User login
Can RCTs be Misleading and Biased?
Randomized controlled trials (RCTs) constitute level 1 evidence, which is widely considered the best data upon which to base medical practice. This is particularly true when the RCTs are published in leading journals like the New England Journal of Medicine or Lancet. Such trials are viewed by many as the Holy Grail of medicine and thus infallible and inviolate.
However, RCTs can have many flaws that render them obsolete, non-applicable or outright misleading. More importantly RCTs can be misinterpreted or spun by their authors or others so that they exert an effect on practice trends or standards unjustified by their data.
Possible flaws in RCTs are of two types:
1. Timeliness flaws can occur when progress is made in the treatment under evaluation arm or the control arm. Examples would be the early trials of carotid stenting (CAS) vs. carotid endarterectomy (CEA). If progress in CAS technology or patient selection occurs, a trial showing CAS inferiority becomes invalid. In contrast, the landmark trials showing CEA to be superior to medical treatment in preventing strokes have become obsolete because dramatic progress has been made with medical treatment.
2. Many design flaws can impair the validity of RCTs. These include patient selection flaws (e.g. in SAPPHIRE, patients were selected for randomization only if they were high risk for CEA). SAPPHIRE also included 71% asymptomatic patients in whom the high adverse event rates for both CEA and CAS were unjustified. Good medical treatment would have served these patients better. CREST also had patient selection flaws. It was originally designed to compare CAS and CEA only in symptomatic patients. When adequate numbers of patients could not be recruited, asymptomatic patients were added, thereby diluting the power of the study and impairing the statistical significance of some of its results.
Other design flaws include questionable competence of operators in a trial (e.g. the CAS operators in the EVA-3S and ICSS trials); problems with randomization (e.g. SAPPHIRE in which only 10% of eligible patients were randomized); and questionable applicability of RCT results to real world practice (e.g. CAS operators in CREST were highly vetted and more skilled than others performing the procedure).
There are also idiosyncratic flaws, as in the EVAR 2 trial in patients unfit for open repair. Although this trial, published in Lancet, showed EVAR to have similar mortality to no treatment, half the deaths in the group randomized to EVAR occurred from rupture during a lengthy (average 57 days) waiting period before treatment. Had these deaths been prevented by a more timely EVAR, the conclusion of EVAR 2 might have been different.
Inappropriate or questionable primary endpoints in RCTS are another design flaw that can lead to misleading conclusions. An example is the inclusion of minor myocardial infarctions (MIs) with strokes and deaths as a composite endpoint in a CAS vs. CEA trial (e.g. SAPPHIRE and CREST).
The components of the primary endpoint in the CAS and CEA arms of CREST were death, stroke, and myocardial infarction. Total stroke and minor strokes were both significantly different in the two groups in favor of CEA, and death and major strokes, although not significantly different between the two groups were both numerically higher for CAS. (See complete table oline at www. vascularspecialistonline.com)
Although it is arguable, it is hard to understand how minor MIs are the equivalent of strokes and deaths, and only when MIs were included were the adverse event rates in the two groups similar (7.2% for CAS vs 6.8% for CEA, P = .051).
So much for the flaws in RCTs. What about good trials or those with only minor weaknesses? Even these can result in misleading conclusions when the authors reach conclusions unjustified by their own data. SAPPHIRE and CREST are two recent examples.
Despite the flaws in these trials, both of which were reported in the New England Journal of Medicine, the authors concluded that "with high risk patients CAS and CEA are equivalent treatments" (SAPPHIRE) and "among patients with symptomatic and asymptomatic carotid stenosis, the risk of the composite primary end-point ... did not differ significantly in the group undergoing CAS and the group undergoing CEA" (CREST).
Although the CREST authors pointed out the higher incidence of stroke with stenting, others have used the CREST study to claim equivalence of CAS and CEA. Nowhere is this more apparent than in the recent American Heart Association (AHA) Guideline on the management of patients with extracranial carotid and vertebral artery disease.
This important and influential document, which was also approved by 13 other organizations including the SVS, stated that "CAS is indicated as an alternative to CEA for symptomatic patients at average or low risk of complications associated from endovascular interventions...." In Webster’s Dictionary one definition of "alternative" is "a choice between 2 things".
This clearly implies equivalence, and it has been so interpreted by many others, particularly those biased toward catheter based treatment. Of note, the AHA Guideline appears to be based largely on CREST, and did not even consider the findings of the ICSS trial, published in Lancet the same day as the main article reporting CREST.
Although ICSS may also have flaws, it showed, in a large group of only symptomatic patients, that CAS produced significantly more strokes and diffusion weighted MRI defects than did CEA. It is hard to understand why these ICSS results did not have more of an influence on the AHA Guideline.
Although my bias as a CAS enthusiast makes me believe that CAS will ultimately have a major role in the treatment of carotid stenosis patients, that bias is not yet sufficient for me to spin the data and believe we are now there. One has to wonder if bias more intense than mine was involved in the conclusion reached in the AHA Guideline.
Thus, it is apparent that misleading conclusions can be reached in articles reporting RCTs in leading journals. These can be the result of flaws in the RCTs and/or unrecognized author bias. More importantly, the results of even good trials can be further misinterpreted by others to guide practice standards in a way unjustified by the data.
It is important for all to recognize the possible role of bias in these misinterpretations. By recognizing the possible flaws in RCTs and that physicians, like all other people, are influenced by bias, we can exercise the judgment to use RCTs fairly to help us treat individual patients optimally.n
Dr. Frank J. Veith is professor of surgery at New York University Medical Center and professor of surgery and William J. von Liebig Chair in vascular surgery at Case Western Reserve University and The Cleveland Clinic.
Randomized controlled trials (RCTs) constitute level 1 evidence, which is widely considered the best data upon which to base medical practice. This is particularly true when the RCTs are published in leading journals like the New England Journal of Medicine or Lancet. Such trials are viewed by many as the Holy Grail of medicine and thus infallible and inviolate.
However, RCTs can have many flaws that render them obsolete, non-applicable or outright misleading. More importantly RCTs can be misinterpreted or spun by their authors or others so that they exert an effect on practice trends or standards unjustified by their data.
Possible flaws in RCTs are of two types:
1. Timeliness flaws can occur when progress is made in the treatment under evaluation arm or the control arm. Examples would be the early trials of carotid stenting (CAS) vs. carotid endarterectomy (CEA). If progress in CAS technology or patient selection occurs, a trial showing CAS inferiority becomes invalid. In contrast, the landmark trials showing CEA to be superior to medical treatment in preventing strokes have become obsolete because dramatic progress has been made with medical treatment.
2. Many design flaws can impair the validity of RCTs. These include patient selection flaws (e.g. in SAPPHIRE, patients were selected for randomization only if they were high risk for CEA). SAPPHIRE also included 71% asymptomatic patients in whom the high adverse event rates for both CEA and CAS were unjustified. Good medical treatment would have served these patients better. CREST also had patient selection flaws. It was originally designed to compare CAS and CEA only in symptomatic patients. When adequate numbers of patients could not be recruited, asymptomatic patients were added, thereby diluting the power of the study and impairing the statistical significance of some of its results.
Other design flaws include questionable competence of operators in a trial (e.g. the CAS operators in the EVA-3S and ICSS trials); problems with randomization (e.g. SAPPHIRE in which only 10% of eligible patients were randomized); and questionable applicability of RCT results to real world practice (e.g. CAS operators in CREST were highly vetted and more skilled than others performing the procedure).
There are also idiosyncratic flaws, as in the EVAR 2 trial in patients unfit for open repair. Although this trial, published in Lancet, showed EVAR to have similar mortality to no treatment, half the deaths in the group randomized to EVAR occurred from rupture during a lengthy (average 57 days) waiting period before treatment. Had these deaths been prevented by a more timely EVAR, the conclusion of EVAR 2 might have been different.
Inappropriate or questionable primary endpoints in RCTS are another design flaw that can lead to misleading conclusions. An example is the inclusion of minor myocardial infarctions (MIs) with strokes and deaths as a composite endpoint in a CAS vs. CEA trial (e.g. SAPPHIRE and CREST).
The components of the primary endpoint in the CAS and CEA arms of CREST were death, stroke, and myocardial infarction. Total stroke and minor strokes were both significantly different in the two groups in favor of CEA, and death and major strokes, although not significantly different between the two groups were both numerically higher for CAS. (See complete table oline at www. vascularspecialistonline.com)
Although it is arguable, it is hard to understand how minor MIs are the equivalent of strokes and deaths, and only when MIs were included were the adverse event rates in the two groups similar (7.2% for CAS vs 6.8% for CEA, P = .051).
So much for the flaws in RCTs. What about good trials or those with only minor weaknesses? Even these can result in misleading conclusions when the authors reach conclusions unjustified by their own data. SAPPHIRE and CREST are two recent examples.
Despite the flaws in these trials, both of which were reported in the New England Journal of Medicine, the authors concluded that "with high risk patients CAS and CEA are equivalent treatments" (SAPPHIRE) and "among patients with symptomatic and asymptomatic carotid stenosis, the risk of the composite primary end-point ... did not differ significantly in the group undergoing CAS and the group undergoing CEA" (CREST).
Although the CREST authors pointed out the higher incidence of stroke with stenting, others have used the CREST study to claim equivalence of CAS and CEA. Nowhere is this more apparent than in the recent American Heart Association (AHA) Guideline on the management of patients with extracranial carotid and vertebral artery disease.
This important and influential document, which was also approved by 13 other organizations including the SVS, stated that "CAS is indicated as an alternative to CEA for symptomatic patients at average or low risk of complications associated from endovascular interventions...." In Webster’s Dictionary one definition of "alternative" is "a choice between 2 things".
This clearly implies equivalence, and it has been so interpreted by many others, particularly those biased toward catheter based treatment. Of note, the AHA Guideline appears to be based largely on CREST, and did not even consider the findings of the ICSS trial, published in Lancet the same day as the main article reporting CREST.
Although ICSS may also have flaws, it showed, in a large group of only symptomatic patients, that CAS produced significantly more strokes and diffusion weighted MRI defects than did CEA. It is hard to understand why these ICSS results did not have more of an influence on the AHA Guideline.
Although my bias as a CAS enthusiast makes me believe that CAS will ultimately have a major role in the treatment of carotid stenosis patients, that bias is not yet sufficient for me to spin the data and believe we are now there. One has to wonder if bias more intense than mine was involved in the conclusion reached in the AHA Guideline.
Thus, it is apparent that misleading conclusions can be reached in articles reporting RCTs in leading journals. These can be the result of flaws in the RCTs and/or unrecognized author bias. More importantly, the results of even good trials can be further misinterpreted by others to guide practice standards in a way unjustified by the data.
It is important for all to recognize the possible role of bias in these misinterpretations. By recognizing the possible flaws in RCTs and that physicians, like all other people, are influenced by bias, we can exercise the judgment to use RCTs fairly to help us treat individual patients optimally.n
Dr. Frank J. Veith is professor of surgery at New York University Medical Center and professor of surgery and William J. von Liebig Chair in vascular surgery at Case Western Reserve University and The Cleveland Clinic.
Randomized controlled trials (RCTs) constitute level 1 evidence, which is widely considered the best data upon which to base medical practice. This is particularly true when the RCTs are published in leading journals like the New England Journal of Medicine or Lancet. Such trials are viewed by many as the Holy Grail of medicine and thus infallible and inviolate.
However, RCTs can have many flaws that render them obsolete, non-applicable or outright misleading. More importantly RCTs can be misinterpreted or spun by their authors or others so that they exert an effect on practice trends or standards unjustified by their data.
Possible flaws in RCTs are of two types:
1. Timeliness flaws can occur when progress is made in the treatment under evaluation arm or the control arm. Examples would be the early trials of carotid stenting (CAS) vs. carotid endarterectomy (CEA). If progress in CAS technology or patient selection occurs, a trial showing CAS inferiority becomes invalid. In contrast, the landmark trials showing CEA to be superior to medical treatment in preventing strokes have become obsolete because dramatic progress has been made with medical treatment.
2. Many design flaws can impair the validity of RCTs. These include patient selection flaws (e.g. in SAPPHIRE, patients were selected for randomization only if they were high risk for CEA). SAPPHIRE also included 71% asymptomatic patients in whom the high adverse event rates for both CEA and CAS were unjustified. Good medical treatment would have served these patients better. CREST also had patient selection flaws. It was originally designed to compare CAS and CEA only in symptomatic patients. When adequate numbers of patients could not be recruited, asymptomatic patients were added, thereby diluting the power of the study and impairing the statistical significance of some of its results.
Other design flaws include questionable competence of operators in a trial (e.g. the CAS operators in the EVA-3S and ICSS trials); problems with randomization (e.g. SAPPHIRE in which only 10% of eligible patients were randomized); and questionable applicability of RCT results to real world practice (e.g. CAS operators in CREST were highly vetted and more skilled than others performing the procedure).
There are also idiosyncratic flaws, as in the EVAR 2 trial in patients unfit for open repair. Although this trial, published in Lancet, showed EVAR to have similar mortality to no treatment, half the deaths in the group randomized to EVAR occurred from rupture during a lengthy (average 57 days) waiting period before treatment. Had these deaths been prevented by a more timely EVAR, the conclusion of EVAR 2 might have been different.
Inappropriate or questionable primary endpoints in RCTS are another design flaw that can lead to misleading conclusions. An example is the inclusion of minor myocardial infarctions (MIs) with strokes and deaths as a composite endpoint in a CAS vs. CEA trial (e.g. SAPPHIRE and CREST).
The components of the primary endpoint in the CAS and CEA arms of CREST were death, stroke, and myocardial infarction. Total stroke and minor strokes were both significantly different in the two groups in favor of CEA, and death and major strokes, although not significantly different between the two groups were both numerically higher for CAS. (See complete table oline at www. vascularspecialistonline.com)
Although it is arguable, it is hard to understand how minor MIs are the equivalent of strokes and deaths, and only when MIs were included were the adverse event rates in the two groups similar (7.2% for CAS vs 6.8% for CEA, P = .051).
So much for the flaws in RCTs. What about good trials or those with only minor weaknesses? Even these can result in misleading conclusions when the authors reach conclusions unjustified by their own data. SAPPHIRE and CREST are two recent examples.
Despite the flaws in these trials, both of which were reported in the New England Journal of Medicine, the authors concluded that "with high risk patients CAS and CEA are equivalent treatments" (SAPPHIRE) and "among patients with symptomatic and asymptomatic carotid stenosis, the risk of the composite primary end-point ... did not differ significantly in the group undergoing CAS and the group undergoing CEA" (CREST).
Although the CREST authors pointed out the higher incidence of stroke with stenting, others have used the CREST study to claim equivalence of CAS and CEA. Nowhere is this more apparent than in the recent American Heart Association (AHA) Guideline on the management of patients with extracranial carotid and vertebral artery disease.
This important and influential document, which was also approved by 13 other organizations including the SVS, stated that "CAS is indicated as an alternative to CEA for symptomatic patients at average or low risk of complications associated from endovascular interventions...." In Webster’s Dictionary one definition of "alternative" is "a choice between 2 things".
This clearly implies equivalence, and it has been so interpreted by many others, particularly those biased toward catheter based treatment. Of note, the AHA Guideline appears to be based largely on CREST, and did not even consider the findings of the ICSS trial, published in Lancet the same day as the main article reporting CREST.
Although ICSS may also have flaws, it showed, in a large group of only symptomatic patients, that CAS produced significantly more strokes and diffusion weighted MRI defects than did CEA. It is hard to understand why these ICSS results did not have more of an influence on the AHA Guideline.
Although my bias as a CAS enthusiast makes me believe that CAS will ultimately have a major role in the treatment of carotid stenosis patients, that bias is not yet sufficient for me to spin the data and believe we are now there. One has to wonder if bias more intense than mine was involved in the conclusion reached in the AHA Guideline.
Thus, it is apparent that misleading conclusions can be reached in articles reporting RCTs in leading journals. These can be the result of flaws in the RCTs and/or unrecognized author bias. More importantly, the results of even good trials can be further misinterpreted by others to guide practice standards in a way unjustified by the data.
It is important for all to recognize the possible role of bias in these misinterpretations. By recognizing the possible flaws in RCTs and that physicians, like all other people, are influenced by bias, we can exercise the judgment to use RCTs fairly to help us treat individual patients optimally.n
Dr. Frank J. Veith is professor of surgery at New York University Medical Center and professor of surgery and William J. von Liebig Chair in vascular surgery at Case Western Reserve University and The Cleveland Clinic.
Continuous Admission Model Reduces LOS
Smooth and timely hospital patient flow can have multiple positive effects including reduced wait times for services, decreased congestion in the Emergency Department (ED), and increased patient and staff satisfaction.14 One way to improve patient flow is to remove variation along the care pathway.57
For teaching hospitals that provide team‐based care, 1 significant source of variation involves the emergent admission process.8, 9 Typically, for services that admit the majority of their patients from the ED, 1 team is assigned to all admitting duties on a particular day; the on‐call team. While teams rotate between designations of on‐call, post‐call, and pre‐call over the course of the week, only the team designated on‐call accepts new admissions. This bolus call structure creates the need for extensive cross‐coverage, large variations in team admissions, and disparate team workloads.1012 Moreover, the effects of these variations may persist and extend along the care pathway, ultimately impacting timely patient discharge. Therefore, interventions aimed at improving the admission process may be candidates for improved patient flow.
The objective of this study is to evaluate the effect of changing the admission process from a bolus admission system to a trickle system that evenly distributes newly admitted patients to each of the physician‐led care teams. We hypothesize that by removing variation within the team admission process, team workload will be smoothed and ultimately result in patients being discharged by the team in a more uniform pattern. We evaluate this hypothesis by measuring length of stay and daily discharge rate.
METHODS
Setting
This retrospective study was conducted on the General Internal Medicine clinical teaching unit (GIM CTU) at a large academic tertiary care center in Toronto, Canada. GIM provides acute, nonsurgical care to a patient population composed primarily of elderly patients with complex chronic illnesses. GIM receives 98% of its inpatient admissions from the ED. On a daily basis, the ED sees approximately 100 patients, of which nearly 20% are admitted to hospital. GIM constitutes the single largest admitting service in the ED, admitting nearly half of all emergent admissions. Surgical and specialized medical services (eg, Cardiology, Oncology, Nephrology) admit the remaining half.
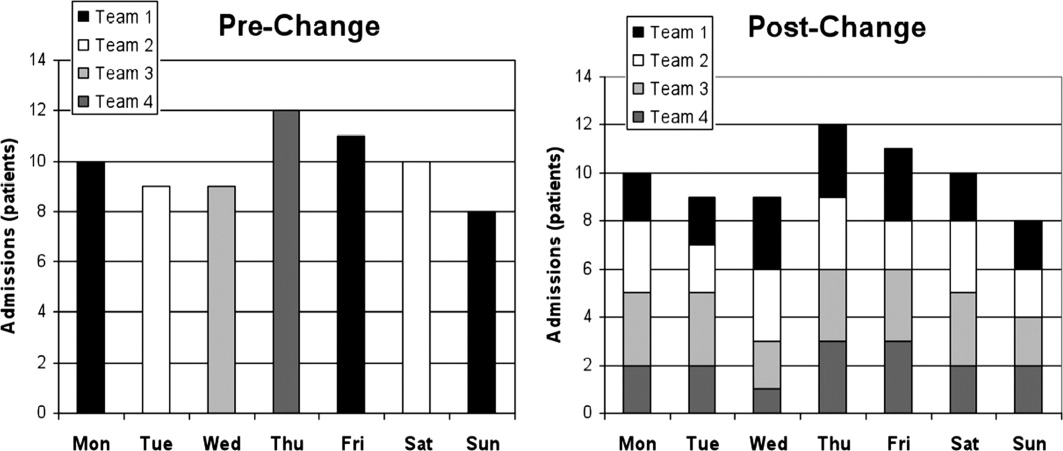
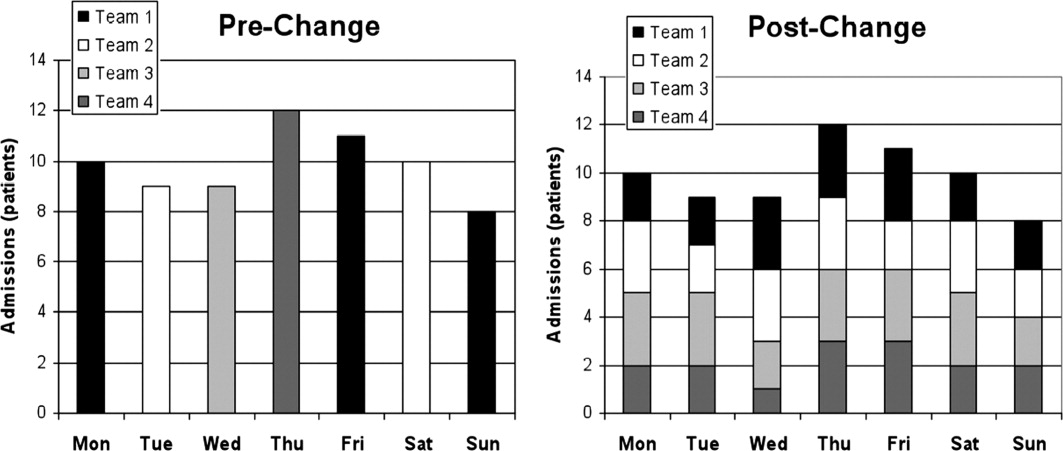
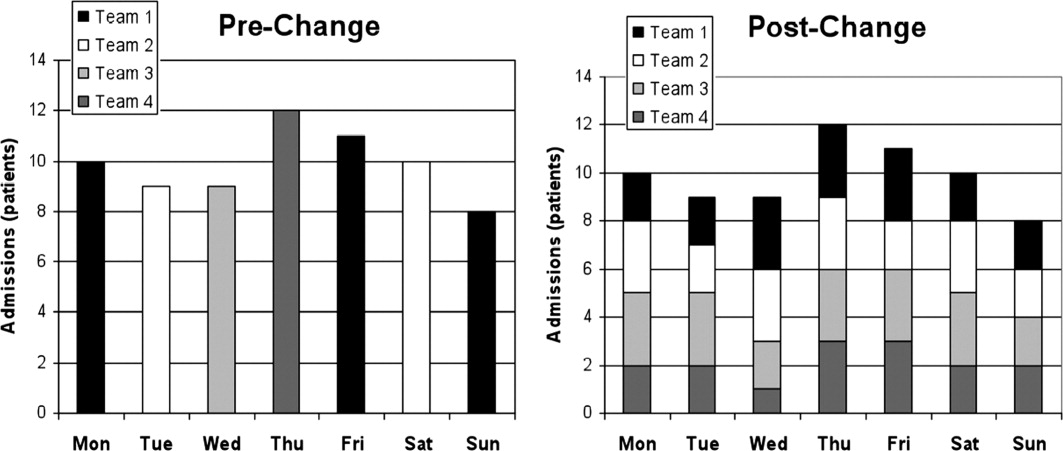
On March 2, 2009, the GIM CTU underwent a structural change from a bolus admission system to a trickle system of admissions to each care team. Figure 1 depicts a typical pre‐change admission pattern where each of the 4 care teams would admit a bolus of patients on a given day (left panel), and a typical post‐change admission pattern where the variation in daily admissions is smoothed out as a result of the trickle admission system (right panel). No change was made to care team members; each team consisted of an attending physician, 1 senior resident, 2 to 3 junior residents, 1 social worker, 1 physiotherapist, 1 occupational therapist, and 1 pharmacist. The Appendix provides a detailed description of the structural change.
Data Collection
Records were obtained from the hospital's Electronic Patient Record, which contains information on socio‐demographics, diagnosis, length of stay (LOS), patient disposition, attending physician, and date of admission and discharge.
Data were collected for 2 time periods, the pre‐change period (March to August 2008) and the post‐change period (March to August 2009). The new system was implemented on March 2, 2009. The same months of 2 consecutive years were used to account for any seasonal variation in patient volumes and diagnoses. During the pre‐change and post‐change periods, the hospital maintained the same admitting and discharge policies and protocols. Similarly, the authors are unaware of any provincial‐wide government policies that would have impacted only 1 of either the pre‐change or post‐change periods.
Outcomes
Two main outcomes were studied, daily discharge rate (DDR)13 and LOS. DDR was expressed as the number of discharges on a particular day divided by the total patient census on that day. DDR was calculated by team, stratified by their call schedule status (on‐call, post‐call, postpost‐call, pre‐call, or none of these), and then aggregated. A day was defined as a 24‐hour period beginning at 8 AM. This was chosen because it better reflects the period when decisions are made and work is completed. Daily team‐specific patient census was measured at 8 AM. LOS was measured in days, calculated for each patient using the admission and discharge dates.
The DDR calculation included only those patients who were admitted and discharged within the study periods. For analysis of LOS, we also included patients admitted prior to, but discharged during, the study periods.
We included all patients admitted to GIM. Patient discharge dispositions were categorized into 5 groups: discharge home, interfacility transfers (discharged to long‐term care, rehabilitation, chronic care, etc), intrafacility transfers (to other inpatient services within the hospital), death, and left against medical advice. To focus on discharges that may be influenced by the team, for analysis of both DDR and LOS, only patients discharged home and interfacility and intrafacility transfers were included (deaths and patients who left against medical advice were not included).
Statistical Analysis
To assess whether the trickle system smoothed discharge rates, we fitted a logistic regression model and compared the variability in the log‐odds of discharge across the 4 main types of call days (on‐call, post‐call, postpost‐call, pre‐call) in the pre‐change and post‐change periods. The number of discharges on a given day was modeled as a binomial outcome with sample size equal to the census for that day and a log‐odds of discharge that depended on type of call day and a random error component. In this model, the effect of type of call day was allowed to be different in the pre‐change and post‐change periods. To account for the fact that data were collected on 180 consecutive days in each time period, we modeled the error component for each team in each time period as an autoregressive time series. We summarized the smoothness of discharge rates across type of call day in each period by calculating the variance of the corresponding regression parameters (the log‐odds ratios). By comparing the variances in the 2 periods, we were able to compute the probability that there was a reduction in variability, or equivalently, a smoothing of DDR. This model was fitted with Bayesian methods, implemented using Markov chain Monte Carlo (MCMC) techniques in the software WinBUGS.14 Uninformative priors were used for all parameters; model convergence was checked with the Gelman‐Brooks Rubin statistics. Further details are available from the authors on request. Summary estimates of discharge rates on the 4 main types of call day were calculated for the pre‐change and post‐change periods and plotted with 95% credible intervals.
Descriptive statistics were calculated for age, case mix group (CMG), total admission and discharges, and LOS. We chose to report median LOS, rather than the mean, because this modulates the influence of outliers in the samples.
KaplanMeier curves were also plotted for LOS. We tested for equality of the KaplanMeier curves using a weighted log‐rank test (G‐rho), which gave more weight to smaller LOS values (giving weight equal to the proportion of patients not yet discharged). This weighting was performed because an improvement in operational efficiency was more likely to have an effect on patients who could be discharged more quickly (7 days) than patients whose discharge was delayed by factors outside the hospital's control.
All other statistical analyses were performed using R (version 2.10.1; R Foundation for Statistical Computing, Vienna, Austria).
This study was approved by The University Health Network Research Ethics Board.
RESULTS
During the 2 study periods, a total of 2734 patients were discharged, 1446 in the pre‐change period (1535 admitted), and 1288 in the post‐change period (1363 admitted). Table 1 presents mean age and primary CMG diagnosis.
| Pre‐Intervention Period (March 3August 29, 2008) 1446 Total Discharges (Mean Age [SD], 66 [18.6]) | Post‐Intervention Period (March 2August 28, 2009) 1288 Total Discharges (Mean Age [SD], 67 [18.8]) | |||
|---|---|---|---|---|
| CMG Rank | CMG Description | N (%) | CMG Description | N (%) |
| ||||
| Pneumonia | 117 (7.4) | Heart failure | 102 (7.4) | |
| 2 | Heart failure | 84 (5.3) | Pneumonia | 65 (4.7) |
| 3 | G.I. hemorrhage | 68 (4.3) | Esoph/gastro/misc digestive disorder | 61 (4.4) |
| 4 | Esoph/gastro/misc digestive disorder | 62 (3.9) | Lower urinary tract infection | 56 (4.1) |
| 5 | Red blood cell disorders | 59 (3.7) | G.I. hemorrhage | 52 (3.8) |
| 6 | Nutrit/misc metabolic disorder | 56 (3.5) | Nutrit/misc metabolic disorder | 47 (3.4) |
| 7 | Reticuloendothelial disorder | 56 (3.5) | Cerebrovascular disorder | 41 (3.0) |
| 8 | Lower urinary tract infection | 50 (3.2) | Red blood cell disorders | 40 (2.9) |
| 9 | Respiratory infect and inflamm | 42 (2.7) | Ungroupable input data | 36 (2.6) |
| 10 | Cerebrovascular disorder | 40 (2.5) | Chronic obstructive pulmonary disease | 33 (2.4) |
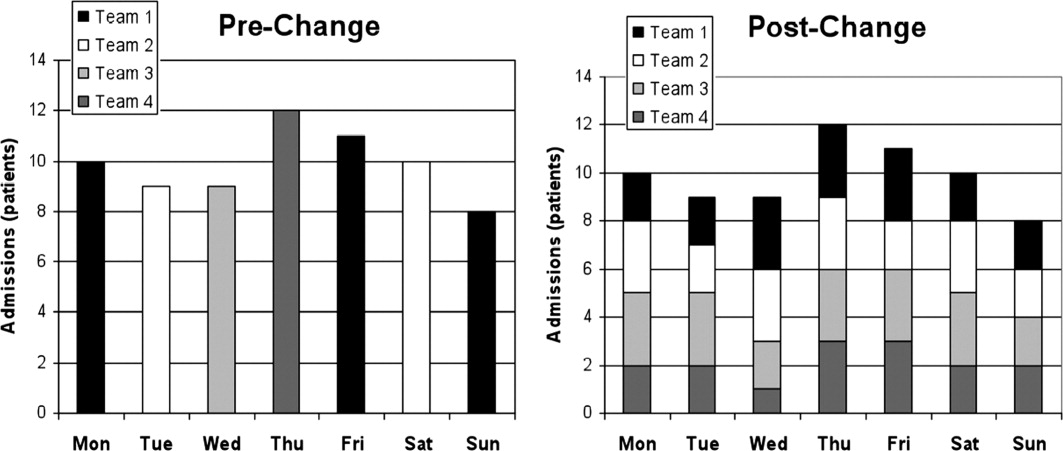
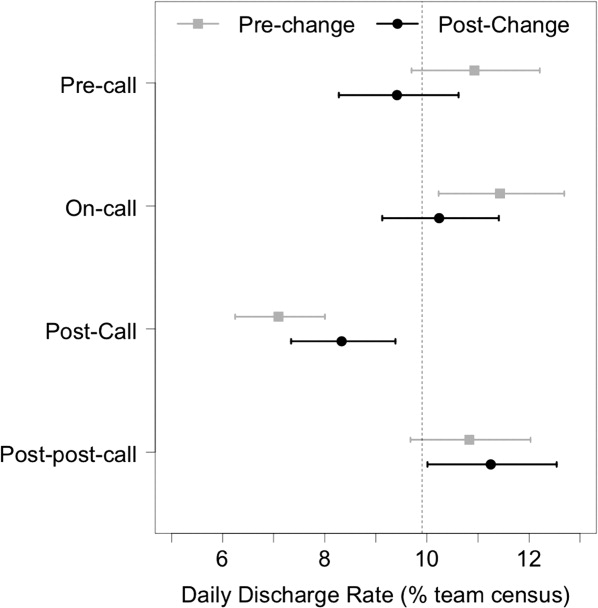
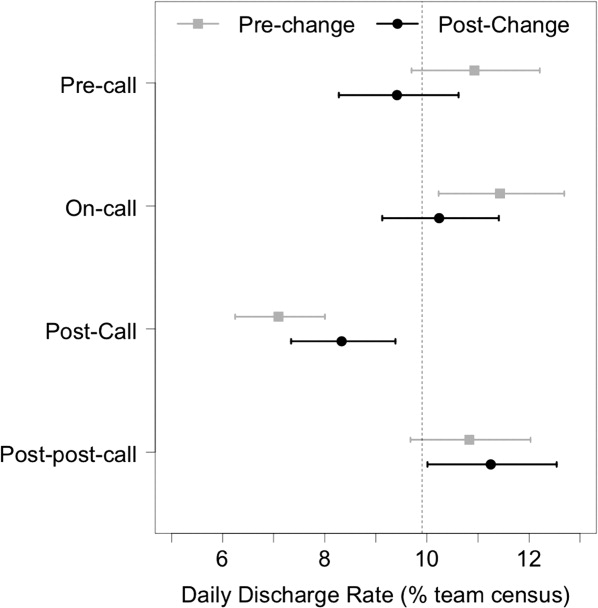
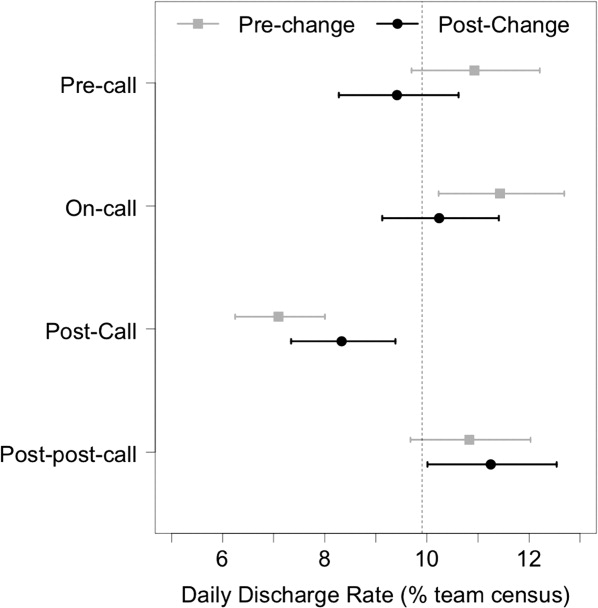
Figure 2 shows the estimated average team‐specific DDR's according to call schedule status, along with 95% credible intervals. With the exception of the postpost‐call day, each black point (2009, post‐change period) is closer to the overall average DDR of 9.9% than each corresponding gray point (2008, pre‐change period). In our Bayesian model, there was a 96.9% probability that the variability across call schedule status was reduced in the post‐change period, substantial evidence of smoother discharge rates across different types of call days.
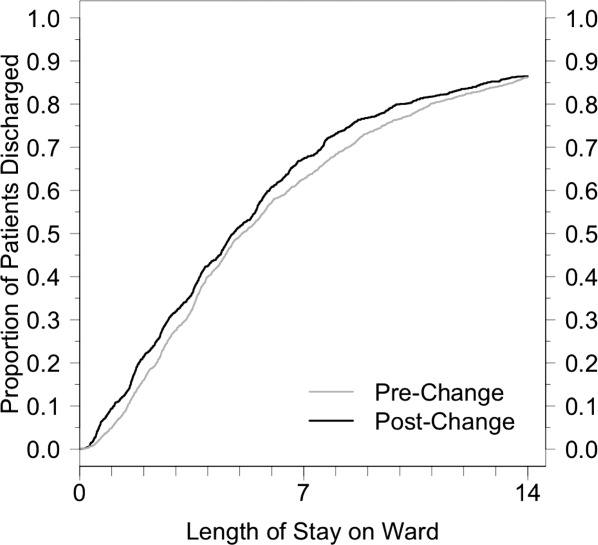
Summary statistics for the LOS for both groups can be seen in Table 2. The median LOS in the post‐change period was statistically significantly shorter than in the pre‐change period (4.8 days vs 5.1 days, P 0.001).
| Pre‐Change | Post‐Change | ||
|---|---|---|---|
| |||
| N | 1446 | 1288 | t Test comparing means |
| Mean LOS (SD) | 8.7 (15) | 8.8 (16) | P = 0.89 |
| Wilcoxon rank‐sum test | |||
| Median LOS | 5.06 | 4.79 | P = 0.0065 |
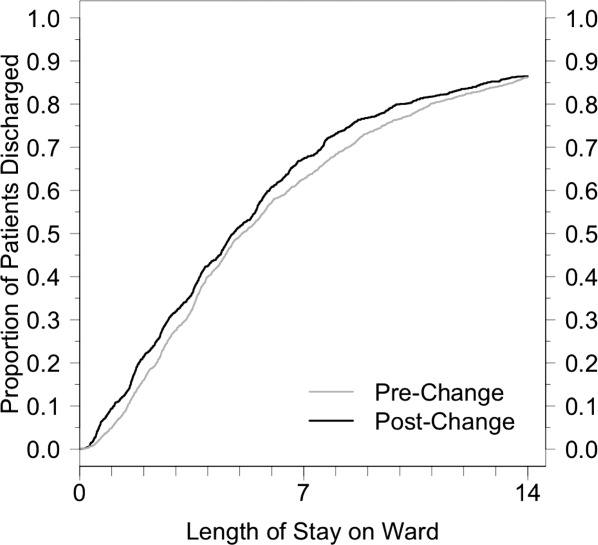
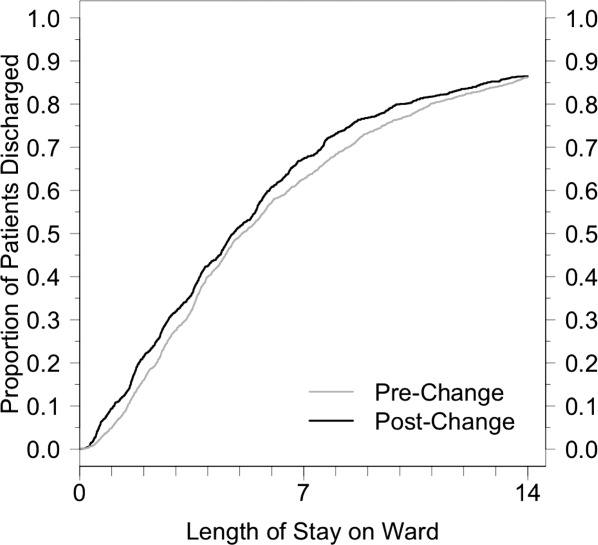
Figure 3 shows the estimated KaplanMeier curves of time to discharge (LOS) in both time periods. Differences between the 2 study periods in the proportion of patients that had been discharged at each time point (the vertical distance between the curves) can be observed, particularly in the shorter LOS times.
DISCUSSION
Previous studies have suggested that systems become more efficient when every day runs the same way.15 Achieving this for the number of daily discharges from the ward should have a positive effect on the flow of patients through the GIM service.16 Wong et al. showed how the on call schedule of medical personnel had a strong effect on the variation in daily discharges.17 A more recent study by the same authors demonstrated, through a computer simulation model, that smoothing patient discharges over the course of the week decreases the number of ED beds occupied by admitted patients.18 After introducing a structural change to our admission system that made the daily admissions of patients to each care team uniform, we showed a significant reduction in the variation of discharge rates from day to day, and the expected improvement in patient flow as shown by a decrease in the median LOS.
This intervention changed only 1 component of a complex patient care process, of which the resident on‐call schedule is only a small part. Nevertheless, this small change, designed to optimize the doctors' contribution to patient flow, was sufficient in effecting a significant reduction in the variation of the DDR. Inpatients follow a usual course in the hospital, requiring an average LOS of 4 to 5 days. In the bolus system of admissions, we observed what was essentially a cohort effect where the same bolus of patients was discharged on roughly the same day, an average of 4 to 5 days after admission. If the daily variation in discharges were only dependent on the daily variation in admissions, by making the influx of inpatients constant, we should have eliminated this cohort effect. Although the variation in discharges was reduced, it was not completely eliminated, suggesting that elements of the old system are retained. It is possible that the senior resident's management of the patients on the team has a stronger influence than that of other members of the team, and the flow of patients may still be affected by their call schedule.
We observed a significant reduction (0.3 days) in median LOS. By making each day look the same for admissions to each care team, and by making each day look more uniform for discharges from each care team, we were able to improve our unit's operational efficiency. Other benefits of the new system included: less cross‐coverage, since after‐hours there was always a member of each team to look after their own patients; the elimination of the post‐call day for the entire team; and the relatively decreased average daily workload.
The bulk of the reduction in median LOS was attributed to short‐stay patients. The flow of very sick patients who require prolonged inpatient treatment, or those waiting for post‐acute care beds (rehabilitation, long‐term care, convalescence, etc) may be less sensitive to improvements in internal efficiencies.
Although the improvement in LOS was modest, it was certainly no worse than in the older system, and the change was accompanied by the many other benefits already mentioned. In fact, ours is not the only hospital in the city that has made this change. Early results of a qualitative study exploring the perceptions of attending staff, residents, and students of the new systemparticularly its effects on the educational experienceare encouraging, showing overall positive opinions about the change. Further studies aimed at analyzing the barriers to efficient patient discharges may help identify important factors, such as those already mentioned, that this change in structure did not address. Policymakers could address other components of the discharge process, particularly the chronic shortage of post‐acute care beds. Finally, an economic analysis could provide insights about the potential savings that such structural changes could represent.
This study has several limitations. It took place in a single teaching hospital in Canada and, therefore, may not be generalizable to community hospitals or to settings that do not provide single‐payer free public healthcare. Nevertheless, most hospital units are subject to the effects of medical personnel scheduling, and the variation in patient flow processes that this produces. The current resident association collective agreement in Ontario still allows trainees to be scheduled for continuous 24‐hour duty periods. An exact replication of our structure would not be possible in settings with more stringent duty‐hour restrictions. Nevertheless, the goal of the structural change was to make the influx of patients to each care team constant, and this is achievable regardless of the length of the trainee call period. Although there is no reason to suspect a systematic difference in the mix of patients from 2008 to 2009, it would have been preferable to use a propensity score to compare clinical characteristics of the 2 patient groups. We used a relatively new metric, DDR, which was created in our institution and already has been used in several studies. However, it has not yet been validated in other centers.
One of the limitations of a before‐and‐after analysis is our inability to adjust for other changes that may have occurred during the study periods. These known and unknown factors may have had effects on the findings.
CONCLUSIONS
A new admission structure was introduced to the GIM CTU in March 2009, with the intention of changing the admissions to each care team from a bolus to a trickle system. This study was a real‐world demonstration of a concept that had, until this point, only been observed in robust simulation models. When the daily influx of patients to a care team becomes constant, the number of discharges from that team experience less daily variation, and the overall efficiency of the team improves, as measured by a reduction in the median LOS. Standardizing the care processes on the GIM inpatient ward improves overall efficiency and capacity.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52(2):126–136.
- ,,, et al.Fewer intensive care unit refusals and a higher capacity utilization by using a cyclic surgical case schedule.J Crit Care.2008;23(2):222–226.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24(4):344–346.
- ,.Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction.J Healthc Manag.2005;50(5):327–342.
- ,,.Managing variation in demand: lessons from the UK National Health Service.J Healthc Manag.2006;51(5):309–322.
- ,,,,,.The timing of neonatal discharge: an example of unwarranted variation?Pediatrics.2001;107(1):73–77.
- ,,,,.Restricted weekend service inappropriately delays discharge after acute myocardial infarction.Heart.2002;87(3):216–219.
- ,,, et al.Effect of short call admission on length of stay and quality of care for acute decompensated heart failure.Circulation.2008;117(20):2637–2644.
- ,,,,.House staff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167(1):47–52.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,,,.Evaluation of a redesign initiative in an internal‐medicine residency.N Engl J Med.2010;362(14):1304–1311.
- ,,, et al.Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities.JAMA.2008;300(10):1146–1153.
- ,,,,.Real‐time operational feedback: daily discharge rate as a novel hospital efficiency metric.Qual Saf Health Care.2010;19(6):e32.
- ,,,.WinBUGS—a Bayesian modelling framework: concepts, structure, and extensibility.Statistics and Computing.2000;10(4):325–337.
- Institute for Healthcare Improvement. Optimizing patient flow: moving patients smoothly through acute care settings;2003. Available at: http://www.ihi.org.
- Canadian Institute for Health Information. Waiting for health care in Canada: what we know and what we don't know;2006. Available at: http://www.cihi.ca.
- ,,, et al.How much do operational processes affect hospital inpatient discharge rates?J Public Health (Oxf).2009;31(4):546–553.
- ,,,,.Smoothing inpatient discharges decreases emergency department congestion: a system dynamics simulation model.Emerg Med J.2010;27(8):593–598.
Smooth and timely hospital patient flow can have multiple positive effects including reduced wait times for services, decreased congestion in the Emergency Department (ED), and increased patient and staff satisfaction.14 One way to improve patient flow is to remove variation along the care pathway.57
For teaching hospitals that provide team‐based care, 1 significant source of variation involves the emergent admission process.8, 9 Typically, for services that admit the majority of their patients from the ED, 1 team is assigned to all admitting duties on a particular day; the on‐call team. While teams rotate between designations of on‐call, post‐call, and pre‐call over the course of the week, only the team designated on‐call accepts new admissions. This bolus call structure creates the need for extensive cross‐coverage, large variations in team admissions, and disparate team workloads.1012 Moreover, the effects of these variations may persist and extend along the care pathway, ultimately impacting timely patient discharge. Therefore, interventions aimed at improving the admission process may be candidates for improved patient flow.
The objective of this study is to evaluate the effect of changing the admission process from a bolus admission system to a trickle system that evenly distributes newly admitted patients to each of the physician‐led care teams. We hypothesize that by removing variation within the team admission process, team workload will be smoothed and ultimately result in patients being discharged by the team in a more uniform pattern. We evaluate this hypothesis by measuring length of stay and daily discharge rate.
METHODS
Setting
This retrospective study was conducted on the General Internal Medicine clinical teaching unit (GIM CTU) at a large academic tertiary care center in Toronto, Canada. GIM provides acute, nonsurgical care to a patient population composed primarily of elderly patients with complex chronic illnesses. GIM receives 98% of its inpatient admissions from the ED. On a daily basis, the ED sees approximately 100 patients, of which nearly 20% are admitted to hospital. GIM constitutes the single largest admitting service in the ED, admitting nearly half of all emergent admissions. Surgical and specialized medical services (eg, Cardiology, Oncology, Nephrology) admit the remaining half.
On March 2, 2009, the GIM CTU underwent a structural change from a bolus admission system to a trickle system of admissions to each care team. Figure 1 depicts a typical pre‐change admission pattern where each of the 4 care teams would admit a bolus of patients on a given day (left panel), and a typical post‐change admission pattern where the variation in daily admissions is smoothed out as a result of the trickle admission system (right panel). No change was made to care team members; each team consisted of an attending physician, 1 senior resident, 2 to 3 junior residents, 1 social worker, 1 physiotherapist, 1 occupational therapist, and 1 pharmacist. The Appendix provides a detailed description of the structural change.
Data Collection
Records were obtained from the hospital's Electronic Patient Record, which contains information on socio‐demographics, diagnosis, length of stay (LOS), patient disposition, attending physician, and date of admission and discharge.
Data were collected for 2 time periods, the pre‐change period (March to August 2008) and the post‐change period (March to August 2009). The new system was implemented on March 2, 2009. The same months of 2 consecutive years were used to account for any seasonal variation in patient volumes and diagnoses. During the pre‐change and post‐change periods, the hospital maintained the same admitting and discharge policies and protocols. Similarly, the authors are unaware of any provincial‐wide government policies that would have impacted only 1 of either the pre‐change or post‐change periods.
Outcomes
Two main outcomes were studied, daily discharge rate (DDR)13 and LOS. DDR was expressed as the number of discharges on a particular day divided by the total patient census on that day. DDR was calculated by team, stratified by their call schedule status (on‐call, post‐call, postpost‐call, pre‐call, or none of these), and then aggregated. A day was defined as a 24‐hour period beginning at 8 AM. This was chosen because it better reflects the period when decisions are made and work is completed. Daily team‐specific patient census was measured at 8 AM. LOS was measured in days, calculated for each patient using the admission and discharge dates.
The DDR calculation included only those patients who were admitted and discharged within the study periods. For analysis of LOS, we also included patients admitted prior to, but discharged during, the study periods.
We included all patients admitted to GIM. Patient discharge dispositions were categorized into 5 groups: discharge home, interfacility transfers (discharged to long‐term care, rehabilitation, chronic care, etc), intrafacility transfers (to other inpatient services within the hospital), death, and left against medical advice. To focus on discharges that may be influenced by the team, for analysis of both DDR and LOS, only patients discharged home and interfacility and intrafacility transfers were included (deaths and patients who left against medical advice were not included).
Statistical Analysis
To assess whether the trickle system smoothed discharge rates, we fitted a logistic regression model and compared the variability in the log‐odds of discharge across the 4 main types of call days (on‐call, post‐call, postpost‐call, pre‐call) in the pre‐change and post‐change periods. The number of discharges on a given day was modeled as a binomial outcome with sample size equal to the census for that day and a log‐odds of discharge that depended on type of call day and a random error component. In this model, the effect of type of call day was allowed to be different in the pre‐change and post‐change periods. To account for the fact that data were collected on 180 consecutive days in each time period, we modeled the error component for each team in each time period as an autoregressive time series. We summarized the smoothness of discharge rates across type of call day in each period by calculating the variance of the corresponding regression parameters (the log‐odds ratios). By comparing the variances in the 2 periods, we were able to compute the probability that there was a reduction in variability, or equivalently, a smoothing of DDR. This model was fitted with Bayesian methods, implemented using Markov chain Monte Carlo (MCMC) techniques in the software WinBUGS.14 Uninformative priors were used for all parameters; model convergence was checked with the Gelman‐Brooks Rubin statistics. Further details are available from the authors on request. Summary estimates of discharge rates on the 4 main types of call day were calculated for the pre‐change and post‐change periods and plotted with 95% credible intervals.
Descriptive statistics were calculated for age, case mix group (CMG), total admission and discharges, and LOS. We chose to report median LOS, rather than the mean, because this modulates the influence of outliers in the samples.
KaplanMeier curves were also plotted for LOS. We tested for equality of the KaplanMeier curves using a weighted log‐rank test (G‐rho), which gave more weight to smaller LOS values (giving weight equal to the proportion of patients not yet discharged). This weighting was performed because an improvement in operational efficiency was more likely to have an effect on patients who could be discharged more quickly (7 days) than patients whose discharge was delayed by factors outside the hospital's control.
All other statistical analyses were performed using R (version 2.10.1; R Foundation for Statistical Computing, Vienna, Austria).
This study was approved by The University Health Network Research Ethics Board.
RESULTS
During the 2 study periods, a total of 2734 patients were discharged, 1446 in the pre‐change period (1535 admitted), and 1288 in the post‐change period (1363 admitted). Table 1 presents mean age and primary CMG diagnosis.
| Pre‐Intervention Period (March 3August 29, 2008) 1446 Total Discharges (Mean Age [SD], 66 [18.6]) | Post‐Intervention Period (March 2August 28, 2009) 1288 Total Discharges (Mean Age [SD], 67 [18.8]) | |||
|---|---|---|---|---|
| CMG Rank | CMG Description | N (%) | CMG Description | N (%) |
| ||||
| Pneumonia | 117 (7.4) | Heart failure | 102 (7.4) | |
| 2 | Heart failure | 84 (5.3) | Pneumonia | 65 (4.7) |
| 3 | G.I. hemorrhage | 68 (4.3) | Esoph/gastro/misc digestive disorder | 61 (4.4) |
| 4 | Esoph/gastro/misc digestive disorder | 62 (3.9) | Lower urinary tract infection | 56 (4.1) |
| 5 | Red blood cell disorders | 59 (3.7) | G.I. hemorrhage | 52 (3.8) |
| 6 | Nutrit/misc metabolic disorder | 56 (3.5) | Nutrit/misc metabolic disorder | 47 (3.4) |
| 7 | Reticuloendothelial disorder | 56 (3.5) | Cerebrovascular disorder | 41 (3.0) |
| 8 | Lower urinary tract infection | 50 (3.2) | Red blood cell disorders | 40 (2.9) |
| 9 | Respiratory infect and inflamm | 42 (2.7) | Ungroupable input data | 36 (2.6) |
| 10 | Cerebrovascular disorder | 40 (2.5) | Chronic obstructive pulmonary disease | 33 (2.4) |
Figure 2 shows the estimated average team‐specific DDR's according to call schedule status, along with 95% credible intervals. With the exception of the postpost‐call day, each black point (2009, post‐change period) is closer to the overall average DDR of 9.9% than each corresponding gray point (2008, pre‐change period). In our Bayesian model, there was a 96.9% probability that the variability across call schedule status was reduced in the post‐change period, substantial evidence of smoother discharge rates across different types of call days.
Summary statistics for the LOS for both groups can be seen in Table 2. The median LOS in the post‐change period was statistically significantly shorter than in the pre‐change period (4.8 days vs 5.1 days, P 0.001).
| Pre‐Change | Post‐Change | ||
|---|---|---|---|
| |||
| N | 1446 | 1288 | t Test comparing means |
| Mean LOS (SD) | 8.7 (15) | 8.8 (16) | P = 0.89 |
| Wilcoxon rank‐sum test | |||
| Median LOS | 5.06 | 4.79 | P = 0.0065 |
Figure 3 shows the estimated KaplanMeier curves of time to discharge (LOS) in both time periods. Differences between the 2 study periods in the proportion of patients that had been discharged at each time point (the vertical distance between the curves) can be observed, particularly in the shorter LOS times.
DISCUSSION
Previous studies have suggested that systems become more efficient when every day runs the same way.15 Achieving this for the number of daily discharges from the ward should have a positive effect on the flow of patients through the GIM service.16 Wong et al. showed how the on call schedule of medical personnel had a strong effect on the variation in daily discharges.17 A more recent study by the same authors demonstrated, through a computer simulation model, that smoothing patient discharges over the course of the week decreases the number of ED beds occupied by admitted patients.18 After introducing a structural change to our admission system that made the daily admissions of patients to each care team uniform, we showed a significant reduction in the variation of discharge rates from day to day, and the expected improvement in patient flow as shown by a decrease in the median LOS.
This intervention changed only 1 component of a complex patient care process, of which the resident on‐call schedule is only a small part. Nevertheless, this small change, designed to optimize the doctors' contribution to patient flow, was sufficient in effecting a significant reduction in the variation of the DDR. Inpatients follow a usual course in the hospital, requiring an average LOS of 4 to 5 days. In the bolus system of admissions, we observed what was essentially a cohort effect where the same bolus of patients was discharged on roughly the same day, an average of 4 to 5 days after admission. If the daily variation in discharges were only dependent on the daily variation in admissions, by making the influx of inpatients constant, we should have eliminated this cohort effect. Although the variation in discharges was reduced, it was not completely eliminated, suggesting that elements of the old system are retained. It is possible that the senior resident's management of the patients on the team has a stronger influence than that of other members of the team, and the flow of patients may still be affected by their call schedule.
We observed a significant reduction (0.3 days) in median LOS. By making each day look the same for admissions to each care team, and by making each day look more uniform for discharges from each care team, we were able to improve our unit's operational efficiency. Other benefits of the new system included: less cross‐coverage, since after‐hours there was always a member of each team to look after their own patients; the elimination of the post‐call day for the entire team; and the relatively decreased average daily workload.
The bulk of the reduction in median LOS was attributed to short‐stay patients. The flow of very sick patients who require prolonged inpatient treatment, or those waiting for post‐acute care beds (rehabilitation, long‐term care, convalescence, etc) may be less sensitive to improvements in internal efficiencies.
Although the improvement in LOS was modest, it was certainly no worse than in the older system, and the change was accompanied by the many other benefits already mentioned. In fact, ours is not the only hospital in the city that has made this change. Early results of a qualitative study exploring the perceptions of attending staff, residents, and students of the new systemparticularly its effects on the educational experienceare encouraging, showing overall positive opinions about the change. Further studies aimed at analyzing the barriers to efficient patient discharges may help identify important factors, such as those already mentioned, that this change in structure did not address. Policymakers could address other components of the discharge process, particularly the chronic shortage of post‐acute care beds. Finally, an economic analysis could provide insights about the potential savings that such structural changes could represent.
This study has several limitations. It took place in a single teaching hospital in Canada and, therefore, may not be generalizable to community hospitals or to settings that do not provide single‐payer free public healthcare. Nevertheless, most hospital units are subject to the effects of medical personnel scheduling, and the variation in patient flow processes that this produces. The current resident association collective agreement in Ontario still allows trainees to be scheduled for continuous 24‐hour duty periods. An exact replication of our structure would not be possible in settings with more stringent duty‐hour restrictions. Nevertheless, the goal of the structural change was to make the influx of patients to each care team constant, and this is achievable regardless of the length of the trainee call period. Although there is no reason to suspect a systematic difference in the mix of patients from 2008 to 2009, it would have been preferable to use a propensity score to compare clinical characteristics of the 2 patient groups. We used a relatively new metric, DDR, which was created in our institution and already has been used in several studies. However, it has not yet been validated in other centers.
One of the limitations of a before‐and‐after analysis is our inability to adjust for other changes that may have occurred during the study periods. These known and unknown factors may have had effects on the findings.
CONCLUSIONS
A new admission structure was introduced to the GIM CTU in March 2009, with the intention of changing the admissions to each care team from a bolus to a trickle system. This study was a real‐world demonstration of a concept that had, until this point, only been observed in robust simulation models. When the daily influx of patients to a care team becomes constant, the number of discharges from that team experience less daily variation, and the overall efficiency of the team improves, as measured by a reduction in the median LOS. Standardizing the care processes on the GIM inpatient ward improves overall efficiency and capacity.
Smooth and timely hospital patient flow can have multiple positive effects including reduced wait times for services, decreased congestion in the Emergency Department (ED), and increased patient and staff satisfaction.14 One way to improve patient flow is to remove variation along the care pathway.57
For teaching hospitals that provide team‐based care, 1 significant source of variation involves the emergent admission process.8, 9 Typically, for services that admit the majority of their patients from the ED, 1 team is assigned to all admitting duties on a particular day; the on‐call team. While teams rotate between designations of on‐call, post‐call, and pre‐call over the course of the week, only the team designated on‐call accepts new admissions. This bolus call structure creates the need for extensive cross‐coverage, large variations in team admissions, and disparate team workloads.1012 Moreover, the effects of these variations may persist and extend along the care pathway, ultimately impacting timely patient discharge. Therefore, interventions aimed at improving the admission process may be candidates for improved patient flow.
The objective of this study is to evaluate the effect of changing the admission process from a bolus admission system to a trickle system that evenly distributes newly admitted patients to each of the physician‐led care teams. We hypothesize that by removing variation within the team admission process, team workload will be smoothed and ultimately result in patients being discharged by the team in a more uniform pattern. We evaluate this hypothesis by measuring length of stay and daily discharge rate.
METHODS
Setting
This retrospective study was conducted on the General Internal Medicine clinical teaching unit (GIM CTU) at a large academic tertiary care center in Toronto, Canada. GIM provides acute, nonsurgical care to a patient population composed primarily of elderly patients with complex chronic illnesses. GIM receives 98% of its inpatient admissions from the ED. On a daily basis, the ED sees approximately 100 patients, of which nearly 20% are admitted to hospital. GIM constitutes the single largest admitting service in the ED, admitting nearly half of all emergent admissions. Surgical and specialized medical services (eg, Cardiology, Oncology, Nephrology) admit the remaining half.
On March 2, 2009, the GIM CTU underwent a structural change from a bolus admission system to a trickle system of admissions to each care team. Figure 1 depicts a typical pre‐change admission pattern where each of the 4 care teams would admit a bolus of patients on a given day (left panel), and a typical post‐change admission pattern where the variation in daily admissions is smoothed out as a result of the trickle admission system (right panel). No change was made to care team members; each team consisted of an attending physician, 1 senior resident, 2 to 3 junior residents, 1 social worker, 1 physiotherapist, 1 occupational therapist, and 1 pharmacist. The Appendix provides a detailed description of the structural change.
Data Collection
Records were obtained from the hospital's Electronic Patient Record, which contains information on socio‐demographics, diagnosis, length of stay (LOS), patient disposition, attending physician, and date of admission and discharge.
Data were collected for 2 time periods, the pre‐change period (March to August 2008) and the post‐change period (March to August 2009). The new system was implemented on March 2, 2009. The same months of 2 consecutive years were used to account for any seasonal variation in patient volumes and diagnoses. During the pre‐change and post‐change periods, the hospital maintained the same admitting and discharge policies and protocols. Similarly, the authors are unaware of any provincial‐wide government policies that would have impacted only 1 of either the pre‐change or post‐change periods.
Outcomes
Two main outcomes were studied, daily discharge rate (DDR)13 and LOS. DDR was expressed as the number of discharges on a particular day divided by the total patient census on that day. DDR was calculated by team, stratified by their call schedule status (on‐call, post‐call, postpost‐call, pre‐call, or none of these), and then aggregated. A day was defined as a 24‐hour period beginning at 8 AM. This was chosen because it better reflects the period when decisions are made and work is completed. Daily team‐specific patient census was measured at 8 AM. LOS was measured in days, calculated for each patient using the admission and discharge dates.
The DDR calculation included only those patients who were admitted and discharged within the study periods. For analysis of LOS, we also included patients admitted prior to, but discharged during, the study periods.
We included all patients admitted to GIM. Patient discharge dispositions were categorized into 5 groups: discharge home, interfacility transfers (discharged to long‐term care, rehabilitation, chronic care, etc), intrafacility transfers (to other inpatient services within the hospital), death, and left against medical advice. To focus on discharges that may be influenced by the team, for analysis of both DDR and LOS, only patients discharged home and interfacility and intrafacility transfers were included (deaths and patients who left against medical advice were not included).
Statistical Analysis
To assess whether the trickle system smoothed discharge rates, we fitted a logistic regression model and compared the variability in the log‐odds of discharge across the 4 main types of call days (on‐call, post‐call, postpost‐call, pre‐call) in the pre‐change and post‐change periods. The number of discharges on a given day was modeled as a binomial outcome with sample size equal to the census for that day and a log‐odds of discharge that depended on type of call day and a random error component. In this model, the effect of type of call day was allowed to be different in the pre‐change and post‐change periods. To account for the fact that data were collected on 180 consecutive days in each time period, we modeled the error component for each team in each time period as an autoregressive time series. We summarized the smoothness of discharge rates across type of call day in each period by calculating the variance of the corresponding regression parameters (the log‐odds ratios). By comparing the variances in the 2 periods, we were able to compute the probability that there was a reduction in variability, or equivalently, a smoothing of DDR. This model was fitted with Bayesian methods, implemented using Markov chain Monte Carlo (MCMC) techniques in the software WinBUGS.14 Uninformative priors were used for all parameters; model convergence was checked with the Gelman‐Brooks Rubin statistics. Further details are available from the authors on request. Summary estimates of discharge rates on the 4 main types of call day were calculated for the pre‐change and post‐change periods and plotted with 95% credible intervals.
Descriptive statistics were calculated for age, case mix group (CMG), total admission and discharges, and LOS. We chose to report median LOS, rather than the mean, because this modulates the influence of outliers in the samples.
KaplanMeier curves were also plotted for LOS. We tested for equality of the KaplanMeier curves using a weighted log‐rank test (G‐rho), which gave more weight to smaller LOS values (giving weight equal to the proportion of patients not yet discharged). This weighting was performed because an improvement in operational efficiency was more likely to have an effect on patients who could be discharged more quickly (7 days) than patients whose discharge was delayed by factors outside the hospital's control.
All other statistical analyses were performed using R (version 2.10.1; R Foundation for Statistical Computing, Vienna, Austria).
This study was approved by The University Health Network Research Ethics Board.
RESULTS
During the 2 study periods, a total of 2734 patients were discharged, 1446 in the pre‐change period (1535 admitted), and 1288 in the post‐change period (1363 admitted). Table 1 presents mean age and primary CMG diagnosis.
| Pre‐Intervention Period (March 3August 29, 2008) 1446 Total Discharges (Mean Age [SD], 66 [18.6]) | Post‐Intervention Period (March 2August 28, 2009) 1288 Total Discharges (Mean Age [SD], 67 [18.8]) | |||
|---|---|---|---|---|
| CMG Rank | CMG Description | N (%) | CMG Description | N (%) |
| ||||
| Pneumonia | 117 (7.4) | Heart failure | 102 (7.4) | |
| 2 | Heart failure | 84 (5.3) | Pneumonia | 65 (4.7) |
| 3 | G.I. hemorrhage | 68 (4.3) | Esoph/gastro/misc digestive disorder | 61 (4.4) |
| 4 | Esoph/gastro/misc digestive disorder | 62 (3.9) | Lower urinary tract infection | 56 (4.1) |
| 5 | Red blood cell disorders | 59 (3.7) | G.I. hemorrhage | 52 (3.8) |
| 6 | Nutrit/misc metabolic disorder | 56 (3.5) | Nutrit/misc metabolic disorder | 47 (3.4) |
| 7 | Reticuloendothelial disorder | 56 (3.5) | Cerebrovascular disorder | 41 (3.0) |
| 8 | Lower urinary tract infection | 50 (3.2) | Red blood cell disorders | 40 (2.9) |
| 9 | Respiratory infect and inflamm | 42 (2.7) | Ungroupable input data | 36 (2.6) |
| 10 | Cerebrovascular disorder | 40 (2.5) | Chronic obstructive pulmonary disease | 33 (2.4) |
Figure 2 shows the estimated average team‐specific DDR's according to call schedule status, along with 95% credible intervals. With the exception of the postpost‐call day, each black point (2009, post‐change period) is closer to the overall average DDR of 9.9% than each corresponding gray point (2008, pre‐change period). In our Bayesian model, there was a 96.9% probability that the variability across call schedule status was reduced in the post‐change period, substantial evidence of smoother discharge rates across different types of call days.
Summary statistics for the LOS for both groups can be seen in Table 2. The median LOS in the post‐change period was statistically significantly shorter than in the pre‐change period (4.8 days vs 5.1 days, P 0.001).
| Pre‐Change | Post‐Change | ||
|---|---|---|---|
| |||
| N | 1446 | 1288 | t Test comparing means |
| Mean LOS (SD) | 8.7 (15) | 8.8 (16) | P = 0.89 |
| Wilcoxon rank‐sum test | |||
| Median LOS | 5.06 | 4.79 | P = 0.0065 |
Figure 3 shows the estimated KaplanMeier curves of time to discharge (LOS) in both time periods. Differences between the 2 study periods in the proportion of patients that had been discharged at each time point (the vertical distance between the curves) can be observed, particularly in the shorter LOS times.
DISCUSSION
Previous studies have suggested that systems become more efficient when every day runs the same way.15 Achieving this for the number of daily discharges from the ward should have a positive effect on the flow of patients through the GIM service.16 Wong et al. showed how the on call schedule of medical personnel had a strong effect on the variation in daily discharges.17 A more recent study by the same authors demonstrated, through a computer simulation model, that smoothing patient discharges over the course of the week decreases the number of ED beds occupied by admitted patients.18 After introducing a structural change to our admission system that made the daily admissions of patients to each care team uniform, we showed a significant reduction in the variation of discharge rates from day to day, and the expected improvement in patient flow as shown by a decrease in the median LOS.
This intervention changed only 1 component of a complex patient care process, of which the resident on‐call schedule is only a small part. Nevertheless, this small change, designed to optimize the doctors' contribution to patient flow, was sufficient in effecting a significant reduction in the variation of the DDR. Inpatients follow a usual course in the hospital, requiring an average LOS of 4 to 5 days. In the bolus system of admissions, we observed what was essentially a cohort effect where the same bolus of patients was discharged on roughly the same day, an average of 4 to 5 days after admission. If the daily variation in discharges were only dependent on the daily variation in admissions, by making the influx of inpatients constant, we should have eliminated this cohort effect. Although the variation in discharges was reduced, it was not completely eliminated, suggesting that elements of the old system are retained. It is possible that the senior resident's management of the patients on the team has a stronger influence than that of other members of the team, and the flow of patients may still be affected by their call schedule.
We observed a significant reduction (0.3 days) in median LOS. By making each day look the same for admissions to each care team, and by making each day look more uniform for discharges from each care team, we were able to improve our unit's operational efficiency. Other benefits of the new system included: less cross‐coverage, since after‐hours there was always a member of each team to look after their own patients; the elimination of the post‐call day for the entire team; and the relatively decreased average daily workload.
The bulk of the reduction in median LOS was attributed to short‐stay patients. The flow of very sick patients who require prolonged inpatient treatment, or those waiting for post‐acute care beds (rehabilitation, long‐term care, convalescence, etc) may be less sensitive to improvements in internal efficiencies.
Although the improvement in LOS was modest, it was certainly no worse than in the older system, and the change was accompanied by the many other benefits already mentioned. In fact, ours is not the only hospital in the city that has made this change. Early results of a qualitative study exploring the perceptions of attending staff, residents, and students of the new systemparticularly its effects on the educational experienceare encouraging, showing overall positive opinions about the change. Further studies aimed at analyzing the barriers to efficient patient discharges may help identify important factors, such as those already mentioned, that this change in structure did not address. Policymakers could address other components of the discharge process, particularly the chronic shortage of post‐acute care beds. Finally, an economic analysis could provide insights about the potential savings that such structural changes could represent.
This study has several limitations. It took place in a single teaching hospital in Canada and, therefore, may not be generalizable to community hospitals or to settings that do not provide single‐payer free public healthcare. Nevertheless, most hospital units are subject to the effects of medical personnel scheduling, and the variation in patient flow processes that this produces. The current resident association collective agreement in Ontario still allows trainees to be scheduled for continuous 24‐hour duty periods. An exact replication of our structure would not be possible in settings with more stringent duty‐hour restrictions. Nevertheless, the goal of the structural change was to make the influx of patients to each care team constant, and this is achievable regardless of the length of the trainee call period. Although there is no reason to suspect a systematic difference in the mix of patients from 2008 to 2009, it would have been preferable to use a propensity score to compare clinical characteristics of the 2 patient groups. We used a relatively new metric, DDR, which was created in our institution and already has been used in several studies. However, it has not yet been validated in other centers.
One of the limitations of a before‐and‐after analysis is our inability to adjust for other changes that may have occurred during the study periods. These known and unknown factors may have had effects on the findings.
CONCLUSIONS
A new admission structure was introduced to the GIM CTU in March 2009, with the intention of changing the admissions to each care team from a bolus to a trickle system. This study was a real‐world demonstration of a concept that had, until this point, only been observed in robust simulation models. When the daily influx of patients to a care team becomes constant, the number of discharges from that team experience less daily variation, and the overall efficiency of the team improves, as measured by a reduction in the median LOS. Standardizing the care processes on the GIM inpatient ward improves overall efficiency and capacity.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52(2):126–136.
- ,,, et al.Fewer intensive care unit refusals and a higher capacity utilization by using a cyclic surgical case schedule.J Crit Care.2008;23(2):222–226.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24(4):344–346.
- ,.Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction.J Healthc Manag.2005;50(5):327–342.
- ,,.Managing variation in demand: lessons from the UK National Health Service.J Healthc Manag.2006;51(5):309–322.
- ,,,,,.The timing of neonatal discharge: an example of unwarranted variation?Pediatrics.2001;107(1):73–77.
- ,,,,.Restricted weekend service inappropriately delays discharge after acute myocardial infarction.Heart.2002;87(3):216–219.
- ,,, et al.Effect of short call admission on length of stay and quality of care for acute decompensated heart failure.Circulation.2008;117(20):2637–2644.
- ,,,,.House staff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167(1):47–52.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,,,.Evaluation of a redesign initiative in an internal‐medicine residency.N Engl J Med.2010;362(14):1304–1311.
- ,,, et al.Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities.JAMA.2008;300(10):1146–1153.
- ,,,,.Real‐time operational feedback: daily discharge rate as a novel hospital efficiency metric.Qual Saf Health Care.2010;19(6):e32.
- ,,,.WinBUGS—a Bayesian modelling framework: concepts, structure, and extensibility.Statistics and Computing.2000;10(4):325–337.
- Institute for Healthcare Improvement. Optimizing patient flow: moving patients smoothly through acute care settings;2003. Available at: http://www.ihi.org.
- Canadian Institute for Health Information. Waiting for health care in Canada: what we know and what we don't know;2006. Available at: http://www.cihi.ca.
- ,,, et al.How much do operational processes affect hospital inpatient discharge rates?J Public Health (Oxf).2009;31(4):546–553.
- ,,,,.Smoothing inpatient discharges decreases emergency department congestion: a system dynamics simulation model.Emerg Med J.2010;27(8):593–598.
- ,.Systematic review of emergency department crowding: causes, effects, and solutions.Ann Emerg Med.2008;52(2):126–136.
- ,,, et al.Fewer intensive care unit refusals and a higher capacity utilization by using a cyclic surgical case schedule.J Crit Care.2008;23(2):222–226.
- .Reengineering hospital discharge: a protocol to improve patient safety, reduce costs, and boost patient satisfaction.Am J Med Qual.2009;24(4):344–346.
- ,.Emergency department overcrowding: the impact of resource scarcity on physician job satisfaction.J Healthc Manag.2005;50(5):327–342.
- ,,.Managing variation in demand: lessons from the UK National Health Service.J Healthc Manag.2006;51(5):309–322.
- ,,,,,.The timing of neonatal discharge: an example of unwarranted variation?Pediatrics.2001;107(1):73–77.
- ,,,,.Restricted weekend service inappropriately delays discharge after acute myocardial infarction.Heart.2002;87(3):216–219.
- ,,, et al.Effect of short call admission on length of stay and quality of care for acute decompensated heart failure.Circulation.2008;117(20):2637–2644.
- ,,,,.House staff team workload and organization effects on patient outcomes in an academic general internal medicine inpatient service.Arch Intern Med.2007;167(1):47–52.
- ,,, et al.Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes.J Hosp Med.2008;3(5):361–368.
- ,,,,.Evaluation of a redesign initiative in an internal‐medicine residency.N Engl J Med.2010;362(14):1304–1311.
- ,,, et al.Association of workload of on‐call medical interns with on‐call sleep duration, shift duration, and participation in educational activities.JAMA.2008;300(10):1146–1153.
- ,,,,.Real‐time operational feedback: daily discharge rate as a novel hospital efficiency metric.Qual Saf Health Care.2010;19(6):e32.
- ,,,.WinBUGS—a Bayesian modelling framework: concepts, structure, and extensibility.Statistics and Computing.2000;10(4):325–337.
- Institute for Healthcare Improvement. Optimizing patient flow: moving patients smoothly through acute care settings;2003. Available at: http://www.ihi.org.
- Canadian Institute for Health Information. Waiting for health care in Canada: what we know and what we don't know;2006. Available at: http://www.cihi.ca.
- ,,, et al.How much do operational processes affect hospital inpatient discharge rates?J Public Health (Oxf).2009;31(4):546–553.
- ,,,,.Smoothing inpatient discharges decreases emergency department congestion: a system dynamics simulation model.Emerg Med J.2010;27(8):593–598.
U.S. Diabetes-Free Life Expectancy on the Decline
Americans are living longer – but not healthier – lives, researchers have found.
While average life expectancy is now higher than ever, the number of years Americans can expect to live without type 2 diabetes is decreasing. A prolonged period of morbidity is more likely to characterize people’s later years now than it was in the 1980s.
The difference was driven by a marked increase in the number of Americans who are obese, according to findings published Sept. 23 by Solveig A. Cunningham, Ph.D., an epidemiologist at Emory University in Atlanta, and colleagues. More than one-third of American adults now have a body-mass index of 30 kg/m2 or higher.
"All of the observed reductions in diabetes-free life expectancy at the population level were actually due to increases in diabetes only among obese individuals," Dr. Cunningham and colleagues reported (Diabetes Care 2011;34:2225-30 [doi:10.2337/dc11-0462]).
The fact that obese individuals would be more likely to be diagnosed with diabetes in the 2000s than in the 1980s, they wrote, may be because obese adults were 3.4% heavier in the latter period, or it may reflect better diagnosis of diabetes in this population group, the researchers hypothesized. Another possible explanation "is that diabetes risks are higher with younger age of obesity onset; indeed, the prevalence of obesity has tripled among children since the 1970s."
For other weight groups, including people classified as overweight (BMI, 25-30), the diabetes-free life expectancy actually improved from the 1980s to the 2000s. However, this was largely thanks to overall mortality decreasing. Life expectancy as a whole was 70.6 years for men and 77.4 years for women in the 1980s, and had increased to 74.3 for men and 79 years for women by 2000-2004.
The proportion of obese individuals had grown enough in the same time period to alter estimates of disease-free life expectancy for the population as a whole, the investigators found.
All together, diabetes-free life expectancy for an 18-year-old U.S. man was 1.7 years longer in the 1980s than it was during 2000-2004; for a woman, it was 1.5 years longer in the 1980s. The proportion of 18-year-olds who would be diagnosed with diabetes in their lifetimes increased by almost 50% among women between 1980-1989 and 2000-2004, and almost doubled among men, Dr. Cunningham and colleagues found.
Obese men lost an average of 5.6 years of diabetes-free life between the 1980s and the early 2000s, whereas women lost 2.5 years in the same interval. "In 2000-2004, obese 18-year-old men and women could expect to live 13.7 and 19.1 fewer years without diabetes, respectively, compared with normal/underweight 18-year-old men and women," the investigators wrote.
For their research, Dr. Cunningham and colleagues examined data from the National Vital Statistics System and the National Health Interview Survey, which collects self-reported health information from the noninstitutionalized, nonmilitary population.
The 1980-1989 NHIS surveys analyzed by Dr. Cunningham and colleagues contained responses from 143,765 adults (507 diagnosed diabetic in the previous year), and the 2000-2004 period surveys contained responses from 150,718 (1,366 diagnosed diabetic in the previous year).
Dr. Cunningham and colleagues examined diabetes and obesity incidence in the survey population in the context of changes in national mortality rates and population aging between the time periods.
Limitations of the study included its reliance on self-reported information about diabetes diagnosis, weight, and height, which is susceptible to bias. However, the investigators wrote that "NHIS data are collected via rigorous in-person interviews, and the differences in reported and measured BMI are not large and do not affect health risk estimates, including those associated with diabetes."
The researchers concluded that their results "suggest that in the face of budgetary or logistic constraints, new efforts to prevent diabetes can have the greatest impact among obese individuals," as all other groups were shown to have improved diabetes-free life expectancy over the decades studied.
Dr. Cunningham and colleagues reported no conflicts of interest.
Americans are living longer – but not healthier – lives, researchers have found.
While average life expectancy is now higher than ever, the number of years Americans can expect to live without type 2 diabetes is decreasing. A prolonged period of morbidity is more likely to characterize people’s later years now than it was in the 1980s.
The difference was driven by a marked increase in the number of Americans who are obese, according to findings published Sept. 23 by Solveig A. Cunningham, Ph.D., an epidemiologist at Emory University in Atlanta, and colleagues. More than one-third of American adults now have a body-mass index of 30 kg/m2 or higher.
"All of the observed reductions in diabetes-free life expectancy at the population level were actually due to increases in diabetes only among obese individuals," Dr. Cunningham and colleagues reported (Diabetes Care 2011;34:2225-30 [doi:10.2337/dc11-0462]).
The fact that obese individuals would be more likely to be diagnosed with diabetes in the 2000s than in the 1980s, they wrote, may be because obese adults were 3.4% heavier in the latter period, or it may reflect better diagnosis of diabetes in this population group, the researchers hypothesized. Another possible explanation "is that diabetes risks are higher with younger age of obesity onset; indeed, the prevalence of obesity has tripled among children since the 1970s."
For other weight groups, including people classified as overweight (BMI, 25-30), the diabetes-free life expectancy actually improved from the 1980s to the 2000s. However, this was largely thanks to overall mortality decreasing. Life expectancy as a whole was 70.6 years for men and 77.4 years for women in the 1980s, and had increased to 74.3 for men and 79 years for women by 2000-2004.
The proportion of obese individuals had grown enough in the same time period to alter estimates of disease-free life expectancy for the population as a whole, the investigators found.
All together, diabetes-free life expectancy for an 18-year-old U.S. man was 1.7 years longer in the 1980s than it was during 2000-2004; for a woman, it was 1.5 years longer in the 1980s. The proportion of 18-year-olds who would be diagnosed with diabetes in their lifetimes increased by almost 50% among women between 1980-1989 and 2000-2004, and almost doubled among men, Dr. Cunningham and colleagues found.
Obese men lost an average of 5.6 years of diabetes-free life between the 1980s and the early 2000s, whereas women lost 2.5 years in the same interval. "In 2000-2004, obese 18-year-old men and women could expect to live 13.7 and 19.1 fewer years without diabetes, respectively, compared with normal/underweight 18-year-old men and women," the investigators wrote.
For their research, Dr. Cunningham and colleagues examined data from the National Vital Statistics System and the National Health Interview Survey, which collects self-reported health information from the noninstitutionalized, nonmilitary population.
The 1980-1989 NHIS surveys analyzed by Dr. Cunningham and colleagues contained responses from 143,765 adults (507 diagnosed diabetic in the previous year), and the 2000-2004 period surveys contained responses from 150,718 (1,366 diagnosed diabetic in the previous year).
Dr. Cunningham and colleagues examined diabetes and obesity incidence in the survey population in the context of changes in national mortality rates and population aging between the time periods.
Limitations of the study included its reliance on self-reported information about diabetes diagnosis, weight, and height, which is susceptible to bias. However, the investigators wrote that "NHIS data are collected via rigorous in-person interviews, and the differences in reported and measured BMI are not large and do not affect health risk estimates, including those associated with diabetes."
The researchers concluded that their results "suggest that in the face of budgetary or logistic constraints, new efforts to prevent diabetes can have the greatest impact among obese individuals," as all other groups were shown to have improved diabetes-free life expectancy over the decades studied.
Dr. Cunningham and colleagues reported no conflicts of interest.
Americans are living longer – but not healthier – lives, researchers have found.
While average life expectancy is now higher than ever, the number of years Americans can expect to live without type 2 diabetes is decreasing. A prolonged period of morbidity is more likely to characterize people’s later years now than it was in the 1980s.
The difference was driven by a marked increase in the number of Americans who are obese, according to findings published Sept. 23 by Solveig A. Cunningham, Ph.D., an epidemiologist at Emory University in Atlanta, and colleagues. More than one-third of American adults now have a body-mass index of 30 kg/m2 or higher.
"All of the observed reductions in diabetes-free life expectancy at the population level were actually due to increases in diabetes only among obese individuals," Dr. Cunningham and colleagues reported (Diabetes Care 2011;34:2225-30 [doi:10.2337/dc11-0462]).
The fact that obese individuals would be more likely to be diagnosed with diabetes in the 2000s than in the 1980s, they wrote, may be because obese adults were 3.4% heavier in the latter period, or it may reflect better diagnosis of diabetes in this population group, the researchers hypothesized. Another possible explanation "is that diabetes risks are higher with younger age of obesity onset; indeed, the prevalence of obesity has tripled among children since the 1970s."
For other weight groups, including people classified as overweight (BMI, 25-30), the diabetes-free life expectancy actually improved from the 1980s to the 2000s. However, this was largely thanks to overall mortality decreasing. Life expectancy as a whole was 70.6 years for men and 77.4 years for women in the 1980s, and had increased to 74.3 for men and 79 years for women by 2000-2004.
The proportion of obese individuals had grown enough in the same time period to alter estimates of disease-free life expectancy for the population as a whole, the investigators found.
All together, diabetes-free life expectancy for an 18-year-old U.S. man was 1.7 years longer in the 1980s than it was during 2000-2004; for a woman, it was 1.5 years longer in the 1980s. The proportion of 18-year-olds who would be diagnosed with diabetes in their lifetimes increased by almost 50% among women between 1980-1989 and 2000-2004, and almost doubled among men, Dr. Cunningham and colleagues found.
Obese men lost an average of 5.6 years of diabetes-free life between the 1980s and the early 2000s, whereas women lost 2.5 years in the same interval. "In 2000-2004, obese 18-year-old men and women could expect to live 13.7 and 19.1 fewer years without diabetes, respectively, compared with normal/underweight 18-year-old men and women," the investigators wrote.
For their research, Dr. Cunningham and colleagues examined data from the National Vital Statistics System and the National Health Interview Survey, which collects self-reported health information from the noninstitutionalized, nonmilitary population.
The 1980-1989 NHIS surveys analyzed by Dr. Cunningham and colleagues contained responses from 143,765 adults (507 diagnosed diabetic in the previous year), and the 2000-2004 period surveys contained responses from 150,718 (1,366 diagnosed diabetic in the previous year).
Dr. Cunningham and colleagues examined diabetes and obesity incidence in the survey population in the context of changes in national mortality rates and population aging between the time periods.
Limitations of the study included its reliance on self-reported information about diabetes diagnosis, weight, and height, which is susceptible to bias. However, the investigators wrote that "NHIS data are collected via rigorous in-person interviews, and the differences in reported and measured BMI are not large and do not affect health risk estimates, including those associated with diabetes."
The researchers concluded that their results "suggest that in the face of budgetary or logistic constraints, new efforts to prevent diabetes can have the greatest impact among obese individuals," as all other groups were shown to have improved diabetes-free life expectancy over the decades studied.
Dr. Cunningham and colleagues reported no conflicts of interest.
FROM DIABETES CARE
Major Findings: While life expectancy increased between the 1980s and the early 2000s for Americans, diabetes-free life expectancy shrank by 1.7 years in men and 1.5 years in women overall, and by 5.6 and 2.5 years, respectively, in the obese.
Data Source: Nearly 300,000 national health interview surveys conducted between 1980 and 2004, along with data collected by the National Vital Statistics System.
Disclosures: Dr. Cunningham and colleagues reported no conflicts of interest.
How Hospitalists Can Team with Nursing to Improve Patient Care
Establishing mutual respect and trust between hospitalists and nurses is an important part of ensuring patient safety, whether you’re on your first job or your 20th, says Angela Beck, RN, director of critical-care services at Nebraska Medical Center in Omaha.
“Nurses are important coordinators of care,” she says. “Recognizing and valuing nurses for that is truly the most important thing for the patient, and can also help hospitalists build relationships.”
Key Partners
Forming a collaborative relationship with the nursing service might depend on where you start. At Northwestern Memorial Hospital in Chicago, the nursing service enjoys a “close and collaborative relationship” with hospitalists, according to Kristin Ramsey, RN, MSN, MPPM, NE-BC, associate chief nurse and executive director of operations. New hospitalists are oriented to the care-delivery models on the inpatient care units. In addition, hospitalists are acculturated into the hospital’s coleadership model.
—Kristin Ramsey, RN, MSN, MPPM, NE-BC, associate chief nurse and executive director of operations, Northwestern Memorial Hospital, Chicago
“We have partnered with our hospitalists to create a model in which the physician and nurse leader collaboratively lead the development of multidisciplinary, subspecialty teams to ensure quality outcomes,” Ramsey says. “The model is so successful with the hospitalists that we are now extending it to other areas in the organization.”
Round Sharing
Absent a formalized training protocol for partnering with nursing, hospitalists still can learn a great deal by listening to and communicating with the nursing staff, says Connie Ogden, RN, MSN, NEA-BC, executive director of adult acute services at Nebraska Medical Center. “Nurses are there around the clock caring for patients and may have a different insight” about patients’ evolving conditions, she says.
Care for the patient improves if everyone is on the same page, Ogden adds. That’s why it makes sense, she says, to include nurses during rounds. Beck agrees: “If nurses aren’t there to hear how the plan of care comes about, there is no reason to believe they can effectively describe it once the physician turns around and walks away to see another patient.”
In critical-care units, according to Beck, nurses can function as a bridge between patients and physicians. For example, they can help patients define and express their goals. Some of these goals can be incremental, she notes, such as “I really want to get out of bed this afternoon,” or “I really want my family here to listen to this message.”
Different Role, Same Goal
As director of adult acute services, Ogden often receives complaints from physicians about calls they receive from nurses. Often, these calls emanate from a concern for the patient (e.g. a 2 a.m. call for a Tylenol order to address a headache) or from the requirement that nurses follow policy and clarify orders. If hospitalists understand the back story of the call, their perception of its purpose can change.
Although there have been strides toward better nurse-physician collaboration, “we still have a lot of opportunities for improvement,” Beck asserts.
Establishing mutual respect and trust is not an overnight accomplishment. As Ogden explains, physicians and nurses have different roles, but they share the same goal: quality outcomes in patient care.
Gretchen Henkel is a freelance writer based in southern California.
► For more career-related articles, visit the SHM Career Center.
BEST WAYS TO IMPROVE HOSPITALIST-NURSING COLLABORATION
“A good portion of nurses are relationship builders,” says Beck, director of critical-care services at Nebraska Medical Center. She urges hospitalists on a new job to just “be physically present, in the beginning, on inpatient units” whenever possible. “Acting like you care is really important, and nurses will respond to that,” she says. “You can create an environment in which nurses’ feedback is valued.”
She also recommends, especially for new hospitalists, Dr. Peter J. Pronovost’s three-part talk “The Science of Safety,” delivered to incoming residents at Johns Hopkins University Medical Center in Baltimore, where Dr. Provonost is medical director of the quality and safety research group.—GH
Establishing mutual respect and trust between hospitalists and nurses is an important part of ensuring patient safety, whether you’re on your first job or your 20th, says Angela Beck, RN, director of critical-care services at Nebraska Medical Center in Omaha.
“Nurses are important coordinators of care,” she says. “Recognizing and valuing nurses for that is truly the most important thing for the patient, and can also help hospitalists build relationships.”
Key Partners
Forming a collaborative relationship with the nursing service might depend on where you start. At Northwestern Memorial Hospital in Chicago, the nursing service enjoys a “close and collaborative relationship” with hospitalists, according to Kristin Ramsey, RN, MSN, MPPM, NE-BC, associate chief nurse and executive director of operations. New hospitalists are oriented to the care-delivery models on the inpatient care units. In addition, hospitalists are acculturated into the hospital’s coleadership model.
—Kristin Ramsey, RN, MSN, MPPM, NE-BC, associate chief nurse and executive director of operations, Northwestern Memorial Hospital, Chicago
“We have partnered with our hospitalists to create a model in which the physician and nurse leader collaboratively lead the development of multidisciplinary, subspecialty teams to ensure quality outcomes,” Ramsey says. “The model is so successful with the hospitalists that we are now extending it to other areas in the organization.”
Round Sharing
Absent a formalized training protocol for partnering with nursing, hospitalists still can learn a great deal by listening to and communicating with the nursing staff, says Connie Ogden, RN, MSN, NEA-BC, executive director of adult acute services at Nebraska Medical Center. “Nurses are there around the clock caring for patients and may have a different insight” about patients’ evolving conditions, she says.
Care for the patient improves if everyone is on the same page, Ogden adds. That’s why it makes sense, she says, to include nurses during rounds. Beck agrees: “If nurses aren’t there to hear how the plan of care comes about, there is no reason to believe they can effectively describe it once the physician turns around and walks away to see another patient.”
In critical-care units, according to Beck, nurses can function as a bridge between patients and physicians. For example, they can help patients define and express their goals. Some of these goals can be incremental, she notes, such as “I really want to get out of bed this afternoon,” or “I really want my family here to listen to this message.”
Different Role, Same Goal
As director of adult acute services, Ogden often receives complaints from physicians about calls they receive from nurses. Often, these calls emanate from a concern for the patient (e.g. a 2 a.m. call for a Tylenol order to address a headache) or from the requirement that nurses follow policy and clarify orders. If hospitalists understand the back story of the call, their perception of its purpose can change.
Although there have been strides toward better nurse-physician collaboration, “we still have a lot of opportunities for improvement,” Beck asserts.
Establishing mutual respect and trust is not an overnight accomplishment. As Ogden explains, physicians and nurses have different roles, but they share the same goal: quality outcomes in patient care.
Gretchen Henkel is a freelance writer based in southern California.
► For more career-related articles, visit the SHM Career Center.
BEST WAYS TO IMPROVE HOSPITALIST-NURSING COLLABORATION
“A good portion of nurses are relationship builders,” says Beck, director of critical-care services at Nebraska Medical Center. She urges hospitalists on a new job to just “be physically present, in the beginning, on inpatient units” whenever possible. “Acting like you care is really important, and nurses will respond to that,” she says. “You can create an environment in which nurses’ feedback is valued.”
She also recommends, especially for new hospitalists, Dr. Peter J. Pronovost’s three-part talk “The Science of Safety,” delivered to incoming residents at Johns Hopkins University Medical Center in Baltimore, where Dr. Provonost is medical director of the quality and safety research group.—GH
Establishing mutual respect and trust between hospitalists and nurses is an important part of ensuring patient safety, whether you’re on your first job or your 20th, says Angela Beck, RN, director of critical-care services at Nebraska Medical Center in Omaha.
“Nurses are important coordinators of care,” she says. “Recognizing and valuing nurses for that is truly the most important thing for the patient, and can also help hospitalists build relationships.”
Key Partners
Forming a collaborative relationship with the nursing service might depend on where you start. At Northwestern Memorial Hospital in Chicago, the nursing service enjoys a “close and collaborative relationship” with hospitalists, according to Kristin Ramsey, RN, MSN, MPPM, NE-BC, associate chief nurse and executive director of operations. New hospitalists are oriented to the care-delivery models on the inpatient care units. In addition, hospitalists are acculturated into the hospital’s coleadership model.
—Kristin Ramsey, RN, MSN, MPPM, NE-BC, associate chief nurse and executive director of operations, Northwestern Memorial Hospital, Chicago
“We have partnered with our hospitalists to create a model in which the physician and nurse leader collaboratively lead the development of multidisciplinary, subspecialty teams to ensure quality outcomes,” Ramsey says. “The model is so successful with the hospitalists that we are now extending it to other areas in the organization.”
Round Sharing
Absent a formalized training protocol for partnering with nursing, hospitalists still can learn a great deal by listening to and communicating with the nursing staff, says Connie Ogden, RN, MSN, NEA-BC, executive director of adult acute services at Nebraska Medical Center. “Nurses are there around the clock caring for patients and may have a different insight” about patients’ evolving conditions, she says.
Care for the patient improves if everyone is on the same page, Ogden adds. That’s why it makes sense, she says, to include nurses during rounds. Beck agrees: “If nurses aren’t there to hear how the plan of care comes about, there is no reason to believe they can effectively describe it once the physician turns around and walks away to see another patient.”
In critical-care units, according to Beck, nurses can function as a bridge between patients and physicians. For example, they can help patients define and express their goals. Some of these goals can be incremental, she notes, such as “I really want to get out of bed this afternoon,” or “I really want my family here to listen to this message.”
Different Role, Same Goal
As director of adult acute services, Ogden often receives complaints from physicians about calls they receive from nurses. Often, these calls emanate from a concern for the patient (e.g. a 2 a.m. call for a Tylenol order to address a headache) or from the requirement that nurses follow policy and clarify orders. If hospitalists understand the back story of the call, their perception of its purpose can change.
Although there have been strides toward better nurse-physician collaboration, “we still have a lot of opportunities for improvement,” Beck asserts.
Establishing mutual respect and trust is not an overnight accomplishment. As Ogden explains, physicians and nurses have different roles, but they share the same goal: quality outcomes in patient care.
Gretchen Henkel is a freelance writer based in southern California.
► For more career-related articles, visit the SHM Career Center.
BEST WAYS TO IMPROVE HOSPITALIST-NURSING COLLABORATION
“A good portion of nurses are relationship builders,” says Beck, director of critical-care services at Nebraska Medical Center. She urges hospitalists on a new job to just “be physically present, in the beginning, on inpatient units” whenever possible. “Acting like you care is really important, and nurses will respond to that,” she says. “You can create an environment in which nurses’ feedback is valued.”
She also recommends, especially for new hospitalists, Dr. Peter J. Pronovost’s three-part talk “The Science of Safety,” delivered to incoming residents at Johns Hopkins University Medical Center in Baltimore, where Dr. Provonost is medical director of the quality and safety research group.—GH
Eculizumab gets accelerated approval for aHUS
The US Food and Drug Administration (FDA) has granted accelerated approval for eculizumab (Soliris) to treat patients with atypical hemolytic uremic syndrome (aHUS).
This rare and chronic disease can lead to renal failure and is associated with an increased risk of death and stroke. It accounts for 5% to 10% of all cases of hemolytic uremic syndrome and disproportionately affects children.
Eculizumab is a targeted therapy that works by inhibiting proteins that play a role in aHUS. The FDA granted accelerated approval for eculizumab based on data suggesting the drug likely confers a clinical benefit for patients with aHUS.
The FDA’s Accelerated Approval Program allows for earlier approval of drugs that treat serious conditions and fill an unmet medical need based on a surrogate endpoint that is thought to predict clinical benefit. The makers of eculizumab, Alexion Pharmaceuticals, are still required to conduct research to confirm the anticipated clinical benefit.
If this research indicates that eculizumab does provide a clinical benefit, the FDA will grant traditional approval for the drug. If research suggests eculizumab does not provide a clinical benefit, the FDA has regulatory procedures in place that could lead to removing the drug from the market.
There are no other FDA-approved treatments for aHUS. The safety and efficacy of the current standard treatment, plasma therapy (plasma exchange or fresh frozen plasma infusion), have not been studied in well-controlled trials.
Researchers have examined the safety and efficacy of eculizumab in 2 single-arm trials of 37 adult and adolescent patients with aHUS and 1 retrospective study of 19 pediatric and 11 adult patients with aHUS.
Patients treated with eculizumab in these studies experienced a favorable improvement in kidney function, including elimination of the requirement for dialysis in several patients who did not respond to plasma therapy.
Patients treated with eculizumab also exhibited improvement in platelet counts and other blood parameters that correlate with aHUS disease activity.
The most common side effects included hypertension, diarrhea, headache, anemia, vomiting, nausea, upper respiratory and urinary tract infections, and leukopenia.
Eculizumab will continue to be available only through a restricted program. Prescribers must enroll in a registration program and provide a medication guide to patients who receive the drug.
Eculizumab is marketed as Soliris by Alexion Pharmaceuticals, located in Cheshire, Connecticut. ![]()
The US Food and Drug Administration (FDA) has granted accelerated approval for eculizumab (Soliris) to treat patients with atypical hemolytic uremic syndrome (aHUS).
This rare and chronic disease can lead to renal failure and is associated with an increased risk of death and stroke. It accounts for 5% to 10% of all cases of hemolytic uremic syndrome and disproportionately affects children.
Eculizumab is a targeted therapy that works by inhibiting proteins that play a role in aHUS. The FDA granted accelerated approval for eculizumab based on data suggesting the drug likely confers a clinical benefit for patients with aHUS.
The FDA’s Accelerated Approval Program allows for earlier approval of drugs that treat serious conditions and fill an unmet medical need based on a surrogate endpoint that is thought to predict clinical benefit. The makers of eculizumab, Alexion Pharmaceuticals, are still required to conduct research to confirm the anticipated clinical benefit.
If this research indicates that eculizumab does provide a clinical benefit, the FDA will grant traditional approval for the drug. If research suggests eculizumab does not provide a clinical benefit, the FDA has regulatory procedures in place that could lead to removing the drug from the market.
There are no other FDA-approved treatments for aHUS. The safety and efficacy of the current standard treatment, plasma therapy (plasma exchange or fresh frozen plasma infusion), have not been studied in well-controlled trials.
Researchers have examined the safety and efficacy of eculizumab in 2 single-arm trials of 37 adult and adolescent patients with aHUS and 1 retrospective study of 19 pediatric and 11 adult patients with aHUS.
Patients treated with eculizumab in these studies experienced a favorable improvement in kidney function, including elimination of the requirement for dialysis in several patients who did not respond to plasma therapy.
Patients treated with eculizumab also exhibited improvement in platelet counts and other blood parameters that correlate with aHUS disease activity.
The most common side effects included hypertension, diarrhea, headache, anemia, vomiting, nausea, upper respiratory and urinary tract infections, and leukopenia.
Eculizumab will continue to be available only through a restricted program. Prescribers must enroll in a registration program and provide a medication guide to patients who receive the drug.
Eculizumab is marketed as Soliris by Alexion Pharmaceuticals, located in Cheshire, Connecticut. ![]()
The US Food and Drug Administration (FDA) has granted accelerated approval for eculizumab (Soliris) to treat patients with atypical hemolytic uremic syndrome (aHUS).
This rare and chronic disease can lead to renal failure and is associated with an increased risk of death and stroke. It accounts for 5% to 10% of all cases of hemolytic uremic syndrome and disproportionately affects children.
Eculizumab is a targeted therapy that works by inhibiting proteins that play a role in aHUS. The FDA granted accelerated approval for eculizumab based on data suggesting the drug likely confers a clinical benefit for patients with aHUS.
The FDA’s Accelerated Approval Program allows for earlier approval of drugs that treat serious conditions and fill an unmet medical need based on a surrogate endpoint that is thought to predict clinical benefit. The makers of eculizumab, Alexion Pharmaceuticals, are still required to conduct research to confirm the anticipated clinical benefit.
If this research indicates that eculizumab does provide a clinical benefit, the FDA will grant traditional approval for the drug. If research suggests eculizumab does not provide a clinical benefit, the FDA has regulatory procedures in place that could lead to removing the drug from the market.
There are no other FDA-approved treatments for aHUS. The safety and efficacy of the current standard treatment, plasma therapy (plasma exchange or fresh frozen plasma infusion), have not been studied in well-controlled trials.
Researchers have examined the safety and efficacy of eculizumab in 2 single-arm trials of 37 adult and adolescent patients with aHUS and 1 retrospective study of 19 pediatric and 11 adult patients with aHUS.
Patients treated with eculizumab in these studies experienced a favorable improvement in kidney function, including elimination of the requirement for dialysis in several patients who did not respond to plasma therapy.
Patients treated with eculizumab also exhibited improvement in platelet counts and other blood parameters that correlate with aHUS disease activity.
The most common side effects included hypertension, diarrhea, headache, anemia, vomiting, nausea, upper respiratory and urinary tract infections, and leukopenia.
Eculizumab will continue to be available only through a restricted program. Prescribers must enroll in a registration program and provide a medication guide to patients who receive the drug.
Eculizumab is marketed as Soliris by Alexion Pharmaceuticals, located in Cheshire, Connecticut. ![]()
DPP-4 Inhibitors May Be Cardioprotective
LISBON – A new meta-analysis offers some tantalizing hints that DPP-4 inhibitors may offer some level of protection against major cardiovascular events in type 2 diabetes patients.
The analysis, which included data on more than 33,000 patients, found a consistent 31% reduction in major cardiovascular events among those who took dipeptidyl peptidase–4 (DPP-4) inhibitors, compared with those taking placebo or other treatments, Dr. Edoardo Mannucci reported at the annual meeting of the European Association for the Study of Diabetes.
Despite the positive findings, Dr. Mannucci, of the Careggi Teaching Hospital in Florence, Italy, warned against taking the data as gospel.
"The limitations here are clear," he said. "Cardiovascular events were not end points in any of these trials, and were [reported only] as major adverse events. Also, since they were not prespecified end points, there is a possibility that some of the cases could have been misclassified."
Additionally, none of the trials enrolled patients who were at a high risk of cardiovascular events. "These subjects are not very likely to be included in trials with metabolic outcomes, so we really don’t know the effect on those people."
Still, he said, the consistency of the findings "suggests the possibility of some unconventional cardiovascular protective effect that deserves further investigation."
Dr. Mannucci and his colleagues examined 42 phase III trials completed through March 2011 that included one of four DPP-4 inhibitors: saxagliptin, sitagliptin, alogliptin, and vildagliptin. (The latter two are not available in the United States.) Among placebo-controlled trials, 137 events occurred, and in comparator trials, 120 occurred.
Overall, the hazard ratios for a major cardiovascular event were 0.63 for alogliptin, 0.66 for saxagliptin, 0.74 for sitagliptin, and 0.67 for vildagliptin, compared with placebo. All the comparisons were statistically significant, he said.
In the comparator trials, none of the difference in cardiovascular events between drug regimens reached statistical significance, but the trend in favor of the DPP-4 inhibitors was similar to the findings in the placebo-controlled studies, he said.
Dr. Mannucci speculated that the lack of significance could be related to the low incidence of a major cardiovascular event in these trials, ranging from one event in an acarbose study to five each in studies with metformin and sulfonylureas.
Considering all of the 26 placebo-controlled and 16 comparator studies, the odds ratio in favor of the DPP-4 drugs was 0.69, "easily reaching statistical significance," with a P value of .006, Dr. Mannucci said.
When the trials were divided by duration, those less than 52 weeks (30) were significantly in favor of the drugs (OR, 0.62). For those 52 weeks or longer, the result was not significant (OR, 0.83).
Despite the analysis’s limitations, the unexpected observation raises intriguing questions, Dr. Mannucci said, including the possible rapidity of a cardiovascular benefit in the shorter trials. "Usually when we treat any risk factor for cardiovascular disease, we need several years to see any effect on major cardiovascular events. This is true for blood pressure, blood lipids, and blood glucose, and here we see agents that work on blood glucose and show an effect in a few months. This points to speculation that some unconventional cardioprotective effect occurs, which does not require a lot of incubation."
There are no proven mechanistic actions for the observed risk reductions, but Dr. Mannucci said that preclinical studies of the DPP-4 drugs provide some hints, including a direct myocardial effect, GLP-1 stimulation, myocardial protection from ischemia, and recruitment of endothelial cell progenitors."
"We are somewhat stretching the data here, because these trials were not designed for this end point," he acknowledged. "These findings are not fully reliable and we must admit that. But we won’t have any data with credible reliability for the next 4-5 years, so in the meanwhile, even data with some problems could give us some further information."
Dr. Carolyn Deacon, a medical physiologist at Panum Institute in Copenhagen, said that the meta-analysis offers some reassurance to those who are concerned about the cardiovascular safety of any drug. "When we get all the data for the DPP-4–inhibitor trials and the GLP-1 analogues, and examine cardiovascular events for these outcomes, we’ll know much more. But we are getting preclinical data that look positive, so we’re moving in the right direction," she noted.
The preclinical data suggest that the DPP-4 inhibitors may act directly on the heart, induce vasodilation, and improve endothelial function, Dr. Deacon added. "But right now, we cannot separate those benefits from the improved metabolic profile that the drugs induce, so I don’t want to raise hopes too much."
Dr. Mannucci disclosed relationships with Astra Zeneca, Boehringer Ingelheim, Eli Lilly Merck, Bristol-Myers Squibb, Novartis, and Takeda. Dr. Deacon disclosed a number of relationships with pharmaceutical companies involved in diabetes research.
This meta-analysis offers some reassurance to those of us who continue to be concerned about the cardiovascular safety of any drug. When we get all the data for the DPP-4–inhibitor trials and the GLP-1 analogues, and examine cardiovascular events for these outcomes, we’ll know much more. But we are getting preclinical data that look positive, so we’re moving in the right direction.
The preclinical data suggest that the DPP-4 inhibitors may act directly on the heart, induce vasodilation, and improve endothelial function. But right now, we cannot separate those benefits from the improved metabolic profile that the drugs induce, so I don’t want to raise hopes too much.
Carolyn Deacon, M.D., is a medical physiologist at Panum Institute in Copenhagen. She disclosed a number of relationships with pharmaceutical companies involved in diabetes research. Her spouse is an employee of Merck.
This meta-analysis offers some reassurance to those of us who continue to be concerned about the cardiovascular safety of any drug. When we get all the data for the DPP-4–inhibitor trials and the GLP-1 analogues, and examine cardiovascular events for these outcomes, we’ll know much more. But we are getting preclinical data that look positive, so we’re moving in the right direction.
The preclinical data suggest that the DPP-4 inhibitors may act directly on the heart, induce vasodilation, and improve endothelial function. But right now, we cannot separate those benefits from the improved metabolic profile that the drugs induce, so I don’t want to raise hopes too much.
Carolyn Deacon, M.D., is a medical physiologist at Panum Institute in Copenhagen. She disclosed a number of relationships with pharmaceutical companies involved in diabetes research. Her spouse is an employee of Merck.
This meta-analysis offers some reassurance to those of us who continue to be concerned about the cardiovascular safety of any drug. When we get all the data for the DPP-4–inhibitor trials and the GLP-1 analogues, and examine cardiovascular events for these outcomes, we’ll know much more. But we are getting preclinical data that look positive, so we’re moving in the right direction.
The preclinical data suggest that the DPP-4 inhibitors may act directly on the heart, induce vasodilation, and improve endothelial function. But right now, we cannot separate those benefits from the improved metabolic profile that the drugs induce, so I don’t want to raise hopes too much.
Carolyn Deacon, M.D., is a medical physiologist at Panum Institute in Copenhagen. She disclosed a number of relationships with pharmaceutical companies involved in diabetes research. Her spouse is an employee of Merck.
LISBON – A new meta-analysis offers some tantalizing hints that DPP-4 inhibitors may offer some level of protection against major cardiovascular events in type 2 diabetes patients.
The analysis, which included data on more than 33,000 patients, found a consistent 31% reduction in major cardiovascular events among those who took dipeptidyl peptidase–4 (DPP-4) inhibitors, compared with those taking placebo or other treatments, Dr. Edoardo Mannucci reported at the annual meeting of the European Association for the Study of Diabetes.
Despite the positive findings, Dr. Mannucci, of the Careggi Teaching Hospital in Florence, Italy, warned against taking the data as gospel.
"The limitations here are clear," he said. "Cardiovascular events were not end points in any of these trials, and were [reported only] as major adverse events. Also, since they were not prespecified end points, there is a possibility that some of the cases could have been misclassified."
Additionally, none of the trials enrolled patients who were at a high risk of cardiovascular events. "These subjects are not very likely to be included in trials with metabolic outcomes, so we really don’t know the effect on those people."
Still, he said, the consistency of the findings "suggests the possibility of some unconventional cardiovascular protective effect that deserves further investigation."
Dr. Mannucci and his colleagues examined 42 phase III trials completed through March 2011 that included one of four DPP-4 inhibitors: saxagliptin, sitagliptin, alogliptin, and vildagliptin. (The latter two are not available in the United States.) Among placebo-controlled trials, 137 events occurred, and in comparator trials, 120 occurred.
Overall, the hazard ratios for a major cardiovascular event were 0.63 for alogliptin, 0.66 for saxagliptin, 0.74 for sitagliptin, and 0.67 for vildagliptin, compared with placebo. All the comparisons were statistically significant, he said.
In the comparator trials, none of the difference in cardiovascular events between drug regimens reached statistical significance, but the trend in favor of the DPP-4 inhibitors was similar to the findings in the placebo-controlled studies, he said.
Dr. Mannucci speculated that the lack of significance could be related to the low incidence of a major cardiovascular event in these trials, ranging from one event in an acarbose study to five each in studies with metformin and sulfonylureas.
Considering all of the 26 placebo-controlled and 16 comparator studies, the odds ratio in favor of the DPP-4 drugs was 0.69, "easily reaching statistical significance," with a P value of .006, Dr. Mannucci said.
When the trials were divided by duration, those less than 52 weeks (30) were significantly in favor of the drugs (OR, 0.62). For those 52 weeks or longer, the result was not significant (OR, 0.83).
Despite the analysis’s limitations, the unexpected observation raises intriguing questions, Dr. Mannucci said, including the possible rapidity of a cardiovascular benefit in the shorter trials. "Usually when we treat any risk factor for cardiovascular disease, we need several years to see any effect on major cardiovascular events. This is true for blood pressure, blood lipids, and blood glucose, and here we see agents that work on blood glucose and show an effect in a few months. This points to speculation that some unconventional cardioprotective effect occurs, which does not require a lot of incubation."
There are no proven mechanistic actions for the observed risk reductions, but Dr. Mannucci said that preclinical studies of the DPP-4 drugs provide some hints, including a direct myocardial effect, GLP-1 stimulation, myocardial protection from ischemia, and recruitment of endothelial cell progenitors."
"We are somewhat stretching the data here, because these trials were not designed for this end point," he acknowledged. "These findings are not fully reliable and we must admit that. But we won’t have any data with credible reliability for the next 4-5 years, so in the meanwhile, even data with some problems could give us some further information."
Dr. Carolyn Deacon, a medical physiologist at Panum Institute in Copenhagen, said that the meta-analysis offers some reassurance to those who are concerned about the cardiovascular safety of any drug. "When we get all the data for the DPP-4–inhibitor trials and the GLP-1 analogues, and examine cardiovascular events for these outcomes, we’ll know much more. But we are getting preclinical data that look positive, so we’re moving in the right direction," she noted.
The preclinical data suggest that the DPP-4 inhibitors may act directly on the heart, induce vasodilation, and improve endothelial function, Dr. Deacon added. "But right now, we cannot separate those benefits from the improved metabolic profile that the drugs induce, so I don’t want to raise hopes too much."
Dr. Mannucci disclosed relationships with Astra Zeneca, Boehringer Ingelheim, Eli Lilly Merck, Bristol-Myers Squibb, Novartis, and Takeda. Dr. Deacon disclosed a number of relationships with pharmaceutical companies involved in diabetes research.
LISBON – A new meta-analysis offers some tantalizing hints that DPP-4 inhibitors may offer some level of protection against major cardiovascular events in type 2 diabetes patients.
The analysis, which included data on more than 33,000 patients, found a consistent 31% reduction in major cardiovascular events among those who took dipeptidyl peptidase–4 (DPP-4) inhibitors, compared with those taking placebo or other treatments, Dr. Edoardo Mannucci reported at the annual meeting of the European Association for the Study of Diabetes.
Despite the positive findings, Dr. Mannucci, of the Careggi Teaching Hospital in Florence, Italy, warned against taking the data as gospel.
"The limitations here are clear," he said. "Cardiovascular events were not end points in any of these trials, and were [reported only] as major adverse events. Also, since they were not prespecified end points, there is a possibility that some of the cases could have been misclassified."
Additionally, none of the trials enrolled patients who were at a high risk of cardiovascular events. "These subjects are not very likely to be included in trials with metabolic outcomes, so we really don’t know the effect on those people."
Still, he said, the consistency of the findings "suggests the possibility of some unconventional cardiovascular protective effect that deserves further investigation."
Dr. Mannucci and his colleagues examined 42 phase III trials completed through March 2011 that included one of four DPP-4 inhibitors: saxagliptin, sitagliptin, alogliptin, and vildagliptin. (The latter two are not available in the United States.) Among placebo-controlled trials, 137 events occurred, and in comparator trials, 120 occurred.
Overall, the hazard ratios for a major cardiovascular event were 0.63 for alogliptin, 0.66 for saxagliptin, 0.74 for sitagliptin, and 0.67 for vildagliptin, compared with placebo. All the comparisons were statistically significant, he said.
In the comparator trials, none of the difference in cardiovascular events between drug regimens reached statistical significance, but the trend in favor of the DPP-4 inhibitors was similar to the findings in the placebo-controlled studies, he said.
Dr. Mannucci speculated that the lack of significance could be related to the low incidence of a major cardiovascular event in these trials, ranging from one event in an acarbose study to five each in studies with metformin and sulfonylureas.
Considering all of the 26 placebo-controlled and 16 comparator studies, the odds ratio in favor of the DPP-4 drugs was 0.69, "easily reaching statistical significance," with a P value of .006, Dr. Mannucci said.
When the trials were divided by duration, those less than 52 weeks (30) were significantly in favor of the drugs (OR, 0.62). For those 52 weeks or longer, the result was not significant (OR, 0.83).
Despite the analysis’s limitations, the unexpected observation raises intriguing questions, Dr. Mannucci said, including the possible rapidity of a cardiovascular benefit in the shorter trials. "Usually when we treat any risk factor for cardiovascular disease, we need several years to see any effect on major cardiovascular events. This is true for blood pressure, blood lipids, and blood glucose, and here we see agents that work on blood glucose and show an effect in a few months. This points to speculation that some unconventional cardioprotective effect occurs, which does not require a lot of incubation."
There are no proven mechanistic actions for the observed risk reductions, but Dr. Mannucci said that preclinical studies of the DPP-4 drugs provide some hints, including a direct myocardial effect, GLP-1 stimulation, myocardial protection from ischemia, and recruitment of endothelial cell progenitors."
"We are somewhat stretching the data here, because these trials were not designed for this end point," he acknowledged. "These findings are not fully reliable and we must admit that. But we won’t have any data with credible reliability for the next 4-5 years, so in the meanwhile, even data with some problems could give us some further information."
Dr. Carolyn Deacon, a medical physiologist at Panum Institute in Copenhagen, said that the meta-analysis offers some reassurance to those who are concerned about the cardiovascular safety of any drug. "When we get all the data for the DPP-4–inhibitor trials and the GLP-1 analogues, and examine cardiovascular events for these outcomes, we’ll know much more. But we are getting preclinical data that look positive, so we’re moving in the right direction," she noted.
The preclinical data suggest that the DPP-4 inhibitors may act directly on the heart, induce vasodilation, and improve endothelial function, Dr. Deacon added. "But right now, we cannot separate those benefits from the improved metabolic profile that the drugs induce, so I don’t want to raise hopes too much."
Dr. Mannucci disclosed relationships with Astra Zeneca, Boehringer Ingelheim, Eli Lilly Merck, Bristol-Myers Squibb, Novartis, and Takeda. Dr. Deacon disclosed a number of relationships with pharmaceutical companies involved in diabetes research.
FROM THE ANNUAL MEETING OF THE EUROPEAN ASSOCIATION FOR THE STUDY OF DIABETES
Major Finding: Type 2 diabetes patients taking DPP-4 inhibitors had a statistically significant 31% reduced incidence of cardiovascular events, compared with those on placebo or comparator drugs.
Data Source: A meta-analysis of 42 phase III studies of four DPP-4–inhibiting drugs in more than 30,000 patients.
Disclosures: Dr. Mannucci disclosed relationships with Astra Zeneca, Boehringer Ingelheim, Eli Lilly, Merck, Bristol-Myers Squibb, Novartis, and Takeda.
Diagnosis, Management of Arthritis in Children and Teens
When you assess a patient with a swollen joint, limited range of motion, and/or pain, consider a diagnosis of juvenile idiopathic arthritis.
Start with a detailed history and physical examination. Questions to ask include: How long have the symptoms been present? Was the onset acute or gradual? What is its severity? Ask the patient to rate the severity of pain. Use a 0-10 rating scale in older children and a faces scale in younger kids. Remember that not all children with oligoarticular juvenile idiopathic arthritis (JIA) experience pain.
Is there interference with school or any other activities? Are the symptoms improving or getting worse?
Also inquire about diurnal variation: Are symptoms more problematic in the morning or evening? Stiffness in the morning or following prolonged inactivity is a classic sign of arthritis in children as well as in adults. Also, what medications or other strategies has the patient tried, and how successful where they?
Inquire about associated symptoms. Fever, cutaneous eruption, weight loss, abdominal pain, diarrhea, and behavioral or visual changes are examples. Ocular inflammation is a common feature of some of the subtypes of juvenile arthritis.
Ask the patient or family about a history of trauma to rule out a fracture or significant intraarticular injury. Keep in mind that even chronic swelling of a joint sometimes may be an orthopedic issue.
One diagnosis you don’t want to miss is malignancy. You think automatically about arthritis when a child presents with joint pain, but all pediatric rheumatologists see a few children each year who turn out to have cancer instead. So be sure that pain truly is localized to the joint, and it’s not bone pain which may reflect the presence of leukemia, lymphoma, or another malignancy.
Remember arthritis is not always the primary disorder. During the initial evaluation you might see a child with inflammation of two of three joints. If you don’t ask about recurrent abdominal pain and/or low-grade fever, you may miss the fact that their arthritis is part of inflammatory bowel disease. If you have any questions about the primary vs. secondary nature of a child’s arthritis, refer the patient to a pediatric rheumatologist for further evaluation. The differential diagnosis for juvenile idiopathic arthritis (now the preferred name replacing "juvenile rheumatoid arthritis") can be lengthy.
Once a diagnosis of JIA is confirmed, a pediatric rheumatologist is best qualified to oversee ongoing care of the patient. Compared with 20 years ago, there are now a great many new agents specifically tailored to treat JIA (particularly biologics), and these medications require that those familiar with dosing schedules and side effects direct their administration. A medication that works well for one subtype of JIA may not work as well for another.
Physical and occupational therapists are critical for a successful approach to children with chronic arthritis. Their involvement helps to maintain range of motion, muscle strength, and endurance while preventing joint contractures and abnormalities of bone growth. The overall goal is to "mainstream" children back to their usual activities. However, if they participated in rugby, ice hockey, or tackle football, we will try to steer these patients to activities with a lower potential for direct trauma. We don’t want a child to be isolated from their peers.
It also is important not to overtest children with suspected arthritis. Laboratory testing is indicated if you strongly suspect an inflammatory process rather than for a child with vague aches and pains. Appropriate initial assays often include a complete blood count, urinalysis, sedimentation rate, and measurement of the C-reactive protein.
Tests such as an ANA (antinuclear antibody) and rheumatoid factor should be reserved for those children with symptoms and signs more likely to be associated with an inflammatory condition. These tests may be misleading with frequent false-positive results that cause undue anxiety for the patient and their family.
For more information on when to refer your patient, see the American College of Rheumatology’s 2010 Guidelines for the Referral of Children and Adolescents to Pediatric Rheumatologists.
Dr. Goldsmith is professor of pediatrics at Drexel University and chief of the rheumatology section at St. Christopher’s Hospital for Children, both in Philadelphia. Dr. Goldsmith said that he has no relevant financial disclosures.
This column, "Subspecialist Consult," appears regularly in Pediatric News, a publication of Elsevier.
When you assess a patient with a swollen joint, limited range of motion, and/or pain, consider a diagnosis of juvenile idiopathic arthritis.
Start with a detailed history and physical examination. Questions to ask include: How long have the symptoms been present? Was the onset acute or gradual? What is its severity? Ask the patient to rate the severity of pain. Use a 0-10 rating scale in older children and a faces scale in younger kids. Remember that not all children with oligoarticular juvenile idiopathic arthritis (JIA) experience pain.
Is there interference with school or any other activities? Are the symptoms improving or getting worse?
Also inquire about diurnal variation: Are symptoms more problematic in the morning or evening? Stiffness in the morning or following prolonged inactivity is a classic sign of arthritis in children as well as in adults. Also, what medications or other strategies has the patient tried, and how successful where they?
Inquire about associated symptoms. Fever, cutaneous eruption, weight loss, abdominal pain, diarrhea, and behavioral or visual changes are examples. Ocular inflammation is a common feature of some of the subtypes of juvenile arthritis.
Ask the patient or family about a history of trauma to rule out a fracture or significant intraarticular injury. Keep in mind that even chronic swelling of a joint sometimes may be an orthopedic issue.
One diagnosis you don’t want to miss is malignancy. You think automatically about arthritis when a child presents with joint pain, but all pediatric rheumatologists see a few children each year who turn out to have cancer instead. So be sure that pain truly is localized to the joint, and it’s not bone pain which may reflect the presence of leukemia, lymphoma, or another malignancy.
Remember arthritis is not always the primary disorder. During the initial evaluation you might see a child with inflammation of two of three joints. If you don’t ask about recurrent abdominal pain and/or low-grade fever, you may miss the fact that their arthritis is part of inflammatory bowel disease. If you have any questions about the primary vs. secondary nature of a child’s arthritis, refer the patient to a pediatric rheumatologist for further evaluation. The differential diagnosis for juvenile idiopathic arthritis (now the preferred name replacing "juvenile rheumatoid arthritis") can be lengthy.
Once a diagnosis of JIA is confirmed, a pediatric rheumatologist is best qualified to oversee ongoing care of the patient. Compared with 20 years ago, there are now a great many new agents specifically tailored to treat JIA (particularly biologics), and these medications require that those familiar with dosing schedules and side effects direct their administration. A medication that works well for one subtype of JIA may not work as well for another.
Physical and occupational therapists are critical for a successful approach to children with chronic arthritis. Their involvement helps to maintain range of motion, muscle strength, and endurance while preventing joint contractures and abnormalities of bone growth. The overall goal is to "mainstream" children back to their usual activities. However, if they participated in rugby, ice hockey, or tackle football, we will try to steer these patients to activities with a lower potential for direct trauma. We don’t want a child to be isolated from their peers.
It also is important not to overtest children with suspected arthritis. Laboratory testing is indicated if you strongly suspect an inflammatory process rather than for a child with vague aches and pains. Appropriate initial assays often include a complete blood count, urinalysis, sedimentation rate, and measurement of the C-reactive protein.
Tests such as an ANA (antinuclear antibody) and rheumatoid factor should be reserved for those children with symptoms and signs more likely to be associated with an inflammatory condition. These tests may be misleading with frequent false-positive results that cause undue anxiety for the patient and their family.
For more information on when to refer your patient, see the American College of Rheumatology’s 2010 Guidelines for the Referral of Children and Adolescents to Pediatric Rheumatologists.
Dr. Goldsmith is professor of pediatrics at Drexel University and chief of the rheumatology section at St. Christopher’s Hospital for Children, both in Philadelphia. Dr. Goldsmith said that he has no relevant financial disclosures.
This column, "Subspecialist Consult," appears regularly in Pediatric News, a publication of Elsevier.
When you assess a patient with a swollen joint, limited range of motion, and/or pain, consider a diagnosis of juvenile idiopathic arthritis.
Start with a detailed history and physical examination. Questions to ask include: How long have the symptoms been present? Was the onset acute or gradual? What is its severity? Ask the patient to rate the severity of pain. Use a 0-10 rating scale in older children and a faces scale in younger kids. Remember that not all children with oligoarticular juvenile idiopathic arthritis (JIA) experience pain.
Is there interference with school or any other activities? Are the symptoms improving or getting worse?
Also inquire about diurnal variation: Are symptoms more problematic in the morning or evening? Stiffness in the morning or following prolonged inactivity is a classic sign of arthritis in children as well as in adults. Also, what medications or other strategies has the patient tried, and how successful where they?
Inquire about associated symptoms. Fever, cutaneous eruption, weight loss, abdominal pain, diarrhea, and behavioral or visual changes are examples. Ocular inflammation is a common feature of some of the subtypes of juvenile arthritis.
Ask the patient or family about a history of trauma to rule out a fracture or significant intraarticular injury. Keep in mind that even chronic swelling of a joint sometimes may be an orthopedic issue.
One diagnosis you don’t want to miss is malignancy. You think automatically about arthritis when a child presents with joint pain, but all pediatric rheumatologists see a few children each year who turn out to have cancer instead. So be sure that pain truly is localized to the joint, and it’s not bone pain which may reflect the presence of leukemia, lymphoma, or another malignancy.
Remember arthritis is not always the primary disorder. During the initial evaluation you might see a child with inflammation of two of three joints. If you don’t ask about recurrent abdominal pain and/or low-grade fever, you may miss the fact that their arthritis is part of inflammatory bowel disease. If you have any questions about the primary vs. secondary nature of a child’s arthritis, refer the patient to a pediatric rheumatologist for further evaluation. The differential diagnosis for juvenile idiopathic arthritis (now the preferred name replacing "juvenile rheumatoid arthritis") can be lengthy.
Once a diagnosis of JIA is confirmed, a pediatric rheumatologist is best qualified to oversee ongoing care of the patient. Compared with 20 years ago, there are now a great many new agents specifically tailored to treat JIA (particularly biologics), and these medications require that those familiar with dosing schedules and side effects direct their administration. A medication that works well for one subtype of JIA may not work as well for another.
Physical and occupational therapists are critical for a successful approach to children with chronic arthritis. Their involvement helps to maintain range of motion, muscle strength, and endurance while preventing joint contractures and abnormalities of bone growth. The overall goal is to "mainstream" children back to their usual activities. However, if they participated in rugby, ice hockey, or tackle football, we will try to steer these patients to activities with a lower potential for direct trauma. We don’t want a child to be isolated from their peers.
It also is important not to overtest children with suspected arthritis. Laboratory testing is indicated if you strongly suspect an inflammatory process rather than for a child with vague aches and pains. Appropriate initial assays often include a complete blood count, urinalysis, sedimentation rate, and measurement of the C-reactive protein.
Tests such as an ANA (antinuclear antibody) and rheumatoid factor should be reserved for those children with symptoms and signs more likely to be associated with an inflammatory condition. These tests may be misleading with frequent false-positive results that cause undue anxiety for the patient and their family.
For more information on when to refer your patient, see the American College of Rheumatology’s 2010 Guidelines for the Referral of Children and Adolescents to Pediatric Rheumatologists.
Dr. Goldsmith is professor of pediatrics at Drexel University and chief of the rheumatology section at St. Christopher’s Hospital for Children, both in Philadelphia. Dr. Goldsmith said that he has no relevant financial disclosures.
This column, "Subspecialist Consult," appears regularly in Pediatric News, a publication of Elsevier.
Deadline Extension for Bundled Payments Program
The Centers for Medicare & Medicaid Services (CMS) on Aug. 23 introduced the Bundled Payments for Care Improvement Initiative, developed as part of the payment bundling provision of the Affordable Care Act (ACA). CMS has invited providers to apply to help test and develop four different models of bundling payments, which allow for great flexibility in selecting conditions, developing the care delivery structure, and determining how payments will be allocated among participating providers.
SHM learned last week that the Center for Medicare & Medicaid Innovation (CMMI) will accept nonbinding letters of intent for Model 1 of the program through Oct. 6. CMMI extended the deadline, originally set for Sept. 22, to give institutions and providers more time. Once institutions submit their letters of intent, the deadline to submit a formal application is Nov. 18.
The deadline for letters of intent for Models 2-4 remains Nov. 4, according to CMMI. The application deadline for those three models is March 15, 2012.
Felix Aguirre, MD, SFHM, vice president of medical affairs for North Hollywood, Calif.-based IPC: The Hospitalist Co., says HM group leaders should continue to monitor the process, but how involved they get depends on their individual situations and their relationship with an institution. “If you’re a private group, there’s a lot of weight on you to try to convince an acute-care facility to go down this risk-bearing road,” he says.
Dr. Aguirre says CMMI’s first three models are all “retrospective,” meaning hospitals and/or providers will be paid fees for service, and once episodic care is completed, as defined by each of the models, reconciliation will be made—and there is the real risk of having to pay back funds to CMS. In Model 4, the lone “prospective” setup, there is a single bundled payment up front “and you live and die by that money,” Dr. Aguirre says. “If it costs you a lot more to provide the service, it’s a true risk arrangement where you take a loss. Of course, if you have reduced costs by providing services a little more efficiently and you’ve saved a few dollars, you get to remain with those dollars.”
Dr. Aguirre also notes that of the four current models, Model 3 is the only one available directly to individual providers or HM groups as a risk-bearing entity, and only for post-acute-care services.
CMMI is expected to introduce at least a few more models in the coming months.
For more about CMS' bundling initiatives, visit our website.
The Centers for Medicare & Medicaid Services (CMS) on Aug. 23 introduced the Bundled Payments for Care Improvement Initiative, developed as part of the payment bundling provision of the Affordable Care Act (ACA). CMS has invited providers to apply to help test and develop four different models of bundling payments, which allow for great flexibility in selecting conditions, developing the care delivery structure, and determining how payments will be allocated among participating providers.
SHM learned last week that the Center for Medicare & Medicaid Innovation (CMMI) will accept nonbinding letters of intent for Model 1 of the program through Oct. 6. CMMI extended the deadline, originally set for Sept. 22, to give institutions and providers more time. Once institutions submit their letters of intent, the deadline to submit a formal application is Nov. 18.
The deadline for letters of intent for Models 2-4 remains Nov. 4, according to CMMI. The application deadline for those three models is March 15, 2012.
Felix Aguirre, MD, SFHM, vice president of medical affairs for North Hollywood, Calif.-based IPC: The Hospitalist Co., says HM group leaders should continue to monitor the process, but how involved they get depends on their individual situations and their relationship with an institution. “If you’re a private group, there’s a lot of weight on you to try to convince an acute-care facility to go down this risk-bearing road,” he says.
Dr. Aguirre says CMMI’s first three models are all “retrospective,” meaning hospitals and/or providers will be paid fees for service, and once episodic care is completed, as defined by each of the models, reconciliation will be made—and there is the real risk of having to pay back funds to CMS. In Model 4, the lone “prospective” setup, there is a single bundled payment up front “and you live and die by that money,” Dr. Aguirre says. “If it costs you a lot more to provide the service, it’s a true risk arrangement where you take a loss. Of course, if you have reduced costs by providing services a little more efficiently and you’ve saved a few dollars, you get to remain with those dollars.”
Dr. Aguirre also notes that of the four current models, Model 3 is the only one available directly to individual providers or HM groups as a risk-bearing entity, and only for post-acute-care services.
CMMI is expected to introduce at least a few more models in the coming months.
For more about CMS' bundling initiatives, visit our website.
The Centers for Medicare & Medicaid Services (CMS) on Aug. 23 introduced the Bundled Payments for Care Improvement Initiative, developed as part of the payment bundling provision of the Affordable Care Act (ACA). CMS has invited providers to apply to help test and develop four different models of bundling payments, which allow for great flexibility in selecting conditions, developing the care delivery structure, and determining how payments will be allocated among participating providers.
SHM learned last week that the Center for Medicare & Medicaid Innovation (CMMI) will accept nonbinding letters of intent for Model 1 of the program through Oct. 6. CMMI extended the deadline, originally set for Sept. 22, to give institutions and providers more time. Once institutions submit their letters of intent, the deadline to submit a formal application is Nov. 18.
The deadline for letters of intent for Models 2-4 remains Nov. 4, according to CMMI. The application deadline for those three models is March 15, 2012.
Felix Aguirre, MD, SFHM, vice president of medical affairs for North Hollywood, Calif.-based IPC: The Hospitalist Co., says HM group leaders should continue to monitor the process, but how involved they get depends on their individual situations and their relationship with an institution. “If you’re a private group, there’s a lot of weight on you to try to convince an acute-care facility to go down this risk-bearing road,” he says.
Dr. Aguirre says CMMI’s first three models are all “retrospective,” meaning hospitals and/or providers will be paid fees for service, and once episodic care is completed, as defined by each of the models, reconciliation will be made—and there is the real risk of having to pay back funds to CMS. In Model 4, the lone “prospective” setup, there is a single bundled payment up front “and you live and die by that money,” Dr. Aguirre says. “If it costs you a lot more to provide the service, it’s a true risk arrangement where you take a loss. Of course, if you have reduced costs by providing services a little more efficiently and you’ve saved a few dollars, you get to remain with those dollars.”
Dr. Aguirre also notes that of the four current models, Model 3 is the only one available directly to individual providers or HM groups as a risk-bearing entity, and only for post-acute-care services.
CMMI is expected to introduce at least a few more models in the coming months.
For more about CMS' bundling initiatives, visit our website.
Anticoagulant Rivaroxaban Clears FDA Panel Hurdle
An FDA advisory panel has recommended the approval of rivaroxaban (Xarelto) for stroke prevention in patients with non-valvular atrial fibrillation, but the panelists raised questions about the methodology of the trial that compared the drug to the gold standard, warfarin (Coumadin).
A final decision on the drug is expected in November.
Rivaroxaban has been developed as a once-a-day oral medication that prevents clotting by inhibiting factor Xa, a key component in the generation of thrombin. It is one medication in a line of drugs trying to position themselves to replace warfarin, which has many contraindications and requires frequent blood draws for monitoring; the new drugs would not require frequent blood draws.
Panelists questioned whether ROCKET-AF—the trial that compared rivaroxaban to warfarin—was sufficient to show noninferiority, as only 55% of the patients on warfarin had international normalized ratio (INR) levels needed for stroke prevention.
Ian Jenkins, MD, assistant professor in the division of hospital medicine at the University of California at San Diego, says that rivaroxaban “will be an option for AF, but probably not my first choice.”
Another oral warfarin alternative—dabigatran, which inhibits thrombin—is already available, he notes. And dabigatran was found to be superior to warfarin, while rivaroxaban was only found to be noninferior. But Dr. Jenkins also notes that dabigatran and rivaroxaban have not been compared head-to-head.
“The low percent of therapeutic INRs in ROCKET-AF does concern me,” Dr. Jenkins adds, “but we have to remember that the patients who will benefit the most from these medications are the ones with difficult-to-control INRs anyway.”
He also explains that patients now doing well on warfarin don’t have a “great reason” to boost their costs by trying another drug.
An FDA advisory panel has recommended the approval of rivaroxaban (Xarelto) for stroke prevention in patients with non-valvular atrial fibrillation, but the panelists raised questions about the methodology of the trial that compared the drug to the gold standard, warfarin (Coumadin).
A final decision on the drug is expected in November.
Rivaroxaban has been developed as a once-a-day oral medication that prevents clotting by inhibiting factor Xa, a key component in the generation of thrombin. It is one medication in a line of drugs trying to position themselves to replace warfarin, which has many contraindications and requires frequent blood draws for monitoring; the new drugs would not require frequent blood draws.
Panelists questioned whether ROCKET-AF—the trial that compared rivaroxaban to warfarin—was sufficient to show noninferiority, as only 55% of the patients on warfarin had international normalized ratio (INR) levels needed for stroke prevention.
Ian Jenkins, MD, assistant professor in the division of hospital medicine at the University of California at San Diego, says that rivaroxaban “will be an option for AF, but probably not my first choice.”
Another oral warfarin alternative—dabigatran, which inhibits thrombin—is already available, he notes. And dabigatran was found to be superior to warfarin, while rivaroxaban was only found to be noninferior. But Dr. Jenkins also notes that dabigatran and rivaroxaban have not been compared head-to-head.
“The low percent of therapeutic INRs in ROCKET-AF does concern me,” Dr. Jenkins adds, “but we have to remember that the patients who will benefit the most from these medications are the ones with difficult-to-control INRs anyway.”
He also explains that patients now doing well on warfarin don’t have a “great reason” to boost their costs by trying another drug.
An FDA advisory panel has recommended the approval of rivaroxaban (Xarelto) for stroke prevention in patients with non-valvular atrial fibrillation, but the panelists raised questions about the methodology of the trial that compared the drug to the gold standard, warfarin (Coumadin).
A final decision on the drug is expected in November.
Rivaroxaban has been developed as a once-a-day oral medication that prevents clotting by inhibiting factor Xa, a key component in the generation of thrombin. It is one medication in a line of drugs trying to position themselves to replace warfarin, which has many contraindications and requires frequent blood draws for monitoring; the new drugs would not require frequent blood draws.
Panelists questioned whether ROCKET-AF—the trial that compared rivaroxaban to warfarin—was sufficient to show noninferiority, as only 55% of the patients on warfarin had international normalized ratio (INR) levels needed for stroke prevention.
Ian Jenkins, MD, assistant professor in the division of hospital medicine at the University of California at San Diego, says that rivaroxaban “will be an option for AF, but probably not my first choice.”
Another oral warfarin alternative—dabigatran, which inhibits thrombin—is already available, he notes. And dabigatran was found to be superior to warfarin, while rivaroxaban was only found to be noninferior. But Dr. Jenkins also notes that dabigatran and rivaroxaban have not been compared head-to-head.
“The low percent of therapeutic INRs in ROCKET-AF does concern me,” Dr. Jenkins adds, “but we have to remember that the patients who will benefit the most from these medications are the ones with difficult-to-control INRs anyway.”
He also explains that patients now doing well on warfarin don’t have a “great reason” to boost their costs by trying another drug.
Continuous Glucose Monitor Accurate Post-Cardiac Surgery
LISBON – Although microcirculation in cardiac surgery patients is impaired during the first few hours of admission to the intensive care unit, the degree of impairment was not great enough to affect the accuracy of continuous glucose monitors in a prospective, observational study of 60 patients.
Hyperglycemia, hypoglycemia, and glucose hypervariability are all associated with increased mortality in critically ill patients following cardiac surgery. Continuous glucose monitoring (CGM) is a potential alternative to frequent, time-consuming fingerstick glucose measurements, and can provide more information about glucose trends. However, the accuracy of these systems in critically ill patients has been uncertain, said Dr. J. Hans DeVries, an endocrinologist at the University of Amsterdam.
Now, "these results support CGM use in cardiac surgery patients, with quite good sensor accuracy in patients with a low severity of illness," he said at the annual meeting of the European Association for the Study of Diabetes (EASD).
The patients had a mean age of 65 years, and 48 of the 60 were male. Nearly a third (27%) had diabetes. Thirty-two (53%) of the patients were undergoing only coronary artery bypass surgery, 16 (27%) were having just valve surgery, and 12 (20%) had both procedures. Their APACHE score predicting mortality was low, 0.01. Total ICU stay was 23 hours. Hemodynamic parameters were fairly good, with a microcirculatory function index of 2.8 (out of 3.0). The proportion of perfused vessels was high, 0.97. However, the patients’ peripheral temperature was low, 32.8 °C.
Two sensors – the Medtronic Guardian REAL-Time and the Abbott FreeStyle Navigator – were placed subcutaneously in the abdominal wall of each patient prior to surgery. The Navigator performed slightly better than did the Guardian. Microcirculation was measured by microvascular flow index (MFI), perfused vessel density (PVD), and proportion of perfused vessels (PPV) using sublingual sidestream dark-field (SDF) imaging; and tissue oxygenation (StO2) was obtained with near-infrared spectroscopy.
While StO2 and PVD were impaired in the first hours after surgery, at no point were any microcirculatory parameters significantly associated with sensor accuracy. For the Navigator CGM, lower peripheral temperature and higher APACHE IV scores were significantly associated with decreased sensor accuracy (P values of .003 and less than .001, respectively). For the Guardian, lower peripheral temperature was significantly associated with decreased sensor accuracy (P = .048).
"Further studies are needed to assess the influence of microcirculation on sensor accuracy in more severely ill patients, such as those with sepsis," Dr. DeVries concluded.
The study was supported by the EASD’s European Foundation for the Study of Diabetes. Dr. DeVries has received research support from, and is on the speakers’ bureau for Dexcom, Abbott, and Medtronic.
LISBON – Although microcirculation in cardiac surgery patients is impaired during the first few hours of admission to the intensive care unit, the degree of impairment was not great enough to affect the accuracy of continuous glucose monitors in a prospective, observational study of 60 patients.
Hyperglycemia, hypoglycemia, and glucose hypervariability are all associated with increased mortality in critically ill patients following cardiac surgery. Continuous glucose monitoring (CGM) is a potential alternative to frequent, time-consuming fingerstick glucose measurements, and can provide more information about glucose trends. However, the accuracy of these systems in critically ill patients has been uncertain, said Dr. J. Hans DeVries, an endocrinologist at the University of Amsterdam.
Now, "these results support CGM use in cardiac surgery patients, with quite good sensor accuracy in patients with a low severity of illness," he said at the annual meeting of the European Association for the Study of Diabetes (EASD).
The patients had a mean age of 65 years, and 48 of the 60 were male. Nearly a third (27%) had diabetes. Thirty-two (53%) of the patients were undergoing only coronary artery bypass surgery, 16 (27%) were having just valve surgery, and 12 (20%) had both procedures. Their APACHE score predicting mortality was low, 0.01. Total ICU stay was 23 hours. Hemodynamic parameters were fairly good, with a microcirculatory function index of 2.8 (out of 3.0). The proportion of perfused vessels was high, 0.97. However, the patients’ peripheral temperature was low, 32.8 °C.
Two sensors – the Medtronic Guardian REAL-Time and the Abbott FreeStyle Navigator – were placed subcutaneously in the abdominal wall of each patient prior to surgery. The Navigator performed slightly better than did the Guardian. Microcirculation was measured by microvascular flow index (MFI), perfused vessel density (PVD), and proportion of perfused vessels (PPV) using sublingual sidestream dark-field (SDF) imaging; and tissue oxygenation (StO2) was obtained with near-infrared spectroscopy.
While StO2 and PVD were impaired in the first hours after surgery, at no point were any microcirculatory parameters significantly associated with sensor accuracy. For the Navigator CGM, lower peripheral temperature and higher APACHE IV scores were significantly associated with decreased sensor accuracy (P values of .003 and less than .001, respectively). For the Guardian, lower peripheral temperature was significantly associated with decreased sensor accuracy (P = .048).
"Further studies are needed to assess the influence of microcirculation on sensor accuracy in more severely ill patients, such as those with sepsis," Dr. DeVries concluded.
The study was supported by the EASD’s European Foundation for the Study of Diabetes. Dr. DeVries has received research support from, and is on the speakers’ bureau for Dexcom, Abbott, and Medtronic.
LISBON – Although microcirculation in cardiac surgery patients is impaired during the first few hours of admission to the intensive care unit, the degree of impairment was not great enough to affect the accuracy of continuous glucose monitors in a prospective, observational study of 60 patients.
Hyperglycemia, hypoglycemia, and glucose hypervariability are all associated with increased mortality in critically ill patients following cardiac surgery. Continuous glucose monitoring (CGM) is a potential alternative to frequent, time-consuming fingerstick glucose measurements, and can provide more information about glucose trends. However, the accuracy of these systems in critically ill patients has been uncertain, said Dr. J. Hans DeVries, an endocrinologist at the University of Amsterdam.
Now, "these results support CGM use in cardiac surgery patients, with quite good sensor accuracy in patients with a low severity of illness," he said at the annual meeting of the European Association for the Study of Diabetes (EASD).
The patients had a mean age of 65 years, and 48 of the 60 were male. Nearly a third (27%) had diabetes. Thirty-two (53%) of the patients were undergoing only coronary artery bypass surgery, 16 (27%) were having just valve surgery, and 12 (20%) had both procedures. Their APACHE score predicting mortality was low, 0.01. Total ICU stay was 23 hours. Hemodynamic parameters were fairly good, with a microcirculatory function index of 2.8 (out of 3.0). The proportion of perfused vessels was high, 0.97. However, the patients’ peripheral temperature was low, 32.8 °C.
Two sensors – the Medtronic Guardian REAL-Time and the Abbott FreeStyle Navigator – were placed subcutaneously in the abdominal wall of each patient prior to surgery. The Navigator performed slightly better than did the Guardian. Microcirculation was measured by microvascular flow index (MFI), perfused vessel density (PVD), and proportion of perfused vessels (PPV) using sublingual sidestream dark-field (SDF) imaging; and tissue oxygenation (StO2) was obtained with near-infrared spectroscopy.
While StO2 and PVD were impaired in the first hours after surgery, at no point were any microcirculatory parameters significantly associated with sensor accuracy. For the Navigator CGM, lower peripheral temperature and higher APACHE IV scores were significantly associated with decreased sensor accuracy (P values of .003 and less than .001, respectively). For the Guardian, lower peripheral temperature was significantly associated with decreased sensor accuracy (P = .048).
"Further studies are needed to assess the influence of microcirculation on sensor accuracy in more severely ill patients, such as those with sepsis," Dr. DeVries concluded.
The study was supported by the EASD’s European Foundation for the Study of Diabetes. Dr. DeVries has received research support from, and is on the speakers’ bureau for Dexcom, Abbott, and Medtronic.
FROM THE ANNUAL MEETING OF THE EUROPEAN ASSOCIATION FOR THE STUDY OF DIABETES (EASD)
Major Finding: While StO2 and PVD were impaired in the first hours after surgery, at no point were any microcirculatory parameters significantly associated with sensor accuracy.
Data Source: Prospective, observational study of 60 patients undergoing cardiac surgery.
Disclosures: The study was supported by the EASD’s European Foundation for the Study of Diabetes. Dr. DeVries has received research support from, and is on the speakers’ bureau for Dexcom, Abbott, and Medtronic.