User login
The Official Newspaper of the American Association for Thoracic Surgery
‘Sobering’ high 10-year mortality post-MI after age 65
WASHINGTON – Patients who experience an acute MI at age 65 or older have unsettlingly high 5- and 10-year mortality in community practice settings despite excellent rates of evidence-based medications being prescribed at discharge, Ajar Kochar, MD, reported at the annual meeting of the American College of Cardiology.
This observation is based upon more than 22,000 patients aged 65 years or older treated for an acute MI during 2004-2006 at 344 U.S. hospitals participating in the CRUSADE registry. Their median age at the time of MI was 77 years. But 10-year all-cause mortality remained high even among relatively younger patients aged 65-74 whom one would expect to have a favorable long-term prognosis because they had additional survival-enhancing factors working in their favor, including having undergone coronary revascularization during their index hospitalization and surviving their first year post-MI, observed Dr. Kochar of the Duke Clinical Research Institute in Durham, N.C.
This unmet need will increasingly clamor for attention as the aging of the American population accelerates like a runaway freight train. By 2030, an estimated 20% of Americans will be aged 65 or older. That’s more than 71 million people. And more than half of all MIs occur in individuals above age 65, he noted.
Dr. Kochar presented a CRUSADE analysis which included 19,755 older Americans with a non–ST elevation MI (NSTEMI) and 2,540 with a STEMI. The overall group’s 1-year mortality was 24%, with a 5-year cumulative mortality of 51% and a whopping 10-year mortality of 72%.
According to the Centers for Disease Control and Prevention, the expected additional lifespan of someone who was 65 years old in 2015 is 19 years. In contrast, the median survival of patients in the CRUSADE registry who were 65-69 at the time of their MI was less than half of that, at 8.3 years.
Among the key findings from the CRUSADE analysis:
• Unadjusted 10-year all-cause mortality was significantly greater in patients with NSTEMI than STEMI, by a margin of 73% versus 60%. Notably, however, NSTEMI patients were far less likely to undergo coronary revascularization: 32% of them had percutaneous coronary intervention during their index hospitalization, and 8.7% underwent coronary artery bypass grafting, in contrast to rates of 65.5% for PCI and 8.0% for CABG in the STEMI patients. After adjustment for these and other differences in care, NSTEMI patients actually had a 7% lower risk of long-term mortality than the STEMI group.
• Even after limiting the analysis to the youngest elderly – patients aged 65-74 when their MI occurred – 10-year mortality remained high, at 53%.
• After excluding the 24% of patients who died within 1 year after MI, 10-year mortality was still quite high, at 63%. Dr. Kochar and his coinvestigators chose to reanalyze the data in this way because the 1-year mark is an important time point clinically, since it’s when decisions regarding extended dual-antiplatelet therapy are made.
Patients who underwent coronary revascularization during their index hospitalization had a much-improved long-term prognosis, compared with those with medical management only. The 10-year cumulative mortality rate was 57% in patients who had PCI, identical at 57% in those who received CABG, and 84% in medically managed patients.
Ninety-five percent of patients were discharged on aspirin, 94% on a beta blocker, 81% on a statin, and 73% on clopidogrel. Discharge prescriptions for statins and clopidogrel were more common for the STEMI group. Unfortunately, the CRUSADE registry doesn’t include data on long-term medication adherence or prescription refill rates.
Dr. Kochar named several potential strategies aimed at reducing the high long-term mortality rates in older patients with MI as documented in this study. These include structured efforts to improve adherence to evidence-based medications for secondary prevention, as well as making percutaneous revascularization more widely available for older patients with NSTEMI. He noted that while in 2004-2006, 32% of CRUSADE participants with NSTEMI underwent PCI during their index hospitalization, by 2011-2012 that rate had inched upward only to 36%.
Several physicians commented that the high long-term all-cause mortality rates in older CRUSADE participants may paint a grim picture, in part because the aged face growing risks of cancer and other noncardiovascular competing causes of death. But Dr. Kochar replied that while the lack of information on specific causes of death is a study limitation, he and his coinvestigators are convinced based upon data from other studies that most of the deaths in CRUSADE were cardiovascular in nature.
He reported having no financial conflicts regarding his study.
WASHINGTON – Patients who experience an acute MI at age 65 or older have unsettlingly high 5- and 10-year mortality in community practice settings despite excellent rates of evidence-based medications being prescribed at discharge, Ajar Kochar, MD, reported at the annual meeting of the American College of Cardiology.
This observation is based upon more than 22,000 patients aged 65 years or older treated for an acute MI during 2004-2006 at 344 U.S. hospitals participating in the CRUSADE registry. Their median age at the time of MI was 77 years. But 10-year all-cause mortality remained high even among relatively younger patients aged 65-74 whom one would expect to have a favorable long-term prognosis because they had additional survival-enhancing factors working in their favor, including having undergone coronary revascularization during their index hospitalization and surviving their first year post-MI, observed Dr. Kochar of the Duke Clinical Research Institute in Durham, N.C.
This unmet need will increasingly clamor for attention as the aging of the American population accelerates like a runaway freight train. By 2030, an estimated 20% of Americans will be aged 65 or older. That’s more than 71 million people. And more than half of all MIs occur in individuals above age 65, he noted.
Dr. Kochar presented a CRUSADE analysis which included 19,755 older Americans with a non–ST elevation MI (NSTEMI) and 2,540 with a STEMI. The overall group’s 1-year mortality was 24%, with a 5-year cumulative mortality of 51% and a whopping 10-year mortality of 72%.
According to the Centers for Disease Control and Prevention, the expected additional lifespan of someone who was 65 years old in 2015 is 19 years. In contrast, the median survival of patients in the CRUSADE registry who were 65-69 at the time of their MI was less than half of that, at 8.3 years.
Among the key findings from the CRUSADE analysis:
• Unadjusted 10-year all-cause mortality was significantly greater in patients with NSTEMI than STEMI, by a margin of 73% versus 60%. Notably, however, NSTEMI patients were far less likely to undergo coronary revascularization: 32% of them had percutaneous coronary intervention during their index hospitalization, and 8.7% underwent coronary artery bypass grafting, in contrast to rates of 65.5% for PCI and 8.0% for CABG in the STEMI patients. After adjustment for these and other differences in care, NSTEMI patients actually had a 7% lower risk of long-term mortality than the STEMI group.
• Even after limiting the analysis to the youngest elderly – patients aged 65-74 when their MI occurred – 10-year mortality remained high, at 53%.
• After excluding the 24% of patients who died within 1 year after MI, 10-year mortality was still quite high, at 63%. Dr. Kochar and his coinvestigators chose to reanalyze the data in this way because the 1-year mark is an important time point clinically, since it’s when decisions regarding extended dual-antiplatelet therapy are made.
Patients who underwent coronary revascularization during their index hospitalization had a much-improved long-term prognosis, compared with those with medical management only. The 10-year cumulative mortality rate was 57% in patients who had PCI, identical at 57% in those who received CABG, and 84% in medically managed patients.
Ninety-five percent of patients were discharged on aspirin, 94% on a beta blocker, 81% on a statin, and 73% on clopidogrel. Discharge prescriptions for statins and clopidogrel were more common for the STEMI group. Unfortunately, the CRUSADE registry doesn’t include data on long-term medication adherence or prescription refill rates.
Dr. Kochar named several potential strategies aimed at reducing the high long-term mortality rates in older patients with MI as documented in this study. These include structured efforts to improve adherence to evidence-based medications for secondary prevention, as well as making percutaneous revascularization more widely available for older patients with NSTEMI. He noted that while in 2004-2006, 32% of CRUSADE participants with NSTEMI underwent PCI during their index hospitalization, by 2011-2012 that rate had inched upward only to 36%.
Several physicians commented that the high long-term all-cause mortality rates in older CRUSADE participants may paint a grim picture, in part because the aged face growing risks of cancer and other noncardiovascular competing causes of death. But Dr. Kochar replied that while the lack of information on specific causes of death is a study limitation, he and his coinvestigators are convinced based upon data from other studies that most of the deaths in CRUSADE were cardiovascular in nature.
He reported having no financial conflicts regarding his study.
WASHINGTON – Patients who experience an acute MI at age 65 or older have unsettlingly high 5- and 10-year mortality in community practice settings despite excellent rates of evidence-based medications being prescribed at discharge, Ajar Kochar, MD, reported at the annual meeting of the American College of Cardiology.
This observation is based upon more than 22,000 patients aged 65 years or older treated for an acute MI during 2004-2006 at 344 U.S. hospitals participating in the CRUSADE registry. Their median age at the time of MI was 77 years. But 10-year all-cause mortality remained high even among relatively younger patients aged 65-74 whom one would expect to have a favorable long-term prognosis because they had additional survival-enhancing factors working in their favor, including having undergone coronary revascularization during their index hospitalization and surviving their first year post-MI, observed Dr. Kochar of the Duke Clinical Research Institute in Durham, N.C.
This unmet need will increasingly clamor for attention as the aging of the American population accelerates like a runaway freight train. By 2030, an estimated 20% of Americans will be aged 65 or older. That’s more than 71 million people. And more than half of all MIs occur in individuals above age 65, he noted.
Dr. Kochar presented a CRUSADE analysis which included 19,755 older Americans with a non–ST elevation MI (NSTEMI) and 2,540 with a STEMI. The overall group’s 1-year mortality was 24%, with a 5-year cumulative mortality of 51% and a whopping 10-year mortality of 72%.
According to the Centers for Disease Control and Prevention, the expected additional lifespan of someone who was 65 years old in 2015 is 19 years. In contrast, the median survival of patients in the CRUSADE registry who were 65-69 at the time of their MI was less than half of that, at 8.3 years.
Among the key findings from the CRUSADE analysis:
• Unadjusted 10-year all-cause mortality was significantly greater in patients with NSTEMI than STEMI, by a margin of 73% versus 60%. Notably, however, NSTEMI patients were far less likely to undergo coronary revascularization: 32% of them had percutaneous coronary intervention during their index hospitalization, and 8.7% underwent coronary artery bypass grafting, in contrast to rates of 65.5% for PCI and 8.0% for CABG in the STEMI patients. After adjustment for these and other differences in care, NSTEMI patients actually had a 7% lower risk of long-term mortality than the STEMI group.
• Even after limiting the analysis to the youngest elderly – patients aged 65-74 when their MI occurred – 10-year mortality remained high, at 53%.
• After excluding the 24% of patients who died within 1 year after MI, 10-year mortality was still quite high, at 63%. Dr. Kochar and his coinvestigators chose to reanalyze the data in this way because the 1-year mark is an important time point clinically, since it’s when decisions regarding extended dual-antiplatelet therapy are made.
Patients who underwent coronary revascularization during their index hospitalization had a much-improved long-term prognosis, compared with those with medical management only. The 10-year cumulative mortality rate was 57% in patients who had PCI, identical at 57% in those who received CABG, and 84% in medically managed patients.
Ninety-five percent of patients were discharged on aspirin, 94% on a beta blocker, 81% on a statin, and 73% on clopidogrel. Discharge prescriptions for statins and clopidogrel were more common for the STEMI group. Unfortunately, the CRUSADE registry doesn’t include data on long-term medication adherence or prescription refill rates.
Dr. Kochar named several potential strategies aimed at reducing the high long-term mortality rates in older patients with MI as documented in this study. These include structured efforts to improve adherence to evidence-based medications for secondary prevention, as well as making percutaneous revascularization more widely available for older patients with NSTEMI. He noted that while in 2004-2006, 32% of CRUSADE participants with NSTEMI underwent PCI during their index hospitalization, by 2011-2012 that rate had inched upward only to 36%.
Several physicians commented that the high long-term all-cause mortality rates in older CRUSADE participants may paint a grim picture, in part because the aged face growing risks of cancer and other noncardiovascular competing causes of death. But Dr. Kochar replied that while the lack of information on specific causes of death is a study limitation, he and his coinvestigators are convinced based upon data from other studies that most of the deaths in CRUSADE were cardiovascular in nature.
He reported having no financial conflicts regarding his study.
AT ACC 17
Key clinical point:
Major finding: The 10-year cumulative mortality rate in patients who had an MI at age 65-74 is 53%.
Data source: This was an analysis of 10-year cumulative mortality in more than 22,000 patients aged 65 or older treated for an acute MI during 2004-2006 at 344 U.S. community hospitals participating in the prospective CRUSADE registry.
Disclosures: The study presenter reported having no financial conflicts.
Osimertinib receives full approval for advanced EGFR-mutated NSCLC
The Food and Drug Administration has converted accelerated approval of osimertinib to full approval for the treatment of patients with metastatic epidermal growth factor receptor (EGFR) T790M mutation–positive non–small cell lung cancer (NSCLC), as detected by an FDA-approved test.
Also included in the indication, disease must have progressed on or after EGFR tyrosine kinase inhibitor (TKI) therapy, the FDA said in a statement.
Full approval was based on an improvement in progression-free survival (PFS) in the phase III AURA3 study, which randomized 419 patients (2:1) to receive osimertinib (n = 279) 80 mg orally once daily or platinum-based doublet chemotherapy (n = 140). The hazard ratio for the investigator-assessed PFS was .30 (95% confidence interval: 0.23, 0.41; P less than .001).
The estimated median PFS was 10.1 months in the osimertinib arm and 4.4 months in the chemotherapy arm. Confirmed ORR was 65% (95% CI: 59%, 70%) and 29% (95% CI: 21%, 37%) in the osimertinib and chemotherapy arms, respectively (P less than .0001). Estimated median response durations were 11 months (95% CI: 8.6, 12.6) and 4.2 months (95% CI: 3.9, 5.9) in the osimertinib and chemotherapy arms, respectively, according to the FDA statement.
Overall survival data are immature, the FDA said.
All patients had metastatic EGFR T790M mutation–positive NSCLC, identified by the cobas EGFR mutation test performed in a central laboratory, and progressive disease following first-line EGFR TKI therapy. Patients in the chemotherapy arm received either pemetrexed, 500 mg/m2 with carboplatin AUC5, or pemetrexed, 500mg/m2 with cisplatin 75 mg/m2), on day 1 of every 21-day cycle for up to six cycles followed by pemetrexed maintenance therapy.
The most serious adverse reactions, evaluated in 833 patients receiving osimertinib, were interstitial lung disease/pneumonitis (3.5%), QTc interval prolongation (0.7%), cardiomyopathy (1.9%), and keratitis (0.7%). The most common adverse reactions were diarrhea, rash, dry skin, nail toxicity, and fatigue.
The recommended dose of osimertinib, to be marketed as Tagrisso by AstraZeneca, is 80 mg orally once daily, with or without food, until disease progression or unacceptable toxicity. The presence of an EGFR T790M mutation in a tumor specimen, or plasma specimen (if tumor tissue is unavailable), should be confirmed by an FDA-approved test prior to initiation of treatment.
Full prescribing information is available here.
The Food and Drug Administration has converted accelerated approval of osimertinib to full approval for the treatment of patients with metastatic epidermal growth factor receptor (EGFR) T790M mutation–positive non–small cell lung cancer (NSCLC), as detected by an FDA-approved test.
Also included in the indication, disease must have progressed on or after EGFR tyrosine kinase inhibitor (TKI) therapy, the FDA said in a statement.
Full approval was based on an improvement in progression-free survival (PFS) in the phase III AURA3 study, which randomized 419 patients (2:1) to receive osimertinib (n = 279) 80 mg orally once daily or platinum-based doublet chemotherapy (n = 140). The hazard ratio for the investigator-assessed PFS was .30 (95% confidence interval: 0.23, 0.41; P less than .001).
The estimated median PFS was 10.1 months in the osimertinib arm and 4.4 months in the chemotherapy arm. Confirmed ORR was 65% (95% CI: 59%, 70%) and 29% (95% CI: 21%, 37%) in the osimertinib and chemotherapy arms, respectively (P less than .0001). Estimated median response durations were 11 months (95% CI: 8.6, 12.6) and 4.2 months (95% CI: 3.9, 5.9) in the osimertinib and chemotherapy arms, respectively, according to the FDA statement.
Overall survival data are immature, the FDA said.
All patients had metastatic EGFR T790M mutation–positive NSCLC, identified by the cobas EGFR mutation test performed in a central laboratory, and progressive disease following first-line EGFR TKI therapy. Patients in the chemotherapy arm received either pemetrexed, 500 mg/m2 with carboplatin AUC5, or pemetrexed, 500mg/m2 with cisplatin 75 mg/m2), on day 1 of every 21-day cycle for up to six cycles followed by pemetrexed maintenance therapy.
The most serious adverse reactions, evaluated in 833 patients receiving osimertinib, were interstitial lung disease/pneumonitis (3.5%), QTc interval prolongation (0.7%), cardiomyopathy (1.9%), and keratitis (0.7%). The most common adverse reactions were diarrhea, rash, dry skin, nail toxicity, and fatigue.
The recommended dose of osimertinib, to be marketed as Tagrisso by AstraZeneca, is 80 mg orally once daily, with or without food, until disease progression or unacceptable toxicity. The presence of an EGFR T790M mutation in a tumor specimen, or plasma specimen (if tumor tissue is unavailable), should be confirmed by an FDA-approved test prior to initiation of treatment.
Full prescribing information is available here.
The Food and Drug Administration has converted accelerated approval of osimertinib to full approval for the treatment of patients with metastatic epidermal growth factor receptor (EGFR) T790M mutation–positive non–small cell lung cancer (NSCLC), as detected by an FDA-approved test.
Also included in the indication, disease must have progressed on or after EGFR tyrosine kinase inhibitor (TKI) therapy, the FDA said in a statement.
Full approval was based on an improvement in progression-free survival (PFS) in the phase III AURA3 study, which randomized 419 patients (2:1) to receive osimertinib (n = 279) 80 mg orally once daily or platinum-based doublet chemotherapy (n = 140). The hazard ratio for the investigator-assessed PFS was .30 (95% confidence interval: 0.23, 0.41; P less than .001).
The estimated median PFS was 10.1 months in the osimertinib arm and 4.4 months in the chemotherapy arm. Confirmed ORR was 65% (95% CI: 59%, 70%) and 29% (95% CI: 21%, 37%) in the osimertinib and chemotherapy arms, respectively (P less than .0001). Estimated median response durations were 11 months (95% CI: 8.6, 12.6) and 4.2 months (95% CI: 3.9, 5.9) in the osimertinib and chemotherapy arms, respectively, according to the FDA statement.
Overall survival data are immature, the FDA said.
All patients had metastatic EGFR T790M mutation–positive NSCLC, identified by the cobas EGFR mutation test performed in a central laboratory, and progressive disease following first-line EGFR TKI therapy. Patients in the chemotherapy arm received either pemetrexed, 500 mg/m2 with carboplatin AUC5, or pemetrexed, 500mg/m2 with cisplatin 75 mg/m2), on day 1 of every 21-day cycle for up to six cycles followed by pemetrexed maintenance therapy.
The most serious adverse reactions, evaluated in 833 patients receiving osimertinib, were interstitial lung disease/pneumonitis (3.5%), QTc interval prolongation (0.7%), cardiomyopathy (1.9%), and keratitis (0.7%). The most common adverse reactions were diarrhea, rash, dry skin, nail toxicity, and fatigue.
The recommended dose of osimertinib, to be marketed as Tagrisso by AstraZeneca, is 80 mg orally once daily, with or without food, until disease progression or unacceptable toxicity. The presence of an EGFR T790M mutation in a tumor specimen, or plasma specimen (if tumor tissue is unavailable), should be confirmed by an FDA-approved test prior to initiation of treatment.
Full prescribing information is available here.
Save the Date: Heart Valve Summit: Medical, Surgical and Interventional Decision Making
The American College of Cardiology and the American Association for Thoracic Surgery are once again partnering to bring together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease.
October 5-7, 2017
Radisson Blu Aqua Hotel
Chicago, IL, USA
Program Overview
With the tradition of interactivity and practical decision making, the unique Heart Valve Summit is designed to engage participants in discussions, debates and potential controversies surrounding real-world cases with renowned faculty on the cutting edge of clinically relevant data for valvular heart disease management.
This interdisciplinary course emphasizes clinical decision making while combining the most relevant medical, surgical and interventional options for patient care. Tools for management are rapidly advancing and can significantly impact the entire care team. Breakout sessions for cardiologists, cardiac surgeons, nurses and physician assistants are designed to help specialists manage their unique challenges from a team perspective.
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
The American College of Cardiology and the American Association for Thoracic Surgery are once again partnering to bring together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease.
October 5-7, 2017
Radisson Blu Aqua Hotel
Chicago, IL, USA
Program Overview
With the tradition of interactivity and practical decision making, the unique Heart Valve Summit is designed to engage participants in discussions, debates and potential controversies surrounding real-world cases with renowned faculty on the cutting edge of clinically relevant data for valvular heart disease management.
This interdisciplinary course emphasizes clinical decision making while combining the most relevant medical, surgical and interventional options for patient care. Tools for management are rapidly advancing and can significantly impact the entire care team. Breakout sessions for cardiologists, cardiac surgeons, nurses and physician assistants are designed to help specialists manage their unique challenges from a team perspective.
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
The American College of Cardiology and the American Association for Thoracic Surgery are once again partnering to bring together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease.
October 5-7, 2017
Radisson Blu Aqua Hotel
Chicago, IL, USA
Program Overview
With the tradition of interactivity and practical decision making, the unique Heart Valve Summit is designed to engage participants in discussions, debates and potential controversies surrounding real-world cases with renowned faculty on the cutting edge of clinically relevant data for valvular heart disease management.
This interdisciplinary course emphasizes clinical decision making while combining the most relevant medical, surgical and interventional options for patient care. Tools for management are rapidly advancing and can significantly impact the entire care team. Breakout sessions for cardiologists, cardiac surgeons, nurses and physician assistants are designed to help specialists manage their unique challenges from a team perspective.
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
Join us at the AATS Innovation Summit
Ignite your spirit for innovation at the 2017 AATS Innovation Summit.
Saturday, April 29, 2017
Boston Marriott Copley Place Hotel
Boston, MA
Course Director
W. Randolph Chitwood, Jr.
Program Overview
This one-day program will assist cardiothoracic surgeons in developing new clinically applicable technology by obtaining the cross-specialty knowledge needed for novel idea generation, protecting intellectual property, developmental funding, clinical trials, regulatory pathways and industry relations.
Target Audience
The summit is aimed at cardiothoracic surgeons who are interested in gaining the knowledge and tools to develop new clinically applicable technology. Attendees will craft new ideas with a long-term focus on creating partnerships with industry and incubators leading to enduring pathways for surgeons to become the architects of the future for cardiothoracic therapy.
Ignite your spirit for innovation at the 2017 AATS Innovation Summit.
Saturday, April 29, 2017
Boston Marriott Copley Place Hotel
Boston, MA
Course Director
W. Randolph Chitwood, Jr.
Program Overview
This one-day program will assist cardiothoracic surgeons in developing new clinically applicable technology by obtaining the cross-specialty knowledge needed for novel idea generation, protecting intellectual property, developmental funding, clinical trials, regulatory pathways and industry relations.
Target Audience
The summit is aimed at cardiothoracic surgeons who are interested in gaining the knowledge and tools to develop new clinically applicable technology. Attendees will craft new ideas with a long-term focus on creating partnerships with industry and incubators leading to enduring pathways for surgeons to become the architects of the future for cardiothoracic therapy.
Ignite your spirit for innovation at the 2017 AATS Innovation Summit.
Saturday, April 29, 2017
Boston Marriott Copley Place Hotel
Boston, MA
Course Director
W. Randolph Chitwood, Jr.
Program Overview
This one-day program will assist cardiothoracic surgeons in developing new clinically applicable technology by obtaining the cross-specialty knowledge needed for novel idea generation, protecting intellectual property, developmental funding, clinical trials, regulatory pathways and industry relations.
Target Audience
The summit is aimed at cardiothoracic surgeons who are interested in gaining the knowledge and tools to develop new clinically applicable technology. Attendees will craft new ideas with a long-term focus on creating partnerships with industry and incubators leading to enduring pathways for surgeons to become the architects of the future for cardiothoracic therapy.
Register for the AATS Mitral Conclave
Registration and housing information is available for AATS Mitral Conclave, which immediately precedes the AATS Centennial. Take a look at the preliminary program that is available online to see the many interesting and novel sessions scheduled for the meeting.
Thursday, April 27 – Friday, April 28, 2017
New York Hilton Midtown Hotel
New York, NY
Program Overview
The AATS Mitral Conclave will bring the world's leading figures in mitral valve disease together for two days to discuss the latest information regarding management guidelines, imaging, pathology, minimally invasive and percutaneous approaches, surgical techniques, devices, and long-term results. Faculty will present the latest available data, techniques, and state of the art reviews, supplemented by abstract and video presentations selected by the program committee from submitted original work.
Course Director
David H. Adams
Program Committee
Anelechi C. Anyanwu
Tirone E. David
Pedro J. del Nido
Gilles D. Dreyfus
Khalil Fattouch
D. Craig Miller
Rakesh M. Suri
Vinod H. Thourani
View the preliminary program, registration & housing information
Registration and housing information is available for AATS Mitral Conclave, which immediately precedes the AATS Centennial. Take a look at the preliminary program that is available online to see the many interesting and novel sessions scheduled for the meeting.
Thursday, April 27 – Friday, April 28, 2017
New York Hilton Midtown Hotel
New York, NY
Program Overview
The AATS Mitral Conclave will bring the world's leading figures in mitral valve disease together for two days to discuss the latest information regarding management guidelines, imaging, pathology, minimally invasive and percutaneous approaches, surgical techniques, devices, and long-term results. Faculty will present the latest available data, techniques, and state of the art reviews, supplemented by abstract and video presentations selected by the program committee from submitted original work.
Course Director
David H. Adams
Program Committee
Anelechi C. Anyanwu
Tirone E. David
Pedro J. del Nido
Gilles D. Dreyfus
Khalil Fattouch
D. Craig Miller
Rakesh M. Suri
Vinod H. Thourani
View the preliminary program, registration & housing information
Registration and housing information is available for AATS Mitral Conclave, which immediately precedes the AATS Centennial. Take a look at the preliminary program that is available online to see the many interesting and novel sessions scheduled for the meeting.
Thursday, April 27 – Friday, April 28, 2017
New York Hilton Midtown Hotel
New York, NY
Program Overview
The AATS Mitral Conclave will bring the world's leading figures in mitral valve disease together for two days to discuss the latest information regarding management guidelines, imaging, pathology, minimally invasive and percutaneous approaches, surgical techniques, devices, and long-term results. Faculty will present the latest available data, techniques, and state of the art reviews, supplemented by abstract and video presentations selected by the program committee from submitted original work.
Course Director
David H. Adams
Program Committee
Anelechi C. Anyanwu
Tirone E. David
Pedro J. del Nido
Gilles D. Dreyfus
Khalil Fattouch
D. Craig Miller
Rakesh M. Suri
Vinod H. Thourani
View the preliminary program, registration & housing information
See you at AATS Week 2017
Join the world’s foremost cardiothoracic surgery scientists and medical professionals during this once-in-a-lifetime week of meetings. Celebrate the history of the American Association for Thoracic Surgery and our specialty through unique events and activities while continuing your commitment to life-long learning at three incredible events.
AATS Mitral Conclave 2017
April 27-28, 2017
New York Hilton Midtown
New York, NY
AATS Innovation Summit
April 29, 2017
Boston Marriott Copley Place Hotel
Boston, MA
AATS Centennial
April 29 – May 3, 2017
Boston Hynes Convention Center
Boston, MA
Register for AATS Week 2017 today & receive a $100 discount off the AATS Mitral Conclave registration fee.
Join the world’s foremost cardiothoracic surgery scientists and medical professionals during this once-in-a-lifetime week of meetings. Celebrate the history of the American Association for Thoracic Surgery and our specialty through unique events and activities while continuing your commitment to life-long learning at three incredible events.
AATS Mitral Conclave 2017
April 27-28, 2017
New York Hilton Midtown
New York, NY
AATS Innovation Summit
April 29, 2017
Boston Marriott Copley Place Hotel
Boston, MA
AATS Centennial
April 29 – May 3, 2017
Boston Hynes Convention Center
Boston, MA
Register for AATS Week 2017 today & receive a $100 discount off the AATS Mitral Conclave registration fee.
Join the world’s foremost cardiothoracic surgery scientists and medical professionals during this once-in-a-lifetime week of meetings. Celebrate the history of the American Association for Thoracic Surgery and our specialty through unique events and activities while continuing your commitment to life-long learning at three incredible events.
AATS Mitral Conclave 2017
April 27-28, 2017
New York Hilton Midtown
New York, NY
AATS Innovation Summit
April 29, 2017
Boston Marriott Copley Place Hotel
Boston, MA
AATS Centennial
April 29 – May 3, 2017
Boston Hynes Convention Center
Boston, MA
Register for AATS Week 2017 today & receive a $100 discount off the AATS Mitral Conclave registration fee.
Moving or starting a practice? Consider Iowa
The federal government may or may not believe in global warming, but when it comes to states’ medical practice climates, Iowa trumps them all, according to the personal finance website WalletHub.
The Hawkeye State came out on top of WalletHub’s list of the Best States to Practice Medicine for 2017 with 68.7 out of a possible 100 points, while New York finished 51st (Washington, D.C., was 50th) with 28.5 points. Minnesota is the second-best state for physicians, followed by Idaho, Wisconsin, and Kansas. The rest of the bottom five included New Jersey at 49th, Maryland at 48th, and Rhode Island at 47th, WalletHub reported.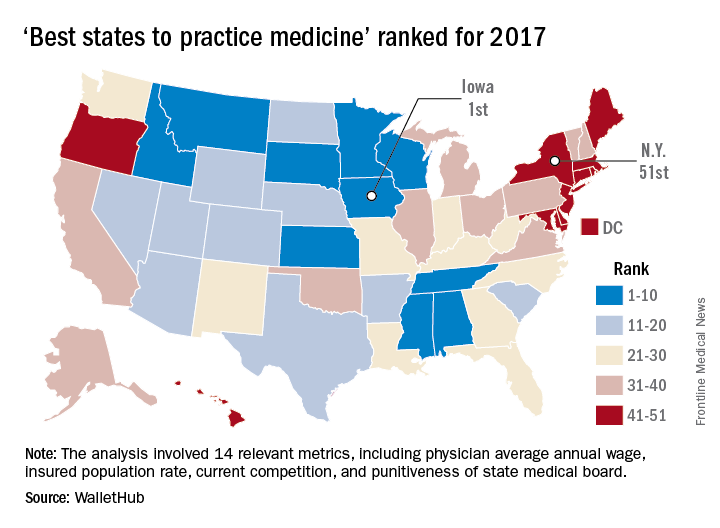
WalletHub compared the 50 states and Washington using 14 different metrics across two broad categories: “opportunity and competition” (70 points) and “medical environment” (30 points). Metrics included physicians’ average annual wage (adjusted for cost of living), hospitals per capita, quality of public hospital system, and annual malpractice liability insurance rate.
The federal government may or may not believe in global warming, but when it comes to states’ medical practice climates, Iowa trumps them all, according to the personal finance website WalletHub.
The Hawkeye State came out on top of WalletHub’s list of the Best States to Practice Medicine for 2017 with 68.7 out of a possible 100 points, while New York finished 51st (Washington, D.C., was 50th) with 28.5 points. Minnesota is the second-best state for physicians, followed by Idaho, Wisconsin, and Kansas. The rest of the bottom five included New Jersey at 49th, Maryland at 48th, and Rhode Island at 47th, WalletHub reported.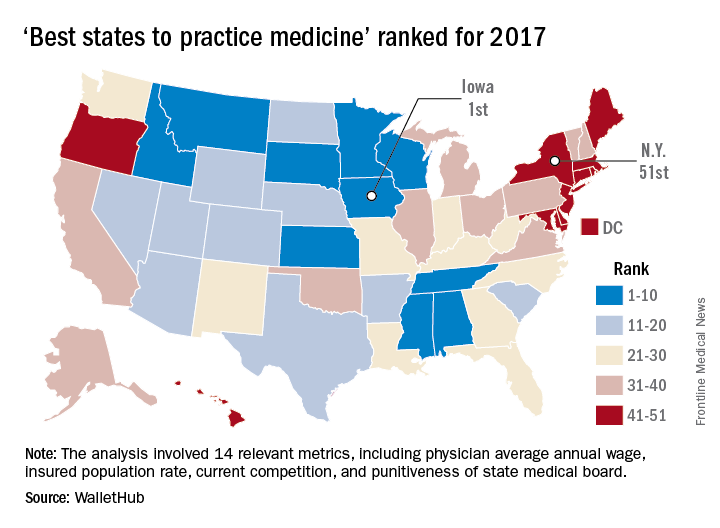
WalletHub compared the 50 states and Washington using 14 different metrics across two broad categories: “opportunity and competition” (70 points) and “medical environment” (30 points). Metrics included physicians’ average annual wage (adjusted for cost of living), hospitals per capita, quality of public hospital system, and annual malpractice liability insurance rate.
The federal government may or may not believe in global warming, but when it comes to states’ medical practice climates, Iowa trumps them all, according to the personal finance website WalletHub.
The Hawkeye State came out on top of WalletHub’s list of the Best States to Practice Medicine for 2017 with 68.7 out of a possible 100 points, while New York finished 51st (Washington, D.C., was 50th) with 28.5 points. Minnesota is the second-best state for physicians, followed by Idaho, Wisconsin, and Kansas. The rest of the bottom five included New Jersey at 49th, Maryland at 48th, and Rhode Island at 47th, WalletHub reported.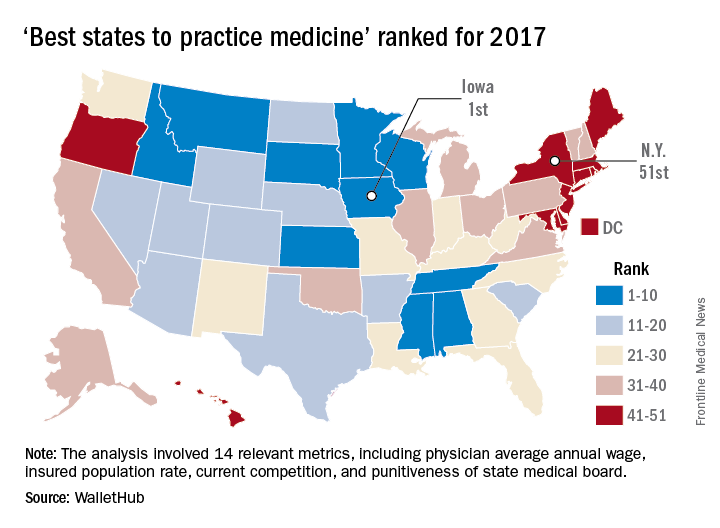
WalletHub compared the 50 states and Washington using 14 different metrics across two broad categories: “opportunity and competition” (70 points) and “medical environment” (30 points). Metrics included physicians’ average annual wage (adjusted for cost of living), hospitals per capita, quality of public hospital system, and annual malpractice liability insurance rate.
BEST PRACTICES: Reinforced Reload Stapling in the Thoracic Space
Air leaks have been reported to be frequent and difficult-to-manage sequelae in some lung resection procedures. Click here to learn about a new device being used in the thoracic space
Author:
Mark Ellis Ginsburg,
MD, FACS
Associate Clinical Professor of Surgery
Division of Cardiothoracic Surgery
Columbia University Medical Center
New York, NY
Faculty Disclosure: Dr. Ginsburg has received compensation from Medtronic Inc. for his participation in this article. He has no other conflicts of interest to disclose.
Air leaks have been reported to be frequent and difficult-to-manage sequelae in some lung resection procedures. Click here to learn about a new device being used in the thoracic space
Author:
Mark Ellis Ginsburg,
MD, FACS
Associate Clinical Professor of Surgery
Division of Cardiothoracic Surgery
Columbia University Medical Center
New York, NY
Faculty Disclosure: Dr. Ginsburg has received compensation from Medtronic Inc. for his participation in this article. He has no other conflicts of interest to disclose.
Air leaks have been reported to be frequent and difficult-to-manage sequelae in some lung resection procedures. Click here to learn about a new device being used in the thoracic space
Author:
Mark Ellis Ginsburg,
MD, FACS
Associate Clinical Professor of Surgery
Division of Cardiothoracic Surgery
Columbia University Medical Center
New York, NY
Faculty Disclosure: Dr. Ginsburg has received compensation from Medtronic Inc. for his participation in this article. He has no other conflicts of interest to disclose.
House leaders ‘came up short’ in effort to kill Obamacare
Despite days of intense negotiations and last-minute concessions to win over wavering GOP conservatives and moderates, House Republican leaders Friday failed to secure enough support to pass their plan to repeal and replace the Affordable Care Act.
House Speaker Paul Ryan pulled the bill from consideration after he rushed to the White House to tell President Donald Trump that there weren’t the 216 votes necessary for passage.
“We came really close today, but we came up short,” he told reporters at a hastily called news conference.
When pressed about what happens to the federal health law, he added, “Obamacare is the law of the land. … We’re going to be living with Obamacare for the foreseeable future.”
President Trump laid the blame at the feet of Democrats, complaining that not one was willing to help Republicans on the measure, and he warned again that the Obamacare insurance markets are in serious danger. “Bad things are going to happen to Obamacare,” he told reporters at the White House. “There’s not much you can do to help it. I’ve been saying that for a year and a half. I said, look, eventually, it’s not sustainable. The insurance companies are leaving.”
But he said the collapse of the bill might allow Republicans and Democrats to work on a replacement. “I honestly believe the Democrats will come to us and say, ‘Look, let’s get together and get a great health care bill or plan that’s really great for the people of our country,’” he said.
Mr. Ryan originally had hoped to hold a floor vote on the measure Thursday – timed to coincide with the 7th anniversary of the ACA – but decided to delay that effort because GOP leaders didn’t have enough “yes” votes. The House was in session Friday, before his announcement, while members debated the bill.
House Democratic leader Nancy Pelosi (Calif.) said the speaker’s decision to pull the bill “is pretty exciting for us … a victory for the Affordable Care Act, more importantly for the American people.”
The legislation was damaged by a variety of issues raised by competing factions of the party. Many members were nervous about reports by the Congressional Budget Office showing that the bill would lead eventually to 24 million people losing insurance, while some moderate Republicans worried that ending the ACA’s Medicaid expansion would hurt low-income Americans.
At the same time, conservatives, especially the hard-right House Freedom Caucus that often has needled party leaders, complained that the bill kept too much of the ACA structure in place. They wanted a straight repeal of Obamacare, but party leaders said that couldn’t pass the Senate, where Republicans don’t have enough votes to stop a filibuster. They were hoping to use a complicated legislative strategy called budget reconciliation that would allow them to repeal parts of the ACA that only affect federal spending.
The decision came after a chaotic week of negotiations, as party leaders sought to woo more conservatives. The president lobbied 120 members through personal meetings or phone calls, according to a count provided Friday by his spokesman, Sean Spicer. “The president and the team here have left everything on the field,” Mr. Spicer said.
On Thursday evening, Mr. Trump dispatched Office of Management and Budget Director Mick Mulvaney to tell his former House GOP colleagues that the president wanted a vote on Friday. It was time to move on to other priorities, including tax reform, he told House Republicans.
“He said the president needs this, the president has said he wants a vote tomorrow, up or down. If for any reason it goes down, we’re just going to move forward with additional parts of his agenda. This is our moment in time,” Rep. Chris Collins (R-N.Y.), a loyal Trump ally, told reporters late Thursday. “If it doesn’t pass, we’re moving beyond health care. … We are done negotiating.”
Trump’s edict clearly irked some lawmakers, including the Freedom Caucus chairman, Rep. Mark Meadows (R-N.C), whose group of more than two dozen members represented the strongest bloc against the measure.
“Anytime you don’t have 216 votes, negotiations are not totally over,” he told reporters who had surrounded him in a Capitol basement hallway as he headed in to the party’s caucus meeting.
President Trump, Speaker Ryan, and other GOP lawmakers tweaked their initial package in a variety of ways to win over both conservatives and moderates. But every time one change was made to win votes in one camp, it repelled support in another.
The White House on Thursday accepted conservatives’ demands that the legislation strip federal guarantees of essential health benefits from insurance policies. But that was another problem for moderates, and Democrats suggested the provision would not survive in the Senate.
Republican moderates in the House – as well as the Senate – objected to the bill’s provisions that would shift Medicaid from an open-ended entitlement to a set amount of funding for states that also would give governors and state lawmakers more flexibility over the program. Moderates also were concerned that the package’s tax credits would not be generous enough to help older Americans – who could be charged five times more for coverage than would their younger counterparts – afford coverage.
The House package also lost the support of key GOP allies, including the Club for Growth and Heritage Action. Physician, patient and hospital groups also opposed it.
But Mr. Ryan’s comments made clear how difficult this decision was. “This is a disappointing day for us,” he said. “Doing big things is hard. All of us. All of us – myself included – we will need time to reflect on how we got to this moment, what we could have done to do it better.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Despite days of intense negotiations and last-minute concessions to win over wavering GOP conservatives and moderates, House Republican leaders Friday failed to secure enough support to pass their plan to repeal and replace the Affordable Care Act.
House Speaker Paul Ryan pulled the bill from consideration after he rushed to the White House to tell President Donald Trump that there weren’t the 216 votes necessary for passage.
“We came really close today, but we came up short,” he told reporters at a hastily called news conference.
When pressed about what happens to the federal health law, he added, “Obamacare is the law of the land. … We’re going to be living with Obamacare for the foreseeable future.”
President Trump laid the blame at the feet of Democrats, complaining that not one was willing to help Republicans on the measure, and he warned again that the Obamacare insurance markets are in serious danger. “Bad things are going to happen to Obamacare,” he told reporters at the White House. “There’s not much you can do to help it. I’ve been saying that for a year and a half. I said, look, eventually, it’s not sustainable. The insurance companies are leaving.”
But he said the collapse of the bill might allow Republicans and Democrats to work on a replacement. “I honestly believe the Democrats will come to us and say, ‘Look, let’s get together and get a great health care bill or plan that’s really great for the people of our country,’” he said.
Mr. Ryan originally had hoped to hold a floor vote on the measure Thursday – timed to coincide with the 7th anniversary of the ACA – but decided to delay that effort because GOP leaders didn’t have enough “yes” votes. The House was in session Friday, before his announcement, while members debated the bill.
House Democratic leader Nancy Pelosi (Calif.) said the speaker’s decision to pull the bill “is pretty exciting for us … a victory for the Affordable Care Act, more importantly for the American people.”
The legislation was damaged by a variety of issues raised by competing factions of the party. Many members were nervous about reports by the Congressional Budget Office showing that the bill would lead eventually to 24 million people losing insurance, while some moderate Republicans worried that ending the ACA’s Medicaid expansion would hurt low-income Americans.
At the same time, conservatives, especially the hard-right House Freedom Caucus that often has needled party leaders, complained that the bill kept too much of the ACA structure in place. They wanted a straight repeal of Obamacare, but party leaders said that couldn’t pass the Senate, where Republicans don’t have enough votes to stop a filibuster. They were hoping to use a complicated legislative strategy called budget reconciliation that would allow them to repeal parts of the ACA that only affect federal spending.
The decision came after a chaotic week of negotiations, as party leaders sought to woo more conservatives. The president lobbied 120 members through personal meetings or phone calls, according to a count provided Friday by his spokesman, Sean Spicer. “The president and the team here have left everything on the field,” Mr. Spicer said.
On Thursday evening, Mr. Trump dispatched Office of Management and Budget Director Mick Mulvaney to tell his former House GOP colleagues that the president wanted a vote on Friday. It was time to move on to other priorities, including tax reform, he told House Republicans.
“He said the president needs this, the president has said he wants a vote tomorrow, up or down. If for any reason it goes down, we’re just going to move forward with additional parts of his agenda. This is our moment in time,” Rep. Chris Collins (R-N.Y.), a loyal Trump ally, told reporters late Thursday. “If it doesn’t pass, we’re moving beyond health care. … We are done negotiating.”
Trump’s edict clearly irked some lawmakers, including the Freedom Caucus chairman, Rep. Mark Meadows (R-N.C), whose group of more than two dozen members represented the strongest bloc against the measure.
“Anytime you don’t have 216 votes, negotiations are not totally over,” he told reporters who had surrounded him in a Capitol basement hallway as he headed in to the party’s caucus meeting.
President Trump, Speaker Ryan, and other GOP lawmakers tweaked their initial package in a variety of ways to win over both conservatives and moderates. But every time one change was made to win votes in one camp, it repelled support in another.
The White House on Thursday accepted conservatives’ demands that the legislation strip federal guarantees of essential health benefits from insurance policies. But that was another problem for moderates, and Democrats suggested the provision would not survive in the Senate.
Republican moderates in the House – as well as the Senate – objected to the bill’s provisions that would shift Medicaid from an open-ended entitlement to a set amount of funding for states that also would give governors and state lawmakers more flexibility over the program. Moderates also were concerned that the package’s tax credits would not be generous enough to help older Americans – who could be charged five times more for coverage than would their younger counterparts – afford coverage.
The House package also lost the support of key GOP allies, including the Club for Growth and Heritage Action. Physician, patient and hospital groups also opposed it.
But Mr. Ryan’s comments made clear how difficult this decision was. “This is a disappointing day for us,” he said. “Doing big things is hard. All of us. All of us – myself included – we will need time to reflect on how we got to this moment, what we could have done to do it better.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Despite days of intense negotiations and last-minute concessions to win over wavering GOP conservatives and moderates, House Republican leaders Friday failed to secure enough support to pass their plan to repeal and replace the Affordable Care Act.
House Speaker Paul Ryan pulled the bill from consideration after he rushed to the White House to tell President Donald Trump that there weren’t the 216 votes necessary for passage.
“We came really close today, but we came up short,” he told reporters at a hastily called news conference.
When pressed about what happens to the federal health law, he added, “Obamacare is the law of the land. … We’re going to be living with Obamacare for the foreseeable future.”
President Trump laid the blame at the feet of Democrats, complaining that not one was willing to help Republicans on the measure, and he warned again that the Obamacare insurance markets are in serious danger. “Bad things are going to happen to Obamacare,” he told reporters at the White House. “There’s not much you can do to help it. I’ve been saying that for a year and a half. I said, look, eventually, it’s not sustainable. The insurance companies are leaving.”
But he said the collapse of the bill might allow Republicans and Democrats to work on a replacement. “I honestly believe the Democrats will come to us and say, ‘Look, let’s get together and get a great health care bill or plan that’s really great for the people of our country,’” he said.
Mr. Ryan originally had hoped to hold a floor vote on the measure Thursday – timed to coincide with the 7th anniversary of the ACA – but decided to delay that effort because GOP leaders didn’t have enough “yes” votes. The House was in session Friday, before his announcement, while members debated the bill.
House Democratic leader Nancy Pelosi (Calif.) said the speaker’s decision to pull the bill “is pretty exciting for us … a victory for the Affordable Care Act, more importantly for the American people.”
The legislation was damaged by a variety of issues raised by competing factions of the party. Many members were nervous about reports by the Congressional Budget Office showing that the bill would lead eventually to 24 million people losing insurance, while some moderate Republicans worried that ending the ACA’s Medicaid expansion would hurt low-income Americans.
At the same time, conservatives, especially the hard-right House Freedom Caucus that often has needled party leaders, complained that the bill kept too much of the ACA structure in place. They wanted a straight repeal of Obamacare, but party leaders said that couldn’t pass the Senate, where Republicans don’t have enough votes to stop a filibuster. They were hoping to use a complicated legislative strategy called budget reconciliation that would allow them to repeal parts of the ACA that only affect federal spending.
The decision came after a chaotic week of negotiations, as party leaders sought to woo more conservatives. The president lobbied 120 members through personal meetings or phone calls, according to a count provided Friday by his spokesman, Sean Spicer. “The president and the team here have left everything on the field,” Mr. Spicer said.
On Thursday evening, Mr. Trump dispatched Office of Management and Budget Director Mick Mulvaney to tell his former House GOP colleagues that the president wanted a vote on Friday. It was time to move on to other priorities, including tax reform, he told House Republicans.
“He said the president needs this, the president has said he wants a vote tomorrow, up or down. If for any reason it goes down, we’re just going to move forward with additional parts of his agenda. This is our moment in time,” Rep. Chris Collins (R-N.Y.), a loyal Trump ally, told reporters late Thursday. “If it doesn’t pass, we’re moving beyond health care. … We are done negotiating.”
Trump’s edict clearly irked some lawmakers, including the Freedom Caucus chairman, Rep. Mark Meadows (R-N.C), whose group of more than two dozen members represented the strongest bloc against the measure.
“Anytime you don’t have 216 votes, negotiations are not totally over,” he told reporters who had surrounded him in a Capitol basement hallway as he headed in to the party’s caucus meeting.
President Trump, Speaker Ryan, and other GOP lawmakers tweaked their initial package in a variety of ways to win over both conservatives and moderates. But every time one change was made to win votes in one camp, it repelled support in another.
The White House on Thursday accepted conservatives’ demands that the legislation strip federal guarantees of essential health benefits from insurance policies. But that was another problem for moderates, and Democrats suggested the provision would not survive in the Senate.
Republican moderates in the House – as well as the Senate – objected to the bill’s provisions that would shift Medicaid from an open-ended entitlement to a set amount of funding for states that also would give governors and state lawmakers more flexibility over the program. Moderates also were concerned that the package’s tax credits would not be generous enough to help older Americans – who could be charged five times more for coverage than would their younger counterparts – afford coverage.
The House package also lost the support of key GOP allies, including the Club for Growth and Heritage Action. Physician, patient and hospital groups also opposed it.
But Mr. Ryan’s comments made clear how difficult this decision was. “This is a disappointing day for us,” he said. “Doing big things is hard. All of us. All of us – myself included – we will need time to reflect on how we got to this moment, what we could have done to do it better.”
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
ACGME finalizes return of trainees’ 24-hour max shift
First-year residents will once again be permitted to work up to 24 consecutive hours following a reversal of a rule implemented in 2011 that restricted them to 16 hours, the Accreditation Council for Graduate Medical Education (ACGME) announced.
According to a memo issued by the ACGME March 10, 2017, the change reverting back to the 24-hour ceiling was evidence based.
“The preponderance of the evidence from a number of studies conducted after the current 16-hour cap was implemented in 2011 suggests that it may not have had an incremental benefit in patient safety, and that there might be significant negative impacts to the quality of physician education and professional development,” the memo states. The work week is still capped at 80 hours worked per week, with 1 day free from clinical experience or education in 7, and in-house call no more frequent than every third night.
An ACGME task force determined “that the hypothesized benefits associated with the changes made to first-year resident scheduled hours in 2011 have not been realized, and the disruption of team-based care and supervisory systems has had a significant negative impact on the professional education of the first-year resident, and the effectiveness of care delivery of the team as a whole.”
Sharmila Dissanaike, MD, FACS, chair and professor of surgery at Texas Tech University, Lubbock, said in an interview that the change back to a 24-hour ceiling provides “an increased flexibility for all residents in order to allow completion of immediate patient care responsibilities, such as finishing an operation, and ensure smooth handoffs. Both of these should improve work flow for both trainees and supervisors.”
Mark A. Malangoni, MD, FACS, associate executive director of the American Board of Surgery, said he believes the change back to 24 hours is a positive thing.
“The 16-hour requirement posed a lot of scheduling problems,” he said in an interview. “In essence, what it meant was you had residents that either couldn’t take call or they did take call, it was very limited in what they could do.”
Complicating the issue of time is the nature of what needs to be taught to residents.
“What has definitely changed is the breadth of knowledge and repertoire of technical skills that must be learned by today’s residents,” Dr. Dissanaike said. “As scientific knowledge and technical capabilities expand, there is ever more to learn and increasingly less time in which to learn it.”
Dr. Malangoni added that the time restraints didn’t allow for residents to see the natural progression of the patient’s condition. “You don’t have the chance to continue to assess that over a longer period of time,” he said. “That is really important in learning when to operate on someone, but also when not to operate on someone because they will get better without an operation.”
Compounding that is a greater need for reporting to meet regulatory requirements.
“Concurrently, we have increased requirements for documentation and clerical tasks, and reduced time available to do it,” Dr. Dissanaike continued. “All of this has led to a severe ‘work-compression’ for the modern resident, and I suspect the high rates of burnout and depression that are being reported in many specialties are at least partly a result of this phenomenon.”
That being said, Dr. Dissanaike was quick to add that this latest change should not be considered a “final solution” and that there are “many ongoing issues around resident fatigue, as well as adequacy of educational experience that still need to be addressed.”
Dr. Malangoni added that residents need to be more mindful and take more responsibility for their own health and well-being.
“I think what residents need to understand is they are really in charge of their own well-being. Making that point is really a key,” he said. “So it’s not only what you do while you are in the hospital, but you are also responsible for what you do when you are not in the hospital. ACGME cannot regulate what people do in their free time. If you work a 24-hour shift and you decide you are not going to sleep the next day for whatever reason, your well-being is likely not going to be what you want it to be and what, I think, your patients want it to be.”
First-year residents will once again be permitted to work up to 24 consecutive hours following a reversal of a rule implemented in 2011 that restricted them to 16 hours, the Accreditation Council for Graduate Medical Education (ACGME) announced.
According to a memo issued by the ACGME March 10, 2017, the change reverting back to the 24-hour ceiling was evidence based.
“The preponderance of the evidence from a number of studies conducted after the current 16-hour cap was implemented in 2011 suggests that it may not have had an incremental benefit in patient safety, and that there might be significant negative impacts to the quality of physician education and professional development,” the memo states. The work week is still capped at 80 hours worked per week, with 1 day free from clinical experience or education in 7, and in-house call no more frequent than every third night.
An ACGME task force determined “that the hypothesized benefits associated with the changes made to first-year resident scheduled hours in 2011 have not been realized, and the disruption of team-based care and supervisory systems has had a significant negative impact on the professional education of the first-year resident, and the effectiveness of care delivery of the team as a whole.”
Sharmila Dissanaike, MD, FACS, chair and professor of surgery at Texas Tech University, Lubbock, said in an interview that the change back to a 24-hour ceiling provides “an increased flexibility for all residents in order to allow completion of immediate patient care responsibilities, such as finishing an operation, and ensure smooth handoffs. Both of these should improve work flow for both trainees and supervisors.”
Mark A. Malangoni, MD, FACS, associate executive director of the American Board of Surgery, said he believes the change back to 24 hours is a positive thing.
“The 16-hour requirement posed a lot of scheduling problems,” he said in an interview. “In essence, what it meant was you had residents that either couldn’t take call or they did take call, it was very limited in what they could do.”
Complicating the issue of time is the nature of what needs to be taught to residents.
“What has definitely changed is the breadth of knowledge and repertoire of technical skills that must be learned by today’s residents,” Dr. Dissanaike said. “As scientific knowledge and technical capabilities expand, there is ever more to learn and increasingly less time in which to learn it.”
Dr. Malangoni added that the time restraints didn’t allow for residents to see the natural progression of the patient’s condition. “You don’t have the chance to continue to assess that over a longer period of time,” he said. “That is really important in learning when to operate on someone, but also when not to operate on someone because they will get better without an operation.”
Compounding that is a greater need for reporting to meet regulatory requirements.
“Concurrently, we have increased requirements for documentation and clerical tasks, and reduced time available to do it,” Dr. Dissanaike continued. “All of this has led to a severe ‘work-compression’ for the modern resident, and I suspect the high rates of burnout and depression that are being reported in many specialties are at least partly a result of this phenomenon.”
That being said, Dr. Dissanaike was quick to add that this latest change should not be considered a “final solution” and that there are “many ongoing issues around resident fatigue, as well as adequacy of educational experience that still need to be addressed.”
Dr. Malangoni added that residents need to be more mindful and take more responsibility for their own health and well-being.
“I think what residents need to understand is they are really in charge of their own well-being. Making that point is really a key,” he said. “So it’s not only what you do while you are in the hospital, but you are also responsible for what you do when you are not in the hospital. ACGME cannot regulate what people do in their free time. If you work a 24-hour shift and you decide you are not going to sleep the next day for whatever reason, your well-being is likely not going to be what you want it to be and what, I think, your patients want it to be.”
First-year residents will once again be permitted to work up to 24 consecutive hours following a reversal of a rule implemented in 2011 that restricted them to 16 hours, the Accreditation Council for Graduate Medical Education (ACGME) announced.
According to a memo issued by the ACGME March 10, 2017, the change reverting back to the 24-hour ceiling was evidence based.
“The preponderance of the evidence from a number of studies conducted after the current 16-hour cap was implemented in 2011 suggests that it may not have had an incremental benefit in patient safety, and that there might be significant negative impacts to the quality of physician education and professional development,” the memo states. The work week is still capped at 80 hours worked per week, with 1 day free from clinical experience or education in 7, and in-house call no more frequent than every third night.
An ACGME task force determined “that the hypothesized benefits associated with the changes made to first-year resident scheduled hours in 2011 have not been realized, and the disruption of team-based care and supervisory systems has had a significant negative impact on the professional education of the first-year resident, and the effectiveness of care delivery of the team as a whole.”
Sharmila Dissanaike, MD, FACS, chair and professor of surgery at Texas Tech University, Lubbock, said in an interview that the change back to a 24-hour ceiling provides “an increased flexibility for all residents in order to allow completion of immediate patient care responsibilities, such as finishing an operation, and ensure smooth handoffs. Both of these should improve work flow for both trainees and supervisors.”
Mark A. Malangoni, MD, FACS, associate executive director of the American Board of Surgery, said he believes the change back to 24 hours is a positive thing.
“The 16-hour requirement posed a lot of scheduling problems,” he said in an interview. “In essence, what it meant was you had residents that either couldn’t take call or they did take call, it was very limited in what they could do.”
Complicating the issue of time is the nature of what needs to be taught to residents.
“What has definitely changed is the breadth of knowledge and repertoire of technical skills that must be learned by today’s residents,” Dr. Dissanaike said. “As scientific knowledge and technical capabilities expand, there is ever more to learn and increasingly less time in which to learn it.”
Dr. Malangoni added that the time restraints didn’t allow for residents to see the natural progression of the patient’s condition. “You don’t have the chance to continue to assess that over a longer period of time,” he said. “That is really important in learning when to operate on someone, but also when not to operate on someone because they will get better without an operation.”
Compounding that is a greater need for reporting to meet regulatory requirements.
“Concurrently, we have increased requirements for documentation and clerical tasks, and reduced time available to do it,” Dr. Dissanaike continued. “All of this has led to a severe ‘work-compression’ for the modern resident, and I suspect the high rates of burnout and depression that are being reported in many specialties are at least partly a result of this phenomenon.”
That being said, Dr. Dissanaike was quick to add that this latest change should not be considered a “final solution” and that there are “many ongoing issues around resident fatigue, as well as adequacy of educational experience that still need to be addressed.”
Dr. Malangoni added that residents need to be more mindful and take more responsibility for their own health and well-being.
“I think what residents need to understand is they are really in charge of their own well-being. Making that point is really a key,” he said. “So it’s not only what you do while you are in the hospital, but you are also responsible for what you do when you are not in the hospital. ACGME cannot regulate what people do in their free time. If you work a 24-hour shift and you decide you are not going to sleep the next day for whatever reason, your well-being is likely not going to be what you want it to be and what, I think, your patients want it to be.”






