User login
Editorial
Insanity: doing the same thing over and over again and expecting different results.Albert Einstein
Diabetes is one of the most common diagnoses in hospitalized patients.1 A third of all persons admitted to urban general hospitals have glucose levels qualifying them for the diagnosis of diabetes, and a third of these hyperglycemic patients have not previously been diagnosed with diabetes.2 The impact of hyperglycemia on the mortality rate of hospitalized patients has been increasingly appreciated. Extensive evidence from observational studies indicates that hyperglycemia in patients with or without a history of diabetes is a marker of a poor clinical outcome.38 In addition, the results of prospective randomized trials in patients with critical illness or those undergoing coronary bypass surgery suggest that aggressive glycemic control improves clinical outcomes including reductions in: a) short‐ and long‐term mortality, b) multiorgan failure and systemic infection, and c) length of hospitalization.7, 911
The importance of glycemic control is not limited to patients in critical care areas but may also apply to patients admitted to general surgical and medical wards. The development of hyperglycemia in such patients with or without a history of diabetes has been associated with prolonged hospital stay, infection, disability after hospital discharge, and death.12, 13 In general‐surgical patients, serum glucose > 220 mg/dL on postoperative day 1 has been shown to be a sensitive, albeit nonspecific, predictor of the development of serious postoperative hospital‐acquired infection.14 A retrospective review of 1886 admissions to a community hospital in Atlanta, Georgia, found an 18‐fold increase in mortality in hyperglycemic patients without a history of diabetes and a 2.5‐fold increase in mortality in patients with known diabetes compared with controls.2 A meta‐analysis of 26 studies identified an association of admission glucose > 110 mg/dL with the increased mortality of patients hospitalized for acute stroke.15 More recently, hyperglycemia on admission was also shown to be independently associated with adverse outcomes in patients with community acquired pneumonia.16, 17
In view of the increasing evidence supporting better glycemic control in the hospital, the American Association of Clinical Endocrinologists (AACE) in late 2003 convened a consensus conference on the inpatient with diabetes, cosponsored or supported by other prominent professional organizations, including the Society of Hospital Medicine (SHM). An expert panel agreed on and published glycemic targets and recommendations for inpatient management of hyperglycemia.18 The American Diabetes Association (ADA) subsequently published an excellent technical review evaluating the evidence and outlining treatment, monitoring, and educational strategies13 for the hospitalized patient, and these recommendations were largely incorporated into the 2005 ADA Clinical Practice Guidelines for Hospitalized Patients.19 The recommended glycemic targets for hospitalized patients in the intensive care unit are between 80 and 110 mg/dL. In noncritical care settings a preprandial glucose of 90130 mg/dL (midpoint 110 mg/dL) and a postprandial or random glucose of less than 180 mg/dL are the recommended glycemic targets. Physiologic and safe insulin regimen strategies for virtually all patient situations were succinctly presented. Although there have been modest (and occasionally dramatic) improvements in glycemic control in several institutions, the reviews and guidelines have not yet resulted in widespread change in clinical practice on the inpatient wards.
Two retrospective studies from prestigious medical institutions reported in this issue of the Journal of Hospital Medicine dramatically illustrate that glycemic control and insulin‐ordering practices in general medicine services continue to be deficient and underscore the contribution of physician inertia in the management of hyperglycemia in noncritically ill patients.20, 21 From their findings and experiences in our institutions, you should expect the following at your institution unless you have embarked on an organized program to improve noncritical care inpatient glycemic control.
-
Around one third of your patients with hyperglycemia have a mean glucose of more than 200 mg/dL during their hospital stay.
-
Despite these out‐of‐control values, 60% of your inpatients will remain on a static regimen of sliding‐scale insulin over the duration of their stay. Unfortunately, this degree of hyperglycemia is not protective for hypoglycemic episodes.
-
Around 10% of your monitored ward inpatients will have at least one hypoglycemic episode during their stay. Many of these episodes will be precipitated by poor coordination of nutrition and insulin administration and nonsensical insulin regimens that lead to insulin stacking.
-
Discharge summaries and plans will include mention and follow‐up of hyperglycemia only a minority of the time.
-
Your nursing and medical staffs are unevenly educated about the proper use of insulin, even though insulin errors are very common, and insulin is one of the top 3 drugs involved in adverse drug events in your institution.
-
Transitions in care will lead to an inconsistent approach to glycemic control, leaving some of your patients confused and others just plain angry.
The ubiquitous use of the insulin sliding scale as the single routine response for controlling hyperglycemia in inpatients has been discredited for a long time.2224 Strong terms have been used the condemnation of this method: mindless medicine, paralysis of thought, and action without benefit, for example.25, 26 Yet this remains the most popular default regimen in most institutions across the country. Clinical inertia is defined as not initiating or intensifying therapy when doing so is indicated,27, 28 and that term certainly applies to glycemic control practices and the continued heavy use of sliding‐scale insulin across the nation.
Why is clinical inertia so strong in this area? Why have well‐done practice guidelines and reviews not eradicated the use of sliding‐scale insulin? First, hyperglycemia is rarely the focus of care during the hospital stay, as the overwhelming majority of hospitalizations of patients with hyperglycemia occur for comorbid conditions.2, 29 Second, fear of hypoglycemia constitutes a major barrier to efforts to improve glycemic control in hospitalized patients, especially in those with poor caloric intake.13, 30 Third, practitioners initiate sliding‐scale insulin regimens, even though this has been a thoroughly discredited approach, simply because it is the easiest thing to do in their current practice environment.31
How do we break this inertia and redesign our practice environment in such a way that using a more physiologic and sensible insulin regimen is the easiest thing to do? It starts with local physician leadership. On noncritical care wards, hospitalists and endocrinologists are the natural candidates to own the issue of inpatient diabetes care. These physician leaders need to garner appropriate institutional support, form a multidisciplinary steering committee or team, and formulate interventions.
Implementing a standardized subcutaneous insulin order set promoting the use of scheduled insulin therapy is a key intervention in the inpatient management of diabetes. These order sets should encourage basal replacement insulin therapy (ie, NPH, glargine, detemir) and scheduled nutritional/prandial short‐/rapid‐acting insulin (ie, regular, aspart, lispro, glulisine). The order set should also state the glycemic target, eliminate improper abbreviations and notations, incorporate a hypoglycemia protocol, and provide a range of default correction insulin dosage scales appropriate for varied levels of insulin sensitivity. Examples of such order sets are widely available.13, 32 This simple intervention can result in a tripling of insulin regimens including scheduled basal insulin, substantial subsequent improvement in glycemic control on the hospital floor, and significant reduction in hypoglycemic event rates.
The standardized order set can be much more effective when it is complemented by institution‐specific algorithms, protocols, and policies that support their effective use. These tools must not merely exist; they must be widely disseminated and used and, if possible, embedded in the order set. They should outline the calculation of insulin dosages, define recommended insulin regimens for patients with different forms of nutritional intake, guide transitions from insulin infusion to subcutaneous regimens, and enhance discharge planning and education.
The SHM, AACE, ADA, and other organizations are partnering to create a compendium of tested tools and strategies to assist hospitalists and their hospitals in these and other interventions and to assist them in devising reliable and practical metrics to gauge the impact of their efforts. These tools and a guidebook to walk teams through the improvement process step by step should be available on the SHM (
Look around and take stock. Does your hospital have standardized subcutaneous insulin order sets, algorithms and protocols supporting the order set, a multidisciplinary team tasked with improving insulin safety and glycemic control, and metrics to gauge whether your efforts are making a difference? Expecting better results without these essential elements is not only foolhardy but fits Einstein's definition of insanity: doing the same thing over and over again and expecting different results. Let's stop this sliding‐scale insulin insanity now.
- ,,, et al.Diabetes trends in the U.S.: 1990–1998.Diabetes Care.2000;23:1278–1283.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,Outcomes and perioperative hyperglycemia in patients with or without diabetes mellitus undergoing coronary artery bypass grafting.Ann Thorac Surg.2003;75:1392–1399.
- ,,,.Glucose control and mortality in critically ill patients.JAMA.2003;290:2041–2047.
- ,,.Admission plasma glucose. Independent risk factor for long‐term prognosis after myocardial infarction even in nondiabetic patients.Diabetes Care.1999;22:1827–1831.
- ,.ICU care for patients with diabetes.Curr Opin Endocrinol.2004;11:75–81.
- ,,, et al.Intensive insulin therapy in the critically ill patients.N Engl J Med.2001;345:1359–1367.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461.
- .Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients.Mayo Clin Proc.2003;78:1471–1478.
- ,,, et al.Randomized trial of insulin‐glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): effects on mortality at 1 year.J Am Coll Cardiol.1995;26(1):57–65.
- ,,, et al.Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting.J Thorac Cardiovasc Surg.2003;125:1007–1021.
- ,,,.Hyperglycemia is associated with adverse outcomes in patients receiving total parenteral nutrition.Diabetes Care.2005;28:2367–2371.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–597.
- ,,, et al.Early postoperative glucose control predicts nosocomial infection rate in diabetic patients.JPEN J Parenter Enteral Nutr.1998;22(2):77–81.
- ,,,,.Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview.Stroke.2001;32:2426–2432.
- ,,,,.Etiology and outcome of community‐acquired pneumonia in patients with diabetes mellitus.Chest.2005;128:3233–3239.
- ,,,,,.The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community‐acquired pneumonia.Diabetes Care.2005;28:810–815.
- ,,, et al.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10(Suppl 2):4–9.
- Standards of medical care in diabetes—2006.Diabetes Care.2006;29(Suppl 1):S4–S42.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1:145–150.
- ,,, et al.Diabetes care in the hospital: Is there clinical inertia?J Hosp Med.2006;1:151–160.
- ,.Are sliding‐scale insulin regimens a recipe for diabetic instability?Lancet.1997;349:1555.
- ,,,.Eliminating inpatient sliding‐scale insulin: a reeducation project with medical house staff.Diabetes Care.2005;28:1008–1011.
- ,,,,.Efficacy of sliding‐scale insulin therapy: a comparison with prospective regimens.Fam Pract Res J.1994;14:313–322.
- .Action without benefit. The sliding scale of insulin use.Arch Intern Med.1997;157:489.
- ,,, et al.Clinical inertia.Ann Intern Med.2001;135:825–834.
- ,,,,.Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians?Diabetes Care.2005;28:600–606.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,,.Drug‐induced hypoglycemic coma in 102 diabetic patients.Arch Intern Med.1999;159:281–284.
- ,.Hospital management of diabetes.Endocrinol Metab Clin North Am.2000;29:745–770.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10(Suppl 2):89–99.
Insanity: doing the same thing over and over again and expecting different results.Albert Einstein
Diabetes is one of the most common diagnoses in hospitalized patients.1 A third of all persons admitted to urban general hospitals have glucose levels qualifying them for the diagnosis of diabetes, and a third of these hyperglycemic patients have not previously been diagnosed with diabetes.2 The impact of hyperglycemia on the mortality rate of hospitalized patients has been increasingly appreciated. Extensive evidence from observational studies indicates that hyperglycemia in patients with or without a history of diabetes is a marker of a poor clinical outcome.38 In addition, the results of prospective randomized trials in patients with critical illness or those undergoing coronary bypass surgery suggest that aggressive glycemic control improves clinical outcomes including reductions in: a) short‐ and long‐term mortality, b) multiorgan failure and systemic infection, and c) length of hospitalization.7, 911
The importance of glycemic control is not limited to patients in critical care areas but may also apply to patients admitted to general surgical and medical wards. The development of hyperglycemia in such patients with or without a history of diabetes has been associated with prolonged hospital stay, infection, disability after hospital discharge, and death.12, 13 In general‐surgical patients, serum glucose > 220 mg/dL on postoperative day 1 has been shown to be a sensitive, albeit nonspecific, predictor of the development of serious postoperative hospital‐acquired infection.14 A retrospective review of 1886 admissions to a community hospital in Atlanta, Georgia, found an 18‐fold increase in mortality in hyperglycemic patients without a history of diabetes and a 2.5‐fold increase in mortality in patients with known diabetes compared with controls.2 A meta‐analysis of 26 studies identified an association of admission glucose > 110 mg/dL with the increased mortality of patients hospitalized for acute stroke.15 More recently, hyperglycemia on admission was also shown to be independently associated with adverse outcomes in patients with community acquired pneumonia.16, 17
In view of the increasing evidence supporting better glycemic control in the hospital, the American Association of Clinical Endocrinologists (AACE) in late 2003 convened a consensus conference on the inpatient with diabetes, cosponsored or supported by other prominent professional organizations, including the Society of Hospital Medicine (SHM). An expert panel agreed on and published glycemic targets and recommendations for inpatient management of hyperglycemia.18 The American Diabetes Association (ADA) subsequently published an excellent technical review evaluating the evidence and outlining treatment, monitoring, and educational strategies13 for the hospitalized patient, and these recommendations were largely incorporated into the 2005 ADA Clinical Practice Guidelines for Hospitalized Patients.19 The recommended glycemic targets for hospitalized patients in the intensive care unit are between 80 and 110 mg/dL. In noncritical care settings a preprandial glucose of 90130 mg/dL (midpoint 110 mg/dL) and a postprandial or random glucose of less than 180 mg/dL are the recommended glycemic targets. Physiologic and safe insulin regimen strategies for virtually all patient situations were succinctly presented. Although there have been modest (and occasionally dramatic) improvements in glycemic control in several institutions, the reviews and guidelines have not yet resulted in widespread change in clinical practice on the inpatient wards.
Two retrospective studies from prestigious medical institutions reported in this issue of the Journal of Hospital Medicine dramatically illustrate that glycemic control and insulin‐ordering practices in general medicine services continue to be deficient and underscore the contribution of physician inertia in the management of hyperglycemia in noncritically ill patients.20, 21 From their findings and experiences in our institutions, you should expect the following at your institution unless you have embarked on an organized program to improve noncritical care inpatient glycemic control.
-
Around one third of your patients with hyperglycemia have a mean glucose of more than 200 mg/dL during their hospital stay.
-
Despite these out‐of‐control values, 60% of your inpatients will remain on a static regimen of sliding‐scale insulin over the duration of their stay. Unfortunately, this degree of hyperglycemia is not protective for hypoglycemic episodes.
-
Around 10% of your monitored ward inpatients will have at least one hypoglycemic episode during their stay. Many of these episodes will be precipitated by poor coordination of nutrition and insulin administration and nonsensical insulin regimens that lead to insulin stacking.
-
Discharge summaries and plans will include mention and follow‐up of hyperglycemia only a minority of the time.
-
Your nursing and medical staffs are unevenly educated about the proper use of insulin, even though insulin errors are very common, and insulin is one of the top 3 drugs involved in adverse drug events in your institution.
-
Transitions in care will lead to an inconsistent approach to glycemic control, leaving some of your patients confused and others just plain angry.
The ubiquitous use of the insulin sliding scale as the single routine response for controlling hyperglycemia in inpatients has been discredited for a long time.2224 Strong terms have been used the condemnation of this method: mindless medicine, paralysis of thought, and action without benefit, for example.25, 26 Yet this remains the most popular default regimen in most institutions across the country. Clinical inertia is defined as not initiating or intensifying therapy when doing so is indicated,27, 28 and that term certainly applies to glycemic control practices and the continued heavy use of sliding‐scale insulin across the nation.
Why is clinical inertia so strong in this area? Why have well‐done practice guidelines and reviews not eradicated the use of sliding‐scale insulin? First, hyperglycemia is rarely the focus of care during the hospital stay, as the overwhelming majority of hospitalizations of patients with hyperglycemia occur for comorbid conditions.2, 29 Second, fear of hypoglycemia constitutes a major barrier to efforts to improve glycemic control in hospitalized patients, especially in those with poor caloric intake.13, 30 Third, practitioners initiate sliding‐scale insulin regimens, even though this has been a thoroughly discredited approach, simply because it is the easiest thing to do in their current practice environment.31
How do we break this inertia and redesign our practice environment in such a way that using a more physiologic and sensible insulin regimen is the easiest thing to do? It starts with local physician leadership. On noncritical care wards, hospitalists and endocrinologists are the natural candidates to own the issue of inpatient diabetes care. These physician leaders need to garner appropriate institutional support, form a multidisciplinary steering committee or team, and formulate interventions.
Implementing a standardized subcutaneous insulin order set promoting the use of scheduled insulin therapy is a key intervention in the inpatient management of diabetes. These order sets should encourage basal replacement insulin therapy (ie, NPH, glargine, detemir) and scheduled nutritional/prandial short‐/rapid‐acting insulin (ie, regular, aspart, lispro, glulisine). The order set should also state the glycemic target, eliminate improper abbreviations and notations, incorporate a hypoglycemia protocol, and provide a range of default correction insulin dosage scales appropriate for varied levels of insulin sensitivity. Examples of such order sets are widely available.13, 32 This simple intervention can result in a tripling of insulin regimens including scheduled basal insulin, substantial subsequent improvement in glycemic control on the hospital floor, and significant reduction in hypoglycemic event rates.
The standardized order set can be much more effective when it is complemented by institution‐specific algorithms, protocols, and policies that support their effective use. These tools must not merely exist; they must be widely disseminated and used and, if possible, embedded in the order set. They should outline the calculation of insulin dosages, define recommended insulin regimens for patients with different forms of nutritional intake, guide transitions from insulin infusion to subcutaneous regimens, and enhance discharge planning and education.
The SHM, AACE, ADA, and other organizations are partnering to create a compendium of tested tools and strategies to assist hospitalists and their hospitals in these and other interventions and to assist them in devising reliable and practical metrics to gauge the impact of their efforts. These tools and a guidebook to walk teams through the improvement process step by step should be available on the SHM (
Look around and take stock. Does your hospital have standardized subcutaneous insulin order sets, algorithms and protocols supporting the order set, a multidisciplinary team tasked with improving insulin safety and glycemic control, and metrics to gauge whether your efforts are making a difference? Expecting better results without these essential elements is not only foolhardy but fits Einstein's definition of insanity: doing the same thing over and over again and expecting different results. Let's stop this sliding‐scale insulin insanity now.
Insanity: doing the same thing over and over again and expecting different results.Albert Einstein
Diabetes is one of the most common diagnoses in hospitalized patients.1 A third of all persons admitted to urban general hospitals have glucose levels qualifying them for the diagnosis of diabetes, and a third of these hyperglycemic patients have not previously been diagnosed with diabetes.2 The impact of hyperglycemia on the mortality rate of hospitalized patients has been increasingly appreciated. Extensive evidence from observational studies indicates that hyperglycemia in patients with or without a history of diabetes is a marker of a poor clinical outcome.38 In addition, the results of prospective randomized trials in patients with critical illness or those undergoing coronary bypass surgery suggest that aggressive glycemic control improves clinical outcomes including reductions in: a) short‐ and long‐term mortality, b) multiorgan failure and systemic infection, and c) length of hospitalization.7, 911
The importance of glycemic control is not limited to patients in critical care areas but may also apply to patients admitted to general surgical and medical wards. The development of hyperglycemia in such patients with or without a history of diabetes has been associated with prolonged hospital stay, infection, disability after hospital discharge, and death.12, 13 In general‐surgical patients, serum glucose > 220 mg/dL on postoperative day 1 has been shown to be a sensitive, albeit nonspecific, predictor of the development of serious postoperative hospital‐acquired infection.14 A retrospective review of 1886 admissions to a community hospital in Atlanta, Georgia, found an 18‐fold increase in mortality in hyperglycemic patients without a history of diabetes and a 2.5‐fold increase in mortality in patients with known diabetes compared with controls.2 A meta‐analysis of 26 studies identified an association of admission glucose > 110 mg/dL with the increased mortality of patients hospitalized for acute stroke.15 More recently, hyperglycemia on admission was also shown to be independently associated with adverse outcomes in patients with community acquired pneumonia.16, 17
In view of the increasing evidence supporting better glycemic control in the hospital, the American Association of Clinical Endocrinologists (AACE) in late 2003 convened a consensus conference on the inpatient with diabetes, cosponsored or supported by other prominent professional organizations, including the Society of Hospital Medicine (SHM). An expert panel agreed on and published glycemic targets and recommendations for inpatient management of hyperglycemia.18 The American Diabetes Association (ADA) subsequently published an excellent technical review evaluating the evidence and outlining treatment, monitoring, and educational strategies13 for the hospitalized patient, and these recommendations were largely incorporated into the 2005 ADA Clinical Practice Guidelines for Hospitalized Patients.19 The recommended glycemic targets for hospitalized patients in the intensive care unit are between 80 and 110 mg/dL. In noncritical care settings a preprandial glucose of 90130 mg/dL (midpoint 110 mg/dL) and a postprandial or random glucose of less than 180 mg/dL are the recommended glycemic targets. Physiologic and safe insulin regimen strategies for virtually all patient situations were succinctly presented. Although there have been modest (and occasionally dramatic) improvements in glycemic control in several institutions, the reviews and guidelines have not yet resulted in widespread change in clinical practice on the inpatient wards.
Two retrospective studies from prestigious medical institutions reported in this issue of the Journal of Hospital Medicine dramatically illustrate that glycemic control and insulin‐ordering practices in general medicine services continue to be deficient and underscore the contribution of physician inertia in the management of hyperglycemia in noncritically ill patients.20, 21 From their findings and experiences in our institutions, you should expect the following at your institution unless you have embarked on an organized program to improve noncritical care inpatient glycemic control.
-
Around one third of your patients with hyperglycemia have a mean glucose of more than 200 mg/dL during their hospital stay.
-
Despite these out‐of‐control values, 60% of your inpatients will remain on a static regimen of sliding‐scale insulin over the duration of their stay. Unfortunately, this degree of hyperglycemia is not protective for hypoglycemic episodes.
-
Around 10% of your monitored ward inpatients will have at least one hypoglycemic episode during their stay. Many of these episodes will be precipitated by poor coordination of nutrition and insulin administration and nonsensical insulin regimens that lead to insulin stacking.
-
Discharge summaries and plans will include mention and follow‐up of hyperglycemia only a minority of the time.
-
Your nursing and medical staffs are unevenly educated about the proper use of insulin, even though insulin errors are very common, and insulin is one of the top 3 drugs involved in adverse drug events in your institution.
-
Transitions in care will lead to an inconsistent approach to glycemic control, leaving some of your patients confused and others just plain angry.
The ubiquitous use of the insulin sliding scale as the single routine response for controlling hyperglycemia in inpatients has been discredited for a long time.2224 Strong terms have been used the condemnation of this method: mindless medicine, paralysis of thought, and action without benefit, for example.25, 26 Yet this remains the most popular default regimen in most institutions across the country. Clinical inertia is defined as not initiating or intensifying therapy when doing so is indicated,27, 28 and that term certainly applies to glycemic control practices and the continued heavy use of sliding‐scale insulin across the nation.
Why is clinical inertia so strong in this area? Why have well‐done practice guidelines and reviews not eradicated the use of sliding‐scale insulin? First, hyperglycemia is rarely the focus of care during the hospital stay, as the overwhelming majority of hospitalizations of patients with hyperglycemia occur for comorbid conditions.2, 29 Second, fear of hypoglycemia constitutes a major barrier to efforts to improve glycemic control in hospitalized patients, especially in those with poor caloric intake.13, 30 Third, practitioners initiate sliding‐scale insulin regimens, even though this has been a thoroughly discredited approach, simply because it is the easiest thing to do in their current practice environment.31
How do we break this inertia and redesign our practice environment in such a way that using a more physiologic and sensible insulin regimen is the easiest thing to do? It starts with local physician leadership. On noncritical care wards, hospitalists and endocrinologists are the natural candidates to own the issue of inpatient diabetes care. These physician leaders need to garner appropriate institutional support, form a multidisciplinary steering committee or team, and formulate interventions.
Implementing a standardized subcutaneous insulin order set promoting the use of scheduled insulin therapy is a key intervention in the inpatient management of diabetes. These order sets should encourage basal replacement insulin therapy (ie, NPH, glargine, detemir) and scheduled nutritional/prandial short‐/rapid‐acting insulin (ie, regular, aspart, lispro, glulisine). The order set should also state the glycemic target, eliminate improper abbreviations and notations, incorporate a hypoglycemia protocol, and provide a range of default correction insulin dosage scales appropriate for varied levels of insulin sensitivity. Examples of such order sets are widely available.13, 32 This simple intervention can result in a tripling of insulin regimens including scheduled basal insulin, substantial subsequent improvement in glycemic control on the hospital floor, and significant reduction in hypoglycemic event rates.
The standardized order set can be much more effective when it is complemented by institution‐specific algorithms, protocols, and policies that support their effective use. These tools must not merely exist; they must be widely disseminated and used and, if possible, embedded in the order set. They should outline the calculation of insulin dosages, define recommended insulin regimens for patients with different forms of nutritional intake, guide transitions from insulin infusion to subcutaneous regimens, and enhance discharge planning and education.
The SHM, AACE, ADA, and other organizations are partnering to create a compendium of tested tools and strategies to assist hospitalists and their hospitals in these and other interventions and to assist them in devising reliable and practical metrics to gauge the impact of their efforts. These tools and a guidebook to walk teams through the improvement process step by step should be available on the SHM (
Look around and take stock. Does your hospital have standardized subcutaneous insulin order sets, algorithms and protocols supporting the order set, a multidisciplinary team tasked with improving insulin safety and glycemic control, and metrics to gauge whether your efforts are making a difference? Expecting better results without these essential elements is not only foolhardy but fits Einstein's definition of insanity: doing the same thing over and over again and expecting different results. Let's stop this sliding‐scale insulin insanity now.
- ,,, et al.Diabetes trends in the U.S.: 1990–1998.Diabetes Care.2000;23:1278–1283.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,Outcomes and perioperative hyperglycemia in patients with or without diabetes mellitus undergoing coronary artery bypass grafting.Ann Thorac Surg.2003;75:1392–1399.
- ,,,.Glucose control and mortality in critically ill patients.JAMA.2003;290:2041–2047.
- ,,.Admission plasma glucose. Independent risk factor for long‐term prognosis after myocardial infarction even in nondiabetic patients.Diabetes Care.1999;22:1827–1831.
- ,.ICU care for patients with diabetes.Curr Opin Endocrinol.2004;11:75–81.
- ,,, et al.Intensive insulin therapy in the critically ill patients.N Engl J Med.2001;345:1359–1367.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461.
- .Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients.Mayo Clin Proc.2003;78:1471–1478.
- ,,, et al.Randomized trial of insulin‐glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): effects on mortality at 1 year.J Am Coll Cardiol.1995;26(1):57–65.
- ,,, et al.Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting.J Thorac Cardiovasc Surg.2003;125:1007–1021.
- ,,,.Hyperglycemia is associated with adverse outcomes in patients receiving total parenteral nutrition.Diabetes Care.2005;28:2367–2371.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–597.
- ,,, et al.Early postoperative glucose control predicts nosocomial infection rate in diabetic patients.JPEN J Parenter Enteral Nutr.1998;22(2):77–81.
- ,,,,.Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview.Stroke.2001;32:2426–2432.
- ,,,,.Etiology and outcome of community‐acquired pneumonia in patients with diabetes mellitus.Chest.2005;128:3233–3239.
- ,,,,,.The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community‐acquired pneumonia.Diabetes Care.2005;28:810–815.
- ,,, et al.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10(Suppl 2):4–9.
- Standards of medical care in diabetes—2006.Diabetes Care.2006;29(Suppl 1):S4–S42.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1:145–150.
- ,,, et al.Diabetes care in the hospital: Is there clinical inertia?J Hosp Med.2006;1:151–160.
- ,.Are sliding‐scale insulin regimens a recipe for diabetic instability?Lancet.1997;349:1555.
- ,,,.Eliminating inpatient sliding‐scale insulin: a reeducation project with medical house staff.Diabetes Care.2005;28:1008–1011.
- ,,,,.Efficacy of sliding‐scale insulin therapy: a comparison with prospective regimens.Fam Pract Res J.1994;14:313–322.
- .Action without benefit. The sliding scale of insulin use.Arch Intern Med.1997;157:489.
- ,,, et al.Clinical inertia.Ann Intern Med.2001;135:825–834.
- ,,,,.Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians?Diabetes Care.2005;28:600–606.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,,.Drug‐induced hypoglycemic coma in 102 diabetic patients.Arch Intern Med.1999;159:281–284.
- ,.Hospital management of diabetes.Endocrinol Metab Clin North Am.2000;29:745–770.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10(Suppl 2):89–99.
- ,,, et al.Diabetes trends in the U.S.: 1990–1998.Diabetes Care.2000;23:1278–1283.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,Outcomes and perioperative hyperglycemia in patients with or without diabetes mellitus undergoing coronary artery bypass grafting.Ann Thorac Surg.2003;75:1392–1399.
- ,,,.Glucose control and mortality in critically ill patients.JAMA.2003;290:2041–2047.
- ,,.Admission plasma glucose. Independent risk factor for long‐term prognosis after myocardial infarction even in nondiabetic patients.Diabetes Care.1999;22:1827–1831.
- ,.ICU care for patients with diabetes.Curr Opin Endocrinol.2004;11:75–81.
- ,,, et al.Intensive insulin therapy in the critically ill patients.N Engl J Med.2001;345:1359–1367.
- ,,, et al.Intensive insulin therapy in the medical ICU.N Engl J Med.2006;354:449–461.
- .Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients.Mayo Clin Proc.2003;78:1471–1478.
- ,,, et al.Randomized trial of insulin‐glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): effects on mortality at 1 year.J Am Coll Cardiol.1995;26(1):57–65.
- ,,, et al.Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting.J Thorac Cardiovasc Surg.2003;125:1007–1021.
- ,,,.Hyperglycemia is associated with adverse outcomes in patients receiving total parenteral nutrition.Diabetes Care.2005;28:2367–2371.
- ,,, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–597.
- ,,, et al.Early postoperative glucose control predicts nosocomial infection rate in diabetic patients.JPEN J Parenter Enteral Nutr.1998;22(2):77–81.
- ,,,,.Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview.Stroke.2001;32:2426–2432.
- ,,,,.Etiology and outcome of community‐acquired pneumonia in patients with diabetes mellitus.Chest.2005;128:3233–3239.
- ,,,,,.The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community‐acquired pneumonia.Diabetes Care.2005;28:810–815.
- ,,, et al.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10(Suppl 2):4–9.
- Standards of medical care in diabetes—2006.Diabetes Care.2006;29(Suppl 1):S4–S42.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- ,,,,.Inpatient management of diabetes and hyperglycemia among general medicine patients at a large teaching hospital.J Hosp Med.2006;1:145–150.
- ,,, et al.Diabetes care in the hospital: Is there clinical inertia?J Hosp Med.2006;1:151–160.
- ,.Are sliding‐scale insulin regimens a recipe for diabetic instability?Lancet.1997;349:1555.
- ,,,.Eliminating inpatient sliding‐scale insulin: a reeducation project with medical house staff.Diabetes Care.2005;28:1008–1011.
- ,,,,.Efficacy of sliding‐scale insulin therapy: a comparison with prospective regimens.Fam Pract Res J.1994;14:313–322.
- .Action without benefit. The sliding scale of insulin use.Arch Intern Med.1997;157:489.
- ,,, et al.Clinical inertia.Ann Intern Med.2001;135:825–834.
- ,,,,.Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians?Diabetes Care.2005;28:600–606.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,,.Drug‐induced hypoglycemic coma in 102 diabetic patients.Arch Intern Med.1999;159:281–284.
- ,.Hospital management of diabetes.Endocrinol Metab Clin North Am.2000;29:745–770.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10(Suppl 2):89–99.
Cost Utility of Enoxaparin for DVT Prophylaxis
Several groups of medical patients at risk for venous thromboembolism (VTE) while hospitalized have been identified. These include patients with certain acute medical illnesses such as acute myocardial infarction, stroke, or chronic obstructive pulmonary disease and those with acute medical illness combined with additional risk factors including advanced age, cancer, obesity, or prior VTE.13
Heparin‐induced thrombocytopenia (HIT) and heparin‐induced thrombocytopenia with thrombosis (HITT), a spectrum of disease also known as type 2 HIT, are potentially devastating hematologic consequences of VTE prophylaxis that result from heparin binding to platelet factor IV, leading to IgG antibodymediated platelet activation.46 These complications manifest along a spectrum from thrombocytopenia alone (HIT) to more severe sequelae that include death, amputation, venous and arterial thrombosis. Unfractionated heparin (UFH) has traditionally been used for VTE prophylaxis in these populations at risk. More recently, evidence has indicated that enoxaparin, a low‐molecular‐weight heparin, is at least as effective for VTE prophylaxis1, 7 and carries a significantly lower risk for the development of the complications of HIT and HITT. Despite the superior side‐effect profile of enoxaparin, many institutions encourage the use of heparin for DVT prophylaxis because of its lower price. However, when the costs of treating these complications are considered, using unfractionated heparin may actually be more costly.
Two studies of the cost effectiveness of heparin compared with enoxaparin when used for VTE prophylaxis in medical inpatients have recently been published.8, 9 However, one of these studies focused only on pharmacy‐related costs and did not consider patient‐related outcomes, and the other was published by a for‐profit research company. Studies of treatment with enoxaparin versus UFH in other medical settings, including non‐Q‐wave myocardial infarction10 and treatment of acute deep‐vein thrombosis,11 suggest that enoxaparin is more cost effective. Studies of prophylaxis of surgical patients have been contradictory. Data suggest that in orthopedic patients the use of enoxaparin is more cost effective for both short‐ and long‐term VTE prophylaxis,1214 but low‐dose heparin appeared more cost effective for patients undergoing colorectal surgery, in large part because of an assumption of a smaller risk of bleeding.15
The purpose of this analysis was to determine the cost utility of heparin compared with enoxaparin for VTE prophylaxis for medical inpatients at risk. In such an analysis, it is important to consider the possibly different meanings that entities may attach to cost utility and effectiveness according to their different roles in the health care system. Individual institutions pay inpatient medication costs, but they often do not directly bear the costs of complications of treatment and may actually receive reimbursements for them. In contrast, payers must provide that reimbursement. For this reason, costs were analyzed from 2 perspectives, that of a payer (Medicare) and that of a health care system or institution.
METHODS
This protocol was declared exempt by the Institutional Review Board at the University of Texas Health Science Center at San Antonio.
Estimates of Effectiveness
Estimates of effectiveness include those related both to efficacy in preventing VTE, and those related to adverse drug events. They are summarized in Table 1.
| Base Case | Range for Sensitivity Analysis | |
|---|---|---|
| Rate of development of HIT on heparin | 2.70% | 0.80%4.90% |
| Rate of development of HIT on enoxaparin | 0.30% | 0.09%0.54% |
| Rate of progression to HITT | 40% | 25%50% |
| Mortality rate despite treatment, HITT | 8% | 0%20% |
| Assumed extension in length of stayHIT | 1 day | 05 days |
| Assumed extension in length of stayHITT | 7 days | 510 days |
| Life expectancy (2001) | 77.2 years | |
| Average age of medical inpatient | 71.9 years | |
| QALY adjustment for: | ||
| CHFsevere | 0.6 | |
| COPD | 0.4 | |
| Cancer | 0.9 |
Assumptions about the efficacy of heparin and enoxaparin when used for VTE prophylaxis were based on the following published data. The rate of development of VTE reported in the Medenox trial, 5.5%,1 is consistent with rates reported for patients receiving heparin (2%13%).1618 More recently, the PRINCE study demonstrated that enoxaparin was at least as effective as heparin in patients with severe heart failure or respiratory disease and was more effective in the former group of patients.7 Finally, data from patients with acute stroke indicated that low‐molecular‐weight heparins are at least as effective as heparin for this indication.19, 20 Equal efficacy was assumed for this analysis for several reasons, primarily to avoid the creation or amplification of errors through the introduction of more assumptions about the proportion of patients with specific diagnoses and about the magnitude and range of differences in efficacy. Only one study has examined the relative efficacy in patients with congestive heart failure, and not all the results of studies in stroke patients pointed to enoxaparin having improved efficacy. Therefore, making valid assumptions about the magnitude of the difference between the drugs on the basis of the available evidence may not be possible.
It was also assumed that aside from HIT and HITT, the 2 drugs had the same rates of adverse events, including bleeding complications, in this patient population.1
A Medline search combining MeSH terms thrombocytopenia and heparin was done to find the appropriate incidence of HIT and HITT. The resulting group was further limited in 3 separate searches using the terms prophylaxis (keyword), incidence (MeSH term), and thromboembolism or venous thrombosis (MeSH terms). Heparin‐induced thrombocytopenia was searched for as a keyword and combined with the MeSH term prophylaxis in a separate search. Finally, reference lists were searched to find additional articles.
The range of reported rates of development of HIT among patients receiving heparin was wide. In part, this is related to the different subgroups of patients studied and to the inclusion of patients receiving both prophylaxis and treatment doses of heparin. The one study that looked specifically at medical inpatients included patients receiving treatment‐dose heparin. The rate of HIT in this study was 0.8%.21 A study of both prophylactic and therapeutic use in neurologic patients reported a rate of 2.5%.22 Studies specific to VTE prophylaxis in surgical patients reported a range of 0.8%4.9%.2326 Based on these results, a rate of 2.7%, the median of the reported ranges, was used for the base case, and 0.8% and 4.9% were used for sensitivity analysis.
The reported rates of progression to thrombosis for patients with HIT ranged from 25 to more than 50%.21, 27, 28 A median rate of 40% was used for the base case, and 25% and 50% were used for sensitivity analysis. It was assumed that 0.3% of patients receiving enoxaparin developed HIT, 1/9 as frequently as those receiving heparin,24, 25, 29 but that the same percentage of those with HIT would develop thrombosis.
Mortality secondary to thrombosis in patients with untreated HIT has been reported to be 4%5%.30, 31 All‐cause mortality in untreated patients with HITT has been reported to be as high as >20%,31, 32 but in treated patients it has been reported as 8%.30 A mortality rate of 8% for HITT despite treatment was assumed with a range in the sensitivity analysis from 0% to 20%.
Life expectancy data were obtained from the National Center for Health Statistics, and the average age of medical inpatients potentially eligible for DVT prophylaxis was calculated from this data. The catalog of preference scores was obtained from the Cost Effectiveness Analysis Registry at the Harvard Center for Risk Analysis.33 These preference scores adjust the quality of a year of life for chronic diseases and provide a more accurate assessment of quality‐adjusted life years.
It was assumed that patients with HIT alone would be treated with argatroban, consistent with evidence that this is superior to withdrawal of heparin alone in patients with HIT.28 Using other agents such as lepirudin for the treatment of HIT was not considered in this analysis because there is no data on which to base their efficacy in patients with HIT.
For treatment of patients with HITT, again only the use of argatroban was considered. Though other agents are as efficacious in treating HITT, they are also more expensive. Therefore, using argatroban allowed for a more conservative estimate.
Platelet counts typically fall after 5 days of heparin administration in patients developing HIT34 and typically recover within 35 days of initiation of treatment.4, 29 In the past, patients may not have been kept in the hospital for resolution of their platelet count. However, with evidence that HIT should be aggressively treated, patients with HIT will likely have a longer length of stay. A study of treatment of HIT reported a mean time on argatroban of 57 days.23 This is greater than the average length of stay for medical diagnosis, which is 45 days.35 Therefore, an additional length of stay of 1 day was assumed for patients given a diagnosis of HIT, with a range of 05 days used for the sensitivity analysis. An additional length of stay totaling 7 days was assumed for those with thrombosis, based on patients requiring 7 days of argatroban therapy for treatment of HITT in a recent study.28
Estimates of Costs
Costs were analyzed from institutional and Medicare perspectives. Only direct medical expenditures related to hospitalization were considered; indirect patient costs resulting from the sequelae of HITT, while potentially severe, were not included. An incremental analysis was performed to express the increase in resources used when a person develops HIT/T, with the final result expressed as a daily cost of each medication. Cost assumptions are summarized in Table 2.
| Medicarerelated | Institutionrelated | |||
|---|---|---|---|---|
| Base case | Range | Base case | Range | |
| Additional reimbursement for HIT (if considered a complicating condition) | $ 765.06 | $ 0.00 | $ 765.06 | $0.00 |
| Additional reimbursement for HITT (if coagulation disorder DRG used) | $1135.56 | $ 0.00 | $1135.56 | $0.00 |
| Primary provider visit (99232) | $ 54.89 | $33.00$ 78.04 | n/a | |
| Consultant initial visit (99254) | $ 140.39 | $35.84$193.03 | n/a | |
| Consultant followup (99263) | $ 44.80 | $22.40$ 66.09 | n/a | |
| Medication (per day) | ||||
| Heparin | n/a | $ 4.00 | ||
| Enoxaparin | n/a | $ 84.00 | ||
| Argatroban | n/a | $ 150.00 | ||
| Coumadin | n/a | $ 0.50 | ||
| Laboratory tests (per test) | ||||
| Complete blood count | n/a | $ 2.14 | ||
| Prothrombin time/partial thromboplastin time | n/a | $ 9.85 | ||
| Opportunity cost per additional day of hospitalization (if hospital at capacity) | n/a | $1096.72 | ||
Medicare Related
Diagnosis‐related group (DRG) reimbursement to institutions and physicians were considered the only payer‐related costs. These were based on the 2005 Medicare reimbursement.36 Costs related to laboratory, medication, or other diagnostic studies were assumed to be covered by the DRG payment and not to be billed separately.
The average Medicare reimbursement to institutions for all diagnosis‐related groups is the national standard number, or $4971.81. To determine the additional potential charges resulting from the development of HIT, it was considered a complicating condition. The average adjustment factor for complicating conditions of medical diagnoses is .1539, leading to an increase in charges of $765.06. No additional adjustments for geographic location were made. Sensitivity analysis was performed with no additional reimbursement for HIT as a complicating condition.
To quantify additional charges related to caring for patients with HITT, we used the amount of additional charges for the coagulation disorder DRG (#397) above those of the average reimbursement. This amount is $1135.56, the difference between the higher charge of $6107.37 for this DRG, and the national standard number. Sensitivity analysis with no additional charges was performed.
Physician charges used were based on the 2004 Medicare reimbursement.36 It was assumed that each patient with HIT would have a daily visit of moderate complexity (CPT 99232), which carries a reimbursement rate of $54.89. Patients with thrombotic complications were assumed to also have a hematology consult consisting of one initial visit and one followup, both of midlevel complexity (CPTs 99253 and 99262). The reimbursement rates for these visits are $97.45 and $44.80. Sensitivity analysis using both lower‐ and higher‐level visits was performed (Table 2).
Based on the above DRG and physician reimbursements, the total cost to Medicare of treating a patient with HIT is $820.05 and of treating a patient with HITT is $1749.98. For the situation in which a patient with HIT also developed HITT, only the cost of reimbursement for HITT was modeled.
Hospital‐Related
To calculate the benefit or cost to an institution, 2 scenarios were modeled. In the first scenario, only the DRG‐related revenues collected and the costs of caring for patients with HIT/T were considered. The revenues used are described above. The cost of medications at a multi‐institutional health care system (MIHCS) was obtained from the pharmacy and used in this analysis. This system is composed of a network of urban and suburban acute care facilities with academic affiliations with 2 universities. Costs are representative of the entire system. The cost of heparin is $2.00 per unit dose; daily cost for b.i.d. prophylaxis is $4.00. The cost of one daily dose of enoxaparin is $84.00. One unit (50 mg) of argatroban costs $50.00. For a 70‐kg man at a standard dosing rate of 2 g/kg per minute, the daily cost would be approximately $150.00. The daily cost of coumadin was estimated at $0.50 regardless of the dose. The cost of laboratory tests within the MIHCS is $2.14 per complete blood count and $9.85 for each PT/PTT.
Other costs, such as those related to the additional time spent by nursing and pharmacy staff in the mixing and administration of argatroban or caring for patients with HIT and HITT were not included in this analysis, as it was believed that they would have no impact on actual staffing levels and would not lead to a tangible or easily quantifiable increase in expenditures.
In the second scenario, the potential loss of income from additional days of hospitalization for HIT and HITT was considered. An institution could potentially lose money if a patient with HIT or HITT stayed longer than the number of days that is economically attractive given the DRG reimbursement. In this scenario, a longer length of stay of a patient with HIT or HITT could lead to the bed not being used by other patients for whom the hospital could be collecting revenue. This would only be applicable with high occupancy rates. The average revenue per day that a hospital could receive for a patient was calculated by dividing the average reimbursement, $4971.81, by the average length of stay for medical inpatients, 4.5 days. This amount is $1096.72. The amount of additional reimbursement for a complicating condition, $754.06, then covers 0.7 days of additional hospitalization. As described above, the average additional reimbursement for using the coagulation disorder DRG for patients with HITT, instead of using the DRG for which they were otherwise admitted, was $1135.56. This would cover an additional 1.04 days of hospitalization. If the hospital stay of patients with HIT/T were to be longer, an amount computed as $1096.72 multiplied by the number of additional days of hospitalization was considered a loss of income borne by the hospital.
Sensitivity Analysis
Sensitivity analysis was performed to ensure the validity of results over a range of values and to assess the effect of medication prices on our findings. The analysis used these parameters, both alone and in combination: rate of development of HIT, rate of development on enoxaparin compared with on heparin, percentage of those with HIT who developed thrombosis, mortality related to HITT, length of stay of patients with both HIT and HITT, reimbursement rates, and costs of medication.
RESULTS
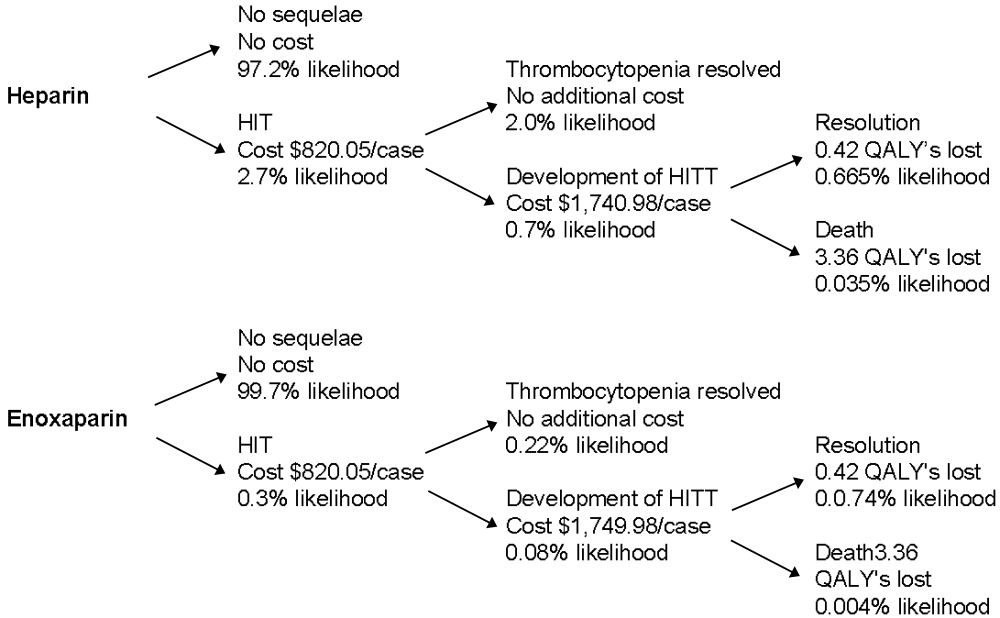
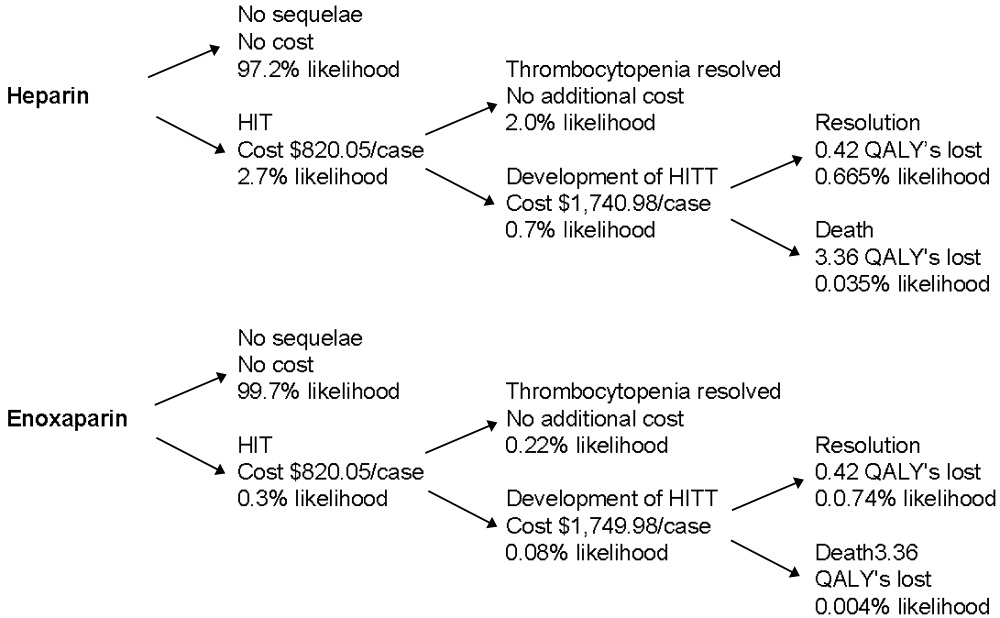
The decision tree used for the base‐case analysis is shown in Figure 1. The gain in quality‐adjusted life years (QALYs) for medical patients who used enoxaparin rather than heparin for VTE prophylaxis was 0.00629 (approximately 55 hours). This was based on the decrease in HITT‐related premature death resulting from the use of enoxaparin. From a payer perspective, the daily cost of enoxaparin is $3.58, compared with $32.18 for heparin. The difference is a savings of $28.61, leading to a savings/QALY of $4550.17. Therefore, the use of enoxaparin is both more effective and less costly.
Sensitivity analysis showed that from a payer perspective, enoxaparin remained both less costly and more effective in all cases. The factors that had the largest impact on cost/QALY were incidence of HIT and rate of thrombosis among those with HIT. Decreasing length of stay to 0 for patients with HIT, decreasing reimbursement to $0 for both HIT and HITT, and billing at a high or low level did not change the general finding. Decreasing the cost of enoxaparin or heparin also did not affect these findings. The results of the sensitivity analysis are summarized in Table 3.
| Enoxaparin (cost/day) | Heparin (cost/day) | QALYs saved | Savings/QALY | |
|---|---|---|---|---|
| Base case | $3.58 | $32.18 | 0.00629 | $4550.17 |
| Sensitivity analysis | ||||
| Incidence of HIT | $1.06$6.49 | $ 9.54$58.11 | 0.001860.01141 | $4550.17 |
| Progression of HIT to HITT | $3.12$3.77 | $28.05$33.95 | 0.003930.00786 | $6344.53$3840.30 |
| Level of physician visit billed | $3.23$3.81 | $28.45$34.27 | 0.00629 | $4021.85$4844.35 |
| HIT length of stay | $3.48$3.64 | $31.30$32.78 | 0.00629 | $4424.46$4633.98 |
| No reimbursement for HIT | $2.13 | $19.20 | 0.00629 | $2713.90 |
| No reimbursement for HITT | $0.77 | $ 6.93 | 0.00629 | $ 980.05 |
From an institutional perspective, the effect of considering the costs of HIT and HITT did not necessarily make enoxaparin a more attractive choice. When potential reimbursement for drug‐related complications was considered, an institution actually make $7.27/day by choosing heparin, whereas the cost of enoxaparin decreases only minimally from $84.00 to $82.75/day (Table 4). Factoring opportunity costs into the analysis showed that an institution does not make money by using heparin, but heparin still costs less on a daily basis. This finding changes only at rates of HIT over 4%.
| Heparin | Enoxaparin | |||
|---|---|---|---|---|
| Drug cost alone | Drug cost + cost of increased LOS | Drug cost alone | Drug cost + cost of increased LOS | |
| Base case | ($7.27) | $72.33 | $82.75 | $91.59 |
| Sensitivity Analysis | ||||
| Incidence of HIT | $ 0.66($16.45) | $24.25$128.01 | $83.63$81.75 | $86.25$ 97.18 |
| Length of stay HIT | ($ 7.27) | $42.72$190.78 | $82.75 | $88.30$104.75 |
| Length of stay HITT | ($ 7.27) | $48.64$101.57 | $82.75 | $88.96$ 95.54 |
| Drug costs below which enoxaparin is more attractive | $ 0.50$ 4.00 | $ 0.50$ 4.00 | $33.00$37.00 | < $1.00 |
Sensitivity analyses of institutional costs are summarized in Table 4. These analyses demonstrated that potential increases in length of stay for patients with HIT or HITT could make heparin less attractive when opportunity costs to the hospital are considered. If the additional length of stay for patients with HIT increased to greater than 1.75 days or the additional length of stay for those with HITT increased to more than 9 days, heparin becomes a less attractive choice. Loss of reimbursement for HIT or HITT alone does not make enoxaparin less costly than heparin.
Sensitivity analysis also demonstrated that variation in the price of enoxaparin could potentially make heparin less attractive. If the price of heparin were held constant at $4.00/day, enoxaparin would become less costly at a price of $37.00. If the price of heparin were to decrease to as low as $0.50/day, the price at which enoxaparin would be more attractive decreased to $33.00. These prices are only applicable when the opportunity costs of having occupied beds are consideredthat is, only when an institution is operating at full capacity. When this is not the case, enoxaparin would have to cost less than $1.00 to be more financially attractive than heparin. In practical terms, unless a hospital is at full capacity and needs hospital beds for other patients, the cost of enoxaparin would have to be less than $1 for an institution to choose it instead of heparin.
DISCUSSION
This study demonstrates that from a payer perspective, there is greater cost utility in the use of enoxaparin in place of heparin for the prevention of venous thromboembolism in at‐risk medical patients. This benefit is based on a single advantage of enoxaparin: its decreased tendency to cause HIT/T. Despite the simplicity of this assumption, it is well supported by published data. Sensitivity analyses supported the finding that enoxaparin was a superior choice in all scenarios modeled. This payer data can be extrapolated to a societal level because the costs used were based on Medicare reimbursements.
The benefit of using enoxaparin when expressed in an absolute number of quality‐adjusted life years was small, approximately 55 hours. This reflects that although the effects of HIT and HITT are potentially devastating, they occur infrequently. However, our calculation was conservative in several respects. We calculated the highest possible average age for a medical inpatient based on the available statistics. This was done to ensure that we were not overestimating the number of QALYs saved by preventing death secondary to HITT. We also considered only 2 outcomes of HITT: death and recovery. This underestimates the significant potential thrombotic complications, notably amputation or other loss of function, which would increase the number of QALYs saved by using enoxaparin. The inclusion of these complications would only strengthen this finding. Finally, we assumed equal efficacy for heparin and enoxaparin. The inclusion of superior efficacy of enoxaparin in subpopulations of medical inpatients would again only strengthen this finding.
Apart from the price of the medication, the incidence of HIT had the largest impact on costs and QALYs saved in the sensitivity analysis. Studies specific to VTE prophylaxis in medical inpatients could better define the incidence of HIT/T in this population, but this would not change our overall finding.
From an institutional perspective, the choice of heparin or enoxaparin is more complicated. In most but not all scenarios, the use of heparin appears to be more financially attractive. The prices of enoxaparin and heparin, the additional length of stay required to care for patients with HIT and HITT, and the percentage of total beds occupied all affect this decision. Several pieces of cost data, specifically those related to medication and laboratory testing, were specific to an MIHCS health care system, the type considered in the analysis and could potentially limit the applicability of this study to other institutions. However, the sensitivity analysis demonstrated that the cost of enoxaparin would have to be at least 60% lower, below $33/day, before affecting our conclusion, and then only if an institution were at full capacity. Thus, we expect that our results are generally applicable.
The potential limitations of this study are related to the assumptions required. However, our efficacy assumptions were conservatively based on published data. It is possible that a decrease in the rate of thrombosis if all cases of HIT were treated with argatroban could affect our findings. However, in the study by Lewis et al., the complication rate for those with HIT in the treatment group was 28% (versus 38.8% in the untreated group), consistent with rates used in our sensitivity analysis. DRG and physician reimbursements are based on published Medicare data. The greatest variation is likely to be in drug cost, as different institutions may negotiate lower prices. From a payer perspective, drug costs do not affect the conclusions; from an institutional perspective, drug cost may make the choice a complicated one. One factor not included in our analysis that may affect this decision is the possible impact of legal action on the medications institutions choose for VTE prophylaxis. Because the potential consequences of HITT can be so devastating, an institution could have difficulty defending the choice of heparin when an equally effective alternative with fewer adverse events was available. A settlement of $1 million could potentially pay for prophylaxis with enoxaparin for at least 2500 patients.
This analysis has highlighted one of the unfortunate paradoxes caused by the different, potentially competing incentives in our health care system. Payers and institutions often face different financial incentives. From a hospital's perspective, it may cost less to use an intervention that can potentially cause a greater number of complications and higher payer costs. We believe that for VTE prophylaxis for medical inpatients, improved patient outcomes coupled with decreased payer/societal costs argue strongly for the use of enoxaparin over unfractionated heparin and outweigh any institutional benefits.
- ,,, et al.A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients.N Eng J Med.1999;322:793–800.
- .Recommendations for prophylaxis of venous thromboembolism: International consensus and the American College of Chest Physicians Fifth Consensus Conference on Antithrombotic therapy.Curr Opin Pulm Med.2000;6:314–320.
- ,,, et al.Risk factors for venous thromboembolism in hospitalized patients with acute medical illness: analysis of the MEDENOX study.Arch Intern Med.2004;164:963–968.
- .Heparin–induced thrombocytopenia: pathogenesis and management.Br J Haematology.1003;121:535–555.
- .Heparin–induced thrombocytopenia diagnosis and management.Circulation.2004;110:e454–e458.
- .New approaches to the diagnosis of heparin–induced thrombocytopenia.Chest.2005;27(2 suppl):35S–45S.
- ,,, et al.Randomized comparison of enoxaparin with unfractionated heparin for the prevention of venous thromboembolism in medical patients with heart failure or severe respiratory disease.Am Heart J.2003;145:614–621.
- ,.Cost–effectiveness analysis of deep vein thrombosis prophylaxis in internal medicine patients.Thrombosis Res.1999;94:65–68.
- ,.,.Cost effectiveness of thromboprophylaxis with low–molecular–weight heparin versus unfractionated heparin in acutely ill medical inpatients.Am J Manag Care.2004;10:632–642.
- ,,, et al.Economic assessment of low–molecular–weight heparin (enoxaparin) versus unfractionated heparin in acute coronary syndrome patients: results from the ESSENCE Randomized Trial.Circulation.1998;97:1702–1707.
- ,, et al.Management of acute proximal deep vein thrombosis: pharmacoeconomic evaluation of outpatient treatment with enoxaparin vs inpatient treatment with unfractionated heparin.Chest.2002;122(1);108–114.
- ,,, et al.Prevention of deep–vein thrombosis following total hip replacement surgery with enoxaparin versus unfractionated heparin: a pharmacoeconomic evaluation.Ann Pharmacother.1994:28(2):271–275.
- ,.Cost–effectiveness of prolonged out–of–hospital prophylaxis with low–molecular–weight heparin following total hip replacement.Haemostasis.2000;30(suppl 2):130–135.
- ,,, et al.Cost effectiveness of a low–molecular–weight heparin in prolonged prophylaxis against deep vein thrombosis after total hip replacement.Pharmacoeconomics.1998;13:81–89.
- ,,, et al.Economic analysis of low–dose heparin vs the low–molecular–weight heparin enoxaparin for prevention of venous thromboembolism after colorectal surgery.Arch Intern Med.1999;159:1221–1228.
- .High risk of the critically ill for venous thromboembolism.Crit Care Med.1982;10:448–450.
- ,,, et al.Prevention of deep vein thrombosis in medical patients by low dose heparin.Scott Med J.1981;26:115–117.
- ,,, et al.Prevalence and prevention of deep venous thrombosis of the lower extremities in high–risk pulmonary patients.Angiology.1988;39:505–513.
- ,,, et al.A double–blind randomized trial of ORG 10172 low–molecular weight heparinoid versus unfractionated heparin in the prevention of deep venous thrombosis in patients with thrombotic stroke.Thromb Haemost.1991;65(suppl):753.
- ,,, et al.A double–blind and randomized placebo controlled trial of low molecular weight heparin once daily to prevent deep vein thrombosis in acute ischemic stroke.Semin Thromb Hemost.1990;16(suppl):25–33.
- ,,, et al.The incidence of heparin–induced thrombocytopenia in hospitalized medical patients treated with subcutaneous unfractionated heparin: a prospective cohort study.Blood.2003;101:2955–2959.
- ,,, et al.Heparin–induced thrombocytopenia in neurologic disease treated with unfractionated heparin.Neurology.2004;62:657–659.
- ,,, et al.Subcutaneous heparin versus low–molecular–weight heparin as thromboprophylaxis in patients undergoing colorectal surgery.Ann Surg2001;233:438–44.
- ,,, et al.Heparin–induced thrombocytopenia inpatients treated with low–molecular weight heparin or unfractionated heparin.N Eng J Med.1995;332:1330–1335.
- ,,, et al.An improved definition of heparin–induced thrombocytopenia in postoperative orthopedic patients.Arch Intern Med.2003;163:2518–2524.
- ,,, et al.Impact of patient population on the risk for heparin–induced thrombocytopenia.Blood.2000;96:1703–1708.
- ,,, et al.Heparin–induced thrombocytopenia and thrombosis: incidence, analysis of risk factors, and clinical outcomes in 108 consecutive patients treated at a single institution.Am J Hematol.1997;56(1):12–16.
- .., et al.Argatroban anticoagulation in patients with heparin–induced thrombocytopenia.Arch Intern Med.2003:163:1849–1856.
- ,,, et al.Antibodies to platelet factor 4–heparin after cardiopulmonary bypass in patients anticoagulated with unfractionated heparin or a low–molecular–weight heparin: clinical implications for heparin–induced thrombocytopenia.Circulation.1999;99:2530–2536.
- ,,, et.Al. Argatroban anticoagulant therapy in patients with heparin–induced thrombocytopenia.Circulation.2001;103:1838–1843.
- ,.A 14 year study of heparin–induced thrombocytopenia.Am J Med.1996;101:502–507.
- ,,, et al.Failure of early heparin cessation as treatment for heparin–induced thrombocytopenia.Am J Med.1999;106:629–635.
- CEA Registry,Harvard Center for Risk Analysis. Available at: http://www.hcra.harvard.edu/pdf/preferencescores.pdf.
- .Temporal aspects of heparin–induced thrombocytopenia.N Eng J Med.2001;344:1286–1292.
- National Center for Health Statistics. Available at: http://www.cdc.gov/nchs/.
- Centers for Medicare and Medicaid Services. Available at: http://www.cms.hhs.gov/.
Several groups of medical patients at risk for venous thromboembolism (VTE) while hospitalized have been identified. These include patients with certain acute medical illnesses such as acute myocardial infarction, stroke, or chronic obstructive pulmonary disease and those with acute medical illness combined with additional risk factors including advanced age, cancer, obesity, or prior VTE.13
Heparin‐induced thrombocytopenia (HIT) and heparin‐induced thrombocytopenia with thrombosis (HITT), a spectrum of disease also known as type 2 HIT, are potentially devastating hematologic consequences of VTE prophylaxis that result from heparin binding to platelet factor IV, leading to IgG antibodymediated platelet activation.46 These complications manifest along a spectrum from thrombocytopenia alone (HIT) to more severe sequelae that include death, amputation, venous and arterial thrombosis. Unfractionated heparin (UFH) has traditionally been used for VTE prophylaxis in these populations at risk. More recently, evidence has indicated that enoxaparin, a low‐molecular‐weight heparin, is at least as effective for VTE prophylaxis1, 7 and carries a significantly lower risk for the development of the complications of HIT and HITT. Despite the superior side‐effect profile of enoxaparin, many institutions encourage the use of heparin for DVT prophylaxis because of its lower price. However, when the costs of treating these complications are considered, using unfractionated heparin may actually be more costly.
Two studies of the cost effectiveness of heparin compared with enoxaparin when used for VTE prophylaxis in medical inpatients have recently been published.8, 9 However, one of these studies focused only on pharmacy‐related costs and did not consider patient‐related outcomes, and the other was published by a for‐profit research company. Studies of treatment with enoxaparin versus UFH in other medical settings, including non‐Q‐wave myocardial infarction10 and treatment of acute deep‐vein thrombosis,11 suggest that enoxaparin is more cost effective. Studies of prophylaxis of surgical patients have been contradictory. Data suggest that in orthopedic patients the use of enoxaparin is more cost effective for both short‐ and long‐term VTE prophylaxis,1214 but low‐dose heparin appeared more cost effective for patients undergoing colorectal surgery, in large part because of an assumption of a smaller risk of bleeding.15
The purpose of this analysis was to determine the cost utility of heparin compared with enoxaparin for VTE prophylaxis for medical inpatients at risk. In such an analysis, it is important to consider the possibly different meanings that entities may attach to cost utility and effectiveness according to their different roles in the health care system. Individual institutions pay inpatient medication costs, but they often do not directly bear the costs of complications of treatment and may actually receive reimbursements for them. In contrast, payers must provide that reimbursement. For this reason, costs were analyzed from 2 perspectives, that of a payer (Medicare) and that of a health care system or institution.
METHODS
This protocol was declared exempt by the Institutional Review Board at the University of Texas Health Science Center at San Antonio.
Estimates of Effectiveness
Estimates of effectiveness include those related both to efficacy in preventing VTE, and those related to adverse drug events. They are summarized in Table 1.
| Base Case | Range for Sensitivity Analysis | |
|---|---|---|
| Rate of development of HIT on heparin | 2.70% | 0.80%4.90% |
| Rate of development of HIT on enoxaparin | 0.30% | 0.09%0.54% |
| Rate of progression to HITT | 40% | 25%50% |
| Mortality rate despite treatment, HITT | 8% | 0%20% |
| Assumed extension in length of stayHIT | 1 day | 05 days |
| Assumed extension in length of stayHITT | 7 days | 510 days |
| Life expectancy (2001) | 77.2 years | |
| Average age of medical inpatient | 71.9 years | |
| QALY adjustment for: | ||
| CHFsevere | 0.6 | |
| COPD | 0.4 | |
| Cancer | 0.9 |
Assumptions about the efficacy of heparin and enoxaparin when used for VTE prophylaxis were based on the following published data. The rate of development of VTE reported in the Medenox trial, 5.5%,1 is consistent with rates reported for patients receiving heparin (2%13%).1618 More recently, the PRINCE study demonstrated that enoxaparin was at least as effective as heparin in patients with severe heart failure or respiratory disease and was more effective in the former group of patients.7 Finally, data from patients with acute stroke indicated that low‐molecular‐weight heparins are at least as effective as heparin for this indication.19, 20 Equal efficacy was assumed for this analysis for several reasons, primarily to avoid the creation or amplification of errors through the introduction of more assumptions about the proportion of patients with specific diagnoses and about the magnitude and range of differences in efficacy. Only one study has examined the relative efficacy in patients with congestive heart failure, and not all the results of studies in stroke patients pointed to enoxaparin having improved efficacy. Therefore, making valid assumptions about the magnitude of the difference between the drugs on the basis of the available evidence may not be possible.
It was also assumed that aside from HIT and HITT, the 2 drugs had the same rates of adverse events, including bleeding complications, in this patient population.1
A Medline search combining MeSH terms thrombocytopenia and heparin was done to find the appropriate incidence of HIT and HITT. The resulting group was further limited in 3 separate searches using the terms prophylaxis (keyword), incidence (MeSH term), and thromboembolism or venous thrombosis (MeSH terms). Heparin‐induced thrombocytopenia was searched for as a keyword and combined with the MeSH term prophylaxis in a separate search. Finally, reference lists were searched to find additional articles.
The range of reported rates of development of HIT among patients receiving heparin was wide. In part, this is related to the different subgroups of patients studied and to the inclusion of patients receiving both prophylaxis and treatment doses of heparin. The one study that looked specifically at medical inpatients included patients receiving treatment‐dose heparin. The rate of HIT in this study was 0.8%.21 A study of both prophylactic and therapeutic use in neurologic patients reported a rate of 2.5%.22 Studies specific to VTE prophylaxis in surgical patients reported a range of 0.8%4.9%.2326 Based on these results, a rate of 2.7%, the median of the reported ranges, was used for the base case, and 0.8% and 4.9% were used for sensitivity analysis.
The reported rates of progression to thrombosis for patients with HIT ranged from 25 to more than 50%.21, 27, 28 A median rate of 40% was used for the base case, and 25% and 50% were used for sensitivity analysis. It was assumed that 0.3% of patients receiving enoxaparin developed HIT, 1/9 as frequently as those receiving heparin,24, 25, 29 but that the same percentage of those with HIT would develop thrombosis.
Mortality secondary to thrombosis in patients with untreated HIT has been reported to be 4%5%.30, 31 All‐cause mortality in untreated patients with HITT has been reported to be as high as >20%,31, 32 but in treated patients it has been reported as 8%.30 A mortality rate of 8% for HITT despite treatment was assumed with a range in the sensitivity analysis from 0% to 20%.
Life expectancy data were obtained from the National Center for Health Statistics, and the average age of medical inpatients potentially eligible for DVT prophylaxis was calculated from this data. The catalog of preference scores was obtained from the Cost Effectiveness Analysis Registry at the Harvard Center for Risk Analysis.33 These preference scores adjust the quality of a year of life for chronic diseases and provide a more accurate assessment of quality‐adjusted life years.
It was assumed that patients with HIT alone would be treated with argatroban, consistent with evidence that this is superior to withdrawal of heparin alone in patients with HIT.28 Using other agents such as lepirudin for the treatment of HIT was not considered in this analysis because there is no data on which to base their efficacy in patients with HIT.
For treatment of patients with HITT, again only the use of argatroban was considered. Though other agents are as efficacious in treating HITT, they are also more expensive. Therefore, using argatroban allowed for a more conservative estimate.
Platelet counts typically fall after 5 days of heparin administration in patients developing HIT34 and typically recover within 35 days of initiation of treatment.4, 29 In the past, patients may not have been kept in the hospital for resolution of their platelet count. However, with evidence that HIT should be aggressively treated, patients with HIT will likely have a longer length of stay. A study of treatment of HIT reported a mean time on argatroban of 57 days.23 This is greater than the average length of stay for medical diagnosis, which is 45 days.35 Therefore, an additional length of stay of 1 day was assumed for patients given a diagnosis of HIT, with a range of 05 days used for the sensitivity analysis. An additional length of stay totaling 7 days was assumed for those with thrombosis, based on patients requiring 7 days of argatroban therapy for treatment of HITT in a recent study.28
Estimates of Costs
Costs were analyzed from institutional and Medicare perspectives. Only direct medical expenditures related to hospitalization were considered; indirect patient costs resulting from the sequelae of HITT, while potentially severe, were not included. An incremental analysis was performed to express the increase in resources used when a person develops HIT/T, with the final result expressed as a daily cost of each medication. Cost assumptions are summarized in Table 2.
| Medicarerelated | Institutionrelated | |||
|---|---|---|---|---|
| Base case | Range | Base case | Range | |
| Additional reimbursement for HIT (if considered a complicating condition) | $ 765.06 | $ 0.00 | $ 765.06 | $0.00 |
| Additional reimbursement for HITT (if coagulation disorder DRG used) | $1135.56 | $ 0.00 | $1135.56 | $0.00 |
| Primary provider visit (99232) | $ 54.89 | $33.00$ 78.04 | n/a | |
| Consultant initial visit (99254) | $ 140.39 | $35.84$193.03 | n/a | |
| Consultant followup (99263) | $ 44.80 | $22.40$ 66.09 | n/a | |
| Medication (per day) | ||||
| Heparin | n/a | $ 4.00 | ||
| Enoxaparin | n/a | $ 84.00 | ||
| Argatroban | n/a | $ 150.00 | ||
| Coumadin | n/a | $ 0.50 | ||
| Laboratory tests (per test) | ||||
| Complete blood count | n/a | $ 2.14 | ||
| Prothrombin time/partial thromboplastin time | n/a | $ 9.85 | ||
| Opportunity cost per additional day of hospitalization (if hospital at capacity) | n/a | $1096.72 | ||
Medicare Related
Diagnosis‐related group (DRG) reimbursement to institutions and physicians were considered the only payer‐related costs. These were based on the 2005 Medicare reimbursement.36 Costs related to laboratory, medication, or other diagnostic studies were assumed to be covered by the DRG payment and not to be billed separately.
The average Medicare reimbursement to institutions for all diagnosis‐related groups is the national standard number, or $4971.81. To determine the additional potential charges resulting from the development of HIT, it was considered a complicating condition. The average adjustment factor for complicating conditions of medical diagnoses is .1539, leading to an increase in charges of $765.06. No additional adjustments for geographic location were made. Sensitivity analysis was performed with no additional reimbursement for HIT as a complicating condition.
To quantify additional charges related to caring for patients with HITT, we used the amount of additional charges for the coagulation disorder DRG (#397) above those of the average reimbursement. This amount is $1135.56, the difference between the higher charge of $6107.37 for this DRG, and the national standard number. Sensitivity analysis with no additional charges was performed.
Physician charges used were based on the 2004 Medicare reimbursement.36 It was assumed that each patient with HIT would have a daily visit of moderate complexity (CPT 99232), which carries a reimbursement rate of $54.89. Patients with thrombotic complications were assumed to also have a hematology consult consisting of one initial visit and one followup, both of midlevel complexity (CPTs 99253 and 99262). The reimbursement rates for these visits are $97.45 and $44.80. Sensitivity analysis using both lower‐ and higher‐level visits was performed (Table 2).
Based on the above DRG and physician reimbursements, the total cost to Medicare of treating a patient with HIT is $820.05 and of treating a patient with HITT is $1749.98. For the situation in which a patient with HIT also developed HITT, only the cost of reimbursement for HITT was modeled.
Hospital‐Related
To calculate the benefit or cost to an institution, 2 scenarios were modeled. In the first scenario, only the DRG‐related revenues collected and the costs of caring for patients with HIT/T were considered. The revenues used are described above. The cost of medications at a multi‐institutional health care system (MIHCS) was obtained from the pharmacy and used in this analysis. This system is composed of a network of urban and suburban acute care facilities with academic affiliations with 2 universities. Costs are representative of the entire system. The cost of heparin is $2.00 per unit dose; daily cost for b.i.d. prophylaxis is $4.00. The cost of one daily dose of enoxaparin is $84.00. One unit (50 mg) of argatroban costs $50.00. For a 70‐kg man at a standard dosing rate of 2 g/kg per minute, the daily cost would be approximately $150.00. The daily cost of coumadin was estimated at $0.50 regardless of the dose. The cost of laboratory tests within the MIHCS is $2.14 per complete blood count and $9.85 for each PT/PTT.
Other costs, such as those related to the additional time spent by nursing and pharmacy staff in the mixing and administration of argatroban or caring for patients with HIT and HITT were not included in this analysis, as it was believed that they would have no impact on actual staffing levels and would not lead to a tangible or easily quantifiable increase in expenditures.
In the second scenario, the potential loss of income from additional days of hospitalization for HIT and HITT was considered. An institution could potentially lose money if a patient with HIT or HITT stayed longer than the number of days that is economically attractive given the DRG reimbursement. In this scenario, a longer length of stay of a patient with HIT or HITT could lead to the bed not being used by other patients for whom the hospital could be collecting revenue. This would only be applicable with high occupancy rates. The average revenue per day that a hospital could receive for a patient was calculated by dividing the average reimbursement, $4971.81, by the average length of stay for medical inpatients, 4.5 days. This amount is $1096.72. The amount of additional reimbursement for a complicating condition, $754.06, then covers 0.7 days of additional hospitalization. As described above, the average additional reimbursement for using the coagulation disorder DRG for patients with HITT, instead of using the DRG for which they were otherwise admitted, was $1135.56. This would cover an additional 1.04 days of hospitalization. If the hospital stay of patients with HIT/T were to be longer, an amount computed as $1096.72 multiplied by the number of additional days of hospitalization was considered a loss of income borne by the hospital.
Sensitivity Analysis
Sensitivity analysis was performed to ensure the validity of results over a range of values and to assess the effect of medication prices on our findings. The analysis used these parameters, both alone and in combination: rate of development of HIT, rate of development on enoxaparin compared with on heparin, percentage of those with HIT who developed thrombosis, mortality related to HITT, length of stay of patients with both HIT and HITT, reimbursement rates, and costs of medication.
RESULTS
The decision tree used for the base‐case analysis is shown in Figure 1. The gain in quality‐adjusted life years (QALYs) for medical patients who used enoxaparin rather than heparin for VTE prophylaxis was 0.00629 (approximately 55 hours). This was based on the decrease in HITT‐related premature death resulting from the use of enoxaparin. From a payer perspective, the daily cost of enoxaparin is $3.58, compared with $32.18 for heparin. The difference is a savings of $28.61, leading to a savings/QALY of $4550.17. Therefore, the use of enoxaparin is both more effective and less costly.
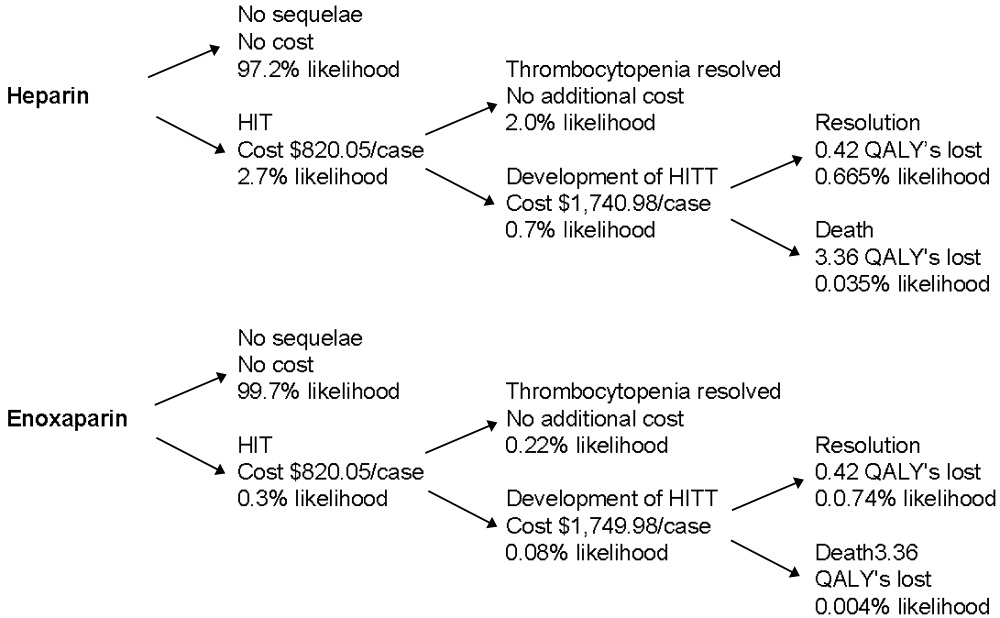
Sensitivity analysis showed that from a payer perspective, enoxaparin remained both less costly and more effective in all cases. The factors that had the largest impact on cost/QALY were incidence of HIT and rate of thrombosis among those with HIT. Decreasing length of stay to 0 for patients with HIT, decreasing reimbursement to $0 for both HIT and HITT, and billing at a high or low level did not change the general finding. Decreasing the cost of enoxaparin or heparin also did not affect these findings. The results of the sensitivity analysis are summarized in Table 3.
| Enoxaparin (cost/day) | Heparin (cost/day) | QALYs saved | Savings/QALY | |
|---|---|---|---|---|
| Base case | $3.58 | $32.18 | 0.00629 | $4550.17 |
| Sensitivity analysis | ||||
| Incidence of HIT | $1.06$6.49 | $ 9.54$58.11 | 0.001860.01141 | $4550.17 |
| Progression of HIT to HITT | $3.12$3.77 | $28.05$33.95 | 0.003930.00786 | $6344.53$3840.30 |
| Level of physician visit billed | $3.23$3.81 | $28.45$34.27 | 0.00629 | $4021.85$4844.35 |
| HIT length of stay | $3.48$3.64 | $31.30$32.78 | 0.00629 | $4424.46$4633.98 |
| No reimbursement for HIT | $2.13 | $19.20 | 0.00629 | $2713.90 |
| No reimbursement for HITT | $0.77 | $ 6.93 | 0.00629 | $ 980.05 |
From an institutional perspective, the effect of considering the costs of HIT and HITT did not necessarily make enoxaparin a more attractive choice. When potential reimbursement for drug‐related complications was considered, an institution actually make $7.27/day by choosing heparin, whereas the cost of enoxaparin decreases only minimally from $84.00 to $82.75/day (Table 4). Factoring opportunity costs into the analysis showed that an institution does not make money by using heparin, but heparin still costs less on a daily basis. This finding changes only at rates of HIT over 4%.
| Heparin | Enoxaparin | |||
|---|---|---|---|---|
| Drug cost alone | Drug cost + cost of increased LOS | Drug cost alone | Drug cost + cost of increased LOS | |
| Base case | ($7.27) | $72.33 | $82.75 | $91.59 |
| Sensitivity Analysis | ||||
| Incidence of HIT | $ 0.66($16.45) | $24.25$128.01 | $83.63$81.75 | $86.25$ 97.18 |
| Length of stay HIT | ($ 7.27) | $42.72$190.78 | $82.75 | $88.30$104.75 |
| Length of stay HITT | ($ 7.27) | $48.64$101.57 | $82.75 | $88.96$ 95.54 |
| Drug costs below which enoxaparin is more attractive | $ 0.50$ 4.00 | $ 0.50$ 4.00 | $33.00$37.00 | < $1.00 |
Sensitivity analyses of institutional costs are summarized in Table 4. These analyses demonstrated that potential increases in length of stay for patients with HIT or HITT could make heparin less attractive when opportunity costs to the hospital are considered. If the additional length of stay for patients with HIT increased to greater than 1.75 days or the additional length of stay for those with HITT increased to more than 9 days, heparin becomes a less attractive choice. Loss of reimbursement for HIT or HITT alone does not make enoxaparin less costly than heparin.
Sensitivity analysis also demonstrated that variation in the price of enoxaparin could potentially make heparin less attractive. If the price of heparin were held constant at $4.00/day, enoxaparin would become less costly at a price of $37.00. If the price of heparin were to decrease to as low as $0.50/day, the price at which enoxaparin would be more attractive decreased to $33.00. These prices are only applicable when the opportunity costs of having occupied beds are consideredthat is, only when an institution is operating at full capacity. When this is not the case, enoxaparin would have to cost less than $1.00 to be more financially attractive than heparin. In practical terms, unless a hospital is at full capacity and needs hospital beds for other patients, the cost of enoxaparin would have to be less than $1 for an institution to choose it instead of heparin.
DISCUSSION
This study demonstrates that from a payer perspective, there is greater cost utility in the use of enoxaparin in place of heparin for the prevention of venous thromboembolism in at‐risk medical patients. This benefit is based on a single advantage of enoxaparin: its decreased tendency to cause HIT/T. Despite the simplicity of this assumption, it is well supported by published data. Sensitivity analyses supported the finding that enoxaparin was a superior choice in all scenarios modeled. This payer data can be extrapolated to a societal level because the costs used were based on Medicare reimbursements.
The benefit of using enoxaparin when expressed in an absolute number of quality‐adjusted life years was small, approximately 55 hours. This reflects that although the effects of HIT and HITT are potentially devastating, they occur infrequently. However, our calculation was conservative in several respects. We calculated the highest possible average age for a medical inpatient based on the available statistics. This was done to ensure that we were not overestimating the number of QALYs saved by preventing death secondary to HITT. We also considered only 2 outcomes of HITT: death and recovery. This underestimates the significant potential thrombotic complications, notably amputation or other loss of function, which would increase the number of QALYs saved by using enoxaparin. The inclusion of these complications would only strengthen this finding. Finally, we assumed equal efficacy for heparin and enoxaparin. The inclusion of superior efficacy of enoxaparin in subpopulations of medical inpatients would again only strengthen this finding.
Apart from the price of the medication, the incidence of HIT had the largest impact on costs and QALYs saved in the sensitivity analysis. Studies specific to VTE prophylaxis in medical inpatients could better define the incidence of HIT/T in this population, but this would not change our overall finding.
From an institutional perspective, the choice of heparin or enoxaparin is more complicated. In most but not all scenarios, the use of heparin appears to be more financially attractive. The prices of enoxaparin and heparin, the additional length of stay required to care for patients with HIT and HITT, and the percentage of total beds occupied all affect this decision. Several pieces of cost data, specifically those related to medication and laboratory testing, were specific to an MIHCS health care system, the type considered in the analysis and could potentially limit the applicability of this study to other institutions. However, the sensitivity analysis demonstrated that the cost of enoxaparin would have to be at least 60% lower, below $33/day, before affecting our conclusion, and then only if an institution were at full capacity. Thus, we expect that our results are generally applicable.
The potential limitations of this study are related to the assumptions required. However, our efficacy assumptions were conservatively based on published data. It is possible that a decrease in the rate of thrombosis if all cases of HIT were treated with argatroban could affect our findings. However, in the study by Lewis et al., the complication rate for those with HIT in the treatment group was 28% (versus 38.8% in the untreated group), consistent with rates used in our sensitivity analysis. DRG and physician reimbursements are based on published Medicare data. The greatest variation is likely to be in drug cost, as different institutions may negotiate lower prices. From a payer perspective, drug costs do not affect the conclusions; from an institutional perspective, drug cost may make the choice a complicated one. One factor not included in our analysis that may affect this decision is the possible impact of legal action on the medications institutions choose for VTE prophylaxis. Because the potential consequences of HITT can be so devastating, an institution could have difficulty defending the choice of heparin when an equally effective alternative with fewer adverse events was available. A settlement of $1 million could potentially pay for prophylaxis with enoxaparin for at least 2500 patients.
This analysis has highlighted one of the unfortunate paradoxes caused by the different, potentially competing incentives in our health care system. Payers and institutions often face different financial incentives. From a hospital's perspective, it may cost less to use an intervention that can potentially cause a greater number of complications and higher payer costs. We believe that for VTE prophylaxis for medical inpatients, improved patient outcomes coupled with decreased payer/societal costs argue strongly for the use of enoxaparin over unfractionated heparin and outweigh any institutional benefits.
Several groups of medical patients at risk for venous thromboembolism (VTE) while hospitalized have been identified. These include patients with certain acute medical illnesses such as acute myocardial infarction, stroke, or chronic obstructive pulmonary disease and those with acute medical illness combined with additional risk factors including advanced age, cancer, obesity, or prior VTE.13
Heparin‐induced thrombocytopenia (HIT) and heparin‐induced thrombocytopenia with thrombosis (HITT), a spectrum of disease also known as type 2 HIT, are potentially devastating hematologic consequences of VTE prophylaxis that result from heparin binding to platelet factor IV, leading to IgG antibodymediated platelet activation.46 These complications manifest along a spectrum from thrombocytopenia alone (HIT) to more severe sequelae that include death, amputation, venous and arterial thrombosis. Unfractionated heparin (UFH) has traditionally been used for VTE prophylaxis in these populations at risk. More recently, evidence has indicated that enoxaparin, a low‐molecular‐weight heparin, is at least as effective for VTE prophylaxis1, 7 and carries a significantly lower risk for the development of the complications of HIT and HITT. Despite the superior side‐effect profile of enoxaparin, many institutions encourage the use of heparin for DVT prophylaxis because of its lower price. However, when the costs of treating these complications are considered, using unfractionated heparin may actually be more costly.
Two studies of the cost effectiveness of heparin compared with enoxaparin when used for VTE prophylaxis in medical inpatients have recently been published.8, 9 However, one of these studies focused only on pharmacy‐related costs and did not consider patient‐related outcomes, and the other was published by a for‐profit research company. Studies of treatment with enoxaparin versus UFH in other medical settings, including non‐Q‐wave myocardial infarction10 and treatment of acute deep‐vein thrombosis,11 suggest that enoxaparin is more cost effective. Studies of prophylaxis of surgical patients have been contradictory. Data suggest that in orthopedic patients the use of enoxaparin is more cost effective for both short‐ and long‐term VTE prophylaxis,1214 but low‐dose heparin appeared more cost effective for patients undergoing colorectal surgery, in large part because of an assumption of a smaller risk of bleeding.15
The purpose of this analysis was to determine the cost utility of heparin compared with enoxaparin for VTE prophylaxis for medical inpatients at risk. In such an analysis, it is important to consider the possibly different meanings that entities may attach to cost utility and effectiveness according to their different roles in the health care system. Individual institutions pay inpatient medication costs, but they often do not directly bear the costs of complications of treatment and may actually receive reimbursements for them. In contrast, payers must provide that reimbursement. For this reason, costs were analyzed from 2 perspectives, that of a payer (Medicare) and that of a health care system or institution.
METHODS
This protocol was declared exempt by the Institutional Review Board at the University of Texas Health Science Center at San Antonio.
Estimates of Effectiveness
Estimates of effectiveness include those related both to efficacy in preventing VTE, and those related to adverse drug events. They are summarized in Table 1.
| Base Case | Range for Sensitivity Analysis | |
|---|---|---|
| Rate of development of HIT on heparin | 2.70% | 0.80%4.90% |
| Rate of development of HIT on enoxaparin | 0.30% | 0.09%0.54% |
| Rate of progression to HITT | 40% | 25%50% |
| Mortality rate despite treatment, HITT | 8% | 0%20% |
| Assumed extension in length of stayHIT | 1 day | 05 days |
| Assumed extension in length of stayHITT | 7 days | 510 days |
| Life expectancy (2001) | 77.2 years | |
| Average age of medical inpatient | 71.9 years | |
| QALY adjustment for: | ||
| CHFsevere | 0.6 | |
| COPD | 0.4 | |
| Cancer | 0.9 |
Assumptions about the efficacy of heparin and enoxaparin when used for VTE prophylaxis were based on the following published data. The rate of development of VTE reported in the Medenox trial, 5.5%,1 is consistent with rates reported for patients receiving heparin (2%13%).1618 More recently, the PRINCE study demonstrated that enoxaparin was at least as effective as heparin in patients with severe heart failure or respiratory disease and was more effective in the former group of patients.7 Finally, data from patients with acute stroke indicated that low‐molecular‐weight heparins are at least as effective as heparin for this indication.19, 20 Equal efficacy was assumed for this analysis for several reasons, primarily to avoid the creation or amplification of errors through the introduction of more assumptions about the proportion of patients with specific diagnoses and about the magnitude and range of differences in efficacy. Only one study has examined the relative efficacy in patients with congestive heart failure, and not all the results of studies in stroke patients pointed to enoxaparin having improved efficacy. Therefore, making valid assumptions about the magnitude of the difference between the drugs on the basis of the available evidence may not be possible.
It was also assumed that aside from HIT and HITT, the 2 drugs had the same rates of adverse events, including bleeding complications, in this patient population.1
A Medline search combining MeSH terms thrombocytopenia and heparin was done to find the appropriate incidence of HIT and HITT. The resulting group was further limited in 3 separate searches using the terms prophylaxis (keyword), incidence (MeSH term), and thromboembolism or venous thrombosis (MeSH terms). Heparin‐induced thrombocytopenia was searched for as a keyword and combined with the MeSH term prophylaxis in a separate search. Finally, reference lists were searched to find additional articles.
The range of reported rates of development of HIT among patients receiving heparin was wide. In part, this is related to the different subgroups of patients studied and to the inclusion of patients receiving both prophylaxis and treatment doses of heparin. The one study that looked specifically at medical inpatients included patients receiving treatment‐dose heparin. The rate of HIT in this study was 0.8%.21 A study of both prophylactic and therapeutic use in neurologic patients reported a rate of 2.5%.22 Studies specific to VTE prophylaxis in surgical patients reported a range of 0.8%4.9%.2326 Based on these results, a rate of 2.7%, the median of the reported ranges, was used for the base case, and 0.8% and 4.9% were used for sensitivity analysis.
The reported rates of progression to thrombosis for patients with HIT ranged from 25 to more than 50%.21, 27, 28 A median rate of 40% was used for the base case, and 25% and 50% were used for sensitivity analysis. It was assumed that 0.3% of patients receiving enoxaparin developed HIT, 1/9 as frequently as those receiving heparin,24, 25, 29 but that the same percentage of those with HIT would develop thrombosis.
Mortality secondary to thrombosis in patients with untreated HIT has been reported to be 4%5%.30, 31 All‐cause mortality in untreated patients with HITT has been reported to be as high as >20%,31, 32 but in treated patients it has been reported as 8%.30 A mortality rate of 8% for HITT despite treatment was assumed with a range in the sensitivity analysis from 0% to 20%.
Life expectancy data were obtained from the National Center for Health Statistics, and the average age of medical inpatients potentially eligible for DVT prophylaxis was calculated from this data. The catalog of preference scores was obtained from the Cost Effectiveness Analysis Registry at the Harvard Center for Risk Analysis.33 These preference scores adjust the quality of a year of life for chronic diseases and provide a more accurate assessment of quality‐adjusted life years.
It was assumed that patients with HIT alone would be treated with argatroban, consistent with evidence that this is superior to withdrawal of heparin alone in patients with HIT.28 Using other agents such as lepirudin for the treatment of HIT was not considered in this analysis because there is no data on which to base their efficacy in patients with HIT.
For treatment of patients with HITT, again only the use of argatroban was considered. Though other agents are as efficacious in treating HITT, they are also more expensive. Therefore, using argatroban allowed for a more conservative estimate.
Platelet counts typically fall after 5 days of heparin administration in patients developing HIT34 and typically recover within 35 days of initiation of treatment.4, 29 In the past, patients may not have been kept in the hospital for resolution of their platelet count. However, with evidence that HIT should be aggressively treated, patients with HIT will likely have a longer length of stay. A study of treatment of HIT reported a mean time on argatroban of 57 days.23 This is greater than the average length of stay for medical diagnosis, which is 45 days.35 Therefore, an additional length of stay of 1 day was assumed for patients given a diagnosis of HIT, with a range of 05 days used for the sensitivity analysis. An additional length of stay totaling 7 days was assumed for those with thrombosis, based on patients requiring 7 days of argatroban therapy for treatment of HITT in a recent study.28
Estimates of Costs
Costs were analyzed from institutional and Medicare perspectives. Only direct medical expenditures related to hospitalization were considered; indirect patient costs resulting from the sequelae of HITT, while potentially severe, were not included. An incremental analysis was performed to express the increase in resources used when a person develops HIT/T, with the final result expressed as a daily cost of each medication. Cost assumptions are summarized in Table 2.
| Medicarerelated | Institutionrelated | |||
|---|---|---|---|---|
| Base case | Range | Base case | Range | |
| Additional reimbursement for HIT (if considered a complicating condition) | $ 765.06 | $ 0.00 | $ 765.06 | $0.00 |
| Additional reimbursement for HITT (if coagulation disorder DRG used) | $1135.56 | $ 0.00 | $1135.56 | $0.00 |
| Primary provider visit (99232) | $ 54.89 | $33.00$ 78.04 | n/a | |
| Consultant initial visit (99254) | $ 140.39 | $35.84$193.03 | n/a | |
| Consultant followup (99263) | $ 44.80 | $22.40$ 66.09 | n/a | |
| Medication (per day) | ||||
| Heparin | n/a | $ 4.00 | ||
| Enoxaparin | n/a | $ 84.00 | ||
| Argatroban | n/a | $ 150.00 | ||
| Coumadin | n/a | $ 0.50 | ||
| Laboratory tests (per test) | ||||
| Complete blood count | n/a | $ 2.14 | ||
| Prothrombin time/partial thromboplastin time | n/a | $ 9.85 | ||
| Opportunity cost per additional day of hospitalization (if hospital at capacity) | n/a | $1096.72 | ||
Medicare Related
Diagnosis‐related group (DRG) reimbursement to institutions and physicians were considered the only payer‐related costs. These were based on the 2005 Medicare reimbursement.36 Costs related to laboratory, medication, or other diagnostic studies were assumed to be covered by the DRG payment and not to be billed separately.
The average Medicare reimbursement to institutions for all diagnosis‐related groups is the national standard number, or $4971.81. To determine the additional potential charges resulting from the development of HIT, it was considered a complicating condition. The average adjustment factor for complicating conditions of medical diagnoses is .1539, leading to an increase in charges of $765.06. No additional adjustments for geographic location were made. Sensitivity analysis was performed with no additional reimbursement for HIT as a complicating condition.
To quantify additional charges related to caring for patients with HITT, we used the amount of additional charges for the coagulation disorder DRG (#397) above those of the average reimbursement. This amount is $1135.56, the difference between the higher charge of $6107.37 for this DRG, and the national standard number. Sensitivity analysis with no additional charges was performed.
Physician charges used were based on the 2004 Medicare reimbursement.36 It was assumed that each patient with HIT would have a daily visit of moderate complexity (CPT 99232), which carries a reimbursement rate of $54.89. Patients with thrombotic complications were assumed to also have a hematology consult consisting of one initial visit and one followup, both of midlevel complexity (CPTs 99253 and 99262). The reimbursement rates for these visits are $97.45 and $44.80. Sensitivity analysis using both lower‐ and higher‐level visits was performed (Table 2).
Based on the above DRG and physician reimbursements, the total cost to Medicare of treating a patient with HIT is $820.05 and of treating a patient with HITT is $1749.98. For the situation in which a patient with HIT also developed HITT, only the cost of reimbursement for HITT was modeled.
Hospital‐Related
To calculate the benefit or cost to an institution, 2 scenarios were modeled. In the first scenario, only the DRG‐related revenues collected and the costs of caring for patients with HIT/T were considered. The revenues used are described above. The cost of medications at a multi‐institutional health care system (MIHCS) was obtained from the pharmacy and used in this analysis. This system is composed of a network of urban and suburban acute care facilities with academic affiliations with 2 universities. Costs are representative of the entire system. The cost of heparin is $2.00 per unit dose; daily cost for b.i.d. prophylaxis is $4.00. The cost of one daily dose of enoxaparin is $84.00. One unit (50 mg) of argatroban costs $50.00. For a 70‐kg man at a standard dosing rate of 2 g/kg per minute, the daily cost would be approximately $150.00. The daily cost of coumadin was estimated at $0.50 regardless of the dose. The cost of laboratory tests within the MIHCS is $2.14 per complete blood count and $9.85 for each PT/PTT.
Other costs, such as those related to the additional time spent by nursing and pharmacy staff in the mixing and administration of argatroban or caring for patients with HIT and HITT were not included in this analysis, as it was believed that they would have no impact on actual staffing levels and would not lead to a tangible or easily quantifiable increase in expenditures.
In the second scenario, the potential loss of income from additional days of hospitalization for HIT and HITT was considered. An institution could potentially lose money if a patient with HIT or HITT stayed longer than the number of days that is economically attractive given the DRG reimbursement. In this scenario, a longer length of stay of a patient with HIT or HITT could lead to the bed not being used by other patients for whom the hospital could be collecting revenue. This would only be applicable with high occupancy rates. The average revenue per day that a hospital could receive for a patient was calculated by dividing the average reimbursement, $4971.81, by the average length of stay for medical inpatients, 4.5 days. This amount is $1096.72. The amount of additional reimbursement for a complicating condition, $754.06, then covers 0.7 days of additional hospitalization. As described above, the average additional reimbursement for using the coagulation disorder DRG for patients with HITT, instead of using the DRG for which they were otherwise admitted, was $1135.56. This would cover an additional 1.04 days of hospitalization. If the hospital stay of patients with HIT/T were to be longer, an amount computed as $1096.72 multiplied by the number of additional days of hospitalization was considered a loss of income borne by the hospital.
Sensitivity Analysis
Sensitivity analysis was performed to ensure the validity of results over a range of values and to assess the effect of medication prices on our findings. The analysis used these parameters, both alone and in combination: rate of development of HIT, rate of development on enoxaparin compared with on heparin, percentage of those with HIT who developed thrombosis, mortality related to HITT, length of stay of patients with both HIT and HITT, reimbursement rates, and costs of medication.
RESULTS
The decision tree used for the base‐case analysis is shown in Figure 1. The gain in quality‐adjusted life years (QALYs) for medical patients who used enoxaparin rather than heparin for VTE prophylaxis was 0.00629 (approximately 55 hours). This was based on the decrease in HITT‐related premature death resulting from the use of enoxaparin. From a payer perspective, the daily cost of enoxaparin is $3.58, compared with $32.18 for heparin. The difference is a savings of $28.61, leading to a savings/QALY of $4550.17. Therefore, the use of enoxaparin is both more effective and less costly.
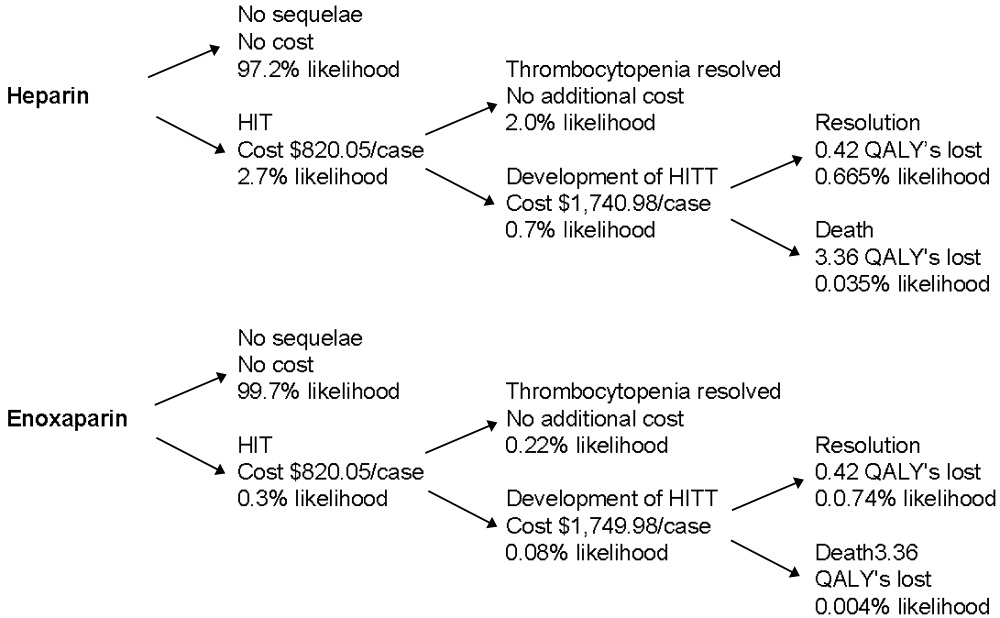
Sensitivity analysis showed that from a payer perspective, enoxaparin remained both less costly and more effective in all cases. The factors that had the largest impact on cost/QALY were incidence of HIT and rate of thrombosis among those with HIT. Decreasing length of stay to 0 for patients with HIT, decreasing reimbursement to $0 for both HIT and HITT, and billing at a high or low level did not change the general finding. Decreasing the cost of enoxaparin or heparin also did not affect these findings. The results of the sensitivity analysis are summarized in Table 3.
| Enoxaparin (cost/day) | Heparin (cost/day) | QALYs saved | Savings/QALY | |
|---|---|---|---|---|
| Base case | $3.58 | $32.18 | 0.00629 | $4550.17 |
| Sensitivity analysis | ||||
| Incidence of HIT | $1.06$6.49 | $ 9.54$58.11 | 0.001860.01141 | $4550.17 |
| Progression of HIT to HITT | $3.12$3.77 | $28.05$33.95 | 0.003930.00786 | $6344.53$3840.30 |
| Level of physician visit billed | $3.23$3.81 | $28.45$34.27 | 0.00629 | $4021.85$4844.35 |
| HIT length of stay | $3.48$3.64 | $31.30$32.78 | 0.00629 | $4424.46$4633.98 |
| No reimbursement for HIT | $2.13 | $19.20 | 0.00629 | $2713.90 |
| No reimbursement for HITT | $0.77 | $ 6.93 | 0.00629 | $ 980.05 |
From an institutional perspective, the effect of considering the costs of HIT and HITT did not necessarily make enoxaparin a more attractive choice. When potential reimbursement for drug‐related complications was considered, an institution actually make $7.27/day by choosing heparin, whereas the cost of enoxaparin decreases only minimally from $84.00 to $82.75/day (Table 4). Factoring opportunity costs into the analysis showed that an institution does not make money by using heparin, but heparin still costs less on a daily basis. This finding changes only at rates of HIT over 4%.
| Heparin | Enoxaparin | |||
|---|---|---|---|---|
| Drug cost alone | Drug cost + cost of increased LOS | Drug cost alone | Drug cost + cost of increased LOS | |
| Base case | ($7.27) | $72.33 | $82.75 | $91.59 |
| Sensitivity Analysis | ||||
| Incidence of HIT | $ 0.66($16.45) | $24.25$128.01 | $83.63$81.75 | $86.25$ 97.18 |
| Length of stay HIT | ($ 7.27) | $42.72$190.78 | $82.75 | $88.30$104.75 |
| Length of stay HITT | ($ 7.27) | $48.64$101.57 | $82.75 | $88.96$ 95.54 |
| Drug costs below which enoxaparin is more attractive | $ 0.50$ 4.00 | $ 0.50$ 4.00 | $33.00$37.00 | < $1.00 |
Sensitivity analyses of institutional costs are summarized in Table 4. These analyses demonstrated that potential increases in length of stay for patients with HIT or HITT could make heparin less attractive when opportunity costs to the hospital are considered. If the additional length of stay for patients with HIT increased to greater than 1.75 days or the additional length of stay for those with HITT increased to more than 9 days, heparin becomes a less attractive choice. Loss of reimbursement for HIT or HITT alone does not make enoxaparin less costly than heparin.
Sensitivity analysis also demonstrated that variation in the price of enoxaparin could potentially make heparin less attractive. If the price of heparin were held constant at $4.00/day, enoxaparin would become less costly at a price of $37.00. If the price of heparin were to decrease to as low as $0.50/day, the price at which enoxaparin would be more attractive decreased to $33.00. These prices are only applicable when the opportunity costs of having occupied beds are consideredthat is, only when an institution is operating at full capacity. When this is not the case, enoxaparin would have to cost less than $1.00 to be more financially attractive than heparin. In practical terms, unless a hospital is at full capacity and needs hospital beds for other patients, the cost of enoxaparin would have to be less than $1 for an institution to choose it instead of heparin.
DISCUSSION
This study demonstrates that from a payer perspective, there is greater cost utility in the use of enoxaparin in place of heparin for the prevention of venous thromboembolism in at‐risk medical patients. This benefit is based on a single advantage of enoxaparin: its decreased tendency to cause HIT/T. Despite the simplicity of this assumption, it is well supported by published data. Sensitivity analyses supported the finding that enoxaparin was a superior choice in all scenarios modeled. This payer data can be extrapolated to a societal level because the costs used were based on Medicare reimbursements.
The benefit of using enoxaparin when expressed in an absolute number of quality‐adjusted life years was small, approximately 55 hours. This reflects that although the effects of HIT and HITT are potentially devastating, they occur infrequently. However, our calculation was conservative in several respects. We calculated the highest possible average age for a medical inpatient based on the available statistics. This was done to ensure that we were not overestimating the number of QALYs saved by preventing death secondary to HITT. We also considered only 2 outcomes of HITT: death and recovery. This underestimates the significant potential thrombotic complications, notably amputation or other loss of function, which would increase the number of QALYs saved by using enoxaparin. The inclusion of these complications would only strengthen this finding. Finally, we assumed equal efficacy for heparin and enoxaparin. The inclusion of superior efficacy of enoxaparin in subpopulations of medical inpatients would again only strengthen this finding.
Apart from the price of the medication, the incidence of HIT had the largest impact on costs and QALYs saved in the sensitivity analysis. Studies specific to VTE prophylaxis in medical inpatients could better define the incidence of HIT/T in this population, but this would not change our overall finding.
From an institutional perspective, the choice of heparin or enoxaparin is more complicated. In most but not all scenarios, the use of heparin appears to be more financially attractive. The prices of enoxaparin and heparin, the additional length of stay required to care for patients with HIT and HITT, and the percentage of total beds occupied all affect this decision. Several pieces of cost data, specifically those related to medication and laboratory testing, were specific to an MIHCS health care system, the type considered in the analysis and could potentially limit the applicability of this study to other institutions. However, the sensitivity analysis demonstrated that the cost of enoxaparin would have to be at least 60% lower, below $33/day, before affecting our conclusion, and then only if an institution were at full capacity. Thus, we expect that our results are generally applicable.
The potential limitations of this study are related to the assumptions required. However, our efficacy assumptions were conservatively based on published data. It is possible that a decrease in the rate of thrombosis if all cases of HIT were treated with argatroban could affect our findings. However, in the study by Lewis et al., the complication rate for those with HIT in the treatment group was 28% (versus 38.8% in the untreated group), consistent with rates used in our sensitivity analysis. DRG and physician reimbursements are based on published Medicare data. The greatest variation is likely to be in drug cost, as different institutions may negotiate lower prices. From a payer perspective, drug costs do not affect the conclusions; from an institutional perspective, drug cost may make the choice a complicated one. One factor not included in our analysis that may affect this decision is the possible impact of legal action on the medications institutions choose for VTE prophylaxis. Because the potential consequences of HITT can be so devastating, an institution could have difficulty defending the choice of heparin when an equally effective alternative with fewer adverse events was available. A settlement of $1 million could potentially pay for prophylaxis with enoxaparin for at least 2500 patients.
This analysis has highlighted one of the unfortunate paradoxes caused by the different, potentially competing incentives in our health care system. Payers and institutions often face different financial incentives. From a hospital's perspective, it may cost less to use an intervention that can potentially cause a greater number of complications and higher payer costs. We believe that for VTE prophylaxis for medical inpatients, improved patient outcomes coupled with decreased payer/societal costs argue strongly for the use of enoxaparin over unfractionated heparin and outweigh any institutional benefits.
- ,,, et al.A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients.N Eng J Med.1999;322:793–800.
- .Recommendations for prophylaxis of venous thromboembolism: International consensus and the American College of Chest Physicians Fifth Consensus Conference on Antithrombotic therapy.Curr Opin Pulm Med.2000;6:314–320.
- ,,, et al.Risk factors for venous thromboembolism in hospitalized patients with acute medical illness: analysis of the MEDENOX study.Arch Intern Med.2004;164:963–968.
- .Heparin–induced thrombocytopenia: pathogenesis and management.Br J Haematology.1003;121:535–555.
- .Heparin–induced thrombocytopenia diagnosis and management.Circulation.2004;110:e454–e458.
- .New approaches to the diagnosis of heparin–induced thrombocytopenia.Chest.2005;27(2 suppl):35S–45S.
- ,,, et al.Randomized comparison of enoxaparin with unfractionated heparin for the prevention of venous thromboembolism in medical patients with heart failure or severe respiratory disease.Am Heart J.2003;145:614–621.
- ,.Cost–effectiveness analysis of deep vein thrombosis prophylaxis in internal medicine patients.Thrombosis Res.1999;94:65–68.
- ,.,.Cost effectiveness of thromboprophylaxis with low–molecular–weight heparin versus unfractionated heparin in acutely ill medical inpatients.Am J Manag Care.2004;10:632–642.
- ,,, et al.Economic assessment of low–molecular–weight heparin (enoxaparin) versus unfractionated heparin in acute coronary syndrome patients: results from the ESSENCE Randomized Trial.Circulation.1998;97:1702–1707.
- ,, et al.Management of acute proximal deep vein thrombosis: pharmacoeconomic evaluation of outpatient treatment with enoxaparin vs inpatient treatment with unfractionated heparin.Chest.2002;122(1);108–114.
- ,,, et al.Prevention of deep–vein thrombosis following total hip replacement surgery with enoxaparin versus unfractionated heparin: a pharmacoeconomic evaluation.Ann Pharmacother.1994:28(2):271–275.
- ,.Cost–effectiveness of prolonged out–of–hospital prophylaxis with low–molecular–weight heparin following total hip replacement.Haemostasis.2000;30(suppl 2):130–135.
- ,,, et al.Cost effectiveness of a low–molecular–weight heparin in prolonged prophylaxis against deep vein thrombosis after total hip replacement.Pharmacoeconomics.1998;13:81–89.
- ,,, et al.Economic analysis of low–dose heparin vs the low–molecular–weight heparin enoxaparin for prevention of venous thromboembolism after colorectal surgery.Arch Intern Med.1999;159:1221–1228.
- .High risk of the critically ill for venous thromboembolism.Crit Care Med.1982;10:448–450.
- ,,, et al.Prevention of deep vein thrombosis in medical patients by low dose heparin.Scott Med J.1981;26:115–117.
- ,,, et al.Prevalence and prevention of deep venous thrombosis of the lower extremities in high–risk pulmonary patients.Angiology.1988;39:505–513.
- ,,, et al.A double–blind randomized trial of ORG 10172 low–molecular weight heparinoid versus unfractionated heparin in the prevention of deep venous thrombosis in patients with thrombotic stroke.Thromb Haemost.1991;65(suppl):753.
- ,,, et al.A double–blind and randomized placebo controlled trial of low molecular weight heparin once daily to prevent deep vein thrombosis in acute ischemic stroke.Semin Thromb Hemost.1990;16(suppl):25–33.
- ,,, et al.The incidence of heparin–induced thrombocytopenia in hospitalized medical patients treated with subcutaneous unfractionated heparin: a prospective cohort study.Blood.2003;101:2955–2959.
- ,,, et al.Heparin–induced thrombocytopenia in neurologic disease treated with unfractionated heparin.Neurology.2004;62:657–659.
- ,,, et al.Subcutaneous heparin versus low–molecular–weight heparin as thromboprophylaxis in patients undergoing colorectal surgery.Ann Surg2001;233:438–44.
- ,,, et al.Heparin–induced thrombocytopenia inpatients treated with low–molecular weight heparin or unfractionated heparin.N Eng J Med.1995;332:1330–1335.
- ,,, et al.An improved definition of heparin–induced thrombocytopenia in postoperative orthopedic patients.Arch Intern Med.2003;163:2518–2524.
- ,,, et al.Impact of patient population on the risk for heparin–induced thrombocytopenia.Blood.2000;96:1703–1708.
- ,,, et al.Heparin–induced thrombocytopenia and thrombosis: incidence, analysis of risk factors, and clinical outcomes in 108 consecutive patients treated at a single institution.Am J Hematol.1997;56(1):12–16.
- .., et al.Argatroban anticoagulation in patients with heparin–induced thrombocytopenia.Arch Intern Med.2003:163:1849–1856.
- ,,, et al.Antibodies to platelet factor 4–heparin after cardiopulmonary bypass in patients anticoagulated with unfractionated heparin or a low–molecular–weight heparin: clinical implications for heparin–induced thrombocytopenia.Circulation.1999;99:2530–2536.
- ,,, et.Al. Argatroban anticoagulant therapy in patients with heparin–induced thrombocytopenia.Circulation.2001;103:1838–1843.
- ,.A 14 year study of heparin–induced thrombocytopenia.Am J Med.1996;101:502–507.
- ,,, et al.Failure of early heparin cessation as treatment for heparin–induced thrombocytopenia.Am J Med.1999;106:629–635.
- CEA Registry,Harvard Center for Risk Analysis. Available at: http://www.hcra.harvard.edu/pdf/preferencescores.pdf.
- .Temporal aspects of heparin–induced thrombocytopenia.N Eng J Med.2001;344:1286–1292.
- National Center for Health Statistics. Available at: http://www.cdc.gov/nchs/.
- Centers for Medicare and Medicaid Services. Available at: http://www.cms.hhs.gov/.
- ,,, et al.A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients.N Eng J Med.1999;322:793–800.
- .Recommendations for prophylaxis of venous thromboembolism: International consensus and the American College of Chest Physicians Fifth Consensus Conference on Antithrombotic therapy.Curr Opin Pulm Med.2000;6:314–320.
- ,,, et al.Risk factors for venous thromboembolism in hospitalized patients with acute medical illness: analysis of the MEDENOX study.Arch Intern Med.2004;164:963–968.
- .Heparin–induced thrombocytopenia: pathogenesis and management.Br J Haematology.1003;121:535–555.
- .Heparin–induced thrombocytopenia diagnosis and management.Circulation.2004;110:e454–e458.
- .New approaches to the diagnosis of heparin–induced thrombocytopenia.Chest.2005;27(2 suppl):35S–45S.
- ,,, et al.Randomized comparison of enoxaparin with unfractionated heparin for the prevention of venous thromboembolism in medical patients with heart failure or severe respiratory disease.Am Heart J.2003;145:614–621.
- ,.Cost–effectiveness analysis of deep vein thrombosis prophylaxis in internal medicine patients.Thrombosis Res.1999;94:65–68.
- ,.,.Cost effectiveness of thromboprophylaxis with low–molecular–weight heparin versus unfractionated heparin in acutely ill medical inpatients.Am J Manag Care.2004;10:632–642.
- ,,, et al.Economic assessment of low–molecular–weight heparin (enoxaparin) versus unfractionated heparin in acute coronary syndrome patients: results from the ESSENCE Randomized Trial.Circulation.1998;97:1702–1707.
- ,, et al.Management of acute proximal deep vein thrombosis: pharmacoeconomic evaluation of outpatient treatment with enoxaparin vs inpatient treatment with unfractionated heparin.Chest.2002;122(1);108–114.
- ,,, et al.Prevention of deep–vein thrombosis following total hip replacement surgery with enoxaparin versus unfractionated heparin: a pharmacoeconomic evaluation.Ann Pharmacother.1994:28(2):271–275.
- ,.Cost–effectiveness of prolonged out–of–hospital prophylaxis with low–molecular–weight heparin following total hip replacement.Haemostasis.2000;30(suppl 2):130–135.
- ,,, et al.Cost effectiveness of a low–molecular–weight heparin in prolonged prophylaxis against deep vein thrombosis after total hip replacement.Pharmacoeconomics.1998;13:81–89.
- ,,, et al.Economic analysis of low–dose heparin vs the low–molecular–weight heparin enoxaparin for prevention of venous thromboembolism after colorectal surgery.Arch Intern Med.1999;159:1221–1228.
- .High risk of the critically ill for venous thromboembolism.Crit Care Med.1982;10:448–450.
- ,,, et al.Prevention of deep vein thrombosis in medical patients by low dose heparin.Scott Med J.1981;26:115–117.
- ,,, et al.Prevalence and prevention of deep venous thrombosis of the lower extremities in high–risk pulmonary patients.Angiology.1988;39:505–513.
- ,,, et al.A double–blind randomized trial of ORG 10172 low–molecular weight heparinoid versus unfractionated heparin in the prevention of deep venous thrombosis in patients with thrombotic stroke.Thromb Haemost.1991;65(suppl):753.
- ,,, et al.A double–blind and randomized placebo controlled trial of low molecular weight heparin once daily to prevent deep vein thrombosis in acute ischemic stroke.Semin Thromb Hemost.1990;16(suppl):25–33.
- ,,, et al.The incidence of heparin–induced thrombocytopenia in hospitalized medical patients treated with subcutaneous unfractionated heparin: a prospective cohort study.Blood.2003;101:2955–2959.
- ,,, et al.Heparin–induced thrombocytopenia in neurologic disease treated with unfractionated heparin.Neurology.2004;62:657–659.
- ,,, et al.Subcutaneous heparin versus low–molecular–weight heparin as thromboprophylaxis in patients undergoing colorectal surgery.Ann Surg2001;233:438–44.
- ,,, et al.Heparin–induced thrombocytopenia inpatients treated with low–molecular weight heparin or unfractionated heparin.N Eng J Med.1995;332:1330–1335.
- ,,, et al.An improved definition of heparin–induced thrombocytopenia in postoperative orthopedic patients.Arch Intern Med.2003;163:2518–2524.
- ,,, et al.Impact of patient population on the risk for heparin–induced thrombocytopenia.Blood.2000;96:1703–1708.
- ,,, et al.Heparin–induced thrombocytopenia and thrombosis: incidence, analysis of risk factors, and clinical outcomes in 108 consecutive patients treated at a single institution.Am J Hematol.1997;56(1):12–16.
- .., et al.Argatroban anticoagulation in patients with heparin–induced thrombocytopenia.Arch Intern Med.2003:163:1849–1856.
- ,,, et al.Antibodies to platelet factor 4–heparin after cardiopulmonary bypass in patients anticoagulated with unfractionated heparin or a low–molecular–weight heparin: clinical implications for heparin–induced thrombocytopenia.Circulation.1999;99:2530–2536.
- ,,, et.Al. Argatroban anticoagulant therapy in patients with heparin–induced thrombocytopenia.Circulation.2001;103:1838–1843.
- ,.A 14 year study of heparin–induced thrombocytopenia.Am J Med.1996;101:502–507.
- ,,, et al.Failure of early heparin cessation as treatment for heparin–induced thrombocytopenia.Am J Med.1999;106:629–635.
- CEA Registry,Harvard Center for Risk Analysis. Available at: http://www.hcra.harvard.edu/pdf/preferencescores.pdf.
- .Temporal aspects of heparin–induced thrombocytopenia.N Eng J Med.2001;344:1286–1292.
- National Center for Health Statistics. Available at: http://www.cdc.gov/nchs/.
- Centers for Medicare and Medicaid Services. Available at: http://www.cms.hhs.gov/.
Copyright © 2006 Society of Hospital Medicine
Editorial
People willingly believe what they wish.
Chinese fortune cookie
Being a hospitalist provides us with many rewards in life: a secure job, decent income, intellectually stimulating experiences at work, and gratification from helping the patients we encounter. Importantly, without patients none of this would be possible. Their role in our work lives and their personal experience in the hospital vary dramatically from ours, and that experience may be relatively invisible to many of us. Be honesthave you fully recognized the apprehension and even terror experienced by some patients when nightfall sweeps through the hospital wards and the commotion and attention of the day shift dissipates?1 Have you been fully aware of the desperate need of patients or their family members for timely communication of understandable information in the midst of critical illness?2 We willingly believe what we wishpatients and their families are having a comforting experience while hospitalized, and we are doing wonderful jobs as hospitalists caring for them. However, the lay press indicates that the patient's perception may differ radically from this reassuring point of view.3
To comprehend fully the hospital experience of patients and their families, we can benefit from them telling us their stories. The narrative stories from a patient1 and the wife of a patient2 clearly convey the apprehension and fear both patients and their loved ones suffer. Without this appreciation, we cannot empathetically deliver the care patients deserve. Not surprisingly, as medical technology guides physicians to focus more on the disease instead of the person, a backlash of an increasing emphasis on patient‐centered care is emerging.4, 5 Through short essays on illuminating experiences of physicians, patients, or families of patients, I hope to bring the patient's perspective to the forefront of hospital medicine care. View from the Hospital Bed can educate us about patients' perspectives on the experience of being hospitalized. We can also learn from the families of patients in View from the Hospital Room. The next time you recognize that a patient or family member has a potent story to tell (good or bad), encourage them to send it to us at the Journal of Hospital Medicine.
For the secret of the care of the patient is in caring for the patient.
Francis W. Peabody, MD
October 21, 1925
- .Uncharted waters.J Hosp Med.2006;1:136–137.
- .Hospitals foreign soil for those who don't work there.J Hosp Med.1006;1:70–72.
- .In the hospital, a degrading shift from person to patient.New York Times. Aug. 16,2005.
- .Towards a global definition of patient centred care.Br Med J.2001;322:444–445.
- ,.Engaging patients in medical decision making.Br Med J.2001;323:584–585.
People willingly believe what they wish.
Chinese fortune cookie
Being a hospitalist provides us with many rewards in life: a secure job, decent income, intellectually stimulating experiences at work, and gratification from helping the patients we encounter. Importantly, without patients none of this would be possible. Their role in our work lives and their personal experience in the hospital vary dramatically from ours, and that experience may be relatively invisible to many of us. Be honesthave you fully recognized the apprehension and even terror experienced by some patients when nightfall sweeps through the hospital wards and the commotion and attention of the day shift dissipates?1 Have you been fully aware of the desperate need of patients or their family members for timely communication of understandable information in the midst of critical illness?2 We willingly believe what we wishpatients and their families are having a comforting experience while hospitalized, and we are doing wonderful jobs as hospitalists caring for them. However, the lay press indicates that the patient's perception may differ radically from this reassuring point of view.3
To comprehend fully the hospital experience of patients and their families, we can benefit from them telling us their stories. The narrative stories from a patient1 and the wife of a patient2 clearly convey the apprehension and fear both patients and their loved ones suffer. Without this appreciation, we cannot empathetically deliver the care patients deserve. Not surprisingly, as medical technology guides physicians to focus more on the disease instead of the person, a backlash of an increasing emphasis on patient‐centered care is emerging.4, 5 Through short essays on illuminating experiences of physicians, patients, or families of patients, I hope to bring the patient's perspective to the forefront of hospital medicine care. View from the Hospital Bed can educate us about patients' perspectives on the experience of being hospitalized. We can also learn from the families of patients in View from the Hospital Room. The next time you recognize that a patient or family member has a potent story to tell (good or bad), encourage them to send it to us at the Journal of Hospital Medicine.
For the secret of the care of the patient is in caring for the patient.
Francis W. Peabody, MD
October 21, 1925
People willingly believe what they wish.
Chinese fortune cookie
Being a hospitalist provides us with many rewards in life: a secure job, decent income, intellectually stimulating experiences at work, and gratification from helping the patients we encounter. Importantly, without patients none of this would be possible. Their role in our work lives and their personal experience in the hospital vary dramatically from ours, and that experience may be relatively invisible to many of us. Be honesthave you fully recognized the apprehension and even terror experienced by some patients when nightfall sweeps through the hospital wards and the commotion and attention of the day shift dissipates?1 Have you been fully aware of the desperate need of patients or their family members for timely communication of understandable information in the midst of critical illness?2 We willingly believe what we wishpatients and their families are having a comforting experience while hospitalized, and we are doing wonderful jobs as hospitalists caring for them. However, the lay press indicates that the patient's perception may differ radically from this reassuring point of view.3
To comprehend fully the hospital experience of patients and their families, we can benefit from them telling us their stories. The narrative stories from a patient1 and the wife of a patient2 clearly convey the apprehension and fear both patients and their loved ones suffer. Without this appreciation, we cannot empathetically deliver the care patients deserve. Not surprisingly, as medical technology guides physicians to focus more on the disease instead of the person, a backlash of an increasing emphasis on patient‐centered care is emerging.4, 5 Through short essays on illuminating experiences of physicians, patients, or families of patients, I hope to bring the patient's perspective to the forefront of hospital medicine care. View from the Hospital Bed can educate us about patients' perspectives on the experience of being hospitalized. We can also learn from the families of patients in View from the Hospital Room. The next time you recognize that a patient or family member has a potent story to tell (good or bad), encourage them to send it to us at the Journal of Hospital Medicine.
For the secret of the care of the patient is in caring for the patient.
Francis W. Peabody, MD
October 21, 1925
- .Uncharted waters.J Hosp Med.2006;1:136–137.
- .Hospitals foreign soil for those who don't work there.J Hosp Med.1006;1:70–72.
- .In the hospital, a degrading shift from person to patient.New York Times. Aug. 16,2005.
- .Towards a global definition of patient centred care.Br Med J.2001;322:444–445.
- ,.Engaging patients in medical decision making.Br Med J.2001;323:584–585.
- .Uncharted waters.J Hosp Med.2006;1:136–137.
- .Hospitals foreign soil for those who don't work there.J Hosp Med.1006;1:70–72.
- .In the hospital, a degrading shift from person to patient.New York Times. Aug. 16,2005.
- .Towards a global definition of patient centred care.Br Med J.2001;322:444–445.
- ,.Engaging patients in medical decision making.Br Med J.2001;323:584–585.
Bluebonnet Revisited
Editor’s note: It has been several years since the story you are about to read took place, but my experiences as a hospitalist have given me a new perspective to this bittersweet tale.
My wife and I never contemplated a future without her. She was a part of our new family. Aside from a few rough black spots that needed to be removed, she seemed in perfect shape. She had been at our wedding, and we had spent countless days sunning on the beach and taking long drives with her through the Texas Hill Country spotting wildflowers. The Hill Country is where she got her nickname. Everyone called her Bluebonnet; the name just seemed to fit her. She brought special meaning to the number 69. People who saw her would just stop and wave. We were proud to be seen with her.
I left the house one fateful morning and found her in the street, motionless. I did everything I could to get her to move. I was sure she was dead. I could not get her to turn over. I ran inside and called for help. It seemed like forever until I could get someone on the phone. It was not long until the emergency vehicle arrived. A few quick maneuvers were made to get her going, but the efforts seemed doomed to failure. My wife and I watched sadly as she was carried away. Driving behind those eerie flashing lights, not a word was spoken.
We spent forever in a cheerless waiting room with antiquated magazines and lukewarm bitter coffee. The television mounted high on the wall blared a moronic game show. Imagining the worst-case scenario was far scarier than knowing the truth. Finally, a young man came to talk to us. His uniform was splattered with stains, and he looked like he hadn’t slept in a few days. He bellowed our name across the waiting room. I guessed there would be no privacy here.
He said that Bluebonnet was not going anywhere soon. He mentioned something about giving fluids and checking levels, but we did not understand the terminology. He said a specimen of fluid looked milky and the differential seemed abnormal and a pressure measurement was high. Was this supposed to mean something to us? He talked so fast, and no matter whether you know the lingo or not, when it’s a loved one it’s hard to concentrate.
Another hour went by. I stared at the receptionist, but she would not let me catch her eye. Sometime later, another man came out to meet with us. He wore a clean uniform and looked less harried. He said he was a Specialist in this kind of problem. What kind of problem was unclear to me. He never told us his name.
He started with the good news. He told us that Bluebonnet was responding now, that her balance was good, though her joints were worn out and that she had no gross motor abnormalities. It could be a disk problem, but probably not. This all seemed like good news. But then came the kicker; he had heard something strange during his evaluation. It was an odd rumbling sound and the Specialist wanted another opinion. He wanted the Expert.
By now we had accepted the fact that we were not going anywhere. We had been absorbed into the system, a fixture in the waiting room. Another set of pale faces was now illuminated by the television screen, searching for information, hoping for good news, but not expecting it. The coffee was starting to seem not that bad.
When the Expert came out he was friendly and invited us to watch while he made his comprehensive evaluation. He seemed thorough and competent. He did not ask us any questions; perhaps his colleagues had filled him in. Bluebonnet was not going to be doing any talking, that was obvious. The Expert’s nonchalant demeanor evaporated as he pulled his hand out from beneath her, his finger covered in something black and tarry. He suggested more testing and hooked her up to an erratically beeping monitor. He told us that his evaluation might take a while, and perhaps we should leave. He would call us when he had a better picture of what was going on. We sadly trudged home.
When we returned the next day we met with the Expert again. He said he had found the problem. Bluebonnet needed her valve replaced. As best I could understand it, there were two problems: The valve would not open completely so flow was obstructed, and the valve would not close completely either. I put my head on my wife’s more stoic shoulder and began to cry. We were not ready to make this kind of decision; Bluebonnet seemed too old for a procedure this aggressive.
We reminisced about the good times and the bad. We considered the cost and risks. There was no guarantee that a valve replacement would do the trick. A time comes in existence when the good memories can outweigh common sense. In the end, however, I had them remove her from the monitors. I drove her home, not knowing what to expect.
The next month was fairly quiet. I made sure she was turned over as much as possible. There were no problems, but she barely went out. It seemed like she was missing her usual spark. One warm Sunday, with much trepidation, I took her shopping. Half way to the mall she started to cough, then shook uncontrollably. I looked frantically around; what would I do if she died right in the street? I was in luck however, there was a small facility right on the corner and I nervously pulled into the entrance.
It was a small, private place. A few friends had gone there and were pleased with the results. It was run by an efficient young woman who immediately helped us. She ran the facility on her own—no big corporation telling her what to do and monitoring her bottom line. She listened to the whole story, and checked out Bluebonnet thoroughly. She patted Bluebonnet affectionately; you could tell she cared. She smiled as she told us that the new valve would last for years. It was not the valve at all, only bad gas.
We had several more years with her, and then she was gone. But we never forgot our time with our 1969 Cadillac convertible, Bluebonnet.
Rust in peace. TH
Jamie Newman, MD, FACP, is the physician editor of The Hospitalist, consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
Editor’s note: It has been several years since the story you are about to read took place, but my experiences as a hospitalist have given me a new perspective to this bittersweet tale.
My wife and I never contemplated a future without her. She was a part of our new family. Aside from a few rough black spots that needed to be removed, she seemed in perfect shape. She had been at our wedding, and we had spent countless days sunning on the beach and taking long drives with her through the Texas Hill Country spotting wildflowers. The Hill Country is where she got her nickname. Everyone called her Bluebonnet; the name just seemed to fit her. She brought special meaning to the number 69. People who saw her would just stop and wave. We were proud to be seen with her.
I left the house one fateful morning and found her in the street, motionless. I did everything I could to get her to move. I was sure she was dead. I could not get her to turn over. I ran inside and called for help. It seemed like forever until I could get someone on the phone. It was not long until the emergency vehicle arrived. A few quick maneuvers were made to get her going, but the efforts seemed doomed to failure. My wife and I watched sadly as she was carried away. Driving behind those eerie flashing lights, not a word was spoken.
We spent forever in a cheerless waiting room with antiquated magazines and lukewarm bitter coffee. The television mounted high on the wall blared a moronic game show. Imagining the worst-case scenario was far scarier than knowing the truth. Finally, a young man came to talk to us. His uniform was splattered with stains, and he looked like he hadn’t slept in a few days. He bellowed our name across the waiting room. I guessed there would be no privacy here.
He said that Bluebonnet was not going anywhere soon. He mentioned something about giving fluids and checking levels, but we did not understand the terminology. He said a specimen of fluid looked milky and the differential seemed abnormal and a pressure measurement was high. Was this supposed to mean something to us? He talked so fast, and no matter whether you know the lingo or not, when it’s a loved one it’s hard to concentrate.
Another hour went by. I stared at the receptionist, but she would not let me catch her eye. Sometime later, another man came out to meet with us. He wore a clean uniform and looked less harried. He said he was a Specialist in this kind of problem. What kind of problem was unclear to me. He never told us his name.
He started with the good news. He told us that Bluebonnet was responding now, that her balance was good, though her joints were worn out and that she had no gross motor abnormalities. It could be a disk problem, but probably not. This all seemed like good news. But then came the kicker; he had heard something strange during his evaluation. It was an odd rumbling sound and the Specialist wanted another opinion. He wanted the Expert.
By now we had accepted the fact that we were not going anywhere. We had been absorbed into the system, a fixture in the waiting room. Another set of pale faces was now illuminated by the television screen, searching for information, hoping for good news, but not expecting it. The coffee was starting to seem not that bad.
When the Expert came out he was friendly and invited us to watch while he made his comprehensive evaluation. He seemed thorough and competent. He did not ask us any questions; perhaps his colleagues had filled him in. Bluebonnet was not going to be doing any talking, that was obvious. The Expert’s nonchalant demeanor evaporated as he pulled his hand out from beneath her, his finger covered in something black and tarry. He suggested more testing and hooked her up to an erratically beeping monitor. He told us that his evaluation might take a while, and perhaps we should leave. He would call us when he had a better picture of what was going on. We sadly trudged home.
When we returned the next day we met with the Expert again. He said he had found the problem. Bluebonnet needed her valve replaced. As best I could understand it, there were two problems: The valve would not open completely so flow was obstructed, and the valve would not close completely either. I put my head on my wife’s more stoic shoulder and began to cry. We were not ready to make this kind of decision; Bluebonnet seemed too old for a procedure this aggressive.
We reminisced about the good times and the bad. We considered the cost and risks. There was no guarantee that a valve replacement would do the trick. A time comes in existence when the good memories can outweigh common sense. In the end, however, I had them remove her from the monitors. I drove her home, not knowing what to expect.
The next month was fairly quiet. I made sure she was turned over as much as possible. There were no problems, but she barely went out. It seemed like she was missing her usual spark. One warm Sunday, with much trepidation, I took her shopping. Half way to the mall she started to cough, then shook uncontrollably. I looked frantically around; what would I do if she died right in the street? I was in luck however, there was a small facility right on the corner and I nervously pulled into the entrance.
It was a small, private place. A few friends had gone there and were pleased with the results. It was run by an efficient young woman who immediately helped us. She ran the facility on her own—no big corporation telling her what to do and monitoring her bottom line. She listened to the whole story, and checked out Bluebonnet thoroughly. She patted Bluebonnet affectionately; you could tell she cared. She smiled as she told us that the new valve would last for years. It was not the valve at all, only bad gas.
We had several more years with her, and then she was gone. But we never forgot our time with our 1969 Cadillac convertible, Bluebonnet.
Rust in peace. TH
Jamie Newman, MD, FACP, is the physician editor of The Hospitalist, consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
Editor’s note: It has been several years since the story you are about to read took place, but my experiences as a hospitalist have given me a new perspective to this bittersweet tale.
My wife and I never contemplated a future without her. She was a part of our new family. Aside from a few rough black spots that needed to be removed, she seemed in perfect shape. She had been at our wedding, and we had spent countless days sunning on the beach and taking long drives with her through the Texas Hill Country spotting wildflowers. The Hill Country is where she got her nickname. Everyone called her Bluebonnet; the name just seemed to fit her. She brought special meaning to the number 69. People who saw her would just stop and wave. We were proud to be seen with her.
I left the house one fateful morning and found her in the street, motionless. I did everything I could to get her to move. I was sure she was dead. I could not get her to turn over. I ran inside and called for help. It seemed like forever until I could get someone on the phone. It was not long until the emergency vehicle arrived. A few quick maneuvers were made to get her going, but the efforts seemed doomed to failure. My wife and I watched sadly as she was carried away. Driving behind those eerie flashing lights, not a word was spoken.
We spent forever in a cheerless waiting room with antiquated magazines and lukewarm bitter coffee. The television mounted high on the wall blared a moronic game show. Imagining the worst-case scenario was far scarier than knowing the truth. Finally, a young man came to talk to us. His uniform was splattered with stains, and he looked like he hadn’t slept in a few days. He bellowed our name across the waiting room. I guessed there would be no privacy here.
He said that Bluebonnet was not going anywhere soon. He mentioned something about giving fluids and checking levels, but we did not understand the terminology. He said a specimen of fluid looked milky and the differential seemed abnormal and a pressure measurement was high. Was this supposed to mean something to us? He talked so fast, and no matter whether you know the lingo or not, when it’s a loved one it’s hard to concentrate.
Another hour went by. I stared at the receptionist, but she would not let me catch her eye. Sometime later, another man came out to meet with us. He wore a clean uniform and looked less harried. He said he was a Specialist in this kind of problem. What kind of problem was unclear to me. He never told us his name.
He started with the good news. He told us that Bluebonnet was responding now, that her balance was good, though her joints were worn out and that she had no gross motor abnormalities. It could be a disk problem, but probably not. This all seemed like good news. But then came the kicker; he had heard something strange during his evaluation. It was an odd rumbling sound and the Specialist wanted another opinion. He wanted the Expert.
By now we had accepted the fact that we were not going anywhere. We had been absorbed into the system, a fixture in the waiting room. Another set of pale faces was now illuminated by the television screen, searching for information, hoping for good news, but not expecting it. The coffee was starting to seem not that bad.
When the Expert came out he was friendly and invited us to watch while he made his comprehensive evaluation. He seemed thorough and competent. He did not ask us any questions; perhaps his colleagues had filled him in. Bluebonnet was not going to be doing any talking, that was obvious. The Expert’s nonchalant demeanor evaporated as he pulled his hand out from beneath her, his finger covered in something black and tarry. He suggested more testing and hooked her up to an erratically beeping monitor. He told us that his evaluation might take a while, and perhaps we should leave. He would call us when he had a better picture of what was going on. We sadly trudged home.
When we returned the next day we met with the Expert again. He said he had found the problem. Bluebonnet needed her valve replaced. As best I could understand it, there were two problems: The valve would not open completely so flow was obstructed, and the valve would not close completely either. I put my head on my wife’s more stoic shoulder and began to cry. We were not ready to make this kind of decision; Bluebonnet seemed too old for a procedure this aggressive.
We reminisced about the good times and the bad. We considered the cost and risks. There was no guarantee that a valve replacement would do the trick. A time comes in existence when the good memories can outweigh common sense. In the end, however, I had them remove her from the monitors. I drove her home, not knowing what to expect.
The next month was fairly quiet. I made sure she was turned over as much as possible. There were no problems, but she barely went out. It seemed like she was missing her usual spark. One warm Sunday, with much trepidation, I took her shopping. Half way to the mall she started to cough, then shook uncontrollably. I looked frantically around; what would I do if she died right in the street? I was in luck however, there was a small facility right on the corner and I nervously pulled into the entrance.
It was a small, private place. A few friends had gone there and were pleased with the results. It was run by an efficient young woman who immediately helped us. She ran the facility on her own—no big corporation telling her what to do and monitoring her bottom line. She listened to the whole story, and checked out Bluebonnet thoroughly. She patted Bluebonnet affectionately; you could tell she cared. She smiled as she told us that the new valve would last for years. It was not the valve at all, only bad gas.
We had several more years with her, and then she was gone. But we never forgot our time with our 1969 Cadillac convertible, Bluebonnet.
Rust in peace. TH
Jamie Newman, MD, FACP, is the physician editor of The Hospitalist, consultant, Hospital Internal Medicine, and assistant professor of internal medicine and medical history, Mayo Clinic College of Medicine, Rochester, Minn.
Hospital Med in the Land of Rocky Top
If a busy doctor is a happy doctor, then the hospitalists in the Methodist Medical Group at Methodist Hospital in Oak Ridge, Tenn., are ecstatic. Chris Frost, MD, the hospital medicine group’s chief hospitalist and medical director, has seen the group’s average daily census climb to 70, then 90, and now 100 patients. Fortunately, the group is growing, too, from nine full-time employees in late October 2005 to 12 before year-end, a projection for 15 by first quarter 2006, and several intensivists to help by March.
The hospital itself has grown as well: It’s in the midst of a $40 million renovation and expansion started in 2004. By August 2006, Methodist Medical will have 230 new private rooms, 12 beds in a new acute care unit, and an emergency department twice the size of its predecessor.

—Chris Frost, MD
How It Started
Methodist Medical Group has been shaped by Oak Ridge’s traditions and demographics. Nestled between the Great Smokey and Cumberland Mountains, Oak Ridge was one of three research and production sites for the Manhattan Project (an effort by the United States, in conjunction with Canada and the United Kingdom to develop nuclear weapons). At its height, Oak Ridge had 75,000 inhabitants. Now its population is 28,000, with a Medicare age group that comprises 42% more of its population than the average Tennessee city. It continues as a magnet for scientists, and its physicians—both office-based and hospitalists—form a close-knit community.
Given its dynamics and demographics, when Oak Ridge’s primary care physicians asked Methodist Hospital in 1993 for help in admitting their patients, the hospital responded affirmatively. Hospital President Jan McNally, BSN, MHA, recalls how things unfolded. “Dr. Richard Dew, a highly respected primary practice physician with a busy office, wanted to change his life. His son had died and he decided to close his office, but he wanted to stay in medicine in Oak Ridge. He agreed to practice inpatient medicine at Methodist,” she explains. “The beauty of it was that he was universally respected. Barriers to the program fell because the admitting doctors and the patients all knew him.”
When Dr. Dew retired in 2002, Anthony Garton, MD, who closed his solo practice to join Dr. Dew as Methodist’s second hospitalist, stayed on. Dr. Garton became a hospitalist because “office procedures just brought me to break even financially. Only the things I did that didn’t have office overhead, such as being medical director at a nursing home and doing physicals for Boeing, made sense financially.” Dr. Garton, who worked with a nephrology group for 13 years, made a smooth transition to a hospitalist career.
From the hospitalist program’s inception, Methodist turned to Team Health, Inc., of Knoxville, an outsourcer of medical personnel, for staffing. Team Health Vice President Kenneth Burns saw a natural fit; his firm already supplied Methodist’s emergency department physicians.
“We understood the problems faced by Methodist’s ED docs,” says Burns. “Patients got stuck there and couldn’t be admitted rapidly to inpatient floors.”
He identified the hospitalist’s necessary skills as an ability to cooperate with community physicians, and an interest in improving processes to boost care quality and decrease costs. Methodist’s hospitalists have been independent contractors since the program’s inception. They receive hourly wages plus incentives based on productivity and metrics negotiated with hospital administrators.
Team Health recently rethought the model as potential recruits balked. In 2006 Methodist’s hospitalists became employees, with health benefits and defined contribution plans. Hospitalist Helen Bidawid, MD, says being employees improves recruiting because many doctors—particularly those just out of residency—find getting loans, buying health insurance, and other business associated with independent contractor status troublesome.
Symbiosis
The relationship of Methodist’s hospitalist program to Oak Ridge’s community physicians has changed over the years. Early on the group hired a hospitalist Dr. Garton describes as “very bright, knew his medicine, and would wow them in academia, but he antagonized the local docs. He left after one year and that was good because our census got low.”
Tact wasn’t that hospitalist’s long suit, and the community doctors who were uncomfortable with him didn’t refer many patients to the hospitalists. With the odd man out, hiring new hospitalists such as Joel Perkerson, MD, put the program back on track.
Dr. Perkerson left an office practice he had been in for 12 years. “I was drowning in paperwork, and it was so frustrating,” he says. “I couldn’t get my homework done or help my son, who was struggling academically.”
Having been both an office- and a hospital-based physician in Oak Ridge, he says it’s too hectic to do both. Being a hospitalist is challenging enough.
“It’s like the movie ‘Field of Dreams.’ Build it, and they will come. Demand keeps growing for our services and we all work a lot of hours,” he says, crediting the increasing load both to Dr. Frost’s leadership, which has made the subspecialists comfortable with the hospitalists’ management of medically complex patients, and to ex-TennCare patients flooding the emergency department. (See “When Politics Collide with Healthcare,” p. 38.)
Under Dr. Frost’s direction (he took over as medical director in 2003 after being recruited as assistant medical director), the hospitalist program has thrived. Dr. Frost has built relationships with Oak Ridge’s subspecialists, particularly pulmonologists, hematologists, oncologists, gastroenterologists, and orthopedists. Typical of Dr. Frost’s leadership is his response to Oak Ridge’s only pulmonary group imploding from six physicians to two. The hospitalists now admit all the group’s patients and Dr. Frost worked with Team Health to recruit intensivists for those very ill patients.
“I’m very pleased with the growth of the hospitalist program,” says Dr. Frost. “We feel empowered that more and more primary care doctors and subspecialists are allowing us to admit and take an active role in managing their patients.”
Tackling one problem that has bedeviled other hospitalist programs, Jan McNally has added a mechanism to ensure cooperation from referring doctors. She expects referring subspecialists to come for consults ASAP when a hospitalist calls.
“We must have that commitment from specialists,” she says. “We have about 15 percent who are laggards, but we will impose disciplinary action if they don’t come when called.”
Dr. Frost favors specialists willing to turn their patients over to the hospitalists in order to improve care quality. He diligently writes care guidelines, focuses on core measures, has deepened discussion of end-of-life care issues, and built such strong esprit de corps that the hospitalists willingly work long and irregular schedules until more physicians arrive. Helen Bidawid, MD, who has been a Methodist hospitalist for about a year, enjoys the hospitalist group, doesn’t mind pitching in to support her colleagues, and says “we function very well together. We watch out for all of our patients, share our responsibilities, and ask each other for help.”
Dr. Bidawid, who was in a non-supportive hospitalist group before her current position, asked herself before she arrived at Methodist: “’Will I be nurtured here or thrown to the wolves?’ Fortunately, I found a very supportive environment.”
With the course set, Dr. Frost still has challenges ahead. There’s growing patient volume, more complex cases to co-manage, carve-outs such as cardiology, neurology, and stroke care, and TennCare disenrollees to contend with.
“Our goal is to add value to Methodist Medical Center,” he says. “As a 24/7 hospitalist program, we help the medical community to be more profitable by enabling them to see more patients in the office and doing more procedures in the hospital. Better communication between physicians, patients, and their families benefits everyone and, we hope, will grow Methodist’s market share.” TH
Marlene Piturro is based in New York.
If a busy doctor is a happy doctor, then the hospitalists in the Methodist Medical Group at Methodist Hospital in Oak Ridge, Tenn., are ecstatic. Chris Frost, MD, the hospital medicine group’s chief hospitalist and medical director, has seen the group’s average daily census climb to 70, then 90, and now 100 patients. Fortunately, the group is growing, too, from nine full-time employees in late October 2005 to 12 before year-end, a projection for 15 by first quarter 2006, and several intensivists to help by March.
The hospital itself has grown as well: It’s in the midst of a $40 million renovation and expansion started in 2004. By August 2006, Methodist Medical will have 230 new private rooms, 12 beds in a new acute care unit, and an emergency department twice the size of its predecessor.

—Chris Frost, MD
How It Started
Methodist Medical Group has been shaped by Oak Ridge’s traditions and demographics. Nestled between the Great Smokey and Cumberland Mountains, Oak Ridge was one of three research and production sites for the Manhattan Project (an effort by the United States, in conjunction with Canada and the United Kingdom to develop nuclear weapons). At its height, Oak Ridge had 75,000 inhabitants. Now its population is 28,000, with a Medicare age group that comprises 42% more of its population than the average Tennessee city. It continues as a magnet for scientists, and its physicians—both office-based and hospitalists—form a close-knit community.
Given its dynamics and demographics, when Oak Ridge’s primary care physicians asked Methodist Hospital in 1993 for help in admitting their patients, the hospital responded affirmatively. Hospital President Jan McNally, BSN, MHA, recalls how things unfolded. “Dr. Richard Dew, a highly respected primary practice physician with a busy office, wanted to change his life. His son had died and he decided to close his office, but he wanted to stay in medicine in Oak Ridge. He agreed to practice inpatient medicine at Methodist,” she explains. “The beauty of it was that he was universally respected. Barriers to the program fell because the admitting doctors and the patients all knew him.”
When Dr. Dew retired in 2002, Anthony Garton, MD, who closed his solo practice to join Dr. Dew as Methodist’s second hospitalist, stayed on. Dr. Garton became a hospitalist because “office procedures just brought me to break even financially. Only the things I did that didn’t have office overhead, such as being medical director at a nursing home and doing physicals for Boeing, made sense financially.” Dr. Garton, who worked with a nephrology group for 13 years, made a smooth transition to a hospitalist career.
From the hospitalist program’s inception, Methodist turned to Team Health, Inc., of Knoxville, an outsourcer of medical personnel, for staffing. Team Health Vice President Kenneth Burns saw a natural fit; his firm already supplied Methodist’s emergency department physicians.
“We understood the problems faced by Methodist’s ED docs,” says Burns. “Patients got stuck there and couldn’t be admitted rapidly to inpatient floors.”
He identified the hospitalist’s necessary skills as an ability to cooperate with community physicians, and an interest in improving processes to boost care quality and decrease costs. Methodist’s hospitalists have been independent contractors since the program’s inception. They receive hourly wages plus incentives based on productivity and metrics negotiated with hospital administrators.
Team Health recently rethought the model as potential recruits balked. In 2006 Methodist’s hospitalists became employees, with health benefits and defined contribution plans. Hospitalist Helen Bidawid, MD, says being employees improves recruiting because many doctors—particularly those just out of residency—find getting loans, buying health insurance, and other business associated with independent contractor status troublesome.
Symbiosis
The relationship of Methodist’s hospitalist program to Oak Ridge’s community physicians has changed over the years. Early on the group hired a hospitalist Dr. Garton describes as “very bright, knew his medicine, and would wow them in academia, but he antagonized the local docs. He left after one year and that was good because our census got low.”
Tact wasn’t that hospitalist’s long suit, and the community doctors who were uncomfortable with him didn’t refer many patients to the hospitalists. With the odd man out, hiring new hospitalists such as Joel Perkerson, MD, put the program back on track.
Dr. Perkerson left an office practice he had been in for 12 years. “I was drowning in paperwork, and it was so frustrating,” he says. “I couldn’t get my homework done or help my son, who was struggling academically.”
Having been both an office- and a hospital-based physician in Oak Ridge, he says it’s too hectic to do both. Being a hospitalist is challenging enough.
“It’s like the movie ‘Field of Dreams.’ Build it, and they will come. Demand keeps growing for our services and we all work a lot of hours,” he says, crediting the increasing load both to Dr. Frost’s leadership, which has made the subspecialists comfortable with the hospitalists’ management of medically complex patients, and to ex-TennCare patients flooding the emergency department. (See “When Politics Collide with Healthcare,” p. 38.)
Under Dr. Frost’s direction (he took over as medical director in 2003 after being recruited as assistant medical director), the hospitalist program has thrived. Dr. Frost has built relationships with Oak Ridge’s subspecialists, particularly pulmonologists, hematologists, oncologists, gastroenterologists, and orthopedists. Typical of Dr. Frost’s leadership is his response to Oak Ridge’s only pulmonary group imploding from six physicians to two. The hospitalists now admit all the group’s patients and Dr. Frost worked with Team Health to recruit intensivists for those very ill patients.
“I’m very pleased with the growth of the hospitalist program,” says Dr. Frost. “We feel empowered that more and more primary care doctors and subspecialists are allowing us to admit and take an active role in managing their patients.”
Tackling one problem that has bedeviled other hospitalist programs, Jan McNally has added a mechanism to ensure cooperation from referring doctors. She expects referring subspecialists to come for consults ASAP when a hospitalist calls.
“We must have that commitment from specialists,” she says. “We have about 15 percent who are laggards, but we will impose disciplinary action if they don’t come when called.”
Dr. Frost favors specialists willing to turn their patients over to the hospitalists in order to improve care quality. He diligently writes care guidelines, focuses on core measures, has deepened discussion of end-of-life care issues, and built such strong esprit de corps that the hospitalists willingly work long and irregular schedules until more physicians arrive. Helen Bidawid, MD, who has been a Methodist hospitalist for about a year, enjoys the hospitalist group, doesn’t mind pitching in to support her colleagues, and says “we function very well together. We watch out for all of our patients, share our responsibilities, and ask each other for help.”
Dr. Bidawid, who was in a non-supportive hospitalist group before her current position, asked herself before she arrived at Methodist: “’Will I be nurtured here or thrown to the wolves?’ Fortunately, I found a very supportive environment.”
With the course set, Dr. Frost still has challenges ahead. There’s growing patient volume, more complex cases to co-manage, carve-outs such as cardiology, neurology, and stroke care, and TennCare disenrollees to contend with.
“Our goal is to add value to Methodist Medical Center,” he says. “As a 24/7 hospitalist program, we help the medical community to be more profitable by enabling them to see more patients in the office and doing more procedures in the hospital. Better communication between physicians, patients, and their families benefits everyone and, we hope, will grow Methodist’s market share.” TH
Marlene Piturro is based in New York.
If a busy doctor is a happy doctor, then the hospitalists in the Methodist Medical Group at Methodist Hospital in Oak Ridge, Tenn., are ecstatic. Chris Frost, MD, the hospital medicine group’s chief hospitalist and medical director, has seen the group’s average daily census climb to 70, then 90, and now 100 patients. Fortunately, the group is growing, too, from nine full-time employees in late October 2005 to 12 before year-end, a projection for 15 by first quarter 2006, and several intensivists to help by March.
The hospital itself has grown as well: It’s in the midst of a $40 million renovation and expansion started in 2004. By August 2006, Methodist Medical will have 230 new private rooms, 12 beds in a new acute care unit, and an emergency department twice the size of its predecessor.

—Chris Frost, MD
How It Started
Methodist Medical Group has been shaped by Oak Ridge’s traditions and demographics. Nestled between the Great Smokey and Cumberland Mountains, Oak Ridge was one of three research and production sites for the Manhattan Project (an effort by the United States, in conjunction with Canada and the United Kingdom to develop nuclear weapons). At its height, Oak Ridge had 75,000 inhabitants. Now its population is 28,000, with a Medicare age group that comprises 42% more of its population than the average Tennessee city. It continues as a magnet for scientists, and its physicians—both office-based and hospitalists—form a close-knit community.
Given its dynamics and demographics, when Oak Ridge’s primary care physicians asked Methodist Hospital in 1993 for help in admitting their patients, the hospital responded affirmatively. Hospital President Jan McNally, BSN, MHA, recalls how things unfolded. “Dr. Richard Dew, a highly respected primary practice physician with a busy office, wanted to change his life. His son had died and he decided to close his office, but he wanted to stay in medicine in Oak Ridge. He agreed to practice inpatient medicine at Methodist,” she explains. “The beauty of it was that he was universally respected. Barriers to the program fell because the admitting doctors and the patients all knew him.”
When Dr. Dew retired in 2002, Anthony Garton, MD, who closed his solo practice to join Dr. Dew as Methodist’s second hospitalist, stayed on. Dr. Garton became a hospitalist because “office procedures just brought me to break even financially. Only the things I did that didn’t have office overhead, such as being medical director at a nursing home and doing physicals for Boeing, made sense financially.” Dr. Garton, who worked with a nephrology group for 13 years, made a smooth transition to a hospitalist career.
From the hospitalist program’s inception, Methodist turned to Team Health, Inc., of Knoxville, an outsourcer of medical personnel, for staffing. Team Health Vice President Kenneth Burns saw a natural fit; his firm already supplied Methodist’s emergency department physicians.
“We understood the problems faced by Methodist’s ED docs,” says Burns. “Patients got stuck there and couldn’t be admitted rapidly to inpatient floors.”
He identified the hospitalist’s necessary skills as an ability to cooperate with community physicians, and an interest in improving processes to boost care quality and decrease costs. Methodist’s hospitalists have been independent contractors since the program’s inception. They receive hourly wages plus incentives based on productivity and metrics negotiated with hospital administrators.
Team Health recently rethought the model as potential recruits balked. In 2006 Methodist’s hospitalists became employees, with health benefits and defined contribution plans. Hospitalist Helen Bidawid, MD, says being employees improves recruiting because many doctors—particularly those just out of residency—find getting loans, buying health insurance, and other business associated with independent contractor status troublesome.
Symbiosis
The relationship of Methodist’s hospitalist program to Oak Ridge’s community physicians has changed over the years. Early on the group hired a hospitalist Dr. Garton describes as “very bright, knew his medicine, and would wow them in academia, but he antagonized the local docs. He left after one year and that was good because our census got low.”
Tact wasn’t that hospitalist’s long suit, and the community doctors who were uncomfortable with him didn’t refer many patients to the hospitalists. With the odd man out, hiring new hospitalists such as Joel Perkerson, MD, put the program back on track.
Dr. Perkerson left an office practice he had been in for 12 years. “I was drowning in paperwork, and it was so frustrating,” he says. “I couldn’t get my homework done or help my son, who was struggling academically.”
Having been both an office- and a hospital-based physician in Oak Ridge, he says it’s too hectic to do both. Being a hospitalist is challenging enough.
“It’s like the movie ‘Field of Dreams.’ Build it, and they will come. Demand keeps growing for our services and we all work a lot of hours,” he says, crediting the increasing load both to Dr. Frost’s leadership, which has made the subspecialists comfortable with the hospitalists’ management of medically complex patients, and to ex-TennCare patients flooding the emergency department. (See “When Politics Collide with Healthcare,” p. 38.)
Under Dr. Frost’s direction (he took over as medical director in 2003 after being recruited as assistant medical director), the hospitalist program has thrived. Dr. Frost has built relationships with Oak Ridge’s subspecialists, particularly pulmonologists, hematologists, oncologists, gastroenterologists, and orthopedists. Typical of Dr. Frost’s leadership is his response to Oak Ridge’s only pulmonary group imploding from six physicians to two. The hospitalists now admit all the group’s patients and Dr. Frost worked with Team Health to recruit intensivists for those very ill patients.
“I’m very pleased with the growth of the hospitalist program,” says Dr. Frost. “We feel empowered that more and more primary care doctors and subspecialists are allowing us to admit and take an active role in managing their patients.”
Tackling one problem that has bedeviled other hospitalist programs, Jan McNally has added a mechanism to ensure cooperation from referring doctors. She expects referring subspecialists to come for consults ASAP when a hospitalist calls.
“We must have that commitment from specialists,” she says. “We have about 15 percent who are laggards, but we will impose disciplinary action if they don’t come when called.”
Dr. Frost favors specialists willing to turn their patients over to the hospitalists in order to improve care quality. He diligently writes care guidelines, focuses on core measures, has deepened discussion of end-of-life care issues, and built such strong esprit de corps that the hospitalists willingly work long and irregular schedules until more physicians arrive. Helen Bidawid, MD, who has been a Methodist hospitalist for about a year, enjoys the hospitalist group, doesn’t mind pitching in to support her colleagues, and says “we function very well together. We watch out for all of our patients, share our responsibilities, and ask each other for help.”
Dr. Bidawid, who was in a non-supportive hospitalist group before her current position, asked herself before she arrived at Methodist: “’Will I be nurtured here or thrown to the wolves?’ Fortunately, I found a very supportive environment.”
With the course set, Dr. Frost still has challenges ahead. There’s growing patient volume, more complex cases to co-manage, carve-outs such as cardiology, neurology, and stroke care, and TennCare disenrollees to contend with.
“Our goal is to add value to Methodist Medical Center,” he says. “As a 24/7 hospitalist program, we help the medical community to be more profitable by enabling them to see more patients in the office and doing more procedures in the hospital. Better communication between physicians, patients, and their families benefits everyone and, we hope, will grow Methodist’s market share.” TH
Marlene Piturro is based in New York.
Principal Investigations
What can you do with a quarter of a million dollars? In some places, that amount can buy a home that can shelter a family for decades. In other places, it is enough to pay annual malpractice insurance premiums for physicians practicing in high-risk specialties—with a little left over.
But if you wanted to use that money for an enduring healthcare project that would provide the most good for the most people, how would you do it? Hospitalists can look to the Agency for Healthcare Research and Quality (AHRQ) for stellar examples of well-invested dollars with excellent return.
AHRQ Funding
With a staff of approximately 300, the tiny AHRQ is the lead federal agency charged with improving the quality, safety, efficiency, and effectiveness of healthcare for all Americans. It creates a priority research agenda annually, and funds studies in areas where improvement is deemed most needed. These include patient safety, data development, pharmaceutical outcomes, and other areas described on its Web site (www.ahrq.gov/).
In 2005, AHRQ announced its Partnerships in Implementing Patient Safety (PIPS) and committed up to $9 million in total costs to fund new grants of less than $300,000 per year, lasting two years. AHRQ indicated that eligible safe practice intervention projects would be required to include “tool kits,” and a comprehensive implementation tool kit to help others overcome barriers and allay adoption concerns. AHRQ’s goal was and is to disseminate funded projects’ perfected tools widely for adaptation and/or adoption by diverse healthcare settings.
AHRQ asked that principal investigators (PIs) be experienced senior level individuals familiar with implementing change in healthcare settings. Their expectation was that PIs would devote at least 15% of their time to the project for its duration. Thus the competitive challenge to potential PIs was great:
- Select a worthy project from among the endless areas where healthcare needs improvement, and then plan specific, realistic, achievable interventions that could create measurable improvement over two years;
- Implement the program; and
- Develop a plan and tools so basic and user-friendly that they could feasibly be applied in not just the local practice setting, but in other healthcare settings.
Although the size and duration of the awards varied, many of the 17 projects they funded received slightly more than a quarter of a million dollars. Among the funded projects, two boast hospitalists as their PIs and address areas of obvious concern in most healthcare settings. Greg Maynard, MD, MS, at the University of California, San Diego, was funded to implement a venous thromboembolism (VTE) intervention program. And Mark V. Williams, MD, FACP, professor of medicine, Emory University School of Medicine, Atlanta, and editor of the Journal of Hospital Medicine, was funded to implement a discharge bundle of patient safety interventions respectively.
Stalking the Silent Killer
Dr. Maynard’s project, “Optimal Prevention of Hospital Acquired Venous Thromboembolism,” focuses on eliminating preventable hospital-acquired VTE at an academic healthcare facility that has a large population of Hispanic patients.
The project’s timeliness and utility is clear: Although the exact incidence of VTE is unknown, experts estimate that approximately 260,000 are clinically recognized annually in acutely hospitalized patients.1 Pulmonary embolism (PE) resulting from deep vein thrombosis (DVT) is the most common cause of preventable hospital death, the majority of hospitalized patients with risk factors for DVT receive no prophylaxis, and the rate of fatal PE more than doubles between age 50 and 80.2,3 The problem is easily recognizable, but “Getting people to do what they need to do to prevent VTE can be hard,” says Dr. Maynard.
This project was carefully planned. It used a rigorous quality improvement process, involving all appropriate clinicians, nurses, managers, and technical support personnel.
Dr. Maynard and his team anticipated roadblocks and negotiated in advance to reduce their effects. They accepted that when patients are hospitalized, things frequently happen that cause physicians to stop VTE prophylaxis: A hemoglobin or platelet count may fall, the patient may have difficulty taking the drug, or the patient’s status may change abruptly. Or the prophylaxis might be accidentally discontinued—perhaps when a patient is transferred.
The team also looked at other institutions’ solutions. Then, using a basic understanding of the ways in which their process was missing VTE prophylaxis opportunities, they built interventions.
This team considered logistics carefully because it was clear that the only intervention that could decrease risk would have to be repetitive in nature. “The process we ultimately selected is very, very quick, yet valid,” says Dr. Maynard, while acknowledging that presenting any intervention repeatedly has the potential to interfere with care. “Other models require the physician to use math and add points. This one does not, and takes only seconds.”
Beginning April 19, 2006, the University of California, San Diego (UCSD) will introduce an intervention that presents a VTE risk assessment screen on every patient who is admitted. This process inquires about the need for prophylaxis every three days for the duration of hospitalization, and physicians cannot skip the screen. If risk factors are present and bleeding risk is not, the screen presents appropriate VTE options.
For example, the system will suggest enoxaparin 40 mg daily, enoxaparin 30 mg twice daily, or appropriately dosed warfarin for a high-risk orthopedic surgery patient who has no bleeding risk. Every three days, the process repeats itself, making explicit decisions or suggestions about appropriate prophylaxis. (Figure 1, below, shows a sample screen for a patient with moderately high risk.
Much evidence about VTE is still being gathered. For example, opinions vary about when to start prophylaxis or how long to continue it. Dr. Maynard and his team also addressed real versus relative contraindications—another area of debate among clinicians. Many clinicians are uncertain about how soon after surgery to restart VTE prophylaxis. After orthopedic spine surgery, for example, some might start it on day five, while others may not restart prophylaxis even after day 10. At UCSD, clinical stakeholders in the process came to consensus, and now all restart by day seven.
The tool kit UCSD is developing recognizes that every institution is unique. Those that choose to implement a similar program must identify their baseline rate of VTE and monitor change over time to determine if progress is being made. Every institution must define adequate VTE prophylaxis and tailor the tools appropriately.
Wait? No Need
One compelling aspect of Dr. Maynard’s project is that some of UCSD’s VTE tools are already available on the SHM Web site in the “VTE Resource Room.” With or without AHRQ funding, UCSD planned to develop and implement a VTE awareness program. UCSD’s grant department provided the support Dr. Maynard and his colleagues needed to apply for the AHRQ funding, and Dr. Maynard says the funding they received helped UCSD “disseminate the program better and to carry it out with more rigor.”
UCSD worked with SHM to develop the tool kit. In return, SHM is providing and promoting the VTE tool kit at no charge to interested parties. Additionally, SHM recently received funding via an unrestricted sponsorship to create a mentored implementation project for the “VTE Resource Room.” Interested institutions will be mentored by UCSD staff who have experience with the tool kit.
Over time, Dr. Maynard will measure the effects of the intervention to ensure it is working. In addition to creating a malleable tool kit, UCSD research hospitalists will examine race, gender, and age to determine the effects of these on the likelihood of getting adequate prophylaxis.
Hospital Patient Safe-D(ischarge)
Dr. Williams and his colleagues at Emory University and the University of Ottawa received funding for “Hospital Patient Safe-D(ischarge): A Discharge Bundle for Patients,” a program that builds on previous AHRQ funding. This intervention implements a “discharge bundle” of patient safety interventions to improve patient transition from the hospital to home or another healthcare setting.
“We hope that every patient will undergo discharge, and of course the majority do, but the discharge process has almost been treated as an afterthought,” explains Dr. Williams. “Doctors spend a lot of time on diagnosis and treatment, but not on discharge. This process of transition from total care with a call button, lots of nursing attention, daily visits from the doctor, and delivered meals to greater independence, has not been well researched.”
What little research exists tends to indicate that discharge processes are very heterogeneous.
So far, Dr. Williams’ team’s examination of the process has produced only one surprise: The team has discovered that the discharge process is even more capricious than they suspected. As patients prepare to leave the hospital, what could and should be an orderly process that educates and prepares patients to assume responsibility for their own care in a new and better way is often interrupted or disjointed.
Preparing patients for discharge once fell to the nursing staff. As nursing faces staffing shortages and expanded roles, the discharge process often belongs to everyone and to no one. That physicians’ discharge visits pay much less than the time required to do it well also complicates the problem. The researchers were not surprised, however, to learn that many patients do not know their diagnosis or treatment plan as discharge is imminent. Their goal is to develop a consistent, comprehensive discharge process that will be a national model.
Here again, the precepts of continuous quality improvement are apparent. Dr. Williams’ team’s effort represents collaboration among physicians, pharmacists, nurses, and patients; involves SHM and several other professional organizations; and calls upon an advisory committee consisting of nationally recognized patient care and safety experts.
The discharge bundle of patient safety interventions—a concept advocated by the Joint Commission on Accreditation of Healthcare Organizations and other quality-promoting groups—adds a post-discharge continuity check to medication reconciliation and patient-centered education at discharge.
The four project phases—implement, evaluate, develop a tool, and disseminate the discharge bundle—overlap and ensure success.
Dr. Williams believes that the group of patients most likely to benefit from this intervention is the elderly. “The elderly bear the greatest burden of chronic disease and typically have several concurrent health problems,” he says.
Educating elders at the time of discharge should decrease the medication error rate and improve adherence to other treatments and recommended lifestyle changes. To gauge the appropriateness of the discharge bundle, John Banja, PhD, an expert in communication and safety, observes the discharge process directly. All communications must be patient-centered, and thus presented in a manner that patients will understand and appreciate. Banja relies on his background in patient safety and disability/rehabilitation to assess the discharge process.
Initial enrollment in this study seems successful. More than 50 patients have consented to participate, but Banja projects a need for 200 to complete the entire process. Recently, the team increased its planned maximum accrual to 300 to increase the statistical power of their findings. The participants like the program because most of them find discharge somewhat discomforting. Patients know they have knowledge gaps and appreciate clinicians’ efforts to fill those gaps seamlessly. A small investment of time can prevent problems after discharge.
Added Value
Clearly, the findings from these AHRQ-funded studies have the potential to reduce morbidity and mortality in a logarithmic manner as other institutions adapt these new tool kits. Dr. Williams indicates that recipients of PIPS funding receive more than just funding and the satisfaction of creating tools that will help all Americans.
“The AHRQ sponsors quarterly conference calls for all participants, regardless of their research topic, and an annual meeting in June to bring all investigators together,” he says.
The opportunity to learn how others address problems, plan interventions, and tackle hurdles proves invaluable. In addition, being privy to interim study results or learning how others handle research dilemmas helps hospitalists expand their skill sets.
Listening to Drs. Maynard and Williams is a not-so-subtle reminder that every hospital needs a well-structured quality improvement plan, and that hospitalists are essential in the plan’s success. Every hospitalist needs an understanding of the precepts these PIs used to earn this well-deserved funding: interdisciplinary and professional organization collaboration, good communication, realistic planning, managing change by measuring, and above all, sharing success. TH
Jeannette Yeznach Wick, RPh, MBA, FASCP, is a freelance medical writer based in Arlington, Va.
References
- Anderson FA Jr, Wheeler HB, Goldberg RJ, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med. 1991 May;151(5):933-938.
- Clagett GP, Anderson FA Jr, Heit J, et al. Prevention of venous thromboembolism. Chest. 1995 Oct;108(4 Suppl):312S-334S.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest. 2001;119(1 Suppl):132S-175S.
What can you do with a quarter of a million dollars? In some places, that amount can buy a home that can shelter a family for decades. In other places, it is enough to pay annual malpractice insurance premiums for physicians practicing in high-risk specialties—with a little left over.
But if you wanted to use that money for an enduring healthcare project that would provide the most good for the most people, how would you do it? Hospitalists can look to the Agency for Healthcare Research and Quality (AHRQ) for stellar examples of well-invested dollars with excellent return.
AHRQ Funding
With a staff of approximately 300, the tiny AHRQ is the lead federal agency charged with improving the quality, safety, efficiency, and effectiveness of healthcare for all Americans. It creates a priority research agenda annually, and funds studies in areas where improvement is deemed most needed. These include patient safety, data development, pharmaceutical outcomes, and other areas described on its Web site (www.ahrq.gov/).
In 2005, AHRQ announced its Partnerships in Implementing Patient Safety (PIPS) and committed up to $9 million in total costs to fund new grants of less than $300,000 per year, lasting two years. AHRQ indicated that eligible safe practice intervention projects would be required to include “tool kits,” and a comprehensive implementation tool kit to help others overcome barriers and allay adoption concerns. AHRQ’s goal was and is to disseminate funded projects’ perfected tools widely for adaptation and/or adoption by diverse healthcare settings.
AHRQ asked that principal investigators (PIs) be experienced senior level individuals familiar with implementing change in healthcare settings. Their expectation was that PIs would devote at least 15% of their time to the project for its duration. Thus the competitive challenge to potential PIs was great:
- Select a worthy project from among the endless areas where healthcare needs improvement, and then plan specific, realistic, achievable interventions that could create measurable improvement over two years;
- Implement the program; and
- Develop a plan and tools so basic and user-friendly that they could feasibly be applied in not just the local practice setting, but in other healthcare settings.
Although the size and duration of the awards varied, many of the 17 projects they funded received slightly more than a quarter of a million dollars. Among the funded projects, two boast hospitalists as their PIs and address areas of obvious concern in most healthcare settings. Greg Maynard, MD, MS, at the University of California, San Diego, was funded to implement a venous thromboembolism (VTE) intervention program. And Mark V. Williams, MD, FACP, professor of medicine, Emory University School of Medicine, Atlanta, and editor of the Journal of Hospital Medicine, was funded to implement a discharge bundle of patient safety interventions respectively.
Stalking the Silent Killer
Dr. Maynard’s project, “Optimal Prevention of Hospital Acquired Venous Thromboembolism,” focuses on eliminating preventable hospital-acquired VTE at an academic healthcare facility that has a large population of Hispanic patients.
The project’s timeliness and utility is clear: Although the exact incidence of VTE is unknown, experts estimate that approximately 260,000 are clinically recognized annually in acutely hospitalized patients.1 Pulmonary embolism (PE) resulting from deep vein thrombosis (DVT) is the most common cause of preventable hospital death, the majority of hospitalized patients with risk factors for DVT receive no prophylaxis, and the rate of fatal PE more than doubles between age 50 and 80.2,3 The problem is easily recognizable, but “Getting people to do what they need to do to prevent VTE can be hard,” says Dr. Maynard.
This project was carefully planned. It used a rigorous quality improvement process, involving all appropriate clinicians, nurses, managers, and technical support personnel.
Dr. Maynard and his team anticipated roadblocks and negotiated in advance to reduce their effects. They accepted that when patients are hospitalized, things frequently happen that cause physicians to stop VTE prophylaxis: A hemoglobin or platelet count may fall, the patient may have difficulty taking the drug, or the patient’s status may change abruptly. Or the prophylaxis might be accidentally discontinued—perhaps when a patient is transferred.
The team also looked at other institutions’ solutions. Then, using a basic understanding of the ways in which their process was missing VTE prophylaxis opportunities, they built interventions.
This team considered logistics carefully because it was clear that the only intervention that could decrease risk would have to be repetitive in nature. “The process we ultimately selected is very, very quick, yet valid,” says Dr. Maynard, while acknowledging that presenting any intervention repeatedly has the potential to interfere with care. “Other models require the physician to use math and add points. This one does not, and takes only seconds.”
Beginning April 19, 2006, the University of California, San Diego (UCSD) will introduce an intervention that presents a VTE risk assessment screen on every patient who is admitted. This process inquires about the need for prophylaxis every three days for the duration of hospitalization, and physicians cannot skip the screen. If risk factors are present and bleeding risk is not, the screen presents appropriate VTE options.
For example, the system will suggest enoxaparin 40 mg daily, enoxaparin 30 mg twice daily, or appropriately dosed warfarin for a high-risk orthopedic surgery patient who has no bleeding risk. Every three days, the process repeats itself, making explicit decisions or suggestions about appropriate prophylaxis. (Figure 1, below, shows a sample screen for a patient with moderately high risk.
Much evidence about VTE is still being gathered. For example, opinions vary about when to start prophylaxis or how long to continue it. Dr. Maynard and his team also addressed real versus relative contraindications—another area of debate among clinicians. Many clinicians are uncertain about how soon after surgery to restart VTE prophylaxis. After orthopedic spine surgery, for example, some might start it on day five, while others may not restart prophylaxis even after day 10. At UCSD, clinical stakeholders in the process came to consensus, and now all restart by day seven.
The tool kit UCSD is developing recognizes that every institution is unique. Those that choose to implement a similar program must identify their baseline rate of VTE and monitor change over time to determine if progress is being made. Every institution must define adequate VTE prophylaxis and tailor the tools appropriately.
Wait? No Need
One compelling aspect of Dr. Maynard’s project is that some of UCSD’s VTE tools are already available on the SHM Web site in the “VTE Resource Room.” With or without AHRQ funding, UCSD planned to develop and implement a VTE awareness program. UCSD’s grant department provided the support Dr. Maynard and his colleagues needed to apply for the AHRQ funding, and Dr. Maynard says the funding they received helped UCSD “disseminate the program better and to carry it out with more rigor.”
UCSD worked with SHM to develop the tool kit. In return, SHM is providing and promoting the VTE tool kit at no charge to interested parties. Additionally, SHM recently received funding via an unrestricted sponsorship to create a mentored implementation project for the “VTE Resource Room.” Interested institutions will be mentored by UCSD staff who have experience with the tool kit.
Over time, Dr. Maynard will measure the effects of the intervention to ensure it is working. In addition to creating a malleable tool kit, UCSD research hospitalists will examine race, gender, and age to determine the effects of these on the likelihood of getting adequate prophylaxis.
Hospital Patient Safe-D(ischarge)
Dr. Williams and his colleagues at Emory University and the University of Ottawa received funding for “Hospital Patient Safe-D(ischarge): A Discharge Bundle for Patients,” a program that builds on previous AHRQ funding. This intervention implements a “discharge bundle” of patient safety interventions to improve patient transition from the hospital to home or another healthcare setting.
“We hope that every patient will undergo discharge, and of course the majority do, but the discharge process has almost been treated as an afterthought,” explains Dr. Williams. “Doctors spend a lot of time on diagnosis and treatment, but not on discharge. This process of transition from total care with a call button, lots of nursing attention, daily visits from the doctor, and delivered meals to greater independence, has not been well researched.”
What little research exists tends to indicate that discharge processes are very heterogeneous.
So far, Dr. Williams’ team’s examination of the process has produced only one surprise: The team has discovered that the discharge process is even more capricious than they suspected. As patients prepare to leave the hospital, what could and should be an orderly process that educates and prepares patients to assume responsibility for their own care in a new and better way is often interrupted or disjointed.
Preparing patients for discharge once fell to the nursing staff. As nursing faces staffing shortages and expanded roles, the discharge process often belongs to everyone and to no one. That physicians’ discharge visits pay much less than the time required to do it well also complicates the problem. The researchers were not surprised, however, to learn that many patients do not know their diagnosis or treatment plan as discharge is imminent. Their goal is to develop a consistent, comprehensive discharge process that will be a national model.
Here again, the precepts of continuous quality improvement are apparent. Dr. Williams’ team’s effort represents collaboration among physicians, pharmacists, nurses, and patients; involves SHM and several other professional organizations; and calls upon an advisory committee consisting of nationally recognized patient care and safety experts.
The discharge bundle of patient safety interventions—a concept advocated by the Joint Commission on Accreditation of Healthcare Organizations and other quality-promoting groups—adds a post-discharge continuity check to medication reconciliation and patient-centered education at discharge.
The four project phases—implement, evaluate, develop a tool, and disseminate the discharge bundle—overlap and ensure success.
Dr. Williams believes that the group of patients most likely to benefit from this intervention is the elderly. “The elderly bear the greatest burden of chronic disease and typically have several concurrent health problems,” he says.
Educating elders at the time of discharge should decrease the medication error rate and improve adherence to other treatments and recommended lifestyle changes. To gauge the appropriateness of the discharge bundle, John Banja, PhD, an expert in communication and safety, observes the discharge process directly. All communications must be patient-centered, and thus presented in a manner that patients will understand and appreciate. Banja relies on his background in patient safety and disability/rehabilitation to assess the discharge process.
Initial enrollment in this study seems successful. More than 50 patients have consented to participate, but Banja projects a need for 200 to complete the entire process. Recently, the team increased its planned maximum accrual to 300 to increase the statistical power of their findings. The participants like the program because most of them find discharge somewhat discomforting. Patients know they have knowledge gaps and appreciate clinicians’ efforts to fill those gaps seamlessly. A small investment of time can prevent problems after discharge.
Added Value
Clearly, the findings from these AHRQ-funded studies have the potential to reduce morbidity and mortality in a logarithmic manner as other institutions adapt these new tool kits. Dr. Williams indicates that recipients of PIPS funding receive more than just funding and the satisfaction of creating tools that will help all Americans.
“The AHRQ sponsors quarterly conference calls for all participants, regardless of their research topic, and an annual meeting in June to bring all investigators together,” he says.
The opportunity to learn how others address problems, plan interventions, and tackle hurdles proves invaluable. In addition, being privy to interim study results or learning how others handle research dilemmas helps hospitalists expand their skill sets.
Listening to Drs. Maynard and Williams is a not-so-subtle reminder that every hospital needs a well-structured quality improvement plan, and that hospitalists are essential in the plan’s success. Every hospitalist needs an understanding of the precepts these PIs used to earn this well-deserved funding: interdisciplinary and professional organization collaboration, good communication, realistic planning, managing change by measuring, and above all, sharing success. TH
Jeannette Yeznach Wick, RPh, MBA, FASCP, is a freelance medical writer based in Arlington, Va.
References
- Anderson FA Jr, Wheeler HB, Goldberg RJ, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med. 1991 May;151(5):933-938.
- Clagett GP, Anderson FA Jr, Heit J, et al. Prevention of venous thromboembolism. Chest. 1995 Oct;108(4 Suppl):312S-334S.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest. 2001;119(1 Suppl):132S-175S.
What can you do with a quarter of a million dollars? In some places, that amount can buy a home that can shelter a family for decades. In other places, it is enough to pay annual malpractice insurance premiums for physicians practicing in high-risk specialties—with a little left over.
But if you wanted to use that money for an enduring healthcare project that would provide the most good for the most people, how would you do it? Hospitalists can look to the Agency for Healthcare Research and Quality (AHRQ) for stellar examples of well-invested dollars with excellent return.
AHRQ Funding
With a staff of approximately 300, the tiny AHRQ is the lead federal agency charged with improving the quality, safety, efficiency, and effectiveness of healthcare for all Americans. It creates a priority research agenda annually, and funds studies in areas where improvement is deemed most needed. These include patient safety, data development, pharmaceutical outcomes, and other areas described on its Web site (www.ahrq.gov/).
In 2005, AHRQ announced its Partnerships in Implementing Patient Safety (PIPS) and committed up to $9 million in total costs to fund new grants of less than $300,000 per year, lasting two years. AHRQ indicated that eligible safe practice intervention projects would be required to include “tool kits,” and a comprehensive implementation tool kit to help others overcome barriers and allay adoption concerns. AHRQ’s goal was and is to disseminate funded projects’ perfected tools widely for adaptation and/or adoption by diverse healthcare settings.
AHRQ asked that principal investigators (PIs) be experienced senior level individuals familiar with implementing change in healthcare settings. Their expectation was that PIs would devote at least 15% of their time to the project for its duration. Thus the competitive challenge to potential PIs was great:
- Select a worthy project from among the endless areas where healthcare needs improvement, and then plan specific, realistic, achievable interventions that could create measurable improvement over two years;
- Implement the program; and
- Develop a plan and tools so basic and user-friendly that they could feasibly be applied in not just the local practice setting, but in other healthcare settings.
Although the size and duration of the awards varied, many of the 17 projects they funded received slightly more than a quarter of a million dollars. Among the funded projects, two boast hospitalists as their PIs and address areas of obvious concern in most healthcare settings. Greg Maynard, MD, MS, at the University of California, San Diego, was funded to implement a venous thromboembolism (VTE) intervention program. And Mark V. Williams, MD, FACP, professor of medicine, Emory University School of Medicine, Atlanta, and editor of the Journal of Hospital Medicine, was funded to implement a discharge bundle of patient safety interventions respectively.
Stalking the Silent Killer
Dr. Maynard’s project, “Optimal Prevention of Hospital Acquired Venous Thromboembolism,” focuses on eliminating preventable hospital-acquired VTE at an academic healthcare facility that has a large population of Hispanic patients.
The project’s timeliness and utility is clear: Although the exact incidence of VTE is unknown, experts estimate that approximately 260,000 are clinically recognized annually in acutely hospitalized patients.1 Pulmonary embolism (PE) resulting from deep vein thrombosis (DVT) is the most common cause of preventable hospital death, the majority of hospitalized patients with risk factors for DVT receive no prophylaxis, and the rate of fatal PE more than doubles between age 50 and 80.2,3 The problem is easily recognizable, but “Getting people to do what they need to do to prevent VTE can be hard,” says Dr. Maynard.
This project was carefully planned. It used a rigorous quality improvement process, involving all appropriate clinicians, nurses, managers, and technical support personnel.
Dr. Maynard and his team anticipated roadblocks and negotiated in advance to reduce their effects. They accepted that when patients are hospitalized, things frequently happen that cause physicians to stop VTE prophylaxis: A hemoglobin or platelet count may fall, the patient may have difficulty taking the drug, or the patient’s status may change abruptly. Or the prophylaxis might be accidentally discontinued—perhaps when a patient is transferred.
The team also looked at other institutions’ solutions. Then, using a basic understanding of the ways in which their process was missing VTE prophylaxis opportunities, they built interventions.
This team considered logistics carefully because it was clear that the only intervention that could decrease risk would have to be repetitive in nature. “The process we ultimately selected is very, very quick, yet valid,” says Dr. Maynard, while acknowledging that presenting any intervention repeatedly has the potential to interfere with care. “Other models require the physician to use math and add points. This one does not, and takes only seconds.”
Beginning April 19, 2006, the University of California, San Diego (UCSD) will introduce an intervention that presents a VTE risk assessment screen on every patient who is admitted. This process inquires about the need for prophylaxis every three days for the duration of hospitalization, and physicians cannot skip the screen. If risk factors are present and bleeding risk is not, the screen presents appropriate VTE options.
For example, the system will suggest enoxaparin 40 mg daily, enoxaparin 30 mg twice daily, or appropriately dosed warfarin for a high-risk orthopedic surgery patient who has no bleeding risk. Every three days, the process repeats itself, making explicit decisions or suggestions about appropriate prophylaxis. (Figure 1, below, shows a sample screen for a patient with moderately high risk.
Much evidence about VTE is still being gathered. For example, opinions vary about when to start prophylaxis or how long to continue it. Dr. Maynard and his team also addressed real versus relative contraindications—another area of debate among clinicians. Many clinicians are uncertain about how soon after surgery to restart VTE prophylaxis. After orthopedic spine surgery, for example, some might start it on day five, while others may not restart prophylaxis even after day 10. At UCSD, clinical stakeholders in the process came to consensus, and now all restart by day seven.
The tool kit UCSD is developing recognizes that every institution is unique. Those that choose to implement a similar program must identify their baseline rate of VTE and monitor change over time to determine if progress is being made. Every institution must define adequate VTE prophylaxis and tailor the tools appropriately.
Wait? No Need
One compelling aspect of Dr. Maynard’s project is that some of UCSD’s VTE tools are already available on the SHM Web site in the “VTE Resource Room.” With or without AHRQ funding, UCSD planned to develop and implement a VTE awareness program. UCSD’s grant department provided the support Dr. Maynard and his colleagues needed to apply for the AHRQ funding, and Dr. Maynard says the funding they received helped UCSD “disseminate the program better and to carry it out with more rigor.”
UCSD worked with SHM to develop the tool kit. In return, SHM is providing and promoting the VTE tool kit at no charge to interested parties. Additionally, SHM recently received funding via an unrestricted sponsorship to create a mentored implementation project for the “VTE Resource Room.” Interested institutions will be mentored by UCSD staff who have experience with the tool kit.
Over time, Dr. Maynard will measure the effects of the intervention to ensure it is working. In addition to creating a malleable tool kit, UCSD research hospitalists will examine race, gender, and age to determine the effects of these on the likelihood of getting adequate prophylaxis.
Hospital Patient Safe-D(ischarge)
Dr. Williams and his colleagues at Emory University and the University of Ottawa received funding for “Hospital Patient Safe-D(ischarge): A Discharge Bundle for Patients,” a program that builds on previous AHRQ funding. This intervention implements a “discharge bundle” of patient safety interventions to improve patient transition from the hospital to home or another healthcare setting.
“We hope that every patient will undergo discharge, and of course the majority do, but the discharge process has almost been treated as an afterthought,” explains Dr. Williams. “Doctors spend a lot of time on diagnosis and treatment, but not on discharge. This process of transition from total care with a call button, lots of nursing attention, daily visits from the doctor, and delivered meals to greater independence, has not been well researched.”
What little research exists tends to indicate that discharge processes are very heterogeneous.
So far, Dr. Williams’ team’s examination of the process has produced only one surprise: The team has discovered that the discharge process is even more capricious than they suspected. As patients prepare to leave the hospital, what could and should be an orderly process that educates and prepares patients to assume responsibility for their own care in a new and better way is often interrupted or disjointed.
Preparing patients for discharge once fell to the nursing staff. As nursing faces staffing shortages and expanded roles, the discharge process often belongs to everyone and to no one. That physicians’ discharge visits pay much less than the time required to do it well also complicates the problem. The researchers were not surprised, however, to learn that many patients do not know their diagnosis or treatment plan as discharge is imminent. Their goal is to develop a consistent, comprehensive discharge process that will be a national model.
Here again, the precepts of continuous quality improvement are apparent. Dr. Williams’ team’s effort represents collaboration among physicians, pharmacists, nurses, and patients; involves SHM and several other professional organizations; and calls upon an advisory committee consisting of nationally recognized patient care and safety experts.
The discharge bundle of patient safety interventions—a concept advocated by the Joint Commission on Accreditation of Healthcare Organizations and other quality-promoting groups—adds a post-discharge continuity check to medication reconciliation and patient-centered education at discharge.
The four project phases—implement, evaluate, develop a tool, and disseminate the discharge bundle—overlap and ensure success.
Dr. Williams believes that the group of patients most likely to benefit from this intervention is the elderly. “The elderly bear the greatest burden of chronic disease and typically have several concurrent health problems,” he says.
Educating elders at the time of discharge should decrease the medication error rate and improve adherence to other treatments and recommended lifestyle changes. To gauge the appropriateness of the discharge bundle, John Banja, PhD, an expert in communication and safety, observes the discharge process directly. All communications must be patient-centered, and thus presented in a manner that patients will understand and appreciate. Banja relies on his background in patient safety and disability/rehabilitation to assess the discharge process.
Initial enrollment in this study seems successful. More than 50 patients have consented to participate, but Banja projects a need for 200 to complete the entire process. Recently, the team increased its planned maximum accrual to 300 to increase the statistical power of their findings. The participants like the program because most of them find discharge somewhat discomforting. Patients know they have knowledge gaps and appreciate clinicians’ efforts to fill those gaps seamlessly. A small investment of time can prevent problems after discharge.
Added Value
Clearly, the findings from these AHRQ-funded studies have the potential to reduce morbidity and mortality in a logarithmic manner as other institutions adapt these new tool kits. Dr. Williams indicates that recipients of PIPS funding receive more than just funding and the satisfaction of creating tools that will help all Americans.
“The AHRQ sponsors quarterly conference calls for all participants, regardless of their research topic, and an annual meeting in June to bring all investigators together,” he says.
The opportunity to learn how others address problems, plan interventions, and tackle hurdles proves invaluable. In addition, being privy to interim study results or learning how others handle research dilemmas helps hospitalists expand their skill sets.
Listening to Drs. Maynard and Williams is a not-so-subtle reminder that every hospital needs a well-structured quality improvement plan, and that hospitalists are essential in the plan’s success. Every hospitalist needs an understanding of the precepts these PIs used to earn this well-deserved funding: interdisciplinary and professional organization collaboration, good communication, realistic planning, managing change by measuring, and above all, sharing success. TH
Jeannette Yeznach Wick, RPh, MBA, FASCP, is a freelance medical writer based in Arlington, Va.
References
- Anderson FA Jr, Wheeler HB, Goldberg RJ, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med. 1991 May;151(5):933-938.
- Clagett GP, Anderson FA Jr, Heit J, et al. Prevention of venous thromboembolism. Chest. 1995 Oct;108(4 Suppl):312S-334S.
- Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest. 2001;119(1 Suppl):132S-175S.
Listen Between the Lines
When an elderly person is admitted to the hospital, Adrienne Green, MD, sees an opportunity for something beyond addressing the medical issues at hand.
“One of the key issues that is important for practical, everyday care is trying to figure out how the elderly are not functioning well at home,” says Dr. Green, an associate clinical professor of medicine at the University of California at San Francisco and a member of UCSF’s hospitalist group. “I think we do a great job of managing their diseases, but what we don’t do very well is helping them out with other things [such as coping with] their losses and the fact that they may be just barely hanging on at home in terms of their ability to care for themselves; and this hospitalization may really have set them back.”
Eva Chittenden, MD, an assistant clinical professor of medicine, also at UCSF, agrees. “Many hospitalists are so focused on the hospital that they’re not thinking about the ‘before the hospital’ and the ‘after the hospital,’” she says.
But after identifying the challenges that elderly patients face, communication itself may be challenging. Elderly individuals struggle with issues of control and allowing people to tell them what they need to change in their lives may not be an easy task. What are the best ways to communicate with hospitalized elderly patients to facilitate the best “whole-person” care?

—David Solie, MS, PA
Under the Radar Screen
The hospitalists interviewed for this article agreed that getting a broader picture of an elderly patient’s health and well-being involves discovering how they are really doing at home. Dr. Green asks simple questions, particularly about activities of daily living, such as whether they’re doing their own shopping and cooking. She also involves the family, “because very frequently the patient will say, ‘I’m doing fine,’ and the family member is in the background shaking their head.”
She also looks for clues about whether the patient needs more help at home, whether they are compliant with their medications, and if not, why (e.g., can they open their medicine bottles)?
“I frequently have the elderly patients evaluated for home care just to get someone into their house … ,” says Dr. Green. “I think that probably 80% of our patients who are over 80 who come into the hospital have things in their homes that are not safe, such as throw rugs.” Even if patients are basically doing OK, “if I can get some home care for them, I know we’ll uncover a ton [of things that can be improved],” she says. “These patients may have … kind of snuck under the radar screen of their families and their primary [care physician], and I think the hospitalization kind of opens that up in some ways.”
Facing Resistance
Even if issues are uncovered by means of interviews and home-health visits, however, many elderly patients present a particular communication challenge. This, says David Solie, MS, PA, author of How to Say It to Seniors: Closing the Communication Gap with Our Elders, is because of the difference in circumstances and current experiences between the elderly and their hospitalist providers.1 It is common knowledge that younger people go through stages of development, but the elderly do, too, says Solie, who is medical director and CEO of Second Opinion Insurance Services in Woodland Hills, Calif., a brokerage that specializes in the insurance needs of impaired-risk, elderly individuals.
The last human developmental stage compels elderly adults to work hard at maintaining control over their lives in the face of almost daily losses. A big part of the losses they experience involve their health and functioning, and the ways different patients cope with loss and the perceived stresses of healthcare have been analyzed and categorized.2-5
But in addition to loss of control, the elderly also face the daunting task of discovering what their legacy will be—what will live on after they die. “The way our elders communicate contains clues to the urgency they feel in trying to resolve these items on their agendas,” writes Solie. “In almost every conversation with older adults, control and legacy issues rise to the surface.”
A Matter of Loss
By the time a person is old (over 70) or old-old (over 85) their losses may have manifested in many areas: They’ve lost:
- Parents;
- Other relatives—perhaps including children;
- Friends;
- Places of residence (both homes and the familiarity of cities or towns);
- Possessions;
- Other relationships (sometimes other healthcare providers);
- Careers;
- Consultative authority (“ours is not a culture that values the wisdom of our elders,” writes Solie);
- Identity;
- Financial independence;
- Habits and pleasures;
- Physical space (the room at their son or daughter’s or in assisted living or the nursing home can’t compare to the homes, gardens, and expanses of view they may have had as younger people), and, of course; and
- Physical and mental capacities.
Sometimes the losses elders sustain occur in rapid-fire sequence, with little or no recovery time in between.1,6
It is no wonder that older adults, in one way or another, exhibit what we consider resistance to their changing lives. In terms of a hospitalization, this may mean saying “no” to medications, individual providers, tests, surgery, home-health visits, or something as small as being talked to or touched in what they perceive as a disturbing, overly familiar, or mechanized manner.
“Many patients are resistant to having people come into their homes and help them, and at the same time they are resistant to going to a skilled nursing care facility,” says Dr. Green, “and it has to do with their [feelings of the] loss of independence and control over their lives.”
“It’s very easy if you’re in medicine to normalize your context of the hospital,” says Solie. “In other words, the hospital seems familiar to you and you’re very comfortable moving around there, and mainly because you’re in control. You’re the doctor … and you move in the hospital in order to make things happen and you never feel all that threatened. But when you bring an older person who already has a heightened sensitivity toward losing control into the hospital—this complex, technological world of medicine—and they have the cumulative disadvantage of being sick,” says Solie, “it’s really important to remember that there will probably be no other state that they’ll be in, except maybe nursing home care, where they will feel so out of control.”
A good first step in communicating with older patients is to quickly develop a rapport with them and show them you recognize what they’re up against.7 “They really want to know whether or not I get it,” says Solie.
The way you communicate that you get it, he says, is fairly straightforward: When I’m first interacting with the patient, I say, “if you are like my [other] elderly patients … I’m sure you’re feeling a lot of anxiety over [not having much] control and, first of all, I want to assure you that I’m going to make sure you understand the choices and help you make all the decisions. And … I’m definitely going to … put everything in a language that you understand. But if I’m not successful, I’m going to employ someone from your family. We’re going to work together. Even though you’re hospitalized and even though you’re fighting this illness (or whatever the condition might be), you still [have] the right to make choices, and my goal is to partner with you. My expertise is medicine, but you have an expertise in your life.”
In other words, you are signaling that you recognize that control is the issue. Acknowledge the loss, ask about the value of the event or decision to the patient, ask what you can do to help them deal with their feelings or make up their minds. It also allows you to remind an older patient’s children that control is a big and normal concern for their mother or father.

—Eva Chittenden, MD
Hospitalists at a Different Time and Place
The elderly desperately need people who can serve them as natural healers, who are not constantly in a hurry, and who care what they are thinking and feeling. How can hospitalists relate to those who are in the midst of life review and who are hanging on to an escaping control? How can they serve their patients in a way that meets all needs?
Fighting—with denial or ignorance—the resistance that patients might put up will more than likely provoke them. A fight for control can undermine and sabotage the best intentions of the provider and the greatest wishes for the patient to experience comfort or regain health and well-being. Rather than justifying wresting control from elderly patients because it’s for their own good, advises Solie, what we must do instead is to “step back, hand them the control baton, and allow them to run with it.”1
A person’s admission to the hospital “might be such a huge crisis for them, whereas for us it’s our routine work,” says Dr. Chittenden, who practices as a hospitalist and also works on her institution’s inpatient palliative care service. “And many people who are hospitalists—who are even in their late 20s, 30s, 40s—have been totally healthy their whole life, so it is hard to relate to what it’s like to be older and to be losing function, losing friends who are also dying, losing their house … . I think that it can be very helpful for the hospitalist to take a little more time and explore some of those issues [of loss and legacy]. I try to meet the person where they’re at and try to understand what their goals, needs, ... and fears are [as well as] their functional status.”
Allowing older patients to engage with you about their lives and their pasts is a privilege for any healthcare provider. Engaging with them in a way that will help facilitate their loosening the reins on control may expedite and allow greater quality into their healthcare. It may provide an opening whereby you can order that home-health visit with less struggle.
Create Openings
“There are a lot of different ‘on-ramps’ to asking the life-review questions, which are extremely comforting,” says Solie. “For example, you might say, ‘Mary, I notice that you were born in Iowa. You know, my family on my father’s side came from Iowa. Where were you raised?’ And ‘Do you have a big family on your farm, because my aunt had cows.’”
Once you get a response that engages the patient, then you “are in the slipstream. Physicians have such a high experience curve, they see so many patients,” he says. “They don’t have to go very far into their inventory of experiences [to find one] that essentially matches up with that patient.”
Any kind of comment that will key you in to their background experience can help establish some kind of foundation for relationship. Another example: “You know, Mary, I was working with this woman who was about your age and she was raised in the Midwest and was dealing with some of these issues of congestive heart failure, and one of her big concerns was something that I didn’t appreciate until I understood what an impact it was having on her life.”
This kind of communication, says Solie, can help to relieve some of the patient’s control anxieties, “because she feels that if I ‘get it,’ she’s open to what I have to say, such as, ‘The first thing, we have to deal with is there is too much fluid going on in your body and it’s putting a big strain on your heart, so the first couple days all we did for that [other] woman was try to pull some fluid off and keep everything in balance.’”
You’ve communicated that you have a plan, that you can be trusted, and that you will help her to exercise as much control as possible. Creating and accessing those openings is also “the ideal way to weave the family into this whole life-review process, which is where the patient lives, psychologically and emotionally, when outside the hospital environment,” he says. “We become so myopic when we’re caught in the hospital environment that the world becomes a narrow tunnel and we forget the greater matrix outside that we’re all connected to.”
The Boon of Biology
Whereas the physiology and anatomy of humans deteriorate with time, some of the changes in mental processes in old age may actually enhance the ability to reflect and make informed judgments. Solie’s view is that what younger people may view as slow behavior, confusing speech patterns, and physical frailty don’t hinder the tasks that are before the elderly. On the contrary, they assist the fulfillment of their developmental agendas to feel in control when they’re losing control and to let go enough to reveal the legacy that will survive after they go.
Research on the aging brain indicates that changes in brain chemistry facilitate the life-review process.1,6 In general, reflection is the normal mode of existence for elderly adults and their primary focus. Thus, viewing them as diminished because they communicate differently than younger people do is doing them a disservice.
Those slowed mental processes, Dr. Chittenden concurs, “are conducive to reflection. Someone younger will pathologize it. … I agree that we don’t value the slowing down process, but I also think that when this population is in the hospital we are tending to look at loss of functional status or the quick mental traits that we value as opposed to [that which is] adaptive [and] that enables them to look at things differently and reflect.”
The key to connecting the dots of where they are and where they need to be (both medically and psychosocially), as well as how they occur to their providers and their families as opposed to how they occur to themselves, is to listen to and speak with them by making use of what you know about this stage of their life as it affects their communication. You can do this, says Solie, by invoking the “access code,” which is “to clearly understand that at the top of their agenda—no matter what else is happening—is the need for control and the need to develop and go after a legacy, and that means life review. If you know that, you will never lose your reference point with them.”
Communication Habits of the Elderly
Solie identifies some verbal behaviors that are common in older people. In many cases these behaviors may reveal something between the lines.
- Lack of urgency. Older people need more time to decide things. Accept that slower pace as normal. Don’t take it personally. Adjust your schedule to allow time to deliver news or ask for choices and then allow time for them to discuss with their families or contemplate on their own; return to them at a later time. Become expert at spontaneous facilitation. Use your access code to get their attention and gain their trust.
- Nonlinear conversations. Although older patients may appear to wander off topic, they may do so in the urge to ground themselves in what their priorities are, what their feelings are, what their choices will be. Signal you’re willing to listen and that you’re tuned in to the content, even if you don’t know where it is leading. (Obviously, someone who is demented or delirious presents a different scenario altogether, and depression is common and frequently overlooked.) Listen for patterns and themes. Nonlinear conversations can lead to spontaneous revelations and great insights for your patients and for yourself and can help patients revisit life dramas that test and clarify values. This, too, is a part of healthcare.
- Repetition and attention to details. In situations when dementia is ruled out, a patient’s repetition may indicate a means to emphasize an important point or value. Keep in mind, too, that as we age, we all repeat stories to some degree. Details in stories may be the means by which older adults connect to their pasts and may also serve as clues to what is important to these people. Don’t assume details demand any action on your part. You are only being asked to listen as the older person sorts things out.
- Uncoupling. Solie describes uncoupling as any time an older person appears to disconnect from you in the course of a conversation. For a professional, this can feel as if you are dismissed or ignored just when you think you’ve hit the mark with a comment or question. Go back and assess the information you’ve gathered by doing some verification. Rethink the objective: Any action that works against their maintaining control and discovering a legacy will produce uncoupling.
“I try to be aware of when I’m losing people,” says Dr. Chittenden of this phenomenon. “I would say, ‘I seem to be losing you and I’m wondering what you’re thinking right now.’ I would try to find out where they’re at and if it was something I said that didn’t gel with them, didn’t make sense to them, or wasn’t their priority.” This is something, she emphasizes, that a hospitalist needs to watch for with patients of all ages. “Whether you’re older or younger,” she says, the communication can be complicated because “you’re … in the hospital culture and the priorities of doctors are so often different from the priorities of patients.”
Conclusion
Older and especially old-old individuals in some ways live in an era other than the one traversed by the young and middle-aged.6 Their purposes, agendas, and mission are different and the slowing down of their functioning can facilitate their attempts to put their lives into perspective and manage what control they can still exercise or are still allowed. Viewing older patients with the utmost respect and acknowledging the challenges they face at these last phases of their lives can better help you to partner with them and their families in their care. TH
Andrea Sattinger also writes about the importance of apology in this issue.
References
- Solie D. How to Say it to Seniors: Closing the Communication Gap with Our Elders. New York: Prentice Hall Press; 2004.
- Chochinov HM, Cann BJ. Interventions to enhance the spiritual aspects of dying. J Palliat Med. 2005;8:Suppl 1:S103-115.
- Dennis KE. Patients' control and the information imperative: clarification and confirmation. Nurs Res. 1990;39(3):162-166.
- Kiesler DJ, Auerbach SM. Integrating measurement of control and affiliation in studies of physician-patient interaction: the interpersonal circumplex. Soc Sci Med. 2003;57(9):1707-1722.
- Breemhaar B, Visser AP, Kleijnen JG. Perceptions and behaviour among elderly hospital patients: description and explanation of age differences in satisfaction, knowledge, emotions and behaviour. Soc Sci Med. 1990;31(12):1377-1385.
- Pipher M. Another Country: Navigating the Emotional Terrain of Our Elders. New York: Riverhead Books; 1999.
- Barnett PB. Rapport and the hospitalist. Am J Med. 2001;111:31S-35S.
When an elderly person is admitted to the hospital, Adrienne Green, MD, sees an opportunity for something beyond addressing the medical issues at hand.
“One of the key issues that is important for practical, everyday care is trying to figure out how the elderly are not functioning well at home,” says Dr. Green, an associate clinical professor of medicine at the University of California at San Francisco and a member of UCSF’s hospitalist group. “I think we do a great job of managing their diseases, but what we don’t do very well is helping them out with other things [such as coping with] their losses and the fact that they may be just barely hanging on at home in terms of their ability to care for themselves; and this hospitalization may really have set them back.”
Eva Chittenden, MD, an assistant clinical professor of medicine, also at UCSF, agrees. “Many hospitalists are so focused on the hospital that they’re not thinking about the ‘before the hospital’ and the ‘after the hospital,’” she says.
But after identifying the challenges that elderly patients face, communication itself may be challenging. Elderly individuals struggle with issues of control and allowing people to tell them what they need to change in their lives may not be an easy task. What are the best ways to communicate with hospitalized elderly patients to facilitate the best “whole-person” care?

—David Solie, MS, PA
Under the Radar Screen
The hospitalists interviewed for this article agreed that getting a broader picture of an elderly patient’s health and well-being involves discovering how they are really doing at home. Dr. Green asks simple questions, particularly about activities of daily living, such as whether they’re doing their own shopping and cooking. She also involves the family, “because very frequently the patient will say, ‘I’m doing fine,’ and the family member is in the background shaking their head.”
She also looks for clues about whether the patient needs more help at home, whether they are compliant with their medications, and if not, why (e.g., can they open their medicine bottles)?
“I frequently have the elderly patients evaluated for home care just to get someone into their house … ,” says Dr. Green. “I think that probably 80% of our patients who are over 80 who come into the hospital have things in their homes that are not safe, such as throw rugs.” Even if patients are basically doing OK, “if I can get some home care for them, I know we’ll uncover a ton [of things that can be improved],” she says. “These patients may have … kind of snuck under the radar screen of their families and their primary [care physician], and I think the hospitalization kind of opens that up in some ways.”
Facing Resistance
Even if issues are uncovered by means of interviews and home-health visits, however, many elderly patients present a particular communication challenge. This, says David Solie, MS, PA, author of How to Say It to Seniors: Closing the Communication Gap with Our Elders, is because of the difference in circumstances and current experiences between the elderly and their hospitalist providers.1 It is common knowledge that younger people go through stages of development, but the elderly do, too, says Solie, who is medical director and CEO of Second Opinion Insurance Services in Woodland Hills, Calif., a brokerage that specializes in the insurance needs of impaired-risk, elderly individuals.
The last human developmental stage compels elderly adults to work hard at maintaining control over their lives in the face of almost daily losses. A big part of the losses they experience involve their health and functioning, and the ways different patients cope with loss and the perceived stresses of healthcare have been analyzed and categorized.2-5
But in addition to loss of control, the elderly also face the daunting task of discovering what their legacy will be—what will live on after they die. “The way our elders communicate contains clues to the urgency they feel in trying to resolve these items on their agendas,” writes Solie. “In almost every conversation with older adults, control and legacy issues rise to the surface.”
A Matter of Loss
By the time a person is old (over 70) or old-old (over 85) their losses may have manifested in many areas: They’ve lost:
- Parents;
- Other relatives—perhaps including children;
- Friends;
- Places of residence (both homes and the familiarity of cities or towns);
- Possessions;
- Other relationships (sometimes other healthcare providers);
- Careers;
- Consultative authority (“ours is not a culture that values the wisdom of our elders,” writes Solie);
- Identity;
- Financial independence;
- Habits and pleasures;
- Physical space (the room at their son or daughter’s or in assisted living or the nursing home can’t compare to the homes, gardens, and expanses of view they may have had as younger people), and, of course; and
- Physical and mental capacities.
Sometimes the losses elders sustain occur in rapid-fire sequence, with little or no recovery time in between.1,6
It is no wonder that older adults, in one way or another, exhibit what we consider resistance to their changing lives. In terms of a hospitalization, this may mean saying “no” to medications, individual providers, tests, surgery, home-health visits, or something as small as being talked to or touched in what they perceive as a disturbing, overly familiar, or mechanized manner.
“Many patients are resistant to having people come into their homes and help them, and at the same time they are resistant to going to a skilled nursing care facility,” says Dr. Green, “and it has to do with their [feelings of the] loss of independence and control over their lives.”
“It’s very easy if you’re in medicine to normalize your context of the hospital,” says Solie. “In other words, the hospital seems familiar to you and you’re very comfortable moving around there, and mainly because you’re in control. You’re the doctor … and you move in the hospital in order to make things happen and you never feel all that threatened. But when you bring an older person who already has a heightened sensitivity toward losing control into the hospital—this complex, technological world of medicine—and they have the cumulative disadvantage of being sick,” says Solie, “it’s really important to remember that there will probably be no other state that they’ll be in, except maybe nursing home care, where they will feel so out of control.”
A good first step in communicating with older patients is to quickly develop a rapport with them and show them you recognize what they’re up against.7 “They really want to know whether or not I get it,” says Solie.
The way you communicate that you get it, he says, is fairly straightforward: When I’m first interacting with the patient, I say, “if you are like my [other] elderly patients … I’m sure you’re feeling a lot of anxiety over [not having much] control and, first of all, I want to assure you that I’m going to make sure you understand the choices and help you make all the decisions. And … I’m definitely going to … put everything in a language that you understand. But if I’m not successful, I’m going to employ someone from your family. We’re going to work together. Even though you’re hospitalized and even though you’re fighting this illness (or whatever the condition might be), you still [have] the right to make choices, and my goal is to partner with you. My expertise is medicine, but you have an expertise in your life.”
In other words, you are signaling that you recognize that control is the issue. Acknowledge the loss, ask about the value of the event or decision to the patient, ask what you can do to help them deal with their feelings or make up their minds. It also allows you to remind an older patient’s children that control is a big and normal concern for their mother or father.

—Eva Chittenden, MD
Hospitalists at a Different Time and Place
The elderly desperately need people who can serve them as natural healers, who are not constantly in a hurry, and who care what they are thinking and feeling. How can hospitalists relate to those who are in the midst of life review and who are hanging on to an escaping control? How can they serve their patients in a way that meets all needs?
Fighting—with denial or ignorance—the resistance that patients might put up will more than likely provoke them. A fight for control can undermine and sabotage the best intentions of the provider and the greatest wishes for the patient to experience comfort or regain health and well-being. Rather than justifying wresting control from elderly patients because it’s for their own good, advises Solie, what we must do instead is to “step back, hand them the control baton, and allow them to run with it.”1
A person’s admission to the hospital “might be such a huge crisis for them, whereas for us it’s our routine work,” says Dr. Chittenden, who practices as a hospitalist and also works on her institution’s inpatient palliative care service. “And many people who are hospitalists—who are even in their late 20s, 30s, 40s—have been totally healthy their whole life, so it is hard to relate to what it’s like to be older and to be losing function, losing friends who are also dying, losing their house … . I think that it can be very helpful for the hospitalist to take a little more time and explore some of those issues [of loss and legacy]. I try to meet the person where they’re at and try to understand what their goals, needs, ... and fears are [as well as] their functional status.”
Allowing older patients to engage with you about their lives and their pasts is a privilege for any healthcare provider. Engaging with them in a way that will help facilitate their loosening the reins on control may expedite and allow greater quality into their healthcare. It may provide an opening whereby you can order that home-health visit with less struggle.
Create Openings
“There are a lot of different ‘on-ramps’ to asking the life-review questions, which are extremely comforting,” says Solie. “For example, you might say, ‘Mary, I notice that you were born in Iowa. You know, my family on my father’s side came from Iowa. Where were you raised?’ And ‘Do you have a big family on your farm, because my aunt had cows.’”
Once you get a response that engages the patient, then you “are in the slipstream. Physicians have such a high experience curve, they see so many patients,” he says. “They don’t have to go very far into their inventory of experiences [to find one] that essentially matches up with that patient.”
Any kind of comment that will key you in to their background experience can help establish some kind of foundation for relationship. Another example: “You know, Mary, I was working with this woman who was about your age and she was raised in the Midwest and was dealing with some of these issues of congestive heart failure, and one of her big concerns was something that I didn’t appreciate until I understood what an impact it was having on her life.”
This kind of communication, says Solie, can help to relieve some of the patient’s control anxieties, “because she feels that if I ‘get it,’ she’s open to what I have to say, such as, ‘The first thing, we have to deal with is there is too much fluid going on in your body and it’s putting a big strain on your heart, so the first couple days all we did for that [other] woman was try to pull some fluid off and keep everything in balance.’”
You’ve communicated that you have a plan, that you can be trusted, and that you will help her to exercise as much control as possible. Creating and accessing those openings is also “the ideal way to weave the family into this whole life-review process, which is where the patient lives, psychologically and emotionally, when outside the hospital environment,” he says. “We become so myopic when we’re caught in the hospital environment that the world becomes a narrow tunnel and we forget the greater matrix outside that we’re all connected to.”
The Boon of Biology
Whereas the physiology and anatomy of humans deteriorate with time, some of the changes in mental processes in old age may actually enhance the ability to reflect and make informed judgments. Solie’s view is that what younger people may view as slow behavior, confusing speech patterns, and physical frailty don’t hinder the tasks that are before the elderly. On the contrary, they assist the fulfillment of their developmental agendas to feel in control when they’re losing control and to let go enough to reveal the legacy that will survive after they go.
Research on the aging brain indicates that changes in brain chemistry facilitate the life-review process.1,6 In general, reflection is the normal mode of existence for elderly adults and their primary focus. Thus, viewing them as diminished because they communicate differently than younger people do is doing them a disservice.
Those slowed mental processes, Dr. Chittenden concurs, “are conducive to reflection. Someone younger will pathologize it. … I agree that we don’t value the slowing down process, but I also think that when this population is in the hospital we are tending to look at loss of functional status or the quick mental traits that we value as opposed to [that which is] adaptive [and] that enables them to look at things differently and reflect.”
The key to connecting the dots of where they are and where they need to be (both medically and psychosocially), as well as how they occur to their providers and their families as opposed to how they occur to themselves, is to listen to and speak with them by making use of what you know about this stage of their life as it affects their communication. You can do this, says Solie, by invoking the “access code,” which is “to clearly understand that at the top of their agenda—no matter what else is happening—is the need for control and the need to develop and go after a legacy, and that means life review. If you know that, you will never lose your reference point with them.”
Communication Habits of the Elderly
Solie identifies some verbal behaviors that are common in older people. In many cases these behaviors may reveal something between the lines.
- Lack of urgency. Older people need more time to decide things. Accept that slower pace as normal. Don’t take it personally. Adjust your schedule to allow time to deliver news or ask for choices and then allow time for them to discuss with their families or contemplate on their own; return to them at a later time. Become expert at spontaneous facilitation. Use your access code to get their attention and gain their trust.
- Nonlinear conversations. Although older patients may appear to wander off topic, they may do so in the urge to ground themselves in what their priorities are, what their feelings are, what their choices will be. Signal you’re willing to listen and that you’re tuned in to the content, even if you don’t know where it is leading. (Obviously, someone who is demented or delirious presents a different scenario altogether, and depression is common and frequently overlooked.) Listen for patterns and themes. Nonlinear conversations can lead to spontaneous revelations and great insights for your patients and for yourself and can help patients revisit life dramas that test and clarify values. This, too, is a part of healthcare.
- Repetition and attention to details. In situations when dementia is ruled out, a patient’s repetition may indicate a means to emphasize an important point or value. Keep in mind, too, that as we age, we all repeat stories to some degree. Details in stories may be the means by which older adults connect to their pasts and may also serve as clues to what is important to these people. Don’t assume details demand any action on your part. You are only being asked to listen as the older person sorts things out.
- Uncoupling. Solie describes uncoupling as any time an older person appears to disconnect from you in the course of a conversation. For a professional, this can feel as if you are dismissed or ignored just when you think you’ve hit the mark with a comment or question. Go back and assess the information you’ve gathered by doing some verification. Rethink the objective: Any action that works against their maintaining control and discovering a legacy will produce uncoupling.
“I try to be aware of when I’m losing people,” says Dr. Chittenden of this phenomenon. “I would say, ‘I seem to be losing you and I’m wondering what you’re thinking right now.’ I would try to find out where they’re at and if it was something I said that didn’t gel with them, didn’t make sense to them, or wasn’t their priority.” This is something, she emphasizes, that a hospitalist needs to watch for with patients of all ages. “Whether you’re older or younger,” she says, the communication can be complicated because “you’re … in the hospital culture and the priorities of doctors are so often different from the priorities of patients.”
Conclusion
Older and especially old-old individuals in some ways live in an era other than the one traversed by the young and middle-aged.6 Their purposes, agendas, and mission are different and the slowing down of their functioning can facilitate their attempts to put their lives into perspective and manage what control they can still exercise or are still allowed. Viewing older patients with the utmost respect and acknowledging the challenges they face at these last phases of their lives can better help you to partner with them and their families in their care. TH
Andrea Sattinger also writes about the importance of apology in this issue.
References
- Solie D. How to Say it to Seniors: Closing the Communication Gap with Our Elders. New York: Prentice Hall Press; 2004.
- Chochinov HM, Cann BJ. Interventions to enhance the spiritual aspects of dying. J Palliat Med. 2005;8:Suppl 1:S103-115.
- Dennis KE. Patients' control and the information imperative: clarification and confirmation. Nurs Res. 1990;39(3):162-166.
- Kiesler DJ, Auerbach SM. Integrating measurement of control and affiliation in studies of physician-patient interaction: the interpersonal circumplex. Soc Sci Med. 2003;57(9):1707-1722.
- Breemhaar B, Visser AP, Kleijnen JG. Perceptions and behaviour among elderly hospital patients: description and explanation of age differences in satisfaction, knowledge, emotions and behaviour. Soc Sci Med. 1990;31(12):1377-1385.
- Pipher M. Another Country: Navigating the Emotional Terrain of Our Elders. New York: Riverhead Books; 1999.
- Barnett PB. Rapport and the hospitalist. Am J Med. 2001;111:31S-35S.
When an elderly person is admitted to the hospital, Adrienne Green, MD, sees an opportunity for something beyond addressing the medical issues at hand.
“One of the key issues that is important for practical, everyday care is trying to figure out how the elderly are not functioning well at home,” says Dr. Green, an associate clinical professor of medicine at the University of California at San Francisco and a member of UCSF’s hospitalist group. “I think we do a great job of managing their diseases, but what we don’t do very well is helping them out with other things [such as coping with] their losses and the fact that they may be just barely hanging on at home in terms of their ability to care for themselves; and this hospitalization may really have set them back.”
Eva Chittenden, MD, an assistant clinical professor of medicine, also at UCSF, agrees. “Many hospitalists are so focused on the hospital that they’re not thinking about the ‘before the hospital’ and the ‘after the hospital,’” she says.
But after identifying the challenges that elderly patients face, communication itself may be challenging. Elderly individuals struggle with issues of control and allowing people to tell them what they need to change in their lives may not be an easy task. What are the best ways to communicate with hospitalized elderly patients to facilitate the best “whole-person” care?

—David Solie, MS, PA
Under the Radar Screen
The hospitalists interviewed for this article agreed that getting a broader picture of an elderly patient’s health and well-being involves discovering how they are really doing at home. Dr. Green asks simple questions, particularly about activities of daily living, such as whether they’re doing their own shopping and cooking. She also involves the family, “because very frequently the patient will say, ‘I’m doing fine,’ and the family member is in the background shaking their head.”
She also looks for clues about whether the patient needs more help at home, whether they are compliant with their medications, and if not, why (e.g., can they open their medicine bottles)?
“I frequently have the elderly patients evaluated for home care just to get someone into their house … ,” says Dr. Green. “I think that probably 80% of our patients who are over 80 who come into the hospital have things in their homes that are not safe, such as throw rugs.” Even if patients are basically doing OK, “if I can get some home care for them, I know we’ll uncover a ton [of things that can be improved],” she says. “These patients may have … kind of snuck under the radar screen of their families and their primary [care physician], and I think the hospitalization kind of opens that up in some ways.”
Facing Resistance
Even if issues are uncovered by means of interviews and home-health visits, however, many elderly patients present a particular communication challenge. This, says David Solie, MS, PA, author of How to Say It to Seniors: Closing the Communication Gap with Our Elders, is because of the difference in circumstances and current experiences between the elderly and their hospitalist providers.1 It is common knowledge that younger people go through stages of development, but the elderly do, too, says Solie, who is medical director and CEO of Second Opinion Insurance Services in Woodland Hills, Calif., a brokerage that specializes in the insurance needs of impaired-risk, elderly individuals.
The last human developmental stage compels elderly adults to work hard at maintaining control over their lives in the face of almost daily losses. A big part of the losses they experience involve their health and functioning, and the ways different patients cope with loss and the perceived stresses of healthcare have been analyzed and categorized.2-5
But in addition to loss of control, the elderly also face the daunting task of discovering what their legacy will be—what will live on after they die. “The way our elders communicate contains clues to the urgency they feel in trying to resolve these items on their agendas,” writes Solie. “In almost every conversation with older adults, control and legacy issues rise to the surface.”
A Matter of Loss
By the time a person is old (over 70) or old-old (over 85) their losses may have manifested in many areas: They’ve lost:
- Parents;
- Other relatives—perhaps including children;
- Friends;
- Places of residence (both homes and the familiarity of cities or towns);
- Possessions;
- Other relationships (sometimes other healthcare providers);
- Careers;
- Consultative authority (“ours is not a culture that values the wisdom of our elders,” writes Solie);
- Identity;
- Financial independence;
- Habits and pleasures;
- Physical space (the room at their son or daughter’s or in assisted living or the nursing home can’t compare to the homes, gardens, and expanses of view they may have had as younger people), and, of course; and
- Physical and mental capacities.
Sometimes the losses elders sustain occur in rapid-fire sequence, with little or no recovery time in between.1,6
It is no wonder that older adults, in one way or another, exhibit what we consider resistance to their changing lives. In terms of a hospitalization, this may mean saying “no” to medications, individual providers, tests, surgery, home-health visits, or something as small as being talked to or touched in what they perceive as a disturbing, overly familiar, or mechanized manner.
“Many patients are resistant to having people come into their homes and help them, and at the same time they are resistant to going to a skilled nursing care facility,” says Dr. Green, “and it has to do with their [feelings of the] loss of independence and control over their lives.”
“It’s very easy if you’re in medicine to normalize your context of the hospital,” says Solie. “In other words, the hospital seems familiar to you and you’re very comfortable moving around there, and mainly because you’re in control. You’re the doctor … and you move in the hospital in order to make things happen and you never feel all that threatened. But when you bring an older person who already has a heightened sensitivity toward losing control into the hospital—this complex, technological world of medicine—and they have the cumulative disadvantage of being sick,” says Solie, “it’s really important to remember that there will probably be no other state that they’ll be in, except maybe nursing home care, where they will feel so out of control.”
A good first step in communicating with older patients is to quickly develop a rapport with them and show them you recognize what they’re up against.7 “They really want to know whether or not I get it,” says Solie.
The way you communicate that you get it, he says, is fairly straightforward: When I’m first interacting with the patient, I say, “if you are like my [other] elderly patients … I’m sure you’re feeling a lot of anxiety over [not having much] control and, first of all, I want to assure you that I’m going to make sure you understand the choices and help you make all the decisions. And … I’m definitely going to … put everything in a language that you understand. But if I’m not successful, I’m going to employ someone from your family. We’re going to work together. Even though you’re hospitalized and even though you’re fighting this illness (or whatever the condition might be), you still [have] the right to make choices, and my goal is to partner with you. My expertise is medicine, but you have an expertise in your life.”
In other words, you are signaling that you recognize that control is the issue. Acknowledge the loss, ask about the value of the event or decision to the patient, ask what you can do to help them deal with their feelings or make up their minds. It also allows you to remind an older patient’s children that control is a big and normal concern for their mother or father.

—Eva Chittenden, MD
Hospitalists at a Different Time and Place
The elderly desperately need people who can serve them as natural healers, who are not constantly in a hurry, and who care what they are thinking and feeling. How can hospitalists relate to those who are in the midst of life review and who are hanging on to an escaping control? How can they serve their patients in a way that meets all needs?
Fighting—with denial or ignorance—the resistance that patients might put up will more than likely provoke them. A fight for control can undermine and sabotage the best intentions of the provider and the greatest wishes for the patient to experience comfort or regain health and well-being. Rather than justifying wresting control from elderly patients because it’s for their own good, advises Solie, what we must do instead is to “step back, hand them the control baton, and allow them to run with it.”1
A person’s admission to the hospital “might be such a huge crisis for them, whereas for us it’s our routine work,” says Dr. Chittenden, who practices as a hospitalist and also works on her institution’s inpatient palliative care service. “And many people who are hospitalists—who are even in their late 20s, 30s, 40s—have been totally healthy their whole life, so it is hard to relate to what it’s like to be older and to be losing function, losing friends who are also dying, losing their house … . I think that it can be very helpful for the hospitalist to take a little more time and explore some of those issues [of loss and legacy]. I try to meet the person where they’re at and try to understand what their goals, needs, ... and fears are [as well as] their functional status.”
Allowing older patients to engage with you about their lives and their pasts is a privilege for any healthcare provider. Engaging with them in a way that will help facilitate their loosening the reins on control may expedite and allow greater quality into their healthcare. It may provide an opening whereby you can order that home-health visit with less struggle.
Create Openings
“There are a lot of different ‘on-ramps’ to asking the life-review questions, which are extremely comforting,” says Solie. “For example, you might say, ‘Mary, I notice that you were born in Iowa. You know, my family on my father’s side came from Iowa. Where were you raised?’ And ‘Do you have a big family on your farm, because my aunt had cows.’”
Once you get a response that engages the patient, then you “are in the slipstream. Physicians have such a high experience curve, they see so many patients,” he says. “They don’t have to go very far into their inventory of experiences [to find one] that essentially matches up with that patient.”
Any kind of comment that will key you in to their background experience can help establish some kind of foundation for relationship. Another example: “You know, Mary, I was working with this woman who was about your age and she was raised in the Midwest and was dealing with some of these issues of congestive heart failure, and one of her big concerns was something that I didn’t appreciate until I understood what an impact it was having on her life.”
This kind of communication, says Solie, can help to relieve some of the patient’s control anxieties, “because she feels that if I ‘get it,’ she’s open to what I have to say, such as, ‘The first thing, we have to deal with is there is too much fluid going on in your body and it’s putting a big strain on your heart, so the first couple days all we did for that [other] woman was try to pull some fluid off and keep everything in balance.’”
You’ve communicated that you have a plan, that you can be trusted, and that you will help her to exercise as much control as possible. Creating and accessing those openings is also “the ideal way to weave the family into this whole life-review process, which is where the patient lives, psychologically and emotionally, when outside the hospital environment,” he says. “We become so myopic when we’re caught in the hospital environment that the world becomes a narrow tunnel and we forget the greater matrix outside that we’re all connected to.”
The Boon of Biology
Whereas the physiology and anatomy of humans deteriorate with time, some of the changes in mental processes in old age may actually enhance the ability to reflect and make informed judgments. Solie’s view is that what younger people may view as slow behavior, confusing speech patterns, and physical frailty don’t hinder the tasks that are before the elderly. On the contrary, they assist the fulfillment of their developmental agendas to feel in control when they’re losing control and to let go enough to reveal the legacy that will survive after they go.
Research on the aging brain indicates that changes in brain chemistry facilitate the life-review process.1,6 In general, reflection is the normal mode of existence for elderly adults and their primary focus. Thus, viewing them as diminished because they communicate differently than younger people do is doing them a disservice.
Those slowed mental processes, Dr. Chittenden concurs, “are conducive to reflection. Someone younger will pathologize it. … I agree that we don’t value the slowing down process, but I also think that when this population is in the hospital we are tending to look at loss of functional status or the quick mental traits that we value as opposed to [that which is] adaptive [and] that enables them to look at things differently and reflect.”
The key to connecting the dots of where they are and where they need to be (both medically and psychosocially), as well as how they occur to their providers and their families as opposed to how they occur to themselves, is to listen to and speak with them by making use of what you know about this stage of their life as it affects their communication. You can do this, says Solie, by invoking the “access code,” which is “to clearly understand that at the top of their agenda—no matter what else is happening—is the need for control and the need to develop and go after a legacy, and that means life review. If you know that, you will never lose your reference point with them.”
Communication Habits of the Elderly
Solie identifies some verbal behaviors that are common in older people. In many cases these behaviors may reveal something between the lines.
- Lack of urgency. Older people need more time to decide things. Accept that slower pace as normal. Don’t take it personally. Adjust your schedule to allow time to deliver news or ask for choices and then allow time for them to discuss with their families or contemplate on their own; return to them at a later time. Become expert at spontaneous facilitation. Use your access code to get their attention and gain their trust.
- Nonlinear conversations. Although older patients may appear to wander off topic, they may do so in the urge to ground themselves in what their priorities are, what their feelings are, what their choices will be. Signal you’re willing to listen and that you’re tuned in to the content, even if you don’t know where it is leading. (Obviously, someone who is demented or delirious presents a different scenario altogether, and depression is common and frequently overlooked.) Listen for patterns and themes. Nonlinear conversations can lead to spontaneous revelations and great insights for your patients and for yourself and can help patients revisit life dramas that test and clarify values. This, too, is a part of healthcare.
- Repetition and attention to details. In situations when dementia is ruled out, a patient’s repetition may indicate a means to emphasize an important point or value. Keep in mind, too, that as we age, we all repeat stories to some degree. Details in stories may be the means by which older adults connect to their pasts and may also serve as clues to what is important to these people. Don’t assume details demand any action on your part. You are only being asked to listen as the older person sorts things out.
- Uncoupling. Solie describes uncoupling as any time an older person appears to disconnect from you in the course of a conversation. For a professional, this can feel as if you are dismissed or ignored just when you think you’ve hit the mark with a comment or question. Go back and assess the information you’ve gathered by doing some verification. Rethink the objective: Any action that works against their maintaining control and discovering a legacy will produce uncoupling.
“I try to be aware of when I’m losing people,” says Dr. Chittenden of this phenomenon. “I would say, ‘I seem to be losing you and I’m wondering what you’re thinking right now.’ I would try to find out where they’re at and if it was something I said that didn’t gel with them, didn’t make sense to them, or wasn’t their priority.” This is something, she emphasizes, that a hospitalist needs to watch for with patients of all ages. “Whether you’re older or younger,” she says, the communication can be complicated because “you’re … in the hospital culture and the priorities of doctors are so often different from the priorities of patients.”
Conclusion
Older and especially old-old individuals in some ways live in an era other than the one traversed by the young and middle-aged.6 Their purposes, agendas, and mission are different and the slowing down of their functioning can facilitate their attempts to put their lives into perspective and manage what control they can still exercise or are still allowed. Viewing older patients with the utmost respect and acknowledging the challenges they face at these last phases of their lives can better help you to partner with them and their families in their care. TH
Andrea Sattinger also writes about the importance of apology in this issue.
References
- Solie D. How to Say it to Seniors: Closing the Communication Gap with Our Elders. New York: Prentice Hall Press; 2004.
- Chochinov HM, Cann BJ. Interventions to enhance the spiritual aspects of dying. J Palliat Med. 2005;8:Suppl 1:S103-115.
- Dennis KE. Patients' control and the information imperative: clarification and confirmation. Nurs Res. 1990;39(3):162-166.
- Kiesler DJ, Auerbach SM. Integrating measurement of control and affiliation in studies of physician-patient interaction: the interpersonal circumplex. Soc Sci Med. 2003;57(9):1707-1722.
- Breemhaar B, Visser AP, Kleijnen JG. Perceptions and behaviour among elderly hospital patients: description and explanation of age differences in satisfaction, knowledge, emotions and behaviour. Soc Sci Med. 1990;31(12):1377-1385.
- Pipher M. Another Country: Navigating the Emotional Terrain of Our Elders. New York: Riverhead Books; 1999.
- Barnett PB. Rapport and the hospitalist. Am J Med. 2001;111:31S-35S.
Conflict Conundrums
Contrary to popular belief, conflicts are not necessarily bad. In fact, conflicts can spark discussions that can lead to improved processes and quality care. They also can help open lines of communication among practitioners and between physicians and patients.
Of course, not all conflict is positive and discord can be detrimental to patients and to relationships in the hospital. It behooves hospitalists to understand how to resolve conflicts constructively and communicate effectively in emotionally charged and controversial situations.
Good Conflict
When resolved effectively, conflicts can lead to positive changes, process improvements, and enhanced quality, says Leonard Marcus, PhD, founding director of the Program for Health Care Negotiation and Conflict Resolution at the Harvard School of Public Health (Boston). In fact, conflict sometimes is necessary because it:
- Raises and resolves problems;
- Focuses change efforts on the most urgent and appropriate issues;
- Motivates people to participate in efforts to create positive changes; and
- Helps people learn to benefit from and recognize their differences.
Conflict is problematic when it:
- Hampers productivity;
- Lowers morale and/or hurts relationships;
- Creates more and continued conflicts; and
- Causes inappropriate and/or dangerous behaviors.
Conflicts often arise from everyday occurrences. Poor communication is one of the most common causes of disputes. However, conflicts also may result from insufficient resources, personality clashes, and leadership problems (e.g., inconsistent, missing, dictatorial, or uninformed leadership).
—Peter Prendergast, MD
Anatomy of a Conflict
A primary care physician, Dr. X, tells a patient, Mrs. Y, that she needs to be admitted to the hospital. If the hospitalist examines Mrs. Y and agrees that admission is necessary, there is no conflict. However, if the hospitalist determines that Mrs. Y doesn’t need to be admitted, the potential for conflict is ripe.
“This can create real tension,” says James W. Leyhane, MD, hospitalist director at Auburn Memorial Hospital, N.Y. “The hospitalist can find himself facing a conflict with the patient or the physician—or both.”
These situations can be highly charged and difficult to resolve. “Sometimes the person is adamant that he or she wants to be admitted,” says Dr. Leyhane. “And the stronger the relationship the patient has with the primary care physician, the greater the resistance they may have to what you are saying.”
The most common approach Dr. Leyhane takes to such a situation is to get on the physician’s side. “I will say something like, ‘I understand why Dr. Jones thought you should be admitted. However, after further examination, we now realize that admission is unnecessary,’” he explains.
Once the hospitalist addresses any anger or frustrations patients feel, most are relieved to avoid a hospitalization. But sometimes this approach doesn’t work, and some patients still insist on being admitted. In those cases, Dr. Leyhane will appeal to their pocketbook instead of their emotions. “I will tell them that I can admit them if they insist,” he says. “However, someone else will review their chart for insurance purposes, and they will have to pay out-of-pocket for the stay because it is not medically necessary. This is very persuasive.”
When Hospitalists and Attendings Clash
When such situations create conflict with physicians, they must be addressed carefully and resolved promptly. Dr. Marcus suggests that such conflicts can be minimized or eliminated altogether when “physicians negotiate expectations of their relationships” up front. “It is best for attendings and hospitalists to be communicating on an ongoing basis and understand each other’s positions before situations occur,” he offers.
Peter Prendergast, MD, chief hospitalist at St. Joseph’s Hospital and associate professor of Medicine at SUNY Upstate Medicine Center in Syracuse, New York, suggests that conflicts with physicians in these situations are not common. “Physicians overwhelmingly understand that we have more information by which to make admitting decisions,” says Dr. Prendergast. “We just need to make sure the patient understands that the physician makes the best possible decision with the data set he or she has and that we have access to more information and assessment tools and may draw a different conclusion.”
Nonetheless, Dr. Prendergast acknowledges that there are other situations that present the potential for attending-hospitalist conflict. “You may run into a problem with the primary care physician when the patient presents with a medical problem that previously was treated in the hospital that now is treated on an outpatient basis,” he notes.
Dr. Leyhane offers another common conflict with attendings. “Sometimes the physician will order a test or procedure that will not be reimbursed because it is unrelated to the patient’s reason for admission,” he says. “When this happens and the patient gets the bill, he or she is unhappy with the hospital and not the attending physician.”
These situations generally occur because the physician doesn’t realize that a service isn’t reimbursable or that a protocol has changed, Dr. Prendergast stresses, and not because the practitioner is being stubborn or contrary. Nonetheless, it presents a conflict.
“You need to let the physician know that there has been a change in treatment standards or that there is a reimbursement issue. Once he or she has the facts, you aren’t likely to have another problem,” says Dr. Prendergast. “The physician needs to get a phone call or at least a note in a timely manner.”
Dr. Marcus actually advises that hospitalists talk with the physician before communicating any information to the patient that conflicts with what the doctor has told him or her. “Otherwise,” he observes, “the conflict already has escalated.” Physicians, he says, don’t want to hear about a difference of opinion after the fact.
Hospitalist-Patient Conflicts
Roger Gildersleeve, MD, administrative hospitalist at Augusta Medical Center, Fishersville, Va., says conflicts with patients or family members are common situations for the hospitalist. “You may see conflicts when there is a disconnect between the patient’s or family’s expectations and the realities of the patient’s prognosis and outcomes,” he says. “We spend a lot of time trying to bring these two things closer together.”
One key to resolving these problems is to make a quick study of the situation. “You usually can read patients and families—by their body language and facial expressions—when you enter the room,” says Dr. Gildersleeve, “and you can detect tension and hostility.”
Dr. Prendergast agrees. “When you see patients and families in certain situations—such as 2 a.m. in the ER—you can make some reasonable assumptions about what they are thinking or feeling,” he says. “You can predict what these people’s concerns are, and you can address them even before they ask. Acknowledging their position and concerns is important.”
When possible, preparing for family and/or patient encounters can make a difference. “Before seeing a new patient, I try to learn as much as I can about him or her,” says Dr. Gildersleeve. “We have a good computer system, so it’s pretty easy. I use some of what I’ve learned in my opening comments, and this gives patients and families more confidence in me and my ability to deal with them as individuals.”
This is especially important for hospitalists, who have to establish patient relationships in a relatively short period of time.
Resolving Conflicts
Of course, it is impossible to prevent or avoid all conflicts. “To some degree, conflicts are inevitable,” says Dr. Marcus. “It’s the nature of medical practice.”
When conflicts occur, many of them can—and should—be resolved before they escalate into a dangerous confrontation or litigation. Listening is key to resolving conflicts quickly. “By listening, you can prevent a lot of conflicts from escalating or even starting,” says Dr. Prendergast. “We teach our physicians to listen, then repeat back what they heard—‘I’m hearing that you’re upset because … .’ If you get it right, the person knows that you are listening and that you understand their concerns. If you miss, they are likely to state their concern directly.”
Dr. Marcus believes conflict resolution may be particularly effective and satisfying when interest-based negotiation (IBN) is employed. IBN is a problem-solving strategy that focuses on satisfying as many interests or needs as possible for all involved parties. Because this technique addresses people’s needs and interests and separates people from the problem, it enables the parties to reach an integrative solution rather than creating a win-lose situation.
IBN enables those involved in a conflict to work together to reach a mutually satisfactory conclusion. The technique commonly results in creative and durable solutions, as well as enhanced relationships.
Conflict resolution efforts are more likely to fail, says Dr. Marcus, when the physicians and others involved apply position-based negotiations. With this conflict-management method, the parties argue only their positions, and their underlying interests may never be stated explicitly or understood. People are more likely to reach an impasse when they employ position-based negotiations, and they are more likely to see the situation as having a clear-cut winner and a loser.
“When you negotiate based on positions,” explains Dr. Marcus, “that is when situations are likely to escalate.”
While clear hospital policies and procedures can help resolve or prevent some conflicts involving physicians, more layers of policy are not necessarily the answer. “I think the time it would take to establish these policies would be better spent developing pathways for easier and better communication,” says Dr. Gildersleeve. “You see few of these hospitalist-physician conflicts when there is good communication between all the players.”
Professional mediator Pat Costello suggests that policy changes actually can help resolve some disputes. “Continued conflicts might suggest a need for a policy change or a new policy,” says Costello. “I have mediated a lot of situations that were resolved by policy changes.”
15 Seconds to Make an Impression
Hospitalists must remain cognizant of mistakes they can make that actually exacerbate conflicts with patients and families. “When physicians use an overbearing approach, they can’t accomplish as much,” says Dr. Marcus. “You have to take care to treat patients and families with care and concern and the same respect they afford their colleagues.”
It is important for hospitalists to be aware of how they come across to others, stressed Carole Houk, Esq., president of Carole Houk International, Alexandria, Va.
“You make a snap judgment of whether or not you like someone in about 15 seconds,” says Houk. “Studies show that physicians who use a dominant tone of voice are more likely to be sued than those who don’t.
“Explain what happens and why—and put a lot of focus on your tone of voice,” she says. “Rather than coming down imperiously, reach out to patients in a compassionate way. You need to be seen as someone with a heart and not a gatekeeper for the insurance company.”
When Hospitalists Can’t Resolve a Conflict
Unfortunately, some conflicts can’t be resolved easily. While hospitalists require some conflict resolution skills, they must also be willing and able to recognize when they need assistance. For example, suggests Houk, “We have ombudsmen in some hospitals who serve as conflict coaches. They are trained for this purpose. Hospitalists and others can go to these people for help resolving conflicts.”
Elsewhere, she notes, “We are training risk managers on conflict skills so that they can help resolve disputes in their hospitals and serve as informal mediators.”
On rare occasions, it may be necessary to seek the involvement of an independent professional mediator. Mediator Costello says this might be necessary in instances where there is an ongoing and escalating lack of communication, repeated conflicts (despite attempts to resolve them), physical altercations or threats of violence, and/or imminent risk to a patent’s safety.
While there may be conflicts that hospitalists cannot resolve, overall they are well equipped to communicate effectively in a way that minimizes disputes. “Many of us were attracted to this profession because of the opportunities and challenges of working with a wide range of situations and colleagues,” says Dr. Leyhane. “We know that communication skills are important, and we get a lot of practice during our interactions with physicians, families, patients, administrators, and ancillary staff.”
Houk agrees: “This field seems to attract people with big hearts. They understand the importance of understanding and acknowledging the needs and feelings of others.” TH
Joanne Kaldy writes regularly for The Hospitalist.
Contrary to popular belief, conflicts are not necessarily bad. In fact, conflicts can spark discussions that can lead to improved processes and quality care. They also can help open lines of communication among practitioners and between physicians and patients.
Of course, not all conflict is positive and discord can be detrimental to patients and to relationships in the hospital. It behooves hospitalists to understand how to resolve conflicts constructively and communicate effectively in emotionally charged and controversial situations.
Good Conflict
When resolved effectively, conflicts can lead to positive changes, process improvements, and enhanced quality, says Leonard Marcus, PhD, founding director of the Program for Health Care Negotiation and Conflict Resolution at the Harvard School of Public Health (Boston). In fact, conflict sometimes is necessary because it:
- Raises and resolves problems;
- Focuses change efforts on the most urgent and appropriate issues;
- Motivates people to participate in efforts to create positive changes; and
- Helps people learn to benefit from and recognize their differences.
Conflict is problematic when it:
- Hampers productivity;
- Lowers morale and/or hurts relationships;
- Creates more and continued conflicts; and
- Causes inappropriate and/or dangerous behaviors.
Conflicts often arise from everyday occurrences. Poor communication is one of the most common causes of disputes. However, conflicts also may result from insufficient resources, personality clashes, and leadership problems (e.g., inconsistent, missing, dictatorial, or uninformed leadership).
—Peter Prendergast, MD
Anatomy of a Conflict
A primary care physician, Dr. X, tells a patient, Mrs. Y, that she needs to be admitted to the hospital. If the hospitalist examines Mrs. Y and agrees that admission is necessary, there is no conflict. However, if the hospitalist determines that Mrs. Y doesn’t need to be admitted, the potential for conflict is ripe.
“This can create real tension,” says James W. Leyhane, MD, hospitalist director at Auburn Memorial Hospital, N.Y. “The hospitalist can find himself facing a conflict with the patient or the physician—or both.”
These situations can be highly charged and difficult to resolve. “Sometimes the person is adamant that he or she wants to be admitted,” says Dr. Leyhane. “And the stronger the relationship the patient has with the primary care physician, the greater the resistance they may have to what you are saying.”
The most common approach Dr. Leyhane takes to such a situation is to get on the physician’s side. “I will say something like, ‘I understand why Dr. Jones thought you should be admitted. However, after further examination, we now realize that admission is unnecessary,’” he explains.
Once the hospitalist addresses any anger or frustrations patients feel, most are relieved to avoid a hospitalization. But sometimes this approach doesn’t work, and some patients still insist on being admitted. In those cases, Dr. Leyhane will appeal to their pocketbook instead of their emotions. “I will tell them that I can admit them if they insist,” he says. “However, someone else will review their chart for insurance purposes, and they will have to pay out-of-pocket for the stay because it is not medically necessary. This is very persuasive.”
When Hospitalists and Attendings Clash
When such situations create conflict with physicians, they must be addressed carefully and resolved promptly. Dr. Marcus suggests that such conflicts can be minimized or eliminated altogether when “physicians negotiate expectations of their relationships” up front. “It is best for attendings and hospitalists to be communicating on an ongoing basis and understand each other’s positions before situations occur,” he offers.
Peter Prendergast, MD, chief hospitalist at St. Joseph’s Hospital and associate professor of Medicine at SUNY Upstate Medicine Center in Syracuse, New York, suggests that conflicts with physicians in these situations are not common. “Physicians overwhelmingly understand that we have more information by which to make admitting decisions,” says Dr. Prendergast. “We just need to make sure the patient understands that the physician makes the best possible decision with the data set he or she has and that we have access to more information and assessment tools and may draw a different conclusion.”
Nonetheless, Dr. Prendergast acknowledges that there are other situations that present the potential for attending-hospitalist conflict. “You may run into a problem with the primary care physician when the patient presents with a medical problem that previously was treated in the hospital that now is treated on an outpatient basis,” he notes.
Dr. Leyhane offers another common conflict with attendings. “Sometimes the physician will order a test or procedure that will not be reimbursed because it is unrelated to the patient’s reason for admission,” he says. “When this happens and the patient gets the bill, he or she is unhappy with the hospital and not the attending physician.”
These situations generally occur because the physician doesn’t realize that a service isn’t reimbursable or that a protocol has changed, Dr. Prendergast stresses, and not because the practitioner is being stubborn or contrary. Nonetheless, it presents a conflict.
“You need to let the physician know that there has been a change in treatment standards or that there is a reimbursement issue. Once he or she has the facts, you aren’t likely to have another problem,” says Dr. Prendergast. “The physician needs to get a phone call or at least a note in a timely manner.”
Dr. Marcus actually advises that hospitalists talk with the physician before communicating any information to the patient that conflicts with what the doctor has told him or her. “Otherwise,” he observes, “the conflict already has escalated.” Physicians, he says, don’t want to hear about a difference of opinion after the fact.
Hospitalist-Patient Conflicts
Roger Gildersleeve, MD, administrative hospitalist at Augusta Medical Center, Fishersville, Va., says conflicts with patients or family members are common situations for the hospitalist. “You may see conflicts when there is a disconnect between the patient’s or family’s expectations and the realities of the patient’s prognosis and outcomes,” he says. “We spend a lot of time trying to bring these two things closer together.”
One key to resolving these problems is to make a quick study of the situation. “You usually can read patients and families—by their body language and facial expressions—when you enter the room,” says Dr. Gildersleeve, “and you can detect tension and hostility.”
Dr. Prendergast agrees. “When you see patients and families in certain situations—such as 2 a.m. in the ER—you can make some reasonable assumptions about what they are thinking or feeling,” he says. “You can predict what these people’s concerns are, and you can address them even before they ask. Acknowledging their position and concerns is important.”
When possible, preparing for family and/or patient encounters can make a difference. “Before seeing a new patient, I try to learn as much as I can about him or her,” says Dr. Gildersleeve. “We have a good computer system, so it’s pretty easy. I use some of what I’ve learned in my opening comments, and this gives patients and families more confidence in me and my ability to deal with them as individuals.”
This is especially important for hospitalists, who have to establish patient relationships in a relatively short period of time.
Resolving Conflicts
Of course, it is impossible to prevent or avoid all conflicts. “To some degree, conflicts are inevitable,” says Dr. Marcus. “It’s the nature of medical practice.”
When conflicts occur, many of them can—and should—be resolved before they escalate into a dangerous confrontation or litigation. Listening is key to resolving conflicts quickly. “By listening, you can prevent a lot of conflicts from escalating or even starting,” says Dr. Prendergast. “We teach our physicians to listen, then repeat back what they heard—‘I’m hearing that you’re upset because … .’ If you get it right, the person knows that you are listening and that you understand their concerns. If you miss, they are likely to state their concern directly.”
Dr. Marcus believes conflict resolution may be particularly effective and satisfying when interest-based negotiation (IBN) is employed. IBN is a problem-solving strategy that focuses on satisfying as many interests or needs as possible for all involved parties. Because this technique addresses people’s needs and interests and separates people from the problem, it enables the parties to reach an integrative solution rather than creating a win-lose situation.
IBN enables those involved in a conflict to work together to reach a mutually satisfactory conclusion. The technique commonly results in creative and durable solutions, as well as enhanced relationships.
Conflict resolution efforts are more likely to fail, says Dr. Marcus, when the physicians and others involved apply position-based negotiations. With this conflict-management method, the parties argue only their positions, and their underlying interests may never be stated explicitly or understood. People are more likely to reach an impasse when they employ position-based negotiations, and they are more likely to see the situation as having a clear-cut winner and a loser.
“When you negotiate based on positions,” explains Dr. Marcus, “that is when situations are likely to escalate.”
While clear hospital policies and procedures can help resolve or prevent some conflicts involving physicians, more layers of policy are not necessarily the answer. “I think the time it would take to establish these policies would be better spent developing pathways for easier and better communication,” says Dr. Gildersleeve. “You see few of these hospitalist-physician conflicts when there is good communication between all the players.”
Professional mediator Pat Costello suggests that policy changes actually can help resolve some disputes. “Continued conflicts might suggest a need for a policy change or a new policy,” says Costello. “I have mediated a lot of situations that were resolved by policy changes.”
15 Seconds to Make an Impression
Hospitalists must remain cognizant of mistakes they can make that actually exacerbate conflicts with patients and families. “When physicians use an overbearing approach, they can’t accomplish as much,” says Dr. Marcus. “You have to take care to treat patients and families with care and concern and the same respect they afford their colleagues.”
It is important for hospitalists to be aware of how they come across to others, stressed Carole Houk, Esq., president of Carole Houk International, Alexandria, Va.
“You make a snap judgment of whether or not you like someone in about 15 seconds,” says Houk. “Studies show that physicians who use a dominant tone of voice are more likely to be sued than those who don’t.
“Explain what happens and why—and put a lot of focus on your tone of voice,” she says. “Rather than coming down imperiously, reach out to patients in a compassionate way. You need to be seen as someone with a heart and not a gatekeeper for the insurance company.”
When Hospitalists Can’t Resolve a Conflict
Unfortunately, some conflicts can’t be resolved easily. While hospitalists require some conflict resolution skills, they must also be willing and able to recognize when they need assistance. For example, suggests Houk, “We have ombudsmen in some hospitals who serve as conflict coaches. They are trained for this purpose. Hospitalists and others can go to these people for help resolving conflicts.”
Elsewhere, she notes, “We are training risk managers on conflict skills so that they can help resolve disputes in their hospitals and serve as informal mediators.”
On rare occasions, it may be necessary to seek the involvement of an independent professional mediator. Mediator Costello says this might be necessary in instances where there is an ongoing and escalating lack of communication, repeated conflicts (despite attempts to resolve them), physical altercations or threats of violence, and/or imminent risk to a patent’s safety.
While there may be conflicts that hospitalists cannot resolve, overall they are well equipped to communicate effectively in a way that minimizes disputes. “Many of us were attracted to this profession because of the opportunities and challenges of working with a wide range of situations and colleagues,” says Dr. Leyhane. “We know that communication skills are important, and we get a lot of practice during our interactions with physicians, families, patients, administrators, and ancillary staff.”
Houk agrees: “This field seems to attract people with big hearts. They understand the importance of understanding and acknowledging the needs and feelings of others.” TH
Joanne Kaldy writes regularly for The Hospitalist.
Contrary to popular belief, conflicts are not necessarily bad. In fact, conflicts can spark discussions that can lead to improved processes and quality care. They also can help open lines of communication among practitioners and between physicians and patients.
Of course, not all conflict is positive and discord can be detrimental to patients and to relationships in the hospital. It behooves hospitalists to understand how to resolve conflicts constructively and communicate effectively in emotionally charged and controversial situations.
Good Conflict
When resolved effectively, conflicts can lead to positive changes, process improvements, and enhanced quality, says Leonard Marcus, PhD, founding director of the Program for Health Care Negotiation and Conflict Resolution at the Harvard School of Public Health (Boston). In fact, conflict sometimes is necessary because it:
- Raises and resolves problems;
- Focuses change efforts on the most urgent and appropriate issues;
- Motivates people to participate in efforts to create positive changes; and
- Helps people learn to benefit from and recognize their differences.
Conflict is problematic when it:
- Hampers productivity;
- Lowers morale and/or hurts relationships;
- Creates more and continued conflicts; and
- Causes inappropriate and/or dangerous behaviors.
Conflicts often arise from everyday occurrences. Poor communication is one of the most common causes of disputes. However, conflicts also may result from insufficient resources, personality clashes, and leadership problems (e.g., inconsistent, missing, dictatorial, or uninformed leadership).
—Peter Prendergast, MD
Anatomy of a Conflict
A primary care physician, Dr. X, tells a patient, Mrs. Y, that she needs to be admitted to the hospital. If the hospitalist examines Mrs. Y and agrees that admission is necessary, there is no conflict. However, if the hospitalist determines that Mrs. Y doesn’t need to be admitted, the potential for conflict is ripe.
“This can create real tension,” says James W. Leyhane, MD, hospitalist director at Auburn Memorial Hospital, N.Y. “The hospitalist can find himself facing a conflict with the patient or the physician—or both.”
These situations can be highly charged and difficult to resolve. “Sometimes the person is adamant that he or she wants to be admitted,” says Dr. Leyhane. “And the stronger the relationship the patient has with the primary care physician, the greater the resistance they may have to what you are saying.”
The most common approach Dr. Leyhane takes to such a situation is to get on the physician’s side. “I will say something like, ‘I understand why Dr. Jones thought you should be admitted. However, after further examination, we now realize that admission is unnecessary,’” he explains.
Once the hospitalist addresses any anger or frustrations patients feel, most are relieved to avoid a hospitalization. But sometimes this approach doesn’t work, and some patients still insist on being admitted. In those cases, Dr. Leyhane will appeal to their pocketbook instead of their emotions. “I will tell them that I can admit them if they insist,” he says. “However, someone else will review their chart for insurance purposes, and they will have to pay out-of-pocket for the stay because it is not medically necessary. This is very persuasive.”
When Hospitalists and Attendings Clash
When such situations create conflict with physicians, they must be addressed carefully and resolved promptly. Dr. Marcus suggests that such conflicts can be minimized or eliminated altogether when “physicians negotiate expectations of their relationships” up front. “It is best for attendings and hospitalists to be communicating on an ongoing basis and understand each other’s positions before situations occur,” he offers.
Peter Prendergast, MD, chief hospitalist at St. Joseph’s Hospital and associate professor of Medicine at SUNY Upstate Medicine Center in Syracuse, New York, suggests that conflicts with physicians in these situations are not common. “Physicians overwhelmingly understand that we have more information by which to make admitting decisions,” says Dr. Prendergast. “We just need to make sure the patient understands that the physician makes the best possible decision with the data set he or she has and that we have access to more information and assessment tools and may draw a different conclusion.”
Nonetheless, Dr. Prendergast acknowledges that there are other situations that present the potential for attending-hospitalist conflict. “You may run into a problem with the primary care physician when the patient presents with a medical problem that previously was treated in the hospital that now is treated on an outpatient basis,” he notes.
Dr. Leyhane offers another common conflict with attendings. “Sometimes the physician will order a test or procedure that will not be reimbursed because it is unrelated to the patient’s reason for admission,” he says. “When this happens and the patient gets the bill, he or she is unhappy with the hospital and not the attending physician.”
These situations generally occur because the physician doesn’t realize that a service isn’t reimbursable or that a protocol has changed, Dr. Prendergast stresses, and not because the practitioner is being stubborn or contrary. Nonetheless, it presents a conflict.
“You need to let the physician know that there has been a change in treatment standards or that there is a reimbursement issue. Once he or she has the facts, you aren’t likely to have another problem,” says Dr. Prendergast. “The physician needs to get a phone call or at least a note in a timely manner.”
Dr. Marcus actually advises that hospitalists talk with the physician before communicating any information to the patient that conflicts with what the doctor has told him or her. “Otherwise,” he observes, “the conflict already has escalated.” Physicians, he says, don’t want to hear about a difference of opinion after the fact.
Hospitalist-Patient Conflicts
Roger Gildersleeve, MD, administrative hospitalist at Augusta Medical Center, Fishersville, Va., says conflicts with patients or family members are common situations for the hospitalist. “You may see conflicts when there is a disconnect between the patient’s or family’s expectations and the realities of the patient’s prognosis and outcomes,” he says. “We spend a lot of time trying to bring these two things closer together.”
One key to resolving these problems is to make a quick study of the situation. “You usually can read patients and families—by their body language and facial expressions—when you enter the room,” says Dr. Gildersleeve, “and you can detect tension and hostility.”
Dr. Prendergast agrees. “When you see patients and families in certain situations—such as 2 a.m. in the ER—you can make some reasonable assumptions about what they are thinking or feeling,” he says. “You can predict what these people’s concerns are, and you can address them even before they ask. Acknowledging their position and concerns is important.”
When possible, preparing for family and/or patient encounters can make a difference. “Before seeing a new patient, I try to learn as much as I can about him or her,” says Dr. Gildersleeve. “We have a good computer system, so it’s pretty easy. I use some of what I’ve learned in my opening comments, and this gives patients and families more confidence in me and my ability to deal with them as individuals.”
This is especially important for hospitalists, who have to establish patient relationships in a relatively short period of time.
Resolving Conflicts
Of course, it is impossible to prevent or avoid all conflicts. “To some degree, conflicts are inevitable,” says Dr. Marcus. “It’s the nature of medical practice.”
When conflicts occur, many of them can—and should—be resolved before they escalate into a dangerous confrontation or litigation. Listening is key to resolving conflicts quickly. “By listening, you can prevent a lot of conflicts from escalating or even starting,” says Dr. Prendergast. “We teach our physicians to listen, then repeat back what they heard—‘I’m hearing that you’re upset because … .’ If you get it right, the person knows that you are listening and that you understand their concerns. If you miss, they are likely to state their concern directly.”
Dr. Marcus believes conflict resolution may be particularly effective and satisfying when interest-based negotiation (IBN) is employed. IBN is a problem-solving strategy that focuses on satisfying as many interests or needs as possible for all involved parties. Because this technique addresses people’s needs and interests and separates people from the problem, it enables the parties to reach an integrative solution rather than creating a win-lose situation.
IBN enables those involved in a conflict to work together to reach a mutually satisfactory conclusion. The technique commonly results in creative and durable solutions, as well as enhanced relationships.
Conflict resolution efforts are more likely to fail, says Dr. Marcus, when the physicians and others involved apply position-based negotiations. With this conflict-management method, the parties argue only their positions, and their underlying interests may never be stated explicitly or understood. People are more likely to reach an impasse when they employ position-based negotiations, and they are more likely to see the situation as having a clear-cut winner and a loser.
“When you negotiate based on positions,” explains Dr. Marcus, “that is when situations are likely to escalate.”
While clear hospital policies and procedures can help resolve or prevent some conflicts involving physicians, more layers of policy are not necessarily the answer. “I think the time it would take to establish these policies would be better spent developing pathways for easier and better communication,” says Dr. Gildersleeve. “You see few of these hospitalist-physician conflicts when there is good communication between all the players.”
Professional mediator Pat Costello suggests that policy changes actually can help resolve some disputes. “Continued conflicts might suggest a need for a policy change or a new policy,” says Costello. “I have mediated a lot of situations that were resolved by policy changes.”
15 Seconds to Make an Impression
Hospitalists must remain cognizant of mistakes they can make that actually exacerbate conflicts with patients and families. “When physicians use an overbearing approach, they can’t accomplish as much,” says Dr. Marcus. “You have to take care to treat patients and families with care and concern and the same respect they afford their colleagues.”
It is important for hospitalists to be aware of how they come across to others, stressed Carole Houk, Esq., president of Carole Houk International, Alexandria, Va.
“You make a snap judgment of whether or not you like someone in about 15 seconds,” says Houk. “Studies show that physicians who use a dominant tone of voice are more likely to be sued than those who don’t.
“Explain what happens and why—and put a lot of focus on your tone of voice,” she says. “Rather than coming down imperiously, reach out to patients in a compassionate way. You need to be seen as someone with a heart and not a gatekeeper for the insurance company.”
When Hospitalists Can’t Resolve a Conflict
Unfortunately, some conflicts can’t be resolved easily. While hospitalists require some conflict resolution skills, they must also be willing and able to recognize when they need assistance. For example, suggests Houk, “We have ombudsmen in some hospitals who serve as conflict coaches. They are trained for this purpose. Hospitalists and others can go to these people for help resolving conflicts.”
Elsewhere, she notes, “We are training risk managers on conflict skills so that they can help resolve disputes in their hospitals and serve as informal mediators.”
On rare occasions, it may be necessary to seek the involvement of an independent professional mediator. Mediator Costello says this might be necessary in instances where there is an ongoing and escalating lack of communication, repeated conflicts (despite attempts to resolve them), physical altercations or threats of violence, and/or imminent risk to a patent’s safety.
While there may be conflicts that hospitalists cannot resolve, overall they are well equipped to communicate effectively in a way that minimizes disputes. “Many of us were attracted to this profession because of the opportunities and challenges of working with a wide range of situations and colleagues,” says Dr. Leyhane. “We know that communication skills are important, and we get a lot of practice during our interactions with physicians, families, patients, administrators, and ancillary staff.”
Houk agrees: “This field seems to attract people with big hearts. They understand the importance of understanding and acknowledging the needs and feelings of others.” TH
Joanne Kaldy writes regularly for The Hospitalist.
I'm Sorry
Apologizing to a patient is the right thing to do,” says Michael S. Woods, MD, a general surgeon at St. Vincent’s Regional Medical Center in Santa Fe, N.M. “It is the respectful thing in any relationship in terms of trust whenever there is a violation, whether it is real or perceived.” Dr. Woods, the author of Healing Words: The Power of Apology in Medicine, teaches and consults with corporations around the country about apology as well as physician leadership.1-2 In fact, his study of apology stemmed from examining the subject of physician leadership, and he and other experts consider the vital components of leadership to be effective communication, integrity, honesty, and respectful treatment of other individuals.3,4
Dr. Woods also works with Doug Wojcieszak, a public relations consultant whose victims’ rights group proposed “Sorry Works!” This program recommends apologies and settlements when medical mistakes occur. (See “A History of Sorry Works!” p. 26.) Dr. Woods says Wojcieszak comes from an interesting angle that he supports. “Something I increasingly try to hammer home when I speak is that one of the most important components of the apology law has nothing to do with the backhand of the reduction of litigation as much as the fact that it gives the physician the green light to say ‘I’m sorry,’” says Dr. Woods.
The Benefit of Healing
Providers may be less than open when things go terribly wrong because of feelings of fear, shame, and guilt regarding the consequences to the patient as well as to themselves.1,3 Apology heals by restoring the patient’s dignity and self-respect, providing assurance of shared values, and assuring patients that they are not at fault, they are now safe, and that the caregiver shares their suffering.4,7
Two Senses of Apology
There are circumstances other than when errors occur in which a physician’s apology may carry the power to improve patient care. Peter Barnett, MD, MPH, a clinical associate professor of medicine at the University of New Mexico in Albuquerque, says that in general there are two senses of apology.
“The first sense of apology regards the situation,” he says. For example, you might say, ‘I’m sorry you have cancer,’ or ‘I’m sorry that our system doesn’t allow your family doctor to be taking care of you in the hospital.’ It’s an expression of sympathy, but I think apology works better.”
The other sense of apology regards responsibility, says Dr. Barnett, citing the example, “I’m sorry I gave you the wrong drug.”
Situational needs for apology include when patients have been waiting a long time, such as when a hospitalist meets them in the emergency department. “In those cases you would say, ‘I’m sorry that you had to wait so long,’” says Dr. Barnett. “It’s not my fault, but I really am sorry.”
Bridging the Gap
Dr. Barnett, who practices hospital medicine part-time along with his major focus in addiction medicine, was formerly the director of the UNM hospitalist team. He explains that one of the primary reasons hospitalists may need to apologize to patients is that the hospitalist and patient have no prior relationship that could serve as a foundation for interpreting each other’s behavior.8
He believes apologizing for the delays and inconveniences that happen in the hospital “can help bridge the relationship gap in hospital medicine. Because what people believe about their primary care physicians is that they know and care about them,” he says. “To minimize their anxiety about you, show them that you do care about them by getting to know them well, and apology is the one of the best ways of doing that.”
When asked to elaborate what he means by “getting to know them well,” Dr. Barnett says, “I might tell someone, ‘I’d like to get to know you better; what can you tell me about yourself that would help bring me up to speed?’” It’s open-ended, he says, and you let the patient choose the topic. “Most people will say something. … It’s empathic inquiry with really good reflective listening; that is probably the simplest way of summarizing what it takes.”
Dr. Barnett suggests this kind of inquiry can mitigate the gaps in relationships that may lead to misunderstandings, edgy situations, and errors that may later call for apology. He recommends asking or saying some of the following to patients:
- What do you know about your illness?
- What do you believe about your illness?
- What are your feelings, values, beliefs, and preferences about/for your treatment?
- What can you tell me about your experiences in the hospital?
For patients who have been ill many times and have had a lot of medical experience, you could ask:
- Could you tell me about your doctors?
- What do you like about doctors?
- What don’t you like about your doctors?
These questions can help you discern who they are as a patient, and it gives patients the opportunity to be candid with you.
“It’s not about finding information that’s embarrassing or critical to your predecessor physicians, but it allows you to not make the same mistakes inadvertently,” says Dr. Barnett, who considers it concrete information. “I want them to have good medical care. I don’t want to make them unhappy. I want to avoid pitfalls. I think the two of us—the patient and I—should avoid pitfalls together.”
Asking the patient in a straightforward way what they want and don’t want gives the patient an opportunity to give the physician advice on how to stay out of trouble with them.
Apology When Disclosing Errors
The matter of assuming responsibility for errors is more complicated as it pertains to the use of apology, but it is an “idea whose time has come.”9 Although it is hard to quantify, plenty of evidence shows that apologizing for errors reduces the number of lawsuits and may reduce the settlement value of malpractice claims.3,5-7,10-26 Although there is not always agreement about the specifics of full disclosure, above all patients have the right to know what happens during their medical care and, therefore, restricting the information that is given to a patient can have legal ramifications.
Beyond this, writes Lucian Leape, MD, adjunct professor of health policy at the Harvard School of Public Health and an internationally recognized leader in the patient safety movement, wrote in the March-April issue of Physician Executive that apology is a “therapeutic necessity” that allows the patient to recognize a physician’s humanity and fallibility as well as his or her remorse at having caused harm.9 In the long run, apologizing to patients defuses more situations than it aggravates, and it pays off emotionally, financially, and in practice morale.5,6,9
Data from studies of medical practices that issue apologies in circumstances where accountability is clearly established show that litigation claims are reduced. In one 1992 study, 24% of people who sued physicians said they did so because the doctor was dishonest and withheld information. Nineteen percent said that they either sued to deter subsequent malpractice or for revenge.11,12 In each case of legal action, the investigators hypothesized that the doctor could have avoided the lawsuit by taking responsibility and apologizing up front and making amends at that time. It has been estimated that more than half of claims relegated to litigation could be avoided with use of prudent disclosure and apology.3,21
“My mantra, if you will,” says Dr. Woods, “is that [when] you apologize because it’s the right thing to do, all the benefits naturally ensue.”
Anticipating Apology
The issue of complications, adverse events, and errors carries its own protocol in terms of whether and how apology is offered. “Hopefully some of these have been anticipated,” says Dr. Barnett. “For instance, when you spoke with the patient about their pneumonia, you’ve said something about the possibility that pneumonias could become complicated, and [they] might have some kind of complications; or if they’ve had a heart attack, [you mentioned that] they might have some complications. So you’re actually already warning people about what could happen and you’ve said you’re going to try to prevent it, but it could [still happen].”
Apology can be appropriately offered when those events do occur and you genuinely express disappointment that you and the patient share.
“There are some quite complicated systematic problems [related to apology and hospital medicine],” says Dr. Barnett. “Some are communication aspects and some are legal ones. What I have heard from the attorneys is that you want to keep the apology relatively simple, … and it shouldn’t include any statements about other people who may have been involved, such as pharmacy or nurses.”
The other important issue related to hospitalists and apology, says Dr. Barnett, is that because of the lack of relationship, the severity of illness of the patients you are treating, and the strangeness of systems, people come to the hospital expecting errors. They expect them and may be afraid of them. In particular, when a medication error is made, they expect those errors to be disclosed to them.7,27 Dr. Barnett believes patients are waiting and watching, and hoping that nothing happens to them. Complicating the issue, he says, is that “many hospitalists are fairly guarded in this respect. The emotional deck is sort of stacked against everybody, so if the hospitalist is sensitive about the situation, that tends actually to make the situation worse. If you can apologize sincerely and simply, the patient may be reassured that you’re not trying to conceal anything, you’re honest, you’re on top of it, and you’ll do your best to deal with it,” he says, adding, “they know that that stuff happens; they hope that it is not hidden, ignored, or mismanaged.”
Start Early and Let It Flow
Dr. Woods’ advice is to offer apology earlier rather than later and to widen the spectrum of those to whom you wish to show your empathy, sympathy, respect, and compassion.
“What I promote to organizations is that they drive this into the consciousness of the organization by getting people to apologize for the least infraction—not waiting for the grave errors.” He interprets this as apologizing “when you’re running 30 minutes late, apologize when you’ve interrupted the patient or the family when they’re speaking. These are the things we would do for our spouse or our significant other or our family members; why is it any different at work?”
He also believes it is inherent for doctors as leaders to “apologize to your staff members, apologize to the nurses.” Because the image you express serves as a role model in this regard and will permeate your practice culture. Drive respectful treatment as a basic common social courtesy into the organizational consciousness, says Dr. Woods, and then in any circumstance where an apology is offered, it is perceived as authentic.
Conclusion
Hospitalists may find a need to apologize to patients and families for situations and circumstances in the hospital environment as well as the gap in relationship that exists when hospitalists and patients first encounter each other. Apologizing early rather than later as well as simply and authentically goes a long way to help achieve the ethical and business objectives held by most hospital physicians. TH
Andrea Sattinger wrote about error reporting in the May issue.
References
- Woods MS, Star JI. Healing Words: The Power of Apology in Medicine. Santa Fe, N.M.: Doctors in Touch; 2004.
- Woods MS. Applying Personal Leadership Principles to Health Care: The DEPO Principle. Orlando, Fl.: American College of Physician Executives; 2001.
- Leape LL. National Patient Safety Foundation. Understanding the power of apology: how saying “I’m sorry" helps heal patients and caregivers. Focus on Patient Safety. 2005;8:1-3.
- Lazare A. On Apology. Oxford, U.K.: Oxford University Press; 2004.
- Boothman RC. Apologies and a strong defense at the University of Michigan Health System. Physician Exec. 2006 Mar-Apr; 32(2):7-10.
- Weber DO. Who’s sorry now? Special report: patient trust and safety. Physician Exec. 2006 Mar-Apr:32(2)6-14.
- When Things Go Wrong: Responding to Adverse Events. A Consensus Statement of the Harvard Hospitals. Burlington, Massachusetts: Massachusetts Coalition for the Prevention of Medical Errors; 2006.
- Barnett PB. Rapport and the hospitalist. Am J Med. 2001;111:31S-35S.
- Leape LL. Full disclosure and apology—an idea whose time has come. Physician Exec. Mar-Apr 2006 32:16-18.
- Beckman HB, Markakis KM, Suchman AL, et al. The doctor-patient relationship and malpractice. Lessons from plaintiff depositions. Arch Intern Med. Jun 27 1994;154(12):1365-1370.
- Cohen JR. Apology and organizations: Exploring an example from medical practice. Fordham Urban Law J. 2000;27(5):1447-1482.
- Cohen JR. Advising clients to apologize. South Calif Law Rev. 1999;72:1009-1069.
- Entman SS, Glass CA, Hickson GB, et al. The relationship between malpractice claims history and subsequent obstetric care. JAMA. 1994 Nov 23-30;272(20):1588-1591.
- Gesensway D. Hospitalists and the malpractice insurance crisis. The Hospitalist. 2002Jul/Aug;11-13.
- Levinson W, Roter D, Mullooly JP, et al. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997 Feb19;227(7):553-559.
- Lo B. Ethical and policy implications of hospitalist systems. Dis Mon. 2002 Apr;48(4):281-290.
- Mello MM, Studdert DM, Brennan TA. The new medical malpractice crisis. New Engl J Med. 2003 Jun 5;348(23):2281-2284.
- Shapiro RS, Simpson DE, Lawrence SL, et al. A survey of sued and nonsued physicians and suing patients. Arch Intern Med. 1989 Oct;149(10):2190-2196.
- Zimmerman R. Doctors' new tool to fight lawsuits: saying 'I'm sorry.' Malpractice insurers find owning up to errors soothes patient anger. 'The risks are extraordinary.' J Okla State Med Assoc. 2004 Jun;97(6):245-247.
- Ambady N, LaPlante D, Nguyen T, et al. Surgeons' tone of voice: a clue to malpractice history. Surgery. 2002 Jul;132(1):5-9.
- Wu AW. Handling hospital errors: is disclosure the best defense? Ann Intern Med. 1999 Dec 21;131(12):970-972.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence. Results of the Harvard Medical Practice Study III. N Engl J Med. 1991 Jul 25;325(4):245-251.
- Brennan TA, Sox CM, Burstin HR. Relation between negligent adverse events and the outcomes of medical-malpractice litigation. N Engl J Med. 1996 Dec;335(26):1963-1967.
- Hickson GB, Federspiel CF, Pichert JW, et al. Patient complaints and malpractice risk. JAMA. 2002 Jun 12;287(22):2951-1957.
- Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005 Oct;118(10):1126-1133.
- Pham HH, Devers KJ, Kuo S, et al. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005 Feb;20(2):101-107.
- Harris Interactive(R). Telephone survey conducted for the American Academy on Physician and Patient, March 3-6, 2006.
Apologizing to a patient is the right thing to do,” says Michael S. Woods, MD, a general surgeon at St. Vincent’s Regional Medical Center in Santa Fe, N.M. “It is the respectful thing in any relationship in terms of trust whenever there is a violation, whether it is real or perceived.” Dr. Woods, the author of Healing Words: The Power of Apology in Medicine, teaches and consults with corporations around the country about apology as well as physician leadership.1-2 In fact, his study of apology stemmed from examining the subject of physician leadership, and he and other experts consider the vital components of leadership to be effective communication, integrity, honesty, and respectful treatment of other individuals.3,4
Dr. Woods also works with Doug Wojcieszak, a public relations consultant whose victims’ rights group proposed “Sorry Works!” This program recommends apologies and settlements when medical mistakes occur. (See “A History of Sorry Works!” p. 26.) Dr. Woods says Wojcieszak comes from an interesting angle that he supports. “Something I increasingly try to hammer home when I speak is that one of the most important components of the apology law has nothing to do with the backhand of the reduction of litigation as much as the fact that it gives the physician the green light to say ‘I’m sorry,’” says Dr. Woods.
The Benefit of Healing
Providers may be less than open when things go terribly wrong because of feelings of fear, shame, and guilt regarding the consequences to the patient as well as to themselves.1,3 Apology heals by restoring the patient’s dignity and self-respect, providing assurance of shared values, and assuring patients that they are not at fault, they are now safe, and that the caregiver shares their suffering.4,7
Two Senses of Apology
There are circumstances other than when errors occur in which a physician’s apology may carry the power to improve patient care. Peter Barnett, MD, MPH, a clinical associate professor of medicine at the University of New Mexico in Albuquerque, says that in general there are two senses of apology.
“The first sense of apology regards the situation,” he says. For example, you might say, ‘I’m sorry you have cancer,’ or ‘I’m sorry that our system doesn’t allow your family doctor to be taking care of you in the hospital.’ It’s an expression of sympathy, but I think apology works better.”
The other sense of apology regards responsibility, says Dr. Barnett, citing the example, “I’m sorry I gave you the wrong drug.”
Situational needs for apology include when patients have been waiting a long time, such as when a hospitalist meets them in the emergency department. “In those cases you would say, ‘I’m sorry that you had to wait so long,’” says Dr. Barnett. “It’s not my fault, but I really am sorry.”
Bridging the Gap
Dr. Barnett, who practices hospital medicine part-time along with his major focus in addiction medicine, was formerly the director of the UNM hospitalist team. He explains that one of the primary reasons hospitalists may need to apologize to patients is that the hospitalist and patient have no prior relationship that could serve as a foundation for interpreting each other’s behavior.8
He believes apologizing for the delays and inconveniences that happen in the hospital “can help bridge the relationship gap in hospital medicine. Because what people believe about their primary care physicians is that they know and care about them,” he says. “To minimize their anxiety about you, show them that you do care about them by getting to know them well, and apology is the one of the best ways of doing that.”
When asked to elaborate what he means by “getting to know them well,” Dr. Barnett says, “I might tell someone, ‘I’d like to get to know you better; what can you tell me about yourself that would help bring me up to speed?’” It’s open-ended, he says, and you let the patient choose the topic. “Most people will say something. … It’s empathic inquiry with really good reflective listening; that is probably the simplest way of summarizing what it takes.”
Dr. Barnett suggests this kind of inquiry can mitigate the gaps in relationships that may lead to misunderstandings, edgy situations, and errors that may later call for apology. He recommends asking or saying some of the following to patients:
- What do you know about your illness?
- What do you believe about your illness?
- What are your feelings, values, beliefs, and preferences about/for your treatment?
- What can you tell me about your experiences in the hospital?
For patients who have been ill many times and have had a lot of medical experience, you could ask:
- Could you tell me about your doctors?
- What do you like about doctors?
- What don’t you like about your doctors?
These questions can help you discern who they are as a patient, and it gives patients the opportunity to be candid with you.
“It’s not about finding information that’s embarrassing or critical to your predecessor physicians, but it allows you to not make the same mistakes inadvertently,” says Dr. Barnett, who considers it concrete information. “I want them to have good medical care. I don’t want to make them unhappy. I want to avoid pitfalls. I think the two of us—the patient and I—should avoid pitfalls together.”
Asking the patient in a straightforward way what they want and don’t want gives the patient an opportunity to give the physician advice on how to stay out of trouble with them.
Apology When Disclosing Errors
The matter of assuming responsibility for errors is more complicated as it pertains to the use of apology, but it is an “idea whose time has come.”9 Although it is hard to quantify, plenty of evidence shows that apologizing for errors reduces the number of lawsuits and may reduce the settlement value of malpractice claims.3,5-7,10-26 Although there is not always agreement about the specifics of full disclosure, above all patients have the right to know what happens during their medical care and, therefore, restricting the information that is given to a patient can have legal ramifications.
Beyond this, writes Lucian Leape, MD, adjunct professor of health policy at the Harvard School of Public Health and an internationally recognized leader in the patient safety movement, wrote in the March-April issue of Physician Executive that apology is a “therapeutic necessity” that allows the patient to recognize a physician’s humanity and fallibility as well as his or her remorse at having caused harm.9 In the long run, apologizing to patients defuses more situations than it aggravates, and it pays off emotionally, financially, and in practice morale.5,6,9
Data from studies of medical practices that issue apologies in circumstances where accountability is clearly established show that litigation claims are reduced. In one 1992 study, 24% of people who sued physicians said they did so because the doctor was dishonest and withheld information. Nineteen percent said that they either sued to deter subsequent malpractice or for revenge.11,12 In each case of legal action, the investigators hypothesized that the doctor could have avoided the lawsuit by taking responsibility and apologizing up front and making amends at that time. It has been estimated that more than half of claims relegated to litigation could be avoided with use of prudent disclosure and apology.3,21
“My mantra, if you will,” says Dr. Woods, “is that [when] you apologize because it’s the right thing to do, all the benefits naturally ensue.”
Anticipating Apology
The issue of complications, adverse events, and errors carries its own protocol in terms of whether and how apology is offered. “Hopefully some of these have been anticipated,” says Dr. Barnett. “For instance, when you spoke with the patient about their pneumonia, you’ve said something about the possibility that pneumonias could become complicated, and [they] might have some kind of complications; or if they’ve had a heart attack, [you mentioned that] they might have some complications. So you’re actually already warning people about what could happen and you’ve said you’re going to try to prevent it, but it could [still happen].”
Apology can be appropriately offered when those events do occur and you genuinely express disappointment that you and the patient share.
“There are some quite complicated systematic problems [related to apology and hospital medicine],” says Dr. Barnett. “Some are communication aspects and some are legal ones. What I have heard from the attorneys is that you want to keep the apology relatively simple, … and it shouldn’t include any statements about other people who may have been involved, such as pharmacy or nurses.”
The other important issue related to hospitalists and apology, says Dr. Barnett, is that because of the lack of relationship, the severity of illness of the patients you are treating, and the strangeness of systems, people come to the hospital expecting errors. They expect them and may be afraid of them. In particular, when a medication error is made, they expect those errors to be disclosed to them.7,27 Dr. Barnett believes patients are waiting and watching, and hoping that nothing happens to them. Complicating the issue, he says, is that “many hospitalists are fairly guarded in this respect. The emotional deck is sort of stacked against everybody, so if the hospitalist is sensitive about the situation, that tends actually to make the situation worse. If you can apologize sincerely and simply, the patient may be reassured that you’re not trying to conceal anything, you’re honest, you’re on top of it, and you’ll do your best to deal with it,” he says, adding, “they know that that stuff happens; they hope that it is not hidden, ignored, or mismanaged.”
Start Early and Let It Flow
Dr. Woods’ advice is to offer apology earlier rather than later and to widen the spectrum of those to whom you wish to show your empathy, sympathy, respect, and compassion.
“What I promote to organizations is that they drive this into the consciousness of the organization by getting people to apologize for the least infraction—not waiting for the grave errors.” He interprets this as apologizing “when you’re running 30 minutes late, apologize when you’ve interrupted the patient or the family when they’re speaking. These are the things we would do for our spouse or our significant other or our family members; why is it any different at work?”
He also believes it is inherent for doctors as leaders to “apologize to your staff members, apologize to the nurses.” Because the image you express serves as a role model in this regard and will permeate your practice culture. Drive respectful treatment as a basic common social courtesy into the organizational consciousness, says Dr. Woods, and then in any circumstance where an apology is offered, it is perceived as authentic.
Conclusion
Hospitalists may find a need to apologize to patients and families for situations and circumstances in the hospital environment as well as the gap in relationship that exists when hospitalists and patients first encounter each other. Apologizing early rather than later as well as simply and authentically goes a long way to help achieve the ethical and business objectives held by most hospital physicians. TH
Andrea Sattinger wrote about error reporting in the May issue.
References
- Woods MS, Star JI. Healing Words: The Power of Apology in Medicine. Santa Fe, N.M.: Doctors in Touch; 2004.
- Woods MS. Applying Personal Leadership Principles to Health Care: The DEPO Principle. Orlando, Fl.: American College of Physician Executives; 2001.
- Leape LL. National Patient Safety Foundation. Understanding the power of apology: how saying “I’m sorry" helps heal patients and caregivers. Focus on Patient Safety. 2005;8:1-3.
- Lazare A. On Apology. Oxford, U.K.: Oxford University Press; 2004.
- Boothman RC. Apologies and a strong defense at the University of Michigan Health System. Physician Exec. 2006 Mar-Apr; 32(2):7-10.
- Weber DO. Who’s sorry now? Special report: patient trust and safety. Physician Exec. 2006 Mar-Apr:32(2)6-14.
- When Things Go Wrong: Responding to Adverse Events. A Consensus Statement of the Harvard Hospitals. Burlington, Massachusetts: Massachusetts Coalition for the Prevention of Medical Errors; 2006.
- Barnett PB. Rapport and the hospitalist. Am J Med. 2001;111:31S-35S.
- Leape LL. Full disclosure and apology—an idea whose time has come. Physician Exec. Mar-Apr 2006 32:16-18.
- Beckman HB, Markakis KM, Suchman AL, et al. The doctor-patient relationship and malpractice. Lessons from plaintiff depositions. Arch Intern Med. Jun 27 1994;154(12):1365-1370.
- Cohen JR. Apology and organizations: Exploring an example from medical practice. Fordham Urban Law J. 2000;27(5):1447-1482.
- Cohen JR. Advising clients to apologize. South Calif Law Rev. 1999;72:1009-1069.
- Entman SS, Glass CA, Hickson GB, et al. The relationship between malpractice claims history and subsequent obstetric care. JAMA. 1994 Nov 23-30;272(20):1588-1591.
- Gesensway D. Hospitalists and the malpractice insurance crisis. The Hospitalist. 2002Jul/Aug;11-13.
- Levinson W, Roter D, Mullooly JP, et al. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997 Feb19;227(7):553-559.
- Lo B. Ethical and policy implications of hospitalist systems. Dis Mon. 2002 Apr;48(4):281-290.
- Mello MM, Studdert DM, Brennan TA. The new medical malpractice crisis. New Engl J Med. 2003 Jun 5;348(23):2281-2284.
- Shapiro RS, Simpson DE, Lawrence SL, et al. A survey of sued and nonsued physicians and suing patients. Arch Intern Med. 1989 Oct;149(10):2190-2196.
- Zimmerman R. Doctors' new tool to fight lawsuits: saying 'I'm sorry.' Malpractice insurers find owning up to errors soothes patient anger. 'The risks are extraordinary.' J Okla State Med Assoc. 2004 Jun;97(6):245-247.
- Ambady N, LaPlante D, Nguyen T, et al. Surgeons' tone of voice: a clue to malpractice history. Surgery. 2002 Jul;132(1):5-9.
- Wu AW. Handling hospital errors: is disclosure the best defense? Ann Intern Med. 1999 Dec 21;131(12):970-972.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence. Results of the Harvard Medical Practice Study III. N Engl J Med. 1991 Jul 25;325(4):245-251.
- Brennan TA, Sox CM, Burstin HR. Relation between negligent adverse events and the outcomes of medical-malpractice litigation. N Engl J Med. 1996 Dec;335(26):1963-1967.
- Hickson GB, Federspiel CF, Pichert JW, et al. Patient complaints and malpractice risk. JAMA. 2002 Jun 12;287(22):2951-1957.
- Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005 Oct;118(10):1126-1133.
- Pham HH, Devers KJ, Kuo S, et al. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005 Feb;20(2):101-107.
- Harris Interactive(R). Telephone survey conducted for the American Academy on Physician and Patient, March 3-6, 2006.
Apologizing to a patient is the right thing to do,” says Michael S. Woods, MD, a general surgeon at St. Vincent’s Regional Medical Center in Santa Fe, N.M. “It is the respectful thing in any relationship in terms of trust whenever there is a violation, whether it is real or perceived.” Dr. Woods, the author of Healing Words: The Power of Apology in Medicine, teaches and consults with corporations around the country about apology as well as physician leadership.1-2 In fact, his study of apology stemmed from examining the subject of physician leadership, and he and other experts consider the vital components of leadership to be effective communication, integrity, honesty, and respectful treatment of other individuals.3,4
Dr. Woods also works with Doug Wojcieszak, a public relations consultant whose victims’ rights group proposed “Sorry Works!” This program recommends apologies and settlements when medical mistakes occur. (See “A History of Sorry Works!” p. 26.) Dr. Woods says Wojcieszak comes from an interesting angle that he supports. “Something I increasingly try to hammer home when I speak is that one of the most important components of the apology law has nothing to do with the backhand of the reduction of litigation as much as the fact that it gives the physician the green light to say ‘I’m sorry,’” says Dr. Woods.
The Benefit of Healing
Providers may be less than open when things go terribly wrong because of feelings of fear, shame, and guilt regarding the consequences to the patient as well as to themselves.1,3 Apology heals by restoring the patient’s dignity and self-respect, providing assurance of shared values, and assuring patients that they are not at fault, they are now safe, and that the caregiver shares their suffering.4,7
Two Senses of Apology
There are circumstances other than when errors occur in which a physician’s apology may carry the power to improve patient care. Peter Barnett, MD, MPH, a clinical associate professor of medicine at the University of New Mexico in Albuquerque, says that in general there are two senses of apology.
“The first sense of apology regards the situation,” he says. For example, you might say, ‘I’m sorry you have cancer,’ or ‘I’m sorry that our system doesn’t allow your family doctor to be taking care of you in the hospital.’ It’s an expression of sympathy, but I think apology works better.”
The other sense of apology regards responsibility, says Dr. Barnett, citing the example, “I’m sorry I gave you the wrong drug.”
Situational needs for apology include when patients have been waiting a long time, such as when a hospitalist meets them in the emergency department. “In those cases you would say, ‘I’m sorry that you had to wait so long,’” says Dr. Barnett. “It’s not my fault, but I really am sorry.”
Bridging the Gap
Dr. Barnett, who practices hospital medicine part-time along with his major focus in addiction medicine, was formerly the director of the UNM hospitalist team. He explains that one of the primary reasons hospitalists may need to apologize to patients is that the hospitalist and patient have no prior relationship that could serve as a foundation for interpreting each other’s behavior.8
He believes apologizing for the delays and inconveniences that happen in the hospital “can help bridge the relationship gap in hospital medicine. Because what people believe about their primary care physicians is that they know and care about them,” he says. “To minimize their anxiety about you, show them that you do care about them by getting to know them well, and apology is the one of the best ways of doing that.”
When asked to elaborate what he means by “getting to know them well,” Dr. Barnett says, “I might tell someone, ‘I’d like to get to know you better; what can you tell me about yourself that would help bring me up to speed?’” It’s open-ended, he says, and you let the patient choose the topic. “Most people will say something. … It’s empathic inquiry with really good reflective listening; that is probably the simplest way of summarizing what it takes.”
Dr. Barnett suggests this kind of inquiry can mitigate the gaps in relationships that may lead to misunderstandings, edgy situations, and errors that may later call for apology. He recommends asking or saying some of the following to patients:
- What do you know about your illness?
- What do you believe about your illness?
- What are your feelings, values, beliefs, and preferences about/for your treatment?
- What can you tell me about your experiences in the hospital?
For patients who have been ill many times and have had a lot of medical experience, you could ask:
- Could you tell me about your doctors?
- What do you like about doctors?
- What don’t you like about your doctors?
These questions can help you discern who they are as a patient, and it gives patients the opportunity to be candid with you.
“It’s not about finding information that’s embarrassing or critical to your predecessor physicians, but it allows you to not make the same mistakes inadvertently,” says Dr. Barnett, who considers it concrete information. “I want them to have good medical care. I don’t want to make them unhappy. I want to avoid pitfalls. I think the two of us—the patient and I—should avoid pitfalls together.”
Asking the patient in a straightforward way what they want and don’t want gives the patient an opportunity to give the physician advice on how to stay out of trouble with them.
Apology When Disclosing Errors
The matter of assuming responsibility for errors is more complicated as it pertains to the use of apology, but it is an “idea whose time has come.”9 Although it is hard to quantify, plenty of evidence shows that apologizing for errors reduces the number of lawsuits and may reduce the settlement value of malpractice claims.3,5-7,10-26 Although there is not always agreement about the specifics of full disclosure, above all patients have the right to know what happens during their medical care and, therefore, restricting the information that is given to a patient can have legal ramifications.
Beyond this, writes Lucian Leape, MD, adjunct professor of health policy at the Harvard School of Public Health and an internationally recognized leader in the patient safety movement, wrote in the March-April issue of Physician Executive that apology is a “therapeutic necessity” that allows the patient to recognize a physician’s humanity and fallibility as well as his or her remorse at having caused harm.9 In the long run, apologizing to patients defuses more situations than it aggravates, and it pays off emotionally, financially, and in practice morale.5,6,9
Data from studies of medical practices that issue apologies in circumstances where accountability is clearly established show that litigation claims are reduced. In one 1992 study, 24% of people who sued physicians said they did so because the doctor was dishonest and withheld information. Nineteen percent said that they either sued to deter subsequent malpractice or for revenge.11,12 In each case of legal action, the investigators hypothesized that the doctor could have avoided the lawsuit by taking responsibility and apologizing up front and making amends at that time. It has been estimated that more than half of claims relegated to litigation could be avoided with use of prudent disclosure and apology.3,21
“My mantra, if you will,” says Dr. Woods, “is that [when] you apologize because it’s the right thing to do, all the benefits naturally ensue.”
Anticipating Apology
The issue of complications, adverse events, and errors carries its own protocol in terms of whether and how apology is offered. “Hopefully some of these have been anticipated,” says Dr. Barnett. “For instance, when you spoke with the patient about their pneumonia, you’ve said something about the possibility that pneumonias could become complicated, and [they] might have some kind of complications; or if they’ve had a heart attack, [you mentioned that] they might have some complications. So you’re actually already warning people about what could happen and you’ve said you’re going to try to prevent it, but it could [still happen].”
Apology can be appropriately offered when those events do occur and you genuinely express disappointment that you and the patient share.
“There are some quite complicated systematic problems [related to apology and hospital medicine],” says Dr. Barnett. “Some are communication aspects and some are legal ones. What I have heard from the attorneys is that you want to keep the apology relatively simple, … and it shouldn’t include any statements about other people who may have been involved, such as pharmacy or nurses.”
The other important issue related to hospitalists and apology, says Dr. Barnett, is that because of the lack of relationship, the severity of illness of the patients you are treating, and the strangeness of systems, people come to the hospital expecting errors. They expect them and may be afraid of them. In particular, when a medication error is made, they expect those errors to be disclosed to them.7,27 Dr. Barnett believes patients are waiting and watching, and hoping that nothing happens to them. Complicating the issue, he says, is that “many hospitalists are fairly guarded in this respect. The emotional deck is sort of stacked against everybody, so if the hospitalist is sensitive about the situation, that tends actually to make the situation worse. If you can apologize sincerely and simply, the patient may be reassured that you’re not trying to conceal anything, you’re honest, you’re on top of it, and you’ll do your best to deal with it,” he says, adding, “they know that that stuff happens; they hope that it is not hidden, ignored, or mismanaged.”
Start Early and Let It Flow
Dr. Woods’ advice is to offer apology earlier rather than later and to widen the spectrum of those to whom you wish to show your empathy, sympathy, respect, and compassion.
“What I promote to organizations is that they drive this into the consciousness of the organization by getting people to apologize for the least infraction—not waiting for the grave errors.” He interprets this as apologizing “when you’re running 30 minutes late, apologize when you’ve interrupted the patient or the family when they’re speaking. These are the things we would do for our spouse or our significant other or our family members; why is it any different at work?”
He also believes it is inherent for doctors as leaders to “apologize to your staff members, apologize to the nurses.” Because the image you express serves as a role model in this regard and will permeate your practice culture. Drive respectful treatment as a basic common social courtesy into the organizational consciousness, says Dr. Woods, and then in any circumstance where an apology is offered, it is perceived as authentic.
Conclusion
Hospitalists may find a need to apologize to patients and families for situations and circumstances in the hospital environment as well as the gap in relationship that exists when hospitalists and patients first encounter each other. Apologizing early rather than later as well as simply and authentically goes a long way to help achieve the ethical and business objectives held by most hospital physicians. TH
Andrea Sattinger wrote about error reporting in the May issue.
References
- Woods MS, Star JI. Healing Words: The Power of Apology in Medicine. Santa Fe, N.M.: Doctors in Touch; 2004.
- Woods MS. Applying Personal Leadership Principles to Health Care: The DEPO Principle. Orlando, Fl.: American College of Physician Executives; 2001.
- Leape LL. National Patient Safety Foundation. Understanding the power of apology: how saying “I’m sorry" helps heal patients and caregivers. Focus on Patient Safety. 2005;8:1-3.
- Lazare A. On Apology. Oxford, U.K.: Oxford University Press; 2004.
- Boothman RC. Apologies and a strong defense at the University of Michigan Health System. Physician Exec. 2006 Mar-Apr; 32(2):7-10.
- Weber DO. Who’s sorry now? Special report: patient trust and safety. Physician Exec. 2006 Mar-Apr:32(2)6-14.
- When Things Go Wrong: Responding to Adverse Events. A Consensus Statement of the Harvard Hospitals. Burlington, Massachusetts: Massachusetts Coalition for the Prevention of Medical Errors; 2006.
- Barnett PB. Rapport and the hospitalist. Am J Med. 2001;111:31S-35S.
- Leape LL. Full disclosure and apology—an idea whose time has come. Physician Exec. Mar-Apr 2006 32:16-18.
- Beckman HB, Markakis KM, Suchman AL, et al. The doctor-patient relationship and malpractice. Lessons from plaintiff depositions. Arch Intern Med. Jun 27 1994;154(12):1365-1370.
- Cohen JR. Apology and organizations: Exploring an example from medical practice. Fordham Urban Law J. 2000;27(5):1447-1482.
- Cohen JR. Advising clients to apologize. South Calif Law Rev. 1999;72:1009-1069.
- Entman SS, Glass CA, Hickson GB, et al. The relationship between malpractice claims history and subsequent obstetric care. JAMA. 1994 Nov 23-30;272(20):1588-1591.
- Gesensway D. Hospitalists and the malpractice insurance crisis. The Hospitalist. 2002Jul/Aug;11-13.
- Levinson W, Roter D, Mullooly JP, et al. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997 Feb19;227(7):553-559.
- Lo B. Ethical and policy implications of hospitalist systems. Dis Mon. 2002 Apr;48(4):281-290.
- Mello MM, Studdert DM, Brennan TA. The new medical malpractice crisis. New Engl J Med. 2003 Jun 5;348(23):2281-2284.
- Shapiro RS, Simpson DE, Lawrence SL, et al. A survey of sued and nonsued physicians and suing patients. Arch Intern Med. 1989 Oct;149(10):2190-2196.
- Zimmerman R. Doctors' new tool to fight lawsuits: saying 'I'm sorry.' Malpractice insurers find owning up to errors soothes patient anger. 'The risks are extraordinary.' J Okla State Med Assoc. 2004 Jun;97(6):245-247.
- Ambady N, LaPlante D, Nguyen T, et al. Surgeons' tone of voice: a clue to malpractice history. Surgery. 2002 Jul;132(1):5-9.
- Wu AW. Handling hospital errors: is disclosure the best defense? Ann Intern Med. 1999 Dec 21;131(12):970-972.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence. Results of the Harvard Medical Practice Study III. N Engl J Med. 1991 Jul 25;325(4):245-251.
- Brennan TA, Sox CM, Burstin HR. Relation between negligent adverse events and the outcomes of medical-malpractice litigation. N Engl J Med. 1996 Dec;335(26):1963-1967.
- Hickson GB, Federspiel CF, Pichert JW, et al. Patient complaints and malpractice risk. JAMA. 2002 Jun 12;287(22):2951-1957.
- Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005 Oct;118(10):1126-1133.
- Pham HH, Devers KJ, Kuo S, et al. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005 Feb;20(2):101-107.
- Harris Interactive(R). Telephone survey conducted for the American Academy on Physician and Patient, March 3-6, 2006.
A Case of Palpebral Purpura and Trouble Swallowing
A48-year-old female was admitted to the hospital with atrial fibrillation. Her medical history was significant for systemic lupus erythematosus (SLE) diagnosed 28 years ago, with low dose prednisone treatment for the past 15 years.
In the past year, the patient had experienced progressive difficulty swallowing and often choked on her food, resulting in a 35-pound weight loss. She also mentioned that she had been bruising easily.
On examination, the patient had bruising around her eyes and a thick, enlarged tongue with clear marks of her teeth visible on the surface.
Which test will most likely lead to a diagnosis?
- Magnetic resonance imaging (MRI) of pituitary gland;
- Abdominal fat pad biopsy;
- Thyroid stimulating hormone (TSH) level;
- Serum Angiotensin converting enzyme (ACE) levels
- Tongue biopsy
Discussion
The answer is B: abdominal fat pad biopsy. Macroglossia, especially in adults, is a rare clinical finding and is most often associated with amyloidosis.1 It has also been rarely described in association with acromegaly, hypothyroidism, and sarcoidosis. In children, macroglossia may be seen in a variety of conditions including cretinism, Down syndrome, Beckwith-Wiedemann syndrome, and various storage diseases.2 Lymphangioma of the tongue may also present with macroglossia.3
Another finding classically seen in amyloidosis is palpebral purpura.4 The occurrence of these two physical findings together in this patient strongly suggests the diagnosis of amyloidosis. The amyloidoses are now considered a group of diseases characterized by extracellular deposition of insoluble fibrillar proteins in various organs secondary to misfolding of proteins.
They include not only primary and secondary amyloidosis but also Alzheimer’s, prion diseases, many other neurodegenerative disorders, and some types of cystic fibroses.5
Traditionally, amyloidosis was described as one of three types: primary, secondary, and heritable. Primary amyloidosis is the most common type and results from deposition of fragments of light chain immunoglobulin deposits. It is most frequently associated with plasma cell dyscrasias. Secondary, or AA, amyloidosis occurs in association with inflammatory conditions and results from deposition of fragments of the acute phase reactant serum amyloid A. Familial amyloidoses or the ATTR amyloidoses are a fairly heterogeneous group with different proteins associated with different disorders.5
The typical findings seen in this case are associated with primary amyloidosis.4 The presence of primary amyloidosis was confirmed in this case by a bone marrow biopsy. This patient had SLE, but SLE is usually not complicated by the development of amyloidosis, although rare cases in literature have been described.6 Also, as mentioned above, secondary amyloidosis is usually characterized by AA rather than AL amyloidosis.
The diagnosis of amyloidosis is made pathologically when an involved organ is biopsied. When clinical suspicion is high and no organ has been biopsied, the simplest procedure is to obtain an abdominal fat pad biopsy and stain it with Congo red. This test is 85% sensitive in patients with primary amyloidosis.4 TH
References
- Xavier SD, Bussoloti IF, Muller H. Macroglossia secondary to systemic amyloidosis: case report and literature review. Ear Nose Throat J. 2005 Jun;84(6):358-361.
- Wolford LM, Cottrell DA. Diagnosis of macroglossia and indications for reduction glossectomy. Am J Orthod Dentofacial Orthop. 1996 Aug;110:170-177.
- Gulemann M, Katz J. Macroglossia combined with lymphangioma: a case report. J Clin Pediatr Dent. 2003 Winter;27(2):167-169.
- Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med 1997; 337: 898-909.
- Merlini G, Bellotti V. Mechanisms of disease: molecular mechanisms of amyloidosis. N Engl J Med. 2003; 349:583-596.
- Al-Hoqail I, Naddaf H, Al-Rikabi A, et al. Systemic lupus erythematosus and amyloidosis. Clin Rheumatol. 1997 Jun;16(4):422-424.on.
A48-year-old female was admitted to the hospital with atrial fibrillation. Her medical history was significant for systemic lupus erythematosus (SLE) diagnosed 28 years ago, with low dose prednisone treatment for the past 15 years.
In the past year, the patient had experienced progressive difficulty swallowing and often choked on her food, resulting in a 35-pound weight loss. She also mentioned that she had been bruising easily.
On examination, the patient had bruising around her eyes and a thick, enlarged tongue with clear marks of her teeth visible on the surface.
Which test will most likely lead to a diagnosis?
- Magnetic resonance imaging (MRI) of pituitary gland;
- Abdominal fat pad biopsy;
- Thyroid stimulating hormone (TSH) level;
- Serum Angiotensin converting enzyme (ACE) levels
- Tongue biopsy
Discussion
The answer is B: abdominal fat pad biopsy. Macroglossia, especially in adults, is a rare clinical finding and is most often associated with amyloidosis.1 It has also been rarely described in association with acromegaly, hypothyroidism, and sarcoidosis. In children, macroglossia may be seen in a variety of conditions including cretinism, Down syndrome, Beckwith-Wiedemann syndrome, and various storage diseases.2 Lymphangioma of the tongue may also present with macroglossia.3
Another finding classically seen in amyloidosis is palpebral purpura.4 The occurrence of these two physical findings together in this patient strongly suggests the diagnosis of amyloidosis. The amyloidoses are now considered a group of diseases characterized by extracellular deposition of insoluble fibrillar proteins in various organs secondary to misfolding of proteins.
They include not only primary and secondary amyloidosis but also Alzheimer’s, prion diseases, many other neurodegenerative disorders, and some types of cystic fibroses.5
Traditionally, amyloidosis was described as one of three types: primary, secondary, and heritable. Primary amyloidosis is the most common type and results from deposition of fragments of light chain immunoglobulin deposits. It is most frequently associated with plasma cell dyscrasias. Secondary, or AA, amyloidosis occurs in association with inflammatory conditions and results from deposition of fragments of the acute phase reactant serum amyloid A. Familial amyloidoses or the ATTR amyloidoses are a fairly heterogeneous group with different proteins associated with different disorders.5
The typical findings seen in this case are associated with primary amyloidosis.4 The presence of primary amyloidosis was confirmed in this case by a bone marrow biopsy. This patient had SLE, but SLE is usually not complicated by the development of amyloidosis, although rare cases in literature have been described.6 Also, as mentioned above, secondary amyloidosis is usually characterized by AA rather than AL amyloidosis.
The diagnosis of amyloidosis is made pathologically when an involved organ is biopsied. When clinical suspicion is high and no organ has been biopsied, the simplest procedure is to obtain an abdominal fat pad biopsy and stain it with Congo red. This test is 85% sensitive in patients with primary amyloidosis.4 TH
References
- Xavier SD, Bussoloti IF, Muller H. Macroglossia secondary to systemic amyloidosis: case report and literature review. Ear Nose Throat J. 2005 Jun;84(6):358-361.
- Wolford LM, Cottrell DA. Diagnosis of macroglossia and indications for reduction glossectomy. Am J Orthod Dentofacial Orthop. 1996 Aug;110:170-177.
- Gulemann M, Katz J. Macroglossia combined with lymphangioma: a case report. J Clin Pediatr Dent. 2003 Winter;27(2):167-169.
- Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med 1997; 337: 898-909.
- Merlini G, Bellotti V. Mechanisms of disease: molecular mechanisms of amyloidosis. N Engl J Med. 2003; 349:583-596.
- Al-Hoqail I, Naddaf H, Al-Rikabi A, et al. Systemic lupus erythematosus and amyloidosis. Clin Rheumatol. 1997 Jun;16(4):422-424.on.
A48-year-old female was admitted to the hospital with atrial fibrillation. Her medical history was significant for systemic lupus erythematosus (SLE) diagnosed 28 years ago, with low dose prednisone treatment for the past 15 years.
In the past year, the patient had experienced progressive difficulty swallowing and often choked on her food, resulting in a 35-pound weight loss. She also mentioned that she had been bruising easily.
On examination, the patient had bruising around her eyes and a thick, enlarged tongue with clear marks of her teeth visible on the surface.
Which test will most likely lead to a diagnosis?
- Magnetic resonance imaging (MRI) of pituitary gland;
- Abdominal fat pad biopsy;
- Thyroid stimulating hormone (TSH) level;
- Serum Angiotensin converting enzyme (ACE) levels
- Tongue biopsy
Discussion
The answer is B: abdominal fat pad biopsy. Macroglossia, especially in adults, is a rare clinical finding and is most often associated with amyloidosis.1 It has also been rarely described in association with acromegaly, hypothyroidism, and sarcoidosis. In children, macroglossia may be seen in a variety of conditions including cretinism, Down syndrome, Beckwith-Wiedemann syndrome, and various storage diseases.2 Lymphangioma of the tongue may also present with macroglossia.3
Another finding classically seen in amyloidosis is palpebral purpura.4 The occurrence of these two physical findings together in this patient strongly suggests the diagnosis of amyloidosis. The amyloidoses are now considered a group of diseases characterized by extracellular deposition of insoluble fibrillar proteins in various organs secondary to misfolding of proteins.
They include not only primary and secondary amyloidosis but also Alzheimer’s, prion diseases, many other neurodegenerative disorders, and some types of cystic fibroses.5
Traditionally, amyloidosis was described as one of three types: primary, secondary, and heritable. Primary amyloidosis is the most common type and results from deposition of fragments of light chain immunoglobulin deposits. It is most frequently associated with plasma cell dyscrasias. Secondary, or AA, amyloidosis occurs in association with inflammatory conditions and results from deposition of fragments of the acute phase reactant serum amyloid A. Familial amyloidoses or the ATTR amyloidoses are a fairly heterogeneous group with different proteins associated with different disorders.5
The typical findings seen in this case are associated with primary amyloidosis.4 The presence of primary amyloidosis was confirmed in this case by a bone marrow biopsy. This patient had SLE, but SLE is usually not complicated by the development of amyloidosis, although rare cases in literature have been described.6 Also, as mentioned above, secondary amyloidosis is usually characterized by AA rather than AL amyloidosis.
The diagnosis of amyloidosis is made pathologically when an involved organ is biopsied. When clinical suspicion is high and no organ has been biopsied, the simplest procedure is to obtain an abdominal fat pad biopsy and stain it with Congo red. This test is 85% sensitive in patients with primary amyloidosis.4 TH
References
- Xavier SD, Bussoloti IF, Muller H. Macroglossia secondary to systemic amyloidosis: case report and literature review. Ear Nose Throat J. 2005 Jun;84(6):358-361.
- Wolford LM, Cottrell DA. Diagnosis of macroglossia and indications for reduction glossectomy. Am J Orthod Dentofacial Orthop. 1996 Aug;110:170-177.
- Gulemann M, Katz J. Macroglossia combined with lymphangioma: a case report. J Clin Pediatr Dent. 2003 Winter;27(2):167-169.
- Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med 1997; 337: 898-909.
- Merlini G, Bellotti V. Mechanisms of disease: molecular mechanisms of amyloidosis. N Engl J Med. 2003; 349:583-596.
- Al-Hoqail I, Naddaf H, Al-Rikabi A, et al. Systemic lupus erythematosus and amyloidosis. Clin Rheumatol. 1997 Jun;16(4):422-424.on.