was between 10 p.m. and 11 p.m.
A secondary analysis examined the circadian distribution of time to treatment with rescue medications. The distribution of time to treatment with the first benzodiazepine did not differ significantly from a uniform distribution. The time to treatment with the first nonbenzodiazepine antiseizure medication, however, was not uniformly distributed. The longest time to treatment occurred between 3 a.m. and 4 a.m., and the shortest time was between 3 p.m. and 4 p.m. “Although fewer refractory status epilepticus episodes occurred at night, the time to antiseizure medication administration was the longest [during that period]. Thus, nighttime refractory status epilepticus episodes may be at higher risk for delayed treatment,” said Ms. Clark. A limitation of this analysis is that it was influenced by outliers, she added.
The Pediatric Epilepsy Research Foundation and the Epilepsy Research Fund supported the study.
SOURCE: Clark J et al. AES 2018. Abstract 3.426.
REPORTING FROM AES 2018
Key clinical point: The onset of pediatric refractory status epilepticus is not distributed uniformly across the day.
Major finding: Episodes peaked between 10 a.m. and 11 a.m.
Study details: A prospective, observational study conducted at 25 hospitals that included 300 patients.
Disclosures: The Pediatric Epilepsy Research Foundation and the Epilepsy Research Fund funded the study.
Source: Clark J et al. AES 2018. Abstract 3.426.
Hippocampal abnormalities seen in epilepsy subtypes may be congenital
NEW ORLEANS – , although to a lesser extent, based on findings from two studies presented at the annual meeting of the American Epilepsy Society.
While the studies suggest an imaging endophenotype associated with these disorders, it’s unclear if a larger degree of abnormality causes disease manifestation, or whether there are other predisposing actors at work.
“What our study tells us is that hippocampal abnormalities can occur in the absence of seizure,” Marian Galovic, MD, said in an interview. “It may be that, in some cases, hippocampal abnormalities could be the cause, rather than the consequence, of seizures.”
Dr. Galovic of University College London was on hand to discuss the work of his colleague, Lili Long, MD, PhD, of the Xiangya Hospital of Central South University, Changsha, China. Visa issues prevented her from attending the meeting.
The study included 18 sibling pairs in which the affected siblings had sporadic, nonlesional temporal lobe epilepsy (TLE), involving the right lobe in 12 and the left in 6. The patients, siblings, and 18 healthy, age-matched controls underwent clinical, electrophysiologic, and high-resolution structural neuroimaging.
The researchers compared overall hippocampal volumes between groups and determined the subregional extent of hippocampal abnormalities using shape analysis. They also looked at whole-brain differences in cortical thickness and folding complexity.
As expected, median hippocampal volumes were largest in the healthy controls (left = 2.82 mL, right = 2.94 mL), and smallest in patients. Patients with left TLE had a median left hippocampal volume of 2.23 mL, while those with right TLE had a median right hippocampal volume of 1.92 mL.
However, volume in the unaffected siblings was a surprise. Like the patients, these subjects also had significant reductions in hippocampal volume when compared with controls (left = 2.47 mL, right = 2.65 mL). “The atrophy was relatively similar in siblings and patients, although not as pronounced in siblings,” Dr. Galovic said. “It was mostly unilateral in the siblings and bilateral in the patients, but it was still more pronounced on the side where the epilepsy of the affected sibling was coming from.”
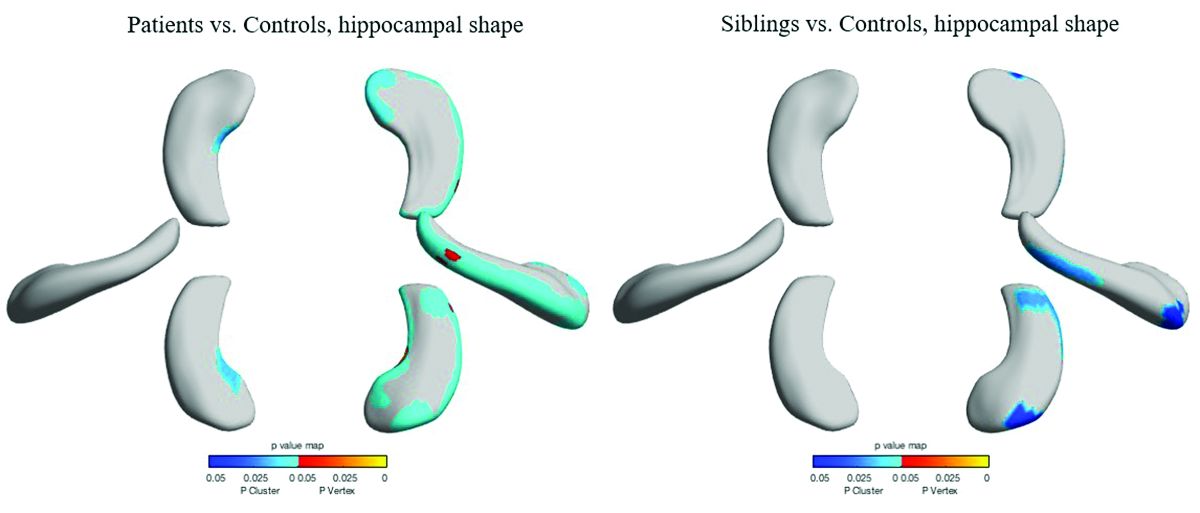
Patients and siblings also shared morphologic variations of the hippocampus, with atrophy more pronounced on the right than the left. The right lateral body and anterior head of the hippocampus were most affected, Dr. Galovic said, with reductions in the right cornu ammonis 1 subfield and subiculum.
Widespread cortical thinning was present in patients, including the pericentral, frontal, and temporal areas. Unaffected siblings also showed cortical thinning, but this was mostly restricted to the right postcentral gyrus. Patients and siblings also demonstrated increased cortical folding complexity, but in different areas: predominantly frontal in patients, but predominantly parieto-occipital in siblings. Both were significantly different than healthy control subjects.
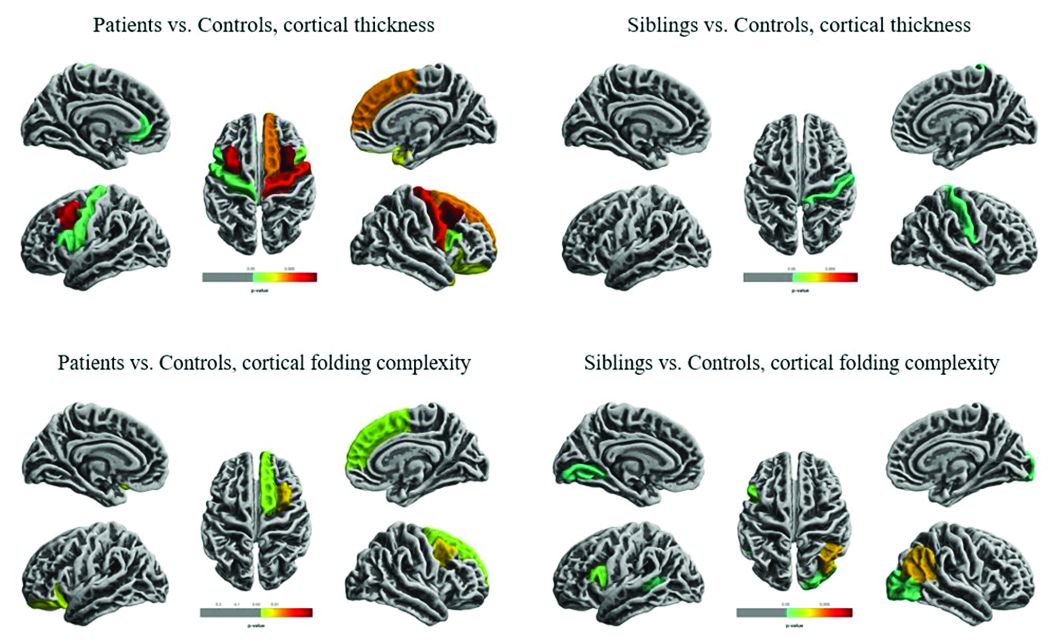
The study didn’t examine any association with memory, which is often impaired in patients with TLE. However, Dr. Galovic said, “We have just submitted for publication a study in which we did find an association between focal hippocampal atrophy and memory performance.”
A different study by a team at University College London looked at hippocampal structure and function in patients with juvenile myoclonic epilepsy (JME) and their unaffected siblings. The imaging study, lead by Lorenzo Caciagli, MD, of the university comprised 37 patients with JME, 16 unaffected siblings, and 20 healthy controls. It employed multimodal MRI and neuropsychological measures to examine the form and function of the mesiotemporal lobe.
The subjects were matched for age, sex, handedness, and hemispheric dominance, which was assessed with language lateralization indices. This measures the number of active voxels on functional MRI, showing which hemisphere is dominant for language.
Both patients and their siblings showed reductions in left hippocampal volume on the order of 5%-8%, significantly smaller than the volumes seen in healthy controls. About half of patients and half of siblings also showed either unilateral or bilateral hippocampal malrotation. This was present in just 15% of controls, another significant difference. The structural differences weren’t associated with seizure control or age at disease onset, or with any impairments in verbal or visual memory. But when the investigators performed functional mapping, they found unusual patterns of hippocampal activation in both patients and siblings, pointing to a dysfunction of verbal encoding. In patients, there appeared to be distinct patterns of underactivation along the hippocampal long axis, regardless of whether malrotation was present. But among patients who had malrotation, the left posterior hippocampus showed more activation during visual memory.
The team concluded that the hippocampal abnormalities in volume, shape, and positioning in patients with JME and their siblings are related to functional reorganization. The abnormalities probably occur during prenatal neurodevelopment, they noted.
“Cosegregation of imaging patterns in patients and their siblings is suggestive of genetic imaging phenotypes, and independent of disease activity,” Dr. Caciagli and his coinvestigators wrote in their abstract.
Funding for the TLE study came from the National Natural Science Foundation of China, the Ministry of Science and Technology of China, and Xiangya Hospital. Funding for the JME study came from a variety of U.K. charities and government agencies.
SOURCES: Long L et al. AES 2018, Abstract 2.183; Caciagli L et al. AES 2018, Abstract 2.166.
NEW ORLEANS – , although to a lesser extent, based on findings from two studies presented at the annual meeting of the American Epilepsy Society.
While the studies suggest an imaging endophenotype associated with these disorders, it’s unclear if a larger degree of abnormality causes disease manifestation, or whether there are other predisposing actors at work.
“What our study tells us is that hippocampal abnormalities can occur in the absence of seizure,” Marian Galovic, MD, said in an interview. “It may be that, in some cases, hippocampal abnormalities could be the cause, rather than the consequence, of seizures.”
Dr. Galovic of University College London was on hand to discuss the work of his colleague, Lili Long, MD, PhD, of the Xiangya Hospital of Central South University, Changsha, China. Visa issues prevented her from attending the meeting.
The study included 18 sibling pairs in which the affected siblings had sporadic, nonlesional temporal lobe epilepsy (TLE), involving the right lobe in 12 and the left in 6. The patients, siblings, and 18 healthy, age-matched controls underwent clinical, electrophysiologic, and high-resolution structural neuroimaging.
The researchers compared overall hippocampal volumes between groups and determined the subregional extent of hippocampal abnormalities using shape analysis. They also looked at whole-brain differences in cortical thickness and folding complexity.
As expected, median hippocampal volumes were largest in the healthy controls (left = 2.82 mL, right = 2.94 mL), and smallest in patients. Patients with left TLE had a median left hippocampal volume of 2.23 mL, while those with right TLE had a median right hippocampal volume of 1.92 mL.
However, volume in the unaffected siblings was a surprise. Like the patients, these subjects also had significant reductions in hippocampal volume when compared with controls (left = 2.47 mL, right = 2.65 mL). “The atrophy was relatively similar in siblings and patients, although not as pronounced in siblings,” Dr. Galovic said. “It was mostly unilateral in the siblings and bilateral in the patients, but it was still more pronounced on the side where the epilepsy of the affected sibling was coming from.”
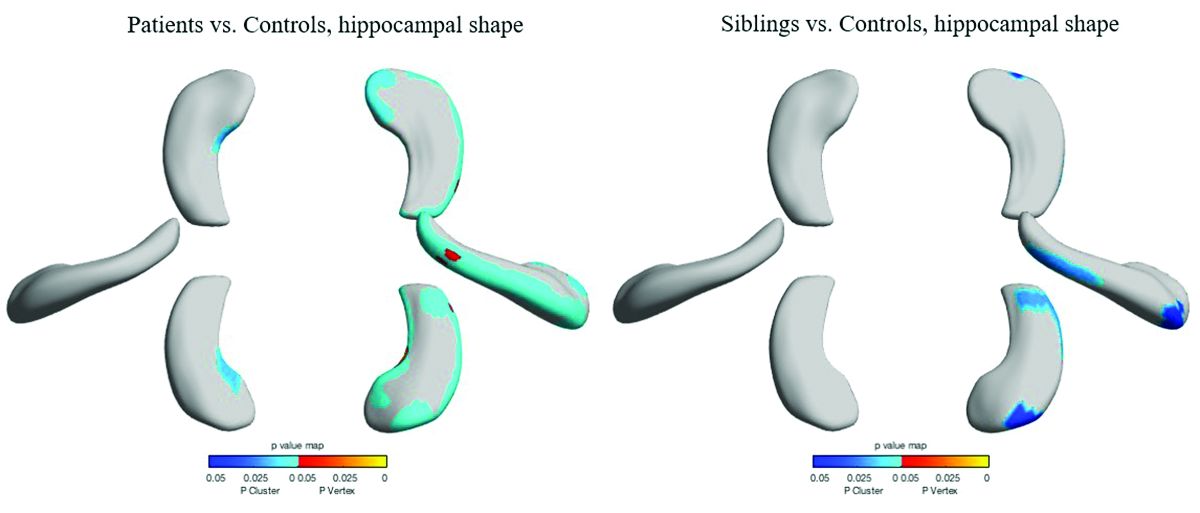
Patients and siblings also shared morphologic variations of the hippocampus, with atrophy more pronounced on the right than the left. The right lateral body and anterior head of the hippocampus were most affected, Dr. Galovic said, with reductions in the right cornu ammonis 1 subfield and subiculum.
Widespread cortical thinning was present in patients, including the pericentral, frontal, and temporal areas. Unaffected siblings also showed cortical thinning, but this was mostly restricted to the right postcentral gyrus. Patients and siblings also demonstrated increased cortical folding complexity, but in different areas: predominantly frontal in patients, but predominantly parieto-occipital in siblings. Both were significantly different than healthy control subjects.
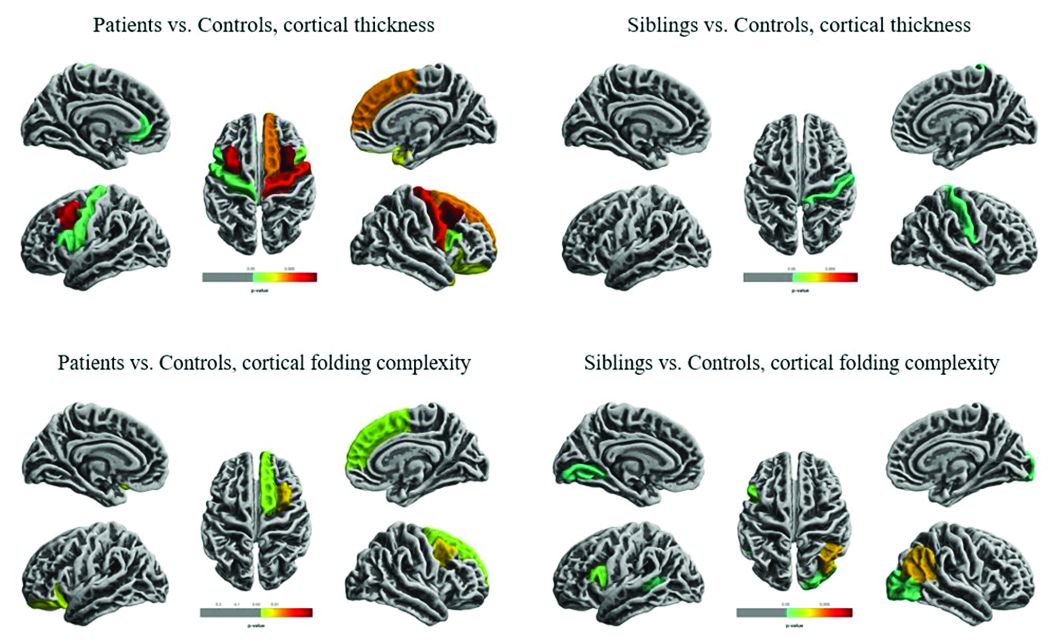
The study didn’t examine any association with memory, which is often impaired in patients with TLE. However, Dr. Galovic said, “We have just submitted for publication a study in which we did find an association between focal hippocampal atrophy and memory performance.”
A different study by a team at University College London looked at hippocampal structure and function in patients with juvenile myoclonic epilepsy (JME) and their unaffected siblings. The imaging study, lead by Lorenzo Caciagli, MD, of the university comprised 37 patients with JME, 16 unaffected siblings, and 20 healthy controls. It employed multimodal MRI and neuropsychological measures to examine the form and function of the mesiotemporal lobe.
The subjects were matched for age, sex, handedness, and hemispheric dominance, which was assessed with language lateralization indices. This measures the number of active voxels on functional MRI, showing which hemisphere is dominant for language.
Both patients and their siblings showed reductions in left hippocampal volume on the order of 5%-8%, significantly smaller than the volumes seen in healthy controls. About half of patients and half of siblings also showed either unilateral or bilateral hippocampal malrotation. This was present in just 15% of controls, another significant difference. The structural differences weren’t associated with seizure control or age at disease onset, or with any impairments in verbal or visual memory. But when the investigators performed functional mapping, they found unusual patterns of hippocampal activation in both patients and siblings, pointing to a dysfunction of verbal encoding. In patients, there appeared to be distinct patterns of underactivation along the hippocampal long axis, regardless of whether malrotation was present. But among patients who had malrotation, the left posterior hippocampus showed more activation during visual memory.
The team concluded that the hippocampal abnormalities in volume, shape, and positioning in patients with JME and their siblings are related to functional reorganization. The abnormalities probably occur during prenatal neurodevelopment, they noted.
“Cosegregation of imaging patterns in patients and their siblings is suggestive of genetic imaging phenotypes, and independent of disease activity,” Dr. Caciagli and his coinvestigators wrote in their abstract.
Funding for the TLE study came from the National Natural Science Foundation of China, the Ministry of Science and Technology of China, and Xiangya Hospital. Funding for the JME study came from a variety of U.K. charities and government agencies.
SOURCES: Long L et al. AES 2018, Abstract 2.183; Caciagli L et al. AES 2018, Abstract 2.166.
NEW ORLEANS – , although to a lesser extent, based on findings from two studies presented at the annual meeting of the American Epilepsy Society.
While the studies suggest an imaging endophenotype associated with these disorders, it’s unclear if a larger degree of abnormality causes disease manifestation, or whether there are other predisposing actors at work.
“What our study tells us is that hippocampal abnormalities can occur in the absence of seizure,” Marian Galovic, MD, said in an interview. “It may be that, in some cases, hippocampal abnormalities could be the cause, rather than the consequence, of seizures.”
Dr. Galovic of University College London was on hand to discuss the work of his colleague, Lili Long, MD, PhD, of the Xiangya Hospital of Central South University, Changsha, China. Visa issues prevented her from attending the meeting.
The study included 18 sibling pairs in which the affected siblings had sporadic, nonlesional temporal lobe epilepsy (TLE), involving the right lobe in 12 and the left in 6. The patients, siblings, and 18 healthy, age-matched controls underwent clinical, electrophysiologic, and high-resolution structural neuroimaging.
The researchers compared overall hippocampal volumes between groups and determined the subregional extent of hippocampal abnormalities using shape analysis. They also looked at whole-brain differences in cortical thickness and folding complexity.
As expected, median hippocampal volumes were largest in the healthy controls (left = 2.82 mL, right = 2.94 mL), and smallest in patients. Patients with left TLE had a median left hippocampal volume of 2.23 mL, while those with right TLE had a median right hippocampal volume of 1.92 mL.
However, volume in the unaffected siblings was a surprise. Like the patients, these subjects also had significant reductions in hippocampal volume when compared with controls (left = 2.47 mL, right = 2.65 mL). “The atrophy was relatively similar in siblings and patients, although not as pronounced in siblings,” Dr. Galovic said. “It was mostly unilateral in the siblings and bilateral in the patients, but it was still more pronounced on the side where the epilepsy of the affected sibling was coming from.”
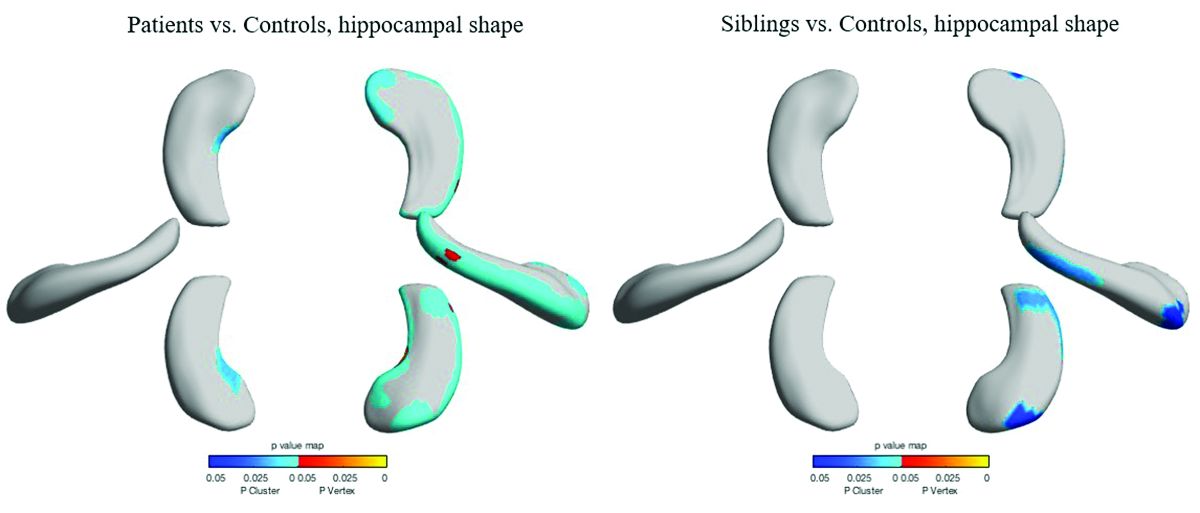
Patients and siblings also shared morphologic variations of the hippocampus, with atrophy more pronounced on the right than the left. The right lateral body and anterior head of the hippocampus were most affected, Dr. Galovic said, with reductions in the right cornu ammonis 1 subfield and subiculum.
Widespread cortical thinning was present in patients, including the pericentral, frontal, and temporal areas. Unaffected siblings also showed cortical thinning, but this was mostly restricted to the right postcentral gyrus. Patients and siblings also demonstrated increased cortical folding complexity, but in different areas: predominantly frontal in patients, but predominantly parieto-occipital in siblings. Both were significantly different than healthy control subjects.
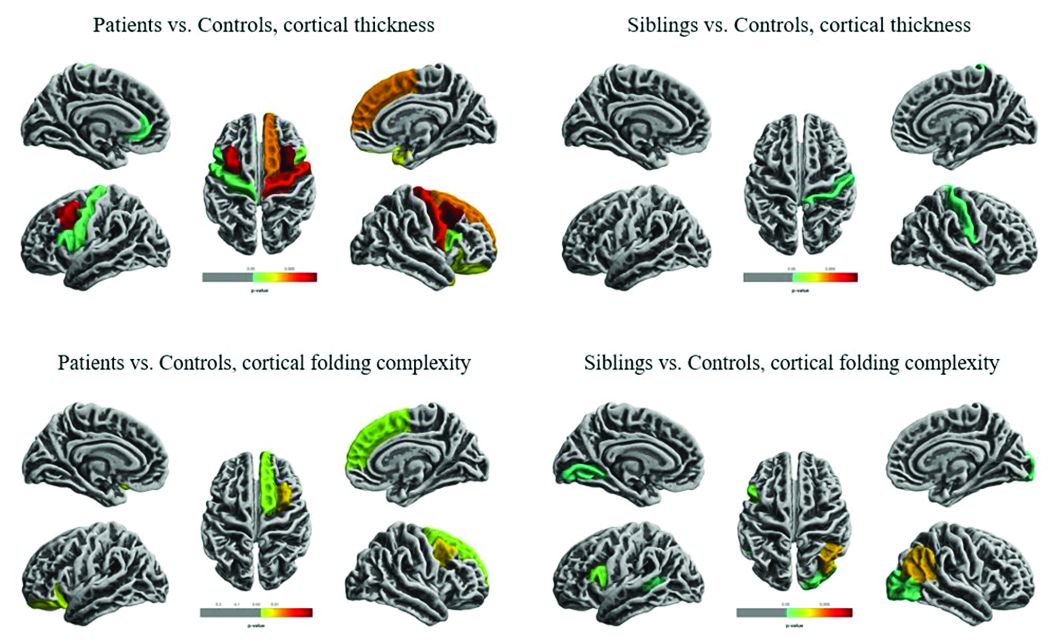
The study didn’t examine any association with memory, which is often impaired in patients with TLE. However, Dr. Galovic said, “We have just submitted for publication a study in which we did find an association between focal hippocampal atrophy and memory performance.”
A different study by a team at University College London looked at hippocampal structure and function in patients with juvenile myoclonic epilepsy (JME) and their unaffected siblings. The imaging study, lead by Lorenzo Caciagli, MD, of the university comprised 37 patients with JME, 16 unaffected siblings, and 20 healthy controls. It employed multimodal MRI and neuropsychological measures to examine the form and function of the mesiotemporal lobe.
The subjects were matched for age, sex, handedness, and hemispheric dominance, which was assessed with language lateralization indices. This measures the number of active voxels on functional MRI, showing which hemisphere is dominant for language.
Both patients and their siblings showed reductions in left hippocampal volume on the order of 5%-8%, significantly smaller than the volumes seen in healthy controls. About half of patients and half of siblings also showed either unilateral or bilateral hippocampal malrotation. This was present in just 15% of controls, another significant difference. The structural differences weren’t associated with seizure control or age at disease onset, or with any impairments in verbal or visual memory. But when the investigators performed functional mapping, they found unusual patterns of hippocampal activation in both patients and siblings, pointing to a dysfunction of verbal encoding. In patients, there appeared to be distinct patterns of underactivation along the hippocampal long axis, regardless of whether malrotation was present. But among patients who had malrotation, the left posterior hippocampus showed more activation during visual memory.
The team concluded that the hippocampal abnormalities in volume, shape, and positioning in patients with JME and their siblings are related to functional reorganization. The abnormalities probably occur during prenatal neurodevelopment, they noted.
“Cosegregation of imaging patterns in patients and their siblings is suggestive of genetic imaging phenotypes, and independent of disease activity,” Dr. Caciagli and his coinvestigators wrote in their abstract.
Funding for the TLE study came from the National Natural Science Foundation of China, the Ministry of Science and Technology of China, and Xiangya Hospital. Funding for the JME study came from a variety of U.K. charities and government agencies.
SOURCES: Long L et al. AES 2018, Abstract 2.183; Caciagli L et al. AES 2018, Abstract 2.166.
REPORTING FROM AES 2018
How often is AED treatment delayed for patients with epilepsy?
NEW ORLEANS – , according to an Australian study presented at the annual meeting of the American Epilepsy Society. Most untreated patients begin an AED after experiencing subsequent seizures, however.
“The decision to start or withhold treatment reflects the complex interplay between factors perceived to influence the predicted risk of seizure recurrence, which remain imprecise, and personal factors,” said lead study author Zhibin Chen, PhD, a biostatistician at the University of Melbourne and colleagues.
Many patients with epilepsy in resource-poor countries may not receive AED therapy for socioeconomic reasons, but little is known about untreated epilepsy in high-income countries. To assess the extent of and reasons for patients not receiving AEDs when treatment is accessible and affordable, Dr. Chen and colleagues prospectively recruited adult patients who attended the first-seizure clinics of publicly funded hospitals in Western Australia between May 1, 1999, and May 31, 2016. The patients had new-onset seizures and were referred by primary care or emergency department physicians. The health care system provided universal coverage for patients’ hospital admissions, outpatient visits, investigations, and treatment.
The researchers identified patients with newly diagnosed epilepsy and reviewed medical records to determine the proportion of untreated patients and the reasons for not starting treatment at each follow-up visit. The investigators compared the sociodemographic factors, neuroimaging, and EEG findings of treated and untreated patients.
In all, 1,317 people attended the clinics during the study period, and 610 patients (61% male; median age, 40) received a diagnosis of epilepsy and met 2014 International League Against Epilepsy (ILAE) diagnostic criteria for epilepsy. Patients were followed for a median of 5.7 years.
Of the 610 patients with epilepsy, 31% did not start AED treatment at the time of diagnosis – 16.4% because the neurologist did not recommend treatment and 14.6% because the patient declined treatment despite a neurologist’s recommendation to start therapy.
Patients’ reasons for not starting treatment included doubts about the need for treatment or about the epilepsy diagnosis, as well as concerns about medication side effects. Neurologists’ reasons for not beginning treatment included a patient having only one seizure and awaiting further results. The presence of seizure-precipitating factors (e.g., flashing lights, sleep deprivation, stress, or alcohol use) was another reason that patients and neurologists commonly cited for not initiating treatment.
Among the 189 initially untreated patients, 62.4% started treatment after a median delay of 95 days, “mainly after further seizures,” the investigators said. Patients with epilepsy who were older, from lower socioeconomic areas, had experienced more seizures, or had epileptogenic lesions on neuroimaging were more likely to initiate AED treatment at diagnosis.
“The percentage of people who were not initially prescribed AEDs was much higher than expected and suggests that untreated epilepsy exists not just in resource-poor, but also in wealthy countries,” said Dr. Chen.
More research is needed to assess the long-term outcomes of patient with seizure-precipitating factors who initiate AEDs immediately, compared with those who try avoidance of precipitating factors alone, said Dr. Chen.
This study was supported by a grant from UCB Pharma.
SOURCE: Chen Z et al. AES 2018, Abstract 3.421.
NEW ORLEANS – , according to an Australian study presented at the annual meeting of the American Epilepsy Society. Most untreated patients begin an AED after experiencing subsequent seizures, however.
“The decision to start or withhold treatment reflects the complex interplay between factors perceived to influence the predicted risk of seizure recurrence, which remain imprecise, and personal factors,” said lead study author Zhibin Chen, PhD, a biostatistician at the University of Melbourne and colleagues.
Many patients with epilepsy in resource-poor countries may not receive AED therapy for socioeconomic reasons, but little is known about untreated epilepsy in high-income countries. To assess the extent of and reasons for patients not receiving AEDs when treatment is accessible and affordable, Dr. Chen and colleagues prospectively recruited adult patients who attended the first-seizure clinics of publicly funded hospitals in Western Australia between May 1, 1999, and May 31, 2016. The patients had new-onset seizures and were referred by primary care or emergency department physicians. The health care system provided universal coverage for patients’ hospital admissions, outpatient visits, investigations, and treatment.
The researchers identified patients with newly diagnosed epilepsy and reviewed medical records to determine the proportion of untreated patients and the reasons for not starting treatment at each follow-up visit. The investigators compared the sociodemographic factors, neuroimaging, and EEG findings of treated and untreated patients.
In all, 1,317 people attended the clinics during the study period, and 610 patients (61% male; median age, 40) received a diagnosis of epilepsy and met 2014 International League Against Epilepsy (ILAE) diagnostic criteria for epilepsy. Patients were followed for a median of 5.7 years.
Of the 610 patients with epilepsy, 31% did not start AED treatment at the time of diagnosis – 16.4% because the neurologist did not recommend treatment and 14.6% because the patient declined treatment despite a neurologist’s recommendation to start therapy.
Patients’ reasons for not starting treatment included doubts about the need for treatment or about the epilepsy diagnosis, as well as concerns about medication side effects. Neurologists’ reasons for not beginning treatment included a patient having only one seizure and awaiting further results. The presence of seizure-precipitating factors (e.g., flashing lights, sleep deprivation, stress, or alcohol use) was another reason that patients and neurologists commonly cited for not initiating treatment.
Among the 189 initially untreated patients, 62.4% started treatment after a median delay of 95 days, “mainly after further seizures,” the investigators said. Patients with epilepsy who were older, from lower socioeconomic areas, had experienced more seizures, or had epileptogenic lesions on neuroimaging were more likely to initiate AED treatment at diagnosis.
“The percentage of people who were not initially prescribed AEDs was much higher than expected and suggests that untreated epilepsy exists not just in resource-poor, but also in wealthy countries,” said Dr. Chen.
More research is needed to assess the long-term outcomes of patient with seizure-precipitating factors who initiate AEDs immediately, compared with those who try avoidance of precipitating factors alone, said Dr. Chen.
This study was supported by a grant from UCB Pharma.
SOURCE: Chen Z et al. AES 2018, Abstract 3.421.
NEW ORLEANS – , according to an Australian study presented at the annual meeting of the American Epilepsy Society. Most untreated patients begin an AED after experiencing subsequent seizures, however.
“The decision to start or withhold treatment reflects the complex interplay between factors perceived to influence the predicted risk of seizure recurrence, which remain imprecise, and personal factors,” said lead study author Zhibin Chen, PhD, a biostatistician at the University of Melbourne and colleagues.
Many patients with epilepsy in resource-poor countries may not receive AED therapy for socioeconomic reasons, but little is known about untreated epilepsy in high-income countries. To assess the extent of and reasons for patients not receiving AEDs when treatment is accessible and affordable, Dr. Chen and colleagues prospectively recruited adult patients who attended the first-seizure clinics of publicly funded hospitals in Western Australia between May 1, 1999, and May 31, 2016. The patients had new-onset seizures and were referred by primary care or emergency department physicians. The health care system provided universal coverage for patients’ hospital admissions, outpatient visits, investigations, and treatment.
The researchers identified patients with newly diagnosed epilepsy and reviewed medical records to determine the proportion of untreated patients and the reasons for not starting treatment at each follow-up visit. The investigators compared the sociodemographic factors, neuroimaging, and EEG findings of treated and untreated patients.
In all, 1,317 people attended the clinics during the study period, and 610 patients (61% male; median age, 40) received a diagnosis of epilepsy and met 2014 International League Against Epilepsy (ILAE) diagnostic criteria for epilepsy. Patients were followed for a median of 5.7 years.
Of the 610 patients with epilepsy, 31% did not start AED treatment at the time of diagnosis – 16.4% because the neurologist did not recommend treatment and 14.6% because the patient declined treatment despite a neurologist’s recommendation to start therapy.
Patients’ reasons for not starting treatment included doubts about the need for treatment or about the epilepsy diagnosis, as well as concerns about medication side effects. Neurologists’ reasons for not beginning treatment included a patient having only one seizure and awaiting further results. The presence of seizure-precipitating factors (e.g., flashing lights, sleep deprivation, stress, or alcohol use) was another reason that patients and neurologists commonly cited for not initiating treatment.
Among the 189 initially untreated patients, 62.4% started treatment after a median delay of 95 days, “mainly after further seizures,” the investigators said. Patients with epilepsy who were older, from lower socioeconomic areas, had experienced more seizures, or had epileptogenic lesions on neuroimaging were more likely to initiate AED treatment at diagnosis.
“The percentage of people who were not initially prescribed AEDs was much higher than expected and suggests that untreated epilepsy exists not just in resource-poor, but also in wealthy countries,” said Dr. Chen.
More research is needed to assess the long-term outcomes of patient with seizure-precipitating factors who initiate AEDs immediately, compared with those who try avoidance of precipitating factors alone, said Dr. Chen.
This study was supported by a grant from UCB Pharma.
SOURCE: Chen Z et al. AES 2018, Abstract 3.421.
REPORTING FROM AES 2018
Key clinical point: Delayed initiation of antiepileptic drug treatment may be more common than thought.
Major finding: More than 30% of patients with epilepsy do not initiate treatment at diagnosis.
Study details: Review of 610 patients with newly diagnosed epilepsy who were seen at clinics in Western Australia.
Disclosures: The study was supported by a grant from UCB Pharma.
Source: Chen Z et al. AES 2018, Abstract 3.421.
Bioequivalents lamotrigine, levetiracetam control new-onset focal seizures equally well
NEW ORLEANS – Bioequivalent generic formulations of levetiracetam and lamotrigine reduced seizures by a similar extent over 2 years in a retrospective study of patients with newly diagnosed focal epilepsy.
Each drug had a specific adverse event profile, with lamotrigine associated with rash and levetiracetam with mood disorders, Sirichai Chayasirisobhon, MD, said at the annual meeting of the American Epilepsy Society. This finding can play into the initial therapeutic decision, said Dr. Chayasirisobhon of Kaiser Permanente Southern California. “If someone comes in with depression or mood disorder, I will start on lamotrigine, not levetiracetam. And we can decrease the chance of rash with a very slow titration, as we did here, starting with just 5 mg/kg and working up over 6 months.”
Although the drugs have a somewhat similar teratogenic profile, Dr. Chayasirisobhon added that he favors lamotrigine for women of childbearing years. “It’s a little bit better choice for them I think.”
His retrospective analysis followed 442 patients from first seizure and medical therapy for 2 years. The generic medications came from Kaiser Permanente’s central pharmacy. They were single-source, with a proven 95% bioequivalence. The main outcome was the percentage of patients who became seizure free and remained so. Any seizure, whether febrile, breakthroughs, or from titration, was considered a failure. These patients were dropped from the study. Any patient who developed a drug-related rash was dropped from the study and started on another medication.
More women than men took lamotrigine (113 vs. 75), whereas more men took levetiracetam (148 vs. 106). Those taking lamotrigine were younger than were those taking levetiracetam (30 vs. 40 years).
At the end of 2 years, there was no statistically significant difference in the primary outcome of being free from seizures (66.5% with lamotrigine vs. 72.4% with levetiracetam). In the lamotrigine group, 33.5% were eliminated from the study, 24% because they had a seizure, and the rest due to an adverse event. In the levetiracetam group, 27.6% were eliminated, 13% because they had a seizure and the rest because of an adverse event.
Adverse events in the lamotrigine group included rash (12), dizziness (3), lethargy (1), and mood changes (2). Among the levetiracetam group, adverse events included dizziness (3), lethargy (7), mood changes (20), slowed thinking (4), depression (2) and headache (1).
“Rash was the main event we saw in this group, and this was even when we did a very slow titration of 5 mg/kg per week,” Dr. Chayasirisobhon said. “Any sign of rash or itching at all, we told them to stop immediately and call us. Fortunately, we had no cases of Steven-Johnson syndrome and all our cases of rash were transient. But in the levetiracetam group, the mood changes are the major thing. Some of the patients became very agitated and aggressive. Whenever we see a patient for the first time, we always ask about mood changes, and we instruct the family to call and report any changes in mood immediately.”
Aside from reproductive age, however, Dr. Chayasirisobhon generally prefers to start new patients on levetiracetam. Its safety profile is remarkable, he said, recounting a case report he published in 2010 (Acta Neurol Taiwan. 2010;19:292-5).
The paper describes a male patient who decided to commit suicide after an argument with his wife. He took his levetiracetam and walked to his father’s grave, swallowing pills the entire time. When he arrived at the grave, he had taken around 65 grams of the medication. “The amazing thing was, he’s still walking, just a little unsteady. Then he decided he’s not ready to die,” Dr. Chayasirisobhon said. “He was able to call 911, so he’s still talking fine. When they checked his level it was so high, but he remained unimpaired except for the unsteady gait and some nystagmus.”
The study did not receive outside funding. Dr. Chayasirisobhon had no financial disclosures.
NEW ORLEANS – Bioequivalent generic formulations of levetiracetam and lamotrigine reduced seizures by a similar extent over 2 years in a retrospective study of patients with newly diagnosed focal epilepsy.
Each drug had a specific adverse event profile, with lamotrigine associated with rash and levetiracetam with mood disorders, Sirichai Chayasirisobhon, MD, said at the annual meeting of the American Epilepsy Society. This finding can play into the initial therapeutic decision, said Dr. Chayasirisobhon of Kaiser Permanente Southern California. “If someone comes in with depression or mood disorder, I will start on lamotrigine, not levetiracetam. And we can decrease the chance of rash with a very slow titration, as we did here, starting with just 5 mg/kg and working up over 6 months.”
Although the drugs have a somewhat similar teratogenic profile, Dr. Chayasirisobhon added that he favors lamotrigine for women of childbearing years. “It’s a little bit better choice for them I think.”
His retrospective analysis followed 442 patients from first seizure and medical therapy for 2 years. The generic medications came from Kaiser Permanente’s central pharmacy. They were single-source, with a proven 95% bioequivalence. The main outcome was the percentage of patients who became seizure free and remained so. Any seizure, whether febrile, breakthroughs, or from titration, was considered a failure. These patients were dropped from the study. Any patient who developed a drug-related rash was dropped from the study and started on another medication.
More women than men took lamotrigine (113 vs. 75), whereas more men took levetiracetam (148 vs. 106). Those taking lamotrigine were younger than were those taking levetiracetam (30 vs. 40 years).
At the end of 2 years, there was no statistically significant difference in the primary outcome of being free from seizures (66.5% with lamotrigine vs. 72.4% with levetiracetam). In the lamotrigine group, 33.5% were eliminated from the study, 24% because they had a seizure, and the rest due to an adverse event. In the levetiracetam group, 27.6% were eliminated, 13% because they had a seizure and the rest because of an adverse event.
Adverse events in the lamotrigine group included rash (12), dizziness (3), lethargy (1), and mood changes (2). Among the levetiracetam group, adverse events included dizziness (3), lethargy (7), mood changes (20), slowed thinking (4), depression (2) and headache (1).
“Rash was the main event we saw in this group, and this was even when we did a very slow titration of 5 mg/kg per week,” Dr. Chayasirisobhon said. “Any sign of rash or itching at all, we told them to stop immediately and call us. Fortunately, we had no cases of Steven-Johnson syndrome and all our cases of rash were transient. But in the levetiracetam group, the mood changes are the major thing. Some of the patients became very agitated and aggressive. Whenever we see a patient for the first time, we always ask about mood changes, and we instruct the family to call and report any changes in mood immediately.”
Aside from reproductive age, however, Dr. Chayasirisobhon generally prefers to start new patients on levetiracetam. Its safety profile is remarkable, he said, recounting a case report he published in 2010 (Acta Neurol Taiwan. 2010;19:292-5).
The paper describes a male patient who decided to commit suicide after an argument with his wife. He took his levetiracetam and walked to his father’s grave, swallowing pills the entire time. When he arrived at the grave, he had taken around 65 grams of the medication. “The amazing thing was, he’s still walking, just a little unsteady. Then he decided he’s not ready to die,” Dr. Chayasirisobhon said. “He was able to call 911, so he’s still talking fine. When they checked his level it was so high, but he remained unimpaired except for the unsteady gait and some nystagmus.”
The study did not receive outside funding. Dr. Chayasirisobhon had no financial disclosures.
NEW ORLEANS – Bioequivalent generic formulations of levetiracetam and lamotrigine reduced seizures by a similar extent over 2 years in a retrospective study of patients with newly diagnosed focal epilepsy.
Each drug had a specific adverse event profile, with lamotrigine associated with rash and levetiracetam with mood disorders, Sirichai Chayasirisobhon, MD, said at the annual meeting of the American Epilepsy Society. This finding can play into the initial therapeutic decision, said Dr. Chayasirisobhon of Kaiser Permanente Southern California. “If someone comes in with depression or mood disorder, I will start on lamotrigine, not levetiracetam. And we can decrease the chance of rash with a very slow titration, as we did here, starting with just 5 mg/kg and working up over 6 months.”
Although the drugs have a somewhat similar teratogenic profile, Dr. Chayasirisobhon added that he favors lamotrigine for women of childbearing years. “It’s a little bit better choice for them I think.”
His retrospective analysis followed 442 patients from first seizure and medical therapy for 2 years. The generic medications came from Kaiser Permanente’s central pharmacy. They were single-source, with a proven 95% bioequivalence. The main outcome was the percentage of patients who became seizure free and remained so. Any seizure, whether febrile, breakthroughs, or from titration, was considered a failure. These patients were dropped from the study. Any patient who developed a drug-related rash was dropped from the study and started on another medication.
More women than men took lamotrigine (113 vs. 75), whereas more men took levetiracetam (148 vs. 106). Those taking lamotrigine were younger than were those taking levetiracetam (30 vs. 40 years).
At the end of 2 years, there was no statistically significant difference in the primary outcome of being free from seizures (66.5% with lamotrigine vs. 72.4% with levetiracetam). In the lamotrigine group, 33.5% were eliminated from the study, 24% because they had a seizure, and the rest due to an adverse event. In the levetiracetam group, 27.6% were eliminated, 13% because they had a seizure and the rest because of an adverse event.
Adverse events in the lamotrigine group included rash (12), dizziness (3), lethargy (1), and mood changes (2). Among the levetiracetam group, adverse events included dizziness (3), lethargy (7), mood changes (20), slowed thinking (4), depression (2) and headache (1).
“Rash was the main event we saw in this group, and this was even when we did a very slow titration of 5 mg/kg per week,” Dr. Chayasirisobhon said. “Any sign of rash or itching at all, we told them to stop immediately and call us. Fortunately, we had no cases of Steven-Johnson syndrome and all our cases of rash were transient. But in the levetiracetam group, the mood changes are the major thing. Some of the patients became very agitated and aggressive. Whenever we see a patient for the first time, we always ask about mood changes, and we instruct the family to call and report any changes in mood immediately.”
Aside from reproductive age, however, Dr. Chayasirisobhon generally prefers to start new patients on levetiracetam. Its safety profile is remarkable, he said, recounting a case report he published in 2010 (Acta Neurol Taiwan. 2010;19:292-5).
The paper describes a male patient who decided to commit suicide after an argument with his wife. He took his levetiracetam and walked to his father’s grave, swallowing pills the entire time. When he arrived at the grave, he had taken around 65 grams of the medication. “The amazing thing was, he’s still walking, just a little unsteady. Then he decided he’s not ready to die,” Dr. Chayasirisobhon said. “He was able to call 911, so he’s still talking fine. When they checked his level it was so high, but he remained unimpaired except for the unsteady gait and some nystagmus.”
The study did not receive outside funding. Dr. Chayasirisobhon had no financial disclosures.
REPORTING FROM AES 2018
Key clinical point:
Major finding: At 2 years, 66.5% of the lamotrigine group and 72.4% of the levetiracetam group were seizure free.
Study details: The retrospective study comprised 442 patients.
Disclosures: The study did not receive outside funding. Dr. Chayasirisobhon had no financial disclosures.
Source: Chayasirisobhon S et al. AES 2018, Abstract 2.147.
Study elicits patients’ most disturbing epilepsy symptoms
NEW ORLEANS – according to a study presented at the annual meeting of the American Epilepsy Society. The most prominent symptoms and effects on daily life may differ in the early, middle, and late stages of the disease, the results suggest.
Lead study author Jacqueline A. French, MD, professor of neurology at New York University, and her colleagues interviewed 62 patients with focal-onset epilepsy to examine patients’ experiences living with epilepsy. The investigators focused on salient symptoms and functional impacts – those that were reported by at least 50% of patients and were associated with a high degree of disturbance (patients rated them 5 or greater on a scale from 0 [no disturbance] to 10 [high disturbance]).
Of 51 symptoms that patients described during the interviews, the following 8 met the salience criteria for the total cohort: twitching or tremors, confusion, difficulty in talking, loss of awareness of others’ presence, stiffening, impaired consciousness or loss of consciousness, difficulty in remembering, and dizziness or lightheadedness. Patients reported salient functional impacts on driving and transportation, work and school, and leisure and social activities. Some symptoms met salience criteria among patients in certain stages of the disease (for example, tongue biting in patients with early-stage epilepsy and anxiety, fear, or panic in late-stage epilepsy) but not among patients in the other cohorts.
“These findings underscore the need to consider all these experiences when developing patient-reported outcome measures for use in clinical trials,” said Dr. French and her colleagues. “It may be useful to tailor measures of patient experiences to the patient’s stage of disease.”
Previous qualitative studies of epilepsy symptoms and burdens were based on small numbers of patients and interviews at a single center. For the present study, the researchers conducted qualitative, semistructured, in-person interviews with adults with focal epilepsy in different areas of the United States (such as California, Minnesota, New York, Ohio, and Pennsylvania). Patients were grouped by early, middle, or late disease stage. Patients in the early cohort (n = 19) had at least two seizures in the past year, a diagnosis of focal epilepsy in the past year, and had not yet received antiepileptic drug (AED) treatment or had received treatment with only one AED and had not failed treatment. Patients in the middle cohort (n = 17) had at least one seizure in the past year, a diagnosis of focal epilepsy within the past 5 years, and had failed one AED because of lack of efficacy or had received their first add-on AED. Patients in the late cohort (n = 26) had at least one seizure every 3 months during the past year, a diagnosis of focal epilepsy at age 12 years or older, and inadequate response to treatment of at least 3 months with two AEDs that were tolerated and appropriately chosen.
Patients’ mean age was 37 years (range, 19-60 years), 73% were female, 79% were white, 69% had a college degree as their highest level of education, and 65% were employed. Patients’ seizure types included simple partial without motor signs (52%), simple partial with motor signs (16%), complex partial (68%), or secondarily generalized (65%).
While driving or transportation was a salient impact for all three groups, memory loss was a salient impact in the early and middle cohorts only. Headaches and sadness or depression were salient impacts for the late cohort only.
This study was funded by Eisai and two of the authors are former or current employees of Eisai.
SOURCE: French JA et al. AES 2018, Abstract 1.196.
NEW ORLEANS – according to a study presented at the annual meeting of the American Epilepsy Society. The most prominent symptoms and effects on daily life may differ in the early, middle, and late stages of the disease, the results suggest.
Lead study author Jacqueline A. French, MD, professor of neurology at New York University, and her colleagues interviewed 62 patients with focal-onset epilepsy to examine patients’ experiences living with epilepsy. The investigators focused on salient symptoms and functional impacts – those that were reported by at least 50% of patients and were associated with a high degree of disturbance (patients rated them 5 or greater on a scale from 0 [no disturbance] to 10 [high disturbance]).
Of 51 symptoms that patients described during the interviews, the following 8 met the salience criteria for the total cohort: twitching or tremors, confusion, difficulty in talking, loss of awareness of others’ presence, stiffening, impaired consciousness or loss of consciousness, difficulty in remembering, and dizziness or lightheadedness. Patients reported salient functional impacts on driving and transportation, work and school, and leisure and social activities. Some symptoms met salience criteria among patients in certain stages of the disease (for example, tongue biting in patients with early-stage epilepsy and anxiety, fear, or panic in late-stage epilepsy) but not among patients in the other cohorts.
“These findings underscore the need to consider all these experiences when developing patient-reported outcome measures for use in clinical trials,” said Dr. French and her colleagues. “It may be useful to tailor measures of patient experiences to the patient’s stage of disease.”
Previous qualitative studies of epilepsy symptoms and burdens were based on small numbers of patients and interviews at a single center. For the present study, the researchers conducted qualitative, semistructured, in-person interviews with adults with focal epilepsy in different areas of the United States (such as California, Minnesota, New York, Ohio, and Pennsylvania). Patients were grouped by early, middle, or late disease stage. Patients in the early cohort (n = 19) had at least two seizures in the past year, a diagnosis of focal epilepsy in the past year, and had not yet received antiepileptic drug (AED) treatment or had received treatment with only one AED and had not failed treatment. Patients in the middle cohort (n = 17) had at least one seizure in the past year, a diagnosis of focal epilepsy within the past 5 years, and had failed one AED because of lack of efficacy or had received their first add-on AED. Patients in the late cohort (n = 26) had at least one seizure every 3 months during the past year, a diagnosis of focal epilepsy at age 12 years or older, and inadequate response to treatment of at least 3 months with two AEDs that were tolerated and appropriately chosen.
Patients’ mean age was 37 years (range, 19-60 years), 73% were female, 79% were white, 69% had a college degree as their highest level of education, and 65% were employed. Patients’ seizure types included simple partial without motor signs (52%), simple partial with motor signs (16%), complex partial (68%), or secondarily generalized (65%).
While driving or transportation was a salient impact for all three groups, memory loss was a salient impact in the early and middle cohorts only. Headaches and sadness or depression were salient impacts for the late cohort only.
This study was funded by Eisai and two of the authors are former or current employees of Eisai.
SOURCE: French JA et al. AES 2018, Abstract 1.196.
NEW ORLEANS – according to a study presented at the annual meeting of the American Epilepsy Society. The most prominent symptoms and effects on daily life may differ in the early, middle, and late stages of the disease, the results suggest.
Lead study author Jacqueline A. French, MD, professor of neurology at New York University, and her colleagues interviewed 62 patients with focal-onset epilepsy to examine patients’ experiences living with epilepsy. The investigators focused on salient symptoms and functional impacts – those that were reported by at least 50% of patients and were associated with a high degree of disturbance (patients rated them 5 or greater on a scale from 0 [no disturbance] to 10 [high disturbance]).
Of 51 symptoms that patients described during the interviews, the following 8 met the salience criteria for the total cohort: twitching or tremors, confusion, difficulty in talking, loss of awareness of others’ presence, stiffening, impaired consciousness or loss of consciousness, difficulty in remembering, and dizziness or lightheadedness. Patients reported salient functional impacts on driving and transportation, work and school, and leisure and social activities. Some symptoms met salience criteria among patients in certain stages of the disease (for example, tongue biting in patients with early-stage epilepsy and anxiety, fear, or panic in late-stage epilepsy) but not among patients in the other cohorts.
“These findings underscore the need to consider all these experiences when developing patient-reported outcome measures for use in clinical trials,” said Dr. French and her colleagues. “It may be useful to tailor measures of patient experiences to the patient’s stage of disease.”
Previous qualitative studies of epilepsy symptoms and burdens were based on small numbers of patients and interviews at a single center. For the present study, the researchers conducted qualitative, semistructured, in-person interviews with adults with focal epilepsy in different areas of the United States (such as California, Minnesota, New York, Ohio, and Pennsylvania). Patients were grouped by early, middle, or late disease stage. Patients in the early cohort (n = 19) had at least two seizures in the past year, a diagnosis of focal epilepsy in the past year, and had not yet received antiepileptic drug (AED) treatment or had received treatment with only one AED and had not failed treatment. Patients in the middle cohort (n = 17) had at least one seizure in the past year, a diagnosis of focal epilepsy within the past 5 years, and had failed one AED because of lack of efficacy or had received their first add-on AED. Patients in the late cohort (n = 26) had at least one seizure every 3 months during the past year, a diagnosis of focal epilepsy at age 12 years or older, and inadequate response to treatment of at least 3 months with two AEDs that were tolerated and appropriately chosen.
Patients’ mean age was 37 years (range, 19-60 years), 73% were female, 79% were white, 69% had a college degree as their highest level of education, and 65% were employed. Patients’ seizure types included simple partial without motor signs (52%), simple partial with motor signs (16%), complex partial (68%), or secondarily generalized (65%).
While driving or transportation was a salient impact for all three groups, memory loss was a salient impact in the early and middle cohorts only. Headaches and sadness or depression were salient impacts for the late cohort only.
This study was funded by Eisai and two of the authors are former or current employees of Eisai.
SOURCE: French JA et al. AES 2018, Abstract 1.196.
REPORTING FROM AES 2018
Key clinical point: The most prominent symptoms and functional impacts of epilepsy may differ in the early, middle, and late stages of the disease.
Major finding: More than 50% of patients reported functional impacts on driving and transportation, work and school, and leisure and social activities.
Study details: An analysis of data from semistructured interviews with 62 adults with focal epilepsy.
Disclosures: This study was funded by Eisai and two of the authors are former or current employees of Eisai.
Source: French JA et al. AES 2018, Abstract 1.196.
Nicotine patch may be an effective precision therapy for select epilepsies
NEW ORLEANS – according to research presented at the annual meeting of the American Epilepsy Society. Of four epilepsy patients at one center who received nicotine-patch treatment, three had a good clinical response, one of whom became seizure free.
“We confirm that, in select patients, treatment with a nicotine patch ... can be an effective precision therapy for epilepsy. We propose consideration of nicotine-patch treatment in refractory patients with known cholinergic nicotine receptor subunit variants, especially those with a clinical history consistent with autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE),” said Jordana Fox, DO, and Alison Dolce, MD, both with the University of Texas Southwestern Medical Center in Dallas.
Gene variants in CHRAn4,CHRNA2, and CHRNB2 can cause ADNFLE. Preclinical and n-of-1 studies have suggested that nicotine may be a precision treatment for ADNFLE.
Dr. Fox and Dr. Dolce reviewed next-generation sequencing epilepsy panels from patients seen at Children’s Medical Center, Dallas, during 2011-2015 to identify patients with nAChR gene variants (CHNRA4, CHRNA2, CHRNB2, and CHRNA7). They reviewed patients’ medical and laboratory records, including genetic variant details and treatment history, and focused on patients who underwent a trial of nicotine-patch treatment.
Of the 21 patients who had nAChR gene variants, 4 tried treatment with a nicotine patch, either 7 mg or 14 mg. The patients who received nicotine-patch treatment had genetic variants in CHRNA4, CHRNB2, and CHRNA2. Three of the patients who tried nicotine-patch treatment had a greater than 50% reduction in seizures, whereas one had no treatment response.
“One patient became seizure free and is now treated with the nicotine patch as monotherapy,” Dr. Fox said.
The patient with complete resolution of seizures had a heterozygous disease–causing mutation in CHRNB2. This patient had nocturnal focal seizures, normal neuroimaging, and had been receiving treatment with oxcarbazepine and zonisamide.
The review identified four patients with nAChR gene variants and the ADNFLE phenotype who have not been treated with nicotine. Further phenotype-genotype characterizations and preclinical studies will help neurologists understand the mechanisms of these complex gene variants.
The researchers received no funding for the study and had no relevant financial disclosures.
SOURCE: Fox J et al. AES 2018, Abstract 1.230.
NEW ORLEANS – according to research presented at the annual meeting of the American Epilepsy Society. Of four epilepsy patients at one center who received nicotine-patch treatment, three had a good clinical response, one of whom became seizure free.
“We confirm that, in select patients, treatment with a nicotine patch ... can be an effective precision therapy for epilepsy. We propose consideration of nicotine-patch treatment in refractory patients with known cholinergic nicotine receptor subunit variants, especially those with a clinical history consistent with autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE),” said Jordana Fox, DO, and Alison Dolce, MD, both with the University of Texas Southwestern Medical Center in Dallas.
Gene variants in CHRAn4,CHRNA2, and CHRNB2 can cause ADNFLE. Preclinical and n-of-1 studies have suggested that nicotine may be a precision treatment for ADNFLE.
Dr. Fox and Dr. Dolce reviewed next-generation sequencing epilepsy panels from patients seen at Children’s Medical Center, Dallas, during 2011-2015 to identify patients with nAChR gene variants (CHNRA4, CHRNA2, CHRNB2, and CHRNA7). They reviewed patients’ medical and laboratory records, including genetic variant details and treatment history, and focused on patients who underwent a trial of nicotine-patch treatment.
Of the 21 patients who had nAChR gene variants, 4 tried treatment with a nicotine patch, either 7 mg or 14 mg. The patients who received nicotine-patch treatment had genetic variants in CHRNA4, CHRNB2, and CHRNA2. Three of the patients who tried nicotine-patch treatment had a greater than 50% reduction in seizures, whereas one had no treatment response.
“One patient became seizure free and is now treated with the nicotine patch as monotherapy,” Dr. Fox said.
The patient with complete resolution of seizures had a heterozygous disease–causing mutation in CHRNB2. This patient had nocturnal focal seizures, normal neuroimaging, and had been receiving treatment with oxcarbazepine and zonisamide.
The review identified four patients with nAChR gene variants and the ADNFLE phenotype who have not been treated with nicotine. Further phenotype-genotype characterizations and preclinical studies will help neurologists understand the mechanisms of these complex gene variants.
The researchers received no funding for the study and had no relevant financial disclosures.
SOURCE: Fox J et al. AES 2018, Abstract 1.230.
NEW ORLEANS – according to research presented at the annual meeting of the American Epilepsy Society. Of four epilepsy patients at one center who received nicotine-patch treatment, three had a good clinical response, one of whom became seizure free.
“We confirm that, in select patients, treatment with a nicotine patch ... can be an effective precision therapy for epilepsy. We propose consideration of nicotine-patch treatment in refractory patients with known cholinergic nicotine receptor subunit variants, especially those with a clinical history consistent with autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE),” said Jordana Fox, DO, and Alison Dolce, MD, both with the University of Texas Southwestern Medical Center in Dallas.
Gene variants in CHRAn4,CHRNA2, and CHRNB2 can cause ADNFLE. Preclinical and n-of-1 studies have suggested that nicotine may be a precision treatment for ADNFLE.
Dr. Fox and Dr. Dolce reviewed next-generation sequencing epilepsy panels from patients seen at Children’s Medical Center, Dallas, during 2011-2015 to identify patients with nAChR gene variants (CHNRA4, CHRNA2, CHRNB2, and CHRNA7). They reviewed patients’ medical and laboratory records, including genetic variant details and treatment history, and focused on patients who underwent a trial of nicotine-patch treatment.
Of the 21 patients who had nAChR gene variants, 4 tried treatment with a nicotine patch, either 7 mg or 14 mg. The patients who received nicotine-patch treatment had genetic variants in CHRNA4, CHRNB2, and CHRNA2. Three of the patients who tried nicotine-patch treatment had a greater than 50% reduction in seizures, whereas one had no treatment response.
“One patient became seizure free and is now treated with the nicotine patch as monotherapy,” Dr. Fox said.
The patient with complete resolution of seizures had a heterozygous disease–causing mutation in CHRNB2. This patient had nocturnal focal seizures, normal neuroimaging, and had been receiving treatment with oxcarbazepine and zonisamide.
The review identified four patients with nAChR gene variants and the ADNFLE phenotype who have not been treated with nicotine. Further phenotype-genotype characterizations and preclinical studies will help neurologists understand the mechanisms of these complex gene variants.
The researchers received no funding for the study and had no relevant financial disclosures.
SOURCE: Fox J et al. AES 2018, Abstract 1.230.
REPORTING FROM AES 2018
Key clinical point: In select patients with epilepsy, nicotine may be an effective precision therapy.
Major finding: Of four patients who received nicotine-patch treatment at one center, three had a good clinical response, one of whom became seizure free.
Study details: Single-center chart review of 21 patients with gene variants in subunits of the nicotinic acetylcholine receptor.
Disclosures: The researchers received no funding for the study and had no relevant financial disclosures.
Source: Fox J et al. AES 2018, Abstract 1.230.
Common AEDs confer modestly increased risk of major congenital malformations
NEW ORLEANS – The most commonly used antiepileptic drugs modestly increased the risk of major congenital malformations among prenatally exposed infants in the MONEAD study.
Malformations occurred among 5% of pregnancies exposed to the medications – higher than the 2% background rate – but this was still much lower than the 9%-10% rate associated with valproate.
Overall, however, the message of the Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic (MONEAD) study is quite reassuring, Kimford J. Meador, MD, said at the annual meeting of the American Epilepsy Society. MONEAD is an ongoing, prospective study to determine both maternal outcomes and long-term childhood neurodevelopmental outcomes associated with the use of antiepileptic drugs (AEDs) during pregnancy.
“The rate of malformations was higher than I thought it would be, and higher than the 2% background rate, but it’s still a modest increase and most babies are born completely normal,” Dr. Meador, professor of neurology and neurosciences at Stanford (Calif.) University, said in an interview. “I think the news here is good, and it’s especially reassuring when you put it in the context that, 60 years ago, there were laws that women with epilepsy couldn’t get married, and some states even had laws to sterilize women. I think that’s absurd when most infants born to these women are without malformations and the risk of miscarriage is very low.”
Another positive finding, he said, is that valproate use among pregnant women is now practically nonexistent. Only 1 of 351 pregnant women with epilepsy and just 2 of a comparator group of 109 nonpregnant women with epilepsy were taking it. That’s great news, said Dr. Meador, who also initiated the NEAD (Neurodevelopmental Effects of Antiepileptic Drugs) study in the early 2000s. NEAD determined the drug’s serious teratogenic potential.
In addition to the cohorts of pregnant and nonpregnant women with epilepsy, 105 healthy pregnant women enrolled in the MONEAD study. Women will be monitored during pregnancy and postpartum to measure maternal outcomes and their children will be monitored from birth through age 6 years to measure their health and developmental outcomes.
The study has six primary outcomes, three for the women and three for their children.
- Determine if women with epilepsy have increased seizures during pregnancy and delineate the contributing factors.
- Determine if C-section rate is increased in women with epilepsy and delineate contributing factors.
- Determine if women with epilepsy have an increased risk for depression during pregnancy and the postpartum period and characterize risk factors.
- Determine the long-term effects of in utero AED exposure on verbal intellectual abilities and other neurobehavioral outcomes.
- Determine if small-for-gestational age and other adverse neonatal outcomes are increased.
- Determine if breastfeeding when taking AEDs impairs the child’s ultimate verbal and other cognitive outcomes.
Rates of miscarriage and neonatal malformations were not primary study outcomes, but the descriptive data were collected and are of high interest, Dr. Meador said.
At baseline, all the women had a mean age of about 30 years. Most (75%) were on monotherapy, 20% were on polytherapy, and the rest were not taking an AED. About 60% had focal epilepsy, 31% had generalized epilepsy, and the remainder had an unclassified seizure disorder. Three subjects had multiple seizure types. The most commonly used AEDs were lamotrigine and levetiracetam (both about 30%); 4% were taking zonisamide, 4% carbamazepine, and 4% oxcarbazepine. Topiramate was being used for 2% of the pregnant woman and 5% of the nonpregnant woman. The combination of lamotrigine and levetiracetam was used for 9.0% of pregnant and 5.5% of nonpregnant women, and other polytherapies in 12.0% of the pregnant and 14.0% of the nonpregnant woman. About 4% of the pregnant and 1% of the nonpregnant women were not taking any AED.
There were 10 (2.8%) spontaneous miscarriages among the pregnant women with epilepsy and none among the healthy pregnant women. Spontaneous miscarriages weren’t associated with acute seizures, and there were no major congenital malformations reported among them. There were also two elective abortions among the pregnant women with epilepsy.
There were 18 major congenital malformations among the pregnant woman with epilepsy (5%). A total of 14 were among pregnancies exposed to monotherapy, 3 were in polytherapy-exposed pregnancies, and 1 was in the group not taking any AEDs.
The malformations were:
- Carbamazepine (one case) – hydronephrosis.
- Gabapentin (one case) – inguinal hernia.
- Lamotrigine (five cases) – aortic coarctation, cryptorchidism, hydronephrosis, pectus excavatum, and morning glory syndrome (a funnel-shaped optic nerve disc associated with impaired visual acuity).
- Levetiracetam (five cases) – atrial septal defect, buried penis syndrome, cryptorchidism, hypoplastic aortic valve, ventricular septal defect.
- Topiramate (one case) – ventricular septal defect.
- Zonisamide (one case) – inguinal hernia, absent pinna.
- Lamotrigine plus clonazepam (one case) – cardiomyopathy.
- Lamotrigine plus levetiracetam (one case) – microcephaly, myelomeningocele, Chiari II malformation.
- Levetiracetam plus phenobarbital (one case) – bilateral inguinal hernia.
MONEAD is funded by the National Institutes of Health; Dr. Meador reported no financial disclosures.
SOURCE: Meador KJ et al. AES 2018, Abstract 3.231.
NEW ORLEANS – The most commonly used antiepileptic drugs modestly increased the risk of major congenital malformations among prenatally exposed infants in the MONEAD study.
Malformations occurred among 5% of pregnancies exposed to the medications – higher than the 2% background rate – but this was still much lower than the 9%-10% rate associated with valproate.
Overall, however, the message of the Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic (MONEAD) study is quite reassuring, Kimford J. Meador, MD, said at the annual meeting of the American Epilepsy Society. MONEAD is an ongoing, prospective study to determine both maternal outcomes and long-term childhood neurodevelopmental outcomes associated with the use of antiepileptic drugs (AEDs) during pregnancy.
“The rate of malformations was higher than I thought it would be, and higher than the 2% background rate, but it’s still a modest increase and most babies are born completely normal,” Dr. Meador, professor of neurology and neurosciences at Stanford (Calif.) University, said in an interview. “I think the news here is good, and it’s especially reassuring when you put it in the context that, 60 years ago, there were laws that women with epilepsy couldn’t get married, and some states even had laws to sterilize women. I think that’s absurd when most infants born to these women are without malformations and the risk of miscarriage is very low.”
Another positive finding, he said, is that valproate use among pregnant women is now practically nonexistent. Only 1 of 351 pregnant women with epilepsy and just 2 of a comparator group of 109 nonpregnant women with epilepsy were taking it. That’s great news, said Dr. Meador, who also initiated the NEAD (Neurodevelopmental Effects of Antiepileptic Drugs) study in the early 2000s. NEAD determined the drug’s serious teratogenic potential.
In addition to the cohorts of pregnant and nonpregnant women with epilepsy, 105 healthy pregnant women enrolled in the MONEAD study. Women will be monitored during pregnancy and postpartum to measure maternal outcomes and their children will be monitored from birth through age 6 years to measure their health and developmental outcomes.
The study has six primary outcomes, three for the women and three for their children.
- Determine if women with epilepsy have increased seizures during pregnancy and delineate the contributing factors.
- Determine if C-section rate is increased in women with epilepsy and delineate contributing factors.
- Determine if women with epilepsy have an increased risk for depression during pregnancy and the postpartum period and characterize risk factors.
- Determine the long-term effects of in utero AED exposure on verbal intellectual abilities and other neurobehavioral outcomes.
- Determine if small-for-gestational age and other adverse neonatal outcomes are increased.
- Determine if breastfeeding when taking AEDs impairs the child’s ultimate verbal and other cognitive outcomes.
Rates of miscarriage and neonatal malformations were not primary study outcomes, but the descriptive data were collected and are of high interest, Dr. Meador said.
At baseline, all the women had a mean age of about 30 years. Most (75%) were on monotherapy, 20% were on polytherapy, and the rest were not taking an AED. About 60% had focal epilepsy, 31% had generalized epilepsy, and the remainder had an unclassified seizure disorder. Three subjects had multiple seizure types. The most commonly used AEDs were lamotrigine and levetiracetam (both about 30%); 4% were taking zonisamide, 4% carbamazepine, and 4% oxcarbazepine. Topiramate was being used for 2% of the pregnant woman and 5% of the nonpregnant woman. The combination of lamotrigine and levetiracetam was used for 9.0% of pregnant and 5.5% of nonpregnant women, and other polytherapies in 12.0% of the pregnant and 14.0% of the nonpregnant woman. About 4% of the pregnant and 1% of the nonpregnant women were not taking any AED.
There were 10 (2.8%) spontaneous miscarriages among the pregnant women with epilepsy and none among the healthy pregnant women. Spontaneous miscarriages weren’t associated with acute seizures, and there were no major congenital malformations reported among them. There were also two elective abortions among the pregnant women with epilepsy.
There were 18 major congenital malformations among the pregnant woman with epilepsy (5%). A total of 14 were among pregnancies exposed to monotherapy, 3 were in polytherapy-exposed pregnancies, and 1 was in the group not taking any AEDs.
The malformations were:
- Carbamazepine (one case) – hydronephrosis.
- Gabapentin (one case) – inguinal hernia.
- Lamotrigine (five cases) – aortic coarctation, cryptorchidism, hydronephrosis, pectus excavatum, and morning glory syndrome (a funnel-shaped optic nerve disc associated with impaired visual acuity).
- Levetiracetam (five cases) – atrial septal defect, buried penis syndrome, cryptorchidism, hypoplastic aortic valve, ventricular septal defect.
- Topiramate (one case) – ventricular septal defect.
- Zonisamide (one case) – inguinal hernia, absent pinna.
- Lamotrigine plus clonazepam (one case) – cardiomyopathy.
- Lamotrigine plus levetiracetam (one case) – microcephaly, myelomeningocele, Chiari II malformation.
- Levetiracetam plus phenobarbital (one case) – bilateral inguinal hernia.
MONEAD is funded by the National Institutes of Health; Dr. Meador reported no financial disclosures.
SOURCE: Meador KJ et al. AES 2018, Abstract 3.231.
NEW ORLEANS – The most commonly used antiepileptic drugs modestly increased the risk of major congenital malformations among prenatally exposed infants in the MONEAD study.
Malformations occurred among 5% of pregnancies exposed to the medications – higher than the 2% background rate – but this was still much lower than the 9%-10% rate associated with valproate.
Overall, however, the message of the Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic (MONEAD) study is quite reassuring, Kimford J. Meador, MD, said at the annual meeting of the American Epilepsy Society. MONEAD is an ongoing, prospective study to determine both maternal outcomes and long-term childhood neurodevelopmental outcomes associated with the use of antiepileptic drugs (AEDs) during pregnancy.
“The rate of malformations was higher than I thought it would be, and higher than the 2% background rate, but it’s still a modest increase and most babies are born completely normal,” Dr. Meador, professor of neurology and neurosciences at Stanford (Calif.) University, said in an interview. “I think the news here is good, and it’s especially reassuring when you put it in the context that, 60 years ago, there were laws that women with epilepsy couldn’t get married, and some states even had laws to sterilize women. I think that’s absurd when most infants born to these women are without malformations and the risk of miscarriage is very low.”
Another positive finding, he said, is that valproate use among pregnant women is now practically nonexistent. Only 1 of 351 pregnant women with epilepsy and just 2 of a comparator group of 109 nonpregnant women with epilepsy were taking it. That’s great news, said Dr. Meador, who also initiated the NEAD (Neurodevelopmental Effects of Antiepileptic Drugs) study in the early 2000s. NEAD determined the drug’s serious teratogenic potential.
In addition to the cohorts of pregnant and nonpregnant women with epilepsy, 105 healthy pregnant women enrolled in the MONEAD study. Women will be monitored during pregnancy and postpartum to measure maternal outcomes and their children will be monitored from birth through age 6 years to measure their health and developmental outcomes.
The study has six primary outcomes, three for the women and three for their children.
- Determine if women with epilepsy have increased seizures during pregnancy and delineate the contributing factors.
- Determine if C-section rate is increased in women with epilepsy and delineate contributing factors.
- Determine if women with epilepsy have an increased risk for depression during pregnancy and the postpartum period and characterize risk factors.
- Determine the long-term effects of in utero AED exposure on verbal intellectual abilities and other neurobehavioral outcomes.
- Determine if small-for-gestational age and other adverse neonatal outcomes are increased.
- Determine if breastfeeding when taking AEDs impairs the child’s ultimate verbal and other cognitive outcomes.
Rates of miscarriage and neonatal malformations were not primary study outcomes, but the descriptive data were collected and are of high interest, Dr. Meador said.
At baseline, all the women had a mean age of about 30 years. Most (75%) were on monotherapy, 20% were on polytherapy, and the rest were not taking an AED. About 60% had focal epilepsy, 31% had generalized epilepsy, and the remainder had an unclassified seizure disorder. Three subjects had multiple seizure types. The most commonly used AEDs were lamotrigine and levetiracetam (both about 30%); 4% were taking zonisamide, 4% carbamazepine, and 4% oxcarbazepine. Topiramate was being used for 2% of the pregnant woman and 5% of the nonpregnant woman. The combination of lamotrigine and levetiracetam was used for 9.0% of pregnant and 5.5% of nonpregnant women, and other polytherapies in 12.0% of the pregnant and 14.0% of the nonpregnant woman. About 4% of the pregnant and 1% of the nonpregnant women were not taking any AED.
There were 10 (2.8%) spontaneous miscarriages among the pregnant women with epilepsy and none among the healthy pregnant women. Spontaneous miscarriages weren’t associated with acute seizures, and there were no major congenital malformations reported among them. There were also two elective abortions among the pregnant women with epilepsy.
There were 18 major congenital malformations among the pregnant woman with epilepsy (5%). A total of 14 were among pregnancies exposed to monotherapy, 3 were in polytherapy-exposed pregnancies, and 1 was in the group not taking any AEDs.
The malformations were:
- Carbamazepine (one case) – hydronephrosis.
- Gabapentin (one case) – inguinal hernia.
- Lamotrigine (five cases) – aortic coarctation, cryptorchidism, hydronephrosis, pectus excavatum, and morning glory syndrome (a funnel-shaped optic nerve disc associated with impaired visual acuity).
- Levetiracetam (five cases) – atrial septal defect, buried penis syndrome, cryptorchidism, hypoplastic aortic valve, ventricular septal defect.
- Topiramate (one case) – ventricular septal defect.
- Zonisamide (one case) – inguinal hernia, absent pinna.
- Lamotrigine plus clonazepam (one case) – cardiomyopathy.
- Lamotrigine plus levetiracetam (one case) – microcephaly, myelomeningocele, Chiari II malformation.
- Levetiracetam plus phenobarbital (one case) – bilateral inguinal hernia.
MONEAD is funded by the National Institutes of Health; Dr. Meador reported no financial disclosures.
SOURCE: Meador KJ et al. AES 2018, Abstract 3.231.
REPORTING FROM AES 2018
Key clinical point:
Major finding: The malformation rate was 5% in exposed pregnancies.
Study details: The MONEAD study comprised 351 pregnant women with epilepsy, 109 nonpregnant women with epilepsy, and 105 healthy pregnant women.
Disclosures: The National Institutes of Health funded the study; Dr. Meador reported no financial disclosures.
Source: Meador KJ et al. AES 2018, Abstract 3.231.