User login
Psych Solutions
Kenneth Duckworth, MD, medical director at Vinfen Corporation in Boston, recalls the frustration he felt when inpatient hospital staff would release his psychiatric patients without contacting him. The lack of communication often led to gaps in his patients’ records and left him scrambling to learn more about the circumstances of the hospitalization.
Those experiences are among the reasons Dr. Duckworth, a triple-board-certified psychiatrist and medical director of the National Alliance on Mental Illness (NAMI), was pleased to hear The Joint Commission had released its Hospital-Based Inpatient Psychiatric Services, or HBIPS, measure set. And he’s not alone. HBIPS provides standardized measures for psychiatric services where previously none existed, and it gives hospitals the ability to use their data as a basis for national comparison.
Ann Watt, associate director, division of quality measurement and research at the Joint Commission, says although it’s still early, the measures seem to be working. “While we don’t have any actual data, we have received positive feedback,” she says. “It seems like the field has accepted them well.”
Standard of Care Guidelines
Comprised of seven main measures that the commission released in October 2008, HBIPS is the result of a determined effort by the nation’s psychiatry leaders, says Noel Mazade, PhD, executive director of the National Association of State Mental Health Program Directors’ Research Institute Inc. HBIPS is available to hospitals accredited under the Comprehensive Accreditation Manual for Hospitals (CAMH), says Celeste Milton, associate project director at the commission’s Department of Quality Measurement. Free-standing psychiatric hospitals and acute-care hospitals with psychiatric units can use the HBIPS measure set to help meet performance requirements under the commission’s ORYX initiative (www. jointcommission.org/AccreditationPrograms/Hospitals/ORYX/).
The Joint Commission’s final HBIPS measure set, which went into effect with Oct. 1, 2008, discharges, followed more than three years’ of field review, public comment, and pilot testing by 196 hospitals across the country. HBIPS’ seven measures address:
—Tim Lineberry, MD, medical director, Mayo Clinic Psychiatric Hospital, Rochester, Minn.
- Admission screening;
- Hours of physical restraint;
- Hours of seclusion;
- Patients discharged on multiple antipsychotic medications;
- Patients discharged on multiple antipsychotic medications with appropriate justification;
- Post-discharge plan creation; and
- Post-discharge plans transmitted to the next level of care provider.
“These are all areas that are of interest to NAMI,” Dr. Duckworth says. “We still have a long way to go, but it’s definitely a step in the right direction.”
The measure set’s effect on psychiatric hospitalists will depend on physicians’ responsibilities at the facilities where they work, Milton says. For example, a psychiatric hospitalist may be asked to screen a patient at admission for violence risk, substance abuse, psychological trauma history, and strengths, such as personal motivation and family involvement (HBIPS Measure 1). Another qualified psychiatric practitioner, such as a psychiatrist, registered nurse, physician’s assistant, or social worker, could perform the screening, she says.
The measures are intended to help unify the screening process used by psychiatric hospitalists; however, traditional hospitalists could be called on to perform a face-to-face evaluation of a patient placed in physical restraint or held in seclusion (Measures 2 and 3). As a result of the evaluation, hospitalists could be asked to write orders to discontinue or renew physical restraint or seclusion, Milton says. The feedback the Joint Commission has received shows psychiatric hospitalists are using the measures. They are most likely to be in charge of managing a patient’s medications and could play a role in documenting appropriate justification for placing a patient on more than one antipsychotic medication at discharge (Measures 4 and 5). Depending on the scope of practice, traditional hospitalists who discharge patients might be responsible for determining a final discharge diagnosis, discharge medications, and next-level-of-care recommendations (Measures 6 and 7). The provider at the next level of care could be an inpatient or outpatient clinician or entity, Milton says.
How It Works
The HBIPS data collection process is similar to other ORYX processes; however, this is the first time the Joint Commission has created a measure set for psychiatric services, says Dr. Mazade, who worked directly with the commission to develop HBIPS. Hospitals using HBIPS will submit data from patients’ medical records to their ORYX vendor. The vendor will submit performance measures to the hospital and the commission, which will provide hospitals with feedback on measure performance, Dr. Mazade says. Initially, the commission will supply acute-care and psychiatric hospitals the option of using HBIPS to meet current ORYX performance measurement requirements, although Dr. Mazade says he expects the commission will eventually mandate use of the measures.
The commission says data collection, analysis, and performance reporting is running behind schedule. Once the commission report is received, hospitals should share the message with their medical staff, Milton says. “This feedback will be useful to all staff involved in patient care to help them improve their practice,” she explains. “The purpose of an initial screening, including a trauma history, is to help the practitioner formulate an individual treatment plan based on information obtained during the initial screening.”
Tim Lineberry, MD, medical director at the Mayo Clinic Psychiatric Hospital in Rochester, Minn., says each HBIPS measure is composed of sub-elements. For example, the assessment measure includes admission screening for violence risk, substance abuse, trauma history, and patient strengths, such as motivation and family involvement. These elements create a more complete picture of the patient and might improve the initial assessment. By improving initial assessment, experts in the field hope hospital staff will be able to better identify problems, Dr. Lineberry says.
“We are all working for improvement in care,” says Dr. Lineberry, noting the Mayo Clinic was one of the pilot sites. “HBIPS is part of that effort.”
Time Is of the Essence
Many of the standards represent areas in which there is consensus among psychiatrists about the need for change, says Anand Pandya, MD, a psychiatric hospitalist and director of inpatient psychiatry at Cedars-Sinai Medical Center in Los Angeles. Many psychiatrists recognize there is a need to improve communication between inpatient psychiatric services and follow-up outpatient providers, Dr. Pandya says. However, a clear consensus has not been reached regarding the standards of tracking patients who take multiple antipsychotic medications, Dr. Pandya says.
“With the low average length of stay in inpatient psychiatric units, it is common for patients to continue a cross-taper between medications after discharge,” Dr. Pandya says. “For most antipsychotic medications, there is insufficient data to determine how fast or slow to cross-taper. I worry that these standards may send the unintentional message that these cross-tapers should be completed quickly during the course of a brief inpatient stay.”
Data suggest individuals using lithium should be tapered off the drug as slowly as possible—probably over months rather than weeks, Dr. Pandya says. “I am concerned that tracking data regarding patients on multiple antipsychotic medications may create incentives to change practice in a sub-optimal direction for some cases,” he says.
Dr. Duckworth also acknowledges patients’ length of stay is getting shorter. Psychiatric hospitalists are under a great deal of pressure to “get people patched up in too short a period of time,” he says. “They really do need more time. There is a temptation to use more than one antipsychotic medication, but people really should not be given two antipsychotic medications unless someone has performed a thoughtful assessment.”
On Board with HBIPS
While HBIPS covers areas of care important to many, the details of implementing the measure set might be challenging, Dr. Lineberry says. The requirements increase the documentation burden for physicians, nurses, and allied health professionals, such as social workers and therapists. Hospitals using electronic medical records might have to modify their records to meet the requirements. And with the new measure comes new, significant personnel costs to audit and collect the data, he says.
“For psychiatric hospitalists who are using HBIPS, it will be helpful to look at the measures from a multidisciplinary standpoint,” Dr. Lineberry says. “Approach HBIPS as a team. Look at the process and see how it works, then adapt it to fit in with your current workflow.”
As of July, more than 274 psychiatric hospitals and psychiatric units had implemented the HBIPS measures. “We don’t usually have numbers until at least six months after,” Milton says, noting the commission is eager to receive quantitative data and report back to the participating hospitals.
Milton anticipates the Joint Commission will submit the HBIPS measure set to the National Quality Forum (NQF) for consideration and endorsement. Although she anticipates the measures will receive NQF endorsement sometime this year, an exact timeline has not been established, she says. The Joint Commission will work closely with the NQF to ensure the HBIPS measure set receives endorsement, and will make necessary modifications that may be required, Milton says.
Once HBIPS receives NQF endorsement, HBIPS data will be publicly reported following the first two quarters of data collection, Milton says. Data on each hospital will be available at www.qualitycheck.org. TH
Gina Gotsill is a freelance medical writer in California. Freelance writer Chris Haliskoe contributed to this report.
Image Source: TIM TEEBKEN/PHOTODISC
Kenneth Duckworth, MD, medical director at Vinfen Corporation in Boston, recalls the frustration he felt when inpatient hospital staff would release his psychiatric patients without contacting him. The lack of communication often led to gaps in his patients’ records and left him scrambling to learn more about the circumstances of the hospitalization.
Those experiences are among the reasons Dr. Duckworth, a triple-board-certified psychiatrist and medical director of the National Alliance on Mental Illness (NAMI), was pleased to hear The Joint Commission had released its Hospital-Based Inpatient Psychiatric Services, or HBIPS, measure set. And he’s not alone. HBIPS provides standardized measures for psychiatric services where previously none existed, and it gives hospitals the ability to use their data as a basis for national comparison.
Ann Watt, associate director, division of quality measurement and research at the Joint Commission, says although it’s still early, the measures seem to be working. “While we don’t have any actual data, we have received positive feedback,” she says. “It seems like the field has accepted them well.”
Standard of Care Guidelines
Comprised of seven main measures that the commission released in October 2008, HBIPS is the result of a determined effort by the nation’s psychiatry leaders, says Noel Mazade, PhD, executive director of the National Association of State Mental Health Program Directors’ Research Institute Inc. HBIPS is available to hospitals accredited under the Comprehensive Accreditation Manual for Hospitals (CAMH), says Celeste Milton, associate project director at the commission’s Department of Quality Measurement. Free-standing psychiatric hospitals and acute-care hospitals with psychiatric units can use the HBIPS measure set to help meet performance requirements under the commission’s ORYX initiative (www. jointcommission.org/AccreditationPrograms/Hospitals/ORYX/).
The Joint Commission’s final HBIPS measure set, which went into effect with Oct. 1, 2008, discharges, followed more than three years’ of field review, public comment, and pilot testing by 196 hospitals across the country. HBIPS’ seven measures address:
—Tim Lineberry, MD, medical director, Mayo Clinic Psychiatric Hospital, Rochester, Minn.
- Admission screening;
- Hours of physical restraint;
- Hours of seclusion;
- Patients discharged on multiple antipsychotic medications;
- Patients discharged on multiple antipsychotic medications with appropriate justification;
- Post-discharge plan creation; and
- Post-discharge plans transmitted to the next level of care provider.
“These are all areas that are of interest to NAMI,” Dr. Duckworth says. “We still have a long way to go, but it’s definitely a step in the right direction.”
The measure set’s effect on psychiatric hospitalists will depend on physicians’ responsibilities at the facilities where they work, Milton says. For example, a psychiatric hospitalist may be asked to screen a patient at admission for violence risk, substance abuse, psychological trauma history, and strengths, such as personal motivation and family involvement (HBIPS Measure 1). Another qualified psychiatric practitioner, such as a psychiatrist, registered nurse, physician’s assistant, or social worker, could perform the screening, she says.
The measures are intended to help unify the screening process used by psychiatric hospitalists; however, traditional hospitalists could be called on to perform a face-to-face evaluation of a patient placed in physical restraint or held in seclusion (Measures 2 and 3). As a result of the evaluation, hospitalists could be asked to write orders to discontinue or renew physical restraint or seclusion, Milton says. The feedback the Joint Commission has received shows psychiatric hospitalists are using the measures. They are most likely to be in charge of managing a patient’s medications and could play a role in documenting appropriate justification for placing a patient on more than one antipsychotic medication at discharge (Measures 4 and 5). Depending on the scope of practice, traditional hospitalists who discharge patients might be responsible for determining a final discharge diagnosis, discharge medications, and next-level-of-care recommendations (Measures 6 and 7). The provider at the next level of care could be an inpatient or outpatient clinician or entity, Milton says.
How It Works
The HBIPS data collection process is similar to other ORYX processes; however, this is the first time the Joint Commission has created a measure set for psychiatric services, says Dr. Mazade, who worked directly with the commission to develop HBIPS. Hospitals using HBIPS will submit data from patients’ medical records to their ORYX vendor. The vendor will submit performance measures to the hospital and the commission, which will provide hospitals with feedback on measure performance, Dr. Mazade says. Initially, the commission will supply acute-care and psychiatric hospitals the option of using HBIPS to meet current ORYX performance measurement requirements, although Dr. Mazade says he expects the commission will eventually mandate use of the measures.
The commission says data collection, analysis, and performance reporting is running behind schedule. Once the commission report is received, hospitals should share the message with their medical staff, Milton says. “This feedback will be useful to all staff involved in patient care to help them improve their practice,” she explains. “The purpose of an initial screening, including a trauma history, is to help the practitioner formulate an individual treatment plan based on information obtained during the initial screening.”
Tim Lineberry, MD, medical director at the Mayo Clinic Psychiatric Hospital in Rochester, Minn., says each HBIPS measure is composed of sub-elements. For example, the assessment measure includes admission screening for violence risk, substance abuse, trauma history, and patient strengths, such as motivation and family involvement. These elements create a more complete picture of the patient and might improve the initial assessment. By improving initial assessment, experts in the field hope hospital staff will be able to better identify problems, Dr. Lineberry says.
“We are all working for improvement in care,” says Dr. Lineberry, noting the Mayo Clinic was one of the pilot sites. “HBIPS is part of that effort.”
Time Is of the Essence
Many of the standards represent areas in which there is consensus among psychiatrists about the need for change, says Anand Pandya, MD, a psychiatric hospitalist and director of inpatient psychiatry at Cedars-Sinai Medical Center in Los Angeles. Many psychiatrists recognize there is a need to improve communication between inpatient psychiatric services and follow-up outpatient providers, Dr. Pandya says. However, a clear consensus has not been reached regarding the standards of tracking patients who take multiple antipsychotic medications, Dr. Pandya says.
“With the low average length of stay in inpatient psychiatric units, it is common for patients to continue a cross-taper between medications after discharge,” Dr. Pandya says. “For most antipsychotic medications, there is insufficient data to determine how fast or slow to cross-taper. I worry that these standards may send the unintentional message that these cross-tapers should be completed quickly during the course of a brief inpatient stay.”
Data suggest individuals using lithium should be tapered off the drug as slowly as possible—probably over months rather than weeks, Dr. Pandya says. “I am concerned that tracking data regarding patients on multiple antipsychotic medications may create incentives to change practice in a sub-optimal direction for some cases,” he says.
Dr. Duckworth also acknowledges patients’ length of stay is getting shorter. Psychiatric hospitalists are under a great deal of pressure to “get people patched up in too short a period of time,” he says. “They really do need more time. There is a temptation to use more than one antipsychotic medication, but people really should not be given two antipsychotic medications unless someone has performed a thoughtful assessment.”
On Board with HBIPS
While HBIPS covers areas of care important to many, the details of implementing the measure set might be challenging, Dr. Lineberry says. The requirements increase the documentation burden for physicians, nurses, and allied health professionals, such as social workers and therapists. Hospitals using electronic medical records might have to modify their records to meet the requirements. And with the new measure comes new, significant personnel costs to audit and collect the data, he says.
“For psychiatric hospitalists who are using HBIPS, it will be helpful to look at the measures from a multidisciplinary standpoint,” Dr. Lineberry says. “Approach HBIPS as a team. Look at the process and see how it works, then adapt it to fit in with your current workflow.”
As of July, more than 274 psychiatric hospitals and psychiatric units had implemented the HBIPS measures. “We don’t usually have numbers until at least six months after,” Milton says, noting the commission is eager to receive quantitative data and report back to the participating hospitals.
Milton anticipates the Joint Commission will submit the HBIPS measure set to the National Quality Forum (NQF) for consideration and endorsement. Although she anticipates the measures will receive NQF endorsement sometime this year, an exact timeline has not been established, she says. The Joint Commission will work closely with the NQF to ensure the HBIPS measure set receives endorsement, and will make necessary modifications that may be required, Milton says.
Once HBIPS receives NQF endorsement, HBIPS data will be publicly reported following the first two quarters of data collection, Milton says. Data on each hospital will be available at www.qualitycheck.org. TH
Gina Gotsill is a freelance medical writer in California. Freelance writer Chris Haliskoe contributed to this report.
Image Source: TIM TEEBKEN/PHOTODISC
Kenneth Duckworth, MD, medical director at Vinfen Corporation in Boston, recalls the frustration he felt when inpatient hospital staff would release his psychiatric patients without contacting him. The lack of communication often led to gaps in his patients’ records and left him scrambling to learn more about the circumstances of the hospitalization.
Those experiences are among the reasons Dr. Duckworth, a triple-board-certified psychiatrist and medical director of the National Alliance on Mental Illness (NAMI), was pleased to hear The Joint Commission had released its Hospital-Based Inpatient Psychiatric Services, or HBIPS, measure set. And he’s not alone. HBIPS provides standardized measures for psychiatric services where previously none existed, and it gives hospitals the ability to use their data as a basis for national comparison.
Ann Watt, associate director, division of quality measurement and research at the Joint Commission, says although it’s still early, the measures seem to be working. “While we don’t have any actual data, we have received positive feedback,” she says. “It seems like the field has accepted them well.”
Standard of Care Guidelines
Comprised of seven main measures that the commission released in October 2008, HBIPS is the result of a determined effort by the nation’s psychiatry leaders, says Noel Mazade, PhD, executive director of the National Association of State Mental Health Program Directors’ Research Institute Inc. HBIPS is available to hospitals accredited under the Comprehensive Accreditation Manual for Hospitals (CAMH), says Celeste Milton, associate project director at the commission’s Department of Quality Measurement. Free-standing psychiatric hospitals and acute-care hospitals with psychiatric units can use the HBIPS measure set to help meet performance requirements under the commission’s ORYX initiative (www. jointcommission.org/AccreditationPrograms/Hospitals/ORYX/).
The Joint Commission’s final HBIPS measure set, which went into effect with Oct. 1, 2008, discharges, followed more than three years’ of field review, public comment, and pilot testing by 196 hospitals across the country. HBIPS’ seven measures address:
—Tim Lineberry, MD, medical director, Mayo Clinic Psychiatric Hospital, Rochester, Minn.
- Admission screening;
- Hours of physical restraint;
- Hours of seclusion;
- Patients discharged on multiple antipsychotic medications;
- Patients discharged on multiple antipsychotic medications with appropriate justification;
- Post-discharge plan creation; and
- Post-discharge plans transmitted to the next level of care provider.
“These are all areas that are of interest to NAMI,” Dr. Duckworth says. “We still have a long way to go, but it’s definitely a step in the right direction.”
The measure set’s effect on psychiatric hospitalists will depend on physicians’ responsibilities at the facilities where they work, Milton says. For example, a psychiatric hospitalist may be asked to screen a patient at admission for violence risk, substance abuse, psychological trauma history, and strengths, such as personal motivation and family involvement (HBIPS Measure 1). Another qualified psychiatric practitioner, such as a psychiatrist, registered nurse, physician’s assistant, or social worker, could perform the screening, she says.
The measures are intended to help unify the screening process used by psychiatric hospitalists; however, traditional hospitalists could be called on to perform a face-to-face evaluation of a patient placed in physical restraint or held in seclusion (Measures 2 and 3). As a result of the evaluation, hospitalists could be asked to write orders to discontinue or renew physical restraint or seclusion, Milton says. The feedback the Joint Commission has received shows psychiatric hospitalists are using the measures. They are most likely to be in charge of managing a patient’s medications and could play a role in documenting appropriate justification for placing a patient on more than one antipsychotic medication at discharge (Measures 4 and 5). Depending on the scope of practice, traditional hospitalists who discharge patients might be responsible for determining a final discharge diagnosis, discharge medications, and next-level-of-care recommendations (Measures 6 and 7). The provider at the next level of care could be an inpatient or outpatient clinician or entity, Milton says.
How It Works
The HBIPS data collection process is similar to other ORYX processes; however, this is the first time the Joint Commission has created a measure set for psychiatric services, says Dr. Mazade, who worked directly with the commission to develop HBIPS. Hospitals using HBIPS will submit data from patients’ medical records to their ORYX vendor. The vendor will submit performance measures to the hospital and the commission, which will provide hospitals with feedback on measure performance, Dr. Mazade says. Initially, the commission will supply acute-care and psychiatric hospitals the option of using HBIPS to meet current ORYX performance measurement requirements, although Dr. Mazade says he expects the commission will eventually mandate use of the measures.
The commission says data collection, analysis, and performance reporting is running behind schedule. Once the commission report is received, hospitals should share the message with their medical staff, Milton says. “This feedback will be useful to all staff involved in patient care to help them improve their practice,” she explains. “The purpose of an initial screening, including a trauma history, is to help the practitioner formulate an individual treatment plan based on information obtained during the initial screening.”
Tim Lineberry, MD, medical director at the Mayo Clinic Psychiatric Hospital in Rochester, Minn., says each HBIPS measure is composed of sub-elements. For example, the assessment measure includes admission screening for violence risk, substance abuse, trauma history, and patient strengths, such as motivation and family involvement. These elements create a more complete picture of the patient and might improve the initial assessment. By improving initial assessment, experts in the field hope hospital staff will be able to better identify problems, Dr. Lineberry says.
“We are all working for improvement in care,” says Dr. Lineberry, noting the Mayo Clinic was one of the pilot sites. “HBIPS is part of that effort.”
Time Is of the Essence
Many of the standards represent areas in which there is consensus among psychiatrists about the need for change, says Anand Pandya, MD, a psychiatric hospitalist and director of inpatient psychiatry at Cedars-Sinai Medical Center in Los Angeles. Many psychiatrists recognize there is a need to improve communication between inpatient psychiatric services and follow-up outpatient providers, Dr. Pandya says. However, a clear consensus has not been reached regarding the standards of tracking patients who take multiple antipsychotic medications, Dr. Pandya says.
“With the low average length of stay in inpatient psychiatric units, it is common for patients to continue a cross-taper between medications after discharge,” Dr. Pandya says. “For most antipsychotic medications, there is insufficient data to determine how fast or slow to cross-taper. I worry that these standards may send the unintentional message that these cross-tapers should be completed quickly during the course of a brief inpatient stay.”
Data suggest individuals using lithium should be tapered off the drug as slowly as possible—probably over months rather than weeks, Dr. Pandya says. “I am concerned that tracking data regarding patients on multiple antipsychotic medications may create incentives to change practice in a sub-optimal direction for some cases,” he says.
Dr. Duckworth also acknowledges patients’ length of stay is getting shorter. Psychiatric hospitalists are under a great deal of pressure to “get people patched up in too short a period of time,” he says. “They really do need more time. There is a temptation to use more than one antipsychotic medication, but people really should not be given two antipsychotic medications unless someone has performed a thoughtful assessment.”
On Board with HBIPS
While HBIPS covers areas of care important to many, the details of implementing the measure set might be challenging, Dr. Lineberry says. The requirements increase the documentation burden for physicians, nurses, and allied health professionals, such as social workers and therapists. Hospitals using electronic medical records might have to modify their records to meet the requirements. And with the new measure comes new, significant personnel costs to audit and collect the data, he says.
“For psychiatric hospitalists who are using HBIPS, it will be helpful to look at the measures from a multidisciplinary standpoint,” Dr. Lineberry says. “Approach HBIPS as a team. Look at the process and see how it works, then adapt it to fit in with your current workflow.”
As of July, more than 274 psychiatric hospitals and psychiatric units had implemented the HBIPS measures. “We don’t usually have numbers until at least six months after,” Milton says, noting the commission is eager to receive quantitative data and report back to the participating hospitals.
Milton anticipates the Joint Commission will submit the HBIPS measure set to the National Quality Forum (NQF) for consideration and endorsement. Although she anticipates the measures will receive NQF endorsement sometime this year, an exact timeline has not been established, she says. The Joint Commission will work closely with the NQF to ensure the HBIPS measure set receives endorsement, and will make necessary modifications that may be required, Milton says.
Once HBIPS receives NQF endorsement, HBIPS data will be publicly reported following the first two quarters of data collection, Milton says. Data on each hospital will be available at www.qualitycheck.org. TH
Gina Gotsill is a freelance medical writer in California. Freelance writer Chris Haliskoe contributed to this report.
Image Source: TIM TEEBKEN/PHOTODISC
How do I keep my elderly patients from falling?
Case
An 85-year-old man with peripheral vascular disease, coronary artery disease, congestive heart failure, dementia, a history of falls, and atrial fibrillation, which was being treated with warfarin, was admitted for a left transmetatarsal amputation. On postoperative day two, the patient slipped as he was getting out of bed to use the bathroom. He hit his head on his IV pole, and a CT scan demonstrated an acute right subdural hemorrhage. He subsequently suffered eight months of delirium before passing away at a skilled nursing facility. How could this incident have been prevented?
Background
Hospitalization represents a vulnerable time for elderly people. The presence of acute illness, an unfamiliar environment, and the frequent addition of new medications predispose an elderly patient to such iatrogenic hazards of hospitalization as falls, pressure ulcers, and delirium.1 Inpatient falls are the most common type of adverse hospital event, accounting for 70% of all inpatient accidents.2 Thirty percent to 40% of inpatient falls result in injury, with 4% to 6% resulting in serious harm.2 Interestingly, 55% of falls occur in patients 60 or younger, but 60% of falls resulting in moderate to severe injury occur in those 70 and older.3
A fall is a seminal event in the life of an elderly person. Even a fall without injury can initiate a vicious circle that begins with a fear of falling and is followed by a self-restriction of mobility, which commonly results in a decline in function.4 Functional decline in the elderly has been shown to predict mortality and nursing home placement.5
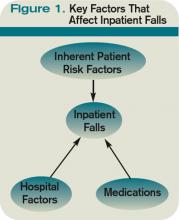
Inpatient falls are thought to occur via a complex interplay between medications, inherent patient susceptibilities, and hospital environmental hazards (see Figure 1, below).
Risk Factors
Medication prescription for the hospitalized elderly patient is perhaps the area where the hospitalist can have the greatest impact in reducing a patient’s fall risk. The most common medications thought to predispose community dwelling elders to falls are psychotropic drugs: neuroleptics, sedatives, hypnotics, antidepressants, and benzodiazepines.6
Limited studies of hospitalized patients indicate similar drugs as culprits. Passaro et al demonstrated that benzodiazepines with a half-life <24 hours (e.g., lorazepam and oxazepam) were strongly associated with falls even after correcting for multiple confounders.7 Furthermore, multivariate logistic regression revealed that the use of other psychotropic drugs in addition to benzodiazepines (OR 2.3; 95% CI, 1.6–3.2) was strongly associated with an increased risk of falls. Taking more than five medications also increased a patient’s fall risk (OR 1.6; 95% CI, 1.02–2.6). Thus, the judicious prescription of medications—aimed at decreasing the number and dosage of medications an elderly patient takes—is essential to minimizing the risk for falls.
Several studies conducted in hospitalized elderly patients have repeatedly demonstrated a core group of inherent patient risk factors for falls: delirium, agitation or impaired judgment, burden of comorbidity, gait instability or lower-extremity weakness, urinary incontinence or frequency, and a history of falls.2,3,8 These risk factors are targeted as part of most inpatient fall prevention programs, as discussed below.
Several environmental hazards have been known to increase the risk of falls and injury. These include high patient-to-nurse ratio, inappropriate use of bedrails, wet floors, and lack of assistance with ambulation and toileting. The most studied of these is assistance with ambulation and toileting. Hitcho et al demonstrated that as many as 50% of falls are toileting-related.3 The study also showed that only 42% of patients who fell and used an assistive device at home had a fall in the hospital. As many as 85% of patients were not assisted with a device or person at the time of a fall.2 Unassisted falls are associated with increased injury risk (adjusted OR 1.70; 95% CI, 1.23-2.36).
Consistent with this, increased patient-to-nurse ratios are keenly associated with an increased risk of falls. Essentially, a patient whose nurse had more than five patients was 2.6 times more likely to fall than a patient whose nurse had five or fewer patients (95% CI, 1.6 to 4.1). Based on this data, hospitals have invested in low-to-the-floor beds and alarms for beds and chairs. Placing patients on a regular toileting schedule, avoiding medications that cause urinary incontinence, and attention to bowel regimens have become standard components of hospital fall prevention programs. Even though these issues have long been thought to be the purview of nurses and support staff, hospitalist involvement and awareness are crucial to ensuring that these issues are consistently addressed and enforced for every at-risk patient.
Inpatient Fall Prevention
Inpatient falls are similar to other geriatric syndromes and are multifactorial in etiology. Studies that report a decrease in the number of falls identify patients at the highest risk for falls and target multiple risk factors simultaneously.
Several inpatient fall risk assessment tools have been developed. The most widely used and validated in the acute hospital setting are the Morse Falls Scale and St. Thomas’ Risk Assessment Tool in Falling Elderly Inpatients (STRATIFY) (see Table 1, p. 24).9 Both tools incorporate the risk factors identified above—namely, the presence of cognitive or sensory deficits, environmental hazards, history of falls, lower-extremity or gait instability/weakness, and level of comorbidity to create a score. Higher scores are associated with increased fall risk. The scales have demonstrated sensitivities and specificities of 70% to 96% and 50% to 85%, respectively, depending on the population tested and the cutoff scores used.
In 2004, Healey et al published the results of one of the few successful randomized, controlled fall-prevention trials in an acute-care setting.10 Pairs of identical hospital units were randomized to intervention and control groups. The sample size was 3,386 patients, with a mean length of stay of 19 days.1 As part of the intervention group, a fall-risk assessment was performed on admission. Patients were screened for deficits in visual acuity (identify a pen, key, or watch from a distance of 2 meters), polypharmacy, orthostatic hypotension, mobility deficits, appropriate bedrail use, footwear safety, bed height, distance of patient from nursing station, loose cables, wet floors, and availability of the nurse call bell.
Interventions for patients who were identified as high fall risks included ophthalmology/optician referral for those for whom reading aides could not be procured, medication review, adjustment of bed rails, and physical therapy. Patients with a history of falls were placed close to nursing stations. Environmental hazards were removed. Patients with orthostatic hypotension were educated on slowly changing body position. Call lights were moved to within easy reach. No additional money was allocated for this study, but by performing these simple interventions, the authors were able to decrease the relative risk of falls by 29% (RR 0.71, 95% CI 0.55–0.90, P=0.006). The incidence of injuries sustained as a result of falling, however, was unchanged.
Two large, prospective studies with historical controls involving 3,000 to 7,000 patients over the course of three years and incorporating similar interventions also demonstrated a decrease in the number of falls.11,12 Fonda and his colleagues were able to demonstrate a 77% reduction in the number of falls resulting in serious injuries.
Even though these studies are promising, a recent cluster-randomized, multifactorial intervention trial involving almost 4,000 patients on a dozen medical floors did not demonstrate a reduction in the incidence of falls or falls with injury.13 Several differences exist between the two randomized trials. In the latter trial, by Cumming et al, a study nurse reviewed the care plan of all of the patients on the intervention wards and made recommendations.13 Also, the study was designed so that each patient on the intervention wards received the intervention, regardless of their fall risk. Additionally, the study period was a mere three months. In the Healey trial, the nurses on the intervention units implemented targeted risk reduction for patients at high risk, and the study period was a full year.
Back to the Case
Our patient had several risk factors for falls on admission. A targeted fall risk assessment on admission would have identified him as high-risk, with a Morse score of 95 given his dementia (15 points), impaired gait status post-transmetatarsal amputation (20 points), secondary diagnoses (multiple comorbidities, 15 points) and history of falls (25 points), and presence of an IV (20 points). The STRATIFY risk assessment tool would have produced similar results.
Frequent toileting assistance, early mobilization, medication review, and environmental modification might have prevented his fall (see Table 2, pg. 24).
Bottom Line
Focused assessment of patients on admission can identify those at risk for falls. Multifactorial inpatient fall-prevention strategies have been shown to reduce the rate of falls in inpatients without increasing costs. TH
Dr. Ölveczky is a geriatric nocturnist in the hospital medicine program, division of medicine, at Beth Israel Deaconess Medical Center in Boston.
References
- Fernandez HM, Callahan KE, Likourezos A, Leipzig RM. House staff member awareness of older inpatients’ risks for hazards of hospitalization. Arch Intern Med. 2008;168(4):390-396.
- Krauss MJ, Evanoff B, Hitcho E, et al. A case control study of patient, medication, and care-related risk factors for inpatient falls. J Gen Intern Med. 2005;20(2):116-122.
- Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med. 2004;19(7):732-739.
- Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348(1):42-49.
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556-561.
- Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47(1):30-39.
- Passaro A, Volpato S, Romagnoni F, Manzoli N, Zuliani G, Fellin R. Benzodiazepines with different half-life and falling in a hospitalized population: The GIFA study. Gruppo Italiano di Farmacovigilanza nell'Anziano. J Clin Epidemiol. 2000;53(12):1222-1229.
- Oliver D, Daly F, Martin FC, McMurdo ME. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing. 2004;33(2):122-130.
- Scott V, Votova K, Scanlan A, Close J. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings. Age Ageing. 2007;36(2):130-139.
- Healey F, Monro A, Cockram A, Adams V, Heseltine D. Using targeted risk factor reduction to prevent falls in older in-patients: a randomised controlled trial. Age Ageing. 2004;33(4):390-395.
- Fonda D, Cook J, Sandler V, Bailey M. Sustained reduction in serious fall-related injuries in older people in hospital. Med J Aust. 2006;184(8):379-382.
- Von Renteln-Kruse W, Krause T. Incidence of in-hospital falls in geriatric patients before and after the introduction of an interdisciplinary team-based fall-prevention intervention. J Am Geriatr Soc. 2007;55(12):2068-2074.
- Cumming RG, Sherrington C, Lord SR, et al. Cluster randomised trial of a targeted multifactorial intervention to prevent falls among older people in hospital. BMJ. 2008;336(7647):758-760.
- Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ. 1997;315(7115):1049-1053.
Case
An 85-year-old man with peripheral vascular disease, coronary artery disease, congestive heart failure, dementia, a history of falls, and atrial fibrillation, which was being treated with warfarin, was admitted for a left transmetatarsal amputation. On postoperative day two, the patient slipped as he was getting out of bed to use the bathroom. He hit his head on his IV pole, and a CT scan demonstrated an acute right subdural hemorrhage. He subsequently suffered eight months of delirium before passing away at a skilled nursing facility. How could this incident have been prevented?
Background
Hospitalization represents a vulnerable time for elderly people. The presence of acute illness, an unfamiliar environment, and the frequent addition of new medications predispose an elderly patient to such iatrogenic hazards of hospitalization as falls, pressure ulcers, and delirium.1 Inpatient falls are the most common type of adverse hospital event, accounting for 70% of all inpatient accidents.2 Thirty percent to 40% of inpatient falls result in injury, with 4% to 6% resulting in serious harm.2 Interestingly, 55% of falls occur in patients 60 or younger, but 60% of falls resulting in moderate to severe injury occur in those 70 and older.3
A fall is a seminal event in the life of an elderly person. Even a fall without injury can initiate a vicious circle that begins with a fear of falling and is followed by a self-restriction of mobility, which commonly results in a decline in function.4 Functional decline in the elderly has been shown to predict mortality and nursing home placement.5
Inpatient falls are thought to occur via a complex interplay between medications, inherent patient susceptibilities, and hospital environmental hazards (see Figure 1, below).
Risk Factors
Medication prescription for the hospitalized elderly patient is perhaps the area where the hospitalist can have the greatest impact in reducing a patient’s fall risk. The most common medications thought to predispose community dwelling elders to falls are psychotropic drugs: neuroleptics, sedatives, hypnotics, antidepressants, and benzodiazepines.6
Limited studies of hospitalized patients indicate similar drugs as culprits. Passaro et al demonstrated that benzodiazepines with a half-life <24 hours (e.g., lorazepam and oxazepam) were strongly associated with falls even after correcting for multiple confounders.7 Furthermore, multivariate logistic regression revealed that the use of other psychotropic drugs in addition to benzodiazepines (OR 2.3; 95% CI, 1.6–3.2) was strongly associated with an increased risk of falls. Taking more than five medications also increased a patient’s fall risk (OR 1.6; 95% CI, 1.02–2.6). Thus, the judicious prescription of medications—aimed at decreasing the number and dosage of medications an elderly patient takes—is essential to minimizing the risk for falls.
Several studies conducted in hospitalized elderly patients have repeatedly demonstrated a core group of inherent patient risk factors for falls: delirium, agitation or impaired judgment, burden of comorbidity, gait instability or lower-extremity weakness, urinary incontinence or frequency, and a history of falls.2,3,8 These risk factors are targeted as part of most inpatient fall prevention programs, as discussed below.
Several environmental hazards have been known to increase the risk of falls and injury. These include high patient-to-nurse ratio, inappropriate use of bedrails, wet floors, and lack of assistance with ambulation and toileting. The most studied of these is assistance with ambulation and toileting. Hitcho et al demonstrated that as many as 50% of falls are toileting-related.3 The study also showed that only 42% of patients who fell and used an assistive device at home had a fall in the hospital. As many as 85% of patients were not assisted with a device or person at the time of a fall.2 Unassisted falls are associated with increased injury risk (adjusted OR 1.70; 95% CI, 1.23-2.36).
Consistent with this, increased patient-to-nurse ratios are keenly associated with an increased risk of falls. Essentially, a patient whose nurse had more than five patients was 2.6 times more likely to fall than a patient whose nurse had five or fewer patients (95% CI, 1.6 to 4.1). Based on this data, hospitals have invested in low-to-the-floor beds and alarms for beds and chairs. Placing patients on a regular toileting schedule, avoiding medications that cause urinary incontinence, and attention to bowel regimens have become standard components of hospital fall prevention programs. Even though these issues have long been thought to be the purview of nurses and support staff, hospitalist involvement and awareness are crucial to ensuring that these issues are consistently addressed and enforced for every at-risk patient.
Inpatient Fall Prevention
Inpatient falls are similar to other geriatric syndromes and are multifactorial in etiology. Studies that report a decrease in the number of falls identify patients at the highest risk for falls and target multiple risk factors simultaneously.
Several inpatient fall risk assessment tools have been developed. The most widely used and validated in the acute hospital setting are the Morse Falls Scale and St. Thomas’ Risk Assessment Tool in Falling Elderly Inpatients (STRATIFY) (see Table 1, p. 24).9 Both tools incorporate the risk factors identified above—namely, the presence of cognitive or sensory deficits, environmental hazards, history of falls, lower-extremity or gait instability/weakness, and level of comorbidity to create a score. Higher scores are associated with increased fall risk. The scales have demonstrated sensitivities and specificities of 70% to 96% and 50% to 85%, respectively, depending on the population tested and the cutoff scores used.
In 2004, Healey et al published the results of one of the few successful randomized, controlled fall-prevention trials in an acute-care setting.10 Pairs of identical hospital units were randomized to intervention and control groups. The sample size was 3,386 patients, with a mean length of stay of 19 days.1 As part of the intervention group, a fall-risk assessment was performed on admission. Patients were screened for deficits in visual acuity (identify a pen, key, or watch from a distance of 2 meters), polypharmacy, orthostatic hypotension, mobility deficits, appropriate bedrail use, footwear safety, bed height, distance of patient from nursing station, loose cables, wet floors, and availability of the nurse call bell.
Interventions for patients who were identified as high fall risks included ophthalmology/optician referral for those for whom reading aides could not be procured, medication review, adjustment of bed rails, and physical therapy. Patients with a history of falls were placed close to nursing stations. Environmental hazards were removed. Patients with orthostatic hypotension were educated on slowly changing body position. Call lights were moved to within easy reach. No additional money was allocated for this study, but by performing these simple interventions, the authors were able to decrease the relative risk of falls by 29% (RR 0.71, 95% CI 0.55–0.90, P=0.006). The incidence of injuries sustained as a result of falling, however, was unchanged.
Two large, prospective studies with historical controls involving 3,000 to 7,000 patients over the course of three years and incorporating similar interventions also demonstrated a decrease in the number of falls.11,12 Fonda and his colleagues were able to demonstrate a 77% reduction in the number of falls resulting in serious injuries.
Even though these studies are promising, a recent cluster-randomized, multifactorial intervention trial involving almost 4,000 patients on a dozen medical floors did not demonstrate a reduction in the incidence of falls or falls with injury.13 Several differences exist between the two randomized trials. In the latter trial, by Cumming et al, a study nurse reviewed the care plan of all of the patients on the intervention wards and made recommendations.13 Also, the study was designed so that each patient on the intervention wards received the intervention, regardless of their fall risk. Additionally, the study period was a mere three months. In the Healey trial, the nurses on the intervention units implemented targeted risk reduction for patients at high risk, and the study period was a full year.
Back to the Case
Our patient had several risk factors for falls on admission. A targeted fall risk assessment on admission would have identified him as high-risk, with a Morse score of 95 given his dementia (15 points), impaired gait status post-transmetatarsal amputation (20 points), secondary diagnoses (multiple comorbidities, 15 points) and history of falls (25 points), and presence of an IV (20 points). The STRATIFY risk assessment tool would have produced similar results.
Frequent toileting assistance, early mobilization, medication review, and environmental modification might have prevented his fall (see Table 2, pg. 24).
Bottom Line
Focused assessment of patients on admission can identify those at risk for falls. Multifactorial inpatient fall-prevention strategies have been shown to reduce the rate of falls in inpatients without increasing costs. TH
Dr. Ölveczky is a geriatric nocturnist in the hospital medicine program, division of medicine, at Beth Israel Deaconess Medical Center in Boston.
References
- Fernandez HM, Callahan KE, Likourezos A, Leipzig RM. House staff member awareness of older inpatients’ risks for hazards of hospitalization. Arch Intern Med. 2008;168(4):390-396.
- Krauss MJ, Evanoff B, Hitcho E, et al. A case control study of patient, medication, and care-related risk factors for inpatient falls. J Gen Intern Med. 2005;20(2):116-122.
- Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med. 2004;19(7):732-739.
- Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348(1):42-49.
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556-561.
- Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47(1):30-39.
- Passaro A, Volpato S, Romagnoni F, Manzoli N, Zuliani G, Fellin R. Benzodiazepines with different half-life and falling in a hospitalized population: The GIFA study. Gruppo Italiano di Farmacovigilanza nell'Anziano. J Clin Epidemiol. 2000;53(12):1222-1229.
- Oliver D, Daly F, Martin FC, McMurdo ME. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing. 2004;33(2):122-130.
- Scott V, Votova K, Scanlan A, Close J. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings. Age Ageing. 2007;36(2):130-139.
- Healey F, Monro A, Cockram A, Adams V, Heseltine D. Using targeted risk factor reduction to prevent falls in older in-patients: a randomised controlled trial. Age Ageing. 2004;33(4):390-395.
- Fonda D, Cook J, Sandler V, Bailey M. Sustained reduction in serious fall-related injuries in older people in hospital. Med J Aust. 2006;184(8):379-382.
- Von Renteln-Kruse W, Krause T. Incidence of in-hospital falls in geriatric patients before and after the introduction of an interdisciplinary team-based fall-prevention intervention. J Am Geriatr Soc. 2007;55(12):2068-2074.
- Cumming RG, Sherrington C, Lord SR, et al. Cluster randomised trial of a targeted multifactorial intervention to prevent falls among older people in hospital. BMJ. 2008;336(7647):758-760.
- Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ. 1997;315(7115):1049-1053.
Case
An 85-year-old man with peripheral vascular disease, coronary artery disease, congestive heart failure, dementia, a history of falls, and atrial fibrillation, which was being treated with warfarin, was admitted for a left transmetatarsal amputation. On postoperative day two, the patient slipped as he was getting out of bed to use the bathroom. He hit his head on his IV pole, and a CT scan demonstrated an acute right subdural hemorrhage. He subsequently suffered eight months of delirium before passing away at a skilled nursing facility. How could this incident have been prevented?
Background
Hospitalization represents a vulnerable time for elderly people. The presence of acute illness, an unfamiliar environment, and the frequent addition of new medications predispose an elderly patient to such iatrogenic hazards of hospitalization as falls, pressure ulcers, and delirium.1 Inpatient falls are the most common type of adverse hospital event, accounting for 70% of all inpatient accidents.2 Thirty percent to 40% of inpatient falls result in injury, with 4% to 6% resulting in serious harm.2 Interestingly, 55% of falls occur in patients 60 or younger, but 60% of falls resulting in moderate to severe injury occur in those 70 and older.3
A fall is a seminal event in the life of an elderly person. Even a fall without injury can initiate a vicious circle that begins with a fear of falling and is followed by a self-restriction of mobility, which commonly results in a decline in function.4 Functional decline in the elderly has been shown to predict mortality and nursing home placement.5
Inpatient falls are thought to occur via a complex interplay between medications, inherent patient susceptibilities, and hospital environmental hazards (see Figure 1, below).
Risk Factors
Medication prescription for the hospitalized elderly patient is perhaps the area where the hospitalist can have the greatest impact in reducing a patient’s fall risk. The most common medications thought to predispose community dwelling elders to falls are psychotropic drugs: neuroleptics, sedatives, hypnotics, antidepressants, and benzodiazepines.6
Limited studies of hospitalized patients indicate similar drugs as culprits. Passaro et al demonstrated that benzodiazepines with a half-life <24 hours (e.g., lorazepam and oxazepam) were strongly associated with falls even after correcting for multiple confounders.7 Furthermore, multivariate logistic regression revealed that the use of other psychotropic drugs in addition to benzodiazepines (OR 2.3; 95% CI, 1.6–3.2) was strongly associated with an increased risk of falls. Taking more than five medications also increased a patient’s fall risk (OR 1.6; 95% CI, 1.02–2.6). Thus, the judicious prescription of medications—aimed at decreasing the number and dosage of medications an elderly patient takes—is essential to minimizing the risk for falls.
Several studies conducted in hospitalized elderly patients have repeatedly demonstrated a core group of inherent patient risk factors for falls: delirium, agitation or impaired judgment, burden of comorbidity, gait instability or lower-extremity weakness, urinary incontinence or frequency, and a history of falls.2,3,8 These risk factors are targeted as part of most inpatient fall prevention programs, as discussed below.
Several environmental hazards have been known to increase the risk of falls and injury. These include high patient-to-nurse ratio, inappropriate use of bedrails, wet floors, and lack of assistance with ambulation and toileting. The most studied of these is assistance with ambulation and toileting. Hitcho et al demonstrated that as many as 50% of falls are toileting-related.3 The study also showed that only 42% of patients who fell and used an assistive device at home had a fall in the hospital. As many as 85% of patients were not assisted with a device or person at the time of a fall.2 Unassisted falls are associated with increased injury risk (adjusted OR 1.70; 95% CI, 1.23-2.36).
Consistent with this, increased patient-to-nurse ratios are keenly associated with an increased risk of falls. Essentially, a patient whose nurse had more than five patients was 2.6 times more likely to fall than a patient whose nurse had five or fewer patients (95% CI, 1.6 to 4.1). Based on this data, hospitals have invested in low-to-the-floor beds and alarms for beds and chairs. Placing patients on a regular toileting schedule, avoiding medications that cause urinary incontinence, and attention to bowel regimens have become standard components of hospital fall prevention programs. Even though these issues have long been thought to be the purview of nurses and support staff, hospitalist involvement and awareness are crucial to ensuring that these issues are consistently addressed and enforced for every at-risk patient.
Inpatient Fall Prevention
Inpatient falls are similar to other geriatric syndromes and are multifactorial in etiology. Studies that report a decrease in the number of falls identify patients at the highest risk for falls and target multiple risk factors simultaneously.
Several inpatient fall risk assessment tools have been developed. The most widely used and validated in the acute hospital setting are the Morse Falls Scale and St. Thomas’ Risk Assessment Tool in Falling Elderly Inpatients (STRATIFY) (see Table 1, p. 24).9 Both tools incorporate the risk factors identified above—namely, the presence of cognitive or sensory deficits, environmental hazards, history of falls, lower-extremity or gait instability/weakness, and level of comorbidity to create a score. Higher scores are associated with increased fall risk. The scales have demonstrated sensitivities and specificities of 70% to 96% and 50% to 85%, respectively, depending on the population tested and the cutoff scores used.
In 2004, Healey et al published the results of one of the few successful randomized, controlled fall-prevention trials in an acute-care setting.10 Pairs of identical hospital units were randomized to intervention and control groups. The sample size was 3,386 patients, with a mean length of stay of 19 days.1 As part of the intervention group, a fall-risk assessment was performed on admission. Patients were screened for deficits in visual acuity (identify a pen, key, or watch from a distance of 2 meters), polypharmacy, orthostatic hypotension, mobility deficits, appropriate bedrail use, footwear safety, bed height, distance of patient from nursing station, loose cables, wet floors, and availability of the nurse call bell.
Interventions for patients who were identified as high fall risks included ophthalmology/optician referral for those for whom reading aides could not be procured, medication review, adjustment of bed rails, and physical therapy. Patients with a history of falls were placed close to nursing stations. Environmental hazards were removed. Patients with orthostatic hypotension were educated on slowly changing body position. Call lights were moved to within easy reach. No additional money was allocated for this study, but by performing these simple interventions, the authors were able to decrease the relative risk of falls by 29% (RR 0.71, 95% CI 0.55–0.90, P=0.006). The incidence of injuries sustained as a result of falling, however, was unchanged.
Two large, prospective studies with historical controls involving 3,000 to 7,000 patients over the course of three years and incorporating similar interventions also demonstrated a decrease in the number of falls.11,12 Fonda and his colleagues were able to demonstrate a 77% reduction in the number of falls resulting in serious injuries.
Even though these studies are promising, a recent cluster-randomized, multifactorial intervention trial involving almost 4,000 patients on a dozen medical floors did not demonstrate a reduction in the incidence of falls or falls with injury.13 Several differences exist between the two randomized trials. In the latter trial, by Cumming et al, a study nurse reviewed the care plan of all of the patients on the intervention wards and made recommendations.13 Also, the study was designed so that each patient on the intervention wards received the intervention, regardless of their fall risk. Additionally, the study period was a mere three months. In the Healey trial, the nurses on the intervention units implemented targeted risk reduction for patients at high risk, and the study period was a full year.
Back to the Case
Our patient had several risk factors for falls on admission. A targeted fall risk assessment on admission would have identified him as high-risk, with a Morse score of 95 given his dementia (15 points), impaired gait status post-transmetatarsal amputation (20 points), secondary diagnoses (multiple comorbidities, 15 points) and history of falls (25 points), and presence of an IV (20 points). The STRATIFY risk assessment tool would have produced similar results.
Frequent toileting assistance, early mobilization, medication review, and environmental modification might have prevented his fall (see Table 2, pg. 24).
Bottom Line
Focused assessment of patients on admission can identify those at risk for falls. Multifactorial inpatient fall-prevention strategies have been shown to reduce the rate of falls in inpatients without increasing costs. TH
Dr. Ölveczky is a geriatric nocturnist in the hospital medicine program, division of medicine, at Beth Israel Deaconess Medical Center in Boston.
References
- Fernandez HM, Callahan KE, Likourezos A, Leipzig RM. House staff member awareness of older inpatients’ risks for hazards of hospitalization. Arch Intern Med. 2008;168(4):390-396.
- Krauss MJ, Evanoff B, Hitcho E, et al. A case control study of patient, medication, and care-related risk factors for inpatient falls. J Gen Intern Med. 2005;20(2):116-122.
- Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med. 2004;19(7):732-739.
- Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348(1):42-49.
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556-561.
- Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47(1):30-39.
- Passaro A, Volpato S, Romagnoni F, Manzoli N, Zuliani G, Fellin R. Benzodiazepines with different half-life and falling in a hospitalized population: The GIFA study. Gruppo Italiano di Farmacovigilanza nell'Anziano. J Clin Epidemiol. 2000;53(12):1222-1229.
- Oliver D, Daly F, Martin FC, McMurdo ME. Risk factors and risk assessment tools for falls in hospital in-patients: a systematic review. Age Ageing. 2004;33(2):122-130.
- Scott V, Votova K, Scanlan A, Close J. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings. Age Ageing. 2007;36(2):130-139.
- Healey F, Monro A, Cockram A, Adams V, Heseltine D. Using targeted risk factor reduction to prevent falls in older in-patients: a randomised controlled trial. Age Ageing. 2004;33(4):390-395.
- Fonda D, Cook J, Sandler V, Bailey M. Sustained reduction in serious fall-related injuries in older people in hospital. Med J Aust. 2006;184(8):379-382.
- Von Renteln-Kruse W, Krause T. Incidence of in-hospital falls in geriatric patients before and after the introduction of an interdisciplinary team-based fall-prevention intervention. J Am Geriatr Soc. 2007;55(12):2068-2074.
- Cumming RG, Sherrington C, Lord SR, et al. Cluster randomised trial of a targeted multifactorial intervention to prevent falls among older people in hospital. BMJ. 2008;336(7647):758-760.
- Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ. 1997;315(7115):1049-1053.
Job Hunter’s Checklist
Apart from the part-time job that provided pocket money while you were in high school or during your undergraduate years, physicians generally have little experience in the job-hunting arena. A physician’s career path requires much skill at applying for such educational endeavors as medical school and residency training, but applying for a “real” job can be a strange concept for most.
Not lost in the equation is the fact that the application process doesn’t begin until most physicians are in their late 20s. While many of our non-physician friends are on their second or third jobs, graduating residents looking to launch their careers often struggle with the transition to the world of HM. In order to help navigate these waters, we have put together a yearlong guide to help make the transition from third-year resident to hospitalist a little smoother.
July-September
The first step in landing a job is to find a mentor who can assist you through the entire process. Choose your mentor wisely; an experienced hospitalist can provide valuable feedback during your job search. If your goal is employment with a private hospitalist group, find a hospitalist with private-practice experience.
Choose your senior-year electives carefully. Consider focusing on areas of weakness or areas that are pertinent to HM (e.g., infectious disease, cardiology, neurology, critical-care medicine). Think about an outside elective in HM.
If you haven’t done so already, now is the time to create a curriculum vitae, also known as a CV, and a cover letter. The CV is a vital document. It might be the key element in determining whether you are worthy of an interview. Work on this document early, as you will need time for edits, updates, and mentor review. The cover letter should clearly describe the type of position you want and confidently state why you would be an asset to a particular hospitalist program. Edit your words carefully; spelling errors or typos in documents can be costly.
Once the Labor Day holiday has passed, you should start requesting letters of recommendation. Think hard about who you want before asking for a letter of recommendation, as these typically carry a lot of weight in the interview selection process. Although program directors, chiefs of medicine, and hospitalists can be good choices, it is important to choose people who know you well, as they tend to generate a more personal and powerful letter. Because letter-writers often are busy people, it is appropriate to give a deadline for when you need the letter.
October-December
Actively start the job search and apply for desired positions. This is the time of year when HM jobs are heavily advertised and programs are looking to fill positions. Hospitalists are in high demand throughout the country. Some great places to find job openings are:
- SHM’s Career Center (www.hospitalmedicine.org/careers);
- Classified ad sections in the Journal of Hospital Medicine, general medicine journals, and HM news magazines like The Hospitalist (see “SHM Career Center,” p. 35); and
- Hospitals and HM groups of interest, even if they are not advertising; contact them personally.
Begin the interview process by researching the hospital and HM group in advance. Prepare appropriate interview questions. When you interview, try to meet with as many people as possible to get a feel for what the job entails. Talk to the everyday hospitalists and try to gauge how satisfied they are in their jobs.
Bring extra copies of your updated CV and look sharp. Shine your shoes. Is it time to replace the suit you used to apply for residency?
Send a thank-you note or e-mail to the person(s) you interviewed with. If possible, do this within three days of your visit. It’s an important step in the process, yet this simple task often is overlooked. Remain in contact with the HM programs you are most interested in. Think about a follow-up visit or phone call to address any unanswered questions.
January-March
Hopefully you will have one or more offers by now. This is the time to negotiate a contract and accept an offer. Review the contract carefully and don’t hesitate to ask for clarification of unclear points. Some applicants prefer to have a lawyer review the contract prior to signing (see “The Art of Negotiation,” December 2008, p. 20).
Register for your board examination. Most specialties, including internal medicine, family medicine, and pediatrics, as well as board exams for osteopathic medicine, have registration deadlines in February. Given the significant cost of applying for these exams, it pays not to be tardy, as late fees can set you back hundreds of dollars.
Apply for state medical licensure. This process varies by state, but it can take several months to complete, especially if you are applying in a state other than where you trained. For example, California recommends starting the application process six to nine months in advance. International medical graduates who require a work visa need to ensure their paperwork is processed in a timely manner.
Each hospital is different, but applications for hospital credentialing generally means filling out a mountain of paperwork. Most hospitals will perform a thorough background check, so don’t be surprised if fingerprinting is required. The hospital or hospitalist group usually helps new hires navigate through this process, which can take several weeks or even months.
April-June
Moving to a different city or state can be exciting—and stressful. Start talking to hospitalists at the facility where you will be working to get a feel for the city and recommendations for places to live. Revisit the location to become more familiar with the surroundings. Some hospitals are very helpful; some provide new hires with a real estate agent. Moving expenses often are covered as a condition of employment, but it depends on your contract.
Consider taking a vacation to either further explore relocation options or to simply relax. If you have followed the recommendations outlined in the previous months, you should have time to unwind as your residency comes to an end. Some future hospitalists like to use this time to intensify board review; others cringe at the thought.
Transitioning from resident to hospitalist is no easy task, and it shouldn’t be taken lightly. It’s not a one-month process, either, so planning is essential. Although it might seem to be a daunting journey, it’s very rewarding in the long run. TH
Dr. Grant is a hospitalist at the University of Michigan Health System in Ann Arbor. Dr. Warren-Marzola is a hospitalist at St. Luke’s Hospital in Toledo, Ohio. Both are members of SHM’s Young Physicians Committee.
Apart from the part-time job that provided pocket money while you were in high school or during your undergraduate years, physicians generally have little experience in the job-hunting arena. A physician’s career path requires much skill at applying for such educational endeavors as medical school and residency training, but applying for a “real” job can be a strange concept for most.
Not lost in the equation is the fact that the application process doesn’t begin until most physicians are in their late 20s. While many of our non-physician friends are on their second or third jobs, graduating residents looking to launch their careers often struggle with the transition to the world of HM. In order to help navigate these waters, we have put together a yearlong guide to help make the transition from third-year resident to hospitalist a little smoother.
July-September
The first step in landing a job is to find a mentor who can assist you through the entire process. Choose your mentor wisely; an experienced hospitalist can provide valuable feedback during your job search. If your goal is employment with a private hospitalist group, find a hospitalist with private-practice experience.
Choose your senior-year electives carefully. Consider focusing on areas of weakness or areas that are pertinent to HM (e.g., infectious disease, cardiology, neurology, critical-care medicine). Think about an outside elective in HM.
If you haven’t done so already, now is the time to create a curriculum vitae, also known as a CV, and a cover letter. The CV is a vital document. It might be the key element in determining whether you are worthy of an interview. Work on this document early, as you will need time for edits, updates, and mentor review. The cover letter should clearly describe the type of position you want and confidently state why you would be an asset to a particular hospitalist program. Edit your words carefully; spelling errors or typos in documents can be costly.
Once the Labor Day holiday has passed, you should start requesting letters of recommendation. Think hard about who you want before asking for a letter of recommendation, as these typically carry a lot of weight in the interview selection process. Although program directors, chiefs of medicine, and hospitalists can be good choices, it is important to choose people who know you well, as they tend to generate a more personal and powerful letter. Because letter-writers often are busy people, it is appropriate to give a deadline for when you need the letter.
October-December
Actively start the job search and apply for desired positions. This is the time of year when HM jobs are heavily advertised and programs are looking to fill positions. Hospitalists are in high demand throughout the country. Some great places to find job openings are:
- SHM’s Career Center (www.hospitalmedicine.org/careers);
- Classified ad sections in the Journal of Hospital Medicine, general medicine journals, and HM news magazines like The Hospitalist (see “SHM Career Center,” p. 35); and
- Hospitals and HM groups of interest, even if they are not advertising; contact them personally.
Begin the interview process by researching the hospital and HM group in advance. Prepare appropriate interview questions. When you interview, try to meet with as many people as possible to get a feel for what the job entails. Talk to the everyday hospitalists and try to gauge how satisfied they are in their jobs.
Bring extra copies of your updated CV and look sharp. Shine your shoes. Is it time to replace the suit you used to apply for residency?
Send a thank-you note or e-mail to the person(s) you interviewed with. If possible, do this within three days of your visit. It’s an important step in the process, yet this simple task often is overlooked. Remain in contact with the HM programs you are most interested in. Think about a follow-up visit or phone call to address any unanswered questions.
January-March
Hopefully you will have one or more offers by now. This is the time to negotiate a contract and accept an offer. Review the contract carefully and don’t hesitate to ask for clarification of unclear points. Some applicants prefer to have a lawyer review the contract prior to signing (see “The Art of Negotiation,” December 2008, p. 20).
Register for your board examination. Most specialties, including internal medicine, family medicine, and pediatrics, as well as board exams for osteopathic medicine, have registration deadlines in February. Given the significant cost of applying for these exams, it pays not to be tardy, as late fees can set you back hundreds of dollars.
Apply for state medical licensure. This process varies by state, but it can take several months to complete, especially if you are applying in a state other than where you trained. For example, California recommends starting the application process six to nine months in advance. International medical graduates who require a work visa need to ensure their paperwork is processed in a timely manner.
Each hospital is different, but applications for hospital credentialing generally means filling out a mountain of paperwork. Most hospitals will perform a thorough background check, so don’t be surprised if fingerprinting is required. The hospital or hospitalist group usually helps new hires navigate through this process, which can take several weeks or even months.
April-June
Moving to a different city or state can be exciting—and stressful. Start talking to hospitalists at the facility where you will be working to get a feel for the city and recommendations for places to live. Revisit the location to become more familiar with the surroundings. Some hospitals are very helpful; some provide new hires with a real estate agent. Moving expenses often are covered as a condition of employment, but it depends on your contract.
Consider taking a vacation to either further explore relocation options or to simply relax. If you have followed the recommendations outlined in the previous months, you should have time to unwind as your residency comes to an end. Some future hospitalists like to use this time to intensify board review; others cringe at the thought.
Transitioning from resident to hospitalist is no easy task, and it shouldn’t be taken lightly. It’s not a one-month process, either, so planning is essential. Although it might seem to be a daunting journey, it’s very rewarding in the long run. TH
Dr. Grant is a hospitalist at the University of Michigan Health System in Ann Arbor. Dr. Warren-Marzola is a hospitalist at St. Luke’s Hospital in Toledo, Ohio. Both are members of SHM’s Young Physicians Committee.
Apart from the part-time job that provided pocket money while you were in high school or during your undergraduate years, physicians generally have little experience in the job-hunting arena. A physician’s career path requires much skill at applying for such educational endeavors as medical school and residency training, but applying for a “real” job can be a strange concept for most.
Not lost in the equation is the fact that the application process doesn’t begin until most physicians are in their late 20s. While many of our non-physician friends are on their second or third jobs, graduating residents looking to launch their careers often struggle with the transition to the world of HM. In order to help navigate these waters, we have put together a yearlong guide to help make the transition from third-year resident to hospitalist a little smoother.
July-September
The first step in landing a job is to find a mentor who can assist you through the entire process. Choose your mentor wisely; an experienced hospitalist can provide valuable feedback during your job search. If your goal is employment with a private hospitalist group, find a hospitalist with private-practice experience.
Choose your senior-year electives carefully. Consider focusing on areas of weakness or areas that are pertinent to HM (e.g., infectious disease, cardiology, neurology, critical-care medicine). Think about an outside elective in HM.
If you haven’t done so already, now is the time to create a curriculum vitae, also known as a CV, and a cover letter. The CV is a vital document. It might be the key element in determining whether you are worthy of an interview. Work on this document early, as you will need time for edits, updates, and mentor review. The cover letter should clearly describe the type of position you want and confidently state why you would be an asset to a particular hospitalist program. Edit your words carefully; spelling errors or typos in documents can be costly.
Once the Labor Day holiday has passed, you should start requesting letters of recommendation. Think hard about who you want before asking for a letter of recommendation, as these typically carry a lot of weight in the interview selection process. Although program directors, chiefs of medicine, and hospitalists can be good choices, it is important to choose people who know you well, as they tend to generate a more personal and powerful letter. Because letter-writers often are busy people, it is appropriate to give a deadline for when you need the letter.
October-December
Actively start the job search and apply for desired positions. This is the time of year when HM jobs are heavily advertised and programs are looking to fill positions. Hospitalists are in high demand throughout the country. Some great places to find job openings are:
- SHM’s Career Center (www.hospitalmedicine.org/careers);
- Classified ad sections in the Journal of Hospital Medicine, general medicine journals, and HM news magazines like The Hospitalist (see “SHM Career Center,” p. 35); and
- Hospitals and HM groups of interest, even if they are not advertising; contact them personally.
Begin the interview process by researching the hospital and HM group in advance. Prepare appropriate interview questions. When you interview, try to meet with as many people as possible to get a feel for what the job entails. Talk to the everyday hospitalists and try to gauge how satisfied they are in their jobs.
Bring extra copies of your updated CV and look sharp. Shine your shoes. Is it time to replace the suit you used to apply for residency?
Send a thank-you note or e-mail to the person(s) you interviewed with. If possible, do this within three days of your visit. It’s an important step in the process, yet this simple task often is overlooked. Remain in contact with the HM programs you are most interested in. Think about a follow-up visit or phone call to address any unanswered questions.
January-March
Hopefully you will have one or more offers by now. This is the time to negotiate a contract and accept an offer. Review the contract carefully and don’t hesitate to ask for clarification of unclear points. Some applicants prefer to have a lawyer review the contract prior to signing (see “The Art of Negotiation,” December 2008, p. 20).
Register for your board examination. Most specialties, including internal medicine, family medicine, and pediatrics, as well as board exams for osteopathic medicine, have registration deadlines in February. Given the significant cost of applying for these exams, it pays not to be tardy, as late fees can set you back hundreds of dollars.
Apply for state medical licensure. This process varies by state, but it can take several months to complete, especially if you are applying in a state other than where you trained. For example, California recommends starting the application process six to nine months in advance. International medical graduates who require a work visa need to ensure their paperwork is processed in a timely manner.
Each hospital is different, but applications for hospital credentialing generally means filling out a mountain of paperwork. Most hospitals will perform a thorough background check, so don’t be surprised if fingerprinting is required. The hospital or hospitalist group usually helps new hires navigate through this process, which can take several weeks or even months.
April-June
Moving to a different city or state can be exciting—and stressful. Start talking to hospitalists at the facility where you will be working to get a feel for the city and recommendations for places to live. Revisit the location to become more familiar with the surroundings. Some hospitals are very helpful; some provide new hires with a real estate agent. Moving expenses often are covered as a condition of employment, but it depends on your contract.
Consider taking a vacation to either further explore relocation options or to simply relax. If you have followed the recommendations outlined in the previous months, you should have time to unwind as your residency comes to an end. Some future hospitalists like to use this time to intensify board review; others cringe at the thought.
Transitioning from resident to hospitalist is no easy task, and it shouldn’t be taken lightly. It’s not a one-month process, either, so planning is essential. Although it might seem to be a daunting journey, it’s very rewarding in the long run. TH
Dr. Grant is a hospitalist at the University of Michigan Health System in Ann Arbor. Dr. Warren-Marzola is a hospitalist at St. Luke’s Hospital in Toledo, Ohio. Both are members of SHM’s Young Physicians Committee.
Facility Transfers
Patient care provided in the acute setting might not always end with discharge to the patient’s home. Frequently, a hospitalist will transfer the patient to a different unit in the hospital or an off-site facility to receive additional services before returning to their home. When the patient’s condition requires a transfer to a physical medicine and rehabilitation (PM&R) unit, a psychiatric unit, a long-term acute-care facility, or a skilled nursing facility, it is important for the hospitalist to identify their role, if any, in the new area of care. Physician billing will depend on several factors:
- A shared medical record;
- The attending of record in each setting; and
- The care rendered by the hospitalist in each setting.
Intrafacility
A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for a 68-year-old male with hypertension and diabetes who sustained a hip fracture. The care plan includes post-discharge therapy and rehabilitation. When the hospitalist transfers care to a PM&R unit within the same facility for which the hospitalist is no longer the attending of record, they might be asked to provide ongoing care for the patient’s medical conditions (e.g., diabetes and hypertension). The hospitalist’s knee-jerk reaction is to bill for an inpatient consultation for the initial service provided in the transferred setting. This would only be appropriate if the request for opinion or advice involved an unrelated, new condition, and the requesting physician’s intent is for opinion or advice on how to manage the patient and not the a priori intent for the hospitalist to assume the patient’s medical care.
If consultation requirements are met (see “Consulataion Reminder,” p. 20), the hospitalist can report an inpatient consultation code (99251-99255). However, when circumstances do not fully represent the intent or need for consultative services but rather a continuity of the medical care provided during the acute phase of the hospitalization, report the most appropriate subsequent hospital care code (99231-99233) for the initial rehab visit and all follow-up services.
On occasion, the hospitalist will be asked to perform and provide the history and physical (H&P) for the patient’s “sub-acute” phase of care, even though the hospitalist is not the attending of record. This usually happens when the attending of record cannot complete the medical requirements of the H&P, either at all or as comprehensively as the hospitalist. When this occurs, the hospitalist should not report an initial hospital care code (99221-99223) because they are not the attending of record—the physician who admits the patient and is responsible for the patient’s stay in the transferred location.
Additionally, a consultation service (99251-99255) should not be reported, because the request involves the completion of a facility-mandated form and not an opinion or advice on caring for the patient. If medical issues require the hospitalist’s evaluation and management, there is medical necessity for capturing the hospitalist’s participation as subsequent hospital care (99231-99233). If no medical conditions present for the hospitalist to manage, the service will not be considered “medically necessary” by the payor.
Interfacility
Hospitalist groups provide patient care and coverage in a variety of facilities. Confusion often arises when the attending of record during acute care and the sub-acute setting are different hospitalists from the same HM group. The hospitalist who receives the patient in the transfer facility may err on the side of caution and report subsequent hospital care (99231-99233) because the group has provided ongoing patient care. In this scenario, the hospitalist group might lose revenue if an admission service (99221-99223) was not reported.
Day of Transfer Billing
A single hospitalist or two hospitalists from the same group might bill both the hospital discharge management code (99238-99239) and an initial hospital care code (99221-99223) when the discharge and admission do not occur on the same day if the transfer is between:
- Different hospitals;
- Different facilities under common ownership that do not have merged records;* or
- Between the acute-care hospital and a prospective payment system (PPS)-exempt unit within the same hospital when there are no merged records.
In all other transfer circumstances that do not meet the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Of note, Medicare Part A covers inpatient care in psychiatric, rehabilitation, critical access, and long-term-care hospitals. Each of these specialty hospitals is exempt from the PPS established for acute-care hospitals in 1983.2 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
*Editor’s note: “Merged record” is not equivalent to commonly accessible charts via an electronic health record system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1E. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
- Department of Health and Human Services. Office of Inspector General: Oversight of Medicare PPS-Exempt Hospital Services. HHS Web site. Available at: www.oig.hhs.gov/oei/reports/oei-12-02-00170.pdf. Accessed June 1, 2009.
- CMS. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1H. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
Patient care provided in the acute setting might not always end with discharge to the patient’s home. Frequently, a hospitalist will transfer the patient to a different unit in the hospital or an off-site facility to receive additional services before returning to their home. When the patient’s condition requires a transfer to a physical medicine and rehabilitation (PM&R) unit, a psychiatric unit, a long-term acute-care facility, or a skilled nursing facility, it is important for the hospitalist to identify their role, if any, in the new area of care. Physician billing will depend on several factors:
- A shared medical record;
- The attending of record in each setting; and
- The care rendered by the hospitalist in each setting.
Intrafacility
A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for a 68-year-old male with hypertension and diabetes who sustained a hip fracture. The care plan includes post-discharge therapy and rehabilitation. When the hospitalist transfers care to a PM&R unit within the same facility for which the hospitalist is no longer the attending of record, they might be asked to provide ongoing care for the patient’s medical conditions (e.g., diabetes and hypertension). The hospitalist’s knee-jerk reaction is to bill for an inpatient consultation for the initial service provided in the transferred setting. This would only be appropriate if the request for opinion or advice involved an unrelated, new condition, and the requesting physician’s intent is for opinion or advice on how to manage the patient and not the a priori intent for the hospitalist to assume the patient’s medical care.
If consultation requirements are met (see “Consulataion Reminder,” p. 20), the hospitalist can report an inpatient consultation code (99251-99255). However, when circumstances do not fully represent the intent or need for consultative services but rather a continuity of the medical care provided during the acute phase of the hospitalization, report the most appropriate subsequent hospital care code (99231-99233) for the initial rehab visit and all follow-up services.
On occasion, the hospitalist will be asked to perform and provide the history and physical (H&P) for the patient’s “sub-acute” phase of care, even though the hospitalist is not the attending of record. This usually happens when the attending of record cannot complete the medical requirements of the H&P, either at all or as comprehensively as the hospitalist. When this occurs, the hospitalist should not report an initial hospital care code (99221-99223) because they are not the attending of record—the physician who admits the patient and is responsible for the patient’s stay in the transferred location.
Additionally, a consultation service (99251-99255) should not be reported, because the request involves the completion of a facility-mandated form and not an opinion or advice on caring for the patient. If medical issues require the hospitalist’s evaluation and management, there is medical necessity for capturing the hospitalist’s participation as subsequent hospital care (99231-99233). If no medical conditions present for the hospitalist to manage, the service will not be considered “medically necessary” by the payor.
Interfacility
Hospitalist groups provide patient care and coverage in a variety of facilities. Confusion often arises when the attending of record during acute care and the sub-acute setting are different hospitalists from the same HM group. The hospitalist who receives the patient in the transfer facility may err on the side of caution and report subsequent hospital care (99231-99233) because the group has provided ongoing patient care. In this scenario, the hospitalist group might lose revenue if an admission service (99221-99223) was not reported.
Day of Transfer Billing
A single hospitalist or two hospitalists from the same group might bill both the hospital discharge management code (99238-99239) and an initial hospital care code (99221-99223) when the discharge and admission do not occur on the same day if the transfer is between:
- Different hospitals;
- Different facilities under common ownership that do not have merged records;* or
- Between the acute-care hospital and a prospective payment system (PPS)-exempt unit within the same hospital when there are no merged records.
In all other transfer circumstances that do not meet the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Of note, Medicare Part A covers inpatient care in psychiatric, rehabilitation, critical access, and long-term-care hospitals. Each of these specialty hospitals is exempt from the PPS established for acute-care hospitals in 1983.2 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
*Editor’s note: “Merged record” is not equivalent to commonly accessible charts via an electronic health record system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1E. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
- Department of Health and Human Services. Office of Inspector General: Oversight of Medicare PPS-Exempt Hospital Services. HHS Web site. Available at: www.oig.hhs.gov/oei/reports/oei-12-02-00170.pdf. Accessed June 1, 2009.
- CMS. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1H. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
Patient care provided in the acute setting might not always end with discharge to the patient’s home. Frequently, a hospitalist will transfer the patient to a different unit in the hospital or an off-site facility to receive additional services before returning to their home. When the patient’s condition requires a transfer to a physical medicine and rehabilitation (PM&R) unit, a psychiatric unit, a long-term acute-care facility, or a skilled nursing facility, it is important for the hospitalist to identify their role, if any, in the new area of care. Physician billing will depend on several factors:
- A shared medical record;
- The attending of record in each setting; and
- The care rendered by the hospitalist in each setting.
Intrafacility
A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for a 68-year-old male with hypertension and diabetes who sustained a hip fracture. The care plan includes post-discharge therapy and rehabilitation. When the hospitalist transfers care to a PM&R unit within the same facility for which the hospitalist is no longer the attending of record, they might be asked to provide ongoing care for the patient’s medical conditions (e.g., diabetes and hypertension). The hospitalist’s knee-jerk reaction is to bill for an inpatient consultation for the initial service provided in the transferred setting. This would only be appropriate if the request for opinion or advice involved an unrelated, new condition, and the requesting physician’s intent is for opinion or advice on how to manage the patient and not the a priori intent for the hospitalist to assume the patient’s medical care.
If consultation requirements are met (see “Consulataion Reminder,” p. 20), the hospitalist can report an inpatient consultation code (99251-99255). However, when circumstances do not fully represent the intent or need for consultative services but rather a continuity of the medical care provided during the acute phase of the hospitalization, report the most appropriate subsequent hospital care code (99231-99233) for the initial rehab visit and all follow-up services.
On occasion, the hospitalist will be asked to perform and provide the history and physical (H&P) for the patient’s “sub-acute” phase of care, even though the hospitalist is not the attending of record. This usually happens when the attending of record cannot complete the medical requirements of the H&P, either at all or as comprehensively as the hospitalist. When this occurs, the hospitalist should not report an initial hospital care code (99221-99223) because they are not the attending of record—the physician who admits the patient and is responsible for the patient’s stay in the transferred location.
Additionally, a consultation service (99251-99255) should not be reported, because the request involves the completion of a facility-mandated form and not an opinion or advice on caring for the patient. If medical issues require the hospitalist’s evaluation and management, there is medical necessity for capturing the hospitalist’s participation as subsequent hospital care (99231-99233). If no medical conditions present for the hospitalist to manage, the service will not be considered “medically necessary” by the payor.
Interfacility
Hospitalist groups provide patient care and coverage in a variety of facilities. Confusion often arises when the attending of record during acute care and the sub-acute setting are different hospitalists from the same HM group. The hospitalist who receives the patient in the transfer facility may err on the side of caution and report subsequent hospital care (99231-99233) because the group has provided ongoing patient care. In this scenario, the hospitalist group might lose revenue if an admission service (99221-99223) was not reported.
Day of Transfer Billing
A single hospitalist or two hospitalists from the same group might bill both the hospital discharge management code (99238-99239) and an initial hospital care code (99221-99223) when the discharge and admission do not occur on the same day if the transfer is between:
- Different hospitals;
- Different facilities under common ownership that do not have merged records;* or
- Between the acute-care hospital and a prospective payment system (PPS)-exempt unit within the same hospital when there are no merged records.
In all other transfer circumstances that do not meet the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Of note, Medicare Part A covers inpatient care in psychiatric, rehabilitation, critical access, and long-term-care hospitals. Each of these specialty hospitals is exempt from the PPS established for acute-care hospitals in 1983.2 TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center in Philadelphia. She is faculty of SHM’s inpatient coding course.
*Editor’s note: “Merged record” is not equivalent to commonly accessible charts via an electronic health record system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
References
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1E. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
- Department of Health and Human Services. Office of Inspector General: Oversight of Medicare PPS-Exempt Hospital Services. HHS Web site. Available at: www.oig.hhs.gov/oei/reports/oei-12-02-00170.pdf. Accessed June 1, 2009.
- CMS. Medicare Claims Processing Manual: Chapter 12, Section 30.6.9.1H. CMS Web site. Available at: www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed June 1, 2009.
Billion-Dollar Questions
On June 30, a new government agency within the Department of Health and Human Services (HHS) called the Federal Coordinating Council for Comparative Effectiveness Research released its first report to President Obama and Congress. Authorized by the American Recovery and Reinvestment Act of 2009, the council is tasked with prioritizing and coordinating how multiple government agencies will spend the stimulus package’s $1.1 billion windfall for comparative effectiveness research (CER), which is aimed at improving healthcare outcomes in the U.S.
Of the funds, $400 million has been directed to the National Institutes of Health (NIH), $300 million to the Agency for Healthcare Research and Quality, and the remaining $400 million to the Office of the Secretary of Health and Human Services.
Patrick Conway, MD, MSc, the federal coordinating council’s executive director, is well versed in the potential impact of comparative effectiveness research on hospitalists. Just as Dr. Conway was joining the Center for Health Care Quality at Cincinnati Children’s Hospital after a fellowship at Children’s Hospital of Philadelphia, the pediatric hospitalist was named a 2007-2008 White House Fellow at HHS—the first hospitalist accepted into the program.

—Patrick Conway, MD, MSc, executive director, HHS’ Federal Coordinating Council for Comparative Effectiveness Research
In August 2008, he was tapped for the post of chief medical officer in the department’s Office of the Assistant Secretary for Planning and Evaluation.
Meanwhile, Dr. Conway still sees patients on weekends at Children’s National Medical Center in Washington, D.C. He recently talked with The Hospitalist about the challenges of coordinating research funding across multiple government agencies, how the Office of the Secretary’s $400 million allocation could be best spent, and what it all means for patient care.
Question: What are the biggest recommendations in the federal coordinating council’s report?
Answer: We approached this as “What unique role can the Office of the Secretary research funds address?” We identified data infrastructure as a potential primary investment. That includes things such as patient registries, distributed data networks, and claims databases.
Traditionally, the federal government has not invested in infrastructure because we have funded independent investigators on a one-question-by-one-question basis. The way I see this infusion of funds is it allows you to invest in data infrastructure that can then be used to answer literally hundreds of questions over time.
Secondly, we identified dissemination and translation, so how do we think about innovative ways to actually communicate directly to patients and physicians at the point of care? We also identified priority populations, including racial and ethnic minorities, persons with multiple chronic conditions, children, and the elderly. And lastly, we identified priority interventions, such as behavioral change, delivery systems, and prevention. So how do we decrease obesity, how do we decrease smoking rates?
Q: How will you address the challenge of coordinating research funding across multiple federal agencies?
A: I think the first step is doing the inventory [of CER], which is going to be an ongoing and iterative process. By doing that, then the council and the HHS have to attempt to avoid duplicating efforts and actually coordinate efforts across the federal government.
Honestly, I think the biggest challenge is these are extremely large, complex government programs. These are hundreds of millions of dollars going out to a huge variety of researchers, academic institutions, etc. One of the systems we’re trying to put in place is a better way to track what’s going on now, so we can actually coordinate going forward. It’s something as simple as we now have a common definition. We tag all money (e.g., CER), so we know exactly what we’re spending money on. That sounds really simple, but it’s actually never been done before. This is a relatively new area of emphasis for the federal government and for healthcare.
Q: What main point should hospitalists take away from this report?
A: This research will address primary questions about which medicine is best for which patient but also address larger issues, such as care coordination and how care is organized within the hospital and outside the hospital, so that we focus on the gamut of questions that have the potential to improve patient outcomes.
Q: What were some common themes you heard in the public listening sessions and online comments you solicited during the report’s preparation?
A: One of them was the importance of engaging stakeholders throughout the process, getting input from patients, physicians, policymakers. … We also heard themes about the need for infrastructure development, also the need for data infrastructure. We also heard a theme about the need for more work on research methodology and training of researchers. And then we heard a strong theme around “This needs to actually be disseminated and translated into care delivery.” So producing knowledge is helpful, but translating that knowledge into better outcomes is the ultimate goal.
Q: The report repeatedly mentions “real world” healthcare settings. Is this meant as a criticism of the idealized outcomes of efficacy research as it is typically conducted?
A: I don’t know that I would frame it as a criticism. I will say that as hospitalists, we are faced with patients every day where there’s unclear evidence about how best to manage that patient. And therefore, we need more evidence on the real questions that patients and physicians encounter in practice. I think we’ve had a long history of strong, well-funded randomized trials in this country, and I think we need to complement that with other methods of research as well, including databases, quality improvement, and measuring interventions.
Q: What are the limitations in translating all of this knowledge to interventions for the patients who need it?
A: I think the research paradigm traditionally has been: We fund an investigator. They go off for years and do their research. And then they publish it in the New England Journal [of Medicine] or JAMA, and we call that a success.
I would argue that we’re at a time where we need to think about a new paradigm, where just publishing it is some middle step. And we need to think about how you actually link the research enterprise to the care delivery enterprise, so research is rapidly implemented and you’re measuring outcomes and ensuring that research actually reaches the patients and clinicians.
Q: Are there any real-world examples of how to do this?
A: Say we had a national patient library and we thought about things that we have not traditionally thought about in healthcare—social networking, Twitter, Facebook, media channels that reach people now. How do you insert health content into those channels to actually change people’s behavior, or at least inform them? The medical establishment thinks we publish it in the New England Journal [of Medicine] and the world changes. That’s just fundamentally not true.
On the provider side, how do we think about the lay media? How do we think about channels that providers use, like UpToDate and Medscape? How do we get comparative effectiveness content into those channels that are used by providers and physicians?
Q: How should CER address the needs of patient groups that are under-represented in traditional medical studies?
A: I think that’s a huge area. Efficacy trials generally will show something works for the average patient. But the issue is, and I’ll give you a concrete example, if you are an elderly, African-American female with a couple of conditions (diabetes and heart disease), how will that treatment work for you? So I think the power of comparative effectiveness is that we, especially with the data sources we just talked about, can look at patient subgroups and get as close as possible to the individual level to really present information. Instead of [saying], this works on average patients, which includes lots of patients that don’t look at all like you, [we can] say we’ve looked and it actually works well for racial and ethnic minorities, or persons with disabilities, or the very elderly.
Q: What do you hope ultimately will come from this report?
A: On the care delivery side, this is an opportunity for hospitalists to test different interventions to improve care in the hospitals. For what I hope to achieve, I think as we invest in all these individual programs, we are building in evaluation components to assess how this impacts patient outcomes.
I think the ultimate goal is to improve patient outcomes in this country, which I know is an unbelievably grand goal, but I think you build up to that by each investment. You track what it produces and ultimately how it affects outcomes, and so you at least start to build a sense of what this program means for the nation’s health. TH
Bryn Nelson is a freelance writer based in Seattle.
On June 30, a new government agency within the Department of Health and Human Services (HHS) called the Federal Coordinating Council for Comparative Effectiveness Research released its first report to President Obama and Congress. Authorized by the American Recovery and Reinvestment Act of 2009, the council is tasked with prioritizing and coordinating how multiple government agencies will spend the stimulus package’s $1.1 billion windfall for comparative effectiveness research (CER), which is aimed at improving healthcare outcomes in the U.S.
Of the funds, $400 million has been directed to the National Institutes of Health (NIH), $300 million to the Agency for Healthcare Research and Quality, and the remaining $400 million to the Office of the Secretary of Health and Human Services.
Patrick Conway, MD, MSc, the federal coordinating council’s executive director, is well versed in the potential impact of comparative effectiveness research on hospitalists. Just as Dr. Conway was joining the Center for Health Care Quality at Cincinnati Children’s Hospital after a fellowship at Children’s Hospital of Philadelphia, the pediatric hospitalist was named a 2007-2008 White House Fellow at HHS—the first hospitalist accepted into the program.

—Patrick Conway, MD, MSc, executive director, HHS’ Federal Coordinating Council for Comparative Effectiveness Research
In August 2008, he was tapped for the post of chief medical officer in the department’s Office of the Assistant Secretary for Planning and Evaluation.
Meanwhile, Dr. Conway still sees patients on weekends at Children’s National Medical Center in Washington, D.C. He recently talked with The Hospitalist about the challenges of coordinating research funding across multiple government agencies, how the Office of the Secretary’s $400 million allocation could be best spent, and what it all means for patient care.
Question: What are the biggest recommendations in the federal coordinating council’s report?
Answer: We approached this as “What unique role can the Office of the Secretary research funds address?” We identified data infrastructure as a potential primary investment. That includes things such as patient registries, distributed data networks, and claims databases.
Traditionally, the federal government has not invested in infrastructure because we have funded independent investigators on a one-question-by-one-question basis. The way I see this infusion of funds is it allows you to invest in data infrastructure that can then be used to answer literally hundreds of questions over time.
Secondly, we identified dissemination and translation, so how do we think about innovative ways to actually communicate directly to patients and physicians at the point of care? We also identified priority populations, including racial and ethnic minorities, persons with multiple chronic conditions, children, and the elderly. And lastly, we identified priority interventions, such as behavioral change, delivery systems, and prevention. So how do we decrease obesity, how do we decrease smoking rates?
Q: How will you address the challenge of coordinating research funding across multiple federal agencies?
A: I think the first step is doing the inventory [of CER], which is going to be an ongoing and iterative process. By doing that, then the council and the HHS have to attempt to avoid duplicating efforts and actually coordinate efforts across the federal government.
Honestly, I think the biggest challenge is these are extremely large, complex government programs. These are hundreds of millions of dollars going out to a huge variety of researchers, academic institutions, etc. One of the systems we’re trying to put in place is a better way to track what’s going on now, so we can actually coordinate going forward. It’s something as simple as we now have a common definition. We tag all money (e.g., CER), so we know exactly what we’re spending money on. That sounds really simple, but it’s actually never been done before. This is a relatively new area of emphasis for the federal government and for healthcare.
Q: What main point should hospitalists take away from this report?
A: This research will address primary questions about which medicine is best for which patient but also address larger issues, such as care coordination and how care is organized within the hospital and outside the hospital, so that we focus on the gamut of questions that have the potential to improve patient outcomes.
Q: What were some common themes you heard in the public listening sessions and online comments you solicited during the report’s preparation?
A: One of them was the importance of engaging stakeholders throughout the process, getting input from patients, physicians, policymakers. … We also heard themes about the need for infrastructure development, also the need for data infrastructure. We also heard a theme about the need for more work on research methodology and training of researchers. And then we heard a strong theme around “This needs to actually be disseminated and translated into care delivery.” So producing knowledge is helpful, but translating that knowledge into better outcomes is the ultimate goal.
Q: The report repeatedly mentions “real world” healthcare settings. Is this meant as a criticism of the idealized outcomes of efficacy research as it is typically conducted?
A: I don’t know that I would frame it as a criticism. I will say that as hospitalists, we are faced with patients every day where there’s unclear evidence about how best to manage that patient. And therefore, we need more evidence on the real questions that patients and physicians encounter in practice. I think we’ve had a long history of strong, well-funded randomized trials in this country, and I think we need to complement that with other methods of research as well, including databases, quality improvement, and measuring interventions.
Q: What are the limitations in translating all of this knowledge to interventions for the patients who need it?
A: I think the research paradigm traditionally has been: We fund an investigator. They go off for years and do their research. And then they publish it in the New England Journal [of Medicine] or JAMA, and we call that a success.
I would argue that we’re at a time where we need to think about a new paradigm, where just publishing it is some middle step. And we need to think about how you actually link the research enterprise to the care delivery enterprise, so research is rapidly implemented and you’re measuring outcomes and ensuring that research actually reaches the patients and clinicians.
Q: Are there any real-world examples of how to do this?
A: Say we had a national patient library and we thought about things that we have not traditionally thought about in healthcare—social networking, Twitter, Facebook, media channels that reach people now. How do you insert health content into those channels to actually change people’s behavior, or at least inform them? The medical establishment thinks we publish it in the New England Journal [of Medicine] and the world changes. That’s just fundamentally not true.
On the provider side, how do we think about the lay media? How do we think about channels that providers use, like UpToDate and Medscape? How do we get comparative effectiveness content into those channels that are used by providers and physicians?
Q: How should CER address the needs of patient groups that are under-represented in traditional medical studies?
A: I think that’s a huge area. Efficacy trials generally will show something works for the average patient. But the issue is, and I’ll give you a concrete example, if you are an elderly, African-American female with a couple of conditions (diabetes and heart disease), how will that treatment work for you? So I think the power of comparative effectiveness is that we, especially with the data sources we just talked about, can look at patient subgroups and get as close as possible to the individual level to really present information. Instead of [saying], this works on average patients, which includes lots of patients that don’t look at all like you, [we can] say we’ve looked and it actually works well for racial and ethnic minorities, or persons with disabilities, or the very elderly.
Q: What do you hope ultimately will come from this report?
A: On the care delivery side, this is an opportunity for hospitalists to test different interventions to improve care in the hospitals. For what I hope to achieve, I think as we invest in all these individual programs, we are building in evaluation components to assess how this impacts patient outcomes.
I think the ultimate goal is to improve patient outcomes in this country, which I know is an unbelievably grand goal, but I think you build up to that by each investment. You track what it produces and ultimately how it affects outcomes, and so you at least start to build a sense of what this program means for the nation’s health. TH
Bryn Nelson is a freelance writer based in Seattle.
On June 30, a new government agency within the Department of Health and Human Services (HHS) called the Federal Coordinating Council for Comparative Effectiveness Research released its first report to President Obama and Congress. Authorized by the American Recovery and Reinvestment Act of 2009, the council is tasked with prioritizing and coordinating how multiple government agencies will spend the stimulus package’s $1.1 billion windfall for comparative effectiveness research (CER), which is aimed at improving healthcare outcomes in the U.S.
Of the funds, $400 million has been directed to the National Institutes of Health (NIH), $300 million to the Agency for Healthcare Research and Quality, and the remaining $400 million to the Office of the Secretary of Health and Human Services.
Patrick Conway, MD, MSc, the federal coordinating council’s executive director, is well versed in the potential impact of comparative effectiveness research on hospitalists. Just as Dr. Conway was joining the Center for Health Care Quality at Cincinnati Children’s Hospital after a fellowship at Children’s Hospital of Philadelphia, the pediatric hospitalist was named a 2007-2008 White House Fellow at HHS—the first hospitalist accepted into the program.

—Patrick Conway, MD, MSc, executive director, HHS’ Federal Coordinating Council for Comparative Effectiveness Research
In August 2008, he was tapped for the post of chief medical officer in the department’s Office of the Assistant Secretary for Planning and Evaluation.
Meanwhile, Dr. Conway still sees patients on weekends at Children’s National Medical Center in Washington, D.C. He recently talked with The Hospitalist about the challenges of coordinating research funding across multiple government agencies, how the Office of the Secretary’s $400 million allocation could be best spent, and what it all means for patient care.
Question: What are the biggest recommendations in the federal coordinating council’s report?
Answer: We approached this as “What unique role can the Office of the Secretary research funds address?” We identified data infrastructure as a potential primary investment. That includes things such as patient registries, distributed data networks, and claims databases.
Traditionally, the federal government has not invested in infrastructure because we have funded independent investigators on a one-question-by-one-question basis. The way I see this infusion of funds is it allows you to invest in data infrastructure that can then be used to answer literally hundreds of questions over time.
Secondly, we identified dissemination and translation, so how do we think about innovative ways to actually communicate directly to patients and physicians at the point of care? We also identified priority populations, including racial and ethnic minorities, persons with multiple chronic conditions, children, and the elderly. And lastly, we identified priority interventions, such as behavioral change, delivery systems, and prevention. So how do we decrease obesity, how do we decrease smoking rates?
Q: How will you address the challenge of coordinating research funding across multiple federal agencies?
A: I think the first step is doing the inventory [of CER], which is going to be an ongoing and iterative process. By doing that, then the council and the HHS have to attempt to avoid duplicating efforts and actually coordinate efforts across the federal government.
Honestly, I think the biggest challenge is these are extremely large, complex government programs. These are hundreds of millions of dollars going out to a huge variety of researchers, academic institutions, etc. One of the systems we’re trying to put in place is a better way to track what’s going on now, so we can actually coordinate going forward. It’s something as simple as we now have a common definition. We tag all money (e.g., CER), so we know exactly what we’re spending money on. That sounds really simple, but it’s actually never been done before. This is a relatively new area of emphasis for the federal government and for healthcare.
Q: What main point should hospitalists take away from this report?
A: This research will address primary questions about which medicine is best for which patient but also address larger issues, such as care coordination and how care is organized within the hospital and outside the hospital, so that we focus on the gamut of questions that have the potential to improve patient outcomes.
Q: What were some common themes you heard in the public listening sessions and online comments you solicited during the report’s preparation?
A: One of them was the importance of engaging stakeholders throughout the process, getting input from patients, physicians, policymakers. … We also heard themes about the need for infrastructure development, also the need for data infrastructure. We also heard a theme about the need for more work on research methodology and training of researchers. And then we heard a strong theme around “This needs to actually be disseminated and translated into care delivery.” So producing knowledge is helpful, but translating that knowledge into better outcomes is the ultimate goal.
Q: The report repeatedly mentions “real world” healthcare settings. Is this meant as a criticism of the idealized outcomes of efficacy research as it is typically conducted?
A: I don’t know that I would frame it as a criticism. I will say that as hospitalists, we are faced with patients every day where there’s unclear evidence about how best to manage that patient. And therefore, we need more evidence on the real questions that patients and physicians encounter in practice. I think we’ve had a long history of strong, well-funded randomized trials in this country, and I think we need to complement that with other methods of research as well, including databases, quality improvement, and measuring interventions.
Q: What are the limitations in translating all of this knowledge to interventions for the patients who need it?
A: I think the research paradigm traditionally has been: We fund an investigator. They go off for years and do their research. And then they publish it in the New England Journal [of Medicine] or JAMA, and we call that a success.
I would argue that we’re at a time where we need to think about a new paradigm, where just publishing it is some middle step. And we need to think about how you actually link the research enterprise to the care delivery enterprise, so research is rapidly implemented and you’re measuring outcomes and ensuring that research actually reaches the patients and clinicians.
Q: Are there any real-world examples of how to do this?
A: Say we had a national patient library and we thought about things that we have not traditionally thought about in healthcare—social networking, Twitter, Facebook, media channels that reach people now. How do you insert health content into those channels to actually change people’s behavior, or at least inform them? The medical establishment thinks we publish it in the New England Journal [of Medicine] and the world changes. That’s just fundamentally not true.
On the provider side, how do we think about the lay media? How do we think about channels that providers use, like UpToDate and Medscape? How do we get comparative effectiveness content into those channels that are used by providers and physicians?
Q: How should CER address the needs of patient groups that are under-represented in traditional medical studies?
A: I think that’s a huge area. Efficacy trials generally will show something works for the average patient. But the issue is, and I’ll give you a concrete example, if you are an elderly, African-American female with a couple of conditions (diabetes and heart disease), how will that treatment work for you? So I think the power of comparative effectiveness is that we, especially with the data sources we just talked about, can look at patient subgroups and get as close as possible to the individual level to really present information. Instead of [saying], this works on average patients, which includes lots of patients that don’t look at all like you, [we can] say we’ve looked and it actually works well for racial and ethnic minorities, or persons with disabilities, or the very elderly.
Q: What do you hope ultimately will come from this report?
A: On the care delivery side, this is an opportunity for hospitalists to test different interventions to improve care in the hospitals. For what I hope to achieve, I think as we invest in all these individual programs, we are building in evaluation components to assess how this impacts patient outcomes.
I think the ultimate goal is to improve patient outcomes in this country, which I know is an unbelievably grand goal, but I think you build up to that by each investment. You track what it produces and ultimately how it affects outcomes, and so you at least start to build a sense of what this program means for the nation’s health. TH
Bryn Nelson is a freelance writer based in Seattle.
The Downtime Dilemma
How do you spend your time off? Do you neglect your to-do list in favor of rest and relaxation, or do you race around trying to get everything done? How you use your free time affects your energy level and on-the-job enthusiasm. Hospitalists who learn to make the most of their time off reduce their stress and master the elusive work-life balance, and are more likely to avoid burnout. It’s especially true of physicians who work long hours followed by multiple days of downtime.
“I tell hospitalists … that they have to know what a sense of ‘work-life balance’ means to them,” says Iris Grimm, creator of the Balanced Physician program and founder of Marietta, Ga.-based Master Performance Inc. (www.balanced physician.com). Understanding what you need to lead a healthy, balanced life is crucial to your happiness and well-being on and off the job.
Hospitalists who work long shifts also face extended stretches of time off that are vital to recharging one’s batteries. “One of the challenges they have is to find a routine,” Grimm says. “As human beings, we prefer to have a daily routine, which is a benefit from a health standpoint. These people have different sleep patterns when they’re off, which can throw off their bodies, which in turn has an effect on health and well-being.”
—Chad Whelan, MD, FHM, assistant professor of medicine, University of Chicago
Plan to Cope
The allure of regular, extended time off—namely, the seven-day-on, seven-day-off schedule model—can factor heavily into a physician’s decision to choose an HM career. A full week off is ideal for some, but not so ideal for others.
Many think the seven-on, seven-off schedule increases the likelihood of physician burnout. Others think the exact opposite. No matter what, the “intense shift” model is not going away anytime soon, says Chad Whelan, MD, FHM, associate professor of medicine and director of the division of hospital medicine at Loyola University Chicago Stritch School of Medicine.
The first step in maximizing your personal time is to accept your schedule. “Whatever schedule you’re working, you’re going to be working when others are not,” Dr. Whelan says. “You have to recognize that, and you have to own it.”
Once you accept the fact that you’ll miss out on some activities—from dinner parties to your child’s Little League baseball games—that fall on your workdays, you can move on to a key component of maximizing your days off: the art of planning.
Planning your days off helps ensure that you don’t end up wasting them. “Your plan could include exercise, visiting with friends, and keeping up with CME,” Grimm says. Dr. Whelan agrees: “You have to do some active planning to schedule things that need to get done.” He knows from personal experience that “the mundane details are easy to drop; instead of grocery shopping, you end up ordering in. I find that if I schedule these things—even at a funky time like late at night—I’ll get them done.”
Planning works both ways. “Part of balance is using time in your off days to prepare for when you’ll be working,” Grimm says. For example, make sure you have food in your refrigerator so that you can have a healthy breakfast and occasionally prepare dinners in advance that you can quickly heat up after your shift.
Focusing your organizational skills and planning on personal “to-dos” will lighten the load of a long workday. “Automate as much as possible—such as paying bills,” Grimm advises, “and delegate what you can. The less you have to keep track of, the less stress you’ll feel and the more energy you’ll find to do what you’re paid to do.”
Time for Self
Physicians, especially those with families, need to remember to make time for themselves “so that you won’t build resentment toward others,” Grimm says. “Doing something for yourself refills your energy tank.” Whether it’s exercising, going fishing, volunteering at the community center, downloading photos from your digital camera, or reading a book, “it’s different for everyone,” Grimm points out. “You have to know what you need.”
Dr. Whelan—who is a runner—focuses on physical activity to relieve stress and re-energize his mind and body. “It’s hard, because people who are serious about exercise, however you define ‘serious,’ are told to exercise on a consistent schedule. Well, we don’t have consistent schedules,” he says. “The key is to recognize that this is a challenge and find a creative way to schedule it, just like we make other decisions creatively. You have to make an upfront commitment.”
Whatever you do to “refill your tank,” there’s a good reason to devote time to it. “The more we do for ourselves, the more we can do for others,” Grimm says. “It’s not an hour-to-hour ratio; you might just need a five-minute meditation at the end of the day. … I always challenge my clients to be aware of what gives them energy and what takes energy away from them. This is essential for work, and essential for life.”
Leave Work Behind
One of the hardest things to learn—a lesson left out of medical school texts—is how to leave the stress and responsibility of the job at the office. “These are intense jobs; they’re high-stress,” Dr. Whelan explains. “The good thing about being a hospitalist is that when you’re off, you’re off. But it’s important to be able to compartmentalize.”
Dr. Whelan learned a couple of simple strategies to help with this concept. “At the end of every work day, after you’ve signed off, dedicate some time to transition. It can be just 10 or 15 minutes. Don’t answer the phone or e-mail; just dedicate that time to transition,” he says. “Run through your day and process each part—whether that’s each patient or each administrative task—emotionally and intellectually. For each one, make a plan for what you’ll do tomorrow. Once you’ve worked through your day this way, you can allow yourself to let it go.”
He also advises hospitalists to use on-the-job time when it’s available, rather than overlapping work and personal time. “There are parts of your business that can be done when you’re not seeing patients, such as reading journals,” Dr. Whelan says. “Try to schedule those things into your [work day], so you don’t end up catching up on them at home.”
Find Your Balance
Make it a point to make the most of your time off. Plan it in advance to ensure you do what you need to do and what you want to do. Think creatively and include all types of activities. And be sure to include time for yourself.
“There are very few of us who can sustain a life made up entirely of work and still be happy,” Dr. Whelan says. “Eventually, you’ll start to resent the work, and that’s the stuff that leads to burnout. You’re also probably not doing as good a job.”
One final piece of advice: Be prepared to change.
“You need to be self-aware, and you need to realize that your definition of balance will shift with age, responsibility, and goals,” Grimm says. TH
Jane Jerrard is a freelance writer based in Chicago.
How do you spend your time off? Do you neglect your to-do list in favor of rest and relaxation, or do you race around trying to get everything done? How you use your free time affects your energy level and on-the-job enthusiasm. Hospitalists who learn to make the most of their time off reduce their stress and master the elusive work-life balance, and are more likely to avoid burnout. It’s especially true of physicians who work long hours followed by multiple days of downtime.
“I tell hospitalists … that they have to know what a sense of ‘work-life balance’ means to them,” says Iris Grimm, creator of the Balanced Physician program and founder of Marietta, Ga.-based Master Performance Inc. (www.balanced physician.com). Understanding what you need to lead a healthy, balanced life is crucial to your happiness and well-being on and off the job.
Hospitalists who work long shifts also face extended stretches of time off that are vital to recharging one’s batteries. “One of the challenges they have is to find a routine,” Grimm says. “As human beings, we prefer to have a daily routine, which is a benefit from a health standpoint. These people have different sleep patterns when they’re off, which can throw off their bodies, which in turn has an effect on health and well-being.”
—Chad Whelan, MD, FHM, assistant professor of medicine, University of Chicago
Plan to Cope
The allure of regular, extended time off—namely, the seven-day-on, seven-day-off schedule model—can factor heavily into a physician’s decision to choose an HM career. A full week off is ideal for some, but not so ideal for others.
Many think the seven-on, seven-off schedule increases the likelihood of physician burnout. Others think the exact opposite. No matter what, the “intense shift” model is not going away anytime soon, says Chad Whelan, MD, FHM, associate professor of medicine and director of the division of hospital medicine at Loyola University Chicago Stritch School of Medicine.
The first step in maximizing your personal time is to accept your schedule. “Whatever schedule you’re working, you’re going to be working when others are not,” Dr. Whelan says. “You have to recognize that, and you have to own it.”
Once you accept the fact that you’ll miss out on some activities—from dinner parties to your child’s Little League baseball games—that fall on your workdays, you can move on to a key component of maximizing your days off: the art of planning.
Planning your days off helps ensure that you don’t end up wasting them. “Your plan could include exercise, visiting with friends, and keeping up with CME,” Grimm says. Dr. Whelan agrees: “You have to do some active planning to schedule things that need to get done.” He knows from personal experience that “the mundane details are easy to drop; instead of grocery shopping, you end up ordering in. I find that if I schedule these things—even at a funky time like late at night—I’ll get them done.”
Planning works both ways. “Part of balance is using time in your off days to prepare for when you’ll be working,” Grimm says. For example, make sure you have food in your refrigerator so that you can have a healthy breakfast and occasionally prepare dinners in advance that you can quickly heat up after your shift.
Focusing your organizational skills and planning on personal “to-dos” will lighten the load of a long workday. “Automate as much as possible—such as paying bills,” Grimm advises, “and delegate what you can. The less you have to keep track of, the less stress you’ll feel and the more energy you’ll find to do what you’re paid to do.”
Time for Self
Physicians, especially those with families, need to remember to make time for themselves “so that you won’t build resentment toward others,” Grimm says. “Doing something for yourself refills your energy tank.” Whether it’s exercising, going fishing, volunteering at the community center, downloading photos from your digital camera, or reading a book, “it’s different for everyone,” Grimm points out. “You have to know what you need.”
Dr. Whelan—who is a runner—focuses on physical activity to relieve stress and re-energize his mind and body. “It’s hard, because people who are serious about exercise, however you define ‘serious,’ are told to exercise on a consistent schedule. Well, we don’t have consistent schedules,” he says. “The key is to recognize that this is a challenge and find a creative way to schedule it, just like we make other decisions creatively. You have to make an upfront commitment.”
Whatever you do to “refill your tank,” there’s a good reason to devote time to it. “The more we do for ourselves, the more we can do for others,” Grimm says. “It’s not an hour-to-hour ratio; you might just need a five-minute meditation at the end of the day. … I always challenge my clients to be aware of what gives them energy and what takes energy away from them. This is essential for work, and essential for life.”
Leave Work Behind
One of the hardest things to learn—a lesson left out of medical school texts—is how to leave the stress and responsibility of the job at the office. “These are intense jobs; they’re high-stress,” Dr. Whelan explains. “The good thing about being a hospitalist is that when you’re off, you’re off. But it’s important to be able to compartmentalize.”
Dr. Whelan learned a couple of simple strategies to help with this concept. “At the end of every work day, after you’ve signed off, dedicate some time to transition. It can be just 10 or 15 minutes. Don’t answer the phone or e-mail; just dedicate that time to transition,” he says. “Run through your day and process each part—whether that’s each patient or each administrative task—emotionally and intellectually. For each one, make a plan for what you’ll do tomorrow. Once you’ve worked through your day this way, you can allow yourself to let it go.”
He also advises hospitalists to use on-the-job time when it’s available, rather than overlapping work and personal time. “There are parts of your business that can be done when you’re not seeing patients, such as reading journals,” Dr. Whelan says. “Try to schedule those things into your [work day], so you don’t end up catching up on them at home.”
Find Your Balance
Make it a point to make the most of your time off. Plan it in advance to ensure you do what you need to do and what you want to do. Think creatively and include all types of activities. And be sure to include time for yourself.
“There are very few of us who can sustain a life made up entirely of work and still be happy,” Dr. Whelan says. “Eventually, you’ll start to resent the work, and that’s the stuff that leads to burnout. You’re also probably not doing as good a job.”
One final piece of advice: Be prepared to change.
“You need to be self-aware, and you need to realize that your definition of balance will shift with age, responsibility, and goals,” Grimm says. TH
Jane Jerrard is a freelance writer based in Chicago.
How do you spend your time off? Do you neglect your to-do list in favor of rest and relaxation, or do you race around trying to get everything done? How you use your free time affects your energy level and on-the-job enthusiasm. Hospitalists who learn to make the most of their time off reduce their stress and master the elusive work-life balance, and are more likely to avoid burnout. It’s especially true of physicians who work long hours followed by multiple days of downtime.
“I tell hospitalists … that they have to know what a sense of ‘work-life balance’ means to them,” says Iris Grimm, creator of the Balanced Physician program and founder of Marietta, Ga.-based Master Performance Inc. (www.balanced physician.com). Understanding what you need to lead a healthy, balanced life is crucial to your happiness and well-being on and off the job.
Hospitalists who work long shifts also face extended stretches of time off that are vital to recharging one’s batteries. “One of the challenges they have is to find a routine,” Grimm says. “As human beings, we prefer to have a daily routine, which is a benefit from a health standpoint. These people have different sleep patterns when they’re off, which can throw off their bodies, which in turn has an effect on health and well-being.”
—Chad Whelan, MD, FHM, assistant professor of medicine, University of Chicago
Plan to Cope
The allure of regular, extended time off—namely, the seven-day-on, seven-day-off schedule model—can factor heavily into a physician’s decision to choose an HM career. A full week off is ideal for some, but not so ideal for others.
Many think the seven-on, seven-off schedule increases the likelihood of physician burnout. Others think the exact opposite. No matter what, the “intense shift” model is not going away anytime soon, says Chad Whelan, MD, FHM, associate professor of medicine and director of the division of hospital medicine at Loyola University Chicago Stritch School of Medicine.
The first step in maximizing your personal time is to accept your schedule. “Whatever schedule you’re working, you’re going to be working when others are not,” Dr. Whelan says. “You have to recognize that, and you have to own it.”
Once you accept the fact that you’ll miss out on some activities—from dinner parties to your child’s Little League baseball games—that fall on your workdays, you can move on to a key component of maximizing your days off: the art of planning.
Planning your days off helps ensure that you don’t end up wasting them. “Your plan could include exercise, visiting with friends, and keeping up with CME,” Grimm says. Dr. Whelan agrees: “You have to do some active planning to schedule things that need to get done.” He knows from personal experience that “the mundane details are easy to drop; instead of grocery shopping, you end up ordering in. I find that if I schedule these things—even at a funky time like late at night—I’ll get them done.”
Planning works both ways. “Part of balance is using time in your off days to prepare for when you’ll be working,” Grimm says. For example, make sure you have food in your refrigerator so that you can have a healthy breakfast and occasionally prepare dinners in advance that you can quickly heat up after your shift.
Focusing your organizational skills and planning on personal “to-dos” will lighten the load of a long workday. “Automate as much as possible—such as paying bills,” Grimm advises, “and delegate what you can. The less you have to keep track of, the less stress you’ll feel and the more energy you’ll find to do what you’re paid to do.”
Time for Self
Physicians, especially those with families, need to remember to make time for themselves “so that you won’t build resentment toward others,” Grimm says. “Doing something for yourself refills your energy tank.” Whether it’s exercising, going fishing, volunteering at the community center, downloading photos from your digital camera, or reading a book, “it’s different for everyone,” Grimm points out. “You have to know what you need.”
Dr. Whelan—who is a runner—focuses on physical activity to relieve stress and re-energize his mind and body. “It’s hard, because people who are serious about exercise, however you define ‘serious,’ are told to exercise on a consistent schedule. Well, we don’t have consistent schedules,” he says. “The key is to recognize that this is a challenge and find a creative way to schedule it, just like we make other decisions creatively. You have to make an upfront commitment.”
Whatever you do to “refill your tank,” there’s a good reason to devote time to it. “The more we do for ourselves, the more we can do for others,” Grimm says. “It’s not an hour-to-hour ratio; you might just need a five-minute meditation at the end of the day. … I always challenge my clients to be aware of what gives them energy and what takes energy away from them. This is essential for work, and essential for life.”
Leave Work Behind
One of the hardest things to learn—a lesson left out of medical school texts—is how to leave the stress and responsibility of the job at the office. “These are intense jobs; they’re high-stress,” Dr. Whelan explains. “The good thing about being a hospitalist is that when you’re off, you’re off. But it’s important to be able to compartmentalize.”
Dr. Whelan learned a couple of simple strategies to help with this concept. “At the end of every work day, after you’ve signed off, dedicate some time to transition. It can be just 10 or 15 minutes. Don’t answer the phone or e-mail; just dedicate that time to transition,” he says. “Run through your day and process each part—whether that’s each patient or each administrative task—emotionally and intellectually. For each one, make a plan for what you’ll do tomorrow. Once you’ve worked through your day this way, you can allow yourself to let it go.”
He also advises hospitalists to use on-the-job time when it’s available, rather than overlapping work and personal time. “There are parts of your business that can be done when you’re not seeing patients, such as reading journals,” Dr. Whelan says. “Try to schedule those things into your [work day], so you don’t end up catching up on them at home.”
Find Your Balance
Make it a point to make the most of your time off. Plan it in advance to ensure you do what you need to do and what you want to do. Think creatively and include all types of activities. And be sure to include time for yourself.
“There are very few of us who can sustain a life made up entirely of work and still be happy,” Dr. Whelan says. “Eventually, you’ll start to resent the work, and that’s the stuff that leads to burnout. You’re also probably not doing as good a job.”
One final piece of advice: Be prepared to change.
“You need to be self-aware, and you need to realize that your definition of balance will shift with age, responsibility, and goals,” Grimm says. TH
Jane Jerrard is a freelance writer based in Chicago.
Simulation Sensation
To Jeffrey Barsuk, MD, FACP, FHM, the concept of simulation-based mastery learning is simplistic to the point of genius. Give a hospitalist—or any other physician—a physical task and let them practice the procedure until they master it. Take care not to fall into the decades-old mind-set that repetition alone will achieve a threshold of competence. Test the competence with a rigorous assessment schedule, which will objectively determine if the skill is truly mastered.
It’s standard operating procedure in many technical fields, such as engineering, computer programming, and aviation. For example, professional pilots undergo countless hours of simulation flying to freshen and further hone the skills they need to succeed in an airplane cockpit. But with tasks as menial as central venous catheter (CVC) insertions, the typical practice most young physicians get is the trial and error of needle passes.
More training, Dr. Barsuk argues, would make everyone involved better off—from the resident nervously seeking a line to the patient who wants the procedure completed as quickly and painlessly as possible.
“It’s very common sense,” says Dr. Barsuk, assistant professor of medicine in the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago. “But no one is doing this. People don’t know that simulators are so effective. At least in the medical profession, we’re probably behind the times in it. … We’re enthusiastic about it because we believe in it so much. We want to see how far it can go. With mastery learning, the sky’s the limit. You can simulate almost anything you want.”
Dr. Barsuk and his colleagues have worked hard to translate “common sense” into empirical literature. Accordingly, the team will publish their latest work, “Use of Simulation-Based Mastery Learning to Improve the Quality of Central Venous Catheter Placement in a Medical Intensive Care Unit,” in September’s Journal of Hospital Medicine. The single-institution cohort study found simulation-based mastery learning increased internal-medicine residents’ skills in simulated CVC insertions, decreased the number of needle passes when performing actual procedures, and increased resident self-confidence.
“It’s always been assumed that experience in and of itself is a proxy for competence,” says William McGaghie, PhD, professor of medical education and preventive medicine at Feinberg, as well as director of evaluation for Northwestern University’s Clinical and Translational Science Institute (NUCATS). “We now know that is not the case … if skill acquisition is the goal. Experience on the wards isn’t enough. We have to have deliberate education interventions to practice in controlled, safe environments.”

—Jeffrey Barsuk, MD, FACP, FHM, Feinberg School of Medicine, Northwestern University, Chicago
The Northwestern study put that theory to the test. It aimed to expand mastery learning to a new skill set and assess quality indicators (number of needle passes, arterial punctures, etc.) and resident confidence before and after training modules. The team studied 41 second- and third-year residents rotating through the medical intensive-care unit (MICU) from October 2006 to February 2007. The university’s Institutional Review Board approved the study, and all of the participants gave informed consent prior to participating. Thirteen of the residents rotated through during a six-week pre-intervention phase, serving as the “traditionally-trained group,” the authors wrote. Twenty-eight residents were trained on Simulab’s CentralLineMan, a model with “ultrasound compatibility, an arterial pulse, and self-sealing veins and skins. Needles, dilators and guidewires can be inserted and realistic venous and arterial pressures demonstrated,” the authors wrote.
The residents who were trained for internal jugular (IJ) and subclavian (SC) CVC insertions received two two-hour education sessions consisting of a lecture, ultrasound training, deliberate practice, and feedback. A 27-item checklist was drafted to measure outcomes; all pre- and post-tests were graded by a single unblended instructor to ensure accuracy. According to the study:
- None of the residents met the minimum passing score (MPS) of 79.1% for CVC insertion at baseline: mean IJ=48.4%, standard deviation=23.1; mean SC=45.2%, standard deviation=26.3;
- All residents met or exceeded the MPS at testing after simulation training: mean IJ=94.8%, standard deviation=10.0; mean SC=91.1%, standard deviation=17.8 (P<0.001);
- In the MICU, simulator-trained residents required fewer needle passes to insert a CVC than traditionally trained residents: mean=1.79, standard deviation=1.0 vs. mean=2.78, standard deviation=1.77 (P=0.04);
- Simulator-trained residents displayed more self-confidence about their procedural skills: mean=81, standard deviation=11 vs. mean=68, standard deviation=20 (P=0.02).
Dr. Barsuk isn’t surprised that confidence increases with training, saying “they hammer this home.” There were several categories for which the authors found no major improvement, though, even with the addition of deliberate training and standardized didactic materials.
Notably, the authors wrote, the resident groups “did not differ in pneumothorax, arterial puncture, or mean number of CVC adjustments.” Some of the lack of disparity was attributed to the small sample size.
In interviews, the authors noted that additional study would help assess such clinical outcomes as reduced CVC-related infections after simulation-based training. Still, Dr. Barsuk says, this pilot report is an important first step to win over skeptics.
“Simulation-based training and deliberate practice in a mastery learning setting improves performance of both simulated and actual CVC insertions by internal medicine residents,” the study reads. “Procedural training remains an important component of internal medicine training although internists are performing fewer invasive procedures now than in years past. Use of a mastery model of CVC insertion requires that trainees demonstrate skill in a simulated environment before independently performing this invasive procedure on patients.”
Another advantage of the training, McGaghie says, is that it helps physicians track their own improvement. He cautions against administrators using the data for more nefarious purposes, lest the testing become unpopular and less useful to quality improvement programs.
“You don’t use these evaluations as a weapon; you use them as a tool,” McGaghie says. “No one is there to beat up the doctors; no one is there to make them look foolish. The whole idea is to be as rigorous as possible to look for improvement—constant improvement.” TH
Richard Quinn is a freelance writer based in New Jersey.
To Jeffrey Barsuk, MD, FACP, FHM, the concept of simulation-based mastery learning is simplistic to the point of genius. Give a hospitalist—or any other physician—a physical task and let them practice the procedure until they master it. Take care not to fall into the decades-old mind-set that repetition alone will achieve a threshold of competence. Test the competence with a rigorous assessment schedule, which will objectively determine if the skill is truly mastered.
It’s standard operating procedure in many technical fields, such as engineering, computer programming, and aviation. For example, professional pilots undergo countless hours of simulation flying to freshen and further hone the skills they need to succeed in an airplane cockpit. But with tasks as menial as central venous catheter (CVC) insertions, the typical practice most young physicians get is the trial and error of needle passes.
More training, Dr. Barsuk argues, would make everyone involved better off—from the resident nervously seeking a line to the patient who wants the procedure completed as quickly and painlessly as possible.
“It’s very common sense,” says Dr. Barsuk, assistant professor of medicine in the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago. “But no one is doing this. People don’t know that simulators are so effective. At least in the medical profession, we’re probably behind the times in it. … We’re enthusiastic about it because we believe in it so much. We want to see how far it can go. With mastery learning, the sky’s the limit. You can simulate almost anything you want.”
Dr. Barsuk and his colleagues have worked hard to translate “common sense” into empirical literature. Accordingly, the team will publish their latest work, “Use of Simulation-Based Mastery Learning to Improve the Quality of Central Venous Catheter Placement in a Medical Intensive Care Unit,” in September’s Journal of Hospital Medicine. The single-institution cohort study found simulation-based mastery learning increased internal-medicine residents’ skills in simulated CVC insertions, decreased the number of needle passes when performing actual procedures, and increased resident self-confidence.
“It’s always been assumed that experience in and of itself is a proxy for competence,” says William McGaghie, PhD, professor of medical education and preventive medicine at Feinberg, as well as director of evaluation for Northwestern University’s Clinical and Translational Science Institute (NUCATS). “We now know that is not the case … if skill acquisition is the goal. Experience on the wards isn’t enough. We have to have deliberate education interventions to practice in controlled, safe environments.”

—Jeffrey Barsuk, MD, FACP, FHM, Feinberg School of Medicine, Northwestern University, Chicago
The Northwestern study put that theory to the test. It aimed to expand mastery learning to a new skill set and assess quality indicators (number of needle passes, arterial punctures, etc.) and resident confidence before and after training modules. The team studied 41 second- and third-year residents rotating through the medical intensive-care unit (MICU) from October 2006 to February 2007. The university’s Institutional Review Board approved the study, and all of the participants gave informed consent prior to participating. Thirteen of the residents rotated through during a six-week pre-intervention phase, serving as the “traditionally-trained group,” the authors wrote. Twenty-eight residents were trained on Simulab’s CentralLineMan, a model with “ultrasound compatibility, an arterial pulse, and self-sealing veins and skins. Needles, dilators and guidewires can be inserted and realistic venous and arterial pressures demonstrated,” the authors wrote.
The residents who were trained for internal jugular (IJ) and subclavian (SC) CVC insertions received two two-hour education sessions consisting of a lecture, ultrasound training, deliberate practice, and feedback. A 27-item checklist was drafted to measure outcomes; all pre- and post-tests were graded by a single unblended instructor to ensure accuracy. According to the study:
- None of the residents met the minimum passing score (MPS) of 79.1% for CVC insertion at baseline: mean IJ=48.4%, standard deviation=23.1; mean SC=45.2%, standard deviation=26.3;
- All residents met or exceeded the MPS at testing after simulation training: mean IJ=94.8%, standard deviation=10.0; mean SC=91.1%, standard deviation=17.8 (P<0.001);
- In the MICU, simulator-trained residents required fewer needle passes to insert a CVC than traditionally trained residents: mean=1.79, standard deviation=1.0 vs. mean=2.78, standard deviation=1.77 (P=0.04);
- Simulator-trained residents displayed more self-confidence about their procedural skills: mean=81, standard deviation=11 vs. mean=68, standard deviation=20 (P=0.02).
Dr. Barsuk isn’t surprised that confidence increases with training, saying “they hammer this home.” There were several categories for which the authors found no major improvement, though, even with the addition of deliberate training and standardized didactic materials.
Notably, the authors wrote, the resident groups “did not differ in pneumothorax, arterial puncture, or mean number of CVC adjustments.” Some of the lack of disparity was attributed to the small sample size.
In interviews, the authors noted that additional study would help assess such clinical outcomes as reduced CVC-related infections after simulation-based training. Still, Dr. Barsuk says, this pilot report is an important first step to win over skeptics.
“Simulation-based training and deliberate practice in a mastery learning setting improves performance of both simulated and actual CVC insertions by internal medicine residents,” the study reads. “Procedural training remains an important component of internal medicine training although internists are performing fewer invasive procedures now than in years past. Use of a mastery model of CVC insertion requires that trainees demonstrate skill in a simulated environment before independently performing this invasive procedure on patients.”
Another advantage of the training, McGaghie says, is that it helps physicians track their own improvement. He cautions against administrators using the data for more nefarious purposes, lest the testing become unpopular and less useful to quality improvement programs.
“You don’t use these evaluations as a weapon; you use them as a tool,” McGaghie says. “No one is there to beat up the doctors; no one is there to make them look foolish. The whole idea is to be as rigorous as possible to look for improvement—constant improvement.” TH
Richard Quinn is a freelance writer based in New Jersey.
To Jeffrey Barsuk, MD, FACP, FHM, the concept of simulation-based mastery learning is simplistic to the point of genius. Give a hospitalist—or any other physician—a physical task and let them practice the procedure until they master it. Take care not to fall into the decades-old mind-set that repetition alone will achieve a threshold of competence. Test the competence with a rigorous assessment schedule, which will objectively determine if the skill is truly mastered.
It’s standard operating procedure in many technical fields, such as engineering, computer programming, and aviation. For example, professional pilots undergo countless hours of simulation flying to freshen and further hone the skills they need to succeed in an airplane cockpit. But with tasks as menial as central venous catheter (CVC) insertions, the typical practice most young physicians get is the trial and error of needle passes.
More training, Dr. Barsuk argues, would make everyone involved better off—from the resident nervously seeking a line to the patient who wants the procedure completed as quickly and painlessly as possible.
“It’s very common sense,” says Dr. Barsuk, assistant professor of medicine in the division of hospital medicine at Northwestern University’s Feinberg School of Medicine in Chicago. “But no one is doing this. People don’t know that simulators are so effective. At least in the medical profession, we’re probably behind the times in it. … We’re enthusiastic about it because we believe in it so much. We want to see how far it can go. With mastery learning, the sky’s the limit. You can simulate almost anything you want.”
Dr. Barsuk and his colleagues have worked hard to translate “common sense” into empirical literature. Accordingly, the team will publish their latest work, “Use of Simulation-Based Mastery Learning to Improve the Quality of Central Venous Catheter Placement in a Medical Intensive Care Unit,” in September’s Journal of Hospital Medicine. The single-institution cohort study found simulation-based mastery learning increased internal-medicine residents’ skills in simulated CVC insertions, decreased the number of needle passes when performing actual procedures, and increased resident self-confidence.
“It’s always been assumed that experience in and of itself is a proxy for competence,” says William McGaghie, PhD, professor of medical education and preventive medicine at Feinberg, as well as director of evaluation for Northwestern University’s Clinical and Translational Science Institute (NUCATS). “We now know that is not the case … if skill acquisition is the goal. Experience on the wards isn’t enough. We have to have deliberate education interventions to practice in controlled, safe environments.”

—Jeffrey Barsuk, MD, FACP, FHM, Feinberg School of Medicine, Northwestern University, Chicago
The Northwestern study put that theory to the test. It aimed to expand mastery learning to a new skill set and assess quality indicators (number of needle passes, arterial punctures, etc.) and resident confidence before and after training modules. The team studied 41 second- and third-year residents rotating through the medical intensive-care unit (MICU) from October 2006 to February 2007. The university’s Institutional Review Board approved the study, and all of the participants gave informed consent prior to participating. Thirteen of the residents rotated through during a six-week pre-intervention phase, serving as the “traditionally-trained group,” the authors wrote. Twenty-eight residents were trained on Simulab’s CentralLineMan, a model with “ultrasound compatibility, an arterial pulse, and self-sealing veins and skins. Needles, dilators and guidewires can be inserted and realistic venous and arterial pressures demonstrated,” the authors wrote.
The residents who were trained for internal jugular (IJ) and subclavian (SC) CVC insertions received two two-hour education sessions consisting of a lecture, ultrasound training, deliberate practice, and feedback. A 27-item checklist was drafted to measure outcomes; all pre- and post-tests were graded by a single unblended instructor to ensure accuracy. According to the study:
- None of the residents met the minimum passing score (MPS) of 79.1% for CVC insertion at baseline: mean IJ=48.4%, standard deviation=23.1; mean SC=45.2%, standard deviation=26.3;
- All residents met or exceeded the MPS at testing after simulation training: mean IJ=94.8%, standard deviation=10.0; mean SC=91.1%, standard deviation=17.8 (P<0.001);
- In the MICU, simulator-trained residents required fewer needle passes to insert a CVC than traditionally trained residents: mean=1.79, standard deviation=1.0 vs. mean=2.78, standard deviation=1.77 (P=0.04);
- Simulator-trained residents displayed more self-confidence about their procedural skills: mean=81, standard deviation=11 vs. mean=68, standard deviation=20 (P=0.02).
Dr. Barsuk isn’t surprised that confidence increases with training, saying “they hammer this home.” There were several categories for which the authors found no major improvement, though, even with the addition of deliberate training and standardized didactic materials.
Notably, the authors wrote, the resident groups “did not differ in pneumothorax, arterial puncture, or mean number of CVC adjustments.” Some of the lack of disparity was attributed to the small sample size.
In interviews, the authors noted that additional study would help assess such clinical outcomes as reduced CVC-related infections after simulation-based training. Still, Dr. Barsuk says, this pilot report is an important first step to win over skeptics.
“Simulation-based training and deliberate practice in a mastery learning setting improves performance of both simulated and actual CVC insertions by internal medicine residents,” the study reads. “Procedural training remains an important component of internal medicine training although internists are performing fewer invasive procedures now than in years past. Use of a mastery model of CVC insertion requires that trainees demonstrate skill in a simulated environment before independently performing this invasive procedure on patients.”
Another advantage of the training, McGaghie says, is that it helps physicians track their own improvement. He cautions against administrators using the data for more nefarious purposes, lest the testing become unpopular and less useful to quality improvement programs.
“You don’t use these evaluations as a weapon; you use them as a tool,” McGaghie says. “No one is there to beat up the doctors; no one is there to make them look foolish. The whole idea is to be as rigorous as possible to look for improvement—constant improvement.” TH
Richard Quinn is a freelance writer based in New Jersey.
In the Literature
In This Edition
- Pharmacists and readmission rates.
- Geriatric discharge bundles and readmission rates.
- Medication reconciliation and risk of adverse drug events.
- End-of-life discussions and care outcomes.
- Effect of case management and housing for homeless adults.
- IV esomeprazole in bleeding ulcers.
- Causes of discharge delays.
- Methods to reduce ICU medication errors.
Addition of Pharmacists to Inpatient Teams Reduces Drug-Related Readmissions, Morbidity, and Costs for Elderly Patients
Clinical question: Would a ward-based pharmacist reduce morbidity, subsequent ED visits, and readmissions for elderly patients?
Background: Adverse drug events can cause significant drug-related morbidity and mortality, and lead to unnecessary healthcare costs. Elderly patients are more vulnerable to these effects given the polypharmacy often associated with their care. The effectiveness of a ward-based pharmacist intervention for elderly patients has not yet been studied.
Study design: Randomized controlled trial.
Setting: Two acute-care, internal-medicine wards at the University Hospital of Uppsala in Uppsala, Sweden.
Synopsis: Three hundred sixty-eight hospitalized patients ages 80 or older were randomized to control or intervention groups. The latter received enhanced services from a pharmacist who was integrated into the inpatient team. This individual performed medication reconciliation, reviewed the medication list, and advised the treating physician. The pharmacist educated and monitored patients during the hospitalization, counseled them at discharge, communicated pertinent medication information to the primary-care physicians (PCPs), and called the patients two months after discharge.
The primary outcome measure was the frequency of all hospital visits (ED visits plus hospital readmissions) during 12-month follow-up. The secondary outcome measure was the cost of hospital care.
The intervention group had a 16% reduction in all hospital visits and a 47% reduction in ED visits. There were five times as many drug-related readmissions in the control group compared with the intervention group, but the study did not have enough power to show a reduction in the total number of readmissions alone. The cost of hospital care minus the cost of the intervention resulted in a net savings of $230 per patient.
Bottom line: For elderly patients, adding a pharmacist to the inpatient team could lead to significant reductions in morbidity and, on a population basis, healthcare costs.
Citation: Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
Geriatric Care Coordination at Discharge Reduces Readmission Rates at 30 Days
Clinical question: Does a discharge planning service package affect readmission rates and ED visits?
Background: Elderly patients are at high risk for readmission after a hospitalization. Coordinated care packages, although effective in congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) management, have yielded inconsistent results in terms of decreasing readmission rates for patients with a broader range of medical issues.
Study design: Randomized controlled pilot study.
Setting: A single large academic medical center in Texas.
Synopsis: Forty-one elderly patients at high risk for readmission—because of their age and comorbidities—were enrolled within 72 hours of admission. Patients randomized to the care bundle arm received daily education about medication reconciliation, health conditions, and self-care provided by study pharmacists and nurses. The intervention required approximately 40 minutes per day: 20 to 25 minutes for the care coordinators and 20 minutes for the pharmacists. A post-discharge phone call to review medication and confirm follow-up instructions was included.
Eight patients in the control group and two patients in the intervention arm were readmitted or seen in the ED within 30 days after discharge (38% vs. 10%, P=0.004). At 60 days, the difference between the two groups was no longer significant. The intervention group had a longer time interval before its first readmission (36.2 days vs. 15.7 days). The sample was too small to determine the effect on length of hospitalization.
Limitations of the study include its small sample size and unclear costs of the intervention.
Bottom line: Geriatric discharge bundles might decrease readmission and ED visits after discharge, but larger studies are needed to confirm this finding.
Citation: Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day post-discharge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Computer-Assisted Medication Reconciliation Might Reduce Unintentional Drug Discrepancies with Potential for Harm
Clinical question: Does a computerized medication reconciliation intervention reduce unintentional medication discrepancies?
Background: Given the high prevalence of unintentional medication discrepancies in hospitalized patients and the potential for harm, medication reconciliation is a national patient safety goal. Little data exist on the efficacy of medication reconciliation interventions for reducing medication discrepancies.
Study design: Cluster-randomized controlled trial.
Setting: Two large academic hospitals in Boston.
Synopsis: Using 14 medical teams, the study enrolled and randomized 322 patients to a floor with intervention or to a floor with traditional care. The intervention teams utilized a computerized order entry application designed to facilitate medication reconciliation, as well as a process redesign for physicians, nurses, and pharmacists.
The primary outcome was the number of unintentional medication discrepancies with the potential for causing harm (PADEs) per patient.
Patients randomized to the intervention group had a 28% reduction in relative risk compared with the control group (1.05 PADEs vs. 1.44 PADEs; absolute relative risk 0.72 (0.52-0.99)). The absolute relative risk reduction between the two arms was 0.39 PADE per patient (NNT=2.6). The intervention was associated with a significant reduction in PADEs at discharge but not at admission. The effects of the intervention were greater in patients with a higher PADE score.
Bottom line: This computerized medication reconciliation program with process redesign was associated with reduced risk of unintentional medication discrepancies with potential for causing harms (PADEs).
Citation: Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169(8):771-780.
End-of-Life Discussions Associated with Lower Healthcare Costs
Clinical question: What is the impact of patient-physician discussions of end-of-life care on healthcare costs in the final week of a patient’s life?
Background: Life-sustaining medical care of patients with advanced cancer is costly, with disproportionate spending at the end of a patient’s life. The link between discussions of end-of-life care preferences and healthcare expenditure has not been studied thoroughly.
Study design: Prospective observational study.
Setting: Seven sites in Connecticut, Texas, New Hampshire, and Massachusetts.
Synopsis: More than 600 patients with advanced cancer were recruited from September 2002 through December 2007 as part of the Coping With Cancer study. The 188 patients (31%) who reported end-of-life discussions with their physicians at baseline were less likely to undergo mechanical ventilator use or resuscitation, or to be admitted or die in an intensive-care unit in the final week of life. They were more likely to receive outpatient hospice care and had less physical distress in the last week than those who did not.
The mean aggregate cost of care in this group was $1,876, which was 36% lower than in the group that did not discuss end-of-life care ($2,917), P=0.002. In addition, higher medical costs were associated with worse quality of death, as reported by caregivers.
This study is limited by its observational design.
Bottom line: Physician communication with patients regarding end-of-life care preferences is associated with lower costs in the final week of life.
Citation: Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480-488.
Reduction of ED Visits and Hospitalizations for Chronically Ill and Homeless Adults
Clinical question: Can a case management and housing program reduce the utilization of ED and hospital medical services among chronically ill homeless adults?
Background: Homeless adults have high rates of chronic illness, have poor access to uninterrupted primary healthcare, and frequently use costly medical services, including those provided by EDs and inpatient hospitalizations. Studies to determine the efficacy of housing and case management services in reducing hospital and ED utilization in this population are lacking.
Study design: Randomized controlled trial.
Setting: A public teaching hospital and a private nonprofit hospital in Chicago.
Synopsis: Four hundred seven chronically ill and homeless adults were randomized to receive a case management and housing intervention or traditional care following an index hospitalization. The intervention group received assistance with stable housing on discharge and biweekly case management services throughout the study period. Traditional care consisted of routine inpatient discharge planning and transportation to a shelter.
Patients were followed for 18 months for the primary outcomes: number of hospitalizations, total hospital days, and number of ED visits.
After adjusting for differences in baseline variables, the intervention group was found to have significantly lower rates of hospitalization (relative reduction 29%), total hospital days (29%), and ED visits (24%). The authors did not find a difference in mortality or quality of life between the two groups.
Limitations of this study include a small sample size, limited geographic distribution of subjects, and the lack of a cost-benefit analysis of the intervention.
Bottom line: Case management and housing interventions can decrease hospitalizations and ED visits among chronically ill homeless adults.
Citation: Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771-1778.
Intravenous Esomeprazole Reduces Recurrent Bleeding from Peptic Ulcers
Clinical question: Does intravenous esomeprazole prevent recurrent peptic ulcer bleeding, compared with placebo?
Background: U.S. hospitals admit more than 300,000 patients per year for peptic ulcer bleeding. Asian studies of proton pump inhibitors have demonstrated improved outcomes in patients with bleeding caused by peptic ulcers, but these results have not been consistently replicated in studies in Western Europe or North America.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Ninety-one hospital EDs in 16 countries.
Synopsis: The study team randomized 764 adult patients with a single bleeding gastric or duodenal ulcer after successful endoscopic hemostasis. The study group received esomeprazole (80 mg bolus, given intravenously over 30 minutes, followed by an 8 mg/hour infusion for 71.5 hours). The second group received placebo. Each group subsequently received 40 mg/day of oral esomeprazole for 27 days.
Recurrent bleeding within 72 hours was reduced by nearly half in the intravenous esomeprazole arm compared with placebo (5.9% vs. 10.3%, P=0.026). This remained significant at seven and 30 days. Intravenous esomeprazole also reduced endoscopic retreatment (6.4% vs. 11.6%; P=0.012) and demonstrated a trend toward reduction in surgery (2.7% vs. 5.4%) and all-cause mortality (0.8% vs. 2.1%).
Study limitations included a lack of standardization of endoscopic therapy across institutions.
Bottom line: Given after endoscopic hemostatis, intravenous esomeprazole followed by oral esomeprazole reduced recurrent bleeding in patients with a single duodenal or gastric ulcer.
Citation: Sung JJ, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2009;150(7):455-464.
Discharge Time and Duration Affected by Several Factors During Hospitalization
Clinical question: What are the factors affecting late and long discharges in a general medical unit?
Background: The mismatch between admission and discharge times is a problem for many hospitals; admissions occur early in the day whereas, discharges occur later in the day. The reasons behind delays in discharge and prolongation of discharges are not fully understood.
Study design: Prospective cohort study.
Setting: A general medical unit without house staff coverage at an academic medical center in Baltimore.
Synopsis: Care providers completed surveys on 201 consecutive discharges from January to April 2005. Outcome variables included time of discharge and discharge duration.
Mean discharge time was 3:09 p.m. Delay in discharge was associated with a need for ambulance transportation (1.5 hours), need for prescriptions to be filled at the hospital (1.4 hours), and for patients whose final test was a procedure (1.2 hours) or consult (1.1 hours).
Median discharge time was 7.6 hours. Longer discharge duration was associated with discharge to a location other than home (28.9 hours), need for consultation (14.8 hours), or need for a procedure (13.4 hours) before discharge.
African-American race, gender, age, and comorbid psychiatric and substance abuse disorders were not associated with either late or prolonged discharges.
Bottom line: Final-day tests, procedures, and consults, as well as complex discharge arrangements, prolong and delay discharges more than the characteristics of patients themselves.
Citation: Chen LM, Freitag MH, Franco M, Sullivan CD, Dickson C, Brancati FL. Natural history of late discharges from a general medical ward. J Hosp Med. 2009;4(4):226-233.
Administration of Parenteral Medication a Common Point at Which Errors Occur in ICUs
Clinical question: To what extent are medication administration errors a problem across ICUs, and what are some ways to prevent them?
Background: High-acuity and complex systems increase the likelihood of medical errors in ICUs. The first multinational Sentinel Events Evaluation study reported an ICU medication error rate of 10.5 per 100 patient days at the prescription and administration stages of medication delivery.
Study design: Multinational observational, prospective, cross-sectional study.
Setting: One hundred thirteen ICUs in 27 countries on five continents.
Synopsis: This study addressed five types of medication error at the administration stage in the ICU in a 24-hour timeframe: wrong drug, wrong dose, wrong route, wrong time, and missed medication. The main outcome measures were the number and impact of administration errors, the distribution of error characteristics, and the distribution of contributing and preventive factors.
In the 1,328 critically ill patients included in the study, 861 medication errors were reported by structured questionnaire; 441 patients were affected by the errors. The prevalence was 74.5 errors per 100 patient days, and 12 patients (0.9%) suffered permanent harm or death. Most medication administration errors occurred during routine care, not during extraordinary situations. Most were omission errors.
This study is limited by its observational design and by the fact that self-reporting also carries the risk of under-reporting.
This study points out several ways to reduce medication errors. An independent predictor of decreased risk of medication errors of all types is an established incident reporting system. Routine checking of infusion pumps at every nursing shift change also reduced this risk.
Bottom line: This study confirmed that the administration of parenteral medications is a vulnerable point across many ICUs, and incident reporting systems and routine checks of infusion pumps are effective ways to reduce the risk of this type of error.
Citation: Valentin A, Capuzzo M, Guidet B, et al. Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ. 2009;338:b814. TH
In This Edition
- Pharmacists and readmission rates.
- Geriatric discharge bundles and readmission rates.
- Medication reconciliation and risk of adverse drug events.
- End-of-life discussions and care outcomes.
- Effect of case management and housing for homeless adults.
- IV esomeprazole in bleeding ulcers.
- Causes of discharge delays.
- Methods to reduce ICU medication errors.
Addition of Pharmacists to Inpatient Teams Reduces Drug-Related Readmissions, Morbidity, and Costs for Elderly Patients
Clinical question: Would a ward-based pharmacist reduce morbidity, subsequent ED visits, and readmissions for elderly patients?
Background: Adverse drug events can cause significant drug-related morbidity and mortality, and lead to unnecessary healthcare costs. Elderly patients are more vulnerable to these effects given the polypharmacy often associated with their care. The effectiveness of a ward-based pharmacist intervention for elderly patients has not yet been studied.
Study design: Randomized controlled trial.
Setting: Two acute-care, internal-medicine wards at the University Hospital of Uppsala in Uppsala, Sweden.
Synopsis: Three hundred sixty-eight hospitalized patients ages 80 or older were randomized to control or intervention groups. The latter received enhanced services from a pharmacist who was integrated into the inpatient team. This individual performed medication reconciliation, reviewed the medication list, and advised the treating physician. The pharmacist educated and monitored patients during the hospitalization, counseled them at discharge, communicated pertinent medication information to the primary-care physicians (PCPs), and called the patients two months after discharge.
The primary outcome measure was the frequency of all hospital visits (ED visits plus hospital readmissions) during 12-month follow-up. The secondary outcome measure was the cost of hospital care.
The intervention group had a 16% reduction in all hospital visits and a 47% reduction in ED visits. There were five times as many drug-related readmissions in the control group compared with the intervention group, but the study did not have enough power to show a reduction in the total number of readmissions alone. The cost of hospital care minus the cost of the intervention resulted in a net savings of $230 per patient.
Bottom line: For elderly patients, adding a pharmacist to the inpatient team could lead to significant reductions in morbidity and, on a population basis, healthcare costs.
Citation: Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
Geriatric Care Coordination at Discharge Reduces Readmission Rates at 30 Days
Clinical question: Does a discharge planning service package affect readmission rates and ED visits?
Background: Elderly patients are at high risk for readmission after a hospitalization. Coordinated care packages, although effective in congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) management, have yielded inconsistent results in terms of decreasing readmission rates for patients with a broader range of medical issues.
Study design: Randomized controlled pilot study.
Setting: A single large academic medical center in Texas.
Synopsis: Forty-one elderly patients at high risk for readmission—because of their age and comorbidities—were enrolled within 72 hours of admission. Patients randomized to the care bundle arm received daily education about medication reconciliation, health conditions, and self-care provided by study pharmacists and nurses. The intervention required approximately 40 minutes per day: 20 to 25 minutes for the care coordinators and 20 minutes for the pharmacists. A post-discharge phone call to review medication and confirm follow-up instructions was included.
Eight patients in the control group and two patients in the intervention arm were readmitted or seen in the ED within 30 days after discharge (38% vs. 10%, P=0.004). At 60 days, the difference between the two groups was no longer significant. The intervention group had a longer time interval before its first readmission (36.2 days vs. 15.7 days). The sample was too small to determine the effect on length of hospitalization.
Limitations of the study include its small sample size and unclear costs of the intervention.
Bottom line: Geriatric discharge bundles might decrease readmission and ED visits after discharge, but larger studies are needed to confirm this finding.
Citation: Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day post-discharge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Computer-Assisted Medication Reconciliation Might Reduce Unintentional Drug Discrepancies with Potential for Harm
Clinical question: Does a computerized medication reconciliation intervention reduce unintentional medication discrepancies?
Background: Given the high prevalence of unintentional medication discrepancies in hospitalized patients and the potential for harm, medication reconciliation is a national patient safety goal. Little data exist on the efficacy of medication reconciliation interventions for reducing medication discrepancies.
Study design: Cluster-randomized controlled trial.
Setting: Two large academic hospitals in Boston.
Synopsis: Using 14 medical teams, the study enrolled and randomized 322 patients to a floor with intervention or to a floor with traditional care. The intervention teams utilized a computerized order entry application designed to facilitate medication reconciliation, as well as a process redesign for physicians, nurses, and pharmacists.
The primary outcome was the number of unintentional medication discrepancies with the potential for causing harm (PADEs) per patient.
Patients randomized to the intervention group had a 28% reduction in relative risk compared with the control group (1.05 PADEs vs. 1.44 PADEs; absolute relative risk 0.72 (0.52-0.99)). The absolute relative risk reduction between the two arms was 0.39 PADE per patient (NNT=2.6). The intervention was associated with a significant reduction in PADEs at discharge but not at admission. The effects of the intervention were greater in patients with a higher PADE score.
Bottom line: This computerized medication reconciliation program with process redesign was associated with reduced risk of unintentional medication discrepancies with potential for causing harms (PADEs).
Citation: Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169(8):771-780.
End-of-Life Discussions Associated with Lower Healthcare Costs
Clinical question: What is the impact of patient-physician discussions of end-of-life care on healthcare costs in the final week of a patient’s life?
Background: Life-sustaining medical care of patients with advanced cancer is costly, with disproportionate spending at the end of a patient’s life. The link between discussions of end-of-life care preferences and healthcare expenditure has not been studied thoroughly.
Study design: Prospective observational study.
Setting: Seven sites in Connecticut, Texas, New Hampshire, and Massachusetts.
Synopsis: More than 600 patients with advanced cancer were recruited from September 2002 through December 2007 as part of the Coping With Cancer study. The 188 patients (31%) who reported end-of-life discussions with their physicians at baseline were less likely to undergo mechanical ventilator use or resuscitation, or to be admitted or die in an intensive-care unit in the final week of life. They were more likely to receive outpatient hospice care and had less physical distress in the last week than those who did not.
The mean aggregate cost of care in this group was $1,876, which was 36% lower than in the group that did not discuss end-of-life care ($2,917), P=0.002. In addition, higher medical costs were associated with worse quality of death, as reported by caregivers.
This study is limited by its observational design.
Bottom line: Physician communication with patients regarding end-of-life care preferences is associated with lower costs in the final week of life.
Citation: Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480-488.
Reduction of ED Visits and Hospitalizations for Chronically Ill and Homeless Adults
Clinical question: Can a case management and housing program reduce the utilization of ED and hospital medical services among chronically ill homeless adults?
Background: Homeless adults have high rates of chronic illness, have poor access to uninterrupted primary healthcare, and frequently use costly medical services, including those provided by EDs and inpatient hospitalizations. Studies to determine the efficacy of housing and case management services in reducing hospital and ED utilization in this population are lacking.
Study design: Randomized controlled trial.
Setting: A public teaching hospital and a private nonprofit hospital in Chicago.
Synopsis: Four hundred seven chronically ill and homeless adults were randomized to receive a case management and housing intervention or traditional care following an index hospitalization. The intervention group received assistance with stable housing on discharge and biweekly case management services throughout the study period. Traditional care consisted of routine inpatient discharge planning and transportation to a shelter.
Patients were followed for 18 months for the primary outcomes: number of hospitalizations, total hospital days, and number of ED visits.
After adjusting for differences in baseline variables, the intervention group was found to have significantly lower rates of hospitalization (relative reduction 29%), total hospital days (29%), and ED visits (24%). The authors did not find a difference in mortality or quality of life between the two groups.
Limitations of this study include a small sample size, limited geographic distribution of subjects, and the lack of a cost-benefit analysis of the intervention.
Bottom line: Case management and housing interventions can decrease hospitalizations and ED visits among chronically ill homeless adults.
Citation: Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771-1778.
Intravenous Esomeprazole Reduces Recurrent Bleeding from Peptic Ulcers
Clinical question: Does intravenous esomeprazole prevent recurrent peptic ulcer bleeding, compared with placebo?
Background: U.S. hospitals admit more than 300,000 patients per year for peptic ulcer bleeding. Asian studies of proton pump inhibitors have demonstrated improved outcomes in patients with bleeding caused by peptic ulcers, but these results have not been consistently replicated in studies in Western Europe or North America.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Ninety-one hospital EDs in 16 countries.
Synopsis: The study team randomized 764 adult patients with a single bleeding gastric or duodenal ulcer after successful endoscopic hemostasis. The study group received esomeprazole (80 mg bolus, given intravenously over 30 minutes, followed by an 8 mg/hour infusion for 71.5 hours). The second group received placebo. Each group subsequently received 40 mg/day of oral esomeprazole for 27 days.
Recurrent bleeding within 72 hours was reduced by nearly half in the intravenous esomeprazole arm compared with placebo (5.9% vs. 10.3%, P=0.026). This remained significant at seven and 30 days. Intravenous esomeprazole also reduced endoscopic retreatment (6.4% vs. 11.6%; P=0.012) and demonstrated a trend toward reduction in surgery (2.7% vs. 5.4%) and all-cause mortality (0.8% vs. 2.1%).
Study limitations included a lack of standardization of endoscopic therapy across institutions.
Bottom line: Given after endoscopic hemostatis, intravenous esomeprazole followed by oral esomeprazole reduced recurrent bleeding in patients with a single duodenal or gastric ulcer.
Citation: Sung JJ, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2009;150(7):455-464.
Discharge Time and Duration Affected by Several Factors During Hospitalization
Clinical question: What are the factors affecting late and long discharges in a general medical unit?
Background: The mismatch between admission and discharge times is a problem for many hospitals; admissions occur early in the day whereas, discharges occur later in the day. The reasons behind delays in discharge and prolongation of discharges are not fully understood.
Study design: Prospective cohort study.
Setting: A general medical unit without house staff coverage at an academic medical center in Baltimore.
Synopsis: Care providers completed surveys on 201 consecutive discharges from January to April 2005. Outcome variables included time of discharge and discharge duration.
Mean discharge time was 3:09 p.m. Delay in discharge was associated with a need for ambulance transportation (1.5 hours), need for prescriptions to be filled at the hospital (1.4 hours), and for patients whose final test was a procedure (1.2 hours) or consult (1.1 hours).
Median discharge time was 7.6 hours. Longer discharge duration was associated with discharge to a location other than home (28.9 hours), need for consultation (14.8 hours), or need for a procedure (13.4 hours) before discharge.
African-American race, gender, age, and comorbid psychiatric and substance abuse disorders were not associated with either late or prolonged discharges.
Bottom line: Final-day tests, procedures, and consults, as well as complex discharge arrangements, prolong and delay discharges more than the characteristics of patients themselves.
Citation: Chen LM, Freitag MH, Franco M, Sullivan CD, Dickson C, Brancati FL. Natural history of late discharges from a general medical ward. J Hosp Med. 2009;4(4):226-233.
Administration of Parenteral Medication a Common Point at Which Errors Occur in ICUs
Clinical question: To what extent are medication administration errors a problem across ICUs, and what are some ways to prevent them?
Background: High-acuity and complex systems increase the likelihood of medical errors in ICUs. The first multinational Sentinel Events Evaluation study reported an ICU medication error rate of 10.5 per 100 patient days at the prescription and administration stages of medication delivery.
Study design: Multinational observational, prospective, cross-sectional study.
Setting: One hundred thirteen ICUs in 27 countries on five continents.
Synopsis: This study addressed five types of medication error at the administration stage in the ICU in a 24-hour timeframe: wrong drug, wrong dose, wrong route, wrong time, and missed medication. The main outcome measures were the number and impact of administration errors, the distribution of error characteristics, and the distribution of contributing and preventive factors.
In the 1,328 critically ill patients included in the study, 861 medication errors were reported by structured questionnaire; 441 patients were affected by the errors. The prevalence was 74.5 errors per 100 patient days, and 12 patients (0.9%) suffered permanent harm or death. Most medication administration errors occurred during routine care, not during extraordinary situations. Most were omission errors.
This study is limited by its observational design and by the fact that self-reporting also carries the risk of under-reporting.
This study points out several ways to reduce medication errors. An independent predictor of decreased risk of medication errors of all types is an established incident reporting system. Routine checking of infusion pumps at every nursing shift change also reduced this risk.
Bottom line: This study confirmed that the administration of parenteral medications is a vulnerable point across many ICUs, and incident reporting systems and routine checks of infusion pumps are effective ways to reduce the risk of this type of error.
Citation: Valentin A, Capuzzo M, Guidet B, et al. Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ. 2009;338:b814. TH
In This Edition
- Pharmacists and readmission rates.
- Geriatric discharge bundles and readmission rates.
- Medication reconciliation and risk of adverse drug events.
- End-of-life discussions and care outcomes.
- Effect of case management and housing for homeless adults.
- IV esomeprazole in bleeding ulcers.
- Causes of discharge delays.
- Methods to reduce ICU medication errors.
Addition of Pharmacists to Inpatient Teams Reduces Drug-Related Readmissions, Morbidity, and Costs for Elderly Patients
Clinical question: Would a ward-based pharmacist reduce morbidity, subsequent ED visits, and readmissions for elderly patients?
Background: Adverse drug events can cause significant drug-related morbidity and mortality, and lead to unnecessary healthcare costs. Elderly patients are more vulnerable to these effects given the polypharmacy often associated with their care. The effectiveness of a ward-based pharmacist intervention for elderly patients has not yet been studied.
Study design: Randomized controlled trial.
Setting: Two acute-care, internal-medicine wards at the University Hospital of Uppsala in Uppsala, Sweden.
Synopsis: Three hundred sixty-eight hospitalized patients ages 80 or older were randomized to control or intervention groups. The latter received enhanced services from a pharmacist who was integrated into the inpatient team. This individual performed medication reconciliation, reviewed the medication list, and advised the treating physician. The pharmacist educated and monitored patients during the hospitalization, counseled them at discharge, communicated pertinent medication information to the primary-care physicians (PCPs), and called the patients two months after discharge.
The primary outcome measure was the frequency of all hospital visits (ED visits plus hospital readmissions) during 12-month follow-up. The secondary outcome measure was the cost of hospital care.
The intervention group had a 16% reduction in all hospital visits and a 47% reduction in ED visits. There were five times as many drug-related readmissions in the control group compared with the intervention group, but the study did not have enough power to show a reduction in the total number of readmissions alone. The cost of hospital care minus the cost of the intervention resulted in a net savings of $230 per patient.
Bottom line: For elderly patients, adding a pharmacist to the inpatient team could lead to significant reductions in morbidity and, on a population basis, healthcare costs.
Citation: Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
Geriatric Care Coordination at Discharge Reduces Readmission Rates at 30 Days
Clinical question: Does a discharge planning service package affect readmission rates and ED visits?
Background: Elderly patients are at high risk for readmission after a hospitalization. Coordinated care packages, although effective in congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD) management, have yielded inconsistent results in terms of decreasing readmission rates for patients with a broader range of medical issues.
Study design: Randomized controlled pilot study.
Setting: A single large academic medical center in Texas.
Synopsis: Forty-one elderly patients at high risk for readmission—because of their age and comorbidities—were enrolled within 72 hours of admission. Patients randomized to the care bundle arm received daily education about medication reconciliation, health conditions, and self-care provided by study pharmacists and nurses. The intervention required approximately 40 minutes per day: 20 to 25 minutes for the care coordinators and 20 minutes for the pharmacists. A post-discharge phone call to review medication and confirm follow-up instructions was included.
Eight patients in the control group and two patients in the intervention arm were readmitted or seen in the ED within 30 days after discharge (38% vs. 10%, P=0.004). At 60 days, the difference between the two groups was no longer significant. The intervention group had a longer time interval before its first readmission (36.2 days vs. 15.7 days). The sample was too small to determine the effect on length of hospitalization.
Limitations of the study include its small sample size and unclear costs of the intervention.
Bottom line: Geriatric discharge bundles might decrease readmission and ED visits after discharge, but larger studies are needed to confirm this finding.
Citation: Koehler BE, Richter KM, Youngblood L, et al. Reduction of 30-day post-discharge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Computer-Assisted Medication Reconciliation Might Reduce Unintentional Drug Discrepancies with Potential for Harm
Clinical question: Does a computerized medication reconciliation intervention reduce unintentional medication discrepancies?
Background: Given the high prevalence of unintentional medication discrepancies in hospitalized patients and the potential for harm, medication reconciliation is a national patient safety goal. Little data exist on the efficacy of medication reconciliation interventions for reducing medication discrepancies.
Study design: Cluster-randomized controlled trial.
Setting: Two large academic hospitals in Boston.
Synopsis: Using 14 medical teams, the study enrolled and randomized 322 patients to a floor with intervention or to a floor with traditional care. The intervention teams utilized a computerized order entry application designed to facilitate medication reconciliation, as well as a process redesign for physicians, nurses, and pharmacists.
The primary outcome was the number of unintentional medication discrepancies with the potential for causing harm (PADEs) per patient.
Patients randomized to the intervention group had a 28% reduction in relative risk compared with the control group (1.05 PADEs vs. 1.44 PADEs; absolute relative risk 0.72 (0.52-0.99)). The absolute relative risk reduction between the two arms was 0.39 PADE per patient (NNT=2.6). The intervention was associated with a significant reduction in PADEs at discharge but not at admission. The effects of the intervention were greater in patients with a higher PADE score.
Bottom line: This computerized medication reconciliation program with process redesign was associated with reduced risk of unintentional medication discrepancies with potential for causing harms (PADEs).
Citation: Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169(8):771-780.
End-of-Life Discussions Associated with Lower Healthcare Costs
Clinical question: What is the impact of patient-physician discussions of end-of-life care on healthcare costs in the final week of a patient’s life?
Background: Life-sustaining medical care of patients with advanced cancer is costly, with disproportionate spending at the end of a patient’s life. The link between discussions of end-of-life care preferences and healthcare expenditure has not been studied thoroughly.
Study design: Prospective observational study.
Setting: Seven sites in Connecticut, Texas, New Hampshire, and Massachusetts.
Synopsis: More than 600 patients with advanced cancer were recruited from September 2002 through December 2007 as part of the Coping With Cancer study. The 188 patients (31%) who reported end-of-life discussions with their physicians at baseline were less likely to undergo mechanical ventilator use or resuscitation, or to be admitted or die in an intensive-care unit in the final week of life. They were more likely to receive outpatient hospice care and had less physical distress in the last week than those who did not.
The mean aggregate cost of care in this group was $1,876, which was 36% lower than in the group that did not discuss end-of-life care ($2,917), P=0.002. In addition, higher medical costs were associated with worse quality of death, as reported by caregivers.
This study is limited by its observational design.
Bottom line: Physician communication with patients regarding end-of-life care preferences is associated with lower costs in the final week of life.
Citation: Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life: associations with end-of-life conversations. Arch Intern Med. 2009;169(5):480-488.
Reduction of ED Visits and Hospitalizations for Chronically Ill and Homeless Adults
Clinical question: Can a case management and housing program reduce the utilization of ED and hospital medical services among chronically ill homeless adults?
Background: Homeless adults have high rates of chronic illness, have poor access to uninterrupted primary healthcare, and frequently use costly medical services, including those provided by EDs and inpatient hospitalizations. Studies to determine the efficacy of housing and case management services in reducing hospital and ED utilization in this population are lacking.
Study design: Randomized controlled trial.
Setting: A public teaching hospital and a private nonprofit hospital in Chicago.
Synopsis: Four hundred seven chronically ill and homeless adults were randomized to receive a case management and housing intervention or traditional care following an index hospitalization. The intervention group received assistance with stable housing on discharge and biweekly case management services throughout the study period. Traditional care consisted of routine inpatient discharge planning and transportation to a shelter.
Patients were followed for 18 months for the primary outcomes: number of hospitalizations, total hospital days, and number of ED visits.
After adjusting for differences in baseline variables, the intervention group was found to have significantly lower rates of hospitalization (relative reduction 29%), total hospital days (29%), and ED visits (24%). The authors did not find a difference in mortality or quality of life between the two groups.
Limitations of this study include a small sample size, limited geographic distribution of subjects, and the lack of a cost-benefit analysis of the intervention.
Bottom line: Case management and housing interventions can decrease hospitalizations and ED visits among chronically ill homeless adults.
Citation: Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009;301(17):1771-1778.
Intravenous Esomeprazole Reduces Recurrent Bleeding from Peptic Ulcers
Clinical question: Does intravenous esomeprazole prevent recurrent peptic ulcer bleeding, compared with placebo?
Background: U.S. hospitals admit more than 300,000 patients per year for peptic ulcer bleeding. Asian studies of proton pump inhibitors have demonstrated improved outcomes in patients with bleeding caused by peptic ulcers, but these results have not been consistently replicated in studies in Western Europe or North America.
Study design: Randomized, placebo-controlled, double-blind trial.
Setting: Ninety-one hospital EDs in 16 countries.
Synopsis: The study team randomized 764 adult patients with a single bleeding gastric or duodenal ulcer after successful endoscopic hemostasis. The study group received esomeprazole (80 mg bolus, given intravenously over 30 minutes, followed by an 8 mg/hour infusion for 71.5 hours). The second group received placebo. Each group subsequently received 40 mg/day of oral esomeprazole for 27 days.
Recurrent bleeding within 72 hours was reduced by nearly half in the intravenous esomeprazole arm compared with placebo (5.9% vs. 10.3%, P=0.026). This remained significant at seven and 30 days. Intravenous esomeprazole also reduced endoscopic retreatment (6.4% vs. 11.6%; P=0.012) and demonstrated a trend toward reduction in surgery (2.7% vs. 5.4%) and all-cause mortality (0.8% vs. 2.1%).
Study limitations included a lack of standardization of endoscopic therapy across institutions.
Bottom line: Given after endoscopic hemostatis, intravenous esomeprazole followed by oral esomeprazole reduced recurrent bleeding in patients with a single duodenal or gastric ulcer.
Citation: Sung JJ, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2009;150(7):455-464.
Discharge Time and Duration Affected by Several Factors During Hospitalization
Clinical question: What are the factors affecting late and long discharges in a general medical unit?
Background: The mismatch between admission and discharge times is a problem for many hospitals; admissions occur early in the day whereas, discharges occur later in the day. The reasons behind delays in discharge and prolongation of discharges are not fully understood.
Study design: Prospective cohort study.
Setting: A general medical unit without house staff coverage at an academic medical center in Baltimore.
Synopsis: Care providers completed surveys on 201 consecutive discharges from January to April 2005. Outcome variables included time of discharge and discharge duration.
Mean discharge time was 3:09 p.m. Delay in discharge was associated with a need for ambulance transportation (1.5 hours), need for prescriptions to be filled at the hospital (1.4 hours), and for patients whose final test was a procedure (1.2 hours) or consult (1.1 hours).
Median discharge time was 7.6 hours. Longer discharge duration was associated with discharge to a location other than home (28.9 hours), need for consultation (14.8 hours), or need for a procedure (13.4 hours) before discharge.
African-American race, gender, age, and comorbid psychiatric and substance abuse disorders were not associated with either late or prolonged discharges.
Bottom line: Final-day tests, procedures, and consults, as well as complex discharge arrangements, prolong and delay discharges more than the characteristics of patients themselves.
Citation: Chen LM, Freitag MH, Franco M, Sullivan CD, Dickson C, Brancati FL. Natural history of late discharges from a general medical ward. J Hosp Med. 2009;4(4):226-233.
Administration of Parenteral Medication a Common Point at Which Errors Occur in ICUs
Clinical question: To what extent are medication administration errors a problem across ICUs, and what are some ways to prevent them?
Background: High-acuity and complex systems increase the likelihood of medical errors in ICUs. The first multinational Sentinel Events Evaluation study reported an ICU medication error rate of 10.5 per 100 patient days at the prescription and administration stages of medication delivery.
Study design: Multinational observational, prospective, cross-sectional study.
Setting: One hundred thirteen ICUs in 27 countries on five continents.
Synopsis: This study addressed five types of medication error at the administration stage in the ICU in a 24-hour timeframe: wrong drug, wrong dose, wrong route, wrong time, and missed medication. The main outcome measures were the number and impact of administration errors, the distribution of error characteristics, and the distribution of contributing and preventive factors.
In the 1,328 critically ill patients included in the study, 861 medication errors were reported by structured questionnaire; 441 patients were affected by the errors. The prevalence was 74.5 errors per 100 patient days, and 12 patients (0.9%) suffered permanent harm or death. Most medication administration errors occurred during routine care, not during extraordinary situations. Most were omission errors.
This study is limited by its observational design and by the fact that self-reporting also carries the risk of under-reporting.
This study points out several ways to reduce medication errors. An independent predictor of decreased risk of medication errors of all types is an established incident reporting system. Routine checking of infusion pumps at every nursing shift change also reduced this risk.
Bottom line: This study confirmed that the administration of parenteral medications is a vulnerable point across many ICUs, and incident reporting systems and routine checks of infusion pumps are effective ways to reduce the risk of this type of error.
Citation: Valentin A, Capuzzo M, Guidet B, et al. Errors in administration of parenteral drugs in intensive care units: multinational prospective study. BMJ. 2009;338:b814. TH
Planned Partnerships
A day in the life of a hospitalist is not spent in a vacuum. Every day in hospitals across the country, hospitalists coordinate patient care with a host of other physicians, caregivers, and administrators. One minute, a hospitalist could be managing a patient’s treatment with a physician assistant; the next minute, the hospitalist could be reviewing a diagnosis from a cardiologist. The same hospitalist might finish the shift by reporting valuable quality-improvement (QI) data to the hospital’s management staff.
It’s that kind of collaboration that is the hallmark of HM, so it makes sense that the same level of collaboration take place between SHM and a bevy of other healthcare-related organizations.
“The delivery of hospital-based care is a team sport,” says Joe Miller, SHM’s executive advisor to the CEO. “It requires coordination across disciplines, from clinical to managerial. Hospital medicine is in the middle of a complex system, and we can’t do it ourselves. If we’re going to be successful, we need to forge partnerships.”
Those partnerships have been critical to SHM’s ability to create educational programs and practice management resources. It also factors into SHM’s efforts to enhance patient satisfaction and advocate for QI in healthcare. The list of SHM’s partner organizations and joint projects is an alphabet soup that includes the nation’s most influential professional societies, academies, and government entities, each of which is working to improve the delivery of care to hospitalized patients.
Small Start, Quick Growth
The relationship between SHM and the American Medical Association (AMA) began as a simple research project and has grown into a deeper collaboration. In 2007, the AMA’s Organized Medical Staff Section (OMSS), the department that advocates on behalf of physicians who are members of medical staffs and other organizations, wanted to increase understanding of how hospitalists, primary-care physicians, and other physicians work together in the hospital setting. The association collaborated with SHM to conduct a survey and obtain feedback from hospitalists.
The 2007 survey found that there was still work to be done between the organizations, namely the need for a set of guiding principles for a successful hospitalist practice. OMSS, SHM, AHA, and the Joint Commission developed the principles, which were recently endorsed by OMSS at the association’s annual conference in June.
“We feel they’re appropriate and make sense,” says Jim DeNuccio, director of AMA’s Organized Medical Staff, Group Practice, and Senior Physician Services.
The 2007 survey and the principles for a hospitalist practice have led to a new survey, conducted this year, to track how the issues and challenges within a hospital have changed. The initiatives are just the beginning of a long-term relationship between SHM and AMA.
“It’s very important for all of us to work together to continue to grow,” says DeNuccio, who cites AMA’s courses in practice management, QI, and patient safety as educational opportunities for hospitalists. “Our interest is in the patient. That’s what this is all about. The AMA and OMSS feel strongly that the profession needs to call the shots about how care is delivered in hospitals. They see that engaging the hospitalist is in the interest of the patient.”
SHM and AAPA: Educating Together
Hospitalists and physician assistants (PAs) work hand in hand to care for their patients. At the national level, SHM and the American Academy of Physician Assistants (AAPA) are coordinating educational programs to ensure PAs and hospitalists are properly informed and learning from the same page.
“It’s a very broad spectrum,” says Sharon Kulesz, AAPA director of alliance development and education. “We provide physician assistants with information about hospitalists, and we provide physicians with information about the benefit of working with physician assistants.”
Along with the American Academy of Nurse Practitioners (AANP), AAPA and SHM have coordinated educational programs at SHM’s annual meeting for hospitalists, and recently developed a stand-alone “Boot Camp” series for nurse practitioners and physician assistants to learn more about HM.
Kulesz notes, however, that not all of the education is exclusively for hospital-based workers. Some of the efforts are geared toward educating the public about hospitals’ patient-care teams. Regardless of the topic or the audience, the key is a comfortable working relationship between teams, she says.
“Our work with SHM is the model that I would like to use in all of our collaborations,” Kulesz says. “SHM gets us. They get what we can do and how a collaborative approach can be of benefit to everyone. It’s like an extended family.”
Patient-First Collaboration
The new Hospital Care Collaborative takes a team approach to hospital-based care. More than simply a partnership, the group brings together groups that represent healthcare professionals in the hospital—hospitalists, nurses, case managers, respiratory therapists, social workers—to find common approaches to QI and patient safety.
“As a group, the Hospital Care Collaborative is looking for ways to work together to improve the care of the hospitalized patient,” says Larry Wellikson, MD, FHM, CEO of SHM. “We’ve developed common principles, which have been ratified by each of our boards. At its core, the collaborative is looking for real-world ways to integrate medical professionals and help hospitals take a new approach to patient care.”
Part of the answer is in the education, development, and promotion of high-performance teams in hospital settings, Dr. Wellikson says. For instance, if a patient is admitted to the hospital with a blood clot, each team member has the opportunity to contribute his or her expertise and coordinate with others. The hospitalist might make the diagnosis, which leads to the prescription from the hospital pharmacist. With the diagnosis and list of prescriptions in hand, a nurse can then explain to the patient how the medications will affect their daily routine.
“In modern healthcare, no one professional or professional society can have all the perspectives you need,” Dr. Wellikson says. “In SHM’s approach, we’re looking at the hospital as a community, not a building. The problems we’re trying to solve are complex, and it requires an all-hands-on-deck approach. Knitting the perspectives and expertise together will be the key to treating the patient in the 21st century.” TH
Brendon Shank is a freelance writer based in Philadelphia.
A day in the life of a hospitalist is not spent in a vacuum. Every day in hospitals across the country, hospitalists coordinate patient care with a host of other physicians, caregivers, and administrators. One minute, a hospitalist could be managing a patient’s treatment with a physician assistant; the next minute, the hospitalist could be reviewing a diagnosis from a cardiologist. The same hospitalist might finish the shift by reporting valuable quality-improvement (QI) data to the hospital’s management staff.
It’s that kind of collaboration that is the hallmark of HM, so it makes sense that the same level of collaboration take place between SHM and a bevy of other healthcare-related organizations.
“The delivery of hospital-based care is a team sport,” says Joe Miller, SHM’s executive advisor to the CEO. “It requires coordination across disciplines, from clinical to managerial. Hospital medicine is in the middle of a complex system, and we can’t do it ourselves. If we’re going to be successful, we need to forge partnerships.”
Those partnerships have been critical to SHM’s ability to create educational programs and practice management resources. It also factors into SHM’s efforts to enhance patient satisfaction and advocate for QI in healthcare. The list of SHM’s partner organizations and joint projects is an alphabet soup that includes the nation’s most influential professional societies, academies, and government entities, each of which is working to improve the delivery of care to hospitalized patients.
Small Start, Quick Growth
The relationship between SHM and the American Medical Association (AMA) began as a simple research project and has grown into a deeper collaboration. In 2007, the AMA’s Organized Medical Staff Section (OMSS), the department that advocates on behalf of physicians who are members of medical staffs and other organizations, wanted to increase understanding of how hospitalists, primary-care physicians, and other physicians work together in the hospital setting. The association collaborated with SHM to conduct a survey and obtain feedback from hospitalists.
The 2007 survey found that there was still work to be done between the organizations, namely the need for a set of guiding principles for a successful hospitalist practice. OMSS, SHM, AHA, and the Joint Commission developed the principles, which were recently endorsed by OMSS at the association’s annual conference in June.
“We feel they’re appropriate and make sense,” says Jim DeNuccio, director of AMA’s Organized Medical Staff, Group Practice, and Senior Physician Services.
The 2007 survey and the principles for a hospitalist practice have led to a new survey, conducted this year, to track how the issues and challenges within a hospital have changed. The initiatives are just the beginning of a long-term relationship between SHM and AMA.
“It’s very important for all of us to work together to continue to grow,” says DeNuccio, who cites AMA’s courses in practice management, QI, and patient safety as educational opportunities for hospitalists. “Our interest is in the patient. That’s what this is all about. The AMA and OMSS feel strongly that the profession needs to call the shots about how care is delivered in hospitals. They see that engaging the hospitalist is in the interest of the patient.”
SHM and AAPA: Educating Together
Hospitalists and physician assistants (PAs) work hand in hand to care for their patients. At the national level, SHM and the American Academy of Physician Assistants (AAPA) are coordinating educational programs to ensure PAs and hospitalists are properly informed and learning from the same page.
“It’s a very broad spectrum,” says Sharon Kulesz, AAPA director of alliance development and education. “We provide physician assistants with information about hospitalists, and we provide physicians with information about the benefit of working with physician assistants.”
Along with the American Academy of Nurse Practitioners (AANP), AAPA and SHM have coordinated educational programs at SHM’s annual meeting for hospitalists, and recently developed a stand-alone “Boot Camp” series for nurse practitioners and physician assistants to learn more about HM.
Kulesz notes, however, that not all of the education is exclusively for hospital-based workers. Some of the efforts are geared toward educating the public about hospitals’ patient-care teams. Regardless of the topic or the audience, the key is a comfortable working relationship between teams, she says.
“Our work with SHM is the model that I would like to use in all of our collaborations,” Kulesz says. “SHM gets us. They get what we can do and how a collaborative approach can be of benefit to everyone. It’s like an extended family.”
Patient-First Collaboration
The new Hospital Care Collaborative takes a team approach to hospital-based care. More than simply a partnership, the group brings together groups that represent healthcare professionals in the hospital—hospitalists, nurses, case managers, respiratory therapists, social workers—to find common approaches to QI and patient safety.
“As a group, the Hospital Care Collaborative is looking for ways to work together to improve the care of the hospitalized patient,” says Larry Wellikson, MD, FHM, CEO of SHM. “We’ve developed common principles, which have been ratified by each of our boards. At its core, the collaborative is looking for real-world ways to integrate medical professionals and help hospitals take a new approach to patient care.”
Part of the answer is in the education, development, and promotion of high-performance teams in hospital settings, Dr. Wellikson says. For instance, if a patient is admitted to the hospital with a blood clot, each team member has the opportunity to contribute his or her expertise and coordinate with others. The hospitalist might make the diagnosis, which leads to the prescription from the hospital pharmacist. With the diagnosis and list of prescriptions in hand, a nurse can then explain to the patient how the medications will affect their daily routine.
“In modern healthcare, no one professional or professional society can have all the perspectives you need,” Dr. Wellikson says. “In SHM’s approach, we’re looking at the hospital as a community, not a building. The problems we’re trying to solve are complex, and it requires an all-hands-on-deck approach. Knitting the perspectives and expertise together will be the key to treating the patient in the 21st century.” TH
Brendon Shank is a freelance writer based in Philadelphia.
A day in the life of a hospitalist is not spent in a vacuum. Every day in hospitals across the country, hospitalists coordinate patient care with a host of other physicians, caregivers, and administrators. One minute, a hospitalist could be managing a patient’s treatment with a physician assistant; the next minute, the hospitalist could be reviewing a diagnosis from a cardiologist. The same hospitalist might finish the shift by reporting valuable quality-improvement (QI) data to the hospital’s management staff.
It’s that kind of collaboration that is the hallmark of HM, so it makes sense that the same level of collaboration take place between SHM and a bevy of other healthcare-related organizations.
“The delivery of hospital-based care is a team sport,” says Joe Miller, SHM’s executive advisor to the CEO. “It requires coordination across disciplines, from clinical to managerial. Hospital medicine is in the middle of a complex system, and we can’t do it ourselves. If we’re going to be successful, we need to forge partnerships.”
Those partnerships have been critical to SHM’s ability to create educational programs and practice management resources. It also factors into SHM’s efforts to enhance patient satisfaction and advocate for QI in healthcare. The list of SHM’s partner organizations and joint projects is an alphabet soup that includes the nation’s most influential professional societies, academies, and government entities, each of which is working to improve the delivery of care to hospitalized patients.
Small Start, Quick Growth
The relationship between SHM and the American Medical Association (AMA) began as a simple research project and has grown into a deeper collaboration. In 2007, the AMA’s Organized Medical Staff Section (OMSS), the department that advocates on behalf of physicians who are members of medical staffs and other organizations, wanted to increase understanding of how hospitalists, primary-care physicians, and other physicians work together in the hospital setting. The association collaborated with SHM to conduct a survey and obtain feedback from hospitalists.
The 2007 survey found that there was still work to be done between the organizations, namely the need for a set of guiding principles for a successful hospitalist practice. OMSS, SHM, AHA, and the Joint Commission developed the principles, which were recently endorsed by OMSS at the association’s annual conference in June.
“We feel they’re appropriate and make sense,” says Jim DeNuccio, director of AMA’s Organized Medical Staff, Group Practice, and Senior Physician Services.
The 2007 survey and the principles for a hospitalist practice have led to a new survey, conducted this year, to track how the issues and challenges within a hospital have changed. The initiatives are just the beginning of a long-term relationship between SHM and AMA.
“It’s very important for all of us to work together to continue to grow,” says DeNuccio, who cites AMA’s courses in practice management, QI, and patient safety as educational opportunities for hospitalists. “Our interest is in the patient. That’s what this is all about. The AMA and OMSS feel strongly that the profession needs to call the shots about how care is delivered in hospitals. They see that engaging the hospitalist is in the interest of the patient.”
SHM and AAPA: Educating Together
Hospitalists and physician assistants (PAs) work hand in hand to care for their patients. At the national level, SHM and the American Academy of Physician Assistants (AAPA) are coordinating educational programs to ensure PAs and hospitalists are properly informed and learning from the same page.
“It’s a very broad spectrum,” says Sharon Kulesz, AAPA director of alliance development and education. “We provide physician assistants with information about hospitalists, and we provide physicians with information about the benefit of working with physician assistants.”
Along with the American Academy of Nurse Practitioners (AANP), AAPA and SHM have coordinated educational programs at SHM’s annual meeting for hospitalists, and recently developed a stand-alone “Boot Camp” series for nurse practitioners and physician assistants to learn more about HM.
Kulesz notes, however, that not all of the education is exclusively for hospital-based workers. Some of the efforts are geared toward educating the public about hospitals’ patient-care teams. Regardless of the topic or the audience, the key is a comfortable working relationship between teams, she says.
“Our work with SHM is the model that I would like to use in all of our collaborations,” Kulesz says. “SHM gets us. They get what we can do and how a collaborative approach can be of benefit to everyone. It’s like an extended family.”
Patient-First Collaboration
The new Hospital Care Collaborative takes a team approach to hospital-based care. More than simply a partnership, the group brings together groups that represent healthcare professionals in the hospital—hospitalists, nurses, case managers, respiratory therapists, social workers—to find common approaches to QI and patient safety.
“As a group, the Hospital Care Collaborative is looking for ways to work together to improve the care of the hospitalized patient,” says Larry Wellikson, MD, FHM, CEO of SHM. “We’ve developed common principles, which have been ratified by each of our boards. At its core, the collaborative is looking for real-world ways to integrate medical professionals and help hospitals take a new approach to patient care.”
Part of the answer is in the education, development, and promotion of high-performance teams in hospital settings, Dr. Wellikson says. For instance, if a patient is admitted to the hospital with a blood clot, each team member has the opportunity to contribute his or her expertise and coordinate with others. The hospitalist might make the diagnosis, which leads to the prescription from the hospital pharmacist. With the diagnosis and list of prescriptions in hand, a nurse can then explain to the patient how the medications will affect their daily routine.
“In modern healthcare, no one professional or professional society can have all the perspectives you need,” Dr. Wellikson says. “In SHM’s approach, we’re looking at the hospital as a community, not a building. The problems we’re trying to solve are complex, and it requires an all-hands-on-deck approach. Knitting the perspectives and expertise together will be the key to treating the patient in the 21st century.” TH
Brendon Shank is a freelance writer based in Philadelphia.
JHM Names Baudendistel CME Editor
Some physicians have an interest in teaching; some are really good at it, and some make a career out of it. For Thomas Baudendistel, MD, FACP, teaching comes second nature and, as one of his former colleagues says, is a definition of who he is.
It’s those qualities, his experience in both academic and community hospital settings, and a passion for innovation that Dr. Baudendistel, the internal-medicine residency program director for Kaiser Permanente in Oakland, Calif., hopes to infuse as CME editor of the Journal of Hospital Medicine (JHM).
He was appointed to the new position in June. The first issue containing article-level CME, the answers to which will be submitted online, is scheduled to appear in the October issue.
“Tom is a superlative educator. He has defined himself that way. He has a passion for it and a talent for it,” says Brian J. Harte, MD, FHM, chair of the department of hospital medicine at The Cleveland Clinic and a deputy editor of JHM.
Dr. Harte, who first met Dr. Baudendistel in 1996 during his residency at the University of California at San Francisco, says his former mentor “can take a submission, drill down to the most important teaching point, and challenge the readership.”
Dr. Baudendistel admits teaching is why he “gets out of bed in the morning.” He says he wants to take advantage of the young, tech-savvy nature of most HM physicians.
“JHM has been an innovative journal. I see the CME piece as being equally innovative,” says Dr. Baudendistel, who served four years as a JHM associate editor. “I’d like to move [CME] past the pencil-and-paper phase.” TH
Some physicians have an interest in teaching; some are really good at it, and some make a career out of it. For Thomas Baudendistel, MD, FACP, teaching comes second nature and, as one of his former colleagues says, is a definition of who he is.
It’s those qualities, his experience in both academic and community hospital settings, and a passion for innovation that Dr. Baudendistel, the internal-medicine residency program director for Kaiser Permanente in Oakland, Calif., hopes to infuse as CME editor of the Journal of Hospital Medicine (JHM).
He was appointed to the new position in June. The first issue containing article-level CME, the answers to which will be submitted online, is scheduled to appear in the October issue.
“Tom is a superlative educator. He has defined himself that way. He has a passion for it and a talent for it,” says Brian J. Harte, MD, FHM, chair of the department of hospital medicine at The Cleveland Clinic and a deputy editor of JHM.
Dr. Harte, who first met Dr. Baudendistel in 1996 during his residency at the University of California at San Francisco, says his former mentor “can take a submission, drill down to the most important teaching point, and challenge the readership.”
Dr. Baudendistel admits teaching is why he “gets out of bed in the morning.” He says he wants to take advantage of the young, tech-savvy nature of most HM physicians.
“JHM has been an innovative journal. I see the CME piece as being equally innovative,” says Dr. Baudendistel, who served four years as a JHM associate editor. “I’d like to move [CME] past the pencil-and-paper phase.” TH
Some physicians have an interest in teaching; some are really good at it, and some make a career out of it. For Thomas Baudendistel, MD, FACP, teaching comes second nature and, as one of his former colleagues says, is a definition of who he is.
It’s those qualities, his experience in both academic and community hospital settings, and a passion for innovation that Dr. Baudendistel, the internal-medicine residency program director for Kaiser Permanente in Oakland, Calif., hopes to infuse as CME editor of the Journal of Hospital Medicine (JHM).
He was appointed to the new position in June. The first issue containing article-level CME, the answers to which will be submitted online, is scheduled to appear in the October issue.
“Tom is a superlative educator. He has defined himself that way. He has a passion for it and a talent for it,” says Brian J. Harte, MD, FHM, chair of the department of hospital medicine at The Cleveland Clinic and a deputy editor of JHM.
Dr. Harte, who first met Dr. Baudendistel in 1996 during his residency at the University of California at San Francisco, says his former mentor “can take a submission, drill down to the most important teaching point, and challenge the readership.”
Dr. Baudendistel admits teaching is why he “gets out of bed in the morning.” He says he wants to take advantage of the young, tech-savvy nature of most HM physicians.
“JHM has been an innovative journal. I see the CME piece as being equally innovative,” says Dr. Baudendistel, who served four years as a JHM associate editor. “I’d like to move [CME] past the pencil-and-paper phase.” TH