User login
Long COVID comes in three forms: Study
, according to a new preprint study published on MedRxiv that hasn’t yet been peer-reviewed.
Long COVID has been hard to define due to its large number of symptoms, but researchers at King’s College London have identified three distinct profiles – with long-term symptoms focused on neurological, respiratory, or physical conditions. So far, they also found patterns among people infected with the original coronavirus strain, the Alpha variant, and the Delta variant.
“These data show clearly that post-COVID syndrome is not just one condition but appears to have several subtypes,” Claire Steves, PhD, one of the study authors and a senior clinical lecturer in King’s College London’s School of Life Course & Population Sciences, said in a statement.
“Understanding the root causes of these subtypes may help in finding treatment strategies,” she said. “Moreover, these data emphasize the need for long-COVID services to incorporate a personalized approach sensitive to the issues of each individual.”
The research team analyzed ZOE COVID app data for 1,459 people who have had symptoms for more than 84 days, or 12 weeks, according to their definition of long COVID or post-COVID syndrome.
They found that the largest group had a cluster of symptoms in the nervous system, such as fatigue, brain fog, and headaches. It was the most common subtype among the Alpha variant, which was dominant in winter 2020-2021, and the Delta variant, which was dominant in 2021.
The second group had respiratory symptoms, such as chest pain and severe shortness of breath, which could suggest lung damage, the researchers wrote. It was the largest cluster for the original coronavirus strain in spring 2020, when people were unvaccinated.
The third group included people who reported a diverse range of physical symptoms, including heart palpitations, muscle aches and pain, and changes to their skin and hair. This group had some of the “most severe and debilitating multi-organ symptoms,” the researchers wrote.
The researchers found that the subtypes were similar in vaccinated and unvaccinated people based on the variants investigated so far. But the data showed that the risk of long COVID was reduced by vaccination.
In addition, although the three subtypes were present in all the variants, other symptom clusters had subtle differences among the variants, such as symptoms in the stomach and intestines. The differences could be due to other things that changed during the pandemic, such as the time of year, social behaviors, and treatments, the researchers said.
“Machine learning approaches, such as clustering analysis, have made it possible to start exploring and identifying different profiles of post-COVID syndrome,” Marc Modat, PhD, who led the analysis and is a senior lecturer at King’s College London’s School of Biomedical Engineering & Imaging Sciences, said in the statement.
“This opens new avenues of research to better understand COVID-19 and to motivate clinical research that might mitigate the long-term effects of the disease,” he said.
A version of this article first appeared on WebMD.com.
, according to a new preprint study published on MedRxiv that hasn’t yet been peer-reviewed.
Long COVID has been hard to define due to its large number of symptoms, but researchers at King’s College London have identified three distinct profiles – with long-term symptoms focused on neurological, respiratory, or physical conditions. So far, they also found patterns among people infected with the original coronavirus strain, the Alpha variant, and the Delta variant.
“These data show clearly that post-COVID syndrome is not just one condition but appears to have several subtypes,” Claire Steves, PhD, one of the study authors and a senior clinical lecturer in King’s College London’s School of Life Course & Population Sciences, said in a statement.
“Understanding the root causes of these subtypes may help in finding treatment strategies,” she said. “Moreover, these data emphasize the need for long-COVID services to incorporate a personalized approach sensitive to the issues of each individual.”
The research team analyzed ZOE COVID app data for 1,459 people who have had symptoms for more than 84 days, or 12 weeks, according to their definition of long COVID or post-COVID syndrome.
They found that the largest group had a cluster of symptoms in the nervous system, such as fatigue, brain fog, and headaches. It was the most common subtype among the Alpha variant, which was dominant in winter 2020-2021, and the Delta variant, which was dominant in 2021.
The second group had respiratory symptoms, such as chest pain and severe shortness of breath, which could suggest lung damage, the researchers wrote. It was the largest cluster for the original coronavirus strain in spring 2020, when people were unvaccinated.
The third group included people who reported a diverse range of physical symptoms, including heart palpitations, muscle aches and pain, and changes to their skin and hair. This group had some of the “most severe and debilitating multi-organ symptoms,” the researchers wrote.
The researchers found that the subtypes were similar in vaccinated and unvaccinated people based on the variants investigated so far. But the data showed that the risk of long COVID was reduced by vaccination.
In addition, although the three subtypes were present in all the variants, other symptom clusters had subtle differences among the variants, such as symptoms in the stomach and intestines. The differences could be due to other things that changed during the pandemic, such as the time of year, social behaviors, and treatments, the researchers said.
“Machine learning approaches, such as clustering analysis, have made it possible to start exploring and identifying different profiles of post-COVID syndrome,” Marc Modat, PhD, who led the analysis and is a senior lecturer at King’s College London’s School of Biomedical Engineering & Imaging Sciences, said in the statement.
“This opens new avenues of research to better understand COVID-19 and to motivate clinical research that might mitigate the long-term effects of the disease,” he said.
A version of this article first appeared on WebMD.com.
, according to a new preprint study published on MedRxiv that hasn’t yet been peer-reviewed.
Long COVID has been hard to define due to its large number of symptoms, but researchers at King’s College London have identified three distinct profiles – with long-term symptoms focused on neurological, respiratory, or physical conditions. So far, they also found patterns among people infected with the original coronavirus strain, the Alpha variant, and the Delta variant.
“These data show clearly that post-COVID syndrome is not just one condition but appears to have several subtypes,” Claire Steves, PhD, one of the study authors and a senior clinical lecturer in King’s College London’s School of Life Course & Population Sciences, said in a statement.
“Understanding the root causes of these subtypes may help in finding treatment strategies,” she said. “Moreover, these data emphasize the need for long-COVID services to incorporate a personalized approach sensitive to the issues of each individual.”
The research team analyzed ZOE COVID app data for 1,459 people who have had symptoms for more than 84 days, or 12 weeks, according to their definition of long COVID or post-COVID syndrome.
They found that the largest group had a cluster of symptoms in the nervous system, such as fatigue, brain fog, and headaches. It was the most common subtype among the Alpha variant, which was dominant in winter 2020-2021, and the Delta variant, which was dominant in 2021.
The second group had respiratory symptoms, such as chest pain and severe shortness of breath, which could suggest lung damage, the researchers wrote. It was the largest cluster for the original coronavirus strain in spring 2020, when people were unvaccinated.
The third group included people who reported a diverse range of physical symptoms, including heart palpitations, muscle aches and pain, and changes to their skin and hair. This group had some of the “most severe and debilitating multi-organ symptoms,” the researchers wrote.
The researchers found that the subtypes were similar in vaccinated and unvaccinated people based on the variants investigated so far. But the data showed that the risk of long COVID was reduced by vaccination.
In addition, although the three subtypes were present in all the variants, other symptom clusters had subtle differences among the variants, such as symptoms in the stomach and intestines. The differences could be due to other things that changed during the pandemic, such as the time of year, social behaviors, and treatments, the researchers said.
“Machine learning approaches, such as clustering analysis, have made it possible to start exploring and identifying different profiles of post-COVID syndrome,” Marc Modat, PhD, who led the analysis and is a senior lecturer at King’s College London’s School of Biomedical Engineering & Imaging Sciences, said in the statement.
“This opens new avenues of research to better understand COVID-19 and to motivate clinical research that might mitigate the long-term effects of the disease,” he said.
A version of this article first appeared on WebMD.com.
Children and COVID: Weekly cases top 95,000, admissions continue to rise
New pediatric COVID-19 cases increased for the third straight week as a substantial number of children under age 5 years started to receive their second doses of the vaccine.
Despite the 3-week trend, however, there are some positive signs. The new-case count for the latest reporting week (July 22-28) was over 95,000, but the 3.9% increase over the previous week’s 92,000 cases is much smaller than that week’s (July 15-21) corresponding jump of almost 22% over the July 8-14 total (75,000), according to the American Academy of Pediatrics and the Children’s Hospital Association.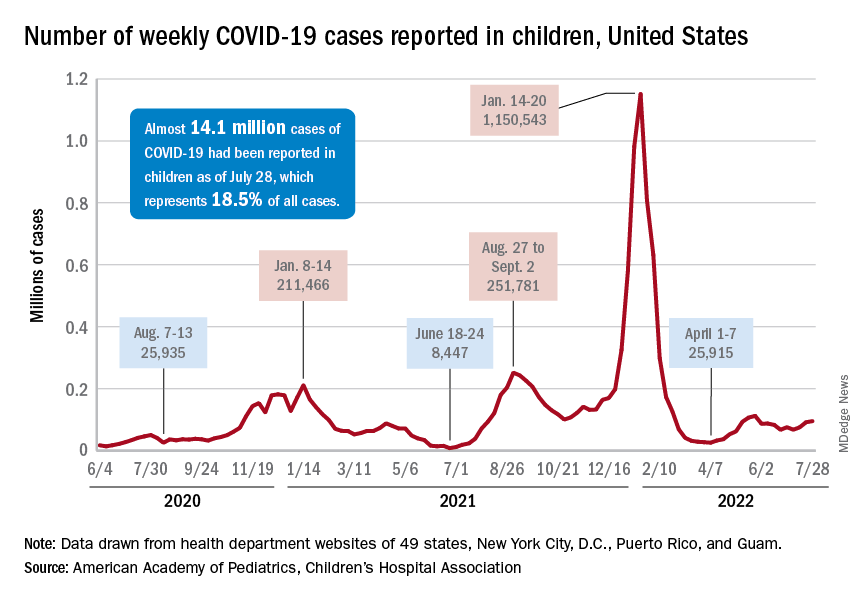
On the not-so-positive side is the trend in admissions among children aged 0-17 years, which continue to climb steadily and have nearly equaled the highest rate seen during the Delta surge in 2021. The rate on July 29 was 0.46 admissions per 100,000 population, and the highest rate over the course of the Delta surge was 0.47 per 100,000, but the all-time high from the Omicron surge – 1.25 per 100,000 in mid-January – is still a long way off, based on data from the Centers for Disease Control and Prevention.
A similar situation is occurring with emergency department visits, but there is differentiation by age group. Among those aged 0-11 years, visits with diagnosed COVID made up 6.5% of all their ED visits on July 25, which was well above the high (4.0%) during the Delta surge, the CDC said.
That is not the case, however, for the older children, for whom rates are rising more slowly. Those aged 12-15 have reached 3.4% so far this summer, as have the 16- to 17-years-olds, versus Delta highs last year of around 7%, the CDC said on its COVID Data Tracker. As with admissions, though, current rates are well below the all-time Omicron high points, the CDC data show.
Joining the ranks of the fully vaccinated
Over the last 2 weeks, the first children to receive the COVID vaccine after its approval for those under age 5 years have been coming back for their second doses. Almost 50,000, about 0.3% of all those in that age group, had done so by July 27. Just over 662,000, about 3.4% of the total under-5 population, have received at least one dose, the CDC said.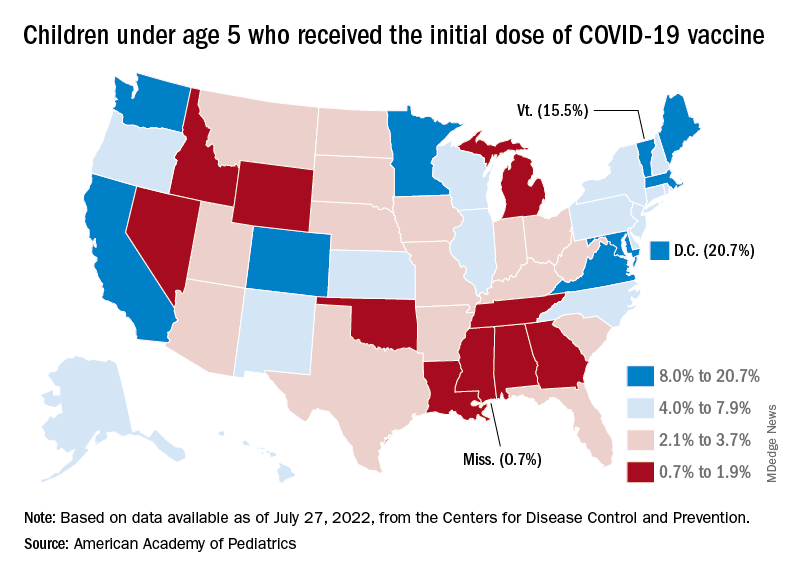
Meanwhile, analysis of “data from the first several weeks following availability of the vaccine in this age group indicate high variability across states,” the AAP said in its weekly vaccination report. In the District of Columbia, 20.7% of all children under age 5 have received an initial dose as of July 27, as have 15.5% of those in Vermont and 12.5% in Massachusetts. No other state was above 10%, but Mississippi, at 0.7%, was the only one below 1%.
The older children, obviously, have a head start, so their numbers are much higher. At the state level, Vermont has the highest initial dose rate, 69%, for those aged 5-11 years, while Alabama, Mississippi, and Wyoming, at 17%, are looking up at everyone else in the country. Among children aged 12-17 years, D.C. is the highest with 100% vaccination – Massachusetts and Rhode Island are at 98% – and Wyoming is the lowest with 40%, the AAP said.
New pediatric COVID-19 cases increased for the third straight week as a substantial number of children under age 5 years started to receive their second doses of the vaccine.
Despite the 3-week trend, however, there are some positive signs. The new-case count for the latest reporting week (July 22-28) was over 95,000, but the 3.9% increase over the previous week’s 92,000 cases is much smaller than that week’s (July 15-21) corresponding jump of almost 22% over the July 8-14 total (75,000), according to the American Academy of Pediatrics and the Children’s Hospital Association.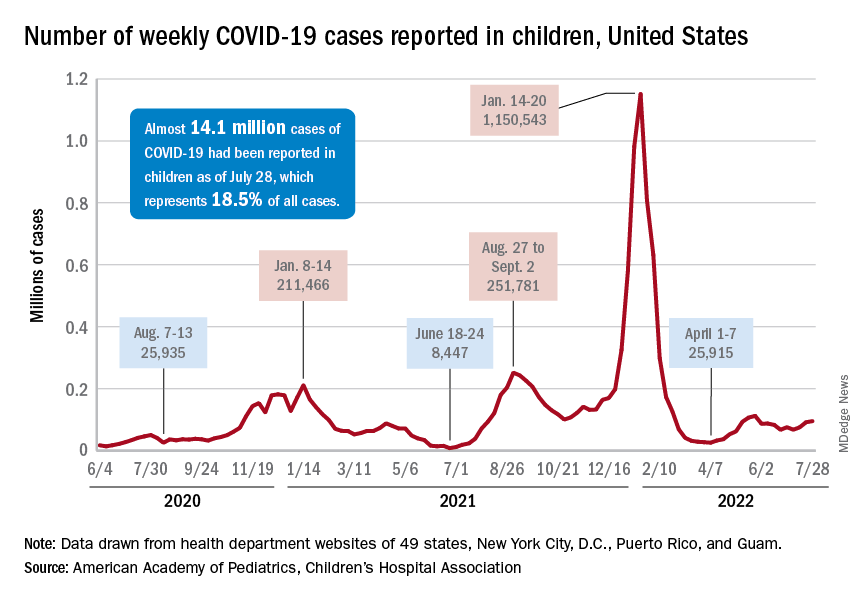
On the not-so-positive side is the trend in admissions among children aged 0-17 years, which continue to climb steadily and have nearly equaled the highest rate seen during the Delta surge in 2021. The rate on July 29 was 0.46 admissions per 100,000 population, and the highest rate over the course of the Delta surge was 0.47 per 100,000, but the all-time high from the Omicron surge – 1.25 per 100,000 in mid-January – is still a long way off, based on data from the Centers for Disease Control and Prevention.
A similar situation is occurring with emergency department visits, but there is differentiation by age group. Among those aged 0-11 years, visits with diagnosed COVID made up 6.5% of all their ED visits on July 25, which was well above the high (4.0%) during the Delta surge, the CDC said.
That is not the case, however, for the older children, for whom rates are rising more slowly. Those aged 12-15 have reached 3.4% so far this summer, as have the 16- to 17-years-olds, versus Delta highs last year of around 7%, the CDC said on its COVID Data Tracker. As with admissions, though, current rates are well below the all-time Omicron high points, the CDC data show.
Joining the ranks of the fully vaccinated
Over the last 2 weeks, the first children to receive the COVID vaccine after its approval for those under age 5 years have been coming back for their second doses. Almost 50,000, about 0.3% of all those in that age group, had done so by July 27. Just over 662,000, about 3.4% of the total under-5 population, have received at least one dose, the CDC said.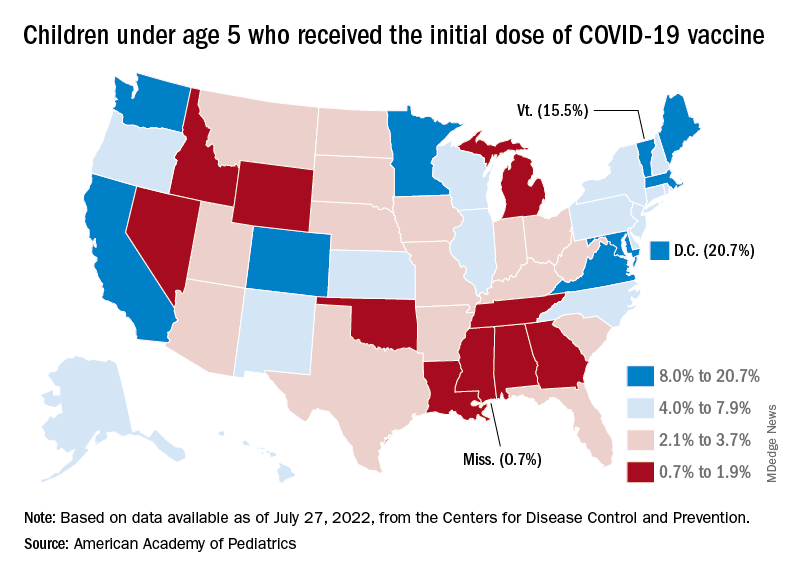
Meanwhile, analysis of “data from the first several weeks following availability of the vaccine in this age group indicate high variability across states,” the AAP said in its weekly vaccination report. In the District of Columbia, 20.7% of all children under age 5 have received an initial dose as of July 27, as have 15.5% of those in Vermont and 12.5% in Massachusetts. No other state was above 10%, but Mississippi, at 0.7%, was the only one below 1%.
The older children, obviously, have a head start, so their numbers are much higher. At the state level, Vermont has the highest initial dose rate, 69%, for those aged 5-11 years, while Alabama, Mississippi, and Wyoming, at 17%, are looking up at everyone else in the country. Among children aged 12-17 years, D.C. is the highest with 100% vaccination – Massachusetts and Rhode Island are at 98% – and Wyoming is the lowest with 40%, the AAP said.
New pediatric COVID-19 cases increased for the third straight week as a substantial number of children under age 5 years started to receive their second doses of the vaccine.
Despite the 3-week trend, however, there are some positive signs. The new-case count for the latest reporting week (July 22-28) was over 95,000, but the 3.9% increase over the previous week’s 92,000 cases is much smaller than that week’s (July 15-21) corresponding jump of almost 22% over the July 8-14 total (75,000), according to the American Academy of Pediatrics and the Children’s Hospital Association.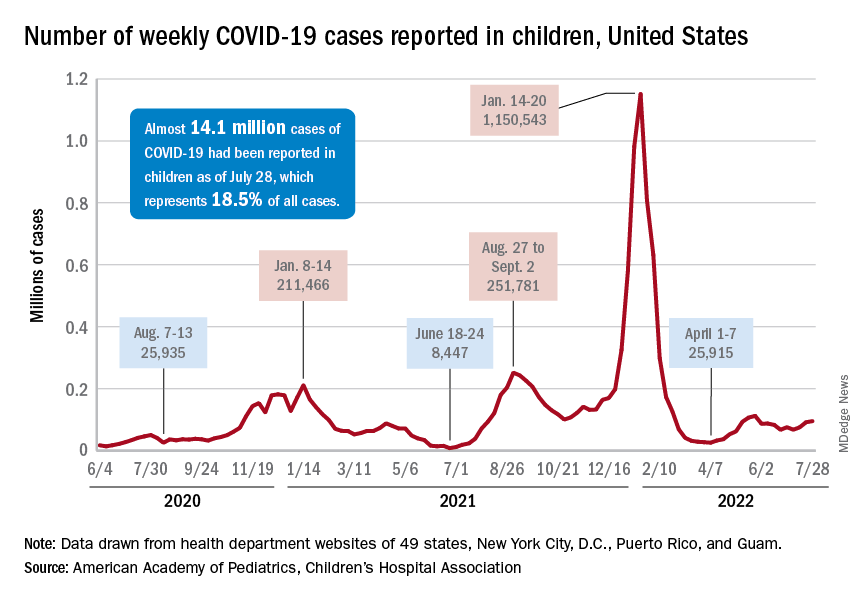
On the not-so-positive side is the trend in admissions among children aged 0-17 years, which continue to climb steadily and have nearly equaled the highest rate seen during the Delta surge in 2021. The rate on July 29 was 0.46 admissions per 100,000 population, and the highest rate over the course of the Delta surge was 0.47 per 100,000, but the all-time high from the Omicron surge – 1.25 per 100,000 in mid-January – is still a long way off, based on data from the Centers for Disease Control and Prevention.
A similar situation is occurring with emergency department visits, but there is differentiation by age group. Among those aged 0-11 years, visits with diagnosed COVID made up 6.5% of all their ED visits on July 25, which was well above the high (4.0%) during the Delta surge, the CDC said.
That is not the case, however, for the older children, for whom rates are rising more slowly. Those aged 12-15 have reached 3.4% so far this summer, as have the 16- to 17-years-olds, versus Delta highs last year of around 7%, the CDC said on its COVID Data Tracker. As with admissions, though, current rates are well below the all-time Omicron high points, the CDC data show.
Joining the ranks of the fully vaccinated
Over the last 2 weeks, the first children to receive the COVID vaccine after its approval for those under age 5 years have been coming back for their second doses. Almost 50,000, about 0.3% of all those in that age group, had done so by July 27. Just over 662,000, about 3.4% of the total under-5 population, have received at least one dose, the CDC said.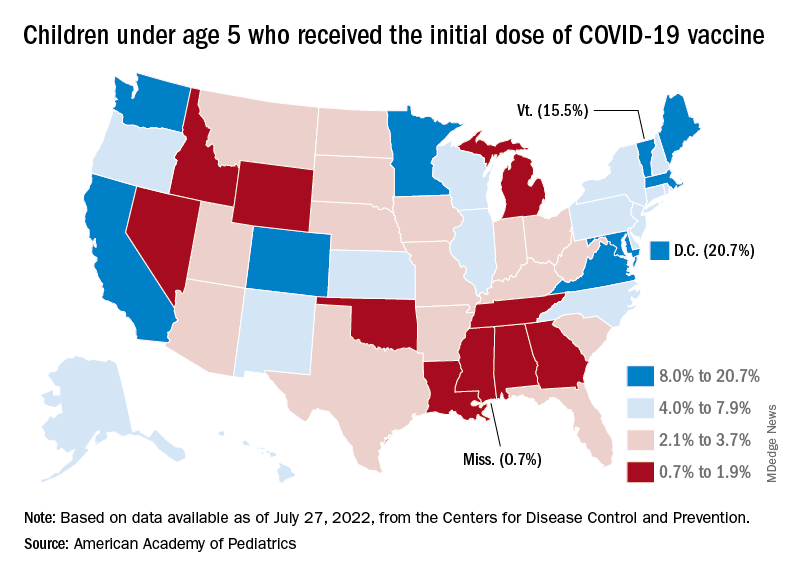
Meanwhile, analysis of “data from the first several weeks following availability of the vaccine in this age group indicate high variability across states,” the AAP said in its weekly vaccination report. In the District of Columbia, 20.7% of all children under age 5 have received an initial dose as of July 27, as have 15.5% of those in Vermont and 12.5% in Massachusetts. No other state was above 10%, but Mississippi, at 0.7%, was the only one below 1%.
The older children, obviously, have a head start, so their numbers are much higher. At the state level, Vermont has the highest initial dose rate, 69%, for those aged 5-11 years, while Alabama, Mississippi, and Wyoming, at 17%, are looking up at everyone else in the country. Among children aged 12-17 years, D.C. is the highest with 100% vaccination – Massachusetts and Rhode Island are at 98% – and Wyoming is the lowest with 40%, the AAP said.
Ongoing debate whether COVID links to new diabetes in kids
compared with the pre-pandemic rate, in new research.
This contrasts with findings from a U.S. study and a German study, but this is “not the final word” about this possible association, lead author Rayzel Shulman, MD, admits, since the study may have been underpowered.
The population-based, cross-sectional study was published recently as a research letter in JAMA Open.
The researchers found a nonsignificant increase in the monthly rate of new diabetes during the first 18 months of the COVID-19 pandemic, compared with the 3 prior years (relative risk 1.09, 95% confidence interval).
New study contrasts with previous reports
This differs from a Morbidity and Mortality Weekly Report from the U.S. Centers for Disease Control and Prevention, in which COVID-19 infection was associated with a significant increase in new onset of diabetes in children during March 2020 through June 2021, “although some experts have criticized the study methods and conclusion validity,” Dr. Shulman and colleagues write.
Another study, from Germany, reported a significant 1.15-fold increase in type 1 diabetes in children during the pandemic, they note.
The current study may have been underpowered and too small to show a significant association between COVID-19 and new diabetes, the researchers acknowledge.
And the 1.30 upper limit of the confidence interval shows that it “cannot rule out a possible 1.3-fold increase” in relative risk of a diagnosis of diabetes related to COVID, Dr. Shulman explained to this news organization.
It will be important to see how the rates have changed since September 2021 (the end of the current study), added Dr. Shulman, an adjunct scientist at the Institute for Clinical Evaluative Sciences (ICES) and a physician and scientist at the Hospital for Sick Children, Toronto.
The current study did find a decreased (delayed) rate of diagnosis of new diabetes during the first months of the pandemic when there were lockdowns, followed by a “catch-up” increase in rates later on, as has been reported earlier.
“Our study is definitely not the final word on this,” Dr. Shulman summarized in a statement from ICES. “However, our findings call into question whether a direct association between COVID-19 and new-onset diabetes in children exists.”
COVID-diabetes link?
The researchers analyzed health administrative data from January 2017 to September 2021.
They identified 2,700,178 children and youth in Ontario who were under age 18 in 2021, who had a mean age of 9.2, and about half were girls.
Between November 2020 and April 2021, an estimated 3.3% of children in Ontario had a SARS-COV-2 infection.
New diagnoses of diabetes in this age group are mostly type 1 diabetes, based on previous studies.
The rate of incident diabetes was 15%-32% lower during the first 3 months of the pandemic, March-May 2020 (1.67-2.34 cases per 100,000), compared with the pre-pandemic monthly rate during 2017, 2018, and 2019 (2.54-2.59 cases per 100,000).
The rate of incident diabetes was 33%-50% higher during February to July 2021 (3.48-4.18 cases per 100,000), compared with the pre-pandemic rate.
The pre-pandemic and pandemic monthly rates of incident diabetes were similar during the other months.
The group concludes: “The lack of both an observable increase in overall diabetes incidence among children during the 18-month pandemic restrictions [in this Ontario study] and a plausible biological mechanism call into question an association between COVID-19 and new-onset diabetes.”
More research is needed. “Given the variability in monthly [relative risks], additional population-based, longer-term data are needed to examine the direct and indirect effects of COVID-19 and diabetes risk among children,” the authors write.
This study was supported by ICES (which is funded by the Ontario Ministry of Health) and by a grant from the Canadian Institutes of Health Research. Dr. Shulman reported receiving fees from Dexcom outside the submitted work, and she and three other authors reported receiving grants from the Canadian Institutes of Health Research outside the submitted work.
A version of this article first appeared on Medscape.com.
compared with the pre-pandemic rate, in new research.
This contrasts with findings from a U.S. study and a German study, but this is “not the final word” about this possible association, lead author Rayzel Shulman, MD, admits, since the study may have been underpowered.
The population-based, cross-sectional study was published recently as a research letter in JAMA Open.
The researchers found a nonsignificant increase in the monthly rate of new diabetes during the first 18 months of the COVID-19 pandemic, compared with the 3 prior years (relative risk 1.09, 95% confidence interval).
New study contrasts with previous reports
This differs from a Morbidity and Mortality Weekly Report from the U.S. Centers for Disease Control and Prevention, in which COVID-19 infection was associated with a significant increase in new onset of diabetes in children during March 2020 through June 2021, “although some experts have criticized the study methods and conclusion validity,” Dr. Shulman and colleagues write.
Another study, from Germany, reported a significant 1.15-fold increase in type 1 diabetes in children during the pandemic, they note.
The current study may have been underpowered and too small to show a significant association between COVID-19 and new diabetes, the researchers acknowledge.
And the 1.30 upper limit of the confidence interval shows that it “cannot rule out a possible 1.3-fold increase” in relative risk of a diagnosis of diabetes related to COVID, Dr. Shulman explained to this news organization.
It will be important to see how the rates have changed since September 2021 (the end of the current study), added Dr. Shulman, an adjunct scientist at the Institute for Clinical Evaluative Sciences (ICES) and a physician and scientist at the Hospital for Sick Children, Toronto.
The current study did find a decreased (delayed) rate of diagnosis of new diabetes during the first months of the pandemic when there were lockdowns, followed by a “catch-up” increase in rates later on, as has been reported earlier.
“Our study is definitely not the final word on this,” Dr. Shulman summarized in a statement from ICES. “However, our findings call into question whether a direct association between COVID-19 and new-onset diabetes in children exists.”
COVID-diabetes link?
The researchers analyzed health administrative data from January 2017 to September 2021.
They identified 2,700,178 children and youth in Ontario who were under age 18 in 2021, who had a mean age of 9.2, and about half were girls.
Between November 2020 and April 2021, an estimated 3.3% of children in Ontario had a SARS-COV-2 infection.
New diagnoses of diabetes in this age group are mostly type 1 diabetes, based on previous studies.
The rate of incident diabetes was 15%-32% lower during the first 3 months of the pandemic, March-May 2020 (1.67-2.34 cases per 100,000), compared with the pre-pandemic monthly rate during 2017, 2018, and 2019 (2.54-2.59 cases per 100,000).
The rate of incident diabetes was 33%-50% higher during February to July 2021 (3.48-4.18 cases per 100,000), compared with the pre-pandemic rate.
The pre-pandemic and pandemic monthly rates of incident diabetes were similar during the other months.
The group concludes: “The lack of both an observable increase in overall diabetes incidence among children during the 18-month pandemic restrictions [in this Ontario study] and a plausible biological mechanism call into question an association between COVID-19 and new-onset diabetes.”
More research is needed. “Given the variability in monthly [relative risks], additional population-based, longer-term data are needed to examine the direct and indirect effects of COVID-19 and diabetes risk among children,” the authors write.
This study was supported by ICES (which is funded by the Ontario Ministry of Health) and by a grant from the Canadian Institutes of Health Research. Dr. Shulman reported receiving fees from Dexcom outside the submitted work, and she and three other authors reported receiving grants from the Canadian Institutes of Health Research outside the submitted work.
A version of this article first appeared on Medscape.com.
compared with the pre-pandemic rate, in new research.
This contrasts with findings from a U.S. study and a German study, but this is “not the final word” about this possible association, lead author Rayzel Shulman, MD, admits, since the study may have been underpowered.
The population-based, cross-sectional study was published recently as a research letter in JAMA Open.
The researchers found a nonsignificant increase in the monthly rate of new diabetes during the first 18 months of the COVID-19 pandemic, compared with the 3 prior years (relative risk 1.09, 95% confidence interval).
New study contrasts with previous reports
This differs from a Morbidity and Mortality Weekly Report from the U.S. Centers for Disease Control and Prevention, in which COVID-19 infection was associated with a significant increase in new onset of diabetes in children during March 2020 through June 2021, “although some experts have criticized the study methods and conclusion validity,” Dr. Shulman and colleagues write.
Another study, from Germany, reported a significant 1.15-fold increase in type 1 diabetes in children during the pandemic, they note.
The current study may have been underpowered and too small to show a significant association between COVID-19 and new diabetes, the researchers acknowledge.
And the 1.30 upper limit of the confidence interval shows that it “cannot rule out a possible 1.3-fold increase” in relative risk of a diagnosis of diabetes related to COVID, Dr. Shulman explained to this news organization.
It will be important to see how the rates have changed since September 2021 (the end of the current study), added Dr. Shulman, an adjunct scientist at the Institute for Clinical Evaluative Sciences (ICES) and a physician and scientist at the Hospital for Sick Children, Toronto.
The current study did find a decreased (delayed) rate of diagnosis of new diabetes during the first months of the pandemic when there were lockdowns, followed by a “catch-up” increase in rates later on, as has been reported earlier.
“Our study is definitely not the final word on this,” Dr. Shulman summarized in a statement from ICES. “However, our findings call into question whether a direct association between COVID-19 and new-onset diabetes in children exists.”
COVID-diabetes link?
The researchers analyzed health administrative data from January 2017 to September 2021.
They identified 2,700,178 children and youth in Ontario who were under age 18 in 2021, who had a mean age of 9.2, and about half were girls.
Between November 2020 and April 2021, an estimated 3.3% of children in Ontario had a SARS-COV-2 infection.
New diagnoses of diabetes in this age group are mostly type 1 diabetes, based on previous studies.
The rate of incident diabetes was 15%-32% lower during the first 3 months of the pandemic, March-May 2020 (1.67-2.34 cases per 100,000), compared with the pre-pandemic monthly rate during 2017, 2018, and 2019 (2.54-2.59 cases per 100,000).
The rate of incident diabetes was 33%-50% higher during February to July 2021 (3.48-4.18 cases per 100,000), compared with the pre-pandemic rate.
The pre-pandemic and pandemic monthly rates of incident diabetes were similar during the other months.
The group concludes: “The lack of both an observable increase in overall diabetes incidence among children during the 18-month pandemic restrictions [in this Ontario study] and a plausible biological mechanism call into question an association between COVID-19 and new-onset diabetes.”
More research is needed. “Given the variability in monthly [relative risks], additional population-based, longer-term data are needed to examine the direct and indirect effects of COVID-19 and diabetes risk among children,” the authors write.
This study was supported by ICES (which is funded by the Ontario Ministry of Health) and by a grant from the Canadian Institutes of Health Research. Dr. Shulman reported receiving fees from Dexcom outside the submitted work, and she and three other authors reported receiving grants from the Canadian Institutes of Health Research outside the submitted work.
A version of this article first appeared on Medscape.com.
FROM JAMA OPEN
Evusheld for COVID-19: Lifesaving and free, but still few takers
Evusheld (AstraZeneca), a medication used to prevent SARS-CoV-2 infection in patients at high risk, has problems: Namely, that supplies of the potentially lifesaving drug outweigh demand.
At least 7 million people who are immunocompromised could benefit from it, as could many others who are undergoing cancer treatment, have received a transplant, or who are allergic to the COVID-19 vaccines. The medication has laboratory-produced antibodies against SARS-CoV-2 and helps the body protect itself. It can slash the chances of becoming infected by 77%, according to the U.S. Food and Drug Administration.
And it’s free to eligible patients (although there may be an out-of-pocket administrative fee in some cases).
To meet demand, the Biden administration secured 1.7 million doses of the medicine, which was granted emergency use authorization by the FDA in December 2021. As of July 25, however, 793,348 doses have been ordered by the administration sites, and only 398,181 doses have been reported as used, a spokesperson for the Department of Health & Human Services tells this news organization.
Each week, a certain amount of doses from the 1.7 million dose stockpile is made available to state and territorial health departments. States have not been asking for their full allotment, the spokesperson said July 28.
Now, HHS and AstraZeneca have taken a number of steps to increase awareness of the medication and access to it.
- On July 27, HHS announced that individual providers and smaller sites of care that don’t currently receive Evusheld through the federal distribution process via the HHS Health Partner Order Portal can now order up to three patient courses of the medicine. These can be
- Health care providers can use the HHS’s COVID-19 Therapeutics Locator to find Evusheld in their area.
- AstraZeneca has launched a new website with educational materials and says it is working closely with patient and professional groups to inform patients and health care providers.
- A direct-to-consumer ad launched on June 22 and will run in the United States online and on TV (Yahoo, Fox, CBS Sports, MSN, ESPN) and be amplified on social and digital channels through year’s end, an AstraZeneca spokesperson said in an interview.
- AstraZeneca set up a toll-free number for providers: 1-833-EVUSHLD.
Evusheld includes two monoclonal antibodies, tixagevimab and cilgavimab. The medication is given as two consecutive intramuscular injections during a single visit to a doctor’s office, infusion center, or other health care facility. The antibodies bind to the SARS-CoV-2 spike protein and prevent the virus from getting into human cells and infecting them. It’s authorized for use in children and adults aged 12 years and older who weigh at least 88 pounds.
Studies have found that the medication decreases the risk of getting COVID-19 for up to 6 months after it is given. The FDA recommends repeat dosing every 6 months with the doses of 300 mg of each monoclonal antibody. In clinical trials, Evusheld reduced the incidence of COVID-19 symptomatic illness by 77%, compared with placebo.
Physicians monitor patients for an hour after administering Evusheld for allergic reactions. Other possible side effects include cardiac events, but they are not common.
Doctors and patients weigh in
Physicians – and patients – from the United States to the United Kingdom and beyond are questioning why the medication is underused while lauding the recent efforts to expand access and increase awareness.
The U.S. federal government may have underestimated the amount of communication needed to increase awareness of the medication and its applications, said infectious disease specialist William Schaffner, MD, professor of preventive medicine at Vanderbilt University School of Medicine, Nashville, Tenn.
“HHS hasn’t made a major educational effort to promote it,” he said in an interview.
Many physicians who need to know about it, such as transplant doctors and rheumatologists, are outside the typical public health communications loop, he said.
Eric Topol, MD, director of the Scripps Research Transational Institute and editor-in-chief of Medscape, has taken to social media to bemoan the lack of awareness.
Another infectious disease expert agrees. “In my experience, the awareness of Evusheld is low amongst many patients as well as many providers,” said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore.
“Initially, there were scarce supplies of the drug, and certain hospital systems tiered eligibility based on degrees of immunosuppression, and only the most immunosuppressed were proactively approached for treatment.”
“Also, many community hospitals never initially ordered Evusheld – they may have been crowded out by academic centers who treat many more immunosuppressed patients and may not currently see it as a priority,” Dr. Adalja said in an interview. “As such, many immunosuppressed patients would have to seek treatment at academic medical centers, where the drug is more likely to be available.”
A version of this article first appeared on Medscape.com.
Evusheld (AstraZeneca), a medication used to prevent SARS-CoV-2 infection in patients at high risk, has problems: Namely, that supplies of the potentially lifesaving drug outweigh demand.
At least 7 million people who are immunocompromised could benefit from it, as could many others who are undergoing cancer treatment, have received a transplant, or who are allergic to the COVID-19 vaccines. The medication has laboratory-produced antibodies against SARS-CoV-2 and helps the body protect itself. It can slash the chances of becoming infected by 77%, according to the U.S. Food and Drug Administration.
And it’s free to eligible patients (although there may be an out-of-pocket administrative fee in some cases).
To meet demand, the Biden administration secured 1.7 million doses of the medicine, which was granted emergency use authorization by the FDA in December 2021. As of July 25, however, 793,348 doses have been ordered by the administration sites, and only 398,181 doses have been reported as used, a spokesperson for the Department of Health & Human Services tells this news organization.
Each week, a certain amount of doses from the 1.7 million dose stockpile is made available to state and territorial health departments. States have not been asking for their full allotment, the spokesperson said July 28.
Now, HHS and AstraZeneca have taken a number of steps to increase awareness of the medication and access to it.
- On July 27, HHS announced that individual providers and smaller sites of care that don’t currently receive Evusheld through the federal distribution process via the HHS Health Partner Order Portal can now order up to three patient courses of the medicine. These can be
- Health care providers can use the HHS’s COVID-19 Therapeutics Locator to find Evusheld in their area.
- AstraZeneca has launched a new website with educational materials and says it is working closely with patient and professional groups to inform patients and health care providers.
- A direct-to-consumer ad launched on June 22 and will run in the United States online and on TV (Yahoo, Fox, CBS Sports, MSN, ESPN) and be amplified on social and digital channels through year’s end, an AstraZeneca spokesperson said in an interview.
- AstraZeneca set up a toll-free number for providers: 1-833-EVUSHLD.
Evusheld includes two monoclonal antibodies, tixagevimab and cilgavimab. The medication is given as two consecutive intramuscular injections during a single visit to a doctor’s office, infusion center, or other health care facility. The antibodies bind to the SARS-CoV-2 spike protein and prevent the virus from getting into human cells and infecting them. It’s authorized for use in children and adults aged 12 years and older who weigh at least 88 pounds.
Studies have found that the medication decreases the risk of getting COVID-19 for up to 6 months after it is given. The FDA recommends repeat dosing every 6 months with the doses of 300 mg of each monoclonal antibody. In clinical trials, Evusheld reduced the incidence of COVID-19 symptomatic illness by 77%, compared with placebo.
Physicians monitor patients for an hour after administering Evusheld for allergic reactions. Other possible side effects include cardiac events, but they are not common.
Doctors and patients weigh in
Physicians – and patients – from the United States to the United Kingdom and beyond are questioning why the medication is underused while lauding the recent efforts to expand access and increase awareness.
The U.S. federal government may have underestimated the amount of communication needed to increase awareness of the medication and its applications, said infectious disease specialist William Schaffner, MD, professor of preventive medicine at Vanderbilt University School of Medicine, Nashville, Tenn.
“HHS hasn’t made a major educational effort to promote it,” he said in an interview.
Many physicians who need to know about it, such as transplant doctors and rheumatologists, are outside the typical public health communications loop, he said.
Eric Topol, MD, director of the Scripps Research Transational Institute and editor-in-chief of Medscape, has taken to social media to bemoan the lack of awareness.
Another infectious disease expert agrees. “In my experience, the awareness of Evusheld is low amongst many patients as well as many providers,” said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore.
“Initially, there were scarce supplies of the drug, and certain hospital systems tiered eligibility based on degrees of immunosuppression, and only the most immunosuppressed were proactively approached for treatment.”
“Also, many community hospitals never initially ordered Evusheld – they may have been crowded out by academic centers who treat many more immunosuppressed patients and may not currently see it as a priority,” Dr. Adalja said in an interview. “As such, many immunosuppressed patients would have to seek treatment at academic medical centers, where the drug is more likely to be available.”
A version of this article first appeared on Medscape.com.
Evusheld (AstraZeneca), a medication used to prevent SARS-CoV-2 infection in patients at high risk, has problems: Namely, that supplies of the potentially lifesaving drug outweigh demand.
At least 7 million people who are immunocompromised could benefit from it, as could many others who are undergoing cancer treatment, have received a transplant, or who are allergic to the COVID-19 vaccines. The medication has laboratory-produced antibodies against SARS-CoV-2 and helps the body protect itself. It can slash the chances of becoming infected by 77%, according to the U.S. Food and Drug Administration.
And it’s free to eligible patients (although there may be an out-of-pocket administrative fee in some cases).
To meet demand, the Biden administration secured 1.7 million doses of the medicine, which was granted emergency use authorization by the FDA in December 2021. As of July 25, however, 793,348 doses have been ordered by the administration sites, and only 398,181 doses have been reported as used, a spokesperson for the Department of Health & Human Services tells this news organization.
Each week, a certain amount of doses from the 1.7 million dose stockpile is made available to state and territorial health departments. States have not been asking for their full allotment, the spokesperson said July 28.
Now, HHS and AstraZeneca have taken a number of steps to increase awareness of the medication and access to it.
- On July 27, HHS announced that individual providers and smaller sites of care that don’t currently receive Evusheld through the federal distribution process via the HHS Health Partner Order Portal can now order up to three patient courses of the medicine. These can be
- Health care providers can use the HHS’s COVID-19 Therapeutics Locator to find Evusheld in their area.
- AstraZeneca has launched a new website with educational materials and says it is working closely with patient and professional groups to inform patients and health care providers.
- A direct-to-consumer ad launched on June 22 and will run in the United States online and on TV (Yahoo, Fox, CBS Sports, MSN, ESPN) and be amplified on social and digital channels through year’s end, an AstraZeneca spokesperson said in an interview.
- AstraZeneca set up a toll-free number for providers: 1-833-EVUSHLD.
Evusheld includes two monoclonal antibodies, tixagevimab and cilgavimab. The medication is given as two consecutive intramuscular injections during a single visit to a doctor’s office, infusion center, or other health care facility. The antibodies bind to the SARS-CoV-2 spike protein and prevent the virus from getting into human cells and infecting them. It’s authorized for use in children and adults aged 12 years and older who weigh at least 88 pounds.
Studies have found that the medication decreases the risk of getting COVID-19 for up to 6 months after it is given. The FDA recommends repeat dosing every 6 months with the doses of 300 mg of each monoclonal antibody. In clinical trials, Evusheld reduced the incidence of COVID-19 symptomatic illness by 77%, compared with placebo.
Physicians monitor patients for an hour after administering Evusheld for allergic reactions. Other possible side effects include cardiac events, but they are not common.
Doctors and patients weigh in
Physicians – and patients – from the United States to the United Kingdom and beyond are questioning why the medication is underused while lauding the recent efforts to expand access and increase awareness.
The U.S. federal government may have underestimated the amount of communication needed to increase awareness of the medication and its applications, said infectious disease specialist William Schaffner, MD, professor of preventive medicine at Vanderbilt University School of Medicine, Nashville, Tenn.
“HHS hasn’t made a major educational effort to promote it,” he said in an interview.
Many physicians who need to know about it, such as transplant doctors and rheumatologists, are outside the typical public health communications loop, he said.
Eric Topol, MD, director of the Scripps Research Transational Institute and editor-in-chief of Medscape, has taken to social media to bemoan the lack of awareness.
Another infectious disease expert agrees. “In my experience, the awareness of Evusheld is low amongst many patients as well as many providers,” said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore.
“Initially, there were scarce supplies of the drug, and certain hospital systems tiered eligibility based on degrees of immunosuppression, and only the most immunosuppressed were proactively approached for treatment.”
“Also, many community hospitals never initially ordered Evusheld – they may have been crowded out by academic centers who treat many more immunosuppressed patients and may not currently see it as a priority,” Dr. Adalja said in an interview. “As such, many immunosuppressed patients would have to seek treatment at academic medical centers, where the drug is more likely to be available.”
A version of this article first appeared on Medscape.com.
‘Striking’ disparities in CVD deaths persist across COVID waves
Cardiovascular disease (CVD) mortality rose significantly during the COVID-19 pandemic and persists more than 2 years on and, once again, Blacks and African Americans have been disproportionately affected, an analysis of death certificates shows.
The findings “suggest that the pandemic may reverse years or decades of work aimed at reducing gaps in cardiovascular outcomes,” Sadeer G. Al-Kindi, MD, Case Western Reserve University, Cleveland, said in an interview.
Although the disparities are in line with previous research, he said, “what was surprising is the persistence of excess cardiovascular mortality approximately 2 years after the pandemic started, even during a period of low COVID-19 mortality.”
“This suggests that the pandemic resulted in a disruption of health care access and, along with disparities in COVID-19 infection and its complications, he said, “may have a long-lasting effect on health care disparities, especially among vulnerable populations.”
The study was published online in Mayo Clinic Proceedings with lead author Scott E. Janus, MD, also of Case Western Reserve University.
Impact consistently greater for Blacks
Dr. Al-Kindi and colleagues used 3,598,352 U.S. death files to investigate trends in deaths caused specifically by CVD as well as its subtypes myocardial infarction, stroke, and heart failure (HF) in 2018 and 2019 (prepandemic) and the pandemic years 2020 and 2021. Baseline demographics showed a higher percentage of older, female, and Black individuals among the CVD subtypes of interest.
Overall, there was an excess CVD mortality of 6.7% during the pandemic, compared with prepandemic years, including a 2.5% rise in MI deaths and an 8.5% rise in stroke deaths. HF mortality remained relatively steady, rising only 0.1%.
Subgroup analyses revealed “striking differences” in excess mortality between Blacks and Whites, the authors noted. Blacks had an overall excess mortality of 13.8% versus 5.1% for Whites, compared with the prepandemic years. The differences were consistent across subtypes: MI (9.6% vs. 1.0%); stroke (14.5% vs. 6.9%); and HF (5.1% vs. –1.2%; P value for all < .001).
When the investigators looked at deaths on a yearly basis with 2018 as the baseline, they found CVD deaths increased by 1.5% in 2019, 15.8% in 2020, and 13.5% in 2021 among Black Americans, compared with 0.5%, 5.1%, and 5.7%, respectively, among White Americans.
Excess deaths from MI rose by 9.5% in 2020 and by 6.7% in 2021 among Blacks but fell by 1.2% in 2020 and by 1.0% in 2021 among Whites.
Disparities in excess HF mortality were similar, rising 9.1% and 4.1% in 2020 and 2021 among Blacks, while dipping 0.1% and 0.8% in 2020 and 2021 among Whites.
The “most striking difference” was in excess stroke mortality, which doubled among Blacks compared with whites in 2020 (14.9% vs. 6.7%) and in 2021 (17.5% vs. 8.1%), according to the authors.
Awareness urged
Although the disparities were expected, “there is clear value in documenting and quantifying the magnitude of these disparities,” Amil M. Shah, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston, said in an interview.
In addition to being observational, the main limitation of the study, he noted, is the quality and resolution of the death certificate data, which may limit the accuracy of the cause of death ascertainment and classification of race or ethnicity. “However, I think these potential inaccuracies are unlikely to materially impact the overall study findings.”
Dr. Shah, who was not involved in the study, said he would like to see additional research into the diversity and heterogeneity in risk among Black communities. “Understanding the environmental, social, and health care factors – both harmful and protective – that influence risk for CVD morbidity and mortality among Black individuals and communities offers the promise to provide actionable insights to mitigate these disparities.”
“Intervention studies testing approaches to mitigate disparities based on race/ethnicity” are also needed, he added. These may be at the policy, community, health system, or individual level, and community involvement in phases will be essential.”
Meanwhile, both Dr. Al-Kindi and Dr. Shah urged clinicians to be aware of the disparities and the need to improve access to care and address social determinants of health in vulnerable populations.
These disparities “are driven by structural factors, and are reinforced by individual behaviors. In this context, implicit bias training is important to help clinicians recognize and mitigate bias in their own practice,” Dr. Shah said. “Supporting diversity, equity, and inclusion efforts, and advocating for anti-racist policies and practices in their health systems” can also help.
Dr. Al-Kindi and Dr. Shah disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiovascular disease (CVD) mortality rose significantly during the COVID-19 pandemic and persists more than 2 years on and, once again, Blacks and African Americans have been disproportionately affected, an analysis of death certificates shows.
The findings “suggest that the pandemic may reverse years or decades of work aimed at reducing gaps in cardiovascular outcomes,” Sadeer G. Al-Kindi, MD, Case Western Reserve University, Cleveland, said in an interview.
Although the disparities are in line with previous research, he said, “what was surprising is the persistence of excess cardiovascular mortality approximately 2 years after the pandemic started, even during a period of low COVID-19 mortality.”
“This suggests that the pandemic resulted in a disruption of health care access and, along with disparities in COVID-19 infection and its complications, he said, “may have a long-lasting effect on health care disparities, especially among vulnerable populations.”
The study was published online in Mayo Clinic Proceedings with lead author Scott E. Janus, MD, also of Case Western Reserve University.
Impact consistently greater for Blacks
Dr. Al-Kindi and colleagues used 3,598,352 U.S. death files to investigate trends in deaths caused specifically by CVD as well as its subtypes myocardial infarction, stroke, and heart failure (HF) in 2018 and 2019 (prepandemic) and the pandemic years 2020 and 2021. Baseline demographics showed a higher percentage of older, female, and Black individuals among the CVD subtypes of interest.
Overall, there was an excess CVD mortality of 6.7% during the pandemic, compared with prepandemic years, including a 2.5% rise in MI deaths and an 8.5% rise in stroke deaths. HF mortality remained relatively steady, rising only 0.1%.
Subgroup analyses revealed “striking differences” in excess mortality between Blacks and Whites, the authors noted. Blacks had an overall excess mortality of 13.8% versus 5.1% for Whites, compared with the prepandemic years. The differences were consistent across subtypes: MI (9.6% vs. 1.0%); stroke (14.5% vs. 6.9%); and HF (5.1% vs. –1.2%; P value for all < .001).
When the investigators looked at deaths on a yearly basis with 2018 as the baseline, they found CVD deaths increased by 1.5% in 2019, 15.8% in 2020, and 13.5% in 2021 among Black Americans, compared with 0.5%, 5.1%, and 5.7%, respectively, among White Americans.
Excess deaths from MI rose by 9.5% in 2020 and by 6.7% in 2021 among Blacks but fell by 1.2% in 2020 and by 1.0% in 2021 among Whites.
Disparities in excess HF mortality were similar, rising 9.1% and 4.1% in 2020 and 2021 among Blacks, while dipping 0.1% and 0.8% in 2020 and 2021 among Whites.
The “most striking difference” was in excess stroke mortality, which doubled among Blacks compared with whites in 2020 (14.9% vs. 6.7%) and in 2021 (17.5% vs. 8.1%), according to the authors.
Awareness urged
Although the disparities were expected, “there is clear value in documenting and quantifying the magnitude of these disparities,” Amil M. Shah, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston, said in an interview.
In addition to being observational, the main limitation of the study, he noted, is the quality and resolution of the death certificate data, which may limit the accuracy of the cause of death ascertainment and classification of race or ethnicity. “However, I think these potential inaccuracies are unlikely to materially impact the overall study findings.”
Dr. Shah, who was not involved in the study, said he would like to see additional research into the diversity and heterogeneity in risk among Black communities. “Understanding the environmental, social, and health care factors – both harmful and protective – that influence risk for CVD morbidity and mortality among Black individuals and communities offers the promise to provide actionable insights to mitigate these disparities.”
“Intervention studies testing approaches to mitigate disparities based on race/ethnicity” are also needed, he added. These may be at the policy, community, health system, or individual level, and community involvement in phases will be essential.”
Meanwhile, both Dr. Al-Kindi and Dr. Shah urged clinicians to be aware of the disparities and the need to improve access to care and address social determinants of health in vulnerable populations.
These disparities “are driven by structural factors, and are reinforced by individual behaviors. In this context, implicit bias training is important to help clinicians recognize and mitigate bias in their own practice,” Dr. Shah said. “Supporting diversity, equity, and inclusion efforts, and advocating for anti-racist policies and practices in their health systems” can also help.
Dr. Al-Kindi and Dr. Shah disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cardiovascular disease (CVD) mortality rose significantly during the COVID-19 pandemic and persists more than 2 years on and, once again, Blacks and African Americans have been disproportionately affected, an analysis of death certificates shows.
The findings “suggest that the pandemic may reverse years or decades of work aimed at reducing gaps in cardiovascular outcomes,” Sadeer G. Al-Kindi, MD, Case Western Reserve University, Cleveland, said in an interview.
Although the disparities are in line with previous research, he said, “what was surprising is the persistence of excess cardiovascular mortality approximately 2 years after the pandemic started, even during a period of low COVID-19 mortality.”
“This suggests that the pandemic resulted in a disruption of health care access and, along with disparities in COVID-19 infection and its complications, he said, “may have a long-lasting effect on health care disparities, especially among vulnerable populations.”
The study was published online in Mayo Clinic Proceedings with lead author Scott E. Janus, MD, also of Case Western Reserve University.
Impact consistently greater for Blacks
Dr. Al-Kindi and colleagues used 3,598,352 U.S. death files to investigate trends in deaths caused specifically by CVD as well as its subtypes myocardial infarction, stroke, and heart failure (HF) in 2018 and 2019 (prepandemic) and the pandemic years 2020 and 2021. Baseline demographics showed a higher percentage of older, female, and Black individuals among the CVD subtypes of interest.
Overall, there was an excess CVD mortality of 6.7% during the pandemic, compared with prepandemic years, including a 2.5% rise in MI deaths and an 8.5% rise in stroke deaths. HF mortality remained relatively steady, rising only 0.1%.
Subgroup analyses revealed “striking differences” in excess mortality between Blacks and Whites, the authors noted. Blacks had an overall excess mortality of 13.8% versus 5.1% for Whites, compared with the prepandemic years. The differences were consistent across subtypes: MI (9.6% vs. 1.0%); stroke (14.5% vs. 6.9%); and HF (5.1% vs. –1.2%; P value for all < .001).
When the investigators looked at deaths on a yearly basis with 2018 as the baseline, they found CVD deaths increased by 1.5% in 2019, 15.8% in 2020, and 13.5% in 2021 among Black Americans, compared with 0.5%, 5.1%, and 5.7%, respectively, among White Americans.
Excess deaths from MI rose by 9.5% in 2020 and by 6.7% in 2021 among Blacks but fell by 1.2% in 2020 and by 1.0% in 2021 among Whites.
Disparities in excess HF mortality were similar, rising 9.1% and 4.1% in 2020 and 2021 among Blacks, while dipping 0.1% and 0.8% in 2020 and 2021 among Whites.
The “most striking difference” was in excess stroke mortality, which doubled among Blacks compared with whites in 2020 (14.9% vs. 6.7%) and in 2021 (17.5% vs. 8.1%), according to the authors.
Awareness urged
Although the disparities were expected, “there is clear value in documenting and quantifying the magnitude of these disparities,” Amil M. Shah, MD, MPH, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston, said in an interview.
In addition to being observational, the main limitation of the study, he noted, is the quality and resolution of the death certificate data, which may limit the accuracy of the cause of death ascertainment and classification of race or ethnicity. “However, I think these potential inaccuracies are unlikely to materially impact the overall study findings.”
Dr. Shah, who was not involved in the study, said he would like to see additional research into the diversity and heterogeneity in risk among Black communities. “Understanding the environmental, social, and health care factors – both harmful and protective – that influence risk for CVD morbidity and mortality among Black individuals and communities offers the promise to provide actionable insights to mitigate these disparities.”
“Intervention studies testing approaches to mitigate disparities based on race/ethnicity” are also needed, he added. These may be at the policy, community, health system, or individual level, and community involvement in phases will be essential.”
Meanwhile, both Dr. Al-Kindi and Dr. Shah urged clinicians to be aware of the disparities and the need to improve access to care and address social determinants of health in vulnerable populations.
These disparities “are driven by structural factors, and are reinforced by individual behaviors. In this context, implicit bias training is important to help clinicians recognize and mitigate bias in their own practice,” Dr. Shah said. “Supporting diversity, equity, and inclusion efforts, and advocating for anti-racist policies and practices in their health systems” can also help.
Dr. Al-Kindi and Dr. Shah disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM MAYO CLINIC PROCEEDINGS
More evidence that COVID-19 started in Wuhan marketplace
The original spread of the virus was a one-two punch, the studies found. Twice, the virus jumped from animals to humans. Virus genetics and outbreak modeling in one study revealed two strains released a few weeks apart in November and December 2019.
“Now I realize it sounds like I just said that a once-in-a-generation event happened twice in short succession, and pandemics are indeed rare,” Joel O. Wertheim, PhD, said at a briefing sponsored by the American Association for the Advancement of Science.
A unique storm of factors had to be present for the outbreak to blow up into a pandemic: Animals carrying a virus that could spread to humans, close human contact with these animals, and a city large enough for the infection to take off before it could be contained are examples.
Unluckily for us humans, this coronavirus – SARS-CoV-2 – is a “generalist virus” capable of infecting many animals, including humans.
“Once all the conditions are in place ... the barriers to spillover have been lowered,” said Dr. Wertheim, a researcher in genetic and molecular networks at the University of California, San Diego. In fact, beyond the two strains of the virus that took hold, there were likely up to two dozen more times where people got the virus but did not spread it far and wide, and it died out.
Overall, the odds were against the virus – 78% of the time, the “introduction” to humans was likely to go extinct, the study showed.
The research revealed the COVID-19 pandemic started small.
“Our model shows that there were likely only a few dozen infections, and only several hospitalizations due to COVID-19, by early December,” said Jonathan Pekar, a graduate student working with Dr. Wertheim.
In Wuhan in late 2019, Mr. Pekar said, there was not a single positive coronavirus sample from thousands of samples from healthy blood donors tested between September and December. Likewise, not one blood sample from patients hospitalized with flu-like illness from October to December 2019 tested positive for SARS-CoV-2.
Mapping the outbreak
A second study published in the journal Science mapped out the earliest COVID-19 cases. This effort showed a tight cluster around the wholesale seafood market inside Wuhan, a city of 11 million residents.
When researchers tried other scenarios – modeling outbreaks in other parts of the city – the pattern did not hold. Again, the Wuhan market appeared to be ground zero for the start of the pandemic.
Michael Worobey, PhD, and colleagues used data from Chinese scientists and the World Health Organization for the study.
“There was this extraordinary pattern where the highest density of cases was both extremely near to and very centered on this market,” said Dr. Worobey, head of ecology and evolutionary biology at the University of Arizona, Tucson.
The highest density of cases, in a city of 8,000 square kilometers, was a “very, very small area of about a third of a kilometer square,” he said.
The outbreak pattern showed the Wuhan market “smack dab in the middle.”
So if it started with infected workers at the market, how did it spread from there? It’s likely the virus got into the community as the vendors at the market went to local shops, infecting people in those stores. Then local community members not linked to the market started getting the virus, Dr. Worobey said.
The investigators also identified which stalls in the market were most likely involved, a sort of internal clustering. “That clustering is very, very specifically in the parts of the market where ... they were selling wildlife, including, for example, raccoon dogs and other animals that we know are susceptible to infection with SARS-CoV-2,” said Kristian Andersen, PhD, director of infectious disease genomics at the Scripps Research Institute in La Jolla, Calif.
What remains unknown is which animal or animals carried the virus, although the raccoon dog – an animal similar to a fox that is native to parts of Asia – remains central to most theories. In addition, many of the farms supplying animals to the market have since been closed, making it challenging for researchers to figure out exactly where infected animals came from.
“We don’t know necessarily, but raccoon dogs were sold at this market all the way up to the beginning of the pandemic,” Dr. Andersen said.
Not ruling out other theories
People who believe SARS-CoV-2 was released from a laboratory in China at first included Dr. Worobey himself. “I’ve in the past been much more open to the lab leak idea,” he said. “And published that in a letter in Science” in November 2021.
The letter was “much more influential than I thought it would be in ways that I think it turned out to be quite damaging,” he said. As more evidence emerged since then, Dr. Worobey said he came around to the Wuhan market source theory.
Dr. Andersen agreed he was more open to the lab-leak theory at first. “I was quite convinced of the lab leak myself until we dove into this very carefully and looked at it much closer,” he said. Newer evidence convinced him “that actually, the data points to this particular market.”
“Have we disproved the lab-leak theory? No,” Dr. Anderson said. “Will we ever be able to? No.” But the Wuhan market origin scenario is more plausible. “I would say these two papers combined present the strongest evidence of that to date.”
Identifying the source of the outbreak that led to the COVID-19 pandemic is based in science, Dr. Andersen said. “What we’re trying to understand is the origin of the pandemic. We’re not trying to place blame.”
Future directions
“With pandemics being pandemics, they affect all of us,” Dr. Andersen said. “We can’t prevent these kinds of events that led to the COVID-19 pandemic. But what we can hope to do is to prevent outbreaks from becoming pandemics.”
Rapid reporting of data and cooperation are needed going forward, Dr. Andersen said. Very strong surveillance systems, including wastewater surveillance, could help monitor for SARS-CoV-2, and other pathogens of potential concern in the future as well.
It should be standard practice for medical professionals to be on alert for unusual respiratory infections too, the researchers said.
“It’s a bloody lucky thing that the doctors at the Shinwa hospital were so on the ball, that they noticed that these cases were something unusual at the end of December,” Dr. Worobey said. “It didn’t have to work out that way.”
A version of this article first appeared on WebMD.com.
The original spread of the virus was a one-two punch, the studies found. Twice, the virus jumped from animals to humans. Virus genetics and outbreak modeling in one study revealed two strains released a few weeks apart in November and December 2019.
“Now I realize it sounds like I just said that a once-in-a-generation event happened twice in short succession, and pandemics are indeed rare,” Joel O. Wertheim, PhD, said at a briefing sponsored by the American Association for the Advancement of Science.
A unique storm of factors had to be present for the outbreak to blow up into a pandemic: Animals carrying a virus that could spread to humans, close human contact with these animals, and a city large enough for the infection to take off before it could be contained are examples.
Unluckily for us humans, this coronavirus – SARS-CoV-2 – is a “generalist virus” capable of infecting many animals, including humans.
“Once all the conditions are in place ... the barriers to spillover have been lowered,” said Dr. Wertheim, a researcher in genetic and molecular networks at the University of California, San Diego. In fact, beyond the two strains of the virus that took hold, there were likely up to two dozen more times where people got the virus but did not spread it far and wide, and it died out.
Overall, the odds were against the virus – 78% of the time, the “introduction” to humans was likely to go extinct, the study showed.
The research revealed the COVID-19 pandemic started small.
“Our model shows that there were likely only a few dozen infections, and only several hospitalizations due to COVID-19, by early December,” said Jonathan Pekar, a graduate student working with Dr. Wertheim.
In Wuhan in late 2019, Mr. Pekar said, there was not a single positive coronavirus sample from thousands of samples from healthy blood donors tested between September and December. Likewise, not one blood sample from patients hospitalized with flu-like illness from October to December 2019 tested positive for SARS-CoV-2.
Mapping the outbreak
A second study published in the journal Science mapped out the earliest COVID-19 cases. This effort showed a tight cluster around the wholesale seafood market inside Wuhan, a city of 11 million residents.
When researchers tried other scenarios – modeling outbreaks in other parts of the city – the pattern did not hold. Again, the Wuhan market appeared to be ground zero for the start of the pandemic.
Michael Worobey, PhD, and colleagues used data from Chinese scientists and the World Health Organization for the study.
“There was this extraordinary pattern where the highest density of cases was both extremely near to and very centered on this market,” said Dr. Worobey, head of ecology and evolutionary biology at the University of Arizona, Tucson.
The highest density of cases, in a city of 8,000 square kilometers, was a “very, very small area of about a third of a kilometer square,” he said.
The outbreak pattern showed the Wuhan market “smack dab in the middle.”
So if it started with infected workers at the market, how did it spread from there? It’s likely the virus got into the community as the vendors at the market went to local shops, infecting people in those stores. Then local community members not linked to the market started getting the virus, Dr. Worobey said.
The investigators also identified which stalls in the market were most likely involved, a sort of internal clustering. “That clustering is very, very specifically in the parts of the market where ... they were selling wildlife, including, for example, raccoon dogs and other animals that we know are susceptible to infection with SARS-CoV-2,” said Kristian Andersen, PhD, director of infectious disease genomics at the Scripps Research Institute in La Jolla, Calif.
What remains unknown is which animal or animals carried the virus, although the raccoon dog – an animal similar to a fox that is native to parts of Asia – remains central to most theories. In addition, many of the farms supplying animals to the market have since been closed, making it challenging for researchers to figure out exactly where infected animals came from.
“We don’t know necessarily, but raccoon dogs were sold at this market all the way up to the beginning of the pandemic,” Dr. Andersen said.
Not ruling out other theories
People who believe SARS-CoV-2 was released from a laboratory in China at first included Dr. Worobey himself. “I’ve in the past been much more open to the lab leak idea,” he said. “And published that in a letter in Science” in November 2021.
The letter was “much more influential than I thought it would be in ways that I think it turned out to be quite damaging,” he said. As more evidence emerged since then, Dr. Worobey said he came around to the Wuhan market source theory.
Dr. Andersen agreed he was more open to the lab-leak theory at first. “I was quite convinced of the lab leak myself until we dove into this very carefully and looked at it much closer,” he said. Newer evidence convinced him “that actually, the data points to this particular market.”
“Have we disproved the lab-leak theory? No,” Dr. Anderson said. “Will we ever be able to? No.” But the Wuhan market origin scenario is more plausible. “I would say these two papers combined present the strongest evidence of that to date.”
Identifying the source of the outbreak that led to the COVID-19 pandemic is based in science, Dr. Andersen said. “What we’re trying to understand is the origin of the pandemic. We’re not trying to place blame.”
Future directions
“With pandemics being pandemics, they affect all of us,” Dr. Andersen said. “We can’t prevent these kinds of events that led to the COVID-19 pandemic. But what we can hope to do is to prevent outbreaks from becoming pandemics.”
Rapid reporting of data and cooperation are needed going forward, Dr. Andersen said. Very strong surveillance systems, including wastewater surveillance, could help monitor for SARS-CoV-2, and other pathogens of potential concern in the future as well.
It should be standard practice for medical professionals to be on alert for unusual respiratory infections too, the researchers said.
“It’s a bloody lucky thing that the doctors at the Shinwa hospital were so on the ball, that they noticed that these cases were something unusual at the end of December,” Dr. Worobey said. “It didn’t have to work out that way.”
A version of this article first appeared on WebMD.com.
The original spread of the virus was a one-two punch, the studies found. Twice, the virus jumped from animals to humans. Virus genetics and outbreak modeling in one study revealed two strains released a few weeks apart in November and December 2019.
“Now I realize it sounds like I just said that a once-in-a-generation event happened twice in short succession, and pandemics are indeed rare,” Joel O. Wertheim, PhD, said at a briefing sponsored by the American Association for the Advancement of Science.
A unique storm of factors had to be present for the outbreak to blow up into a pandemic: Animals carrying a virus that could spread to humans, close human contact with these animals, and a city large enough for the infection to take off before it could be contained are examples.
Unluckily for us humans, this coronavirus – SARS-CoV-2 – is a “generalist virus” capable of infecting many animals, including humans.
“Once all the conditions are in place ... the barriers to spillover have been lowered,” said Dr. Wertheim, a researcher in genetic and molecular networks at the University of California, San Diego. In fact, beyond the two strains of the virus that took hold, there were likely up to two dozen more times where people got the virus but did not spread it far and wide, and it died out.
Overall, the odds were against the virus – 78% of the time, the “introduction” to humans was likely to go extinct, the study showed.
The research revealed the COVID-19 pandemic started small.
“Our model shows that there were likely only a few dozen infections, and only several hospitalizations due to COVID-19, by early December,” said Jonathan Pekar, a graduate student working with Dr. Wertheim.
In Wuhan in late 2019, Mr. Pekar said, there was not a single positive coronavirus sample from thousands of samples from healthy blood donors tested between September and December. Likewise, not one blood sample from patients hospitalized with flu-like illness from October to December 2019 tested positive for SARS-CoV-2.
Mapping the outbreak
A second study published in the journal Science mapped out the earliest COVID-19 cases. This effort showed a tight cluster around the wholesale seafood market inside Wuhan, a city of 11 million residents.
When researchers tried other scenarios – modeling outbreaks in other parts of the city – the pattern did not hold. Again, the Wuhan market appeared to be ground zero for the start of the pandemic.
Michael Worobey, PhD, and colleagues used data from Chinese scientists and the World Health Organization for the study.
“There was this extraordinary pattern where the highest density of cases was both extremely near to and very centered on this market,” said Dr. Worobey, head of ecology and evolutionary biology at the University of Arizona, Tucson.
The highest density of cases, in a city of 8,000 square kilometers, was a “very, very small area of about a third of a kilometer square,” he said.
The outbreak pattern showed the Wuhan market “smack dab in the middle.”
So if it started with infected workers at the market, how did it spread from there? It’s likely the virus got into the community as the vendors at the market went to local shops, infecting people in those stores. Then local community members not linked to the market started getting the virus, Dr. Worobey said.
The investigators also identified which stalls in the market were most likely involved, a sort of internal clustering. “That clustering is very, very specifically in the parts of the market where ... they were selling wildlife, including, for example, raccoon dogs and other animals that we know are susceptible to infection with SARS-CoV-2,” said Kristian Andersen, PhD, director of infectious disease genomics at the Scripps Research Institute in La Jolla, Calif.
What remains unknown is which animal or animals carried the virus, although the raccoon dog – an animal similar to a fox that is native to parts of Asia – remains central to most theories. In addition, many of the farms supplying animals to the market have since been closed, making it challenging for researchers to figure out exactly where infected animals came from.
“We don’t know necessarily, but raccoon dogs were sold at this market all the way up to the beginning of the pandemic,” Dr. Andersen said.
Not ruling out other theories
People who believe SARS-CoV-2 was released from a laboratory in China at first included Dr. Worobey himself. “I’ve in the past been much more open to the lab leak idea,” he said. “And published that in a letter in Science” in November 2021.
The letter was “much more influential than I thought it would be in ways that I think it turned out to be quite damaging,” he said. As more evidence emerged since then, Dr. Worobey said he came around to the Wuhan market source theory.
Dr. Andersen agreed he was more open to the lab-leak theory at first. “I was quite convinced of the lab leak myself until we dove into this very carefully and looked at it much closer,” he said. Newer evidence convinced him “that actually, the data points to this particular market.”
“Have we disproved the lab-leak theory? No,” Dr. Anderson said. “Will we ever be able to? No.” But the Wuhan market origin scenario is more plausible. “I would say these two papers combined present the strongest evidence of that to date.”
Identifying the source of the outbreak that led to the COVID-19 pandemic is based in science, Dr. Andersen said. “What we’re trying to understand is the origin of the pandemic. We’re not trying to place blame.”
Future directions
“With pandemics being pandemics, they affect all of us,” Dr. Andersen said. “We can’t prevent these kinds of events that led to the COVID-19 pandemic. But what we can hope to do is to prevent outbreaks from becoming pandemics.”
Rapid reporting of data and cooperation are needed going forward, Dr. Andersen said. Very strong surveillance systems, including wastewater surveillance, could help monitor for SARS-CoV-2, and other pathogens of potential concern in the future as well.
It should be standard practice for medical professionals to be on alert for unusual respiratory infections too, the researchers said.
“It’s a bloody lucky thing that the doctors at the Shinwa hospital were so on the ball, that they noticed that these cases were something unusual at the end of December,” Dr. Worobey said. “It didn’t have to work out that way.”
A version of this article first appeared on WebMD.com.
Scientists aim to combat COVID with a shot in the nose
Scientists seeking to stay ahead of an evolving SARS-Cov-2 virus are looking at new strategies, including developing intranasal vaccines, according to speakers at a conference on July 26.
inviting researchers to provide a public update on efforts to try to keep ahead of SARS-CoV-2.
Scientists and federal officials are looking to build on the successes seen in developing the original crop of COVID vaccines, which were authorized for use in the United States less than a year after the pandemic took hold.
But emerging variants are eroding these gains. For months now, officials at the Centers for Disease Control and Prevention and Food and Drug Administration have been keeping an eye on how the level of effectiveness of COVID vaccines has waned during the rise of the Omicron strain. And there’s continual concern about how SARS-CoV-2 might evolve over time.
“Our vaccines are terrific,” Ashish K. Jha, MD, the White House’s COVID-19 response coordinator, said at the summit. “[But] we have to do better.”
Among the approaches being considered are vaccines that would be applied intranasally, with the idea that this might be able to boost the immune response to SARS-CoV-2.
At the summit, Akiko Iwasaki, PhD, of Yale University, New Haven, Conn., said the intranasal approach might be helpful in preventing transmission as well as reducing the burden of illness for those who are infected with SARS-CoV-2.
“We’re stopping the virus from spreading right at the border,” Dr. Iwasaki said at the summit. “This is akin to putting a guard outside of the house in order to patrol for invaders compared to putting the guards in the hallway of the building in the hope that they capture the invader.”
Dr. Iwasaki is one of the founders of Xanadu Bio, a private company created last year to focus on ways to kill SARS-CoV-2 in the nasosinus before it spreads deeper into the respiratory tract. In an editorial in Science Immunology, Dr. Iwasaki and Eric J. Topol, MD, director of the Scripps Research Translational Institute, urged greater federal investment in this approach to fighting SARS-CoV-2. (Dr. Topol is editor-in-chief of Medscape.)
Titled “Operation Nasal Vaccine – Lightning speed to counter COVID-19,” their editorial noted the “unprecedented success” seen in the rapid development of the first two mRNA shots. Dr. Iwasaki and Dr. Topol noted that these victories had been “fueled by the $10 billion governmental investment in Operation Warp Speed.
“During the first year of the pandemic, meaningful evolution of the virus was slow-paced, without any functional consequences, but since that time we have seen a succession of important variants of concern, with increasing transmissibility and immune evasion, culminating in the Omicron lineages,” wrote Dr. Iwasaki and Dr. Topol.
Recent developments have “spotlighted the possibility of nasal vaccines, with their allure for achieving mucosal immunity, complementing, and likely bolstering the circulating immunity achieved via intramuscular shots,” they added.
An early setback
Scientists at the National Institutes of Health and the Biomedical Advanced Research and Development Authority (BARDA) have for some time been looking to vet an array of next-generation vaccine concepts, including ones that trigger mucosal immunity, the Washington Post reported in April.
At the summit on July 26, several participants, including Dr. Jha, stressed the role that public-private partnerships were key to the rapid development of the initial COVID vaccines. They said continued U.S. government support will be needed to make advances in this field.
One of the presenters, Biao He, PhD, founder and president of CyanVac and Blue Lake Biotechnology, spoke of the federal support that his efforts have received over the years to develop intranasal vaccines. His Georgia-based firm already has an experimental intranasal vaccine candidate, CVXGA1-001, in phase 1 testing (NCT04954287).
The CVXGA-001 builds on technology already used in a veterinary product, an intranasal vaccine long used to prevent kennel cough in dogs, he said at the summit.
The emerging field of experimental intranasal COVID vaccines already has had at least one setback.
The biotech firm Altimmune in June 2021 announced that it would discontinue development of its experimental intranasal AdCOVID vaccine following disappointing phase 1 results. The vaccine appeared to be well tolerated in the test, but the immunogenicity data demonstrated lower than expected results in healthy volunteers, especially in light of the responses seen to already cleared vaccines, Altimmune said in a release.
In the statement, Scot Roberts, PhD, chief scientific officer at Altimmune, noted that the study participants lacked immunity from prior infection or vaccination. “We believe that prior immunity in humans may be important for a robust immune response to intranasal dosing with AdCOVID,” he said.
At the summit, Marty Moore, PhD, cofounder and chief scientific officer for Redwood City, Calif.–based Meissa Vaccines, noted the challenges that remain ahead for intranasal COVID vaccines, while also highlighting what he sees as the potential of this approach.
Meissa also has advanced an experimental intranasal COVID vaccine as far as phase 1 testing (NCT04798001).
“No one here today can tell you that mucosal COVID vaccines work. We’re not there yet. We need clinical efficacy data to answer that question,” Dr. Moore said.
But there’s a potential for a “knockout blow to COVID, a transmission-blocking vaccine” from the intranasal approach, he said.
“The virus is mutating faster than our ability to manage vaccines and not enough people are getting boosters. These injectable vaccines do a great job of preventing severe disease, but they do little to prevent infection” from spreading, Dr. Moore said.
A version of this article first appeared on Medscape.com.
Scientists seeking to stay ahead of an evolving SARS-Cov-2 virus are looking at new strategies, including developing intranasal vaccines, according to speakers at a conference on July 26.
inviting researchers to provide a public update on efforts to try to keep ahead of SARS-CoV-2.
Scientists and federal officials are looking to build on the successes seen in developing the original crop of COVID vaccines, which were authorized for use in the United States less than a year after the pandemic took hold.
But emerging variants are eroding these gains. For months now, officials at the Centers for Disease Control and Prevention and Food and Drug Administration have been keeping an eye on how the level of effectiveness of COVID vaccines has waned during the rise of the Omicron strain. And there’s continual concern about how SARS-CoV-2 might evolve over time.
“Our vaccines are terrific,” Ashish K. Jha, MD, the White House’s COVID-19 response coordinator, said at the summit. “[But] we have to do better.”
Among the approaches being considered are vaccines that would be applied intranasally, with the idea that this might be able to boost the immune response to SARS-CoV-2.
At the summit, Akiko Iwasaki, PhD, of Yale University, New Haven, Conn., said the intranasal approach might be helpful in preventing transmission as well as reducing the burden of illness for those who are infected with SARS-CoV-2.
“We’re stopping the virus from spreading right at the border,” Dr. Iwasaki said at the summit. “This is akin to putting a guard outside of the house in order to patrol for invaders compared to putting the guards in the hallway of the building in the hope that they capture the invader.”
Dr. Iwasaki is one of the founders of Xanadu Bio, a private company created last year to focus on ways to kill SARS-CoV-2 in the nasosinus before it spreads deeper into the respiratory tract. In an editorial in Science Immunology, Dr. Iwasaki and Eric J. Topol, MD, director of the Scripps Research Translational Institute, urged greater federal investment in this approach to fighting SARS-CoV-2. (Dr. Topol is editor-in-chief of Medscape.)
Titled “Operation Nasal Vaccine – Lightning speed to counter COVID-19,” their editorial noted the “unprecedented success” seen in the rapid development of the first two mRNA shots. Dr. Iwasaki and Dr. Topol noted that these victories had been “fueled by the $10 billion governmental investment in Operation Warp Speed.
“During the first year of the pandemic, meaningful evolution of the virus was slow-paced, without any functional consequences, but since that time we have seen a succession of important variants of concern, with increasing transmissibility and immune evasion, culminating in the Omicron lineages,” wrote Dr. Iwasaki and Dr. Topol.
Recent developments have “spotlighted the possibility of nasal vaccines, with their allure for achieving mucosal immunity, complementing, and likely bolstering the circulating immunity achieved via intramuscular shots,” they added.
An early setback
Scientists at the National Institutes of Health and the Biomedical Advanced Research and Development Authority (BARDA) have for some time been looking to vet an array of next-generation vaccine concepts, including ones that trigger mucosal immunity, the Washington Post reported in April.
At the summit on July 26, several participants, including Dr. Jha, stressed the role that public-private partnerships were key to the rapid development of the initial COVID vaccines. They said continued U.S. government support will be needed to make advances in this field.
One of the presenters, Biao He, PhD, founder and president of CyanVac and Blue Lake Biotechnology, spoke of the federal support that his efforts have received over the years to develop intranasal vaccines. His Georgia-based firm already has an experimental intranasal vaccine candidate, CVXGA1-001, in phase 1 testing (NCT04954287).
The CVXGA-001 builds on technology already used in a veterinary product, an intranasal vaccine long used to prevent kennel cough in dogs, he said at the summit.
The emerging field of experimental intranasal COVID vaccines already has had at least one setback.
The biotech firm Altimmune in June 2021 announced that it would discontinue development of its experimental intranasal AdCOVID vaccine following disappointing phase 1 results. The vaccine appeared to be well tolerated in the test, but the immunogenicity data demonstrated lower than expected results in healthy volunteers, especially in light of the responses seen to already cleared vaccines, Altimmune said in a release.
In the statement, Scot Roberts, PhD, chief scientific officer at Altimmune, noted that the study participants lacked immunity from prior infection or vaccination. “We believe that prior immunity in humans may be important for a robust immune response to intranasal dosing with AdCOVID,” he said.
At the summit, Marty Moore, PhD, cofounder and chief scientific officer for Redwood City, Calif.–based Meissa Vaccines, noted the challenges that remain ahead for intranasal COVID vaccines, while also highlighting what he sees as the potential of this approach.
Meissa also has advanced an experimental intranasal COVID vaccine as far as phase 1 testing (NCT04798001).
“No one here today can tell you that mucosal COVID vaccines work. We’re not there yet. We need clinical efficacy data to answer that question,” Dr. Moore said.
But there’s a potential for a “knockout blow to COVID, a transmission-blocking vaccine” from the intranasal approach, he said.
“The virus is mutating faster than our ability to manage vaccines and not enough people are getting boosters. These injectable vaccines do a great job of preventing severe disease, but they do little to prevent infection” from spreading, Dr. Moore said.
A version of this article first appeared on Medscape.com.
Scientists seeking to stay ahead of an evolving SARS-Cov-2 virus are looking at new strategies, including developing intranasal vaccines, according to speakers at a conference on July 26.
inviting researchers to provide a public update on efforts to try to keep ahead of SARS-CoV-2.
Scientists and federal officials are looking to build on the successes seen in developing the original crop of COVID vaccines, which were authorized for use in the United States less than a year after the pandemic took hold.
But emerging variants are eroding these gains. For months now, officials at the Centers for Disease Control and Prevention and Food and Drug Administration have been keeping an eye on how the level of effectiveness of COVID vaccines has waned during the rise of the Omicron strain. And there’s continual concern about how SARS-CoV-2 might evolve over time.
“Our vaccines are terrific,” Ashish K. Jha, MD, the White House’s COVID-19 response coordinator, said at the summit. “[But] we have to do better.”
Among the approaches being considered are vaccines that would be applied intranasally, with the idea that this might be able to boost the immune response to SARS-CoV-2.
At the summit, Akiko Iwasaki, PhD, of Yale University, New Haven, Conn., said the intranasal approach might be helpful in preventing transmission as well as reducing the burden of illness for those who are infected with SARS-CoV-2.
“We’re stopping the virus from spreading right at the border,” Dr. Iwasaki said at the summit. “This is akin to putting a guard outside of the house in order to patrol for invaders compared to putting the guards in the hallway of the building in the hope that they capture the invader.”
Dr. Iwasaki is one of the founders of Xanadu Bio, a private company created last year to focus on ways to kill SARS-CoV-2 in the nasosinus before it spreads deeper into the respiratory tract. In an editorial in Science Immunology, Dr. Iwasaki and Eric J. Topol, MD, director of the Scripps Research Translational Institute, urged greater federal investment in this approach to fighting SARS-CoV-2. (Dr. Topol is editor-in-chief of Medscape.)
Titled “Operation Nasal Vaccine – Lightning speed to counter COVID-19,” their editorial noted the “unprecedented success” seen in the rapid development of the first two mRNA shots. Dr. Iwasaki and Dr. Topol noted that these victories had been “fueled by the $10 billion governmental investment in Operation Warp Speed.
“During the first year of the pandemic, meaningful evolution of the virus was slow-paced, without any functional consequences, but since that time we have seen a succession of important variants of concern, with increasing transmissibility and immune evasion, culminating in the Omicron lineages,” wrote Dr. Iwasaki and Dr. Topol.
Recent developments have “spotlighted the possibility of nasal vaccines, with their allure for achieving mucosal immunity, complementing, and likely bolstering the circulating immunity achieved via intramuscular shots,” they added.
An early setback
Scientists at the National Institutes of Health and the Biomedical Advanced Research and Development Authority (BARDA) have for some time been looking to vet an array of next-generation vaccine concepts, including ones that trigger mucosal immunity, the Washington Post reported in April.
At the summit on July 26, several participants, including Dr. Jha, stressed the role that public-private partnerships were key to the rapid development of the initial COVID vaccines. They said continued U.S. government support will be needed to make advances in this field.
One of the presenters, Biao He, PhD, founder and president of CyanVac and Blue Lake Biotechnology, spoke of the federal support that his efforts have received over the years to develop intranasal vaccines. His Georgia-based firm already has an experimental intranasal vaccine candidate, CVXGA1-001, in phase 1 testing (NCT04954287).
The CVXGA-001 builds on technology already used in a veterinary product, an intranasal vaccine long used to prevent kennel cough in dogs, he said at the summit.
The emerging field of experimental intranasal COVID vaccines already has had at least one setback.
The biotech firm Altimmune in June 2021 announced that it would discontinue development of its experimental intranasal AdCOVID vaccine following disappointing phase 1 results. The vaccine appeared to be well tolerated in the test, but the immunogenicity data demonstrated lower than expected results in healthy volunteers, especially in light of the responses seen to already cleared vaccines, Altimmune said in a release.
In the statement, Scot Roberts, PhD, chief scientific officer at Altimmune, noted that the study participants lacked immunity from prior infection or vaccination. “We believe that prior immunity in humans may be important for a robust immune response to intranasal dosing with AdCOVID,” he said.
At the summit, Marty Moore, PhD, cofounder and chief scientific officer for Redwood City, Calif.–based Meissa Vaccines, noted the challenges that remain ahead for intranasal COVID vaccines, while also highlighting what he sees as the potential of this approach.
Meissa also has advanced an experimental intranasal COVID vaccine as far as phase 1 testing (NCT04798001).
“No one here today can tell you that mucosal COVID vaccines work. We’re not there yet. We need clinical efficacy data to answer that question,” Dr. Moore said.
But there’s a potential for a “knockout blow to COVID, a transmission-blocking vaccine” from the intranasal approach, he said.
“The virus is mutating faster than our ability to manage vaccines and not enough people are getting boosters. These injectable vaccines do a great job of preventing severe disease, but they do little to prevent infection” from spreading, Dr. Moore said.
A version of this article first appeared on Medscape.com.
VA foster program helps older vets manage COVID challenges
Susan Snead used to live in an apartment complex for older adults. The complex had a nice dayroom, and neighbors would knock on her door every now and then to check in.
But despite not being lonely, Ms. Snead, 89, did live alone in downtown Charleston, S.C. Eventually, that became dangerous.
“I fell a few times,” she says. “I had to call somebody to come and get me up.”
Sometimes help would come from the apartment complex’s office. Sometimes it came with a police escort.
Over time, needing to make those calls became a burden. Making and keeping appointments with her doctor, something she had to do regularly, as she has diabetes, got harder, too.
“It kind of wore me out,” she says. “Like you’re going up a hill.”
As she was beginning to accept she could no longer live alone, Ms. Snead, an Air Force veteran, learned about a program run by the Department of Veterans Affairs called Medical Foster Home.
Caregivers help aging veterans with activities of daily living like bathing, cooking, making and getting to appointments, getting dressed, and taking daily medication.
Caregivers can take care of up to three residents in their home at a time. While most residents are veterans, caregivers sometimes care for non-veteran residents, such as a veteran’s spouse or a caregiver’s family member.
Veterans typically pay about $1,500 to $3,000 out-of-pocket per month for the service, depending on location.
According to the VA, the concept of medical foster homes has been around since 1999, when VA hospitals across the country began reaching out to people willing to provide live-in care for veterans. The option is led by local VA hospitals, which approve caregivers and provide administrative services. There are now 517 medical foster homes, the VA says.
Much like other residential care facilities, medical foster homes get regular inspections for safety, nutrition, and more.
In 2019, Ms. Snead signed up for the program. She expected to be cared for, but she found a sense of family with her caregiver, Wilhelmina Brown, and another veteran in the home.
Ms. Brown started taking care of people – but not necessarily veterans – in 1997 when her grandmother was unable to care for herself, she says.
“My grandmama carried me to church every Sunday, she carried me to the beach – everywhere she went, she took me with her,” Ms. Brown says. As her grandmother got older, “I said, ‘I’m going to take care of her in my home.’ ”
Caring for others must come from the heart, Ms. Brown says.
She cooks her residents’ meals three times a day with dietary restrictions in mind, washes their dishes, does their laundry, remembers birthdays, and plans little parties.
“That’s my family,” Ms. Brown says.
In 2020, the COVID-19 pandemic upended the world – but at the same time, it highlighted the advantages of the medical foster home model.
Home-based primary care keeps veterans out of nursing homes – something that became particularly important as COVID-19 hit nursing homes and long-term care facilities.
Caregivers in the system were also able to help veterans, often living in rural areas, pivot and adapt to telehealth during a time of crisis.
One study, published in the journal Geriatrics, set out to identify how medical foster homes were able to deliver safe, effective health care during the early stages of the pandemic.
Researchers interviewed 37 VA care providers at 16 rural medical foster home programs across the country. The interviews took place between December 2020 and February 2021. They found medical foster home caregivers, coordinators, and health care providers communicated to move office visits to the home, helped veterans navigate telehealth, advocated to get veterans vaccinated in-home, and relied on each other to fight social isolation.
Caregivers also adapted quickly to telehealth, according to Leah Haverhals, PhD, a health research scientist and communications director for the Seattle-Denver Center of Innovation for Veteran Centered and Value Driven Care, who led the study.
Most veterans in the foster home program are older and find new technology difficult to use.
Caregivers, coordinators, and health care providers were largely new to the technology, too.
While the study found that most veterans and caregivers preferred in-person care, they were able to work together to make the best of telehealth.
“That speaks to the nature of the care being given, being able to pivot in a crisis like that,” Dr. Haverhals says.
If caregivers didn’t already have computers or telehealth-compatible devices, the VA provided iPads that would connect to the internet using cellular signals. According to the study, this helped to overcome connectivity issues that may have caused problems in rural areas.
Ms. Snead says Ms. Brown helped a lot with her telehealth calls.
“If we had to do things over the phone or with video, she was able to set that up to work with the person on the other end. She knows a lot about that stuff – about computers and things like that,” Ms. Snead says, adding that she hadn’t worked with computers since retirement in 1998.
Telehealth helped health care providers identify infections and quickly prescribe antibiotics to veterans in rural areas and provide other care that was more safely delivered in private homes.
“The findings from our study highlighted that when working together for the common goal of keeping vulnerable populations like veterans in MFHs [medical foster homes] safe during times of crisis, adaptation and collaboration facilitated the ongoing provision of high-quality care,” Dr. Haverhals’s group wrote. “Such collaboration has been shown to be critical in recent research in the United States on supporting older adults during the pandemic.”
Cari Levy, MD, PhD, a professor at the University of Colorado at Denver, Aurora, and a co-author of the study, specializes in palliative and telenursing home care for the VA.
Dr. Levy, who has worked for the VA for about 20 years, says how medical foster homes provided care during the pandemic carries lessons for civilian clinics. One of the most important lessons, she says, is that medical professionals will need to provide more care where people are, especially in populations that are too sick to get to the clinic.
“For years, there was all this hope that telehealth would expand,” but it took a pandemic to authorize approval from federal agencies to explode, she says. “I shudder to think what would have happened if we didn’t have telehealth. Fortunately, it was the right time to be able to flip a switch.”
Crisis aside, Dr. Levy says her dream would be for health care providers to do more home-based care. The model allows people to preserve the relational aspects of medicine, which can counteract a lot of the moral injury and burnout in the field, she says, adding:
“I see this as the kind of medicine many people intended to do when they got into medicine.”
A version of this article first appeared on WebMD.com.
Susan Snead used to live in an apartment complex for older adults. The complex had a nice dayroom, and neighbors would knock on her door every now and then to check in.
But despite not being lonely, Ms. Snead, 89, did live alone in downtown Charleston, S.C. Eventually, that became dangerous.
“I fell a few times,” she says. “I had to call somebody to come and get me up.”
Sometimes help would come from the apartment complex’s office. Sometimes it came with a police escort.
Over time, needing to make those calls became a burden. Making and keeping appointments with her doctor, something she had to do regularly, as she has diabetes, got harder, too.
“It kind of wore me out,” she says. “Like you’re going up a hill.”
As she was beginning to accept she could no longer live alone, Ms. Snead, an Air Force veteran, learned about a program run by the Department of Veterans Affairs called Medical Foster Home.
Caregivers help aging veterans with activities of daily living like bathing, cooking, making and getting to appointments, getting dressed, and taking daily medication.
Caregivers can take care of up to three residents in their home at a time. While most residents are veterans, caregivers sometimes care for non-veteran residents, such as a veteran’s spouse or a caregiver’s family member.
Veterans typically pay about $1,500 to $3,000 out-of-pocket per month for the service, depending on location.
According to the VA, the concept of medical foster homes has been around since 1999, when VA hospitals across the country began reaching out to people willing to provide live-in care for veterans. The option is led by local VA hospitals, which approve caregivers and provide administrative services. There are now 517 medical foster homes, the VA says.
Much like other residential care facilities, medical foster homes get regular inspections for safety, nutrition, and more.
In 2019, Ms. Snead signed up for the program. She expected to be cared for, but she found a sense of family with her caregiver, Wilhelmina Brown, and another veteran in the home.
Ms. Brown started taking care of people – but not necessarily veterans – in 1997 when her grandmother was unable to care for herself, she says.
“My grandmama carried me to church every Sunday, she carried me to the beach – everywhere she went, she took me with her,” Ms. Brown says. As her grandmother got older, “I said, ‘I’m going to take care of her in my home.’ ”
Caring for others must come from the heart, Ms. Brown says.
She cooks her residents’ meals three times a day with dietary restrictions in mind, washes their dishes, does their laundry, remembers birthdays, and plans little parties.
“That’s my family,” Ms. Brown says.
In 2020, the COVID-19 pandemic upended the world – but at the same time, it highlighted the advantages of the medical foster home model.
Home-based primary care keeps veterans out of nursing homes – something that became particularly important as COVID-19 hit nursing homes and long-term care facilities.
Caregivers in the system were also able to help veterans, often living in rural areas, pivot and adapt to telehealth during a time of crisis.
One study, published in the journal Geriatrics, set out to identify how medical foster homes were able to deliver safe, effective health care during the early stages of the pandemic.
Researchers interviewed 37 VA care providers at 16 rural medical foster home programs across the country. The interviews took place between December 2020 and February 2021. They found medical foster home caregivers, coordinators, and health care providers communicated to move office visits to the home, helped veterans navigate telehealth, advocated to get veterans vaccinated in-home, and relied on each other to fight social isolation.
Caregivers also adapted quickly to telehealth, according to Leah Haverhals, PhD, a health research scientist and communications director for the Seattle-Denver Center of Innovation for Veteran Centered and Value Driven Care, who led the study.
Most veterans in the foster home program are older and find new technology difficult to use.
Caregivers, coordinators, and health care providers were largely new to the technology, too.
While the study found that most veterans and caregivers preferred in-person care, they were able to work together to make the best of telehealth.
“That speaks to the nature of the care being given, being able to pivot in a crisis like that,” Dr. Haverhals says.
If caregivers didn’t already have computers or telehealth-compatible devices, the VA provided iPads that would connect to the internet using cellular signals. According to the study, this helped to overcome connectivity issues that may have caused problems in rural areas.
Ms. Snead says Ms. Brown helped a lot with her telehealth calls.
“If we had to do things over the phone or with video, she was able to set that up to work with the person on the other end. She knows a lot about that stuff – about computers and things like that,” Ms. Snead says, adding that she hadn’t worked with computers since retirement in 1998.
Telehealth helped health care providers identify infections and quickly prescribe antibiotics to veterans in rural areas and provide other care that was more safely delivered in private homes.
“The findings from our study highlighted that when working together for the common goal of keeping vulnerable populations like veterans in MFHs [medical foster homes] safe during times of crisis, adaptation and collaboration facilitated the ongoing provision of high-quality care,” Dr. Haverhals’s group wrote. “Such collaboration has been shown to be critical in recent research in the United States on supporting older adults during the pandemic.”
Cari Levy, MD, PhD, a professor at the University of Colorado at Denver, Aurora, and a co-author of the study, specializes in palliative and telenursing home care for the VA.
Dr. Levy, who has worked for the VA for about 20 years, says how medical foster homes provided care during the pandemic carries lessons for civilian clinics. One of the most important lessons, she says, is that medical professionals will need to provide more care where people are, especially in populations that are too sick to get to the clinic.
“For years, there was all this hope that telehealth would expand,” but it took a pandemic to authorize approval from federal agencies to explode, she says. “I shudder to think what would have happened if we didn’t have telehealth. Fortunately, it was the right time to be able to flip a switch.”
Crisis aside, Dr. Levy says her dream would be for health care providers to do more home-based care. The model allows people to preserve the relational aspects of medicine, which can counteract a lot of the moral injury and burnout in the field, she says, adding:
“I see this as the kind of medicine many people intended to do when they got into medicine.”
A version of this article first appeared on WebMD.com.
Susan Snead used to live in an apartment complex for older adults. The complex had a nice dayroom, and neighbors would knock on her door every now and then to check in.
But despite not being lonely, Ms. Snead, 89, did live alone in downtown Charleston, S.C. Eventually, that became dangerous.
“I fell a few times,” she says. “I had to call somebody to come and get me up.”
Sometimes help would come from the apartment complex’s office. Sometimes it came with a police escort.
Over time, needing to make those calls became a burden. Making and keeping appointments with her doctor, something she had to do regularly, as she has diabetes, got harder, too.
“It kind of wore me out,” she says. “Like you’re going up a hill.”
As she was beginning to accept she could no longer live alone, Ms. Snead, an Air Force veteran, learned about a program run by the Department of Veterans Affairs called Medical Foster Home.
Caregivers help aging veterans with activities of daily living like bathing, cooking, making and getting to appointments, getting dressed, and taking daily medication.
Caregivers can take care of up to three residents in their home at a time. While most residents are veterans, caregivers sometimes care for non-veteran residents, such as a veteran’s spouse or a caregiver’s family member.
Veterans typically pay about $1,500 to $3,000 out-of-pocket per month for the service, depending on location.
According to the VA, the concept of medical foster homes has been around since 1999, when VA hospitals across the country began reaching out to people willing to provide live-in care for veterans. The option is led by local VA hospitals, which approve caregivers and provide administrative services. There are now 517 medical foster homes, the VA says.
Much like other residential care facilities, medical foster homes get regular inspections for safety, nutrition, and more.
In 2019, Ms. Snead signed up for the program. She expected to be cared for, but she found a sense of family with her caregiver, Wilhelmina Brown, and another veteran in the home.
Ms. Brown started taking care of people – but not necessarily veterans – in 1997 when her grandmother was unable to care for herself, she says.
“My grandmama carried me to church every Sunday, she carried me to the beach – everywhere she went, she took me with her,” Ms. Brown says. As her grandmother got older, “I said, ‘I’m going to take care of her in my home.’ ”
Caring for others must come from the heart, Ms. Brown says.
She cooks her residents’ meals three times a day with dietary restrictions in mind, washes their dishes, does their laundry, remembers birthdays, and plans little parties.
“That’s my family,” Ms. Brown says.
In 2020, the COVID-19 pandemic upended the world – but at the same time, it highlighted the advantages of the medical foster home model.
Home-based primary care keeps veterans out of nursing homes – something that became particularly important as COVID-19 hit nursing homes and long-term care facilities.
Caregivers in the system were also able to help veterans, often living in rural areas, pivot and adapt to telehealth during a time of crisis.
One study, published in the journal Geriatrics, set out to identify how medical foster homes were able to deliver safe, effective health care during the early stages of the pandemic.
Researchers interviewed 37 VA care providers at 16 rural medical foster home programs across the country. The interviews took place between December 2020 and February 2021. They found medical foster home caregivers, coordinators, and health care providers communicated to move office visits to the home, helped veterans navigate telehealth, advocated to get veterans vaccinated in-home, and relied on each other to fight social isolation.
Caregivers also adapted quickly to telehealth, according to Leah Haverhals, PhD, a health research scientist and communications director for the Seattle-Denver Center of Innovation for Veteran Centered and Value Driven Care, who led the study.
Most veterans in the foster home program are older and find new technology difficult to use.
Caregivers, coordinators, and health care providers were largely new to the technology, too.
While the study found that most veterans and caregivers preferred in-person care, they were able to work together to make the best of telehealth.
“That speaks to the nature of the care being given, being able to pivot in a crisis like that,” Dr. Haverhals says.
If caregivers didn’t already have computers or telehealth-compatible devices, the VA provided iPads that would connect to the internet using cellular signals. According to the study, this helped to overcome connectivity issues that may have caused problems in rural areas.
Ms. Snead says Ms. Brown helped a lot with her telehealth calls.
“If we had to do things over the phone or with video, she was able to set that up to work with the person on the other end. She knows a lot about that stuff – about computers and things like that,” Ms. Snead says, adding that she hadn’t worked with computers since retirement in 1998.
Telehealth helped health care providers identify infections and quickly prescribe antibiotics to veterans in rural areas and provide other care that was more safely delivered in private homes.
“The findings from our study highlighted that when working together for the common goal of keeping vulnerable populations like veterans in MFHs [medical foster homes] safe during times of crisis, adaptation and collaboration facilitated the ongoing provision of high-quality care,” Dr. Haverhals’s group wrote. “Such collaboration has been shown to be critical in recent research in the United States on supporting older adults during the pandemic.”
Cari Levy, MD, PhD, a professor at the University of Colorado at Denver, Aurora, and a co-author of the study, specializes in palliative and telenursing home care for the VA.
Dr. Levy, who has worked for the VA for about 20 years, says how medical foster homes provided care during the pandemic carries lessons for civilian clinics. One of the most important lessons, she says, is that medical professionals will need to provide more care where people are, especially in populations that are too sick to get to the clinic.
“For years, there was all this hope that telehealth would expand,” but it took a pandemic to authorize approval from federal agencies to explode, she says. “I shudder to think what would have happened if we didn’t have telehealth. Fortunately, it was the right time to be able to flip a switch.”
Crisis aside, Dr. Levy says her dream would be for health care providers to do more home-based care. The model allows people to preserve the relational aspects of medicine, which can counteract a lot of the moral injury and burnout in the field, she says, adding:
“I see this as the kind of medicine many people intended to do when they got into medicine.”
A version of this article first appeared on WebMD.com.
Children and COVID: Many parents see vaccine as the greater risk
New COVID-19 cases rose for the second week in a row as cumulative cases among U.S. children passed the 14-million mark, but a recent survey shows that more than half of parents believe that the vaccine is a greater risk to children under age 5 years than the virus.
In a Kaiser Family Foundation survey conducted July 7-17, 53% of parents with children aged 6 months to 5 years said that the vaccine is “a bigger risk to their child’s health than getting infected with COVID-19, compared to 44% who say getting infected is the bigger risk,” KFF reported July 26.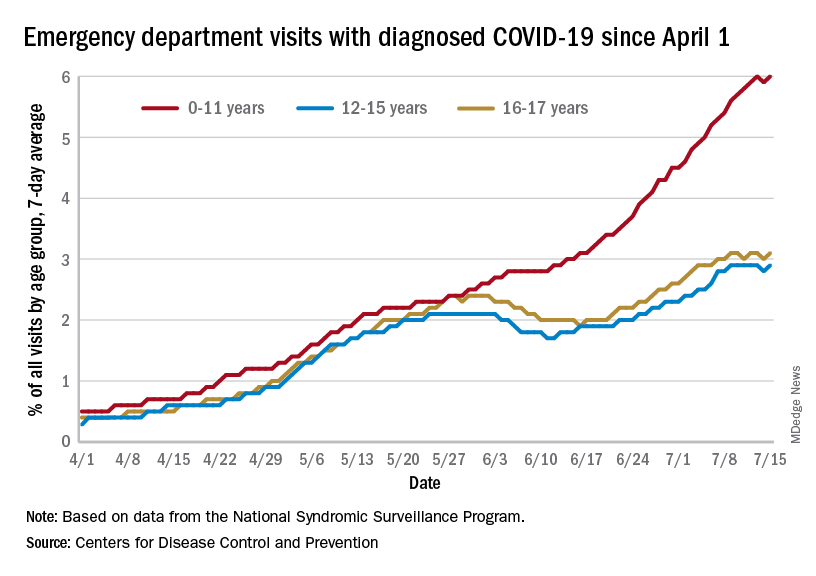
More than 4 out of 10 of respondents (43%) said that they will “definitely not” get their eligible children vaccinated, while only 7% said that their children had already received it and 10% said their children would get it as soon as possible, according to the KFF survey, which had an overall sample size of 1,847 adults, including an oversample of 471 parents of children under age 5.
Vaccine initiation has been slow in the first month since it was approved for the youngest children. Just 2.8% of all eligible children under age 5 had received an initial dose as of July 19, compared with first-month uptake figures of more than 18% for the 5- to 11-year-olds and 27% for those aged 12-15, based on data from the Centers for Disease Control and Prevention.
The current rates for vaccination in those aged 5 and older look like this: 70.2% of 12- to 17-year-olds have received at least one dose, versus 37.1% of those aged 5-11. Just over 60% of the older children were fully vaccinated as of July 19, as were 30.2% of the 5- to 11-year-olds, the CDC reported on its COVID Data Tracker.
Number of new cases hits 2-month high
Despite the vaccine, SARS-CoV-2 and its various mutations have continued with their summer travels. With 92,000 newly infected children added for the week of July 15-21, there have now been a total of 14,003,497 pediatric cases reported since the start of the pandemic, which works out to 18.6% of cases in all ages, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
The 92,000 new cases represent an increase of almost 22% over the previous week and mark the highest 1-week count since May, when the total passed 100,000 for 2 consecutive weeks. More recently the trend had seemed more stable as weekly cases dropped twice and rose twice as the total hovered around 70,000, based on the data collected by the AAP and CHA from state and territorial health departments.
A different scenario has played out for emergency department visits and hospital admissions, which have risen steadily since the beginning of April. The admission rate for children aged 0-17, which was just 0.13 new patients per 100,000 population on April 11, was up to 0.44 per 100,000 on July 21. By comparison, the highest rate reached last year during the Delta surge was 0.47 per 100,000, based on CDC data.
The 7-day average of emergency dept. visits among the youngest age group, 0-11 years, shows the same general increase as hospital admissions, but the older children have diverged form that path (see graph). For those aged 12-15 and 16-17, hospitalizations started dropping in late May and into mid-June before climbing again, although more slowly than for the youngest group, the CDC data show.
The ED visit rate with diagnosed COVID among those aged 0-11, measured at 6.1% of all visits on July 19, is, in fact, considerably higher than at any time during the Delta surge last year, when it never passed 4.0%, although much lower than peak Omicron (14.1%). That 6.1% was also higher than any other age group on that day, adults included, the CDC said.
New COVID-19 cases rose for the second week in a row as cumulative cases among U.S. children passed the 14-million mark, but a recent survey shows that more than half of parents believe that the vaccine is a greater risk to children under age 5 years than the virus.
In a Kaiser Family Foundation survey conducted July 7-17, 53% of parents with children aged 6 months to 5 years said that the vaccine is “a bigger risk to their child’s health than getting infected with COVID-19, compared to 44% who say getting infected is the bigger risk,” KFF reported July 26.
More than 4 out of 10 of respondents (43%) said that they will “definitely not” get their eligible children vaccinated, while only 7% said that their children had already received it and 10% said their children would get it as soon as possible, according to the KFF survey, which had an overall sample size of 1,847 adults, including an oversample of 471 parents of children under age 5.
Vaccine initiation has been slow in the first month since it was approved for the youngest children. Just 2.8% of all eligible children under age 5 had received an initial dose as of July 19, compared with first-month uptake figures of more than 18% for the 5- to 11-year-olds and 27% for those aged 12-15, based on data from the Centers for Disease Control and Prevention.
The current rates for vaccination in those aged 5 and older look like this: 70.2% of 12- to 17-year-olds have received at least one dose, versus 37.1% of those aged 5-11. Just over 60% of the older children were fully vaccinated as of July 19, as were 30.2% of the 5- to 11-year-olds, the CDC reported on its COVID Data Tracker.
Number of new cases hits 2-month high
Despite the vaccine, SARS-CoV-2 and its various mutations have continued with their summer travels. With 92,000 newly infected children added for the week of July 15-21, there have now been a total of 14,003,497 pediatric cases reported since the start of the pandemic, which works out to 18.6% of cases in all ages, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
The 92,000 new cases represent an increase of almost 22% over the previous week and mark the highest 1-week count since May, when the total passed 100,000 for 2 consecutive weeks. More recently the trend had seemed more stable as weekly cases dropped twice and rose twice as the total hovered around 70,000, based on the data collected by the AAP and CHA from state and territorial health departments.
A different scenario has played out for emergency department visits and hospital admissions, which have risen steadily since the beginning of April. The admission rate for children aged 0-17, which was just 0.13 new patients per 100,000 population on April 11, was up to 0.44 per 100,000 on July 21. By comparison, the highest rate reached last year during the Delta surge was 0.47 per 100,000, based on CDC data.
The 7-day average of emergency dept. visits among the youngest age group, 0-11 years, shows the same general increase as hospital admissions, but the older children have diverged form that path (see graph). For those aged 12-15 and 16-17, hospitalizations started dropping in late May and into mid-June before climbing again, although more slowly than for the youngest group, the CDC data show.
The ED visit rate with diagnosed COVID among those aged 0-11, measured at 6.1% of all visits on July 19, is, in fact, considerably higher than at any time during the Delta surge last year, when it never passed 4.0%, although much lower than peak Omicron (14.1%). That 6.1% was also higher than any other age group on that day, adults included, the CDC said.
New COVID-19 cases rose for the second week in a row as cumulative cases among U.S. children passed the 14-million mark, but a recent survey shows that more than half of parents believe that the vaccine is a greater risk to children under age 5 years than the virus.
In a Kaiser Family Foundation survey conducted July 7-17, 53% of parents with children aged 6 months to 5 years said that the vaccine is “a bigger risk to their child’s health than getting infected with COVID-19, compared to 44% who say getting infected is the bigger risk,” KFF reported July 26.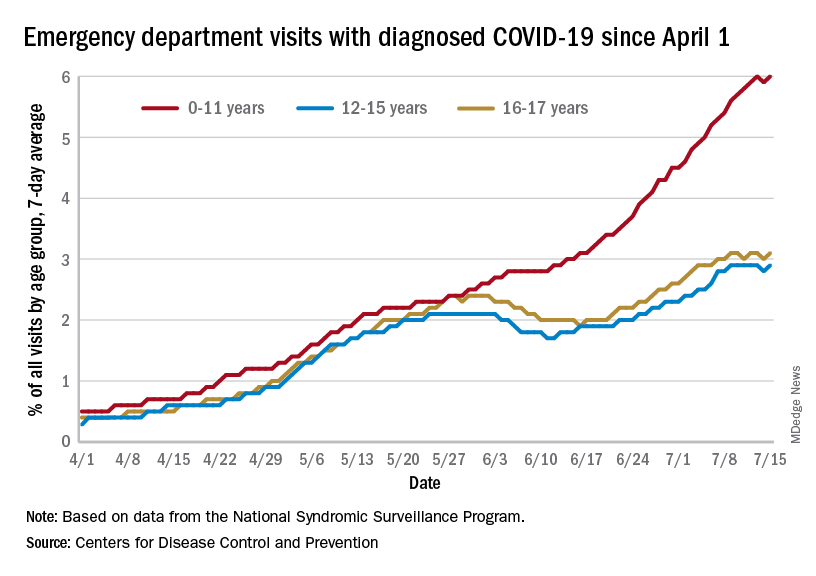
More than 4 out of 10 of respondents (43%) said that they will “definitely not” get their eligible children vaccinated, while only 7% said that their children had already received it and 10% said their children would get it as soon as possible, according to the KFF survey, which had an overall sample size of 1,847 adults, including an oversample of 471 parents of children under age 5.
Vaccine initiation has been slow in the first month since it was approved for the youngest children. Just 2.8% of all eligible children under age 5 had received an initial dose as of July 19, compared with first-month uptake figures of more than 18% for the 5- to 11-year-olds and 27% for those aged 12-15, based on data from the Centers for Disease Control and Prevention.
The current rates for vaccination in those aged 5 and older look like this: 70.2% of 12- to 17-year-olds have received at least one dose, versus 37.1% of those aged 5-11. Just over 60% of the older children were fully vaccinated as of July 19, as were 30.2% of the 5- to 11-year-olds, the CDC reported on its COVID Data Tracker.
Number of new cases hits 2-month high
Despite the vaccine, SARS-CoV-2 and its various mutations have continued with their summer travels. With 92,000 newly infected children added for the week of July 15-21, there have now been a total of 14,003,497 pediatric cases reported since the start of the pandemic, which works out to 18.6% of cases in all ages, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
The 92,000 new cases represent an increase of almost 22% over the previous week and mark the highest 1-week count since May, when the total passed 100,000 for 2 consecutive weeks. More recently the trend had seemed more stable as weekly cases dropped twice and rose twice as the total hovered around 70,000, based on the data collected by the AAP and CHA from state and territorial health departments.
A different scenario has played out for emergency department visits and hospital admissions, which have risen steadily since the beginning of April. The admission rate for children aged 0-17, which was just 0.13 new patients per 100,000 population on April 11, was up to 0.44 per 100,000 on July 21. By comparison, the highest rate reached last year during the Delta surge was 0.47 per 100,000, based on CDC data.
The 7-day average of emergency dept. visits among the youngest age group, 0-11 years, shows the same general increase as hospital admissions, but the older children have diverged form that path (see graph). For those aged 12-15 and 16-17, hospitalizations started dropping in late May and into mid-June before climbing again, although more slowly than for the youngest group, the CDC data show.
The ED visit rate with diagnosed COVID among those aged 0-11, measured at 6.1% of all visits on July 19, is, in fact, considerably higher than at any time during the Delta surge last year, when it never passed 4.0%, although much lower than peak Omicron (14.1%). That 6.1% was also higher than any other age group on that day, adults included, the CDC said.
Two distinct phenotypes of COVID-related myocarditis emerge
Researchers from France have identified two distinct phenotypes of fulminant COVID-19–related myocarditis in adults, with different clinical presentations, immunologic profiles, and outcomes.
Differentiation between the two bioclinical entities is important to understand for patient management and further pathophysiological studies, they said.
The first phenotype occurs early (within a few days) in acute SARS-CoV-2 infection, with active viral replication (polymerase chain reaction positive) in adults who meet criteria for multisystem inflammatory syndrome (MIS-A+).
In this early phenotype, there is “limited systemic inflammation without skin and mucosal involvement, but myocardial dysfunction is fulminant and frequently associated with large pericardial effusions. These cases more often require extracorporeal membrane oxygenation [ECMO],” Guy Gorochov, MD, PhD, Sorbonne University, Paris, said in an interview.
The second is a delayed, postinfectious, immune-driven phenotype that occurs in adults who fail to meet the criteria for MIS-A (MIS-A–).
This phenotype occurs weeks after SARS-CoV-2 infection, usually beyond detectable active viral replication (PCR–) in the context of specific immune response and severe systemic inflammation with skin and mucosal involvement. Myocardial dysfunction is more progressive and rarely associated with large pericardial effusions, Dr. Gorochov explained.
The study was published in the Journal of the American College of Cardiology.
Evolving understanding
The findings are based on a retrospective analysis of 38 patients without a history of COVID-19 vaccination who were admitted to the intensive care unit from March 2020 to June 2021 for suspected fulminant COVID-19 myocarditis.
Patients were confirmed to have SARS-CoV-2 infection by PCR and/or by serologic testing. As noted in other studies, the patients were predominantly young men (66%; median age, 27.5 years). Twenty-five (66%) patients were MIS-A+ and 13 (34%) were MIS-A–.
In general, the MIS-A– patients were sicker and had worse outcomes.
Specifically, compared with the MIS-A+ patients, MIS-A– patients had a shorter time between the onset of COVID-19 symptoms and the development of myocarditis, a shorter time to ICU admission, and more severe presentations assessed using lower left ventricular ejection fraction and sequential organ failure assessment scores.
MIS-A– patients also had higher lactate levels, were more likely to need venoarterial ECMO (92% vs 16%), had higher ICU mortality (31% vs. 4%), and a had lower probability of survival at 3 months (68% vs. 96%), compared with their MIS-A+ peers.
Immunologic differences
The immunologic profiles of these two distinct clinical phenotypes also differed.
In MIS-A– early-type COVID-19 myocarditis, RNA polymerase III autoantibodies are frequently positive and serum levels of antiviral interferon-alpha and granulocyte-attracting interleukin-8 are elevated.
In contrast, in MIS-A+ delayed-type COVID-19 myocarditis, RNA polymerase III autoantibodies are negative and serum levels of IL-17 and IL-22 are highly elevated.
“We suggest that IL-17 and IL-22 are novel criteria that should help to assess in adults the recently recognized MIS-A,” Dr. Gorochov told this news organization. “It should be tested whether IL-17 and IL-22 are also elevated in children with MIS-C.”
The researchers also observed “extremely” high serum IL-10 levels in both patient groups. This has been previously associated with severe myocardial injury and an increase in the risk for death in severe COVID-19 patients.
The researchers said the phenotypic clustering of patients with fulminant COVID-19–related myocarditis “seems relevant” for their management.
MIS-A– cases, owing to the high risk for evolution toward refractory cardiogenic shock, should be “urgently” referred to a center with venoarterial ECMO and closely monitored to prevent a “too-late” cannulation, especially under cardiopulmonary resuscitation, known to be associated with poor outcomes, they advised.
They noted that the five patients who died in their series had late venoarterial ECMO implantation, while undergoing multiple organ failures or resuscitation.
Conversely, the risk for evolution to refractory cardiogenic shock is lower in MIS-A+ cases. However, identifying MIS-A+ cases is “all the more important given that numerous data support the efficacy of corticosteroids and/or intravenous immunoglobulins in MIS-C,” Dr. Gorochov and colleagues wrote.
The authors of a linked editorial said the French team should be “commended on their work in furthering our understanding of fulminant myocarditis related to COVID-19 infection.”
Ajith Nair, MD, Baylor College of Medicine, and Anita Deswal, MD, MPH, University of Texas M.D. Anderson Cancer Center, both in Houston, noted that fulminant myocarditis is rare and can result from either of two mechanisms: viral tropism or an immune-mediated mechanism.
“It remains to be seen whether using antiviral therapy versus immunomodulatory therapy on the basis of clinical and cytokine profiles will yield benefits,” they wrote.
“Fulminant myocarditis invariably requires hemodynamic support and carries a high mortality risk if it is recognized late. However, the long-term prognosis in patients who survive the critical period is favorable, with recovery of myocardial function,” they added.
“This study highlights the ever-shifting understanding of the pathophysiology and therapeutic approaches to fulminant myocarditis,” Dr. Nair and Dr. Deswal concluded.
This research was supported in part by the Foundation of France, French National Research Agency, Sorbonne University, and Clinical Research Hospital. The researchers have filed a patent application based on these results. Dr. Nair and Dr. Deswal have no relevant disclosures.
A version of this article first appeared on Medscape.com.
Researchers from France have identified two distinct phenotypes of fulminant COVID-19–related myocarditis in adults, with different clinical presentations, immunologic profiles, and outcomes.
Differentiation between the two bioclinical entities is important to understand for patient management and further pathophysiological studies, they said.
The first phenotype occurs early (within a few days) in acute SARS-CoV-2 infection, with active viral replication (polymerase chain reaction positive) in adults who meet criteria for multisystem inflammatory syndrome (MIS-A+).
In this early phenotype, there is “limited systemic inflammation without skin and mucosal involvement, but myocardial dysfunction is fulminant and frequently associated with large pericardial effusions. These cases more often require extracorporeal membrane oxygenation [ECMO],” Guy Gorochov, MD, PhD, Sorbonne University, Paris, said in an interview.
The second is a delayed, postinfectious, immune-driven phenotype that occurs in adults who fail to meet the criteria for MIS-A (MIS-A–).
This phenotype occurs weeks after SARS-CoV-2 infection, usually beyond detectable active viral replication (PCR–) in the context of specific immune response and severe systemic inflammation with skin and mucosal involvement. Myocardial dysfunction is more progressive and rarely associated with large pericardial effusions, Dr. Gorochov explained.
The study was published in the Journal of the American College of Cardiology.
Evolving understanding
The findings are based on a retrospective analysis of 38 patients without a history of COVID-19 vaccination who were admitted to the intensive care unit from March 2020 to June 2021 for suspected fulminant COVID-19 myocarditis.
Patients were confirmed to have SARS-CoV-2 infection by PCR and/or by serologic testing. As noted in other studies, the patients were predominantly young men (66%; median age, 27.5 years). Twenty-five (66%) patients were MIS-A+ and 13 (34%) were MIS-A–.
In general, the MIS-A– patients were sicker and had worse outcomes.
Specifically, compared with the MIS-A+ patients, MIS-A– patients had a shorter time between the onset of COVID-19 symptoms and the development of myocarditis, a shorter time to ICU admission, and more severe presentations assessed using lower left ventricular ejection fraction and sequential organ failure assessment scores.
MIS-A– patients also had higher lactate levels, were more likely to need venoarterial ECMO (92% vs 16%), had higher ICU mortality (31% vs. 4%), and a had lower probability of survival at 3 months (68% vs. 96%), compared with their MIS-A+ peers.
Immunologic differences
The immunologic profiles of these two distinct clinical phenotypes also differed.
In MIS-A– early-type COVID-19 myocarditis, RNA polymerase III autoantibodies are frequently positive and serum levels of antiviral interferon-alpha and granulocyte-attracting interleukin-8 are elevated.
In contrast, in MIS-A+ delayed-type COVID-19 myocarditis, RNA polymerase III autoantibodies are negative and serum levels of IL-17 and IL-22 are highly elevated.
“We suggest that IL-17 and IL-22 are novel criteria that should help to assess in adults the recently recognized MIS-A,” Dr. Gorochov told this news organization. “It should be tested whether IL-17 and IL-22 are also elevated in children with MIS-C.”
The researchers also observed “extremely” high serum IL-10 levels in both patient groups. This has been previously associated with severe myocardial injury and an increase in the risk for death in severe COVID-19 patients.
The researchers said the phenotypic clustering of patients with fulminant COVID-19–related myocarditis “seems relevant” for their management.
MIS-A– cases, owing to the high risk for evolution toward refractory cardiogenic shock, should be “urgently” referred to a center with venoarterial ECMO and closely monitored to prevent a “too-late” cannulation, especially under cardiopulmonary resuscitation, known to be associated with poor outcomes, they advised.
They noted that the five patients who died in their series had late venoarterial ECMO implantation, while undergoing multiple organ failures or resuscitation.
Conversely, the risk for evolution to refractory cardiogenic shock is lower in MIS-A+ cases. However, identifying MIS-A+ cases is “all the more important given that numerous data support the efficacy of corticosteroids and/or intravenous immunoglobulins in MIS-C,” Dr. Gorochov and colleagues wrote.
The authors of a linked editorial said the French team should be “commended on their work in furthering our understanding of fulminant myocarditis related to COVID-19 infection.”
Ajith Nair, MD, Baylor College of Medicine, and Anita Deswal, MD, MPH, University of Texas M.D. Anderson Cancer Center, both in Houston, noted that fulminant myocarditis is rare and can result from either of two mechanisms: viral tropism or an immune-mediated mechanism.
“It remains to be seen whether using antiviral therapy versus immunomodulatory therapy on the basis of clinical and cytokine profiles will yield benefits,” they wrote.
“Fulminant myocarditis invariably requires hemodynamic support and carries a high mortality risk if it is recognized late. However, the long-term prognosis in patients who survive the critical period is favorable, with recovery of myocardial function,” they added.
“This study highlights the ever-shifting understanding of the pathophysiology and therapeutic approaches to fulminant myocarditis,” Dr. Nair and Dr. Deswal concluded.
This research was supported in part by the Foundation of France, French National Research Agency, Sorbonne University, and Clinical Research Hospital. The researchers have filed a patent application based on these results. Dr. Nair and Dr. Deswal have no relevant disclosures.
A version of this article first appeared on Medscape.com.
Researchers from France have identified two distinct phenotypes of fulminant COVID-19–related myocarditis in adults, with different clinical presentations, immunologic profiles, and outcomes.
Differentiation between the two bioclinical entities is important to understand for patient management and further pathophysiological studies, they said.
The first phenotype occurs early (within a few days) in acute SARS-CoV-2 infection, with active viral replication (polymerase chain reaction positive) in adults who meet criteria for multisystem inflammatory syndrome (MIS-A+).
In this early phenotype, there is “limited systemic inflammation without skin and mucosal involvement, but myocardial dysfunction is fulminant and frequently associated with large pericardial effusions. These cases more often require extracorporeal membrane oxygenation [ECMO],” Guy Gorochov, MD, PhD, Sorbonne University, Paris, said in an interview.
The second is a delayed, postinfectious, immune-driven phenotype that occurs in adults who fail to meet the criteria for MIS-A (MIS-A–).
This phenotype occurs weeks after SARS-CoV-2 infection, usually beyond detectable active viral replication (PCR–) in the context of specific immune response and severe systemic inflammation with skin and mucosal involvement. Myocardial dysfunction is more progressive and rarely associated with large pericardial effusions, Dr. Gorochov explained.
The study was published in the Journal of the American College of Cardiology.
Evolving understanding
The findings are based on a retrospective analysis of 38 patients without a history of COVID-19 vaccination who were admitted to the intensive care unit from March 2020 to June 2021 for suspected fulminant COVID-19 myocarditis.
Patients were confirmed to have SARS-CoV-2 infection by PCR and/or by serologic testing. As noted in other studies, the patients were predominantly young men (66%; median age, 27.5 years). Twenty-five (66%) patients were MIS-A+ and 13 (34%) were MIS-A–.
In general, the MIS-A– patients were sicker and had worse outcomes.
Specifically, compared with the MIS-A+ patients, MIS-A– patients had a shorter time between the onset of COVID-19 symptoms and the development of myocarditis, a shorter time to ICU admission, and more severe presentations assessed using lower left ventricular ejection fraction and sequential organ failure assessment scores.
MIS-A– patients also had higher lactate levels, were more likely to need venoarterial ECMO (92% vs 16%), had higher ICU mortality (31% vs. 4%), and a had lower probability of survival at 3 months (68% vs. 96%), compared with their MIS-A+ peers.
Immunologic differences
The immunologic profiles of these two distinct clinical phenotypes also differed.
In MIS-A– early-type COVID-19 myocarditis, RNA polymerase III autoantibodies are frequently positive and serum levels of antiviral interferon-alpha and granulocyte-attracting interleukin-8 are elevated.
In contrast, in MIS-A+ delayed-type COVID-19 myocarditis, RNA polymerase III autoantibodies are negative and serum levels of IL-17 and IL-22 are highly elevated.
“We suggest that IL-17 and IL-22 are novel criteria that should help to assess in adults the recently recognized MIS-A,” Dr. Gorochov told this news organization. “It should be tested whether IL-17 and IL-22 are also elevated in children with MIS-C.”
The researchers also observed “extremely” high serum IL-10 levels in both patient groups. This has been previously associated with severe myocardial injury and an increase in the risk for death in severe COVID-19 patients.
The researchers said the phenotypic clustering of patients with fulminant COVID-19–related myocarditis “seems relevant” for their management.
MIS-A– cases, owing to the high risk for evolution toward refractory cardiogenic shock, should be “urgently” referred to a center with venoarterial ECMO and closely monitored to prevent a “too-late” cannulation, especially under cardiopulmonary resuscitation, known to be associated with poor outcomes, they advised.
They noted that the five patients who died in their series had late venoarterial ECMO implantation, while undergoing multiple organ failures or resuscitation.
Conversely, the risk for evolution to refractory cardiogenic shock is lower in MIS-A+ cases. However, identifying MIS-A+ cases is “all the more important given that numerous data support the efficacy of corticosteroids and/or intravenous immunoglobulins in MIS-C,” Dr. Gorochov and colleagues wrote.
The authors of a linked editorial said the French team should be “commended on their work in furthering our understanding of fulminant myocarditis related to COVID-19 infection.”
Ajith Nair, MD, Baylor College of Medicine, and Anita Deswal, MD, MPH, University of Texas M.D. Anderson Cancer Center, both in Houston, noted that fulminant myocarditis is rare and can result from either of two mechanisms: viral tropism or an immune-mediated mechanism.
“It remains to be seen whether using antiviral therapy versus immunomodulatory therapy on the basis of clinical and cytokine profiles will yield benefits,” they wrote.
“Fulminant myocarditis invariably requires hemodynamic support and carries a high mortality risk if it is recognized late. However, the long-term prognosis in patients who survive the critical period is favorable, with recovery of myocardial function,” they added.
“This study highlights the ever-shifting understanding of the pathophysiology and therapeutic approaches to fulminant myocarditis,” Dr. Nair and Dr. Deswal concluded.
This research was supported in part by the Foundation of France, French National Research Agency, Sorbonne University, and Clinical Research Hospital. The researchers have filed a patent application based on these results. Dr. Nair and Dr. Deswal have no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY

