User login
Acne and rosacea management for men
In a report released March 2014 by the American Society of Aesthetic Plastic Surgery, the top five surgical procedures for men were liposuction, eyelid surgery, rhinoplasty, male breast reduction, and ear surgery. However, the rate of noninvasive cosmetic procedures and sales of men’s grooming products is one of the leading segments of the beauty industry.
Although most scientific research and media are focused on the female aesthetic, understanding the specific needs of your male patients is key to patient satisfaction. Most men are generally less aware than are women of the treatment options and risks and benefits of procedures. Men also prefer treatments with less downtime and natural-looking results. This column continues our miniseries on aesthetic dermatology for the male patient.
In a general dermatology practice, there are several skin concerns often identified by male patients, and acne and rosacea are among them.
Acne: Men generally have thicker, more sebaceous skin than that of women. Although acne is a very common problem in teens and young men, there is a growing trend of cases of cystic acne in adult men who consume popular protein meal replacement or muscle enhancing shakes that contain whey protein. Whey is a protein derived from cow’s milk. Milk and dairy products act by increasing insulin-like growth factor 1, which has been linked to acne. Although few case reports have shown a link between dietary whey supplementation and acne, in my practice, men with cystic acne who report using whey supplementation products have had almost complete resolution of their acne without medical intervention after discontinuing these products.
Rosacea: Men have a higher density of facial blood vessels than women do, and often seek treatment for telangiectasias and overall facial erythema. For papulopustular rosacea, common treatments include oral antibiotics, topical antibiotics, topical azaleic acid, and topical anti-inflammatory medications. For erythematotelangiectatic rosacea, Mirvaso (brimonidine), a topical vasoconstrictor, can be applied to the skin for 8-12 hours of marked reduction in facial erythema. Although theoretically a great option for patients suffering from erythema, the effects of topical brimonidine are transient, and the gel requires daily application with no long-term benefit. Vascular laser treatments are effective for telangiectasias for both men and women. However, men with more granulomatous or phymatous rosacea often need a combination of treatments including antibiotics, oral isotretinoin and fractional ablative lasers.
Resources:
American Society for Plastic Surgery 2012 statistics.
“Whey protein precipitating moderate to severe acne flares in 5 teenaged athletes,” Cutis 2012;90:70-2.
Dr. Talakoub and Dr. Wesley are cocontributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
In a report released March 2014 by the American Society of Aesthetic Plastic Surgery, the top five surgical procedures for men were liposuction, eyelid surgery, rhinoplasty, male breast reduction, and ear surgery. However, the rate of noninvasive cosmetic procedures and sales of men’s grooming products is one of the leading segments of the beauty industry.
Although most scientific research and media are focused on the female aesthetic, understanding the specific needs of your male patients is key to patient satisfaction. Most men are generally less aware than are women of the treatment options and risks and benefits of procedures. Men also prefer treatments with less downtime and natural-looking results. This column continues our miniseries on aesthetic dermatology for the male patient.
In a general dermatology practice, there are several skin concerns often identified by male patients, and acne and rosacea are among them.
Acne: Men generally have thicker, more sebaceous skin than that of women. Although acne is a very common problem in teens and young men, there is a growing trend of cases of cystic acne in adult men who consume popular protein meal replacement or muscle enhancing shakes that contain whey protein. Whey is a protein derived from cow’s milk. Milk and dairy products act by increasing insulin-like growth factor 1, which has been linked to acne. Although few case reports have shown a link between dietary whey supplementation and acne, in my practice, men with cystic acne who report using whey supplementation products have had almost complete resolution of their acne without medical intervention after discontinuing these products.
Rosacea: Men have a higher density of facial blood vessels than women do, and often seek treatment for telangiectasias and overall facial erythema. For papulopustular rosacea, common treatments include oral antibiotics, topical antibiotics, topical azaleic acid, and topical anti-inflammatory medications. For erythematotelangiectatic rosacea, Mirvaso (brimonidine), a topical vasoconstrictor, can be applied to the skin for 8-12 hours of marked reduction in facial erythema. Although theoretically a great option for patients suffering from erythema, the effects of topical brimonidine are transient, and the gel requires daily application with no long-term benefit. Vascular laser treatments are effective for telangiectasias for both men and women. However, men with more granulomatous or phymatous rosacea often need a combination of treatments including antibiotics, oral isotretinoin and fractional ablative lasers.
Resources:
American Society for Plastic Surgery 2012 statistics.
“Whey protein precipitating moderate to severe acne flares in 5 teenaged athletes,” Cutis 2012;90:70-2.
Dr. Talakoub and Dr. Wesley are cocontributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
In a report released March 2014 by the American Society of Aesthetic Plastic Surgery, the top five surgical procedures for men were liposuction, eyelid surgery, rhinoplasty, male breast reduction, and ear surgery. However, the rate of noninvasive cosmetic procedures and sales of men’s grooming products is one of the leading segments of the beauty industry.
Although most scientific research and media are focused on the female aesthetic, understanding the specific needs of your male patients is key to patient satisfaction. Most men are generally less aware than are women of the treatment options and risks and benefits of procedures. Men also prefer treatments with less downtime and natural-looking results. This column continues our miniseries on aesthetic dermatology for the male patient.
In a general dermatology practice, there are several skin concerns often identified by male patients, and acne and rosacea are among them.
Acne: Men generally have thicker, more sebaceous skin than that of women. Although acne is a very common problem in teens and young men, there is a growing trend of cases of cystic acne in adult men who consume popular protein meal replacement or muscle enhancing shakes that contain whey protein. Whey is a protein derived from cow’s milk. Milk and dairy products act by increasing insulin-like growth factor 1, which has been linked to acne. Although few case reports have shown a link between dietary whey supplementation and acne, in my practice, men with cystic acne who report using whey supplementation products have had almost complete resolution of their acne without medical intervention after discontinuing these products.
Rosacea: Men have a higher density of facial blood vessels than women do, and often seek treatment for telangiectasias and overall facial erythema. For papulopustular rosacea, common treatments include oral antibiotics, topical antibiotics, topical azaleic acid, and topical anti-inflammatory medications. For erythematotelangiectatic rosacea, Mirvaso (brimonidine), a topical vasoconstrictor, can be applied to the skin for 8-12 hours of marked reduction in facial erythema. Although theoretically a great option for patients suffering from erythema, the effects of topical brimonidine are transient, and the gel requires daily application with no long-term benefit. Vascular laser treatments are effective for telangiectasias for both men and women. However, men with more granulomatous or phymatous rosacea often need a combination of treatments including antibiotics, oral isotretinoin and fractional ablative lasers.
Resources:
American Society for Plastic Surgery 2012 statistics.
“Whey protein precipitating moderate to severe acne flares in 5 teenaged athletes,” Cutis 2012;90:70-2.
Dr. Talakoub and Dr. Wesley are cocontributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
Botulinum toxin for men
Men make up an increasing number of dermatology patients seeking cosmetic procedures. According to data from the American Society for Dermatologic Surgery and the American Society of Plastic Surgery, 9%-10% of all cosmetic procedures performed in the United States in 2013 were on men, a 104% increase since 2000. Botulinum toxin is currently the most common minimally invasive cosmetic procedure performed in men. While the overall percentage of men undergoing treatment, compared with women, is relatively small, more than 385,000 botulinum toxin treatments were performed on men last year in the United States, an increase of 310% since 2000.
Studies have shown that men often require more units of onabotulinumtoxinA than women when treating the glabella. In a 2005 study by Alstair and Jean Carruthers, 80 men were randomized to receive 20, 40, 60, or 80 units of onabotulinumtoxinA (Botox or Vistabel). The 40-, 60-, and 80-U doses were consistently more effective than the 20-U dose was in reducing glabellar lines (duration, peak response rate, and improvement from baseline). I find this to be true in my practice. Men may often require 20-60 U in the superficial corrugator and procerus muscles, compared with 20-30 units of onabotulinumtoxinA in the same muscles in women. For the frontalis muscles, I may use 5-20 U in men, compared with 5-10 U of onabotulinumtoxinA in women, but I take care not to inject too inferiorly to avoid a heavy brow or brow ptosis. The orbicularis oculi muscles often require the similar doses of between 6-15 U (most often 12 U/side) depending on degree of muscle contraction and severity of rhytids.
In addition to differences in botulinum toxin dosing between men and women, placement of toxin also may vary. Placement in the superficial corrugator, procerus, frontalis, and orbicularis oculi muscles are often the similar and patient dependent, based on a visual assessment of where their muscles move/contract. The superficial corrugator may insert more laterally in some men, and the brow is often straighter or less arched. The difference in injection site is often at the lateral brow. In women, botulinum toxin is often injected at the lateral brow at the junction where the lateral superior portion of the orbicularis oculi muscle and frontalis meet, in order to help give the brow a "lift." Men, however, often do not want raised or arched brow. Therefore, an injection is often placed about 1 cm above the lateral brow to maintain brow position and avoid overarching, or what some may regard as feminization of the male brow.
The depressor anguli oris and orbicularis oris muscles are injected less frequently in men than in women in my practice because of seemingly decreased rhytid formation in men in these locations. The platysmal muscles may be injected in men, but their average age is older compared with women who receive injections in this location.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley.
Men make up an increasing number of dermatology patients seeking cosmetic procedures. According to data from the American Society for Dermatologic Surgery and the American Society of Plastic Surgery, 9%-10% of all cosmetic procedures performed in the United States in 2013 were on men, a 104% increase since 2000. Botulinum toxin is currently the most common minimally invasive cosmetic procedure performed in men. While the overall percentage of men undergoing treatment, compared with women, is relatively small, more than 385,000 botulinum toxin treatments were performed on men last year in the United States, an increase of 310% since 2000.
Studies have shown that men often require more units of onabotulinumtoxinA than women when treating the glabella. In a 2005 study by Alstair and Jean Carruthers, 80 men were randomized to receive 20, 40, 60, or 80 units of onabotulinumtoxinA (Botox or Vistabel). The 40-, 60-, and 80-U doses were consistently more effective than the 20-U dose was in reducing glabellar lines (duration, peak response rate, and improvement from baseline). I find this to be true in my practice. Men may often require 20-60 U in the superficial corrugator and procerus muscles, compared with 20-30 units of onabotulinumtoxinA in the same muscles in women. For the frontalis muscles, I may use 5-20 U in men, compared with 5-10 U of onabotulinumtoxinA in women, but I take care not to inject too inferiorly to avoid a heavy brow or brow ptosis. The orbicularis oculi muscles often require the similar doses of between 6-15 U (most often 12 U/side) depending on degree of muscle contraction and severity of rhytids.
In addition to differences in botulinum toxin dosing between men and women, placement of toxin also may vary. Placement in the superficial corrugator, procerus, frontalis, and orbicularis oculi muscles are often the similar and patient dependent, based on a visual assessment of where their muscles move/contract. The superficial corrugator may insert more laterally in some men, and the brow is often straighter or less arched. The difference in injection site is often at the lateral brow. In women, botulinum toxin is often injected at the lateral brow at the junction where the lateral superior portion of the orbicularis oculi muscle and frontalis meet, in order to help give the brow a "lift." Men, however, often do not want raised or arched brow. Therefore, an injection is often placed about 1 cm above the lateral brow to maintain brow position and avoid overarching, or what some may regard as feminization of the male brow.
The depressor anguli oris and orbicularis oris muscles are injected less frequently in men than in women in my practice because of seemingly decreased rhytid formation in men in these locations. The platysmal muscles may be injected in men, but their average age is older compared with women who receive injections in this location.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley.
Men make up an increasing number of dermatology patients seeking cosmetic procedures. According to data from the American Society for Dermatologic Surgery and the American Society of Plastic Surgery, 9%-10% of all cosmetic procedures performed in the United States in 2013 were on men, a 104% increase since 2000. Botulinum toxin is currently the most common minimally invasive cosmetic procedure performed in men. While the overall percentage of men undergoing treatment, compared with women, is relatively small, more than 385,000 botulinum toxin treatments were performed on men last year in the United States, an increase of 310% since 2000.
Studies have shown that men often require more units of onabotulinumtoxinA than women when treating the glabella. In a 2005 study by Alstair and Jean Carruthers, 80 men were randomized to receive 20, 40, 60, or 80 units of onabotulinumtoxinA (Botox or Vistabel). The 40-, 60-, and 80-U doses were consistently more effective than the 20-U dose was in reducing glabellar lines (duration, peak response rate, and improvement from baseline). I find this to be true in my practice. Men may often require 20-60 U in the superficial corrugator and procerus muscles, compared with 20-30 units of onabotulinumtoxinA in the same muscles in women. For the frontalis muscles, I may use 5-20 U in men, compared with 5-10 U of onabotulinumtoxinA in women, but I take care not to inject too inferiorly to avoid a heavy brow or brow ptosis. The orbicularis oculi muscles often require the similar doses of between 6-15 U (most often 12 U/side) depending on degree of muscle contraction and severity of rhytids.
In addition to differences in botulinum toxin dosing between men and women, placement of toxin also may vary. Placement in the superficial corrugator, procerus, frontalis, and orbicularis oculi muscles are often the similar and patient dependent, based on a visual assessment of where their muscles move/contract. The superficial corrugator may insert more laterally in some men, and the brow is often straighter or less arched. The difference in injection site is often at the lateral brow. In women, botulinum toxin is often injected at the lateral brow at the junction where the lateral superior portion of the orbicularis oculi muscle and frontalis meet, in order to help give the brow a "lift." Men, however, often do not want raised or arched brow. Therefore, an injection is often placed about 1 cm above the lateral brow to maintain brow position and avoid overarching, or what some may regard as feminization of the male brow.
The depressor anguli oris and orbicularis oris muscles are injected less frequently in men than in women in my practice because of seemingly decreased rhytid formation in men in these locations. The platysmal muscles may be injected in men, but their average age is older compared with women who receive injections in this location.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Wesley.
Summer care for atopic skin
Summer months can be dreadful for patients with atopic dermatitis. The chlorine, heat, and humidity can lead to flares. Furthermore, noncompliance with skin care regimens because of changing summer routines, travel, and the use of hotel products can exacerbate even the calmest skin disease.
Share these tips with your patients to help them keep their atopic skin under control in the summer heat, and stop flares before they start.
• Rinse the skin well after swimming. Chlorine and saltwater can dry out the skin. Showers after swimming in chlorinated pools can help retain the skin’s natural oils.
• Avoid hot tubs. Cracks and fissures in atopic skin can become infected in hot tubs with Staphylococcus and Pseudomonas. Advise your atopic patients to avoid hot tubs, even if they claim the tubs have been cleaned.
• Bring your own products. Many soaps and shower gels available in hotels and resorts are extremely drying, and may contain ingredients that could irritate atopic skin.
• Don’t switch from thick creams to thin lotions just because it is summer. Remind your patients that a thin lotion does not provide the same occlusive and humectant properties as thicker creams, although they are not as easy to apply, and can feel thick and sticky on the skin with humidity.
• In case of an active eczema flare, topical steroids should be used and sun exposure should be avoided. Topical steroids are the most effective treatment when used correctly. However, any occurrence of hypopigmentation as a result of their use becomes more evident if the skin tans around the area of treatment.
• Wear physical sunscreen. This seems obvious, but most chemical blockers – even the formulations made for babies – can burn on cracked, inflamed skin. Instead, stress to your patients that they use a physical blocker made of pure titanium dioxide or zinc oxide on inflamed skin.
• Oral steroids and sun do not mix. Oral steroids can be potent photosensitizers. If they are needed, UV exposure should be avoided.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice at McLean (Va.) Dermatology Center. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
Summer months can be dreadful for patients with atopic dermatitis. The chlorine, heat, and humidity can lead to flares. Furthermore, noncompliance with skin care regimens because of changing summer routines, travel, and the use of hotel products can exacerbate even the calmest skin disease.
Share these tips with your patients to help them keep their atopic skin under control in the summer heat, and stop flares before they start.
• Rinse the skin well after swimming. Chlorine and saltwater can dry out the skin. Showers after swimming in chlorinated pools can help retain the skin’s natural oils.
• Avoid hot tubs. Cracks and fissures in atopic skin can become infected in hot tubs with Staphylococcus and Pseudomonas. Advise your atopic patients to avoid hot tubs, even if they claim the tubs have been cleaned.
• Bring your own products. Many soaps and shower gels available in hotels and resorts are extremely drying, and may contain ingredients that could irritate atopic skin.
• Don’t switch from thick creams to thin lotions just because it is summer. Remind your patients that a thin lotion does not provide the same occlusive and humectant properties as thicker creams, although they are not as easy to apply, and can feel thick and sticky on the skin with humidity.
• In case of an active eczema flare, topical steroids should be used and sun exposure should be avoided. Topical steroids are the most effective treatment when used correctly. However, any occurrence of hypopigmentation as a result of their use becomes more evident if the skin tans around the area of treatment.
• Wear physical sunscreen. This seems obvious, but most chemical blockers – even the formulations made for babies – can burn on cracked, inflamed skin. Instead, stress to your patients that they use a physical blocker made of pure titanium dioxide or zinc oxide on inflamed skin.
• Oral steroids and sun do not mix. Oral steroids can be potent photosensitizers. If they are needed, UV exposure should be avoided.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice at McLean (Va.) Dermatology Center. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
Summer months can be dreadful for patients with atopic dermatitis. The chlorine, heat, and humidity can lead to flares. Furthermore, noncompliance with skin care regimens because of changing summer routines, travel, and the use of hotel products can exacerbate even the calmest skin disease.
Share these tips with your patients to help them keep their atopic skin under control in the summer heat, and stop flares before they start.
• Rinse the skin well after swimming. Chlorine and saltwater can dry out the skin. Showers after swimming in chlorinated pools can help retain the skin’s natural oils.
• Avoid hot tubs. Cracks and fissures in atopic skin can become infected in hot tubs with Staphylococcus and Pseudomonas. Advise your atopic patients to avoid hot tubs, even if they claim the tubs have been cleaned.
• Bring your own products. Many soaps and shower gels available in hotels and resorts are extremely drying, and may contain ingredients that could irritate atopic skin.
• Don’t switch from thick creams to thin lotions just because it is summer. Remind your patients that a thin lotion does not provide the same occlusive and humectant properties as thicker creams, although they are not as easy to apply, and can feel thick and sticky on the skin with humidity.
• In case of an active eczema flare, topical steroids should be used and sun exposure should be avoided. Topical steroids are the most effective treatment when used correctly. However, any occurrence of hypopigmentation as a result of their use becomes more evident if the skin tans around the area of treatment.
• Wear physical sunscreen. This seems obvious, but most chemical blockers – even the formulations made for babies – can burn on cracked, inflamed skin. Instead, stress to your patients that they use a physical blocker made of pure titanium dioxide or zinc oxide on inflamed skin.
• Oral steroids and sun do not mix. Oral steroids can be potent photosensitizers. If they are needed, UV exposure should be avoided.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice at McLean (Va.) Dermatology Center. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
Cryolipolysis
Cryolipolysis has emerged as a popular noninvasive treatment option for reducing localized areas of fat. The technology was developed on the premise that cold temperatures can selectively damage subcutaneous fat while leaving the overlying skin unharmed, as demonstrated by popsicle panniculitis. In this process, when subcutaneous fat is cooled below body temperature but above freezing, the fat undergoes cell death followed by a local inflammatory response, a localized panniculitis, that gradually results in a reduction of fat in that area.
Dr. Dieter Manstein and Dr. R. Rox Anderson pioneered the concept of cryolipolysis in 2008. The technology was approved by the Food and Drug Administration in 2010 in the form of the Zeltiq device. The device has different-sized hand pieces with a vacuum connection that, after it is applied to the skin, cools the subcutaneous fat without damaging the top layers of skin. Each area is treated for 1 hour, and 20%-30% of the fat cells are expected to be reduced with a single treatment. Typical responses after treatment include numbness, but some patients may also experience bruising and discomfort, all of which typically last no longer than 2-3 weeks.
If discomfort occurs in my patients, I find they report it more often in the lower abdomen than the love handles. Paradoxical adipose hyperplasia was recently reported for the first time in a male patient in his 40s (in the lower abdomen) (JAMA Dermatol. 2014;150:317-9).
In my experience, there is no difference in efficacy or adverse events seen in patients of different ethnicities. One study found no difference in efficacy or adverse events of cryolipolysis in Chinese patients (Lasers Surg. Med. 2012;44:125-30), but no other study of cryolipolysis in ethnic patients has been published.
I was involved in the clinical trials for this device prior to FDA approval where one love handle was treated on a patient and the other side was used as a control. Based on this experience and my experience using the device in practice, it is not a replacement for abdominoplasty or liposuction, but it is a useful technology in the right candidate. The patients who seem to do the best are those who are 10-15 pounds from their goal weight, are not obese (body mass index less than 30 kg/m2), and have a discrete bulge (typically love handles or abdomen) that they can’t get rid of with good diet and exercise alone. Massage for a few minutes after treatment seems to increase efficacy (Lasers Surg. Med. 2014;46:20-6).
Some patients may require more than one treatment to achieve their desired results, but I recommend waiting at least 2-3 months before opting for additional treatment. Choosing the right candidates and providing patients with realistic expectations seem to be the most helpful in this process.
Dr. Wesley practices dermatology in Beverly Hills, Calif.
Cryolipolysis has emerged as a popular noninvasive treatment option for reducing localized areas of fat. The technology was developed on the premise that cold temperatures can selectively damage subcutaneous fat while leaving the overlying skin unharmed, as demonstrated by popsicle panniculitis. In this process, when subcutaneous fat is cooled below body temperature but above freezing, the fat undergoes cell death followed by a local inflammatory response, a localized panniculitis, that gradually results in a reduction of fat in that area.
Dr. Dieter Manstein and Dr. R. Rox Anderson pioneered the concept of cryolipolysis in 2008. The technology was approved by the Food and Drug Administration in 2010 in the form of the Zeltiq device. The device has different-sized hand pieces with a vacuum connection that, after it is applied to the skin, cools the subcutaneous fat without damaging the top layers of skin. Each area is treated for 1 hour, and 20%-30% of the fat cells are expected to be reduced with a single treatment. Typical responses after treatment include numbness, but some patients may also experience bruising and discomfort, all of which typically last no longer than 2-3 weeks.
If discomfort occurs in my patients, I find they report it more often in the lower abdomen than the love handles. Paradoxical adipose hyperplasia was recently reported for the first time in a male patient in his 40s (in the lower abdomen) (JAMA Dermatol. 2014;150:317-9).
In my experience, there is no difference in efficacy or adverse events seen in patients of different ethnicities. One study found no difference in efficacy or adverse events of cryolipolysis in Chinese patients (Lasers Surg. Med. 2012;44:125-30), but no other study of cryolipolysis in ethnic patients has been published.
I was involved in the clinical trials for this device prior to FDA approval where one love handle was treated on a patient and the other side was used as a control. Based on this experience and my experience using the device in practice, it is not a replacement for abdominoplasty or liposuction, but it is a useful technology in the right candidate. The patients who seem to do the best are those who are 10-15 pounds from their goal weight, are not obese (body mass index less than 30 kg/m2), and have a discrete bulge (typically love handles or abdomen) that they can’t get rid of with good diet and exercise alone. Massage for a few minutes after treatment seems to increase efficacy (Lasers Surg. Med. 2014;46:20-6).
Some patients may require more than one treatment to achieve their desired results, but I recommend waiting at least 2-3 months before opting for additional treatment. Choosing the right candidates and providing patients with realistic expectations seem to be the most helpful in this process.
Dr. Wesley practices dermatology in Beverly Hills, Calif.
Cryolipolysis has emerged as a popular noninvasive treatment option for reducing localized areas of fat. The technology was developed on the premise that cold temperatures can selectively damage subcutaneous fat while leaving the overlying skin unharmed, as demonstrated by popsicle panniculitis. In this process, when subcutaneous fat is cooled below body temperature but above freezing, the fat undergoes cell death followed by a local inflammatory response, a localized panniculitis, that gradually results in a reduction of fat in that area.
Dr. Dieter Manstein and Dr. R. Rox Anderson pioneered the concept of cryolipolysis in 2008. The technology was approved by the Food and Drug Administration in 2010 in the form of the Zeltiq device. The device has different-sized hand pieces with a vacuum connection that, after it is applied to the skin, cools the subcutaneous fat without damaging the top layers of skin. Each area is treated for 1 hour, and 20%-30% of the fat cells are expected to be reduced with a single treatment. Typical responses after treatment include numbness, but some patients may also experience bruising and discomfort, all of which typically last no longer than 2-3 weeks.
If discomfort occurs in my patients, I find they report it more often in the lower abdomen than the love handles. Paradoxical adipose hyperplasia was recently reported for the first time in a male patient in his 40s (in the lower abdomen) (JAMA Dermatol. 2014;150:317-9).
In my experience, there is no difference in efficacy or adverse events seen in patients of different ethnicities. One study found no difference in efficacy or adverse events of cryolipolysis in Chinese patients (Lasers Surg. Med. 2012;44:125-30), but no other study of cryolipolysis in ethnic patients has been published.
I was involved in the clinical trials for this device prior to FDA approval where one love handle was treated on a patient and the other side was used as a control. Based on this experience and my experience using the device in practice, it is not a replacement for abdominoplasty or liposuction, but it is a useful technology in the right candidate. The patients who seem to do the best are those who are 10-15 pounds from their goal weight, are not obese (body mass index less than 30 kg/m2), and have a discrete bulge (typically love handles or abdomen) that they can’t get rid of with good diet and exercise alone. Massage for a few minutes after treatment seems to increase efficacy (Lasers Surg. Med. 2014;46:20-6).
Some patients may require more than one treatment to achieve their desired results, but I recommend waiting at least 2-3 months before opting for additional treatment. Choosing the right candidates and providing patients with realistic expectations seem to be the most helpful in this process.
Dr. Wesley practices dermatology in Beverly Hills, Calif.
The springtime eruptions
The spectrum of idiopathic ultraviolet-induced dermatoses includes the most severe variant, polymorphous light eruption (PMLE), in which erythematous papules, papulovesicles, and plaques form from a delayed type IV hypersensitivity reaction to the sun. Its milder cousins, benign summer light eruption and juvenile springtime eruption, are milder, more transient variants.
Patients may experience sudden-onset, pruritic, sometimes painful papules and papulovesicles or cheilitis within 30 minutes to several hours of exposure to UV light in areas normally covered in the winter months. The rash subsides over 1-7 days (or sooner with effective topical steroid administration and strict sun avoidance) and without scarring. Occasionally, patients experience systemic flulike symptoms after sun exposure. Triggers can be UVA, UVB, or UVC. However, because most cases appear in the spring, describing these variants as benign summer light eruption is something of a misnomer.
These seasonal rashes are often underrecognized in skin of color patients, particularly those with Fitzpatrick skin types III-VI, because many practitioners assume a protective role of melanin (Photochem. Photobiol. Sci. 2013;12:65-77). A study by Kerr and Lim identified 280 patients with photodermatoses; 135 (48%) were African American, 110 (40%) were white, and 35 (12%) were other ethnicities. They noted a significantly higher proportion of African Americans with PMLE, compared with whites (J. Am. Acad. Dermatol. 2007;57:638-43). Also, Native Americans have a hereditary form of PMLE with autosomal dominant inheritance that can involve the face and is most common in patients with Fitzpatrick skin types III-VI.
For sun-sensitive patients, and especially skin of color patients, diagnosis and treatment include ruling out other photosensitive diseases such as systemic lupus, and then counseling about the importance of sun avoidance and the use of sunscreens, which include both UVA and UVB protection. Prophylactic phototherapy or photochemotherapy at the beginning of spring for several weeks may prevent flare-ups throughout the summer. PUVA (psoralen and UVA) therapy, as well as UVB phototherapy, have been successful at preventing flares in several studies. Topical steroids, antihistamines, and oral prednisone are mainstays of treatment for severe flares, alone or in combination with phototherapy. For severe cases, or those recalcitrant to first-line treatment, antimalarials, azathioprine, and thalidomide have been used with variable efficacy.
Particularly at this time of year, I always ask patients with photo-distributed rashes about their ethnicities. One can never assume ethnicity, culture, skin type, background, or even photosensitivity based on skin color alone. I have been surprised by the many patients with dark skin who may have Native American origins who present with photosensitive rashes, or the many patients with hereditary photosensitive rashes with fair skin. Our beautiful, multicultural society makes it harder to define or categorize dermatoses by skin type alone, based on the definitions we have set for skin type in our literature today.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice at McLean (Va.) Dermatology Center. Dr. Wesley practices dermatology in Beverly Hills, Calif.
The spectrum of idiopathic ultraviolet-induced dermatoses includes the most severe variant, polymorphous light eruption (PMLE), in which erythematous papules, papulovesicles, and plaques form from a delayed type IV hypersensitivity reaction to the sun. Its milder cousins, benign summer light eruption and juvenile springtime eruption, are milder, more transient variants.
Patients may experience sudden-onset, pruritic, sometimes painful papules and papulovesicles or cheilitis within 30 minutes to several hours of exposure to UV light in areas normally covered in the winter months. The rash subsides over 1-7 days (or sooner with effective topical steroid administration and strict sun avoidance) and without scarring. Occasionally, patients experience systemic flulike symptoms after sun exposure. Triggers can be UVA, UVB, or UVC. However, because most cases appear in the spring, describing these variants as benign summer light eruption is something of a misnomer.
These seasonal rashes are often underrecognized in skin of color patients, particularly those with Fitzpatrick skin types III-VI, because many practitioners assume a protective role of melanin (Photochem. Photobiol. Sci. 2013;12:65-77). A study by Kerr and Lim identified 280 patients with photodermatoses; 135 (48%) were African American, 110 (40%) were white, and 35 (12%) were other ethnicities. They noted a significantly higher proportion of African Americans with PMLE, compared with whites (J. Am. Acad. Dermatol. 2007;57:638-43). Also, Native Americans have a hereditary form of PMLE with autosomal dominant inheritance that can involve the face and is most common in patients with Fitzpatrick skin types III-VI.
For sun-sensitive patients, and especially skin of color patients, diagnosis and treatment include ruling out other photosensitive diseases such as systemic lupus, and then counseling about the importance of sun avoidance and the use of sunscreens, which include both UVA and UVB protection. Prophylactic phototherapy or photochemotherapy at the beginning of spring for several weeks may prevent flare-ups throughout the summer. PUVA (psoralen and UVA) therapy, as well as UVB phototherapy, have been successful at preventing flares in several studies. Topical steroids, antihistamines, and oral prednisone are mainstays of treatment for severe flares, alone or in combination with phototherapy. For severe cases, or those recalcitrant to first-line treatment, antimalarials, azathioprine, and thalidomide have been used with variable efficacy.
Particularly at this time of year, I always ask patients with photo-distributed rashes about their ethnicities. One can never assume ethnicity, culture, skin type, background, or even photosensitivity based on skin color alone. I have been surprised by the many patients with dark skin who may have Native American origins who present with photosensitive rashes, or the many patients with hereditary photosensitive rashes with fair skin. Our beautiful, multicultural society makes it harder to define or categorize dermatoses by skin type alone, based on the definitions we have set for skin type in our literature today.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice at McLean (Va.) Dermatology Center. Dr. Wesley practices dermatology in Beverly Hills, Calif.
The spectrum of idiopathic ultraviolet-induced dermatoses includes the most severe variant, polymorphous light eruption (PMLE), in which erythematous papules, papulovesicles, and plaques form from a delayed type IV hypersensitivity reaction to the sun. Its milder cousins, benign summer light eruption and juvenile springtime eruption, are milder, more transient variants.
Patients may experience sudden-onset, pruritic, sometimes painful papules and papulovesicles or cheilitis within 30 minutes to several hours of exposure to UV light in areas normally covered in the winter months. The rash subsides over 1-7 days (or sooner with effective topical steroid administration and strict sun avoidance) and without scarring. Occasionally, patients experience systemic flulike symptoms after sun exposure. Triggers can be UVA, UVB, or UVC. However, because most cases appear in the spring, describing these variants as benign summer light eruption is something of a misnomer.
These seasonal rashes are often underrecognized in skin of color patients, particularly those with Fitzpatrick skin types III-VI, because many practitioners assume a protective role of melanin (Photochem. Photobiol. Sci. 2013;12:65-77). A study by Kerr and Lim identified 280 patients with photodermatoses; 135 (48%) were African American, 110 (40%) were white, and 35 (12%) were other ethnicities. They noted a significantly higher proportion of African Americans with PMLE, compared with whites (J. Am. Acad. Dermatol. 2007;57:638-43). Also, Native Americans have a hereditary form of PMLE with autosomal dominant inheritance that can involve the face and is most common in patients with Fitzpatrick skin types III-VI.
For sun-sensitive patients, and especially skin of color patients, diagnosis and treatment include ruling out other photosensitive diseases such as systemic lupus, and then counseling about the importance of sun avoidance and the use of sunscreens, which include both UVA and UVB protection. Prophylactic phototherapy or photochemotherapy at the beginning of spring for several weeks may prevent flare-ups throughout the summer. PUVA (psoralen and UVA) therapy, as well as UVB phototherapy, have been successful at preventing flares in several studies. Topical steroids, antihistamines, and oral prednisone are mainstays of treatment for severe flares, alone or in combination with phototherapy. For severe cases, or those recalcitrant to first-line treatment, antimalarials, azathioprine, and thalidomide have been used with variable efficacy.
Particularly at this time of year, I always ask patients with photo-distributed rashes about their ethnicities. One can never assume ethnicity, culture, skin type, background, or even photosensitivity based on skin color alone. I have been surprised by the many patients with dark skin who may have Native American origins who present with photosensitive rashes, or the many patients with hereditary photosensitive rashes with fair skin. Our beautiful, multicultural society makes it harder to define or categorize dermatoses by skin type alone, based on the definitions we have set for skin type in our literature today.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice at McLean (Va.) Dermatology Center. Dr. Wesley practices dermatology in Beverly Hills, Calif.
Discrepancies in dyschromia
Dyschromias are one of the most common skin concerns among women and persons of color. In the April issue of Journal of Drugs in Dermatology, Dr. S.J. Kang and associates conducted an excellent study to determine whether racial or ethnic groups are treated differently for dyschromia.
The investigators searched the National Ambulatory Medical Care Survey (NAMCS) database for visits including the diagnosis of dyschromia (ICD-9 codes 709.00 or 709.09) during an 18-year period (1993-2010). They found 24.7 million visits for dyschromia and 5,531,000 patients with a sole diagnosis of dyschromia. Of those with a sole diagnosis of dyschromia, 76% were seen by a dermatologist, and more than half were female. Seventy-five percent were white, 11% African American, 7% Asian/Pacific Islander, and 9% Hispanic, although Asians demonstrated the highest number of visits per 100,000 persons.
In this review, hydroquinone monotherapy was the most commonly prescribed medication by dermatologists. Combination therapy with hydroquinone plus a retinoid and corticosteroid was utilized for women 10 times more than for men. African American patients were less likely to be prescribed combination therapy or receive procedures (such as cryotherapy, chemical peels or lasers). Additionally, sunscreens were recommended less often to black and Asian patients, compared with white patients.
While the underlying reason for dyschromia plays a role in the type of treatment given, overall combination therapies are often more effective than therapy with hydroquinone alone. This study demonstrates that combination therapy may be under-utilized in patients of color.
In my practice, I find that unless the patient’s skin is completely hydroquinone-naive, combination therapy with hydroquinone, retinoid, and corticosteroid is often a first-line treatment that may achieve faster results. Sun protection is a vital component in the treatment of dyschromia, and it is recommended for every patient, regardless of race or ethnicity. Nonhydroquinone topical agents containing ingredients such as kojic acid, arbutin, licorice, niacinamide, resveratrol, and superficial chemical peels are also used in all ethnic groups. In my Asian, Hispanic, and African American or darker-skinned patients, I do use caution with deeper peels and lasers and often perform a test spot first if this type of therapy is considered.
Dr. Wesley practices dermatology in Beverly Hills, Calif.
Dyschromias are one of the most common skin concerns among women and persons of color. In the April issue of Journal of Drugs in Dermatology, Dr. S.J. Kang and associates conducted an excellent study to determine whether racial or ethnic groups are treated differently for dyschromia.
The investigators searched the National Ambulatory Medical Care Survey (NAMCS) database for visits including the diagnosis of dyschromia (ICD-9 codes 709.00 or 709.09) during an 18-year period (1993-2010). They found 24.7 million visits for dyschromia and 5,531,000 patients with a sole diagnosis of dyschromia. Of those with a sole diagnosis of dyschromia, 76% were seen by a dermatologist, and more than half were female. Seventy-five percent were white, 11% African American, 7% Asian/Pacific Islander, and 9% Hispanic, although Asians demonstrated the highest number of visits per 100,000 persons.
In this review, hydroquinone monotherapy was the most commonly prescribed medication by dermatologists. Combination therapy with hydroquinone plus a retinoid and corticosteroid was utilized for women 10 times more than for men. African American patients were less likely to be prescribed combination therapy or receive procedures (such as cryotherapy, chemical peels or lasers). Additionally, sunscreens were recommended less often to black and Asian patients, compared with white patients.
While the underlying reason for dyschromia plays a role in the type of treatment given, overall combination therapies are often more effective than therapy with hydroquinone alone. This study demonstrates that combination therapy may be under-utilized in patients of color.
In my practice, I find that unless the patient’s skin is completely hydroquinone-naive, combination therapy with hydroquinone, retinoid, and corticosteroid is often a first-line treatment that may achieve faster results. Sun protection is a vital component in the treatment of dyschromia, and it is recommended for every patient, regardless of race or ethnicity. Nonhydroquinone topical agents containing ingredients such as kojic acid, arbutin, licorice, niacinamide, resveratrol, and superficial chemical peels are also used in all ethnic groups. In my Asian, Hispanic, and African American or darker-skinned patients, I do use caution with deeper peels and lasers and often perform a test spot first if this type of therapy is considered.
Dr. Wesley practices dermatology in Beverly Hills, Calif.
Dyschromias are one of the most common skin concerns among women and persons of color. In the April issue of Journal of Drugs in Dermatology, Dr. S.J. Kang and associates conducted an excellent study to determine whether racial or ethnic groups are treated differently for dyschromia.
The investigators searched the National Ambulatory Medical Care Survey (NAMCS) database for visits including the diagnosis of dyschromia (ICD-9 codes 709.00 or 709.09) during an 18-year period (1993-2010). They found 24.7 million visits for dyschromia and 5,531,000 patients with a sole diagnosis of dyschromia. Of those with a sole diagnosis of dyschromia, 76% were seen by a dermatologist, and more than half were female. Seventy-five percent were white, 11% African American, 7% Asian/Pacific Islander, and 9% Hispanic, although Asians demonstrated the highest number of visits per 100,000 persons.
In this review, hydroquinone monotherapy was the most commonly prescribed medication by dermatologists. Combination therapy with hydroquinone plus a retinoid and corticosteroid was utilized for women 10 times more than for men. African American patients were less likely to be prescribed combination therapy or receive procedures (such as cryotherapy, chemical peels or lasers). Additionally, sunscreens were recommended less often to black and Asian patients, compared with white patients.
While the underlying reason for dyschromia plays a role in the type of treatment given, overall combination therapies are often more effective than therapy with hydroquinone alone. This study demonstrates that combination therapy may be under-utilized in patients of color.
In my practice, I find that unless the patient’s skin is completely hydroquinone-naive, combination therapy with hydroquinone, retinoid, and corticosteroid is often a first-line treatment that may achieve faster results. Sun protection is a vital component in the treatment of dyschromia, and it is recommended for every patient, regardless of race or ethnicity. Nonhydroquinone topical agents containing ingredients such as kojic acid, arbutin, licorice, niacinamide, resveratrol, and superficial chemical peels are also used in all ethnic groups. In my Asian, Hispanic, and African American or darker-skinned patients, I do use caution with deeper peels and lasers and often perform a test spot first if this type of therapy is considered.
Dr. Wesley practices dermatology in Beverly Hills, Calif.
VIDEO: Concise guide to lasers: cellulite, tattoo removal, and skin tightening
DENVER – In 15 minutes, Dr. M. Christine Lee brings you a definitive guide to lasers for various patient needs, including tattoo removal, treatment of cellulite, skin tightening, and skin resurfacing. Learn more about lasers that you might want to add to your practice and get ideas on how to make the most of devices you already have.
Dr. Lee is with the department of dermatologic surgery at the University of California, San Francisco, and director of East Bay Laser & Skin Care Center in Walnut Creek, Calif. In this video, she also shares clinical pearls about different types of laser procedures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
DENVER – In 15 minutes, Dr. M. Christine Lee brings you a definitive guide to lasers for various patient needs, including tattoo removal, treatment of cellulite, skin tightening, and skin resurfacing. Learn more about lasers that you might want to add to your practice and get ideas on how to make the most of devices you already have.
Dr. Lee is with the department of dermatologic surgery at the University of California, San Francisco, and director of East Bay Laser & Skin Care Center in Walnut Creek, Calif. In this video, she also shares clinical pearls about different types of laser procedures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
DENVER – In 15 minutes, Dr. M. Christine Lee brings you a definitive guide to lasers for various patient needs, including tattoo removal, treatment of cellulite, skin tightening, and skin resurfacing. Learn more about lasers that you might want to add to your practice and get ideas on how to make the most of devices you already have.
Dr. Lee is with the department of dermatologic surgery at the University of California, San Francisco, and director of East Bay Laser & Skin Care Center in Walnut Creek, Calif. In this video, she also shares clinical pearls about different types of laser procedures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @naseemmiller
EXPERT ANALYSIS FROM THE AAD ANNUAL MEETING
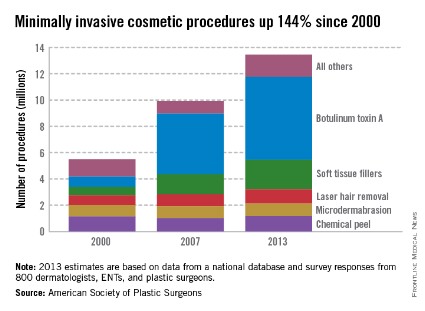
Botulinum toxin A tops list of nonsurgical cosmetic procedures in 2013
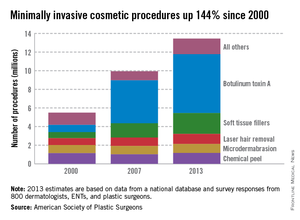
Injection of botulinum toxin type A continues to be the most popular form of minimally invasive cosmetic surgery, with a total of more than 6.3 million procedures performed in 2013, the American Society of Plastic Surgeons reported.
Overall, botulinum toxins such as Botox and Dysport accounted for 47% of the market for minimally invasive procedures, which totaled 13.4 million procedures in 2013, according to the ASPS.
The second most popular surgery was injection of soft tissue fillers, with 2.2 million procedures performed, followed by chemical peels (1.2 million procedures), laser hair removal (1.1 million), and microdermabrasion (970,000), the ASPS said.
The total number of minimally invasive procedures increased by 3% from 2012, as did the number of botulinum injections. The largest increase for a single type of procedure was seen for the soft tissue fillers, with hyaluronic acid injections up 18% from 2012 to 2013, the ASPS noted.
The estimates for 2013 are based on data from a national database and survey responses from 800 dermatologists, ENTs, and plastic surgeons.
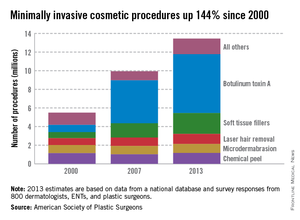
Injection of botulinum toxin type A continues to be the most popular form of minimally invasive cosmetic surgery, with a total of more than 6.3 million procedures performed in 2013, the American Society of Plastic Surgeons reported.
Overall, botulinum toxins such as Botox and Dysport accounted for 47% of the market for minimally invasive procedures, which totaled 13.4 million procedures in 2013, according to the ASPS.
The second most popular surgery was injection of soft tissue fillers, with 2.2 million procedures performed, followed by chemical peels (1.2 million procedures), laser hair removal (1.1 million), and microdermabrasion (970,000), the ASPS said.
The total number of minimally invasive procedures increased by 3% from 2012, as did the number of botulinum injections. The largest increase for a single type of procedure was seen for the soft tissue fillers, with hyaluronic acid injections up 18% from 2012 to 2013, the ASPS noted.
The estimates for 2013 are based on data from a national database and survey responses from 800 dermatologists, ENTs, and plastic surgeons.
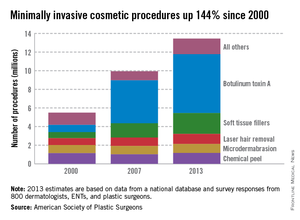
Injection of botulinum toxin type A continues to be the most popular form of minimally invasive cosmetic surgery, with a total of more than 6.3 million procedures performed in 2013, the American Society of Plastic Surgeons reported.
Overall, botulinum toxins such as Botox and Dysport accounted for 47% of the market for minimally invasive procedures, which totaled 13.4 million procedures in 2013, according to the ASPS.
The second most popular surgery was injection of soft tissue fillers, with 2.2 million procedures performed, followed by chemical peels (1.2 million procedures), laser hair removal (1.1 million), and microdermabrasion (970,000), the ASPS said.
The total number of minimally invasive procedures increased by 3% from 2012, as did the number of botulinum injections. The largest increase for a single type of procedure was seen for the soft tissue fillers, with hyaluronic acid injections up 18% from 2012 to 2013, the ASPS noted.
The estimates for 2013 are based on data from a national database and survey responses from 800 dermatologists, ENTs, and plastic surgeons.
More ways to make the most of lasers in clinical practice
PHOENIX – What’s the latest in lasers? The most stubborn tattoos – those with blue or green ink – are now the easiest to remove with new laser technology and techniques. Microwave treatment for armpit hair is a real option, even on difficult-to-remove blond hair. Cutaneous laser expert Dr. Roy Geronemus, director of the Laser and Skin Surgery Center of New York, describes what dermatologists need to know about these and other innovative cosmetic treatments in an interview at the annual meeting of the American Society for Laser Medicine and Surgery.
But that’s not all. More data support the use of lasers for common medical conditions, says Dr. Geronemus. Hear his description of how the same new laser used for tattoo removal can be a noninvasive treatment to reduce either hypertrophic or atrophic scarring in any skin type, with practically no downtime. He also explains several new approaches that show promise as acne therapy.
On Twitter @sherryboschert
PHOENIX – What’s the latest in lasers? The most stubborn tattoos – those with blue or green ink – are now the easiest to remove with new laser technology and techniques. Microwave treatment for armpit hair is a real option, even on difficult-to-remove blond hair. Cutaneous laser expert Dr. Roy Geronemus, director of the Laser and Skin Surgery Center of New York, describes what dermatologists need to know about these and other innovative cosmetic treatments in an interview at the annual meeting of the American Society for Laser Medicine and Surgery.
But that’s not all. More data support the use of lasers for common medical conditions, says Dr. Geronemus. Hear his description of how the same new laser used for tattoo removal can be a noninvasive treatment to reduce either hypertrophic or atrophic scarring in any skin type, with practically no downtime. He also explains several new approaches that show promise as acne therapy.
On Twitter @sherryboschert
PHOENIX – What’s the latest in lasers? The most stubborn tattoos – those with blue or green ink – are now the easiest to remove with new laser technology and techniques. Microwave treatment for armpit hair is a real option, even on difficult-to-remove blond hair. Cutaneous laser expert Dr. Roy Geronemus, director of the Laser and Skin Surgery Center of New York, describes what dermatologists need to know about these and other innovative cosmetic treatments in an interview at the annual meeting of the American Society for Laser Medicine and Surgery.
But that’s not all. More data support the use of lasers for common medical conditions, says Dr. Geronemus. Hear his description of how the same new laser used for tattoo removal can be a noninvasive treatment to reduce either hypertrophic or atrophic scarring in any skin type, with practically no downtime. He also explains several new approaches that show promise as acne therapy.
On Twitter @sherryboschert
AT LASER 2014
How an expert uses Voluma
WAIKOLOA, HAWAII – A key point to understand about Juvederm Voluma XC, the recently approved filler for age-related midface volume deficit, is that it’s a pillar or lift product, according to Dr. Sue Ellen Cox.
"Voluma loves to lift. It works great when placed on bone, such as the malar bone. With a supraperiosteal vertical puncture, you’ll see the skin lift right in front of your eyes," said Dr. Cox, a dermatologist at the University of North Carolina at Chapel Hill and principal investigator in the pivotal clinical trial that led to Food and Drug Administration approval of Voluma.
This characteristic of the highly cohesive 20-mg/mL hyaluronic acid filler has important implications for the product’s optimal use and achieving maximal patient satisfaction. For one, Voluma absolutely should not be used for patients with thin skin. For these patients, a more effective option is a product containing monophasic monodensified hyaluronic acids, such as Juvederm Ultra or Ultra Plus, Dr. Cox said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
As a rule of thumb, approximately 40% of Voluma is needed compared with the amount of monophasic monodensified hyaluronic acid fillers dermatologists are accustomed to working with, she said.
It’s crucial to inject Voluma extremely slowly, Dr. Cox emphasized. She advised scheduling 30 minutes for a patient’s first volumizing session. It’s also important to avoid using a large bolus, and be sure not to overcorrect. Voluma loves water and will draw it from tissue, Dr. Cox noted. Therefore it’s important to use the exact correction. Remember that at 9 months post treatment, 50% or more of the original correction will remain, so the 9-month mark is a good time to schedule a touch-up, she added.
Another pearl: Inject struts or pillars from the periostium; then blend and mold them, Dr. Cox continued.
She urged her colleagues to be conservative in using Voluma around the eyes. In her experience, too much Voluma in this area causes the product to migrate anteriorly on the cheek, which could result in an unwelcome doughy appearance.
To achieve improvement in the submalar area, it’s best to utilize tangential microdroplets of Voluma after reconstitution with saline so the filler doesn’t affect the nerve and cause a lip drop, according to Dr. Cox.
Should it become necessary to dissolve Voluma, use twice as much hyaluronidase (Hylenex).
Dr. Cox reported serving as a consultant to Allergan and Medicis and serving as principal investigator in trials funded by those companies, as well as in studies funded by Revance and Kythera.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – A key point to understand about Juvederm Voluma XC, the recently approved filler for age-related midface volume deficit, is that it’s a pillar or lift product, according to Dr. Sue Ellen Cox.
"Voluma loves to lift. It works great when placed on bone, such as the malar bone. With a supraperiosteal vertical puncture, you’ll see the skin lift right in front of your eyes," said Dr. Cox, a dermatologist at the University of North Carolina at Chapel Hill and principal investigator in the pivotal clinical trial that led to Food and Drug Administration approval of Voluma.
This characteristic of the highly cohesive 20-mg/mL hyaluronic acid filler has important implications for the product’s optimal use and achieving maximal patient satisfaction. For one, Voluma absolutely should not be used for patients with thin skin. For these patients, a more effective option is a product containing monophasic monodensified hyaluronic acids, such as Juvederm Ultra or Ultra Plus, Dr. Cox said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
As a rule of thumb, approximately 40% of Voluma is needed compared with the amount of monophasic monodensified hyaluronic acid fillers dermatologists are accustomed to working with, she said.
It’s crucial to inject Voluma extremely slowly, Dr. Cox emphasized. She advised scheduling 30 minutes for a patient’s first volumizing session. It’s also important to avoid using a large bolus, and be sure not to overcorrect. Voluma loves water and will draw it from tissue, Dr. Cox noted. Therefore it’s important to use the exact correction. Remember that at 9 months post treatment, 50% or more of the original correction will remain, so the 9-month mark is a good time to schedule a touch-up, she added.
Another pearl: Inject struts or pillars from the periostium; then blend and mold them, Dr. Cox continued.
She urged her colleagues to be conservative in using Voluma around the eyes. In her experience, too much Voluma in this area causes the product to migrate anteriorly on the cheek, which could result in an unwelcome doughy appearance.
To achieve improvement in the submalar area, it’s best to utilize tangential microdroplets of Voluma after reconstitution with saline so the filler doesn’t affect the nerve and cause a lip drop, according to Dr. Cox.
Should it become necessary to dissolve Voluma, use twice as much hyaluronidase (Hylenex).
Dr. Cox reported serving as a consultant to Allergan and Medicis and serving as principal investigator in trials funded by those companies, as well as in studies funded by Revance and Kythera.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – A key point to understand about Juvederm Voluma XC, the recently approved filler for age-related midface volume deficit, is that it’s a pillar or lift product, according to Dr. Sue Ellen Cox.
"Voluma loves to lift. It works great when placed on bone, such as the malar bone. With a supraperiosteal vertical puncture, you’ll see the skin lift right in front of your eyes," said Dr. Cox, a dermatologist at the University of North Carolina at Chapel Hill and principal investigator in the pivotal clinical trial that led to Food and Drug Administration approval of Voluma.
This characteristic of the highly cohesive 20-mg/mL hyaluronic acid filler has important implications for the product’s optimal use and achieving maximal patient satisfaction. For one, Voluma absolutely should not be used for patients with thin skin. For these patients, a more effective option is a product containing monophasic monodensified hyaluronic acids, such as Juvederm Ultra or Ultra Plus, Dr. Cox said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
As a rule of thumb, approximately 40% of Voluma is needed compared with the amount of monophasic monodensified hyaluronic acid fillers dermatologists are accustomed to working with, she said.
It’s crucial to inject Voluma extremely slowly, Dr. Cox emphasized. She advised scheduling 30 minutes for a patient’s first volumizing session. It’s also important to avoid using a large bolus, and be sure not to overcorrect. Voluma loves water and will draw it from tissue, Dr. Cox noted. Therefore it’s important to use the exact correction. Remember that at 9 months post treatment, 50% or more of the original correction will remain, so the 9-month mark is a good time to schedule a touch-up, she added.
Another pearl: Inject struts or pillars from the periostium; then blend and mold them, Dr. Cox continued.
She urged her colleagues to be conservative in using Voluma around the eyes. In her experience, too much Voluma in this area causes the product to migrate anteriorly on the cheek, which could result in an unwelcome doughy appearance.
To achieve improvement in the submalar area, it’s best to utilize tangential microdroplets of Voluma after reconstitution with saline so the filler doesn’t affect the nerve and cause a lip drop, according to Dr. Cox.
Should it become necessary to dissolve Voluma, use twice as much hyaluronidase (Hylenex).
Dr. Cox reported serving as a consultant to Allergan and Medicis and serving as principal investigator in trials funded by those companies, as well as in studies funded by Revance and Kythera.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR