User login
American Urogynecologic Society (AUGS)/ International Urogynecology Association (IUGA): Annual Scientific Meeting
Successful Bariatric Surgery Also May Improve Urinary Incontinence
WASHINGTON – The majority of obese women who had urinary incontinence before bariatric surgery had complete or near-complete resolution of symptoms for up to 3 years after surgery in a study of more than 1,500 women, Dr. Leslee Subak reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
These results indicate that "improvement in incontinence may be another long-term benefit of weight loss, in this case surgical weight loss," said Dr. Subak, professor of obstetrics and gynecology and reproductive sciences, epidemiology and biostatistics, and urology at the University of California, San Francisco.
The study evaluated the effect of surgery on urinary incontinence in 1,565 severely obese women who were part of the multicenter Longitudinal Cohort Study of Bariatric Surgery-2 and had completed self-administered questionnaires about urinary incontinence episodes before surgery and at one or more annual follow-up assessments within 3 years of surgery.
The results were based on outcomes of the 772 women who reported experiencing episodes of incontinence at least weekly, with an average of about 11 incontinence episodes per week. Their median age was 46 years and most were white; about 7% had undergone previous incontinence surgery and about 8% had received or were receiving behavioral treatment or medication for incontinence.
Most of the patients underwent a Roux-en-Y gastric bypass (71%) or laparoscopic adjustable gastric banding (25%). After the first year, they had lost a median of about 30% of their baseline weight, which was maintained through the third year.
At all follow-up times after surgery, there were significantly fewer incontinence episodes, compared with baseline, with a remission rate of 60%-65%, Dr. Subak said.
Urinary incontinence episodes dropped from an average of about 11 episodes per week before surgery to an average of almost 3 episodes per week at 1 year and 4 episodes per week at 2 and 3 years, she noted. Episodes of stress incontinence also decreased from an average of about 5 episodes per week at baseline to about 1 episode per week at 1 year and almost 2 episodes per week at 2 and 3 years.
The remission rate – defined as less than 1 weekly urinary incontinence episode over the past 3 months – was 70% at 1 year, dropping to and stabilizing at about 61%-62% at 2 and 3 years. Moreover, 25% of the women had a complete remission (no episodes of incontinence during the past 3 months) at 3 years, a slight increase from almost 27% at 1 year, Dr. Subak said.
"The magnitude of weight loss was the strongest predictor of improvement in incontinence over time," she noted. "Incontinence and BMI [body mass index] seemed to track together, as [whenever] there’s a reduction in BMI ... there’s a reduction in urinary incontinence episode frequency."
A younger age also was significantly associated with a reduction in the frequency or a remission of urinary incontinence, while being pregnant in the previous year and having had a hysterectomy were associated with a lower likelihood of having a remission.
Dr. Subak noted that limitations of the study included the observational design and the lack of a control group, as well as the fact that data were based on self-reports.
She referred to urinary incontinence and obesity as "twin epidemics," with about a fourfold increased risk of urinary incontinence associated with obesity. About one-third of women in the United States are obese and about 70% of women with incontinence are obese, she pointed out.
The Longitudinal Cohort Study of Bariatric Surgery-2 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Subak received additional funding from the NIDDK; she had no other disclosures.
WASHINGTON – The majority of obese women who had urinary incontinence before bariatric surgery had complete or near-complete resolution of symptoms for up to 3 years after surgery in a study of more than 1,500 women, Dr. Leslee Subak reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
These results indicate that "improvement in incontinence may be another long-term benefit of weight loss, in this case surgical weight loss," said Dr. Subak, professor of obstetrics and gynecology and reproductive sciences, epidemiology and biostatistics, and urology at the University of California, San Francisco.
The study evaluated the effect of surgery on urinary incontinence in 1,565 severely obese women who were part of the multicenter Longitudinal Cohort Study of Bariatric Surgery-2 and had completed self-administered questionnaires about urinary incontinence episodes before surgery and at one or more annual follow-up assessments within 3 years of surgery.
The results were based on outcomes of the 772 women who reported experiencing episodes of incontinence at least weekly, with an average of about 11 incontinence episodes per week. Their median age was 46 years and most were white; about 7% had undergone previous incontinence surgery and about 8% had received or were receiving behavioral treatment or medication for incontinence.
Most of the patients underwent a Roux-en-Y gastric bypass (71%) or laparoscopic adjustable gastric banding (25%). After the first year, they had lost a median of about 30% of their baseline weight, which was maintained through the third year.
At all follow-up times after surgery, there were significantly fewer incontinence episodes, compared with baseline, with a remission rate of 60%-65%, Dr. Subak said.
Urinary incontinence episodes dropped from an average of about 11 episodes per week before surgery to an average of almost 3 episodes per week at 1 year and 4 episodes per week at 2 and 3 years, she noted. Episodes of stress incontinence also decreased from an average of about 5 episodes per week at baseline to about 1 episode per week at 1 year and almost 2 episodes per week at 2 and 3 years.
The remission rate – defined as less than 1 weekly urinary incontinence episode over the past 3 months – was 70% at 1 year, dropping to and stabilizing at about 61%-62% at 2 and 3 years. Moreover, 25% of the women had a complete remission (no episodes of incontinence during the past 3 months) at 3 years, a slight increase from almost 27% at 1 year, Dr. Subak said.
"The magnitude of weight loss was the strongest predictor of improvement in incontinence over time," she noted. "Incontinence and BMI [body mass index] seemed to track together, as [whenever] there’s a reduction in BMI ... there’s a reduction in urinary incontinence episode frequency."
A younger age also was significantly associated with a reduction in the frequency or a remission of urinary incontinence, while being pregnant in the previous year and having had a hysterectomy were associated with a lower likelihood of having a remission.
Dr. Subak noted that limitations of the study included the observational design and the lack of a control group, as well as the fact that data were based on self-reports.
She referred to urinary incontinence and obesity as "twin epidemics," with about a fourfold increased risk of urinary incontinence associated with obesity. About one-third of women in the United States are obese and about 70% of women with incontinence are obese, she pointed out.
The Longitudinal Cohort Study of Bariatric Surgery-2 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Subak received additional funding from the NIDDK; she had no other disclosures.
WASHINGTON – The majority of obese women who had urinary incontinence before bariatric surgery had complete or near-complete resolution of symptoms for up to 3 years after surgery in a study of more than 1,500 women, Dr. Leslee Subak reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
These results indicate that "improvement in incontinence may be another long-term benefit of weight loss, in this case surgical weight loss," said Dr. Subak, professor of obstetrics and gynecology and reproductive sciences, epidemiology and biostatistics, and urology at the University of California, San Francisco.
The study evaluated the effect of surgery on urinary incontinence in 1,565 severely obese women who were part of the multicenter Longitudinal Cohort Study of Bariatric Surgery-2 and had completed self-administered questionnaires about urinary incontinence episodes before surgery and at one or more annual follow-up assessments within 3 years of surgery.
The results were based on outcomes of the 772 women who reported experiencing episodes of incontinence at least weekly, with an average of about 11 incontinence episodes per week. Their median age was 46 years and most were white; about 7% had undergone previous incontinence surgery and about 8% had received or were receiving behavioral treatment or medication for incontinence.
Most of the patients underwent a Roux-en-Y gastric bypass (71%) or laparoscopic adjustable gastric banding (25%). After the first year, they had lost a median of about 30% of their baseline weight, which was maintained through the third year.
At all follow-up times after surgery, there were significantly fewer incontinence episodes, compared with baseline, with a remission rate of 60%-65%, Dr. Subak said.
Urinary incontinence episodes dropped from an average of about 11 episodes per week before surgery to an average of almost 3 episodes per week at 1 year and 4 episodes per week at 2 and 3 years, she noted. Episodes of stress incontinence also decreased from an average of about 5 episodes per week at baseline to about 1 episode per week at 1 year and almost 2 episodes per week at 2 and 3 years.
The remission rate – defined as less than 1 weekly urinary incontinence episode over the past 3 months – was 70% at 1 year, dropping to and stabilizing at about 61%-62% at 2 and 3 years. Moreover, 25% of the women had a complete remission (no episodes of incontinence during the past 3 months) at 3 years, a slight increase from almost 27% at 1 year, Dr. Subak said.
"The magnitude of weight loss was the strongest predictor of improvement in incontinence over time," she noted. "Incontinence and BMI [body mass index] seemed to track together, as [whenever] there’s a reduction in BMI ... there’s a reduction in urinary incontinence episode frequency."
A younger age also was significantly associated with a reduction in the frequency or a remission of urinary incontinence, while being pregnant in the previous year and having had a hysterectomy were associated with a lower likelihood of having a remission.
Dr. Subak noted that limitations of the study included the observational design and the lack of a control group, as well as the fact that data were based on self-reports.
She referred to urinary incontinence and obesity as "twin epidemics," with about a fourfold increased risk of urinary incontinence associated with obesity. About one-third of women in the United States are obese and about 70% of women with incontinence are obese, she pointed out.
The Longitudinal Cohort Study of Bariatric Surgery-2 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Subak received additional funding from the NIDDK; she had no other disclosures.
AT AUGS/IUGA 2014
No unexpected leiomyosarcomas in chart review of TVH and LAVH cases
WASHINGTON – There were no cases of unexpected leiomyosarcomas in a retrospective chart study of about 1,600 cases of vaginal or laparoscopic-assisted vaginal hysterectomies performed over a 7-year period.
In the study, the rate of endometrial adenocarcinomas was about 1 in 200, and while the overall manual vaginal morcellation rate was 19%, no uterine malignancies were morcellated, said Dr. Pedro Maldonado of the division of female pelvic medicine and reconstructive surgery at the University of Texas Southwestern Medical Center, Dallas.
The review looked at all total vaginal hysterectomy (TVH) and laparoscopic-assisted vaginal hysterectomy (LAVH) cases performed at the three main teaching hospitals of the university from July 2006 through March 2013. Malignancies known before surgery were excluded.
There were a total of 1,608 cases: 1,091 TVH and 517 LAVH procedures. The overall morcellation rate was 19%: 32% in the TVH group and 13% in the LAVH group, Dr. Maldonado reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
Among the 1,608 cases, there were no cases of leiomyosarcoma (LMS) diagnosed on pathology. There was one case of an endometrial adenosarcoma (0.06%) in a 37-year-old patient with a preoperative diagnosis of menorrhagia and fibroids, and one case of a low-grade endometrial stromal tumor (0.06%) in a 39-year-old patient also diagnosed with menorrhagia and fibroids preoperatively. Neither of these patients underwent morcellation.
Three patients (0.19%) – aged 32, 38, and 47 years – who had preoperative diagnoses of menorrhagia, fibroids, and/or anemia had a pathologic diagnosis of smooth muscle tumor of uncertain malignant potential. One of these three patients underwent morcellation.
Another 8 (0.50%) of the patients with a preoperative diagnosis of endometrial hyperplasia were diagnosed with endometrial adenocarcinoma on pathology; none of them underwent morcellation, Dr. Maldonado said.
The risk of intraperitoneal dissemination of an unexpected LMS during endoscopic power morcellation has become a major issue since the Food and Drug Administration recommended in April 2014 that the use of power morcellation during a hysterectomy or myomectomy for uterine fibroids be discouraged because of the risk of disseminating cancerous tissue and upstaging disease. The FDA estimates that about 1 in 350 women undergoing hysterectomy or myomectomy for presumed fibroids have an unsuspected uterine sarcoma and that the risk of an unsuspected LMS is about 1 in 500.
Dr. Maldonado said he had no relevant financial disclosures.
WASHINGTON – There were no cases of unexpected leiomyosarcomas in a retrospective chart study of about 1,600 cases of vaginal or laparoscopic-assisted vaginal hysterectomies performed over a 7-year period.
In the study, the rate of endometrial adenocarcinomas was about 1 in 200, and while the overall manual vaginal morcellation rate was 19%, no uterine malignancies were morcellated, said Dr. Pedro Maldonado of the division of female pelvic medicine and reconstructive surgery at the University of Texas Southwestern Medical Center, Dallas.
The review looked at all total vaginal hysterectomy (TVH) and laparoscopic-assisted vaginal hysterectomy (LAVH) cases performed at the three main teaching hospitals of the university from July 2006 through March 2013. Malignancies known before surgery were excluded.
There were a total of 1,608 cases: 1,091 TVH and 517 LAVH procedures. The overall morcellation rate was 19%: 32% in the TVH group and 13% in the LAVH group, Dr. Maldonado reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
Among the 1,608 cases, there were no cases of leiomyosarcoma (LMS) diagnosed on pathology. There was one case of an endometrial adenosarcoma (0.06%) in a 37-year-old patient with a preoperative diagnosis of menorrhagia and fibroids, and one case of a low-grade endometrial stromal tumor (0.06%) in a 39-year-old patient also diagnosed with menorrhagia and fibroids preoperatively. Neither of these patients underwent morcellation.
Three patients (0.19%) – aged 32, 38, and 47 years – who had preoperative diagnoses of menorrhagia, fibroids, and/or anemia had a pathologic diagnosis of smooth muscle tumor of uncertain malignant potential. One of these three patients underwent morcellation.
Another 8 (0.50%) of the patients with a preoperative diagnosis of endometrial hyperplasia were diagnosed with endometrial adenocarcinoma on pathology; none of them underwent morcellation, Dr. Maldonado said.
The risk of intraperitoneal dissemination of an unexpected LMS during endoscopic power morcellation has become a major issue since the Food and Drug Administration recommended in April 2014 that the use of power morcellation during a hysterectomy or myomectomy for uterine fibroids be discouraged because of the risk of disseminating cancerous tissue and upstaging disease. The FDA estimates that about 1 in 350 women undergoing hysterectomy or myomectomy for presumed fibroids have an unsuspected uterine sarcoma and that the risk of an unsuspected LMS is about 1 in 500.
Dr. Maldonado said he had no relevant financial disclosures.
WASHINGTON – There were no cases of unexpected leiomyosarcomas in a retrospective chart study of about 1,600 cases of vaginal or laparoscopic-assisted vaginal hysterectomies performed over a 7-year period.
In the study, the rate of endometrial adenocarcinomas was about 1 in 200, and while the overall manual vaginal morcellation rate was 19%, no uterine malignancies were morcellated, said Dr. Pedro Maldonado of the division of female pelvic medicine and reconstructive surgery at the University of Texas Southwestern Medical Center, Dallas.
The review looked at all total vaginal hysterectomy (TVH) and laparoscopic-assisted vaginal hysterectomy (LAVH) cases performed at the three main teaching hospitals of the university from July 2006 through March 2013. Malignancies known before surgery were excluded.
There were a total of 1,608 cases: 1,091 TVH and 517 LAVH procedures. The overall morcellation rate was 19%: 32% in the TVH group and 13% in the LAVH group, Dr. Maldonado reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
Among the 1,608 cases, there were no cases of leiomyosarcoma (LMS) diagnosed on pathology. There was one case of an endometrial adenosarcoma (0.06%) in a 37-year-old patient with a preoperative diagnosis of menorrhagia and fibroids, and one case of a low-grade endometrial stromal tumor (0.06%) in a 39-year-old patient also diagnosed with menorrhagia and fibroids preoperatively. Neither of these patients underwent morcellation.
Three patients (0.19%) – aged 32, 38, and 47 years – who had preoperative diagnoses of menorrhagia, fibroids, and/or anemia had a pathologic diagnosis of smooth muscle tumor of uncertain malignant potential. One of these three patients underwent morcellation.
Another 8 (0.50%) of the patients with a preoperative diagnosis of endometrial hyperplasia were diagnosed with endometrial adenocarcinoma on pathology; none of them underwent morcellation, Dr. Maldonado said.
The risk of intraperitoneal dissemination of an unexpected LMS during endoscopic power morcellation has become a major issue since the Food and Drug Administration recommended in April 2014 that the use of power morcellation during a hysterectomy or myomectomy for uterine fibroids be discouraged because of the risk of disseminating cancerous tissue and upstaging disease. The FDA estimates that about 1 in 350 women undergoing hysterectomy or myomectomy for presumed fibroids have an unsuspected uterine sarcoma and that the risk of an unsuspected LMS is about 1 in 500.
Dr. Maldonado said he had no relevant financial disclosures.
AT AUGS/IUGA 2014
Key clinical point: This study provides another estimate of the rate of unexpected leiomyosarcomas in women undergoing hysterectomy for presumably benign conditions, an issue that is currently under FDA review because of heightened concerns over the risk of spreading malignancies if morcellation also is performed during these procedures.
Major finding: There were no unexpected leiomyosarcomas, and no uterine malignancies were morcellated in a series of 1,608 cases of vaginal or laparoscopic-assisted vaginal hysterectomies performed for presumably benign conditions over a 7-year period
Data source: A retrospective study of 1,608 cases of TVH or LAVH performed over 7 years at three teaching hospitals that looked at the rate of unexpected uterine malignancies and cases of malignancies that were morcellated.
Disclosures: Dr. Maldonado said he had no disclosures.
Disposable, self-administered new anal insert device effective for anal leakage
WASHINGTON – A single-use, self-administered anal insert made of soft silicone was effective and safe in reducing episodes of accidental bowel leakage, in a multi-center, prospective open-label single-arm study, Dr. Emily Lukacz reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
The device provides a nonsurgical option for managing accidental bowel leakage (ABL), as an alternative or as an adjunct to invasive therapy, said Dr. Lukacz, professor of clinical reproductive medicine at the University of California, San Diego.
The device is designed to prevent leakage of solid and liquid stool, and is expelled with each bowel movement and subsequently replaced. The manufacturer, Renew Medical, hopes to make it available by the end of 2014 and is negotiating with the Centers for Medicare & Medicaid Services for coverage, she noted.
The study enrolled 91 people with moderate to severe bowel incontinence, who experienced at least weekly leakage of solid and/or liquid stool, with a Wexner severity score of 12 or greater (ranging from 0, fully continent, to 20, full incontinence); most were female (90%) and white (91%); their mean age was almost 69 years. Seven participants withdrew because they were not satisfied with the device.
Among the 85 participants who completed at least 1 week of treatment, the frequency of ABL dropped from eight episodes per week at baseline to one-two episodes per week at 12 weeks, an 82% reduction that was statistically significant (P less than or equal to .001), Dr. Lukacz said. Of the 85 participants, 78% experienced at least a 50% reduction in ABL frequency, and 8 (9%) achieved total continence.
The mean Wexner scores improved by about 32% after treatment, from about 16 to about 11, which was also statistically significant (P less than or equal to .001). Of the 73 who completed the full 12 weeks of the study, 57 (78%) were "very or extremely satisfied with the device," Dr. Lukacz noted.
There were no serious adverse events. The three moderate adverse events were fecal urgency, soreness, and bleeding related to the use of the insert in two participants. Almost one-quarter of the patients had episodes where the device was displaced "upward into the anal canal," but was expelled with the next bowel movement, she said.
Dr. Lukacz’s disclosures included being a paid consultant to Pfizer and Renew Medical. The study was sponsored by Renew.
WASHINGTON – A single-use, self-administered anal insert made of soft silicone was effective and safe in reducing episodes of accidental bowel leakage, in a multi-center, prospective open-label single-arm study, Dr. Emily Lukacz reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
The device provides a nonsurgical option for managing accidental bowel leakage (ABL), as an alternative or as an adjunct to invasive therapy, said Dr. Lukacz, professor of clinical reproductive medicine at the University of California, San Diego.
The device is designed to prevent leakage of solid and liquid stool, and is expelled with each bowel movement and subsequently replaced. The manufacturer, Renew Medical, hopes to make it available by the end of 2014 and is negotiating with the Centers for Medicare & Medicaid Services for coverage, she noted.
The study enrolled 91 people with moderate to severe bowel incontinence, who experienced at least weekly leakage of solid and/or liquid stool, with a Wexner severity score of 12 or greater (ranging from 0, fully continent, to 20, full incontinence); most were female (90%) and white (91%); their mean age was almost 69 years. Seven participants withdrew because they were not satisfied with the device.
Among the 85 participants who completed at least 1 week of treatment, the frequency of ABL dropped from eight episodes per week at baseline to one-two episodes per week at 12 weeks, an 82% reduction that was statistically significant (P less than or equal to .001), Dr. Lukacz said. Of the 85 participants, 78% experienced at least a 50% reduction in ABL frequency, and 8 (9%) achieved total continence.
The mean Wexner scores improved by about 32% after treatment, from about 16 to about 11, which was also statistically significant (P less than or equal to .001). Of the 73 who completed the full 12 weeks of the study, 57 (78%) were "very or extremely satisfied with the device," Dr. Lukacz noted.
There were no serious adverse events. The three moderate adverse events were fecal urgency, soreness, and bleeding related to the use of the insert in two participants. Almost one-quarter of the patients had episodes where the device was displaced "upward into the anal canal," but was expelled with the next bowel movement, she said.
Dr. Lukacz’s disclosures included being a paid consultant to Pfizer and Renew Medical. The study was sponsored by Renew.
WASHINGTON – A single-use, self-administered anal insert made of soft silicone was effective and safe in reducing episodes of accidental bowel leakage, in a multi-center, prospective open-label single-arm study, Dr. Emily Lukacz reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
The device provides a nonsurgical option for managing accidental bowel leakage (ABL), as an alternative or as an adjunct to invasive therapy, said Dr. Lukacz, professor of clinical reproductive medicine at the University of California, San Diego.
The device is designed to prevent leakage of solid and liquid stool, and is expelled with each bowel movement and subsequently replaced. The manufacturer, Renew Medical, hopes to make it available by the end of 2014 and is negotiating with the Centers for Medicare & Medicaid Services for coverage, she noted.
The study enrolled 91 people with moderate to severe bowel incontinence, who experienced at least weekly leakage of solid and/or liquid stool, with a Wexner severity score of 12 or greater (ranging from 0, fully continent, to 20, full incontinence); most were female (90%) and white (91%); their mean age was almost 69 years. Seven participants withdrew because they were not satisfied with the device.
Among the 85 participants who completed at least 1 week of treatment, the frequency of ABL dropped from eight episodes per week at baseline to one-two episodes per week at 12 weeks, an 82% reduction that was statistically significant (P less than or equal to .001), Dr. Lukacz said. Of the 85 participants, 78% experienced at least a 50% reduction in ABL frequency, and 8 (9%) achieved total continence.
The mean Wexner scores improved by about 32% after treatment, from about 16 to about 11, which was also statistically significant (P less than or equal to .001). Of the 73 who completed the full 12 weeks of the study, 57 (78%) were "very or extremely satisfied with the device," Dr. Lukacz noted.
There were no serious adverse events. The three moderate adverse events were fecal urgency, soreness, and bleeding related to the use of the insert in two participants. Almost one-quarter of the patients had episodes where the device was displaced "upward into the anal canal," but was expelled with the next bowel movement, she said.
Dr. Lukacz’s disclosures included being a paid consultant to Pfizer and Renew Medical. The study was sponsored by Renew.
AT AUGS/IUGA 2014
Major finding: Once available, this soft silicone, self-administered anal insert could be an effective, safe alternative or adjunct to invasive treatment of accidental bowel leakage (ABL).
Key numerical finding: The frequency of ABL dropped by 82% after 12 weeks of using the anal insert, from 8 weekly episodes at baseline to 1-2 episodes per week.
Data source: A multicenter, prospective, open-label, single-arm study evaluated the effect of the device on the reduction of ABL episodes per week and severity of ABL over 12 weeks in 91 mostly female, white patients with moderate to severe anal leakage at baseline.
Disclosures: Dr. Lukacz’s disclosures included being a paid consultant to Pfizer and Renew Medical, the manufacturer of the anal insert. The study was sponsored by Renew.
Successful bariatric surgery also may improve urinary incontinence
WASHINGTON – The majority of obese women who had urinary incontinence before bariatric surgery had complete or near-complete resolution of symptoms for up to 3 years after surgery in a study of more than 1,500 women, Dr. Leslee Subak reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
These results indicate that "improvement in incontinence may be another long-term benefit of weight loss, in this case surgical weight loss," said Dr. Subak, professor of obstetrics and gynecology and reproductive sciences, epidemiology and biostatistics, and urology at the University of California, San Francisco.
The study evaluated the effect of surgery on urinary incontinence in 1,565 severely obese women who were part of the multicenter Longitudinal Cohort Study of Bariatric Surgery-2 and had completed self-administered questionnaires about urinary incontinence episodes before surgery and at one or more annual follow-up assessments within 3 years of surgery.
The results were based on outcomes of the 772 women who reported experiencing episodes of incontinence at least weekly, with an average of about 11 incontinence episodes per week. Their median age was 46 years and most were white; about 7% had undergone previous incontinence surgery and about 8% had received or were receiving behavioral treatment or medication for incontinence.
Most of the patients underwent a Roux-en-Y gastric bypass (71%) or laparoscopic adjustable gastric banding (25%). After the first year, they had lost a median of about 30% of their baseline weight, which was maintained through the third year.
At all follow-up times after surgery, there were significantly fewer incontinence episodes, compared with baseline, with a remission rate of 60%-65%, Dr. Subak said.
Urinary incontinence episodes dropped from an average of about 11 episodes per week before surgery to an average of almost 3 episodes per week at 1 year and 4 episodes per week at 2 and 3 years, she noted. Episodes of stress incontinence also decreased from an average of about 5 episodes per week at baseline to about 1 episode per week at 1 year and almost 2 episodes per week at 2 and 3 years.
The remission rate – defined as less than 1 weekly urinary incontinence episode over the past 3 months – was 70% at 1 year, dropping to and stabilizing at about 61%-62% at 2 and 3 years. Moreover, 25% of the women had a complete remission (no episodes of incontinence during the past 3 months) at 3 years, a slight increase from almost 27% at 1 year, Dr. Subak said.
"The magnitude of weight loss was the strongest predictor of improvement in incontinence over time," she noted. "Incontinence and BMI [body mass index] seemed to track together, as [whenever] there’s a reduction in BMI ... there’s a reduction in urinary incontinence episode frequency."
A younger age also was significantly associated with a reduction in the frequency or a remission of urinary incontinence, while being pregnant in the previous year and having had a hysterectomy were associated with a lower likelihood of having a remission.
Dr. Subak noted that limitations of the study included the observational design and the lack of a control group, as well as the fact that data were based on self-reports.
She referred to urinary incontinence and obesity as "twin epidemics," with about a fourfold increased risk of urinary incontinence associated with obesity. About one-third of women in the United States are obese and about 70% of women with incontinence are obese, she pointed out.
The Longitudinal Cohort Study of Bariatric Surgery-2 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Subak received additional funding from the NIDDK; she had no other disclosures.
WASHINGTON – The majority of obese women who had urinary incontinence before bariatric surgery had complete or near-complete resolution of symptoms for up to 3 years after surgery in a study of more than 1,500 women, Dr. Leslee Subak reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
These results indicate that "improvement in incontinence may be another long-term benefit of weight loss, in this case surgical weight loss," said Dr. Subak, professor of obstetrics and gynecology and reproductive sciences, epidemiology and biostatistics, and urology at the University of California, San Francisco.
The study evaluated the effect of surgery on urinary incontinence in 1,565 severely obese women who were part of the multicenter Longitudinal Cohort Study of Bariatric Surgery-2 and had completed self-administered questionnaires about urinary incontinence episodes before surgery and at one or more annual follow-up assessments within 3 years of surgery.
The results were based on outcomes of the 772 women who reported experiencing episodes of incontinence at least weekly, with an average of about 11 incontinence episodes per week. Their median age was 46 years and most were white; about 7% had undergone previous incontinence surgery and about 8% had received or were receiving behavioral treatment or medication for incontinence.
Most of the patients underwent a Roux-en-Y gastric bypass (71%) or laparoscopic adjustable gastric banding (25%). After the first year, they had lost a median of about 30% of their baseline weight, which was maintained through the third year.
At all follow-up times after surgery, there were significantly fewer incontinence episodes, compared with baseline, with a remission rate of 60%-65%, Dr. Subak said.
Urinary incontinence episodes dropped from an average of about 11 episodes per week before surgery to an average of almost 3 episodes per week at 1 year and 4 episodes per week at 2 and 3 years, she noted. Episodes of stress incontinence also decreased from an average of about 5 episodes per week at baseline to about 1 episode per week at 1 year and almost 2 episodes per week at 2 and 3 years.
The remission rate – defined as less than 1 weekly urinary incontinence episode over the past 3 months – was 70% at 1 year, dropping to and stabilizing at about 61%-62% at 2 and 3 years. Moreover, 25% of the women had a complete remission (no episodes of incontinence during the past 3 months) at 3 years, a slight increase from almost 27% at 1 year, Dr. Subak said.
"The magnitude of weight loss was the strongest predictor of improvement in incontinence over time," she noted. "Incontinence and BMI [body mass index] seemed to track together, as [whenever] there’s a reduction in BMI ... there’s a reduction in urinary incontinence episode frequency."
A younger age also was significantly associated with a reduction in the frequency or a remission of urinary incontinence, while being pregnant in the previous year and having had a hysterectomy were associated with a lower likelihood of having a remission.
Dr. Subak noted that limitations of the study included the observational design and the lack of a control group, as well as the fact that data were based on self-reports.
She referred to urinary incontinence and obesity as "twin epidemics," with about a fourfold increased risk of urinary incontinence associated with obesity. About one-third of women in the United States are obese and about 70% of women with incontinence are obese, she pointed out.
The Longitudinal Cohort Study of Bariatric Surgery-2 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Subak received additional funding from the NIDDK; she had no other disclosures.
WASHINGTON – The majority of obese women who had urinary incontinence before bariatric surgery had complete or near-complete resolution of symptoms for up to 3 years after surgery in a study of more than 1,500 women, Dr. Leslee Subak reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
These results indicate that "improvement in incontinence may be another long-term benefit of weight loss, in this case surgical weight loss," said Dr. Subak, professor of obstetrics and gynecology and reproductive sciences, epidemiology and biostatistics, and urology at the University of California, San Francisco.
The study evaluated the effect of surgery on urinary incontinence in 1,565 severely obese women who were part of the multicenter Longitudinal Cohort Study of Bariatric Surgery-2 and had completed self-administered questionnaires about urinary incontinence episodes before surgery and at one or more annual follow-up assessments within 3 years of surgery.
The results were based on outcomes of the 772 women who reported experiencing episodes of incontinence at least weekly, with an average of about 11 incontinence episodes per week. Their median age was 46 years and most were white; about 7% had undergone previous incontinence surgery and about 8% had received or were receiving behavioral treatment or medication for incontinence.
Most of the patients underwent a Roux-en-Y gastric bypass (71%) or laparoscopic adjustable gastric banding (25%). After the first year, they had lost a median of about 30% of their baseline weight, which was maintained through the third year.
At all follow-up times after surgery, there were significantly fewer incontinence episodes, compared with baseline, with a remission rate of 60%-65%, Dr. Subak said.
Urinary incontinence episodes dropped from an average of about 11 episodes per week before surgery to an average of almost 3 episodes per week at 1 year and 4 episodes per week at 2 and 3 years, she noted. Episodes of stress incontinence also decreased from an average of about 5 episodes per week at baseline to about 1 episode per week at 1 year and almost 2 episodes per week at 2 and 3 years.
The remission rate – defined as less than 1 weekly urinary incontinence episode over the past 3 months – was 70% at 1 year, dropping to and stabilizing at about 61%-62% at 2 and 3 years. Moreover, 25% of the women had a complete remission (no episodes of incontinence during the past 3 months) at 3 years, a slight increase from almost 27% at 1 year, Dr. Subak said.
"The magnitude of weight loss was the strongest predictor of improvement in incontinence over time," she noted. "Incontinence and BMI [body mass index] seemed to track together, as [whenever] there’s a reduction in BMI ... there’s a reduction in urinary incontinence episode frequency."
A younger age also was significantly associated with a reduction in the frequency or a remission of urinary incontinence, while being pregnant in the previous year and having had a hysterectomy were associated with a lower likelihood of having a remission.
Dr. Subak noted that limitations of the study included the observational design and the lack of a control group, as well as the fact that data were based on self-reports.
She referred to urinary incontinence and obesity as "twin epidemics," with about a fourfold increased risk of urinary incontinence associated with obesity. About one-third of women in the United States are obese and about 70% of women with incontinence are obese, she pointed out.
The Longitudinal Cohort Study of Bariatric Surgery-2 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Subak received additional funding from the NIDDK; she had no other disclosures.
AT AUGS/IUGA 2014
Key clinical point: Obese women who report urinary incontinence may experience improvement or even resolution of symptoms after bariatric surgery.
Major finding: About one-quarter of the 772 severely obese women who reported having urinary incontinence before undergoing bariatric surgery had complete remission of urinary incontinence 3 years after surgery.
Data source: The frequency of urinary incontinence symptoms at baseline and for up to 3 years after bariatric surgery was evaluated in a substudy of 1,565 severely obese women who were enrolled in a multicenter, longitudinal cohort study based on self-administered questionnaires.
Disclosures: The Longitudinal Cohort Study of Bariatric Surgery-2 is funded by the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Subak received additional funding from the NIDDK; she had no other disclosures.
Bariatric Surgery Results may Include Improved Sexual Function for Female Patients
WASHINGTON – Obese women experienced significant improvements in sexual function over 6-24 months after bariatric surgery in a multistudy review, indicating that this outcome should be listed among the possible benefits of surgery in this patient population, Dr. Kalaivani Ramalingam said at a joint annual meeting of the American Urogynecologic Society.
In a review of studies published between 1996 and 2013, Dr. Ramalingam of the department of gynecology at Kingston Hospital, Kingston upon Thames, England, and her associates identified five original studies of 254 obese women undergoing bariatric surgery that reported Female Sexual Function Index (FSFI) scores before and after surgery. Studies of nonsurgical weight loss treatments and those that included both men and women were not included. The FSFI evaluates sexual function in six domains: desire, arousal, lubrication, orgasm, satisfaction, and pain.
Patients in the studies had statistically significant reductions in body mass index over 6-24 months of follow-up (P = .001). In one of the five studies, which enrolled 36 patients, FSFI scores did not improve after surgery.
But in the remaining four studies, there were statistically significant improvements in the overall FSFI scores after surgery (P = .003), Dr. Ramalingam said. In addition, statistically significant improvements in all domains of the score were observed after surgery: increased desire (P = .005), arousal (P = .001), lubrication (P = .003), satisfaction (P = .012) and orgasm (P =.003) – and a decrease in the levels of pain during intercourse (P = .014).
She noted that in one of the five studies, sexual function improved in women with pelvic floor dysfunction and that further studies in this specific group of patients are needed to evaluate the effect of surgery among obese women who are undergoing bariatric surgery and have pelvic floor dysfunction.
An estimated 51% of female bariatric surgery patients report sexual dysfunction, she said.
Dr. Ramalingam and one of her coauthors had no relevant disclosures. The third author disclosed being a speaker for and receiving honoraria from Pfizer, Astellas, and Shire; and serving on an advisory committee for Allergan.
WASHINGTON – Obese women experienced significant improvements in sexual function over 6-24 months after bariatric surgery in a multistudy review, indicating that this outcome should be listed among the possible benefits of surgery in this patient population, Dr. Kalaivani Ramalingam said at a joint annual meeting of the American Urogynecologic Society.
In a review of studies published between 1996 and 2013, Dr. Ramalingam of the department of gynecology at Kingston Hospital, Kingston upon Thames, England, and her associates identified five original studies of 254 obese women undergoing bariatric surgery that reported Female Sexual Function Index (FSFI) scores before and after surgery. Studies of nonsurgical weight loss treatments and those that included both men and women were not included. The FSFI evaluates sexual function in six domains: desire, arousal, lubrication, orgasm, satisfaction, and pain.
Patients in the studies had statistically significant reductions in body mass index over 6-24 months of follow-up (P = .001). In one of the five studies, which enrolled 36 patients, FSFI scores did not improve after surgery.
But in the remaining four studies, there were statistically significant improvements in the overall FSFI scores after surgery (P = .003), Dr. Ramalingam said. In addition, statistically significant improvements in all domains of the score were observed after surgery: increased desire (P = .005), arousal (P = .001), lubrication (P = .003), satisfaction (P = .012) and orgasm (P =.003) – and a decrease in the levels of pain during intercourse (P = .014).
She noted that in one of the five studies, sexual function improved in women with pelvic floor dysfunction and that further studies in this specific group of patients are needed to evaluate the effect of surgery among obese women who are undergoing bariatric surgery and have pelvic floor dysfunction.
An estimated 51% of female bariatric surgery patients report sexual dysfunction, she said.
Dr. Ramalingam and one of her coauthors had no relevant disclosures. The third author disclosed being a speaker for and receiving honoraria from Pfizer, Astellas, and Shire; and serving on an advisory committee for Allergan.
WASHINGTON – Obese women experienced significant improvements in sexual function over 6-24 months after bariatric surgery in a multistudy review, indicating that this outcome should be listed among the possible benefits of surgery in this patient population, Dr. Kalaivani Ramalingam said at a joint annual meeting of the American Urogynecologic Society.
In a review of studies published between 1996 and 2013, Dr. Ramalingam of the department of gynecology at Kingston Hospital, Kingston upon Thames, England, and her associates identified five original studies of 254 obese women undergoing bariatric surgery that reported Female Sexual Function Index (FSFI) scores before and after surgery. Studies of nonsurgical weight loss treatments and those that included both men and women were not included. The FSFI evaluates sexual function in six domains: desire, arousal, lubrication, orgasm, satisfaction, and pain.
Patients in the studies had statistically significant reductions in body mass index over 6-24 months of follow-up (P = .001). In one of the five studies, which enrolled 36 patients, FSFI scores did not improve after surgery.
But in the remaining four studies, there were statistically significant improvements in the overall FSFI scores after surgery (P = .003), Dr. Ramalingam said. In addition, statistically significant improvements in all domains of the score were observed after surgery: increased desire (P = .005), arousal (P = .001), lubrication (P = .003), satisfaction (P = .012) and orgasm (P =.003) – and a decrease in the levels of pain during intercourse (P = .014).
She noted that in one of the five studies, sexual function improved in women with pelvic floor dysfunction and that further studies in this specific group of patients are needed to evaluate the effect of surgery among obese women who are undergoing bariatric surgery and have pelvic floor dysfunction.
An estimated 51% of female bariatric surgery patients report sexual dysfunction, she said.
Dr. Ramalingam and one of her coauthors had no relevant disclosures. The third author disclosed being a speaker for and receiving honoraria from Pfizer, Astellas, and Shire; and serving on an advisory committee for Allergan.
AT THE AUGS ANNUAL MEETING
Women Are Not Seeking Care for Urinary Incontinence
WASHINGTON – Women are not seeking care for even moderate to severe urinary incontinence because they have a fear of treatment and lack knowledge of the etiology of the condition and available treatment options, according to a qualitative focus group study at Kaiser Permanente Orange County (Calif.).
Embarrassment is another barrier. So are physicians themselves, said Dr. Jennifer K. Lee, a urogynecologist at Kaiser in Anaheim, Calif., who reported the findings at the annual meeting of the American Urogynecologic Society.
"Providers were mentioned (in the focus groups) to be barriers," Dr. Lee said. "Patients were either dismissed, or they were given misinformation."
By 2050, an estimated 50 million Americans will have urinary incontinence. Previous research has shown, however, that less than 50% of women with moderate incontinence seek care.
The focus group study involved 19 women – 11 who had not sought care but were found after recruitment to have moderate to severe incontinence by the Sandvik severity index, and 8 who had previous treatment or had been evaluated for urinary incontinence.
A moderator led discussions among small groups of these women, all of whom were fluent in English and most of whom (90%) had a college education or higher. The participants were of varying ethnicities, including Caucasian, Hispanic, and Asian.
A fear of medical or surgical treatment, including medication side effects and recovery time for surgery, was one of the themes to emerge. Women also said they felt embarrassed and were therefore not likely to raise the issue, particularly with time constraints in their medical visits.
There was a prevailing idea that urinary incontinence is a normal part of aging or childbearing, or that it is hereditary, and that other health issues take priority. Physicians, moreover, did not ask about the issue, and in cases in which it was mentioned, physicians were dismissive or gave misinformation, the study showed.
Dr. Lee said the barriers are significant, and that "there’s a lot of work to be done" to facilitate communication and change practices.
Leaders at Kaiser Permanente Orange County, Anaheim, Calif., plan to give physicians question prompts to incorporate into routine and primary care visits, she noted during a press conference at the meeting. "We also want to work on educational tools for the public," she said.
"There are urinary incontinence questions [for] the Medicare wellness visit, but these are for women over 65," she said. "There certainly are plenty of women under 65 who have incontinence."
Food and Drug Administration warnings about complications associated with transvaginal placement of surgical mesh did not come up in the focus group discussions, but Dr. Lee said that in her practice she has seen this controversy feed patients’ fear of incontinence and its treatment.
Study participants were recruited through e-mail research announcements and flyers, as well as more actively through the offices of urogynecology providers.
Dr. Lee said she had no disclosures to report. Her coauthors and research colleagues at the University of California, Irvine, reported numerous disclosures ranging from speakers’ bureau participation and consulting fees at Hospira and Cadence Pharmaceuticals to consultant positions with Medtronic and Boston Scientific.
WASHINGTON – Women are not seeking care for even moderate to severe urinary incontinence because they have a fear of treatment and lack knowledge of the etiology of the condition and available treatment options, according to a qualitative focus group study at Kaiser Permanente Orange County (Calif.).
Embarrassment is another barrier. So are physicians themselves, said Dr. Jennifer K. Lee, a urogynecologist at Kaiser in Anaheim, Calif., who reported the findings at the annual meeting of the American Urogynecologic Society.
"Providers were mentioned (in the focus groups) to be barriers," Dr. Lee said. "Patients were either dismissed, or they were given misinformation."
By 2050, an estimated 50 million Americans will have urinary incontinence. Previous research has shown, however, that less than 50% of women with moderate incontinence seek care.
The focus group study involved 19 women – 11 who had not sought care but were found after recruitment to have moderate to severe incontinence by the Sandvik severity index, and 8 who had previous treatment or had been evaluated for urinary incontinence.
A moderator led discussions among small groups of these women, all of whom were fluent in English and most of whom (90%) had a college education or higher. The participants were of varying ethnicities, including Caucasian, Hispanic, and Asian.
A fear of medical or surgical treatment, including medication side effects and recovery time for surgery, was one of the themes to emerge. Women also said they felt embarrassed and were therefore not likely to raise the issue, particularly with time constraints in their medical visits.
There was a prevailing idea that urinary incontinence is a normal part of aging or childbearing, or that it is hereditary, and that other health issues take priority. Physicians, moreover, did not ask about the issue, and in cases in which it was mentioned, physicians were dismissive or gave misinformation, the study showed.
Dr. Lee said the barriers are significant, and that "there’s a lot of work to be done" to facilitate communication and change practices.
Leaders at Kaiser Permanente Orange County, Anaheim, Calif., plan to give physicians question prompts to incorporate into routine and primary care visits, she noted during a press conference at the meeting. "We also want to work on educational tools for the public," she said.
"There are urinary incontinence questions [for] the Medicare wellness visit, but these are for women over 65," she said. "There certainly are plenty of women under 65 who have incontinence."
Food and Drug Administration warnings about complications associated with transvaginal placement of surgical mesh did not come up in the focus group discussions, but Dr. Lee said that in her practice she has seen this controversy feed patients’ fear of incontinence and its treatment.
Study participants were recruited through e-mail research announcements and flyers, as well as more actively through the offices of urogynecology providers.
Dr. Lee said she had no disclosures to report. Her coauthors and research colleagues at the University of California, Irvine, reported numerous disclosures ranging from speakers’ bureau participation and consulting fees at Hospira and Cadence Pharmaceuticals to consultant positions with Medtronic and Boston Scientific.
WASHINGTON – Women are not seeking care for even moderate to severe urinary incontinence because they have a fear of treatment and lack knowledge of the etiology of the condition and available treatment options, according to a qualitative focus group study at Kaiser Permanente Orange County (Calif.).
Embarrassment is another barrier. So are physicians themselves, said Dr. Jennifer K. Lee, a urogynecologist at Kaiser in Anaheim, Calif., who reported the findings at the annual meeting of the American Urogynecologic Society.
"Providers were mentioned (in the focus groups) to be barriers," Dr. Lee said. "Patients were either dismissed, or they were given misinformation."
By 2050, an estimated 50 million Americans will have urinary incontinence. Previous research has shown, however, that less than 50% of women with moderate incontinence seek care.
The focus group study involved 19 women – 11 who had not sought care but were found after recruitment to have moderate to severe incontinence by the Sandvik severity index, and 8 who had previous treatment or had been evaluated for urinary incontinence.
A moderator led discussions among small groups of these women, all of whom were fluent in English and most of whom (90%) had a college education or higher. The participants were of varying ethnicities, including Caucasian, Hispanic, and Asian.
A fear of medical or surgical treatment, including medication side effects and recovery time for surgery, was one of the themes to emerge. Women also said they felt embarrassed and were therefore not likely to raise the issue, particularly with time constraints in their medical visits.
There was a prevailing idea that urinary incontinence is a normal part of aging or childbearing, or that it is hereditary, and that other health issues take priority. Physicians, moreover, did not ask about the issue, and in cases in which it was mentioned, physicians were dismissive or gave misinformation, the study showed.
Dr. Lee said the barriers are significant, and that "there’s a lot of work to be done" to facilitate communication and change practices.
Leaders at Kaiser Permanente Orange County, Anaheim, Calif., plan to give physicians question prompts to incorporate into routine and primary care visits, she noted during a press conference at the meeting. "We also want to work on educational tools for the public," she said.
"There are urinary incontinence questions [for] the Medicare wellness visit, but these are for women over 65," she said. "There certainly are plenty of women under 65 who have incontinence."
Food and Drug Administration warnings about complications associated with transvaginal placement of surgical mesh did not come up in the focus group discussions, but Dr. Lee said that in her practice she has seen this controversy feed patients’ fear of incontinence and its treatment.
Study participants were recruited through e-mail research announcements and flyers, as well as more actively through the offices of urogynecology providers.
Dr. Lee said she had no disclosures to report. Her coauthors and research colleagues at the University of California, Irvine, reported numerous disclosures ranging from speakers’ bureau participation and consulting fees at Hospira and Cadence Pharmaceuticals to consultant positions with Medtronic and Boston Scientific.
AT THE AUGS ANNUAL MEETING
Mediolateral episiotomy shines in 10-year Netherlands analysis
WASHINGTON – The use of mediolateral episiotomy in women undergoing operative vaginal delivery – a common practice in the Netherlands – was associated with a large reduction in the risk of obstetrical anal sphincter injuries, according to an analysis of 10 years of data from the Netherlands Perinatal Registry.
For physicians and other obstetrical providers in the small European country, the findings reinforce current practice of favoring mediolateral episiotomies in operative vaginal deliveries as protection against obstetrical anal sphincter injuries (OASIS) – a risk factor for fecal incontinence, the investigators said.
"In the Netherlands, a mediolateral episiotomy is common practice. ... Our opinion is that the mediolateral episiotomies are causing less morbidity than an anal sphincter rupture would cause," Dr. Jeroen van Bavel reported during a press conference at the scientific meetings of the American Urogynecologic Society (AUGS) and the International Urogynecological Association.
But for physicians here in the United States, the risks are weighed differently. "It’s not that we don’t know that a mediolateral episiotomy decreases the risk of sphincter injury," Dr. Haywood Brown, professor and chair of obstetrics and gynecology at Duke University, Durham, N.C., said in a telephone interview after the conference.
"The problem is, mediolateral incisions are so uncomfortable," said Dr. Brown, who also is chair of the American College of Obstetricians and Gynecologists, District IV.
"They heal poorly, they heal with defects, ... and as a result the patient has more pain related to the mediolateral [episiotomy] than they would have with a third- or fourth-degree tear," he said. "Doing the mediolateral is really not the answer."
The Netherlands Perinatal Registry contains information on 96% of the 1.5 million deliveries that occurred during 2000-2009. Dr. van Bavel, of Amphia Hospital in Breda, the Netherlands, and his coinvestigators focused their analysis on the 170,974 women who had operative vaginal deliveries, comparing the rates of OASIS in women who had mediolateral episiotomies with those who did not.
Among primiparous women who had vacuum deliveries, OASIS occurred in 2.5% of those who had mediolateral episiotomies, compared with 14% who did not. Among multiparous women who had vacuum deliveries, OASIS rates were 2.1% with mediolateral episiotomy versus 7.5% without.
The differences were more striking with forceps deliveries. Anal sphincter injuries occurred in 3.4% versus 26.7% in primiparous women with and without mediolateral episiotomies, respectively. Among multiparous women, the risk of OASIS was 2.6% versus 14.2%.
For primiparous women, the number of mediolateral episiotomies needed to prevent one OASIS was 8 for vacuum delivery and 4 for forceps delivery, according to the analysis. For multiparous women, 18 mediolateral episiotomies were needed to prevent one OASIS for vacuum delivery, and 8 for forceps delivery.
ACOG’s Practice Bulletin No. 71 on episiotomy, which was written in 2006 (Obstet. Gynecol. 2006;107:957-62) and reaffirmed in 2013, states that median episiotomy is associated with higher rates of injury to the anal sphincter and rectum than mediolateral episiotomy (level A evidence), and that mediolateral episiotomy may be preferable in selected cases (level B evidence).
Overall, "restricted use of episiotomy is preferable to routine use of episiotomy," the guidelines say (level A evidence). Postpartum recovery, the guidelines note, is an area of obstetrics that lacks systematic study and analysis.
Dr. Brown said he stands firmly with his belief that mediolateral episiotomy as a routine prophylactic procedure in operative vaginal deliveries cannot be justified. "Having lived through an era of mediolaterals and seeing how long they take to heal, and the discomfort that patients have, I can’t justify it," he said.
"We’ve moved away from episiotomies [in the United States], period," he said. "We’ve moved away from them primarily because of the data showing that midline episiotomies increase the risk of sphincter injury. And the mediolateral episiotomies are just too painful."
The risk of OASIS can be minimized through good delivery technique, he noted.
"The trend here is toward more vacuum deliveries, which have [been shown to be less risky] than forceps deliveries, although its depends on the type of forceps used and the skill of the [obstetrician]," Dr. Brown said. "The challenge we face is that we don’t have enough forceps and vacuum deliveries to easily keep skill levels up."
Dr. Charles W. Nager, president of AUGS and director the urogynecological and reconstructive pelvic surgery division at the University of California, San Diego, said that rates of both episiotomy and operative vaginal delivery have been declining in the United States, and that simultaneously, "there’s been a parallel drop in OASIS."
There also is more training ongoing in U.S. hospitals on repairing third- and fourth-degree obstetric lacerations, he said in an interview at the meeting.
The Netherlands analysis excluded women with preterm delivery, stillbirth, multiple gestation, transverse position, and breech delivery, as well as women whose deliveries involved both forceps and vacuum and women who had a midline episiotomy.
Factors controlled for in the study included parity, fetal position, birth weight, augmentation with oxytocin, and duration of the second stage of labor.
Dr. van Bavel and all but one of his coinvestigators reported no disclosures.
WASHINGTON – The use of mediolateral episiotomy in women undergoing operative vaginal delivery – a common practice in the Netherlands – was associated with a large reduction in the risk of obstetrical anal sphincter injuries, according to an analysis of 10 years of data from the Netherlands Perinatal Registry.
For physicians and other obstetrical providers in the small European country, the findings reinforce current practice of favoring mediolateral episiotomies in operative vaginal deliveries as protection against obstetrical anal sphincter injuries (OASIS) – a risk factor for fecal incontinence, the investigators said.
"In the Netherlands, a mediolateral episiotomy is common practice. ... Our opinion is that the mediolateral episiotomies are causing less morbidity than an anal sphincter rupture would cause," Dr. Jeroen van Bavel reported during a press conference at the scientific meetings of the American Urogynecologic Society (AUGS) and the International Urogynecological Association.
But for physicians here in the United States, the risks are weighed differently. "It’s not that we don’t know that a mediolateral episiotomy decreases the risk of sphincter injury," Dr. Haywood Brown, professor and chair of obstetrics and gynecology at Duke University, Durham, N.C., said in a telephone interview after the conference.
"The problem is, mediolateral incisions are so uncomfortable," said Dr. Brown, who also is chair of the American College of Obstetricians and Gynecologists, District IV.
"They heal poorly, they heal with defects, ... and as a result the patient has more pain related to the mediolateral [episiotomy] than they would have with a third- or fourth-degree tear," he said. "Doing the mediolateral is really not the answer."
The Netherlands Perinatal Registry contains information on 96% of the 1.5 million deliveries that occurred during 2000-2009. Dr. van Bavel, of Amphia Hospital in Breda, the Netherlands, and his coinvestigators focused their analysis on the 170,974 women who had operative vaginal deliveries, comparing the rates of OASIS in women who had mediolateral episiotomies with those who did not.
Among primiparous women who had vacuum deliveries, OASIS occurred in 2.5% of those who had mediolateral episiotomies, compared with 14% who did not. Among multiparous women who had vacuum deliveries, OASIS rates were 2.1% with mediolateral episiotomy versus 7.5% without.
The differences were more striking with forceps deliveries. Anal sphincter injuries occurred in 3.4% versus 26.7% in primiparous women with and without mediolateral episiotomies, respectively. Among multiparous women, the risk of OASIS was 2.6% versus 14.2%.
For primiparous women, the number of mediolateral episiotomies needed to prevent one OASIS was 8 for vacuum delivery and 4 for forceps delivery, according to the analysis. For multiparous women, 18 mediolateral episiotomies were needed to prevent one OASIS for vacuum delivery, and 8 for forceps delivery.
ACOG’s Practice Bulletin No. 71 on episiotomy, which was written in 2006 (Obstet. Gynecol. 2006;107:957-62) and reaffirmed in 2013, states that median episiotomy is associated with higher rates of injury to the anal sphincter and rectum than mediolateral episiotomy (level A evidence), and that mediolateral episiotomy may be preferable in selected cases (level B evidence).
Overall, "restricted use of episiotomy is preferable to routine use of episiotomy," the guidelines say (level A evidence). Postpartum recovery, the guidelines note, is an area of obstetrics that lacks systematic study and analysis.
Dr. Brown said he stands firmly with his belief that mediolateral episiotomy as a routine prophylactic procedure in operative vaginal deliveries cannot be justified. "Having lived through an era of mediolaterals and seeing how long they take to heal, and the discomfort that patients have, I can’t justify it," he said.
"We’ve moved away from episiotomies [in the United States], period," he said. "We’ve moved away from them primarily because of the data showing that midline episiotomies increase the risk of sphincter injury. And the mediolateral episiotomies are just too painful."
The risk of OASIS can be minimized through good delivery technique, he noted.
"The trend here is toward more vacuum deliveries, which have [been shown to be less risky] than forceps deliveries, although its depends on the type of forceps used and the skill of the [obstetrician]," Dr. Brown said. "The challenge we face is that we don’t have enough forceps and vacuum deliveries to easily keep skill levels up."
Dr. Charles W. Nager, president of AUGS and director the urogynecological and reconstructive pelvic surgery division at the University of California, San Diego, said that rates of both episiotomy and operative vaginal delivery have been declining in the United States, and that simultaneously, "there’s been a parallel drop in OASIS."
There also is more training ongoing in U.S. hospitals on repairing third- and fourth-degree obstetric lacerations, he said in an interview at the meeting.
The Netherlands analysis excluded women with preterm delivery, stillbirth, multiple gestation, transverse position, and breech delivery, as well as women whose deliveries involved both forceps and vacuum and women who had a midline episiotomy.
Factors controlled for in the study included parity, fetal position, birth weight, augmentation with oxytocin, and duration of the second stage of labor.
Dr. van Bavel and all but one of his coinvestigators reported no disclosures.
WASHINGTON – The use of mediolateral episiotomy in women undergoing operative vaginal delivery – a common practice in the Netherlands – was associated with a large reduction in the risk of obstetrical anal sphincter injuries, according to an analysis of 10 years of data from the Netherlands Perinatal Registry.
For physicians and other obstetrical providers in the small European country, the findings reinforce current practice of favoring mediolateral episiotomies in operative vaginal deliveries as protection against obstetrical anal sphincter injuries (OASIS) – a risk factor for fecal incontinence, the investigators said.
"In the Netherlands, a mediolateral episiotomy is common practice. ... Our opinion is that the mediolateral episiotomies are causing less morbidity than an anal sphincter rupture would cause," Dr. Jeroen van Bavel reported during a press conference at the scientific meetings of the American Urogynecologic Society (AUGS) and the International Urogynecological Association.
But for physicians here in the United States, the risks are weighed differently. "It’s not that we don’t know that a mediolateral episiotomy decreases the risk of sphincter injury," Dr. Haywood Brown, professor and chair of obstetrics and gynecology at Duke University, Durham, N.C., said in a telephone interview after the conference.
"The problem is, mediolateral incisions are so uncomfortable," said Dr. Brown, who also is chair of the American College of Obstetricians and Gynecologists, District IV.
"They heal poorly, they heal with defects, ... and as a result the patient has more pain related to the mediolateral [episiotomy] than they would have with a third- or fourth-degree tear," he said. "Doing the mediolateral is really not the answer."
The Netherlands Perinatal Registry contains information on 96% of the 1.5 million deliveries that occurred during 2000-2009. Dr. van Bavel, of Amphia Hospital in Breda, the Netherlands, and his coinvestigators focused their analysis on the 170,974 women who had operative vaginal deliveries, comparing the rates of OASIS in women who had mediolateral episiotomies with those who did not.
Among primiparous women who had vacuum deliveries, OASIS occurred in 2.5% of those who had mediolateral episiotomies, compared with 14% who did not. Among multiparous women who had vacuum deliveries, OASIS rates were 2.1% with mediolateral episiotomy versus 7.5% without.
The differences were more striking with forceps deliveries. Anal sphincter injuries occurred in 3.4% versus 26.7% in primiparous women with and without mediolateral episiotomies, respectively. Among multiparous women, the risk of OASIS was 2.6% versus 14.2%.
For primiparous women, the number of mediolateral episiotomies needed to prevent one OASIS was 8 for vacuum delivery and 4 for forceps delivery, according to the analysis. For multiparous women, 18 mediolateral episiotomies were needed to prevent one OASIS for vacuum delivery, and 8 for forceps delivery.
ACOG’s Practice Bulletin No. 71 on episiotomy, which was written in 2006 (Obstet. Gynecol. 2006;107:957-62) and reaffirmed in 2013, states that median episiotomy is associated with higher rates of injury to the anal sphincter and rectum than mediolateral episiotomy (level A evidence), and that mediolateral episiotomy may be preferable in selected cases (level B evidence).
Overall, "restricted use of episiotomy is preferable to routine use of episiotomy," the guidelines say (level A evidence). Postpartum recovery, the guidelines note, is an area of obstetrics that lacks systematic study and analysis.
Dr. Brown said he stands firmly with his belief that mediolateral episiotomy as a routine prophylactic procedure in operative vaginal deliveries cannot be justified. "Having lived through an era of mediolaterals and seeing how long they take to heal, and the discomfort that patients have, I can’t justify it," he said.
"We’ve moved away from episiotomies [in the United States], period," he said. "We’ve moved away from them primarily because of the data showing that midline episiotomies increase the risk of sphincter injury. And the mediolateral episiotomies are just too painful."
The risk of OASIS can be minimized through good delivery technique, he noted.
"The trend here is toward more vacuum deliveries, which have [been shown to be less risky] than forceps deliveries, although its depends on the type of forceps used and the skill of the [obstetrician]," Dr. Brown said. "The challenge we face is that we don’t have enough forceps and vacuum deliveries to easily keep skill levels up."
Dr. Charles W. Nager, president of AUGS and director the urogynecological and reconstructive pelvic surgery division at the University of California, San Diego, said that rates of both episiotomy and operative vaginal delivery have been declining in the United States, and that simultaneously, "there’s been a parallel drop in OASIS."
There also is more training ongoing in U.S. hospitals on repairing third- and fourth-degree obstetric lacerations, he said in an interview at the meeting.
The Netherlands analysis excluded women with preterm delivery, stillbirth, multiple gestation, transverse position, and breech delivery, as well as women whose deliveries involved both forceps and vacuum and women who had a midline episiotomy.
Factors controlled for in the study included parity, fetal position, birth weight, augmentation with oxytocin, and duration of the second stage of labor.
Dr. van Bavel and all but one of his coinvestigators reported no disclosures.
AT AUGS/IUGA 2014
Key clinical point: The findings reinforce the Dutch practice of favoring mediolateral episiotomies in operative vaginal deliveries as protection against obstetrical anal sphincter injuries, but American obstetricians disagree on the basis that mediolateral episiotomies are quite painful and vacuum and forceps deliveries are becoming less common in the United States.
Major finding: The use of mediolateral episiotomy in vaginal operative deliveries is associated with significant reductions in the risk of obstetric anal sphincter injuries, across vacuum and forceps deliveries and primiparous and multiparous births.
Data source: A retrospective cohort study of 170,974 vaginal operative deliveries in the Netherlands.
Disclosures: Dr. Jeroen van Bavel and all but one of his coinvestigators reported no disclosures.
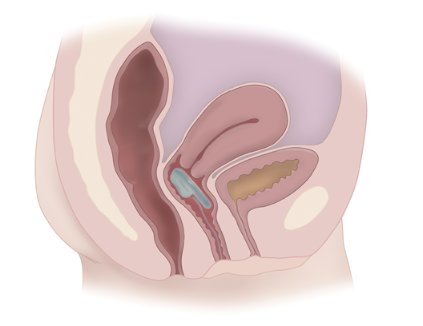
Vaginal bowel control device shown safe, effective in pivotal trial
WASHINGTON – Use of a vaginal bowel control device currently under review by the Food and Drug Administration resulted in a significant reduction of fecal incontinence episodes and significant improvement in quality of life, with only mild and transient adverse events, a pivotal study has shown.
The device – the Vaginal Bowel Control (VBC) System made by Pelvalon (Sunnyvale, Calif.) – consists of a silicone base and a posteriorly directed balloon. The patient controls the inflation pump, inflating the balloon to deflect the rectovaginal septum and interrupt stool passage, and deflating it to allow bowel movements.
"It provides [the patient with] dynamic control of the rectum," said Holly E. Richter, Ph.D., M.D., who served as the national principal investigator of the study. "It’s a new paradigm for treating patients with fecal incontinence."
At the 1-month primary endpoint, 79% of the 61 patients in the study’s intent-to-treat cohort – and 86% of patients in the per-protocol cohort – had experienced treatment success, which was defined as a 50% or greater reduction in fecal incontinence episodes, Dr. Richter reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
Mean weekly fecal incontinence episodes were reduced from 5.9 per week at baseline to 1.1 at 1 month.
After the 1-month treatment period, women were given the option of continuing with an additional 2-month study period. The rate of treatment success held steady among the 44 women who continued, with 86% seeing a 50% or greater reduction in fecal incontinence at 3 months, said Dr. Richter, director of the division of urogynecology and pelvic reconstructive surgery at the University of Alabama at Birmingham.
Total continence was achieved in approximately 40% of women in the 1-month and 3-month per-protocol cohorts, she noted.
Scores on the Fecal Incontinence Quality of Life survey and the Modified Manchester Health Questionnaire improved significantly across all subscales. At 1 month, 86% reported their fecal incontinence to be "very much better" (57%) or "much better" (29%). Almost all – 96% – reported their insert to be comfortable, and half said they could not feel it.
To qualify for the six-center study, women had to have a history of fecal incontinence of at least 6 months, with 4 or more incontinence episodes recorded during a 2-week baseline bowel diary.
Study participants had a mean age of 61 years and a mean of 5.9 weekly fecal incontinence episodes (or 12 in their diaries).Thirty percent were obese. Nearly 50% had prior hysterectomy, 8% had prior pelvic prolapse surgery, and 15% had prior urinary incontinence surgery.
There were no device-related serious adverse events. The most common complaint was cramping or discomfort, which most often occurred during the fitting period. There were approximately a half-dozen reported changes in urinary incontinence or overactive bladder symptoms.
"We believe that the Vaginal Bowel Control System can be tried early in the algorithm of treatment for fecal incontinence," Dr. Richter said.
It won’t be a good option for everyone, however. After being fitted with the device (it is made with three base sizes and two balloon sizes), women in the study were instructed to try it for a week before entering the 1-month treatment period. Approximately 40 women who were screened and fitted did not continue. This rate of discomfort or nonacceptance is similar to that associated with pessaries, Dr. Richter noted.
The initial fitting procedure for the new bowel control device "requires a little more provider and patient training, beyond [what is needed] for use of a traditional vaginal pessary," she said.
"Patients in the study could put the device in and take it out as they wished. Most patients used it all day long, and some took it out at night," she said. Patients were instructed to "take it out once or twice a week to wash it."
Dr. Richter is a paid consultant for Pelvalon. Her coinvestigators reported consulting for Pelvalon and other companies.
Fecal incontinence is one of the most emotionally devastating of all nonfatal medical conditions, and there is a need for new and effective strategies when medical therapy fails. The vaginal bowel control device appears to hold promise for some women with fecal incontinence by mechanically impeding stool passage to the anorectum by means of an inflatable balloon inserted into the vagina. The premise is that it can be used during times when the patient is not near to toileting facilities, can be inserted and removed at will, and is not a safety concern.
It is important to emphasize that this was not a randomized, placebo-controlled trial but rather a proof-of-concept study. The 40% complete continence response is 1) similar to that observed with the sacral nerve stimulation trial that resulted in Food and Drug Administration approval in the absence of a double-blind, controlled trial (Ann. Surg. 2010;1251:441), and 2) superior to the injectable bulking agent (6% complete continence), which was approved on the basis of a randomized, double-blind, sham-controlled trial (Lancet 2011;377:997).
However, complete continence is not necessary to improve quality of life in patients with incontinence. All three of these techniques require future studies to determine which incontinent patients are likely to benefit from each of these modalities. It must be recognized that there are many causes of incontinence, which often require different therapeutic approaches.
I look forward to reading a peer-reviewed paper on this new technique and to future randomized, controlled studies on this innovative approach to a condition with a large unmet need.
Dr. Arnold Wald is professor of medicine at the University of Wisconsin School of Medicine and Public Health, Madison.
Fecal incontinence is one of the most emotionally devastating of all nonfatal medical conditions, and there is a need for new and effective strategies when medical therapy fails. The vaginal bowel control device appears to hold promise for some women with fecal incontinence by mechanically impeding stool passage to the anorectum by means of an inflatable balloon inserted into the vagina. The premise is that it can be used during times when the patient is not near to toileting facilities, can be inserted and removed at will, and is not a safety concern.
It is important to emphasize that this was not a randomized, placebo-controlled trial but rather a proof-of-concept study. The 40% complete continence response is 1) similar to that observed with the sacral nerve stimulation trial that resulted in Food and Drug Administration approval in the absence of a double-blind, controlled trial (Ann. Surg. 2010;1251:441), and 2) superior to the injectable bulking agent (6% complete continence), which was approved on the basis of a randomized, double-blind, sham-controlled trial (Lancet 2011;377:997).
However, complete continence is not necessary to improve quality of life in patients with incontinence. All three of these techniques require future studies to determine which incontinent patients are likely to benefit from each of these modalities. It must be recognized that there are many causes of incontinence, which often require different therapeutic approaches.
I look forward to reading a peer-reviewed paper on this new technique and to future randomized, controlled studies on this innovative approach to a condition with a large unmet need.
Dr. Arnold Wald is professor of medicine at the University of Wisconsin School of Medicine and Public Health, Madison.
Fecal incontinence is one of the most emotionally devastating of all nonfatal medical conditions, and there is a need for new and effective strategies when medical therapy fails. The vaginal bowel control device appears to hold promise for some women with fecal incontinence by mechanically impeding stool passage to the anorectum by means of an inflatable balloon inserted into the vagina. The premise is that it can be used during times when the patient is not near to toileting facilities, can be inserted and removed at will, and is not a safety concern.
It is important to emphasize that this was not a randomized, placebo-controlled trial but rather a proof-of-concept study. The 40% complete continence response is 1) similar to that observed with the sacral nerve stimulation trial that resulted in Food and Drug Administration approval in the absence of a double-blind, controlled trial (Ann. Surg. 2010;1251:441), and 2) superior to the injectable bulking agent (6% complete continence), which was approved on the basis of a randomized, double-blind, sham-controlled trial (Lancet 2011;377:997).
However, complete continence is not necessary to improve quality of life in patients with incontinence. All three of these techniques require future studies to determine which incontinent patients are likely to benefit from each of these modalities. It must be recognized that there are many causes of incontinence, which often require different therapeutic approaches.
I look forward to reading a peer-reviewed paper on this new technique and to future randomized, controlled studies on this innovative approach to a condition with a large unmet need.
Dr. Arnold Wald is professor of medicine at the University of Wisconsin School of Medicine and Public Health, Madison.
WASHINGTON – Use of a vaginal bowel control device currently under review by the Food and Drug Administration resulted in a significant reduction of fecal incontinence episodes and significant improvement in quality of life, with only mild and transient adverse events, a pivotal study has shown.
The device – the Vaginal Bowel Control (VBC) System made by Pelvalon (Sunnyvale, Calif.) – consists of a silicone base and a posteriorly directed balloon. The patient controls the inflation pump, inflating the balloon to deflect the rectovaginal septum and interrupt stool passage, and deflating it to allow bowel movements.
"It provides [the patient with] dynamic control of the rectum," said Holly E. Richter, Ph.D., M.D., who served as the national principal investigator of the study. "It’s a new paradigm for treating patients with fecal incontinence."
At the 1-month primary endpoint, 79% of the 61 patients in the study’s intent-to-treat cohort – and 86% of patients in the per-protocol cohort – had experienced treatment success, which was defined as a 50% or greater reduction in fecal incontinence episodes, Dr. Richter reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
Mean weekly fecal incontinence episodes were reduced from 5.9 per week at baseline to 1.1 at 1 month.
After the 1-month treatment period, women were given the option of continuing with an additional 2-month study period. The rate of treatment success held steady among the 44 women who continued, with 86% seeing a 50% or greater reduction in fecal incontinence at 3 months, said Dr. Richter, director of the division of urogynecology and pelvic reconstructive surgery at the University of Alabama at Birmingham.
Total continence was achieved in approximately 40% of women in the 1-month and 3-month per-protocol cohorts, she noted.
Scores on the Fecal Incontinence Quality of Life survey and the Modified Manchester Health Questionnaire improved significantly across all subscales. At 1 month, 86% reported their fecal incontinence to be "very much better" (57%) or "much better" (29%). Almost all – 96% – reported their insert to be comfortable, and half said they could not feel it.
To qualify for the six-center study, women had to have a history of fecal incontinence of at least 6 months, with 4 or more incontinence episodes recorded during a 2-week baseline bowel diary.
Study participants had a mean age of 61 years and a mean of 5.9 weekly fecal incontinence episodes (or 12 in their diaries).Thirty percent were obese. Nearly 50% had prior hysterectomy, 8% had prior pelvic prolapse surgery, and 15% had prior urinary incontinence surgery.
There were no device-related serious adverse events. The most common complaint was cramping or discomfort, which most often occurred during the fitting period. There were approximately a half-dozen reported changes in urinary incontinence or overactive bladder symptoms.
"We believe that the Vaginal Bowel Control System can be tried early in the algorithm of treatment for fecal incontinence," Dr. Richter said.
It won’t be a good option for everyone, however. After being fitted with the device (it is made with three base sizes and two balloon sizes), women in the study were instructed to try it for a week before entering the 1-month treatment period. Approximately 40 women who were screened and fitted did not continue. This rate of discomfort or nonacceptance is similar to that associated with pessaries, Dr. Richter noted.
The initial fitting procedure for the new bowel control device "requires a little more provider and patient training, beyond [what is needed] for use of a traditional vaginal pessary," she said.
"Patients in the study could put the device in and take it out as they wished. Most patients used it all day long, and some took it out at night," she said. Patients were instructed to "take it out once or twice a week to wash it."
Dr. Richter is a paid consultant for Pelvalon. Her coinvestigators reported consulting for Pelvalon and other companies.
WASHINGTON – Use of a vaginal bowel control device currently under review by the Food and Drug Administration resulted in a significant reduction of fecal incontinence episodes and significant improvement in quality of life, with only mild and transient adverse events, a pivotal study has shown.
The device – the Vaginal Bowel Control (VBC) System made by Pelvalon (Sunnyvale, Calif.) – consists of a silicone base and a posteriorly directed balloon. The patient controls the inflation pump, inflating the balloon to deflect the rectovaginal septum and interrupt stool passage, and deflating it to allow bowel movements.
"It provides [the patient with] dynamic control of the rectum," said Holly E. Richter, Ph.D., M.D., who served as the national principal investigator of the study. "It’s a new paradigm for treating patients with fecal incontinence."
At the 1-month primary endpoint, 79% of the 61 patients in the study’s intent-to-treat cohort – and 86% of patients in the per-protocol cohort – had experienced treatment success, which was defined as a 50% or greater reduction in fecal incontinence episodes, Dr. Richter reported at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
Mean weekly fecal incontinence episodes were reduced from 5.9 per week at baseline to 1.1 at 1 month.
After the 1-month treatment period, women were given the option of continuing with an additional 2-month study period. The rate of treatment success held steady among the 44 women who continued, with 86% seeing a 50% or greater reduction in fecal incontinence at 3 months, said Dr. Richter, director of the division of urogynecology and pelvic reconstructive surgery at the University of Alabama at Birmingham.
Total continence was achieved in approximately 40% of women in the 1-month and 3-month per-protocol cohorts, she noted.
Scores on the Fecal Incontinence Quality of Life survey and the Modified Manchester Health Questionnaire improved significantly across all subscales. At 1 month, 86% reported their fecal incontinence to be "very much better" (57%) or "much better" (29%). Almost all – 96% – reported their insert to be comfortable, and half said they could not feel it.
To qualify for the six-center study, women had to have a history of fecal incontinence of at least 6 months, with 4 or more incontinence episodes recorded during a 2-week baseline bowel diary.
Study participants had a mean age of 61 years and a mean of 5.9 weekly fecal incontinence episodes (or 12 in their diaries).Thirty percent were obese. Nearly 50% had prior hysterectomy, 8% had prior pelvic prolapse surgery, and 15% had prior urinary incontinence surgery.
There were no device-related serious adverse events. The most common complaint was cramping or discomfort, which most often occurred during the fitting period. There were approximately a half-dozen reported changes in urinary incontinence or overactive bladder symptoms.
"We believe that the Vaginal Bowel Control System can be tried early in the algorithm of treatment for fecal incontinence," Dr. Richter said.
It won’t be a good option for everyone, however. After being fitted with the device (it is made with three base sizes and two balloon sizes), women in the study were instructed to try it for a week before entering the 1-month treatment period. Approximately 40 women who were screened and fitted did not continue. This rate of discomfort or nonacceptance is similar to that associated with pessaries, Dr. Richter noted.
The initial fitting procedure for the new bowel control device "requires a little more provider and patient training, beyond [what is needed] for use of a traditional vaginal pessary," she said.
"Patients in the study could put the device in and take it out as they wished. Most patients used it all day long, and some took it out at night," she said. Patients were instructed to "take it out once or twice a week to wash it."
Dr. Richter is a paid consultant for Pelvalon. Her coinvestigators reported consulting for Pelvalon and other companies.
AT AUGS/IUGA 2014
Key clinical finding: A controllable vaginal approach to bowel continence may be useful in the future.
Major finding: Almost 80% of 61 patients in an intent-to-treat cohort saw a 50% or greater reduction in fecal incontinence episodes with use of the Vaginal Bowel Control System, a device placed in the vagina to restore bowel control.
Data source: A multicenter, prospective, open-label study of women with fecal incontinence.
Disclosures: Dr. Richter is a paid consultant for Pelvalon. Her coinvestigators reported consulting for Pelvalon and other companies.
Repeat Botox treatments sustain improvements for overactive bladder
WASHINGTON – Repeat treatment with onabotulinumtoxin A provided sustained improvements in the symptoms of overactive bladder and was well tolerated in women who were followed for a median 2.4 years beyond their participation in one of the two large clinical trials that established the agent’s effectiveness and safety for this indication.
"This treatment remains a safe and effective therapeutic option" for patients with overactive bladder, said Dr. Tomasz Rechberger of the Medical University of Lublin (Poland). It’s "an attractive alternative [in the longer term] for patients who were inadequately treated with anticholinergics."
Women who completed either of the placebo-controlled, multicenter phase III studies were given the option of entering a 3-year open-label extension study in which they could receive additional treatments upon request and as needed to maintain symptom control. The intradetrusor injections of 100 U of onabotulinumtoxin A (Botox) needed to be at least 12 weeks apart.
At the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association, Dr. Rechberger reported on an interim analysis of this extension study, which was scheduled to end in August 2014.
As of June 2014, the overall discontinuation rate among the 749 patients who entered the extension study was 38%, but only 4.5% discontinued because of adverse effects or a lack of efficacy. "It was extremely low – much lower than [we expected]," said Dr. Rechberger.
The women had a mean age of 60 and had experienced symptoms of overactive bladder (OAB) for more than 6 years. At the start of the extension study, they had a mean of 5.6 episodes per day of urinary incontinence, 11.6 micturitions per day, and 8.4 urgency episodes per day.
In the original studies, the results after 12 weeks showed that patients treated with Botox experienced urinary incontinence an average of 1.6-1.9 times fewer per day than did patients treated with placebo, and they needed to urinate on average 1.0-1.7 times fewer per day, according to the Food and Drug Administration. In 2013, the FDA approved the use of Botox to treat adults with OAB who cannot use or do not adequately respond to anticholinergics.
Consistent reductions in symptoms were seen after the one to five treatments evaluated as part of the interim analysis of the extension study. Investigators checked all endpoints against the baseline 12 weeks after each treatment. The number of urinary incontinence episodes per day, for instance, was reduced by 3.3 after the first treatment cycle, 3.7 after two treatments, 3.9 after the third treatment, and 3.2 after the fourth and fifth treatment cycles.
Approximately 63%-72% of patients achieved a reduction of incontinence episodes of at least 50% across the treatment cycles.
Additionally, women saw mean reductions in micturition ranging from 2.4 to 3 over the five treatment cycles, and mean reductions in urgency episodes ranging from 3.6 to 4.2. A consistent increase in the volume voided per micturition also was seen.
Urinary tract infection was the most common side effect in each repeat treatment, as was the case in the original studies, but declined slightly with each treatment cycle, from approximately 30% after the first treatment to approximately 20% after the fifth. There were no new safety signals, Dr. Rechberger reported.
Each treatment consisted of 20 cystoscopic injections of 0.5 mL each. The median time between treatments ranged from 24 to 33 weeks – significantly longer than the required 12-week minimum.
Dr. Rechberger is an advisory committee member for Allergan (maker of Botox) and consults for Astellas and Johnson & Johnson. The study was funded by Allergan.
WASHINGTON – Repeat treatment with onabotulinumtoxin A provided sustained improvements in the symptoms of overactive bladder and was well tolerated in women who were followed for a median 2.4 years beyond their participation in one of the two large clinical trials that established the agent’s effectiveness and safety for this indication.
"This treatment remains a safe and effective therapeutic option" for patients with overactive bladder, said Dr. Tomasz Rechberger of the Medical University of Lublin (Poland). It’s "an attractive alternative [in the longer term] for patients who were inadequately treated with anticholinergics."
Women who completed either of the placebo-controlled, multicenter phase III studies were given the option of entering a 3-year open-label extension study in which they could receive additional treatments upon request and as needed to maintain symptom control. The intradetrusor injections of 100 U of onabotulinumtoxin A (Botox) needed to be at least 12 weeks apart.
At the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association, Dr. Rechberger reported on an interim analysis of this extension study, which was scheduled to end in August 2014.
As of June 2014, the overall discontinuation rate among the 749 patients who entered the extension study was 38%, but only 4.5% discontinued because of adverse effects or a lack of efficacy. "It was extremely low – much lower than [we expected]," said Dr. Rechberger.
The women had a mean age of 60 and had experienced symptoms of overactive bladder (OAB) for more than 6 years. At the start of the extension study, they had a mean of 5.6 episodes per day of urinary incontinence, 11.6 micturitions per day, and 8.4 urgency episodes per day.
In the original studies, the results after 12 weeks showed that patients treated with Botox experienced urinary incontinence an average of 1.6-1.9 times fewer per day than did patients treated with placebo, and they needed to urinate on average 1.0-1.7 times fewer per day, according to the Food and Drug Administration. In 2013, the FDA approved the use of Botox to treat adults with OAB who cannot use or do not adequately respond to anticholinergics.
Consistent reductions in symptoms were seen after the one to five treatments evaluated as part of the interim analysis of the extension study. Investigators checked all endpoints against the baseline 12 weeks after each treatment. The number of urinary incontinence episodes per day, for instance, was reduced by 3.3 after the first treatment cycle, 3.7 after two treatments, 3.9 after the third treatment, and 3.2 after the fourth and fifth treatment cycles.
Approximately 63%-72% of patients achieved a reduction of incontinence episodes of at least 50% across the treatment cycles.
Additionally, women saw mean reductions in micturition ranging from 2.4 to 3 over the five treatment cycles, and mean reductions in urgency episodes ranging from 3.6 to 4.2. A consistent increase in the volume voided per micturition also was seen.
Urinary tract infection was the most common side effect in each repeat treatment, as was the case in the original studies, but declined slightly with each treatment cycle, from approximately 30% after the first treatment to approximately 20% after the fifth. There were no new safety signals, Dr. Rechberger reported.
Each treatment consisted of 20 cystoscopic injections of 0.5 mL each. The median time between treatments ranged from 24 to 33 weeks – significantly longer than the required 12-week minimum.
Dr. Rechberger is an advisory committee member for Allergan (maker of Botox) and consults for Astellas and Johnson & Johnson. The study was funded by Allergan.
WASHINGTON – Repeat treatment with onabotulinumtoxin A provided sustained improvements in the symptoms of overactive bladder and was well tolerated in women who were followed for a median 2.4 years beyond their participation in one of the two large clinical trials that established the agent’s effectiveness and safety for this indication.
"This treatment remains a safe and effective therapeutic option" for patients with overactive bladder, said Dr. Tomasz Rechberger of the Medical University of Lublin (Poland). It’s "an attractive alternative [in the longer term] for patients who were inadequately treated with anticholinergics."
Women who completed either of the placebo-controlled, multicenter phase III studies were given the option of entering a 3-year open-label extension study in which they could receive additional treatments upon request and as needed to maintain symptom control. The intradetrusor injections of 100 U of onabotulinumtoxin A (Botox) needed to be at least 12 weeks apart.
At the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association, Dr. Rechberger reported on an interim analysis of this extension study, which was scheduled to end in August 2014.
As of June 2014, the overall discontinuation rate among the 749 patients who entered the extension study was 38%, but only 4.5% discontinued because of adverse effects or a lack of efficacy. "It was extremely low – much lower than [we expected]," said Dr. Rechberger.
The women had a mean age of 60 and had experienced symptoms of overactive bladder (OAB) for more than 6 years. At the start of the extension study, they had a mean of 5.6 episodes per day of urinary incontinence, 11.6 micturitions per day, and 8.4 urgency episodes per day.
In the original studies, the results after 12 weeks showed that patients treated with Botox experienced urinary incontinence an average of 1.6-1.9 times fewer per day than did patients treated with placebo, and they needed to urinate on average 1.0-1.7 times fewer per day, according to the Food and Drug Administration. In 2013, the FDA approved the use of Botox to treat adults with OAB who cannot use or do not adequately respond to anticholinergics.
Consistent reductions in symptoms were seen after the one to five treatments evaluated as part of the interim analysis of the extension study. Investigators checked all endpoints against the baseline 12 weeks after each treatment. The number of urinary incontinence episodes per day, for instance, was reduced by 3.3 after the first treatment cycle, 3.7 after two treatments, 3.9 after the third treatment, and 3.2 after the fourth and fifth treatment cycles.
Approximately 63%-72% of patients achieved a reduction of incontinence episodes of at least 50% across the treatment cycles.
Additionally, women saw mean reductions in micturition ranging from 2.4 to 3 over the five treatment cycles, and mean reductions in urgency episodes ranging from 3.6 to 4.2. A consistent increase in the volume voided per micturition also was seen.
Urinary tract infection was the most common side effect in each repeat treatment, as was the case in the original studies, but declined slightly with each treatment cycle, from approximately 30% after the first treatment to approximately 20% after the fifth. There were no new safety signals, Dr. Rechberger reported.
Each treatment consisted of 20 cystoscopic injections of 0.5 mL each. The median time between treatments ranged from 24 to 33 weeks – significantly longer than the required 12-week minimum.
Dr. Rechberger is an advisory committee member for Allergan (maker of Botox) and consults for Astellas and Johnson & Johnson. The study was funded by Allergan.
AT AUGS/IUGA 2014
Key clinical point: Consider Botox treatments in women with overactive bladder who could not use or did not adequately respond to anticholinergics.
Major finding: Repeat treatments of 100 U of onabotulinumtoxin A sustained improvements and led to consistent reductions in symptoms overall in a group of almost 750 women with overactive bladder who could not use or did not adequately respond to anticholinergics.
Data source: An interim analysis of an open-label, multicenter extension study of two placebo-controlled phase III trials.
Disclosures: Dr. Rechberger is an advisory committee member of Allergan and consults for Astellas and Johnson & Johnson. The study was funded by Allergan.
Pelvic floor disorders prevalent in female triathletes
WASHINGTON – A large proportion of female triathletes who responded to a national Web-based survey have symptoms of pelvic floor disorders, and one in four screened positive for the female athlete triad.
These findings from women in the general population, with a median age range of 35-44 years, echo findings from studies of Olympic and professional athletes, and "show that even young, thin, and otherwise healthy endurance athletes [who are not professional athletes] have pelvic floor disorders," said Dr. Johnny Yi after presenting his findings in a press conference at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
Currently, "these women may not get screened because they are not believed to be in a high-risk group," said Dr. Yi, a urogynecologist in group practice in Denver.
Of 311 women who responded to the survey, 37% reported symptoms of stress urinary incontinence, and 16% reported symptoms of urgency urinary incontinence. Anal incontinence was also a problem, with 37% reporting symptoms of this condition. Pelvic organ prolapse symptoms were reported by 5%.
Most of the participants were white (90%), nonsmokers (99%), and premenopausal (80%), and had a mean body mass index of 22 kg/m2. About half had borne children, almost all of them had vaginal deliveries.
The women were invited to participate through a database of nationwide triathlon interest groups and a triathlete Internet forum. The survey included the Epidemiology of Prolapse and Incontinence Questionnaire (EPIQ) and the Pelvic Girdle Pain Questionnaire (PGPQ), both of which are validated tools; the Female Athlete Triad Screening Questionnaire, which is endorsed by the National Collegiate Athletic Association; and various medical and demographic questions.
Approximately 18% of the women had pelvic girdle pain, although the mean score on the PGPQ (35.6) was relatively low. Respondents with various types of incontinence reported higher levels of pelvic girdle pain, Dr. Yi said.
Of the 75% of respondents who completed the triad questionnaire, 22% screened positive for low energy availability, 24% for menstrual irregularities, and 29% for abnormal bone strength. Eight percent screened positive for all three components of the female athlete triad, which is characterized by a hypoestrogenic state similar to menopause.
Dr. Yi said he is particularly interested in possible associations between the female athlete triad and pelvic floor disorders, and in the pelvic floor consequences of coupling high-impact, high-endurance activity with the potential for a hypoestrogenic state.
This study showed no significant association between the triad and pelvic floor disorders, but the findings emphasize that "both disorders are prevalent" and should be screened for and treated to avoid long-term sequelae and improve quality of life, he said.
Weekly training of the study participants consisted of running for a mean of 3.7 days, biking for a mean of 2.9 days, and swimming for a mean of 2.4 days. Training mileage and intensity were not associated with pelvic floor disorders. Not unexpectedly, parity was associated with a higher prevalence of stress urinary incontinence and pelvic organ prolapse.
Dr. Yi and his coinvestigators reported no disclosures.
WASHINGTON – A large proportion of female triathletes who responded to a national Web-based survey have symptoms of pelvic floor disorders, and one in four screened positive for the female athlete triad.
These findings from women in the general population, with a median age range of 35-44 years, echo findings from studies of Olympic and professional athletes, and "show that even young, thin, and otherwise healthy endurance athletes [who are not professional athletes] have pelvic floor disorders," said Dr. Johnny Yi after presenting his findings in a press conference at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
Currently, "these women may not get screened because they are not believed to be in a high-risk group," said Dr. Yi, a urogynecologist in group practice in Denver.
Of 311 women who responded to the survey, 37% reported symptoms of stress urinary incontinence, and 16% reported symptoms of urgency urinary incontinence. Anal incontinence was also a problem, with 37% reporting symptoms of this condition. Pelvic organ prolapse symptoms were reported by 5%.
Most of the participants were white (90%), nonsmokers (99%), and premenopausal (80%), and had a mean body mass index of 22 kg/m2. About half had borne children, almost all of them had vaginal deliveries.
The women were invited to participate through a database of nationwide triathlon interest groups and a triathlete Internet forum. The survey included the Epidemiology of Prolapse and Incontinence Questionnaire (EPIQ) and the Pelvic Girdle Pain Questionnaire (PGPQ), both of which are validated tools; the Female Athlete Triad Screening Questionnaire, which is endorsed by the National Collegiate Athletic Association; and various medical and demographic questions.
Approximately 18% of the women had pelvic girdle pain, although the mean score on the PGPQ (35.6) was relatively low. Respondents with various types of incontinence reported higher levels of pelvic girdle pain, Dr. Yi said.
Of the 75% of respondents who completed the triad questionnaire, 22% screened positive for low energy availability, 24% for menstrual irregularities, and 29% for abnormal bone strength. Eight percent screened positive for all three components of the female athlete triad, which is characterized by a hypoestrogenic state similar to menopause.
Dr. Yi said he is particularly interested in possible associations between the female athlete triad and pelvic floor disorders, and in the pelvic floor consequences of coupling high-impact, high-endurance activity with the potential for a hypoestrogenic state.
This study showed no significant association between the triad and pelvic floor disorders, but the findings emphasize that "both disorders are prevalent" and should be screened for and treated to avoid long-term sequelae and improve quality of life, he said.
Weekly training of the study participants consisted of running for a mean of 3.7 days, biking for a mean of 2.9 days, and swimming for a mean of 2.4 days. Training mileage and intensity were not associated with pelvic floor disorders. Not unexpectedly, parity was associated with a higher prevalence of stress urinary incontinence and pelvic organ prolapse.
Dr. Yi and his coinvestigators reported no disclosures.
WASHINGTON – A large proportion of female triathletes who responded to a national Web-based survey have symptoms of pelvic floor disorders, and one in four screened positive for the female athlete triad.
These findings from women in the general population, with a median age range of 35-44 years, echo findings from studies of Olympic and professional athletes, and "show that even young, thin, and otherwise healthy endurance athletes [who are not professional athletes] have pelvic floor disorders," said Dr. Johnny Yi after presenting his findings in a press conference at the scientific meetings of the American Urogynecologic Society and the International Urogynecological Association.
Currently, "these women may not get screened because they are not believed to be in a high-risk group," said Dr. Yi, a urogynecologist in group practice in Denver.
Of 311 women who responded to the survey, 37% reported symptoms of stress urinary incontinence, and 16% reported symptoms of urgency urinary incontinence. Anal incontinence was also a problem, with 37% reporting symptoms of this condition. Pelvic organ prolapse symptoms were reported by 5%.
Most of the participants were white (90%), nonsmokers (99%), and premenopausal (80%), and had a mean body mass index of 22 kg/m2. About half had borne children, almost all of them had vaginal deliveries.
The women were invited to participate through a database of nationwide triathlon interest groups and a triathlete Internet forum. The survey included the Epidemiology of Prolapse and Incontinence Questionnaire (EPIQ) and the Pelvic Girdle Pain Questionnaire (PGPQ), both of which are validated tools; the Female Athlete Triad Screening Questionnaire, which is endorsed by the National Collegiate Athletic Association; and various medical and demographic questions.
Approximately 18% of the women had pelvic girdle pain, although the mean score on the PGPQ (35.6) was relatively low. Respondents with various types of incontinence reported higher levels of pelvic girdle pain, Dr. Yi said.
Of the 75% of respondents who completed the triad questionnaire, 22% screened positive for low energy availability, 24% for menstrual irregularities, and 29% for abnormal bone strength. Eight percent screened positive for all three components of the female athlete triad, which is characterized by a hypoestrogenic state similar to menopause.
Dr. Yi said he is particularly interested in possible associations between the female athlete triad and pelvic floor disorders, and in the pelvic floor consequences of coupling high-impact, high-endurance activity with the potential for a hypoestrogenic state.
This study showed no significant association between the triad and pelvic floor disorders, but the findings emphasize that "both disorders are prevalent" and should be screened for and treated to avoid long-term sequelae and improve quality of life, he said.
Weekly training of the study participants consisted of running for a mean of 3.7 days, biking for a mean of 2.9 days, and swimming for a mean of 2.4 days. Training mileage and intensity were not associated with pelvic floor disorders. Not unexpectedly, parity was associated with a higher prevalence of stress urinary incontinence and pelvic organ prolapse.
Dr. Yi and his coinvestigators reported no disclosures.
AT AUGS/IUGA 2014
Key clinical point: Consider stress urinary incontinence and pelvic floor disorders in female triathletes.
Major finding: Women training for triathlons have a high prevalence of stress urinary incontinence (37%), urgency urinary incontinence (16%), anal incontinence (37%), and components of the female athlete triad.
Data source: A survey of 311 female triathletes with a median age range of 35-44 years.
Disclosures: Dr. Yi and his colleagues reported no disclosures.