User login
AGA News
AGA journals select new editorial fellows
Congrats to the six GIs selected for this competitive program.
The AGA journals – Gastroenterology, Clinical Gastroenterology and Hepatology (CGH), and Cellular and Molecular Gastroenterology and Hepatology (CMGH) – are pleased to announce their 2019-2020 editorial fellows.
Gastroenterology
Feng Su, MD
University of Washington, Seattle
Victoria Weis, PhD
Wake Forest University, Winston-Salem, N.C.
CGH
Austin Chiang, MD, MPH
Jefferson Medical College, Philadelphia, Penn.
Jennifer Kolb, MD
University of Colorado at Denver, Aurora
CMGH
Cambrian Liu, PhD
The Saban Research Institute, Children’s Hospital Los Angeles, Calif.
Tirthadipa Pradhan-Sundd, PhD
University of Pittsburgh, Penn.
The editorial fellows will be mentored on their respective journals’ editorial processes, including peer review and the publication process from manuscript submission to acceptance. They will participate in discussions and conferences with the boards of editors and work closely with the AGA editorial staff. Additionally, the fellows will participate in AGA’s new reviewer education program and will also be offered the opportunity to contribute content to their respective journals. The newly expanded program builds on the success of the previous 2 years when Gastroenterology had an editorial fellow.
The journals’ board of editors and editorial staff congratulate the fellows and are excited to work with them over the next year.
Get to know this rock star IBS researcher and mom
AGA Research Foundation pilot awards are an invaluable tool for investigators – they provide seed funding to explore promising new lines of research and generate preliminary data for larger grants. So, when Meenakshi Rao, MD, PhD, received the 2016 AGA–Takeda Pharmaceuticals International Research Scholar Award in Neurogastroenterology, she was able to double down on a project to identify why men and women with irritable bowel syndrome (IBS), the most common but least understood of all digestive disorders, report different symptoms and respond differently to treatment. Based on her recent accomplishments, we’re excited for you to get to know Dr. Rao, assistant professor of pediatrics at Harvard Medical School, Boston, and our AGA Research Foundation researcher of the month.
The Rao lab AGA-funded project focused on building upon Dr. Rao’s previous findings, which showed that disrupting nerves in the bowel had vastly different effects on males and females. These surprising results led Dr. Rao to explore whether sex hormones, such as testosterone and estrogen, might regulate how well things move through the bowel. Dr. Rao believes that identifying the underlying causes for sex differences in bowel function could lead to more effective and personalized treatments for patients with IBS. You can read the specifics of Dr. Rao’s research in the October 2017 issue of Gastroenterology and the October 2018 issue of Journal of Neuroscience.
IBS symptoms in women more typically involve constipation while young men with IBS more commonly report diarrhea. Over time, as men age, however, they tend to experience more constipation, Dr. Rao said. “Sex hormones might be signaling directly to the nerves in our gut and playing a role in these sex differences,” Dr. Rao said. “It might mean we can’t think of this as one disorder. IBS in a male may be different than IBS in a female, and that could change how we approach diagnosis and treatment.”
The AGA grant laid the groundwork for Dr. Rao’s findings, which led to a new understanding of how different types of cells in the gut nervous system regulate bowel functions – and how this regulation is different in males and females. The AGA grant helped Dr. Rao secure funding from the National Institutes of Health to launch new projects focused on how disruption of the gut nervous system causes disease.
Dr. Rao received the AGA award in 2015, when her son, Avinash, was aged 2 years. She acknowledged the delicate balancing act of raising a family and advancing her research.
“A lot of things were happening at once,” she said. “As a young parent, having the support of this award and having a technician (made possible by the award) made a big difference.”
Her son, now 5 years old, is growing up in a science-centric household because Dr. Rao’s husband is also a scientist. Not surprisingly, Dr. Rao says, her son is becoming a budding scientist.
“He talks about experiments all the time,” she says. “He even articulated to me the other day why we work on mice to learn how to help people. I never taught him that. I was floored.”
Five new GI technologies to know
The AGA Tech Summit Shark Tank is our annual reminder that the field of GI is ripe for innovation. Continue reading for an overview of the five new technologies pitched to our panel of sharks.
The smart toilet seat. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that capture images of bowel movements and urination for subsequent analysis. The company describes TrueLoo as a low-cost disease-screening tool that has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.
AI to aid screening endoscopy. A new tool called Ultivision, being developed by the startup Docbot, was described as a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia in either screening colonoscopy or in surveillance of Barrett’s esophagus. The tool integrates with existing endoscopic tools. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist.
Obesity phenotyping tool. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes: hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates). With this knowledge, treatment can be tailored appropriately leading to better outcomes.
Capsule diagnostic tool. The Atmo Gas Capsule from Atmo Biosciences is an ingestible capsule that measures gases at the source, which can accelerate the diagnosis of diseases such as IBS and inflammatory bowel disease (IBD). According to the company, this technique is highly accurate and offers an alternative to more invasive and expensive diagnostic tools.
Winner: “all-in-one” IBD app. Our Shark Tank winner by both popular vote from AGA Tech Summit attendees and the six-member Shark Tank panel was Oshi Health, selected for its IBD app. The app allows patients to track symptoms, a first step in understanding personalized flare pattern, as well as find resources to learn about their disease and communicate with other patients about their experiences. In a future iteration, information gathered by the app will be made available to physicians to provide current information about disease status to better individualize therapy.
2020 Crohn’s & Colitis Congress now open for registration
Join the Crohn’s & Colitis Foundation and AGA next January in Austin, Tex., for the premier conference on IBD.
The Crohn’s & Colitis Congress combines the strengths of the nation’s leading IBD patient organization, the Crohn’s & Colitis Foundation, and the premier GI professional organization, AGA, to bring together IBD professionals, across all disciplines, to transform IBD care.
The 2020 Congress Committee Chair David T. Rubin, MD, AGAF, University of Chicago, and Cochair Uma Mahadevan, MD, AGAF, University of California, San Francisco, lead a faculty that includes thought leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The congress’s agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators. In addition, opening breakout sessions, taking place Jan. 23, will be available for selection free of charge.
Attendees of the 2020 congress will be able to meet with IBD leaders, discover different perspectives, leave with practical information they can immediately implement to take care of their next IBD patient and hear what’s on the horizon in potential treatment.
There will also be plenty of social events and plenty of time to build a strong network, including a Friday night Welcome Reception that should not be missed.
In addition, the 2020 congress is taking place in Austin, Tex. The capital of Texas and the Live Music Capital of the World, Austin is famous for its inspiring and enticing entertainment, culture, cuisine, and outdoor settings. Make a week of it and enjoy all Austin has to offer.
Early-bird registration ends Sept. 18. General abstract submissions for basic, translational, and clinical research begin Aug. 28 and end Oct. 23. To learn more and register, visit www.crohnscolitiscongress.org.
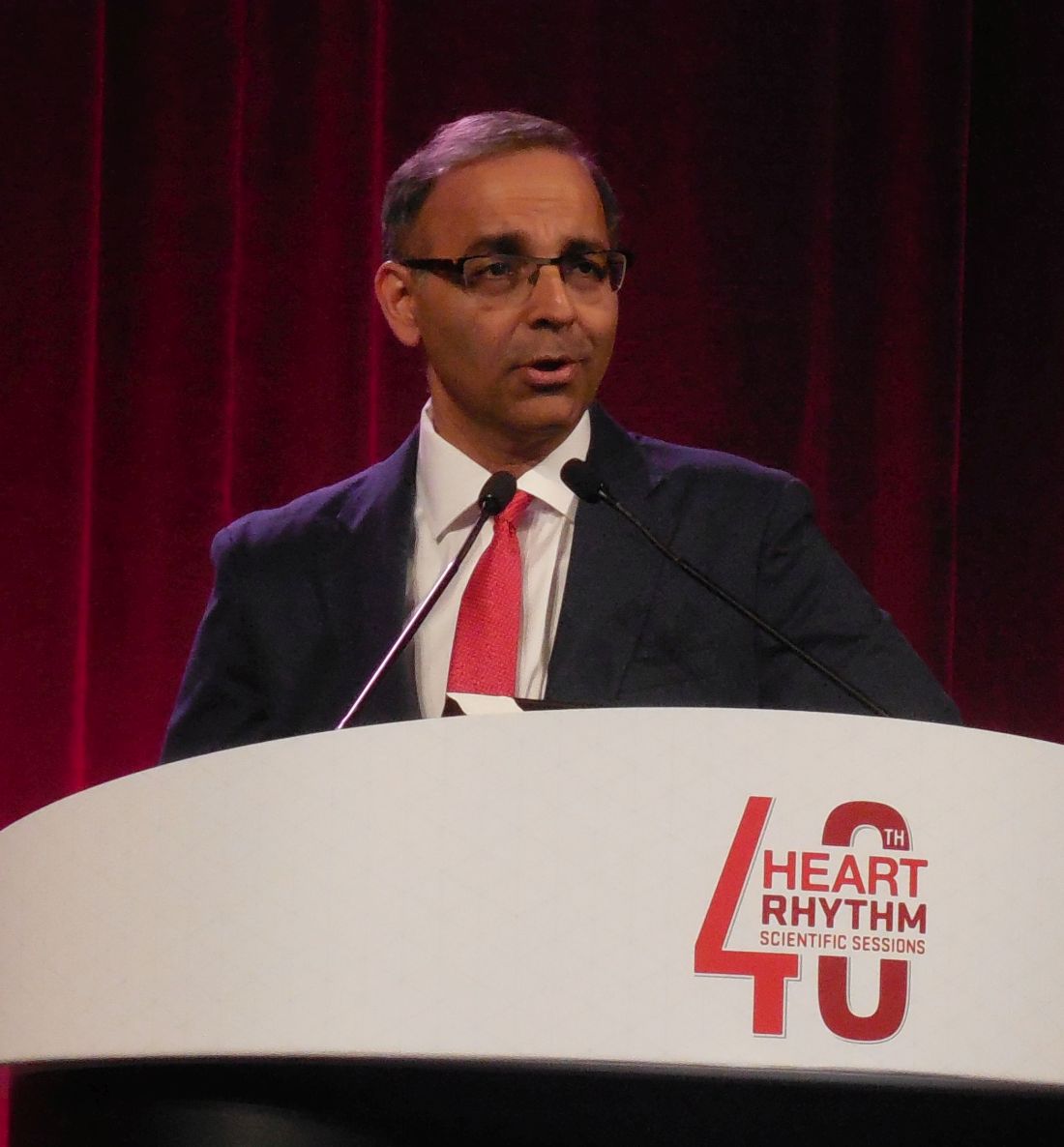
AGA welcomes new president, Hashem B. El-Serag, MD, MPH, AGAF
Hashem B. El-Serag, MD, MPH, AGAF, began his term as the 114th president of the AGA Institute at Digestive Disease Week® (DDW 2019).
Dr. El-Serag is former editor in chief of Clinical Gastroenterology and Hepatology. He currently serves as chair of the department of medicine at Baylor College of Medicine, Houston, following a decade leading and expanding Baylor’s gastroenterology and hepatology section. He is one of the few academic gastroenterologists serving as a chair of a department of medicine in the United States.
Originally Palestinian, Dr. El-Serag became a U.S. citizen in the early 2000s after medical school in Libya. He completed his training at community hospitals in the United States. His path from Benghazi to Baylor is described in the May issue of Gastroenterology by Baylor colleague Dr. Fasiha Kanwal.
“I firmly believe that the success I achieved in the United States would not have been possible anywhere else in the world, and it is as much a testament to the accepting society and medical system as to whatever intrinsic ability or skill I have,” noted Dr. El-Serag.
The major focus of Dr. El-Serag’s scholarly work is the epidemiology and clinical outcomes of hepatocellular carcinoma. Much of the modern literature on this topic includes his more than 100 publications. Since 2014, Dr. El-Serag has been named by Thomson Reuter as among the top 1% of clinical scientists.
Dr. El-Serag “is an innovative scientist, a compassionate physician, and a gifted educator. He is a relentless advocate of science and training, with an astute political sense — all key to influencing and shaping policy,” said Dr. Kanwal.
Dr. El-Serag’s term as AGA president concludes May 2020. Follow him on twitter at @SeragHashem.
AGA journals select new editorial fellows
Congrats to the six GIs selected for this competitive program.
The AGA journals – Gastroenterology, Clinical Gastroenterology and Hepatology (CGH), and Cellular and Molecular Gastroenterology and Hepatology (CMGH) – are pleased to announce their 2019-2020 editorial fellows.
Gastroenterology
Feng Su, MD
University of Washington, Seattle
Victoria Weis, PhD
Wake Forest University, Winston-Salem, N.C.
CGH
Austin Chiang, MD, MPH
Jefferson Medical College, Philadelphia, Penn.
Jennifer Kolb, MD
University of Colorado at Denver, Aurora
CMGH
Cambrian Liu, PhD
The Saban Research Institute, Children’s Hospital Los Angeles, Calif.
Tirthadipa Pradhan-Sundd, PhD
University of Pittsburgh, Penn.
The editorial fellows will be mentored on their respective journals’ editorial processes, including peer review and the publication process from manuscript submission to acceptance. They will participate in discussions and conferences with the boards of editors and work closely with the AGA editorial staff. Additionally, the fellows will participate in AGA’s new reviewer education program and will also be offered the opportunity to contribute content to their respective journals. The newly expanded program builds on the success of the previous 2 years when Gastroenterology had an editorial fellow.
The journals’ board of editors and editorial staff congratulate the fellows and are excited to work with them over the next year.
Get to know this rock star IBS researcher and mom
AGA Research Foundation pilot awards are an invaluable tool for investigators – they provide seed funding to explore promising new lines of research and generate preliminary data for larger grants. So, when Meenakshi Rao, MD, PhD, received the 2016 AGA–Takeda Pharmaceuticals International Research Scholar Award in Neurogastroenterology, she was able to double down on a project to identify why men and women with irritable bowel syndrome (IBS), the most common but least understood of all digestive disorders, report different symptoms and respond differently to treatment. Based on her recent accomplishments, we’re excited for you to get to know Dr. Rao, assistant professor of pediatrics at Harvard Medical School, Boston, and our AGA Research Foundation researcher of the month.
The Rao lab AGA-funded project focused on building upon Dr. Rao’s previous findings, which showed that disrupting nerves in the bowel had vastly different effects on males and females. These surprising results led Dr. Rao to explore whether sex hormones, such as testosterone and estrogen, might regulate how well things move through the bowel. Dr. Rao believes that identifying the underlying causes for sex differences in bowel function could lead to more effective and personalized treatments for patients with IBS. You can read the specifics of Dr. Rao’s research in the October 2017 issue of Gastroenterology and the October 2018 issue of Journal of Neuroscience.
IBS symptoms in women more typically involve constipation while young men with IBS more commonly report diarrhea. Over time, as men age, however, they tend to experience more constipation, Dr. Rao said. “Sex hormones might be signaling directly to the nerves in our gut and playing a role in these sex differences,” Dr. Rao said. “It might mean we can’t think of this as one disorder. IBS in a male may be different than IBS in a female, and that could change how we approach diagnosis and treatment.”
The AGA grant laid the groundwork for Dr. Rao’s findings, which led to a new understanding of how different types of cells in the gut nervous system regulate bowel functions – and how this regulation is different in males and females. The AGA grant helped Dr. Rao secure funding from the National Institutes of Health to launch new projects focused on how disruption of the gut nervous system causes disease.
Dr. Rao received the AGA award in 2015, when her son, Avinash, was aged 2 years. She acknowledged the delicate balancing act of raising a family and advancing her research.
“A lot of things were happening at once,” she said. “As a young parent, having the support of this award and having a technician (made possible by the award) made a big difference.”
Her son, now 5 years old, is growing up in a science-centric household because Dr. Rao’s husband is also a scientist. Not surprisingly, Dr. Rao says, her son is becoming a budding scientist.
“He talks about experiments all the time,” she says. “He even articulated to me the other day why we work on mice to learn how to help people. I never taught him that. I was floored.”
Five new GI technologies to know
The AGA Tech Summit Shark Tank is our annual reminder that the field of GI is ripe for innovation. Continue reading for an overview of the five new technologies pitched to our panel of sharks.
The smart toilet seat. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that capture images of bowel movements and urination for subsequent analysis. The company describes TrueLoo as a low-cost disease-screening tool that has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.
AI to aid screening endoscopy. A new tool called Ultivision, being developed by the startup Docbot, was described as a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia in either screening colonoscopy or in surveillance of Barrett’s esophagus. The tool integrates with existing endoscopic tools. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist.
Obesity phenotyping tool. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes: hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates). With this knowledge, treatment can be tailored appropriately leading to better outcomes.
Capsule diagnostic tool. The Atmo Gas Capsule from Atmo Biosciences is an ingestible capsule that measures gases at the source, which can accelerate the diagnosis of diseases such as IBS and inflammatory bowel disease (IBD). According to the company, this technique is highly accurate and offers an alternative to more invasive and expensive diagnostic tools.
Winner: “all-in-one” IBD app. Our Shark Tank winner by both popular vote from AGA Tech Summit attendees and the six-member Shark Tank panel was Oshi Health, selected for its IBD app. The app allows patients to track symptoms, a first step in understanding personalized flare pattern, as well as find resources to learn about their disease and communicate with other patients about their experiences. In a future iteration, information gathered by the app will be made available to physicians to provide current information about disease status to better individualize therapy.
2020 Crohn’s & Colitis Congress now open for registration
Join the Crohn’s & Colitis Foundation and AGA next January in Austin, Tex., for the premier conference on IBD.
The Crohn’s & Colitis Congress combines the strengths of the nation’s leading IBD patient organization, the Crohn’s & Colitis Foundation, and the premier GI professional organization, AGA, to bring together IBD professionals, across all disciplines, to transform IBD care.
The 2020 Congress Committee Chair David T. Rubin, MD, AGAF, University of Chicago, and Cochair Uma Mahadevan, MD, AGAF, University of California, San Francisco, lead a faculty that includes thought leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The congress’s agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators. In addition, opening breakout sessions, taking place Jan. 23, will be available for selection free of charge.
Attendees of the 2020 congress will be able to meet with IBD leaders, discover different perspectives, leave with practical information they can immediately implement to take care of their next IBD patient and hear what’s on the horizon in potential treatment.
There will also be plenty of social events and plenty of time to build a strong network, including a Friday night Welcome Reception that should not be missed.
In addition, the 2020 congress is taking place in Austin, Tex. The capital of Texas and the Live Music Capital of the World, Austin is famous for its inspiring and enticing entertainment, culture, cuisine, and outdoor settings. Make a week of it and enjoy all Austin has to offer.
Early-bird registration ends Sept. 18. General abstract submissions for basic, translational, and clinical research begin Aug. 28 and end Oct. 23. To learn more and register, visit www.crohnscolitiscongress.org.
AGA welcomes new president, Hashem B. El-Serag, MD, MPH, AGAF
Hashem B. El-Serag, MD, MPH, AGAF, began his term as the 114th president of the AGA Institute at Digestive Disease Week® (DDW 2019).
Dr. El-Serag is former editor in chief of Clinical Gastroenterology and Hepatology. He currently serves as chair of the department of medicine at Baylor College of Medicine, Houston, following a decade leading and expanding Baylor’s gastroenterology and hepatology section. He is one of the few academic gastroenterologists serving as a chair of a department of medicine in the United States.
Originally Palestinian, Dr. El-Serag became a U.S. citizen in the early 2000s after medical school in Libya. He completed his training at community hospitals in the United States. His path from Benghazi to Baylor is described in the May issue of Gastroenterology by Baylor colleague Dr. Fasiha Kanwal.
“I firmly believe that the success I achieved in the United States would not have been possible anywhere else in the world, and it is as much a testament to the accepting society and medical system as to whatever intrinsic ability or skill I have,” noted Dr. El-Serag.
The major focus of Dr. El-Serag’s scholarly work is the epidemiology and clinical outcomes of hepatocellular carcinoma. Much of the modern literature on this topic includes his more than 100 publications. Since 2014, Dr. El-Serag has been named by Thomson Reuter as among the top 1% of clinical scientists.
Dr. El-Serag “is an innovative scientist, a compassionate physician, and a gifted educator. He is a relentless advocate of science and training, with an astute political sense — all key to influencing and shaping policy,” said Dr. Kanwal.
Dr. El-Serag’s term as AGA president concludes May 2020. Follow him on twitter at @SeragHashem.
AGA journals select new editorial fellows
Congrats to the six GIs selected for this competitive program.
The AGA journals – Gastroenterology, Clinical Gastroenterology and Hepatology (CGH), and Cellular and Molecular Gastroenterology and Hepatology (CMGH) – are pleased to announce their 2019-2020 editorial fellows.
Gastroenterology
Feng Su, MD
University of Washington, Seattle
Victoria Weis, PhD
Wake Forest University, Winston-Salem, N.C.
CGH
Austin Chiang, MD, MPH
Jefferson Medical College, Philadelphia, Penn.
Jennifer Kolb, MD
University of Colorado at Denver, Aurora
CMGH
Cambrian Liu, PhD
The Saban Research Institute, Children’s Hospital Los Angeles, Calif.
Tirthadipa Pradhan-Sundd, PhD
University of Pittsburgh, Penn.
The editorial fellows will be mentored on their respective journals’ editorial processes, including peer review and the publication process from manuscript submission to acceptance. They will participate in discussions and conferences with the boards of editors and work closely with the AGA editorial staff. Additionally, the fellows will participate in AGA’s new reviewer education program and will also be offered the opportunity to contribute content to their respective journals. The newly expanded program builds on the success of the previous 2 years when Gastroenterology had an editorial fellow.
The journals’ board of editors and editorial staff congratulate the fellows and are excited to work with them over the next year.
Get to know this rock star IBS researcher and mom
AGA Research Foundation pilot awards are an invaluable tool for investigators – they provide seed funding to explore promising new lines of research and generate preliminary data for larger grants. So, when Meenakshi Rao, MD, PhD, received the 2016 AGA–Takeda Pharmaceuticals International Research Scholar Award in Neurogastroenterology, she was able to double down on a project to identify why men and women with irritable bowel syndrome (IBS), the most common but least understood of all digestive disorders, report different symptoms and respond differently to treatment. Based on her recent accomplishments, we’re excited for you to get to know Dr. Rao, assistant professor of pediatrics at Harvard Medical School, Boston, and our AGA Research Foundation researcher of the month.
The Rao lab AGA-funded project focused on building upon Dr. Rao’s previous findings, which showed that disrupting nerves in the bowel had vastly different effects on males and females. These surprising results led Dr. Rao to explore whether sex hormones, such as testosterone and estrogen, might regulate how well things move through the bowel. Dr. Rao believes that identifying the underlying causes for sex differences in bowel function could lead to more effective and personalized treatments for patients with IBS. You can read the specifics of Dr. Rao’s research in the October 2017 issue of Gastroenterology and the October 2018 issue of Journal of Neuroscience.
IBS symptoms in women more typically involve constipation while young men with IBS more commonly report diarrhea. Over time, as men age, however, they tend to experience more constipation, Dr. Rao said. “Sex hormones might be signaling directly to the nerves in our gut and playing a role in these sex differences,” Dr. Rao said. “It might mean we can’t think of this as one disorder. IBS in a male may be different than IBS in a female, and that could change how we approach diagnosis and treatment.”
The AGA grant laid the groundwork for Dr. Rao’s findings, which led to a new understanding of how different types of cells in the gut nervous system regulate bowel functions – and how this regulation is different in males and females. The AGA grant helped Dr. Rao secure funding from the National Institutes of Health to launch new projects focused on how disruption of the gut nervous system causes disease.
Dr. Rao received the AGA award in 2015, when her son, Avinash, was aged 2 years. She acknowledged the delicate balancing act of raising a family and advancing her research.
“A lot of things were happening at once,” she said. “As a young parent, having the support of this award and having a technician (made possible by the award) made a big difference.”
Her son, now 5 years old, is growing up in a science-centric household because Dr. Rao’s husband is also a scientist. Not surprisingly, Dr. Rao says, her son is becoming a budding scientist.
“He talks about experiments all the time,” she says. “He even articulated to me the other day why we work on mice to learn how to help people. I never taught him that. I was floored.”
Five new GI technologies to know
The AGA Tech Summit Shark Tank is our annual reminder that the field of GI is ripe for innovation. Continue reading for an overview of the five new technologies pitched to our panel of sharks.
The smart toilet seat. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that capture images of bowel movements and urination for subsequent analysis. The company describes TrueLoo as a low-cost disease-screening tool that has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.
AI to aid screening endoscopy. A new tool called Ultivision, being developed by the startup Docbot, was described as a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia in either screening colonoscopy or in surveillance of Barrett’s esophagus. The tool integrates with existing endoscopic tools. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist.
Obesity phenotyping tool. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes: hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates). With this knowledge, treatment can be tailored appropriately leading to better outcomes.
Capsule diagnostic tool. The Atmo Gas Capsule from Atmo Biosciences is an ingestible capsule that measures gases at the source, which can accelerate the diagnosis of diseases such as IBS and inflammatory bowel disease (IBD). According to the company, this technique is highly accurate and offers an alternative to more invasive and expensive diagnostic tools.
Winner: “all-in-one” IBD app. Our Shark Tank winner by both popular vote from AGA Tech Summit attendees and the six-member Shark Tank panel was Oshi Health, selected for its IBD app. The app allows patients to track symptoms, a first step in understanding personalized flare pattern, as well as find resources to learn about their disease and communicate with other patients about their experiences. In a future iteration, information gathered by the app will be made available to physicians to provide current information about disease status to better individualize therapy.
2020 Crohn’s & Colitis Congress now open for registration
Join the Crohn’s & Colitis Foundation and AGA next January in Austin, Tex., for the premier conference on IBD.
The Crohn’s & Colitis Congress combines the strengths of the nation’s leading IBD patient organization, the Crohn’s & Colitis Foundation, and the premier GI professional organization, AGA, to bring together IBD professionals, across all disciplines, to transform IBD care.
The 2020 Congress Committee Chair David T. Rubin, MD, AGAF, University of Chicago, and Cochair Uma Mahadevan, MD, AGAF, University of California, San Francisco, lead a faculty that includes thought leaders in the fields of GI, research investigation, surgery, pediatrics, advanced practice, IBD nursing, diet and nutrition, mental health, radiology, and pathology.
The congress’s agenda includes main sessions that will emphasize case studies and panel discussions. There will also be parallel sessions on basic and translational science for senior and junior investigators. In addition, opening breakout sessions, taking place Jan. 23, will be available for selection free of charge.
Attendees of the 2020 congress will be able to meet with IBD leaders, discover different perspectives, leave with practical information they can immediately implement to take care of their next IBD patient and hear what’s on the horizon in potential treatment.
There will also be plenty of social events and plenty of time to build a strong network, including a Friday night Welcome Reception that should not be missed.
In addition, the 2020 congress is taking place in Austin, Tex. The capital of Texas and the Live Music Capital of the World, Austin is famous for its inspiring and enticing entertainment, culture, cuisine, and outdoor settings. Make a week of it and enjoy all Austin has to offer.
Early-bird registration ends Sept. 18. General abstract submissions for basic, translational, and clinical research begin Aug. 28 and end Oct. 23. To learn more and register, visit www.crohnscolitiscongress.org.
AGA welcomes new president, Hashem B. El-Serag, MD, MPH, AGAF
Hashem B. El-Serag, MD, MPH, AGAF, began his term as the 114th president of the AGA Institute at Digestive Disease Week® (DDW 2019).
Dr. El-Serag is former editor in chief of Clinical Gastroenterology and Hepatology. He currently serves as chair of the department of medicine at Baylor College of Medicine, Houston, following a decade leading and expanding Baylor’s gastroenterology and hepatology section. He is one of the few academic gastroenterologists serving as a chair of a department of medicine in the United States.
Originally Palestinian, Dr. El-Serag became a U.S. citizen in the early 2000s after medical school in Libya. He completed his training at community hospitals in the United States. His path from Benghazi to Baylor is described in the May issue of Gastroenterology by Baylor colleague Dr. Fasiha Kanwal.
“I firmly believe that the success I achieved in the United States would not have been possible anywhere else in the world, and it is as much a testament to the accepting society and medical system as to whatever intrinsic ability or skill I have,” noted Dr. El-Serag.
The major focus of Dr. El-Serag’s scholarly work is the epidemiology and clinical outcomes of hepatocellular carcinoma. Much of the modern literature on this topic includes his more than 100 publications. Since 2014, Dr. El-Serag has been named by Thomson Reuter as among the top 1% of clinical scientists.
Dr. El-Serag “is an innovative scientist, a compassionate physician, and a gifted educator. He is a relentless advocate of science and training, with an astute political sense — all key to influencing and shaping policy,” said Dr. Kanwal.
Dr. El-Serag’s term as AGA president concludes May 2020. Follow him on twitter at @SeragHashem.
Lipoprotein(a) levels can guide CV risk assessment and treatment
Lipoprotein(a) is an independent risk factor for atherosclerotic cardiovascular disease–related events, and plasma levels of Lp(a) could help refine risk assessment and influence treatment decisions, say the authors of a scientific statement from the National Lipid Association.
Don P. Wilson, MD, of Cook Children’s Medical Center, Fort Worth, Tex., and coauthors reviewed the evidence around testing of Lp(a) in clinical practice and its use in guiding treatment for both primary and secondary prevention. Their report is in the Journal of Clinical Lipidology.
Prospective, population-based studies point to a clear link between high Lp(a) levels and high risk of myocardial infarction, coronary heart disease, coronary artery stenosis, carotid stenosis, valvular aortic stenosis, ischemic stroke, cardiovascular mortality, and all-cause mortality, the authors wrote. This association was independent of the effect of other risk factors, including LDL cholesterol.
However, existing Lp(a) assays have not been globally standardized, and there is only incomplete evidence for age, sex, or ethnicity-specific cutoff points for high risk.
The authors suggested Lp(a) levels greater than 50 mg/dL (100 nmol/L) could be considered a risk factor that justifies the initiation of statin therapy. However ,they pointed out this level corresponded to the 80th population percentile in predominantly white populations, while in African American populations the equivalent cutoff was around 150 nmol/L.
On the issue of whom to test for Lp(a) serum levels, the authors said testing could reasonably be used to refine risk assessment for atherosclerotic cardiovascular disease in adults with first-degree relatives who experienced premature atherosclerotic cardiovascular disease, those with a personal history of the disease, or in those with severe hypercholesterolemia or suspected familial hypercholesterolemia.
However, statin therapy does not decrease Lp(a) levels, and there is also evidence that patients with high Lp(a) levels may not show as much LDL-C lowering in response to statin therapy.
“There is a lack of current evidence demonstrating that lowering Lp(a), independently of LDL-C, reduces ASCVD events in individuals with established ASCVD,” the authors wrote. “It appears that large absolute reductions in Lp(a) may be needed to demonstrate a significant clinical benefit.”
Despite this, the authors argued that in primary prevention, it was reasonable to use a Lp(a) level greater than 50 mg/dL (100 nmol/L) as a “risk-enhancing factor,” and in high-risk or very-high-risk patients with elevated LDL-C, it could prompt use of more intensive therapies.
Five authors disclosed honorarium or advisory board positions with the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Wilson D et al. J Clin Lipidol. 2019 May 17. doi: 10.1016/j.jacl.2019.04.010.
Lipoprotein(a) is an independent risk factor for atherosclerotic cardiovascular disease–related events, and plasma levels of Lp(a) could help refine risk assessment and influence treatment decisions, say the authors of a scientific statement from the National Lipid Association.
Don P. Wilson, MD, of Cook Children’s Medical Center, Fort Worth, Tex., and coauthors reviewed the evidence around testing of Lp(a) in clinical practice and its use in guiding treatment for both primary and secondary prevention. Their report is in the Journal of Clinical Lipidology.
Prospective, population-based studies point to a clear link between high Lp(a) levels and high risk of myocardial infarction, coronary heart disease, coronary artery stenosis, carotid stenosis, valvular aortic stenosis, ischemic stroke, cardiovascular mortality, and all-cause mortality, the authors wrote. This association was independent of the effect of other risk factors, including LDL cholesterol.
However, existing Lp(a) assays have not been globally standardized, and there is only incomplete evidence for age, sex, or ethnicity-specific cutoff points for high risk.
The authors suggested Lp(a) levels greater than 50 mg/dL (100 nmol/L) could be considered a risk factor that justifies the initiation of statin therapy. However ,they pointed out this level corresponded to the 80th population percentile in predominantly white populations, while in African American populations the equivalent cutoff was around 150 nmol/L.
On the issue of whom to test for Lp(a) serum levels, the authors said testing could reasonably be used to refine risk assessment for atherosclerotic cardiovascular disease in adults with first-degree relatives who experienced premature atherosclerotic cardiovascular disease, those with a personal history of the disease, or in those with severe hypercholesterolemia or suspected familial hypercholesterolemia.
However, statin therapy does not decrease Lp(a) levels, and there is also evidence that patients with high Lp(a) levels may not show as much LDL-C lowering in response to statin therapy.
“There is a lack of current evidence demonstrating that lowering Lp(a), independently of LDL-C, reduces ASCVD events in individuals with established ASCVD,” the authors wrote. “It appears that large absolute reductions in Lp(a) may be needed to demonstrate a significant clinical benefit.”
Despite this, the authors argued that in primary prevention, it was reasonable to use a Lp(a) level greater than 50 mg/dL (100 nmol/L) as a “risk-enhancing factor,” and in high-risk or very-high-risk patients with elevated LDL-C, it could prompt use of more intensive therapies.
Five authors disclosed honorarium or advisory board positions with the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Wilson D et al. J Clin Lipidol. 2019 May 17. doi: 10.1016/j.jacl.2019.04.010.
Lipoprotein(a) is an independent risk factor for atherosclerotic cardiovascular disease–related events, and plasma levels of Lp(a) could help refine risk assessment and influence treatment decisions, say the authors of a scientific statement from the National Lipid Association.
Don P. Wilson, MD, of Cook Children’s Medical Center, Fort Worth, Tex., and coauthors reviewed the evidence around testing of Lp(a) in clinical practice and its use in guiding treatment for both primary and secondary prevention. Their report is in the Journal of Clinical Lipidology.
Prospective, population-based studies point to a clear link between high Lp(a) levels and high risk of myocardial infarction, coronary heart disease, coronary artery stenosis, carotid stenosis, valvular aortic stenosis, ischemic stroke, cardiovascular mortality, and all-cause mortality, the authors wrote. This association was independent of the effect of other risk factors, including LDL cholesterol.
However, existing Lp(a) assays have not been globally standardized, and there is only incomplete evidence for age, sex, or ethnicity-specific cutoff points for high risk.
The authors suggested Lp(a) levels greater than 50 mg/dL (100 nmol/L) could be considered a risk factor that justifies the initiation of statin therapy. However ,they pointed out this level corresponded to the 80th population percentile in predominantly white populations, while in African American populations the equivalent cutoff was around 150 nmol/L.
On the issue of whom to test for Lp(a) serum levels, the authors said testing could reasonably be used to refine risk assessment for atherosclerotic cardiovascular disease in adults with first-degree relatives who experienced premature atherosclerotic cardiovascular disease, those with a personal history of the disease, or in those with severe hypercholesterolemia or suspected familial hypercholesterolemia.
However, statin therapy does not decrease Lp(a) levels, and there is also evidence that patients with high Lp(a) levels may not show as much LDL-C lowering in response to statin therapy.
“There is a lack of current evidence demonstrating that lowering Lp(a), independently of LDL-C, reduces ASCVD events in individuals with established ASCVD,” the authors wrote. “It appears that large absolute reductions in Lp(a) may be needed to demonstrate a significant clinical benefit.”
Despite this, the authors argued that in primary prevention, it was reasonable to use a Lp(a) level greater than 50 mg/dL (100 nmol/L) as a “risk-enhancing factor,” and in high-risk or very-high-risk patients with elevated LDL-C, it could prompt use of more intensive therapies.
Five authors disclosed honorarium or advisory board positions with the pharmaceutical sector. No other conflicts of interest were declared.
SOURCE: Wilson D et al. J Clin Lipidol. 2019 May 17. doi: 10.1016/j.jacl.2019.04.010.
FROM THE JOURNAL OF CLINICAL LIPIDOLOGY
Calendar
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Aug. 9-10, 2019
2019 Freston Conference: Food at the Intersection of Gut Health and Disease
GI clinicians and allied health professionals are increasingly focused on how nutrients influence GI physiology and how diet can promote sound gut health. In response to this growing body of knowledge, the 2019 James W. Freston Conference — Food at the Intersection of Gut Health and Disease, Aug. 9-10, 2019, in Chicago — will examine how nutrition management therapies can combat GI disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease and how diet supports improvement across the care continuum.
Chicago, Illinois
Aug. 9–11, 2019
2019 Principles of GI for the NP and PA
The Principles of Gastroenterology for the Nurse Practitioner and Physician Assistant (NPPA) is the medical industry’s premiere course guiding and enabling nurse practitioners and physician assistants with the intricacies of identifying, treating, and managing GI disorders. Designed and taught by expert clinicians and advanced practice providers, NPPA provides the latest insights, knowledge, and research on how to improve GI patient care. Attendees will leave with stronger diagnostic and therapeutic skills, a more robust professional network, and an enhanced value for their practices.
Chicago, Illinois
Sept. 18-19, 2019; Oct. 9-10. 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Atlanta, GA (9/18-19); Las Vegas, NV (10/9-10)
Oct. 4, 2019
2019 AGA Partners in Value
Join GI trailblazers and leaders from AGA and DHPA to network and discuss strategies that will help your practice succeed in the changing business of health care. Leave equipped to make better decisions for the future.
Chicago, Illinois
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Illinois
AWARDS APPLICATION DEADLINES
AGA-Elsevier Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing research in gastroenterology- or hepatology-related areas.
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of inflammatory bowel disease (IBD).
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Nonalcoholic Fatty Liver Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of nonalcoholic fatty liver disease (NAFLD).
Application Deadline: Sept. 4, 2019
AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to recipients at any career stage researching new directions focused on improving the diagnosis and treatment of inflammatory bowel disease.
Application Deadline: Sept. 4, 2019
AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing clinical or translational research pertaining to functional GI and motility disorders.
Application Deadline: Sept. 4, 2019
AGA Research Scholar Award (RSA)
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in digestive disease research.
Application Deadline: Nov. 13, 2019
AGA-Gastric Cancer Foundation Ben Feinstein Memorial Research Scholar Award in Gastric Cancer
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in gastric cancer research. Research involving precancerous lesions will be considered if relevance to gastric cancer is explicitly outlined.
Application Deadline: Nov. 13, 2019
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $100,000 per year for 3 years (total $300,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Nov. 13, 2019
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Aug. 9-10, 2019
2019 Freston Conference: Food at the Intersection of Gut Health and Disease
GI clinicians and allied health professionals are increasingly focused on how nutrients influence GI physiology and how diet can promote sound gut health. In response to this growing body of knowledge, the 2019 James W. Freston Conference — Food at the Intersection of Gut Health and Disease, Aug. 9-10, 2019, in Chicago — will examine how nutrition management therapies can combat GI disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease and how diet supports improvement across the care continuum.
Chicago, Illinois
Aug. 9–11, 2019
2019 Principles of GI for the NP and PA
The Principles of Gastroenterology for the Nurse Practitioner and Physician Assistant (NPPA) is the medical industry’s premiere course guiding and enabling nurse practitioners and physician assistants with the intricacies of identifying, treating, and managing GI disorders. Designed and taught by expert clinicians and advanced practice providers, NPPA provides the latest insights, knowledge, and research on how to improve GI patient care. Attendees will leave with stronger diagnostic and therapeutic skills, a more robust professional network, and an enhanced value for their practices.
Chicago, Illinois
Sept. 18-19, 2019; Oct. 9-10. 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Atlanta, GA (9/18-19); Las Vegas, NV (10/9-10)
Oct. 4, 2019
2019 AGA Partners in Value
Join GI trailblazers and leaders from AGA and DHPA to network and discuss strategies that will help your practice succeed in the changing business of health care. Leave equipped to make better decisions for the future.
Chicago, Illinois
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Illinois
AWARDS APPLICATION DEADLINES
AGA-Elsevier Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing research in gastroenterology- or hepatology-related areas.
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of inflammatory bowel disease (IBD).
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Nonalcoholic Fatty Liver Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of nonalcoholic fatty liver disease (NAFLD).
Application Deadline: Sept. 4, 2019
AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to recipients at any career stage researching new directions focused on improving the diagnosis and treatment of inflammatory bowel disease.
Application Deadline: Sept. 4, 2019
AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing clinical or translational research pertaining to functional GI and motility disorders.
Application Deadline: Sept. 4, 2019
AGA Research Scholar Award (RSA)
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in digestive disease research.
Application Deadline: Nov. 13, 2019
AGA-Gastric Cancer Foundation Ben Feinstein Memorial Research Scholar Award in Gastric Cancer
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in gastric cancer research. Research involving precancerous lesions will be considered if relevance to gastric cancer is explicitly outlined.
Application Deadline: Nov. 13, 2019
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $100,000 per year for 3 years (total $300,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Nov. 13, 2019
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
For more information about upcoming events and award deadlines, please visit http://agau.gastro.org and http://www.gastro.org/research-funding.
UPCOMING EVENTS
Aug. 9-10, 2019
2019 Freston Conference: Food at the Intersection of Gut Health and Disease
GI clinicians and allied health professionals are increasingly focused on how nutrients influence GI physiology and how diet can promote sound gut health. In response to this growing body of knowledge, the 2019 James W. Freston Conference — Food at the Intersection of Gut Health and Disease, Aug. 9-10, 2019, in Chicago — will examine how nutrition management therapies can combat GI disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and celiac disease and how diet supports improvement across the care continuum.
Chicago, Illinois
Aug. 9–11, 2019
2019 Principles of GI for the NP and PA
The Principles of Gastroenterology for the Nurse Practitioner and Physician Assistant (NPPA) is the medical industry’s premiere course guiding and enabling nurse practitioners and physician assistants with the intricacies of identifying, treating, and managing GI disorders. Designed and taught by expert clinicians and advanced practice providers, NPPA provides the latest insights, knowledge, and research on how to improve GI patient care. Attendees will leave with stronger diagnostic and therapeutic skills, a more robust professional network, and an enhanced value for their practices.
Chicago, Illinois
Sept. 18-19, 2019; Oct. 9-10. 2019
Two-Day, In-Depth Coding Seminar by McVey Associates, Inc.
Become a certified GI coder with a two-day, in-depth training course provided by McVey Associates, Inc.
Atlanta, GA (9/18-19); Las Vegas, NV (10/9-10)
Oct. 4, 2019
2019 AGA Partners in Value
Join GI trailblazers and leaders from AGA and DHPA to network and discuss strategies that will help your practice succeed in the changing business of health care. Leave equipped to make better decisions for the future.
Chicago, Illinois
May 2-5, 2020
Digestive Disease Week® (DDW)
Digestive Disease Week® (DDW) is the world’s leading educational forum for academicians, clinicians, researchers, students, and trainees working in gastroenterology, hepatology, GI endoscopy, gastrointestinal surgery, and related fields. Whether you work in patient care, research, education, or administration, the DDW program offers something for you. Abstract submissions will be due on Dec. 1, and registration will open in January 2020.
Chicago, Illinois
AWARDS APPLICATION DEADLINES
AGA-Elsevier Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing research in gastroenterology- or hepatology-related areas.
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of inflammatory bowel disease (IBD).
Application Deadline: Sept. 4, 2019
AGA-Allergan Foundation Pilot Research Award in Nonalcoholic Fatty Liver Disease
This award provides $30,000 for 1 year to an investigator at any career stage researching the pathophysiology and/or treatment of nonalcoholic fatty liver disease (NAFLD).
Application Deadline: Sept. 4, 2019
AGA-Pfizer Pilot Research Award in Inflammatory Bowel Disease
This award provides $30,000 for 1 year to recipients at any career stage researching new directions focused on improving the diagnosis and treatment of inflammatory bowel disease.
Application Deadline: Sept. 4, 2019
AGA-Rome Foundation Functional GI and Motility Disorders Pilot Research Award
This award provides $30,000 for 1 year to a recipient at any career stage performing clinical or translational research pertaining to functional GI and motility disorders.
Application Deadline: Sept. 4, 2019
AGA Research Scholar Award (RSA)
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in digestive disease research.
Application Deadline: Nov. 13, 2019
AGA-Gastric Cancer Foundation Ben Feinstein Memorial Research Scholar Award in Gastric Cancer
This award provides $100,000 per year for 3 years (total $300,000) to early career faculty (i.e., investigator, instructor, research associate or equivalent) working toward an independent career in gastric cancer research. Research involving precancerous lesions will be considered if relevance to gastric cancer is explicitly outlined.
Application Deadline: Nov. 13, 2019
AGA-Takeda Pharmaceuticals Research Scholar Award in Inflammatory Bowel Disease
This award provides $100,000 per year for 3 years (total $300,000) to a young investigator, instructor, research associate or equivalent working toward an independent career in inflammatory bowel disease research.
Application Deadline: Nov. 13, 2019
AGA Fellow Abstract Award
This $500 travel award supports recipients who are MD, PhD or equivalent fellows giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW). The top-scoring abstract will be designated the Fellow Abstract of the Year and receive a $1,000 award.
Application Deadline: Feb. 26, 2020
AGA Student Abstract Award
This $500 travel award supports recipients who are graduate students, medical students, or medical residents (residents up to postgraduate year three) giving abstract-based oral or poster presentations at Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
AGA-Moti L. & Kamla Rustgi International Travel Awards
This $750 travel award supports recipients who are young (i.e., 35 years of age or younger at the time of DDW) basic, translational, or clinical investigators residing outside North America to support travel and related expenses to attend Digestive Disease Week® (DDW).
Application Deadline: Feb. 26, 2020
Nephrectomy may benefit select renal cancer patients based on risk factors
CHICAGO – While cytoreductive nephrectomy is generally still inadvisable in metastatic renal cell carcinoma patients who require medical therapy, an update of the CARMENA trial suggests the procedure may provide benefit for certain patients.
Patients with only one International Metastatic Renal Cell Carcinoma Database Consortium (IMDC) risk factor may benefit from cytoreductive nephrectomy, said CARMENA investigator Arnaud Méjean, MD, PhD, in a presentation at the annual meeting of the American Society of Clinical Oncology.
Among patients in CARMENA treated with nephrectomy plus sunitinib, median overall survival was 31.4 months for those with just one risk factor, and 17.6 months for those with two or more (hazard ratio, 1.68; 95% confidence interval, 1.10-2.57; P = .01), suggesting the procedure was “detrimental” to perform in the presence of multiple risk factors, the investigator said.
By contrast, among patients treated with sunitinib alone, there was no significant difference in median overall survival for patients with one risk factor versus those with two or more risk factors, said Dr. Méjean, who is with the Hôpital Européen Georges-Pompidou and Paris Descartes University.
In another analysis of the data, delayed nephrectomy after initial systemic therapy was associated with long overall survival in good responders, supporting that approach as a “good therapeutic strategy,” he said.
Based on these results, Dr. Méjean told ASCO attendees he would “go back to the operating theater to operate just very selected patients.”
In a podium discussion, Alexander Kutikov, MD, FACS, said CARMENA makes it “undeniable” that up-front cytoreductive therapy should be applied to a “very select group” of patients.
While that select group may be defined as the one IMDC risk factor group, Dr. Kutkov said it is also appropriate to offer cytoreductive nephrectomy to carefully selected patients who do not need immediate systemic therapy.
“If the plan is to observe without systemic therapy, proceed with cytoreductive nephrectomy, and for everybody else, I think we take great caution in offering cytoreductive nephrectomy, because it absolutely can harm,” said Dr. Kutikov, professor and chief of urologic oncology at Fox Chase Cancer Center, Philadelphia.
The CARMENA update confirmed that, in general, cytoreductive nephrectomy should not be the standard of care, according to Dr. Méjean.
With follow-up of 61.5 months, or longer than what was previously reported for the 450-patient trial, cytoreductive nephrectomy followed by sunitinib was again found to be not superior to sunitinib alone, he said. Median overall survival was 15.6 months for the nephrectomy plus sunitinib arm versus 19.8 months for the sunitinib arm, showing that sunitinib alone was noninferior based on the statistical design of the trial (hazard ratio, 0.97; 95% CI, 0.79-1.19, with a fixed upper limit for noninferiority of 1.20).
Dr. Méjean reported disclosures related to Ipsen, Novartis, Pfizer, Bristol-Myers Squibb, Janssen, Sanofi and Roche.
SOURCE: Méjean A et al. ASCO 2019, Abstract 4508.
CHICAGO – While cytoreductive nephrectomy is generally still inadvisable in metastatic renal cell carcinoma patients who require medical therapy, an update of the CARMENA trial suggests the procedure may provide benefit for certain patients.
Patients with only one International Metastatic Renal Cell Carcinoma Database Consortium (IMDC) risk factor may benefit from cytoreductive nephrectomy, said CARMENA investigator Arnaud Méjean, MD, PhD, in a presentation at the annual meeting of the American Society of Clinical Oncology.
Among patients in CARMENA treated with nephrectomy plus sunitinib, median overall survival was 31.4 months for those with just one risk factor, and 17.6 months for those with two or more (hazard ratio, 1.68; 95% confidence interval, 1.10-2.57; P = .01), suggesting the procedure was “detrimental” to perform in the presence of multiple risk factors, the investigator said.
By contrast, among patients treated with sunitinib alone, there was no significant difference in median overall survival for patients with one risk factor versus those with two or more risk factors, said Dr. Méjean, who is with the Hôpital Européen Georges-Pompidou and Paris Descartes University.
In another analysis of the data, delayed nephrectomy after initial systemic therapy was associated with long overall survival in good responders, supporting that approach as a “good therapeutic strategy,” he said.
Based on these results, Dr. Méjean told ASCO attendees he would “go back to the operating theater to operate just very selected patients.”
In a podium discussion, Alexander Kutikov, MD, FACS, said CARMENA makes it “undeniable” that up-front cytoreductive therapy should be applied to a “very select group” of patients.
While that select group may be defined as the one IMDC risk factor group, Dr. Kutkov said it is also appropriate to offer cytoreductive nephrectomy to carefully selected patients who do not need immediate systemic therapy.
“If the plan is to observe without systemic therapy, proceed with cytoreductive nephrectomy, and for everybody else, I think we take great caution in offering cytoreductive nephrectomy, because it absolutely can harm,” said Dr. Kutikov, professor and chief of urologic oncology at Fox Chase Cancer Center, Philadelphia.
The CARMENA update confirmed that, in general, cytoreductive nephrectomy should not be the standard of care, according to Dr. Méjean.
With follow-up of 61.5 months, or longer than what was previously reported for the 450-patient trial, cytoreductive nephrectomy followed by sunitinib was again found to be not superior to sunitinib alone, he said. Median overall survival was 15.6 months for the nephrectomy plus sunitinib arm versus 19.8 months for the sunitinib arm, showing that sunitinib alone was noninferior based on the statistical design of the trial (hazard ratio, 0.97; 95% CI, 0.79-1.19, with a fixed upper limit for noninferiority of 1.20).
Dr. Méjean reported disclosures related to Ipsen, Novartis, Pfizer, Bristol-Myers Squibb, Janssen, Sanofi and Roche.
SOURCE: Méjean A et al. ASCO 2019, Abstract 4508.
CHICAGO – While cytoreductive nephrectomy is generally still inadvisable in metastatic renal cell carcinoma patients who require medical therapy, an update of the CARMENA trial suggests the procedure may provide benefit for certain patients.
Patients with only one International Metastatic Renal Cell Carcinoma Database Consortium (IMDC) risk factor may benefit from cytoreductive nephrectomy, said CARMENA investigator Arnaud Méjean, MD, PhD, in a presentation at the annual meeting of the American Society of Clinical Oncology.
Among patients in CARMENA treated with nephrectomy plus sunitinib, median overall survival was 31.4 months for those with just one risk factor, and 17.6 months for those with two or more (hazard ratio, 1.68; 95% confidence interval, 1.10-2.57; P = .01), suggesting the procedure was “detrimental” to perform in the presence of multiple risk factors, the investigator said.
By contrast, among patients treated with sunitinib alone, there was no significant difference in median overall survival for patients with one risk factor versus those with two or more risk factors, said Dr. Méjean, who is with the Hôpital Européen Georges-Pompidou and Paris Descartes University.
In another analysis of the data, delayed nephrectomy after initial systemic therapy was associated with long overall survival in good responders, supporting that approach as a “good therapeutic strategy,” he said.
Based on these results, Dr. Méjean told ASCO attendees he would “go back to the operating theater to operate just very selected patients.”
In a podium discussion, Alexander Kutikov, MD, FACS, said CARMENA makes it “undeniable” that up-front cytoreductive therapy should be applied to a “very select group” of patients.
While that select group may be defined as the one IMDC risk factor group, Dr. Kutkov said it is also appropriate to offer cytoreductive nephrectomy to carefully selected patients who do not need immediate systemic therapy.
“If the plan is to observe without systemic therapy, proceed with cytoreductive nephrectomy, and for everybody else, I think we take great caution in offering cytoreductive nephrectomy, because it absolutely can harm,” said Dr. Kutikov, professor and chief of urologic oncology at Fox Chase Cancer Center, Philadelphia.
The CARMENA update confirmed that, in general, cytoreductive nephrectomy should not be the standard of care, according to Dr. Méjean.
With follow-up of 61.5 months, or longer than what was previously reported for the 450-patient trial, cytoreductive nephrectomy followed by sunitinib was again found to be not superior to sunitinib alone, he said. Median overall survival was 15.6 months for the nephrectomy plus sunitinib arm versus 19.8 months for the sunitinib arm, showing that sunitinib alone was noninferior based on the statistical design of the trial (hazard ratio, 0.97; 95% CI, 0.79-1.19, with a fixed upper limit for noninferiority of 1.20).
Dr. Méjean reported disclosures related to Ipsen, Novartis, Pfizer, Bristol-Myers Squibb, Janssen, Sanofi and Roche.
SOURCE: Méjean A et al. ASCO 2019, Abstract 4508.
REPORTING FROM ASCO 2019
DOACs surpass warfarin in low-weight AFib patients
SAN FRANCISCO – The direct-acting anticoagulants, as a class, were more effective and at least as safe as warfarin in low-weight and very-low-weight patients with atrial fibrillation in an adjusted analysis of real-world outcomes data from more than 21,000 Korean patients.
The analysis also showed that the direct-acting oral anticoagulants (DOACs) had the best safety and efficacy on low-weight patients when used at the labeled dosages, with blunted efficacy and safety at dosages that either exceeded or fell short of labeled levels, So-Ryoung Lee, MD, said at the annual scientific sessions of the Heart Rhythm Society.
The overall superiority of DOACs by both efficacy and safety also generally extended to the subgroup of very-low-weight patients, those with weights of less than 50 kg. In this subgroup, which was 28% of the total population studied, the composite adverse event outcome occurred 33% less often among patients treated with a DOAC relative to patients treated with warfarin, a statistically significant difference, said Dr. Lee, a cardiologist at Seoul (South Korea) National University Hospital. Among all patients with weights of 60 kg (132 pounds) or less, the composite outcome occurred 34% less often in the DOAC-treated patients relative to the warfarin-treated patients, also a statistically significant difference.
Dr. Lee and colleagues used a Korean National Health Insurance database that included information on more than 600,000 adults with atrial fibrillation (AFib) as of January 2013. The researchers whittled this down to 21,678 patients who began for the first time treatment with an oral anticoagulant starting during or after January 2014; had no history of a stroke, intracranial hemorrhage, or gastrointestinal bleed; and weighed no more than 60 kg. This cohort included 7,575 (35%) who received warfarin treatment, and 14,103 (65%) who received a DOAC. Within the DOAC-treated group, 42% received rivaroxaban (Xarelto), 26% dabigatran (Pradaxa), 24% apixaban (Eliquis), and 8% edoxaban (Savaysa).
To account for baseline differences in demographics and comorbidities between the patients treated with a DOAC and those who received warfarin, Dr. Lee and her associates did propensity score adjustment, which resulted in similar cohorts of 6,692 patients treated with warfarin and 12,810 patients treated with a DOAC. The average age of these patients was 73 years, a third were men, and the average body mass index was just over 22 kg/m2.
The events that the researchers tallied during follow-up through December 2016 included rates of all-cause death, ischemic stroke, intracranial hemorrhage, hospitalization for GI bleeding, hospitalization for major bleeding, and the composite of these five outcomes.
In the propensity-score adjusted full cohort of all patients who weighed 60 kg or less, the rate of each of these five outcomes, as well as the composite outcome, occurred statistically significantly less often among the DOAC-treated patients than in those on warfarin. The reductions ranged from a 41% lower incidence of ischemic stroke on DOAC treatment compared with warfarin treatment, to an 18% reduced rate of hospitalization for a GI bleed, compared with warfarin-treated patients. In the subgroup of patients who weighed less than 50 kg (110 pounds), the reductions ranged from a 41% cut in ischemic stroke on a DOAC compared with warfarin to a 24% relative reduction in the rate of hospitalization for a major bleed, a difference that just reached statistical significance. The outcome of hospitalization for a GI bleed showed no significant between-group difference among very-low-weight patients, but the rates of intracranial hemorrhage and all-cause death also showed statistically significant lower rates among DOAC-treated patients.
Nearly two-thirds of the patients on a DOAC received the label-appropriate dose of the drug, but 31% received a dosage that was below the labeled level while 4% received a dosage above the labeled level. An analysis that divided the NOAC patients by the appropriateness of their treatment dosages showed that patients on the correct dosages fared best. For example, in the total cohort of patients who weighed 60 kg or less, those on the correct DOAC dosage had a 9.1% rate of the combined endpoint. Patients on a low DOAC dosage did about as well as did the patients on warfarin, with a combined event rate of 11.6% in each of these subgroups. The worst outcomes occurred among the small number of patients on an inappropriately-high DOAC dosage, with a combined event rate of 15.4%. The researchers found a similar pattern among patients who weighed less than 50 kg.
Dr. Lee had no disclosures.
SOURCE: Lee SR et al. HRS 2019, Abstract S-AB30-05.
SAN FRANCISCO – The direct-acting anticoagulants, as a class, were more effective and at least as safe as warfarin in low-weight and very-low-weight patients with atrial fibrillation in an adjusted analysis of real-world outcomes data from more than 21,000 Korean patients.
The analysis also showed that the direct-acting oral anticoagulants (DOACs) had the best safety and efficacy on low-weight patients when used at the labeled dosages, with blunted efficacy and safety at dosages that either exceeded or fell short of labeled levels, So-Ryoung Lee, MD, said at the annual scientific sessions of the Heart Rhythm Society.
The overall superiority of DOACs by both efficacy and safety also generally extended to the subgroup of very-low-weight patients, those with weights of less than 50 kg. In this subgroup, which was 28% of the total population studied, the composite adverse event outcome occurred 33% less often among patients treated with a DOAC relative to patients treated with warfarin, a statistically significant difference, said Dr. Lee, a cardiologist at Seoul (South Korea) National University Hospital. Among all patients with weights of 60 kg (132 pounds) or less, the composite outcome occurred 34% less often in the DOAC-treated patients relative to the warfarin-treated patients, also a statistically significant difference.
Dr. Lee and colleagues used a Korean National Health Insurance database that included information on more than 600,000 adults with atrial fibrillation (AFib) as of January 2013. The researchers whittled this down to 21,678 patients who began for the first time treatment with an oral anticoagulant starting during or after January 2014; had no history of a stroke, intracranial hemorrhage, or gastrointestinal bleed; and weighed no more than 60 kg. This cohort included 7,575 (35%) who received warfarin treatment, and 14,103 (65%) who received a DOAC. Within the DOAC-treated group, 42% received rivaroxaban (Xarelto), 26% dabigatran (Pradaxa), 24% apixaban (Eliquis), and 8% edoxaban (Savaysa).
To account for baseline differences in demographics and comorbidities between the patients treated with a DOAC and those who received warfarin, Dr. Lee and her associates did propensity score adjustment, which resulted in similar cohorts of 6,692 patients treated with warfarin and 12,810 patients treated with a DOAC. The average age of these patients was 73 years, a third were men, and the average body mass index was just over 22 kg/m2.
The events that the researchers tallied during follow-up through December 2016 included rates of all-cause death, ischemic stroke, intracranial hemorrhage, hospitalization for GI bleeding, hospitalization for major bleeding, and the composite of these five outcomes.
In the propensity-score adjusted full cohort of all patients who weighed 60 kg or less, the rate of each of these five outcomes, as well as the composite outcome, occurred statistically significantly less often among the DOAC-treated patients than in those on warfarin. The reductions ranged from a 41% lower incidence of ischemic stroke on DOAC treatment compared with warfarin treatment, to an 18% reduced rate of hospitalization for a GI bleed, compared with warfarin-treated patients. In the subgroup of patients who weighed less than 50 kg (110 pounds), the reductions ranged from a 41% cut in ischemic stroke on a DOAC compared with warfarin to a 24% relative reduction in the rate of hospitalization for a major bleed, a difference that just reached statistical significance. The outcome of hospitalization for a GI bleed showed no significant between-group difference among very-low-weight patients, but the rates of intracranial hemorrhage and all-cause death also showed statistically significant lower rates among DOAC-treated patients.
Nearly two-thirds of the patients on a DOAC received the label-appropriate dose of the drug, but 31% received a dosage that was below the labeled level while 4% received a dosage above the labeled level. An analysis that divided the NOAC patients by the appropriateness of their treatment dosages showed that patients on the correct dosages fared best. For example, in the total cohort of patients who weighed 60 kg or less, those on the correct DOAC dosage had a 9.1% rate of the combined endpoint. Patients on a low DOAC dosage did about as well as did the patients on warfarin, with a combined event rate of 11.6% in each of these subgroups. The worst outcomes occurred among the small number of patients on an inappropriately-high DOAC dosage, with a combined event rate of 15.4%. The researchers found a similar pattern among patients who weighed less than 50 kg.
Dr. Lee had no disclosures.
SOURCE: Lee SR et al. HRS 2019, Abstract S-AB30-05.
SAN FRANCISCO – The direct-acting anticoagulants, as a class, were more effective and at least as safe as warfarin in low-weight and very-low-weight patients with atrial fibrillation in an adjusted analysis of real-world outcomes data from more than 21,000 Korean patients.
The analysis also showed that the direct-acting oral anticoagulants (DOACs) had the best safety and efficacy on low-weight patients when used at the labeled dosages, with blunted efficacy and safety at dosages that either exceeded or fell short of labeled levels, So-Ryoung Lee, MD, said at the annual scientific sessions of the Heart Rhythm Society.
The overall superiority of DOACs by both efficacy and safety also generally extended to the subgroup of very-low-weight patients, those with weights of less than 50 kg. In this subgroup, which was 28% of the total population studied, the composite adverse event outcome occurred 33% less often among patients treated with a DOAC relative to patients treated with warfarin, a statistically significant difference, said Dr. Lee, a cardiologist at Seoul (South Korea) National University Hospital. Among all patients with weights of 60 kg (132 pounds) or less, the composite outcome occurred 34% less often in the DOAC-treated patients relative to the warfarin-treated patients, also a statistically significant difference.
Dr. Lee and colleagues used a Korean National Health Insurance database that included information on more than 600,000 adults with atrial fibrillation (AFib) as of January 2013. The researchers whittled this down to 21,678 patients who began for the first time treatment with an oral anticoagulant starting during or after January 2014; had no history of a stroke, intracranial hemorrhage, or gastrointestinal bleed; and weighed no more than 60 kg. This cohort included 7,575 (35%) who received warfarin treatment, and 14,103 (65%) who received a DOAC. Within the DOAC-treated group, 42% received rivaroxaban (Xarelto), 26% dabigatran (Pradaxa), 24% apixaban (Eliquis), and 8% edoxaban (Savaysa).
To account for baseline differences in demographics and comorbidities between the patients treated with a DOAC and those who received warfarin, Dr. Lee and her associates did propensity score adjustment, which resulted in similar cohorts of 6,692 patients treated with warfarin and 12,810 patients treated with a DOAC. The average age of these patients was 73 years, a third were men, and the average body mass index was just over 22 kg/m2.
The events that the researchers tallied during follow-up through December 2016 included rates of all-cause death, ischemic stroke, intracranial hemorrhage, hospitalization for GI bleeding, hospitalization for major bleeding, and the composite of these five outcomes.
In the propensity-score adjusted full cohort of all patients who weighed 60 kg or less, the rate of each of these five outcomes, as well as the composite outcome, occurred statistically significantly less often among the DOAC-treated patients than in those on warfarin. The reductions ranged from a 41% lower incidence of ischemic stroke on DOAC treatment compared with warfarin treatment, to an 18% reduced rate of hospitalization for a GI bleed, compared with warfarin-treated patients. In the subgroup of patients who weighed less than 50 kg (110 pounds), the reductions ranged from a 41% cut in ischemic stroke on a DOAC compared with warfarin to a 24% relative reduction in the rate of hospitalization for a major bleed, a difference that just reached statistical significance. The outcome of hospitalization for a GI bleed showed no significant between-group difference among very-low-weight patients, but the rates of intracranial hemorrhage and all-cause death also showed statistically significant lower rates among DOAC-treated patients.
Nearly two-thirds of the patients on a DOAC received the label-appropriate dose of the drug, but 31% received a dosage that was below the labeled level while 4% received a dosage above the labeled level. An analysis that divided the NOAC patients by the appropriateness of their treatment dosages showed that patients on the correct dosages fared best. For example, in the total cohort of patients who weighed 60 kg or less, those on the correct DOAC dosage had a 9.1% rate of the combined endpoint. Patients on a low DOAC dosage did about as well as did the patients on warfarin, with a combined event rate of 11.6% in each of these subgroups. The worst outcomes occurred among the small number of patients on an inappropriately-high DOAC dosage, with a combined event rate of 15.4%. The researchers found a similar pattern among patients who weighed less than 50 kg.
Dr. Lee had no disclosures.
SOURCE: Lee SR et al. HRS 2019, Abstract S-AB30-05.
REPORTING FROM HEART RHYTHM 2019
More liberal criteria could greatly expand clinical trial participation
CHICAGO – Fewer than 1 in 20 adults with cancer enroll in clinical trials, and even when cancer patients are willing to participate in a trial, they are often excluded because of comorbidities, prior therapies, or a host of other factors that could confound results.
But as a team of investigators shows in a proof-of-concept study, more generous exclusion criteria in some trials could nearly double the number of participants. Using retrospective, deidentified electronic health record data from the American Society of Clinical Oncology CancerLinQ Discovery database, R. Donald Harvey, PharmD and colleagues found that when they applied broader inclusion criteria for patients with advanced non–small cell lung cancer (NSCLC), the number of patients who would be eligible for clinical trials nearly doubled from 5,495 to 10,349.
In this video interview from the ASCO annual meeting, Dr. Harvey of the Winship Cancer Institute of Emory University in Atlanta discusses collaborations between the oncology community, federal agencies, and the pharmaceutical industry that could improve clinical trials by safely increasing sample sizes.
The study received funding from ASCO. Dr. Harvey disclosed consulting or advisory roles with and institutional research funding from multiple entities.
CHICAGO – Fewer than 1 in 20 adults with cancer enroll in clinical trials, and even when cancer patients are willing to participate in a trial, they are often excluded because of comorbidities, prior therapies, or a host of other factors that could confound results.
But as a team of investigators shows in a proof-of-concept study, more generous exclusion criteria in some trials could nearly double the number of participants. Using retrospective, deidentified electronic health record data from the American Society of Clinical Oncology CancerLinQ Discovery database, R. Donald Harvey, PharmD and colleagues found that when they applied broader inclusion criteria for patients with advanced non–small cell lung cancer (NSCLC), the number of patients who would be eligible for clinical trials nearly doubled from 5,495 to 10,349.
In this video interview from the ASCO annual meeting, Dr. Harvey of the Winship Cancer Institute of Emory University in Atlanta discusses collaborations between the oncology community, federal agencies, and the pharmaceutical industry that could improve clinical trials by safely increasing sample sizes.
The study received funding from ASCO. Dr. Harvey disclosed consulting or advisory roles with and institutional research funding from multiple entities.
CHICAGO – Fewer than 1 in 20 adults with cancer enroll in clinical trials, and even when cancer patients are willing to participate in a trial, they are often excluded because of comorbidities, prior therapies, or a host of other factors that could confound results.
But as a team of investigators shows in a proof-of-concept study, more generous exclusion criteria in some trials could nearly double the number of participants. Using retrospective, deidentified electronic health record data from the American Society of Clinical Oncology CancerLinQ Discovery database, R. Donald Harvey, PharmD and colleagues found that when they applied broader inclusion criteria for patients with advanced non–small cell lung cancer (NSCLC), the number of patients who would be eligible for clinical trials nearly doubled from 5,495 to 10,349.
In this video interview from the ASCO annual meeting, Dr. Harvey of the Winship Cancer Institute of Emory University in Atlanta discusses collaborations between the oncology community, federal agencies, and the pharmaceutical industry that could improve clinical trials by safely increasing sample sizes.
The study received funding from ASCO. Dr. Harvey disclosed consulting or advisory roles with and institutional research funding from multiple entities.
REPORTING FROM ASCO 2019
CDC Updates Cancer Cluster Guidelines
In 2013, the CDC published guidelines to help state, tribal, local, and territorial public health agencies apply a systematic approach when responding to inquiries about suspected cancer clusters.
But since then, the CDC says, there have been technical and scientific advances that may be useful—so it is time to update Investigating Suspected Cancer Clusters and Responding to Community Concerns: Guidelines from CDC and the Council of State and Territorial Epidemiologists.
The CDC is working with the Agency for Toxic Substances and Disease Registry (ATSDR) to update the 2013 guidelines to ensure that users have access to current scientific tools and approaches. The new version will include input from subject matter experts, public health agencies, the public, and other stakeholders.
“We don’t yet know how the guidelines will change,” the CDC says. Once they are written, though, the public will have the opportunity to comment. In the meantime, the public and interested organizations are invited to participate by submitting written views, information, recommendations, and data. The CDC and ATSDR are looking for answers to questions such as, “What are the best approaches to respond to community concerns about potential cancer clusters?” and “What gaps and challenges exist in the 2013 guidelines? What are possible solutions to overcoming them?” Comments will be posted on https://www.regulations.gov.
The request for comment was posted May 15 in the Federal Register and will be available for public comment through July 15, 2019. For more information and to provide comment, visit https://www.federalregister.gov/documents/2019/05/15/2019-09998/updating-federal-guidelines-used-by-public-health-agencies-to-assess-and-respond-to-potential-cancer.
In 2013, the CDC published guidelines to help state, tribal, local, and territorial public health agencies apply a systematic approach when responding to inquiries about suspected cancer clusters.
But since then, the CDC says, there have been technical and scientific advances that may be useful—so it is time to update Investigating Suspected Cancer Clusters and Responding to Community Concerns: Guidelines from CDC and the Council of State and Territorial Epidemiologists.
The CDC is working with the Agency for Toxic Substances and Disease Registry (ATSDR) to update the 2013 guidelines to ensure that users have access to current scientific tools and approaches. The new version will include input from subject matter experts, public health agencies, the public, and other stakeholders.
“We don’t yet know how the guidelines will change,” the CDC says. Once they are written, though, the public will have the opportunity to comment. In the meantime, the public and interested organizations are invited to participate by submitting written views, information, recommendations, and data. The CDC and ATSDR are looking for answers to questions such as, “What are the best approaches to respond to community concerns about potential cancer clusters?” and “What gaps and challenges exist in the 2013 guidelines? What are possible solutions to overcoming them?” Comments will be posted on https://www.regulations.gov.
The request for comment was posted May 15 in the Federal Register and will be available for public comment through July 15, 2019. For more information and to provide comment, visit https://www.federalregister.gov/documents/2019/05/15/2019-09998/updating-federal-guidelines-used-by-public-health-agencies-to-assess-and-respond-to-potential-cancer.
In 2013, the CDC published guidelines to help state, tribal, local, and territorial public health agencies apply a systematic approach when responding to inquiries about suspected cancer clusters.
But since then, the CDC says, there have been technical and scientific advances that may be useful—so it is time to update Investigating Suspected Cancer Clusters and Responding to Community Concerns: Guidelines from CDC and the Council of State and Territorial Epidemiologists.
The CDC is working with the Agency for Toxic Substances and Disease Registry (ATSDR) to update the 2013 guidelines to ensure that users have access to current scientific tools and approaches. The new version will include input from subject matter experts, public health agencies, the public, and other stakeholders.
“We don’t yet know how the guidelines will change,” the CDC says. Once they are written, though, the public will have the opportunity to comment. In the meantime, the public and interested organizations are invited to participate by submitting written views, information, recommendations, and data. The CDC and ATSDR are looking for answers to questions such as, “What are the best approaches to respond to community concerns about potential cancer clusters?” and “What gaps and challenges exist in the 2013 guidelines? What are possible solutions to overcoming them?” Comments will be posted on https://www.regulations.gov.
The request for comment was posted May 15 in the Federal Register and will be available for public comment through July 15, 2019. For more information and to provide comment, visit https://www.federalregister.gov/documents/2019/05/15/2019-09998/updating-federal-guidelines-used-by-public-health-agencies-to-assess-and-respond-to-potential-cancer.
August 2019 – ICYMI
Gastroenterology
Promoting leadership by women in gastroenterology: Lessons learned and future directions. Pascua M et al. 2019 May;156(6):1548-52. doi. org/10.1053/j.gastro.2019.03.012.
How to incorporate esophageal manometry teaching in your fellowship program. Kraft C et al. 2019 June;156(8):2120-3. doi. org/10.1053/j.gastro.2019.04.024.
How to incorporate bariatric training into your fellowship program. Jirapinyo P et al. 2019 July;157(1):9-13. doi. org/10.1053/j.gastro.2019.05.034.
Clin Gastroenterol Hepatol.
Preparing for large-scale disruptions in health care delivery: Nursing strikes and beyond. Allen JI et al. 2019 July;17(8):1424-7. doi. org/10.1016/j.cgh.2019.02.001.
Optimal management of malignant polyps, from endoscopic assessment and resection to decisions about surgery. Rex DK et al. 2019 July;17(8):1428-37. doi. org/10.1016/j.cgh.2018.09.040.
Bowel cleansing strategies after suboptimal bowel preparation. Sharara AI et al. 2019 June;17(7):1239-41. doi. org/10.1016/j.cgh.2018.12.042.
Holding gastroenterologists accountable for colonoscopy through MACRA episode–based cost measure. Siddique SM et al. 2019 May;17(6):1015-8. doi. org/10.1016/j.cgh.2019.01.009.
Endoscopic mucosal resection vs endoscopic submucosal dissection for Barrett’s esophagus and colorectal neoplasia. Yang D et al. May;17(6):1019-28. doi. org/10.1016/j.cgh.2018.09.030.
Metal biliary stents in benign disease. Haseeb A et al. 2019 May;17(6):1029-32. doi. org/10.1016/j.cgh.2018.12.010.
Cell Mol Gastroenterol Hepatol.
Rigor, reproducibility, and responsibility: A quantum of solace. Turner JR. 2019;7(4):869-71. doi. org/10.1016/j.jcmgh.2019.03.006.
Gastroenterology
Promoting leadership by women in gastroenterology: Lessons learned and future directions. Pascua M et al. 2019 May;156(6):1548-52. doi. org/10.1053/j.gastro.2019.03.012.
How to incorporate esophageal manometry teaching in your fellowship program. Kraft C et al. 2019 June;156(8):2120-3. doi. org/10.1053/j.gastro.2019.04.024.
How to incorporate bariatric training into your fellowship program. Jirapinyo P et al. 2019 July;157(1):9-13. doi. org/10.1053/j.gastro.2019.05.034.
Clin Gastroenterol Hepatol.
Preparing for large-scale disruptions in health care delivery: Nursing strikes and beyond. Allen JI et al. 2019 July;17(8):1424-7. doi. org/10.1016/j.cgh.2019.02.001.
Optimal management of malignant polyps, from endoscopic assessment and resection to decisions about surgery. Rex DK et al. 2019 July;17(8):1428-37. doi. org/10.1016/j.cgh.2018.09.040.
Bowel cleansing strategies after suboptimal bowel preparation. Sharara AI et al. 2019 June;17(7):1239-41. doi. org/10.1016/j.cgh.2018.12.042.
Holding gastroenterologists accountable for colonoscopy through MACRA episode–based cost measure. Siddique SM et al. 2019 May;17(6):1015-8. doi. org/10.1016/j.cgh.2019.01.009.
Endoscopic mucosal resection vs endoscopic submucosal dissection for Barrett’s esophagus and colorectal neoplasia. Yang D et al. May;17(6):1019-28. doi. org/10.1016/j.cgh.2018.09.030.
Metal biliary stents in benign disease. Haseeb A et al. 2019 May;17(6):1029-32. doi. org/10.1016/j.cgh.2018.12.010.
Cell Mol Gastroenterol Hepatol.
Rigor, reproducibility, and responsibility: A quantum of solace. Turner JR. 2019;7(4):869-71. doi. org/10.1016/j.jcmgh.2019.03.006.
Gastroenterology
Promoting leadership by women in gastroenterology: Lessons learned and future directions. Pascua M et al. 2019 May;156(6):1548-52. doi. org/10.1053/j.gastro.2019.03.012.
How to incorporate esophageal manometry teaching in your fellowship program. Kraft C et al. 2019 June;156(8):2120-3. doi. org/10.1053/j.gastro.2019.04.024.
How to incorporate bariatric training into your fellowship program. Jirapinyo P et al. 2019 July;157(1):9-13. doi. org/10.1053/j.gastro.2019.05.034.
Clin Gastroenterol Hepatol.
Preparing for large-scale disruptions in health care delivery: Nursing strikes and beyond. Allen JI et al. 2019 July;17(8):1424-7. doi. org/10.1016/j.cgh.2019.02.001.
Optimal management of malignant polyps, from endoscopic assessment and resection to decisions about surgery. Rex DK et al. 2019 July;17(8):1428-37. doi. org/10.1016/j.cgh.2018.09.040.
Bowel cleansing strategies after suboptimal bowel preparation. Sharara AI et al. 2019 June;17(7):1239-41. doi. org/10.1016/j.cgh.2018.12.042.
Holding gastroenterologists accountable for colonoscopy through MACRA episode–based cost measure. Siddique SM et al. 2019 May;17(6):1015-8. doi. org/10.1016/j.cgh.2019.01.009.
Endoscopic mucosal resection vs endoscopic submucosal dissection for Barrett’s esophagus and colorectal neoplasia. Yang D et al. May;17(6):1019-28. doi. org/10.1016/j.cgh.2018.09.030.
Metal biliary stents in benign disease. Haseeb A et al. 2019 May;17(6):1029-32. doi. org/10.1016/j.cgh.2018.12.010.
Cell Mol Gastroenterol Hepatol.
Rigor, reproducibility, and responsibility: A quantum of solace. Turner JR. 2019;7(4):869-71. doi. org/10.1016/j.jcmgh.2019.03.006.
MADIT-CHIC: CRT aids patients with chemotherapy-induced cardiomyopathy
SAN FRANCISCO – Patients with cardiomyopathy secondary to cancer chemotherapy who qualified for cardiac resynchronization therapy (CRT) by having a wide QRS interval showed a virtually uniform, positive response to this treatment in a multicenter study with 30 patients.
This is the first time this therapy has been prospectively assessed in this patient population.
The results “show for the first time that patients with chemotherapy-induced cardiomyopathy [CHIC] who meet criteria for CRT show significant improvement in left ventricular function and clinical symptoms in the short term” during follow-up of 6 months, Jagmeet P. Singh, MD, said at the annual scientific sessions of the Heart Rhythm Society.
Dr. Singh acknowledged that, with 30 patients, the study was small, uncontrolled, had a brief follow-up of 6 months, and was highly selective. It took collaborating investigators at 12 U.S. centers more than 3.5 years to find the 30 participating patients, who had to meet very specific criteria designed to identify true CHIC. Nonetheless, Dr. Singh considered the results convincing enough to shift practice.
Based on the results, “I would certainly feel comfortable using CRT in patients with CHIC,” said Dr. Singh, associate chief of cardiology at Massachusetts General Hospital and professor of medicine at Harvard Medical School, both in Boston. “If a patient has CHIC with a wide QRS interval and evidence for a conduction defect on their ECG, they are a great candidate for CRT. The results highlight that there is a cohort of patients who develop cardiomyopathy after chemotherapy, and these patients are often written off” and until now have generally received little follow-up for their potential development of cardiomyopathy. Dr. Singh expressed hope that the recent emergence of cardio-oncology as a subspecialty will focus attention on CHIC patients.
The MADIT-CHIC (Multicenter Automatic Defibrillator Implantation Trial – Chemotherapy-Induced Cardiomyopathy) study enrolled patients with a history of exposure to a cancer chemotherapy regimen known to cause cardiomyopathy who had no history of heart failure prior to the chemotherapy. All patients had developed clinically apparent heart failure (New York Heart Association functional class II, III, or IV) at least 6 months after completing chemotherapy, had no other apparent cause of the cardiomyopathy as ascertained by a cardio-oncologist, and were on guideline-directed medical therapy. Enrolled patients also had to have a class I or II indication for CRT, with a left ventricular ejection fraction of 35% or less, a QRS interval of at least 120 milliseconds, sinus rhythm and left bundle branch block, or no left bundle branch block and a QRS of at least 150 milliseconds.
Just over three-quarters of the patients had received an anthracycline drug, and 73% had a history of breast cancer, 20% a history of leukemia or lymphoma, and 7% had a history of sarcoma. The patients averaged 64 years of age, and 87% were women. CRT placement occurred 18-256 months after the end of chemotherapy, with a median of 188 months.
The study’s primary endpoint was the change in left ventricular ejection fraction after 6 months, which increased from an average of 28% at baseline to 39% at follow-up, a statistically significant change. Ejection fraction increased in 29 of the 30 patients, with one patient showing a flat response to CRT. Cardiac function and geometry significantly improved by seven other measures, including left ventricular mass and left atrial volume, and the improved ejection fraction was consistent across several subgroup analyses. Patients’ NYHA functional class improved by at least one level in 41% of patients, and 83% of the patients stopped showing clinical features of heart failure after 6 months on CRT.
MADIT-CHIC received funding from Boston Scientific. Dr. Singh has been a consultant to Abbott, Back Beat, Biotronik, Boston Scientific, EBR, Impulse Dynamics, Medtronic, Microport, St. Jude, and Toray, and he has received research support from Abbott and Boston Scientific.
SOURCE: Singh JP et al. HRS 2019, Abstract S-LBCT02-04.
No guideline currently addresses using cardiac resynchronization therapy to treat chemotherapy-induced cardiomyopathy. The findings from MADIT-CHIC showed a striking benefit from treatment with cardiac resynchronization therapy of a magnitude we would expect to see in patients with nonischemic cardiomyopathy. Patients showed improvements in all measures of cardiac performance.
It appears that CHIC can take as long as decades to appear in a patient, but we now need to have a high level of suspicion for this complication. We need to come up with better ways to monitor development of CHIC in patients who have received cancer chemotherapy so that we can give eligible patients this beneficial treatment. We can be optimistic about the potential for benefit from CRT in these patients.
Kenneth A. Ellenbogen, MD , is chief of cardiology and a professor of medicine at Virginia Commonwealth University in Richmond, Va. He has been a consultant to Boston Scientific, Medtronic, and St. Jude; he has received honoraria from Biotronik; and he has received research funding from Boston Scientific and Medtronic. He made these comments as the designated discussant for the MADIT-CHIC report.
No guideline currently addresses using cardiac resynchronization therapy to treat chemotherapy-induced cardiomyopathy. The findings from MADIT-CHIC showed a striking benefit from treatment with cardiac resynchronization therapy of a magnitude we would expect to see in patients with nonischemic cardiomyopathy. Patients showed improvements in all measures of cardiac performance.
It appears that CHIC can take as long as decades to appear in a patient, but we now need to have a high level of suspicion for this complication. We need to come up with better ways to monitor development of CHIC in patients who have received cancer chemotherapy so that we can give eligible patients this beneficial treatment. We can be optimistic about the potential for benefit from CRT in these patients.
Kenneth A. Ellenbogen, MD , is chief of cardiology and a professor of medicine at Virginia Commonwealth University in Richmond, Va. He has been a consultant to Boston Scientific, Medtronic, and St. Jude; he has received honoraria from Biotronik; and he has received research funding from Boston Scientific and Medtronic. He made these comments as the designated discussant for the MADIT-CHIC report.
No guideline currently addresses using cardiac resynchronization therapy to treat chemotherapy-induced cardiomyopathy. The findings from MADIT-CHIC showed a striking benefit from treatment with cardiac resynchronization therapy of a magnitude we would expect to see in patients with nonischemic cardiomyopathy. Patients showed improvements in all measures of cardiac performance.
It appears that CHIC can take as long as decades to appear in a patient, but we now need to have a high level of suspicion for this complication. We need to come up with better ways to monitor development of CHIC in patients who have received cancer chemotherapy so that we can give eligible patients this beneficial treatment. We can be optimistic about the potential for benefit from CRT in these patients.
Kenneth A. Ellenbogen, MD , is chief of cardiology and a professor of medicine at Virginia Commonwealth University in Richmond, Va. He has been a consultant to Boston Scientific, Medtronic, and St. Jude; he has received honoraria from Biotronik; and he has received research funding from Boston Scientific and Medtronic. He made these comments as the designated discussant for the MADIT-CHIC report.
SAN FRANCISCO – Patients with cardiomyopathy secondary to cancer chemotherapy who qualified for cardiac resynchronization therapy (CRT) by having a wide QRS interval showed a virtually uniform, positive response to this treatment in a multicenter study with 30 patients.
This is the first time this therapy has been prospectively assessed in this patient population.
The results “show for the first time that patients with chemotherapy-induced cardiomyopathy [CHIC] who meet criteria for CRT show significant improvement in left ventricular function and clinical symptoms in the short term” during follow-up of 6 months, Jagmeet P. Singh, MD, said at the annual scientific sessions of the Heart Rhythm Society.
Dr. Singh acknowledged that, with 30 patients, the study was small, uncontrolled, had a brief follow-up of 6 months, and was highly selective. It took collaborating investigators at 12 U.S. centers more than 3.5 years to find the 30 participating patients, who had to meet very specific criteria designed to identify true CHIC. Nonetheless, Dr. Singh considered the results convincing enough to shift practice.
Based on the results, “I would certainly feel comfortable using CRT in patients with CHIC,” said Dr. Singh, associate chief of cardiology at Massachusetts General Hospital and professor of medicine at Harvard Medical School, both in Boston. “If a patient has CHIC with a wide QRS interval and evidence for a conduction defect on their ECG, they are a great candidate for CRT. The results highlight that there is a cohort of patients who develop cardiomyopathy after chemotherapy, and these patients are often written off” and until now have generally received little follow-up for their potential development of cardiomyopathy. Dr. Singh expressed hope that the recent emergence of cardio-oncology as a subspecialty will focus attention on CHIC patients.
The MADIT-CHIC (Multicenter Automatic Defibrillator Implantation Trial – Chemotherapy-Induced Cardiomyopathy) study enrolled patients with a history of exposure to a cancer chemotherapy regimen known to cause cardiomyopathy who had no history of heart failure prior to the chemotherapy. All patients had developed clinically apparent heart failure (New York Heart Association functional class II, III, or IV) at least 6 months after completing chemotherapy, had no other apparent cause of the cardiomyopathy as ascertained by a cardio-oncologist, and were on guideline-directed medical therapy. Enrolled patients also had to have a class I or II indication for CRT, with a left ventricular ejection fraction of 35% or less, a QRS interval of at least 120 milliseconds, sinus rhythm and left bundle branch block, or no left bundle branch block and a QRS of at least 150 milliseconds.
Just over three-quarters of the patients had received an anthracycline drug, and 73% had a history of breast cancer, 20% a history of leukemia or lymphoma, and 7% had a history of sarcoma. The patients averaged 64 years of age, and 87% were women. CRT placement occurred 18-256 months after the end of chemotherapy, with a median of 188 months.
The study’s primary endpoint was the change in left ventricular ejection fraction after 6 months, which increased from an average of 28% at baseline to 39% at follow-up, a statistically significant change. Ejection fraction increased in 29 of the 30 patients, with one patient showing a flat response to CRT. Cardiac function and geometry significantly improved by seven other measures, including left ventricular mass and left atrial volume, and the improved ejection fraction was consistent across several subgroup analyses. Patients’ NYHA functional class improved by at least one level in 41% of patients, and 83% of the patients stopped showing clinical features of heart failure after 6 months on CRT.
MADIT-CHIC received funding from Boston Scientific. Dr. Singh has been a consultant to Abbott, Back Beat, Biotronik, Boston Scientific, EBR, Impulse Dynamics, Medtronic, Microport, St. Jude, and Toray, and he has received research support from Abbott and Boston Scientific.
SOURCE: Singh JP et al. HRS 2019, Abstract S-LBCT02-04.
SAN FRANCISCO – Patients with cardiomyopathy secondary to cancer chemotherapy who qualified for cardiac resynchronization therapy (CRT) by having a wide QRS interval showed a virtually uniform, positive response to this treatment in a multicenter study with 30 patients.
This is the first time this therapy has been prospectively assessed in this patient population.
The results “show for the first time that patients with chemotherapy-induced cardiomyopathy [CHIC] who meet criteria for CRT show significant improvement in left ventricular function and clinical symptoms in the short term” during follow-up of 6 months, Jagmeet P. Singh, MD, said at the annual scientific sessions of the Heart Rhythm Society.
Dr. Singh acknowledged that, with 30 patients, the study was small, uncontrolled, had a brief follow-up of 6 months, and was highly selective. It took collaborating investigators at 12 U.S. centers more than 3.5 years to find the 30 participating patients, who had to meet very specific criteria designed to identify true CHIC. Nonetheless, Dr. Singh considered the results convincing enough to shift practice.
Based on the results, “I would certainly feel comfortable using CRT in patients with CHIC,” said Dr. Singh, associate chief of cardiology at Massachusetts General Hospital and professor of medicine at Harvard Medical School, both in Boston. “If a patient has CHIC with a wide QRS interval and evidence for a conduction defect on their ECG, they are a great candidate for CRT. The results highlight that there is a cohort of patients who develop cardiomyopathy after chemotherapy, and these patients are often written off” and until now have generally received little follow-up for their potential development of cardiomyopathy. Dr. Singh expressed hope that the recent emergence of cardio-oncology as a subspecialty will focus attention on CHIC patients.
The MADIT-CHIC (Multicenter Automatic Defibrillator Implantation Trial – Chemotherapy-Induced Cardiomyopathy) study enrolled patients with a history of exposure to a cancer chemotherapy regimen known to cause cardiomyopathy who had no history of heart failure prior to the chemotherapy. All patients had developed clinically apparent heart failure (New York Heart Association functional class II, III, or IV) at least 6 months after completing chemotherapy, had no other apparent cause of the cardiomyopathy as ascertained by a cardio-oncologist, and were on guideline-directed medical therapy. Enrolled patients also had to have a class I or II indication for CRT, with a left ventricular ejection fraction of 35% or less, a QRS interval of at least 120 milliseconds, sinus rhythm and left bundle branch block, or no left bundle branch block and a QRS of at least 150 milliseconds.
Just over three-quarters of the patients had received an anthracycline drug, and 73% had a history of breast cancer, 20% a history of leukemia or lymphoma, and 7% had a history of sarcoma. The patients averaged 64 years of age, and 87% were women. CRT placement occurred 18-256 months after the end of chemotherapy, with a median of 188 months.
The study’s primary endpoint was the change in left ventricular ejection fraction after 6 months, which increased from an average of 28% at baseline to 39% at follow-up, a statistically significant change. Ejection fraction increased in 29 of the 30 patients, with one patient showing a flat response to CRT. Cardiac function and geometry significantly improved by seven other measures, including left ventricular mass and left atrial volume, and the improved ejection fraction was consistent across several subgroup analyses. Patients’ NYHA functional class improved by at least one level in 41% of patients, and 83% of the patients stopped showing clinical features of heart failure after 6 months on CRT.
MADIT-CHIC received funding from Boston Scientific. Dr. Singh has been a consultant to Abbott, Back Beat, Biotronik, Boston Scientific, EBR, Impulse Dynamics, Medtronic, Microport, St. Jude, and Toray, and he has received research support from Abbott and Boston Scientific.
SOURCE: Singh JP et al. HRS 2019, Abstract S-LBCT02-04.
REPORTING FROM HEART RHYTHM 2019
An app to help women and clinicians manage menopausal symptoms
In North America, women experience menopause (the permanent cessation of menstruation due to loss of ovarian activity) at a median age of 51 years. They may experience symptoms of perimenopause, or the menopause transition, for several years before menstruation ceases. Menopausal symptoms include vasomotor symptoms, such as hot flushes, and vaginal symptoms, such as vaginal dryness and pain during intercourse.1
Women may have questions about treating menopausal symptoms, maintaining their health, and preventing such age-related diseases as osteoporosis and cardiovascular disease. The decision to treat menopausal symptoms is challenging for women as well as their clinicians given that recommendations have changed over the past few years.
A free app with multiple features. The North American Menopause Society (NAMS) has developed a no-cost mobile health application called MenoPro for menopausal symptom management based on the organization’s 2017 recommendations.2 The app has 2 modes: one for clinicians and one for women/patients to support shared decision making.
For clinicians, the app helps identify which patients with menopausal symptoms are candidates for pharmacologic treatment and the options for optimal therapy. The app also can be used to calculate a 10-year cardiovascular disease (heart disease and stroke) risk assessment. In addition, it contains links to a breast cancer risk assessment as well as an osteoporosis/bone fracture risk assessment tool (FRAX model calculator). Finally, MenoPro includes NAMS’s educational materials and information pages on lifestyle modifications to reduce hot flushes, contraindications and cautions to hormone therapy, pros and cons of hormonal versus nonhormonal options, a comparison of oral (pills) and transdermal (patches, gels, sprays) therapies, treatment options for vaginal dryness and pain with sexual activities, and direct links to tables with the various formulations and doses of medications.
The TABLE details the features of the MenoPro app based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).3 I hope that the app described here will assist you in caring for women in the menopausal transition.

1. American College of Obstetricians and Gynecologists. Practice bulletin no. 141: Management of menopausal symptoms. Obstet Gynecol. 2014;123:202-216.
2. The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2018;25:13621387.
3. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
In North America, women experience menopause (the permanent cessation of menstruation due to loss of ovarian activity) at a median age of 51 years. They may experience symptoms of perimenopause, or the menopause transition, for several years before menstruation ceases. Menopausal symptoms include vasomotor symptoms, such as hot flushes, and vaginal symptoms, such as vaginal dryness and pain during intercourse.1
Women may have questions about treating menopausal symptoms, maintaining their health, and preventing such age-related diseases as osteoporosis and cardiovascular disease. The decision to treat menopausal symptoms is challenging for women as well as their clinicians given that recommendations have changed over the past few years.
A free app with multiple features. The North American Menopause Society (NAMS) has developed a no-cost mobile health application called MenoPro for menopausal symptom management based on the organization’s 2017 recommendations.2 The app has 2 modes: one for clinicians and one for women/patients to support shared decision making.
For clinicians, the app helps identify which patients with menopausal symptoms are candidates for pharmacologic treatment and the options for optimal therapy. The app also can be used to calculate a 10-year cardiovascular disease (heart disease and stroke) risk assessment. In addition, it contains links to a breast cancer risk assessment as well as an osteoporosis/bone fracture risk assessment tool (FRAX model calculator). Finally, MenoPro includes NAMS’s educational materials and information pages on lifestyle modifications to reduce hot flushes, contraindications and cautions to hormone therapy, pros and cons of hormonal versus nonhormonal options, a comparison of oral (pills) and transdermal (patches, gels, sprays) therapies, treatment options for vaginal dryness and pain with sexual activities, and direct links to tables with the various formulations and doses of medications.
The TABLE details the features of the MenoPro app based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).3 I hope that the app described here will assist you in caring for women in the menopausal transition.

In North America, women experience menopause (the permanent cessation of menstruation due to loss of ovarian activity) at a median age of 51 years. They may experience symptoms of perimenopause, or the menopause transition, for several years before menstruation ceases. Menopausal symptoms include vasomotor symptoms, such as hot flushes, and vaginal symptoms, such as vaginal dryness and pain during intercourse.1
Women may have questions about treating menopausal symptoms, maintaining their health, and preventing such age-related diseases as osteoporosis and cardiovascular disease. The decision to treat menopausal symptoms is challenging for women as well as their clinicians given that recommendations have changed over the past few years.
A free app with multiple features. The North American Menopause Society (NAMS) has developed a no-cost mobile health application called MenoPro for menopausal symptom management based on the organization’s 2017 recommendations.2 The app has 2 modes: one for clinicians and one for women/patients to support shared decision making.
For clinicians, the app helps identify which patients with menopausal symptoms are candidates for pharmacologic treatment and the options for optimal therapy. The app also can be used to calculate a 10-year cardiovascular disease (heart disease and stroke) risk assessment. In addition, it contains links to a breast cancer risk assessment as well as an osteoporosis/bone fracture risk assessment tool (FRAX model calculator). Finally, MenoPro includes NAMS’s educational materials and information pages on lifestyle modifications to reduce hot flushes, contraindications and cautions to hormone therapy, pros and cons of hormonal versus nonhormonal options, a comparison of oral (pills) and transdermal (patches, gels, sprays) therapies, treatment options for vaginal dryness and pain with sexual activities, and direct links to tables with the various formulations and doses of medications.
The TABLE details the features of the MenoPro app based on a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature used, and important special features).3 I hope that the app described here will assist you in caring for women in the menopausal transition.

1. American College of Obstetricians and Gynecologists. Practice bulletin no. 141: Management of menopausal symptoms. Obstet Gynecol. 2014;123:202-216.
2. The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2018;25:13621387.
3. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.
1. American College of Obstetricians and Gynecologists. Practice bulletin no. 141: Management of menopausal symptoms. Obstet Gynecol. 2014;123:202-216.
2. The 2017 hormone therapy position statement of The North American Menopause Society. Menopause. 2018;25:13621387.
3. Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483.