User login
Endometriosis pain stemming from pelvic spasms improved with botulinum toxin
LOS ANGELES – Women treated surgically and with hormones for endometriosis may continue to experience pain, say investigators, and that pain frequently extends beyond the pelvis.
At the annual meeting of the American Academy of Neurology, Barbara Karp, MD, of the National Institute of Neurological Disorders and Stroke, presented results from an ongoing randomized trial of women with endometriosis receiving botulinum toxin to treat endometriosis-related chronic pelvic pain and pelvic spasm.
All 28 women currently enrolled in the trial (median age, 29 years) were evaluated by a gynecologist to confirm pelvic muscle spasm as their primary source of pain. Each also underwent a neuromuscular examination to identify pain points beyond the pelvis.
All subjects had myofascial dysfunction. Most reported headaches and half reported orofacial pain, while 13 subjects reported myofascial trigger points in all the 26 spots assessed, which included head and facial muscles, shoulder and back muscles, and muscles in the buttocks, abdomen, and upper legs.
Dr. Karp said her group hypothesized that for patients with endometriosis, the widespread pain seen in the study “probably has some origin in sensitization initiated by pain associated with the endometriosis lesions, and that gives us a mechanism to think about peripheral and central sensitization.” But she noted that such sensitization can be easily missed in the clinic.
“One of the things that’s really underappreciated is how much women with chronic pelvic pain have pain elsewhere. So the neurologist or pain specialist may say, ‘that’s not my body territory, there’s something going on with your pelvis.’ And the gynecologist may be focused on the endometriosis and the endometriosis lesions. So you have these women with really widespread pain problems whose care is being fractionated.”
In another aspect of the study she also presented at the meeting, Dr. Karp, a neurologist who has studied the therapeutic use of neurotoxins such as botulinum for 30 years, showed results from an open-label extension of a randomized trial of botulinum toxin injections to treat pelvic spasm in the same cohort of women with confirmed endometriosis and confirmed pelvic muscle spasm.
A month after the open-label injection, spasm was reduced or absent in all subjects (P = .0005), with 11 of 13 rating pain as absent or mild (P = .0001), Dr. Karp and her colleagues reported. Between 5 and 11 months post injection, five women requested a repeat of the treatment.
Besides the data on pain and disability collected as part of the trial, Dr. Karp and her colleagues are also looking at biomarkers for pain and inflammation, and changes in medication and hormone use. They are preparing a separate literature review on injection techniques and dosages of toxin to the pelvic floor muscles.
“It’s an area of the body neurologists don’t feel comfortable injecting, and I don’t necessarily feel comfortable doing it myself,” Dr. Karp said.
The researchers had to develop their own procedure because at the time they started the research there was almost nothing in the literature on how to inject botulinum toxin for pelvic pain in women. “People in different specialties have been doing it [to relieve pelvic pain] and it’s really widespread, but they’re doing it all different ways,” Dr. Karp said. “We’re hoping to find a best approach.”
Dr. Karp and her colleagues’ research is supported by the NINDS and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. OnabotulinumtoxinA for the clinical trial is supplied by Allergan. Dr. Karp has received research support from Allergan and Merz.
SOURCE: Karp B et al. AAN 2018, Abstract P2.096; Karp B et al. AAN 2018, Abstract P2.098.
LOS ANGELES – Women treated surgically and with hormones for endometriosis may continue to experience pain, say investigators, and that pain frequently extends beyond the pelvis.
At the annual meeting of the American Academy of Neurology, Barbara Karp, MD, of the National Institute of Neurological Disorders and Stroke, presented results from an ongoing randomized trial of women with endometriosis receiving botulinum toxin to treat endometriosis-related chronic pelvic pain and pelvic spasm.
All 28 women currently enrolled in the trial (median age, 29 years) were evaluated by a gynecologist to confirm pelvic muscle spasm as their primary source of pain. Each also underwent a neuromuscular examination to identify pain points beyond the pelvis.
All subjects had myofascial dysfunction. Most reported headaches and half reported orofacial pain, while 13 subjects reported myofascial trigger points in all the 26 spots assessed, which included head and facial muscles, shoulder and back muscles, and muscles in the buttocks, abdomen, and upper legs.
Dr. Karp said her group hypothesized that for patients with endometriosis, the widespread pain seen in the study “probably has some origin in sensitization initiated by pain associated with the endometriosis lesions, and that gives us a mechanism to think about peripheral and central sensitization.” But she noted that such sensitization can be easily missed in the clinic.
“One of the things that’s really underappreciated is how much women with chronic pelvic pain have pain elsewhere. So the neurologist or pain specialist may say, ‘that’s not my body territory, there’s something going on with your pelvis.’ And the gynecologist may be focused on the endometriosis and the endometriosis lesions. So you have these women with really widespread pain problems whose care is being fractionated.”
In another aspect of the study she also presented at the meeting, Dr. Karp, a neurologist who has studied the therapeutic use of neurotoxins such as botulinum for 30 years, showed results from an open-label extension of a randomized trial of botulinum toxin injections to treat pelvic spasm in the same cohort of women with confirmed endometriosis and confirmed pelvic muscle spasm.
A month after the open-label injection, spasm was reduced or absent in all subjects (P = .0005), with 11 of 13 rating pain as absent or mild (P = .0001), Dr. Karp and her colleagues reported. Between 5 and 11 months post injection, five women requested a repeat of the treatment.
Besides the data on pain and disability collected as part of the trial, Dr. Karp and her colleagues are also looking at biomarkers for pain and inflammation, and changes in medication and hormone use. They are preparing a separate literature review on injection techniques and dosages of toxin to the pelvic floor muscles.
“It’s an area of the body neurologists don’t feel comfortable injecting, and I don’t necessarily feel comfortable doing it myself,” Dr. Karp said.
The researchers had to develop their own procedure because at the time they started the research there was almost nothing in the literature on how to inject botulinum toxin for pelvic pain in women. “People in different specialties have been doing it [to relieve pelvic pain] and it’s really widespread, but they’re doing it all different ways,” Dr. Karp said. “We’re hoping to find a best approach.”
Dr. Karp and her colleagues’ research is supported by the NINDS and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. OnabotulinumtoxinA for the clinical trial is supplied by Allergan. Dr. Karp has received research support from Allergan and Merz.
SOURCE: Karp B et al. AAN 2018, Abstract P2.096; Karp B et al. AAN 2018, Abstract P2.098.
LOS ANGELES – Women treated surgically and with hormones for endometriosis may continue to experience pain, say investigators, and that pain frequently extends beyond the pelvis.
At the annual meeting of the American Academy of Neurology, Barbara Karp, MD, of the National Institute of Neurological Disorders and Stroke, presented results from an ongoing randomized trial of women with endometriosis receiving botulinum toxin to treat endometriosis-related chronic pelvic pain and pelvic spasm.
All 28 women currently enrolled in the trial (median age, 29 years) were evaluated by a gynecologist to confirm pelvic muscle spasm as their primary source of pain. Each also underwent a neuromuscular examination to identify pain points beyond the pelvis.
All subjects had myofascial dysfunction. Most reported headaches and half reported orofacial pain, while 13 subjects reported myofascial trigger points in all the 26 spots assessed, which included head and facial muscles, shoulder and back muscles, and muscles in the buttocks, abdomen, and upper legs.
Dr. Karp said her group hypothesized that for patients with endometriosis, the widespread pain seen in the study “probably has some origin in sensitization initiated by pain associated with the endometriosis lesions, and that gives us a mechanism to think about peripheral and central sensitization.” But she noted that such sensitization can be easily missed in the clinic.
“One of the things that’s really underappreciated is how much women with chronic pelvic pain have pain elsewhere. So the neurologist or pain specialist may say, ‘that’s not my body territory, there’s something going on with your pelvis.’ And the gynecologist may be focused on the endometriosis and the endometriosis lesions. So you have these women with really widespread pain problems whose care is being fractionated.”
In another aspect of the study she also presented at the meeting, Dr. Karp, a neurologist who has studied the therapeutic use of neurotoxins such as botulinum for 30 years, showed results from an open-label extension of a randomized trial of botulinum toxin injections to treat pelvic spasm in the same cohort of women with confirmed endometriosis and confirmed pelvic muscle spasm.
A month after the open-label injection, spasm was reduced or absent in all subjects (P = .0005), with 11 of 13 rating pain as absent or mild (P = .0001), Dr. Karp and her colleagues reported. Between 5 and 11 months post injection, five women requested a repeat of the treatment.
Besides the data on pain and disability collected as part of the trial, Dr. Karp and her colleagues are also looking at biomarkers for pain and inflammation, and changes in medication and hormone use. They are preparing a separate literature review on injection techniques and dosages of toxin to the pelvic floor muscles.
“It’s an area of the body neurologists don’t feel comfortable injecting, and I don’t necessarily feel comfortable doing it myself,” Dr. Karp said.
The researchers had to develop their own procedure because at the time they started the research there was almost nothing in the literature on how to inject botulinum toxin for pelvic pain in women. “People in different specialties have been doing it [to relieve pelvic pain] and it’s really widespread, but they’re doing it all different ways,” Dr. Karp said. “We’re hoping to find a best approach.”
Dr. Karp and her colleagues’ research is supported by the NINDS and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. OnabotulinumtoxinA for the clinical trial is supplied by Allergan. Dr. Karp has received research support from Allergan and Merz.
SOURCE: Karp B et al. AAN 2018, Abstract P2.096; Karp B et al. AAN 2018, Abstract P2.098.
REPORTING FROM AAN 2018
Key clinical point:
Major finding: A month after the open-label injection, spasm was reduced or absent in all subjects (P = .0005), with 11 of 13 rating pain as absent or mild (P = .0001).
Study details: An open-label extension in 13 of 28 patients enrolled in a randomized trial.
Disclosures: Dr. Karp and her colleagues’ research is supported by the NINDS and the Eunice Kennedy Shriver National Institute of Child Health and Human Development. OnabotulinumtoxinA for the clinical trial is supplied by Allergan. Dr. Karp has received research support from Allergan and Merz.
Source: Karp B et al. AAN 2018, Abstract P2.096; Karp B et al. AAN 2018, Abstract P2.098.
VIDEOS: High-priced drugs, out-of-pocket costs raise challenges for neurologists
LOS ANGELES – Neurologists can play an important role in helping patients gain access to high-cost, breakthrough drugs, while at the same time guiding patients to lower-cost options whenever possible, speakers said at the annual meeting of the American Academy of Neurology.
The use of the Orphan Drug approval pathway established in 1983 has gained a great deal of steam for rare neurologic diseases in recent years with the approval of a number of drugs, such as nusinersen (Spinraza) for spinal muscular atrophy, eteplirsen (Exondys 51) for Duchenne muscular dystrophy, and edaravone (Radicava) for amyotrophic lateral sclerosis, said Nicholas Johnson, MD, a pediatric neuromuscular disease specialist at the University of Utah, Salt Lake City.
But given that only 2% of U.S. physicians are neurologists, yet 18% of rare diseases are neurologic and 11% of drugs in development overall are for neurologic diseases, there are a great deal of challenges arising for neurologists in getting access to these new high-priced drugs for their patients, said Dr. Johnson, who leads the AAN’s Neurology Drug Pricing Task Force and is also chair of the AAN Government Relations Committee.
These challenges range from increased administrative burden on staff, getting insurance approval, finding administration sites, and the ability to perform special patient assessments, he said in an interview.
Dr. Nicholas Johnson’s interview:
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Brian Callaghan’s interview:
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Many high-priced drugs commonly prescribed for chronic neurologic conditions and diagnostic tests also have high out-of-pocket costs for patients, but it is remarkably hard even for well-informed experts to find the actual costs that patients will pay out of pocket for such drugs and tests, according to Brian Callaghan, MD, a neuromuscular disease specialist at the University of Michigan, Ann Arbor.
Neurologist can seek to find more affordable alternatives to drugs when the out-of-pocket expenses are too great, said Dr. Callaghan, who also serves on the Neurology Drug Pricing Task Force. It may be advisable to put certain drugs lower on a list of potential treatment options than others for a chronic condition such as epilepsy because of their out-of-pocket costs, but it can be frustratingly hard to determine these costs in advance.
The University of Michigan Health System is unique in having drug cost data provided as part of information presented to physicians in electronic health records, but this is not the case in most other clinics. Until doctors can regularly access patient-specific drug and diagnostic testing out-of-pocket costs through EHRs, finding the best affordable medications for patients will remain a costly and time-consuming process, he said in an interview.
LOS ANGELES – Neurologists can play an important role in helping patients gain access to high-cost, breakthrough drugs, while at the same time guiding patients to lower-cost options whenever possible, speakers said at the annual meeting of the American Academy of Neurology.
The use of the Orphan Drug approval pathway established in 1983 has gained a great deal of steam for rare neurologic diseases in recent years with the approval of a number of drugs, such as nusinersen (Spinraza) for spinal muscular atrophy, eteplirsen (Exondys 51) for Duchenne muscular dystrophy, and edaravone (Radicava) for amyotrophic lateral sclerosis, said Nicholas Johnson, MD, a pediatric neuromuscular disease specialist at the University of Utah, Salt Lake City.
But given that only 2% of U.S. physicians are neurologists, yet 18% of rare diseases are neurologic and 11% of drugs in development overall are for neurologic diseases, there are a great deal of challenges arising for neurologists in getting access to these new high-priced drugs for their patients, said Dr. Johnson, who leads the AAN’s Neurology Drug Pricing Task Force and is also chair of the AAN Government Relations Committee.
These challenges range from increased administrative burden on staff, getting insurance approval, finding administration sites, and the ability to perform special patient assessments, he said in an interview.
Dr. Nicholas Johnson’s interview:
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Brian Callaghan’s interview:
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Many high-priced drugs commonly prescribed for chronic neurologic conditions and diagnostic tests also have high out-of-pocket costs for patients, but it is remarkably hard even for well-informed experts to find the actual costs that patients will pay out of pocket for such drugs and tests, according to Brian Callaghan, MD, a neuromuscular disease specialist at the University of Michigan, Ann Arbor.
Neurologist can seek to find more affordable alternatives to drugs when the out-of-pocket expenses are too great, said Dr. Callaghan, who also serves on the Neurology Drug Pricing Task Force. It may be advisable to put certain drugs lower on a list of potential treatment options than others for a chronic condition such as epilepsy because of their out-of-pocket costs, but it can be frustratingly hard to determine these costs in advance.
The University of Michigan Health System is unique in having drug cost data provided as part of information presented to physicians in electronic health records, but this is not the case in most other clinics. Until doctors can regularly access patient-specific drug and diagnostic testing out-of-pocket costs through EHRs, finding the best affordable medications for patients will remain a costly and time-consuming process, he said in an interview.
LOS ANGELES – Neurologists can play an important role in helping patients gain access to high-cost, breakthrough drugs, while at the same time guiding patients to lower-cost options whenever possible, speakers said at the annual meeting of the American Academy of Neurology.
The use of the Orphan Drug approval pathway established in 1983 has gained a great deal of steam for rare neurologic diseases in recent years with the approval of a number of drugs, such as nusinersen (Spinraza) for spinal muscular atrophy, eteplirsen (Exondys 51) for Duchenne muscular dystrophy, and edaravone (Radicava) for amyotrophic lateral sclerosis, said Nicholas Johnson, MD, a pediatric neuromuscular disease specialist at the University of Utah, Salt Lake City.
But given that only 2% of U.S. physicians are neurologists, yet 18% of rare diseases are neurologic and 11% of drugs in development overall are for neurologic diseases, there are a great deal of challenges arising for neurologists in getting access to these new high-priced drugs for their patients, said Dr. Johnson, who leads the AAN’s Neurology Drug Pricing Task Force and is also chair of the AAN Government Relations Committee.
These challenges range from increased administrative burden on staff, getting insurance approval, finding administration sites, and the ability to perform special patient assessments, he said in an interview.
Dr. Nicholas Johnson’s interview:
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Brian Callaghan’s interview:
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Many high-priced drugs commonly prescribed for chronic neurologic conditions and diagnostic tests also have high out-of-pocket costs for patients, but it is remarkably hard even for well-informed experts to find the actual costs that patients will pay out of pocket for such drugs and tests, according to Brian Callaghan, MD, a neuromuscular disease specialist at the University of Michigan, Ann Arbor.
Neurologist can seek to find more affordable alternatives to drugs when the out-of-pocket expenses are too great, said Dr. Callaghan, who also serves on the Neurology Drug Pricing Task Force. It may be advisable to put certain drugs lower on a list of potential treatment options than others for a chronic condition such as epilepsy because of their out-of-pocket costs, but it can be frustratingly hard to determine these costs in advance.
The University of Michigan Health System is unique in having drug cost data provided as part of information presented to physicians in electronic health records, but this is not the case in most other clinics. Until doctors can regularly access patient-specific drug and diagnostic testing out-of-pocket costs through EHRs, finding the best affordable medications for patients will remain a costly and time-consuming process, he said in an interview.
REPORTING FROM AAN 2018
Real-world data so far support pimavanserin trial results
LOS ANGELES – Two studies of real-world use of pimavanserin after its approval in March 2016 for the treatment of Parkinson’s disease–associated psychosis indicate its effectiveness, tolerability, and safety in line with clinical trial results, according to reports presented at the annual meeting of the American Academy of Neurology.
In the first study, 102 patients were prescribed pimavanserin (Nuplazid) during May 2016-March 2018. Of the 88 patients who actually took the drug, 83% had Parkinson’s, and 78% were men. Participants’ mean age was 79 years. Nearly a third had deep brain stimulation.
About two-thirds of the patients started taking pimavanserin after failing prior antipsychotic therapy, whereas the other third had not previously taken an antipsychotic. Quetiapine had been used by 91% of previous antipsychotic users, and another 20% had taken clozapine. Other antipsychotics were less commonly used.
There was no consistent strategy implemented for starting pimavanserin: 17 stopped or were advised to stop their other antipsychotic before starting pimavanserin, 15 were told to taper off their other antipsychotic for 1 week or for up to 3 months, and 22 were told to keep taking their other antipsychotic after starting pimavanserin.
The mean treatment duration has been nearly 11 months for the two-thirds of patients who remain on pimavanserin, including 38 who take it alone and another 20 who take it with another antipsychotic.
A total of 10 patients were unable to tolerate pimavanserin because of adverse events, 5 of whom had generalized weakness/gait instability. This adverse event was the only difference in adverse events that was seen from the clinical trials, said lead author Jessie Sellers, a nurse practitioner at Vanderbilt University Medical Center in Nashville, Tenn.
“But overall the drug was really well tolerated and was effective,” she said.
There also was no increase in mortality detected in users, providing evidence against an association with mortality in older people with dementia-related psychosis that previously led to a boxed warning for atypical antipsychotics, noted senior author Daniel O. Claassen, MD. A total of 6 of the 88 patients died, compared with 5 of the 14 patients who never started the drug.
Patients who stopped pimavanserin and started another antipsychotic had only limited success. Of 11 patients who stopped pimavanserin and started another antipsychotic, only 5 were successful. Another six who stopped pimavanserin did not take another antipsychotic drug, primarily because of the resolution of their symptoms.
The pimavanserin status was unknown for four patients, and another three patients who stopped the drug had not returned for follow-up.
Abhimanyu Mahajan, MD, and other researchers from Henry Ford Hospital in Detroit reported similar results with pimavanserin at the AAN annual meeting in a separate, smaller, retrospective chart review of 16 patients with Parkinson’s disease–associated psychosis and 1 with Lewy body dementia.
These patients had a mean duration of parkinsonism of nearly 12 years and more than 2 years of psychotic symptoms, which consisted of daily or continuous hallucinations in all but one patient.
Telephone interviews with patients and caregivers revealed that 10 of 14 had improvement in hallucinations, and 3 had stopped taking it because of either no benefit or remission. Of six patients who took pimavanserin monotherapy, half improved from severe to mild hallucination severity (less than one episode per week), two had no change, and one improved from severe to moderate. For the other eight patients who took pimavanserin with another antipsychotic, two had no change in hallucination severity, two went from severe to mild, three improved from severe to moderate, and one went from moderate to mild. The patients reported no major adverse events.
Ms. Sellers and another author had no disclosures. Dr. Claassen disclosed personal compensation for consulting, serving on a scientific advisory board, speaking, or other activities with several companies, including Acadia, which markets pimavanserin.
Two of the authors of Dr. Mahajan’s study reported financial ties to Acadia and other companies.
SOURCE: Sellers J et al. AAN 2018, abstract P1.040 and Mahajan A et al. AAN 2018, abstract P5.065
LOS ANGELES – Two studies of real-world use of pimavanserin after its approval in March 2016 for the treatment of Parkinson’s disease–associated psychosis indicate its effectiveness, tolerability, and safety in line with clinical trial results, according to reports presented at the annual meeting of the American Academy of Neurology.
In the first study, 102 patients were prescribed pimavanserin (Nuplazid) during May 2016-March 2018. Of the 88 patients who actually took the drug, 83% had Parkinson’s, and 78% were men. Participants’ mean age was 79 years. Nearly a third had deep brain stimulation.
About two-thirds of the patients started taking pimavanserin after failing prior antipsychotic therapy, whereas the other third had not previously taken an antipsychotic. Quetiapine had been used by 91% of previous antipsychotic users, and another 20% had taken clozapine. Other antipsychotics were less commonly used.
There was no consistent strategy implemented for starting pimavanserin: 17 stopped or were advised to stop their other antipsychotic before starting pimavanserin, 15 were told to taper off their other antipsychotic for 1 week or for up to 3 months, and 22 were told to keep taking their other antipsychotic after starting pimavanserin.
The mean treatment duration has been nearly 11 months for the two-thirds of patients who remain on pimavanserin, including 38 who take it alone and another 20 who take it with another antipsychotic.
A total of 10 patients were unable to tolerate pimavanserin because of adverse events, 5 of whom had generalized weakness/gait instability. This adverse event was the only difference in adverse events that was seen from the clinical trials, said lead author Jessie Sellers, a nurse practitioner at Vanderbilt University Medical Center in Nashville, Tenn.
“But overall the drug was really well tolerated and was effective,” she said.
There also was no increase in mortality detected in users, providing evidence against an association with mortality in older people with dementia-related psychosis that previously led to a boxed warning for atypical antipsychotics, noted senior author Daniel O. Claassen, MD. A total of 6 of the 88 patients died, compared with 5 of the 14 patients who never started the drug.
Patients who stopped pimavanserin and started another antipsychotic had only limited success. Of 11 patients who stopped pimavanserin and started another antipsychotic, only 5 were successful. Another six who stopped pimavanserin did not take another antipsychotic drug, primarily because of the resolution of their symptoms.
The pimavanserin status was unknown for four patients, and another three patients who stopped the drug had not returned for follow-up.
Abhimanyu Mahajan, MD, and other researchers from Henry Ford Hospital in Detroit reported similar results with pimavanserin at the AAN annual meeting in a separate, smaller, retrospective chart review of 16 patients with Parkinson’s disease–associated psychosis and 1 with Lewy body dementia.
These patients had a mean duration of parkinsonism of nearly 12 years and more than 2 years of psychotic symptoms, which consisted of daily or continuous hallucinations in all but one patient.
Telephone interviews with patients and caregivers revealed that 10 of 14 had improvement in hallucinations, and 3 had stopped taking it because of either no benefit or remission. Of six patients who took pimavanserin monotherapy, half improved from severe to mild hallucination severity (less than one episode per week), two had no change, and one improved from severe to moderate. For the other eight patients who took pimavanserin with another antipsychotic, two had no change in hallucination severity, two went from severe to mild, three improved from severe to moderate, and one went from moderate to mild. The patients reported no major adverse events.
Ms. Sellers and another author had no disclosures. Dr. Claassen disclosed personal compensation for consulting, serving on a scientific advisory board, speaking, or other activities with several companies, including Acadia, which markets pimavanserin.
Two of the authors of Dr. Mahajan’s study reported financial ties to Acadia and other companies.
SOURCE: Sellers J et al. AAN 2018, abstract P1.040 and Mahajan A et al. AAN 2018, abstract P5.065
LOS ANGELES – Two studies of real-world use of pimavanserin after its approval in March 2016 for the treatment of Parkinson’s disease–associated psychosis indicate its effectiveness, tolerability, and safety in line with clinical trial results, according to reports presented at the annual meeting of the American Academy of Neurology.
In the first study, 102 patients were prescribed pimavanserin (Nuplazid) during May 2016-March 2018. Of the 88 patients who actually took the drug, 83% had Parkinson’s, and 78% were men. Participants’ mean age was 79 years. Nearly a third had deep brain stimulation.
About two-thirds of the patients started taking pimavanserin after failing prior antipsychotic therapy, whereas the other third had not previously taken an antipsychotic. Quetiapine had been used by 91% of previous antipsychotic users, and another 20% had taken clozapine. Other antipsychotics were less commonly used.
There was no consistent strategy implemented for starting pimavanserin: 17 stopped or were advised to stop their other antipsychotic before starting pimavanserin, 15 were told to taper off their other antipsychotic for 1 week or for up to 3 months, and 22 were told to keep taking their other antipsychotic after starting pimavanserin.
The mean treatment duration has been nearly 11 months for the two-thirds of patients who remain on pimavanserin, including 38 who take it alone and another 20 who take it with another antipsychotic.
A total of 10 patients were unable to tolerate pimavanserin because of adverse events, 5 of whom had generalized weakness/gait instability. This adverse event was the only difference in adverse events that was seen from the clinical trials, said lead author Jessie Sellers, a nurse practitioner at Vanderbilt University Medical Center in Nashville, Tenn.
“But overall the drug was really well tolerated and was effective,” she said.
There also was no increase in mortality detected in users, providing evidence against an association with mortality in older people with dementia-related psychosis that previously led to a boxed warning for atypical antipsychotics, noted senior author Daniel O. Claassen, MD. A total of 6 of the 88 patients died, compared with 5 of the 14 patients who never started the drug.
Patients who stopped pimavanserin and started another antipsychotic had only limited success. Of 11 patients who stopped pimavanserin and started another antipsychotic, only 5 were successful. Another six who stopped pimavanserin did not take another antipsychotic drug, primarily because of the resolution of their symptoms.
The pimavanserin status was unknown for four patients, and another three patients who stopped the drug had not returned for follow-up.
Abhimanyu Mahajan, MD, and other researchers from Henry Ford Hospital in Detroit reported similar results with pimavanserin at the AAN annual meeting in a separate, smaller, retrospective chart review of 16 patients with Parkinson’s disease–associated psychosis and 1 with Lewy body dementia.
These patients had a mean duration of parkinsonism of nearly 12 years and more than 2 years of psychotic symptoms, which consisted of daily or continuous hallucinations in all but one patient.
Telephone interviews with patients and caregivers revealed that 10 of 14 had improvement in hallucinations, and 3 had stopped taking it because of either no benefit or remission. Of six patients who took pimavanserin monotherapy, half improved from severe to mild hallucination severity (less than one episode per week), two had no change, and one improved from severe to moderate. For the other eight patients who took pimavanserin with another antipsychotic, two had no change in hallucination severity, two went from severe to mild, three improved from severe to moderate, and one went from moderate to mild. The patients reported no major adverse events.
Ms. Sellers and another author had no disclosures. Dr. Claassen disclosed personal compensation for consulting, serving on a scientific advisory board, speaking, or other activities with several companies, including Acadia, which markets pimavanserin.
Two of the authors of Dr. Mahajan’s study reported financial ties to Acadia and other companies.
SOURCE: Sellers J et al. AAN 2018, abstract P1.040 and Mahajan A et al. AAN 2018, abstract P5.065
REPORTING FROM AAN 2018
Key clinical point:
Major finding: Psychotic symptoms improved in 71%-88% of patients taking pimavanserin.
Study details: Two retrospective chart reviews totaling 105 patients who took pimavanserin.
Disclosures: One or more authors in each study reported financial ties to Acadia, which markets pimavanserin.
Source: Sellers J et al. AAN 2018, abstract P1.040, and Mahajan A et al. AAN 2018, abstract P5.065.
VIDEO: AAN MS guidelines aim to help clinicians weigh expanding drug choices
LOS ANGELES – A new clinical guideline for adults with multiple sclerosis is designed to help clinicians navigate an increasingly complex landscape of treatment options, its authors say.
The new American Academy of Neurology (AAN) guideline includes some 30 recommendations related to starting a disease-modifying therapy (DMT), switching therapies, or stopping treatment. The guideline, presented April 23 at the AAN annual meeting and published online simultaneously in Neurology, is the first full MS practice guideline issued by AAN since 2002, when only a handful of medications were licensed for use in MS.
The new guideline does not present a hierarchy of DMTs to start but instead weighs evidence for 21 medications or formulations, including 8 used off label, with the idea that clinicians will tailor their choices by considering patient needs, preferences, potential adverse affects, cost of medicines, comorbidities (including depression), and likelihood of adherence, among other factors addressed.
“It’s a dramatically different landscape of the choices clinicians have,” guideline lead author Alexander Rae-Grant, MD, of the Cleveland Clinic, said at a press conference announcing the guideline.
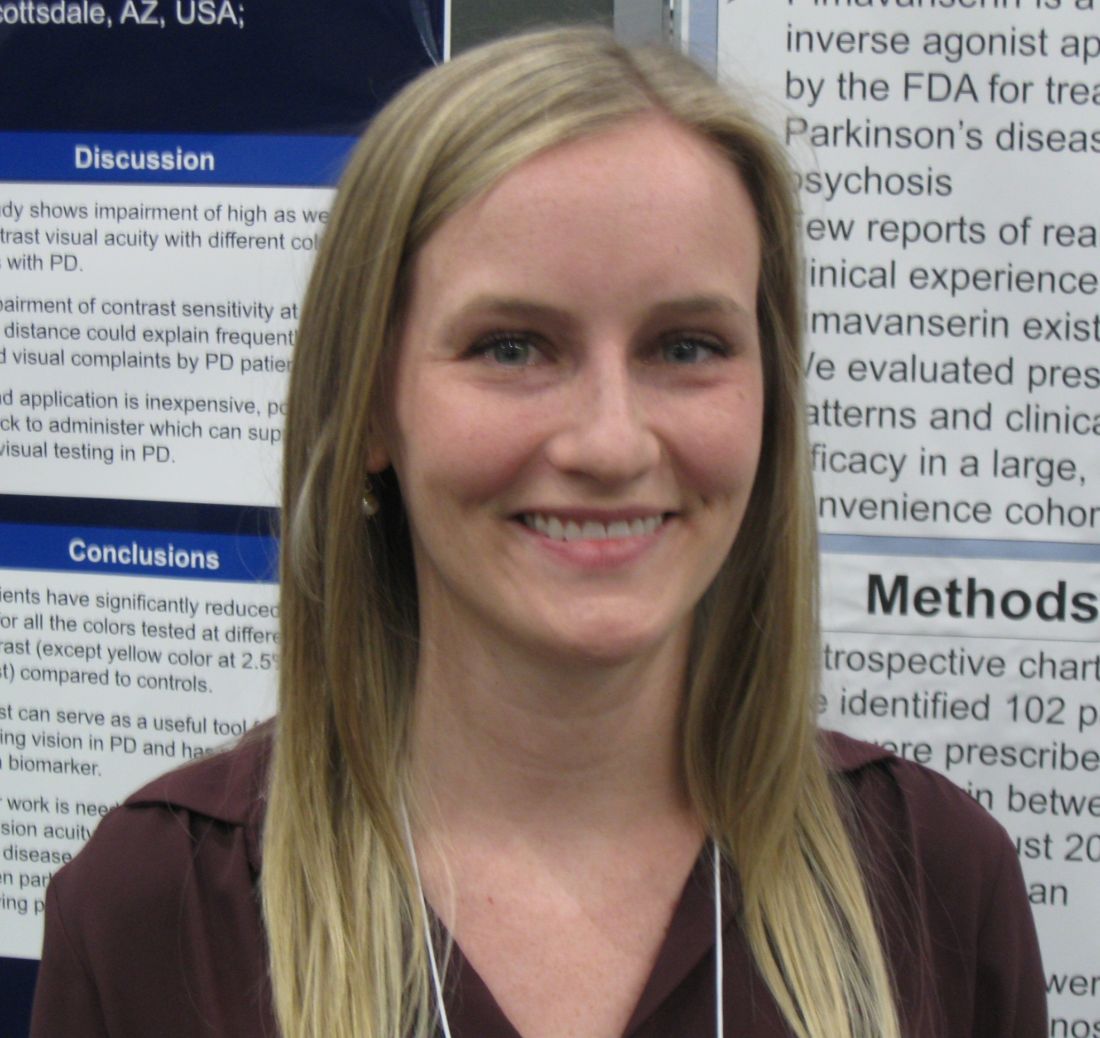
The guideline encourages clinicians and patients “to have a detailed discussion of the risks and benefits of different therapies,” guideline coauthor Ruth Ann Marrie, MD, PhD, of the University of Manitoba, Winnipeg, said at the press conference. “You need to have that informed ... discussion to share decision making – the guideline provides information for each provider-patient dyad to make decisions specific to that patient.”
The guideline incorporates findings from nearly 50 randomized trials, although few of these were head-to-head comparisons of therapies. The authors graded evidence for each DMT as compared with placebo or other DMTs in lowering relapse rate, taking into consideration study design and size. The guideline reflects changes to diagnostic criteria made in 2010, and a classification scheme issued in 2014 for MS subtypes, both of which have complicated the extension of clinical trial findings to some patient groups. It stresses early treatment, recommending that clinicians start DMTs in people with a single clinical demyelinating event and two or more brain lesions characteristic of MS.
Several drugs used off label in MS, including azathioprine and cladribine, were included in the evidence review, with cladribine described as a cost-effective option for patients without the resources to obtain approved agents.
Patients with a new diagnosis of MS should be counseled on starting DMTs not at the time of diagnosis but in a dedicated follow-up visit, the guideline says. Dr. Rae-Grant said that there’s a reasonable amount of “literature to suggest that at the time of diagnosis, what people hear after diagnosis is zero – and that deciding what medication to use is such a weighty decision, we did feel it was important to do that at a different time.”
Dr. Marrie said the AAN guideline “shares some strong similarities” with guidelines released in 2017 by the European Academy of Neurology, including recommendations for early initiation of therapy, for maintaining therapies, and for switching DMTs in individuals not responding or who have breakthrough relapses or changes on MRI.
Dr. Marrie disclosed no conflicts of interest related to her work on the guidelines. Dr. Rae-Grant disclosed income from textbooks on neurology and MS, and no other financial conflicts of interest.
SOURCE: Rae-Grant A et al. Neurology. 2018;90:777-88.
LOS ANGELES – A new clinical guideline for adults with multiple sclerosis is designed to help clinicians navigate an increasingly complex landscape of treatment options, its authors say.
The new American Academy of Neurology (AAN) guideline includes some 30 recommendations related to starting a disease-modifying therapy (DMT), switching therapies, or stopping treatment. The guideline, presented April 23 at the AAN annual meeting and published online simultaneously in Neurology, is the first full MS practice guideline issued by AAN since 2002, when only a handful of medications were licensed for use in MS.
The new guideline does not present a hierarchy of DMTs to start but instead weighs evidence for 21 medications or formulations, including 8 used off label, with the idea that clinicians will tailor their choices by considering patient needs, preferences, potential adverse affects, cost of medicines, comorbidities (including depression), and likelihood of adherence, among other factors addressed.
“It’s a dramatically different landscape of the choices clinicians have,” guideline lead author Alexander Rae-Grant, MD, of the Cleveland Clinic, said at a press conference announcing the guideline.
The guideline encourages clinicians and patients “to have a detailed discussion of the risks and benefits of different therapies,” guideline coauthor Ruth Ann Marrie, MD, PhD, of the University of Manitoba, Winnipeg, said at the press conference. “You need to have that informed ... discussion to share decision making – the guideline provides information for each provider-patient dyad to make decisions specific to that patient.”
The guideline incorporates findings from nearly 50 randomized trials, although few of these were head-to-head comparisons of therapies. The authors graded evidence for each DMT as compared with placebo or other DMTs in lowering relapse rate, taking into consideration study design and size. The guideline reflects changes to diagnostic criteria made in 2010, and a classification scheme issued in 2014 for MS subtypes, both of which have complicated the extension of clinical trial findings to some patient groups. It stresses early treatment, recommending that clinicians start DMTs in people with a single clinical demyelinating event and two or more brain lesions characteristic of MS.
Several drugs used off label in MS, including azathioprine and cladribine, were included in the evidence review, with cladribine described as a cost-effective option for patients without the resources to obtain approved agents.
Patients with a new diagnosis of MS should be counseled on starting DMTs not at the time of diagnosis but in a dedicated follow-up visit, the guideline says. Dr. Rae-Grant said that there’s a reasonable amount of “literature to suggest that at the time of diagnosis, what people hear after diagnosis is zero – and that deciding what medication to use is such a weighty decision, we did feel it was important to do that at a different time.”
Dr. Marrie said the AAN guideline “shares some strong similarities” with guidelines released in 2017 by the European Academy of Neurology, including recommendations for early initiation of therapy, for maintaining therapies, and for switching DMTs in individuals not responding or who have breakthrough relapses or changes on MRI.
Dr. Marrie disclosed no conflicts of interest related to her work on the guidelines. Dr. Rae-Grant disclosed income from textbooks on neurology and MS, and no other financial conflicts of interest.
SOURCE: Rae-Grant A et al. Neurology. 2018;90:777-88.
LOS ANGELES – A new clinical guideline for adults with multiple sclerosis is designed to help clinicians navigate an increasingly complex landscape of treatment options, its authors say.
The new American Academy of Neurology (AAN) guideline includes some 30 recommendations related to starting a disease-modifying therapy (DMT), switching therapies, or stopping treatment. The guideline, presented April 23 at the AAN annual meeting and published online simultaneously in Neurology, is the first full MS practice guideline issued by AAN since 2002, when only a handful of medications were licensed for use in MS.
The new guideline does not present a hierarchy of DMTs to start but instead weighs evidence for 21 medications or formulations, including 8 used off label, with the idea that clinicians will tailor their choices by considering patient needs, preferences, potential adverse affects, cost of medicines, comorbidities (including depression), and likelihood of adherence, among other factors addressed.
“It’s a dramatically different landscape of the choices clinicians have,” guideline lead author Alexander Rae-Grant, MD, of the Cleveland Clinic, said at a press conference announcing the guideline.
The guideline encourages clinicians and patients “to have a detailed discussion of the risks and benefits of different therapies,” guideline coauthor Ruth Ann Marrie, MD, PhD, of the University of Manitoba, Winnipeg, said at the press conference. “You need to have that informed ... discussion to share decision making – the guideline provides information for each provider-patient dyad to make decisions specific to that patient.”
The guideline incorporates findings from nearly 50 randomized trials, although few of these were head-to-head comparisons of therapies. The authors graded evidence for each DMT as compared with placebo or other DMTs in lowering relapse rate, taking into consideration study design and size. The guideline reflects changes to diagnostic criteria made in 2010, and a classification scheme issued in 2014 for MS subtypes, both of which have complicated the extension of clinical trial findings to some patient groups. It stresses early treatment, recommending that clinicians start DMTs in people with a single clinical demyelinating event and two or more brain lesions characteristic of MS.
Several drugs used off label in MS, including azathioprine and cladribine, were included in the evidence review, with cladribine described as a cost-effective option for patients without the resources to obtain approved agents.
Patients with a new diagnosis of MS should be counseled on starting DMTs not at the time of diagnosis but in a dedicated follow-up visit, the guideline says. Dr. Rae-Grant said that there’s a reasonable amount of “literature to suggest that at the time of diagnosis, what people hear after diagnosis is zero – and that deciding what medication to use is such a weighty decision, we did feel it was important to do that at a different time.”
Dr. Marrie said the AAN guideline “shares some strong similarities” with guidelines released in 2017 by the European Academy of Neurology, including recommendations for early initiation of therapy, for maintaining therapies, and for switching DMTs in individuals not responding or who have breakthrough relapses or changes on MRI.
Dr. Marrie disclosed no conflicts of interest related to her work on the guidelines. Dr. Rae-Grant disclosed income from textbooks on neurology and MS, and no other financial conflicts of interest.
SOURCE: Rae-Grant A et al. Neurology. 2018;90:777-88.
REPORTING FROM AAN 2018
VIDEO: Encouraging results reported for novel Huntington’s disease therapy
LOS ANGELES – Results from the first-in-human trial of the investigational antisense oligonucleotide therapy IONIS-HTTRx showed strong dose-dependent reductions in the toxic huntingtin protein in Huntington’s disease patients’ cerebrospinal fluid when compared with placebo.
An exploratory analysis also showed signals of clinical improvement among patients receiving the therapy, the study’s lead author, Sarah Tabrizi, MD, PhD, of University College London, reported at the annual meeting of the American Academy of Neurology.
The findings represent a potential breakthrough in the way Huntington’s – and possibly other neurodegenerative diseases – are treated, said Dr. Tabrizi of University College London. The intrathecally-delivered drug binds to mutant huntingtin protein mRNA to reduce the level of the toxic protein being made.
In the phase 1/2a trial, Dr. Tabrizi and her colleagues enrolled 46 patients with early-stage Huntington’s disease and randomized them to four doses of IONIS-HTTRx or placebo. Patients received four monthly injections of the study drug into the cerebrospinal fluid followed by a 4-month untreated follow-up period. IONIS-HTTRx was delivered in five ascending-dose cohorts.
IONIS-HTTRx was safe and well tolerated and all patients completed the study, Dr. Tabrizi reported. “Our results show that we had significant lowering of the toxic mutant huntingtin protein in the spinal fluid of the patients,” she said, noting that patients receiving the highest doses saw 40%-60% lowering of the protein, which preclinical work suggests correlates to reductions of the protein in the brain.
Dr. Tabrizi stressed that the main outcome measures in the study were reduction of the mutant protein in the CSF and safety and tolerance of the study drug. The investigators did not expect to see clinical measures to change in such a short, small study, she said.
“But then when we looked more carefully at the data with exploratory analysis we found a link between lowering of CSF mutant huntingtin and improvement in total motor score, which is a measure of neurological function, and also, improvement in the Symbol Digit Modalities Test.”
The clinical results are exploratory and require confirmation in larger studies, Dr. Tabrizi stressed.
The study was supported by Ionis Pharmaceuticals. Roche will develop the drug in further clinical trials.
SOURCE: Tabrizi S et al. AAN 2018 abstract CT.002.
LOS ANGELES – Results from the first-in-human trial of the investigational antisense oligonucleotide therapy IONIS-HTTRx showed strong dose-dependent reductions in the toxic huntingtin protein in Huntington’s disease patients’ cerebrospinal fluid when compared with placebo.
An exploratory analysis also showed signals of clinical improvement among patients receiving the therapy, the study’s lead author, Sarah Tabrizi, MD, PhD, of University College London, reported at the annual meeting of the American Academy of Neurology.
The findings represent a potential breakthrough in the way Huntington’s – and possibly other neurodegenerative diseases – are treated, said Dr. Tabrizi of University College London. The intrathecally-delivered drug binds to mutant huntingtin protein mRNA to reduce the level of the toxic protein being made.
In the phase 1/2a trial, Dr. Tabrizi and her colleagues enrolled 46 patients with early-stage Huntington’s disease and randomized them to four doses of IONIS-HTTRx or placebo. Patients received four monthly injections of the study drug into the cerebrospinal fluid followed by a 4-month untreated follow-up period. IONIS-HTTRx was delivered in five ascending-dose cohorts.
IONIS-HTTRx was safe and well tolerated and all patients completed the study, Dr. Tabrizi reported. “Our results show that we had significant lowering of the toxic mutant huntingtin protein in the spinal fluid of the patients,” she said, noting that patients receiving the highest doses saw 40%-60% lowering of the protein, which preclinical work suggests correlates to reductions of the protein in the brain.
Dr. Tabrizi stressed that the main outcome measures in the study were reduction of the mutant protein in the CSF and safety and tolerance of the study drug. The investigators did not expect to see clinical measures to change in such a short, small study, she said.
“But then when we looked more carefully at the data with exploratory analysis we found a link between lowering of CSF mutant huntingtin and improvement in total motor score, which is a measure of neurological function, and also, improvement in the Symbol Digit Modalities Test.”
The clinical results are exploratory and require confirmation in larger studies, Dr. Tabrizi stressed.
The study was supported by Ionis Pharmaceuticals. Roche will develop the drug in further clinical trials.
SOURCE: Tabrizi S et al. AAN 2018 abstract CT.002.
LOS ANGELES – Results from the first-in-human trial of the investigational antisense oligonucleotide therapy IONIS-HTTRx showed strong dose-dependent reductions in the toxic huntingtin protein in Huntington’s disease patients’ cerebrospinal fluid when compared with placebo.
An exploratory analysis also showed signals of clinical improvement among patients receiving the therapy, the study’s lead author, Sarah Tabrizi, MD, PhD, of University College London, reported at the annual meeting of the American Academy of Neurology.
The findings represent a potential breakthrough in the way Huntington’s – and possibly other neurodegenerative diseases – are treated, said Dr. Tabrizi of University College London. The intrathecally-delivered drug binds to mutant huntingtin protein mRNA to reduce the level of the toxic protein being made.
In the phase 1/2a trial, Dr. Tabrizi and her colleagues enrolled 46 patients with early-stage Huntington’s disease and randomized them to four doses of IONIS-HTTRx or placebo. Patients received four monthly injections of the study drug into the cerebrospinal fluid followed by a 4-month untreated follow-up period. IONIS-HTTRx was delivered in five ascending-dose cohorts.
IONIS-HTTRx was safe and well tolerated and all patients completed the study, Dr. Tabrizi reported. “Our results show that we had significant lowering of the toxic mutant huntingtin protein in the spinal fluid of the patients,” she said, noting that patients receiving the highest doses saw 40%-60% lowering of the protein, which preclinical work suggests correlates to reductions of the protein in the brain.
Dr. Tabrizi stressed that the main outcome measures in the study were reduction of the mutant protein in the CSF and safety and tolerance of the study drug. The investigators did not expect to see clinical measures to change in such a short, small study, she said.
“But then when we looked more carefully at the data with exploratory analysis we found a link between lowering of CSF mutant huntingtin and improvement in total motor score, which is a measure of neurological function, and also, improvement in the Symbol Digit Modalities Test.”
The clinical results are exploratory and require confirmation in larger studies, Dr. Tabrizi stressed.
The study was supported by Ionis Pharmaceuticals. Roche will develop the drug in further clinical trials.
SOURCE: Tabrizi S et al. AAN 2018 abstract CT.002.
REPORTING FROM AAN 2018
VIDEO: Ubrogepant reduced pain, related symptoms of a migraine attack
LOS ANGELES – The investigational oral calcitonin gene-related peptide (CGRP) blocker ubrogepant proved superior to placebo in treating a single, acute, moderate to severe migraine attack in the phase 3 ACHIEVE I trial.
Blocking the function of CGRP when it is pathologically released during a migraine attack is the mechanism of a bevy of antagonists under development for treating migraine, and the ACHIEVE I trial results are the first to be reported from a phase 3 trial of an oral small molecule to treat single migraine attacks rather than prevent attacks with monoclonal antibodies targeting CGRP or its receptor, according to the lead author of ACHIEVE I, Joel M. Trugman, MD, director of clinical development for Allergan.
Dr. Trugman and his colleagues recruited 1,672 adult patients (88% female, mean age 41) with a history of migraine with or without aura, and randomized them to placebo, ubrogepant 50 mg, or ubrogepant 100 mg. Patients were instructed to treat a single migraine attack of moderate to severe pain intensity and record symptoms, such as pain, light sensitivity, and sound sensitivity, before and after taking the medication.
“The paradigm for this type of trial is to treat a single, well characterized migraine attack in a large population of patients,” Dr. Trugman said in a press conference at the annual meeting of the American Academy of Neurology.
At 2 hours after dosing, the percentage of ubrogepant-treated patients achieving freedom from pain was significantly greater than the percentage of those treated with placebo (50 mg: 19.2%, P = .0023; 100 mg: 21.2%, P = .0003; placebo: 11.8%).
The percentage of ubrogepant-treated patients achieving absence of their most bothersome symptom was also significantly greater than that of placebo (50 mg: 38.6%, P = .0023; 100 mg: 37.7%, P = .0023; placebo: 27.8%).
Adverse events in the ubrogepant groups were similar to those of placebo, the most reported to be nausea, somnolence, and dry mouth.
Several authors are employees of Allergan, which sponsored the study.
SOURCE: Trugman J et al. AAN 2018 emerging science abstract 008.
LOS ANGELES – The investigational oral calcitonin gene-related peptide (CGRP) blocker ubrogepant proved superior to placebo in treating a single, acute, moderate to severe migraine attack in the phase 3 ACHIEVE I trial.
Blocking the function of CGRP when it is pathologically released during a migraine attack is the mechanism of a bevy of antagonists under development for treating migraine, and the ACHIEVE I trial results are the first to be reported from a phase 3 trial of an oral small molecule to treat single migraine attacks rather than prevent attacks with monoclonal antibodies targeting CGRP or its receptor, according to the lead author of ACHIEVE I, Joel M. Trugman, MD, director of clinical development for Allergan.
Dr. Trugman and his colleagues recruited 1,672 adult patients (88% female, mean age 41) with a history of migraine with or without aura, and randomized them to placebo, ubrogepant 50 mg, or ubrogepant 100 mg. Patients were instructed to treat a single migraine attack of moderate to severe pain intensity and record symptoms, such as pain, light sensitivity, and sound sensitivity, before and after taking the medication.
“The paradigm for this type of trial is to treat a single, well characterized migraine attack in a large population of patients,” Dr. Trugman said in a press conference at the annual meeting of the American Academy of Neurology.
At 2 hours after dosing, the percentage of ubrogepant-treated patients achieving freedom from pain was significantly greater than the percentage of those treated with placebo (50 mg: 19.2%, P = .0023; 100 mg: 21.2%, P = .0003; placebo: 11.8%).
The percentage of ubrogepant-treated patients achieving absence of their most bothersome symptom was also significantly greater than that of placebo (50 mg: 38.6%, P = .0023; 100 mg: 37.7%, P = .0023; placebo: 27.8%).
Adverse events in the ubrogepant groups were similar to those of placebo, the most reported to be nausea, somnolence, and dry mouth.
Several authors are employees of Allergan, which sponsored the study.
SOURCE: Trugman J et al. AAN 2018 emerging science abstract 008.
LOS ANGELES – The investigational oral calcitonin gene-related peptide (CGRP) blocker ubrogepant proved superior to placebo in treating a single, acute, moderate to severe migraine attack in the phase 3 ACHIEVE I trial.
Blocking the function of CGRP when it is pathologically released during a migraine attack is the mechanism of a bevy of antagonists under development for treating migraine, and the ACHIEVE I trial results are the first to be reported from a phase 3 trial of an oral small molecule to treat single migraine attacks rather than prevent attacks with monoclonal antibodies targeting CGRP or its receptor, according to the lead author of ACHIEVE I, Joel M. Trugman, MD, director of clinical development for Allergan.
Dr. Trugman and his colleagues recruited 1,672 adult patients (88% female, mean age 41) with a history of migraine with or without aura, and randomized them to placebo, ubrogepant 50 mg, or ubrogepant 100 mg. Patients were instructed to treat a single migraine attack of moderate to severe pain intensity and record symptoms, such as pain, light sensitivity, and sound sensitivity, before and after taking the medication.
“The paradigm for this type of trial is to treat a single, well characterized migraine attack in a large population of patients,” Dr. Trugman said in a press conference at the annual meeting of the American Academy of Neurology.
At 2 hours after dosing, the percentage of ubrogepant-treated patients achieving freedom from pain was significantly greater than the percentage of those treated with placebo (50 mg: 19.2%, P = .0023; 100 mg: 21.2%, P = .0003; placebo: 11.8%).
The percentage of ubrogepant-treated patients achieving absence of their most bothersome symptom was also significantly greater than that of placebo (50 mg: 38.6%, P = .0023; 100 mg: 37.7%, P = .0023; placebo: 27.8%).
Adverse events in the ubrogepant groups were similar to those of placebo, the most reported to be nausea, somnolence, and dry mouth.
Several authors are employees of Allergan, which sponsored the study.
SOURCE: Trugman J et al. AAN 2018 emerging science abstract 008.
REPORTING FROM AAN 2018
Multiple sclerosis “top picks” from AAN 2018
Clinical Neurology News editorial advisory board member Jonathan L. Carter, MD, scoured the pages of the American Academy of Neurology’s annual meeting program for his “top picks” in multiple sclerosis at this year’s meeting.
NFLCs in serum as a biomarker for MS and treatment response. Multiple abstracts explore the use of NFLCs as a marker for disease progression and response to MS therapies, including:
- Hot Topics Plenary Session presentation: “Monitoring Multiple Sclerosis Using Blood Neurofilament Light Protein” by Jens Kuhle, MD.
- P5.036, Serum and CSF Neurofilament Light Chain levels normalise following Bone Marrow Transplant in MS Patients.
- S24.002, Interim Analysis of the OBOE (Ocrelizumab Biomarker Outcome Evaluation) Study in Multiple Sclerosis (MS).
- S24.003, Serum Neurofilament Light (NfL): Towards a Blood Test for Prognosis and Disease/Treatment Monitoring in Multiple Sclerosis Patients.
- S24.004, Long-term Prognosis of Disease Evolution and Evidence for Sustained Fingolimod Treatment Effect by Blood Neurofilament Light in RRMS Patients.
- S24.007, Including Blood Neurofilament Light Chain in the NEDA Concept in Relapsing Remitting Multiple Sclerosis Trials.
- S8.006, Siponimod Reduces Neurofilament Light Chain Blood Levels in Secondary Progressive Multiple Sclerosis Patients.
Cognitive function as an outcome measure in MS clinical trials. Several abstracts examine cognition as an outcome measure in clinical trials and show slowing of cognitive worsening in patients on MS disease-modifying therapies:
- S44.004, Impact of Siponimod on Cognition in Patients With Secondary Progressive Multiple Sclerosis: Results From Phase 3 EXPAND Study.
- S44.005, Time to Cognitive Worsening in Patients With Relapsing Multiple Sclerosis in Ocrelizumab Phase 3 Trials.
- S44.007, Benchmarks of Cognitive Performance in a Large, Representative Patient Population.
Improved disability outcome measures and predictors of disability in MS. Several abstracts assess novel disability outcome measures and neuroimaging techniques to better predict progression of clinical disability:
- P4.380, Overall Response Score: A Novel Disability Endpoint That Allows for the Integrated Assessment of Improvement and Worsening over Time in Patients with MS.
- S47.001, Longitudinal Changes in Quantitative Spinal Cord MRI in Multiple Sclerosis Patients: Results of a 5-year Study.
- P6.354, Effect of Fingolimod 0.5 mg/day versus Placebo on Two Newly Developed Expanded Disability Status Scale (EDSS) Subscales for Patients with Relapsing Remitting MS: EDSS Factor Analysis.
Is treatment response in MS an age-dependent or relapse-driven phenomenon, and is it safe to discontinue MS therapies with advancing age? Several abstracts address this question:
- S47.004, Meta-Analysis of the Age-Dependent Efficacy of Multiple Sclerosis Treatments.
- S8.005, Uncoupling the Impact on Relapses and Disability Progression: Siponimod in Relapsing and Nonrelapsing Patients With Secondary Progressive Multiple Sclerosis in the Phase 3 EXPAND Study.
- S8.008, Discontinuation of Disease Modifying Therapies in Stable MS Patients is Associated with Disability Progression Regardless of Age.
Neuromyelitis optica spectrum disorders and MS mimics. Multiple abstracts explore the differences between neuromyelitis optica spectrum disorder because of aquaporin-4 versus myelin oligodendrocyte glycoprotein antibodies; describe unique features of another recently described autoimmune disorder, autoimmune GFAP astrocytopathy; and explore the differential diagnosis of idiopathic transverse myelitis:
- S13.002, Clinical Characteristics of MOG and AQP associated Neuromyelitis Optica Spectrum Disorder (NMOSD) in Adults, through S13.008, It’s Not All Transverse Myelitis: The Differential Diagnosis of Spinal Cord Myelopathy.
- P6.409, The Mayo Clinic Glial Autoimmunity Study: Glial autoantibody (AQP4/MOG/GFAP) serostatus in recurrent longitudinally extensive transverse myelitis.
- P6.417, Evaluation of idiopathic transverse myelitis revealing specific myelopathy diagnoses.
- S6.003, Brain and Spinal Cord Imaging Features in Neuromyelitis Optica Spectrum Disorders.
Updated safety and efficacy data for recently approved or investigational MS therapies. Multiple abstracts report updated safety and efficacy data from MS clinical trials of ozanimod, ocrelizumab (Ocrevus), and hematopoietic stem cell transplantation:
- Clinical Trials Plenary Session presentation: “A Phase 2 Trial of Ibudilast in Progressive Multiple Sclerosis” by Robert J. Fox, MD.
- Contemporary Clinical Issues Plenary Session presentation: “Biosimilars and Nonbiologic Complex Drugs” by Jeffrey Allan Cohen, MD.
- S6.002, Brain MRI Activity and Atrophy Measures in Patients Receiving Continuous Ocrelizumab or Switching From Interferon Beta-1a to Ocrelizumab Therapy in the Open-Label Extension Period of the Phase 3 Trials of Ocrelizumab in Patients With Relapsing Multiple Sclerosis.
- P3.410, Clinical and Magnetic Resonance Imaging Results From RADIANCE Part B, a Multicenter, Randomized, Double-Blind, Phase 3 Trial of Ozanimod Versus Intramuscular Interferon beta-1a in Relapsing Multiple Sclerosis (RMS).
- P3.396, Ozanimod Demonstrates Efficacy and Safety in a Multicenter, Randomized, Double-Blind, Double-Dummy, Active-Controlled Phase 3 Trial of Relapsing Multiple Sclerosis (SUNBEAM).
- S36.001, Safety of Ocrelizumab in Multiple Sclerosis: Updated Analysis in Patients With Relapsing and Primary Progressive Multiple Sclerosis.
- S36.004, Nonmyeloablative hematopoietic stem cell transplantation (HSCT) is superior to disease modifying drug (DMD) treatment in highly active Relapsing Remitting Multiple Sclerosis (RRMS): interim results of the Multiple Sclerosis International Stem cell Transplant (MIST) Randomized Trial.
- S36.005, Efficacy of Ozanimod Versus Interferon beta-1a by Prior Treatment and Baseline Disability in Two Multicenter, Randomized, Double-Blind, Parallel-Group, Active-Controlled, Double-Dummy Phase 3 Studies in Relapsing Multiple Sclerosis (SUNBEAM and RADIANCE Part B).
- S36.006, Safety of Ozanimod Versus Interferon beta-1a in Two Multicenter, Randomized, Double-Blind, Parallel-Group, Active-Controlled, Double-Dummy Phase 3 Studies in Relapsing Multiple Sclerosis (SUNBEAM and RADIANCE Part B).
New thoughts on MS pathogenesis.
- Frontiers in Neuroscience Plenary Session presentation: “Pediatric MS: A Unique Window into Environmental and Genetic Risk Factors for MS” by Emmanuelle Waubant, MD.
Dr. Carter has received personal compensation for consulting, serving on a scientific advisory board, speaking, or other activities with Alder Pharmaceuticals. He has received research support from Roche/Genentech and MedDay Pharmaceuticals.
Clinical Neurology News editorial advisory board member Jonathan L. Carter, MD, scoured the pages of the American Academy of Neurology’s annual meeting program for his “top picks” in multiple sclerosis at this year’s meeting.
NFLCs in serum as a biomarker for MS and treatment response. Multiple abstracts explore the use of NFLCs as a marker for disease progression and response to MS therapies, including:
- Hot Topics Plenary Session presentation: “Monitoring Multiple Sclerosis Using Blood Neurofilament Light Protein” by Jens Kuhle, MD.
- P5.036, Serum and CSF Neurofilament Light Chain levels normalise following Bone Marrow Transplant in MS Patients.
- S24.002, Interim Analysis of the OBOE (Ocrelizumab Biomarker Outcome Evaluation) Study in Multiple Sclerosis (MS).
- S24.003, Serum Neurofilament Light (NfL): Towards a Blood Test for Prognosis and Disease/Treatment Monitoring in Multiple Sclerosis Patients.
- S24.004, Long-term Prognosis of Disease Evolution and Evidence for Sustained Fingolimod Treatment Effect by Blood Neurofilament Light in RRMS Patients.
- S24.007, Including Blood Neurofilament Light Chain in the NEDA Concept in Relapsing Remitting Multiple Sclerosis Trials.
- S8.006, Siponimod Reduces Neurofilament Light Chain Blood Levels in Secondary Progressive Multiple Sclerosis Patients.
Cognitive function as an outcome measure in MS clinical trials. Several abstracts examine cognition as an outcome measure in clinical trials and show slowing of cognitive worsening in patients on MS disease-modifying therapies:
- S44.004, Impact of Siponimod on Cognition in Patients With Secondary Progressive Multiple Sclerosis: Results From Phase 3 EXPAND Study.
- S44.005, Time to Cognitive Worsening in Patients With Relapsing Multiple Sclerosis in Ocrelizumab Phase 3 Trials.
- S44.007, Benchmarks of Cognitive Performance in a Large, Representative Patient Population.
Improved disability outcome measures and predictors of disability in MS. Several abstracts assess novel disability outcome measures and neuroimaging techniques to better predict progression of clinical disability:
- P4.380, Overall Response Score: A Novel Disability Endpoint That Allows for the Integrated Assessment of Improvement and Worsening over Time in Patients with MS.
- S47.001, Longitudinal Changes in Quantitative Spinal Cord MRI in Multiple Sclerosis Patients: Results of a 5-year Study.
- P6.354, Effect of Fingolimod 0.5 mg/day versus Placebo on Two Newly Developed Expanded Disability Status Scale (EDSS) Subscales for Patients with Relapsing Remitting MS: EDSS Factor Analysis.
Is treatment response in MS an age-dependent or relapse-driven phenomenon, and is it safe to discontinue MS therapies with advancing age? Several abstracts address this question:
- S47.004, Meta-Analysis of the Age-Dependent Efficacy of Multiple Sclerosis Treatments.
- S8.005, Uncoupling the Impact on Relapses and Disability Progression: Siponimod in Relapsing and Nonrelapsing Patients With Secondary Progressive Multiple Sclerosis in the Phase 3 EXPAND Study.
- S8.008, Discontinuation of Disease Modifying Therapies in Stable MS Patients is Associated with Disability Progression Regardless of Age.
Neuromyelitis optica spectrum disorders and MS mimics. Multiple abstracts explore the differences between neuromyelitis optica spectrum disorder because of aquaporin-4 versus myelin oligodendrocyte glycoprotein antibodies; describe unique features of another recently described autoimmune disorder, autoimmune GFAP astrocytopathy; and explore the differential diagnosis of idiopathic transverse myelitis:
- S13.002, Clinical Characteristics of MOG and AQP associated Neuromyelitis Optica Spectrum Disorder (NMOSD) in Adults, through S13.008, It’s Not All Transverse Myelitis: The Differential Diagnosis of Spinal Cord Myelopathy.
- P6.409, The Mayo Clinic Glial Autoimmunity Study: Glial autoantibody (AQP4/MOG/GFAP) serostatus in recurrent longitudinally extensive transverse myelitis.
- P6.417, Evaluation of idiopathic transverse myelitis revealing specific myelopathy diagnoses.
- S6.003, Brain and Spinal Cord Imaging Features in Neuromyelitis Optica Spectrum Disorders.
Updated safety and efficacy data for recently approved or investigational MS therapies. Multiple abstracts report updated safety and efficacy data from MS clinical trials of ozanimod, ocrelizumab (Ocrevus), and hematopoietic stem cell transplantation:
- Clinical Trials Plenary Session presentation: “A Phase 2 Trial of Ibudilast in Progressive Multiple Sclerosis” by Robert J. Fox, MD.
- Contemporary Clinical Issues Plenary Session presentation: “Biosimilars and Nonbiologic Complex Drugs” by Jeffrey Allan Cohen, MD.
- S6.002, Brain MRI Activity and Atrophy Measures in Patients Receiving Continuous Ocrelizumab or Switching From Interferon Beta-1a to Ocrelizumab Therapy in the Open-Label Extension Period of the Phase 3 Trials of Ocrelizumab in Patients With Relapsing Multiple Sclerosis.
- P3.410, Clinical and Magnetic Resonance Imaging Results From RADIANCE Part B, a Multicenter, Randomized, Double-Blind, Phase 3 Trial of Ozanimod Versus Intramuscular Interferon beta-1a in Relapsing Multiple Sclerosis (RMS).
- P3.396, Ozanimod Demonstrates Efficacy and Safety in a Multicenter, Randomized, Double-Blind, Double-Dummy, Active-Controlled Phase 3 Trial of Relapsing Multiple Sclerosis (SUNBEAM).
- S36.001, Safety of Ocrelizumab in Multiple Sclerosis: Updated Analysis in Patients With Relapsing and Primary Progressive Multiple Sclerosis.
- S36.004, Nonmyeloablative hematopoietic stem cell transplantation (HSCT) is superior to disease modifying drug (DMD) treatment in highly active Relapsing Remitting Multiple Sclerosis (RRMS): interim results of the Multiple Sclerosis International Stem cell Transplant (MIST) Randomized Trial.
- S36.005, Efficacy of Ozanimod Versus Interferon beta-1a by Prior Treatment and Baseline Disability in Two Multicenter, Randomized, Double-Blind, Parallel-Group, Active-Controlled, Double-Dummy Phase 3 Studies in Relapsing Multiple Sclerosis (SUNBEAM and RADIANCE Part B).
- S36.006, Safety of Ozanimod Versus Interferon beta-1a in Two Multicenter, Randomized, Double-Blind, Parallel-Group, Active-Controlled, Double-Dummy Phase 3 Studies in Relapsing Multiple Sclerosis (SUNBEAM and RADIANCE Part B).
New thoughts on MS pathogenesis.
- Frontiers in Neuroscience Plenary Session presentation: “Pediatric MS: A Unique Window into Environmental and Genetic Risk Factors for MS” by Emmanuelle Waubant, MD.
Dr. Carter has received personal compensation for consulting, serving on a scientific advisory board, speaking, or other activities with Alder Pharmaceuticals. He has received research support from Roche/Genentech and MedDay Pharmaceuticals.
Clinical Neurology News editorial advisory board member Jonathan L. Carter, MD, scoured the pages of the American Academy of Neurology’s annual meeting program for his “top picks” in multiple sclerosis at this year’s meeting.
NFLCs in serum as a biomarker for MS and treatment response. Multiple abstracts explore the use of NFLCs as a marker for disease progression and response to MS therapies, including:
- Hot Topics Plenary Session presentation: “Monitoring Multiple Sclerosis Using Blood Neurofilament Light Protein” by Jens Kuhle, MD.
- P5.036, Serum and CSF Neurofilament Light Chain levels normalise following Bone Marrow Transplant in MS Patients.
- S24.002, Interim Analysis of the OBOE (Ocrelizumab Biomarker Outcome Evaluation) Study in Multiple Sclerosis (MS).
- S24.003, Serum Neurofilament Light (NfL): Towards a Blood Test for Prognosis and Disease/Treatment Monitoring in Multiple Sclerosis Patients.
- S24.004, Long-term Prognosis of Disease Evolution and Evidence for Sustained Fingolimod Treatment Effect by Blood Neurofilament Light in RRMS Patients.
- S24.007, Including Blood Neurofilament Light Chain in the NEDA Concept in Relapsing Remitting Multiple Sclerosis Trials.
- S8.006, Siponimod Reduces Neurofilament Light Chain Blood Levels in Secondary Progressive Multiple Sclerosis Patients.
Cognitive function as an outcome measure in MS clinical trials. Several abstracts examine cognition as an outcome measure in clinical trials and show slowing of cognitive worsening in patients on MS disease-modifying therapies:
- S44.004, Impact of Siponimod on Cognition in Patients With Secondary Progressive Multiple Sclerosis: Results From Phase 3 EXPAND Study.
- S44.005, Time to Cognitive Worsening in Patients With Relapsing Multiple Sclerosis in Ocrelizumab Phase 3 Trials.
- S44.007, Benchmarks of Cognitive Performance in a Large, Representative Patient Population.
Improved disability outcome measures and predictors of disability in MS. Several abstracts assess novel disability outcome measures and neuroimaging techniques to better predict progression of clinical disability:
- P4.380, Overall Response Score: A Novel Disability Endpoint That Allows for the Integrated Assessment of Improvement and Worsening over Time in Patients with MS.
- S47.001, Longitudinal Changes in Quantitative Spinal Cord MRI in Multiple Sclerosis Patients: Results of a 5-year Study.
- P6.354, Effect of Fingolimod 0.5 mg/day versus Placebo on Two Newly Developed Expanded Disability Status Scale (EDSS) Subscales for Patients with Relapsing Remitting MS: EDSS Factor Analysis.
Is treatment response in MS an age-dependent or relapse-driven phenomenon, and is it safe to discontinue MS therapies with advancing age? Several abstracts address this question:
- S47.004, Meta-Analysis of the Age-Dependent Efficacy of Multiple Sclerosis Treatments.
- S8.005, Uncoupling the Impact on Relapses and Disability Progression: Siponimod in Relapsing and Nonrelapsing Patients With Secondary Progressive Multiple Sclerosis in the Phase 3 EXPAND Study.
- S8.008, Discontinuation of Disease Modifying Therapies in Stable MS Patients is Associated with Disability Progression Regardless of Age.
Neuromyelitis optica spectrum disorders and MS mimics. Multiple abstracts explore the differences between neuromyelitis optica spectrum disorder because of aquaporin-4 versus myelin oligodendrocyte glycoprotein antibodies; describe unique features of another recently described autoimmune disorder, autoimmune GFAP astrocytopathy; and explore the differential diagnosis of idiopathic transverse myelitis:
- S13.002, Clinical Characteristics of MOG and AQP associated Neuromyelitis Optica Spectrum Disorder (NMOSD) in Adults, through S13.008, It’s Not All Transverse Myelitis: The Differential Diagnosis of Spinal Cord Myelopathy.
- P6.409, The Mayo Clinic Glial Autoimmunity Study: Glial autoantibody (AQP4/MOG/GFAP) serostatus in recurrent longitudinally extensive transverse myelitis.
- P6.417, Evaluation of idiopathic transverse myelitis revealing specific myelopathy diagnoses.
- S6.003, Brain and Spinal Cord Imaging Features in Neuromyelitis Optica Spectrum Disorders.
Updated safety and efficacy data for recently approved or investigational MS therapies. Multiple abstracts report updated safety and efficacy data from MS clinical trials of ozanimod, ocrelizumab (Ocrevus), and hematopoietic stem cell transplantation:
- Clinical Trials Plenary Session presentation: “A Phase 2 Trial of Ibudilast in Progressive Multiple Sclerosis” by Robert J. Fox, MD.
- Contemporary Clinical Issues Plenary Session presentation: “Biosimilars and Nonbiologic Complex Drugs” by Jeffrey Allan Cohen, MD.
- S6.002, Brain MRI Activity and Atrophy Measures in Patients Receiving Continuous Ocrelizumab or Switching From Interferon Beta-1a to Ocrelizumab Therapy in the Open-Label Extension Period of the Phase 3 Trials of Ocrelizumab in Patients With Relapsing Multiple Sclerosis.
- P3.410, Clinical and Magnetic Resonance Imaging Results From RADIANCE Part B, a Multicenter, Randomized, Double-Blind, Phase 3 Trial of Ozanimod Versus Intramuscular Interferon beta-1a in Relapsing Multiple Sclerosis (RMS).
- P3.396, Ozanimod Demonstrates Efficacy and Safety in a Multicenter, Randomized, Double-Blind, Double-Dummy, Active-Controlled Phase 3 Trial of Relapsing Multiple Sclerosis (SUNBEAM).
- S36.001, Safety of Ocrelizumab in Multiple Sclerosis: Updated Analysis in Patients With Relapsing and Primary Progressive Multiple Sclerosis.
- S36.004, Nonmyeloablative hematopoietic stem cell transplantation (HSCT) is superior to disease modifying drug (DMD) treatment in highly active Relapsing Remitting Multiple Sclerosis (RRMS): interim results of the Multiple Sclerosis International Stem cell Transplant (MIST) Randomized Trial.
- S36.005, Efficacy of Ozanimod Versus Interferon beta-1a by Prior Treatment and Baseline Disability in Two Multicenter, Randomized, Double-Blind, Parallel-Group, Active-Controlled, Double-Dummy Phase 3 Studies in Relapsing Multiple Sclerosis (SUNBEAM and RADIANCE Part B).
- S36.006, Safety of Ozanimod Versus Interferon beta-1a in Two Multicenter, Randomized, Double-Blind, Parallel-Group, Active-Controlled, Double-Dummy Phase 3 Studies in Relapsing Multiple Sclerosis (SUNBEAM and RADIANCE Part B).
New thoughts on MS pathogenesis.
- Frontiers in Neuroscience Plenary Session presentation: “Pediatric MS: A Unique Window into Environmental and Genetic Risk Factors for MS” by Emmanuelle Waubant, MD.
Dr. Carter has received personal compensation for consulting, serving on a scientific advisory board, speaking, or other activities with Alder Pharmaceuticals. He has received research support from Roche/Genentech and MedDay Pharmaceuticals.
Erenumab found beneficial to migraine patients with unsuccessful preventive treatment history
Results from the phase 3b LIBERTY trial of the investigational migraine-prevention drug erenumab indicate its potential effectiveness in patients with episodic migraine attacks who have unsuccessfully tried other migraine-prevention drugs to reduce the frequency of migraine days.
Erenumab, a fully human monoclonal antibody that is designed to block the calcitonin gene-related peptide (CGRP) receptor, reduced the average number of monthly migraine headaches by half or more for 30% of study participants, which is a level of improvement that “can greatly improve a person’s quality of life,” first author Uwe Reuter, MD, of Charité–University Medicine Berlin said in a press release. Dr. Reuter will present the full results of the study during the Emerging Science Platform Session at the annual meeting of the American Academy of Neurology in Los Angeles on April 24.
At 3 months, patients treated with erenumab significantly more often met the study’s primary endpoint of the proportion of patients achieving a 50% or greater reduction in mean monthly migraine days (MMDs) during weeks 9-12: At week 12, 30% on erenumab vs. 14% on placebo (odds ratio, 2.73; 95% confidence interval, 1.43-5.19) met the endpoint.
Those treated with erenumab also had a greater average reduction in MMDs in several secondary endpoints. For those on erenumab, there was an overall mean difference of –1.61 MMDs, compared with placebo. Erenumab-treated patients also had an overall mean difference of –1.73 acute medication days, compared with placebo.
The authors reported that erenumab had safety and tolerability comparable to placebo, and none of the patients taking erenumab discontinued because of adverse events.
Dr. Reuter cautioned that additional studies will need to be conducted to determine if the effects last longer than 3 months and to identify patients most likely to respond.
The study was funded by Novartis, which is developing erenumab.
SOURCE: Reuter E et al. AAN 2018, Emerging Science Abstract 009.
Results from the phase 3b LIBERTY trial of the investigational migraine-prevention drug erenumab indicate its potential effectiveness in patients with episodic migraine attacks who have unsuccessfully tried other migraine-prevention drugs to reduce the frequency of migraine days.
Erenumab, a fully human monoclonal antibody that is designed to block the calcitonin gene-related peptide (CGRP) receptor, reduced the average number of monthly migraine headaches by half or more for 30% of study participants, which is a level of improvement that “can greatly improve a person’s quality of life,” first author Uwe Reuter, MD, of Charité–University Medicine Berlin said in a press release. Dr. Reuter will present the full results of the study during the Emerging Science Platform Session at the annual meeting of the American Academy of Neurology in Los Angeles on April 24.
At 3 months, patients treated with erenumab significantly more often met the study’s primary endpoint of the proportion of patients achieving a 50% or greater reduction in mean monthly migraine days (MMDs) during weeks 9-12: At week 12, 30% on erenumab vs. 14% on placebo (odds ratio, 2.73; 95% confidence interval, 1.43-5.19) met the endpoint.
Those treated with erenumab also had a greater average reduction in MMDs in several secondary endpoints. For those on erenumab, there was an overall mean difference of –1.61 MMDs, compared with placebo. Erenumab-treated patients also had an overall mean difference of –1.73 acute medication days, compared with placebo.
The authors reported that erenumab had safety and tolerability comparable to placebo, and none of the patients taking erenumab discontinued because of adverse events.
Dr. Reuter cautioned that additional studies will need to be conducted to determine if the effects last longer than 3 months and to identify patients most likely to respond.
The study was funded by Novartis, which is developing erenumab.
SOURCE: Reuter E et al. AAN 2018, Emerging Science Abstract 009.
Results from the phase 3b LIBERTY trial of the investigational migraine-prevention drug erenumab indicate its potential effectiveness in patients with episodic migraine attacks who have unsuccessfully tried other migraine-prevention drugs to reduce the frequency of migraine days.
Erenumab, a fully human monoclonal antibody that is designed to block the calcitonin gene-related peptide (CGRP) receptor, reduced the average number of monthly migraine headaches by half or more for 30% of study participants, which is a level of improvement that “can greatly improve a person’s quality of life,” first author Uwe Reuter, MD, of Charité–University Medicine Berlin said in a press release. Dr. Reuter will present the full results of the study during the Emerging Science Platform Session at the annual meeting of the American Academy of Neurology in Los Angeles on April 24.
At 3 months, patients treated with erenumab significantly more often met the study’s primary endpoint of the proportion of patients achieving a 50% or greater reduction in mean monthly migraine days (MMDs) during weeks 9-12: At week 12, 30% on erenumab vs. 14% on placebo (odds ratio, 2.73; 95% confidence interval, 1.43-5.19) met the endpoint.
Those treated with erenumab also had a greater average reduction in MMDs in several secondary endpoints. For those on erenumab, there was an overall mean difference of –1.61 MMDs, compared with placebo. Erenumab-treated patients also had an overall mean difference of –1.73 acute medication days, compared with placebo.
The authors reported that erenumab had safety and tolerability comparable to placebo, and none of the patients taking erenumab discontinued because of adverse events.
Dr. Reuter cautioned that additional studies will need to be conducted to determine if the effects last longer than 3 months and to identify patients most likely to respond.
The study was funded by Novartis, which is developing erenumab.
SOURCE: Reuter E et al. AAN 2018, Emerging Science Abstract 009.
FROM AAN 2018
Key clinical point:
Major finding: Patients treated with erenumab significantly more often achieved a 50% or greater reduction in mean monthly migraine days during weeks 9-12: At week 12, 30% with erenumab vs. 14% with placebo met the endpoint.
Study details: A 12-week, double-blind study of 246 patients with episodic migraine randomized to receive erenumab 140 mg or placebo.
Disclosures: The study was funded by Novartis, which is developing erenumab.
Source: Reuter E et al. AAN 2018, Emerging Science Abstract 009.
Top AAN picks from Clinical Neurology News’ medical editor
Standout presentations at this year’s American Academy of Neurology annual meeting range from targeting tau in Alzheimer’s disease, to new treatments for spinal muscular atrophy, to the controversial topic of allowing your child to play contact sports, but all are sure to have an impact, according to Clinical Neurology News Medical Editor Richard J. Caselli, MD.
“There are a lot of good talks and papers being presented, and it is impossible without having seen and heard them all to accurately predict what will be the real standouts, but from a purely personal perspective, and with all due apologies to any others not mentioned below, these are some of the ones I think could have large and, in some cases, almost immediate impact or potential impact,” said Dr. Caselli, professor of neurology at the Mayo Clinic Arizona in Scottsdale and also associate director and clinical core director of the Arizona Alzheimer’s Disease Center.
Targeting tau in Alzheimer’s
The measuring of plasma tau to detect preclinical Alzheimer’s, as is described in the abstract from Pase and colleagues, is an “intriguing” approach, Dr. Caselli said. In that study, higher plasma tau levels were observed across correlates of preclinical Alzheimer’s: poorer cognitive function and smaller hippocampal volumes on MRI. Plasma tau level was also a strong predictor of future dementia. It will be presented Friday, April 27, 1:00-3:00 in S48, “Novel Biomarkers in Aging and Dementia.”
Focus continues on SMA
More advancements continue to be made in the treatment of various forms of spinal muscular trophy. In Monday morning’s Presidential Plenary Session, Richard Finkel’s presentation in receipt of the Sidney Carter Award in Child Neurology, should chart the development, current state, and future of antisense oligonucleotide therapy for SMA.
In the Emerging Science poster program on Wednesday, April 25, attendees will get an update on trial results for a different approach to the treatment of SMA using AVXS-101 gene replacement therapy for SMA type 1. John W. Day, MD, PhD, will provide longer-term outcomes after last year’s presentation of results in 15 patients.
Big news in stroke
Gregory Albers, MD, will describe in the Clinical Trials Plenary Session how new evidence from stroke thrombectomy trials such as DEFUSE 3 have led to new recommendations for extending the time window for thrombectomy. The results of DEFUSE 3 were first reported in January at the International Stroke Conference.
Other plenary presentations
In Wednesday’s Frontiers in Neuroscience Session, Dr. Caselli recommended Alan Evans’ discussion of the development and current and upcoming work to use and update the giant, freely accessible “BigBrain” High Resolution 3D Digital Human Brain Atlas.
In the always “fun and interesting” Controversies in Neurology on the morning of Thursday, April 26, the debate on “Should We Use Biomarkers Alone For Diagnosis of Alzheimer’s?” takes on greater interest now that the National Institute on Aging and the Alzheimer’s Association have defined Alzheimer’s disease as a diagnosis based on biomarkers. The separate debate of “Would You Let Your Child Play Contact Sports?” should also bring lots of interesting questions to the forefront of attendees’ minds.
Dr. Steven R. Messé’s talk, “Finally, Some Closure on PFO Closure,” at the Neurology Year in Review on Friday morning, April 27, is “of immediate relevance” as recent clinical trials have begun to determine patient groups for whom PFO closure appears worthwhile, Dr. Caselli said.
He has no relevant disclosures.
Standout presentations at this year’s American Academy of Neurology annual meeting range from targeting tau in Alzheimer’s disease, to new treatments for spinal muscular atrophy, to the controversial topic of allowing your child to play contact sports, but all are sure to have an impact, according to Clinical Neurology News Medical Editor Richard J. Caselli, MD.
“There are a lot of good talks and papers being presented, and it is impossible without having seen and heard them all to accurately predict what will be the real standouts, but from a purely personal perspective, and with all due apologies to any others not mentioned below, these are some of the ones I think could have large and, in some cases, almost immediate impact or potential impact,” said Dr. Caselli, professor of neurology at the Mayo Clinic Arizona in Scottsdale and also associate director and clinical core director of the Arizona Alzheimer’s Disease Center.
Targeting tau in Alzheimer’s
The measuring of plasma tau to detect preclinical Alzheimer’s, as is described in the abstract from Pase and colleagues, is an “intriguing” approach, Dr. Caselli said. In that study, higher plasma tau levels were observed across correlates of preclinical Alzheimer’s: poorer cognitive function and smaller hippocampal volumes on MRI. Plasma tau level was also a strong predictor of future dementia. It will be presented Friday, April 27, 1:00-3:00 in S48, “Novel Biomarkers in Aging and Dementia.”
Focus continues on SMA
More advancements continue to be made in the treatment of various forms of spinal muscular trophy. In Monday morning’s Presidential Plenary Session, Richard Finkel’s presentation in receipt of the Sidney Carter Award in Child Neurology, should chart the development, current state, and future of antisense oligonucleotide therapy for SMA.
In the Emerging Science poster program on Wednesday, April 25, attendees will get an update on trial results for a different approach to the treatment of SMA using AVXS-101 gene replacement therapy for SMA type 1. John W. Day, MD, PhD, will provide longer-term outcomes after last year’s presentation of results in 15 patients.
Big news in stroke
Gregory Albers, MD, will describe in the Clinical Trials Plenary Session how new evidence from stroke thrombectomy trials such as DEFUSE 3 have led to new recommendations for extending the time window for thrombectomy. The results of DEFUSE 3 were first reported in January at the International Stroke Conference.
Other plenary presentations
In Wednesday’s Frontiers in Neuroscience Session, Dr. Caselli recommended Alan Evans’ discussion of the development and current and upcoming work to use and update the giant, freely accessible “BigBrain” High Resolution 3D Digital Human Brain Atlas.
In the always “fun and interesting” Controversies in Neurology on the morning of Thursday, April 26, the debate on “Should We Use Biomarkers Alone For Diagnosis of Alzheimer’s?” takes on greater interest now that the National Institute on Aging and the Alzheimer’s Association have defined Alzheimer’s disease as a diagnosis based on biomarkers. The separate debate of “Would You Let Your Child Play Contact Sports?” should also bring lots of interesting questions to the forefront of attendees’ minds.
Dr. Steven R. Messé’s talk, “Finally, Some Closure on PFO Closure,” at the Neurology Year in Review on Friday morning, April 27, is “of immediate relevance” as recent clinical trials have begun to determine patient groups for whom PFO closure appears worthwhile, Dr. Caselli said.
He has no relevant disclosures.
Standout presentations at this year’s American Academy of Neurology annual meeting range from targeting tau in Alzheimer’s disease, to new treatments for spinal muscular atrophy, to the controversial topic of allowing your child to play contact sports, but all are sure to have an impact, according to Clinical Neurology News Medical Editor Richard J. Caselli, MD.
“There are a lot of good talks and papers being presented, and it is impossible without having seen and heard them all to accurately predict what will be the real standouts, but from a purely personal perspective, and with all due apologies to any others not mentioned below, these are some of the ones I think could have large and, in some cases, almost immediate impact or potential impact,” said Dr. Caselli, professor of neurology at the Mayo Clinic Arizona in Scottsdale and also associate director and clinical core director of the Arizona Alzheimer’s Disease Center.
Targeting tau in Alzheimer’s
The measuring of plasma tau to detect preclinical Alzheimer’s, as is described in the abstract from Pase and colleagues, is an “intriguing” approach, Dr. Caselli said. In that study, higher plasma tau levels were observed across correlates of preclinical Alzheimer’s: poorer cognitive function and smaller hippocampal volumes on MRI. Plasma tau level was also a strong predictor of future dementia. It will be presented Friday, April 27, 1:00-3:00 in S48, “Novel Biomarkers in Aging and Dementia.”
Focus continues on SMA
More advancements continue to be made in the treatment of various forms of spinal muscular trophy. In Monday morning’s Presidential Plenary Session, Richard Finkel’s presentation in receipt of the Sidney Carter Award in Child Neurology, should chart the development, current state, and future of antisense oligonucleotide therapy for SMA.
In the Emerging Science poster program on Wednesday, April 25, attendees will get an update on trial results for a different approach to the treatment of SMA using AVXS-101 gene replacement therapy for SMA type 1. John W. Day, MD, PhD, will provide longer-term outcomes after last year’s presentation of results in 15 patients.
Big news in stroke
Gregory Albers, MD, will describe in the Clinical Trials Plenary Session how new evidence from stroke thrombectomy trials such as DEFUSE 3 have led to new recommendations for extending the time window for thrombectomy. The results of DEFUSE 3 were first reported in January at the International Stroke Conference.
Other plenary presentations
In Wednesday’s Frontiers in Neuroscience Session, Dr. Caselli recommended Alan Evans’ discussion of the development and current and upcoming work to use and update the giant, freely accessible “BigBrain” High Resolution 3D Digital Human Brain Atlas.
In the always “fun and interesting” Controversies in Neurology on the morning of Thursday, April 26, the debate on “Should We Use Biomarkers Alone For Diagnosis of Alzheimer’s?” takes on greater interest now that the National Institute on Aging and the Alzheimer’s Association have defined Alzheimer’s disease as a diagnosis based on biomarkers. The separate debate of “Would You Let Your Child Play Contact Sports?” should also bring lots of interesting questions to the forefront of attendees’ minds.
Dr. Steven R. Messé’s talk, “Finally, Some Closure on PFO Closure,” at the Neurology Year in Review on Friday morning, April 27, is “of immediate relevance” as recent clinical trials have begun to determine patient groups for whom PFO closure appears worthwhile, Dr. Caselli said.
He has no relevant disclosures.