User login
Elderly Stroke Patients Have High Atrial Fibrillation Prevalence
NEW ORLEANS – Nearly half of elderly patients who have an ischemic stroke also have atrial fibrillation, based on a review of 527 stroke patients aged 75 or older at a single U.S. center.
Atrial fibrillation (AF) "should be meticulously searched for" in elderly stroke patients who have not already been diagnosed with the arrhythmia so that they can be considered for anticoagulation treatment to prevent future strokes, Dr. Jacob I. Haft and Dr. Louis E. Teichholz said in a poster presentation at the International Stroke Conference.
The findings "suggest that atrial fibriilation plays a more important role in the etiology of stroke than previously considered," said Dr. Haft and Dr. Teichholz, who are both cardiologists at Hackensack (N.J.) University Medical Center.
The prevalence of AF among elderly stroke patients was even higher among patients with other comorbidities that also predispose to atrial arrhythmia. For example, among the 130 elderly stroke patients studied who also had heart failure, the AF prevalence was 68%. Among elderly patients with a cardiac abnormality detected by echocardiography, the prevalence of AF was 56%. Among the elderly with coronary artery disease, the AF prevalence was 53%, they reported.
In contrast, among 458 stroke patients included in the study who were younger than 75 years old, the AF prevalence was 15%. Gender was not linked to AF prevalence.
The investigators reviewed patients admitted to the medical center from January 2005 to December 2007 with a diagnosis of ischemic stroke and retrospectively diagnosed AF in these patients based on a 14-year database of ECG recordings available at the hospital. Because the AF diagnoses depended on "serendipitous" identification of AF episodes and did not come from a systematic, prospective study, the analysis likely underestimated the true prevalence of AF in these stroke patients, the researchers said at the meeting, which was sponsored by the American Heart Association.
Dr. Haft and Dr. Teichholz said that they had no disclosures.
NEW ORLEANS – Nearly half of elderly patients who have an ischemic stroke also have atrial fibrillation, based on a review of 527 stroke patients aged 75 or older at a single U.S. center.
Atrial fibrillation (AF) "should be meticulously searched for" in elderly stroke patients who have not already been diagnosed with the arrhythmia so that they can be considered for anticoagulation treatment to prevent future strokes, Dr. Jacob I. Haft and Dr. Louis E. Teichholz said in a poster presentation at the International Stroke Conference.
The findings "suggest that atrial fibriilation plays a more important role in the etiology of stroke than previously considered," said Dr. Haft and Dr. Teichholz, who are both cardiologists at Hackensack (N.J.) University Medical Center.
The prevalence of AF among elderly stroke patients was even higher among patients with other comorbidities that also predispose to atrial arrhythmia. For example, among the 130 elderly stroke patients studied who also had heart failure, the AF prevalence was 68%. Among elderly patients with a cardiac abnormality detected by echocardiography, the prevalence of AF was 56%. Among the elderly with coronary artery disease, the AF prevalence was 53%, they reported.
In contrast, among 458 stroke patients included in the study who were younger than 75 years old, the AF prevalence was 15%. Gender was not linked to AF prevalence.
The investigators reviewed patients admitted to the medical center from January 2005 to December 2007 with a diagnosis of ischemic stroke and retrospectively diagnosed AF in these patients based on a 14-year database of ECG recordings available at the hospital. Because the AF diagnoses depended on "serendipitous" identification of AF episodes and did not come from a systematic, prospective study, the analysis likely underestimated the true prevalence of AF in these stroke patients, the researchers said at the meeting, which was sponsored by the American Heart Association.
Dr. Haft and Dr. Teichholz said that they had no disclosures.
NEW ORLEANS – Nearly half of elderly patients who have an ischemic stroke also have atrial fibrillation, based on a review of 527 stroke patients aged 75 or older at a single U.S. center.
Atrial fibrillation (AF) "should be meticulously searched for" in elderly stroke patients who have not already been diagnosed with the arrhythmia so that they can be considered for anticoagulation treatment to prevent future strokes, Dr. Jacob I. Haft and Dr. Louis E. Teichholz said in a poster presentation at the International Stroke Conference.
The findings "suggest that atrial fibriilation plays a more important role in the etiology of stroke than previously considered," said Dr. Haft and Dr. Teichholz, who are both cardiologists at Hackensack (N.J.) University Medical Center.
The prevalence of AF among elderly stroke patients was even higher among patients with other comorbidities that also predispose to atrial arrhythmia. For example, among the 130 elderly stroke patients studied who also had heart failure, the AF prevalence was 68%. Among elderly patients with a cardiac abnormality detected by echocardiography, the prevalence of AF was 56%. Among the elderly with coronary artery disease, the AF prevalence was 53%, they reported.
In contrast, among 458 stroke patients included in the study who were younger than 75 years old, the AF prevalence was 15%. Gender was not linked to AF prevalence.
The investigators reviewed patients admitted to the medical center from January 2005 to December 2007 with a diagnosis of ischemic stroke and retrospectively diagnosed AF in these patients based on a 14-year database of ECG recordings available at the hospital. Because the AF diagnoses depended on "serendipitous" identification of AF episodes and did not come from a systematic, prospective study, the analysis likely underestimated the true prevalence of AF in these stroke patients, the researchers said at the meeting, which was sponsored by the American Heart Association.
Dr. Haft and Dr. Teichholz said that they had no disclosures.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Ischemic stroke patients who were at least 75 years old had a 45% prevalence of atrial fibrillation.
Data Source: The findings came from a review of 527 stroke patients at least 75 years old and 458 stroke patients less than 75 years old at a single U.S. medical center.
Disclosures: Dr. Haft and Dr. Teichholz said that they had no disclosures.
Embolectomy May Help Despite Infarct Size
NEW ORLEANS – Improving the outcomes of endovascular stroke intervention lies – at least in part – in selecting the best candidates.
But even those who are at the highest risk of harm from the treatment still may reap some benefit when compared with the grim alternative, researchers said at the International Stroke Conference, which was sponsored by the American Heart Association.
The oldest patients and those with large ischemic infarcts are at exceedingly high risk of very poor outcomes with mechanical embolectomy, according to Dr. Albert Yoo and Dr. Yogesh Moradiya. But their analyses of stroke study cohorts indicate that clinicians might be able to predict and screen for patients who will benefit most from endovascular stroke treatment.
Patients with the lowest scores on the ASPECTS (Alberta Stroke Program Early CT Score) assessment are known to have "dismal outcomes, and should probably be excluded from this therapy," said Dr. Yoo, a vascular radiologist at Massachusetts General Hospital, Boston. But, he said, his analysis identified a subgroup of patients he now believes should be treated, despite their prior reputation as barely salvageable.
"If you take the wrong person, and the procedure goes bad and they die on the table, this is not helping the brain."
In the prediction of outcome by ASPECTS, patients with ischemic stroke are grouped by the size of their initial infarct, as seen on noncontrast CT scan. The 10-point score has conventionally dichotomized patients into those destined to have poor outcomes (ASPECTS 0-7) and those with much better outcomes (APSECTS 8-10).
Dr. Yoo examined outcomes in two stroke study cohorts that used ASPECTS as a predictor of outcome. The pooled analysis included 215 patients with a mean age of 66 years. Their mean National Institutes of Health Stroke Scale score was 17. Most of the strokes (77%) were in the middle cerebral artery.
The pretreatment ASPECTS score was 0-4 in 16% of patients, 5-7 in 34%, and 8-10 in the remainder. The median ASPECTS score was 7, which is the widely accepted cutoff level for using mechanical embolectomy with a reasonable hope of good outcome.
The procedure was successful in most patients, with 83% achieving a TIMI (thrombolysis in myocardial infarction) score of 2 or 3. Most of the reperfusions occurred in a timely manner as well (within 6 hours for 27% and shortly thereafter for the rest).
Dr. Yoo said that, generally, those with the lowest scores on ASPECTS fared significantly worse, as expected. In the conventional split, 24% of those with scores of 0-7 had a good 90-day outcome (defined as discharge home with self-care), compared with 44% of those with scores of 8-10. Time to reperfusion did not affect outcomes in the lower-scoring group. The patients who reperfused early had almost exactly the same poor outcome as did those who reperfused late and those who never received the intervention.
But when Dr. Yoo split the scores of the cohorts into three groups, he found that the vast majority of poor outcomes occurred in the 0- to 4-point range. Among these patients, only 4% had good outcomes, and no one in the 0- to 3-point group had a good outcome.
Patients who had a score of 5, 6, or 7 points on ASPECTS, however, fared significantly better, with good outcomes in about 20%, 30%, and 40%, respectively. Time to reperfusion was important in these patients: Outcomes were good in 53% of early reperfusions, 31% of late reperfusions, and 20% of those who were not reperfused.
The results for patients with 8-10 points on ASPECTS – generally considered the group most likely to benefit – were similar to those seen in the 5- to 7-point group. Good outcomes occurred in 54% of those in the 8- to 10-point group with early perfusion. The rates were 46% in those with later reperfusions and 17% in those with no reperfusion.
When Dr. Yoo combined patients with 5-7 points and 8-10 points on ASPECTS, the outcomes still looked positive. "Almost all [85%] of the patients in these groups who achieved a TIMI 2-3 reperfusion had good outcomes," he said. This was a threefold increase over similar patients with a TIMI score of 0-1.
"The ASPECTS score does identify a group of patients highly likely to have dismal outcomes who probably will not benefit from reperfusion therapy and should be excluded from it," he said. "But patients with ASPECTS scores of 5-7 do appear to benefit, and treatment should not be withheld from this group."
Age as the determining factor of who should undergo reperfusion therapy proved a tougher sell for Dr. Yogesh Moradiya, a neurology fellow at the SUNY Downstate Medical Center, Brooklyn, N.Y.
He examined the relationship between advanced age and functional outcome after ischemic stroke treatment in a sample of 6,700 patients in the Nationwide Inpatient Sample. Of those patients, 20% were older than 80 years.
"Not surprisingly, most [68%] of these elderly old were female," said Dr. Moradiya. Those older than 80 years also had more comorbidity, leading to a higher Elixhauser comorbidity index than that in young patients (mean, 3.4 vs. 1.6).
Mortality was significantly higher in the older patients than the younger patients (31% vs. 22%), although there were no differences between the age groups in the rates of symptomatic and asymptomatic intracranial hemorrhage, mechanical ventilation, and tracheostomy.
The older patients were more likely to receive intravenous or intra-arterial thrombolysis in addition to embolectomy, probably because of an unsuccessful initial endovascular procedure. But the octogenarians did not withstand their treatment and hospitalization very well. Compared with younger patients, the older patients had significantly higher rates of heart attack (7% vs. 5%), acute kidney injury (9% vs. 6%), gastrointestinal bleeding (3% vs. 2%), urinary tract infections (22% vs. 15%), and transfusions (10% vs. 8%).
Patients older than 80 years had several comorbidities that significantly predicted mortality after ischemic stroke, including the following:
• Chronic pulmonary disease (odds ratio, 2.7).
• Acute kidney injury (OR, 3.8).
• Myocardial infarction (OR, 3.2).
• Intracranial hemorrhage (OR, 3).
• Sepsis (OR, 8).
Thrombolytic treatment lowered the risk of death by 68% in older patients, but this was not significantly different from the treatment effect in younger patients. Dr. Moradiya suggested that selecting younger or healthier patients would improve endovascular stroke treatment outcomes. "This is screening in the sense that people with this higher comorbidity profile should not undergo embolectomy, compared to the more healthy elderly."
This summation rankled some audience members, including Dr. James L. Frey, director of the stroke center at Barrow Neurological Institute, Phoenix.
"I don’t like this concept of reducing complications by screening people for these procedures," he said during the discussion. "It seems obvious that the medical complications are the problem, and not the procedure itself, so when you talk about screening, how are you going to do that?"
Very elderly stroke patients want treatment just as much as younger patients do, he said. "They don’t like what’s going wrong with their brain and they want someone to do something about it. They don’t mind so much if you try this and they die, but they do not want to live with a brain hemorrhage. It sounds like you’re saying they are better off having a clot in their middle cerebral artery than having someone try to remove it. Is this what you’re saying?"
Dr. Felipe Albuquerque, a session moderator, added his take on the issue.
"Absolutely, the brain is paramount and all other organs are secondary, so we should do all we can for the brain. But if you take the wrong person, and the procedure goes bad and they die on the table, this is not helping the brain. There are simply patients who are too high risk, and for these you might think about a different procedure."
"I don’t do these procedures with anesthesia on board," because of the extra burden it places on an elderly patient, said Dr. Albuquerque, a neurosurgeon who is also with the Barrow Neurological Institute.
"So in that sense, screening does help your approach and should perhaps obviate intervention for people who are going to die, no matter what you do."
Dr. Moradiya had no financial disclosures. Dr. Yoo said that he has received research funding from Penumbra Inc. Dr. Frey and Dr. Albuquerque said they had no relevant disclosures.
NEW ORLEANS – Improving the outcomes of endovascular stroke intervention lies – at least in part – in selecting the best candidates.
But even those who are at the highest risk of harm from the treatment still may reap some benefit when compared with the grim alternative, researchers said at the International Stroke Conference, which was sponsored by the American Heart Association.
The oldest patients and those with large ischemic infarcts are at exceedingly high risk of very poor outcomes with mechanical embolectomy, according to Dr. Albert Yoo and Dr. Yogesh Moradiya. But their analyses of stroke study cohorts indicate that clinicians might be able to predict and screen for patients who will benefit most from endovascular stroke treatment.
Patients with the lowest scores on the ASPECTS (Alberta Stroke Program Early CT Score) assessment are known to have "dismal outcomes, and should probably be excluded from this therapy," said Dr. Yoo, a vascular radiologist at Massachusetts General Hospital, Boston. But, he said, his analysis identified a subgroup of patients he now believes should be treated, despite their prior reputation as barely salvageable.
"If you take the wrong person, and the procedure goes bad and they die on the table, this is not helping the brain."
In the prediction of outcome by ASPECTS, patients with ischemic stroke are grouped by the size of their initial infarct, as seen on noncontrast CT scan. The 10-point score has conventionally dichotomized patients into those destined to have poor outcomes (ASPECTS 0-7) and those with much better outcomes (APSECTS 8-10).
Dr. Yoo examined outcomes in two stroke study cohorts that used ASPECTS as a predictor of outcome. The pooled analysis included 215 patients with a mean age of 66 years. Their mean National Institutes of Health Stroke Scale score was 17. Most of the strokes (77%) were in the middle cerebral artery.
The pretreatment ASPECTS score was 0-4 in 16% of patients, 5-7 in 34%, and 8-10 in the remainder. The median ASPECTS score was 7, which is the widely accepted cutoff level for using mechanical embolectomy with a reasonable hope of good outcome.
The procedure was successful in most patients, with 83% achieving a TIMI (thrombolysis in myocardial infarction) score of 2 or 3. Most of the reperfusions occurred in a timely manner as well (within 6 hours for 27% and shortly thereafter for the rest).
Dr. Yoo said that, generally, those with the lowest scores on ASPECTS fared significantly worse, as expected. In the conventional split, 24% of those with scores of 0-7 had a good 90-day outcome (defined as discharge home with self-care), compared with 44% of those with scores of 8-10. Time to reperfusion did not affect outcomes in the lower-scoring group. The patients who reperfused early had almost exactly the same poor outcome as did those who reperfused late and those who never received the intervention.
But when Dr. Yoo split the scores of the cohorts into three groups, he found that the vast majority of poor outcomes occurred in the 0- to 4-point range. Among these patients, only 4% had good outcomes, and no one in the 0- to 3-point group had a good outcome.
Patients who had a score of 5, 6, or 7 points on ASPECTS, however, fared significantly better, with good outcomes in about 20%, 30%, and 40%, respectively. Time to reperfusion was important in these patients: Outcomes were good in 53% of early reperfusions, 31% of late reperfusions, and 20% of those who were not reperfused.
The results for patients with 8-10 points on ASPECTS – generally considered the group most likely to benefit – were similar to those seen in the 5- to 7-point group. Good outcomes occurred in 54% of those in the 8- to 10-point group with early perfusion. The rates were 46% in those with later reperfusions and 17% in those with no reperfusion.
When Dr. Yoo combined patients with 5-7 points and 8-10 points on ASPECTS, the outcomes still looked positive. "Almost all [85%] of the patients in these groups who achieved a TIMI 2-3 reperfusion had good outcomes," he said. This was a threefold increase over similar patients with a TIMI score of 0-1.
"The ASPECTS score does identify a group of patients highly likely to have dismal outcomes who probably will not benefit from reperfusion therapy and should be excluded from it," he said. "But patients with ASPECTS scores of 5-7 do appear to benefit, and treatment should not be withheld from this group."
Age as the determining factor of who should undergo reperfusion therapy proved a tougher sell for Dr. Yogesh Moradiya, a neurology fellow at the SUNY Downstate Medical Center, Brooklyn, N.Y.
He examined the relationship between advanced age and functional outcome after ischemic stroke treatment in a sample of 6,700 patients in the Nationwide Inpatient Sample. Of those patients, 20% were older than 80 years.
"Not surprisingly, most [68%] of these elderly old were female," said Dr. Moradiya. Those older than 80 years also had more comorbidity, leading to a higher Elixhauser comorbidity index than that in young patients (mean, 3.4 vs. 1.6).
Mortality was significantly higher in the older patients than the younger patients (31% vs. 22%), although there were no differences between the age groups in the rates of symptomatic and asymptomatic intracranial hemorrhage, mechanical ventilation, and tracheostomy.
The older patients were more likely to receive intravenous or intra-arterial thrombolysis in addition to embolectomy, probably because of an unsuccessful initial endovascular procedure. But the octogenarians did not withstand their treatment and hospitalization very well. Compared with younger patients, the older patients had significantly higher rates of heart attack (7% vs. 5%), acute kidney injury (9% vs. 6%), gastrointestinal bleeding (3% vs. 2%), urinary tract infections (22% vs. 15%), and transfusions (10% vs. 8%).
Patients older than 80 years had several comorbidities that significantly predicted mortality after ischemic stroke, including the following:
• Chronic pulmonary disease (odds ratio, 2.7).
• Acute kidney injury (OR, 3.8).
• Myocardial infarction (OR, 3.2).
• Intracranial hemorrhage (OR, 3).
• Sepsis (OR, 8).
Thrombolytic treatment lowered the risk of death by 68% in older patients, but this was not significantly different from the treatment effect in younger patients. Dr. Moradiya suggested that selecting younger or healthier patients would improve endovascular stroke treatment outcomes. "This is screening in the sense that people with this higher comorbidity profile should not undergo embolectomy, compared to the more healthy elderly."
This summation rankled some audience members, including Dr. James L. Frey, director of the stroke center at Barrow Neurological Institute, Phoenix.
"I don’t like this concept of reducing complications by screening people for these procedures," he said during the discussion. "It seems obvious that the medical complications are the problem, and not the procedure itself, so when you talk about screening, how are you going to do that?"
Very elderly stroke patients want treatment just as much as younger patients do, he said. "They don’t like what’s going wrong with their brain and they want someone to do something about it. They don’t mind so much if you try this and they die, but they do not want to live with a brain hemorrhage. It sounds like you’re saying they are better off having a clot in their middle cerebral artery than having someone try to remove it. Is this what you’re saying?"
Dr. Felipe Albuquerque, a session moderator, added his take on the issue.
"Absolutely, the brain is paramount and all other organs are secondary, so we should do all we can for the brain. But if you take the wrong person, and the procedure goes bad and they die on the table, this is not helping the brain. There are simply patients who are too high risk, and for these you might think about a different procedure."
"I don’t do these procedures with anesthesia on board," because of the extra burden it places on an elderly patient, said Dr. Albuquerque, a neurosurgeon who is also with the Barrow Neurological Institute.
"So in that sense, screening does help your approach and should perhaps obviate intervention for people who are going to die, no matter what you do."
Dr. Moradiya had no financial disclosures. Dr. Yoo said that he has received research funding from Penumbra Inc. Dr. Frey and Dr. Albuquerque said they had no relevant disclosures.
NEW ORLEANS – Improving the outcomes of endovascular stroke intervention lies – at least in part – in selecting the best candidates.
But even those who are at the highest risk of harm from the treatment still may reap some benefit when compared with the grim alternative, researchers said at the International Stroke Conference, which was sponsored by the American Heart Association.
The oldest patients and those with large ischemic infarcts are at exceedingly high risk of very poor outcomes with mechanical embolectomy, according to Dr. Albert Yoo and Dr. Yogesh Moradiya. But their analyses of stroke study cohorts indicate that clinicians might be able to predict and screen for patients who will benefit most from endovascular stroke treatment.
Patients with the lowest scores on the ASPECTS (Alberta Stroke Program Early CT Score) assessment are known to have "dismal outcomes, and should probably be excluded from this therapy," said Dr. Yoo, a vascular radiologist at Massachusetts General Hospital, Boston. But, he said, his analysis identified a subgroup of patients he now believes should be treated, despite their prior reputation as barely salvageable.
"If you take the wrong person, and the procedure goes bad and they die on the table, this is not helping the brain."
In the prediction of outcome by ASPECTS, patients with ischemic stroke are grouped by the size of their initial infarct, as seen on noncontrast CT scan. The 10-point score has conventionally dichotomized patients into those destined to have poor outcomes (ASPECTS 0-7) and those with much better outcomes (APSECTS 8-10).
Dr. Yoo examined outcomes in two stroke study cohorts that used ASPECTS as a predictor of outcome. The pooled analysis included 215 patients with a mean age of 66 years. Their mean National Institutes of Health Stroke Scale score was 17. Most of the strokes (77%) were in the middle cerebral artery.
The pretreatment ASPECTS score was 0-4 in 16% of patients, 5-7 in 34%, and 8-10 in the remainder. The median ASPECTS score was 7, which is the widely accepted cutoff level for using mechanical embolectomy with a reasonable hope of good outcome.
The procedure was successful in most patients, with 83% achieving a TIMI (thrombolysis in myocardial infarction) score of 2 or 3. Most of the reperfusions occurred in a timely manner as well (within 6 hours for 27% and shortly thereafter for the rest).
Dr. Yoo said that, generally, those with the lowest scores on ASPECTS fared significantly worse, as expected. In the conventional split, 24% of those with scores of 0-7 had a good 90-day outcome (defined as discharge home with self-care), compared with 44% of those with scores of 8-10. Time to reperfusion did not affect outcomes in the lower-scoring group. The patients who reperfused early had almost exactly the same poor outcome as did those who reperfused late and those who never received the intervention.
But when Dr. Yoo split the scores of the cohorts into three groups, he found that the vast majority of poor outcomes occurred in the 0- to 4-point range. Among these patients, only 4% had good outcomes, and no one in the 0- to 3-point group had a good outcome.
Patients who had a score of 5, 6, or 7 points on ASPECTS, however, fared significantly better, with good outcomes in about 20%, 30%, and 40%, respectively. Time to reperfusion was important in these patients: Outcomes were good in 53% of early reperfusions, 31% of late reperfusions, and 20% of those who were not reperfused.
The results for patients with 8-10 points on ASPECTS – generally considered the group most likely to benefit – were similar to those seen in the 5- to 7-point group. Good outcomes occurred in 54% of those in the 8- to 10-point group with early perfusion. The rates were 46% in those with later reperfusions and 17% in those with no reperfusion.
When Dr. Yoo combined patients with 5-7 points and 8-10 points on ASPECTS, the outcomes still looked positive. "Almost all [85%] of the patients in these groups who achieved a TIMI 2-3 reperfusion had good outcomes," he said. This was a threefold increase over similar patients with a TIMI score of 0-1.
"The ASPECTS score does identify a group of patients highly likely to have dismal outcomes who probably will not benefit from reperfusion therapy and should be excluded from it," he said. "But patients with ASPECTS scores of 5-7 do appear to benefit, and treatment should not be withheld from this group."
Age as the determining factor of who should undergo reperfusion therapy proved a tougher sell for Dr. Yogesh Moradiya, a neurology fellow at the SUNY Downstate Medical Center, Brooklyn, N.Y.
He examined the relationship between advanced age and functional outcome after ischemic stroke treatment in a sample of 6,700 patients in the Nationwide Inpatient Sample. Of those patients, 20% were older than 80 years.
"Not surprisingly, most [68%] of these elderly old were female," said Dr. Moradiya. Those older than 80 years also had more comorbidity, leading to a higher Elixhauser comorbidity index than that in young patients (mean, 3.4 vs. 1.6).
Mortality was significantly higher in the older patients than the younger patients (31% vs. 22%), although there were no differences between the age groups in the rates of symptomatic and asymptomatic intracranial hemorrhage, mechanical ventilation, and tracheostomy.
The older patients were more likely to receive intravenous or intra-arterial thrombolysis in addition to embolectomy, probably because of an unsuccessful initial endovascular procedure. But the octogenarians did not withstand their treatment and hospitalization very well. Compared with younger patients, the older patients had significantly higher rates of heart attack (7% vs. 5%), acute kidney injury (9% vs. 6%), gastrointestinal bleeding (3% vs. 2%), urinary tract infections (22% vs. 15%), and transfusions (10% vs. 8%).
Patients older than 80 years had several comorbidities that significantly predicted mortality after ischemic stroke, including the following:
• Chronic pulmonary disease (odds ratio, 2.7).
• Acute kidney injury (OR, 3.8).
• Myocardial infarction (OR, 3.2).
• Intracranial hemorrhage (OR, 3).
• Sepsis (OR, 8).
Thrombolytic treatment lowered the risk of death by 68% in older patients, but this was not significantly different from the treatment effect in younger patients. Dr. Moradiya suggested that selecting younger or healthier patients would improve endovascular stroke treatment outcomes. "This is screening in the sense that people with this higher comorbidity profile should not undergo embolectomy, compared to the more healthy elderly."
This summation rankled some audience members, including Dr. James L. Frey, director of the stroke center at Barrow Neurological Institute, Phoenix.
"I don’t like this concept of reducing complications by screening people for these procedures," he said during the discussion. "It seems obvious that the medical complications are the problem, and not the procedure itself, so when you talk about screening, how are you going to do that?"
Very elderly stroke patients want treatment just as much as younger patients do, he said. "They don’t like what’s going wrong with their brain and they want someone to do something about it. They don’t mind so much if you try this and they die, but they do not want to live with a brain hemorrhage. It sounds like you’re saying they are better off having a clot in their middle cerebral artery than having someone try to remove it. Is this what you’re saying?"
Dr. Felipe Albuquerque, a session moderator, added his take on the issue.
"Absolutely, the brain is paramount and all other organs are secondary, so we should do all we can for the brain. But if you take the wrong person, and the procedure goes bad and they die on the table, this is not helping the brain. There are simply patients who are too high risk, and for these you might think about a different procedure."
"I don’t do these procedures with anesthesia on board," because of the extra burden it places on an elderly patient, said Dr. Albuquerque, a neurosurgeon who is also with the Barrow Neurological Institute.
"So in that sense, screening does help your approach and should perhaps obviate intervention for people who are going to die, no matter what you do."
Dr. Moradiya had no financial disclosures. Dr. Yoo said that he has received research funding from Penumbra Inc. Dr. Frey and Dr. Albuquerque said they had no relevant disclosures.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Embolectomy could help up to 70% of patients whose ischemic stroke infarct size may have previously disqualified them from treatment.
Data Source: Two database studies identified additional patients who could benefit from mechanical embolectomy.
Disclosures: Dr. Moradiya had no financial disclosures. Dr. Yoo said that he has received research funding from Penumbra. Dr. Frey and Dr. Albuquerque said they had no relevant disclosures.
Surgical Removal of Brain Thrombus Boosts Recovery
NEW ORLEANS – An investigative, minimally invasive surgery for reducing intracranial clot volume following an intracerebral hemorrhage showed promise in results from a phase II study.
In the controlled study, 54 patients who underwent clot removal by minimally-invasive surgery (MIS) had a 10% increased rate of achieving a modified Rankin Scale (mRS) score of 1-3 at 180 days, compared with 39 patients managed by conventional, medical therapy, Dr. Daniel F. Hanley said at the meeting.
"These data may establish a surgical goal for MIS of reducing clot burden to 15 mL or less by 3-4 days" after the intracerebral hemorrhage (ICH), said Dr. Hanley, a professor of neurology and neurosurgery at Johns Hopkins University in Baltimore. The study enrolled patients within a day of their ICH with a clot volume of at least 20 mL; the average volume for the 93 patients was 40 mL.
The next step will be a pivotal, controlled study planned to enroll 500 patients at 35-50 centers, with an expected study duration of 5 years. Dr. Hanley and his associates are seeking funding for the phase III trial from the National Institutes of Health.
The MISTIE (Minimally Invasive [Stereotactic] Surgery and rTPA for ICH Extraction) study used a combination of intracerebrally infused recombinant tissue plasminogen activator (rTPA) and placement of a cannula into a patient’s skull to remove thrombolysed clot, a method that "has been around" for several years, but never before underwent assessment as a standardized procedure and in a prospective, controlled study, Dr. Hanley said in an interview. "MIS is widely available, and could be practical to use on ICH patients" once it is clearly shown to be safe and effective.
The study enrolled patients at 35 international sites who were 18-75 years old and had a spontaneous, supratentorial ICH with a stable clot. They also had received rTPA within 54 hours of their first diagnostic CT examination. The mean age of the enrolled patients was 61 years, two-thirds were men, and the patients randomized to MIS received their initial rTPA treatment an average of 48 hours after the ICH began. During an initial phase of the study patients received 0.3 mg of rTPA, but during the later phase the dose increased to 1.0 mg, the amount that most of the MIS patients received.
Safety data showed that patients treated with MIS had a 7-day mortality rate of 2 and a 30-day mortality of 15%, compared with a rate of 8% at 30 days in the medically-treated control patients. Symptomatic bleeds occurred in two of the MIS patients and one of the controls, and a brain infection occurred in none of the MIS patients and in one control patient. During follow-up out to 180 days, mortality rates were virtually identical, about 20%, in both arms of the study, and dropouts also reached similar levels in both arms, about 45%.
During their first 4 days in the study, MIS patients had an average 65% reduction in their intracerebral clot volume, compared with no change in the control patients. The two-thirds reduction with MIS corresponded to an average 28 mL drop in volume. Twenty-four surgeons participated in the study, and the analysis showed very little surgeon-to-surgeon variation in their ability to achieve clot-volume reductions. Roughly two-thirds of the surgeons had never previously performed the procedure, but each surgeon treated a run-in patient before the study formally began.
The study’s primary outcome was mRS at 180 days, with data available for 50 MIS patients and 33 controls. No patients in either group had an mRS of 0. An mRS of 1 occurred in two MIS patients and none of the controls. An mRS of 1-3 occurred in about 35% of the MIS patients and about 25% of the controls.
An analysis of all patients showed a strong link between clot volume after 4 days in the study and 180-day outcomes. The prespecified goal of MIS was removal of at least 15 mL of clot, and surgeons achieved this in about a third of the MIS patients. When patients attained that level of clot reduction, they had a statistically significant, 3.7-fold increased rate of having an mRS of 1-3 at 180 days, compared with patients who did not reach this goal.
The impact of MIS on outcome was even stronger in patients who entered the study with larger clots. Among the subgroup with a clot burden of at least 50 mL, MIS led to a 17% increased rate of patients achieving an mRS of 1-3, compared with the controls, Dr. Hanley said. Among patients treated medically, those with a clot burden on entry of about 20 mL often had an mRS of 1-3 at 180 days, but among those who began with a clot of at least 30 mL, only three patients reached an mRS of 1-3.
The MIS tested in the study used a frameless stereotactic technique that relied on an electromagnetic wave or infrared light system to guide surgical navigation. Several commercial forms of these systems exist; surgeons could use whichever they preferred, Dr. Hanley said.
The National Institute of Neurological Disorders and Stroke funded the trial. Dr. Hanley said that Johns Hopkins Medical Institutions holds a patent on intracerebral treatment with rTPA. He had no other disclosures.
The minimally invasive surgery tested in MISTIE is probably the most promising approach developed for treating the devastating disease of intracerebral hemorrhage.
The results showed a 10% increase in the rate of patients recovering to a modified Rankin Scale score of 1-3, is a pretty significant result. It results in less disability for patients and less burden to their families.

|
|
The most important predictor of outcome was the size of the clot; if you can do anything meaningful to reduce the size, it should benefit patients. But aggressiveness in removing clot must be balanced against minimizing manipulation of brain tissue. The goal is to remove as much clot as possible without doing damage. The results did not include information on brain edema following surgery, but it looks like despite the trauma of intervention patients on balance had better outcomes.
This was a phase II study, so the results now need to be replicated in additional patients. At this point, it remains ethical to randomize patients to receive either this treatment or conventional therapy. This is a very important treatment to further examine.
Dr. Steven R. Levine is professor of neurology and emergency medicine at State University of New York, Brooklyn. He said that he had no disclosures. Dr. Levine made these comments in an interview.
The minimally invasive surgery tested in MISTIE is probably the most promising approach developed for treating the devastating disease of intracerebral hemorrhage.
The results showed a 10% increase in the rate of patients recovering to a modified Rankin Scale score of 1-3, is a pretty significant result. It results in less disability for patients and less burden to their families.

|
|
The most important predictor of outcome was the size of the clot; if you can do anything meaningful to reduce the size, it should benefit patients. But aggressiveness in removing clot must be balanced against minimizing manipulation of brain tissue. The goal is to remove as much clot as possible without doing damage. The results did not include information on brain edema following surgery, but it looks like despite the trauma of intervention patients on balance had better outcomes.
This was a phase II study, so the results now need to be replicated in additional patients. At this point, it remains ethical to randomize patients to receive either this treatment or conventional therapy. This is a very important treatment to further examine.
Dr. Steven R. Levine is professor of neurology and emergency medicine at State University of New York, Brooklyn. He said that he had no disclosures. Dr. Levine made these comments in an interview.
The minimally invasive surgery tested in MISTIE is probably the most promising approach developed for treating the devastating disease of intracerebral hemorrhage.
The results showed a 10% increase in the rate of patients recovering to a modified Rankin Scale score of 1-3, is a pretty significant result. It results in less disability for patients and less burden to their families.

|
|
The most important predictor of outcome was the size of the clot; if you can do anything meaningful to reduce the size, it should benefit patients. But aggressiveness in removing clot must be balanced against minimizing manipulation of brain tissue. The goal is to remove as much clot as possible without doing damage. The results did not include information on brain edema following surgery, but it looks like despite the trauma of intervention patients on balance had better outcomes.
This was a phase II study, so the results now need to be replicated in additional patients. At this point, it remains ethical to randomize patients to receive either this treatment or conventional therapy. This is a very important treatment to further examine.
Dr. Steven R. Levine is professor of neurology and emergency medicine at State University of New York, Brooklyn. He said that he had no disclosures. Dr. Levine made these comments in an interview.
NEW ORLEANS – An investigative, minimally invasive surgery for reducing intracranial clot volume following an intracerebral hemorrhage showed promise in results from a phase II study.
In the controlled study, 54 patients who underwent clot removal by minimally-invasive surgery (MIS) had a 10% increased rate of achieving a modified Rankin Scale (mRS) score of 1-3 at 180 days, compared with 39 patients managed by conventional, medical therapy, Dr. Daniel F. Hanley said at the meeting.
"These data may establish a surgical goal for MIS of reducing clot burden to 15 mL or less by 3-4 days" after the intracerebral hemorrhage (ICH), said Dr. Hanley, a professor of neurology and neurosurgery at Johns Hopkins University in Baltimore. The study enrolled patients within a day of their ICH with a clot volume of at least 20 mL; the average volume for the 93 patients was 40 mL.
The next step will be a pivotal, controlled study planned to enroll 500 patients at 35-50 centers, with an expected study duration of 5 years. Dr. Hanley and his associates are seeking funding for the phase III trial from the National Institutes of Health.
The MISTIE (Minimally Invasive [Stereotactic] Surgery and rTPA for ICH Extraction) study used a combination of intracerebrally infused recombinant tissue plasminogen activator (rTPA) and placement of a cannula into a patient’s skull to remove thrombolysed clot, a method that "has been around" for several years, but never before underwent assessment as a standardized procedure and in a prospective, controlled study, Dr. Hanley said in an interview. "MIS is widely available, and could be practical to use on ICH patients" once it is clearly shown to be safe and effective.
The study enrolled patients at 35 international sites who were 18-75 years old and had a spontaneous, supratentorial ICH with a stable clot. They also had received rTPA within 54 hours of their first diagnostic CT examination. The mean age of the enrolled patients was 61 years, two-thirds were men, and the patients randomized to MIS received their initial rTPA treatment an average of 48 hours after the ICH began. During an initial phase of the study patients received 0.3 mg of rTPA, but during the later phase the dose increased to 1.0 mg, the amount that most of the MIS patients received.
Safety data showed that patients treated with MIS had a 7-day mortality rate of 2 and a 30-day mortality of 15%, compared with a rate of 8% at 30 days in the medically-treated control patients. Symptomatic bleeds occurred in two of the MIS patients and one of the controls, and a brain infection occurred in none of the MIS patients and in one control patient. During follow-up out to 180 days, mortality rates were virtually identical, about 20%, in both arms of the study, and dropouts also reached similar levels in both arms, about 45%.
During their first 4 days in the study, MIS patients had an average 65% reduction in their intracerebral clot volume, compared with no change in the control patients. The two-thirds reduction with MIS corresponded to an average 28 mL drop in volume. Twenty-four surgeons participated in the study, and the analysis showed very little surgeon-to-surgeon variation in their ability to achieve clot-volume reductions. Roughly two-thirds of the surgeons had never previously performed the procedure, but each surgeon treated a run-in patient before the study formally began.
The study’s primary outcome was mRS at 180 days, with data available for 50 MIS patients and 33 controls. No patients in either group had an mRS of 0. An mRS of 1 occurred in two MIS patients and none of the controls. An mRS of 1-3 occurred in about 35% of the MIS patients and about 25% of the controls.
An analysis of all patients showed a strong link between clot volume after 4 days in the study and 180-day outcomes. The prespecified goal of MIS was removal of at least 15 mL of clot, and surgeons achieved this in about a third of the MIS patients. When patients attained that level of clot reduction, they had a statistically significant, 3.7-fold increased rate of having an mRS of 1-3 at 180 days, compared with patients who did not reach this goal.
The impact of MIS on outcome was even stronger in patients who entered the study with larger clots. Among the subgroup with a clot burden of at least 50 mL, MIS led to a 17% increased rate of patients achieving an mRS of 1-3, compared with the controls, Dr. Hanley said. Among patients treated medically, those with a clot burden on entry of about 20 mL often had an mRS of 1-3 at 180 days, but among those who began with a clot of at least 30 mL, only three patients reached an mRS of 1-3.
The MIS tested in the study used a frameless stereotactic technique that relied on an electromagnetic wave or infrared light system to guide surgical navigation. Several commercial forms of these systems exist; surgeons could use whichever they preferred, Dr. Hanley said.
The National Institute of Neurological Disorders and Stroke funded the trial. Dr. Hanley said that Johns Hopkins Medical Institutions holds a patent on intracerebral treatment with rTPA. He had no other disclosures.
NEW ORLEANS – An investigative, minimally invasive surgery for reducing intracranial clot volume following an intracerebral hemorrhage showed promise in results from a phase II study.
In the controlled study, 54 patients who underwent clot removal by minimally-invasive surgery (MIS) had a 10% increased rate of achieving a modified Rankin Scale (mRS) score of 1-3 at 180 days, compared with 39 patients managed by conventional, medical therapy, Dr. Daniel F. Hanley said at the meeting.
"These data may establish a surgical goal for MIS of reducing clot burden to 15 mL or less by 3-4 days" after the intracerebral hemorrhage (ICH), said Dr. Hanley, a professor of neurology and neurosurgery at Johns Hopkins University in Baltimore. The study enrolled patients within a day of their ICH with a clot volume of at least 20 mL; the average volume for the 93 patients was 40 mL.
The next step will be a pivotal, controlled study planned to enroll 500 patients at 35-50 centers, with an expected study duration of 5 years. Dr. Hanley and his associates are seeking funding for the phase III trial from the National Institutes of Health.
The MISTIE (Minimally Invasive [Stereotactic] Surgery and rTPA for ICH Extraction) study used a combination of intracerebrally infused recombinant tissue plasminogen activator (rTPA) and placement of a cannula into a patient’s skull to remove thrombolysed clot, a method that "has been around" for several years, but never before underwent assessment as a standardized procedure and in a prospective, controlled study, Dr. Hanley said in an interview. "MIS is widely available, and could be practical to use on ICH patients" once it is clearly shown to be safe and effective.
The study enrolled patients at 35 international sites who were 18-75 years old and had a spontaneous, supratentorial ICH with a stable clot. They also had received rTPA within 54 hours of their first diagnostic CT examination. The mean age of the enrolled patients was 61 years, two-thirds were men, and the patients randomized to MIS received their initial rTPA treatment an average of 48 hours after the ICH began. During an initial phase of the study patients received 0.3 mg of rTPA, but during the later phase the dose increased to 1.0 mg, the amount that most of the MIS patients received.
Safety data showed that patients treated with MIS had a 7-day mortality rate of 2 and a 30-day mortality of 15%, compared with a rate of 8% at 30 days in the medically-treated control patients. Symptomatic bleeds occurred in two of the MIS patients and one of the controls, and a brain infection occurred in none of the MIS patients and in one control patient. During follow-up out to 180 days, mortality rates were virtually identical, about 20%, in both arms of the study, and dropouts also reached similar levels in both arms, about 45%.
During their first 4 days in the study, MIS patients had an average 65% reduction in their intracerebral clot volume, compared with no change in the control patients. The two-thirds reduction with MIS corresponded to an average 28 mL drop in volume. Twenty-four surgeons participated in the study, and the analysis showed very little surgeon-to-surgeon variation in their ability to achieve clot-volume reductions. Roughly two-thirds of the surgeons had never previously performed the procedure, but each surgeon treated a run-in patient before the study formally began.
The study’s primary outcome was mRS at 180 days, with data available for 50 MIS patients and 33 controls. No patients in either group had an mRS of 0. An mRS of 1 occurred in two MIS patients and none of the controls. An mRS of 1-3 occurred in about 35% of the MIS patients and about 25% of the controls.
An analysis of all patients showed a strong link between clot volume after 4 days in the study and 180-day outcomes. The prespecified goal of MIS was removal of at least 15 mL of clot, and surgeons achieved this in about a third of the MIS patients. When patients attained that level of clot reduction, they had a statistically significant, 3.7-fold increased rate of having an mRS of 1-3 at 180 days, compared with patients who did not reach this goal.
The impact of MIS on outcome was even stronger in patients who entered the study with larger clots. Among the subgroup with a clot burden of at least 50 mL, MIS led to a 17% increased rate of patients achieving an mRS of 1-3, compared with the controls, Dr. Hanley said. Among patients treated medically, those with a clot burden on entry of about 20 mL often had an mRS of 1-3 at 180 days, but among those who began with a clot of at least 30 mL, only three patients reached an mRS of 1-3.
The MIS tested in the study used a frameless stereotactic technique that relied on an electromagnetic wave or infrared light system to guide surgical navigation. Several commercial forms of these systems exist; surgeons could use whichever they preferred, Dr. Hanley said.
The National Institute of Neurological Disorders and Stroke funded the trial. Dr. Hanley said that Johns Hopkins Medical Institutions holds a patent on intracerebral treatment with rTPA. He had no other disclosures.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Treating intracerebral hemorrhage with minimally invasive surgery plus intracerebral rTPA increased mRS 1-3 recoveries by 10% compared with medical treatment.
Data Source: Data are from MISTIE, a prospective, randomized, phase 2 trial included 93 patients treated at 35 international sites.
Disclosures: The National Institute of Neurological Disorders and Stroke funded the trial. Dr. Hanley said that Johns Hopkins Medical Institutions holds a patent on intracerebral treatment with rtPA. He had no other disclosures.
Asymptomatic Carotid Disease Impairs Cognitive Function
NEW ORLEANS – Patients with "asymptomatic" carotid-artery disease may still have important sequelae from their arterial stenosis.
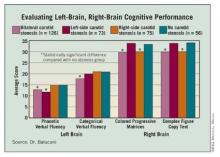
Patients with substantial carotid-artery stenosis and no history of stroke or transient ischemic attack had significant cognitive impairments, compared with people without carotid disease, in a single-center, prospective study of 330 people, Dr. Clotilde Balucani said at the International Stroke Conference.
Notably, patients with severe, unilateral carotid stenosis showed cognitive impairments for functions linked with the brain hemisphere that received its blood supply from an occluded carotid, while the same people with an unimpeded contralateral carotid showed no impairment on cognitive tests that tested their contralateral brain function, said Dr. Balucani, a neurologist at Downstate Medical Center in Brooklyn, N.Y. Patients with bilateral carotid disease had impairments on all of the cognitive tests she used in this study, whereas control subjects without carotid disease showed no impairments on any of the cognitive tests.
"Asymptomatic carotid stenosis may not be truly asymptomatic," she said. "There appears to be an association between cognitive dysfunction and cerebral hemodynamic impairment. Cognitive function could be considered a potential outcome measure, and its improvement by treatment of asymptomatic carotid stenosis may be worthy of further investigation." Adding improved cognitive dysfunction to stroke prevention as another potential beneficial outcome of carotid revascularization may "better help risk stratify patients," Dr. Balucani said.
As of today, no study results have clearly documented that carotid revascularization improves cognition, so this hypothesis needs further testing, she cautioned.
Her study enrolled people during 2005-2010 who had no history of stroke or transient ischemic attack, who were also negative for other markers of poor cognitive function: heart failure, proximal internal carotid artery occlusion, a low score (less than 26) on the Mini Mental State Examination (MMSE), and severe stenosis of an intracranial or vertebro/basilar artery. The study group included 126 patients with ultrasound evidence for at least 60% occlusion of both carotid arteries, 73 patients with this level of occlusion in their left carotid, 75 with this occlusion in their right carotid, and 56 controls without occlusion in either carotid. Patients’ average age was 70 years, two-thirds were men, and their average MMSE score was 27.
All participants underwent assessment by four cognitive evaluations: the phonemic verbal fluency test and the categorical verbal fluency test – both designed to assess cognition in the left brain – and the Raven Colored Progressive Matrices Test and the Rey-Osterrieth Complex Figure Test, both of which assess right-brain function. The researchers also quantified cerebrovascular reactivity during hypercapnia using transcranial Doppler to assess cerebral hemodynamics during breath holding, the Breath Holding Index.
In each of the four cognitive evaluations, patients with bilateral carotid stenosis showed significant impairments, compared with the controls, in both brain hemispheres. In comparison, the patients with unilateral stenosis showed significant impairments only in the brain hemisphere directly connected to their stenotic carotid artery.
A similar pattern occurred in a subgroup of patients assessed for cerebrovascular reactivity. Patients with impaired reactivity in the left hemisphere showed impaired cognition in the two evaluations of left-brain function, whereas patients with impaired reactivity in the right hemisphere showed impaired cognition in the right-brain evaluations.
Dr. Balucani said that she had no disclosures.
NEW ORLEANS – Patients with "asymptomatic" carotid-artery disease may still have important sequelae from their arterial stenosis.
Patients with substantial carotid-artery stenosis and no history of stroke or transient ischemic attack had significant cognitive impairments, compared with people without carotid disease, in a single-center, prospective study of 330 people, Dr. Clotilde Balucani said at the International Stroke Conference.
Notably, patients with severe, unilateral carotid stenosis showed cognitive impairments for functions linked with the brain hemisphere that received its blood supply from an occluded carotid, while the same people with an unimpeded contralateral carotid showed no impairment on cognitive tests that tested their contralateral brain function, said Dr. Balucani, a neurologist at Downstate Medical Center in Brooklyn, N.Y. Patients with bilateral carotid disease had impairments on all of the cognitive tests she used in this study, whereas control subjects without carotid disease showed no impairments on any of the cognitive tests.
"Asymptomatic carotid stenosis may not be truly asymptomatic," she said. "There appears to be an association between cognitive dysfunction and cerebral hemodynamic impairment. Cognitive function could be considered a potential outcome measure, and its improvement by treatment of asymptomatic carotid stenosis may be worthy of further investigation." Adding improved cognitive dysfunction to stroke prevention as another potential beneficial outcome of carotid revascularization may "better help risk stratify patients," Dr. Balucani said.
As of today, no study results have clearly documented that carotid revascularization improves cognition, so this hypothesis needs further testing, she cautioned.
Her study enrolled people during 2005-2010 who had no history of stroke or transient ischemic attack, who were also negative for other markers of poor cognitive function: heart failure, proximal internal carotid artery occlusion, a low score (less than 26) on the Mini Mental State Examination (MMSE), and severe stenosis of an intracranial or vertebro/basilar artery. The study group included 126 patients with ultrasound evidence for at least 60% occlusion of both carotid arteries, 73 patients with this level of occlusion in their left carotid, 75 with this occlusion in their right carotid, and 56 controls without occlusion in either carotid. Patients’ average age was 70 years, two-thirds were men, and their average MMSE score was 27.
All participants underwent assessment by four cognitive evaluations: the phonemic verbal fluency test and the categorical verbal fluency test – both designed to assess cognition in the left brain – and the Raven Colored Progressive Matrices Test and the Rey-Osterrieth Complex Figure Test, both of which assess right-brain function. The researchers also quantified cerebrovascular reactivity during hypercapnia using transcranial Doppler to assess cerebral hemodynamics during breath holding, the Breath Holding Index.
In each of the four cognitive evaluations, patients with bilateral carotid stenosis showed significant impairments, compared with the controls, in both brain hemispheres. In comparison, the patients with unilateral stenosis showed significant impairments only in the brain hemisphere directly connected to their stenotic carotid artery.
A similar pattern occurred in a subgroup of patients assessed for cerebrovascular reactivity. Patients with impaired reactivity in the left hemisphere showed impaired cognition in the two evaluations of left-brain function, whereas patients with impaired reactivity in the right hemisphere showed impaired cognition in the right-brain evaluations.
Dr. Balucani said that she had no disclosures.
NEW ORLEANS – Patients with "asymptomatic" carotid-artery disease may still have important sequelae from their arterial stenosis.
Patients with substantial carotid-artery stenosis and no history of stroke or transient ischemic attack had significant cognitive impairments, compared with people without carotid disease, in a single-center, prospective study of 330 people, Dr. Clotilde Balucani said at the International Stroke Conference.
Notably, patients with severe, unilateral carotid stenosis showed cognitive impairments for functions linked with the brain hemisphere that received its blood supply from an occluded carotid, while the same people with an unimpeded contralateral carotid showed no impairment on cognitive tests that tested their contralateral brain function, said Dr. Balucani, a neurologist at Downstate Medical Center in Brooklyn, N.Y. Patients with bilateral carotid disease had impairments on all of the cognitive tests she used in this study, whereas control subjects without carotid disease showed no impairments on any of the cognitive tests.
"Asymptomatic carotid stenosis may not be truly asymptomatic," she said. "There appears to be an association between cognitive dysfunction and cerebral hemodynamic impairment. Cognitive function could be considered a potential outcome measure, and its improvement by treatment of asymptomatic carotid stenosis may be worthy of further investigation." Adding improved cognitive dysfunction to stroke prevention as another potential beneficial outcome of carotid revascularization may "better help risk stratify patients," Dr. Balucani said.
As of today, no study results have clearly documented that carotid revascularization improves cognition, so this hypothesis needs further testing, she cautioned.
Her study enrolled people during 2005-2010 who had no history of stroke or transient ischemic attack, who were also negative for other markers of poor cognitive function: heart failure, proximal internal carotid artery occlusion, a low score (less than 26) on the Mini Mental State Examination (MMSE), and severe stenosis of an intracranial or vertebro/basilar artery. The study group included 126 patients with ultrasound evidence for at least 60% occlusion of both carotid arteries, 73 patients with this level of occlusion in their left carotid, 75 with this occlusion in their right carotid, and 56 controls without occlusion in either carotid. Patients’ average age was 70 years, two-thirds were men, and their average MMSE score was 27.
All participants underwent assessment by four cognitive evaluations: the phonemic verbal fluency test and the categorical verbal fluency test – both designed to assess cognition in the left brain – and the Raven Colored Progressive Matrices Test and the Rey-Osterrieth Complex Figure Test, both of which assess right-brain function. The researchers also quantified cerebrovascular reactivity during hypercapnia using transcranial Doppler to assess cerebral hemodynamics during breath holding, the Breath Holding Index.
In each of the four cognitive evaluations, patients with bilateral carotid stenosis showed significant impairments, compared with the controls, in both brain hemispheres. In comparison, the patients with unilateral stenosis showed significant impairments only in the brain hemisphere directly connected to their stenotic carotid artery.
A similar pattern occurred in a subgroup of patients assessed for cerebrovascular reactivity. Patients with impaired reactivity in the left hemisphere showed impaired cognition in the two evaluations of left-brain function, whereas patients with impaired reactivity in the right hemisphere showed impaired cognition in the right-brain evaluations.
Dr. Balucani said that she had no disclosures.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: Patients with unilateral or bilateral asymptomatic carotid stenosis of at least 60% had significant cognitive-function impairment in the corresponding brain hemisphere(s).
Data Source: Data are from a prospective, single-center study of 329 patients with bilateral or unilateral asymptomatic carotid stenosis and controls with no carotid stenosis.
Disclosures: Dr. Balucani said that she had no disclosures.
Role of Patent Foramen Ovale Varies in Cryptogenic Strokes
NEW ORLEANS – When results from a major trial with more than 900 patients failed to show that closure of a patent foramen ovale in patients who had a cryptogenic stroke worked better than medical therapy for preventing a future stroke, some experts suggested that the problem was patient selection. Researchers now have evidence that this explanation was right.
"Among patients with cryptogenic stroke, there is considerable variation in PFO [patent foramen ovale] prevalence, based on easily obtainable clinical characteristics." Dr. David M. Kent said at the International Stroke Conference, which was sponsored by the American Heart Association. This wide variation suggests that the risk for cryptogenic stroke attributable to a PFO can vary from 0% to nearly 90%, said Dr. Kent, an internal medicine physician at Tufts Medical Center in Boston.
"It’s very compelling that a patient has a stroke; you don’t know what caused it, and the patient has a hole in his heart and you have a safe way to close it. Do you close it? Of course, why not? The flaw is that the patient is 40 years old and had the hole in his heart for his entire life with no stroke. When a stroke then happens, maybe something else caused it," Dr. Kent said in an interview.
His analysis showed that cryptogenic stroke patients who have a PFO often have one or more additional stroke risk factors – including diabetes, coronary artery disease, hypertension, smoking, and older age – that could as easily have been the culprit.
"There are cryptogenic stroke patients with a PFO who did not have paradoxical emboli; they had something else. The question is, can we identify the important PFOs? Can we find the PFOs that caused the first stroke? And, having found the PFOs that likely caused the first stroke, can we divide those patients into those with a high or low risk for having a second stroke? Not all PFOs are the same," said Dr. David E. Thaler, a neurologist and director of the comprehensive stoke center at Tufts, as well as a collaborator with Dr. Kent on the ROPE (Risk of Paradoxical Embolism) project.
Results from the CLOSURE I (Evaluation of the STARFlex Septal Closure System in Patients With a Stroke or TIA [Transient Ischemic Attack] Due to the Possible Passage of a Clot of Unknown Origin Through a Patent Foramen Ovale) trial showcased the problem with presuming that when a patient has a cryptogenic stroke and also has a PFO the two are causally related. As Dr. Anthony J. Furlan reported at the American Heart Association scientific sessions in November 2010*, CLOSURE I randomized 909 patients who had a recent cryptogenic stroke or TIA as well as a PFO. Patients either received medical therapy with warfarin, aspirin, or a combination of both drugs, or underwent endovascular PFO closure using the device developed by the study’s sponsor. After 2 years of follow-up, the combined rate of new-onset stroke or TIA (the study’s primary end point) was 6% in the patients whose PFO had been closed and 8% in the control group, a difference that was not statistically significant. The study will be published in the New England Journal of Medicine on March 14. **
To explore what other stroke risk factors might exist in patients with a history of cryptogenic stroke, Dr. Kent and his associates pooled data for 3,023 cryptogenic strokes from 12 international data sets. All patients underwent assessment for a PFO, which existed in 1,274 patients and was not present in the remaining 1,749. About 30% of the patients were older than 65 years, and 59% were men.
The researchers analyzed all the patients by a list of other stroke risk factors, comparing the prevalence of each factor in the subgroups with and without PFOs.
They then performed a multivariate analysis, which identified six factors that each posed a significant, independent risk for a cryptogenic stroke: older age, diabetes, hypertension, current smoking, a history of a stroke or TIA, and a history of a deep stroke. The analysis showed that the presence of each of these risk factors reduced the likelihood by about 30% that the cryptogenic stroke resulting from the patient’s PFO.
Because the risk from each factor was roughly similar, Dr. Kent and his associates developed a point system to estimate the likelihood that a PFO caused a stroke in a cryptogenic stroke patient with a PFO. For example, in patients with none of these other risk factors, their PFO-attributable risk for their prior cryptogenic stroke was 88%, and their estimated 2-year risk for another stroke was about 5%. In contrast, among patients with all six of these risk factors, their PFO-attributable risk for their index cryptogenic stroke was 0%, and their estimated 2-year risk for having another stroke was 20%.
The researchers plan next to apply their new model for PFO-attributable stroke risk to the CLOSURE I data set. "We may be able to figure out why CLOSURE I didn’t work, and whether this approach could identify the patients who should have been in the trial" Dr. Thaler said. If the scoring method looks promising in the retrospective analysis, it might then be suitable for selecting patients to enroll into a new prospective study of PFO closure.
"The idea is that we’ll stratify patients in clinical studies, and – if all the stars align – we’ll be able to say that these are the patients who have the potential to benefit" from PFO closure, Dr. Kent said.
If these studies also find parameters that identify the types of PFOs that pose the greatest risk for causing strokes, the implications could extend beyond patients who already had a cryptogenic stroke.
"A quarter of the entire population has a PFO. Wouldn’t it be interesting if we could identify high-risk PFOs in the general population, among people who never had a stroke?" Dr. Thaler asked.
Dr. Kent said that he is a consultant to W.L. Gore & Associates. Dr. Thaler said that he is a consultant to W.L. Gore & Associates and AGA Medical.
*Correction, 3/12/2012: An earlier version of this article misstated the timing of the American Heart Association's annual scientific sessions at which the data were presented.
**Correction, 3/12/012: An earlier version of this article incorrectly stated that the study had already been published.
NEW ORLEANS – When results from a major trial with more than 900 patients failed to show that closure of a patent foramen ovale in patients who had a cryptogenic stroke worked better than medical therapy for preventing a future stroke, some experts suggested that the problem was patient selection. Researchers now have evidence that this explanation was right.
"Among patients with cryptogenic stroke, there is considerable variation in PFO [patent foramen ovale] prevalence, based on easily obtainable clinical characteristics." Dr. David M. Kent said at the International Stroke Conference, which was sponsored by the American Heart Association. This wide variation suggests that the risk for cryptogenic stroke attributable to a PFO can vary from 0% to nearly 90%, said Dr. Kent, an internal medicine physician at Tufts Medical Center in Boston.
"It’s very compelling that a patient has a stroke; you don’t know what caused it, and the patient has a hole in his heart and you have a safe way to close it. Do you close it? Of course, why not? The flaw is that the patient is 40 years old and had the hole in his heart for his entire life with no stroke. When a stroke then happens, maybe something else caused it," Dr. Kent said in an interview.
His analysis showed that cryptogenic stroke patients who have a PFO often have one or more additional stroke risk factors – including diabetes, coronary artery disease, hypertension, smoking, and older age – that could as easily have been the culprit.
"There are cryptogenic stroke patients with a PFO who did not have paradoxical emboli; they had something else. The question is, can we identify the important PFOs? Can we find the PFOs that caused the first stroke? And, having found the PFOs that likely caused the first stroke, can we divide those patients into those with a high or low risk for having a second stroke? Not all PFOs are the same," said Dr. David E. Thaler, a neurologist and director of the comprehensive stoke center at Tufts, as well as a collaborator with Dr. Kent on the ROPE (Risk of Paradoxical Embolism) project.
Results from the CLOSURE I (Evaluation of the STARFlex Septal Closure System in Patients With a Stroke or TIA [Transient Ischemic Attack] Due to the Possible Passage of a Clot of Unknown Origin Through a Patent Foramen Ovale) trial showcased the problem with presuming that when a patient has a cryptogenic stroke and also has a PFO the two are causally related. As Dr. Anthony J. Furlan reported at the American Heart Association scientific sessions in November 2010*, CLOSURE I randomized 909 patients who had a recent cryptogenic stroke or TIA as well as a PFO. Patients either received medical therapy with warfarin, aspirin, or a combination of both drugs, or underwent endovascular PFO closure using the device developed by the study’s sponsor. After 2 years of follow-up, the combined rate of new-onset stroke or TIA (the study’s primary end point) was 6% in the patients whose PFO had been closed and 8% in the control group, a difference that was not statistically significant. The study will be published in the New England Journal of Medicine on March 14. **
To explore what other stroke risk factors might exist in patients with a history of cryptogenic stroke, Dr. Kent and his associates pooled data for 3,023 cryptogenic strokes from 12 international data sets. All patients underwent assessment for a PFO, which existed in 1,274 patients and was not present in the remaining 1,749. About 30% of the patients were older than 65 years, and 59% were men.
The researchers analyzed all the patients by a list of other stroke risk factors, comparing the prevalence of each factor in the subgroups with and without PFOs.
They then performed a multivariate analysis, which identified six factors that each posed a significant, independent risk for a cryptogenic stroke: older age, diabetes, hypertension, current smoking, a history of a stroke or TIA, and a history of a deep stroke. The analysis showed that the presence of each of these risk factors reduced the likelihood by about 30% that the cryptogenic stroke resulting from the patient’s PFO.
Because the risk from each factor was roughly similar, Dr. Kent and his associates developed a point system to estimate the likelihood that a PFO caused a stroke in a cryptogenic stroke patient with a PFO. For example, in patients with none of these other risk factors, their PFO-attributable risk for their prior cryptogenic stroke was 88%, and their estimated 2-year risk for another stroke was about 5%. In contrast, among patients with all six of these risk factors, their PFO-attributable risk for their index cryptogenic stroke was 0%, and their estimated 2-year risk for having another stroke was 20%.
The researchers plan next to apply their new model for PFO-attributable stroke risk to the CLOSURE I data set. "We may be able to figure out why CLOSURE I didn’t work, and whether this approach could identify the patients who should have been in the trial" Dr. Thaler said. If the scoring method looks promising in the retrospective analysis, it might then be suitable for selecting patients to enroll into a new prospective study of PFO closure.
"The idea is that we’ll stratify patients in clinical studies, and – if all the stars align – we’ll be able to say that these are the patients who have the potential to benefit" from PFO closure, Dr. Kent said.
If these studies also find parameters that identify the types of PFOs that pose the greatest risk for causing strokes, the implications could extend beyond patients who already had a cryptogenic stroke.
"A quarter of the entire population has a PFO. Wouldn’t it be interesting if we could identify high-risk PFOs in the general population, among people who never had a stroke?" Dr. Thaler asked.
Dr. Kent said that he is a consultant to W.L. Gore & Associates. Dr. Thaler said that he is a consultant to W.L. Gore & Associates and AGA Medical.
*Correction, 3/12/2012: An earlier version of this article misstated the timing of the American Heart Association's annual scientific sessions at which the data were presented.
**Correction, 3/12/012: An earlier version of this article incorrectly stated that the study had already been published.
NEW ORLEANS – When results from a major trial with more than 900 patients failed to show that closure of a patent foramen ovale in patients who had a cryptogenic stroke worked better than medical therapy for preventing a future stroke, some experts suggested that the problem was patient selection. Researchers now have evidence that this explanation was right.
"Among patients with cryptogenic stroke, there is considerable variation in PFO [patent foramen ovale] prevalence, based on easily obtainable clinical characteristics." Dr. David M. Kent said at the International Stroke Conference, which was sponsored by the American Heart Association. This wide variation suggests that the risk for cryptogenic stroke attributable to a PFO can vary from 0% to nearly 90%, said Dr. Kent, an internal medicine physician at Tufts Medical Center in Boston.
"It’s very compelling that a patient has a stroke; you don’t know what caused it, and the patient has a hole in his heart and you have a safe way to close it. Do you close it? Of course, why not? The flaw is that the patient is 40 years old and had the hole in his heart for his entire life with no stroke. When a stroke then happens, maybe something else caused it," Dr. Kent said in an interview.
His analysis showed that cryptogenic stroke patients who have a PFO often have one or more additional stroke risk factors – including diabetes, coronary artery disease, hypertension, smoking, and older age – that could as easily have been the culprit.
"There are cryptogenic stroke patients with a PFO who did not have paradoxical emboli; they had something else. The question is, can we identify the important PFOs? Can we find the PFOs that caused the first stroke? And, having found the PFOs that likely caused the first stroke, can we divide those patients into those with a high or low risk for having a second stroke? Not all PFOs are the same," said Dr. David E. Thaler, a neurologist and director of the comprehensive stoke center at Tufts, as well as a collaborator with Dr. Kent on the ROPE (Risk of Paradoxical Embolism) project.
Results from the CLOSURE I (Evaluation of the STARFlex Septal Closure System in Patients With a Stroke or TIA [Transient Ischemic Attack] Due to the Possible Passage of a Clot of Unknown Origin Through a Patent Foramen Ovale) trial showcased the problem with presuming that when a patient has a cryptogenic stroke and also has a PFO the two are causally related. As Dr. Anthony J. Furlan reported at the American Heart Association scientific sessions in November 2010*, CLOSURE I randomized 909 patients who had a recent cryptogenic stroke or TIA as well as a PFO. Patients either received medical therapy with warfarin, aspirin, or a combination of both drugs, or underwent endovascular PFO closure using the device developed by the study’s sponsor. After 2 years of follow-up, the combined rate of new-onset stroke or TIA (the study’s primary end point) was 6% in the patients whose PFO had been closed and 8% in the control group, a difference that was not statistically significant. The study will be published in the New England Journal of Medicine on March 14. **
To explore what other stroke risk factors might exist in patients with a history of cryptogenic stroke, Dr. Kent and his associates pooled data for 3,023 cryptogenic strokes from 12 international data sets. All patients underwent assessment for a PFO, which existed in 1,274 patients and was not present in the remaining 1,749. About 30% of the patients were older than 65 years, and 59% were men.
The researchers analyzed all the patients by a list of other stroke risk factors, comparing the prevalence of each factor in the subgroups with and without PFOs.
They then performed a multivariate analysis, which identified six factors that each posed a significant, independent risk for a cryptogenic stroke: older age, diabetes, hypertension, current smoking, a history of a stroke or TIA, and a history of a deep stroke. The analysis showed that the presence of each of these risk factors reduced the likelihood by about 30% that the cryptogenic stroke resulting from the patient’s PFO.
Because the risk from each factor was roughly similar, Dr. Kent and his associates developed a point system to estimate the likelihood that a PFO caused a stroke in a cryptogenic stroke patient with a PFO. For example, in patients with none of these other risk factors, their PFO-attributable risk for their prior cryptogenic stroke was 88%, and their estimated 2-year risk for another stroke was about 5%. In contrast, among patients with all six of these risk factors, their PFO-attributable risk for their index cryptogenic stroke was 0%, and their estimated 2-year risk for having another stroke was 20%.
The researchers plan next to apply their new model for PFO-attributable stroke risk to the CLOSURE I data set. "We may be able to figure out why CLOSURE I didn’t work, and whether this approach could identify the patients who should have been in the trial" Dr. Thaler said. If the scoring method looks promising in the retrospective analysis, it might then be suitable for selecting patients to enroll into a new prospective study of PFO closure.
"The idea is that we’ll stratify patients in clinical studies, and – if all the stars align – we’ll be able to say that these are the patients who have the potential to benefit" from PFO closure, Dr. Kent said.
If these studies also find parameters that identify the types of PFOs that pose the greatest risk for causing strokes, the implications could extend beyond patients who already had a cryptogenic stroke.
"A quarter of the entire population has a PFO. Wouldn’t it be interesting if we could identify high-risk PFOs in the general population, among people who never had a stroke?" Dr. Thaler asked.
Dr. Kent said that he is a consultant to W.L. Gore & Associates. Dr. Thaler said that he is a consultant to W.L. Gore & Associates and AGA Medical.
*Correction, 3/12/2012: An earlier version of this article misstated the timing of the American Heart Association's annual scientific sessions at which the data were presented.
**Correction, 3/12/012: An earlier version of this article incorrectly stated that the study had already been published.
FROM THE ANNUAL INTERNATIONAL STROKE CONFERENCE
Major Finding: The PFO-attributable risk for a previous cryptogenic stroke varied between 0% in some patients with a PFO to 88% in others.
Data Source: Data are from a review of 12 international data sets containing 3,023 patients who had a cryptogenic stroke.
Disclosures: Dr. Kent said that he is a consultant to W.L. Gore & Associates. Dr. Thaler said that he is a consultant to W.L. Gore & Associates and AGA Medical.
Epilepsy Incidence High Following Pediatric Stroke
NEW ORLEANS – Pediatric stroke survivors had an absolute risk of 39% for developing epilepsy in the 10 years following their stroke in a review of 371 patients in Northern California.
Two factors significantly boosted a child’s risk of developing epilepsy following a stroke: A seizure at the time of stroke, and a neurologic deficit at the time of hospital discharge following the index stroke, Dr. Christine Fox said at the International Stroke Conference (Stroke 2012;43:A41).
Although these findings have no immediate management implications, the information could help parents know what to expect when their child has a stroke.
Epilepsy "is not always one of the first outcomes we think about when we speak with parents," said Dr. Fox, a neurologist at the University of California, San Francisco. "If there is such a high incidence of epilepsy after stroke, maybe it’s something to talk about with parents," she said in an interview.
The study reviewed used data collected in the Kaiser Pediatric Stroke Study, run by Kaiser Permanente of Northern California, and included children who ranged from neonates to 19 years old and had a clinical presentation and brain imaging results consistent with a stroke. The group included hemorrhagic and ischemic strokes occurring during 1993-2003, and arterial ischemic strokes during 2003-2007. This cohort consisted of 371 children who survived a stroke to hospital discharge, including 110 neonates and 261 older children who had 226 ischemic strokes and 145 hemorrhagic strokes.
During a median follow-up of 4.5 years, 89 of these children developed epilepsy, defined as a confirmed, unprovoked seizure occurring more than 30 days following the index stroke. The researchers excluded 7 of the 89 incident epilepsy cases because they had a history of seizures prior to their stroke. Survivor analysis of the 82 new-onset cases showed an average annual incidence of 6%, with a cumulative 5-year incidence of 23% and a cumulative 10-year rate of 39%, Dr. Fox said.
A multivariate adjusted analysis that controlled for factors such as age, sex, race, and type of stroke identified two parameters linked with a significantly higher risk for developing epilepsy following stroke: a seizure concurrent with the stroke ictus, which boosted the risk of subsequent epilepsy 3.6-fold, and a neurologic deficit at discharge, which increased the risk for later epilepsy twofold.
In contrast to these findings, previous reports documented a much lower incidence of epilepsy in adults following a stroke, with a 3% rate after 1 year, and an 8% rate after 5 years, Dr. Fox said.
Dr. Fox said that she had no disclosures. The conference was sponsored by the American Heart Association.
NEW ORLEANS – Pediatric stroke survivors had an absolute risk of 39% for developing epilepsy in the 10 years following their stroke in a review of 371 patients in Northern California.
Two factors significantly boosted a child’s risk of developing epilepsy following a stroke: A seizure at the time of stroke, and a neurologic deficit at the time of hospital discharge following the index stroke, Dr. Christine Fox said at the International Stroke Conference (Stroke 2012;43:A41).
Although these findings have no immediate management implications, the information could help parents know what to expect when their child has a stroke.
Epilepsy "is not always one of the first outcomes we think about when we speak with parents," said Dr. Fox, a neurologist at the University of California, San Francisco. "If there is such a high incidence of epilepsy after stroke, maybe it’s something to talk about with parents," she said in an interview.
The study reviewed used data collected in the Kaiser Pediatric Stroke Study, run by Kaiser Permanente of Northern California, and included children who ranged from neonates to 19 years old and had a clinical presentation and brain imaging results consistent with a stroke. The group included hemorrhagic and ischemic strokes occurring during 1993-2003, and arterial ischemic strokes during 2003-2007. This cohort consisted of 371 children who survived a stroke to hospital discharge, including 110 neonates and 261 older children who had 226 ischemic strokes and 145 hemorrhagic strokes.
During a median follow-up of 4.5 years, 89 of these children developed epilepsy, defined as a confirmed, unprovoked seizure occurring more than 30 days following the index stroke. The researchers excluded 7 of the 89 incident epilepsy cases because they had a history of seizures prior to their stroke. Survivor analysis of the 82 new-onset cases showed an average annual incidence of 6%, with a cumulative 5-year incidence of 23% and a cumulative 10-year rate of 39%, Dr. Fox said.
A multivariate adjusted analysis that controlled for factors such as age, sex, race, and type of stroke identified two parameters linked with a significantly higher risk for developing epilepsy following stroke: a seizure concurrent with the stroke ictus, which boosted the risk of subsequent epilepsy 3.6-fold, and a neurologic deficit at discharge, which increased the risk for later epilepsy twofold.
In contrast to these findings, previous reports documented a much lower incidence of epilepsy in adults following a stroke, with a 3% rate after 1 year, and an 8% rate after 5 years, Dr. Fox said.
Dr. Fox said that she had no disclosures. The conference was sponsored by the American Heart Association.
NEW ORLEANS – Pediatric stroke survivors had an absolute risk of 39% for developing epilepsy in the 10 years following their stroke in a review of 371 patients in Northern California.
Two factors significantly boosted a child’s risk of developing epilepsy following a stroke: A seizure at the time of stroke, and a neurologic deficit at the time of hospital discharge following the index stroke, Dr. Christine Fox said at the International Stroke Conference (Stroke 2012;43:A41).
Although these findings have no immediate management implications, the information could help parents know what to expect when their child has a stroke.
Epilepsy "is not always one of the first outcomes we think about when we speak with parents," said Dr. Fox, a neurologist at the University of California, San Francisco. "If there is such a high incidence of epilepsy after stroke, maybe it’s something to talk about with parents," she said in an interview.
The study reviewed used data collected in the Kaiser Pediatric Stroke Study, run by Kaiser Permanente of Northern California, and included children who ranged from neonates to 19 years old and had a clinical presentation and brain imaging results consistent with a stroke. The group included hemorrhagic and ischemic strokes occurring during 1993-2003, and arterial ischemic strokes during 2003-2007. This cohort consisted of 371 children who survived a stroke to hospital discharge, including 110 neonates and 261 older children who had 226 ischemic strokes and 145 hemorrhagic strokes.
During a median follow-up of 4.5 years, 89 of these children developed epilepsy, defined as a confirmed, unprovoked seizure occurring more than 30 days following the index stroke. The researchers excluded 7 of the 89 incident epilepsy cases because they had a history of seizures prior to their stroke. Survivor analysis of the 82 new-onset cases showed an average annual incidence of 6%, with a cumulative 5-year incidence of 23% and a cumulative 10-year rate of 39%, Dr. Fox said.
A multivariate adjusted analysis that controlled for factors such as age, sex, race, and type of stroke identified two parameters linked with a significantly higher risk for developing epilepsy following stroke: a seizure concurrent with the stroke ictus, which boosted the risk of subsequent epilepsy 3.6-fold, and a neurologic deficit at discharge, which increased the risk for later epilepsy twofold.
In contrast to these findings, previous reports documented a much lower incidence of epilepsy in adults following a stroke, with a 3% rate after 1 year, and an 8% rate after 5 years, Dr. Fox said.
Dr. Fox said that she had no disclosures. The conference was sponsored by the American Heart Association.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: During the 10 years following a stroke, the cumulative incidence of epilepsy in children aged 19 years and younger was 39%.
Data Source: The review included 371 pediatric strokes included in the Kaiser Pediatric Stroke Study.
Disclosures: Dr. Fox said that she had no disclosures.
Tenecteplase Edges TPA in Acute Stroke
NEW ORLEANS – The potential advantages of tenecteplase, a modified form of tissue plasminogen activator engineered to outperform the native molecule, finally shone through for treating patients with acute ischemic stroke.
A head-to-head comparison of tenecteplase against recombinant tissue plasminogen activator (TPA; alteplase) showed that the modified molecule produced better reperfusion and better clinical recovery 24 hours after treatment in a randomized trial of 75 Australian patients whose treatment was guided by CT brain imaging, Dr. Bill O’Brien reported at the International Stroke Conference.
Although Dr. O’Brien cautioned that this pilot study did not produce definitive results, the superiority of tenecteplase eclipsed its failure to surpass TPA in a randomized comparison of 112 patients reported in 2010.
The results "support using advanced imaging to identify the patients who are most likely to benefit" from tenecteplase, he said. The use of systematic CT brain imaging to select patients appeared to be the main factor that distinguished this study from the previous trial where tenecteplase failed to show an advantage, said Dr. O’Brien, a stroke physician at John Hunter Hospital in Newcastle, Australia.
Targeted patient selection may also explain why the tenecteplase treatment was so safe, resulting in a trend toward a reduced rate of type 2 parenchymal hemorrhages, compared with TPA, despite the superior thrombolytic activity shown by tenecteplase, he said.
Although the current trial had "compelling results," another study will follow to compare the two drugs by several 3-month outcomes, Dr. O’Brien said in an interview. The successful dosages of tenecteplase tested also have the advantage of being cheaper than the standard TPA dosage, he added.
Developed in the 1990s, tenecteplase resulted from three targeted amino acid substitutions in conventional TPA. This produced a molecule with increased fibrin specificity, and longer plasma half-life due to increased resistance to enzymatic degradation, which meant that it could be administered by an intravenous bolus instead of requiring continuous infusion like TPA. When used to treat myocardial infarctions, tenecteplase has also resulted in fewer bleeding complications than TPA.
The study enrolled 75 patients within 6 hours of onset of an ischemic stroke at any of three Australian hospitals, following selection by CT imaging to identify patients with a small infarct core and a large penumbra of salvageable brain. Researchers randomized patients to receive 0.1 mg/kg tenecteplase or 0.25 mg/kg tenecteplase by an intravenous bolus injection, or standard infusion with 0.9 mg/kg TPA. The patients averaged 70 years old, their average NIHSS (National Institutes of Health Stroke Scale) score at entry was about 14, and patients received treatment an average of about 3 hours after symptom onset.
The reperfusion rate after 24 hours was 78% among all 50 patients treated with tenecteplase, and 55% among the TPA treated patients, a statistically significant difference for one of the study’s two primary end points, Dr. O’Brien said. The second primary end point, change in NIHSS score after 24 hours, improved by an average of 8 points in all 50 tenecteplase patients, and by an average of 3 points in the TPA patients, also a significant difference.
The results appeared to show a dose-response relationship for tenecteplase, with the 25 patients who received the 0.25-mg/kg dosage having better reperfusion rates and reductions in their NIHSS scores than the 25 patients who received a 0.1-mg/kg dosage as well as the patients treated with TPA, but Dr. O’Brien did not report specific numbers from this analysis.
Of the 50 tenecteplase patients, 2 (4%) developed a type 2 parenchymal hemorrhage within 24 hours, compared with 4 (16%) of the 25 TPA-treated patients, a difference that trended toward significance. The rates of symptomatic intracerebral hemorrhages and death at 24 hours were similar with both drugs. But at 90 days after treatment, the combined rate of death or severe disability was 10% in the 50 tenecteplase patients and 25% in the TPA patients, a difference that also trended toward significance.
These findings contrast with a 2010 report from a randomized trial that compared three different tenecteplase dosages with TPA in a multicenter U.S. study of 112 patients (Stroke 2010;41:707-11). The results showed no significant differences between any of the tenecteplase dosages and TPA for any of the outcomes measured out to 90 days after treatment.
The major difference between the U.S. study and the new Australian study was in patient selection, Dr. O’Brien said. "We used imaging to balance the groups," and to select patients who stood to benefit most from effective reperfusion, he said.
Dr. O’Brien said that he and his associates had no disclosures.
NEW ORLEANS – The potential advantages of tenecteplase, a modified form of tissue plasminogen activator engineered to outperform the native molecule, finally shone through for treating patients with acute ischemic stroke.
A head-to-head comparison of tenecteplase against recombinant tissue plasminogen activator (TPA; alteplase) showed that the modified molecule produced better reperfusion and better clinical recovery 24 hours after treatment in a randomized trial of 75 Australian patients whose treatment was guided by CT brain imaging, Dr. Bill O’Brien reported at the International Stroke Conference.
Although Dr. O’Brien cautioned that this pilot study did not produce definitive results, the superiority of tenecteplase eclipsed its failure to surpass TPA in a randomized comparison of 112 patients reported in 2010.
The results "support using advanced imaging to identify the patients who are most likely to benefit" from tenecteplase, he said. The use of systematic CT brain imaging to select patients appeared to be the main factor that distinguished this study from the previous trial where tenecteplase failed to show an advantage, said Dr. O’Brien, a stroke physician at John Hunter Hospital in Newcastle, Australia.
Targeted patient selection may also explain why the tenecteplase treatment was so safe, resulting in a trend toward a reduced rate of type 2 parenchymal hemorrhages, compared with TPA, despite the superior thrombolytic activity shown by tenecteplase, he said.
Although the current trial had "compelling results," another study will follow to compare the two drugs by several 3-month outcomes, Dr. O’Brien said in an interview. The successful dosages of tenecteplase tested also have the advantage of being cheaper than the standard TPA dosage, he added.
Developed in the 1990s, tenecteplase resulted from three targeted amino acid substitutions in conventional TPA. This produced a molecule with increased fibrin specificity, and longer plasma half-life due to increased resistance to enzymatic degradation, which meant that it could be administered by an intravenous bolus instead of requiring continuous infusion like TPA. When used to treat myocardial infarctions, tenecteplase has also resulted in fewer bleeding complications than TPA.
The study enrolled 75 patients within 6 hours of onset of an ischemic stroke at any of three Australian hospitals, following selection by CT imaging to identify patients with a small infarct core and a large penumbra of salvageable brain. Researchers randomized patients to receive 0.1 mg/kg tenecteplase or 0.25 mg/kg tenecteplase by an intravenous bolus injection, or standard infusion with 0.9 mg/kg TPA. The patients averaged 70 years old, their average NIHSS (National Institutes of Health Stroke Scale) score at entry was about 14, and patients received treatment an average of about 3 hours after symptom onset.
The reperfusion rate after 24 hours was 78% among all 50 patients treated with tenecteplase, and 55% among the TPA treated patients, a statistically significant difference for one of the study’s two primary end points, Dr. O’Brien said. The second primary end point, change in NIHSS score after 24 hours, improved by an average of 8 points in all 50 tenecteplase patients, and by an average of 3 points in the TPA patients, also a significant difference.
The results appeared to show a dose-response relationship for tenecteplase, with the 25 patients who received the 0.25-mg/kg dosage having better reperfusion rates and reductions in their NIHSS scores than the 25 patients who received a 0.1-mg/kg dosage as well as the patients treated with TPA, but Dr. O’Brien did not report specific numbers from this analysis.
Of the 50 tenecteplase patients, 2 (4%) developed a type 2 parenchymal hemorrhage within 24 hours, compared with 4 (16%) of the 25 TPA-treated patients, a difference that trended toward significance. The rates of symptomatic intracerebral hemorrhages and death at 24 hours were similar with both drugs. But at 90 days after treatment, the combined rate of death or severe disability was 10% in the 50 tenecteplase patients and 25% in the TPA patients, a difference that also trended toward significance.
These findings contrast with a 2010 report from a randomized trial that compared three different tenecteplase dosages with TPA in a multicenter U.S. study of 112 patients (Stroke 2010;41:707-11). The results showed no significant differences between any of the tenecteplase dosages and TPA for any of the outcomes measured out to 90 days after treatment.
The major difference between the U.S. study and the new Australian study was in patient selection, Dr. O’Brien said. "We used imaging to balance the groups," and to select patients who stood to benefit most from effective reperfusion, he said.
Dr. O’Brien said that he and his associates had no disclosures.
NEW ORLEANS – The potential advantages of tenecteplase, a modified form of tissue plasminogen activator engineered to outperform the native molecule, finally shone through for treating patients with acute ischemic stroke.
A head-to-head comparison of tenecteplase against recombinant tissue plasminogen activator (TPA; alteplase) showed that the modified molecule produced better reperfusion and better clinical recovery 24 hours after treatment in a randomized trial of 75 Australian patients whose treatment was guided by CT brain imaging, Dr. Bill O’Brien reported at the International Stroke Conference.
Although Dr. O’Brien cautioned that this pilot study did not produce definitive results, the superiority of tenecteplase eclipsed its failure to surpass TPA in a randomized comparison of 112 patients reported in 2010.
The results "support using advanced imaging to identify the patients who are most likely to benefit" from tenecteplase, he said. The use of systematic CT brain imaging to select patients appeared to be the main factor that distinguished this study from the previous trial where tenecteplase failed to show an advantage, said Dr. O’Brien, a stroke physician at John Hunter Hospital in Newcastle, Australia.
Targeted patient selection may also explain why the tenecteplase treatment was so safe, resulting in a trend toward a reduced rate of type 2 parenchymal hemorrhages, compared with TPA, despite the superior thrombolytic activity shown by tenecteplase, he said.
Although the current trial had "compelling results," another study will follow to compare the two drugs by several 3-month outcomes, Dr. O’Brien said in an interview. The successful dosages of tenecteplase tested also have the advantage of being cheaper than the standard TPA dosage, he added.
Developed in the 1990s, tenecteplase resulted from three targeted amino acid substitutions in conventional TPA. This produced a molecule with increased fibrin specificity, and longer plasma half-life due to increased resistance to enzymatic degradation, which meant that it could be administered by an intravenous bolus instead of requiring continuous infusion like TPA. When used to treat myocardial infarctions, tenecteplase has also resulted in fewer bleeding complications than TPA.
The study enrolled 75 patients within 6 hours of onset of an ischemic stroke at any of three Australian hospitals, following selection by CT imaging to identify patients with a small infarct core and a large penumbra of salvageable brain. Researchers randomized patients to receive 0.1 mg/kg tenecteplase or 0.25 mg/kg tenecteplase by an intravenous bolus injection, or standard infusion with 0.9 mg/kg TPA. The patients averaged 70 years old, their average NIHSS (National Institutes of Health Stroke Scale) score at entry was about 14, and patients received treatment an average of about 3 hours after symptom onset.
The reperfusion rate after 24 hours was 78% among all 50 patients treated with tenecteplase, and 55% among the TPA treated patients, a statistically significant difference for one of the study’s two primary end points, Dr. O’Brien said. The second primary end point, change in NIHSS score after 24 hours, improved by an average of 8 points in all 50 tenecteplase patients, and by an average of 3 points in the TPA patients, also a significant difference.
The results appeared to show a dose-response relationship for tenecteplase, with the 25 patients who received the 0.25-mg/kg dosage having better reperfusion rates and reductions in their NIHSS scores than the 25 patients who received a 0.1-mg/kg dosage as well as the patients treated with TPA, but Dr. O’Brien did not report specific numbers from this analysis.
Of the 50 tenecteplase patients, 2 (4%) developed a type 2 parenchymal hemorrhage within 24 hours, compared with 4 (16%) of the 25 TPA-treated patients, a difference that trended toward significance. The rates of symptomatic intracerebral hemorrhages and death at 24 hours were similar with both drugs. But at 90 days after treatment, the combined rate of death or severe disability was 10% in the 50 tenecteplase patients and 25% in the TPA patients, a difference that also trended toward significance.
These findings contrast with a 2010 report from a randomized trial that compared three different tenecteplase dosages with TPA in a multicenter U.S. study of 112 patients (Stroke 2010;41:707-11). The results showed no significant differences between any of the tenecteplase dosages and TPA for any of the outcomes measured out to 90 days after treatment.
The major difference between the U.S. study and the new Australian study was in patient selection, Dr. O’Brien said. "We used imaging to balance the groups," and to select patients who stood to benefit most from effective reperfusion, he said.
Dr. O’Brien said that he and his associates had no disclosures.
FROM THE INTERNATIONAL STROKE CONFERENCE
'Drip and Ship' Proves Safe for Stroke
NEW ORLEANS – "Drip and ship" is a safe way to manage patients with acute ischemic stroke, according to results from two separate studies.
A review of 145 ischemic stroke patients who began receiving an intravenous infusion of tissue plasminogen activator (TPA) at a community hospital, followed by transport to a regional primary stroke center, showed a 63% rate of good stroke recoveries and a 3% rate of spontaneous intracranial hemorrhage, Dr. Marilyn M. Rymer reported at the International Stroke Conference.
And a review of 129 acute ischemic stroke patients treated by "drip and ship" throughout Minnesota during October 2008–December 2009 showed that initiating a TPA drip at a community hospital and then shifting the patient to a regional center led to outcomes that were generally identical to those of 473 similar patients who received TPA at a primary center and remained there, Dr. Saqib A. Chaudhry and his associates reported in a poster at the meeting, which was sponsored by the American Heart Association.
The review by Dr. Rymer and her associates included 145 consecutive ischemic stroke patients who arrived at the Mid-American Brain and Stroke Institute at Saint Luke’s Hospital in Kansas City, Mo., in 2008-2010. They came from 63 referring hospitals, including 40 hospitals located more than 50 miles away from Saint Luke’s. In all, 29 of the referring hospitals had 25 or fewer beds, indicating that despite their small size, these community facilities had "pretty sophisticated emergency [department] staffing," said Dr. Rymer, the institute’s medical director.
The shipped patients were an average of 68 years old, and their mean National Institutes of Health Stroke Scale score at admission to Mid-America was 10.4. On arrival, 14 (10%) of the shipped patients had blood pressure higher than 180/105 mm Hg, the maximum level recommended for treatment with IV TPA.
Among the 114 patients in the series who were assessed for their modified Rankin Scale (mRS) score at 90 days after their stroke, 72 patients (63%) had an mRS score of 0-2, a "good" outcome. (The 31 patients who were treated during 2008 did not have an mRS score available at 90 days.) Of all 145 patients in the series, 14% (20 patients) died.
Four of the 145 patients (3%) had a spontaneous intracerebral hemorrhage on arrival to the referral center, which in two cases resulted in death. One of these patients arrived with a blood pressure of 183/77 mm Hg; the other three intracranial hemorrhages occurred in patients with blood pressures below the limit for receiving TPA. Six patients (4%) received an inaccurate diagnosis when they were initially evaluated at a community hospital, but all six of these patients had "excellent" clinical outcomes.
These results show that immediate transfer of patients treated with IV TPA is "safe, with a low rate of spontaneous intracranial hemorrhage en route," said Dr. Rymer, who is also a professor of medicine at the University of Missouri–Kansas City. "The 63% rate of good outcomes may, in part, relate to early treatment with IV TPA at the referring hospitals. Hospitals of every size and location can safely treat stroke patients with IV TPA if they have access to consultation and transfer agreements with experienced stroke centers," she concluded.
The Minnesota study used data collected by the Minnesota Hospital Association; researchers identified patients with ischemic stroke and those treated with IV TPA who were then transported to a referral hospital according to the ICD-9-CM codes in their medical records, said Dr. Chaudhry, a researcher at the stroke research center of the University of Minnesota in Minneapolis.
Among more than 21,000 patients with acute ischemic strokes who were seen at Minnesota hospitals during the 14-month study period, 602 received thrombolytic therapy at 30 different hospitals, with 129 (21%) undergoing "drip and ship" management at 13 of these hospitals, while the other 473 (79%) remained at the centers where they began treatment with IV TPA. The patients averaged about 70 years old, and nearly half were women.
Patient profiles of the shipped and unshipped patients were similar, as were most outcomes including in-hospital mortality and length of stay. The only significant difference in clinical outcomes between these two subgroups during hospitalization was in the rate of intracerebral or subarachnoid hemorrhage, which occurred in 9% of the patients who remained at the site where they first received TPA and in 3% of the shipped patients, a statistically significant difference.
"Drip and ship" was also substantially cheaper. Average hospital charges for the untransported patients ran more than $65,000, whereas patients managed by "drip and ship" had average hospitalization charges of just under $48,000, a statistically significant difference.
Dr. Rymer said that she has been a speaker for Genentech and Concentric Medical. Dr. Chaudhry and his associates had no disclosures.
NEW ORLEANS – "Drip and ship" is a safe way to manage patients with acute ischemic stroke, according to results from two separate studies.
A review of 145 ischemic stroke patients who began receiving an intravenous infusion of tissue plasminogen activator (TPA) at a community hospital, followed by transport to a regional primary stroke center, showed a 63% rate of good stroke recoveries and a 3% rate of spontaneous intracranial hemorrhage, Dr. Marilyn M. Rymer reported at the International Stroke Conference.
And a review of 129 acute ischemic stroke patients treated by "drip and ship" throughout Minnesota during October 2008–December 2009 showed that initiating a TPA drip at a community hospital and then shifting the patient to a regional center led to outcomes that were generally identical to those of 473 similar patients who received TPA at a primary center and remained there, Dr. Saqib A. Chaudhry and his associates reported in a poster at the meeting, which was sponsored by the American Heart Association.
The review by Dr. Rymer and her associates included 145 consecutive ischemic stroke patients who arrived at the Mid-American Brain and Stroke Institute at Saint Luke’s Hospital in Kansas City, Mo., in 2008-2010. They came from 63 referring hospitals, including 40 hospitals located more than 50 miles away from Saint Luke’s. In all, 29 of the referring hospitals had 25 or fewer beds, indicating that despite their small size, these community facilities had "pretty sophisticated emergency [department] staffing," said Dr. Rymer, the institute’s medical director.
The shipped patients were an average of 68 years old, and their mean National Institutes of Health Stroke Scale score at admission to Mid-America was 10.4. On arrival, 14 (10%) of the shipped patients had blood pressure higher than 180/105 mm Hg, the maximum level recommended for treatment with IV TPA.
Among the 114 patients in the series who were assessed for their modified Rankin Scale (mRS) score at 90 days after their stroke, 72 patients (63%) had an mRS score of 0-2, a "good" outcome. (The 31 patients who were treated during 2008 did not have an mRS score available at 90 days.) Of all 145 patients in the series, 14% (20 patients) died.
Four of the 145 patients (3%) had a spontaneous intracerebral hemorrhage on arrival to the referral center, which in two cases resulted in death. One of these patients arrived with a blood pressure of 183/77 mm Hg; the other three intracranial hemorrhages occurred in patients with blood pressures below the limit for receiving TPA. Six patients (4%) received an inaccurate diagnosis when they were initially evaluated at a community hospital, but all six of these patients had "excellent" clinical outcomes.
These results show that immediate transfer of patients treated with IV TPA is "safe, with a low rate of spontaneous intracranial hemorrhage en route," said Dr. Rymer, who is also a professor of medicine at the University of Missouri–Kansas City. "The 63% rate of good outcomes may, in part, relate to early treatment with IV TPA at the referring hospitals. Hospitals of every size and location can safely treat stroke patients with IV TPA if they have access to consultation and transfer agreements with experienced stroke centers," she concluded.
The Minnesota study used data collected by the Minnesota Hospital Association; researchers identified patients with ischemic stroke and those treated with IV TPA who were then transported to a referral hospital according to the ICD-9-CM codes in their medical records, said Dr. Chaudhry, a researcher at the stroke research center of the University of Minnesota in Minneapolis.
Among more than 21,000 patients with acute ischemic strokes who were seen at Minnesota hospitals during the 14-month study period, 602 received thrombolytic therapy at 30 different hospitals, with 129 (21%) undergoing "drip and ship" management at 13 of these hospitals, while the other 473 (79%) remained at the centers where they began treatment with IV TPA. The patients averaged about 70 years old, and nearly half were women.
Patient profiles of the shipped and unshipped patients were similar, as were most outcomes including in-hospital mortality and length of stay. The only significant difference in clinical outcomes between these two subgroups during hospitalization was in the rate of intracerebral or subarachnoid hemorrhage, which occurred in 9% of the patients who remained at the site where they first received TPA and in 3% of the shipped patients, a statistically significant difference.
"Drip and ship" was also substantially cheaper. Average hospital charges for the untransported patients ran more than $65,000, whereas patients managed by "drip and ship" had average hospitalization charges of just under $48,000, a statistically significant difference.
Dr. Rymer said that she has been a speaker for Genentech and Concentric Medical. Dr. Chaudhry and his associates had no disclosures.
NEW ORLEANS – "Drip and ship" is a safe way to manage patients with acute ischemic stroke, according to results from two separate studies.
A review of 145 ischemic stroke patients who began receiving an intravenous infusion of tissue plasminogen activator (TPA) at a community hospital, followed by transport to a regional primary stroke center, showed a 63% rate of good stroke recoveries and a 3% rate of spontaneous intracranial hemorrhage, Dr. Marilyn M. Rymer reported at the International Stroke Conference.
And a review of 129 acute ischemic stroke patients treated by "drip and ship" throughout Minnesota during October 2008–December 2009 showed that initiating a TPA drip at a community hospital and then shifting the patient to a regional center led to outcomes that were generally identical to those of 473 similar patients who received TPA at a primary center and remained there, Dr. Saqib A. Chaudhry and his associates reported in a poster at the meeting, which was sponsored by the American Heart Association.
The review by Dr. Rymer and her associates included 145 consecutive ischemic stroke patients who arrived at the Mid-American Brain and Stroke Institute at Saint Luke’s Hospital in Kansas City, Mo., in 2008-2010. They came from 63 referring hospitals, including 40 hospitals located more than 50 miles away from Saint Luke’s. In all, 29 of the referring hospitals had 25 or fewer beds, indicating that despite their small size, these community facilities had "pretty sophisticated emergency [department] staffing," said Dr. Rymer, the institute’s medical director.
The shipped patients were an average of 68 years old, and their mean National Institutes of Health Stroke Scale score at admission to Mid-America was 10.4. On arrival, 14 (10%) of the shipped patients had blood pressure higher than 180/105 mm Hg, the maximum level recommended for treatment with IV TPA.
Among the 114 patients in the series who were assessed for their modified Rankin Scale (mRS) score at 90 days after their stroke, 72 patients (63%) had an mRS score of 0-2, a "good" outcome. (The 31 patients who were treated during 2008 did not have an mRS score available at 90 days.) Of all 145 patients in the series, 14% (20 patients) died.
Four of the 145 patients (3%) had a spontaneous intracerebral hemorrhage on arrival to the referral center, which in two cases resulted in death. One of these patients arrived with a blood pressure of 183/77 mm Hg; the other three intracranial hemorrhages occurred in patients with blood pressures below the limit for receiving TPA. Six patients (4%) received an inaccurate diagnosis when they were initially evaluated at a community hospital, but all six of these patients had "excellent" clinical outcomes.
These results show that immediate transfer of patients treated with IV TPA is "safe, with a low rate of spontaneous intracranial hemorrhage en route," said Dr. Rymer, who is also a professor of medicine at the University of Missouri–Kansas City. "The 63% rate of good outcomes may, in part, relate to early treatment with IV TPA at the referring hospitals. Hospitals of every size and location can safely treat stroke patients with IV TPA if they have access to consultation and transfer agreements with experienced stroke centers," she concluded.
The Minnesota study used data collected by the Minnesota Hospital Association; researchers identified patients with ischemic stroke and those treated with IV TPA who were then transported to a referral hospital according to the ICD-9-CM codes in their medical records, said Dr. Chaudhry, a researcher at the stroke research center of the University of Minnesota in Minneapolis.
Among more than 21,000 patients with acute ischemic strokes who were seen at Minnesota hospitals during the 14-month study period, 602 received thrombolytic therapy at 30 different hospitals, with 129 (21%) undergoing "drip and ship" management at 13 of these hospitals, while the other 473 (79%) remained at the centers where they began treatment with IV TPA. The patients averaged about 70 years old, and nearly half were women.
Patient profiles of the shipped and unshipped patients were similar, as were most outcomes including in-hospital mortality and length of stay. The only significant difference in clinical outcomes between these two subgroups during hospitalization was in the rate of intracerebral or subarachnoid hemorrhage, which occurred in 9% of the patients who remained at the site where they first received TPA and in 3% of the shipped patients, a statistically significant difference.
"Drip and ship" was also substantially cheaper. Average hospital charges for the untransported patients ran more than $65,000, whereas patients managed by "drip and ship" had average hospitalization charges of just under $48,000, a statistically significant difference.
Dr. Rymer said that she has been a speaker for Genentech and Concentric Medical. Dr. Chaudhry and his associates had no disclosures.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: In
acute ischemic stroke patients, 63% in one review had an mRS score of 0-2 at 90
days after TPA and transfer to a stroke center; in another review, 129 “ship
and drip” patients had outcomes similar to those of 473 patients who had TPA
but remained in place.
Data Source: Data
are from two reviews, one of 145 patients transferred to a single stroke center
in Missouri, and another of more than 21,000
patients in Minnesota.
Disclosures: Dr.
Rymer said that she has been a speaker for Genentech and Concentric Medical.
Dr. Chaudhry and his associates had no disclosures.
Patients Hit Web Survey When TIAs Threaten
NEW ORLEANS – A brief online evaluation may prompt patients to seek quick medical attention if they experience symptoms of stroke or transient ischemic attack.
Researchers are evaluating the WebTIA Program, a 26-item questionnaire that identifies risk factors and symptoms common to stroke and TIA. The investigative deployment has enrolled more than 251 people from across the country, who came upon WebTIA when searching for information on symptoms, Dr. Anthony Kim said at an international stroke conference.
Immediate medical attention offers the best outcomes for patients, said Dr. Kim, medical director of the University of California, San Francisco, Stroke Center. But because TIA symptoms can come and go suddenly, they may not be enough to prompt a patient to visit to the emergency department, or even a call to the physician.
"There is a perception that because the symptoms resolved or improved, they are not as serious," he said at the meeting, sponsored by the American Stroke Association. "Even when the symptoms are correctly recognized as a TIA or stroke, people tend to underappreciate the need for urgent evaluation."
The Internet could improve this understanding, because it’s available 24 hours a day and there are no barriers to access, as there can be with a doctor’s or emergency department visit.
The ongoing WebTIA survey aims to test the utility of the Internet as a resource for helping people identify serious cerebrovascular symptoms. The survey page comes up as an option when people search for key words or phrases, such as "Am I having a ministroke." A click-through ad also appears on some other sites with stroke information.
The WebTIA site includes videos and text explanations of the TIA and stroke, and describes how taking the survey helps researchers create an effective Web-based risk-evaluation tool. The step-by-step program begins with six qualification questions and then guides visitors through the process of informed consent and explains Internet privacy terms. If patients agree, they answer a 26-item questionnaire that incorporates the ABCD2 score, as well as questions that give some hint about the brain territory affected. If visitors indicate that symptoms are occurring at the moment, the survey urges them to stop reading and seek emergency help.
The concluding page gives visitors the option to contact a study neurologist immediately, by phone or by computer, and reminds them that they’ll get a follow-up call from a neurologist participating in the study.
In the first 3 months, the WebTIA site received an average of 200 hits per day. More than 250 people completed the online interview; there were 175 follow-up interviews. The mean age was 59 years; the oldest visitor was aged 88 years, showing that elderly people can easily use the Internet to access information.
About two-thirds of the visitors had sought medical advice for their symptoms. Many noted that their symptoms had occurred within the prior 30 minutes and subsided. One man, vacationing in a recreational vehicle, completed the survey from his phone. About a quarter of visitors were sent to the hospital within minutes, hours, or a day.
Follow-up interviews determined that 43 (25%) had suffered a TIA and that 67 (39%) had either a TIA or a stroke. "There was good agreement between the online tool and our neurologists’ assessment," Dr. Kim remarked.
The ABCD2 score itself, however, was only moderately predictive, with a discrimination rate of 69%. "One of the 12 patients with a risk score of 0 had a cerebrovascular event of isolated diplopia," Dr. Kim said. Incorporating a question about diplopia and one about prior TIA or stroke improved the discrimination rate to 78%. By this calculation, seven patients had a risk score of 0, and none of those had an event.
"We identified a population of patients with possible TIA or stroke that might be a promising target for a computer-based public health intervention that could reduce delays to medical intervention." Such interventions would involve minimal cost and have the potential to reach a very large population, Dr. Kim said.
The project was funded by a grant from the National Stroke Association and Boehringer Ingelheim. Dr. Kim said he received a research grant from the company.
NEW ORLEANS – A brief online evaluation may prompt patients to seek quick medical attention if they experience symptoms of stroke or transient ischemic attack.
Researchers are evaluating the WebTIA Program, a 26-item questionnaire that identifies risk factors and symptoms common to stroke and TIA. The investigative deployment has enrolled more than 251 people from across the country, who came upon WebTIA when searching for information on symptoms, Dr. Anthony Kim said at an international stroke conference.
Immediate medical attention offers the best outcomes for patients, said Dr. Kim, medical director of the University of California, San Francisco, Stroke Center. But because TIA symptoms can come and go suddenly, they may not be enough to prompt a patient to visit to the emergency department, or even a call to the physician.
"There is a perception that because the symptoms resolved or improved, they are not as serious," he said at the meeting, sponsored by the American Stroke Association. "Even when the symptoms are correctly recognized as a TIA or stroke, people tend to underappreciate the need for urgent evaluation."
The Internet could improve this understanding, because it’s available 24 hours a day and there are no barriers to access, as there can be with a doctor’s or emergency department visit.
The ongoing WebTIA survey aims to test the utility of the Internet as a resource for helping people identify serious cerebrovascular symptoms. The survey page comes up as an option when people search for key words or phrases, such as "Am I having a ministroke." A click-through ad also appears on some other sites with stroke information.
The WebTIA site includes videos and text explanations of the TIA and stroke, and describes how taking the survey helps researchers create an effective Web-based risk-evaluation tool. The step-by-step program begins with six qualification questions and then guides visitors through the process of informed consent and explains Internet privacy terms. If patients agree, they answer a 26-item questionnaire that incorporates the ABCD2 score, as well as questions that give some hint about the brain territory affected. If visitors indicate that symptoms are occurring at the moment, the survey urges them to stop reading and seek emergency help.
The concluding page gives visitors the option to contact a study neurologist immediately, by phone or by computer, and reminds them that they’ll get a follow-up call from a neurologist participating in the study.
In the first 3 months, the WebTIA site received an average of 200 hits per day. More than 250 people completed the online interview; there were 175 follow-up interviews. The mean age was 59 years; the oldest visitor was aged 88 years, showing that elderly people can easily use the Internet to access information.
About two-thirds of the visitors had sought medical advice for their symptoms. Many noted that their symptoms had occurred within the prior 30 minutes and subsided. One man, vacationing in a recreational vehicle, completed the survey from his phone. About a quarter of visitors were sent to the hospital within minutes, hours, or a day.
Follow-up interviews determined that 43 (25%) had suffered a TIA and that 67 (39%) had either a TIA or a stroke. "There was good agreement between the online tool and our neurologists’ assessment," Dr. Kim remarked.
The ABCD2 score itself, however, was only moderately predictive, with a discrimination rate of 69%. "One of the 12 patients with a risk score of 0 had a cerebrovascular event of isolated diplopia," Dr. Kim said. Incorporating a question about diplopia and one about prior TIA or stroke improved the discrimination rate to 78%. By this calculation, seven patients had a risk score of 0, and none of those had an event.
"We identified a population of patients with possible TIA or stroke that might be a promising target for a computer-based public health intervention that could reduce delays to medical intervention." Such interventions would involve minimal cost and have the potential to reach a very large population, Dr. Kim said.
The project was funded by a grant from the National Stroke Association and Boehringer Ingelheim. Dr. Kim said he received a research grant from the company.
NEW ORLEANS – A brief online evaluation may prompt patients to seek quick medical attention if they experience symptoms of stroke or transient ischemic attack.
Researchers are evaluating the WebTIA Program, a 26-item questionnaire that identifies risk factors and symptoms common to stroke and TIA. The investigative deployment has enrolled more than 251 people from across the country, who came upon WebTIA when searching for information on symptoms, Dr. Anthony Kim said at an international stroke conference.
Immediate medical attention offers the best outcomes for patients, said Dr. Kim, medical director of the University of California, San Francisco, Stroke Center. But because TIA symptoms can come and go suddenly, they may not be enough to prompt a patient to visit to the emergency department, or even a call to the physician.
"There is a perception that because the symptoms resolved or improved, they are not as serious," he said at the meeting, sponsored by the American Stroke Association. "Even when the symptoms are correctly recognized as a TIA or stroke, people tend to underappreciate the need for urgent evaluation."
The Internet could improve this understanding, because it’s available 24 hours a day and there are no barriers to access, as there can be with a doctor’s or emergency department visit.
The ongoing WebTIA survey aims to test the utility of the Internet as a resource for helping people identify serious cerebrovascular symptoms. The survey page comes up as an option when people search for key words or phrases, such as "Am I having a ministroke." A click-through ad also appears on some other sites with stroke information.
The WebTIA site includes videos and text explanations of the TIA and stroke, and describes how taking the survey helps researchers create an effective Web-based risk-evaluation tool. The step-by-step program begins with six qualification questions and then guides visitors through the process of informed consent and explains Internet privacy terms. If patients agree, they answer a 26-item questionnaire that incorporates the ABCD2 score, as well as questions that give some hint about the brain territory affected. If visitors indicate that symptoms are occurring at the moment, the survey urges them to stop reading and seek emergency help.
The concluding page gives visitors the option to contact a study neurologist immediately, by phone or by computer, and reminds them that they’ll get a follow-up call from a neurologist participating in the study.
In the first 3 months, the WebTIA site received an average of 200 hits per day. More than 250 people completed the online interview; there were 175 follow-up interviews. The mean age was 59 years; the oldest visitor was aged 88 years, showing that elderly people can easily use the Internet to access information.
About two-thirds of the visitors had sought medical advice for their symptoms. Many noted that their symptoms had occurred within the prior 30 minutes and subsided. One man, vacationing in a recreational vehicle, completed the survey from his phone. About a quarter of visitors were sent to the hospital within minutes, hours, or a day.
Follow-up interviews determined that 43 (25%) had suffered a TIA and that 67 (39%) had either a TIA or a stroke. "There was good agreement between the online tool and our neurologists’ assessment," Dr. Kim remarked.
The ABCD2 score itself, however, was only moderately predictive, with a discrimination rate of 69%. "One of the 12 patients with a risk score of 0 had a cerebrovascular event of isolated diplopia," Dr. Kim said. Incorporating a question about diplopia and one about prior TIA or stroke improved the discrimination rate to 78%. By this calculation, seven patients had a risk score of 0, and none of those had an event.
"We identified a population of patients with possible TIA or stroke that might be a promising target for a computer-based public health intervention that could reduce delays to medical intervention." Such interventions would involve minimal cost and have the potential to reach a very large population, Dr. Kim said.
The project was funded by a grant from the National Stroke Association and Boehringer Ingelheim. Dr. Kim said he received a research grant from the company.
FROM THE INTERNATIONAL STROKE CONFERENCE
Major Finding: An investigational Web-based survey can identify symptoms of TIA or stroke in up to 78% of people who visit the site and fill out a questionnaire.
Data Source: The pilot WebTIA program, which has so far enrolled more than 250 patients.
Disclosures: The project was funded by a grant from the National Stroke Association and Boehringer Ingelheim. Dr. Kim said he received a research grant from the company
CT Perfusion in Acute Stroke Questioned
NEW ORLEANS – The extra time needed for CT perfusion imaging in patients with an acute ischemic stroke may not be warranted, based on a retrospective analysis of 418 patients treated at nine U.S. tertiary stroke centers.
The analysis showed that the outcomes in patients assessed using CT perfusion (CTP) were very similar to those in patients worked up with noncontrast CT (NCCT), and that CTP added an average of 48 minutes to the time elapsed between the start of imaging and the completion of the reperfusion procedure, Dr. Rishi Gupta said at the annual International Stroke Conference.
"Additional imaging did not translate into better clinical outcomes or reduced hemorrhage rates, raising the question of whether NCCT is good enough," said Dr. Gupta, a neurologist at Emory University and director of the acute stroke network at Grady Health System, both in Atlanta.
Because the analysis was retrospective, the next step is a prospective, randomized study to compare the impact of NCCT and CT perfusion, Dr. Gupta noted. Despite this limitation, he said he and his associates at Grady Health are convinced by the findings and have already scaled back their use of CTP to rely more on NCCT.
"CTP better demarcates the area of irreversible brain damage, but we stopped doing a lot of CTP because we were cognizant of the time delay. We didn’t feel we got additional, helpful information. We cut back quite a lot on our CTP based on these findings," although a majority of centers that perform endovascular perfusion on acute stroke patients "tolerate the delay and get CTP," he said in an interview. "We need to do a randomized study" to settle the question, he added.
The data set compiled from the nine participating U.S. centers included 418 eligible patients who underwent imaging prior to endovascular reperfusion therapy between September 2009 and December 2011. Of these, 227 (54%) had CTP and 191 (46%) had NCCT.
The study included consecutive patients with an occlusion of the middle cerebral or internal carotid artery treated within 8 hours of symptom onset. The analysis excluded patients with a posterior circulation stroke, those who underwent MRI, and those with a thrombus in their anterior cerebral or distal middle cerebral artery. The patients’ average age was 67 years, and their average National Institutes of Health Stroke Scale score was 18.
The analysis showed successful reperfusion in 65% of the NCCT patients and in 71% of those imaged with CTP. A good clinical outcome – a modified Rankin Scale score of 0-2 at 90 days after hospitalization – was achieved in 37% of the NCCT and 38% of the CTP patients. Mortality was 23% in the NCCT and 21% in the CTP patients. The rates of symptomatic and asymptomatic hemorrhage were also similar in the two subgroups. None of these between-group differences were statistically significant. In a multivariate analysis, the use of CTP was not a significant determinant of a good clinical outcome.
Average time from the start of CT imaging to reperfusion was 175 minutes in the NCCT patients and 223 minutes in the CTP group – an average of 48 minutes additional time with CTP.
Dr. Gupta presented two additional analyses designed to compare outcomes using the two imaging methods in closely matched subgroups. In one analysis, he focused exclusively on the 291 patients in the database who had occlusions at the M1 site of the middle cerebral artery. In these patients, NCCT saved an average of 40 minutes, compared with CTP, and outcomes were not significantly better with CTP. In the second analysis, he categorized patients by their Alberta Stroke Program Early CT Score (ASPECTS). In the subgroup of 198 patients with an ASPECTS of more than 7 on a scale of 10, with 10 being normal, CTP did not lead to significant improvement in outcomes and took an average of 45 minutes longer to reperfusion, compared with NCCT.
Dr. Gupta said that he has been a consultant to Concentric Medical, CoAxia, Rapid Medical, and Codman.
NEW ORLEANS – The extra time needed for CT perfusion imaging in patients with an acute ischemic stroke may not be warranted, based on a retrospective analysis of 418 patients treated at nine U.S. tertiary stroke centers.
The analysis showed that the outcomes in patients assessed using CT perfusion (CTP) were very similar to those in patients worked up with noncontrast CT (NCCT), and that CTP added an average of 48 minutes to the time elapsed between the start of imaging and the completion of the reperfusion procedure, Dr. Rishi Gupta said at the annual International Stroke Conference.
"Additional imaging did not translate into better clinical outcomes or reduced hemorrhage rates, raising the question of whether NCCT is good enough," said Dr. Gupta, a neurologist at Emory University and director of the acute stroke network at Grady Health System, both in Atlanta.
Because the analysis was retrospective, the next step is a prospective, randomized study to compare the impact of NCCT and CT perfusion, Dr. Gupta noted. Despite this limitation, he said he and his associates at Grady Health are convinced by the findings and have already scaled back their use of CTP to rely more on NCCT.
"CTP better demarcates the area of irreversible brain damage, but we stopped doing a lot of CTP because we were cognizant of the time delay. We didn’t feel we got additional, helpful information. We cut back quite a lot on our CTP based on these findings," although a majority of centers that perform endovascular perfusion on acute stroke patients "tolerate the delay and get CTP," he said in an interview. "We need to do a randomized study" to settle the question, he added.
The data set compiled from the nine participating U.S. centers included 418 eligible patients who underwent imaging prior to endovascular reperfusion therapy between September 2009 and December 2011. Of these, 227 (54%) had CTP and 191 (46%) had NCCT.
The study included consecutive patients with an occlusion of the middle cerebral or internal carotid artery treated within 8 hours of symptom onset. The analysis excluded patients with a posterior circulation stroke, those who underwent MRI, and those with a thrombus in their anterior cerebral or distal middle cerebral artery. The patients’ average age was 67 years, and their average National Institutes of Health Stroke Scale score was 18.
The analysis showed successful reperfusion in 65% of the NCCT patients and in 71% of those imaged with CTP. A good clinical outcome – a modified Rankin Scale score of 0-2 at 90 days after hospitalization – was achieved in 37% of the NCCT and 38% of the CTP patients. Mortality was 23% in the NCCT and 21% in the CTP patients. The rates of symptomatic and asymptomatic hemorrhage were also similar in the two subgroups. None of these between-group differences were statistically significant. In a multivariate analysis, the use of CTP was not a significant determinant of a good clinical outcome.
Average time from the start of CT imaging to reperfusion was 175 minutes in the NCCT patients and 223 minutes in the CTP group – an average of 48 minutes additional time with CTP.
Dr. Gupta presented two additional analyses designed to compare outcomes using the two imaging methods in closely matched subgroups. In one analysis, he focused exclusively on the 291 patients in the database who had occlusions at the M1 site of the middle cerebral artery. In these patients, NCCT saved an average of 40 minutes, compared with CTP, and outcomes were not significantly better with CTP. In the second analysis, he categorized patients by their Alberta Stroke Program Early CT Score (ASPECTS). In the subgroup of 198 patients with an ASPECTS of more than 7 on a scale of 10, with 10 being normal, CTP did not lead to significant improvement in outcomes and took an average of 45 minutes longer to reperfusion, compared with NCCT.
Dr. Gupta said that he has been a consultant to Concentric Medical, CoAxia, Rapid Medical, and Codman.
NEW ORLEANS – The extra time needed for CT perfusion imaging in patients with an acute ischemic stroke may not be warranted, based on a retrospective analysis of 418 patients treated at nine U.S. tertiary stroke centers.
The analysis showed that the outcomes in patients assessed using CT perfusion (CTP) were very similar to those in patients worked up with noncontrast CT (NCCT), and that CTP added an average of 48 minutes to the time elapsed between the start of imaging and the completion of the reperfusion procedure, Dr. Rishi Gupta said at the annual International Stroke Conference.
"Additional imaging did not translate into better clinical outcomes or reduced hemorrhage rates, raising the question of whether NCCT is good enough," said Dr. Gupta, a neurologist at Emory University and director of the acute stroke network at Grady Health System, both in Atlanta.
Because the analysis was retrospective, the next step is a prospective, randomized study to compare the impact of NCCT and CT perfusion, Dr. Gupta noted. Despite this limitation, he said he and his associates at Grady Health are convinced by the findings and have already scaled back their use of CTP to rely more on NCCT.
"CTP better demarcates the area of irreversible brain damage, but we stopped doing a lot of CTP because we were cognizant of the time delay. We didn’t feel we got additional, helpful information. We cut back quite a lot on our CTP based on these findings," although a majority of centers that perform endovascular perfusion on acute stroke patients "tolerate the delay and get CTP," he said in an interview. "We need to do a randomized study" to settle the question, he added.
The data set compiled from the nine participating U.S. centers included 418 eligible patients who underwent imaging prior to endovascular reperfusion therapy between September 2009 and December 2011. Of these, 227 (54%) had CTP and 191 (46%) had NCCT.
The study included consecutive patients with an occlusion of the middle cerebral or internal carotid artery treated within 8 hours of symptom onset. The analysis excluded patients with a posterior circulation stroke, those who underwent MRI, and those with a thrombus in their anterior cerebral or distal middle cerebral artery. The patients’ average age was 67 years, and their average National Institutes of Health Stroke Scale score was 18.
The analysis showed successful reperfusion in 65% of the NCCT patients and in 71% of those imaged with CTP. A good clinical outcome – a modified Rankin Scale score of 0-2 at 90 days after hospitalization – was achieved in 37% of the NCCT and 38% of the CTP patients. Mortality was 23% in the NCCT and 21% in the CTP patients. The rates of symptomatic and asymptomatic hemorrhage were also similar in the two subgroups. None of these between-group differences were statistically significant. In a multivariate analysis, the use of CTP was not a significant determinant of a good clinical outcome.
Average time from the start of CT imaging to reperfusion was 175 minutes in the NCCT patients and 223 minutes in the CTP group – an average of 48 minutes additional time with CTP.
Dr. Gupta presented two additional analyses designed to compare outcomes using the two imaging methods in closely matched subgroups. In one analysis, he focused exclusively on the 291 patients in the database who had occlusions at the M1 site of the middle cerebral artery. In these patients, NCCT saved an average of 40 minutes, compared with CTP, and outcomes were not significantly better with CTP. In the second analysis, he categorized patients by their Alberta Stroke Program Early CT Score (ASPECTS). In the subgroup of 198 patients with an ASPECTS of more than 7 on a scale of 10, with 10 being normal, CTP did not lead to significant improvement in outcomes and took an average of 45 minutes longer to reperfusion, compared with NCCT.
Dr. Gupta said that he has been a consultant to Concentric Medical, CoAxia, Rapid Medical, and Codman.
FROM THE ANNUAL INTERNATIONAL STROKE CONFERENCE
Major Finding: CT perfusion imaging of ischemic stroke patients boosted average time to reperfusion by 48 minutes, compared with noncontrast CT, without improving outcomes.
Data Source: A retrospective analysis of 418 consecutive patients with an acute ischemic stroke treated with endovascular reperfusion therapy was performed at nine U.S. centers during 2009-2011.
Disclosures: Dr. Gupta said that he has been a consultant to Concentric Medical, CoAxia, Rapid Medical, and Codman.