User login
Mid-life cardiovascular risk factors set stage for later-life dementia
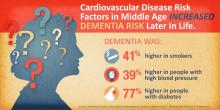
HOUSTON – Cardiovascular risk factors present in middle age may presage dementia in later years, a subanalysis of a 25-year atherosclerosis study has determined.
Diabetes conferred the greatest dementia risk, nearly doubling the chance of dementia, Rebecca Gottesman, MD, PhD, said at the International Stroke Conference, sponsored by the American Heart Association.
“In fact, the risk associated with diabetes nears the increased risk associated with having an APOE4 [apolipoprotein E epsilon 4] allele,” said Dr. Gottesman of Johns Hopkins University, Baltimore.
Her subanalysis of the biracial ARIC-NCS (Atherosclerosis Risk in Communities Neurocognitive Study) also identified some racial differences in risk, with blacks being more vulnerable to the risk imposed by diabetes, and whites more vulnerable to the hypertension-associated risk.
The ARIC study, sponsored by the National Heart, Lung, and Blood Institute, is a prospective epidemiologic study conducted in four U.S. communities. ARIC is designed to investigate the causes of atherosclerosis and its clinical outcomes, and variation in cardiovascular risk factors, medical care, and disease by race, gender, location, and date. To date, the ARIC project has published over 800 articles in peer-reviewed journals. A total of 15,792 participants received an extensive examination, including medical, social, and demographic data. These participants were reexamined every 3 years with the first screen occurring in 1987-1989. Follow-up occurs yearly by telephone to maintain contact with participants and to assess the health status of the cohort.
ARIC-NCS comprises about 10,000 of these subjects. Of these, 6,471 completed the fifth visit, which occurred during 2011-2013. They have undergone cognitive, neurologic, and brain imaging assessments to diagnose mild cognitive impairment or dementia and assign an etiology for the cognitive disorder. Last year, investigators published the study’s primary findings: Nearly 30% had a diagnosis of either dementia or mild cognitive impairment.
Dr. Gottesman sought to determine the extent to which these subjects’ baseline cardiovascular risk factors influenced their chances of cognitive decline or dementia. She assessed risk for the entire cohort, and then for black and white subjects separately.
Dementia was present in 1,516 cases (23%). In the total cohort, dementia was – not surprisingly – significantly associated with increasing age. Subjects aged 50-54 years had twice the risk for dementia when compared with younger subjects, while those aged 60-66 years had eight times greater risk. Black race conferred a 30% increased risk, compared with white race (hazard ratio, 1.3). Education of less than a high school degree was associated with a 40% increased risk. Having at least one copy of the APOE4 allele doubled the risk.
Diabetes was second only to genetic status, increasing the risk by 80%.
Dr. Gottesman then divided the cohort by race and reexamined these risk factors separately. She found some significant differences in the way these factors affected risk in white and black subjects.
Age exerted a greater influence on dementia risks in whites than it did in blacks. The risk was about doubled in both groups for people aged 50-54 years. But at age 55-59 years, it was significantly higher in whites than in blacks (HR, 4.37 vs. 3.53). The risk differential was even greater between whites and blacks aged 60-66 years (HR, 9.5 vs. 6.2).
Blacks with low education were more vulnerable to dementia than were whites (HR, 1.6 vs. 1.29). APOE4 status (at least one allele) more than doubled the risk of dementia for whites (HR, 2.23) but was not as strong in blacks (HR, 1.61).
Obesity was riskier for whites, increasing the risk of dementia by 22%, but it had no influence on risk among blacks. Current smoking increased the risk for whites by 62% but was not a significant risk factor for blacks. Prehypertension also affected whites more, increasing the risk by 35%, compared with a nonsignificant 17% for blacks. Full-blown hypertension increased the risk of dementia similarly in both groups (37% and 36%, respectively).
Diabetes increased the risk of dementia more in blacks than it did in whites (85% vs. 69%).
“We don’t have a clear explanation of these disparities in dementia risk with regard to race,” Dr. Gottesman said. “It could be, though, that even if a risk factor has the same relationship with dementia in both groups, if it is more prevalent in one group, that may somewhat account for this larger population attributable risk.”
She had no financial disclosures.
On Twitter @alz_gal
HOUSTON – Cardiovascular risk factors present in middle age may presage dementia in later years, a subanalysis of a 25-year atherosclerosis study has determined.
Diabetes conferred the greatest dementia risk, nearly doubling the chance of dementia, Rebecca Gottesman, MD, PhD, said at the International Stroke Conference, sponsored by the American Heart Association.
“In fact, the risk associated with diabetes nears the increased risk associated with having an APOE4 [apolipoprotein E epsilon 4] allele,” said Dr. Gottesman of Johns Hopkins University, Baltimore.
Her subanalysis of the biracial ARIC-NCS (Atherosclerosis Risk in Communities Neurocognitive Study) also identified some racial differences in risk, with blacks being more vulnerable to the risk imposed by diabetes, and whites more vulnerable to the hypertension-associated risk.
The ARIC study, sponsored by the National Heart, Lung, and Blood Institute, is a prospective epidemiologic study conducted in four U.S. communities. ARIC is designed to investigate the causes of atherosclerosis and its clinical outcomes, and variation in cardiovascular risk factors, medical care, and disease by race, gender, location, and date. To date, the ARIC project has published over 800 articles in peer-reviewed journals. A total of 15,792 participants received an extensive examination, including medical, social, and demographic data. These participants were reexamined every 3 years with the first screen occurring in 1987-1989. Follow-up occurs yearly by telephone to maintain contact with participants and to assess the health status of the cohort.
ARIC-NCS comprises about 10,000 of these subjects. Of these, 6,471 completed the fifth visit, which occurred during 2011-2013. They have undergone cognitive, neurologic, and brain imaging assessments to diagnose mild cognitive impairment or dementia and assign an etiology for the cognitive disorder. Last year, investigators published the study’s primary findings: Nearly 30% had a diagnosis of either dementia or mild cognitive impairment.
Dr. Gottesman sought to determine the extent to which these subjects’ baseline cardiovascular risk factors influenced their chances of cognitive decline or dementia. She assessed risk for the entire cohort, and then for black and white subjects separately.
Dementia was present in 1,516 cases (23%). In the total cohort, dementia was – not surprisingly – significantly associated with increasing age. Subjects aged 50-54 years had twice the risk for dementia when compared with younger subjects, while those aged 60-66 years had eight times greater risk. Black race conferred a 30% increased risk, compared with white race (hazard ratio, 1.3). Education of less than a high school degree was associated with a 40% increased risk. Having at least one copy of the APOE4 allele doubled the risk.
Diabetes was second only to genetic status, increasing the risk by 80%.
Dr. Gottesman then divided the cohort by race and reexamined these risk factors separately. She found some significant differences in the way these factors affected risk in white and black subjects.
Age exerted a greater influence on dementia risks in whites than it did in blacks. The risk was about doubled in both groups for people aged 50-54 years. But at age 55-59 years, it was significantly higher in whites than in blacks (HR, 4.37 vs. 3.53). The risk differential was even greater between whites and blacks aged 60-66 years (HR, 9.5 vs. 6.2).
Blacks with low education were more vulnerable to dementia than were whites (HR, 1.6 vs. 1.29). APOE4 status (at least one allele) more than doubled the risk of dementia for whites (HR, 2.23) but was not as strong in blacks (HR, 1.61).
Obesity was riskier for whites, increasing the risk of dementia by 22%, but it had no influence on risk among blacks. Current smoking increased the risk for whites by 62% but was not a significant risk factor for blacks. Prehypertension also affected whites more, increasing the risk by 35%, compared with a nonsignificant 17% for blacks. Full-blown hypertension increased the risk of dementia similarly in both groups (37% and 36%, respectively).
Diabetes increased the risk of dementia more in blacks than it did in whites (85% vs. 69%).
“We don’t have a clear explanation of these disparities in dementia risk with regard to race,” Dr. Gottesman said. “It could be, though, that even if a risk factor has the same relationship with dementia in both groups, if it is more prevalent in one group, that may somewhat account for this larger population attributable risk.”
She had no financial disclosures.
On Twitter @alz_gal
HOUSTON – Cardiovascular risk factors present in middle age may presage dementia in later years, a subanalysis of a 25-year atherosclerosis study has determined.
Diabetes conferred the greatest dementia risk, nearly doubling the chance of dementia, Rebecca Gottesman, MD, PhD, said at the International Stroke Conference, sponsored by the American Heart Association.
“In fact, the risk associated with diabetes nears the increased risk associated with having an APOE4 [apolipoprotein E epsilon 4] allele,” said Dr. Gottesman of Johns Hopkins University, Baltimore.
Her subanalysis of the biracial ARIC-NCS (Atherosclerosis Risk in Communities Neurocognitive Study) also identified some racial differences in risk, with blacks being more vulnerable to the risk imposed by diabetes, and whites more vulnerable to the hypertension-associated risk.
The ARIC study, sponsored by the National Heart, Lung, and Blood Institute, is a prospective epidemiologic study conducted in four U.S. communities. ARIC is designed to investigate the causes of atherosclerosis and its clinical outcomes, and variation in cardiovascular risk factors, medical care, and disease by race, gender, location, and date. To date, the ARIC project has published over 800 articles in peer-reviewed journals. A total of 15,792 participants received an extensive examination, including medical, social, and demographic data. These participants were reexamined every 3 years with the first screen occurring in 1987-1989. Follow-up occurs yearly by telephone to maintain contact with participants and to assess the health status of the cohort.
ARIC-NCS comprises about 10,000 of these subjects. Of these, 6,471 completed the fifth visit, which occurred during 2011-2013. They have undergone cognitive, neurologic, and brain imaging assessments to diagnose mild cognitive impairment or dementia and assign an etiology for the cognitive disorder. Last year, investigators published the study’s primary findings: Nearly 30% had a diagnosis of either dementia or mild cognitive impairment.
Dr. Gottesman sought to determine the extent to which these subjects’ baseline cardiovascular risk factors influenced their chances of cognitive decline or dementia. She assessed risk for the entire cohort, and then for black and white subjects separately.
Dementia was present in 1,516 cases (23%). In the total cohort, dementia was – not surprisingly – significantly associated with increasing age. Subjects aged 50-54 years had twice the risk for dementia when compared with younger subjects, while those aged 60-66 years had eight times greater risk. Black race conferred a 30% increased risk, compared with white race (hazard ratio, 1.3). Education of less than a high school degree was associated with a 40% increased risk. Having at least one copy of the APOE4 allele doubled the risk.
Diabetes was second only to genetic status, increasing the risk by 80%.
Dr. Gottesman then divided the cohort by race and reexamined these risk factors separately. She found some significant differences in the way these factors affected risk in white and black subjects.
Age exerted a greater influence on dementia risks in whites than it did in blacks. The risk was about doubled in both groups for people aged 50-54 years. But at age 55-59 years, it was significantly higher in whites than in blacks (HR, 4.37 vs. 3.53). The risk differential was even greater between whites and blacks aged 60-66 years (HR, 9.5 vs. 6.2).
Blacks with low education were more vulnerable to dementia than were whites (HR, 1.6 vs. 1.29). APOE4 status (at least one allele) more than doubled the risk of dementia for whites (HR, 2.23) but was not as strong in blacks (HR, 1.61).
Obesity was riskier for whites, increasing the risk of dementia by 22%, but it had no influence on risk among blacks. Current smoking increased the risk for whites by 62% but was not a significant risk factor for blacks. Prehypertension also affected whites more, increasing the risk by 35%, compared with a nonsignificant 17% for blacks. Full-blown hypertension increased the risk of dementia similarly in both groups (37% and 36%, respectively).
Diabetes increased the risk of dementia more in blacks than it did in whites (85% vs. 69%).
“We don’t have a clear explanation of these disparities in dementia risk with regard to race,” Dr. Gottesman said. “It could be, though, that even if a risk factor has the same relationship with dementia in both groups, if it is more prevalent in one group, that may somewhat account for this larger population attributable risk.”
She had no financial disclosures.
On Twitter @alz_gal
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point:
Major finding: Smoking and hypertension increased the risk of dementia by 40% each; diabetes, by 80%.
Data source: The Atherosclerosis Risk in Communities Neurocognitive Study study comprised more than 6,000 people.
Disclosures: Dr. Gottesman had no financial disclosures.
Personalized coaching program controls blood pressure for black patients
HOUSTON – A personalized lifestyle coaching program focused on healthy eating increased blood pressure control by 7%, compared with usual care, among black patients with persistent hypertension.
A year after the program was instituted, the rate of blood pressure control was 69% in the intervention group, compared with 62% in the group that had the usual care offered to hypertensive patients, Mai Nguyen-Huynh, MD, said at the International Stroke Conference sponsored by the American Heart Association.
Still, the intervention worked, said Dr. Nguyen-Huynh, a vascular neurologist with the Kaiser Permanente Northern California Division of Research. More analyses will follow to try to tease out just how.
Kaiser Permanente of Northern California was already in a fairly good place with blood pressure control in 2012, when researchers first started considering the project, she said. That was directly related to a system-wide intensification of hypertension identification and treatment, implemented in the early 2000s. The company started a hypertension registry, added free blood pressure checks for all members, and promoted single-pill combination therapy. For patients with persistent hypertension, the company added free hypertension consultations with pharmacists and primary care providers.
By 2012, 85% of its enrollees had blood pressure control, classified as below 140/90 mm Hg. But for at least a decade, black participants had been lagging behind whites in that regard. And despite these intensified, group-wide efforts to target hypertension, a 5% gap in hypertension control among blacks paralleled rates among whites (80%-85% vs. 85%-90% over 10 years).
“Even with equal utilization and access to care, we continued to see this clear disparity in blacks vs. whites,” Dr. Nguyen-Huynh said.
The “Shake, Rattle, and Roll” blood pressure control trial was an effort to identify a treatment paradigm that could reduce this disparity by 4% within 1 year. The program moniker describes its three goals:
• “Shake” the salt habit.
• “Rattle” the intensity of the existing blood pressure control protocol.
• “Roll” out the results and incorporate into clinical practice.
The study was organized into three arms. Usual care was Kaiser’s typical intensified hypertension management. Patients filled out health and diet questionnaires and could voluntarily undergo a 24-hour urine sodium test.
The enhanced monitoring arm consisted of usual care, plus an in-person session with a nurse to discuss resources and possible barriers to treatment; regular blood pressure checks; intensification of pharmacotherapy, focusing on thiazides; and the addition of spironolactone for patients who had persistent hypertension despite being on three or more medications.
The lifestyle intervention arm consisted of usual care plus personalized coaching, both on the phone and in person. Participants could have up to 16 phone sessions with a specially trained counselor, with the option of bimonthly in-person group sessions.
These were accompanied by a workbook that emphasized healthy eating, from meal planning to shopping and cooking. Restaurant dining was tackled as well, including fast food and carryout. The workbook covered eight sessions. Each session ended with goal-setting for the next meeting, and opened with a review of how the prior month’s goals were accomplished.
Individualization was an important part of the lifestyle intervention program, Dr. Nguyen-Huynh said. Counselors didn’t strive to make each participant fit into a cookie-cutter solution. Instead, they worked as a team to build interventions that would work for each person.
The study group comprised 1,660 subjects. About 70% were women. Diabetes was common (about 33%), and around 10% had a history of coronary artery disease. The mean body mass index was 34 kg/m2.
The primary outcome was rate of blood pressure control in the usual care vs. enhanced monitoring groups, and the usual care vs. lifestyle modification groups after 1 year.
At the end of follow-up, there was no difference in the rate of control between the usual care group and the enhanced monitoring group (62% vs. 64%). However, there was a significant difference in the rate of control between the usual care and the lifestyle modification groups (62% vs. 69%).
Again, Dr. Nguyen-Huynh said, it was tough to pinpoint any particular reason for the improvement. There was no apparent increase in compliance with antihypertensive medication. The Morisky scale, an 8-point self-reported measure of medication compliance, was not different from baseline. Participants didn’t report any big changes in salt intake or salt use in food. This was borne out in the 24-hour urine sodium screens, which were also not different from baseline. There were no significant weight changes and no changes in the use of outpatient primary care.
“What we can say is that it apparently worked,” she said. “This culturally appropriate, telephone-based lifestyle intervention, that focuses on the DASH eating plan, may be something that can help African-Americans with uncontrolled hypertension manage their condition.”
She added that Kaiser will continue to drill down in the data to discover the source of its benefit and follow the participants for at least another year to assess the longevity of the its clinical effect.
Dr. Nguyen-Huynh had no financial disclosures.
[email protected]
On Twitter @alz_gal
HOUSTON – A personalized lifestyle coaching program focused on healthy eating increased blood pressure control by 7%, compared with usual care, among black patients with persistent hypertension.
A year after the program was instituted, the rate of blood pressure control was 69% in the intervention group, compared with 62% in the group that had the usual care offered to hypertensive patients, Mai Nguyen-Huynh, MD, said at the International Stroke Conference sponsored by the American Heart Association.
Still, the intervention worked, said Dr. Nguyen-Huynh, a vascular neurologist with the Kaiser Permanente Northern California Division of Research. More analyses will follow to try to tease out just how.
Kaiser Permanente of Northern California was already in a fairly good place with blood pressure control in 2012, when researchers first started considering the project, she said. That was directly related to a system-wide intensification of hypertension identification and treatment, implemented in the early 2000s. The company started a hypertension registry, added free blood pressure checks for all members, and promoted single-pill combination therapy. For patients with persistent hypertension, the company added free hypertension consultations with pharmacists and primary care providers.
By 2012, 85% of its enrollees had blood pressure control, classified as below 140/90 mm Hg. But for at least a decade, black participants had been lagging behind whites in that regard. And despite these intensified, group-wide efforts to target hypertension, a 5% gap in hypertension control among blacks paralleled rates among whites (80%-85% vs. 85%-90% over 10 years).
“Even with equal utilization and access to care, we continued to see this clear disparity in blacks vs. whites,” Dr. Nguyen-Huynh said.
The “Shake, Rattle, and Roll” blood pressure control trial was an effort to identify a treatment paradigm that could reduce this disparity by 4% within 1 year. The program moniker describes its three goals:
• “Shake” the salt habit.
• “Rattle” the intensity of the existing blood pressure control protocol.
• “Roll” out the results and incorporate into clinical practice.
The study was organized into three arms. Usual care was Kaiser’s typical intensified hypertension management. Patients filled out health and diet questionnaires and could voluntarily undergo a 24-hour urine sodium test.
The enhanced monitoring arm consisted of usual care, plus an in-person session with a nurse to discuss resources and possible barriers to treatment; regular blood pressure checks; intensification of pharmacotherapy, focusing on thiazides; and the addition of spironolactone for patients who had persistent hypertension despite being on three or more medications.
The lifestyle intervention arm consisted of usual care plus personalized coaching, both on the phone and in person. Participants could have up to 16 phone sessions with a specially trained counselor, with the option of bimonthly in-person group sessions.
These were accompanied by a workbook that emphasized healthy eating, from meal planning to shopping and cooking. Restaurant dining was tackled as well, including fast food and carryout. The workbook covered eight sessions. Each session ended with goal-setting for the next meeting, and opened with a review of how the prior month’s goals were accomplished.
Individualization was an important part of the lifestyle intervention program, Dr. Nguyen-Huynh said. Counselors didn’t strive to make each participant fit into a cookie-cutter solution. Instead, they worked as a team to build interventions that would work for each person.
The study group comprised 1,660 subjects. About 70% were women. Diabetes was common (about 33%), and around 10% had a history of coronary artery disease. The mean body mass index was 34 kg/m2.
The primary outcome was rate of blood pressure control in the usual care vs. enhanced monitoring groups, and the usual care vs. lifestyle modification groups after 1 year.
At the end of follow-up, there was no difference in the rate of control between the usual care group and the enhanced monitoring group (62% vs. 64%). However, there was a significant difference in the rate of control between the usual care and the lifestyle modification groups (62% vs. 69%).
Again, Dr. Nguyen-Huynh said, it was tough to pinpoint any particular reason for the improvement. There was no apparent increase in compliance with antihypertensive medication. The Morisky scale, an 8-point self-reported measure of medication compliance, was not different from baseline. Participants didn’t report any big changes in salt intake or salt use in food. This was borne out in the 24-hour urine sodium screens, which were also not different from baseline. There were no significant weight changes and no changes in the use of outpatient primary care.
“What we can say is that it apparently worked,” she said. “This culturally appropriate, telephone-based lifestyle intervention, that focuses on the DASH eating plan, may be something that can help African-Americans with uncontrolled hypertension manage their condition.”
She added that Kaiser will continue to drill down in the data to discover the source of its benefit and follow the participants for at least another year to assess the longevity of the its clinical effect.
Dr. Nguyen-Huynh had no financial disclosures.
[email protected]
On Twitter @alz_gal
HOUSTON – A personalized lifestyle coaching program focused on healthy eating increased blood pressure control by 7%, compared with usual care, among black patients with persistent hypertension.
A year after the program was instituted, the rate of blood pressure control was 69% in the intervention group, compared with 62% in the group that had the usual care offered to hypertensive patients, Mai Nguyen-Huynh, MD, said at the International Stroke Conference sponsored by the American Heart Association.
Still, the intervention worked, said Dr. Nguyen-Huynh, a vascular neurologist with the Kaiser Permanente Northern California Division of Research. More analyses will follow to try to tease out just how.
Kaiser Permanente of Northern California was already in a fairly good place with blood pressure control in 2012, when researchers first started considering the project, she said. That was directly related to a system-wide intensification of hypertension identification and treatment, implemented in the early 2000s. The company started a hypertension registry, added free blood pressure checks for all members, and promoted single-pill combination therapy. For patients with persistent hypertension, the company added free hypertension consultations with pharmacists and primary care providers.
By 2012, 85% of its enrollees had blood pressure control, classified as below 140/90 mm Hg. But for at least a decade, black participants had been lagging behind whites in that regard. And despite these intensified, group-wide efforts to target hypertension, a 5% gap in hypertension control among blacks paralleled rates among whites (80%-85% vs. 85%-90% over 10 years).
“Even with equal utilization and access to care, we continued to see this clear disparity in blacks vs. whites,” Dr. Nguyen-Huynh said.
The “Shake, Rattle, and Roll” blood pressure control trial was an effort to identify a treatment paradigm that could reduce this disparity by 4% within 1 year. The program moniker describes its three goals:
• “Shake” the salt habit.
• “Rattle” the intensity of the existing blood pressure control protocol.
• “Roll” out the results and incorporate into clinical practice.
The study was organized into three arms. Usual care was Kaiser’s typical intensified hypertension management. Patients filled out health and diet questionnaires and could voluntarily undergo a 24-hour urine sodium test.
The enhanced monitoring arm consisted of usual care, plus an in-person session with a nurse to discuss resources and possible barriers to treatment; regular blood pressure checks; intensification of pharmacotherapy, focusing on thiazides; and the addition of spironolactone for patients who had persistent hypertension despite being on three or more medications.
The lifestyle intervention arm consisted of usual care plus personalized coaching, both on the phone and in person. Participants could have up to 16 phone sessions with a specially trained counselor, with the option of bimonthly in-person group sessions.
These were accompanied by a workbook that emphasized healthy eating, from meal planning to shopping and cooking. Restaurant dining was tackled as well, including fast food and carryout. The workbook covered eight sessions. Each session ended with goal-setting for the next meeting, and opened with a review of how the prior month’s goals were accomplished.
Individualization was an important part of the lifestyle intervention program, Dr. Nguyen-Huynh said. Counselors didn’t strive to make each participant fit into a cookie-cutter solution. Instead, they worked as a team to build interventions that would work for each person.
The study group comprised 1,660 subjects. About 70% were women. Diabetes was common (about 33%), and around 10% had a history of coronary artery disease. The mean body mass index was 34 kg/m2.
The primary outcome was rate of blood pressure control in the usual care vs. enhanced monitoring groups, and the usual care vs. lifestyle modification groups after 1 year.
At the end of follow-up, there was no difference in the rate of control between the usual care group and the enhanced monitoring group (62% vs. 64%). However, there was a significant difference in the rate of control between the usual care and the lifestyle modification groups (62% vs. 69%).
Again, Dr. Nguyen-Huynh said, it was tough to pinpoint any particular reason for the improvement. There was no apparent increase in compliance with antihypertensive medication. The Morisky scale, an 8-point self-reported measure of medication compliance, was not different from baseline. Participants didn’t report any big changes in salt intake or salt use in food. This was borne out in the 24-hour urine sodium screens, which were also not different from baseline. There were no significant weight changes and no changes in the use of outpatient primary care.
“What we can say is that it apparently worked,” she said. “This culturally appropriate, telephone-based lifestyle intervention, that focuses on the DASH eating plan, may be something that can help African-Americans with uncontrolled hypertension manage their condition.”
She added that Kaiser will continue to drill down in the data to discover the source of its benefit and follow the participants for at least another year to assess the longevity of the its clinical effect.
Dr. Nguyen-Huynh had no financial disclosures.
[email protected]
On Twitter @alz_gal
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point:
Major finding: A year after launching “Shake, Rattle, and Roll,” blood pressure control rates improved from 62% with usual care to 69%, compared with a lifestyle intervention program.
Data source: The program randomized 1,660 patients with persistent uncontrolled hypertension.
Disclosures: Dr. Nguyen-Huynh had no financial disclosures.
Ticagrelor beats aspirin for recurrent stroke in patients with atherosclerosis
HOUSTON – Ticagrelor outperformed aspirin in preventing a combination of recurrent stroke, heart attack, and death – but only in patients whose index stroke was probably related to atherosclerosis.
The antiplatelet drug reduced the risk of the composite endpoint by 32%, compared with aspirin, in stroke patients with proven ipsilateral atherosclerotic stenosis (hazard ratio, 0.68). But ticagrelor (Brilinta) had no effect at all in those without stenosis (HR, 0.97), Pierre Amarenco, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
The study was simultaneously published in Lancet Neurology (Lancet Neurol. 2017 Feb 23. doi: 10.1016/S1474-4422[17]30038-8). “The interaction that we found suggests what we already know in clinical practice: An understanding of stroke mechanisms and their causes is important to being able to deliver safe and effective treatment of early stroke prevention,” said Dr. Amarenco of Paris-Diderot Sorbonne University, Paris.
The findings come from a preplanned subgroup analysis of the large SOCRATES trial, published in 2016. The study determined that ticagrelor was no better than aspirin in preventing recurrent stroke, heart attack or death in patients who had a transient ischemic attack.
SOCRATES randomized 13,199 patients with a nonsevere ischemic stroke or high-risk transient ischemic attack to ticagrelor (180 mg loading dose on day 1 followed by 90 mg twice daily for days 2-90) or aspirin (300 mg on day 1 followed by 100 mg daily for days 2-90). The primary endpoint was the time to the occurrence of stroke, myocardial infarction, or death within 90 days.
The search for a potentially responsive group made sense, Dr. Amarenco said, because ticagrelor “is an effective antiplatelet therapy in patients with coronary atherosclerotic disease.” Therefore, investigators reasoned, it might be most effective in patients whose strokes were of atherosclerotic origin.
The substudy focused on 3,081 of the patients with proven ipsilateral atherosclerotic stenosis and/or a mobile thrombus or plaque in the aortic arch that was judged to potentially have caused their index stroke. Generally, the atherosclerotic patients were older and more likely to have dyslipidemia, hypertension, diabetes, coronary artery disease, and heart failure than were the patients with strokes of nonatherosclerotic origin. Atherosclerotic patients also were significantly more likely to have had a prior stroke or heart attack.
In the group with atherosclerosis, ticagrelor was significantly more effective at preventing the composite primary endpoint than was aspirin. There were 103 events in 1,542 patients in the ticagrelor group and 147 in 1,539 patients in the aspirin group (6.7% vs. 9.6%) – a “very impressive” risk reduction of 32% (HR, 0.68), Dr. Amarenco said.
In the group of patients without ipsilateral atherosclerotic stenosis, ticagrelor exerted no benefit over aspirin, with an event rate of 6.7% vs. 6.9% (HR, 0.97).
The rate of recurrent ischemic stroke was the driving force behind the significant between-group difference. Ischemic stroke occurred in 6.4% of those taking ticagrelor and 8.5% of those taking aspirin – a significant risk reduction of 27% (HR, 0.73). The drug exerted no benefit for recurrent ischemic stroke over aspirin in the group without atherosclerosis (5.8% vs. 6.1%; HR, 0.93).
There were no differences in the rate of heart attack or death, or in the secondary endpoints of all stroke, disabling stroke, or fatal stroke.
Ticagrelor was not associated with any major bleeding, compared with aspirin in either group, Dr. Amarenco noted.
The higher event rate in the patients with atherosclerosis is not surprising, he said.
“We had the exact same finding in our recent study with TIAregistry.org, which we found that patients with large artery atherosclerosis were at much higher risk than patients with other stroke subtypes.”
Dr. Amarenco disclosed financial relationships with numerous pharmaceutical companies, including AstraZeneca, which sponsored the study.
[email protected]
On Twitter @alz_gal
HOUSTON – Ticagrelor outperformed aspirin in preventing a combination of recurrent stroke, heart attack, and death – but only in patients whose index stroke was probably related to atherosclerosis.
The antiplatelet drug reduced the risk of the composite endpoint by 32%, compared with aspirin, in stroke patients with proven ipsilateral atherosclerotic stenosis (hazard ratio, 0.68). But ticagrelor (Brilinta) had no effect at all in those without stenosis (HR, 0.97), Pierre Amarenco, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
The study was simultaneously published in Lancet Neurology (Lancet Neurol. 2017 Feb 23. doi: 10.1016/S1474-4422[17]30038-8). “The interaction that we found suggests what we already know in clinical practice: An understanding of stroke mechanisms and their causes is important to being able to deliver safe and effective treatment of early stroke prevention,” said Dr. Amarenco of Paris-Diderot Sorbonne University, Paris.
The findings come from a preplanned subgroup analysis of the large SOCRATES trial, published in 2016. The study determined that ticagrelor was no better than aspirin in preventing recurrent stroke, heart attack or death in patients who had a transient ischemic attack.
SOCRATES randomized 13,199 patients with a nonsevere ischemic stroke or high-risk transient ischemic attack to ticagrelor (180 mg loading dose on day 1 followed by 90 mg twice daily for days 2-90) or aspirin (300 mg on day 1 followed by 100 mg daily for days 2-90). The primary endpoint was the time to the occurrence of stroke, myocardial infarction, or death within 90 days.
The search for a potentially responsive group made sense, Dr. Amarenco said, because ticagrelor “is an effective antiplatelet therapy in patients with coronary atherosclerotic disease.” Therefore, investigators reasoned, it might be most effective in patients whose strokes were of atherosclerotic origin.
The substudy focused on 3,081 of the patients with proven ipsilateral atherosclerotic stenosis and/or a mobile thrombus or plaque in the aortic arch that was judged to potentially have caused their index stroke. Generally, the atherosclerotic patients were older and more likely to have dyslipidemia, hypertension, diabetes, coronary artery disease, and heart failure than were the patients with strokes of nonatherosclerotic origin. Atherosclerotic patients also were significantly more likely to have had a prior stroke or heart attack.
In the group with atherosclerosis, ticagrelor was significantly more effective at preventing the composite primary endpoint than was aspirin. There were 103 events in 1,542 patients in the ticagrelor group and 147 in 1,539 patients in the aspirin group (6.7% vs. 9.6%) – a “very impressive” risk reduction of 32% (HR, 0.68), Dr. Amarenco said.
In the group of patients without ipsilateral atherosclerotic stenosis, ticagrelor exerted no benefit over aspirin, with an event rate of 6.7% vs. 6.9% (HR, 0.97).
The rate of recurrent ischemic stroke was the driving force behind the significant between-group difference. Ischemic stroke occurred in 6.4% of those taking ticagrelor and 8.5% of those taking aspirin – a significant risk reduction of 27% (HR, 0.73). The drug exerted no benefit for recurrent ischemic stroke over aspirin in the group without atherosclerosis (5.8% vs. 6.1%; HR, 0.93).
There were no differences in the rate of heart attack or death, or in the secondary endpoints of all stroke, disabling stroke, or fatal stroke.
Ticagrelor was not associated with any major bleeding, compared with aspirin in either group, Dr. Amarenco noted.
The higher event rate in the patients with atherosclerosis is not surprising, he said.
“We had the exact same finding in our recent study with TIAregistry.org, which we found that patients with large artery atherosclerosis were at much higher risk than patients with other stroke subtypes.”
Dr. Amarenco disclosed financial relationships with numerous pharmaceutical companies, including AstraZeneca, which sponsored the study.
[email protected]
On Twitter @alz_gal
HOUSTON – Ticagrelor outperformed aspirin in preventing a combination of recurrent stroke, heart attack, and death – but only in patients whose index stroke was probably related to atherosclerosis.
The antiplatelet drug reduced the risk of the composite endpoint by 32%, compared with aspirin, in stroke patients with proven ipsilateral atherosclerotic stenosis (hazard ratio, 0.68). But ticagrelor (Brilinta) had no effect at all in those without stenosis (HR, 0.97), Pierre Amarenco, MD, said at the International Stroke Conference, sponsored by the American Heart Association.
The study was simultaneously published in Lancet Neurology (Lancet Neurol. 2017 Feb 23. doi: 10.1016/S1474-4422[17]30038-8). “The interaction that we found suggests what we already know in clinical practice: An understanding of stroke mechanisms and their causes is important to being able to deliver safe and effective treatment of early stroke prevention,” said Dr. Amarenco of Paris-Diderot Sorbonne University, Paris.
The findings come from a preplanned subgroup analysis of the large SOCRATES trial, published in 2016. The study determined that ticagrelor was no better than aspirin in preventing recurrent stroke, heart attack or death in patients who had a transient ischemic attack.
SOCRATES randomized 13,199 patients with a nonsevere ischemic stroke or high-risk transient ischemic attack to ticagrelor (180 mg loading dose on day 1 followed by 90 mg twice daily for days 2-90) or aspirin (300 mg on day 1 followed by 100 mg daily for days 2-90). The primary endpoint was the time to the occurrence of stroke, myocardial infarction, or death within 90 days.
The search for a potentially responsive group made sense, Dr. Amarenco said, because ticagrelor “is an effective antiplatelet therapy in patients with coronary atherosclerotic disease.” Therefore, investigators reasoned, it might be most effective in patients whose strokes were of atherosclerotic origin.
The substudy focused on 3,081 of the patients with proven ipsilateral atherosclerotic stenosis and/or a mobile thrombus or plaque in the aortic arch that was judged to potentially have caused their index stroke. Generally, the atherosclerotic patients were older and more likely to have dyslipidemia, hypertension, diabetes, coronary artery disease, and heart failure than were the patients with strokes of nonatherosclerotic origin. Atherosclerotic patients also were significantly more likely to have had a prior stroke or heart attack.
In the group with atherosclerosis, ticagrelor was significantly more effective at preventing the composite primary endpoint than was aspirin. There were 103 events in 1,542 patients in the ticagrelor group and 147 in 1,539 patients in the aspirin group (6.7% vs. 9.6%) – a “very impressive” risk reduction of 32% (HR, 0.68), Dr. Amarenco said.
In the group of patients without ipsilateral atherosclerotic stenosis, ticagrelor exerted no benefit over aspirin, with an event rate of 6.7% vs. 6.9% (HR, 0.97).
The rate of recurrent ischemic stroke was the driving force behind the significant between-group difference. Ischemic stroke occurred in 6.4% of those taking ticagrelor and 8.5% of those taking aspirin – a significant risk reduction of 27% (HR, 0.73). The drug exerted no benefit for recurrent ischemic stroke over aspirin in the group without atherosclerosis (5.8% vs. 6.1%; HR, 0.93).
There were no differences in the rate of heart attack or death, or in the secondary endpoints of all stroke, disabling stroke, or fatal stroke.
Ticagrelor was not associated with any major bleeding, compared with aspirin in either group, Dr. Amarenco noted.
The higher event rate in the patients with atherosclerosis is not surprising, he said.
“We had the exact same finding in our recent study with TIAregistry.org, which we found that patients with large artery atherosclerosis were at much higher risk than patients with other stroke subtypes.”
Dr. Amarenco disclosed financial relationships with numerous pharmaceutical companies, including AstraZeneca, which sponsored the study.
[email protected]
On Twitter @alz_gal
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point:
Major finding: The drug cut risk of a combination of recurrent stroke, heart attack, and death by 32% among these patients, but was not better than aspirin for patients without atherosclerosis.
Data source: The subanalysis of the SOCRATES trial, comprising 3,081 patients with atherosclerosis and 10,118 without.
Disclosures: Dr. Amarenco disclosed financial relationships with numerous pharmaceutical companies, including AstraZeneca, which sponsored the study.
rFVII didn’t improve hemorrhagic stroke outcomes in twin trials
HOUSTON – Acute hemostatic treatment with a clotting protein didn’t improve either short- or long-term outcomes in patients with intracerebral hemorrhage (ICH), according to findings from twin studies.
When given to patients who displayed a high-risk imaging marker suggestive of active bleeding, recombinant activated blood coagulation factor VII (rFVII) didn’t significantly reduce 24-hour hemorrhage volume or improve 90-day stroke outcomes, relative to placebo, David Gladstone, MD, said at the International Stroke Conference sponsored by the American Heart Association.
This isn’t the first time rFVII has been investigated as an acute treatment for ICH, said Dr. Gladstone, director of the Sunnybrook Regional Stroke Prevention Clinic and the Rapid Transient Ischemic Attack Clinic, Toronto. In the large phase III FAST trial, rFVII reduced growth of the hematoma but did not improve survival or functional outcome in an unselected population.
Their determination was the genesis of the two studies, SPOTLIGHT (Canada) and STOP-IT (United States), that Dr. Gladstone reported at the meeting.
Both studies stratified patients using the “spot sign,” a relatively new imaging biomarker thought to reflect active bleeding in the ICH hematoma. The hyperintense signal can be easily seen on cerebral angiography.
“It shows up like a flashlight as a bright spot in the margin of the hematoma,” Dr. Gladstone said. “When we see this, we know this patient has a possible active bleed that is likely to expand and get worse. They are at highest risk for ICH expansion and should be the best candidates for hemostatic therapy.”
Spot-negative patients, on the other hand, are at low risk for ICH expansion and would not benefit from hemostatic therapy, he said.
Both SPOTLIGHT and STOP-IT stratified their subjects by the presence of this sign. Spot-positive patients were randomized to placebo or to a single intravenous bolus of 80 mcg/kg rFVII given in the emergency department and within 6.5 hours of stroke onset. Spot-negative patients were enrolled in a prospective observational cohort, which provided data to support the sign’s use as a predictor of outcome.
In order to obtain the most focused patient population, the investigators imposed a number of exclusion criteria – a choice that may have contributed to the lackluster results, Dr. Gladstone noted. Exclusion criteria were brain stem ICH; ICH with secondary cause, such as a tumor or trauma; additional treatments such as plasma or prothrombin; acute coronary ischemia; history of other strokes, angioplasty, or stenting; past thrombotic events; a Glasgow Coma Scale of less than 8; or a modified Rankin Scale (mRS) score more than 2.
These stringent criteria, plus the uncommon nature of ICH events, compared with other cerebrovascular events, made recruitment a struggle, Dr. Gladstone said. After 6 years, the trials together managed to enroll only 69 spot-positive and 72 spot-negative patients. At that point, both studies were stopped because of the low numbers and because they had run out of money.
The studies’ primary efficacy endpoint was 24-hour ICH volume. Secondary outcomes were 24-hour total ICH plus intraventricular hemorrhage volumes, 90-day mRS of 5-6, and comparisons between the spot-negative and spot-positive groups. The primary safety outcome was acute myocardial infarction, ischemic stroke, or pulmonary embolism within 4 days of treatment.
Patients were a mean of about 70 years, although spot-positive patients were older than were spot-negative patients (71 years vs. 61 years). Spot-positive patients were also less likely to have a Glasgow coma score of 15-16 (56% vs. 66%). The National Institutes of Health Stroke Scale score was a mean of 16 in the spot-positive group and 10 in the spot-negative group. Intraventricular hemorrhage was also more common in the spot-positive group (44% vs. 18%).
After researchers adjusted for baseline ICH volume and onset-to-needle time, rFVII exerted no significant effect on either 24-hour ICH volume or 24-hour total volume.
In the treated group, median ICH volume increased from 16 mL at baseline to 22 mL by 24 hours. In the placebo group, it increased from 20 mL at baseline to 29 mL at 24 hours (between-group difference, P = 0.9).
In the treated group, the median total volume (ICH plus intraventricular hemorrhage) increased from 24 mL at baseline to 26 mL at 24 hours. In the placebo group, it increased from 25 mL at baseline to 31 mL at 24 hours later (between-group difference, P = .9).
There was no significant difference in the number of patients who had a volume increase of more than 6 mL or more than 33% (41% vs. 43%, respectively).
In contrast, spot-negative patients had lower baseline and 24-hour total hematoma volumes. In the spot-negative group, total volumes increased from a median of 13 mL at baseline to 14 mL at 24 hours. Significantly fewer spot-negative patients than spot-positive patients experienced hematoma growth of more than 6 mL or 33% (11% vs. 43%, respectively.)
However, the spot sign was a very good predictor of continued bleeding. In all spot-positive patients, median ICH volume expanded 9 mL over 24 hours (from 20 mL at baseline to 29 mL at 24 hours), compared with a median ICH expansion of only 1 mL over 24 hours (from 12 mL to 13 mL) for spot-negative patients.
There were no significant differences in 90-day mRS scores between the treated and placebo groups. One-fifth of each group (20%) had a score of 1-2, and one-fifth died. mRS scores of 3-5 were also similar between the groups.
Despite similar scores, other factors showed that the spot-negative patients did significantly better. Only 6% of this group died. More than a third (38%) had an mRS of 0-1 at 90 days.
Dr. Gladstone was not pleased about the treatment time intervals, which were prolonged, compared with those that have been achieved with antithrombotic therapy in ischemic stroke.
Time from stroke onset to the emergency department was similar in both spot-positive groups taking rFVIIa and spot-positive placebo patients (64 and 66 minutes, respectively). Onset-to-CT time was significantly longer in the rFVIIa patients than in placebo patients (89 vs. 83 minutes, respectively). Door-to-needle time also was longer in the rFVIIa patients than in the placebo patients (104 vs. 87 minutes, respectively), as was onset-to-needle time (195 vs. 161 minutes, respectively).
Only 37% of spot-positive patients receiving rFVIIa were treated in less than 3 hours – significantly less than the 65% that were treated that quickly in the spot-positive placebo group.
rFVII had a positive safety profile, with no significant events related to the study medication. No patient had a heart attack or pulmonary embolism within 4 days. An ischemic stroke developed in one patient in the placebo group. One patient had a possible thrombosis in the middle cerebral artery, but this was asymptomatic.
“What we are left with is that the spot sign predicted final ICH volume, but the magnitude of ICH expansion was small, less than we expected,” Dr. Gladstone said. “The median absolute ICH volume increase overall was only 2.5 mm, which is surprisingly small for this group of patients. And I do believe that treatment was administered too late, after most of the ICH expansion had already happened.”
Nonetheless, “there is much to learn here,” he said. “The biggest issue I think is that treatment was just too little, too late. We need to be catching these patients at a much earlier phase to make a difference, and that is probably the largest reason we didn’t see a difference.”
On the upside, the spot sign “was a statistically significant predictor of final ICH volumes,” Dr. Gladstone said. It’s an easy sign to catch, and it’s obvious on an imaging study that’s routinely acquired for stroke patients.
“We are also beginning to understand that there are many different types of spot signs associated with different kinds of bleeding at different times,” he noted. “We need to understand this variation further, and this should allow us to characterize the patients who are likely to be big bleeders.”
SPOTLIGHT was funded by the Canadian Institutes of Health Research, the Ontario Stroke Network, and the Ontario Ministry of Research, Innovation, and Science. STOP-IT was funded by the National Institute of Neurological Disorders and Stroke.
Dr. Gladstone had no financial disclosures.
[email protected]
On Twitter @alz_gal
HOUSTON – Acute hemostatic treatment with a clotting protein didn’t improve either short- or long-term outcomes in patients with intracerebral hemorrhage (ICH), according to findings from twin studies.
When given to patients who displayed a high-risk imaging marker suggestive of active bleeding, recombinant activated blood coagulation factor VII (rFVII) didn’t significantly reduce 24-hour hemorrhage volume or improve 90-day stroke outcomes, relative to placebo, David Gladstone, MD, said at the International Stroke Conference sponsored by the American Heart Association.
This isn’t the first time rFVII has been investigated as an acute treatment for ICH, said Dr. Gladstone, director of the Sunnybrook Regional Stroke Prevention Clinic and the Rapid Transient Ischemic Attack Clinic, Toronto. In the large phase III FAST trial, rFVII reduced growth of the hematoma but did not improve survival or functional outcome in an unselected population.
Their determination was the genesis of the two studies, SPOTLIGHT (Canada) and STOP-IT (United States), that Dr. Gladstone reported at the meeting.
Both studies stratified patients using the “spot sign,” a relatively new imaging biomarker thought to reflect active bleeding in the ICH hematoma. The hyperintense signal can be easily seen on cerebral angiography.
“It shows up like a flashlight as a bright spot in the margin of the hematoma,” Dr. Gladstone said. “When we see this, we know this patient has a possible active bleed that is likely to expand and get worse. They are at highest risk for ICH expansion and should be the best candidates for hemostatic therapy.”
Spot-negative patients, on the other hand, are at low risk for ICH expansion and would not benefit from hemostatic therapy, he said.
Both SPOTLIGHT and STOP-IT stratified their subjects by the presence of this sign. Spot-positive patients were randomized to placebo or to a single intravenous bolus of 80 mcg/kg rFVII given in the emergency department and within 6.5 hours of stroke onset. Spot-negative patients were enrolled in a prospective observational cohort, which provided data to support the sign’s use as a predictor of outcome.
In order to obtain the most focused patient population, the investigators imposed a number of exclusion criteria – a choice that may have contributed to the lackluster results, Dr. Gladstone noted. Exclusion criteria were brain stem ICH; ICH with secondary cause, such as a tumor or trauma; additional treatments such as plasma or prothrombin; acute coronary ischemia; history of other strokes, angioplasty, or stenting; past thrombotic events; a Glasgow Coma Scale of less than 8; or a modified Rankin Scale (mRS) score more than 2.
These stringent criteria, plus the uncommon nature of ICH events, compared with other cerebrovascular events, made recruitment a struggle, Dr. Gladstone said. After 6 years, the trials together managed to enroll only 69 spot-positive and 72 spot-negative patients. At that point, both studies were stopped because of the low numbers and because they had run out of money.
The studies’ primary efficacy endpoint was 24-hour ICH volume. Secondary outcomes were 24-hour total ICH plus intraventricular hemorrhage volumes, 90-day mRS of 5-6, and comparisons between the spot-negative and spot-positive groups. The primary safety outcome was acute myocardial infarction, ischemic stroke, or pulmonary embolism within 4 days of treatment.
Patients were a mean of about 70 years, although spot-positive patients were older than were spot-negative patients (71 years vs. 61 years). Spot-positive patients were also less likely to have a Glasgow coma score of 15-16 (56% vs. 66%). The National Institutes of Health Stroke Scale score was a mean of 16 in the spot-positive group and 10 in the spot-negative group. Intraventricular hemorrhage was also more common in the spot-positive group (44% vs. 18%).
After researchers adjusted for baseline ICH volume and onset-to-needle time, rFVII exerted no significant effect on either 24-hour ICH volume or 24-hour total volume.
In the treated group, median ICH volume increased from 16 mL at baseline to 22 mL by 24 hours. In the placebo group, it increased from 20 mL at baseline to 29 mL at 24 hours (between-group difference, P = 0.9).
In the treated group, the median total volume (ICH plus intraventricular hemorrhage) increased from 24 mL at baseline to 26 mL at 24 hours. In the placebo group, it increased from 25 mL at baseline to 31 mL at 24 hours later (between-group difference, P = .9).
There was no significant difference in the number of patients who had a volume increase of more than 6 mL or more than 33% (41% vs. 43%, respectively).
In contrast, spot-negative patients had lower baseline and 24-hour total hematoma volumes. In the spot-negative group, total volumes increased from a median of 13 mL at baseline to 14 mL at 24 hours. Significantly fewer spot-negative patients than spot-positive patients experienced hematoma growth of more than 6 mL or 33% (11% vs. 43%, respectively.)
However, the spot sign was a very good predictor of continued bleeding. In all spot-positive patients, median ICH volume expanded 9 mL over 24 hours (from 20 mL at baseline to 29 mL at 24 hours), compared with a median ICH expansion of only 1 mL over 24 hours (from 12 mL to 13 mL) for spot-negative patients.
There were no significant differences in 90-day mRS scores between the treated and placebo groups. One-fifth of each group (20%) had a score of 1-2, and one-fifth died. mRS scores of 3-5 were also similar between the groups.
Despite similar scores, other factors showed that the spot-negative patients did significantly better. Only 6% of this group died. More than a third (38%) had an mRS of 0-1 at 90 days.
Dr. Gladstone was not pleased about the treatment time intervals, which were prolonged, compared with those that have been achieved with antithrombotic therapy in ischemic stroke.
Time from stroke onset to the emergency department was similar in both spot-positive groups taking rFVIIa and spot-positive placebo patients (64 and 66 minutes, respectively). Onset-to-CT time was significantly longer in the rFVIIa patients than in placebo patients (89 vs. 83 minutes, respectively). Door-to-needle time also was longer in the rFVIIa patients than in the placebo patients (104 vs. 87 minutes, respectively), as was onset-to-needle time (195 vs. 161 minutes, respectively).
Only 37% of spot-positive patients receiving rFVIIa were treated in less than 3 hours – significantly less than the 65% that were treated that quickly in the spot-positive placebo group.
rFVII had a positive safety profile, with no significant events related to the study medication. No patient had a heart attack or pulmonary embolism within 4 days. An ischemic stroke developed in one patient in the placebo group. One patient had a possible thrombosis in the middle cerebral artery, but this was asymptomatic.
“What we are left with is that the spot sign predicted final ICH volume, but the magnitude of ICH expansion was small, less than we expected,” Dr. Gladstone said. “The median absolute ICH volume increase overall was only 2.5 mm, which is surprisingly small for this group of patients. And I do believe that treatment was administered too late, after most of the ICH expansion had already happened.”
Nonetheless, “there is much to learn here,” he said. “The biggest issue I think is that treatment was just too little, too late. We need to be catching these patients at a much earlier phase to make a difference, and that is probably the largest reason we didn’t see a difference.”
On the upside, the spot sign “was a statistically significant predictor of final ICH volumes,” Dr. Gladstone said. It’s an easy sign to catch, and it’s obvious on an imaging study that’s routinely acquired for stroke patients.
“We are also beginning to understand that there are many different types of spot signs associated with different kinds of bleeding at different times,” he noted. “We need to understand this variation further, and this should allow us to characterize the patients who are likely to be big bleeders.”
SPOTLIGHT was funded by the Canadian Institutes of Health Research, the Ontario Stroke Network, and the Ontario Ministry of Research, Innovation, and Science. STOP-IT was funded by the National Institute of Neurological Disorders and Stroke.
Dr. Gladstone had no financial disclosures.
[email protected]
On Twitter @alz_gal
HOUSTON – Acute hemostatic treatment with a clotting protein didn’t improve either short- or long-term outcomes in patients with intracerebral hemorrhage (ICH), according to findings from twin studies.
When given to patients who displayed a high-risk imaging marker suggestive of active bleeding, recombinant activated blood coagulation factor VII (rFVII) didn’t significantly reduce 24-hour hemorrhage volume or improve 90-day stroke outcomes, relative to placebo, David Gladstone, MD, said at the International Stroke Conference sponsored by the American Heart Association.
This isn’t the first time rFVII has been investigated as an acute treatment for ICH, said Dr. Gladstone, director of the Sunnybrook Regional Stroke Prevention Clinic and the Rapid Transient Ischemic Attack Clinic, Toronto. In the large phase III FAST trial, rFVII reduced growth of the hematoma but did not improve survival or functional outcome in an unselected population.
Their determination was the genesis of the two studies, SPOTLIGHT (Canada) and STOP-IT (United States), that Dr. Gladstone reported at the meeting.
Both studies stratified patients using the “spot sign,” a relatively new imaging biomarker thought to reflect active bleeding in the ICH hematoma. The hyperintense signal can be easily seen on cerebral angiography.
“It shows up like a flashlight as a bright spot in the margin of the hematoma,” Dr. Gladstone said. “When we see this, we know this patient has a possible active bleed that is likely to expand and get worse. They are at highest risk for ICH expansion and should be the best candidates for hemostatic therapy.”
Spot-negative patients, on the other hand, are at low risk for ICH expansion and would not benefit from hemostatic therapy, he said.
Both SPOTLIGHT and STOP-IT stratified their subjects by the presence of this sign. Spot-positive patients were randomized to placebo or to a single intravenous bolus of 80 mcg/kg rFVII given in the emergency department and within 6.5 hours of stroke onset. Spot-negative patients were enrolled in a prospective observational cohort, which provided data to support the sign’s use as a predictor of outcome.
In order to obtain the most focused patient population, the investigators imposed a number of exclusion criteria – a choice that may have contributed to the lackluster results, Dr. Gladstone noted. Exclusion criteria were brain stem ICH; ICH with secondary cause, such as a tumor or trauma; additional treatments such as plasma or prothrombin; acute coronary ischemia; history of other strokes, angioplasty, or stenting; past thrombotic events; a Glasgow Coma Scale of less than 8; or a modified Rankin Scale (mRS) score more than 2.
These stringent criteria, plus the uncommon nature of ICH events, compared with other cerebrovascular events, made recruitment a struggle, Dr. Gladstone said. After 6 years, the trials together managed to enroll only 69 spot-positive and 72 spot-negative patients. At that point, both studies were stopped because of the low numbers and because they had run out of money.
The studies’ primary efficacy endpoint was 24-hour ICH volume. Secondary outcomes were 24-hour total ICH plus intraventricular hemorrhage volumes, 90-day mRS of 5-6, and comparisons between the spot-negative and spot-positive groups. The primary safety outcome was acute myocardial infarction, ischemic stroke, or pulmonary embolism within 4 days of treatment.
Patients were a mean of about 70 years, although spot-positive patients were older than were spot-negative patients (71 years vs. 61 years). Spot-positive patients were also less likely to have a Glasgow coma score of 15-16 (56% vs. 66%). The National Institutes of Health Stroke Scale score was a mean of 16 in the spot-positive group and 10 in the spot-negative group. Intraventricular hemorrhage was also more common in the spot-positive group (44% vs. 18%).
After researchers adjusted for baseline ICH volume and onset-to-needle time, rFVII exerted no significant effect on either 24-hour ICH volume or 24-hour total volume.
In the treated group, median ICH volume increased from 16 mL at baseline to 22 mL by 24 hours. In the placebo group, it increased from 20 mL at baseline to 29 mL at 24 hours (between-group difference, P = 0.9).
In the treated group, the median total volume (ICH plus intraventricular hemorrhage) increased from 24 mL at baseline to 26 mL at 24 hours. In the placebo group, it increased from 25 mL at baseline to 31 mL at 24 hours later (between-group difference, P = .9).
There was no significant difference in the number of patients who had a volume increase of more than 6 mL or more than 33% (41% vs. 43%, respectively).
In contrast, spot-negative patients had lower baseline and 24-hour total hematoma volumes. In the spot-negative group, total volumes increased from a median of 13 mL at baseline to 14 mL at 24 hours. Significantly fewer spot-negative patients than spot-positive patients experienced hematoma growth of more than 6 mL or 33% (11% vs. 43%, respectively.)
However, the spot sign was a very good predictor of continued bleeding. In all spot-positive patients, median ICH volume expanded 9 mL over 24 hours (from 20 mL at baseline to 29 mL at 24 hours), compared with a median ICH expansion of only 1 mL over 24 hours (from 12 mL to 13 mL) for spot-negative patients.
There were no significant differences in 90-day mRS scores between the treated and placebo groups. One-fifth of each group (20%) had a score of 1-2, and one-fifth died. mRS scores of 3-5 were also similar between the groups.
Despite similar scores, other factors showed that the spot-negative patients did significantly better. Only 6% of this group died. More than a third (38%) had an mRS of 0-1 at 90 days.
Dr. Gladstone was not pleased about the treatment time intervals, which were prolonged, compared with those that have been achieved with antithrombotic therapy in ischemic stroke.
Time from stroke onset to the emergency department was similar in both spot-positive groups taking rFVIIa and spot-positive placebo patients (64 and 66 minutes, respectively). Onset-to-CT time was significantly longer in the rFVIIa patients than in placebo patients (89 vs. 83 minutes, respectively). Door-to-needle time also was longer in the rFVIIa patients than in the placebo patients (104 vs. 87 minutes, respectively), as was onset-to-needle time (195 vs. 161 minutes, respectively).
Only 37% of spot-positive patients receiving rFVIIa were treated in less than 3 hours – significantly less than the 65% that were treated that quickly in the spot-positive placebo group.
rFVII had a positive safety profile, with no significant events related to the study medication. No patient had a heart attack or pulmonary embolism within 4 days. An ischemic stroke developed in one patient in the placebo group. One patient had a possible thrombosis in the middle cerebral artery, but this was asymptomatic.
“What we are left with is that the spot sign predicted final ICH volume, but the magnitude of ICH expansion was small, less than we expected,” Dr. Gladstone said. “The median absolute ICH volume increase overall was only 2.5 mm, which is surprisingly small for this group of patients. And I do believe that treatment was administered too late, after most of the ICH expansion had already happened.”
Nonetheless, “there is much to learn here,” he said. “The biggest issue I think is that treatment was just too little, too late. We need to be catching these patients at a much earlier phase to make a difference, and that is probably the largest reason we didn’t see a difference.”
On the upside, the spot sign “was a statistically significant predictor of final ICH volumes,” Dr. Gladstone said. It’s an easy sign to catch, and it’s obvious on an imaging study that’s routinely acquired for stroke patients.
“We are also beginning to understand that there are many different types of spot signs associated with different kinds of bleeding at different times,” he noted. “We need to understand this variation further, and this should allow us to characterize the patients who are likely to be big bleeders.”
SPOTLIGHT was funded by the Canadian Institutes of Health Research, the Ontario Stroke Network, and the Ontario Ministry of Research, Innovation, and Science. STOP-IT was funded by the National Institute of Neurological Disorders and Stroke.
Dr. Gladstone had no financial disclosures.
[email protected]
On Twitter @alz_gal
Key clinical point:
Major finding: In the treated group, median ICH volume increased from 16 mL at baseline to 22 mL at 24 hours. In the placebo group, it increased from 20 mL to 29 mL (between-group difference, P = .9).
Data source: SPOTLIGHT and STOP-IT enrolled 141 patients.
Disclosures: SPOTLIGHT was funded by the Canadian Institutes of Health Research, the Ontario Stroke Network, and the Ontario Ministry of Research, Innovation, and Science. STOP-IT was funded by the National Institute of Neurological Disorders and Stroke.
Hydrogel coils improve outcomes in medium-sized intracranial aneurysms
HOUSTON – Hydrogel coils significantly outperformed bare platinum coils in treating patients with medium-sized intracranial aneurysms, reducing the incidence of adverse outcomes by about 9% in an open-label, randomized trial.
Compared against the platinum coils, the self-expandable, hydrophilic coils scored significantly better on a composite endpoint of aneurysm recurrence at 18 months, re-treatment by 18 months, serious morbidity that prevented angiographic follow-up, and death, Christian Taschner, MD, said at the International Stroke Conference sponsored by the America Heart Association.
These are the company’s second-generation products, said Dr. Taschner, a neuroradiologist at University Hospital Freiburg (Germany). The initial hydrogel-coated coils were not well received because they were too stiff, he said in an interview.
The 18-month study comprised 513 patients and was conducted in 15 centers in France and 7 in Germany. Patients with medium-sized aneurysms (4-12 mm) were randomized to coiling with either the hydrogel coils or bare platinum coils and followed for 18 months. The cohort was stratified by rupture status in the analysis.
Angiographic images of the aneurysm were obtained before treatment, immediately after treatment, at 6 months, and at 18 months. All images were reviewed by an independent laboratory that was blinded to the treatment.
In addition to the primary composite outcome, the study assessed secondary endpoints of modified Rankin Scale (mRS) score at 18 months and coil packing density.
The final analysis included 484 patients. They were a mean of 52 years old, and about 70% were women. The aneurysms were ruptured at baseline in about 43% of cases. The mean aneurysm size was 7 mm, and the mean neck size, 3.5 mm. The dome-to-neck ratio was less than 1.5 in about a third of the group. Most lesions (89%) had anterior circulation.
Most patients needed some kind of adjunctive endovascular-assisting device during the procedure. These included balloon remodeling, which was necessary in about 50% of cases to help keep the coils from extruding into the parent vessel, and stents in 22%.
Intraoperative adverse events were uncommon in both groups. They were numerically, but not significantly, less common in the hydrogel group. These included thromboembolism (8 vs. 12), intraoperative rupture (3 vs. 7), parent vessel occlusion (1 vs. 3), and vessel perforation (one in each group). There were no vessel dissections.
By 18 months, 20% of the hydrogel group and 29% of the platinum coil group had experienced the composite primary endpoint. The 9% absolute difference was statistically significant. It was largely driven by the subcomponents of major recurrence (12% vs. 18%) and re-treatment (3% vs. 6%).
An mRS of 3-5 was used as the proxy for patients whose clinical status prevented them from having angiographic follow-up. That endpoint occurred in three patients in the hydrogel group but in none of the platinum coil group. Dr. Taschner said that difference was not statistically significant.
In an analysis that stratified by baseline rupture status and by aneurysm size, the hydrogel coils were largely superior to bare platinum. However, the hydrogel coils were not significantly more effective than the platinum coils for aneurysms 10 mm or larger, Dr. Taschner noted.
There was no significant difference in the secondary endpoint of mRS at 18 months. Most patients (85% vs. 86%) did well, with an mRS of 0. Scores of 1-2 were seen in 9% of each group. An mRS of 3-5 occurred in 3% of the hydrogel group and 1% of the platinum coil group. There were 17 deaths: 7 in the hydrogel group and 10 in the platinum coil group (3% vs. 4%). This was not a significant difference.
Patients whose aneurysms were unruptured at baseline did significantly better than did those with ruptured lesions, although the mRS scores did not vary significantly between treatment groups. Among those with intact lesions, 90% of the hydrogel and 94% of the platinum coil group achieved an mRS of 0, and 2% of each group died. Among those with ruptured lesions at baseline, 78% of the hydrogel group and 75% of the platinum coil group achieved an mRS of 0. Five patients in the hydrogel group and seven in the platinum coil group died.
On the technical outcome of coil volume, hydrogel did somewhat better (0.041 cm3 vs. 0.038 cm3). The mean packing density was significantly higher (39% vs. 31%).
Dr. Taschner said the study provides good support for using the hydrogel coils in medium-sized aneurysms, and that other recent data reaffirm this.
“A recent trial in Canada and the U.S. looked at hydrogel coils in aneurysms 12 mm or larger, with broad necks, and it failed to show a benefit of the hydrogel coils.”
Additionally, a study published in January found that hydrogel coils were no better than platinum coils in 250 patients with large or recurrent aneurysms (AJNR Am J Neuroradiol. 2017 Jan 12. doi: 10.3174/ajnr.A5101).
“I myself would use them in medium-sized aneurysms with an unfavorable dome-to-neck ratio, and in those that have a broad neck. In those instances, I do think that hydrogel coils have their place. I wouldn’t use them in really large aneurysms. I don’t think they are well suited for that. In those cases, I would probably use platinum coils in combination with a flow diverter. That really provides very stable aneurysm occlusion with acceptable complication rates.”
Dr. Taschner said that he received research support from MicroVention during the study.
[email protected]
On Twitter @alz_gal
HOUSTON – Hydrogel coils significantly outperformed bare platinum coils in treating patients with medium-sized intracranial aneurysms, reducing the incidence of adverse outcomes by about 9% in an open-label, randomized trial.
Compared against the platinum coils, the self-expandable, hydrophilic coils scored significantly better on a composite endpoint of aneurysm recurrence at 18 months, re-treatment by 18 months, serious morbidity that prevented angiographic follow-up, and death, Christian Taschner, MD, said at the International Stroke Conference sponsored by the America Heart Association.
These are the company’s second-generation products, said Dr. Taschner, a neuroradiologist at University Hospital Freiburg (Germany). The initial hydrogel-coated coils were not well received because they were too stiff, he said in an interview.
The 18-month study comprised 513 patients and was conducted in 15 centers in France and 7 in Germany. Patients with medium-sized aneurysms (4-12 mm) were randomized to coiling with either the hydrogel coils or bare platinum coils and followed for 18 months. The cohort was stratified by rupture status in the analysis.
Angiographic images of the aneurysm were obtained before treatment, immediately after treatment, at 6 months, and at 18 months. All images were reviewed by an independent laboratory that was blinded to the treatment.
In addition to the primary composite outcome, the study assessed secondary endpoints of modified Rankin Scale (mRS) score at 18 months and coil packing density.
The final analysis included 484 patients. They were a mean of 52 years old, and about 70% were women. The aneurysms were ruptured at baseline in about 43% of cases. The mean aneurysm size was 7 mm, and the mean neck size, 3.5 mm. The dome-to-neck ratio was less than 1.5 in about a third of the group. Most lesions (89%) had anterior circulation.
Most patients needed some kind of adjunctive endovascular-assisting device during the procedure. These included balloon remodeling, which was necessary in about 50% of cases to help keep the coils from extruding into the parent vessel, and stents in 22%.
Intraoperative adverse events were uncommon in both groups. They were numerically, but not significantly, less common in the hydrogel group. These included thromboembolism (8 vs. 12), intraoperative rupture (3 vs. 7), parent vessel occlusion (1 vs. 3), and vessel perforation (one in each group). There were no vessel dissections.
By 18 months, 20% of the hydrogel group and 29% of the platinum coil group had experienced the composite primary endpoint. The 9% absolute difference was statistically significant. It was largely driven by the subcomponents of major recurrence (12% vs. 18%) and re-treatment (3% vs. 6%).
An mRS of 3-5 was used as the proxy for patients whose clinical status prevented them from having angiographic follow-up. That endpoint occurred in three patients in the hydrogel group but in none of the platinum coil group. Dr. Taschner said that difference was not statistically significant.
In an analysis that stratified by baseline rupture status and by aneurysm size, the hydrogel coils were largely superior to bare platinum. However, the hydrogel coils were not significantly more effective than the platinum coils for aneurysms 10 mm or larger, Dr. Taschner noted.
There was no significant difference in the secondary endpoint of mRS at 18 months. Most patients (85% vs. 86%) did well, with an mRS of 0. Scores of 1-2 were seen in 9% of each group. An mRS of 3-5 occurred in 3% of the hydrogel group and 1% of the platinum coil group. There were 17 deaths: 7 in the hydrogel group and 10 in the platinum coil group (3% vs. 4%). This was not a significant difference.
Patients whose aneurysms were unruptured at baseline did significantly better than did those with ruptured lesions, although the mRS scores did not vary significantly between treatment groups. Among those with intact lesions, 90% of the hydrogel and 94% of the platinum coil group achieved an mRS of 0, and 2% of each group died. Among those with ruptured lesions at baseline, 78% of the hydrogel group and 75% of the platinum coil group achieved an mRS of 0. Five patients in the hydrogel group and seven in the platinum coil group died.
On the technical outcome of coil volume, hydrogel did somewhat better (0.041 cm3 vs. 0.038 cm3). The mean packing density was significantly higher (39% vs. 31%).
Dr. Taschner said the study provides good support for using the hydrogel coils in medium-sized aneurysms, and that other recent data reaffirm this.
“A recent trial in Canada and the U.S. looked at hydrogel coils in aneurysms 12 mm or larger, with broad necks, and it failed to show a benefit of the hydrogel coils.”
Additionally, a study published in January found that hydrogel coils were no better than platinum coils in 250 patients with large or recurrent aneurysms (AJNR Am J Neuroradiol. 2017 Jan 12. doi: 10.3174/ajnr.A5101).
“I myself would use them in medium-sized aneurysms with an unfavorable dome-to-neck ratio, and in those that have a broad neck. In those instances, I do think that hydrogel coils have their place. I wouldn’t use them in really large aneurysms. I don’t think they are well suited for that. In those cases, I would probably use platinum coils in combination with a flow diverter. That really provides very stable aneurysm occlusion with acceptable complication rates.”
Dr. Taschner said that he received research support from MicroVention during the study.
[email protected]
On Twitter @alz_gal
HOUSTON – Hydrogel coils significantly outperformed bare platinum coils in treating patients with medium-sized intracranial aneurysms, reducing the incidence of adverse outcomes by about 9% in an open-label, randomized trial.
Compared against the platinum coils, the self-expandable, hydrophilic coils scored significantly better on a composite endpoint of aneurysm recurrence at 18 months, re-treatment by 18 months, serious morbidity that prevented angiographic follow-up, and death, Christian Taschner, MD, said at the International Stroke Conference sponsored by the America Heart Association.
These are the company’s second-generation products, said Dr. Taschner, a neuroradiologist at University Hospital Freiburg (Germany). The initial hydrogel-coated coils were not well received because they were too stiff, he said in an interview.
The 18-month study comprised 513 patients and was conducted in 15 centers in France and 7 in Germany. Patients with medium-sized aneurysms (4-12 mm) were randomized to coiling with either the hydrogel coils or bare platinum coils and followed for 18 months. The cohort was stratified by rupture status in the analysis.
Angiographic images of the aneurysm were obtained before treatment, immediately after treatment, at 6 months, and at 18 months. All images were reviewed by an independent laboratory that was blinded to the treatment.
In addition to the primary composite outcome, the study assessed secondary endpoints of modified Rankin Scale (mRS) score at 18 months and coil packing density.
The final analysis included 484 patients. They were a mean of 52 years old, and about 70% were women. The aneurysms were ruptured at baseline in about 43% of cases. The mean aneurysm size was 7 mm, and the mean neck size, 3.5 mm. The dome-to-neck ratio was less than 1.5 in about a third of the group. Most lesions (89%) had anterior circulation.
Most patients needed some kind of adjunctive endovascular-assisting device during the procedure. These included balloon remodeling, which was necessary in about 50% of cases to help keep the coils from extruding into the parent vessel, and stents in 22%.
Intraoperative adverse events were uncommon in both groups. They were numerically, but not significantly, less common in the hydrogel group. These included thromboembolism (8 vs. 12), intraoperative rupture (3 vs. 7), parent vessel occlusion (1 vs. 3), and vessel perforation (one in each group). There were no vessel dissections.
By 18 months, 20% of the hydrogel group and 29% of the platinum coil group had experienced the composite primary endpoint. The 9% absolute difference was statistically significant. It was largely driven by the subcomponents of major recurrence (12% vs. 18%) and re-treatment (3% vs. 6%).
An mRS of 3-5 was used as the proxy for patients whose clinical status prevented them from having angiographic follow-up. That endpoint occurred in three patients in the hydrogel group but in none of the platinum coil group. Dr. Taschner said that difference was not statistically significant.
In an analysis that stratified by baseline rupture status and by aneurysm size, the hydrogel coils were largely superior to bare platinum. However, the hydrogel coils were not significantly more effective than the platinum coils for aneurysms 10 mm or larger, Dr. Taschner noted.
There was no significant difference in the secondary endpoint of mRS at 18 months. Most patients (85% vs. 86%) did well, with an mRS of 0. Scores of 1-2 were seen in 9% of each group. An mRS of 3-5 occurred in 3% of the hydrogel group and 1% of the platinum coil group. There were 17 deaths: 7 in the hydrogel group and 10 in the platinum coil group (3% vs. 4%). This was not a significant difference.
Patients whose aneurysms were unruptured at baseline did significantly better than did those with ruptured lesions, although the mRS scores did not vary significantly between treatment groups. Among those with intact lesions, 90% of the hydrogel and 94% of the platinum coil group achieved an mRS of 0, and 2% of each group died. Among those with ruptured lesions at baseline, 78% of the hydrogel group and 75% of the platinum coil group achieved an mRS of 0. Five patients in the hydrogel group and seven in the platinum coil group died.
On the technical outcome of coil volume, hydrogel did somewhat better (0.041 cm3 vs. 0.038 cm3). The mean packing density was significantly higher (39% vs. 31%).
Dr. Taschner said the study provides good support for using the hydrogel coils in medium-sized aneurysms, and that other recent data reaffirm this.
“A recent trial in Canada and the U.S. looked at hydrogel coils in aneurysms 12 mm or larger, with broad necks, and it failed to show a benefit of the hydrogel coils.”
Additionally, a study published in January found that hydrogel coils were no better than platinum coils in 250 patients with large or recurrent aneurysms (AJNR Am J Neuroradiol. 2017 Jan 12. doi: 10.3174/ajnr.A5101).
“I myself would use them in medium-sized aneurysms with an unfavorable dome-to-neck ratio, and in those that have a broad neck. In those instances, I do think that hydrogel coils have their place. I wouldn’t use them in really large aneurysms. I don’t think they are well suited for that. In those cases, I would probably use platinum coils in combination with a flow diverter. That really provides very stable aneurysm occlusion with acceptable complication rates.”
Dr. Taschner said that he received research support from MicroVention during the study.
[email protected]
On Twitter @alz_gal
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point:
Major finding: Compared with bare-metal coils, hydrogel coils reduced by 9% the incidence of a composite primary outcome of recurrence, re-treatment, morbidity, and death.
Data source: An 18-month, open-label, randomized study of 513 patients.
Disclosures: MicroVention sponsored the study. Dr. Taschner said that he received research support from the company during the study.
Anticoagulant resumption after ICH aids patients
HOUSTON – Even when patients on an oral anticoagulant have the dreaded complication of an intracerebral hemorrhage, resumption of their oral anticoagulation regimen appears to produce the best midterm outcomes, based on a meta-analysis of data from more than 1,000 patients collected in three observational studies.
Resumption of oral anticoagulation therapy (OAT) is a “major dilemma” when managing patients who developed an intracerebral hemorrhage (ICH) while on OAT, said Alessandro Biffi, MD, explaining why he performed this meta-analysis that he presented at the International Stroke Conference sponsored by the American Heart Association.
He used individual patient data collected from a total of 1,027 patients enrolled in any of three different observational studies: the German-wide Multicenter Analysis of Oral Anticoagulation Associated Intracerebral Hemorrhage (RETRACE) study, the MGH longitudinal ICH study, or the Ethnic/Racial Variations of Intracerebral Hemorrhage (ERICH) study. Overall 26% of the patients resumed OAT following their ICH, although the rate ranged from a low of 20% in one study to a high of 42% in another. The vast majority of patients received a vitamin K antagonist as their anticoagulant; very few received a new oral anticoagulant.
Using propensity score matching to compare similar patients who resumed or stayed off OAT, Dr. Biffi found that, during the year following the index ICH, mortality was 71%-74% lower among patients who resumed OAT. Recurrent all-cause stroke was 49%-55% lower with resumed OAT, and favorable functional outcomes (a score of 0-3 on the modified Rankin scale) were more than fourfold higher with OAT resumption, he reported.
Dr. Biffi calculated these relative rates, both for patients with a lumbar location of their ICH and for those with a nonlumbar location, and found that location had no influence on responsiveness to OAT. Patients with an index ICH in a lumbar location had a trend toward more recurrent ICH on OAT, a 26% higher rate relative to patients not resumed on OAT, but this difference fell short of statistical significance.
The only factor he found that linked with whether or not patients resumed OAT was the severity of their index ICH. The more severe their bleed, the less likely were patients to resume. Aside from that, “there is a lot of variation in practice,” he said. “We are gathering additional data” to try to further address this question.
Dr. Biffi had no disclosures.
[email protected]
On Twitter @mitchelzoler
Resuming oral anticoagulation following an intracerebral hemorrhage is one of the most vexing problems today in vascular neurology. It’s a situation that often happens, and it will grow increasingly more common as the number of patients with atrial fibrillation escalates and even more people start oral anticoagulation.
It’s also very important to remember that patients like these who need oral anticoagulation but now have a history of ICH must have all their other cardiovascular disease risk factors very well controlled: their blood pressure, their diabetes, their smoking, etc. Oral anticoagulation may be important for these patients, but tight risk factor control is even more important.
I agree with Dr. Biffi that a prospective, randomized trial is the best way to get more information to help guide resuming oral anticoagulation. Observational studies are significantly limited by ascertainment bias, and for these patients there are also many variables – at least a dozen – that can influence whether or not a patient resumes oral anticoagulation. Dr. Biffi’s findings are interesting, but the limitations of his data prevent the results from being truly compelling.
It would be very helpful to have data from a trial that randomized ICH patients who required anticoagulation to a full-dose NOAC, a reduced-dose NOAC, or aspirin and see which group had the best long-term outcome. Whatever the results, it would change practice. It’s intriguing to speculate that a reduced-dose NOAC might provide adequate ischemic protection with a reduced risk for more bleeding.
Mark J. Alberts, MD , is chief of neurology at Hartford (Conn.) Hospital. He had no disclosures. He made these comments in an interview and during a press conference.
Resuming oral anticoagulation following an intracerebral hemorrhage is one of the most vexing problems today in vascular neurology. It’s a situation that often happens, and it will grow increasingly more common as the number of patients with atrial fibrillation escalates and even more people start oral anticoagulation.
It’s also very important to remember that patients like these who need oral anticoagulation but now have a history of ICH must have all their other cardiovascular disease risk factors very well controlled: their blood pressure, their diabetes, their smoking, etc. Oral anticoagulation may be important for these patients, but tight risk factor control is even more important.
I agree with Dr. Biffi that a prospective, randomized trial is the best way to get more information to help guide resuming oral anticoagulation. Observational studies are significantly limited by ascertainment bias, and for these patients there are also many variables – at least a dozen – that can influence whether or not a patient resumes oral anticoagulation. Dr. Biffi’s findings are interesting, but the limitations of his data prevent the results from being truly compelling.
It would be very helpful to have data from a trial that randomized ICH patients who required anticoagulation to a full-dose NOAC, a reduced-dose NOAC, or aspirin and see which group had the best long-term outcome. Whatever the results, it would change practice. It’s intriguing to speculate that a reduced-dose NOAC might provide adequate ischemic protection with a reduced risk for more bleeding.
Mark J. Alberts, MD , is chief of neurology at Hartford (Conn.) Hospital. He had no disclosures. He made these comments in an interview and during a press conference.
Resuming oral anticoagulation following an intracerebral hemorrhage is one of the most vexing problems today in vascular neurology. It’s a situation that often happens, and it will grow increasingly more common as the number of patients with atrial fibrillation escalates and even more people start oral anticoagulation.
It’s also very important to remember that patients like these who need oral anticoagulation but now have a history of ICH must have all their other cardiovascular disease risk factors very well controlled: their blood pressure, their diabetes, their smoking, etc. Oral anticoagulation may be important for these patients, but tight risk factor control is even more important.
I agree with Dr. Biffi that a prospective, randomized trial is the best way to get more information to help guide resuming oral anticoagulation. Observational studies are significantly limited by ascertainment bias, and for these patients there are also many variables – at least a dozen – that can influence whether or not a patient resumes oral anticoagulation. Dr. Biffi’s findings are interesting, but the limitations of his data prevent the results from being truly compelling.
It would be very helpful to have data from a trial that randomized ICH patients who required anticoagulation to a full-dose NOAC, a reduced-dose NOAC, or aspirin and see which group had the best long-term outcome. Whatever the results, it would change practice. It’s intriguing to speculate that a reduced-dose NOAC might provide adequate ischemic protection with a reduced risk for more bleeding.
Mark J. Alberts, MD , is chief of neurology at Hartford (Conn.) Hospital. He had no disclosures. He made these comments in an interview and during a press conference.
HOUSTON – Even when patients on an oral anticoagulant have the dreaded complication of an intracerebral hemorrhage, resumption of their oral anticoagulation regimen appears to produce the best midterm outcomes, based on a meta-analysis of data from more than 1,000 patients collected in three observational studies.
Resumption of oral anticoagulation therapy (OAT) is a “major dilemma” when managing patients who developed an intracerebral hemorrhage (ICH) while on OAT, said Alessandro Biffi, MD, explaining why he performed this meta-analysis that he presented at the International Stroke Conference sponsored by the American Heart Association.
He used individual patient data collected from a total of 1,027 patients enrolled in any of three different observational studies: the German-wide Multicenter Analysis of Oral Anticoagulation Associated Intracerebral Hemorrhage (RETRACE) study, the MGH longitudinal ICH study, or the Ethnic/Racial Variations of Intracerebral Hemorrhage (ERICH) study. Overall 26% of the patients resumed OAT following their ICH, although the rate ranged from a low of 20% in one study to a high of 42% in another. The vast majority of patients received a vitamin K antagonist as their anticoagulant; very few received a new oral anticoagulant.
Using propensity score matching to compare similar patients who resumed or stayed off OAT, Dr. Biffi found that, during the year following the index ICH, mortality was 71%-74% lower among patients who resumed OAT. Recurrent all-cause stroke was 49%-55% lower with resumed OAT, and favorable functional outcomes (a score of 0-3 on the modified Rankin scale) were more than fourfold higher with OAT resumption, he reported.
Dr. Biffi calculated these relative rates, both for patients with a lumbar location of their ICH and for those with a nonlumbar location, and found that location had no influence on responsiveness to OAT. Patients with an index ICH in a lumbar location had a trend toward more recurrent ICH on OAT, a 26% higher rate relative to patients not resumed on OAT, but this difference fell short of statistical significance.
The only factor he found that linked with whether or not patients resumed OAT was the severity of their index ICH. The more severe their bleed, the less likely were patients to resume. Aside from that, “there is a lot of variation in practice,” he said. “We are gathering additional data” to try to further address this question.
Dr. Biffi had no disclosures.
[email protected]
On Twitter @mitchelzoler
HOUSTON – Even when patients on an oral anticoagulant have the dreaded complication of an intracerebral hemorrhage, resumption of their oral anticoagulation regimen appears to produce the best midterm outcomes, based on a meta-analysis of data from more than 1,000 patients collected in three observational studies.
Resumption of oral anticoagulation therapy (OAT) is a “major dilemma” when managing patients who developed an intracerebral hemorrhage (ICH) while on OAT, said Alessandro Biffi, MD, explaining why he performed this meta-analysis that he presented at the International Stroke Conference sponsored by the American Heart Association.
He used individual patient data collected from a total of 1,027 patients enrolled in any of three different observational studies: the German-wide Multicenter Analysis of Oral Anticoagulation Associated Intracerebral Hemorrhage (RETRACE) study, the MGH longitudinal ICH study, or the Ethnic/Racial Variations of Intracerebral Hemorrhage (ERICH) study. Overall 26% of the patients resumed OAT following their ICH, although the rate ranged from a low of 20% in one study to a high of 42% in another. The vast majority of patients received a vitamin K antagonist as their anticoagulant; very few received a new oral anticoagulant.
Using propensity score matching to compare similar patients who resumed or stayed off OAT, Dr. Biffi found that, during the year following the index ICH, mortality was 71%-74% lower among patients who resumed OAT. Recurrent all-cause stroke was 49%-55% lower with resumed OAT, and favorable functional outcomes (a score of 0-3 on the modified Rankin scale) were more than fourfold higher with OAT resumption, he reported.
Dr. Biffi calculated these relative rates, both for patients with a lumbar location of their ICH and for those with a nonlumbar location, and found that location had no influence on responsiveness to OAT. Patients with an index ICH in a lumbar location had a trend toward more recurrent ICH on OAT, a 26% higher rate relative to patients not resumed on OAT, but this difference fell short of statistical significance.
The only factor he found that linked with whether or not patients resumed OAT was the severity of their index ICH. The more severe their bleed, the less likely were patients to resume. Aside from that, “there is a lot of variation in practice,” he said. “We are gathering additional data” to try to further address this question.
Dr. Biffi had no disclosures.
[email protected]
On Twitter @mitchelzoler
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point:
Major finding: One-year mortality was 71%-74% lower among patients who resumed oral anticoagulation relative to those who did not.
Data source: Meta-analysis of data from 1,027 patients collected in three observational studies.
Disclosures: Dr. Biffi had no disclosures.
VIDEO: Clot aspiration equals retrieval for ischemic stroke
HOUSTON – Intracerebral clot aspiration was as safe and effective as stent retriever thrombectomy for restoring cerebral blood flow in a French multicenter, randomized trial with 381 acute ischemic stroke patients.
This study is the “first direct comparison of aspiration versus stent retrieval” as the initial strategy for clot removal in acute ischemic stroke, and it “opens the door to add a new tool” for clot removal, Bertrand Lapergue, MD, said at the International Stroke Conference sponsored by the American Heart Association.
The new results “are the first to show that aspiration first is as good as a stent retriever, but we need to also see the results from COMPASS,” a U.S. multicenter trial that is in the process of making the same comparison, commented Ricardo A. Hanel, MD, a vascular neurosurgeon at Baptist Health in Jacksonville, Fla. The COMPASS Trial: a Direct Aspiration First Pass Technique has now enrolled about two-thirds of its target patient number, and until the study is complete the role of direct aspiration for clot removal in stroke remains investigational for U.S. practice, said Dr. Hanel, a COMPASS investigator.
The aspiration catheter tested in ASTER is marketed by Penumbra and has already received Food and Drug Administration approval for revascularization of ischemic stroke patients. U.S. use of aspiration for treating acute ischemic stroke, however, has remained limited because there is no clear evidence of the method’s efficacy. Dr. Hanel said that he occasionally uses aspiration as an adjunct to clot removal with a stent retriever.
ASTER’s primary endpoint was the percentage of patients who achieved thrombolysis in cerebral infarction (TICI) 2b or 3 flow at the end of treatment, which occurred in 85% of patients treated with aspiration first and in 83% of those treated by clot removal first, a difference that was not statistically significant, Dr. Lapergue reported. The rate of patients who achieved either TICI 2b or 3 flow after the initial strategy only was 63% with aspiration and 68% with clot removal, also a nonsignificant difference. The two strategies also showed no significant difference for any measured safety parameter. The results showed a trend toward more vasospasm with clot removal – a 6% rate, versus 3% with clot aspiration – but this did not reach statistical significance.
Results from additional analyses of the clinical outcomes of patients in the trial and of cost efficacy will be reported later in 2017, Dr. Lapergue said.
ASTER received an unrestricted research grant from Penumbra, a company that markets clot removal aspiration catheters. Dr. Lapergue had no personal disclosures. Dr. Hanel has been a consultant to and received grant support from Medtronic. He has received research grants from MicroVention and has an ownership interest in InNeuroCo.
[email protected]
On Twitter @mitchelzoler
ASTER is an important trial. It shows for the first time that an aspiration device is probably as safe and reasonable for opening an acute occlusion in a large cerebral artery as is a stent retriever.
ASTER, however, was done entirely in a French population, making it uncertain whether the results are applicable to other populations. For example, U.S. acute ischemic stroke patients, especially African Americans and Hispanics, generally have more intracerebral atherostenotic disease than do patients from European countries, while French patients tend to have more embolic disease. Will aspiration be as effective in U.S. patients with atherostenotic blockages? I would love to see this study repeated in a U.S. population of ischemic stroke patients, and that is now happening in the COMPASS trial. It would be helpful to know if there are selected U.S. patients who might be better treated using either aspiration or a stent retriever first.
Although aspiration catheters have already received Food and Drug Administration approval for clot removal in acute ischemic stroke patients, many U.S. interventionalists have moved to deploying stent retrievers based on the very positive results reported with these devices about 2 years ago. For the moment, stent retrievers remain the most prominent devices to open large vessel occlusions.
Ralph L. Sacco, MD, is professor and chairman of neurology at the University of Miami. He had no relevant disclosures. He made these comments in a video interview and during a press conference.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ASTER is an important trial. It shows for the first time that an aspiration device is probably as safe and reasonable for opening an acute occlusion in a large cerebral artery as is a stent retriever.
ASTER, however, was done entirely in a French population, making it uncertain whether the results are applicable to other populations. For example, U.S. acute ischemic stroke patients, especially African Americans and Hispanics, generally have more intracerebral atherostenotic disease than do patients from European countries, while French patients tend to have more embolic disease. Will aspiration be as effective in U.S. patients with atherostenotic blockages? I would love to see this study repeated in a U.S. population of ischemic stroke patients, and that is now happening in the COMPASS trial. It would be helpful to know if there are selected U.S. patients who might be better treated using either aspiration or a stent retriever first.
Although aspiration catheters have already received Food and Drug Administration approval for clot removal in acute ischemic stroke patients, many U.S. interventionalists have moved to deploying stent retrievers based on the very positive results reported with these devices about 2 years ago. For the moment, stent retrievers remain the most prominent devices to open large vessel occlusions.
Ralph L. Sacco, MD, is professor and chairman of neurology at the University of Miami. He had no relevant disclosures. He made these comments in a video interview and during a press conference.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
ASTER is an important trial. It shows for the first time that an aspiration device is probably as safe and reasonable for opening an acute occlusion in a large cerebral artery as is a stent retriever.
ASTER, however, was done entirely in a French population, making it uncertain whether the results are applicable to other populations. For example, U.S. acute ischemic stroke patients, especially African Americans and Hispanics, generally have more intracerebral atherostenotic disease than do patients from European countries, while French patients tend to have more embolic disease. Will aspiration be as effective in U.S. patients with atherostenotic blockages? I would love to see this study repeated in a U.S. population of ischemic stroke patients, and that is now happening in the COMPASS trial. It would be helpful to know if there are selected U.S. patients who might be better treated using either aspiration or a stent retriever first.
Although aspiration catheters have already received Food and Drug Administration approval for clot removal in acute ischemic stroke patients, many U.S. interventionalists have moved to deploying stent retrievers based on the very positive results reported with these devices about 2 years ago. For the moment, stent retrievers remain the most prominent devices to open large vessel occlusions.
Ralph L. Sacco, MD, is professor and chairman of neurology at the University of Miami. He had no relevant disclosures. He made these comments in a video interview and during a press conference.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
HOUSTON – Intracerebral clot aspiration was as safe and effective as stent retriever thrombectomy for restoring cerebral blood flow in a French multicenter, randomized trial with 381 acute ischemic stroke patients.
This study is the “first direct comparison of aspiration versus stent retrieval” as the initial strategy for clot removal in acute ischemic stroke, and it “opens the door to add a new tool” for clot removal, Bertrand Lapergue, MD, said at the International Stroke Conference sponsored by the American Heart Association.
The new results “are the first to show that aspiration first is as good as a stent retriever, but we need to also see the results from COMPASS,” a U.S. multicenter trial that is in the process of making the same comparison, commented Ricardo A. Hanel, MD, a vascular neurosurgeon at Baptist Health in Jacksonville, Fla. The COMPASS Trial: a Direct Aspiration First Pass Technique has now enrolled about two-thirds of its target patient number, and until the study is complete the role of direct aspiration for clot removal in stroke remains investigational for U.S. practice, said Dr. Hanel, a COMPASS investigator.
The aspiration catheter tested in ASTER is marketed by Penumbra and has already received Food and Drug Administration approval for revascularization of ischemic stroke patients. U.S. use of aspiration for treating acute ischemic stroke, however, has remained limited because there is no clear evidence of the method’s efficacy. Dr. Hanel said that he occasionally uses aspiration as an adjunct to clot removal with a stent retriever.
ASTER’s primary endpoint was the percentage of patients who achieved thrombolysis in cerebral infarction (TICI) 2b or 3 flow at the end of treatment, which occurred in 85% of patients treated with aspiration first and in 83% of those treated by clot removal first, a difference that was not statistically significant, Dr. Lapergue reported. The rate of patients who achieved either TICI 2b or 3 flow after the initial strategy only was 63% with aspiration and 68% with clot removal, also a nonsignificant difference. The two strategies also showed no significant difference for any measured safety parameter. The results showed a trend toward more vasospasm with clot removal – a 6% rate, versus 3% with clot aspiration – but this did not reach statistical significance.
Results from additional analyses of the clinical outcomes of patients in the trial and of cost efficacy will be reported later in 2017, Dr. Lapergue said.
ASTER received an unrestricted research grant from Penumbra, a company that markets clot removal aspiration catheters. Dr. Lapergue had no personal disclosures. Dr. Hanel has been a consultant to and received grant support from Medtronic. He has received research grants from MicroVention and has an ownership interest in InNeuroCo.
[email protected]
On Twitter @mitchelzoler
HOUSTON – Intracerebral clot aspiration was as safe and effective as stent retriever thrombectomy for restoring cerebral blood flow in a French multicenter, randomized trial with 381 acute ischemic stroke patients.
This study is the “first direct comparison of aspiration versus stent retrieval” as the initial strategy for clot removal in acute ischemic stroke, and it “opens the door to add a new tool” for clot removal, Bertrand Lapergue, MD, said at the International Stroke Conference sponsored by the American Heart Association.
The new results “are the first to show that aspiration first is as good as a stent retriever, but we need to also see the results from COMPASS,” a U.S. multicenter trial that is in the process of making the same comparison, commented Ricardo A. Hanel, MD, a vascular neurosurgeon at Baptist Health in Jacksonville, Fla. The COMPASS Trial: a Direct Aspiration First Pass Technique has now enrolled about two-thirds of its target patient number, and until the study is complete the role of direct aspiration for clot removal in stroke remains investigational for U.S. practice, said Dr. Hanel, a COMPASS investigator.
The aspiration catheter tested in ASTER is marketed by Penumbra and has already received Food and Drug Administration approval for revascularization of ischemic stroke patients. U.S. use of aspiration for treating acute ischemic stroke, however, has remained limited because there is no clear evidence of the method’s efficacy. Dr. Hanel said that he occasionally uses aspiration as an adjunct to clot removal with a stent retriever.
ASTER’s primary endpoint was the percentage of patients who achieved thrombolysis in cerebral infarction (TICI) 2b or 3 flow at the end of treatment, which occurred in 85% of patients treated with aspiration first and in 83% of those treated by clot removal first, a difference that was not statistically significant, Dr. Lapergue reported. The rate of patients who achieved either TICI 2b or 3 flow after the initial strategy only was 63% with aspiration and 68% with clot removal, also a nonsignificant difference. The two strategies also showed no significant difference for any measured safety parameter. The results showed a trend toward more vasospasm with clot removal – a 6% rate, versus 3% with clot aspiration – but this did not reach statistical significance.
Results from additional analyses of the clinical outcomes of patients in the trial and of cost efficacy will be reported later in 2017, Dr. Lapergue said.
ASTER received an unrestricted research grant from Penumbra, a company that markets clot removal aspiration catheters. Dr. Lapergue had no personal disclosures. Dr. Hanel has been a consultant to and received grant support from Medtronic. He has received research grants from MicroVention and has an ownership interest in InNeuroCo.
[email protected]
On Twitter @mitchelzoler
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point:
Major finding: Recanalization occurred in 85% of patients treated with aspiration first and 83% treated with clot removal first.
Data source: ASTER, a multicenter, randomized French trial with 381 patients.
Disclosures: ASTER received an unrestricted research grant from Penumbra, a company that markets clot removal aspiration catheters. Dr. Lapergue had no personal disclosures. Dr. Hanel has been a consultant to and received grant support from Medtronic. He has received research grants from MicroVention and has an ownership interest in InNeuroCo.
Exercise can boost cognition after stroke
HOUSTON – Exercise seems to improve some of the cognitive difficulties that can manifest in stroke survivors, even if patients don’t hit the gym for a couple of years after the incident.
A meta-analysis of 14 randomized, controlled studies has determined that the combination of aerobic and weight-bearing exercises is most effective at boosting brain function. The studies showed a moderate, but consistent, effect of exercise in both the acute and chronic phase, Lauren Oberlin said at the International Stroke Conference sponsored by the American Heart Association.
“This is an important message for stroke survivors who have experienced cognitive deficits for a long time: These may not be permanent, and they can be modified with physical activity,” she said.
Long-term cognitive impairment is a very common problem after stroke, she said, occurring to some degree in up to 85% of survivors. The most commonly affected domains are executive function, attention, processing speed, and memory.
“These deficits can also be highly persistent, and remain in the years after a stroke,” Ms. Oberlin said. “And they represent a major health and economic burden. Stroke survivors with cognitive deficits are at an increased risk for long-term disability, functional decline, dependent living, hospitalization, and even mortality. Despite all this, there is an absence of effective treatments. There are no effective pharmaceutical treatments and cognitive rehabilitation training has not been widely successful.”
Exercise has not been as well-studied in stroke as it has in other neurological disorders, including Parkinson’s disease, multiple sclerosis, and more recently, Alzheimer’s disease. Physical activity has also been shown to help maintain and boost cognitive function and memory in healthy aging populations.
Ms. Oberlin and her colleagues conducted a meta-analysis of 14 randomized, controlled studies conducted during 2001-2016. The studies enrolled a total of 736 subjects. All of them randomized subjects to 3-6 months of an active exercise arm or a control arm that did not involve physical training.
The researchers assessed effect sizes by Hedges’ g, calculated separately for intervention and control conditions within each trial. The results were interpreted as follows:
• Small effect = 0.2
• Moderate effect = 0.5
• Large effect = 0.8
Only four of the studies demonstrated a statistically significant benefit between the active and control arms. Seven trended strongly toward the positive, but had wide confidence intervals that crossed the null. Three studies showed no significant benefit. The overall effects size was 0.56 (moderate).
Ms. Oberlin and her colleagues then parsed the data to examine the effect of when the program was initiated after the stroke, the program’s duration, and the type of exercise it studied.
Length of the intervention (less than 3 months and more than 3 months) was not significantly related to cognitive outcome. However, the combination of aerobic and strength training exerted a significantly greater effect size (0.45) than did aerobic training or weight training alone (0.2 and 0.34, respectively). Programs that started more than 3 months after the stroke were also more effective than were those started earlier in recovery (0.45 vs. 0.16).
Finally, in a subset of five studies, she evaluated whether particular cognitive domains benefited most from physical activity. Attention and processing speed improved the most (0.4). Changes in memory and executive function were not significant.
“I will say this was only five studies, so we may have been underpowered to see any effects on these other domains,” Ms. Oberlin said.
The mechanistic link between physical activity and improved cognition has not been fully elucidated in humans, she said. However, animal studies have identified a number of associations. “In rodent studies, we see that exercise improves blood flow to the brain, and promotes both neurogenesis and synaptogenesis. This has been confirmed in imaging studies of healthy older adults. Exercise was associated with increased structural connectivity, changes in functional connectivity, and increases in brain volume in some regions, including the hippocampus and prefrontal cortex.”
She also acknowledged that preaching exercise in clinic is much easier than actually getting patients into the gym. “Stroke survivors often have mobility limitations, and these studies were primarily conducted in subjects who did not have those issues and who could work out on a treadmill or exercise bike. How we can adapt these programs to patients with limited mobility is certainly a challenge.”
Ms. Oberlin had no financial disclosures.
[email protected]
On Twitter @alz_gal
HOUSTON – Exercise seems to improve some of the cognitive difficulties that can manifest in stroke survivors, even if patients don’t hit the gym for a couple of years after the incident.
A meta-analysis of 14 randomized, controlled studies has determined that the combination of aerobic and weight-bearing exercises is most effective at boosting brain function. The studies showed a moderate, but consistent, effect of exercise in both the acute and chronic phase, Lauren Oberlin said at the International Stroke Conference sponsored by the American Heart Association.
“This is an important message for stroke survivors who have experienced cognitive deficits for a long time: These may not be permanent, and they can be modified with physical activity,” she said.
Long-term cognitive impairment is a very common problem after stroke, she said, occurring to some degree in up to 85% of survivors. The most commonly affected domains are executive function, attention, processing speed, and memory.
“These deficits can also be highly persistent, and remain in the years after a stroke,” Ms. Oberlin said. “And they represent a major health and economic burden. Stroke survivors with cognitive deficits are at an increased risk for long-term disability, functional decline, dependent living, hospitalization, and even mortality. Despite all this, there is an absence of effective treatments. There are no effective pharmaceutical treatments and cognitive rehabilitation training has not been widely successful.”
Exercise has not been as well-studied in stroke as it has in other neurological disorders, including Parkinson’s disease, multiple sclerosis, and more recently, Alzheimer’s disease. Physical activity has also been shown to help maintain and boost cognitive function and memory in healthy aging populations.
Ms. Oberlin and her colleagues conducted a meta-analysis of 14 randomized, controlled studies conducted during 2001-2016. The studies enrolled a total of 736 subjects. All of them randomized subjects to 3-6 months of an active exercise arm or a control arm that did not involve physical training.
The researchers assessed effect sizes by Hedges’ g, calculated separately for intervention and control conditions within each trial. The results were interpreted as follows:
• Small effect = 0.2
• Moderate effect = 0.5
• Large effect = 0.8
Only four of the studies demonstrated a statistically significant benefit between the active and control arms. Seven trended strongly toward the positive, but had wide confidence intervals that crossed the null. Three studies showed no significant benefit. The overall effects size was 0.56 (moderate).
Ms. Oberlin and her colleagues then parsed the data to examine the effect of when the program was initiated after the stroke, the program’s duration, and the type of exercise it studied.
Length of the intervention (less than 3 months and more than 3 months) was not significantly related to cognitive outcome. However, the combination of aerobic and strength training exerted a significantly greater effect size (0.45) than did aerobic training or weight training alone (0.2 and 0.34, respectively). Programs that started more than 3 months after the stroke were also more effective than were those started earlier in recovery (0.45 vs. 0.16).
Finally, in a subset of five studies, she evaluated whether particular cognitive domains benefited most from physical activity. Attention and processing speed improved the most (0.4). Changes in memory and executive function were not significant.
“I will say this was only five studies, so we may have been underpowered to see any effects on these other domains,” Ms. Oberlin said.
The mechanistic link between physical activity and improved cognition has not been fully elucidated in humans, she said. However, animal studies have identified a number of associations. “In rodent studies, we see that exercise improves blood flow to the brain, and promotes both neurogenesis and synaptogenesis. This has been confirmed in imaging studies of healthy older adults. Exercise was associated with increased structural connectivity, changes in functional connectivity, and increases in brain volume in some regions, including the hippocampus and prefrontal cortex.”
She also acknowledged that preaching exercise in clinic is much easier than actually getting patients into the gym. “Stroke survivors often have mobility limitations, and these studies were primarily conducted in subjects who did not have those issues and who could work out on a treadmill or exercise bike. How we can adapt these programs to patients with limited mobility is certainly a challenge.”
Ms. Oberlin had no financial disclosures.
[email protected]
On Twitter @alz_gal
HOUSTON – Exercise seems to improve some of the cognitive difficulties that can manifest in stroke survivors, even if patients don’t hit the gym for a couple of years after the incident.
A meta-analysis of 14 randomized, controlled studies has determined that the combination of aerobic and weight-bearing exercises is most effective at boosting brain function. The studies showed a moderate, but consistent, effect of exercise in both the acute and chronic phase, Lauren Oberlin said at the International Stroke Conference sponsored by the American Heart Association.
“This is an important message for stroke survivors who have experienced cognitive deficits for a long time: These may not be permanent, and they can be modified with physical activity,” she said.
Long-term cognitive impairment is a very common problem after stroke, she said, occurring to some degree in up to 85% of survivors. The most commonly affected domains are executive function, attention, processing speed, and memory.
“These deficits can also be highly persistent, and remain in the years after a stroke,” Ms. Oberlin said. “And they represent a major health and economic burden. Stroke survivors with cognitive deficits are at an increased risk for long-term disability, functional decline, dependent living, hospitalization, and even mortality. Despite all this, there is an absence of effective treatments. There are no effective pharmaceutical treatments and cognitive rehabilitation training has not been widely successful.”
Exercise has not been as well-studied in stroke as it has in other neurological disorders, including Parkinson’s disease, multiple sclerosis, and more recently, Alzheimer’s disease. Physical activity has also been shown to help maintain and boost cognitive function and memory in healthy aging populations.
Ms. Oberlin and her colleagues conducted a meta-analysis of 14 randomized, controlled studies conducted during 2001-2016. The studies enrolled a total of 736 subjects. All of them randomized subjects to 3-6 months of an active exercise arm or a control arm that did not involve physical training.
The researchers assessed effect sizes by Hedges’ g, calculated separately for intervention and control conditions within each trial. The results were interpreted as follows:
• Small effect = 0.2
• Moderate effect = 0.5
• Large effect = 0.8
Only four of the studies demonstrated a statistically significant benefit between the active and control arms. Seven trended strongly toward the positive, but had wide confidence intervals that crossed the null. Three studies showed no significant benefit. The overall effects size was 0.56 (moderate).
Ms. Oberlin and her colleagues then parsed the data to examine the effect of when the program was initiated after the stroke, the program’s duration, and the type of exercise it studied.
Length of the intervention (less than 3 months and more than 3 months) was not significantly related to cognitive outcome. However, the combination of aerobic and strength training exerted a significantly greater effect size (0.45) than did aerobic training or weight training alone (0.2 and 0.34, respectively). Programs that started more than 3 months after the stroke were also more effective than were those started earlier in recovery (0.45 vs. 0.16).
Finally, in a subset of five studies, she evaluated whether particular cognitive domains benefited most from physical activity. Attention and processing speed improved the most (0.4). Changes in memory and executive function were not significant.
“I will say this was only five studies, so we may have been underpowered to see any effects on these other domains,” Ms. Oberlin said.
The mechanistic link between physical activity and improved cognition has not been fully elucidated in humans, she said. However, animal studies have identified a number of associations. “In rodent studies, we see that exercise improves blood flow to the brain, and promotes both neurogenesis and synaptogenesis. This has been confirmed in imaging studies of healthy older adults. Exercise was associated with increased structural connectivity, changes in functional connectivity, and increases in brain volume in some regions, including the hippocampus and prefrontal cortex.”
She also acknowledged that preaching exercise in clinic is much easier than actually getting patients into the gym. “Stroke survivors often have mobility limitations, and these studies were primarily conducted in subjects who did not have those issues and who could work out on a treadmill or exercise bike. How we can adapt these programs to patients with limited mobility is certainly a challenge.”
Ms. Oberlin had no financial disclosures.
[email protected]
On Twitter @alz_gal
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point:
Major finding: Overall, exercise after stroke exerted a moderate effect size of 0.56 on cognition.
Data source: The meta-analysis comprised 14 studies and 736 subjects.
Disclosures: Ms. Oberlin had no financial disclosures.
Mesh cylinder effective for small to medium wide-necked aneurysms
HOUSTON – An expandable mesh cylinder that is approved to treat large, wide-necked carotid aneurysms has now proved successful in treating small lesions of the internal carotid or vertebral artery up to 12 mm in diameter.
The Pipeline Embolization Device (PED, Medtronic) completely occluded 84% of such lesions without significant stenosis or retreatment within 1 year in the PREMIER trial, Ricardo Hanel, MD, PhD, said at the International Stroke Conference sponsored by the American Heart Association.
Overall morbidity and mortality in the year-long trial was very low (2.2%). However, within the first year, three patients had a major stroke in brain regions supplied by the treated artery; one of these was related to device deployment and was fatal, said Dr. Hanel, director of the Baptist Neurological Institute, Jacksonville, Fla.
Counseling patients with these lesions is not easy, Dr. Hanel said. Treatment decisions must take into account not only the patient’s current clinical status and comorbidities, but family history and personal preference. In fact, patient preference was the largest driver of treatment (63%) in the PREMIER study.
In an interview, Dr. Hanel illustrated the importance of individualized decision making. A middle-aged female had been monitored for a small aneurysm for 7 years. When the patient was 6 years old, her mother died during an open operation to treat an aneurysm.
“We had tried to treat this patient with coiling [when the lesion was first detected], but it was unsuccessful,” Dr. Hanel said. “And since her mother had died during surgery, she did not want to go for an open approach. Now, 6 years later, we have the technology to cure her with a single device, and the odds of [recurrence over 10 years] are virtually zero. It is a very personal decision, and we take a lot of factors under consideration before we decide to expose the patient to the risks of this treatment.”
The PED is a flexible 75% cobalt-chromium/25% platinum-tungsten mesh with a braided configuration. It is advanced slightly beyond the aneurysm neck and then deployed. As it opens, it partially occludes the lesion, immediately decreasing the amount of blood entering the sac. Within a month, vascular remodeling is well underway; as endothelium grows throughout the mesh, blood flow into the aneurysm is gradually cut off. Eventually the aneurysmal sac recedes, and the normal vascular architecture is restored.
“Within 4 weeks you can’t see the metal at all,” Dr. Hanel said. “It’s covered by a thin layer of endothelial cells. This device allows the patient’s body to heal and close the aneurysm, and we don’t have to deal with the reoccurrence problem we have with stent coils. The pipeline treats the entire circumference of the vessel.”
The PED is used in combination with dual-antiplatelet therapy (DAP, aspirin/clopidogrel). Dr. Hanel initiates DAP 7 days before the procedure and continues it for 3 months. At that time, clopidogrel may be discontinued. “I advise my patients to then take a baby aspirin every day for the rest of their lives,” and they are regularly monitored, he said. “Aspirin seems to protect against the formation and rupture of aneurysms.”
PREMIER followed 141 patients with unruptured, wide-necked small aneurysms of the internal carotid (up to the terminus) or the vertebral artery segment up to and including the posterior inferior cerebellar artery. The primary efficacy endpoint was complete aneurysm occlusion and absence of significant parent artery stenosis at 1 year. The secondary endpoint was successful device deployment.
The primary safety endpoint was major stroke in the territory supplied by the treated artery or neurologic death at 1 year. There were two secondary safety endpoints: major stroke or neurologic death within 30 days, attributable to procedural complications, and intracerebral hemorrhage more than 30 days later.
The patients were largely female (88%) with a mean age of 55 years. They were asymptomatic with a mean modified Rankin Scale score of 0.2 and National Institutes of Health Stroke Scale score of 0.1. Nearly half of the patients had hypertension, and 38% had hyperlipidemia. About 28% were current smokers, and another 16% had a history of smoking.
The patients’ mean maximal aneurysm diameter was 4.6 mm, with a mean neck width of 3.7 mm. The majority of lesions (84%) were less than 7 mm in diameter, but they ranged up to 12 mm.
Internal carotid artery aneurysms comprised 95% of all in the study; 5% were in the vertebral artery. Most involved the side wall (84%), while the remainder involved a side branch (12%) or were fusiform (4%).
There was only one unsuccessful initial deployment, resulting in a 99.3% deployment success rate. The mean procedure time was 78 minutes. While most patients received just one PED, 10 received multiple devices. The PED completely covered the entire neck of the lesion in 97%. There were no intraoperative aneurysm ruptures and no intraoperative deaths.
At 1 year after implantation, 84% of the aneurysms were completely occluded, with the aneurysmal sac eliminated in 92%. A residual aneurysm remained in 11 patients (8%), and a residual neck in 8 patients (6%). Two patients (1.4%) had arterial stenosis of more than 50%. Three patients (2.2%) required retreatment.
There were three major strokes in the region supplied by the target artery in three patients.
The fatal stroke occurred in a patient who had an aneurysm on the right ophthalmic carotid segment. The first device failed to deploy correctly and was removed. A second device was implanted. The next day the patient developed a facial droop, slurred speech, and a headache. She experienced a distal intraparenchymal hemorrhage and underwent hemicraniotomy, but did not survive.
The second stroke occurred in a patient who needed two devices to occlude a lesion in the left ophthalmic segment of the carotid. The patient developed an intraparenchymal hemorrhage on postoperative day 15. The stroke resolved with sequelae and the clopidogrel dose was increased.
The third stroke was associated with treatment of a right communicating segment aneurysm. The patient stopped taking the recommended DAP and experienced an acute ischemic stroke 169 days after the procedure. This stroke also resolved with sequelae.
Based on the results of PREMIER, Medtronic will pursue Food and Drug Administration approval of the PED for small to medium wide-necked aneurysms, Dr. Hanel noted.
Medtronic sponsored the study. Dr. Hanel is an adviser to the company and has received research funds from it.
[email protected]
On Twitter @alz_gal
HOUSTON – An expandable mesh cylinder that is approved to treat large, wide-necked carotid aneurysms has now proved successful in treating small lesions of the internal carotid or vertebral artery up to 12 mm in diameter.
The Pipeline Embolization Device (PED, Medtronic) completely occluded 84% of such lesions without significant stenosis or retreatment within 1 year in the PREMIER trial, Ricardo Hanel, MD, PhD, said at the International Stroke Conference sponsored by the American Heart Association.
Overall morbidity and mortality in the year-long trial was very low (2.2%). However, within the first year, three patients had a major stroke in brain regions supplied by the treated artery; one of these was related to device deployment and was fatal, said Dr. Hanel, director of the Baptist Neurological Institute, Jacksonville, Fla.
Counseling patients with these lesions is not easy, Dr. Hanel said. Treatment decisions must take into account not only the patient’s current clinical status and comorbidities, but family history and personal preference. In fact, patient preference was the largest driver of treatment (63%) in the PREMIER study.
In an interview, Dr. Hanel illustrated the importance of individualized decision making. A middle-aged female had been monitored for a small aneurysm for 7 years. When the patient was 6 years old, her mother died during an open operation to treat an aneurysm.
“We had tried to treat this patient with coiling [when the lesion was first detected], but it was unsuccessful,” Dr. Hanel said. “And since her mother had died during surgery, she did not want to go for an open approach. Now, 6 years later, we have the technology to cure her with a single device, and the odds of [recurrence over 10 years] are virtually zero. It is a very personal decision, and we take a lot of factors under consideration before we decide to expose the patient to the risks of this treatment.”
The PED is a flexible 75% cobalt-chromium/25% platinum-tungsten mesh with a braided configuration. It is advanced slightly beyond the aneurysm neck and then deployed. As it opens, it partially occludes the lesion, immediately decreasing the amount of blood entering the sac. Within a month, vascular remodeling is well underway; as endothelium grows throughout the mesh, blood flow into the aneurysm is gradually cut off. Eventually the aneurysmal sac recedes, and the normal vascular architecture is restored.
“Within 4 weeks you can’t see the metal at all,” Dr. Hanel said. “It’s covered by a thin layer of endothelial cells. This device allows the patient’s body to heal and close the aneurysm, and we don’t have to deal with the reoccurrence problem we have with stent coils. The pipeline treats the entire circumference of the vessel.”
The PED is used in combination with dual-antiplatelet therapy (DAP, aspirin/clopidogrel). Dr. Hanel initiates DAP 7 days before the procedure and continues it for 3 months. At that time, clopidogrel may be discontinued. “I advise my patients to then take a baby aspirin every day for the rest of their lives,” and they are regularly monitored, he said. “Aspirin seems to protect against the formation and rupture of aneurysms.”
PREMIER followed 141 patients with unruptured, wide-necked small aneurysms of the internal carotid (up to the terminus) or the vertebral artery segment up to and including the posterior inferior cerebellar artery. The primary efficacy endpoint was complete aneurysm occlusion and absence of significant parent artery stenosis at 1 year. The secondary endpoint was successful device deployment.
The primary safety endpoint was major stroke in the territory supplied by the treated artery or neurologic death at 1 year. There were two secondary safety endpoints: major stroke or neurologic death within 30 days, attributable to procedural complications, and intracerebral hemorrhage more than 30 days later.
The patients were largely female (88%) with a mean age of 55 years. They were asymptomatic with a mean modified Rankin Scale score of 0.2 and National Institutes of Health Stroke Scale score of 0.1. Nearly half of the patients had hypertension, and 38% had hyperlipidemia. About 28% were current smokers, and another 16% had a history of smoking.
The patients’ mean maximal aneurysm diameter was 4.6 mm, with a mean neck width of 3.7 mm. The majority of lesions (84%) were less than 7 mm in diameter, but they ranged up to 12 mm.
Internal carotid artery aneurysms comprised 95% of all in the study; 5% were in the vertebral artery. Most involved the side wall (84%), while the remainder involved a side branch (12%) or were fusiform (4%).
There was only one unsuccessful initial deployment, resulting in a 99.3% deployment success rate. The mean procedure time was 78 minutes. While most patients received just one PED, 10 received multiple devices. The PED completely covered the entire neck of the lesion in 97%. There were no intraoperative aneurysm ruptures and no intraoperative deaths.
At 1 year after implantation, 84% of the aneurysms were completely occluded, with the aneurysmal sac eliminated in 92%. A residual aneurysm remained in 11 patients (8%), and a residual neck in 8 patients (6%). Two patients (1.4%) had arterial stenosis of more than 50%. Three patients (2.2%) required retreatment.
There were three major strokes in the region supplied by the target artery in three patients.
The fatal stroke occurred in a patient who had an aneurysm on the right ophthalmic carotid segment. The first device failed to deploy correctly and was removed. A second device was implanted. The next day the patient developed a facial droop, slurred speech, and a headache. She experienced a distal intraparenchymal hemorrhage and underwent hemicraniotomy, but did not survive.
The second stroke occurred in a patient who needed two devices to occlude a lesion in the left ophthalmic segment of the carotid. The patient developed an intraparenchymal hemorrhage on postoperative day 15. The stroke resolved with sequelae and the clopidogrel dose was increased.
The third stroke was associated with treatment of a right communicating segment aneurysm. The patient stopped taking the recommended DAP and experienced an acute ischemic stroke 169 days after the procedure. This stroke also resolved with sequelae.
Based on the results of PREMIER, Medtronic will pursue Food and Drug Administration approval of the PED for small to medium wide-necked aneurysms, Dr. Hanel noted.
Medtronic sponsored the study. Dr. Hanel is an adviser to the company and has received research funds from it.
[email protected]
On Twitter @alz_gal
HOUSTON – An expandable mesh cylinder that is approved to treat large, wide-necked carotid aneurysms has now proved successful in treating small lesions of the internal carotid or vertebral artery up to 12 mm in diameter.
The Pipeline Embolization Device (PED, Medtronic) completely occluded 84% of such lesions without significant stenosis or retreatment within 1 year in the PREMIER trial, Ricardo Hanel, MD, PhD, said at the International Stroke Conference sponsored by the American Heart Association.
Overall morbidity and mortality in the year-long trial was very low (2.2%). However, within the first year, three patients had a major stroke in brain regions supplied by the treated artery; one of these was related to device deployment and was fatal, said Dr. Hanel, director of the Baptist Neurological Institute, Jacksonville, Fla.
Counseling patients with these lesions is not easy, Dr. Hanel said. Treatment decisions must take into account not only the patient’s current clinical status and comorbidities, but family history and personal preference. In fact, patient preference was the largest driver of treatment (63%) in the PREMIER study.
In an interview, Dr. Hanel illustrated the importance of individualized decision making. A middle-aged female had been monitored for a small aneurysm for 7 years. When the patient was 6 years old, her mother died during an open operation to treat an aneurysm.
“We had tried to treat this patient with coiling [when the lesion was first detected], but it was unsuccessful,” Dr. Hanel said. “And since her mother had died during surgery, she did not want to go for an open approach. Now, 6 years later, we have the technology to cure her with a single device, and the odds of [recurrence over 10 years] are virtually zero. It is a very personal decision, and we take a lot of factors under consideration before we decide to expose the patient to the risks of this treatment.”
The PED is a flexible 75% cobalt-chromium/25% platinum-tungsten mesh with a braided configuration. It is advanced slightly beyond the aneurysm neck and then deployed. As it opens, it partially occludes the lesion, immediately decreasing the amount of blood entering the sac. Within a month, vascular remodeling is well underway; as endothelium grows throughout the mesh, blood flow into the aneurysm is gradually cut off. Eventually the aneurysmal sac recedes, and the normal vascular architecture is restored.
“Within 4 weeks you can’t see the metal at all,” Dr. Hanel said. “It’s covered by a thin layer of endothelial cells. This device allows the patient’s body to heal and close the aneurysm, and we don’t have to deal with the reoccurrence problem we have with stent coils. The pipeline treats the entire circumference of the vessel.”
The PED is used in combination with dual-antiplatelet therapy (DAP, aspirin/clopidogrel). Dr. Hanel initiates DAP 7 days before the procedure and continues it for 3 months. At that time, clopidogrel may be discontinued. “I advise my patients to then take a baby aspirin every day for the rest of their lives,” and they are regularly monitored, he said. “Aspirin seems to protect against the formation and rupture of aneurysms.”
PREMIER followed 141 patients with unruptured, wide-necked small aneurysms of the internal carotid (up to the terminus) or the vertebral artery segment up to and including the posterior inferior cerebellar artery. The primary efficacy endpoint was complete aneurysm occlusion and absence of significant parent artery stenosis at 1 year. The secondary endpoint was successful device deployment.
The primary safety endpoint was major stroke in the territory supplied by the treated artery or neurologic death at 1 year. There were two secondary safety endpoints: major stroke or neurologic death within 30 days, attributable to procedural complications, and intracerebral hemorrhage more than 30 days later.
The patients were largely female (88%) with a mean age of 55 years. They were asymptomatic with a mean modified Rankin Scale score of 0.2 and National Institutes of Health Stroke Scale score of 0.1. Nearly half of the patients had hypertension, and 38% had hyperlipidemia. About 28% were current smokers, and another 16% had a history of smoking.
The patients’ mean maximal aneurysm diameter was 4.6 mm, with a mean neck width of 3.7 mm. The majority of lesions (84%) were less than 7 mm in diameter, but they ranged up to 12 mm.
Internal carotid artery aneurysms comprised 95% of all in the study; 5% were in the vertebral artery. Most involved the side wall (84%), while the remainder involved a side branch (12%) or were fusiform (4%).
There was only one unsuccessful initial deployment, resulting in a 99.3% deployment success rate. The mean procedure time was 78 minutes. While most patients received just one PED, 10 received multiple devices. The PED completely covered the entire neck of the lesion in 97%. There were no intraoperative aneurysm ruptures and no intraoperative deaths.
At 1 year after implantation, 84% of the aneurysms were completely occluded, with the aneurysmal sac eliminated in 92%. A residual aneurysm remained in 11 patients (8%), and a residual neck in 8 patients (6%). Two patients (1.4%) had arterial stenosis of more than 50%. Three patients (2.2%) required retreatment.
There were three major strokes in the region supplied by the target artery in three patients.
The fatal stroke occurred in a patient who had an aneurysm on the right ophthalmic carotid segment. The first device failed to deploy correctly and was removed. A second device was implanted. The next day the patient developed a facial droop, slurred speech, and a headache. She experienced a distal intraparenchymal hemorrhage and underwent hemicraniotomy, but did not survive.
The second stroke occurred in a patient who needed two devices to occlude a lesion in the left ophthalmic segment of the carotid. The patient developed an intraparenchymal hemorrhage on postoperative day 15. The stroke resolved with sequelae and the clopidogrel dose was increased.
The third stroke was associated with treatment of a right communicating segment aneurysm. The patient stopped taking the recommended DAP and experienced an acute ischemic stroke 169 days after the procedure. This stroke also resolved with sequelae.
Based on the results of PREMIER, Medtronic will pursue Food and Drug Administration approval of the PED for small to medium wide-necked aneurysms, Dr. Hanel noted.
Medtronic sponsored the study. Dr. Hanel is an adviser to the company and has received research funds from it.
[email protected]
On Twitter @alz_gal
AT THE INTERNATIONAL STROKE CONFERENCE
Key clinical point:
Major finding: The PED completely occluded 84% of aneurysms of the internal carotid or vertebral artery up to 12 mm in diameter at 1 year.
Data source: PREMIER investigators prospectively evaluated the PED in 141 patients.
Disclosures: Medtronic sponsored the study. Dr. Hanel is an adviser to the company and has received research funds from it.