User login
Is there a doctor on the plane? Tips for providing in-flight assistance
In most cases, passengers on an airline flight are representative of the general population, which means that anyone could have an emergency at any time.
as determined on the basis of in-flight medical emergencies that resulted in calls to a physician-directed medical communications center, said Amy Faith Ho, MD, MPH of Integrative Emergency Services, Dallas–Fort Worth, in a presentation at the annual meeting of the American College of Emergency Physicians.
The study authors reviewed records of 11,920 in-flight medical emergencies between Jan. 1, 2008, and Oct. 31, 2010. The data showed that physician passengers provided medical assistance in nearly half of in-flight emergencies (48.1%) and that flights were diverted because of the emergency in 7.3% of cases.
The majority of the in-flight emergencies involved syncope or presyncope (37.4% of cases), followed by respiratory symptoms (12.1%) and nausea or vomiting (9.5%), according to the study.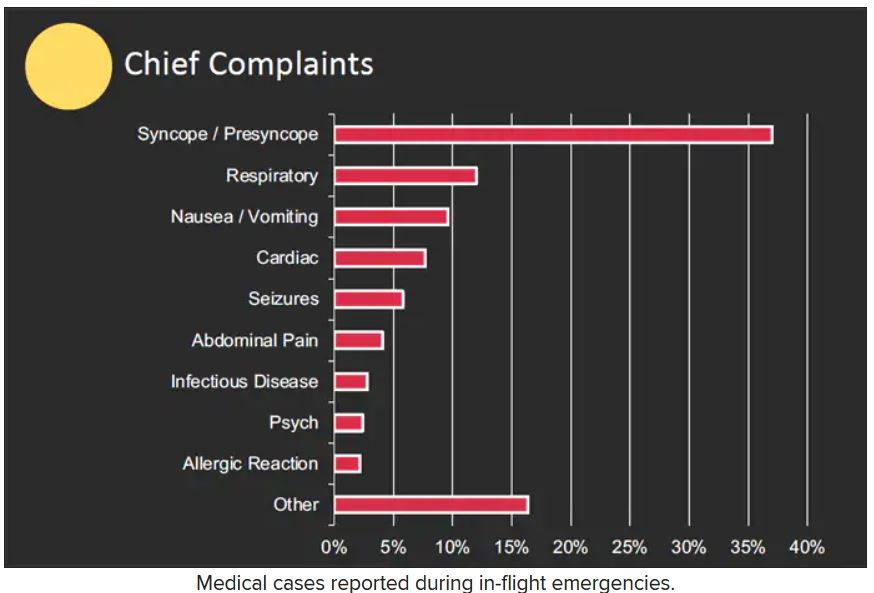
When a physician is faced with an in-flight emergency, the medical team includes the physician himself, medical ground control, and the flight attendants, said Dr. Ho. Requirements may vary among airlines, but all flight attendants will be trained in cardiopulmonary resuscitation (CPR) or basic life support, as well as use of automated external defibrillators (AEDs).
Physician call centers (medical ground control) can provide additional assistance remotely, she said.
The in-flight medical bag
Tools in a physician’s in-flight toolbox start with the first-aid kit. Airplanes also have an emergency medical kit (EMK), an oxygen tank, and an AED.
The minimum EMK contents are mandated by the Federal Aviation Administration, said Dr. Ho. The standard equipment includes a stethoscope, a sphygmomanometer, and three sizes of oropharyngeal airways. Other items include self-inflating manual resuscitation devices and CPR masks in thee sizes, alcohol sponges, gloves, adhesive tape, scissors, a tourniquet, as well as saline solution, needles, syringes, and an intravenous administration set consisting of tubing and two Y connectors.
An EMK also should contain the following medications: nonnarcotic analgesic tablets, antihistamine tablets, an injectable antihistamine, atropine, aspirin tablets, a bronchodilator, and epinephrine (both 1:1000; 1 injectable cc and 1:10,000; two injectable cc). Nitroglycerin tablets and 5 cc of 20 mg/mL injectable cardiac lidocaine are part of the mandated kit as well, according to Dr. Ho.
Some airlines carry additional supplies on all their flights, said Dr. Ho. Notably, American Airlines and British Airways carry EpiPens for adults and children, as well as opioid reversal medication (naloxone) and glucose for managing low blood sugar. American Airlines and Delta stock antiemetics, and Delta also carries naloxone. British Airways is unique in stocking additional cardiac medications, both oral and injectable.
How to handle an in-flight emergency
Physicians should always carry a copy of their medical license when traveling for documentation by the airline if they assist in a medical emergency during a flight, Dr. Ho emphasized. “Staff” personnel should be used. These include the flight attendants, medical ground control, and other passengers who might have useful skills, such as nursing, the ability to perform CPR, or therapy/counseling to calm a frightened patient. If needed, “crowdsource additional supplies from passengers,” such as a glucometer or pulse oximeter.
Legal lessons
Physicians are not obligated to assist during an in-flight medical emergency, said Dr. Ho. Legal jurisdiction can vary. In the United States, a bystander who assists in an emergency is generally protected by Good Samaritan laws; for international airlines, the laws may vary; those where the airline is based usually apply.
The Aviation Medical Assistance Act, passed in 1998, protects individuals from being sued for negligence while providing medical assistance, “unless the individual, while rendering such assistance, is guilty of gross negligence of willful misconduct,” Dr. Ho noted. The Aviation Medical Assistance Act also protects the airline itself “if the carrier in good faith believes that the passenger is a medically qualified individual.”
Dr. Ho disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In most cases, passengers on an airline flight are representative of the general population, which means that anyone could have an emergency at any time.
as determined on the basis of in-flight medical emergencies that resulted in calls to a physician-directed medical communications center, said Amy Faith Ho, MD, MPH of Integrative Emergency Services, Dallas–Fort Worth, in a presentation at the annual meeting of the American College of Emergency Physicians.
The study authors reviewed records of 11,920 in-flight medical emergencies between Jan. 1, 2008, and Oct. 31, 2010. The data showed that physician passengers provided medical assistance in nearly half of in-flight emergencies (48.1%) and that flights were diverted because of the emergency in 7.3% of cases.
The majority of the in-flight emergencies involved syncope or presyncope (37.4% of cases), followed by respiratory symptoms (12.1%) and nausea or vomiting (9.5%), according to the study.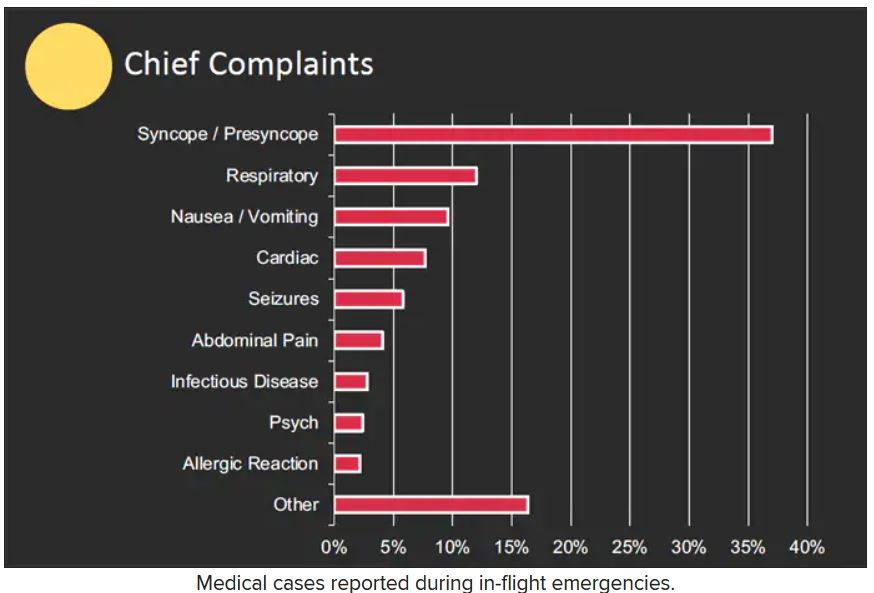
When a physician is faced with an in-flight emergency, the medical team includes the physician himself, medical ground control, and the flight attendants, said Dr. Ho. Requirements may vary among airlines, but all flight attendants will be trained in cardiopulmonary resuscitation (CPR) or basic life support, as well as use of automated external defibrillators (AEDs).
Physician call centers (medical ground control) can provide additional assistance remotely, she said.
The in-flight medical bag
Tools in a physician’s in-flight toolbox start with the first-aid kit. Airplanes also have an emergency medical kit (EMK), an oxygen tank, and an AED.
The minimum EMK contents are mandated by the Federal Aviation Administration, said Dr. Ho. The standard equipment includes a stethoscope, a sphygmomanometer, and three sizes of oropharyngeal airways. Other items include self-inflating manual resuscitation devices and CPR masks in thee sizes, alcohol sponges, gloves, adhesive tape, scissors, a tourniquet, as well as saline solution, needles, syringes, and an intravenous administration set consisting of tubing and two Y connectors.
An EMK also should contain the following medications: nonnarcotic analgesic tablets, antihistamine tablets, an injectable antihistamine, atropine, aspirin tablets, a bronchodilator, and epinephrine (both 1:1000; 1 injectable cc and 1:10,000; two injectable cc). Nitroglycerin tablets and 5 cc of 20 mg/mL injectable cardiac lidocaine are part of the mandated kit as well, according to Dr. Ho.
Some airlines carry additional supplies on all their flights, said Dr. Ho. Notably, American Airlines and British Airways carry EpiPens for adults and children, as well as opioid reversal medication (naloxone) and glucose for managing low blood sugar. American Airlines and Delta stock antiemetics, and Delta also carries naloxone. British Airways is unique in stocking additional cardiac medications, both oral and injectable.
How to handle an in-flight emergency
Physicians should always carry a copy of their medical license when traveling for documentation by the airline if they assist in a medical emergency during a flight, Dr. Ho emphasized. “Staff” personnel should be used. These include the flight attendants, medical ground control, and other passengers who might have useful skills, such as nursing, the ability to perform CPR, or therapy/counseling to calm a frightened patient. If needed, “crowdsource additional supplies from passengers,” such as a glucometer or pulse oximeter.
Legal lessons
Physicians are not obligated to assist during an in-flight medical emergency, said Dr. Ho. Legal jurisdiction can vary. In the United States, a bystander who assists in an emergency is generally protected by Good Samaritan laws; for international airlines, the laws may vary; those where the airline is based usually apply.
The Aviation Medical Assistance Act, passed in 1998, protects individuals from being sued for negligence while providing medical assistance, “unless the individual, while rendering such assistance, is guilty of gross negligence of willful misconduct,” Dr. Ho noted. The Aviation Medical Assistance Act also protects the airline itself “if the carrier in good faith believes that the passenger is a medically qualified individual.”
Dr. Ho disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In most cases, passengers on an airline flight are representative of the general population, which means that anyone could have an emergency at any time.
as determined on the basis of in-flight medical emergencies that resulted in calls to a physician-directed medical communications center, said Amy Faith Ho, MD, MPH of Integrative Emergency Services, Dallas–Fort Worth, in a presentation at the annual meeting of the American College of Emergency Physicians.
The study authors reviewed records of 11,920 in-flight medical emergencies between Jan. 1, 2008, and Oct. 31, 2010. The data showed that physician passengers provided medical assistance in nearly half of in-flight emergencies (48.1%) and that flights were diverted because of the emergency in 7.3% of cases.
The majority of the in-flight emergencies involved syncope or presyncope (37.4% of cases), followed by respiratory symptoms (12.1%) and nausea or vomiting (9.5%), according to the study.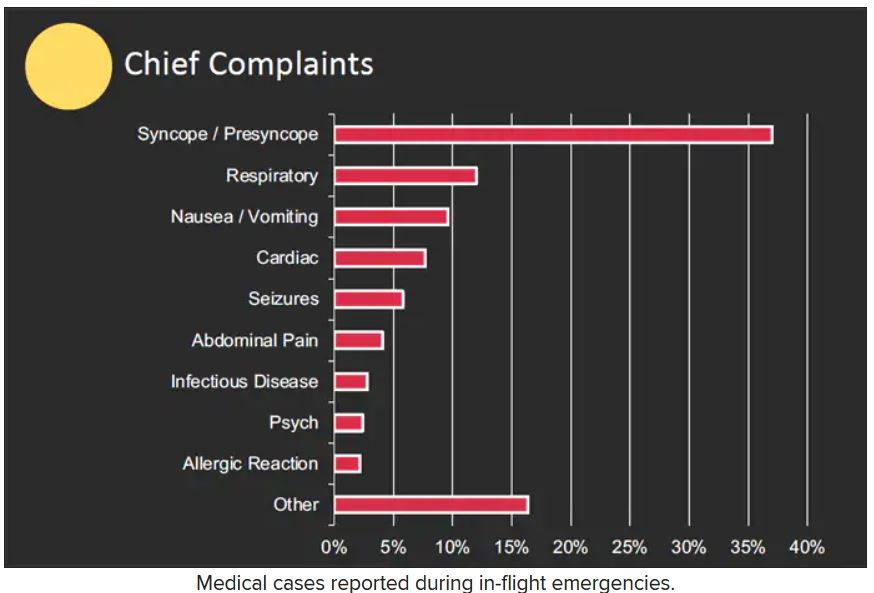
When a physician is faced with an in-flight emergency, the medical team includes the physician himself, medical ground control, and the flight attendants, said Dr. Ho. Requirements may vary among airlines, but all flight attendants will be trained in cardiopulmonary resuscitation (CPR) or basic life support, as well as use of automated external defibrillators (AEDs).
Physician call centers (medical ground control) can provide additional assistance remotely, she said.
The in-flight medical bag
Tools in a physician’s in-flight toolbox start with the first-aid kit. Airplanes also have an emergency medical kit (EMK), an oxygen tank, and an AED.
The minimum EMK contents are mandated by the Federal Aviation Administration, said Dr. Ho. The standard equipment includes a stethoscope, a sphygmomanometer, and three sizes of oropharyngeal airways. Other items include self-inflating manual resuscitation devices and CPR masks in thee sizes, alcohol sponges, gloves, adhesive tape, scissors, a tourniquet, as well as saline solution, needles, syringes, and an intravenous administration set consisting of tubing and two Y connectors.
An EMK also should contain the following medications: nonnarcotic analgesic tablets, antihistamine tablets, an injectable antihistamine, atropine, aspirin tablets, a bronchodilator, and epinephrine (both 1:1000; 1 injectable cc and 1:10,000; two injectable cc). Nitroglycerin tablets and 5 cc of 20 mg/mL injectable cardiac lidocaine are part of the mandated kit as well, according to Dr. Ho.
Some airlines carry additional supplies on all their flights, said Dr. Ho. Notably, American Airlines and British Airways carry EpiPens for adults and children, as well as opioid reversal medication (naloxone) and glucose for managing low blood sugar. American Airlines and Delta stock antiemetics, and Delta also carries naloxone. British Airways is unique in stocking additional cardiac medications, both oral and injectable.
How to handle an in-flight emergency
Physicians should always carry a copy of their medical license when traveling for documentation by the airline if they assist in a medical emergency during a flight, Dr. Ho emphasized. “Staff” personnel should be used. These include the flight attendants, medical ground control, and other passengers who might have useful skills, such as nursing, the ability to perform CPR, or therapy/counseling to calm a frightened patient. If needed, “crowdsource additional supplies from passengers,” such as a glucometer or pulse oximeter.
Legal lessons
Physicians are not obligated to assist during an in-flight medical emergency, said Dr. Ho. Legal jurisdiction can vary. In the United States, a bystander who assists in an emergency is generally protected by Good Samaritan laws; for international airlines, the laws may vary; those where the airline is based usually apply.
The Aviation Medical Assistance Act, passed in 1998, protects individuals from being sued for negligence while providing medical assistance, “unless the individual, while rendering such assistance, is guilty of gross negligence of willful misconduct,” Dr. Ho noted. The Aviation Medical Assistance Act also protects the airline itself “if the carrier in good faith believes that the passenger is a medically qualified individual.”
Dr. Ho disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACEP 2022
Asthma ED visits predict failed housing inspections
, according to a new study presented at the annual meeting of the American College of Emergency Physicians.
While links between asthma and low-quality housing prone to harboring allergens have been well-documented, the current study takes the extra step of looking at housing down to the level of individual land parcels and suggests that asthma hospital visits can be used to identify hazardous housing earlier.
“Emergency department visits for asthma provide a leading indicator that can be used by health departments or housing authorities to direct housing inspections and remediation of poor housing conditions, track improvements in housing quality, measure housing department performance, support resident grievances, and inform funding allocation decisions,” said the study’s lead researcher, Elizabeth Samuels, MD, who is assistant professor of epidemiology and emergency medicine at Brown University, Providence, R.I.
Researchers retrospectively looked at cases of children and adults in the Greater New Haven area of Connecticut seen at the Yale New Haven Hospital ED for asthma-related problems between March 2013 and August 2017. The region has the fifth-highest prevalence of asthma in the United States, the researchers point out, due to its air quality, pollens, and quality of its housing. More than half of residences were built before 1,940, compared with about 13% nationally. Patient addresses were matched with HUD inspection records.
The review encompassed 11,429 ED visits by 6,366 individuals; 54% were insured by Medicaid, and 42% were Black. Controlling for patient and neighborhood data, researchers found that increased asthma ED visits at the parcel level were associated with decreased HUD inspection scores to a highly significant degree (P < .001).
They also found that there was a relationship in terms of timing between asthma ED visits and inspection scores: asthma ED visits increased more than 1 year before a failed HUD inspection. They also found that asthma ED visits were not elevated at housing units that passed inspection. Using asthma ED visits to predict failed housing inspections produced a specificity rate of 92.3% in an adjusted model, Dr. Samuels noted.
“This approach represents a novel method of early identification of dangerous housing conditions, which could aid in the prevention of asthma-related morbidity and mortality,” Dr. Samuels said.
The investigators noted that, of the parcels with the top three incidence rates of asthma ED visits, “all of them have been closed or demolished.”
In addition to limiting exposure of patients with asthma to the allergens of mold, mice and rats, and cockroaches, improving poor-quality housing earlier could help asthma by reducing stress, she said.
“There is also an increasing evidence base that psychosocial stress increases the risk of asthma attacks, and it’s therefore possible that living in poor housing conditions – often highly stressful situations – drives exacerbation risk via this pathway,” she said. “Synergistic effects between these pathways are also possible or even likely.”
Neeta Thakur, MD, associate professor of medicine at the University of California, San Francisco, who researches asthma, said the findings could lead to a strategy for improving poor-quality housing more quickly. As it is, inspections are too infrequent, often prompted by resident complaints.
“Once the complaints get to a certain threshold, then there might be an inspection that happens, and if there is a periodic review of the buildings, they often happen few and far between,” she said. “We could actually use some of the information that we’re already getting from something like ED visits and see if there is a pattern.”
An important follow-up would be to see whether asthma outcomes improve after housing deficiencies are addressed and whether the predictive capacity of ED visits occurs in other places.
“Would you then see a decline in the ED visit rates from individuals living in those buildings?” Dr. Thakur said. “It’s important to find a leading indicator, but you want to be sure that that leading indicator is useful as something that can be intervened upon.”
Dr. Samuels and Dr. Thakur have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a new study presented at the annual meeting of the American College of Emergency Physicians.
While links between asthma and low-quality housing prone to harboring allergens have been well-documented, the current study takes the extra step of looking at housing down to the level of individual land parcels and suggests that asthma hospital visits can be used to identify hazardous housing earlier.
“Emergency department visits for asthma provide a leading indicator that can be used by health departments or housing authorities to direct housing inspections and remediation of poor housing conditions, track improvements in housing quality, measure housing department performance, support resident grievances, and inform funding allocation decisions,” said the study’s lead researcher, Elizabeth Samuels, MD, who is assistant professor of epidemiology and emergency medicine at Brown University, Providence, R.I.
Researchers retrospectively looked at cases of children and adults in the Greater New Haven area of Connecticut seen at the Yale New Haven Hospital ED for asthma-related problems between March 2013 and August 2017. The region has the fifth-highest prevalence of asthma in the United States, the researchers point out, due to its air quality, pollens, and quality of its housing. More than half of residences were built before 1,940, compared with about 13% nationally. Patient addresses were matched with HUD inspection records.
The review encompassed 11,429 ED visits by 6,366 individuals; 54% were insured by Medicaid, and 42% were Black. Controlling for patient and neighborhood data, researchers found that increased asthma ED visits at the parcel level were associated with decreased HUD inspection scores to a highly significant degree (P < .001).
They also found that there was a relationship in terms of timing between asthma ED visits and inspection scores: asthma ED visits increased more than 1 year before a failed HUD inspection. They also found that asthma ED visits were not elevated at housing units that passed inspection. Using asthma ED visits to predict failed housing inspections produced a specificity rate of 92.3% in an adjusted model, Dr. Samuels noted.
“This approach represents a novel method of early identification of dangerous housing conditions, which could aid in the prevention of asthma-related morbidity and mortality,” Dr. Samuels said.
The investigators noted that, of the parcels with the top three incidence rates of asthma ED visits, “all of them have been closed or demolished.”
In addition to limiting exposure of patients with asthma to the allergens of mold, mice and rats, and cockroaches, improving poor-quality housing earlier could help asthma by reducing stress, she said.
“There is also an increasing evidence base that psychosocial stress increases the risk of asthma attacks, and it’s therefore possible that living in poor housing conditions – often highly stressful situations – drives exacerbation risk via this pathway,” she said. “Synergistic effects between these pathways are also possible or even likely.”
Neeta Thakur, MD, associate professor of medicine at the University of California, San Francisco, who researches asthma, said the findings could lead to a strategy for improving poor-quality housing more quickly. As it is, inspections are too infrequent, often prompted by resident complaints.
“Once the complaints get to a certain threshold, then there might be an inspection that happens, and if there is a periodic review of the buildings, they often happen few and far between,” she said. “We could actually use some of the information that we’re already getting from something like ED visits and see if there is a pattern.”
An important follow-up would be to see whether asthma outcomes improve after housing deficiencies are addressed and whether the predictive capacity of ED visits occurs in other places.
“Would you then see a decline in the ED visit rates from individuals living in those buildings?” Dr. Thakur said. “It’s important to find a leading indicator, but you want to be sure that that leading indicator is useful as something that can be intervened upon.”
Dr. Samuels and Dr. Thakur have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a new study presented at the annual meeting of the American College of Emergency Physicians.
While links between asthma and low-quality housing prone to harboring allergens have been well-documented, the current study takes the extra step of looking at housing down to the level of individual land parcels and suggests that asthma hospital visits can be used to identify hazardous housing earlier.
“Emergency department visits for asthma provide a leading indicator that can be used by health departments or housing authorities to direct housing inspections and remediation of poor housing conditions, track improvements in housing quality, measure housing department performance, support resident grievances, and inform funding allocation decisions,” said the study’s lead researcher, Elizabeth Samuels, MD, who is assistant professor of epidemiology and emergency medicine at Brown University, Providence, R.I.
Researchers retrospectively looked at cases of children and adults in the Greater New Haven area of Connecticut seen at the Yale New Haven Hospital ED for asthma-related problems between March 2013 and August 2017. The region has the fifth-highest prevalence of asthma in the United States, the researchers point out, due to its air quality, pollens, and quality of its housing. More than half of residences were built before 1,940, compared with about 13% nationally. Patient addresses were matched with HUD inspection records.
The review encompassed 11,429 ED visits by 6,366 individuals; 54% were insured by Medicaid, and 42% were Black. Controlling for patient and neighborhood data, researchers found that increased asthma ED visits at the parcel level were associated with decreased HUD inspection scores to a highly significant degree (P < .001).
They also found that there was a relationship in terms of timing between asthma ED visits and inspection scores: asthma ED visits increased more than 1 year before a failed HUD inspection. They also found that asthma ED visits were not elevated at housing units that passed inspection. Using asthma ED visits to predict failed housing inspections produced a specificity rate of 92.3% in an adjusted model, Dr. Samuels noted.
“This approach represents a novel method of early identification of dangerous housing conditions, which could aid in the prevention of asthma-related morbidity and mortality,” Dr. Samuels said.
The investigators noted that, of the parcels with the top three incidence rates of asthma ED visits, “all of them have been closed or demolished.”
In addition to limiting exposure of patients with asthma to the allergens of mold, mice and rats, and cockroaches, improving poor-quality housing earlier could help asthma by reducing stress, she said.
“There is also an increasing evidence base that psychosocial stress increases the risk of asthma attacks, and it’s therefore possible that living in poor housing conditions – often highly stressful situations – drives exacerbation risk via this pathway,” she said. “Synergistic effects between these pathways are also possible or even likely.”
Neeta Thakur, MD, associate professor of medicine at the University of California, San Francisco, who researches asthma, said the findings could lead to a strategy for improving poor-quality housing more quickly. As it is, inspections are too infrequent, often prompted by resident complaints.
“Once the complaints get to a certain threshold, then there might be an inspection that happens, and if there is a periodic review of the buildings, they often happen few and far between,” she said. “We could actually use some of the information that we’re already getting from something like ED visits and see if there is a pattern.”
An important follow-up would be to see whether asthma outcomes improve after housing deficiencies are addressed and whether the predictive capacity of ED visits occurs in other places.
“Would you then see a decline in the ED visit rates from individuals living in those buildings?” Dr. Thakur said. “It’s important to find a leading indicator, but you want to be sure that that leading indicator is useful as something that can be intervened upon.”
Dr. Samuels and Dr. Thakur have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACEP 2022
Novel head-up CPR position raises odds of survival of out-of-hospital heart attacks
Individuals who experience out-of-hospital cardiac arrest (OHCA) with nonshockable presentations have a better chance of survival when first responders use a novel CPR approach that includes gradual head-up positioning combined with basic but effective circulation-enhancing adjuncts, as shown from data from more than 2,000 patients.
In a study presented at the annual meeting of the American College of Emergency Physicians, Paul Pepe, MD, medical director for Dallas County Emergency Medical Services, reviewed data from five EMS systems that had adopted the new approach. Data were collected prospectively over the past 2 years from a national registry of patients who had received what Dr. Pepe called a “neuroprotective CPR bundle” (NP-CPR).
The study compared 380 NP-CPR case patients to 1,852 control patients who had received conventional CPR. Control data came from high-performance EMS systems that had participated in well-monitored, published OHCA trials funded by the National Institutes of Health. The primary outcome that was used for comparison was successful survival to hospital discharge with neurologically intact status (SURV-NI).
Traditional CPR supine chest compression techniques, if performed early and properly, can be lifesaving, but they are suboptimal, Dr. Pepe said. “Current techniques create pressure waves that run up the arterial side, but they also create back-pressure on the venous side, increasing intracranial pressure (ICP), thus compromising optimal cerebral blood flow,” he told this news organization.
For that reason, a modified physiologic approach to CPR was designed. It involves an airway adjunct called an impedance threshold device (ITD) and active compression-decompression (ACD) with a device “resembling a toilet plunger,” Dr. Pepe said.
The devices draw more blood out of the brain and into the thorax in a complementary fashion. The combination of these two adjuncts had dramatically improved SURV-NI by 50% in a clinical trial, Dr. Pepe said.
The new technology uses automated gradual head-up/torso-up positioning (AHUP) after first “priming the pump” with ITD-ACD–enhanced circulation. It was found to markedly augment that effect even further. In the laboratory setting, this synergistic NP-CPR bundle has been shown to help normalize cerebral perfusion pressure, further promoting neuro-intact survival. Normalization of end-tidal CO2 is routinely observed, according to Dr. Pepe.
In contrast to patients who present with ventricular fibrillation (shockable cases), patients with nonshockable presentations always have had grim prognoses, Dr. Pepe said. Until now, lifesaving advances had not been found, despite the fact that nonshockable presentations (asystole or electrical activity with no pulse) constitute approximately 80% of OHCA cases, or about 250,000 to 300,00 cases a year in the United States, he said.
In the study, approximately 60% of both the NP-CPR patients and control patients had asystole (flatline) presentations. The NP-CPR group had a significant threefold improvement in SURV-NI, compared with patients treated with conventional CPR in the high-functioning systems (odds ratio, 3.09). In a propensity-scored analysis matching all variables known to affect outcome, the OR increased to nearly fourfold higher (OR, 3.87; 95% confidence interval, 1.27-11.78), Dr. Pepe said.
The researchers also found that the time from receipt of a 911 call to initiation of AHUP was associated with progressively higher chances of survival. The median time for application was 11 minutes; when the elapsed time was less than 11 minutes, the SURV-NI was nearly 11-fold higher for NP-CPR patients than for control patients (OR, 10.59), with survival chances of 6% versus 0.5%. ORs were even higher when the time to treatment was less than 16 minutes (OR, 13.58), with survival rates of 5% versus 0.4%.
The findings not only demonstrate proof of concept in these most futile cases but also that implementation is feasible for the majority of patients, considering that the median time to the start of any CPR by a first responder was 8 minutes for both NP-CPR patients and control patients, “let alone 11 minutes for the AHUP initiation,” Dr. Pepe said. “This finally gives some hope for these nonshockable cases,” he emphasized.
“All of these devices have now been cleared by the Food and Drug Administration and should be adopted by all first-in responders,” said Dr. Pepe. “But they should be implemented as a bundle and in the proper sequence and as soon as feasible.”
Training and implementation efforts continue to expand, and more lives can be saved as more firefighters and first-in response teams acquire equipment and training, which can cut the time to response, he said.
The registry will continue to monitor outcomes with NP-CPR – the term was suggested by a patient who survived through this new approach – and Dr. Pepe and colleagues expect the statistics to improve further with wider adoption and faster implementation with the fastest responders.
A recent study by Dr. Pepe’s team, published in Resuscitation, showed the effectiveness of the neuroprotective bundle in improving survival for OHCA patients overall. The current study confirmed its impact on neuro-intact survival for the subgroup of patients with nonshockable cases.
One other take-home message is that head-up CPR cannot yet be performed by lay bystanders. “Also, do not implement this unless you are going to do it right,” Dr. Pepe emphasized in an interview.
Advanced CPR Solutions provided some materials and research funding for an independent data collector. No other relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
Individuals who experience out-of-hospital cardiac arrest (OHCA) with nonshockable presentations have a better chance of survival when first responders use a novel CPR approach that includes gradual head-up positioning combined with basic but effective circulation-enhancing adjuncts, as shown from data from more than 2,000 patients.
In a study presented at the annual meeting of the American College of Emergency Physicians, Paul Pepe, MD, medical director for Dallas County Emergency Medical Services, reviewed data from five EMS systems that had adopted the new approach. Data were collected prospectively over the past 2 years from a national registry of patients who had received what Dr. Pepe called a “neuroprotective CPR bundle” (NP-CPR).
The study compared 380 NP-CPR case patients to 1,852 control patients who had received conventional CPR. Control data came from high-performance EMS systems that had participated in well-monitored, published OHCA trials funded by the National Institutes of Health. The primary outcome that was used for comparison was successful survival to hospital discharge with neurologically intact status (SURV-NI).
Traditional CPR supine chest compression techniques, if performed early and properly, can be lifesaving, but they are suboptimal, Dr. Pepe said. “Current techniques create pressure waves that run up the arterial side, but they also create back-pressure on the venous side, increasing intracranial pressure (ICP), thus compromising optimal cerebral blood flow,” he told this news organization.
For that reason, a modified physiologic approach to CPR was designed. It involves an airway adjunct called an impedance threshold device (ITD) and active compression-decompression (ACD) with a device “resembling a toilet plunger,” Dr. Pepe said.
The devices draw more blood out of the brain and into the thorax in a complementary fashion. The combination of these two adjuncts had dramatically improved SURV-NI by 50% in a clinical trial, Dr. Pepe said.
The new technology uses automated gradual head-up/torso-up positioning (AHUP) after first “priming the pump” with ITD-ACD–enhanced circulation. It was found to markedly augment that effect even further. In the laboratory setting, this synergistic NP-CPR bundle has been shown to help normalize cerebral perfusion pressure, further promoting neuro-intact survival. Normalization of end-tidal CO2 is routinely observed, according to Dr. Pepe.
In contrast to patients who present with ventricular fibrillation (shockable cases), patients with nonshockable presentations always have had grim prognoses, Dr. Pepe said. Until now, lifesaving advances had not been found, despite the fact that nonshockable presentations (asystole or electrical activity with no pulse) constitute approximately 80% of OHCA cases, or about 250,000 to 300,00 cases a year in the United States, he said.
In the study, approximately 60% of both the NP-CPR patients and control patients had asystole (flatline) presentations. The NP-CPR group had a significant threefold improvement in SURV-NI, compared with patients treated with conventional CPR in the high-functioning systems (odds ratio, 3.09). In a propensity-scored analysis matching all variables known to affect outcome, the OR increased to nearly fourfold higher (OR, 3.87; 95% confidence interval, 1.27-11.78), Dr. Pepe said.
The researchers also found that the time from receipt of a 911 call to initiation of AHUP was associated with progressively higher chances of survival. The median time for application was 11 minutes; when the elapsed time was less than 11 minutes, the SURV-NI was nearly 11-fold higher for NP-CPR patients than for control patients (OR, 10.59), with survival chances of 6% versus 0.5%. ORs were even higher when the time to treatment was less than 16 minutes (OR, 13.58), with survival rates of 5% versus 0.4%.
The findings not only demonstrate proof of concept in these most futile cases but also that implementation is feasible for the majority of patients, considering that the median time to the start of any CPR by a first responder was 8 minutes for both NP-CPR patients and control patients, “let alone 11 minutes for the AHUP initiation,” Dr. Pepe said. “This finally gives some hope for these nonshockable cases,” he emphasized.
“All of these devices have now been cleared by the Food and Drug Administration and should be adopted by all first-in responders,” said Dr. Pepe. “But they should be implemented as a bundle and in the proper sequence and as soon as feasible.”
Training and implementation efforts continue to expand, and more lives can be saved as more firefighters and first-in response teams acquire equipment and training, which can cut the time to response, he said.
The registry will continue to monitor outcomes with NP-CPR – the term was suggested by a patient who survived through this new approach – and Dr. Pepe and colleagues expect the statistics to improve further with wider adoption and faster implementation with the fastest responders.
A recent study by Dr. Pepe’s team, published in Resuscitation, showed the effectiveness of the neuroprotective bundle in improving survival for OHCA patients overall. The current study confirmed its impact on neuro-intact survival for the subgroup of patients with nonshockable cases.
One other take-home message is that head-up CPR cannot yet be performed by lay bystanders. “Also, do not implement this unless you are going to do it right,” Dr. Pepe emphasized in an interview.
Advanced CPR Solutions provided some materials and research funding for an independent data collector. No other relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
Individuals who experience out-of-hospital cardiac arrest (OHCA) with nonshockable presentations have a better chance of survival when first responders use a novel CPR approach that includes gradual head-up positioning combined with basic but effective circulation-enhancing adjuncts, as shown from data from more than 2,000 patients.
In a study presented at the annual meeting of the American College of Emergency Physicians, Paul Pepe, MD, medical director for Dallas County Emergency Medical Services, reviewed data from five EMS systems that had adopted the new approach. Data were collected prospectively over the past 2 years from a national registry of patients who had received what Dr. Pepe called a “neuroprotective CPR bundle” (NP-CPR).
The study compared 380 NP-CPR case patients to 1,852 control patients who had received conventional CPR. Control data came from high-performance EMS systems that had participated in well-monitored, published OHCA trials funded by the National Institutes of Health. The primary outcome that was used for comparison was successful survival to hospital discharge with neurologically intact status (SURV-NI).
Traditional CPR supine chest compression techniques, if performed early and properly, can be lifesaving, but they are suboptimal, Dr. Pepe said. “Current techniques create pressure waves that run up the arterial side, but they also create back-pressure on the venous side, increasing intracranial pressure (ICP), thus compromising optimal cerebral blood flow,” he told this news organization.
For that reason, a modified physiologic approach to CPR was designed. It involves an airway adjunct called an impedance threshold device (ITD) and active compression-decompression (ACD) with a device “resembling a toilet plunger,” Dr. Pepe said.
The devices draw more blood out of the brain and into the thorax in a complementary fashion. The combination of these two adjuncts had dramatically improved SURV-NI by 50% in a clinical trial, Dr. Pepe said.
The new technology uses automated gradual head-up/torso-up positioning (AHUP) after first “priming the pump” with ITD-ACD–enhanced circulation. It was found to markedly augment that effect even further. In the laboratory setting, this synergistic NP-CPR bundle has been shown to help normalize cerebral perfusion pressure, further promoting neuro-intact survival. Normalization of end-tidal CO2 is routinely observed, according to Dr. Pepe.
In contrast to patients who present with ventricular fibrillation (shockable cases), patients with nonshockable presentations always have had grim prognoses, Dr. Pepe said. Until now, lifesaving advances had not been found, despite the fact that nonshockable presentations (asystole or electrical activity with no pulse) constitute approximately 80% of OHCA cases, or about 250,000 to 300,00 cases a year in the United States, he said.
In the study, approximately 60% of both the NP-CPR patients and control patients had asystole (flatline) presentations. The NP-CPR group had a significant threefold improvement in SURV-NI, compared with patients treated with conventional CPR in the high-functioning systems (odds ratio, 3.09). In a propensity-scored analysis matching all variables known to affect outcome, the OR increased to nearly fourfold higher (OR, 3.87; 95% confidence interval, 1.27-11.78), Dr. Pepe said.
The researchers also found that the time from receipt of a 911 call to initiation of AHUP was associated with progressively higher chances of survival. The median time for application was 11 minutes; when the elapsed time was less than 11 minutes, the SURV-NI was nearly 11-fold higher for NP-CPR patients than for control patients (OR, 10.59), with survival chances of 6% versus 0.5%. ORs were even higher when the time to treatment was less than 16 minutes (OR, 13.58), with survival rates of 5% versus 0.4%.
The findings not only demonstrate proof of concept in these most futile cases but also that implementation is feasible for the majority of patients, considering that the median time to the start of any CPR by a first responder was 8 minutes for both NP-CPR patients and control patients, “let alone 11 minutes for the AHUP initiation,” Dr. Pepe said. “This finally gives some hope for these nonshockable cases,” he emphasized.
“All of these devices have now been cleared by the Food and Drug Administration and should be adopted by all first-in responders,” said Dr. Pepe. “But they should be implemented as a bundle and in the proper sequence and as soon as feasible.”
Training and implementation efforts continue to expand, and more lives can be saved as more firefighters and first-in response teams acquire equipment and training, which can cut the time to response, he said.
The registry will continue to monitor outcomes with NP-CPR – the term was suggested by a patient who survived through this new approach – and Dr. Pepe and colleagues expect the statistics to improve further with wider adoption and faster implementation with the fastest responders.
A recent study by Dr. Pepe’s team, published in Resuscitation, showed the effectiveness of the neuroprotective bundle in improving survival for OHCA patients overall. The current study confirmed its impact on neuro-intact survival for the subgroup of patients with nonshockable cases.
One other take-home message is that head-up CPR cannot yet be performed by lay bystanders. “Also, do not implement this unless you are going to do it right,” Dr. Pepe emphasized in an interview.
Advanced CPR Solutions provided some materials and research funding for an independent data collector. No other relevant financial relationships have been disclosed.
A version of this article first appeared on Medscape.com.
FROM ACEP 2022
Longer boarding times predict patient processing in ED
on the basis of data from nearly 900 facilities presented at the annual meeting of the American College of Emergency Physicians.
The study was important to conduct at this time because ED boarding is significantly limiting ED physicians to provide optimal care, said Camila Tyminski, MD, of Brown University, Providence, R.I., who presented the findings at the meeting.
“Boarding had steadily been rising prior to the COVID-19 pandemic due to increased ED use. As our data show, boarding had a detrimental impact on ED throughput measures, including increased door to provider time, increased length of stay of the patient discharged from the ED, and increased rate of patients that left before completion of treatment,” she said.
“It was important to understand these trends prior to 2019-2020 because the COVID-19 pandemic and national nursing shortage have drastically worsened boarding. This study provided a framework for future studies on boarding across ED’s nationally since the start of the pandemic,” she added.
“Post-pandemic, we have hit a crisis point,” lead author Anthony Napoli, MD, also of Brown University, said in an interview. “Boarding is largely a hospital capacity problem, but one key fix germane to EM [emergency medicine] is the provider in triage model (PIT). While PIT has been shown to improve efficiency of ED care, a single institution study demonstrated that it was unable to mitigate the effects of boarding. The study of the association of boarding and efficiency of ED operations and intake needed to be shown on a national scale,” he said.
The researchers reviewed cross-sectional ED operational data from the ED Department Benchmarking Alliance (EDBA), a voluntary database that includes self-reports of operational metrics from approximately half of EDs in the United States.
The data set included 892 EDs; freestanding and pediatric EDs, as well as those with missing boarding data, were excluded.
The primary outcome was boarding time, door-to-provider time (D2P), length of stay for discharged patients (LOSD) and the percentage of patients who left the hospital before treatment was complete (LBTC).
In a multivariate analysis, increased boarding time was significantly associated with longer D2P time, LOSD time, and rates of LBTC.
Overall, D2P and LOSD increased by 0.8 minutes and 2.8 minutes, respectively, for each additional 10 minutes of boarding time. LBTC rates increased by 0.1% for each additional 10 minutes of boarding time.
However, boarding did not have a significant impact on operational metrics among hospitals with fewer than 20,000 visits per year.
Although more research is needed, the results indicate that boarding reduces the throughput of nonboarded patients at a ratio of approximately 4:1. The limited impact of ED efficiency measures on operations highlights the need for hospital-based solutions to boarding, Dr. Tyminski concluded.
“Overall, we expected that there would be an association between boarding and reductions in ED intake and operational efficiency,” said Dr. Napoli in an interview. “However, we were surprised the relationship continued to be as strong in a national study of nearly a quarter of all EDs, as it did in our prior local study,” he said. “Every 10 minutes of boarding in an ED is associated with an approximate 0.1% increase in LWBS and a 3-minute increase in LOSD. Extrapolating this association across the country, we predicted that nearly one million patients may have potentially not received ED care due to boarding,” he explained. “Not only does this potentially have a huge impact on hospital finances but also the overall health of our patients,” he added.
The key takeaway from the study is that boarding is a hospital capacity management issue, said Dr. Napoli. Hospital leadership must be directly involved in plans to mitigate or eliminate it to the extent possible; until then, boarding will continue to result in inefficient ED operations, he explained.
“As ED providers, we are limited in what we can do, but one area where we might be able to make the most impact is to optimize the care and throughput of the LOSD patients,” Dr. Tyminski said. More research is needed to see if interventions to reduce boarding correspond with equivalent improvements in emergency department intake and improved ED throughput, she noted.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
on the basis of data from nearly 900 facilities presented at the annual meeting of the American College of Emergency Physicians.
The study was important to conduct at this time because ED boarding is significantly limiting ED physicians to provide optimal care, said Camila Tyminski, MD, of Brown University, Providence, R.I., who presented the findings at the meeting.
“Boarding had steadily been rising prior to the COVID-19 pandemic due to increased ED use. As our data show, boarding had a detrimental impact on ED throughput measures, including increased door to provider time, increased length of stay of the patient discharged from the ED, and increased rate of patients that left before completion of treatment,” she said.
“It was important to understand these trends prior to 2019-2020 because the COVID-19 pandemic and national nursing shortage have drastically worsened boarding. This study provided a framework for future studies on boarding across ED’s nationally since the start of the pandemic,” she added.
“Post-pandemic, we have hit a crisis point,” lead author Anthony Napoli, MD, also of Brown University, said in an interview. “Boarding is largely a hospital capacity problem, but one key fix germane to EM [emergency medicine] is the provider in triage model (PIT). While PIT has been shown to improve efficiency of ED care, a single institution study demonstrated that it was unable to mitigate the effects of boarding. The study of the association of boarding and efficiency of ED operations and intake needed to be shown on a national scale,” he said.
The researchers reviewed cross-sectional ED operational data from the ED Department Benchmarking Alliance (EDBA), a voluntary database that includes self-reports of operational metrics from approximately half of EDs in the United States.
The data set included 892 EDs; freestanding and pediatric EDs, as well as those with missing boarding data, were excluded.
The primary outcome was boarding time, door-to-provider time (D2P), length of stay for discharged patients (LOSD) and the percentage of patients who left the hospital before treatment was complete (LBTC).
In a multivariate analysis, increased boarding time was significantly associated with longer D2P time, LOSD time, and rates of LBTC.
Overall, D2P and LOSD increased by 0.8 minutes and 2.8 minutes, respectively, for each additional 10 minutes of boarding time. LBTC rates increased by 0.1% for each additional 10 minutes of boarding time.
However, boarding did not have a significant impact on operational metrics among hospitals with fewer than 20,000 visits per year.
Although more research is needed, the results indicate that boarding reduces the throughput of nonboarded patients at a ratio of approximately 4:1. The limited impact of ED efficiency measures on operations highlights the need for hospital-based solutions to boarding, Dr. Tyminski concluded.
“Overall, we expected that there would be an association between boarding and reductions in ED intake and operational efficiency,” said Dr. Napoli in an interview. “However, we were surprised the relationship continued to be as strong in a national study of nearly a quarter of all EDs, as it did in our prior local study,” he said. “Every 10 minutes of boarding in an ED is associated with an approximate 0.1% increase in LWBS and a 3-minute increase in LOSD. Extrapolating this association across the country, we predicted that nearly one million patients may have potentially not received ED care due to boarding,” he explained. “Not only does this potentially have a huge impact on hospital finances but also the overall health of our patients,” he added.
The key takeaway from the study is that boarding is a hospital capacity management issue, said Dr. Napoli. Hospital leadership must be directly involved in plans to mitigate or eliminate it to the extent possible; until then, boarding will continue to result in inefficient ED operations, he explained.
“As ED providers, we are limited in what we can do, but one area where we might be able to make the most impact is to optimize the care and throughput of the LOSD patients,” Dr. Tyminski said. More research is needed to see if interventions to reduce boarding correspond with equivalent improvements in emergency department intake and improved ED throughput, she noted.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
on the basis of data from nearly 900 facilities presented at the annual meeting of the American College of Emergency Physicians.
The study was important to conduct at this time because ED boarding is significantly limiting ED physicians to provide optimal care, said Camila Tyminski, MD, of Brown University, Providence, R.I., who presented the findings at the meeting.
“Boarding had steadily been rising prior to the COVID-19 pandemic due to increased ED use. As our data show, boarding had a detrimental impact on ED throughput measures, including increased door to provider time, increased length of stay of the patient discharged from the ED, and increased rate of patients that left before completion of treatment,” she said.
“It was important to understand these trends prior to 2019-2020 because the COVID-19 pandemic and national nursing shortage have drastically worsened boarding. This study provided a framework for future studies on boarding across ED’s nationally since the start of the pandemic,” she added.
“Post-pandemic, we have hit a crisis point,” lead author Anthony Napoli, MD, also of Brown University, said in an interview. “Boarding is largely a hospital capacity problem, but one key fix germane to EM [emergency medicine] is the provider in triage model (PIT). While PIT has been shown to improve efficiency of ED care, a single institution study demonstrated that it was unable to mitigate the effects of boarding. The study of the association of boarding and efficiency of ED operations and intake needed to be shown on a national scale,” he said.
The researchers reviewed cross-sectional ED operational data from the ED Department Benchmarking Alliance (EDBA), a voluntary database that includes self-reports of operational metrics from approximately half of EDs in the United States.
The data set included 892 EDs; freestanding and pediatric EDs, as well as those with missing boarding data, were excluded.
The primary outcome was boarding time, door-to-provider time (D2P), length of stay for discharged patients (LOSD) and the percentage of patients who left the hospital before treatment was complete (LBTC).
In a multivariate analysis, increased boarding time was significantly associated with longer D2P time, LOSD time, and rates of LBTC.
Overall, D2P and LOSD increased by 0.8 minutes and 2.8 minutes, respectively, for each additional 10 minutes of boarding time. LBTC rates increased by 0.1% for each additional 10 minutes of boarding time.
However, boarding did not have a significant impact on operational metrics among hospitals with fewer than 20,000 visits per year.
Although more research is needed, the results indicate that boarding reduces the throughput of nonboarded patients at a ratio of approximately 4:1. The limited impact of ED efficiency measures on operations highlights the need for hospital-based solutions to boarding, Dr. Tyminski concluded.
“Overall, we expected that there would be an association between boarding and reductions in ED intake and operational efficiency,” said Dr. Napoli in an interview. “However, we were surprised the relationship continued to be as strong in a national study of nearly a quarter of all EDs, as it did in our prior local study,” he said. “Every 10 minutes of boarding in an ED is associated with an approximate 0.1% increase in LWBS and a 3-minute increase in LOSD. Extrapolating this association across the country, we predicted that nearly one million patients may have potentially not received ED care due to boarding,” he explained. “Not only does this potentially have a huge impact on hospital finances but also the overall health of our patients,” he added.
The key takeaway from the study is that boarding is a hospital capacity management issue, said Dr. Napoli. Hospital leadership must be directly involved in plans to mitigate or eliminate it to the extent possible; until then, boarding will continue to result in inefficient ED operations, he explained.
“As ED providers, we are limited in what we can do, but one area where we might be able to make the most impact is to optimize the care and throughput of the LOSD patients,” Dr. Tyminski said. More research is needed to see if interventions to reduce boarding correspond with equivalent improvements in emergency department intake and improved ED throughput, she noted.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACEP 2022
Long-acting naltrexone effective in alcohol use disorder
according to findings presented at the annual meeting of the American College of Emergency Physicians.
The results show the feasibility of such a program and underscore the importance of the ED in combating AUD, said the researchers, from the University of California, San Francisco.
“According to the National Institute on Alcohol Abuse and Alcoholism, 18% of ED visits had alcohol as a contributing factor – the volume of alcohol-related ED visits has been climbing every year, and it is a significant public health problem,” said Maria Raven, MD, MPH, professor of emergency medicine at UCSF. “Right now, we do very little for people who come to the ED with AUD, so it is a missed opportunity to intervene, especially given the volume of visits we see and that our patient population is one that often has significant barriers to accessing outpatient treatment.”
The findings come from a 12-week, prospective, single-arm study of ED patients who were actively drinking adults with known or suspected AUD and who had positive scores on a screening test. Of 179 patients who were approached, 32 agreed to enroll; the enrollment yield was 18%. Participants were given monthly extended-release naltrexone and case management services.
Of the 32 participants, 25 completed all their study visits and 22 (69%) continued taking naltrexone after the 12 weeks.
The researchers said the results surprised them. The average daily alcohol consumption at baseline was 7.6 drinks a day, and it fell by 7.5 drinks a day – in other words, to almost no consumption.
“The median alcohol consumption when measured over the last 2 weeks of the study was zero,” Dr. Raven said. “This doesn’t mean everyone was at zero, but this was the median and reflects that many participants stopped drinking altogether. We were pleasantly surprised by this. I don’t know that we thought so many people who participated would actually fully abstain.”
On the Kemp Quality of Life Scale – with scores from 1 to 7, with 1 being “life is very distressing,” 4 being “life is so-so,” and 7 being “life is great” – the average baseline score was 3.6. That score rose by 1.2 points by the study’s end.
Dr. Raven said she hoped more would enroll but that “a number of people actually did not want the injection or were not ready to think about stopping.” Still, the 18% enrollment is “a major improvement,” considering that no attempt was made to initiate treatment with naltrexone prior to the study. Oral naltrexone, rather than the injection, could be offered to improve participation, but oral naltrexone has to be taken daily.
She said a larger study is planned at UCSF and that other institutions are interested in starting a similar program.
“When someone is in the ED for an AUD-related issue, it can serve as a turning point for them in some cases,” she said.
Erik S. Anderson, MD, associate research director at Oakland, Calif.–based Alameda Health System, who has studied naltrexone in the ED, said the findings dovetail with what his team has found at his center. He added that psychosocial support is important as well and that his team has found that navigation services are the most important factor in connecting patients with follow-up care – even more so than providing medications.
“In my mind, this is a situation where we have treatment options and approaches that work, and it’s really about implementing these services in a novel care setting,” he said. “ED patients are at higher risk of complications for AUD simply because they are in the ED in the first place – initiating AUD treatment in this setting is the right thing to do.”
Dr. Raven and Dr. Anderson disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to findings presented at the annual meeting of the American College of Emergency Physicians.
The results show the feasibility of such a program and underscore the importance of the ED in combating AUD, said the researchers, from the University of California, San Francisco.
“According to the National Institute on Alcohol Abuse and Alcoholism, 18% of ED visits had alcohol as a contributing factor – the volume of alcohol-related ED visits has been climbing every year, and it is a significant public health problem,” said Maria Raven, MD, MPH, professor of emergency medicine at UCSF. “Right now, we do very little for people who come to the ED with AUD, so it is a missed opportunity to intervene, especially given the volume of visits we see and that our patient population is one that often has significant barriers to accessing outpatient treatment.”
The findings come from a 12-week, prospective, single-arm study of ED patients who were actively drinking adults with known or suspected AUD and who had positive scores on a screening test. Of 179 patients who were approached, 32 agreed to enroll; the enrollment yield was 18%. Participants were given monthly extended-release naltrexone and case management services.
Of the 32 participants, 25 completed all their study visits and 22 (69%) continued taking naltrexone after the 12 weeks.
The researchers said the results surprised them. The average daily alcohol consumption at baseline was 7.6 drinks a day, and it fell by 7.5 drinks a day – in other words, to almost no consumption.
“The median alcohol consumption when measured over the last 2 weeks of the study was zero,” Dr. Raven said. “This doesn’t mean everyone was at zero, but this was the median and reflects that many participants stopped drinking altogether. We were pleasantly surprised by this. I don’t know that we thought so many people who participated would actually fully abstain.”
On the Kemp Quality of Life Scale – with scores from 1 to 7, with 1 being “life is very distressing,” 4 being “life is so-so,” and 7 being “life is great” – the average baseline score was 3.6. That score rose by 1.2 points by the study’s end.
Dr. Raven said she hoped more would enroll but that “a number of people actually did not want the injection or were not ready to think about stopping.” Still, the 18% enrollment is “a major improvement,” considering that no attempt was made to initiate treatment with naltrexone prior to the study. Oral naltrexone, rather than the injection, could be offered to improve participation, but oral naltrexone has to be taken daily.
She said a larger study is planned at UCSF and that other institutions are interested in starting a similar program.
“When someone is in the ED for an AUD-related issue, it can serve as a turning point for them in some cases,” she said.
Erik S. Anderson, MD, associate research director at Oakland, Calif.–based Alameda Health System, who has studied naltrexone in the ED, said the findings dovetail with what his team has found at his center. He added that psychosocial support is important as well and that his team has found that navigation services are the most important factor in connecting patients with follow-up care – even more so than providing medications.
“In my mind, this is a situation where we have treatment options and approaches that work, and it’s really about implementing these services in a novel care setting,” he said. “ED patients are at higher risk of complications for AUD simply because they are in the ED in the first place – initiating AUD treatment in this setting is the right thing to do.”
Dr. Raven and Dr. Anderson disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to findings presented at the annual meeting of the American College of Emergency Physicians.
The results show the feasibility of such a program and underscore the importance of the ED in combating AUD, said the researchers, from the University of California, San Francisco.
“According to the National Institute on Alcohol Abuse and Alcoholism, 18% of ED visits had alcohol as a contributing factor – the volume of alcohol-related ED visits has been climbing every year, and it is a significant public health problem,” said Maria Raven, MD, MPH, professor of emergency medicine at UCSF. “Right now, we do very little for people who come to the ED with AUD, so it is a missed opportunity to intervene, especially given the volume of visits we see and that our patient population is one that often has significant barriers to accessing outpatient treatment.”
The findings come from a 12-week, prospective, single-arm study of ED patients who were actively drinking adults with known or suspected AUD and who had positive scores on a screening test. Of 179 patients who were approached, 32 agreed to enroll; the enrollment yield was 18%. Participants were given monthly extended-release naltrexone and case management services.
Of the 32 participants, 25 completed all their study visits and 22 (69%) continued taking naltrexone after the 12 weeks.
The researchers said the results surprised them. The average daily alcohol consumption at baseline was 7.6 drinks a day, and it fell by 7.5 drinks a day – in other words, to almost no consumption.
“The median alcohol consumption when measured over the last 2 weeks of the study was zero,” Dr. Raven said. “This doesn’t mean everyone was at zero, but this was the median and reflects that many participants stopped drinking altogether. We were pleasantly surprised by this. I don’t know that we thought so many people who participated would actually fully abstain.”
On the Kemp Quality of Life Scale – with scores from 1 to 7, with 1 being “life is very distressing,” 4 being “life is so-so,” and 7 being “life is great” – the average baseline score was 3.6. That score rose by 1.2 points by the study’s end.
Dr. Raven said she hoped more would enroll but that “a number of people actually did not want the injection or were not ready to think about stopping.” Still, the 18% enrollment is “a major improvement,” considering that no attempt was made to initiate treatment with naltrexone prior to the study. Oral naltrexone, rather than the injection, could be offered to improve participation, but oral naltrexone has to be taken daily.
She said a larger study is planned at UCSF and that other institutions are interested in starting a similar program.
“When someone is in the ED for an AUD-related issue, it can serve as a turning point for them in some cases,” she said.
Erik S. Anderson, MD, associate research director at Oakland, Calif.–based Alameda Health System, who has studied naltrexone in the ED, said the findings dovetail with what his team has found at his center. He added that psychosocial support is important as well and that his team has found that navigation services are the most important factor in connecting patients with follow-up care – even more so than providing medications.
“In my mind, this is a situation where we have treatment options and approaches that work, and it’s really about implementing these services in a novel care setting,” he said. “ED patients are at higher risk of complications for AUD simply because they are in the ED in the first place – initiating AUD treatment in this setting is the right thing to do.”
Dr. Raven and Dr. Anderson disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACEP 2022