User login
Is quetiapine effective for anxiety?
Discuss this article at www.facebook.com/CurrentPsychiatry
The rate of off-label prescribing of second-generation antipsychotics (SGAs) is estimated to have doubled in the past decade.1,2 In 2010, quetiapine was the most commonly used SGA in the United States with >10 million prescriptions dispensed.2 Clinical experience and reports from patients indicate quetiapine may be useful for treating anxiety. When making medication choices, it can be useful to combine anecdotal evidence with the facts (or lack thereof). Does evidence support or contradict the use of quetiapine for anxiety?
What the research shows
Quetiapine is FDA-approved for treating:
- adults and adolescents with schizophrenia
- adults, children, and adolescents with acute manic episodes associated with bipolar I disorder (BDI) as monotherapy or as an adjunct to lithium or divalproex
- adults with an acute depressive episode associated with bipolar disorder
- adjunctive treatment of major depressive disorder (MDD) in adults
- maintenance treatment of BDI as an adjunct to lithium or divalproex in adults.3
In addition, quetiapine extended-release (XR) is approved as an adjunctive treatment for MDD in adults.4
Neither the immediate-release or XR formulation is indicated for treating anxiety, but quetiapine has been studied as a treatment for several anxiety disorders, including posttraumatic stress disorder, social phobia, obsessive-compulsive disorder, and anxiety secondary to mood disorders. It has been most extensively studied as treatment for generalized anxiety disorder (GAD).
Three trials that involved >2,100 patients found quetiapine XR monotherapy is effective for GAD in doses of 50 to 300 mg/d.5-7 In 2 of the studies, quetiapine XR was as effective as paroxetine and escitalopram for GAD.5,6 Reviews of off-label SGA use have found that compared with placebo, quetiapine XR monotherapy is effective for GAD (number needed to treat=8).8,9 Side effects reported in clinical trials of quetiapine included headache, somnolence, sedation, fatigue, dizziness, dry mouth, weight gain, hyperlipidemia, and elevated glucose levels.
What did the FDA say?
In April 2009, the FDA’s Psychopharmacologic Drugs Advisory Committee reviewed whether evidence supported quetiapine XR for treating MDD and GAD.10 Although the committee found that quetiapine XR monotherapy effectively treated GAD, it concluded it was not acceptably safe.11 The committee expressed concerns over exposing a greatly expanded population to a drug with substantial metabolic side effects, including weight gain (incidence 3% to 23%), increased cholesterol (incidence 7% to 18%), and hyperglycemia.12-14 Weight gain and metabolic effects have been reported even when quetiapine is prescribed at low doses (≤100 mg/d).15,16 The FDA did not approve expanding the indication of quetiapine XR to include treatment of GAD.
Our opinion
Quetiapine XR is effective for treating GAD. However, even at low doses, it is associated with substantial side effects and should be reserved for patients with poor response or contraindications (eg, mania) to traditional GAD treatments such as selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors. Published studies assessed quetiapine XR only when used on a scheduled basis, and did not address use of quetiapine immediate release or XR on an as-needed basis for GAD.
Related Resources
- AstraZeneca. Seroquel prescribing information. www1.astrazeneca-us.com/pi/seroquel.pdf.
- AstraZeneca. Seroquel XR prescribing information. www1.astrazeneca-us.com/pi/seroquelxr.pdf.
Drug Brand Names
- Divalproex • Depakote
- Paroxetine • Paxil
- Escitalopram • Lexapro
- Quetiapine • Seroquel
- Lithium • Eskalith, Lithobid
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Alexander GC, Gallagher SA, Mascola A, et al. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiol Drug Saf. 2011;20(2):177-184.
2. Drug Topics. 2010 Top 200 branded drugs by total prescriptions. http://drugtopics.modernmedicine.com/drugtopics/data/articlestandard/drugtopics/252011/727256/article.pdf. Published June 2011. Accessed June 26 2012.
3. Seroquel [package insert]. Wilmington DE: AstraZeneca; 2012.
4. Seroquel XR [package insert]. Wilmington DE: AstraZeneca; 2012.
5. Merideth C, Cutler A, Neijber A, et al. Efficacy and tolerability of extended release quetiapine fumarate monotherapy in the treatment of GAD. Eur Neuropsychopharmacol. 2008;18(suppl 4):S499-S500.
6. Bandelow B, Chouinard G, Bobes J, et al. Extended-release quetiapine fumarate (quetiapine XR): a once-daily monotherapy effective in generalized anxiety disorder. Data from a randomized, double-blind, placebo- and active-controlled study. Int J Neuropsychopharmacol. 2010;13(3):305-320.
7. Katzman MA, Brawman-Mintzer O, Reyes EB, et al. Extended release quetiapine fumarate (quetiapine XR) monotherapy as maintenance treatment for generalized anxiety disorder: a long-term, randomized, placebo-controlled trial. Int Clin Psychopharmacol. 2011;26(1):11-24.
8. Maglione M, Ruelaz Maher A, Hu J, et al. Agency for Healthcare Research and Quality. Off-label use of atypical antipsychotics: an update. http://www.effectivehealthcare.ahrq.gov/ehc/products/150/786/CER43_Off-LabelAntipsychotics_execsumm_20110928.pdf. Published September 2011. Accessed June 26 2012.
9. Maher AR, Maglione M, Bagley S, et al. Efficacy and comparative effectiveness of atypical antipsychotic medications for off-label uses in adults: a systematic review and meta-analysis. JAMA. 2011;306(12):1359-1369.
10. U.S. Food and Drug Administration. Psychopharmacologic Drugs Advisory Committee meeting announcement. http://www.fda.gov/AdvisoryCommittees/Calendar/ucm136250.htm. Updated June 18, 2009. Accessed June 26, 2012.
11. FDA advisory committee recommendation on Seroquel XR supplemental new drug applications [news release]. Wilmington DE: AstraZeneca; April 9, 2009. http://www.astrazeneca.com/Media/Press-releases/Article/20090409—FDA-Advisory-Committee-Recommendation-on-Seroquel-XR-. Accessed June 26, 2012.
12. Meyer JM, Koro CE. The effects of antipsychotic therapy on serum lipids: a comprehensive review. Schizophr Res. 2004;70(1):1-17.
13. Newcomer JW. Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry. 2007;68(suppl 1):20-27.
14. Chen WY, Chen CC, Hung GC. Hyperglycemic hyperosmolar state associated with low-dose quetiapine treatment in a patient with bipolar disorder. Curr Drug Saf. 2011;6(3):207-208.
15. Williams SG, Alinejad NA, Williams JA, et al. Statistically significant increase in weight caused by low-dose quetiapine. Pharmacotherapy. 2010;30(10):1011-1015.
16. Simon V, van Winkel R, De Hert M. Are weight gain and metabolic side effects of atypical antipsychotics dose dependent? A literature review. J Clin Psychiatry. 2009;70(7):1041-1050.
Discuss this article at www.facebook.com/CurrentPsychiatry
The rate of off-label prescribing of second-generation antipsychotics (SGAs) is estimated to have doubled in the past decade.1,2 In 2010, quetiapine was the most commonly used SGA in the United States with >10 million prescriptions dispensed.2 Clinical experience and reports from patients indicate quetiapine may be useful for treating anxiety. When making medication choices, it can be useful to combine anecdotal evidence with the facts (or lack thereof). Does evidence support or contradict the use of quetiapine for anxiety?
What the research shows
Quetiapine is FDA-approved for treating:
- adults and adolescents with schizophrenia
- adults, children, and adolescents with acute manic episodes associated with bipolar I disorder (BDI) as monotherapy or as an adjunct to lithium or divalproex
- adults with an acute depressive episode associated with bipolar disorder
- adjunctive treatment of major depressive disorder (MDD) in adults
- maintenance treatment of BDI as an adjunct to lithium or divalproex in adults.3
In addition, quetiapine extended-release (XR) is approved as an adjunctive treatment for MDD in adults.4
Neither the immediate-release or XR formulation is indicated for treating anxiety, but quetiapine has been studied as a treatment for several anxiety disorders, including posttraumatic stress disorder, social phobia, obsessive-compulsive disorder, and anxiety secondary to mood disorders. It has been most extensively studied as treatment for generalized anxiety disorder (GAD).
Three trials that involved >2,100 patients found quetiapine XR monotherapy is effective for GAD in doses of 50 to 300 mg/d.5-7 In 2 of the studies, quetiapine XR was as effective as paroxetine and escitalopram for GAD.5,6 Reviews of off-label SGA use have found that compared with placebo, quetiapine XR monotherapy is effective for GAD (number needed to treat=8).8,9 Side effects reported in clinical trials of quetiapine included headache, somnolence, sedation, fatigue, dizziness, dry mouth, weight gain, hyperlipidemia, and elevated glucose levels.
What did the FDA say?
In April 2009, the FDA’s Psychopharmacologic Drugs Advisory Committee reviewed whether evidence supported quetiapine XR for treating MDD and GAD.10 Although the committee found that quetiapine XR monotherapy effectively treated GAD, it concluded it was not acceptably safe.11 The committee expressed concerns over exposing a greatly expanded population to a drug with substantial metabolic side effects, including weight gain (incidence 3% to 23%), increased cholesterol (incidence 7% to 18%), and hyperglycemia.12-14 Weight gain and metabolic effects have been reported even when quetiapine is prescribed at low doses (≤100 mg/d).15,16 The FDA did not approve expanding the indication of quetiapine XR to include treatment of GAD.
Our opinion
Quetiapine XR is effective for treating GAD. However, even at low doses, it is associated with substantial side effects and should be reserved for patients with poor response or contraindications (eg, mania) to traditional GAD treatments such as selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors. Published studies assessed quetiapine XR only when used on a scheduled basis, and did not address use of quetiapine immediate release or XR on an as-needed basis for GAD.
Related Resources
- AstraZeneca. Seroquel prescribing information. www1.astrazeneca-us.com/pi/seroquel.pdf.
- AstraZeneca. Seroquel XR prescribing information. www1.astrazeneca-us.com/pi/seroquelxr.pdf.
Drug Brand Names
- Divalproex • Depakote
- Paroxetine • Paxil
- Escitalopram • Lexapro
- Quetiapine • Seroquel
- Lithium • Eskalith, Lithobid
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
The rate of off-label prescribing of second-generation antipsychotics (SGAs) is estimated to have doubled in the past decade.1,2 In 2010, quetiapine was the most commonly used SGA in the United States with >10 million prescriptions dispensed.2 Clinical experience and reports from patients indicate quetiapine may be useful for treating anxiety. When making medication choices, it can be useful to combine anecdotal evidence with the facts (or lack thereof). Does evidence support or contradict the use of quetiapine for anxiety?
What the research shows
Quetiapine is FDA-approved for treating:
- adults and adolescents with schizophrenia
- adults, children, and adolescents with acute manic episodes associated with bipolar I disorder (BDI) as monotherapy or as an adjunct to lithium or divalproex
- adults with an acute depressive episode associated with bipolar disorder
- adjunctive treatment of major depressive disorder (MDD) in adults
- maintenance treatment of BDI as an adjunct to lithium or divalproex in adults.3
In addition, quetiapine extended-release (XR) is approved as an adjunctive treatment for MDD in adults.4
Neither the immediate-release or XR formulation is indicated for treating anxiety, but quetiapine has been studied as a treatment for several anxiety disorders, including posttraumatic stress disorder, social phobia, obsessive-compulsive disorder, and anxiety secondary to mood disorders. It has been most extensively studied as treatment for generalized anxiety disorder (GAD).
Three trials that involved >2,100 patients found quetiapine XR monotherapy is effective for GAD in doses of 50 to 300 mg/d.5-7 In 2 of the studies, quetiapine XR was as effective as paroxetine and escitalopram for GAD.5,6 Reviews of off-label SGA use have found that compared with placebo, quetiapine XR monotherapy is effective for GAD (number needed to treat=8).8,9 Side effects reported in clinical trials of quetiapine included headache, somnolence, sedation, fatigue, dizziness, dry mouth, weight gain, hyperlipidemia, and elevated glucose levels.
What did the FDA say?
In April 2009, the FDA’s Psychopharmacologic Drugs Advisory Committee reviewed whether evidence supported quetiapine XR for treating MDD and GAD.10 Although the committee found that quetiapine XR monotherapy effectively treated GAD, it concluded it was not acceptably safe.11 The committee expressed concerns over exposing a greatly expanded population to a drug with substantial metabolic side effects, including weight gain (incidence 3% to 23%), increased cholesterol (incidence 7% to 18%), and hyperglycemia.12-14 Weight gain and metabolic effects have been reported even when quetiapine is prescribed at low doses (≤100 mg/d).15,16 The FDA did not approve expanding the indication of quetiapine XR to include treatment of GAD.
Our opinion
Quetiapine XR is effective for treating GAD. However, even at low doses, it is associated with substantial side effects and should be reserved for patients with poor response or contraindications (eg, mania) to traditional GAD treatments such as selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors. Published studies assessed quetiapine XR only when used on a scheduled basis, and did not address use of quetiapine immediate release or XR on an as-needed basis for GAD.
Related Resources
- AstraZeneca. Seroquel prescribing information. www1.astrazeneca-us.com/pi/seroquel.pdf.
- AstraZeneca. Seroquel XR prescribing information. www1.astrazeneca-us.com/pi/seroquelxr.pdf.
Drug Brand Names
- Divalproex • Depakote
- Paroxetine • Paxil
- Escitalopram • Lexapro
- Quetiapine • Seroquel
- Lithium • Eskalith, Lithobid
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Alexander GC, Gallagher SA, Mascola A, et al. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiol Drug Saf. 2011;20(2):177-184.
2. Drug Topics. 2010 Top 200 branded drugs by total prescriptions. http://drugtopics.modernmedicine.com/drugtopics/data/articlestandard/drugtopics/252011/727256/article.pdf. Published June 2011. Accessed June 26 2012.
3. Seroquel [package insert]. Wilmington DE: AstraZeneca; 2012.
4. Seroquel XR [package insert]. Wilmington DE: AstraZeneca; 2012.
5. Merideth C, Cutler A, Neijber A, et al. Efficacy and tolerability of extended release quetiapine fumarate monotherapy in the treatment of GAD. Eur Neuropsychopharmacol. 2008;18(suppl 4):S499-S500.
6. Bandelow B, Chouinard G, Bobes J, et al. Extended-release quetiapine fumarate (quetiapine XR): a once-daily monotherapy effective in generalized anxiety disorder. Data from a randomized, double-blind, placebo- and active-controlled study. Int J Neuropsychopharmacol. 2010;13(3):305-320.
7. Katzman MA, Brawman-Mintzer O, Reyes EB, et al. Extended release quetiapine fumarate (quetiapine XR) monotherapy as maintenance treatment for generalized anxiety disorder: a long-term, randomized, placebo-controlled trial. Int Clin Psychopharmacol. 2011;26(1):11-24.
8. Maglione M, Ruelaz Maher A, Hu J, et al. Agency for Healthcare Research and Quality. Off-label use of atypical antipsychotics: an update. http://www.effectivehealthcare.ahrq.gov/ehc/products/150/786/CER43_Off-LabelAntipsychotics_execsumm_20110928.pdf. Published September 2011. Accessed June 26 2012.
9. Maher AR, Maglione M, Bagley S, et al. Efficacy and comparative effectiveness of atypical antipsychotic medications for off-label uses in adults: a systematic review and meta-analysis. JAMA. 2011;306(12):1359-1369.
10. U.S. Food and Drug Administration. Psychopharmacologic Drugs Advisory Committee meeting announcement. http://www.fda.gov/AdvisoryCommittees/Calendar/ucm136250.htm. Updated June 18, 2009. Accessed June 26, 2012.
11. FDA advisory committee recommendation on Seroquel XR supplemental new drug applications [news release]. Wilmington DE: AstraZeneca; April 9, 2009. http://www.astrazeneca.com/Media/Press-releases/Article/20090409—FDA-Advisory-Committee-Recommendation-on-Seroquel-XR-. Accessed June 26, 2012.
12. Meyer JM, Koro CE. The effects of antipsychotic therapy on serum lipids: a comprehensive review. Schizophr Res. 2004;70(1):1-17.
13. Newcomer JW. Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry. 2007;68(suppl 1):20-27.
14. Chen WY, Chen CC, Hung GC. Hyperglycemic hyperosmolar state associated with low-dose quetiapine treatment in a patient with bipolar disorder. Curr Drug Saf. 2011;6(3):207-208.
15. Williams SG, Alinejad NA, Williams JA, et al. Statistically significant increase in weight caused by low-dose quetiapine. Pharmacotherapy. 2010;30(10):1011-1015.
16. Simon V, van Winkel R, De Hert M. Are weight gain and metabolic side effects of atypical antipsychotics dose dependent? A literature review. J Clin Psychiatry. 2009;70(7):1041-1050.
1. Alexander GC, Gallagher SA, Mascola A, et al. Increasing off-label use of antipsychotic medications in the United States, 1995-2008. Pharmacoepidemiol Drug Saf. 2011;20(2):177-184.
2. Drug Topics. 2010 Top 200 branded drugs by total prescriptions. http://drugtopics.modernmedicine.com/drugtopics/data/articlestandard/drugtopics/252011/727256/article.pdf. Published June 2011. Accessed June 26 2012.
3. Seroquel [package insert]. Wilmington DE: AstraZeneca; 2012.
4. Seroquel XR [package insert]. Wilmington DE: AstraZeneca; 2012.
5. Merideth C, Cutler A, Neijber A, et al. Efficacy and tolerability of extended release quetiapine fumarate monotherapy in the treatment of GAD. Eur Neuropsychopharmacol. 2008;18(suppl 4):S499-S500.
6. Bandelow B, Chouinard G, Bobes J, et al. Extended-release quetiapine fumarate (quetiapine XR): a once-daily monotherapy effective in generalized anxiety disorder. Data from a randomized, double-blind, placebo- and active-controlled study. Int J Neuropsychopharmacol. 2010;13(3):305-320.
7. Katzman MA, Brawman-Mintzer O, Reyes EB, et al. Extended release quetiapine fumarate (quetiapine XR) monotherapy as maintenance treatment for generalized anxiety disorder: a long-term, randomized, placebo-controlled trial. Int Clin Psychopharmacol. 2011;26(1):11-24.
8. Maglione M, Ruelaz Maher A, Hu J, et al. Agency for Healthcare Research and Quality. Off-label use of atypical antipsychotics: an update. http://www.effectivehealthcare.ahrq.gov/ehc/products/150/786/CER43_Off-LabelAntipsychotics_execsumm_20110928.pdf. Published September 2011. Accessed June 26 2012.
9. Maher AR, Maglione M, Bagley S, et al. Efficacy and comparative effectiveness of atypical antipsychotic medications for off-label uses in adults: a systematic review and meta-analysis. JAMA. 2011;306(12):1359-1369.
10. U.S. Food and Drug Administration. Psychopharmacologic Drugs Advisory Committee meeting announcement. http://www.fda.gov/AdvisoryCommittees/Calendar/ucm136250.htm. Updated June 18, 2009. Accessed June 26, 2012.
11. FDA advisory committee recommendation on Seroquel XR supplemental new drug applications [news release]. Wilmington DE: AstraZeneca; April 9, 2009. http://www.astrazeneca.com/Media/Press-releases/Article/20090409—FDA-Advisory-Committee-Recommendation-on-Seroquel-XR-. Accessed June 26, 2012.
12. Meyer JM, Koro CE. The effects of antipsychotic therapy on serum lipids: a comprehensive review. Schizophr Res. 2004;70(1):1-17.
13. Newcomer JW. Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry. 2007;68(suppl 1):20-27.
14. Chen WY, Chen CC, Hung GC. Hyperglycemic hyperosmolar state associated with low-dose quetiapine treatment in a patient with bipolar disorder. Curr Drug Saf. 2011;6(3):207-208.
15. Williams SG, Alinejad NA, Williams JA, et al. Statistically significant increase in weight caused by low-dose quetiapine. Pharmacotherapy. 2010;30(10):1011-1015.
16. Simon V, van Winkel R, De Hert M. Are weight gain and metabolic side effects of atypical antipsychotics dose dependent? A literature review. J Clin Psychiatry. 2009;70(7):1041-1050.
Meningococcal vaccine for infants?
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
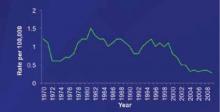
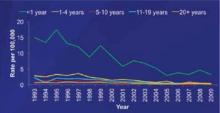
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
Meningococcal vaccine for infants?
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
Nutrition and exercise in cancer survivors
Obesity has reached epidemic proportions in the United States in the past 2 decades. According to a recent report, 36% of the adult population currently has a body mass index of more than 30 kg/m2, which is the diagnostic for obesity.1 If we focus only on the US adult cancer survivor population, then the magnitude of being overweight or obese is notably higher, ranging from 52% to 68%.2 In adult survivors of childhood cancer, several factors are associated with increased risk for obesity, such as hypothalamic or pituitary radiation, the use of certain antidepressants, and lifestyle factors.3
*For a PDF of the full article, click on the link to the left of this introduction.
Obesity has reached epidemic proportions in the United States in the past 2 decades. According to a recent report, 36% of the adult population currently has a body mass index of more than 30 kg/m2, which is the diagnostic for obesity.1 If we focus only on the US adult cancer survivor population, then the magnitude of being overweight or obese is notably higher, ranging from 52% to 68%.2 In adult survivors of childhood cancer, several factors are associated with increased risk for obesity, such as hypothalamic or pituitary radiation, the use of certain antidepressants, and lifestyle factors.3
*For a PDF of the full article, click on the link to the left of this introduction.
Obesity has reached epidemic proportions in the United States in the past 2 decades. According to a recent report, 36% of the adult population currently has a body mass index of more than 30 kg/m2, which is the diagnostic for obesity.1 If we focus only on the US adult cancer survivor population, then the magnitude of being overweight or obese is notably higher, ranging from 52% to 68%.2 In adult survivors of childhood cancer, several factors are associated with increased risk for obesity, such as hypothalamic or pituitary radiation, the use of certain antidepressants, and lifestyle factors.3
*For a PDF of the full article, click on the link to the left of this introduction.
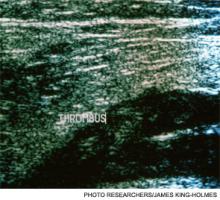
PCA3 permutation increases the prostate biopsy yield
Background: A direct correlation between the preoperative prostate cancer antigen 3 (PCA3) gene and total tumor volume in postprostatectomy specimens has recently been reported. This suggests that the PCA3 score could serve as a surrogate for tumor burden in patients with prostate cancer. Accordingly, the PCA3 density (that is, the ratio of the PCA3 score to prostate volume) is representative of the degree of prostate volume occupied by tumor.
Objective: To show that the PCA3 density would be directly related to the likelihood of finding cancer on prostate biopsy, given that larger tumors in smaller glands would be more likely to be detected through prostate biopsy.
Methods: We identified 288 men referred for prostate biopsy for an elevated prostate-specific antigen (PSA) level, high PSA velocity, low free- to total-PSA ratio, or suspicious digital rectal exam. All of the patients had had a urinary PCA3 test performed no more than 4 weeks before biopsy, and prostate volume was recorded by transrectal ultrasound determination at the time of biopsy. The diagnostic yield of PSA level, PSA density (PSAD), PCA3 score, and PCA3 density in detecting cancer was evaluated using a receiver operating characteristic (ROC) curve.
Results: Of the 288 patients included for analysis, 183 (63.5%) underwent an initial prostate biopsy and 105 (36.5%) had at least 1 previous negative biopsy. Cancer was detected in 74 (25.7%) patients. The area under the curve was 0.486 for PSA level, 0.590 for PSAD, 0.687 for PCA3 score, and 0.717 for PCA3 density.
Conclusion: PCA3 density is strongly correlated with cancer detection and may be useful in selecting patients for biopsy.
*For a PDF of the full article, click on the link to the left of this introduction.
Background: A direct correlation between the preoperative prostate cancer antigen 3 (PCA3) gene and total tumor volume in postprostatectomy specimens has recently been reported. This suggests that the PCA3 score could serve as a surrogate for tumor burden in patients with prostate cancer. Accordingly, the PCA3 density (that is, the ratio of the PCA3 score to prostate volume) is representative of the degree of prostate volume occupied by tumor.
Objective: To show that the PCA3 density would be directly related to the likelihood of finding cancer on prostate biopsy, given that larger tumors in smaller glands would be more likely to be detected through prostate biopsy.
Methods: We identified 288 men referred for prostate biopsy for an elevated prostate-specific antigen (PSA) level, high PSA velocity, low free- to total-PSA ratio, or suspicious digital rectal exam. All of the patients had had a urinary PCA3 test performed no more than 4 weeks before biopsy, and prostate volume was recorded by transrectal ultrasound determination at the time of biopsy. The diagnostic yield of PSA level, PSA density (PSAD), PCA3 score, and PCA3 density in detecting cancer was evaluated using a receiver operating characteristic (ROC) curve.
Results: Of the 288 patients included for analysis, 183 (63.5%) underwent an initial prostate biopsy and 105 (36.5%) had at least 1 previous negative biopsy. Cancer was detected in 74 (25.7%) patients. The area under the curve was 0.486 for PSA level, 0.590 for PSAD, 0.687 for PCA3 score, and 0.717 for PCA3 density.
Conclusion: PCA3 density is strongly correlated with cancer detection and may be useful in selecting patients for biopsy.
*For a PDF of the full article, click on the link to the left of this introduction.
Background: A direct correlation between the preoperative prostate cancer antigen 3 (PCA3) gene and total tumor volume in postprostatectomy specimens has recently been reported. This suggests that the PCA3 score could serve as a surrogate for tumor burden in patients with prostate cancer. Accordingly, the PCA3 density (that is, the ratio of the PCA3 score to prostate volume) is representative of the degree of prostate volume occupied by tumor.
Objective: To show that the PCA3 density would be directly related to the likelihood of finding cancer on prostate biopsy, given that larger tumors in smaller glands would be more likely to be detected through prostate biopsy.
Methods: We identified 288 men referred for prostate biopsy for an elevated prostate-specific antigen (PSA) level, high PSA velocity, low free- to total-PSA ratio, or suspicious digital rectal exam. All of the patients had had a urinary PCA3 test performed no more than 4 weeks before biopsy, and prostate volume was recorded by transrectal ultrasound determination at the time of biopsy. The diagnostic yield of PSA level, PSA density (PSAD), PCA3 score, and PCA3 density in detecting cancer was evaluated using a receiver operating characteristic (ROC) curve.
Results: Of the 288 patients included for analysis, 183 (63.5%) underwent an initial prostate biopsy and 105 (36.5%) had at least 1 previous negative biopsy. Cancer was detected in 74 (25.7%) patients. The area under the curve was 0.486 for PSA level, 0.590 for PSAD, 0.687 for PCA3 score, and 0.717 for PCA3 density.
Conclusion: PCA3 density is strongly correlated with cancer detection and may be useful in selecting patients for biopsy.
*For a PDF of the full article, click on the link to the left of this introduction.
Maintenance therapy in solid tumors
The concept of maintenance therapy has been well studied in hematologic malignancies, and now, an increasing number of clinical trials explore the role of maintenance therapy in solid cancers. Both biological and lower-intensity chemotherapeutic agents are currently being evaluated as maintenance therapy. However, despite the increase in research in this area, there has not been consensus about the definition and timing of maintenance therapy. In this review, we will focus on continuation maintenance therapy and switch maintenance therapy in patients with metastatic solid tumors who have achieved stable disease, partial response, or complete response after first-line treatment.
*For a PDF of the full article, click on the link to the left of this introduction.
The concept of maintenance therapy has been well studied in hematologic malignancies, and now, an increasing number of clinical trials explore the role of maintenance therapy in solid cancers. Both biological and lower-intensity chemotherapeutic agents are currently being evaluated as maintenance therapy. However, despite the increase in research in this area, there has not been consensus about the definition and timing of maintenance therapy. In this review, we will focus on continuation maintenance therapy and switch maintenance therapy in patients with metastatic solid tumors who have achieved stable disease, partial response, or complete response after first-line treatment.
*For a PDF of the full article, click on the link to the left of this introduction.
The concept of maintenance therapy has been well studied in hematologic malignancies, and now, an increasing number of clinical trials explore the role of maintenance therapy in solid cancers. Both biological and lower-intensity chemotherapeutic agents are currently being evaluated as maintenance therapy. However, despite the increase in research in this area, there has not been consensus about the definition and timing of maintenance therapy. In this review, we will focus on continuation maintenance therapy and switch maintenance therapy in patients with metastatic solid tumors who have achieved stable disease, partial response, or complete response after first-line treatment.
*For a PDF of the full article, click on the link to the left of this introduction.
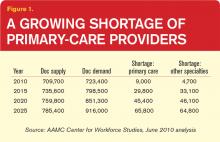
Workforce Shortages, Increased Patient Populations, and Funding Woes Pressure U.S. Primary-Care System
It’s been about 15 years since the last surge of interest in primary care as a career, when U.S. medical graduates temporarily reversed a long decline by flocking to family medicine, general internal medicine, and pediatrics. Newly minted doctors responded enthusiastically to a widely held perception in the mid-1990s that primary care would be central to a brave new paradigm of managed healthcare delivery.
That profound change never materialized, and the primary-care workforce has since resumed a downward slide that is sounding alarm bells throughout the country. Even more distressing, the medical profession’s recent misfortunes have spread far beyond the doctor’s office.
“What we’re looking at now is that there’s a shortage of somewhere around 90,000 physicians in the next 10 years, increasing in the five years beyond that to 125,000 or more,” says Atul Grover, MD, PhD, chief public policy officer of the Association of American Medical Colleges. The association’s estimates suggest that the 10- and 15-year shortfalls will be split nearly evenly between primary care and other specialties.
Hospitalists could feel that widening gap as well. With increasing numbers of aging baby boomers reaching Medicare eligibility and 32 million Americans set to join the ranks of the insured by 2019 through the Affordable Care Act, primary care’s difficulties arguably are the closest to a full-blown crisis. “Primary care in the United States needs a lifeline,” began a 2009 editorial in the New England Journal of Medicine.1 And that was before an estimate suggesting that new insurance mandates will require an additional 4,307 to 6,940 primary-care physicians to meet demand before the end of the decade contributing about 15% to the expected shortfall.2
Why should hospitalists care about the fate of their counterparts? For starters, what’s good for outpatient providers is good for a sound healthcare system. Researchers have linked strong
primary care to lower overall spending, fewer health disparities, and higher quality of care.3
Hospitalists and primary-care physicians (PCPs) also are inexorably linked. They follow similar training and education pathways, and need each other to ensure safe transitions of care. And despite the evidence pointing to a slew of contributing factors, HM regularly is blamed for many of primary care’s mounting woes.
Based on well-functioning healthcare systems around the world, analysts say the ideal primary-care-to-specialty-care-provider ratio should be roughly 40:60 or 50:50. According to Kathleen Klink, MD, director of the Division of Medicine and Dentistry in the Health Resources and Services Administration (HRSA), only about 32% of physicians in the U.S. are practicing primary care. Unless something changes, that percentage will erode even further. “We’re going in the wrong direction,” Dr. Klink says.
Opinions differ on the extent of the current PCP shortage. Nevertheless, there is clearly a “huge maldistribution problem,” says Robert Phillips, MD, MSPH, director of the Washington, D.C.-based Robert Graham Center, a primary-care research center. Rural and underserved areas already are being shortchanged as more doctors locate in more affluent and desirable areas, he says.
That phenomenon is hardly unique to primary care, but Dr. Phillips says the deficit in frontline doctors could cause disproportionately more hardships in rural and underserved communities given the shrinking pipeline for medical trainees. A decade ago, almost a third of all medical graduates were placed into primary-care residency training slots. Now, he says, that figure is a bit less than 22%. “We can’t even replace the primary-care workforce we have now with that kind of output,” Dr. Phillips says.
Already, many doctors are no longer accepting new Medicaid or Medicare patients because their practices are losing money from low reimbursement rates. The Affordable Care Act’s significant expansion of insurance benefits, Dr. Grover says, will effectively accelerate the timetable of growing imbalances between supply and demand. “I think the challenge you face is, Will the ACA efforts to expand access fail because you’re giving people an insurance card but you have nobody there to take care of them?”
Reasons Aplenty
Some medical students simply aren’t interested in primary care. For the rest, however, interviews with doctors, analysts, and federal officials suggest that the pipeline has been battered throughout its length. Of all the contributing factors, Dr. Phillips says, the main one might be income disparity. In a 2009 study, the center found that the growing gulf in salaries between primary care and subspecialty medicine “cuts in half the likelihood that a student will choose to go into primary care,” he says. Over a career, that gap translates into a difference of $3.5 million. “It dissuades them strongly,” Dr. Phillips says.
At the same time, medical school tuitions have increased at a rate far outstripping the consumer price index. “What we found is that when you hit somewhere between $200,000 and $250,000 in debt, that’s where you see the dropoff really happen,” he says. “Because it becomes almost unfathomable that you can, on a primary-care income, pay off your debts without it severely cutting into your lifestyle.”
Lori Heim, MD, former president of the American Academy of Family Physicians and a hospitalist at Scotland Memorial Hospital in Laurinburg, N.C., says the prevailing fee-for-service payment model has failed primary-care providers, requiring them to work more to meet soaring outpatient demand but reimbursing them less. “People talk about the hamster wheel,” she says. “And that has created more workplace dissatisfaction. Not only does it impact students, but it also impacts the number of primary-care physicians who want to stay in the community, practicing.”
Frederick Chen, MD, MPH, associate professor of family medicine at the University of Washington in Seattle, can relate. “I came from community practice, where you’re seeing 30 to 35 patients a day, and the pressure was entirely on your productivity, and that’s not fun,” he says. “So we’re burning out a lot of primary-care physicians, and students are seeing that very easily.”
The larger theme, several doctors say, is one of perceived worth. Leora Horwitz, MD, assistant professor of internal medicine at Yale School of Medicine in New Haven, Conn., says she has to think holistically about her patients’ symptoms, medication lists, family history, home situation, and other factors during her limited time with them. She bristles at the notion that specialists might spend their time considering only one aspect of her patients’ care yet bill twice as much.
“Realistically, I am providing better value to the healthcare system than a specialist does, and yet we pay specialists much more,” she says. “And until that’s different, people go where the money is and they also go where the respect is, and I think it’s going to be very hard to recruit more people to primary care.”
Despite research pointing to financial concerns, lifestyle perceptions, and training inadequacies as key factors in the decline of primary care, perceptions that HM is poaching young talent have been hard to shake. A recent article in The Atlantic asserts that HM might be a “rational choice” given the profession’s more favorable training, lifestyle, and financial considerations.4 The author, a general internist, contrasts those enticements “to the realities of office practice: Fifteen-minute visits with patients on multiple medications, oodles of paperwork that cause office docs to run a gauntlet just to get through their day, and more documentation and regulatory burdens than ever before.”
Nevertheless, the article describes PCPs who resist hospitals’ calls to move to a hospitalist system as honorable “holdouts” who are committed to being directly involved in their patients’ care.
In her blog post at KevinMD.com, “Hospitalists are Killing Primary Care, and other Myths Debunked,” Vineet Arora, MD, MPP, FHM, a hospitalist at the University of Chicago, addresses those perceptions head-on. “If hospitalists did not exist, there would still be declining interest in primary care among medical students and residents,” she writes.
In a subsequent interview, Dr. Arora contends that both primary care and HM instead might be losing out to higher-paying subspecialties, especially the “ROAD” quartet of radiology, ophthalmology, anesthesiology, and dermatology. She also questions the notion that the professions draw from the same talent pool. “Anecdotally, I can tell you that I don’t see a lot of people choosing between primary care and hospital medicine,” she says. “They’re thinking, ‘Do I want to do critical care, hospital medicine, or cardiology?’ Because the type of person who does hospital medicine is more attracted to that inpatient, acute environment.”
Dr. Horwitz agrees that the choice between a career in primary care and HM might not be as clear-cut as some detractors have suggested. Even so, she describes hospitalists as a “double-edged sword” for PCPs. “On the one hand, primary-care docs get paid so little for their outpatient visits that most need to see a high volume of patients in a day just to break even. So they have less and less time to go to the hospital to see hospitalizations,” Dr. Horwitz says. “The hospitalist movement was really a godsend in that respect, because it allowed primary-care docs to focus on their outpatient practice and not spend all that travel time going to the hospital.”
Other PCPs have lamented the erosion of their inpatient roles while recognizing that current economic realities are gradually pushing them out of the hospital. In fact, Dr. Horwitz says, PCPs often don’t know when their patients have been hospitalized, leading to a breakdown in the continuity of care. A weak primary-care infrastructure in a community, hospitalists say, can likewise imperil safe transitions. With the partitioning of inpatient and outpatient responsibilities, the potential for such miscommunications and lapses has clearly grown.
“We’re all in the same workforce; we’re all trying to take care of patients,” Dr. Heim says. “The discussion needs to be on how do we coordinate, not over turf wars.”
Signs of Life
Experts are focusing more on team-based approaches among the few potential short-term solutions, a common theme in HM circles. Advanced-practice registered nurses, physician assistants, and other providers can be trained more quickly than doctors, potentially extending the reach of primary care. In turn, the concept of team-based care could be beefed up during medical residencies.
Primary-care advocates say more equitable reimbursements also could help to ease the crisis, as would more federal support of residency training. But with many politicians focused on deficit reduction, new government incentives are debuting even as existing programs are being threatened or dismantled.
The Affordable Care Act, for example, more than doubled the capacity of the well-regarded National Health Service Corps, which provides scholarships and loan repayments to doctors who agree to practice in underserved communities. The law also created primary-care incentive payments that added $500 million to physician incomes in 2011. “So that’s a pretty strong message of value, and it’s some real value, too,” Dr. Phillips says.
—Atul Grover, MD, PhD, chief public policy officer, Association of American Medical Colleges
The Affordable Care Act, however, cuts $155 billion to hospital payments over 10 years, adding to the downward pressure on reimbursements. And President Obama’s fiscal-year 2013 budget proposal trims an additional $1 billion, or 10%, from Medicare’s annual payments for patient care, which could impact graduate medical education as hospitals seek to balance out the cuts.
Amid the challenges, primary care is showing some encouraging signs of life. Medical school enrollments are on pace to increase by 30% over their 2002 levels within the next three to five years. In both 2010 and 2011, the number of U.S. medical graduates going into family medicine increased by roughly 10% (followed by a more modest increase of 1% this year). Residency matches in general internal medicine also have been climbing. Dr. Heim and others say it’s no coincidence that students’ interest in primary care began rising again amid public discussions on healthcare reform that focused on the value of primary care.
In the end, the profession’s fate could depend in large part on whether the affirmations continue this time around. “There are some rock stars and heroes of primary care that are not as well-known to medical students as they should be,” says Elbert Huang, MD, associate professor of medicine at the University of Chicago. Highlighting some of those individual leaders, Dr. Huang believes, might significantly improve the profession’s standing among students.
“We need a Michael Jordan of primary care,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
References
- Bodenheimer T, Grumbach K, Berenson RA. A lifeline for primary care. New Engl J Med. 2009;360(26):2693-2696.
- Hofer AN, Abraham JM, Moscovice I. Expansion of coverage under the Patient Protection and Affordable Care Act and primary care utilization. Milbank Q. 2011;89(1):69-89.
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502.
- Henning Schumann, J. The doctor is out: young talent is turning away from primary care. The Atlantic; March 12, 2012.
It’s been about 15 years since the last surge of interest in primary care as a career, when U.S. medical graduates temporarily reversed a long decline by flocking to family medicine, general internal medicine, and pediatrics. Newly minted doctors responded enthusiastically to a widely held perception in the mid-1990s that primary care would be central to a brave new paradigm of managed healthcare delivery.
That profound change never materialized, and the primary-care workforce has since resumed a downward slide that is sounding alarm bells throughout the country. Even more distressing, the medical profession’s recent misfortunes have spread far beyond the doctor’s office.
“What we’re looking at now is that there’s a shortage of somewhere around 90,000 physicians in the next 10 years, increasing in the five years beyond that to 125,000 or more,” says Atul Grover, MD, PhD, chief public policy officer of the Association of American Medical Colleges. The association’s estimates suggest that the 10- and 15-year shortfalls will be split nearly evenly between primary care and other specialties.
Hospitalists could feel that widening gap as well. With increasing numbers of aging baby boomers reaching Medicare eligibility and 32 million Americans set to join the ranks of the insured by 2019 through the Affordable Care Act, primary care’s difficulties arguably are the closest to a full-blown crisis. “Primary care in the United States needs a lifeline,” began a 2009 editorial in the New England Journal of Medicine.1 And that was before an estimate suggesting that new insurance mandates will require an additional 4,307 to 6,940 primary-care physicians to meet demand before the end of the decade contributing about 15% to the expected shortfall.2
Why should hospitalists care about the fate of their counterparts? For starters, what’s good for outpatient providers is good for a sound healthcare system. Researchers have linked strong
primary care to lower overall spending, fewer health disparities, and higher quality of care.3
Hospitalists and primary-care physicians (PCPs) also are inexorably linked. They follow similar training and education pathways, and need each other to ensure safe transitions of care. And despite the evidence pointing to a slew of contributing factors, HM regularly is blamed for many of primary care’s mounting woes.
Based on well-functioning healthcare systems around the world, analysts say the ideal primary-care-to-specialty-care-provider ratio should be roughly 40:60 or 50:50. According to Kathleen Klink, MD, director of the Division of Medicine and Dentistry in the Health Resources and Services Administration (HRSA), only about 32% of physicians in the U.S. are practicing primary care. Unless something changes, that percentage will erode even further. “We’re going in the wrong direction,” Dr. Klink says.
Opinions differ on the extent of the current PCP shortage. Nevertheless, there is clearly a “huge maldistribution problem,” says Robert Phillips, MD, MSPH, director of the Washington, D.C.-based Robert Graham Center, a primary-care research center. Rural and underserved areas already are being shortchanged as more doctors locate in more affluent and desirable areas, he says.
That phenomenon is hardly unique to primary care, but Dr. Phillips says the deficit in frontline doctors could cause disproportionately more hardships in rural and underserved communities given the shrinking pipeline for medical trainees. A decade ago, almost a third of all medical graduates were placed into primary-care residency training slots. Now, he says, that figure is a bit less than 22%. “We can’t even replace the primary-care workforce we have now with that kind of output,” Dr. Phillips says.
Already, many doctors are no longer accepting new Medicaid or Medicare patients because their practices are losing money from low reimbursement rates. The Affordable Care Act’s significant expansion of insurance benefits, Dr. Grover says, will effectively accelerate the timetable of growing imbalances between supply and demand. “I think the challenge you face is, Will the ACA efforts to expand access fail because you’re giving people an insurance card but you have nobody there to take care of them?”
Reasons Aplenty
Some medical students simply aren’t interested in primary care. For the rest, however, interviews with doctors, analysts, and federal officials suggest that the pipeline has been battered throughout its length. Of all the contributing factors, Dr. Phillips says, the main one might be income disparity. In a 2009 study, the center found that the growing gulf in salaries between primary care and subspecialty medicine “cuts in half the likelihood that a student will choose to go into primary care,” he says. Over a career, that gap translates into a difference of $3.5 million. “It dissuades them strongly,” Dr. Phillips says.
At the same time, medical school tuitions have increased at a rate far outstripping the consumer price index. “What we found is that when you hit somewhere between $200,000 and $250,000 in debt, that’s where you see the dropoff really happen,” he says. “Because it becomes almost unfathomable that you can, on a primary-care income, pay off your debts without it severely cutting into your lifestyle.”
Lori Heim, MD, former president of the American Academy of Family Physicians and a hospitalist at Scotland Memorial Hospital in Laurinburg, N.C., says the prevailing fee-for-service payment model has failed primary-care providers, requiring them to work more to meet soaring outpatient demand but reimbursing them less. “People talk about the hamster wheel,” she says. “And that has created more workplace dissatisfaction. Not only does it impact students, but it also impacts the number of primary-care physicians who want to stay in the community, practicing.”
Frederick Chen, MD, MPH, associate professor of family medicine at the University of Washington in Seattle, can relate. “I came from community practice, where you’re seeing 30 to 35 patients a day, and the pressure was entirely on your productivity, and that’s not fun,” he says. “So we’re burning out a lot of primary-care physicians, and students are seeing that very easily.”
The larger theme, several doctors say, is one of perceived worth. Leora Horwitz, MD, assistant professor of internal medicine at Yale School of Medicine in New Haven, Conn., says she has to think holistically about her patients’ symptoms, medication lists, family history, home situation, and other factors during her limited time with them. She bristles at the notion that specialists might spend their time considering only one aspect of her patients’ care yet bill twice as much.
“Realistically, I am providing better value to the healthcare system than a specialist does, and yet we pay specialists much more,” she says. “And until that’s different, people go where the money is and they also go where the respect is, and I think it’s going to be very hard to recruit more people to primary care.”
Despite research pointing to financial concerns, lifestyle perceptions, and training inadequacies as key factors in the decline of primary care, perceptions that HM is poaching young talent have been hard to shake. A recent article in The Atlantic asserts that HM might be a “rational choice” given the profession’s more favorable training, lifestyle, and financial considerations.4 The author, a general internist, contrasts those enticements “to the realities of office practice: Fifteen-minute visits with patients on multiple medications, oodles of paperwork that cause office docs to run a gauntlet just to get through their day, and more documentation and regulatory burdens than ever before.”
Nevertheless, the article describes PCPs who resist hospitals’ calls to move to a hospitalist system as honorable “holdouts” who are committed to being directly involved in their patients’ care.
In her blog post at KevinMD.com, “Hospitalists are Killing Primary Care, and other Myths Debunked,” Vineet Arora, MD, MPP, FHM, a hospitalist at the University of Chicago, addresses those perceptions head-on. “If hospitalists did not exist, there would still be declining interest in primary care among medical students and residents,” she writes.
In a subsequent interview, Dr. Arora contends that both primary care and HM instead might be losing out to higher-paying subspecialties, especially the “ROAD” quartet of radiology, ophthalmology, anesthesiology, and dermatology. She also questions the notion that the professions draw from the same talent pool. “Anecdotally, I can tell you that I don’t see a lot of people choosing between primary care and hospital medicine,” she says. “They’re thinking, ‘Do I want to do critical care, hospital medicine, or cardiology?’ Because the type of person who does hospital medicine is more attracted to that inpatient, acute environment.”
Dr. Horwitz agrees that the choice between a career in primary care and HM might not be as clear-cut as some detractors have suggested. Even so, she describes hospitalists as a “double-edged sword” for PCPs. “On the one hand, primary-care docs get paid so little for their outpatient visits that most need to see a high volume of patients in a day just to break even. So they have less and less time to go to the hospital to see hospitalizations,” Dr. Horwitz says. “The hospitalist movement was really a godsend in that respect, because it allowed primary-care docs to focus on their outpatient practice and not spend all that travel time going to the hospital.”
Other PCPs have lamented the erosion of their inpatient roles while recognizing that current economic realities are gradually pushing them out of the hospital. In fact, Dr. Horwitz says, PCPs often don’t know when their patients have been hospitalized, leading to a breakdown in the continuity of care. A weak primary-care infrastructure in a community, hospitalists say, can likewise imperil safe transitions. With the partitioning of inpatient and outpatient responsibilities, the potential for such miscommunications and lapses has clearly grown.
“We’re all in the same workforce; we’re all trying to take care of patients,” Dr. Heim says. “The discussion needs to be on how do we coordinate, not over turf wars.”
Signs of Life
Experts are focusing more on team-based approaches among the few potential short-term solutions, a common theme in HM circles. Advanced-practice registered nurses, physician assistants, and other providers can be trained more quickly than doctors, potentially extending the reach of primary care. In turn, the concept of team-based care could be beefed up during medical residencies.
Primary-care advocates say more equitable reimbursements also could help to ease the crisis, as would more federal support of residency training. But with many politicians focused on deficit reduction, new government incentives are debuting even as existing programs are being threatened or dismantled.
The Affordable Care Act, for example, more than doubled the capacity of the well-regarded National Health Service Corps, which provides scholarships and loan repayments to doctors who agree to practice in underserved communities. The law also created primary-care incentive payments that added $500 million to physician incomes in 2011. “So that’s a pretty strong message of value, and it’s some real value, too,” Dr. Phillips says.
—Atul Grover, MD, PhD, chief public policy officer, Association of American Medical Colleges
The Affordable Care Act, however, cuts $155 billion to hospital payments over 10 years, adding to the downward pressure on reimbursements. And President Obama’s fiscal-year 2013 budget proposal trims an additional $1 billion, or 10%, from Medicare’s annual payments for patient care, which could impact graduate medical education as hospitals seek to balance out the cuts.
Amid the challenges, primary care is showing some encouraging signs of life. Medical school enrollments are on pace to increase by 30% over their 2002 levels within the next three to five years. In both 2010 and 2011, the number of U.S. medical graduates going into family medicine increased by roughly 10% (followed by a more modest increase of 1% this year). Residency matches in general internal medicine also have been climbing. Dr. Heim and others say it’s no coincidence that students’ interest in primary care began rising again amid public discussions on healthcare reform that focused on the value of primary care.
In the end, the profession’s fate could depend in large part on whether the affirmations continue this time around. “There are some rock stars and heroes of primary care that are not as well-known to medical students as they should be,” says Elbert Huang, MD, associate professor of medicine at the University of Chicago. Highlighting some of those individual leaders, Dr. Huang believes, might significantly improve the profession’s standing among students.
“We need a Michael Jordan of primary care,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
References
- Bodenheimer T, Grumbach K, Berenson RA. A lifeline for primary care. New Engl J Med. 2009;360(26):2693-2696.
- Hofer AN, Abraham JM, Moscovice I. Expansion of coverage under the Patient Protection and Affordable Care Act and primary care utilization. Milbank Q. 2011;89(1):69-89.
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502.
- Henning Schumann, J. The doctor is out: young talent is turning away from primary care. The Atlantic; March 12, 2012.
It’s been about 15 years since the last surge of interest in primary care as a career, when U.S. medical graduates temporarily reversed a long decline by flocking to family medicine, general internal medicine, and pediatrics. Newly minted doctors responded enthusiastically to a widely held perception in the mid-1990s that primary care would be central to a brave new paradigm of managed healthcare delivery.
That profound change never materialized, and the primary-care workforce has since resumed a downward slide that is sounding alarm bells throughout the country. Even more distressing, the medical profession’s recent misfortunes have spread far beyond the doctor’s office.
“What we’re looking at now is that there’s a shortage of somewhere around 90,000 physicians in the next 10 years, increasing in the five years beyond that to 125,000 or more,” says Atul Grover, MD, PhD, chief public policy officer of the Association of American Medical Colleges. The association’s estimates suggest that the 10- and 15-year shortfalls will be split nearly evenly between primary care and other specialties.
Hospitalists could feel that widening gap as well. With increasing numbers of aging baby boomers reaching Medicare eligibility and 32 million Americans set to join the ranks of the insured by 2019 through the Affordable Care Act, primary care’s difficulties arguably are the closest to a full-blown crisis. “Primary care in the United States needs a lifeline,” began a 2009 editorial in the New England Journal of Medicine.1 And that was before an estimate suggesting that new insurance mandates will require an additional 4,307 to 6,940 primary-care physicians to meet demand before the end of the decade contributing about 15% to the expected shortfall.2
Why should hospitalists care about the fate of their counterparts? For starters, what’s good for outpatient providers is good for a sound healthcare system. Researchers have linked strong
primary care to lower overall spending, fewer health disparities, and higher quality of care.3
Hospitalists and primary-care physicians (PCPs) also are inexorably linked. They follow similar training and education pathways, and need each other to ensure safe transitions of care. And despite the evidence pointing to a slew of contributing factors, HM regularly is blamed for many of primary care’s mounting woes.
Based on well-functioning healthcare systems around the world, analysts say the ideal primary-care-to-specialty-care-provider ratio should be roughly 40:60 or 50:50. According to Kathleen Klink, MD, director of the Division of Medicine and Dentistry in the Health Resources and Services Administration (HRSA), only about 32% of physicians in the U.S. are practicing primary care. Unless something changes, that percentage will erode even further. “We’re going in the wrong direction,” Dr. Klink says.
Opinions differ on the extent of the current PCP shortage. Nevertheless, there is clearly a “huge maldistribution problem,” says Robert Phillips, MD, MSPH, director of the Washington, D.C.-based Robert Graham Center, a primary-care research center. Rural and underserved areas already are being shortchanged as more doctors locate in more affluent and desirable areas, he says.
That phenomenon is hardly unique to primary care, but Dr. Phillips says the deficit in frontline doctors could cause disproportionately more hardships in rural and underserved communities given the shrinking pipeline for medical trainees. A decade ago, almost a third of all medical graduates were placed into primary-care residency training slots. Now, he says, that figure is a bit less than 22%. “We can’t even replace the primary-care workforce we have now with that kind of output,” Dr. Phillips says.
Already, many doctors are no longer accepting new Medicaid or Medicare patients because their practices are losing money from low reimbursement rates. The Affordable Care Act’s significant expansion of insurance benefits, Dr. Grover says, will effectively accelerate the timetable of growing imbalances between supply and demand. “I think the challenge you face is, Will the ACA efforts to expand access fail because you’re giving people an insurance card but you have nobody there to take care of them?”
Reasons Aplenty
Some medical students simply aren’t interested in primary care. For the rest, however, interviews with doctors, analysts, and federal officials suggest that the pipeline has been battered throughout its length. Of all the contributing factors, Dr. Phillips says, the main one might be income disparity. In a 2009 study, the center found that the growing gulf in salaries between primary care and subspecialty medicine “cuts in half the likelihood that a student will choose to go into primary care,” he says. Over a career, that gap translates into a difference of $3.5 million. “It dissuades them strongly,” Dr. Phillips says.
At the same time, medical school tuitions have increased at a rate far outstripping the consumer price index. “What we found is that when you hit somewhere between $200,000 and $250,000 in debt, that’s where you see the dropoff really happen,” he says. “Because it becomes almost unfathomable that you can, on a primary-care income, pay off your debts without it severely cutting into your lifestyle.”
Lori Heim, MD, former president of the American Academy of Family Physicians and a hospitalist at Scotland Memorial Hospital in Laurinburg, N.C., says the prevailing fee-for-service payment model has failed primary-care providers, requiring them to work more to meet soaring outpatient demand but reimbursing them less. “People talk about the hamster wheel,” she says. “And that has created more workplace dissatisfaction. Not only does it impact students, but it also impacts the number of primary-care physicians who want to stay in the community, practicing.”
Frederick Chen, MD, MPH, associate professor of family medicine at the University of Washington in Seattle, can relate. “I came from community practice, where you’re seeing 30 to 35 patients a day, and the pressure was entirely on your productivity, and that’s not fun,” he says. “So we’re burning out a lot of primary-care physicians, and students are seeing that very easily.”
The larger theme, several doctors say, is one of perceived worth. Leora Horwitz, MD, assistant professor of internal medicine at Yale School of Medicine in New Haven, Conn., says she has to think holistically about her patients’ symptoms, medication lists, family history, home situation, and other factors during her limited time with them. She bristles at the notion that specialists might spend their time considering only one aspect of her patients’ care yet bill twice as much.
“Realistically, I am providing better value to the healthcare system than a specialist does, and yet we pay specialists much more,” she says. “And until that’s different, people go where the money is and they also go where the respect is, and I think it’s going to be very hard to recruit more people to primary care.”
Despite research pointing to financial concerns, lifestyle perceptions, and training inadequacies as key factors in the decline of primary care, perceptions that HM is poaching young talent have been hard to shake. A recent article in The Atlantic asserts that HM might be a “rational choice” given the profession’s more favorable training, lifestyle, and financial considerations.4 The author, a general internist, contrasts those enticements “to the realities of office practice: Fifteen-minute visits with patients on multiple medications, oodles of paperwork that cause office docs to run a gauntlet just to get through their day, and more documentation and regulatory burdens than ever before.”
Nevertheless, the article describes PCPs who resist hospitals’ calls to move to a hospitalist system as honorable “holdouts” who are committed to being directly involved in their patients’ care.
In her blog post at KevinMD.com, “Hospitalists are Killing Primary Care, and other Myths Debunked,” Vineet Arora, MD, MPP, FHM, a hospitalist at the University of Chicago, addresses those perceptions head-on. “If hospitalists did not exist, there would still be declining interest in primary care among medical students and residents,” she writes.
In a subsequent interview, Dr. Arora contends that both primary care and HM instead might be losing out to higher-paying subspecialties, especially the “ROAD” quartet of radiology, ophthalmology, anesthesiology, and dermatology. She also questions the notion that the professions draw from the same talent pool. “Anecdotally, I can tell you that I don’t see a lot of people choosing between primary care and hospital medicine,” she says. “They’re thinking, ‘Do I want to do critical care, hospital medicine, or cardiology?’ Because the type of person who does hospital medicine is more attracted to that inpatient, acute environment.”
Dr. Horwitz agrees that the choice between a career in primary care and HM might not be as clear-cut as some detractors have suggested. Even so, she describes hospitalists as a “double-edged sword” for PCPs. “On the one hand, primary-care docs get paid so little for their outpatient visits that most need to see a high volume of patients in a day just to break even. So they have less and less time to go to the hospital to see hospitalizations,” Dr. Horwitz says. “The hospitalist movement was really a godsend in that respect, because it allowed primary-care docs to focus on their outpatient practice and not spend all that travel time going to the hospital.”
Other PCPs have lamented the erosion of their inpatient roles while recognizing that current economic realities are gradually pushing them out of the hospital. In fact, Dr. Horwitz says, PCPs often don’t know when their patients have been hospitalized, leading to a breakdown in the continuity of care. A weak primary-care infrastructure in a community, hospitalists say, can likewise imperil safe transitions. With the partitioning of inpatient and outpatient responsibilities, the potential for such miscommunications and lapses has clearly grown.
“We’re all in the same workforce; we’re all trying to take care of patients,” Dr. Heim says. “The discussion needs to be on how do we coordinate, not over turf wars.”
Signs of Life
Experts are focusing more on team-based approaches among the few potential short-term solutions, a common theme in HM circles. Advanced-practice registered nurses, physician assistants, and other providers can be trained more quickly than doctors, potentially extending the reach of primary care. In turn, the concept of team-based care could be beefed up during medical residencies.
Primary-care advocates say more equitable reimbursements also could help to ease the crisis, as would more federal support of residency training. But with many politicians focused on deficit reduction, new government incentives are debuting even as existing programs are being threatened or dismantled.
The Affordable Care Act, for example, more than doubled the capacity of the well-regarded National Health Service Corps, which provides scholarships and loan repayments to doctors who agree to practice in underserved communities. The law also created primary-care incentive payments that added $500 million to physician incomes in 2011. “So that’s a pretty strong message of value, and it’s some real value, too,” Dr. Phillips says.
—Atul Grover, MD, PhD, chief public policy officer, Association of American Medical Colleges
The Affordable Care Act, however, cuts $155 billion to hospital payments over 10 years, adding to the downward pressure on reimbursements. And President Obama’s fiscal-year 2013 budget proposal trims an additional $1 billion, or 10%, from Medicare’s annual payments for patient care, which could impact graduate medical education as hospitals seek to balance out the cuts.
Amid the challenges, primary care is showing some encouraging signs of life. Medical school enrollments are on pace to increase by 30% over their 2002 levels within the next three to five years. In both 2010 and 2011, the number of U.S. medical graduates going into family medicine increased by roughly 10% (followed by a more modest increase of 1% this year). Residency matches in general internal medicine also have been climbing. Dr. Heim and others say it’s no coincidence that students’ interest in primary care began rising again amid public discussions on healthcare reform that focused on the value of primary care.
In the end, the profession’s fate could depend in large part on whether the affirmations continue this time around. “There are some rock stars and heroes of primary care that are not as well-known to medical students as they should be,” says Elbert Huang, MD, associate professor of medicine at the University of Chicago. Highlighting some of those individual leaders, Dr. Huang believes, might significantly improve the profession’s standing among students.
“We need a Michael Jordan of primary care,” he says.
Bryn Nelson is a freelance medical writer in Seattle.
References
- Bodenheimer T, Grumbach K, Berenson RA. A lifeline for primary care. New Engl J Med. 2009;360(26):2693-2696.
- Hofer AN, Abraham JM, Moscovice I. Expansion of coverage under the Patient Protection and Affordable Care Act and primary care utilization. Milbank Q. 2011;89(1):69-89.
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502.
- Henning Schumann, J. The doctor is out: young talent is turning away from primary care. The Atlantic; March 12, 2012.
Most Adverse Events at Hospitals Still Go Unreported
Nearly 13 years after the release of the Institute of Medicine’s landmark report To Err Is Human, which called national attention to the rate of preventable errors in U.S. hospitals and galvanized the patient-safety movement, 6 out of every 7 hospital-based errors, accidents, and other adverse events still go unreported.
That’s the troubling conclusion of a report released in January by the Department of Health and Human Services’ Office of the Inspector General (OIG). According to the OIG, the report the National Incident Study on Adverse Events in Hospitals Among Medicare Beneficiaries, is the first truly national adverse-event study in the nation documenting hospital-based adverse events among Medicare beneficiaries.1
Previous studies assessing errors and adverse events had tracked the number of events reported, but they had no denominator; in other words, one hospital might have 1,000 reports of adverse events and errors in a given month, while another might have 50, but there was no way to know how many adverse events had been missed and how much harm had actually occurred.
The OIG study dug deeper, conducting in-depth, yearlong reviews led by independent physicians to first identify the rates of harm, then returning to the hospitals in the study where they knew harm had occurred to find out if it had been reported or not.
Overall, the inspector general estimated that more than 130,000 Medicare beneficiaries experienced one or more adverse events in hospitals in a single month. Perhaps one of the most surprising findings was that even some of the most serious, egregious adverse events were not reported. Of the 12 deaths in the sample that were iatrogenic, only two were reported as errors. More serious errors were no more likely to be captured as errors than mild reactions, such as breaking out in hives as the result of a medication.
Why aren’t more hospital-based errors and adverse events being reported, and how can this situation be changed? The OIG’s report provides some insight into the underlying problem: The dominant reason that events weren’t reported was that they weren’t perceived as adverse events. (Not all adverse events are medical errors: A medical error is a preventable adverse event.) A urinary catheter infection, while not necessarily a medical error, is always an adverse event—and yet, only one of the 17 urinary catheter infections identified by doctors in medical review was reported.
Lack of recognition—seeing adverse events and errors as just part of routine care—is only one part of the problem, says Rosemary Gibson, MSc, a former senior program officer at the Robert Wood Johnson Foundation and author of “The Treatment Trap” and “Wall of Silence.” Other issues include:
- Fear of retribution. “You have to feel safe to report someone else’s error, or your own,” Gibson says. “Most hospitals have yet to create a safety culture.”
- A sense of disbelief. “I remember talking to a hospital CEO once right after the IOM report,” Gibson recalls. “He said that after a significant error, he would get up in the morning and look in the mirror and think, ‘Did this really happen here?’ There’s almost a sense that if you don’t see it, it didn’t exist.”
- Competing pressures. “The requirements of healthcare reform have taken up so much time and energy that I fear safety has moved to the back burner,” Gibson says. “Someone in a quality and safety leadership role at one hospital said to me, ‘Safety was just a fad. We’re not doing that anymore.’”
- Productivity demands. “Healthcare’s mantra today has become volume, volume, volume. If you already have an environment that’s not as safe as we would like, and you ramp up the volume so people have to do more in the name of productivity, what’s going to happen?” asks Gibson.
The Hospitalist Perspective
Greg Maynard, MD, SFHM, director of the University of California San Diego Center for Innovation and Improvement Science (CIIS) and senior vice president of SHM’s Center for Healthcare Improvement and Innovation, says hospitalists face multiple barriers to regular reporting. Some errors, he says, are so pervasive that they are “considered routine” and “happen all the time.”
“Hypoglycemic events, for example, don’t always get entered into adverse-event reporting systems because they’re so common,” he explains, “even though you should be entering and examining them all.”
—Dan Budnitz, MD, MPH, director, Medication Safety Program, Centers for Disease Control and Prevention
Improper coding is another hospitalist-centric issue. Since Oct. 1, 2008, the Centers for Medicare & Medicaid Services (CMS) has reduced payment for acute-care inpatient cases when designated hospital-acquired conditions are not present on admission and the condition would have increased the reimbursement.
“CMS went to a lot of trouble to implement codes that could help them identify, in the coding process, patients who had an iatrogenic event,” Dr. Maynard says. “But those codes simply aren’t being used properly, and administrative coding is always a problem with regard to accuracy.”
Hospitalists can be particularly vulnerable to errors due to the nature of their work—multiple tasks, multiple team members, multiple interruptions. “[Hospitalists] are prone to the type of errors that are related to the hectic nature of being a doctor and an air traffic controller at the same time,” Dr. Maynard says. “You’re in the middle of admitting someone and get two urgent calls on two other patients, so you have to switch out of what you’re doing on that patient, issue orders on the other two, and immediately switch back. It’s hard to keep your focus when dealing with many complex patients, many of whom you’re seeing for the first time, and try to remember all the things you should not omit.”
One area that has, in recent years, become more important to hospitalists in terms of error prevention—and reporting—is discharge planning.
“When you’re sending your patient out of the hospital, they may have started on new medications or changed medications while an inpatient,” says Dan Budnitz, MD, MPH, director of the Medication Safety Program at the Centers for Disease Control and Prevention. “A recent report in the New England Journal of Medicine looked at drug-only causes of emergency hospitalizations, and the most common drugs involved are blood thinners, insulin, and some diabetes pills. The implication for the hospitalist is clear: If you start a patient on these medications in the hospital, or change them, you need to pay particular attention, because they’re two of the top drugs that may put your patient back in the hospital.”
National Models
One institution that is far ahead of the curve in error reporting is the University of Michigan Health System. In 2001, just two years after To Err is Human was published, the health system adopted a process of full disclosure of medical errors. The process involves multiple components, including an online incident reporting system, a multidisciplinary claims review committee, open and honest communication with patients and families, and quality-improvement (QI) initiatives guided by reported errors.
“They’ll get 7,000 or 8,000 reports a year from staff,” Gibson says. “That’s what you want. Most of them are minor or near-misses, and you want to know about those so you can learn from them and prevent the larger errors. But you have to create a space where it’s safe for people to report.”
She says that hospitals must adhere to the principle of “just culture” in error reporting, a philosophy that recognizes that even competent professionals make mistakes. Quality-improvement leader and Harvard School of Public Health professor Lucian Leape, MD, has said that the biggest impediment to error reporting and prevention in medicine is “that we punish people for making mistakes.”2
“If I made a mistake and anybody else in my position could have made that same mistake, the chances are the system contributed to my making that mistake, and just culture would suggest I shouldn’t bear all the blame for it,” Gibson says. “That’s different from a case in which I did something that was truly negligent. Hospitals often do not make this distinction, and [they] lack a just culture.”
—Greg Maynard, MD, SFHM, director, University of California San Diego Center for Innovation and Improvement Science, senior vice president, SHM’s Center for Healthcare Improvement and Innovation
Traditional reporting systems in healthcare, however, often do not support a just-culture model or a true patient-safety-focused approach, says Brian Nussenbaum, MD, associate professor of otolaryngology and head and neck surgery at Washington University School of Medicine in Seattle. “Paper or online reports are sent to hospital risk management departments, whose concerns are primarily to limit the potential legal risk,” he says. “There is little emphasis on systems improvement or prevention. Dissemination of incidents to others in the organization is unusual, and the impact on clinical care is often not felt by providers.”
Who should be reporting errors? The responsibility ideally lies with everyone involved in patient care, Dr. Nussenbaum says. In practice, physicians are more likely to report events that caused permanent harm or the death or near-death of a patient, but overall, they report only 1% of adverse events.3 Nurses, on the other hand, are more likely to report events that cause no harm or harm that’s only temporary, and report about 45% of events. Residents, in the same study, reported only a little more than half of adverse events to attending physicians.
“Nurses and pharmacists have a lot more training in how to fill out the voluntary reporting,” Dr. Maynard says. “Nurses and pharmacists report the overwhelming majority of adverse events and errors. I think physicians need to take some responsibility for ensuring that errors are reported into the voluntary reporting system. When I get called about something that happens on one of my patients, or detect it, I don’t necessarily enter it myself, but I will specify with whoever is calling me that it should be reported.”
Society Initiatives
SHM has taken an aggressive stance that is more focused on improving quality and safety than that of most professional organizations, according to Dr. Maynard. “We feel that the best way to build hospitalists in their careers is to increase their value by helping them take care of patients and being part of the solution to these problems,” he says. “We have quality and safety modules for learning about error and medical harm and ways to prevent it.”
SHM’s website (www.hospitalmedicine.org)
features resources and tools for DVT prevention, glycemic control, and anticoagulation—all well-known areas for medical errors. “We’re about ready to embark on putting together an adverse-drug-events module, and Project BOOST [Better Outcomes for Older Adults through Safe Transitions] provides materials to help optimize transitions of care,” Dr. Maynard says. “We want to build this into the daily fabric of the hospitalist’s career.”
At the CDC’s medication safety program, Dr. Budnitz says, his focus is less on error reporting and more on tracking backward to see what could have been the cause of harm to a patient—error or not.
“Sometimes, medication-induced harms are caused by things that we classically think of as errors, and sometimes they are not,” he says. “Error reporting is important, but sometimes things don’t fit neatly into the ‘healthcare error’ box—like when a patient misses a follow-up appointment to get their blood thinner level checked, and [the] patient has an unintended bleeding event.”
—Rosemary Gibson, MSc, author, former senior program officer, Robert Wood Johnson Foundation
Gibson believes that what’s needed is a public system for the reporting of adverse events in hospitals—like a Consumer Product Safety Commission for healthcare.
“If your child gets injured by a defective crib, there’s a system for you to report that,” she says. “We need that for hospitals. There should be an open capability for reporting events online, in person, any way you want, whether you’re on the hospital staff, a patient, or a family member. Such a system should acknowledge the report, provide for an immediate action step in urgent situations, and offer assistance and support to the person doing the reporting.”
But overall, the response in the healthcare industry to the OIG’s report has been “we need to do more research,” Gibson notes. “We don’t need more research; we need to apply what is known. There are institutions that have made pockets of progress, and patients are alive today and home with their families because we’ve made care safer, but safety still hasn’t become a system property in healthcare.”
Gina Shaw is a freelance writer in New York City.
References
- Levinson DR. Adverse events in hospitals: national incidence among Medicare beneficiaries. U.S. Department of Health and Human Services’ Office of Inspector General website. Available at: http://oig.hhs.gov/oei/reports/oei-06-09-00090.pdf. Accessed May 31, 2012.
- Leape LL. Testimony, United States Congress, House Committee on Veterans’ Affairs; Oct. 12, 1997.
- Rowin EJ. Does error and adverse event reporting by physicians and nurses differ? Jt Comm J Qual Patient Saf. 2008;34(9):537-545.
Nearly 13 years after the release of the Institute of Medicine’s landmark report To Err Is Human, which called national attention to the rate of preventable errors in U.S. hospitals and galvanized the patient-safety movement, 6 out of every 7 hospital-based errors, accidents, and other adverse events still go unreported.
That’s the troubling conclusion of a report released in January by the Department of Health and Human Services’ Office of the Inspector General (OIG). According to the OIG, the report the National Incident Study on Adverse Events in Hospitals Among Medicare Beneficiaries, is the first truly national adverse-event study in the nation documenting hospital-based adverse events among Medicare beneficiaries.1
Previous studies assessing errors and adverse events had tracked the number of events reported, but they had no denominator; in other words, one hospital might have 1,000 reports of adverse events and errors in a given month, while another might have 50, but there was no way to know how many adverse events had been missed and how much harm had actually occurred.
The OIG study dug deeper, conducting in-depth, yearlong reviews led by independent physicians to first identify the rates of harm, then returning to the hospitals in the study where they knew harm had occurred to find out if it had been reported or not.
Overall, the inspector general estimated that more than 130,000 Medicare beneficiaries experienced one or more adverse events in hospitals in a single month. Perhaps one of the most surprising findings was that even some of the most serious, egregious adverse events were not reported. Of the 12 deaths in the sample that were iatrogenic, only two were reported as errors. More serious errors were no more likely to be captured as errors than mild reactions, such as breaking out in hives as the result of a medication.
Why aren’t more hospital-based errors and adverse events being reported, and how can this situation be changed? The OIG’s report provides some insight into the underlying problem: The dominant reason that events weren’t reported was that they weren’t perceived as adverse events. (Not all adverse events are medical errors: A medical error is a preventable adverse event.) A urinary catheter infection, while not necessarily a medical error, is always an adverse event—and yet, only one of the 17 urinary catheter infections identified by doctors in medical review was reported.
Lack of recognition—seeing adverse events and errors as just part of routine care—is only one part of the problem, says Rosemary Gibson, MSc, a former senior program officer at the Robert Wood Johnson Foundation and author of “The Treatment Trap” and “Wall of Silence.” Other issues include:
- Fear of retribution. “You have to feel safe to report someone else’s error, or your own,” Gibson says. “Most hospitals have yet to create a safety culture.”
- A sense of disbelief. “I remember talking to a hospital CEO once right after the IOM report,” Gibson recalls. “He said that after a significant error, he would get up in the morning and look in the mirror and think, ‘Did this really happen here?’ There’s almost a sense that if you don’t see it, it didn’t exist.”
- Competing pressures. “The requirements of healthcare reform have taken up so much time and energy that I fear safety has moved to the back burner,” Gibson says. “Someone in a quality and safety leadership role at one hospital said to me, ‘Safety was just a fad. We’re not doing that anymore.’”
- Productivity demands. “Healthcare’s mantra today has become volume, volume, volume. If you already have an environment that’s not as safe as we would like, and you ramp up the volume so people have to do more in the name of productivity, what’s going to happen?” asks Gibson.
The Hospitalist Perspective
Greg Maynard, MD, SFHM, director of the University of California San Diego Center for Innovation and Improvement Science (CIIS) and senior vice president of SHM’s Center for Healthcare Improvement and Innovation, says hospitalists face multiple barriers to regular reporting. Some errors, he says, are so pervasive that they are “considered routine” and “happen all the time.”
“Hypoglycemic events, for example, don’t always get entered into adverse-event reporting systems because they’re so common,” he explains, “even though you should be entering and examining them all.”
—Dan Budnitz, MD, MPH, director, Medication Safety Program, Centers for Disease Control and Prevention
Improper coding is another hospitalist-centric issue. Since Oct. 1, 2008, the Centers for Medicare & Medicaid Services (CMS) has reduced payment for acute-care inpatient cases when designated hospital-acquired conditions are not present on admission and the condition would have increased the reimbursement.
“CMS went to a lot of trouble to implement codes that could help them identify, in the coding process, patients who had an iatrogenic event,” Dr. Maynard says. “But those codes simply aren’t being used properly, and administrative coding is always a problem with regard to accuracy.”
Hospitalists can be particularly vulnerable to errors due to the nature of their work—multiple tasks, multiple team members, multiple interruptions. “[Hospitalists] are prone to the type of errors that are related to the hectic nature of being a doctor and an air traffic controller at the same time,” Dr. Maynard says. “You’re in the middle of admitting someone and get two urgent calls on two other patients, so you have to switch out of what you’re doing on that patient, issue orders on the other two, and immediately switch back. It’s hard to keep your focus when dealing with many complex patients, many of whom you’re seeing for the first time, and try to remember all the things you should not omit.”
One area that has, in recent years, become more important to hospitalists in terms of error prevention—and reporting—is discharge planning.
“When you’re sending your patient out of the hospital, they may have started on new medications or changed medications while an inpatient,” says Dan Budnitz, MD, MPH, director of the Medication Safety Program at the Centers for Disease Control and Prevention. “A recent report in the New England Journal of Medicine looked at drug-only causes of emergency hospitalizations, and the most common drugs involved are blood thinners, insulin, and some diabetes pills. The implication for the hospitalist is clear: If you start a patient on these medications in the hospital, or change them, you need to pay particular attention, because they’re two of the top drugs that may put your patient back in the hospital.”
National Models
One institution that is far ahead of the curve in error reporting is the University of Michigan Health System. In 2001, just two years after To Err is Human was published, the health system adopted a process of full disclosure of medical errors. The process involves multiple components, including an online incident reporting system, a multidisciplinary claims review committee, open and honest communication with patients and families, and quality-improvement (QI) initiatives guided by reported errors.
“They’ll get 7,000 or 8,000 reports a year from staff,” Gibson says. “That’s what you want. Most of them are minor or near-misses, and you want to know about those so you can learn from them and prevent the larger errors. But you have to create a space where it’s safe for people to report.”
She says that hospitals must adhere to the principle of “just culture” in error reporting, a philosophy that recognizes that even competent professionals make mistakes. Quality-improvement leader and Harvard School of Public Health professor Lucian Leape, MD, has said that the biggest impediment to error reporting and prevention in medicine is “that we punish people for making mistakes.”2
“If I made a mistake and anybody else in my position could have made that same mistake, the chances are the system contributed to my making that mistake, and just culture would suggest I shouldn’t bear all the blame for it,” Gibson says. “That’s different from a case in which I did something that was truly negligent. Hospitals often do not make this distinction, and [they] lack a just culture.”
—Greg Maynard, MD, SFHM, director, University of California San Diego Center for Innovation and Improvement Science, senior vice president, SHM’s Center for Healthcare Improvement and Innovation
Traditional reporting systems in healthcare, however, often do not support a just-culture model or a true patient-safety-focused approach, says Brian Nussenbaum, MD, associate professor of otolaryngology and head and neck surgery at Washington University School of Medicine in Seattle. “Paper or online reports are sent to hospital risk management departments, whose concerns are primarily to limit the potential legal risk,” he says. “There is little emphasis on systems improvement or prevention. Dissemination of incidents to others in the organization is unusual, and the impact on clinical care is often not felt by providers.”
Who should be reporting errors? The responsibility ideally lies with everyone involved in patient care, Dr. Nussenbaum says. In practice, physicians are more likely to report events that caused permanent harm or the death or near-death of a patient, but overall, they report only 1% of adverse events.3 Nurses, on the other hand, are more likely to report events that cause no harm or harm that’s only temporary, and report about 45% of events. Residents, in the same study, reported only a little more than half of adverse events to attending physicians.
“Nurses and pharmacists have a lot more training in how to fill out the voluntary reporting,” Dr. Maynard says. “Nurses and pharmacists report the overwhelming majority of adverse events and errors. I think physicians need to take some responsibility for ensuring that errors are reported into the voluntary reporting system. When I get called about something that happens on one of my patients, or detect it, I don’t necessarily enter it myself, but I will specify with whoever is calling me that it should be reported.”
Society Initiatives
SHM has taken an aggressive stance that is more focused on improving quality and safety than that of most professional organizations, according to Dr. Maynard. “We feel that the best way to build hospitalists in their careers is to increase their value by helping them take care of patients and being part of the solution to these problems,” he says. “We have quality and safety modules for learning about error and medical harm and ways to prevent it.”
SHM’s website (www.hospitalmedicine.org)
features resources and tools for DVT prevention, glycemic control, and anticoagulation—all well-known areas for medical errors. “We’re about ready to embark on putting together an adverse-drug-events module, and Project BOOST [Better Outcomes for Older Adults through Safe Transitions] provides materials to help optimize transitions of care,” Dr. Maynard says. “We want to build this into the daily fabric of the hospitalist’s career.”
At the CDC’s medication safety program, Dr. Budnitz says, his focus is less on error reporting and more on tracking backward to see what could have been the cause of harm to a patient—error or not.
“Sometimes, medication-induced harms are caused by things that we classically think of as errors, and sometimes they are not,” he says. “Error reporting is important, but sometimes things don’t fit neatly into the ‘healthcare error’ box—like when a patient misses a follow-up appointment to get their blood thinner level checked, and [the] patient has an unintended bleeding event.”
—Rosemary Gibson, MSc, author, former senior program officer, Robert Wood Johnson Foundation
Gibson believes that what’s needed is a public system for the reporting of adverse events in hospitals—like a Consumer Product Safety Commission for healthcare.
“If your child gets injured by a defective crib, there’s a system for you to report that,” she says. “We need that for hospitals. There should be an open capability for reporting events online, in person, any way you want, whether you’re on the hospital staff, a patient, or a family member. Such a system should acknowledge the report, provide for an immediate action step in urgent situations, and offer assistance and support to the person doing the reporting.”
But overall, the response in the healthcare industry to the OIG’s report has been “we need to do more research,” Gibson notes. “We don’t need more research; we need to apply what is known. There are institutions that have made pockets of progress, and patients are alive today and home with their families because we’ve made care safer, but safety still hasn’t become a system property in healthcare.”
Gina Shaw is a freelance writer in New York City.
References
- Levinson DR. Adverse events in hospitals: national incidence among Medicare beneficiaries. U.S. Department of Health and Human Services’ Office of Inspector General website. Available at: http://oig.hhs.gov/oei/reports/oei-06-09-00090.pdf. Accessed May 31, 2012.
- Leape LL. Testimony, United States Congress, House Committee on Veterans’ Affairs; Oct. 12, 1997.
- Rowin EJ. Does error and adverse event reporting by physicians and nurses differ? Jt Comm J Qual Patient Saf. 2008;34(9):537-545.
Nearly 13 years after the release of the Institute of Medicine’s landmark report To Err Is Human, which called national attention to the rate of preventable errors in U.S. hospitals and galvanized the patient-safety movement, 6 out of every 7 hospital-based errors, accidents, and other adverse events still go unreported.
That’s the troubling conclusion of a report released in January by the Department of Health and Human Services’ Office of the Inspector General (OIG). According to the OIG, the report the National Incident Study on Adverse Events in Hospitals Among Medicare Beneficiaries, is the first truly national adverse-event study in the nation documenting hospital-based adverse events among Medicare beneficiaries.1
Previous studies assessing errors and adverse events had tracked the number of events reported, but they had no denominator; in other words, one hospital might have 1,000 reports of adverse events and errors in a given month, while another might have 50, but there was no way to know how many adverse events had been missed and how much harm had actually occurred.
The OIG study dug deeper, conducting in-depth, yearlong reviews led by independent physicians to first identify the rates of harm, then returning to the hospitals in the study where they knew harm had occurred to find out if it had been reported or not.
Overall, the inspector general estimated that more than 130,000 Medicare beneficiaries experienced one or more adverse events in hospitals in a single month. Perhaps one of the most surprising findings was that even some of the most serious, egregious adverse events were not reported. Of the 12 deaths in the sample that were iatrogenic, only two were reported as errors. More serious errors were no more likely to be captured as errors than mild reactions, such as breaking out in hives as the result of a medication.
Why aren’t more hospital-based errors and adverse events being reported, and how can this situation be changed? The OIG’s report provides some insight into the underlying problem: The dominant reason that events weren’t reported was that they weren’t perceived as adverse events. (Not all adverse events are medical errors: A medical error is a preventable adverse event.) A urinary catheter infection, while not necessarily a medical error, is always an adverse event—and yet, only one of the 17 urinary catheter infections identified by doctors in medical review was reported.
Lack of recognition—seeing adverse events and errors as just part of routine care—is only one part of the problem, says Rosemary Gibson, MSc, a former senior program officer at the Robert Wood Johnson Foundation and author of “The Treatment Trap” and “Wall of Silence.” Other issues include:
- Fear of retribution. “You have to feel safe to report someone else’s error, or your own,” Gibson says. “Most hospitals have yet to create a safety culture.”
- A sense of disbelief. “I remember talking to a hospital CEO once right after the IOM report,” Gibson recalls. “He said that after a significant error, he would get up in the morning and look in the mirror and think, ‘Did this really happen here?’ There’s almost a sense that if you don’t see it, it didn’t exist.”
- Competing pressures. “The requirements of healthcare reform have taken up so much time and energy that I fear safety has moved to the back burner,” Gibson says. “Someone in a quality and safety leadership role at one hospital said to me, ‘Safety was just a fad. We’re not doing that anymore.’”
- Productivity demands. “Healthcare’s mantra today has become volume, volume, volume. If you already have an environment that’s not as safe as we would like, and you ramp up the volume so people have to do more in the name of productivity, what’s going to happen?” asks Gibson.
The Hospitalist Perspective
Greg Maynard, MD, SFHM, director of the University of California San Diego Center for Innovation and Improvement Science (CIIS) and senior vice president of SHM’s Center for Healthcare Improvement and Innovation, says hospitalists face multiple barriers to regular reporting. Some errors, he says, are so pervasive that they are “considered routine” and “happen all the time.”
“Hypoglycemic events, for example, don’t always get entered into adverse-event reporting systems because they’re so common,” he explains, “even though you should be entering and examining them all.”
—Dan Budnitz, MD, MPH, director, Medication Safety Program, Centers for Disease Control and Prevention
Improper coding is another hospitalist-centric issue. Since Oct. 1, 2008, the Centers for Medicare & Medicaid Services (CMS) has reduced payment for acute-care inpatient cases when designated hospital-acquired conditions are not present on admission and the condition would have increased the reimbursement.
“CMS went to a lot of trouble to implement codes that could help them identify, in the coding process, patients who had an iatrogenic event,” Dr. Maynard says. “But those codes simply aren’t being used properly, and administrative coding is always a problem with regard to accuracy.”
Hospitalists can be particularly vulnerable to errors due to the nature of their work—multiple tasks, multiple team members, multiple interruptions. “[Hospitalists] are prone to the type of errors that are related to the hectic nature of being a doctor and an air traffic controller at the same time,” Dr. Maynard says. “You’re in the middle of admitting someone and get two urgent calls on two other patients, so you have to switch out of what you’re doing on that patient, issue orders on the other two, and immediately switch back. It’s hard to keep your focus when dealing with many complex patients, many of whom you’re seeing for the first time, and try to remember all the things you should not omit.”
One area that has, in recent years, become more important to hospitalists in terms of error prevention—and reporting—is discharge planning.
“When you’re sending your patient out of the hospital, they may have started on new medications or changed medications while an inpatient,” says Dan Budnitz, MD, MPH, director of the Medication Safety Program at the Centers for Disease Control and Prevention. “A recent report in the New England Journal of Medicine looked at drug-only causes of emergency hospitalizations, and the most common drugs involved are blood thinners, insulin, and some diabetes pills. The implication for the hospitalist is clear: If you start a patient on these medications in the hospital, or change them, you need to pay particular attention, because they’re two of the top drugs that may put your patient back in the hospital.”
National Models
One institution that is far ahead of the curve in error reporting is the University of Michigan Health System. In 2001, just two years after To Err is Human was published, the health system adopted a process of full disclosure of medical errors. The process involves multiple components, including an online incident reporting system, a multidisciplinary claims review committee, open and honest communication with patients and families, and quality-improvement (QI) initiatives guided by reported errors.
“They’ll get 7,000 or 8,000 reports a year from staff,” Gibson says. “That’s what you want. Most of them are minor or near-misses, and you want to know about those so you can learn from them and prevent the larger errors. But you have to create a space where it’s safe for people to report.”
She says that hospitals must adhere to the principle of “just culture” in error reporting, a philosophy that recognizes that even competent professionals make mistakes. Quality-improvement leader and Harvard School of Public Health professor Lucian Leape, MD, has said that the biggest impediment to error reporting and prevention in medicine is “that we punish people for making mistakes.”2
“If I made a mistake and anybody else in my position could have made that same mistake, the chances are the system contributed to my making that mistake, and just culture would suggest I shouldn’t bear all the blame for it,” Gibson says. “That’s different from a case in which I did something that was truly negligent. Hospitals often do not make this distinction, and [they] lack a just culture.”
—Greg Maynard, MD, SFHM, director, University of California San Diego Center for Innovation and Improvement Science, senior vice president, SHM’s Center for Healthcare Improvement and Innovation
Traditional reporting systems in healthcare, however, often do not support a just-culture model or a true patient-safety-focused approach, says Brian Nussenbaum, MD, associate professor of otolaryngology and head and neck surgery at Washington University School of Medicine in Seattle. “Paper or online reports are sent to hospital risk management departments, whose concerns are primarily to limit the potential legal risk,” he says. “There is little emphasis on systems improvement or prevention. Dissemination of incidents to others in the organization is unusual, and the impact on clinical care is often not felt by providers.”
Who should be reporting errors? The responsibility ideally lies with everyone involved in patient care, Dr. Nussenbaum says. In practice, physicians are more likely to report events that caused permanent harm or the death or near-death of a patient, but overall, they report only 1% of adverse events.3 Nurses, on the other hand, are more likely to report events that cause no harm or harm that’s only temporary, and report about 45% of events. Residents, in the same study, reported only a little more than half of adverse events to attending physicians.
“Nurses and pharmacists have a lot more training in how to fill out the voluntary reporting,” Dr. Maynard says. “Nurses and pharmacists report the overwhelming majority of adverse events and errors. I think physicians need to take some responsibility for ensuring that errors are reported into the voluntary reporting system. When I get called about something that happens on one of my patients, or detect it, I don’t necessarily enter it myself, but I will specify with whoever is calling me that it should be reported.”
Society Initiatives
SHM has taken an aggressive stance that is more focused on improving quality and safety than that of most professional organizations, according to Dr. Maynard. “We feel that the best way to build hospitalists in their careers is to increase their value by helping them take care of patients and being part of the solution to these problems,” he says. “We have quality and safety modules for learning about error and medical harm and ways to prevent it.”
SHM’s website (www.hospitalmedicine.org)
features resources and tools for DVT prevention, glycemic control, and anticoagulation—all well-known areas for medical errors. “We’re about ready to embark on putting together an adverse-drug-events module, and Project BOOST [Better Outcomes for Older Adults through Safe Transitions] provides materials to help optimize transitions of care,” Dr. Maynard says. “We want to build this into the daily fabric of the hospitalist’s career.”
At the CDC’s medication safety program, Dr. Budnitz says, his focus is less on error reporting and more on tracking backward to see what could have been the cause of harm to a patient—error or not.
“Sometimes, medication-induced harms are caused by things that we classically think of as errors, and sometimes they are not,” he says. “Error reporting is important, but sometimes things don’t fit neatly into the ‘healthcare error’ box—like when a patient misses a follow-up appointment to get their blood thinner level checked, and [the] patient has an unintended bleeding event.”
—Rosemary Gibson, MSc, author, former senior program officer, Robert Wood Johnson Foundation
Gibson believes that what’s needed is a public system for the reporting of adverse events in hospitals—like a Consumer Product Safety Commission for healthcare.
“If your child gets injured by a defective crib, there’s a system for you to report that,” she says. “We need that for hospitals. There should be an open capability for reporting events online, in person, any way you want, whether you’re on the hospital staff, a patient, or a family member. Such a system should acknowledge the report, provide for an immediate action step in urgent situations, and offer assistance and support to the person doing the reporting.”
But overall, the response in the healthcare industry to the OIG’s report has been “we need to do more research,” Gibson notes. “We don’t need more research; we need to apply what is known. There are institutions that have made pockets of progress, and patients are alive today and home with their families because we’ve made care safer, but safety still hasn’t become a system property in healthcare.”
Gina Shaw is a freelance writer in New York City.
References
- Levinson DR. Adverse events in hospitals: national incidence among Medicare beneficiaries. U.S. Department of Health and Human Services’ Office of Inspector General website. Available at: http://oig.hhs.gov/oei/reports/oei-06-09-00090.pdf. Accessed May 31, 2012.
- Leape LL. Testimony, United States Congress, House Committee on Veterans’ Affairs; Oct. 12, 1997.
- Rowin EJ. Does error and adverse event reporting by physicians and nurses differ? Jt Comm J Qual Patient Saf. 2008;34(9):537-545.
What Is the Optimal Therapy for Acute DVT?
The Case
A 55-year-old female undergoes cholecystectomy. On post-operative Day 2, she develops right-lower-extremity swelling and pain; venous ultrasound detects a proximal deep venous thrombosis (DVT). The patient denies smoking or use of hormonal medications. She has no history of venous thromboembolism (VTE), although her brother had a DVT at age 60. The hospitalist team is consulted for management of acute DVT.
Overview
VTE, including lower- and upper-extremity DVT and pulmonary embolism (PE), is one of the most common and preventable hospital diseases. DVT with PE is associated with a 10% mortality rate, and DVT with post-thrombotic syndrome can be associated with significant morbidity, including pain, edema, skin/pigment change, venous dilation, and ulcer development.1,2 Recognition of clinical symptoms and risk factors for DVT (see Table 1) in conjunction with validated clinical scoring predictors (such as the Wells Prediction Rule) and a high-sensitivity D-dimer assay can help diagnose the condition and determine the need for ultrasound.3-7
Pharmacologic Treatment
Anticoagulation should be initiated in all patients with VTE, regardless of patient symptoms. Anticoagulant options include:
- Intravenous (IV) or subcutaneous (SC) unfractionated heparin (UFH);
- SC low-molecular-weight heparins (LMWH), such as enoxaparin and dalteparin; and
- Fondaparinux (as effective as LMWH for acute treatment of VTE).8
These agents can be used while transitioning to oral vitamin K antagonists (VKA), such as warfarin.3
The 2012 American College of Chest Physicians (ACCP) guidelines on antithrombotic therapy for VTE recommend initial therapy with LMWH or fondaparinux (rather than IV or SC UFH). The guidelines suggest that LMWH once-daily dosing is favored over twice-daily dosing, based mainly on patient convenience, although this is a weak recommendation (2C) based on the overall quality of the data. The recommendation applies only if the daily dosing of the LMWH, including tinzaparin, dalteparin, and nadroparin, is equivalent to the twice-daily dosing (i.e., dalteparin may be dosed at 100 units/kg BID vs. 200 units/kg daily). Of importance, enoxaparin has not been studied at a once-daily dose (2 mg/kg), which is equivalent to the twice-daily dosing regimen (1 mg/kg twice daily). Additionally, one study suggests that once-daily dosing of enoxaparin 1.5mg/kg might be inferior to 1 mg/kg twice-daily dosing; therefore, caution must be exercised in applying this recommendation to the LMWH enoxaparin at this time.3,27,28 (updated Aug. 28, 2012)
Warfarin should be started simultaneously at a usual daily dose of 5 mg for the first two days, with subsequent doses adjusted to achieve a goal international normalized ratio (INR) of 2.0 to 3.0. Parenteral agents should be given for a minimum of five days and until the INR has been >2.0 for at least 24 hours.3
The new factor-Xa inhibitor rivaroxaban and the direct thrombin inhibitor dabigatran are promising oral alternatives to warfarin.9-11 However, neither drug is currently FDA-approved for the treatment of VTE, nor are they recommended by current guidelines (given limited data for DVT treatment and concerns of bleeding risk).3,12,13 See Table 2 (above) for comparisons of common anticoagulants.3,14-17
Duration of anticoagulation. Anticoagulant treatment of acute DVT should continue for at least three months, as shorter durations are associated with higher recurrence rates. Longer treatment may be indicated depending on the patient’s risk of recurrence.3
The ACCP guidelines estimate risk of recurrence using primary, secondary, and additional factors (see Table 3, p. 19) and recommend the following durations:
- First episode provoked: three months (proximal or distal, provoked by surgery or a nonsurgical transient risk factor);
- First episode unprovoked distal: three months (see “Considerations for isolated distal DVT,” below);
- First episode unprovoked proximal: Indefinite if low to moderate bleeding risk, three months if high bleeding risk;
- Recurrent unprovoked: Indefinite if low to moderate bleeding risk, three months if high bleeding risk; and
- With active cancer: Indefinite with LMWH due to higher risk of recurrence.3,18
These treatment duration guidelines might need to be individualized based on other factors including patient preference, ability to obtain accurate INR monitoring (for those on warfarin), treatment cost, and comorbidities.3
Considerations for isolated distal DVT. Patients with an initial episode of distal DVT, without significant symptoms or risk factors for extension (e.g. positive D-dimer, extensive clot near proximal veins, absence of a reversible provoking factor, active cancer, inpatient status, or previous VTE) might not need anticoagulation.
The DVT can be followed with serial ultrasounds for the first two weeks; anticoagulation is recommended only if the thrombus extends during that time period. The development of significant symptoms or risk factors of extension might indicate the need for anticoagulation.3
Considerations for upper-extremity DVT (UEDVT). Anticoagulation for an UEDVT is generally consistent with the above guidelines for lower-extremity DVT, with a few caveats. If an UEDVT is associated with a central venous catheter (CVC), the CVC should be removed if possible; there are no recommendations to determine whether CVC removal should be preceded by a period of anticoagulation.
A catheter-associated UEDVT requires a minimum of three months of anticoagulation; if the CVC remains in place beyond three months, anticoagulation should be continued until the catheter is removed. Unprovoked UEDVT has a lower risk of recurrence than lower-extremity DVT and three months of anticoagulation, rather than indefinite therapy, is recommended.3
Mechanical Treatment
Non-pharmacologic therapies, such as knee-high graduated compression stockings with pressure of 30 mmHg to 40 mmHg at the ankle, can help reduce the morbidity of post-thrombotic syndrome (PTS) when combined with anticoagulation. Symptomatic patients who use compression stockings as soon as feasible and for a minimum of two years can reduce their incidence of PTS by 50%.3,19,20
Thigh-length stockings are not more effective than knee-high, and while multilayer compression bandages might relieve symptoms during the first-week post-DVT, they do not reduce the one-year incidence of PTS.21,22 Early mobilization is not associated with an increased risk of PE, extension of DVT, or death; patients should ambulate as soon as physically able.23,24
Pharmacomechanical Thrombolysis
For acute DVT, ACCP guidelines recommend anticoagulation alone over pharmacomechanical thrombolysis (either systemic or catheter-directed thrombolysis and mechanical thrombus fragmentation). The rare patient with impending venous gangrene despite anticoagulation is the only clinical scenario in which thrombolysis is clearly indicated. Patients who undergo pharmacomechanical thrombolysis still need a standard course of anticoagulation.3
Role for Inferior Vena Cava Filters
The optimal role of inferior vena cava (IVC) filters remains uncertain. Only one randomized trial found that IVC filters, in conjunction with systemic anticoagulation versus systemic anticoagulation alone, were associated with short-term reductions in the incidence of PE but long-term increases in recurrent DVT, with no differences in mortality or major bleeding. However, no trials have compared anticoagulation plus IVC filter placement with IVC filter placement alone.25,26
ACCP guidelines recommend IVC filter placement only in patients with acute, proximal DVT of the lower extremity, and a contraindication to anticoagulant therapy. If the contraindication resolves, a conventional course of anticoagulation can commence. Combining an IVC filter with an anticoagulant is not recommended. The risks and benefits of retrievable filters require further investigation.3
Back to the Case
Our patient has a provoked DVT secondary to a reversible risk factor (surgery) without additional clinical risk factors. Her family history of DVT is not significant (her brother was >age 50 when it occurred). This patient should be treated with LMWH or fondaparinux with initiation of warfarin with goal INR of 2.0 to 3.0 for at least three months. She does not need an IVC filter, and she should use compression stockings to reduce the risk of PTS.
Bottom Line
In hospitalized patients, treatment of DVT should include immediate anticoagulation with LMWH, fondaparinux, or IV heparin (in patients with renal failure) with transition to warfarin and a goal INR of 2.0 to 3.0. New oral anticoagulants could prove beneficial in acute treatment of DVT but require further testing. Duration of treatment is patient-specific, but most should be anticoagulated for at least three months; some warrant indefinite therapy based on risk factors.
Dr. Sebasky is an assistant professor and Dr. DeKorte is assistant professor of medicine in the division of hospital medicine at the University of California at San Diego.
References
- Agency for Healthcare Research and Quality. Talking Points to Attract Administration Support for Venous Thromboembolism Prevention Programs. U.S. Department of Health & Human Services website. Available at: http://www.ahrq.gov/qual/vtguide/vtguideapa.htm. Accessed Feb. 4, 2012.
- Kahn SR, Shbaklo H, Lamping DL, et al. Determinants of health-related quality of life during the 2 years following deep vein thrombosis. J Thromb Haemost. 2008;6:1105-1112.
- Kearon C, Akl E, Comerota AJ, et al. Antithrombotic Therapy for VTE Disease. Antithrombotic Therapy and Prevention of Thrombosis, 9th ed.: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e419S-e494S.
- Hirsh J, Hull RD, Raskob GE. Clinical features and diagnosis of venous thrombosis. J Am Coll Cardiol. 1986;8(6 Suppl B):114B-127B.
- Qaseem A, Snow V, Barry P, et al. Current diagnosis of venous thromboembolism in primary care: a clinical practice guideline from the American Academy of Family Physicians and the American College of Physicians. Ann Int Med. 2007;146:454-458.
- Tapson VF, Carroll BA, Davidson BL, et al. The diagnostic approach to acute venous thromboembolism. Clinical practice guideline. American Thoracic Society. Am J Respir Crit Care Med. 1999;160:1043-1066.
- Wells PS, Owen C, Doucette S, Fergusson D, Tran H. Does this patient have deep vein thrombosis? JAMA. 2006;295:199-207.
- Büller HR, Davidson BL, Decousus H, et al. Fondaparinux or enoxaparin for the initial treatment of symptomatic deep venous thrombosis: a randomized trial. Ann Intern Med. 2004;140:867-873.
- EINSTEIN Investigators, Bauersachs R, Berkowitz SD, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363:2499-25
- Garcia, D, Libby E, Crowther M. The new oral anticoagulants. Blood. 2010;115:15-20.
- Douketis JD. Pharmacologic properties of the new oral anticoagulants: a clinician-oriented review with a focus on perioperative management. Curr Pharm Des. 2010;16:3436-3441.
- U.S. Food and Drug Administration. Pradaxa (dabigatran etexilate mesylate): Drug Safety Communication—Safety Review of Post-Market Reports of Serious Bleeding Events. U.S. Food and Drug Administration website. Available at: http://www.fda.gov/Safety/MedWatch/SafetyInformation/
SafetyAlertsforHumanMedicalProducts/ucm282820.htm. Accessed March 12, 2012.
- Levi M, Erenberg E, Kamphuisen PW. Bleeding risk and reversal strategies for old and new anticoagulants and antiplatelet agents. J Thromb Haemost. 2011;9:1705.
- Erkens PM, Prins MH. Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism. Cochrane Database Syst Rev. 2010;8(9);CD001100.Vardi M, Zittan E, Bitterman H. Subcutaneous unfractionated heparin for the initial treatment of venous thromboembolism. Cochrane Database Syst Rev. 2009;(4):CD006771.
- Hirsh J, Levine MN. Low molecular weight heparin. Blood. 1992;79:1-17.
- Schulman S, Kearon C, Kakkar AK, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361;2342-2352.
- Bauer KA. Long-term management of venous thromboembolism. JAMA. 2011;305:1336-1345.
- Prandoni P, Lensing AW, Prins MH, et al. Below-knee elastic compression stockings to prevent the postthrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004;141:249-256.
- Brandjes DP, Büller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349:759-762.
- Prandoni P, Noventa F, Quintavalla R, et al. Thigh-length versus below-knee compression elastic stockings for prevention of the post-thrombotic syndrome in patients with proximal-venous thrombosis: a randomized trial. Blood. 2012;119:1561-1565.
- Roumen-Klappe EM, den Heijer M, van Rossum J, et al. Multilayer compression bandaging in the acute phase of deep-vein thrombosis has no effect on the development of the post-thrombotic syndrome. J Thromb Thrombolysis. 2009;27:400-405.
- Aissaoui N, Martins E, Mouly S, Weber S, Meune C. A meta-analysis of bed rest versus early ambulation in the management of pulmonary embolism, deep venous thrombosis, or both. Int J Cardiol. 2009;137:37-41.
- Anderson CM, Overend TJ, Godwin J, Sealy C, Sunderji A. Ambulation after deep vein thrombosis: a systematic review. Physiother Can. 2009;61:133-140.
- Hann CL, Streiff MB. The role of vena caval filters in the management of venous thromboembolism. Blood Rev. 2005;19:179-202.
- Decousus H, Leizorovicz A, Page Y, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. N Engl J Med. 1998;338:409-415.
The Case
A 55-year-old female undergoes cholecystectomy. On post-operative Day 2, she develops right-lower-extremity swelling and pain; venous ultrasound detects a proximal deep venous thrombosis (DVT). The patient denies smoking or use of hormonal medications. She has no history of venous thromboembolism (VTE), although her brother had a DVT at age 60. The hospitalist team is consulted for management of acute DVT.
Overview
VTE, including lower- and upper-extremity DVT and pulmonary embolism (PE), is one of the most common and preventable hospital diseases. DVT with PE is associated with a 10% mortality rate, and DVT with post-thrombotic syndrome can be associated with significant morbidity, including pain, edema, skin/pigment change, venous dilation, and ulcer development.1,2 Recognition of clinical symptoms and risk factors for DVT (see Table 1) in conjunction with validated clinical scoring predictors (such as the Wells Prediction Rule) and a high-sensitivity D-dimer assay can help diagnose the condition and determine the need for ultrasound.3-7
Pharmacologic Treatment
Anticoagulation should be initiated in all patients with VTE, regardless of patient symptoms. Anticoagulant options include:
- Intravenous (IV) or subcutaneous (SC) unfractionated heparin (UFH);
- SC low-molecular-weight heparins (LMWH), such as enoxaparin and dalteparin; and
- Fondaparinux (as effective as LMWH for acute treatment of VTE).8
These agents can be used while transitioning to oral vitamin K antagonists (VKA), such as warfarin.3
The 2012 American College of Chest Physicians (ACCP) guidelines on antithrombotic therapy for VTE recommend initial therapy with LMWH or fondaparinux (rather than IV or SC UFH). The guidelines suggest that LMWH once-daily dosing is favored over twice-daily dosing, based mainly on patient convenience, although this is a weak recommendation (2C) based on the overall quality of the data. The recommendation applies only if the daily dosing of the LMWH, including tinzaparin, dalteparin, and nadroparin, is equivalent to the twice-daily dosing (i.e., dalteparin may be dosed at 100 units/kg BID vs. 200 units/kg daily). Of importance, enoxaparin has not been studied at a once-daily dose (2 mg/kg), which is equivalent to the twice-daily dosing regimen (1 mg/kg twice daily). Additionally, one study suggests that once-daily dosing of enoxaparin 1.5mg/kg might be inferior to 1 mg/kg twice-daily dosing; therefore, caution must be exercised in applying this recommendation to the LMWH enoxaparin at this time.3,27,28 (updated Aug. 28, 2012)
Warfarin should be started simultaneously at a usual daily dose of 5 mg for the first two days, with subsequent doses adjusted to achieve a goal international normalized ratio (INR) of 2.0 to 3.0. Parenteral agents should be given for a minimum of five days and until the INR has been >2.0 for at least 24 hours.3
The new factor-Xa inhibitor rivaroxaban and the direct thrombin inhibitor dabigatran are promising oral alternatives to warfarin.9-11 However, neither drug is currently FDA-approved for the treatment of VTE, nor are they recommended by current guidelines (given limited data for DVT treatment and concerns of bleeding risk).3,12,13 See Table 2 (above) for comparisons of common anticoagulants.3,14-17
Duration of anticoagulation. Anticoagulant treatment of acute DVT should continue for at least three months, as shorter durations are associated with higher recurrence rates. Longer treatment may be indicated depending on the patient’s risk of recurrence.3
The ACCP guidelines estimate risk of recurrence using primary, secondary, and additional factors (see Table 3, p. 19) and recommend the following durations:
- First episode provoked: three months (proximal or distal, provoked by surgery or a nonsurgical transient risk factor);
- First episode unprovoked distal: three months (see “Considerations for isolated distal DVT,” below);
- First episode unprovoked proximal: Indefinite if low to moderate bleeding risk, three months if high bleeding risk;
- Recurrent unprovoked: Indefinite if low to moderate bleeding risk, three months if high bleeding risk; and
- With active cancer: Indefinite with LMWH due to higher risk of recurrence.3,18
These treatment duration guidelines might need to be individualized based on other factors including patient preference, ability to obtain accurate INR monitoring (for those on warfarin), treatment cost, and comorbidities.3
Considerations for isolated distal DVT. Patients with an initial episode of distal DVT, without significant symptoms or risk factors for extension (e.g. positive D-dimer, extensive clot near proximal veins, absence of a reversible provoking factor, active cancer, inpatient status, or previous VTE) might not need anticoagulation.
The DVT can be followed with serial ultrasounds for the first two weeks; anticoagulation is recommended only if the thrombus extends during that time period. The development of significant symptoms or risk factors of extension might indicate the need for anticoagulation.3
Considerations for upper-extremity DVT (UEDVT). Anticoagulation for an UEDVT is generally consistent with the above guidelines for lower-extremity DVT, with a few caveats. If an UEDVT is associated with a central venous catheter (CVC), the CVC should be removed if possible; there are no recommendations to determine whether CVC removal should be preceded by a period of anticoagulation.
A catheter-associated UEDVT requires a minimum of three months of anticoagulation; if the CVC remains in place beyond three months, anticoagulation should be continued until the catheter is removed. Unprovoked UEDVT has a lower risk of recurrence than lower-extremity DVT and three months of anticoagulation, rather than indefinite therapy, is recommended.3
Mechanical Treatment
Non-pharmacologic therapies, such as knee-high graduated compression stockings with pressure of 30 mmHg to 40 mmHg at the ankle, can help reduce the morbidity of post-thrombotic syndrome (PTS) when combined with anticoagulation. Symptomatic patients who use compression stockings as soon as feasible and for a minimum of two years can reduce their incidence of PTS by 50%.3,19,20
Thigh-length stockings are not more effective than knee-high, and while multilayer compression bandages might relieve symptoms during the first-week post-DVT, they do not reduce the one-year incidence of PTS.21,22 Early mobilization is not associated with an increased risk of PE, extension of DVT, or death; patients should ambulate as soon as physically able.23,24
Pharmacomechanical Thrombolysis
For acute DVT, ACCP guidelines recommend anticoagulation alone over pharmacomechanical thrombolysis (either systemic or catheter-directed thrombolysis and mechanical thrombus fragmentation). The rare patient with impending venous gangrene despite anticoagulation is the only clinical scenario in which thrombolysis is clearly indicated. Patients who undergo pharmacomechanical thrombolysis still need a standard course of anticoagulation.3
Role for Inferior Vena Cava Filters
The optimal role of inferior vena cava (IVC) filters remains uncertain. Only one randomized trial found that IVC filters, in conjunction with systemic anticoagulation versus systemic anticoagulation alone, were associated with short-term reductions in the incidence of PE but long-term increases in recurrent DVT, with no differences in mortality or major bleeding. However, no trials have compared anticoagulation plus IVC filter placement with IVC filter placement alone.25,26
ACCP guidelines recommend IVC filter placement only in patients with acute, proximal DVT of the lower extremity, and a contraindication to anticoagulant therapy. If the contraindication resolves, a conventional course of anticoagulation can commence. Combining an IVC filter with an anticoagulant is not recommended. The risks and benefits of retrievable filters require further investigation.3
Back to the Case
Our patient has a provoked DVT secondary to a reversible risk factor (surgery) without additional clinical risk factors. Her family history of DVT is not significant (her brother was >age 50 when it occurred). This patient should be treated with LMWH or fondaparinux with initiation of warfarin with goal INR of 2.0 to 3.0 for at least three months. She does not need an IVC filter, and she should use compression stockings to reduce the risk of PTS.
Bottom Line
In hospitalized patients, treatment of DVT should include immediate anticoagulation with LMWH, fondaparinux, or IV heparin (in patients with renal failure) with transition to warfarin and a goal INR of 2.0 to 3.0. New oral anticoagulants could prove beneficial in acute treatment of DVT but require further testing. Duration of treatment is patient-specific, but most should be anticoagulated for at least three months; some warrant indefinite therapy based on risk factors.
Dr. Sebasky is an assistant professor and Dr. DeKorte is assistant professor of medicine in the division of hospital medicine at the University of California at San Diego.
References
- Agency for Healthcare Research and Quality. Talking Points to Attract Administration Support for Venous Thromboembolism Prevention Programs. U.S. Department of Health & Human Services website. Available at: http://www.ahrq.gov/qual/vtguide/vtguideapa.htm. Accessed Feb. 4, 2012.
- Kahn SR, Shbaklo H, Lamping DL, et al. Determinants of health-related quality of life during the 2 years following deep vein thrombosis. J Thromb Haemost. 2008;6:1105-1112.
- Kearon C, Akl E, Comerota AJ, et al. Antithrombotic Therapy for VTE Disease. Antithrombotic Therapy and Prevention of Thrombosis, 9th ed.: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e419S-e494S.
- Hirsh J, Hull RD, Raskob GE. Clinical features and diagnosis of venous thrombosis. J Am Coll Cardiol. 1986;8(6 Suppl B):114B-127B.
- Qaseem A, Snow V, Barry P, et al. Current diagnosis of venous thromboembolism in primary care: a clinical practice guideline from the American Academy of Family Physicians and the American College of Physicians. Ann Int Med. 2007;146:454-458.
- Tapson VF, Carroll BA, Davidson BL, et al. The diagnostic approach to acute venous thromboembolism. Clinical practice guideline. American Thoracic Society. Am J Respir Crit Care Med. 1999;160:1043-1066.
- Wells PS, Owen C, Doucette S, Fergusson D, Tran H. Does this patient have deep vein thrombosis? JAMA. 2006;295:199-207.
- Büller HR, Davidson BL, Decousus H, et al. Fondaparinux or enoxaparin for the initial treatment of symptomatic deep venous thrombosis: a randomized trial. Ann Intern Med. 2004;140:867-873.
- EINSTEIN Investigators, Bauersachs R, Berkowitz SD, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363:2499-25
- Garcia, D, Libby E, Crowther M. The new oral anticoagulants. Blood. 2010;115:15-20.
- Douketis JD. Pharmacologic properties of the new oral anticoagulants: a clinician-oriented review with a focus on perioperative management. Curr Pharm Des. 2010;16:3436-3441.
- U.S. Food and Drug Administration. Pradaxa (dabigatran etexilate mesylate): Drug Safety Communication—Safety Review of Post-Market Reports of Serious Bleeding Events. U.S. Food and Drug Administration website. Available at: http://www.fda.gov/Safety/MedWatch/SafetyInformation/
SafetyAlertsforHumanMedicalProducts/ucm282820.htm. Accessed March 12, 2012.
- Levi M, Erenberg E, Kamphuisen PW. Bleeding risk and reversal strategies for old and new anticoagulants and antiplatelet agents. J Thromb Haemost. 2011;9:1705.
- Erkens PM, Prins MH. Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism. Cochrane Database Syst Rev. 2010;8(9);CD001100.Vardi M, Zittan E, Bitterman H. Subcutaneous unfractionated heparin for the initial treatment of venous thromboembolism. Cochrane Database Syst Rev. 2009;(4):CD006771.
- Hirsh J, Levine MN. Low molecular weight heparin. Blood. 1992;79:1-17.
- Schulman S, Kearon C, Kakkar AK, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361;2342-2352.
- Bauer KA. Long-term management of venous thromboembolism. JAMA. 2011;305:1336-1345.
- Prandoni P, Lensing AW, Prins MH, et al. Below-knee elastic compression stockings to prevent the postthrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004;141:249-256.
- Brandjes DP, Büller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349:759-762.
- Prandoni P, Noventa F, Quintavalla R, et al. Thigh-length versus below-knee compression elastic stockings for prevention of the post-thrombotic syndrome in patients with proximal-venous thrombosis: a randomized trial. Blood. 2012;119:1561-1565.
- Roumen-Klappe EM, den Heijer M, van Rossum J, et al. Multilayer compression bandaging in the acute phase of deep-vein thrombosis has no effect on the development of the post-thrombotic syndrome. J Thromb Thrombolysis. 2009;27:400-405.
- Aissaoui N, Martins E, Mouly S, Weber S, Meune C. A meta-analysis of bed rest versus early ambulation in the management of pulmonary embolism, deep venous thrombosis, or both. Int J Cardiol. 2009;137:37-41.
- Anderson CM, Overend TJ, Godwin J, Sealy C, Sunderji A. Ambulation after deep vein thrombosis: a systematic review. Physiother Can. 2009;61:133-140.
- Hann CL, Streiff MB. The role of vena caval filters in the management of venous thromboembolism. Blood Rev. 2005;19:179-202.
- Decousus H, Leizorovicz A, Page Y, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. N Engl J Med. 1998;338:409-415.
The Case
A 55-year-old female undergoes cholecystectomy. On post-operative Day 2, she develops right-lower-extremity swelling and pain; venous ultrasound detects a proximal deep venous thrombosis (DVT). The patient denies smoking or use of hormonal medications. She has no history of venous thromboembolism (VTE), although her brother had a DVT at age 60. The hospitalist team is consulted for management of acute DVT.
Overview
VTE, including lower- and upper-extremity DVT and pulmonary embolism (PE), is one of the most common and preventable hospital diseases. DVT with PE is associated with a 10% mortality rate, and DVT with post-thrombotic syndrome can be associated with significant morbidity, including pain, edema, skin/pigment change, venous dilation, and ulcer development.1,2 Recognition of clinical symptoms and risk factors for DVT (see Table 1) in conjunction with validated clinical scoring predictors (such as the Wells Prediction Rule) and a high-sensitivity D-dimer assay can help diagnose the condition and determine the need for ultrasound.3-7
Pharmacologic Treatment
Anticoagulation should be initiated in all patients with VTE, regardless of patient symptoms. Anticoagulant options include:
- Intravenous (IV) or subcutaneous (SC) unfractionated heparin (UFH);
- SC low-molecular-weight heparins (LMWH), such as enoxaparin and dalteparin; and
- Fondaparinux (as effective as LMWH for acute treatment of VTE).8
These agents can be used while transitioning to oral vitamin K antagonists (VKA), such as warfarin.3
The 2012 American College of Chest Physicians (ACCP) guidelines on antithrombotic therapy for VTE recommend initial therapy with LMWH or fondaparinux (rather than IV or SC UFH). The guidelines suggest that LMWH once-daily dosing is favored over twice-daily dosing, based mainly on patient convenience, although this is a weak recommendation (2C) based on the overall quality of the data. The recommendation applies only if the daily dosing of the LMWH, including tinzaparin, dalteparin, and nadroparin, is equivalent to the twice-daily dosing (i.e., dalteparin may be dosed at 100 units/kg BID vs. 200 units/kg daily). Of importance, enoxaparin has not been studied at a once-daily dose (2 mg/kg), which is equivalent to the twice-daily dosing regimen (1 mg/kg twice daily). Additionally, one study suggests that once-daily dosing of enoxaparin 1.5mg/kg might be inferior to 1 mg/kg twice-daily dosing; therefore, caution must be exercised in applying this recommendation to the LMWH enoxaparin at this time.3,27,28 (updated Aug. 28, 2012)
Warfarin should be started simultaneously at a usual daily dose of 5 mg for the first two days, with subsequent doses adjusted to achieve a goal international normalized ratio (INR) of 2.0 to 3.0. Parenteral agents should be given for a minimum of five days and until the INR has been >2.0 for at least 24 hours.3
The new factor-Xa inhibitor rivaroxaban and the direct thrombin inhibitor dabigatran are promising oral alternatives to warfarin.9-11 However, neither drug is currently FDA-approved for the treatment of VTE, nor are they recommended by current guidelines (given limited data for DVT treatment and concerns of bleeding risk).3,12,13 See Table 2 (above) for comparisons of common anticoagulants.3,14-17
Duration of anticoagulation. Anticoagulant treatment of acute DVT should continue for at least three months, as shorter durations are associated with higher recurrence rates. Longer treatment may be indicated depending on the patient’s risk of recurrence.3
The ACCP guidelines estimate risk of recurrence using primary, secondary, and additional factors (see Table 3, p. 19) and recommend the following durations:
- First episode provoked: three months (proximal or distal, provoked by surgery or a nonsurgical transient risk factor);
- First episode unprovoked distal: three months (see “Considerations for isolated distal DVT,” below);
- First episode unprovoked proximal: Indefinite if low to moderate bleeding risk, three months if high bleeding risk;
- Recurrent unprovoked: Indefinite if low to moderate bleeding risk, three months if high bleeding risk; and
- With active cancer: Indefinite with LMWH due to higher risk of recurrence.3,18
These treatment duration guidelines might need to be individualized based on other factors including patient preference, ability to obtain accurate INR monitoring (for those on warfarin), treatment cost, and comorbidities.3
Considerations for isolated distal DVT. Patients with an initial episode of distal DVT, without significant symptoms or risk factors for extension (e.g. positive D-dimer, extensive clot near proximal veins, absence of a reversible provoking factor, active cancer, inpatient status, or previous VTE) might not need anticoagulation.
The DVT can be followed with serial ultrasounds for the first two weeks; anticoagulation is recommended only if the thrombus extends during that time period. The development of significant symptoms or risk factors of extension might indicate the need for anticoagulation.3
Considerations for upper-extremity DVT (UEDVT). Anticoagulation for an UEDVT is generally consistent with the above guidelines for lower-extremity DVT, with a few caveats. If an UEDVT is associated with a central venous catheter (CVC), the CVC should be removed if possible; there are no recommendations to determine whether CVC removal should be preceded by a period of anticoagulation.
A catheter-associated UEDVT requires a minimum of three months of anticoagulation; if the CVC remains in place beyond three months, anticoagulation should be continued until the catheter is removed. Unprovoked UEDVT has a lower risk of recurrence than lower-extremity DVT and three months of anticoagulation, rather than indefinite therapy, is recommended.3
Mechanical Treatment
Non-pharmacologic therapies, such as knee-high graduated compression stockings with pressure of 30 mmHg to 40 mmHg at the ankle, can help reduce the morbidity of post-thrombotic syndrome (PTS) when combined with anticoagulation. Symptomatic patients who use compression stockings as soon as feasible and for a minimum of two years can reduce their incidence of PTS by 50%.3,19,20
Thigh-length stockings are not more effective than knee-high, and while multilayer compression bandages might relieve symptoms during the first-week post-DVT, they do not reduce the one-year incidence of PTS.21,22 Early mobilization is not associated with an increased risk of PE, extension of DVT, or death; patients should ambulate as soon as physically able.23,24
Pharmacomechanical Thrombolysis
For acute DVT, ACCP guidelines recommend anticoagulation alone over pharmacomechanical thrombolysis (either systemic or catheter-directed thrombolysis and mechanical thrombus fragmentation). The rare patient with impending venous gangrene despite anticoagulation is the only clinical scenario in which thrombolysis is clearly indicated. Patients who undergo pharmacomechanical thrombolysis still need a standard course of anticoagulation.3
Role for Inferior Vena Cava Filters
The optimal role of inferior vena cava (IVC) filters remains uncertain. Only one randomized trial found that IVC filters, in conjunction with systemic anticoagulation versus systemic anticoagulation alone, were associated with short-term reductions in the incidence of PE but long-term increases in recurrent DVT, with no differences in mortality or major bleeding. However, no trials have compared anticoagulation plus IVC filter placement with IVC filter placement alone.25,26
ACCP guidelines recommend IVC filter placement only in patients with acute, proximal DVT of the lower extremity, and a contraindication to anticoagulant therapy. If the contraindication resolves, a conventional course of anticoagulation can commence. Combining an IVC filter with an anticoagulant is not recommended. The risks and benefits of retrievable filters require further investigation.3
Back to the Case
Our patient has a provoked DVT secondary to a reversible risk factor (surgery) without additional clinical risk factors. Her family history of DVT is not significant (her brother was >age 50 when it occurred). This patient should be treated with LMWH or fondaparinux with initiation of warfarin with goal INR of 2.0 to 3.0 for at least three months. She does not need an IVC filter, and she should use compression stockings to reduce the risk of PTS.
Bottom Line
In hospitalized patients, treatment of DVT should include immediate anticoagulation with LMWH, fondaparinux, or IV heparin (in patients with renal failure) with transition to warfarin and a goal INR of 2.0 to 3.0. New oral anticoagulants could prove beneficial in acute treatment of DVT but require further testing. Duration of treatment is patient-specific, but most should be anticoagulated for at least three months; some warrant indefinite therapy based on risk factors.
Dr. Sebasky is an assistant professor and Dr. DeKorte is assistant professor of medicine in the division of hospital medicine at the University of California at San Diego.
References
- Agency for Healthcare Research and Quality. Talking Points to Attract Administration Support for Venous Thromboembolism Prevention Programs. U.S. Department of Health & Human Services website. Available at: http://www.ahrq.gov/qual/vtguide/vtguideapa.htm. Accessed Feb. 4, 2012.
- Kahn SR, Shbaklo H, Lamping DL, et al. Determinants of health-related quality of life during the 2 years following deep vein thrombosis. J Thromb Haemost. 2008;6:1105-1112.
- Kearon C, Akl E, Comerota AJ, et al. Antithrombotic Therapy for VTE Disease. Antithrombotic Therapy and Prevention of Thrombosis, 9th ed.: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e419S-e494S.
- Hirsh J, Hull RD, Raskob GE. Clinical features and diagnosis of venous thrombosis. J Am Coll Cardiol. 1986;8(6 Suppl B):114B-127B.
- Qaseem A, Snow V, Barry P, et al. Current diagnosis of venous thromboembolism in primary care: a clinical practice guideline from the American Academy of Family Physicians and the American College of Physicians. Ann Int Med. 2007;146:454-458.
- Tapson VF, Carroll BA, Davidson BL, et al. The diagnostic approach to acute venous thromboembolism. Clinical practice guideline. American Thoracic Society. Am J Respir Crit Care Med. 1999;160:1043-1066.
- Wells PS, Owen C, Doucette S, Fergusson D, Tran H. Does this patient have deep vein thrombosis? JAMA. 2006;295:199-207.
- Büller HR, Davidson BL, Decousus H, et al. Fondaparinux or enoxaparin for the initial treatment of symptomatic deep venous thrombosis: a randomized trial. Ann Intern Med. 2004;140:867-873.
- EINSTEIN Investigators, Bauersachs R, Berkowitz SD, et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363:2499-25
- Garcia, D, Libby E, Crowther M. The new oral anticoagulants. Blood. 2010;115:15-20.
- Douketis JD. Pharmacologic properties of the new oral anticoagulants: a clinician-oriented review with a focus on perioperative management. Curr Pharm Des. 2010;16:3436-3441.
- U.S. Food and Drug Administration. Pradaxa (dabigatran etexilate mesylate): Drug Safety Communication—Safety Review of Post-Market Reports of Serious Bleeding Events. U.S. Food and Drug Administration website. Available at: http://www.fda.gov/Safety/MedWatch/SafetyInformation/
SafetyAlertsforHumanMedicalProducts/ucm282820.htm. Accessed March 12, 2012.
- Levi M, Erenberg E, Kamphuisen PW. Bleeding risk and reversal strategies for old and new anticoagulants and antiplatelet agents. J Thromb Haemost. 2011;9:1705.
- Erkens PM, Prins MH. Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism. Cochrane Database Syst Rev. 2010;8(9);CD001100.Vardi M, Zittan E, Bitterman H. Subcutaneous unfractionated heparin for the initial treatment of venous thromboembolism. Cochrane Database Syst Rev. 2009;(4):CD006771.
- Hirsh J, Levine MN. Low molecular weight heparin. Blood. 1992;79:1-17.
- Schulman S, Kearon C, Kakkar AK, et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361;2342-2352.
- Bauer KA. Long-term management of venous thromboembolism. JAMA. 2011;305:1336-1345.
- Prandoni P, Lensing AW, Prins MH, et al. Below-knee elastic compression stockings to prevent the postthrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004;141:249-256.
- Brandjes DP, Büller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349:759-762.
- Prandoni P, Noventa F, Quintavalla R, et al. Thigh-length versus below-knee compression elastic stockings for prevention of the post-thrombotic syndrome in patients with proximal-venous thrombosis: a randomized trial. Blood. 2012;119:1561-1565.
- Roumen-Klappe EM, den Heijer M, van Rossum J, et al. Multilayer compression bandaging in the acute phase of deep-vein thrombosis has no effect on the development of the post-thrombotic syndrome. J Thromb Thrombolysis. 2009;27:400-405.
- Aissaoui N, Martins E, Mouly S, Weber S, Meune C. A meta-analysis of bed rest versus early ambulation in the management of pulmonary embolism, deep venous thrombosis, or both. Int J Cardiol. 2009;137:37-41.
- Anderson CM, Overend TJ, Godwin J, Sealy C, Sunderji A. Ambulation after deep vein thrombosis: a systematic review. Physiother Can. 2009;61:133-140.
- Hann CL, Streiff MB. The role of vena caval filters in the management of venous thromboembolism. Blood Rev. 2005;19:179-202.
- Decousus H, Leizorovicz A, Page Y, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. N Engl J Med. 1998;338:409-415.
ITL: Physician Reviews of HM-Relevant Research
In This Edition
Literature At A Glance
A guide to this month’s studies
- Neutral head position safe for internal jugular vein cannulation
- Thrombolysis decreases mortality in unstable patients with acute PE
- Rectal indomethacin decreases incidence of post-ERCP pancreatitis
- CHADS2-VASc and HAS-BLED as predictors in afib patients
- No readmission, mortality decreases with self-supported COPD management
- Medicare Premier P4P initiatives do not decrease mortality
- In-hospital rate of DVT/PE after hip and knee arthroplasty
- Sodium chloride prevents contrast-induced nephropathy
Neutral Head Position Is Safe for Internal Jugular Vein Cannulation
Clinical question: Is there a difference in the complication rate between neutral head position and 45-degree neck rotation during ultrasound-guided internal jugular vein cannulation?
Background: Cannulation of the internal jugular vein using ultrasound decreases the rate of major complications (carotid artery puncture, pneumothorax, and hemothorax). The relative positions of the internal jugular vein and the carotid artery change based on degree of neck rotation. The optimal position for ultrasound-guided vein puncture has not been shown.
Study design: Prospective, randomized, controlled, non-blinded study.
Setting: Tertiary neurosurgical center in Milan, Italy.
Synopsis: One thousand, three hundred thirty-two patients undergoing major neurosurgical procedures who needed central venous catheter placement were randomized to a neutral head position (NH) or a 45-degree neck rotation (HT) during ultrasound-guided internal jugular vein cannulation. Exclusion criteria were consent refusal, age <12 years, and coagulopathy. Six experienced anesthesiologists performed the procedures; blinding was not possible.
There was no difference in the rate of major complications (carotid artery puncture, pneumothorax, or hemothorax) based on head position (0.9% in NH vs. 0.6% in HT). Minor complications (multiple skin punctures, multiple vein punctures, difficulty inserting the guidewire) were similar in the two groups (13.2% in NG vs. 12.6% in HT). Neck rotation was not associated with operator-reported difficulty or vascular access time.
Limitations of the study include the inability to blind the operator. Additionally, the study involved six experienced anesthesiologists at one center who performed the procedure on patients needing an elective central line. The ability to generalize the findings to other settings, less experienced providers, and patients who need an emergency line is not certain.
Bottom line: Neutral head position is as safe as 45-degree neck rotation for elective ultrasound-guided internal jugular vein cannulation.
Citation: Lamperti M, Subert M, Cortellazzi P, et al. Is a neutral head position safer than 45-degree neck rotation during ultrasound-guided internal jugular vein cannulation? Results of a randomized controlled clinical trial. Anesth Analg. 2012;114:777-784.
Thrombolysis Decreases Mortality in Unstable Patients with Acute Pulmonary Embolism
Clinical question: Does thrombolytic therapy decrease mortality in unstable patients with acute pulmonary embolism (PE)?
Background: PE is a common problem; associated mortality is high. Despite this fact, the data supporting thrombolytic therapy in hemodynamically unstable patients are not robust, and randomized, controlled trials are unlikely to be performed.
Study design: Retrospective cohort study.
Setting: One thousand nonfederal, short-term U.S. hospitals.
Synopsis: Using data from the Nationwide Inpatient Sample database from 1999-2008, investigators found that thrombolysis decreased both all-cause and PE-specific mortality for unstable patients, defined as those either in shock or on a ventilator. Specifically for all-cause mortality, 15% of patients who received thrombolysis died vs. 47% of those who did not (RR 0.31, 95% CI 0.30-0.32). Placement of an inferior vena cava (IVC) filter further reduced mortality, to only 7.6% in patients who received both IVC filter and thrombolysis.
For PE-specific mortality, patients who received thrombolysis also had decreased rates, from 42% to 8.4% (RR 0.20; 95% CI 0.19-0.22). Across all age groups, patients who received thrombolysis had decreased all-cause and PE-specific mortality. Patients who did not receive thrombolysis had additional comorbidities.
As this study is retrospective, it might be affected by unknown confounding. In addition, it relies on coding data to identify patient stability and treatment. Despite this limitation, a randomized, controlled trial is unlikely to be performed at this stage. This study provides evidence to support use of thrombolysis in unstable patients.
Bottom line: Thrombolysis might reduce mortality in unstable patients with acute PE. In combination with IVC filters, the mortality reduction might be even greater.
Citation: Stein PD, Matta F. Thrombolytic therapy in unstable patients with acute pulmonary embolism: saves lives but underused. Am J Med. 2012;125(5):465-470.
Rectal Indomethacin Decreases Incidence of Post-ERCP Pancreatitis
Clinical question: Does rectal indomethacin reduce the incidence of pancreatitis after ERCP?
Background: Acute pancreatitis is the most common complication from endoscopic retrograde cholangiopancreatography (ERCP). No pharmacologic treatment has proven to reduce the incidence of pancreatitis. Preliminary studies, including a meta-analysis, suggest that the use of NSAIDs might reduce the incidence of post-ERCP pancreatitis.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Multicenter trial at four university-affiliated medical centers in the U.S.
Synopsis: More than 600 patients at high risk for post-ERCP pancreatitis were randomized to receive either two 50-mg indomethacin suppositories or two identical-appearing placebo suppositories. Patients were considered at high risk for pancreatitis based on previously identified patient- and procedure-related risk factors. Most of the participants had sphincter of Oddi dysfunction (84.4% of the indomethacin group and 80.5% of the placebo group). Exclusion criteria included elevated creatinine and active peptic ulcer disease. The indomethacin or placebo suppositories were given immediately following the ERCP.
Post-ERCP pancreatitis, defined by upper abdominal pain, elevation of pancreatic enzymes, and hospitalization for at least two nights, was significantly higher in the placebo group compared with the indomethacin group (16.9% vs. 9.2%, P=0.005). Moderate or severe post-ERCP pancreatitis was significantly higher in the placebo group compared with the indomethacin group (8.8% vs. 4.4%, P=0.03).
There were no significant differences in the rates of clinically significant bleeding or acute renal failure between the two groups. The ability to generalize these findings to patients without risk factors for post-ERCP pancreatitis is not clear.
Bottom line: Rectal indomethacin decreases the rate of post-ERCP pancreatitis in patients who are at high risk for this complication.
Citation: Elmunzer BJ, Scheiman JM, Lehman GA, et al. A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med. 2012;366(15):1414-1422.
CHADS2-VASc and HAS-BLED Can Predict Thromboembolism and Bleeding Risk in Afib Patients
Clinical question: What are the risk factors for stroke/thromboembolism and bleeding from atrial fibrillation (afib), and how well do the CHADS2-VASc and HAS-BLED stroke and bleeding risk-assessment tools perform against other published stroke and bleeding risk-assessment tools (CHADS2 and HEMORR2HAGES) for patients with afib?
Background: In afib patients, the CHADS2-VASc tool might offer more comprehensive stroke assessment over the CHADS2 by identifying truly-low-risk patients with afib who might not even need antiplatelet therapy. HAS-BLED, a newer bleeding-risk-assessment tool, has been validated in previous trials and is more user-friendly than others. Use of CHADS2-VASc and HAS-BLED are recommended by the European Society of Cardiology to assess stroke and bleeding risks for patients with afib.
Study design: Prospective cohort study.
Setting: All hospitals in Sweden.
Synopsis: Investigators identified 182,678 afib patients via ICD-10 data from Sweden’s National Hospital Discharge Registry ICD-10 from 2005 to 2008. Approximately half the patients were not taking anticoagulants. Analysis assessed risk factors for stroke and bleeding and the performance of CHADS2-VASc and HAS-BLED against CHADS2 and HEMORR2HAGES stroke and bleeding risk-assessment tools.
Risk of composite thromboembolism (unspecified stroke, TIA, systemic embolism) was significantly higher in patients with increased age, peripheral arterial disease, prior myocardial infarction (MI), prior coronary artery bypass grafting (CABG), female gender, renal failure, and aspirin use, as well as hypertension, diabetes, prior thromboembolic event, or prior intracranial hemorrhage (ICH). Interestingly, a statistically increased risk was seen with aspirin use.
Conversely, history of heart failure, thyroid disease, and obesity were not associated with increased composite thromboembolic risk. The use of CHADS2-VASc was marginally better than CHADS2 in predicting stroke risk.
ICH risk was increased in patients with older age, prior ischemic stroke, prior ICH, and hypertension. Risk of composite bleeding (from ICH or other major bleeding) was significantly higher in patients with these risk factors, as well as renal failure, liver disease, anemia, dysfunctional platelets, alcohol use, and cancer. Ischemic heart disease was associated with a statistically significant lower risk of ICH, but not of composite bleeding risk.
HAS-BLED usage was as good as, and easier to use than, HEMORR2HAGES in predicting bleeding risk.
Bottom line: CHADS2-VASc might be better than CHADS2 in predicting truly-low-risk patients with nonvalvular afib; HAS-BLED is just as good as, and easier to use than, HEMORR2HAGES in predicting bleeding risk for patients with nonvalvular afib who are to receive antithrombotic therapy.
Citation: Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182,678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33(12):1500-10 [Epub 2012 Jan 13].
Supported Self-Management of COPD Does Not Decrease Readmission or Mortality Rates
Clinical question: Does supported self-management of patients with chronic obstructive pulmonary disease (COPD) decrease COPD-related hospital readmission or death?
Clinical background: Supported self-management has benefited patients with such chronic diseases as heart failure and asthma. Evidence to support such a strategy for patients with COPD is relatively lacking.
Study design: Randomized, controlled trial.
Setting: Community-based care following urban hospitalization in western Scotland.
Synopsis: From June 2007 to May 2009, and following hospitalization for COPD exacerbation, 464 patients were randomized to receive routine community-based care with or without 12 months of support and training to detect, and promptly treat, recurrent exacerbations. Independent of disease severity or demographics, investigators found no difference in combined readmission (48% vs. 47%, 95% confidence interval [CI] 0.80-1.38) or death (10% vs. 7%, 95% CI 0.71-2.61).
Based on review of appropriateness of self-management strategies used by the intervention group, unplanned exploratory subgroup analysis classified a minority of the intervention group as “successful” (42%) supported self-managers, and demonstrated decreased COPD readmissions and death (27% vs. 49%, 95% CI 0.25-0.76, P=0.003) vs. “unsuccessful” self-managers. This successful group was younger and tended to live with others. Further research to define characteristics of patients who benefit from self-management is needed.
Bottom line: Supported self-management of COPD does not reduce COPD-related readmission or death in a large population.
Citation: Bucknall CE, Miller G, Lloyd SM, et al. Glasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trial. BMJ. 2012;344:e1060 [Epub ahead of print].
Medicare Premier P4P Initiatives Do Not Decrease Mortality
Clinical question: Has the Medicare Premier Hospital Quality Incentive Demonstration (HQID) resulted in lower mortality?
Background: The Centers for Medicare & Medicaid Services’ (CMS) value-based purchasing program will expand to include 30-day mortality in 2013, but do pay-for-performance (P4P) initiatives result in improved mortality? Studies have demonstrated improvement in process of care but have not demonstrated mortality benefit thus far.
Study design: Cohort study.
Setting: Two hundred fifty-two hospitals participating in the Premier HQID compared with 3,363 control hospitals participating in the Hospital Compare program.
Synopsis: Researchers examined 30-day mortality for patients admitted with acute myocardial infarction, congestive heart failure, pneumonia, and for coronary artery bypass grafting (CABG) from 2003 to 2009. Results showed no difference in 30-day mortality rates over the six-year span of the program for any of the conditions studied in the Premier hospitals (participating in the voluntary pay-for-performance program) vs. non-Premier hospitals (11.82% vs. 11.74%). This held true for each condition measured individually, with a higher mortality rate for patients undergoing CABG at the Premier hospitals.
In addition, in the hospitals that underperformed initially, there was no difference with respect to rate of improvement when comparing Premier vs. non-Premier hospitals. Furthermore, mortality rate trends did not differ between those conditions that were incentivized (acute MI and CABG) compared with those that were not (congestive heart failure and pneumonia).
The authors concluded that there was “little evidence” that the Premier HQID pay-for-performance program resulted in reduced 30-day mortality.
Bottom line: Programs participating in the Medicare Premier HQID pay-for-performance program had similar 30-day mortality compared with nonparticipating programs.
Citation: Jha AK, Joynt KE, Orav EJ, Epstein AM. The long-term effect of premier pay for performance on patient outcomes. N Engl J Med. 2012;366:1606-1615.
In-Hospital Rate of DVT/PE After Hip and Knee Arthroplasty with Guideline-Recommended Prophylaxis
Clinical question: What is the rate of symptomatic DVT/PE after total or partial hip (TPHA) or knee (TPKA) arthroplasty using currently recommended prophylaxis?
Background: The rate of postoperative DVT/PE after TPHA/TPKA has dropped dramatically with use of pharmacologic prophylaxis. However, the current rate of symptomatic DVT/PE using current pharmacologic prophylaxis is not known. Such rates are needed for informed patient consent and development of patient safety benchmarks.
Study design: Systematic review.
Setting: Randomized clinical trials (RCTs) and observational studies worldwide of adult inpatients undergoing TPHA and/or TPKA from 1996 to 2011.
Synopsis: Forty-seven studies were included, of which 41 were RCTs and six were observational studies. Twenty-one studies evaluated rates after TPHA, 20 after TPKA, and six after both. More than 44,000 patients were included, with ages ranging from 58 to 74 years. The mean duration of prophylaxis was eight days, with a mean follow-up of 13 days.
In-hospital rates of symptomatic venous thromboembolism (VTE) were higher in patients undergoing TPKA than TPHA (1.09% vs. 0.53% for VTE, 0.63% vs. 0.26% for DVT, and 0.27% vs. 0.14% for PE). This is in contrast to the higher rates of VTE observed after TPHA when the post-discharge period is included. The pooled incidence of VTE was lower with use of direct inhibitors of Factors Xa or IIa when compared to low-molecular-weight heparin, although a direct efficacy comparison could not be made.
Because the majority of studies were RCTs with restrictive inclusion criteria, rates of DVT/PE in actual practice might be higher.
Bottom line: When informing patients of postoperative VTE risk, or establishing benchmarks to evaluate patient safety, one can anticipate an in-hospital VTE rate of 0.5% following TPHA and 1% following TPKA.
Citation: Januel JM, Chen G, Ruffieux C, et al. Symptomatic in-hospital deep vein thrombosis and pulmonary embolism following hip and knee arthroplasty among patients receiving recommended prophylaxis: a systematic review. JAMA. 2012;307(3):294-303.
Sodium Chloride Prevents Contrast-Induced Nephropathy
Clinical question: Is sodium chloride more effective than sodium bicarbonate for preventing contrast-induced nephropathy?
Background: Contrast-induced nephropathy can be prevented with precontrast hydration. Study authors sought to compare sodium chloride administered over 24 hours with sodium bicarbonate administered over seven hours, and with sodium bicarbonate administered orally.
Study design: Randomized, open-label, controlled trial.
Setting: Three European medical centers.
Synopsis: The study examined 258 patients with an estimated glomerular filtration rate <60mL/min/1.73m2 undergoing intravenous or intra-arterial contrast procedure. Patients with Class III or IV heart failure were excluded. The remaining patients were randomized to receive one of three regimens: sodium chloride at 1 ml/kg/hr for 12 hours prior to and 12 hours following the procedure; intravenous sodium bicarbonate for one hour prior to and six hours following the procedure; or intravenous and oral sodium bicarbonate 20 minutes prior to the procedure.
The group that received saline had a lower incidence of contrast-induced nephropathy than the bicarbonate groups (1% vs. 9% vs. 10%). The oral bicarbonate strategy was noninferior to the seven-hour intravenous bicarbonate strategy.
The authors postulated that saline should be used for high-risk patients, but that given the overall low incidence of contrast-induced nephropathy, the short-term bicarbonate strategy (intravenous followed by oral) is a viable alternative for low-risk patients.
Bottom line: Sodium chloride is more effective than sodium bicarbonate for preventing contrast-induced nephropathy, but in light of the low incidence, a short course of sodium bicarbonate is a possible convenient alternative for low-risk patients.
Citation: Klima T, Christ A, Marana I, et al. Sodium chloride vs. sodium bicarbonate for the prevention of contrast medium-induced nephropathy: a randomized controlled trial. Eur Heart J. 2012 Jan 19 [Epub ahead of print].
In This Edition
Literature At A Glance
A guide to this month’s studies
- Neutral head position safe for internal jugular vein cannulation
- Thrombolysis decreases mortality in unstable patients with acute PE
- Rectal indomethacin decreases incidence of post-ERCP pancreatitis
- CHADS2-VASc and HAS-BLED as predictors in afib patients
- No readmission, mortality decreases with self-supported COPD management
- Medicare Premier P4P initiatives do not decrease mortality
- In-hospital rate of DVT/PE after hip and knee arthroplasty
- Sodium chloride prevents contrast-induced nephropathy
Neutral Head Position Is Safe for Internal Jugular Vein Cannulation
Clinical question: Is there a difference in the complication rate between neutral head position and 45-degree neck rotation during ultrasound-guided internal jugular vein cannulation?
Background: Cannulation of the internal jugular vein using ultrasound decreases the rate of major complications (carotid artery puncture, pneumothorax, and hemothorax). The relative positions of the internal jugular vein and the carotid artery change based on degree of neck rotation. The optimal position for ultrasound-guided vein puncture has not been shown.
Study design: Prospective, randomized, controlled, non-blinded study.
Setting: Tertiary neurosurgical center in Milan, Italy.
Synopsis: One thousand, three hundred thirty-two patients undergoing major neurosurgical procedures who needed central venous catheter placement were randomized to a neutral head position (NH) or a 45-degree neck rotation (HT) during ultrasound-guided internal jugular vein cannulation. Exclusion criteria were consent refusal, age <12 years, and coagulopathy. Six experienced anesthesiologists performed the procedures; blinding was not possible.
There was no difference in the rate of major complications (carotid artery puncture, pneumothorax, or hemothorax) based on head position (0.9% in NH vs. 0.6% in HT). Minor complications (multiple skin punctures, multiple vein punctures, difficulty inserting the guidewire) were similar in the two groups (13.2% in NG vs. 12.6% in HT). Neck rotation was not associated with operator-reported difficulty or vascular access time.
Limitations of the study include the inability to blind the operator. Additionally, the study involved six experienced anesthesiologists at one center who performed the procedure on patients needing an elective central line. The ability to generalize the findings to other settings, less experienced providers, and patients who need an emergency line is not certain.
Bottom line: Neutral head position is as safe as 45-degree neck rotation for elective ultrasound-guided internal jugular vein cannulation.
Citation: Lamperti M, Subert M, Cortellazzi P, et al. Is a neutral head position safer than 45-degree neck rotation during ultrasound-guided internal jugular vein cannulation? Results of a randomized controlled clinical trial. Anesth Analg. 2012;114:777-784.
Thrombolysis Decreases Mortality in Unstable Patients with Acute Pulmonary Embolism
Clinical question: Does thrombolytic therapy decrease mortality in unstable patients with acute pulmonary embolism (PE)?
Background: PE is a common problem; associated mortality is high. Despite this fact, the data supporting thrombolytic therapy in hemodynamically unstable patients are not robust, and randomized, controlled trials are unlikely to be performed.
Study design: Retrospective cohort study.
Setting: One thousand nonfederal, short-term U.S. hospitals.
Synopsis: Using data from the Nationwide Inpatient Sample database from 1999-2008, investigators found that thrombolysis decreased both all-cause and PE-specific mortality for unstable patients, defined as those either in shock or on a ventilator. Specifically for all-cause mortality, 15% of patients who received thrombolysis died vs. 47% of those who did not (RR 0.31, 95% CI 0.30-0.32). Placement of an inferior vena cava (IVC) filter further reduced mortality, to only 7.6% in patients who received both IVC filter and thrombolysis.
For PE-specific mortality, patients who received thrombolysis also had decreased rates, from 42% to 8.4% (RR 0.20; 95% CI 0.19-0.22). Across all age groups, patients who received thrombolysis had decreased all-cause and PE-specific mortality. Patients who did not receive thrombolysis had additional comorbidities.
As this study is retrospective, it might be affected by unknown confounding. In addition, it relies on coding data to identify patient stability and treatment. Despite this limitation, a randomized, controlled trial is unlikely to be performed at this stage. This study provides evidence to support use of thrombolysis in unstable patients.
Bottom line: Thrombolysis might reduce mortality in unstable patients with acute PE. In combination with IVC filters, the mortality reduction might be even greater.
Citation: Stein PD, Matta F. Thrombolytic therapy in unstable patients with acute pulmonary embolism: saves lives but underused. Am J Med. 2012;125(5):465-470.
Rectal Indomethacin Decreases Incidence of Post-ERCP Pancreatitis
Clinical question: Does rectal indomethacin reduce the incidence of pancreatitis after ERCP?
Background: Acute pancreatitis is the most common complication from endoscopic retrograde cholangiopancreatography (ERCP). No pharmacologic treatment has proven to reduce the incidence of pancreatitis. Preliminary studies, including a meta-analysis, suggest that the use of NSAIDs might reduce the incidence of post-ERCP pancreatitis.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Multicenter trial at four university-affiliated medical centers in the U.S.
Synopsis: More than 600 patients at high risk for post-ERCP pancreatitis were randomized to receive either two 50-mg indomethacin suppositories or two identical-appearing placebo suppositories. Patients were considered at high risk for pancreatitis based on previously identified patient- and procedure-related risk factors. Most of the participants had sphincter of Oddi dysfunction (84.4% of the indomethacin group and 80.5% of the placebo group). Exclusion criteria included elevated creatinine and active peptic ulcer disease. The indomethacin or placebo suppositories were given immediately following the ERCP.
Post-ERCP pancreatitis, defined by upper abdominal pain, elevation of pancreatic enzymes, and hospitalization for at least two nights, was significantly higher in the placebo group compared with the indomethacin group (16.9% vs. 9.2%, P=0.005). Moderate or severe post-ERCP pancreatitis was significantly higher in the placebo group compared with the indomethacin group (8.8% vs. 4.4%, P=0.03).
There were no significant differences in the rates of clinically significant bleeding or acute renal failure between the two groups. The ability to generalize these findings to patients without risk factors for post-ERCP pancreatitis is not clear.
Bottom line: Rectal indomethacin decreases the rate of post-ERCP pancreatitis in patients who are at high risk for this complication.
Citation: Elmunzer BJ, Scheiman JM, Lehman GA, et al. A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med. 2012;366(15):1414-1422.
CHADS2-VASc and HAS-BLED Can Predict Thromboembolism and Bleeding Risk in Afib Patients
Clinical question: What are the risk factors for stroke/thromboembolism and bleeding from atrial fibrillation (afib), and how well do the CHADS2-VASc and HAS-BLED stroke and bleeding risk-assessment tools perform against other published stroke and bleeding risk-assessment tools (CHADS2 and HEMORR2HAGES) for patients with afib?
Background: In afib patients, the CHADS2-VASc tool might offer more comprehensive stroke assessment over the CHADS2 by identifying truly-low-risk patients with afib who might not even need antiplatelet therapy. HAS-BLED, a newer bleeding-risk-assessment tool, has been validated in previous trials and is more user-friendly than others. Use of CHADS2-VASc and HAS-BLED are recommended by the European Society of Cardiology to assess stroke and bleeding risks for patients with afib.
Study design: Prospective cohort study.
Setting: All hospitals in Sweden.
Synopsis: Investigators identified 182,678 afib patients via ICD-10 data from Sweden’s National Hospital Discharge Registry ICD-10 from 2005 to 2008. Approximately half the patients were not taking anticoagulants. Analysis assessed risk factors for stroke and bleeding and the performance of CHADS2-VASc and HAS-BLED against CHADS2 and HEMORR2HAGES stroke and bleeding risk-assessment tools.
Risk of composite thromboembolism (unspecified stroke, TIA, systemic embolism) was significantly higher in patients with increased age, peripheral arterial disease, prior myocardial infarction (MI), prior coronary artery bypass grafting (CABG), female gender, renal failure, and aspirin use, as well as hypertension, diabetes, prior thromboembolic event, or prior intracranial hemorrhage (ICH). Interestingly, a statistically increased risk was seen with aspirin use.
Conversely, history of heart failure, thyroid disease, and obesity were not associated with increased composite thromboembolic risk. The use of CHADS2-VASc was marginally better than CHADS2 in predicting stroke risk.
ICH risk was increased in patients with older age, prior ischemic stroke, prior ICH, and hypertension. Risk of composite bleeding (from ICH or other major bleeding) was significantly higher in patients with these risk factors, as well as renal failure, liver disease, anemia, dysfunctional platelets, alcohol use, and cancer. Ischemic heart disease was associated with a statistically significant lower risk of ICH, but not of composite bleeding risk.
HAS-BLED usage was as good as, and easier to use than, HEMORR2HAGES in predicting bleeding risk.
Bottom line: CHADS2-VASc might be better than CHADS2 in predicting truly-low-risk patients with nonvalvular afib; HAS-BLED is just as good as, and easier to use than, HEMORR2HAGES in predicting bleeding risk for patients with nonvalvular afib who are to receive antithrombotic therapy.
Citation: Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182,678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33(12):1500-10 [Epub 2012 Jan 13].
Supported Self-Management of COPD Does Not Decrease Readmission or Mortality Rates
Clinical question: Does supported self-management of patients with chronic obstructive pulmonary disease (COPD) decrease COPD-related hospital readmission or death?
Clinical background: Supported self-management has benefited patients with such chronic diseases as heart failure and asthma. Evidence to support such a strategy for patients with COPD is relatively lacking.
Study design: Randomized, controlled trial.
Setting: Community-based care following urban hospitalization in western Scotland.
Synopsis: From June 2007 to May 2009, and following hospitalization for COPD exacerbation, 464 patients were randomized to receive routine community-based care with or without 12 months of support and training to detect, and promptly treat, recurrent exacerbations. Independent of disease severity or demographics, investigators found no difference in combined readmission (48% vs. 47%, 95% confidence interval [CI] 0.80-1.38) or death (10% vs. 7%, 95% CI 0.71-2.61).
Based on review of appropriateness of self-management strategies used by the intervention group, unplanned exploratory subgroup analysis classified a minority of the intervention group as “successful” (42%) supported self-managers, and demonstrated decreased COPD readmissions and death (27% vs. 49%, 95% CI 0.25-0.76, P=0.003) vs. “unsuccessful” self-managers. This successful group was younger and tended to live with others. Further research to define characteristics of patients who benefit from self-management is needed.
Bottom line: Supported self-management of COPD does not reduce COPD-related readmission or death in a large population.
Citation: Bucknall CE, Miller G, Lloyd SM, et al. Glasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trial. BMJ. 2012;344:e1060 [Epub ahead of print].
Medicare Premier P4P Initiatives Do Not Decrease Mortality
Clinical question: Has the Medicare Premier Hospital Quality Incentive Demonstration (HQID) resulted in lower mortality?
Background: The Centers for Medicare & Medicaid Services’ (CMS) value-based purchasing program will expand to include 30-day mortality in 2013, but do pay-for-performance (P4P) initiatives result in improved mortality? Studies have demonstrated improvement in process of care but have not demonstrated mortality benefit thus far.
Study design: Cohort study.
Setting: Two hundred fifty-two hospitals participating in the Premier HQID compared with 3,363 control hospitals participating in the Hospital Compare program.
Synopsis: Researchers examined 30-day mortality for patients admitted with acute myocardial infarction, congestive heart failure, pneumonia, and for coronary artery bypass grafting (CABG) from 2003 to 2009. Results showed no difference in 30-day mortality rates over the six-year span of the program for any of the conditions studied in the Premier hospitals (participating in the voluntary pay-for-performance program) vs. non-Premier hospitals (11.82% vs. 11.74%). This held true for each condition measured individually, with a higher mortality rate for patients undergoing CABG at the Premier hospitals.
In addition, in the hospitals that underperformed initially, there was no difference with respect to rate of improvement when comparing Premier vs. non-Premier hospitals. Furthermore, mortality rate trends did not differ between those conditions that were incentivized (acute MI and CABG) compared with those that were not (congestive heart failure and pneumonia).
The authors concluded that there was “little evidence” that the Premier HQID pay-for-performance program resulted in reduced 30-day mortality.
Bottom line: Programs participating in the Medicare Premier HQID pay-for-performance program had similar 30-day mortality compared with nonparticipating programs.
Citation: Jha AK, Joynt KE, Orav EJ, Epstein AM. The long-term effect of premier pay for performance on patient outcomes. N Engl J Med. 2012;366:1606-1615.
In-Hospital Rate of DVT/PE After Hip and Knee Arthroplasty with Guideline-Recommended Prophylaxis
Clinical question: What is the rate of symptomatic DVT/PE after total or partial hip (TPHA) or knee (TPKA) arthroplasty using currently recommended prophylaxis?
Background: The rate of postoperative DVT/PE after TPHA/TPKA has dropped dramatically with use of pharmacologic prophylaxis. However, the current rate of symptomatic DVT/PE using current pharmacologic prophylaxis is not known. Such rates are needed for informed patient consent and development of patient safety benchmarks.
Study design: Systematic review.
Setting: Randomized clinical trials (RCTs) and observational studies worldwide of adult inpatients undergoing TPHA and/or TPKA from 1996 to 2011.
Synopsis: Forty-seven studies were included, of which 41 were RCTs and six were observational studies. Twenty-one studies evaluated rates after TPHA, 20 after TPKA, and six after both. More than 44,000 patients were included, with ages ranging from 58 to 74 years. The mean duration of prophylaxis was eight days, with a mean follow-up of 13 days.
In-hospital rates of symptomatic venous thromboembolism (VTE) were higher in patients undergoing TPKA than TPHA (1.09% vs. 0.53% for VTE, 0.63% vs. 0.26% for DVT, and 0.27% vs. 0.14% for PE). This is in contrast to the higher rates of VTE observed after TPHA when the post-discharge period is included. The pooled incidence of VTE was lower with use of direct inhibitors of Factors Xa or IIa when compared to low-molecular-weight heparin, although a direct efficacy comparison could not be made.
Because the majority of studies were RCTs with restrictive inclusion criteria, rates of DVT/PE in actual practice might be higher.
Bottom line: When informing patients of postoperative VTE risk, or establishing benchmarks to evaluate patient safety, one can anticipate an in-hospital VTE rate of 0.5% following TPHA and 1% following TPKA.
Citation: Januel JM, Chen G, Ruffieux C, et al. Symptomatic in-hospital deep vein thrombosis and pulmonary embolism following hip and knee arthroplasty among patients receiving recommended prophylaxis: a systematic review. JAMA. 2012;307(3):294-303.
Sodium Chloride Prevents Contrast-Induced Nephropathy
Clinical question: Is sodium chloride more effective than sodium bicarbonate for preventing contrast-induced nephropathy?
Background: Contrast-induced nephropathy can be prevented with precontrast hydration. Study authors sought to compare sodium chloride administered over 24 hours with sodium bicarbonate administered over seven hours, and with sodium bicarbonate administered orally.
Study design: Randomized, open-label, controlled trial.
Setting: Three European medical centers.
Synopsis: The study examined 258 patients with an estimated glomerular filtration rate <60mL/min/1.73m2 undergoing intravenous or intra-arterial contrast procedure. Patients with Class III or IV heart failure were excluded. The remaining patients were randomized to receive one of three regimens: sodium chloride at 1 ml/kg/hr for 12 hours prior to and 12 hours following the procedure; intravenous sodium bicarbonate for one hour prior to and six hours following the procedure; or intravenous and oral sodium bicarbonate 20 minutes prior to the procedure.
The group that received saline had a lower incidence of contrast-induced nephropathy than the bicarbonate groups (1% vs. 9% vs. 10%). The oral bicarbonate strategy was noninferior to the seven-hour intravenous bicarbonate strategy.
The authors postulated that saline should be used for high-risk patients, but that given the overall low incidence of contrast-induced nephropathy, the short-term bicarbonate strategy (intravenous followed by oral) is a viable alternative for low-risk patients.
Bottom line: Sodium chloride is more effective than sodium bicarbonate for preventing contrast-induced nephropathy, but in light of the low incidence, a short course of sodium bicarbonate is a possible convenient alternative for low-risk patients.
Citation: Klima T, Christ A, Marana I, et al. Sodium chloride vs. sodium bicarbonate for the prevention of contrast medium-induced nephropathy: a randomized controlled trial. Eur Heart J. 2012 Jan 19 [Epub ahead of print].
In This Edition
Literature At A Glance
A guide to this month’s studies
- Neutral head position safe for internal jugular vein cannulation
- Thrombolysis decreases mortality in unstable patients with acute PE
- Rectal indomethacin decreases incidence of post-ERCP pancreatitis
- CHADS2-VASc and HAS-BLED as predictors in afib patients
- No readmission, mortality decreases with self-supported COPD management
- Medicare Premier P4P initiatives do not decrease mortality
- In-hospital rate of DVT/PE after hip and knee arthroplasty
- Sodium chloride prevents contrast-induced nephropathy
Neutral Head Position Is Safe for Internal Jugular Vein Cannulation
Clinical question: Is there a difference in the complication rate between neutral head position and 45-degree neck rotation during ultrasound-guided internal jugular vein cannulation?
Background: Cannulation of the internal jugular vein using ultrasound decreases the rate of major complications (carotid artery puncture, pneumothorax, and hemothorax). The relative positions of the internal jugular vein and the carotid artery change based on degree of neck rotation. The optimal position for ultrasound-guided vein puncture has not been shown.
Study design: Prospective, randomized, controlled, non-blinded study.
Setting: Tertiary neurosurgical center in Milan, Italy.
Synopsis: One thousand, three hundred thirty-two patients undergoing major neurosurgical procedures who needed central venous catheter placement were randomized to a neutral head position (NH) or a 45-degree neck rotation (HT) during ultrasound-guided internal jugular vein cannulation. Exclusion criteria were consent refusal, age <12 years, and coagulopathy. Six experienced anesthesiologists performed the procedures; blinding was not possible.
There was no difference in the rate of major complications (carotid artery puncture, pneumothorax, or hemothorax) based on head position (0.9% in NH vs. 0.6% in HT). Minor complications (multiple skin punctures, multiple vein punctures, difficulty inserting the guidewire) were similar in the two groups (13.2% in NG vs. 12.6% in HT). Neck rotation was not associated with operator-reported difficulty or vascular access time.
Limitations of the study include the inability to blind the operator. Additionally, the study involved six experienced anesthesiologists at one center who performed the procedure on patients needing an elective central line. The ability to generalize the findings to other settings, less experienced providers, and patients who need an emergency line is not certain.
Bottom line: Neutral head position is as safe as 45-degree neck rotation for elective ultrasound-guided internal jugular vein cannulation.
Citation: Lamperti M, Subert M, Cortellazzi P, et al. Is a neutral head position safer than 45-degree neck rotation during ultrasound-guided internal jugular vein cannulation? Results of a randomized controlled clinical trial. Anesth Analg. 2012;114:777-784.
Thrombolysis Decreases Mortality in Unstable Patients with Acute Pulmonary Embolism
Clinical question: Does thrombolytic therapy decrease mortality in unstable patients with acute pulmonary embolism (PE)?
Background: PE is a common problem; associated mortality is high. Despite this fact, the data supporting thrombolytic therapy in hemodynamically unstable patients are not robust, and randomized, controlled trials are unlikely to be performed.
Study design: Retrospective cohort study.
Setting: One thousand nonfederal, short-term U.S. hospitals.
Synopsis: Using data from the Nationwide Inpatient Sample database from 1999-2008, investigators found that thrombolysis decreased both all-cause and PE-specific mortality for unstable patients, defined as those either in shock or on a ventilator. Specifically for all-cause mortality, 15% of patients who received thrombolysis died vs. 47% of those who did not (RR 0.31, 95% CI 0.30-0.32). Placement of an inferior vena cava (IVC) filter further reduced mortality, to only 7.6% in patients who received both IVC filter and thrombolysis.
For PE-specific mortality, patients who received thrombolysis also had decreased rates, from 42% to 8.4% (RR 0.20; 95% CI 0.19-0.22). Across all age groups, patients who received thrombolysis had decreased all-cause and PE-specific mortality. Patients who did not receive thrombolysis had additional comorbidities.
As this study is retrospective, it might be affected by unknown confounding. In addition, it relies on coding data to identify patient stability and treatment. Despite this limitation, a randomized, controlled trial is unlikely to be performed at this stage. This study provides evidence to support use of thrombolysis in unstable patients.
Bottom line: Thrombolysis might reduce mortality in unstable patients with acute PE. In combination with IVC filters, the mortality reduction might be even greater.
Citation: Stein PD, Matta F. Thrombolytic therapy in unstable patients with acute pulmonary embolism: saves lives but underused. Am J Med. 2012;125(5):465-470.
Rectal Indomethacin Decreases Incidence of Post-ERCP Pancreatitis
Clinical question: Does rectal indomethacin reduce the incidence of pancreatitis after ERCP?
Background: Acute pancreatitis is the most common complication from endoscopic retrograde cholangiopancreatography (ERCP). No pharmacologic treatment has proven to reduce the incidence of pancreatitis. Preliminary studies, including a meta-analysis, suggest that the use of NSAIDs might reduce the incidence of post-ERCP pancreatitis.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Multicenter trial at four university-affiliated medical centers in the U.S.
Synopsis: More than 600 patients at high risk for post-ERCP pancreatitis were randomized to receive either two 50-mg indomethacin suppositories or two identical-appearing placebo suppositories. Patients were considered at high risk for pancreatitis based on previously identified patient- and procedure-related risk factors. Most of the participants had sphincter of Oddi dysfunction (84.4% of the indomethacin group and 80.5% of the placebo group). Exclusion criteria included elevated creatinine and active peptic ulcer disease. The indomethacin or placebo suppositories were given immediately following the ERCP.
Post-ERCP pancreatitis, defined by upper abdominal pain, elevation of pancreatic enzymes, and hospitalization for at least two nights, was significantly higher in the placebo group compared with the indomethacin group (16.9% vs. 9.2%, P=0.005). Moderate or severe post-ERCP pancreatitis was significantly higher in the placebo group compared with the indomethacin group (8.8% vs. 4.4%, P=0.03).
There were no significant differences in the rates of clinically significant bleeding or acute renal failure between the two groups. The ability to generalize these findings to patients without risk factors for post-ERCP pancreatitis is not clear.
Bottom line: Rectal indomethacin decreases the rate of post-ERCP pancreatitis in patients who are at high risk for this complication.
Citation: Elmunzer BJ, Scheiman JM, Lehman GA, et al. A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med. 2012;366(15):1414-1422.
CHADS2-VASc and HAS-BLED Can Predict Thromboembolism and Bleeding Risk in Afib Patients
Clinical question: What are the risk factors for stroke/thromboembolism and bleeding from atrial fibrillation (afib), and how well do the CHADS2-VASc and HAS-BLED stroke and bleeding risk-assessment tools perform against other published stroke and bleeding risk-assessment tools (CHADS2 and HEMORR2HAGES) for patients with afib?
Background: In afib patients, the CHADS2-VASc tool might offer more comprehensive stroke assessment over the CHADS2 by identifying truly-low-risk patients with afib who might not even need antiplatelet therapy. HAS-BLED, a newer bleeding-risk-assessment tool, has been validated in previous trials and is more user-friendly than others. Use of CHADS2-VASc and HAS-BLED are recommended by the European Society of Cardiology to assess stroke and bleeding risks for patients with afib.
Study design: Prospective cohort study.
Setting: All hospitals in Sweden.
Synopsis: Investigators identified 182,678 afib patients via ICD-10 data from Sweden’s National Hospital Discharge Registry ICD-10 from 2005 to 2008. Approximately half the patients were not taking anticoagulants. Analysis assessed risk factors for stroke and bleeding and the performance of CHADS2-VASc and HAS-BLED against CHADS2 and HEMORR2HAGES stroke and bleeding risk-assessment tools.
Risk of composite thromboembolism (unspecified stroke, TIA, systemic embolism) was significantly higher in patients with increased age, peripheral arterial disease, prior myocardial infarction (MI), prior coronary artery bypass grafting (CABG), female gender, renal failure, and aspirin use, as well as hypertension, diabetes, prior thromboembolic event, or prior intracranial hemorrhage (ICH). Interestingly, a statistically increased risk was seen with aspirin use.
Conversely, history of heart failure, thyroid disease, and obesity were not associated with increased composite thromboembolic risk. The use of CHADS2-VASc was marginally better than CHADS2 in predicting stroke risk.
ICH risk was increased in patients with older age, prior ischemic stroke, prior ICH, and hypertension. Risk of composite bleeding (from ICH or other major bleeding) was significantly higher in patients with these risk factors, as well as renal failure, liver disease, anemia, dysfunctional platelets, alcohol use, and cancer. Ischemic heart disease was associated with a statistically significant lower risk of ICH, but not of composite bleeding risk.
HAS-BLED usage was as good as, and easier to use than, HEMORR2HAGES in predicting bleeding risk.
Bottom line: CHADS2-VASc might be better than CHADS2 in predicting truly-low-risk patients with nonvalvular afib; HAS-BLED is just as good as, and easier to use than, HEMORR2HAGES in predicting bleeding risk for patients with nonvalvular afib who are to receive antithrombotic therapy.
Citation: Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182,678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33(12):1500-10 [Epub 2012 Jan 13].
Supported Self-Management of COPD Does Not Decrease Readmission or Mortality Rates
Clinical question: Does supported self-management of patients with chronic obstructive pulmonary disease (COPD) decrease COPD-related hospital readmission or death?
Clinical background: Supported self-management has benefited patients with such chronic diseases as heart failure and asthma. Evidence to support such a strategy for patients with COPD is relatively lacking.
Study design: Randomized, controlled trial.
Setting: Community-based care following urban hospitalization in western Scotland.
Synopsis: From June 2007 to May 2009, and following hospitalization for COPD exacerbation, 464 patients were randomized to receive routine community-based care with or without 12 months of support and training to detect, and promptly treat, recurrent exacerbations. Independent of disease severity or demographics, investigators found no difference in combined readmission (48% vs. 47%, 95% confidence interval [CI] 0.80-1.38) or death (10% vs. 7%, 95% CI 0.71-2.61).
Based on review of appropriateness of self-management strategies used by the intervention group, unplanned exploratory subgroup analysis classified a minority of the intervention group as “successful” (42%) supported self-managers, and demonstrated decreased COPD readmissions and death (27% vs. 49%, 95% CI 0.25-0.76, P=0.003) vs. “unsuccessful” self-managers. This successful group was younger and tended to live with others. Further research to define characteristics of patients who benefit from self-management is needed.
Bottom line: Supported self-management of COPD does not reduce COPD-related readmission or death in a large population.
Citation: Bucknall CE, Miller G, Lloyd SM, et al. Glasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trial. BMJ. 2012;344:e1060 [Epub ahead of print].
Medicare Premier P4P Initiatives Do Not Decrease Mortality
Clinical question: Has the Medicare Premier Hospital Quality Incentive Demonstration (HQID) resulted in lower mortality?
Background: The Centers for Medicare & Medicaid Services’ (CMS) value-based purchasing program will expand to include 30-day mortality in 2013, but do pay-for-performance (P4P) initiatives result in improved mortality? Studies have demonstrated improvement in process of care but have not demonstrated mortality benefit thus far.
Study design: Cohort study.
Setting: Two hundred fifty-two hospitals participating in the Premier HQID compared with 3,363 control hospitals participating in the Hospital Compare program.
Synopsis: Researchers examined 30-day mortality for patients admitted with acute myocardial infarction, congestive heart failure, pneumonia, and for coronary artery bypass grafting (CABG) from 2003 to 2009. Results showed no difference in 30-day mortality rates over the six-year span of the program for any of the conditions studied in the Premier hospitals (participating in the voluntary pay-for-performance program) vs. non-Premier hospitals (11.82% vs. 11.74%). This held true for each condition measured individually, with a higher mortality rate for patients undergoing CABG at the Premier hospitals.
In addition, in the hospitals that underperformed initially, there was no difference with respect to rate of improvement when comparing Premier vs. non-Premier hospitals. Furthermore, mortality rate trends did not differ between those conditions that were incentivized (acute MI and CABG) compared with those that were not (congestive heart failure and pneumonia).
The authors concluded that there was “little evidence” that the Premier HQID pay-for-performance program resulted in reduced 30-day mortality.
Bottom line: Programs participating in the Medicare Premier HQID pay-for-performance program had similar 30-day mortality compared with nonparticipating programs.
Citation: Jha AK, Joynt KE, Orav EJ, Epstein AM. The long-term effect of premier pay for performance on patient outcomes. N Engl J Med. 2012;366:1606-1615.
In-Hospital Rate of DVT/PE After Hip and Knee Arthroplasty with Guideline-Recommended Prophylaxis
Clinical question: What is the rate of symptomatic DVT/PE after total or partial hip (TPHA) or knee (TPKA) arthroplasty using currently recommended prophylaxis?
Background: The rate of postoperative DVT/PE after TPHA/TPKA has dropped dramatically with use of pharmacologic prophylaxis. However, the current rate of symptomatic DVT/PE using current pharmacologic prophylaxis is not known. Such rates are needed for informed patient consent and development of patient safety benchmarks.
Study design: Systematic review.
Setting: Randomized clinical trials (RCTs) and observational studies worldwide of adult inpatients undergoing TPHA and/or TPKA from 1996 to 2011.
Synopsis: Forty-seven studies were included, of which 41 were RCTs and six were observational studies. Twenty-one studies evaluated rates after TPHA, 20 after TPKA, and six after both. More than 44,000 patients were included, with ages ranging from 58 to 74 years. The mean duration of prophylaxis was eight days, with a mean follow-up of 13 days.
In-hospital rates of symptomatic venous thromboembolism (VTE) were higher in patients undergoing TPKA than TPHA (1.09% vs. 0.53% for VTE, 0.63% vs. 0.26% for DVT, and 0.27% vs. 0.14% for PE). This is in contrast to the higher rates of VTE observed after TPHA when the post-discharge period is included. The pooled incidence of VTE was lower with use of direct inhibitors of Factors Xa or IIa when compared to low-molecular-weight heparin, although a direct efficacy comparison could not be made.
Because the majority of studies were RCTs with restrictive inclusion criteria, rates of DVT/PE in actual practice might be higher.
Bottom line: When informing patients of postoperative VTE risk, or establishing benchmarks to evaluate patient safety, one can anticipate an in-hospital VTE rate of 0.5% following TPHA and 1% following TPKA.
Citation: Januel JM, Chen G, Ruffieux C, et al. Symptomatic in-hospital deep vein thrombosis and pulmonary embolism following hip and knee arthroplasty among patients receiving recommended prophylaxis: a systematic review. JAMA. 2012;307(3):294-303.
Sodium Chloride Prevents Contrast-Induced Nephropathy
Clinical question: Is sodium chloride more effective than sodium bicarbonate for preventing contrast-induced nephropathy?
Background: Contrast-induced nephropathy can be prevented with precontrast hydration. Study authors sought to compare sodium chloride administered over 24 hours with sodium bicarbonate administered over seven hours, and with sodium bicarbonate administered orally.
Study design: Randomized, open-label, controlled trial.
Setting: Three European medical centers.
Synopsis: The study examined 258 patients with an estimated glomerular filtration rate <60mL/min/1.73m2 undergoing intravenous or intra-arterial contrast procedure. Patients with Class III or IV heart failure were excluded. The remaining patients were randomized to receive one of three regimens: sodium chloride at 1 ml/kg/hr for 12 hours prior to and 12 hours following the procedure; intravenous sodium bicarbonate for one hour prior to and six hours following the procedure; or intravenous and oral sodium bicarbonate 20 minutes prior to the procedure.
The group that received saline had a lower incidence of contrast-induced nephropathy than the bicarbonate groups (1% vs. 9% vs. 10%). The oral bicarbonate strategy was noninferior to the seven-hour intravenous bicarbonate strategy.
The authors postulated that saline should be used for high-risk patients, but that given the overall low incidence of contrast-induced nephropathy, the short-term bicarbonate strategy (intravenous followed by oral) is a viable alternative for low-risk patients.
Bottom line: Sodium chloride is more effective than sodium bicarbonate for preventing contrast-induced nephropathy, but in light of the low incidence, a short course of sodium bicarbonate is a possible convenient alternative for low-risk patients.
Citation: Klima T, Christ A, Marana I, et al. Sodium chloride vs. sodium bicarbonate for the prevention of contrast medium-induced nephropathy: a randomized controlled trial. Eur Heart J. 2012 Jan 19 [Epub ahead of print].