User login
MRI Is an Important Tool in Identifying Silent JIA
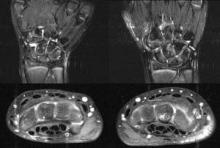
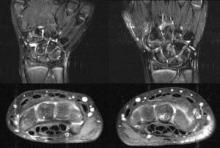
Magnetic resonance imaging is an important tool for detecting subclinical arthritis in children with juvenile idiopathic arthritis. In addition, MRI is a useful way to determine if there is disease persistence or silent progression before discontinuing treatment, according to a study of children who have clinically inactive JIA or are in remission on medication, according to Dr. Nikolay Tzaribachev.
All of the patients with clinically defined persistent oligoarticular juvenile idiopathic arthritis (JIA) were found to have polyarticular disease on MRI, according to Dr. Tzaribachev, head of the pediatric rheumatology department at the Center for Rheumatic Diseases in Bad Bramstedt, Germany.
"JIA tends to have an insidious onset and disease course. Subclinical JIA can elude the human tactile senses and clinical capacity to detect arthritis. In patients who are on drug treatment, symptoms may drop beyond clinical activity and disease may only become detectable by imaging techniques," said Dr. Tzaribachev in an interview.
"Remission criteria appear to be insufficient to detect the real extent of disease, which is of high importance to prevent joint damage, especially in growing children, who are supposed to become healthy adults.
"Furthermore, differentiation between oligo- and polyarticular disease at the first clinical evaluation after onset of symptoms is indispensable, since according to the ACR 2011 treatment guidelines [Arthritis Care Res. (Hoboken) 2011;63:465-82], oligo- and polyarticular disease have different treatment approaches," he noted.
During the last few years, silent arthritis in adults with RA has been detected only through the use of different imaging techniques, according to Dr. Tzaribachev. This fact led him and his colleagues to speculate that silent arthritis might also be the cause of the high percentage of disabilities in young adults with JIA, and that the clinical criteria for inactive disease and remission in JIA might be inadequate for detecting silent arthritis.
"We saw the huge discrepancy between clinical examination and MRI results, and understood the urgent need for more knowledge about the real extent of disease and silent disease progression, in order to protect the children from joint damage," said Dr. Tzaribachev.
The study included 21 patients with JIA (median age, 10.2 years at enrollment), who were on medications including NSAIDs, methotrexate, and/or tumor necrosis factor antagonists.
Clinically inactive disease or remission on medication were defined according to the Wallace criteria (J. Rheumatol. 2006;33:789-95). Patients underwent clinical examination, laboratory tests, and MRIs, and were asked to fill out a child health assessment questionnaire at every visit. The joints examined included wrists, knees, and ankles. Clinical and MRI exams and laboratory investigations were performed on the same day. Joint counts included those done clinically, as well as those based on MRI findings.
JIA subtype distribution included persistent oligoarticular (five patients), extended oligoarticular (four), polyarthritis (six), psoriatic arthritis (five), and undifferentiated arthritis (one). The median follow up time was 2.5 years.
Overall, 45 events were documented, 29 of which involved silent arthritis.
In all events, MRI revealed the following findings: 36 events with joint effusion, 39 with synovitis, 42 with synovial hypertrophy, 15 with bone marrow edema, 14 with osteitis, 15 with erosions, and 3 with tenosynovitis. All the silent arthritis events involved signs of arthritis that could be seen on MRI. Silent arthritis events were followed after a delay by clinical activity, according to the study.
In patients with JIA who present with clinically inactive disease or remission on medication, flares are preceded by arthritis detected on MRI. "In those cases, clinical examination and laboratory parameters remain normal despite ongoing disease activity, and remission criteria fail to show the real extent of disease," said Dr. Tzaribachev. "The lack of symptoms may also lead to silent disease progression, explaining the high percentage of physical disabilities in young adults with JIA. Imaging seems to be an important tool for defining disease activity, which should be included in the remission criteria and performed before treatment discontinuation."
The JIA classification probably needs to be redefined and remission criteria need to be reviewed to allow for the use of MRI and ultrasound, said Dr. Tzaribachev. Imaging techniques and protocols also need to be improved to become more child friendly, he noted. In addition, more studies are needed to define normal findings with respect to the growing musculoskeletal system in children and to allow for differentiation from mild pathology, especially for new imaging techniques like Xiralite. "Last, but not least, as in adult rheumatology, imaging should probably find its place in all clinical trials of children with inflammatory arthritis," he said.
Dr. Tzaribachev has received a research grant from Pfizer on temporomandibular joint arthritis in patients with JIA. His coauthors reported no disclosures.
Magnetic resonance imaging is an important tool for detecting subclinical arthritis in children with juvenile idiopathic arthritis. In addition, MRI is a useful way to determine if there is disease persistence or silent progression before discontinuing treatment, according to a study of children who have clinically inactive JIA or are in remission on medication, according to Dr. Nikolay Tzaribachev.
All of the patients with clinically defined persistent oligoarticular juvenile idiopathic arthritis (JIA) were found to have polyarticular disease on MRI, according to Dr. Tzaribachev, head of the pediatric rheumatology department at the Center for Rheumatic Diseases in Bad Bramstedt, Germany.
"JIA tends to have an insidious onset and disease course. Subclinical JIA can elude the human tactile senses and clinical capacity to detect arthritis. In patients who are on drug treatment, symptoms may drop beyond clinical activity and disease may only become detectable by imaging techniques," said Dr. Tzaribachev in an interview.
"Remission criteria appear to be insufficient to detect the real extent of disease, which is of high importance to prevent joint damage, especially in growing children, who are supposed to become healthy adults.
"Furthermore, differentiation between oligo- and polyarticular disease at the first clinical evaluation after onset of symptoms is indispensable, since according to the ACR 2011 treatment guidelines [Arthritis Care Res. (Hoboken) 2011;63:465-82], oligo- and polyarticular disease have different treatment approaches," he noted.
During the last few years, silent arthritis in adults with RA has been detected only through the use of different imaging techniques, according to Dr. Tzaribachev. This fact led him and his colleagues to speculate that silent arthritis might also be the cause of the high percentage of disabilities in young adults with JIA, and that the clinical criteria for inactive disease and remission in JIA might be inadequate for detecting silent arthritis.
"We saw the huge discrepancy between clinical examination and MRI results, and understood the urgent need for more knowledge about the real extent of disease and silent disease progression, in order to protect the children from joint damage," said Dr. Tzaribachev.
The study included 21 patients with JIA (median age, 10.2 years at enrollment), who were on medications including NSAIDs, methotrexate, and/or tumor necrosis factor antagonists.
Clinically inactive disease or remission on medication were defined according to the Wallace criteria (J. Rheumatol. 2006;33:789-95). Patients underwent clinical examination, laboratory tests, and MRIs, and were asked to fill out a child health assessment questionnaire at every visit. The joints examined included wrists, knees, and ankles. Clinical and MRI exams and laboratory investigations were performed on the same day. Joint counts included those done clinically, as well as those based on MRI findings.
JIA subtype distribution included persistent oligoarticular (five patients), extended oligoarticular (four), polyarthritis (six), psoriatic arthritis (five), and undifferentiated arthritis (one). The median follow up time was 2.5 years.
Overall, 45 events were documented, 29 of which involved silent arthritis.
In all events, MRI revealed the following findings: 36 events with joint effusion, 39 with synovitis, 42 with synovial hypertrophy, 15 with bone marrow edema, 14 with osteitis, 15 with erosions, and 3 with tenosynovitis. All the silent arthritis events involved signs of arthritis that could be seen on MRI. Silent arthritis events were followed after a delay by clinical activity, according to the study.
In patients with JIA who present with clinically inactive disease or remission on medication, flares are preceded by arthritis detected on MRI. "In those cases, clinical examination and laboratory parameters remain normal despite ongoing disease activity, and remission criteria fail to show the real extent of disease," said Dr. Tzaribachev. "The lack of symptoms may also lead to silent disease progression, explaining the high percentage of physical disabilities in young adults with JIA. Imaging seems to be an important tool for defining disease activity, which should be included in the remission criteria and performed before treatment discontinuation."
The JIA classification probably needs to be redefined and remission criteria need to be reviewed to allow for the use of MRI and ultrasound, said Dr. Tzaribachev. Imaging techniques and protocols also need to be improved to become more child friendly, he noted. In addition, more studies are needed to define normal findings with respect to the growing musculoskeletal system in children and to allow for differentiation from mild pathology, especially for new imaging techniques like Xiralite. "Last, but not least, as in adult rheumatology, imaging should probably find its place in all clinical trials of children with inflammatory arthritis," he said.
Dr. Tzaribachev has received a research grant from Pfizer on temporomandibular joint arthritis in patients with JIA. His coauthors reported no disclosures.
Magnetic resonance imaging is an important tool for detecting subclinical arthritis in children with juvenile idiopathic arthritis. In addition, MRI is a useful way to determine if there is disease persistence or silent progression before discontinuing treatment, according to a study of children who have clinically inactive JIA or are in remission on medication, according to Dr. Nikolay Tzaribachev.
All of the patients with clinically defined persistent oligoarticular juvenile idiopathic arthritis (JIA) were found to have polyarticular disease on MRI, according to Dr. Tzaribachev, head of the pediatric rheumatology department at the Center for Rheumatic Diseases in Bad Bramstedt, Germany.
"JIA tends to have an insidious onset and disease course. Subclinical JIA can elude the human tactile senses and clinical capacity to detect arthritis. In patients who are on drug treatment, symptoms may drop beyond clinical activity and disease may only become detectable by imaging techniques," said Dr. Tzaribachev in an interview.
"Remission criteria appear to be insufficient to detect the real extent of disease, which is of high importance to prevent joint damage, especially in growing children, who are supposed to become healthy adults.
"Furthermore, differentiation between oligo- and polyarticular disease at the first clinical evaluation after onset of symptoms is indispensable, since according to the ACR 2011 treatment guidelines [Arthritis Care Res. (Hoboken) 2011;63:465-82], oligo- and polyarticular disease have different treatment approaches," he noted.
During the last few years, silent arthritis in adults with RA has been detected only through the use of different imaging techniques, according to Dr. Tzaribachev. This fact led him and his colleagues to speculate that silent arthritis might also be the cause of the high percentage of disabilities in young adults with JIA, and that the clinical criteria for inactive disease and remission in JIA might be inadequate for detecting silent arthritis.
"We saw the huge discrepancy between clinical examination and MRI results, and understood the urgent need for more knowledge about the real extent of disease and silent disease progression, in order to protect the children from joint damage," said Dr. Tzaribachev.
The study included 21 patients with JIA (median age, 10.2 years at enrollment), who were on medications including NSAIDs, methotrexate, and/or tumor necrosis factor antagonists.
Clinically inactive disease or remission on medication were defined according to the Wallace criteria (J. Rheumatol. 2006;33:789-95). Patients underwent clinical examination, laboratory tests, and MRIs, and were asked to fill out a child health assessment questionnaire at every visit. The joints examined included wrists, knees, and ankles. Clinical and MRI exams and laboratory investigations were performed on the same day. Joint counts included those done clinically, as well as those based on MRI findings.
JIA subtype distribution included persistent oligoarticular (five patients), extended oligoarticular (four), polyarthritis (six), psoriatic arthritis (five), and undifferentiated arthritis (one). The median follow up time was 2.5 years.
Overall, 45 events were documented, 29 of which involved silent arthritis.
In all events, MRI revealed the following findings: 36 events with joint effusion, 39 with synovitis, 42 with synovial hypertrophy, 15 with bone marrow edema, 14 with osteitis, 15 with erosions, and 3 with tenosynovitis. All the silent arthritis events involved signs of arthritis that could be seen on MRI. Silent arthritis events were followed after a delay by clinical activity, according to the study.
In patients with JIA who present with clinically inactive disease or remission on medication, flares are preceded by arthritis detected on MRI. "In those cases, clinical examination and laboratory parameters remain normal despite ongoing disease activity, and remission criteria fail to show the real extent of disease," said Dr. Tzaribachev. "The lack of symptoms may also lead to silent disease progression, explaining the high percentage of physical disabilities in young adults with JIA. Imaging seems to be an important tool for defining disease activity, which should be included in the remission criteria and performed before treatment discontinuation."
The JIA classification probably needs to be redefined and remission criteria need to be reviewed to allow for the use of MRI and ultrasound, said Dr. Tzaribachev. Imaging techniques and protocols also need to be improved to become more child friendly, he noted. In addition, more studies are needed to define normal findings with respect to the growing musculoskeletal system in children and to allow for differentiation from mild pathology, especially for new imaging techniques like Xiralite. "Last, but not least, as in adult rheumatology, imaging should probably find its place in all clinical trials of children with inflammatory arthritis," he said.
Dr. Tzaribachev has received a research grant from Pfizer on temporomandibular joint arthritis in patients with JIA. His coauthors reported no disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: All of the patients with clinically defined persistent oligoarticular
juvenile idiopathic arthritis (JIA) were found to have polyarticular
disease on MRI.
Data Source: A study of 21 patients with JIA (median age, 10.2 years at
enrollment), who were on medications including NSAIDs, methotrexate,
and/or tumor necrosis factor antagonists
Disclosures: Dr. Tzaribachev has received a research grant from Pfizer on
temporomandibular joint arthritis in patients with JIA. His coauthors
reported no disclosures.
MRI Is an Important Tool in Identifying Silent JIA
Magnetic resonance imaging is an important tool for detecting subclinical arthritis in children with juvenile idiopathic arthritis. In addition, MRI is a useful way to determine if there is disease persistence or silent progression before discontinuing treatment, according to a study of children who have clinically inactive JIA or are in remission on medication, according to Dr. Nikolay Tzaribachev.
All of the patients with clinically defined persistent oligoarticular juvenile idiopathic arthritis (JIA) were found to have polyarticular disease on MRI, according to Dr. Tzaribachev, head of the pediatric rheumatology department at the Center for Rheumatic Diseases in Bad Bramstedt, Germany.
"JIA tends to have an insidious onset and disease course. Subclinical JIA can elude the human tactile senses and clinical capacity to detect arthritis. In patients who are on drug treatment, symptoms may drop beyond clinical activity and disease may only become detectable by imaging techniques," said Dr. Tzaribachev in an interview.
"Remission criteria appear to be insufficient to detect the real extent of disease, which is of high importance to prevent joint damage, especially in growing children, who are supposed to become healthy adults.
"Furthermore, differentiation between oligo- and polyarticular disease at the first clinical evaluation after onset of symptoms is indispensable, since according to the ACR 2011 treatment guidelines [Arthritis Care Res. (Hoboken) 2011;63:465-82], oligo- and polyarticular disease have different treatment approaches," he noted.
During the last few years, silent arthritis in adults with RA has been detected only through the use of different imaging techniques, according to Dr. Tzaribachev. This fact led him and his colleagues to speculate that silent arthritis might also be the cause of the high percentage of disabilities in young adults with JIA, and that the clinical criteria for inactive disease and remission in JIA might be inadequate for detecting silent arthritis.
"We saw the huge discrepancy between clinical examination and MRI results, and understood the urgent need for more knowledge about the real extent of disease and silent disease progression, in order to protect the children from joint damage," said Dr. Tzaribachev.
The study included 21 patients with JIA (median age, 10.2 years at enrollment), who were on medications including NSAIDs, methotrexate, and/or tumor necrosis factor antagonists.
Clinically inactive disease or remission on medication were defined according to the Wallace criteria (J. Rheumatol. 2006;33:789-95). Patients underwent clinical examination, laboratory tests, and MRIs, and were asked to fill out a child health assessment questionnaire at every visit. The joints examined included wrists, knees, and ankles. Clinical and MRI exams and laboratory investigations were performed on the same day. Joint counts included those done clinically, as well as those based on MRI findings.
JIA subtype distribution included persistent oligoarticular (five patients), extended oligoarticular (four), polyarthritis (six), psoriatic arthritis (five), and undifferentiated arthritis (one). The median follow up time was 2.5 years.
Overall, 45 events were documented, 29 of which involved silent arthritis.
In all events, MRI revealed the following findings: 36 events with joint effusion, 39 with synovitis, 42 with synovial hypertrophy, 15 with bone marrow edema, 14 with osteitis, 15 with erosions, and 3 with tenosynovitis. All the silent arthritis events involved signs of arthritis that could be seen on MRI. Silent arthritis events were followed after a delay by clinical activity, according to the study.
In patients with JIA who present with clinically inactive disease or remission on medication, flares are preceded by arthritis detected on MRI. "In those cases, clinical examination and laboratory parameters remain normal despite ongoing disease activity, and remission criteria fail to show the real extent of disease," said Dr. Tzaribachev. "The lack of symptoms may also lead to silent disease progression, explaining the high percentage of physical disabilities in young adults with JIA. Imaging seems to be an important tool for defining disease activity, which should be included in the remission criteria and performed before treatment discontinuation."
The JIA classification probably needs to be redefined and remission criteria need to be reviewed to allow for the use of MRI and ultrasound, said Dr. Tzaribachev. Imaging techniques and protocols also need to be improved to become more child friendly, he noted. In addition, more studies are needed to define normal findings with respect to the growing musculoskeletal system in children and to allow for differentiation from mild pathology, especially for new imaging techniques like Xiralite. "Last, but not least, as in adult rheumatology, imaging should probably find its place in all clinical trials of children with inflammatory arthritis," he said.
Dr. Tzaribachev has received a research grant from Pfizer on temporomandibular joint arthritis in patients with JIA. His coauthors reported no disclosures.
Magnetic resonance imaging is an important tool for detecting subclinical arthritis in children with juvenile idiopathic arthritis. In addition, MRI is a useful way to determine if there is disease persistence or silent progression before discontinuing treatment, according to a study of children who have clinically inactive JIA or are in remission on medication, according to Dr. Nikolay Tzaribachev.
All of the patients with clinically defined persistent oligoarticular juvenile idiopathic arthritis (JIA) were found to have polyarticular disease on MRI, according to Dr. Tzaribachev, head of the pediatric rheumatology department at the Center for Rheumatic Diseases in Bad Bramstedt, Germany.
"JIA tends to have an insidious onset and disease course. Subclinical JIA can elude the human tactile senses and clinical capacity to detect arthritis. In patients who are on drug treatment, symptoms may drop beyond clinical activity and disease may only become detectable by imaging techniques," said Dr. Tzaribachev in an interview.
"Remission criteria appear to be insufficient to detect the real extent of disease, which is of high importance to prevent joint damage, especially in growing children, who are supposed to become healthy adults.
"Furthermore, differentiation between oligo- and polyarticular disease at the first clinical evaluation after onset of symptoms is indispensable, since according to the ACR 2011 treatment guidelines [Arthritis Care Res. (Hoboken) 2011;63:465-82], oligo- and polyarticular disease have different treatment approaches," he noted.
During the last few years, silent arthritis in adults with RA has been detected only through the use of different imaging techniques, according to Dr. Tzaribachev. This fact led him and his colleagues to speculate that silent arthritis might also be the cause of the high percentage of disabilities in young adults with JIA, and that the clinical criteria for inactive disease and remission in JIA might be inadequate for detecting silent arthritis.
"We saw the huge discrepancy between clinical examination and MRI results, and understood the urgent need for more knowledge about the real extent of disease and silent disease progression, in order to protect the children from joint damage," said Dr. Tzaribachev.
The study included 21 patients with JIA (median age, 10.2 years at enrollment), who were on medications including NSAIDs, methotrexate, and/or tumor necrosis factor antagonists.
Clinically inactive disease or remission on medication were defined according to the Wallace criteria (J. Rheumatol. 2006;33:789-95). Patients underwent clinical examination, laboratory tests, and MRIs, and were asked to fill out a child health assessment questionnaire at every visit. The joints examined included wrists, knees, and ankles. Clinical and MRI exams and laboratory investigations were performed on the same day. Joint counts included those done clinically, as well as those based on MRI findings.
JIA subtype distribution included persistent oligoarticular (five patients), extended oligoarticular (four), polyarthritis (six), psoriatic arthritis (five), and undifferentiated arthritis (one). The median follow up time was 2.5 years.
Overall, 45 events were documented, 29 of which involved silent arthritis.
In all events, MRI revealed the following findings: 36 events with joint effusion, 39 with synovitis, 42 with synovial hypertrophy, 15 with bone marrow edema, 14 with osteitis, 15 with erosions, and 3 with tenosynovitis. All the silent arthritis events involved signs of arthritis that could be seen on MRI. Silent arthritis events were followed after a delay by clinical activity, according to the study.
In patients with JIA who present with clinically inactive disease or remission on medication, flares are preceded by arthritis detected on MRI. "In those cases, clinical examination and laboratory parameters remain normal despite ongoing disease activity, and remission criteria fail to show the real extent of disease," said Dr. Tzaribachev. "The lack of symptoms may also lead to silent disease progression, explaining the high percentage of physical disabilities in young adults with JIA. Imaging seems to be an important tool for defining disease activity, which should be included in the remission criteria and performed before treatment discontinuation."
The JIA classification probably needs to be redefined and remission criteria need to be reviewed to allow for the use of MRI and ultrasound, said Dr. Tzaribachev. Imaging techniques and protocols also need to be improved to become more child friendly, he noted. In addition, more studies are needed to define normal findings with respect to the growing musculoskeletal system in children and to allow for differentiation from mild pathology, especially for new imaging techniques like Xiralite. "Last, but not least, as in adult rheumatology, imaging should probably find its place in all clinical trials of children with inflammatory arthritis," he said.
Dr. Tzaribachev has received a research grant from Pfizer on temporomandibular joint arthritis in patients with JIA. His coauthors reported no disclosures.
Magnetic resonance imaging is an important tool for detecting subclinical arthritis in children with juvenile idiopathic arthritis. In addition, MRI is a useful way to determine if there is disease persistence or silent progression before discontinuing treatment, according to a study of children who have clinically inactive JIA or are in remission on medication, according to Dr. Nikolay Tzaribachev.
All of the patients with clinically defined persistent oligoarticular juvenile idiopathic arthritis (JIA) were found to have polyarticular disease on MRI, according to Dr. Tzaribachev, head of the pediatric rheumatology department at the Center for Rheumatic Diseases in Bad Bramstedt, Germany.
"JIA tends to have an insidious onset and disease course. Subclinical JIA can elude the human tactile senses and clinical capacity to detect arthritis. In patients who are on drug treatment, symptoms may drop beyond clinical activity and disease may only become detectable by imaging techniques," said Dr. Tzaribachev in an interview.
"Remission criteria appear to be insufficient to detect the real extent of disease, which is of high importance to prevent joint damage, especially in growing children, who are supposed to become healthy adults.
"Furthermore, differentiation between oligo- and polyarticular disease at the first clinical evaluation after onset of symptoms is indispensable, since according to the ACR 2011 treatment guidelines [Arthritis Care Res. (Hoboken) 2011;63:465-82], oligo- and polyarticular disease have different treatment approaches," he noted.
During the last few years, silent arthritis in adults with RA has been detected only through the use of different imaging techniques, according to Dr. Tzaribachev. This fact led him and his colleagues to speculate that silent arthritis might also be the cause of the high percentage of disabilities in young adults with JIA, and that the clinical criteria for inactive disease and remission in JIA might be inadequate for detecting silent arthritis.
"We saw the huge discrepancy between clinical examination and MRI results, and understood the urgent need for more knowledge about the real extent of disease and silent disease progression, in order to protect the children from joint damage," said Dr. Tzaribachev.
The study included 21 patients with JIA (median age, 10.2 years at enrollment), who were on medications including NSAIDs, methotrexate, and/or tumor necrosis factor antagonists.
Clinically inactive disease or remission on medication were defined according to the Wallace criteria (J. Rheumatol. 2006;33:789-95). Patients underwent clinical examination, laboratory tests, and MRIs, and were asked to fill out a child health assessment questionnaire at every visit. The joints examined included wrists, knees, and ankles. Clinical and MRI exams and laboratory investigations were performed on the same day. Joint counts included those done clinically, as well as those based on MRI findings.
JIA subtype distribution included persistent oligoarticular (five patients), extended oligoarticular (four), polyarthritis (six), psoriatic arthritis (five), and undifferentiated arthritis (one). The median follow up time was 2.5 years.
Overall, 45 events were documented, 29 of which involved silent arthritis.
In all events, MRI revealed the following findings: 36 events with joint effusion, 39 with synovitis, 42 with synovial hypertrophy, 15 with bone marrow edema, 14 with osteitis, 15 with erosions, and 3 with tenosynovitis. All the silent arthritis events involved signs of arthritis that could be seen on MRI. Silent arthritis events were followed after a delay by clinical activity, according to the study.
In patients with JIA who present with clinically inactive disease or remission on medication, flares are preceded by arthritis detected on MRI. "In those cases, clinical examination and laboratory parameters remain normal despite ongoing disease activity, and remission criteria fail to show the real extent of disease," said Dr. Tzaribachev. "The lack of symptoms may also lead to silent disease progression, explaining the high percentage of physical disabilities in young adults with JIA. Imaging seems to be an important tool for defining disease activity, which should be included in the remission criteria and performed before treatment discontinuation."
The JIA classification probably needs to be redefined and remission criteria need to be reviewed to allow for the use of MRI and ultrasound, said Dr. Tzaribachev. Imaging techniques and protocols also need to be improved to become more child friendly, he noted. In addition, more studies are needed to define normal findings with respect to the growing musculoskeletal system in children and to allow for differentiation from mild pathology, especially for new imaging techniques like Xiralite. "Last, but not least, as in adult rheumatology, imaging should probably find its place in all clinical trials of children with inflammatory arthritis," he said.
Dr. Tzaribachev has received a research grant from Pfizer on temporomandibular joint arthritis in patients with JIA. His coauthors reported no disclosures.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
WHO Data Shows Worldwide Uptick in Osteoarthritis
Updated World Health Organization estimates are showing a downward trend in the incidence of gout in North America among 65-year-olds, but men in that age group on the continent are far more likely to suffer from gout than are men in Africa.
That’s a sampling of the updated data on a host of musculoskeletal disorders worldwide, including rheumatoid arthritis, said Dr. Lyn March at the Annual European Congress of Rheumatology.
She presented a preliminary report from the Musculoskeletal Expert Group that’s part of the new Global Burden of Diseases, Injuries, and Risk Factors Study, which began in the spring of 2007. This is the first major effort since the original Global Burden of Disease in 1990 study to carry out a complete systematic assessment of the data on all diseases and injuries, and to produce comprehensive and comparable estimates of the burden of diseases, injuries, and risk factors for two time periods (1990 and 2005), according to the WHO. The project is due to produce final estimates in the spring, said Dr. March of the Royal North Shore Hospital in Sydney.
Dr. March said the specific aims for the Musculoskeletal Expert Group are to include more population-based self-report data; to develop health-state descriptions for different levels of severity of osteoarthritis, rheumatoid arthritis, back pain, neck pain, gout, and other musculoskeletal disorders; and to update systematic literature reviews of incidence, prevalence, and mortality risk for these conditions. The group will also evaluate bone mineral density (g/cm2) as a risk factor for disability-adjusted life-year (DALY) burden, "which will put the [degenerative] bone condition on the map for policy making," she said.
"The methodology employed in the systematic review, development of lay health state descriptions, and generation of data estimates for calculating [DALYs] will be revealed," Dr. March said.
In 2000, the beginning of what the WHO declared "the Bone and Joint Decade," results from the previous Global Burden of Disease (GBD) study reported that rheumatoid arthritis accounted for 0.3% of global DALYs (a time-based measure that combined years of life lost to premature mortality and years of life lost to time lived in health states of less-than-ideal health). "These data enable, in part, an evaluation of the impact of the Bone and Joint Decade and the setting of the research agenda for the next decade," Dr. March said.
The GBD study investigated the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions. In 2000, the WHO reported that osteoarthritis accounted for 1.1% of global DALYs, ranking 19th among all diseases and disorders, and rheumatoid arthritis accounted for 0.3% of DALYs. All musculoskeletal disorders combined had a prevalence of 2.1% of the worldwide population and ranked 12th in DALYs among all disorders, according to Dr. March. Preliminary data from the 2005 study show trends toward increases in the prevalence of osteoarthritis of the knee and hip, rheumatoid arthritis, and other musculoskeletal disease, and slight decreases in low-back pain and gout, she said, noting that the findings will likely have policy implications.
A 2005 update reported that musculoskeletal disorders are more common in developed countries.
Dr. March had no disclosures to report. The study received funding from the Bill and Melinda Gates Foundation and the Australian Commonwealth Government’s Department of Health and Aging.
Updated World Health Organization estimates are showing a downward trend in the incidence of gout in North America among 65-year-olds, but men in that age group on the continent are far more likely to suffer from gout than are men in Africa.
That’s a sampling of the updated data on a host of musculoskeletal disorders worldwide, including rheumatoid arthritis, said Dr. Lyn March at the Annual European Congress of Rheumatology.
She presented a preliminary report from the Musculoskeletal Expert Group that’s part of the new Global Burden of Diseases, Injuries, and Risk Factors Study, which began in the spring of 2007. This is the first major effort since the original Global Burden of Disease in 1990 study to carry out a complete systematic assessment of the data on all diseases and injuries, and to produce comprehensive and comparable estimates of the burden of diseases, injuries, and risk factors for two time periods (1990 and 2005), according to the WHO. The project is due to produce final estimates in the spring, said Dr. March of the Royal North Shore Hospital in Sydney.
Dr. March said the specific aims for the Musculoskeletal Expert Group are to include more population-based self-report data; to develop health-state descriptions for different levels of severity of osteoarthritis, rheumatoid arthritis, back pain, neck pain, gout, and other musculoskeletal disorders; and to update systematic literature reviews of incidence, prevalence, and mortality risk for these conditions. The group will also evaluate bone mineral density (g/cm2) as a risk factor for disability-adjusted life-year (DALY) burden, "which will put the [degenerative] bone condition on the map for policy making," she said.
"The methodology employed in the systematic review, development of lay health state descriptions, and generation of data estimates for calculating [DALYs] will be revealed," Dr. March said.
In 2000, the beginning of what the WHO declared "the Bone and Joint Decade," results from the previous Global Burden of Disease (GBD) study reported that rheumatoid arthritis accounted for 0.3% of global DALYs (a time-based measure that combined years of life lost to premature mortality and years of life lost to time lived in health states of less-than-ideal health). "These data enable, in part, an evaluation of the impact of the Bone and Joint Decade and the setting of the research agenda for the next decade," Dr. March said.
The GBD study investigated the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions. In 2000, the WHO reported that osteoarthritis accounted for 1.1% of global DALYs, ranking 19th among all diseases and disorders, and rheumatoid arthritis accounted for 0.3% of DALYs. All musculoskeletal disorders combined had a prevalence of 2.1% of the worldwide population and ranked 12th in DALYs among all disorders, according to Dr. March. Preliminary data from the 2005 study show trends toward increases in the prevalence of osteoarthritis of the knee and hip, rheumatoid arthritis, and other musculoskeletal disease, and slight decreases in low-back pain and gout, she said, noting that the findings will likely have policy implications.
A 2005 update reported that musculoskeletal disorders are more common in developed countries.
Dr. March had no disclosures to report. The study received funding from the Bill and Melinda Gates Foundation and the Australian Commonwealth Government’s Department of Health and Aging.
Updated World Health Organization estimates are showing a downward trend in the incidence of gout in North America among 65-year-olds, but men in that age group on the continent are far more likely to suffer from gout than are men in Africa.
That’s a sampling of the updated data on a host of musculoskeletal disorders worldwide, including rheumatoid arthritis, said Dr. Lyn March at the Annual European Congress of Rheumatology.
She presented a preliminary report from the Musculoskeletal Expert Group that’s part of the new Global Burden of Diseases, Injuries, and Risk Factors Study, which began in the spring of 2007. This is the first major effort since the original Global Burden of Disease in 1990 study to carry out a complete systematic assessment of the data on all diseases and injuries, and to produce comprehensive and comparable estimates of the burden of diseases, injuries, and risk factors for two time periods (1990 and 2005), according to the WHO. The project is due to produce final estimates in the spring, said Dr. March of the Royal North Shore Hospital in Sydney.
Dr. March said the specific aims for the Musculoskeletal Expert Group are to include more population-based self-report data; to develop health-state descriptions for different levels of severity of osteoarthritis, rheumatoid arthritis, back pain, neck pain, gout, and other musculoskeletal disorders; and to update systematic literature reviews of incidence, prevalence, and mortality risk for these conditions. The group will also evaluate bone mineral density (g/cm2) as a risk factor for disability-adjusted life-year (DALY) burden, "which will put the [degenerative] bone condition on the map for policy making," she said.
"The methodology employed in the systematic review, development of lay health state descriptions, and generation of data estimates for calculating [DALYs] will be revealed," Dr. March said.
In 2000, the beginning of what the WHO declared "the Bone and Joint Decade," results from the previous Global Burden of Disease (GBD) study reported that rheumatoid arthritis accounted for 0.3% of global DALYs (a time-based measure that combined years of life lost to premature mortality and years of life lost to time lived in health states of less-than-ideal health). "These data enable, in part, an evaluation of the impact of the Bone and Joint Decade and the setting of the research agenda for the next decade," Dr. March said.
The GBD study investigated the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions. In 2000, the WHO reported that osteoarthritis accounted for 1.1% of global DALYs, ranking 19th among all diseases and disorders, and rheumatoid arthritis accounted for 0.3% of DALYs. All musculoskeletal disorders combined had a prevalence of 2.1% of the worldwide population and ranked 12th in DALYs among all disorders, according to Dr. March. Preliminary data from the 2005 study show trends toward increases in the prevalence of osteoarthritis of the knee and hip, rheumatoid arthritis, and other musculoskeletal disease, and slight decreases in low-back pain and gout, she said, noting that the findings will likely have policy implications.
A 2005 update reported that musculoskeletal disorders are more common in developed countries.
Dr. March had no disclosures to report. The study received funding from the Bill and Melinda Gates Foundation and the Australian Commonwealth Government’s Department of Health and Aging.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: All musculoskeletal disorders combined had a prevalence of 2.1% of the
worldwide population and ranked 12th in disability-adjusted life-year (DALY) burden among all disorders. Preliminary data from the 2005 study show trends
toward increases in the prevalence of osteoarthritis of the knee and
hip, rheumatoid arthritis, and other musculoskeletal disease.
Data Source: The Global Burden of Diseases, Injuries, and Risk Factors Study investigating the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions.
Disclosures: Dr. March had no disclosures to report. The study received funding from
the Bill and Melinda Gates Foundation and the Australian Commonwealth
Government’s Department of Health and Aging.
WHO Data Shows Worldwide Uptick in Osteoarthritis
Updated World Health Organization estimates are showing a downward trend in the incidence of gout in North America among 65-year-olds, but men in that age group on the continent are far more likely to suffer from gout than are men in Africa.
That’s a sampling of the updated data on a host of musculoskeletal disorders worldwide, including rheumatoid arthritis, said Dr. Lyn March at the Annual European Congress of Rheumatology.
She presented a preliminary report from the Musculoskeletal Expert Group that’s part of the new Global Burden of Diseases, Injuries, and Risk Factors Study, which began in the spring of 2007. This is the first major effort since the original Global Burden of Disease in 1990 study to carry out a complete systematic assessment of the data on all diseases and injuries, and to produce comprehensive and comparable estimates of the burden of diseases, injuries, and risk factors for two time periods (1990 and 2005), according to the WHO. The project is due to produce final estimates in the spring, said Dr. March of the Royal North Shore Hospital in Sydney.
Dr. March said the specific aims for the Musculoskeletal Expert Group are to include more population-based self-report data; to develop health-state descriptions for different levels of severity of osteoarthritis, rheumatoid arthritis, back pain, neck pain, gout, and other musculoskeletal disorders; and to update systematic literature reviews of incidence, prevalence, and mortality risk for these conditions. The group will also evaluate bone mineral density (g/cm2) as a risk factor for disability-adjusted life-year (DALY) burden, "which will put the [degenerative] bone condition on the map for policy making," she said.
"The methodology employed in the systematic review, development of lay health state descriptions, and generation of data estimates for calculating [DALYs] will be revealed," Dr. March said.
In 2000, the beginning of what the WHO declared "the Bone and Joint Decade," results from the previous Global Burden of Disease (GBD) study reported that rheumatoid arthritis accounted for 0.3% of global DALYs (a time-based measure that combined years of life lost to premature mortality and years of life lost to time lived in health states of less-than-ideal health). "These data enable, in part, an evaluation of the impact of the Bone and Joint Decade and the setting of the research agenda for the next decade," Dr. March said.
The GBD study investigated the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions. In 2000, the WHO reported that osteoarthritis accounted for 1.1% of global DALYs, ranking 19th among all diseases and disorders, and rheumatoid arthritis accounted for 0.3% of DALYs. All musculoskeletal disorders combined had a prevalence of 2.1% of the worldwide population and ranked 12th in DALYs among all disorders, according to Dr. March. Preliminary data from the 2005 study show trends toward increases in the prevalence of osteoarthritis of the knee and hip, rheumatoid arthritis, and other musculoskeletal disease, and slight decreases in low-back pain and gout, she said, noting that the findings will likely have policy implications.
A 2005 update reported that musculoskeletal disorders are more common in developed countries.
Dr. March had no disclosures to report. The study received funding from the Bill and Melinda Gates Foundation and the Australian Commonwealth Government’s Department of Health and Aging.
Updated World Health Organization estimates are showing a downward trend in the incidence of gout in North America among 65-year-olds, but men in that age group on the continent are far more likely to suffer from gout than are men in Africa.
That’s a sampling of the updated data on a host of musculoskeletal disorders worldwide, including rheumatoid arthritis, said Dr. Lyn March at the Annual European Congress of Rheumatology.
She presented a preliminary report from the Musculoskeletal Expert Group that’s part of the new Global Burden of Diseases, Injuries, and Risk Factors Study, which began in the spring of 2007. This is the first major effort since the original Global Burden of Disease in 1990 study to carry out a complete systematic assessment of the data on all diseases and injuries, and to produce comprehensive and comparable estimates of the burden of diseases, injuries, and risk factors for two time periods (1990 and 2005), according to the WHO. The project is due to produce final estimates in the spring, said Dr. March of the Royal North Shore Hospital in Sydney.
Dr. March said the specific aims for the Musculoskeletal Expert Group are to include more population-based self-report data; to develop health-state descriptions for different levels of severity of osteoarthritis, rheumatoid arthritis, back pain, neck pain, gout, and other musculoskeletal disorders; and to update systematic literature reviews of incidence, prevalence, and mortality risk for these conditions. The group will also evaluate bone mineral density (g/cm2) as a risk factor for disability-adjusted life-year (DALY) burden, "which will put the [degenerative] bone condition on the map for policy making," she said.
"The methodology employed in the systematic review, development of lay health state descriptions, and generation of data estimates for calculating [DALYs] will be revealed," Dr. March said.
In 2000, the beginning of what the WHO declared "the Bone and Joint Decade," results from the previous Global Burden of Disease (GBD) study reported that rheumatoid arthritis accounted for 0.3% of global DALYs (a time-based measure that combined years of life lost to premature mortality and years of life lost to time lived in health states of less-than-ideal health). "These data enable, in part, an evaluation of the impact of the Bone and Joint Decade and the setting of the research agenda for the next decade," Dr. March said.
The GBD study investigated the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions. In 2000, the WHO reported that osteoarthritis accounted for 1.1% of global DALYs, ranking 19th among all diseases and disorders, and rheumatoid arthritis accounted for 0.3% of DALYs. All musculoskeletal disorders combined had a prevalence of 2.1% of the worldwide population and ranked 12th in DALYs among all disorders, according to Dr. March. Preliminary data from the 2005 study show trends toward increases in the prevalence of osteoarthritis of the knee and hip, rheumatoid arthritis, and other musculoskeletal disease, and slight decreases in low-back pain and gout, she said, noting that the findings will likely have policy implications.
A 2005 update reported that musculoskeletal disorders are more common in developed countries.
Dr. March had no disclosures to report. The study received funding from the Bill and Melinda Gates Foundation and the Australian Commonwealth Government’s Department of Health and Aging.
Updated World Health Organization estimates are showing a downward trend in the incidence of gout in North America among 65-year-olds, but men in that age group on the continent are far more likely to suffer from gout than are men in Africa.
That’s a sampling of the updated data on a host of musculoskeletal disorders worldwide, including rheumatoid arthritis, said Dr. Lyn March at the Annual European Congress of Rheumatology.
She presented a preliminary report from the Musculoskeletal Expert Group that’s part of the new Global Burden of Diseases, Injuries, and Risk Factors Study, which began in the spring of 2007. This is the first major effort since the original Global Burden of Disease in 1990 study to carry out a complete systematic assessment of the data on all diseases and injuries, and to produce comprehensive and comparable estimates of the burden of diseases, injuries, and risk factors for two time periods (1990 and 2005), according to the WHO. The project is due to produce final estimates in the spring, said Dr. March of the Royal North Shore Hospital in Sydney.
Dr. March said the specific aims for the Musculoskeletal Expert Group are to include more population-based self-report data; to develop health-state descriptions for different levels of severity of osteoarthritis, rheumatoid arthritis, back pain, neck pain, gout, and other musculoskeletal disorders; and to update systematic literature reviews of incidence, prevalence, and mortality risk for these conditions. The group will also evaluate bone mineral density (g/cm2) as a risk factor for disability-adjusted life-year (DALY) burden, "which will put the [degenerative] bone condition on the map for policy making," she said.
"The methodology employed in the systematic review, development of lay health state descriptions, and generation of data estimates for calculating [DALYs] will be revealed," Dr. March said.
In 2000, the beginning of what the WHO declared "the Bone and Joint Decade," results from the previous Global Burden of Disease (GBD) study reported that rheumatoid arthritis accounted for 0.3% of global DALYs (a time-based measure that combined years of life lost to premature mortality and years of life lost to time lived in health states of less-than-ideal health). "These data enable, in part, an evaluation of the impact of the Bone and Joint Decade and the setting of the research agenda for the next decade," Dr. March said.
The GBD study investigated the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions. In 2000, the WHO reported that osteoarthritis accounted for 1.1% of global DALYs, ranking 19th among all diseases and disorders, and rheumatoid arthritis accounted for 0.3% of DALYs. All musculoskeletal disorders combined had a prevalence of 2.1% of the worldwide population and ranked 12th in DALYs among all disorders, according to Dr. March. Preliminary data from the 2005 study show trends toward increases in the prevalence of osteoarthritis of the knee and hip, rheumatoid arthritis, and other musculoskeletal disease, and slight decreases in low-back pain and gout, she said, noting that the findings will likely have policy implications.
A 2005 update reported that musculoskeletal disorders are more common in developed countries.
Dr. March had no disclosures to report. The study received funding from the Bill and Melinda Gates Foundation and the Australian Commonwealth Government’s Department of Health and Aging.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Finding: All musculoskeletal disorders combined had a prevalence of 2.1% of the
worldwide population and ranked 12th in disability-adjusted life-year (DALY) burden among all disorders. Preliminary data from the 2005 study show trends
toward increases in the prevalence of osteoarthritis of the knee and
hip, rheumatoid arthritis, and other musculoskeletal disease.
Data Source: The Global Burden of Diseases, Injuries, and Risk Factors Study investigating the incidence of 109 diseases and injuries and 10 risk factors across eight World Bank regions.
Disclosures: Dr. March had no disclosures to report. The study received funding from
the Bill and Melinda Gates Foundation and the Australian Commonwealth
Government’s Department of Health and Aging.
Gum Disease Tied to Worsening Rheumatoid Arthritis
Recent laboratory findings from Australia have shown a strong correlation between gum disease and worsening signs and symptoms of rheumatoid arthritis, one of the lead investigators reported May 25.
During his presentation at the annual European Congress of Rheumatology, Mark Bartold, Ph.D., who is a periodontist and the director of the Colgate Dental Research Centre at the University of Adelaide (South Australia), discussed his group’s recently published study of laboratory mice with preexisting periodontitis and worsening RA. "Emerging evidence now suggests a strong relationship between the extent and severity of periodontal disease and rheumatoid arthritis," Dr. Bartold said in an interview.
The experiments showed that mice with coexisting periodontitis and RA exhibited more severe joint inflammation than did the mice with just RA, he said. Also, mice with both periodontitis and RA were more likely to demonstrate signs of arthritis in their rear paws, compared with mice with arthritis only. The progress of RA in mice with both conditions followed a more rapid course than it did in mice with just RA or just periodontitis, he reported.
Gum disease and RA could be related through common underlying dysfunction of fundamental inflammatory mechanisms. The nature of the dysfunction remains unknown, but recent scientific studies have suggested a link between the two, he said.
Although this relationship is unlikely to be causal, it is clear that individuals with advanced RA are more likely to have significant periodontal problems, compared with their nonrheumatoid counterparts. Likewise, people with severe gingivitis are more likely to have severe RA. Data from earlier studies have shown that individuals with RA had a 3.6-fold greater risk of moderate to severe periodontitis, and those with gum disease had a 2.2-fold greater risk of RA than did the general population.
Other studies have demonstrated that OPG (osteoprotegerin) and RANKL (receptor-activated nuclear factor–kappaB ligand) are highly expressed in both RA synovium and periodontitis lesions. Dr. Bartold noted pilot studies that have confirmed the potential to identify periodontal pathogen DNA in synovial tissues and inflamed human periodontal tissues. "It remains to be established whether treatment of periodontal disease and reduction of periodontal inflammation in patients with chronic rheumatoid arthritis will reduce the disease activity of rheumatoid arthritis," Dr. Bartold said.
Dr. Bartold’s research suggests that periodontitis and rheumatoid arthritis share a common development pathway within the RANK/RANKL/OPG axis, where a drop in OPG leads to reduced vascular protection. "Increases in RANKL levels within inflamed tissues may result in not only the development of vascular damage, but also activation of osteoclasts and subsequent bone resorption," he said.
The role of bacteria in arthritis has also garnered considerable attention, noted Dr. Bartold. Animal studies have demonstrated that arthritis can develop in response to different stimuli and through different effector pathways, including exogenous infections or microbial antigens. "If these observations are also applicable to human rheumatoid arthritis, we might expect that different types of infections – as well as other environmental exposures with the capacity to induce excessive proinflammatory cytokines in genetically susceptible individuals – may contribute to disease," he said.
Among the pathogens that have been implicated in rheumatoid arthritis patients are periodontopathic bacteria including Porphyromonas gingivalis, Prevotella intermedia, Prevotella melaninogenica, Bacteroides forsythus, and Aggregatibacter actinomycetemcomitans. Elevated antibodies to B. forsythus and P. intermedia have also been found in synovial fluid, he added.
The ultimate goal of emerging research is to determine whether the reduction of periodontal inflammation improves the disease activity of RA, he said. The clinical implications of these findings are that early intervention strategies to aid in the overall management of rheumatoid arthritis could include a periodontal assessment.
Dr. Bartold disclosed that he receives research support from the National Health and Medical Research Council of Australia, and acts as a consultant for Colgate and Nobel Biocare.
Recent laboratory findings from Australia have shown a strong correlation between gum disease and worsening signs and symptoms of rheumatoid arthritis, one of the lead investigators reported May 25.
During his presentation at the annual European Congress of Rheumatology, Mark Bartold, Ph.D., who is a periodontist and the director of the Colgate Dental Research Centre at the University of Adelaide (South Australia), discussed his group’s recently published study of laboratory mice with preexisting periodontitis and worsening RA. "Emerging evidence now suggests a strong relationship between the extent and severity of periodontal disease and rheumatoid arthritis," Dr. Bartold said in an interview.
The experiments showed that mice with coexisting periodontitis and RA exhibited more severe joint inflammation than did the mice with just RA, he said. Also, mice with both periodontitis and RA were more likely to demonstrate signs of arthritis in their rear paws, compared with mice with arthritis only. The progress of RA in mice with both conditions followed a more rapid course than it did in mice with just RA or just periodontitis, he reported.
Gum disease and RA could be related through common underlying dysfunction of fundamental inflammatory mechanisms. The nature of the dysfunction remains unknown, but recent scientific studies have suggested a link between the two, he said.
Although this relationship is unlikely to be causal, it is clear that individuals with advanced RA are more likely to have significant periodontal problems, compared with their nonrheumatoid counterparts. Likewise, people with severe gingivitis are more likely to have severe RA. Data from earlier studies have shown that individuals with RA had a 3.6-fold greater risk of moderate to severe periodontitis, and those with gum disease had a 2.2-fold greater risk of RA than did the general population.
Other studies have demonstrated that OPG (osteoprotegerin) and RANKL (receptor-activated nuclear factor–kappaB ligand) are highly expressed in both RA synovium and periodontitis lesions. Dr. Bartold noted pilot studies that have confirmed the potential to identify periodontal pathogen DNA in synovial tissues and inflamed human periodontal tissues. "It remains to be established whether treatment of periodontal disease and reduction of periodontal inflammation in patients with chronic rheumatoid arthritis will reduce the disease activity of rheumatoid arthritis," Dr. Bartold said.
Dr. Bartold’s research suggests that periodontitis and rheumatoid arthritis share a common development pathway within the RANK/RANKL/OPG axis, where a drop in OPG leads to reduced vascular protection. "Increases in RANKL levels within inflamed tissues may result in not only the development of vascular damage, but also activation of osteoclasts and subsequent bone resorption," he said.
The role of bacteria in arthritis has also garnered considerable attention, noted Dr. Bartold. Animal studies have demonstrated that arthritis can develop in response to different stimuli and through different effector pathways, including exogenous infections or microbial antigens. "If these observations are also applicable to human rheumatoid arthritis, we might expect that different types of infections – as well as other environmental exposures with the capacity to induce excessive proinflammatory cytokines in genetically susceptible individuals – may contribute to disease," he said.
Among the pathogens that have been implicated in rheumatoid arthritis patients are periodontopathic bacteria including Porphyromonas gingivalis, Prevotella intermedia, Prevotella melaninogenica, Bacteroides forsythus, and Aggregatibacter actinomycetemcomitans. Elevated antibodies to B. forsythus and P. intermedia have also been found in synovial fluid, he added.
The ultimate goal of emerging research is to determine whether the reduction of periodontal inflammation improves the disease activity of RA, he said. The clinical implications of these findings are that early intervention strategies to aid in the overall management of rheumatoid arthritis could include a periodontal assessment.
Dr. Bartold disclosed that he receives research support from the National Health and Medical Research Council of Australia, and acts as a consultant for Colgate and Nobel Biocare.
Recent laboratory findings from Australia have shown a strong correlation between gum disease and worsening signs and symptoms of rheumatoid arthritis, one of the lead investigators reported May 25.
During his presentation at the annual European Congress of Rheumatology, Mark Bartold, Ph.D., who is a periodontist and the director of the Colgate Dental Research Centre at the University of Adelaide (South Australia), discussed his group’s recently published study of laboratory mice with preexisting periodontitis and worsening RA. "Emerging evidence now suggests a strong relationship between the extent and severity of periodontal disease and rheumatoid arthritis," Dr. Bartold said in an interview.
The experiments showed that mice with coexisting periodontitis and RA exhibited more severe joint inflammation than did the mice with just RA, he said. Also, mice with both periodontitis and RA were more likely to demonstrate signs of arthritis in their rear paws, compared with mice with arthritis only. The progress of RA in mice with both conditions followed a more rapid course than it did in mice with just RA or just periodontitis, he reported.
Gum disease and RA could be related through common underlying dysfunction of fundamental inflammatory mechanisms. The nature of the dysfunction remains unknown, but recent scientific studies have suggested a link between the two, he said.
Although this relationship is unlikely to be causal, it is clear that individuals with advanced RA are more likely to have significant periodontal problems, compared with their nonrheumatoid counterparts. Likewise, people with severe gingivitis are more likely to have severe RA. Data from earlier studies have shown that individuals with RA had a 3.6-fold greater risk of moderate to severe periodontitis, and those with gum disease had a 2.2-fold greater risk of RA than did the general population.
Other studies have demonstrated that OPG (osteoprotegerin) and RANKL (receptor-activated nuclear factor–kappaB ligand) are highly expressed in both RA synovium and periodontitis lesions. Dr. Bartold noted pilot studies that have confirmed the potential to identify periodontal pathogen DNA in synovial tissues and inflamed human periodontal tissues. "It remains to be established whether treatment of periodontal disease and reduction of periodontal inflammation in patients with chronic rheumatoid arthritis will reduce the disease activity of rheumatoid arthritis," Dr. Bartold said.
Dr. Bartold’s research suggests that periodontitis and rheumatoid arthritis share a common development pathway within the RANK/RANKL/OPG axis, where a drop in OPG leads to reduced vascular protection. "Increases in RANKL levels within inflamed tissues may result in not only the development of vascular damage, but also activation of osteoclasts and subsequent bone resorption," he said.
The role of bacteria in arthritis has also garnered considerable attention, noted Dr. Bartold. Animal studies have demonstrated that arthritis can develop in response to different stimuli and through different effector pathways, including exogenous infections or microbial antigens. "If these observations are also applicable to human rheumatoid arthritis, we might expect that different types of infections – as well as other environmental exposures with the capacity to induce excessive proinflammatory cytokines in genetically susceptible individuals – may contribute to disease," he said.
Among the pathogens that have been implicated in rheumatoid arthritis patients are periodontopathic bacteria including Porphyromonas gingivalis, Prevotella intermedia, Prevotella melaninogenica, Bacteroides forsythus, and Aggregatibacter actinomycetemcomitans. Elevated antibodies to B. forsythus and P. intermedia have also been found in synovial fluid, he added.
The ultimate goal of emerging research is to determine whether the reduction of periodontal inflammation improves the disease activity of RA, he said. The clinical implications of these findings are that early intervention strategies to aid in the overall management of rheumatoid arthritis could include a periodontal assessment.
Dr. Bartold disclosed that he receives research support from the National Health and Medical Research Council of Australia, and acts as a consultant for Colgate and Nobel Biocare.
EXPERT ANALYSIS FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Gum Disease Tied to Worsening Rheumatoid Arthritis
Recent laboratory findings from Australia have shown a strong correlation between gum disease and worsening signs and symptoms of rheumatoid arthritis, one of the lead investigators reported May 25.
During his presentation at the annual European Congress of Rheumatology, Mark Bartold, Ph.D., who is a periodontist and the director of the Colgate Dental Research Centre at the University of Adelaide (South Australia), discussed his group’s recently published study of laboratory mice with preexisting periodontitis and worsening RA. "Emerging evidence now suggests a strong relationship between the extent and severity of periodontal disease and rheumatoid arthritis," Dr. Bartold said in an interview.
The experiments showed that mice with coexisting periodontitis and RA exhibited more severe joint inflammation than did the mice with just RA, he said. Also, mice with both periodontitis and RA were more likely to demonstrate signs of arthritis in their rear paws, compared with mice with arthritis only. The progress of RA in mice with both conditions followed a more rapid course than it did in mice with just RA or just periodontitis, he reported.
Gum disease and RA could be related through common underlying dysfunction of fundamental inflammatory mechanisms. The nature of the dysfunction remains unknown, but recent scientific studies have suggested a link between the two, he said.
Although this relationship is unlikely to be causal, it is clear that individuals with advanced RA are more likely to have significant periodontal problems, compared with their nonrheumatoid counterparts. Likewise, people with severe gingivitis are more likely to have severe RA. Data from earlier studies have shown that individuals with RA had a 3.6-fold greater risk of moderate to severe periodontitis, and those with gum disease had a 2.2-fold greater risk of RA than did the general population.
Other studies have demonstrated that OPG (osteoprotegerin) and RANKL (receptor-activated nuclear factor–kappaB ligand) are highly expressed in both RA synovium and periodontitis lesions. Dr. Bartold noted pilot studies that have confirmed the potential to identify periodontal pathogen DNA in synovial tissues and inflamed human periodontal tissues. "It remains to be established whether treatment of periodontal disease and reduction of periodontal inflammation in patients with chronic rheumatoid arthritis will reduce the disease activity of rheumatoid arthritis," Dr. Bartold said.
Dr. Bartold’s research suggests that periodontitis and rheumatoid arthritis share a common development pathway within the RANK/RANKL/OPG axis, where a drop in OPG leads to reduced vascular protection. "Increases in RANKL levels within inflamed tissues may result in not only the development of vascular damage, but also activation of osteoclasts and subsequent bone resorption," he said.
The role of bacteria in arthritis has also garnered considerable attention, noted Dr. Bartold. Animal studies have demonstrated that arthritis can develop in response to different stimuli and through different effector pathways, including exogenous infections or microbial antigens. "If these observations are also applicable to human rheumatoid arthritis, we might expect that different types of infections – as well as other environmental exposures with the capacity to induce excessive proinflammatory cytokines in genetically susceptible individuals – may contribute to disease," he said.
Among the pathogens that have been implicated in rheumatoid arthritis patients are periodontopathic bacteria including Porphyromonas gingivalis, Prevotella intermedia, Prevotella melaninogenica, Bacteroides forsythus, and Aggregatibacter actinomycetemcomitans. Elevated antibodies to B. forsythus and P. intermedia have also been found in synovial fluid, he added.
The ultimate goal of emerging research is to determine whether the reduction of periodontal inflammation improves the disease activity of RA, he said. The clinical implications of these findings are that early intervention strategies to aid in the overall management of rheumatoid arthritis could include a periodontal assessment.
Dr. Bartold disclosed that he receives research support from the National Health and Medical Research Council of Australia, and acts as a consultant for Colgate and Nobel Biocare.
Recent laboratory findings from Australia have shown a strong correlation between gum disease and worsening signs and symptoms of rheumatoid arthritis, one of the lead investigators reported May 25.
During his presentation at the annual European Congress of Rheumatology, Mark Bartold, Ph.D., who is a periodontist and the director of the Colgate Dental Research Centre at the University of Adelaide (South Australia), discussed his group’s recently published study of laboratory mice with preexisting periodontitis and worsening RA. "Emerging evidence now suggests a strong relationship between the extent and severity of periodontal disease and rheumatoid arthritis," Dr. Bartold said in an interview.
The experiments showed that mice with coexisting periodontitis and RA exhibited more severe joint inflammation than did the mice with just RA, he said. Also, mice with both periodontitis and RA were more likely to demonstrate signs of arthritis in their rear paws, compared with mice with arthritis only. The progress of RA in mice with both conditions followed a more rapid course than it did in mice with just RA or just periodontitis, he reported.
Gum disease and RA could be related through common underlying dysfunction of fundamental inflammatory mechanisms. The nature of the dysfunction remains unknown, but recent scientific studies have suggested a link between the two, he said.
Although this relationship is unlikely to be causal, it is clear that individuals with advanced RA are more likely to have significant periodontal problems, compared with their nonrheumatoid counterparts. Likewise, people with severe gingivitis are more likely to have severe RA. Data from earlier studies have shown that individuals with RA had a 3.6-fold greater risk of moderate to severe periodontitis, and those with gum disease had a 2.2-fold greater risk of RA than did the general population.
Other studies have demonstrated that OPG (osteoprotegerin) and RANKL (receptor-activated nuclear factor–kappaB ligand) are highly expressed in both RA synovium and periodontitis lesions. Dr. Bartold noted pilot studies that have confirmed the potential to identify periodontal pathogen DNA in synovial tissues and inflamed human periodontal tissues. "It remains to be established whether treatment of periodontal disease and reduction of periodontal inflammation in patients with chronic rheumatoid arthritis will reduce the disease activity of rheumatoid arthritis," Dr. Bartold said.
Dr. Bartold’s research suggests that periodontitis and rheumatoid arthritis share a common development pathway within the RANK/RANKL/OPG axis, where a drop in OPG leads to reduced vascular protection. "Increases in RANKL levels within inflamed tissues may result in not only the development of vascular damage, but also activation of osteoclasts and subsequent bone resorption," he said.
The role of bacteria in arthritis has also garnered considerable attention, noted Dr. Bartold. Animal studies have demonstrated that arthritis can develop in response to different stimuli and through different effector pathways, including exogenous infections or microbial antigens. "If these observations are also applicable to human rheumatoid arthritis, we might expect that different types of infections – as well as other environmental exposures with the capacity to induce excessive proinflammatory cytokines in genetically susceptible individuals – may contribute to disease," he said.
Among the pathogens that have been implicated in rheumatoid arthritis patients are periodontopathic bacteria including Porphyromonas gingivalis, Prevotella intermedia, Prevotella melaninogenica, Bacteroides forsythus, and Aggregatibacter actinomycetemcomitans. Elevated antibodies to B. forsythus and P. intermedia have also been found in synovial fluid, he added.
The ultimate goal of emerging research is to determine whether the reduction of periodontal inflammation improves the disease activity of RA, he said. The clinical implications of these findings are that early intervention strategies to aid in the overall management of rheumatoid arthritis could include a periodontal assessment.
Dr. Bartold disclosed that he receives research support from the National Health and Medical Research Council of Australia, and acts as a consultant for Colgate and Nobel Biocare.
Recent laboratory findings from Australia have shown a strong correlation between gum disease and worsening signs and symptoms of rheumatoid arthritis, one of the lead investigators reported May 25.
During his presentation at the annual European Congress of Rheumatology, Mark Bartold, Ph.D., who is a periodontist and the director of the Colgate Dental Research Centre at the University of Adelaide (South Australia), discussed his group’s recently published study of laboratory mice with preexisting periodontitis and worsening RA. "Emerging evidence now suggests a strong relationship between the extent and severity of periodontal disease and rheumatoid arthritis," Dr. Bartold said in an interview.
The experiments showed that mice with coexisting periodontitis and RA exhibited more severe joint inflammation than did the mice with just RA, he said. Also, mice with both periodontitis and RA were more likely to demonstrate signs of arthritis in their rear paws, compared with mice with arthritis only. The progress of RA in mice with both conditions followed a more rapid course than it did in mice with just RA or just periodontitis, he reported.
Gum disease and RA could be related through common underlying dysfunction of fundamental inflammatory mechanisms. The nature of the dysfunction remains unknown, but recent scientific studies have suggested a link between the two, he said.
Although this relationship is unlikely to be causal, it is clear that individuals with advanced RA are more likely to have significant periodontal problems, compared with their nonrheumatoid counterparts. Likewise, people with severe gingivitis are more likely to have severe RA. Data from earlier studies have shown that individuals with RA had a 3.6-fold greater risk of moderate to severe periodontitis, and those with gum disease had a 2.2-fold greater risk of RA than did the general population.
Other studies have demonstrated that OPG (osteoprotegerin) and RANKL (receptor-activated nuclear factor–kappaB ligand) are highly expressed in both RA synovium and periodontitis lesions. Dr. Bartold noted pilot studies that have confirmed the potential to identify periodontal pathogen DNA in synovial tissues and inflamed human periodontal tissues. "It remains to be established whether treatment of periodontal disease and reduction of periodontal inflammation in patients with chronic rheumatoid arthritis will reduce the disease activity of rheumatoid arthritis," Dr. Bartold said.
Dr. Bartold’s research suggests that periodontitis and rheumatoid arthritis share a common development pathway within the RANK/RANKL/OPG axis, where a drop in OPG leads to reduced vascular protection. "Increases in RANKL levels within inflamed tissues may result in not only the development of vascular damage, but also activation of osteoclasts and subsequent bone resorption," he said.
The role of bacteria in arthritis has also garnered considerable attention, noted Dr. Bartold. Animal studies have demonstrated that arthritis can develop in response to different stimuli and through different effector pathways, including exogenous infections or microbial antigens. "If these observations are also applicable to human rheumatoid arthritis, we might expect that different types of infections – as well as other environmental exposures with the capacity to induce excessive proinflammatory cytokines in genetically susceptible individuals – may contribute to disease," he said.
Among the pathogens that have been implicated in rheumatoid arthritis patients are periodontopathic bacteria including Porphyromonas gingivalis, Prevotella intermedia, Prevotella melaninogenica, Bacteroides forsythus, and Aggregatibacter actinomycetemcomitans. Elevated antibodies to B. forsythus and P. intermedia have also been found in synovial fluid, he added.
The ultimate goal of emerging research is to determine whether the reduction of periodontal inflammation improves the disease activity of RA, he said. The clinical implications of these findings are that early intervention strategies to aid in the overall management of rheumatoid arthritis could include a periodontal assessment.
Dr. Bartold disclosed that he receives research support from the National Health and Medical Research Council of Australia, and acts as a consultant for Colgate and Nobel Biocare.
EXPERT ANALYSIS FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
New Recommendations Outline Nurses' Role in Arthritis Care
The role of the nurse in rheumatology varies widely among countries, in large part because of differences in legal regulations, as well as nurses’ educational background and funding issues related to overall health care provision.
However, a new set of recommendations aims to standardize – and optimize – nursing care for patients with arthritis.
The recommendations, presented May 25 at the annual European Congress of Rheumatology by Yvonne van Eijk-Hustings, were developed by the EULAR Nursing Task Force, which consists of nurses, rheumatologists, an occupational therapist, a physiotherapist, a psychologist, an epidemiologist, and patient representatives from 14 European countries.
"The role of the nurse in rheumatology is undergoing great changes," said Ms. van Eijk-Hustings. "Nurses should participate in comprehensive disease management to control disease activity, reduce symptoms, and improve outcomes."
The panel conducted a systematic literature search of the Medline, Embase, Cochrane library, CINAHL, and PscychINFO databases, plus abstracts from the last three American College of Rheumatology and EULAR conferences. They ultimately consulted a total of 54 studies.
In general, said Ms. van Eijk-Hustings, the researchers’ findings support the conclusion that nurses play an important part of a necessarily multidisciplinary team of caregivers that – in addition to rheumatologists – also includes physical therapists, occupational therapists, and psychologists.
"Being involved in the disease process provides nurses with the opportunity to recognize and point out problems in an early stage, which ensures timely interventions and timely referral to other members of the multidisciplinary team," said Ms. van Eijk-Hustings of the department of integrated care at Maastricht (the Netherlands) University Medical Centre.
However, "our project showed that the contribution of nurses to multidisciplinary care is not clearly stated and that competencies and skills of nurses are often not optimally used," according to Ms. Van Eijk-Hustings.
Ultimately, the panel developed 10 recommendations, 7 of which deal with nurses’ ideal contribution to the areas of patient education, satisfaction with care, access to care, psychosocial support, disease management, self-management, and efficiency of care.
Three additional recommendations outline the need for professional support for nurses, including increasing the availability of guidelines or nursing protocols, increasing access to education, and encouraging nurses to undertake extended roles in rheumatology.
"In general, it is of importance that patients have access to rheumatology nurses for various reasons and that rheumatology nurses have access to appropriate training and education in order to maintain and improve their knowledge and skills," said Ms. Van Eijk-Hustings, a registered nurse and doctoral candidate whose own current research deals with the evolving roles of nurses in changing health care systems in different countries.
"This includes advanced, more autonomous roles for nurses, as well as substitution of tasks in the management of chronic disorders without loss of typical nursing skills," she added.
The task force also highlighted ten topics for future research, including the need for high-quality quantitative and qualitative studies with clear descriptions of nursing roles and interventions.
"One important area to mention is the contribution of the nurse in improving patient-preferred outcomes," added Ms. Van Eijk-Hustings.
The researchers cautioned that although the recommendations are likely to be applicable to the role of nurses in other rheumatic diseases, "in the present project, we focused on rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis, and most evidence was found with regard to rheumatoid arthritis."
EULAR support is needed for further dissemination and evaluation of the recommendations, she added.
The researchers reported having no disclosures to make in relation to this study.
The role of the nurse in rheumatology varies widely among countries, in large part because of differences in legal regulations, as well as nurses’ educational background and funding issues related to overall health care provision.
However, a new set of recommendations aims to standardize – and optimize – nursing care for patients with arthritis.
The recommendations, presented May 25 at the annual European Congress of Rheumatology by Yvonne van Eijk-Hustings, were developed by the EULAR Nursing Task Force, which consists of nurses, rheumatologists, an occupational therapist, a physiotherapist, a psychologist, an epidemiologist, and patient representatives from 14 European countries.
"The role of the nurse in rheumatology is undergoing great changes," said Ms. van Eijk-Hustings. "Nurses should participate in comprehensive disease management to control disease activity, reduce symptoms, and improve outcomes."
The panel conducted a systematic literature search of the Medline, Embase, Cochrane library, CINAHL, and PscychINFO databases, plus abstracts from the last three American College of Rheumatology and EULAR conferences. They ultimately consulted a total of 54 studies.
In general, said Ms. van Eijk-Hustings, the researchers’ findings support the conclusion that nurses play an important part of a necessarily multidisciplinary team of caregivers that – in addition to rheumatologists – also includes physical therapists, occupational therapists, and psychologists.
"Being involved in the disease process provides nurses with the opportunity to recognize and point out problems in an early stage, which ensures timely interventions and timely referral to other members of the multidisciplinary team," said Ms. van Eijk-Hustings of the department of integrated care at Maastricht (the Netherlands) University Medical Centre.
However, "our project showed that the contribution of nurses to multidisciplinary care is not clearly stated and that competencies and skills of nurses are often not optimally used," according to Ms. Van Eijk-Hustings.
Ultimately, the panel developed 10 recommendations, 7 of which deal with nurses’ ideal contribution to the areas of patient education, satisfaction with care, access to care, psychosocial support, disease management, self-management, and efficiency of care.
Three additional recommendations outline the need for professional support for nurses, including increasing the availability of guidelines or nursing protocols, increasing access to education, and encouraging nurses to undertake extended roles in rheumatology.
"In general, it is of importance that patients have access to rheumatology nurses for various reasons and that rheumatology nurses have access to appropriate training and education in order to maintain and improve their knowledge and skills," said Ms. Van Eijk-Hustings, a registered nurse and doctoral candidate whose own current research deals with the evolving roles of nurses in changing health care systems in different countries.
"This includes advanced, more autonomous roles for nurses, as well as substitution of tasks in the management of chronic disorders without loss of typical nursing skills," she added.
The task force also highlighted ten topics for future research, including the need for high-quality quantitative and qualitative studies with clear descriptions of nursing roles and interventions.
"One important area to mention is the contribution of the nurse in improving patient-preferred outcomes," added Ms. Van Eijk-Hustings.
The researchers cautioned that although the recommendations are likely to be applicable to the role of nurses in other rheumatic diseases, "in the present project, we focused on rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis, and most evidence was found with regard to rheumatoid arthritis."
EULAR support is needed for further dissemination and evaluation of the recommendations, she added.
The researchers reported having no disclosures to make in relation to this study.
The role of the nurse in rheumatology varies widely among countries, in large part because of differences in legal regulations, as well as nurses’ educational background and funding issues related to overall health care provision.
However, a new set of recommendations aims to standardize – and optimize – nursing care for patients with arthritis.
The recommendations, presented May 25 at the annual European Congress of Rheumatology by Yvonne van Eijk-Hustings, were developed by the EULAR Nursing Task Force, which consists of nurses, rheumatologists, an occupational therapist, a physiotherapist, a psychologist, an epidemiologist, and patient representatives from 14 European countries.
"The role of the nurse in rheumatology is undergoing great changes," said Ms. van Eijk-Hustings. "Nurses should participate in comprehensive disease management to control disease activity, reduce symptoms, and improve outcomes."
The panel conducted a systematic literature search of the Medline, Embase, Cochrane library, CINAHL, and PscychINFO databases, plus abstracts from the last three American College of Rheumatology and EULAR conferences. They ultimately consulted a total of 54 studies.
In general, said Ms. van Eijk-Hustings, the researchers’ findings support the conclusion that nurses play an important part of a necessarily multidisciplinary team of caregivers that – in addition to rheumatologists – also includes physical therapists, occupational therapists, and psychologists.
"Being involved in the disease process provides nurses with the opportunity to recognize and point out problems in an early stage, which ensures timely interventions and timely referral to other members of the multidisciplinary team," said Ms. van Eijk-Hustings of the department of integrated care at Maastricht (the Netherlands) University Medical Centre.
However, "our project showed that the contribution of nurses to multidisciplinary care is not clearly stated and that competencies and skills of nurses are often not optimally used," according to Ms. Van Eijk-Hustings.
Ultimately, the panel developed 10 recommendations, 7 of which deal with nurses’ ideal contribution to the areas of patient education, satisfaction with care, access to care, psychosocial support, disease management, self-management, and efficiency of care.
Three additional recommendations outline the need for professional support for nurses, including increasing the availability of guidelines or nursing protocols, increasing access to education, and encouraging nurses to undertake extended roles in rheumatology.
"In general, it is of importance that patients have access to rheumatology nurses for various reasons and that rheumatology nurses have access to appropriate training and education in order to maintain and improve their knowledge and skills," said Ms. Van Eijk-Hustings, a registered nurse and doctoral candidate whose own current research deals with the evolving roles of nurses in changing health care systems in different countries.
"This includes advanced, more autonomous roles for nurses, as well as substitution of tasks in the management of chronic disorders without loss of typical nursing skills," she added.
The task force also highlighted ten topics for future research, including the need for high-quality quantitative and qualitative studies with clear descriptions of nursing roles and interventions.
"One important area to mention is the contribution of the nurse in improving patient-preferred outcomes," added Ms. Van Eijk-Hustings.
The researchers cautioned that although the recommendations are likely to be applicable to the role of nurses in other rheumatic diseases, "in the present project, we focused on rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis, and most evidence was found with regard to rheumatoid arthritis."
EULAR support is needed for further dissemination and evaluation of the recommendations, she added.
The researchers reported having no disclosures to make in relation to this study.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
New Recommendations Outline Nurses' Role in Arthritis Care
The role of the nurse in rheumatology varies widely among countries, in large part because of differences in legal regulations, as well as nurses’ educational background and funding issues related to overall health care provision.
However, a new set of recommendations aims to standardize – and optimize – nursing care for patients with arthritis.
The recommendations, presented May 25 at the annual European Congress of Rheumatology by Yvonne van Eijk-Hustings, were developed by the EULAR Nursing Task Force, which consists of nurses, rheumatologists, an occupational therapist, a physiotherapist, a psychologist, an epidemiologist, and patient representatives from 14 European countries.
"The role of the nurse in rheumatology is undergoing great changes," said Ms. van Eijk-Hustings. "Nurses should participate in comprehensive disease management to control disease activity, reduce symptoms, and improve outcomes."
The panel conducted a systematic literature search of the Medline, Embase, Cochrane library, CINAHL, and PscychINFO databases, plus abstracts from the last three American College of Rheumatology and EULAR conferences. They ultimately consulted a total of 54 studies.
In general, said Ms. van Eijk-Hustings, the researchers’ findings support the conclusion that nurses play an important part of a necessarily multidisciplinary team of caregivers that – in addition to rheumatologists – also includes physical therapists, occupational therapists, and psychologists.
"Being involved in the disease process provides nurses with the opportunity to recognize and point out problems in an early stage, which ensures timely interventions and timely referral to other members of the multidisciplinary team," said Ms. van Eijk-Hustings of the department of integrated care at Maastricht (the Netherlands) University Medical Centre.
However, "our project showed that the contribution of nurses to multidisciplinary care is not clearly stated and that competencies and skills of nurses are often not optimally used," according to Ms. Van Eijk-Hustings.
Ultimately, the panel developed 10 recommendations, 7 of which deal with nurses’ ideal contribution to the areas of patient education, satisfaction with care, access to care, psychosocial support, disease management, self-management, and efficiency of care.
Three additional recommendations outline the need for professional support for nurses, including increasing the availability of guidelines or nursing protocols, increasing access to education, and encouraging nurses to undertake extended roles in rheumatology.
"In general, it is of importance that patients have access to rheumatology nurses for various reasons and that rheumatology nurses have access to appropriate training and education in order to maintain and improve their knowledge and skills," said Ms. Van Eijk-Hustings, a registered nurse and doctoral candidate whose own current research deals with the evolving roles of nurses in changing health care systems in different countries.
"This includes advanced, more autonomous roles for nurses, as well as substitution of tasks in the management of chronic disorders without loss of typical nursing skills," she added.
The task force also highlighted ten topics for future research, including the need for high-quality quantitative and qualitative studies with clear descriptions of nursing roles and interventions.
"One important area to mention is the contribution of the nurse in improving patient-preferred outcomes," added Ms. Van Eijk-Hustings.
The researchers cautioned that although the recommendations are likely to be applicable to the role of nurses in other rheumatic diseases, "in the present project, we focused on rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis, and most evidence was found with regard to rheumatoid arthritis."
EULAR support is needed for further dissemination and evaluation of the recommendations, she added.
The researchers reported having no disclosures to make in relation to this study.
The role of the nurse in rheumatology varies widely among countries, in large part because of differences in legal regulations, as well as nurses’ educational background and funding issues related to overall health care provision.
However, a new set of recommendations aims to standardize – and optimize – nursing care for patients with arthritis.
The recommendations, presented May 25 at the annual European Congress of Rheumatology by Yvonne van Eijk-Hustings, were developed by the EULAR Nursing Task Force, which consists of nurses, rheumatologists, an occupational therapist, a physiotherapist, a psychologist, an epidemiologist, and patient representatives from 14 European countries.
"The role of the nurse in rheumatology is undergoing great changes," said Ms. van Eijk-Hustings. "Nurses should participate in comprehensive disease management to control disease activity, reduce symptoms, and improve outcomes."
The panel conducted a systematic literature search of the Medline, Embase, Cochrane library, CINAHL, and PscychINFO databases, plus abstracts from the last three American College of Rheumatology and EULAR conferences. They ultimately consulted a total of 54 studies.
In general, said Ms. van Eijk-Hustings, the researchers’ findings support the conclusion that nurses play an important part of a necessarily multidisciplinary team of caregivers that – in addition to rheumatologists – also includes physical therapists, occupational therapists, and psychologists.
"Being involved in the disease process provides nurses with the opportunity to recognize and point out problems in an early stage, which ensures timely interventions and timely referral to other members of the multidisciplinary team," said Ms. van Eijk-Hustings of the department of integrated care at Maastricht (the Netherlands) University Medical Centre.
However, "our project showed that the contribution of nurses to multidisciplinary care is not clearly stated and that competencies and skills of nurses are often not optimally used," according to Ms. Van Eijk-Hustings.
Ultimately, the panel developed 10 recommendations, 7 of which deal with nurses’ ideal contribution to the areas of patient education, satisfaction with care, access to care, psychosocial support, disease management, self-management, and efficiency of care.
Three additional recommendations outline the need for professional support for nurses, including increasing the availability of guidelines or nursing protocols, increasing access to education, and encouraging nurses to undertake extended roles in rheumatology.
"In general, it is of importance that patients have access to rheumatology nurses for various reasons and that rheumatology nurses have access to appropriate training and education in order to maintain and improve their knowledge and skills," said Ms. Van Eijk-Hustings, a registered nurse and doctoral candidate whose own current research deals with the evolving roles of nurses in changing health care systems in different countries.
"This includes advanced, more autonomous roles for nurses, as well as substitution of tasks in the management of chronic disorders without loss of typical nursing skills," she added.
The task force also highlighted ten topics for future research, including the need for high-quality quantitative and qualitative studies with clear descriptions of nursing roles and interventions.
"One important area to mention is the contribution of the nurse in improving patient-preferred outcomes," added Ms. Van Eijk-Hustings.
The researchers cautioned that although the recommendations are likely to be applicable to the role of nurses in other rheumatic diseases, "in the present project, we focused on rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis, and most evidence was found with regard to rheumatoid arthritis."
EULAR support is needed for further dissemination and evaluation of the recommendations, she added.
The researchers reported having no disclosures to make in relation to this study.
The role of the nurse in rheumatology varies widely among countries, in large part because of differences in legal regulations, as well as nurses’ educational background and funding issues related to overall health care provision.
However, a new set of recommendations aims to standardize – and optimize – nursing care for patients with arthritis.
The recommendations, presented May 25 at the annual European Congress of Rheumatology by Yvonne van Eijk-Hustings, were developed by the EULAR Nursing Task Force, which consists of nurses, rheumatologists, an occupational therapist, a physiotherapist, a psychologist, an epidemiologist, and patient representatives from 14 European countries.
"The role of the nurse in rheumatology is undergoing great changes," said Ms. van Eijk-Hustings. "Nurses should participate in comprehensive disease management to control disease activity, reduce symptoms, and improve outcomes."
The panel conducted a systematic literature search of the Medline, Embase, Cochrane library, CINAHL, and PscychINFO databases, plus abstracts from the last three American College of Rheumatology and EULAR conferences. They ultimately consulted a total of 54 studies.
In general, said Ms. van Eijk-Hustings, the researchers’ findings support the conclusion that nurses play an important part of a necessarily multidisciplinary team of caregivers that – in addition to rheumatologists – also includes physical therapists, occupational therapists, and psychologists.
"Being involved in the disease process provides nurses with the opportunity to recognize and point out problems in an early stage, which ensures timely interventions and timely referral to other members of the multidisciplinary team," said Ms. van Eijk-Hustings of the department of integrated care at Maastricht (the Netherlands) University Medical Centre.
However, "our project showed that the contribution of nurses to multidisciplinary care is not clearly stated and that competencies and skills of nurses are often not optimally used," according to Ms. Van Eijk-Hustings.
Ultimately, the panel developed 10 recommendations, 7 of which deal with nurses’ ideal contribution to the areas of patient education, satisfaction with care, access to care, psychosocial support, disease management, self-management, and efficiency of care.
Three additional recommendations outline the need for professional support for nurses, including increasing the availability of guidelines or nursing protocols, increasing access to education, and encouraging nurses to undertake extended roles in rheumatology.
"In general, it is of importance that patients have access to rheumatology nurses for various reasons and that rheumatology nurses have access to appropriate training and education in order to maintain and improve their knowledge and skills," said Ms. Van Eijk-Hustings, a registered nurse and doctoral candidate whose own current research deals with the evolving roles of nurses in changing health care systems in different countries.
"This includes advanced, more autonomous roles for nurses, as well as substitution of tasks in the management of chronic disorders without loss of typical nursing skills," she added.
The task force also highlighted ten topics for future research, including the need for high-quality quantitative and qualitative studies with clear descriptions of nursing roles and interventions.
"One important area to mention is the contribution of the nurse in improving patient-preferred outcomes," added Ms. Van Eijk-Hustings.
The researchers cautioned that although the recommendations are likely to be applicable to the role of nurses in other rheumatic diseases, "in the present project, we focused on rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis, and most evidence was found with regard to rheumatoid arthritis."
EULAR support is needed for further dissemination and evaluation of the recommendations, she added.
The researchers reported having no disclosures to make in relation to this study.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Tofacitinib Effective for RA in Phase III Study
The use of tofacitinib in combination with conventional background disease-modifying antirheumatic drugs is associated with rapid, significant, and clinically meaningful reductions in signs and symptoms of rheumatoid arthritis, as well as with improvement in physical function, according to findings from a phase III study.
The data were presented by Dr. Joel M. Kremer at a press briefing during the annual meeting of the European Congress of Rheumatology.
"The very rapid responses were sustained beyond 6 months to 12 months," Dr. Kremer noted.
The findings from the 12-month, placebo-controlled study are consistent with those from phase II studies and a phase III monotherapy study of the novel oral JAK inhibitor, and no new safety signals were detected, said Dr. Kremer, a rheumatologist and the Pfaff Family Professor of Medicine at Albany (N.Y.) Medical College.
In 792 patients with inadequate response to nonbiologic background DMARDs – most often methotrexate – who were randomized to receive either 5 mg or 10 mg of tofacitinib or placebo twice daily, tofacitinib was statistically superior to placebo for all primary efficacy end points, including an ACR 20 response (that is, an American College of Rheumatology score based on a 20% improvement in specified parameters), a DAS28-4(ESR) response (that is, a disease activity score based on a 28-joint count and the erythrocyte sedimentation rate) of less than 2.6 at month 6, and a change in HAQ-DI (Health and Quality of Life–Disability Index) at month 3.
In the 5-mg, 10-mg, and placebo groups, respectively, ACR 20 responses at 6 months were 52.7%, 58.3%, and 31.2%; DAS28-4(ESR) responses of less than 2.6 at 6 months were 11.0%, 14.8% and 2.7%; and changes in HAQ-DI at 3 months were –0.46, –0.56, and –0.21.
Significant differences between the treatment and placebo groups were seen by week 2, Dr. Kremer noted.
The most common adverse events included infections and infestations, which were generally mild. However, four deaths and four opportunistic infections occurred. Deaths included one from acute heart failure and one from respiratory failure in the 10-mg treatment group, and one from traumatic brain injury and one from RA in the 5-mg treatment group, both following discontinuation of treatment (at 22 and 42 days, respectively). Serious infectious events (including opportunistic infections, such as TB, Cryptococcus, and herpes zoster) occurred in two patients in the 5-mg group and in four patients in the 10-mg group during months 0-4, and in one patient in each group during months 3-6. Other adverse events included decreases in neutrophils, increases in LDL and HDL cholesterol levels, small increases in serum creatinine, and anemia.
Patients in the study were mostly women (81.4%) with a mean age in the treatment and placebo groups, respectively, of 50.8 and 53.3 years at baseline, and a mean disease duration of 8.1 and 10.2 years. Nonresponders in the placebo group at month 3 were advanced to tofacitinib, and all remaining patients in the placebo group were advanced at 6 months.
"This large, phase III trial adds to the body of evidence on the efficacy of tofacitinib," Dr. Kremer concluded.
There were four deaths but only one was thought to be treatment related, Dr. Kremer noted. The patient’s spouse refused to grant permission for an autopsy, he added.
Dr. Kremer reported receiving grant and/or research support from Pfizer Inc. and serving as a consultant for Pfizer. Other study authors disclosed having similar relationships with Pfizer, as well as serving on the speakers bureau and/or being a shareholder or employee of Pfizer.
The use of tofacitinib in combination with conventional background disease-modifying antirheumatic drugs is associated with rapid, significant, and clinically meaningful reductions in signs and symptoms of rheumatoid arthritis, as well as with improvement in physical function, according to findings from a phase III study.
The data were presented by Dr. Joel M. Kremer at a press briefing during the annual meeting of the European Congress of Rheumatology.
"The very rapid responses were sustained beyond 6 months to 12 months," Dr. Kremer noted.
The findings from the 12-month, placebo-controlled study are consistent with those from phase II studies and a phase III monotherapy study of the novel oral JAK inhibitor, and no new safety signals were detected, said Dr. Kremer, a rheumatologist and the Pfaff Family Professor of Medicine at Albany (N.Y.) Medical College.
In 792 patients with inadequate response to nonbiologic background DMARDs – most often methotrexate – who were randomized to receive either 5 mg or 10 mg of tofacitinib or placebo twice daily, tofacitinib was statistically superior to placebo for all primary efficacy end points, including an ACR 20 response (that is, an American College of Rheumatology score based on a 20% improvement in specified parameters), a DAS28-4(ESR) response (that is, a disease activity score based on a 28-joint count and the erythrocyte sedimentation rate) of less than 2.6 at month 6, and a change in HAQ-DI (Health and Quality of Life–Disability Index) at month 3.
In the 5-mg, 10-mg, and placebo groups, respectively, ACR 20 responses at 6 months were 52.7%, 58.3%, and 31.2%; DAS28-4(ESR) responses of less than 2.6 at 6 months were 11.0%, 14.8% and 2.7%; and changes in HAQ-DI at 3 months were –0.46, –0.56, and –0.21.
Significant differences between the treatment and placebo groups were seen by week 2, Dr. Kremer noted.
The most common adverse events included infections and infestations, which were generally mild. However, four deaths and four opportunistic infections occurred. Deaths included one from acute heart failure and one from respiratory failure in the 10-mg treatment group, and one from traumatic brain injury and one from RA in the 5-mg treatment group, both following discontinuation of treatment (at 22 and 42 days, respectively). Serious infectious events (including opportunistic infections, such as TB, Cryptococcus, and herpes zoster) occurred in two patients in the 5-mg group and in four patients in the 10-mg group during months 0-4, and in one patient in each group during months 3-6. Other adverse events included decreases in neutrophils, increases in LDL and HDL cholesterol levels, small increases in serum creatinine, and anemia.
Patients in the study were mostly women (81.4%) with a mean age in the treatment and placebo groups, respectively, of 50.8 and 53.3 years at baseline, and a mean disease duration of 8.1 and 10.2 years. Nonresponders in the placebo group at month 3 were advanced to tofacitinib, and all remaining patients in the placebo group were advanced at 6 months.
"This large, phase III trial adds to the body of evidence on the efficacy of tofacitinib," Dr. Kremer concluded.
There were four deaths but only one was thought to be treatment related, Dr. Kremer noted. The patient’s spouse refused to grant permission for an autopsy, he added.
Dr. Kremer reported receiving grant and/or research support from Pfizer Inc. and serving as a consultant for Pfizer. Other study authors disclosed having similar relationships with Pfizer, as well as serving on the speakers bureau and/or being a shareholder or employee of Pfizer.
The use of tofacitinib in combination with conventional background disease-modifying antirheumatic drugs is associated with rapid, significant, and clinically meaningful reductions in signs and symptoms of rheumatoid arthritis, as well as with improvement in physical function, according to findings from a phase III study.
The data were presented by Dr. Joel M. Kremer at a press briefing during the annual meeting of the European Congress of Rheumatology.
"The very rapid responses were sustained beyond 6 months to 12 months," Dr. Kremer noted.
The findings from the 12-month, placebo-controlled study are consistent with those from phase II studies and a phase III monotherapy study of the novel oral JAK inhibitor, and no new safety signals were detected, said Dr. Kremer, a rheumatologist and the Pfaff Family Professor of Medicine at Albany (N.Y.) Medical College.
In 792 patients with inadequate response to nonbiologic background DMARDs – most often methotrexate – who were randomized to receive either 5 mg or 10 mg of tofacitinib or placebo twice daily, tofacitinib was statistically superior to placebo for all primary efficacy end points, including an ACR 20 response (that is, an American College of Rheumatology score based on a 20% improvement in specified parameters), a DAS28-4(ESR) response (that is, a disease activity score based on a 28-joint count and the erythrocyte sedimentation rate) of less than 2.6 at month 6, and a change in HAQ-DI (Health and Quality of Life–Disability Index) at month 3.
In the 5-mg, 10-mg, and placebo groups, respectively, ACR 20 responses at 6 months were 52.7%, 58.3%, and 31.2%; DAS28-4(ESR) responses of less than 2.6 at 6 months were 11.0%, 14.8% and 2.7%; and changes in HAQ-DI at 3 months were –0.46, –0.56, and –0.21.
Significant differences between the treatment and placebo groups were seen by week 2, Dr. Kremer noted.
The most common adverse events included infections and infestations, which were generally mild. However, four deaths and four opportunistic infections occurred. Deaths included one from acute heart failure and one from respiratory failure in the 10-mg treatment group, and one from traumatic brain injury and one from RA in the 5-mg treatment group, both following discontinuation of treatment (at 22 and 42 days, respectively). Serious infectious events (including opportunistic infections, such as TB, Cryptococcus, and herpes zoster) occurred in two patients in the 5-mg group and in four patients in the 10-mg group during months 0-4, and in one patient in each group during months 3-6. Other adverse events included decreases in neutrophils, increases in LDL and HDL cholesterol levels, small increases in serum creatinine, and anemia.
Patients in the study were mostly women (81.4%) with a mean age in the treatment and placebo groups, respectively, of 50.8 and 53.3 years at baseline, and a mean disease duration of 8.1 and 10.2 years. Nonresponders in the placebo group at month 3 were advanced to tofacitinib, and all remaining patients in the placebo group were advanced at 6 months.
"This large, phase III trial adds to the body of evidence on the efficacy of tofacitinib," Dr. Kremer concluded.
There were four deaths but only one was thought to be treatment related, Dr. Kremer noted. The patient’s spouse refused to grant permission for an autopsy, he added.
Dr. Kremer reported receiving grant and/or research support from Pfizer Inc. and serving as a consultant for Pfizer. Other study authors disclosed having similar relationships with Pfizer, as well as serving on the speakers bureau and/or being a shareholder or employee of Pfizer.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Findings: In the 5-mg, 10-mg, and placebo groups, respectively, ACR 20
responses at 6 months were 52.7%, 58.3%, and 31.2%; DAS28-4(ESR)
responses of less than 2.6 at 6 months were 11.0%, 14.8% and 2.7%; and
changes in HAQ-DI at 3 months were –0.46, –0.56, and –0.21. Significant differences between the treatment and placebo groups were seen by week 2
Data Source: A phase III 12-month, placebo-controlled study. A total of 792 patients with inadequate response to nonbiologic background DMARDs –
most often methotrexate – who were randomized to receive either 5 mg or
10 mg of tofacitinib or placebo twice daily.
Disclosures: Dr. Kremer reported receiving grant and/or research support from Pfizer
Inc. and serving as a consultant for Pfizer. Other study authors
disclosed having similar relationships with Pfizer, as well as serving
on the speakers bureau and/or being a shareholder or employee of Pfizer.
Tofacitinib Effective for RA in Phase III Study
The use of tofacitinib in combination with conventional background disease-modifying antirheumatic drugs is associated with rapid, significant, and clinically meaningful reductions in signs and symptoms of rheumatoid arthritis, as well as with improvement in physical function, according to findings from a phase III study.
The data were presented by Dr. Joel M. Kremer at a press briefing during the annual meeting of the European Congress of Rheumatology.
"The very rapid responses were sustained beyond 6 months to 12 months," Dr. Kremer noted.
The findings from the 12-month, placebo-controlled study are consistent with those from phase II studies and a phase III monotherapy study of the novel oral JAK inhibitor, and no new safety signals were detected, said Dr. Kremer, a rheumatologist and the Pfaff Family Professor of Medicine at Albany (N.Y.) Medical College.
In 792 patients with inadequate response to nonbiologic background DMARDs – most often methotrexate – who were randomized to receive either 5 mg or 10 mg of tofacitinib or placebo twice daily, tofacitinib was statistically superior to placebo for all primary efficacy end points, including an ACR 20 response (that is, an American College of Rheumatology score based on a 20% improvement in specified parameters), a DAS28-4(ESR) response (that is, a disease activity score based on a 28-joint count and the erythrocyte sedimentation rate) of less than 2.6 at month 6, and a change in HAQ-DI (Health and Quality of Life–Disability Index) at month 3.
In the 5-mg, 10-mg, and placebo groups, respectively, ACR 20 responses at 6 months were 52.7%, 58.3%, and 31.2%; DAS28-4(ESR) responses of less than 2.6 at 6 months were 11.0%, 14.8% and 2.7%; and changes in HAQ-DI at 3 months were –0.46, –0.56, and –0.21.
Significant differences between the treatment and placebo groups were seen by week 2, Dr. Kremer noted.
The most common adverse events included infections and infestations, which were generally mild. However, four deaths and four opportunistic infections occurred. Deaths included one from acute heart failure and one from respiratory failure in the 10-mg treatment group, and one from traumatic brain injury and one from RA in the 5-mg treatment group, both following discontinuation of treatment (at 22 and 42 days, respectively). Serious infectious events (including opportunistic infections, such as TB, Cryptococcus, and herpes zoster) occurred in two patients in the 5-mg group and in four patients in the 10-mg group during months 0-4, and in one patient in each group during months 3-6. Other adverse events included decreases in neutrophils, increases in LDL and HDL cholesterol levels, small increases in serum creatinine, and anemia.
Patients in the study were mostly women (81.4%) with a mean age in the treatment and placebo groups, respectively, of 50.8 and 53.3 years at baseline, and a mean disease duration of 8.1 and 10.2 years. Nonresponders in the placebo group at month 3 were advanced to tofacitinib, and all remaining patients in the placebo group were advanced at 6 months.
"This large, phase III trial adds to the body of evidence on the efficacy of tofacitinib," Dr. Kremer concluded.
There were four deaths but only one was thought to be treatment related, Dr. Kremer noted. The patient’s spouse refused to grant permission for an autopsy, he added.
Dr. Kremer reported receiving grant and/or research support from Pfizer Inc. and serving as a consultant for Pfizer. Other study authors disclosed having similar relationships with Pfizer, as well as serving on the speakers bureau and/or being a shareholder or employee of Pfizer.
The use of tofacitinib in combination with conventional background disease-modifying antirheumatic drugs is associated with rapid, significant, and clinically meaningful reductions in signs and symptoms of rheumatoid arthritis, as well as with improvement in physical function, according to findings from a phase III study.
The data were presented by Dr. Joel M. Kremer at a press briefing during the annual meeting of the European Congress of Rheumatology.
"The very rapid responses were sustained beyond 6 months to 12 months," Dr. Kremer noted.
The findings from the 12-month, placebo-controlled study are consistent with those from phase II studies and a phase III monotherapy study of the novel oral JAK inhibitor, and no new safety signals were detected, said Dr. Kremer, a rheumatologist and the Pfaff Family Professor of Medicine at Albany (N.Y.) Medical College.
In 792 patients with inadequate response to nonbiologic background DMARDs – most often methotrexate – who were randomized to receive either 5 mg or 10 mg of tofacitinib or placebo twice daily, tofacitinib was statistically superior to placebo for all primary efficacy end points, including an ACR 20 response (that is, an American College of Rheumatology score based on a 20% improvement in specified parameters), a DAS28-4(ESR) response (that is, a disease activity score based on a 28-joint count and the erythrocyte sedimentation rate) of less than 2.6 at month 6, and a change in HAQ-DI (Health and Quality of Life–Disability Index) at month 3.
In the 5-mg, 10-mg, and placebo groups, respectively, ACR 20 responses at 6 months were 52.7%, 58.3%, and 31.2%; DAS28-4(ESR) responses of less than 2.6 at 6 months were 11.0%, 14.8% and 2.7%; and changes in HAQ-DI at 3 months were –0.46, –0.56, and –0.21.
Significant differences between the treatment and placebo groups were seen by week 2, Dr. Kremer noted.
The most common adverse events included infections and infestations, which were generally mild. However, four deaths and four opportunistic infections occurred. Deaths included one from acute heart failure and one from respiratory failure in the 10-mg treatment group, and one from traumatic brain injury and one from RA in the 5-mg treatment group, both following discontinuation of treatment (at 22 and 42 days, respectively). Serious infectious events (including opportunistic infections, such as TB, Cryptococcus, and herpes zoster) occurred in two patients in the 5-mg group and in four patients in the 10-mg group during months 0-4, and in one patient in each group during months 3-6. Other adverse events included decreases in neutrophils, increases in LDL and HDL cholesterol levels, small increases in serum creatinine, and anemia.
Patients in the study were mostly women (81.4%) with a mean age in the treatment and placebo groups, respectively, of 50.8 and 53.3 years at baseline, and a mean disease duration of 8.1 and 10.2 years. Nonresponders in the placebo group at month 3 were advanced to tofacitinib, and all remaining patients in the placebo group were advanced at 6 months.
"This large, phase III trial adds to the body of evidence on the efficacy of tofacitinib," Dr. Kremer concluded.
There were four deaths but only one was thought to be treatment related, Dr. Kremer noted. The patient’s spouse refused to grant permission for an autopsy, he added.
Dr. Kremer reported receiving grant and/or research support from Pfizer Inc. and serving as a consultant for Pfizer. Other study authors disclosed having similar relationships with Pfizer, as well as serving on the speakers bureau and/or being a shareholder or employee of Pfizer.
The use of tofacitinib in combination with conventional background disease-modifying antirheumatic drugs is associated with rapid, significant, and clinically meaningful reductions in signs and symptoms of rheumatoid arthritis, as well as with improvement in physical function, according to findings from a phase III study.
The data were presented by Dr. Joel M. Kremer at a press briefing during the annual meeting of the European Congress of Rheumatology.
"The very rapid responses were sustained beyond 6 months to 12 months," Dr. Kremer noted.
The findings from the 12-month, placebo-controlled study are consistent with those from phase II studies and a phase III monotherapy study of the novel oral JAK inhibitor, and no new safety signals were detected, said Dr. Kremer, a rheumatologist and the Pfaff Family Professor of Medicine at Albany (N.Y.) Medical College.
In 792 patients with inadequate response to nonbiologic background DMARDs – most often methotrexate – who were randomized to receive either 5 mg or 10 mg of tofacitinib or placebo twice daily, tofacitinib was statistically superior to placebo for all primary efficacy end points, including an ACR 20 response (that is, an American College of Rheumatology score based on a 20% improvement in specified parameters), a DAS28-4(ESR) response (that is, a disease activity score based on a 28-joint count and the erythrocyte sedimentation rate) of less than 2.6 at month 6, and a change in HAQ-DI (Health and Quality of Life–Disability Index) at month 3.
In the 5-mg, 10-mg, and placebo groups, respectively, ACR 20 responses at 6 months were 52.7%, 58.3%, and 31.2%; DAS28-4(ESR) responses of less than 2.6 at 6 months were 11.0%, 14.8% and 2.7%; and changes in HAQ-DI at 3 months were –0.46, –0.56, and –0.21.
Significant differences between the treatment and placebo groups were seen by week 2, Dr. Kremer noted.
The most common adverse events included infections and infestations, which were generally mild. However, four deaths and four opportunistic infections occurred. Deaths included one from acute heart failure and one from respiratory failure in the 10-mg treatment group, and one from traumatic brain injury and one from RA in the 5-mg treatment group, both following discontinuation of treatment (at 22 and 42 days, respectively). Serious infectious events (including opportunistic infections, such as TB, Cryptococcus, and herpes zoster) occurred in two patients in the 5-mg group and in four patients in the 10-mg group during months 0-4, and in one patient in each group during months 3-6. Other adverse events included decreases in neutrophils, increases in LDL and HDL cholesterol levels, small increases in serum creatinine, and anemia.
Patients in the study were mostly women (81.4%) with a mean age in the treatment and placebo groups, respectively, of 50.8 and 53.3 years at baseline, and a mean disease duration of 8.1 and 10.2 years. Nonresponders in the placebo group at month 3 were advanced to tofacitinib, and all remaining patients in the placebo group were advanced at 6 months.
"This large, phase III trial adds to the body of evidence on the efficacy of tofacitinib," Dr. Kremer concluded.
There were four deaths but only one was thought to be treatment related, Dr. Kremer noted. The patient’s spouse refused to grant permission for an autopsy, he added.
Dr. Kremer reported receiving grant and/or research support from Pfizer Inc. and serving as a consultant for Pfizer. Other study authors disclosed having similar relationships with Pfizer, as well as serving on the speakers bureau and/or being a shareholder or employee of Pfizer.
FROM THE ANNUAL EUROPEAN CONGRESS OF RHEUMATOLOGY
Major Findings: In the 5-mg, 10-mg, and placebo groups,
respectively, ACR 20
responses at 6 months were 52.7%, 58.3%, and 31.2%; DAS28-4(ESR)
responses of less than 2.6 at 6 months were 11.0%, 14.8% and 2.7%; and
changes in HAQ-DI at 3 months were –0.46, –0.56, and –0.21. Significant
differences between the treatment and placebo groups were seen by week 2
Data Source:
A phase III 12-month, placebo-controlled study. A total of 792
patients with inadequate response to nonbiologic background DMARDs –
most often methotrexate – who were randomized to receive either 5 mg or
10 mg of tofacitinib or placebo twice daily.
Disclosures: Dr. Kremer reported receiving grant and/or research support from Pfizer
Inc. and serving as a consultant for Pfizer. Other study authors
disclosed having similar relationships with Pfizer, as well as serving
on the speakers bureau and/or being a shareholder or employee of Pfizer.