User login
Guidelines for Thyroid Nodule Evaluation
Adolescent Androgenic Alopecia
Erratum (2007;80:113-120)
Is there a link between aripiprazole and treatment-emergent psychosis?
Discuss this article at www.facebook.com/CurrentPsychiatry
• Aripiprazole may interact preferentially with distinct conformations of the D2 receptor, leading to a spectrum of pharmacologic effects, including acting as a full agonist, partial agonist, or antagonist.
• Clinical predictors of aripiprazole-associated worsening of psychosis include low baseline level of psychopathology and previous treatment with high-dose antipsychotics.
• Rapid transition from a medication with significant anticholinergic properties to 1 without these properties may result in symptoms of activation, including restlessness, insomnia, and anxiety, which can be mistaken for worsening psychosis.
• Akathisia, a common adverse effect of aripiprazole, may masquerade as treatment-emergent worsening of psychotic symptoms.
Mr. N, age 29, presents to the emergency department at the urging of his family because of poor self-care, bizarre behavior, and disturbed sleep. He first experienced psychiatric symptoms 10 years ago after his mother died. He became dysphoric and paranoid, displaying bizarre responses and behaviors with poor self-care and a gradual functional decline. He has been taking sertraline, 100 mg/d, for 10 years.
Upon arrival at the hospital’s inpatient unit, Mr. N is unkempt, oddly related, and paranoid. His affect is constricted. Mr. N displays thought blocking and possibly is responding to internal stimuli. Sertraline is continued and haloperidol, 1 mg/d, is initiated. For the next 2 weeks, Mr. N continues to be oddly related, irritable, and paranoid, and experiences disturbed sleep and thought blocking. After an episode of impulsive aggression, the treatment team initiates aripiprazole, which is titrated to 30 mg/d for 1 week. Mr. N’s clinical status worsens; he is menacing toward other patients and his thinking is more disorganized, with loose associations and ideas of reference. He requires 4 injections of IM haloperidol, 5 mg, and several visits to the seclusion room over the next week. Haloperidol is increased to 30 mg/d over the next 10 days, then aripiprazole is discontinued because of a putative drug interaction with haloperidol. Following the medication changes Mr. N demonstrates better behavioral control, but still is grossly psychotic. While awaiting transfer to a state hospital, Mr. N receives a trial of olanzapine, 20 to 40 mg/d, for 2 weeks without significant benefit.
Several clinical trials demonstrate a significant reduction in intensity of psychotic symptoms with aripiprazole, which has a unique mechanism of action.1 However, since its FDA approval in 2002, several case reports have described treatment-emergent psychotic symptoms associated with aripiprazole initiation. Over the past 40 years, reports of worsening psychosis associated with antipsychotics have been limited to patients with schizophrenia who were taking high dosages or who had high plasma concentrations, when anticholinergic delirium may have explained increased psychotic symptoms.2-4
How can a drug effectively treat psychotic symptoms and occasionally worsen them? In this article, we discuss the relevant pharmacology and clinical literature on aripiprazole and try to make sense of this apparent paradox.
Unique pharmacologic profile
Antipsychotics have been reported to be either neutral antagonists or inverse agonists at the D2 receptor, based on in vitro data.5 Aripiprazole and its main metabolite, dehydroaripiprazole, originally were described as partial agonists at D2 dopamine receptors.6,7 However, it appears aripiprazole’s pharmacologic action is better explained by the concept of functional selectivity. Aripiprazole may interact preferentially with distinct conformations of the D2 receptor, leading to a spectrum of pharmacologic effects, including acting as a full agonist, partial agonist, or antagonistic.5
Researchers have hypothesized that the pathophysiology of schizophrenia may, in part, be caused by dysfunction of mesocorticolimbic dopaminergic neurons characterized by an enhanced sensitivity of postsynaptic D2 receptors and increased sensitivity to dopaminergic drugs.8,9 In addition, chronic treatment with a D2 receptor antagonist is associated with increases in postsynaptic dopamine receptor density (ie, an increase in receptor reserve).10,11 Upregulation of D2 receptors may explain several features seen in patients chronically treated with antipsychotics, including tardive dyskinesia12 and rapid psychotic relapse after discontinuing an antipsychotic (supersensitivity psychosis).13 Because chronic antipsychotic treatment leads to high postsynaptic receptor reserve, aripiprazole initiation may produce overactivation of D2 receptors, which might worsen a patient’s condition.14 In vitro data15-18 and clinical observations indicate that aripiprazole has intrinsic efficacy at D2 receptors, as do clinical observations, such as:
- its propensity to reduce serum prolactin19
- a decreased likelihood of producing extrapyramidal side effects despite >80% occupancy of D2 receptors6
- case reports documenting aripiprazole-associated mania,20 improvement of risperidone-associated cognitive impairment,21 and pathologic gambling.22
Emergence or worsening of psychotic symptoms or a marginal antipsychotic effect may occur if aripiprazole is indeed a postsynaptic D2 receptor agonist. An individual patient’s outcome likely would depend on his or her sensitivity to psychosis and concurrent or previous exposure to a D2 receptor antagonist. For example, stimulation of postsynaptic D2 receptors may be further augmented if the dosage of the previous antipsychotic was reduced or withdrawn before initiating aripiprazole because additional receptors would be available for interaction with aripiprazole.
Case reports
A literature review revealed 23 reports of treatment-emergent psychosis associated with aripiprazole initiation (Table). The mean age of the patients was 47 (range: 17 to 69) and 57% were men. Most patients (87%) were diagnosed with a schizophrenia-spectrum illness before aripiprazole initiation. Most (57%) had mild, stable, or no psychotic symptoms before aripiprazole initiation. Most were receiving relatively high doses of antipsychotics (average chlorpromazine equivalents [CPZE]: 648 mg/d) before aripiprazole initiation. This medication was either decreased or discontinued in 70% of patients.
Emergence or worsening of psychotic symptoms included agitation, aggressive behavior, and increased psychomotor activity. However, akathisia evaluation was described in only 2 reports: 1 author identified akathisia symptoms, but attributed them to a concomitant antipsychotic (fluphenazine)23 and the other report specifically excluded the possibility of akathisia.24 Two systematic studies have attempted to establish risk factors for aripiprazole-associated worsening psychosis (Box).14,25
In our literature review, the mean final dose of aripiprazole was 21.5 mg/d (range: 2 to 60 mg/d). In the cases describing subsequent treatment, all but 1 patient were switched to another antipsychotic, including 2 whose psychotic symptoms stabilized with continuation of aripiprazole and addition of a second antipsychotic. Interestingly, in the case reported by Adan-Manes et al,26 initial treatment with aripiprazole monotherapy was efficacious, but a subsequent trial of adjunctive aripiprazole resulted in worsening psychosis.
Table
Case reports: Treatment-emergent psychosis associated with aripiprazole
| Study | Age, sex | Diagnosis | Before aripiprazole initiation | Pre-aripiprazole treatment | Aripiprazole dose | Concomitant psychotropic treatment | Subsequent treatment |
|---|---|---|---|---|---|---|---|
| Chiu et al, 2011a | 39, M | Schizophrenia | Psychiatrically stable, tardive dystonia | Clozapine, 300 mg/d | 10 mg/d | Valproic acid, 1,000 mg/d, clonazepam, 2 mg/d, mephenoxalone, 800 mg/d | Clozapine |
| Ekinci et al, 2010b | 17, M | ADHD | Inattention and impulsive aggression | Tapered and discontinued risperidone, 2.5 mg/d | 5 mg/d | Methylphenidate, 54 mg/d | Risperidone, 2 mg/d, methylphenidate, 36 mg/d |
| Selvaraj et al, 2010c | 49, F | Chronic depression | Depressive symptoms, suicidal ideation | None stated | 2 mg/d | Duloxetine, 80 mg/d, clonazepam, 2 mg/d | Duloxetine, 120 mg/d |
| Adan-Manes et al, 2009d | 23, M | Schizophrenia | No psychotic symptoms | Abrupt decrease of amisulpride dose from 800 mg/d to 400 mg/d | 20 mg/d | Biperiden, 4 mg/d | Amisulpride, 800 mg/d |
| Cho et al, 2009e | 45, F | Schizophrenia | Persistent psychotic symptoms, new onset diabetes with acute ketoacidosis | Haloperidol, 20 mg/d, abrupt clozapine discontinuation | 15 mg/d | Valproic acid, nortriptyline | Molindone, 150 mg/d |
| Ahuja et al, 2007f | 35, F | Schizoaffective disorder | Stable before medication change | Tapered amisulpride, 400 mg/d, over 6 weeks | 15 mg/d | None | Amisulpride, 600 mg/d |
| Lea et al, 2007g | 57, M | Schizophrenia | Persistent psychotic symptoms, treatment resistance, recent recovery from NMS | Discontinued ziprasidone, 200 mg/d | 30 mg/d | Lorazepam, 2 mg/d, amantadine, 100 mg, sertraline, 50 mg/d | Clozapine |
| Lea et al, 2007g | 49, M | Schizoaffective disorder | Delusions, verbal aggression, substance abuse, HCV | Decreased quetiapine dose from 800 mg/d to 400 mg/d | 15 mg/d | Divalproex, 1,000 mg/d, fluvoxamine, 200 mg/d, clonazepam, 2 mg/d | Lithium, quetiapine, 500 mg/d, haloperidol, 2 mg/d |
| Lea et al, 2007g | 60, M | Schizophrenia | Delusions, labile mood, aggression | Risperidone, 3 mg/d, interruption of fluphenazine, 75 mg/d | 20 mg/d | Divalproex, 4,500 mg/d, benztropine, 3 mg/d | Not discussed |
| Raja, 2007h | 30, M | Schizoaffective disorder | Negative symptoms, otherwise stable, recent citalopram discontinuation | Discontinued amisulpride, 800 mg/d over 2 weeks | 30 mg/d | Lithium | Amisulpride, 500 mg/d |
| Raja, 2007h | 69, F | Bipolar disorder | History of multiple relapses; presented with tremor, akathisia, weight gain | Discontinued risperidone, 2 mg/d, over 2 weeks | 15 mg/d | Lithium | Risperidone, 4 mg |
| Raja, 2007h | 59, F | Schizophrenia | Negative symptoms, otherwise stable | Reduced risperidone dosage from 5 mg/d to 4 mg/d | 7.5 mg/d | None | Risperidone, 5 mg/d |
| Thone, 2007i | 31, M | Schizophrenia | Confusion, agitation, delusions worsened with aripiprazole dose increase | None | 60 mg/d | None | Aripiprazole dose reduction to 15 mg/d, olanzapine, 10 mg/d |
| Glick et al, 2006j | 55, F | Schizophrenia | Stable before medication change | Tapered and discontinued thioridazine, 600 mg/d, over 3 months | 30 mg/d | None | Chlorpromazine, 200 mg/d, aripiprazole, 30 mg/d |
| Glick et al, 2006j | 52, M | Schizophrenia | Negative symptoms | Decreased olanzapine dose from 30 mg/d to 20 mg/d | 30 mg/d | None | Olanzapine, 30 mg/d |
| Barnas et al, 2005k | 57, F | Schizoaffective disorder | Stable before medication change | Discontinued perphenazine, 8 mg/d | 30 mg/d | None | Quetiapine, 350 mg/d |
| DeQuardo, 2004l | 54, M | Schizophrenia | History of aggression, residual paranoia, severe EPS | Haloperidol, 200 mg/d | 15 mg/d | Benztropine | Haloperidol |
| DeQuardo, 2004l | 51, M | Schizophrenia | History of aggression, persistent psychotic symptoms, treatment resistance | Olanzapine, 60 mg/d | 10 mg/d | None | Olanzapine |
| Ramaswamy et al, 2004m | 43, F | Schizoaffective disorder | Psychiatrically stable, multiple medication changes, including substituting carbamazepine for valproic acid | Discontinued ziprasidone, 160 mg/d, discontinued quetiapine, 400 mg/d, over 2 weeks | 30 mg/d | Propranolol, 30 mg/d, l-thyroxine, .05 mg/d, carbamazepine, 600 mg/d | Not available |
| Ramaswawamy et al, 2004m | 57, F | Schizoaffective disorder | History of multiple hospitalizations, but stable before medication change | Decreased olanzapine dose from 20 mg/d to 15 mg/d | 30 mg/d | Valproic acid, 2,000 mg/d | Ziprasidone |
| Ramaswawamy et al, 2004m | 67, F | Schizophrenia | Remote hospitalizations, recent worsened psychosis | Decreased ziprasidone dose from 200 mg/d to 160 mg/d 2 months previously | 30 mg/d | Carbamazepine, 200 mg/d | Not discussed |
| Ramaswamy et al, 2004m | 46, M | Schizophrenia | Persistent delusions while receiving risperidone, TD | Risperidone, 3 mg/d | 15 mg/d | Valproic acid, 1,500 mg/d | Risperidone, 3 mg/d |
| Reeves et al, 2004n | 50, M | Schizoaffective disorder | Relatively stable with nonthreatening delusions, hallucinations | Quetiapine, 800 mg/d | 30 mg/d | Divalproex, 2,000 mg/d | Olanzapine, 20 mg/d |
| ADHD: attention-deficit/hyperactivity disorder; EPS: extrapyramidal symptoms; HCV: hepatitis C virus; NMS: neuroleptic malignant syndrome; TD: tardive dyskinesia Source: References a. Chiu YH, Chen CH, Lu ML. Worsening psychosis after adding aripiprazole to clozapine. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(1):291-292. b. Ekinci O, Sabuncuoglu O. Psychosis associated with switching from risperidone to aripiprazole in an adolescent on methylphenidate treatment. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(2):648-649. c. Selvaraj V, Ramaswamy S, Sharma A, et al. New-onset psychosis and emergence of suicidal ideation with aripiprazole. Am J Psychiatry. 2010;167(12):1535-1536. d. Adan-Manes J, Garcia-Parajua P. Aripiprazole in combination with other antipsychotic drugs may worsen psychosis. J Clin Pharm Ther. 2009;34(2):245-246. e. Cho DY, Lindenmayer JP. Aripiprazole-induced agitation after clozapine discontinuation: a case report. J Clin Psychiatry. 2009;70(1):141-143. f. Ahuja N, Lloyd AJ. Aripiprazole and worsening of psychosis: a case report. J Clin Psychiatry. 2007;68(5):805-806. g. Lea JW, Stoner SC, Lafollette J. Agitation associated with aripiprazole initiation. Pharmacotherapy. 2007;27(9):1339-1342. h. Raja M. Improvement or worsening of psychotic symptoms after treatment with low doses of aripiprazole. Int J Neuropsychopharmacol. 2007;10(1):107-110. i. Thone J. Worsened agitation and confusion in schizophrenia subsequent to high-dose aripiprazole. J Neuropsychiatry Clin Neurosci. 2007;19(4):481-482. j. Glick ID, Duggal V, Hodulik C. Aripiprazole as a dopamine partial agonist: positive and negative effects. J Clin Psychopharmacol. 2006;26(1):101-103. k. Barnas ME, Hussain N, Petrides G. Treatment-emergent psychosis with aripiprazole. J Clin Psychiatry. 2005;66(10):1339. l. DeQuardo JR. Worsened agitation with aripiprazole: adverse effect of dopamine partial agonism? J Clin Psychiatry. 2004;65(1):132-133. m. Ramaswamy S, Vijay D, William M, et al. Aripiprazole possibly worsens psychosis. Int Clin Psychopharmacol. 2004;19(1):45-48. n. Reeves RR, Mack JE. Worsening schizoaffective disorder with aripiprazole. Am J Psychiatry. 2004;161(7):1308. | |||||||
Takeuchi et al14 aimed to establish predictors of worsening psychosis in a naturalistic setting where patients slowly transitioned to aripiprazole from previous antipsychotic treatment. Patients were required to be on a stable dose of an antipsychotic before participating in the study. Aripiprazole was started at 12 mg/d for 2 weeks with flexible dosing from weeks 2 to 52. Previous antipsychotic therapy was reduced biweekly by 25%. The incidence of worsening psychopathology after aripiprazole initiation was higher in the group of patients who had previously received high-dose antipsychotic therapy (average chlorpromazine equivalents [CPZE]: 727 mg/d) compared with the group on low dosages (average CPZE: 382 mg/d). It is possible that previous high-dose antipsychotic therapy was indicative of more significant baseline psychopathology; however, the worsened group and stabilized group had similar baseline Clinical Global Impressions-Severity scores.
Pae et al25 aimed to find predictors of worsening psychosis with aripiprazole in patients whose previous antipsychotic therapy was immediately discontinued. They found lower baseline disease severity was associated with significant worsening during the first month of aripiprazole treatment.
Other potential explanations
Aripiprazole’s manufacturer reported the incidence of psychosis-related adverse events in an analysis of 9 randomized schizophrenia trials.27 The rates of psychosis-related adverse events ranged from 0.6% to 18%, but there was no apparent relationship to study design or method of transitioning to aripiprazole. Rates of psychosis-related adverse events were similar between aripiprazole and the control group (placebo in 3 studies, another antipsychotic in 2 studies).
Emergence or worsening of psychotic symptoms temporally associated with aripiprazole initiation does not necessarily imply causation. As in Mr. N’s case, it is not always possible to determine whether worsening psychosis is the natural disease course or a treatment effect. In addition, it is not possible to differentiate lack of efficacy from a true propensity for aripiprazole to worsen psychosis.
It also is conceivable discontinuation or dosage reduction of a previous antipsychotic would worsen psychotic symptoms or cause side effects. When significant changes in psychopathology or side effects develop during the transition from 1 antipsychotic to another, it is difficult to determine etiology. Specifically, rapid transition from a medication with significant anticholinergic and antihistaminic properties—such as quetiapine or olanzapine—to 1 without these properties—such as aripiprazole—may result in symptoms of activation, including restlessness, insomnia, and anxiety. Consequently, these symptoms could be mistaken for worsening psychosis.28 Only 1 patient in this series was reported to abruptly discontinue an antipsychotic with significant anticholinergic properties (clozapine) before initiating aripiprazole.24 Studies by Takeuchi et al14 and Pae et al25 did not report the relative baseline use of antipsychotic medication with anticholinergic properties.
In a pooled analysis of treatment-emergent adverse events in 5 randomized clinical trials of patients receiving aripiprazole for acute relapse of schizophrenia, the incidence of akathisia was 10%, although it is not clear if this is a dose-related adverse effect.29 Because akathisia may be confused for worsening psychosis,30 it is possible akathisia was mistakenly identified as worsening psychotic symptoms in Mr. N’s case, as well as several reports from our literature review.
Covert akathisia is unlikely to explain worsening psychopathology observed in all patients in our literature review because confusion of akathisia and worsening psychosis is not a widespread phenomenon. In a post hoc analysis of pooled safety data from aripiprazole trials, Kane et al31 did not find a correlation between presence of akathisia and aripiprazole efficacy as measured by the Positive and Negative Syndrome Scale (PANSS) total, PANSS positive, PANSS negative, Clinical Global Impressions-Severity, Clinical Global Impressions-Improvement, and percentage of responders. Pae et al25 also noted there was no correlation between scores on the Barnes Akathisia Rating Scale and worsening psychopathology in patients switched to aripiprazole.
An antagonist always is an antagonist and clinicians have appreciated this concept since the days of chlorpromazine. The activity of aripiprazole, however, is on a pharmacologic continuum between a neutral antagonist and full agonist and currently there is no way to precisely determine the level of D2 receptor agonist action in a patient.
Although it is interesting to speculate that aripiprazole’s D2 receptor agonist action may contribute to worsening psychosis,32-34 there are other plausible explanations to consider. Rapid transition from a drug with significant anticholinergic properties and aripiprazole-associated akathisia may contribute to worsening psychopathology in patients starting aripiprazole. Because covert side effects may be incorrectly identified as psychotic agitation, we cannot exclude this as a possible etiologic factor in Mr. N’s case as well as the cases in our literature review.
Related Resource
- Abilify [package insert]. Princeton, NJ: Bristol-Myers Squibb; 2011.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Benztropine • Cogentin
- Biperiden • Akineton
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Clonazepam • Klonopin
- Clozapine • Clozaril
- Divalproex • Depakote
- Duloxetine • Cymbalta
- Fluphenazine • Permitil, Prolixin
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Nortriptyline • Aventyl, Pamelor
- Methylphenidate • Concerta
- Molindone • Moban
- Olanzapine • Zyprexa
- Perphenazine • Trilafon
- Propranolol • Inderal
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Thyroxine • Synthroid
- Valproic acid • Depakene
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Citrome L. A review of aripiprazole in the treatment of patients with schizophrenia or bipolar I disorder. Neuropsychiatr Dis Treat. 2006;2(4):427-443.
2. Chong SA, Tan CH, Lee HS. Worsening of psychosis with clozapine and selective serotonin reuptake inhibitor combination: two case reports. J Clin Psychopharmacol. 1997;17(1):68-69.
3. Bowers MB Jr, Swigar ME. Psychotic patients who become worse on neuroleptics. J Clin Psychopharmacol. 1988;8(6):417-421.
4. Tornatore FL, Lee D, Sramek JJ. Psychotic exacerbation with haloperidol. Drug Intell Clin Pharm. 1981;15(3):209-213.
5. Beaulieu JM, Gainetdinov RR. The physiology signaling, and pharmacology of dopamine receptors. Pharmacol Rev. 2011;63(1):182-217.
6. Grunder G, Carlsson A, Wong DF. Mechanism of new antipsychotic medications: occupancy is not just antagonism. Arch Gen Psychiatry. 2003;60(10):974-977.
7. Wood MD, Scott C, Clarke K, et al. Aripiprazole and its human metabolite are partial agonists at the human dopamine D2 receptor, but the rodent metabolite displays antagonist properties. Eur J Pharmacol. 2006;546(1-3):88-94.
8. Seeman P, Weinshenker D, Quirion R, et al. Dopamine supersensitivity correlates with D2High states, implying many paths to psychosis. Proc Natl Acad Sci U S A. 2005;102(9):3513-3518.
9. Seeman P, Ko F, Jack E, et al. Consistent with dopamine supersensitivity, RGS9 expression is diminished in the amphetamine-treated animal model of schizophrenia and in postmortem schizophrenia brain. Synapse. 2007;61(5):303-309.
10. Burt DR, Creese I, Snyder SH. Antischizophrenic drugs: chronic treatment elevates dopamine receptor binding in brain. Science. 1977;196(4287):326-328.
11. Silvestri S, Seeman MV, Negrete JC, et al. Increased dopamine D2 receptor binding after long-term treatment with antipsychotics in humans: a clinical PET study. Psychopharmacology (Berl). 2000;152(2):174-180.
12. Sayers AC, Bürki HR, Ruch W, et al. Neuroleptic-induced hypersensitivity of striatal dopamine receptors in the rat as a model of tardive dyskinesias. Effects of clozapine, haloperidol, loxapine and chlorpromazine. Psychopharmacologia. 1975;41(2):97-104.
13. Moncrieff J. Does antipsychotic withdrawal provoke psychosis? Review of the literature on rapid onset psychosis (supersensitivity psychosis) and withdrawal-related relapse. Acta Psychiatr Scand. 2006;114(1):3-13.
14. Takeuchi H, Uchida H, Suzuki T, et al. Predictors of clinical worsening after a switch to aripiprazole in patients with schizophrenia: a 1-year naturalistic follow-up study. J Clin Psychopharmacol. 2009;29(4):394-395.
15. Shapiro DA, Renock S, Arrington E, et al. Aripiprazole, a novel atypical antipsychotic drug with a unique and robust pharmacology. Neuropsychopharmacology. 2003;28(8):1400-1411.
16. Urban JD, Vargas GA, von Zastrow M, et al. Aripiprazole has functionally selective actions at dopamine D2 receptor-mediated signaling pathways. Neuropsychopharmacology. 2007;32(1):67-77.
17. Klewe IV, Nielsen SM, Tarpo L, et al. Recruitment of beta-arrestin2 to the dopamine D2 receptor: Insights into anti-psychotic and anti-parkinsonian drug receptor signaling. Neuropharmacology. 2008;54(8):1215-1222.
18. Masri B, Salahpour A, Didriksen M, et al. Antagonism of dopamine D2 receptor/beta-arrestin 2 interaction is a common property of clinically effective antipsychotics. Proc Natl Acad Sci U S A. 2008;105(36):13656-13661.
19. Shim JC, Shin JG, Kelly DL, et al. Adjunctive treatment with a dopamine partial agonist, aripiprazole, for antipsychotic-induced hyperprolactinemia: a placebo-controlled trial. Am J Psychiatry. 2007;164(9):1404-1410.
20. Padala PR, Wengel SP, Petty F. Manic episode during treatment with aripiprazole. Am J Psychiatry. 2007;164(1):172-173.
21. Hu CH, Pai N, Huang XF, et al. Potential control of risperidone-related cognitive deficits by adjunctive aripiprazole treatment. J Clin Psychopharmacol. 2011;31(1):135-136;author reply 136–137.
22. Cohen J, Magalon D, Boyer L, et al. Aripiprazole-induced pathological gambling: a report of 3 cases. Curr Drug Saf. 2011;6(1):51-53.
23. Lea JW, Stoner SC, Lafollette J. Agitation associated with aripiprazole initiation. Pharmacotherapy. 2007;27(9):1339-1342.
24. Cho DY, Lindenmayer JP. Aripiprazole-induced agitation after clozapine discontinuation: a case report. J Clin Psychiatry. 2009;70(1):141-143.
25. Pae CU, Chiesa A, Mandelli L, et al. Predictors of early worsening after switch to aripiprazole: a randomized, controlled, open-label study. Clin Drug Investig. 2010;30(3):187-193.
26. Adan-Manes J, Garcia-Parajua P. Aripiprazole in combination with other antipsychotic drugs may worsen psychosis. J Clin Pharm Ther. 2009;34(2):245-246.
27. Cognata-Smith C, Baker RA, Pikalov A, et al. Analysis of nine aripiprazole trials to evaluate strategies for switching patients with schizophrenia to aripiprazole. Paper presented at: 162nd Annual Meeting American Psychiatric Association; May 16-21, 2009; San Francisco, CA.
28. Lieberman J. Cholinergic rebound in neuroleptic withdrawal syndromes. Psychosomatics. 1981;22(3):253-254.
29. Marder SR, McQuade RD, Stock E, et al. Aripiprazole in the treatment of schizophrenia: Safety and tolerability in short-term, placebo-controlled trials. Schizophr Res. 2003;61(2-3):123-136.
30. Kane JM, Fleischhacker WW, Hansen L, et al. Akathisia: an updated review focusing on second-generation antipsychotics. J Clin Psychiatry. 2009;70(5):627-643.
31. Kane JM, Barnes TR, Correll CU, et al. Evaluation of akathisia in patients with schizophrenia, schizoaffective disorder, or bipolar I disorder: A post hoc analysis of pooled data from short- and long-term aripiprazole trials. J Psychopharmacol. 2010;24(7):1019-1029.
32. Fleischhacker WW, McQuade RD, Marcus RN, et al. A double-blind, randomized comparative study of aripiprazole and olanzapine in patients with schizophrenia. Biol Psychiatry. 2009;65(6):510-517.
33. Kane JM, Osuntokun O, Kryzhanovskaya LA, et al. A 28-week, randomized, double-blind study of olanzapine versus aripiprazole in the treatment of schizophrenia. J Clin Psychiatry. 2009;70(4):572-581.
34. Kane JM, Correll CU, Goff DC, et al. A multicenter, randomized, double-blind, placebo-controlled, 16-week study of adjunctive aripiprazole for schizophrenia or schizoaffective disorder inadequately treated with quetiapine or risperidone monotherapy. J Clin Psychiatry. 2009;70(10):1348-1357.
Discuss this article at www.facebook.com/CurrentPsychiatry
• Aripiprazole may interact preferentially with distinct conformations of the D2 receptor, leading to a spectrum of pharmacologic effects, including acting as a full agonist, partial agonist, or antagonist.
• Clinical predictors of aripiprazole-associated worsening of psychosis include low baseline level of psychopathology and previous treatment with high-dose antipsychotics.
• Rapid transition from a medication with significant anticholinergic properties to 1 without these properties may result in symptoms of activation, including restlessness, insomnia, and anxiety, which can be mistaken for worsening psychosis.
• Akathisia, a common adverse effect of aripiprazole, may masquerade as treatment-emergent worsening of psychotic symptoms.
Mr. N, age 29, presents to the emergency department at the urging of his family because of poor self-care, bizarre behavior, and disturbed sleep. He first experienced psychiatric symptoms 10 years ago after his mother died. He became dysphoric and paranoid, displaying bizarre responses and behaviors with poor self-care and a gradual functional decline. He has been taking sertraline, 100 mg/d, for 10 years.
Upon arrival at the hospital’s inpatient unit, Mr. N is unkempt, oddly related, and paranoid. His affect is constricted. Mr. N displays thought blocking and possibly is responding to internal stimuli. Sertraline is continued and haloperidol, 1 mg/d, is initiated. For the next 2 weeks, Mr. N continues to be oddly related, irritable, and paranoid, and experiences disturbed sleep and thought blocking. After an episode of impulsive aggression, the treatment team initiates aripiprazole, which is titrated to 30 mg/d for 1 week. Mr. N’s clinical status worsens; he is menacing toward other patients and his thinking is more disorganized, with loose associations and ideas of reference. He requires 4 injections of IM haloperidol, 5 mg, and several visits to the seclusion room over the next week. Haloperidol is increased to 30 mg/d over the next 10 days, then aripiprazole is discontinued because of a putative drug interaction with haloperidol. Following the medication changes Mr. N demonstrates better behavioral control, but still is grossly psychotic. While awaiting transfer to a state hospital, Mr. N receives a trial of olanzapine, 20 to 40 mg/d, for 2 weeks without significant benefit.
Several clinical trials demonstrate a significant reduction in intensity of psychotic symptoms with aripiprazole, which has a unique mechanism of action.1 However, since its FDA approval in 2002, several case reports have described treatment-emergent psychotic symptoms associated with aripiprazole initiation. Over the past 40 years, reports of worsening psychosis associated with antipsychotics have been limited to patients with schizophrenia who were taking high dosages or who had high plasma concentrations, when anticholinergic delirium may have explained increased psychotic symptoms.2-4
How can a drug effectively treat psychotic symptoms and occasionally worsen them? In this article, we discuss the relevant pharmacology and clinical literature on aripiprazole and try to make sense of this apparent paradox.
Unique pharmacologic profile
Antipsychotics have been reported to be either neutral antagonists or inverse agonists at the D2 receptor, based on in vitro data.5 Aripiprazole and its main metabolite, dehydroaripiprazole, originally were described as partial agonists at D2 dopamine receptors.6,7 However, it appears aripiprazole’s pharmacologic action is better explained by the concept of functional selectivity. Aripiprazole may interact preferentially with distinct conformations of the D2 receptor, leading to a spectrum of pharmacologic effects, including acting as a full agonist, partial agonist, or antagonistic.5
Researchers have hypothesized that the pathophysiology of schizophrenia may, in part, be caused by dysfunction of mesocorticolimbic dopaminergic neurons characterized by an enhanced sensitivity of postsynaptic D2 receptors and increased sensitivity to dopaminergic drugs.8,9 In addition, chronic treatment with a D2 receptor antagonist is associated with increases in postsynaptic dopamine receptor density (ie, an increase in receptor reserve).10,11 Upregulation of D2 receptors may explain several features seen in patients chronically treated with antipsychotics, including tardive dyskinesia12 and rapid psychotic relapse after discontinuing an antipsychotic (supersensitivity psychosis).13 Because chronic antipsychotic treatment leads to high postsynaptic receptor reserve, aripiprazole initiation may produce overactivation of D2 receptors, which might worsen a patient’s condition.14 In vitro data15-18 and clinical observations indicate that aripiprazole has intrinsic efficacy at D2 receptors, as do clinical observations, such as:
- its propensity to reduce serum prolactin19
- a decreased likelihood of producing extrapyramidal side effects despite >80% occupancy of D2 receptors6
- case reports documenting aripiprazole-associated mania,20 improvement of risperidone-associated cognitive impairment,21 and pathologic gambling.22
Emergence or worsening of psychotic symptoms or a marginal antipsychotic effect may occur if aripiprazole is indeed a postsynaptic D2 receptor agonist. An individual patient’s outcome likely would depend on his or her sensitivity to psychosis and concurrent or previous exposure to a D2 receptor antagonist. For example, stimulation of postsynaptic D2 receptors may be further augmented if the dosage of the previous antipsychotic was reduced or withdrawn before initiating aripiprazole because additional receptors would be available for interaction with aripiprazole.
Case reports
A literature review revealed 23 reports of treatment-emergent psychosis associated with aripiprazole initiation (Table). The mean age of the patients was 47 (range: 17 to 69) and 57% were men. Most patients (87%) were diagnosed with a schizophrenia-spectrum illness before aripiprazole initiation. Most (57%) had mild, stable, or no psychotic symptoms before aripiprazole initiation. Most were receiving relatively high doses of antipsychotics (average chlorpromazine equivalents [CPZE]: 648 mg/d) before aripiprazole initiation. This medication was either decreased or discontinued in 70% of patients.
Emergence or worsening of psychotic symptoms included agitation, aggressive behavior, and increased psychomotor activity. However, akathisia evaluation was described in only 2 reports: 1 author identified akathisia symptoms, but attributed them to a concomitant antipsychotic (fluphenazine)23 and the other report specifically excluded the possibility of akathisia.24 Two systematic studies have attempted to establish risk factors for aripiprazole-associated worsening psychosis (Box).14,25
In our literature review, the mean final dose of aripiprazole was 21.5 mg/d (range: 2 to 60 mg/d). In the cases describing subsequent treatment, all but 1 patient were switched to another antipsychotic, including 2 whose psychotic symptoms stabilized with continuation of aripiprazole and addition of a second antipsychotic. Interestingly, in the case reported by Adan-Manes et al,26 initial treatment with aripiprazole monotherapy was efficacious, but a subsequent trial of adjunctive aripiprazole resulted in worsening psychosis.
Table
Case reports: Treatment-emergent psychosis associated with aripiprazole
| Study | Age, sex | Diagnosis | Before aripiprazole initiation | Pre-aripiprazole treatment | Aripiprazole dose | Concomitant psychotropic treatment | Subsequent treatment |
|---|---|---|---|---|---|---|---|
| Chiu et al, 2011a | 39, M | Schizophrenia | Psychiatrically stable, tardive dystonia | Clozapine, 300 mg/d | 10 mg/d | Valproic acid, 1,000 mg/d, clonazepam, 2 mg/d, mephenoxalone, 800 mg/d | Clozapine |
| Ekinci et al, 2010b | 17, M | ADHD | Inattention and impulsive aggression | Tapered and discontinued risperidone, 2.5 mg/d | 5 mg/d | Methylphenidate, 54 mg/d | Risperidone, 2 mg/d, methylphenidate, 36 mg/d |
| Selvaraj et al, 2010c | 49, F | Chronic depression | Depressive symptoms, suicidal ideation | None stated | 2 mg/d | Duloxetine, 80 mg/d, clonazepam, 2 mg/d | Duloxetine, 120 mg/d |
| Adan-Manes et al, 2009d | 23, M | Schizophrenia | No psychotic symptoms | Abrupt decrease of amisulpride dose from 800 mg/d to 400 mg/d | 20 mg/d | Biperiden, 4 mg/d | Amisulpride, 800 mg/d |
| Cho et al, 2009e | 45, F | Schizophrenia | Persistent psychotic symptoms, new onset diabetes with acute ketoacidosis | Haloperidol, 20 mg/d, abrupt clozapine discontinuation | 15 mg/d | Valproic acid, nortriptyline | Molindone, 150 mg/d |
| Ahuja et al, 2007f | 35, F | Schizoaffective disorder | Stable before medication change | Tapered amisulpride, 400 mg/d, over 6 weeks | 15 mg/d | None | Amisulpride, 600 mg/d |
| Lea et al, 2007g | 57, M | Schizophrenia | Persistent psychotic symptoms, treatment resistance, recent recovery from NMS | Discontinued ziprasidone, 200 mg/d | 30 mg/d | Lorazepam, 2 mg/d, amantadine, 100 mg, sertraline, 50 mg/d | Clozapine |
| Lea et al, 2007g | 49, M | Schizoaffective disorder | Delusions, verbal aggression, substance abuse, HCV | Decreased quetiapine dose from 800 mg/d to 400 mg/d | 15 mg/d | Divalproex, 1,000 mg/d, fluvoxamine, 200 mg/d, clonazepam, 2 mg/d | Lithium, quetiapine, 500 mg/d, haloperidol, 2 mg/d |
| Lea et al, 2007g | 60, M | Schizophrenia | Delusions, labile mood, aggression | Risperidone, 3 mg/d, interruption of fluphenazine, 75 mg/d | 20 mg/d | Divalproex, 4,500 mg/d, benztropine, 3 mg/d | Not discussed |
| Raja, 2007h | 30, M | Schizoaffective disorder | Negative symptoms, otherwise stable, recent citalopram discontinuation | Discontinued amisulpride, 800 mg/d over 2 weeks | 30 mg/d | Lithium | Amisulpride, 500 mg/d |
| Raja, 2007h | 69, F | Bipolar disorder | History of multiple relapses; presented with tremor, akathisia, weight gain | Discontinued risperidone, 2 mg/d, over 2 weeks | 15 mg/d | Lithium | Risperidone, 4 mg |
| Raja, 2007h | 59, F | Schizophrenia | Negative symptoms, otherwise stable | Reduced risperidone dosage from 5 mg/d to 4 mg/d | 7.5 mg/d | None | Risperidone, 5 mg/d |
| Thone, 2007i | 31, M | Schizophrenia | Confusion, agitation, delusions worsened with aripiprazole dose increase | None | 60 mg/d | None | Aripiprazole dose reduction to 15 mg/d, olanzapine, 10 mg/d |
| Glick et al, 2006j | 55, F | Schizophrenia | Stable before medication change | Tapered and discontinued thioridazine, 600 mg/d, over 3 months | 30 mg/d | None | Chlorpromazine, 200 mg/d, aripiprazole, 30 mg/d |
| Glick et al, 2006j | 52, M | Schizophrenia | Negative symptoms | Decreased olanzapine dose from 30 mg/d to 20 mg/d | 30 mg/d | None | Olanzapine, 30 mg/d |
| Barnas et al, 2005k | 57, F | Schizoaffective disorder | Stable before medication change | Discontinued perphenazine, 8 mg/d | 30 mg/d | None | Quetiapine, 350 mg/d |
| DeQuardo, 2004l | 54, M | Schizophrenia | History of aggression, residual paranoia, severe EPS | Haloperidol, 200 mg/d | 15 mg/d | Benztropine | Haloperidol |
| DeQuardo, 2004l | 51, M | Schizophrenia | History of aggression, persistent psychotic symptoms, treatment resistance | Olanzapine, 60 mg/d | 10 mg/d | None | Olanzapine |
| Ramaswamy et al, 2004m | 43, F | Schizoaffective disorder | Psychiatrically stable, multiple medication changes, including substituting carbamazepine for valproic acid | Discontinued ziprasidone, 160 mg/d, discontinued quetiapine, 400 mg/d, over 2 weeks | 30 mg/d | Propranolol, 30 mg/d, l-thyroxine, .05 mg/d, carbamazepine, 600 mg/d | Not available |
| Ramaswawamy et al, 2004m | 57, F | Schizoaffective disorder | History of multiple hospitalizations, but stable before medication change | Decreased olanzapine dose from 20 mg/d to 15 mg/d | 30 mg/d | Valproic acid, 2,000 mg/d | Ziprasidone |
| Ramaswawamy et al, 2004m | 67, F | Schizophrenia | Remote hospitalizations, recent worsened psychosis | Decreased ziprasidone dose from 200 mg/d to 160 mg/d 2 months previously | 30 mg/d | Carbamazepine, 200 mg/d | Not discussed |
| Ramaswamy et al, 2004m | 46, M | Schizophrenia | Persistent delusions while receiving risperidone, TD | Risperidone, 3 mg/d | 15 mg/d | Valproic acid, 1,500 mg/d | Risperidone, 3 mg/d |
| Reeves et al, 2004n | 50, M | Schizoaffective disorder | Relatively stable with nonthreatening delusions, hallucinations | Quetiapine, 800 mg/d | 30 mg/d | Divalproex, 2,000 mg/d | Olanzapine, 20 mg/d |
| ADHD: attention-deficit/hyperactivity disorder; EPS: extrapyramidal symptoms; HCV: hepatitis C virus; NMS: neuroleptic malignant syndrome; TD: tardive dyskinesia Source: References a. Chiu YH, Chen CH, Lu ML. Worsening psychosis after adding aripiprazole to clozapine. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(1):291-292. b. Ekinci O, Sabuncuoglu O. Psychosis associated with switching from risperidone to aripiprazole in an adolescent on methylphenidate treatment. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(2):648-649. c. Selvaraj V, Ramaswamy S, Sharma A, et al. New-onset psychosis and emergence of suicidal ideation with aripiprazole. Am J Psychiatry. 2010;167(12):1535-1536. d. Adan-Manes J, Garcia-Parajua P. Aripiprazole in combination with other antipsychotic drugs may worsen psychosis. J Clin Pharm Ther. 2009;34(2):245-246. e. Cho DY, Lindenmayer JP. Aripiprazole-induced agitation after clozapine discontinuation: a case report. J Clin Psychiatry. 2009;70(1):141-143. f. Ahuja N, Lloyd AJ. Aripiprazole and worsening of psychosis: a case report. J Clin Psychiatry. 2007;68(5):805-806. g. Lea JW, Stoner SC, Lafollette J. Agitation associated with aripiprazole initiation. Pharmacotherapy. 2007;27(9):1339-1342. h. Raja M. Improvement or worsening of psychotic symptoms after treatment with low doses of aripiprazole. Int J Neuropsychopharmacol. 2007;10(1):107-110. i. Thone J. Worsened agitation and confusion in schizophrenia subsequent to high-dose aripiprazole. J Neuropsychiatry Clin Neurosci. 2007;19(4):481-482. j. Glick ID, Duggal V, Hodulik C. Aripiprazole as a dopamine partial agonist: positive and negative effects. J Clin Psychopharmacol. 2006;26(1):101-103. k. Barnas ME, Hussain N, Petrides G. Treatment-emergent psychosis with aripiprazole. J Clin Psychiatry. 2005;66(10):1339. l. DeQuardo JR. Worsened agitation with aripiprazole: adverse effect of dopamine partial agonism? J Clin Psychiatry. 2004;65(1):132-133. m. Ramaswamy S, Vijay D, William M, et al. Aripiprazole possibly worsens psychosis. Int Clin Psychopharmacol. 2004;19(1):45-48. n. Reeves RR, Mack JE. Worsening schizoaffective disorder with aripiprazole. Am J Psychiatry. 2004;161(7):1308. | |||||||
Takeuchi et al14 aimed to establish predictors of worsening psychosis in a naturalistic setting where patients slowly transitioned to aripiprazole from previous antipsychotic treatment. Patients were required to be on a stable dose of an antipsychotic before participating in the study. Aripiprazole was started at 12 mg/d for 2 weeks with flexible dosing from weeks 2 to 52. Previous antipsychotic therapy was reduced biweekly by 25%. The incidence of worsening psychopathology after aripiprazole initiation was higher in the group of patients who had previously received high-dose antipsychotic therapy (average chlorpromazine equivalents [CPZE]: 727 mg/d) compared with the group on low dosages (average CPZE: 382 mg/d). It is possible that previous high-dose antipsychotic therapy was indicative of more significant baseline psychopathology; however, the worsened group and stabilized group had similar baseline Clinical Global Impressions-Severity scores.
Pae et al25 aimed to find predictors of worsening psychosis with aripiprazole in patients whose previous antipsychotic therapy was immediately discontinued. They found lower baseline disease severity was associated with significant worsening during the first month of aripiprazole treatment.
Other potential explanations
Aripiprazole’s manufacturer reported the incidence of psychosis-related adverse events in an analysis of 9 randomized schizophrenia trials.27 The rates of psychosis-related adverse events ranged from 0.6% to 18%, but there was no apparent relationship to study design or method of transitioning to aripiprazole. Rates of psychosis-related adverse events were similar between aripiprazole and the control group (placebo in 3 studies, another antipsychotic in 2 studies).
Emergence or worsening of psychotic symptoms temporally associated with aripiprazole initiation does not necessarily imply causation. As in Mr. N’s case, it is not always possible to determine whether worsening psychosis is the natural disease course or a treatment effect. In addition, it is not possible to differentiate lack of efficacy from a true propensity for aripiprazole to worsen psychosis.
It also is conceivable discontinuation or dosage reduction of a previous antipsychotic would worsen psychotic symptoms or cause side effects. When significant changes in psychopathology or side effects develop during the transition from 1 antipsychotic to another, it is difficult to determine etiology. Specifically, rapid transition from a medication with significant anticholinergic and antihistaminic properties—such as quetiapine or olanzapine—to 1 without these properties—such as aripiprazole—may result in symptoms of activation, including restlessness, insomnia, and anxiety. Consequently, these symptoms could be mistaken for worsening psychosis.28 Only 1 patient in this series was reported to abruptly discontinue an antipsychotic with significant anticholinergic properties (clozapine) before initiating aripiprazole.24 Studies by Takeuchi et al14 and Pae et al25 did not report the relative baseline use of antipsychotic medication with anticholinergic properties.
In a pooled analysis of treatment-emergent adverse events in 5 randomized clinical trials of patients receiving aripiprazole for acute relapse of schizophrenia, the incidence of akathisia was 10%, although it is not clear if this is a dose-related adverse effect.29 Because akathisia may be confused for worsening psychosis,30 it is possible akathisia was mistakenly identified as worsening psychotic symptoms in Mr. N’s case, as well as several reports from our literature review.
Covert akathisia is unlikely to explain worsening psychopathology observed in all patients in our literature review because confusion of akathisia and worsening psychosis is not a widespread phenomenon. In a post hoc analysis of pooled safety data from aripiprazole trials, Kane et al31 did not find a correlation between presence of akathisia and aripiprazole efficacy as measured by the Positive and Negative Syndrome Scale (PANSS) total, PANSS positive, PANSS negative, Clinical Global Impressions-Severity, Clinical Global Impressions-Improvement, and percentage of responders. Pae et al25 also noted there was no correlation between scores on the Barnes Akathisia Rating Scale and worsening psychopathology in patients switched to aripiprazole.
An antagonist always is an antagonist and clinicians have appreciated this concept since the days of chlorpromazine. The activity of aripiprazole, however, is on a pharmacologic continuum between a neutral antagonist and full agonist and currently there is no way to precisely determine the level of D2 receptor agonist action in a patient.
Although it is interesting to speculate that aripiprazole’s D2 receptor agonist action may contribute to worsening psychosis,32-34 there are other plausible explanations to consider. Rapid transition from a drug with significant anticholinergic properties and aripiprazole-associated akathisia may contribute to worsening psychopathology in patients starting aripiprazole. Because covert side effects may be incorrectly identified as psychotic agitation, we cannot exclude this as a possible etiologic factor in Mr. N’s case as well as the cases in our literature review.
Related Resource
- Abilify [package insert]. Princeton, NJ: Bristol-Myers Squibb; 2011.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Benztropine • Cogentin
- Biperiden • Akineton
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Clonazepam • Klonopin
- Clozapine • Clozaril
- Divalproex • Depakote
- Duloxetine • Cymbalta
- Fluphenazine • Permitil, Prolixin
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Nortriptyline • Aventyl, Pamelor
- Methylphenidate • Concerta
- Molindone • Moban
- Olanzapine • Zyprexa
- Perphenazine • Trilafon
- Propranolol • Inderal
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Thyroxine • Synthroid
- Valproic acid • Depakene
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
• Aripiprazole may interact preferentially with distinct conformations of the D2 receptor, leading to a spectrum of pharmacologic effects, including acting as a full agonist, partial agonist, or antagonist.
• Clinical predictors of aripiprazole-associated worsening of psychosis include low baseline level of psychopathology and previous treatment with high-dose antipsychotics.
• Rapid transition from a medication with significant anticholinergic properties to 1 without these properties may result in symptoms of activation, including restlessness, insomnia, and anxiety, which can be mistaken for worsening psychosis.
• Akathisia, a common adverse effect of aripiprazole, may masquerade as treatment-emergent worsening of psychotic symptoms.
Mr. N, age 29, presents to the emergency department at the urging of his family because of poor self-care, bizarre behavior, and disturbed sleep. He first experienced psychiatric symptoms 10 years ago after his mother died. He became dysphoric and paranoid, displaying bizarre responses and behaviors with poor self-care and a gradual functional decline. He has been taking sertraline, 100 mg/d, for 10 years.
Upon arrival at the hospital’s inpatient unit, Mr. N is unkempt, oddly related, and paranoid. His affect is constricted. Mr. N displays thought blocking and possibly is responding to internal stimuli. Sertraline is continued and haloperidol, 1 mg/d, is initiated. For the next 2 weeks, Mr. N continues to be oddly related, irritable, and paranoid, and experiences disturbed sleep and thought blocking. After an episode of impulsive aggression, the treatment team initiates aripiprazole, which is titrated to 30 mg/d for 1 week. Mr. N’s clinical status worsens; he is menacing toward other patients and his thinking is more disorganized, with loose associations and ideas of reference. He requires 4 injections of IM haloperidol, 5 mg, and several visits to the seclusion room over the next week. Haloperidol is increased to 30 mg/d over the next 10 days, then aripiprazole is discontinued because of a putative drug interaction with haloperidol. Following the medication changes Mr. N demonstrates better behavioral control, but still is grossly psychotic. While awaiting transfer to a state hospital, Mr. N receives a trial of olanzapine, 20 to 40 mg/d, for 2 weeks without significant benefit.
Several clinical trials demonstrate a significant reduction in intensity of psychotic symptoms with aripiprazole, which has a unique mechanism of action.1 However, since its FDA approval in 2002, several case reports have described treatment-emergent psychotic symptoms associated with aripiprazole initiation. Over the past 40 years, reports of worsening psychosis associated with antipsychotics have been limited to patients with schizophrenia who were taking high dosages or who had high plasma concentrations, when anticholinergic delirium may have explained increased psychotic symptoms.2-4
How can a drug effectively treat psychotic symptoms and occasionally worsen them? In this article, we discuss the relevant pharmacology and clinical literature on aripiprazole and try to make sense of this apparent paradox.
Unique pharmacologic profile
Antipsychotics have been reported to be either neutral antagonists or inverse agonists at the D2 receptor, based on in vitro data.5 Aripiprazole and its main metabolite, dehydroaripiprazole, originally were described as partial agonists at D2 dopamine receptors.6,7 However, it appears aripiprazole’s pharmacologic action is better explained by the concept of functional selectivity. Aripiprazole may interact preferentially with distinct conformations of the D2 receptor, leading to a spectrum of pharmacologic effects, including acting as a full agonist, partial agonist, or antagonistic.5
Researchers have hypothesized that the pathophysiology of schizophrenia may, in part, be caused by dysfunction of mesocorticolimbic dopaminergic neurons characterized by an enhanced sensitivity of postsynaptic D2 receptors and increased sensitivity to dopaminergic drugs.8,9 In addition, chronic treatment with a D2 receptor antagonist is associated with increases in postsynaptic dopamine receptor density (ie, an increase in receptor reserve).10,11 Upregulation of D2 receptors may explain several features seen in patients chronically treated with antipsychotics, including tardive dyskinesia12 and rapid psychotic relapse after discontinuing an antipsychotic (supersensitivity psychosis).13 Because chronic antipsychotic treatment leads to high postsynaptic receptor reserve, aripiprazole initiation may produce overactivation of D2 receptors, which might worsen a patient’s condition.14 In vitro data15-18 and clinical observations indicate that aripiprazole has intrinsic efficacy at D2 receptors, as do clinical observations, such as:
- its propensity to reduce serum prolactin19
- a decreased likelihood of producing extrapyramidal side effects despite >80% occupancy of D2 receptors6
- case reports documenting aripiprazole-associated mania,20 improvement of risperidone-associated cognitive impairment,21 and pathologic gambling.22
Emergence or worsening of psychotic symptoms or a marginal antipsychotic effect may occur if aripiprazole is indeed a postsynaptic D2 receptor agonist. An individual patient’s outcome likely would depend on his or her sensitivity to psychosis and concurrent or previous exposure to a D2 receptor antagonist. For example, stimulation of postsynaptic D2 receptors may be further augmented if the dosage of the previous antipsychotic was reduced or withdrawn before initiating aripiprazole because additional receptors would be available for interaction with aripiprazole.
Case reports
A literature review revealed 23 reports of treatment-emergent psychosis associated with aripiprazole initiation (Table). The mean age of the patients was 47 (range: 17 to 69) and 57% were men. Most patients (87%) were diagnosed with a schizophrenia-spectrum illness before aripiprazole initiation. Most (57%) had mild, stable, or no psychotic symptoms before aripiprazole initiation. Most were receiving relatively high doses of antipsychotics (average chlorpromazine equivalents [CPZE]: 648 mg/d) before aripiprazole initiation. This medication was either decreased or discontinued in 70% of patients.
Emergence or worsening of psychotic symptoms included agitation, aggressive behavior, and increased psychomotor activity. However, akathisia evaluation was described in only 2 reports: 1 author identified akathisia symptoms, but attributed them to a concomitant antipsychotic (fluphenazine)23 and the other report specifically excluded the possibility of akathisia.24 Two systematic studies have attempted to establish risk factors for aripiprazole-associated worsening psychosis (Box).14,25
In our literature review, the mean final dose of aripiprazole was 21.5 mg/d (range: 2 to 60 mg/d). In the cases describing subsequent treatment, all but 1 patient were switched to another antipsychotic, including 2 whose psychotic symptoms stabilized with continuation of aripiprazole and addition of a second antipsychotic. Interestingly, in the case reported by Adan-Manes et al,26 initial treatment with aripiprazole monotherapy was efficacious, but a subsequent trial of adjunctive aripiprazole resulted in worsening psychosis.
Table
Case reports: Treatment-emergent psychosis associated with aripiprazole
| Study | Age, sex | Diagnosis | Before aripiprazole initiation | Pre-aripiprazole treatment | Aripiprazole dose | Concomitant psychotropic treatment | Subsequent treatment |
|---|---|---|---|---|---|---|---|
| Chiu et al, 2011a | 39, M | Schizophrenia | Psychiatrically stable, tardive dystonia | Clozapine, 300 mg/d | 10 mg/d | Valproic acid, 1,000 mg/d, clonazepam, 2 mg/d, mephenoxalone, 800 mg/d | Clozapine |
| Ekinci et al, 2010b | 17, M | ADHD | Inattention and impulsive aggression | Tapered and discontinued risperidone, 2.5 mg/d | 5 mg/d | Methylphenidate, 54 mg/d | Risperidone, 2 mg/d, methylphenidate, 36 mg/d |
| Selvaraj et al, 2010c | 49, F | Chronic depression | Depressive symptoms, suicidal ideation | None stated | 2 mg/d | Duloxetine, 80 mg/d, clonazepam, 2 mg/d | Duloxetine, 120 mg/d |
| Adan-Manes et al, 2009d | 23, M | Schizophrenia | No psychotic symptoms | Abrupt decrease of amisulpride dose from 800 mg/d to 400 mg/d | 20 mg/d | Biperiden, 4 mg/d | Amisulpride, 800 mg/d |
| Cho et al, 2009e | 45, F | Schizophrenia | Persistent psychotic symptoms, new onset diabetes with acute ketoacidosis | Haloperidol, 20 mg/d, abrupt clozapine discontinuation | 15 mg/d | Valproic acid, nortriptyline | Molindone, 150 mg/d |
| Ahuja et al, 2007f | 35, F | Schizoaffective disorder | Stable before medication change | Tapered amisulpride, 400 mg/d, over 6 weeks | 15 mg/d | None | Amisulpride, 600 mg/d |
| Lea et al, 2007g | 57, M | Schizophrenia | Persistent psychotic symptoms, treatment resistance, recent recovery from NMS | Discontinued ziprasidone, 200 mg/d | 30 mg/d | Lorazepam, 2 mg/d, amantadine, 100 mg, sertraline, 50 mg/d | Clozapine |
| Lea et al, 2007g | 49, M | Schizoaffective disorder | Delusions, verbal aggression, substance abuse, HCV | Decreased quetiapine dose from 800 mg/d to 400 mg/d | 15 mg/d | Divalproex, 1,000 mg/d, fluvoxamine, 200 mg/d, clonazepam, 2 mg/d | Lithium, quetiapine, 500 mg/d, haloperidol, 2 mg/d |
| Lea et al, 2007g | 60, M | Schizophrenia | Delusions, labile mood, aggression | Risperidone, 3 mg/d, interruption of fluphenazine, 75 mg/d | 20 mg/d | Divalproex, 4,500 mg/d, benztropine, 3 mg/d | Not discussed |
| Raja, 2007h | 30, M | Schizoaffective disorder | Negative symptoms, otherwise stable, recent citalopram discontinuation | Discontinued amisulpride, 800 mg/d over 2 weeks | 30 mg/d | Lithium | Amisulpride, 500 mg/d |
| Raja, 2007h | 69, F | Bipolar disorder | History of multiple relapses; presented with tremor, akathisia, weight gain | Discontinued risperidone, 2 mg/d, over 2 weeks | 15 mg/d | Lithium | Risperidone, 4 mg |
| Raja, 2007h | 59, F | Schizophrenia | Negative symptoms, otherwise stable | Reduced risperidone dosage from 5 mg/d to 4 mg/d | 7.5 mg/d | None | Risperidone, 5 mg/d |
| Thone, 2007i | 31, M | Schizophrenia | Confusion, agitation, delusions worsened with aripiprazole dose increase | None | 60 mg/d | None | Aripiprazole dose reduction to 15 mg/d, olanzapine, 10 mg/d |
| Glick et al, 2006j | 55, F | Schizophrenia | Stable before medication change | Tapered and discontinued thioridazine, 600 mg/d, over 3 months | 30 mg/d | None | Chlorpromazine, 200 mg/d, aripiprazole, 30 mg/d |
| Glick et al, 2006j | 52, M | Schizophrenia | Negative symptoms | Decreased olanzapine dose from 30 mg/d to 20 mg/d | 30 mg/d | None | Olanzapine, 30 mg/d |
| Barnas et al, 2005k | 57, F | Schizoaffective disorder | Stable before medication change | Discontinued perphenazine, 8 mg/d | 30 mg/d | None | Quetiapine, 350 mg/d |
| DeQuardo, 2004l | 54, M | Schizophrenia | History of aggression, residual paranoia, severe EPS | Haloperidol, 200 mg/d | 15 mg/d | Benztropine | Haloperidol |
| DeQuardo, 2004l | 51, M | Schizophrenia | History of aggression, persistent psychotic symptoms, treatment resistance | Olanzapine, 60 mg/d | 10 mg/d | None | Olanzapine |
| Ramaswamy et al, 2004m | 43, F | Schizoaffective disorder | Psychiatrically stable, multiple medication changes, including substituting carbamazepine for valproic acid | Discontinued ziprasidone, 160 mg/d, discontinued quetiapine, 400 mg/d, over 2 weeks | 30 mg/d | Propranolol, 30 mg/d, l-thyroxine, .05 mg/d, carbamazepine, 600 mg/d | Not available |
| Ramaswawamy et al, 2004m | 57, F | Schizoaffective disorder | History of multiple hospitalizations, but stable before medication change | Decreased olanzapine dose from 20 mg/d to 15 mg/d | 30 mg/d | Valproic acid, 2,000 mg/d | Ziprasidone |
| Ramaswawamy et al, 2004m | 67, F | Schizophrenia | Remote hospitalizations, recent worsened psychosis | Decreased ziprasidone dose from 200 mg/d to 160 mg/d 2 months previously | 30 mg/d | Carbamazepine, 200 mg/d | Not discussed |
| Ramaswamy et al, 2004m | 46, M | Schizophrenia | Persistent delusions while receiving risperidone, TD | Risperidone, 3 mg/d | 15 mg/d | Valproic acid, 1,500 mg/d | Risperidone, 3 mg/d |
| Reeves et al, 2004n | 50, M | Schizoaffective disorder | Relatively stable with nonthreatening delusions, hallucinations | Quetiapine, 800 mg/d | 30 mg/d | Divalproex, 2,000 mg/d | Olanzapine, 20 mg/d |
| ADHD: attention-deficit/hyperactivity disorder; EPS: extrapyramidal symptoms; HCV: hepatitis C virus; NMS: neuroleptic malignant syndrome; TD: tardive dyskinesia Source: References a. Chiu YH, Chen CH, Lu ML. Worsening psychosis after adding aripiprazole to clozapine. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(1):291-292. b. Ekinci O, Sabuncuoglu O. Psychosis associated with switching from risperidone to aripiprazole in an adolescent on methylphenidate treatment. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(2):648-649. c. Selvaraj V, Ramaswamy S, Sharma A, et al. New-onset psychosis and emergence of suicidal ideation with aripiprazole. Am J Psychiatry. 2010;167(12):1535-1536. d. Adan-Manes J, Garcia-Parajua P. Aripiprazole in combination with other antipsychotic drugs may worsen psychosis. J Clin Pharm Ther. 2009;34(2):245-246. e. Cho DY, Lindenmayer JP. Aripiprazole-induced agitation after clozapine discontinuation: a case report. J Clin Psychiatry. 2009;70(1):141-143. f. Ahuja N, Lloyd AJ. Aripiprazole and worsening of psychosis: a case report. J Clin Psychiatry. 2007;68(5):805-806. g. Lea JW, Stoner SC, Lafollette J. Agitation associated with aripiprazole initiation. Pharmacotherapy. 2007;27(9):1339-1342. h. Raja M. Improvement or worsening of psychotic symptoms after treatment with low doses of aripiprazole. Int J Neuropsychopharmacol. 2007;10(1):107-110. i. Thone J. Worsened agitation and confusion in schizophrenia subsequent to high-dose aripiprazole. J Neuropsychiatry Clin Neurosci. 2007;19(4):481-482. j. Glick ID, Duggal V, Hodulik C. Aripiprazole as a dopamine partial agonist: positive and negative effects. J Clin Psychopharmacol. 2006;26(1):101-103. k. Barnas ME, Hussain N, Petrides G. Treatment-emergent psychosis with aripiprazole. J Clin Psychiatry. 2005;66(10):1339. l. DeQuardo JR. Worsened agitation with aripiprazole: adverse effect of dopamine partial agonism? J Clin Psychiatry. 2004;65(1):132-133. m. Ramaswamy S, Vijay D, William M, et al. Aripiprazole possibly worsens psychosis. Int Clin Psychopharmacol. 2004;19(1):45-48. n. Reeves RR, Mack JE. Worsening schizoaffective disorder with aripiprazole. Am J Psychiatry. 2004;161(7):1308. | |||||||
Takeuchi et al14 aimed to establish predictors of worsening psychosis in a naturalistic setting where patients slowly transitioned to aripiprazole from previous antipsychotic treatment. Patients were required to be on a stable dose of an antipsychotic before participating in the study. Aripiprazole was started at 12 mg/d for 2 weeks with flexible dosing from weeks 2 to 52. Previous antipsychotic therapy was reduced biweekly by 25%. The incidence of worsening psychopathology after aripiprazole initiation was higher in the group of patients who had previously received high-dose antipsychotic therapy (average chlorpromazine equivalents [CPZE]: 727 mg/d) compared with the group on low dosages (average CPZE: 382 mg/d). It is possible that previous high-dose antipsychotic therapy was indicative of more significant baseline psychopathology; however, the worsened group and stabilized group had similar baseline Clinical Global Impressions-Severity scores.
Pae et al25 aimed to find predictors of worsening psychosis with aripiprazole in patients whose previous antipsychotic therapy was immediately discontinued. They found lower baseline disease severity was associated with significant worsening during the first month of aripiprazole treatment.
Other potential explanations
Aripiprazole’s manufacturer reported the incidence of psychosis-related adverse events in an analysis of 9 randomized schizophrenia trials.27 The rates of psychosis-related adverse events ranged from 0.6% to 18%, but there was no apparent relationship to study design or method of transitioning to aripiprazole. Rates of psychosis-related adverse events were similar between aripiprazole and the control group (placebo in 3 studies, another antipsychotic in 2 studies).
Emergence or worsening of psychotic symptoms temporally associated with aripiprazole initiation does not necessarily imply causation. As in Mr. N’s case, it is not always possible to determine whether worsening psychosis is the natural disease course or a treatment effect. In addition, it is not possible to differentiate lack of efficacy from a true propensity for aripiprazole to worsen psychosis.
It also is conceivable discontinuation or dosage reduction of a previous antipsychotic would worsen psychotic symptoms or cause side effects. When significant changes in psychopathology or side effects develop during the transition from 1 antipsychotic to another, it is difficult to determine etiology. Specifically, rapid transition from a medication with significant anticholinergic and antihistaminic properties—such as quetiapine or olanzapine—to 1 without these properties—such as aripiprazole—may result in symptoms of activation, including restlessness, insomnia, and anxiety. Consequently, these symptoms could be mistaken for worsening psychosis.28 Only 1 patient in this series was reported to abruptly discontinue an antipsychotic with significant anticholinergic properties (clozapine) before initiating aripiprazole.24 Studies by Takeuchi et al14 and Pae et al25 did not report the relative baseline use of antipsychotic medication with anticholinergic properties.
In a pooled analysis of treatment-emergent adverse events in 5 randomized clinical trials of patients receiving aripiprazole for acute relapse of schizophrenia, the incidence of akathisia was 10%, although it is not clear if this is a dose-related adverse effect.29 Because akathisia may be confused for worsening psychosis,30 it is possible akathisia was mistakenly identified as worsening psychotic symptoms in Mr. N’s case, as well as several reports from our literature review.
Covert akathisia is unlikely to explain worsening psychopathology observed in all patients in our literature review because confusion of akathisia and worsening psychosis is not a widespread phenomenon. In a post hoc analysis of pooled safety data from aripiprazole trials, Kane et al31 did not find a correlation between presence of akathisia and aripiprazole efficacy as measured by the Positive and Negative Syndrome Scale (PANSS) total, PANSS positive, PANSS negative, Clinical Global Impressions-Severity, Clinical Global Impressions-Improvement, and percentage of responders. Pae et al25 also noted there was no correlation between scores on the Barnes Akathisia Rating Scale and worsening psychopathology in patients switched to aripiprazole.
An antagonist always is an antagonist and clinicians have appreciated this concept since the days of chlorpromazine. The activity of aripiprazole, however, is on a pharmacologic continuum between a neutral antagonist and full agonist and currently there is no way to precisely determine the level of D2 receptor agonist action in a patient.
Although it is interesting to speculate that aripiprazole’s D2 receptor agonist action may contribute to worsening psychosis,32-34 there are other plausible explanations to consider. Rapid transition from a drug with significant anticholinergic properties and aripiprazole-associated akathisia may contribute to worsening psychopathology in patients starting aripiprazole. Because covert side effects may be incorrectly identified as psychotic agitation, we cannot exclude this as a possible etiologic factor in Mr. N’s case as well as the cases in our literature review.
Related Resource
- Abilify [package insert]. Princeton, NJ: Bristol-Myers Squibb; 2011.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Benztropine • Cogentin
- Biperiden • Akineton
- Carbamazepine • Tegretol
- Chlorpromazine • Thorazine
- Clonazepam • Klonopin
- Clozapine • Clozaril
- Divalproex • Depakote
- Duloxetine • Cymbalta
- Fluphenazine • Permitil, Prolixin
- Fluvoxamine • Luvox
- Haloperidol • Haldol
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Nortriptyline • Aventyl, Pamelor
- Methylphenidate • Concerta
- Molindone • Moban
- Olanzapine • Zyprexa
- Perphenazine • Trilafon
- Propranolol • Inderal
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Thioridazine • Mellaril
- Thyroxine • Synthroid
- Valproic acid • Depakene
- Ziprasidone • Geodon
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Citrome L. A review of aripiprazole in the treatment of patients with schizophrenia or bipolar I disorder. Neuropsychiatr Dis Treat. 2006;2(4):427-443.
2. Chong SA, Tan CH, Lee HS. Worsening of psychosis with clozapine and selective serotonin reuptake inhibitor combination: two case reports. J Clin Psychopharmacol. 1997;17(1):68-69.
3. Bowers MB Jr, Swigar ME. Psychotic patients who become worse on neuroleptics. J Clin Psychopharmacol. 1988;8(6):417-421.
4. Tornatore FL, Lee D, Sramek JJ. Psychotic exacerbation with haloperidol. Drug Intell Clin Pharm. 1981;15(3):209-213.
5. Beaulieu JM, Gainetdinov RR. The physiology signaling, and pharmacology of dopamine receptors. Pharmacol Rev. 2011;63(1):182-217.
6. Grunder G, Carlsson A, Wong DF. Mechanism of new antipsychotic medications: occupancy is not just antagonism. Arch Gen Psychiatry. 2003;60(10):974-977.
7. Wood MD, Scott C, Clarke K, et al. Aripiprazole and its human metabolite are partial agonists at the human dopamine D2 receptor, but the rodent metabolite displays antagonist properties. Eur J Pharmacol. 2006;546(1-3):88-94.
8. Seeman P, Weinshenker D, Quirion R, et al. Dopamine supersensitivity correlates with D2High states, implying many paths to psychosis. Proc Natl Acad Sci U S A. 2005;102(9):3513-3518.
9. Seeman P, Ko F, Jack E, et al. Consistent with dopamine supersensitivity, RGS9 expression is diminished in the amphetamine-treated animal model of schizophrenia and in postmortem schizophrenia brain. Synapse. 2007;61(5):303-309.
10. Burt DR, Creese I, Snyder SH. Antischizophrenic drugs: chronic treatment elevates dopamine receptor binding in brain. Science. 1977;196(4287):326-328.
11. Silvestri S, Seeman MV, Negrete JC, et al. Increased dopamine D2 receptor binding after long-term treatment with antipsychotics in humans: a clinical PET study. Psychopharmacology (Berl). 2000;152(2):174-180.
12. Sayers AC, Bürki HR, Ruch W, et al. Neuroleptic-induced hypersensitivity of striatal dopamine receptors in the rat as a model of tardive dyskinesias. Effects of clozapine, haloperidol, loxapine and chlorpromazine. Psychopharmacologia. 1975;41(2):97-104.
13. Moncrieff J. Does antipsychotic withdrawal provoke psychosis? Review of the literature on rapid onset psychosis (supersensitivity psychosis) and withdrawal-related relapse. Acta Psychiatr Scand. 2006;114(1):3-13.
14. Takeuchi H, Uchida H, Suzuki T, et al. Predictors of clinical worsening after a switch to aripiprazole in patients with schizophrenia: a 1-year naturalistic follow-up study. J Clin Psychopharmacol. 2009;29(4):394-395.
15. Shapiro DA, Renock S, Arrington E, et al. Aripiprazole, a novel atypical antipsychotic drug with a unique and robust pharmacology. Neuropsychopharmacology. 2003;28(8):1400-1411.
16. Urban JD, Vargas GA, von Zastrow M, et al. Aripiprazole has functionally selective actions at dopamine D2 receptor-mediated signaling pathways. Neuropsychopharmacology. 2007;32(1):67-77.
17. Klewe IV, Nielsen SM, Tarpo L, et al. Recruitment of beta-arrestin2 to the dopamine D2 receptor: Insights into anti-psychotic and anti-parkinsonian drug receptor signaling. Neuropharmacology. 2008;54(8):1215-1222.
18. Masri B, Salahpour A, Didriksen M, et al. Antagonism of dopamine D2 receptor/beta-arrestin 2 interaction is a common property of clinically effective antipsychotics. Proc Natl Acad Sci U S A. 2008;105(36):13656-13661.
19. Shim JC, Shin JG, Kelly DL, et al. Adjunctive treatment with a dopamine partial agonist, aripiprazole, for antipsychotic-induced hyperprolactinemia: a placebo-controlled trial. Am J Psychiatry. 2007;164(9):1404-1410.
20. Padala PR, Wengel SP, Petty F. Manic episode during treatment with aripiprazole. Am J Psychiatry. 2007;164(1):172-173.
21. Hu CH, Pai N, Huang XF, et al. Potential control of risperidone-related cognitive deficits by adjunctive aripiprazole treatment. J Clin Psychopharmacol. 2011;31(1):135-136;author reply 136–137.
22. Cohen J, Magalon D, Boyer L, et al. Aripiprazole-induced pathological gambling: a report of 3 cases. Curr Drug Saf. 2011;6(1):51-53.
23. Lea JW, Stoner SC, Lafollette J. Agitation associated with aripiprazole initiation. Pharmacotherapy. 2007;27(9):1339-1342.
24. Cho DY, Lindenmayer JP. Aripiprazole-induced agitation after clozapine discontinuation: a case report. J Clin Psychiatry. 2009;70(1):141-143.
25. Pae CU, Chiesa A, Mandelli L, et al. Predictors of early worsening after switch to aripiprazole: a randomized, controlled, open-label study. Clin Drug Investig. 2010;30(3):187-193.
26. Adan-Manes J, Garcia-Parajua P. Aripiprazole in combination with other antipsychotic drugs may worsen psychosis. J Clin Pharm Ther. 2009;34(2):245-246.
27. Cognata-Smith C, Baker RA, Pikalov A, et al. Analysis of nine aripiprazole trials to evaluate strategies for switching patients with schizophrenia to aripiprazole. Paper presented at: 162nd Annual Meeting American Psychiatric Association; May 16-21, 2009; San Francisco, CA.
28. Lieberman J. Cholinergic rebound in neuroleptic withdrawal syndromes. Psychosomatics. 1981;22(3):253-254.
29. Marder SR, McQuade RD, Stock E, et al. Aripiprazole in the treatment of schizophrenia: Safety and tolerability in short-term, placebo-controlled trials. Schizophr Res. 2003;61(2-3):123-136.
30. Kane JM, Fleischhacker WW, Hansen L, et al. Akathisia: an updated review focusing on second-generation antipsychotics. J Clin Psychiatry. 2009;70(5):627-643.
31. Kane JM, Barnes TR, Correll CU, et al. Evaluation of akathisia in patients with schizophrenia, schizoaffective disorder, or bipolar I disorder: A post hoc analysis of pooled data from short- and long-term aripiprazole trials. J Psychopharmacol. 2010;24(7):1019-1029.
32. Fleischhacker WW, McQuade RD, Marcus RN, et al. A double-blind, randomized comparative study of aripiprazole and olanzapine in patients with schizophrenia. Biol Psychiatry. 2009;65(6):510-517.
33. Kane JM, Osuntokun O, Kryzhanovskaya LA, et al. A 28-week, randomized, double-blind study of olanzapine versus aripiprazole in the treatment of schizophrenia. J Clin Psychiatry. 2009;70(4):572-581.
34. Kane JM, Correll CU, Goff DC, et al. A multicenter, randomized, double-blind, placebo-controlled, 16-week study of adjunctive aripiprazole for schizophrenia or schizoaffective disorder inadequately treated with quetiapine or risperidone monotherapy. J Clin Psychiatry. 2009;70(10):1348-1357.
1. Citrome L. A review of aripiprazole in the treatment of patients with schizophrenia or bipolar I disorder. Neuropsychiatr Dis Treat. 2006;2(4):427-443.
2. Chong SA, Tan CH, Lee HS. Worsening of psychosis with clozapine and selective serotonin reuptake inhibitor combination: two case reports. J Clin Psychopharmacol. 1997;17(1):68-69.
3. Bowers MB Jr, Swigar ME. Psychotic patients who become worse on neuroleptics. J Clin Psychopharmacol. 1988;8(6):417-421.
4. Tornatore FL, Lee D, Sramek JJ. Psychotic exacerbation with haloperidol. Drug Intell Clin Pharm. 1981;15(3):209-213.
5. Beaulieu JM, Gainetdinov RR. The physiology signaling, and pharmacology of dopamine receptors. Pharmacol Rev. 2011;63(1):182-217.
6. Grunder G, Carlsson A, Wong DF. Mechanism of new antipsychotic medications: occupancy is not just antagonism. Arch Gen Psychiatry. 2003;60(10):974-977.
7. Wood MD, Scott C, Clarke K, et al. Aripiprazole and its human metabolite are partial agonists at the human dopamine D2 receptor, but the rodent metabolite displays antagonist properties. Eur J Pharmacol. 2006;546(1-3):88-94.
8. Seeman P, Weinshenker D, Quirion R, et al. Dopamine supersensitivity correlates with D2High states, implying many paths to psychosis. Proc Natl Acad Sci U S A. 2005;102(9):3513-3518.
9. Seeman P, Ko F, Jack E, et al. Consistent with dopamine supersensitivity, RGS9 expression is diminished in the amphetamine-treated animal model of schizophrenia and in postmortem schizophrenia brain. Synapse. 2007;61(5):303-309.
10. Burt DR, Creese I, Snyder SH. Antischizophrenic drugs: chronic treatment elevates dopamine receptor binding in brain. Science. 1977;196(4287):326-328.
11. Silvestri S, Seeman MV, Negrete JC, et al. Increased dopamine D2 receptor binding after long-term treatment with antipsychotics in humans: a clinical PET study. Psychopharmacology (Berl). 2000;152(2):174-180.
12. Sayers AC, Bürki HR, Ruch W, et al. Neuroleptic-induced hypersensitivity of striatal dopamine receptors in the rat as a model of tardive dyskinesias. Effects of clozapine, haloperidol, loxapine and chlorpromazine. Psychopharmacologia. 1975;41(2):97-104.
13. Moncrieff J. Does antipsychotic withdrawal provoke psychosis? Review of the literature on rapid onset psychosis (supersensitivity psychosis) and withdrawal-related relapse. Acta Psychiatr Scand. 2006;114(1):3-13.
14. Takeuchi H, Uchida H, Suzuki T, et al. Predictors of clinical worsening after a switch to aripiprazole in patients with schizophrenia: a 1-year naturalistic follow-up study. J Clin Psychopharmacol. 2009;29(4):394-395.
15. Shapiro DA, Renock S, Arrington E, et al. Aripiprazole, a novel atypical antipsychotic drug with a unique and robust pharmacology. Neuropsychopharmacology. 2003;28(8):1400-1411.
16. Urban JD, Vargas GA, von Zastrow M, et al. Aripiprazole has functionally selective actions at dopamine D2 receptor-mediated signaling pathways. Neuropsychopharmacology. 2007;32(1):67-77.
17. Klewe IV, Nielsen SM, Tarpo L, et al. Recruitment of beta-arrestin2 to the dopamine D2 receptor: Insights into anti-psychotic and anti-parkinsonian drug receptor signaling. Neuropharmacology. 2008;54(8):1215-1222.
18. Masri B, Salahpour A, Didriksen M, et al. Antagonism of dopamine D2 receptor/beta-arrestin 2 interaction is a common property of clinically effective antipsychotics. Proc Natl Acad Sci U S A. 2008;105(36):13656-13661.
19. Shim JC, Shin JG, Kelly DL, et al. Adjunctive treatment with a dopamine partial agonist, aripiprazole, for antipsychotic-induced hyperprolactinemia: a placebo-controlled trial. Am J Psychiatry. 2007;164(9):1404-1410.
20. Padala PR, Wengel SP, Petty F. Manic episode during treatment with aripiprazole. Am J Psychiatry. 2007;164(1):172-173.
21. Hu CH, Pai N, Huang XF, et al. Potential control of risperidone-related cognitive deficits by adjunctive aripiprazole treatment. J Clin Psychopharmacol. 2011;31(1):135-136;author reply 136–137.
22. Cohen J, Magalon D, Boyer L, et al. Aripiprazole-induced pathological gambling: a report of 3 cases. Curr Drug Saf. 2011;6(1):51-53.
23. Lea JW, Stoner SC, Lafollette J. Agitation associated with aripiprazole initiation. Pharmacotherapy. 2007;27(9):1339-1342.
24. Cho DY, Lindenmayer JP. Aripiprazole-induced agitation after clozapine discontinuation: a case report. J Clin Psychiatry. 2009;70(1):141-143.
25. Pae CU, Chiesa A, Mandelli L, et al. Predictors of early worsening after switch to aripiprazole: a randomized, controlled, open-label study. Clin Drug Investig. 2010;30(3):187-193.
26. Adan-Manes J, Garcia-Parajua P. Aripiprazole in combination with other antipsychotic drugs may worsen psychosis. J Clin Pharm Ther. 2009;34(2):245-246.
27. Cognata-Smith C, Baker RA, Pikalov A, et al. Analysis of nine aripiprazole trials to evaluate strategies for switching patients with schizophrenia to aripiprazole. Paper presented at: 162nd Annual Meeting American Psychiatric Association; May 16-21, 2009; San Francisco, CA.
28. Lieberman J. Cholinergic rebound in neuroleptic withdrawal syndromes. Psychosomatics. 1981;22(3):253-254.
29. Marder SR, McQuade RD, Stock E, et al. Aripiprazole in the treatment of schizophrenia: Safety and tolerability in short-term, placebo-controlled trials. Schizophr Res. 2003;61(2-3):123-136.
30. Kane JM, Fleischhacker WW, Hansen L, et al. Akathisia: an updated review focusing on second-generation antipsychotics. J Clin Psychiatry. 2009;70(5):627-643.
31. Kane JM, Barnes TR, Correll CU, et al. Evaluation of akathisia in patients with schizophrenia, schizoaffective disorder, or bipolar I disorder: A post hoc analysis of pooled data from short- and long-term aripiprazole trials. J Psychopharmacol. 2010;24(7):1019-1029.
32. Fleischhacker WW, McQuade RD, Marcus RN, et al. A double-blind, randomized comparative study of aripiprazole and olanzapine in patients with schizophrenia. Biol Psychiatry. 2009;65(6):510-517.
33. Kane JM, Osuntokun O, Kryzhanovskaya LA, et al. A 28-week, randomized, double-blind study of olanzapine versus aripiprazole in the treatment of schizophrenia. J Clin Psychiatry. 2009;70(4):572-581.
34. Kane JM, Correll CU, Goff DC, et al. A multicenter, randomized, double-blind, placebo-controlled, 16-week study of adjunctive aripiprazole for schizophrenia or schizoaffective disorder inadequately treated with quetiapine or risperidone monotherapy. J Clin Psychiatry. 2009;70(10):1348-1357.
UPDATE ON PELVIC FLOOR DYSFUNCTION
Vulvar Pain Syndromes 3-Part Series
- Making the correct diagnosis
(September 2011) - A bounty of treatments-but not all of them are proven
(October 2011) - Provoked vestibulodynia
(Coming in November 2011)
Chronic pelvic pain: 11 critical questions about causes and care
Fred M. Howard, MD (August 2009)
Vague symptoms. Unexpected flares. Inconsistent manifestations. These characteristics can make diagnosis and treatment of chronic pelvic pain frustrating for both patient and physician. Most patients undergo myriad tests and studies to uncover the source of their pain—but a targeted pelvic exam may be all that is necessary to identify a prevalent but commonly overlooked cause of pelvic pain. Levator myalgia, myofascial pelvic pain syndrome, and pelvic floor spasm are all terms that describe a condition that may affect as many as 78% of women who are given a diagnosis of chronic pelvic pain.1 This syndrome may be represented by an array of symptoms, including pelvic pressure, dyspareunia, rectal discomfort, and irritative urinary symptoms such as spasms, frequency, and urgency. It is characterized by the presence of tight, band-like pelvic muscles that reproduce the patient’s pain when palpated.2
Diagnosis of this syndrome often surprises the patient. Although the concept of a muscle spasm is not foreign, the location is unexpected. Patients and physicians alike may forget that there is a large complex of muscles that completely lines the pelvic girdle. To complicate matters, the patient often associates the onset of her symptoms with an acute event such as a “bad” urinary tract infection or pelvic or vaginal surgery, which may divert attention from the musculature. Although a muscle spasm may be the cause of the patient’s pain, it’s important to realize that an underlying process may have triggered the original spasm. To provide effective treatment of pain, therefore, you must identify the fundamental cause, assuming that it is reversible, rather than focus exclusively on symptoms.
Although there are many therapeutic options for levator myalgia, an appraisal of the extensive literature on these medications is beyond the scope of this article. Rather, we will review alternative treatment modalities and summarize the results of five trials that explored physical therapy, trigger-point or chemodenervation injection, and neuromodulation (TABLE).
Weighing the nonpharmaceutical options for treatment
of myofascial pelvic pain
| Treatment | Pros | Cons |
|---|---|---|
| Physical therapy | Minimally invasive Moderate long-term success | Requires highly specialized therapist |
| Trigger-point injection | Minimally invasive Performed in clinic Immediate short-term success | Optimal injectable agent is unknown Botulinum toxin A lacks FDA approval for this indication Limited information on adverse events and long-term efficacy |
| Percutaneous tibial nerve stimulation | Minimally invasive Performed in clinic | Requires numerous office visits for treatment Lacks FDA approval for this indication Limited information on long-term efficacy |
| Sacral neuromodulation | Moderately invasive Permanent implant | Requires implantation in operating room Lacks FDA approval for this indication Limited information on long-term efficacy |
Pelvic myofascial therapy offers relief—but qualified therapists may be scarce
FitzGerald MP, Anderson RU, Potts J, et al; Urological Pelvic Pain Collaborative Research Network. Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. J Urology. 2009;182(2):570–580.
Physical therapy of the pelvic floor—otherwise known as pelvic myofascial therapy—requires a therapist who is highly trained and specialized in this technique. It is more invasive than other forms of rehabilitative therapy because of the need to perform transvaginal maneuvers (FIGURE 1).
This pilot study by the Urological Pelvic Pain Collaborative Research Network evaluated the ability of patients to adhere to pelvic myofascial therapy, the response of their pain to therapy, and adverse events associated with manual therapy. It found that patients were willing to undergo the therapy, despite the invasive nature of the maneuvers, because it was significantly effective.
Details of the study
Patients (both men and women) were randomized to myofascial physical therapy or global therapeutic massage. Myofascial therapy consisted of internal or vaginal manipulation of the trigger-point muscle bundles and tissues of the pelvic floor. It also focused on muscles of the hip girdle and abdomen. The comparison group underwent traditional Western full-body massage. In both groups, treatment lasted 1 hour every week, and participants agreed to 10 full treatments.
Patients were eligible for the study if they experienced pelvic pain, urinary frequency, or bladder discomfort in the previous 6 months. In addition, an examiner must have been able to elicit tenderness upon palpation of the pelvic floor during examination. Patients were excluded if they showed signs of urinary tract infection or dysmenorrhea.
A total of 47 patients were randomized—24 to global massage and 23 to myofascial physical therapy. Overall, the myofascial group experienced a significantly higher rate of improvement in the global response at 12 weeks than did patients in the global-massage group (57% vs 21%; P=.03). Patients were willing to engage in myofascial pelvic therapy, and adverse events were minor.
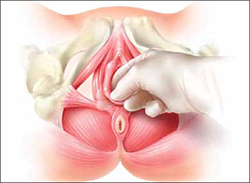
FIGURE 1 Transvaginal myofascial therapy
Physical therapy of the pelvic floor is more invasive than other forms of rehabilitative therapy because of the need to perform transvaginal maneuvers.
Need for specialized training may limit number of therapists
The randomized controlled study design renders these findings fairly reliable. Therapists were unmasked and aware of the treatment arms but were trained to make the different therapy sessions appear as similar as possible.
Although investigators were enthusiastic about their initial findings, additional studies are needed to validate the results. Moreover, these findings may be difficult to generalize because women who volunteer to participate in such a study may differ from the general population.
Nevertheless, patients who suffer from chronic pelvic pain may take heart that there is a nonpharmaceutical alternative to manage their symptoms, although availability is likely limited in many areas. Given the nature of the physical therapy required for this particular location of myofascial pain, specialized training is necessary for therapists. Despite motivated patients and well-informed providers, it may be difficult to find specialized therapists within local vicinities. Referrals to centers where this type of therapy is offered may be necessary.
Pelvic myofascial therapy is an effective and acceptable intervention for the treatment of levator myalgia.
The ideal agent for trigger-point injections remains a mystery
Langford CF, Udvari Nagy S, Ghoniem G M. Levator ani trigger point injections: An underutilized treatment for chronic pelvic pain. Neurourol Urodyn. 2007;26(1):59–62.
Abbott JA, Jarvis SK, Lyons SD, Thomson A, Vancaille TG. Botulinum toxin type A for chronic pain and pelvic floor spasm in women: a randomized controlled trial. Obstet Gynecol. 2006;108(4):915–923.
Trigger points are discrete, tender areas within a ridge of contracted muscle. These points may cause focal pain or referred pain upon irritation of the muscle.2 Trigger-point injection therapy aims to anesthetize or relax these points by infiltrating the muscle with medications.
These two studies evaluated the value of trigger-point injections in the treatment of pelvic myofascial pain; they found that the injections provide relief, although the mechanism of action and the ideal agent remain to be determined.
Langford et al: Details of the study
In this prospective study, 18 women who had pelvic pain of at least 6 months’ duration and confirmed trigger points on examination underwent transvaginal injection of a solution of bupivacaine, lidocaine, and triamcinolone. They were assessed by questionnaire at baseline and 3 months after injection. Assessment included a visual analog scale for pain severity. Investigators defined success as a decrease in pain of 50% or more and global-satisfaction and global-cure visual scores of 60% or higher.
Thirteen of the 18 women (72.2%) improved after their first injection, with six women reporting a complete absence of pain. Overall, women reported significant decreases in pain and increases in the rates of satisfaction and cure, meeting the definition of success at 3 months after the injection.
Among the theories proposed to explain the mechanism of action of trigger-point injections are:
- disruption of reflex arcs within skeletal muscle
- release of endorphins
- mechanical changes in abnormally contracted muscle fibers.
This last theory highlights one of the limitations of this study—lack of a placebo arm. Could it be possible that the injection of any fluid produces the same effect?
This study was not designed to investigate the causal relationship between the injection of a particular solution and pain relief, but it does highlight the need for studies to clarify the mechanism of action, including use of a placebo. It also prompts questions about the duration of effect after a single injection.
Goal of chemodenervation is blocking of muscle activity
Botulinum toxin type A (Botox) blocks the release of acetylcholine from presynaptic neurons. The release of acetylcholine stimulates muscle contractions; therefore, blockage of its release reduces muscle activity. This type of chemodenervation has found widespread use, and botulinum toxin A now has approval from the Food and Drug Administration (FDA) for treatment of chronic migraine, limb spasticity, cervical dystonia, strabismus, hyperhidrosis, and facial cosmesis.3 Although it is not approved for pelvic floor levator spasm, its success in treating other myotonic disorders suggests that its application may be relevant.
Abbott et al: Details of the study
Abbott and colleagues performed a double-blind, randomized, controlled trial to compare injection of botulinum toxin A with injection of saline. They measured changes in the pain scale, quality of life, and vaginal pressure.
Women were eligible for the study if they had subjectively reported pelvic pain of more than 2 years’ duration and objective evidence of trigger points (on examination) and elevated vaginal resting pressure (by vaginal manometry). Neither the clinical research staff nor the patient knew the contents of the injections, but all women received a total of four—two at sites in the puborectalis muscle and two in the pubococcygeus muscle.
After periodic assessment by questionnaire and examination through 6 months after injection, no differences were found in the pain score or resting vaginal pressure between the group of women who received botulinum toxin A and the group who received placebo. However, each group experienced a significant reduction in pain and vaginal pressure, compared with baseline. And both groups reported improved quality of life, compared with baseline. Neither group reported voiding dysfunction.
These two studies support the use of trigger-point injection into pelvic floor muscles to reduce pelvic myofascial pain. The findings of Abbott and colleagues, in particular, suggest that the substance that is injected may not be as important as the actual needling of the muscle. Larger studies and comparisons between placebo, botulinum toxin A, and anesthetic solutions are needed to elucidate the therapeutic benefit of these particular medications.
Neuromodulation shows promise as treatment for pelvic myofascial pain
van Balken MR, Vandoninck V, Messelink, BJ, et al. Percutaneous tibial nerve stimulation as neuromodulative treatment of chronic pelvic pain. Eur Urol. 2003;43(2):158–163.
Zabihi N, Mourtzinos A, Maher MG, Raz S, Rodriguez LV. Short-term results of bilateral S2-S4 sacral neuromodulation for the treatment of refractory interstitial cystitis, painful bladder syndrome, and chronic pelvic pain. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(4):553–557.
Neuromodulation is the science of using electrical impulses to alter neuronal activities. The exact mechanisms of action are unclear, but the technology has been utilized to control symptoms of overactive bladder and urinary retention caused by poor relaxation of the urethral and pelvic floor muscles. While studying the effects of sacral nerve root neuromodulation on the bladder, investigators noted improvements in other symptoms, such as pelvic pain.
Neuromodulation of the sacral nerve roots may be achieved by direct conduction of electrical impulses from a lead implanted in the sacrum (sacral neuromodulation) or by the retrograde conduction of these impulses through the posterior tibial nerve (percutaneous tibial nerve stimulation, or PTNS) (FIGURE 2). The tibial nerve arises from sacral nerves L5 to S3 and is one of the larger branches of the sciatic nerve.
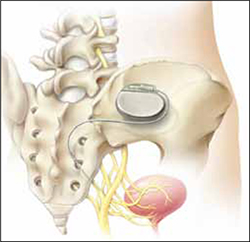
FIGURE 2 InterStim therapy
Stimulation of the sacral nerve has been used successfully to manage overactive bladder and urinary retention and may prove useful in the treatment of pelvic myofascial pain.
Van Balken et al: Details of the study
In this prospective observational study, 33 patients (both male and female) who had chronic pelvic pain by history and examination were treated with weekly, 30-minute outpatient sessions of PTNS for 12 weeks. Participants were asked to provide baseline pain scores and keep a diary of their pain. Quality-of-life questionnaires were also administered at baseline and at 12 weeks.
Investigators considered both subjective and objective success in their outcomes. If a patient elected to continue therapy, he or she was classified as a subjective success. Objective success required a decrease of at least 50% in the pain score. At the end of 12 weeks, although 33 patients (42%) wanted to continue therapy, only seven (21%) met the definition for objective success. Of those seven, six elected to continue therapy.
This study sheds light on a treatment modality that has not been studied adequately for the indication of pelvic pain but that may be promising in patients who have levator myalgia. Limitations of this study include the lack of a placebo arm, short-term outcome, and lack of localization of pain. Furthermore, although PTNS has FDA approval for treatment of urinary urgency, frequency, and urge incontinence, it is not approved for the treatment of pelvic pain. These preliminary findings demonstrate potential but, as with any new indication, long-term comparative studies are needed.
Zabihi et al: Details of the study
Patients in this retrospective study had a diagnosis of interstitial cystitis or chronic pelvic pain. Pelvic myofascial pain and trigger points were not required for eligibility. Thirty patients (21 women and nine men) had temporary placement of a lead containing four small electrodes along the S2 to S4 sacral nerve roots on both sides of the sacrum. They were then followed for a trial period of 2 to 4 weeks. To qualify for the final stage of the study, in which the leads were connected internally to a generator implanted in the buttocks, patients had to report improvement of at least 50% in their symptoms. If their improvement did not meet that threshold, the leads were removed.
Twenty-three patients (77%) met the criteria for permanent implantation. Of these patients, 42% reported improvement of more than 50% at 6 postoperative months. Quality-of-life scores also improved significantly.
Sacral neuromodulation is not FDA-approved for the treatment of chronic pelvic pain; further studies are needed before it can be recommended for this indication.
Neither of these studies required objective evidence of myofascial pain for inclusion. Therefore, although the benefits they demonstrated may be theorized to extend to the relief of myofascial pain, this fact cannot be corroborated.
We want to hear from you! Tell us what you think.
1. Bassaly R, Tidwell N, Bertolino S, Hoyte L, Downes K, Hart S. Myofascial pain and pelvic floor dysfunction in patients with interstitial cystitis. Int Urogynecol J. 2011;22(4):413-418.
2. Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65(4):653-660.
3. Allergan, Inc. Medication Guide: BOTOX. US Food and Drug Administration Web site. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM176360.pdf. Published October 2010. Accessed August 30, 2011.
Vulvar Pain Syndromes 3-Part Series
- Making the correct diagnosis
(September 2011) - A bounty of treatments-but not all of them are proven
(October 2011) - Provoked vestibulodynia
(Coming in November 2011)
Chronic pelvic pain: 11 critical questions about causes and care
Fred M. Howard, MD (August 2009)
Vague symptoms. Unexpected flares. Inconsistent manifestations. These characteristics can make diagnosis and treatment of chronic pelvic pain frustrating for both patient and physician. Most patients undergo myriad tests and studies to uncover the source of their pain—but a targeted pelvic exam may be all that is necessary to identify a prevalent but commonly overlooked cause of pelvic pain. Levator myalgia, myofascial pelvic pain syndrome, and pelvic floor spasm are all terms that describe a condition that may affect as many as 78% of women who are given a diagnosis of chronic pelvic pain.1 This syndrome may be represented by an array of symptoms, including pelvic pressure, dyspareunia, rectal discomfort, and irritative urinary symptoms such as spasms, frequency, and urgency. It is characterized by the presence of tight, band-like pelvic muscles that reproduce the patient’s pain when palpated.2
Diagnosis of this syndrome often surprises the patient. Although the concept of a muscle spasm is not foreign, the location is unexpected. Patients and physicians alike may forget that there is a large complex of muscles that completely lines the pelvic girdle. To complicate matters, the patient often associates the onset of her symptoms with an acute event such as a “bad” urinary tract infection or pelvic or vaginal surgery, which may divert attention from the musculature. Although a muscle spasm may be the cause of the patient’s pain, it’s important to realize that an underlying process may have triggered the original spasm. To provide effective treatment of pain, therefore, you must identify the fundamental cause, assuming that it is reversible, rather than focus exclusively on symptoms.
Although there are many therapeutic options for levator myalgia, an appraisal of the extensive literature on these medications is beyond the scope of this article. Rather, we will review alternative treatment modalities and summarize the results of five trials that explored physical therapy, trigger-point or chemodenervation injection, and neuromodulation (TABLE).
Weighing the nonpharmaceutical options for treatment
of myofascial pelvic pain
| Treatment | Pros | Cons |
|---|---|---|
| Physical therapy | Minimally invasive Moderate long-term success | Requires highly specialized therapist |
| Trigger-point injection | Minimally invasive Performed in clinic Immediate short-term success | Optimal injectable agent is unknown Botulinum toxin A lacks FDA approval for this indication Limited information on adverse events and long-term efficacy |
| Percutaneous tibial nerve stimulation | Minimally invasive Performed in clinic | Requires numerous office visits for treatment Lacks FDA approval for this indication Limited information on long-term efficacy |
| Sacral neuromodulation | Moderately invasive Permanent implant | Requires implantation in operating room Lacks FDA approval for this indication Limited information on long-term efficacy |
Pelvic myofascial therapy offers relief—but qualified therapists may be scarce
FitzGerald MP, Anderson RU, Potts J, et al; Urological Pelvic Pain Collaborative Research Network. Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. J Urology. 2009;182(2):570–580.
Physical therapy of the pelvic floor—otherwise known as pelvic myofascial therapy—requires a therapist who is highly trained and specialized in this technique. It is more invasive than other forms of rehabilitative therapy because of the need to perform transvaginal maneuvers (FIGURE 1).
This pilot study by the Urological Pelvic Pain Collaborative Research Network evaluated the ability of patients to adhere to pelvic myofascial therapy, the response of their pain to therapy, and adverse events associated with manual therapy. It found that patients were willing to undergo the therapy, despite the invasive nature of the maneuvers, because it was significantly effective.
Details of the study
Patients (both men and women) were randomized to myofascial physical therapy or global therapeutic massage. Myofascial therapy consisted of internal or vaginal manipulation of the trigger-point muscle bundles and tissues of the pelvic floor. It also focused on muscles of the hip girdle and abdomen. The comparison group underwent traditional Western full-body massage. In both groups, treatment lasted 1 hour every week, and participants agreed to 10 full treatments.
Patients were eligible for the study if they experienced pelvic pain, urinary frequency, or bladder discomfort in the previous 6 months. In addition, an examiner must have been able to elicit tenderness upon palpation of the pelvic floor during examination. Patients were excluded if they showed signs of urinary tract infection or dysmenorrhea.
A total of 47 patients were randomized—24 to global massage and 23 to myofascial physical therapy. Overall, the myofascial group experienced a significantly higher rate of improvement in the global response at 12 weeks than did patients in the global-massage group (57% vs 21%; P=.03). Patients were willing to engage in myofascial pelvic therapy, and adverse events were minor.
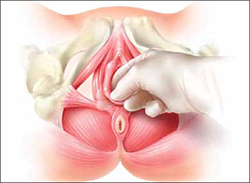
FIGURE 1 Transvaginal myofascial therapy
Physical therapy of the pelvic floor is more invasive than other forms of rehabilitative therapy because of the need to perform transvaginal maneuvers.
Need for specialized training may limit number of therapists
The randomized controlled study design renders these findings fairly reliable. Therapists were unmasked and aware of the treatment arms but were trained to make the different therapy sessions appear as similar as possible.
Although investigators were enthusiastic about their initial findings, additional studies are needed to validate the results. Moreover, these findings may be difficult to generalize because women who volunteer to participate in such a study may differ from the general population.
Nevertheless, patients who suffer from chronic pelvic pain may take heart that there is a nonpharmaceutical alternative to manage their symptoms, although availability is likely limited in many areas. Given the nature of the physical therapy required for this particular location of myofascial pain, specialized training is necessary for therapists. Despite motivated patients and well-informed providers, it may be difficult to find specialized therapists within local vicinities. Referrals to centers where this type of therapy is offered may be necessary.
Pelvic myofascial therapy is an effective and acceptable intervention for the treatment of levator myalgia.
The ideal agent for trigger-point injections remains a mystery
Langford CF, Udvari Nagy S, Ghoniem G M. Levator ani trigger point injections: An underutilized treatment for chronic pelvic pain. Neurourol Urodyn. 2007;26(1):59–62.
Abbott JA, Jarvis SK, Lyons SD, Thomson A, Vancaille TG. Botulinum toxin type A for chronic pain and pelvic floor spasm in women: a randomized controlled trial. Obstet Gynecol. 2006;108(4):915–923.
Trigger points are discrete, tender areas within a ridge of contracted muscle. These points may cause focal pain or referred pain upon irritation of the muscle.2 Trigger-point injection therapy aims to anesthetize or relax these points by infiltrating the muscle with medications.
These two studies evaluated the value of trigger-point injections in the treatment of pelvic myofascial pain; they found that the injections provide relief, although the mechanism of action and the ideal agent remain to be determined.
Langford et al: Details of the study
In this prospective study, 18 women who had pelvic pain of at least 6 months’ duration and confirmed trigger points on examination underwent transvaginal injection of a solution of bupivacaine, lidocaine, and triamcinolone. They were assessed by questionnaire at baseline and 3 months after injection. Assessment included a visual analog scale for pain severity. Investigators defined success as a decrease in pain of 50% or more and global-satisfaction and global-cure visual scores of 60% or higher.
Thirteen of the 18 women (72.2%) improved after their first injection, with six women reporting a complete absence of pain. Overall, women reported significant decreases in pain and increases in the rates of satisfaction and cure, meeting the definition of success at 3 months after the injection.
Among the theories proposed to explain the mechanism of action of trigger-point injections are:
- disruption of reflex arcs within skeletal muscle
- release of endorphins
- mechanical changes in abnormally contracted muscle fibers.
This last theory highlights one of the limitations of this study—lack of a placebo arm. Could it be possible that the injection of any fluid produces the same effect?
This study was not designed to investigate the causal relationship between the injection of a particular solution and pain relief, but it does highlight the need for studies to clarify the mechanism of action, including use of a placebo. It also prompts questions about the duration of effect after a single injection.
Goal of chemodenervation is blocking of muscle activity
Botulinum toxin type A (Botox) blocks the release of acetylcholine from presynaptic neurons. The release of acetylcholine stimulates muscle contractions; therefore, blockage of its release reduces muscle activity. This type of chemodenervation has found widespread use, and botulinum toxin A now has approval from the Food and Drug Administration (FDA) for treatment of chronic migraine, limb spasticity, cervical dystonia, strabismus, hyperhidrosis, and facial cosmesis.3 Although it is not approved for pelvic floor levator spasm, its success in treating other myotonic disorders suggests that its application may be relevant.
Abbott et al: Details of the study
Abbott and colleagues performed a double-blind, randomized, controlled trial to compare injection of botulinum toxin A with injection of saline. They measured changes in the pain scale, quality of life, and vaginal pressure.
Women were eligible for the study if they had subjectively reported pelvic pain of more than 2 years’ duration and objective evidence of trigger points (on examination) and elevated vaginal resting pressure (by vaginal manometry). Neither the clinical research staff nor the patient knew the contents of the injections, but all women received a total of four—two at sites in the puborectalis muscle and two in the pubococcygeus muscle.
After periodic assessment by questionnaire and examination through 6 months after injection, no differences were found in the pain score or resting vaginal pressure between the group of women who received botulinum toxin A and the group who received placebo. However, each group experienced a significant reduction in pain and vaginal pressure, compared with baseline. And both groups reported improved quality of life, compared with baseline. Neither group reported voiding dysfunction.
These two studies support the use of trigger-point injection into pelvic floor muscles to reduce pelvic myofascial pain. The findings of Abbott and colleagues, in particular, suggest that the substance that is injected may not be as important as the actual needling of the muscle. Larger studies and comparisons between placebo, botulinum toxin A, and anesthetic solutions are needed to elucidate the therapeutic benefit of these particular medications.
Neuromodulation shows promise as treatment for pelvic myofascial pain
van Balken MR, Vandoninck V, Messelink, BJ, et al. Percutaneous tibial nerve stimulation as neuromodulative treatment of chronic pelvic pain. Eur Urol. 2003;43(2):158–163.
Zabihi N, Mourtzinos A, Maher MG, Raz S, Rodriguez LV. Short-term results of bilateral S2-S4 sacral neuromodulation for the treatment of refractory interstitial cystitis, painful bladder syndrome, and chronic pelvic pain. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(4):553–557.
Neuromodulation is the science of using electrical impulses to alter neuronal activities. The exact mechanisms of action are unclear, but the technology has been utilized to control symptoms of overactive bladder and urinary retention caused by poor relaxation of the urethral and pelvic floor muscles. While studying the effects of sacral nerve root neuromodulation on the bladder, investigators noted improvements in other symptoms, such as pelvic pain.
Neuromodulation of the sacral nerve roots may be achieved by direct conduction of electrical impulses from a lead implanted in the sacrum (sacral neuromodulation) or by the retrograde conduction of these impulses through the posterior tibial nerve (percutaneous tibial nerve stimulation, or PTNS) (FIGURE 2). The tibial nerve arises from sacral nerves L5 to S3 and is one of the larger branches of the sciatic nerve.
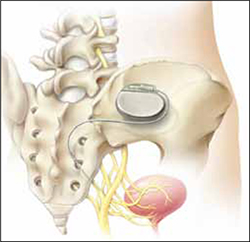
FIGURE 2 InterStim therapy
Stimulation of the sacral nerve has been used successfully to manage overactive bladder and urinary retention and may prove useful in the treatment of pelvic myofascial pain.
Van Balken et al: Details of the study
In this prospective observational study, 33 patients (both male and female) who had chronic pelvic pain by history and examination were treated with weekly, 30-minute outpatient sessions of PTNS for 12 weeks. Participants were asked to provide baseline pain scores and keep a diary of their pain. Quality-of-life questionnaires were also administered at baseline and at 12 weeks.
Investigators considered both subjective and objective success in their outcomes. If a patient elected to continue therapy, he or she was classified as a subjective success. Objective success required a decrease of at least 50% in the pain score. At the end of 12 weeks, although 33 patients (42%) wanted to continue therapy, only seven (21%) met the definition for objective success. Of those seven, six elected to continue therapy.
This study sheds light on a treatment modality that has not been studied adequately for the indication of pelvic pain but that may be promising in patients who have levator myalgia. Limitations of this study include the lack of a placebo arm, short-term outcome, and lack of localization of pain. Furthermore, although PTNS has FDA approval for treatment of urinary urgency, frequency, and urge incontinence, it is not approved for the treatment of pelvic pain. These preliminary findings demonstrate potential but, as with any new indication, long-term comparative studies are needed.
Zabihi et al: Details of the study
Patients in this retrospective study had a diagnosis of interstitial cystitis or chronic pelvic pain. Pelvic myofascial pain and trigger points were not required for eligibility. Thirty patients (21 women and nine men) had temporary placement of a lead containing four small electrodes along the S2 to S4 sacral nerve roots on both sides of the sacrum. They were then followed for a trial period of 2 to 4 weeks. To qualify for the final stage of the study, in which the leads were connected internally to a generator implanted in the buttocks, patients had to report improvement of at least 50% in their symptoms. If their improvement did not meet that threshold, the leads were removed.
Twenty-three patients (77%) met the criteria for permanent implantation. Of these patients, 42% reported improvement of more than 50% at 6 postoperative months. Quality-of-life scores also improved significantly.
Sacral neuromodulation is not FDA-approved for the treatment of chronic pelvic pain; further studies are needed before it can be recommended for this indication.
Neither of these studies required objective evidence of myofascial pain for inclusion. Therefore, although the benefits they demonstrated may be theorized to extend to the relief of myofascial pain, this fact cannot be corroborated.
We want to hear from you! Tell us what you think.
Vulvar Pain Syndromes 3-Part Series
- Making the correct diagnosis
(September 2011) - A bounty of treatments-but not all of them are proven
(October 2011) - Provoked vestibulodynia
(Coming in November 2011)
Chronic pelvic pain: 11 critical questions about causes and care
Fred M. Howard, MD (August 2009)
Vague symptoms. Unexpected flares. Inconsistent manifestations. These characteristics can make diagnosis and treatment of chronic pelvic pain frustrating for both patient and physician. Most patients undergo myriad tests and studies to uncover the source of their pain—but a targeted pelvic exam may be all that is necessary to identify a prevalent but commonly overlooked cause of pelvic pain. Levator myalgia, myofascial pelvic pain syndrome, and pelvic floor spasm are all terms that describe a condition that may affect as many as 78% of women who are given a diagnosis of chronic pelvic pain.1 This syndrome may be represented by an array of symptoms, including pelvic pressure, dyspareunia, rectal discomfort, and irritative urinary symptoms such as spasms, frequency, and urgency. It is characterized by the presence of tight, band-like pelvic muscles that reproduce the patient’s pain when palpated.2
Diagnosis of this syndrome often surprises the patient. Although the concept of a muscle spasm is not foreign, the location is unexpected. Patients and physicians alike may forget that there is a large complex of muscles that completely lines the pelvic girdle. To complicate matters, the patient often associates the onset of her symptoms with an acute event such as a “bad” urinary tract infection or pelvic or vaginal surgery, which may divert attention from the musculature. Although a muscle spasm may be the cause of the patient’s pain, it’s important to realize that an underlying process may have triggered the original spasm. To provide effective treatment of pain, therefore, you must identify the fundamental cause, assuming that it is reversible, rather than focus exclusively on symptoms.
Although there are many therapeutic options for levator myalgia, an appraisal of the extensive literature on these medications is beyond the scope of this article. Rather, we will review alternative treatment modalities and summarize the results of five trials that explored physical therapy, trigger-point or chemodenervation injection, and neuromodulation (TABLE).
Weighing the nonpharmaceutical options for treatment
of myofascial pelvic pain
| Treatment | Pros | Cons |
|---|---|---|
| Physical therapy | Minimally invasive Moderate long-term success | Requires highly specialized therapist |
| Trigger-point injection | Minimally invasive Performed in clinic Immediate short-term success | Optimal injectable agent is unknown Botulinum toxin A lacks FDA approval for this indication Limited information on adverse events and long-term efficacy |
| Percutaneous tibial nerve stimulation | Minimally invasive Performed in clinic | Requires numerous office visits for treatment Lacks FDA approval for this indication Limited information on long-term efficacy |
| Sacral neuromodulation | Moderately invasive Permanent implant | Requires implantation in operating room Lacks FDA approval for this indication Limited information on long-term efficacy |
Pelvic myofascial therapy offers relief—but qualified therapists may be scarce
FitzGerald MP, Anderson RU, Potts J, et al; Urological Pelvic Pain Collaborative Research Network. Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. J Urology. 2009;182(2):570–580.
Physical therapy of the pelvic floor—otherwise known as pelvic myofascial therapy—requires a therapist who is highly trained and specialized in this technique. It is more invasive than other forms of rehabilitative therapy because of the need to perform transvaginal maneuvers (FIGURE 1).
This pilot study by the Urological Pelvic Pain Collaborative Research Network evaluated the ability of patients to adhere to pelvic myofascial therapy, the response of their pain to therapy, and adverse events associated with manual therapy. It found that patients were willing to undergo the therapy, despite the invasive nature of the maneuvers, because it was significantly effective.
Details of the study
Patients (both men and women) were randomized to myofascial physical therapy or global therapeutic massage. Myofascial therapy consisted of internal or vaginal manipulation of the trigger-point muscle bundles and tissues of the pelvic floor. It also focused on muscles of the hip girdle and abdomen. The comparison group underwent traditional Western full-body massage. In both groups, treatment lasted 1 hour every week, and participants agreed to 10 full treatments.
Patients were eligible for the study if they experienced pelvic pain, urinary frequency, or bladder discomfort in the previous 6 months. In addition, an examiner must have been able to elicit tenderness upon palpation of the pelvic floor during examination. Patients were excluded if they showed signs of urinary tract infection or dysmenorrhea.
A total of 47 patients were randomized—24 to global massage and 23 to myofascial physical therapy. Overall, the myofascial group experienced a significantly higher rate of improvement in the global response at 12 weeks than did patients in the global-massage group (57% vs 21%; P=.03). Patients were willing to engage in myofascial pelvic therapy, and adverse events were minor.
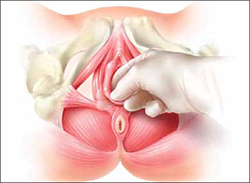
FIGURE 1 Transvaginal myofascial therapy
Physical therapy of the pelvic floor is more invasive than other forms of rehabilitative therapy because of the need to perform transvaginal maneuvers.
Need for specialized training may limit number of therapists
The randomized controlled study design renders these findings fairly reliable. Therapists were unmasked and aware of the treatment arms but were trained to make the different therapy sessions appear as similar as possible.
Although investigators were enthusiastic about their initial findings, additional studies are needed to validate the results. Moreover, these findings may be difficult to generalize because women who volunteer to participate in such a study may differ from the general population.
Nevertheless, patients who suffer from chronic pelvic pain may take heart that there is a nonpharmaceutical alternative to manage their symptoms, although availability is likely limited in many areas. Given the nature of the physical therapy required for this particular location of myofascial pain, specialized training is necessary for therapists. Despite motivated patients and well-informed providers, it may be difficult to find specialized therapists within local vicinities. Referrals to centers where this type of therapy is offered may be necessary.
Pelvic myofascial therapy is an effective and acceptable intervention for the treatment of levator myalgia.
The ideal agent for trigger-point injections remains a mystery
Langford CF, Udvari Nagy S, Ghoniem G M. Levator ani trigger point injections: An underutilized treatment for chronic pelvic pain. Neurourol Urodyn. 2007;26(1):59–62.
Abbott JA, Jarvis SK, Lyons SD, Thomson A, Vancaille TG. Botulinum toxin type A for chronic pain and pelvic floor spasm in women: a randomized controlled trial. Obstet Gynecol. 2006;108(4):915–923.
Trigger points are discrete, tender areas within a ridge of contracted muscle. These points may cause focal pain or referred pain upon irritation of the muscle.2 Trigger-point injection therapy aims to anesthetize or relax these points by infiltrating the muscle with medications.
These two studies evaluated the value of trigger-point injections in the treatment of pelvic myofascial pain; they found that the injections provide relief, although the mechanism of action and the ideal agent remain to be determined.
Langford et al: Details of the study
In this prospective study, 18 women who had pelvic pain of at least 6 months’ duration and confirmed trigger points on examination underwent transvaginal injection of a solution of bupivacaine, lidocaine, and triamcinolone. They were assessed by questionnaire at baseline and 3 months after injection. Assessment included a visual analog scale for pain severity. Investigators defined success as a decrease in pain of 50% or more and global-satisfaction and global-cure visual scores of 60% or higher.
Thirteen of the 18 women (72.2%) improved after their first injection, with six women reporting a complete absence of pain. Overall, women reported significant decreases in pain and increases in the rates of satisfaction and cure, meeting the definition of success at 3 months after the injection.
Among the theories proposed to explain the mechanism of action of trigger-point injections are:
- disruption of reflex arcs within skeletal muscle
- release of endorphins
- mechanical changes in abnormally contracted muscle fibers.
This last theory highlights one of the limitations of this study—lack of a placebo arm. Could it be possible that the injection of any fluid produces the same effect?
This study was not designed to investigate the causal relationship between the injection of a particular solution and pain relief, but it does highlight the need for studies to clarify the mechanism of action, including use of a placebo. It also prompts questions about the duration of effect after a single injection.
Goal of chemodenervation is blocking of muscle activity
Botulinum toxin type A (Botox) blocks the release of acetylcholine from presynaptic neurons. The release of acetylcholine stimulates muscle contractions; therefore, blockage of its release reduces muscle activity. This type of chemodenervation has found widespread use, and botulinum toxin A now has approval from the Food and Drug Administration (FDA) for treatment of chronic migraine, limb spasticity, cervical dystonia, strabismus, hyperhidrosis, and facial cosmesis.3 Although it is not approved for pelvic floor levator spasm, its success in treating other myotonic disorders suggests that its application may be relevant.
Abbott et al: Details of the study
Abbott and colleagues performed a double-blind, randomized, controlled trial to compare injection of botulinum toxin A with injection of saline. They measured changes in the pain scale, quality of life, and vaginal pressure.
Women were eligible for the study if they had subjectively reported pelvic pain of more than 2 years’ duration and objective evidence of trigger points (on examination) and elevated vaginal resting pressure (by vaginal manometry). Neither the clinical research staff nor the patient knew the contents of the injections, but all women received a total of four—two at sites in the puborectalis muscle and two in the pubococcygeus muscle.
After periodic assessment by questionnaire and examination through 6 months after injection, no differences were found in the pain score or resting vaginal pressure between the group of women who received botulinum toxin A and the group who received placebo. However, each group experienced a significant reduction in pain and vaginal pressure, compared with baseline. And both groups reported improved quality of life, compared with baseline. Neither group reported voiding dysfunction.
These two studies support the use of trigger-point injection into pelvic floor muscles to reduce pelvic myofascial pain. The findings of Abbott and colleagues, in particular, suggest that the substance that is injected may not be as important as the actual needling of the muscle. Larger studies and comparisons between placebo, botulinum toxin A, and anesthetic solutions are needed to elucidate the therapeutic benefit of these particular medications.
Neuromodulation shows promise as treatment for pelvic myofascial pain
van Balken MR, Vandoninck V, Messelink, BJ, et al. Percutaneous tibial nerve stimulation as neuromodulative treatment of chronic pelvic pain. Eur Urol. 2003;43(2):158–163.
Zabihi N, Mourtzinos A, Maher MG, Raz S, Rodriguez LV. Short-term results of bilateral S2-S4 sacral neuromodulation for the treatment of refractory interstitial cystitis, painful bladder syndrome, and chronic pelvic pain. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(4):553–557.
Neuromodulation is the science of using electrical impulses to alter neuronal activities. The exact mechanisms of action are unclear, but the technology has been utilized to control symptoms of overactive bladder and urinary retention caused by poor relaxation of the urethral and pelvic floor muscles. While studying the effects of sacral nerve root neuromodulation on the bladder, investigators noted improvements in other symptoms, such as pelvic pain.
Neuromodulation of the sacral nerve roots may be achieved by direct conduction of electrical impulses from a lead implanted in the sacrum (sacral neuromodulation) or by the retrograde conduction of these impulses through the posterior tibial nerve (percutaneous tibial nerve stimulation, or PTNS) (FIGURE 2). The tibial nerve arises from sacral nerves L5 to S3 and is one of the larger branches of the sciatic nerve.
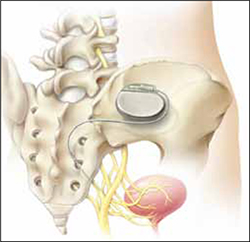
FIGURE 2 InterStim therapy
Stimulation of the sacral nerve has been used successfully to manage overactive bladder and urinary retention and may prove useful in the treatment of pelvic myofascial pain.
Van Balken et al: Details of the study
In this prospective observational study, 33 patients (both male and female) who had chronic pelvic pain by history and examination were treated with weekly, 30-minute outpatient sessions of PTNS for 12 weeks. Participants were asked to provide baseline pain scores and keep a diary of their pain. Quality-of-life questionnaires were also administered at baseline and at 12 weeks.
Investigators considered both subjective and objective success in their outcomes. If a patient elected to continue therapy, he or she was classified as a subjective success. Objective success required a decrease of at least 50% in the pain score. At the end of 12 weeks, although 33 patients (42%) wanted to continue therapy, only seven (21%) met the definition for objective success. Of those seven, six elected to continue therapy.
This study sheds light on a treatment modality that has not been studied adequately for the indication of pelvic pain but that may be promising in patients who have levator myalgia. Limitations of this study include the lack of a placebo arm, short-term outcome, and lack of localization of pain. Furthermore, although PTNS has FDA approval for treatment of urinary urgency, frequency, and urge incontinence, it is not approved for the treatment of pelvic pain. These preliminary findings demonstrate potential but, as with any new indication, long-term comparative studies are needed.
Zabihi et al: Details of the study
Patients in this retrospective study had a diagnosis of interstitial cystitis or chronic pelvic pain. Pelvic myofascial pain and trigger points were not required for eligibility. Thirty patients (21 women and nine men) had temporary placement of a lead containing four small electrodes along the S2 to S4 sacral nerve roots on both sides of the sacrum. They were then followed for a trial period of 2 to 4 weeks. To qualify for the final stage of the study, in which the leads were connected internally to a generator implanted in the buttocks, patients had to report improvement of at least 50% in their symptoms. If their improvement did not meet that threshold, the leads were removed.
Twenty-three patients (77%) met the criteria for permanent implantation. Of these patients, 42% reported improvement of more than 50% at 6 postoperative months. Quality-of-life scores also improved significantly.
Sacral neuromodulation is not FDA-approved for the treatment of chronic pelvic pain; further studies are needed before it can be recommended for this indication.
Neither of these studies required objective evidence of myofascial pain for inclusion. Therefore, although the benefits they demonstrated may be theorized to extend to the relief of myofascial pain, this fact cannot be corroborated.
We want to hear from you! Tell us what you think.
1. Bassaly R, Tidwell N, Bertolino S, Hoyte L, Downes K, Hart S. Myofascial pain and pelvic floor dysfunction in patients with interstitial cystitis. Int Urogynecol J. 2011;22(4):413-418.
2. Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65(4):653-660.
3. Allergan, Inc. Medication Guide: BOTOX. US Food and Drug Administration Web site. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM176360.pdf. Published October 2010. Accessed August 30, 2011.
1. Bassaly R, Tidwell N, Bertolino S, Hoyte L, Downes K, Hart S. Myofascial pain and pelvic floor dysfunction in patients with interstitial cystitis. Int Urogynecol J. 2011;22(4):413-418.
2. Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65(4):653-660.
3. Allergan, Inc. Medication Guide: BOTOX. US Food and Drug Administration Web site. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM176360.pdf. Published October 2010. Accessed August 30, 2011.
Colon cleansing: Not dangerous if done right
As a scientist and certified colon therapist with a colon hydrotherapy practice, I was concerned by the lack of objectivity in your recent article, “The dangers of colon cleansing” (J Fam Pract. 2011;60:454-457). The authors cited literature describing adverse effects associated with common laxative preparations used prior to colonoscopy exams, such as oral sodium phosphate or polyethylene glycol, but neither one is generally used by patients looking to colon cleanse to “enhance their well-being.” Ironically, the use of colon hydrotherapy is growing in popularity as an alternative to these laxatives for colonoscopy prep,1 yet the authors made no mention of this.
The article also contained jumps in logic that misrepresent colon cleansing in general, and colon hydrotherapy in particular. For example, the first case study involved a 31-year-old with Crohn’s disease—a specific contraindication for colon therapy. Therapists certified by the Global Professional Association for Colon Therapy (http://GPACT.org) are taught to give extensive health background questionnaires before administering colon hydrotherapy, so it is difficult to determine whether the therapist or the patient was at fault for failure to disclose her health status. Other case reports the authors cited described isolated events that either involved people who already had severe health problems or could not be attributed to colon hydrotherapy with certainty.
While there is no denying the paucity of studies on the potential benefits of colonic irrigation, it is unfortunate that the authors chose to omit the few studies that have been conducted. One study found that daily water irrigations in patients who underwent sigmoidostomies for rectal cancer were not associated with alterations in the colonic mucosa structure.2 Others determined that colonic irrigation was an effective alternative for the treatment of persistent fecal incontinence after dynamic graciloplasty3 and low anterior resection for a rectal carcinoma.4 In addition, the potential benefits of colonic irrigation have been shown in rats following the induction of pancreatitis by intraduodenal injection of sodium taurocholate.5
There are inherent risks to most, if not all, medical treatments, whether given by an allopathic doctor or alternative health practitioner. However, the huge number of colon hydrotherapy sessions performed worldwide has resulted in a vast database of testimonials to the positive effects of this therapy.
Melisa Bunderson-Schelvan, PhD
Missoula, Mont
1. Fiorito J, Culpepper-Morgan A, Estabrook SG, et al. Hydrotherapy compared with PEG-ES lavage and aqueous sodium phosphate as bowel preparation for elective colonoscopy. American College of Gastroenterology Annual Meeting; Las Vegas, Nev; October 2006.
2. Galliani I, Santi P, Barratta B, et al. Effect of water irrigations on human colonic mucosa structure after sigmoidostomy. Dis Colon Rectum. 1987;30:453-456.
3. Koch SM, Uldao O, El Naggar K, et al. Colonic irrigation for defecation disorders after dynamic graciloplasty. Int J Colorectal Dis. 2008;23:195-200.
4. Koch SM, Rietveld MP, Govaert B, et al. Retrograde colonic irrigation for faecal incontinence after low anterior resection. Int J Colorectal Dis. 2009;24:1019-1022.
5. Sulkowski U, Boin C, Brockmann J, et al. The influence of caecostomy and colonic irrigation on pathophysiology and prognosis in acute experimental pancreatitis. Eur J Surg. 1993;159:287-291.
As a scientist and certified colon therapist with a colon hydrotherapy practice, I was concerned by the lack of objectivity in your recent article, “The dangers of colon cleansing” (J Fam Pract. 2011;60:454-457). The authors cited literature describing adverse effects associated with common laxative preparations used prior to colonoscopy exams, such as oral sodium phosphate or polyethylene glycol, but neither one is generally used by patients looking to colon cleanse to “enhance their well-being.” Ironically, the use of colon hydrotherapy is growing in popularity as an alternative to these laxatives for colonoscopy prep,1 yet the authors made no mention of this.
The article also contained jumps in logic that misrepresent colon cleansing in general, and colon hydrotherapy in particular. For example, the first case study involved a 31-year-old with Crohn’s disease—a specific contraindication for colon therapy. Therapists certified by the Global Professional Association for Colon Therapy (http://GPACT.org) are taught to give extensive health background questionnaires before administering colon hydrotherapy, so it is difficult to determine whether the therapist or the patient was at fault for failure to disclose her health status. Other case reports the authors cited described isolated events that either involved people who already had severe health problems or could not be attributed to colon hydrotherapy with certainty.
While there is no denying the paucity of studies on the potential benefits of colonic irrigation, it is unfortunate that the authors chose to omit the few studies that have been conducted. One study found that daily water irrigations in patients who underwent sigmoidostomies for rectal cancer were not associated with alterations in the colonic mucosa structure.2 Others determined that colonic irrigation was an effective alternative for the treatment of persistent fecal incontinence after dynamic graciloplasty3 and low anterior resection for a rectal carcinoma.4 In addition, the potential benefits of colonic irrigation have been shown in rats following the induction of pancreatitis by intraduodenal injection of sodium taurocholate.5
There are inherent risks to most, if not all, medical treatments, whether given by an allopathic doctor or alternative health practitioner. However, the huge number of colon hydrotherapy sessions performed worldwide has resulted in a vast database of testimonials to the positive effects of this therapy.
Melisa Bunderson-Schelvan, PhD
Missoula, Mont
As a scientist and certified colon therapist with a colon hydrotherapy practice, I was concerned by the lack of objectivity in your recent article, “The dangers of colon cleansing” (J Fam Pract. 2011;60:454-457). The authors cited literature describing adverse effects associated with common laxative preparations used prior to colonoscopy exams, such as oral sodium phosphate or polyethylene glycol, but neither one is generally used by patients looking to colon cleanse to “enhance their well-being.” Ironically, the use of colon hydrotherapy is growing in popularity as an alternative to these laxatives for colonoscopy prep,1 yet the authors made no mention of this.
The article also contained jumps in logic that misrepresent colon cleansing in general, and colon hydrotherapy in particular. For example, the first case study involved a 31-year-old with Crohn’s disease—a specific contraindication for colon therapy. Therapists certified by the Global Professional Association for Colon Therapy (http://GPACT.org) are taught to give extensive health background questionnaires before administering colon hydrotherapy, so it is difficult to determine whether the therapist or the patient was at fault for failure to disclose her health status. Other case reports the authors cited described isolated events that either involved people who already had severe health problems or could not be attributed to colon hydrotherapy with certainty.
While there is no denying the paucity of studies on the potential benefits of colonic irrigation, it is unfortunate that the authors chose to omit the few studies that have been conducted. One study found that daily water irrigations in patients who underwent sigmoidostomies for rectal cancer were not associated with alterations in the colonic mucosa structure.2 Others determined that colonic irrigation was an effective alternative for the treatment of persistent fecal incontinence after dynamic graciloplasty3 and low anterior resection for a rectal carcinoma.4 In addition, the potential benefits of colonic irrigation have been shown in rats following the induction of pancreatitis by intraduodenal injection of sodium taurocholate.5
There are inherent risks to most, if not all, medical treatments, whether given by an allopathic doctor or alternative health practitioner. However, the huge number of colon hydrotherapy sessions performed worldwide has resulted in a vast database of testimonials to the positive effects of this therapy.
Melisa Bunderson-Schelvan, PhD
Missoula, Mont
1. Fiorito J, Culpepper-Morgan A, Estabrook SG, et al. Hydrotherapy compared with PEG-ES lavage and aqueous sodium phosphate as bowel preparation for elective colonoscopy. American College of Gastroenterology Annual Meeting; Las Vegas, Nev; October 2006.
2. Galliani I, Santi P, Barratta B, et al. Effect of water irrigations on human colonic mucosa structure after sigmoidostomy. Dis Colon Rectum. 1987;30:453-456.
3. Koch SM, Uldao O, El Naggar K, et al. Colonic irrigation for defecation disorders after dynamic graciloplasty. Int J Colorectal Dis. 2008;23:195-200.
4. Koch SM, Rietveld MP, Govaert B, et al. Retrograde colonic irrigation for faecal incontinence after low anterior resection. Int J Colorectal Dis. 2009;24:1019-1022.
5. Sulkowski U, Boin C, Brockmann J, et al. The influence of caecostomy and colonic irrigation on pathophysiology and prognosis in acute experimental pancreatitis. Eur J Surg. 1993;159:287-291.
1. Fiorito J, Culpepper-Morgan A, Estabrook SG, et al. Hydrotherapy compared with PEG-ES lavage and aqueous sodium phosphate as bowel preparation for elective colonoscopy. American College of Gastroenterology Annual Meeting; Las Vegas, Nev; October 2006.
2. Galliani I, Santi P, Barratta B, et al. Effect of water irrigations on human colonic mucosa structure after sigmoidostomy. Dis Colon Rectum. 1987;30:453-456.
3. Koch SM, Uldao O, El Naggar K, et al. Colonic irrigation for defecation disorders after dynamic graciloplasty. Int J Colorectal Dis. 2008;23:195-200.
4. Koch SM, Rietveld MP, Govaert B, et al. Retrograde colonic irrigation for faecal incontinence after low anterior resection. Int J Colorectal Dis. 2009;24:1019-1022.
5. Sulkowski U, Boin C, Brockmann J, et al. The influence of caecostomy and colonic irrigation on pathophysiology and prognosis in acute experimental pancreatitis. Eur J Surg. 1993;159:287-291.
Arthritis pain? These supplements provide little relief
Tell patients with large joint arthritis that glucosamine and chondroitin have been found to be little better than placebo.1
Wandel S, Juni P, Tendal B, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ .2010;314:c4675.
STRENGTH OF RECOMMENDATION
A: Based on a good-quality meta-analysis.
ILLUSTRATIVE CASE
A 64-year-old woman with osteoarthritis (OA) of both knees reports that acetaminophen does not relieve the pain, and both ibuprofen and naproxen give her an upset stomach. She wonders if glucosamine and chondroitin would help relieve the pain. How should you respond?
Degenerative joint disease is a common and frustrating problem for patients and clinicians. Symptomatic knee OA has a prevalence of 16% among adults older than 45 years, and is one of the top 5 reasons for disability in noninstitutionalized adults.2 With no highly effective treatment for OA of the hip or knee other than joint replacement surgery, patients often turn to unproven over-the-counter remedies. Individuals with OA spend about $2600 per year out-of-pocket on disease-related expenses.2
Trials of these supplements have had mixed results
Glucosamine and chondroitin have been touted as beneficial, and sales have grown rapidly over the last decade, reaching nearly $900 million in the United States in 2008 alone.3 There have been many randomized trials of these supplements, with inconsistent results.
Larger and higher quality studies have found little or no effect, while smaller studies reported that glucosamine and chondroitin helped to relieve joint pain. A meta-analysis published in 2000 found 15 studies and reported moderate to large effect sizes, but the authors noted that quality issues and publication bias probably exaggerated the benefit.4 An updated Cochrane meta-analysis of 25 randomized controlled trials (RCTs), published in 2009, found little benefit from glucosamine. A subgroup analysis found that one company’s preparation appeared to be beneficial, but all 14 studies of that particular formulation had some connection with the manufacturer.5
STUDY SUMMARY: Effects of glucosamine and chondroitin, alone or together, were small
The meta-analysis we review in this PURL only included RCTs with an average of ≥100 patients with hip or knee OA in each group.1 This was based on the minimum sample size needed to detect a small or moderate difference between the 2 groups (roughly 1 cm on a 10-cm visual analogue scale [VAS]). The authors found 10 eligible RCTs with a total of 3803 patients; the average age of participants ranged from 58 to 66 years. Most of the trials studied knee arthritis, and most were sponsored by pharmaceutical firms.
Included studies had to compare glucosamine sulphate, glucosamine hydrochloride, chondroitin sulphate, or a combination, either with a placebo or head-to-head. Minimum daily doses were 800 mg chondroitin and 1500 mg glucosamine. The primary outcome was absolute pain intensity over the duration of the study. The authors summarized pain scores every 3 months for up to 2 years; they also analyzed changes in joint space narrowing in the studies reporting that measure.
The authors used a sophisticated framework that adjusted for comparisons over time and between studies, allowing them to increase the power, and likely the accuracy, of their comparisons. They reported outcomes as effect sizes, then translated the findings to a real-world outcome by converting results to a 10-cm VAS. Typically, an effect size of 0.2 standard deviation (SD) units is considered small, 0.5 SD units is a moderate difference, and 0.8 SD units is large. The authors set their threshold for a clinically important difference at 0.37 SD units, which translated to a 0.9 cm change on a 10-cm VAS—a generally accepted minimal clinically significant difference in pain.
They found that all 3 interventions (glucosamine alone, chondroitin alone, and a combination) were statistically better than placebo, with very little difference in outcomes over time. Compared with placebo, VAS improvements were 0.4 cm for glucosamine (95% confidence interval [CI], 0.1-0.7), 0.3 cm for chondroitin (95% CI, 0-0.7) and 0.5 cm for the combination (95% CI, 0-0.9). All of these improvements in pain were less than the authors’ defined minimum clinically significant improvement of 0.9 cm on a 10-cm scale.
Among the 6 trials that reported on joint space narrowing, the changes were minute and not statistically significant. There was a net difference between treatment and placebo groups of less than 0.2 mm (an effect size ≤0.16 SD units). There was no evidence of increased risk of adverse effects or increased dropout rates with any of the substances.
WHAT’S NEW: Study results leave little room for doubt
This meta-analysis used more sophisticated comparison techniques and used only larger (and probably better quality) studies than previous meta-analyses. However, inclusion and exclusion were not based on any study quality criteria.
The authors found that glucosamine and chondroitin, used alone or in combination, provide little benefit in terms of pain relief of OA of the knee or hip compared with placebo, and contend that we should recommend against patients buying them. This meta-analysis is consistent with the American Academy of Orthopedic Surgeons 2008 guideline for knee OA, which recommends not using glucosamine and/or chondroitin based on good evidence.6
CAVEATS: Rate of joint replacement was not considered
This meta-analysis did not study the effect of these supplements on joint replacement. In a 5-year follow-up study after completion of 2 of the RCTs included in this meta-analysis, the relative risk of total joint replacement was 0.43 (95% CI, 0.2-0.92) for those in the glucosamine group (who had taken 1500 mg glucosamine sulphate for 12-36 months) compared with placebo (NNT=12).7 However, the authors were only able to follow up with 81% of the original participants. In the meta-analysis reported here, the difference in joint space narrowing was unlikely to be clinically significant or to lead to a difference in joint replacement rates.
Among the studies included in the meta-analysis, commercially funded trials had a greater decrease in pain with glucosamine or chondroitin compared with independent trials. This did not change the overall outcome of the meta-analysis, thereby supporting the validity of the results.
CHALLENGES TO IMPLEMENTATION: These supplements are available OTC
There are few barriers to advising patients not to use these products. Since glucosamine and chondroitin are available over-the-counter, however, patients have ready access to them, even if their doctors don’t recommend them. Several meta-analyses have not found an increased risk of harm from these products (other than the expense).1,5
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Wandel S, Juni P, Tendal B, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ. 2010;341:c4675.-
2. Centers for Disease Control and Prevention (CDC). Arthritis. Last updated June 25, 2010. Available at: http://www.cdc.gov/arthritis/basics/osteoarthritis.htm. Accessed June 5, 2011.
3. Heller L. US glucosamine grows slow, lags global sales. Last updated March 2, 2009. Available at: http://www.nutraingredientsusa.com/Consumer-Trends/US-glucosamine-grows-slow-lags-global-sales. Accessed May 7, 2011.
4. McAlindon TE, LaValley MP, Gulin JP, et al. Glucosamine and chondroitin for treatment of osteoarthritis: a systematic quality assessment and meta-analysis. JAMA. 2000;283:1469-1475.
5. Towheed TE, Maxwell L, Anastassiades TP, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev. 2009;(2):CD002946.-
6. National Guideline Clearinghouse (NGC). Guideline summary: American Academy of Orthopaedic Surgeons treatment of osteoarthritis of the knee (non-arthroplasty). Rockville, MD: Agency for Healthcare Research and Quality, 2008. Last updated December 6, 2008. Available at: http://www.guidelines.gov/content.aspx?id=14279. Accessed May 16, 2011.
7. Bruyere O, Pavelka K, Rovati LC, et al. Total joint replacement after glucosamine sulphate treatment in knee osteoarthritis: results of a mean 8-year observation of patients from two previous 3-year, randomised, placebo-controlled trials. Osteo Cartilage. 2008;16:254-260.
Tell patients with large joint arthritis that glucosamine and chondroitin have been found to be little better than placebo.1
Wandel S, Juni P, Tendal B, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ .2010;314:c4675.
STRENGTH OF RECOMMENDATION
A: Based on a good-quality meta-analysis.
ILLUSTRATIVE CASE
A 64-year-old woman with osteoarthritis (OA) of both knees reports that acetaminophen does not relieve the pain, and both ibuprofen and naproxen give her an upset stomach. She wonders if glucosamine and chondroitin would help relieve the pain. How should you respond?
Degenerative joint disease is a common and frustrating problem for patients and clinicians. Symptomatic knee OA has a prevalence of 16% among adults older than 45 years, and is one of the top 5 reasons for disability in noninstitutionalized adults.2 With no highly effective treatment for OA of the hip or knee other than joint replacement surgery, patients often turn to unproven over-the-counter remedies. Individuals with OA spend about $2600 per year out-of-pocket on disease-related expenses.2
Trials of these supplements have had mixed results
Glucosamine and chondroitin have been touted as beneficial, and sales have grown rapidly over the last decade, reaching nearly $900 million in the United States in 2008 alone.3 There have been many randomized trials of these supplements, with inconsistent results.
Larger and higher quality studies have found little or no effect, while smaller studies reported that glucosamine and chondroitin helped to relieve joint pain. A meta-analysis published in 2000 found 15 studies and reported moderate to large effect sizes, but the authors noted that quality issues and publication bias probably exaggerated the benefit.4 An updated Cochrane meta-analysis of 25 randomized controlled trials (RCTs), published in 2009, found little benefit from glucosamine. A subgroup analysis found that one company’s preparation appeared to be beneficial, but all 14 studies of that particular formulation had some connection with the manufacturer.5
STUDY SUMMARY: Effects of glucosamine and chondroitin, alone or together, were small
The meta-analysis we review in this PURL only included RCTs with an average of ≥100 patients with hip or knee OA in each group.1 This was based on the minimum sample size needed to detect a small or moderate difference between the 2 groups (roughly 1 cm on a 10-cm visual analogue scale [VAS]). The authors found 10 eligible RCTs with a total of 3803 patients; the average age of participants ranged from 58 to 66 years. Most of the trials studied knee arthritis, and most were sponsored by pharmaceutical firms.
Included studies had to compare glucosamine sulphate, glucosamine hydrochloride, chondroitin sulphate, or a combination, either with a placebo or head-to-head. Minimum daily doses were 800 mg chondroitin and 1500 mg glucosamine. The primary outcome was absolute pain intensity over the duration of the study. The authors summarized pain scores every 3 months for up to 2 years; they also analyzed changes in joint space narrowing in the studies reporting that measure.
The authors used a sophisticated framework that adjusted for comparisons over time and between studies, allowing them to increase the power, and likely the accuracy, of their comparisons. They reported outcomes as effect sizes, then translated the findings to a real-world outcome by converting results to a 10-cm VAS. Typically, an effect size of 0.2 standard deviation (SD) units is considered small, 0.5 SD units is a moderate difference, and 0.8 SD units is large. The authors set their threshold for a clinically important difference at 0.37 SD units, which translated to a 0.9 cm change on a 10-cm VAS—a generally accepted minimal clinically significant difference in pain.
They found that all 3 interventions (glucosamine alone, chondroitin alone, and a combination) were statistically better than placebo, with very little difference in outcomes over time. Compared with placebo, VAS improvements were 0.4 cm for glucosamine (95% confidence interval [CI], 0.1-0.7), 0.3 cm for chondroitin (95% CI, 0-0.7) and 0.5 cm for the combination (95% CI, 0-0.9). All of these improvements in pain were less than the authors’ defined minimum clinically significant improvement of 0.9 cm on a 10-cm scale.
Among the 6 trials that reported on joint space narrowing, the changes were minute and not statistically significant. There was a net difference between treatment and placebo groups of less than 0.2 mm (an effect size ≤0.16 SD units). There was no evidence of increased risk of adverse effects or increased dropout rates with any of the substances.
WHAT’S NEW: Study results leave little room for doubt
This meta-analysis used more sophisticated comparison techniques and used only larger (and probably better quality) studies than previous meta-analyses. However, inclusion and exclusion were not based on any study quality criteria.
The authors found that glucosamine and chondroitin, used alone or in combination, provide little benefit in terms of pain relief of OA of the knee or hip compared with placebo, and contend that we should recommend against patients buying them. This meta-analysis is consistent with the American Academy of Orthopedic Surgeons 2008 guideline for knee OA, which recommends not using glucosamine and/or chondroitin based on good evidence.6
CAVEATS: Rate of joint replacement was not considered
This meta-analysis did not study the effect of these supplements on joint replacement. In a 5-year follow-up study after completion of 2 of the RCTs included in this meta-analysis, the relative risk of total joint replacement was 0.43 (95% CI, 0.2-0.92) for those in the glucosamine group (who had taken 1500 mg glucosamine sulphate for 12-36 months) compared with placebo (NNT=12).7 However, the authors were only able to follow up with 81% of the original participants. In the meta-analysis reported here, the difference in joint space narrowing was unlikely to be clinically significant or to lead to a difference in joint replacement rates.
Among the studies included in the meta-analysis, commercially funded trials had a greater decrease in pain with glucosamine or chondroitin compared with independent trials. This did not change the overall outcome of the meta-analysis, thereby supporting the validity of the results.
CHALLENGES TO IMPLEMENTATION: These supplements are available OTC
There are few barriers to advising patients not to use these products. Since glucosamine and chondroitin are available over-the-counter, however, patients have ready access to them, even if their doctors don’t recommend them. Several meta-analyses have not found an increased risk of harm from these products (other than the expense).1,5
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
Tell patients with large joint arthritis that glucosamine and chondroitin have been found to be little better than placebo.1
Wandel S, Juni P, Tendal B, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ .2010;314:c4675.
STRENGTH OF RECOMMENDATION
A: Based on a good-quality meta-analysis.
ILLUSTRATIVE CASE
A 64-year-old woman with osteoarthritis (OA) of both knees reports that acetaminophen does not relieve the pain, and both ibuprofen and naproxen give her an upset stomach. She wonders if glucosamine and chondroitin would help relieve the pain. How should you respond?
Degenerative joint disease is a common and frustrating problem for patients and clinicians. Symptomatic knee OA has a prevalence of 16% among adults older than 45 years, and is one of the top 5 reasons for disability in noninstitutionalized adults.2 With no highly effective treatment for OA of the hip or knee other than joint replacement surgery, patients often turn to unproven over-the-counter remedies. Individuals with OA spend about $2600 per year out-of-pocket on disease-related expenses.2
Trials of these supplements have had mixed results
Glucosamine and chondroitin have been touted as beneficial, and sales have grown rapidly over the last decade, reaching nearly $900 million in the United States in 2008 alone.3 There have been many randomized trials of these supplements, with inconsistent results.
Larger and higher quality studies have found little or no effect, while smaller studies reported that glucosamine and chondroitin helped to relieve joint pain. A meta-analysis published in 2000 found 15 studies and reported moderate to large effect sizes, but the authors noted that quality issues and publication bias probably exaggerated the benefit.4 An updated Cochrane meta-analysis of 25 randomized controlled trials (RCTs), published in 2009, found little benefit from glucosamine. A subgroup analysis found that one company’s preparation appeared to be beneficial, but all 14 studies of that particular formulation had some connection with the manufacturer.5
STUDY SUMMARY: Effects of glucosamine and chondroitin, alone or together, were small
The meta-analysis we review in this PURL only included RCTs with an average of ≥100 patients with hip or knee OA in each group.1 This was based on the minimum sample size needed to detect a small or moderate difference between the 2 groups (roughly 1 cm on a 10-cm visual analogue scale [VAS]). The authors found 10 eligible RCTs with a total of 3803 patients; the average age of participants ranged from 58 to 66 years. Most of the trials studied knee arthritis, and most were sponsored by pharmaceutical firms.
Included studies had to compare glucosamine sulphate, glucosamine hydrochloride, chondroitin sulphate, or a combination, either with a placebo or head-to-head. Minimum daily doses were 800 mg chondroitin and 1500 mg glucosamine. The primary outcome was absolute pain intensity over the duration of the study. The authors summarized pain scores every 3 months for up to 2 years; they also analyzed changes in joint space narrowing in the studies reporting that measure.
The authors used a sophisticated framework that adjusted for comparisons over time and between studies, allowing them to increase the power, and likely the accuracy, of their comparisons. They reported outcomes as effect sizes, then translated the findings to a real-world outcome by converting results to a 10-cm VAS. Typically, an effect size of 0.2 standard deviation (SD) units is considered small, 0.5 SD units is a moderate difference, and 0.8 SD units is large. The authors set their threshold for a clinically important difference at 0.37 SD units, which translated to a 0.9 cm change on a 10-cm VAS—a generally accepted minimal clinically significant difference in pain.
They found that all 3 interventions (glucosamine alone, chondroitin alone, and a combination) were statistically better than placebo, with very little difference in outcomes over time. Compared with placebo, VAS improvements were 0.4 cm for glucosamine (95% confidence interval [CI], 0.1-0.7), 0.3 cm for chondroitin (95% CI, 0-0.7) and 0.5 cm for the combination (95% CI, 0-0.9). All of these improvements in pain were less than the authors’ defined minimum clinically significant improvement of 0.9 cm on a 10-cm scale.
Among the 6 trials that reported on joint space narrowing, the changes were minute and not statistically significant. There was a net difference between treatment and placebo groups of less than 0.2 mm (an effect size ≤0.16 SD units). There was no evidence of increased risk of adverse effects or increased dropout rates with any of the substances.
WHAT’S NEW: Study results leave little room for doubt
This meta-analysis used more sophisticated comparison techniques and used only larger (and probably better quality) studies than previous meta-analyses. However, inclusion and exclusion were not based on any study quality criteria.
The authors found that glucosamine and chondroitin, used alone or in combination, provide little benefit in terms of pain relief of OA of the knee or hip compared with placebo, and contend that we should recommend against patients buying them. This meta-analysis is consistent with the American Academy of Orthopedic Surgeons 2008 guideline for knee OA, which recommends not using glucosamine and/or chondroitin based on good evidence.6
CAVEATS: Rate of joint replacement was not considered
This meta-analysis did not study the effect of these supplements on joint replacement. In a 5-year follow-up study after completion of 2 of the RCTs included in this meta-analysis, the relative risk of total joint replacement was 0.43 (95% CI, 0.2-0.92) for those in the glucosamine group (who had taken 1500 mg glucosamine sulphate for 12-36 months) compared with placebo (NNT=12).7 However, the authors were only able to follow up with 81% of the original participants. In the meta-analysis reported here, the difference in joint space narrowing was unlikely to be clinically significant or to lead to a difference in joint replacement rates.
Among the studies included in the meta-analysis, commercially funded trials had a greater decrease in pain with glucosamine or chondroitin compared with independent trials. This did not change the overall outcome of the meta-analysis, thereby supporting the validity of the results.
CHALLENGES TO IMPLEMENTATION: These supplements are available OTC
There are few barriers to advising patients not to use these products. Since glucosamine and chondroitin are available over-the-counter, however, patients have ready access to them, even if their doctors don’t recommend them. Several meta-analyses have not found an increased risk of harm from these products (other than the expense).1,5
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Click here to view PURL METHODOLOGY
1. Wandel S, Juni P, Tendal B, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ. 2010;341:c4675.-
2. Centers for Disease Control and Prevention (CDC). Arthritis. Last updated June 25, 2010. Available at: http://www.cdc.gov/arthritis/basics/osteoarthritis.htm. Accessed June 5, 2011.
3. Heller L. US glucosamine grows slow, lags global sales. Last updated March 2, 2009. Available at: http://www.nutraingredientsusa.com/Consumer-Trends/US-glucosamine-grows-slow-lags-global-sales. Accessed May 7, 2011.
4. McAlindon TE, LaValley MP, Gulin JP, et al. Glucosamine and chondroitin for treatment of osteoarthritis: a systematic quality assessment and meta-analysis. JAMA. 2000;283:1469-1475.
5. Towheed TE, Maxwell L, Anastassiades TP, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev. 2009;(2):CD002946.-
6. National Guideline Clearinghouse (NGC). Guideline summary: American Academy of Orthopaedic Surgeons treatment of osteoarthritis of the knee (non-arthroplasty). Rockville, MD: Agency for Healthcare Research and Quality, 2008. Last updated December 6, 2008. Available at: http://www.guidelines.gov/content.aspx?id=14279. Accessed May 16, 2011.
7. Bruyere O, Pavelka K, Rovati LC, et al. Total joint replacement after glucosamine sulphate treatment in knee osteoarthritis: results of a mean 8-year observation of patients from two previous 3-year, randomised, placebo-controlled trials. Osteo Cartilage. 2008;16:254-260.
1. Wandel S, Juni P, Tendal B, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ. 2010;341:c4675.-
2. Centers for Disease Control and Prevention (CDC). Arthritis. Last updated June 25, 2010. Available at: http://www.cdc.gov/arthritis/basics/osteoarthritis.htm. Accessed June 5, 2011.
3. Heller L. US glucosamine grows slow, lags global sales. Last updated March 2, 2009. Available at: http://www.nutraingredientsusa.com/Consumer-Trends/US-glucosamine-grows-slow-lags-global-sales. Accessed May 7, 2011.
4. McAlindon TE, LaValley MP, Gulin JP, et al. Glucosamine and chondroitin for treatment of osteoarthritis: a systematic quality assessment and meta-analysis. JAMA. 2000;283:1469-1475.
5. Towheed TE, Maxwell L, Anastassiades TP, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev. 2009;(2):CD002946.-
6. National Guideline Clearinghouse (NGC). Guideline summary: American Academy of Orthopaedic Surgeons treatment of osteoarthritis of the knee (non-arthroplasty). Rockville, MD: Agency for Healthcare Research and Quality, 2008. Last updated December 6, 2008. Available at: http://www.guidelines.gov/content.aspx?id=14279. Accessed May 16, 2011.
7. Bruyere O, Pavelka K, Rovati LC, et al. Total joint replacement after glucosamine sulphate treatment in knee osteoarthritis: results of a mean 8-year observation of patients from two previous 3-year, randomised, placebo-controlled trials. Osteo Cartilage. 2008;16:254-260.
Copyright © 2011 The Family Physicians Inquiries Network.
All rights reserved.
Postcholecystectomy diarrhea: What relieves it?
A TRIAL OF A BILE ACID BINDER such as cholestyramine or colestipol may benefit patients with postcholecystectomy diarrhea (strength of recommendation [SOR]: C, case series).
Although postcholecystectomy diarrhea is uncommon and rarely severe, it can be debilitating (SOR: B, prospective case-control study).
Evidence summary
A prospective study compared the bowel function of 106 adults (85 women) who underwent laparoscopic cholecystectomy with bowel function of 37 women who had laparoscopic sterilization (and served as controls).1 The investigators gave bowel function questionnaires to both groups before surgery and 2 to 6 months afterward. They found no significant differences in bowel function between the groups.
Of the 6 women in the cholecystectomy group who reported diarrhea, only one had new-onset diarrhea, and it was “mild.” No men reported bowel function changes.1
Case studies suggest benefit from bile acid binders
When postcholecystectomy diarrhea does occur, the best treatment is unclear in the absence of randomized controlled trials. Case reports and case series support using bile acid binders based on the hypothesis that bile acid malabsorption causes the diarrhea.
The largest case series followed 26 postcholecystectomy patients with chronic diarrhea, defined as more than 3 liquid stools in 24 hours for an average of 3.9 years (range, 3 months to 13 years). Twenty-five of the 26 (96%) had severe bile acid malabsorption.
Cholestyramine, in doses of 2 to 12 g/d “normalized bowel movements” in 23 of the 25 patients with malabsorption (92%). When treatment was suspended, diarrhea recurred in 9 of the 23 (39%); bowel habits remained regular in 14 (61%).2
A smaller case series studied 8 patients who had postcholecystectomy diarrhea, defined as more than 4 loose stools in a 24-hour period for 1 to 20 years. Six of the 8 had elevated stool bile acids and stool weight greater than 200 g/24 hours. All 6 had less frequent bowel movements within 72 hours of starting oral cholestyramine at 4 to 16 g/d (adjusting the dose to maintain 1 bowel movement daily). Diarrhea recurred in all of the patients after they stopped cholestyramine.3
A single case report of a 71-year-old man who had 4 to 6 loose stools a day for 4 years after cholecystectomy noted improvement to 2 to 3 stools daily when he was treated with either colestipol or psyllium hydrophilic mucilloid.4
Recommendations
We found no consensus statements regarding treatment of postcholecystectomy diarrhea. A gastroenterology textbook notes that diarrhea occurs in as many as 20% of patients.5 The authors recommend nightly bile acid binders and, in refractory cases, opiate antidiarrheals.
An internal medicine textbook states that postcholecystectomy diarrhea—defined as 3 or more watery bowel movements per day—occurs in 5% to 10% of patients.6 The authors recommend treatment with cholestyramine or colestipol.
1. Hearing SD, Thomas LA, Heaton KW, et al. Effect of cholecystectomy on bowel function: a prospective, controlled study. Gut. 1999;45:889-894.
2. Sciarretta G, Furno A, Mazzoni M, et al. Post-cholecystectomy diarrhea: evidence of bile acid malabsorption assessed by SeHCAT test. Am J Gastroenterol. 1992;87:1852-1854.
3. Arlow FL, Dekovich AA, Priest RJ, et al. Bile acid-mediated postcholecystectomy diarrhea. Arch Intern Med. 1987;147:1327-1329.
4. Strommen GL, Dorworth TE, Walker PR, et al. Treatment of suspected postcholecystectomy diarrhea with psyllium hydrophilic mucilloid. Clin Pharm. 1990;9:206-208.
5. Schiller LR, Sellin JH. Diarrhea. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 8th ed. Philadelphia, PA: Saunders; 2006:159–186.
6. Greenberger NJ, Paumgartner G. Diseases of the gallbladder and bile ducts. In: Fauci AS, Braunwald E, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 17th ed. New York: McGraw-Hill Medical; 2008. Available at: www.accessmedicine.com/content.aspx?aID=2874111. Accessed February 2008.
A TRIAL OF A BILE ACID BINDER such as cholestyramine or colestipol may benefit patients with postcholecystectomy diarrhea (strength of recommendation [SOR]: C, case series).
Although postcholecystectomy diarrhea is uncommon and rarely severe, it can be debilitating (SOR: B, prospective case-control study).
Evidence summary
A prospective study compared the bowel function of 106 adults (85 women) who underwent laparoscopic cholecystectomy with bowel function of 37 women who had laparoscopic sterilization (and served as controls).1 The investigators gave bowel function questionnaires to both groups before surgery and 2 to 6 months afterward. They found no significant differences in bowel function between the groups.
Of the 6 women in the cholecystectomy group who reported diarrhea, only one had new-onset diarrhea, and it was “mild.” No men reported bowel function changes.1
Case studies suggest benefit from bile acid binders
When postcholecystectomy diarrhea does occur, the best treatment is unclear in the absence of randomized controlled trials. Case reports and case series support using bile acid binders based on the hypothesis that bile acid malabsorption causes the diarrhea.
The largest case series followed 26 postcholecystectomy patients with chronic diarrhea, defined as more than 3 liquid stools in 24 hours for an average of 3.9 years (range, 3 months to 13 years). Twenty-five of the 26 (96%) had severe bile acid malabsorption.
Cholestyramine, in doses of 2 to 12 g/d “normalized bowel movements” in 23 of the 25 patients with malabsorption (92%). When treatment was suspended, diarrhea recurred in 9 of the 23 (39%); bowel habits remained regular in 14 (61%).2
A smaller case series studied 8 patients who had postcholecystectomy diarrhea, defined as more than 4 loose stools in a 24-hour period for 1 to 20 years. Six of the 8 had elevated stool bile acids and stool weight greater than 200 g/24 hours. All 6 had less frequent bowel movements within 72 hours of starting oral cholestyramine at 4 to 16 g/d (adjusting the dose to maintain 1 bowel movement daily). Diarrhea recurred in all of the patients after they stopped cholestyramine.3
A single case report of a 71-year-old man who had 4 to 6 loose stools a day for 4 years after cholecystectomy noted improvement to 2 to 3 stools daily when he was treated with either colestipol or psyllium hydrophilic mucilloid.4
Recommendations
We found no consensus statements regarding treatment of postcholecystectomy diarrhea. A gastroenterology textbook notes that diarrhea occurs in as many as 20% of patients.5 The authors recommend nightly bile acid binders and, in refractory cases, opiate antidiarrheals.
An internal medicine textbook states that postcholecystectomy diarrhea—defined as 3 or more watery bowel movements per day—occurs in 5% to 10% of patients.6 The authors recommend treatment with cholestyramine or colestipol.
A TRIAL OF A BILE ACID BINDER such as cholestyramine or colestipol may benefit patients with postcholecystectomy diarrhea (strength of recommendation [SOR]: C, case series).
Although postcholecystectomy diarrhea is uncommon and rarely severe, it can be debilitating (SOR: B, prospective case-control study).
Evidence summary
A prospective study compared the bowel function of 106 adults (85 women) who underwent laparoscopic cholecystectomy with bowel function of 37 women who had laparoscopic sterilization (and served as controls).1 The investigators gave bowel function questionnaires to both groups before surgery and 2 to 6 months afterward. They found no significant differences in bowel function between the groups.
Of the 6 women in the cholecystectomy group who reported diarrhea, only one had new-onset diarrhea, and it was “mild.” No men reported bowel function changes.1
Case studies suggest benefit from bile acid binders
When postcholecystectomy diarrhea does occur, the best treatment is unclear in the absence of randomized controlled trials. Case reports and case series support using bile acid binders based on the hypothesis that bile acid malabsorption causes the diarrhea.
The largest case series followed 26 postcholecystectomy patients with chronic diarrhea, defined as more than 3 liquid stools in 24 hours for an average of 3.9 years (range, 3 months to 13 years). Twenty-five of the 26 (96%) had severe bile acid malabsorption.
Cholestyramine, in doses of 2 to 12 g/d “normalized bowel movements” in 23 of the 25 patients with malabsorption (92%). When treatment was suspended, diarrhea recurred in 9 of the 23 (39%); bowel habits remained regular in 14 (61%).2
A smaller case series studied 8 patients who had postcholecystectomy diarrhea, defined as more than 4 loose stools in a 24-hour period for 1 to 20 years. Six of the 8 had elevated stool bile acids and stool weight greater than 200 g/24 hours. All 6 had less frequent bowel movements within 72 hours of starting oral cholestyramine at 4 to 16 g/d (adjusting the dose to maintain 1 bowel movement daily). Diarrhea recurred in all of the patients after they stopped cholestyramine.3
A single case report of a 71-year-old man who had 4 to 6 loose stools a day for 4 years after cholecystectomy noted improvement to 2 to 3 stools daily when he was treated with either colestipol or psyllium hydrophilic mucilloid.4
Recommendations
We found no consensus statements regarding treatment of postcholecystectomy diarrhea. A gastroenterology textbook notes that diarrhea occurs in as many as 20% of patients.5 The authors recommend nightly bile acid binders and, in refractory cases, opiate antidiarrheals.
An internal medicine textbook states that postcholecystectomy diarrhea—defined as 3 or more watery bowel movements per day—occurs in 5% to 10% of patients.6 The authors recommend treatment with cholestyramine or colestipol.
1. Hearing SD, Thomas LA, Heaton KW, et al. Effect of cholecystectomy on bowel function: a prospective, controlled study. Gut. 1999;45:889-894.
2. Sciarretta G, Furno A, Mazzoni M, et al. Post-cholecystectomy diarrhea: evidence of bile acid malabsorption assessed by SeHCAT test. Am J Gastroenterol. 1992;87:1852-1854.
3. Arlow FL, Dekovich AA, Priest RJ, et al. Bile acid-mediated postcholecystectomy diarrhea. Arch Intern Med. 1987;147:1327-1329.
4. Strommen GL, Dorworth TE, Walker PR, et al. Treatment of suspected postcholecystectomy diarrhea with psyllium hydrophilic mucilloid. Clin Pharm. 1990;9:206-208.
5. Schiller LR, Sellin JH. Diarrhea. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 8th ed. Philadelphia, PA: Saunders; 2006:159–186.
6. Greenberger NJ, Paumgartner G. Diseases of the gallbladder and bile ducts. In: Fauci AS, Braunwald E, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 17th ed. New York: McGraw-Hill Medical; 2008. Available at: www.accessmedicine.com/content.aspx?aID=2874111. Accessed February 2008.
1. Hearing SD, Thomas LA, Heaton KW, et al. Effect of cholecystectomy on bowel function: a prospective, controlled study. Gut. 1999;45:889-894.
2. Sciarretta G, Furno A, Mazzoni M, et al. Post-cholecystectomy diarrhea: evidence of bile acid malabsorption assessed by SeHCAT test. Am J Gastroenterol. 1992;87:1852-1854.
3. Arlow FL, Dekovich AA, Priest RJ, et al. Bile acid-mediated postcholecystectomy diarrhea. Arch Intern Med. 1987;147:1327-1329.
4. Strommen GL, Dorworth TE, Walker PR, et al. Treatment of suspected postcholecystectomy diarrhea with psyllium hydrophilic mucilloid. Clin Pharm. 1990;9:206-208.
5. Schiller LR, Sellin JH. Diarrhea. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 8th ed. Philadelphia, PA: Saunders; 2006:159–186.
6. Greenberger NJ, Paumgartner G. Diseases of the gallbladder and bile ducts. In: Fauci AS, Braunwald E, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 17th ed. New York: McGraw-Hill Medical; 2008. Available at: www.accessmedicine.com/content.aspx?aID=2874111. Accessed February 2008.
Evidence-based answers from the Family Physicians Inquiries Network
Elbow injuries: Getting kids back in the game
• Administer the valgus stress test, the “milking maneuver,” and the moving valgus stress test to athletes suspected of having ulnar collateral ligament injury. C
• Treat Little League elbow with nonsteroidal anti-inflammatory drugs, ice, brief immobilization, and a 4- to 6-week “break” from throwing. A
• Advise young baseball players (and their parents) to avoid pitching year-round, and to get 3 months of rest per year. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The growing popularity of club teams and year-round participation in sports has spawned an epidemic of elbow injuries in primary and secondary school students and young adults alike. The incidence of elbow pain in children engaged in sports that require overhead throwing, such as baseball, football, volleyball, tennis, and javelin, ranges from 45% to 78%.1
Fortunately, acute traumatic elbow injury, with pain severe enough to force the athlete to cease participation entirely, is relatively rare, accounting for only 1% to 5% of cases.1,2 Far more often, elbow pain is associated with overuse, resulting in a gradual onset of medial elbow soreness that does not prevent the athlete from playing.
When an athlete seeks care for elbow pain, there are a number of things to consider, including the patient’s age, skeletal maturity, and type and frequency of throwing. Younger “throwers” typically incur injuries related to the physes, while adolescents and adults are more likely to sustain injuries to the ligaments and tendons.3 In both cases, repetitive valgus stress is the mechanism of injury. This review—of elbow anatomy (see the box),4-6 injury, differential diagnosis, and treatment—will make it easier for you to get injured athletes back in the game.
The elbow has 3 articulations—ulnohumeral, radiocapitellar, and proximal radioulnar—that provide primary stability to valgus stress. The elbow’s soft tissue restraints include 2 ligament complexes (medial and lateral collateral), 4 muscle groups (flexors, extensors, pronators, supinators), and 3 major nerves (radial, median, ulnar) and their branches.
The ulnar collateral ligament (UCL) complex—which consists of the anterior and posterior bundles and the transverse ligament—is the main source of medial elbow stability. 4 Mechanical stability for overhead throwing is provided by both bony and soft tissue restraints. During the pitching motion, the forces generated exceed the UCL’s tensile strength, and protective flexor muscles are activated.5,6
And the pitch…There are 6 stages of throwing: windup, early cocking, late cocking, acceleration, deceleration, and follow-through. Elbow pain is most likely during the late-cocking or early acceleration phase of a throw, the point of ball/javelin release, or the moment the racquet hits the ball.4
Is it Little League elbow? Start with a targeted history
In skeletally immature athletes, open physes result in the epicondylar apophysis being the weakest structure on the medial aspect of the elbow. Thus, repetitive valgus stress and tension overload often lead to “Little League elbow”—an umbrella term with a differential diagnosis that encompasses medial epicondylar fragmentation, delayed or accelerated growth of the medial epicondyle, and delayed closure of its growth plate, among other conditions (TABLE 1).3,7,8
In more mature athletes, repetitive microtrauma to the ulnar collateral ligament (UCL) leads to its gradual attenuation or complete failure.7 This increases the stress on the radiocapitellar joint and olecranon, and can lead to edema, scarring, calcification, osteophyte formation, medial epicondylitis, ulnar nerve neurapraxia, or radiocapitellar chondral damage.9 Extended practices and tournaments, with no substantial rest period throughout the year, put adolescents at increased risk for UCL injuries.10
Regardless of age, the medical history of an athlete with elbow pain should elicit information about the mechanism of injury; the location, duration, and quality of the pain; factors that alleviate or exacerbate the pain; the presence of weakness or paresthesias; and the extent to which the pain has affected the patient’s ability to throw. Patients with chronic UCL injuries, for example, often report a loss of arm control and decrease in throwing speed. It is also important to address hand dominance, level of participation, the position played, changes in technique or training regimen, prior injuries, and the effects of any previous treatment.11
TABLE 1
Differential diagnosis of elbow injuries
| Location | Differential diagnosis |
|---|---|
| Medial | Little League elbow
|
| Anterior | Anterior capsule strain Biceps tendon rupture Biceps tendonitis Dislocation Median nerve compression (pronator) syndrome |
| Posterior | Olecranon bursitis Olecranon process or tip stress fracture Triceps rupture/olecranon avulsion Triceps tendonitis Trochlear rupture Valgus overload syndrome (posterior olecranon impingement syndrome) |
| Lateral | Capitellum fracture Lateral epicondylitis Lateral ulnar collateral ligament injury Osteochondritis dissecans Posterior interosseous nerve syndrome Posterolateral rotary instability Radial head fracture Radiocapitellar chondromalacia |
| Adapted from: McKeag DB, Moeller JL. ACSM’s Primary Care Sports Medicine. 2nd ed.3 | |
Compare the affected and uninjured extremities
Inspect, palpate, and assess the active and passive range of motion, strength, and neurovascular status of both arms, with the uninjured side serving as a comparison. The scapula, shoulder, and wrist are also involved in throwing, so these joints should be examined along with the elbow.
Measure range of motion. Normal ranges for the flexion-extension arc are 0 to 140°, with 75° of pronation and 82° of supination.12 Use a goniometer, if available, to ensure accuracy and reproducibility,1 and pay close attention to the position that elicits pain.
In medial epicondylitis, the full range of motion should be preserved. Patients experience pain at the medial epicondyle and overlying flexor-pronator mass proximately, and pain or weakness with resisted wrist flexion, and resisted pronation, at full extension.4,11 Flexor-pronator strain will produce similar findings, but edema or ecchymosis may be present and there may be pain immediately distal to the medial epicondyle.11
Pain associated with injury to the UCL—which courses distal and slightly posterior to the medial epicondyle—typically occurs 2 cm distal to the medial epicondyle over the anterior bundle. Tenderness over the UCL has a sensitivity of 81% to 94% for UCL tears, but a specificity of only 22%.13
Physical maneuvers can help identify source of elbow pain
A complete UCL tear can cause valgus gapping as small as 3 mm, which makes it difficult to detect on physical exam alone.4 Orthopedic and sports medicine literature recommend that 3 maneuvers be used to identify UCL pathology:4,14,15
The valgus stress test (FIGURE 1) assesses the effects of valgus stress on the UCL. Gapping >3 mm signifies UCL instability. The test has a sensitivity of 66% and a specificity of 60% for detecting a UCL strain or tear.13,16
The milking maneuver (FIGURE 2), performed by the patient (or by a clinician if the patient lacks flexibility), reproduces a common pitching exercise. Medial elbow pain or apprehension indicates UCL injury.13,16
The moving valgus stress test (FIGURE 3A-C) is done in an effort to recreate the flexion angles of the elbow during the late cocking and early acceleration phases of throwing. Pain anywhere in the arc of motion suggests a UCL injury; pain elicited at 45° of flexion suggests osteochondrosis of the humeral capitellum, while pain closer to full extension suggests osteochondrosis of the trochlea.13,16
FIGURE 1
Valgus stress test
With the injured elbow at 30° of flexion, the shoulder abducted and fully externally rotated, and the patient’s wrist under your arm, place one hand laterally over the elbow. Place the other hand under the ulna and the thumb over the ulnar collateral ligament and apply valgus stress. Gapping >3 mm is abnormal.
FIGURE 2
Milking maneuver
The patient grasps the thumb of the affected arm and pulls downward, with the affected elbow positioned as shown, stressing the ulnar collateral ligament (UCL). Elbow pain or apprehension is positive for UCL injury.
FIGURE 3
Moving valgus stress test
With the shoulder in abduction and maximum external rotation (A), place the elbow in maximum flexion and apply valgus force (B), and extend the elbow from full flexion to full extension (C) in an attempt to reproduce the medial pain.
Does your patient have 2 positive valgus tests and posterior pain?
Valgus extension overload syndrome, which is caused by repetitive stress and results in osteophytes, chondromalacia of the medial olecranon fossa, tension in the UCL, and compression of the radiocapitellar joint, will also produce positive valgus stress and positive moving valgus stress tests. Keep in mind, however, that patients with valgus extension overload often have loss of full extension and posterior elbow pain with forced elbow hyperextension.17
Look for ulnar nerve injury
The physical examination should also be used to test for ulnar nerve injury. The elbow flexion test—a provocative maneuver in which the patient flexes the elbow as far as possible and reports any tingling or numbness of the hand—should be included in the work-up. Symptoms that develop in <60 seconds indicate a positive test for ulnar nerve compression, with the pinky and ulnar half of the ring finger most likely to have loss of vibration and light touch perception. A positive Tinel’s sign over the cubital tunnel is an indication of ulnar neuritis.18
If the ulnar nerve moves out of the ulnar groove when the groove is palpated as the elbow is flexed and extended, subluxating ulnar nerve is the likely diagnosis. If 2 structures displace over the medial epicondyle with elbow flexion, the first will be the ulnar nerve and the second will be the medial head of the triceps—an indication of a snapping medial head of triceps.18
Imaging studies may require a second look
Imaging studies are sometimes used to further aid in diagnosis of elbow injury. However, standard elbow x-rays, including an anteroposterior view in full extension, an oblique view, and a lateral view at 90° flexion, can be deceiving, as they often appear normal in conditions causing medial elbow pain associated with overhead throwing.
Careful review of the images may be needed to rule out fracture and other conditions, keeping the following factors in mind:
- A supracondylar fracture is likely if the anterior humeral line that is drawn along the anterior surface of the humeral cortex (on a lateral view) does not transect the middle third of the midcapitellum.3,11,18
- Dislocation of the radial head is suggested if the radiocapitellar line (drawn through the center of the radial head and neck) does not transect the midcapitellum on a lateral view.3,11,18
- Intra-articular injury with a joint effusion is indicated when an enlarged anterior fat pad, which is slightly anterior to the distal humeral diaphysis, is visible (the “sail sign”) on a normal elbow radiograph.3,11,18
- A fracture is likely if a posterior fat pad (which lies in the olecranon fossa and is not usually visible unless an effusion elevates the fat pad away from the cortex) is visible on an elbow x-ray. 3,11,18
- A chronic UCL tear is suggested by heterotropic calcification of the UCL.19
It is useful to x-ray both the injured and the unaffected elbows in skeletally immature athletes to compare secondary ossification centers. Little League elbow demonstrates a widening of the medial epicondyle physis, for example, when the x-rays are compared.3 Secondary ossification centers of the elbow appear first at the capitellum (age 2), followed by the radial head (age 5), medial epicondyle (age 7), trochlea (age 9), and lateral epicondyle (age 11). Most ossification centers fuse between 14 and 17 years of age.3
Computed tomography arthrograms, magnetic resonance imaging (MRI), and ultrasonography are also used to identify UCL tears. MRI, which can reveal injuries to cartilage and tendons as well, is the most commonly used imaging technique for musculoskeletal diagnosis of the elbow.16,20
Treatment gets most athletes back on track
Most medial elbow injuries respond to conservative treatment—typically, with some combination of activity modification, nonsteroidal anti-inflammatory drugs (NSAIDs), icing, physical therapy aimed at flexor-pronator strengthening, and counterforce bracing.11 Medial epicondylosis and flexor-pronator strain injuries have an excellent prognosis, with more than 90% of patients back to their previous level of activity at 1 year. Initial treatment consists of a 2- to 3-week rest period, followed by a 6- to 12-week rehabilitation protocol.11
Randomized controlled trials have found limited evidence of short-term improvement in symptoms with corticosteroid injections compared with placebo or no treatment, local anesthetic, orthosis, physical therapy, and NSAIDs. However, corticosteroids were less effective than physiotherapy or oral NSAIDs in improving long-term outcomes.21 Despite a paucity of well-designed studies to prove their use, autologous blood, platelet-rich plasma, and botulinum toxin are sometimes used for refractory elbow pain.21
Treatment of Little League elbow consists of cessation of throwing for at least 4 to 6 weeks, with a gradual return to throwing and emphasis on proper throwing mechanics after the pain resolves. Most throwers are out of competition for 2 to 3 months, but fully recover with nonoperative management.21
UCL injuries, too, are initially treated with rest, NSAIDs, icing, bracing, and physical therapy, typically with 2 to 3 months of no throwing. Some patients also use a splint at 90° flexion at night and as needed for pain during the day. Patients whose symptoms last more than a year despite treatment may be candidates for arthroscopic debridement.11
Consider reconstruction when nonsurgical management fails
UCL reconstruction was introduced in 1974, when reconstruction was performed on professional pitcher Tommy John, who went on to win 164 games.4,9 The procedure has since undergone numerous modifications. Surgery is indicated for acute rupture, significant chronic instability, insufficient UCL tissue after debridement, or recurrent pain and valgus instability with throwing after rehabilitation.2,4,6,9
Reconstruction generally entails fixing a tendon graft through bone tunnels in the medial epicondyle of the humerus and sublime tubercle of the ulna to reestablish valgus stability. A recent systematic review of reconstruction methods found a 76% to 95% rate of excellent results, with patients returned to their prior level of activity at a mean follow-up of 1 year.22 Rehabilitation typically begins 7 days postop; throwing (without windup) may begin in 4 to 5 months, with a gradual increase in speed and force and a return to the game at 12 months.
A stepped-up focus on prevention
The increase in UCL injuries in adolescents highlights the need for greater emphasis on prevention.10 Several governing bodies, including USA Baseball and the American Academy of Pediatrics, have developed research-based guidelines for young athletes (TABLE 2).1,10,23-25
One of the easiest to follow is to limit an athlete’s weekly pitch count to 10 times his age. Thus, a 10 year old should pitch no more than 100 pitches in a given 7-day period. Another important measure—in addition to ensuring that young athletes receive instruction in proper pitching mechanics (see http://www.littleleague.org/Little_League_Online.htm)—is to urge coaches and parents to require players to get at least 3 months of rest after each season and to stop throwing if they have pain or fatigue.24
TABLE 2
Keeping young pitchers injury-free1,10,23-25
| Recommendations for coaches and parents |
|---|
| Record the number of pitches thrown at each outing/sports event for all young pitchers |
| Avoid allowing young athletes to pitch competitively >8 months per year |
| Limit the number of pitches to ≤2500 per year and 10 × the pitcher’s age per week, or 90 per outing |
| Ensure that young pitchers are instructed in proper pitching mechanics |
| Restrict throwing breaking ball pitches* prior to puberty |
| Ensure that young pitchers get 3 months of rest per year. |
| *A pitch that changes direction either sideways or downwards as it approaches the batter, eg, a slider or curve ball. |
CORRESPONDENCE
Jennifer A. Southard, MD, MSc, Saint Alphonsus Medical Group, 6533 Emerald Street, Boise, ID 83704; [email protected]
1. American Academy of Pediatrics Committee on Sports Medicine and Fitness. Risk of injury from baseball and softball in children. Pediatrics. 2001;107:782-784.
2. Maloney MD, Morhr KJ, el Attrache NS, et al. Elbow injuries in the throwing athlete. Clin Sports Med. 1999;18:795-809.
3. McKeag DB, Moeller JL. ACSM’s Primary Care Sports Medicine. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:387–402.
4. Hariri S, Safran MR. Ulnar collateral ligament injury in the overhead athlete. Clin Sports Med. 2010;29:619-644.
5. Park MJ, Kim HG, Lee JY. Surgical treatment of post-traumatic stiffness of the elbow. J Bone Joint Surg Br. 2004;86:1158-1162.
6. Lin F, Kohli N, Perlmutter S, et al. Muscle contribution to elbow joint valgus stability. J Shoulder Elbow Surg. 2007;16:795-802.
7. Fleisig GS, Andrews JR, Dillman CJ, et al. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233-239.
8. Baker CL, Romero AA. Osteochondritis dissecans of the capitellum. Am J Sports Med. 2010;38:1917-1928.
9. Cain EL, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38:2426-2434.
10. Fleisig GS, Andrews JR, Cutter GR, et al. Prevention of elbow injuries in youth baseball pitchers. Curr Sports Med Rep. 2009;8:250-254.
11. Madden CC, Putukian M, McCarty E, et al. Netter’s Sports Medicine. Philadelphia, PA: Saunders Elsevier; 2010:360–367.
12. Boone DC, Azen SP. Normal range of motion of joints in male subjects. J Bone Joint Surg Am. 1979;61:756-759.
13. Timmerman LA, Schwartz ML, Andrews JR. Preoperative evaluation of the ulnar collateral ligament by magnetic resonance imaging and computed tomography arthrography. Evaluation in 25 baseball players with surgical confirmation. Am J Sports Med. 1994;22:26-31.
14. Mehlhoff TL, Bennet JB. Elbow injuries. In: Mellion MB, Walsh WM, Shelton GI, eds. The Team Physician’s Handbook. 2nd ed. Philadelphia, PA: Hanley & Belfus; 1997:461–473.
15. O’Connor FG, Ollivierre CO, Nirschl RP. Elbow and forearm injuries. In: Lillegard WA, Butcher KS, eds. Handbook of Sports Medicine: A Symptom-Oriented Approach. 2nd ed. Boston, MA: Butterworth-Heinemann; 1999:141–157.
16. Safran MR, Greene H, Lee TQ. Comparison of elbow valgus laxity using radiographic and non-radiographic objective measurement. 73rd Annual Meeting of the American Academy of Orthopaedic Surgeons; May 22, 2006; Chicago, IL.
17. Ahmad CS, El Attrache NS. Valgus extension overload syndrome and stress injury of the olecranon. Clin Sports Med. 2004;23:665-676.
18. Sarwart JF. Essentials of Musculoskeletal Care. 4th ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010:384–387.
19. Mulligan SA, Schwartz ML, Broussard MF, et al. Heterotopic calcification and tears of the ulnar collateral ligament: radiographic and MR imaging findings. AJR Am J Roentgenol. 2000;175:1099-1102.
20. Tuite MJ, Kijowski R. Sports related injures of the elbow: an approach to MRI interpretation. Clin Sports Med. 2006;25:387-408.
21. Rineer CA, Ruch DS. Elbow tendinopathy and tendon ruptures: epicondylitis, biceps and triceps ruptures. J Hand Surg Am. 2009;34:566-576.
22. Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008;36:1993-205.
23. Olsen SJ, Fleisig GS, Dun S, et al. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34:905-912.
24. Lyman S, Fleisig GS, Andrews JR, et al. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30:463-468.
25. Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011;39:253-257.
• Administer the valgus stress test, the “milking maneuver,” and the moving valgus stress test to athletes suspected of having ulnar collateral ligament injury. C
• Treat Little League elbow with nonsteroidal anti-inflammatory drugs, ice, brief immobilization, and a 4- to 6-week “break” from throwing. A
• Advise young baseball players (and their parents) to avoid pitching year-round, and to get 3 months of rest per year. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The growing popularity of club teams and year-round participation in sports has spawned an epidemic of elbow injuries in primary and secondary school students and young adults alike. The incidence of elbow pain in children engaged in sports that require overhead throwing, such as baseball, football, volleyball, tennis, and javelin, ranges from 45% to 78%.1
Fortunately, acute traumatic elbow injury, with pain severe enough to force the athlete to cease participation entirely, is relatively rare, accounting for only 1% to 5% of cases.1,2 Far more often, elbow pain is associated with overuse, resulting in a gradual onset of medial elbow soreness that does not prevent the athlete from playing.
When an athlete seeks care for elbow pain, there are a number of things to consider, including the patient’s age, skeletal maturity, and type and frequency of throwing. Younger “throwers” typically incur injuries related to the physes, while adolescents and adults are more likely to sustain injuries to the ligaments and tendons.3 In both cases, repetitive valgus stress is the mechanism of injury. This review—of elbow anatomy (see the box),4-6 injury, differential diagnosis, and treatment—will make it easier for you to get injured athletes back in the game.
The elbow has 3 articulations—ulnohumeral, radiocapitellar, and proximal radioulnar—that provide primary stability to valgus stress. The elbow’s soft tissue restraints include 2 ligament complexes (medial and lateral collateral), 4 muscle groups (flexors, extensors, pronators, supinators), and 3 major nerves (radial, median, ulnar) and their branches.
The ulnar collateral ligament (UCL) complex—which consists of the anterior and posterior bundles and the transverse ligament—is the main source of medial elbow stability. 4 Mechanical stability for overhead throwing is provided by both bony and soft tissue restraints. During the pitching motion, the forces generated exceed the UCL’s tensile strength, and protective flexor muscles are activated.5,6
And the pitch…There are 6 stages of throwing: windup, early cocking, late cocking, acceleration, deceleration, and follow-through. Elbow pain is most likely during the late-cocking or early acceleration phase of a throw, the point of ball/javelin release, or the moment the racquet hits the ball.4
Is it Little League elbow? Start with a targeted history
In skeletally immature athletes, open physes result in the epicondylar apophysis being the weakest structure on the medial aspect of the elbow. Thus, repetitive valgus stress and tension overload often lead to “Little League elbow”—an umbrella term with a differential diagnosis that encompasses medial epicondylar fragmentation, delayed or accelerated growth of the medial epicondyle, and delayed closure of its growth plate, among other conditions (TABLE 1).3,7,8
In more mature athletes, repetitive microtrauma to the ulnar collateral ligament (UCL) leads to its gradual attenuation or complete failure.7 This increases the stress on the radiocapitellar joint and olecranon, and can lead to edema, scarring, calcification, osteophyte formation, medial epicondylitis, ulnar nerve neurapraxia, or radiocapitellar chondral damage.9 Extended practices and tournaments, with no substantial rest period throughout the year, put adolescents at increased risk for UCL injuries.10
Regardless of age, the medical history of an athlete with elbow pain should elicit information about the mechanism of injury; the location, duration, and quality of the pain; factors that alleviate or exacerbate the pain; the presence of weakness or paresthesias; and the extent to which the pain has affected the patient’s ability to throw. Patients with chronic UCL injuries, for example, often report a loss of arm control and decrease in throwing speed. It is also important to address hand dominance, level of participation, the position played, changes in technique or training regimen, prior injuries, and the effects of any previous treatment.11
TABLE 1
Differential diagnosis of elbow injuries
| Location | Differential diagnosis |
|---|---|
| Medial | Little League elbow
|
| Anterior | Anterior capsule strain Biceps tendon rupture Biceps tendonitis Dislocation Median nerve compression (pronator) syndrome |
| Posterior | Olecranon bursitis Olecranon process or tip stress fracture Triceps rupture/olecranon avulsion Triceps tendonitis Trochlear rupture Valgus overload syndrome (posterior olecranon impingement syndrome) |
| Lateral | Capitellum fracture Lateral epicondylitis Lateral ulnar collateral ligament injury Osteochondritis dissecans Posterior interosseous nerve syndrome Posterolateral rotary instability Radial head fracture Radiocapitellar chondromalacia |
| Adapted from: McKeag DB, Moeller JL. ACSM’s Primary Care Sports Medicine. 2nd ed.3 | |
Compare the affected and uninjured extremities
Inspect, palpate, and assess the active and passive range of motion, strength, and neurovascular status of both arms, with the uninjured side serving as a comparison. The scapula, shoulder, and wrist are also involved in throwing, so these joints should be examined along with the elbow.
Measure range of motion. Normal ranges for the flexion-extension arc are 0 to 140°, with 75° of pronation and 82° of supination.12 Use a goniometer, if available, to ensure accuracy and reproducibility,1 and pay close attention to the position that elicits pain.
In medial epicondylitis, the full range of motion should be preserved. Patients experience pain at the medial epicondyle and overlying flexor-pronator mass proximately, and pain or weakness with resisted wrist flexion, and resisted pronation, at full extension.4,11 Flexor-pronator strain will produce similar findings, but edema or ecchymosis may be present and there may be pain immediately distal to the medial epicondyle.11
Pain associated with injury to the UCL—which courses distal and slightly posterior to the medial epicondyle—typically occurs 2 cm distal to the medial epicondyle over the anterior bundle. Tenderness over the UCL has a sensitivity of 81% to 94% for UCL tears, but a specificity of only 22%.13
Physical maneuvers can help identify source of elbow pain
A complete UCL tear can cause valgus gapping as small as 3 mm, which makes it difficult to detect on physical exam alone.4 Orthopedic and sports medicine literature recommend that 3 maneuvers be used to identify UCL pathology:4,14,15
The valgus stress test (FIGURE 1) assesses the effects of valgus stress on the UCL. Gapping >3 mm signifies UCL instability. The test has a sensitivity of 66% and a specificity of 60% for detecting a UCL strain or tear.13,16
The milking maneuver (FIGURE 2), performed by the patient (or by a clinician if the patient lacks flexibility), reproduces a common pitching exercise. Medial elbow pain or apprehension indicates UCL injury.13,16
The moving valgus stress test (FIGURE 3A-C) is done in an effort to recreate the flexion angles of the elbow during the late cocking and early acceleration phases of throwing. Pain anywhere in the arc of motion suggests a UCL injury; pain elicited at 45° of flexion suggests osteochondrosis of the humeral capitellum, while pain closer to full extension suggests osteochondrosis of the trochlea.13,16
FIGURE 1
Valgus stress test
With the injured elbow at 30° of flexion, the shoulder abducted and fully externally rotated, and the patient’s wrist under your arm, place one hand laterally over the elbow. Place the other hand under the ulna and the thumb over the ulnar collateral ligament and apply valgus stress. Gapping >3 mm is abnormal.
FIGURE 2
Milking maneuver
The patient grasps the thumb of the affected arm and pulls downward, with the affected elbow positioned as shown, stressing the ulnar collateral ligament (UCL). Elbow pain or apprehension is positive for UCL injury.
FIGURE 3
Moving valgus stress test
With the shoulder in abduction and maximum external rotation (A), place the elbow in maximum flexion and apply valgus force (B), and extend the elbow from full flexion to full extension (C) in an attempt to reproduce the medial pain.
Does your patient have 2 positive valgus tests and posterior pain?
Valgus extension overload syndrome, which is caused by repetitive stress and results in osteophytes, chondromalacia of the medial olecranon fossa, tension in the UCL, and compression of the radiocapitellar joint, will also produce positive valgus stress and positive moving valgus stress tests. Keep in mind, however, that patients with valgus extension overload often have loss of full extension and posterior elbow pain with forced elbow hyperextension.17
Look for ulnar nerve injury
The physical examination should also be used to test for ulnar nerve injury. The elbow flexion test—a provocative maneuver in which the patient flexes the elbow as far as possible and reports any tingling or numbness of the hand—should be included in the work-up. Symptoms that develop in <60 seconds indicate a positive test for ulnar nerve compression, with the pinky and ulnar half of the ring finger most likely to have loss of vibration and light touch perception. A positive Tinel’s sign over the cubital tunnel is an indication of ulnar neuritis.18
If the ulnar nerve moves out of the ulnar groove when the groove is palpated as the elbow is flexed and extended, subluxating ulnar nerve is the likely diagnosis. If 2 structures displace over the medial epicondyle with elbow flexion, the first will be the ulnar nerve and the second will be the medial head of the triceps—an indication of a snapping medial head of triceps.18
Imaging studies may require a second look
Imaging studies are sometimes used to further aid in diagnosis of elbow injury. However, standard elbow x-rays, including an anteroposterior view in full extension, an oblique view, and a lateral view at 90° flexion, can be deceiving, as they often appear normal in conditions causing medial elbow pain associated with overhead throwing.
Careful review of the images may be needed to rule out fracture and other conditions, keeping the following factors in mind:
- A supracondylar fracture is likely if the anterior humeral line that is drawn along the anterior surface of the humeral cortex (on a lateral view) does not transect the middle third of the midcapitellum.3,11,18
- Dislocation of the radial head is suggested if the radiocapitellar line (drawn through the center of the radial head and neck) does not transect the midcapitellum on a lateral view.3,11,18
- Intra-articular injury with a joint effusion is indicated when an enlarged anterior fat pad, which is slightly anterior to the distal humeral diaphysis, is visible (the “sail sign”) on a normal elbow radiograph.3,11,18
- A fracture is likely if a posterior fat pad (which lies in the olecranon fossa and is not usually visible unless an effusion elevates the fat pad away from the cortex) is visible on an elbow x-ray. 3,11,18
- A chronic UCL tear is suggested by heterotropic calcification of the UCL.19
It is useful to x-ray both the injured and the unaffected elbows in skeletally immature athletes to compare secondary ossification centers. Little League elbow demonstrates a widening of the medial epicondyle physis, for example, when the x-rays are compared.3 Secondary ossification centers of the elbow appear first at the capitellum (age 2), followed by the radial head (age 5), medial epicondyle (age 7), trochlea (age 9), and lateral epicondyle (age 11). Most ossification centers fuse between 14 and 17 years of age.3
Computed tomography arthrograms, magnetic resonance imaging (MRI), and ultrasonography are also used to identify UCL tears. MRI, which can reveal injuries to cartilage and tendons as well, is the most commonly used imaging technique for musculoskeletal diagnosis of the elbow.16,20
Treatment gets most athletes back on track
Most medial elbow injuries respond to conservative treatment—typically, with some combination of activity modification, nonsteroidal anti-inflammatory drugs (NSAIDs), icing, physical therapy aimed at flexor-pronator strengthening, and counterforce bracing.11 Medial epicondylosis and flexor-pronator strain injuries have an excellent prognosis, with more than 90% of patients back to their previous level of activity at 1 year. Initial treatment consists of a 2- to 3-week rest period, followed by a 6- to 12-week rehabilitation protocol.11
Randomized controlled trials have found limited evidence of short-term improvement in symptoms with corticosteroid injections compared with placebo or no treatment, local anesthetic, orthosis, physical therapy, and NSAIDs. However, corticosteroids were less effective than physiotherapy or oral NSAIDs in improving long-term outcomes.21 Despite a paucity of well-designed studies to prove their use, autologous blood, platelet-rich plasma, and botulinum toxin are sometimes used for refractory elbow pain.21
Treatment of Little League elbow consists of cessation of throwing for at least 4 to 6 weeks, with a gradual return to throwing and emphasis on proper throwing mechanics after the pain resolves. Most throwers are out of competition for 2 to 3 months, but fully recover with nonoperative management.21
UCL injuries, too, are initially treated with rest, NSAIDs, icing, bracing, and physical therapy, typically with 2 to 3 months of no throwing. Some patients also use a splint at 90° flexion at night and as needed for pain during the day. Patients whose symptoms last more than a year despite treatment may be candidates for arthroscopic debridement.11
Consider reconstruction when nonsurgical management fails
UCL reconstruction was introduced in 1974, when reconstruction was performed on professional pitcher Tommy John, who went on to win 164 games.4,9 The procedure has since undergone numerous modifications. Surgery is indicated for acute rupture, significant chronic instability, insufficient UCL tissue after debridement, or recurrent pain and valgus instability with throwing after rehabilitation.2,4,6,9
Reconstruction generally entails fixing a tendon graft through bone tunnels in the medial epicondyle of the humerus and sublime tubercle of the ulna to reestablish valgus stability. A recent systematic review of reconstruction methods found a 76% to 95% rate of excellent results, with patients returned to their prior level of activity at a mean follow-up of 1 year.22 Rehabilitation typically begins 7 days postop; throwing (without windup) may begin in 4 to 5 months, with a gradual increase in speed and force and a return to the game at 12 months.
A stepped-up focus on prevention
The increase in UCL injuries in adolescents highlights the need for greater emphasis on prevention.10 Several governing bodies, including USA Baseball and the American Academy of Pediatrics, have developed research-based guidelines for young athletes (TABLE 2).1,10,23-25
One of the easiest to follow is to limit an athlete’s weekly pitch count to 10 times his age. Thus, a 10 year old should pitch no more than 100 pitches in a given 7-day period. Another important measure—in addition to ensuring that young athletes receive instruction in proper pitching mechanics (see http://www.littleleague.org/Little_League_Online.htm)—is to urge coaches and parents to require players to get at least 3 months of rest after each season and to stop throwing if they have pain or fatigue.24
TABLE 2
Keeping young pitchers injury-free1,10,23-25
| Recommendations for coaches and parents |
|---|
| Record the number of pitches thrown at each outing/sports event for all young pitchers |
| Avoid allowing young athletes to pitch competitively >8 months per year |
| Limit the number of pitches to ≤2500 per year and 10 × the pitcher’s age per week, or 90 per outing |
| Ensure that young pitchers are instructed in proper pitching mechanics |
| Restrict throwing breaking ball pitches* prior to puberty |
| Ensure that young pitchers get 3 months of rest per year. |
| *A pitch that changes direction either sideways or downwards as it approaches the batter, eg, a slider or curve ball. |
CORRESPONDENCE
Jennifer A. Southard, MD, MSc, Saint Alphonsus Medical Group, 6533 Emerald Street, Boise, ID 83704; [email protected]
• Administer the valgus stress test, the “milking maneuver,” and the moving valgus stress test to athletes suspected of having ulnar collateral ligament injury. C
• Treat Little League elbow with nonsteroidal anti-inflammatory drugs, ice, brief immobilization, and a 4- to 6-week “break” from throwing. A
• Advise young baseball players (and their parents) to avoid pitching year-round, and to get 3 months of rest per year. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The growing popularity of club teams and year-round participation in sports has spawned an epidemic of elbow injuries in primary and secondary school students and young adults alike. The incidence of elbow pain in children engaged in sports that require overhead throwing, such as baseball, football, volleyball, tennis, and javelin, ranges from 45% to 78%.1
Fortunately, acute traumatic elbow injury, with pain severe enough to force the athlete to cease participation entirely, is relatively rare, accounting for only 1% to 5% of cases.1,2 Far more often, elbow pain is associated with overuse, resulting in a gradual onset of medial elbow soreness that does not prevent the athlete from playing.
When an athlete seeks care for elbow pain, there are a number of things to consider, including the patient’s age, skeletal maturity, and type and frequency of throwing. Younger “throwers” typically incur injuries related to the physes, while adolescents and adults are more likely to sustain injuries to the ligaments and tendons.3 In both cases, repetitive valgus stress is the mechanism of injury. This review—of elbow anatomy (see the box),4-6 injury, differential diagnosis, and treatment—will make it easier for you to get injured athletes back in the game.
The elbow has 3 articulations—ulnohumeral, radiocapitellar, and proximal radioulnar—that provide primary stability to valgus stress. The elbow’s soft tissue restraints include 2 ligament complexes (medial and lateral collateral), 4 muscle groups (flexors, extensors, pronators, supinators), and 3 major nerves (radial, median, ulnar) and their branches.
The ulnar collateral ligament (UCL) complex—which consists of the anterior and posterior bundles and the transverse ligament—is the main source of medial elbow stability. 4 Mechanical stability for overhead throwing is provided by both bony and soft tissue restraints. During the pitching motion, the forces generated exceed the UCL’s tensile strength, and protective flexor muscles are activated.5,6
And the pitch…There are 6 stages of throwing: windup, early cocking, late cocking, acceleration, deceleration, and follow-through. Elbow pain is most likely during the late-cocking or early acceleration phase of a throw, the point of ball/javelin release, or the moment the racquet hits the ball.4
Is it Little League elbow? Start with a targeted history
In skeletally immature athletes, open physes result in the epicondylar apophysis being the weakest structure on the medial aspect of the elbow. Thus, repetitive valgus stress and tension overload often lead to “Little League elbow”—an umbrella term with a differential diagnosis that encompasses medial epicondylar fragmentation, delayed or accelerated growth of the medial epicondyle, and delayed closure of its growth plate, among other conditions (TABLE 1).3,7,8
In more mature athletes, repetitive microtrauma to the ulnar collateral ligament (UCL) leads to its gradual attenuation or complete failure.7 This increases the stress on the radiocapitellar joint and olecranon, and can lead to edema, scarring, calcification, osteophyte formation, medial epicondylitis, ulnar nerve neurapraxia, or radiocapitellar chondral damage.9 Extended practices and tournaments, with no substantial rest period throughout the year, put adolescents at increased risk for UCL injuries.10
Regardless of age, the medical history of an athlete with elbow pain should elicit information about the mechanism of injury; the location, duration, and quality of the pain; factors that alleviate or exacerbate the pain; the presence of weakness or paresthesias; and the extent to which the pain has affected the patient’s ability to throw. Patients with chronic UCL injuries, for example, often report a loss of arm control and decrease in throwing speed. It is also important to address hand dominance, level of participation, the position played, changes in technique or training regimen, prior injuries, and the effects of any previous treatment.11
TABLE 1
Differential diagnosis of elbow injuries
| Location | Differential diagnosis |
|---|---|
| Medial | Little League elbow
|
| Anterior | Anterior capsule strain Biceps tendon rupture Biceps tendonitis Dislocation Median nerve compression (pronator) syndrome |
| Posterior | Olecranon bursitis Olecranon process or tip stress fracture Triceps rupture/olecranon avulsion Triceps tendonitis Trochlear rupture Valgus overload syndrome (posterior olecranon impingement syndrome) |
| Lateral | Capitellum fracture Lateral epicondylitis Lateral ulnar collateral ligament injury Osteochondritis dissecans Posterior interosseous nerve syndrome Posterolateral rotary instability Radial head fracture Radiocapitellar chondromalacia |
| Adapted from: McKeag DB, Moeller JL. ACSM’s Primary Care Sports Medicine. 2nd ed.3 | |
Compare the affected and uninjured extremities
Inspect, palpate, and assess the active and passive range of motion, strength, and neurovascular status of both arms, with the uninjured side serving as a comparison. The scapula, shoulder, and wrist are also involved in throwing, so these joints should be examined along with the elbow.
Measure range of motion. Normal ranges for the flexion-extension arc are 0 to 140°, with 75° of pronation and 82° of supination.12 Use a goniometer, if available, to ensure accuracy and reproducibility,1 and pay close attention to the position that elicits pain.
In medial epicondylitis, the full range of motion should be preserved. Patients experience pain at the medial epicondyle and overlying flexor-pronator mass proximately, and pain or weakness with resisted wrist flexion, and resisted pronation, at full extension.4,11 Flexor-pronator strain will produce similar findings, but edema or ecchymosis may be present and there may be pain immediately distal to the medial epicondyle.11
Pain associated with injury to the UCL—which courses distal and slightly posterior to the medial epicondyle—typically occurs 2 cm distal to the medial epicondyle over the anterior bundle. Tenderness over the UCL has a sensitivity of 81% to 94% for UCL tears, but a specificity of only 22%.13
Physical maneuvers can help identify source of elbow pain
A complete UCL tear can cause valgus gapping as small as 3 mm, which makes it difficult to detect on physical exam alone.4 Orthopedic and sports medicine literature recommend that 3 maneuvers be used to identify UCL pathology:4,14,15
The valgus stress test (FIGURE 1) assesses the effects of valgus stress on the UCL. Gapping >3 mm signifies UCL instability. The test has a sensitivity of 66% and a specificity of 60% for detecting a UCL strain or tear.13,16
The milking maneuver (FIGURE 2), performed by the patient (or by a clinician if the patient lacks flexibility), reproduces a common pitching exercise. Medial elbow pain or apprehension indicates UCL injury.13,16
The moving valgus stress test (FIGURE 3A-C) is done in an effort to recreate the flexion angles of the elbow during the late cocking and early acceleration phases of throwing. Pain anywhere in the arc of motion suggests a UCL injury; pain elicited at 45° of flexion suggests osteochondrosis of the humeral capitellum, while pain closer to full extension suggests osteochondrosis of the trochlea.13,16
FIGURE 1
Valgus stress test
With the injured elbow at 30° of flexion, the shoulder abducted and fully externally rotated, and the patient’s wrist under your arm, place one hand laterally over the elbow. Place the other hand under the ulna and the thumb over the ulnar collateral ligament and apply valgus stress. Gapping >3 mm is abnormal.
FIGURE 2
Milking maneuver
The patient grasps the thumb of the affected arm and pulls downward, with the affected elbow positioned as shown, stressing the ulnar collateral ligament (UCL). Elbow pain or apprehension is positive for UCL injury.
FIGURE 3
Moving valgus stress test
With the shoulder in abduction and maximum external rotation (A), place the elbow in maximum flexion and apply valgus force (B), and extend the elbow from full flexion to full extension (C) in an attempt to reproduce the medial pain.
Does your patient have 2 positive valgus tests and posterior pain?
Valgus extension overload syndrome, which is caused by repetitive stress and results in osteophytes, chondromalacia of the medial olecranon fossa, tension in the UCL, and compression of the radiocapitellar joint, will also produce positive valgus stress and positive moving valgus stress tests. Keep in mind, however, that patients with valgus extension overload often have loss of full extension and posterior elbow pain with forced elbow hyperextension.17
Look for ulnar nerve injury
The physical examination should also be used to test for ulnar nerve injury. The elbow flexion test—a provocative maneuver in which the patient flexes the elbow as far as possible and reports any tingling or numbness of the hand—should be included in the work-up. Symptoms that develop in <60 seconds indicate a positive test for ulnar nerve compression, with the pinky and ulnar half of the ring finger most likely to have loss of vibration and light touch perception. A positive Tinel’s sign over the cubital tunnel is an indication of ulnar neuritis.18
If the ulnar nerve moves out of the ulnar groove when the groove is palpated as the elbow is flexed and extended, subluxating ulnar nerve is the likely diagnosis. If 2 structures displace over the medial epicondyle with elbow flexion, the first will be the ulnar nerve and the second will be the medial head of the triceps—an indication of a snapping medial head of triceps.18
Imaging studies may require a second look
Imaging studies are sometimes used to further aid in diagnosis of elbow injury. However, standard elbow x-rays, including an anteroposterior view in full extension, an oblique view, and a lateral view at 90° flexion, can be deceiving, as they often appear normal in conditions causing medial elbow pain associated with overhead throwing.
Careful review of the images may be needed to rule out fracture and other conditions, keeping the following factors in mind:
- A supracondylar fracture is likely if the anterior humeral line that is drawn along the anterior surface of the humeral cortex (on a lateral view) does not transect the middle third of the midcapitellum.3,11,18
- Dislocation of the radial head is suggested if the radiocapitellar line (drawn through the center of the radial head and neck) does not transect the midcapitellum on a lateral view.3,11,18
- Intra-articular injury with a joint effusion is indicated when an enlarged anterior fat pad, which is slightly anterior to the distal humeral diaphysis, is visible (the “sail sign”) on a normal elbow radiograph.3,11,18
- A fracture is likely if a posterior fat pad (which lies in the olecranon fossa and is not usually visible unless an effusion elevates the fat pad away from the cortex) is visible on an elbow x-ray. 3,11,18
- A chronic UCL tear is suggested by heterotropic calcification of the UCL.19
It is useful to x-ray both the injured and the unaffected elbows in skeletally immature athletes to compare secondary ossification centers. Little League elbow demonstrates a widening of the medial epicondyle physis, for example, when the x-rays are compared.3 Secondary ossification centers of the elbow appear first at the capitellum (age 2), followed by the radial head (age 5), medial epicondyle (age 7), trochlea (age 9), and lateral epicondyle (age 11). Most ossification centers fuse between 14 and 17 years of age.3
Computed tomography arthrograms, magnetic resonance imaging (MRI), and ultrasonography are also used to identify UCL tears. MRI, which can reveal injuries to cartilage and tendons as well, is the most commonly used imaging technique for musculoskeletal diagnosis of the elbow.16,20
Treatment gets most athletes back on track
Most medial elbow injuries respond to conservative treatment—typically, with some combination of activity modification, nonsteroidal anti-inflammatory drugs (NSAIDs), icing, physical therapy aimed at flexor-pronator strengthening, and counterforce bracing.11 Medial epicondylosis and flexor-pronator strain injuries have an excellent prognosis, with more than 90% of patients back to their previous level of activity at 1 year. Initial treatment consists of a 2- to 3-week rest period, followed by a 6- to 12-week rehabilitation protocol.11
Randomized controlled trials have found limited evidence of short-term improvement in symptoms with corticosteroid injections compared with placebo or no treatment, local anesthetic, orthosis, physical therapy, and NSAIDs. However, corticosteroids were less effective than physiotherapy or oral NSAIDs in improving long-term outcomes.21 Despite a paucity of well-designed studies to prove their use, autologous blood, platelet-rich plasma, and botulinum toxin are sometimes used for refractory elbow pain.21
Treatment of Little League elbow consists of cessation of throwing for at least 4 to 6 weeks, with a gradual return to throwing and emphasis on proper throwing mechanics after the pain resolves. Most throwers are out of competition for 2 to 3 months, but fully recover with nonoperative management.21
UCL injuries, too, are initially treated with rest, NSAIDs, icing, bracing, and physical therapy, typically with 2 to 3 months of no throwing. Some patients also use a splint at 90° flexion at night and as needed for pain during the day. Patients whose symptoms last more than a year despite treatment may be candidates for arthroscopic debridement.11
Consider reconstruction when nonsurgical management fails
UCL reconstruction was introduced in 1974, when reconstruction was performed on professional pitcher Tommy John, who went on to win 164 games.4,9 The procedure has since undergone numerous modifications. Surgery is indicated for acute rupture, significant chronic instability, insufficient UCL tissue after debridement, or recurrent pain and valgus instability with throwing after rehabilitation.2,4,6,9
Reconstruction generally entails fixing a tendon graft through bone tunnels in the medial epicondyle of the humerus and sublime tubercle of the ulna to reestablish valgus stability. A recent systematic review of reconstruction methods found a 76% to 95% rate of excellent results, with patients returned to their prior level of activity at a mean follow-up of 1 year.22 Rehabilitation typically begins 7 days postop; throwing (without windup) may begin in 4 to 5 months, with a gradual increase in speed and force and a return to the game at 12 months.
A stepped-up focus on prevention
The increase in UCL injuries in adolescents highlights the need for greater emphasis on prevention.10 Several governing bodies, including USA Baseball and the American Academy of Pediatrics, have developed research-based guidelines for young athletes (TABLE 2).1,10,23-25
One of the easiest to follow is to limit an athlete’s weekly pitch count to 10 times his age. Thus, a 10 year old should pitch no more than 100 pitches in a given 7-day period. Another important measure—in addition to ensuring that young athletes receive instruction in proper pitching mechanics (see http://www.littleleague.org/Little_League_Online.htm)—is to urge coaches and parents to require players to get at least 3 months of rest after each season and to stop throwing if they have pain or fatigue.24
TABLE 2
Keeping young pitchers injury-free1,10,23-25
| Recommendations for coaches and parents |
|---|
| Record the number of pitches thrown at each outing/sports event for all young pitchers |
| Avoid allowing young athletes to pitch competitively >8 months per year |
| Limit the number of pitches to ≤2500 per year and 10 × the pitcher’s age per week, or 90 per outing |
| Ensure that young pitchers are instructed in proper pitching mechanics |
| Restrict throwing breaking ball pitches* prior to puberty |
| Ensure that young pitchers get 3 months of rest per year. |
| *A pitch that changes direction either sideways or downwards as it approaches the batter, eg, a slider or curve ball. |
CORRESPONDENCE
Jennifer A. Southard, MD, MSc, Saint Alphonsus Medical Group, 6533 Emerald Street, Boise, ID 83704; [email protected]
1. American Academy of Pediatrics Committee on Sports Medicine and Fitness. Risk of injury from baseball and softball in children. Pediatrics. 2001;107:782-784.
2. Maloney MD, Morhr KJ, el Attrache NS, et al. Elbow injuries in the throwing athlete. Clin Sports Med. 1999;18:795-809.
3. McKeag DB, Moeller JL. ACSM’s Primary Care Sports Medicine. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:387–402.
4. Hariri S, Safran MR. Ulnar collateral ligament injury in the overhead athlete. Clin Sports Med. 2010;29:619-644.
5. Park MJ, Kim HG, Lee JY. Surgical treatment of post-traumatic stiffness of the elbow. J Bone Joint Surg Br. 2004;86:1158-1162.
6. Lin F, Kohli N, Perlmutter S, et al. Muscle contribution to elbow joint valgus stability. J Shoulder Elbow Surg. 2007;16:795-802.
7. Fleisig GS, Andrews JR, Dillman CJ, et al. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233-239.
8. Baker CL, Romero AA. Osteochondritis dissecans of the capitellum. Am J Sports Med. 2010;38:1917-1928.
9. Cain EL, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38:2426-2434.
10. Fleisig GS, Andrews JR, Cutter GR, et al. Prevention of elbow injuries in youth baseball pitchers. Curr Sports Med Rep. 2009;8:250-254.
11. Madden CC, Putukian M, McCarty E, et al. Netter’s Sports Medicine. Philadelphia, PA: Saunders Elsevier; 2010:360–367.
12. Boone DC, Azen SP. Normal range of motion of joints in male subjects. J Bone Joint Surg Am. 1979;61:756-759.
13. Timmerman LA, Schwartz ML, Andrews JR. Preoperative evaluation of the ulnar collateral ligament by magnetic resonance imaging and computed tomography arthrography. Evaluation in 25 baseball players with surgical confirmation. Am J Sports Med. 1994;22:26-31.
14. Mehlhoff TL, Bennet JB. Elbow injuries. In: Mellion MB, Walsh WM, Shelton GI, eds. The Team Physician’s Handbook. 2nd ed. Philadelphia, PA: Hanley & Belfus; 1997:461–473.
15. O’Connor FG, Ollivierre CO, Nirschl RP. Elbow and forearm injuries. In: Lillegard WA, Butcher KS, eds. Handbook of Sports Medicine: A Symptom-Oriented Approach. 2nd ed. Boston, MA: Butterworth-Heinemann; 1999:141–157.
16. Safran MR, Greene H, Lee TQ. Comparison of elbow valgus laxity using radiographic and non-radiographic objective measurement. 73rd Annual Meeting of the American Academy of Orthopaedic Surgeons; May 22, 2006; Chicago, IL.
17. Ahmad CS, El Attrache NS. Valgus extension overload syndrome and stress injury of the olecranon. Clin Sports Med. 2004;23:665-676.
18. Sarwart JF. Essentials of Musculoskeletal Care. 4th ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010:384–387.
19. Mulligan SA, Schwartz ML, Broussard MF, et al. Heterotopic calcification and tears of the ulnar collateral ligament: radiographic and MR imaging findings. AJR Am J Roentgenol. 2000;175:1099-1102.
20. Tuite MJ, Kijowski R. Sports related injures of the elbow: an approach to MRI interpretation. Clin Sports Med. 2006;25:387-408.
21. Rineer CA, Ruch DS. Elbow tendinopathy and tendon ruptures: epicondylitis, biceps and triceps ruptures. J Hand Surg Am. 2009;34:566-576.
22. Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008;36:1993-205.
23. Olsen SJ, Fleisig GS, Dun S, et al. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34:905-912.
24. Lyman S, Fleisig GS, Andrews JR, et al. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30:463-468.
25. Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011;39:253-257.
1. American Academy of Pediatrics Committee on Sports Medicine and Fitness. Risk of injury from baseball and softball in children. Pediatrics. 2001;107:782-784.
2. Maloney MD, Morhr KJ, el Attrache NS, et al. Elbow injuries in the throwing athlete. Clin Sports Med. 1999;18:795-809.
3. McKeag DB, Moeller JL. ACSM’s Primary Care Sports Medicine. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:387–402.
4. Hariri S, Safran MR. Ulnar collateral ligament injury in the overhead athlete. Clin Sports Med. 2010;29:619-644.
5. Park MJ, Kim HG, Lee JY. Surgical treatment of post-traumatic stiffness of the elbow. J Bone Joint Surg Br. 2004;86:1158-1162.
6. Lin F, Kohli N, Perlmutter S, et al. Muscle contribution to elbow joint valgus stability. J Shoulder Elbow Surg. 2007;16:795-802.
7. Fleisig GS, Andrews JR, Dillman CJ, et al. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233-239.
8. Baker CL, Romero AA. Osteochondritis dissecans of the capitellum. Am J Sports Med. 2010;38:1917-1928.
9. Cain EL, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38:2426-2434.
10. Fleisig GS, Andrews JR, Cutter GR, et al. Prevention of elbow injuries in youth baseball pitchers. Curr Sports Med Rep. 2009;8:250-254.
11. Madden CC, Putukian M, McCarty E, et al. Netter’s Sports Medicine. Philadelphia, PA: Saunders Elsevier; 2010:360–367.
12. Boone DC, Azen SP. Normal range of motion of joints in male subjects. J Bone Joint Surg Am. 1979;61:756-759.
13. Timmerman LA, Schwartz ML, Andrews JR. Preoperative evaluation of the ulnar collateral ligament by magnetic resonance imaging and computed tomography arthrography. Evaluation in 25 baseball players with surgical confirmation. Am J Sports Med. 1994;22:26-31.
14. Mehlhoff TL, Bennet JB. Elbow injuries. In: Mellion MB, Walsh WM, Shelton GI, eds. The Team Physician’s Handbook. 2nd ed. Philadelphia, PA: Hanley & Belfus; 1997:461–473.
15. O’Connor FG, Ollivierre CO, Nirschl RP. Elbow and forearm injuries. In: Lillegard WA, Butcher KS, eds. Handbook of Sports Medicine: A Symptom-Oriented Approach. 2nd ed. Boston, MA: Butterworth-Heinemann; 1999:141–157.
16. Safran MR, Greene H, Lee TQ. Comparison of elbow valgus laxity using radiographic and non-radiographic objective measurement. 73rd Annual Meeting of the American Academy of Orthopaedic Surgeons; May 22, 2006; Chicago, IL.
17. Ahmad CS, El Attrache NS. Valgus extension overload syndrome and stress injury of the olecranon. Clin Sports Med. 2004;23:665-676.
18. Sarwart JF. Essentials of Musculoskeletal Care. 4th ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2010:384–387.
19. Mulligan SA, Schwartz ML, Broussard MF, et al. Heterotopic calcification and tears of the ulnar collateral ligament: radiographic and MR imaging findings. AJR Am J Roentgenol. 2000;175:1099-1102.
20. Tuite MJ, Kijowski R. Sports related injures of the elbow: an approach to MRI interpretation. Clin Sports Med. 2006;25:387-408.
21. Rineer CA, Ruch DS. Elbow tendinopathy and tendon ruptures: epicondylitis, biceps and triceps ruptures. J Hand Surg Am. 2009;34:566-576.
22. Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008;36:1993-205.
23. Olsen SJ, Fleisig GS, Dun S, et al. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34:905-912.
24. Lyman S, Fleisig GS, Andrews JR, et al. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30:463-468.
25. Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011;39:253-257.
The Where and Why of Postsurgical Adhesions
The prevention of postsurgical adhesions is one of the greatest unmet needs in medicine today. Surgical series have shown that adhesions are present after 80%-90% of abdominal and pelvic surgeries, and that these abnormal fibrous connections have a tremendous propensity to reform after adhesiolysis. (We will define adhesions here as “attachments between surfaces at nonanatomical locations.”)
In gynecologic surgery, postoperative adhesions are a frequent cause of infertility, pain, bowel obstruction, and difficulty in later procedures. Adhesions can occur after minimally invasive procedures, which have the potential for trocar injury to structures adherent to the anterior abdominal wall. Other intraoperative injuries can occur due to obscured normal anatomy or restricted access. A significant number of patients also undergo second surgeries to treat sequelae that are directly related to adhesions.
The literature is replete with studies of adhesion development and reports of its incidence and its consequences. Still, the problem of postoperative adhesion development often goes underestimated or unrecognized. This is because we don't routinely perform early second-look operations to assess adhesion development, and because there are no serum markers or sensitive imaging techniques to allow their identification. In addition, we do not follow our patients who seek care from other providers as insurance coverage changes or as other health problems arise, such as bowel obstruction being treated by a general surgeon.
As gynecologic surgeons, we must appreciate that while infections, endometriosis, and other peritoneal insults may contribute to adhesion development, surgery is the most common cause. We also must appreciate how tissue injury leads to the development of adhesions, and why adhesion reformation so commonly occurs.
This understanding is critical to our consideration and use of the “barrier” products currently available for reducing postsurgical adhesions — and critical to our efforts to employ the tenets of gynecologic microsurgery and to achieve as optimal a surgical outcome as possible. At this point in time, use of approved surgical adjuvants in combination with good surgical technique offers the best chance at adhesion reduction and prevention.
Incidence of Adhesions
A series of reports published in the early to mid-1980s documented how commonly adhesions develop after various types of reproductive pelvic surgery. Through early second-look laparoscopy, postoperative adhesions were found to occur, in these studies, in 55%–100% of patients after their primary gynecologic surgery.
In a multicenter study published in 1987, my colleagues and I also showed that gynecologic surgeries performed at the time of laparotomy are frequently complicated by both adhesion reformation and de novo adhesion formation. More than half of the 161 women (51%) who had a second-look laparoscopy 1–12 weeks after reproductive pelvic surgery were found to have de novo adhesion formation (adhesions in at least one new location). Adhesion reformation was also widespread: At the initial laparotomy, 121 of the patients (all of whom were treated for infertility) were noted to have some form of adhesion, and adhesion reformation subsequently occurred at the site of adhesiolysis in 85% of these women, with no differences with respect to adhesion type (Fertil. Steril. 1987;47;864–6).
It was hoped, and largely expected, that the growth of laparoscopy and minimally invasive surgery approaches in more recent years would reduce postoperative adhesion development — that minimally invasive techniques would prove to be less adhesiogenic than laparotomy. Questions remain, but thus far, such hopes have diminished and our expectations for significant improvement have gone unsubstantiated.
One multicenter study on adhesion development after initial laparoscopic procedures found that the incidence of adhesions at an early second-look procedure was 97% — no lower than in prior reports of second-look laparoscopy after laparotomy.
In this study, 68 women underwent operative laparoscopic procedures, including adhesiolysis, and had second-look procedures within 90 days. The good news was that de novo adhesion formation between the two laparoscopic procedures occurred in only 8 of the women (12%) and at 11 of 47 possible sites — much less frequently than after laparotomy. Adhesion scores also decreased at the second look compared with the status of the pelvis at the initial procedure. Still, with the high rate of adhesion reformation, almost all of the women developed postoperative adhesions.
Thus, even when the initial procedure was performed laparoscopically, adhesion development was an all-too-common occurrence, and appeared to be independent of the character of the initial adhesion (Fertil. Steril. 1991;55:700–4).
More recently, data from randomized studies of various adhesion barriers and potential anti-adhesion adjuvants have further dashed hopes that laparoscopy per se can reduce adhesion development.
For instance, in a recent small pilot study of a fibrin-based product called Adhexil, “control” ovaries that were not treated had a 27% increase in the mean adhesion score between an initial laparoscopic procedure and second-look laparoscopy. The women in the study had undergone bilateral ovarian surgery, with ovaries randomized for application of the product or no treatment (Fertil. Steril. 2011;95:1086–90). Clearly, a laparoscopic approach to their procedures did not prevent the development of adhesions.
Many of the initial studies on adhesion development were comprised of patients with infertility, but more recent observations have been extended to women without infertility and to men. Studies have covered patients undergoing colectomies, for instance, as well as neonates undergoing cardiothoracic procedures.
In a recent review article on adhesion prevention and reduction, members of an interdisciplinary consensus conference stated that adhesions develop after “nearly all” abdominal and pelvic procedures performed through either standard laparotomy or laparoscopic approaches. With respect to gynecologic surgery, they point out, research has shown that the most common site for postsurgical adhesion development is the ovary (Surg. Innov. 2010;17:183–8).
Consequences
Pelvic adhesions are a well-recognized cause of infertility, contributing to up to an estimated 40% of the cases of infertility in women. Adhesions are also a leading cause of bowel obstruction and a significant cause of chronic or recurrent pelvic pain.
The contribution of pelvic adhesions to chronic pelvic pain is not completely understood. Adhesions may be the cause of pain in some women, and in other women, an incidental finding that is not contributing to pain. In patients who have endometriosis as well, the question remains as to the contribution of endometriosis per se, or adhesions, to the pain. Endometriosis can cause adhesions and chronic pelvic pain, presumably through the cyclic generation of inflammatory molecules.
The relationship between chronic pain and adhesions is further complicated by ensuing questions about the efficacy of adhesiolysis. The two randomized trials that have thus far examined the role of adhesiolysis in the reduction of chronic pelvic pain failed to demonstrate a significant improvement in pain after adhesiolysis; however, the high failure rates after follow-up may be due to adhesion reformation and de novo adhesion formation (Fertil. Steril. 2004;82:1483–91). Performance of more randomized comparisons in the future may yield improved outcomes when adhesiolysis is paired with postprocedure use of anti-adhesion adjuvants.
Despite the uncertainties, multiple studies support the current estimation that adhesions cause or significantly contribute to chronic pelvic pain in up to 30% of women with the problem. As the Ovarian Adhesion Study Group noted in one of its reports, adhesions have been reported as a primary cause of chronic pelvic pain in 13%-36% of women, depending on the study (Obstet. Gynecol. 1995;86:335–40). Economic analyses also have quantified the impact of adhesion-related hospital readmissions. A study done in the United Kingdom, for instance, concluded that 6% of all hospital readmissions in patients who had undergone abdominal or pelvic surgery were directly related to adhesions (Lancet 1999;353:1476–80).httother report on hospitalizations for lower abdominal adhesiolysis in the United States estimated that in 1988, the cost of adhesions stemming from gynecologic procedures alone was almost $1.2 billion. This estimate did not include outpatient and indirect costs (Surg. Gynecol. Obstet. 1993;176:271–6).
Why, How Adhesions Develop
Our current understanding is that adhesions develop as a result of injury to and devascularization of the peritoneum, and the subsequent inflammatory response and peritoneal wound healing process. Tissue hypoxia triggers a cascade of intracellular responses that, in combination with the fibrinous collection of blood and serosanguinous fluid at the tissue surface, may result in adhesion development.
In the initial postsurgical period, either overt bleeding or oozing may occur at the site(s) of tissue injury, forming clots. In combination with serosanguinous fluid, which may leak from damaged peritoneal surfaces, a fibrinous mass thus develops at the surgical sites and sites of tissue injury. This represents an initial step in peritoneal repair.
When surrounding tissue is normal and there is a sufficient amount of plasminogen activator present in the peritoneum — and when numerous other events and conditions are optimal — the resulting fibrinous mass can be degraded. As that occurs, and tissue healing continues, fibroblasts are recruited to the surface of the injury site from underlying tissues.
If the fibrinous mass is no longer present, fibroblasts “stop” at the tissue surfaces, and become covered by mesothelial cells which line the peritoneal surface as the process of remesothelialization occurs. This process appears to be initiated within hours after surgery and is generally believed to be completed in 3–5 days. (In such instances, healing would have occurred without adhesions, although subperitoneal fibrosis may have occurred.)
Various hypoxia-driven responses, however, such as a reduction in plasminogen activator activity, can cause the fibrinous mass to persist during the healing process, before remesothelialization occurs. In this case, fibroblasts migrate not only to, but through, the injury site, and into the persisting fibrinous mass. This is subsequently followed by deposition of collagen, fibronectin, and other extracellular matrix materials — creating the beginnings of a true adhesion.
In such cases, remesothelialization still occurs, but the mesothelial cells cover the adhesion as well as the normal tissue surfaces, forming adhesive bands and other types of connections between opposing serosal tissue surfaces. Angiogenesis then occurs as the hypoxic tissue in the adhesion sends signals (such as vascular endothelial growth factor) in an attempt to reestablish a supply of oxygen and nutrients to the injured and devascularized tissues. Subsequently, as the tissue remodels, there is a propensity for the adhesion to become more vascular and denser.
Understanding this process is important because the products currently available for reducing adhesions act as barriers during this critical period of remesothelialization, keeping peritoneal surfaces apart and minimizing the potential development of a fibrinous mass that bridges tissue surfaces. If an adhesion does not form during the 3–5-day period of remesothelialization, it is theorized that there will not be any adhesion development — unless there's new injury to the tissue surfaces.
Once an adhesion forms, however, it has acquired a particular “adhesion phenotype” — different from that of normal peritoneum — that appears to be irreversible. This is likely why it is so difficult to prevent adhesion reformation after adhesiolysis. Rates of adhesion reformation — even in the best of surgical hands — run between 80% and 90%, compared with a 50% chance of de novo adhesion development after surgery (at new sites of injury).
The identification of an adhesion phenotype came originally from comparisons of normal peritoneal and adhesion tissues harvested from the same patient, and were later confirmed in cell culture studies in which normal peritoneal fibroblasts were subjected to hypoxia (2% O2 conditions). Fibroblasts cultured under hypoxic conditions were subsequently found to have developed particular molecular biologic characterizations that are different from those of normal peritoneal fibroblasts.
When exposed to normal amounts of oxygen again, the fibroblasts did not go back to being normal fibroblasts — they continued to manifest the adhesion phenotype (J. Am Assoc. Gynecol. Laparosc. 2004;11:307–14). These findings have been confirmed in animal and human studies, and such relationships have also been identified in other peritoneal tissue types such as mesothelial cells and macrophages.
Further research on the pathogenesis of adhesions and the molecular biologic differences between normal peritoneum and adhesions may allow identification of which patients, and which sites within a patient, are most at risk for adhesion development, as well as the discovery of new ways to reduce the development of postoperative adhesions and their clinical sequelae.
It is possible that a future generation of barrier products not only will work as a barrier separating surfaces prior to remesothelialization, but will also have local biologic effects — delivering adhesion-reducing drugs or biologics, for instance, to specific localized tissue sites. A personalized approach to adhesion prevention also might be possible, with particular factors deemed to increase adhesion risk in individual patients (a deficiency of plasminogen activator, for instance) being corrected.
In the meantime, as we've learned more about the pathophysiological state under which adhesions develop, we have found that adhesion development may occur faster than we had thought. In one recent rodent study, we identified postoperative tissue attachments as early as 2 hours after cecal abrasion. We noted considerable local edema and vessel dilatation within 2 hours of injury, angiogenesis and fibrin deposition at 8 hours, and cell proliferation at 24 hours (Fertil. Steril. 2010;93:2734–7). And interestingly, recent studies in mice have shown that laparoscopic insufflation per se can induce peritoneal adhesions, with the adhesions increasing proportionally with both increasing duration of insufflation and an increase in intraperitoneal pressure.
Prevention in Practice
During the past decade a variety of surgical adjuvants — from procoagulants and fibrinolytic agents to anti-inflammatory drugs and antibiotics — have been investigated for use in reducing the occurrence, extent, and severity of adhesions. Unfortunately, most approaches seemingly have been futile. Some products have shown trends toward efficacy in animal or early human studies and need further investigation.
The three synthetic products that are approved by the Food and Drug Administration—Gynecare Interceed, Seprafilm, and Adept — can help reduce postoperative adhesions after gynecologic procedures, and should be considered as potentially useful surgical adjuvants. A meta-analysis of studies of Gynecare Interceed, for instance, found that approximately twice as many operative sites were adhesion free after use of the barrier than after surgery alone (J. Reprod. Med. 1999;44:325–31).
Gynecare Interceed (Johnson & Johnson) and Seprafilm (Genzyme) are approved for use only at laparotomy, while Adept (Baxter International), an icodextrin solution that disperses throughout the abdominopelvic cavity, is approved for use only in laparoscopic surgery.
The key consideration to make when using Interceed — a biodegradable woven fabric composed of oxidized, regenerated cellulose — is the importance of achieving meticulous hemostasis. Its efficacy is reduced, or can even be lost, in the presence of blood. Care also must be taken not to stretch the material or alter its shape and the spacing between the weaves. Otherwise, the material, once gelated, will have a greater potential for spaces in which the tissue surfaces would not be separated and thus a greater potential for blood coagulation and fibroblast in-growth. Multiple pieces of the material may be overlapped, but there have been no benefits demonstrated (at least in animal studies) to using double layers.
Care in application also is critically important for Seprafilm, a film composed of modified hyaluronic acid and carboxymethylcellulose. Seprafilm is brittle and is difficult to apply through small incisions. While it's not impossible to deliver the product laparoscopically, many surgeons have found this very difficult. And in the United States, it is approved for use with laparotomy only.
In applying Seprafilm, it is critical to first get good exposure of the field and then position the film very carefully. Attempts to reposition the product will often result in tears or breaks. Of course, just as with Interceed, this device is believed to work primarily by separating tissue surfaces, and thus it has little to no chance of success if it does not completely separate the surgically injured tissue from other tissue surfaces in the initial postoperative period while remesothelialization is occurring.
The use of adjuvants, moreover, is no substitute for good surgical technique that aims to minimize tissue injury, tissue devascularization, and inflammation. This is easier to achieve, of course, during a microsurgical procedure such as a tubal anastomosis than in a patient with severe endometriosis or many large fibroids. Still, to the extent possible for the procedure being conducted, the tenets of gynecologic microsurgery should always be considered:
▸ Handle as little tissue as possible, as minimally as possible. To the extent possible, handle only those portions that will subsequently be excised.
▸ Keep tissues moist. Tissue drying leads to injury and loss of mesothelial cells. Raw surfaces are more prone to develop adhesions.
▸ Take special care in the use of suture. Consider whether clinical situations will allow use of less reactive and smaller-caliber suture. When using suture to tie off blood vessels, skeletonize the vessels so as to minimize the amount of tissue distal to the suture that will become hypoxic and serve as a nidus to adhesion development.
▸ Target the use of electrosurgery and other energy sources. Use it in specific localized sites where it's needed, such as to stop bleeding, but avoid widely dispersed use, when possible, again to minimize the amount of residual devitalized tissue remaining in the pelvis at the conclusion of the surgical procedure.
Pelvic Adhesions — An Update
“A number of human interventional trials and animal studies have evaluated techniques and materials designed to prevent and reduce postsurgical adhesions. The results have been inconclusive and sometimes contradictory. Thus, preventing postsurgical adhesions remains an art, rather than a science.” So I began my introduction to the program on adhesion prevention at the 2010 Congress of the Society of Laparoscopic Surgeons in New York City.
Patients with adhesions can present with small bowel obstruction or with complaints of infertility, chronic pain, or dyspareunia. Unfortunately, adhesive disease is problematic. Four percent of the patients undergoing abdominal and pelvic surgery will be readmitted due to adhesion-related complications. In excess of 400,000 surgical procedures are performed annually in the United States for lysis of adhesions. In a Scottish National Health Service Study of nearly 9,000 women who previously underwent open gynecologic surgery, just less than 3% were readmitted secondary to adhesions; the highest readmit rate was ovarian surgery (BJOG 2000;107:855–62).
While one would expect a reduction in the number of patients undergoing laparoscopic surgery, in reality, the verdict is not yet clear. A 1998 meta-analysis showed a decrease in both reformed (26.6% vs. 14.3%) and de novo adhesions (45.2% vs. 37.2%) in the laparoscopic group, compared with laparotomy (Fertil. Steril. 1998;70:702–11).
Despite this, other authors cite pneumoperitoneum, prolonged surgery, high insufflation pressure, and overzealous use of energy to cut and coagulate as reasons why laparoscopic surgery increases risk of adhesions.
The economic impact of adhesions is staggering, in excess of $1.3 billion in the United States per year.
For this current excerpt of the Master Class in Gynecologic Surgery, I have solicited the wisdom of Dr. Michael Diamond. He is the Kamran S. Moghissi Professor of Obstetrics and Gynecology and associate chairman of the department of obstetrics and gynecology at Wayne State University, Detroit. Dr. Diamond also is director of the division of reproductive endocrinology and infertility and assistant dean for clinical and translational research at the university. Dr. Diamond has spent much of his academic career involved in the pathogenesis, prevention, and treatment of pelvic adhesions. He is truly considered the world's leader in this area, and we are honored to have Dr. Diamond as guest author of this important area of our surgical arena.
The prevention of postsurgical adhesions is one of the greatest unmet needs in medicine today. Surgical series have shown that adhesions are present after 80%-90% of abdominal and pelvic surgeries, and that these abnormal fibrous connections have a tremendous propensity to reform after adhesiolysis. (We will define adhesions here as “attachments between surfaces at nonanatomical locations.”)
In gynecologic surgery, postoperative adhesions are a frequent cause of infertility, pain, bowel obstruction, and difficulty in later procedures. Adhesions can occur after minimally invasive procedures, which have the potential for trocar injury to structures adherent to the anterior abdominal wall. Other intraoperative injuries can occur due to obscured normal anatomy or restricted access. A significant number of patients also undergo second surgeries to treat sequelae that are directly related to adhesions.
The literature is replete with studies of adhesion development and reports of its incidence and its consequences. Still, the problem of postoperative adhesion development often goes underestimated or unrecognized. This is because we don't routinely perform early second-look operations to assess adhesion development, and because there are no serum markers or sensitive imaging techniques to allow their identification. In addition, we do not follow our patients who seek care from other providers as insurance coverage changes or as other health problems arise, such as bowel obstruction being treated by a general surgeon.
As gynecologic surgeons, we must appreciate that while infections, endometriosis, and other peritoneal insults may contribute to adhesion development, surgery is the most common cause. We also must appreciate how tissue injury leads to the development of adhesions, and why adhesion reformation so commonly occurs.
This understanding is critical to our consideration and use of the “barrier” products currently available for reducing postsurgical adhesions — and critical to our efforts to employ the tenets of gynecologic microsurgery and to achieve as optimal a surgical outcome as possible. At this point in time, use of approved surgical adjuvants in combination with good surgical technique offers the best chance at adhesion reduction and prevention.
Incidence of Adhesions
A series of reports published in the early to mid-1980s documented how commonly adhesions develop after various types of reproductive pelvic surgery. Through early second-look laparoscopy, postoperative adhesions were found to occur, in these studies, in 55%–100% of patients after their primary gynecologic surgery.
In a multicenter study published in 1987, my colleagues and I also showed that gynecologic surgeries performed at the time of laparotomy are frequently complicated by both adhesion reformation and de novo adhesion formation. More than half of the 161 women (51%) who had a second-look laparoscopy 1–12 weeks after reproductive pelvic surgery were found to have de novo adhesion formation (adhesions in at least one new location). Adhesion reformation was also widespread: At the initial laparotomy, 121 of the patients (all of whom were treated for infertility) were noted to have some form of adhesion, and adhesion reformation subsequently occurred at the site of adhesiolysis in 85% of these women, with no differences with respect to adhesion type (Fertil. Steril. 1987;47;864–6).
It was hoped, and largely expected, that the growth of laparoscopy and minimally invasive surgery approaches in more recent years would reduce postoperative adhesion development — that minimally invasive techniques would prove to be less adhesiogenic than laparotomy. Questions remain, but thus far, such hopes have diminished and our expectations for significant improvement have gone unsubstantiated.
One multicenter study on adhesion development after initial laparoscopic procedures found that the incidence of adhesions at an early second-look procedure was 97% — no lower than in prior reports of second-look laparoscopy after laparotomy.
In this study, 68 women underwent operative laparoscopic procedures, including adhesiolysis, and had second-look procedures within 90 days. The good news was that de novo adhesion formation between the two laparoscopic procedures occurred in only 8 of the women (12%) and at 11 of 47 possible sites — much less frequently than after laparotomy. Adhesion scores also decreased at the second look compared with the status of the pelvis at the initial procedure. Still, with the high rate of adhesion reformation, almost all of the women developed postoperative adhesions.
Thus, even when the initial procedure was performed laparoscopically, adhesion development was an all-too-common occurrence, and appeared to be independent of the character of the initial adhesion (Fertil. Steril. 1991;55:700–4).
More recently, data from randomized studies of various adhesion barriers and potential anti-adhesion adjuvants have further dashed hopes that laparoscopy per se can reduce adhesion development.
For instance, in a recent small pilot study of a fibrin-based product called Adhexil, “control” ovaries that were not treated had a 27% increase in the mean adhesion score between an initial laparoscopic procedure and second-look laparoscopy. The women in the study had undergone bilateral ovarian surgery, with ovaries randomized for application of the product or no treatment (Fertil. Steril. 2011;95:1086–90). Clearly, a laparoscopic approach to their procedures did not prevent the development of adhesions.
Many of the initial studies on adhesion development were comprised of patients with infertility, but more recent observations have been extended to women without infertility and to men. Studies have covered patients undergoing colectomies, for instance, as well as neonates undergoing cardiothoracic procedures.
In a recent review article on adhesion prevention and reduction, members of an interdisciplinary consensus conference stated that adhesions develop after “nearly all” abdominal and pelvic procedures performed through either standard laparotomy or laparoscopic approaches. With respect to gynecologic surgery, they point out, research has shown that the most common site for postsurgical adhesion development is the ovary (Surg. Innov. 2010;17:183–8).
Consequences
Pelvic adhesions are a well-recognized cause of infertility, contributing to up to an estimated 40% of the cases of infertility in women. Adhesions are also a leading cause of bowel obstruction and a significant cause of chronic or recurrent pelvic pain.
The contribution of pelvic adhesions to chronic pelvic pain is not completely understood. Adhesions may be the cause of pain in some women, and in other women, an incidental finding that is not contributing to pain. In patients who have endometriosis as well, the question remains as to the contribution of endometriosis per se, or adhesions, to the pain. Endometriosis can cause adhesions and chronic pelvic pain, presumably through the cyclic generation of inflammatory molecules.
The relationship between chronic pain and adhesions is further complicated by ensuing questions about the efficacy of adhesiolysis. The two randomized trials that have thus far examined the role of adhesiolysis in the reduction of chronic pelvic pain failed to demonstrate a significant improvement in pain after adhesiolysis; however, the high failure rates after follow-up may be due to adhesion reformation and de novo adhesion formation (Fertil. Steril. 2004;82:1483–91). Performance of more randomized comparisons in the future may yield improved outcomes when adhesiolysis is paired with postprocedure use of anti-adhesion adjuvants.
Despite the uncertainties, multiple studies support the current estimation that adhesions cause or significantly contribute to chronic pelvic pain in up to 30% of women with the problem. As the Ovarian Adhesion Study Group noted in one of its reports, adhesions have been reported as a primary cause of chronic pelvic pain in 13%-36% of women, depending on the study (Obstet. Gynecol. 1995;86:335–40). Economic analyses also have quantified the impact of adhesion-related hospital readmissions. A study done in the United Kingdom, for instance, concluded that 6% of all hospital readmissions in patients who had undergone abdominal or pelvic surgery were directly related to adhesions (Lancet 1999;353:1476–80).httother report on hospitalizations for lower abdominal adhesiolysis in the United States estimated that in 1988, the cost of adhesions stemming from gynecologic procedures alone was almost $1.2 billion. This estimate did not include outpatient and indirect costs (Surg. Gynecol. Obstet. 1993;176:271–6).
Why, How Adhesions Develop
Our current understanding is that adhesions develop as a result of injury to and devascularization of the peritoneum, and the subsequent inflammatory response and peritoneal wound healing process. Tissue hypoxia triggers a cascade of intracellular responses that, in combination with the fibrinous collection of blood and serosanguinous fluid at the tissue surface, may result in adhesion development.
In the initial postsurgical period, either overt bleeding or oozing may occur at the site(s) of tissue injury, forming clots. In combination with serosanguinous fluid, which may leak from damaged peritoneal surfaces, a fibrinous mass thus develops at the surgical sites and sites of tissue injury. This represents an initial step in peritoneal repair.
When surrounding tissue is normal and there is a sufficient amount of plasminogen activator present in the peritoneum — and when numerous other events and conditions are optimal — the resulting fibrinous mass can be degraded. As that occurs, and tissue healing continues, fibroblasts are recruited to the surface of the injury site from underlying tissues.
If the fibrinous mass is no longer present, fibroblasts “stop” at the tissue surfaces, and become covered by mesothelial cells which line the peritoneal surface as the process of remesothelialization occurs. This process appears to be initiated within hours after surgery and is generally believed to be completed in 3–5 days. (In such instances, healing would have occurred without adhesions, although subperitoneal fibrosis may have occurred.)
Various hypoxia-driven responses, however, such as a reduction in plasminogen activator activity, can cause the fibrinous mass to persist during the healing process, before remesothelialization occurs. In this case, fibroblasts migrate not only to, but through, the injury site, and into the persisting fibrinous mass. This is subsequently followed by deposition of collagen, fibronectin, and other extracellular matrix materials — creating the beginnings of a true adhesion.
In such cases, remesothelialization still occurs, but the mesothelial cells cover the adhesion as well as the normal tissue surfaces, forming adhesive bands and other types of connections between opposing serosal tissue surfaces. Angiogenesis then occurs as the hypoxic tissue in the adhesion sends signals (such as vascular endothelial growth factor) in an attempt to reestablish a supply of oxygen and nutrients to the injured and devascularized tissues. Subsequently, as the tissue remodels, there is a propensity for the adhesion to become more vascular and denser.
Understanding this process is important because the products currently available for reducing adhesions act as barriers during this critical period of remesothelialization, keeping peritoneal surfaces apart and minimizing the potential development of a fibrinous mass that bridges tissue surfaces. If an adhesion does not form during the 3–5-day period of remesothelialization, it is theorized that there will not be any adhesion development — unless there's new injury to the tissue surfaces.
Once an adhesion forms, however, it has acquired a particular “adhesion phenotype” — different from that of normal peritoneum — that appears to be irreversible. This is likely why it is so difficult to prevent adhesion reformation after adhesiolysis. Rates of adhesion reformation — even in the best of surgical hands — run between 80% and 90%, compared with a 50% chance of de novo adhesion development after surgery (at new sites of injury).
The identification of an adhesion phenotype came originally from comparisons of normal peritoneal and adhesion tissues harvested from the same patient, and were later confirmed in cell culture studies in which normal peritoneal fibroblasts were subjected to hypoxia (2% O2 conditions). Fibroblasts cultured under hypoxic conditions were subsequently found to have developed particular molecular biologic characterizations that are different from those of normal peritoneal fibroblasts.
When exposed to normal amounts of oxygen again, the fibroblasts did not go back to being normal fibroblasts — they continued to manifest the adhesion phenotype (J. Am Assoc. Gynecol. Laparosc. 2004;11:307–14). These findings have been confirmed in animal and human studies, and such relationships have also been identified in other peritoneal tissue types such as mesothelial cells and macrophages.
Further research on the pathogenesis of adhesions and the molecular biologic differences between normal peritoneum and adhesions may allow identification of which patients, and which sites within a patient, are most at risk for adhesion development, as well as the discovery of new ways to reduce the development of postoperative adhesions and their clinical sequelae.
It is possible that a future generation of barrier products not only will work as a barrier separating surfaces prior to remesothelialization, but will also have local biologic effects — delivering adhesion-reducing drugs or biologics, for instance, to specific localized tissue sites. A personalized approach to adhesion prevention also might be possible, with particular factors deemed to increase adhesion risk in individual patients (a deficiency of plasminogen activator, for instance) being corrected.
In the meantime, as we've learned more about the pathophysiological state under which adhesions develop, we have found that adhesion development may occur faster than we had thought. In one recent rodent study, we identified postoperative tissue attachments as early as 2 hours after cecal abrasion. We noted considerable local edema and vessel dilatation within 2 hours of injury, angiogenesis and fibrin deposition at 8 hours, and cell proliferation at 24 hours (Fertil. Steril. 2010;93:2734–7). And interestingly, recent studies in mice have shown that laparoscopic insufflation per se can induce peritoneal adhesions, with the adhesions increasing proportionally with both increasing duration of insufflation and an increase in intraperitoneal pressure.
Prevention in Practice
During the past decade a variety of surgical adjuvants — from procoagulants and fibrinolytic agents to anti-inflammatory drugs and antibiotics — have been investigated for use in reducing the occurrence, extent, and severity of adhesions. Unfortunately, most approaches seemingly have been futile. Some products have shown trends toward efficacy in animal or early human studies and need further investigation.
The three synthetic products that are approved by the Food and Drug Administration—Gynecare Interceed, Seprafilm, and Adept — can help reduce postoperative adhesions after gynecologic procedures, and should be considered as potentially useful surgical adjuvants. A meta-analysis of studies of Gynecare Interceed, for instance, found that approximately twice as many operative sites were adhesion free after use of the barrier than after surgery alone (J. Reprod. Med. 1999;44:325–31).
Gynecare Interceed (Johnson & Johnson) and Seprafilm (Genzyme) are approved for use only at laparotomy, while Adept (Baxter International), an icodextrin solution that disperses throughout the abdominopelvic cavity, is approved for use only in laparoscopic surgery.
The key consideration to make when using Interceed — a biodegradable woven fabric composed of oxidized, regenerated cellulose — is the importance of achieving meticulous hemostasis. Its efficacy is reduced, or can even be lost, in the presence of blood. Care also must be taken not to stretch the material or alter its shape and the spacing between the weaves. Otherwise, the material, once gelated, will have a greater potential for spaces in which the tissue surfaces would not be separated and thus a greater potential for blood coagulation and fibroblast in-growth. Multiple pieces of the material may be overlapped, but there have been no benefits demonstrated (at least in animal studies) to using double layers.
Care in application also is critically important for Seprafilm, a film composed of modified hyaluronic acid and carboxymethylcellulose. Seprafilm is brittle and is difficult to apply through small incisions. While it's not impossible to deliver the product laparoscopically, many surgeons have found this very difficult. And in the United States, it is approved for use with laparotomy only.
In applying Seprafilm, it is critical to first get good exposure of the field and then position the film very carefully. Attempts to reposition the product will often result in tears or breaks. Of course, just as with Interceed, this device is believed to work primarily by separating tissue surfaces, and thus it has little to no chance of success if it does not completely separate the surgically injured tissue from other tissue surfaces in the initial postoperative period while remesothelialization is occurring.
The use of adjuvants, moreover, is no substitute for good surgical technique that aims to minimize tissue injury, tissue devascularization, and inflammation. This is easier to achieve, of course, during a microsurgical procedure such as a tubal anastomosis than in a patient with severe endometriosis or many large fibroids. Still, to the extent possible for the procedure being conducted, the tenets of gynecologic microsurgery should always be considered:
▸ Handle as little tissue as possible, as minimally as possible. To the extent possible, handle only those portions that will subsequently be excised.
▸ Keep tissues moist. Tissue drying leads to injury and loss of mesothelial cells. Raw surfaces are more prone to develop adhesions.
▸ Take special care in the use of suture. Consider whether clinical situations will allow use of less reactive and smaller-caliber suture. When using suture to tie off blood vessels, skeletonize the vessels so as to minimize the amount of tissue distal to the suture that will become hypoxic and serve as a nidus to adhesion development.
▸ Target the use of electrosurgery and other energy sources. Use it in specific localized sites where it's needed, such as to stop bleeding, but avoid widely dispersed use, when possible, again to minimize the amount of residual devitalized tissue remaining in the pelvis at the conclusion of the surgical procedure.
Pelvic Adhesions — An Update
“A number of human interventional trials and animal studies have evaluated techniques and materials designed to prevent and reduce postsurgical adhesions. The results have been inconclusive and sometimes contradictory. Thus, preventing postsurgical adhesions remains an art, rather than a science.” So I began my introduction to the program on adhesion prevention at the 2010 Congress of the Society of Laparoscopic Surgeons in New York City.
Patients with adhesions can present with small bowel obstruction or with complaints of infertility, chronic pain, or dyspareunia. Unfortunately, adhesive disease is problematic. Four percent of the patients undergoing abdominal and pelvic surgery will be readmitted due to adhesion-related complications. In excess of 400,000 surgical procedures are performed annually in the United States for lysis of adhesions. In a Scottish National Health Service Study of nearly 9,000 women who previously underwent open gynecologic surgery, just less than 3% were readmitted secondary to adhesions; the highest readmit rate was ovarian surgery (BJOG 2000;107:855–62).
While one would expect a reduction in the number of patients undergoing laparoscopic surgery, in reality, the verdict is not yet clear. A 1998 meta-analysis showed a decrease in both reformed (26.6% vs. 14.3%) and de novo adhesions (45.2% vs. 37.2%) in the laparoscopic group, compared with laparotomy (Fertil. Steril. 1998;70:702–11).
Despite this, other authors cite pneumoperitoneum, prolonged surgery, high insufflation pressure, and overzealous use of energy to cut and coagulate as reasons why laparoscopic surgery increases risk of adhesions.
The economic impact of adhesions is staggering, in excess of $1.3 billion in the United States per year.
For this current excerpt of the Master Class in Gynecologic Surgery, I have solicited the wisdom of Dr. Michael Diamond. He is the Kamran S. Moghissi Professor of Obstetrics and Gynecology and associate chairman of the department of obstetrics and gynecology at Wayne State University, Detroit. Dr. Diamond also is director of the division of reproductive endocrinology and infertility and assistant dean for clinical and translational research at the university. Dr. Diamond has spent much of his academic career involved in the pathogenesis, prevention, and treatment of pelvic adhesions. He is truly considered the world's leader in this area, and we are honored to have Dr. Diamond as guest author of this important area of our surgical arena.
The prevention of postsurgical adhesions is one of the greatest unmet needs in medicine today. Surgical series have shown that adhesions are present after 80%-90% of abdominal and pelvic surgeries, and that these abnormal fibrous connections have a tremendous propensity to reform after adhesiolysis. (We will define adhesions here as “attachments between surfaces at nonanatomical locations.”)
In gynecologic surgery, postoperative adhesions are a frequent cause of infertility, pain, bowel obstruction, and difficulty in later procedures. Adhesions can occur after minimally invasive procedures, which have the potential for trocar injury to structures adherent to the anterior abdominal wall. Other intraoperative injuries can occur due to obscured normal anatomy or restricted access. A significant number of patients also undergo second surgeries to treat sequelae that are directly related to adhesions.
The literature is replete with studies of adhesion development and reports of its incidence and its consequences. Still, the problem of postoperative adhesion development often goes underestimated or unrecognized. This is because we don't routinely perform early second-look operations to assess adhesion development, and because there are no serum markers or sensitive imaging techniques to allow their identification. In addition, we do not follow our patients who seek care from other providers as insurance coverage changes or as other health problems arise, such as bowel obstruction being treated by a general surgeon.
As gynecologic surgeons, we must appreciate that while infections, endometriosis, and other peritoneal insults may contribute to adhesion development, surgery is the most common cause. We also must appreciate how tissue injury leads to the development of adhesions, and why adhesion reformation so commonly occurs.
This understanding is critical to our consideration and use of the “barrier” products currently available for reducing postsurgical adhesions — and critical to our efforts to employ the tenets of gynecologic microsurgery and to achieve as optimal a surgical outcome as possible. At this point in time, use of approved surgical adjuvants in combination with good surgical technique offers the best chance at adhesion reduction and prevention.
Incidence of Adhesions
A series of reports published in the early to mid-1980s documented how commonly adhesions develop after various types of reproductive pelvic surgery. Through early second-look laparoscopy, postoperative adhesions were found to occur, in these studies, in 55%–100% of patients after their primary gynecologic surgery.
In a multicenter study published in 1987, my colleagues and I also showed that gynecologic surgeries performed at the time of laparotomy are frequently complicated by both adhesion reformation and de novo adhesion formation. More than half of the 161 women (51%) who had a second-look laparoscopy 1–12 weeks after reproductive pelvic surgery were found to have de novo adhesion formation (adhesions in at least one new location). Adhesion reformation was also widespread: At the initial laparotomy, 121 of the patients (all of whom were treated for infertility) were noted to have some form of adhesion, and adhesion reformation subsequently occurred at the site of adhesiolysis in 85% of these women, with no differences with respect to adhesion type (Fertil. Steril. 1987;47;864–6).
It was hoped, and largely expected, that the growth of laparoscopy and minimally invasive surgery approaches in more recent years would reduce postoperative adhesion development — that minimally invasive techniques would prove to be less adhesiogenic than laparotomy. Questions remain, but thus far, such hopes have diminished and our expectations for significant improvement have gone unsubstantiated.
One multicenter study on adhesion development after initial laparoscopic procedures found that the incidence of adhesions at an early second-look procedure was 97% — no lower than in prior reports of second-look laparoscopy after laparotomy.
In this study, 68 women underwent operative laparoscopic procedures, including adhesiolysis, and had second-look procedures within 90 days. The good news was that de novo adhesion formation between the two laparoscopic procedures occurred in only 8 of the women (12%) and at 11 of 47 possible sites — much less frequently than after laparotomy. Adhesion scores also decreased at the second look compared with the status of the pelvis at the initial procedure. Still, with the high rate of adhesion reformation, almost all of the women developed postoperative adhesions.
Thus, even when the initial procedure was performed laparoscopically, adhesion development was an all-too-common occurrence, and appeared to be independent of the character of the initial adhesion (Fertil. Steril. 1991;55:700–4).
More recently, data from randomized studies of various adhesion barriers and potential anti-adhesion adjuvants have further dashed hopes that laparoscopy per se can reduce adhesion development.
For instance, in a recent small pilot study of a fibrin-based product called Adhexil, “control” ovaries that were not treated had a 27% increase in the mean adhesion score between an initial laparoscopic procedure and second-look laparoscopy. The women in the study had undergone bilateral ovarian surgery, with ovaries randomized for application of the product or no treatment (Fertil. Steril. 2011;95:1086–90). Clearly, a laparoscopic approach to their procedures did not prevent the development of adhesions.
Many of the initial studies on adhesion development were comprised of patients with infertility, but more recent observations have been extended to women without infertility and to men. Studies have covered patients undergoing colectomies, for instance, as well as neonates undergoing cardiothoracic procedures.
In a recent review article on adhesion prevention and reduction, members of an interdisciplinary consensus conference stated that adhesions develop after “nearly all” abdominal and pelvic procedures performed through either standard laparotomy or laparoscopic approaches. With respect to gynecologic surgery, they point out, research has shown that the most common site for postsurgical adhesion development is the ovary (Surg. Innov. 2010;17:183–8).
Consequences
Pelvic adhesions are a well-recognized cause of infertility, contributing to up to an estimated 40% of the cases of infertility in women. Adhesions are also a leading cause of bowel obstruction and a significant cause of chronic or recurrent pelvic pain.
The contribution of pelvic adhesions to chronic pelvic pain is not completely understood. Adhesions may be the cause of pain in some women, and in other women, an incidental finding that is not contributing to pain. In patients who have endometriosis as well, the question remains as to the contribution of endometriosis per se, or adhesions, to the pain. Endometriosis can cause adhesions and chronic pelvic pain, presumably through the cyclic generation of inflammatory molecules.
The relationship between chronic pain and adhesions is further complicated by ensuing questions about the efficacy of adhesiolysis. The two randomized trials that have thus far examined the role of adhesiolysis in the reduction of chronic pelvic pain failed to demonstrate a significant improvement in pain after adhesiolysis; however, the high failure rates after follow-up may be due to adhesion reformation and de novo adhesion formation (Fertil. Steril. 2004;82:1483–91). Performance of more randomized comparisons in the future may yield improved outcomes when adhesiolysis is paired with postprocedure use of anti-adhesion adjuvants.
Despite the uncertainties, multiple studies support the current estimation that adhesions cause or significantly contribute to chronic pelvic pain in up to 30% of women with the problem. As the Ovarian Adhesion Study Group noted in one of its reports, adhesions have been reported as a primary cause of chronic pelvic pain in 13%-36% of women, depending on the study (Obstet. Gynecol. 1995;86:335–40). Economic analyses also have quantified the impact of adhesion-related hospital readmissions. A study done in the United Kingdom, for instance, concluded that 6% of all hospital readmissions in patients who had undergone abdominal or pelvic surgery were directly related to adhesions (Lancet 1999;353:1476–80).httother report on hospitalizations for lower abdominal adhesiolysis in the United States estimated that in 1988, the cost of adhesions stemming from gynecologic procedures alone was almost $1.2 billion. This estimate did not include outpatient and indirect costs (Surg. Gynecol. Obstet. 1993;176:271–6).
Why, How Adhesions Develop
Our current understanding is that adhesions develop as a result of injury to and devascularization of the peritoneum, and the subsequent inflammatory response and peritoneal wound healing process. Tissue hypoxia triggers a cascade of intracellular responses that, in combination with the fibrinous collection of blood and serosanguinous fluid at the tissue surface, may result in adhesion development.
In the initial postsurgical period, either overt bleeding or oozing may occur at the site(s) of tissue injury, forming clots. In combination with serosanguinous fluid, which may leak from damaged peritoneal surfaces, a fibrinous mass thus develops at the surgical sites and sites of tissue injury. This represents an initial step in peritoneal repair.
When surrounding tissue is normal and there is a sufficient amount of plasminogen activator present in the peritoneum — and when numerous other events and conditions are optimal — the resulting fibrinous mass can be degraded. As that occurs, and tissue healing continues, fibroblasts are recruited to the surface of the injury site from underlying tissues.
If the fibrinous mass is no longer present, fibroblasts “stop” at the tissue surfaces, and become covered by mesothelial cells which line the peritoneal surface as the process of remesothelialization occurs. This process appears to be initiated within hours after surgery and is generally believed to be completed in 3–5 days. (In such instances, healing would have occurred without adhesions, although subperitoneal fibrosis may have occurred.)
Various hypoxia-driven responses, however, such as a reduction in plasminogen activator activity, can cause the fibrinous mass to persist during the healing process, before remesothelialization occurs. In this case, fibroblasts migrate not only to, but through, the injury site, and into the persisting fibrinous mass. This is subsequently followed by deposition of collagen, fibronectin, and other extracellular matrix materials — creating the beginnings of a true adhesion.
In such cases, remesothelialization still occurs, but the mesothelial cells cover the adhesion as well as the normal tissue surfaces, forming adhesive bands and other types of connections between opposing serosal tissue surfaces. Angiogenesis then occurs as the hypoxic tissue in the adhesion sends signals (such as vascular endothelial growth factor) in an attempt to reestablish a supply of oxygen and nutrients to the injured and devascularized tissues. Subsequently, as the tissue remodels, there is a propensity for the adhesion to become more vascular and denser.
Understanding this process is important because the products currently available for reducing adhesions act as barriers during this critical period of remesothelialization, keeping peritoneal surfaces apart and minimizing the potential development of a fibrinous mass that bridges tissue surfaces. If an adhesion does not form during the 3–5-day period of remesothelialization, it is theorized that there will not be any adhesion development — unless there's new injury to the tissue surfaces.
Once an adhesion forms, however, it has acquired a particular “adhesion phenotype” — different from that of normal peritoneum — that appears to be irreversible. This is likely why it is so difficult to prevent adhesion reformation after adhesiolysis. Rates of adhesion reformation — even in the best of surgical hands — run between 80% and 90%, compared with a 50% chance of de novo adhesion development after surgery (at new sites of injury).
The identification of an adhesion phenotype came originally from comparisons of normal peritoneal and adhesion tissues harvested from the same patient, and were later confirmed in cell culture studies in which normal peritoneal fibroblasts were subjected to hypoxia (2% O2 conditions). Fibroblasts cultured under hypoxic conditions were subsequently found to have developed particular molecular biologic characterizations that are different from those of normal peritoneal fibroblasts.
When exposed to normal amounts of oxygen again, the fibroblasts did not go back to being normal fibroblasts — they continued to manifest the adhesion phenotype (J. Am Assoc. Gynecol. Laparosc. 2004;11:307–14). These findings have been confirmed in animal and human studies, and such relationships have also been identified in other peritoneal tissue types such as mesothelial cells and macrophages.
Further research on the pathogenesis of adhesions and the molecular biologic differences between normal peritoneum and adhesions may allow identification of which patients, and which sites within a patient, are most at risk for adhesion development, as well as the discovery of new ways to reduce the development of postoperative adhesions and their clinical sequelae.
It is possible that a future generation of barrier products not only will work as a barrier separating surfaces prior to remesothelialization, but will also have local biologic effects — delivering adhesion-reducing drugs or biologics, for instance, to specific localized tissue sites. A personalized approach to adhesion prevention also might be possible, with particular factors deemed to increase adhesion risk in individual patients (a deficiency of plasminogen activator, for instance) being corrected.
In the meantime, as we've learned more about the pathophysiological state under which adhesions develop, we have found that adhesion development may occur faster than we had thought. In one recent rodent study, we identified postoperative tissue attachments as early as 2 hours after cecal abrasion. We noted considerable local edema and vessel dilatation within 2 hours of injury, angiogenesis and fibrin deposition at 8 hours, and cell proliferation at 24 hours (Fertil. Steril. 2010;93:2734–7). And interestingly, recent studies in mice have shown that laparoscopic insufflation per se can induce peritoneal adhesions, with the adhesions increasing proportionally with both increasing duration of insufflation and an increase in intraperitoneal pressure.
Prevention in Practice
During the past decade a variety of surgical adjuvants — from procoagulants and fibrinolytic agents to anti-inflammatory drugs and antibiotics — have been investigated for use in reducing the occurrence, extent, and severity of adhesions. Unfortunately, most approaches seemingly have been futile. Some products have shown trends toward efficacy in animal or early human studies and need further investigation.
The three synthetic products that are approved by the Food and Drug Administration—Gynecare Interceed, Seprafilm, and Adept — can help reduce postoperative adhesions after gynecologic procedures, and should be considered as potentially useful surgical adjuvants. A meta-analysis of studies of Gynecare Interceed, for instance, found that approximately twice as many operative sites were adhesion free after use of the barrier than after surgery alone (J. Reprod. Med. 1999;44:325–31).
Gynecare Interceed (Johnson & Johnson) and Seprafilm (Genzyme) are approved for use only at laparotomy, while Adept (Baxter International), an icodextrin solution that disperses throughout the abdominopelvic cavity, is approved for use only in laparoscopic surgery.
The key consideration to make when using Interceed — a biodegradable woven fabric composed of oxidized, regenerated cellulose — is the importance of achieving meticulous hemostasis. Its efficacy is reduced, or can even be lost, in the presence of blood. Care also must be taken not to stretch the material or alter its shape and the spacing between the weaves. Otherwise, the material, once gelated, will have a greater potential for spaces in which the tissue surfaces would not be separated and thus a greater potential for blood coagulation and fibroblast in-growth. Multiple pieces of the material may be overlapped, but there have been no benefits demonstrated (at least in animal studies) to using double layers.
Care in application also is critically important for Seprafilm, a film composed of modified hyaluronic acid and carboxymethylcellulose. Seprafilm is brittle and is difficult to apply through small incisions. While it's not impossible to deliver the product laparoscopically, many surgeons have found this very difficult. And in the United States, it is approved for use with laparotomy only.
In applying Seprafilm, it is critical to first get good exposure of the field and then position the film very carefully. Attempts to reposition the product will often result in tears or breaks. Of course, just as with Interceed, this device is believed to work primarily by separating tissue surfaces, and thus it has little to no chance of success if it does not completely separate the surgically injured tissue from other tissue surfaces in the initial postoperative period while remesothelialization is occurring.
The use of adjuvants, moreover, is no substitute for good surgical technique that aims to minimize tissue injury, tissue devascularization, and inflammation. This is easier to achieve, of course, during a microsurgical procedure such as a tubal anastomosis than in a patient with severe endometriosis or many large fibroids. Still, to the extent possible for the procedure being conducted, the tenets of gynecologic microsurgery should always be considered:
▸ Handle as little tissue as possible, as minimally as possible. To the extent possible, handle only those portions that will subsequently be excised.
▸ Keep tissues moist. Tissue drying leads to injury and loss of mesothelial cells. Raw surfaces are more prone to develop adhesions.
▸ Take special care in the use of suture. Consider whether clinical situations will allow use of less reactive and smaller-caliber suture. When using suture to tie off blood vessels, skeletonize the vessels so as to minimize the amount of tissue distal to the suture that will become hypoxic and serve as a nidus to adhesion development.
▸ Target the use of electrosurgery and other energy sources. Use it in specific localized sites where it's needed, such as to stop bleeding, but avoid widely dispersed use, when possible, again to minimize the amount of residual devitalized tissue remaining in the pelvis at the conclusion of the surgical procedure.
Pelvic Adhesions — An Update
“A number of human interventional trials and animal studies have evaluated techniques and materials designed to prevent and reduce postsurgical adhesions. The results have been inconclusive and sometimes contradictory. Thus, preventing postsurgical adhesions remains an art, rather than a science.” So I began my introduction to the program on adhesion prevention at the 2010 Congress of the Society of Laparoscopic Surgeons in New York City.
Patients with adhesions can present with small bowel obstruction or with complaints of infertility, chronic pain, or dyspareunia. Unfortunately, adhesive disease is problematic. Four percent of the patients undergoing abdominal and pelvic surgery will be readmitted due to adhesion-related complications. In excess of 400,000 surgical procedures are performed annually in the United States for lysis of adhesions. In a Scottish National Health Service Study of nearly 9,000 women who previously underwent open gynecologic surgery, just less than 3% were readmitted secondary to adhesions; the highest readmit rate was ovarian surgery (BJOG 2000;107:855–62).
While one would expect a reduction in the number of patients undergoing laparoscopic surgery, in reality, the verdict is not yet clear. A 1998 meta-analysis showed a decrease in both reformed (26.6% vs. 14.3%) and de novo adhesions (45.2% vs. 37.2%) in the laparoscopic group, compared with laparotomy (Fertil. Steril. 1998;70:702–11).
Despite this, other authors cite pneumoperitoneum, prolonged surgery, high insufflation pressure, and overzealous use of energy to cut and coagulate as reasons why laparoscopic surgery increases risk of adhesions.
The economic impact of adhesions is staggering, in excess of $1.3 billion in the United States per year.
For this current excerpt of the Master Class in Gynecologic Surgery, I have solicited the wisdom of Dr. Michael Diamond. He is the Kamran S. Moghissi Professor of Obstetrics and Gynecology and associate chairman of the department of obstetrics and gynecology at Wayne State University, Detroit. Dr. Diamond also is director of the division of reproductive endocrinology and infertility and assistant dean for clinical and translational research at the university. Dr. Diamond has spent much of his academic career involved in the pathogenesis, prevention, and treatment of pelvic adhesions. He is truly considered the world's leader in this area, and we are honored to have Dr. Diamond as guest author of this important area of our surgical arena.






