User login
Treating sleep disorders in chronic opioid users
BALTIMORE – Given the prevalence of opioid use in the general population, sleep specialists need to be alert to the effects of opioid use on sleep and the link between chronic use and sleep disorders, a pulmonologist recommended at the annual meeting of the Associated Professional Sleep Societies.
Chronic opioid use has multiple effects on sleep that render continuous positive airway pressure (CPAP) all but ineffective, said Bernardo J. Selim, MD, of Mayo Clinic, Rochester, Minn. Characteristic signs of the effects of chronic opioid use on sleep include ataxic central sleep apnea (CSA) and sustained hypoxemia, for which CPAP is generally not effective. Obtaining arterial blood gas measures in these patients is also important to rule out a hypoventilative condition, he added.
In his review of opioid-induced sleep disorders, Dr. Selim cited a small “landmark” study of 24 chronic pain patients on opioids that found 46% had sleep disordered breathing and that the risk rose with the morphine equivalent dose they were taking (J Clin Sleep Med. 2014 Aug 15; 10[8]:847-52).
A meta-analysis also found a dose-dependent relationship with the severity of CSA in patients on opioids, Dr. Selim noted (Anesth Analg. 2015 Jun;120[6]:1273-85). The prevalence of CSA was 24% in the study, which defined two risk factors for CSA severity: a morphine equivalent dose exceeding 200 mg/day and a low or normal body mass index.
Dr. Selim noted that opioids reduce respiration rate more than tidal volume and cause changes to respiratory rhythm. “[Opioids] decrease hypercapnia but increase hypoxic ventilatory response, decrease the arousal index, decrease upper-airway muscle tone, and decrease and also act on chest and abdominal wall compliance.”
Further, different opioids and injection methods can influence breathing. For example, REM and slow-wave sleep decreased across all three categories – intravenous morphine, oral morphine or methadone, and heroin use.
Sleep specialists should be aware that all opioid receptor agonists, whether legal or illegal, have respiratory side effects, Dr. Selim said. “They can present in any way, in any form – CSA, obstructive sleep apnea [OSA], ataxic breathing or sustained hypoxemia. Most of the time [respiratory side effects] present as a combination of complex respiratory patterns.”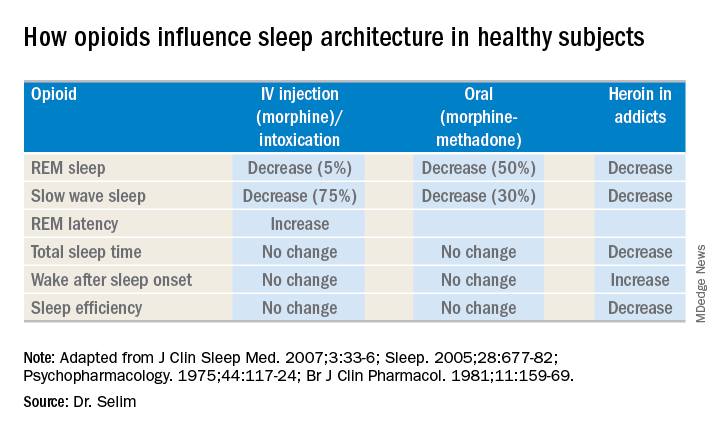
In one meta-analysis, CSA was significantly more prevalent in OSA patients on opioids than it was in nonusers, Dr. Selim said, with increased sleep apnea severity as well (J Clin Sleep Med. 2016 Apr 15;12[4]:617-25). Another study found that ataxic breathing was more frequent in non-REM sleep in chronic opioid users (odds ratio, 15.4; P = .017; J Clin Sleep Med. 2007 Aug 15;3[5]:455-61).
The key rule for treating sleep disorders in opioid-dependent patients is to change to nonopioid analgesics, Dr. Selim said. In that regard, ampakines are experimental drugs which have been shown to improve opioid-induced ventilation without loss of the analgesic effect (Clin Pharmacol Ther. 2010 Feb;87[2]:204-11). “Ampakines modulate the action of the glutamate neurotransmitter, decreasing opiate-induced respiratory depression,” Dr. Selim said. An emerging technology, adaptive servo-ventilation (ASV), has been as effective in the treatment of central and complex sleep apnea in chronic opioid users as it is in patients with congestive heart failure, Dr. Selim said (J Clin Sleep Med. 2016 May 15;12[5]:757-61). “ASV can be very effective in these patients; lower body mass index being a predictor for ASV success,” he said.
Dr. Selim reported having no financial relationships.
BALTIMORE – Given the prevalence of opioid use in the general population, sleep specialists need to be alert to the effects of opioid use on sleep and the link between chronic use and sleep disorders, a pulmonologist recommended at the annual meeting of the Associated Professional Sleep Societies.
Chronic opioid use has multiple effects on sleep that render continuous positive airway pressure (CPAP) all but ineffective, said Bernardo J. Selim, MD, of Mayo Clinic, Rochester, Minn. Characteristic signs of the effects of chronic opioid use on sleep include ataxic central sleep apnea (CSA) and sustained hypoxemia, for which CPAP is generally not effective. Obtaining arterial blood gas measures in these patients is also important to rule out a hypoventilative condition, he added.
In his review of opioid-induced sleep disorders, Dr. Selim cited a small “landmark” study of 24 chronic pain patients on opioids that found 46% had sleep disordered breathing and that the risk rose with the morphine equivalent dose they were taking (J Clin Sleep Med. 2014 Aug 15; 10[8]:847-52).
A meta-analysis also found a dose-dependent relationship with the severity of CSA in patients on opioids, Dr. Selim noted (Anesth Analg. 2015 Jun;120[6]:1273-85). The prevalence of CSA was 24% in the study, which defined two risk factors for CSA severity: a morphine equivalent dose exceeding 200 mg/day and a low or normal body mass index.
Dr. Selim noted that opioids reduce respiration rate more than tidal volume and cause changes to respiratory rhythm. “[Opioids] decrease hypercapnia but increase hypoxic ventilatory response, decrease the arousal index, decrease upper-airway muscle tone, and decrease and also act on chest and abdominal wall compliance.”
Further, different opioids and injection methods can influence breathing. For example, REM and slow-wave sleep decreased across all three categories – intravenous morphine, oral morphine or methadone, and heroin use.
Sleep specialists should be aware that all opioid receptor agonists, whether legal or illegal, have respiratory side effects, Dr. Selim said. “They can present in any way, in any form – CSA, obstructive sleep apnea [OSA], ataxic breathing or sustained hypoxemia. Most of the time [respiratory side effects] present as a combination of complex respiratory patterns.”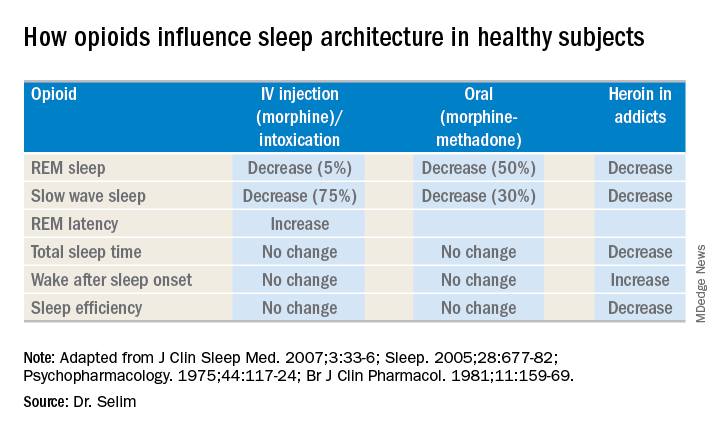
In one meta-analysis, CSA was significantly more prevalent in OSA patients on opioids than it was in nonusers, Dr. Selim said, with increased sleep apnea severity as well (J Clin Sleep Med. 2016 Apr 15;12[4]:617-25). Another study found that ataxic breathing was more frequent in non-REM sleep in chronic opioid users (odds ratio, 15.4; P = .017; J Clin Sleep Med. 2007 Aug 15;3[5]:455-61).
The key rule for treating sleep disorders in opioid-dependent patients is to change to nonopioid analgesics, Dr. Selim said. In that regard, ampakines are experimental drugs which have been shown to improve opioid-induced ventilation without loss of the analgesic effect (Clin Pharmacol Ther. 2010 Feb;87[2]:204-11). “Ampakines modulate the action of the glutamate neurotransmitter, decreasing opiate-induced respiratory depression,” Dr. Selim said. An emerging technology, adaptive servo-ventilation (ASV), has been as effective in the treatment of central and complex sleep apnea in chronic opioid users as it is in patients with congestive heart failure, Dr. Selim said (J Clin Sleep Med. 2016 May 15;12[5]:757-61). “ASV can be very effective in these patients; lower body mass index being a predictor for ASV success,” he said.
Dr. Selim reported having no financial relationships.
BALTIMORE – Given the prevalence of opioid use in the general population, sleep specialists need to be alert to the effects of opioid use on sleep and the link between chronic use and sleep disorders, a pulmonologist recommended at the annual meeting of the Associated Professional Sleep Societies.
Chronic opioid use has multiple effects on sleep that render continuous positive airway pressure (CPAP) all but ineffective, said Bernardo J. Selim, MD, of Mayo Clinic, Rochester, Minn. Characteristic signs of the effects of chronic opioid use on sleep include ataxic central sleep apnea (CSA) and sustained hypoxemia, for which CPAP is generally not effective. Obtaining arterial blood gas measures in these patients is also important to rule out a hypoventilative condition, he added.
In his review of opioid-induced sleep disorders, Dr. Selim cited a small “landmark” study of 24 chronic pain patients on opioids that found 46% had sleep disordered breathing and that the risk rose with the morphine equivalent dose they were taking (J Clin Sleep Med. 2014 Aug 15; 10[8]:847-52).
A meta-analysis also found a dose-dependent relationship with the severity of CSA in patients on opioids, Dr. Selim noted (Anesth Analg. 2015 Jun;120[6]:1273-85). The prevalence of CSA was 24% in the study, which defined two risk factors for CSA severity: a morphine equivalent dose exceeding 200 mg/day and a low or normal body mass index.
Dr. Selim noted that opioids reduce respiration rate more than tidal volume and cause changes to respiratory rhythm. “[Opioids] decrease hypercapnia but increase hypoxic ventilatory response, decrease the arousal index, decrease upper-airway muscle tone, and decrease and also act on chest and abdominal wall compliance.”
Further, different opioids and injection methods can influence breathing. For example, REM and slow-wave sleep decreased across all three categories – intravenous morphine, oral morphine or methadone, and heroin use.
Sleep specialists should be aware that all opioid receptor agonists, whether legal or illegal, have respiratory side effects, Dr. Selim said. “They can present in any way, in any form – CSA, obstructive sleep apnea [OSA], ataxic breathing or sustained hypoxemia. Most of the time [respiratory side effects] present as a combination of complex respiratory patterns.”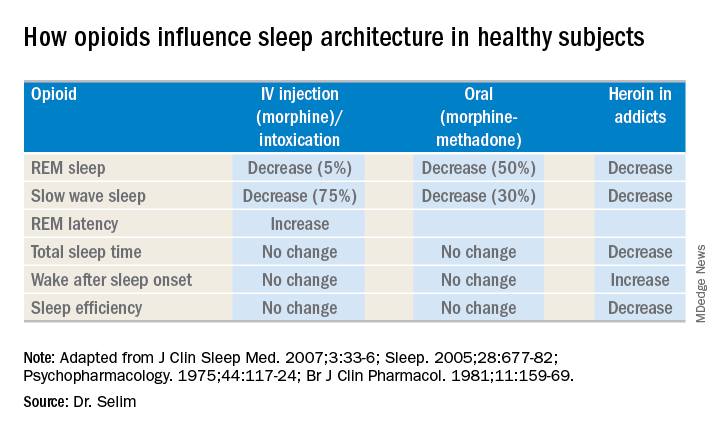
In one meta-analysis, CSA was significantly more prevalent in OSA patients on opioids than it was in nonusers, Dr. Selim said, with increased sleep apnea severity as well (J Clin Sleep Med. 2016 Apr 15;12[4]:617-25). Another study found that ataxic breathing was more frequent in non-REM sleep in chronic opioid users (odds ratio, 15.4; P = .017; J Clin Sleep Med. 2007 Aug 15;3[5]:455-61).
The key rule for treating sleep disorders in opioid-dependent patients is to change to nonopioid analgesics, Dr. Selim said. In that regard, ampakines are experimental drugs which have been shown to improve opioid-induced ventilation without loss of the analgesic effect (Clin Pharmacol Ther. 2010 Feb;87[2]:204-11). “Ampakines modulate the action of the glutamate neurotransmitter, decreasing opiate-induced respiratory depression,” Dr. Selim said. An emerging technology, adaptive servo-ventilation (ASV), has been as effective in the treatment of central and complex sleep apnea in chronic opioid users as it is in patients with congestive heart failure, Dr. Selim said (J Clin Sleep Med. 2016 May 15;12[5]:757-61). “ASV can be very effective in these patients; lower body mass index being a predictor for ASV success,” he said.
Dr. Selim reported having no financial relationships.
EXPERT ANALYSIS FROM SLEEP 2018
Sleep may mediate healthy behavior in children
BALTIMORE – a 6-year follow-up of children in the Infant Feeding Practices Study II determined.
However, improving health in these children is more than a matter of simply seeing that they get more sleep, said lead investigator Jill Landsbaugh Kaar, PhD, of Children’s Hospital Colorado, Aurora, in presenting the results at the annual meeting of the Associated Professional Sleep Societies. “Perhaps there’s a potential pathway linking healthy eaters and obesity in children that may be mediated through sleep duration.”
The relationship between sleep, diet, and activity level may be more cyclical, rather than linear, Dr. Kaar said. “Poor sleep is typically linked to a poor diet or low levels of physical activity, and then linked to some outcome or disease,” she said. But her research indicates that those three factors – sleep, diet and activity – are more interrelated than one being causative of the others.
Noting that one in three adults and one in six children in the United States are either overweight or obese (JAMA. 2014 Feb 26;311[8]:806-14), Dr. Kaar said, “Childhood obesity prevention has really not been effective in reducing weight or preventing or limiting weight gain.” Such programs typically focus on one health behavior when each child has a unique pattern of health behaviors that influence weight.
Dr. Kaar’s research used data collected by the Centers for Disease Control and Prevention as part of a 6-year follow-up study of women from the Infant Feeding Practices Study II. Some 1,542 women completed mailed questionnaires about their 6-year-olds’ diet, activity, screen time, sleep duration, height, and weight. The statistical analysis grouped the children into health behavior patterns of diet, activity, and screen time and used a three-step mediation regression model to examine their hypothesis.
The analysis characterized children into three health behavior pattern groups: poorest eaters (22%), healthy children (37%), and active supereaters with the highest screen time (41%). The poorest eaters were more likely to be female (58%) and obese (18%) than the other groups, but even 10% of the healthy children group were obese.
In the first model, the poorest eaters had the highest risk of obesity. In the second model, both the poorest eaters and active supereaters had shorter sleep duration than healthy children – 9.46 and 9.59 hours a night, respectively, versus 9.97 hours for healthy children – “thus telling me that sleep was really driving that relationship,” Dr. Kaar said.
“Future interventions should consider that improving health behavior patterns by targeting someone’s diet or physical activity, that you’re also targeting them to improve sleep, and then through increasing sleep you will be influencing obesity,” she said. “Interventions and research studies in general really need to measure all of those health behaviors because they’re all related; it’s not just one of them leading to obesity risk.”
The next step for her research is to branch out beyond a one-center study, Dr. Kaar said.
Dr. Kaar reported having no financial relationships. An American Heart Association Scientist Development Award provided funding for the study.
BALTIMORE – a 6-year follow-up of children in the Infant Feeding Practices Study II determined.
However, improving health in these children is more than a matter of simply seeing that they get more sleep, said lead investigator Jill Landsbaugh Kaar, PhD, of Children’s Hospital Colorado, Aurora, in presenting the results at the annual meeting of the Associated Professional Sleep Societies. “Perhaps there’s a potential pathway linking healthy eaters and obesity in children that may be mediated through sleep duration.”
The relationship between sleep, diet, and activity level may be more cyclical, rather than linear, Dr. Kaar said. “Poor sleep is typically linked to a poor diet or low levels of physical activity, and then linked to some outcome or disease,” she said. But her research indicates that those three factors – sleep, diet and activity – are more interrelated than one being causative of the others.
Noting that one in three adults and one in six children in the United States are either overweight or obese (JAMA. 2014 Feb 26;311[8]:806-14), Dr. Kaar said, “Childhood obesity prevention has really not been effective in reducing weight or preventing or limiting weight gain.” Such programs typically focus on one health behavior when each child has a unique pattern of health behaviors that influence weight.
Dr. Kaar’s research used data collected by the Centers for Disease Control and Prevention as part of a 6-year follow-up study of women from the Infant Feeding Practices Study II. Some 1,542 women completed mailed questionnaires about their 6-year-olds’ diet, activity, screen time, sleep duration, height, and weight. The statistical analysis grouped the children into health behavior patterns of diet, activity, and screen time and used a three-step mediation regression model to examine their hypothesis.
The analysis characterized children into three health behavior pattern groups: poorest eaters (22%), healthy children (37%), and active supereaters with the highest screen time (41%). The poorest eaters were more likely to be female (58%) and obese (18%) than the other groups, but even 10% of the healthy children group were obese.
In the first model, the poorest eaters had the highest risk of obesity. In the second model, both the poorest eaters and active supereaters had shorter sleep duration than healthy children – 9.46 and 9.59 hours a night, respectively, versus 9.97 hours for healthy children – “thus telling me that sleep was really driving that relationship,” Dr. Kaar said.
“Future interventions should consider that improving health behavior patterns by targeting someone’s diet or physical activity, that you’re also targeting them to improve sleep, and then through increasing sleep you will be influencing obesity,” she said. “Interventions and research studies in general really need to measure all of those health behaviors because they’re all related; it’s not just one of them leading to obesity risk.”
The next step for her research is to branch out beyond a one-center study, Dr. Kaar said.
Dr. Kaar reported having no financial relationships. An American Heart Association Scientist Development Award provided funding for the study.
BALTIMORE – a 6-year follow-up of children in the Infant Feeding Practices Study II determined.
However, improving health in these children is more than a matter of simply seeing that they get more sleep, said lead investigator Jill Landsbaugh Kaar, PhD, of Children’s Hospital Colorado, Aurora, in presenting the results at the annual meeting of the Associated Professional Sleep Societies. “Perhaps there’s a potential pathway linking healthy eaters and obesity in children that may be mediated through sleep duration.”
The relationship between sleep, diet, and activity level may be more cyclical, rather than linear, Dr. Kaar said. “Poor sleep is typically linked to a poor diet or low levels of physical activity, and then linked to some outcome or disease,” she said. But her research indicates that those three factors – sleep, diet and activity – are more interrelated than one being causative of the others.
Noting that one in three adults and one in six children in the United States are either overweight or obese (JAMA. 2014 Feb 26;311[8]:806-14), Dr. Kaar said, “Childhood obesity prevention has really not been effective in reducing weight or preventing or limiting weight gain.” Such programs typically focus on one health behavior when each child has a unique pattern of health behaviors that influence weight.
Dr. Kaar’s research used data collected by the Centers for Disease Control and Prevention as part of a 6-year follow-up study of women from the Infant Feeding Practices Study II. Some 1,542 women completed mailed questionnaires about their 6-year-olds’ diet, activity, screen time, sleep duration, height, and weight. The statistical analysis grouped the children into health behavior patterns of diet, activity, and screen time and used a three-step mediation regression model to examine their hypothesis.
The analysis characterized children into three health behavior pattern groups: poorest eaters (22%), healthy children (37%), and active supereaters with the highest screen time (41%). The poorest eaters were more likely to be female (58%) and obese (18%) than the other groups, but even 10% of the healthy children group were obese.
In the first model, the poorest eaters had the highest risk of obesity. In the second model, both the poorest eaters and active supereaters had shorter sleep duration than healthy children – 9.46 and 9.59 hours a night, respectively, versus 9.97 hours for healthy children – “thus telling me that sleep was really driving that relationship,” Dr. Kaar said.
“Future interventions should consider that improving health behavior patterns by targeting someone’s diet or physical activity, that you’re also targeting them to improve sleep, and then through increasing sleep you will be influencing obesity,” she said. “Interventions and research studies in general really need to measure all of those health behaviors because they’re all related; it’s not just one of them leading to obesity risk.”
The next step for her research is to branch out beyond a one-center study, Dr. Kaar said.
Dr. Kaar reported having no financial relationships. An American Heart Association Scientist Development Award provided funding for the study.
REPORTING FROM SLEEP 2018
Key clinical point: Sleep may mediate how diet and activity influence weight in children.
Major finding: Healthy children had 9.97 hours of sleep per night versus 9.46 hours for poorest eaters.
Study details: A 6-year follow-up of 1,542 children in the Infant Feeding Practices Study II whose health behaviors were self-reported by mothers.
Disclosures: Dr. Kaar reported having no financial relationships. The study was funded through an American Heart Association Scientist Development Award.
Algorithm shows promise in calculating CV risk in sleep apnea patients
BALTIMORE – Researchers have developed an algorithm to calculate circulation time during sleep that may provide another tool to identify the risk of underlying cardiac vascular disease in patients with sleep apnea, one of the study’s lead investigators reported at the annual meeting of the Associated Professional Sleep Societies.
“There’s always been a question that there could be some global or untapped physiological indices that might give us some glimpse into future cardiovascular events or instantaneous cardiovascular vulnerability during sleep apnea events,” said Younghoon Kwon, MD, assistant professor of cardiovascular medicine at the University of Virginia, Charlottesville. “Circulation time that can be derived from a sleep study may be one of these novel indices. Although it has been examined in patients with heart failure with Cheyne-Stokes respiration, it has rarely been studied in patients with obstructive sleep apnea without heart failure.”
He noted that in this study, which utilized a cohort of 686 patients from the Multi-Ethnic Study of Atherosclerosis (MESA), all with an apnea-hypopnea index greater than 15, the automated algorithm the researchers developed to calculate lung-to-finger circulation was correlated highly with visual measurement.
The algorithm used randomly selected polysomnograms from the MESA cohort. It employed the airflow/nasal signal and the oxygen saturation signal, using the visually scored start and endpoint of apnea/hypopnea as a starting point. For each event, the calculation identified two key points: the endpoint of apnea/hypopnea and the endpoint of desaturation to arrive at a calculation of lung-to-finger circulation, Dr. Kwon explained.
The significance of the findings was the correlation between the visual and automated methods of calculating lung-to-finder circulation time. In a matched subgroup of 25 subjects, the correlation was around 95% (P less than .0001); in all cases, the correlation was around 69% (P less than .001). In matched cases, the average lung-to-finger circulation times were identical with visual and automated techniques: 19.5 seconds (P = .92), whereas in all cases the averages differed: 19.6 seconds for visual versus 18.6 seconds for automated (P = .42). “The results showed that the visual against the automated circulatory time measurement was very good,” Dr. Kwon said.
With this algorithm, multiple circulation time measures were automatically derived for each sleep study. Subsequently, average circulation time was derived for each study participant. The average circulation time was 19.4 seconds in the entire cohort, versus 21.0 seconds in those with apnea and 17.6 seconds in patients with hypopnea.
“Older age, male gender, and higher obstructive sleep apnea severity appeared to be independently associated with higher than average lung-to-finger circulation times,” Dr. Kwon said. “However, there was no apparent association between the obstructive event length or the severity of oxygen desaturation and the respective circulation time within subjects. Similarly, sleep positions and sleep stages do not seem to bear any association.”
One of the limitations of the study, he noted, was its assumption of the automated algorithm as the threshold and somewhat limited candidate variables. Future studies should involve more diverse cohorts with prevalent cardiovascular disease to determine the utility of the algorithm in predicting cardiovascular events, he said.
Dr. Kwon reported having no financial relationships, and the American Academy of Sleep Medicine Foundation provided study funding.
SOURCE: Kwon Y et al. SLEEP 2018, Abstract #0450.
BALTIMORE – Researchers have developed an algorithm to calculate circulation time during sleep that may provide another tool to identify the risk of underlying cardiac vascular disease in patients with sleep apnea, one of the study’s lead investigators reported at the annual meeting of the Associated Professional Sleep Societies.
“There’s always been a question that there could be some global or untapped physiological indices that might give us some glimpse into future cardiovascular events or instantaneous cardiovascular vulnerability during sleep apnea events,” said Younghoon Kwon, MD, assistant professor of cardiovascular medicine at the University of Virginia, Charlottesville. “Circulation time that can be derived from a sleep study may be one of these novel indices. Although it has been examined in patients with heart failure with Cheyne-Stokes respiration, it has rarely been studied in patients with obstructive sleep apnea without heart failure.”
He noted that in this study, which utilized a cohort of 686 patients from the Multi-Ethnic Study of Atherosclerosis (MESA), all with an apnea-hypopnea index greater than 15, the automated algorithm the researchers developed to calculate lung-to-finger circulation was correlated highly with visual measurement.
The algorithm used randomly selected polysomnograms from the MESA cohort. It employed the airflow/nasal signal and the oxygen saturation signal, using the visually scored start and endpoint of apnea/hypopnea as a starting point. For each event, the calculation identified two key points: the endpoint of apnea/hypopnea and the endpoint of desaturation to arrive at a calculation of lung-to-finger circulation, Dr. Kwon explained.
The significance of the findings was the correlation between the visual and automated methods of calculating lung-to-finder circulation time. In a matched subgroup of 25 subjects, the correlation was around 95% (P less than .0001); in all cases, the correlation was around 69% (P less than .001). In matched cases, the average lung-to-finger circulation times were identical with visual and automated techniques: 19.5 seconds (P = .92), whereas in all cases the averages differed: 19.6 seconds for visual versus 18.6 seconds for automated (P = .42). “The results showed that the visual against the automated circulatory time measurement was very good,” Dr. Kwon said.
With this algorithm, multiple circulation time measures were automatically derived for each sleep study. Subsequently, average circulation time was derived for each study participant. The average circulation time was 19.4 seconds in the entire cohort, versus 21.0 seconds in those with apnea and 17.6 seconds in patients with hypopnea.
“Older age, male gender, and higher obstructive sleep apnea severity appeared to be independently associated with higher than average lung-to-finger circulation times,” Dr. Kwon said. “However, there was no apparent association between the obstructive event length or the severity of oxygen desaturation and the respective circulation time within subjects. Similarly, sleep positions and sleep stages do not seem to bear any association.”
One of the limitations of the study, he noted, was its assumption of the automated algorithm as the threshold and somewhat limited candidate variables. Future studies should involve more diverse cohorts with prevalent cardiovascular disease to determine the utility of the algorithm in predicting cardiovascular events, he said.
Dr. Kwon reported having no financial relationships, and the American Academy of Sleep Medicine Foundation provided study funding.
SOURCE: Kwon Y et al. SLEEP 2018, Abstract #0450.
BALTIMORE – Researchers have developed an algorithm to calculate circulation time during sleep that may provide another tool to identify the risk of underlying cardiac vascular disease in patients with sleep apnea, one of the study’s lead investigators reported at the annual meeting of the Associated Professional Sleep Societies.
“There’s always been a question that there could be some global or untapped physiological indices that might give us some glimpse into future cardiovascular events or instantaneous cardiovascular vulnerability during sleep apnea events,” said Younghoon Kwon, MD, assistant professor of cardiovascular medicine at the University of Virginia, Charlottesville. “Circulation time that can be derived from a sleep study may be one of these novel indices. Although it has been examined in patients with heart failure with Cheyne-Stokes respiration, it has rarely been studied in patients with obstructive sleep apnea without heart failure.”
He noted that in this study, which utilized a cohort of 686 patients from the Multi-Ethnic Study of Atherosclerosis (MESA), all with an apnea-hypopnea index greater than 15, the automated algorithm the researchers developed to calculate lung-to-finger circulation was correlated highly with visual measurement.
The algorithm used randomly selected polysomnograms from the MESA cohort. It employed the airflow/nasal signal and the oxygen saturation signal, using the visually scored start and endpoint of apnea/hypopnea as a starting point. For each event, the calculation identified two key points: the endpoint of apnea/hypopnea and the endpoint of desaturation to arrive at a calculation of lung-to-finger circulation, Dr. Kwon explained.
The significance of the findings was the correlation between the visual and automated methods of calculating lung-to-finder circulation time. In a matched subgroup of 25 subjects, the correlation was around 95% (P less than .0001); in all cases, the correlation was around 69% (P less than .001). In matched cases, the average lung-to-finger circulation times were identical with visual and automated techniques: 19.5 seconds (P = .92), whereas in all cases the averages differed: 19.6 seconds for visual versus 18.6 seconds for automated (P = .42). “The results showed that the visual against the automated circulatory time measurement was very good,” Dr. Kwon said.
With this algorithm, multiple circulation time measures were automatically derived for each sleep study. Subsequently, average circulation time was derived for each study participant. The average circulation time was 19.4 seconds in the entire cohort, versus 21.0 seconds in those with apnea and 17.6 seconds in patients with hypopnea.
“Older age, male gender, and higher obstructive sleep apnea severity appeared to be independently associated with higher than average lung-to-finger circulation times,” Dr. Kwon said. “However, there was no apparent association between the obstructive event length or the severity of oxygen desaturation and the respective circulation time within subjects. Similarly, sleep positions and sleep stages do not seem to bear any association.”
One of the limitations of the study, he noted, was its assumption of the automated algorithm as the threshold and somewhat limited candidate variables. Future studies should involve more diverse cohorts with prevalent cardiovascular disease to determine the utility of the algorithm in predicting cardiovascular events, he said.
Dr. Kwon reported having no financial relationships, and the American Academy of Sleep Medicine Foundation provided study funding.
SOURCE: Kwon Y et al. SLEEP 2018, Abstract #0450.
REPORTING FROM SLEEP 2018
Key clinical point: An automated algorithm to calculate sleep-study circulation times correlated with visual review.
Major finding: The correlation between visual and automated methods for calculating lung-to-finger circulation times was around 95% (P less than .0001).
Study details: A cohort of 686 participants in the Multi-Ethnic Study of Atherosclerosis.
Disclosures: Dr. Kwon reported no financial disclosures, and the American Academy of Sleep Medicine Foundation provided study funding.
Source: Kwon Y et al. SLEEP 2018, Abstract #0450.
New insights into sleep, pregnancy weight gain
BALTIMORE – Pregnant women who are overweight and obese are like the general population in that the less they sleep, the more weight they gain, particularly in the first half of pregnancy. However, unlike in the larger adult population, prolonged daily total eating time was not associated with gestational weight gain in these women, particularly early in pregnancy, according to findings from a small study presented at the Associated Professional Sleep Societies annual meeting.
Those findings point to a need to further study the , said Rachel P. Kolko, PhD, a postdoctoral scholar at the University of Pittsburgh, Western Psychiatric Institute and Clinic.
“The association with total sleep time was found to be significant, such that if you had less sleep, you had higher amounts of weight gain; we did not find a significant relation with our eating window variable,” Dr. Kolko said.
She reported on research involving 62 pregnant women, 53% of whom were overweight with a body mass index of 25-29.9 kg/m2 and 47% of whom were obese with BMI greater than 30. Forty-seven percent of the study population was nonwhite.
The research grew out of a need to identify potentially modifiable factors to curtail excessive gestational weight gain during pregnancy, she said. The study hypotheses were that both shorter total sleep time and longer total eating time would lead to higher gestational weight gain, but the study confirmed only the former as a contributing factor.
The women in the study were at 12-20 weeks of pregnancy. Gestational weight gain was calculated as the difference between self-reported prepregnancy weight and current weight. Total sleep time was based on the Pittsburgh Sleep Quality Index, and total eating time was calculated as the time difference between the day’s first meal or snack of more than 50 calories and the last, as self-reported.
Average total sleep time was 7.8 hours, with total eating time spanning 10.8 hours. On average, study participants gained 9.7 pounds through the first half of pregnancy, Dr. Kolko said. She noted that the Institute of Medicine, now known as the National Academy of Medicine, recommends that women who are overweight women gain 15-25 pounds during pregnancy and women who are obese gain 11-20 pounds (JAMA. 2017;317:2207-25). “Already about 20% of our sample has gained that amount of weight within the first half of pregnancy,” she said.
“Total sleep time was related to a higher early gestational weight in women with overweight and obesity, and it’s possible that addressing this may affect and hopefully improve women’s weight gain during early pregnancy to fit within those guidelines,” she said.
Future research should look at the entire gestational period – possibly targeting sleep patterns during pregnancy – and should expand to include women who are not overweight or obese, Dr. Kolko noted.
Dr. Kolko reported having no financial relationships to disclose.
SOURCE: Kolko RP, et al., SLEEP 2018, Abstract 0692.
BALTIMORE – Pregnant women who are overweight and obese are like the general population in that the less they sleep, the more weight they gain, particularly in the first half of pregnancy. However, unlike in the larger adult population, prolonged daily total eating time was not associated with gestational weight gain in these women, particularly early in pregnancy, according to findings from a small study presented at the Associated Professional Sleep Societies annual meeting.
Those findings point to a need to further study the , said Rachel P. Kolko, PhD, a postdoctoral scholar at the University of Pittsburgh, Western Psychiatric Institute and Clinic.
“The association with total sleep time was found to be significant, such that if you had less sleep, you had higher amounts of weight gain; we did not find a significant relation with our eating window variable,” Dr. Kolko said.
She reported on research involving 62 pregnant women, 53% of whom were overweight with a body mass index of 25-29.9 kg/m2 and 47% of whom were obese with BMI greater than 30. Forty-seven percent of the study population was nonwhite.
The research grew out of a need to identify potentially modifiable factors to curtail excessive gestational weight gain during pregnancy, she said. The study hypotheses were that both shorter total sleep time and longer total eating time would lead to higher gestational weight gain, but the study confirmed only the former as a contributing factor.
The women in the study were at 12-20 weeks of pregnancy. Gestational weight gain was calculated as the difference between self-reported prepregnancy weight and current weight. Total sleep time was based on the Pittsburgh Sleep Quality Index, and total eating time was calculated as the time difference between the day’s first meal or snack of more than 50 calories and the last, as self-reported.
Average total sleep time was 7.8 hours, with total eating time spanning 10.8 hours. On average, study participants gained 9.7 pounds through the first half of pregnancy, Dr. Kolko said. She noted that the Institute of Medicine, now known as the National Academy of Medicine, recommends that women who are overweight women gain 15-25 pounds during pregnancy and women who are obese gain 11-20 pounds (JAMA. 2017;317:2207-25). “Already about 20% of our sample has gained that amount of weight within the first half of pregnancy,” she said.
“Total sleep time was related to a higher early gestational weight in women with overweight and obesity, and it’s possible that addressing this may affect and hopefully improve women’s weight gain during early pregnancy to fit within those guidelines,” she said.
Future research should look at the entire gestational period – possibly targeting sleep patterns during pregnancy – and should expand to include women who are not overweight or obese, Dr. Kolko noted.
Dr. Kolko reported having no financial relationships to disclose.
SOURCE: Kolko RP, et al., SLEEP 2018, Abstract 0692.
BALTIMORE – Pregnant women who are overweight and obese are like the general population in that the less they sleep, the more weight they gain, particularly in the first half of pregnancy. However, unlike in the larger adult population, prolonged daily total eating time was not associated with gestational weight gain in these women, particularly early in pregnancy, according to findings from a small study presented at the Associated Professional Sleep Societies annual meeting.
Those findings point to a need to further study the , said Rachel P. Kolko, PhD, a postdoctoral scholar at the University of Pittsburgh, Western Psychiatric Institute and Clinic.
“The association with total sleep time was found to be significant, such that if you had less sleep, you had higher amounts of weight gain; we did not find a significant relation with our eating window variable,” Dr. Kolko said.
She reported on research involving 62 pregnant women, 53% of whom were overweight with a body mass index of 25-29.9 kg/m2 and 47% of whom were obese with BMI greater than 30. Forty-seven percent of the study population was nonwhite.
The research grew out of a need to identify potentially modifiable factors to curtail excessive gestational weight gain during pregnancy, she said. The study hypotheses were that both shorter total sleep time and longer total eating time would lead to higher gestational weight gain, but the study confirmed only the former as a contributing factor.
The women in the study were at 12-20 weeks of pregnancy. Gestational weight gain was calculated as the difference between self-reported prepregnancy weight and current weight. Total sleep time was based on the Pittsburgh Sleep Quality Index, and total eating time was calculated as the time difference between the day’s first meal or snack of more than 50 calories and the last, as self-reported.
Average total sleep time was 7.8 hours, with total eating time spanning 10.8 hours. On average, study participants gained 9.7 pounds through the first half of pregnancy, Dr. Kolko said. She noted that the Institute of Medicine, now known as the National Academy of Medicine, recommends that women who are overweight women gain 15-25 pounds during pregnancy and women who are obese gain 11-20 pounds (JAMA. 2017;317:2207-25). “Already about 20% of our sample has gained that amount of weight within the first half of pregnancy,” she said.
“Total sleep time was related to a higher early gestational weight in women with overweight and obesity, and it’s possible that addressing this may affect and hopefully improve women’s weight gain during early pregnancy to fit within those guidelines,” she said.
Future research should look at the entire gestational period – possibly targeting sleep patterns during pregnancy – and should expand to include women who are not overweight or obese, Dr. Kolko noted.
Dr. Kolko reported having no financial relationships to disclose.
SOURCE: Kolko RP, et al., SLEEP 2018, Abstract 0692.
REPORTING FROM SLEEP 2018
Key clinical point: In overweight/obese women, shorter sleep times are linked to early gestational weight gain.
Major finding: Overweight/obese women slept 30% less and had higher gestational weight gain in early pregnancy.
Study details: Study of 62 women between 12 and 20 weeks’ gestation with prepregnancy BMI greater than 25 kg/m2.
Disclosures: Dr. Kolko reported having no financial relationships.
Source: Kolko RP et al. SLEEP 2018, Abstract 0692.
Trial finds link between OSA, aortic diameter
BALTIMORE – Individuals with moderate to severe and thus may be at a heightened risk of cardiovascular events, according to an analysis of a national, multisite research study presented at the annual meeting of the Associated Professional Sleep Societies.
The study evaluated a subgroup of 708 patients with no history of cardiovascular disease (CVD) from the Multi-Ethnic Study of Atherosclerosis (MESA).
Dr. Kwon noted that previous studies have shown that patients with thoracic aortopathy have a high rate of obstructive sleep apnea (OSA) (Am J Respir Crit Care Med. 2003;168:1528-31), and those with OSA tend to have higher thoracic aortic size (J Am Coll Cardiol. 2008;52:885-6). “There’s also a degree of evidence suggesting that OSA is associated with high arterial stiffness, which is a marker of primary organ damage and a major cardiovascular risk that is predictive of cardiovascular disease,” Dr. Kwon said (J Intl Med Res. 2011;39:228-38). However, he also noted that some studies have found no relationship between OSA and aortic disease (Respiration. 2006;73:741-50). “The question can be raised as to whether sleep apnea may have implications” in thoracic aortic disease, he said.
Dr. Kwon’s study evaluated three groups: patients with no OSA (apnea hypopnea index [AHI] less than 5, n = 87); mild OSA (AHI 5-15, n = 215); and severe OSA (AHI greater than 15, n = 406). All patients had polysomnography as part of an ancillary study. Cardiac MRI measured these three features of aortic function and physiology (unadjusted results):
Diameter at the pulmonary artery bifurcation, which ranged from 3.13 cm in patients with no OSA to 3.37 cm in those with severe OSA (P = .0017).
Pulse wave velocity, which averaged 8.07 m/s in the no-OSA group and 9.11 m/s in the severe group (P less than .0001).
Distensibility, or aortic stiffness, which was 1.73%/mm Hg in the no-OSA group, 1.54%/mm Hg in the mild group and 1.68%/mm Hg in the severe group (P = .0141).
“There was maybe some higher pulse wave velocity across the significant OSA group,” Dr. Kwon said. “However, with aortic distensibility, there did not seem to be any significant trend.”
In the adjusted analysis of aortic diameter, “there did appear to be a small but significant difference in the significant OSA group, compared with the reference group,” Dr. Kwon said. He also noted that women with OSA typically had significantly larger aortic diameters than did non-OSA counterparts, whereas that trend was not as pronounced in men.
“Thoracic aorta size does seem to increase with OSA severity, but this has a sex-interaction component; it’s more pronounced in women,” Dr. Kwon said. He also noted a discrepancy in the results: “The functional properties of the aorta did not seem to bear a significant association with OSA severity.”
In explaining why these results differed from previous studies, Dr. Kwon said the study populations or their characteristics may be the cause, or that MRI-based measures of aortic properties have not been extensively studied before. “This is probably the first study to look at an unselected population, use a large sample size that was ethnically diverse, and use cardiac MRI technology,” he said.
Limitations he noted were the study’s cross-sectional nature and its small population of patients with enlarged thoracic aorta size, which left it underpowered to evaluate that population.
Dr. Kwon reported having no financial relationships.
SOURCE: Kwon Y et al. SLEEP 2018, Abstract #0465.
BALTIMORE – Individuals with moderate to severe and thus may be at a heightened risk of cardiovascular events, according to an analysis of a national, multisite research study presented at the annual meeting of the Associated Professional Sleep Societies.
The study evaluated a subgroup of 708 patients with no history of cardiovascular disease (CVD) from the Multi-Ethnic Study of Atherosclerosis (MESA).
Dr. Kwon noted that previous studies have shown that patients with thoracic aortopathy have a high rate of obstructive sleep apnea (OSA) (Am J Respir Crit Care Med. 2003;168:1528-31), and those with OSA tend to have higher thoracic aortic size (J Am Coll Cardiol. 2008;52:885-6). “There’s also a degree of evidence suggesting that OSA is associated with high arterial stiffness, which is a marker of primary organ damage and a major cardiovascular risk that is predictive of cardiovascular disease,” Dr. Kwon said (J Intl Med Res. 2011;39:228-38). However, he also noted that some studies have found no relationship between OSA and aortic disease (Respiration. 2006;73:741-50). “The question can be raised as to whether sleep apnea may have implications” in thoracic aortic disease, he said.
Dr. Kwon’s study evaluated three groups: patients with no OSA (apnea hypopnea index [AHI] less than 5, n = 87); mild OSA (AHI 5-15, n = 215); and severe OSA (AHI greater than 15, n = 406). All patients had polysomnography as part of an ancillary study. Cardiac MRI measured these three features of aortic function and physiology (unadjusted results):
Diameter at the pulmonary artery bifurcation, which ranged from 3.13 cm in patients with no OSA to 3.37 cm in those with severe OSA (P = .0017).
Pulse wave velocity, which averaged 8.07 m/s in the no-OSA group and 9.11 m/s in the severe group (P less than .0001).
Distensibility, or aortic stiffness, which was 1.73%/mm Hg in the no-OSA group, 1.54%/mm Hg in the mild group and 1.68%/mm Hg in the severe group (P = .0141).
“There was maybe some higher pulse wave velocity across the significant OSA group,” Dr. Kwon said. “However, with aortic distensibility, there did not seem to be any significant trend.”
In the adjusted analysis of aortic diameter, “there did appear to be a small but significant difference in the significant OSA group, compared with the reference group,” Dr. Kwon said. He also noted that women with OSA typically had significantly larger aortic diameters than did non-OSA counterparts, whereas that trend was not as pronounced in men.
“Thoracic aorta size does seem to increase with OSA severity, but this has a sex-interaction component; it’s more pronounced in women,” Dr. Kwon said. He also noted a discrepancy in the results: “The functional properties of the aorta did not seem to bear a significant association with OSA severity.”
In explaining why these results differed from previous studies, Dr. Kwon said the study populations or their characteristics may be the cause, or that MRI-based measures of aortic properties have not been extensively studied before. “This is probably the first study to look at an unselected population, use a large sample size that was ethnically diverse, and use cardiac MRI technology,” he said.
Limitations he noted were the study’s cross-sectional nature and its small population of patients with enlarged thoracic aorta size, which left it underpowered to evaluate that population.
Dr. Kwon reported having no financial relationships.
SOURCE: Kwon Y et al. SLEEP 2018, Abstract #0465.
BALTIMORE – Individuals with moderate to severe and thus may be at a heightened risk of cardiovascular events, according to an analysis of a national, multisite research study presented at the annual meeting of the Associated Professional Sleep Societies.
The study evaluated a subgroup of 708 patients with no history of cardiovascular disease (CVD) from the Multi-Ethnic Study of Atherosclerosis (MESA).
Dr. Kwon noted that previous studies have shown that patients with thoracic aortopathy have a high rate of obstructive sleep apnea (OSA) (Am J Respir Crit Care Med. 2003;168:1528-31), and those with OSA tend to have higher thoracic aortic size (J Am Coll Cardiol. 2008;52:885-6). “There’s also a degree of evidence suggesting that OSA is associated with high arterial stiffness, which is a marker of primary organ damage and a major cardiovascular risk that is predictive of cardiovascular disease,” Dr. Kwon said (J Intl Med Res. 2011;39:228-38). However, he also noted that some studies have found no relationship between OSA and aortic disease (Respiration. 2006;73:741-50). “The question can be raised as to whether sleep apnea may have implications” in thoracic aortic disease, he said.
Dr. Kwon’s study evaluated three groups: patients with no OSA (apnea hypopnea index [AHI] less than 5, n = 87); mild OSA (AHI 5-15, n = 215); and severe OSA (AHI greater than 15, n = 406). All patients had polysomnography as part of an ancillary study. Cardiac MRI measured these three features of aortic function and physiology (unadjusted results):
Diameter at the pulmonary artery bifurcation, which ranged from 3.13 cm in patients with no OSA to 3.37 cm in those with severe OSA (P = .0017).
Pulse wave velocity, which averaged 8.07 m/s in the no-OSA group and 9.11 m/s in the severe group (P less than .0001).
Distensibility, or aortic stiffness, which was 1.73%/mm Hg in the no-OSA group, 1.54%/mm Hg in the mild group and 1.68%/mm Hg in the severe group (P = .0141).
“There was maybe some higher pulse wave velocity across the significant OSA group,” Dr. Kwon said. “However, with aortic distensibility, there did not seem to be any significant trend.”
In the adjusted analysis of aortic diameter, “there did appear to be a small but significant difference in the significant OSA group, compared with the reference group,” Dr. Kwon said. He also noted that women with OSA typically had significantly larger aortic diameters than did non-OSA counterparts, whereas that trend was not as pronounced in men.
“Thoracic aorta size does seem to increase with OSA severity, but this has a sex-interaction component; it’s more pronounced in women,” Dr. Kwon said. He also noted a discrepancy in the results: “The functional properties of the aorta did not seem to bear a significant association with OSA severity.”
In explaining why these results differed from previous studies, Dr. Kwon said the study populations or their characteristics may be the cause, or that MRI-based measures of aortic properties have not been extensively studied before. “This is probably the first study to look at an unselected population, use a large sample size that was ethnically diverse, and use cardiac MRI technology,” he said.
Limitations he noted were the study’s cross-sectional nature and its small population of patients with enlarged thoracic aorta size, which left it underpowered to evaluate that population.
Dr. Kwon reported having no financial relationships.
SOURCE: Kwon Y et al. SLEEP 2018, Abstract #0465.
REPORTING FROM SLEEP 2018
Key clinical point: Obstructive sleep apnea severity is related to increased aortic artery size.
Major finding: Ascending aortic diameter measured 3.37 cm in patients with severe OSA vs. 3.13 cm with no OSA.
Study details: Subgroup of 708 patients with OSA but no history of cardiovascular disease from the Multi-Ethnic Study of Atherosclerosis.
Disclosures: Dr. Kwon reported having no financial relationships.
Source: Kwon Y et al. SLEEP 2018, Abstract #0465.
Investigational solriamfetol may improve multiple sleep measures
BALTIMORE – Multiple studies based on phase 3 clinical trials of the investigational drug solriamfetol have found that it may be effective for improving next-day wakefulness and work productivity in people with narcolepsy and obstructive sleep apnea, and that the drug can maintain its effect throughout the day as well as for up to 6 months, investigators reported at the annual meeting of the Associated Professional Sleep Societies.
Solriamfetol, developed by Jazz Pharmaceuticals, is the subject of a new drug application accepted by the Food and Drug Administration in March of 2018 for the treatment of excessive sleepiness due to narcolepsy or obstructive sleep apnea (OSA). Solriamfetol is a selective dopamine and norepinephrine reuptake inhibitor.
The drug was the subject of four different studies presented at SLEEP 2018 that drilled down into its effect on specific aspects of narcolepsy or OSA, or both. One study explored results in narcoleptic patients with and without cataplexy. Another study investigated the drug’s maintenance of efficacy after 6 months of treatment. A third study looked at the drug’s impact on next-day function, work productivity, and quality of life in patients with narcolepsy. And the fourth study researched how solriamfetol helped maintain wakefulness throughout the day.
Yves Dauvilliers, MD, reported that the 150- and 300-mg doses of solriamfetol were effective in improving both sleep latency, as measured with maintenance of wakefulness test (MWT), and Epworth Sleepiness Scale (ESS) scores in both cataplexic (n = 117) and noncataplexic (n = 114) narcolepsy. The objective of the study was to reevaluate the safety of solriamfetol in these narcoleptic subgroups from the phase 3 trial, said Dr. Dauvilliers, a faculty member at Centre Hospitalier Universitaire de Montpellier (France).
In patients with cataplexy, the 150-mg dose increased sleep latency from a baseline of 0 to 7.9 after a week and sustained that for 12 weeks; doubling the dose raised that to 10.3 after a week, reaching 10.7 in week 12. Gains were even more dramatic in noncataplexic patients, with the 150-mg dose improving sleep latency to 12.8 at week 1 and 11.6 at week 12, and the 300-mg dose resulting in a gain of 16.8 after a week, trailing off to 13.8 after 12 weeks, Dr. Dauvilliers said.
The study also evaluated ESS scores for three dosing levels – 75, 150, and 300 mg – plus placebo. In the group with cataplexy, ESS at week 12 improved from a baseline of 0 to –3.1, –5.6, and –6.3 for the three dosing groups, respectively, vs. –1.8 for placebo. In the noncataplexy patients with narcolepsy, the improvements in ESS at week 12 were –4.5, –5.2 and –6.4, respectively, vs. –1.5 for placebo.
“At 150 mg and 300 mg, solriamfetol seems to be very effective in treating excessive sleepiness with narcolepsy, with the same efficacy in the group with and without cataplexy – with efficacy even after just 1 week of treatment,” Dr. Dauvilliers said.
Atul Malhotra, MD, and his coresearchers investigated the long-term safety and efficacy of solriamfetol out to 42 weeks in patients with narcolepsy or OSA who completed previous clinical trials, which were 6- and 12-week trials. The study involved an open-label phase from weeks 14 to 27, a 2-week randomized withdrawal phase and then safety follow-up after week 40. In the open-label phase, ESS scores for the overall treatment group (n = 519) improved from 15.9 at baseline to 8.3 at week 40, with variation between the OSA (n = 333) and narcolepsy (n = 186) groups: from 15.2 at baseline to 6.5 at week 40 for the former and from 17.3 to 11.4 for the latter.
In the randomized withdrawal phase, ESS scores for those on solriamfetol (n = 139) migrated upward from 7.3 to 8.5 – but for the placebo group (n = 141) ESS rose from 7.8 to 12.6, a difference of 3.7 favoring the treatment group, said Dr. Malhotra, chief of pulmonary and critical care medicine and the Kenneth M. Moser Professor in the department of medicine, University of California San Diego, La Jolla. Most patients in the placebo group had worsening of symptoms based on global impression of change – 64.5% vs. 28.2% in the treatment group in the self-reported cohort, and 63.8% vs. 28.7% in the clinician-evaluated cohort.
“The open-label phase demonstrated maintenance-of-efficacy after 1 year,” Dr. Malhotra said. “The safety profile was consistent with prior placebo-controlled studies of solriamfetol. Epworth sleepiness score and adverse event data demonstrated a lack of rebound sleepiness or withdrawal after abrupt discontinuation of solriamfetol during the randomized washout phase. So the bottom line is it looks to be a durable, effective treatment without major side effects.”
Helene A. Emsellem, MD, led a study into how solriamfetol can impact daily activity in patients with narcolepsy. “Solriamfetol at 300 mg reduced activity impairment outside the workplace and, at 150 mg, reduced activity and work impairment from baseline to week 12 on the measures of functionality at work and in private life,” said Dr. Emsellem, of George Washington University Medical Center, Washington. She is medical director of the Center for Sleep & Wake Disorders, Chevy Chase, Md.
Patients on 300 mg solriamfetol (n = 43) gained an average 3.01 on the Functional Outcomes of Sleep Questionnaire short version (FOSQ-10) total score from baseline to week 12. That compares with gains of 2.57 in the 150-mg group (n = 51), 2.39 in the 75-mg group (n = 49), and 1.56 in the placebo group (n = 52, P = .05). The study looked at activity across four different measures in terms of reduced impairment, as measured by percentage reductions in the negative. The 150-mg group showed most improvement in impairment while working and overall work impairment, with changes of –22.02% and –19.77%, respectively, vs. –11.62% and –10.59% for the 300-mg dose. However, the higher dose showed greater improvement in general activity impairment: –21.17% vs. –17.84% in the 150-mg dose (P less than .05).
Notably, there was little difference across the dosing groups in improvement in work time missed, “I think mostly because there wasn’t much absenteeism to start with,” Dr. Emsellem said.
The 300-mg group also showed greater gains in physical component summary, based on answers to the 36-item Short Form Health Survey, averaging a gain of 3.29 from baseline vs. 2.65 for 150 mg, 2.54 for 75 mg, and 1.06 for placebo. However, on the mental component summary of the survey, the 300-mg group showed the smallest increase: 0.68 vs. 2.05 (150 mg), 1.55 (75 mg), and 0.78 (placebo), respectively (P less than . 05).
In reporting on the effects of solriamfetol through the day, Paula K. Schweitzer, PhD, director of research at the Sleep Medicine and Research Center at St. Luke’s Hospital, Chesterfield, Mo., noted that sustained full-day efficacy may be a limitation of other wake-promoting medications (Clin Neuropharmacol. 2003;26:252-57; Curr Med Res Opin. 2006;22:761-74). The objective of her study was to evaluate the efficacy of solriamfetol through the day over five sequential MWT trials. Her research involved two double-blind, 12-week studies in patients with either narcolepsy (n = 231) or OSA (n = 459) who were randomized to placebo or one of four doses of solriamfetol: 37.5 mg (in OSA only) and 75, 150, and 300 mg. Patients took the drug orally in the morning.
“Solriamfetol significantly increased sleep latency on all five sequential MWT trials at doses of 150 and 300 mg in the narcolepsy patients, and at doses of 75, 150, and 300 mg in the OSA patients.” Dr. Schweitzer said.
The 150- and 300-mg doses showed the greatest improvement over smaller doses and placebo in both the narcolepsy and OSA groups. In the narcolepsy patients, changes from baseline in MWT sleep latency in the first trial, at approximately 1 hour post dose, were 9.9 (150 mg), 9.9 (300 mg), and –0.6 (placebo) minutes; and in the fifth trial, approximately 9 hours post dose, were 9.3 (150 mg), 12.3 (300 mg), and 3.1 (placebo) minutes. In the OSA patients, changes from baseline in the first trial were 10.9 (150 mg), 12.5 (300 mg), and –0.4 (placebo) minutes; and in the fifth trial, changes were 8.1 (150 mg), 7.6 (300 mg), and 0.2 (placebo) minutes.
“These data demonstrate sustained efficacy over approximately 9 hours following morning dosing for solriamfetol at 150-300 mg in narcolepsy patients and 75-300 mg in OSA patients.” Dr. Schweitzer said.
She also noted that rates of insomnia through the day were less than 5% in each study population combined across dose groups.
Reporting of adverse events was similar across treatment groups in all four studies. The most common adverse event was headache, ranging from around 10% for OSA to 24.2% in patients with cataplexic narcolepsy (n = 91), followed by nausea, decreased appetite, anxiety, and nasopharyngitis. Dr. Malhotra’s study, which involved the largest population of OSA (n = 417) and narcolepsy (n = 226) patients, showed overall rates of at least one adverse event of 75.1% and 74.8%, respectively. His study also showed an overall rate of 5% for respiratory tract infection, and nine patients (1.4%) who had serious cardiovascular adverse events – two cases of atrial fibrillation, and one each of acute MI, angina pectoris, chest discomfort, chest pain, noncardiac chest pain, cerebrovascular accident, and pulmonary embolism.
Dr. Schweitzer noted that the adverse events were mild to moderate in severity, with discontinuation rates of 5% to 7% in the treatment group. Dr. Dauvilliers said the safety results were consistent with previous studies.
All four researchers reported receiving grant/research support from Jazz Pharmaceuticals, sponsor of the study.
SOURCE: Dauvilliers Y et al. Abstract 0619; Malhotra A et al. Abstract 0620; Emsellem H et al. Abstract 0621; Schweitzer PK et al. Abstract 0622. Presented at Sleep 2018.
BALTIMORE – Multiple studies based on phase 3 clinical trials of the investigational drug solriamfetol have found that it may be effective for improving next-day wakefulness and work productivity in people with narcolepsy and obstructive sleep apnea, and that the drug can maintain its effect throughout the day as well as for up to 6 months, investigators reported at the annual meeting of the Associated Professional Sleep Societies.
Solriamfetol, developed by Jazz Pharmaceuticals, is the subject of a new drug application accepted by the Food and Drug Administration in March of 2018 for the treatment of excessive sleepiness due to narcolepsy or obstructive sleep apnea (OSA). Solriamfetol is a selective dopamine and norepinephrine reuptake inhibitor.
The drug was the subject of four different studies presented at SLEEP 2018 that drilled down into its effect on specific aspects of narcolepsy or OSA, or both. One study explored results in narcoleptic patients with and without cataplexy. Another study investigated the drug’s maintenance of efficacy after 6 months of treatment. A third study looked at the drug’s impact on next-day function, work productivity, and quality of life in patients with narcolepsy. And the fourth study researched how solriamfetol helped maintain wakefulness throughout the day.
Yves Dauvilliers, MD, reported that the 150- and 300-mg doses of solriamfetol were effective in improving both sleep latency, as measured with maintenance of wakefulness test (MWT), and Epworth Sleepiness Scale (ESS) scores in both cataplexic (n = 117) and noncataplexic (n = 114) narcolepsy. The objective of the study was to reevaluate the safety of solriamfetol in these narcoleptic subgroups from the phase 3 trial, said Dr. Dauvilliers, a faculty member at Centre Hospitalier Universitaire de Montpellier (France).
In patients with cataplexy, the 150-mg dose increased sleep latency from a baseline of 0 to 7.9 after a week and sustained that for 12 weeks; doubling the dose raised that to 10.3 after a week, reaching 10.7 in week 12. Gains were even more dramatic in noncataplexic patients, with the 150-mg dose improving sleep latency to 12.8 at week 1 and 11.6 at week 12, and the 300-mg dose resulting in a gain of 16.8 after a week, trailing off to 13.8 after 12 weeks, Dr. Dauvilliers said.
The study also evaluated ESS scores for three dosing levels – 75, 150, and 300 mg – plus placebo. In the group with cataplexy, ESS at week 12 improved from a baseline of 0 to –3.1, –5.6, and –6.3 for the three dosing groups, respectively, vs. –1.8 for placebo. In the noncataplexy patients with narcolepsy, the improvements in ESS at week 12 were –4.5, –5.2 and –6.4, respectively, vs. –1.5 for placebo.
“At 150 mg and 300 mg, solriamfetol seems to be very effective in treating excessive sleepiness with narcolepsy, with the same efficacy in the group with and without cataplexy – with efficacy even after just 1 week of treatment,” Dr. Dauvilliers said.
Atul Malhotra, MD, and his coresearchers investigated the long-term safety and efficacy of solriamfetol out to 42 weeks in patients with narcolepsy or OSA who completed previous clinical trials, which were 6- and 12-week trials. The study involved an open-label phase from weeks 14 to 27, a 2-week randomized withdrawal phase and then safety follow-up after week 40. In the open-label phase, ESS scores for the overall treatment group (n = 519) improved from 15.9 at baseline to 8.3 at week 40, with variation between the OSA (n = 333) and narcolepsy (n = 186) groups: from 15.2 at baseline to 6.5 at week 40 for the former and from 17.3 to 11.4 for the latter.
In the randomized withdrawal phase, ESS scores for those on solriamfetol (n = 139) migrated upward from 7.3 to 8.5 – but for the placebo group (n = 141) ESS rose from 7.8 to 12.6, a difference of 3.7 favoring the treatment group, said Dr. Malhotra, chief of pulmonary and critical care medicine and the Kenneth M. Moser Professor in the department of medicine, University of California San Diego, La Jolla. Most patients in the placebo group had worsening of symptoms based on global impression of change – 64.5% vs. 28.2% in the treatment group in the self-reported cohort, and 63.8% vs. 28.7% in the clinician-evaluated cohort.
“The open-label phase demonstrated maintenance-of-efficacy after 1 year,” Dr. Malhotra said. “The safety profile was consistent with prior placebo-controlled studies of solriamfetol. Epworth sleepiness score and adverse event data demonstrated a lack of rebound sleepiness or withdrawal after abrupt discontinuation of solriamfetol during the randomized washout phase. So the bottom line is it looks to be a durable, effective treatment without major side effects.”
Helene A. Emsellem, MD, led a study into how solriamfetol can impact daily activity in patients with narcolepsy. “Solriamfetol at 300 mg reduced activity impairment outside the workplace and, at 150 mg, reduced activity and work impairment from baseline to week 12 on the measures of functionality at work and in private life,” said Dr. Emsellem, of George Washington University Medical Center, Washington. She is medical director of the Center for Sleep & Wake Disorders, Chevy Chase, Md.
Patients on 300 mg solriamfetol (n = 43) gained an average 3.01 on the Functional Outcomes of Sleep Questionnaire short version (FOSQ-10) total score from baseline to week 12. That compares with gains of 2.57 in the 150-mg group (n = 51), 2.39 in the 75-mg group (n = 49), and 1.56 in the placebo group (n = 52, P = .05). The study looked at activity across four different measures in terms of reduced impairment, as measured by percentage reductions in the negative. The 150-mg group showed most improvement in impairment while working and overall work impairment, with changes of –22.02% and –19.77%, respectively, vs. –11.62% and –10.59% for the 300-mg dose. However, the higher dose showed greater improvement in general activity impairment: –21.17% vs. –17.84% in the 150-mg dose (P less than .05).
Notably, there was little difference across the dosing groups in improvement in work time missed, “I think mostly because there wasn’t much absenteeism to start with,” Dr. Emsellem said.
The 300-mg group also showed greater gains in physical component summary, based on answers to the 36-item Short Form Health Survey, averaging a gain of 3.29 from baseline vs. 2.65 for 150 mg, 2.54 for 75 mg, and 1.06 for placebo. However, on the mental component summary of the survey, the 300-mg group showed the smallest increase: 0.68 vs. 2.05 (150 mg), 1.55 (75 mg), and 0.78 (placebo), respectively (P less than . 05).
In reporting on the effects of solriamfetol through the day, Paula K. Schweitzer, PhD, director of research at the Sleep Medicine and Research Center at St. Luke’s Hospital, Chesterfield, Mo., noted that sustained full-day efficacy may be a limitation of other wake-promoting medications (Clin Neuropharmacol. 2003;26:252-57; Curr Med Res Opin. 2006;22:761-74). The objective of her study was to evaluate the efficacy of solriamfetol through the day over five sequential MWT trials. Her research involved two double-blind, 12-week studies in patients with either narcolepsy (n = 231) or OSA (n = 459) who were randomized to placebo or one of four doses of solriamfetol: 37.5 mg (in OSA only) and 75, 150, and 300 mg. Patients took the drug orally in the morning.
“Solriamfetol significantly increased sleep latency on all five sequential MWT trials at doses of 150 and 300 mg in the narcolepsy patients, and at doses of 75, 150, and 300 mg in the OSA patients.” Dr. Schweitzer said.
The 150- and 300-mg doses showed the greatest improvement over smaller doses and placebo in both the narcolepsy and OSA groups. In the narcolepsy patients, changes from baseline in MWT sleep latency in the first trial, at approximately 1 hour post dose, were 9.9 (150 mg), 9.9 (300 mg), and –0.6 (placebo) minutes; and in the fifth trial, approximately 9 hours post dose, were 9.3 (150 mg), 12.3 (300 mg), and 3.1 (placebo) minutes. In the OSA patients, changes from baseline in the first trial were 10.9 (150 mg), 12.5 (300 mg), and –0.4 (placebo) minutes; and in the fifth trial, changes were 8.1 (150 mg), 7.6 (300 mg), and 0.2 (placebo) minutes.
“These data demonstrate sustained efficacy over approximately 9 hours following morning dosing for solriamfetol at 150-300 mg in narcolepsy patients and 75-300 mg in OSA patients.” Dr. Schweitzer said.
She also noted that rates of insomnia through the day were less than 5% in each study population combined across dose groups.
Reporting of adverse events was similar across treatment groups in all four studies. The most common adverse event was headache, ranging from around 10% for OSA to 24.2% in patients with cataplexic narcolepsy (n = 91), followed by nausea, decreased appetite, anxiety, and nasopharyngitis. Dr. Malhotra’s study, which involved the largest population of OSA (n = 417) and narcolepsy (n = 226) patients, showed overall rates of at least one adverse event of 75.1% and 74.8%, respectively. His study also showed an overall rate of 5% for respiratory tract infection, and nine patients (1.4%) who had serious cardiovascular adverse events – two cases of atrial fibrillation, and one each of acute MI, angina pectoris, chest discomfort, chest pain, noncardiac chest pain, cerebrovascular accident, and pulmonary embolism.
Dr. Schweitzer noted that the adverse events were mild to moderate in severity, with discontinuation rates of 5% to 7% in the treatment group. Dr. Dauvilliers said the safety results were consistent with previous studies.
All four researchers reported receiving grant/research support from Jazz Pharmaceuticals, sponsor of the study.
SOURCE: Dauvilliers Y et al. Abstract 0619; Malhotra A et al. Abstract 0620; Emsellem H et al. Abstract 0621; Schweitzer PK et al. Abstract 0622. Presented at Sleep 2018.
BALTIMORE – Multiple studies based on phase 3 clinical trials of the investigational drug solriamfetol have found that it may be effective for improving next-day wakefulness and work productivity in people with narcolepsy and obstructive sleep apnea, and that the drug can maintain its effect throughout the day as well as for up to 6 months, investigators reported at the annual meeting of the Associated Professional Sleep Societies.
Solriamfetol, developed by Jazz Pharmaceuticals, is the subject of a new drug application accepted by the Food and Drug Administration in March of 2018 for the treatment of excessive sleepiness due to narcolepsy or obstructive sleep apnea (OSA). Solriamfetol is a selective dopamine and norepinephrine reuptake inhibitor.
The drug was the subject of four different studies presented at SLEEP 2018 that drilled down into its effect on specific aspects of narcolepsy or OSA, or both. One study explored results in narcoleptic patients with and without cataplexy. Another study investigated the drug’s maintenance of efficacy after 6 months of treatment. A third study looked at the drug’s impact on next-day function, work productivity, and quality of life in patients with narcolepsy. And the fourth study researched how solriamfetol helped maintain wakefulness throughout the day.
Yves Dauvilliers, MD, reported that the 150- and 300-mg doses of solriamfetol were effective in improving both sleep latency, as measured with maintenance of wakefulness test (MWT), and Epworth Sleepiness Scale (ESS) scores in both cataplexic (n = 117) and noncataplexic (n = 114) narcolepsy. The objective of the study was to reevaluate the safety of solriamfetol in these narcoleptic subgroups from the phase 3 trial, said Dr. Dauvilliers, a faculty member at Centre Hospitalier Universitaire de Montpellier (France).
In patients with cataplexy, the 150-mg dose increased sleep latency from a baseline of 0 to 7.9 after a week and sustained that for 12 weeks; doubling the dose raised that to 10.3 after a week, reaching 10.7 in week 12. Gains were even more dramatic in noncataplexic patients, with the 150-mg dose improving sleep latency to 12.8 at week 1 and 11.6 at week 12, and the 300-mg dose resulting in a gain of 16.8 after a week, trailing off to 13.8 after 12 weeks, Dr. Dauvilliers said.
The study also evaluated ESS scores for three dosing levels – 75, 150, and 300 mg – plus placebo. In the group with cataplexy, ESS at week 12 improved from a baseline of 0 to –3.1, –5.6, and –6.3 for the three dosing groups, respectively, vs. –1.8 for placebo. In the noncataplexy patients with narcolepsy, the improvements in ESS at week 12 were –4.5, –5.2 and –6.4, respectively, vs. –1.5 for placebo.
“At 150 mg and 300 mg, solriamfetol seems to be very effective in treating excessive sleepiness with narcolepsy, with the same efficacy in the group with and without cataplexy – with efficacy even after just 1 week of treatment,” Dr. Dauvilliers said.
Atul Malhotra, MD, and his coresearchers investigated the long-term safety and efficacy of solriamfetol out to 42 weeks in patients with narcolepsy or OSA who completed previous clinical trials, which were 6- and 12-week trials. The study involved an open-label phase from weeks 14 to 27, a 2-week randomized withdrawal phase and then safety follow-up after week 40. In the open-label phase, ESS scores for the overall treatment group (n = 519) improved from 15.9 at baseline to 8.3 at week 40, with variation between the OSA (n = 333) and narcolepsy (n = 186) groups: from 15.2 at baseline to 6.5 at week 40 for the former and from 17.3 to 11.4 for the latter.
In the randomized withdrawal phase, ESS scores for those on solriamfetol (n = 139) migrated upward from 7.3 to 8.5 – but for the placebo group (n = 141) ESS rose from 7.8 to 12.6, a difference of 3.7 favoring the treatment group, said Dr. Malhotra, chief of pulmonary and critical care medicine and the Kenneth M. Moser Professor in the department of medicine, University of California San Diego, La Jolla. Most patients in the placebo group had worsening of symptoms based on global impression of change – 64.5% vs. 28.2% in the treatment group in the self-reported cohort, and 63.8% vs. 28.7% in the clinician-evaluated cohort.
“The open-label phase demonstrated maintenance-of-efficacy after 1 year,” Dr. Malhotra said. “The safety profile was consistent with prior placebo-controlled studies of solriamfetol. Epworth sleepiness score and adverse event data demonstrated a lack of rebound sleepiness or withdrawal after abrupt discontinuation of solriamfetol during the randomized washout phase. So the bottom line is it looks to be a durable, effective treatment without major side effects.”
Helene A. Emsellem, MD, led a study into how solriamfetol can impact daily activity in patients with narcolepsy. “Solriamfetol at 300 mg reduced activity impairment outside the workplace and, at 150 mg, reduced activity and work impairment from baseline to week 12 on the measures of functionality at work and in private life,” said Dr. Emsellem, of George Washington University Medical Center, Washington. She is medical director of the Center for Sleep & Wake Disorders, Chevy Chase, Md.
Patients on 300 mg solriamfetol (n = 43) gained an average 3.01 on the Functional Outcomes of Sleep Questionnaire short version (FOSQ-10) total score from baseline to week 12. That compares with gains of 2.57 in the 150-mg group (n = 51), 2.39 in the 75-mg group (n = 49), and 1.56 in the placebo group (n = 52, P = .05). The study looked at activity across four different measures in terms of reduced impairment, as measured by percentage reductions in the negative. The 150-mg group showed most improvement in impairment while working and overall work impairment, with changes of –22.02% and –19.77%, respectively, vs. –11.62% and –10.59% for the 300-mg dose. However, the higher dose showed greater improvement in general activity impairment: –21.17% vs. –17.84% in the 150-mg dose (P less than .05).
Notably, there was little difference across the dosing groups in improvement in work time missed, “I think mostly because there wasn’t much absenteeism to start with,” Dr. Emsellem said.
The 300-mg group also showed greater gains in physical component summary, based on answers to the 36-item Short Form Health Survey, averaging a gain of 3.29 from baseline vs. 2.65 for 150 mg, 2.54 for 75 mg, and 1.06 for placebo. However, on the mental component summary of the survey, the 300-mg group showed the smallest increase: 0.68 vs. 2.05 (150 mg), 1.55 (75 mg), and 0.78 (placebo), respectively (P less than . 05).
In reporting on the effects of solriamfetol through the day, Paula K. Schweitzer, PhD, director of research at the Sleep Medicine and Research Center at St. Luke’s Hospital, Chesterfield, Mo., noted that sustained full-day efficacy may be a limitation of other wake-promoting medications (Clin Neuropharmacol. 2003;26:252-57; Curr Med Res Opin. 2006;22:761-74). The objective of her study was to evaluate the efficacy of solriamfetol through the day over five sequential MWT trials. Her research involved two double-blind, 12-week studies in patients with either narcolepsy (n = 231) or OSA (n = 459) who were randomized to placebo or one of four doses of solriamfetol: 37.5 mg (in OSA only) and 75, 150, and 300 mg. Patients took the drug orally in the morning.
“Solriamfetol significantly increased sleep latency on all five sequential MWT trials at doses of 150 and 300 mg in the narcolepsy patients, and at doses of 75, 150, and 300 mg in the OSA patients.” Dr. Schweitzer said.
The 150- and 300-mg doses showed the greatest improvement over smaller doses and placebo in both the narcolepsy and OSA groups. In the narcolepsy patients, changes from baseline in MWT sleep latency in the first trial, at approximately 1 hour post dose, were 9.9 (150 mg), 9.9 (300 mg), and –0.6 (placebo) minutes; and in the fifth trial, approximately 9 hours post dose, were 9.3 (150 mg), 12.3 (300 mg), and 3.1 (placebo) minutes. In the OSA patients, changes from baseline in the first trial were 10.9 (150 mg), 12.5 (300 mg), and –0.4 (placebo) minutes; and in the fifth trial, changes were 8.1 (150 mg), 7.6 (300 mg), and 0.2 (placebo) minutes.
“These data demonstrate sustained efficacy over approximately 9 hours following morning dosing for solriamfetol at 150-300 mg in narcolepsy patients and 75-300 mg in OSA patients.” Dr. Schweitzer said.
She also noted that rates of insomnia through the day were less than 5% in each study population combined across dose groups.
Reporting of adverse events was similar across treatment groups in all four studies. The most common adverse event was headache, ranging from around 10% for OSA to 24.2% in patients with cataplexic narcolepsy (n = 91), followed by nausea, decreased appetite, anxiety, and nasopharyngitis. Dr. Malhotra’s study, which involved the largest population of OSA (n = 417) and narcolepsy (n = 226) patients, showed overall rates of at least one adverse event of 75.1% and 74.8%, respectively. His study also showed an overall rate of 5% for respiratory tract infection, and nine patients (1.4%) who had serious cardiovascular adverse events – two cases of atrial fibrillation, and one each of acute MI, angina pectoris, chest discomfort, chest pain, noncardiac chest pain, cerebrovascular accident, and pulmonary embolism.
Dr. Schweitzer noted that the adverse events were mild to moderate in severity, with discontinuation rates of 5% to 7% in the treatment group. Dr. Dauvilliers said the safety results were consistent with previous studies.
All four researchers reported receiving grant/research support from Jazz Pharmaceuticals, sponsor of the study.
SOURCE: Dauvilliers Y et al. Abstract 0619; Malhotra A et al. Abstract 0620; Emsellem H et al. Abstract 0621; Schweitzer PK et al. Abstract 0622. Presented at Sleep 2018.
REPORTING FROM SLEEP 2018
Key clinical point: Solriamfetol seems effective for improving multiple measures of wakefulness in narcolepsy and obstructive sleep apnea.
Major finding: Individuals with narcolepsy in the 150-mg and 300-mg dosing groups had average increase in maintenance of wakefulness test scores of 9.9 vs. a loss of 0.6 for the placebo group.
Data source: Four studies of data from two phase 3 trials of adults with excessive sleepiness and narcolepsy or excessive sleepiness and obstructive sleep apnea, with study populations ranging in size from 231 to 643.
Disclosures: All presenters reported receiving support from Jazz Pharmaceuticals, sponsor of the studies. Dr. Dauvilliers reported being a consultant to UCB Pharma, Bioprojet, Theranexus, Flamel and Harmony Biosciences. Dr. Emsellem reported financial relationships with Vanda Pharmaceuticals, Eisai, Flamel (Avadel), Balance Therapeutics, Merck, NightBalance, Novartis, Phillips Respironics, and Harmony Biosciences. Dr. Schweitzer reported relationships with Phillips Respironics and NightBalance. Dr. Malhotra reported that ResMed provided a philanthropic donation to his institution, University of California San Diego.
Sources: Dauvilliers Y et al. Abstract 0619; Malhotra A et al. Abstract 620; Emsellem H et al. Abstract 0621; Schweitzer PK et al. Abstract 0622. Presented at Sleep 2018.
Study profiles sleep disruption in depression
Waking theta reduced in depression
BALTIMORE – Disruption of slow-wave activity may potentially explain the positive influence that sleep deprivation may have on major depressive disorder, according to results of a study presented at the annual meeting of the Associated Professional Sleep Societies.
Jennifer Goldschmied, PhD, of the University of Pennsylvania, Philadelphia, reported preliminary results of a study of slow-wave activity (SWA) disruption in 26 subjects – 12 healthy controls and 14 people diagnosed with major depressive disorder – that found a significant decrease of about 20% in waking theta activity, as measured with EEG, in the MDD group. In the 3-night sleep study, conducted at the University of Michigan, Ann Arbor, an adaptation night was followed by baseline and SWA disruption nights with EEGs performed each night. After the baseline night, patients also had a morning and afternoon EEG.
Across the baseline day, patients with depression showed “no modulation of theta activity whatsoever,” Dr. Goldschmied said. “And then we see, following slow-wave disruption, a significant decrease in theta activity,” whereas, healthy controls showed no change in waking theta following slow-wave disruption. “So what this means is that the presence of SWA may actually be facilitating the reduction of theta or sleep propensity during typical sleep in healthy individuals,” she added. In MDD patients, the decline in theta power following slow-wave disruption was from around 5.4 to 4.3.
Dr. Goldschmied noted that this finding somewhat supports what is known as the synaptic homeostasis hypothesis that University of Wisconsin researchers Giulio Tononi, MD, PhD, and Chiara Cirelli, MD, PhD, reported (Brain Res Bull. 2003;62:143-50). This hypothesis holds that SWA is a marker of synaptic strength and promotes the downscaling of synaptic strength during sleep. No method for measuring synaptic strength in humans exists, Dr. Goldschmied added, but waking theta can be considered a proxy for net synaptic strength across the cortex.
Dr. Goldschmied noted other research that has found SWA disruption improves mood (Psychiatry Res. 2015;228:715-8; J Psychiatr Res. 2011;45:1019-26), but the study she reported on found no role of decreased theta activity in that change. “To go even further,” she said, “we looked at the entire data set and found no relationship between the decrease in theta and any of the measures of sleep architecture – so there’s really no way to predict this decrease in our sample of people with depression.”
SWA plays a significant role in depression and merits more study, Dr. Goldschmied said. She noted that future research should examine the effects of SWA disruption in a larger sample, investigate theta findings with other proxy measures of synaptic strength such as brain-derived neurotrophic factor and transcranial magnetic stimulation, explore differences in SWA between sexes, and explore how SWA enhancement influences mood and theta activity.
Dr. Goldschmied reported having no financial relationships.
SOURCE: Goldschmied J et al. Sleep 2018, Abstract 0245.
Waking theta reduced in depression
Waking theta reduced in depression
BALTIMORE – Disruption of slow-wave activity may potentially explain the positive influence that sleep deprivation may have on major depressive disorder, according to results of a study presented at the annual meeting of the Associated Professional Sleep Societies.
Jennifer Goldschmied, PhD, of the University of Pennsylvania, Philadelphia, reported preliminary results of a study of slow-wave activity (SWA) disruption in 26 subjects – 12 healthy controls and 14 people diagnosed with major depressive disorder – that found a significant decrease of about 20% in waking theta activity, as measured with EEG, in the MDD group. In the 3-night sleep study, conducted at the University of Michigan, Ann Arbor, an adaptation night was followed by baseline and SWA disruption nights with EEGs performed each night. After the baseline night, patients also had a morning and afternoon EEG.
Across the baseline day, patients with depression showed “no modulation of theta activity whatsoever,” Dr. Goldschmied said. “And then we see, following slow-wave disruption, a significant decrease in theta activity,” whereas, healthy controls showed no change in waking theta following slow-wave disruption. “So what this means is that the presence of SWA may actually be facilitating the reduction of theta or sleep propensity during typical sleep in healthy individuals,” she added. In MDD patients, the decline in theta power following slow-wave disruption was from around 5.4 to 4.3.
Dr. Goldschmied noted that this finding somewhat supports what is known as the synaptic homeostasis hypothesis that University of Wisconsin researchers Giulio Tononi, MD, PhD, and Chiara Cirelli, MD, PhD, reported (Brain Res Bull. 2003;62:143-50). This hypothesis holds that SWA is a marker of synaptic strength and promotes the downscaling of synaptic strength during sleep. No method for measuring synaptic strength in humans exists, Dr. Goldschmied added, but waking theta can be considered a proxy for net synaptic strength across the cortex.
Dr. Goldschmied noted other research that has found SWA disruption improves mood (Psychiatry Res. 2015;228:715-8; J Psychiatr Res. 2011;45:1019-26), but the study she reported on found no role of decreased theta activity in that change. “To go even further,” she said, “we looked at the entire data set and found no relationship between the decrease in theta and any of the measures of sleep architecture – so there’s really no way to predict this decrease in our sample of people with depression.”
SWA plays a significant role in depression and merits more study, Dr. Goldschmied said. She noted that future research should examine the effects of SWA disruption in a larger sample, investigate theta findings with other proxy measures of synaptic strength such as brain-derived neurotrophic factor and transcranial magnetic stimulation, explore differences in SWA between sexes, and explore how SWA enhancement influences mood and theta activity.
Dr. Goldschmied reported having no financial relationships.
SOURCE: Goldschmied J et al. Sleep 2018, Abstract 0245.
BALTIMORE – Disruption of slow-wave activity may potentially explain the positive influence that sleep deprivation may have on major depressive disorder, according to results of a study presented at the annual meeting of the Associated Professional Sleep Societies.
Jennifer Goldschmied, PhD, of the University of Pennsylvania, Philadelphia, reported preliminary results of a study of slow-wave activity (SWA) disruption in 26 subjects – 12 healthy controls and 14 people diagnosed with major depressive disorder – that found a significant decrease of about 20% in waking theta activity, as measured with EEG, in the MDD group. In the 3-night sleep study, conducted at the University of Michigan, Ann Arbor, an adaptation night was followed by baseline and SWA disruption nights with EEGs performed each night. After the baseline night, patients also had a morning and afternoon EEG.
Across the baseline day, patients with depression showed “no modulation of theta activity whatsoever,” Dr. Goldschmied said. “And then we see, following slow-wave disruption, a significant decrease in theta activity,” whereas, healthy controls showed no change in waking theta following slow-wave disruption. “So what this means is that the presence of SWA may actually be facilitating the reduction of theta or sleep propensity during typical sleep in healthy individuals,” she added. In MDD patients, the decline in theta power following slow-wave disruption was from around 5.4 to 4.3.
Dr. Goldschmied noted that this finding somewhat supports what is known as the synaptic homeostasis hypothesis that University of Wisconsin researchers Giulio Tononi, MD, PhD, and Chiara Cirelli, MD, PhD, reported (Brain Res Bull. 2003;62:143-50). This hypothesis holds that SWA is a marker of synaptic strength and promotes the downscaling of synaptic strength during sleep. No method for measuring synaptic strength in humans exists, Dr. Goldschmied added, but waking theta can be considered a proxy for net synaptic strength across the cortex.
Dr. Goldschmied noted other research that has found SWA disruption improves mood (Psychiatry Res. 2015;228:715-8; J Psychiatr Res. 2011;45:1019-26), but the study she reported on found no role of decreased theta activity in that change. “To go even further,” she said, “we looked at the entire data set and found no relationship between the decrease in theta and any of the measures of sleep architecture – so there’s really no way to predict this decrease in our sample of people with depression.”
SWA plays a significant role in depression and merits more study, Dr. Goldschmied said. She noted that future research should examine the effects of SWA disruption in a larger sample, investigate theta findings with other proxy measures of synaptic strength such as brain-derived neurotrophic factor and transcranial magnetic stimulation, explore differences in SWA between sexes, and explore how SWA enhancement influences mood and theta activity.
Dr. Goldschmied reported having no financial relationships.
SOURCE: Goldschmied J et al. Sleep 2018, Abstract 0245.
REPORTING FROM SLEEP 2018
Key clinical point: Patients with major depression have reduced brain activity after sleep disruption.
Major finding: Morning theta activity was 20% lower following slow-wave disruption in patients with major depressive disorder than in healthy controls.
Data source: EEG measures of 14 individuals with major depressive disorder and 12 healthy controls in the evening before sleep and the morning following sleep after 1 night of baseline and 1 night of selective slow-wave disrupted sleep.
Disclosure: Dr. Goldschmied had no financial relationships to disclose.
Source: Goldschmied J et al. Sleep 2018, Abstract 0245.
Emerging CPAP options show sustained benefits
BALTIMORE – Emerging developments for the treatment of obstructive sleep apnea have shown promise in providing options beyond continuous-positive airway pressure, investigators reported at the annual meeting of the Associated Professional Sleep Societies. These developments include a single-use nasopharyngeal airway stent, upper-airway stimulation using a pacemaker-like device, a negative-pressure device that opens the airway, and an artificial intelligence approach that can predict outcomes of oral appliance therapy.
Nasopharyngeal airway stent
Clete A. Kushida, MD, of Stanford (Calif.) University reported on recent results of a trial of the nasopharyngeal airway stent (NAS) single-use disposable insert (Seven Dreamers Laboratories, Tokyo). This device consists of a flexible semi-rigid silicone rubber tube 120-145 mm in length and coated with a hydrophilic gel. The patient inserts the distal end of the tube into the nostril, and it positions itself within the nasopharynx and retropalatal oropharynx to open the airway. A clip attaches to the exterior septum to keep the device in place. The patient removes the NAS in the morning. The device is commercially available in Japan and some European countries.
Dr. Kushida reported on two posters that were presented at Sleep 2018. The first by the Osaka University Graduate School of Dentistry in Japan investigated the predictability of NAS efficacy in patients with a velopharynx that was narrower than the hypopharynx (Sleep. 2018;41 (suppl 1):A207: doi.org/10.1093/sleep/zsy061.554). The study showed that 11 responders had a narrow velopharynx while 18 nonresponders had a narrow hypopharynx. Response was defined as 50% or greater reduction of apnea-hypopnea index (AHI) from baseline. “The success rate of NAS for the patients with narrowing of the velopharynx is 83.3%,” Dr. Kushida said.
He also reported on a study he led of NAS in patients with obstructive sleep apnea and healthy controls (Sleep. 2018;41 (suppl 1):A207: doi.org/10.1093/sleep/zsy061.555). The trial was conducted at Stanford and Tokyo sleep medical centers, with healthy controls at the Tokyo site only. AHI improved in all three obstructive sleep apnea (OSA) groups, but most significantly in those with moderate (n = 23) and severe (n = 21) OSA: 7.2 (P = .0038) and 11.7 (P = .0069), respectively. In the Stanford cohort, 2 of 32 patients originally enrolled dropped out because they found the NAS uncomfortable; none dropped out of the Tokyo cohort.
“NAS can be effective in treatment of snoring and OSA, in particular those with moderate/severe OSA, with significant improvement in mean obstructive apnea index,” Dr. Kushida said. He also noted the device is more effective in patients with narrowing of the oropharynx/velopharynx rather than the hypopharynx.
Dr. Kushida reported he had a financial relationship with the Seven Dreamers Laboratories.
Continuous negative external pressure
Jerrold A. Kram, MD, reported on a device that employs continuous negative external pressure – known as cNEP – that uses a silicone collar covering the front of the throat and a pump that applies suction to keep the airway open from the outside. He cited a small 2015 study out of Japan that found the device was effective in keeping the pharyngeal airway open in nonobese women (J Appl Physiol. 2015;118:912-20). Another small U.S. study found cNEP reduces respiratory impairment during screening colonoscopy (Endoscopy. 2016;48:584-7). Sommetrics, which has patented the technology, is developing a version of the product for obstructive sleep apnea, Dr. Kram said. The company already has a Food and Drug Administration–approved product to treat apneas that people experience when under mild to moderate sedation, such as a colonoscopy. It is approved for sale in Canada, but not in the United States.
“It gives us another tool in the box,” Dr. Kram said. “It’s very small and portable, easy to take on an airplane with you, and it reduces the chance for claustrophobia” that comes with continuous-positive airway pressure (CPAP), said Dr. Kram. There are no tubes or masks and no humidifier to deal with.
Dr. Kram conducted a small study of 15 OSA patients using cNEP last year. Among nine excellent responders, the lowest AHI was 1.5 on average, from an average baseline of 43.9; among four partial responders, the lowest observed AHI averaged 11.75 (J Clin Sleep Med. 2017;13:1009-12).
The cNEP device is also the subject of a home study of patients with OSA in Canada, Dr. Kram said. Unpublished results indicate that 46% (27/59) of patients had an initial response rate to either -25 or -30 characteristic moment waveform (cmw) of negative airway pressure. For those who completed 3 weeks of treatment, the response rate was 64% (16/25). “Seventy-six percent of subjects felt their overall experience with cNEP was better than with CPAP,” Dr. Kram said.
However, studies have noted some minor issues with cNEP, Dr. Kram said. They include mild skin irritation, choking sensation if not properly placed, limited size availability, and absence of efficacy data. Dr. Kram said a U.S. pivotal trial is scheduled to start soon.
Dr. Kram disclosed he is a paid adviser for Sommetrics.
Oral appliance therapy
Oral appliance therapy (OAT) has been very effective in some patients and has been endorsed by the American Academy of Sleep Medicine since 2006, but it has been underutilized predominantly for two reasons, noted John Remmers, MD, because fitting the device requires a trial-and-error approach that can discourage patients; and the therapeutic success rate is 50%-60%.
To predict which patients are likely to succeed with OAT, Dr. Remmers and his colleagues at Zephyr Sleep Technologies have developed an artificial intelligence (AI) platform that uses a feedback-controlled mandibular positioner, a mouthpiece-like device that opens the airway during sleep. Dr. Remmers is chief medical officer and cofounder of Zephyr Sleep Technologies, based in Calgary, Alta.
While imaging has been used in awake patients to fit OAT devices, Dr. Remmers noted a number of shortcomings with this modality. “Sleep apnea results from an anatomic problem – i.e., structural encroachment on the pharyngeal airway, which is neurally compensated when the patient is awake,” he said. “Because of this, we need to do the test when the patient is asleep.”
The AI platform with feedback-controlled mandibular positioner uses temporary dental trays to create impressions for the mouthpiece the patient uses during sleep. The mouthpiece connects to a remote-controlled device that makes real-time adjustments in the mandibular position without disturbing the patient’s sleep. “The computer identifies respiratory events all night long, adjusting the position of the mandible,” he said in explaining the AI component of the device. “Just think of it as similar to autotitration with CPAP.”
Dr. Remmers reported results of a phase 2 study of the platform presented as a poster reporting on a study of 101 patients with OSA participants. The study reported sensitivity of 86% and specificity of 92% in predicting success with the feedback-controlled mandibular positioner, he said.
“The sensitivity and overall predictive accuracy of the AI-based approach was greater than an intuitive approach using a pretreatment, temporary appliance, indicating that feedback-controlled mandibular positioning test outperformed the intuitive approach,” he said. The device has been approved by Health Canada and is awaiting clearance in the United States.
Upper airway stimulation
Upper airway stimulation (UAS) is emerging as a new class of therapy, said Patrick J. Strollo Jr., MD, of the University of Pittsburgh. The therapy involves an impulse generator (IPG) similar to a pacemaker that is implanted in the left side of the chest and connected to a stimulation lead secured to the distal hypoglossal nerve in the neck. The UAS system also incorporates a sensing lead that is implanted between the intercostal muscles and attached to the IPG allowing for phasic stimulation of the genioglossal muscle. The patient uses a remote control to turn the device on at night and off in the morning.
Dr. Strollo was lead author of the Stimulation Therapy for Apnea Reduction (STAR) trial (N Engl J Med. 2014:370;139-49), a prospective multicenter trial with a randomized therapy withdrawal arm. In 126 participants, he said, the median AHI score declined 68% in 12 months, from 29.3 at baseline to 9 (P less than .0001).
He provided updated results that showed 80% of patients continued to use the device after 5 years (Otolaryngol Head Neck Surg. 2018; doi: 10.1177/0194599818762383). Median AHI at 5 years was 6.9, Dr. Strollo said, and median Epworth Sleepiness Scale scores declined from 11.6 at baseline to 6.9 at 5 years.
Another postapproval study of UAS, the ADHERE registry, has enrolled 348 patients at 10 centers with a goal of 2,500, Dr. Strollo said (Otolaryngol Head Neck Surg. 2018: doi: 10.1177/0194599818764896). Twelve-month study results have shown reductions in AHI and Epworth Sleepiness Scale scores comparable to previous reports. ADHERE also reported that 92% of patients were satisfied with UAS.
The latest innovation for UAS is the ability to download data from the implant at office visits so the physician can review patient adherence patterns, along with energy levels and settings for sensing and stimulation, Dr. Strollo said.
“Upper airway stimulation is an additional tool in the management of properly selected, at-risk apnea patients who do not accept or adhere to positive pressure therapy,” Dr. Strollo said. “The STAR trial has provided robust evidence that upper airway stimulation is safe and effective in participants with moderate to severe OSA, and the treatment effect is maintained beyond the 12-month endpoint.”
Dr. Strollo disclosed a financial relationship with Inspire Medical Systems, manufacturer of the UAS device.
BALTIMORE – Emerging developments for the treatment of obstructive sleep apnea have shown promise in providing options beyond continuous-positive airway pressure, investigators reported at the annual meeting of the Associated Professional Sleep Societies. These developments include a single-use nasopharyngeal airway stent, upper-airway stimulation using a pacemaker-like device, a negative-pressure device that opens the airway, and an artificial intelligence approach that can predict outcomes of oral appliance therapy.
Nasopharyngeal airway stent
Clete A. Kushida, MD, of Stanford (Calif.) University reported on recent results of a trial of the nasopharyngeal airway stent (NAS) single-use disposable insert (Seven Dreamers Laboratories, Tokyo). This device consists of a flexible semi-rigid silicone rubber tube 120-145 mm in length and coated with a hydrophilic gel. The patient inserts the distal end of the tube into the nostril, and it positions itself within the nasopharynx and retropalatal oropharynx to open the airway. A clip attaches to the exterior septum to keep the device in place. The patient removes the NAS in the morning. The device is commercially available in Japan and some European countries.
Dr. Kushida reported on two posters that were presented at Sleep 2018. The first by the Osaka University Graduate School of Dentistry in Japan investigated the predictability of NAS efficacy in patients with a velopharynx that was narrower than the hypopharynx (Sleep. 2018;41 (suppl 1):A207: doi.org/10.1093/sleep/zsy061.554). The study showed that 11 responders had a narrow velopharynx while 18 nonresponders had a narrow hypopharynx. Response was defined as 50% or greater reduction of apnea-hypopnea index (AHI) from baseline. “The success rate of NAS for the patients with narrowing of the velopharynx is 83.3%,” Dr. Kushida said.
He also reported on a study he led of NAS in patients with obstructive sleep apnea and healthy controls (Sleep. 2018;41 (suppl 1):A207: doi.org/10.1093/sleep/zsy061.555). The trial was conducted at Stanford and Tokyo sleep medical centers, with healthy controls at the Tokyo site only. AHI improved in all three obstructive sleep apnea (OSA) groups, but most significantly in those with moderate (n = 23) and severe (n = 21) OSA: 7.2 (P = .0038) and 11.7 (P = .0069), respectively. In the Stanford cohort, 2 of 32 patients originally enrolled dropped out because they found the NAS uncomfortable; none dropped out of the Tokyo cohort.
“NAS can be effective in treatment of snoring and OSA, in particular those with moderate/severe OSA, with significant improvement in mean obstructive apnea index,” Dr. Kushida said. He also noted the device is more effective in patients with narrowing of the oropharynx/velopharynx rather than the hypopharynx.
Dr. Kushida reported he had a financial relationship with the Seven Dreamers Laboratories.
Continuous negative external pressure
Jerrold A. Kram, MD, reported on a device that employs continuous negative external pressure – known as cNEP – that uses a silicone collar covering the front of the throat and a pump that applies suction to keep the airway open from the outside. He cited a small 2015 study out of Japan that found the device was effective in keeping the pharyngeal airway open in nonobese women (J Appl Physiol. 2015;118:912-20). Another small U.S. study found cNEP reduces respiratory impairment during screening colonoscopy (Endoscopy. 2016;48:584-7). Sommetrics, which has patented the technology, is developing a version of the product for obstructive sleep apnea, Dr. Kram said. The company already has a Food and Drug Administration–approved product to treat apneas that people experience when under mild to moderate sedation, such as a colonoscopy. It is approved for sale in Canada, but not in the United States.
“It gives us another tool in the box,” Dr. Kram said. “It’s very small and portable, easy to take on an airplane with you, and it reduces the chance for claustrophobia” that comes with continuous-positive airway pressure (CPAP), said Dr. Kram. There are no tubes or masks and no humidifier to deal with.
Dr. Kram conducted a small study of 15 OSA patients using cNEP last year. Among nine excellent responders, the lowest AHI was 1.5 on average, from an average baseline of 43.9; among four partial responders, the lowest observed AHI averaged 11.75 (J Clin Sleep Med. 2017;13:1009-12).
The cNEP device is also the subject of a home study of patients with OSA in Canada, Dr. Kram said. Unpublished results indicate that 46% (27/59) of patients had an initial response rate to either -25 or -30 characteristic moment waveform (cmw) of negative airway pressure. For those who completed 3 weeks of treatment, the response rate was 64% (16/25). “Seventy-six percent of subjects felt their overall experience with cNEP was better than with CPAP,” Dr. Kram said.
However, studies have noted some minor issues with cNEP, Dr. Kram said. They include mild skin irritation, choking sensation if not properly placed, limited size availability, and absence of efficacy data. Dr. Kram said a U.S. pivotal trial is scheduled to start soon.
Dr. Kram disclosed he is a paid adviser for Sommetrics.
Oral appliance therapy
Oral appliance therapy (OAT) has been very effective in some patients and has been endorsed by the American Academy of Sleep Medicine since 2006, but it has been underutilized predominantly for two reasons, noted John Remmers, MD, because fitting the device requires a trial-and-error approach that can discourage patients; and the therapeutic success rate is 50%-60%.
To predict which patients are likely to succeed with OAT, Dr. Remmers and his colleagues at Zephyr Sleep Technologies have developed an artificial intelligence (AI) platform that uses a feedback-controlled mandibular positioner, a mouthpiece-like device that opens the airway during sleep. Dr. Remmers is chief medical officer and cofounder of Zephyr Sleep Technologies, based in Calgary, Alta.
While imaging has been used in awake patients to fit OAT devices, Dr. Remmers noted a number of shortcomings with this modality. “Sleep apnea results from an anatomic problem – i.e., structural encroachment on the pharyngeal airway, which is neurally compensated when the patient is awake,” he said. “Because of this, we need to do the test when the patient is asleep.”
The AI platform with feedback-controlled mandibular positioner uses temporary dental trays to create impressions for the mouthpiece the patient uses during sleep. The mouthpiece connects to a remote-controlled device that makes real-time adjustments in the mandibular position without disturbing the patient’s sleep. “The computer identifies respiratory events all night long, adjusting the position of the mandible,” he said in explaining the AI component of the device. “Just think of it as similar to autotitration with CPAP.”
Dr. Remmers reported results of a phase 2 study of the platform presented as a poster reporting on a study of 101 patients with OSA participants. The study reported sensitivity of 86% and specificity of 92% in predicting success with the feedback-controlled mandibular positioner, he said.
“The sensitivity and overall predictive accuracy of the AI-based approach was greater than an intuitive approach using a pretreatment, temporary appliance, indicating that feedback-controlled mandibular positioning test outperformed the intuitive approach,” he said. The device has been approved by Health Canada and is awaiting clearance in the United States.
Upper airway stimulation
Upper airway stimulation (UAS) is emerging as a new class of therapy, said Patrick J. Strollo Jr., MD, of the University of Pittsburgh. The therapy involves an impulse generator (IPG) similar to a pacemaker that is implanted in the left side of the chest and connected to a stimulation lead secured to the distal hypoglossal nerve in the neck. The UAS system also incorporates a sensing lead that is implanted between the intercostal muscles and attached to the IPG allowing for phasic stimulation of the genioglossal muscle. The patient uses a remote control to turn the device on at night and off in the morning.
Dr. Strollo was lead author of the Stimulation Therapy for Apnea Reduction (STAR) trial (N Engl J Med. 2014:370;139-49), a prospective multicenter trial with a randomized therapy withdrawal arm. In 126 participants, he said, the median AHI score declined 68% in 12 months, from 29.3 at baseline to 9 (P less than .0001).
He provided updated results that showed 80% of patients continued to use the device after 5 years (Otolaryngol Head Neck Surg. 2018; doi: 10.1177/0194599818762383). Median AHI at 5 years was 6.9, Dr. Strollo said, and median Epworth Sleepiness Scale scores declined from 11.6 at baseline to 6.9 at 5 years.
Another postapproval study of UAS, the ADHERE registry, has enrolled 348 patients at 10 centers with a goal of 2,500, Dr. Strollo said (Otolaryngol Head Neck Surg. 2018: doi: 10.1177/0194599818764896). Twelve-month study results have shown reductions in AHI and Epworth Sleepiness Scale scores comparable to previous reports. ADHERE also reported that 92% of patients were satisfied with UAS.
The latest innovation for UAS is the ability to download data from the implant at office visits so the physician can review patient adherence patterns, along with energy levels and settings for sensing and stimulation, Dr. Strollo said.
“Upper airway stimulation is an additional tool in the management of properly selected, at-risk apnea patients who do not accept or adhere to positive pressure therapy,” Dr. Strollo said. “The STAR trial has provided robust evidence that upper airway stimulation is safe and effective in participants with moderate to severe OSA, and the treatment effect is maintained beyond the 12-month endpoint.”
Dr. Strollo disclosed a financial relationship with Inspire Medical Systems, manufacturer of the UAS device.
BALTIMORE – Emerging developments for the treatment of obstructive sleep apnea have shown promise in providing options beyond continuous-positive airway pressure, investigators reported at the annual meeting of the Associated Professional Sleep Societies. These developments include a single-use nasopharyngeal airway stent, upper-airway stimulation using a pacemaker-like device, a negative-pressure device that opens the airway, and an artificial intelligence approach that can predict outcomes of oral appliance therapy.
Nasopharyngeal airway stent
Clete A. Kushida, MD, of Stanford (Calif.) University reported on recent results of a trial of the nasopharyngeal airway stent (NAS) single-use disposable insert (Seven Dreamers Laboratories, Tokyo). This device consists of a flexible semi-rigid silicone rubber tube 120-145 mm in length and coated with a hydrophilic gel. The patient inserts the distal end of the tube into the nostril, and it positions itself within the nasopharynx and retropalatal oropharynx to open the airway. A clip attaches to the exterior septum to keep the device in place. The patient removes the NAS in the morning. The device is commercially available in Japan and some European countries.
Dr. Kushida reported on two posters that were presented at Sleep 2018. The first by the Osaka University Graduate School of Dentistry in Japan investigated the predictability of NAS efficacy in patients with a velopharynx that was narrower than the hypopharynx (Sleep. 2018;41 (suppl 1):A207: doi.org/10.1093/sleep/zsy061.554). The study showed that 11 responders had a narrow velopharynx while 18 nonresponders had a narrow hypopharynx. Response was defined as 50% or greater reduction of apnea-hypopnea index (AHI) from baseline. “The success rate of NAS for the patients with narrowing of the velopharynx is 83.3%,” Dr. Kushida said.
He also reported on a study he led of NAS in patients with obstructive sleep apnea and healthy controls (Sleep. 2018;41 (suppl 1):A207: doi.org/10.1093/sleep/zsy061.555). The trial was conducted at Stanford and Tokyo sleep medical centers, with healthy controls at the Tokyo site only. AHI improved in all three obstructive sleep apnea (OSA) groups, but most significantly in those with moderate (n = 23) and severe (n = 21) OSA: 7.2 (P = .0038) and 11.7 (P = .0069), respectively. In the Stanford cohort, 2 of 32 patients originally enrolled dropped out because they found the NAS uncomfortable; none dropped out of the Tokyo cohort.
“NAS can be effective in treatment of snoring and OSA, in particular those with moderate/severe OSA, with significant improvement in mean obstructive apnea index,” Dr. Kushida said. He also noted the device is more effective in patients with narrowing of the oropharynx/velopharynx rather than the hypopharynx.
Dr. Kushida reported he had a financial relationship with the Seven Dreamers Laboratories.
Continuous negative external pressure
Jerrold A. Kram, MD, reported on a device that employs continuous negative external pressure – known as cNEP – that uses a silicone collar covering the front of the throat and a pump that applies suction to keep the airway open from the outside. He cited a small 2015 study out of Japan that found the device was effective in keeping the pharyngeal airway open in nonobese women (J Appl Physiol. 2015;118:912-20). Another small U.S. study found cNEP reduces respiratory impairment during screening colonoscopy (Endoscopy. 2016;48:584-7). Sommetrics, which has patented the technology, is developing a version of the product for obstructive sleep apnea, Dr. Kram said. The company already has a Food and Drug Administration–approved product to treat apneas that people experience when under mild to moderate sedation, such as a colonoscopy. It is approved for sale in Canada, but not in the United States.
“It gives us another tool in the box,” Dr. Kram said. “It’s very small and portable, easy to take on an airplane with you, and it reduces the chance for claustrophobia” that comes with continuous-positive airway pressure (CPAP), said Dr. Kram. There are no tubes or masks and no humidifier to deal with.
Dr. Kram conducted a small study of 15 OSA patients using cNEP last year. Among nine excellent responders, the lowest AHI was 1.5 on average, from an average baseline of 43.9; among four partial responders, the lowest observed AHI averaged 11.75 (J Clin Sleep Med. 2017;13:1009-12).
The cNEP device is also the subject of a home study of patients with OSA in Canada, Dr. Kram said. Unpublished results indicate that 46% (27/59) of patients had an initial response rate to either -25 or -30 characteristic moment waveform (cmw) of negative airway pressure. For those who completed 3 weeks of treatment, the response rate was 64% (16/25). “Seventy-six percent of subjects felt their overall experience with cNEP was better than with CPAP,” Dr. Kram said.
However, studies have noted some minor issues with cNEP, Dr. Kram said. They include mild skin irritation, choking sensation if not properly placed, limited size availability, and absence of efficacy data. Dr. Kram said a U.S. pivotal trial is scheduled to start soon.
Dr. Kram disclosed he is a paid adviser for Sommetrics.
Oral appliance therapy
Oral appliance therapy (OAT) has been very effective in some patients and has been endorsed by the American Academy of Sleep Medicine since 2006, but it has been underutilized predominantly for two reasons, noted John Remmers, MD, because fitting the device requires a trial-and-error approach that can discourage patients; and the therapeutic success rate is 50%-60%.
To predict which patients are likely to succeed with OAT, Dr. Remmers and his colleagues at Zephyr Sleep Technologies have developed an artificial intelligence (AI) platform that uses a feedback-controlled mandibular positioner, a mouthpiece-like device that opens the airway during sleep. Dr. Remmers is chief medical officer and cofounder of Zephyr Sleep Technologies, based in Calgary, Alta.
While imaging has been used in awake patients to fit OAT devices, Dr. Remmers noted a number of shortcomings with this modality. “Sleep apnea results from an anatomic problem – i.e., structural encroachment on the pharyngeal airway, which is neurally compensated when the patient is awake,” he said. “Because of this, we need to do the test when the patient is asleep.”
The AI platform with feedback-controlled mandibular positioner uses temporary dental trays to create impressions for the mouthpiece the patient uses during sleep. The mouthpiece connects to a remote-controlled device that makes real-time adjustments in the mandibular position without disturbing the patient’s sleep. “The computer identifies respiratory events all night long, adjusting the position of the mandible,” he said in explaining the AI component of the device. “Just think of it as similar to autotitration with CPAP.”
Dr. Remmers reported results of a phase 2 study of the platform presented as a poster reporting on a study of 101 patients with OSA participants. The study reported sensitivity of 86% and specificity of 92% in predicting success with the feedback-controlled mandibular positioner, he said.
“The sensitivity and overall predictive accuracy of the AI-based approach was greater than an intuitive approach using a pretreatment, temporary appliance, indicating that feedback-controlled mandibular positioning test outperformed the intuitive approach,” he said. The device has been approved by Health Canada and is awaiting clearance in the United States.
Upper airway stimulation
Upper airway stimulation (UAS) is emerging as a new class of therapy, said Patrick J. Strollo Jr., MD, of the University of Pittsburgh. The therapy involves an impulse generator (IPG) similar to a pacemaker that is implanted in the left side of the chest and connected to a stimulation lead secured to the distal hypoglossal nerve in the neck. The UAS system also incorporates a sensing lead that is implanted between the intercostal muscles and attached to the IPG allowing for phasic stimulation of the genioglossal muscle. The patient uses a remote control to turn the device on at night and off in the morning.
Dr. Strollo was lead author of the Stimulation Therapy for Apnea Reduction (STAR) trial (N Engl J Med. 2014:370;139-49), a prospective multicenter trial with a randomized therapy withdrawal arm. In 126 participants, he said, the median AHI score declined 68% in 12 months, from 29.3 at baseline to 9 (P less than .0001).
He provided updated results that showed 80% of patients continued to use the device after 5 years (Otolaryngol Head Neck Surg. 2018; doi: 10.1177/0194599818762383). Median AHI at 5 years was 6.9, Dr. Strollo said, and median Epworth Sleepiness Scale scores declined from 11.6 at baseline to 6.9 at 5 years.
Another postapproval study of UAS, the ADHERE registry, has enrolled 348 patients at 10 centers with a goal of 2,500, Dr. Strollo said (Otolaryngol Head Neck Surg. 2018: doi: 10.1177/0194599818764896). Twelve-month study results have shown reductions in AHI and Epworth Sleepiness Scale scores comparable to previous reports. ADHERE also reported that 92% of patients were satisfied with UAS.
The latest innovation for UAS is the ability to download data from the implant at office visits so the physician can review patient adherence patterns, along with energy levels and settings for sensing and stimulation, Dr. Strollo said.
“Upper airway stimulation is an additional tool in the management of properly selected, at-risk apnea patients who do not accept or adhere to positive pressure therapy,” Dr. Strollo said. “The STAR trial has provided robust evidence that upper airway stimulation is safe and effective in participants with moderate to severe OSA, and the treatment effect is maintained beyond the 12-month endpoint.”
Dr. Strollo disclosed a financial relationship with Inspire Medical Systems, manufacturer of the UAS device.
REPORTING FROM SLEEP 2018
Key clinical point: Alternative treatments have shown sustained improvement in sleep apnea symptoms.
Major finding: The negative-pressure device improved oxygen flow in OSA to 64% vs. 25% for continuous-positive airway pressure.
Data source: Multiple abstracts presented at Sleep 2018 and published studies, including ADHERE study of 326 patients and a multicenter study of 430 patients using the upper airway stimulation device; a trial of 67 patients using the nasopharyngeal airway stent; and 101 patients in the artificial intelligence study.
Disclosures: Dr. Kushida disclosed a relationship with Seven Dreamers Laboratories. Dr. Kram is a paid adviser for Sommetrics. Dr. Remmers is founder of Zephyr Sleep Technologies. Dr. Strollo is an investigator in the STAR trial, supported by Inspire Medical Systems.
Phase 3 trial: Tasimelteon effective for jet lag disorder
BALTIMORE – Tasimelteon, a drug approved for non–24-hour sleep-wake disorder, has been shown to increase sleep times in travelers with jet lag, according to results from a phase 3 trial.
“Tasimelteon demonstrated an increase in total sleep time of 85 minutes versus placebo and also demonstrated improvement in next-day alertness versus placebo,” Christos Polymeropoulos, MD, medical director of Vanda Pharmaceuticals, said in presenting results of the JET8 trial during the late-breaking abstracts session at the annual meeting of the Associated Professional Sleep Societies.
Tasimelteon, sold under the trade name Hetlioz, is a melatonin receptor agonist that is Food and Drug Administration–approved for non-24-hour sleep-wake disorder – but not for treatment of jet lag disorder (JLD). Dr. Polymeropoulos noted there is no FDA-approved treatment for JLD.
“Jet lag disorder is a circadian disorder frequently observed in millions of travelers who cross multiple time zones,” Dr. Polymeropoulos said. “JLD is characterized by nighttime sleep disruption, decrease in daytime alertness, and impairment in social and occupational function.”
JET8 induced the circadian challenge equivalent to crossing eight time zones. The study involved 318 individuals randomized evenly to 20 mg tasimelteon or placebo 30 minutes before bedtime. The primary endpoint of the study was total sleep time in the first two-thirds of night measured by polysomnography.
Those on tasimelteon averaged 216.4 minutes of total sleep time in the first two-thirds of night versus 156.1 for those on placebo (P less than .0001), Dr. Polymeropoulos said. Full total sleep times were 315.8 minutes versus 230.3 minutes (P less than .0001), respectively.
“For total sleep time, the tasimelteon subjects gained about an hour and a half, as measured by PSG [polysomnography],” Dr. Polymeropoulos said.
Other key markers the trial measured were latency to persistent sleep and wakefulness after sleep onset. They measured 15 minutes less and 74.6 minutes less, respectively, in the tasimelteon arm.
Dr. Polymeropoulos also disclosed early results of a second trial of tasimelteon in JLD: the JET Study, a two-phase transatlantic travel study of 25 patients. The subjects flew from four U.S. cities to London for 3 nights, receiving tasimelteon or placebo each night in London. The study was terminated before reaching its enrollment goal of 90 patients because of its complexity, Vanda said in a separate press release. Over 3 nights of study, the tasimelteon arm gained a total of about 130 minutes of sleep versus 40 minutes for the placebo arm, Dr. Polymeropoulos said.
Vanda has said it plans to file a supplemental new drug application for tasimelteon for treatment of JLD in the second half of this year.
Dr. Polymeropoulos is an employee of Vanda Pharmaceuticals.
BALTIMORE – Tasimelteon, a drug approved for non–24-hour sleep-wake disorder, has been shown to increase sleep times in travelers with jet lag, according to results from a phase 3 trial.
“Tasimelteon demonstrated an increase in total sleep time of 85 minutes versus placebo and also demonstrated improvement in next-day alertness versus placebo,” Christos Polymeropoulos, MD, medical director of Vanda Pharmaceuticals, said in presenting results of the JET8 trial during the late-breaking abstracts session at the annual meeting of the Associated Professional Sleep Societies.
Tasimelteon, sold under the trade name Hetlioz, is a melatonin receptor agonist that is Food and Drug Administration–approved for non-24-hour sleep-wake disorder – but not for treatment of jet lag disorder (JLD). Dr. Polymeropoulos noted there is no FDA-approved treatment for JLD.
“Jet lag disorder is a circadian disorder frequently observed in millions of travelers who cross multiple time zones,” Dr. Polymeropoulos said. “JLD is characterized by nighttime sleep disruption, decrease in daytime alertness, and impairment in social and occupational function.”
JET8 induced the circadian challenge equivalent to crossing eight time zones. The study involved 318 individuals randomized evenly to 20 mg tasimelteon or placebo 30 minutes before bedtime. The primary endpoint of the study was total sleep time in the first two-thirds of night measured by polysomnography.
Those on tasimelteon averaged 216.4 minutes of total sleep time in the first two-thirds of night versus 156.1 for those on placebo (P less than .0001), Dr. Polymeropoulos said. Full total sleep times were 315.8 minutes versus 230.3 minutes (P less than .0001), respectively.
“For total sleep time, the tasimelteon subjects gained about an hour and a half, as measured by PSG [polysomnography],” Dr. Polymeropoulos said.
Other key markers the trial measured were latency to persistent sleep and wakefulness after sleep onset. They measured 15 minutes less and 74.6 minutes less, respectively, in the tasimelteon arm.
Dr. Polymeropoulos also disclosed early results of a second trial of tasimelteon in JLD: the JET Study, a two-phase transatlantic travel study of 25 patients. The subjects flew from four U.S. cities to London for 3 nights, receiving tasimelteon or placebo each night in London. The study was terminated before reaching its enrollment goal of 90 patients because of its complexity, Vanda said in a separate press release. Over 3 nights of study, the tasimelteon arm gained a total of about 130 minutes of sleep versus 40 minutes for the placebo arm, Dr. Polymeropoulos said.
Vanda has said it plans to file a supplemental new drug application for tasimelteon for treatment of JLD in the second half of this year.
Dr. Polymeropoulos is an employee of Vanda Pharmaceuticals.
BALTIMORE – Tasimelteon, a drug approved for non–24-hour sleep-wake disorder, has been shown to increase sleep times in travelers with jet lag, according to results from a phase 3 trial.
“Tasimelteon demonstrated an increase in total sleep time of 85 minutes versus placebo and also demonstrated improvement in next-day alertness versus placebo,” Christos Polymeropoulos, MD, medical director of Vanda Pharmaceuticals, said in presenting results of the JET8 trial during the late-breaking abstracts session at the annual meeting of the Associated Professional Sleep Societies.
Tasimelteon, sold under the trade name Hetlioz, is a melatonin receptor agonist that is Food and Drug Administration–approved for non-24-hour sleep-wake disorder – but not for treatment of jet lag disorder (JLD). Dr. Polymeropoulos noted there is no FDA-approved treatment for JLD.
“Jet lag disorder is a circadian disorder frequently observed in millions of travelers who cross multiple time zones,” Dr. Polymeropoulos said. “JLD is characterized by nighttime sleep disruption, decrease in daytime alertness, and impairment in social and occupational function.”
JET8 induced the circadian challenge equivalent to crossing eight time zones. The study involved 318 individuals randomized evenly to 20 mg tasimelteon or placebo 30 minutes before bedtime. The primary endpoint of the study was total sleep time in the first two-thirds of night measured by polysomnography.
Those on tasimelteon averaged 216.4 minutes of total sleep time in the first two-thirds of night versus 156.1 for those on placebo (P less than .0001), Dr. Polymeropoulos said. Full total sleep times were 315.8 minutes versus 230.3 minutes (P less than .0001), respectively.
“For total sleep time, the tasimelteon subjects gained about an hour and a half, as measured by PSG [polysomnography],” Dr. Polymeropoulos said.
Other key markers the trial measured were latency to persistent sleep and wakefulness after sleep onset. They measured 15 minutes less and 74.6 minutes less, respectively, in the tasimelteon arm.
Dr. Polymeropoulos also disclosed early results of a second trial of tasimelteon in JLD: the JET Study, a two-phase transatlantic travel study of 25 patients. The subjects flew from four U.S. cities to London for 3 nights, receiving tasimelteon or placebo each night in London. The study was terminated before reaching its enrollment goal of 90 patients because of its complexity, Vanda said in a separate press release. Over 3 nights of study, the tasimelteon arm gained a total of about 130 minutes of sleep versus 40 minutes for the placebo arm, Dr. Polymeropoulos said.
Vanda has said it plans to file a supplemental new drug application for tasimelteon for treatment of JLD in the second half of this year.
Dr. Polymeropoulos is an employee of Vanda Pharmaceuticals.
REPORTING FROM SLEEP 2018
Key clinical point: The melatonin receptor agonist tasimelteon may improve sleep in jet lag.
Major finding: Total sleep times were 315.8 minutes for tasimelteon versus 230.3 for placebo.
Study details: JET8 randomized, double-blind, placebo-controlled, multicenter trial of 318 healthy subjects with induced jet lag disorder.
Disclosures: Dr. Polymeropoulos is an employee of Vanda Pharmaceuticals.
CPAP and oxygen have different cardiac effects in OSA
BALTIMORE – Continuous positive airway pressure (CPAP) may supersede supplemental oxygen and patient education for improving one key marker of cardiac electrophysiological autonomic function during sleep, but supplemental oxygen may have the upper hand in improving a second key electrophysiological biomarker, according to results of a multicenter, randomized clinical trial presented at the annual meeting of the Associated Professional Sleep Societies.
“Based on these findings, it appears that there are opposing alterations in both frequency and time domain in heart rate variability indices in the CPAP versus oxygen groups,” said Jenie George, MD, of the Cleveland Clinic.
The study evaluated 3-month outcomes of frequency-based heart rate variability (HRV) indices obtained with ECG from sleep studies in 203 patients with obstructive sleep apnea and increased cardiovascular risk in the Heart Biomarker Elevation in Apnea Treatment (HeartBEAT) trial. The interventions were either CPAP, supplemental oxygen, or healthy lifestyle education. Dr. George noted that HRV is a noninvasive tool to evaluate autonomic function by quantifying changes in intervals between sinus beats during sleep.
On the high-frequency power index, patients on CPAP had a 9% reduction versus a 19% increase for those on supplemental oxygen, Dr. George said. However for the low frequency to high frequency ratio, the CPAP group had a 4% increase, whereas the oxygen group had a 34% reduction.
The increase of low frequency to high frequency ratio in the CPAP group is a reflection of sympathovagal balance – the ratio between low-frequency and high-frequency powers – while the changes in high-frequency power in the CPAP patients reflect changes in sinoatrial node electrophysiological function, Dr. George said.
Strengths of the study were its use of data from a large clinical trial, careful preprocessing of ECG data, and consideration of the influence of oxygen in sleep apnea and of confounding influences, such as medications. Limitations of the study, Dr. George noted, include the absence of sleep-wake data and acknowledgment that HRV measures are accepted surrogates of autonomic imbalance but that they are not direct measures.
The next steps for the current research, Dr. George said, include an analysis of how respiratory events influence HRV indices in CPAP and supplemental oxygen. Future trials should be designed to examine how the two interventions affect direct measures of autonomic function and consider a longer follow-up duration, she said.
Dr. George had no financial relationships to disclose. The trial received support from the National Heart, Lung, and Blood Institute and the National Center for Research Resources.
SOURCE: George J et al. Sleep 2018, Abstract 0444.
BALTIMORE – Continuous positive airway pressure (CPAP) may supersede supplemental oxygen and patient education for improving one key marker of cardiac electrophysiological autonomic function during sleep, but supplemental oxygen may have the upper hand in improving a second key electrophysiological biomarker, according to results of a multicenter, randomized clinical trial presented at the annual meeting of the Associated Professional Sleep Societies.
“Based on these findings, it appears that there are opposing alterations in both frequency and time domain in heart rate variability indices in the CPAP versus oxygen groups,” said Jenie George, MD, of the Cleveland Clinic.
The study evaluated 3-month outcomes of frequency-based heart rate variability (HRV) indices obtained with ECG from sleep studies in 203 patients with obstructive sleep apnea and increased cardiovascular risk in the Heart Biomarker Elevation in Apnea Treatment (HeartBEAT) trial. The interventions were either CPAP, supplemental oxygen, or healthy lifestyle education. Dr. George noted that HRV is a noninvasive tool to evaluate autonomic function by quantifying changes in intervals between sinus beats during sleep.
On the high-frequency power index, patients on CPAP had a 9% reduction versus a 19% increase for those on supplemental oxygen, Dr. George said. However for the low frequency to high frequency ratio, the CPAP group had a 4% increase, whereas the oxygen group had a 34% reduction.
The increase of low frequency to high frequency ratio in the CPAP group is a reflection of sympathovagal balance – the ratio between low-frequency and high-frequency powers – while the changes in high-frequency power in the CPAP patients reflect changes in sinoatrial node electrophysiological function, Dr. George said.
Strengths of the study were its use of data from a large clinical trial, careful preprocessing of ECG data, and consideration of the influence of oxygen in sleep apnea and of confounding influences, such as medications. Limitations of the study, Dr. George noted, include the absence of sleep-wake data and acknowledgment that HRV measures are accepted surrogates of autonomic imbalance but that they are not direct measures.
The next steps for the current research, Dr. George said, include an analysis of how respiratory events influence HRV indices in CPAP and supplemental oxygen. Future trials should be designed to examine how the two interventions affect direct measures of autonomic function and consider a longer follow-up duration, she said.
Dr. George had no financial relationships to disclose. The trial received support from the National Heart, Lung, and Blood Institute and the National Center for Research Resources.
SOURCE: George J et al. Sleep 2018, Abstract 0444.
BALTIMORE – Continuous positive airway pressure (CPAP) may supersede supplemental oxygen and patient education for improving one key marker of cardiac electrophysiological autonomic function during sleep, but supplemental oxygen may have the upper hand in improving a second key electrophysiological biomarker, according to results of a multicenter, randomized clinical trial presented at the annual meeting of the Associated Professional Sleep Societies.
“Based on these findings, it appears that there are opposing alterations in both frequency and time domain in heart rate variability indices in the CPAP versus oxygen groups,” said Jenie George, MD, of the Cleveland Clinic.
The study evaluated 3-month outcomes of frequency-based heart rate variability (HRV) indices obtained with ECG from sleep studies in 203 patients with obstructive sleep apnea and increased cardiovascular risk in the Heart Biomarker Elevation in Apnea Treatment (HeartBEAT) trial. The interventions were either CPAP, supplemental oxygen, or healthy lifestyle education. Dr. George noted that HRV is a noninvasive tool to evaluate autonomic function by quantifying changes in intervals between sinus beats during sleep.
On the high-frequency power index, patients on CPAP had a 9% reduction versus a 19% increase for those on supplemental oxygen, Dr. George said. However for the low frequency to high frequency ratio, the CPAP group had a 4% increase, whereas the oxygen group had a 34% reduction.
The increase of low frequency to high frequency ratio in the CPAP group is a reflection of sympathovagal balance – the ratio between low-frequency and high-frequency powers – while the changes in high-frequency power in the CPAP patients reflect changes in sinoatrial node electrophysiological function, Dr. George said.
Strengths of the study were its use of data from a large clinical trial, careful preprocessing of ECG data, and consideration of the influence of oxygen in sleep apnea and of confounding influences, such as medications. Limitations of the study, Dr. George noted, include the absence of sleep-wake data and acknowledgment that HRV measures are accepted surrogates of autonomic imbalance but that they are not direct measures.
The next steps for the current research, Dr. George said, include an analysis of how respiratory events influence HRV indices in CPAP and supplemental oxygen. Future trials should be designed to examine how the two interventions affect direct measures of autonomic function and consider a longer follow-up duration, she said.
Dr. George had no financial relationships to disclose. The trial received support from the National Heart, Lung, and Blood Institute and the National Center for Research Resources.
SOURCE: George J et al. Sleep 2018, Abstract 0444.
REPORTING FROM SLEEP 2018
Key clinical point: CPAP and oxygen in sleep apnea have countering effects on ECG.
Major finding: CPAP conferred a 9% reduction in high-frequency power but a 4% increase in low-frequency power.
Study details: Evaluation of 203 participants in the multicenter, randomized controlled Heart Biomarker Elevation in Apnea Treatment (HeartBEAT) trial.
Disclosures: Dr. George reported no financial relationships. The trial received support from the National Heart, Lung, and Blood Institute and the National Center for Research Resources.
Source: George J et al. Sleep 2018, Abstract 0444.