User login
Held every two years International Headache Society (IHS): International Headache Congress (IHC 2015)
Sexual abuse history may promote migraine transformation
VALENCIA, SPAIN – A history of childhood sexual abuse is nearly fourfold more common among chronic migraine patients than in those with episodic migraine, Dr. Brad Torphy reported at the International Headache Congress.
This association raises the possibility that prior sexual abuse is a contributing factor in the transformation from episodic migraine – defined as fewer than 15 headache days per month – to the more serious and difficult-to-treat chronic migraine, which entails headaches on 15 or more days monthly, said Dr. Torphy of Diamond Headache Clinic in Chicago.
“The clinical implications of these findings, and what I’m stressing, is the importance of intervention – such as psychological counseling – in episodic migraine patients who have a history of abuse. The other key point is that patients who have episodic migraine may warrant more aggressive therapy, including going on preventive medications sooner, if they have a history of sexual abuse, because they’re probably at risk for progression to chronic migraine,” he said in an interview at the meeting.
Dr. Torphy presented a retrospective study of all new patients seen at the Diamond Headache Clinic during the final 4 months of last year. The new-patient questionnaire includes a section about past sexual abuse. Such a history was reported by 6 (4.4%) of the 135 episodic migraine patients, compared with 30 (15.5%) of the 194 patients with chronic migraine.
“What made me think about doing this study is that at the Diamond Clinic every week we have a meeting with our psychology group, and it just seemed like week after week so many patients had these horrifying stories of their childhood. I thought there must be a connection between that history of sexual abuse and progression to chronic migraine,” he said.
He added that, based upon his experience in the clinic, he suspects that the true proportion of patients with a positive history for sexual abuse is considerably higher than the rates the new-patient questionnaire would suggest.
“A lot of factors would lead to that being a very low number. It’s the patient’s first visit, and it’s a paper questionnaire so patients may not be comfortable checking that box when they don’t know who’s going to see the results. I’ve had cases where patients shared with me only after two or three visits that, yes, I do have that history. I think it’s underreported across the board,” Dr. Torphy continued.
In his review of the literature he found that other investigators have tended either to lump together all kinds of abuse – physical, emotional, and sexual – in analyzing an association with migraine, or if they looked at sexual abuse in particular it was in association with all types of chronic pain, not specifically migraine.
The meeting was sponsored by the International Headache Society and the American Headache Society. Dr. Torphy reported no financial conflicts.
VALENCIA, SPAIN – A history of childhood sexual abuse is nearly fourfold more common among chronic migraine patients than in those with episodic migraine, Dr. Brad Torphy reported at the International Headache Congress.
This association raises the possibility that prior sexual abuse is a contributing factor in the transformation from episodic migraine – defined as fewer than 15 headache days per month – to the more serious and difficult-to-treat chronic migraine, which entails headaches on 15 or more days monthly, said Dr. Torphy of Diamond Headache Clinic in Chicago.
“The clinical implications of these findings, and what I’m stressing, is the importance of intervention – such as psychological counseling – in episodic migraine patients who have a history of abuse. The other key point is that patients who have episodic migraine may warrant more aggressive therapy, including going on preventive medications sooner, if they have a history of sexual abuse, because they’re probably at risk for progression to chronic migraine,” he said in an interview at the meeting.
Dr. Torphy presented a retrospective study of all new patients seen at the Diamond Headache Clinic during the final 4 months of last year. The new-patient questionnaire includes a section about past sexual abuse. Such a history was reported by 6 (4.4%) of the 135 episodic migraine patients, compared with 30 (15.5%) of the 194 patients with chronic migraine.
“What made me think about doing this study is that at the Diamond Clinic every week we have a meeting with our psychology group, and it just seemed like week after week so many patients had these horrifying stories of their childhood. I thought there must be a connection between that history of sexual abuse and progression to chronic migraine,” he said.
He added that, based upon his experience in the clinic, he suspects that the true proportion of patients with a positive history for sexual abuse is considerably higher than the rates the new-patient questionnaire would suggest.
“A lot of factors would lead to that being a very low number. It’s the patient’s first visit, and it’s a paper questionnaire so patients may not be comfortable checking that box when they don’t know who’s going to see the results. I’ve had cases where patients shared with me only after two or three visits that, yes, I do have that history. I think it’s underreported across the board,” Dr. Torphy continued.
In his review of the literature he found that other investigators have tended either to lump together all kinds of abuse – physical, emotional, and sexual – in analyzing an association with migraine, or if they looked at sexual abuse in particular it was in association with all types of chronic pain, not specifically migraine.
The meeting was sponsored by the International Headache Society and the American Headache Society. Dr. Torphy reported no financial conflicts.
VALENCIA, SPAIN – A history of childhood sexual abuse is nearly fourfold more common among chronic migraine patients than in those with episodic migraine, Dr. Brad Torphy reported at the International Headache Congress.
This association raises the possibility that prior sexual abuse is a contributing factor in the transformation from episodic migraine – defined as fewer than 15 headache days per month – to the more serious and difficult-to-treat chronic migraine, which entails headaches on 15 or more days monthly, said Dr. Torphy of Diamond Headache Clinic in Chicago.
“The clinical implications of these findings, and what I’m stressing, is the importance of intervention – such as psychological counseling – in episodic migraine patients who have a history of abuse. The other key point is that patients who have episodic migraine may warrant more aggressive therapy, including going on preventive medications sooner, if they have a history of sexual abuse, because they’re probably at risk for progression to chronic migraine,” he said in an interview at the meeting.
Dr. Torphy presented a retrospective study of all new patients seen at the Diamond Headache Clinic during the final 4 months of last year. The new-patient questionnaire includes a section about past sexual abuse. Such a history was reported by 6 (4.4%) of the 135 episodic migraine patients, compared with 30 (15.5%) of the 194 patients with chronic migraine.
“What made me think about doing this study is that at the Diamond Clinic every week we have a meeting with our psychology group, and it just seemed like week after week so many patients had these horrifying stories of their childhood. I thought there must be a connection between that history of sexual abuse and progression to chronic migraine,” he said.
He added that, based upon his experience in the clinic, he suspects that the true proportion of patients with a positive history for sexual abuse is considerably higher than the rates the new-patient questionnaire would suggest.
“A lot of factors would lead to that being a very low number. It’s the patient’s first visit, and it’s a paper questionnaire so patients may not be comfortable checking that box when they don’t know who’s going to see the results. I’ve had cases where patients shared with me only after two or three visits that, yes, I do have that history. I think it’s underreported across the board,” Dr. Torphy continued.
In his review of the literature he found that other investigators have tended either to lump together all kinds of abuse – physical, emotional, and sexual – in analyzing an association with migraine, or if they looked at sexual abuse in particular it was in association with all types of chronic pain, not specifically migraine.
The meeting was sponsored by the International Headache Society and the American Headache Society. Dr. Torphy reported no financial conflicts.
AT IHC 2015
Key clinical point: Episodic migraine patients with a history of childhood sexual abuse may be at increased risk of transformation to chronic migraine.
Major finding: A history of childhood sexual abuse was self-reported by 4.4% of episodic migraine patients, compared with 15.5% chronic migraineurs.
Data source: A retrospective chart review of 329 consecutive migraine patients seen at a specialized headache clinic.
Disclosures: The presenter reported no financial conflicts.
IHC: Botox for migraine also improves depression
VALENCIA, SPAIN – OnabotulinumtoxinA injections given for treatment of chronic migraine provide a major side benefit: clinically meaningful improvement in comorbid moderate to severe depression, Dr. Stewart J. Tepper reported at the International Headache Congress.
He presented an uncontrolled, retrospective study with prospectively collected patient-reported outcomes data in 429 chronic migraine patients who underwent two or more sessions of onabotulinumtoxinA (Botox) injections, a treatment approved by the Food and Drug Administration for chronic migraine since 2010.
Since the safety and efficacy of the treatment for chronic migraine are already well established, the goal of this study was to examine change in depression, a common comorbid condition in this population. The primary outcome measure was change in Patient Health Questionnaire-9 (PHQ-9) scores from baseline to follow-up at 6-12 months.
In the overall study population, PHQ-9 scores improved significantly, from a mean of 14.4 at baseline to 11.3 post Botox. But the results became considerably more intriguing when broken by baseline level of depression, according to Dr. Tepper, professor of medicine (neurology) at Case Western Reserve University, Cleveland, and director of research at the Neurological Center for Pain at the Cleveland Clinic.
Seventy percent of the chronic migraine patients had at least mild depression as reflected in a baseline PHQ-9 score of 5 or more. Among the 145 patients with mild depression as evidenced by a PHQ-9 of 5-9, Botox therapy wasn’t associated with any impact on depression scores: a mean of 6.8 at baseline and 6.8 at follow-up.
In contrast, among the 75 patients with moderate depression as defined by a PHQ-9 score of 10-14, depression scores improved significantly from 11.8 to 9.6. Moreover, in the 30 patients with baseline moderate/severe depression as evidenced by a PHQ-9 of 15-19, scores improved from 17 at pretreatment to 13.4 at follow-up. The largest absolute improvement in depression scores was seen in those who were most severely depressed: in the 16 patients with baseline severe depression as defined by a PHQ-9 score of 20-27, mean scores improved from 21.8 at baseline to 15.2, Dr. Tepper reported at the meeting sponsored by the International Headache Society and the American Headache Society.
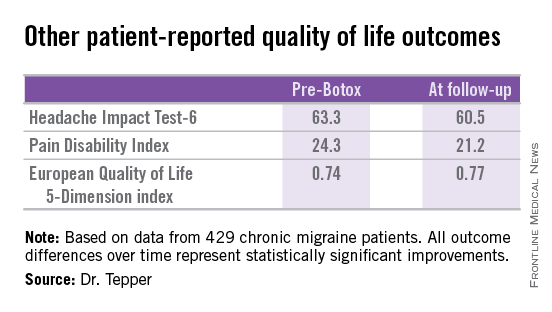
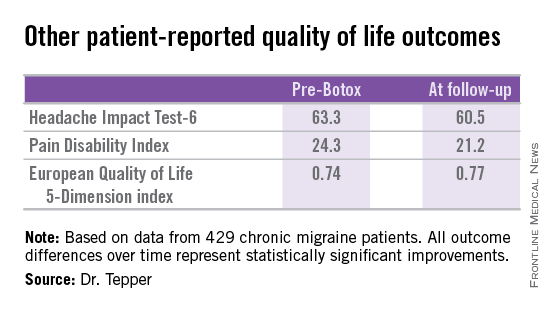
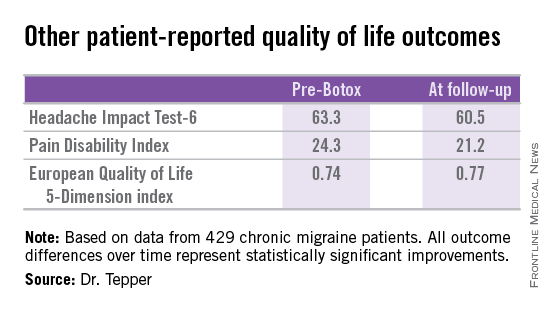
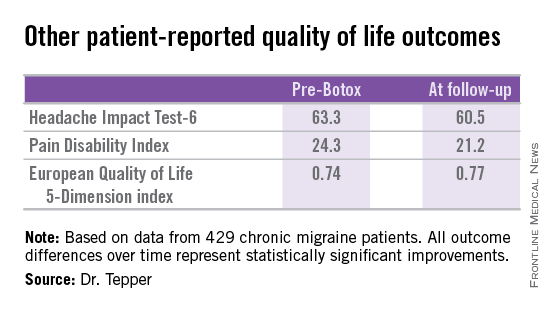
Other patient-reported outcomes also improved significantly following two or more onabotulinumtoxinA treatment sessions.
Dr. Tepper reported no financial conflicts regarding this study, which was conducted exclusively with institutional funds.
VALENCIA, SPAIN – OnabotulinumtoxinA injections given for treatment of chronic migraine provide a major side benefit: clinically meaningful improvement in comorbid moderate to severe depression, Dr. Stewart J. Tepper reported at the International Headache Congress.
He presented an uncontrolled, retrospective study with prospectively collected patient-reported outcomes data in 429 chronic migraine patients who underwent two or more sessions of onabotulinumtoxinA (Botox) injections, a treatment approved by the Food and Drug Administration for chronic migraine since 2010.
Since the safety and efficacy of the treatment for chronic migraine are already well established, the goal of this study was to examine change in depression, a common comorbid condition in this population. The primary outcome measure was change in Patient Health Questionnaire-9 (PHQ-9) scores from baseline to follow-up at 6-12 months.
In the overall study population, PHQ-9 scores improved significantly, from a mean of 14.4 at baseline to 11.3 post Botox. But the results became considerably more intriguing when broken by baseline level of depression, according to Dr. Tepper, professor of medicine (neurology) at Case Western Reserve University, Cleveland, and director of research at the Neurological Center for Pain at the Cleveland Clinic.
Seventy percent of the chronic migraine patients had at least mild depression as reflected in a baseline PHQ-9 score of 5 or more. Among the 145 patients with mild depression as evidenced by a PHQ-9 of 5-9, Botox therapy wasn’t associated with any impact on depression scores: a mean of 6.8 at baseline and 6.8 at follow-up.
In contrast, among the 75 patients with moderate depression as defined by a PHQ-9 score of 10-14, depression scores improved significantly from 11.8 to 9.6. Moreover, in the 30 patients with baseline moderate/severe depression as evidenced by a PHQ-9 of 15-19, scores improved from 17 at pretreatment to 13.4 at follow-up. The largest absolute improvement in depression scores was seen in those who were most severely depressed: in the 16 patients with baseline severe depression as defined by a PHQ-9 score of 20-27, mean scores improved from 21.8 at baseline to 15.2, Dr. Tepper reported at the meeting sponsored by the International Headache Society and the American Headache Society.
Other patient-reported outcomes also improved significantly following two or more onabotulinumtoxinA treatment sessions.
Dr. Tepper reported no financial conflicts regarding this study, which was conducted exclusively with institutional funds.
VALENCIA, SPAIN – OnabotulinumtoxinA injections given for treatment of chronic migraine provide a major side benefit: clinically meaningful improvement in comorbid moderate to severe depression, Dr. Stewart J. Tepper reported at the International Headache Congress.
He presented an uncontrolled, retrospective study with prospectively collected patient-reported outcomes data in 429 chronic migraine patients who underwent two or more sessions of onabotulinumtoxinA (Botox) injections, a treatment approved by the Food and Drug Administration for chronic migraine since 2010.
Since the safety and efficacy of the treatment for chronic migraine are already well established, the goal of this study was to examine change in depression, a common comorbid condition in this population. The primary outcome measure was change in Patient Health Questionnaire-9 (PHQ-9) scores from baseline to follow-up at 6-12 months.
In the overall study population, PHQ-9 scores improved significantly, from a mean of 14.4 at baseline to 11.3 post Botox. But the results became considerably more intriguing when broken by baseline level of depression, according to Dr. Tepper, professor of medicine (neurology) at Case Western Reserve University, Cleveland, and director of research at the Neurological Center for Pain at the Cleveland Clinic.
Seventy percent of the chronic migraine patients had at least mild depression as reflected in a baseline PHQ-9 score of 5 or more. Among the 145 patients with mild depression as evidenced by a PHQ-9 of 5-9, Botox therapy wasn’t associated with any impact on depression scores: a mean of 6.8 at baseline and 6.8 at follow-up.
In contrast, among the 75 patients with moderate depression as defined by a PHQ-9 score of 10-14, depression scores improved significantly from 11.8 to 9.6. Moreover, in the 30 patients with baseline moderate/severe depression as evidenced by a PHQ-9 of 15-19, scores improved from 17 at pretreatment to 13.4 at follow-up. The largest absolute improvement in depression scores was seen in those who were most severely depressed: in the 16 patients with baseline severe depression as defined by a PHQ-9 score of 20-27, mean scores improved from 21.8 at baseline to 15.2, Dr. Tepper reported at the meeting sponsored by the International Headache Society and the American Headache Society.
Other patient-reported outcomes also improved significantly following two or more onabotulinumtoxinA treatment sessions.
Dr. Tepper reported no financial conflicts regarding this study, which was conducted exclusively with institutional funds.
AT IHC 2015
Key clinical point: OnabotulinumtoxinA injections for chronic migraine significantly improved depression scores in patients with moderate or severe depression at baseline.
Major finding: Mean depression scores on the Patient Health Questionnaire-9 in chronic migraine patients with baseline severe depression improved from 21.8 out of a possible 27 at baseline to 15.2 at 6-12 months’ follow-up after two or more onabotulinumtoxinA treatment sessions.
Data source: This was an uncontrolled, retrospective study of 429 patients who underwent two or more sessions of onabotulinumtoxinA injections for chronic migraine and were assessed for change in depression scores.
Disclosures: This study was conducted entirely with institutional funds. The presenter reported having no financial conflicts.
IHC: Infantile colic portends adolescent migraine
VALENCIA, SPAIN – Infantile colic appears to be a potent predictor of subsequent adolescent migraine without aura, according to a large, prospective, population-based Finnish study.
This is the latest of several studies to document a relationship between infantile colic and later migraine. It’s particularly persuasive by virtue of its 18 years of prospective follow-up, Dr. Kenneth J. Mack commented at the International Headache Congress.
Indeed, he hailed the Finnish study (Cephalalgia. 2015 Mar 9. pii: 0333102415576225.) led by investigators at the University of Turku as one of the top developments in the field of pediatric headache within the past year.
The Finnish investigators followed 1,267 infants, all the first-born in their families, and 13% of whom were diagnosed with colic by age 3 months. Of the 787 subjects captured at follow-up at age 18 years, 129 had been diagnosed with migraine, and 96 of the 787 had a history of infantile colic.
Migraine was present in 23% of the 18-year-olds with a history of infantile colic but in only 11% of those without such a history, noted Dr. Mack, professor of neurology and pediatrics at the Mayo Clinic, Rochester, Minn.
Fourteen of 22 adolescent migraineurs with a history of infantile colic had migraine without aura. The remaining eight had migraine with aura. Thus, infantile colic was associated with a highly significant 2.8-fold increased risk for adolescent migraine without aura but no increased risk for developing migraine with aura, Dr. Mack continued at the meeting sponsored by the International Headache Society and the American Headache Society.
This study solidifies the link between infantile colic and subsequent migraine, but Dr. Mack said he has long suspected the existence of such an association based upon personal experience: “In my own family, two out of three colicky boys developed migraine.”
As the Finnish investigators noted, their study leaves unanswered the question of whether infantile colic is through some as-yet unknown mechanism a risk factor for the subsequent development of migraine or, alternatively, infantile colic might actually be an expression of infantile migraine.
The study was sponsored by the University of Turku, Finland. Dr. Mack reported having no financial conflicts regarding the Finnish study.
VALENCIA, SPAIN – Infantile colic appears to be a potent predictor of subsequent adolescent migraine without aura, according to a large, prospective, population-based Finnish study.
This is the latest of several studies to document a relationship between infantile colic and later migraine. It’s particularly persuasive by virtue of its 18 years of prospective follow-up, Dr. Kenneth J. Mack commented at the International Headache Congress.
Indeed, he hailed the Finnish study (Cephalalgia. 2015 Mar 9. pii: 0333102415576225.) led by investigators at the University of Turku as one of the top developments in the field of pediatric headache within the past year.
The Finnish investigators followed 1,267 infants, all the first-born in their families, and 13% of whom were diagnosed with colic by age 3 months. Of the 787 subjects captured at follow-up at age 18 years, 129 had been diagnosed with migraine, and 96 of the 787 had a history of infantile colic.
Migraine was present in 23% of the 18-year-olds with a history of infantile colic but in only 11% of those without such a history, noted Dr. Mack, professor of neurology and pediatrics at the Mayo Clinic, Rochester, Minn.
Fourteen of 22 adolescent migraineurs with a history of infantile colic had migraine without aura. The remaining eight had migraine with aura. Thus, infantile colic was associated with a highly significant 2.8-fold increased risk for adolescent migraine without aura but no increased risk for developing migraine with aura, Dr. Mack continued at the meeting sponsored by the International Headache Society and the American Headache Society.
This study solidifies the link between infantile colic and subsequent migraine, but Dr. Mack said he has long suspected the existence of such an association based upon personal experience: “In my own family, two out of three colicky boys developed migraine.”
As the Finnish investigators noted, their study leaves unanswered the question of whether infantile colic is through some as-yet unknown mechanism a risk factor for the subsequent development of migraine or, alternatively, infantile colic might actually be an expression of infantile migraine.
The study was sponsored by the University of Turku, Finland. Dr. Mack reported having no financial conflicts regarding the Finnish study.
VALENCIA, SPAIN – Infantile colic appears to be a potent predictor of subsequent adolescent migraine without aura, according to a large, prospective, population-based Finnish study.
This is the latest of several studies to document a relationship between infantile colic and later migraine. It’s particularly persuasive by virtue of its 18 years of prospective follow-up, Dr. Kenneth J. Mack commented at the International Headache Congress.
Indeed, he hailed the Finnish study (Cephalalgia. 2015 Mar 9. pii: 0333102415576225.) led by investigators at the University of Turku as one of the top developments in the field of pediatric headache within the past year.
The Finnish investigators followed 1,267 infants, all the first-born in their families, and 13% of whom were diagnosed with colic by age 3 months. Of the 787 subjects captured at follow-up at age 18 years, 129 had been diagnosed with migraine, and 96 of the 787 had a history of infantile colic.
Migraine was present in 23% of the 18-year-olds with a history of infantile colic but in only 11% of those without such a history, noted Dr. Mack, professor of neurology and pediatrics at the Mayo Clinic, Rochester, Minn.
Fourteen of 22 adolescent migraineurs with a history of infantile colic had migraine without aura. The remaining eight had migraine with aura. Thus, infantile colic was associated with a highly significant 2.8-fold increased risk for adolescent migraine without aura but no increased risk for developing migraine with aura, Dr. Mack continued at the meeting sponsored by the International Headache Society and the American Headache Society.
This study solidifies the link between infantile colic and subsequent migraine, but Dr. Mack said he has long suspected the existence of such an association based upon personal experience: “In my own family, two out of three colicky boys developed migraine.”
As the Finnish investigators noted, their study leaves unanswered the question of whether infantile colic is through some as-yet unknown mechanism a risk factor for the subsequent development of migraine or, alternatively, infantile colic might actually be an expression of infantile migraine.
The study was sponsored by the University of Turku, Finland. Dr. Mack reported having no financial conflicts regarding the Finnish study.
AT IHC 2015
Key clinical point: Infantile colic is associated with a nearly threefold increased risk of having migraine by age 18 years.
Major finding: Migraine was present at age 18 in 23% of a group of Finnish youths with a history of infantile colic but in only 11% of subjects without such a history.
Data source: This was a prospective, population-based cohort study involving 18 years of follow-up of 1,267 Finnish infants.
Disclosures: The study was sponsored by the University of Turku, Finland. The presenter reported having no financial conflicts.
IHC: Sucked clonazepam douses burning mouth syndrome
VALENCIA, SPAIN – Sucking on a clonazepam tablet for 3 minutes after every meal effectively reduced pain, paresthesia, dry mouth, and altered sense of taste in patients with burning mouth syndrome in a retrospective study.
Seventy-two patients who met International Headache Society criteria for burning mouth syndrome were instructed to place a 1-mg tablet of clonazepam in their mouths after each meal and suck on it for 3 minutes, holding their saliva in the painful areas of the mouth all the while without swallowing. After the 3 minutes were up, the dregs of the tablet and the saliva were to be spit out, Dr. Maialen Mendizabal reported at the International Headache Congress.
Controlled trials previously have shown orally ingested clonazepam to be effective in patients with burning mouth syndrome. Sucked clonazepam provides the advantages of a topical therapy, added Dr. Mendizabal of the University of the Basque Country, Bilbao, Spain.
Pain was assessed via the validated Brief Pain Inventory at baseline, 2 months, and 6 months, as were the sensory disturbances and other symptoms that are often featured prominently in patients with burning mouth syndrome.
At 2 months, 31% of patients reported a greater than 50% reduction from baseline in pain scores, and an additional 10% had a 30%-50% reduction in pain. At 6 months, 39% of patients reported a greater than 50% reduction in pain, and 8% had a 30%-50% decrease.
Fifteen patients (20%) were completely asymptomatic at 6 months. An additional three patients were pain free but continued to experience dry mouth or other symptoms associated with burning mouth syndrome, she reported at the meeting sponsored by the International Headache Society and the American Headache Society.
Dry mouth and altered taste showed a particularly favorable response to topical clonazepam. Two-thirds of subjects had an altered sense of taste at baseline, one-third after 2 months of clonazepam sucking, and none at 6 months. Likewise, two-thirds of patients reported dry mouth at baseline, 47% at 2 months, and just 13% at 6 months.
Although this retrospective, uncontrolled study certainly can’t be considered the final word, the results are sufficiently encouraging to warrant a randomized trial, Dr. Mendizabal said.
The International Headache Society diagnostic criteria for burning mouth syndrome require the presence of pain in the mouth on a daily basis and persisting for most of the day, normal appearing oral mucosa, and exclusion of other local and systemic diseases.
Burning mouth syndrome is mainly a disorder of postmenopausal women. In this study, the mean age of the population was 63 years, and 82% were female.
Dr. Mendizabal reported having no financial conflicts regarding this study, which was conducted free of commercial support.
VALENCIA, SPAIN – Sucking on a clonazepam tablet for 3 minutes after every meal effectively reduced pain, paresthesia, dry mouth, and altered sense of taste in patients with burning mouth syndrome in a retrospective study.
Seventy-two patients who met International Headache Society criteria for burning mouth syndrome were instructed to place a 1-mg tablet of clonazepam in their mouths after each meal and suck on it for 3 minutes, holding their saliva in the painful areas of the mouth all the while without swallowing. After the 3 minutes were up, the dregs of the tablet and the saliva were to be spit out, Dr. Maialen Mendizabal reported at the International Headache Congress.
Controlled trials previously have shown orally ingested clonazepam to be effective in patients with burning mouth syndrome. Sucked clonazepam provides the advantages of a topical therapy, added Dr. Mendizabal of the University of the Basque Country, Bilbao, Spain.
Pain was assessed via the validated Brief Pain Inventory at baseline, 2 months, and 6 months, as were the sensory disturbances and other symptoms that are often featured prominently in patients with burning mouth syndrome.
At 2 months, 31% of patients reported a greater than 50% reduction from baseline in pain scores, and an additional 10% had a 30%-50% reduction in pain. At 6 months, 39% of patients reported a greater than 50% reduction in pain, and 8% had a 30%-50% decrease.
Fifteen patients (20%) were completely asymptomatic at 6 months. An additional three patients were pain free but continued to experience dry mouth or other symptoms associated with burning mouth syndrome, she reported at the meeting sponsored by the International Headache Society and the American Headache Society.
Dry mouth and altered taste showed a particularly favorable response to topical clonazepam. Two-thirds of subjects had an altered sense of taste at baseline, one-third after 2 months of clonazepam sucking, and none at 6 months. Likewise, two-thirds of patients reported dry mouth at baseline, 47% at 2 months, and just 13% at 6 months.
Although this retrospective, uncontrolled study certainly can’t be considered the final word, the results are sufficiently encouraging to warrant a randomized trial, Dr. Mendizabal said.
The International Headache Society diagnostic criteria for burning mouth syndrome require the presence of pain in the mouth on a daily basis and persisting for most of the day, normal appearing oral mucosa, and exclusion of other local and systemic diseases.
Burning mouth syndrome is mainly a disorder of postmenopausal women. In this study, the mean age of the population was 63 years, and 82% were female.
Dr. Mendizabal reported having no financial conflicts regarding this study, which was conducted free of commercial support.
VALENCIA, SPAIN – Sucking on a clonazepam tablet for 3 minutes after every meal effectively reduced pain, paresthesia, dry mouth, and altered sense of taste in patients with burning mouth syndrome in a retrospective study.
Seventy-two patients who met International Headache Society criteria for burning mouth syndrome were instructed to place a 1-mg tablet of clonazepam in their mouths after each meal and suck on it for 3 minutes, holding their saliva in the painful areas of the mouth all the while without swallowing. After the 3 minutes were up, the dregs of the tablet and the saliva were to be spit out, Dr. Maialen Mendizabal reported at the International Headache Congress.
Controlled trials previously have shown orally ingested clonazepam to be effective in patients with burning mouth syndrome. Sucked clonazepam provides the advantages of a topical therapy, added Dr. Mendizabal of the University of the Basque Country, Bilbao, Spain.
Pain was assessed via the validated Brief Pain Inventory at baseline, 2 months, and 6 months, as were the sensory disturbances and other symptoms that are often featured prominently in patients with burning mouth syndrome.
At 2 months, 31% of patients reported a greater than 50% reduction from baseline in pain scores, and an additional 10% had a 30%-50% reduction in pain. At 6 months, 39% of patients reported a greater than 50% reduction in pain, and 8% had a 30%-50% decrease.
Fifteen patients (20%) were completely asymptomatic at 6 months. An additional three patients were pain free but continued to experience dry mouth or other symptoms associated with burning mouth syndrome, she reported at the meeting sponsored by the International Headache Society and the American Headache Society.
Dry mouth and altered taste showed a particularly favorable response to topical clonazepam. Two-thirds of subjects had an altered sense of taste at baseline, one-third after 2 months of clonazepam sucking, and none at 6 months. Likewise, two-thirds of patients reported dry mouth at baseline, 47% at 2 months, and just 13% at 6 months.
Although this retrospective, uncontrolled study certainly can’t be considered the final word, the results are sufficiently encouraging to warrant a randomized trial, Dr. Mendizabal said.
The International Headache Society diagnostic criteria for burning mouth syndrome require the presence of pain in the mouth on a daily basis and persisting for most of the day, normal appearing oral mucosa, and exclusion of other local and systemic diseases.
Burning mouth syndrome is mainly a disorder of postmenopausal women. In this study, the mean age of the population was 63 years, and 82% were female.
Dr. Mendizabal reported having no financial conflicts regarding this study, which was conducted free of commercial support.
AT IHC 2015
Key clinical point: Sucking on clonazepam tablets reduces the pain and other symptoms of burning mouth syndrome.
Major finding: After 6 months of sucking on a clonazepam tablet for 3 minutes after every meal, 28 of 72 patients with burning mouth syndrome reported a greater than 50% reduction in pain compared with baseline, including 15 patients with no pain at all.
Data source: This was a retrospective uncontrolled study of 72 patients with burning mouth syndrome treated with topical clonazepam and followed for 6 months.
Disclosures: The presenter reported having no financial conflicts regarding this study, which was conducted free of commercial support.
Growing buzz surrounds CGRP inhibitors in migraine
VALENCIA, SPAIN – In the lecture halls and corridors at the International Headache Congress, far and away the dominant topic of conversation was the latest highly promising data for the CGRP (calcitonin gene–related peptide)-inhibiting monoclonal antibodies being developed for migraine prophylaxis.
“The question of efficacy, to me, has been resolved: They’re spectacularly effective. The whole reason for the phase III studies is to establish safety,” Dr. Marcelo E. Bigal, a vice president at Teva Pharmaceuticals, said in the opening plenary session.
“This is the second revolution in the history of migraine therapy,” declared another opening plenary speaker, Dr. Messoud Ashina, professor of neurology at the University of Copenhagen.
“It is a really exciting emerging field. It kind of reminds me of the triptan story,” observed Richard J. Hargreaves, Ph.D., vice president for discovery science at Biogen in Cambridge, Mass.
With a long track record of success in new drug development and having conducted research on CGRP for more than 2 decades, it fell to Dr. Hargreaves to provide an introductory overview of the CGRP inhibitors. Each of the monoclonal antibodies has a different mechanism of action. However, they share several key characteristics: They are highly specific in their mechanisms of action, they have long circulating plasma half-lives, they are largely peripherally restricted rather than acting at the level of the central nervous system, and they typically have a low toxicity profile. Indeed, in phase I and -II studies the type and frequency of adverse events was essentially indistinguishable from placebo.
Now advancing through the developmental pipeline are three CGRP ligand-neutralizing antibodies and one CGRP receptor antibody.
“The race is on. It’s estimated that 40% of migraine patients are candidates for prophylaxis. That’s 14 million U.S. patients. And preventive therapy represents a significant unmet medical need,” Dr. Hargreaves said at the meeting sponsored by the International Headache Society and the American Headache Society.
“Clearly the CGRP monoclonal antibodies aren’t going to be used for acute migraine therapy. That’s going to be the province for oral small-molecule CGRP inhibitors because of the need for rapid activity. But if the antibodies prevent well, then hopefully the need for acute medications will go down,” he continued.
A particularly impressive feature of the investigational agents is that a substantial proportion of treated patients are hyperresponders – that is, individuals who experience at least a 75% and in some cases a 100% reduction in migraine days per month.
“Understanding these hyperresponders in the antibody trials is a real goal for the field. What’s the biomarker that predicts you can cure a patient of migraine headaches? How can you match an individual’s phenotype to the pharmacology of the medicine you’re giving them and get a better outcome?” he asked.
Dr. Hargreaves left his audience of headache specialists with another question to ponder: “If triptans inhibit CGRP release, and CGRP modulators, such as the monoclonal antibodies block CGRP’s action, then why aren’t triptans useful preventive agents? It’s something for the field to think about. I’ll leave you with the thought that maybe CGRP is the volume control for trigeminovascular sensory transmission.”
New data on three CGRP inhibitors was presented at the congress:
ALD403: A single 1,000-mg IV dose of this humanized IgG1 CGRP antibody produced lasting efficacy for 6 months in a phase II, randomized, double-blind, placebo-controlled study.
The study, conducted at 28 U.S. sites, included 163 patients with high-frequency episodic migraine, defined as an average of 5-14 migraine days per month.
One month post infusion, 51% of ALD403-treated patients and 24% of controls had a 75% reduction in monthly migraine days; in addition, 26% of the ALD403 group and 5% of controls had a 100% response, meaning they had no migraines.
At 12 weeks, 33% of the ALD403 group and 9% of controls had a 75% response, while 16% of ALD403-treated patients and zero controls had a 100% response.
At 24 weeks – again, after just a single dose – 26% of the ALD403 group and 7% of controls had a 75% response, while 11% of the active treatment group and no controls had a 100% response.
“There is relatively little difference between the 3-month and 24-week data. So in initial responders, the antibody is still working at 6 months. Some patients simply never had a migraine from the end of the needle to the end of the study,” said Dr. Jeffrey T.L. Smith, senior vice president at Alden BioPharmaceuticals in Bothell, Wash.
One audience member asked how the antibody can reduce the frequency of migraines so swiftly – starting within the first several weeks – when conventional prophylactic medications take months and months to work.
“An antibody having this high an affinity will shut down the biology of CGRP very quickly. The same is true for the very high–affinity anti-TNF and anti-interleukin-6 antibodies used in rheumatology. ALD403 will not only bind to free CGRP, it will actually pull CGRP off the receptor. Everything goes towards the antibody; it acts as a sink,” Dr. Smith replied.
This study was too small to identify predictors of hyperresponsiveness. Investigators hope to hunt down useful biomarkers in the large upcoming phase III studies, he added.
TEV-48125: Dr. Bigal presented the first-ever clinical trial of any CGRP-inhibiting antibody in patients with chronic migraine, defined as 15 or more headache days per month. All other studies to date have been conducted in patients with episodic migraine, who typically have far less cardiovascular disease and other comorbidities. Another unique feature of this trial was that current users of migraine preventive medications weren’t excluded; indeed, roughly half of participants were current users.
In this 263-patient, multicenter, double-blind, placebo-controlled, 3-month, phase II study, once-monthly subcutaneous TEV-48125 at 900 mg resulted in a 6.3-day reduction in the monthly number of moderate to severe headache days, while a regimen consisting of a 675-mg loading dose followed by 225 mg achieved a 6-day reduction, compared with baseline. Both of these outcomes were significantly better than the 4-day reduction seen with placebo.
Moreover, efficacy was evident just 1 week into the study. At that point, patients on either the high or low dose of TEV-48125 already showed a significantly greater reduction in the number of headache hours recorded in an electronic headache diary than did controls.
The monoclonal antibody–treated patients also resorted to acute medications significantly less frequently than did controls by a margin of roughly 2 fewer days per month.
The benefit of both TEV-48125 dosing regimens was equally robust regardless of whether they were on conventional prophylactic medications.
A 75% or greater reduction in monthly headache days was achieved in 32% of patients on the 900-mg dose, in nearly 30% of those on 675/225 mg, and in 16% of controls.
“These patients had suffered with frequent migraine for an average of 18 years, and now they come in and say, ‘I’m basically free of headaches for the first time in my life,’” Dr. Bigal said.
AMG 334: This fully human monoclonal antibody to the CGRP receptor was the focus of a multicenter, phase IIb, double-blind, dose-ranging study in 483 patients with 4-14 migraine days per month at baseline. Patients with comorbid depression and/or anxiety disorders were eligible to participate.
The most effective dose, and the one being carried forward into phase III, was 70 mg given subcutaneously once per month. The mean number of monthly migraine days was reduced by 3.4 days in patients on that regimen from a baseline of 8.7 days, significantly better than the 2.28-day reduction with placebo. In a prespecified secondary analysis, there was no difference in efficacy between patients with more than 8 monthly migraine days at baseline and those with fewer than 8 days, reported Dr. Robert Lenz of Amgen in Thousand Oaks, Calif.
The safety data showed no signal of any adverse event. Fewer than 3% of patients of the AMG 334 group discontinued treatment for any reason.
VALENCIA, SPAIN – In the lecture halls and corridors at the International Headache Congress, far and away the dominant topic of conversation was the latest highly promising data for the CGRP (calcitonin gene–related peptide)-inhibiting monoclonal antibodies being developed for migraine prophylaxis.
“The question of efficacy, to me, has been resolved: They’re spectacularly effective. The whole reason for the phase III studies is to establish safety,” Dr. Marcelo E. Bigal, a vice president at Teva Pharmaceuticals, said in the opening plenary session.
“This is the second revolution in the history of migraine therapy,” declared another opening plenary speaker, Dr. Messoud Ashina, professor of neurology at the University of Copenhagen.
“It is a really exciting emerging field. It kind of reminds me of the triptan story,” observed Richard J. Hargreaves, Ph.D., vice president for discovery science at Biogen in Cambridge, Mass.
With a long track record of success in new drug development and having conducted research on CGRP for more than 2 decades, it fell to Dr. Hargreaves to provide an introductory overview of the CGRP inhibitors. Each of the monoclonal antibodies has a different mechanism of action. However, they share several key characteristics: They are highly specific in their mechanisms of action, they have long circulating plasma half-lives, they are largely peripherally restricted rather than acting at the level of the central nervous system, and they typically have a low toxicity profile. Indeed, in phase I and -II studies the type and frequency of adverse events was essentially indistinguishable from placebo.
Now advancing through the developmental pipeline are three CGRP ligand-neutralizing antibodies and one CGRP receptor antibody.
“The race is on. It’s estimated that 40% of migraine patients are candidates for prophylaxis. That’s 14 million U.S. patients. And preventive therapy represents a significant unmet medical need,” Dr. Hargreaves said at the meeting sponsored by the International Headache Society and the American Headache Society.
“Clearly the CGRP monoclonal antibodies aren’t going to be used for acute migraine therapy. That’s going to be the province for oral small-molecule CGRP inhibitors because of the need for rapid activity. But if the antibodies prevent well, then hopefully the need for acute medications will go down,” he continued.
A particularly impressive feature of the investigational agents is that a substantial proportion of treated patients are hyperresponders – that is, individuals who experience at least a 75% and in some cases a 100% reduction in migraine days per month.
“Understanding these hyperresponders in the antibody trials is a real goal for the field. What’s the biomarker that predicts you can cure a patient of migraine headaches? How can you match an individual’s phenotype to the pharmacology of the medicine you’re giving them and get a better outcome?” he asked.
Dr. Hargreaves left his audience of headache specialists with another question to ponder: “If triptans inhibit CGRP release, and CGRP modulators, such as the monoclonal antibodies block CGRP’s action, then why aren’t triptans useful preventive agents? It’s something for the field to think about. I’ll leave you with the thought that maybe CGRP is the volume control for trigeminovascular sensory transmission.”
New data on three CGRP inhibitors was presented at the congress:
ALD403: A single 1,000-mg IV dose of this humanized IgG1 CGRP antibody produced lasting efficacy for 6 months in a phase II, randomized, double-blind, placebo-controlled study.
The study, conducted at 28 U.S. sites, included 163 patients with high-frequency episodic migraine, defined as an average of 5-14 migraine days per month.
One month post infusion, 51% of ALD403-treated patients and 24% of controls had a 75% reduction in monthly migraine days; in addition, 26% of the ALD403 group and 5% of controls had a 100% response, meaning they had no migraines.
At 12 weeks, 33% of the ALD403 group and 9% of controls had a 75% response, while 16% of ALD403-treated patients and zero controls had a 100% response.
At 24 weeks – again, after just a single dose – 26% of the ALD403 group and 7% of controls had a 75% response, while 11% of the active treatment group and no controls had a 100% response.
“There is relatively little difference between the 3-month and 24-week data. So in initial responders, the antibody is still working at 6 months. Some patients simply never had a migraine from the end of the needle to the end of the study,” said Dr. Jeffrey T.L. Smith, senior vice president at Alden BioPharmaceuticals in Bothell, Wash.
One audience member asked how the antibody can reduce the frequency of migraines so swiftly – starting within the first several weeks – when conventional prophylactic medications take months and months to work.
“An antibody having this high an affinity will shut down the biology of CGRP very quickly. The same is true for the very high–affinity anti-TNF and anti-interleukin-6 antibodies used in rheumatology. ALD403 will not only bind to free CGRP, it will actually pull CGRP off the receptor. Everything goes towards the antibody; it acts as a sink,” Dr. Smith replied.
This study was too small to identify predictors of hyperresponsiveness. Investigators hope to hunt down useful biomarkers in the large upcoming phase III studies, he added.
TEV-48125: Dr. Bigal presented the first-ever clinical trial of any CGRP-inhibiting antibody in patients with chronic migraine, defined as 15 or more headache days per month. All other studies to date have been conducted in patients with episodic migraine, who typically have far less cardiovascular disease and other comorbidities. Another unique feature of this trial was that current users of migraine preventive medications weren’t excluded; indeed, roughly half of participants were current users.
In this 263-patient, multicenter, double-blind, placebo-controlled, 3-month, phase II study, once-monthly subcutaneous TEV-48125 at 900 mg resulted in a 6.3-day reduction in the monthly number of moderate to severe headache days, while a regimen consisting of a 675-mg loading dose followed by 225 mg achieved a 6-day reduction, compared with baseline. Both of these outcomes were significantly better than the 4-day reduction seen with placebo.
Moreover, efficacy was evident just 1 week into the study. At that point, patients on either the high or low dose of TEV-48125 already showed a significantly greater reduction in the number of headache hours recorded in an electronic headache diary than did controls.
The monoclonal antibody–treated patients also resorted to acute medications significantly less frequently than did controls by a margin of roughly 2 fewer days per month.
The benefit of both TEV-48125 dosing regimens was equally robust regardless of whether they were on conventional prophylactic medications.
A 75% or greater reduction in monthly headache days was achieved in 32% of patients on the 900-mg dose, in nearly 30% of those on 675/225 mg, and in 16% of controls.
“These patients had suffered with frequent migraine for an average of 18 years, and now they come in and say, ‘I’m basically free of headaches for the first time in my life,’” Dr. Bigal said.
AMG 334: This fully human monoclonal antibody to the CGRP receptor was the focus of a multicenter, phase IIb, double-blind, dose-ranging study in 483 patients with 4-14 migraine days per month at baseline. Patients with comorbid depression and/or anxiety disorders were eligible to participate.
The most effective dose, and the one being carried forward into phase III, was 70 mg given subcutaneously once per month. The mean number of monthly migraine days was reduced by 3.4 days in patients on that regimen from a baseline of 8.7 days, significantly better than the 2.28-day reduction with placebo. In a prespecified secondary analysis, there was no difference in efficacy between patients with more than 8 monthly migraine days at baseline and those with fewer than 8 days, reported Dr. Robert Lenz of Amgen in Thousand Oaks, Calif.
The safety data showed no signal of any adverse event. Fewer than 3% of patients of the AMG 334 group discontinued treatment for any reason.
VALENCIA, SPAIN – In the lecture halls and corridors at the International Headache Congress, far and away the dominant topic of conversation was the latest highly promising data for the CGRP (calcitonin gene–related peptide)-inhibiting monoclonal antibodies being developed for migraine prophylaxis.
“The question of efficacy, to me, has been resolved: They’re spectacularly effective. The whole reason for the phase III studies is to establish safety,” Dr. Marcelo E. Bigal, a vice president at Teva Pharmaceuticals, said in the opening plenary session.
“This is the second revolution in the history of migraine therapy,” declared another opening plenary speaker, Dr. Messoud Ashina, professor of neurology at the University of Copenhagen.
“It is a really exciting emerging field. It kind of reminds me of the triptan story,” observed Richard J. Hargreaves, Ph.D., vice president for discovery science at Biogen in Cambridge, Mass.
With a long track record of success in new drug development and having conducted research on CGRP for more than 2 decades, it fell to Dr. Hargreaves to provide an introductory overview of the CGRP inhibitors. Each of the monoclonal antibodies has a different mechanism of action. However, they share several key characteristics: They are highly specific in their mechanisms of action, they have long circulating plasma half-lives, they are largely peripherally restricted rather than acting at the level of the central nervous system, and they typically have a low toxicity profile. Indeed, in phase I and -II studies the type and frequency of adverse events was essentially indistinguishable from placebo.
Now advancing through the developmental pipeline are three CGRP ligand-neutralizing antibodies and one CGRP receptor antibody.
“The race is on. It’s estimated that 40% of migraine patients are candidates for prophylaxis. That’s 14 million U.S. patients. And preventive therapy represents a significant unmet medical need,” Dr. Hargreaves said at the meeting sponsored by the International Headache Society and the American Headache Society.
“Clearly the CGRP monoclonal antibodies aren’t going to be used for acute migraine therapy. That’s going to be the province for oral small-molecule CGRP inhibitors because of the need for rapid activity. But if the antibodies prevent well, then hopefully the need for acute medications will go down,” he continued.
A particularly impressive feature of the investigational agents is that a substantial proportion of treated patients are hyperresponders – that is, individuals who experience at least a 75% and in some cases a 100% reduction in migraine days per month.
“Understanding these hyperresponders in the antibody trials is a real goal for the field. What’s the biomarker that predicts you can cure a patient of migraine headaches? How can you match an individual’s phenotype to the pharmacology of the medicine you’re giving them and get a better outcome?” he asked.
Dr. Hargreaves left his audience of headache specialists with another question to ponder: “If triptans inhibit CGRP release, and CGRP modulators, such as the monoclonal antibodies block CGRP’s action, then why aren’t triptans useful preventive agents? It’s something for the field to think about. I’ll leave you with the thought that maybe CGRP is the volume control for trigeminovascular sensory transmission.”
New data on three CGRP inhibitors was presented at the congress:
ALD403: A single 1,000-mg IV dose of this humanized IgG1 CGRP antibody produced lasting efficacy for 6 months in a phase II, randomized, double-blind, placebo-controlled study.
The study, conducted at 28 U.S. sites, included 163 patients with high-frequency episodic migraine, defined as an average of 5-14 migraine days per month.
One month post infusion, 51% of ALD403-treated patients and 24% of controls had a 75% reduction in monthly migraine days; in addition, 26% of the ALD403 group and 5% of controls had a 100% response, meaning they had no migraines.
At 12 weeks, 33% of the ALD403 group and 9% of controls had a 75% response, while 16% of ALD403-treated patients and zero controls had a 100% response.
At 24 weeks – again, after just a single dose – 26% of the ALD403 group and 7% of controls had a 75% response, while 11% of the active treatment group and no controls had a 100% response.
“There is relatively little difference between the 3-month and 24-week data. So in initial responders, the antibody is still working at 6 months. Some patients simply never had a migraine from the end of the needle to the end of the study,” said Dr. Jeffrey T.L. Smith, senior vice president at Alden BioPharmaceuticals in Bothell, Wash.
One audience member asked how the antibody can reduce the frequency of migraines so swiftly – starting within the first several weeks – when conventional prophylactic medications take months and months to work.
“An antibody having this high an affinity will shut down the biology of CGRP very quickly. The same is true for the very high–affinity anti-TNF and anti-interleukin-6 antibodies used in rheumatology. ALD403 will not only bind to free CGRP, it will actually pull CGRP off the receptor. Everything goes towards the antibody; it acts as a sink,” Dr. Smith replied.
This study was too small to identify predictors of hyperresponsiveness. Investigators hope to hunt down useful biomarkers in the large upcoming phase III studies, he added.
TEV-48125: Dr. Bigal presented the first-ever clinical trial of any CGRP-inhibiting antibody in patients with chronic migraine, defined as 15 or more headache days per month. All other studies to date have been conducted in patients with episodic migraine, who typically have far less cardiovascular disease and other comorbidities. Another unique feature of this trial was that current users of migraine preventive medications weren’t excluded; indeed, roughly half of participants were current users.
In this 263-patient, multicenter, double-blind, placebo-controlled, 3-month, phase II study, once-monthly subcutaneous TEV-48125 at 900 mg resulted in a 6.3-day reduction in the monthly number of moderate to severe headache days, while a regimen consisting of a 675-mg loading dose followed by 225 mg achieved a 6-day reduction, compared with baseline. Both of these outcomes were significantly better than the 4-day reduction seen with placebo.
Moreover, efficacy was evident just 1 week into the study. At that point, patients on either the high or low dose of TEV-48125 already showed a significantly greater reduction in the number of headache hours recorded in an electronic headache diary than did controls.
The monoclonal antibody–treated patients also resorted to acute medications significantly less frequently than did controls by a margin of roughly 2 fewer days per month.
The benefit of both TEV-48125 dosing regimens was equally robust regardless of whether they were on conventional prophylactic medications.
A 75% or greater reduction in monthly headache days was achieved in 32% of patients on the 900-mg dose, in nearly 30% of those on 675/225 mg, and in 16% of controls.
“These patients had suffered with frequent migraine for an average of 18 years, and now they come in and say, ‘I’m basically free of headaches for the first time in my life,’” Dr. Bigal said.
AMG 334: This fully human monoclonal antibody to the CGRP receptor was the focus of a multicenter, phase IIb, double-blind, dose-ranging study in 483 patients with 4-14 migraine days per month at baseline. Patients with comorbid depression and/or anxiety disorders were eligible to participate.
The most effective dose, and the one being carried forward into phase III, was 70 mg given subcutaneously once per month. The mean number of monthly migraine days was reduced by 3.4 days in patients on that regimen from a baseline of 8.7 days, significantly better than the 2.28-day reduction with placebo. In a prespecified secondary analysis, there was no difference in efficacy between patients with more than 8 monthly migraine days at baseline and those with fewer than 8 days, reported Dr. Robert Lenz of Amgen in Thousand Oaks, Calif.
The safety data showed no signal of any adverse event. Fewer than 3% of patients of the AMG 334 group discontinued treatment for any reason.
AT IHC 2015
IHC: Acupuncture deflates migraine
VALENCIA, SPAIN – Acupuncture is as effective as standard pharmacotherapy for migraine prophylaxis, according to a randomized, clinical trial. Forty-four percent of patients in the acupuncture group were deemed treatment responders based upon at least a 50% reduction in headache days per month at 4 months of follow-up, compared with baseline, Dr. Giulia Giannini reported at the International Headache Congress.
The responder rate in the prophylactic pharmacotherapy group was similar at 38%. However, it must be noted that half of the migraineurs assigned to the medication group dropped out of the study for various reasons – No. 1 being treatment side effects – and in this study the responder rate was based upon patients who made it to the 4-month mark, noted Dr. Giannini of the University of Bologna (Italy).
The study included 85 patients, none of whom had been on prophylactic medication during the previous 3 months. They were randomized to a series of 12 acupuncture sessions or to whatever conventional prophylactic drug the physician and patient agreed was most appropriate.
Eight of 42 patients in the acupuncture group and 21 of 43 controls discontinued the study.
Among the study completers in the acupuncture group, migraine frequency dropped from 9.26 headache days per month at baseline to 6 days per month at 4 months. The group on prophylactic pharmacotherapy improved from 7.95 to 6.24 headache days per month.
These results are consistent with the findings of several published clinical trials comparing acupuncture with prophylactic antimigraine drugs, including one in which acupuncture proved more effective than valproic acid (Minerva Anestesiol. 2013;79:634-42). The published data prompted a Cochrane systematic review which concluded that acupuncture is at least as effective as prophylactic drug therapy, has fewer adverse effects, and should be considered a legitimate treatment option (Cochrane Database Syst. Rev. 2009 [doi:10.1002/14651858.CD001218.pub2]). Dr. Giannini noted at the meeting sponsored by the International Headache Society and the American Headache Society.
No serious adverse events occurred in either study arm.
The study was funded by the Emilia-Romagna (Italy) Department of Health. Dr. Giannini reported having no financial conflicts.
VALENCIA, SPAIN – Acupuncture is as effective as standard pharmacotherapy for migraine prophylaxis, according to a randomized, clinical trial. Forty-four percent of patients in the acupuncture group were deemed treatment responders based upon at least a 50% reduction in headache days per month at 4 months of follow-up, compared with baseline, Dr. Giulia Giannini reported at the International Headache Congress.
The responder rate in the prophylactic pharmacotherapy group was similar at 38%. However, it must be noted that half of the migraineurs assigned to the medication group dropped out of the study for various reasons – No. 1 being treatment side effects – and in this study the responder rate was based upon patients who made it to the 4-month mark, noted Dr. Giannini of the University of Bologna (Italy).
The study included 85 patients, none of whom had been on prophylactic medication during the previous 3 months. They were randomized to a series of 12 acupuncture sessions or to whatever conventional prophylactic drug the physician and patient agreed was most appropriate.
Eight of 42 patients in the acupuncture group and 21 of 43 controls discontinued the study.
Among the study completers in the acupuncture group, migraine frequency dropped from 9.26 headache days per month at baseline to 6 days per month at 4 months. The group on prophylactic pharmacotherapy improved from 7.95 to 6.24 headache days per month.
These results are consistent with the findings of several published clinical trials comparing acupuncture with prophylactic antimigraine drugs, including one in which acupuncture proved more effective than valproic acid (Minerva Anestesiol. 2013;79:634-42). The published data prompted a Cochrane systematic review which concluded that acupuncture is at least as effective as prophylactic drug therapy, has fewer adverse effects, and should be considered a legitimate treatment option (Cochrane Database Syst. Rev. 2009 [doi:10.1002/14651858.CD001218.pub2]). Dr. Giannini noted at the meeting sponsored by the International Headache Society and the American Headache Society.
No serious adverse events occurred in either study arm.
The study was funded by the Emilia-Romagna (Italy) Department of Health. Dr. Giannini reported having no financial conflicts.
VALENCIA, SPAIN – Acupuncture is as effective as standard pharmacotherapy for migraine prophylaxis, according to a randomized, clinical trial. Forty-four percent of patients in the acupuncture group were deemed treatment responders based upon at least a 50% reduction in headache days per month at 4 months of follow-up, compared with baseline, Dr. Giulia Giannini reported at the International Headache Congress.
The responder rate in the prophylactic pharmacotherapy group was similar at 38%. However, it must be noted that half of the migraineurs assigned to the medication group dropped out of the study for various reasons – No. 1 being treatment side effects – and in this study the responder rate was based upon patients who made it to the 4-month mark, noted Dr. Giannini of the University of Bologna (Italy).
The study included 85 patients, none of whom had been on prophylactic medication during the previous 3 months. They were randomized to a series of 12 acupuncture sessions or to whatever conventional prophylactic drug the physician and patient agreed was most appropriate.
Eight of 42 patients in the acupuncture group and 21 of 43 controls discontinued the study.
Among the study completers in the acupuncture group, migraine frequency dropped from 9.26 headache days per month at baseline to 6 days per month at 4 months. The group on prophylactic pharmacotherapy improved from 7.95 to 6.24 headache days per month.
These results are consistent with the findings of several published clinical trials comparing acupuncture with prophylactic antimigraine drugs, including one in which acupuncture proved more effective than valproic acid (Minerva Anestesiol. 2013;79:634-42). The published data prompted a Cochrane systematic review which concluded that acupuncture is at least as effective as prophylactic drug therapy, has fewer adverse effects, and should be considered a legitimate treatment option (Cochrane Database Syst. Rev. 2009 [doi:10.1002/14651858.CD001218.pub2]). Dr. Giannini noted at the meeting sponsored by the International Headache Society and the American Headache Society.
No serious adverse events occurred in either study arm.
The study was funded by the Emilia-Romagna (Italy) Department of Health. Dr. Giannini reported having no financial conflicts.
AT IHC 2015
Key clinical point: Acupuncture is at least as effective for migraine prophylaxis as standard preventive medications.
Major finding: Forty-four percent of migraine patients who completed 12 sessions of acupuncture had at least a 50% reduction in headache days per month at 4 months of follow-up, similar to the 38% rate in patients randomized to prophylactic medication.
Data source: This was a prospective, unblinded, randomized trial involving 85 migraineurs.
Disclosures: The study was funded by the Emilia-Romagna (Italy) Department of Health. The presenter reported having no financial conflicts.
Intranasal evaporative cooling quickly quelled migraine
VALENCIA, SPAIN – The day may be coming when physicians simply advise their patients experiencing migraine onset to “just chill.”
Literally.
A few minutes of intranasal evaporative cooling brought rapid improvement in headache pain and other migraine-associated symptoms, sustained for 24 hours, in 87% of patients in a small proof-of-concept study, Dr. Jitka Vanderpol reported at the International Headache Congress.
The novel migraine therapy, which also shows potential for treatment of cluster headaches, utilizes the same proprietary therapeutic hypothermia technology approved by European regulators as a method to increase neurologically intact survival after cardiac arrest. The RhinoChill technology, marketed by BeneChill International, utilizes an intranasal cooling catheter to deliver cooling. And it’s portable: The system weighs less than 5 kg, making it suitable for prehospital therapeutic cooling by first responders in cases of cardiac arrest.
While the current device is being used in the ongoing migraine studies, it’s bulkier and more powerful than necessary for this purpose, which doesn’t necessitate lowering core temperature. The company is developing a much smaller, more portable version specifically for treatment of headaches, explained Dr. Vanderpol, a neurologist at Cumbria Partnership National Health Service Foundation Trust in Penrith, England.
The proof-of-concept study involved 20 cryotherapy sessions in 15 patients. Participants were hospitalized for treatment so Dr. Vanderpol and coinvestigators could monitor its safety. The two efficacy endpoints were change from admission through 24 hours in headache pain scores on a 0-10 scale, and change in migraine-associated symptom severity, also self-rated on a 0-10 scale.
* Headache pain: From a mean baseline score of 5.96 at admission, scores improved significantly at every evaluation point: 4.28 after 5 minutes of intranasal cooling; 3.79 after 15 minutes of cooling, at which point treatment stopped; 3.12 immediately after treatment halted; 2.42 at 2 hours post-treatment; and 1.97 at 24 hours post-treatment.
* Migraine-associated symptom severity: From a mean score of 4.25 at baseline, scores dropped to 1.9 immediately after treatment, 0.9 at 2 hours, and 0.7 at 24 hours post-treatment.
Two hours post-treatment, 9 of 20 treatments had resulted in dual zero scores – that is, complete freedom both from headache pain and other migraine-associated symptoms. Another 9 of the 20 treatment applications provided partial improvement on both measures.
When patients were asked how intranasal cooling compared with their current rescue medications, 9 of the 15 rated intranasal cooling as superior, and 4 deemed it equal. There were no side effects in the study.
The cooling of the nasal passages and their associated blood vessels is achieved using medicinal air at a temperature of 2 degrees Celsius. Tympanic temperature didn’t change.
“We were not cooling the head, brain, or patient’s body,” Dr. Vanderpol said at the meeting sponsored by the International Headache Society and the American Headache Society.
In an interview, she cited several possible mechanisms of benefit.
One draws upon the neurovascular theory of migraine: Because of the configuration of vascular anatomy, cooled venous blood from the nasal and paranasal mucous membranes can flow to the dura matter. There is also some preliminary evidence to suggest cooling can affect certain calcitonin gene-related peptide receptors. In addition, cooling tissue results in reduced demand for adenosine triphosphate and oxygen.
The sphenopalatine ganglion is another possible site of action, although this would be more relevant for the treatment of cluster headaches, the neurologist added.
In an ongoing clinical trial, patients received instruction in use of the RhinoChill cooling device and were sent home with a loaner for self treatment. A large, definitive, randomized, controlled trial to confirm the therapeutic benefits and safety will be conducted once the mini-cooling system is available.
The pilot study received partial support from Benechill International in the form of loaner equipment and funding for a research nurse. Dr. Vanderpol reported having no financial conflicts.
bjancin@frontlinemedcom
VALENCIA, SPAIN – The day may be coming when physicians simply advise their patients experiencing migraine onset to “just chill.”
Literally.
A few minutes of intranasal evaporative cooling brought rapid improvement in headache pain and other migraine-associated symptoms, sustained for 24 hours, in 87% of patients in a small proof-of-concept study, Dr. Jitka Vanderpol reported at the International Headache Congress.
The novel migraine therapy, which also shows potential for treatment of cluster headaches, utilizes the same proprietary therapeutic hypothermia technology approved by European regulators as a method to increase neurologically intact survival after cardiac arrest. The RhinoChill technology, marketed by BeneChill International, utilizes an intranasal cooling catheter to deliver cooling. And it’s portable: The system weighs less than 5 kg, making it suitable for prehospital therapeutic cooling by first responders in cases of cardiac arrest.
While the current device is being used in the ongoing migraine studies, it’s bulkier and more powerful than necessary for this purpose, which doesn’t necessitate lowering core temperature. The company is developing a much smaller, more portable version specifically for treatment of headaches, explained Dr. Vanderpol, a neurologist at Cumbria Partnership National Health Service Foundation Trust in Penrith, England.
The proof-of-concept study involved 20 cryotherapy sessions in 15 patients. Participants were hospitalized for treatment so Dr. Vanderpol and coinvestigators could monitor its safety. The two efficacy endpoints were change from admission through 24 hours in headache pain scores on a 0-10 scale, and change in migraine-associated symptom severity, also self-rated on a 0-10 scale.
* Headache pain: From a mean baseline score of 5.96 at admission, scores improved significantly at every evaluation point: 4.28 after 5 minutes of intranasal cooling; 3.79 after 15 minutes of cooling, at which point treatment stopped; 3.12 immediately after treatment halted; 2.42 at 2 hours post-treatment; and 1.97 at 24 hours post-treatment.
* Migraine-associated symptom severity: From a mean score of 4.25 at baseline, scores dropped to 1.9 immediately after treatment, 0.9 at 2 hours, and 0.7 at 24 hours post-treatment.
Two hours post-treatment, 9 of 20 treatments had resulted in dual zero scores – that is, complete freedom both from headache pain and other migraine-associated symptoms. Another 9 of the 20 treatment applications provided partial improvement on both measures.
When patients were asked how intranasal cooling compared with their current rescue medications, 9 of the 15 rated intranasal cooling as superior, and 4 deemed it equal. There were no side effects in the study.
The cooling of the nasal passages and their associated blood vessels is achieved using medicinal air at a temperature of 2 degrees Celsius. Tympanic temperature didn’t change.
“We were not cooling the head, brain, or patient’s body,” Dr. Vanderpol said at the meeting sponsored by the International Headache Society and the American Headache Society.
In an interview, she cited several possible mechanisms of benefit.
One draws upon the neurovascular theory of migraine: Because of the configuration of vascular anatomy, cooled venous blood from the nasal and paranasal mucous membranes can flow to the dura matter. There is also some preliminary evidence to suggest cooling can affect certain calcitonin gene-related peptide receptors. In addition, cooling tissue results in reduced demand for adenosine triphosphate and oxygen.
The sphenopalatine ganglion is another possible site of action, although this would be more relevant for the treatment of cluster headaches, the neurologist added.
In an ongoing clinical trial, patients received instruction in use of the RhinoChill cooling device and were sent home with a loaner for self treatment. A large, definitive, randomized, controlled trial to confirm the therapeutic benefits and safety will be conducted once the mini-cooling system is available.
The pilot study received partial support from Benechill International in the form of loaner equipment and funding for a research nurse. Dr. Vanderpol reported having no financial conflicts.
bjancin@frontlinemedcom
VALENCIA, SPAIN – The day may be coming when physicians simply advise their patients experiencing migraine onset to “just chill.”
Literally.
A few minutes of intranasal evaporative cooling brought rapid improvement in headache pain and other migraine-associated symptoms, sustained for 24 hours, in 87% of patients in a small proof-of-concept study, Dr. Jitka Vanderpol reported at the International Headache Congress.
The novel migraine therapy, which also shows potential for treatment of cluster headaches, utilizes the same proprietary therapeutic hypothermia technology approved by European regulators as a method to increase neurologically intact survival after cardiac arrest. The RhinoChill technology, marketed by BeneChill International, utilizes an intranasal cooling catheter to deliver cooling. And it’s portable: The system weighs less than 5 kg, making it suitable for prehospital therapeutic cooling by first responders in cases of cardiac arrest.
While the current device is being used in the ongoing migraine studies, it’s bulkier and more powerful than necessary for this purpose, which doesn’t necessitate lowering core temperature. The company is developing a much smaller, more portable version specifically for treatment of headaches, explained Dr. Vanderpol, a neurologist at Cumbria Partnership National Health Service Foundation Trust in Penrith, England.
The proof-of-concept study involved 20 cryotherapy sessions in 15 patients. Participants were hospitalized for treatment so Dr. Vanderpol and coinvestigators could monitor its safety. The two efficacy endpoints were change from admission through 24 hours in headache pain scores on a 0-10 scale, and change in migraine-associated symptom severity, also self-rated on a 0-10 scale.
* Headache pain: From a mean baseline score of 5.96 at admission, scores improved significantly at every evaluation point: 4.28 after 5 minutes of intranasal cooling; 3.79 after 15 minutes of cooling, at which point treatment stopped; 3.12 immediately after treatment halted; 2.42 at 2 hours post-treatment; and 1.97 at 24 hours post-treatment.
* Migraine-associated symptom severity: From a mean score of 4.25 at baseline, scores dropped to 1.9 immediately after treatment, 0.9 at 2 hours, and 0.7 at 24 hours post-treatment.
Two hours post-treatment, 9 of 20 treatments had resulted in dual zero scores – that is, complete freedom both from headache pain and other migraine-associated symptoms. Another 9 of the 20 treatment applications provided partial improvement on both measures.
When patients were asked how intranasal cooling compared with their current rescue medications, 9 of the 15 rated intranasal cooling as superior, and 4 deemed it equal. There were no side effects in the study.
The cooling of the nasal passages and their associated blood vessels is achieved using medicinal air at a temperature of 2 degrees Celsius. Tympanic temperature didn’t change.
“We were not cooling the head, brain, or patient’s body,” Dr. Vanderpol said at the meeting sponsored by the International Headache Society and the American Headache Society.
In an interview, she cited several possible mechanisms of benefit.
One draws upon the neurovascular theory of migraine: Because of the configuration of vascular anatomy, cooled venous blood from the nasal and paranasal mucous membranes can flow to the dura matter. There is also some preliminary evidence to suggest cooling can affect certain calcitonin gene-related peptide receptors. In addition, cooling tissue results in reduced demand for adenosine triphosphate and oxygen.
The sphenopalatine ganglion is another possible site of action, although this would be more relevant for the treatment of cluster headaches, the neurologist added.
In an ongoing clinical trial, patients received instruction in use of the RhinoChill cooling device and were sent home with a loaner for self treatment. A large, definitive, randomized, controlled trial to confirm the therapeutic benefits and safety will be conducted once the mini-cooling system is available.
The pilot study received partial support from Benechill International in the form of loaner equipment and funding for a research nurse. Dr. Vanderpol reported having no financial conflicts.
bjancin@frontlinemedcom
AT IHC 2015
Key clinical point: A few minutes of concentrated intranasal hypothermia shows promise as rescue therapy for migraine attacks.
Major finding: After 5 minutes of intranasal evaporative cooling, mean scores on measures of headache pain and migraine-associated symptoms decreased significantly, and they dropped further continuously through 24 hours.
Data source: This was a prospective, single-arm, proof-of-concept study involving 15 migraine patients who collectively received 20 intranasal cooling treatments.
Disclosures: The presenter reported having no financial conflicts regarding the study.
IHC: Lifestyle regularity helps quell migraine
VALENCIA, SPAIN – Following a schedule of regular daily mealtimes, bedtimes, and aerobic exercise is an effective yet underutilized tool for the management of migraine, Dr. Yohannes W. Woldeamanuel said at the International Headache Congress.
“We call these three ‘the RLB [regular lifestyle behavior] triumvirate’: daily regular sleep times, mealtime hours, and aerobic exercise. This is something physicians should be advocating ... it provides the patient with a tool to help control his or her own migraine problems. Along with avoidance of daily headache medications, it has added value for clinical practice,” according to Dr. Woldeamanuel, an Ethiopian neurologist who is currently a fellow in the Stanford (Calif.) University Headache and Facial Pain Program.
He presented a retrospective study of 100 patients with chronic migraine aged 15 and older and 100 age- and gender-matched patients with episodic migraine treated at the headache center. Collectively, the chronic migraine patients averaged 2,497 migraine attacks per month, while the episodic migraine group averaged 578.
Although all migraine patients seen at the Stanford center are encouraged to pursue RLB, only 6% of the chronic migraine group did so regularly, compared with a 10-fold higher rate among those with episodic migraine. Slicing the data another way, only 9% of patients who were on the RLB bandwagon had chronic migraine, compared with 70% of those without regular lifestyle behavior.
An observational study such as this cannot establish causality. Yet Dr. Woldeamanuel saw evidence suggestive of cause and effect with regard to RLB.
“Interestingly, among the small cohort of chronic migraineurs who were following the RLB, they were progressively month after month converting into episodic migraineurs, while the episodic migraineurs who were not following the RLB were converting to chronic migraine, month after month,” the neurologist said in an interview at the meeting sponsored by the International Headache Society and the American Headache Society.
By definition, patients with chronic migraine take headache medications most days of the month, raising the possibility that medication use might be a study confounder. To check that out, Dr. Woldeamanuel stratified patients who adhered to the RLB triumvirate into those who regularly used rescue and/or preventive medications and those who didn’t. The two subgroups didn’t differ significantly in terms of the prevalence of chronic migraine.
“This supports the genuine impact of RLB as a migraine management modality. It’s therapeutic. That’s the message,” he declared.
What’s the mechanism of benefit?
“We have biological rhythms that maintain our health: ultradian, circadian, diurnal, infradian. RLB promotes release of endorphins and keeps levels stable, increasing the threshold for sensory change and peripheral pain,” he explained.
Dr. Woldeamanuel reported having no financial conflicts with regard to this study, conducted with institutional funds.
VALENCIA, SPAIN – Following a schedule of regular daily mealtimes, bedtimes, and aerobic exercise is an effective yet underutilized tool for the management of migraine, Dr. Yohannes W. Woldeamanuel said at the International Headache Congress.
“We call these three ‘the RLB [regular lifestyle behavior] triumvirate’: daily regular sleep times, mealtime hours, and aerobic exercise. This is something physicians should be advocating ... it provides the patient with a tool to help control his or her own migraine problems. Along with avoidance of daily headache medications, it has added value for clinical practice,” according to Dr. Woldeamanuel, an Ethiopian neurologist who is currently a fellow in the Stanford (Calif.) University Headache and Facial Pain Program.
He presented a retrospective study of 100 patients with chronic migraine aged 15 and older and 100 age- and gender-matched patients with episodic migraine treated at the headache center. Collectively, the chronic migraine patients averaged 2,497 migraine attacks per month, while the episodic migraine group averaged 578.
Although all migraine patients seen at the Stanford center are encouraged to pursue RLB, only 6% of the chronic migraine group did so regularly, compared with a 10-fold higher rate among those with episodic migraine. Slicing the data another way, only 9% of patients who were on the RLB bandwagon had chronic migraine, compared with 70% of those without regular lifestyle behavior.
An observational study such as this cannot establish causality. Yet Dr. Woldeamanuel saw evidence suggestive of cause and effect with regard to RLB.
“Interestingly, among the small cohort of chronic migraineurs who were following the RLB, they were progressively month after month converting into episodic migraineurs, while the episodic migraineurs who were not following the RLB were converting to chronic migraine, month after month,” the neurologist said in an interview at the meeting sponsored by the International Headache Society and the American Headache Society.
By definition, patients with chronic migraine take headache medications most days of the month, raising the possibility that medication use might be a study confounder. To check that out, Dr. Woldeamanuel stratified patients who adhered to the RLB triumvirate into those who regularly used rescue and/or preventive medications and those who didn’t. The two subgroups didn’t differ significantly in terms of the prevalence of chronic migraine.
“This supports the genuine impact of RLB as a migraine management modality. It’s therapeutic. That’s the message,” he declared.
What’s the mechanism of benefit?
“We have biological rhythms that maintain our health: ultradian, circadian, diurnal, infradian. RLB promotes release of endorphins and keeps levels stable, increasing the threshold for sensory change and peripheral pain,” he explained.
Dr. Woldeamanuel reported having no financial conflicts with regard to this study, conducted with institutional funds.
VALENCIA, SPAIN – Following a schedule of regular daily mealtimes, bedtimes, and aerobic exercise is an effective yet underutilized tool for the management of migraine, Dr. Yohannes W. Woldeamanuel said at the International Headache Congress.
“We call these three ‘the RLB [regular lifestyle behavior] triumvirate’: daily regular sleep times, mealtime hours, and aerobic exercise. This is something physicians should be advocating ... it provides the patient with a tool to help control his or her own migraine problems. Along with avoidance of daily headache medications, it has added value for clinical practice,” according to Dr. Woldeamanuel, an Ethiopian neurologist who is currently a fellow in the Stanford (Calif.) University Headache and Facial Pain Program.
He presented a retrospective study of 100 patients with chronic migraine aged 15 and older and 100 age- and gender-matched patients with episodic migraine treated at the headache center. Collectively, the chronic migraine patients averaged 2,497 migraine attacks per month, while the episodic migraine group averaged 578.
Although all migraine patients seen at the Stanford center are encouraged to pursue RLB, only 6% of the chronic migraine group did so regularly, compared with a 10-fold higher rate among those with episodic migraine. Slicing the data another way, only 9% of patients who were on the RLB bandwagon had chronic migraine, compared with 70% of those without regular lifestyle behavior.
An observational study such as this cannot establish causality. Yet Dr. Woldeamanuel saw evidence suggestive of cause and effect with regard to RLB.
“Interestingly, among the small cohort of chronic migraineurs who were following the RLB, they were progressively month after month converting into episodic migraineurs, while the episodic migraineurs who were not following the RLB were converting to chronic migraine, month after month,” the neurologist said in an interview at the meeting sponsored by the International Headache Society and the American Headache Society.
By definition, patients with chronic migraine take headache medications most days of the month, raising the possibility that medication use might be a study confounder. To check that out, Dr. Woldeamanuel stratified patients who adhered to the RLB triumvirate into those who regularly used rescue and/or preventive medications and those who didn’t. The two subgroups didn’t differ significantly in terms of the prevalence of chronic migraine.
“This supports the genuine impact of RLB as a migraine management modality. It’s therapeutic. That’s the message,” he declared.
What’s the mechanism of benefit?
“We have biological rhythms that maintain our health: ultradian, circadian, diurnal, infradian. RLB promotes release of endorphins and keeps levels stable, increasing the threshold for sensory change and peripheral pain,” he explained.
Dr. Woldeamanuel reported having no financial conflicts with regard to this study, conducted with institutional funds.
AT IHC 2015
Key clinical point: Regular lifestyle behavior in terms of mealtimes, bedtimes, and daily aerobic exercise is a self-management tool with a therapeutic effect in migraine patients.
Major finding: Migraine patients who follow regular lifestyle behavior with regard to mealtimes, bedtimes, and daily aerobic exercise are 10-fold more likely to have episodic than chronic migraine.
Data source: This was a retrospective study of 100 chronic migraineurs and 100 patients with episodic migraine.
Disclosures: The presenter reported having no financial conflicts regarding the study, conducted with institutional funds.
IHCC: Childhood migraine hurts school performance
VALENCIA, SPAIN – Pediatric migraine often has a markedly adverse effect upon school performance and psychosocial adjustment, according to a landmark series of Brazilian studies.
“This is a series of articles that has certainly changed my own practice,” Dr. Kenneth J. Mack said at the International Headache Congress.
The Brazilian investigators are following a nationally representative sample of 5,671 Brazilian 5- to 12-year-olds. They found the prevalence of episodic migraine was 9%, while 17.6% of the youths were categorized as having probable migraine, 12.8% had periodic tensiontype headaches, and 0.6% had chronic migraine as defined by migraine headaches on at least 15 days per month, a rate Dr. Mack said was disturbingly high in such a young population.
In their most recent analysis, the Brazilian investigators reported that the children with episodic or chronic migraine had significantly higher rates of abnormal scores on various measures of psychosocial adjustment. They also had increased rates of attention-deficit/hyperactivity disorder, dyslexia, and other learning disabilities (Headache 2015;55 [suppl. 1]:39-50).
Previously, the investigators reported that the children with migraine were at significantly elevated risk of impaired school performance, as assessed by their teachers as well as on standardized tests of academic competencies. The more frequent, severe, and/or longer-lasting the migraines, the poorer the school performance (Neurology 2012;79:1881-8).
“I’ve always asked about school problems, but since these studies I’ve spent much more time delving into school problems in younger kids with chronic headaches. And I’m surprised by how often they really do have school problems – how often they need extra support and help at school,” said Dr. Mack, professor of neurology and pediatrics at the Mayo Clinic in Rochester, Minn.
Another recent research focus in the field of pediatric headache has been its seasonality, which appears to be strongly tied to the school year, he added at the meeting sponsored by the International Headache Society and the American Headache Society.
One good way to look at how severe headaches are and when they occur is by examining pediatric emergency department visits. In a single-center study of 2,731 visits to a Pittsburgh pediatric emergency department by children aged 4 years and older with a chief complaint of headache, there was a clear peak incidence in September and October – the start of the school year – and a nadir in May and June, when school lets out for the summer. This applied to headaches of all types and to patients of all ages and races and to both sexes (Pediatr. Emerg. Care 2014;30:174-6).
This report was soon followed by a nationwide study of ED visits recorded in the U.S. National Hospital Ambulatory Medical Care Survey. The investigators concluded that 5- to 18-year-olds in the United States collectively make an estimated 250,000 ED visits annually related to various types of primary headache. Indeed, headache accounted for 2.1% of all ED visits in this age group during the study years. Looking at rates on a month-by-month basis, the investigators found that ED visits for headache were highest in September (odds ratio, 1.64) and January (OR, 1.92), when children and adolescents start the academic year and return from winter break, respectively, and lowest in April (OR, 0.42) (Cephalalgia 2014;34:473-8).
In an effort to nail down the apparent link between seeking care for a headache and the school year, Dr. Mack and a coinvestigator, in a soon-to-be-published study, looked retrospectively at 103 pediatric patients diagnosed with new daily persistent headache. They focused on this particular type of headache because its onset can be traced to a particular day. Twenty-two percent of patients presented in September and another 18% in January, the school-start months. And just 1 of 103 patients presented in May or June, Dr. Mack reported.
He said he had no relevant financial conflicts.
VALENCIA, SPAIN – Pediatric migraine often has a markedly adverse effect upon school performance and psychosocial adjustment, according to a landmark series of Brazilian studies.
“This is a series of articles that has certainly changed my own practice,” Dr. Kenneth J. Mack said at the International Headache Congress.
The Brazilian investigators are following a nationally representative sample of 5,671 Brazilian 5- to 12-year-olds. They found the prevalence of episodic migraine was 9%, while 17.6% of the youths were categorized as having probable migraine, 12.8% had periodic tensiontype headaches, and 0.6% had chronic migraine as defined by migraine headaches on at least 15 days per month, a rate Dr. Mack said was disturbingly high in such a young population.
In their most recent analysis, the Brazilian investigators reported that the children with episodic or chronic migraine had significantly higher rates of abnormal scores on various measures of psychosocial adjustment. They also had increased rates of attention-deficit/hyperactivity disorder, dyslexia, and other learning disabilities (Headache 2015;55 [suppl. 1]:39-50).
Previously, the investigators reported that the children with migraine were at significantly elevated risk of impaired school performance, as assessed by their teachers as well as on standardized tests of academic competencies. The more frequent, severe, and/or longer-lasting the migraines, the poorer the school performance (Neurology 2012;79:1881-8).
“I’ve always asked about school problems, but since these studies I’ve spent much more time delving into school problems in younger kids with chronic headaches. And I’m surprised by how often they really do have school problems – how often they need extra support and help at school,” said Dr. Mack, professor of neurology and pediatrics at the Mayo Clinic in Rochester, Minn.
Another recent research focus in the field of pediatric headache has been its seasonality, which appears to be strongly tied to the school year, he added at the meeting sponsored by the International Headache Society and the American Headache Society.
One good way to look at how severe headaches are and when they occur is by examining pediatric emergency department visits. In a single-center study of 2,731 visits to a Pittsburgh pediatric emergency department by children aged 4 years and older with a chief complaint of headache, there was a clear peak incidence in September and October – the start of the school year – and a nadir in May and June, when school lets out for the summer. This applied to headaches of all types and to patients of all ages and races and to both sexes (Pediatr. Emerg. Care 2014;30:174-6).
This report was soon followed by a nationwide study of ED visits recorded in the U.S. National Hospital Ambulatory Medical Care Survey. The investigators concluded that 5- to 18-year-olds in the United States collectively make an estimated 250,000 ED visits annually related to various types of primary headache. Indeed, headache accounted for 2.1% of all ED visits in this age group during the study years. Looking at rates on a month-by-month basis, the investigators found that ED visits for headache were highest in September (odds ratio, 1.64) and January (OR, 1.92), when children and adolescents start the academic year and return from winter break, respectively, and lowest in April (OR, 0.42) (Cephalalgia 2014;34:473-8).
In an effort to nail down the apparent link between seeking care for a headache and the school year, Dr. Mack and a coinvestigator, in a soon-to-be-published study, looked retrospectively at 103 pediatric patients diagnosed with new daily persistent headache. They focused on this particular type of headache because its onset can be traced to a particular day. Twenty-two percent of patients presented in September and another 18% in January, the school-start months. And just 1 of 103 patients presented in May or June, Dr. Mack reported.
He said he had no relevant financial conflicts.
VALENCIA, SPAIN – Pediatric migraine often has a markedly adverse effect upon school performance and psychosocial adjustment, according to a landmark series of Brazilian studies.
“This is a series of articles that has certainly changed my own practice,” Dr. Kenneth J. Mack said at the International Headache Congress.
The Brazilian investigators are following a nationally representative sample of 5,671 Brazilian 5- to 12-year-olds. They found the prevalence of episodic migraine was 9%, while 17.6% of the youths were categorized as having probable migraine, 12.8% had periodic tensiontype headaches, and 0.6% had chronic migraine as defined by migraine headaches on at least 15 days per month, a rate Dr. Mack said was disturbingly high in such a young population.
In their most recent analysis, the Brazilian investigators reported that the children with episodic or chronic migraine had significantly higher rates of abnormal scores on various measures of psychosocial adjustment. They also had increased rates of attention-deficit/hyperactivity disorder, dyslexia, and other learning disabilities (Headache 2015;55 [suppl. 1]:39-50).
Previously, the investigators reported that the children with migraine were at significantly elevated risk of impaired school performance, as assessed by their teachers as well as on standardized tests of academic competencies. The more frequent, severe, and/or longer-lasting the migraines, the poorer the school performance (Neurology 2012;79:1881-8).
“I’ve always asked about school problems, but since these studies I’ve spent much more time delving into school problems in younger kids with chronic headaches. And I’m surprised by how often they really do have school problems – how often they need extra support and help at school,” said Dr. Mack, professor of neurology and pediatrics at the Mayo Clinic in Rochester, Minn.
Another recent research focus in the field of pediatric headache has been its seasonality, which appears to be strongly tied to the school year, he added at the meeting sponsored by the International Headache Society and the American Headache Society.
One good way to look at how severe headaches are and when they occur is by examining pediatric emergency department visits. In a single-center study of 2,731 visits to a Pittsburgh pediatric emergency department by children aged 4 years and older with a chief complaint of headache, there was a clear peak incidence in September and October – the start of the school year – and a nadir in May and June, when school lets out for the summer. This applied to headaches of all types and to patients of all ages and races and to both sexes (Pediatr. Emerg. Care 2014;30:174-6).
This report was soon followed by a nationwide study of ED visits recorded in the U.S. National Hospital Ambulatory Medical Care Survey. The investigators concluded that 5- to 18-year-olds in the United States collectively make an estimated 250,000 ED visits annually related to various types of primary headache. Indeed, headache accounted for 2.1% of all ED visits in this age group during the study years. Looking at rates on a month-by-month basis, the investigators found that ED visits for headache were highest in September (odds ratio, 1.64) and January (OR, 1.92), when children and adolescents start the academic year and return from winter break, respectively, and lowest in April (OR, 0.42) (Cephalalgia 2014;34:473-8).
In an effort to nail down the apparent link between seeking care for a headache and the school year, Dr. Mack and a coinvestigator, in a soon-to-be-published study, looked retrospectively at 103 pediatric patients diagnosed with new daily persistent headache. They focused on this particular type of headache because its onset can be traced to a particular day. Twenty-two percent of patients presented in September and another 18% in January, the school-start months. And just 1 of 103 patients presented in May or June, Dr. Mack reported.
He said he had no relevant financial conflicts.
EXPERT ANALYSIS FROM IHC 2015
IHC: Promising new drug cuts pain in trigeminal neuralgia
VALENCIA, SPAIN – The prospect of a new and effective oral medication for trigeminal neuralgia with much better patient tolerability than what’s currently available caused a stir at the International Headache Congress.
In a double-blind, randomized, 7-week, phase II, proof-of-concept study of 31 patients with frequent daily paroxysmic episodes of trigeminal neuralgia, the investigational agent known for now as CNV1014802 had a treatment failure rate that was half the rate seen in placebo-treated controls, Dr. Joanna Zakrzewska reported at the meeting, which was sponsored by the International Headache Society and the American Headache Society.
“We saw remarkably few adverse events. Drug-related adverse events were confined to a couple of episodes of mild dizziness/headache. There was no cognitive impairment. With the good tolerability, we think these results are encouraging enough to plan further randomized controlled trials,” said Dr. Zakrzewska of University College London.
Trigeminal neuralgia is an uncommon but severe form of unilateral episodic facial pain typically occurring in sudden, stabbing bursts lasting less than 2 minutes. The current first-line treatments – carbamazepine and other anticonvulsants – are quite effective, but often poorly tolerated, have significant drug-drug interactions, and require lengthy titration. All of this adds up to a high treatment failure rate.
CNV1014802 is a state-dependent sodium channel blocker that can be started at its target dose and has selectivity for the Nav 1.7 sodium channel.
The proof-of-concept study had an unusual design. All 31 participants were known to be responders to the novel agent because they were among the 70% of patients who responded to the drug during an open-label screening period. They were then randomized double-blind to CNV1014802 at 150 mg three times a day or placebo.
The primary endpoint in the study was treatment failure, defined as at least a 50% increase from baseline in frequency of paroxysms, a 50% worsening of the associated pain severity, and a physician global impression that a patient was “much worse” or “very much worse.” This occurred in one-third of patients on the novel drug and 64% of those on placebo. The time to treatment failure, when it occurred, was significantly longer in the active treatment group as well, according to Dr. Zakrzewska.
The treatment failure rate was 33% in patients with trigeminal neuralgia randomized to oral CNV1014802 and 64% in placebo-treated controls.
Patients in the active treatment arm experienced a mean 60% decrease in their number of pain paroxysms per day through week 7 as recorded in patient diaries, compared with a 13% reduction in placebo-treated controls. The CNV1014802 group also had a mean 55% reduction in pain severity versus an 18% improvement in controls.
The study results met with an enthusiastic audience response. “This is fantastic news for patients with trigeminal neuralgia,” said Dr. Peter J. Goadsby, chair of the British Association for the Study of Headache, who was charged with summing up the IHC Congress highlights.
Dr. Zakrzewska received a research grant from Convergence Pharmaceuticals, which sponsored the study.
VALENCIA, SPAIN – The prospect of a new and effective oral medication for trigeminal neuralgia with much better patient tolerability than what’s currently available caused a stir at the International Headache Congress.
In a double-blind, randomized, 7-week, phase II, proof-of-concept study of 31 patients with frequent daily paroxysmic episodes of trigeminal neuralgia, the investigational agent known for now as CNV1014802 had a treatment failure rate that was half the rate seen in placebo-treated controls, Dr. Joanna Zakrzewska reported at the meeting, which was sponsored by the International Headache Society and the American Headache Society.
“We saw remarkably few adverse events. Drug-related adverse events were confined to a couple of episodes of mild dizziness/headache. There was no cognitive impairment. With the good tolerability, we think these results are encouraging enough to plan further randomized controlled trials,” said Dr. Zakrzewska of University College London.
Trigeminal neuralgia is an uncommon but severe form of unilateral episodic facial pain typically occurring in sudden, stabbing bursts lasting less than 2 minutes. The current first-line treatments – carbamazepine and other anticonvulsants – are quite effective, but often poorly tolerated, have significant drug-drug interactions, and require lengthy titration. All of this adds up to a high treatment failure rate.
CNV1014802 is a state-dependent sodium channel blocker that can be started at its target dose and has selectivity for the Nav 1.7 sodium channel.
The proof-of-concept study had an unusual design. All 31 participants were known to be responders to the novel agent because they were among the 70% of patients who responded to the drug during an open-label screening period. They were then randomized double-blind to CNV1014802 at 150 mg three times a day or placebo.
The primary endpoint in the study was treatment failure, defined as at least a 50% increase from baseline in frequency of paroxysms, a 50% worsening of the associated pain severity, and a physician global impression that a patient was “much worse” or “very much worse.” This occurred in one-third of patients on the novel drug and 64% of those on placebo. The time to treatment failure, when it occurred, was significantly longer in the active treatment group as well, according to Dr. Zakrzewska.
The treatment failure rate was 33% in patients with trigeminal neuralgia randomized to oral CNV1014802 and 64% in placebo-treated controls.
Patients in the active treatment arm experienced a mean 60% decrease in their number of pain paroxysms per day through week 7 as recorded in patient diaries, compared with a 13% reduction in placebo-treated controls. The CNV1014802 group also had a mean 55% reduction in pain severity versus an 18% improvement in controls.
The study results met with an enthusiastic audience response. “This is fantastic news for patients with trigeminal neuralgia,” said Dr. Peter J. Goadsby, chair of the British Association for the Study of Headache, who was charged with summing up the IHC Congress highlights.
Dr. Zakrzewska received a research grant from Convergence Pharmaceuticals, which sponsored the study.
VALENCIA, SPAIN – The prospect of a new and effective oral medication for trigeminal neuralgia with much better patient tolerability than what’s currently available caused a stir at the International Headache Congress.
In a double-blind, randomized, 7-week, phase II, proof-of-concept study of 31 patients with frequent daily paroxysmic episodes of trigeminal neuralgia, the investigational agent known for now as CNV1014802 had a treatment failure rate that was half the rate seen in placebo-treated controls, Dr. Joanna Zakrzewska reported at the meeting, which was sponsored by the International Headache Society and the American Headache Society.
“We saw remarkably few adverse events. Drug-related adverse events were confined to a couple of episodes of mild dizziness/headache. There was no cognitive impairment. With the good tolerability, we think these results are encouraging enough to plan further randomized controlled trials,” said Dr. Zakrzewska of University College London.
Trigeminal neuralgia is an uncommon but severe form of unilateral episodic facial pain typically occurring in sudden, stabbing bursts lasting less than 2 minutes. The current first-line treatments – carbamazepine and other anticonvulsants – are quite effective, but often poorly tolerated, have significant drug-drug interactions, and require lengthy titration. All of this adds up to a high treatment failure rate.
CNV1014802 is a state-dependent sodium channel blocker that can be started at its target dose and has selectivity for the Nav 1.7 sodium channel.
The proof-of-concept study had an unusual design. All 31 participants were known to be responders to the novel agent because they were among the 70% of patients who responded to the drug during an open-label screening period. They were then randomized double-blind to CNV1014802 at 150 mg three times a day or placebo.
The primary endpoint in the study was treatment failure, defined as at least a 50% increase from baseline in frequency of paroxysms, a 50% worsening of the associated pain severity, and a physician global impression that a patient was “much worse” or “very much worse.” This occurred in one-third of patients on the novel drug and 64% of those on placebo. The time to treatment failure, when it occurred, was significantly longer in the active treatment group as well, according to Dr. Zakrzewska.
The treatment failure rate was 33% in patients with trigeminal neuralgia randomized to oral CNV1014802 and 64% in placebo-treated controls.
Patients in the active treatment arm experienced a mean 60% decrease in their number of pain paroxysms per day through week 7 as recorded in patient diaries, compared with a 13% reduction in placebo-treated controls. The CNV1014802 group also had a mean 55% reduction in pain severity versus an 18% improvement in controls.
The study results met with an enthusiastic audience response. “This is fantastic news for patients with trigeminal neuralgia,” said Dr. Peter J. Goadsby, chair of the British Association for the Study of Headache, who was charged with summing up the IHC Congress highlights.
Dr. Zakrzewska received a research grant from Convergence Pharmaceuticals, which sponsored the study.
AT IHC 2015
Key clinical point: Novel sodium channel blocker could fill treatment gap in trigeminal neuralgia.
Major finding: The treatment failure rate was 33% in patients with trigeminal neuralgia randomized to oral CNV1014802 and 64% in placebo-treated controls.
Data source: A double-blind, randomized, 7-week, phase II, proof-of-concept study of 31 patients.
Disclosures: Dr. Zakrzewska received a research grant from Convergence Pharmaceuticals, which sponsored the study.