User login
Five enter the Shark Tank, one emerges
SAN FRANCISCO – All five innovative startups pitched at the Shark Tank at the 2019 AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology, are in advanced stages of development, but only one is given the opportunity to be declared the winner of the competition. The ideas ranged from a smart toilet for early disease detection to a unique strategy for obesity phenotyping, but the winner by both official decision and popular vote was a smartphone app to help patients with inflammatory bowel disease (IBD) manage the condition.
“As always, this year’s Shark Tank was a highlight of the AGA Tech Summit and represents the progress our field is making when it comes to innovation. Our panel of sharks was focused on understanding the problem each innovation solved – that’s the key when determining if an idea is novel or innovation for innovation’s sake. We were impressed with all of the technologies presented, but ultimately chose the Oshi Health IBD app as our winner because of the impact it is already having on improving the health and care of IBD patients,” said V. Raman Muthusamy, MD, AGAF, chair of the AGA Center for GI Innovation and Technology.
The winner: Oshi pitches “all-in-one” IBD app
By both popular vote from those attending the AGA Tech Summit as well as the six-member Shark Tank panel, Oshi Health was selected as the 2019 Shark Tank winner for its IBD app. The app was designed to help patients track symptoms, a first step in understanding flare patterns, which differ substantially between patients and emphasize the need for a personalized plan for controlling disease.

“Since we launched last June at DDW® we have had 40,000 downloads. We are the number one IBD management app,” reported Dan Weinstein, MBA, CEO of Oshi Health.
The available app represents the first of three phases as the functionality is expanded. Currently, in addition to using the app as a tracking tool, patients can find resources to learn about their disease and to communicate with other patients about their experiences. In a second phase, information gathered by the app will be made available to physicians to provide accurate current information about disease status to better individualize therapy.
Ultimately, the app is expected to guide treatment based on information it has collected on symptom patterns and other data collected over time, although this application is further down the road and will require regulatory approval if it is designed to provide clinical advice as expected, according to Mr. Weinstein.
However, benefits have already been seen. Mr. Weinstein cited data that associated the app with a 40% improvement in medication adherence and a nearly 60-day reduction in flare duration. Calling the app “the next chapter in treat-to-target” IBD management, he believes that this is an important step forward in digital health that will improve IBD outcomes. The Shark Tank panel agreed.
Runners-up: Other potential innovations to improve GI health
With or without Shark Tank endorsement, the other four startups described in the competition are moving forward. Each is designed to address an important unmet need with the potential to improve patient outcomes, which is a criterion for their inclusion in the competition.
The smart toilet seat
One involves a technologically advanced toilet seat. The new seat is based on the fact that fecal matter provides insight into a broad array of disease states, but specimen collection is a hurdle for a variety of reasons, including patient resistance. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that captures images of bowel movements and urination for subsequent analysis.
“The toilet seat sees what the eye cannot,” according to Vikram Kashyap, CEO of Toi Labs. He believes it has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.

Others agree. According to Mr. Kashyap, executives of a chain of senior living facilities have already expressed interest in installing this seat to better monitor health among residents. The seat is bolted into position in place of any standard toilet seat. It collects images and data that are transmitted directly to a cellular network.
“Using our technology, the goal is to catch disease states early before they progress,” said Mr. Kashyap, who called the surveillance system a low-cost disease-screening tool. He believes the smart toilet seat could be of the most important disease detection devices developed in recent years.
AI to aid screening endoscopy
A third entrant in this year’s Shark Tank described a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia. The tool is called Ultivision and is being developed by a startup called Docbot. The CEO, Andrew Ninh, and a senior executive, Jason B. Samarasena, MD, outlined an idea that could be used in either screening colonoscopy or in surveillance of Barrett’s esophagus).
“Dysplasia is difficult to find. It is subtle and it is often missed. With better detection of dysplasia, artificial intelligence offers an opportunity to reduce risk of cancer,” Dr. Samarasena said.
The tool integrates seamlessly with existing endoscopic tools, according to Mr. Ninh. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist. The colonoscopy application is a more advanced stage of development and might be submitted for regulatory approval this year, he said. The same technology will be adapted for Barrett’s esophagus.
“It is like facial recognition for dysplasia,” said Dr. Samarasena.
Obesity phenotyping tool
A fourth Shark Tank entrant employs technology to phenotype obese patients to better tailor therapy. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes. When therapy is tailored to the phenotype, weight loss is greater, according to Andres J. Acosta, MD, PhD, assistant professor of medicine and consultant in gastroenterology and hepatology at Mayo Clinic, Rochester, Minn.
In an initial study that compared weight loss in 55 patients treated based on phenotype with 175 patients managed with standard of care, the total body weight loss “more than doubled,” Dr. Acosta reported.
According to Dr. Acosta, obesity is driven by very different mechanisms. He described the four major phenotypes identified with his test as hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates).
With the blood test, which utilizes hormones, metabolites, DNA, and other biomarkers to separate these phenotypes, treatment can be tailored appropriately, according to Dr. Acosta. His company is now seeking Food and Drug Administration clearance of the test, which he believes will have a major impact on obesity control.
Capsule diagnostic tool
The final entrant selected to participate in this year’s Shark Tank described an ingestible capsule that diagnoses diseases by detecting gases as it descends the gastrointestinal tract. The Atmo Gas Capsule from Atmo Biosciences measures gases at the source, accelerating the diagnosis of such diseases as irritable bowel syndrome (IBS) and IBD.
“By measuring gases at their source, the accuracy is far better than a breath test,” said Malcolm Hebblewhite, MBA, CEO of Atmo Biosciences. The capsule is an alternative to more invasive and expensive diagnostic tools and it is highly accurate.
Providing examples, Mr. Hebblewhite said that elevated levels of oxygen suggest a disorder of motility while an elevated level of carbon dioxide and hydrogen suggest IBS. The capsule transmits data to a small receiver and then on to a smartphone.
“The real-time data is displayed for the user with more complex information accessible by the practitioner remotely via the cloud,” Mr. Hebblewhite said. He cited several papers that have already been published documenting the potential of this technology.
“The capsule is a single-use disposable device that is not retrieved,” according to Mr. Hebblewhite. He reported that his company plans to pursue the diagnosis of motility as an initial clinical application. The diagnosis of IBS and other GI conditions will follow. Clinical studies are already planned.
SAN FRANCISCO – All five innovative startups pitched at the Shark Tank at the 2019 AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology, are in advanced stages of development, but only one is given the opportunity to be declared the winner of the competition. The ideas ranged from a smart toilet for early disease detection to a unique strategy for obesity phenotyping, but the winner by both official decision and popular vote was a smartphone app to help patients with inflammatory bowel disease (IBD) manage the condition.
“As always, this year’s Shark Tank was a highlight of the AGA Tech Summit and represents the progress our field is making when it comes to innovation. Our panel of sharks was focused on understanding the problem each innovation solved – that’s the key when determining if an idea is novel or innovation for innovation’s sake. We were impressed with all of the technologies presented, but ultimately chose the Oshi Health IBD app as our winner because of the impact it is already having on improving the health and care of IBD patients,” said V. Raman Muthusamy, MD, AGAF, chair of the AGA Center for GI Innovation and Technology.
The winner: Oshi pitches “all-in-one” IBD app
By both popular vote from those attending the AGA Tech Summit as well as the six-member Shark Tank panel, Oshi Health was selected as the 2019 Shark Tank winner for its IBD app. The app was designed to help patients track symptoms, a first step in understanding flare patterns, which differ substantially between patients and emphasize the need for a personalized plan for controlling disease.

“Since we launched last June at DDW® we have had 40,000 downloads. We are the number one IBD management app,” reported Dan Weinstein, MBA, CEO of Oshi Health.
The available app represents the first of three phases as the functionality is expanded. Currently, in addition to using the app as a tracking tool, patients can find resources to learn about their disease and to communicate with other patients about their experiences. In a second phase, information gathered by the app will be made available to physicians to provide accurate current information about disease status to better individualize therapy.
Ultimately, the app is expected to guide treatment based on information it has collected on symptom patterns and other data collected over time, although this application is further down the road and will require regulatory approval if it is designed to provide clinical advice as expected, according to Mr. Weinstein.
However, benefits have already been seen. Mr. Weinstein cited data that associated the app with a 40% improvement in medication adherence and a nearly 60-day reduction in flare duration. Calling the app “the next chapter in treat-to-target” IBD management, he believes that this is an important step forward in digital health that will improve IBD outcomes. The Shark Tank panel agreed.
Runners-up: Other potential innovations to improve GI health
With or without Shark Tank endorsement, the other four startups described in the competition are moving forward. Each is designed to address an important unmet need with the potential to improve patient outcomes, which is a criterion for their inclusion in the competition.
The smart toilet seat
One involves a technologically advanced toilet seat. The new seat is based on the fact that fecal matter provides insight into a broad array of disease states, but specimen collection is a hurdle for a variety of reasons, including patient resistance. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that captures images of bowel movements and urination for subsequent analysis.
“The toilet seat sees what the eye cannot,” according to Vikram Kashyap, CEO of Toi Labs. He believes it has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.

Others agree. According to Mr. Kashyap, executives of a chain of senior living facilities have already expressed interest in installing this seat to better monitor health among residents. The seat is bolted into position in place of any standard toilet seat. It collects images and data that are transmitted directly to a cellular network.
“Using our technology, the goal is to catch disease states early before they progress,” said Mr. Kashyap, who called the surveillance system a low-cost disease-screening tool. He believes the smart toilet seat could be of the most important disease detection devices developed in recent years.
AI to aid screening endoscopy
A third entrant in this year’s Shark Tank described a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia. The tool is called Ultivision and is being developed by a startup called Docbot. The CEO, Andrew Ninh, and a senior executive, Jason B. Samarasena, MD, outlined an idea that could be used in either screening colonoscopy or in surveillance of Barrett’s esophagus).
“Dysplasia is difficult to find. It is subtle and it is often missed. With better detection of dysplasia, artificial intelligence offers an opportunity to reduce risk of cancer,” Dr. Samarasena said.
The tool integrates seamlessly with existing endoscopic tools, according to Mr. Ninh. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist. The colonoscopy application is a more advanced stage of development and might be submitted for regulatory approval this year, he said. The same technology will be adapted for Barrett’s esophagus.
“It is like facial recognition for dysplasia,” said Dr. Samarasena.
Obesity phenotyping tool
A fourth Shark Tank entrant employs technology to phenotype obese patients to better tailor therapy. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes. When therapy is tailored to the phenotype, weight loss is greater, according to Andres J. Acosta, MD, PhD, assistant professor of medicine and consultant in gastroenterology and hepatology at Mayo Clinic, Rochester, Minn.
In an initial study that compared weight loss in 55 patients treated based on phenotype with 175 patients managed with standard of care, the total body weight loss “more than doubled,” Dr. Acosta reported.
According to Dr. Acosta, obesity is driven by very different mechanisms. He described the four major phenotypes identified with his test as hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates).
With the blood test, which utilizes hormones, metabolites, DNA, and other biomarkers to separate these phenotypes, treatment can be tailored appropriately, according to Dr. Acosta. His company is now seeking Food and Drug Administration clearance of the test, which he believes will have a major impact on obesity control.
Capsule diagnostic tool
The final entrant selected to participate in this year’s Shark Tank described an ingestible capsule that diagnoses diseases by detecting gases as it descends the gastrointestinal tract. The Atmo Gas Capsule from Atmo Biosciences measures gases at the source, accelerating the diagnosis of such diseases as irritable bowel syndrome (IBS) and IBD.
“By measuring gases at their source, the accuracy is far better than a breath test,” said Malcolm Hebblewhite, MBA, CEO of Atmo Biosciences. The capsule is an alternative to more invasive and expensive diagnostic tools and it is highly accurate.
Providing examples, Mr. Hebblewhite said that elevated levels of oxygen suggest a disorder of motility while an elevated level of carbon dioxide and hydrogen suggest IBS. The capsule transmits data to a small receiver and then on to a smartphone.
“The real-time data is displayed for the user with more complex information accessible by the practitioner remotely via the cloud,” Mr. Hebblewhite said. He cited several papers that have already been published documenting the potential of this technology.
“The capsule is a single-use disposable device that is not retrieved,” according to Mr. Hebblewhite. He reported that his company plans to pursue the diagnosis of motility as an initial clinical application. The diagnosis of IBS and other GI conditions will follow. Clinical studies are already planned.
SAN FRANCISCO – All five innovative startups pitched at the Shark Tank at the 2019 AGA Tech Summit, sponsored by the AGA Center for GI Innovation and Technology, are in advanced stages of development, but only one is given the opportunity to be declared the winner of the competition. The ideas ranged from a smart toilet for early disease detection to a unique strategy for obesity phenotyping, but the winner by both official decision and popular vote was a smartphone app to help patients with inflammatory bowel disease (IBD) manage the condition.
“As always, this year’s Shark Tank was a highlight of the AGA Tech Summit and represents the progress our field is making when it comes to innovation. Our panel of sharks was focused on understanding the problem each innovation solved – that’s the key when determining if an idea is novel or innovation for innovation’s sake. We were impressed with all of the technologies presented, but ultimately chose the Oshi Health IBD app as our winner because of the impact it is already having on improving the health and care of IBD patients,” said V. Raman Muthusamy, MD, AGAF, chair of the AGA Center for GI Innovation and Technology.
The winner: Oshi pitches “all-in-one” IBD app
By both popular vote from those attending the AGA Tech Summit as well as the six-member Shark Tank panel, Oshi Health was selected as the 2019 Shark Tank winner for its IBD app. The app was designed to help patients track symptoms, a first step in understanding flare patterns, which differ substantially between patients and emphasize the need for a personalized plan for controlling disease.

“Since we launched last June at DDW® we have had 40,000 downloads. We are the number one IBD management app,” reported Dan Weinstein, MBA, CEO of Oshi Health.
The available app represents the first of three phases as the functionality is expanded. Currently, in addition to using the app as a tracking tool, patients can find resources to learn about their disease and to communicate with other patients about their experiences. In a second phase, information gathered by the app will be made available to physicians to provide accurate current information about disease status to better individualize therapy.
Ultimately, the app is expected to guide treatment based on information it has collected on symptom patterns and other data collected over time, although this application is further down the road and will require regulatory approval if it is designed to provide clinical advice as expected, according to Mr. Weinstein.
However, benefits have already been seen. Mr. Weinstein cited data that associated the app with a 40% improvement in medication adherence and a nearly 60-day reduction in flare duration. Calling the app “the next chapter in treat-to-target” IBD management, he believes that this is an important step forward in digital health that will improve IBD outcomes. The Shark Tank panel agreed.
Runners-up: Other potential innovations to improve GI health
With or without Shark Tank endorsement, the other four startups described in the competition are moving forward. Each is designed to address an important unmet need with the potential to improve patient outcomes, which is a criterion for their inclusion in the competition.
The smart toilet seat
One involves a technologically advanced toilet seat. The new seat is based on the fact that fecal matter provides insight into a broad array of disease states, but specimen collection is a hurdle for a variety of reasons, including patient resistance. A toilet seat developed by Toi Labs, called TrueLoo, is equipped with lighting and cameras that captures images of bowel movements and urination for subsequent analysis.
“The toilet seat sees what the eye cannot,” according to Vikram Kashyap, CEO of Toi Labs. He believes it has major potential for early detection of conditions ranging from dehydration to gastrointestinal cancer.

Others agree. According to Mr. Kashyap, executives of a chain of senior living facilities have already expressed interest in installing this seat to better monitor health among residents. The seat is bolted into position in place of any standard toilet seat. It collects images and data that are transmitted directly to a cellular network.
“Using our technology, the goal is to catch disease states early before they progress,” said Mr. Kashyap, who called the surveillance system a low-cost disease-screening tool. He believes the smart toilet seat could be of the most important disease detection devices developed in recent years.
AI to aid screening endoscopy
A third entrant in this year’s Shark Tank described a strategy to employ artificial intelligence (AI) to aid endoscopists in screening for dysplasia. The tool is called Ultivision and is being developed by a startup called Docbot. The CEO, Andrew Ninh, and a senior executive, Jason B. Samarasena, MD, outlined an idea that could be used in either screening colonoscopy or in surveillance of Barrett’s esophagus).
“Dysplasia is difficult to find. It is subtle and it is often missed. With better detection of dysplasia, artificial intelligence offers an opportunity to reduce risk of cancer,” Dr. Samarasena said.
The tool integrates seamlessly with existing endoscopic tools, according to Mr. Ninh. As tissue is visualized, the AI is programmed to highlight suspected dysplasia with a colored box to alert the endoscopist. The colonoscopy application is a more advanced stage of development and might be submitted for regulatory approval this year, he said. The same technology will be adapted for Barrett’s esophagus.
“It is like facial recognition for dysplasia,” said Dr. Samarasena.
Obesity phenotyping tool
A fourth Shark Tank entrant employs technology to phenotype obese patients to better tailor therapy. The Pheno Test, developed by Phenomix Sciences, applies “multi-omics” to a blood-based test to separate patients with obesity into four phenotypes. When therapy is tailored to the phenotype, weight loss is greater, according to Andres J. Acosta, MD, PhD, assistant professor of medicine and consultant in gastroenterology and hepatology at Mayo Clinic, Rochester, Minn.
In an initial study that compared weight loss in 55 patients treated based on phenotype with 175 patients managed with standard of care, the total body weight loss “more than doubled,” Dr. Acosta reported.
According to Dr. Acosta, obesity is driven by very different mechanisms. He described the four major phenotypes identified with his test as hungry brain (satiation signal is impaired), hungry gut (signals to eat are upregulated), emotional hunger (psychological reasons drive eating behavior), and slow metabolism (failure to burn fat at normal rates).
With the blood test, which utilizes hormones, metabolites, DNA, and other biomarkers to separate these phenotypes, treatment can be tailored appropriately, according to Dr. Acosta. His company is now seeking Food and Drug Administration clearance of the test, which he believes will have a major impact on obesity control.
Capsule diagnostic tool
The final entrant selected to participate in this year’s Shark Tank described an ingestible capsule that diagnoses diseases by detecting gases as it descends the gastrointestinal tract. The Atmo Gas Capsule from Atmo Biosciences measures gases at the source, accelerating the diagnosis of such diseases as irritable bowel syndrome (IBS) and IBD.
“By measuring gases at their source, the accuracy is far better than a breath test,” said Malcolm Hebblewhite, MBA, CEO of Atmo Biosciences. The capsule is an alternative to more invasive and expensive diagnostic tools and it is highly accurate.
Providing examples, Mr. Hebblewhite said that elevated levels of oxygen suggest a disorder of motility while an elevated level of carbon dioxide and hydrogen suggest IBS. The capsule transmits data to a small receiver and then on to a smartphone.
“The real-time data is displayed for the user with more complex information accessible by the practitioner remotely via the cloud,” Mr. Hebblewhite said. He cited several papers that have already been published documenting the potential of this technology.
“The capsule is a single-use disposable device that is not retrieved,” according to Mr. Hebblewhite. He reported that his company plans to pursue the diagnosis of motility as an initial clinical application. The diagnosis of IBS and other GI conditions will follow. Clinical studies are already planned.
REPORTING FROM 2019 AGA TECH SUMMIT
BWH classification system better predicts outcomes in HNCSCC
For patients with head and neck cutaneous squamous cell carcinoma (HNCSCC), the Brigham and Women’s Hospital (BWH) tumor classification system is better at predicting metastases and death than the American Joint Committee on Cancer Staging Manual, 8th edition (AJCC 8), based on a study involving 459 patients.
Using the AJCC 8 system, twice as many tumors were considered to be in a high tumor class, compared with the BWH system, reported lead author Emily Stamell Ruiz, MD, of Brigham and Women’s Hospital in Boston, and her colleagues. Using the BWH system could minimize the number of patients undergoing intensive monitoring and possibly therapy without missing those at high risk for poor outcomes.
“Identification of … tumors with significant risk of recurrence, progression to unresectability, or death is challenging owing to lack of accurate [cutaneous squamous cell carcinoma] risk stratification,” the investigators wrote in JAMA Dermatology.
Although AJCC 7 offered a method of classifying such tumors, validation and refinement have been challenging because of a lack of relevant data in the Surveillance, Epidemiology, and End Results Program. A previous study showed that the BWH system outperformed AJCC 7; however, until now, no study has compared the BWH system with AJCC 8, which was released in January 2018 with updated HNCSCC classifications. The BWH has four possible classifications defined by number of high-risk factors and presence or absence of bone invasion: T1, T2a, T2b, and T3. In comparison, the AJCC 8 has five possible classifications defined by tumor size and level of invasion: T1, T2, T3, T4a, and T4b.
The present study involved 459 patients with 680 HNCSCCs. The patients were staged by both BWH and AJCC 8 systems, then compared for accuracy of predicting poor outcomes, including nodal metastases, local recurrence, disease specific death, and overall survival.
The analysis showed that the BWH system had a specificity of 93% for predicting metastases or death, compared with 85% for the AJCC 8 (P less than .001). Sensitivity was not statistically significant between the two groups; however, the BWH system had a better positive predictive value, at 30%, compared with 17% from the AJCC 8. Of note, the AJCC 8 system grouped almost one-quarter of patients (23%) into the T2 and T3 groups, which led to poorer risk prediction, according to the investigators. These patients had a 13% risk of nodal metastasis and an 8% risk of disease-specific death. In contrast, the BWH system confined most poor outcomes into the T2b and T3 groups, which included just 9% of patients, raising risk of disease-specific death to 17% and risk of nodal metastasis to 24%, the latter of which aligns with previously published data.
“One reason for the equivalent outcomes in AJCC 8 T2 and T3 is that poor differentiation is not a risk factor,” the investigators explained. “Approximately 50% of nodal metastasis and overall death in AJCC 8 T2 occurred in patients with poorly differentiated tumors, increasing the risk of poor outcomes in this group. The risk of poor outcomes was lower in AJCC 8 T3, compared with BWH T2b because AJCC 8 T3 tumors are only required to have one of four risk factors whereas two risk factors are required for BWH T2b tumor class.”
The investigators concluded by highlighting the real-world benefits of the BWH system. “Use of BWH tumor classification may minimize the number of patients recommended for radiologic evaluation, close surveillance, and possible adjuvant therapy while still identifying most patients at risk for recurrence, metastasis, and death.”
The investigators reported no conflicts of interest.
SOURCE: Ruiz ES et al. JAMA Dermatol. 2019 Apr 10. doi: 10.1001/jamadermatol.2019.0032.
For patients with head and neck cutaneous squamous cell carcinoma (HNCSCC), the Brigham and Women’s Hospital (BWH) tumor classification system is better at predicting metastases and death than the American Joint Committee on Cancer Staging Manual, 8th edition (AJCC 8), based on a study involving 459 patients.
Using the AJCC 8 system, twice as many tumors were considered to be in a high tumor class, compared with the BWH system, reported lead author Emily Stamell Ruiz, MD, of Brigham and Women’s Hospital in Boston, and her colleagues. Using the BWH system could minimize the number of patients undergoing intensive monitoring and possibly therapy without missing those at high risk for poor outcomes.
“Identification of … tumors with significant risk of recurrence, progression to unresectability, or death is challenging owing to lack of accurate [cutaneous squamous cell carcinoma] risk stratification,” the investigators wrote in JAMA Dermatology.
Although AJCC 7 offered a method of classifying such tumors, validation and refinement have been challenging because of a lack of relevant data in the Surveillance, Epidemiology, and End Results Program. A previous study showed that the BWH system outperformed AJCC 7; however, until now, no study has compared the BWH system with AJCC 8, which was released in January 2018 with updated HNCSCC classifications. The BWH has four possible classifications defined by number of high-risk factors and presence or absence of bone invasion: T1, T2a, T2b, and T3. In comparison, the AJCC 8 has five possible classifications defined by tumor size and level of invasion: T1, T2, T3, T4a, and T4b.
The present study involved 459 patients with 680 HNCSCCs. The patients were staged by both BWH and AJCC 8 systems, then compared for accuracy of predicting poor outcomes, including nodal metastases, local recurrence, disease specific death, and overall survival.
The analysis showed that the BWH system had a specificity of 93% for predicting metastases or death, compared with 85% for the AJCC 8 (P less than .001). Sensitivity was not statistically significant between the two groups; however, the BWH system had a better positive predictive value, at 30%, compared with 17% from the AJCC 8. Of note, the AJCC 8 system grouped almost one-quarter of patients (23%) into the T2 and T3 groups, which led to poorer risk prediction, according to the investigators. These patients had a 13% risk of nodal metastasis and an 8% risk of disease-specific death. In contrast, the BWH system confined most poor outcomes into the T2b and T3 groups, which included just 9% of patients, raising risk of disease-specific death to 17% and risk of nodal metastasis to 24%, the latter of which aligns with previously published data.
“One reason for the equivalent outcomes in AJCC 8 T2 and T3 is that poor differentiation is not a risk factor,” the investigators explained. “Approximately 50% of nodal metastasis and overall death in AJCC 8 T2 occurred in patients with poorly differentiated tumors, increasing the risk of poor outcomes in this group. The risk of poor outcomes was lower in AJCC 8 T3, compared with BWH T2b because AJCC 8 T3 tumors are only required to have one of four risk factors whereas two risk factors are required for BWH T2b tumor class.”
The investigators concluded by highlighting the real-world benefits of the BWH system. “Use of BWH tumor classification may minimize the number of patients recommended for radiologic evaluation, close surveillance, and possible adjuvant therapy while still identifying most patients at risk for recurrence, metastasis, and death.”
The investigators reported no conflicts of interest.
SOURCE: Ruiz ES et al. JAMA Dermatol. 2019 Apr 10. doi: 10.1001/jamadermatol.2019.0032.
For patients with head and neck cutaneous squamous cell carcinoma (HNCSCC), the Brigham and Women’s Hospital (BWH) tumor classification system is better at predicting metastases and death than the American Joint Committee on Cancer Staging Manual, 8th edition (AJCC 8), based on a study involving 459 patients.
Using the AJCC 8 system, twice as many tumors were considered to be in a high tumor class, compared with the BWH system, reported lead author Emily Stamell Ruiz, MD, of Brigham and Women’s Hospital in Boston, and her colleagues. Using the BWH system could minimize the number of patients undergoing intensive monitoring and possibly therapy without missing those at high risk for poor outcomes.
“Identification of … tumors with significant risk of recurrence, progression to unresectability, or death is challenging owing to lack of accurate [cutaneous squamous cell carcinoma] risk stratification,” the investigators wrote in JAMA Dermatology.
Although AJCC 7 offered a method of classifying such tumors, validation and refinement have been challenging because of a lack of relevant data in the Surveillance, Epidemiology, and End Results Program. A previous study showed that the BWH system outperformed AJCC 7; however, until now, no study has compared the BWH system with AJCC 8, which was released in January 2018 with updated HNCSCC classifications. The BWH has four possible classifications defined by number of high-risk factors and presence or absence of bone invasion: T1, T2a, T2b, and T3. In comparison, the AJCC 8 has five possible classifications defined by tumor size and level of invasion: T1, T2, T3, T4a, and T4b.
The present study involved 459 patients with 680 HNCSCCs. The patients were staged by both BWH and AJCC 8 systems, then compared for accuracy of predicting poor outcomes, including nodal metastases, local recurrence, disease specific death, and overall survival.
The analysis showed that the BWH system had a specificity of 93% for predicting metastases or death, compared with 85% for the AJCC 8 (P less than .001). Sensitivity was not statistically significant between the two groups; however, the BWH system had a better positive predictive value, at 30%, compared with 17% from the AJCC 8. Of note, the AJCC 8 system grouped almost one-quarter of patients (23%) into the T2 and T3 groups, which led to poorer risk prediction, according to the investigators. These patients had a 13% risk of nodal metastasis and an 8% risk of disease-specific death. In contrast, the BWH system confined most poor outcomes into the T2b and T3 groups, which included just 9% of patients, raising risk of disease-specific death to 17% and risk of nodal metastasis to 24%, the latter of which aligns with previously published data.
“One reason for the equivalent outcomes in AJCC 8 T2 and T3 is that poor differentiation is not a risk factor,” the investigators explained. “Approximately 50% of nodal metastasis and overall death in AJCC 8 T2 occurred in patients with poorly differentiated tumors, increasing the risk of poor outcomes in this group. The risk of poor outcomes was lower in AJCC 8 T3, compared with BWH T2b because AJCC 8 T3 tumors are only required to have one of four risk factors whereas two risk factors are required for BWH T2b tumor class.”
The investigators concluded by highlighting the real-world benefits of the BWH system. “Use of BWH tumor classification may minimize the number of patients recommended for radiologic evaluation, close surveillance, and possible adjuvant therapy while still identifying most patients at risk for recurrence, metastasis, and death.”
The investigators reported no conflicts of interest.
SOURCE: Ruiz ES et al. JAMA Dermatol. 2019 Apr 10. doi: 10.1001/jamadermatol.2019.0032.
FROM JAMA DERMATOLOGY
Tips for preventing complications in resurfacing skin of color
DENVER – In the opinion of
“You have to have the right patients and the right indication,” Dr. Brauer said at the annual conference of the American Society for Laser Medicine and Surgery. “What are they coming in for? Are they asking for what they really need?”
Taking a thorough medical history during consultations and follow-up visits is also key. “What medical or surgical problems do they have?” he asked. “Do they have a history of keloid formation? Are they on isotretinoin? What allergies do they have? What are their expectations, and are they realistic? For example, do they believe that you are going to erase all of their acne scars? On physical exam, be sure that what you’re looking at is what they’re concerned about, so that you agree upon what can and can’t be effectively treated.”
Above all else, stay true to your gut. “If you perceive that someone is not a suitable candidate for resurfacing or has unrealistic expectations, and they are insistent, it is important to stand your ground, and even find a way to politely walk away,” said Dr. Brauer of the department of dermatology at New York University.
Most complications from laser resurfacing are not unique to skin of color, he continued. A review of the topic revealed that mild complications may include prolonged erythema, acne and milia, delayed purpura, superficial erosions, contact dermatitis, and recall phenomenon (Dermatol Surg. 2010;36[3]:299-306). Moderate complications may include infection, pigmentary alteration, anesthesia toxicity, and eruptive keratoacanthomas, while severe complications may include hypertrophic scarring, ectropion formation, and disseminated infection.
An earlier analysis of fractional laser treatment found that patients with darker skin types had a significantly higher proportion of certain side effects, namely postinflammatory hyperpigmentation (Dermatol Surg. 2008;34[3]:301-7). “Additionally, the researchers found that this presented both later and lasted longer than in individuals with lighter skin types,” said Dr. Brauer, who was not involved with the study.
He listed pigmentary alterations and hypertrophic scarring/keloid formation as the potential complications from resurfacing to be most concerned about in skin of color patients. “In addition to appropriate device selection, the correct device parameters are key,” he said. “You have to make sure you use appropriate energy, but you can use higher energies with lower densities to minimize the risk of postinflammatory pigmentation. You also want to protect the epidermis by use of epidermal cooling, avoid bulk heating, and perform sessions at prolonged treatment intervals, to safely achieve optimal results.”
Dr. Brauer reported having received honoraria or being a member of the medical advisory board for Cutera, Cynosure/Hologic, and Merz.
DENVER – In the opinion of
“You have to have the right patients and the right indication,” Dr. Brauer said at the annual conference of the American Society for Laser Medicine and Surgery. “What are they coming in for? Are they asking for what they really need?”
Taking a thorough medical history during consultations and follow-up visits is also key. “What medical or surgical problems do they have?” he asked. “Do they have a history of keloid formation? Are they on isotretinoin? What allergies do they have? What are their expectations, and are they realistic? For example, do they believe that you are going to erase all of their acne scars? On physical exam, be sure that what you’re looking at is what they’re concerned about, so that you agree upon what can and can’t be effectively treated.”
Above all else, stay true to your gut. “If you perceive that someone is not a suitable candidate for resurfacing or has unrealistic expectations, and they are insistent, it is important to stand your ground, and even find a way to politely walk away,” said Dr. Brauer of the department of dermatology at New York University.
Most complications from laser resurfacing are not unique to skin of color, he continued. A review of the topic revealed that mild complications may include prolonged erythema, acne and milia, delayed purpura, superficial erosions, contact dermatitis, and recall phenomenon (Dermatol Surg. 2010;36[3]:299-306). Moderate complications may include infection, pigmentary alteration, anesthesia toxicity, and eruptive keratoacanthomas, while severe complications may include hypertrophic scarring, ectropion formation, and disseminated infection.
An earlier analysis of fractional laser treatment found that patients with darker skin types had a significantly higher proportion of certain side effects, namely postinflammatory hyperpigmentation (Dermatol Surg. 2008;34[3]:301-7). “Additionally, the researchers found that this presented both later and lasted longer than in individuals with lighter skin types,” said Dr. Brauer, who was not involved with the study.
He listed pigmentary alterations and hypertrophic scarring/keloid formation as the potential complications from resurfacing to be most concerned about in skin of color patients. “In addition to appropriate device selection, the correct device parameters are key,” he said. “You have to make sure you use appropriate energy, but you can use higher energies with lower densities to minimize the risk of postinflammatory pigmentation. You also want to protect the epidermis by use of epidermal cooling, avoid bulk heating, and perform sessions at prolonged treatment intervals, to safely achieve optimal results.”
Dr. Brauer reported having received honoraria or being a member of the medical advisory board for Cutera, Cynosure/Hologic, and Merz.
DENVER – In the opinion of
“You have to have the right patients and the right indication,” Dr. Brauer said at the annual conference of the American Society for Laser Medicine and Surgery. “What are they coming in for? Are they asking for what they really need?”
Taking a thorough medical history during consultations and follow-up visits is also key. “What medical or surgical problems do they have?” he asked. “Do they have a history of keloid formation? Are they on isotretinoin? What allergies do they have? What are their expectations, and are they realistic? For example, do they believe that you are going to erase all of their acne scars? On physical exam, be sure that what you’re looking at is what they’re concerned about, so that you agree upon what can and can’t be effectively treated.”
Above all else, stay true to your gut. “If you perceive that someone is not a suitable candidate for resurfacing or has unrealistic expectations, and they are insistent, it is important to stand your ground, and even find a way to politely walk away,” said Dr. Brauer of the department of dermatology at New York University.
Most complications from laser resurfacing are not unique to skin of color, he continued. A review of the topic revealed that mild complications may include prolonged erythema, acne and milia, delayed purpura, superficial erosions, contact dermatitis, and recall phenomenon (Dermatol Surg. 2010;36[3]:299-306). Moderate complications may include infection, pigmentary alteration, anesthesia toxicity, and eruptive keratoacanthomas, while severe complications may include hypertrophic scarring, ectropion formation, and disseminated infection.
An earlier analysis of fractional laser treatment found that patients with darker skin types had a significantly higher proportion of certain side effects, namely postinflammatory hyperpigmentation (Dermatol Surg. 2008;34[3]:301-7). “Additionally, the researchers found that this presented both later and lasted longer than in individuals with lighter skin types,” said Dr. Brauer, who was not involved with the study.
He listed pigmentary alterations and hypertrophic scarring/keloid formation as the potential complications from resurfacing to be most concerned about in skin of color patients. “In addition to appropriate device selection, the correct device parameters are key,” he said. “You have to make sure you use appropriate energy, but you can use higher energies with lower densities to minimize the risk of postinflammatory pigmentation. You also want to protect the epidermis by use of epidermal cooling, avoid bulk heating, and perform sessions at prolonged treatment intervals, to safely achieve optimal results.”
Dr. Brauer reported having received honoraria or being a member of the medical advisory board for Cutera, Cynosure/Hologic, and Merz.
EXPERT ANALYSIS FROM ASLMS 2019
Split-face trial compares outcomes of two different lasers on photoaging
DENVER – The fractionated picosecond Nd:YAG laser and fractionated thulium fiber laser can be equally effective for facial rejuvenation, results from a small split-face trial showed. However, the fractionated picosecond Nd:YAG laser may result in significantly less postoperative downtime, compared with the fractionated thulium fiber laser.
The findings from the prospective, evaluator-blinded trial were presented by Douglas C. Wu, MD, PhD, at the annual conference of the American Society for Laser Medicine and Surgery. Dr. Wu, of San Diego–based Cosmetic Laser Dermatology, and his colleague, Mitchel P. Goldman, MD, enrolled 20 subjects with at least moderate photoaging who randomly received three treatments with either the 1064/532-nm fractionated picosecond Nd:YAG laser or with the 1927-nm fractionated thulium fiber laser on each side of the face, 4 weeks apart. The primary endpoint was the degree of rhytids, laxity, dyschromia, erythema-telangiectasia, keratoses, and texture rated on a four-point scale and performed by a blinded evaluator at baseline, and 12, 20, and 30 weeks from baseline. Secondary endpoints were the global aesthetic improvement score, investigator satisfaction questionnaire, and a subject satisfaction questionnaire administered at weeks 12, 20, and 30. Recovery time and adverse events were assessed through a 14-day subject diary administered after each treatment.
All but 1 of the 20 patients were female and their mean age was 57 years. Six had Fitzpatrick skin type II, seven had type III, six had type IV, and one had type V. The device settings were on medium for both devices. The researchers observed significant improvements in elastosis, erythema, dyschromia, and texture at all treatment follow-up time points (P less than .01 for all endpoints).
There were no differences between the two lasers in terms of efficacy. “Clinically, the efficacy was rated to be the same,” Dr. Wu said. “However, when we analyzed the patient diaries, we found some very interesting results. In terms of redness, at days 3 and 4, there was a consistently increased amount of redness on the side treated with the fractionated thulium fiber laser, with swelling also being significantly increased at day 5.” Similarly, he said, the side treated with the fractionated picosecond laser experienced significantly less crusting on posttreatment days 1 through 9, less peeling on days 3 through 5, and less itching on day 4. Posttreatment pain was minimal on both sides and did not differ significantly.
Dr. Wu disclosed having numerous financial ties to pharmaceutical and device companies.
DENVER – The fractionated picosecond Nd:YAG laser and fractionated thulium fiber laser can be equally effective for facial rejuvenation, results from a small split-face trial showed. However, the fractionated picosecond Nd:YAG laser may result in significantly less postoperative downtime, compared with the fractionated thulium fiber laser.
The findings from the prospective, evaluator-blinded trial were presented by Douglas C. Wu, MD, PhD, at the annual conference of the American Society for Laser Medicine and Surgery. Dr. Wu, of San Diego–based Cosmetic Laser Dermatology, and his colleague, Mitchel P. Goldman, MD, enrolled 20 subjects with at least moderate photoaging who randomly received three treatments with either the 1064/532-nm fractionated picosecond Nd:YAG laser or with the 1927-nm fractionated thulium fiber laser on each side of the face, 4 weeks apart. The primary endpoint was the degree of rhytids, laxity, dyschromia, erythema-telangiectasia, keratoses, and texture rated on a four-point scale and performed by a blinded evaluator at baseline, and 12, 20, and 30 weeks from baseline. Secondary endpoints were the global aesthetic improvement score, investigator satisfaction questionnaire, and a subject satisfaction questionnaire administered at weeks 12, 20, and 30. Recovery time and adverse events were assessed through a 14-day subject diary administered after each treatment.
All but 1 of the 20 patients were female and their mean age was 57 years. Six had Fitzpatrick skin type II, seven had type III, six had type IV, and one had type V. The device settings were on medium for both devices. The researchers observed significant improvements in elastosis, erythema, dyschromia, and texture at all treatment follow-up time points (P less than .01 for all endpoints).
There were no differences between the two lasers in terms of efficacy. “Clinically, the efficacy was rated to be the same,” Dr. Wu said. “However, when we analyzed the patient diaries, we found some very interesting results. In terms of redness, at days 3 and 4, there was a consistently increased amount of redness on the side treated with the fractionated thulium fiber laser, with swelling also being significantly increased at day 5.” Similarly, he said, the side treated with the fractionated picosecond laser experienced significantly less crusting on posttreatment days 1 through 9, less peeling on days 3 through 5, and less itching on day 4. Posttreatment pain was minimal on both sides and did not differ significantly.
Dr. Wu disclosed having numerous financial ties to pharmaceutical and device companies.
DENVER – The fractionated picosecond Nd:YAG laser and fractionated thulium fiber laser can be equally effective for facial rejuvenation, results from a small split-face trial showed. However, the fractionated picosecond Nd:YAG laser may result in significantly less postoperative downtime, compared with the fractionated thulium fiber laser.
The findings from the prospective, evaluator-blinded trial were presented by Douglas C. Wu, MD, PhD, at the annual conference of the American Society for Laser Medicine and Surgery. Dr. Wu, of San Diego–based Cosmetic Laser Dermatology, and his colleague, Mitchel P. Goldman, MD, enrolled 20 subjects with at least moderate photoaging who randomly received three treatments with either the 1064/532-nm fractionated picosecond Nd:YAG laser or with the 1927-nm fractionated thulium fiber laser on each side of the face, 4 weeks apart. The primary endpoint was the degree of rhytids, laxity, dyschromia, erythema-telangiectasia, keratoses, and texture rated on a four-point scale and performed by a blinded evaluator at baseline, and 12, 20, and 30 weeks from baseline. Secondary endpoints were the global aesthetic improvement score, investigator satisfaction questionnaire, and a subject satisfaction questionnaire administered at weeks 12, 20, and 30. Recovery time and adverse events were assessed through a 14-day subject diary administered after each treatment.
All but 1 of the 20 patients were female and their mean age was 57 years. Six had Fitzpatrick skin type II, seven had type III, six had type IV, and one had type V. The device settings were on medium for both devices. The researchers observed significant improvements in elastosis, erythema, dyschromia, and texture at all treatment follow-up time points (P less than .01 for all endpoints).
There were no differences between the two lasers in terms of efficacy. “Clinically, the efficacy was rated to be the same,” Dr. Wu said. “However, when we analyzed the patient diaries, we found some very interesting results. In terms of redness, at days 3 and 4, there was a consistently increased amount of redness on the side treated with the fractionated thulium fiber laser, with swelling also being significantly increased at day 5.” Similarly, he said, the side treated with the fractionated picosecond laser experienced significantly less crusting on posttreatment days 1 through 9, less peeling on days 3 through 5, and less itching on day 4. Posttreatment pain was minimal on both sides and did not differ significantly.
Dr. Wu disclosed having numerous financial ties to pharmaceutical and device companies.
REPORTING FROM ASLMS 2019
Chronic urticaria population identified
Half a million people. That’s pretty close to the population of Sacramento. It’s also the estimated number of adults living with chronic urticaria in the United States, according to analysis of a database including over 55 million individuals.
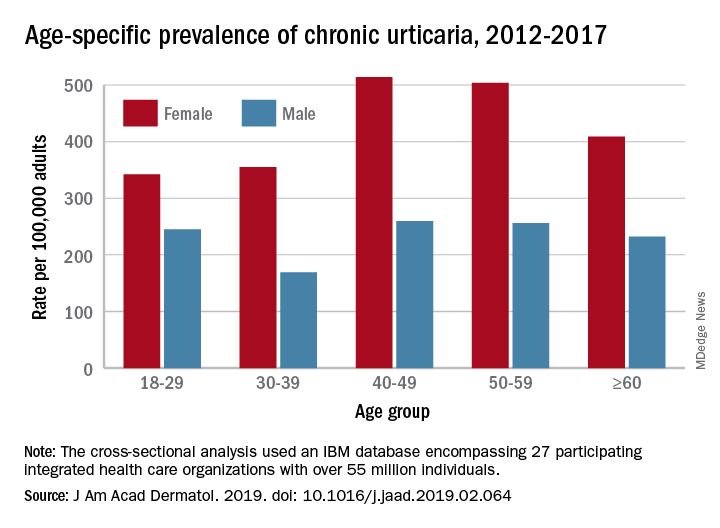
That cross-sectional analysis put the overall standardized at 309.3 per 100,000 (0.31%) and men well below at 145.5 per 100,000 (0.15%), Sara Wertenteil, BA, and her associates at Hofstra University, Hempstead, N.Y., wrote in the Journal of the American Academy of Dermatology.
Overall prevalence of chronic urticaria was similar for all age groups, ranging from 0.21% for those aged 18-29 years and those aged 30-39 years to 0.26% for those aged 40-49, and prevalence was higher for females than males in all age groups, the investigators reported.
“Epidemiologic studies estimating disease burden for chronic urticaria are sparse, [but this study] is based on one of the largest and most ethnically diversified population samples in the United States. It is also drawn from patients with all insurance types and self-pay patients across various types of health care settings and from all census regions,” Ms. Wertenteil and her associates wrote.
The study involved an IBM Watson Health database encompassing 27 participating integrated health care organizations and representing approximately 17% of the population. The analysis identified 69,570 adult patients with chronic urticaria, and the ratio of women to men was 2.7:1.
The senior author, Amit Garg, MD, has served as an advisor for AbbVie, Pfizer, Janssen, and Asana Biosciences.
SOURCE: Wertenteil S et al. J Am Acad Dermatol. 2019. doi: 10.1016/j.jaad.2019.02.064.
Half a million people. That’s pretty close to the population of Sacramento. It’s also the estimated number of adults living with chronic urticaria in the United States, according to analysis of a database including over 55 million individuals.
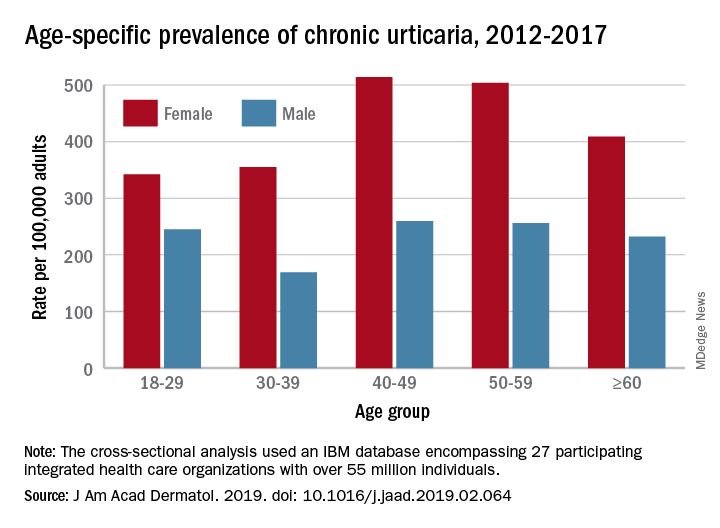
That cross-sectional analysis put the overall standardized at 309.3 per 100,000 (0.31%) and men well below at 145.5 per 100,000 (0.15%), Sara Wertenteil, BA, and her associates at Hofstra University, Hempstead, N.Y., wrote in the Journal of the American Academy of Dermatology.
Overall prevalence of chronic urticaria was similar for all age groups, ranging from 0.21% for those aged 18-29 years and those aged 30-39 years to 0.26% for those aged 40-49, and prevalence was higher for females than males in all age groups, the investigators reported.
“Epidemiologic studies estimating disease burden for chronic urticaria are sparse, [but this study] is based on one of the largest and most ethnically diversified population samples in the United States. It is also drawn from patients with all insurance types and self-pay patients across various types of health care settings and from all census regions,” Ms. Wertenteil and her associates wrote.
The study involved an IBM Watson Health database encompassing 27 participating integrated health care organizations and representing approximately 17% of the population. The analysis identified 69,570 adult patients with chronic urticaria, and the ratio of women to men was 2.7:1.
The senior author, Amit Garg, MD, has served as an advisor for AbbVie, Pfizer, Janssen, and Asana Biosciences.
SOURCE: Wertenteil S et al. J Am Acad Dermatol. 2019. doi: 10.1016/j.jaad.2019.02.064.
Half a million people. That’s pretty close to the population of Sacramento. It’s also the estimated number of adults living with chronic urticaria in the United States, according to analysis of a database including over 55 million individuals.
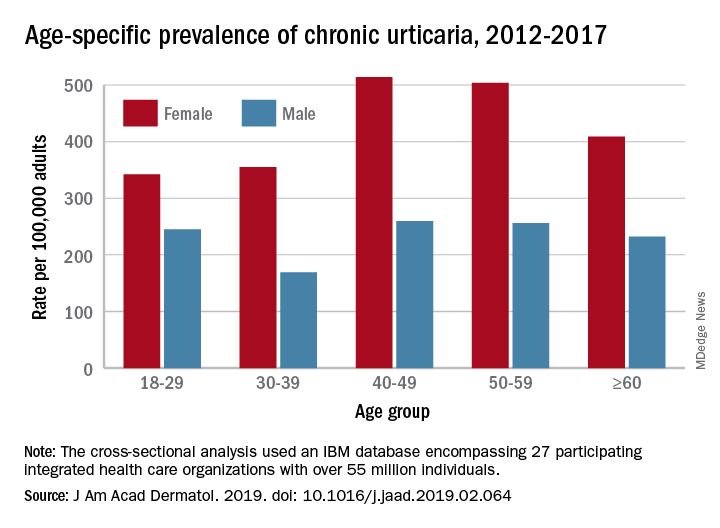
That cross-sectional analysis put the overall standardized at 309.3 per 100,000 (0.31%) and men well below at 145.5 per 100,000 (0.15%), Sara Wertenteil, BA, and her associates at Hofstra University, Hempstead, N.Y., wrote in the Journal of the American Academy of Dermatology.
Overall prevalence of chronic urticaria was similar for all age groups, ranging from 0.21% for those aged 18-29 years and those aged 30-39 years to 0.26% for those aged 40-49, and prevalence was higher for females than males in all age groups, the investigators reported.
“Epidemiologic studies estimating disease burden for chronic urticaria are sparse, [but this study] is based on one of the largest and most ethnically diversified population samples in the United States. It is also drawn from patients with all insurance types and self-pay patients across various types of health care settings and from all census regions,” Ms. Wertenteil and her associates wrote.
The study involved an IBM Watson Health database encompassing 27 participating integrated health care organizations and representing approximately 17% of the population. The analysis identified 69,570 adult patients with chronic urticaria, and the ratio of women to men was 2.7:1.
The senior author, Amit Garg, MD, has served as an advisor for AbbVie, Pfizer, Janssen, and Asana Biosciences.
SOURCE: Wertenteil S et al. J Am Acad Dermatol. 2019. doi: 10.1016/j.jaad.2019.02.064.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
‘Exergaming’ boosts motivation in schizophrenia patients
Attrition rates encouraging in community program
ORLANDO – Using games to promote exercise – or “exergaming” – is proving to boost the motivation of schizophrenia patients to engage in physical activity and help with symptoms, researchers said at the annual congress of the Schizophrenia International Research Society.
Physical fitness has been shown to boost cognitive function in people with schizophrenia – a particularly attractive option because it does not create stigma in the way that engaging in in-person therapy or taking medications might – and it is essentially free of side effects, said Jimmy Choi, PsyD, a senior scientist at the Olin Neuropsychiatry Research Center and staff neuropsychologist at the Institute of Living’s Schizophrenia Rehabilitation Program in Hartford, Conn.
The problem, Dr. Choi said, is that many studies have shown that compliance – or completion of half of an exercise program by participants – is fairly low, at 65%-68%. Among those who are not compliant, the benefits of exercise programs on cognition, psychosis symptoms, and mental status are conspicuously lower.
Effect sizes in laboratory trials on the efficacy of physical fitness are much higher than effectiveness seen in studies of community programs, Dr. Choi said, likely because laboratory trials offer participants a monetary reward for participation, while community studies might offer less attractive incentives, such as tickets for weekly or monthly raffles.
At Olin, a more true-to-life community program of exergaming – which included the use of virtual reality – was created by recreational therapists, exercise physiologists, psychologists, and technology experts to optimize the experience and outcomes, each with a distinct role – either developing the overall experience to promote enjoyment, achieving exhaustion but without an injury risk, incorporating patients’ baseline cognitive profile to make the programs suitable, or tailoring virtual experiences for each participant.
With 35 participants, researchers saw encouraging effects on working memory, processing speed, as well as positive and negative schizophrenia symptoms – with effect sizes ranging from 0.54 for working memory scores to 0.19 for positive schizophrenia symptoms, such as hallucinations.
The attrition rate of 14% was the same for those assessed as having low motivation as it was for those assessed as having high motivation, suggesting that exergaming helped boost and sustain motivation among patients for whom it is usually difficult, said Dr. Choi, who added that he and his colleagues have a paper in press outlining these results in Schizophrenia Research: Cognition.
“Exergaming shows promise in improving adherence to physical exercise and reducing attrition,” he said. “Highly motivated participants benefited more in terms of cognition and symptoms, but even those with low motivation saw improvements in working memory and negative symptoms.”
Dr. Choi added that his center is continuing to evaluate exergaming.
“A nice bike exercise or treadmill, that’s still more portable and cheaper for community clinics to do,” he said. “That’s one of the reasons ... we’re currently doing a randomized, controlled trial looking to see if exergaming could stand up to doing a singular exercise aerobic program.”
The study and Exergame equipment were funded by a Hartford Hospital auxiliary special projects grant. Dr. Choi reported having no financial conflicts.
Attrition rates encouraging in community program
Attrition rates encouraging in community program
ORLANDO – Using games to promote exercise – or “exergaming” – is proving to boost the motivation of schizophrenia patients to engage in physical activity and help with symptoms, researchers said at the annual congress of the Schizophrenia International Research Society.
Physical fitness has been shown to boost cognitive function in people with schizophrenia – a particularly attractive option because it does not create stigma in the way that engaging in in-person therapy or taking medications might – and it is essentially free of side effects, said Jimmy Choi, PsyD, a senior scientist at the Olin Neuropsychiatry Research Center and staff neuropsychologist at the Institute of Living’s Schizophrenia Rehabilitation Program in Hartford, Conn.
The problem, Dr. Choi said, is that many studies have shown that compliance – or completion of half of an exercise program by participants – is fairly low, at 65%-68%. Among those who are not compliant, the benefits of exercise programs on cognition, psychosis symptoms, and mental status are conspicuously lower.
Effect sizes in laboratory trials on the efficacy of physical fitness are much higher than effectiveness seen in studies of community programs, Dr. Choi said, likely because laboratory trials offer participants a monetary reward for participation, while community studies might offer less attractive incentives, such as tickets for weekly or monthly raffles.
At Olin, a more true-to-life community program of exergaming – which included the use of virtual reality – was created by recreational therapists, exercise physiologists, psychologists, and technology experts to optimize the experience and outcomes, each with a distinct role – either developing the overall experience to promote enjoyment, achieving exhaustion but without an injury risk, incorporating patients’ baseline cognitive profile to make the programs suitable, or tailoring virtual experiences for each participant.
With 35 participants, researchers saw encouraging effects on working memory, processing speed, as well as positive and negative schizophrenia symptoms – with effect sizes ranging from 0.54 for working memory scores to 0.19 for positive schizophrenia symptoms, such as hallucinations.
The attrition rate of 14% was the same for those assessed as having low motivation as it was for those assessed as having high motivation, suggesting that exergaming helped boost and sustain motivation among patients for whom it is usually difficult, said Dr. Choi, who added that he and his colleagues have a paper in press outlining these results in Schizophrenia Research: Cognition.
“Exergaming shows promise in improving adherence to physical exercise and reducing attrition,” he said. “Highly motivated participants benefited more in terms of cognition and symptoms, but even those with low motivation saw improvements in working memory and negative symptoms.”
Dr. Choi added that his center is continuing to evaluate exergaming.
“A nice bike exercise or treadmill, that’s still more portable and cheaper for community clinics to do,” he said. “That’s one of the reasons ... we’re currently doing a randomized, controlled trial looking to see if exergaming could stand up to doing a singular exercise aerobic program.”
The study and Exergame equipment were funded by a Hartford Hospital auxiliary special projects grant. Dr. Choi reported having no financial conflicts.
ORLANDO – Using games to promote exercise – or “exergaming” – is proving to boost the motivation of schizophrenia patients to engage in physical activity and help with symptoms, researchers said at the annual congress of the Schizophrenia International Research Society.
Physical fitness has been shown to boost cognitive function in people with schizophrenia – a particularly attractive option because it does not create stigma in the way that engaging in in-person therapy or taking medications might – and it is essentially free of side effects, said Jimmy Choi, PsyD, a senior scientist at the Olin Neuropsychiatry Research Center and staff neuropsychologist at the Institute of Living’s Schizophrenia Rehabilitation Program in Hartford, Conn.
The problem, Dr. Choi said, is that many studies have shown that compliance – or completion of half of an exercise program by participants – is fairly low, at 65%-68%. Among those who are not compliant, the benefits of exercise programs on cognition, psychosis symptoms, and mental status are conspicuously lower.
Effect sizes in laboratory trials on the efficacy of physical fitness are much higher than effectiveness seen in studies of community programs, Dr. Choi said, likely because laboratory trials offer participants a monetary reward for participation, while community studies might offer less attractive incentives, such as tickets for weekly or monthly raffles.
At Olin, a more true-to-life community program of exergaming – which included the use of virtual reality – was created by recreational therapists, exercise physiologists, psychologists, and technology experts to optimize the experience and outcomes, each with a distinct role – either developing the overall experience to promote enjoyment, achieving exhaustion but without an injury risk, incorporating patients’ baseline cognitive profile to make the programs suitable, or tailoring virtual experiences for each participant.
With 35 participants, researchers saw encouraging effects on working memory, processing speed, as well as positive and negative schizophrenia symptoms – with effect sizes ranging from 0.54 for working memory scores to 0.19 for positive schizophrenia symptoms, such as hallucinations.
The attrition rate of 14% was the same for those assessed as having low motivation as it was for those assessed as having high motivation, suggesting that exergaming helped boost and sustain motivation among patients for whom it is usually difficult, said Dr. Choi, who added that he and his colleagues have a paper in press outlining these results in Schizophrenia Research: Cognition.
“Exergaming shows promise in improving adherence to physical exercise and reducing attrition,” he said. “Highly motivated participants benefited more in terms of cognition and symptoms, but even those with low motivation saw improvements in working memory and negative symptoms.”
Dr. Choi added that his center is continuing to evaluate exergaming.
“A nice bike exercise or treadmill, that’s still more portable and cheaper for community clinics to do,” he said. “That’s one of the reasons ... we’re currently doing a randomized, controlled trial looking to see if exergaming could stand up to doing a singular exercise aerobic program.”
The study and Exergame equipment were funded by a Hartford Hospital auxiliary special projects grant. Dr. Choi reported having no financial conflicts.
REPORTING FROM SIRS 2019
Measles cases for 2019 now at postelimination high
according to the Centers for Disease Control and Prevention.
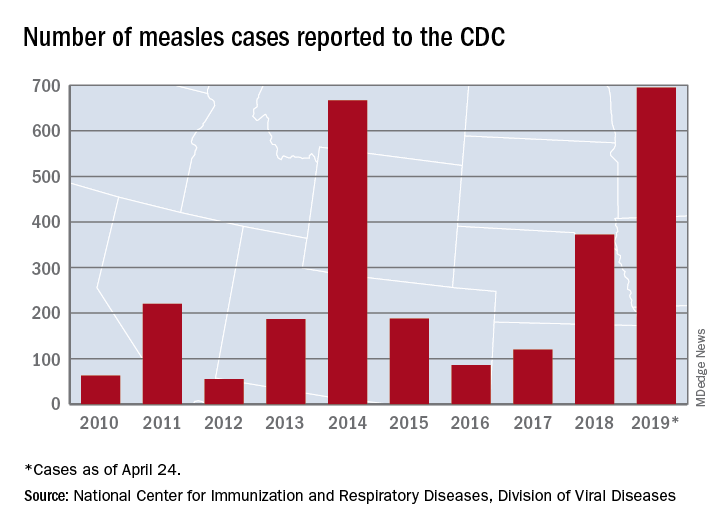
As of Wednesday, April 24, the case count for measles is 695, which eclipses the mark of 667 cases that had been the highest since the disease was declared to be eliminated from this country in 2000, the CDC reported.
“The high number of cases in 2019 is primarily the result of a few large outbreaks – one in Washington State and two large outbreaks in New York that started in late 2018. The outbreaks in New York City and New York State are among the largest and longest lasting since measles elimination in 2000. The longer these outbreaks continue, the greater the chance measles will again get a sustained foothold in the United States,” according to a written statement by the CDC.
Although these outbreaks began when the virus was brought into this country by unvaccinated travelers from other countries where there is widespread transmission, “a significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine. Some organizations are deliberately targeting these communities with inaccurate and misleading information about vaccines,” according to the statement.
“Measles is not a harmless childhood illness, but a highly contagious, potentially life-threatening disease,” Health and Human Services Secretary Alex Azar said in a separate statement. “We have the ability to safely protect our children and our communities. Vaccines are a safe, highly effective public health solution that can prevent this disease. The measles vaccines are among the most extensively studied medical products we have, and their safety has been firmly established over many years in some of the largest vaccine studies ever undertaken. With a safe and effective vaccine that protects against measles, the suffering we are seeing is avoidable.”
according to the Centers for Disease Control and Prevention.
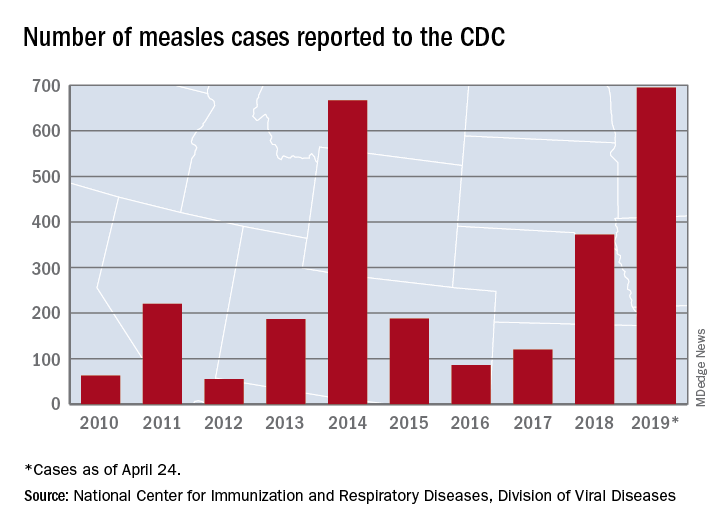
As of Wednesday, April 24, the case count for measles is 695, which eclipses the mark of 667 cases that had been the highest since the disease was declared to be eliminated from this country in 2000, the CDC reported.
“The high number of cases in 2019 is primarily the result of a few large outbreaks – one in Washington State and two large outbreaks in New York that started in late 2018. The outbreaks in New York City and New York State are among the largest and longest lasting since measles elimination in 2000. The longer these outbreaks continue, the greater the chance measles will again get a sustained foothold in the United States,” according to a written statement by the CDC.
Although these outbreaks began when the virus was brought into this country by unvaccinated travelers from other countries where there is widespread transmission, “a significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine. Some organizations are deliberately targeting these communities with inaccurate and misleading information about vaccines,” according to the statement.
“Measles is not a harmless childhood illness, but a highly contagious, potentially life-threatening disease,” Health and Human Services Secretary Alex Azar said in a separate statement. “We have the ability to safely protect our children and our communities. Vaccines are a safe, highly effective public health solution that can prevent this disease. The measles vaccines are among the most extensively studied medical products we have, and their safety has been firmly established over many years in some of the largest vaccine studies ever undertaken. With a safe and effective vaccine that protects against measles, the suffering we are seeing is avoidable.”
according to the Centers for Disease Control and Prevention.
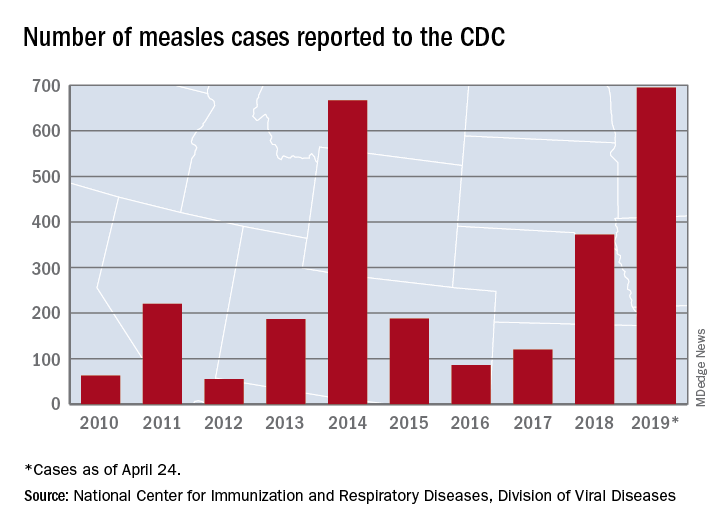
As of Wednesday, April 24, the case count for measles is 695, which eclipses the mark of 667 cases that had been the highest since the disease was declared to be eliminated from this country in 2000, the CDC reported.
“The high number of cases in 2019 is primarily the result of a few large outbreaks – one in Washington State and two large outbreaks in New York that started in late 2018. The outbreaks in New York City and New York State are among the largest and longest lasting since measles elimination in 2000. The longer these outbreaks continue, the greater the chance measles will again get a sustained foothold in the United States,” according to a written statement by the CDC.
Although these outbreaks began when the virus was brought into this country by unvaccinated travelers from other countries where there is widespread transmission, “a significant factor contributing to the outbreaks in New York is misinformation in the communities about the safety of the measles/mumps/rubella vaccine. Some organizations are deliberately targeting these communities with inaccurate and misleading information about vaccines,” according to the statement.
“Measles is not a harmless childhood illness, but a highly contagious, potentially life-threatening disease,” Health and Human Services Secretary Alex Azar said in a separate statement. “We have the ability to safely protect our children and our communities. Vaccines are a safe, highly effective public health solution that can prevent this disease. The measles vaccines are among the most extensively studied medical products we have, and their safety has been firmly established over many years in some of the largest vaccine studies ever undertaken. With a safe and effective vaccine that protects against measles, the suffering we are seeing is avoidable.”
TTP death linked to elevated troponin and neurological signs
GLASGOW – , according to retrospective analysis of 475 patients from the United Kingdom TTP registry.
In addition, low ADAMTS13 activity (less than 10%) was present in 92% of immune-mediated of TTP upon acute presentation, reported lead author Jin-Sup Shin, MD, of University College London Hospital, and colleagues.
Presenting at the annual meeting of the British Society for Haematology, Dr. Shin provided some background on TTP, a condition that most clinicians encounter infrequently.
“As recently as the 1980s and 90s, when etiology was not that well understood, TTP was associated with an untreated mortality of up to 90%,” Dr. Shin said. “However, based on improved understanding of pathophysiology, and through the creation of TTP registries worldwide, there have been major advances in diagnosis, treatment, and outcomes.”
To gain insight into diagnostic and prognostic characteristics of TTP, the investigators turned to data from 602 patients with clinically suspected TTP, based on an ADAMTS13 activity level less than 10% of normal and associated clinical signs. Out of these 602 patients, 475 consented to registry participation and data analysis.
The analysis revealed a mortality rate of 4%, although Dr. Shin said that “this is probably an underestimate of the true figure,” as it excludes those who died before treatment could be initiated.
Nearly three-quarters of patients were female. The median age at presentation was 43 years, with a range of 1-93 years. The most commonly represented racial/ethnic groups were white (60%) and Afro-Caribbean (22%). Some cases were congenital (16%), but the majority were immune mediated (84%).
The immune-mediated group was the primary focus of Dr. Shin’s report. In this cohort, 76% of cases were idiopathic, while the remainder had a defined precipitant; most common were infection, autoimmune disease, pregnancy, and HIV. The relapse rate among those with immune-mediated TTP was 19%, after a median time to relapse of 26 months.
In total, 71% of patients presented with neurological abnormalities, while slightly less than half (48%) had symptomatic thrombocytopenia (bleeding/petechiae).
Diagnostic tools showed that 64% of patients had an elevated troponin level, 92% had ADAMTS13 activity less than 10%, and 25% had a platelet count lower than 10 x 109/L.
Median platelet count upon presentation was 15 x 109/L, and median lactate dehydrogenase (LDH) exceeded 1,000 units/L. After 7 days of therapy, 58% of patients were still severely deficient in ADAMTS13 activity and 36% of patients still had a platelet count lower than 150 x 109/L.
Where information was available, 30% of patients had positive auto-antibody screens, although not necessarily with signs or symptoms of autoimmune disease. A total of 93% of patients had elevated ADAMTS13 IgG antibody upon presentation. The median ADAMTS13 IgG antibody level at presentation was 37%, with a normal value being less than 6%.
Nearly half of patients with immune-mediated TTP (45%) required intensive care, and 10% of these patients were intubated and ventilated. Most patients were treated with steroids upon admission (81%). On average, 11 plasma exchanges (PEXs) were required before remission.
The investigators noted that “[t]he number of PEXs to remission appears to have decreased over the years.” As an example, a median of 14 PEXs were needed from 2009 to 2010, compared with 8 from 2017 to 2018.
Although rituximab usage in the acute setting held steady over the 10-year period, elective use increased. Out of 89 instances of subacute relapse, elective rituximab was given twice from 2009 to 2010, compared with 26 times from 2017 to 2018.
Comparing features of survival, the investigators found that the median ADAMTS13 IgG antibody level was higher among those who died. Other factors related to increased mortality risk included raised troponin (sevenfold increased risk) and neurological abnormalities, defined by reduced Glasgow Coma Scale score (sixfold increased risk).
“Our data confirm other registries worldwide; in particular, increased susceptibility in women, the Afro-Caribbean population, and those who are middle-aged,” Dr. Shin said. “Our data also show that elevated cardiac troponin and neurological involvement are indicators of poor prognosis. Also, raised antibody levels appear to be associated with a worse clinical outcome and increased mortality rate. These are clearly valuable markers in clinical practice, allowing for intensive care of high-risk patients.”
The investigators reported having no conflicts of interest.
GLASGOW – , according to retrospective analysis of 475 patients from the United Kingdom TTP registry.
In addition, low ADAMTS13 activity (less than 10%) was present in 92% of immune-mediated of TTP upon acute presentation, reported lead author Jin-Sup Shin, MD, of University College London Hospital, and colleagues.
Presenting at the annual meeting of the British Society for Haematology, Dr. Shin provided some background on TTP, a condition that most clinicians encounter infrequently.
“As recently as the 1980s and 90s, when etiology was not that well understood, TTP was associated with an untreated mortality of up to 90%,” Dr. Shin said. “However, based on improved understanding of pathophysiology, and through the creation of TTP registries worldwide, there have been major advances in diagnosis, treatment, and outcomes.”
To gain insight into diagnostic and prognostic characteristics of TTP, the investigators turned to data from 602 patients with clinically suspected TTP, based on an ADAMTS13 activity level less than 10% of normal and associated clinical signs. Out of these 602 patients, 475 consented to registry participation and data analysis.
The analysis revealed a mortality rate of 4%, although Dr. Shin said that “this is probably an underestimate of the true figure,” as it excludes those who died before treatment could be initiated.
Nearly three-quarters of patients were female. The median age at presentation was 43 years, with a range of 1-93 years. The most commonly represented racial/ethnic groups were white (60%) and Afro-Caribbean (22%). Some cases were congenital (16%), but the majority were immune mediated (84%).
The immune-mediated group was the primary focus of Dr. Shin’s report. In this cohort, 76% of cases were idiopathic, while the remainder had a defined precipitant; most common were infection, autoimmune disease, pregnancy, and HIV. The relapse rate among those with immune-mediated TTP was 19%, after a median time to relapse of 26 months.
In total, 71% of patients presented with neurological abnormalities, while slightly less than half (48%) had symptomatic thrombocytopenia (bleeding/petechiae).
Diagnostic tools showed that 64% of patients had an elevated troponin level, 92% had ADAMTS13 activity less than 10%, and 25% had a platelet count lower than 10 x 109/L.
Median platelet count upon presentation was 15 x 109/L, and median lactate dehydrogenase (LDH) exceeded 1,000 units/L. After 7 days of therapy, 58% of patients were still severely deficient in ADAMTS13 activity and 36% of patients still had a platelet count lower than 150 x 109/L.
Where information was available, 30% of patients had positive auto-antibody screens, although not necessarily with signs or symptoms of autoimmune disease. A total of 93% of patients had elevated ADAMTS13 IgG antibody upon presentation. The median ADAMTS13 IgG antibody level at presentation was 37%, with a normal value being less than 6%.
Nearly half of patients with immune-mediated TTP (45%) required intensive care, and 10% of these patients were intubated and ventilated. Most patients were treated with steroids upon admission (81%). On average, 11 plasma exchanges (PEXs) were required before remission.
The investigators noted that “[t]he number of PEXs to remission appears to have decreased over the years.” As an example, a median of 14 PEXs were needed from 2009 to 2010, compared with 8 from 2017 to 2018.
Although rituximab usage in the acute setting held steady over the 10-year period, elective use increased. Out of 89 instances of subacute relapse, elective rituximab was given twice from 2009 to 2010, compared with 26 times from 2017 to 2018.
Comparing features of survival, the investigators found that the median ADAMTS13 IgG antibody level was higher among those who died. Other factors related to increased mortality risk included raised troponin (sevenfold increased risk) and neurological abnormalities, defined by reduced Glasgow Coma Scale score (sixfold increased risk).
“Our data confirm other registries worldwide; in particular, increased susceptibility in women, the Afro-Caribbean population, and those who are middle-aged,” Dr. Shin said. “Our data also show that elevated cardiac troponin and neurological involvement are indicators of poor prognosis. Also, raised antibody levels appear to be associated with a worse clinical outcome and increased mortality rate. These are clearly valuable markers in clinical practice, allowing for intensive care of high-risk patients.”
The investigators reported having no conflicts of interest.
GLASGOW – , according to retrospective analysis of 475 patients from the United Kingdom TTP registry.
In addition, low ADAMTS13 activity (less than 10%) was present in 92% of immune-mediated of TTP upon acute presentation, reported lead author Jin-Sup Shin, MD, of University College London Hospital, and colleagues.
Presenting at the annual meeting of the British Society for Haematology, Dr. Shin provided some background on TTP, a condition that most clinicians encounter infrequently.
“As recently as the 1980s and 90s, when etiology was not that well understood, TTP was associated with an untreated mortality of up to 90%,” Dr. Shin said. “However, based on improved understanding of pathophysiology, and through the creation of TTP registries worldwide, there have been major advances in diagnosis, treatment, and outcomes.”
To gain insight into diagnostic and prognostic characteristics of TTP, the investigators turned to data from 602 patients with clinically suspected TTP, based on an ADAMTS13 activity level less than 10% of normal and associated clinical signs. Out of these 602 patients, 475 consented to registry participation and data analysis.
The analysis revealed a mortality rate of 4%, although Dr. Shin said that “this is probably an underestimate of the true figure,” as it excludes those who died before treatment could be initiated.
Nearly three-quarters of patients were female. The median age at presentation was 43 years, with a range of 1-93 years. The most commonly represented racial/ethnic groups were white (60%) and Afro-Caribbean (22%). Some cases were congenital (16%), but the majority were immune mediated (84%).
The immune-mediated group was the primary focus of Dr. Shin’s report. In this cohort, 76% of cases were idiopathic, while the remainder had a defined precipitant; most common were infection, autoimmune disease, pregnancy, and HIV. The relapse rate among those with immune-mediated TTP was 19%, after a median time to relapse of 26 months.
In total, 71% of patients presented with neurological abnormalities, while slightly less than half (48%) had symptomatic thrombocytopenia (bleeding/petechiae).
Diagnostic tools showed that 64% of patients had an elevated troponin level, 92% had ADAMTS13 activity less than 10%, and 25% had a platelet count lower than 10 x 109/L.
Median platelet count upon presentation was 15 x 109/L, and median lactate dehydrogenase (LDH) exceeded 1,000 units/L. After 7 days of therapy, 58% of patients were still severely deficient in ADAMTS13 activity and 36% of patients still had a platelet count lower than 150 x 109/L.
Where information was available, 30% of patients had positive auto-antibody screens, although not necessarily with signs or symptoms of autoimmune disease. A total of 93% of patients had elevated ADAMTS13 IgG antibody upon presentation. The median ADAMTS13 IgG antibody level at presentation was 37%, with a normal value being less than 6%.
Nearly half of patients with immune-mediated TTP (45%) required intensive care, and 10% of these patients were intubated and ventilated. Most patients were treated with steroids upon admission (81%). On average, 11 plasma exchanges (PEXs) were required before remission.
The investigators noted that “[t]he number of PEXs to remission appears to have decreased over the years.” As an example, a median of 14 PEXs were needed from 2009 to 2010, compared with 8 from 2017 to 2018.
Although rituximab usage in the acute setting held steady over the 10-year period, elective use increased. Out of 89 instances of subacute relapse, elective rituximab was given twice from 2009 to 2010, compared with 26 times from 2017 to 2018.
Comparing features of survival, the investigators found that the median ADAMTS13 IgG antibody level was higher among those who died. Other factors related to increased mortality risk included raised troponin (sevenfold increased risk) and neurological abnormalities, defined by reduced Glasgow Coma Scale score (sixfold increased risk).
“Our data confirm other registries worldwide; in particular, increased susceptibility in women, the Afro-Caribbean population, and those who are middle-aged,” Dr. Shin said. “Our data also show that elevated cardiac troponin and neurological involvement are indicators of poor prognosis. Also, raised antibody levels appear to be associated with a worse clinical outcome and increased mortality rate. These are clearly valuable markers in clinical practice, allowing for intensive care of high-risk patients.”
The investigators reported having no conflicts of interest.
REPORTING FROM BSH 2019
Key clinical point: Neurological abnormalities and elevated troponin predict mortality in patients with thrombotic thrombocytopenic purpura (TTP).
Major finding: ADAMTS13 IgG antibody level, elevated troponin, and neurological abnormalities were all linked to an increased mortality risk.
Study details: A retrospective analysis of 475 patients with clinically suspected thrombotic thrombocytopenic purpura (TTP) from the U.K. registry (2009-2018).
Disclosures: The investigators reported having no conflicts of interest.
Study finds increase in dermatologic prescriptions for postsurgical antibiotics
WASHINGTON – , according to an analysis presented at the annual meeting of the American Academy of Dermatology.
John Barbieri, MD, a dermatologist and postdoctoral research fellow at the University of Pennsylvania, Philadelphia, who presented the results, and colleagues examined data about antibiotic use in dermatology between 2008 and 2016. Overall, antibiotic use decreased during this period, primarily for chronic conditions such as acne and rosacea. On the other hand, antibiotic use associated with surgical visits increased by approximately 70%.
Using data from 2008 to 2016 in the Optum Clinformatics DataMart deidentified commercial claims database, the researchers performed a repeated cross-sectional analysis of oral antibiotic prescriptions associated with encounters for surgical procedures performed by dermatologists. They found that oral antibiotic prescriptions increased from 2.9% to 4.4% of visits for benign excisions, from 4.2% to 6.3% of visits for malignant excisions, and from 9.9% to 13.8% of visits for Mohs procedures during this time period. Oral antibiotic prescribing was more common for procedures that entailed a flap or graft and among patients with diabetes, female patients, and younger patients.
The investigators observed greater than twofold variation in antibiotic-prescribing rates across geographic census divisions. “If higher-prescribing divisions were to develop antibiotic prescribing rates similar to [those of] lower-prescribing divisions, antibiotic use could be decreased by over 50%,” Dr. Barbieri said. Before prescribing antibiotic prophylaxis, dermatologists should consider which patients benefit most from it, he added.
The investigators also examined the duration of antibiotic courses. The median course duration of postoperative antibiotics was 7 days. Randomized, controlled trials that collectively included more than 600 patients have failed to demonstrate a benefit of long postoperative courses of antibiotics, compared with perioperative antibiotics alone, said Dr. Barbieri. “While it may be hard to have true perioperative antibiotics available in a dermatology surgical clinic, there likely are opportunities to reduce these postoperative courses to a day or 3 days from this mean of 7 days that we observed in the study.” Reducing these courses would decrease the risk of antibiotic-associated complications such as nausea, diarrhea, and skin rashes, he added.
SOURCE: AAD 2019, Abstract 11356.
WASHINGTON – , according to an analysis presented at the annual meeting of the American Academy of Dermatology.
John Barbieri, MD, a dermatologist and postdoctoral research fellow at the University of Pennsylvania, Philadelphia, who presented the results, and colleagues examined data about antibiotic use in dermatology between 2008 and 2016. Overall, antibiotic use decreased during this period, primarily for chronic conditions such as acne and rosacea. On the other hand, antibiotic use associated with surgical visits increased by approximately 70%.
Using data from 2008 to 2016 in the Optum Clinformatics DataMart deidentified commercial claims database, the researchers performed a repeated cross-sectional analysis of oral antibiotic prescriptions associated with encounters for surgical procedures performed by dermatologists. They found that oral antibiotic prescriptions increased from 2.9% to 4.4% of visits for benign excisions, from 4.2% to 6.3% of visits for malignant excisions, and from 9.9% to 13.8% of visits for Mohs procedures during this time period. Oral antibiotic prescribing was more common for procedures that entailed a flap or graft and among patients with diabetes, female patients, and younger patients.
The investigators observed greater than twofold variation in antibiotic-prescribing rates across geographic census divisions. “If higher-prescribing divisions were to develop antibiotic prescribing rates similar to [those of] lower-prescribing divisions, antibiotic use could be decreased by over 50%,” Dr. Barbieri said. Before prescribing antibiotic prophylaxis, dermatologists should consider which patients benefit most from it, he added.
The investigators also examined the duration of antibiotic courses. The median course duration of postoperative antibiotics was 7 days. Randomized, controlled trials that collectively included more than 600 patients have failed to demonstrate a benefit of long postoperative courses of antibiotics, compared with perioperative antibiotics alone, said Dr. Barbieri. “While it may be hard to have true perioperative antibiotics available in a dermatology surgical clinic, there likely are opportunities to reduce these postoperative courses to a day or 3 days from this mean of 7 days that we observed in the study.” Reducing these courses would decrease the risk of antibiotic-associated complications such as nausea, diarrhea, and skin rashes, he added.
SOURCE: AAD 2019, Abstract 11356.
WASHINGTON – , according to an analysis presented at the annual meeting of the American Academy of Dermatology.
John Barbieri, MD, a dermatologist and postdoctoral research fellow at the University of Pennsylvania, Philadelphia, who presented the results, and colleagues examined data about antibiotic use in dermatology between 2008 and 2016. Overall, antibiotic use decreased during this period, primarily for chronic conditions such as acne and rosacea. On the other hand, antibiotic use associated with surgical visits increased by approximately 70%.
Using data from 2008 to 2016 in the Optum Clinformatics DataMart deidentified commercial claims database, the researchers performed a repeated cross-sectional analysis of oral antibiotic prescriptions associated with encounters for surgical procedures performed by dermatologists. They found that oral antibiotic prescriptions increased from 2.9% to 4.4% of visits for benign excisions, from 4.2% to 6.3% of visits for malignant excisions, and from 9.9% to 13.8% of visits for Mohs procedures during this time period. Oral antibiotic prescribing was more common for procedures that entailed a flap or graft and among patients with diabetes, female patients, and younger patients.
The investigators observed greater than twofold variation in antibiotic-prescribing rates across geographic census divisions. “If higher-prescribing divisions were to develop antibiotic prescribing rates similar to [those of] lower-prescribing divisions, antibiotic use could be decreased by over 50%,” Dr. Barbieri said. Before prescribing antibiotic prophylaxis, dermatologists should consider which patients benefit most from it, he added.
The investigators also examined the duration of antibiotic courses. The median course duration of postoperative antibiotics was 7 days. Randomized, controlled trials that collectively included more than 600 patients have failed to demonstrate a benefit of long postoperative courses of antibiotics, compared with perioperative antibiotics alone, said Dr. Barbieri. “While it may be hard to have true perioperative antibiotics available in a dermatology surgical clinic, there likely are opportunities to reduce these postoperative courses to a day or 3 days from this mean of 7 days that we observed in the study.” Reducing these courses would decrease the risk of antibiotic-associated complications such as nausea, diarrhea, and skin rashes, he added.
SOURCE: AAD 2019, Abstract 11356.
REPORTING FROM AAD 2019
Indoor Tanning: Turning First-Time Clients Into Repeat Customers
Nearly 10 million people use indoor tanning (IT) even though it increases the risk of skin cancer. Young white women are particularly at risk—almost 1 in 3 reports using indoor tanning in the past year, and nearly 1 in 5 reports regular use (that is, > 10 times in the past year), according to researchers from Rutgers University in New Brunswick, New Jersey.
Research has already shown that most people use IT to enhance their appearance. But a tan is not only seen as attractive: It “plays an important part of youth culture,” the researchers note, especially when it comes to special events, like high school proms. Still, some IT users might remain “special event” users, not regular clients. What makes the difference? To find out, the researchers conducted 6 interviews with a salon employee who also used tanning beds. Their purpose was not to produce “generalizable knowledge of the experiences of many users” but to provide insights into the behavior and to propose working hypotheses for future examination.
The researchers found that the incentive to use IT mostly comes down to—as many health-related decisions do—how it is advertised. The first encounter is likely to be the most important one. That is when the sell begins, designed to “guide” the patron into coming back, and back again. For instance, the salon employee may be trained to establish rapport, to personalize the interaction, and to ask about “tan goals,” setting the stage for a process, rather than a 1-time purchase. The employee describes the steps of creating a “base tan,” maintaining the tan, deepening the tan. Framing tanning as a process sends the message that frequent visits are needed. The researchers cite self-regulation theories that posit for a habit to take hold, the individual must develop a mental model or plans for how to use the habitual behavior to achieve desired goals.
The US Federal Trade Commission and other agencies have enacted restrictions on IT industry advertisements, the researchers say. But the policy efforts have not addressed greater regulation at the point-of-purchase, other than requiring the provision of standardized risk warnings. The interview findings suggest ways to help reduce IT use. Pricing controls, for instance: If patrons had to buy single sessions—instead of in bulk—they might feel less pressured to “get their money’s worth.” Restrictions on advertisement might require salon employees also to provide information on unnecessary exposure. The researchers contrast the salon employee to a convenience store clerk who “simply serves as a cashier for purchasing cigarettes or unhealthy food options.”
The researchers suggest that their findings be followed up in larger, more representational samples.
Nearly 10 million people use indoor tanning (IT) even though it increases the risk of skin cancer. Young white women are particularly at risk—almost 1 in 3 reports using indoor tanning in the past year, and nearly 1 in 5 reports regular use (that is, > 10 times in the past year), according to researchers from Rutgers University in New Brunswick, New Jersey.
Research has already shown that most people use IT to enhance their appearance. But a tan is not only seen as attractive: It “plays an important part of youth culture,” the researchers note, especially when it comes to special events, like high school proms. Still, some IT users might remain “special event” users, not regular clients. What makes the difference? To find out, the researchers conducted 6 interviews with a salon employee who also used tanning beds. Their purpose was not to produce “generalizable knowledge of the experiences of many users” but to provide insights into the behavior and to propose working hypotheses for future examination.
The researchers found that the incentive to use IT mostly comes down to—as many health-related decisions do—how it is advertised. The first encounter is likely to be the most important one. That is when the sell begins, designed to “guide” the patron into coming back, and back again. For instance, the salon employee may be trained to establish rapport, to personalize the interaction, and to ask about “tan goals,” setting the stage for a process, rather than a 1-time purchase. The employee describes the steps of creating a “base tan,” maintaining the tan, deepening the tan. Framing tanning as a process sends the message that frequent visits are needed. The researchers cite self-regulation theories that posit for a habit to take hold, the individual must develop a mental model or plans for how to use the habitual behavior to achieve desired goals.
The US Federal Trade Commission and other agencies have enacted restrictions on IT industry advertisements, the researchers say. But the policy efforts have not addressed greater regulation at the point-of-purchase, other than requiring the provision of standardized risk warnings. The interview findings suggest ways to help reduce IT use. Pricing controls, for instance: If patrons had to buy single sessions—instead of in bulk—they might feel less pressured to “get their money’s worth.” Restrictions on advertisement might require salon employees also to provide information on unnecessary exposure. The researchers contrast the salon employee to a convenience store clerk who “simply serves as a cashier for purchasing cigarettes or unhealthy food options.”
The researchers suggest that their findings be followed up in larger, more representational samples.
Nearly 10 million people use indoor tanning (IT) even though it increases the risk of skin cancer. Young white women are particularly at risk—almost 1 in 3 reports using indoor tanning in the past year, and nearly 1 in 5 reports regular use (that is, > 10 times in the past year), according to researchers from Rutgers University in New Brunswick, New Jersey.
Research has already shown that most people use IT to enhance their appearance. But a tan is not only seen as attractive: It “plays an important part of youth culture,” the researchers note, especially when it comes to special events, like high school proms. Still, some IT users might remain “special event” users, not regular clients. What makes the difference? To find out, the researchers conducted 6 interviews with a salon employee who also used tanning beds. Their purpose was not to produce “generalizable knowledge of the experiences of many users” but to provide insights into the behavior and to propose working hypotheses for future examination.
The researchers found that the incentive to use IT mostly comes down to—as many health-related decisions do—how it is advertised. The first encounter is likely to be the most important one. That is when the sell begins, designed to “guide” the patron into coming back, and back again. For instance, the salon employee may be trained to establish rapport, to personalize the interaction, and to ask about “tan goals,” setting the stage for a process, rather than a 1-time purchase. The employee describes the steps of creating a “base tan,” maintaining the tan, deepening the tan. Framing tanning as a process sends the message that frequent visits are needed. The researchers cite self-regulation theories that posit for a habit to take hold, the individual must develop a mental model or plans for how to use the habitual behavior to achieve desired goals.
The US Federal Trade Commission and other agencies have enacted restrictions on IT industry advertisements, the researchers say. But the policy efforts have not addressed greater regulation at the point-of-purchase, other than requiring the provision of standardized risk warnings. The interview findings suggest ways to help reduce IT use. Pricing controls, for instance: If patrons had to buy single sessions—instead of in bulk—they might feel less pressured to “get their money’s worth.” Restrictions on advertisement might require salon employees also to provide information on unnecessary exposure. The researchers contrast the salon employee to a convenience store clerk who “simply serves as a cashier for purchasing cigarettes or unhealthy food options.”
The researchers suggest that their findings be followed up in larger, more representational samples.






