User login
The Official Newspaper of the American Association for Thoracic Surgery
Advance Your Knowledge at the 2017 AATS International Cardiovascular Symposium
December 8-9, 2017
Renaissance São Paulo Hotel
São Paulo, Brazil
Join renowned cardiologists and surgeons at the 2017 AATS International Cardiovascular Symposium in São Paulo, Brazil, on December 8-9, 2017, to advance your clinical knowledge in heart valve disease — aortic and ascending aorta, coronary, mitral, pulmonary and tricuspid.
The two-day symposium will bring together international leaders to discuss state-of the-art information on devices, long-term results and surgical techniques with a focus on preventing, diagnosing and treating heart valve disease. The meeting will have Spanish and Portuguese translations available.
Program Directors
Joseph S. Coselli
Walter J. Gomes
Marc R. Moon
Thoralf M. Sundt III
Registration and Housing now available, go to: aats.org/ics
December 8-9, 2017
Renaissance São Paulo Hotel
São Paulo, Brazil
Join renowned cardiologists and surgeons at the 2017 AATS International Cardiovascular Symposium in São Paulo, Brazil, on December 8-9, 2017, to advance your clinical knowledge in heart valve disease — aortic and ascending aorta, coronary, mitral, pulmonary and tricuspid.
The two-day symposium will bring together international leaders to discuss state-of the-art information on devices, long-term results and surgical techniques with a focus on preventing, diagnosing and treating heart valve disease. The meeting will have Spanish and Portuguese translations available.
Program Directors
Joseph S. Coselli
Walter J. Gomes
Marc R. Moon
Thoralf M. Sundt III
Registration and Housing now available, go to: aats.org/ics
December 8-9, 2017
Renaissance São Paulo Hotel
São Paulo, Brazil
Join renowned cardiologists and surgeons at the 2017 AATS International Cardiovascular Symposium in São Paulo, Brazil, on December 8-9, 2017, to advance your clinical knowledge in heart valve disease — aortic and ascending aorta, coronary, mitral, pulmonary and tricuspid.
The two-day symposium will bring together international leaders to discuss state-of the-art information on devices, long-term results and surgical techniques with a focus on preventing, diagnosing and treating heart valve disease. The meeting will have Spanish and Portuguese translations available.
Program Directors
Joseph S. Coselli
Walter J. Gomes
Marc R. Moon
Thoralf M. Sundt III
Registration and Housing now available, go to: aats.org/ics
Head to Miami for the AATS Surgical Treatment of Arrhythmias and Rhythm Disorders 2017
November 17-18, 2017
Nobu Eden Roc Hotel
Miami Beach, FL USA
Don’t miss this two-day, interactive forum that supports the exchange of information between electrophysiologists and surgeons. The AATS Surgical Treatment of Arrhythmias and Rhythm Disorders provides a comprehensive, unbiased review of the surgical treatment of cardiac arrhythmias and rhythm disorders. The meeting will cover basic underlying mechanisms, cardiac recording and mapping techniques, clinical electrophysiology, operative techniques, cardiac monitoring and appropriate follow-up.
Sessions include:
• Concomitant Ablation – How I Do it and Why
• Hybrid Ablation and Other Alternative Approaches for Lone Atrial Fibrillation
• Lead Extraction: Modern Techniques in Management of Complications
• Management of the Left Atrial Appendage
• Mechanisms of Atrial Fibrillation
• Special Issues and Controversies in Surgical Ablation
• Surgical Ablation Guidelines
• Surgical Treatment of Arrhythmias: The Basics
• Surgical Treatment of Lone Atrial Fibrillation: How I Do It
• Ventricular Tachycardia Ablation
Program Directors
Ralph J. Damiano, Jr.
A. Marc Gillinov
Program Committee
Niv Ad
Vinay Badhwar
Manuel Castella
James L. Cox
Mark LaMeir
Patrick M. McCarthy
Takashi Nitta
Harold G. Roberts
Richard Schuessler
To register and reserve housing, go to: www.aats.org/stars
November 17-18, 2017
Nobu Eden Roc Hotel
Miami Beach, FL USA
Don’t miss this two-day, interactive forum that supports the exchange of information between electrophysiologists and surgeons. The AATS Surgical Treatment of Arrhythmias and Rhythm Disorders provides a comprehensive, unbiased review of the surgical treatment of cardiac arrhythmias and rhythm disorders. The meeting will cover basic underlying mechanisms, cardiac recording and mapping techniques, clinical electrophysiology, operative techniques, cardiac monitoring and appropriate follow-up.
Sessions include:
• Concomitant Ablation – How I Do it and Why
• Hybrid Ablation and Other Alternative Approaches for Lone Atrial Fibrillation
• Lead Extraction: Modern Techniques in Management of Complications
• Management of the Left Atrial Appendage
• Mechanisms of Atrial Fibrillation
• Special Issues and Controversies in Surgical Ablation
• Surgical Ablation Guidelines
• Surgical Treatment of Arrhythmias: The Basics
• Surgical Treatment of Lone Atrial Fibrillation: How I Do It
• Ventricular Tachycardia Ablation
Program Directors
Ralph J. Damiano, Jr.
A. Marc Gillinov
Program Committee
Niv Ad
Vinay Badhwar
Manuel Castella
James L. Cox
Mark LaMeir
Patrick M. McCarthy
Takashi Nitta
Harold G. Roberts
Richard Schuessler
To register and reserve housing, go to: www.aats.org/stars
November 17-18, 2017
Nobu Eden Roc Hotel
Miami Beach, FL USA
Don’t miss this two-day, interactive forum that supports the exchange of information between electrophysiologists and surgeons. The AATS Surgical Treatment of Arrhythmias and Rhythm Disorders provides a comprehensive, unbiased review of the surgical treatment of cardiac arrhythmias and rhythm disorders. The meeting will cover basic underlying mechanisms, cardiac recording and mapping techniques, clinical electrophysiology, operative techniques, cardiac monitoring and appropriate follow-up.
Sessions include:
• Concomitant Ablation – How I Do it and Why
• Hybrid Ablation and Other Alternative Approaches for Lone Atrial Fibrillation
• Lead Extraction: Modern Techniques in Management of Complications
• Management of the Left Atrial Appendage
• Mechanisms of Atrial Fibrillation
• Special Issues and Controversies in Surgical Ablation
• Surgical Ablation Guidelines
• Surgical Treatment of Arrhythmias: The Basics
• Surgical Treatment of Lone Atrial Fibrillation: How I Do It
• Ventricular Tachycardia Ablation
Program Directors
Ralph J. Damiano, Jr.
A. Marc Gillinov
Program Committee
Niv Ad
Vinay Badhwar
Manuel Castella
James L. Cox
Mark LaMeir
Patrick M. McCarthy
Takashi Nitta
Harold G. Roberts
Richard Schuessler
To register and reserve housing, go to: www.aats.org/stars
Learn About the Latest Technologies at AATS Focus on Thoracic Surgery: Mastering Surgical Innovation 2017
October 27-28, 2017
Encore at Wynn Las Vegas
Las Vegas, Nevada, USA
The most elite experts in the field will be presenting the latest information on new and emerging technologies for thoracic surgical diseases at the AATS Focus on Thoracic Surgery: Mastering Surgical Innovation 2017. The two-day meeting in Las Vegas provides surgeons with an opportunity to learn the latest advances in diagnostic and therapeutic techniques, minimally invasive surgery and robotic surgeries.
Concentrating on two major areas that are undergoing dynamic changes due to technological advances – benign and malignant esophageal disease, and lung cancer and related diseases – the sessions will not only give attendees insight into the latest innovations but also includes an interactive format that will enable them to incorporate these technologies into their own practices, and information on how surgical innovation can impact patient outcomes and excellence in patient care.
Program Directors
G. Alexander Patterson
David S. Sugarbaker
Program Committee
Thomas A. D’Amico
Shaf Keshavjee
James D. Luketich
Bryan F. Meyers
Scott J. Swanson
Traves D. Crabtree
To register and reserve housing, go to: aats.org/focus
October 27-28, 2017
Encore at Wynn Las Vegas
Las Vegas, Nevada, USA
The most elite experts in the field will be presenting the latest information on new and emerging technologies for thoracic surgical diseases at the AATS Focus on Thoracic Surgery: Mastering Surgical Innovation 2017. The two-day meeting in Las Vegas provides surgeons with an opportunity to learn the latest advances in diagnostic and therapeutic techniques, minimally invasive surgery and robotic surgeries.
Concentrating on two major areas that are undergoing dynamic changes due to technological advances – benign and malignant esophageal disease, and lung cancer and related diseases – the sessions will not only give attendees insight into the latest innovations but also includes an interactive format that will enable them to incorporate these technologies into their own practices, and information on how surgical innovation can impact patient outcomes and excellence in patient care.
Program Directors
G. Alexander Patterson
David S. Sugarbaker
Program Committee
Thomas A. D’Amico
Shaf Keshavjee
James D. Luketich
Bryan F. Meyers
Scott J. Swanson
Traves D. Crabtree
To register and reserve housing, go to: aats.org/focus
October 27-28, 2017
Encore at Wynn Las Vegas
Las Vegas, Nevada, USA
The most elite experts in the field will be presenting the latest information on new and emerging technologies for thoracic surgical diseases at the AATS Focus on Thoracic Surgery: Mastering Surgical Innovation 2017. The two-day meeting in Las Vegas provides surgeons with an opportunity to learn the latest advances in diagnostic and therapeutic techniques, minimally invasive surgery and robotic surgeries.
Concentrating on two major areas that are undergoing dynamic changes due to technological advances – benign and malignant esophageal disease, and lung cancer and related diseases – the sessions will not only give attendees insight into the latest innovations but also includes an interactive format that will enable them to incorporate these technologies into their own practices, and information on how surgical innovation can impact patient outcomes and excellence in patient care.
Program Directors
G. Alexander Patterson
David S. Sugarbaker
Program Committee
Thomas A. D’Amico
Shaf Keshavjee
James D. Luketich
Bryan F. Meyers
Scott J. Swanson
Traves D. Crabtree
To register and reserve housing, go to: aats.org/focus
Register for the Heart Valve Summit: Medical, Surgical and Interventional Decision Making
October 5-7, 2017
Radisson Blu Aqua Hotel
Chicago, IL, USA
The American College of Cardiology and the American Association for Thoracic Surgery are once again bringing together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease.
With the tradition of interactivity and practical decision making, the unique Heart Valve Summit is designed to engage participants in discussions, debates and potential controversies surrounding real-world cases. A renowned faculty on the cutting edge of clinically relevant data for valvular heart disease management will lead this interdisciplinary course that combines the most relevant medical, surgical and interventional options for patient care.
The Heart Valve Summit will highlight:
• Basics of the Aortic Valve
• Cardiac Network Trials
• Decision Making: Recurrent Mitral Valve Regurgitation
• Degenerative Mitral Anatomy and Physiology
• Difficult Choices and Scenarios
• Ischemic Mitral Regurgitation
• Mitral Endocarditis
• Mitral Valve Replacement
• Preparing for the Future in Mitral Valve Treatment
• TAVR
• The Future of Transcatheter Mitral Interventions
• Transcatheter Aortic Valve Replacement - Indications and Devices
• The Asymptomatic Patient with Advanced Valve Disease
• Treatment of Aortic Valve Disease
• Valve Disease and the Right Ventricle
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
To register and reserve housing, visit:
www.aats.org/valve
October 5-7, 2017
Radisson Blu Aqua Hotel
Chicago, IL, USA
The American College of Cardiology and the American Association for Thoracic Surgery are once again bringing together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease.
With the tradition of interactivity and practical decision making, the unique Heart Valve Summit is designed to engage participants in discussions, debates and potential controversies surrounding real-world cases. A renowned faculty on the cutting edge of clinically relevant data for valvular heart disease management will lead this interdisciplinary course that combines the most relevant medical, surgical and interventional options for patient care.
The Heart Valve Summit will highlight:
• Basics of the Aortic Valve
• Cardiac Network Trials
• Decision Making: Recurrent Mitral Valve Regurgitation
• Degenerative Mitral Anatomy and Physiology
• Difficult Choices and Scenarios
• Ischemic Mitral Regurgitation
• Mitral Endocarditis
• Mitral Valve Replacement
• Preparing for the Future in Mitral Valve Treatment
• TAVR
• The Future of Transcatheter Mitral Interventions
• Transcatheter Aortic Valve Replacement - Indications and Devices
• The Asymptomatic Patient with Advanced Valve Disease
• Treatment of Aortic Valve Disease
• Valve Disease and the Right Ventricle
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
To register and reserve housing, visit:
www.aats.org/valve
October 5-7, 2017
Radisson Blu Aqua Hotel
Chicago, IL, USA
The American College of Cardiology and the American Association for Thoracic Surgery are once again bringing together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease.
With the tradition of interactivity and practical decision making, the unique Heart Valve Summit is designed to engage participants in discussions, debates and potential controversies surrounding real-world cases. A renowned faculty on the cutting edge of clinically relevant data for valvular heart disease management will lead this interdisciplinary course that combines the most relevant medical, surgical and interventional options for patient care.
The Heart Valve Summit will highlight:
• Basics of the Aortic Valve
• Cardiac Network Trials
• Decision Making: Recurrent Mitral Valve Regurgitation
• Degenerative Mitral Anatomy and Physiology
• Difficult Choices and Scenarios
• Ischemic Mitral Regurgitation
• Mitral Endocarditis
• Mitral Valve Replacement
• Preparing for the Future in Mitral Valve Treatment
• TAVR
• The Future of Transcatheter Mitral Interventions
• Transcatheter Aortic Valve Replacement - Indications and Devices
• The Asymptomatic Patient with Advanced Valve Disease
• Treatment of Aortic Valve Disease
• Valve Disease and the Right Ventricle
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
To register and reserve housing, visit:
www.aats.org/valve
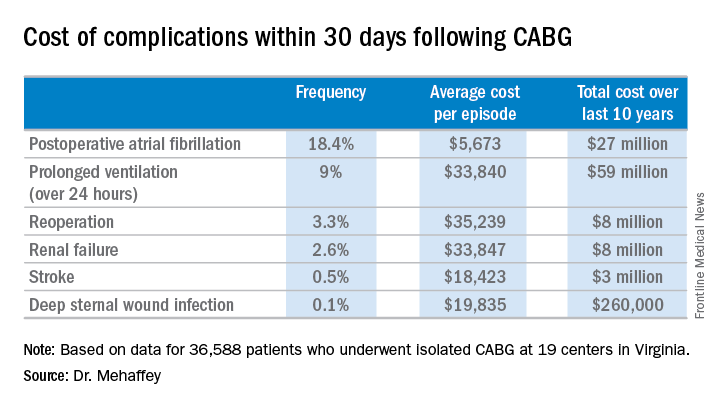
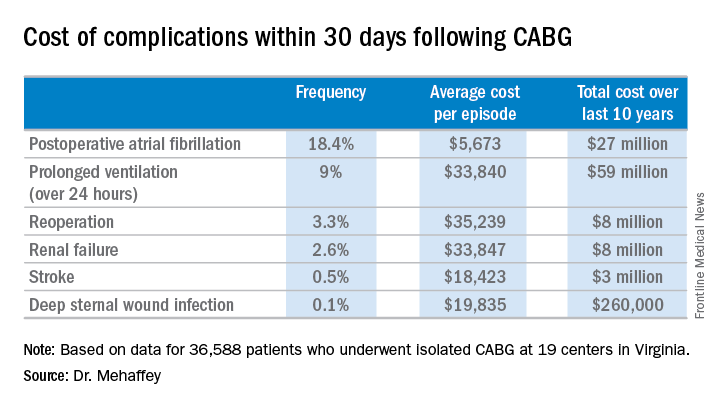
Hidden CABG costs will disrupt bundled payment systems
COLORADO SPRINGS – With bundled payment models for coronary artery bypass graft surgery looming ahead, it’s vital that cardiac surgeons take a hard look at the procedure’s hidden costs – namely, the steep price tag for postoperative complications, James H. Mehaffey, MD, said at the annual meeting of the Western Thoracic Surgical Association.
He presented a retrospective study of the 30-day hospital costs for all 36,588 patients who underwent isolated CABG during 2006-2015 at the 19 Virginia centers where the surgery is performed. This was a typical CABG population, with an average predicted risk of mortality of 1.9%. The actual 30-day mortality was 0.6%, so the surgical performance was better than expected.
“The population of patients experiencing one or more major comorbidities demonstrated a significant and dramatic increase in total hospital costs. It was an exponential increase with each additional major morbidity,” reported Dr. Mehaffey of the University of Virginia, Charlottesville.
Indeed, the average cost jumped from $36,580 for uncomplicated surgery to $64,542 with one major complication, $111,239 with two, and $194,043 with three.
The two most frequent major complications were postoperative atrial fibrillation, which occurred in 18.4% of patients, and prolonged ventilation for longer than 24 hours, which occurred in 9%. Over the course of the decade-long study period, the 19 medical centers in the Virginia Cardiac Surgery Quality Initiative collectively spent roughly $59 million on prolonged ventilation and $27 million for postoperative atrial fibrillation.
The cost of CABG during the study years outpaced the CMS health care–specific inflation rate, and this escalating cost was driven primarily by postoperative complications.
For the Virginia cardiac surgery collaborative, these data on the cost of postoperative complications will be utilized to prioritize quality improvement projects.
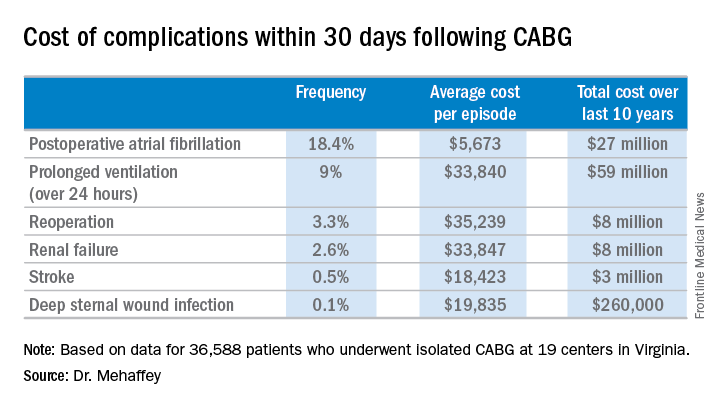
For example, during the past decade, the Virginia collaborative made reduction in the rate of postoperative atrial fibrillation a priority. Toward that end, the collaborative developed a protocol for routine perioperative prophylactic amiodarone therapy.
“At the beginning of the study decade we had postoperative atrial fibrillation rates above 25%. The average for the entire decade was just over 18%, and in the last couple years we’ve been in the 15%-16% range. So I think we are moving the needle on this. We are making a meaningful impact,” Dr. Mehaffey said.
“We’ve already used the complication cost data to do a cost-effectiveness analysis of our prophylactic amiodarone innovation. We showed we saved an average of $250 per patient, even though we’re treating a bunch of patients who’d never get that complication,” he continued.
This sort of data on the cost of adverse events is also critical to accurately risk-adjust bundled payment models.
Discussant Richard J. Shemin, MD, asked if there was much variability in postoperative complication costs between the CABG centers in the Virginia collaborative.
The variability is enormous, Dr. Mehaffey replied. Investigators recently plugged the last 5 years worth of hospital cost and complication rate data into a proposed CABG bundled payment model and extrapolated what that would mean over the next 5 years.
“There were some institutions that would be positive by a couple million dollars from this payment system and some that were losing more than $20 million, just because of the cost variability,” said Dr. Mehaffey.
Dr. Shemin also noted that the Virginia collaborative was able to collect 30-day outcome data only through the STS database, yet the bundled payment programs are based on the 90-day postoperative experience.
“How do we capture the costs in that full 90 days that we’ll be responsible for?” asked Dr. Shemin, professor of surgery and codirector of the UCLA Cardiovascular Center.
Dr. Mehaffey said that’s indeed an important question, since a major complication such as stroke or deep sternal wound infection typically entails considerable long-term costs and repeated hospital admissions beyond the 30-day window. In Virginia, the cardiac surgery collaborative is working with payers to gain access to the 90 days worth of patient data.
He reported having no financial conflicts regarding his study.
COLORADO SPRINGS – With bundled payment models for coronary artery bypass graft surgery looming ahead, it’s vital that cardiac surgeons take a hard look at the procedure’s hidden costs – namely, the steep price tag for postoperative complications, James H. Mehaffey, MD, said at the annual meeting of the Western Thoracic Surgical Association.
He presented a retrospective study of the 30-day hospital costs for all 36,588 patients who underwent isolated CABG during 2006-2015 at the 19 Virginia centers where the surgery is performed. This was a typical CABG population, with an average predicted risk of mortality of 1.9%. The actual 30-day mortality was 0.6%, so the surgical performance was better than expected.
“The population of patients experiencing one or more major comorbidities demonstrated a significant and dramatic increase in total hospital costs. It was an exponential increase with each additional major morbidity,” reported Dr. Mehaffey of the University of Virginia, Charlottesville.
Indeed, the average cost jumped from $36,580 for uncomplicated surgery to $64,542 with one major complication, $111,239 with two, and $194,043 with three.
The two most frequent major complications were postoperative atrial fibrillation, which occurred in 18.4% of patients, and prolonged ventilation for longer than 24 hours, which occurred in 9%. Over the course of the decade-long study period, the 19 medical centers in the Virginia Cardiac Surgery Quality Initiative collectively spent roughly $59 million on prolonged ventilation and $27 million for postoperative atrial fibrillation.
The cost of CABG during the study years outpaced the CMS health care–specific inflation rate, and this escalating cost was driven primarily by postoperative complications.
For the Virginia cardiac surgery collaborative, these data on the cost of postoperative complications will be utilized to prioritize quality improvement projects.
For example, during the past decade, the Virginia collaborative made reduction in the rate of postoperative atrial fibrillation a priority. Toward that end, the collaborative developed a protocol for routine perioperative prophylactic amiodarone therapy.
“At the beginning of the study decade we had postoperative atrial fibrillation rates above 25%. The average for the entire decade was just over 18%, and in the last couple years we’ve been in the 15%-16% range. So I think we are moving the needle on this. We are making a meaningful impact,” Dr. Mehaffey said.
“We’ve already used the complication cost data to do a cost-effectiveness analysis of our prophylactic amiodarone innovation. We showed we saved an average of $250 per patient, even though we’re treating a bunch of patients who’d never get that complication,” he continued.
This sort of data on the cost of adverse events is also critical to accurately risk-adjust bundled payment models.
Discussant Richard J. Shemin, MD, asked if there was much variability in postoperative complication costs between the CABG centers in the Virginia collaborative.
The variability is enormous, Dr. Mehaffey replied. Investigators recently plugged the last 5 years worth of hospital cost and complication rate data into a proposed CABG bundled payment model and extrapolated what that would mean over the next 5 years.
“There were some institutions that would be positive by a couple million dollars from this payment system and some that were losing more than $20 million, just because of the cost variability,” said Dr. Mehaffey.
Dr. Shemin also noted that the Virginia collaborative was able to collect 30-day outcome data only through the STS database, yet the bundled payment programs are based on the 90-day postoperative experience.
“How do we capture the costs in that full 90 days that we’ll be responsible for?” asked Dr. Shemin, professor of surgery and codirector of the UCLA Cardiovascular Center.
Dr. Mehaffey said that’s indeed an important question, since a major complication such as stroke or deep sternal wound infection typically entails considerable long-term costs and repeated hospital admissions beyond the 30-day window. In Virginia, the cardiac surgery collaborative is working with payers to gain access to the 90 days worth of patient data.
He reported having no financial conflicts regarding his study.
COLORADO SPRINGS – With bundled payment models for coronary artery bypass graft surgery looming ahead, it’s vital that cardiac surgeons take a hard look at the procedure’s hidden costs – namely, the steep price tag for postoperative complications, James H. Mehaffey, MD, said at the annual meeting of the Western Thoracic Surgical Association.
He presented a retrospective study of the 30-day hospital costs for all 36,588 patients who underwent isolated CABG during 2006-2015 at the 19 Virginia centers where the surgery is performed. This was a typical CABG population, with an average predicted risk of mortality of 1.9%. The actual 30-day mortality was 0.6%, so the surgical performance was better than expected.
“The population of patients experiencing one or more major comorbidities demonstrated a significant and dramatic increase in total hospital costs. It was an exponential increase with each additional major morbidity,” reported Dr. Mehaffey of the University of Virginia, Charlottesville.
Indeed, the average cost jumped from $36,580 for uncomplicated surgery to $64,542 with one major complication, $111,239 with two, and $194,043 with three.
The two most frequent major complications were postoperative atrial fibrillation, which occurred in 18.4% of patients, and prolonged ventilation for longer than 24 hours, which occurred in 9%. Over the course of the decade-long study period, the 19 medical centers in the Virginia Cardiac Surgery Quality Initiative collectively spent roughly $59 million on prolonged ventilation and $27 million for postoperative atrial fibrillation.
The cost of CABG during the study years outpaced the CMS health care–specific inflation rate, and this escalating cost was driven primarily by postoperative complications.
For the Virginia cardiac surgery collaborative, these data on the cost of postoperative complications will be utilized to prioritize quality improvement projects.
For example, during the past decade, the Virginia collaborative made reduction in the rate of postoperative atrial fibrillation a priority. Toward that end, the collaborative developed a protocol for routine perioperative prophylactic amiodarone therapy.
“At the beginning of the study decade we had postoperative atrial fibrillation rates above 25%. The average for the entire decade was just over 18%, and in the last couple years we’ve been in the 15%-16% range. So I think we are moving the needle on this. We are making a meaningful impact,” Dr. Mehaffey said.
“We’ve already used the complication cost data to do a cost-effectiveness analysis of our prophylactic amiodarone innovation. We showed we saved an average of $250 per patient, even though we’re treating a bunch of patients who’d never get that complication,” he continued.
This sort of data on the cost of adverse events is also critical to accurately risk-adjust bundled payment models.
Discussant Richard J. Shemin, MD, asked if there was much variability in postoperative complication costs between the CABG centers in the Virginia collaborative.
The variability is enormous, Dr. Mehaffey replied. Investigators recently plugged the last 5 years worth of hospital cost and complication rate data into a proposed CABG bundled payment model and extrapolated what that would mean over the next 5 years.
“There were some institutions that would be positive by a couple million dollars from this payment system and some that were losing more than $20 million, just because of the cost variability,” said Dr. Mehaffey.
Dr. Shemin also noted that the Virginia collaborative was able to collect 30-day outcome data only through the STS database, yet the bundled payment programs are based on the 90-day postoperative experience.
“How do we capture the costs in that full 90 days that we’ll be responsible for?” asked Dr. Shemin, professor of surgery and codirector of the UCLA Cardiovascular Center.
Dr. Mehaffey said that’s indeed an important question, since a major complication such as stroke or deep sternal wound infection typically entails considerable long-term costs and repeated hospital admissions beyond the 30-day window. In Virginia, the cardiac surgery collaborative is working with payers to gain access to the 90 days worth of patient data.
He reported having no financial conflicts regarding his study.
AT THE WTSA ANNUAL MEETING
Key clinical point:
Major finding: The average 30-day total hospital cost of an isolated CABG procedure during 2006-2015 in Virginia was $36,580 if there were no postoperative complications, jumping to $64,542 with one major complication and $111,239 with two.
Data source: A retrospective study of the 30-day total hospital costs for all isolated CABG procedures performed in Virginia during 2006-2015.
Disclosures: The study presenter reported having no financial conflicts.
Medicare Part D premiums dip as drug costs continue to rise
As insurance premiums in other sectors of the health care industry continue to soar, seniors enrolled in the Medicare Part D prescription drug plan will see a slight decrease in the average premium for their drug coverage.
The Centers for Medicare & Medicaid Services announced Aug. 2 that the average basic premium for drug coverage is projected to drop to $33.50 per month in 2018, down $1.20 from 2017’s average monthly premium of $34.70.
Average premiums are falling despite the rise in drug spending, according to the 2017 Medicare Trustees report, which details the solvency of the Medicare program.
The report notes, however, that drug costs are lower than previous reports due to higher manufacturer rebates and decreased use of direct acting antiviral therapies for hepatitis C virus. Overall, Medicare Part D expenditures per enrollee are estimated to increase by an average of 4.7% annually from 2017 through 2026.
As insurance premiums in other sectors of the health care industry continue to soar, seniors enrolled in the Medicare Part D prescription drug plan will see a slight decrease in the average premium for their drug coverage.
The Centers for Medicare & Medicaid Services announced Aug. 2 that the average basic premium for drug coverage is projected to drop to $33.50 per month in 2018, down $1.20 from 2017’s average monthly premium of $34.70.
Average premiums are falling despite the rise in drug spending, according to the 2017 Medicare Trustees report, which details the solvency of the Medicare program.
The report notes, however, that drug costs are lower than previous reports due to higher manufacturer rebates and decreased use of direct acting antiviral therapies for hepatitis C virus. Overall, Medicare Part D expenditures per enrollee are estimated to increase by an average of 4.7% annually from 2017 through 2026.
As insurance premiums in other sectors of the health care industry continue to soar, seniors enrolled in the Medicare Part D prescription drug plan will see a slight decrease in the average premium for their drug coverage.
The Centers for Medicare & Medicaid Services announced Aug. 2 that the average basic premium for drug coverage is projected to drop to $33.50 per month in 2018, down $1.20 from 2017’s average monthly premium of $34.70.
Average premiums are falling despite the rise in drug spending, according to the 2017 Medicare Trustees report, which details the solvency of the Medicare program.
The report notes, however, that drug costs are lower than previous reports due to higher manufacturer rebates and decreased use of direct acting antiviral therapies for hepatitis C virus. Overall, Medicare Part D expenditures per enrollee are estimated to increase by an average of 4.7% annually from 2017 through 2026.
Malperfusion key in aortic dissection repair outcomes
Early repair is the standard of care for patients with type A aortic dissection, but the presence of malperfusion rather than the timing of surgery may be a major determinant in patient survival both in the hospital and in the long term, according to an analysis of patients with acute type A aortic dissection over a 17-year period at the University of Bristol (England).
“Malperfusion at presentation rather than the timing of intervention is the major risk factor for death in both the short term and long term in patients undergoing surgical repair of type A aortic dissection,” Pradeep Narayan, FRCS, and his colleagues said in reporting their findings in the July issue of the Journal of Thoracic and Cardiovascular Surgery (154:81-6). Nonetheless, Dr. Narayan and his colleagues acknowledged that early operation prevents the development of malperfusion and is the best option for restoring normal perfusion for patients who already have malperfusion.
Their study analyzed results from two different groups of patients who had surgery for repair of acute type A aortic dissection over a 17-year period: 72 in the early surgery group that had operative repair within 12 hours of symptom onset; and 80 in the late-surgery group that had the operation 12 hours or more after symptoms first appeared. A total of 205 patients underwent surgical repair for acute type A aortic dissection in that period, but only 152 cases had recorded the timing of surgery from onset of symptoms. The median time between arrival at the center and surgery was 3 hours.
Dr. Narayan and his coauthors reported that 39% (60) of the 152 patients had malperfusion. Organ malperfusion was actually more common in the early surgery group, although the difference was not significant: 48.6% vs. 31.3% in the late-surgery group (P = .29). Early mortality was also similar between the two groups: 19.4% in the early surgery group and 13.8% in the late surgery group (P = .8). In terms of late survival, the study found no difference between the two groups.
Dr. Narayan and his coauthors reported that malperfusion and concomitant coronary artery bypass grafting were independent predictors of survival, with hazard ratios of 2.65 (P = .01) and 3.03 (P = .03), respectively. As a nonlinear variable, time to surgery showed an inverse relationship with late mortality (HR, 0.51; P = .26), but as a linear variable when adjusted for other covariates, including malperfusion, it did not affect survival (HR, 1.01; P = .09).
“The main finding of the present study is that almost 40% of patients undergoing repair of type A aortic dissection had evidence of malperfusion,” Dr. Narayan and his coauthors said. “The second important finding is that the presence of malperfusion was associated with significantly increased risk of death in both the short-term and long-term follow-up.” While a delayed operation was associated with a reduced risk of death, it was not significant when accounting for malperfusion.
Dr. Narayan and his coauthors acknowledged limitations of their study, the most important of which was the including of different types of malperfusion as a single variable. Also, the small sample size may explain the lack of statistically significant differences between the two groups.
Dr. Narayan and his coauthors had no financial relationships to disclose.
Malperfusion has the potential to serve as a marker for the need for surgery in type A aortic dissection, but the inability to identify the true risk of developing malperfusion in the first 12-24 hours after acute type A dissection means that the indication for early surgery will remain unchanged, James I. Fann, MD, of Stanford (Calif.) University says in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:87-8).
“The findings of Narayan and colleagues impel us to review the history of the development of the classification and treatment (or in fact vice versa) of acute type A dissection and to acknowledge that early timing of surgery in these high-risk patients was originally proposed to prevent malperfusion and to respond to the most catastrophic complications,” Dr. Fann said.
But Dr. Fann cautioned against “being dismissive” of their findings, because such questioning and re-evaluation are essential in developing appropriate treatments. “Now, the question is whether we can identify the cohort of patients who are at lower risk for the development of malperfusion and tailor their treatment,” he said.
Dr. Fann had no financial relationships to disclose.
Malperfusion has the potential to serve as a marker for the need for surgery in type A aortic dissection, but the inability to identify the true risk of developing malperfusion in the first 12-24 hours after acute type A dissection means that the indication for early surgery will remain unchanged, James I. Fann, MD, of Stanford (Calif.) University says in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:87-8).
“The findings of Narayan and colleagues impel us to review the history of the development of the classification and treatment (or in fact vice versa) of acute type A dissection and to acknowledge that early timing of surgery in these high-risk patients was originally proposed to prevent malperfusion and to respond to the most catastrophic complications,” Dr. Fann said.
But Dr. Fann cautioned against “being dismissive” of their findings, because such questioning and re-evaluation are essential in developing appropriate treatments. “Now, the question is whether we can identify the cohort of patients who are at lower risk for the development of malperfusion and tailor their treatment,” he said.
Dr. Fann had no financial relationships to disclose.
Malperfusion has the potential to serve as a marker for the need for surgery in type A aortic dissection, but the inability to identify the true risk of developing malperfusion in the first 12-24 hours after acute type A dissection means that the indication for early surgery will remain unchanged, James I. Fann, MD, of Stanford (Calif.) University says in his invited commentary (J Thorac Cardiovasc Surg. 2017;154:87-8).
“The findings of Narayan and colleagues impel us to review the history of the development of the classification and treatment (or in fact vice versa) of acute type A dissection and to acknowledge that early timing of surgery in these high-risk patients was originally proposed to prevent malperfusion and to respond to the most catastrophic complications,” Dr. Fann said.
But Dr. Fann cautioned against “being dismissive” of their findings, because such questioning and re-evaluation are essential in developing appropriate treatments. “Now, the question is whether we can identify the cohort of patients who are at lower risk for the development of malperfusion and tailor their treatment,” he said.
Dr. Fann had no financial relationships to disclose.
Early repair is the standard of care for patients with type A aortic dissection, but the presence of malperfusion rather than the timing of surgery may be a major determinant in patient survival both in the hospital and in the long term, according to an analysis of patients with acute type A aortic dissection over a 17-year period at the University of Bristol (England).
“Malperfusion at presentation rather than the timing of intervention is the major risk factor for death in both the short term and long term in patients undergoing surgical repair of type A aortic dissection,” Pradeep Narayan, FRCS, and his colleagues said in reporting their findings in the July issue of the Journal of Thoracic and Cardiovascular Surgery (154:81-6). Nonetheless, Dr. Narayan and his colleagues acknowledged that early operation prevents the development of malperfusion and is the best option for restoring normal perfusion for patients who already have malperfusion.
Their study analyzed results from two different groups of patients who had surgery for repair of acute type A aortic dissection over a 17-year period: 72 in the early surgery group that had operative repair within 12 hours of symptom onset; and 80 in the late-surgery group that had the operation 12 hours or more after symptoms first appeared. A total of 205 patients underwent surgical repair for acute type A aortic dissection in that period, but only 152 cases had recorded the timing of surgery from onset of symptoms. The median time between arrival at the center and surgery was 3 hours.
Dr. Narayan and his coauthors reported that 39% (60) of the 152 patients had malperfusion. Organ malperfusion was actually more common in the early surgery group, although the difference was not significant: 48.6% vs. 31.3% in the late-surgery group (P = .29). Early mortality was also similar between the two groups: 19.4% in the early surgery group and 13.8% in the late surgery group (P = .8). In terms of late survival, the study found no difference between the two groups.
Dr. Narayan and his coauthors reported that malperfusion and concomitant coronary artery bypass grafting were independent predictors of survival, with hazard ratios of 2.65 (P = .01) and 3.03 (P = .03), respectively. As a nonlinear variable, time to surgery showed an inverse relationship with late mortality (HR, 0.51; P = .26), but as a linear variable when adjusted for other covariates, including malperfusion, it did not affect survival (HR, 1.01; P = .09).
“The main finding of the present study is that almost 40% of patients undergoing repair of type A aortic dissection had evidence of malperfusion,” Dr. Narayan and his coauthors said. “The second important finding is that the presence of malperfusion was associated with significantly increased risk of death in both the short-term and long-term follow-up.” While a delayed operation was associated with a reduced risk of death, it was not significant when accounting for malperfusion.
Dr. Narayan and his coauthors acknowledged limitations of their study, the most important of which was the including of different types of malperfusion as a single variable. Also, the small sample size may explain the lack of statistically significant differences between the two groups.
Dr. Narayan and his coauthors had no financial relationships to disclose.
Early repair is the standard of care for patients with type A aortic dissection, but the presence of malperfusion rather than the timing of surgery may be a major determinant in patient survival both in the hospital and in the long term, according to an analysis of patients with acute type A aortic dissection over a 17-year period at the University of Bristol (England).
“Malperfusion at presentation rather than the timing of intervention is the major risk factor for death in both the short term and long term in patients undergoing surgical repair of type A aortic dissection,” Pradeep Narayan, FRCS, and his colleagues said in reporting their findings in the July issue of the Journal of Thoracic and Cardiovascular Surgery (154:81-6). Nonetheless, Dr. Narayan and his colleagues acknowledged that early operation prevents the development of malperfusion and is the best option for restoring normal perfusion for patients who already have malperfusion.
Their study analyzed results from two different groups of patients who had surgery for repair of acute type A aortic dissection over a 17-year period: 72 in the early surgery group that had operative repair within 12 hours of symptom onset; and 80 in the late-surgery group that had the operation 12 hours or more after symptoms first appeared. A total of 205 patients underwent surgical repair for acute type A aortic dissection in that period, but only 152 cases had recorded the timing of surgery from onset of symptoms. The median time between arrival at the center and surgery was 3 hours.
Dr. Narayan and his coauthors reported that 39% (60) of the 152 patients had malperfusion. Organ malperfusion was actually more common in the early surgery group, although the difference was not significant: 48.6% vs. 31.3% in the late-surgery group (P = .29). Early mortality was also similar between the two groups: 19.4% in the early surgery group and 13.8% in the late surgery group (P = .8). In terms of late survival, the study found no difference between the two groups.
Dr. Narayan and his coauthors reported that malperfusion and concomitant coronary artery bypass grafting were independent predictors of survival, with hazard ratios of 2.65 (P = .01) and 3.03 (P = .03), respectively. As a nonlinear variable, time to surgery showed an inverse relationship with late mortality (HR, 0.51; P = .26), but as a linear variable when adjusted for other covariates, including malperfusion, it did not affect survival (HR, 1.01; P = .09).
“The main finding of the present study is that almost 40% of patients undergoing repair of type A aortic dissection had evidence of malperfusion,” Dr. Narayan and his coauthors said. “The second important finding is that the presence of malperfusion was associated with significantly increased risk of death in both the short-term and long-term follow-up.” While a delayed operation was associated with a reduced risk of death, it was not significant when accounting for malperfusion.
Dr. Narayan and his coauthors acknowledged limitations of their study, the most important of which was the including of different types of malperfusion as a single variable. Also, the small sample size may explain the lack of statistically significant differences between the two groups.
Dr. Narayan and his coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Malperfusion is a main determinant of outcomes for patients having surgical repair for acute type A aortic dissection.
Major finding: Patients in the early surgery group (surgery within 12 hours of onset) were more likely to have malperfusion than those who had surgery later, 47% vs. 31%.
Data source: Single-center analysis of 152 operations for repair of acute type A aortic dissections over a 17-year period.
Disclosures: Dr. Narayan and his coauthors had no financial relationships to disclose.
Short, simple antibiotic courses effective in latent TB
Latent tuberculosis infection can be safely and effectively treated with 3- and 4-month medication regimens, including those using once-weekly dosing, according to results from a new meta-analysis.
The findings, published online July 31 in Annals of Internal Medicine, bolster evidence that shorter antibiotic regimens using rifamycins alone or in combination with other drugs are a viable alternative to the longer courses (Ann Intern Med. 2017;167:248-55).
For their research, Dominik Zenner, MD, an epidemiologist with Public Health England in London, and his colleagues updated a meta-analysis they published in 2014. The team added 8 new randomized studies to the 53 that had been included in the earlier paper (Ann Intern Med. 2014 Sep;161:419-28).
Using pairwise comparisons and a Bayesian network analysis, Dr. Zenner and his colleagues found comparable efficacy among isoniazid regimens of 6 months or more; rifampicin-isoniazid regimens of 3 or 4 months, rifampicin-only regimens, and rifampicin-pyrazinamide regimens, compared with placebo (P less than .05 for all).
Importantly, a rifapentine-based regimen in which patients took a weekly dose for 12 weeks was as effective as the others.
“We think that you can get away with shorter regimens,” Dr. Zenner said in an interview. Although 3- to 4-month courses are already recommended in some countries, including the United Kingdom, for most patients with latent TB, “clinicians in some settings have been quite slow to adopt them,” he said.
The U.S. Centers for Disease Control and Prevention currently recommend multiple treatment strategies for latent TB, depending on patient characteristics. These include 6 or 9 months of isoniazid; 3 months of once-weekly isoniazid and rifapentine; or 4 months of daily rifampin.
In the meta-analysis, rifamycin-only regimens performed as well as did those regimens that also used isoniazid, the study showed, suggesting that, for most patients who can safely be treated with rifamycins, “there is no added gain of using isoniazid,” Dr. Zenner said.
He noted that the longer isoniazid-alone regimens are nonetheless effective and appropriate for some, including people who might have potential drug interactions, such as HIV patients taking antiretroviral medications.
About 2 billion people worldwide are estimated to have latent TB, and most will not go on to develop active TB. However, because latent TB acts as the reservoir for active TB, screening of high-risk groups and close contacts of TB patients and treating latent infections is a public health priority.
But many of these asymptomatic patients will get lost between a positive screen result and successful treatment completion, Dr. Zenner said.
“We have huge drop-offs in the cascade of treatment, and treatment completion is one of the worries,” he said. “Whether it makes a huge difference in compliance to take only 12 doses is not sufficiently studied, but it does make a lot of sense. By reducing the pill burden, as we call it, we think that we will see quite good adherence rates – but that’s a subject of further detailed study.”
The investigators noted as a limitation of their study that hepatotoxicity outcomes were not available for all studies and that some of the included trials had a potential for bias. They did not see statistically significant differences in treatment efficacy between regimens in HIV-positive and HIV-negative patients, but noted in their analysis that “efficacy may have been weaker in HIV-positive populations.”
The U.K. National Institute for Health Research provided some funding for Dr. Zenner and his colleagues’ study. One coauthor, Helen Stagg, PhD, reported nonfinancial support from Sanofi during the study, and financial support from Otsuka for unrelated work.
Latent tuberculosis infection can be safely and effectively treated with 3- and 4-month medication regimens, including those using once-weekly dosing, according to results from a new meta-analysis.
The findings, published online July 31 in Annals of Internal Medicine, bolster evidence that shorter antibiotic regimens using rifamycins alone or in combination with other drugs are a viable alternative to the longer courses (Ann Intern Med. 2017;167:248-55).
For their research, Dominik Zenner, MD, an epidemiologist with Public Health England in London, and his colleagues updated a meta-analysis they published in 2014. The team added 8 new randomized studies to the 53 that had been included in the earlier paper (Ann Intern Med. 2014 Sep;161:419-28).
Using pairwise comparisons and a Bayesian network analysis, Dr. Zenner and his colleagues found comparable efficacy among isoniazid regimens of 6 months or more; rifampicin-isoniazid regimens of 3 or 4 months, rifampicin-only regimens, and rifampicin-pyrazinamide regimens, compared with placebo (P less than .05 for all).
Importantly, a rifapentine-based regimen in which patients took a weekly dose for 12 weeks was as effective as the others.
“We think that you can get away with shorter regimens,” Dr. Zenner said in an interview. Although 3- to 4-month courses are already recommended in some countries, including the United Kingdom, for most patients with latent TB, “clinicians in some settings have been quite slow to adopt them,” he said.
The U.S. Centers for Disease Control and Prevention currently recommend multiple treatment strategies for latent TB, depending on patient characteristics. These include 6 or 9 months of isoniazid; 3 months of once-weekly isoniazid and rifapentine; or 4 months of daily rifampin.
In the meta-analysis, rifamycin-only regimens performed as well as did those regimens that also used isoniazid, the study showed, suggesting that, for most patients who can safely be treated with rifamycins, “there is no added gain of using isoniazid,” Dr. Zenner said.
He noted that the longer isoniazid-alone regimens are nonetheless effective and appropriate for some, including people who might have potential drug interactions, such as HIV patients taking antiretroviral medications.
About 2 billion people worldwide are estimated to have latent TB, and most will not go on to develop active TB. However, because latent TB acts as the reservoir for active TB, screening of high-risk groups and close contacts of TB patients and treating latent infections is a public health priority.
But many of these asymptomatic patients will get lost between a positive screen result and successful treatment completion, Dr. Zenner said.
“We have huge drop-offs in the cascade of treatment, and treatment completion is one of the worries,” he said. “Whether it makes a huge difference in compliance to take only 12 doses is not sufficiently studied, but it does make a lot of sense. By reducing the pill burden, as we call it, we think that we will see quite good adherence rates – but that’s a subject of further detailed study.”
The investigators noted as a limitation of their study that hepatotoxicity outcomes were not available for all studies and that some of the included trials had a potential for bias. They did not see statistically significant differences in treatment efficacy between regimens in HIV-positive and HIV-negative patients, but noted in their analysis that “efficacy may have been weaker in HIV-positive populations.”
The U.K. National Institute for Health Research provided some funding for Dr. Zenner and his colleagues’ study. One coauthor, Helen Stagg, PhD, reported nonfinancial support from Sanofi during the study, and financial support from Otsuka for unrelated work.
Latent tuberculosis infection can be safely and effectively treated with 3- and 4-month medication regimens, including those using once-weekly dosing, according to results from a new meta-analysis.
The findings, published online July 31 in Annals of Internal Medicine, bolster evidence that shorter antibiotic regimens using rifamycins alone or in combination with other drugs are a viable alternative to the longer courses (Ann Intern Med. 2017;167:248-55).
For their research, Dominik Zenner, MD, an epidemiologist with Public Health England in London, and his colleagues updated a meta-analysis they published in 2014. The team added 8 new randomized studies to the 53 that had been included in the earlier paper (Ann Intern Med. 2014 Sep;161:419-28).
Using pairwise comparisons and a Bayesian network analysis, Dr. Zenner and his colleagues found comparable efficacy among isoniazid regimens of 6 months or more; rifampicin-isoniazid regimens of 3 or 4 months, rifampicin-only regimens, and rifampicin-pyrazinamide regimens, compared with placebo (P less than .05 for all).
Importantly, a rifapentine-based regimen in which patients took a weekly dose for 12 weeks was as effective as the others.
“We think that you can get away with shorter regimens,” Dr. Zenner said in an interview. Although 3- to 4-month courses are already recommended in some countries, including the United Kingdom, for most patients with latent TB, “clinicians in some settings have been quite slow to adopt them,” he said.
The U.S. Centers for Disease Control and Prevention currently recommend multiple treatment strategies for latent TB, depending on patient characteristics. These include 6 or 9 months of isoniazid; 3 months of once-weekly isoniazid and rifapentine; or 4 months of daily rifampin.
In the meta-analysis, rifamycin-only regimens performed as well as did those regimens that also used isoniazid, the study showed, suggesting that, for most patients who can safely be treated with rifamycins, “there is no added gain of using isoniazid,” Dr. Zenner said.
He noted that the longer isoniazid-alone regimens are nonetheless effective and appropriate for some, including people who might have potential drug interactions, such as HIV patients taking antiretroviral medications.
About 2 billion people worldwide are estimated to have latent TB, and most will not go on to develop active TB. However, because latent TB acts as the reservoir for active TB, screening of high-risk groups and close contacts of TB patients and treating latent infections is a public health priority.
But many of these asymptomatic patients will get lost between a positive screen result and successful treatment completion, Dr. Zenner said.
“We have huge drop-offs in the cascade of treatment, and treatment completion is one of the worries,” he said. “Whether it makes a huge difference in compliance to take only 12 doses is not sufficiently studied, but it does make a lot of sense. By reducing the pill burden, as we call it, we think that we will see quite good adherence rates – but that’s a subject of further detailed study.”
The investigators noted as a limitation of their study that hepatotoxicity outcomes were not available for all studies and that some of the included trials had a potential for bias. They did not see statistically significant differences in treatment efficacy between regimens in HIV-positive and HIV-negative patients, but noted in their analysis that “efficacy may have been weaker in HIV-positive populations.”
The U.K. National Institute for Health Research provided some funding for Dr. Zenner and his colleagues’ study. One coauthor, Helen Stagg, PhD, reported nonfinancial support from Sanofi during the study, and financial support from Otsuka for unrelated work.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Rifamycin-only treatment of latent TB works as well as combination regimens, and shorter dosing schedules show no loss in efficacy vs. longer ones.
Major finding: Rifamycin-only regimens, rifampicin-isoniazid regimens of 3 or 4 months, rifampicin-pyrazinamide regimens were all effective, compared with placebo and with isoniazid regimens of 6, 12 and 72 months.
Data source: A network meta-analysis of 61 randomized trials, 8 of them published in last 3 years
Disclosures: The National Institute for Health Research (UK) funded some co-authors; one co-author disclosed a financial relationship with a pharmaceutical firm.
VIDEO: Less follow-up proposed for low-risk thyroid cancer
BOSTON – , Bryan R. Haugen, MD, suggested in a keynote lecture during the World Congress on Thyroid Cancer.
Traditionally, thyroid cancer specialists have monitored these patients for persistent or recurrent disease as often as every 6 or 12 months. “But what we’ve realized with recent assessments of response to treatment is that some patients do well without a recurrence over many years; so, the concept of doing less monitoring and less imaging, especially in patients with an excellent response [to their initial treatment], is being studied,” Dr. Haugen said in a video interview following his talk.
He estimated that perhaps two-thirds or as many as three-quarters of patients with differentiated thyroid cancer fall into the category of having low- or intermediate-risk disease with an excellent or good response to treatment, and hence they are potential candidates for eventually transitioning to less frequent follow-up.
During his talk, Dr. Haugen suggested that after several years with no sign of disease recurrence, lower-risk patients with an excellent treatment response may be able to stop undergoing regular monitoring, and those with a good treatment response may be able to safely have their monitoring intervals extended.
According to the most recent (2015) guidelines for differentiated thyroid cancer management from the American Thyroid Association, lower-risk patients with an excellent treatment response should have their serum thyroglobulin measured every 12-24 months and undergo an ultrasound examination every 3-5 years, while patients with a good response are targeted for serum thyroglobulin measurement annually with an ultrasound every 1-3 years (Thyroid. 2016 Jan;26[1]:1-133). Dr. Haugen chaired the expert panel that wrote these guidelines.
In another provocative suggestion, Dr. Haugen proposed that once well-responsive, lower-risk patients have remained disease free for several years, their less frequent follow-up monitoring could be continued by a primary care physician or another less specialized clinician.
At some time in the future, “a patient’s primary care physician could follow a simple tumor marker, thyroglobulin, maybe once every 5 years,” said Dr. Haugen, professor of medicine and head of the division of endocrinology, metabolism, and diabetes at the University of Colorado in Aurora. “At the University of Colorado, we use advanced-practice providers to do long-term follow-up” for lower-risk, treatment-responsive patients, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
BOSTON – , Bryan R. Haugen, MD, suggested in a keynote lecture during the World Congress on Thyroid Cancer.
Traditionally, thyroid cancer specialists have monitored these patients for persistent or recurrent disease as often as every 6 or 12 months. “But what we’ve realized with recent assessments of response to treatment is that some patients do well without a recurrence over many years; so, the concept of doing less monitoring and less imaging, especially in patients with an excellent response [to their initial treatment], is being studied,” Dr. Haugen said in a video interview following his talk.
He estimated that perhaps two-thirds or as many as three-quarters of patients with differentiated thyroid cancer fall into the category of having low- or intermediate-risk disease with an excellent or good response to treatment, and hence they are potential candidates for eventually transitioning to less frequent follow-up.
During his talk, Dr. Haugen suggested that after several years with no sign of disease recurrence, lower-risk patients with an excellent treatment response may be able to stop undergoing regular monitoring, and those with a good treatment response may be able to safely have their monitoring intervals extended.
According to the most recent (2015) guidelines for differentiated thyroid cancer management from the American Thyroid Association, lower-risk patients with an excellent treatment response should have their serum thyroglobulin measured every 12-24 months and undergo an ultrasound examination every 3-5 years, while patients with a good response are targeted for serum thyroglobulin measurement annually with an ultrasound every 1-3 years (Thyroid. 2016 Jan;26[1]:1-133). Dr. Haugen chaired the expert panel that wrote these guidelines.
In another provocative suggestion, Dr. Haugen proposed that once well-responsive, lower-risk patients have remained disease free for several years, their less frequent follow-up monitoring could be continued by a primary care physician or another less specialized clinician.
At some time in the future, “a patient’s primary care physician could follow a simple tumor marker, thyroglobulin, maybe once every 5 years,” said Dr. Haugen, professor of medicine and head of the division of endocrinology, metabolism, and diabetes at the University of Colorado in Aurora. “At the University of Colorado, we use advanced-practice providers to do long-term follow-up” for lower-risk, treatment-responsive patients, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
BOSTON – , Bryan R. Haugen, MD, suggested in a keynote lecture during the World Congress on Thyroid Cancer.
Traditionally, thyroid cancer specialists have monitored these patients for persistent or recurrent disease as often as every 6 or 12 months. “But what we’ve realized with recent assessments of response to treatment is that some patients do well without a recurrence over many years; so, the concept of doing less monitoring and less imaging, especially in patients with an excellent response [to their initial treatment], is being studied,” Dr. Haugen said in a video interview following his talk.
He estimated that perhaps two-thirds or as many as three-quarters of patients with differentiated thyroid cancer fall into the category of having low- or intermediate-risk disease with an excellent or good response to treatment, and hence they are potential candidates for eventually transitioning to less frequent follow-up.
During his talk, Dr. Haugen suggested that after several years with no sign of disease recurrence, lower-risk patients with an excellent treatment response may be able to stop undergoing regular monitoring, and those with a good treatment response may be able to safely have their monitoring intervals extended.
According to the most recent (2015) guidelines for differentiated thyroid cancer management from the American Thyroid Association, lower-risk patients with an excellent treatment response should have their serum thyroglobulin measured every 12-24 months and undergo an ultrasound examination every 3-5 years, while patients with a good response are targeted for serum thyroglobulin measurement annually with an ultrasound every 1-3 years (Thyroid. 2016 Jan;26[1]:1-133). Dr. Haugen chaired the expert panel that wrote these guidelines.
In another provocative suggestion, Dr. Haugen proposed that once well-responsive, lower-risk patients have remained disease free for several years, their less frequent follow-up monitoring could be continued by a primary care physician or another less specialized clinician.
At some time in the future, “a patient’s primary care physician could follow a simple tumor marker, thyroglobulin, maybe once every 5 years,” said Dr. Haugen, professor of medicine and head of the division of endocrinology, metabolism, and diabetes at the University of Colorado in Aurora. “At the University of Colorado, we use advanced-practice providers to do long-term follow-up” for lower-risk, treatment-responsive patients, he said.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT WCTC 2017
Senate sinks GOP health care reform effort
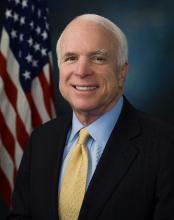
After casting the deciding vote to begin debate in the Senate on the Republican effort to repeal and replace the Affordable Care Act, Sen. John McCain (R-Ariz.) brought the effort to an end when he voted against the so-called “skinny repeal” bill introduced by Senate Majority Leader Mitch McConnell (R-Ky.).
Sen. McCain crossed the aisle with Sen. Susan Collins (R-Maine) and Sen. Lisa Murkowski (R-Alaska) and voted with the 48 members of the chamber’s Democratic caucus to kill the bill. Republicans would have needed 50 votes to pass the measure, with Vice President Mike Pence on hand to cast a tie-breaking vote if necessary. With three senators voting against the measure, however, the 49 votes were not enough.
In the early evening on July 27, however, Sen. McCain made it clear during a press conference that he would not vote for a skinny repeal. Other senators expressed concern over the skinny repeal but said they would vote for it if there were assurances that the House would actually go to conference committee (a procedure used when the House and Senate pass different versions of the same bill to allow a bipartisan group to find consensus and create a unified bill) and work out a final bill and not simply move the skinny repeal straight to the president’s desk.
Speaker of the House Paul Ryan (R-Wisc.) had issued a statement to that effect, but the House was laying a path to simply move any bill passed by the Senate, leaving it up in the air as to whether a conference committee would actually be created.
Despite a reported phone call from Speaker Ryan and conversations directly with Vice President Pence on the Senate floor, Sen. McCain ultimately could not be convinced to vote with the majority of Republicans.
“From the beginning, I have believed that Obamacare should be repealed and replaced with a solution that increases competition, lowers costs, and improves care for the American people,” Sen. McCain said in a statement issued July 28, following the early-morning vote. “The so-called ‘skinny repeal’ amendment the Senate voted on today would not accomplish those goals. While the amendment would have repealed some of Obamacare’s most burdensome regulations, it offered no replacement to actually reform our health care system and deliver affordable, quality health care to our citizens. The Speaker’s statement that the House would be ‘willing’ to go to conference does not ease my concern that this shell of a bill could be taken up and passed at any time.”
The vote brought to an end a few days of minimal activity. Every attempt by the GOP to pass some form of amendment to move the process forward – from the tweaked version of the Better Care Replacement Act to a straight repeal of the ACA – failed. Sen. Steve Daines (R-Mont.) even introduced a single-payer amendment, but that failed to get a single yes vote, with all 52 GOP members and five Democrats voting against it and the remaining 43 Democrats voting “present.”
Very few amendments were proposed, though one did get passed in the process that would have permanently repealed the so-called “Cadillac tax,” which levies a 40% tax on plans that exceed a certain value. That amendment passed along party lines by a 52-48 vote.
The future of the ACA and future reform efforts remain unclear at the moment. Following the vote, a defeated Majority Leader McConnell asked the minority party what plan they have to offer. Senate Minority Leader Charles E. Schumer (D-N.Y.) echoed Sen. McCain’s speech earlier in the week after the vote was cast to start the debate to return to regular and hammer out a bipartisan solution though the committee process.
Meanwhile, President Donald Trump advocated via Twitter to simply let the ACA continue to crumble and when it failed, then to work on a deal.
The American Medical Association called on Congress to continue its work on fixing the health care system. “While we are relieved that the Senate did not adopt legislation that would have harmed patients and critical safety net programs, the status quo is not acceptable,” AMA President David Barbe said in a statement. “We urge Congress to initiate a bipartisan effort to address shortcomings in the Affordable Care Act. The first priority should be to stabilize the individual marketplace to achieve the goal of providing access to quality, affordable health coverage for more Americans.”
After casting the deciding vote to begin debate in the Senate on the Republican effort to repeal and replace the Affordable Care Act, Sen. John McCain (R-Ariz.) brought the effort to an end when he voted against the so-called “skinny repeal” bill introduced by Senate Majority Leader Mitch McConnell (R-Ky.).
Sen. McCain crossed the aisle with Sen. Susan Collins (R-Maine) and Sen. Lisa Murkowski (R-Alaska) and voted with the 48 members of the chamber’s Democratic caucus to kill the bill. Republicans would have needed 50 votes to pass the measure, with Vice President Mike Pence on hand to cast a tie-breaking vote if necessary. With three senators voting against the measure, however, the 49 votes were not enough.
In the early evening on July 27, however, Sen. McCain made it clear during a press conference that he would not vote for a skinny repeal. Other senators expressed concern over the skinny repeal but said they would vote for it if there were assurances that the House would actually go to conference committee (a procedure used when the House and Senate pass different versions of the same bill to allow a bipartisan group to find consensus and create a unified bill) and work out a final bill and not simply move the skinny repeal straight to the president’s desk.
Speaker of the House Paul Ryan (R-Wisc.) had issued a statement to that effect, but the House was laying a path to simply move any bill passed by the Senate, leaving it up in the air as to whether a conference committee would actually be created.
Despite a reported phone call from Speaker Ryan and conversations directly with Vice President Pence on the Senate floor, Sen. McCain ultimately could not be convinced to vote with the majority of Republicans.
“From the beginning, I have believed that Obamacare should be repealed and replaced with a solution that increases competition, lowers costs, and improves care for the American people,” Sen. McCain said in a statement issued July 28, following the early-morning vote. “The so-called ‘skinny repeal’ amendment the Senate voted on today would not accomplish those goals. While the amendment would have repealed some of Obamacare’s most burdensome regulations, it offered no replacement to actually reform our health care system and deliver affordable, quality health care to our citizens. The Speaker’s statement that the House would be ‘willing’ to go to conference does not ease my concern that this shell of a bill could be taken up and passed at any time.”
The vote brought to an end a few days of minimal activity. Every attempt by the GOP to pass some form of amendment to move the process forward – from the tweaked version of the Better Care Replacement Act to a straight repeal of the ACA – failed. Sen. Steve Daines (R-Mont.) even introduced a single-payer amendment, but that failed to get a single yes vote, with all 52 GOP members and five Democrats voting against it and the remaining 43 Democrats voting “present.”
Very few amendments were proposed, though one did get passed in the process that would have permanently repealed the so-called “Cadillac tax,” which levies a 40% tax on plans that exceed a certain value. That amendment passed along party lines by a 52-48 vote.
The future of the ACA and future reform efforts remain unclear at the moment. Following the vote, a defeated Majority Leader McConnell asked the minority party what plan they have to offer. Senate Minority Leader Charles E. Schumer (D-N.Y.) echoed Sen. McCain’s speech earlier in the week after the vote was cast to start the debate to return to regular and hammer out a bipartisan solution though the committee process.
Meanwhile, President Donald Trump advocated via Twitter to simply let the ACA continue to crumble and when it failed, then to work on a deal.
The American Medical Association called on Congress to continue its work on fixing the health care system. “While we are relieved that the Senate did not adopt legislation that would have harmed patients and critical safety net programs, the status quo is not acceptable,” AMA President David Barbe said in a statement. “We urge Congress to initiate a bipartisan effort to address shortcomings in the Affordable Care Act. The first priority should be to stabilize the individual marketplace to achieve the goal of providing access to quality, affordable health coverage for more Americans.”
After casting the deciding vote to begin debate in the Senate on the Republican effort to repeal and replace the Affordable Care Act, Sen. John McCain (R-Ariz.) brought the effort to an end when he voted against the so-called “skinny repeal” bill introduced by Senate Majority Leader Mitch McConnell (R-Ky.).
Sen. McCain crossed the aisle with Sen. Susan Collins (R-Maine) and Sen. Lisa Murkowski (R-Alaska) and voted with the 48 members of the chamber’s Democratic caucus to kill the bill. Republicans would have needed 50 votes to pass the measure, with Vice President Mike Pence on hand to cast a tie-breaking vote if necessary. With three senators voting against the measure, however, the 49 votes were not enough.
In the early evening on July 27, however, Sen. McCain made it clear during a press conference that he would not vote for a skinny repeal. Other senators expressed concern over the skinny repeal but said they would vote for it if there were assurances that the House would actually go to conference committee (a procedure used when the House and Senate pass different versions of the same bill to allow a bipartisan group to find consensus and create a unified bill) and work out a final bill and not simply move the skinny repeal straight to the president’s desk.
Speaker of the House Paul Ryan (R-Wisc.) had issued a statement to that effect, but the House was laying a path to simply move any bill passed by the Senate, leaving it up in the air as to whether a conference committee would actually be created.
Despite a reported phone call from Speaker Ryan and conversations directly with Vice President Pence on the Senate floor, Sen. McCain ultimately could not be convinced to vote with the majority of Republicans.
“From the beginning, I have believed that Obamacare should be repealed and replaced with a solution that increases competition, lowers costs, and improves care for the American people,” Sen. McCain said in a statement issued July 28, following the early-morning vote. “The so-called ‘skinny repeal’ amendment the Senate voted on today would not accomplish those goals. While the amendment would have repealed some of Obamacare’s most burdensome regulations, it offered no replacement to actually reform our health care system and deliver affordable, quality health care to our citizens. The Speaker’s statement that the House would be ‘willing’ to go to conference does not ease my concern that this shell of a bill could be taken up and passed at any time.”
The vote brought to an end a few days of minimal activity. Every attempt by the GOP to pass some form of amendment to move the process forward – from the tweaked version of the Better Care Replacement Act to a straight repeal of the ACA – failed. Sen. Steve Daines (R-Mont.) even introduced a single-payer amendment, but that failed to get a single yes vote, with all 52 GOP members and five Democrats voting against it and the remaining 43 Democrats voting “present.”
Very few amendments were proposed, though one did get passed in the process that would have permanently repealed the so-called “Cadillac tax,” which levies a 40% tax on plans that exceed a certain value. That amendment passed along party lines by a 52-48 vote.
The future of the ACA and future reform efforts remain unclear at the moment. Following the vote, a defeated Majority Leader McConnell asked the minority party what plan they have to offer. Senate Minority Leader Charles E. Schumer (D-N.Y.) echoed Sen. McCain’s speech earlier in the week after the vote was cast to start the debate to return to regular and hammer out a bipartisan solution though the committee process.
Meanwhile, President Donald Trump advocated via Twitter to simply let the ACA continue to crumble and when it failed, then to work on a deal.
The American Medical Association called on Congress to continue its work on fixing the health care system. “While we are relieved that the Senate did not adopt legislation that would have harmed patients and critical safety net programs, the status quo is not acceptable,” AMA President David Barbe said in a statement. “We urge Congress to initiate a bipartisan effort to address shortcomings in the Affordable Care Act. The first priority should be to stabilize the individual marketplace to achieve the goal of providing access to quality, affordable health coverage for more Americans.”