User login
The Official Newspaper of the American Association for Thoracic Surgery
Osimertinib helps NSCLC that progresses despite EGFR-TKIs
Osimertinib, an epidermal growth factor receptor tyrosine kinase inhibitor selective for both EGFR and T790M mutations that render cancers resistant to EGFR-TKIs, yielded a high overall response rate, “encouraging” progression-free survival, and a durable treatment response in advanced non–small cell lung cancer (NSCLC) that had progressed despite EGFR-TKI therapy, according to a report published online Feb. 21 in the Journal of Clinical Oncology.
In a manufacturer-sponsored, open-label phase II trial, 198 patients in 10 countries took 80 mg of oral osimertinib once daily for a median duration of 13.2 months (range, 1-18 months). The overall response rate was 62%, and the median duration of response was 15.2 months. The disease control rate was 90%, said James Chih-Hsin Yang, MD, PhD, of National Taiwan Hospital, Taipei, and his associates.
The median progression-free survival was 12.3 months, and the treatment benefit was generally consistent across all subgroups of patients regardless of age, smoking status, previous therapies, and duration of treatment. Questionnaire responses showed that patients “had consistent and sustained improvements in key lung cancer symptoms including dyspnea, cough, chest pain, and pain in the arm or shoulder,” as well as in global health status and physical functioning. This is particularly noteworthy because some patients had received “many (up to 11) lines of cancer therapy before osimertinib,” the investigators reported (J Clin Oncol. 2017 Feb 21. doi: 10.1200/jco.2016.70.3223).
“We also report encouraging systemic progression-free survival with osimertinib in patients with CNS metastases, and a high CNS response rate (64%) in those with measurable CNS lesions,” they wrote. This finding is particularly important “because new pharmacologic strategies are needed to treat brain metastases, given the long-term complications of brain radiation,” they added.
Osimertinib was generally well tolerated, with 21% of patients having adverse effects leading to dose interruptions and 5% to dose reductions. Nine patients (3%) discontinued the agent because of adverse effects, which included interstitial lung disease (3 fatal cases), QT prolongation, a reduced neutrophil count, and severe vomiting and diarrhea.
This trial was sponsored by AstraZeneca. Dr. Yang and his associates reported ties to numerous industry sources.
Osimertinib, an epidermal growth factor receptor tyrosine kinase inhibitor selective for both EGFR and T790M mutations that render cancers resistant to EGFR-TKIs, yielded a high overall response rate, “encouraging” progression-free survival, and a durable treatment response in advanced non–small cell lung cancer (NSCLC) that had progressed despite EGFR-TKI therapy, according to a report published online Feb. 21 in the Journal of Clinical Oncology.
In a manufacturer-sponsored, open-label phase II trial, 198 patients in 10 countries took 80 mg of oral osimertinib once daily for a median duration of 13.2 months (range, 1-18 months). The overall response rate was 62%, and the median duration of response was 15.2 months. The disease control rate was 90%, said James Chih-Hsin Yang, MD, PhD, of National Taiwan Hospital, Taipei, and his associates.
The median progression-free survival was 12.3 months, and the treatment benefit was generally consistent across all subgroups of patients regardless of age, smoking status, previous therapies, and duration of treatment. Questionnaire responses showed that patients “had consistent and sustained improvements in key lung cancer symptoms including dyspnea, cough, chest pain, and pain in the arm or shoulder,” as well as in global health status and physical functioning. This is particularly noteworthy because some patients had received “many (up to 11) lines of cancer therapy before osimertinib,” the investigators reported (J Clin Oncol. 2017 Feb 21. doi: 10.1200/jco.2016.70.3223).
“We also report encouraging systemic progression-free survival with osimertinib in patients with CNS metastases, and a high CNS response rate (64%) in those with measurable CNS lesions,” they wrote. This finding is particularly important “because new pharmacologic strategies are needed to treat brain metastases, given the long-term complications of brain radiation,” they added.
Osimertinib was generally well tolerated, with 21% of patients having adverse effects leading to dose interruptions and 5% to dose reductions. Nine patients (3%) discontinued the agent because of adverse effects, which included interstitial lung disease (3 fatal cases), QT prolongation, a reduced neutrophil count, and severe vomiting and diarrhea.
This trial was sponsored by AstraZeneca. Dr. Yang and his associates reported ties to numerous industry sources.
Osimertinib, an epidermal growth factor receptor tyrosine kinase inhibitor selective for both EGFR and T790M mutations that render cancers resistant to EGFR-TKIs, yielded a high overall response rate, “encouraging” progression-free survival, and a durable treatment response in advanced non–small cell lung cancer (NSCLC) that had progressed despite EGFR-TKI therapy, according to a report published online Feb. 21 in the Journal of Clinical Oncology.
In a manufacturer-sponsored, open-label phase II trial, 198 patients in 10 countries took 80 mg of oral osimertinib once daily for a median duration of 13.2 months (range, 1-18 months). The overall response rate was 62%, and the median duration of response was 15.2 months. The disease control rate was 90%, said James Chih-Hsin Yang, MD, PhD, of National Taiwan Hospital, Taipei, and his associates.
The median progression-free survival was 12.3 months, and the treatment benefit was generally consistent across all subgroups of patients regardless of age, smoking status, previous therapies, and duration of treatment. Questionnaire responses showed that patients “had consistent and sustained improvements in key lung cancer symptoms including dyspnea, cough, chest pain, and pain in the arm or shoulder,” as well as in global health status and physical functioning. This is particularly noteworthy because some patients had received “many (up to 11) lines of cancer therapy before osimertinib,” the investigators reported (J Clin Oncol. 2017 Feb 21. doi: 10.1200/jco.2016.70.3223).
“We also report encouraging systemic progression-free survival with osimertinib in patients with CNS metastases, and a high CNS response rate (64%) in those with measurable CNS lesions,” they wrote. This finding is particularly important “because new pharmacologic strategies are needed to treat brain metastases, given the long-term complications of brain radiation,” they added.
Osimertinib was generally well tolerated, with 21% of patients having adverse effects leading to dose interruptions and 5% to dose reductions. Nine patients (3%) discontinued the agent because of adverse effects, which included interstitial lung disease (3 fatal cases), QT prolongation, a reduced neutrophil count, and severe vomiting and diarrhea.
This trial was sponsored by AstraZeneca. Dr. Yang and his associates reported ties to numerous industry sources.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Osimertinib yielded a high overall response rate, “encouraging” progression-free survival, and a durable treatment response in advanced non–small cell lung cancer that had progressed despite EGFR-TKI therapy.
Major finding: The overall response rate was 62%, and the median duration of response was 15.2 months.
Data source: An international manufacturer-sponsored, open-label phase II trial involving 198 patients treated for a mean of 13.2 months.
Disclosures: This trial was sponsored by AstraZeneca. Dr. Yang and his associates reported ties to numerous industry sources.
Aortic repair in Loeys-Dietz syndrome requires close follow-up
The knowledge about Loeys-Dietz syndrome has evolved quickly since Hal Dietz, MD, and Bart Loeys, MD, at Johns Hopkins University, Baltimore, first reported on it in 2005. Now, another team of Johns Hopkins investigators have reported that an aggressive approach with aortic root replacement coupled with valve-sparing whenever possible produces favorable results, but that clinicians must follow these patients closely with cardiovascular imaging.
“Growing experience with Loeys-Dietz syndrome has confirmed early impressions of its aggressive nature and proclivity toward aortic catastrophe,” Nishant D. Patel, MD, and his coauthors said in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:406-12). They reported on results of all 79 patients with Loeys-Dietz syndrome (LDS) who had cardiovascular surgery at Johns Hopkins. There were two (3%) deaths during surgery and eight (10%) late deaths.
Patients with LDS are at risk for dissection early when the aortic root reaches 4 cm. Despite what they termed “favorable” outcomes of surgery, Dr. Patel and his coauthors acknowledged that reintervention rates for this population are high – 19 patients (24%) had subsequent operations. That suggests cardiac surgeons must closely monitor these patients. “Meticulous follow-up with cardiovascular surveillance imaging remains important for management, particularly as clinical LDS subtypes are characterized and more tailored treatment is developed,” Dr. Patel and his coauthors reported.
They advise echocardiography every 3 to 6 months for the first year after surgery and then every 6 to 12 months afterward. Full-body imaging should occur at least every 2 years.
“In particular, patients with type B dissections should be monitored aggressively for aneurysm growth,” Dr. Patel and his coauthors said. They recommend imaging at seven to 14 days after dissection, then repeat imaging at 1, 3, 6, and 12 months, and then yearly thereafter.
They noted that four LDS subtypes have been identified. Although those with LDS1 and 2 subtypes are prone to aortic rupture at an earlier age and at smaller aortic diameters than other connective tissue disorders, the medical and surgical management for all subtypes are similar, Dr. Patel and his coauthors indicated.
“Certain congenital heart defects are more common among patients with LDS, compared with the normal population, including patent ductus arteriosus and mitral valve prolapse/insufficiency,” they said. Genotype is one factor that determines the need for surgery in LDS patients, Dr. Patel and his coauthors said. Others are growth rate, aortic valve function, family history, and severity of noncardiac phenotype.
The 79 patients in the study were divided almost evenly between gender, and the average age at first operation was 24.9 years; 38 were children younger than 18 years and 20 had a previous sternotomy.
Aortic root replacement represented the predominant operation in the group, accounting for 65 operations (82.3%), of which 52 (80%) were valve-sparing procedures and the remainder were composite valve-graft procedures. The other procedures the researchers performed were nine aortic arch replacements (11.4%), three open thoracoabdominal repairs (3.8%) and two ascending aorta replacements (2.5%).
“Valve-sparing root replacement has become a safe and reliable option for appropriately selected younger patients with LDS,” Dr. Patel and his coauthors wrote. Five patients needed a second operation on the aortic valve or root; three of them had a Florida sleeve procedure. “Based on these initial outcomes with the Florida sleeve at our institution, we have abandoned this procedure in favor of conventional valve-sparing root replacement,” Dr. Patel and his coauthors stated.
Dr. Patel and his coauthors had no financial relationships to disclose.
This report by Dr. Patel and his coauthors confirms the need for close surveillance of individuals with Loeys-Dietz syndrome who have had aortic operations, John S. Ikonomidis, MD, PhD, of the Medical University of South Carolina, Charleston, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:413-4).
Dr. Ikonomidis noted this study is important because of its population size. “This is probably the largest single-center surgical report of this kind in the world,” he said.
The study highlighted a number of issues germane to LDS patients who have cardiovascular surgery, among them a critical need for genetic testing to help cardiac surgeons determine the disease genotype and what operation to perform, Dr. Ikonomidis said.
But Dr. Ikonomidis also pointed out the variation in aortic root size in the study patients. The smallest root in the series was 2 cm and 21 of 65 patients with a maximum root diameter smaller than 4 cm had root surgery. “This is a testament to the fact that surgical decision making in this population is dependent not just on the known genotype and aortic dimensions, but also on the rate of growth, aortic valve function, severity of noncardiac phenotype, and family history,” Dr. Ikonomidis said.
Dr. Ikonomidis had no financial relationships to disclose.
This report by Dr. Patel and his coauthors confirms the need for close surveillance of individuals with Loeys-Dietz syndrome who have had aortic operations, John S. Ikonomidis, MD, PhD, of the Medical University of South Carolina, Charleston, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:413-4).
Dr. Ikonomidis noted this study is important because of its population size. “This is probably the largest single-center surgical report of this kind in the world,” he said.
The study highlighted a number of issues germane to LDS patients who have cardiovascular surgery, among them a critical need for genetic testing to help cardiac surgeons determine the disease genotype and what operation to perform, Dr. Ikonomidis said.
But Dr. Ikonomidis also pointed out the variation in aortic root size in the study patients. The smallest root in the series was 2 cm and 21 of 65 patients with a maximum root diameter smaller than 4 cm had root surgery. “This is a testament to the fact that surgical decision making in this population is dependent not just on the known genotype and aortic dimensions, but also on the rate of growth, aortic valve function, severity of noncardiac phenotype, and family history,” Dr. Ikonomidis said.
Dr. Ikonomidis had no financial relationships to disclose.
This report by Dr. Patel and his coauthors confirms the need for close surveillance of individuals with Loeys-Dietz syndrome who have had aortic operations, John S. Ikonomidis, MD, PhD, of the Medical University of South Carolina, Charleston, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:413-4).
Dr. Ikonomidis noted this study is important because of its population size. “This is probably the largest single-center surgical report of this kind in the world,” he said.
The study highlighted a number of issues germane to LDS patients who have cardiovascular surgery, among them a critical need for genetic testing to help cardiac surgeons determine the disease genotype and what operation to perform, Dr. Ikonomidis said.
But Dr. Ikonomidis also pointed out the variation in aortic root size in the study patients. The smallest root in the series was 2 cm and 21 of 65 patients with a maximum root diameter smaller than 4 cm had root surgery. “This is a testament to the fact that surgical decision making in this population is dependent not just on the known genotype and aortic dimensions, but also on the rate of growth, aortic valve function, severity of noncardiac phenotype, and family history,” Dr. Ikonomidis said.
Dr. Ikonomidis had no financial relationships to disclose.
The knowledge about Loeys-Dietz syndrome has evolved quickly since Hal Dietz, MD, and Bart Loeys, MD, at Johns Hopkins University, Baltimore, first reported on it in 2005. Now, another team of Johns Hopkins investigators have reported that an aggressive approach with aortic root replacement coupled with valve-sparing whenever possible produces favorable results, but that clinicians must follow these patients closely with cardiovascular imaging.
“Growing experience with Loeys-Dietz syndrome has confirmed early impressions of its aggressive nature and proclivity toward aortic catastrophe,” Nishant D. Patel, MD, and his coauthors said in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:406-12). They reported on results of all 79 patients with Loeys-Dietz syndrome (LDS) who had cardiovascular surgery at Johns Hopkins. There were two (3%) deaths during surgery and eight (10%) late deaths.
Patients with LDS are at risk for dissection early when the aortic root reaches 4 cm. Despite what they termed “favorable” outcomes of surgery, Dr. Patel and his coauthors acknowledged that reintervention rates for this population are high – 19 patients (24%) had subsequent operations. That suggests cardiac surgeons must closely monitor these patients. “Meticulous follow-up with cardiovascular surveillance imaging remains important for management, particularly as clinical LDS subtypes are characterized and more tailored treatment is developed,” Dr. Patel and his coauthors reported.
They advise echocardiography every 3 to 6 months for the first year after surgery and then every 6 to 12 months afterward. Full-body imaging should occur at least every 2 years.
“In particular, patients with type B dissections should be monitored aggressively for aneurysm growth,” Dr. Patel and his coauthors said. They recommend imaging at seven to 14 days after dissection, then repeat imaging at 1, 3, 6, and 12 months, and then yearly thereafter.
They noted that four LDS subtypes have been identified. Although those with LDS1 and 2 subtypes are prone to aortic rupture at an earlier age and at smaller aortic diameters than other connective tissue disorders, the medical and surgical management for all subtypes are similar, Dr. Patel and his coauthors indicated.
“Certain congenital heart defects are more common among patients with LDS, compared with the normal population, including patent ductus arteriosus and mitral valve prolapse/insufficiency,” they said. Genotype is one factor that determines the need for surgery in LDS patients, Dr. Patel and his coauthors said. Others are growth rate, aortic valve function, family history, and severity of noncardiac phenotype.
The 79 patients in the study were divided almost evenly between gender, and the average age at first operation was 24.9 years; 38 were children younger than 18 years and 20 had a previous sternotomy.
Aortic root replacement represented the predominant operation in the group, accounting for 65 operations (82.3%), of which 52 (80%) were valve-sparing procedures and the remainder were composite valve-graft procedures. The other procedures the researchers performed were nine aortic arch replacements (11.4%), three open thoracoabdominal repairs (3.8%) and two ascending aorta replacements (2.5%).
“Valve-sparing root replacement has become a safe and reliable option for appropriately selected younger patients with LDS,” Dr. Patel and his coauthors wrote. Five patients needed a second operation on the aortic valve or root; three of them had a Florida sleeve procedure. “Based on these initial outcomes with the Florida sleeve at our institution, we have abandoned this procedure in favor of conventional valve-sparing root replacement,” Dr. Patel and his coauthors stated.
Dr. Patel and his coauthors had no financial relationships to disclose.
The knowledge about Loeys-Dietz syndrome has evolved quickly since Hal Dietz, MD, and Bart Loeys, MD, at Johns Hopkins University, Baltimore, first reported on it in 2005. Now, another team of Johns Hopkins investigators have reported that an aggressive approach with aortic root replacement coupled with valve-sparing whenever possible produces favorable results, but that clinicians must follow these patients closely with cardiovascular imaging.
“Growing experience with Loeys-Dietz syndrome has confirmed early impressions of its aggressive nature and proclivity toward aortic catastrophe,” Nishant D. Patel, MD, and his coauthors said in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:406-12). They reported on results of all 79 patients with Loeys-Dietz syndrome (LDS) who had cardiovascular surgery at Johns Hopkins. There were two (3%) deaths during surgery and eight (10%) late deaths.
Patients with LDS are at risk for dissection early when the aortic root reaches 4 cm. Despite what they termed “favorable” outcomes of surgery, Dr. Patel and his coauthors acknowledged that reintervention rates for this population are high – 19 patients (24%) had subsequent operations. That suggests cardiac surgeons must closely monitor these patients. “Meticulous follow-up with cardiovascular surveillance imaging remains important for management, particularly as clinical LDS subtypes are characterized and more tailored treatment is developed,” Dr. Patel and his coauthors reported.
They advise echocardiography every 3 to 6 months for the first year after surgery and then every 6 to 12 months afterward. Full-body imaging should occur at least every 2 years.
“In particular, patients with type B dissections should be monitored aggressively for aneurysm growth,” Dr. Patel and his coauthors said. They recommend imaging at seven to 14 days after dissection, then repeat imaging at 1, 3, 6, and 12 months, and then yearly thereafter.
They noted that four LDS subtypes have been identified. Although those with LDS1 and 2 subtypes are prone to aortic rupture at an earlier age and at smaller aortic diameters than other connective tissue disorders, the medical and surgical management for all subtypes are similar, Dr. Patel and his coauthors indicated.
“Certain congenital heart defects are more common among patients with LDS, compared with the normal population, including patent ductus arteriosus and mitral valve prolapse/insufficiency,” they said. Genotype is one factor that determines the need for surgery in LDS patients, Dr. Patel and his coauthors said. Others are growth rate, aortic valve function, family history, and severity of noncardiac phenotype.
The 79 patients in the study were divided almost evenly between gender, and the average age at first operation was 24.9 years; 38 were children younger than 18 years and 20 had a previous sternotomy.
Aortic root replacement represented the predominant operation in the group, accounting for 65 operations (82.3%), of which 52 (80%) were valve-sparing procedures and the remainder were composite valve-graft procedures. The other procedures the researchers performed were nine aortic arch replacements (11.4%), three open thoracoabdominal repairs (3.8%) and two ascending aorta replacements (2.5%).
“Valve-sparing root replacement has become a safe and reliable option for appropriately selected younger patients with LDS,” Dr. Patel and his coauthors wrote. Five patients needed a second operation on the aortic valve or root; three of them had a Florida sleeve procedure. “Based on these initial outcomes with the Florida sleeve at our institution, we have abandoned this procedure in favor of conventional valve-sparing root replacement,” Dr. Patel and his coauthors stated.
Dr. Patel and his coauthors had no financial relationships to disclose.
Key clinical point: Outcomes for aortic surgery in Loeys-Dietz syndrome are favorable, but reintervention rates are high.
Major finding: Patients require close postoperative follow-up with cardiovascular imaging.
Data source: Retrospective review of 79 patients who had cardiovascular surgery for LDS over 26 years at Johns Hopkins University.
Disclosure: Dr. Patel and his coauthors reported having no relevant financial disclosures.
Can a nomogram foretell invasive pulmonary adenocarcinoma?
The diagnosis of solitary peripheral subsolid nodule carries with it an undefined risk of invasive pulmonary carcinoma, but clinicians have not had a tool that can help guide their planning for surgery. However, researchers in China have developed a nomogram that they said may aid clinicians to predict the risk of invasive pulmonary adenocarcinoma in these patients.
“Validation by the use of bootstrap resampling revealed optimal discrimination and calibration, indicating that the nomogram may have clinical utility,” said Chenghua Jin, MD, and Jinlin Cao, MD, of Zhejiang University, Hangzhou, China, and coauthors. They reported their findings in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:42-9).
The nomogram accounts for the following factors: computed tomography attenuation; nodule size; spiculation; signs of vascular convergence; pleural tags; and solid proportion. “The nomogram showed a robust discrimination with an area under the receiver operating characteristic curve of 0.894,” Dr. Jin and coauthors reported. An area under the curve of 1 is equivalent to 100%, so the area under the curve this study reported shows close to 90% accuracy.
The study involved a retrospective analysis of 273 consecutive patients who had resection of a solitary peripheral subsolid nodule at Zhejiang University School of Medicine from January 2013 to December 2014. Subsolid pulmonary nodules include pure ground-glass nodules and part-solid nodules that feature both solid and ground-glass components. “The optimal management of patients with a subsolid nodule is of growing clinical concern, because the most common diagnosis for resected subsolid nodules is lung adenocarcinoma,” Dr. Jin and colleagues indicated.
Of the study population, 58% were diagnosed with invasive pulmonary adenocarcinoma. Other diagnoses within the group were benign (13%), atypical adenomatous hyperplasia (1%), adenocarcinoma in situ (6.5%) and minimally invasive adenocarcinoma (21%).
Results of the multivariable analyses showed that invasive pulmonary adenocarcinoma correlated with the following characteristics: lesion size; spiculation; vascular convergence; and pleural tag. Factors that were not significant included age, family history of lung cancer, CT attenuation, and solid proportion. However, the researchers did include CT attenuation, along with solid proportion, in the final regression analysis based on their contributions to the statistical analysis.
For the model, CT attenuation of –500 to –200 Hounsfield units carried an odds ratio of 1.690 (P = .228) while CT attenuation greater than –200 HU had an OR of 1.791 (P = .645). Positive spiculation had an OR of 3.312 (no P value given) and negative vascular convergence an OR of 0.300 (no P value given).
While a number of prediction models have been devised and validated to evaluate the likelihood of malignancy in pulmonary nodules, they have not given subsolid nodules “specific or detailed consideration,” Dr. Jin and and coauthors said. “To our knowledge, this study was the first to construct a quantitative nomogram to predict the probability of invasive pulmonary adenocarcinoma in patients with subsolid nodules,” the researchers wrote.
One limitation of the study is its selection bias toward patients with a greater probability of having a malignancy. Also, validation of the nomogram requires external analysis with additional databases from other countries and with more diverse ethnic groups. Another shortcoming is the retrospective nature of the study and a small number of patients who had positron emission tomography. “Further data collection, wider geographic recruitment, and incorporation of positron emission tomography results and some molecular factors could improve this model for future use,” Dr. Jin and coauthors concluded.
Dr. Jin and Dr. Cao had no relevant financial disclosures. The study received funding from the Zhejiang Province Science and Technology Plan.
The nomogram Dr. Jin and coauthors present can be a valuable tool for determining the extent of resection of subsolid pulmonary nodules and to distinguish invasive from preinvasive disease where preoperative needle biopsy and intraopertiave frozen section typically cannot, Bryan Burt, MD, of Baylor College of Medicine, Houston, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:460-1).
“However,” Dr. Burt added, “as the accuracy of frozen section for this disease improves, as it has in select centers, the clinical utility of such a nomogram will diminish.”
Use of the nomogram relies on experienced chest radiologists to aid in scoring variables and a validation methodology that a retrospective trial cannot meet, Dr. Burt said. “Of note, this nomogram was constructed from a dataset composed of only surgically resected lesions, and it will be imperative to validate these methods among a larger cohort of individuals with subsolid pulmonary nodules treated both surgically and nonsurgically, ideally in a prospective trial,” Dr. Burt concluded.
Dr. Burt had no relevant financial disclosures.
The nomogram Dr. Jin and coauthors present can be a valuable tool for determining the extent of resection of subsolid pulmonary nodules and to distinguish invasive from preinvasive disease where preoperative needle biopsy and intraopertiave frozen section typically cannot, Bryan Burt, MD, of Baylor College of Medicine, Houston, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:460-1).
“However,” Dr. Burt added, “as the accuracy of frozen section for this disease improves, as it has in select centers, the clinical utility of such a nomogram will diminish.”
Use of the nomogram relies on experienced chest radiologists to aid in scoring variables and a validation methodology that a retrospective trial cannot meet, Dr. Burt said. “Of note, this nomogram was constructed from a dataset composed of only surgically resected lesions, and it will be imperative to validate these methods among a larger cohort of individuals with subsolid pulmonary nodules treated both surgically and nonsurgically, ideally in a prospective trial,” Dr. Burt concluded.
Dr. Burt had no relevant financial disclosures.
The nomogram Dr. Jin and coauthors present can be a valuable tool for determining the extent of resection of subsolid pulmonary nodules and to distinguish invasive from preinvasive disease where preoperative needle biopsy and intraopertiave frozen section typically cannot, Bryan Burt, MD, of Baylor College of Medicine, Houston, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:460-1).
“However,” Dr. Burt added, “as the accuracy of frozen section for this disease improves, as it has in select centers, the clinical utility of such a nomogram will diminish.”
Use of the nomogram relies on experienced chest radiologists to aid in scoring variables and a validation methodology that a retrospective trial cannot meet, Dr. Burt said. “Of note, this nomogram was constructed from a dataset composed of only surgically resected lesions, and it will be imperative to validate these methods among a larger cohort of individuals with subsolid pulmonary nodules treated both surgically and nonsurgically, ideally in a prospective trial,” Dr. Burt concluded.
Dr. Burt had no relevant financial disclosures.
The diagnosis of solitary peripheral subsolid nodule carries with it an undefined risk of invasive pulmonary carcinoma, but clinicians have not had a tool that can help guide their planning for surgery. However, researchers in China have developed a nomogram that they said may aid clinicians to predict the risk of invasive pulmonary adenocarcinoma in these patients.
“Validation by the use of bootstrap resampling revealed optimal discrimination and calibration, indicating that the nomogram may have clinical utility,” said Chenghua Jin, MD, and Jinlin Cao, MD, of Zhejiang University, Hangzhou, China, and coauthors. They reported their findings in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:42-9).
The nomogram accounts for the following factors: computed tomography attenuation; nodule size; spiculation; signs of vascular convergence; pleural tags; and solid proportion. “The nomogram showed a robust discrimination with an area under the receiver operating characteristic curve of 0.894,” Dr. Jin and coauthors reported. An area under the curve of 1 is equivalent to 100%, so the area under the curve this study reported shows close to 90% accuracy.
The study involved a retrospective analysis of 273 consecutive patients who had resection of a solitary peripheral subsolid nodule at Zhejiang University School of Medicine from January 2013 to December 2014. Subsolid pulmonary nodules include pure ground-glass nodules and part-solid nodules that feature both solid and ground-glass components. “The optimal management of patients with a subsolid nodule is of growing clinical concern, because the most common diagnosis for resected subsolid nodules is lung adenocarcinoma,” Dr. Jin and colleagues indicated.
Of the study population, 58% were diagnosed with invasive pulmonary adenocarcinoma. Other diagnoses within the group were benign (13%), atypical adenomatous hyperplasia (1%), adenocarcinoma in situ (6.5%) and minimally invasive adenocarcinoma (21%).
Results of the multivariable analyses showed that invasive pulmonary adenocarcinoma correlated with the following characteristics: lesion size; spiculation; vascular convergence; and pleural tag. Factors that were not significant included age, family history of lung cancer, CT attenuation, and solid proportion. However, the researchers did include CT attenuation, along with solid proportion, in the final regression analysis based on their contributions to the statistical analysis.
For the model, CT attenuation of –500 to –200 Hounsfield units carried an odds ratio of 1.690 (P = .228) while CT attenuation greater than –200 HU had an OR of 1.791 (P = .645). Positive spiculation had an OR of 3.312 (no P value given) and negative vascular convergence an OR of 0.300 (no P value given).
While a number of prediction models have been devised and validated to evaluate the likelihood of malignancy in pulmonary nodules, they have not given subsolid nodules “specific or detailed consideration,” Dr. Jin and and coauthors said. “To our knowledge, this study was the first to construct a quantitative nomogram to predict the probability of invasive pulmonary adenocarcinoma in patients with subsolid nodules,” the researchers wrote.
One limitation of the study is its selection bias toward patients with a greater probability of having a malignancy. Also, validation of the nomogram requires external analysis with additional databases from other countries and with more diverse ethnic groups. Another shortcoming is the retrospective nature of the study and a small number of patients who had positron emission tomography. “Further data collection, wider geographic recruitment, and incorporation of positron emission tomography results and some molecular factors could improve this model for future use,” Dr. Jin and coauthors concluded.
Dr. Jin and Dr. Cao had no relevant financial disclosures. The study received funding from the Zhejiang Province Science and Technology Plan.
The diagnosis of solitary peripheral subsolid nodule carries with it an undefined risk of invasive pulmonary carcinoma, but clinicians have not had a tool that can help guide their planning for surgery. However, researchers in China have developed a nomogram that they said may aid clinicians to predict the risk of invasive pulmonary adenocarcinoma in these patients.
“Validation by the use of bootstrap resampling revealed optimal discrimination and calibration, indicating that the nomogram may have clinical utility,” said Chenghua Jin, MD, and Jinlin Cao, MD, of Zhejiang University, Hangzhou, China, and coauthors. They reported their findings in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:42-9).
The nomogram accounts for the following factors: computed tomography attenuation; nodule size; spiculation; signs of vascular convergence; pleural tags; and solid proportion. “The nomogram showed a robust discrimination with an area under the receiver operating characteristic curve of 0.894,” Dr. Jin and coauthors reported. An area under the curve of 1 is equivalent to 100%, so the area under the curve this study reported shows close to 90% accuracy.
The study involved a retrospective analysis of 273 consecutive patients who had resection of a solitary peripheral subsolid nodule at Zhejiang University School of Medicine from January 2013 to December 2014. Subsolid pulmonary nodules include pure ground-glass nodules and part-solid nodules that feature both solid and ground-glass components. “The optimal management of patients with a subsolid nodule is of growing clinical concern, because the most common diagnosis for resected subsolid nodules is lung adenocarcinoma,” Dr. Jin and colleagues indicated.
Of the study population, 58% were diagnosed with invasive pulmonary adenocarcinoma. Other diagnoses within the group were benign (13%), atypical adenomatous hyperplasia (1%), adenocarcinoma in situ (6.5%) and minimally invasive adenocarcinoma (21%).
Results of the multivariable analyses showed that invasive pulmonary adenocarcinoma correlated with the following characteristics: lesion size; spiculation; vascular convergence; and pleural tag. Factors that were not significant included age, family history of lung cancer, CT attenuation, and solid proportion. However, the researchers did include CT attenuation, along with solid proportion, in the final regression analysis based on their contributions to the statistical analysis.
For the model, CT attenuation of –500 to –200 Hounsfield units carried an odds ratio of 1.690 (P = .228) while CT attenuation greater than –200 HU had an OR of 1.791 (P = .645). Positive spiculation had an OR of 3.312 (no P value given) and negative vascular convergence an OR of 0.300 (no P value given).
While a number of prediction models have been devised and validated to evaluate the likelihood of malignancy in pulmonary nodules, they have not given subsolid nodules “specific or detailed consideration,” Dr. Jin and and coauthors said. “To our knowledge, this study was the first to construct a quantitative nomogram to predict the probability of invasive pulmonary adenocarcinoma in patients with subsolid nodules,” the researchers wrote.
One limitation of the study is its selection bias toward patients with a greater probability of having a malignancy. Also, validation of the nomogram requires external analysis with additional databases from other countries and with more diverse ethnic groups. Another shortcoming is the retrospective nature of the study and a small number of patients who had positron emission tomography. “Further data collection, wider geographic recruitment, and incorporation of positron emission tomography results and some molecular factors could improve this model for future use,” Dr. Jin and coauthors concluded.
Dr. Jin and Dr. Cao had no relevant financial disclosures. The study received funding from the Zhejiang Province Science and Technology Plan.
EXPERT ANALYSIS FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Investigators developed a nomogram that may help predict the risk of invasive pulmonary adenocarcinoma for patients with a solitary peripheral subsolid nodule.
Major finding: This nomogram may help clinicians individualize each patient’s prognosis for invasive pulmonary adenocarcinoma and develop treatment plans accordingly.
Data source: Retrospective analysis of 273 consecutive patients who had surgery to remove a solitary peripheral subsolid nodule at a single center.
Disclosure: The investigators received support from the Zhejiang Province Science and Technology Plan. Dr. Jin and Dr. Cao reported having no relevant financial disclosures.
CMS spending projections come with a caveat
The Centers for Medicare & Medicaid Services is predicting an average annual growth rate of 5.6% in health care expenditures over the next 10 years – but with a big asterisk.
The projections are based on current law and make no assumptions about potential repair, repeal, or replacement of the Affordable Care Act, leaving the projections to serve as a benchmark rather than a forecast.
In the short term, growth rates in 2016 and 2017 are the slowest in the forecast period, at 4.8% and 5.4%, respectively. For 2018 and beyond, the growth rate picks up, with both Medicare and Medicaid projected to grow faster and more rapidly, compared with private health insurance spending.
The CMS actuaries attribute this to the increase in Medicare spending over recent historic lows, a Medicaid population that is expected to become older and sicker, additional Baby Boomers entering the Medicare program, and decreased demand for health services as prices increase.
The percentage of population with either public or private health insurance coverage is expected to grow under current law from 90.9% in 2015 to 91.5% in 2025, “mainly a result of continued growth in enrollment in private health insurance – in particular, employer-sponsored health insurance – in the first year of the projection period, as well as enrollment growth in public programs throughout the period,” Mr. Keegan and colleagues wrote.
The Centers for Medicare & Medicaid Services is predicting an average annual growth rate of 5.6% in health care expenditures over the next 10 years – but with a big asterisk.
The projections are based on current law and make no assumptions about potential repair, repeal, or replacement of the Affordable Care Act, leaving the projections to serve as a benchmark rather than a forecast.
In the short term, growth rates in 2016 and 2017 are the slowest in the forecast period, at 4.8% and 5.4%, respectively. For 2018 and beyond, the growth rate picks up, with both Medicare and Medicaid projected to grow faster and more rapidly, compared with private health insurance spending.
The CMS actuaries attribute this to the increase in Medicare spending over recent historic lows, a Medicaid population that is expected to become older and sicker, additional Baby Boomers entering the Medicare program, and decreased demand for health services as prices increase.
The percentage of population with either public or private health insurance coverage is expected to grow under current law from 90.9% in 2015 to 91.5% in 2025, “mainly a result of continued growth in enrollment in private health insurance – in particular, employer-sponsored health insurance – in the first year of the projection period, as well as enrollment growth in public programs throughout the period,” Mr. Keegan and colleagues wrote.
The Centers for Medicare & Medicaid Services is predicting an average annual growth rate of 5.6% in health care expenditures over the next 10 years – but with a big asterisk.
The projections are based on current law and make no assumptions about potential repair, repeal, or replacement of the Affordable Care Act, leaving the projections to serve as a benchmark rather than a forecast.
In the short term, growth rates in 2016 and 2017 are the slowest in the forecast period, at 4.8% and 5.4%, respectively. For 2018 and beyond, the growth rate picks up, with both Medicare and Medicaid projected to grow faster and more rapidly, compared with private health insurance spending.
The CMS actuaries attribute this to the increase in Medicare spending over recent historic lows, a Medicaid population that is expected to become older and sicker, additional Baby Boomers entering the Medicare program, and decreased demand for health services as prices increase.
The percentage of population with either public or private health insurance coverage is expected to grow under current law from 90.9% in 2015 to 91.5% in 2025, “mainly a result of continued growth in enrollment in private health insurance – in particular, employer-sponsored health insurance – in the first year of the projection period, as well as enrollment growth in public programs throughout the period,” Mr. Keegan and colleagues wrote.
Will genome editing advance animal-to-human transplantation?
Advances in gene editing are pushing the possibility of raising pigs for organs that may be transplanted into humans with immunosuppression regimens comparable to those now used in human-to-human transplants, coauthors James Butler, MD, and A. Joseph Tector, MD, PhD, stated in an expert opinion in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:488-92).
Developments in genome editing could bring new approaches to management of cardiopulmonary diseases, Dr. Butler and Dr. Tector noted. “Recently, cardiac-specific and lung-specific applications have been described, which will allow for the rapid creation of new models of heart and lung disease,” they said. Specifically, they noted gene targeting might eventually offer a way to treat challenging genetic problems “like the heterogeneous nature of nonsquamous cell lung cancer.”
Dr. Butler is with the department of surgery at Indiana University, Indianapolis, and Dr. Tector is with the department of surgery at the University of Alabama at Birmingham.
CRISPR technology has been used in developing multiple gene knockout pigs and neutralizing three separate porcine genes that encode human xenoantigens in a single reaction, leading to efficient methods for creating pigs with multiple genetic modifications.
According to the website of the Broad Institute of MIT and Harvard, Cambridge, Mass., where researchers perfected the system to work in eukaryotes, CRISPR works by using short RNA sequences designed by researchers to guide the system to matching sequences of DNA. When the target DNA is found, Cas9 – one of the enzymes produced by the CRISPR system – binds to the DNA and cuts it, shutting the targeted gene off.
“By facilitating high-throughput model creation, CRISPR has elucidated which modifications are necessary and which are not; despite the ability to alter many loci concurrently, recent evidence has implicated three porcine genes that are responsible for the majority of human-antiporcine humoral immunity,” Dr. Butler and Dr. Tector wrote.
Those genes are the Gal[alpha]1-3 epitope (Gal-alpha), CMAH and B4GaINT2 genes. “Each of these three genes is expressed in pigs but has been evolutionarily silenced in humans,” the coauthors added.
While CRISPR genome editing has yet to reach its full potential, researchers and clinicians should pay attention, according to Dr. Butler and Dr. Tector.
More recent modifications of CRISPR technology have shown promise in not just knocking out or turning off specific genes, but rather guiding directed replacement of genes with researcher-designed substitutes. This can enable permanent transformation of functional genes with altered behavior, according to the Broad Institute website.
Dr. Tector disclosed he has received funding from United Therapeutics and founded Xenobridge with patents for xenotransplantation. Dr. Butler has no relevant financial relationships to disclose.
CRISPR and CRISPR-associated proteins have emerged as effective genome editing techniques that may lead to cardiac and lung models and possibly xenotransplantation, Ari A. Mennander, MD, PhD, of the Tampere (Finland) University Heart Hospital, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:492).
The concept Dr. Butler and Dr. Tector discuss involves not using antibodies to ameliorate porcine antibodies that cause rejection in humans, but rather reengineering the genetic composition of pigs to eliminate those antibodies. “According to the wildest of dreams, these genes affecting porcine glycan expression may be silenced, and the human–antiporcine humoral immunity is controlled down to the level comparable with human allograft rejection,” Dr. Mennander said.
However, such a breakthrough carries with it consequences, Dr. Mennander said. “Should one worry about the induction of zoonosis, as well as the ethical aspects of transplanting the patient a whole organ of a pig? Would even a successful xenotransplant program seriously compete with artificial hearts or allografts?” Embracing the method too early would open its advocates to ridicule, he said.
“We are to applaud the researchers for ever-lasting and exemplary enthusiasm for a futuristic new surgical solution; the future may lie as much in current clinical solutions as in innovative discoveries based on persistent scientific experiments,” Dr. Mennander said.
Dr. Mennander had no relevant financial relationships to disclose.
CRISPR and CRISPR-associated proteins have emerged as effective genome editing techniques that may lead to cardiac and lung models and possibly xenotransplantation, Ari A. Mennander, MD, PhD, of the Tampere (Finland) University Heart Hospital, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:492).
The concept Dr. Butler and Dr. Tector discuss involves not using antibodies to ameliorate porcine antibodies that cause rejection in humans, but rather reengineering the genetic composition of pigs to eliminate those antibodies. “According to the wildest of dreams, these genes affecting porcine glycan expression may be silenced, and the human–antiporcine humoral immunity is controlled down to the level comparable with human allograft rejection,” Dr. Mennander said.
However, such a breakthrough carries with it consequences, Dr. Mennander said. “Should one worry about the induction of zoonosis, as well as the ethical aspects of transplanting the patient a whole organ of a pig? Would even a successful xenotransplant program seriously compete with artificial hearts or allografts?” Embracing the method too early would open its advocates to ridicule, he said.
“We are to applaud the researchers for ever-lasting and exemplary enthusiasm for a futuristic new surgical solution; the future may lie as much in current clinical solutions as in innovative discoveries based on persistent scientific experiments,” Dr. Mennander said.
Dr. Mennander had no relevant financial relationships to disclose.
CRISPR and CRISPR-associated proteins have emerged as effective genome editing techniques that may lead to cardiac and lung models and possibly xenotransplantation, Ari A. Mennander, MD, PhD, of the Tampere (Finland) University Heart Hospital, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:492).
The concept Dr. Butler and Dr. Tector discuss involves not using antibodies to ameliorate porcine antibodies that cause rejection in humans, but rather reengineering the genetic composition of pigs to eliminate those antibodies. “According to the wildest of dreams, these genes affecting porcine glycan expression may be silenced, and the human–antiporcine humoral immunity is controlled down to the level comparable with human allograft rejection,” Dr. Mennander said.
However, such a breakthrough carries with it consequences, Dr. Mennander said. “Should one worry about the induction of zoonosis, as well as the ethical aspects of transplanting the patient a whole organ of a pig? Would even a successful xenotransplant program seriously compete with artificial hearts or allografts?” Embracing the method too early would open its advocates to ridicule, he said.
“We are to applaud the researchers for ever-lasting and exemplary enthusiasm for a futuristic new surgical solution; the future may lie as much in current clinical solutions as in innovative discoveries based on persistent scientific experiments,” Dr. Mennander said.
Dr. Mennander had no relevant financial relationships to disclose.
Advances in gene editing are pushing the possibility of raising pigs for organs that may be transplanted into humans with immunosuppression regimens comparable to those now used in human-to-human transplants, coauthors James Butler, MD, and A. Joseph Tector, MD, PhD, stated in an expert opinion in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:488-92).
Developments in genome editing could bring new approaches to management of cardiopulmonary diseases, Dr. Butler and Dr. Tector noted. “Recently, cardiac-specific and lung-specific applications have been described, which will allow for the rapid creation of new models of heart and lung disease,” they said. Specifically, they noted gene targeting might eventually offer a way to treat challenging genetic problems “like the heterogeneous nature of nonsquamous cell lung cancer.”
Dr. Butler is with the department of surgery at Indiana University, Indianapolis, and Dr. Tector is with the department of surgery at the University of Alabama at Birmingham.
CRISPR technology has been used in developing multiple gene knockout pigs and neutralizing three separate porcine genes that encode human xenoantigens in a single reaction, leading to efficient methods for creating pigs with multiple genetic modifications.
According to the website of the Broad Institute of MIT and Harvard, Cambridge, Mass., where researchers perfected the system to work in eukaryotes, CRISPR works by using short RNA sequences designed by researchers to guide the system to matching sequences of DNA. When the target DNA is found, Cas9 – one of the enzymes produced by the CRISPR system – binds to the DNA and cuts it, shutting the targeted gene off.
“By facilitating high-throughput model creation, CRISPR has elucidated which modifications are necessary and which are not; despite the ability to alter many loci concurrently, recent evidence has implicated three porcine genes that are responsible for the majority of human-antiporcine humoral immunity,” Dr. Butler and Dr. Tector wrote.
Those genes are the Gal[alpha]1-3 epitope (Gal-alpha), CMAH and B4GaINT2 genes. “Each of these three genes is expressed in pigs but has been evolutionarily silenced in humans,” the coauthors added.
While CRISPR genome editing has yet to reach its full potential, researchers and clinicians should pay attention, according to Dr. Butler and Dr. Tector.
More recent modifications of CRISPR technology have shown promise in not just knocking out or turning off specific genes, but rather guiding directed replacement of genes with researcher-designed substitutes. This can enable permanent transformation of functional genes with altered behavior, according to the Broad Institute website.
Dr. Tector disclosed he has received funding from United Therapeutics and founded Xenobridge with patents for xenotransplantation. Dr. Butler has no relevant financial relationships to disclose.
Advances in gene editing are pushing the possibility of raising pigs for organs that may be transplanted into humans with immunosuppression regimens comparable to those now used in human-to-human transplants, coauthors James Butler, MD, and A. Joseph Tector, MD, PhD, stated in an expert opinion in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:488-92).
Developments in genome editing could bring new approaches to management of cardiopulmonary diseases, Dr. Butler and Dr. Tector noted. “Recently, cardiac-specific and lung-specific applications have been described, which will allow for the rapid creation of new models of heart and lung disease,” they said. Specifically, they noted gene targeting might eventually offer a way to treat challenging genetic problems “like the heterogeneous nature of nonsquamous cell lung cancer.”
Dr. Butler is with the department of surgery at Indiana University, Indianapolis, and Dr. Tector is with the department of surgery at the University of Alabama at Birmingham.
CRISPR technology has been used in developing multiple gene knockout pigs and neutralizing three separate porcine genes that encode human xenoantigens in a single reaction, leading to efficient methods for creating pigs with multiple genetic modifications.
According to the website of the Broad Institute of MIT and Harvard, Cambridge, Mass., where researchers perfected the system to work in eukaryotes, CRISPR works by using short RNA sequences designed by researchers to guide the system to matching sequences of DNA. When the target DNA is found, Cas9 – one of the enzymes produced by the CRISPR system – binds to the DNA and cuts it, shutting the targeted gene off.
“By facilitating high-throughput model creation, CRISPR has elucidated which modifications are necessary and which are not; despite the ability to alter many loci concurrently, recent evidence has implicated three porcine genes that are responsible for the majority of human-antiporcine humoral immunity,” Dr. Butler and Dr. Tector wrote.
Those genes are the Gal[alpha]1-3 epitope (Gal-alpha), CMAH and B4GaINT2 genes. “Each of these three genes is expressed in pigs but has been evolutionarily silenced in humans,” the coauthors added.
While CRISPR genome editing has yet to reach its full potential, researchers and clinicians should pay attention, according to Dr. Butler and Dr. Tector.
More recent modifications of CRISPR technology have shown promise in not just knocking out or turning off specific genes, but rather guiding directed replacement of genes with researcher-designed substitutes. This can enable permanent transformation of functional genes with altered behavior, according to the Broad Institute website.
Dr. Tector disclosed he has received funding from United Therapeutics and founded Xenobridge with patents for xenotransplantation. Dr. Butler has no relevant financial relationships to disclose.
Key clinical point: CRISPR/Cas9 genome editing is advancing the creation of animal models for xenotransplantation into humans.
Major finding: Genome editing tools are moving xenotransplantation models quickly toward potential treatments for cardiopulmonary disease.
Data source: Expert opinion with literature review.
Disclosures: Dr. Tector disclosed he has received funding from United Therapeutics and founded Xenobridge with patents for xenotransplantation. Dr. Butler reported having no relevant financial disclosures.
Seema Verma dodges questions on how to improve CMS
If confirmed as Centers for Medicare & Medicaid Services administrator, Seema Verma vowed to modernize CMS programs, improve Medicaid access, and leverage technology to drive better care, but she stopped short of explaining how she would do so during her confirmation hearing Feb. 16 before the Senate Finance Committee.
Legislators grilled Ms. Verma on Medicare improvements, the fate of the Affordable Care Act (ACA), Medicaid reform, and the execution of value-based care. At every turn. Ms. Verma pledged to review current processes and work toward enhancing programs, but she declined to support or oppose specific changes. Instead, she promised to help make health care more affordable and to allow patients more flexibility in making health insurance decisions.
Much of the committee’s questioning centered on Ms. Verma’s work on the Healthy Indiana Plan (HIP), Indiana’s Medicaid expansion under the ACA. The conservative plan requires patients to pay a small amount to receive health coverage and includes a lockout period if payments are missed. Legislators repeatedly asked if Ms. Verma planned to use HIP as a model to alter the Medicaid program.
Ms. Verma countered that each state has different needs and should be allowed to develop individualized Medicaid programs that provide flexibility.
“This is about putting states in a leadership role so that they can manage their programs better,” she said. “States are closer to the people that they serve and have a better understanding of what can work in their state than the federal government. I think states should have that flexibility.”
Legislators raised concerns about Ms. Verma’s past consulting agreements with states while working for Hewlett Packard (HP), a company that had financial interests in the health programs she designed. Ms. Verma’s company, SVC, advises clients on Medicaid waivers and state plan amendment development.
Ms. Verma argued that she never negotiated on behalf of Hewlett Packard, and that the work she conducted for the states did not overlap with work she completed for HP. Her company sought an ethics opinion to ensure the arrangement was not problematic, she said.
“I hold honesty and integrity and adherence to a high ethical standard as part of my personal philosophy. That’s for me, I demand that from my employees, and I set that example for my own children,” she said. “We were never in a position where we were negotiating on behalf of HP or any other contractor with the state that we had a relationship with. If there was the potential [for a conflict], we would recuse ourselves.”
Ms. Verma dodged many specific questions, including whether she supported block grants for Medicaid, how she might improve the problem of prescription drug prices, and whether she supported Medicare as a voucher program. When asked by Sen. Sherrod Campbell Brown (D-Ohio) whether she supported an extension of the current Children’s Health Insurance Program (CHIP) for another 8 years, Ms. Verma said she supported “the reauthorization of CHIP for as long as possible.”
When asked about the value-based reforms included in MACRA (the Medicare Access & CHIP Reauthorization Act of 2015), Ms. Verma said she applauded passage of the law, but she would not go into detail about potential changes to the statute.
“I think it’s an important step forward, not only to providing more stability for providers, but also moving us to better outcomes,” she said.
Sen. Wyden grew visibly frustrated with Ms. Verma’s vague answers, saying he was disappointed that, after many questions, the stances she took in many areas were still unclear.
“You’ve been asked a lot of questions and they were not ‘gotcha’ questions,” Sen. Wyden said during the hearing. “These were questions that were appropriate given the fact that if you’re confirmed, you’re going to head an agency that’s involved with a trillion [dollars] of spending in the health care of 100 million people. We’re not really getting much of a sense of how you’d approach [these issues]. I think this committee needs answers and I think the public needs answers.”
“It is critical that we get a strong, skilled leader as CMS administrator,” he said. “Here you are, somebody who has proven to be a tremendous leader in health care, not only to Indiana but as an example to the rest of the states. All I can say is you will be a strong, skilled leader as CMS administrator.”
A relative unknown before her nomination, Ms. Verma spent 20 years designing policy projects involving Medicaid, including HIP, the nation’s first consumer-directed Medicaid program under Indiana Governor Mitch Daniels and then-Gov. Mike Pence’s HIP 2.0 waiver proposal.
Prior to consulting, Ms. Verma served as vice president of planning for the Health and Hospital Corporation of Marion County (Ind.) and as a director with the Association of State and Territorial Health Officials in Washington.
Senators have asked that Ms. Verma submit written answers to their questions, which they will review before voting on her nomination.
[email protected]
On Twitter @legal_med
If confirmed as Centers for Medicare & Medicaid Services administrator, Seema Verma vowed to modernize CMS programs, improve Medicaid access, and leverage technology to drive better care, but she stopped short of explaining how she would do so during her confirmation hearing Feb. 16 before the Senate Finance Committee.
Legislators grilled Ms. Verma on Medicare improvements, the fate of the Affordable Care Act (ACA), Medicaid reform, and the execution of value-based care. At every turn. Ms. Verma pledged to review current processes and work toward enhancing programs, but she declined to support or oppose specific changes. Instead, she promised to help make health care more affordable and to allow patients more flexibility in making health insurance decisions.
Much of the committee’s questioning centered on Ms. Verma’s work on the Healthy Indiana Plan (HIP), Indiana’s Medicaid expansion under the ACA. The conservative plan requires patients to pay a small amount to receive health coverage and includes a lockout period if payments are missed. Legislators repeatedly asked if Ms. Verma planned to use HIP as a model to alter the Medicaid program.
Ms. Verma countered that each state has different needs and should be allowed to develop individualized Medicaid programs that provide flexibility.
“This is about putting states in a leadership role so that they can manage their programs better,” she said. “States are closer to the people that they serve and have a better understanding of what can work in their state than the federal government. I think states should have that flexibility.”
Legislators raised concerns about Ms. Verma’s past consulting agreements with states while working for Hewlett Packard (HP), a company that had financial interests in the health programs she designed. Ms. Verma’s company, SVC, advises clients on Medicaid waivers and state plan amendment development.
Ms. Verma argued that she never negotiated on behalf of Hewlett Packard, and that the work she conducted for the states did not overlap with work she completed for HP. Her company sought an ethics opinion to ensure the arrangement was not problematic, she said.
“I hold honesty and integrity and adherence to a high ethical standard as part of my personal philosophy. That’s for me, I demand that from my employees, and I set that example for my own children,” she said. “We were never in a position where we were negotiating on behalf of HP or any other contractor with the state that we had a relationship with. If there was the potential [for a conflict], we would recuse ourselves.”
Ms. Verma dodged many specific questions, including whether she supported block grants for Medicaid, how she might improve the problem of prescription drug prices, and whether she supported Medicare as a voucher program. When asked by Sen. Sherrod Campbell Brown (D-Ohio) whether she supported an extension of the current Children’s Health Insurance Program (CHIP) for another 8 years, Ms. Verma said she supported “the reauthorization of CHIP for as long as possible.”
When asked about the value-based reforms included in MACRA (the Medicare Access & CHIP Reauthorization Act of 2015), Ms. Verma said she applauded passage of the law, but she would not go into detail about potential changes to the statute.
“I think it’s an important step forward, not only to providing more stability for providers, but also moving us to better outcomes,” she said.
Sen. Wyden grew visibly frustrated with Ms. Verma’s vague answers, saying he was disappointed that, after many questions, the stances she took in many areas were still unclear.
“You’ve been asked a lot of questions and they were not ‘gotcha’ questions,” Sen. Wyden said during the hearing. “These were questions that were appropriate given the fact that if you’re confirmed, you’re going to head an agency that’s involved with a trillion [dollars] of spending in the health care of 100 million people. We’re not really getting much of a sense of how you’d approach [these issues]. I think this committee needs answers and I think the public needs answers.”
“It is critical that we get a strong, skilled leader as CMS administrator,” he said. “Here you are, somebody who has proven to be a tremendous leader in health care, not only to Indiana but as an example to the rest of the states. All I can say is you will be a strong, skilled leader as CMS administrator.”
A relative unknown before her nomination, Ms. Verma spent 20 years designing policy projects involving Medicaid, including HIP, the nation’s first consumer-directed Medicaid program under Indiana Governor Mitch Daniels and then-Gov. Mike Pence’s HIP 2.0 waiver proposal.
Prior to consulting, Ms. Verma served as vice president of planning for the Health and Hospital Corporation of Marion County (Ind.) and as a director with the Association of State and Territorial Health Officials in Washington.
Senators have asked that Ms. Verma submit written answers to their questions, which they will review before voting on her nomination.
[email protected]
On Twitter @legal_med
If confirmed as Centers for Medicare & Medicaid Services administrator, Seema Verma vowed to modernize CMS programs, improve Medicaid access, and leverage technology to drive better care, but she stopped short of explaining how she would do so during her confirmation hearing Feb. 16 before the Senate Finance Committee.
Legislators grilled Ms. Verma on Medicare improvements, the fate of the Affordable Care Act (ACA), Medicaid reform, and the execution of value-based care. At every turn. Ms. Verma pledged to review current processes and work toward enhancing programs, but she declined to support or oppose specific changes. Instead, she promised to help make health care more affordable and to allow patients more flexibility in making health insurance decisions.
Much of the committee’s questioning centered on Ms. Verma’s work on the Healthy Indiana Plan (HIP), Indiana’s Medicaid expansion under the ACA. The conservative plan requires patients to pay a small amount to receive health coverage and includes a lockout period if payments are missed. Legislators repeatedly asked if Ms. Verma planned to use HIP as a model to alter the Medicaid program.
Ms. Verma countered that each state has different needs and should be allowed to develop individualized Medicaid programs that provide flexibility.
“This is about putting states in a leadership role so that they can manage their programs better,” she said. “States are closer to the people that they serve and have a better understanding of what can work in their state than the federal government. I think states should have that flexibility.”
Legislators raised concerns about Ms. Verma’s past consulting agreements with states while working for Hewlett Packard (HP), a company that had financial interests in the health programs she designed. Ms. Verma’s company, SVC, advises clients on Medicaid waivers and state plan amendment development.
Ms. Verma argued that she never negotiated on behalf of Hewlett Packard, and that the work she conducted for the states did not overlap with work she completed for HP. Her company sought an ethics opinion to ensure the arrangement was not problematic, she said.
“I hold honesty and integrity and adherence to a high ethical standard as part of my personal philosophy. That’s for me, I demand that from my employees, and I set that example for my own children,” she said. “We were never in a position where we were negotiating on behalf of HP or any other contractor with the state that we had a relationship with. If there was the potential [for a conflict], we would recuse ourselves.”
Ms. Verma dodged many specific questions, including whether she supported block grants for Medicaid, how she might improve the problem of prescription drug prices, and whether she supported Medicare as a voucher program. When asked by Sen. Sherrod Campbell Brown (D-Ohio) whether she supported an extension of the current Children’s Health Insurance Program (CHIP) for another 8 years, Ms. Verma said she supported “the reauthorization of CHIP for as long as possible.”
When asked about the value-based reforms included in MACRA (the Medicare Access & CHIP Reauthorization Act of 2015), Ms. Verma said she applauded passage of the law, but she would not go into detail about potential changes to the statute.
“I think it’s an important step forward, not only to providing more stability for providers, but also moving us to better outcomes,” she said.
Sen. Wyden grew visibly frustrated with Ms. Verma’s vague answers, saying he was disappointed that, after many questions, the stances she took in many areas were still unclear.
“You’ve been asked a lot of questions and they were not ‘gotcha’ questions,” Sen. Wyden said during the hearing. “These were questions that were appropriate given the fact that if you’re confirmed, you’re going to head an agency that’s involved with a trillion [dollars] of spending in the health care of 100 million people. We’re not really getting much of a sense of how you’d approach [these issues]. I think this committee needs answers and I think the public needs answers.”
“It is critical that we get a strong, skilled leader as CMS administrator,” he said. “Here you are, somebody who has proven to be a tremendous leader in health care, not only to Indiana but as an example to the rest of the states. All I can say is you will be a strong, skilled leader as CMS administrator.”
A relative unknown before her nomination, Ms. Verma spent 20 years designing policy projects involving Medicaid, including HIP, the nation’s first consumer-directed Medicaid program under Indiana Governor Mitch Daniels and then-Gov. Mike Pence’s HIP 2.0 waiver proposal.
Prior to consulting, Ms. Verma served as vice president of planning for the Health and Hospital Corporation of Marion County (Ind.) and as a director with the Association of State and Territorial Health Officials in Washington.
Senators have asked that Ms. Verma submit written answers to their questions, which they will review before voting on her nomination.
[email protected]
On Twitter @legal_med
CMS proposal seeks to stabilize individual insurance market
Proposed regulations from the Centers for Medicare & Medicaid Services aim to provide short-term stabilization to the individual and small group insurance markets under the Affordable Care Act.
The proposal issued Feb. 15 would make changes to special enrollment periods, open enrollment, guaranteed availability, network adequacy rules, essential community providers, and actuarial value requirements. It also changes the timeline for when insurers would need to get their qualified health plan certification. It represents a first step toward fulfilling President Trump’s Inauguration Day executive order to “minimize the unwarranted economic and regulatory burdens of the [ACA], and prepare to afford the states more flexibility and control to create a more free and open health care market.”
However, the proposed rule, if finalized as is, may not have any dramatic effect on the decision by insurers to serve the individual and small group markets.
“A plan that was going to stay is probably going to stay and be a little bit happier about these regs and a plan that was going to decide to leave, like Humana, would have left anyway,” Caroline Pearson, senior vice president at Avalere Health said in an interview. “I don’t know if it is going to materially change plan participation.”
The proposed rule would shorten open enrollment for plans purchased in the ACA marketplace. Currently, plans can be purchased from Nov. 1 to Jan. 31; the proposal would move the deadline up to Dec. 15.
“We anticipate this change could improve the risk pool because it would reduce opportunities for adverse selection by those who learn they will need services in late December and January; and will encourage healthier individuals who might have previously enrolled in partial year coverage after Dec. 15th to instead enroll in coverage for the full year,” according to the proposed rule.
CMS also proposes to tighten special enrollment by requiring preverification of special enrollment period status for all people applicants. Currently, only 50% of those seeking coverage through special enrollment are verified. The agency also is proposing to limit the plan choices available to individuals who are enrolling via a special enrollment period as a way of minimizing adverse selection.
Another proposal aimed at keeping people covered is one that allows insurers to collect unpaid premiums in the prior coverage year before enrolling a patient in the next year’s plan with the same insurer.
CMS noted in the rule that a recent survey “concluded that approximately 21% of consumers stopped premium payments in 2015. Approximately 87% of those individuals repurchased plans in 2016, while 49% of these consumers purchased the same plan they had previously stopped payment on.”
On the network adequacy front, CMS is shifting the conduct of network adequacy reviews to states, or to an accrediting entity recognized by the Department of Health & Human Services in the case of states that do not have sufficient resources to conduct adequacy reviews. Further, the proposal reduces the minimum percentage of essential community providers (those who serve predominantly low-income and medically underserved populations) in a network to 20% from the 30% instituted in 2015.
CMS said in the proposal that if these rules are finalized, it will issue separate guidance on changes to the timeline for plans to submit their bids for 2018.
Avalere’s Ms. Pearson said that she sees these proposed changes merely as a stopgap measure.
“This reg is intended to stand up the exchange markets and keep them functional while the ACA replacement plan is approved and implemented,” she said. “This is meant to prevent there from being a total loss of coverage before the ACA replacement can be put into effect.”
She added that while insurers will welcome the changes, consumers and patient advocates could push back on the proposal, particularly the actuarial flexibility that could result in smaller networks and shrinking benefits.
Indeed, America’s Health Insurance Plans offered its support of the regulation. “We commend the Administration for proposing these regulatory actions as Congress considers other critical actions necessary to help stabilize and improve the individual market for 2018,” AHIP President and CEO Marilyn Tavenner said in a statement.
The proposed changes were released online Feb. 15 and are scheduled for publication in the Federal Register on Feb. 17. Comments on the proposed changes are due to CMS by March 7.
Proposed regulations from the Centers for Medicare & Medicaid Services aim to provide short-term stabilization to the individual and small group insurance markets under the Affordable Care Act.
The proposal issued Feb. 15 would make changes to special enrollment periods, open enrollment, guaranteed availability, network adequacy rules, essential community providers, and actuarial value requirements. It also changes the timeline for when insurers would need to get their qualified health plan certification. It represents a first step toward fulfilling President Trump’s Inauguration Day executive order to “minimize the unwarranted economic and regulatory burdens of the [ACA], and prepare to afford the states more flexibility and control to create a more free and open health care market.”
However, the proposed rule, if finalized as is, may not have any dramatic effect on the decision by insurers to serve the individual and small group markets.
“A plan that was going to stay is probably going to stay and be a little bit happier about these regs and a plan that was going to decide to leave, like Humana, would have left anyway,” Caroline Pearson, senior vice president at Avalere Health said in an interview. “I don’t know if it is going to materially change plan participation.”
The proposed rule would shorten open enrollment for plans purchased in the ACA marketplace. Currently, plans can be purchased from Nov. 1 to Jan. 31; the proposal would move the deadline up to Dec. 15.
“We anticipate this change could improve the risk pool because it would reduce opportunities for adverse selection by those who learn they will need services in late December and January; and will encourage healthier individuals who might have previously enrolled in partial year coverage after Dec. 15th to instead enroll in coverage for the full year,” according to the proposed rule.
CMS also proposes to tighten special enrollment by requiring preverification of special enrollment period status for all people applicants. Currently, only 50% of those seeking coverage through special enrollment are verified. The agency also is proposing to limit the plan choices available to individuals who are enrolling via a special enrollment period as a way of minimizing adverse selection.
Another proposal aimed at keeping people covered is one that allows insurers to collect unpaid premiums in the prior coverage year before enrolling a patient in the next year’s plan with the same insurer.
CMS noted in the rule that a recent survey “concluded that approximately 21% of consumers stopped premium payments in 2015. Approximately 87% of those individuals repurchased plans in 2016, while 49% of these consumers purchased the same plan they had previously stopped payment on.”
On the network adequacy front, CMS is shifting the conduct of network adequacy reviews to states, or to an accrediting entity recognized by the Department of Health & Human Services in the case of states that do not have sufficient resources to conduct adequacy reviews. Further, the proposal reduces the minimum percentage of essential community providers (those who serve predominantly low-income and medically underserved populations) in a network to 20% from the 30% instituted in 2015.
CMS said in the proposal that if these rules are finalized, it will issue separate guidance on changes to the timeline for plans to submit their bids for 2018.
Avalere’s Ms. Pearson said that she sees these proposed changes merely as a stopgap measure.
“This reg is intended to stand up the exchange markets and keep them functional while the ACA replacement plan is approved and implemented,” she said. “This is meant to prevent there from being a total loss of coverage before the ACA replacement can be put into effect.”
She added that while insurers will welcome the changes, consumers and patient advocates could push back on the proposal, particularly the actuarial flexibility that could result in smaller networks and shrinking benefits.
Indeed, America’s Health Insurance Plans offered its support of the regulation. “We commend the Administration for proposing these regulatory actions as Congress considers other critical actions necessary to help stabilize and improve the individual market for 2018,” AHIP President and CEO Marilyn Tavenner said in a statement.
The proposed changes were released online Feb. 15 and are scheduled for publication in the Federal Register on Feb. 17. Comments on the proposed changes are due to CMS by March 7.
Proposed regulations from the Centers for Medicare & Medicaid Services aim to provide short-term stabilization to the individual and small group insurance markets under the Affordable Care Act.
The proposal issued Feb. 15 would make changes to special enrollment periods, open enrollment, guaranteed availability, network adequacy rules, essential community providers, and actuarial value requirements. It also changes the timeline for when insurers would need to get their qualified health plan certification. It represents a first step toward fulfilling President Trump’s Inauguration Day executive order to “minimize the unwarranted economic and regulatory burdens of the [ACA], and prepare to afford the states more flexibility and control to create a more free and open health care market.”
However, the proposed rule, if finalized as is, may not have any dramatic effect on the decision by insurers to serve the individual and small group markets.
“A plan that was going to stay is probably going to stay and be a little bit happier about these regs and a plan that was going to decide to leave, like Humana, would have left anyway,” Caroline Pearson, senior vice president at Avalere Health said in an interview. “I don’t know if it is going to materially change plan participation.”
The proposed rule would shorten open enrollment for plans purchased in the ACA marketplace. Currently, plans can be purchased from Nov. 1 to Jan. 31; the proposal would move the deadline up to Dec. 15.
“We anticipate this change could improve the risk pool because it would reduce opportunities for adverse selection by those who learn they will need services in late December and January; and will encourage healthier individuals who might have previously enrolled in partial year coverage after Dec. 15th to instead enroll in coverage for the full year,” according to the proposed rule.
CMS also proposes to tighten special enrollment by requiring preverification of special enrollment period status for all people applicants. Currently, only 50% of those seeking coverage through special enrollment are verified. The agency also is proposing to limit the plan choices available to individuals who are enrolling via a special enrollment period as a way of minimizing adverse selection.
Another proposal aimed at keeping people covered is one that allows insurers to collect unpaid premiums in the prior coverage year before enrolling a patient in the next year’s plan with the same insurer.
CMS noted in the rule that a recent survey “concluded that approximately 21% of consumers stopped premium payments in 2015. Approximately 87% of those individuals repurchased plans in 2016, while 49% of these consumers purchased the same plan they had previously stopped payment on.”
On the network adequacy front, CMS is shifting the conduct of network adequacy reviews to states, or to an accrediting entity recognized by the Department of Health & Human Services in the case of states that do not have sufficient resources to conduct adequacy reviews. Further, the proposal reduces the minimum percentage of essential community providers (those who serve predominantly low-income and medically underserved populations) in a network to 20% from the 30% instituted in 2015.
CMS said in the proposal that if these rules are finalized, it will issue separate guidance on changes to the timeline for plans to submit their bids for 2018.
Avalere’s Ms. Pearson said that she sees these proposed changes merely as a stopgap measure.
“This reg is intended to stand up the exchange markets and keep them functional while the ACA replacement plan is approved and implemented,” she said. “This is meant to prevent there from being a total loss of coverage before the ACA replacement can be put into effect.”
She added that while insurers will welcome the changes, consumers and patient advocates could push back on the proposal, particularly the actuarial flexibility that could result in smaller networks and shrinking benefits.
Indeed, America’s Health Insurance Plans offered its support of the regulation. “We commend the Administration for proposing these regulatory actions as Congress considers other critical actions necessary to help stabilize and improve the individual market for 2018,” AHIP President and CEO Marilyn Tavenner said in a statement.
The proposed changes were released online Feb. 15 and are scheduled for publication in the Federal Register on Feb. 17. Comments on the proposed changes are due to CMS by March 7.
Malpractice 2017: Do we need reform?
Malpractice reforms long espoused by Thomas E. Price, MD, Health & Human Services secretary, are fostering debate on whether national fixes are necessary in an improving liability landscape. Claims against health providers have decreased twofold and doctors nationwide have seen their premiums decrease steadily for a decade. But the numbers tell just part of the story, liability experts say.
“Most health policy and medical malpractice scholars would not describe the environment we’re in right now as a state of crisis, at least not compared to what we observed a decade ago,” said Anupam B. Jena, MD, PhD, health care policy professor at Harvard University, Boston, and a medical liability researcher.“But I would argue that malpractice is still a salient fact for most physicians. What’s much more important than focusing on changes over time is taking a static perspective and understanding the risk that a physician faces when it comes to malpractice.”
During just over 12 years in Congress, Dr. Price (R-Ga.) has consistently advocated for tort reform, proposing legislation that would restructure the lawsuit process. He supports damage caps and has recommended the creation of health care tribunals that would hear cases only after medical review. He has also proposed the development of national practice guidelines for doctors, which if followed could be used defensively.
“From exorbitant malpractice insurance premiums to the remarkably expensive practice of defensive medicine, it is my experience that the current culture of litigation costs patients hundreds of billions of dollars,” Dr. Price wrote in a 2009 commentary about his Empowering Patients First Act. “These costs do nothing to provide better care, but rather serve only as a defense against unyielding personal injury lawyers ...When malpractice suits are brought through specialized courts and viewed through the perspective of medically appropriate care, rather than a lottery mentality, we will see a decline in frivolous lawsuits.”
Data show lawsuits down
Claims data however, show that lawsuits against doctors are on the decline – and have been for more than 10 years. The rate of paid claims against physicians dropped from 18.6 to 9.9 paid claims per 1,000 physicians between 2002 and 2013, according to 2014 study by Michelle Mello of Stanford (Calif.) University and colleagues (JAMA. 2014;312(20):2146-2155. doi:10.1001/jama.2014.10705). Another analysis found that claims decreased from 12 claims per 100 doctors in 2003 to 6 per 100 doctors in 2016, according to a study of claims from The Doctors Company database.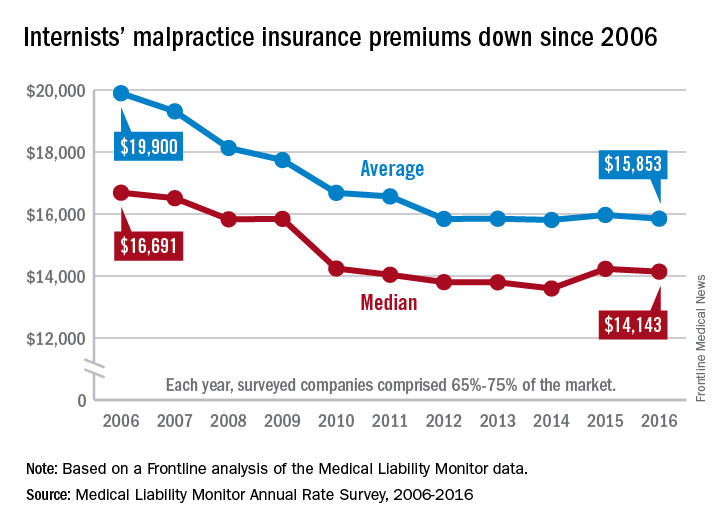
The sharp decline in claims is directly affecting premiums, which have remained nearly unchanged for years, said Michael Matray, editor of the Medical Liability Monitor (MLM), which tracks premium rates. In 2003, rate increases of 49% were commonplace, he noted, with some states reporting rises of 100%. But premiums started to fall in 2006, he said.
“We are in the midst of a 10-year soft market, the longest we’ve ever had,” Mr. Matray said in an interview. “In 2006, we started to soften. We have been soft or flat with no change since. It’s definitely unprecedented.”
In 2016, U.S. internists paid an average premium of $15,853, compared to an average premium payment of $19,900 in 2006 without inflation adjustment, according to this news organization’s analysis of MLM data. General surgeons meanwhile, paid an average of $52,905 in premiums in 2016, compared to a 2006 average of $68,186. Ob.gyns. paid an average premium of $72,999 in 2016, a drop from $93,230 in 2006.
“Generally speaking, it’s great for doctors,” Mr. Matray said. “Even if you remove the inflationary factor, there are some states where they are paying less now than they were 10 years ago.”
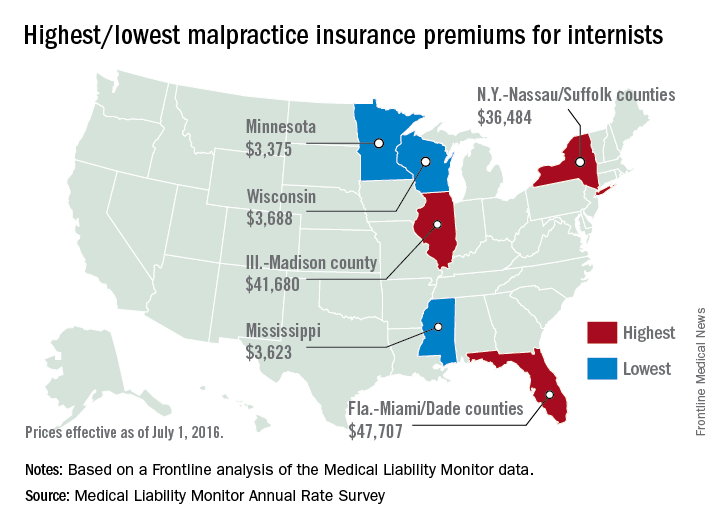
But stable premiums do not mean inexpensive insurance, noted Mike Stinson, vice president of government relations and public policy for the PIAA, a national trade association for medical liability insurers.
“They’ve certainly come down over the last few years,” Mr. Stinson said in an interview. “But they certainly are not low.”
South Florida doctors for example, are paying among the highest premiums in the nation despite an overall drop in the last 10 years. Internists in Dade County, Fla., paid $47,707 for insurance in 2016, $27,000 less than in 2006, according to MLM data. Coverage is still is not affordable, said Jason M. Goldman, MD, an internist in private practice in Coral Springs, Fla., and governor for the American College of Physicians Florida chapter.
The premiums are ridiculous,” he said in an interview. “That’s one of the reasons I went bare. Having medical insurance makes you a target, because lawyers think, ‘We can sue the insurance company and the insurance company is going to pay.’ ”
State reforms driving lawsuit decline
A combination of state reforms and patient safety initiatives are fueling the lawsuit down slide, said Paul A. Greve Jr. senior vice president/senior consultant for Willis Towers Watson Health Care Practice and coauthor of the 2016 MLM Survey report.
More than 25 states now have laws that enforce caps on noneconomic damages in medical liability cases, and in the last 15 years, a large majority have upheld such limits, Mr. Greve said. In addition, a number of states require a certificate of merit before suits can move forward, which mandate that a qualified physician verify that a defendant’s actions were likely negligent.
Patient safety programs such as internal patient safety committees, enhanced provider education, safety protocols, and communication and resolution programs, are also making an impact.
“There have been many efforts toward thinking innovatively about how we should be compensating patients more fairly and more quickly,” said Harvard’s Dr. Jena, who practices at Massachusetts General Hospital. “There are early disclosure programs that many hospitals have adopted as a movement toward that goal. The system is evolving.”
The high expense of filing a medical malpractice lawsuit is another factor detouring lawsuits, Mr. Greve added.
“It’s very expensive for [plaintiffs’ attorneys] to pursue these cases,” he said. “They have to invest a large amount of money into them and they can’t afford to take cases that have questionable liability, or they’re going to end up shelling out a lot of money and not getting anything in return.”
Malpractice system remains broken
While lawsuit and premium data paint a positive picture, the medical malpractice system remains dysfunctional for doctors and patients, said PIAA’s Mr. Stinson.
A majority of medical malpractice claims against physicians are determined to be nonmeritorious yet an average lawsuit takes roughly 4 years to resolve, he noted. Suits against doctors are dismissed by the court 54% of the time across all specialties, and among cases that go to trial, 80% end in the physician’s favor, according to a 2012 study by Dr. Jena and colleagues (JAMA Intern Med. 2012 Jun. 11 doi: 10.1001/jamainternmed.2012.1416)
“We think that’s a huge amount of resources both in time and money and human capital to get poured into cases where no payment is ever deemed appropriate,” Mr. Stinson said. “We would like to see [malpractice] reforms in part because we think you can weed out some of these claims in advance, so more of the resources can be used to determine whether or not there was negligence and if so, making that patient whole as fast as possible.”
Regardless of declining claims, most physicians will still be sued in their lifetime, Dr. Jena said. By age 65, 75% of physicians in low-risk specialties have faced a malpractice claim, and 99% of doctors in high-risk specialties have been sued, according to a 2011 study by Dr. Jena and colleagues (N Engl J Med. 2011 Aug. 18. doi: 10.1056/NEJMsa1012370)
“What really matters for physicians is not only whether they win or lose a malpractice suit, but whether they are sued in the first place,” Dr. Jena said. “Lawsuits happen quite often and over the course of a physician’s career they are quite common. So whether or not we’re in a state of malpractice crisis or not, the lifetime risk for physicians is quite real.”
The cost of defending claims continues to rise, noted Richard E. Anderson, MD, chair and CEO of The Doctors Company. At the same time, multi-million dollar malpractice verdicts have become more common.
“There’s still way too much malpractice litigation,” Dr. Anderson said. “The majority of it is fruitless, and the total cost burden borne by physicians has not decreased as much as the frequency because of the ongoing increase in severity.”
“The bottom line is defensive medicine is a huge and growing cost to all Americans,” he said. “We’re all on the hook for America’s rising health care bills. And as my increasingly infirm Baby Boomer generation gets older and weaker and sicker, those bills are going to rise that much faster. So the notion advanced by some so-called experts that we can nonetheless afford to spend a half trillion dollars a year or more on largely unnecessary testing driven in significant part by fear of litigation and giant outlier verdicts seems rather inane, and it suggests perhaps that those experts aren’t so expert.”
What would Dr. Price do?
Opinions are mixed about whether Dr. Price’s proposed reforms are the right changes for the medical liability system.
Expert panels to review claims for validity are a promising suggestion, Dr. Jena said. “Administrative courts to help identify malpractice cases that are truly malpractice early on is a good idea,” he said. “We want to have a system that prevents less meritorious cases from soaking up resources.”
But the idea may be easier said than done, said Dr. Anderson of The Doctors Company. “The devil is always in the details There is a lot of merit in [health courts] and they make a lot of sense. However, the notion of going from where we are today to an untested system, which would have to be a compromise between adversaries, would be a very challenging one.”
National clinical standards for physicians to follow and use as a safeguard could backfire, Mr. Stinson said. Bureaucracy could slow the guidelines from being promptly updated, and the standards could fail to keep up with the latest medical developments. As doctors know, medicine is not a one-size-fits-all approach, he added.
“[Guidelines] could encourage doctors to practice cookbook medicine, where they’re just going to follow the standard along without being given the opportunity to use their training and clinical experience to see whether that’s actually in the patient’s best interest,” Mr. Stinson said. “We certainly wouldn’t want to see a situation where a doctor feels diverting from a guidelines is in a patient’s best interest, but they don’t dare do it because it could subject them to a lawsuit.”
When enacting malpractice reforms, it will be critical to evaluate the intervention first to ensure the right objections are met, Dr. Jena added.
“At the end of the day, if the [legal] environment is such that it’s uncomfortable to practice medicine, that’s going to have implications for who goes into medicine and implications for ordering tests and procedures,” he said. “Any reform that attempts to make the process more efficient is a good idea because it lowers cost to the system and makes the experience better for patients and physicians.”
This article was updated 2/15/17.
[email protected]
On Twitter @legal_med
Malpractice reforms long espoused by Thomas E. Price, MD, Health & Human Services secretary, are fostering debate on whether national fixes are necessary in an improving liability landscape. Claims against health providers have decreased twofold and doctors nationwide have seen their premiums decrease steadily for a decade. But the numbers tell just part of the story, liability experts say.
“Most health policy and medical malpractice scholars would not describe the environment we’re in right now as a state of crisis, at least not compared to what we observed a decade ago,” said Anupam B. Jena, MD, PhD, health care policy professor at Harvard University, Boston, and a medical liability researcher.“But I would argue that malpractice is still a salient fact for most physicians. What’s much more important than focusing on changes over time is taking a static perspective and understanding the risk that a physician faces when it comes to malpractice.”
During just over 12 years in Congress, Dr. Price (R-Ga.) has consistently advocated for tort reform, proposing legislation that would restructure the lawsuit process. He supports damage caps and has recommended the creation of health care tribunals that would hear cases only after medical review. He has also proposed the development of national practice guidelines for doctors, which if followed could be used defensively.
“From exorbitant malpractice insurance premiums to the remarkably expensive practice of defensive medicine, it is my experience that the current culture of litigation costs patients hundreds of billions of dollars,” Dr. Price wrote in a 2009 commentary about his Empowering Patients First Act. “These costs do nothing to provide better care, but rather serve only as a defense against unyielding personal injury lawyers ...When malpractice suits are brought through specialized courts and viewed through the perspective of medically appropriate care, rather than a lottery mentality, we will see a decline in frivolous lawsuits.”
Data show lawsuits down
Claims data however, show that lawsuits against doctors are on the decline – and have been for more than 10 years. The rate of paid claims against physicians dropped from 18.6 to 9.9 paid claims per 1,000 physicians between 2002 and 2013, according to 2014 study by Michelle Mello of Stanford (Calif.) University and colleagues (JAMA. 2014;312(20):2146-2155. doi:10.1001/jama.2014.10705). Another analysis found that claims decreased from 12 claims per 100 doctors in 2003 to 6 per 100 doctors in 2016, according to a study of claims from The Doctors Company database.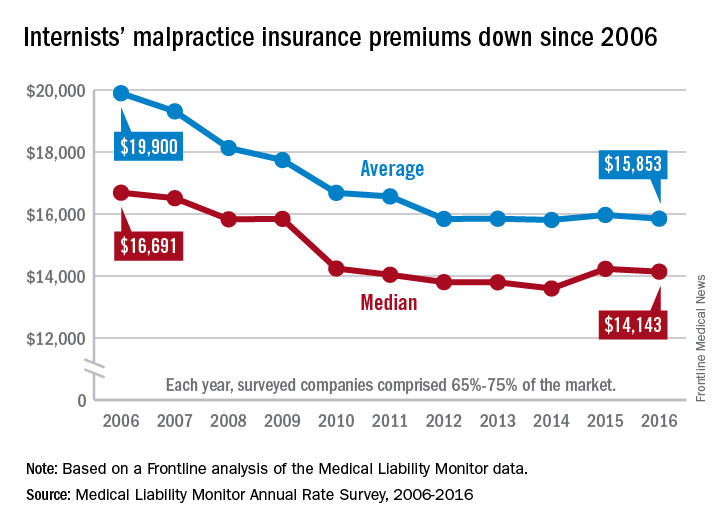
The sharp decline in claims is directly affecting premiums, which have remained nearly unchanged for years, said Michael Matray, editor of the Medical Liability Monitor (MLM), which tracks premium rates. In 2003, rate increases of 49% were commonplace, he noted, with some states reporting rises of 100%. But premiums started to fall in 2006, he said.
“We are in the midst of a 10-year soft market, the longest we’ve ever had,” Mr. Matray said in an interview. “In 2006, we started to soften. We have been soft or flat with no change since. It’s definitely unprecedented.”
In 2016, U.S. internists paid an average premium of $15,853, compared to an average premium payment of $19,900 in 2006 without inflation adjustment, according to this news organization’s analysis of MLM data. General surgeons meanwhile, paid an average of $52,905 in premiums in 2016, compared to a 2006 average of $68,186. Ob.gyns. paid an average premium of $72,999 in 2016, a drop from $93,230 in 2006.
“Generally speaking, it’s great for doctors,” Mr. Matray said. “Even if you remove the inflationary factor, there are some states where they are paying less now than they were 10 years ago.”
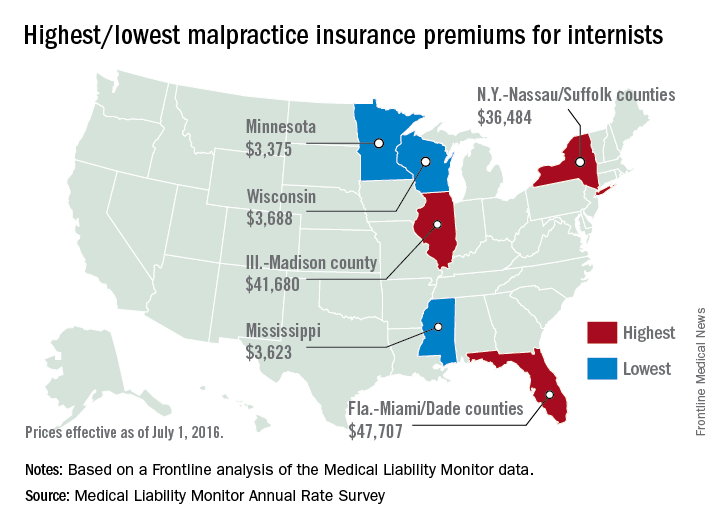
But stable premiums do not mean inexpensive insurance, noted Mike Stinson, vice president of government relations and public policy for the PIAA, a national trade association for medical liability insurers.
“They’ve certainly come down over the last few years,” Mr. Stinson said in an interview. “But they certainly are not low.”
South Florida doctors for example, are paying among the highest premiums in the nation despite an overall drop in the last 10 years. Internists in Dade County, Fla., paid $47,707 for insurance in 2016, $27,000 less than in 2006, according to MLM data. Coverage is still is not affordable, said Jason M. Goldman, MD, an internist in private practice in Coral Springs, Fla., and governor for the American College of Physicians Florida chapter.
The premiums are ridiculous,” he said in an interview. “That’s one of the reasons I went bare. Having medical insurance makes you a target, because lawyers think, ‘We can sue the insurance company and the insurance company is going to pay.’ ”
State reforms driving lawsuit decline
A combination of state reforms and patient safety initiatives are fueling the lawsuit down slide, said Paul A. Greve Jr. senior vice president/senior consultant for Willis Towers Watson Health Care Practice and coauthor of the 2016 MLM Survey report.
More than 25 states now have laws that enforce caps on noneconomic damages in medical liability cases, and in the last 15 years, a large majority have upheld such limits, Mr. Greve said. In addition, a number of states require a certificate of merit before suits can move forward, which mandate that a qualified physician verify that a defendant’s actions were likely negligent.
Patient safety programs such as internal patient safety committees, enhanced provider education, safety protocols, and communication and resolution programs, are also making an impact.
“There have been many efforts toward thinking innovatively about how we should be compensating patients more fairly and more quickly,” said Harvard’s Dr. Jena, who practices at Massachusetts General Hospital. “There are early disclosure programs that many hospitals have adopted as a movement toward that goal. The system is evolving.”
The high expense of filing a medical malpractice lawsuit is another factor detouring lawsuits, Mr. Greve added.
“It’s very expensive for [plaintiffs’ attorneys] to pursue these cases,” he said. “They have to invest a large amount of money into them and they can’t afford to take cases that have questionable liability, or they’re going to end up shelling out a lot of money and not getting anything in return.”
Malpractice system remains broken
While lawsuit and premium data paint a positive picture, the medical malpractice system remains dysfunctional for doctors and patients, said PIAA’s Mr. Stinson.
A majority of medical malpractice claims against physicians are determined to be nonmeritorious yet an average lawsuit takes roughly 4 years to resolve, he noted. Suits against doctors are dismissed by the court 54% of the time across all specialties, and among cases that go to trial, 80% end in the physician’s favor, according to a 2012 study by Dr. Jena and colleagues (JAMA Intern Med. 2012 Jun. 11 doi: 10.1001/jamainternmed.2012.1416)
“We think that’s a huge amount of resources both in time and money and human capital to get poured into cases where no payment is ever deemed appropriate,” Mr. Stinson said. “We would like to see [malpractice] reforms in part because we think you can weed out some of these claims in advance, so more of the resources can be used to determine whether or not there was negligence and if so, making that patient whole as fast as possible.”
Regardless of declining claims, most physicians will still be sued in their lifetime, Dr. Jena said. By age 65, 75% of physicians in low-risk specialties have faced a malpractice claim, and 99% of doctors in high-risk specialties have been sued, according to a 2011 study by Dr. Jena and colleagues (N Engl J Med. 2011 Aug. 18. doi: 10.1056/NEJMsa1012370)
“What really matters for physicians is not only whether they win or lose a malpractice suit, but whether they are sued in the first place,” Dr. Jena said. “Lawsuits happen quite often and over the course of a physician’s career they are quite common. So whether or not we’re in a state of malpractice crisis or not, the lifetime risk for physicians is quite real.”
The cost of defending claims continues to rise, noted Richard E. Anderson, MD, chair and CEO of The Doctors Company. At the same time, multi-million dollar malpractice verdicts have become more common.
“There’s still way too much malpractice litigation,” Dr. Anderson said. “The majority of it is fruitless, and the total cost burden borne by physicians has not decreased as much as the frequency because of the ongoing increase in severity.”
“The bottom line is defensive medicine is a huge and growing cost to all Americans,” he said. “We’re all on the hook for America’s rising health care bills. And as my increasingly infirm Baby Boomer generation gets older and weaker and sicker, those bills are going to rise that much faster. So the notion advanced by some so-called experts that we can nonetheless afford to spend a half trillion dollars a year or more on largely unnecessary testing driven in significant part by fear of litigation and giant outlier verdicts seems rather inane, and it suggests perhaps that those experts aren’t so expert.”
What would Dr. Price do?
Opinions are mixed about whether Dr. Price’s proposed reforms are the right changes for the medical liability system.
Expert panels to review claims for validity are a promising suggestion, Dr. Jena said. “Administrative courts to help identify malpractice cases that are truly malpractice early on is a good idea,” he said. “We want to have a system that prevents less meritorious cases from soaking up resources.”
But the idea may be easier said than done, said Dr. Anderson of The Doctors Company. “The devil is always in the details There is a lot of merit in [health courts] and they make a lot of sense. However, the notion of going from where we are today to an untested system, which would have to be a compromise between adversaries, would be a very challenging one.”
National clinical standards for physicians to follow and use as a safeguard could backfire, Mr. Stinson said. Bureaucracy could slow the guidelines from being promptly updated, and the standards could fail to keep up with the latest medical developments. As doctors know, medicine is not a one-size-fits-all approach, he added.
“[Guidelines] could encourage doctors to practice cookbook medicine, where they’re just going to follow the standard along without being given the opportunity to use their training and clinical experience to see whether that’s actually in the patient’s best interest,” Mr. Stinson said. “We certainly wouldn’t want to see a situation where a doctor feels diverting from a guidelines is in a patient’s best interest, but they don’t dare do it because it could subject them to a lawsuit.”
When enacting malpractice reforms, it will be critical to evaluate the intervention first to ensure the right objections are met, Dr. Jena added.
“At the end of the day, if the [legal] environment is such that it’s uncomfortable to practice medicine, that’s going to have implications for who goes into medicine and implications for ordering tests and procedures,” he said. “Any reform that attempts to make the process more efficient is a good idea because it lowers cost to the system and makes the experience better for patients and physicians.”
This article was updated 2/15/17.
[email protected]
On Twitter @legal_med
Malpractice reforms long espoused by Thomas E. Price, MD, Health & Human Services secretary, are fostering debate on whether national fixes are necessary in an improving liability landscape. Claims against health providers have decreased twofold and doctors nationwide have seen their premiums decrease steadily for a decade. But the numbers tell just part of the story, liability experts say.
“Most health policy and medical malpractice scholars would not describe the environment we’re in right now as a state of crisis, at least not compared to what we observed a decade ago,” said Anupam B. Jena, MD, PhD, health care policy professor at Harvard University, Boston, and a medical liability researcher.“But I would argue that malpractice is still a salient fact for most physicians. What’s much more important than focusing on changes over time is taking a static perspective and understanding the risk that a physician faces when it comes to malpractice.”
During just over 12 years in Congress, Dr. Price (R-Ga.) has consistently advocated for tort reform, proposing legislation that would restructure the lawsuit process. He supports damage caps and has recommended the creation of health care tribunals that would hear cases only after medical review. He has also proposed the development of national practice guidelines for doctors, which if followed could be used defensively.
“From exorbitant malpractice insurance premiums to the remarkably expensive practice of defensive medicine, it is my experience that the current culture of litigation costs patients hundreds of billions of dollars,” Dr. Price wrote in a 2009 commentary about his Empowering Patients First Act. “These costs do nothing to provide better care, but rather serve only as a defense against unyielding personal injury lawyers ...When malpractice suits are brought through specialized courts and viewed through the perspective of medically appropriate care, rather than a lottery mentality, we will see a decline in frivolous lawsuits.”
Data show lawsuits down
Claims data however, show that lawsuits against doctors are on the decline – and have been for more than 10 years. The rate of paid claims against physicians dropped from 18.6 to 9.9 paid claims per 1,000 physicians between 2002 and 2013, according to 2014 study by Michelle Mello of Stanford (Calif.) University and colleagues (JAMA. 2014;312(20):2146-2155. doi:10.1001/jama.2014.10705). Another analysis found that claims decreased from 12 claims per 100 doctors in 2003 to 6 per 100 doctors in 2016, according to a study of claims from The Doctors Company database.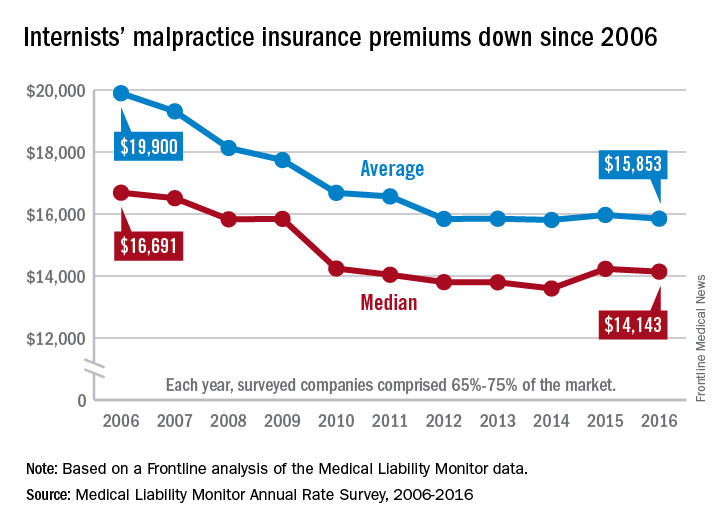
The sharp decline in claims is directly affecting premiums, which have remained nearly unchanged for years, said Michael Matray, editor of the Medical Liability Monitor (MLM), which tracks premium rates. In 2003, rate increases of 49% were commonplace, he noted, with some states reporting rises of 100%. But premiums started to fall in 2006, he said.
“We are in the midst of a 10-year soft market, the longest we’ve ever had,” Mr. Matray said in an interview. “In 2006, we started to soften. We have been soft or flat with no change since. It’s definitely unprecedented.”
In 2016, U.S. internists paid an average premium of $15,853, compared to an average premium payment of $19,900 in 2006 without inflation adjustment, according to this news organization’s analysis of MLM data. General surgeons meanwhile, paid an average of $52,905 in premiums in 2016, compared to a 2006 average of $68,186. Ob.gyns. paid an average premium of $72,999 in 2016, a drop from $93,230 in 2006.
“Generally speaking, it’s great for doctors,” Mr. Matray said. “Even if you remove the inflationary factor, there are some states where they are paying less now than they were 10 years ago.”
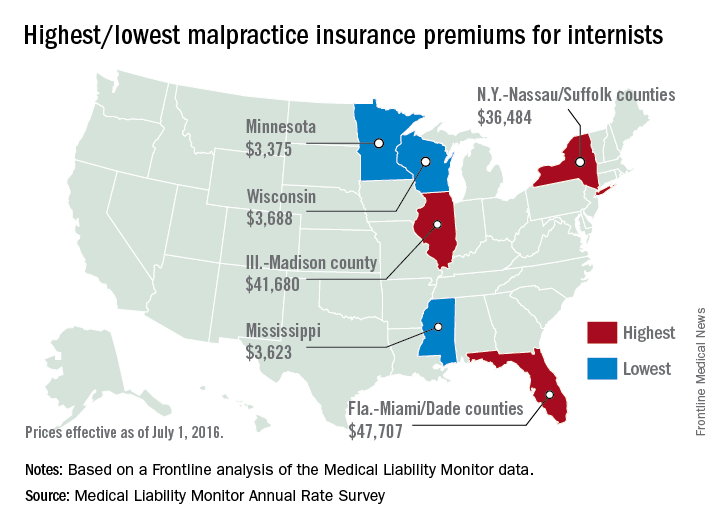
But stable premiums do not mean inexpensive insurance, noted Mike Stinson, vice president of government relations and public policy for the PIAA, a national trade association for medical liability insurers.
“They’ve certainly come down over the last few years,” Mr. Stinson said in an interview. “But they certainly are not low.”
South Florida doctors for example, are paying among the highest premiums in the nation despite an overall drop in the last 10 years. Internists in Dade County, Fla., paid $47,707 for insurance in 2016, $27,000 less than in 2006, according to MLM data. Coverage is still is not affordable, said Jason M. Goldman, MD, an internist in private practice in Coral Springs, Fla., and governor for the American College of Physicians Florida chapter.
The premiums are ridiculous,” he said in an interview. “That’s one of the reasons I went bare. Having medical insurance makes you a target, because lawyers think, ‘We can sue the insurance company and the insurance company is going to pay.’ ”
State reforms driving lawsuit decline
A combination of state reforms and patient safety initiatives are fueling the lawsuit down slide, said Paul A. Greve Jr. senior vice president/senior consultant for Willis Towers Watson Health Care Practice and coauthor of the 2016 MLM Survey report.
More than 25 states now have laws that enforce caps on noneconomic damages in medical liability cases, and in the last 15 years, a large majority have upheld such limits, Mr. Greve said. In addition, a number of states require a certificate of merit before suits can move forward, which mandate that a qualified physician verify that a defendant’s actions were likely negligent.
Patient safety programs such as internal patient safety committees, enhanced provider education, safety protocols, and communication and resolution programs, are also making an impact.
“There have been many efforts toward thinking innovatively about how we should be compensating patients more fairly and more quickly,” said Harvard’s Dr. Jena, who practices at Massachusetts General Hospital. “There are early disclosure programs that many hospitals have adopted as a movement toward that goal. The system is evolving.”
The high expense of filing a medical malpractice lawsuit is another factor detouring lawsuits, Mr. Greve added.
“It’s very expensive for [plaintiffs’ attorneys] to pursue these cases,” he said. “They have to invest a large amount of money into them and they can’t afford to take cases that have questionable liability, or they’re going to end up shelling out a lot of money and not getting anything in return.”
Malpractice system remains broken
While lawsuit and premium data paint a positive picture, the medical malpractice system remains dysfunctional for doctors and patients, said PIAA’s Mr. Stinson.
A majority of medical malpractice claims against physicians are determined to be nonmeritorious yet an average lawsuit takes roughly 4 years to resolve, he noted. Suits against doctors are dismissed by the court 54% of the time across all specialties, and among cases that go to trial, 80% end in the physician’s favor, according to a 2012 study by Dr. Jena and colleagues (JAMA Intern Med. 2012 Jun. 11 doi: 10.1001/jamainternmed.2012.1416)
“We think that’s a huge amount of resources both in time and money and human capital to get poured into cases where no payment is ever deemed appropriate,” Mr. Stinson said. “We would like to see [malpractice] reforms in part because we think you can weed out some of these claims in advance, so more of the resources can be used to determine whether or not there was negligence and if so, making that patient whole as fast as possible.”
Regardless of declining claims, most physicians will still be sued in their lifetime, Dr. Jena said. By age 65, 75% of physicians in low-risk specialties have faced a malpractice claim, and 99% of doctors in high-risk specialties have been sued, according to a 2011 study by Dr. Jena and colleagues (N Engl J Med. 2011 Aug. 18. doi: 10.1056/NEJMsa1012370)
“What really matters for physicians is not only whether they win or lose a malpractice suit, but whether they are sued in the first place,” Dr. Jena said. “Lawsuits happen quite often and over the course of a physician’s career they are quite common. So whether or not we’re in a state of malpractice crisis or not, the lifetime risk for physicians is quite real.”
The cost of defending claims continues to rise, noted Richard E. Anderson, MD, chair and CEO of The Doctors Company. At the same time, multi-million dollar malpractice verdicts have become more common.
“There’s still way too much malpractice litigation,” Dr. Anderson said. “The majority of it is fruitless, and the total cost burden borne by physicians has not decreased as much as the frequency because of the ongoing increase in severity.”
“The bottom line is defensive medicine is a huge and growing cost to all Americans,” he said. “We’re all on the hook for America’s rising health care bills. And as my increasingly infirm Baby Boomer generation gets older and weaker and sicker, those bills are going to rise that much faster. So the notion advanced by some so-called experts that we can nonetheless afford to spend a half trillion dollars a year or more on largely unnecessary testing driven in significant part by fear of litigation and giant outlier verdicts seems rather inane, and it suggests perhaps that those experts aren’t so expert.”
What would Dr. Price do?
Opinions are mixed about whether Dr. Price’s proposed reforms are the right changes for the medical liability system.
Expert panels to review claims for validity are a promising suggestion, Dr. Jena said. “Administrative courts to help identify malpractice cases that are truly malpractice early on is a good idea,” he said. “We want to have a system that prevents less meritorious cases from soaking up resources.”
But the idea may be easier said than done, said Dr. Anderson of The Doctors Company. “The devil is always in the details There is a lot of merit in [health courts] and they make a lot of sense. However, the notion of going from where we are today to an untested system, which would have to be a compromise between adversaries, would be a very challenging one.”
National clinical standards for physicians to follow and use as a safeguard could backfire, Mr. Stinson said. Bureaucracy could slow the guidelines from being promptly updated, and the standards could fail to keep up with the latest medical developments. As doctors know, medicine is not a one-size-fits-all approach, he added.
“[Guidelines] could encourage doctors to practice cookbook medicine, where they’re just going to follow the standard along without being given the opportunity to use their training and clinical experience to see whether that’s actually in the patient’s best interest,” Mr. Stinson said. “We certainly wouldn’t want to see a situation where a doctor feels diverting from a guidelines is in a patient’s best interest, but they don’t dare do it because it could subject them to a lawsuit.”
When enacting malpractice reforms, it will be critical to evaluate the intervention first to ensure the right objections are met, Dr. Jena added.
“At the end of the day, if the [legal] environment is such that it’s uncomfortable to practice medicine, that’s going to have implications for who goes into medicine and implications for ordering tests and procedures,” he said. “Any reform that attempts to make the process more efficient is a good idea because it lowers cost to the system and makes the experience better for patients and physicians.”
This article was updated 2/15/17.
[email protected]
On Twitter @legal_med
Use of bilateral internal mammary arteries in CABG stagnates
HOUSTON – Over the past 5 years there has been no growth in bilateral internal mammary artery use among Medicare beneficiaries, and the frequency of bilateral internal mammary artery use during coronary artery bypass grafting remained low, according to a large observational analysis.
“Despite a growing evidence base supporting bilateral internal mammary artery use with regard to long-term survival and freedom from repeat revascularization, rates of bilateral internal mammary artery [BIMA] use remain low, with no evidence of growth,” Alexander Iribarne, MD, said during an interview at the annual meeting of the Society of Thoracic Surgeons. “Therefore, there is significant opportunity for adoption of bilateral internal mammary artery grafting in the United States.”
The most recent report of CABG trends in the United States published from the STS database showed that in 2009, fewer than 5% of patients who underwent CABG received a BIMA (J Thorac Cardiovasc Surg. 2012 Feb;143[2]:273-81). In an effort to characterize the adoption rate and regional variation of BIMA use in the United States, Dr. Iribarne, director of cardiac surgical research in the section of cardiac surgery at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and his associates examined records from nearly 150 million Medicare beneficiaries from 2009-2014. “This work is unique in that we not only looked at trends in rates of usage but also how this varied by geographic location,” he said.
“I was surprised to find that despite the growing literature supporting BIMA use, there was no growth in rates of usage over the 5-year study period, with rates remaining low,” Dr. Iribarne said. “I was also surprised to see that there was significant regional variation in use that appeared to correlate, in part, with overall CABG volume, although the moderate correlation coefficient indicates that additional factors beyond CABG volume are involved.”
A key limitation of the study, he said, was that its patients were aged 65 and older. Dr. Iribarne disclosed that he receives grant funding from the American Association for Thoracic Surgery Graham Foundation and the Dartmouth SYNERGY Clinical and Translational Science Institute.
HOUSTON – Over the past 5 years there has been no growth in bilateral internal mammary artery use among Medicare beneficiaries, and the frequency of bilateral internal mammary artery use during coronary artery bypass grafting remained low, according to a large observational analysis.
“Despite a growing evidence base supporting bilateral internal mammary artery use with regard to long-term survival and freedom from repeat revascularization, rates of bilateral internal mammary artery [BIMA] use remain low, with no evidence of growth,” Alexander Iribarne, MD, said during an interview at the annual meeting of the Society of Thoracic Surgeons. “Therefore, there is significant opportunity for adoption of bilateral internal mammary artery grafting in the United States.”
The most recent report of CABG trends in the United States published from the STS database showed that in 2009, fewer than 5% of patients who underwent CABG received a BIMA (J Thorac Cardiovasc Surg. 2012 Feb;143[2]:273-81). In an effort to characterize the adoption rate and regional variation of BIMA use in the United States, Dr. Iribarne, director of cardiac surgical research in the section of cardiac surgery at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and his associates examined records from nearly 150 million Medicare beneficiaries from 2009-2014. “This work is unique in that we not only looked at trends in rates of usage but also how this varied by geographic location,” he said.
“I was surprised to find that despite the growing literature supporting BIMA use, there was no growth in rates of usage over the 5-year study period, with rates remaining low,” Dr. Iribarne said. “I was also surprised to see that there was significant regional variation in use that appeared to correlate, in part, with overall CABG volume, although the moderate correlation coefficient indicates that additional factors beyond CABG volume are involved.”
A key limitation of the study, he said, was that its patients were aged 65 and older. Dr. Iribarne disclosed that he receives grant funding from the American Association for Thoracic Surgery Graham Foundation and the Dartmouth SYNERGY Clinical and Translational Science Institute.
HOUSTON – Over the past 5 years there has been no growth in bilateral internal mammary artery use among Medicare beneficiaries, and the frequency of bilateral internal mammary artery use during coronary artery bypass grafting remained low, according to a large observational analysis.
“Despite a growing evidence base supporting bilateral internal mammary artery use with regard to long-term survival and freedom from repeat revascularization, rates of bilateral internal mammary artery [BIMA] use remain low, with no evidence of growth,” Alexander Iribarne, MD, said during an interview at the annual meeting of the Society of Thoracic Surgeons. “Therefore, there is significant opportunity for adoption of bilateral internal mammary artery grafting in the United States.”
The most recent report of CABG trends in the United States published from the STS database showed that in 2009, fewer than 5% of patients who underwent CABG received a BIMA (J Thorac Cardiovasc Surg. 2012 Feb;143[2]:273-81). In an effort to characterize the adoption rate and regional variation of BIMA use in the United States, Dr. Iribarne, director of cardiac surgical research in the section of cardiac surgery at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and his associates examined records from nearly 150 million Medicare beneficiaries from 2009-2014. “This work is unique in that we not only looked at trends in rates of usage but also how this varied by geographic location,” he said.
“I was surprised to find that despite the growing literature supporting BIMA use, there was no growth in rates of usage over the 5-year study period, with rates remaining low,” Dr. Iribarne said. “I was also surprised to see that there was significant regional variation in use that appeared to correlate, in part, with overall CABG volume, although the moderate correlation coefficient indicates that additional factors beyond CABG volume are involved.”
A key limitation of the study, he said, was that its patients were aged 65 and older. Dr. Iribarne disclosed that he receives grant funding from the American Association for Thoracic Surgery Graham Foundation and the Dartmouth SYNERGY Clinical and Translational Science Institute.
AT THE STS ANNUAL MEETING
Key clinical point:
Major finding: The absolute national rate of BIMA use fell from 0.216 claims per 1,000 beneficiaries in 2009 to 0.143 in 2014 (P less than .001).
Data source: An analysis of medical records from nearly 150 million Medicare beneficiaries during 2009-2014.
Disclosures: Dr. Iribarne disclosed that he receives grant funding from the American Association for Thoracic Surgery Graham Foundation and the Dartmouth SYNERGY Clinical and Translational Science Institute.
Comorbid mental illness linked to worse surgical outcomes
LAS VEGAS – A comorbid mental illness may predispose surgical patients to poor outcomes, increasing the risk of postoperative complications, a prolonged length of stay, and – in some cases – even in-hospital mortality.
The link between mental illness and physical response to surgery is not well elucidated, and is likely an extremely complicated one, Elizabeth Bailey, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Dr. Bailey said there is an extreme paucity of data on the relationship between mental illness and surgical outcomes. To investigate it, she examined 580,000 patient records contained in the National Inpatient Sample.
The cases spanned 2009-2011 and represented the four most common surgical procedures in the United States: cholecystectomy, appendectomy, adhesion excision/lysis, and colorectal resection.
She compared surgical outcomes among patients without a DSM-IV diagnosis and those with one of the five most common: mood disorder, anxiety, impulse control, schizophrenia, and substance abuse disorder.
The study’s primary outcomes were length of hospital stay, in-hospital mortality, and postoperative complications. Her analysis controlled for age, gender, race, admission status, operative approach, non–mental health comorbidities, insurance, and income.
Of the 580,000 in the study group 7% (39,000) had at least one of the mental health comorbidities. Mood disorder was the most common (59%), followed by substance abuse (24%), schizophrenia (13%), anxiety disorder (12%), and impulse control disorder (5%).
There were a number of significant baseline differences between those with a mental diagnosis and those without. Those with a DSM-IV diagnosis were younger (52 vs. 54 years), more often women (61% vs. 57%), and white (78% vs. 69%). They more often had additional physical comorbidities (80% vs. 68%). They were more likely to be admitted through the emergency room (74% vs. 71%), to have nonlaparoscopic surgery (60% vs 63%), to be on public insurance (53% vs. 43%), and to be in the lowest income quartile (28% vs. 25%).
Surgical outcomes were almost universally significantly worse among these patients. They were 41% more likely to experience a prolonged length of stay and 18% more likely to experience a complication. These included wound disruption, ileus, and small bowel obstruction. They faced a 24% increased risk for needing total parenteral nutrition; a 29% increased risk of abdominal pain; an 18% increased risk of percutaneous abdominal drainage; and a 15% increased risk of needing another operation in the same admission.
Dr. Bailey also broke down overall risks by DSM-IV diagnosis.
• Patients with a mood disorder were 35% more likely to have a prolonged length of stay and 13% more likely to have a surgical complication.
• Patients with an anxiety disorder were 16% more likely to have a prolonged length of stay and 10% more likely to have a complication.
• Patients with schizophrenia were 77% more likely to have a prolonged length of stay, 3% more likely to die, and 28% more likely to have a complication.
• Patients with substance abuse were 70% more likely to have a prolonged length of stay, 6% more likely to die, and 39% more likely to have a complication.
Interestingly, Dr. Bailey said, the risk of in-hospital death was 16% lower in patients with a mood disorder, 59% lower in those with an anxiety disorder, and 77% lower in those with an impulse control disorder.
She stressed that the National Inpatient Sample provides a limited look into a patient’s hospital experience. The study can’t assess how long patients were sick before they came to the hospital, their medications or medication adherence, or how well they managed their mental and physical comorbidities.
“While we lacked the means to delve into potential clinical mediators, look at unplanned readmissions, or the use of inpatient psychiatric consults, we can clearly see the association with worse surgical outcomes,” Dr. Bailey said. “Recognizing this is the first step in learning how to optimize care for this frequently marginalized population.”
She had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
LAS VEGAS – A comorbid mental illness may predispose surgical patients to poor outcomes, increasing the risk of postoperative complications, a prolonged length of stay, and – in some cases – even in-hospital mortality.
The link between mental illness and physical response to surgery is not well elucidated, and is likely an extremely complicated one, Elizabeth Bailey, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Dr. Bailey said there is an extreme paucity of data on the relationship between mental illness and surgical outcomes. To investigate it, she examined 580,000 patient records contained in the National Inpatient Sample.
The cases spanned 2009-2011 and represented the four most common surgical procedures in the United States: cholecystectomy, appendectomy, adhesion excision/lysis, and colorectal resection.
She compared surgical outcomes among patients without a DSM-IV diagnosis and those with one of the five most common: mood disorder, anxiety, impulse control, schizophrenia, and substance abuse disorder.
The study’s primary outcomes were length of hospital stay, in-hospital mortality, and postoperative complications. Her analysis controlled for age, gender, race, admission status, operative approach, non–mental health comorbidities, insurance, and income.
Of the 580,000 in the study group 7% (39,000) had at least one of the mental health comorbidities. Mood disorder was the most common (59%), followed by substance abuse (24%), schizophrenia (13%), anxiety disorder (12%), and impulse control disorder (5%).
There were a number of significant baseline differences between those with a mental diagnosis and those without. Those with a DSM-IV diagnosis were younger (52 vs. 54 years), more often women (61% vs. 57%), and white (78% vs. 69%). They more often had additional physical comorbidities (80% vs. 68%). They were more likely to be admitted through the emergency room (74% vs. 71%), to have nonlaparoscopic surgery (60% vs 63%), to be on public insurance (53% vs. 43%), and to be in the lowest income quartile (28% vs. 25%).
Surgical outcomes were almost universally significantly worse among these patients. They were 41% more likely to experience a prolonged length of stay and 18% more likely to experience a complication. These included wound disruption, ileus, and small bowel obstruction. They faced a 24% increased risk for needing total parenteral nutrition; a 29% increased risk of abdominal pain; an 18% increased risk of percutaneous abdominal drainage; and a 15% increased risk of needing another operation in the same admission.
Dr. Bailey also broke down overall risks by DSM-IV diagnosis.
• Patients with a mood disorder were 35% more likely to have a prolonged length of stay and 13% more likely to have a surgical complication.
• Patients with an anxiety disorder were 16% more likely to have a prolonged length of stay and 10% more likely to have a complication.
• Patients with schizophrenia were 77% more likely to have a prolonged length of stay, 3% more likely to die, and 28% more likely to have a complication.
• Patients with substance abuse were 70% more likely to have a prolonged length of stay, 6% more likely to die, and 39% more likely to have a complication.
Interestingly, Dr. Bailey said, the risk of in-hospital death was 16% lower in patients with a mood disorder, 59% lower in those with an anxiety disorder, and 77% lower in those with an impulse control disorder.
She stressed that the National Inpatient Sample provides a limited look into a patient’s hospital experience. The study can’t assess how long patients were sick before they came to the hospital, their medications or medication adherence, or how well they managed their mental and physical comorbidities.
“While we lacked the means to delve into potential clinical mediators, look at unplanned readmissions, or the use of inpatient psychiatric consults, we can clearly see the association with worse surgical outcomes,” Dr. Bailey said. “Recognizing this is the first step in learning how to optimize care for this frequently marginalized population.”
She had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
LAS VEGAS – A comorbid mental illness may predispose surgical patients to poor outcomes, increasing the risk of postoperative complications, a prolonged length of stay, and – in some cases – even in-hospital mortality.
The link between mental illness and physical response to surgery is not well elucidated, and is likely an extremely complicated one, Elizabeth Bailey, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
Dr. Bailey said there is an extreme paucity of data on the relationship between mental illness and surgical outcomes. To investigate it, she examined 580,000 patient records contained in the National Inpatient Sample.
The cases spanned 2009-2011 and represented the four most common surgical procedures in the United States: cholecystectomy, appendectomy, adhesion excision/lysis, and colorectal resection.
She compared surgical outcomes among patients without a DSM-IV diagnosis and those with one of the five most common: mood disorder, anxiety, impulse control, schizophrenia, and substance abuse disorder.
The study’s primary outcomes were length of hospital stay, in-hospital mortality, and postoperative complications. Her analysis controlled for age, gender, race, admission status, operative approach, non–mental health comorbidities, insurance, and income.
Of the 580,000 in the study group 7% (39,000) had at least one of the mental health comorbidities. Mood disorder was the most common (59%), followed by substance abuse (24%), schizophrenia (13%), anxiety disorder (12%), and impulse control disorder (5%).
There were a number of significant baseline differences between those with a mental diagnosis and those without. Those with a DSM-IV diagnosis were younger (52 vs. 54 years), more often women (61% vs. 57%), and white (78% vs. 69%). They more often had additional physical comorbidities (80% vs. 68%). They were more likely to be admitted through the emergency room (74% vs. 71%), to have nonlaparoscopic surgery (60% vs 63%), to be on public insurance (53% vs. 43%), and to be in the lowest income quartile (28% vs. 25%).
Surgical outcomes were almost universally significantly worse among these patients. They were 41% more likely to experience a prolonged length of stay and 18% more likely to experience a complication. These included wound disruption, ileus, and small bowel obstruction. They faced a 24% increased risk for needing total parenteral nutrition; a 29% increased risk of abdominal pain; an 18% increased risk of percutaneous abdominal drainage; and a 15% increased risk of needing another operation in the same admission.
Dr. Bailey also broke down overall risks by DSM-IV diagnosis.
• Patients with a mood disorder were 35% more likely to have a prolonged length of stay and 13% more likely to have a surgical complication.
• Patients with an anxiety disorder were 16% more likely to have a prolonged length of stay and 10% more likely to have a complication.
• Patients with schizophrenia were 77% more likely to have a prolonged length of stay, 3% more likely to die, and 28% more likely to have a complication.
• Patients with substance abuse were 70% more likely to have a prolonged length of stay, 6% more likely to die, and 39% more likely to have a complication.
Interestingly, Dr. Bailey said, the risk of in-hospital death was 16% lower in patients with a mood disorder, 59% lower in those with an anxiety disorder, and 77% lower in those with an impulse control disorder.
She stressed that the National Inpatient Sample provides a limited look into a patient’s hospital experience. The study can’t assess how long patients were sick before they came to the hospital, their medications or medication adherence, or how well they managed their mental and physical comorbidities.
“While we lacked the means to delve into potential clinical mediators, look at unplanned readmissions, or the use of inpatient psychiatric consults, we can clearly see the association with worse surgical outcomes,” Dr. Bailey said. “Recognizing this is the first step in learning how to optimize care for this frequently marginalized population.”
She had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point:
Major finding: They were 41% more likely to experience a prolonged length of stay and 18% more likely to experience a complication.
Data source: The database review comprised 580,000 patients.
Disclosures: Dr. Bailey had no financial disclosures.