User login
Lesson of the Titanic
Author’s note: More than 1,500 passengers died in the Titanic, a disaster that resonates nearly a hundred years later. The equivalent of about 50 Titanics capsize annually in U.S. hospitals, nearly one every week (based on the Institute of Medicine’s estimate of 44,000-98,000 deaths per year from hospital adverse events). As hospitalists, it is our obligation to ensure the hull is solid, the crow’s nest properly manned, and the ship is turning in the right direction.
I’m the Rev. John Harper, and it’s April 10, 1912.
As I grasp my boarding pass I can’t contain my awe and excitement. Imagine me aboard the world’s most luxurious cruise liner heading to America. Granted, I’m booked in second class. But as everyone knows, second class on the Titanic outstrips first class on most liners these days. It should—for $66 this is an expensive way to travel. Still, it’s less than the cheapest first-class ticket of $125 and much less than a $4,500 booking in the millionaire’s suite. I could buy several houses for $4,500.
Walking along the gangway I recall hearing that this ship—the largest ever built—weighs nearly 47,000 tons and cost $7.5 million. Outside my cabin door I encounter a fellow passenger who exults over the ship’s amenities. The liner has a heated indoor swimming pool, four electric elevators, two libraries, a Turkish bath, a squash court and gymnasium, and ample room to move about. The White Star Line has thoughtfully limited the amount of lifeboats to 20 to preserve precious deck space for passengers.
I’m Jeff Glasheen, and it’s Sept. 15, 2007.
As my wife prepares to deliver our first child in the coming weeks, we visit the labor and delivery deck of the hospital.
It will be our first major interaction with the healthcare system as patients. It’s the largest healthcare system ever and costs nearly $2 trillion a year to operate. We have chosen a new hospital that features an amazing array of amenities, including a birthing center with private suites, in-room baths with oversize soaking tubs, an in-room sleeping area for family and friends, and a DVD player and flat-screen television. There are even Internet connections.
Room service is available 24 hours a day, and the staff is top-notch. I’m told some choose to stay in the VIP suites for an extra $1,000 a night. This restricted-access area offers 600-square-foot rooms with original art on the walls, luxury mattresses and 350-thread count linens, complimentary robes and slippers, and an office area supplied with newspapers, a printer, fax, voicemail, and teleconferencing capabilities. There is a family room as well as a private refrigerator, an assortment of beverages and a dedicated chef. Unfortunately the cost is too steep, so we’ll spend this voyage in second class. However, as everyone knows, second class on this vessel outstrips first class in most hospitals these days.
Midnight, April 14, 1912
Something has gone wrong; the ship just hiccupped a bit. From my cabin I clearly hear a grinding that could happen only when two large objects come into contact. It’s strange, but I assure my bunkmates there is nothing to worry about. The Titanic is unsinkable, built with every feasible safety feature. The ship’s hull is made of inch-thick steel and held together with nearly 3 million steel rivets. In the unlikely event the hull is breached, the ship contains 15 watertight bulkheads to contain the leakage. Further, 3,560 life vests, 48 life buoys, and the aforementioned 20 lifeboats (four more than required by British law) allay my concerns.
On the off chance something should go wrong, the ship is outfitted with the recently developed Marconi wireless telegraph capable of communicating with any ship or shore within 500 miles.
5 p.m., Sept. 17, 2007
As I write this column I consider that something could go wrong during our hospital stay. The Institute of Medicine reports that medications harm 1.5 million people annually (400,000 incidents occur in the hospital) and that nearly 100,000 die annually in adverse hospital events.
I assure myself there is nothing to worry about. The hospital of today is unsinkable, built with every feasible safety measure. Today’s hospitals require two patient identifiers, time-outs before procedures, read-backs, standardized abbreviations, rules for reporting of critical results, standardized approaches to hand-offs, awareness of look-alike/sound-alike medications, hand-hygiene guidelines, medication reconciliation, core measures, quality and patient safety committees—and, on the off chance that something should go wrong, requirements for communicating sentinel event reviews with regulatory agencies.
1:30 a.m., April 14, 1912
The scuttlebutt is that the Titanic has hit an iceberg, tearing open the hull, flooding the bulkheads, and overcoming the ship’s pumps. Apparently the crow’s nest spotted the iceberg only 30 seconds before the impact. The crew tried to change course immediately. But the unprecedented size and speed of the ship (there is a rumor that the captain may have been trying to set a new trans-Atlantic crossing record) made it impossible to avoid our destiny.
We are clearly sinking. As I anxiously pace the deck waiting for a spot on a lifeboat, I chat with a crew member who assures me help is coming. The ship’s band plays on deck, the music soothing in the night air.
1 p.m., Aug. 26, 2007
I’m about halfway through the Titanic exhibit at the local museum of nature and science. The display is designed to give you the experience of being a passenger aboard the RMS Titanic.
Prior to entering, visitors receive a boarding pass with information about one of the actual passengers. I am the Rev. John Harper, traveling to America with my young daughter to begin a series of revival meetings in Chicago. At the end of the tour I’ll view the passenger manifest to discover my outcome.
Reluctantly, I board the ship, anxiously awaiting my fate. I gaze upon thousands of trinkets and treasures rescued from the Titanic since its remains were discovered 2.5 miles below the ocean’s surface 900 miles off the coast of New York in 1985.
I marvel at dioramas of first- and third-class cabins with recovered china settings, uncorked and still-full bottles of champagne, toiletries, jewelry, and clothing.
One of the most fascinating pieces is a chunk of ice the size and shape of a small whale. The display represents the iceberg that doomed the Titanic and simulates the temperature of the water that fateful night. At approximately 28 degrees Fahrenheit, the average person would survive less than 15 minutes in the water. I was able to hold my hand on the ice only a few moments, quickly understanding the horrific way most passengers would die.
As I complete the tour and nervously approach the passenger manifest I am struck by how many lessons from the Titanic can be applied to modern medicine.
We operate in a system surrounded by perilous obstacles in a huge vessel that is slow to change course even in the face of extreme danger and poor outcomes.
We steam along at unparalleled speed embracing new, relatively untested technologies, procedures, and medications. Modern healthcare, like the Titanic, values building technologically advanced, well-adorned vessels rather than investing in the basic infrastructure to make it safer. We eschew quality for appearance.
We spend money on heated indoor pools, squash courts, and Turkish baths rather than computerized provider order entry, bar code administration, and hand-off improvements. Despite all of this, our passengers trust the vessel is safe. They trust that we will protect them—that we have enough lifeboats.
The Rev. John Harper perished on April 14, 1912; unlike him, as I cross the threshold of the healthcare Titanic I am not filled with awe and excitement. I feel fear and dread. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver and Health Sciences Center, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Author’s note: More than 1,500 passengers died in the Titanic, a disaster that resonates nearly a hundred years later. The equivalent of about 50 Titanics capsize annually in U.S. hospitals, nearly one every week (based on the Institute of Medicine’s estimate of 44,000-98,000 deaths per year from hospital adverse events). As hospitalists, it is our obligation to ensure the hull is solid, the crow’s nest properly manned, and the ship is turning in the right direction.
I’m the Rev. John Harper, and it’s April 10, 1912.
As I grasp my boarding pass I can’t contain my awe and excitement. Imagine me aboard the world’s most luxurious cruise liner heading to America. Granted, I’m booked in second class. But as everyone knows, second class on the Titanic outstrips first class on most liners these days. It should—for $66 this is an expensive way to travel. Still, it’s less than the cheapest first-class ticket of $125 and much less than a $4,500 booking in the millionaire’s suite. I could buy several houses for $4,500.
Walking along the gangway I recall hearing that this ship—the largest ever built—weighs nearly 47,000 tons and cost $7.5 million. Outside my cabin door I encounter a fellow passenger who exults over the ship’s amenities. The liner has a heated indoor swimming pool, four electric elevators, two libraries, a Turkish bath, a squash court and gymnasium, and ample room to move about. The White Star Line has thoughtfully limited the amount of lifeboats to 20 to preserve precious deck space for passengers.
I’m Jeff Glasheen, and it’s Sept. 15, 2007.
As my wife prepares to deliver our first child in the coming weeks, we visit the labor and delivery deck of the hospital.
It will be our first major interaction with the healthcare system as patients. It’s the largest healthcare system ever and costs nearly $2 trillion a year to operate. We have chosen a new hospital that features an amazing array of amenities, including a birthing center with private suites, in-room baths with oversize soaking tubs, an in-room sleeping area for family and friends, and a DVD player and flat-screen television. There are even Internet connections.
Room service is available 24 hours a day, and the staff is top-notch. I’m told some choose to stay in the VIP suites for an extra $1,000 a night. This restricted-access area offers 600-square-foot rooms with original art on the walls, luxury mattresses and 350-thread count linens, complimentary robes and slippers, and an office area supplied with newspapers, a printer, fax, voicemail, and teleconferencing capabilities. There is a family room as well as a private refrigerator, an assortment of beverages and a dedicated chef. Unfortunately the cost is too steep, so we’ll spend this voyage in second class. However, as everyone knows, second class on this vessel outstrips first class in most hospitals these days.
Midnight, April 14, 1912
Something has gone wrong; the ship just hiccupped a bit. From my cabin I clearly hear a grinding that could happen only when two large objects come into contact. It’s strange, but I assure my bunkmates there is nothing to worry about. The Titanic is unsinkable, built with every feasible safety feature. The ship’s hull is made of inch-thick steel and held together with nearly 3 million steel rivets. In the unlikely event the hull is breached, the ship contains 15 watertight bulkheads to contain the leakage. Further, 3,560 life vests, 48 life buoys, and the aforementioned 20 lifeboats (four more than required by British law) allay my concerns.
On the off chance something should go wrong, the ship is outfitted with the recently developed Marconi wireless telegraph capable of communicating with any ship or shore within 500 miles.
5 p.m., Sept. 17, 2007
As I write this column I consider that something could go wrong during our hospital stay. The Institute of Medicine reports that medications harm 1.5 million people annually (400,000 incidents occur in the hospital) and that nearly 100,000 die annually in adverse hospital events.
I assure myself there is nothing to worry about. The hospital of today is unsinkable, built with every feasible safety measure. Today’s hospitals require two patient identifiers, time-outs before procedures, read-backs, standardized abbreviations, rules for reporting of critical results, standardized approaches to hand-offs, awareness of look-alike/sound-alike medications, hand-hygiene guidelines, medication reconciliation, core measures, quality and patient safety committees—and, on the off chance that something should go wrong, requirements for communicating sentinel event reviews with regulatory agencies.
1:30 a.m., April 14, 1912
The scuttlebutt is that the Titanic has hit an iceberg, tearing open the hull, flooding the bulkheads, and overcoming the ship’s pumps. Apparently the crow’s nest spotted the iceberg only 30 seconds before the impact. The crew tried to change course immediately. But the unprecedented size and speed of the ship (there is a rumor that the captain may have been trying to set a new trans-Atlantic crossing record) made it impossible to avoid our destiny.
We are clearly sinking. As I anxiously pace the deck waiting for a spot on a lifeboat, I chat with a crew member who assures me help is coming. The ship’s band plays on deck, the music soothing in the night air.
1 p.m., Aug. 26, 2007
I’m about halfway through the Titanic exhibit at the local museum of nature and science. The display is designed to give you the experience of being a passenger aboard the RMS Titanic.
Prior to entering, visitors receive a boarding pass with information about one of the actual passengers. I am the Rev. John Harper, traveling to America with my young daughter to begin a series of revival meetings in Chicago. At the end of the tour I’ll view the passenger manifest to discover my outcome.
Reluctantly, I board the ship, anxiously awaiting my fate. I gaze upon thousands of trinkets and treasures rescued from the Titanic since its remains were discovered 2.5 miles below the ocean’s surface 900 miles off the coast of New York in 1985.
I marvel at dioramas of first- and third-class cabins with recovered china settings, uncorked and still-full bottles of champagne, toiletries, jewelry, and clothing.
One of the most fascinating pieces is a chunk of ice the size and shape of a small whale. The display represents the iceberg that doomed the Titanic and simulates the temperature of the water that fateful night. At approximately 28 degrees Fahrenheit, the average person would survive less than 15 minutes in the water. I was able to hold my hand on the ice only a few moments, quickly understanding the horrific way most passengers would die.
As I complete the tour and nervously approach the passenger manifest I am struck by how many lessons from the Titanic can be applied to modern medicine.
We operate in a system surrounded by perilous obstacles in a huge vessel that is slow to change course even in the face of extreme danger and poor outcomes.
We steam along at unparalleled speed embracing new, relatively untested technologies, procedures, and medications. Modern healthcare, like the Titanic, values building technologically advanced, well-adorned vessels rather than investing in the basic infrastructure to make it safer. We eschew quality for appearance.
We spend money on heated indoor pools, squash courts, and Turkish baths rather than computerized provider order entry, bar code administration, and hand-off improvements. Despite all of this, our passengers trust the vessel is safe. They trust that we will protect them—that we have enough lifeboats.
The Rev. John Harper perished on April 14, 1912; unlike him, as I cross the threshold of the healthcare Titanic I am not filled with awe and excitement. I feel fear and dread. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver and Health Sciences Center, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Author’s note: More than 1,500 passengers died in the Titanic, a disaster that resonates nearly a hundred years later. The equivalent of about 50 Titanics capsize annually in U.S. hospitals, nearly one every week (based on the Institute of Medicine’s estimate of 44,000-98,000 deaths per year from hospital adverse events). As hospitalists, it is our obligation to ensure the hull is solid, the crow’s nest properly manned, and the ship is turning in the right direction.
I’m the Rev. John Harper, and it’s April 10, 1912.
As I grasp my boarding pass I can’t contain my awe and excitement. Imagine me aboard the world’s most luxurious cruise liner heading to America. Granted, I’m booked in second class. But as everyone knows, second class on the Titanic outstrips first class on most liners these days. It should—for $66 this is an expensive way to travel. Still, it’s less than the cheapest first-class ticket of $125 and much less than a $4,500 booking in the millionaire’s suite. I could buy several houses for $4,500.
Walking along the gangway I recall hearing that this ship—the largest ever built—weighs nearly 47,000 tons and cost $7.5 million. Outside my cabin door I encounter a fellow passenger who exults over the ship’s amenities. The liner has a heated indoor swimming pool, four electric elevators, two libraries, a Turkish bath, a squash court and gymnasium, and ample room to move about. The White Star Line has thoughtfully limited the amount of lifeboats to 20 to preserve precious deck space for passengers.
I’m Jeff Glasheen, and it’s Sept. 15, 2007.
As my wife prepares to deliver our first child in the coming weeks, we visit the labor and delivery deck of the hospital.
It will be our first major interaction with the healthcare system as patients. It’s the largest healthcare system ever and costs nearly $2 trillion a year to operate. We have chosen a new hospital that features an amazing array of amenities, including a birthing center with private suites, in-room baths with oversize soaking tubs, an in-room sleeping area for family and friends, and a DVD player and flat-screen television. There are even Internet connections.
Room service is available 24 hours a day, and the staff is top-notch. I’m told some choose to stay in the VIP suites for an extra $1,000 a night. This restricted-access area offers 600-square-foot rooms with original art on the walls, luxury mattresses and 350-thread count linens, complimentary robes and slippers, and an office area supplied with newspapers, a printer, fax, voicemail, and teleconferencing capabilities. There is a family room as well as a private refrigerator, an assortment of beverages and a dedicated chef. Unfortunately the cost is too steep, so we’ll spend this voyage in second class. However, as everyone knows, second class on this vessel outstrips first class in most hospitals these days.
Midnight, April 14, 1912
Something has gone wrong; the ship just hiccupped a bit. From my cabin I clearly hear a grinding that could happen only when two large objects come into contact. It’s strange, but I assure my bunkmates there is nothing to worry about. The Titanic is unsinkable, built with every feasible safety feature. The ship’s hull is made of inch-thick steel and held together with nearly 3 million steel rivets. In the unlikely event the hull is breached, the ship contains 15 watertight bulkheads to contain the leakage. Further, 3,560 life vests, 48 life buoys, and the aforementioned 20 lifeboats (four more than required by British law) allay my concerns.
On the off chance something should go wrong, the ship is outfitted with the recently developed Marconi wireless telegraph capable of communicating with any ship or shore within 500 miles.
5 p.m., Sept. 17, 2007
As I write this column I consider that something could go wrong during our hospital stay. The Institute of Medicine reports that medications harm 1.5 million people annually (400,000 incidents occur in the hospital) and that nearly 100,000 die annually in adverse hospital events.
I assure myself there is nothing to worry about. The hospital of today is unsinkable, built with every feasible safety measure. Today’s hospitals require two patient identifiers, time-outs before procedures, read-backs, standardized abbreviations, rules for reporting of critical results, standardized approaches to hand-offs, awareness of look-alike/sound-alike medications, hand-hygiene guidelines, medication reconciliation, core measures, quality and patient safety committees—and, on the off chance that something should go wrong, requirements for communicating sentinel event reviews with regulatory agencies.
1:30 a.m., April 14, 1912
The scuttlebutt is that the Titanic has hit an iceberg, tearing open the hull, flooding the bulkheads, and overcoming the ship’s pumps. Apparently the crow’s nest spotted the iceberg only 30 seconds before the impact. The crew tried to change course immediately. But the unprecedented size and speed of the ship (there is a rumor that the captain may have been trying to set a new trans-Atlantic crossing record) made it impossible to avoid our destiny.
We are clearly sinking. As I anxiously pace the deck waiting for a spot on a lifeboat, I chat with a crew member who assures me help is coming. The ship’s band plays on deck, the music soothing in the night air.
1 p.m., Aug. 26, 2007
I’m about halfway through the Titanic exhibit at the local museum of nature and science. The display is designed to give you the experience of being a passenger aboard the RMS Titanic.
Prior to entering, visitors receive a boarding pass with information about one of the actual passengers. I am the Rev. John Harper, traveling to America with my young daughter to begin a series of revival meetings in Chicago. At the end of the tour I’ll view the passenger manifest to discover my outcome.
Reluctantly, I board the ship, anxiously awaiting my fate. I gaze upon thousands of trinkets and treasures rescued from the Titanic since its remains were discovered 2.5 miles below the ocean’s surface 900 miles off the coast of New York in 1985.
I marvel at dioramas of first- and third-class cabins with recovered china settings, uncorked and still-full bottles of champagne, toiletries, jewelry, and clothing.
One of the most fascinating pieces is a chunk of ice the size and shape of a small whale. The display represents the iceberg that doomed the Titanic and simulates the temperature of the water that fateful night. At approximately 28 degrees Fahrenheit, the average person would survive less than 15 minutes in the water. I was able to hold my hand on the ice only a few moments, quickly understanding the horrific way most passengers would die.
As I complete the tour and nervously approach the passenger manifest I am struck by how many lessons from the Titanic can be applied to modern medicine.
We operate in a system surrounded by perilous obstacles in a huge vessel that is slow to change course even in the face of extreme danger and poor outcomes.
We steam along at unparalleled speed embracing new, relatively untested technologies, procedures, and medications. Modern healthcare, like the Titanic, values building technologically advanced, well-adorned vessels rather than investing in the basic infrastructure to make it safer. We eschew quality for appearance.
We spend money on heated indoor pools, squash courts, and Turkish baths rather than computerized provider order entry, bar code administration, and hand-off improvements. Despite all of this, our passengers trust the vessel is safe. They trust that we will protect them—that we have enough lifeboats.
The Rev. John Harper perished on April 14, 1912; unlike him, as I cross the threshold of the healthcare Titanic I am not filled with awe and excitement. I feel fear and dread. TH
Dr. Glasheen is associate professor of medicine at the University of Colorado at Denver and Health Sciences Center, where he serves as director of the Hospital Medicine Program and the Hospitalist Training Program, and as associate program director of the Internal Medicine Residency Program.
Where Loyalty Lies
The question that nearly stumped me came from the back of the room.
I was giving a presentation on the hospital medicine movement to 350 physicians with an organization interested in our rapidly developing specialty. The evolution of hospital medicine is a great story, and I relish telling it. My biggest problem is usually curbing my enthusiasm to fit the time allotted. As an old colleague once told me when I launched into an exhaustive explanation of a simple medical problem: “Rusty, don’t build the watch—just tell me the time!” For this talk, I behaved myself and had managed with 10 minutes to spare for questions.
Then came the question:
“With more than a third of hospitalists directly employed by the hospital I have concerns that the loyalty of the physician will be to the best interests of the institution instead of the patient, don’t you?”
It was certainly thought provoking. The questioner was asking if the source of a physician’s paycheck trumped patient needs. For many hospitalists, our employer is technically not the patient, but the hospital.
Some referring physicians, who put their patients in our care when they hospitalize them, wonder which master we serve. Can that hospitalist in charge of my patient resist the institutional pull to drive down length of stay (LOS) and curtail costs? Whose interests will that physician favor when there is a clash between what my patients might need and the hospital’s bottom line?
I could have simply said: “No, I’m not concerned. Physicians should always act in the interest of their patients over that of the hospital.” But the real answer is far more complex—a synthesis of complementary interests that can appear mutually exclusive.
How? While my response was somewhat less well organized than this column, I attempted to address the complexity of the question by including the profile of hospitalists’ employers, the obligations of the medical staff in any hospital, physician incentives, transparency of performance, checks and balances, and the general principle of managing polarities.
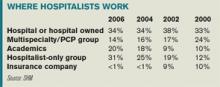
Let’s look at the scope of the issue. Who pays the hospitalist? A third are employed directly by hospitals, a fifth by academic medical centers, and nearly half by multispecialty or hospitalist-only medical groups. Two points emerge from the data. First, employment percentage by hospitals has remained stable, while academic centers and hospitalist-only groups have grown. Second, this employment model is not unique to hospitalists. These same types of practice groups and institutions employ physicians in other specialties, too.
All physicians working in a hospital are members of the active medical staff and must uphold certain core responsibilities. Chief among these are the quality and safety of care, treatment, and services delivered at the institution. That duty applies whether they are solo practitioners or employees of a hospital or independent medical group.
These core obligations are enforced by the organized medical staff through by-laws, rules, and regulations. Further, the medical staff is beholden to operate with the cooperation of hospital administration/management and hospital governance (i.e., the board) to support quality of care within the institution.
These elements are intended to provide a structure for optimizing patient care. But they often collide with the real world in which we physicians operate—a world of competing interests we face daily. While a physician’s fiduciary responsibility is always to the patient, there are often other interests to consider. Who among us has not tried to balance the often conflicting opinions and agendas of the:
- Patient;
- Caregivers/family;
- Hospital;
- Primary care physician;
- Consulting specialists; and
- Insurers.
These conflicts are usually over methods rather than outcomes. If hospitals want to cut LOS, so do patients, who want to sleep in their own beds. Hospitals want to manage costly and scarce resources wisely; patients want judicious use of treatments and tests. Hospitals want to keep costs down; patients want to keep out-of-pocket expenses down.
Are the loyalties of doctors to their patients sometimes at odds? The honest answer is, “Sometimes, yes.” Sometimes hospitals make providing care more challenging. Incentives affect how doctors behave. If bonuses accrue to good infection control, infection rates fall. If bonuses are aligned with keeping costs down, costs likely go down.
But such incentives play a role in how all doctors behave, not just hospitalists employed by a hospital. Self-employed physicians (hospitalists or otherwise) and members of a large medical practice group respond to incentives, as well.
One could argue these doctors might have a greater conflict of interest than hospital-based physicians. Think of the time pressures under which many physicians work, the complexity of the hospital environment, and the burden of paperwork.
Solo private practitioners whose only source of revenue is professional service fees may be inclined to keep patients in the hospital longer because that generates higher fees. They may also have a secondary agenda: Drive higher patient satisfaction by keeping patients in the hospital until they feel completely well, “protecting” them from hospital administrators who want to “prematurely” discharge them.
The real problem with incentives is aligning them with optimal care.
Once we establish that incentives are important, that their ultimate goal is optimal care, the next step is to create transparent, explicit performance criteria. There should be no mystery concerning which behaviors and outcomes physicians are expected to achieve, including those involving quality and safety. Finally, incentives need good checks and balances. There must be a good measurement system for desired performance and a method for keeping tabs to mitigate or eliminate unintended consequences.
All physicians must simultaneously manage the interests of the patient and the interests of the healthcare system—especially the hospital. When these goals are met, patient and system benefit by maximally utilizing precious resources such as inpatient beds, diagnostic and treatment technologies, and drugs. These resources are not limitless and should never be used without a great deal of critical thinking and consideration of alternatives.
There will always be tension between optimizing resources and treatment. Balancing these interests is not a problem to be solved, but a polarity to manage. Polarities are unsolvable because neither pole alone is the right answer. Focusing on one pole to the neglect of the other undermines our efforts to optimize patient needs and propagate a sustainable hospital care system. These alternatives are ongoing and interdependent and must be managed together.
To achieve the right balance, we must establish measures to alert us when one pole “tips” over the other. While I believe physicians, in the face of conflict of interests, must do what is right for the patient, it is also our duty to find ways to balance the interests of all involved. This is the key to a more sustainable, reliable, satisfying healthcare system—and to fulfilling our promise to monitor and self-govern the quality and safety of care we deliver. TH
Dr. Holman is president of SHM. He can be reached at [email protected]
The question that nearly stumped me came from the back of the room.
I was giving a presentation on the hospital medicine movement to 350 physicians with an organization interested in our rapidly developing specialty. The evolution of hospital medicine is a great story, and I relish telling it. My biggest problem is usually curbing my enthusiasm to fit the time allotted. As an old colleague once told me when I launched into an exhaustive explanation of a simple medical problem: “Rusty, don’t build the watch—just tell me the time!” For this talk, I behaved myself and had managed with 10 minutes to spare for questions.
Then came the question:
“With more than a third of hospitalists directly employed by the hospital I have concerns that the loyalty of the physician will be to the best interests of the institution instead of the patient, don’t you?”
It was certainly thought provoking. The questioner was asking if the source of a physician’s paycheck trumped patient needs. For many hospitalists, our employer is technically not the patient, but the hospital.
Some referring physicians, who put their patients in our care when they hospitalize them, wonder which master we serve. Can that hospitalist in charge of my patient resist the institutional pull to drive down length of stay (LOS) and curtail costs? Whose interests will that physician favor when there is a clash between what my patients might need and the hospital’s bottom line?
I could have simply said: “No, I’m not concerned. Physicians should always act in the interest of their patients over that of the hospital.” But the real answer is far more complex—a synthesis of complementary interests that can appear mutually exclusive.
How? While my response was somewhat less well organized than this column, I attempted to address the complexity of the question by including the profile of hospitalists’ employers, the obligations of the medical staff in any hospital, physician incentives, transparency of performance, checks and balances, and the general principle of managing polarities.
Let’s look at the scope of the issue. Who pays the hospitalist? A third are employed directly by hospitals, a fifth by academic medical centers, and nearly half by multispecialty or hospitalist-only medical groups. Two points emerge from the data. First, employment percentage by hospitals has remained stable, while academic centers and hospitalist-only groups have grown. Second, this employment model is not unique to hospitalists. These same types of practice groups and institutions employ physicians in other specialties, too.
All physicians working in a hospital are members of the active medical staff and must uphold certain core responsibilities. Chief among these are the quality and safety of care, treatment, and services delivered at the institution. That duty applies whether they are solo practitioners or employees of a hospital or independent medical group.
These core obligations are enforced by the organized medical staff through by-laws, rules, and regulations. Further, the medical staff is beholden to operate with the cooperation of hospital administration/management and hospital governance (i.e., the board) to support quality of care within the institution.
These elements are intended to provide a structure for optimizing patient care. But they often collide with the real world in which we physicians operate—a world of competing interests we face daily. While a physician’s fiduciary responsibility is always to the patient, there are often other interests to consider. Who among us has not tried to balance the often conflicting opinions and agendas of the:
- Patient;
- Caregivers/family;
- Hospital;
- Primary care physician;
- Consulting specialists; and
- Insurers.
These conflicts are usually over methods rather than outcomes. If hospitals want to cut LOS, so do patients, who want to sleep in their own beds. Hospitals want to manage costly and scarce resources wisely; patients want judicious use of treatments and tests. Hospitals want to keep costs down; patients want to keep out-of-pocket expenses down.
Are the loyalties of doctors to their patients sometimes at odds? The honest answer is, “Sometimes, yes.” Sometimes hospitals make providing care more challenging. Incentives affect how doctors behave. If bonuses accrue to good infection control, infection rates fall. If bonuses are aligned with keeping costs down, costs likely go down.
But such incentives play a role in how all doctors behave, not just hospitalists employed by a hospital. Self-employed physicians (hospitalists or otherwise) and members of a large medical practice group respond to incentives, as well.
One could argue these doctors might have a greater conflict of interest than hospital-based physicians. Think of the time pressures under which many physicians work, the complexity of the hospital environment, and the burden of paperwork.
Solo private practitioners whose only source of revenue is professional service fees may be inclined to keep patients in the hospital longer because that generates higher fees. They may also have a secondary agenda: Drive higher patient satisfaction by keeping patients in the hospital until they feel completely well, “protecting” them from hospital administrators who want to “prematurely” discharge them.
The real problem with incentives is aligning them with optimal care.
Once we establish that incentives are important, that their ultimate goal is optimal care, the next step is to create transparent, explicit performance criteria. There should be no mystery concerning which behaviors and outcomes physicians are expected to achieve, including those involving quality and safety. Finally, incentives need good checks and balances. There must be a good measurement system for desired performance and a method for keeping tabs to mitigate or eliminate unintended consequences.
All physicians must simultaneously manage the interests of the patient and the interests of the healthcare system—especially the hospital. When these goals are met, patient and system benefit by maximally utilizing precious resources such as inpatient beds, diagnostic and treatment technologies, and drugs. These resources are not limitless and should never be used without a great deal of critical thinking and consideration of alternatives.
There will always be tension between optimizing resources and treatment. Balancing these interests is not a problem to be solved, but a polarity to manage. Polarities are unsolvable because neither pole alone is the right answer. Focusing on one pole to the neglect of the other undermines our efforts to optimize patient needs and propagate a sustainable hospital care system. These alternatives are ongoing and interdependent and must be managed together.
To achieve the right balance, we must establish measures to alert us when one pole “tips” over the other. While I believe physicians, in the face of conflict of interests, must do what is right for the patient, it is also our duty to find ways to balance the interests of all involved. This is the key to a more sustainable, reliable, satisfying healthcare system—and to fulfilling our promise to monitor and self-govern the quality and safety of care we deliver. TH
Dr. Holman is president of SHM. He can be reached at [email protected]
The question that nearly stumped me came from the back of the room.
I was giving a presentation on the hospital medicine movement to 350 physicians with an organization interested in our rapidly developing specialty. The evolution of hospital medicine is a great story, and I relish telling it. My biggest problem is usually curbing my enthusiasm to fit the time allotted. As an old colleague once told me when I launched into an exhaustive explanation of a simple medical problem: “Rusty, don’t build the watch—just tell me the time!” For this talk, I behaved myself and had managed with 10 minutes to spare for questions.
Then came the question:
“With more than a third of hospitalists directly employed by the hospital I have concerns that the loyalty of the physician will be to the best interests of the institution instead of the patient, don’t you?”
It was certainly thought provoking. The questioner was asking if the source of a physician’s paycheck trumped patient needs. For many hospitalists, our employer is technically not the patient, but the hospital.
Some referring physicians, who put their patients in our care when they hospitalize them, wonder which master we serve. Can that hospitalist in charge of my patient resist the institutional pull to drive down length of stay (LOS) and curtail costs? Whose interests will that physician favor when there is a clash between what my patients might need and the hospital’s bottom line?
I could have simply said: “No, I’m not concerned. Physicians should always act in the interest of their patients over that of the hospital.” But the real answer is far more complex—a synthesis of complementary interests that can appear mutually exclusive.
How? While my response was somewhat less well organized than this column, I attempted to address the complexity of the question by including the profile of hospitalists’ employers, the obligations of the medical staff in any hospital, physician incentives, transparency of performance, checks and balances, and the general principle of managing polarities.
Let’s look at the scope of the issue. Who pays the hospitalist? A third are employed directly by hospitals, a fifth by academic medical centers, and nearly half by multispecialty or hospitalist-only medical groups. Two points emerge from the data. First, employment percentage by hospitals has remained stable, while academic centers and hospitalist-only groups have grown. Second, this employment model is not unique to hospitalists. These same types of practice groups and institutions employ physicians in other specialties, too.
All physicians working in a hospital are members of the active medical staff and must uphold certain core responsibilities. Chief among these are the quality and safety of care, treatment, and services delivered at the institution. That duty applies whether they are solo practitioners or employees of a hospital or independent medical group.
These core obligations are enforced by the organized medical staff through by-laws, rules, and regulations. Further, the medical staff is beholden to operate with the cooperation of hospital administration/management and hospital governance (i.e., the board) to support quality of care within the institution.
These elements are intended to provide a structure for optimizing patient care. But they often collide with the real world in which we physicians operate—a world of competing interests we face daily. While a physician’s fiduciary responsibility is always to the patient, there are often other interests to consider. Who among us has not tried to balance the often conflicting opinions and agendas of the:
- Patient;
- Caregivers/family;
- Hospital;
- Primary care physician;
- Consulting specialists; and
- Insurers.
These conflicts are usually over methods rather than outcomes. If hospitals want to cut LOS, so do patients, who want to sleep in their own beds. Hospitals want to manage costly and scarce resources wisely; patients want judicious use of treatments and tests. Hospitals want to keep costs down; patients want to keep out-of-pocket expenses down.
Are the loyalties of doctors to their patients sometimes at odds? The honest answer is, “Sometimes, yes.” Sometimes hospitals make providing care more challenging. Incentives affect how doctors behave. If bonuses accrue to good infection control, infection rates fall. If bonuses are aligned with keeping costs down, costs likely go down.
But such incentives play a role in how all doctors behave, not just hospitalists employed by a hospital. Self-employed physicians (hospitalists or otherwise) and members of a large medical practice group respond to incentives, as well.
One could argue these doctors might have a greater conflict of interest than hospital-based physicians. Think of the time pressures under which many physicians work, the complexity of the hospital environment, and the burden of paperwork.
Solo private practitioners whose only source of revenue is professional service fees may be inclined to keep patients in the hospital longer because that generates higher fees. They may also have a secondary agenda: Drive higher patient satisfaction by keeping patients in the hospital until they feel completely well, “protecting” them from hospital administrators who want to “prematurely” discharge them.
The real problem with incentives is aligning them with optimal care.
Once we establish that incentives are important, that their ultimate goal is optimal care, the next step is to create transparent, explicit performance criteria. There should be no mystery concerning which behaviors and outcomes physicians are expected to achieve, including those involving quality and safety. Finally, incentives need good checks and balances. There must be a good measurement system for desired performance and a method for keeping tabs to mitigate or eliminate unintended consequences.
All physicians must simultaneously manage the interests of the patient and the interests of the healthcare system—especially the hospital. When these goals are met, patient and system benefit by maximally utilizing precious resources such as inpatient beds, diagnostic and treatment technologies, and drugs. These resources are not limitless and should never be used without a great deal of critical thinking and consideration of alternatives.
There will always be tension between optimizing resources and treatment. Balancing these interests is not a problem to be solved, but a polarity to manage. Polarities are unsolvable because neither pole alone is the right answer. Focusing on one pole to the neglect of the other undermines our efforts to optimize patient needs and propagate a sustainable hospital care system. These alternatives are ongoing and interdependent and must be managed together.
To achieve the right balance, we must establish measures to alert us when one pole “tips” over the other. While I believe physicians, in the face of conflict of interests, must do what is right for the patient, it is also our duty to find ways to balance the interests of all involved. This is the key to a more sustainable, reliable, satisfying healthcare system—and to fulfilling our promise to monitor and self-govern the quality and safety of care we deliver. TH
Dr. Holman is president of SHM. He can be reached at [email protected]
The Hospitalist as Teacher
In addition to being expert in acute care clinical issues, hospitalists are knowledgeable in the ways and means of the hospital.
As teachers, hospitalists are ideally situated to improve house staff’s proficiency in areas such as evidence-based medicine, effective teamwork, communication, and quality improvement.1 These areas meld with hospitalist core competencies, writes David M. Pressel, MD, PhD, director of Inpatient Service and General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del.
What makes a great hospitalist a great teacher? “I don’t think there is anything special about a hospitalist [that would make him or her] a great teacher as opposed to another kind of physician,” Dr. Pressel says. “The only caveat to that is that presumably the hospitalist has specialized knowledge that they can impart similarly to [how] another doc can [impart information] in their specialized knowledge.”
Good teaching in all specialties has the same core features. But the key component a hospitalist would want to impart, he says, is that the hospitalist should maintain a holistic view of the patient.
In Dr. Pressel’s view, a great teacher loves what he does, has a sense of humor and makes learning fun or enjoyable, makes his lessons interactive, continually learns alongside his students, and knows his strengths and weaknesses.
“A great teacher has a sense of self-awareness as to what they do well and what they don’t do well,” he says. “Some people can be dynamic speakers for a mass audience and hold a lecture hall of 200 in thrall, but one on one, they’re not that strong. Others are the opposite. It is easy to teach people who are smart, dynamic, and interested; it is more challenging for someone who is a bit slower and [finds it] harder to get it.”
A good teacher also models for his trainees, especially in more delicate conversations, such as when giving bad news or asking patients and families to make difficult decisions.
“Residents should be watching you have those kinds of conversations,” says Howard Epstein, MD, a hospitalist and the medical director of the palliative care program at Regions Hospital, St. Paul, Minn. “[Rather than saying], ‘I’m just going to go have a family conference so why don’t you go take care of this, that, and the other thing,’ we should be saying, ‘This is really important. You need to come in and watch me do this now. This is just as important as putting in those discharge orders or putting in that central line.’ ”
Teach versus Coach
Jeffery G. Wiese, MD, associate professor of medicine at Tulane University in New Orleans, has thought a lot about what makes a great teacher and the differences between teaching information and teaching skills. To him it is the difference between teaching and coaching.
Dr. Wiese, who is on SHM’s board of directors, believes medical education is less about the dissemination of knowledge and more about how to apply that knowledge.
“Dissemination of knowledge is requisite but not sufficient,” says Dr. Wiese. “Clinical education is about performance because ultimately it doesn’t matter if the student knows a lot if he or she can’t put it in act for the benefit of their patient. And when you change that paradigm, then you move from being a good teacher to being a great coach.”
Dr. Wiese, who is also director of the Internal Medicine Residency Program and the chief of medicine at Tulane, presented a workshop at the SHM’s annual meeting in May, titled “Great Hospitalist to Great Teacher: Clinical Coaching.”
The five main points of the presentation are represented by the mnemonic VACUM: visualization, anticipation, choosing content that has utility, and motivation.
Visualization
Great teachers empower trainees to visualize how they will use the skill or knowledge for the benefit of the patient. The average lecture on hypotension, for example, disseminates the causes of hypotension and the treatment for each. The great coaching session, however, begins with getting the student to visualize using the skill. “Picture this: You are awakened from sleep on call to see a hypotensive patient,” Dr. Wiese says. “Do you see yourself in the room? Do you see the panic, the fear of those around you? Now visualize feeling the warmth of the patient’s extremities to exclude causes of low vascular resistance. Now imagine feeling the pulse to exclude bradycardia. Are you there? Now see yourself lowering the head of the bed and starting the IV to increase his preload.” The vision makes the content stick in the student’s memory.
Anticipation
“It’s not enough to teach a trainee how to do the skill,” says Dr. Wiese. “You have to anticipate where the trainee is going to get it confused and where the pitfalls are going to be in performing that skill down the road.”
This concept is analogous to that of someone giving directions to their house. Merely giving the student the destination (i.e., what they need to know) is not sufficient. Providing a heads up on where they might take a wrong turn ensures that they arrive at the destination.
In teaching hyperosmolar nonketotic coma (HONKC), for example, a great coach will begin with the warning: “Listen, this is where you could get confused. You might be tempted to ascribe a patient’s delirium to the osmotic effects of the high glucose, and while this can happen, it does not happen with a serum osmolarity of less than 340. You could forget that the cortisol surge that comes from infection is the leading cause of HONKC. Do you see yourself in the emergency department with that patient with HONKC? OK, when it happens, make sure you check the osmolarity; if it’s less than 340, do the lumbar puncture. Meningitis may just be the cause of the delirium and the infection that has caused the HONKC.”
—Jeffery G. Wiese, MD, associate professor of medicine, Tulane University Health Sciences Center, New Orleans
Content With Utility
Teaching the oppressive details about a disease beyond what the student learns from textbooks probably does not have the same utility for them as learning the fundamental principles of how to diagnose, treat, and prognosticate a disease, says Dr. Wiese.
Although most hospitalists train in internal medicine, with a lesser number training in pediatrics or family practice, all hospitalist instructors are still responsible for all students—including those who may be headed for radiology or orthopedics, for instance.
“I can teach the medical content that is of utility to that student’s performance,” Dr. Wiese says, “and I still share responsibility for their performance as an orthopedic surgeon, particularly with respect to how they manage medical disease.” The important lesson is that utility is defined by the learner. “If my student has chosen a future career in orthopedics, the content of the lectures will shift away from high-end internal medicine topics and toward what I think the future orthopedist before me needs to know.”
Motivation
“Should we have to motivate students to be great physicians both professionally and in terms of patient care and knowledge competence?” asks Dr. Wiese. “At the end of the day, the answer should be no; everyone has responsibility for motivating themselves. But, like a great coach, it is still the coach’s responsibly to ensure that when the players are tired, when they’re hungry, when they’ve got other things on their mind, they will stay motivated to want to learn the skill—even before we begin to teach the skill.
“A big portion of that motivation comes from figuring out what their career goals are and helping to link the medical knowledge or the skill that you’re teaching to those hooks, those things that are going to be of interest to them.”
There are four key components to motivation, says Dr. Wiese.
“First, remember the student’s name and use it often,” he says. “Remember that they will not care what you know, until they know that you care. Second, be physical. Reach out with the handshake or pat on the shoulder when things get done correctly. Third, stay focused on their hooks: Couch all content in terms of how they will use it in their future careers, and focus your analogies on their personal interests. For example, if a student likes music, my teaching of heart murmurs is going to use analogies of the song writer and performer.”
Game Time
“The medical knowledge is analogous to the play that the team will run or the skill of throwing the ball, but [there are a lot of other factors that influence what’s needed for] the game-time scenario,” Dr. Wiese says. “It’s how you interact with the clock for the game, how you interact with the referees, how you interact with your team mates, how you interact against the defense.”
To teach in order to prepare your “players” for the realities of the challenge—or the challenges of reality, as the case may be—teachers need to do more than unwittingly repeat the methods used when they were students.
“A student who is learning about a disease from Harrison’s or Cecil’s [textbooks] can focus on all the details and knowledge they need to know,” says Dr. Wiese. “But the thing that they can’t get out of the book and that they really need from the hospitalist coach is all that game-time instruction.”
In other words, hospitalists must consider with their students how to integrate their knowledge into their interactions with the hospital system.
In this era of PDAs, wireless networking, and access to the Internet, hospitalists are way past the point of having to keep all their acquired information in their heads, Dr. Wiese says. “The issue now is how do you ask the right questions and then access that knowledge—and then more importantly, how do you take that knowledge and put it into the ‘play’ that is the patient?” And that is what a student can’t get out of a book, he says—and what they need to get from their coach.
Be an Agent for Change
Don’t automatically transfer the way you learned or the ways you were taught into how you teach your own students. “Learning and teaching are very different,” says Dr. Wiese. “Learning knowledge is focused on the details. Teaching is much more [about] how you put that knowledge into play.”
That kind of transference is easily recognizable in a situation where a student asks “Can you teach me something this afternoon?” and the hospitalist replies, “Well, let me go home tonight and prepare, and then I’ll teach you.”
“What they’re saying is, ‘Let me read up, make a list of facts—maybe worse, maybe put it in PowerPoint,’ ” says Dr. Wiese. “The student could have done that on his or her own.”
Because hospitalists are intimately familiar with the hospital system, they serve as agents of change, Dr. Wiese says.
“Hospitalists are the key group at the first level of being able to take a student or resident or fellow and say, ‘These are the patients, we’re on hospital wards, and let me show you how to put in action the knowledge and skills you have to make a success for your patients,’ ” he says.
Hospitalists know where the system doesn’t work. “The great hospitalist doesn’t [face a problem and think], ‘Oh, woe is me; I’m hopelessly at the whim of the system that is broken,” says Dr. Wiese. “A great hospitalist consistently looks at [the situation] and asks, ‘How can I improve this system?’ The only way that medical students and residents can move out of the helpless role where [they see themselves as] servants of the system is to have hospitalist teachers who have a perspective of themselves as owners and who take responsibility for improving the system. Nothing has to be the way that it is,” says Dr. Wiese. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Pressel DM. Hospitalists in medical education: coming to an academic medical center near you. J Natl Med Assoc. 2006 Sep;98(9):1501-1504.
In addition to being expert in acute care clinical issues, hospitalists are knowledgeable in the ways and means of the hospital.
As teachers, hospitalists are ideally situated to improve house staff’s proficiency in areas such as evidence-based medicine, effective teamwork, communication, and quality improvement.1 These areas meld with hospitalist core competencies, writes David M. Pressel, MD, PhD, director of Inpatient Service and General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del.
What makes a great hospitalist a great teacher? “I don’t think there is anything special about a hospitalist [that would make him or her] a great teacher as opposed to another kind of physician,” Dr. Pressel says. “The only caveat to that is that presumably the hospitalist has specialized knowledge that they can impart similarly to [how] another doc can [impart information] in their specialized knowledge.”
Good teaching in all specialties has the same core features. But the key component a hospitalist would want to impart, he says, is that the hospitalist should maintain a holistic view of the patient.
In Dr. Pressel’s view, a great teacher loves what he does, has a sense of humor and makes learning fun or enjoyable, makes his lessons interactive, continually learns alongside his students, and knows his strengths and weaknesses.
“A great teacher has a sense of self-awareness as to what they do well and what they don’t do well,” he says. “Some people can be dynamic speakers for a mass audience and hold a lecture hall of 200 in thrall, but one on one, they’re not that strong. Others are the opposite. It is easy to teach people who are smart, dynamic, and interested; it is more challenging for someone who is a bit slower and [finds it] harder to get it.”
A good teacher also models for his trainees, especially in more delicate conversations, such as when giving bad news or asking patients and families to make difficult decisions.
“Residents should be watching you have those kinds of conversations,” says Howard Epstein, MD, a hospitalist and the medical director of the palliative care program at Regions Hospital, St. Paul, Minn. “[Rather than saying], ‘I’m just going to go have a family conference so why don’t you go take care of this, that, and the other thing,’ we should be saying, ‘This is really important. You need to come in and watch me do this now. This is just as important as putting in those discharge orders or putting in that central line.’ ”
Teach versus Coach
Jeffery G. Wiese, MD, associate professor of medicine at Tulane University in New Orleans, has thought a lot about what makes a great teacher and the differences between teaching information and teaching skills. To him it is the difference between teaching and coaching.
Dr. Wiese, who is on SHM’s board of directors, believes medical education is less about the dissemination of knowledge and more about how to apply that knowledge.
“Dissemination of knowledge is requisite but not sufficient,” says Dr. Wiese. “Clinical education is about performance because ultimately it doesn’t matter if the student knows a lot if he or she can’t put it in act for the benefit of their patient. And when you change that paradigm, then you move from being a good teacher to being a great coach.”
Dr. Wiese, who is also director of the Internal Medicine Residency Program and the chief of medicine at Tulane, presented a workshop at the SHM’s annual meeting in May, titled “Great Hospitalist to Great Teacher: Clinical Coaching.”
The five main points of the presentation are represented by the mnemonic VACUM: visualization, anticipation, choosing content that has utility, and motivation.
Visualization
Great teachers empower trainees to visualize how they will use the skill or knowledge for the benefit of the patient. The average lecture on hypotension, for example, disseminates the causes of hypotension and the treatment for each. The great coaching session, however, begins with getting the student to visualize using the skill. “Picture this: You are awakened from sleep on call to see a hypotensive patient,” Dr. Wiese says. “Do you see yourself in the room? Do you see the panic, the fear of those around you? Now visualize feeling the warmth of the patient’s extremities to exclude causes of low vascular resistance. Now imagine feeling the pulse to exclude bradycardia. Are you there? Now see yourself lowering the head of the bed and starting the IV to increase his preload.” The vision makes the content stick in the student’s memory.
Anticipation
“It’s not enough to teach a trainee how to do the skill,” says Dr. Wiese. “You have to anticipate where the trainee is going to get it confused and where the pitfalls are going to be in performing that skill down the road.”
This concept is analogous to that of someone giving directions to their house. Merely giving the student the destination (i.e., what they need to know) is not sufficient. Providing a heads up on where they might take a wrong turn ensures that they arrive at the destination.
In teaching hyperosmolar nonketotic coma (HONKC), for example, a great coach will begin with the warning: “Listen, this is where you could get confused. You might be tempted to ascribe a patient’s delirium to the osmotic effects of the high glucose, and while this can happen, it does not happen with a serum osmolarity of less than 340. You could forget that the cortisol surge that comes from infection is the leading cause of HONKC. Do you see yourself in the emergency department with that patient with HONKC? OK, when it happens, make sure you check the osmolarity; if it’s less than 340, do the lumbar puncture. Meningitis may just be the cause of the delirium and the infection that has caused the HONKC.”
—Jeffery G. Wiese, MD, associate professor of medicine, Tulane University Health Sciences Center, New Orleans
Content With Utility
Teaching the oppressive details about a disease beyond what the student learns from textbooks probably does not have the same utility for them as learning the fundamental principles of how to diagnose, treat, and prognosticate a disease, says Dr. Wiese.
Although most hospitalists train in internal medicine, with a lesser number training in pediatrics or family practice, all hospitalist instructors are still responsible for all students—including those who may be headed for radiology or orthopedics, for instance.
“I can teach the medical content that is of utility to that student’s performance,” Dr. Wiese says, “and I still share responsibility for their performance as an orthopedic surgeon, particularly with respect to how they manage medical disease.” The important lesson is that utility is defined by the learner. “If my student has chosen a future career in orthopedics, the content of the lectures will shift away from high-end internal medicine topics and toward what I think the future orthopedist before me needs to know.”
Motivation
“Should we have to motivate students to be great physicians both professionally and in terms of patient care and knowledge competence?” asks Dr. Wiese. “At the end of the day, the answer should be no; everyone has responsibility for motivating themselves. But, like a great coach, it is still the coach’s responsibly to ensure that when the players are tired, when they’re hungry, when they’ve got other things on their mind, they will stay motivated to want to learn the skill—even before we begin to teach the skill.
“A big portion of that motivation comes from figuring out what their career goals are and helping to link the medical knowledge or the skill that you’re teaching to those hooks, those things that are going to be of interest to them.”
There are four key components to motivation, says Dr. Wiese.
“First, remember the student’s name and use it often,” he says. “Remember that they will not care what you know, until they know that you care. Second, be physical. Reach out with the handshake or pat on the shoulder when things get done correctly. Third, stay focused on their hooks: Couch all content in terms of how they will use it in their future careers, and focus your analogies on their personal interests. For example, if a student likes music, my teaching of heart murmurs is going to use analogies of the song writer and performer.”
Game Time
“The medical knowledge is analogous to the play that the team will run or the skill of throwing the ball, but [there are a lot of other factors that influence what’s needed for] the game-time scenario,” Dr. Wiese says. “It’s how you interact with the clock for the game, how you interact with the referees, how you interact with your team mates, how you interact against the defense.”
To teach in order to prepare your “players” for the realities of the challenge—or the challenges of reality, as the case may be—teachers need to do more than unwittingly repeat the methods used when they were students.
“A student who is learning about a disease from Harrison’s or Cecil’s [textbooks] can focus on all the details and knowledge they need to know,” says Dr. Wiese. “But the thing that they can’t get out of the book and that they really need from the hospitalist coach is all that game-time instruction.”
In other words, hospitalists must consider with their students how to integrate their knowledge into their interactions with the hospital system.
In this era of PDAs, wireless networking, and access to the Internet, hospitalists are way past the point of having to keep all their acquired information in their heads, Dr. Wiese says. “The issue now is how do you ask the right questions and then access that knowledge—and then more importantly, how do you take that knowledge and put it into the ‘play’ that is the patient?” And that is what a student can’t get out of a book, he says—and what they need to get from their coach.
Be an Agent for Change
Don’t automatically transfer the way you learned or the ways you were taught into how you teach your own students. “Learning and teaching are very different,” says Dr. Wiese. “Learning knowledge is focused on the details. Teaching is much more [about] how you put that knowledge into play.”
That kind of transference is easily recognizable in a situation where a student asks “Can you teach me something this afternoon?” and the hospitalist replies, “Well, let me go home tonight and prepare, and then I’ll teach you.”
“What they’re saying is, ‘Let me read up, make a list of facts—maybe worse, maybe put it in PowerPoint,’ ” says Dr. Wiese. “The student could have done that on his or her own.”
Because hospitalists are intimately familiar with the hospital system, they serve as agents of change, Dr. Wiese says.
“Hospitalists are the key group at the first level of being able to take a student or resident or fellow and say, ‘These are the patients, we’re on hospital wards, and let me show you how to put in action the knowledge and skills you have to make a success for your patients,’ ” he says.
Hospitalists know where the system doesn’t work. “The great hospitalist doesn’t [face a problem and think], ‘Oh, woe is me; I’m hopelessly at the whim of the system that is broken,” says Dr. Wiese. “A great hospitalist consistently looks at [the situation] and asks, ‘How can I improve this system?’ The only way that medical students and residents can move out of the helpless role where [they see themselves as] servants of the system is to have hospitalist teachers who have a perspective of themselves as owners and who take responsibility for improving the system. Nothing has to be the way that it is,” says Dr. Wiese. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Pressel DM. Hospitalists in medical education: coming to an academic medical center near you. J Natl Med Assoc. 2006 Sep;98(9):1501-1504.
In addition to being expert in acute care clinical issues, hospitalists are knowledgeable in the ways and means of the hospital.
As teachers, hospitalists are ideally situated to improve house staff’s proficiency in areas such as evidence-based medicine, effective teamwork, communication, and quality improvement.1 These areas meld with hospitalist core competencies, writes David M. Pressel, MD, PhD, director of Inpatient Service and General Pediatrics at Alfred I. duPont Hospital for Children in Wilmington, Del.
What makes a great hospitalist a great teacher? “I don’t think there is anything special about a hospitalist [that would make him or her] a great teacher as opposed to another kind of physician,” Dr. Pressel says. “The only caveat to that is that presumably the hospitalist has specialized knowledge that they can impart similarly to [how] another doc can [impart information] in their specialized knowledge.”
Good teaching in all specialties has the same core features. But the key component a hospitalist would want to impart, he says, is that the hospitalist should maintain a holistic view of the patient.
In Dr. Pressel’s view, a great teacher loves what he does, has a sense of humor and makes learning fun or enjoyable, makes his lessons interactive, continually learns alongside his students, and knows his strengths and weaknesses.
“A great teacher has a sense of self-awareness as to what they do well and what they don’t do well,” he says. “Some people can be dynamic speakers for a mass audience and hold a lecture hall of 200 in thrall, but one on one, they’re not that strong. Others are the opposite. It is easy to teach people who are smart, dynamic, and interested; it is more challenging for someone who is a bit slower and [finds it] harder to get it.”
A good teacher also models for his trainees, especially in more delicate conversations, such as when giving bad news or asking patients and families to make difficult decisions.
“Residents should be watching you have those kinds of conversations,” says Howard Epstein, MD, a hospitalist and the medical director of the palliative care program at Regions Hospital, St. Paul, Minn. “[Rather than saying], ‘I’m just going to go have a family conference so why don’t you go take care of this, that, and the other thing,’ we should be saying, ‘This is really important. You need to come in and watch me do this now. This is just as important as putting in those discharge orders or putting in that central line.’ ”
Teach versus Coach
Jeffery G. Wiese, MD, associate professor of medicine at Tulane University in New Orleans, has thought a lot about what makes a great teacher and the differences between teaching information and teaching skills. To him it is the difference between teaching and coaching.
Dr. Wiese, who is on SHM’s board of directors, believes medical education is less about the dissemination of knowledge and more about how to apply that knowledge.
“Dissemination of knowledge is requisite but not sufficient,” says Dr. Wiese. “Clinical education is about performance because ultimately it doesn’t matter if the student knows a lot if he or she can’t put it in act for the benefit of their patient. And when you change that paradigm, then you move from being a good teacher to being a great coach.”
Dr. Wiese, who is also director of the Internal Medicine Residency Program and the chief of medicine at Tulane, presented a workshop at the SHM’s annual meeting in May, titled “Great Hospitalist to Great Teacher: Clinical Coaching.”
The five main points of the presentation are represented by the mnemonic VACUM: visualization, anticipation, choosing content that has utility, and motivation.
Visualization
Great teachers empower trainees to visualize how they will use the skill or knowledge for the benefit of the patient. The average lecture on hypotension, for example, disseminates the causes of hypotension and the treatment for each. The great coaching session, however, begins with getting the student to visualize using the skill. “Picture this: You are awakened from sleep on call to see a hypotensive patient,” Dr. Wiese says. “Do you see yourself in the room? Do you see the panic, the fear of those around you? Now visualize feeling the warmth of the patient’s extremities to exclude causes of low vascular resistance. Now imagine feeling the pulse to exclude bradycardia. Are you there? Now see yourself lowering the head of the bed and starting the IV to increase his preload.” The vision makes the content stick in the student’s memory.
Anticipation
“It’s not enough to teach a trainee how to do the skill,” says Dr. Wiese. “You have to anticipate where the trainee is going to get it confused and where the pitfalls are going to be in performing that skill down the road.”
This concept is analogous to that of someone giving directions to their house. Merely giving the student the destination (i.e., what they need to know) is not sufficient. Providing a heads up on where they might take a wrong turn ensures that they arrive at the destination.
In teaching hyperosmolar nonketotic coma (HONKC), for example, a great coach will begin with the warning: “Listen, this is where you could get confused. You might be tempted to ascribe a patient’s delirium to the osmotic effects of the high glucose, and while this can happen, it does not happen with a serum osmolarity of less than 340. You could forget that the cortisol surge that comes from infection is the leading cause of HONKC. Do you see yourself in the emergency department with that patient with HONKC? OK, when it happens, make sure you check the osmolarity; if it’s less than 340, do the lumbar puncture. Meningitis may just be the cause of the delirium and the infection that has caused the HONKC.”
—Jeffery G. Wiese, MD, associate professor of medicine, Tulane University Health Sciences Center, New Orleans
Content With Utility
Teaching the oppressive details about a disease beyond what the student learns from textbooks probably does not have the same utility for them as learning the fundamental principles of how to diagnose, treat, and prognosticate a disease, says Dr. Wiese.
Although most hospitalists train in internal medicine, with a lesser number training in pediatrics or family practice, all hospitalist instructors are still responsible for all students—including those who may be headed for radiology or orthopedics, for instance.
“I can teach the medical content that is of utility to that student’s performance,” Dr. Wiese says, “and I still share responsibility for their performance as an orthopedic surgeon, particularly with respect to how they manage medical disease.” The important lesson is that utility is defined by the learner. “If my student has chosen a future career in orthopedics, the content of the lectures will shift away from high-end internal medicine topics and toward what I think the future orthopedist before me needs to know.”
Motivation
“Should we have to motivate students to be great physicians both professionally and in terms of patient care and knowledge competence?” asks Dr. Wiese. “At the end of the day, the answer should be no; everyone has responsibility for motivating themselves. But, like a great coach, it is still the coach’s responsibly to ensure that when the players are tired, when they’re hungry, when they’ve got other things on their mind, they will stay motivated to want to learn the skill—even before we begin to teach the skill.
“A big portion of that motivation comes from figuring out what their career goals are and helping to link the medical knowledge or the skill that you’re teaching to those hooks, those things that are going to be of interest to them.”
There are four key components to motivation, says Dr. Wiese.
“First, remember the student’s name and use it often,” he says. “Remember that they will not care what you know, until they know that you care. Second, be physical. Reach out with the handshake or pat on the shoulder when things get done correctly. Third, stay focused on their hooks: Couch all content in terms of how they will use it in their future careers, and focus your analogies on their personal interests. For example, if a student likes music, my teaching of heart murmurs is going to use analogies of the song writer and performer.”
Game Time
“The medical knowledge is analogous to the play that the team will run or the skill of throwing the ball, but [there are a lot of other factors that influence what’s needed for] the game-time scenario,” Dr. Wiese says. “It’s how you interact with the clock for the game, how you interact with the referees, how you interact with your team mates, how you interact against the defense.”
To teach in order to prepare your “players” for the realities of the challenge—or the challenges of reality, as the case may be—teachers need to do more than unwittingly repeat the methods used when they were students.
“A student who is learning about a disease from Harrison’s or Cecil’s [textbooks] can focus on all the details and knowledge they need to know,” says Dr. Wiese. “But the thing that they can’t get out of the book and that they really need from the hospitalist coach is all that game-time instruction.”
In other words, hospitalists must consider with their students how to integrate their knowledge into their interactions with the hospital system.
In this era of PDAs, wireless networking, and access to the Internet, hospitalists are way past the point of having to keep all their acquired information in their heads, Dr. Wiese says. “The issue now is how do you ask the right questions and then access that knowledge—and then more importantly, how do you take that knowledge and put it into the ‘play’ that is the patient?” And that is what a student can’t get out of a book, he says—and what they need to get from their coach.
Be an Agent for Change
Don’t automatically transfer the way you learned or the ways you were taught into how you teach your own students. “Learning and teaching are very different,” says Dr. Wiese. “Learning knowledge is focused on the details. Teaching is much more [about] how you put that knowledge into play.”
That kind of transference is easily recognizable in a situation where a student asks “Can you teach me something this afternoon?” and the hospitalist replies, “Well, let me go home tonight and prepare, and then I’ll teach you.”
“What they’re saying is, ‘Let me read up, make a list of facts—maybe worse, maybe put it in PowerPoint,’ ” says Dr. Wiese. “The student could have done that on his or her own.”
Because hospitalists are intimately familiar with the hospital system, they serve as agents of change, Dr. Wiese says.
“Hospitalists are the key group at the first level of being able to take a student or resident or fellow and say, ‘These are the patients, we’re on hospital wards, and let me show you how to put in action the knowledge and skills you have to make a success for your patients,’ ” he says.
Hospitalists know where the system doesn’t work. “The great hospitalist doesn’t [face a problem and think], ‘Oh, woe is me; I’m hopelessly at the whim of the system that is broken,” says Dr. Wiese. “A great hospitalist consistently looks at [the situation] and asks, ‘How can I improve this system?’ The only way that medical students and residents can move out of the helpless role where [they see themselves as] servants of the system is to have hospitalist teachers who have a perspective of themselves as owners and who take responsibility for improving the system. Nothing has to be the way that it is,” says Dr. Wiese. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Pressel DM. Hospitalists in medical education: coming to an academic medical center near you. J Natl Med Assoc. 2006 Sep;98(9):1501-1504.
Transition Talk
Charles A. Crecelius, MD, of Saint Louis, has experienced best- and worst-case scenarios when his frail elderly patients have been admitted and discharged by local hospitalists.
Best case, he says: “My patient is admitted. I get a call. I’m told what is going on. I’m notified of meaningful changes, and at discharge, I get another call [from the hospitalist].”
But there are wide variations in hospitalist/nursing home relationships, notes Dr. Crecelius, a long-term care physician and president-elect of the American Medical Director’s Association (AMDA).
This was brought home by the case of a patient with a well-documented history of dystonic reaction to toxic lithium levels. The patient was later misdiagnosed as having tardive dyskinesia, a movement disorder. Her much-needed medication was discontinued, and the hospital transferred the patient back to the nursing home in worse condition than before.
“We wasted an entire hospitalization,” Dr. Crecelius recalls ruefully.
The above scenario underscores the importance of a thorough transfer of information when elderly patients move from facility to facility. Interaction between hospitalists and nursing home staff will become increasingly important in light of the growing frail elderly population and the Joint Commission on Accreditation of Health Care Organization’s (JCAHO) push for improved discharge communications.1
By applying a customer service model and continually upgrading transfer documentation, hospital medicine groups can “keep the level of communication where it needs to be,” says Susan S. Cumming, MD, associate medical director of Marin Hospitalist Medical Group at Marin General Hospital in Greenbrae, Calif.
Running a Risk
Dan Osterweil, MD, CMD, is familiar with the hospitalist model through his medical training in Israel during the late 1970s and early 1980s. Hospitalists there routinely handled inpatient care.
Dr. Osterweil, a clinical professor of medicine/geriatric medicine at UCLA, research associate with the UCLA Borun Center for Gerontological Research, and former medical director of the Jewish Home for the Aging in Reseda, Calif., has the opportunity to observe hospitalists deal with nursing homes in his current capacity as a consultant for managed care corporations in Southern California.
“Hospitalists have an excellent understanding of acute care management,” he says. “They do a good on-site job of dealing with immediate problems of the individual, and they’re very efficient and very responsive. But while hospitalists are providing higher competency in the management of intra-hospital care, I think that those I’ve interfaced with fall short on the transitions of care, which is so critical with the nursing home patient.”
Dr. Osterweil recalls one patient who had in place do not resuscitate (DNR) and do not intubate (DNI) orders. But when he was hospitalized, the patient was intubated. “If [the hospitalist] had asked one question of the individual or the caregiver—‘What is the goal of care?’—they would have been able to plan a much smoother transition for that person back to the facility.”
At Lower Bucks Hospital in Bristol, Pa., where long-term care physician Daniel Haimowitz, MD, CMD serves as chairman of internal medicine and chairs the utilization committee, the surrounding community of physicians has responded in a mostly positive way to a new hospitalist program.
However, Dr. Haimowitz has concerns that transitioning admissions of nursing home patients to hospitalists can hinder continuity of care.
Different hospitalists work each shift, and unless the patient has been on the hospitalist service in the past, the admitting hospitalist may know nothing about the patient—and most probably has no relationship with the patient’s family (as the primary care physician would have).
“The family doctor has seen the patient for 20 or 30 years and knows what he or she wants,” Dr. Haimowitz says. “But this patient is brand new to the hospitalist. Unless the hospitalist is really good with communication and takes the extra step to call the physician at the nursing home, I think you run the real risk of duplicating workup or actually not doing what is in the best interest of the patient.”
“While demonstrating improved quality of care for the acutely ill hospitalized patient, hospital medicine has struggled with the fact that it inherently adds more patient hand-offs into the mix,” says Bryce Gartland, MD, medical director for care coordination and director of hospital medicine for Emory University Hospital in Atlanta. “We experience this internally, within our facility and externally when transferring patients into or out of the hospital.”
There is always a potential for what has been called the “voltage drop” when hand-offs occur, agrees Dr. Cumming, whether they’re between hospitalists in the same facility or from hospitalist back to the primary care provider. “We function in a healthcare system that is very individualized,” she says. “When you’re dealing with many different community hospitals that may not be part of the same system, it’s very hard to standardize [transfer processes].”
The standard of care for transferring patients from Marin General Hospital to subacute rehabilitation facilities or to skilled nursing facilities entails a detailed inter-facility transfer form. The form includes a thorough discharge summary, with a separate medication reconciliation form, photocopies of any relevant consultations, and a list of pending lab tests. In concert with the hospital’s case managers, Dr. Cumming and hospitalists on her team also make every effort to speak with patients’ receiving providers to relay a synopsis of what has occurred during their patients’ stay in the hospital.
—Daniel Haimowitz, MD, CMD, chairman of internal medicine, Lower Bucks Hospital, Bristol, Pa.
Avoid Assumptions
Especially in the case of patients with dementia or severe illness prohibiting communication about their condition, a thorough transfer sheet or discharge summary—arriving with the patient or faxed in a timely manner—can help reduce errors and contribute to more seamless resumption of care at the next facility.
Without access to a patient’s history, the opportunity for errors increases. One of Dr. Crecelius’ pet peeves is seeing “history not obtainable” on the hospital’s patient transfer sheet. “A history is always obtainable,” Dr. Crecelius asserts. “You can call the nursing home, the family, or the patient’s physician. That phrase equals, ‘We didn’t bother to take the time.’ There is no such thing as ‘history not obtainable,’ and legally, that will not fly in a court of law.”
Missing or incomplete records necessitate communication between facilities. Dr. Crecelius has also found that hospitalists may not understand the nuances of medication prescription for the elderly—a situation that can be rectified with a phone call.
A case in point: Dr. Crecelius once prescribed theophylline for a bradycardic patient who refused a pacemaker but frequently lost consciousness when his pulse and blood pressure dropped. Although this was an obscure use of the drug, which is primarily a bronchodilator, “it worked to keep the patient’s pulse up so he was not passing out. When he went to the hospital, they stopped the drug, and it took forever to get him discharged. The patient came back to the nursing home in horrible shape. I assume the providers at the hospital thought I was crazy for prescribing theophylline to a frail old person!”
Dr. Crecelius’ prescription for avoiding the above scenario: “If you think the medicine is an odd choice, ask the prescriber why the patient is on it. We need to respect each other and get the information when there is a question.”
Cornerstones of Continuity
Medical directors have addressed continuity of care issues in their own ways. Whenever possible, Dr. Crecelius sees his patients in the hospital. He has also been working as a representative of the Missouri Association of Long-Term Care Physicians with a statewide transition planning committee. The committee is drafting new transfer forms for hospitals and post-acute care facilities.
The Asheville Hospitalist Group, PA has “gone to extraordinary lengths to address the issue of inter-facility transfers,” says Marc Westle, DO, FACP, president and managing partner for the large private group in N.C. His group has coordinated efforts with another group of hospitalists who specialize in managing patients in the Asheville area’s 20-plus nursing homes.
To facilitate transfers to a hospital, the nursing homes send paperwork (including history, physical, and medication records) with patients to the emergency department. When patients are ready for discharge, discharge summaries are dictated stat and faxed to the nursing home. Hospitalists discharging patients pre-order diagnostic tests that will be necessary when the patient returns to the nursing home by noting those tests on discharge orders. In addition, “The nursing home group has a list of all our beeper numbers for direct contact should a question arise,” says Dr. Westle.
Every patient transferred to another facility from Emory University Hospital in Atlanta is accompanied by a three-page transfer form, says Dr. Gartland. Included is a one-page summary of detailed nursing care; a second page listing hospitalization events, including pertinent consults, procedures, diagnoses, pending lab tests, and recommended follow-up; and a detailed medication sheet with discontinuation dates for such medication as antibiotics.
During his time as medical director at the Jewish Home for the Aging, Dr. Osterweil created what he calls his own “pseudo-hospitalist arrangement” to ensure continuity of care. He identified multiphysician groups comprising internists and nephrologists who, between them, could offer 24 hours on-call coverage.
When patients were transported to a local community hospital, Dr. Osterweil or his staff would call one of these physicians, who would take care of the patients when they were admitted to the floor. That arrangement is still in place.
“Any major decisions that are made, we are kept in the loop,” says Dr. Osterweil. “Twenty-four hours before readmission back to the skilled nursing facility, we receive a call letting us know the patient is coming back and his or her issues. The physician group executes a ‘stat’ dictated discharge summary, and the patient leaves the hospital with those orders. This ensures the continuity of care when the patient goes back to the nursing home or the board and care facility.”
Beef Up Communication
Dr. Crecelius concedes that certified medical directors (CMDs) are also often guilty of dropping the ball when it comes to communicating with inpatient provider colleagues.
Care of nursing home patients can be improved if hospitalists and medical directors of nursing homes talk directly on the phone, he says. “I met one wonderful hospitalist who actually showed up at the nursing home to see how the patients that he’d been sending out of the hospital were doing,’’ he recalls. “It was so nice to see the face behind the voice. You can’t get mad at a face!”
However, again demonstrating the range of practice techniques, another hospitalist group in Dr. Crecelius’ area does not do anything beyond faxing him the patient’s diagnosis. “Well, I knew the diagnosis, so that fax is not telling me anything,’’ he says. “And unfortunately, that is their idea of communication.”
The Marin Hospitalist Medical Group makes every effort to ensure communications with receiving facilities are timely and thorough. According to Dr. Cumming, the group has surveyed—and will continue to survey—its referring primary care physicians, whether office or facility-based, for feedback on their performance. Hospital case managers also relay feedback to the hospitalist group, she notes. “We’ve tried to use the customer service model across all the groups of physicians who transfer patients to us and to whom we transfer patients, to keep that level of communication where it needs to be,” she says. Some of the questions they ask of their facilities:
- Are we sending the information you need?
- Do you want to receive all documents with the patient when he or she is transferred, or just a small subset of documents?
- How do you want information delivered? Do you want forms, discharge summaries and other documents faxed to you? Would you prefer a phone call?
- What can we do better?
Dr. Haimowitz’s advice to hospitalists might parallel the advice he recently gave to local a hospital administrators who were considering starting an intensivist program. “If you’re going to do this right, you must have physicians who are sensitive to older patients and what they want,” he says. Quality of life, DNR orders, and goals of care take on subtle gradations when applied to the elderly, he emphasizes.
Absent the time to visit the area nursing homes, hospitalists can always at least call, Dr. Crecelius notes.
Just as a hospitalist or emergency department physician would contact the family to corroborate patient history, they should also call the nursing home. “Speaking with the nurse at the skilled nursing facility, you can access a wealth of information—and save time and effort,” he says.
Improve Transfers
Dr. Haimowitz believes communication—on a form or by phone—is essential. He sees even more opportunity for miscommunication between hospitals and nursing homes because of different recordkeeping systems.
Hospitals are moving increasingly to electronic health records, while nursing homes still rely on paper documentation. “How do you foster communication?” Dr. Haimowitz asks. “How do you get the right people on the same bus? The best transfer sheet in the world is no good if one, it’s not filled out, and two, if it’s not read.”
Disparate systems can be a barrier, but it does not mean you should not try to optimize communication within whatever system you have, says Dr. Cumming.
The Marin Hospitalist Medical Group is setting up a communication system to alert all primary care physicians of pending lab results so such tests do not fall through the cracks after patients are discharged.
In another initiative, the hospital will set up a system to note that any pneumonia or influenza vaccinations performed while the patient was hospitalized are communicated either to PCP or outside facility. The group is also working to urge all local nursing facilities to include records of patients’ recent vaccinations when they are transferred to the hospital.
It’s clear that effective transfers of elderly patients require a concerted effort by all involved. “If you perform a root cause analysis of [transfer] errors, most occur not because of any negligence, but because communication—written or verbal—was not handled as best as it could have been,” Dr. Gartland notes. “Oftentimes, we are just as frustrated as they [nursing facilities] are when patients return to the emergency room unable to communicate their medical conditions, wishes, and the like,” he says. As medical director of care coordination at Emory, he has worked to improve relationships with administrators and physicians in nursing facilities used most often by the hospital. “If people have a vested interest in a relationship, they are more likely to be diligent about the transfer of patients,” he asserts.
Above all, emphasizes Dr. Cumming, “it important to always solicit feedback from your primary care physician ‘clientele.’ They are your clients, much as your patients are, and your hospital is. We’re providing services to all these various groups. Quality patient care is the most important thing that we do, and part of that means that we have to have good transfer of information. Our group recognizes that we are far from perfect; we know we can always do better; and we always have to reassess to make sure that we’re on the right track.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ouslander JG, Osterweil D, Morley J. Medical Care in the Nursing Home. 2nd ed. New York, New York: McGraw-Hill Publishers;1997.
Charles A. Crecelius, MD, of Saint Louis, has experienced best- and worst-case scenarios when his frail elderly patients have been admitted and discharged by local hospitalists.
Best case, he says: “My patient is admitted. I get a call. I’m told what is going on. I’m notified of meaningful changes, and at discharge, I get another call [from the hospitalist].”
But there are wide variations in hospitalist/nursing home relationships, notes Dr. Crecelius, a long-term care physician and president-elect of the American Medical Director’s Association (AMDA).
This was brought home by the case of a patient with a well-documented history of dystonic reaction to toxic lithium levels. The patient was later misdiagnosed as having tardive dyskinesia, a movement disorder. Her much-needed medication was discontinued, and the hospital transferred the patient back to the nursing home in worse condition than before.
“We wasted an entire hospitalization,” Dr. Crecelius recalls ruefully.
The above scenario underscores the importance of a thorough transfer of information when elderly patients move from facility to facility. Interaction between hospitalists and nursing home staff will become increasingly important in light of the growing frail elderly population and the Joint Commission on Accreditation of Health Care Organization’s (JCAHO) push for improved discharge communications.1
By applying a customer service model and continually upgrading transfer documentation, hospital medicine groups can “keep the level of communication where it needs to be,” says Susan S. Cumming, MD, associate medical director of Marin Hospitalist Medical Group at Marin General Hospital in Greenbrae, Calif.
Running a Risk
Dan Osterweil, MD, CMD, is familiar with the hospitalist model through his medical training in Israel during the late 1970s and early 1980s. Hospitalists there routinely handled inpatient care.
Dr. Osterweil, a clinical professor of medicine/geriatric medicine at UCLA, research associate with the UCLA Borun Center for Gerontological Research, and former medical director of the Jewish Home for the Aging in Reseda, Calif., has the opportunity to observe hospitalists deal with nursing homes in his current capacity as a consultant for managed care corporations in Southern California.
“Hospitalists have an excellent understanding of acute care management,” he says. “They do a good on-site job of dealing with immediate problems of the individual, and they’re very efficient and very responsive. But while hospitalists are providing higher competency in the management of intra-hospital care, I think that those I’ve interfaced with fall short on the transitions of care, which is so critical with the nursing home patient.”
Dr. Osterweil recalls one patient who had in place do not resuscitate (DNR) and do not intubate (DNI) orders. But when he was hospitalized, the patient was intubated. “If [the hospitalist] had asked one question of the individual or the caregiver—‘What is the goal of care?’—they would have been able to plan a much smoother transition for that person back to the facility.”
At Lower Bucks Hospital in Bristol, Pa., where long-term care physician Daniel Haimowitz, MD, CMD serves as chairman of internal medicine and chairs the utilization committee, the surrounding community of physicians has responded in a mostly positive way to a new hospitalist program.
However, Dr. Haimowitz has concerns that transitioning admissions of nursing home patients to hospitalists can hinder continuity of care.
Different hospitalists work each shift, and unless the patient has been on the hospitalist service in the past, the admitting hospitalist may know nothing about the patient—and most probably has no relationship with the patient’s family (as the primary care physician would have).
“The family doctor has seen the patient for 20 or 30 years and knows what he or she wants,” Dr. Haimowitz says. “But this patient is brand new to the hospitalist. Unless the hospitalist is really good with communication and takes the extra step to call the physician at the nursing home, I think you run the real risk of duplicating workup or actually not doing what is in the best interest of the patient.”
“While demonstrating improved quality of care for the acutely ill hospitalized patient, hospital medicine has struggled with the fact that it inherently adds more patient hand-offs into the mix,” says Bryce Gartland, MD, medical director for care coordination and director of hospital medicine for Emory University Hospital in Atlanta. “We experience this internally, within our facility and externally when transferring patients into or out of the hospital.”
There is always a potential for what has been called the “voltage drop” when hand-offs occur, agrees Dr. Cumming, whether they’re between hospitalists in the same facility or from hospitalist back to the primary care provider. “We function in a healthcare system that is very individualized,” she says. “When you’re dealing with many different community hospitals that may not be part of the same system, it’s very hard to standardize [transfer processes].”
The standard of care for transferring patients from Marin General Hospital to subacute rehabilitation facilities or to skilled nursing facilities entails a detailed inter-facility transfer form. The form includes a thorough discharge summary, with a separate medication reconciliation form, photocopies of any relevant consultations, and a list of pending lab tests. In concert with the hospital’s case managers, Dr. Cumming and hospitalists on her team also make every effort to speak with patients’ receiving providers to relay a synopsis of what has occurred during their patients’ stay in the hospital.
—Daniel Haimowitz, MD, CMD, chairman of internal medicine, Lower Bucks Hospital, Bristol, Pa.
Avoid Assumptions
Especially in the case of patients with dementia or severe illness prohibiting communication about their condition, a thorough transfer sheet or discharge summary—arriving with the patient or faxed in a timely manner—can help reduce errors and contribute to more seamless resumption of care at the next facility.
Without access to a patient’s history, the opportunity for errors increases. One of Dr. Crecelius’ pet peeves is seeing “history not obtainable” on the hospital’s patient transfer sheet. “A history is always obtainable,” Dr. Crecelius asserts. “You can call the nursing home, the family, or the patient’s physician. That phrase equals, ‘We didn’t bother to take the time.’ There is no such thing as ‘history not obtainable,’ and legally, that will not fly in a court of law.”
Missing or incomplete records necessitate communication between facilities. Dr. Crecelius has also found that hospitalists may not understand the nuances of medication prescription for the elderly—a situation that can be rectified with a phone call.
A case in point: Dr. Crecelius once prescribed theophylline for a bradycardic patient who refused a pacemaker but frequently lost consciousness when his pulse and blood pressure dropped. Although this was an obscure use of the drug, which is primarily a bronchodilator, “it worked to keep the patient’s pulse up so he was not passing out. When he went to the hospital, they stopped the drug, and it took forever to get him discharged. The patient came back to the nursing home in horrible shape. I assume the providers at the hospital thought I was crazy for prescribing theophylline to a frail old person!”
Dr. Crecelius’ prescription for avoiding the above scenario: “If you think the medicine is an odd choice, ask the prescriber why the patient is on it. We need to respect each other and get the information when there is a question.”
Cornerstones of Continuity
Medical directors have addressed continuity of care issues in their own ways. Whenever possible, Dr. Crecelius sees his patients in the hospital. He has also been working as a representative of the Missouri Association of Long-Term Care Physicians with a statewide transition planning committee. The committee is drafting new transfer forms for hospitals and post-acute care facilities.
The Asheville Hospitalist Group, PA has “gone to extraordinary lengths to address the issue of inter-facility transfers,” says Marc Westle, DO, FACP, president and managing partner for the large private group in N.C. His group has coordinated efforts with another group of hospitalists who specialize in managing patients in the Asheville area’s 20-plus nursing homes.
To facilitate transfers to a hospital, the nursing homes send paperwork (including history, physical, and medication records) with patients to the emergency department. When patients are ready for discharge, discharge summaries are dictated stat and faxed to the nursing home. Hospitalists discharging patients pre-order diagnostic tests that will be necessary when the patient returns to the nursing home by noting those tests on discharge orders. In addition, “The nursing home group has a list of all our beeper numbers for direct contact should a question arise,” says Dr. Westle.
Every patient transferred to another facility from Emory University Hospital in Atlanta is accompanied by a three-page transfer form, says Dr. Gartland. Included is a one-page summary of detailed nursing care; a second page listing hospitalization events, including pertinent consults, procedures, diagnoses, pending lab tests, and recommended follow-up; and a detailed medication sheet with discontinuation dates for such medication as antibiotics.
During his time as medical director at the Jewish Home for the Aging, Dr. Osterweil created what he calls his own “pseudo-hospitalist arrangement” to ensure continuity of care. He identified multiphysician groups comprising internists and nephrologists who, between them, could offer 24 hours on-call coverage.
When patients were transported to a local community hospital, Dr. Osterweil or his staff would call one of these physicians, who would take care of the patients when they were admitted to the floor. That arrangement is still in place.
“Any major decisions that are made, we are kept in the loop,” says Dr. Osterweil. “Twenty-four hours before readmission back to the skilled nursing facility, we receive a call letting us know the patient is coming back and his or her issues. The physician group executes a ‘stat’ dictated discharge summary, and the patient leaves the hospital with those orders. This ensures the continuity of care when the patient goes back to the nursing home or the board and care facility.”
Beef Up Communication
Dr. Crecelius concedes that certified medical directors (CMDs) are also often guilty of dropping the ball when it comes to communicating with inpatient provider colleagues.
Care of nursing home patients can be improved if hospitalists and medical directors of nursing homes talk directly on the phone, he says. “I met one wonderful hospitalist who actually showed up at the nursing home to see how the patients that he’d been sending out of the hospital were doing,’’ he recalls. “It was so nice to see the face behind the voice. You can’t get mad at a face!”
However, again demonstrating the range of practice techniques, another hospitalist group in Dr. Crecelius’ area does not do anything beyond faxing him the patient’s diagnosis. “Well, I knew the diagnosis, so that fax is not telling me anything,’’ he says. “And unfortunately, that is their idea of communication.”
The Marin Hospitalist Medical Group makes every effort to ensure communications with receiving facilities are timely and thorough. According to Dr. Cumming, the group has surveyed—and will continue to survey—its referring primary care physicians, whether office or facility-based, for feedback on their performance. Hospital case managers also relay feedback to the hospitalist group, she notes. “We’ve tried to use the customer service model across all the groups of physicians who transfer patients to us and to whom we transfer patients, to keep that level of communication where it needs to be,” she says. Some of the questions they ask of their facilities:
- Are we sending the information you need?
- Do you want to receive all documents with the patient when he or she is transferred, or just a small subset of documents?
- How do you want information delivered? Do you want forms, discharge summaries and other documents faxed to you? Would you prefer a phone call?
- What can we do better?
Dr. Haimowitz’s advice to hospitalists might parallel the advice he recently gave to local a hospital administrators who were considering starting an intensivist program. “If you’re going to do this right, you must have physicians who are sensitive to older patients and what they want,” he says. Quality of life, DNR orders, and goals of care take on subtle gradations when applied to the elderly, he emphasizes.
Absent the time to visit the area nursing homes, hospitalists can always at least call, Dr. Crecelius notes.
Just as a hospitalist or emergency department physician would contact the family to corroborate patient history, they should also call the nursing home. “Speaking with the nurse at the skilled nursing facility, you can access a wealth of information—and save time and effort,” he says.
Improve Transfers
Dr. Haimowitz believes communication—on a form or by phone—is essential. He sees even more opportunity for miscommunication between hospitals and nursing homes because of different recordkeeping systems.
Hospitals are moving increasingly to electronic health records, while nursing homes still rely on paper documentation. “How do you foster communication?” Dr. Haimowitz asks. “How do you get the right people on the same bus? The best transfer sheet in the world is no good if one, it’s not filled out, and two, if it’s not read.”
Disparate systems can be a barrier, but it does not mean you should not try to optimize communication within whatever system you have, says Dr. Cumming.
The Marin Hospitalist Medical Group is setting up a communication system to alert all primary care physicians of pending lab results so such tests do not fall through the cracks after patients are discharged.
In another initiative, the hospital will set up a system to note that any pneumonia or influenza vaccinations performed while the patient was hospitalized are communicated either to PCP or outside facility. The group is also working to urge all local nursing facilities to include records of patients’ recent vaccinations when they are transferred to the hospital.
It’s clear that effective transfers of elderly patients require a concerted effort by all involved. “If you perform a root cause analysis of [transfer] errors, most occur not because of any negligence, but because communication—written or verbal—was not handled as best as it could have been,” Dr. Gartland notes. “Oftentimes, we are just as frustrated as they [nursing facilities] are when patients return to the emergency room unable to communicate their medical conditions, wishes, and the like,” he says. As medical director of care coordination at Emory, he has worked to improve relationships with administrators and physicians in nursing facilities used most often by the hospital. “If people have a vested interest in a relationship, they are more likely to be diligent about the transfer of patients,” he asserts.
Above all, emphasizes Dr. Cumming, “it important to always solicit feedback from your primary care physician ‘clientele.’ They are your clients, much as your patients are, and your hospital is. We’re providing services to all these various groups. Quality patient care is the most important thing that we do, and part of that means that we have to have good transfer of information. Our group recognizes that we are far from perfect; we know we can always do better; and we always have to reassess to make sure that we’re on the right track.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ouslander JG, Osterweil D, Morley J. Medical Care in the Nursing Home. 2nd ed. New York, New York: McGraw-Hill Publishers;1997.
Charles A. Crecelius, MD, of Saint Louis, has experienced best- and worst-case scenarios when his frail elderly patients have been admitted and discharged by local hospitalists.
Best case, he says: “My patient is admitted. I get a call. I’m told what is going on. I’m notified of meaningful changes, and at discharge, I get another call [from the hospitalist].”
But there are wide variations in hospitalist/nursing home relationships, notes Dr. Crecelius, a long-term care physician and president-elect of the American Medical Director’s Association (AMDA).
This was brought home by the case of a patient with a well-documented history of dystonic reaction to toxic lithium levels. The patient was later misdiagnosed as having tardive dyskinesia, a movement disorder. Her much-needed medication was discontinued, and the hospital transferred the patient back to the nursing home in worse condition than before.
“We wasted an entire hospitalization,” Dr. Crecelius recalls ruefully.
The above scenario underscores the importance of a thorough transfer of information when elderly patients move from facility to facility. Interaction between hospitalists and nursing home staff will become increasingly important in light of the growing frail elderly population and the Joint Commission on Accreditation of Health Care Organization’s (JCAHO) push for improved discharge communications.1
By applying a customer service model and continually upgrading transfer documentation, hospital medicine groups can “keep the level of communication where it needs to be,” says Susan S. Cumming, MD, associate medical director of Marin Hospitalist Medical Group at Marin General Hospital in Greenbrae, Calif.
Running a Risk
Dan Osterweil, MD, CMD, is familiar with the hospitalist model through his medical training in Israel during the late 1970s and early 1980s. Hospitalists there routinely handled inpatient care.
Dr. Osterweil, a clinical professor of medicine/geriatric medicine at UCLA, research associate with the UCLA Borun Center for Gerontological Research, and former medical director of the Jewish Home for the Aging in Reseda, Calif., has the opportunity to observe hospitalists deal with nursing homes in his current capacity as a consultant for managed care corporations in Southern California.
“Hospitalists have an excellent understanding of acute care management,” he says. “They do a good on-site job of dealing with immediate problems of the individual, and they’re very efficient and very responsive. But while hospitalists are providing higher competency in the management of intra-hospital care, I think that those I’ve interfaced with fall short on the transitions of care, which is so critical with the nursing home patient.”
Dr. Osterweil recalls one patient who had in place do not resuscitate (DNR) and do not intubate (DNI) orders. But when he was hospitalized, the patient was intubated. “If [the hospitalist] had asked one question of the individual or the caregiver—‘What is the goal of care?’—they would have been able to plan a much smoother transition for that person back to the facility.”
At Lower Bucks Hospital in Bristol, Pa., where long-term care physician Daniel Haimowitz, MD, CMD serves as chairman of internal medicine and chairs the utilization committee, the surrounding community of physicians has responded in a mostly positive way to a new hospitalist program.
However, Dr. Haimowitz has concerns that transitioning admissions of nursing home patients to hospitalists can hinder continuity of care.
Different hospitalists work each shift, and unless the patient has been on the hospitalist service in the past, the admitting hospitalist may know nothing about the patient—and most probably has no relationship with the patient’s family (as the primary care physician would have).
“The family doctor has seen the patient for 20 or 30 years and knows what he or she wants,” Dr. Haimowitz says. “But this patient is brand new to the hospitalist. Unless the hospitalist is really good with communication and takes the extra step to call the physician at the nursing home, I think you run the real risk of duplicating workup or actually not doing what is in the best interest of the patient.”
“While demonstrating improved quality of care for the acutely ill hospitalized patient, hospital medicine has struggled with the fact that it inherently adds more patient hand-offs into the mix,” says Bryce Gartland, MD, medical director for care coordination and director of hospital medicine for Emory University Hospital in Atlanta. “We experience this internally, within our facility and externally when transferring patients into or out of the hospital.”
There is always a potential for what has been called the “voltage drop” when hand-offs occur, agrees Dr. Cumming, whether they’re between hospitalists in the same facility or from hospitalist back to the primary care provider. “We function in a healthcare system that is very individualized,” she says. “When you’re dealing with many different community hospitals that may not be part of the same system, it’s very hard to standardize [transfer processes].”
The standard of care for transferring patients from Marin General Hospital to subacute rehabilitation facilities or to skilled nursing facilities entails a detailed inter-facility transfer form. The form includes a thorough discharge summary, with a separate medication reconciliation form, photocopies of any relevant consultations, and a list of pending lab tests. In concert with the hospital’s case managers, Dr. Cumming and hospitalists on her team also make every effort to speak with patients’ receiving providers to relay a synopsis of what has occurred during their patients’ stay in the hospital.
—Daniel Haimowitz, MD, CMD, chairman of internal medicine, Lower Bucks Hospital, Bristol, Pa.
Avoid Assumptions
Especially in the case of patients with dementia or severe illness prohibiting communication about their condition, a thorough transfer sheet or discharge summary—arriving with the patient or faxed in a timely manner—can help reduce errors and contribute to more seamless resumption of care at the next facility.
Without access to a patient’s history, the opportunity for errors increases. One of Dr. Crecelius’ pet peeves is seeing “history not obtainable” on the hospital’s patient transfer sheet. “A history is always obtainable,” Dr. Crecelius asserts. “You can call the nursing home, the family, or the patient’s physician. That phrase equals, ‘We didn’t bother to take the time.’ There is no such thing as ‘history not obtainable,’ and legally, that will not fly in a court of law.”
Missing or incomplete records necessitate communication between facilities. Dr. Crecelius has also found that hospitalists may not understand the nuances of medication prescription for the elderly—a situation that can be rectified with a phone call.
A case in point: Dr. Crecelius once prescribed theophylline for a bradycardic patient who refused a pacemaker but frequently lost consciousness when his pulse and blood pressure dropped. Although this was an obscure use of the drug, which is primarily a bronchodilator, “it worked to keep the patient’s pulse up so he was not passing out. When he went to the hospital, they stopped the drug, and it took forever to get him discharged. The patient came back to the nursing home in horrible shape. I assume the providers at the hospital thought I was crazy for prescribing theophylline to a frail old person!”
Dr. Crecelius’ prescription for avoiding the above scenario: “If you think the medicine is an odd choice, ask the prescriber why the patient is on it. We need to respect each other and get the information when there is a question.”
Cornerstones of Continuity
Medical directors have addressed continuity of care issues in their own ways. Whenever possible, Dr. Crecelius sees his patients in the hospital. He has also been working as a representative of the Missouri Association of Long-Term Care Physicians with a statewide transition planning committee. The committee is drafting new transfer forms for hospitals and post-acute care facilities.
The Asheville Hospitalist Group, PA has “gone to extraordinary lengths to address the issue of inter-facility transfers,” says Marc Westle, DO, FACP, president and managing partner for the large private group in N.C. His group has coordinated efforts with another group of hospitalists who specialize in managing patients in the Asheville area’s 20-plus nursing homes.
To facilitate transfers to a hospital, the nursing homes send paperwork (including history, physical, and medication records) with patients to the emergency department. When patients are ready for discharge, discharge summaries are dictated stat and faxed to the nursing home. Hospitalists discharging patients pre-order diagnostic tests that will be necessary when the patient returns to the nursing home by noting those tests on discharge orders. In addition, “The nursing home group has a list of all our beeper numbers for direct contact should a question arise,” says Dr. Westle.
Every patient transferred to another facility from Emory University Hospital in Atlanta is accompanied by a three-page transfer form, says Dr. Gartland. Included is a one-page summary of detailed nursing care; a second page listing hospitalization events, including pertinent consults, procedures, diagnoses, pending lab tests, and recommended follow-up; and a detailed medication sheet with discontinuation dates for such medication as antibiotics.
During his time as medical director at the Jewish Home for the Aging, Dr. Osterweil created what he calls his own “pseudo-hospitalist arrangement” to ensure continuity of care. He identified multiphysician groups comprising internists and nephrologists who, between them, could offer 24 hours on-call coverage.
When patients were transported to a local community hospital, Dr. Osterweil or his staff would call one of these physicians, who would take care of the patients when they were admitted to the floor. That arrangement is still in place.
“Any major decisions that are made, we are kept in the loop,” says Dr. Osterweil. “Twenty-four hours before readmission back to the skilled nursing facility, we receive a call letting us know the patient is coming back and his or her issues. The physician group executes a ‘stat’ dictated discharge summary, and the patient leaves the hospital with those orders. This ensures the continuity of care when the patient goes back to the nursing home or the board and care facility.”
Beef Up Communication
Dr. Crecelius concedes that certified medical directors (CMDs) are also often guilty of dropping the ball when it comes to communicating with inpatient provider colleagues.
Care of nursing home patients can be improved if hospitalists and medical directors of nursing homes talk directly on the phone, he says. “I met one wonderful hospitalist who actually showed up at the nursing home to see how the patients that he’d been sending out of the hospital were doing,’’ he recalls. “It was so nice to see the face behind the voice. You can’t get mad at a face!”
However, again demonstrating the range of practice techniques, another hospitalist group in Dr. Crecelius’ area does not do anything beyond faxing him the patient’s diagnosis. “Well, I knew the diagnosis, so that fax is not telling me anything,’’ he says. “And unfortunately, that is their idea of communication.”
The Marin Hospitalist Medical Group makes every effort to ensure communications with receiving facilities are timely and thorough. According to Dr. Cumming, the group has surveyed—and will continue to survey—its referring primary care physicians, whether office or facility-based, for feedback on their performance. Hospital case managers also relay feedback to the hospitalist group, she notes. “We’ve tried to use the customer service model across all the groups of physicians who transfer patients to us and to whom we transfer patients, to keep that level of communication where it needs to be,” she says. Some of the questions they ask of their facilities:
- Are we sending the information you need?
- Do you want to receive all documents with the patient when he or she is transferred, or just a small subset of documents?
- How do you want information delivered? Do you want forms, discharge summaries and other documents faxed to you? Would you prefer a phone call?
- What can we do better?
Dr. Haimowitz’s advice to hospitalists might parallel the advice he recently gave to local a hospital administrators who were considering starting an intensivist program. “If you’re going to do this right, you must have physicians who are sensitive to older patients and what they want,” he says. Quality of life, DNR orders, and goals of care take on subtle gradations when applied to the elderly, he emphasizes.
Absent the time to visit the area nursing homes, hospitalists can always at least call, Dr. Crecelius notes.
Just as a hospitalist or emergency department physician would contact the family to corroborate patient history, they should also call the nursing home. “Speaking with the nurse at the skilled nursing facility, you can access a wealth of information—and save time and effort,” he says.
Improve Transfers
Dr. Haimowitz believes communication—on a form or by phone—is essential. He sees even more opportunity for miscommunication between hospitals and nursing homes because of different recordkeeping systems.
Hospitals are moving increasingly to electronic health records, while nursing homes still rely on paper documentation. “How do you foster communication?” Dr. Haimowitz asks. “How do you get the right people on the same bus? The best transfer sheet in the world is no good if one, it’s not filled out, and two, if it’s not read.”
Disparate systems can be a barrier, but it does not mean you should not try to optimize communication within whatever system you have, says Dr. Cumming.
The Marin Hospitalist Medical Group is setting up a communication system to alert all primary care physicians of pending lab results so such tests do not fall through the cracks after patients are discharged.
In another initiative, the hospital will set up a system to note that any pneumonia or influenza vaccinations performed while the patient was hospitalized are communicated either to PCP or outside facility. The group is also working to urge all local nursing facilities to include records of patients’ recent vaccinations when they are transferred to the hospital.
It’s clear that effective transfers of elderly patients require a concerted effort by all involved. “If you perform a root cause analysis of [transfer] errors, most occur not because of any negligence, but because communication—written or verbal—was not handled as best as it could have been,” Dr. Gartland notes. “Oftentimes, we are just as frustrated as they [nursing facilities] are when patients return to the emergency room unable to communicate their medical conditions, wishes, and the like,” he says. As medical director of care coordination at Emory, he has worked to improve relationships with administrators and physicians in nursing facilities used most often by the hospital. “If people have a vested interest in a relationship, they are more likely to be diligent about the transfer of patients,” he asserts.
Above all, emphasizes Dr. Cumming, “it important to always solicit feedback from your primary care physician ‘clientele.’ They are your clients, much as your patients are, and your hospital is. We’re providing services to all these various groups. Quality patient care is the most important thing that we do, and part of that means that we have to have good transfer of information. Our group recognizes that we are far from perfect; we know we can always do better; and we always have to reassess to make sure that we’re on the right track.” TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Reference
- Ouslander JG, Osterweil D, Morley J. Medical Care in the Nursing Home. 2nd ed. New York, New York: McGraw-Hill Publishers;1997.
The Family Way
Although the vast majority of physicians who practice hospital medicine in the United States are board certified in internal medicine, about 3% of hospitalists have their certification in family medicine.
How do differences in training, general outlook on the practice of medicine, or other factors affect their roles as hospitalists? Do practitioners of family medicine bring special skills to inpatient care? Why do they choose to become hospitalists instead of community-based family doctors? Does their certification in family practice give them a particular bond with the patient’s primary care doctor who may also be a family practitioner? How do they fit into the hospitalist picture, which is—at least in the U.S.—so dominated by internists?
To find out, we asked six hospitalists certified in family medicine:
- Jasen W. Gundersen, MD, division chief of hospital medicine, University of Massachusetts Memorial Medical Center, and assistant professor, UMass. Medical School, Worcester, Mass.
- Michael Kedansky, MD, lead hospitalist at the Kino Campus of University Physicians Healthcare Hospital in Tucson, Ariz., and clinical assistant professor of family and community medicine at the University of Arizona College of Medicine;
- Elizabeth Chmelik, MD, director of the Inpatient Medical Program at Scott and White University Medical Campus at Texas A&M University in Austin;
- Echo-Marie Enns, MD, a family practice hospitalist at the Peter Lougheed Center in Calgary, Alberta, Canada.
- Felix Aguirre, MD, vice president of medical affairs at IPC-the Hospitalist Company, San Antonio, Texas; and
- Jennifer Cameron, MD, a family medicine hospitalist with Central Texas Hospitalist who practices at St. David’s Hospital, Round Rock, Texas.
Drs. Gundersen, Kedansky, and Chmelik are members of SHM’s Family Practice Task Force.
Training And Decisions
Most of the experts we spoke with agree training influenced their decision to become hospitalists. They cite the diversity of cases in family practice residency (adult, pediatric, and obstetric/gynecologic), which they felt they would also find in hospital medicine.
Dr. Gundersen, chair of SHM’s Family Practice Task Force, suspects internists and family physicians probably share one motivator for opting into hospital medicine: the hospital environment. “Even in residency, I liked my time in the hospital,” Dr. Gundersen says. Echoing that sentiment, Dr. Kedansky says he missed hospital work when he was in community practice.
Family medicine is about people and relationships, says Dr. Chmelik. “You can get that same satisfaction on an inpatient basis,” she says. “I’ve always liked seeing the same patients from day to day. You get instant gratification.”
The higher levels of support and resources available in a hospital environment as opposed to those in a community-based practice appeal to Dr. Enns.
Dr. Gundersen adds that some physicians don’t like all the paperwork office practice entails; others favor the regulated hours of hospital practice. “People often evolve into it as they get more experience,” he says. “They feel that hospital medicine gives them a chance to really make a difference.”
Dr. Cameron agrees about the paperwork. “Out of residency, I became a primary care physician in Tucson,” she says. “When the local hospital group became unexpectedly short-handed, they asked me to fill in on weekends. Once I proved myself with my eagerness and team spirit, they asked me to join their group. The timing was just right: the office management, billings, paperwork, employee issues, and 24/7 schedule were just killing me, and I was ready to try something else.”
Dr. Aguirre says his hospitalist career grew out of his work with a primary care group. His primary aim was standardizing the care of the hospitalized patients in the group.
Whole-Patient View
What special skills do family medicine physicians bring to hospital medicine? The experts quickly pointed out that though training and backgrounds might differ somewhat between internists and family medicine hospitalists they view their respective skills as complementary.
“Family medicine physicians bring a wider breadth of general knowledge in more medical areas than a traditional internal medicine physician, but an internal medicine physician is expected to have a greater depth of knowledge in general adult medicine, which is the current mainstay of hospital medicine,” says Dr. Aguirre. But he suggests that the knowledge base tends to equalize with experience as internal medicine (IM) and family medicine hospitalists cover each other.
However, he also believes a family physician initially brings more knowledge and practical experience in gynecology, behavioral science, pediatric, orthopedic, and family medicine. “These experiences can be especially useful when crafting hospitalist programs to serve these specific target audiences and to help staff pediatric or IM/pediatric hospitalist programs as well,” he says.
Family medicine covers a lot of bases, these experts say. “Family medicine hospitalists have training in family dynamics, end-of-life issues, and family counseling,” says Dr. Chmelik. “These skills frequently come into play with hospitalized patients.” For Dr. Kedansky, family medicine residency training focuses on treating the whole patient “from birth to death.”
Dr. Gundersen knows how broad that role is. “We have the ability to treat adult, newborn, pediatric, and obstetric/gynecologic patients,” he says. “Some family medicine hospitalists even do labor management,” he says.
According to him, a family practice hospitalist gives a hospital special value because one hospitalist can take care of children as well as adults.
Community is important in the hospitalist-patient relationship. “Family practitioners learn how patients fit into the community,” says Dr. Enns. “We can picture patients in a home setting. This helps us in getting patients ready for discharge.”
The outpatient perspective gives family practitioners more foresight, says Dr. Cameron. Family practitioners “see possible roadblocks to a successful discharge to the home and are more willing to jump through the necessary hoops to ensure things go as planned once the patient is discharged,” she says. “As prior outpatient physicians, we know the frustration of having a patient just discharged from the hospital land in our clinic Monday morning with many issues unaddressed.”
Many family physicians had office practices before becoming hospitalists. “We understand how the continuum works,” says Dr. Kedansky.
—Elizabeth Chmelik, MD, director of the Inpatient Medical Program at Scott and White University Medical Campus at Texas A&M University, Austin
Bond with Primary Docs
Does belonging to the same “fraternity”—family medicine—create a special relationship between a primary care doctor and a hospitalist with a similar background and training?
From the Canadian perspective, Dr. Enns thinks it may. She says resource constraints may apply to the primary care physician working in the community. “When I am treating a patient, I sometimes find a condition that is unrelated to the patient’s hospitalization,” she says. “I have better access to resources, so I might be able to accomplish a lot for my colleague. I’ll call and ask if the doctor would like me to run an appropriate test, for example. Usually the primary care doctor is extremely grateful for the help.”
In the U.S., Dr. Gundersen suggests that the specialty of neither the primary care doctor nor the hospitalist is particularly important. “Continuity of care is the critical thing,” he says. “The point is to have good communication and a smooth handoff back to the primary care doctor.”
Dr. Kedansky agrees on the necessity for good communication but feels a greater sense of connectivity with the primary care physician, partly because he has been one. “I also know many of the docs personally, so that helps,” he says.
For Drs. Aguirre and Cameron, having worked as a primary care physician helps them empathize with their concerns about continuity and quality of care.
“I have been in their shoes, so to speak,” says Dr. Cameron. “I know the frustrations they deal with daily.”
Some primary care doctors seem pleased the hospitalist shares their background, Dr. Chmelik notes, but she also emphasizes that continuity of care is much more important.
Everyone agreed that, in most cases, primary care doctors are grateful hospitalists are there to take over inpatient care, but Dr. Kedansky notes that some family physicians still want to do it all. “I give those docs credit if they want to maintain care of their patients when they’re in the hospital,” he says. “But most simply can’t keep up with it.”
Improved Training
Dr. Enns says that in Canada, family physicians have training in palliative care, but internists don’t. (They do in the U.S.)
“Family physicians have training in the broader aspects of patient care,” she says. “They view patients in terms of the goal to be achieved rather than the diagnosis.” However, she feels internists have superior training in differential diagnosis.
In her view, family physicians and internists learn skills they originally lacked as they evolve as hospitalists. “I know I’ve learned a lot about diagnosis since I’ve been a hospitalist,” she confesses. She feels that both groups—internists and family physicians—would benefit as hospitalists if they had cross-training in each other’s specialties.
More training on the business side would have been helpful, suggests Dr. Chmelik. “We learned how to be doctors,” she says, “but we also need to know how to function in a hospital setting.” She mentioned billing, length-of-stay protocols, and Joint Commission on Accreditation of Healthcare Organizations (JCAHO) rules as examples. She also would have liked more training in infection control.
Family practice physicians fear the specialty has been slower than internal medicine in developing a program that would offer credentialing for hospitalists.
The U.S. family medicine hospitalists worry that because they are such a small part of the hospitalist family their position will be further eroded unless they can offer a similar credential.
Further, all cited the urgency of expanding fellowships in hospital medicine as a means of training that could lead to credentialing.
It is unlikely any sort of joint credential will be developed, given that the certifying boards of family medicine and internal medicine are individual entities, they say.
In the Minority
Being a minority in the ranks of hospitalists has its disadvantages. Some family medicine hospitalists feel they have to struggle to achieve recognition. But all agreed there is no problem with colleagues.
“I manage a mixed group of internists and family physicians,” says Dr. Kedansky, “and there is no distinction.”
Patient respect is not at issue, either. The panelists say patients are curious about the term hospitalist but seem largely oblivious to any further distinction. If there is any preference for internist hospitalists—and not everyone agrees there is—it seems to be on the part of the people who hire hospitalists.
Some potential employers specify in their employment ads that an applicant be certified in internal medicine, but Dr. Kedansky suggests that because most hospitalists are internists, many hirers assume that is the standard. “The person’s skills are what’s important, not the specialty,” he says. “If the doctor wants the job, he should persist.” But Dr. Gundersen, who thinks there is bias in some cases, says he has found that some hirers will not even interview candidates with family physician boards. “This situation limits a family physician hospitalist’s ability to move around or even get a job in the first place,” he says.
Dr. Cameron knows whereof he speaks. “I had a few hospital groups and hospitals dismiss my [resume] without even talking to me despite my experience and stellar references,” she says of her frustrating year-and-a-half search for her present position.
Family physician hospitalists may have a bigger hurdle to overcome, acknowledges Dr. Chmelik. “We may have to prove more, but it is possible to earn recognition,” she believes. Dr. Aguirre concurs: “Respect is earned and not a predetermined right.”
In Canada there is no hiring issue because almost all hospitalists are family physicians, but Dr. Enns says her U.S. colleagues should “feel their own worth more. They add great value to the skills that internists bring.”
Outlook
Fewer doctors are opting to take the family medicine boards, but leaders are rising to the challenge to redefine and reassert the importance of the needs served by family physicians. At the same time, there is increasing demand for hospitalists.
According to Dr. Aguirre, demand may double—or go even higher—within the next 10 years.
“There are not enough internal medicine physicians, family medicine physicians, pediatric physicians, and physician extenders completing training or leaving private practice to become hospitalists in the near future to fill the oncoming void,” he warns.
Even if this situation proves true and hospitalist jobs are everywhere for the taking, it’s unclear whether that will rekindle interest in family practice as a path to becoming a hospitalist. But one thing seems certain: There will be credentialing processes for family physician and internist hospitalists.
Dr. Kedansky is concerned that family medicine is playing catch-up on this issue, and he wonders what effect credentialing will have. “Now it’s on the radar screen, though,” he says.
Dr. Cameron shares his concerns. She fears that if family physicians lack equal footing with internists as hospitalists, many rural and smaller hospitals will be without hospitalist coverage.
Early on, the medical community in Canada considered that the role of family medicine hospitalist might be a temporary one, taken to give family practice medicine time to regain strength, says Dr. Enns. “Now, there are no signs that it’s temporary,” she says. “It’s an effective method of patient care, and the community has embraced it. There are no more naysayers.”
Getting new physicians interested in the specialty is key, says Dr. Chmelik.
“Fellowships for further training are important,” she says. “We need to work with medical students too, show them there are options within the field. They want choices.”
Dr. Gundersen suggests that whether one is an internist or a family-physician hospitalist may not make much difference in years to come. “I think that in the future physicians will be classified on the basis of whether they are outpatient or inpatient doctors, rather than all these other designations,” he says. “It’s getting harder and harder to be both.” TH
Joen Kinnan is a frequent contributor to The Hospitalist.
Although the vast majority of physicians who practice hospital medicine in the United States are board certified in internal medicine, about 3% of hospitalists have their certification in family medicine.
How do differences in training, general outlook on the practice of medicine, or other factors affect their roles as hospitalists? Do practitioners of family medicine bring special skills to inpatient care? Why do they choose to become hospitalists instead of community-based family doctors? Does their certification in family practice give them a particular bond with the patient’s primary care doctor who may also be a family practitioner? How do they fit into the hospitalist picture, which is—at least in the U.S.—so dominated by internists?
To find out, we asked six hospitalists certified in family medicine:
- Jasen W. Gundersen, MD, division chief of hospital medicine, University of Massachusetts Memorial Medical Center, and assistant professor, UMass. Medical School, Worcester, Mass.
- Michael Kedansky, MD, lead hospitalist at the Kino Campus of University Physicians Healthcare Hospital in Tucson, Ariz., and clinical assistant professor of family and community medicine at the University of Arizona College of Medicine;
- Elizabeth Chmelik, MD, director of the Inpatient Medical Program at Scott and White University Medical Campus at Texas A&M University in Austin;
- Echo-Marie Enns, MD, a family practice hospitalist at the Peter Lougheed Center in Calgary, Alberta, Canada.
- Felix Aguirre, MD, vice president of medical affairs at IPC-the Hospitalist Company, San Antonio, Texas; and
- Jennifer Cameron, MD, a family medicine hospitalist with Central Texas Hospitalist who practices at St. David’s Hospital, Round Rock, Texas.
Drs. Gundersen, Kedansky, and Chmelik are members of SHM’s Family Practice Task Force.
Training And Decisions
Most of the experts we spoke with agree training influenced their decision to become hospitalists. They cite the diversity of cases in family practice residency (adult, pediatric, and obstetric/gynecologic), which they felt they would also find in hospital medicine.
Dr. Gundersen, chair of SHM’s Family Practice Task Force, suspects internists and family physicians probably share one motivator for opting into hospital medicine: the hospital environment. “Even in residency, I liked my time in the hospital,” Dr. Gundersen says. Echoing that sentiment, Dr. Kedansky says he missed hospital work when he was in community practice.
Family medicine is about people and relationships, says Dr. Chmelik. “You can get that same satisfaction on an inpatient basis,” she says. “I’ve always liked seeing the same patients from day to day. You get instant gratification.”
The higher levels of support and resources available in a hospital environment as opposed to those in a community-based practice appeal to Dr. Enns.
Dr. Gundersen adds that some physicians don’t like all the paperwork office practice entails; others favor the regulated hours of hospital practice. “People often evolve into it as they get more experience,” he says. “They feel that hospital medicine gives them a chance to really make a difference.”
Dr. Cameron agrees about the paperwork. “Out of residency, I became a primary care physician in Tucson,” she says. “When the local hospital group became unexpectedly short-handed, they asked me to fill in on weekends. Once I proved myself with my eagerness and team spirit, they asked me to join their group. The timing was just right: the office management, billings, paperwork, employee issues, and 24/7 schedule were just killing me, and I was ready to try something else.”
Dr. Aguirre says his hospitalist career grew out of his work with a primary care group. His primary aim was standardizing the care of the hospitalized patients in the group.
Whole-Patient View
What special skills do family medicine physicians bring to hospital medicine? The experts quickly pointed out that though training and backgrounds might differ somewhat between internists and family medicine hospitalists they view their respective skills as complementary.
“Family medicine physicians bring a wider breadth of general knowledge in more medical areas than a traditional internal medicine physician, but an internal medicine physician is expected to have a greater depth of knowledge in general adult medicine, which is the current mainstay of hospital medicine,” says Dr. Aguirre. But he suggests that the knowledge base tends to equalize with experience as internal medicine (IM) and family medicine hospitalists cover each other.
However, he also believes a family physician initially brings more knowledge and practical experience in gynecology, behavioral science, pediatric, orthopedic, and family medicine. “These experiences can be especially useful when crafting hospitalist programs to serve these specific target audiences and to help staff pediatric or IM/pediatric hospitalist programs as well,” he says.
Family medicine covers a lot of bases, these experts say. “Family medicine hospitalists have training in family dynamics, end-of-life issues, and family counseling,” says Dr. Chmelik. “These skills frequently come into play with hospitalized patients.” For Dr. Kedansky, family medicine residency training focuses on treating the whole patient “from birth to death.”
Dr. Gundersen knows how broad that role is. “We have the ability to treat adult, newborn, pediatric, and obstetric/gynecologic patients,” he says. “Some family medicine hospitalists even do labor management,” he says.
According to him, a family practice hospitalist gives a hospital special value because one hospitalist can take care of children as well as adults.
Community is important in the hospitalist-patient relationship. “Family practitioners learn how patients fit into the community,” says Dr. Enns. “We can picture patients in a home setting. This helps us in getting patients ready for discharge.”
The outpatient perspective gives family practitioners more foresight, says Dr. Cameron. Family practitioners “see possible roadblocks to a successful discharge to the home and are more willing to jump through the necessary hoops to ensure things go as planned once the patient is discharged,” she says. “As prior outpatient physicians, we know the frustration of having a patient just discharged from the hospital land in our clinic Monday morning with many issues unaddressed.”
Many family physicians had office practices before becoming hospitalists. “We understand how the continuum works,” says Dr. Kedansky.
—Elizabeth Chmelik, MD, director of the Inpatient Medical Program at Scott and White University Medical Campus at Texas A&M University, Austin
Bond with Primary Docs
Does belonging to the same “fraternity”—family medicine—create a special relationship between a primary care doctor and a hospitalist with a similar background and training?
From the Canadian perspective, Dr. Enns thinks it may. She says resource constraints may apply to the primary care physician working in the community. “When I am treating a patient, I sometimes find a condition that is unrelated to the patient’s hospitalization,” she says. “I have better access to resources, so I might be able to accomplish a lot for my colleague. I’ll call and ask if the doctor would like me to run an appropriate test, for example. Usually the primary care doctor is extremely grateful for the help.”
In the U.S., Dr. Gundersen suggests that the specialty of neither the primary care doctor nor the hospitalist is particularly important. “Continuity of care is the critical thing,” he says. “The point is to have good communication and a smooth handoff back to the primary care doctor.”
Dr. Kedansky agrees on the necessity for good communication but feels a greater sense of connectivity with the primary care physician, partly because he has been one. “I also know many of the docs personally, so that helps,” he says.
For Drs. Aguirre and Cameron, having worked as a primary care physician helps them empathize with their concerns about continuity and quality of care.
“I have been in their shoes, so to speak,” says Dr. Cameron. “I know the frustrations they deal with daily.”
Some primary care doctors seem pleased the hospitalist shares their background, Dr. Chmelik notes, but she also emphasizes that continuity of care is much more important.
Everyone agreed that, in most cases, primary care doctors are grateful hospitalists are there to take over inpatient care, but Dr. Kedansky notes that some family physicians still want to do it all. “I give those docs credit if they want to maintain care of their patients when they’re in the hospital,” he says. “But most simply can’t keep up with it.”
Improved Training
Dr. Enns says that in Canada, family physicians have training in palliative care, but internists don’t. (They do in the U.S.)
“Family physicians have training in the broader aspects of patient care,” she says. “They view patients in terms of the goal to be achieved rather than the diagnosis.” However, she feels internists have superior training in differential diagnosis.
In her view, family physicians and internists learn skills they originally lacked as they evolve as hospitalists. “I know I’ve learned a lot about diagnosis since I’ve been a hospitalist,” she confesses. She feels that both groups—internists and family physicians—would benefit as hospitalists if they had cross-training in each other’s specialties.
More training on the business side would have been helpful, suggests Dr. Chmelik. “We learned how to be doctors,” she says, “but we also need to know how to function in a hospital setting.” She mentioned billing, length-of-stay protocols, and Joint Commission on Accreditation of Healthcare Organizations (JCAHO) rules as examples. She also would have liked more training in infection control.
Family practice physicians fear the specialty has been slower than internal medicine in developing a program that would offer credentialing for hospitalists.
The U.S. family medicine hospitalists worry that because they are such a small part of the hospitalist family their position will be further eroded unless they can offer a similar credential.
Further, all cited the urgency of expanding fellowships in hospital medicine as a means of training that could lead to credentialing.
It is unlikely any sort of joint credential will be developed, given that the certifying boards of family medicine and internal medicine are individual entities, they say.
In the Minority
Being a minority in the ranks of hospitalists has its disadvantages. Some family medicine hospitalists feel they have to struggle to achieve recognition. But all agreed there is no problem with colleagues.
“I manage a mixed group of internists and family physicians,” says Dr. Kedansky, “and there is no distinction.”
Patient respect is not at issue, either. The panelists say patients are curious about the term hospitalist but seem largely oblivious to any further distinction. If there is any preference for internist hospitalists—and not everyone agrees there is—it seems to be on the part of the people who hire hospitalists.
Some potential employers specify in their employment ads that an applicant be certified in internal medicine, but Dr. Kedansky suggests that because most hospitalists are internists, many hirers assume that is the standard. “The person’s skills are what’s important, not the specialty,” he says. “If the doctor wants the job, he should persist.” But Dr. Gundersen, who thinks there is bias in some cases, says he has found that some hirers will not even interview candidates with family physician boards. “This situation limits a family physician hospitalist’s ability to move around or even get a job in the first place,” he says.
Dr. Cameron knows whereof he speaks. “I had a few hospital groups and hospitals dismiss my [resume] without even talking to me despite my experience and stellar references,” she says of her frustrating year-and-a-half search for her present position.
Family physician hospitalists may have a bigger hurdle to overcome, acknowledges Dr. Chmelik. “We may have to prove more, but it is possible to earn recognition,” she believes. Dr. Aguirre concurs: “Respect is earned and not a predetermined right.”
In Canada there is no hiring issue because almost all hospitalists are family physicians, but Dr. Enns says her U.S. colleagues should “feel their own worth more. They add great value to the skills that internists bring.”
Outlook
Fewer doctors are opting to take the family medicine boards, but leaders are rising to the challenge to redefine and reassert the importance of the needs served by family physicians. At the same time, there is increasing demand for hospitalists.
According to Dr. Aguirre, demand may double—or go even higher—within the next 10 years.
“There are not enough internal medicine physicians, family medicine physicians, pediatric physicians, and physician extenders completing training or leaving private practice to become hospitalists in the near future to fill the oncoming void,” he warns.
Even if this situation proves true and hospitalist jobs are everywhere for the taking, it’s unclear whether that will rekindle interest in family practice as a path to becoming a hospitalist. But one thing seems certain: There will be credentialing processes for family physician and internist hospitalists.
Dr. Kedansky is concerned that family medicine is playing catch-up on this issue, and he wonders what effect credentialing will have. “Now it’s on the radar screen, though,” he says.
Dr. Cameron shares his concerns. She fears that if family physicians lack equal footing with internists as hospitalists, many rural and smaller hospitals will be without hospitalist coverage.
Early on, the medical community in Canada considered that the role of family medicine hospitalist might be a temporary one, taken to give family practice medicine time to regain strength, says Dr. Enns. “Now, there are no signs that it’s temporary,” she says. “It’s an effective method of patient care, and the community has embraced it. There are no more naysayers.”
Getting new physicians interested in the specialty is key, says Dr. Chmelik.
“Fellowships for further training are important,” she says. “We need to work with medical students too, show them there are options within the field. They want choices.”
Dr. Gundersen suggests that whether one is an internist or a family-physician hospitalist may not make much difference in years to come. “I think that in the future physicians will be classified on the basis of whether they are outpatient or inpatient doctors, rather than all these other designations,” he says. “It’s getting harder and harder to be both.” TH
Joen Kinnan is a frequent contributor to The Hospitalist.
Although the vast majority of physicians who practice hospital medicine in the United States are board certified in internal medicine, about 3% of hospitalists have their certification in family medicine.
How do differences in training, general outlook on the practice of medicine, or other factors affect their roles as hospitalists? Do practitioners of family medicine bring special skills to inpatient care? Why do they choose to become hospitalists instead of community-based family doctors? Does their certification in family practice give them a particular bond with the patient’s primary care doctor who may also be a family practitioner? How do they fit into the hospitalist picture, which is—at least in the U.S.—so dominated by internists?
To find out, we asked six hospitalists certified in family medicine:
- Jasen W. Gundersen, MD, division chief of hospital medicine, University of Massachusetts Memorial Medical Center, and assistant professor, UMass. Medical School, Worcester, Mass.
- Michael Kedansky, MD, lead hospitalist at the Kino Campus of University Physicians Healthcare Hospital in Tucson, Ariz., and clinical assistant professor of family and community medicine at the University of Arizona College of Medicine;
- Elizabeth Chmelik, MD, director of the Inpatient Medical Program at Scott and White University Medical Campus at Texas A&M University in Austin;
- Echo-Marie Enns, MD, a family practice hospitalist at the Peter Lougheed Center in Calgary, Alberta, Canada.
- Felix Aguirre, MD, vice president of medical affairs at IPC-the Hospitalist Company, San Antonio, Texas; and
- Jennifer Cameron, MD, a family medicine hospitalist with Central Texas Hospitalist who practices at St. David’s Hospital, Round Rock, Texas.
Drs. Gundersen, Kedansky, and Chmelik are members of SHM’s Family Practice Task Force.
Training And Decisions
Most of the experts we spoke with agree training influenced their decision to become hospitalists. They cite the diversity of cases in family practice residency (adult, pediatric, and obstetric/gynecologic), which they felt they would also find in hospital medicine.
Dr. Gundersen, chair of SHM’s Family Practice Task Force, suspects internists and family physicians probably share one motivator for opting into hospital medicine: the hospital environment. “Even in residency, I liked my time in the hospital,” Dr. Gundersen says. Echoing that sentiment, Dr. Kedansky says he missed hospital work when he was in community practice.
Family medicine is about people and relationships, says Dr. Chmelik. “You can get that same satisfaction on an inpatient basis,” she says. “I’ve always liked seeing the same patients from day to day. You get instant gratification.”
The higher levels of support and resources available in a hospital environment as opposed to those in a community-based practice appeal to Dr. Enns.
Dr. Gundersen adds that some physicians don’t like all the paperwork office practice entails; others favor the regulated hours of hospital practice. “People often evolve into it as they get more experience,” he says. “They feel that hospital medicine gives them a chance to really make a difference.”
Dr. Cameron agrees about the paperwork. “Out of residency, I became a primary care physician in Tucson,” she says. “When the local hospital group became unexpectedly short-handed, they asked me to fill in on weekends. Once I proved myself with my eagerness and team spirit, they asked me to join their group. The timing was just right: the office management, billings, paperwork, employee issues, and 24/7 schedule were just killing me, and I was ready to try something else.”
Dr. Aguirre says his hospitalist career grew out of his work with a primary care group. His primary aim was standardizing the care of the hospitalized patients in the group.
Whole-Patient View
What special skills do family medicine physicians bring to hospital medicine? The experts quickly pointed out that though training and backgrounds might differ somewhat between internists and family medicine hospitalists they view their respective skills as complementary.
“Family medicine physicians bring a wider breadth of general knowledge in more medical areas than a traditional internal medicine physician, but an internal medicine physician is expected to have a greater depth of knowledge in general adult medicine, which is the current mainstay of hospital medicine,” says Dr. Aguirre. But he suggests that the knowledge base tends to equalize with experience as internal medicine (IM) and family medicine hospitalists cover each other.
However, he also believes a family physician initially brings more knowledge and practical experience in gynecology, behavioral science, pediatric, orthopedic, and family medicine. “These experiences can be especially useful when crafting hospitalist programs to serve these specific target audiences and to help staff pediatric or IM/pediatric hospitalist programs as well,” he says.
Family medicine covers a lot of bases, these experts say. “Family medicine hospitalists have training in family dynamics, end-of-life issues, and family counseling,” says Dr. Chmelik. “These skills frequently come into play with hospitalized patients.” For Dr. Kedansky, family medicine residency training focuses on treating the whole patient “from birth to death.”
Dr. Gundersen knows how broad that role is. “We have the ability to treat adult, newborn, pediatric, and obstetric/gynecologic patients,” he says. “Some family medicine hospitalists even do labor management,” he says.
According to him, a family practice hospitalist gives a hospital special value because one hospitalist can take care of children as well as adults.
Community is important in the hospitalist-patient relationship. “Family practitioners learn how patients fit into the community,” says Dr. Enns. “We can picture patients in a home setting. This helps us in getting patients ready for discharge.”
The outpatient perspective gives family practitioners more foresight, says Dr. Cameron. Family practitioners “see possible roadblocks to a successful discharge to the home and are more willing to jump through the necessary hoops to ensure things go as planned once the patient is discharged,” she says. “As prior outpatient physicians, we know the frustration of having a patient just discharged from the hospital land in our clinic Monday morning with many issues unaddressed.”
Many family physicians had office practices before becoming hospitalists. “We understand how the continuum works,” says Dr. Kedansky.
—Elizabeth Chmelik, MD, director of the Inpatient Medical Program at Scott and White University Medical Campus at Texas A&M University, Austin
Bond with Primary Docs
Does belonging to the same “fraternity”—family medicine—create a special relationship between a primary care doctor and a hospitalist with a similar background and training?
From the Canadian perspective, Dr. Enns thinks it may. She says resource constraints may apply to the primary care physician working in the community. “When I am treating a patient, I sometimes find a condition that is unrelated to the patient’s hospitalization,” she says. “I have better access to resources, so I might be able to accomplish a lot for my colleague. I’ll call and ask if the doctor would like me to run an appropriate test, for example. Usually the primary care doctor is extremely grateful for the help.”
In the U.S., Dr. Gundersen suggests that the specialty of neither the primary care doctor nor the hospitalist is particularly important. “Continuity of care is the critical thing,” he says. “The point is to have good communication and a smooth handoff back to the primary care doctor.”
Dr. Kedansky agrees on the necessity for good communication but feels a greater sense of connectivity with the primary care physician, partly because he has been one. “I also know many of the docs personally, so that helps,” he says.
For Drs. Aguirre and Cameron, having worked as a primary care physician helps them empathize with their concerns about continuity and quality of care.
“I have been in their shoes, so to speak,” says Dr. Cameron. “I know the frustrations they deal with daily.”
Some primary care doctors seem pleased the hospitalist shares their background, Dr. Chmelik notes, but she also emphasizes that continuity of care is much more important.
Everyone agreed that, in most cases, primary care doctors are grateful hospitalists are there to take over inpatient care, but Dr. Kedansky notes that some family physicians still want to do it all. “I give those docs credit if they want to maintain care of their patients when they’re in the hospital,” he says. “But most simply can’t keep up with it.”
Improved Training
Dr. Enns says that in Canada, family physicians have training in palliative care, but internists don’t. (They do in the U.S.)
“Family physicians have training in the broader aspects of patient care,” she says. “They view patients in terms of the goal to be achieved rather than the diagnosis.” However, she feels internists have superior training in differential diagnosis.
In her view, family physicians and internists learn skills they originally lacked as they evolve as hospitalists. “I know I’ve learned a lot about diagnosis since I’ve been a hospitalist,” she confesses. She feels that both groups—internists and family physicians—would benefit as hospitalists if they had cross-training in each other’s specialties.
More training on the business side would have been helpful, suggests Dr. Chmelik. “We learned how to be doctors,” she says, “but we also need to know how to function in a hospital setting.” She mentioned billing, length-of-stay protocols, and Joint Commission on Accreditation of Healthcare Organizations (JCAHO) rules as examples. She also would have liked more training in infection control.
Family practice physicians fear the specialty has been slower than internal medicine in developing a program that would offer credentialing for hospitalists.
The U.S. family medicine hospitalists worry that because they are such a small part of the hospitalist family their position will be further eroded unless they can offer a similar credential.
Further, all cited the urgency of expanding fellowships in hospital medicine as a means of training that could lead to credentialing.
It is unlikely any sort of joint credential will be developed, given that the certifying boards of family medicine and internal medicine are individual entities, they say.
In the Minority
Being a minority in the ranks of hospitalists has its disadvantages. Some family medicine hospitalists feel they have to struggle to achieve recognition. But all agreed there is no problem with colleagues.
“I manage a mixed group of internists and family physicians,” says Dr. Kedansky, “and there is no distinction.”
Patient respect is not at issue, either. The panelists say patients are curious about the term hospitalist but seem largely oblivious to any further distinction. If there is any preference for internist hospitalists—and not everyone agrees there is—it seems to be on the part of the people who hire hospitalists.
Some potential employers specify in their employment ads that an applicant be certified in internal medicine, but Dr. Kedansky suggests that because most hospitalists are internists, many hirers assume that is the standard. “The person’s skills are what’s important, not the specialty,” he says. “If the doctor wants the job, he should persist.” But Dr. Gundersen, who thinks there is bias in some cases, says he has found that some hirers will not even interview candidates with family physician boards. “This situation limits a family physician hospitalist’s ability to move around or even get a job in the first place,” he says.
Dr. Cameron knows whereof he speaks. “I had a few hospital groups and hospitals dismiss my [resume] without even talking to me despite my experience and stellar references,” she says of her frustrating year-and-a-half search for her present position.
Family physician hospitalists may have a bigger hurdle to overcome, acknowledges Dr. Chmelik. “We may have to prove more, but it is possible to earn recognition,” she believes. Dr. Aguirre concurs: “Respect is earned and not a predetermined right.”
In Canada there is no hiring issue because almost all hospitalists are family physicians, but Dr. Enns says her U.S. colleagues should “feel their own worth more. They add great value to the skills that internists bring.”
Outlook
Fewer doctors are opting to take the family medicine boards, but leaders are rising to the challenge to redefine and reassert the importance of the needs served by family physicians. At the same time, there is increasing demand for hospitalists.
According to Dr. Aguirre, demand may double—or go even higher—within the next 10 years.
“There are not enough internal medicine physicians, family medicine physicians, pediatric physicians, and physician extenders completing training or leaving private practice to become hospitalists in the near future to fill the oncoming void,” he warns.
Even if this situation proves true and hospitalist jobs are everywhere for the taking, it’s unclear whether that will rekindle interest in family practice as a path to becoming a hospitalist. But one thing seems certain: There will be credentialing processes for family physician and internist hospitalists.
Dr. Kedansky is concerned that family medicine is playing catch-up on this issue, and he wonders what effect credentialing will have. “Now it’s on the radar screen, though,” he says.
Dr. Cameron shares his concerns. She fears that if family physicians lack equal footing with internists as hospitalists, many rural and smaller hospitals will be without hospitalist coverage.
Early on, the medical community in Canada considered that the role of family medicine hospitalist might be a temporary one, taken to give family practice medicine time to regain strength, says Dr. Enns. “Now, there are no signs that it’s temporary,” she says. “It’s an effective method of patient care, and the community has embraced it. There are no more naysayers.”
Getting new physicians interested in the specialty is key, says Dr. Chmelik.
“Fellowships for further training are important,” she says. “We need to work with medical students too, show them there are options within the field. They want choices.”
Dr. Gundersen suggests that whether one is an internist or a family-physician hospitalist may not make much difference in years to come. “I think that in the future physicians will be classified on the basis of whether they are outpatient or inpatient doctors, rather than all these other designations,” he says. “It’s getting harder and harder to be both.” TH
Joen Kinnan is a frequent contributor to The Hospitalist.
What is the best surgical therapy for the secondary prevention of stroke?
Case
A 62-year-old obese woman with type 2 diabetes, hypertension, and a pack-a-day smoking habit presents to the emergency department for acute onset of left-side arm and leg weakness and sensory loss on awakening.
She reports taking a baby aspirin daily to “prevent heart attacks.” Her electrocardiogram demonstrates a left bundle branch block and frequent premature atrial contractions. She recovers partially but has residual mild hemiparesis. A duplex carotid ultrasound shows 80% stenosis of the right internal carotid artery.
Overview
In the United States each year approximately 700,000 cerebrovascular accidents (CVA) constitute the largest cause of age-adjusted morbidity of any illness.1 About 200,000 of these strokes are recurrent events.
CVA is the third-leading cause of death. Hospitalists increasingly are responsible for the inpatient care of patients with acute CVA. Atheroembolism from carotid atherosclerosis is the suspected cause for about one in five ischemic strokes.2
The link between carotid stenosis and stroke has been recognized for many years. The first carotid endarterectomy (CEA) was reported more than 50 years ago.3
This targeted review covers the natural history of symptomatic carotid stenosis, the key efficacy trials of CEA and carotid angioplasty and stenting (CAS) among symptomatic patients, and pitfalls for properly diagnosing the severity of carotid stenosis. The medical therapy of carotid stenosis and the secondary prevention of CVA were recently reviewed in The Hospitalist (October 2007, p. 34).
Natural History
The presence or absence of referable neurological symptoms is pivotal to understanding the near-term risk for recurrent CVA related to carotid stenosis. In the absence of symptoms, the risk for future CVA is essentially constant over years.
However, once symptoms occur, the risk for a second event accelerates substantially. Among patients with newly symptomatic carotid stenosis, the risk for another transient ischemic attack (TIA) or stroke within the following 24 months is 26%.4 This risk peaks within the first month or two following the index event, underscoring the time-dependent nature of carotid evaluation and intervention.
Guidelines from the American Heart Association and the American College of Cardiology on the management of ischemic stroke assign early carotid intervention, defined as within two weeks from the index event, a Class 2 indication.5 Hospitalists must rapidly identify the severity of carotid stenosis and make timely referrals to meet this recommended therapeutic window.
Carotid Endarterectomy
CEA is perhaps the best-studied surgical procedure, with multiple well-conducted prospective randomized trials demonstrating its efficacy. The procedure had been performed for hundreds of thousands of patients prior to this data being published in the early 1990s. The North American Symptomatic Carotid Endarterectomy Trial (NASCET) was the landmark study demonstrating the efficacy of intervention. The trial of patients with symptomatic carotid stenosis was stopped early for patients with severe stenosis, defined as 70% to 99% narrowing by conventional angiography. At two years, the rate of ipsilateral stroke or post-operative death in patients with severe stenosis decreased from 26% in the medical arm to 9% in the CEA arm [an absolute risk reduction of 17% and number needed to treat of six (p<0.001)].
Rarely has any medical or surgical procedure had such a robust effect over so short an interval for such an important outcome. Patients with less severe stenosis were followed out to five years, with the final results showing benefit among patients with moderate stenosis (50% to 69%).6 The Veterans Affairs Cooperative Trial 309 and the European Carotid Stenosis Trial (ECST) were combined with NASCET in a pooled analysis of more than 6,000 patients and about 35,000 patient-years of follow-up.7-9
Among patients with 70% or greater stenosis, CEA reduced the absolute five-year risk of ipsilateral ischemic stroke and any operative stroke or death by 16% (95% confidence interval 11.2% to 20.8%). The benefit was less pronounced among patients with 50% to 69% stenosis, in whom CEA conferred a 4.6% (95% confidence interval 0.6% to 8.6%) absolute five-year risk reduction.
The medical aspect of these trials required only the use of aspirin. Intensive lipid control and tight glycemic and blood pressure control would probably reduce the rate of events. The 30-day operative risk was consistently less than 6% across these trials, with the benefit seen by two years among patients with 70% to 99% stenosis and by five years among patients with 50% to 69% stenosis.
Referring hospitalists should know the operative event rates of the surgeons to whom they are referring. Hospitalists should also refer those patients whose anticipated life expectancy is at least two years for patients with 70% to 99% stenosis and at least five years for patients with 50% to 69% stenosis.
Carotid Angioplasty and Stenting
CAS is increasingly used as an alternative to CEA among selected patients. Two procedural developments have improved the safety of percutaneous carotid revascularization.
First, distal embolic protection filters deployed prior to angioplasty collect debris associated with the mechanical intervention and limit the risk of peri-procedural stroke. (See Figures 1 and 2, p. 36.)
Second, the use of self-expanding stents has improved long-term patency over balloon-expanding stents, which can be damaged by neck movement and external pressure.
The Stenting and Angioplasty with [distal embolic] Protection in Patients at High Risk for Endarterectomy trial demonstrated the noninferiority of CAS versus CEA among high-risk patients.10 Inclusion criteria were symptomatic carotid stenosis of greater than 50% or asymptomatic stenosis greater than 80%. Patients had to have one of several high-risk features to be included. (See Table 1, above)
The cumulative incidence of post-operative stroke, myocardial infarction, death, and ipsilateral stroke within one year after the procedure was 20.1% in the CEA arm and 12.2% in the CAS arm (p=0.004 for noninferiority and p=0.053 for superiority). The rate of post-procedural cranial nerve injury was substantially lower (zero) in the CEA arm.
However, among those patients with symptomatic carotid stenosis, the cumulative incidence of the primary endpoint was 16.8% in the CAS arm and 16.5% in the CEA arm. Based upon this trial, CAS has equivalent one-year outcomes versus CEA in a high-risk population.
The Carotid and Vertebral Artery Transluminal Angioplasty Study trial was the first large prospective trial comparing CEA and CAS among symptomatic patients with severe carotid stenosis (mean 86.4% stenosis).11 At 30 days, the rate of death or disabling stroke was 6.4% with CAS and 5.9% with CEA, which were not significantly different in this trial of about 500 patients.
The trial was begun in 1994, with a large portion of angioplasty performed without stents or distal embolic protection. There were fewer local complications but higher rates of restenosis in the CAS arm. The authors noted “no substantial difference in the rate of ipsilateral stroke … up to three years after randomization” but cautioned that the confidence intervals were wide.
Two recently published trials of CAS versus CEA in lower-risk populations do not support the overall safety of CAS among symptomatic patients. The Stent-Protected Angioplasty versus Carotid Endarterectomy trial randomized 1,200 average-risk patients with symptomatic carotid stenosis of 50% or greater by angiography or 70% of greater by ultrasound to either CAS or CEA.12
The trial design stipulated that both surgeons and percutaneous interventionalists perform at least 25 procedures prior to inclusion in the study and that independent quality committees review these procedures. The use of distal embolic protection devices was left to the discretion of the operators. The 30-day rate of death or ipsilateral ischemic stroke was 6.34% in the CEA arm and 6.84% in the CAS arm (p=0.09 for noninferiority).
The investigators concluded that CAS is not non-inferior to CEA (i.e., that CAS is inferior). The Endarterectomy versus Angioplasty in Patients with Symptomatic Severe Carotid Stenosis trial randomized 527 patients with symptomatic carotid stenosis of 70% or greater by angiography or magnetic resonance angiography (MRA) to either CAS or CEA within two weeks of the index event.13
This trial design also stipulated that surgeons had performed at least 25 CEAs in the prior year. Percutaneous interventionalists did not have similar numeric procedure requirements, although the investigators provided for tutoring of less experienced operators. The trial was stopped prematurely due to futility (in terms of noninferiority) and harm within the CAS arm.
The 30-day cumulative incidence of death or any stroke was 3.9% in the CEA arm and 9.6% in the CAS arm (p=0.01 for superiority of CEA). The trial was powered to detect only large differences among low- and high-volume operators. Nearly 10% of patients did not have distal embolic protection devices used during their CAS procedures. Ongoing trials will further define the role of CAS versus CEA in the interventional treatment of carotid stenosis.
Accurate Diagnosis
Different trials used different criteria for defining the percent stenosis of the diseased carotid arterial segment. These differences were based primarily on the mode of testing (i.e., conventional angiography versus ultrasound), and on what portion of the carotid artery was used as the reference or baseline segment to calculate the percent stenosis.
A meta-analysis of various non-invasive modes of testing for carotid stenosis concluded that duplex ultrasound had a pooled sensitivity and specificity of 86% and 87%, respectively, to distinguish 70% to 99% stenosis from less than 70% stenosis.14 MRA had a pooled sensitivity and specificity of 95% and 90%, respectively.
The authors selected trials comparing these non-invasive methods with the gold standard of digital subtraction angiography. Using ultrasonography to first identify patients with at least 50% stenosis, followed by MRA or conventional angiography to more accurately confirm the degree of stenosis has been shown to be cost-effective.15
Back to the Case
For the patient in the vignette, the positive ultrasonography should lead to an MRA or conventional angiography to more precisely determine the percent stenosis. Current guidelines would suggest referring the patient for CEA to be completed within the next two weeks to treat a 50% or greater stenosis. That’s provided the surgeons have an operative morbidity and mortality rate less than 6% and her life expectancy is at least five years. If the patient had high-risk features as listed in Table 1 (left), referral for CAS in the hands of an experienced operator would be an alternative. TH
Dr. Anderson is an assistant professor of medicine at the University of Colorado, Denver, and an associate program director of the internal medicine residency program.
References
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics-2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69-e171.
- White H, Boden-Albala B, Wang C, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005;111(10):1327-1331.
- Eastcott HH, Pickering GW, Rob CG. Reconstruction of internal carotid artery in a patient with intermittent attacks of hemiplegia. Lancet. 1954;267(6846):994-996.
- Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis: North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1991; 325(7):445-453.
- Sacco RL, Adams R, Albers G, et al. American Heart Association/American Stroke Association Council on Stroke; Council on Cardiovascular Radiology and Intervention; American Academy of Neurology. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention. Circulation. 2006;113:e409-e449.
- North American Symptomatic Carotid Endarterectomy Trialists’ Collaborative Group. The final results of the NASCET trial. N Engl J Med. 1998;339:1415-1425.
- Mayberg MR, Wilson E, Yatsu F, et al. Carotid endarterectomy and prevention of cerebral ischemia in symptomatic carotid stenosis. JAMA. 1991;266:3289-3294.
- European Carotid Surgery Trialists’ Investigators. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998;351:1379-1387.
- Rothwell P, Eliasziw M, Gutnikov A, et al. Analysis of pooled data from the randomised controlled trials of endarterectomy for symptomatic carotid stenosis. Lancet. 2003;361(9352):107-116.
- Yadav JS, Wholey MH, Kuntz, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004;351(15):1493-1501.
- Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): a randomised trial. Lancet. 2001;357:1729-1737.
- SPACE Collaborative Group. 30-day results from the SPACE trial of stent-protected angioplasty versus carotid endarterectomy in symptomatic patients: a randomised noninferiority trial. Lancet. 2006;368:1239-1247.
- Mas J, Chatellier G, Beyssen B, et al. EVA-3S Investigators. Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. N Engl J Med. 2006;355:1660-1671.
- Nederkoorn PJ, van der Graaf Y, Hunink MG. Duplex ultrasound and magnetic resonance angiography compared with digital subtraction angiography in carotid artery stenosis: a systematic review. Stroke. 2003;34:1324-1332.
- U-King-Im JM, Hollingworth W, Trivedi RA, et al. Cost-effectiveness of diagnostic strategies prior to carotid endarterectomy. Ann Neurol. 2005;58(4):506-515.
Case
A 62-year-old obese woman with type 2 diabetes, hypertension, and a pack-a-day smoking habit presents to the emergency department for acute onset of left-side arm and leg weakness and sensory loss on awakening.
She reports taking a baby aspirin daily to “prevent heart attacks.” Her electrocardiogram demonstrates a left bundle branch block and frequent premature atrial contractions. She recovers partially but has residual mild hemiparesis. A duplex carotid ultrasound shows 80% stenosis of the right internal carotid artery.
Overview
In the United States each year approximately 700,000 cerebrovascular accidents (CVA) constitute the largest cause of age-adjusted morbidity of any illness.1 About 200,000 of these strokes are recurrent events.
CVA is the third-leading cause of death. Hospitalists increasingly are responsible for the inpatient care of patients with acute CVA. Atheroembolism from carotid atherosclerosis is the suspected cause for about one in five ischemic strokes.2
The link between carotid stenosis and stroke has been recognized for many years. The first carotid endarterectomy (CEA) was reported more than 50 years ago.3
This targeted review covers the natural history of symptomatic carotid stenosis, the key efficacy trials of CEA and carotid angioplasty and stenting (CAS) among symptomatic patients, and pitfalls for properly diagnosing the severity of carotid stenosis. The medical therapy of carotid stenosis and the secondary prevention of CVA were recently reviewed in The Hospitalist (October 2007, p. 34).
Natural History
The presence or absence of referable neurological symptoms is pivotal to understanding the near-term risk for recurrent CVA related to carotid stenosis. In the absence of symptoms, the risk for future CVA is essentially constant over years.
However, once symptoms occur, the risk for a second event accelerates substantially. Among patients with newly symptomatic carotid stenosis, the risk for another transient ischemic attack (TIA) or stroke within the following 24 months is 26%.4 This risk peaks within the first month or two following the index event, underscoring the time-dependent nature of carotid evaluation and intervention.
Guidelines from the American Heart Association and the American College of Cardiology on the management of ischemic stroke assign early carotid intervention, defined as within two weeks from the index event, a Class 2 indication.5 Hospitalists must rapidly identify the severity of carotid stenosis and make timely referrals to meet this recommended therapeutic window.
Carotid Endarterectomy
CEA is perhaps the best-studied surgical procedure, with multiple well-conducted prospective randomized trials demonstrating its efficacy. The procedure had been performed for hundreds of thousands of patients prior to this data being published in the early 1990s. The North American Symptomatic Carotid Endarterectomy Trial (NASCET) was the landmark study demonstrating the efficacy of intervention. The trial of patients with symptomatic carotid stenosis was stopped early for patients with severe stenosis, defined as 70% to 99% narrowing by conventional angiography. At two years, the rate of ipsilateral stroke or post-operative death in patients with severe stenosis decreased from 26% in the medical arm to 9% in the CEA arm [an absolute risk reduction of 17% and number needed to treat of six (p<0.001)].
Rarely has any medical or surgical procedure had such a robust effect over so short an interval for such an important outcome. Patients with less severe stenosis were followed out to five years, with the final results showing benefit among patients with moderate stenosis (50% to 69%).6 The Veterans Affairs Cooperative Trial 309 and the European Carotid Stenosis Trial (ECST) were combined with NASCET in a pooled analysis of more than 6,000 patients and about 35,000 patient-years of follow-up.7-9
Among patients with 70% or greater stenosis, CEA reduced the absolute five-year risk of ipsilateral ischemic stroke and any operative stroke or death by 16% (95% confidence interval 11.2% to 20.8%). The benefit was less pronounced among patients with 50% to 69% stenosis, in whom CEA conferred a 4.6% (95% confidence interval 0.6% to 8.6%) absolute five-year risk reduction.
The medical aspect of these trials required only the use of aspirin. Intensive lipid control and tight glycemic and blood pressure control would probably reduce the rate of events. The 30-day operative risk was consistently less than 6% across these trials, with the benefit seen by two years among patients with 70% to 99% stenosis and by five years among patients with 50% to 69% stenosis.
Referring hospitalists should know the operative event rates of the surgeons to whom they are referring. Hospitalists should also refer those patients whose anticipated life expectancy is at least two years for patients with 70% to 99% stenosis and at least five years for patients with 50% to 69% stenosis.
Carotid Angioplasty and Stenting
CAS is increasingly used as an alternative to CEA among selected patients. Two procedural developments have improved the safety of percutaneous carotid revascularization.
First, distal embolic protection filters deployed prior to angioplasty collect debris associated with the mechanical intervention and limit the risk of peri-procedural stroke. (See Figures 1 and 2, p. 36.)
Second, the use of self-expanding stents has improved long-term patency over balloon-expanding stents, which can be damaged by neck movement and external pressure.
The Stenting and Angioplasty with [distal embolic] Protection in Patients at High Risk for Endarterectomy trial demonstrated the noninferiority of CAS versus CEA among high-risk patients.10 Inclusion criteria were symptomatic carotid stenosis of greater than 50% or asymptomatic stenosis greater than 80%. Patients had to have one of several high-risk features to be included. (See Table 1, above)
The cumulative incidence of post-operative stroke, myocardial infarction, death, and ipsilateral stroke within one year after the procedure was 20.1% in the CEA arm and 12.2% in the CAS arm (p=0.004 for noninferiority and p=0.053 for superiority). The rate of post-procedural cranial nerve injury was substantially lower (zero) in the CEA arm.
However, among those patients with symptomatic carotid stenosis, the cumulative incidence of the primary endpoint was 16.8% in the CAS arm and 16.5% in the CEA arm. Based upon this trial, CAS has equivalent one-year outcomes versus CEA in a high-risk population.
The Carotid and Vertebral Artery Transluminal Angioplasty Study trial was the first large prospective trial comparing CEA and CAS among symptomatic patients with severe carotid stenosis (mean 86.4% stenosis).11 At 30 days, the rate of death or disabling stroke was 6.4% with CAS and 5.9% with CEA, which were not significantly different in this trial of about 500 patients.
The trial was begun in 1994, with a large portion of angioplasty performed without stents or distal embolic protection. There were fewer local complications but higher rates of restenosis in the CAS arm. The authors noted “no substantial difference in the rate of ipsilateral stroke … up to three years after randomization” but cautioned that the confidence intervals were wide.
Two recently published trials of CAS versus CEA in lower-risk populations do not support the overall safety of CAS among symptomatic patients. The Stent-Protected Angioplasty versus Carotid Endarterectomy trial randomized 1,200 average-risk patients with symptomatic carotid stenosis of 50% or greater by angiography or 70% of greater by ultrasound to either CAS or CEA.12
The trial design stipulated that both surgeons and percutaneous interventionalists perform at least 25 procedures prior to inclusion in the study and that independent quality committees review these procedures. The use of distal embolic protection devices was left to the discretion of the operators. The 30-day rate of death or ipsilateral ischemic stroke was 6.34% in the CEA arm and 6.84% in the CAS arm (p=0.09 for noninferiority).
The investigators concluded that CAS is not non-inferior to CEA (i.e., that CAS is inferior). The Endarterectomy versus Angioplasty in Patients with Symptomatic Severe Carotid Stenosis trial randomized 527 patients with symptomatic carotid stenosis of 70% or greater by angiography or magnetic resonance angiography (MRA) to either CAS or CEA within two weeks of the index event.13
This trial design also stipulated that surgeons had performed at least 25 CEAs in the prior year. Percutaneous interventionalists did not have similar numeric procedure requirements, although the investigators provided for tutoring of less experienced operators. The trial was stopped prematurely due to futility (in terms of noninferiority) and harm within the CAS arm.
The 30-day cumulative incidence of death or any stroke was 3.9% in the CEA arm and 9.6% in the CAS arm (p=0.01 for superiority of CEA). The trial was powered to detect only large differences among low- and high-volume operators. Nearly 10% of patients did not have distal embolic protection devices used during their CAS procedures. Ongoing trials will further define the role of CAS versus CEA in the interventional treatment of carotid stenosis.
Accurate Diagnosis
Different trials used different criteria for defining the percent stenosis of the diseased carotid arterial segment. These differences were based primarily on the mode of testing (i.e., conventional angiography versus ultrasound), and on what portion of the carotid artery was used as the reference or baseline segment to calculate the percent stenosis.
A meta-analysis of various non-invasive modes of testing for carotid stenosis concluded that duplex ultrasound had a pooled sensitivity and specificity of 86% and 87%, respectively, to distinguish 70% to 99% stenosis from less than 70% stenosis.14 MRA had a pooled sensitivity and specificity of 95% and 90%, respectively.
The authors selected trials comparing these non-invasive methods with the gold standard of digital subtraction angiography. Using ultrasonography to first identify patients with at least 50% stenosis, followed by MRA or conventional angiography to more accurately confirm the degree of stenosis has been shown to be cost-effective.15
Back to the Case
For the patient in the vignette, the positive ultrasonography should lead to an MRA or conventional angiography to more precisely determine the percent stenosis. Current guidelines would suggest referring the patient for CEA to be completed within the next two weeks to treat a 50% or greater stenosis. That’s provided the surgeons have an operative morbidity and mortality rate less than 6% and her life expectancy is at least five years. If the patient had high-risk features as listed in Table 1 (left), referral for CAS in the hands of an experienced operator would be an alternative. TH
Dr. Anderson is an assistant professor of medicine at the University of Colorado, Denver, and an associate program director of the internal medicine residency program.
References
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics-2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69-e171.
- White H, Boden-Albala B, Wang C, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005;111(10):1327-1331.
- Eastcott HH, Pickering GW, Rob CG. Reconstruction of internal carotid artery in a patient with intermittent attacks of hemiplegia. Lancet. 1954;267(6846):994-996.
- Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis: North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1991; 325(7):445-453.
- Sacco RL, Adams R, Albers G, et al. American Heart Association/American Stroke Association Council on Stroke; Council on Cardiovascular Radiology and Intervention; American Academy of Neurology. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention. Circulation. 2006;113:e409-e449.
- North American Symptomatic Carotid Endarterectomy Trialists’ Collaborative Group. The final results of the NASCET trial. N Engl J Med. 1998;339:1415-1425.
- Mayberg MR, Wilson E, Yatsu F, et al. Carotid endarterectomy and prevention of cerebral ischemia in symptomatic carotid stenosis. JAMA. 1991;266:3289-3294.
- European Carotid Surgery Trialists’ Investigators. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998;351:1379-1387.
- Rothwell P, Eliasziw M, Gutnikov A, et al. Analysis of pooled data from the randomised controlled trials of endarterectomy for symptomatic carotid stenosis. Lancet. 2003;361(9352):107-116.
- Yadav JS, Wholey MH, Kuntz, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004;351(15):1493-1501.
- Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): a randomised trial. Lancet. 2001;357:1729-1737.
- SPACE Collaborative Group. 30-day results from the SPACE trial of stent-protected angioplasty versus carotid endarterectomy in symptomatic patients: a randomised noninferiority trial. Lancet. 2006;368:1239-1247.
- Mas J, Chatellier G, Beyssen B, et al. EVA-3S Investigators. Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. N Engl J Med. 2006;355:1660-1671.
- Nederkoorn PJ, van der Graaf Y, Hunink MG. Duplex ultrasound and magnetic resonance angiography compared with digital subtraction angiography in carotid artery stenosis: a systematic review. Stroke. 2003;34:1324-1332.
- U-King-Im JM, Hollingworth W, Trivedi RA, et al. Cost-effectiveness of diagnostic strategies prior to carotid endarterectomy. Ann Neurol. 2005;58(4):506-515.
Case
A 62-year-old obese woman with type 2 diabetes, hypertension, and a pack-a-day smoking habit presents to the emergency department for acute onset of left-side arm and leg weakness and sensory loss on awakening.
She reports taking a baby aspirin daily to “prevent heart attacks.” Her electrocardiogram demonstrates a left bundle branch block and frequent premature atrial contractions. She recovers partially but has residual mild hemiparesis. A duplex carotid ultrasound shows 80% stenosis of the right internal carotid artery.
Overview
In the United States each year approximately 700,000 cerebrovascular accidents (CVA) constitute the largest cause of age-adjusted morbidity of any illness.1 About 200,000 of these strokes are recurrent events.
CVA is the third-leading cause of death. Hospitalists increasingly are responsible for the inpatient care of patients with acute CVA. Atheroembolism from carotid atherosclerosis is the suspected cause for about one in five ischemic strokes.2
The link between carotid stenosis and stroke has been recognized for many years. The first carotid endarterectomy (CEA) was reported more than 50 years ago.3
This targeted review covers the natural history of symptomatic carotid stenosis, the key efficacy trials of CEA and carotid angioplasty and stenting (CAS) among symptomatic patients, and pitfalls for properly diagnosing the severity of carotid stenosis. The medical therapy of carotid stenosis and the secondary prevention of CVA were recently reviewed in The Hospitalist (October 2007, p. 34).
Natural History
The presence or absence of referable neurological symptoms is pivotal to understanding the near-term risk for recurrent CVA related to carotid stenosis. In the absence of symptoms, the risk for future CVA is essentially constant over years.
However, once symptoms occur, the risk for a second event accelerates substantially. Among patients with newly symptomatic carotid stenosis, the risk for another transient ischemic attack (TIA) or stroke within the following 24 months is 26%.4 This risk peaks within the first month or two following the index event, underscoring the time-dependent nature of carotid evaluation and intervention.
Guidelines from the American Heart Association and the American College of Cardiology on the management of ischemic stroke assign early carotid intervention, defined as within two weeks from the index event, a Class 2 indication.5 Hospitalists must rapidly identify the severity of carotid stenosis and make timely referrals to meet this recommended therapeutic window.
Carotid Endarterectomy
CEA is perhaps the best-studied surgical procedure, with multiple well-conducted prospective randomized trials demonstrating its efficacy. The procedure had been performed for hundreds of thousands of patients prior to this data being published in the early 1990s. The North American Symptomatic Carotid Endarterectomy Trial (NASCET) was the landmark study demonstrating the efficacy of intervention. The trial of patients with symptomatic carotid stenosis was stopped early for patients with severe stenosis, defined as 70% to 99% narrowing by conventional angiography. At two years, the rate of ipsilateral stroke or post-operative death in patients with severe stenosis decreased from 26% in the medical arm to 9% in the CEA arm [an absolute risk reduction of 17% and number needed to treat of six (p<0.001)].
Rarely has any medical or surgical procedure had such a robust effect over so short an interval for such an important outcome. Patients with less severe stenosis were followed out to five years, with the final results showing benefit among patients with moderate stenosis (50% to 69%).6 The Veterans Affairs Cooperative Trial 309 and the European Carotid Stenosis Trial (ECST) were combined with NASCET in a pooled analysis of more than 6,000 patients and about 35,000 patient-years of follow-up.7-9
Among patients with 70% or greater stenosis, CEA reduced the absolute five-year risk of ipsilateral ischemic stroke and any operative stroke or death by 16% (95% confidence interval 11.2% to 20.8%). The benefit was less pronounced among patients with 50% to 69% stenosis, in whom CEA conferred a 4.6% (95% confidence interval 0.6% to 8.6%) absolute five-year risk reduction.
The medical aspect of these trials required only the use of aspirin. Intensive lipid control and tight glycemic and blood pressure control would probably reduce the rate of events. The 30-day operative risk was consistently less than 6% across these trials, with the benefit seen by two years among patients with 70% to 99% stenosis and by five years among patients with 50% to 69% stenosis.
Referring hospitalists should know the operative event rates of the surgeons to whom they are referring. Hospitalists should also refer those patients whose anticipated life expectancy is at least two years for patients with 70% to 99% stenosis and at least five years for patients with 50% to 69% stenosis.
Carotid Angioplasty and Stenting
CAS is increasingly used as an alternative to CEA among selected patients. Two procedural developments have improved the safety of percutaneous carotid revascularization.
First, distal embolic protection filters deployed prior to angioplasty collect debris associated with the mechanical intervention and limit the risk of peri-procedural stroke. (See Figures 1 and 2, p. 36.)
Second, the use of self-expanding stents has improved long-term patency over balloon-expanding stents, which can be damaged by neck movement and external pressure.
The Stenting and Angioplasty with [distal embolic] Protection in Patients at High Risk for Endarterectomy trial demonstrated the noninferiority of CAS versus CEA among high-risk patients.10 Inclusion criteria were symptomatic carotid stenosis of greater than 50% or asymptomatic stenosis greater than 80%. Patients had to have one of several high-risk features to be included. (See Table 1, above)
The cumulative incidence of post-operative stroke, myocardial infarction, death, and ipsilateral stroke within one year after the procedure was 20.1% in the CEA arm and 12.2% in the CAS arm (p=0.004 for noninferiority and p=0.053 for superiority). The rate of post-procedural cranial nerve injury was substantially lower (zero) in the CEA arm.
However, among those patients with symptomatic carotid stenosis, the cumulative incidence of the primary endpoint was 16.8% in the CAS arm and 16.5% in the CEA arm. Based upon this trial, CAS has equivalent one-year outcomes versus CEA in a high-risk population.
The Carotid and Vertebral Artery Transluminal Angioplasty Study trial was the first large prospective trial comparing CEA and CAS among symptomatic patients with severe carotid stenosis (mean 86.4% stenosis).11 At 30 days, the rate of death or disabling stroke was 6.4% with CAS and 5.9% with CEA, which were not significantly different in this trial of about 500 patients.
The trial was begun in 1994, with a large portion of angioplasty performed without stents or distal embolic protection. There were fewer local complications but higher rates of restenosis in the CAS arm. The authors noted “no substantial difference in the rate of ipsilateral stroke … up to three years after randomization” but cautioned that the confidence intervals were wide.
Two recently published trials of CAS versus CEA in lower-risk populations do not support the overall safety of CAS among symptomatic patients. The Stent-Protected Angioplasty versus Carotid Endarterectomy trial randomized 1,200 average-risk patients with symptomatic carotid stenosis of 50% or greater by angiography or 70% of greater by ultrasound to either CAS or CEA.12
The trial design stipulated that both surgeons and percutaneous interventionalists perform at least 25 procedures prior to inclusion in the study and that independent quality committees review these procedures. The use of distal embolic protection devices was left to the discretion of the operators. The 30-day rate of death or ipsilateral ischemic stroke was 6.34% in the CEA arm and 6.84% in the CAS arm (p=0.09 for noninferiority).
The investigators concluded that CAS is not non-inferior to CEA (i.e., that CAS is inferior). The Endarterectomy versus Angioplasty in Patients with Symptomatic Severe Carotid Stenosis trial randomized 527 patients with symptomatic carotid stenosis of 70% or greater by angiography or magnetic resonance angiography (MRA) to either CAS or CEA within two weeks of the index event.13
This trial design also stipulated that surgeons had performed at least 25 CEAs in the prior year. Percutaneous interventionalists did not have similar numeric procedure requirements, although the investigators provided for tutoring of less experienced operators. The trial was stopped prematurely due to futility (in terms of noninferiority) and harm within the CAS arm.
The 30-day cumulative incidence of death or any stroke was 3.9% in the CEA arm and 9.6% in the CAS arm (p=0.01 for superiority of CEA). The trial was powered to detect only large differences among low- and high-volume operators. Nearly 10% of patients did not have distal embolic protection devices used during their CAS procedures. Ongoing trials will further define the role of CAS versus CEA in the interventional treatment of carotid stenosis.
Accurate Diagnosis
Different trials used different criteria for defining the percent stenosis of the diseased carotid arterial segment. These differences were based primarily on the mode of testing (i.e., conventional angiography versus ultrasound), and on what portion of the carotid artery was used as the reference or baseline segment to calculate the percent stenosis.
A meta-analysis of various non-invasive modes of testing for carotid stenosis concluded that duplex ultrasound had a pooled sensitivity and specificity of 86% and 87%, respectively, to distinguish 70% to 99% stenosis from less than 70% stenosis.14 MRA had a pooled sensitivity and specificity of 95% and 90%, respectively.
The authors selected trials comparing these non-invasive methods with the gold standard of digital subtraction angiography. Using ultrasonography to first identify patients with at least 50% stenosis, followed by MRA or conventional angiography to more accurately confirm the degree of stenosis has been shown to be cost-effective.15
Back to the Case
For the patient in the vignette, the positive ultrasonography should lead to an MRA or conventional angiography to more precisely determine the percent stenosis. Current guidelines would suggest referring the patient for CEA to be completed within the next two weeks to treat a 50% or greater stenosis. That’s provided the surgeons have an operative morbidity and mortality rate less than 6% and her life expectancy is at least five years. If the patient had high-risk features as listed in Table 1 (left), referral for CAS in the hands of an experienced operator would be an alternative. TH
Dr. Anderson is an assistant professor of medicine at the University of Colorado, Denver, and an associate program director of the internal medicine residency program.
References
- Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics-2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69-e171.
- White H, Boden-Albala B, Wang C, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics: the Northern Manhattan Study. Circulation. 2005;111(10):1327-1331.
- Eastcott HH, Pickering GW, Rob CG. Reconstruction of internal carotid artery in a patient with intermittent attacks of hemiplegia. Lancet. 1954;267(6846):994-996.
- Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis: North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1991; 325(7):445-453.
- Sacco RL, Adams R, Albers G, et al. American Heart Association/American Stroke Association Council on Stroke; Council on Cardiovascular Radiology and Intervention; American Academy of Neurology. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention. Circulation. 2006;113:e409-e449.
- North American Symptomatic Carotid Endarterectomy Trialists’ Collaborative Group. The final results of the NASCET trial. N Engl J Med. 1998;339:1415-1425.
- Mayberg MR, Wilson E, Yatsu F, et al. Carotid endarterectomy and prevention of cerebral ischemia in symptomatic carotid stenosis. JAMA. 1991;266:3289-3294.
- European Carotid Surgery Trialists’ Investigators. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998;351:1379-1387.
- Rothwell P, Eliasziw M, Gutnikov A, et al. Analysis of pooled data from the randomised controlled trials of endarterectomy for symptomatic carotid stenosis. Lancet. 2003;361(9352):107-116.
- Yadav JS, Wholey MH, Kuntz, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004;351(15):1493-1501.
- Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): a randomised trial. Lancet. 2001;357:1729-1737.
- SPACE Collaborative Group. 30-day results from the SPACE trial of stent-protected angioplasty versus carotid endarterectomy in symptomatic patients: a randomised noninferiority trial. Lancet. 2006;368:1239-1247.
- Mas J, Chatellier G, Beyssen B, et al. EVA-3S Investigators. Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. N Engl J Med. 2006;355:1660-1671.
- Nederkoorn PJ, van der Graaf Y, Hunink MG. Duplex ultrasound and magnetic resonance angiography compared with digital subtraction angiography in carotid artery stenosis: a systematic review. Stroke. 2003;34:1324-1332.
- U-King-Im JM, Hollingworth W, Trivedi RA, et al. Cost-effectiveness of diagnostic strategies prior to carotid endarterectomy. Ann Neurol. 2005;58(4):506-515.
The Psychology of Error
What do your patient care errors have in common with financial mistakes that may compromise your retirement? Both have their underpinnings in the psychological strategies and tendencies we call heuristics.
The word derives from the Greek term “heuriskein” for discovery, but in the medical context we frequently think of these as these as mental shortcuts. Heuristics allow us to operate quickly despite the bewildering degree of complexity and uncertainty we encounter as we operate in the world but also lay the groundwork for disaster when they lead us astray. Let’s examine two mistakes and look at what they have in common: one that led to a drubbing in the stock market and the other that cost a patient his life.
A Market Misadventure
During the height of the market boom a young internist purchased shares of an exciting new biotech company poised at the forefront of tailored medical therapy based on genetic sequencing.
The stock nearly doubled, but as he rode the wild ride of the market’s fluctuations it became evident that the overall trend had changed. Almost daily monitoring of the press releases from the dynamic CEO helped reinforce his decision to hold the stock even after the dizzying drop that changed a strong gain to a significant loss. Finally after waiting months for the stock ticker to nudge back up to his entry point, he was glumly forced to face the loss.
The field of behavioral finance suggests humans are subject to cognitive predispositions leading to predictable errors. The first heuristic failure demonstrated by the unfortunate internist in our example is that of anchoring (see sidebar, p. 35).
The initial impression of the value of the company or particular price at which he purchased the stock has significance to him but is completely irrelevant to the value of the company once events and profit prospects changed. Thus, when new information about the company came to light, the focus should have been exclusively on the future valuation without regard to the past. That didn’t happen in this case. Our hapless investor had become anchored to the original price and refused to sell as it plummeted in the vain hopes that it would rise again despite the absence of evidence that this was likely.
Anchoring bias affects all of us and is as true in medicine as it is in the markets. The first diagnosis, which seems likely as we hear a case described, can be surprisingly hard to shake even when the facts on the ground have changed.
A second human tendency we see leading to both financial and medical calamity is the desire to be right. A strong self-image (and many physicians have a strong one, indeed) is bolstered by seeking information that confirms prior beliefs.
Unfortunately this confirmation bias can also cause us to overvalue the positive press about a company we are invested in and discount or not read at all things that might change our minds. Back in the clinical environment, examples abound where a physician becomes fixed on a diagnosis and orders tests designed to confirm the initial impression but fails to explore alternatives. The more invested in a diagnosis we become, the more selective we tend to be in seeking and interpreting data to reinforce our convictions.
Higher Stakes
Years later and hundreds of miles away a nocturnist gets a call from the emergency department (ED) on the seventh new admission of the night.
“I’ve got another rule-out myocardial infarction (MI) for you” said the ED physician, who briefly provided the assessment that the patient was low risk, with negative enzymes, chest X-ray, and electrocardiogram.
The nocturnist noted the atypical severity of the pain, systolic blood pressure more than 200, and positive cocaine history. But this did not alter the plan as the patient was passed from the ED physician to the nocturnist and then to the hospitalist who assumed care the next morning. Unfortunately, it took the patient experiencing a severe increase in tearing pain radiating to his back during the exercise stress test to prompt the discovery of his ascending aortic dissection. The patient died on the operating room table, leaving all three physicians wondering how they could have missed the diagnosis when in retrospect it seemed so obvious.
Present the same clinical scenario at grand rounds and the third-year medical students could tell you dissection should have been considered. How did three smart experienced people all make the same fatal mistake?
This case demonstrates a number of heuristic failures. Availability bias is a form of pattern recognition and arises from our habit of perceiving the things we see often as more likely than those which we have not seen or thought about recently. Hoof beats in Kentucky, as they say, are usually not a herd of zebra. ED physicians see what at times seems like hordes of patients with low-risk chest pain, the vast majority of which lack a life-threatening etiology. Thus, we can become complacent in assuming that the next admission for chest pain reflects the same cause as the seven before.
Pattern recognition serves a vital role. Most expert physicians rely on this more than classic deductive reasoning and, much less, Bayesian analysis. Casino operators exploit this tendency to see false patterns to their profit by installing displays that show the last 10 to 20 results over the roulette table. However, just as each turn of the roulette wheel is not influenced by prior spins, each patient is unique. One must beware of the misleading power of the availability bias.
Once the initial misdiagnosis had been made, the anchoring bias and confirmation bias continued the cascade of events—turning a mistake from a temporary error to a disaster. The phrase “chest pain rule out MI” not only encourages the physician to minimize the potential severity of the symptom via the framing effect but also telegraphs the anchoring phenomenon by fixing on a single disease concern for a symptom whose etiologies are legion.
However, even accepting that the initial diagnosis by the ED doctor was influenced by the availability bias, why was this not corrected by the nocturnist or by the hospitalist on the next day? The answer lies in diagnosis momentum.
Each physician does not evaluate the patient in isolation but rather has a tendency to include the assessment of the prior clinician as part of their own decision-making process. The more people who have seen the patient and agreed with the diagnosis, the higher the mental hurdle becomes to disagree and take the work-up in a different direction.
What You Can Do
Does the mere existence of these many heuristics condemn the physician to a career of repeating these potentially fatal errors? The obvious answer is no, but the solution requires a concerted effort on the part of the physician to avoid these mistakes.
Step one is to recognize that many heuristics are essentially abbreviations of full conscious reasoning. Now take a physician who is tired, stressed, or inundated with multiple tasks. In an effort to organize the seemingly chaotic world of medicine the mind seeks a crutch. These mental shortcuts allow us to quickly process massive amounts of information and come up with a reasonable plan that will be right most of the time.
When rushed, stressed, and distracted, we are most prone to use these shortcuts. These times of pressure are exactly when it is most important to pause and consider whether we’re acting on gut feeling or on full consideration of all the evidence. Awareness of the predictable circumstances that create the set-up for heuristic failures allows for a moment of reflection to prevent falling into one of these psychological traps. This process of deliberately considering our own decision-making is referred to as meta-cognition.
An additional familiar tool available to the physician is differential diagnosis. This is essentially a form of cognitive forcing strategy designed to guard against availability and anchoring biases. By deliberately creating a list of alternative possibilities, we become less prone to anchor on a single diagnosis.
By briefly reviewing the rare possibilities we have not seen recently and bringing them to the forefront of memory, we diminish the power of the availability bias. Spending a second or two considering the differential—even in seemingly routine cases—will defuse the hold of these particular heuristics.
Hospitalists by the nature of our practice tend to have multiple transitions in patient care. At times this offers a fresh perspective to correct mistakes, but it also offers potential to compound them via diagnosis momentum.
We habitually convey diagnosis and treatment plans to our partners at handoffs. Including a level of uncertainty as part of checkout would create a cue for the accepting physician to decrease the risk of this heuristic failure. One might imagine the patient in the case above would have had a greater probability of survival if the nocturnist had conveyed a diagnosis of “chest pain of uncertain etiology” to his partner rather than “chest pain rule-out MI.”
As illustrated by the cases above, heuristics are not mistakes in and of themselves. They are the assumptions and pattern-recognition techniques that serve us well the majority of the time in and out of medicine. Recognizing when you take one of these mental shortcuts, being aware of the circumstances that predispose to error creation, and evaluating your decision-making process allows the astute physician to guard against the times when they fail. Greater self-awareness of the process of your own cognition can make for a better clinician—and perhaps even make you a better investor. TH
Drs. Cumbler and Trosterman are assistant professors in the Section of Hospital Medicine at the University of Colorado.
What do your patient care errors have in common with financial mistakes that may compromise your retirement? Both have their underpinnings in the psychological strategies and tendencies we call heuristics.
The word derives from the Greek term “heuriskein” for discovery, but in the medical context we frequently think of these as these as mental shortcuts. Heuristics allow us to operate quickly despite the bewildering degree of complexity and uncertainty we encounter as we operate in the world but also lay the groundwork for disaster when they lead us astray. Let’s examine two mistakes and look at what they have in common: one that led to a drubbing in the stock market and the other that cost a patient his life.
A Market Misadventure
During the height of the market boom a young internist purchased shares of an exciting new biotech company poised at the forefront of tailored medical therapy based on genetic sequencing.
The stock nearly doubled, but as he rode the wild ride of the market’s fluctuations it became evident that the overall trend had changed. Almost daily monitoring of the press releases from the dynamic CEO helped reinforce his decision to hold the stock even after the dizzying drop that changed a strong gain to a significant loss. Finally after waiting months for the stock ticker to nudge back up to his entry point, he was glumly forced to face the loss.
The field of behavioral finance suggests humans are subject to cognitive predispositions leading to predictable errors. The first heuristic failure demonstrated by the unfortunate internist in our example is that of anchoring (see sidebar, p. 35).
The initial impression of the value of the company or particular price at which he purchased the stock has significance to him but is completely irrelevant to the value of the company once events and profit prospects changed. Thus, when new information about the company came to light, the focus should have been exclusively on the future valuation without regard to the past. That didn’t happen in this case. Our hapless investor had become anchored to the original price and refused to sell as it plummeted in the vain hopes that it would rise again despite the absence of evidence that this was likely.
Anchoring bias affects all of us and is as true in medicine as it is in the markets. The first diagnosis, which seems likely as we hear a case described, can be surprisingly hard to shake even when the facts on the ground have changed.
A second human tendency we see leading to both financial and medical calamity is the desire to be right. A strong self-image (and many physicians have a strong one, indeed) is bolstered by seeking information that confirms prior beliefs.
Unfortunately this confirmation bias can also cause us to overvalue the positive press about a company we are invested in and discount or not read at all things that might change our minds. Back in the clinical environment, examples abound where a physician becomes fixed on a diagnosis and orders tests designed to confirm the initial impression but fails to explore alternatives. The more invested in a diagnosis we become, the more selective we tend to be in seeking and interpreting data to reinforce our convictions.
Higher Stakes
Years later and hundreds of miles away a nocturnist gets a call from the emergency department (ED) on the seventh new admission of the night.
“I’ve got another rule-out myocardial infarction (MI) for you” said the ED physician, who briefly provided the assessment that the patient was low risk, with negative enzymes, chest X-ray, and electrocardiogram.
The nocturnist noted the atypical severity of the pain, systolic blood pressure more than 200, and positive cocaine history. But this did not alter the plan as the patient was passed from the ED physician to the nocturnist and then to the hospitalist who assumed care the next morning. Unfortunately, it took the patient experiencing a severe increase in tearing pain radiating to his back during the exercise stress test to prompt the discovery of his ascending aortic dissection. The patient died on the operating room table, leaving all three physicians wondering how they could have missed the diagnosis when in retrospect it seemed so obvious.
Present the same clinical scenario at grand rounds and the third-year medical students could tell you dissection should have been considered. How did three smart experienced people all make the same fatal mistake?
This case demonstrates a number of heuristic failures. Availability bias is a form of pattern recognition and arises from our habit of perceiving the things we see often as more likely than those which we have not seen or thought about recently. Hoof beats in Kentucky, as they say, are usually not a herd of zebra. ED physicians see what at times seems like hordes of patients with low-risk chest pain, the vast majority of which lack a life-threatening etiology. Thus, we can become complacent in assuming that the next admission for chest pain reflects the same cause as the seven before.
Pattern recognition serves a vital role. Most expert physicians rely on this more than classic deductive reasoning and, much less, Bayesian analysis. Casino operators exploit this tendency to see false patterns to their profit by installing displays that show the last 10 to 20 results over the roulette table. However, just as each turn of the roulette wheel is not influenced by prior spins, each patient is unique. One must beware of the misleading power of the availability bias.
Once the initial misdiagnosis had been made, the anchoring bias and confirmation bias continued the cascade of events—turning a mistake from a temporary error to a disaster. The phrase “chest pain rule out MI” not only encourages the physician to minimize the potential severity of the symptom via the framing effect but also telegraphs the anchoring phenomenon by fixing on a single disease concern for a symptom whose etiologies are legion.
However, even accepting that the initial diagnosis by the ED doctor was influenced by the availability bias, why was this not corrected by the nocturnist or by the hospitalist on the next day? The answer lies in diagnosis momentum.
Each physician does not evaluate the patient in isolation but rather has a tendency to include the assessment of the prior clinician as part of their own decision-making process. The more people who have seen the patient and agreed with the diagnosis, the higher the mental hurdle becomes to disagree and take the work-up in a different direction.
What You Can Do
Does the mere existence of these many heuristics condemn the physician to a career of repeating these potentially fatal errors? The obvious answer is no, but the solution requires a concerted effort on the part of the physician to avoid these mistakes.
Step one is to recognize that many heuristics are essentially abbreviations of full conscious reasoning. Now take a physician who is tired, stressed, or inundated with multiple tasks. In an effort to organize the seemingly chaotic world of medicine the mind seeks a crutch. These mental shortcuts allow us to quickly process massive amounts of information and come up with a reasonable plan that will be right most of the time.
When rushed, stressed, and distracted, we are most prone to use these shortcuts. These times of pressure are exactly when it is most important to pause and consider whether we’re acting on gut feeling or on full consideration of all the evidence. Awareness of the predictable circumstances that create the set-up for heuristic failures allows for a moment of reflection to prevent falling into one of these psychological traps. This process of deliberately considering our own decision-making is referred to as meta-cognition.
An additional familiar tool available to the physician is differential diagnosis. This is essentially a form of cognitive forcing strategy designed to guard against availability and anchoring biases. By deliberately creating a list of alternative possibilities, we become less prone to anchor on a single diagnosis.
By briefly reviewing the rare possibilities we have not seen recently and bringing them to the forefront of memory, we diminish the power of the availability bias. Spending a second or two considering the differential—even in seemingly routine cases—will defuse the hold of these particular heuristics.
Hospitalists by the nature of our practice tend to have multiple transitions in patient care. At times this offers a fresh perspective to correct mistakes, but it also offers potential to compound them via diagnosis momentum.
We habitually convey diagnosis and treatment plans to our partners at handoffs. Including a level of uncertainty as part of checkout would create a cue for the accepting physician to decrease the risk of this heuristic failure. One might imagine the patient in the case above would have had a greater probability of survival if the nocturnist had conveyed a diagnosis of “chest pain of uncertain etiology” to his partner rather than “chest pain rule-out MI.”
As illustrated by the cases above, heuristics are not mistakes in and of themselves. They are the assumptions and pattern-recognition techniques that serve us well the majority of the time in and out of medicine. Recognizing when you take one of these mental shortcuts, being aware of the circumstances that predispose to error creation, and evaluating your decision-making process allows the astute physician to guard against the times when they fail. Greater self-awareness of the process of your own cognition can make for a better clinician—and perhaps even make you a better investor. TH
Drs. Cumbler and Trosterman are assistant professors in the Section of Hospital Medicine at the University of Colorado.
What do your patient care errors have in common with financial mistakes that may compromise your retirement? Both have their underpinnings in the psychological strategies and tendencies we call heuristics.
The word derives from the Greek term “heuriskein” for discovery, but in the medical context we frequently think of these as these as mental shortcuts. Heuristics allow us to operate quickly despite the bewildering degree of complexity and uncertainty we encounter as we operate in the world but also lay the groundwork for disaster when they lead us astray. Let’s examine two mistakes and look at what they have in common: one that led to a drubbing in the stock market and the other that cost a patient his life.
A Market Misadventure
During the height of the market boom a young internist purchased shares of an exciting new biotech company poised at the forefront of tailored medical therapy based on genetic sequencing.
The stock nearly doubled, but as he rode the wild ride of the market’s fluctuations it became evident that the overall trend had changed. Almost daily monitoring of the press releases from the dynamic CEO helped reinforce his decision to hold the stock even after the dizzying drop that changed a strong gain to a significant loss. Finally after waiting months for the stock ticker to nudge back up to his entry point, he was glumly forced to face the loss.
The field of behavioral finance suggests humans are subject to cognitive predispositions leading to predictable errors. The first heuristic failure demonstrated by the unfortunate internist in our example is that of anchoring (see sidebar, p. 35).
The initial impression of the value of the company or particular price at which he purchased the stock has significance to him but is completely irrelevant to the value of the company once events and profit prospects changed. Thus, when new information about the company came to light, the focus should have been exclusively on the future valuation without regard to the past. That didn’t happen in this case. Our hapless investor had become anchored to the original price and refused to sell as it plummeted in the vain hopes that it would rise again despite the absence of evidence that this was likely.
Anchoring bias affects all of us and is as true in medicine as it is in the markets. The first diagnosis, which seems likely as we hear a case described, can be surprisingly hard to shake even when the facts on the ground have changed.
A second human tendency we see leading to both financial and medical calamity is the desire to be right. A strong self-image (and many physicians have a strong one, indeed) is bolstered by seeking information that confirms prior beliefs.
Unfortunately this confirmation bias can also cause us to overvalue the positive press about a company we are invested in and discount or not read at all things that might change our minds. Back in the clinical environment, examples abound where a physician becomes fixed on a diagnosis and orders tests designed to confirm the initial impression but fails to explore alternatives. The more invested in a diagnosis we become, the more selective we tend to be in seeking and interpreting data to reinforce our convictions.
Higher Stakes
Years later and hundreds of miles away a nocturnist gets a call from the emergency department (ED) on the seventh new admission of the night.
“I’ve got another rule-out myocardial infarction (MI) for you” said the ED physician, who briefly provided the assessment that the patient was low risk, with negative enzymes, chest X-ray, and electrocardiogram.
The nocturnist noted the atypical severity of the pain, systolic blood pressure more than 200, and positive cocaine history. But this did not alter the plan as the patient was passed from the ED physician to the nocturnist and then to the hospitalist who assumed care the next morning. Unfortunately, it took the patient experiencing a severe increase in tearing pain radiating to his back during the exercise stress test to prompt the discovery of his ascending aortic dissection. The patient died on the operating room table, leaving all three physicians wondering how they could have missed the diagnosis when in retrospect it seemed so obvious.
Present the same clinical scenario at grand rounds and the third-year medical students could tell you dissection should have been considered. How did three smart experienced people all make the same fatal mistake?
This case demonstrates a number of heuristic failures. Availability bias is a form of pattern recognition and arises from our habit of perceiving the things we see often as more likely than those which we have not seen or thought about recently. Hoof beats in Kentucky, as they say, are usually not a herd of zebra. ED physicians see what at times seems like hordes of patients with low-risk chest pain, the vast majority of which lack a life-threatening etiology. Thus, we can become complacent in assuming that the next admission for chest pain reflects the same cause as the seven before.
Pattern recognition serves a vital role. Most expert physicians rely on this more than classic deductive reasoning and, much less, Bayesian analysis. Casino operators exploit this tendency to see false patterns to their profit by installing displays that show the last 10 to 20 results over the roulette table. However, just as each turn of the roulette wheel is not influenced by prior spins, each patient is unique. One must beware of the misleading power of the availability bias.
Once the initial misdiagnosis had been made, the anchoring bias and confirmation bias continued the cascade of events—turning a mistake from a temporary error to a disaster. The phrase “chest pain rule out MI” not only encourages the physician to minimize the potential severity of the symptom via the framing effect but also telegraphs the anchoring phenomenon by fixing on a single disease concern for a symptom whose etiologies are legion.
However, even accepting that the initial diagnosis by the ED doctor was influenced by the availability bias, why was this not corrected by the nocturnist or by the hospitalist on the next day? The answer lies in diagnosis momentum.
Each physician does not evaluate the patient in isolation but rather has a tendency to include the assessment of the prior clinician as part of their own decision-making process. The more people who have seen the patient and agreed with the diagnosis, the higher the mental hurdle becomes to disagree and take the work-up in a different direction.
What You Can Do
Does the mere existence of these many heuristics condemn the physician to a career of repeating these potentially fatal errors? The obvious answer is no, but the solution requires a concerted effort on the part of the physician to avoid these mistakes.
Step one is to recognize that many heuristics are essentially abbreviations of full conscious reasoning. Now take a physician who is tired, stressed, or inundated with multiple tasks. In an effort to organize the seemingly chaotic world of medicine the mind seeks a crutch. These mental shortcuts allow us to quickly process massive amounts of information and come up with a reasonable plan that will be right most of the time.
When rushed, stressed, and distracted, we are most prone to use these shortcuts. These times of pressure are exactly when it is most important to pause and consider whether we’re acting on gut feeling or on full consideration of all the evidence. Awareness of the predictable circumstances that create the set-up for heuristic failures allows for a moment of reflection to prevent falling into one of these psychological traps. This process of deliberately considering our own decision-making is referred to as meta-cognition.
An additional familiar tool available to the physician is differential diagnosis. This is essentially a form of cognitive forcing strategy designed to guard against availability and anchoring biases. By deliberately creating a list of alternative possibilities, we become less prone to anchor on a single diagnosis.
By briefly reviewing the rare possibilities we have not seen recently and bringing them to the forefront of memory, we diminish the power of the availability bias. Spending a second or two considering the differential—even in seemingly routine cases—will defuse the hold of these particular heuristics.
Hospitalists by the nature of our practice tend to have multiple transitions in patient care. At times this offers a fresh perspective to correct mistakes, but it also offers potential to compound them via diagnosis momentum.
We habitually convey diagnosis and treatment plans to our partners at handoffs. Including a level of uncertainty as part of checkout would create a cue for the accepting physician to decrease the risk of this heuristic failure. One might imagine the patient in the case above would have had a greater probability of survival if the nocturnist had conveyed a diagnosis of “chest pain of uncertain etiology” to his partner rather than “chest pain rule-out MI.”
As illustrated by the cases above, heuristics are not mistakes in and of themselves. They are the assumptions and pattern-recognition techniques that serve us well the majority of the time in and out of medicine. Recognizing when you take one of these mental shortcuts, being aware of the circumstances that predispose to error creation, and evaluating your decision-making process allows the astute physician to guard against the times when they fail. Greater self-awareness of the process of your own cognition can make for a better clinician—and perhaps even make you a better investor. TH
Drs. Cumbler and Trosterman are assistant professors in the Section of Hospital Medicine at the University of Colorado.
Close the Loop
This is the second of a two-part series examining medical errors. Part 1 addressed thought processes hospitalists use that may lead to mistaken diagnoses (October 2007, p. 36). Part 2 examines what healthcare corporations are doing to improve diagnoses and reduce errors.
Pilots taking off, Swiss cheese, low-hanging fruit. Talk to hospitalists about the issue of medical errors and the analogies come quickly.
Ever since 2000’s landmark Institute of Medicine report “To Err is Human: Building a Safer Health System” found that anywhere from 40,000 to 100,000 patients incur injury or die every year because of medical errors, debate has been constant.
Medical literature is abundant on this topic. The Joint Commission, National Center for Patient Safety, Agency for Health Care Research and Quality, and myriad other organizations and institutions, including SHM, are all helping providers and hospitals solve the problems by establishing goals, standards, guidelines, and policies.
—Evan Falchuk, president, Best Doctors Inc., Boston
Definitions and Paradigms
Best-practice recommendations for reducing errors are generally based on two essential principles: using a systems-based approach to patient safety and creating an environment that supports open dialogue about errors, their causes, and strategies for prevention.
Terminology is a key factor. The terms “error” and “mistake” carry an emotional component associated with embarrassment and shame. Healthcare providers don’t like to be associated with errors. There is an accompanying fear of litigation, and people, perhaps especially physicians, don’t want to be known as someone who was sued.
“The language we use to talk about these issues is important,” says Janet Nagamine, MD, part-time hospitalist at Kaiser Permanente Santa Clara Medical Center in Calif. and current chair of SHM’s quality and patient safety committee. In fact, because of the negativity around the terms “misdiagnosis” and “delay in diagnosis” she advocates using the term “unintended adverse event” in order to appear more neutral.
“The term error is extremely threatening and scary to any health professional because it implies a personal failure,” says Dr. Nagamine. The goal when it comes to errors is essentially to look for the how—not the who.
Reporting medical errors is one thing, but reporting misdiagnoses is another, says Lakshmi Halasyamani, MD, vice chair for the department of internal medicine at St. Joseph’s Mercy Hospital in Ann Arbor, Mich., and SHM board member. “We don’t really talk about misdiagnosis,” she says. “That’s partly because we have tended to assign more individual blame for misdiagnoses.”
Drs. Nagamine and Halasyamani agree that altering the way of viewing errors means nurturing culture change.
“We have made very little headway helping physicians understand that in the course of their careers there will be misdiagnoses and the best of physicians have misdiagnoses,” says Dr. Halasyamani. “We are not developmentally at the same stage that we are with talking about medical errors.”
She believes this is largely a professionalism issue that first means normalizing the issue of misdiagnosis. “It is kind of ludicrous to think that you will practice medicine over 40 years and not have a misdiagnosis,” she says. “But we don’t look at it from that perspective when we begin to orient trainees.”
National Efforts
To the people at the U.S. Pharmacopeia Center for the Advancement of Patient Safety (USP), the arrival of universal electronic medical records (EMR) in the coming decade will be a boon to the error-reduction effort.
“Eventually we will all have our health information stored electronically for easy retrieval,” says Rodney W. Hicks, PhD, ARNP, manager, patient safety research and practice for the USP and first author on its most recent report. The beginning of regional networks for EMR is taking hold.
“Even before the IOM report, the USP was familiar with intensivists,” says Dr. Hicks. “We recognize hospitalists as experts who bring efficiency and effectiveness to the healthcare system.”
The USP maintains perhaps the largest database of medication errors in the world.1 Each year the USP issues a report that focuses on one topic and builds its knowledge base.
This year’s report focuses exclusively on the perioperative continuum of care. Last year’s covered ICU- and radiology-related errors. Two years ago the report was a five-year data summary of errors occurring primarily in hospitals.
“The area of errors due to breakdowns in handoffs remains a huge problem for diagnosis and the continuity of care,” says Shawn C. Becker, MS, BSN, RN, director of patient safety initiatives for the USP.
Classification
In general, errors are divided into those that stem from individual factors and those that are system-related, which include environmental and organizational factors.
Environmental risks are often related to human factors. Dr. Nagamine offers an aviation analogy to demonstrate the many pulls on caregivers’ attention.
“What happens in a cockpit at take off is that you are not allowed to talk about anything other than the take-off checklist,” she says. “In medicine, we have nurses’ stations or medication carts in the middle of the hallway, so nurses are preparing meds and people are tugging on their shoulder and interrupting them during a critical task.”
Organizational factors involve culture and priorities. If your organization says it values quality and safety but doesn’t put in place policies and processes to support it, that affects diagnostics and error-free performance.
Market Drivers
“The discussion about quality is driven by medical error,” says Evan Falchuk, president of Best Doctors Inc., based in Boston. “But the issue is more interesting than simply looking for mistakes.”
Best Doctors partners with employers and health plans to help members with serious illnesses make sure they have the right diagnosis and treatment. Members can consult with specialists who assess diagnoses and can recommend treatment. The firm believes this is the best way to measure quality, and consumers around the world increasingly agree: The company serves more than 10 million people in 30 countries.
Best Doctors was founded in 1989 by two internists: Falchuk’s father, Kenneth H. Falchuk, MD, a professor of medicine at Harvard University Medical School, and Jose Halperin, MD, an associate professor of medicine at Harvard. The service they created is one in which doctors review a patient’s medical information, identify the important issues, and consult with leading experts from their peer-reviewed database. The company then has clinicians work with the patient and his or her doctor to ensure that the patient is getting appropriate care. The process has identified incorrect diagnosis or treatment in more than half of reviewed cases.
“Hospitalists should think about quality in terms of things happening outside the hospital,” says Falchuk. “The informed, demanding consumer is coming to healthcare, and their expectations are clear: to be paid attention to, to have all of their questions answered, and to be certain that their diagnosis and treatment are correct.” These sentiments affect how hospitals do business.
The increasing amount of medical information patients can find on the Internet can raise questions in their minds. “Patients want to trust their doctors,” Falchuk says. “But when the patient has lots of information and questions and finds it difficult to spend as much time as they would like with their doctor, trust is eroded—and patients start to wonder if their doctor is doing the right thing.”
The complexity of modern medicine, with new diagnoses, treatments, and testing, and ultra-specialized experts, can sometimes—ironically—lead to lesser quality.
“It is more important than ever before that doctors with differing perspectives discuss each case,” says Falchuk. “But doctors complain that the system, often because of constraints imposed by managed care, only allows for episodic interactions like that. If that kind of interaction can be made the norm, it will give patients an extraordinary amount of comfort as to the quality of their care.”
Falchuk believes the tipping point for combating errors is being reached—at least from the business point of view.
“With major employers, as many as one in 200 employees call us for help,” he says. “That is close to the incidence rate of the illnesses we commonly see: cancer, heart problems, and undiagnosed situations. When you see this flood of demand, you say, ‘Something is going on that is driving this.’ ”
These market-based factors are driving hospitals to publish and compare rates for process of care and mortality, and many medical centers are publishing report cards. With the advent of advanced technology, hospital and provider performance will be increasingly apparent and transparent. Corporations and institutions will have to be less guarded about what they share publicly as their public accountability is increased.
Interventions, Feedback
The healthcare industry has embraced British psychologist James Reason’s 1990 Swiss cheese model of error as a means of tackling the cumulative effects that cause adverse events. The model conceptualizes the factors that contributed to an error as holes in slices of Swiss cheese. Only when the holes line up does the adverse event occur; placing barriers at one or more of the holes “traps the error” from being realized.
For instance, Best Doctors notes “potholes” in the reading stage of pathology.
“We see many cases of underdiagnosis or even misdiagnosis based on one of the most difficult steps: a pathology review,” says Falchuk. “With new, specifically targeted treatments, getting that right is extremely significant.” Best Doctors experts often recommend having pathology re-reviewed. “I wouldn’t call this error, but patients view it as a question of quality,” he says.
Integrating technology with observation skills is an important way hospitals are working to improve diagnostics and reduce error.
Because the same factors contribute to a near miss as to an actual event, studying the patterns of near misses can provide a wealth of information.
“I heard some statistics that for every 19 near misses, you’re going to have one event,” says Dr. Nagamine. If on a particular day, a provider was fatigued or overtaxed and didn’t catch a contributing factor that is a risk—termed a “latent condition”—that’s when the holes line up. “An event is never just the result of one thing or one person; it is a combination of factors,” says Dr. Nagamine.
One example of this concerns an element in the policy for discharge bundles that institutions establish to better manage transfer of care. When lab results become available only after a patient’s discharge, it increases the risk for delays in diagnosis. Electronically placing the test results into the primary care physician’s e-mail inbox helps to “close the loop,” says Dr. Nagamine. “That information gets to somebody, and we’re clear on who that somebody is. We are putting in place those types of interventions—which are really the low-hanging fruit.”
Culture Change
Opening up about adverse events and providing feedback creates a different awareness about the risks surrounding the event.
“The look-alike, sound-alike medications are an example,” Dr. Nagamine says. “I went up to the unit and said, ‘A nurse recorded that she almost gave hydralazine instead of hydroxyzine—has that ever happened to you?’ The first three nurses I asked said, ‘Yes,’ ‘Yes,’ ‘Yes.’ Until I ask these types of questions, I don’t know. And until you can make it safe for your staff to talk, you will not have good information.”
Although this is the approach most of the safety world and quality world is embracing, it is not how most clinicians on the frontline view it.
“We are trying to educate people about a framework in which to think about this,” says Dr. Nagamine. “It is not constructive to point fingers, but it is important to give people feedback about how the event happened. It is far more constructive to look at the entire system and ask, ‘How did we fail here? What was your piece of it? What was the system’s piece of it?’ ”
Because of the connection between litigation and adverse events, changing the culture is a complex imperative. But providers must recognize that systems failures are involved in about 75% to 80% of medical malpractice cases—whether that involves communication breakdowns, inadequate availability of information, or a host of other factors. The individual, environment, and organization are linked.
Reducing negativity and sensitivity around the terms associated with error and reframing thinking toward prevention are important.
“There is a richness of information that comes once you change the culture from blaming to fixing,” says Dr. Nagamine. Providing feedback to frontline practitioners is key, as is thanking those who report. “It increases providers’ awareness about where the hot spots and vulnerabilities are and how to stay out of trouble. Simply by giving them information about an event raises their awareness of the magnitude of certain types of issues,” she explains.
When Dr. Nagamine led a safety initiative on the ICU floor consisting of human factors training and a new system for reporting events, the number of reports “went through roof,” she says. “My new problem was not that people were not reporting; it was being overwhelmed with the information that was coming in. We were able to create a culture of safety that made it safe to report and consequently had much better information from which we could devise prevention strategies.”
SHM, in planning to co-create standards for focused practice with the American Board of Internal Medicine, intends to promote the standards of professionalism along with other standards. The issue of personal accountability, although a part of that, has been less of a focus to date. In the future, all institutions may have technology hospitalists can use to learn whether the discharge diagnosis was correct in the months and years that followed. Will the culture be emotionally ready to handle what technology can offer?
“We will need to own it when things go well and when things don’t go well or when we are wrong,” says Dr. Halasyamani. “We need to be able to investigate the distribution of the reasons for misdiagnosis, determine how many of those problems are systems issues, and devise strategies to address them.” In a sense, she says, everything can be viewed as a system issue unless actions are egregious and malicious.
Yet when physicians are associated with an adverse event, research shows they feel they have little support to talk about it.
“The system we have in place has begun to try to address some of the issues related to system errors,” says Dr. Halasyamani. “But what if an individual does have an error? What systems do we have in place to support that person in the recovery? And along the way if we find people who are having these issues over and over again, we need to design processes to deal with that.”
One particular focus of SHM’s transfer-of-care initiative concerns communication surrounding handoffs. “We are setting those standards and thinking about what kinds of technology tools can help make those standards easier to adhere to and easier to implement,” says Dr. Halasyamani. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
This is the second of a two-part series examining medical errors. Part 1 addressed thought processes hospitalists use that may lead to mistaken diagnoses (October 2007, p. 36). Part 2 examines what healthcare corporations are doing to improve diagnoses and reduce errors.
Pilots taking off, Swiss cheese, low-hanging fruit. Talk to hospitalists about the issue of medical errors and the analogies come quickly.
Ever since 2000’s landmark Institute of Medicine report “To Err is Human: Building a Safer Health System” found that anywhere from 40,000 to 100,000 patients incur injury or die every year because of medical errors, debate has been constant.
Medical literature is abundant on this topic. The Joint Commission, National Center for Patient Safety, Agency for Health Care Research and Quality, and myriad other organizations and institutions, including SHM, are all helping providers and hospitals solve the problems by establishing goals, standards, guidelines, and policies.
—Evan Falchuk, president, Best Doctors Inc., Boston
Definitions and Paradigms
Best-practice recommendations for reducing errors are generally based on two essential principles: using a systems-based approach to patient safety and creating an environment that supports open dialogue about errors, their causes, and strategies for prevention.
Terminology is a key factor. The terms “error” and “mistake” carry an emotional component associated with embarrassment and shame. Healthcare providers don’t like to be associated with errors. There is an accompanying fear of litigation, and people, perhaps especially physicians, don’t want to be known as someone who was sued.
“The language we use to talk about these issues is important,” says Janet Nagamine, MD, part-time hospitalist at Kaiser Permanente Santa Clara Medical Center in Calif. and current chair of SHM’s quality and patient safety committee. In fact, because of the negativity around the terms “misdiagnosis” and “delay in diagnosis” she advocates using the term “unintended adverse event” in order to appear more neutral.
“The term error is extremely threatening and scary to any health professional because it implies a personal failure,” says Dr. Nagamine. The goal when it comes to errors is essentially to look for the how—not the who.
Reporting medical errors is one thing, but reporting misdiagnoses is another, says Lakshmi Halasyamani, MD, vice chair for the department of internal medicine at St. Joseph’s Mercy Hospital in Ann Arbor, Mich., and SHM board member. “We don’t really talk about misdiagnosis,” she says. “That’s partly because we have tended to assign more individual blame for misdiagnoses.”
Drs. Nagamine and Halasyamani agree that altering the way of viewing errors means nurturing culture change.
“We have made very little headway helping physicians understand that in the course of their careers there will be misdiagnoses and the best of physicians have misdiagnoses,” says Dr. Halasyamani. “We are not developmentally at the same stage that we are with talking about medical errors.”
She believes this is largely a professionalism issue that first means normalizing the issue of misdiagnosis. “It is kind of ludicrous to think that you will practice medicine over 40 years and not have a misdiagnosis,” she says. “But we don’t look at it from that perspective when we begin to orient trainees.”
National Efforts
To the people at the U.S. Pharmacopeia Center for the Advancement of Patient Safety (USP), the arrival of universal electronic medical records (EMR) in the coming decade will be a boon to the error-reduction effort.
“Eventually we will all have our health information stored electronically for easy retrieval,” says Rodney W. Hicks, PhD, ARNP, manager, patient safety research and practice for the USP and first author on its most recent report. The beginning of regional networks for EMR is taking hold.
“Even before the IOM report, the USP was familiar with intensivists,” says Dr. Hicks. “We recognize hospitalists as experts who bring efficiency and effectiveness to the healthcare system.”
The USP maintains perhaps the largest database of medication errors in the world.1 Each year the USP issues a report that focuses on one topic and builds its knowledge base.
This year’s report focuses exclusively on the perioperative continuum of care. Last year’s covered ICU- and radiology-related errors. Two years ago the report was a five-year data summary of errors occurring primarily in hospitals.
“The area of errors due to breakdowns in handoffs remains a huge problem for diagnosis and the continuity of care,” says Shawn C. Becker, MS, BSN, RN, director of patient safety initiatives for the USP.
Classification
In general, errors are divided into those that stem from individual factors and those that are system-related, which include environmental and organizational factors.
Environmental risks are often related to human factors. Dr. Nagamine offers an aviation analogy to demonstrate the many pulls on caregivers’ attention.
“What happens in a cockpit at take off is that you are not allowed to talk about anything other than the take-off checklist,” she says. “In medicine, we have nurses’ stations or medication carts in the middle of the hallway, so nurses are preparing meds and people are tugging on their shoulder and interrupting them during a critical task.”
Organizational factors involve culture and priorities. If your organization says it values quality and safety but doesn’t put in place policies and processes to support it, that affects diagnostics and error-free performance.
Market Drivers
“The discussion about quality is driven by medical error,” says Evan Falchuk, president of Best Doctors Inc., based in Boston. “But the issue is more interesting than simply looking for mistakes.”
Best Doctors partners with employers and health plans to help members with serious illnesses make sure they have the right diagnosis and treatment. Members can consult with specialists who assess diagnoses and can recommend treatment. The firm believes this is the best way to measure quality, and consumers around the world increasingly agree: The company serves more than 10 million people in 30 countries.
Best Doctors was founded in 1989 by two internists: Falchuk’s father, Kenneth H. Falchuk, MD, a professor of medicine at Harvard University Medical School, and Jose Halperin, MD, an associate professor of medicine at Harvard. The service they created is one in which doctors review a patient’s medical information, identify the important issues, and consult with leading experts from their peer-reviewed database. The company then has clinicians work with the patient and his or her doctor to ensure that the patient is getting appropriate care. The process has identified incorrect diagnosis or treatment in more than half of reviewed cases.
“Hospitalists should think about quality in terms of things happening outside the hospital,” says Falchuk. “The informed, demanding consumer is coming to healthcare, and their expectations are clear: to be paid attention to, to have all of their questions answered, and to be certain that their diagnosis and treatment are correct.” These sentiments affect how hospitals do business.
The increasing amount of medical information patients can find on the Internet can raise questions in their minds. “Patients want to trust their doctors,” Falchuk says. “But when the patient has lots of information and questions and finds it difficult to spend as much time as they would like with their doctor, trust is eroded—and patients start to wonder if their doctor is doing the right thing.”
The complexity of modern medicine, with new diagnoses, treatments, and testing, and ultra-specialized experts, can sometimes—ironically—lead to lesser quality.
“It is more important than ever before that doctors with differing perspectives discuss each case,” says Falchuk. “But doctors complain that the system, often because of constraints imposed by managed care, only allows for episodic interactions like that. If that kind of interaction can be made the norm, it will give patients an extraordinary amount of comfort as to the quality of their care.”
Falchuk believes the tipping point for combating errors is being reached—at least from the business point of view.
“With major employers, as many as one in 200 employees call us for help,” he says. “That is close to the incidence rate of the illnesses we commonly see: cancer, heart problems, and undiagnosed situations. When you see this flood of demand, you say, ‘Something is going on that is driving this.’ ”
These market-based factors are driving hospitals to publish and compare rates for process of care and mortality, and many medical centers are publishing report cards. With the advent of advanced technology, hospital and provider performance will be increasingly apparent and transparent. Corporations and institutions will have to be less guarded about what they share publicly as their public accountability is increased.
Interventions, Feedback
The healthcare industry has embraced British psychologist James Reason’s 1990 Swiss cheese model of error as a means of tackling the cumulative effects that cause adverse events. The model conceptualizes the factors that contributed to an error as holes in slices of Swiss cheese. Only when the holes line up does the adverse event occur; placing barriers at one or more of the holes “traps the error” from being realized.
For instance, Best Doctors notes “potholes” in the reading stage of pathology.
“We see many cases of underdiagnosis or even misdiagnosis based on one of the most difficult steps: a pathology review,” says Falchuk. “With new, specifically targeted treatments, getting that right is extremely significant.” Best Doctors experts often recommend having pathology re-reviewed. “I wouldn’t call this error, but patients view it as a question of quality,” he says.
Integrating technology with observation skills is an important way hospitals are working to improve diagnostics and reduce error.
Because the same factors contribute to a near miss as to an actual event, studying the patterns of near misses can provide a wealth of information.
“I heard some statistics that for every 19 near misses, you’re going to have one event,” says Dr. Nagamine. If on a particular day, a provider was fatigued or overtaxed and didn’t catch a contributing factor that is a risk—termed a “latent condition”—that’s when the holes line up. “An event is never just the result of one thing or one person; it is a combination of factors,” says Dr. Nagamine.
One example of this concerns an element in the policy for discharge bundles that institutions establish to better manage transfer of care. When lab results become available only after a patient’s discharge, it increases the risk for delays in diagnosis. Electronically placing the test results into the primary care physician’s e-mail inbox helps to “close the loop,” says Dr. Nagamine. “That information gets to somebody, and we’re clear on who that somebody is. We are putting in place those types of interventions—which are really the low-hanging fruit.”
Culture Change
Opening up about adverse events and providing feedback creates a different awareness about the risks surrounding the event.
“The look-alike, sound-alike medications are an example,” Dr. Nagamine says. “I went up to the unit and said, ‘A nurse recorded that she almost gave hydralazine instead of hydroxyzine—has that ever happened to you?’ The first three nurses I asked said, ‘Yes,’ ‘Yes,’ ‘Yes.’ Until I ask these types of questions, I don’t know. And until you can make it safe for your staff to talk, you will not have good information.”
Although this is the approach most of the safety world and quality world is embracing, it is not how most clinicians on the frontline view it.
“We are trying to educate people about a framework in which to think about this,” says Dr. Nagamine. “It is not constructive to point fingers, but it is important to give people feedback about how the event happened. It is far more constructive to look at the entire system and ask, ‘How did we fail here? What was your piece of it? What was the system’s piece of it?’ ”
Because of the connection between litigation and adverse events, changing the culture is a complex imperative. But providers must recognize that systems failures are involved in about 75% to 80% of medical malpractice cases—whether that involves communication breakdowns, inadequate availability of information, or a host of other factors. The individual, environment, and organization are linked.
Reducing negativity and sensitivity around the terms associated with error and reframing thinking toward prevention are important.
“There is a richness of information that comes once you change the culture from blaming to fixing,” says Dr. Nagamine. Providing feedback to frontline practitioners is key, as is thanking those who report. “It increases providers’ awareness about where the hot spots and vulnerabilities are and how to stay out of trouble. Simply by giving them information about an event raises their awareness of the magnitude of certain types of issues,” she explains.
When Dr. Nagamine led a safety initiative on the ICU floor consisting of human factors training and a new system for reporting events, the number of reports “went through roof,” she says. “My new problem was not that people were not reporting; it was being overwhelmed with the information that was coming in. We were able to create a culture of safety that made it safe to report and consequently had much better information from which we could devise prevention strategies.”
SHM, in planning to co-create standards for focused practice with the American Board of Internal Medicine, intends to promote the standards of professionalism along with other standards. The issue of personal accountability, although a part of that, has been less of a focus to date. In the future, all institutions may have technology hospitalists can use to learn whether the discharge diagnosis was correct in the months and years that followed. Will the culture be emotionally ready to handle what technology can offer?
“We will need to own it when things go well and when things don’t go well or when we are wrong,” says Dr. Halasyamani. “We need to be able to investigate the distribution of the reasons for misdiagnosis, determine how many of those problems are systems issues, and devise strategies to address them.” In a sense, she says, everything can be viewed as a system issue unless actions are egregious and malicious.
Yet when physicians are associated with an adverse event, research shows they feel they have little support to talk about it.
“The system we have in place has begun to try to address some of the issues related to system errors,” says Dr. Halasyamani. “But what if an individual does have an error? What systems do we have in place to support that person in the recovery? And along the way if we find people who are having these issues over and over again, we need to design processes to deal with that.”
One particular focus of SHM’s transfer-of-care initiative concerns communication surrounding handoffs. “We are setting those standards and thinking about what kinds of technology tools can help make those standards easier to adhere to and easier to implement,” says Dr. Halasyamani. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
This is the second of a two-part series examining medical errors. Part 1 addressed thought processes hospitalists use that may lead to mistaken diagnoses (October 2007, p. 36). Part 2 examines what healthcare corporations are doing to improve diagnoses and reduce errors.
Pilots taking off, Swiss cheese, low-hanging fruit. Talk to hospitalists about the issue of medical errors and the analogies come quickly.
Ever since 2000’s landmark Institute of Medicine report “To Err is Human: Building a Safer Health System” found that anywhere from 40,000 to 100,000 patients incur injury or die every year because of medical errors, debate has been constant.
Medical literature is abundant on this topic. The Joint Commission, National Center for Patient Safety, Agency for Health Care Research and Quality, and myriad other organizations and institutions, including SHM, are all helping providers and hospitals solve the problems by establishing goals, standards, guidelines, and policies.
—Evan Falchuk, president, Best Doctors Inc., Boston
Definitions and Paradigms
Best-practice recommendations for reducing errors are generally based on two essential principles: using a systems-based approach to patient safety and creating an environment that supports open dialogue about errors, their causes, and strategies for prevention.
Terminology is a key factor. The terms “error” and “mistake” carry an emotional component associated with embarrassment and shame. Healthcare providers don’t like to be associated with errors. There is an accompanying fear of litigation, and people, perhaps especially physicians, don’t want to be known as someone who was sued.
“The language we use to talk about these issues is important,” says Janet Nagamine, MD, part-time hospitalist at Kaiser Permanente Santa Clara Medical Center in Calif. and current chair of SHM’s quality and patient safety committee. In fact, because of the negativity around the terms “misdiagnosis” and “delay in diagnosis” she advocates using the term “unintended adverse event” in order to appear more neutral.
“The term error is extremely threatening and scary to any health professional because it implies a personal failure,” says Dr. Nagamine. The goal when it comes to errors is essentially to look for the how—not the who.
Reporting medical errors is one thing, but reporting misdiagnoses is another, says Lakshmi Halasyamani, MD, vice chair for the department of internal medicine at St. Joseph’s Mercy Hospital in Ann Arbor, Mich., and SHM board member. “We don’t really talk about misdiagnosis,” she says. “That’s partly because we have tended to assign more individual blame for misdiagnoses.”
Drs. Nagamine and Halasyamani agree that altering the way of viewing errors means nurturing culture change.
“We have made very little headway helping physicians understand that in the course of their careers there will be misdiagnoses and the best of physicians have misdiagnoses,” says Dr. Halasyamani. “We are not developmentally at the same stage that we are with talking about medical errors.”
She believes this is largely a professionalism issue that first means normalizing the issue of misdiagnosis. “It is kind of ludicrous to think that you will practice medicine over 40 years and not have a misdiagnosis,” she says. “But we don’t look at it from that perspective when we begin to orient trainees.”
National Efforts
To the people at the U.S. Pharmacopeia Center for the Advancement of Patient Safety (USP), the arrival of universal electronic medical records (EMR) in the coming decade will be a boon to the error-reduction effort.
“Eventually we will all have our health information stored electronically for easy retrieval,” says Rodney W. Hicks, PhD, ARNP, manager, patient safety research and practice for the USP and first author on its most recent report. The beginning of regional networks for EMR is taking hold.
“Even before the IOM report, the USP was familiar with intensivists,” says Dr. Hicks. “We recognize hospitalists as experts who bring efficiency and effectiveness to the healthcare system.”
The USP maintains perhaps the largest database of medication errors in the world.1 Each year the USP issues a report that focuses on one topic and builds its knowledge base.
This year’s report focuses exclusively on the perioperative continuum of care. Last year’s covered ICU- and radiology-related errors. Two years ago the report was a five-year data summary of errors occurring primarily in hospitals.
“The area of errors due to breakdowns in handoffs remains a huge problem for diagnosis and the continuity of care,” says Shawn C. Becker, MS, BSN, RN, director of patient safety initiatives for the USP.
Classification
In general, errors are divided into those that stem from individual factors and those that are system-related, which include environmental and organizational factors.
Environmental risks are often related to human factors. Dr. Nagamine offers an aviation analogy to demonstrate the many pulls on caregivers’ attention.
“What happens in a cockpit at take off is that you are not allowed to talk about anything other than the take-off checklist,” she says. “In medicine, we have nurses’ stations or medication carts in the middle of the hallway, so nurses are preparing meds and people are tugging on their shoulder and interrupting them during a critical task.”
Organizational factors involve culture and priorities. If your organization says it values quality and safety but doesn’t put in place policies and processes to support it, that affects diagnostics and error-free performance.
Market Drivers
“The discussion about quality is driven by medical error,” says Evan Falchuk, president of Best Doctors Inc., based in Boston. “But the issue is more interesting than simply looking for mistakes.”
Best Doctors partners with employers and health plans to help members with serious illnesses make sure they have the right diagnosis and treatment. Members can consult with specialists who assess diagnoses and can recommend treatment. The firm believes this is the best way to measure quality, and consumers around the world increasingly agree: The company serves more than 10 million people in 30 countries.
Best Doctors was founded in 1989 by two internists: Falchuk’s father, Kenneth H. Falchuk, MD, a professor of medicine at Harvard University Medical School, and Jose Halperin, MD, an associate professor of medicine at Harvard. The service they created is one in which doctors review a patient’s medical information, identify the important issues, and consult with leading experts from their peer-reviewed database. The company then has clinicians work with the patient and his or her doctor to ensure that the patient is getting appropriate care. The process has identified incorrect diagnosis or treatment in more than half of reviewed cases.
“Hospitalists should think about quality in terms of things happening outside the hospital,” says Falchuk. “The informed, demanding consumer is coming to healthcare, and their expectations are clear: to be paid attention to, to have all of their questions answered, and to be certain that their diagnosis and treatment are correct.” These sentiments affect how hospitals do business.
The increasing amount of medical information patients can find on the Internet can raise questions in their minds. “Patients want to trust their doctors,” Falchuk says. “But when the patient has lots of information and questions and finds it difficult to spend as much time as they would like with their doctor, trust is eroded—and patients start to wonder if their doctor is doing the right thing.”
The complexity of modern medicine, with new diagnoses, treatments, and testing, and ultra-specialized experts, can sometimes—ironically—lead to lesser quality.
“It is more important than ever before that doctors with differing perspectives discuss each case,” says Falchuk. “But doctors complain that the system, often because of constraints imposed by managed care, only allows for episodic interactions like that. If that kind of interaction can be made the norm, it will give patients an extraordinary amount of comfort as to the quality of their care.”
Falchuk believes the tipping point for combating errors is being reached—at least from the business point of view.
“With major employers, as many as one in 200 employees call us for help,” he says. “That is close to the incidence rate of the illnesses we commonly see: cancer, heart problems, and undiagnosed situations. When you see this flood of demand, you say, ‘Something is going on that is driving this.’ ”
These market-based factors are driving hospitals to publish and compare rates for process of care and mortality, and many medical centers are publishing report cards. With the advent of advanced technology, hospital and provider performance will be increasingly apparent and transparent. Corporations and institutions will have to be less guarded about what they share publicly as their public accountability is increased.
Interventions, Feedback
The healthcare industry has embraced British psychologist James Reason’s 1990 Swiss cheese model of error as a means of tackling the cumulative effects that cause adverse events. The model conceptualizes the factors that contributed to an error as holes in slices of Swiss cheese. Only when the holes line up does the adverse event occur; placing barriers at one or more of the holes “traps the error” from being realized.
For instance, Best Doctors notes “potholes” in the reading stage of pathology.
“We see many cases of underdiagnosis or even misdiagnosis based on one of the most difficult steps: a pathology review,” says Falchuk. “With new, specifically targeted treatments, getting that right is extremely significant.” Best Doctors experts often recommend having pathology re-reviewed. “I wouldn’t call this error, but patients view it as a question of quality,” he says.
Integrating technology with observation skills is an important way hospitals are working to improve diagnostics and reduce error.
Because the same factors contribute to a near miss as to an actual event, studying the patterns of near misses can provide a wealth of information.
“I heard some statistics that for every 19 near misses, you’re going to have one event,” says Dr. Nagamine. If on a particular day, a provider was fatigued or overtaxed and didn’t catch a contributing factor that is a risk—termed a “latent condition”—that’s when the holes line up. “An event is never just the result of one thing or one person; it is a combination of factors,” says Dr. Nagamine.
One example of this concerns an element in the policy for discharge bundles that institutions establish to better manage transfer of care. When lab results become available only after a patient’s discharge, it increases the risk for delays in diagnosis. Electronically placing the test results into the primary care physician’s e-mail inbox helps to “close the loop,” says Dr. Nagamine. “That information gets to somebody, and we’re clear on who that somebody is. We are putting in place those types of interventions—which are really the low-hanging fruit.”
Culture Change
Opening up about adverse events and providing feedback creates a different awareness about the risks surrounding the event.
“The look-alike, sound-alike medications are an example,” Dr. Nagamine says. “I went up to the unit and said, ‘A nurse recorded that she almost gave hydralazine instead of hydroxyzine—has that ever happened to you?’ The first three nurses I asked said, ‘Yes,’ ‘Yes,’ ‘Yes.’ Until I ask these types of questions, I don’t know. And until you can make it safe for your staff to talk, you will not have good information.”
Although this is the approach most of the safety world and quality world is embracing, it is not how most clinicians on the frontline view it.
“We are trying to educate people about a framework in which to think about this,” says Dr. Nagamine. “It is not constructive to point fingers, but it is important to give people feedback about how the event happened. It is far more constructive to look at the entire system and ask, ‘How did we fail here? What was your piece of it? What was the system’s piece of it?’ ”
Because of the connection between litigation and adverse events, changing the culture is a complex imperative. But providers must recognize that systems failures are involved in about 75% to 80% of medical malpractice cases—whether that involves communication breakdowns, inadequate availability of information, or a host of other factors. The individual, environment, and organization are linked.
Reducing negativity and sensitivity around the terms associated with error and reframing thinking toward prevention are important.
“There is a richness of information that comes once you change the culture from blaming to fixing,” says Dr. Nagamine. Providing feedback to frontline practitioners is key, as is thanking those who report. “It increases providers’ awareness about where the hot spots and vulnerabilities are and how to stay out of trouble. Simply by giving them information about an event raises their awareness of the magnitude of certain types of issues,” she explains.
When Dr. Nagamine led a safety initiative on the ICU floor consisting of human factors training and a new system for reporting events, the number of reports “went through roof,” she says. “My new problem was not that people were not reporting; it was being overwhelmed with the information that was coming in. We were able to create a culture of safety that made it safe to report and consequently had much better information from which we could devise prevention strategies.”
SHM, in planning to co-create standards for focused practice with the American Board of Internal Medicine, intends to promote the standards of professionalism along with other standards. The issue of personal accountability, although a part of that, has been less of a focus to date. In the future, all institutions may have technology hospitalists can use to learn whether the discharge diagnosis was correct in the months and years that followed. Will the culture be emotionally ready to handle what technology can offer?
“We will need to own it when things go well and when things don’t go well or when we are wrong,” says Dr. Halasyamani. “We need to be able to investigate the distribution of the reasons for misdiagnosis, determine how many of those problems are systems issues, and devise strategies to address them.” In a sense, she says, everything can be viewed as a system issue unless actions are egregious and malicious.
Yet when physicians are associated with an adverse event, research shows they feel they have little support to talk about it.
“The system we have in place has begun to try to address some of the issues related to system errors,” says Dr. Halasyamani. “But what if an individual does have an error? What systems do we have in place to support that person in the recovery? And along the way if we find people who are having these issues over and over again, we need to design processes to deal with that.”
One particular focus of SHM’s transfer-of-care initiative concerns communication surrounding handoffs. “We are setting those standards and thinking about what kinds of technology tools can help make those standards easier to adhere to and easier to implement,” says Dr. Halasyamani. TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
Prudent Partners
In an ideal world, the directors of hospitalist programs and residency programs would be perfectly aligned in their efforts to advance the hospital’s financial health, education initiatives, and quality of patient care. In reality, friction among them is common.
The roots of the tensions lie in their differing responsibilities.
“The goals for residency programs, which are governed by rules of the ACGME [Accreditation Council for Graduate Medical Education], don’t necessarily always match with those of the hospitalists for patient care delivery,” notes Alpesh Amin, MD, MBA, FACP, professor and chief, general internal medicine, executive director and founder of the hospitalist program at the University of California Irvine (UCI), and also associate program director of the UCI internal medicine residency program. Dr. Amin is also a member of SHM’s board of directors.
In teaching hospitals, residency program directors must ensure their residents comply with the ACGME work hour and patient load caps. These requirements limit residents to an 80-hour workweek and continuous on-site duty no longer than 24 consecutive hours, and multiresident internal medicine teams to no more than 24 patients at a time.
Compliance can pressure house staff hospitalists to pick up the slack. In addition, to advance the educational mission, a residency program director might want to have his or her residents read three hours a day. But the hospitalist, charged with caring for as many patients as possible, may want residents on his or her service to spend that time admitting, managing, and discharging patients.
William Iobst, MD, designated institutional official at Lehigh Valley Hospital in Allentown, Pa., and associate program director of the hospital medicine program, knows these issues firsthand. “The conflict usually comes up in that most hospitalist programs are put in place to provide streamlined and efficient service in the hospital,” he says. “To that end, they have targeted goals of improving efficiency, reducing length of stay, and using their expertise in repetitive treatments of the same condition [such as congestive heart failure or pneumonia] over time.”
Hospitalists, says Dr. Iobst, “get very efficient at providing care. In some ways, asking a hospitalist to serve as an educator potentially disrupts that charge of efficiency, quality, and rapid transit through the hospital. So, they may be put in a position of having conflicting bosses.”
—Alpesh Amin, MD, MBA, FACP, professor and chief, general internal medicine, executive director and founder of the hospitalist program at the University of California Irvine
Dual Roles
Some hospitalists work in both worlds: They serve as associate program directors for residency programs as well as directors of hospitalist programs. This can set the stage for conflicts.
Such is the case with Michael Pistoria, DO, chief of the division of hospital medicine at Lehigh Valley Hospital and associate program director for the free-standing medicine residency program.
“There are times when something in one area is impacting—sometimes adversely—the other areas for which I’m responsible,” he says. “One big issue that we really struggle with is how to deal with the [sometimes overwhelming] volume of patients when residents are able to do less and less according to ACGME rules.”
This is especially tricky, he says, when mapping coverage for overnight shifts. Not only are residents’ work hours capped, but the Residency Review Committee (RRC), which provides ACGME oversight, also stipulates that residents must have continuity with patients. They are not supposed to admit patients who won’t be seen by a resident the next day. This can create tension between the resident and hospitalist programs—especially when the latter face high patient loads.
One solution at Lehigh Valley has been to rotate resident teams admitting patients in the afternoon and evening hours, but only to their service. This ensures resident continuity for those patients and meets ACGME requirements. All other patients are admitted through the hospitalist service.
Capitalize on Uniqueness
It’s crucial to identify areas where hospitalists and program directors can dovetail efforts so the programs are not at loggerheads.
Program directors and medical directors can have a positive effect on meshing residency and private hospitalist programs. “We have to talk with our hospitalists, explain that we have no way around this [ACGME guideline], how it will impact them, and figure out a way [together] to help minimize that impact,” says Dr. Pistoria.
Dr. Amin believes the goals of the residency and hospital medicine programs can be mutually beneficial. “Some people may have inherent biases against the concept of hospital medicine,” he says. “But hopefully, as time goes on, you’ll find more and more hospitalists serving in program director or associate program director roles. My view is that the residency program ought to turn to the hospitalist when they’re looking for general inpatient, consultative, and perioperative curricular development. They could turn to hospitalists in the same way that they ask nephrology groups to help design a nephrology curriculum.”
The situation requires planning to make sure all stakeholders can accept the impact of having residents, Dr. Iobst points out. “The program director’s role is to work with the hospitalists and make sure that they understand that the residents have to adhere to their service caps,’’ he says. “The issue then would be to find other meaningful learning opportunities for residents that would not involve admitting patients.”
Dr. Iobst agrees with Dr. Amin. Some opportunities, he says, “are to ensure that a program director is capitalizing on what a hospitalist does.” If hospitalists are offering only “another general internal medicine inpatient service rotation to residents,” they are not capitalizing on their own uniqueness. Instead, hospitalists could offer hospital medicine as a senior rotation for residents. The residents could receive training and exposure to quality improvement; the business aspects of medicine, including the importance of length of stay and appropriate ICD-9 coding; and an evidence-based approach to care.
Embrace Teaching
Although ACGME work-hour caps sometimes create pressures, it’s up to hospitalists to be flexible with residents on their service, says Hasan Shabbir, MD, a hospitalist and associate medical director of quality at Emory Johns Creek Hospital in Duluth, Ga., and an assistant professor of medicine at Emory University in Atlanta.
This is especially true when particular residents are on night float rotation; admitting and managing patients into the early morning can bring them close to their work-hour caps. “We have to be cognizant of that [the ACGME guidelines], give them leeway, and let them go early whenever possible,” he says.
Having the right attitude toward residents is key. “I think we’ve approached [teaching residents] with the attitude that we’re quite fortunate to have residents to do a lot of the upfront work and to be able to help and teach them along the way,” explains Dr. Shabbir. “I think the negative feeling [about residents] is often tied to expectations. If one comes into our program, for example, and expects to just lie back and let the residents do all the work, that would be a bad expectation to have. All of us, having been [residents] at some point, can understand what residents go through. Not every hospitalist has the good fortune of having residents with them.”
There is value to having residents, agrees Dr. Iobst. “There’s the value of serving as a mentor; of training future colleagues; and the value for people who are enthused by the opportunity to teach. The key is to clearly establish all the boundaries and get them on the table to begin with, define which ones are absolutely required and are not flexible, and to ensure that the administration of the hospital that is supporting the hospitalists understands that need.”
Dr. Amin believes program directors need hospitalists to serve as faculty and that hospitalists need to take into account residency rules and regulations so the program can retain accreditation status.
“It’s a two-way street,” he says. “It doesn’t help anybody if the residency program is not accredited, and it doesn’t help anybody if the hospitalist faculty members don’t have good morale.” At UC Irvine, he says: “We try not to develop systems that overwhelm the residents; we also try not to develop systems that allow faculty to be overwhelmed. On the other hand, patient care is not predictable all the time, so some of the ACGME rules may put people into difficult situations.”
Goals and Relationships
Dr. Amin believes that if hospitalists and residency program directors can advocate for their own programs and work together for the greater good, they can craft an exponentially better team model.
One way to achieve this is to encourage more hospitalist directors to also serve as associate program directors/program directors of residency programs. This, he says, “could potentially help facilitate a stronger bridge between both programs.”
Within hospitalist groups, directors can encourage understanding about the dual sets of goals. It’s important for group leaders to involve everyone in the group when making decisions so people feel they are part of the process, says Alan L. Wang, MD, chief medical officer at Emory Johns Creek Hospital in Ga., and co-director of the hospitalist program.
Another tool for aligning hospitalists on their team with hospital goals, he says, is to share the patient workload. “One of the most important ways for medical directors to increase their credibility with the team members is to do shift work,” he asserts. “Getting in the trenches allows you to understand the day-to-day issues and problems that your hospitalists face.”
Dr. Shabbir notes that the burden of good relationship building should not fall solely to the group leaders. “There has to be an effort on all sides,” he says. “It can’t work with the leader alone trying. As a hospitalist, I think the focus has to be not only patient care, but also system efficiency, because, in the end, that makes for better overall patient care.”
Dr. Amin and others believe tensions between residency and hospitalist programs will resolve over time, in part due to hospitalists taking associate program director and program director roles, and in part to increased cooperation.
“The hospitalist could be the program director’s best friend and viewed as a vehicle for developing and training residents in system-based practice, competency-based learning and refinement of communication skills,” he says. TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
In an ideal world, the directors of hospitalist programs and residency programs would be perfectly aligned in their efforts to advance the hospital’s financial health, education initiatives, and quality of patient care. In reality, friction among them is common.
The roots of the tensions lie in their differing responsibilities.
“The goals for residency programs, which are governed by rules of the ACGME [Accreditation Council for Graduate Medical Education], don’t necessarily always match with those of the hospitalists for patient care delivery,” notes Alpesh Amin, MD, MBA, FACP, professor and chief, general internal medicine, executive director and founder of the hospitalist program at the University of California Irvine (UCI), and also associate program director of the UCI internal medicine residency program. Dr. Amin is also a member of SHM’s board of directors.
In teaching hospitals, residency program directors must ensure their residents comply with the ACGME work hour and patient load caps. These requirements limit residents to an 80-hour workweek and continuous on-site duty no longer than 24 consecutive hours, and multiresident internal medicine teams to no more than 24 patients at a time.
Compliance can pressure house staff hospitalists to pick up the slack. In addition, to advance the educational mission, a residency program director might want to have his or her residents read three hours a day. But the hospitalist, charged with caring for as many patients as possible, may want residents on his or her service to spend that time admitting, managing, and discharging patients.
William Iobst, MD, designated institutional official at Lehigh Valley Hospital in Allentown, Pa., and associate program director of the hospital medicine program, knows these issues firsthand. “The conflict usually comes up in that most hospitalist programs are put in place to provide streamlined and efficient service in the hospital,” he says. “To that end, they have targeted goals of improving efficiency, reducing length of stay, and using their expertise in repetitive treatments of the same condition [such as congestive heart failure or pneumonia] over time.”
Hospitalists, says Dr. Iobst, “get very efficient at providing care. In some ways, asking a hospitalist to serve as an educator potentially disrupts that charge of efficiency, quality, and rapid transit through the hospital. So, they may be put in a position of having conflicting bosses.”
—Alpesh Amin, MD, MBA, FACP, professor and chief, general internal medicine, executive director and founder of the hospitalist program at the University of California Irvine
Dual Roles
Some hospitalists work in both worlds: They serve as associate program directors for residency programs as well as directors of hospitalist programs. This can set the stage for conflicts.
Such is the case with Michael Pistoria, DO, chief of the division of hospital medicine at Lehigh Valley Hospital and associate program director for the free-standing medicine residency program.
“There are times when something in one area is impacting—sometimes adversely—the other areas for which I’m responsible,” he says. “One big issue that we really struggle with is how to deal with the [sometimes overwhelming] volume of patients when residents are able to do less and less according to ACGME rules.”
This is especially tricky, he says, when mapping coverage for overnight shifts. Not only are residents’ work hours capped, but the Residency Review Committee (RRC), which provides ACGME oversight, also stipulates that residents must have continuity with patients. They are not supposed to admit patients who won’t be seen by a resident the next day. This can create tension between the resident and hospitalist programs—especially when the latter face high patient loads.
One solution at Lehigh Valley has been to rotate resident teams admitting patients in the afternoon and evening hours, but only to their service. This ensures resident continuity for those patients and meets ACGME requirements. All other patients are admitted through the hospitalist service.
Capitalize on Uniqueness
It’s crucial to identify areas where hospitalists and program directors can dovetail efforts so the programs are not at loggerheads.
Program directors and medical directors can have a positive effect on meshing residency and private hospitalist programs. “We have to talk with our hospitalists, explain that we have no way around this [ACGME guideline], how it will impact them, and figure out a way [together] to help minimize that impact,” says Dr. Pistoria.
Dr. Amin believes the goals of the residency and hospital medicine programs can be mutually beneficial. “Some people may have inherent biases against the concept of hospital medicine,” he says. “But hopefully, as time goes on, you’ll find more and more hospitalists serving in program director or associate program director roles. My view is that the residency program ought to turn to the hospitalist when they’re looking for general inpatient, consultative, and perioperative curricular development. They could turn to hospitalists in the same way that they ask nephrology groups to help design a nephrology curriculum.”
The situation requires planning to make sure all stakeholders can accept the impact of having residents, Dr. Iobst points out. “The program director’s role is to work with the hospitalists and make sure that they understand that the residents have to adhere to their service caps,’’ he says. “The issue then would be to find other meaningful learning opportunities for residents that would not involve admitting patients.”
Dr. Iobst agrees with Dr. Amin. Some opportunities, he says, “are to ensure that a program director is capitalizing on what a hospitalist does.” If hospitalists are offering only “another general internal medicine inpatient service rotation to residents,” they are not capitalizing on their own uniqueness. Instead, hospitalists could offer hospital medicine as a senior rotation for residents. The residents could receive training and exposure to quality improvement; the business aspects of medicine, including the importance of length of stay and appropriate ICD-9 coding; and an evidence-based approach to care.
Embrace Teaching
Although ACGME work-hour caps sometimes create pressures, it’s up to hospitalists to be flexible with residents on their service, says Hasan Shabbir, MD, a hospitalist and associate medical director of quality at Emory Johns Creek Hospital in Duluth, Ga., and an assistant professor of medicine at Emory University in Atlanta.
This is especially true when particular residents are on night float rotation; admitting and managing patients into the early morning can bring them close to their work-hour caps. “We have to be cognizant of that [the ACGME guidelines], give them leeway, and let them go early whenever possible,” he says.
Having the right attitude toward residents is key. “I think we’ve approached [teaching residents] with the attitude that we’re quite fortunate to have residents to do a lot of the upfront work and to be able to help and teach them along the way,” explains Dr. Shabbir. “I think the negative feeling [about residents] is often tied to expectations. If one comes into our program, for example, and expects to just lie back and let the residents do all the work, that would be a bad expectation to have. All of us, having been [residents] at some point, can understand what residents go through. Not every hospitalist has the good fortune of having residents with them.”
There is value to having residents, agrees Dr. Iobst. “There’s the value of serving as a mentor; of training future colleagues; and the value for people who are enthused by the opportunity to teach. The key is to clearly establish all the boundaries and get them on the table to begin with, define which ones are absolutely required and are not flexible, and to ensure that the administration of the hospital that is supporting the hospitalists understands that need.”
Dr. Amin believes program directors need hospitalists to serve as faculty and that hospitalists need to take into account residency rules and regulations so the program can retain accreditation status.
“It’s a two-way street,” he says. “It doesn’t help anybody if the residency program is not accredited, and it doesn’t help anybody if the hospitalist faculty members don’t have good morale.” At UC Irvine, he says: “We try not to develop systems that overwhelm the residents; we also try not to develop systems that allow faculty to be overwhelmed. On the other hand, patient care is not predictable all the time, so some of the ACGME rules may put people into difficult situations.”
Goals and Relationships
Dr. Amin believes that if hospitalists and residency program directors can advocate for their own programs and work together for the greater good, they can craft an exponentially better team model.
One way to achieve this is to encourage more hospitalist directors to also serve as associate program directors/program directors of residency programs. This, he says, “could potentially help facilitate a stronger bridge between both programs.”
Within hospitalist groups, directors can encourage understanding about the dual sets of goals. It’s important for group leaders to involve everyone in the group when making decisions so people feel they are part of the process, says Alan L. Wang, MD, chief medical officer at Emory Johns Creek Hospital in Ga., and co-director of the hospitalist program.
Another tool for aligning hospitalists on their team with hospital goals, he says, is to share the patient workload. “One of the most important ways for medical directors to increase their credibility with the team members is to do shift work,” he asserts. “Getting in the trenches allows you to understand the day-to-day issues and problems that your hospitalists face.”
Dr. Shabbir notes that the burden of good relationship building should not fall solely to the group leaders. “There has to be an effort on all sides,” he says. “It can’t work with the leader alone trying. As a hospitalist, I think the focus has to be not only patient care, but also system efficiency, because, in the end, that makes for better overall patient care.”
Dr. Amin and others believe tensions between residency and hospitalist programs will resolve over time, in part due to hospitalists taking associate program director and program director roles, and in part to increased cooperation.
“The hospitalist could be the program director’s best friend and viewed as a vehicle for developing and training residents in system-based practice, competency-based learning and refinement of communication skills,” he says. TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
In an ideal world, the directors of hospitalist programs and residency programs would be perfectly aligned in their efforts to advance the hospital’s financial health, education initiatives, and quality of patient care. In reality, friction among them is common.
The roots of the tensions lie in their differing responsibilities.
“The goals for residency programs, which are governed by rules of the ACGME [Accreditation Council for Graduate Medical Education], don’t necessarily always match with those of the hospitalists for patient care delivery,” notes Alpesh Amin, MD, MBA, FACP, professor and chief, general internal medicine, executive director and founder of the hospitalist program at the University of California Irvine (UCI), and also associate program director of the UCI internal medicine residency program. Dr. Amin is also a member of SHM’s board of directors.
In teaching hospitals, residency program directors must ensure their residents comply with the ACGME work hour and patient load caps. These requirements limit residents to an 80-hour workweek and continuous on-site duty no longer than 24 consecutive hours, and multiresident internal medicine teams to no more than 24 patients at a time.
Compliance can pressure house staff hospitalists to pick up the slack. In addition, to advance the educational mission, a residency program director might want to have his or her residents read three hours a day. But the hospitalist, charged with caring for as many patients as possible, may want residents on his or her service to spend that time admitting, managing, and discharging patients.
William Iobst, MD, designated institutional official at Lehigh Valley Hospital in Allentown, Pa., and associate program director of the hospital medicine program, knows these issues firsthand. “The conflict usually comes up in that most hospitalist programs are put in place to provide streamlined and efficient service in the hospital,” he says. “To that end, they have targeted goals of improving efficiency, reducing length of stay, and using their expertise in repetitive treatments of the same condition [such as congestive heart failure or pneumonia] over time.”
Hospitalists, says Dr. Iobst, “get very efficient at providing care. In some ways, asking a hospitalist to serve as an educator potentially disrupts that charge of efficiency, quality, and rapid transit through the hospital. So, they may be put in a position of having conflicting bosses.”
—Alpesh Amin, MD, MBA, FACP, professor and chief, general internal medicine, executive director and founder of the hospitalist program at the University of California Irvine
Dual Roles
Some hospitalists work in both worlds: They serve as associate program directors for residency programs as well as directors of hospitalist programs. This can set the stage for conflicts.
Such is the case with Michael Pistoria, DO, chief of the division of hospital medicine at Lehigh Valley Hospital and associate program director for the free-standing medicine residency program.
“There are times when something in one area is impacting—sometimes adversely—the other areas for which I’m responsible,” he says. “One big issue that we really struggle with is how to deal with the [sometimes overwhelming] volume of patients when residents are able to do less and less according to ACGME rules.”
This is especially tricky, he says, when mapping coverage for overnight shifts. Not only are residents’ work hours capped, but the Residency Review Committee (RRC), which provides ACGME oversight, also stipulates that residents must have continuity with patients. They are not supposed to admit patients who won’t be seen by a resident the next day. This can create tension between the resident and hospitalist programs—especially when the latter face high patient loads.
One solution at Lehigh Valley has been to rotate resident teams admitting patients in the afternoon and evening hours, but only to their service. This ensures resident continuity for those patients and meets ACGME requirements. All other patients are admitted through the hospitalist service.
Capitalize on Uniqueness
It’s crucial to identify areas where hospitalists and program directors can dovetail efforts so the programs are not at loggerheads.
Program directors and medical directors can have a positive effect on meshing residency and private hospitalist programs. “We have to talk with our hospitalists, explain that we have no way around this [ACGME guideline], how it will impact them, and figure out a way [together] to help minimize that impact,” says Dr. Pistoria.
Dr. Amin believes the goals of the residency and hospital medicine programs can be mutually beneficial. “Some people may have inherent biases against the concept of hospital medicine,” he says. “But hopefully, as time goes on, you’ll find more and more hospitalists serving in program director or associate program director roles. My view is that the residency program ought to turn to the hospitalist when they’re looking for general inpatient, consultative, and perioperative curricular development. They could turn to hospitalists in the same way that they ask nephrology groups to help design a nephrology curriculum.”
The situation requires planning to make sure all stakeholders can accept the impact of having residents, Dr. Iobst points out. “The program director’s role is to work with the hospitalists and make sure that they understand that the residents have to adhere to their service caps,’’ he says. “The issue then would be to find other meaningful learning opportunities for residents that would not involve admitting patients.”
Dr. Iobst agrees with Dr. Amin. Some opportunities, he says, “are to ensure that a program director is capitalizing on what a hospitalist does.” If hospitalists are offering only “another general internal medicine inpatient service rotation to residents,” they are not capitalizing on their own uniqueness. Instead, hospitalists could offer hospital medicine as a senior rotation for residents. The residents could receive training and exposure to quality improvement; the business aspects of medicine, including the importance of length of stay and appropriate ICD-9 coding; and an evidence-based approach to care.
Embrace Teaching
Although ACGME work-hour caps sometimes create pressures, it’s up to hospitalists to be flexible with residents on their service, says Hasan Shabbir, MD, a hospitalist and associate medical director of quality at Emory Johns Creek Hospital in Duluth, Ga., and an assistant professor of medicine at Emory University in Atlanta.
This is especially true when particular residents are on night float rotation; admitting and managing patients into the early morning can bring them close to their work-hour caps. “We have to be cognizant of that [the ACGME guidelines], give them leeway, and let them go early whenever possible,” he says.
Having the right attitude toward residents is key. “I think we’ve approached [teaching residents] with the attitude that we’re quite fortunate to have residents to do a lot of the upfront work and to be able to help and teach them along the way,” explains Dr. Shabbir. “I think the negative feeling [about residents] is often tied to expectations. If one comes into our program, for example, and expects to just lie back and let the residents do all the work, that would be a bad expectation to have. All of us, having been [residents] at some point, can understand what residents go through. Not every hospitalist has the good fortune of having residents with them.”
There is value to having residents, agrees Dr. Iobst. “There’s the value of serving as a mentor; of training future colleagues; and the value for people who are enthused by the opportunity to teach. The key is to clearly establish all the boundaries and get them on the table to begin with, define which ones are absolutely required and are not flexible, and to ensure that the administration of the hospital that is supporting the hospitalists understands that need.”
Dr. Amin believes program directors need hospitalists to serve as faculty and that hospitalists need to take into account residency rules and regulations so the program can retain accreditation status.
“It’s a two-way street,” he says. “It doesn’t help anybody if the residency program is not accredited, and it doesn’t help anybody if the hospitalist faculty members don’t have good morale.” At UC Irvine, he says: “We try not to develop systems that overwhelm the residents; we also try not to develop systems that allow faculty to be overwhelmed. On the other hand, patient care is not predictable all the time, so some of the ACGME rules may put people into difficult situations.”
Goals and Relationships
Dr. Amin believes that if hospitalists and residency program directors can advocate for their own programs and work together for the greater good, they can craft an exponentially better team model.
One way to achieve this is to encourage more hospitalist directors to also serve as associate program directors/program directors of residency programs. This, he says, “could potentially help facilitate a stronger bridge between both programs.”
Within hospitalist groups, directors can encourage understanding about the dual sets of goals. It’s important for group leaders to involve everyone in the group when making decisions so people feel they are part of the process, says Alan L. Wang, MD, chief medical officer at Emory Johns Creek Hospital in Ga., and co-director of the hospitalist program.
Another tool for aligning hospitalists on their team with hospital goals, he says, is to share the patient workload. “One of the most important ways for medical directors to increase their credibility with the team members is to do shift work,” he asserts. “Getting in the trenches allows you to understand the day-to-day issues and problems that your hospitalists face.”
Dr. Shabbir notes that the burden of good relationship building should not fall solely to the group leaders. “There has to be an effort on all sides,” he says. “It can’t work with the leader alone trying. As a hospitalist, I think the focus has to be not only patient care, but also system efficiency, because, in the end, that makes for better overall patient care.”
Dr. Amin and others believe tensions between residency and hospitalist programs will resolve over time, in part due to hospitalists taking associate program director and program director roles, and in part to increased cooperation.
“The hospitalist could be the program director’s best friend and viewed as a vehicle for developing and training residents in system-based practice, competency-based learning and refinement of communication skills,” he says. TH
Gretchen Henkel is a frequent contributor to The Hospitalist.
Tackle Technology
Dennis Deruelle, MD, a hospitalist at University Community Hospital in Tampa, Fla., once needed reliable medical information in a hurry while treating a young woman admitted to the hospital with cellulitis.
The woman was later diagnosed with methicillin-resistant staphylococcus aureus (MRSA). After Dr. Deruelle administered prochlorperazine (Compazine), she had a severe dystonic reaction.
“She was going rigid right before my eyes,” Dr. Deruelle says. There was no instantly accessible hospital clearinghouse of medical information, although he had called the pharmacy department and was waiting for a call back. So he opened his laptop and turned to an aid available to anyone with a computer and Internet access: Google. “I immediately looked up information on reactions to Compazine and the correct dose for counteracting it. I administered the dose, and within minutes [the patient] was getting better.”
Dr. Deruelle is not alone among physicians in answering medical questions with Google. (See The Hospitalist, July 2007, p. 33.)
He has been interested in medical applications of computer technology for years and serves on SHM’s advisory committee on technology. He receives tech support from his employer, IPC-The Hospitalist Company, based in North Hollywood, Calif. IPC offers its physicians a Web-accessible network called IPC Link—a “virtual office” to help with billing, medical decision support, reference software, continuing medical education, and even blogs written by company CEO Adam Singer, MD.
But Dr. Deruelle has also developed his own applications, including an off-the-shelf voice recognition software loaded onto his company-supplied, 2.5-lb. Tablet PC. He uses it to dictate brief notes to give attending physicians a heads-up about patients being discharged. These notes are uploaded to the company’s network, which automatically generates a fax to the attending within minutes.
The formal discharge summary, produced by the hospital’s medical transcription department, may take 48 hours to arrive.
Dr. Deruelle has wireless Internet access at four of the five hospitals he visits as a hospitalist practice leader.
“As soon as I walk in the door I’m ‘hot,’ ” he says. At the fifth hospital, he uses workstation computers to connect with IPC Link.
Array of Options
A dizzying range of communications technology is available to working hospitalists, typically accessed through personal digital assistants (PDAs), smartphones, computer tablets, pocket PCs, and laptops.
The Palm Pilot, introduced in 1996, is a well-known example of this technology, as are the Palm Treo and BlackBerry. PDAs combine the functions of cell phones, video phones, cameras, video recorders, media players, Web browsers, reference tools, bar code scanners, and global positioning system (GPS) devices—all in a palm-size package.
Hardware and supporting software vary in terms of ease of use, in particular, the ability to interface with the Web or the hospital, practice, or employer network the physician needs to connect with.
The technology is evolving rapidly. But anomalies abound, such as dependence on the fax machine as a staple of communication with attending physicians. Through all of these changes, hospitalists are responsible for learning what works and how best to take advantage of the technology to make their jobs easier.
Hospitalists also vary tremendously in terms of their comfort levels and openness to new technology.
“There is a considerable gap between those of us who ‘Palm’ and those who don’t,” says Timothy Hartzog, MD, pediatric hospitalist at Medical University of South Carolina (MUSC) in Charleston and a medical technology consultant. “Physicians want their patient data in different ways. Some want it printed out or in a paper chart.”
—Steven Liu, MD, of Emory University Medical Center in Atlanta
But implementation of technology, such as hospital electronic health records or computerized physician order entry, inevitably changes their relationships with information technology and patient information.
Some hospitalists, like Dr. Deruelle, are interested in what communication technology can bring their work and how to adapt it to their needs. Others, like Dr. Hartzog, medical director of Information Technology at MUSC, have taken added responsibilities for technology within their institutions.
And a few, such as Steven Liu, MD, of Emory University Medical Center in Atlanta, have taken their interest in computer technology a step further. In 1999, Dr. Liu founded Ingenious Med, an Atlanta software company that offers a suite of inpatient practice management applications to working hospitalists.
“Often the hospitalist is already on the forefront of technology,” Dr. Liu says. “The demographic is typically younger and techno-savvy. They may get tapped by their hospitals to help customize the electronic health record to make sure it satisfies the needs of clinicians. Conversely, if an electronic project does not involve strong physician feedback and collaboration, physicians can be the Achilles’ heel impeding successful implementation. Even though they are the ones who stand to gain most from the potential efficiency, physicians will not adopt technology that does not fit their workflow.”
State of the Art?
Russell Cucina, MD, MS, a hospitalist at the University of California-San Francisco Medical Center, San Francisco, is also the associate medical director for information technology at UCSF.
Dr. Cucina quips that a good example of a state-of-the-art, stand-alone patient data management system offering rapid data entry, long battery life, and high mobility is the paper index card, the longtime standard for making rounding notes.
“Plenty of doctors, including me, use it every day,” he says. But growing numbers of hospitalists also use PDAs, smartphones, and laptops to access information and support applications. Among the plethora of reference applications readily available to physicians by PDA or laptop are UpToDate, Epocrates, the Pocket Sanford Guide to Anti-Microbial Therapy, and Merck Medicus.
“I use many different resources as a hospitalist,” Dr. Cucina says. “I Google all the time.” Hospitalists still have opportunities to innovate, although increasingly their “home-grown” solutions will compete with multinational technology conglomerates entering the medical market.
The use of technology and equipment also varies depending on whether the hospitalist is employed by the hospital or part of an independent medical group.
Another factor is whether that hospital is academic, community-based, or part of a system like the Veterans Affairs or a staff-model HMO such as Kaiser Permanente. But all hospitalists are used to working on the run, Dr. Cucina says. And in their daily jobs, workflow is everything.
Tech in Use
“I use medical technology on the job to a moderate degree,” reports Latha Sivaprasad, MD, a hospitalist at Beth Israel Medical Center in New York City. “This is my sixth year working as a hospitalist, and for the first five years I didn’t use a specific device. Now I have a Palm-based program with MD Everywhere, Epocrates, UpToDate, and the ability to do billing. The hospital’s tech support staff trained us on the new system and how to use the PDA for tasks like developing rounding lists, accessing our colleagues’ lists and creating system-based memos.”
Dr. Sivaprasad also has GPS in her car, a cell phone, and a laptop at home. “We probably aren’t using medical technology as much as we could,” she says. “Many physicians still write prescriptions by hand. I’ve never used voice-recognition software. In a previous hospital, we used the hospital’s transcription service for dictated notes.”
Karim Godamunne, MD, MBA, a hospitalist with Eagle Hospital Physicians and a practice medical director at South Fulton Medical Center in Atlanta, uses a PDA at work for billing.
“I don’t use the PDA intensively,’’ he says. “I’d like to see our hospital create a wireless network like the one I have at home. Our sister hospital has wireless.” He notes, however, that there are computer workstations for him to use at his hospital.
Dr. Godamunne’s group has a practice coordinator who faxes discharge summaries to attending physicians.
“Fax is kind of what they expect these days,” he says. “I’m not sure e-mail would be as reliable for the community we serve. I’d be concerned that the attendings wouldn’t read their e-mails.” He says he sometimes gives written notes to patients at discharge with instructions to hand the note to their physician on their next office visit.
Michelle Pezzani, MD, is part of a 10-member hospital medicine group that practices at El Camino Hospital in Mountain View, Calif., in the heart of Silicon Valley. The hospital tries to stay on the cutting edge with technology, and its hospitalists were given Microsoft XP Tablet laptops a few years ago. “I access the Web two to four times a day at work,” Dr. Pezzani says. “It helps keep us current. The great thing about the laptop is I also take it home with me, and I can use it to check or reorder labs from home. We’re all connected to the hospital’s Intranet from home.”
“One of the issues we’re struggling with is how to achieve the best sign-out possible,” with up to four hospitalists on the day shift checking out and handing over patient responsibilities to the night shift, Dr. Pezzani says. For her, the ideal sign-out is face to face because it permits asking questions and reading nonverbal cues about how sick the patients really are. However, the logistics of multiple physicians and patients makes this ideal difficult to achieve.
Second best (if all group members used a Palm Pilot), would be to send sign-outs via text messaging—although that would also present logistical challenges. “Texting is easier,” she says. “You know who is sending the message. We could beam the written sign-out to each other in a matter of seconds, making it quick and easy. Furthermore, any day-to-day changes on a specific patient would be easy to amend and easy to send. It’s also a quick way to let a colleague know, ‘I need you right now!’ ”
The hospitalists at El Camino use voicemail to record sign-outs. But these messages can take a long time to record and play back, multiplied by the four physicians signing out. “Ideally, there would be a different voice mail for every patient, so I wouldn’t have to listen to patients A, B, C, D, and E to get to the pertinent information about patient F, who is crashing upstairs,” she says. Dr. Pezzani’s group is still exploring how to balance these considerations.
She says her hospitalist group is tight-knit and collaborative. “We leave our cell phones on all the time and answer each other’s calls after hours,” she says. “For example, I’m now on vacation with my family in San Diego and I have gotten at least two calls a day from my partners, either business related, or something like: ‘Do you remember that patient you admitted? Can you give me some information on them?’”
The Wired Hospital
Dr. Cucina is excited about the extra large, easy-to-grip handle on the 3-lb. Motion Computing C5 portable PC that UCSF hospitalists are field-testing. He’s also intrigued by the ever-expanding opportunities for interfacing with the hospital’s technology.
In August he gave a tour of Unit 13L at UCSF’s Moffitt/Long Hospital, a new ward that opened in June and is being used as a technology demonstration site.
The 32-bed unit has a narrow corridor lined with 10 computer workstations for the nurses. All 10 are in use. In an adjacent cubicle, several physicians are typing on their laptops.
On the unit, portable vital signs monitors are attached to rolling stands that also have docking ports for the laptops, offering real-time point-of-care acquisition of vital-signs data directly into the hospital’s medical record.
A nurse or physician can grab the big-handled Tablet PC and run to another room while remaining connected to the patient’s vital signs. The docking ports in patients’ rooms are also linked to a 37-inch, high-definition television. “A clinician can show the patient radiographic studies here or bring up interactive patient education programs,” he explains.
One of the most exciting potentials for this emerging technology is to find ways for embedding medical decision support in physicians’ workflow. “We know that the barriers to physicians routinely consulting decision support applications are high,” Dr. Cucina says.
For Dr. Deruelle, who had to look outside of hospital channels to answer his question about a dystonic patient, medicine has a serious information gap. “I believe we will move to where the technology will put that information at my fingertips,” he says. “Why aren’t we there yet? Not enough people are using the technology, and we don’t agree on what information should be included. But I think we can start with basic things and work up from there. What excites me is that we’re closing the information gap—although medicine is still in the Stone Age compared with other professions.” TH
Larry Beresford is a frequent contributor to The Hospitalist.
Dennis Deruelle, MD, a hospitalist at University Community Hospital in Tampa, Fla., once needed reliable medical information in a hurry while treating a young woman admitted to the hospital with cellulitis.
The woman was later diagnosed with methicillin-resistant staphylococcus aureus (MRSA). After Dr. Deruelle administered prochlorperazine (Compazine), she had a severe dystonic reaction.
“She was going rigid right before my eyes,” Dr. Deruelle says. There was no instantly accessible hospital clearinghouse of medical information, although he had called the pharmacy department and was waiting for a call back. So he opened his laptop and turned to an aid available to anyone with a computer and Internet access: Google. “I immediately looked up information on reactions to Compazine and the correct dose for counteracting it. I administered the dose, and within minutes [the patient] was getting better.”
Dr. Deruelle is not alone among physicians in answering medical questions with Google. (See The Hospitalist, July 2007, p. 33.)
He has been interested in medical applications of computer technology for years and serves on SHM’s advisory committee on technology. He receives tech support from his employer, IPC-The Hospitalist Company, based in North Hollywood, Calif. IPC offers its physicians a Web-accessible network called IPC Link—a “virtual office” to help with billing, medical decision support, reference software, continuing medical education, and even blogs written by company CEO Adam Singer, MD.
But Dr. Deruelle has also developed his own applications, including an off-the-shelf voice recognition software loaded onto his company-supplied, 2.5-lb. Tablet PC. He uses it to dictate brief notes to give attending physicians a heads-up about patients being discharged. These notes are uploaded to the company’s network, which automatically generates a fax to the attending within minutes.
The formal discharge summary, produced by the hospital’s medical transcription department, may take 48 hours to arrive.
Dr. Deruelle has wireless Internet access at four of the five hospitals he visits as a hospitalist practice leader.
“As soon as I walk in the door I’m ‘hot,’ ” he says. At the fifth hospital, he uses workstation computers to connect with IPC Link.
Array of Options
A dizzying range of communications technology is available to working hospitalists, typically accessed through personal digital assistants (PDAs), smartphones, computer tablets, pocket PCs, and laptops.
The Palm Pilot, introduced in 1996, is a well-known example of this technology, as are the Palm Treo and BlackBerry. PDAs combine the functions of cell phones, video phones, cameras, video recorders, media players, Web browsers, reference tools, bar code scanners, and global positioning system (GPS) devices—all in a palm-size package.
Hardware and supporting software vary in terms of ease of use, in particular, the ability to interface with the Web or the hospital, practice, or employer network the physician needs to connect with.
The technology is evolving rapidly. But anomalies abound, such as dependence on the fax machine as a staple of communication with attending physicians. Through all of these changes, hospitalists are responsible for learning what works and how best to take advantage of the technology to make their jobs easier.
Hospitalists also vary tremendously in terms of their comfort levels and openness to new technology.
“There is a considerable gap between those of us who ‘Palm’ and those who don’t,” says Timothy Hartzog, MD, pediatric hospitalist at Medical University of South Carolina (MUSC) in Charleston and a medical technology consultant. “Physicians want their patient data in different ways. Some want it printed out or in a paper chart.”
—Steven Liu, MD, of Emory University Medical Center in Atlanta
But implementation of technology, such as hospital electronic health records or computerized physician order entry, inevitably changes their relationships with information technology and patient information.
Some hospitalists, like Dr. Deruelle, are interested in what communication technology can bring their work and how to adapt it to their needs. Others, like Dr. Hartzog, medical director of Information Technology at MUSC, have taken added responsibilities for technology within their institutions.
And a few, such as Steven Liu, MD, of Emory University Medical Center in Atlanta, have taken their interest in computer technology a step further. In 1999, Dr. Liu founded Ingenious Med, an Atlanta software company that offers a suite of inpatient practice management applications to working hospitalists.
“Often the hospitalist is already on the forefront of technology,” Dr. Liu says. “The demographic is typically younger and techno-savvy. They may get tapped by their hospitals to help customize the electronic health record to make sure it satisfies the needs of clinicians. Conversely, if an electronic project does not involve strong physician feedback and collaboration, physicians can be the Achilles’ heel impeding successful implementation. Even though they are the ones who stand to gain most from the potential efficiency, physicians will not adopt technology that does not fit their workflow.”
State of the Art?
Russell Cucina, MD, MS, a hospitalist at the University of California-San Francisco Medical Center, San Francisco, is also the associate medical director for information technology at UCSF.
Dr. Cucina quips that a good example of a state-of-the-art, stand-alone patient data management system offering rapid data entry, long battery life, and high mobility is the paper index card, the longtime standard for making rounding notes.
“Plenty of doctors, including me, use it every day,” he says. But growing numbers of hospitalists also use PDAs, smartphones, and laptops to access information and support applications. Among the plethora of reference applications readily available to physicians by PDA or laptop are UpToDate, Epocrates, the Pocket Sanford Guide to Anti-Microbial Therapy, and Merck Medicus.
“I use many different resources as a hospitalist,” Dr. Cucina says. “I Google all the time.” Hospitalists still have opportunities to innovate, although increasingly their “home-grown” solutions will compete with multinational technology conglomerates entering the medical market.
The use of technology and equipment also varies depending on whether the hospitalist is employed by the hospital or part of an independent medical group.
Another factor is whether that hospital is academic, community-based, or part of a system like the Veterans Affairs or a staff-model HMO such as Kaiser Permanente. But all hospitalists are used to working on the run, Dr. Cucina says. And in their daily jobs, workflow is everything.
Tech in Use
“I use medical technology on the job to a moderate degree,” reports Latha Sivaprasad, MD, a hospitalist at Beth Israel Medical Center in New York City. “This is my sixth year working as a hospitalist, and for the first five years I didn’t use a specific device. Now I have a Palm-based program with MD Everywhere, Epocrates, UpToDate, and the ability to do billing. The hospital’s tech support staff trained us on the new system and how to use the PDA for tasks like developing rounding lists, accessing our colleagues’ lists and creating system-based memos.”
Dr. Sivaprasad also has GPS in her car, a cell phone, and a laptop at home. “We probably aren’t using medical technology as much as we could,” she says. “Many physicians still write prescriptions by hand. I’ve never used voice-recognition software. In a previous hospital, we used the hospital’s transcription service for dictated notes.”
Karim Godamunne, MD, MBA, a hospitalist with Eagle Hospital Physicians and a practice medical director at South Fulton Medical Center in Atlanta, uses a PDA at work for billing.
“I don’t use the PDA intensively,’’ he says. “I’d like to see our hospital create a wireless network like the one I have at home. Our sister hospital has wireless.” He notes, however, that there are computer workstations for him to use at his hospital.
Dr. Godamunne’s group has a practice coordinator who faxes discharge summaries to attending physicians.
“Fax is kind of what they expect these days,” he says. “I’m not sure e-mail would be as reliable for the community we serve. I’d be concerned that the attendings wouldn’t read their e-mails.” He says he sometimes gives written notes to patients at discharge with instructions to hand the note to their physician on their next office visit.
Michelle Pezzani, MD, is part of a 10-member hospital medicine group that practices at El Camino Hospital in Mountain View, Calif., in the heart of Silicon Valley. The hospital tries to stay on the cutting edge with technology, and its hospitalists were given Microsoft XP Tablet laptops a few years ago. “I access the Web two to four times a day at work,” Dr. Pezzani says. “It helps keep us current. The great thing about the laptop is I also take it home with me, and I can use it to check or reorder labs from home. We’re all connected to the hospital’s Intranet from home.”
“One of the issues we’re struggling with is how to achieve the best sign-out possible,” with up to four hospitalists on the day shift checking out and handing over patient responsibilities to the night shift, Dr. Pezzani says. For her, the ideal sign-out is face to face because it permits asking questions and reading nonverbal cues about how sick the patients really are. However, the logistics of multiple physicians and patients makes this ideal difficult to achieve.
Second best (if all group members used a Palm Pilot), would be to send sign-outs via text messaging—although that would also present logistical challenges. “Texting is easier,” she says. “You know who is sending the message. We could beam the written sign-out to each other in a matter of seconds, making it quick and easy. Furthermore, any day-to-day changes on a specific patient would be easy to amend and easy to send. It’s also a quick way to let a colleague know, ‘I need you right now!’ ”
The hospitalists at El Camino use voicemail to record sign-outs. But these messages can take a long time to record and play back, multiplied by the four physicians signing out. “Ideally, there would be a different voice mail for every patient, so I wouldn’t have to listen to patients A, B, C, D, and E to get to the pertinent information about patient F, who is crashing upstairs,” she says. Dr. Pezzani’s group is still exploring how to balance these considerations.
She says her hospitalist group is tight-knit and collaborative. “We leave our cell phones on all the time and answer each other’s calls after hours,” she says. “For example, I’m now on vacation with my family in San Diego and I have gotten at least two calls a day from my partners, either business related, or something like: ‘Do you remember that patient you admitted? Can you give me some information on them?’”
The Wired Hospital
Dr. Cucina is excited about the extra large, easy-to-grip handle on the 3-lb. Motion Computing C5 portable PC that UCSF hospitalists are field-testing. He’s also intrigued by the ever-expanding opportunities for interfacing with the hospital’s technology.
In August he gave a tour of Unit 13L at UCSF’s Moffitt/Long Hospital, a new ward that opened in June and is being used as a technology demonstration site.
The 32-bed unit has a narrow corridor lined with 10 computer workstations for the nurses. All 10 are in use. In an adjacent cubicle, several physicians are typing on their laptops.
On the unit, portable vital signs monitors are attached to rolling stands that also have docking ports for the laptops, offering real-time point-of-care acquisition of vital-signs data directly into the hospital’s medical record.
A nurse or physician can grab the big-handled Tablet PC and run to another room while remaining connected to the patient’s vital signs. The docking ports in patients’ rooms are also linked to a 37-inch, high-definition television. “A clinician can show the patient radiographic studies here or bring up interactive patient education programs,” he explains.
One of the most exciting potentials for this emerging technology is to find ways for embedding medical decision support in physicians’ workflow. “We know that the barriers to physicians routinely consulting decision support applications are high,” Dr. Cucina says.
For Dr. Deruelle, who had to look outside of hospital channels to answer his question about a dystonic patient, medicine has a serious information gap. “I believe we will move to where the technology will put that information at my fingertips,” he says. “Why aren’t we there yet? Not enough people are using the technology, and we don’t agree on what information should be included. But I think we can start with basic things and work up from there. What excites me is that we’re closing the information gap—although medicine is still in the Stone Age compared with other professions.” TH
Larry Beresford is a frequent contributor to The Hospitalist.
Dennis Deruelle, MD, a hospitalist at University Community Hospital in Tampa, Fla., once needed reliable medical information in a hurry while treating a young woman admitted to the hospital with cellulitis.
The woman was later diagnosed with methicillin-resistant staphylococcus aureus (MRSA). After Dr. Deruelle administered prochlorperazine (Compazine), she had a severe dystonic reaction.
“She was going rigid right before my eyes,” Dr. Deruelle says. There was no instantly accessible hospital clearinghouse of medical information, although he had called the pharmacy department and was waiting for a call back. So he opened his laptop and turned to an aid available to anyone with a computer and Internet access: Google. “I immediately looked up information on reactions to Compazine and the correct dose for counteracting it. I administered the dose, and within minutes [the patient] was getting better.”
Dr. Deruelle is not alone among physicians in answering medical questions with Google. (See The Hospitalist, July 2007, p. 33.)
He has been interested in medical applications of computer technology for years and serves on SHM’s advisory committee on technology. He receives tech support from his employer, IPC-The Hospitalist Company, based in North Hollywood, Calif. IPC offers its physicians a Web-accessible network called IPC Link—a “virtual office” to help with billing, medical decision support, reference software, continuing medical education, and even blogs written by company CEO Adam Singer, MD.
But Dr. Deruelle has also developed his own applications, including an off-the-shelf voice recognition software loaded onto his company-supplied, 2.5-lb. Tablet PC. He uses it to dictate brief notes to give attending physicians a heads-up about patients being discharged. These notes are uploaded to the company’s network, which automatically generates a fax to the attending within minutes.
The formal discharge summary, produced by the hospital’s medical transcription department, may take 48 hours to arrive.
Dr. Deruelle has wireless Internet access at four of the five hospitals he visits as a hospitalist practice leader.
“As soon as I walk in the door I’m ‘hot,’ ” he says. At the fifth hospital, he uses workstation computers to connect with IPC Link.
Array of Options
A dizzying range of communications technology is available to working hospitalists, typically accessed through personal digital assistants (PDAs), smartphones, computer tablets, pocket PCs, and laptops.
The Palm Pilot, introduced in 1996, is a well-known example of this technology, as are the Palm Treo and BlackBerry. PDAs combine the functions of cell phones, video phones, cameras, video recorders, media players, Web browsers, reference tools, bar code scanners, and global positioning system (GPS) devices—all in a palm-size package.
Hardware and supporting software vary in terms of ease of use, in particular, the ability to interface with the Web or the hospital, practice, or employer network the physician needs to connect with.
The technology is evolving rapidly. But anomalies abound, such as dependence on the fax machine as a staple of communication with attending physicians. Through all of these changes, hospitalists are responsible for learning what works and how best to take advantage of the technology to make their jobs easier.
Hospitalists also vary tremendously in terms of their comfort levels and openness to new technology.
“There is a considerable gap between those of us who ‘Palm’ and those who don’t,” says Timothy Hartzog, MD, pediatric hospitalist at Medical University of South Carolina (MUSC) in Charleston and a medical technology consultant. “Physicians want their patient data in different ways. Some want it printed out or in a paper chart.”
—Steven Liu, MD, of Emory University Medical Center in Atlanta
But implementation of technology, such as hospital electronic health records or computerized physician order entry, inevitably changes their relationships with information technology and patient information.
Some hospitalists, like Dr. Deruelle, are interested in what communication technology can bring their work and how to adapt it to their needs. Others, like Dr. Hartzog, medical director of Information Technology at MUSC, have taken added responsibilities for technology within their institutions.
And a few, such as Steven Liu, MD, of Emory University Medical Center in Atlanta, have taken their interest in computer technology a step further. In 1999, Dr. Liu founded Ingenious Med, an Atlanta software company that offers a suite of inpatient practice management applications to working hospitalists.
“Often the hospitalist is already on the forefront of technology,” Dr. Liu says. “The demographic is typically younger and techno-savvy. They may get tapped by their hospitals to help customize the electronic health record to make sure it satisfies the needs of clinicians. Conversely, if an electronic project does not involve strong physician feedback and collaboration, physicians can be the Achilles’ heel impeding successful implementation. Even though they are the ones who stand to gain most from the potential efficiency, physicians will not adopt technology that does not fit their workflow.”
State of the Art?
Russell Cucina, MD, MS, a hospitalist at the University of California-San Francisco Medical Center, San Francisco, is also the associate medical director for information technology at UCSF.
Dr. Cucina quips that a good example of a state-of-the-art, stand-alone patient data management system offering rapid data entry, long battery life, and high mobility is the paper index card, the longtime standard for making rounding notes.
“Plenty of doctors, including me, use it every day,” he says. But growing numbers of hospitalists also use PDAs, smartphones, and laptops to access information and support applications. Among the plethora of reference applications readily available to physicians by PDA or laptop are UpToDate, Epocrates, the Pocket Sanford Guide to Anti-Microbial Therapy, and Merck Medicus.
“I use many different resources as a hospitalist,” Dr. Cucina says. “I Google all the time.” Hospitalists still have opportunities to innovate, although increasingly their “home-grown” solutions will compete with multinational technology conglomerates entering the medical market.
The use of technology and equipment also varies depending on whether the hospitalist is employed by the hospital or part of an independent medical group.
Another factor is whether that hospital is academic, community-based, or part of a system like the Veterans Affairs or a staff-model HMO such as Kaiser Permanente. But all hospitalists are used to working on the run, Dr. Cucina says. And in their daily jobs, workflow is everything.
Tech in Use
“I use medical technology on the job to a moderate degree,” reports Latha Sivaprasad, MD, a hospitalist at Beth Israel Medical Center in New York City. “This is my sixth year working as a hospitalist, and for the first five years I didn’t use a specific device. Now I have a Palm-based program with MD Everywhere, Epocrates, UpToDate, and the ability to do billing. The hospital’s tech support staff trained us on the new system and how to use the PDA for tasks like developing rounding lists, accessing our colleagues’ lists and creating system-based memos.”
Dr. Sivaprasad also has GPS in her car, a cell phone, and a laptop at home. “We probably aren’t using medical technology as much as we could,” she says. “Many physicians still write prescriptions by hand. I’ve never used voice-recognition software. In a previous hospital, we used the hospital’s transcription service for dictated notes.”
Karim Godamunne, MD, MBA, a hospitalist with Eagle Hospital Physicians and a practice medical director at South Fulton Medical Center in Atlanta, uses a PDA at work for billing.
“I don’t use the PDA intensively,’’ he says. “I’d like to see our hospital create a wireless network like the one I have at home. Our sister hospital has wireless.” He notes, however, that there are computer workstations for him to use at his hospital.
Dr. Godamunne’s group has a practice coordinator who faxes discharge summaries to attending physicians.
“Fax is kind of what they expect these days,” he says. “I’m not sure e-mail would be as reliable for the community we serve. I’d be concerned that the attendings wouldn’t read their e-mails.” He says he sometimes gives written notes to patients at discharge with instructions to hand the note to their physician on their next office visit.
Michelle Pezzani, MD, is part of a 10-member hospital medicine group that practices at El Camino Hospital in Mountain View, Calif., in the heart of Silicon Valley. The hospital tries to stay on the cutting edge with technology, and its hospitalists were given Microsoft XP Tablet laptops a few years ago. “I access the Web two to four times a day at work,” Dr. Pezzani says. “It helps keep us current. The great thing about the laptop is I also take it home with me, and I can use it to check or reorder labs from home. We’re all connected to the hospital’s Intranet from home.”
“One of the issues we’re struggling with is how to achieve the best sign-out possible,” with up to four hospitalists on the day shift checking out and handing over patient responsibilities to the night shift, Dr. Pezzani says. For her, the ideal sign-out is face to face because it permits asking questions and reading nonverbal cues about how sick the patients really are. However, the logistics of multiple physicians and patients makes this ideal difficult to achieve.
Second best (if all group members used a Palm Pilot), would be to send sign-outs via text messaging—although that would also present logistical challenges. “Texting is easier,” she says. “You know who is sending the message. We could beam the written sign-out to each other in a matter of seconds, making it quick and easy. Furthermore, any day-to-day changes on a specific patient would be easy to amend and easy to send. It’s also a quick way to let a colleague know, ‘I need you right now!’ ”
The hospitalists at El Camino use voicemail to record sign-outs. But these messages can take a long time to record and play back, multiplied by the four physicians signing out. “Ideally, there would be a different voice mail for every patient, so I wouldn’t have to listen to patients A, B, C, D, and E to get to the pertinent information about patient F, who is crashing upstairs,” she says. Dr. Pezzani’s group is still exploring how to balance these considerations.
She says her hospitalist group is tight-knit and collaborative. “We leave our cell phones on all the time and answer each other’s calls after hours,” she says. “For example, I’m now on vacation with my family in San Diego and I have gotten at least two calls a day from my partners, either business related, or something like: ‘Do you remember that patient you admitted? Can you give me some information on them?’”
The Wired Hospital
Dr. Cucina is excited about the extra large, easy-to-grip handle on the 3-lb. Motion Computing C5 portable PC that UCSF hospitalists are field-testing. He’s also intrigued by the ever-expanding opportunities for interfacing with the hospital’s technology.
In August he gave a tour of Unit 13L at UCSF’s Moffitt/Long Hospital, a new ward that opened in June and is being used as a technology demonstration site.
The 32-bed unit has a narrow corridor lined with 10 computer workstations for the nurses. All 10 are in use. In an adjacent cubicle, several physicians are typing on their laptops.
On the unit, portable vital signs monitors are attached to rolling stands that also have docking ports for the laptops, offering real-time point-of-care acquisition of vital-signs data directly into the hospital’s medical record.
A nurse or physician can grab the big-handled Tablet PC and run to another room while remaining connected to the patient’s vital signs. The docking ports in patients’ rooms are also linked to a 37-inch, high-definition television. “A clinician can show the patient radiographic studies here or bring up interactive patient education programs,” he explains.
One of the most exciting potentials for this emerging technology is to find ways for embedding medical decision support in physicians’ workflow. “We know that the barriers to physicians routinely consulting decision support applications are high,” Dr. Cucina says.
For Dr. Deruelle, who had to look outside of hospital channels to answer his question about a dystonic patient, medicine has a serious information gap. “I believe we will move to where the technology will put that information at my fingertips,” he says. “Why aren’t we there yet? Not enough people are using the technology, and we don’t agree on what information should be included. But I think we can start with basic things and work up from there. What excites me is that we’re closing the information gap—although medicine is still in the Stone Age compared with other professions.” TH
Larry Beresford is a frequent contributor to The Hospitalist.