User login
Blocking a lipoprotein lipase inhibitor improves lipid profiles
Two different approaches to shutting down the function of a human liver protein that inhibits lipoprotein lipase showed preliminary evidence of safely producing favorable lipid changes in healthy volunteers in two separate, phase 1 studies.
These findings, coupled with promising observational data from people who carry loss-of-function mutations in the gene for this protein, angiopoietin-like 3 (ANGPTL3), have raised hopes that interventions that interfere with the function of the ANGPTL3 protein may provide new and effective ways to improve lipid levels and cut the incidence of cardiovascular disease events.
“There is now a growing body of epidemiologic, genetic, and genomewide association studies supporting the hypothesis that lowering levels of ANGPTL3 in plasma by inhibiting hepatic ANGPTL3 synthesis will be beneficial in terms of reducing plasma levels of atherogenic apolipoprotein B and in improving metabolic measures associated with dyslipidemia,” wrote Mark J. Graham and his associates in a recently published article (N Engl J Med. 2017 Jul 20;377[3]:222-32).
The phase 1 study results reported by this group came from 44 healthy adults aged 18-65 years who received varying doses of a commercially developed antisense drug, ANGPTL3-LRX, as either single or serial subcutaneous injections. ANGPTL3-LRX is an oligonucleotide designed to inhibit production of messenger RNA for the ANGPTL3 protein.
Six people received the highest ANGPTL3-LRX dosage administered, 60 mg given as a weekly injection for 6 weeks, and after this regimen they showed an average 50% cut in triglycerides levels, compared with baseline, and an average 33% drop in their low LDL cholesterol levels from baseline. None of the 33 people treated with ANGPTL3-LRX in the trial had a documented serious adverse event, and the only treatment dropout was a patient who was lost to follow-up during the treatment phase, reported Mr. Graham, a researcher at Ionis Pharmaceuticals, the sponsor of the study and the company developing the antisense drug, and his associates.
The second phase 1 study examined a different way to block ANGPTL3 activity, with a human monoclonal antibody to this protein. The study involved 83 healthy adults aged 18-65 years with fasting triglyceride levels of 150-450 mg/dL and fasting LDL cholesterol levels of at least 100 mg/dL. Each participant received a single subcutaneous injection or intravenous dose of the antibody, evinacumab, at varying amounts or placebo. The maximum observed lipid changes seen was a drop in triglycerides of 76% and a fall in LDL cholesterol by 23%. Treatment also produced a maximum drop in HDL cholesterol of 18%. No person left the study because of an adverse event. The most common adverse event was headache, in seven people (11% of evinacumab recipients), reported Frederick E. Dewey, MD, a researcher at Regeneron Pharmaceuticals, the company developing evinacumab, and his associates (N Engl J Med. 2017 Jul 20;377[3]:211-21).
The Regeneron report also included results from population studies they ran. They reported performing genome sequencing on specimens from 58,335 adults enrolled in the DiscovEHR study, and identified 13 distinct loss-of-function variants in the ANGPTL3 genes that occurred individually in a small number of these people.
They then ran analyses of lipid levels and coronary artery disease prevalence rates in people who carry one of these 13 loss-of-function genetic signatures in one of their ANGTPL3 genes. Among 45,226 of the people in DiscovEHR those with a variant had on average a 27% lower triglyceride level, a 9% lower LDL cholesterol level, and a 4% lower HDL cholesterol level than noncarriers, after adjustment for covariates. Analysis of coronary artery disease prevalence showed that, after adjusting for age, sex, and ancestry, carrying a loss-of-function variant was linked with a statistically significant 41% lower prevalence of all coronary artery disease, and a 34% lower prevalence of myocardial infarction that fell short of statistical significance.
A second population study looked at links between loss-of-function variants and coronary artery disease in more than 130,000 Danish people. This showed a nonsignificant 37% lower prevalence of coronary artery disease in people with a variant. Two different types of meta-analyses of the data from both the DiscovEHR and Danish studies showed coronary disease rates reduced by either 31% or 39% in variant carriers depending on which meta-analysis approach the researchers used, both statistically significant reductions.
[email protected]
On Twitter @mitchelzoler
The findings from these two studies together with other recent study results open a new therapeutic window for reducing elevated levels of triglyceride-rich lipoproteins by activating lipoprotein lipase.
The findings also suggest that inhibition of the ANGPTL3 gene or protein is potentially an effective way to treat patients with familial hypercholesterolemia because of a deficiency in the receptor for low density lipoprotein. It is likely that lowering triglyceride levels with an agent that boosts the activity of lipoprotein lipase will result in a different spectrum of benefits and adverse effects, compared with agents that boost the number of LDL receptors.
New approaches to boost lipoprotein lipase activity, such as inhibiting ANGPTL3 function as was done in these two reports, represents a fresh frontier for treatment of hypertriglyceridemia and coronary artery disease.
Alan R. Tall, MD , professor of medicine at Columbia University, New York, made these comments in an editorial ( N Engl J Med. 2017 Jul 20;377[3]:280-3 ).
The findings from these two studies together with other recent study results open a new therapeutic window for reducing elevated levels of triglyceride-rich lipoproteins by activating lipoprotein lipase.
The findings also suggest that inhibition of the ANGPTL3 gene or protein is potentially an effective way to treat patients with familial hypercholesterolemia because of a deficiency in the receptor for low density lipoprotein. It is likely that lowering triglyceride levels with an agent that boosts the activity of lipoprotein lipase will result in a different spectrum of benefits and adverse effects, compared with agents that boost the number of LDL receptors.
New approaches to boost lipoprotein lipase activity, such as inhibiting ANGPTL3 function as was done in these two reports, represents a fresh frontier for treatment of hypertriglyceridemia and coronary artery disease.
Alan R. Tall, MD , professor of medicine at Columbia University, New York, made these comments in an editorial ( N Engl J Med. 2017 Jul 20;377[3]:280-3 ).
The findings from these two studies together with other recent study results open a new therapeutic window for reducing elevated levels of triglyceride-rich lipoproteins by activating lipoprotein lipase.
The findings also suggest that inhibition of the ANGPTL3 gene or protein is potentially an effective way to treat patients with familial hypercholesterolemia because of a deficiency in the receptor for low density lipoprotein. It is likely that lowering triglyceride levels with an agent that boosts the activity of lipoprotein lipase will result in a different spectrum of benefits and adverse effects, compared with agents that boost the number of LDL receptors.
New approaches to boost lipoprotein lipase activity, such as inhibiting ANGPTL3 function as was done in these two reports, represents a fresh frontier for treatment of hypertriglyceridemia and coronary artery disease.
Alan R. Tall, MD , professor of medicine at Columbia University, New York, made these comments in an editorial ( N Engl J Med. 2017 Jul 20;377[3]:280-3 ).
Two different approaches to shutting down the function of a human liver protein that inhibits lipoprotein lipase showed preliminary evidence of safely producing favorable lipid changes in healthy volunteers in two separate, phase 1 studies.
These findings, coupled with promising observational data from people who carry loss-of-function mutations in the gene for this protein, angiopoietin-like 3 (ANGPTL3), have raised hopes that interventions that interfere with the function of the ANGPTL3 protein may provide new and effective ways to improve lipid levels and cut the incidence of cardiovascular disease events.
“There is now a growing body of epidemiologic, genetic, and genomewide association studies supporting the hypothesis that lowering levels of ANGPTL3 in plasma by inhibiting hepatic ANGPTL3 synthesis will be beneficial in terms of reducing plasma levels of atherogenic apolipoprotein B and in improving metabolic measures associated with dyslipidemia,” wrote Mark J. Graham and his associates in a recently published article (N Engl J Med. 2017 Jul 20;377[3]:222-32).
The phase 1 study results reported by this group came from 44 healthy adults aged 18-65 years who received varying doses of a commercially developed antisense drug, ANGPTL3-LRX, as either single or serial subcutaneous injections. ANGPTL3-LRX is an oligonucleotide designed to inhibit production of messenger RNA for the ANGPTL3 protein.
Six people received the highest ANGPTL3-LRX dosage administered, 60 mg given as a weekly injection for 6 weeks, and after this regimen they showed an average 50% cut in triglycerides levels, compared with baseline, and an average 33% drop in their low LDL cholesterol levels from baseline. None of the 33 people treated with ANGPTL3-LRX in the trial had a documented serious adverse event, and the only treatment dropout was a patient who was lost to follow-up during the treatment phase, reported Mr. Graham, a researcher at Ionis Pharmaceuticals, the sponsor of the study and the company developing the antisense drug, and his associates.
The second phase 1 study examined a different way to block ANGPTL3 activity, with a human monoclonal antibody to this protein. The study involved 83 healthy adults aged 18-65 years with fasting triglyceride levels of 150-450 mg/dL and fasting LDL cholesterol levels of at least 100 mg/dL. Each participant received a single subcutaneous injection or intravenous dose of the antibody, evinacumab, at varying amounts or placebo. The maximum observed lipid changes seen was a drop in triglycerides of 76% and a fall in LDL cholesterol by 23%. Treatment also produced a maximum drop in HDL cholesterol of 18%. No person left the study because of an adverse event. The most common adverse event was headache, in seven people (11% of evinacumab recipients), reported Frederick E. Dewey, MD, a researcher at Regeneron Pharmaceuticals, the company developing evinacumab, and his associates (N Engl J Med. 2017 Jul 20;377[3]:211-21).
The Regeneron report also included results from population studies they ran. They reported performing genome sequencing on specimens from 58,335 adults enrolled in the DiscovEHR study, and identified 13 distinct loss-of-function variants in the ANGPTL3 genes that occurred individually in a small number of these people.
They then ran analyses of lipid levels and coronary artery disease prevalence rates in people who carry one of these 13 loss-of-function genetic signatures in one of their ANGTPL3 genes. Among 45,226 of the people in DiscovEHR those with a variant had on average a 27% lower triglyceride level, a 9% lower LDL cholesterol level, and a 4% lower HDL cholesterol level than noncarriers, after adjustment for covariates. Analysis of coronary artery disease prevalence showed that, after adjusting for age, sex, and ancestry, carrying a loss-of-function variant was linked with a statistically significant 41% lower prevalence of all coronary artery disease, and a 34% lower prevalence of myocardial infarction that fell short of statistical significance.
A second population study looked at links between loss-of-function variants and coronary artery disease in more than 130,000 Danish people. This showed a nonsignificant 37% lower prevalence of coronary artery disease in people with a variant. Two different types of meta-analyses of the data from both the DiscovEHR and Danish studies showed coronary disease rates reduced by either 31% or 39% in variant carriers depending on which meta-analysis approach the researchers used, both statistically significant reductions.
[email protected]
On Twitter @mitchelzoler
Two different approaches to shutting down the function of a human liver protein that inhibits lipoprotein lipase showed preliminary evidence of safely producing favorable lipid changes in healthy volunteers in two separate, phase 1 studies.
These findings, coupled with promising observational data from people who carry loss-of-function mutations in the gene for this protein, angiopoietin-like 3 (ANGPTL3), have raised hopes that interventions that interfere with the function of the ANGPTL3 protein may provide new and effective ways to improve lipid levels and cut the incidence of cardiovascular disease events.
“There is now a growing body of epidemiologic, genetic, and genomewide association studies supporting the hypothesis that lowering levels of ANGPTL3 in plasma by inhibiting hepatic ANGPTL3 synthesis will be beneficial in terms of reducing plasma levels of atherogenic apolipoprotein B and in improving metabolic measures associated with dyslipidemia,” wrote Mark J. Graham and his associates in a recently published article (N Engl J Med. 2017 Jul 20;377[3]:222-32).
The phase 1 study results reported by this group came from 44 healthy adults aged 18-65 years who received varying doses of a commercially developed antisense drug, ANGPTL3-LRX, as either single or serial subcutaneous injections. ANGPTL3-LRX is an oligonucleotide designed to inhibit production of messenger RNA for the ANGPTL3 protein.
Six people received the highest ANGPTL3-LRX dosage administered, 60 mg given as a weekly injection for 6 weeks, and after this regimen they showed an average 50% cut in triglycerides levels, compared with baseline, and an average 33% drop in their low LDL cholesterol levels from baseline. None of the 33 people treated with ANGPTL3-LRX in the trial had a documented serious adverse event, and the only treatment dropout was a patient who was lost to follow-up during the treatment phase, reported Mr. Graham, a researcher at Ionis Pharmaceuticals, the sponsor of the study and the company developing the antisense drug, and his associates.
The second phase 1 study examined a different way to block ANGPTL3 activity, with a human monoclonal antibody to this protein. The study involved 83 healthy adults aged 18-65 years with fasting triglyceride levels of 150-450 mg/dL and fasting LDL cholesterol levels of at least 100 mg/dL. Each participant received a single subcutaneous injection or intravenous dose of the antibody, evinacumab, at varying amounts or placebo. The maximum observed lipid changes seen was a drop in triglycerides of 76% and a fall in LDL cholesterol by 23%. Treatment also produced a maximum drop in HDL cholesterol of 18%. No person left the study because of an adverse event. The most common adverse event was headache, in seven people (11% of evinacumab recipients), reported Frederick E. Dewey, MD, a researcher at Regeneron Pharmaceuticals, the company developing evinacumab, and his associates (N Engl J Med. 2017 Jul 20;377[3]:211-21).
The Regeneron report also included results from population studies they ran. They reported performing genome sequencing on specimens from 58,335 adults enrolled in the DiscovEHR study, and identified 13 distinct loss-of-function variants in the ANGPTL3 genes that occurred individually in a small number of these people.
They then ran analyses of lipid levels and coronary artery disease prevalence rates in people who carry one of these 13 loss-of-function genetic signatures in one of their ANGTPL3 genes. Among 45,226 of the people in DiscovEHR those with a variant had on average a 27% lower triglyceride level, a 9% lower LDL cholesterol level, and a 4% lower HDL cholesterol level than noncarriers, after adjustment for covariates. Analysis of coronary artery disease prevalence showed that, after adjusting for age, sex, and ancestry, carrying a loss-of-function variant was linked with a statistically significant 41% lower prevalence of all coronary artery disease, and a 34% lower prevalence of myocardial infarction that fell short of statistical significance.
A second population study looked at links between loss-of-function variants and coronary artery disease in more than 130,000 Danish people. This showed a nonsignificant 37% lower prevalence of coronary artery disease in people with a variant. Two different types of meta-analyses of the data from both the DiscovEHR and Danish studies showed coronary disease rates reduced by either 31% or 39% in variant carriers depending on which meta-analysis approach the researchers used, both statistically significant reductions.
[email protected]
On Twitter @mitchelzoler
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Serial doses of the antisense oligonucleotide ANGPTL3-LRX produced an average 50% cut in triglycerides and 33% cut in LDL cholesterol.
Data source: The ANGPTL3-LRX phase 1 trial enrolled 44 healthy adults. The evinacumab phase 1 trial enrolled 83 healthy adults.
Disclosures: The ANGPTL3-LRX study was funded by Ionis. Mr. Graham is an employee of Ionis. The evinacumab study was funded by Regeneron. Dr. Dewey is an employee of Regeneron.
Cord Blood and Cord Tissue Preservation Information for Your Patients
Your patients may be overwhelmed with so many decisions as they prepare for their newborn to arrive. We want to help make one decision easier. The Cord Blood and Cord Tissue Preservation Patient Handout provides simple and clear education about their cord blood and cord tissue preservation options.
Access and print the handout now and give it to your patients so they can review the information at their own pace.
Your patients may be overwhelmed with so many decisions as they prepare for their newborn to arrive. We want to help make one decision easier. The Cord Blood and Cord Tissue Preservation Patient Handout provides simple and clear education about their cord blood and cord tissue preservation options.
Access and print the handout now and give it to your patients so they can review the information at their own pace.
Your patients may be overwhelmed with so many decisions as they prepare for their newborn to arrive. We want to help make one decision easier. The Cord Blood and Cord Tissue Preservation Patient Handout provides simple and clear education about their cord blood and cord tissue preservation options.
Access and print the handout now and give it to your patients so they can review the information at their own pace.
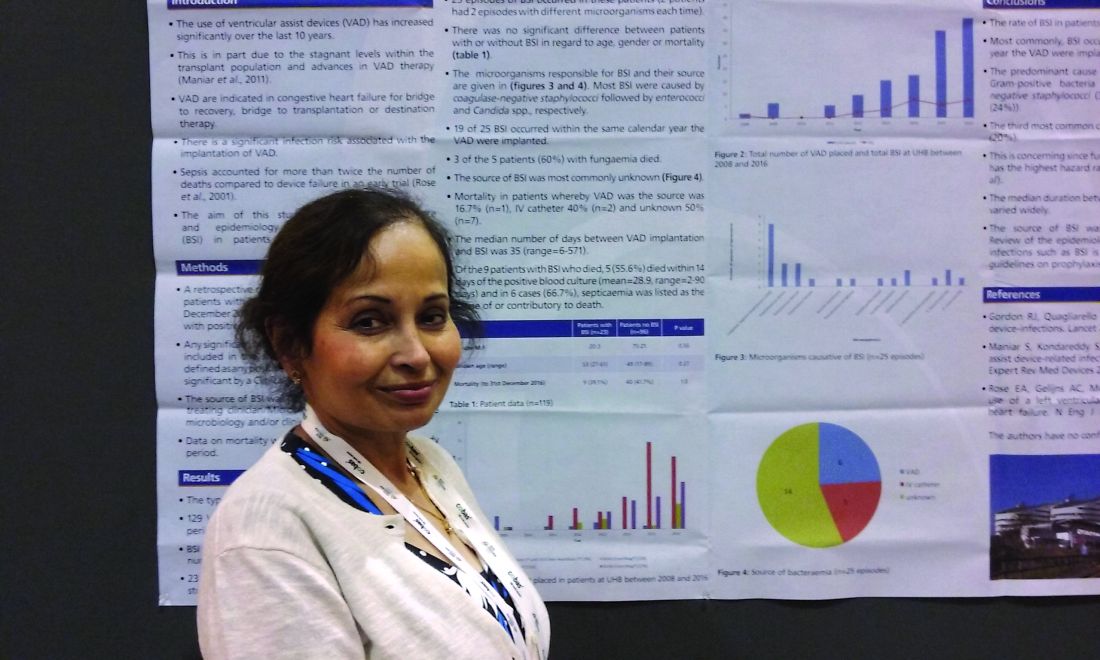
Ventricular assist devices linked to sepsis
NEW ORLEANS – Back in 2008, there was only one case.
Since then, however, the number of patients with ventricular assist devices who developed sepsis while being treated in the cardiac unit at Queen Elizabeth Hospital in Birmingham, England, appeared to be noticeably growing. So, investigators launched a study to confirm their suspicions and to learn more about the underlying causes.
“Bloodstream infection is a serious infection, so I thought, ‘Let’s see what’s happening,’ ” explained Ira Das, MD, a consultant microbiologist at Queen Elizabeth Hospital.
Coagulase-negative staphylococci were the most common cause, present in 32% of the 25 cases. Sepsis was caused by Enterococcus faecium in 12%, Candida parapsilosis in 8%, and Staphylococcus aureus in 2%. Another 4% were either Enterococcus faecalis, Serratia marcescens, Pseudomonas aeruginosa, C. guilliermondii, or C. orthopsilosis. The remaining 16% of bloodstream infections were polymicrobial.
Less certain was the source of these infections.
“In the majority of cases, we didn’t know where it was coming from,” Dr. Das said at the annual meeting of the American Society for Microbiology. In 6 of the 25 cases, VAD was confirmed to be the focus of infection, either through imaging or because a failing component of the explanted device was examined later. An intravascular catheter was the source in another 5 patients, and in 14 cases, the source remained a mystery.
“Some of these infections just might have been hard to see,” Dr. Das said. “If the infection is inside the device, it’s not always easy to visualize.”
The study supports earlier findings from a review article that points to a significant infection risk associated with the implantation of VADs (Expert Rev Med Devices. 2011 Sep;8[5]:627-34). That article’s authors noted, “Despite recent improvements in outcomes, device-related infections remain a significant complication of LVAD [left ventricular assist device] therapy.”
In a previous study of people with end-stage heart failure, other investigators noted that, “despite the substantial survival benefit, the morbidity and mortality associated with the use of the left ventricular assist device were considerable. In particular, infection and mechanical failure of the device were major factors in the 2-year survival rate of only 23%” (N Engl J Med. 2001 Nov 15;345[20]:1435-43).
Similarly, in the current study, mortality was higher among those with sepsis and a VAD. Mortality was 39% – including eight patients who died with a VAD in situ and one following cardiac transplantation. However, Dr. Das cautioned, “It’s a small number, and there are other factors that could have contributed. They all go on anticoagulants so they have bleeding tendencies, and many of the patients are in the ICU with multiorgan failure.”
Infection prevention remains paramount to minimize mortality and other adverse events associated with a patient’s having a VAD. “We have to make sure that infection control procedures and our treatments are up to the optimal standard,” Dr. Das said. “It’s not easy to remove the device.”
Of the 129 VADs implanted, 68 were long-term LVADs, 11 were short-term LVADs, 15 were right ventricular devices, and 35 were biventricular devices.
The study is ongoing. The data presented at the meeting were collected up until December 2016.
“Since then, I’ve seen two more cases, and – very interestingly – one was Haemophilus influenzae,” Dr. Das said. “The patient was on the device, he was at home, and he came in with bacteremia.” Again, the source of infection proved elusive. “With H. influenzae, you would think it was coming from his chest, but the chest x-ray was normal.”
The second case, a patient with a coagulase-negative staphylococci bloodstream infection, was scheduled for a PET scan at the time of Dr. Das’ presentation to try to identify the source of infection.
Dr. Das had no relevant disclosures.
Modern technology saves our patients' lives, but there is always another side to the coin. Reports that LVAD devices are associated with a high incidence of bloodstream infections is important for future clinical practice. The fact that the causes and risk factors for these infections are unknown make this phenomena one of high interest.
Modern technology saves our patients' lives, but there is always another side to the coin. Reports that LVAD devices are associated with a high incidence of bloodstream infections is important for future clinical practice. The fact that the causes and risk factors for these infections are unknown make this phenomena one of high interest.
Modern technology saves our patients' lives, but there is always another side to the coin. Reports that LVAD devices are associated with a high incidence of bloodstream infections is important for future clinical practice. The fact that the causes and risk factors for these infections are unknown make this phenomena one of high interest.
NEW ORLEANS – Back in 2008, there was only one case.
Since then, however, the number of patients with ventricular assist devices who developed sepsis while being treated in the cardiac unit at Queen Elizabeth Hospital in Birmingham, England, appeared to be noticeably growing. So, investigators launched a study to confirm their suspicions and to learn more about the underlying causes.
“Bloodstream infection is a serious infection, so I thought, ‘Let’s see what’s happening,’ ” explained Ira Das, MD, a consultant microbiologist at Queen Elizabeth Hospital.
Coagulase-negative staphylococci were the most common cause, present in 32% of the 25 cases. Sepsis was caused by Enterococcus faecium in 12%, Candida parapsilosis in 8%, and Staphylococcus aureus in 2%. Another 4% were either Enterococcus faecalis, Serratia marcescens, Pseudomonas aeruginosa, C. guilliermondii, or C. orthopsilosis. The remaining 16% of bloodstream infections were polymicrobial.
Less certain was the source of these infections.
“In the majority of cases, we didn’t know where it was coming from,” Dr. Das said at the annual meeting of the American Society for Microbiology. In 6 of the 25 cases, VAD was confirmed to be the focus of infection, either through imaging or because a failing component of the explanted device was examined later. An intravascular catheter was the source in another 5 patients, and in 14 cases, the source remained a mystery.
“Some of these infections just might have been hard to see,” Dr. Das said. “If the infection is inside the device, it’s not always easy to visualize.”
The study supports earlier findings from a review article that points to a significant infection risk associated with the implantation of VADs (Expert Rev Med Devices. 2011 Sep;8[5]:627-34). That article’s authors noted, “Despite recent improvements in outcomes, device-related infections remain a significant complication of LVAD [left ventricular assist device] therapy.”
In a previous study of people with end-stage heart failure, other investigators noted that, “despite the substantial survival benefit, the morbidity and mortality associated with the use of the left ventricular assist device were considerable. In particular, infection and mechanical failure of the device were major factors in the 2-year survival rate of only 23%” (N Engl J Med. 2001 Nov 15;345[20]:1435-43).
Similarly, in the current study, mortality was higher among those with sepsis and a VAD. Mortality was 39% – including eight patients who died with a VAD in situ and one following cardiac transplantation. However, Dr. Das cautioned, “It’s a small number, and there are other factors that could have contributed. They all go on anticoagulants so they have bleeding tendencies, and many of the patients are in the ICU with multiorgan failure.”
Infection prevention remains paramount to minimize mortality and other adverse events associated with a patient’s having a VAD. “We have to make sure that infection control procedures and our treatments are up to the optimal standard,” Dr. Das said. “It’s not easy to remove the device.”
Of the 129 VADs implanted, 68 were long-term LVADs, 11 were short-term LVADs, 15 were right ventricular devices, and 35 were biventricular devices.
The study is ongoing. The data presented at the meeting were collected up until December 2016.
“Since then, I’ve seen two more cases, and – very interestingly – one was Haemophilus influenzae,” Dr. Das said. “The patient was on the device, he was at home, and he came in with bacteremia.” Again, the source of infection proved elusive. “With H. influenzae, you would think it was coming from his chest, but the chest x-ray was normal.”
The second case, a patient with a coagulase-negative staphylococci bloodstream infection, was scheduled for a PET scan at the time of Dr. Das’ presentation to try to identify the source of infection.
Dr. Das had no relevant disclosures.
NEW ORLEANS – Back in 2008, there was only one case.
Since then, however, the number of patients with ventricular assist devices who developed sepsis while being treated in the cardiac unit at Queen Elizabeth Hospital in Birmingham, England, appeared to be noticeably growing. So, investigators launched a study to confirm their suspicions and to learn more about the underlying causes.
“Bloodstream infection is a serious infection, so I thought, ‘Let’s see what’s happening,’ ” explained Ira Das, MD, a consultant microbiologist at Queen Elizabeth Hospital.
Coagulase-negative staphylococci were the most common cause, present in 32% of the 25 cases. Sepsis was caused by Enterococcus faecium in 12%, Candida parapsilosis in 8%, and Staphylococcus aureus in 2%. Another 4% were either Enterococcus faecalis, Serratia marcescens, Pseudomonas aeruginosa, C. guilliermondii, or C. orthopsilosis. The remaining 16% of bloodstream infections were polymicrobial.
Less certain was the source of these infections.
“In the majority of cases, we didn’t know where it was coming from,” Dr. Das said at the annual meeting of the American Society for Microbiology. In 6 of the 25 cases, VAD was confirmed to be the focus of infection, either through imaging or because a failing component of the explanted device was examined later. An intravascular catheter was the source in another 5 patients, and in 14 cases, the source remained a mystery.
“Some of these infections just might have been hard to see,” Dr. Das said. “If the infection is inside the device, it’s not always easy to visualize.”
The study supports earlier findings from a review article that points to a significant infection risk associated with the implantation of VADs (Expert Rev Med Devices. 2011 Sep;8[5]:627-34). That article’s authors noted, “Despite recent improvements in outcomes, device-related infections remain a significant complication of LVAD [left ventricular assist device] therapy.”
In a previous study of people with end-stage heart failure, other investigators noted that, “despite the substantial survival benefit, the morbidity and mortality associated with the use of the left ventricular assist device were considerable. In particular, infection and mechanical failure of the device were major factors in the 2-year survival rate of only 23%” (N Engl J Med. 2001 Nov 15;345[20]:1435-43).
Similarly, in the current study, mortality was higher among those with sepsis and a VAD. Mortality was 39% – including eight patients who died with a VAD in situ and one following cardiac transplantation. However, Dr. Das cautioned, “It’s a small number, and there are other factors that could have contributed. They all go on anticoagulants so they have bleeding tendencies, and many of the patients are in the ICU with multiorgan failure.”
Infection prevention remains paramount to minimize mortality and other adverse events associated with a patient’s having a VAD. “We have to make sure that infection control procedures and our treatments are up to the optimal standard,” Dr. Das said. “It’s not easy to remove the device.”
Of the 129 VADs implanted, 68 were long-term LVADs, 11 were short-term LVADs, 15 were right ventricular devices, and 35 were biventricular devices.
The study is ongoing. The data presented at the meeting were collected up until December 2016.
“Since then, I’ve seen two more cases, and – very interestingly – one was Haemophilus influenzae,” Dr. Das said. “The patient was on the device, he was at home, and he came in with bacteremia.” Again, the source of infection proved elusive. “With H. influenzae, you would think it was coming from his chest, but the chest x-ray was normal.”
The second case, a patient with a coagulase-negative staphylococci bloodstream infection, was scheduled for a PET scan at the time of Dr. Das’ presentation to try to identify the source of infection.
Dr. Das had no relevant disclosures.
AT ASM MICROBE 2017
Key clinical point: There may be a significant rate of bloodstream infections among people with a ventricular assist device.
Major finding: A total of 20% of the 118 people with a VAD had a bloodstream infection.
Data source: A retrospective study of 129 ventricular assist devices placed in 118 people between 2008 and 2016.
Disclosures: Dr. Das had no relevant disclosures.
Online intervention aims to prevent teen depression
AT PAS 17
SAN FRANCISCO – One in eight teenagers experienced at least one major depressive episode in 2015, according to the National Institute for Mental Health. Yet the recent uptick in teen suicide rates suggests that U.S. mental health care services are not meeting their needs.
A team at the University of Illinois in Chicago, led by Benjamin Van Voorhees, MD, MPH, hopes so, and they have spent the past several years developing and testing such a program with a National Institute of Mental Health (NIMH) grant.
“Adolescents are in a really plastic moment in their psychobehavioral repertoire and brain development as they program themselves to adapt to adult life,” Dr. Van Voorhees said in an interview. “Right now we have nothing to offer those individuals other than an occasional referral to an overtaxed mental health system. The only rational strategy is a mass dissemination model, which is going to have to be technology.”
The CATCH-IT program is aimed at teens showing early signs of depression or predepressive symptoms as determined through screening during well checks or other visits for acute or chronic concerns. The study uses multiple screening tools in selecting participants, but Dr. Van Voorhees estimates that screening in practice would require about 1-2 minutes of a medical assistant’s or nurse’s time, followed by 1-2 minutes of the practitioner’s time for positive screens – “and one in five of those screens is going to be positive,” he said.
“The thing we want to convey to primary care practitioners is that these individuals are coming through your office every day, we’re doing nothing for them, and in some ways we are ignoring their enormous future potential adverse trajectory toward mental disorders,” he said.
The program includes 14 modules drawing on cognitive behavioral therapy, behavioral activation, interpersonal psychotherapy, and community resiliency. Six archetypal teens – such as teen living with a single mom or one whose parents are divorcing – are featured in each of the modules to demonstrate six ways of applying the strategies taught in that module. The archetypal teens are around 14-15 years old, but the program is aimed at teens aged 13-18 years, with a reading level at about grade 6, Dr. Van Voorhees said.
Two and a half years after those teens used the CATCH-IT intervention, they showed “a sustained reduction in automatic negative thoughts and educational impairment,” but no difference in their perceptions of support from family or friends. The lack of a control group in that pilot limits what conclusions can be drawn about the program’s effectiveness, but the researchers did learn that motivational interviewing led to greater engagement with the program, compared with teens who received a brief recommendation of it.
Therefore, in the subsequent – and still ongoing – study, physicians used motivational interviewing when offering teens the opportunity to join the program. That study does include a control group, in which participants are assigned a generic health education program online instead of CATCH-IT, and the randomized participants have been stratified by site, gender, and depression risk level.
The researchers first assessed the baseline characteristics of the population, recruited from 38 clinics in two cities. The study enrolled 369 teens aged 13-18 years – 248 in Chicago and 121 in Boston. All were identified as high risk for depression based on elevated scores on the Center for Epidemiological Studies Depression (CES-D) scale or the Kiddie Schedule for Affective Disorders Scale (K-SADS). Two thirds (68%) of participants are female, and most (63%) are in high school. About a third (34%) are in middle school. The racial/ethnic breakdown of the sample is 21% Hispanic, 26% black, 43% white, 4% Asian, 6% multiracial, and 1% other (which adds up to 101% due to rounding). More than half of the participants’ mothers (60%) and fathers (53%) were college graduates.
The teens completed the CES-D, the Screen for Child Related Anxiety Disorders (SCARED), the Beck Hopelessness Scale (BHS), the CRAFFT screening for adolescent substance misuse and the Disruptive Behaviors Disorder Scale (DBD-A). A parent of each teen also filled out the CES-D and DBD-A.
The baseline results did not suggest any concerns about substance use, hopelessness, or disruptive behaviors such as ADHD or conduct disorder. But the average scores on the CES-D and SCARED sat just at the threshold for a potential depressive or anxiety disorders. A CES-D score of at least 16 suggests a possible depressive disorder, and a SCARED score of at least 25 suggests a possible anxiety disorder. The mean scores on the teens’ CES-D were 17.7 in the Chicago cohort, 15.4 in the Boston cohort and 16.9 for the whole group. Similarly, the SCARED mean scores were 26.3 in the Chicago cohort, 23.5 in the Boston cohort and 25.3 overall.
Scores from K-SADS showed subthreshold levels of depressed mood in 36% of teens in both cities, and a nearly identical subthreshold level of irritability. Subthreshold anhedonia was identified in 20% of the overall population. One percent of the overall population had current suicidal ideation.
The next steps are to analyze outcomes among the participants, as the team is doing currently. They have just passed the 1-year anniversary of the trial and are analyzing the data they collected over the past year. The study will run an additional year for longer-term data collection.
One of the abstracts presented at PAS explored the economic implications of incorporating CATCH-IT in primary care.
“The cost for implementation is where the challenge is,” Dr. Van Voorhees said. “Screening takes time, and calling people takes time.” But when spread across a practice’s overall clientele in a year, the costs drop considerably, he said, and savings from effective identification and depression prevention may outweigh costs. The researchers have not yet conducted a cost-effectiveness study because they still are analyzing data on outcomes.
But Dr. Van Voorhees is optimistic about the possibilities of the program.
“What this entire model is about is, how do we understand what’s going on in the environment of the primary care clinic to find these people, identify them, and motivate them, and how can we give them something relevant enough to actually complete,” Dr. Van Voorhees said in the interview. “Then, let’s actually see if it changes their behavioral trajectory.”
The National Institute of Mental Health funded the research. Dr. Van Voorhees has consulted for Prevail Health Solutions, Mevident, Social Kinetics, and Hong Kong University on development of Internet-based interventions.
AT PAS 17
SAN FRANCISCO – One in eight teenagers experienced at least one major depressive episode in 2015, according to the National Institute for Mental Health. Yet the recent uptick in teen suicide rates suggests that U.S. mental health care services are not meeting their needs.
A team at the University of Illinois in Chicago, led by Benjamin Van Voorhees, MD, MPH, hopes so, and they have spent the past several years developing and testing such a program with a National Institute of Mental Health (NIMH) grant.
“Adolescents are in a really plastic moment in their psychobehavioral repertoire and brain development as they program themselves to adapt to adult life,” Dr. Van Voorhees said in an interview. “Right now we have nothing to offer those individuals other than an occasional referral to an overtaxed mental health system. The only rational strategy is a mass dissemination model, which is going to have to be technology.”
The CATCH-IT program is aimed at teens showing early signs of depression or predepressive symptoms as determined through screening during well checks or other visits for acute or chronic concerns. The study uses multiple screening tools in selecting participants, but Dr. Van Voorhees estimates that screening in practice would require about 1-2 minutes of a medical assistant’s or nurse’s time, followed by 1-2 minutes of the practitioner’s time for positive screens – “and one in five of those screens is going to be positive,” he said.
“The thing we want to convey to primary care practitioners is that these individuals are coming through your office every day, we’re doing nothing for them, and in some ways we are ignoring their enormous future potential adverse trajectory toward mental disorders,” he said.
The program includes 14 modules drawing on cognitive behavioral therapy, behavioral activation, interpersonal psychotherapy, and community resiliency. Six archetypal teens – such as teen living with a single mom or one whose parents are divorcing – are featured in each of the modules to demonstrate six ways of applying the strategies taught in that module. The archetypal teens are around 14-15 years old, but the program is aimed at teens aged 13-18 years, with a reading level at about grade 6, Dr. Van Voorhees said.
Two and a half years after those teens used the CATCH-IT intervention, they showed “a sustained reduction in automatic negative thoughts and educational impairment,” but no difference in their perceptions of support from family or friends. The lack of a control group in that pilot limits what conclusions can be drawn about the program’s effectiveness, but the researchers did learn that motivational interviewing led to greater engagement with the program, compared with teens who received a brief recommendation of it.
Therefore, in the subsequent – and still ongoing – study, physicians used motivational interviewing when offering teens the opportunity to join the program. That study does include a control group, in which participants are assigned a generic health education program online instead of CATCH-IT, and the randomized participants have been stratified by site, gender, and depression risk level.
The researchers first assessed the baseline characteristics of the population, recruited from 38 clinics in two cities. The study enrolled 369 teens aged 13-18 years – 248 in Chicago and 121 in Boston. All were identified as high risk for depression based on elevated scores on the Center for Epidemiological Studies Depression (CES-D) scale or the Kiddie Schedule for Affective Disorders Scale (K-SADS). Two thirds (68%) of participants are female, and most (63%) are in high school. About a third (34%) are in middle school. The racial/ethnic breakdown of the sample is 21% Hispanic, 26% black, 43% white, 4% Asian, 6% multiracial, and 1% other (which adds up to 101% due to rounding). More than half of the participants’ mothers (60%) and fathers (53%) were college graduates.
The teens completed the CES-D, the Screen for Child Related Anxiety Disorders (SCARED), the Beck Hopelessness Scale (BHS), the CRAFFT screening for adolescent substance misuse and the Disruptive Behaviors Disorder Scale (DBD-A). A parent of each teen also filled out the CES-D and DBD-A.
The baseline results did not suggest any concerns about substance use, hopelessness, or disruptive behaviors such as ADHD or conduct disorder. But the average scores on the CES-D and SCARED sat just at the threshold for a potential depressive or anxiety disorders. A CES-D score of at least 16 suggests a possible depressive disorder, and a SCARED score of at least 25 suggests a possible anxiety disorder. The mean scores on the teens’ CES-D were 17.7 in the Chicago cohort, 15.4 in the Boston cohort and 16.9 for the whole group. Similarly, the SCARED mean scores were 26.3 in the Chicago cohort, 23.5 in the Boston cohort and 25.3 overall.
Scores from K-SADS showed subthreshold levels of depressed mood in 36% of teens in both cities, and a nearly identical subthreshold level of irritability. Subthreshold anhedonia was identified in 20% of the overall population. One percent of the overall population had current suicidal ideation.
The next steps are to analyze outcomes among the participants, as the team is doing currently. They have just passed the 1-year anniversary of the trial and are analyzing the data they collected over the past year. The study will run an additional year for longer-term data collection.
One of the abstracts presented at PAS explored the economic implications of incorporating CATCH-IT in primary care.
“The cost for implementation is where the challenge is,” Dr. Van Voorhees said. “Screening takes time, and calling people takes time.” But when spread across a practice’s overall clientele in a year, the costs drop considerably, he said, and savings from effective identification and depression prevention may outweigh costs. The researchers have not yet conducted a cost-effectiveness study because they still are analyzing data on outcomes.
But Dr. Van Voorhees is optimistic about the possibilities of the program.
“What this entire model is about is, how do we understand what’s going on in the environment of the primary care clinic to find these people, identify them, and motivate them, and how can we give them something relevant enough to actually complete,” Dr. Van Voorhees said in the interview. “Then, let’s actually see if it changes their behavioral trajectory.”
The National Institute of Mental Health funded the research. Dr. Van Voorhees has consulted for Prevail Health Solutions, Mevident, Social Kinetics, and Hong Kong University on development of Internet-based interventions.
AT PAS 17
SAN FRANCISCO – One in eight teenagers experienced at least one major depressive episode in 2015, according to the National Institute for Mental Health. Yet the recent uptick in teen suicide rates suggests that U.S. mental health care services are not meeting their needs.
A team at the University of Illinois in Chicago, led by Benjamin Van Voorhees, MD, MPH, hopes so, and they have spent the past several years developing and testing such a program with a National Institute of Mental Health (NIMH) grant.
“Adolescents are in a really plastic moment in their psychobehavioral repertoire and brain development as they program themselves to adapt to adult life,” Dr. Van Voorhees said in an interview. “Right now we have nothing to offer those individuals other than an occasional referral to an overtaxed mental health system. The only rational strategy is a mass dissemination model, which is going to have to be technology.”
The CATCH-IT program is aimed at teens showing early signs of depression or predepressive symptoms as determined through screening during well checks or other visits for acute or chronic concerns. The study uses multiple screening tools in selecting participants, but Dr. Van Voorhees estimates that screening in practice would require about 1-2 minutes of a medical assistant’s or nurse’s time, followed by 1-2 minutes of the practitioner’s time for positive screens – “and one in five of those screens is going to be positive,” he said.
“The thing we want to convey to primary care practitioners is that these individuals are coming through your office every day, we’re doing nothing for them, and in some ways we are ignoring their enormous future potential adverse trajectory toward mental disorders,” he said.
The program includes 14 modules drawing on cognitive behavioral therapy, behavioral activation, interpersonal psychotherapy, and community resiliency. Six archetypal teens – such as teen living with a single mom or one whose parents are divorcing – are featured in each of the modules to demonstrate six ways of applying the strategies taught in that module. The archetypal teens are around 14-15 years old, but the program is aimed at teens aged 13-18 years, with a reading level at about grade 6, Dr. Van Voorhees said.
Two and a half years after those teens used the CATCH-IT intervention, they showed “a sustained reduction in automatic negative thoughts and educational impairment,” but no difference in their perceptions of support from family or friends. The lack of a control group in that pilot limits what conclusions can be drawn about the program’s effectiveness, but the researchers did learn that motivational interviewing led to greater engagement with the program, compared with teens who received a brief recommendation of it.
Therefore, in the subsequent – and still ongoing – study, physicians used motivational interviewing when offering teens the opportunity to join the program. That study does include a control group, in which participants are assigned a generic health education program online instead of CATCH-IT, and the randomized participants have been stratified by site, gender, and depression risk level.
The researchers first assessed the baseline characteristics of the population, recruited from 38 clinics in two cities. The study enrolled 369 teens aged 13-18 years – 248 in Chicago and 121 in Boston. All were identified as high risk for depression based on elevated scores on the Center for Epidemiological Studies Depression (CES-D) scale or the Kiddie Schedule for Affective Disorders Scale (K-SADS). Two thirds (68%) of participants are female, and most (63%) are in high school. About a third (34%) are in middle school. The racial/ethnic breakdown of the sample is 21% Hispanic, 26% black, 43% white, 4% Asian, 6% multiracial, and 1% other (which adds up to 101% due to rounding). More than half of the participants’ mothers (60%) and fathers (53%) were college graduates.
The teens completed the CES-D, the Screen for Child Related Anxiety Disorders (SCARED), the Beck Hopelessness Scale (BHS), the CRAFFT screening for adolescent substance misuse and the Disruptive Behaviors Disorder Scale (DBD-A). A parent of each teen also filled out the CES-D and DBD-A.
The baseline results did not suggest any concerns about substance use, hopelessness, or disruptive behaviors such as ADHD or conduct disorder. But the average scores on the CES-D and SCARED sat just at the threshold for a potential depressive or anxiety disorders. A CES-D score of at least 16 suggests a possible depressive disorder, and a SCARED score of at least 25 suggests a possible anxiety disorder. The mean scores on the teens’ CES-D were 17.7 in the Chicago cohort, 15.4 in the Boston cohort and 16.9 for the whole group. Similarly, the SCARED mean scores were 26.3 in the Chicago cohort, 23.5 in the Boston cohort and 25.3 overall.
Scores from K-SADS showed subthreshold levels of depressed mood in 36% of teens in both cities, and a nearly identical subthreshold level of irritability. Subthreshold anhedonia was identified in 20% of the overall population. One percent of the overall population had current suicidal ideation.
The next steps are to analyze outcomes among the participants, as the team is doing currently. They have just passed the 1-year anniversary of the trial and are analyzing the data they collected over the past year. The study will run an additional year for longer-term data collection.
One of the abstracts presented at PAS explored the economic implications of incorporating CATCH-IT in primary care.
“The cost for implementation is where the challenge is,” Dr. Van Voorhees said. “Screening takes time, and calling people takes time.” But when spread across a practice’s overall clientele in a year, the costs drop considerably, he said, and savings from effective identification and depression prevention may outweigh costs. The researchers have not yet conducted a cost-effectiveness study because they still are analyzing data on outcomes.
But Dr. Van Voorhees is optimistic about the possibilities of the program.
“What this entire model is about is, how do we understand what’s going on in the environment of the primary care clinic to find these people, identify them, and motivate them, and how can we give them something relevant enough to actually complete,” Dr. Van Voorhees said in the interview. “Then, let’s actually see if it changes their behavioral trajectory.”
The National Institute of Mental Health funded the research. Dr. Van Voorhees has consulted for Prevail Health Solutions, Mevident, Social Kinetics, and Hong Kong University on development of Internet-based interventions.
Pegboard test useful in upper-extremity motor assessments in Parkinson’s
Pegboard tests are an effective way to assess the progression of upper-extremity motor deficits in patients with early-stage Parkinson’s disease (PD), according to a research letter from Sebastian Heitzel, PhD, and his associates.
As part of the prospective MODEP study, motor performance of early-stage PD patients, midstage PD patients, and a healthy control group were assessed biannually over a 4-year period using the pegboard test. E-PD and M-PD patients performed significantly worse on all pegboard tasks than did people in the control group.
Movement Disorder Society Unified Parkinson’s Disease Rating Scale part III scores worsened in E-PD patients, compared with controls, but slightly improved in M-PD patients.
“Pegboard is cost- and time-effective, does not require medically trained staff, and provides objective and reliable markers of upper-extremity motor deficits,” the investigators noted.
Find the full research letter in Movement Disorders (2017. doi: 10.1002/mds.27062).
Pegboard tests are an effective way to assess the progression of upper-extremity motor deficits in patients with early-stage Parkinson’s disease (PD), according to a research letter from Sebastian Heitzel, PhD, and his associates.
As part of the prospective MODEP study, motor performance of early-stage PD patients, midstage PD patients, and a healthy control group were assessed biannually over a 4-year period using the pegboard test. E-PD and M-PD patients performed significantly worse on all pegboard tasks than did people in the control group.
Movement Disorder Society Unified Parkinson’s Disease Rating Scale part III scores worsened in E-PD patients, compared with controls, but slightly improved in M-PD patients.
“Pegboard is cost- and time-effective, does not require medically trained staff, and provides objective and reliable markers of upper-extremity motor deficits,” the investigators noted.
Find the full research letter in Movement Disorders (2017. doi: 10.1002/mds.27062).
Pegboard tests are an effective way to assess the progression of upper-extremity motor deficits in patients with early-stage Parkinson’s disease (PD), according to a research letter from Sebastian Heitzel, PhD, and his associates.
As part of the prospective MODEP study, motor performance of early-stage PD patients, midstage PD patients, and a healthy control group were assessed biannually over a 4-year period using the pegboard test. E-PD and M-PD patients performed significantly worse on all pegboard tasks than did people in the control group.
Movement Disorder Society Unified Parkinson’s Disease Rating Scale part III scores worsened in E-PD patients, compared with controls, but slightly improved in M-PD patients.
“Pegboard is cost- and time-effective, does not require medically trained staff, and provides objective and reliable markers of upper-extremity motor deficits,” the investigators noted.
Find the full research letter in Movement Disorders (2017. doi: 10.1002/mds.27062).
FROM MOVEMENT DISORDERS
Coping when a patient commits suicide
SAN DIEGO – Most psychiatrists raised their hands in a conference room at the annual meeting of the American Psychiatric Association when a presenter asked whether they’d ever had a patient die from suicide. Moments later, one rose and described her own devastating experience with a patient who killed himself.
“We’d talked for 100 nights over 12 years. If a call came in at night, I knew who it was,” she said. Then he committed suicide, forcing her to question her assumptions about her ability to help others.
“I had this unconscious fantasy that I could will people to keep on living,” she said.
“We spend so much time with our patients,” added another audience member, that “it’s almost like a family member dying. Just overwhelming sadness.”
A 2015 meta-analysis estimated that there is 1 suicide for every 676 inpatient admissions, and a 20-year prospective study found that 1% of 6,891 psychiatric outpatients committed suicide (Acta Psychiatr Scand. 2015 Mar;131[3]:174-84), (J Consult Clin Psychol. 2000 Jun;68[3]:371-7).
To make things more complex for psychiatrists, suicides and attempted suicides are frequent triggers for malpractice suits, accounting for 5.4% overall and 17% of those directed at psychiatrists, said psychologist and copresenter Jane Tillman, PhD, director of the Erikson Institute for Education and Research of the Austen Riggs Center in Stockbridge, Mass., and assistant clinical professor at the Yale Child Study Center in New Haven, Conn. (However, a 2014 U.S. study found that “in malpractice, psychiatry accounted for a small percentage of overall claims and settlements” (Ann Clin Psychiatry. 2014 May;26[2]:91-6).
“They spoke to me about affective experiences like feeling incredibly sad. Some felt angry and rageful,” Dr. Tillman told the APA audience. “One young therapist, a trainee, told me that her patient’s father called to tell her the patient had died by suicide. ‘After I spoke to the patient’s father,’ the therapist recalled, ‘the mother got onto the phone and screamed. I broke down and started crying. Hearing the sound of a mother who had lost her child went right through me.’ ”
Another therapist felt “angry at everyone” and guilty, too, after a patient killed herself without calling for help. And Dr. Tillman heard from therapists who worried about their professional lives, how they’d be viewed, and whether they’d be cut off from their peers.
“I had the sense of people pulling away from me and me pulling away from them,” one therapist told Dr. Tillman. “Some reached out to me early but they didn’t follow through, and I didn’t follow through.”
Young therapists face unique challenges, Dr. Tillman said. “They felt foolish, as if they’d been grandiose,” she said. “They pathologize hope.”
Copresenter Dr. Plakun, associate medical director and director of biopsychosocial advocacy at Austen Riggs, offered these tips to psychiatrists:
• Support colleagues whose patients kill themselves. “Convene and participate in a nonjudgmental review of the suicide. Be there, try to be part of this discussion, share your own experiences. And [be] aware of the inevitability of countertransference of guilt, anger, and blaming.”
• “If you are the person who had a patient die by suicide, avoid isolation; call your insurance carrier for consultation about risk management issues, and prepare yourself for contact with the family.”
• Take special care before meetings with family: Understand the confidentiality issues and remember where the focus belongs. “You’re there to meet the family’s needs, not yours primarily. There’s no reason to castigate yourself and take blame. But that doesn’t mean you can’t express genuine sorrow about the loss.”
• Seek professional support and focus on self-care. “Try to preserve a space in our families and in our personal friendships where we can continue to live our lives and not be haunted by these things in our relationships with partners, spouses, children. And we need to grieve well. It’s a terrible loss, and it’s something that we need to pay attention to and take seriously.”
Dr. Plakun and Dr. Tillman reported no relevant disclosures.
SAN DIEGO – Most psychiatrists raised their hands in a conference room at the annual meeting of the American Psychiatric Association when a presenter asked whether they’d ever had a patient die from suicide. Moments later, one rose and described her own devastating experience with a patient who killed himself.
“We’d talked for 100 nights over 12 years. If a call came in at night, I knew who it was,” she said. Then he committed suicide, forcing her to question her assumptions about her ability to help others.
“I had this unconscious fantasy that I could will people to keep on living,” she said.
“We spend so much time with our patients,” added another audience member, that “it’s almost like a family member dying. Just overwhelming sadness.”
A 2015 meta-analysis estimated that there is 1 suicide for every 676 inpatient admissions, and a 20-year prospective study found that 1% of 6,891 psychiatric outpatients committed suicide (Acta Psychiatr Scand. 2015 Mar;131[3]:174-84), (J Consult Clin Psychol. 2000 Jun;68[3]:371-7).
To make things more complex for psychiatrists, suicides and attempted suicides are frequent triggers for malpractice suits, accounting for 5.4% overall and 17% of those directed at psychiatrists, said psychologist and copresenter Jane Tillman, PhD, director of the Erikson Institute for Education and Research of the Austen Riggs Center in Stockbridge, Mass., and assistant clinical professor at the Yale Child Study Center in New Haven, Conn. (However, a 2014 U.S. study found that “in malpractice, psychiatry accounted for a small percentage of overall claims and settlements” (Ann Clin Psychiatry. 2014 May;26[2]:91-6).
“They spoke to me about affective experiences like feeling incredibly sad. Some felt angry and rageful,” Dr. Tillman told the APA audience. “One young therapist, a trainee, told me that her patient’s father called to tell her the patient had died by suicide. ‘After I spoke to the patient’s father,’ the therapist recalled, ‘the mother got onto the phone and screamed. I broke down and started crying. Hearing the sound of a mother who had lost her child went right through me.’ ”
Another therapist felt “angry at everyone” and guilty, too, after a patient killed herself without calling for help. And Dr. Tillman heard from therapists who worried about their professional lives, how they’d be viewed, and whether they’d be cut off from their peers.
“I had the sense of people pulling away from me and me pulling away from them,” one therapist told Dr. Tillman. “Some reached out to me early but they didn’t follow through, and I didn’t follow through.”
Young therapists face unique challenges, Dr. Tillman said. “They felt foolish, as if they’d been grandiose,” she said. “They pathologize hope.”
Copresenter Dr. Plakun, associate medical director and director of biopsychosocial advocacy at Austen Riggs, offered these tips to psychiatrists:
• Support colleagues whose patients kill themselves. “Convene and participate in a nonjudgmental review of the suicide. Be there, try to be part of this discussion, share your own experiences. And [be] aware of the inevitability of countertransference of guilt, anger, and blaming.”
• “If you are the person who had a patient die by suicide, avoid isolation; call your insurance carrier for consultation about risk management issues, and prepare yourself for contact with the family.”
• Take special care before meetings with family: Understand the confidentiality issues and remember where the focus belongs. “You’re there to meet the family’s needs, not yours primarily. There’s no reason to castigate yourself and take blame. But that doesn’t mean you can’t express genuine sorrow about the loss.”
• Seek professional support and focus on self-care. “Try to preserve a space in our families and in our personal friendships where we can continue to live our lives and not be haunted by these things in our relationships with partners, spouses, children. And we need to grieve well. It’s a terrible loss, and it’s something that we need to pay attention to and take seriously.”
Dr. Plakun and Dr. Tillman reported no relevant disclosures.
SAN DIEGO – Most psychiatrists raised their hands in a conference room at the annual meeting of the American Psychiatric Association when a presenter asked whether they’d ever had a patient die from suicide. Moments later, one rose and described her own devastating experience with a patient who killed himself.
“We’d talked for 100 nights over 12 years. If a call came in at night, I knew who it was,” she said. Then he committed suicide, forcing her to question her assumptions about her ability to help others.
“I had this unconscious fantasy that I could will people to keep on living,” she said.
“We spend so much time with our patients,” added another audience member, that “it’s almost like a family member dying. Just overwhelming sadness.”
A 2015 meta-analysis estimated that there is 1 suicide for every 676 inpatient admissions, and a 20-year prospective study found that 1% of 6,891 psychiatric outpatients committed suicide (Acta Psychiatr Scand. 2015 Mar;131[3]:174-84), (J Consult Clin Psychol. 2000 Jun;68[3]:371-7).
To make things more complex for psychiatrists, suicides and attempted suicides are frequent triggers for malpractice suits, accounting for 5.4% overall and 17% of those directed at psychiatrists, said psychologist and copresenter Jane Tillman, PhD, director of the Erikson Institute for Education and Research of the Austen Riggs Center in Stockbridge, Mass., and assistant clinical professor at the Yale Child Study Center in New Haven, Conn. (However, a 2014 U.S. study found that “in malpractice, psychiatry accounted for a small percentage of overall claims and settlements” (Ann Clin Psychiatry. 2014 May;26[2]:91-6).
“They spoke to me about affective experiences like feeling incredibly sad. Some felt angry and rageful,” Dr. Tillman told the APA audience. “One young therapist, a trainee, told me that her patient’s father called to tell her the patient had died by suicide. ‘After I spoke to the patient’s father,’ the therapist recalled, ‘the mother got onto the phone and screamed. I broke down and started crying. Hearing the sound of a mother who had lost her child went right through me.’ ”
Another therapist felt “angry at everyone” and guilty, too, after a patient killed herself without calling for help. And Dr. Tillman heard from therapists who worried about their professional lives, how they’d be viewed, and whether they’d be cut off from their peers.
“I had the sense of people pulling away from me and me pulling away from them,” one therapist told Dr. Tillman. “Some reached out to me early but they didn’t follow through, and I didn’t follow through.”
Young therapists face unique challenges, Dr. Tillman said. “They felt foolish, as if they’d been grandiose,” she said. “They pathologize hope.”
Copresenter Dr. Plakun, associate medical director and director of biopsychosocial advocacy at Austen Riggs, offered these tips to psychiatrists:
• Support colleagues whose patients kill themselves. “Convene and participate in a nonjudgmental review of the suicide. Be there, try to be part of this discussion, share your own experiences. And [be] aware of the inevitability of countertransference of guilt, anger, and blaming.”
• “If you are the person who had a patient die by suicide, avoid isolation; call your insurance carrier for consultation about risk management issues, and prepare yourself for contact with the family.”
• Take special care before meetings with family: Understand the confidentiality issues and remember where the focus belongs. “You’re there to meet the family’s needs, not yours primarily. There’s no reason to castigate yourself and take blame. But that doesn’t mean you can’t express genuine sorrow about the loss.”
• Seek professional support and focus on self-care. “Try to preserve a space in our families and in our personal friendships where we can continue to live our lives and not be haunted by these things in our relationships with partners, spouses, children. And we need to grieve well. It’s a terrible loss, and it’s something that we need to pay attention to and take seriously.”
Dr. Plakun and Dr. Tillman reported no relevant disclosures.
AT APA
... The mother of direction
If you weren’t a young male living in the United States in the 1960s, it may be hard for you to understand my situation. It was a little more than 6 months from my college graduation. Because I couldn’t think of anything else to do, I had applied for and been accepted in a postgraduate fellowship in art history. However, it was clear that this country was becoming entangled in a confusing, unpopular – and from my personal perspective – a dangerous war.
While I was in college I was protected from the draft. But upon graduation, if I were to pursue my studies in something as unrelated to the war effort as art history, I would be ripe for the picking. I’m not sure why, but luckily I had been banking science credits for a rainy day. And in the winter of 1965-1966, it was raining big time.
I was not alone. Even if the term “gap year” had been coined, taking a year off to “find oneself” was not an option for young American males on the verge of high school or college graduation. I share this unflattering anecdote as evidence that there are times when circumstances can provide a floundering young person with a much needed sense of direction.
In May 2017, the Chicago Board of Education approved a plan sponsored by Mayor Rahm Emanuel that will require all high school students planning to graduate to provide evidence that they have secured a job or have been accepted by a college, trade apprenticeship, structured gap year program, or the military. (“Chicago won’t allow high school students to graduate without a plan for the future,” by Emma Brown, the Washington Post, July 3, 2017). Critics of the plan complain, probably with good reason, that the cash-strapped school system with more than 300,000 students doesn’t have the resources to provide its students with the counseling they will need to create the required post-graduation plans.
Even if there are too many devils in too many details in the Chicago plan, the principle underlying it is worth a try and deserves consideration by other school systems. It is not a universal military service requirement. Although, I wonder at times if this country should consider such a thing. It also is not a scheme cooked up by the business community to provide itself with cheap labor, although, it probably will.
In my mind, . Hopefully something that is productive or creative or at least something that improves your chances of living a life that is more likely to provide you with some degree of happiness. It offers a broad enough range of choices so that it is not overly prescriptive. If well administered, the plan would send the message to the graduating student that you must at least have a Plan A.
Regardless of whether a student’s patients come from affluent families with a myriad of post-graduation opportunities or from an economically challenged neighborhood in Chicago, I suspect that many of them would benefit from an artificial dose of necessity in the form of a message that doing nothing is not going to be an option.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
If you weren’t a young male living in the United States in the 1960s, it may be hard for you to understand my situation. It was a little more than 6 months from my college graduation. Because I couldn’t think of anything else to do, I had applied for and been accepted in a postgraduate fellowship in art history. However, it was clear that this country was becoming entangled in a confusing, unpopular – and from my personal perspective – a dangerous war.
While I was in college I was protected from the draft. But upon graduation, if I were to pursue my studies in something as unrelated to the war effort as art history, I would be ripe for the picking. I’m not sure why, but luckily I had been banking science credits for a rainy day. And in the winter of 1965-1966, it was raining big time.
I was not alone. Even if the term “gap year” had been coined, taking a year off to “find oneself” was not an option for young American males on the verge of high school or college graduation. I share this unflattering anecdote as evidence that there are times when circumstances can provide a floundering young person with a much needed sense of direction.
In May 2017, the Chicago Board of Education approved a plan sponsored by Mayor Rahm Emanuel that will require all high school students planning to graduate to provide evidence that they have secured a job or have been accepted by a college, trade apprenticeship, structured gap year program, or the military. (“Chicago won’t allow high school students to graduate without a plan for the future,” by Emma Brown, the Washington Post, July 3, 2017). Critics of the plan complain, probably with good reason, that the cash-strapped school system with more than 300,000 students doesn’t have the resources to provide its students with the counseling they will need to create the required post-graduation plans.
Even if there are too many devils in too many details in the Chicago plan, the principle underlying it is worth a try and deserves consideration by other school systems. It is not a universal military service requirement. Although, I wonder at times if this country should consider such a thing. It also is not a scheme cooked up by the business community to provide itself with cheap labor, although, it probably will.
In my mind, . Hopefully something that is productive or creative or at least something that improves your chances of living a life that is more likely to provide you with some degree of happiness. It offers a broad enough range of choices so that it is not overly prescriptive. If well administered, the plan would send the message to the graduating student that you must at least have a Plan A.
Regardless of whether a student’s patients come from affluent families with a myriad of post-graduation opportunities or from an economically challenged neighborhood in Chicago, I suspect that many of them would benefit from an artificial dose of necessity in the form of a message that doing nothing is not going to be an option.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
If you weren’t a young male living in the United States in the 1960s, it may be hard for you to understand my situation. It was a little more than 6 months from my college graduation. Because I couldn’t think of anything else to do, I had applied for and been accepted in a postgraduate fellowship in art history. However, it was clear that this country was becoming entangled in a confusing, unpopular – and from my personal perspective – a dangerous war.
While I was in college I was protected from the draft. But upon graduation, if I were to pursue my studies in something as unrelated to the war effort as art history, I would be ripe for the picking. I’m not sure why, but luckily I had been banking science credits for a rainy day. And in the winter of 1965-1966, it was raining big time.
I was not alone. Even if the term “gap year” had been coined, taking a year off to “find oneself” was not an option for young American males on the verge of high school or college graduation. I share this unflattering anecdote as evidence that there are times when circumstances can provide a floundering young person with a much needed sense of direction.
In May 2017, the Chicago Board of Education approved a plan sponsored by Mayor Rahm Emanuel that will require all high school students planning to graduate to provide evidence that they have secured a job or have been accepted by a college, trade apprenticeship, structured gap year program, or the military. (“Chicago won’t allow high school students to graduate without a plan for the future,” by Emma Brown, the Washington Post, July 3, 2017). Critics of the plan complain, probably with good reason, that the cash-strapped school system with more than 300,000 students doesn’t have the resources to provide its students with the counseling they will need to create the required post-graduation plans.
Even if there are too many devils in too many details in the Chicago plan, the principle underlying it is worth a try and deserves consideration by other school systems. It is not a universal military service requirement. Although, I wonder at times if this country should consider such a thing. It also is not a scheme cooked up by the business community to provide itself with cheap labor, although, it probably will.
In my mind, . Hopefully something that is productive or creative or at least something that improves your chances of living a life that is more likely to provide you with some degree of happiness. It offers a broad enough range of choices so that it is not overly prescriptive. If well administered, the plan would send the message to the graduating student that you must at least have a Plan A.
Regardless of whether a student’s patients come from affluent families with a myriad of post-graduation opportunities or from an economically challenged neighborhood in Chicago, I suspect that many of them would benefit from an artificial dose of necessity in the form of a message that doing nothing is not going to be an option.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
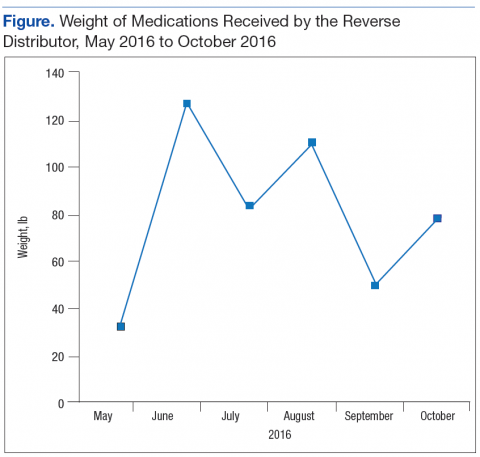
Implementation of a Patient Medication Disposal Program at a VA Medical Center
Opioid overdoses have quadrupled since 1999, with 78 Americans dying every day of opioid overdoses. More than half of all opioid overdose deaths involve prescription opioids.1 Attacking this problem from both ends—prescribing and disposal—can have a greater impact than focusing on a single strategy.
Background
In 2016, the CDC issued opioid prescription guidelines that included encouraging health care providers to discuss “options for safe disposal of unused opioids.”2 Pharmacies are prohibited from directly taking possession of controlled substances from a user. Historically, the Richard L. Roudebush VAMC (RLRVAMC) in Indianapolis, Indiana, recommended that patients follow FDA guidance for household medication disposal, which includes a list of medications that should be flushed down the toilet.3 As more data became available about the negative downstream environmental effects of pharmaceuticals on the water supply, this method of destruction made many patients feel uncomfortable.4,5
The Secure and Responsible Drug Disposal Act of 2010 presented additional options for hospitals and pharmacies to assist the public with medication disposal.6,7 These options offer convenience and anonymity for the end user, reduce potential for diversion, and enhance patient safety by ridding homes of unwanted and expired medications.
Prior to the 2010 act, the only legal methods of controlled substance disposal were via trash disposal, flushing, or delivery to law enforcement, typically at a community-based drug take-back event. These methods were not always convenient, environmentally friendly, or safe for other family members and pets in the home. The Secure and Responsible Drug Disposal Act of 2010 added 2 additional collection options for pharmacies: collection receptacles and mail-back programs.
The RLRVAMC treats > 62,000 veterans annually. The RLRVAMC Pharmacy Service had been providing pharmaceutical mail-back envelopes to patients since May 2015 with moderate success (271 lb of medications returned and a 22.8% envelope return rate through September 2016). Although the mail-back envelopes offer at-home convenience, there was no on-site disposal option. It is not uncommon for patients to bring medications to their appointment or the emergency department (ED). When medication reconciliation is performed, some medications are discontinued, and the prescriber wants them to be safely out of the patient’s possession to avoid confusion and/or accidental overdose. The purpose of this project was to offer more disposal options to patients through the addition of an on-site medication collection receptacle that would be in compliance with U.S. Drug Enforcement Agency (DEA) regulations.
Methods
A policy was developed between the RLRVAMC pharmacy and police departments for the management of a medication collection receptacle. Police would oversee the disposal program so that the pharmacy would not have to change its DEA registration to collector status. The 2 access keys to the receptacle were maintained by police and secured within a key accountability system in the police station.
Full liners are removed from the receptacle by 2 police officers and sealed securely according to vendor guidelines. In accordance with DEA regulations, a form is completed that documents the dates the inner liner was acquired, installed, removed, and transferred for destruction as well as the unique identification number and size of the liner, the address of the location where it was installed, and the names and signatures of the 2 employees that witnessed the removal.
Arrangements are made to have a mail courier present during the removal of the liner. Once removed, the liner is immediately sealed and released to the mail courier who transports the liner to the DEA authorized reverse distributor. The reverse distributor is a licensed entity that has the authority to take control of the medications, including controlled substances, for disposal. The liner tracking numbers are kept in a police log book so that delivery can be confirmed and destruction certificates obtained from the vendor’s website at a later date. The records are kept for 3 years.
Funding was obtained for a 38-gallon collection receptacle and 12 liners from Pharmacy Benefits Management Services (PBM). Approval was obtained from RLRVAMC leadership to locate the receptacle in a high-traffic area, anchored to the floor, under video surveillance, and away from the ED entrance (a DEA requirement). Public Affairs promoted the receptacle to veterans. E-mails were sent to staff to provide education on regulatory requirements. Weight and frequency of medications returned were obtained from data collected by the reverse distributor. Descriptive statistics are reported.
Results
The Federal Supply Schedule cost to procure a DEA-compliant receptacle was $1,450. The additional 12 inner liners cost $2,024.97.8 Staff from Engineering Service were able to install the receptacle at no additional cost to the facility. The collection receptacle was opened to the public in May 2016. From May through October 2016, the facility collected and returned 10 liners to the reverse distributor containing 452 lb of medications. An additional 30 lb of drugs were returned through the mailback envelope program for a total weight of 482 lb over the 6-month period (Figure). The average time between inner liner changes was 2.6 weeks.
Discussion
The most challenging aspect of implementation was identification of a location for the receptacle. The location chosen, an alcove in the hallway between the coffee shop and outpatient pharmacy, was most appropriate. It is a high-traffic area, under video surveillance, and provides easy access for patients. Another challenge was determining the frequency of liner changes. There was no historic data to assist with predicting how quickly the liner would fill up. Initially, Police Service checked the receptacle every week, and it was emptied about every 2 weeks. Aspatients cleaned out their medicine cabinets, the liner needed to be replaced closer to every 4 weeks. An ongoing challenge has been determining how full the liner is without requiring the police to open the receptacle. Consideration is being given to installing a scale in the receptacle under the liner and having the display affixed to the outside of the container.
The receptacle seemed to be the preferred method of disposal, considering that it generated nearly 15 times more waste than did the mail-back envelopes during the same time period. Anecdotal patient feedback has been extremely positive on social media and by word-of-mouth.
Limitations
One limitation of this disposal program is that the specific amount of controlled substance waste vs noncontrolled substance waste cannot be determined since the liner contents are not inventoried. The University of Findlay in Ohio partnered with local law enforcement to host 7 community medication take-back events over a 3-year period, inventoried the drugs, and found that about one-third of the dosing units (eg, tablet or capsule) returned in the analgesic category were controlled substances, suggesting that take-back events may play a role in reducing unauthorized access to prescription painkillers.9 By witnessing the changing of inner liners, it can be anecdotally confirmed that a significant amount of controlled substances were collected and returned at RLRVAMC. These results have been shared with respective VISN leadership, and additional facilities are installing receptacles.
Conclusion
Changes to DEA regulations offer medical centers more options for developing a comprehensive drug disposal program. Implementation of a pharmaceutical take-back program can assist patients with disposal of unwanted and expired medications, promote safety and environmental stewardship, and reduce the risk of diversion.
1. Centers for Disease Control and Prevention. Opioid overdose. http://www.cdc.gov/drugoverdose/index.html. Updated April 16, 2017. Accessed June 5, 2017.
2. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65(1):1-49.
3. U.S. Food and Drug Administration. Disposal of unused medicines: what you should know. http://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/EnsuringSafeUseofMedicine/SafeDisposalofMedicines/ucm186187.htm#Flush_List. Updated April 21, 2017. Accessed June 5, 2017.
4. Li WC. Occurrence, sources, and fate of pharmaceuticals in aquatic environment and soil. Environ Pollut. 2014;187:193-201.
5. Boxall AB. The environmental side effects of medication. EMBO Rep. 2004;5(12):1110-1116.
6. Peterson DM. New DEA rules expand options for controlled substance disposal. J Pain Palliat Care Pharmacother. 2015;29(1):22-26.
7. U.S. Department of Justice, Drug Enforcement Administration. Drug disposal information. https:// www.deadiversion.usdoj.gov/drug_disposal/index.html. Accessed June 5, 2016.
8. GSA Advantage! Online shopping. https://www.gsaadvantage.gov. Accessed June 5, 2017.
9. Perry LA, Shinn BW, Stanovich J. Quantification of an ongoing community-based medication take-back program. J Am Pharm Assoc (2003). 2014;54(3):275-279.
Opioid overdoses have quadrupled since 1999, with 78 Americans dying every day of opioid overdoses. More than half of all opioid overdose deaths involve prescription opioids.1 Attacking this problem from both ends—prescribing and disposal—can have a greater impact than focusing on a single strategy.
Background
In 2016, the CDC issued opioid prescription guidelines that included encouraging health care providers to discuss “options for safe disposal of unused opioids.”2 Pharmacies are prohibited from directly taking possession of controlled substances from a user. Historically, the Richard L. Roudebush VAMC (RLRVAMC) in Indianapolis, Indiana, recommended that patients follow FDA guidance for household medication disposal, which includes a list of medications that should be flushed down the toilet.3 As more data became available about the negative downstream environmental effects of pharmaceuticals on the water supply, this method of destruction made many patients feel uncomfortable.4,5
The Secure and Responsible Drug Disposal Act of 2010 presented additional options for hospitals and pharmacies to assist the public with medication disposal.6,7 These options offer convenience and anonymity for the end user, reduce potential for diversion, and enhance patient safety by ridding homes of unwanted and expired medications.
Prior to the 2010 act, the only legal methods of controlled substance disposal were via trash disposal, flushing, or delivery to law enforcement, typically at a community-based drug take-back event. These methods were not always convenient, environmentally friendly, or safe for other family members and pets in the home. The Secure and Responsible Drug Disposal Act of 2010 added 2 additional collection options for pharmacies: collection receptacles and mail-back programs.
The RLRVAMC treats > 62,000 veterans annually. The RLRVAMC Pharmacy Service had been providing pharmaceutical mail-back envelopes to patients since May 2015 with moderate success (271 lb of medications returned and a 22.8% envelope return rate through September 2016). Although the mail-back envelopes offer at-home convenience, there was no on-site disposal option. It is not uncommon for patients to bring medications to their appointment or the emergency department (ED). When medication reconciliation is performed, some medications are discontinued, and the prescriber wants them to be safely out of the patient’s possession to avoid confusion and/or accidental overdose. The purpose of this project was to offer more disposal options to patients through the addition of an on-site medication collection receptacle that would be in compliance with U.S. Drug Enforcement Agency (DEA) regulations.
Methods
A policy was developed between the RLRVAMC pharmacy and police departments for the management of a medication collection receptacle. Police would oversee the disposal program so that the pharmacy would not have to change its DEA registration to collector status. The 2 access keys to the receptacle were maintained by police and secured within a key accountability system in the police station.
Full liners are removed from the receptacle by 2 police officers and sealed securely according to vendor guidelines. In accordance with DEA regulations, a form is completed that documents the dates the inner liner was acquired, installed, removed, and transferred for destruction as well as the unique identification number and size of the liner, the address of the location where it was installed, and the names and signatures of the 2 employees that witnessed the removal.
Arrangements are made to have a mail courier present during the removal of the liner. Once removed, the liner is immediately sealed and released to the mail courier who transports the liner to the DEA authorized reverse distributor. The reverse distributor is a licensed entity that has the authority to take control of the medications, including controlled substances, for disposal. The liner tracking numbers are kept in a police log book so that delivery can be confirmed and destruction certificates obtained from the vendor’s website at a later date. The records are kept for 3 years.
Funding was obtained for a 38-gallon collection receptacle and 12 liners from Pharmacy Benefits Management Services (PBM). Approval was obtained from RLRVAMC leadership to locate the receptacle in a high-traffic area, anchored to the floor, under video surveillance, and away from the ED entrance (a DEA requirement). Public Affairs promoted the receptacle to veterans. E-mails were sent to staff to provide education on regulatory requirements. Weight and frequency of medications returned were obtained from data collected by the reverse distributor. Descriptive statistics are reported.
Results
The Federal Supply Schedule cost to procure a DEA-compliant receptacle was $1,450. The additional 12 inner liners cost $2,024.97.8 Staff from Engineering Service were able to install the receptacle at no additional cost to the facility. The collection receptacle was opened to the public in May 2016. From May through October 2016, the facility collected and returned 10 liners to the reverse distributor containing 452 lb of medications. An additional 30 lb of drugs were returned through the mailback envelope program for a total weight of 482 lb over the 6-month period (Figure). The average time between inner liner changes was 2.6 weeks.
Discussion
The most challenging aspect of implementation was identification of a location for the receptacle. The location chosen, an alcove in the hallway between the coffee shop and outpatient pharmacy, was most appropriate. It is a high-traffic area, under video surveillance, and provides easy access for patients. Another challenge was determining the frequency of liner changes. There was no historic data to assist with predicting how quickly the liner would fill up. Initially, Police Service checked the receptacle every week, and it was emptied about every 2 weeks. Aspatients cleaned out their medicine cabinets, the liner needed to be replaced closer to every 4 weeks. An ongoing challenge has been determining how full the liner is without requiring the police to open the receptacle. Consideration is being given to installing a scale in the receptacle under the liner and having the display affixed to the outside of the container.
The receptacle seemed to be the preferred method of disposal, considering that it generated nearly 15 times more waste than did the mail-back envelopes during the same time period. Anecdotal patient feedback has been extremely positive on social media and by word-of-mouth.
Limitations
One limitation of this disposal program is that the specific amount of controlled substance waste vs noncontrolled substance waste cannot be determined since the liner contents are not inventoried. The University of Findlay in Ohio partnered with local law enforcement to host 7 community medication take-back events over a 3-year period, inventoried the drugs, and found that about one-third of the dosing units (eg, tablet or capsule) returned in the analgesic category were controlled substances, suggesting that take-back events may play a role in reducing unauthorized access to prescription painkillers.9 By witnessing the changing of inner liners, it can be anecdotally confirmed that a significant amount of controlled substances were collected and returned at RLRVAMC. These results have been shared with respective VISN leadership, and additional facilities are installing receptacles.
Conclusion
Changes to DEA regulations offer medical centers more options for developing a comprehensive drug disposal program. Implementation of a pharmaceutical take-back program can assist patients with disposal of unwanted and expired medications, promote safety and environmental stewardship, and reduce the risk of diversion.
Opioid overdoses have quadrupled since 1999, with 78 Americans dying every day of opioid overdoses. More than half of all opioid overdose deaths involve prescription opioids.1 Attacking this problem from both ends—prescribing and disposal—can have a greater impact than focusing on a single strategy.
Background
In 2016, the CDC issued opioid prescription guidelines that included encouraging health care providers to discuss “options for safe disposal of unused opioids.”2 Pharmacies are prohibited from directly taking possession of controlled substances from a user. Historically, the Richard L. Roudebush VAMC (RLRVAMC) in Indianapolis, Indiana, recommended that patients follow FDA guidance for household medication disposal, which includes a list of medications that should be flushed down the toilet.3 As more data became available about the negative downstream environmental effects of pharmaceuticals on the water supply, this method of destruction made many patients feel uncomfortable.4,5
The Secure and Responsible Drug Disposal Act of 2010 presented additional options for hospitals and pharmacies to assist the public with medication disposal.6,7 These options offer convenience and anonymity for the end user, reduce potential for diversion, and enhance patient safety by ridding homes of unwanted and expired medications.
Prior to the 2010 act, the only legal methods of controlled substance disposal were via trash disposal, flushing, or delivery to law enforcement, typically at a community-based drug take-back event. These methods were not always convenient, environmentally friendly, or safe for other family members and pets in the home. The Secure and Responsible Drug Disposal Act of 2010 added 2 additional collection options for pharmacies: collection receptacles and mail-back programs.
The RLRVAMC treats > 62,000 veterans annually. The RLRVAMC Pharmacy Service had been providing pharmaceutical mail-back envelopes to patients since May 2015 with moderate success (271 lb of medications returned and a 22.8% envelope return rate through September 2016). Although the mail-back envelopes offer at-home convenience, there was no on-site disposal option. It is not uncommon for patients to bring medications to their appointment or the emergency department (ED). When medication reconciliation is performed, some medications are discontinued, and the prescriber wants them to be safely out of the patient’s possession to avoid confusion and/or accidental overdose. The purpose of this project was to offer more disposal options to patients through the addition of an on-site medication collection receptacle that would be in compliance with U.S. Drug Enforcement Agency (DEA) regulations.
Methods
A policy was developed between the RLRVAMC pharmacy and police departments for the management of a medication collection receptacle. Police would oversee the disposal program so that the pharmacy would not have to change its DEA registration to collector status. The 2 access keys to the receptacle were maintained by police and secured within a key accountability system in the police station.
Full liners are removed from the receptacle by 2 police officers and sealed securely according to vendor guidelines. In accordance with DEA regulations, a form is completed that documents the dates the inner liner was acquired, installed, removed, and transferred for destruction as well as the unique identification number and size of the liner, the address of the location where it was installed, and the names and signatures of the 2 employees that witnessed the removal.
Arrangements are made to have a mail courier present during the removal of the liner. Once removed, the liner is immediately sealed and released to the mail courier who transports the liner to the DEA authorized reverse distributor. The reverse distributor is a licensed entity that has the authority to take control of the medications, including controlled substances, for disposal. The liner tracking numbers are kept in a police log book so that delivery can be confirmed and destruction certificates obtained from the vendor’s website at a later date. The records are kept for 3 years.
Funding was obtained for a 38-gallon collection receptacle and 12 liners from Pharmacy Benefits Management Services (PBM). Approval was obtained from RLRVAMC leadership to locate the receptacle in a high-traffic area, anchored to the floor, under video surveillance, and away from the ED entrance (a DEA requirement). Public Affairs promoted the receptacle to veterans. E-mails were sent to staff to provide education on regulatory requirements. Weight and frequency of medications returned were obtained from data collected by the reverse distributor. Descriptive statistics are reported.
Results
The Federal Supply Schedule cost to procure a DEA-compliant receptacle was $1,450. The additional 12 inner liners cost $2,024.97.8 Staff from Engineering Service were able to install the receptacle at no additional cost to the facility. The collection receptacle was opened to the public in May 2016. From May through October 2016, the facility collected and returned 10 liners to the reverse distributor containing 452 lb of medications. An additional 30 lb of drugs were returned through the mailback envelope program for a total weight of 482 lb over the 6-month period (Figure). The average time between inner liner changes was 2.6 weeks.
Discussion
The most challenging aspect of implementation was identification of a location for the receptacle. The location chosen, an alcove in the hallway between the coffee shop and outpatient pharmacy, was most appropriate. It is a high-traffic area, under video surveillance, and provides easy access for patients. Another challenge was determining the frequency of liner changes. There was no historic data to assist with predicting how quickly the liner would fill up. Initially, Police Service checked the receptacle every week, and it was emptied about every 2 weeks. Aspatients cleaned out their medicine cabinets, the liner needed to be replaced closer to every 4 weeks. An ongoing challenge has been determining how full the liner is without requiring the police to open the receptacle. Consideration is being given to installing a scale in the receptacle under the liner and having the display affixed to the outside of the container.
The receptacle seemed to be the preferred method of disposal, considering that it generated nearly 15 times more waste than did the mail-back envelopes during the same time period. Anecdotal patient feedback has been extremely positive on social media and by word-of-mouth.
Limitations
One limitation of this disposal program is that the specific amount of controlled substance waste vs noncontrolled substance waste cannot be determined since the liner contents are not inventoried. The University of Findlay in Ohio partnered with local law enforcement to host 7 community medication take-back events over a 3-year period, inventoried the drugs, and found that about one-third of the dosing units (eg, tablet or capsule) returned in the analgesic category were controlled substances, suggesting that take-back events may play a role in reducing unauthorized access to prescription painkillers.9 By witnessing the changing of inner liners, it can be anecdotally confirmed that a significant amount of controlled substances were collected and returned at RLRVAMC. These results have been shared with respective VISN leadership, and additional facilities are installing receptacles.
Conclusion
Changes to DEA regulations offer medical centers more options for developing a comprehensive drug disposal program. Implementation of a pharmaceutical take-back program can assist patients with disposal of unwanted and expired medications, promote safety and environmental stewardship, and reduce the risk of diversion.
1. Centers for Disease Control and Prevention. Opioid overdose. http://www.cdc.gov/drugoverdose/index.html. Updated April 16, 2017. Accessed June 5, 2017.
2. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65(1):1-49.
3. U.S. Food and Drug Administration. Disposal of unused medicines: what you should know. http://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/EnsuringSafeUseofMedicine/SafeDisposalofMedicines/ucm186187.htm#Flush_List. Updated April 21, 2017. Accessed June 5, 2017.
4. Li WC. Occurrence, sources, and fate of pharmaceuticals in aquatic environment and soil. Environ Pollut. 2014;187:193-201.
5. Boxall AB. The environmental side effects of medication. EMBO Rep. 2004;5(12):1110-1116.
6. Peterson DM. New DEA rules expand options for controlled substance disposal. J Pain Palliat Care Pharmacother. 2015;29(1):22-26.
7. U.S. Department of Justice, Drug Enforcement Administration. Drug disposal information. https:// www.deadiversion.usdoj.gov/drug_disposal/index.html. Accessed June 5, 2016.
8. GSA Advantage! Online shopping. https://www.gsaadvantage.gov. Accessed June 5, 2017.
9. Perry LA, Shinn BW, Stanovich J. Quantification of an ongoing community-based medication take-back program. J Am Pharm Assoc (2003). 2014;54(3):275-279.
1. Centers for Disease Control and Prevention. Opioid overdose. http://www.cdc.gov/drugoverdose/index.html. Updated April 16, 2017. Accessed June 5, 2017.
2. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016;65(1):1-49.
3. U.S. Food and Drug Administration. Disposal of unused medicines: what you should know. http://www.fda.gov/Drugs/ResourcesForYou/Consumers/BuyingUsingMedicineSafely/EnsuringSafeUseofMedicine/SafeDisposalofMedicines/ucm186187.htm#Flush_List. Updated April 21, 2017. Accessed June 5, 2017.
4. Li WC. Occurrence, sources, and fate of pharmaceuticals in aquatic environment and soil. Environ Pollut. 2014;187:193-201.
5. Boxall AB. The environmental side effects of medication. EMBO Rep. 2004;5(12):1110-1116.
6. Peterson DM. New DEA rules expand options for controlled substance disposal. J Pain Palliat Care Pharmacother. 2015;29(1):22-26.
7. U.S. Department of Justice, Drug Enforcement Administration. Drug disposal information. https:// www.deadiversion.usdoj.gov/drug_disposal/index.html. Accessed June 5, 2016.
8. GSA Advantage! Online shopping. https://www.gsaadvantage.gov. Accessed June 5, 2017.
9. Perry LA, Shinn BW, Stanovich J. Quantification of an ongoing community-based medication take-back program. J Am Pharm Assoc (2003). 2014;54(3):275-279.
Modified, CB-derived NK cells target CLL and BL
Natural killer (NK) cells derived from cord blood (CB) can be modified to fight chronic lymphocytic leukemia (CLL) and Burkitt lymphoma (BL), according to research published in Leukemia.
Using a viral vector, researchers transduced CB-derived NK cells with a chimeric antigen receptor (CAR), interleukin-15 (IL-15), and an inducible caspase-9-based suicide gene.
The CAR directed the NK cells to kill CD19-expressing cells, IL-15 prolonged the NK cells’ survival and enhanced their antitumor activity, and the suicide gene allowed researchers to kill off the NK cells in the event of a severe inflammatory response.
“Natural killer cells are the immune system’s most potent killers, but they are short-lived, and cancers manage to evade a patient’s own NK cells to progress,” said study author Katy Rezvani, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston.
“Our cord-blood derived NK cells, genetically equipped with a receptor that focuses them on B-cell malignancies and with interleukin-15 to help them persist longer—potentially for months instead of 2 or 3 weeks—are designed to address these challenges.”
Dr Rezvani and her colleagues tested their CB-derived CAR NK cells in primary CLL cells and a mouse model of BL. Compared to unmodified NK cells, the CAR NK cells killed malignant cells more efficiently and extended the survival of mice.
Another experiment showed the CB-derived CAR NK cells killed CLL cells more efficiently than NK cells that were taken from CLL patients and modified in the same way. The researchers said this highlights the need to transplant CAR-engineered NK cells derived from healthy CB rather than using a patient’s own cells.
Additional experiments in the mouse model of BL showed that a single infusion of low-dose CAR NK cells resulted in prolonged survival.
When CAR NK cells were given at a higher dose, none of the mice died of BL. Half of them survived 100 days and beyond. However, all mice treated with other types of NK cells died by day 41.
Some mice treated with the higher dose of CAR NK cells died of cytokine release syndrome (CRS).
To counteract this toxicity, the researchers activated the suicide gene (iC9) via treatment with a small-molecule dimerizer, AP1903.
The team found that adding as little as 10 nM of AP1903 to cell cultures induced apoptosis/necrosis of the CAR NK cells within 4 hours but had no effect on non-CAR CB-derived NK cells. Similar results were observed in the mouse model.
Next steps
A phase 1/2 trial of these CB-derived CAR NK cells opened at MD Anderson in June for patients with relapsed or refractory CLL, acute lymphocytic leukemia, or non-Hodgkin lymphoma.
Dr Rezvani, the principal investigator of the trial, said the protocol calls for vigilance for signs of CRS, treatment with steroids and tocilizumab for low-grade CRS, and AP1903 added to activate the suicide gene for grade 3 or 4 CRS.
She and her colleagues noted that CB-derived NK cells do not cause graft-vs-host disease. Therefore, they can be an off-the-shelf product, prepared in advance with the necessary receptor and given to patients promptly.
The researchers are developing CB-derived CAR NK cells for other targets in hematologic and solid tumor malignancies.
MD Anderson and the researchers have intellectual property related to the engineered NK cells, which is being managed in accordance with the institution’s conflict-of-interest rules.
Funding for this research was provided by MD Anderson’s Moon Shots Program, the National Cancer Institute of the National Institutes of Health Cancer Center Support Grant (CA016672) to MD Anderson, and grants from the Leukemia and Lymphoma Society and the American Cancer Society. ![]()
Natural killer (NK) cells derived from cord blood (CB) can be modified to fight chronic lymphocytic leukemia (CLL) and Burkitt lymphoma (BL), according to research published in Leukemia.
Using a viral vector, researchers transduced CB-derived NK cells with a chimeric antigen receptor (CAR), interleukin-15 (IL-15), and an inducible caspase-9-based suicide gene.
The CAR directed the NK cells to kill CD19-expressing cells, IL-15 prolonged the NK cells’ survival and enhanced their antitumor activity, and the suicide gene allowed researchers to kill off the NK cells in the event of a severe inflammatory response.
“Natural killer cells are the immune system’s most potent killers, but they are short-lived, and cancers manage to evade a patient’s own NK cells to progress,” said study author Katy Rezvani, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston.
“Our cord-blood derived NK cells, genetically equipped with a receptor that focuses them on B-cell malignancies and with interleukin-15 to help them persist longer—potentially for months instead of 2 or 3 weeks—are designed to address these challenges.”
Dr Rezvani and her colleagues tested their CB-derived CAR NK cells in primary CLL cells and a mouse model of BL. Compared to unmodified NK cells, the CAR NK cells killed malignant cells more efficiently and extended the survival of mice.
Another experiment showed the CB-derived CAR NK cells killed CLL cells more efficiently than NK cells that were taken from CLL patients and modified in the same way. The researchers said this highlights the need to transplant CAR-engineered NK cells derived from healthy CB rather than using a patient’s own cells.
Additional experiments in the mouse model of BL showed that a single infusion of low-dose CAR NK cells resulted in prolonged survival.
When CAR NK cells were given at a higher dose, none of the mice died of BL. Half of them survived 100 days and beyond. However, all mice treated with other types of NK cells died by day 41.
Some mice treated with the higher dose of CAR NK cells died of cytokine release syndrome (CRS).
To counteract this toxicity, the researchers activated the suicide gene (iC9) via treatment with a small-molecule dimerizer, AP1903.
The team found that adding as little as 10 nM of AP1903 to cell cultures induced apoptosis/necrosis of the CAR NK cells within 4 hours but had no effect on non-CAR CB-derived NK cells. Similar results were observed in the mouse model.
Next steps
A phase 1/2 trial of these CB-derived CAR NK cells opened at MD Anderson in June for patients with relapsed or refractory CLL, acute lymphocytic leukemia, or non-Hodgkin lymphoma.
Dr Rezvani, the principal investigator of the trial, said the protocol calls for vigilance for signs of CRS, treatment with steroids and tocilizumab for low-grade CRS, and AP1903 added to activate the suicide gene for grade 3 or 4 CRS.
She and her colleagues noted that CB-derived NK cells do not cause graft-vs-host disease. Therefore, they can be an off-the-shelf product, prepared in advance with the necessary receptor and given to patients promptly.
The researchers are developing CB-derived CAR NK cells for other targets in hematologic and solid tumor malignancies.
MD Anderson and the researchers have intellectual property related to the engineered NK cells, which is being managed in accordance with the institution’s conflict-of-interest rules.
Funding for this research was provided by MD Anderson’s Moon Shots Program, the National Cancer Institute of the National Institutes of Health Cancer Center Support Grant (CA016672) to MD Anderson, and grants from the Leukemia and Lymphoma Society and the American Cancer Society. ![]()
Natural killer (NK) cells derived from cord blood (CB) can be modified to fight chronic lymphocytic leukemia (CLL) and Burkitt lymphoma (BL), according to research published in Leukemia.
Using a viral vector, researchers transduced CB-derived NK cells with a chimeric antigen receptor (CAR), interleukin-15 (IL-15), and an inducible caspase-9-based suicide gene.
The CAR directed the NK cells to kill CD19-expressing cells, IL-15 prolonged the NK cells’ survival and enhanced their antitumor activity, and the suicide gene allowed researchers to kill off the NK cells in the event of a severe inflammatory response.
“Natural killer cells are the immune system’s most potent killers, but they are short-lived, and cancers manage to evade a patient’s own NK cells to progress,” said study author Katy Rezvani, MD, PhD, of The University of Texas MD Anderson Cancer Center in Houston.
“Our cord-blood derived NK cells, genetically equipped with a receptor that focuses them on B-cell malignancies and with interleukin-15 to help them persist longer—potentially for months instead of 2 or 3 weeks—are designed to address these challenges.”
Dr Rezvani and her colleagues tested their CB-derived CAR NK cells in primary CLL cells and a mouse model of BL. Compared to unmodified NK cells, the CAR NK cells killed malignant cells more efficiently and extended the survival of mice.
Another experiment showed the CB-derived CAR NK cells killed CLL cells more efficiently than NK cells that were taken from CLL patients and modified in the same way. The researchers said this highlights the need to transplant CAR-engineered NK cells derived from healthy CB rather than using a patient’s own cells.
Additional experiments in the mouse model of BL showed that a single infusion of low-dose CAR NK cells resulted in prolonged survival.
When CAR NK cells were given at a higher dose, none of the mice died of BL. Half of them survived 100 days and beyond. However, all mice treated with other types of NK cells died by day 41.
Some mice treated with the higher dose of CAR NK cells died of cytokine release syndrome (CRS).
To counteract this toxicity, the researchers activated the suicide gene (iC9) via treatment with a small-molecule dimerizer, AP1903.
The team found that adding as little as 10 nM of AP1903 to cell cultures induced apoptosis/necrosis of the CAR NK cells within 4 hours but had no effect on non-CAR CB-derived NK cells. Similar results were observed in the mouse model.
Next steps
A phase 1/2 trial of these CB-derived CAR NK cells opened at MD Anderson in June for patients with relapsed or refractory CLL, acute lymphocytic leukemia, or non-Hodgkin lymphoma.
Dr Rezvani, the principal investigator of the trial, said the protocol calls for vigilance for signs of CRS, treatment with steroids and tocilizumab for low-grade CRS, and AP1903 added to activate the suicide gene for grade 3 or 4 CRS.
She and her colleagues noted that CB-derived NK cells do not cause graft-vs-host disease. Therefore, they can be an off-the-shelf product, prepared in advance with the necessary receptor and given to patients promptly.
The researchers are developing CB-derived CAR NK cells for other targets in hematologic and solid tumor malignancies.
MD Anderson and the researchers have intellectual property related to the engineered NK cells, which is being managed in accordance with the institution’s conflict-of-interest rules.
Funding for this research was provided by MD Anderson’s Moon Shots Program, the National Cancer Institute of the National Institutes of Health Cancer Center Support Grant (CA016672) to MD Anderson, and grants from the Leukemia and Lymphoma Society and the American Cancer Society. ![]()
AYA cancer survivors struggle with social functioning
New research suggests young cancer survivors struggle to get their social lives “back to normal” within the first 2 years of their diagnosis.
The study showed that adolescents and young adults (AYAs) with cancer had significantly worse social functioning than the general population around the time of cancer diagnosis as well as 1 year and 2 years later.
These findings were published in Cancer.
“The research is important to help these young survivors better reintegrate into society,” said study author Brad Zebrack, PhD, of the University of Michigan in Ann Arbor.
He and his colleagues collected data from 141 AYA cancer patients (ages 14 to 39) who visited 1 of 5 US medical facilities between March 2008 and April 2010.
The patients completed a self-report measure of social functioning within the first 4 months of diagnosis, then again at 12 months and 24 months.
Compared to the general population, the AYA cancer patients had significantly worse social functioning scores at all time points:
- Around the time of diagnosis—52.0 vs 85.1 (P<0.001)
- At 12 months—73.1 vs 85.1 (P<0.001)
- At 24 months—69.2 vs 85.1 (P<0.001).
Overall, the patients did experience improvements in social functioning from baseline to the 12-month time point, but their scores remained stable after that.
The researchers noted that 9% of patients had consistently high/normal social functioning, 47% had improvements in social functioning over time, 13% had worsening social functioning over time, and 32% had consistently low social functioning.
“This finding highlights the need to screen, identify, and respond to the needs of high-risk young adult-adolescent patients at the time of diagnosis and then monitor them over time,” Dr Zebrack said.
“They are likely the ones most in need of help in managing work, school, and potentially problematic relationships with family members and friends.”![]()
New research suggests young cancer survivors struggle to get their social lives “back to normal” within the first 2 years of their diagnosis.
The study showed that adolescents and young adults (AYAs) with cancer had significantly worse social functioning than the general population around the time of cancer diagnosis as well as 1 year and 2 years later.
These findings were published in Cancer.
“The research is important to help these young survivors better reintegrate into society,” said study author Brad Zebrack, PhD, of the University of Michigan in Ann Arbor.
He and his colleagues collected data from 141 AYA cancer patients (ages 14 to 39) who visited 1 of 5 US medical facilities between March 2008 and April 2010.
The patients completed a self-report measure of social functioning within the first 4 months of diagnosis, then again at 12 months and 24 months.
Compared to the general population, the AYA cancer patients had significantly worse social functioning scores at all time points:
- Around the time of diagnosis—52.0 vs 85.1 (P<0.001)
- At 12 months—73.1 vs 85.1 (P<0.001)
- At 24 months—69.2 vs 85.1 (P<0.001).
Overall, the patients did experience improvements in social functioning from baseline to the 12-month time point, but their scores remained stable after that.
The researchers noted that 9% of patients had consistently high/normal social functioning, 47% had improvements in social functioning over time, 13% had worsening social functioning over time, and 32% had consistently low social functioning.
“This finding highlights the need to screen, identify, and respond to the needs of high-risk young adult-adolescent patients at the time of diagnosis and then monitor them over time,” Dr Zebrack said.
“They are likely the ones most in need of help in managing work, school, and potentially problematic relationships with family members and friends.”![]()
New research suggests young cancer survivors struggle to get their social lives “back to normal” within the first 2 years of their diagnosis.
The study showed that adolescents and young adults (AYAs) with cancer had significantly worse social functioning than the general population around the time of cancer diagnosis as well as 1 year and 2 years later.
These findings were published in Cancer.
“The research is important to help these young survivors better reintegrate into society,” said study author Brad Zebrack, PhD, of the University of Michigan in Ann Arbor.
He and his colleagues collected data from 141 AYA cancer patients (ages 14 to 39) who visited 1 of 5 US medical facilities between March 2008 and April 2010.
The patients completed a self-report measure of social functioning within the first 4 months of diagnosis, then again at 12 months and 24 months.
Compared to the general population, the AYA cancer patients had significantly worse social functioning scores at all time points:
- Around the time of diagnosis—52.0 vs 85.1 (P<0.001)
- At 12 months—73.1 vs 85.1 (P<0.001)
- At 24 months—69.2 vs 85.1 (P<0.001).
Overall, the patients did experience improvements in social functioning from baseline to the 12-month time point, but their scores remained stable after that.
The researchers noted that 9% of patients had consistently high/normal social functioning, 47% had improvements in social functioning over time, 13% had worsening social functioning over time, and 32% had consistently low social functioning.
“This finding highlights the need to screen, identify, and respond to the needs of high-risk young adult-adolescent patients at the time of diagnosis and then monitor them over time,” Dr Zebrack said.
“They are likely the ones most in need of help in managing work, school, and potentially problematic relationships with family members and friends.”![]()