User login
Optimizing combination therapy for type 2 diabetes in adolescents and adults: A case-based approach
- Children and adolescents who are overweight and have additional risk factors (ie, high-risk ethnic group or signs of insulin resistance) should be screened for diabetes every 2 years (SOR: C).
- Management of type 2 diabetes in all age groups requires a multifactorial approach that addresses not only glycemic control (A1C <7%) but also other cardiovascular risk factors such as hypertension, dyslipidemia, and obesity (SOR: A).1
- Most patients with type 2 diabetes will eventually require combination therapy with 2 or more agents to attain and maintain glycemic control (SOR: A).2,3
- Combining an insulin secretagogue (ie, sulfonylurea or meglitinide) and an insulin sensitizer (ie, metformin or a glitazone) capitalizes on unique mechanisms of action and results in Significant A1C lowering (SOR: C).
- If a patient is unable to achieve glycemic control on 2 oral agents, insulin therapy is an appropriate consideration and should be added to oral agents (rather than substituted) (SOR: B).4
Diabetes affects 18.2 million people in the United States.5 It is a leading cause of morbidity and mortality.5 Diabetes is associated with more than $90 billion in direct medical costs and with an estimated $40 billion in indirect costs (ie, disability, work loss, and premature mortality).5 Type 2 diabetes accounts for 90% to 95% of total cases. It disproportionately affects certain minority populations, and it is increasingly being identified in children and adolescents.5-7
The obesity epidemic has received tremendous media and public attention and has sobering implications for the development of metabolic syndrome, which is often the precursor to diabetes, and cardiovascular disease (CVD).8,9 In 1 study, the hazard ratio for development of diabetes was 3.85 for individuals who gained 20 kg or more over approximately 10 years, as compared with individuals whose weight remained relatively stable over the same period.10 Obesity is associated with elevations in free fatty acid levels and in other compounds which contribute to insulin resistance11 —a key underlying defect in metabolic syndrome and type 2 diabetes. Thus, particularly in genetically predisposed individuals, obesity (through elevated fatty acids) may be the factor that drives insulin resistance to clinical diabetes. In addition, elevated free fatty acid levels also may contribute to the other key underlying defect in type 2 diabetes: progressive pancreatic β-cell loss which results in insulin deficiency.12 Similar to the trend in adults, childhood obesity has now reached epidemic proportions and has been associated with the increased prevalence of glucose intolerance, metabolic syndrome, and biomarkers of increased CVD risk in this young population.13-15
Type 2 diabetes in adolescents
CASE 1 Suspected new-onset type 2 diabetes
A 16-year-old Hispanic boy presents for treatment of weight loss. He is a defensive tackle on the high school football team and has a strong appetite. His height is 6 ft 1 in and he weighs 250 lb; his body mass index (BMI) is 32 kg/m2, and most of the fat is abdominally distributed (waist circumference, 42 in). Both of his parents are obese, and a grandfather and aunt have type 2 diabetes. Further examination reveals a blood pressure (BP) level of 135/87 mm Hg and acanthosis nigricans. A random fingerstick test shows a blood glucose level of 240 mg/dL.
Until recently, type 2 diabetes rarely was observed in children, occurring in only 1% to 2% of children with new-onset diabetes.16 However, depending on the sampling strategy, race or ethnicity of the population, and the region of the country sampled, it now has been estimated that type 2 diabetes accounts for anywhere from 8% to 45% of all diabetes reported among children and adolescents.6,16 Prevalence estimates of pediatric type 2 diabetes in population-based studies range from 4.1 per 1,000 in the National Health and Nutrition Survey (NHANES III) to 50.9 per 1,000 among Pima Indians in Arizona.17 Unlike the trends of increasing incidence and prevalence of type 2 diabetes in the pediatric population, a similar trend in type 1 diabetes has not been observed.7
The diagnosis and treatment of type 2 diabetes in pediatric patients can be challenging. Type 2 diabetes is associated with an increased BMI and is more common in adolescents than in younger children.6 Puberty is associated with relative insulin resistance and, along with the time-related effects of obesity, resistance may play a role in the subsequent onset of type 2 diabetes in pediatric patients. However, as an increasing number of children become obese at an earlier age, the onset of disease may occur earlier.
Other risk factors for type 2 diabetes in childhood include having a first- or second-degree relative with the disease or non-European ancestry (Americans of African, Hispanic, Asian, Pacific Islander, or Native American descent). In addition, acanthosis nigricans is a skin condition that serves as a specific, though insensitive, marker of insulin resistance. Among adolescent females, polycystic ovary syndrome has been associated with insulin resistance irrespective of excess weight or frank obesity18 and may be associated with an increased risk of type 2 diabetes.6
TABLE 1 provides criteria for screening for type 2 diabetes in children. The adolescent in the case presented has several risk factors for type 2 diabetes, including obesity, a positive family history, Hispanic descent, and acanthosis nigricans. To more definitively diagnose type 2 diabetes, additional laboratory tests are needed, including assessment of blood glucose and insulin production, as well as the presence of autoantibodies.
TABLE 1
Screening recommendations for type 2 diabetes in children
| Testing for type 2 diabetes is recommended every 2 years at onset of puberty or aged >10 years (whichever comes first) if the child* |
|
| *Clinical judgment should be used to test for diabetes in high-risk patients who do not meet these criteria. |
| †Overweight is defined as BMI >85th percentile for age and sex, weight for height >85th percentile, or weight >120% of ideal for height. |
| Copyright © 2004 American Diabetes Association from Diabetes Care,2004;27(suppl 1):S15-S35. Reprinted with permission. |
CASE 1 Laboratory assessment
The patient has a fasting plasma glucose (FPG) level of 215 mg/dL. β-Cell or insulin autoantibodies are not detected. He has a normal-to-high fasting C-peptide level, microalbuminuria, and a serum creatinine level of 0.8 mg/dL. His lipid panel results include: total cholesterol, 234 mg/dL; low-density lipoprotein (LDL) cholesterol, 159 mg/dL; high-density lipoprotein (HDL) cholesterol, 45 mg/dL; and triglycerides, 150 mg/dL.
A comparison of the typical presentation and laboratory findings in pediatric type 1 and type 2 diabetes is listed in TABLE 2. This information underscores that there is significant overlap between the 2 disease classifications.
The laboratory results for this patient confirm a diagnosis of type 2 diabetes. C peptide is a marker of endogenous insulin production and is particularly helpful in the classification of diabetes when it is high, which is indicative of type 2 diabetes. However, it should be noted that a finding of low C-peptide levels does not rule out type 2 diabetes since there is a possibility that glucose toxicity is temporarily limiting insulin production. Indeed, in such a case, insulin therapy can be initiated to establish glycemic control and promote endogenous insulin production by reducing glucose toxicity. Similarly, although the absence of pancreatic β-cells and insulin autoantibodies is consistent with a diagnosis of type 2 diabetes, the presence of such antibodies does not completely rule out type 2 diabetes.19
Like many patients with type 2 diabetes, the current patient exhibits a cluster of CVD risk factors that characterize the metabolic syndrome, including dyslipidemia (elevated total cholesterol, LDL cholesterol, triglyceride levels, and low HDL cholesterol levels), hypertension, glucose intolerance, hyperinsulinemia, and central or abdominal obesity. This is not surprising as an estimated 30% of overweight adolescents, defined as those with BMI at or above the 95th percentile, meet the criteria for metabolic syndrome.14
TABLE 2
Classification of type 1 and type 2 diabetes in pediatric patients
| TYPE 1 DIABETES | TYPE 2 DIABETES | |
|---|---|---|
| Age | Throughout childhood | Pubertal |
| Onset | Acute, severe | Mild to severe, often insidious |
| Insulin secretion | Very low | Variable |
| C-peptide level | Absent | Variable |
| Insulin sensitivity* | Normal | Decreased |
| Insulin dependence† | Permanent | No |
| Genetics | Polygenic | Polygenic |
| Race/ethnic distribution | All (low frequency in Asians) | African American, Hispanic, Asian, American Indian, Pacific Islanders |
| Association | ||
| Obesity | No | Yes, strong |
| Acanthosis nigricans | No | Yes |
| Autoimmunity | Yes | No |
| Presence of autoantibodies | Yes | No‡ |
| *Insulin sensitivity is given as a pathogenic factor. | ||
| † In the absence of acute illness or other stress. | ||
| ‡ Although autoimmunity is not a cause of type 2 diabetes, diabetic autoimmune markers can be present at times and should not be used to rule out a diagnosis of type 2 diabetes in children and adolescents.19 | ||
| Copyright © 2004 American Diabetes Association from Diabetes Care, 1999;22:345-354. Reprinted with permission. | ||
CASE 1 Initial therapy
The patient is provided with education on lifestyle modifications to reduce weight and obtain better control of glucose, lipids, and BP. Instructions include ways to improve his eating habits and to increase his physical activity when away from the football field, such as limiting time spent watching TV and playing video games and increasing exercise time and effort. The patient also is instructed on self-monitoring for blood glucose (SMBG) and is given a referral to an ophthalmologist to determine whether there is any baseline retinopathy.
At his 3-month follow-up, the patient’s A1C is 8.7%, and his weight has not changed. At this point, lifestyle modifications are reinforced, and pharmacotherapy with extended-release metformin is initiated and titrated to 2,000 mg/d.
Typically, the first approach to managing type 2 diabetes involves dietary changes and instituting an exercise program to reduce weight and to improve insulin sensitivity. This was the approach used in the patient described above. However, as is frequently the case, lifestyle modifications by themselves are insufficient to meet the American Diabetes Association (ADA) or American Association of Clinical Endocrinologists targets for glycemic control (A1C <7% and <6.5%, respectively).20,21 It is important to note here that the ADA does recommend less stringent glycemic control guidelines in very young children (ie, those aged less than 13 years).16 As is the case for adults with diabetes, pharmacologic therapies typically are needed in addition to lifestyle changes to lower elevated blood glucose levels. However, unlike the situation with adults, the list of drugs approved by the Food and Drug Administration for use in pediatric patients is limited (ie, currently only metformin and insulin preparations are approved for pediatric use).
Metformin was chosen as the initial therapy in this adolescent for several reasons, including demonstrated efficacy and tolerability in pediatric studies, approval for use in this population, and because it is generally not associated with weight gain. The patient needs a 1.7% reduction in A1C; therefore, metformin was titrated to the maximum daily dosage of 2,000 mg (expected to, on average, reduce A1C by 1% to 2%). In a recent, randomized, double-blind, placebo-controlled trial of pediatric patients (aged 10 to 16 years) with type 2 diabetes,22 metformin 1,000 mg bid significantly reduced baseline-adjusted mean A1C values compared with placebo (7.5% vs 8.6%, P<0.001) without negatively affecting body weight or lipid levels. The adverse events profile of metformin in children was similar to that observed in adults, primarily involving gastrointestinal events.
CASE 1 Monotherapy inadequate
After 6 months on metformin therapy, the patient returns for follow-up. His A1C measure has improved to 7.7%, but his weight remains unchanged. At this point, a discussion is initiated about using combination therapy to bring his diabetes under control.
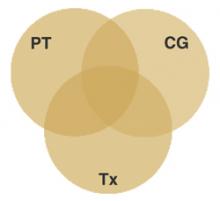
This case study illustrates an important point about the treatment of type 2 diabetes: pharmacologic therapy with a single antidiabetic agent often is insufficient to reach target goals for glycemic control.2 Frequently, this reflects the insidious, progressive nature of the disease, which may be present for years before being recognized. As a general rule, combination therapy involves the use of drugs with different mechanisms of action. Clinical trials evaluating combination therapy generally follow this rationale.
Since there are limited pediatric data for the majority of oral agents, the clinical decision regarding which agents to use in combination often is based on the available data in adults. Information regarding efficacy, safety, and tolerability for the different oral antidiabetic drugs used in adults with type 2 diabetes is provided in TABLE 3.
Secretagogues (ie, sulfonylureas and meglitinides) have been reported to typically reduce A1C values by 1% to 2% at maximal doses. Generally, the shorteracting meglitinides have been considered useful for reducing postprandial hyperglycemia and are taken before meals.23 Unlike traditional sulfonylureas, glimepiride also has demonstrated efficacy in controlling postprandial hyperglycemia.24 All patients starting therapy with a secretagogue should be counseled on recognition of hypoglycemic symptoms and appropriate self-treatment. While severe hypoglycemia is not common in type 2 diabetes, it can occur with any agent that increases insulin secretion.
The glitazones lower A1C levels by an estimated 1% to 1.5%. Although they primarily reduce insulin resistance, they also may have beneficial effects on blood lipids, BP, and inflammatory markers associated with CVD, suggesting a theoretical benefit for reducing macrovascular complications.25 Glitazones, however, have been associated with weight gain and fluid retention, which in adults may unmask or exacerbate congestive heart failure.25 Additionally, although pioglitazone and rosiglitazone do not appear to carry the same risk of hepatotoxicity as the first member of the class, troglitazone, there have been a few case reports of liver injury or failure in patients treated with pioglitazone26-28 or rosiglitazone.29-31 In the absence of pediatric and long-term data, caution is warranted with use of these agents in this population.
α-Glucosidase inhibitors are helpful in controlling mealtime glycemic excursions and may have utility in patients who require smaller reductions in A1C. Use of these relatively safe agents is limited due to gastrointestinal side effects (ie, diarrhea and flatulence are common),32 which can prevent titration to optimal doses. Since the primary mechanism of action is inhibition of carbohydrate digestion, patients who are using these agents in combination with therapies that can cause hypoglycemia should be counseled to use simple sugars (ie, glucose tablets) rather than complex carbohydrates to self-treat hypoglycemia.
If oral agents cannot achieve adequate glycemic control, addition of insulin is a rational, well-tolerated, and effective option.3,4,33 Insulin therapy is often underutilized and delayed in patients with type 2 diabetes who would benefit from earlier introduction of such therapy.34 The pediatric experience with insulin is extensive, but mostly in type 1 diabetes. The potential need for and benefits of insulin therapy may be discussed with patients as early as at the time of diagnosis to help alleviate some of the anxiety patients have regarding this therapy.35
TABLE 3
Available oral antidiabetic agents
| DRUG | DAILY DOSE (MG) | DOSES/DAY | PRIMARY MECHANISM(S) | EXPECTED A1C REDUCTION (%) | COMMON ADVERSE EFFECTS |
|---|---|---|---|---|---|
| Sulfonylureas | Augment insulin secretion | 1–2 | Hypoglycemia, weight gain* | ||
| Glimepiride | 1–8 | 1 | |||
| Glipizide | 2.5–40 | 1–2 | |||
| Glipizide controlled release | 2.5–20 | 1 | |||
| Glyburide | 2.5–20 | 1–2 | |||
| Glyburide micronized | 3–12 | 1–2 | |||
| Meglitinides | Augment insulin secretion | 1–2 | Hypoglycemia, weight gain | ||
| Repaglinide | 0.5–16 | 2–4 | |||
| Nateglinide | 360 | 2–4 | |||
| Biguanides | Increase sensitivity to insulin, decrease hepatic glucose production | 1–2 | Gastrointestinal symptoms† | ||
| Metformin† | Adults: 500–2,550 Children (10–16 yr) 500–2,000 | 2–3 | |||
| Thiazolidinediones | Increase sensitivity to insulin | 1–1.5 | Fluid retention, weight gain‡ | ||
| Rosiglitazone | 2–8 | 1–2 | |||
| Pioglitazone | 15–45 | 1 | |||
| α-Glucosidase Inhibitors | Slow digestion of carbohydrates | 0.5–1 | Flatulence, gastro-intestinal discomfort, weight gain | ||
| Acarbose | 75–300 | 3 | |||
| Miglitol | 75–300 | 3 | |||
| *Glimepiride had a neutral effect on weight in clinical studies and was associated with a lower incidence of hypoglycemia than other sulfonylureas.49-51 | |||||
| † Lactic acidosis has been reported with metformin use, but is extremely rare. The risk may be related to an underlying predisposition to lactic acidosis. | |||||
| ‡ There have been some reports of liver toxicity with second-generation thiazolidinediones. | |||||
| Adapted from American Association of Clinical Endocrinologists;21 Nathan DM. Clinical practice. Initial Management of glycemia in type 2 diabetes mellitus.N Engl J Med. 2002;347:1342-1349. | |||||
Type 2 diabetes in adults
CASE 2 Woman with chronic diabetes
A 60-year-old woman presents for her annual checkup complaining of weight gain, fatigue, and tingling in her feet. Her recent history includes recurrent urinary tract and yeast infections. When initially diagnosed with type 2 diabetes 5 years ago, she had been counseled to increase activity to reduce weight; however, she had been unable to maintain consistent effort. She is 5 ft 4 in tall and weighs 230 lb (BMI, 39.5 kg/m2) with a waist circumference of 40 in. Her weight has fluctuated, but she has had a net gain of 30 lb over the last 5 years. Education and lifestyle modification efforts were reinitiated 1 year ago. The patient is a smoker and has cut her habit to 5 cigarettes per day. Her A1C and total cholesterol levels 1 year ago were 7.8% and 203 mg/dL, respectively. The patient also had cataract surgery 1 year ago. Her current medications include lisinopril 40 mg/d, furosemide 40 mg bid, and rosiglitazone 4 mg/d. She performs SMBG infrequently.
On examination, her BP is 125/72 mm Hg. A random fingerstick blood glucose test shows 210 mg/dL. She exhibits normal monofilament sensation, vibratory sensation, and ankle jerks. She also shows signs of mild pedal edema with no foot lesions and normal pedal pulses.
There are a number of signs suggesting this patient’s diabetes is inadequately controlled, including her complaints of fatigue and repeated yeast infections. Poorly controlled diabetes also is associated with peripheral neuropathy, which may manifest as a tingling sensation or numbness that begins in the feet and moves upward; however, her physical examination is negative for neuropathy.36 A random blood glucose level is of limited value and should not be relied upon as an indicator of the patient’s glycemic status. An A1C measurement is overdue for this patient and will reflect her overall glycemic control in recent months.
A total cholesterol level is rarely adequate for clinical decision making and thus a follow-up lipid profile is warranted. Her BP is well controlled with her current antihypertension regimen. The ADA guidelines recommend adequate treatment of hypertension (target BP, <130/80 mm Hg) in diabetic patients and suggest use of an angiotensin-converting enzyme (ACE) inhibitor or angiotensin-receptor blocker (ARB) because, in addition to their antihypertensive effects, these agents may provide renal benefits for patients with albuminuria or renal insufficiency.20 More typically, a thiazide rather than a loop diuretic is used in combination with an ACE inhibitor (or another antihypertensive drug class) as treatment for hypertension but, since the patient’s BP is well controlled with her current regimen and she has mild pedal edema, the loop diuretic may be maintained.
Her weight gain and peripheral edema may in part be due to rosiglitazone treatment. Edema that is not caused by congestive heart failure is not a contraindication for glitazone use but requires close monitoring and should lead to a consideration of alternate therapy.25
CASE 2 Laboratory assessment
The patient’s glycemic indices are: FPG, 184 mg/dL; A1C, 9.4%; postprandial glucose (PPG), 311 mg/dL. A random urine sample reveals microalbuminuria (protein/creatinine, 38 μg/mg). Her serum creatinine is 1.6 mg/dL. Her lipid panel reveals: total cholesterol, 271 mg/dL; LDL cholesterol, 165 mg/dL; HDL cholesterol, 35 mg/dL; and triglycerides, 355 mg/dL. Liver function tests are within normal limits. Further evaluation indicates that she does not have congestive heart failure.
The laboratory results indicate very poor control of overall and postmeal glucose levels. In addition, she now has microalbuminuria. Although poor adherence with therapy should be ruled out, the loss of control with a previously effective therapy is not unusual and underscores the progressive nature of diabetes.
Collectively, this patient’s poor glycemic control, dyslipidemia and central obesity, place her at a very high risk for CVD.37
CASE 2 Therapy adjusted
Glimepiride 4 mg/d is added to the rosiglitazone; in addition, atorvastatin 20 mg/d and fenofibrate 160 mg/d are prescribed. Lifestyle modifications (eg, dietary changes, exercise, smoking cessation) are reinforced, and the patient is referred to a certified diabetes educator.
The comprehensive approach taken for this patient is consistent with that advocated by the results in the Steno-2 Study. Gaede et al1 demonstrated that a targeted, intensified, multifactorial, interventional approach to improving macrovascular and microvascular risk factors in patients with type 2 diabetes reduces the risk of macrovascular and microvascular diabetic complications by about 50% compared with conventional treatment.1 Specifically, patients receiving intensive therapy had a significantly lower risk of CVD, nephropathy, retinopathy and autonomic neuropathy.1 Intensive, multifactorial therapy involved dietary interventions; a consistent exercise program; smoking cessation; use of ACE inhibitors (or ARBs for patients intolerant to ACE inhibitors) for renal benefits and combined with diuretics and other agents, if necessary, to treat hypertension; lipid-lowering therapy to treat hyperlipidemia (statins, plus fibrates for isolated cases of hypertriglyceridemia); pharmacotherapy for glucose control; daily vitamin-mineral supplements; and daily aspirin as a secondary measure for the prevention of CVD.
In general, pharmacotherapy of diabetes should be individualized, since not all agents are equally appropriate for all patients. A variety of studies have demonstrated that adding a second antidiabetic agent to a first typically results in additional improvements in glycemic control.38-47 In the example here, a sulfonylurea was chosen because of its complementary mechanism of action with an insulin sensitizer. Since the patient had an elevated serum creatinine, metformin was not considered to be an appropriate choice. In addition, the combination of a glitazone with sulfonylurea therapy has been reported to achieve reductions in A1C40,48 at least comparable to those reported in analyses of the combination of a glitazone with metformin.40,45 TABLE 4 provides reported reductions in A1C that have been observed in clinical trials of various combination regimens in type 2 diabetes. Since these are not head-to-head comparisons of the various regimens, the data simply illustrate the range of A1C reductions that may be achieved with combination therapy. In this patient, glimepiride was chosen because of its weight neutral effect,49 potentially lower incidence of hypoglycemia,50,51 favorable effect on postprandial glucose (that may ameliorate cardiovascular risk),52-56 and once-daily dosing.
Given the progressive natural history of type 2 diabetes, and the fact that this patient currently requires a >2% A1C reduction, it is reasonable to anticipate that she will eventually need insulin to attain glycemic control. Recently, Riddle et al4 demonstrated that addition of a basal insulin (neutral protamine Hagedorn [NPH] or glargine) to existing oral agents reduced the A1C to <7% in the majority of patients with type 2 diabetes. Insulin glargine was associated with significantly less hypoglycemia than NPH insulin. This is an important consideration since hypoglycemia remains a major barrier to insulin therapy in type 2 diabetes.57 Sulfonylurea therapy should be maintained when insulin is initiated, as this combination has been demonstrated to be highly effective in improving glycemic control and is associated with a low incidence of hypoglycemia.3,33 In the current patient, the addition of basal insulin glargine would complement her other antidiabetic therapies. Insulin glargine would primarily normalize her FBG, while glimepiride controls PPG and rosiglitazone improves insulin sensitivity. Thus, this regimen would address the 2 most important defects in type 2 diabetes—insulin deficiency and insulin resistance.
Clinical trials have shown that combination therapy with oral agents and insulin, as well as with multiple oral agents, is effective.4,38,39 However, more long-term and comparative studies of these multiple-agent combinations are needed. It is important to set expectations with patients that gaining good control of diabetes frequently requires combination therapy with multiple agents with the ultimate goal of avoiding the onset of new complications or of delaying progression of existing complications.
TABLE 4
A1C reductions noted in clinical trials and reports of combination therapy for type 2 diabetes
| REGIMEN | A1C REDUCTION (%) |
|---|---|
| Sulfonylurea + metformin58 | ~1.7 |
| Sulfonylurea + glitazone40,48 | ~1.3 |
| Sulfonylurea + α-glucosidase inhibitor59 | ~0.9 |
| Metformin + meglitinide46 | ~1.4 |
| Metformin + glitazone40,45 | ~1 |
| Insulin + oral agents4 | Open to target |
Summary
The increased prevalence of obesity, metabolic syndrome, and type 2 diabetes in adolescents and adults is an ominous sign of more serious disease in the future. A concerted effort on the part of health care professionals to improve the care of patients with type 2 diabetes is needed to bring this burgeoning problem under better control. Diabetes is a recognized coronary risk equivalent; thus, a comprehensive multifactorial approach that rigorously addresses glycemia, as well as elevated BP and lipids, is recommended.
Most patients with type 2 diabetes will eventually require combination therapy with 2 or more agents to attain and maintain glycemic control.2,3 In particular, combinations of agents with complementary mechanisms of action (eg, an insulin sensitizer with a secretagogue) demonstrate greater improvements in glycemic control. Based on the progressive nature of diabetes, a principle in the pharmacotherapy of glucose control is that, in absence of untoward effects, if a given agent is secondarily unable to provide adequate glycemic control (ie, there was initial improvement in glucose control and then subsequent deterioration), additional agents—whether oral agents or insulin—should be added rather than substituted.
Disclosures:
Dr. Elasy has done consultation for Aventis Pharmaceuticals. Dr. Levy has received grants/research support from Aventis Pharmaceuticals, Eli Lilly and Co., Merck & Co., Novartis Pharmaceuticals, Novo Nordisk Pharmaceuticals Inc., and Pfizer Inc. He is a consultant and on the speaker’s bureau for Aventis Pharmaceuticals, Eli Lilly and Co., Novartis Pharmaceuticals, Novo Nordisk Pharmaceuticals Inc, Pfizer Inc, Takeda Pharmaceuticals America, Inc., Bristol-Myers Squibb Company, GlaxoSmithKline, and Wyeth-Ayerst Pharmaceuticals. Dr. Davis has received research grants from Aventis Pharmaceuticals, Eli Lilly and Co., and Bayer Pharmaceuticals Corporation.
1. Gaede P, Vedel P, Larsen N, Jensen GVH, Parving H-H, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383-393.
2. Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA. 1999;281:2005-2012.
3. Wright A, Burden AC, Paisey RB, Cull CA, Holman RR. Sulfonylurea inadequacy. Efficacy of addition of insulin over 6 years in patients with type 2 diabetes in the U.K. Prospective Diabetes Study (UKPDS 57). Diabetes Care. 2002;25:330-336.
4. Riddle MC, Rosenstock J, Gerich J. The Treat-to-Target Trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26:3080-3086.
5. National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics fact sheet: general information and national estimates on diabetes in the United States, 2003. 1-14. 2003.
6. Aye T, Levitsky LL. Type 2 diabetes: an epidemic disease in childhood. Curr Opin Pediatr. 2003;15:411-415.
7. Rosenbloom AL. Increasing incidence of type 2 diabetes in children and adolescents: treatment considerations. Paediatr Drugs. 2002;4:209-221.
8. Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291:2847-2850.
9. Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723-1727.
10. Ford ES, Williamson DF, Liu S. Weight change and diabetes incidence: findings from a national cohort of US adults. Am J Epidemiol. 1997;146:214-222.
11. Leong KS, Wilding JP. Obesity and diabetes. Baillieres Best Pract Res Clin Endocrinol Metab. 1999;13:221-237.
12. Shimabukuro M, Zhou YT, Levi M, Unger RH. Fatty acid-induced β-cell apoptosis: a link between obesity and diabetes. Proc Natl Acad Sci U S A. 1998;95:2498-2502.
13. Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362-2374.
14. Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003;157:821-827.
15. Sinha R, Fisch G, Teague B, et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med. 2002;346:802-810.
16. American Diabetes Association. Type 2 diabetes in children and adolescents. Diabetes Care. 2000;23:381-389.
17. Fagot-Campagna A, Pettitt DJ, Engelgau MM, et al. Type 2 diabetes among North American children and adolescents: an epidemiologic review and a public health perspective. J Pediatr. 2000;136:664-672.
18. Pugeat M, Ducluzeau PH. Insulin resistance, polycystic ovary syndrome and metformin. Drugs. 1999;58(suppl 1):41-46.
19. Hathout EH, Thomas W, El Shahawy M, Nahab F, Mace JW. Diabetic autoimmune markers in children and adolescents with type 2 diabetes. Pediatrics. 2001;107:E102.-
20. ADA. American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2004;27(suppl 1):S15-S35.
21. American Association of Clinical Endocrinologists. The American Association of Clinical Endocrinologists Medical Guidelines for the Management of Diabetes Mellitus: the AACE system of intensive diabetes self-management-2002 update. Endocr Pract. 2002;8(suppl 1):40-82.
22. Jones KL, Arslanian S, Peterokova VA, Park JS, Tomlinson MJ. Effect of metformin in pediatric patients with type 2 diabetes: a randomized controlled trial. Diabetes Care. 2002;25:89-94.
23. Monnier L. Is postprandial glucose a neglected cardiovascular risk factor in type 2 diabetes? Eur J Clin Invest. 2000;30(suppl 2):3-11.
24. Sonnenberg GE, Garg DC, Weidler DJ, et al. Short-term comparison of once- versus twice-daily administration of glimepiride in patients with non-insulin-dependent diabetes mellitus. Ann Pharmacother. 1997;31:671-676.
25. Nesto RW, Bell D, Bonow RO, et al. Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American Heart Association and American Diabetes Association. Diabetes Care. 2004;27:256-263.
26. May LD, Lefkowitch JH, Kram MT, Rubin DE. Mixed hepatocellular-cholestatic liver injury after pioglitazone therapy. Ann Intern Med. 2002;136:449-452.
27. Pinto AG, Cummings OW, Chalasani N. Severe but reversible cholestatic liver injury after pioglitazone therapy. Ann Intern Med. 2002;137:857.-
28. Maeda K. Hepatocellular injury in a patient receiving pioglitazone. Ann Intern Med. 2001;135:306.-
29. Dhawan M, Agrawal R, Ravi J, et al. Rosiglitazone-induced granulomatous hepatitis. J Clin Gastroenterol. 2002;34:582-584.
30. Forman LM, Simmons DA, Diamond RH. Hepatic failure in a patient taking rosiglitazone. Ann Intern Med. 2000;132:118-121.
31. Al Salman J, Arjomand H, Kemp DG, Mittal M. Hepatocellular injury in a patient receiving rosiglitazone. A case report. Ann Intern Med. 2000;132:121-124.
32. Coniff RF, Shapiro JA, Robbins D, et al. Reduction of glycosylated hemoglobin and postprandial hyperglycemia by acarbose in patients with NIDDM. A placebo-controlled dose-comparison study. Diabetes Care. 1995;18:817-824.
33. Fritsche A, Schweitzer MA, Haring HU. Glimepiride combined with morning insulin glargine, bedtime neutral protamine hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes. A randomized, controlled trial. Ann Intern Med. 2003;138:952-959.
34. Hirsch IB. Treatment of patients with severe insulin deficiency; what we have learned over the past 2 years. Am J Med. 2004;116(suppl 3A):17S-22S.
35. Hunt LM, Valenzuela MA, Pugh JA. NIDDM patients’ fears and hopes about insulin therapy. The basis of patient reluctance. Diabetes Care. 1997;20:292-298.
36. Frykberg RG. Diabetic foot ulcers: pathogenesis and management. Am Fam Physician. 2002;66:1655-1662.
37. Lagrand WK, Visser CA, Hermens WT, et al. C-reactive protein as a cardiovascular risk factor: more than an epiphenomenon? Circulation. 1999;100:96-102.
38. Dailey GE, III, Noor MA, Park JS, Bruce S, Fiedorek FT. Glycemic control with glyburide/metformin tablets in combination with rosiglitazone in patients with type 2 diabetes: a randomized, double-blind trial. Am J Med. 2004;116:223-229.
39. Aljabri K, Kozak SE, Thompson DM. Addition of pioglitazone or bedtime insulin to maximal doses of sulfonylurea and metformin in type 2 diabetes patients with poor glucose control: a prospective, randomized trial. Am J Med. 2004;116:230-235.
40. Rendell MS, Glazer NB, Ye Z. Combination therapy with pioglitazone plus metformin or sulfonylurea in patients with Type 2 diabetes: influence of prior antidiabetic drug regimen. J Diabetes Complications. 2003;17:211-217.
41. Fonseca V, Grunberger G, Gupta S, Shen S, Foley JE. Addition of nateglinide to rosiglitazone monotherapy suppresses mealtime hyperglycemia and improves overall glycemic control. Diabetes Care. 2003;26:1685-1690.
42. Raskin P, Klaff L, McGill J, et al. Efficacy and safety of combination therapy: repaglinide plus metformin versus nateglinide plus metformin. Diabetes Care. 2003;26:2063-2068.
43. Schwartz S, Sievers R, Strange P, Lyness WH, Hollander P. Insulin 70/30 mix plus metformin versus triple oral therapy in the treatment of type 2 diabetes after failure of two oral drugs: efficacy, safety, and cost analysis. Diabetes Care. 2003;26:2238-2243.
44. Wolffenbuttel BH, Gomis R, Squatrito S, Jones NP, Patwardhan RN. Addition of low-dose rosiglitazone to sulphonylurea therapy improves glycaemic control in type 2 diabetic patients. Diabet Med. 2000;17:40-47.
45. Fonseca V, Rosenstock J, Patwardhan R, Salzman A. Effect of metformin and rosiglitazone combination therapy in patients with type 2 diabetes mellitus: a randomized controlled trial. JAMA. 2000;283:1695-1702.
46. Moses R, Slobodniuk R, Boyages S, et al. Effect of repaglinide addition to metformin monotherapy on glycemic control in patients with type 2 diabetes. Diabetes Care. 1999;22:119-124.
47. Rosenstock J, Brown A, Fischer J, et al. Efficacy and safety of acarbose in metformin-treated patients with type 2 diabetes. Diabetes Care. 1998;21:2050-2055.
48. Kipnes MS, Krosnick A, Rendell MS, Egan JW, Mathisen AL, Schneider RL. Pioglitazone hydrochloride in combination with sulfonylurea therapy improves glycemic control in patients with type 2 diabetes mellitus: a randomized, placebo-controlled study. Am J Med. 2001;111:10-17.
49. Weitgasser R, Lechleitner M, Luger A, Klingler A. Effects of glimepiride on HbA(1c) and body weight in Type 2 diabetes: results of a 1.5-year follow-up study. Diabetes Res Clin Pract. 2003;61:13-19.
50. Holstein A, Plaschke A, Egberts EH. Lower incidence of severe hypoglycaemia in patients with type 2 diabetes treated with glimepiride versus glibenclamide. Diabetes Metab Res Rev. 2001;17:467-473.
51. Dills DG, Schneider J. Clinical evaluation of glimepiride versus glyburide in NIDDM in a double-blind comparative study. Glimepiride/Glyburide Research Group. Horm Metab Res. 1996;28:426-429.
52. Gerich JE. Clinical significance, pathogenesis, and management of postprandial hyperglycemia. Arch Intern Med. 2003;163:1306-1316.
53. Shaw JE, Hodge AM, de Court, Chitson P, Zimmet PZ. Isolated post-challenge hyperglycaemia confirmed as a risk factor for mortality. Diabetologia. 1999;42:1050-1054.
54. Saydah SH, Miret M, Sung J, Varas C, Gause D, Brancati FL. Postchallenge hyperglycemia and mortality in a national sample of U.S. adults. Diabetes Care. 2001;24:1397-1402.
55. Decode Study Group. Glucose tolerance and cardiovascular mortality: comparison of fasting and 2-hour diagnostic criteria. Arch Intern Med. 2001;161:397-405.
56. Korytkowski M, Thomas A, Reid L, Tedesco MB, Gooding WE, Gerich J. Glimepiride improves both first and second phases of insulin secretion in type 2 diabetes. Diabetes Care. 2002;25:1607-1611.
57. Riddle MC. The underuse of insulin therapy in North America. Diabetes Metab Res Rev. 2002;18:S42-S49.
58. DeFronzo RA, Goodman AM. The Multicenter Metformin Study Group. Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. N Engl J Med. 1995;333:541-549.
59. Lin BJ, Wu HP, Huang HS, et al. Efficacy and tolerability of acarbose in Asian patients with type 2 diabetes inadequately controlled with diet and sulfonylureas. J Diabetes Complications. 2003;17:179-185.
- Children and adolescents who are overweight and have additional risk factors (ie, high-risk ethnic group or signs of insulin resistance) should be screened for diabetes every 2 years (SOR: C).
- Management of type 2 diabetes in all age groups requires a multifactorial approach that addresses not only glycemic control (A1C <7%) but also other cardiovascular risk factors such as hypertension, dyslipidemia, and obesity (SOR: A).1
- Most patients with type 2 diabetes will eventually require combination therapy with 2 or more agents to attain and maintain glycemic control (SOR: A).2,3
- Combining an insulin secretagogue (ie, sulfonylurea or meglitinide) and an insulin sensitizer (ie, metformin or a glitazone) capitalizes on unique mechanisms of action and results in Significant A1C lowering (SOR: C).
- If a patient is unable to achieve glycemic control on 2 oral agents, insulin therapy is an appropriate consideration and should be added to oral agents (rather than substituted) (SOR: B).4
Diabetes affects 18.2 million people in the United States.5 It is a leading cause of morbidity and mortality.5 Diabetes is associated with more than $90 billion in direct medical costs and with an estimated $40 billion in indirect costs (ie, disability, work loss, and premature mortality).5 Type 2 diabetes accounts for 90% to 95% of total cases. It disproportionately affects certain minority populations, and it is increasingly being identified in children and adolescents.5-7
The obesity epidemic has received tremendous media and public attention and has sobering implications for the development of metabolic syndrome, which is often the precursor to diabetes, and cardiovascular disease (CVD).8,9 In 1 study, the hazard ratio for development of diabetes was 3.85 for individuals who gained 20 kg or more over approximately 10 years, as compared with individuals whose weight remained relatively stable over the same period.10 Obesity is associated with elevations in free fatty acid levels and in other compounds which contribute to insulin resistance11 —a key underlying defect in metabolic syndrome and type 2 diabetes. Thus, particularly in genetically predisposed individuals, obesity (through elevated fatty acids) may be the factor that drives insulin resistance to clinical diabetes. In addition, elevated free fatty acid levels also may contribute to the other key underlying defect in type 2 diabetes: progressive pancreatic β-cell loss which results in insulin deficiency.12 Similar to the trend in adults, childhood obesity has now reached epidemic proportions and has been associated with the increased prevalence of glucose intolerance, metabolic syndrome, and biomarkers of increased CVD risk in this young population.13-15
Type 2 diabetes in adolescents
CASE 1 Suspected new-onset type 2 diabetes
A 16-year-old Hispanic boy presents for treatment of weight loss. He is a defensive tackle on the high school football team and has a strong appetite. His height is 6 ft 1 in and he weighs 250 lb; his body mass index (BMI) is 32 kg/m2, and most of the fat is abdominally distributed (waist circumference, 42 in). Both of his parents are obese, and a grandfather and aunt have type 2 diabetes. Further examination reveals a blood pressure (BP) level of 135/87 mm Hg and acanthosis nigricans. A random fingerstick test shows a blood glucose level of 240 mg/dL.
Until recently, type 2 diabetes rarely was observed in children, occurring in only 1% to 2% of children with new-onset diabetes.16 However, depending on the sampling strategy, race or ethnicity of the population, and the region of the country sampled, it now has been estimated that type 2 diabetes accounts for anywhere from 8% to 45% of all diabetes reported among children and adolescents.6,16 Prevalence estimates of pediatric type 2 diabetes in population-based studies range from 4.1 per 1,000 in the National Health and Nutrition Survey (NHANES III) to 50.9 per 1,000 among Pima Indians in Arizona.17 Unlike the trends of increasing incidence and prevalence of type 2 diabetes in the pediatric population, a similar trend in type 1 diabetes has not been observed.7
The diagnosis and treatment of type 2 diabetes in pediatric patients can be challenging. Type 2 diabetes is associated with an increased BMI and is more common in adolescents than in younger children.6 Puberty is associated with relative insulin resistance and, along with the time-related effects of obesity, resistance may play a role in the subsequent onset of type 2 diabetes in pediatric patients. However, as an increasing number of children become obese at an earlier age, the onset of disease may occur earlier.
Other risk factors for type 2 diabetes in childhood include having a first- or second-degree relative with the disease or non-European ancestry (Americans of African, Hispanic, Asian, Pacific Islander, or Native American descent). In addition, acanthosis nigricans is a skin condition that serves as a specific, though insensitive, marker of insulin resistance. Among adolescent females, polycystic ovary syndrome has been associated with insulin resistance irrespective of excess weight or frank obesity18 and may be associated with an increased risk of type 2 diabetes.6
TABLE 1 provides criteria for screening for type 2 diabetes in children. The adolescent in the case presented has several risk factors for type 2 diabetes, including obesity, a positive family history, Hispanic descent, and acanthosis nigricans. To more definitively diagnose type 2 diabetes, additional laboratory tests are needed, including assessment of blood glucose and insulin production, as well as the presence of autoantibodies.
TABLE 1
Screening recommendations for type 2 diabetes in children
| Testing for type 2 diabetes is recommended every 2 years at onset of puberty or aged >10 years (whichever comes first) if the child* |
|
| *Clinical judgment should be used to test for diabetes in high-risk patients who do not meet these criteria. |
| †Overweight is defined as BMI >85th percentile for age and sex, weight for height >85th percentile, or weight >120% of ideal for height. |
| Copyright © 2004 American Diabetes Association from Diabetes Care,2004;27(suppl 1):S15-S35. Reprinted with permission. |
CASE 1 Laboratory assessment
The patient has a fasting plasma glucose (FPG) level of 215 mg/dL. β-Cell or insulin autoantibodies are not detected. He has a normal-to-high fasting C-peptide level, microalbuminuria, and a serum creatinine level of 0.8 mg/dL. His lipid panel results include: total cholesterol, 234 mg/dL; low-density lipoprotein (LDL) cholesterol, 159 mg/dL; high-density lipoprotein (HDL) cholesterol, 45 mg/dL; and triglycerides, 150 mg/dL.
A comparison of the typical presentation and laboratory findings in pediatric type 1 and type 2 diabetes is listed in TABLE 2. This information underscores that there is significant overlap between the 2 disease classifications.
The laboratory results for this patient confirm a diagnosis of type 2 diabetes. C peptide is a marker of endogenous insulin production and is particularly helpful in the classification of diabetes when it is high, which is indicative of type 2 diabetes. However, it should be noted that a finding of low C-peptide levels does not rule out type 2 diabetes since there is a possibility that glucose toxicity is temporarily limiting insulin production. Indeed, in such a case, insulin therapy can be initiated to establish glycemic control and promote endogenous insulin production by reducing glucose toxicity. Similarly, although the absence of pancreatic β-cells and insulin autoantibodies is consistent with a diagnosis of type 2 diabetes, the presence of such antibodies does not completely rule out type 2 diabetes.19
Like many patients with type 2 diabetes, the current patient exhibits a cluster of CVD risk factors that characterize the metabolic syndrome, including dyslipidemia (elevated total cholesterol, LDL cholesterol, triglyceride levels, and low HDL cholesterol levels), hypertension, glucose intolerance, hyperinsulinemia, and central or abdominal obesity. This is not surprising as an estimated 30% of overweight adolescents, defined as those with BMI at or above the 95th percentile, meet the criteria for metabolic syndrome.14
TABLE 2
Classification of type 1 and type 2 diabetes in pediatric patients
| TYPE 1 DIABETES | TYPE 2 DIABETES | |
|---|---|---|
| Age | Throughout childhood | Pubertal |
| Onset | Acute, severe | Mild to severe, often insidious |
| Insulin secretion | Very low | Variable |
| C-peptide level | Absent | Variable |
| Insulin sensitivity* | Normal | Decreased |
| Insulin dependence† | Permanent | No |
| Genetics | Polygenic | Polygenic |
| Race/ethnic distribution | All (low frequency in Asians) | African American, Hispanic, Asian, American Indian, Pacific Islanders |
| Association | ||
| Obesity | No | Yes, strong |
| Acanthosis nigricans | No | Yes |
| Autoimmunity | Yes | No |
| Presence of autoantibodies | Yes | No‡ |
| *Insulin sensitivity is given as a pathogenic factor. | ||
| † In the absence of acute illness or other stress. | ||
| ‡ Although autoimmunity is not a cause of type 2 diabetes, diabetic autoimmune markers can be present at times and should not be used to rule out a diagnosis of type 2 diabetes in children and adolescents.19 | ||
| Copyright © 2004 American Diabetes Association from Diabetes Care, 1999;22:345-354. Reprinted with permission. | ||
CASE 1 Initial therapy
The patient is provided with education on lifestyle modifications to reduce weight and obtain better control of glucose, lipids, and BP. Instructions include ways to improve his eating habits and to increase his physical activity when away from the football field, such as limiting time spent watching TV and playing video games and increasing exercise time and effort. The patient also is instructed on self-monitoring for blood glucose (SMBG) and is given a referral to an ophthalmologist to determine whether there is any baseline retinopathy.
At his 3-month follow-up, the patient’s A1C is 8.7%, and his weight has not changed. At this point, lifestyle modifications are reinforced, and pharmacotherapy with extended-release metformin is initiated and titrated to 2,000 mg/d.
Typically, the first approach to managing type 2 diabetes involves dietary changes and instituting an exercise program to reduce weight and to improve insulin sensitivity. This was the approach used in the patient described above. However, as is frequently the case, lifestyle modifications by themselves are insufficient to meet the American Diabetes Association (ADA) or American Association of Clinical Endocrinologists targets for glycemic control (A1C <7% and <6.5%, respectively).20,21 It is important to note here that the ADA does recommend less stringent glycemic control guidelines in very young children (ie, those aged less than 13 years).16 As is the case for adults with diabetes, pharmacologic therapies typically are needed in addition to lifestyle changes to lower elevated blood glucose levels. However, unlike the situation with adults, the list of drugs approved by the Food and Drug Administration for use in pediatric patients is limited (ie, currently only metformin and insulin preparations are approved for pediatric use).
Metformin was chosen as the initial therapy in this adolescent for several reasons, including demonstrated efficacy and tolerability in pediatric studies, approval for use in this population, and because it is generally not associated with weight gain. The patient needs a 1.7% reduction in A1C; therefore, metformin was titrated to the maximum daily dosage of 2,000 mg (expected to, on average, reduce A1C by 1% to 2%). In a recent, randomized, double-blind, placebo-controlled trial of pediatric patients (aged 10 to 16 years) with type 2 diabetes,22 metformin 1,000 mg bid significantly reduced baseline-adjusted mean A1C values compared with placebo (7.5% vs 8.6%, P<0.001) without negatively affecting body weight or lipid levels. The adverse events profile of metformin in children was similar to that observed in adults, primarily involving gastrointestinal events.
CASE 1 Monotherapy inadequate
After 6 months on metformin therapy, the patient returns for follow-up. His A1C measure has improved to 7.7%, but his weight remains unchanged. At this point, a discussion is initiated about using combination therapy to bring his diabetes under control.
This case study illustrates an important point about the treatment of type 2 diabetes: pharmacologic therapy with a single antidiabetic agent often is insufficient to reach target goals for glycemic control.2 Frequently, this reflects the insidious, progressive nature of the disease, which may be present for years before being recognized. As a general rule, combination therapy involves the use of drugs with different mechanisms of action. Clinical trials evaluating combination therapy generally follow this rationale.
Since there are limited pediatric data for the majority of oral agents, the clinical decision regarding which agents to use in combination often is based on the available data in adults. Information regarding efficacy, safety, and tolerability for the different oral antidiabetic drugs used in adults with type 2 diabetes is provided in TABLE 3.
Secretagogues (ie, sulfonylureas and meglitinides) have been reported to typically reduce A1C values by 1% to 2% at maximal doses. Generally, the shorteracting meglitinides have been considered useful for reducing postprandial hyperglycemia and are taken before meals.23 Unlike traditional sulfonylureas, glimepiride also has demonstrated efficacy in controlling postprandial hyperglycemia.24 All patients starting therapy with a secretagogue should be counseled on recognition of hypoglycemic symptoms and appropriate self-treatment. While severe hypoglycemia is not common in type 2 diabetes, it can occur with any agent that increases insulin secretion.
The glitazones lower A1C levels by an estimated 1% to 1.5%. Although they primarily reduce insulin resistance, they also may have beneficial effects on blood lipids, BP, and inflammatory markers associated with CVD, suggesting a theoretical benefit for reducing macrovascular complications.25 Glitazones, however, have been associated with weight gain and fluid retention, which in adults may unmask or exacerbate congestive heart failure.25 Additionally, although pioglitazone and rosiglitazone do not appear to carry the same risk of hepatotoxicity as the first member of the class, troglitazone, there have been a few case reports of liver injury or failure in patients treated with pioglitazone26-28 or rosiglitazone.29-31 In the absence of pediatric and long-term data, caution is warranted with use of these agents in this population.
α-Glucosidase inhibitors are helpful in controlling mealtime glycemic excursions and may have utility in patients who require smaller reductions in A1C. Use of these relatively safe agents is limited due to gastrointestinal side effects (ie, diarrhea and flatulence are common),32 which can prevent titration to optimal doses. Since the primary mechanism of action is inhibition of carbohydrate digestion, patients who are using these agents in combination with therapies that can cause hypoglycemia should be counseled to use simple sugars (ie, glucose tablets) rather than complex carbohydrates to self-treat hypoglycemia.
If oral agents cannot achieve adequate glycemic control, addition of insulin is a rational, well-tolerated, and effective option.3,4,33 Insulin therapy is often underutilized and delayed in patients with type 2 diabetes who would benefit from earlier introduction of such therapy.34 The pediatric experience with insulin is extensive, but mostly in type 1 diabetes. The potential need for and benefits of insulin therapy may be discussed with patients as early as at the time of diagnosis to help alleviate some of the anxiety patients have regarding this therapy.35
TABLE 3
Available oral antidiabetic agents
| DRUG | DAILY DOSE (MG) | DOSES/DAY | PRIMARY MECHANISM(S) | EXPECTED A1C REDUCTION (%) | COMMON ADVERSE EFFECTS |
|---|---|---|---|---|---|
| Sulfonylureas | Augment insulin secretion | 1–2 | Hypoglycemia, weight gain* | ||
| Glimepiride | 1–8 | 1 | |||
| Glipizide | 2.5–40 | 1–2 | |||
| Glipizide controlled release | 2.5–20 | 1 | |||
| Glyburide | 2.5–20 | 1–2 | |||
| Glyburide micronized | 3–12 | 1–2 | |||
| Meglitinides | Augment insulin secretion | 1–2 | Hypoglycemia, weight gain | ||
| Repaglinide | 0.5–16 | 2–4 | |||
| Nateglinide | 360 | 2–4 | |||
| Biguanides | Increase sensitivity to insulin, decrease hepatic glucose production | 1–2 | Gastrointestinal symptoms† | ||
| Metformin† | Adults: 500–2,550 Children (10–16 yr) 500–2,000 | 2–3 | |||
| Thiazolidinediones | Increase sensitivity to insulin | 1–1.5 | Fluid retention, weight gain‡ | ||
| Rosiglitazone | 2–8 | 1–2 | |||
| Pioglitazone | 15–45 | 1 | |||
| α-Glucosidase Inhibitors | Slow digestion of carbohydrates | 0.5–1 | Flatulence, gastro-intestinal discomfort, weight gain | ||
| Acarbose | 75–300 | 3 | |||
| Miglitol | 75–300 | 3 | |||
| *Glimepiride had a neutral effect on weight in clinical studies and was associated with a lower incidence of hypoglycemia than other sulfonylureas.49-51 | |||||
| † Lactic acidosis has been reported with metformin use, but is extremely rare. The risk may be related to an underlying predisposition to lactic acidosis. | |||||
| ‡ There have been some reports of liver toxicity with second-generation thiazolidinediones. | |||||
| Adapted from American Association of Clinical Endocrinologists;21 Nathan DM. Clinical practice. Initial Management of glycemia in type 2 diabetes mellitus.N Engl J Med. 2002;347:1342-1349. | |||||
Type 2 diabetes in adults
CASE 2 Woman with chronic diabetes
A 60-year-old woman presents for her annual checkup complaining of weight gain, fatigue, and tingling in her feet. Her recent history includes recurrent urinary tract and yeast infections. When initially diagnosed with type 2 diabetes 5 years ago, she had been counseled to increase activity to reduce weight; however, she had been unable to maintain consistent effort. She is 5 ft 4 in tall and weighs 230 lb (BMI, 39.5 kg/m2) with a waist circumference of 40 in. Her weight has fluctuated, but she has had a net gain of 30 lb over the last 5 years. Education and lifestyle modification efforts were reinitiated 1 year ago. The patient is a smoker and has cut her habit to 5 cigarettes per day. Her A1C and total cholesterol levels 1 year ago were 7.8% and 203 mg/dL, respectively. The patient also had cataract surgery 1 year ago. Her current medications include lisinopril 40 mg/d, furosemide 40 mg bid, and rosiglitazone 4 mg/d. She performs SMBG infrequently.
On examination, her BP is 125/72 mm Hg. A random fingerstick blood glucose test shows 210 mg/dL. She exhibits normal monofilament sensation, vibratory sensation, and ankle jerks. She also shows signs of mild pedal edema with no foot lesions and normal pedal pulses.
There are a number of signs suggesting this patient’s diabetes is inadequately controlled, including her complaints of fatigue and repeated yeast infections. Poorly controlled diabetes also is associated with peripheral neuropathy, which may manifest as a tingling sensation or numbness that begins in the feet and moves upward; however, her physical examination is negative for neuropathy.36 A random blood glucose level is of limited value and should not be relied upon as an indicator of the patient’s glycemic status. An A1C measurement is overdue for this patient and will reflect her overall glycemic control in recent months.
A total cholesterol level is rarely adequate for clinical decision making and thus a follow-up lipid profile is warranted. Her BP is well controlled with her current antihypertension regimen. The ADA guidelines recommend adequate treatment of hypertension (target BP, <130/80 mm Hg) in diabetic patients and suggest use of an angiotensin-converting enzyme (ACE) inhibitor or angiotensin-receptor blocker (ARB) because, in addition to their antihypertensive effects, these agents may provide renal benefits for patients with albuminuria or renal insufficiency.20 More typically, a thiazide rather than a loop diuretic is used in combination with an ACE inhibitor (or another antihypertensive drug class) as treatment for hypertension but, since the patient’s BP is well controlled with her current regimen and she has mild pedal edema, the loop diuretic may be maintained.
Her weight gain and peripheral edema may in part be due to rosiglitazone treatment. Edema that is not caused by congestive heart failure is not a contraindication for glitazone use but requires close monitoring and should lead to a consideration of alternate therapy.25
CASE 2 Laboratory assessment
The patient’s glycemic indices are: FPG, 184 mg/dL; A1C, 9.4%; postprandial glucose (PPG), 311 mg/dL. A random urine sample reveals microalbuminuria (protein/creatinine, 38 μg/mg). Her serum creatinine is 1.6 mg/dL. Her lipid panel reveals: total cholesterol, 271 mg/dL; LDL cholesterol, 165 mg/dL; HDL cholesterol, 35 mg/dL; and triglycerides, 355 mg/dL. Liver function tests are within normal limits. Further evaluation indicates that she does not have congestive heart failure.
The laboratory results indicate very poor control of overall and postmeal glucose levels. In addition, she now has microalbuminuria. Although poor adherence with therapy should be ruled out, the loss of control with a previously effective therapy is not unusual and underscores the progressive nature of diabetes.
Collectively, this patient’s poor glycemic control, dyslipidemia and central obesity, place her at a very high risk for CVD.37
CASE 2 Therapy adjusted
Glimepiride 4 mg/d is added to the rosiglitazone; in addition, atorvastatin 20 mg/d and fenofibrate 160 mg/d are prescribed. Lifestyle modifications (eg, dietary changes, exercise, smoking cessation) are reinforced, and the patient is referred to a certified diabetes educator.
The comprehensive approach taken for this patient is consistent with that advocated by the results in the Steno-2 Study. Gaede et al1 demonstrated that a targeted, intensified, multifactorial, interventional approach to improving macrovascular and microvascular risk factors in patients with type 2 diabetes reduces the risk of macrovascular and microvascular diabetic complications by about 50% compared with conventional treatment.1 Specifically, patients receiving intensive therapy had a significantly lower risk of CVD, nephropathy, retinopathy and autonomic neuropathy.1 Intensive, multifactorial therapy involved dietary interventions; a consistent exercise program; smoking cessation; use of ACE inhibitors (or ARBs for patients intolerant to ACE inhibitors) for renal benefits and combined with diuretics and other agents, if necessary, to treat hypertension; lipid-lowering therapy to treat hyperlipidemia (statins, plus fibrates for isolated cases of hypertriglyceridemia); pharmacotherapy for glucose control; daily vitamin-mineral supplements; and daily aspirin as a secondary measure for the prevention of CVD.
In general, pharmacotherapy of diabetes should be individualized, since not all agents are equally appropriate for all patients. A variety of studies have demonstrated that adding a second antidiabetic agent to a first typically results in additional improvements in glycemic control.38-47 In the example here, a sulfonylurea was chosen because of its complementary mechanism of action with an insulin sensitizer. Since the patient had an elevated serum creatinine, metformin was not considered to be an appropriate choice. In addition, the combination of a glitazone with sulfonylurea therapy has been reported to achieve reductions in A1C40,48 at least comparable to those reported in analyses of the combination of a glitazone with metformin.40,45 TABLE 4 provides reported reductions in A1C that have been observed in clinical trials of various combination regimens in type 2 diabetes. Since these are not head-to-head comparisons of the various regimens, the data simply illustrate the range of A1C reductions that may be achieved with combination therapy. In this patient, glimepiride was chosen because of its weight neutral effect,49 potentially lower incidence of hypoglycemia,50,51 favorable effect on postprandial glucose (that may ameliorate cardiovascular risk),52-56 and once-daily dosing.
Given the progressive natural history of type 2 diabetes, and the fact that this patient currently requires a >2% A1C reduction, it is reasonable to anticipate that she will eventually need insulin to attain glycemic control. Recently, Riddle et al4 demonstrated that addition of a basal insulin (neutral protamine Hagedorn [NPH] or glargine) to existing oral agents reduced the A1C to <7% in the majority of patients with type 2 diabetes. Insulin glargine was associated with significantly less hypoglycemia than NPH insulin. This is an important consideration since hypoglycemia remains a major barrier to insulin therapy in type 2 diabetes.57 Sulfonylurea therapy should be maintained when insulin is initiated, as this combination has been demonstrated to be highly effective in improving glycemic control and is associated with a low incidence of hypoglycemia.3,33 In the current patient, the addition of basal insulin glargine would complement her other antidiabetic therapies. Insulin glargine would primarily normalize her FBG, while glimepiride controls PPG and rosiglitazone improves insulin sensitivity. Thus, this regimen would address the 2 most important defects in type 2 diabetes—insulin deficiency and insulin resistance.
Clinical trials have shown that combination therapy with oral agents and insulin, as well as with multiple oral agents, is effective.4,38,39 However, more long-term and comparative studies of these multiple-agent combinations are needed. It is important to set expectations with patients that gaining good control of diabetes frequently requires combination therapy with multiple agents with the ultimate goal of avoiding the onset of new complications or of delaying progression of existing complications.
TABLE 4
A1C reductions noted in clinical trials and reports of combination therapy for type 2 diabetes
| REGIMEN | A1C REDUCTION (%) |
|---|---|
| Sulfonylurea + metformin58 | ~1.7 |
| Sulfonylurea + glitazone40,48 | ~1.3 |
| Sulfonylurea + α-glucosidase inhibitor59 | ~0.9 |
| Metformin + meglitinide46 | ~1.4 |
| Metformin + glitazone40,45 | ~1 |
| Insulin + oral agents4 | Open to target |
Summary
The increased prevalence of obesity, metabolic syndrome, and type 2 diabetes in adolescents and adults is an ominous sign of more serious disease in the future. A concerted effort on the part of health care professionals to improve the care of patients with type 2 diabetes is needed to bring this burgeoning problem under better control. Diabetes is a recognized coronary risk equivalent; thus, a comprehensive multifactorial approach that rigorously addresses glycemia, as well as elevated BP and lipids, is recommended.
Most patients with type 2 diabetes will eventually require combination therapy with 2 or more agents to attain and maintain glycemic control.2,3 In particular, combinations of agents with complementary mechanisms of action (eg, an insulin sensitizer with a secretagogue) demonstrate greater improvements in glycemic control. Based on the progressive nature of diabetes, a principle in the pharmacotherapy of glucose control is that, in absence of untoward effects, if a given agent is secondarily unable to provide adequate glycemic control (ie, there was initial improvement in glucose control and then subsequent deterioration), additional agents—whether oral agents or insulin—should be added rather than substituted.
Disclosures:
Dr. Elasy has done consultation for Aventis Pharmaceuticals. Dr. Levy has received grants/research support from Aventis Pharmaceuticals, Eli Lilly and Co., Merck & Co., Novartis Pharmaceuticals, Novo Nordisk Pharmaceuticals Inc., and Pfizer Inc. He is a consultant and on the speaker’s bureau for Aventis Pharmaceuticals, Eli Lilly and Co., Novartis Pharmaceuticals, Novo Nordisk Pharmaceuticals Inc, Pfizer Inc, Takeda Pharmaceuticals America, Inc., Bristol-Myers Squibb Company, GlaxoSmithKline, and Wyeth-Ayerst Pharmaceuticals. Dr. Davis has received research grants from Aventis Pharmaceuticals, Eli Lilly and Co., and Bayer Pharmaceuticals Corporation.
- Children and adolescents who are overweight and have additional risk factors (ie, high-risk ethnic group or signs of insulin resistance) should be screened for diabetes every 2 years (SOR: C).
- Management of type 2 diabetes in all age groups requires a multifactorial approach that addresses not only glycemic control (A1C <7%) but also other cardiovascular risk factors such as hypertension, dyslipidemia, and obesity (SOR: A).1
- Most patients with type 2 diabetes will eventually require combination therapy with 2 or more agents to attain and maintain glycemic control (SOR: A).2,3
- Combining an insulin secretagogue (ie, sulfonylurea or meglitinide) and an insulin sensitizer (ie, metformin or a glitazone) capitalizes on unique mechanisms of action and results in Significant A1C lowering (SOR: C).
- If a patient is unable to achieve glycemic control on 2 oral agents, insulin therapy is an appropriate consideration and should be added to oral agents (rather than substituted) (SOR: B).4
Diabetes affects 18.2 million people in the United States.5 It is a leading cause of morbidity and mortality.5 Diabetes is associated with more than $90 billion in direct medical costs and with an estimated $40 billion in indirect costs (ie, disability, work loss, and premature mortality).5 Type 2 diabetes accounts for 90% to 95% of total cases. It disproportionately affects certain minority populations, and it is increasingly being identified in children and adolescents.5-7
The obesity epidemic has received tremendous media and public attention and has sobering implications for the development of metabolic syndrome, which is often the precursor to diabetes, and cardiovascular disease (CVD).8,9 In 1 study, the hazard ratio for development of diabetes was 3.85 for individuals who gained 20 kg or more over approximately 10 years, as compared with individuals whose weight remained relatively stable over the same period.10 Obesity is associated with elevations in free fatty acid levels and in other compounds which contribute to insulin resistance11 —a key underlying defect in metabolic syndrome and type 2 diabetes. Thus, particularly in genetically predisposed individuals, obesity (through elevated fatty acids) may be the factor that drives insulin resistance to clinical diabetes. In addition, elevated free fatty acid levels also may contribute to the other key underlying defect in type 2 diabetes: progressive pancreatic β-cell loss which results in insulin deficiency.12 Similar to the trend in adults, childhood obesity has now reached epidemic proportions and has been associated with the increased prevalence of glucose intolerance, metabolic syndrome, and biomarkers of increased CVD risk in this young population.13-15
Type 2 diabetes in adolescents
CASE 1 Suspected new-onset type 2 diabetes
A 16-year-old Hispanic boy presents for treatment of weight loss. He is a defensive tackle on the high school football team and has a strong appetite. His height is 6 ft 1 in and he weighs 250 lb; his body mass index (BMI) is 32 kg/m2, and most of the fat is abdominally distributed (waist circumference, 42 in). Both of his parents are obese, and a grandfather and aunt have type 2 diabetes. Further examination reveals a blood pressure (BP) level of 135/87 mm Hg and acanthosis nigricans. A random fingerstick test shows a blood glucose level of 240 mg/dL.
Until recently, type 2 diabetes rarely was observed in children, occurring in only 1% to 2% of children with new-onset diabetes.16 However, depending on the sampling strategy, race or ethnicity of the population, and the region of the country sampled, it now has been estimated that type 2 diabetes accounts for anywhere from 8% to 45% of all diabetes reported among children and adolescents.6,16 Prevalence estimates of pediatric type 2 diabetes in population-based studies range from 4.1 per 1,000 in the National Health and Nutrition Survey (NHANES III) to 50.9 per 1,000 among Pima Indians in Arizona.17 Unlike the trends of increasing incidence and prevalence of type 2 diabetes in the pediatric population, a similar trend in type 1 diabetes has not been observed.7
The diagnosis and treatment of type 2 diabetes in pediatric patients can be challenging. Type 2 diabetes is associated with an increased BMI and is more common in adolescents than in younger children.6 Puberty is associated with relative insulin resistance and, along with the time-related effects of obesity, resistance may play a role in the subsequent onset of type 2 diabetes in pediatric patients. However, as an increasing number of children become obese at an earlier age, the onset of disease may occur earlier.
Other risk factors for type 2 diabetes in childhood include having a first- or second-degree relative with the disease or non-European ancestry (Americans of African, Hispanic, Asian, Pacific Islander, or Native American descent). In addition, acanthosis nigricans is a skin condition that serves as a specific, though insensitive, marker of insulin resistance. Among adolescent females, polycystic ovary syndrome has been associated with insulin resistance irrespective of excess weight or frank obesity18 and may be associated with an increased risk of type 2 diabetes.6
TABLE 1 provides criteria for screening for type 2 diabetes in children. The adolescent in the case presented has several risk factors for type 2 diabetes, including obesity, a positive family history, Hispanic descent, and acanthosis nigricans. To more definitively diagnose type 2 diabetes, additional laboratory tests are needed, including assessment of blood glucose and insulin production, as well as the presence of autoantibodies.
TABLE 1
Screening recommendations for type 2 diabetes in children
| Testing for type 2 diabetes is recommended every 2 years at onset of puberty or aged >10 years (whichever comes first) if the child* |
|
| *Clinical judgment should be used to test for diabetes in high-risk patients who do not meet these criteria. |
| †Overweight is defined as BMI >85th percentile for age and sex, weight for height >85th percentile, or weight >120% of ideal for height. |
| Copyright © 2004 American Diabetes Association from Diabetes Care,2004;27(suppl 1):S15-S35. Reprinted with permission. |
CASE 1 Laboratory assessment
The patient has a fasting plasma glucose (FPG) level of 215 mg/dL. β-Cell or insulin autoantibodies are not detected. He has a normal-to-high fasting C-peptide level, microalbuminuria, and a serum creatinine level of 0.8 mg/dL. His lipid panel results include: total cholesterol, 234 mg/dL; low-density lipoprotein (LDL) cholesterol, 159 mg/dL; high-density lipoprotein (HDL) cholesterol, 45 mg/dL; and triglycerides, 150 mg/dL.
A comparison of the typical presentation and laboratory findings in pediatric type 1 and type 2 diabetes is listed in TABLE 2. This information underscores that there is significant overlap between the 2 disease classifications.
The laboratory results for this patient confirm a diagnosis of type 2 diabetes. C peptide is a marker of endogenous insulin production and is particularly helpful in the classification of diabetes when it is high, which is indicative of type 2 diabetes. However, it should be noted that a finding of low C-peptide levels does not rule out type 2 diabetes since there is a possibility that glucose toxicity is temporarily limiting insulin production. Indeed, in such a case, insulin therapy can be initiated to establish glycemic control and promote endogenous insulin production by reducing glucose toxicity. Similarly, although the absence of pancreatic β-cells and insulin autoantibodies is consistent with a diagnosis of type 2 diabetes, the presence of such antibodies does not completely rule out type 2 diabetes.19
Like many patients with type 2 diabetes, the current patient exhibits a cluster of CVD risk factors that characterize the metabolic syndrome, including dyslipidemia (elevated total cholesterol, LDL cholesterol, triglyceride levels, and low HDL cholesterol levels), hypertension, glucose intolerance, hyperinsulinemia, and central or abdominal obesity. This is not surprising as an estimated 30% of overweight adolescents, defined as those with BMI at or above the 95th percentile, meet the criteria for metabolic syndrome.14
TABLE 2
Classification of type 1 and type 2 diabetes in pediatric patients
| TYPE 1 DIABETES | TYPE 2 DIABETES | |
|---|---|---|
| Age | Throughout childhood | Pubertal |
| Onset | Acute, severe | Mild to severe, often insidious |
| Insulin secretion | Very low | Variable |
| C-peptide level | Absent | Variable |
| Insulin sensitivity* | Normal | Decreased |
| Insulin dependence† | Permanent | No |
| Genetics | Polygenic | Polygenic |
| Race/ethnic distribution | All (low frequency in Asians) | African American, Hispanic, Asian, American Indian, Pacific Islanders |
| Association | ||
| Obesity | No | Yes, strong |
| Acanthosis nigricans | No | Yes |
| Autoimmunity | Yes | No |
| Presence of autoantibodies | Yes | No‡ |
| *Insulin sensitivity is given as a pathogenic factor. | ||
| † In the absence of acute illness or other stress. | ||
| ‡ Although autoimmunity is not a cause of type 2 diabetes, diabetic autoimmune markers can be present at times and should not be used to rule out a diagnosis of type 2 diabetes in children and adolescents.19 | ||
| Copyright © 2004 American Diabetes Association from Diabetes Care, 1999;22:345-354. Reprinted with permission. | ||
CASE 1 Initial therapy
The patient is provided with education on lifestyle modifications to reduce weight and obtain better control of glucose, lipids, and BP. Instructions include ways to improve his eating habits and to increase his physical activity when away from the football field, such as limiting time spent watching TV and playing video games and increasing exercise time and effort. The patient also is instructed on self-monitoring for blood glucose (SMBG) and is given a referral to an ophthalmologist to determine whether there is any baseline retinopathy.
At his 3-month follow-up, the patient’s A1C is 8.7%, and his weight has not changed. At this point, lifestyle modifications are reinforced, and pharmacotherapy with extended-release metformin is initiated and titrated to 2,000 mg/d.
Typically, the first approach to managing type 2 diabetes involves dietary changes and instituting an exercise program to reduce weight and to improve insulin sensitivity. This was the approach used in the patient described above. However, as is frequently the case, lifestyle modifications by themselves are insufficient to meet the American Diabetes Association (ADA) or American Association of Clinical Endocrinologists targets for glycemic control (A1C <7% and <6.5%, respectively).20,21 It is important to note here that the ADA does recommend less stringent glycemic control guidelines in very young children (ie, those aged less than 13 years).16 As is the case for adults with diabetes, pharmacologic therapies typically are needed in addition to lifestyle changes to lower elevated blood glucose levels. However, unlike the situation with adults, the list of drugs approved by the Food and Drug Administration for use in pediatric patients is limited (ie, currently only metformin and insulin preparations are approved for pediatric use).
Metformin was chosen as the initial therapy in this adolescent for several reasons, including demonstrated efficacy and tolerability in pediatric studies, approval for use in this population, and because it is generally not associated with weight gain. The patient needs a 1.7% reduction in A1C; therefore, metformin was titrated to the maximum daily dosage of 2,000 mg (expected to, on average, reduce A1C by 1% to 2%). In a recent, randomized, double-blind, placebo-controlled trial of pediatric patients (aged 10 to 16 years) with type 2 diabetes,22 metformin 1,000 mg bid significantly reduced baseline-adjusted mean A1C values compared with placebo (7.5% vs 8.6%, P<0.001) without negatively affecting body weight or lipid levels. The adverse events profile of metformin in children was similar to that observed in adults, primarily involving gastrointestinal events.
CASE 1 Monotherapy inadequate
After 6 months on metformin therapy, the patient returns for follow-up. His A1C measure has improved to 7.7%, but his weight remains unchanged. At this point, a discussion is initiated about using combination therapy to bring his diabetes under control.
This case study illustrates an important point about the treatment of type 2 diabetes: pharmacologic therapy with a single antidiabetic agent often is insufficient to reach target goals for glycemic control.2 Frequently, this reflects the insidious, progressive nature of the disease, which may be present for years before being recognized. As a general rule, combination therapy involves the use of drugs with different mechanisms of action. Clinical trials evaluating combination therapy generally follow this rationale.
Since there are limited pediatric data for the majority of oral agents, the clinical decision regarding which agents to use in combination often is based on the available data in adults. Information regarding efficacy, safety, and tolerability for the different oral antidiabetic drugs used in adults with type 2 diabetes is provided in TABLE 3.
Secretagogues (ie, sulfonylureas and meglitinides) have been reported to typically reduce A1C values by 1% to 2% at maximal doses. Generally, the shorteracting meglitinides have been considered useful for reducing postprandial hyperglycemia and are taken before meals.23 Unlike traditional sulfonylureas, glimepiride also has demonstrated efficacy in controlling postprandial hyperglycemia.24 All patients starting therapy with a secretagogue should be counseled on recognition of hypoglycemic symptoms and appropriate self-treatment. While severe hypoglycemia is not common in type 2 diabetes, it can occur with any agent that increases insulin secretion.
The glitazones lower A1C levels by an estimated 1% to 1.5%. Although they primarily reduce insulin resistance, they also may have beneficial effects on blood lipids, BP, and inflammatory markers associated with CVD, suggesting a theoretical benefit for reducing macrovascular complications.25 Glitazones, however, have been associated with weight gain and fluid retention, which in adults may unmask or exacerbate congestive heart failure.25 Additionally, although pioglitazone and rosiglitazone do not appear to carry the same risk of hepatotoxicity as the first member of the class, troglitazone, there have been a few case reports of liver injury or failure in patients treated with pioglitazone26-28 or rosiglitazone.29-31 In the absence of pediatric and long-term data, caution is warranted with use of these agents in this population.
α-Glucosidase inhibitors are helpful in controlling mealtime glycemic excursions and may have utility in patients who require smaller reductions in A1C. Use of these relatively safe agents is limited due to gastrointestinal side effects (ie, diarrhea and flatulence are common),32 which can prevent titration to optimal doses. Since the primary mechanism of action is inhibition of carbohydrate digestion, patients who are using these agents in combination with therapies that can cause hypoglycemia should be counseled to use simple sugars (ie, glucose tablets) rather than complex carbohydrates to self-treat hypoglycemia.
If oral agents cannot achieve adequate glycemic control, addition of insulin is a rational, well-tolerated, and effective option.3,4,33 Insulin therapy is often underutilized and delayed in patients with type 2 diabetes who would benefit from earlier introduction of such therapy.34 The pediatric experience with insulin is extensive, but mostly in type 1 diabetes. The potential need for and benefits of insulin therapy may be discussed with patients as early as at the time of diagnosis to help alleviate some of the anxiety patients have regarding this therapy.35
TABLE 3
Available oral antidiabetic agents
| DRUG | DAILY DOSE (MG) | DOSES/DAY | PRIMARY MECHANISM(S) | EXPECTED A1C REDUCTION (%) | COMMON ADVERSE EFFECTS |
|---|---|---|---|---|---|
| Sulfonylureas | Augment insulin secretion | 1–2 | Hypoglycemia, weight gain* | ||
| Glimepiride | 1–8 | 1 | |||
| Glipizide | 2.5–40 | 1–2 | |||
| Glipizide controlled release | 2.5–20 | 1 | |||
| Glyburide | 2.5–20 | 1–2 | |||
| Glyburide micronized | 3–12 | 1–2 | |||
| Meglitinides | Augment insulin secretion | 1–2 | Hypoglycemia, weight gain | ||
| Repaglinide | 0.5–16 | 2–4 | |||
| Nateglinide | 360 | 2–4 | |||
| Biguanides | Increase sensitivity to insulin, decrease hepatic glucose production | 1–2 | Gastrointestinal symptoms† | ||
| Metformin† | Adults: 500–2,550 Children (10–16 yr) 500–2,000 | 2–3 | |||
| Thiazolidinediones | Increase sensitivity to insulin | 1–1.5 | Fluid retention, weight gain‡ | ||
| Rosiglitazone | 2–8 | 1–2 | |||
| Pioglitazone | 15–45 | 1 | |||
| α-Glucosidase Inhibitors | Slow digestion of carbohydrates | 0.5–1 | Flatulence, gastro-intestinal discomfort, weight gain | ||
| Acarbose | 75–300 | 3 | |||
| Miglitol | 75–300 | 3 | |||
| *Glimepiride had a neutral effect on weight in clinical studies and was associated with a lower incidence of hypoglycemia than other sulfonylureas.49-51 | |||||
| † Lactic acidosis has been reported with metformin use, but is extremely rare. The risk may be related to an underlying predisposition to lactic acidosis. | |||||
| ‡ There have been some reports of liver toxicity with second-generation thiazolidinediones. | |||||
| Adapted from American Association of Clinical Endocrinologists;21 Nathan DM. Clinical practice. Initial Management of glycemia in type 2 diabetes mellitus.N Engl J Med. 2002;347:1342-1349. | |||||
Type 2 diabetes in adults
CASE 2 Woman with chronic diabetes
A 60-year-old woman presents for her annual checkup complaining of weight gain, fatigue, and tingling in her feet. Her recent history includes recurrent urinary tract and yeast infections. When initially diagnosed with type 2 diabetes 5 years ago, she had been counseled to increase activity to reduce weight; however, she had been unable to maintain consistent effort. She is 5 ft 4 in tall and weighs 230 lb (BMI, 39.5 kg/m2) with a waist circumference of 40 in. Her weight has fluctuated, but she has had a net gain of 30 lb over the last 5 years. Education and lifestyle modification efforts were reinitiated 1 year ago. The patient is a smoker and has cut her habit to 5 cigarettes per day. Her A1C and total cholesterol levels 1 year ago were 7.8% and 203 mg/dL, respectively. The patient also had cataract surgery 1 year ago. Her current medications include lisinopril 40 mg/d, furosemide 40 mg bid, and rosiglitazone 4 mg/d. She performs SMBG infrequently.
On examination, her BP is 125/72 mm Hg. A random fingerstick blood glucose test shows 210 mg/dL. She exhibits normal monofilament sensation, vibratory sensation, and ankle jerks. She also shows signs of mild pedal edema with no foot lesions and normal pedal pulses.
There are a number of signs suggesting this patient’s diabetes is inadequately controlled, including her complaints of fatigue and repeated yeast infections. Poorly controlled diabetes also is associated with peripheral neuropathy, which may manifest as a tingling sensation or numbness that begins in the feet and moves upward; however, her physical examination is negative for neuropathy.36 A random blood glucose level is of limited value and should not be relied upon as an indicator of the patient’s glycemic status. An A1C measurement is overdue for this patient and will reflect her overall glycemic control in recent months.
A total cholesterol level is rarely adequate for clinical decision making and thus a follow-up lipid profile is warranted. Her BP is well controlled with her current antihypertension regimen. The ADA guidelines recommend adequate treatment of hypertension (target BP, <130/80 mm Hg) in diabetic patients and suggest use of an angiotensin-converting enzyme (ACE) inhibitor or angiotensin-receptor blocker (ARB) because, in addition to their antihypertensive effects, these agents may provide renal benefits for patients with albuminuria or renal insufficiency.20 More typically, a thiazide rather than a loop diuretic is used in combination with an ACE inhibitor (or another antihypertensive drug class) as treatment for hypertension but, since the patient’s BP is well controlled with her current regimen and she has mild pedal edema, the loop diuretic may be maintained.
Her weight gain and peripheral edema may in part be due to rosiglitazone treatment. Edema that is not caused by congestive heart failure is not a contraindication for glitazone use but requires close monitoring and should lead to a consideration of alternate therapy.25
CASE 2 Laboratory assessment
The patient’s glycemic indices are: FPG, 184 mg/dL; A1C, 9.4%; postprandial glucose (PPG), 311 mg/dL. A random urine sample reveals microalbuminuria (protein/creatinine, 38 μg/mg). Her serum creatinine is 1.6 mg/dL. Her lipid panel reveals: total cholesterol, 271 mg/dL; LDL cholesterol, 165 mg/dL; HDL cholesterol, 35 mg/dL; and triglycerides, 355 mg/dL. Liver function tests are within normal limits. Further evaluation indicates that she does not have congestive heart failure.
The laboratory results indicate very poor control of overall and postmeal glucose levels. In addition, she now has microalbuminuria. Although poor adherence with therapy should be ruled out, the loss of control with a previously effective therapy is not unusual and underscores the progressive nature of diabetes.
Collectively, this patient’s poor glycemic control, dyslipidemia and central obesity, place her at a very high risk for CVD.37
CASE 2 Therapy adjusted
Glimepiride 4 mg/d is added to the rosiglitazone; in addition, atorvastatin 20 mg/d and fenofibrate 160 mg/d are prescribed. Lifestyle modifications (eg, dietary changes, exercise, smoking cessation) are reinforced, and the patient is referred to a certified diabetes educator.
The comprehensive approach taken for this patient is consistent with that advocated by the results in the Steno-2 Study. Gaede et al1 demonstrated that a targeted, intensified, multifactorial, interventional approach to improving macrovascular and microvascular risk factors in patients with type 2 diabetes reduces the risk of macrovascular and microvascular diabetic complications by about 50% compared with conventional treatment.1 Specifically, patients receiving intensive therapy had a significantly lower risk of CVD, nephropathy, retinopathy and autonomic neuropathy.1 Intensive, multifactorial therapy involved dietary interventions; a consistent exercise program; smoking cessation; use of ACE inhibitors (or ARBs for patients intolerant to ACE inhibitors) for renal benefits and combined with diuretics and other agents, if necessary, to treat hypertension; lipid-lowering therapy to treat hyperlipidemia (statins, plus fibrates for isolated cases of hypertriglyceridemia); pharmacotherapy for glucose control; daily vitamin-mineral supplements; and daily aspirin as a secondary measure for the prevention of CVD.
In general, pharmacotherapy of diabetes should be individualized, since not all agents are equally appropriate for all patients. A variety of studies have demonstrated that adding a second antidiabetic agent to a first typically results in additional improvements in glycemic control.38-47 In the example here, a sulfonylurea was chosen because of its complementary mechanism of action with an insulin sensitizer. Since the patient had an elevated serum creatinine, metformin was not considered to be an appropriate choice. In addition, the combination of a glitazone with sulfonylurea therapy has been reported to achieve reductions in A1C40,48 at least comparable to those reported in analyses of the combination of a glitazone with metformin.40,45 TABLE 4 provides reported reductions in A1C that have been observed in clinical trials of various combination regimens in type 2 diabetes. Since these are not head-to-head comparisons of the various regimens, the data simply illustrate the range of A1C reductions that may be achieved with combination therapy. In this patient, glimepiride was chosen because of its weight neutral effect,49 potentially lower incidence of hypoglycemia,50,51 favorable effect on postprandial glucose (that may ameliorate cardiovascular risk),52-56 and once-daily dosing.
Given the progressive natural history of type 2 diabetes, and the fact that this patient currently requires a >2% A1C reduction, it is reasonable to anticipate that she will eventually need insulin to attain glycemic control. Recently, Riddle et al4 demonstrated that addition of a basal insulin (neutral protamine Hagedorn [NPH] or glargine) to existing oral agents reduced the A1C to <7% in the majority of patients with type 2 diabetes. Insulin glargine was associated with significantly less hypoglycemia than NPH insulin. This is an important consideration since hypoglycemia remains a major barrier to insulin therapy in type 2 diabetes.57 Sulfonylurea therapy should be maintained when insulin is initiated, as this combination has been demonstrated to be highly effective in improving glycemic control and is associated with a low incidence of hypoglycemia.3,33 In the current patient, the addition of basal insulin glargine would complement her other antidiabetic therapies. Insulin glargine would primarily normalize her FBG, while glimepiride controls PPG and rosiglitazone improves insulin sensitivity. Thus, this regimen would address the 2 most important defects in type 2 diabetes—insulin deficiency and insulin resistance.
Clinical trials have shown that combination therapy with oral agents and insulin, as well as with multiple oral agents, is effective.4,38,39 However, more long-term and comparative studies of these multiple-agent combinations are needed. It is important to set expectations with patients that gaining good control of diabetes frequently requires combination therapy with multiple agents with the ultimate goal of avoiding the onset of new complications or of delaying progression of existing complications.
TABLE 4
A1C reductions noted in clinical trials and reports of combination therapy for type 2 diabetes
| REGIMEN | A1C REDUCTION (%) |
|---|---|
| Sulfonylurea + metformin58 | ~1.7 |
| Sulfonylurea + glitazone40,48 | ~1.3 |
| Sulfonylurea + α-glucosidase inhibitor59 | ~0.9 |
| Metformin + meglitinide46 | ~1.4 |
| Metformin + glitazone40,45 | ~1 |
| Insulin + oral agents4 | Open to target |
Summary
The increased prevalence of obesity, metabolic syndrome, and type 2 diabetes in adolescents and adults is an ominous sign of more serious disease in the future. A concerted effort on the part of health care professionals to improve the care of patients with type 2 diabetes is needed to bring this burgeoning problem under better control. Diabetes is a recognized coronary risk equivalent; thus, a comprehensive multifactorial approach that rigorously addresses glycemia, as well as elevated BP and lipids, is recommended.
Most patients with type 2 diabetes will eventually require combination therapy with 2 or more agents to attain and maintain glycemic control.2,3 In particular, combinations of agents with complementary mechanisms of action (eg, an insulin sensitizer with a secretagogue) demonstrate greater improvements in glycemic control. Based on the progressive nature of diabetes, a principle in the pharmacotherapy of glucose control is that, in absence of untoward effects, if a given agent is secondarily unable to provide adequate glycemic control (ie, there was initial improvement in glucose control and then subsequent deterioration), additional agents—whether oral agents or insulin—should be added rather than substituted.
Disclosures:
Dr. Elasy has done consultation for Aventis Pharmaceuticals. Dr. Levy has received grants/research support from Aventis Pharmaceuticals, Eli Lilly and Co., Merck & Co., Novartis Pharmaceuticals, Novo Nordisk Pharmaceuticals Inc., and Pfizer Inc. He is a consultant and on the speaker’s bureau for Aventis Pharmaceuticals, Eli Lilly and Co., Novartis Pharmaceuticals, Novo Nordisk Pharmaceuticals Inc, Pfizer Inc, Takeda Pharmaceuticals America, Inc., Bristol-Myers Squibb Company, GlaxoSmithKline, and Wyeth-Ayerst Pharmaceuticals. Dr. Davis has received research grants from Aventis Pharmaceuticals, Eli Lilly and Co., and Bayer Pharmaceuticals Corporation.
1. Gaede P, Vedel P, Larsen N, Jensen GVH, Parving H-H, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383-393.
2. Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA. 1999;281:2005-2012.
3. Wright A, Burden AC, Paisey RB, Cull CA, Holman RR. Sulfonylurea inadequacy. Efficacy of addition of insulin over 6 years in patients with type 2 diabetes in the U.K. Prospective Diabetes Study (UKPDS 57). Diabetes Care. 2002;25:330-336.
4. Riddle MC, Rosenstock J, Gerich J. The Treat-to-Target Trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26:3080-3086.
5. National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics fact sheet: general information and national estimates on diabetes in the United States, 2003. 1-14. 2003.
6. Aye T, Levitsky LL. Type 2 diabetes: an epidemic disease in childhood. Curr Opin Pediatr. 2003;15:411-415.
7. Rosenbloom AL. Increasing incidence of type 2 diabetes in children and adolescents: treatment considerations. Paediatr Drugs. 2002;4:209-221.
8. Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291:2847-2850.
9. Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723-1727.
10. Ford ES, Williamson DF, Liu S. Weight change and diabetes incidence: findings from a national cohort of US adults. Am J Epidemiol. 1997;146:214-222.
11. Leong KS, Wilding JP. Obesity and diabetes. Baillieres Best Pract Res Clin Endocrinol Metab. 1999;13:221-237.
12. Shimabukuro M, Zhou YT, Levi M, Unger RH. Fatty acid-induced β-cell apoptosis: a link between obesity and diabetes. Proc Natl Acad Sci U S A. 1998;95:2498-2502.
13. Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362-2374.
14. Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003;157:821-827.
15. Sinha R, Fisch G, Teague B, et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med. 2002;346:802-810.
16. American Diabetes Association. Type 2 diabetes in children and adolescents. Diabetes Care. 2000;23:381-389.
17. Fagot-Campagna A, Pettitt DJ, Engelgau MM, et al. Type 2 diabetes among North American children and adolescents: an epidemiologic review and a public health perspective. J Pediatr. 2000;136:664-672.
18. Pugeat M, Ducluzeau PH. Insulin resistance, polycystic ovary syndrome and metformin. Drugs. 1999;58(suppl 1):41-46.
19. Hathout EH, Thomas W, El Shahawy M, Nahab F, Mace JW. Diabetic autoimmune markers in children and adolescents with type 2 diabetes. Pediatrics. 2001;107:E102.-
20. ADA. American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2004;27(suppl 1):S15-S35.
21. American Association of Clinical Endocrinologists. The American Association of Clinical Endocrinologists Medical Guidelines for the Management of Diabetes Mellitus: the AACE system of intensive diabetes self-management-2002 update. Endocr Pract. 2002;8(suppl 1):40-82.
22. Jones KL, Arslanian S, Peterokova VA, Park JS, Tomlinson MJ. Effect of metformin in pediatric patients with type 2 diabetes: a randomized controlled trial. Diabetes Care. 2002;25:89-94.
23. Monnier L. Is postprandial glucose a neglected cardiovascular risk factor in type 2 diabetes? Eur J Clin Invest. 2000;30(suppl 2):3-11.
24. Sonnenberg GE, Garg DC, Weidler DJ, et al. Short-term comparison of once- versus twice-daily administration of glimepiride in patients with non-insulin-dependent diabetes mellitus. Ann Pharmacother. 1997;31:671-676.
25. Nesto RW, Bell D, Bonow RO, et al. Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American Heart Association and American Diabetes Association. Diabetes Care. 2004;27:256-263.
26. May LD, Lefkowitch JH, Kram MT, Rubin DE. Mixed hepatocellular-cholestatic liver injury after pioglitazone therapy. Ann Intern Med. 2002;136:449-452.
27. Pinto AG, Cummings OW, Chalasani N. Severe but reversible cholestatic liver injury after pioglitazone therapy. Ann Intern Med. 2002;137:857.-
28. Maeda K. Hepatocellular injury in a patient receiving pioglitazone. Ann Intern Med. 2001;135:306.-
29. Dhawan M, Agrawal R, Ravi J, et al. Rosiglitazone-induced granulomatous hepatitis. J Clin Gastroenterol. 2002;34:582-584.
30. Forman LM, Simmons DA, Diamond RH. Hepatic failure in a patient taking rosiglitazone. Ann Intern Med. 2000;132:118-121.
31. Al Salman J, Arjomand H, Kemp DG, Mittal M. Hepatocellular injury in a patient receiving rosiglitazone. A case report. Ann Intern Med. 2000;132:121-124.
32. Coniff RF, Shapiro JA, Robbins D, et al. Reduction of glycosylated hemoglobin and postprandial hyperglycemia by acarbose in patients with NIDDM. A placebo-controlled dose-comparison study. Diabetes Care. 1995;18:817-824.
33. Fritsche A, Schweitzer MA, Haring HU. Glimepiride combined with morning insulin glargine, bedtime neutral protamine hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes. A randomized, controlled trial. Ann Intern Med. 2003;138:952-959.
34. Hirsch IB. Treatment of patients with severe insulin deficiency; what we have learned over the past 2 years. Am J Med. 2004;116(suppl 3A):17S-22S.
35. Hunt LM, Valenzuela MA, Pugh JA. NIDDM patients’ fears and hopes about insulin therapy. The basis of patient reluctance. Diabetes Care. 1997;20:292-298.
36. Frykberg RG. Diabetic foot ulcers: pathogenesis and management. Am Fam Physician. 2002;66:1655-1662.
37. Lagrand WK, Visser CA, Hermens WT, et al. C-reactive protein as a cardiovascular risk factor: more than an epiphenomenon? Circulation. 1999;100:96-102.
38. Dailey GE, III, Noor MA, Park JS, Bruce S, Fiedorek FT. Glycemic control with glyburide/metformin tablets in combination with rosiglitazone in patients with type 2 diabetes: a randomized, double-blind trial. Am J Med. 2004;116:223-229.
39. Aljabri K, Kozak SE, Thompson DM. Addition of pioglitazone or bedtime insulin to maximal doses of sulfonylurea and metformin in type 2 diabetes patients with poor glucose control: a prospective, randomized trial. Am J Med. 2004;116:230-235.
40. Rendell MS, Glazer NB, Ye Z. Combination therapy with pioglitazone plus metformin or sulfonylurea in patients with Type 2 diabetes: influence of prior antidiabetic drug regimen. J Diabetes Complications. 2003;17:211-217.
41. Fonseca V, Grunberger G, Gupta S, Shen S, Foley JE. Addition of nateglinide to rosiglitazone monotherapy suppresses mealtime hyperglycemia and improves overall glycemic control. Diabetes Care. 2003;26:1685-1690.
42. Raskin P, Klaff L, McGill J, et al. Efficacy and safety of combination therapy: repaglinide plus metformin versus nateglinide plus metformin. Diabetes Care. 2003;26:2063-2068.
43. Schwartz S, Sievers R, Strange P, Lyness WH, Hollander P. Insulin 70/30 mix plus metformin versus triple oral therapy in the treatment of type 2 diabetes after failure of two oral drugs: efficacy, safety, and cost analysis. Diabetes Care. 2003;26:2238-2243.
44. Wolffenbuttel BH, Gomis R, Squatrito S, Jones NP, Patwardhan RN. Addition of low-dose rosiglitazone to sulphonylurea therapy improves glycaemic control in type 2 diabetic patients. Diabet Med. 2000;17:40-47.
45. Fonseca V, Rosenstock J, Patwardhan R, Salzman A. Effect of metformin and rosiglitazone combination therapy in patients with type 2 diabetes mellitus: a randomized controlled trial. JAMA. 2000;283:1695-1702.
46. Moses R, Slobodniuk R, Boyages S, et al. Effect of repaglinide addition to metformin monotherapy on glycemic control in patients with type 2 diabetes. Diabetes Care. 1999;22:119-124.
47. Rosenstock J, Brown A, Fischer J, et al. Efficacy and safety of acarbose in metformin-treated patients with type 2 diabetes. Diabetes Care. 1998;21:2050-2055.
48. Kipnes MS, Krosnick A, Rendell MS, Egan JW, Mathisen AL, Schneider RL. Pioglitazone hydrochloride in combination with sulfonylurea therapy improves glycemic control in patients with type 2 diabetes mellitus: a randomized, placebo-controlled study. Am J Med. 2001;111:10-17.
49. Weitgasser R, Lechleitner M, Luger A, Klingler A. Effects of glimepiride on HbA(1c) and body weight in Type 2 diabetes: results of a 1.5-year follow-up study. Diabetes Res Clin Pract. 2003;61:13-19.
50. Holstein A, Plaschke A, Egberts EH. Lower incidence of severe hypoglycaemia in patients with type 2 diabetes treated with glimepiride versus glibenclamide. Diabetes Metab Res Rev. 2001;17:467-473.
51. Dills DG, Schneider J. Clinical evaluation of glimepiride versus glyburide in NIDDM in a double-blind comparative study. Glimepiride/Glyburide Research Group. Horm Metab Res. 1996;28:426-429.
52. Gerich JE. Clinical significance, pathogenesis, and management of postprandial hyperglycemia. Arch Intern Med. 2003;163:1306-1316.
53. Shaw JE, Hodge AM, de Court, Chitson P, Zimmet PZ. Isolated post-challenge hyperglycaemia confirmed as a risk factor for mortality. Diabetologia. 1999;42:1050-1054.
54. Saydah SH, Miret M, Sung J, Varas C, Gause D, Brancati FL. Postchallenge hyperglycemia and mortality in a national sample of U.S. adults. Diabetes Care. 2001;24:1397-1402.
55. Decode Study Group. Glucose tolerance and cardiovascular mortality: comparison of fasting and 2-hour diagnostic criteria. Arch Intern Med. 2001;161:397-405.
56. Korytkowski M, Thomas A, Reid L, Tedesco MB, Gooding WE, Gerich J. Glimepiride improves both first and second phases of insulin secretion in type 2 diabetes. Diabetes Care. 2002;25:1607-1611.
57. Riddle MC. The underuse of insulin therapy in North America. Diabetes Metab Res Rev. 2002;18:S42-S49.
58. DeFronzo RA, Goodman AM. The Multicenter Metformin Study Group. Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. N Engl J Med. 1995;333:541-549.
59. Lin BJ, Wu HP, Huang HS, et al. Efficacy and tolerability of acarbose in Asian patients with type 2 diabetes inadequately controlled with diet and sulfonylureas. J Diabetes Complications. 2003;17:179-185.
1. Gaede P, Vedel P, Larsen N, Jensen GVH, Parving H-H, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383-393.
2. Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA. 1999;281:2005-2012.
3. Wright A, Burden AC, Paisey RB, Cull CA, Holman RR. Sulfonylurea inadequacy. Efficacy of addition of insulin over 6 years in patients with type 2 diabetes in the U.K. Prospective Diabetes Study (UKPDS 57). Diabetes Care. 2002;25:330-336.
4. Riddle MC, Rosenstock J, Gerich J. The Treat-to-Target Trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26:3080-3086.
5. National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics fact sheet: general information and national estimates on diabetes in the United States, 2003. 1-14. 2003.
6. Aye T, Levitsky LL. Type 2 diabetes: an epidemic disease in childhood. Curr Opin Pediatr. 2003;15:411-415.
7. Rosenbloom AL. Increasing incidence of type 2 diabetes in children and adolescents: treatment considerations. Paediatr Drugs. 2002;4:209-221.
8. Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291:2847-2850.
9. Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723-1727.
10. Ford ES, Williamson DF, Liu S. Weight change and diabetes incidence: findings from a national cohort of US adults. Am J Epidemiol. 1997;146:214-222.
11. Leong KS, Wilding JP. Obesity and diabetes. Baillieres Best Pract Res Clin Endocrinol Metab. 1999;13:221-237.
12. Shimabukuro M, Zhou YT, Levi M, Unger RH. Fatty acid-induced β-cell apoptosis: a link between obesity and diabetes. Proc Natl Acad Sci U S A. 1998;95:2498-2502.
13. Weiss R, Dziura J, Burgert TS, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362-2374.
14. Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003;157:821-827.
15. Sinha R, Fisch G, Teague B, et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med. 2002;346:802-810.
16. American Diabetes Association. Type 2 diabetes in children and adolescents. Diabetes Care. 2000;23:381-389.
17. Fagot-Campagna A, Pettitt DJ, Engelgau MM, et al. Type 2 diabetes among North American children and adolescents: an epidemiologic review and a public health perspective. J Pediatr. 2000;136:664-672.
18. Pugeat M, Ducluzeau PH. Insulin resistance, polycystic ovary syndrome and metformin. Drugs. 1999;58(suppl 1):41-46.
19. Hathout EH, Thomas W, El Shahawy M, Nahab F, Mace JW. Diabetic autoimmune markers in children and adolescents with type 2 diabetes. Pediatrics. 2001;107:E102.-
20. ADA. American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2004;27(suppl 1):S15-S35.
21. American Association of Clinical Endocrinologists. The American Association of Clinical Endocrinologists Medical Guidelines for the Management of Diabetes Mellitus: the AACE system of intensive diabetes self-management-2002 update. Endocr Pract. 2002;8(suppl 1):40-82.
22. Jones KL, Arslanian S, Peterokova VA, Park JS, Tomlinson MJ. Effect of metformin in pediatric patients with type 2 diabetes: a randomized controlled trial. Diabetes Care. 2002;25:89-94.
23. Monnier L. Is postprandial glucose a neglected cardiovascular risk factor in type 2 diabetes? Eur J Clin Invest. 2000;30(suppl 2):3-11.
24. Sonnenberg GE, Garg DC, Weidler DJ, et al. Short-term comparison of once- versus twice-daily administration of glimepiride in patients with non-insulin-dependent diabetes mellitus. Ann Pharmacother. 1997;31:671-676.
25. Nesto RW, Bell D, Bonow RO, et al. Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American Heart Association and American Diabetes Association. Diabetes Care. 2004;27:256-263.
26. May LD, Lefkowitch JH, Kram MT, Rubin DE. Mixed hepatocellular-cholestatic liver injury after pioglitazone therapy. Ann Intern Med. 2002;136:449-452.
27. Pinto AG, Cummings OW, Chalasani N. Severe but reversible cholestatic liver injury after pioglitazone therapy. Ann Intern Med. 2002;137:857.-
28. Maeda K. Hepatocellular injury in a patient receiving pioglitazone. Ann Intern Med. 2001;135:306.-
29. Dhawan M, Agrawal R, Ravi J, et al. Rosiglitazone-induced granulomatous hepatitis. J Clin Gastroenterol. 2002;34:582-584.
30. Forman LM, Simmons DA, Diamond RH. Hepatic failure in a patient taking rosiglitazone. Ann Intern Med. 2000;132:118-121.
31. Al Salman J, Arjomand H, Kemp DG, Mittal M. Hepatocellular injury in a patient receiving rosiglitazone. A case report. Ann Intern Med. 2000;132:121-124.
32. Coniff RF, Shapiro JA, Robbins D, et al. Reduction of glycosylated hemoglobin and postprandial hyperglycemia by acarbose in patients with NIDDM. A placebo-controlled dose-comparison study. Diabetes Care. 1995;18:817-824.
33. Fritsche A, Schweitzer MA, Haring HU. Glimepiride combined with morning insulin glargine, bedtime neutral protamine hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes. A randomized, controlled trial. Ann Intern Med. 2003;138:952-959.
34. Hirsch IB. Treatment of patients with severe insulin deficiency; what we have learned over the past 2 years. Am J Med. 2004;116(suppl 3A):17S-22S.
35. Hunt LM, Valenzuela MA, Pugh JA. NIDDM patients’ fears and hopes about insulin therapy. The basis of patient reluctance. Diabetes Care. 1997;20:292-298.
36. Frykberg RG. Diabetic foot ulcers: pathogenesis and management. Am Fam Physician. 2002;66:1655-1662.
37. Lagrand WK, Visser CA, Hermens WT, et al. C-reactive protein as a cardiovascular risk factor: more than an epiphenomenon? Circulation. 1999;100:96-102.
38. Dailey GE, III, Noor MA, Park JS, Bruce S, Fiedorek FT. Glycemic control with glyburide/metformin tablets in combination with rosiglitazone in patients with type 2 diabetes: a randomized, double-blind trial. Am J Med. 2004;116:223-229.
39. Aljabri K, Kozak SE, Thompson DM. Addition of pioglitazone or bedtime insulin to maximal doses of sulfonylurea and metformin in type 2 diabetes patients with poor glucose control: a prospective, randomized trial. Am J Med. 2004;116:230-235.
40. Rendell MS, Glazer NB, Ye Z. Combination therapy with pioglitazone plus metformin or sulfonylurea in patients with Type 2 diabetes: influence of prior antidiabetic drug regimen. J Diabetes Complications. 2003;17:211-217.
41. Fonseca V, Grunberger G, Gupta S, Shen S, Foley JE. Addition of nateglinide to rosiglitazone monotherapy suppresses mealtime hyperglycemia and improves overall glycemic control. Diabetes Care. 2003;26:1685-1690.
42. Raskin P, Klaff L, McGill J, et al. Efficacy and safety of combination therapy: repaglinide plus metformin versus nateglinide plus metformin. Diabetes Care. 2003;26:2063-2068.
43. Schwartz S, Sievers R, Strange P, Lyness WH, Hollander P. Insulin 70/30 mix plus metformin versus triple oral therapy in the treatment of type 2 diabetes after failure of two oral drugs: efficacy, safety, and cost analysis. Diabetes Care. 2003;26:2238-2243.
44. Wolffenbuttel BH, Gomis R, Squatrito S, Jones NP, Patwardhan RN. Addition of low-dose rosiglitazone to sulphonylurea therapy improves glycaemic control in type 2 diabetic patients. Diabet Med. 2000;17:40-47.
45. Fonseca V, Rosenstock J, Patwardhan R, Salzman A. Effect of metformin and rosiglitazone combination therapy in patients with type 2 diabetes mellitus: a randomized controlled trial. JAMA. 2000;283:1695-1702.
46. Moses R, Slobodniuk R, Boyages S, et al. Effect of repaglinide addition to metformin monotherapy on glycemic control in patients with type 2 diabetes. Diabetes Care. 1999;22:119-124.
47. Rosenstock J, Brown A, Fischer J, et al. Efficacy and safety of acarbose in metformin-treated patients with type 2 diabetes. Diabetes Care. 1998;21:2050-2055.
48. Kipnes MS, Krosnick A, Rendell MS, Egan JW, Mathisen AL, Schneider RL. Pioglitazone hydrochloride in combination with sulfonylurea therapy improves glycemic control in patients with type 2 diabetes mellitus: a randomized, placebo-controlled study. Am J Med. 2001;111:10-17.
49. Weitgasser R, Lechleitner M, Luger A, Klingler A. Effects of glimepiride on HbA(1c) and body weight in Type 2 diabetes: results of a 1.5-year follow-up study. Diabetes Res Clin Pract. 2003;61:13-19.
50. Holstein A, Plaschke A, Egberts EH. Lower incidence of severe hypoglycaemia in patients with type 2 diabetes treated with glimepiride versus glibenclamide. Diabetes Metab Res Rev. 2001;17:467-473.
51. Dills DG, Schneider J. Clinical evaluation of glimepiride versus glyburide in NIDDM in a double-blind comparative study. Glimepiride/Glyburide Research Group. Horm Metab Res. 1996;28:426-429.
52. Gerich JE. Clinical significance, pathogenesis, and management of postprandial hyperglycemia. Arch Intern Med. 2003;163:1306-1316.
53. Shaw JE, Hodge AM, de Court, Chitson P, Zimmet PZ. Isolated post-challenge hyperglycaemia confirmed as a risk factor for mortality. Diabetologia. 1999;42:1050-1054.
54. Saydah SH, Miret M, Sung J, Varas C, Gause D, Brancati FL. Postchallenge hyperglycemia and mortality in a national sample of U.S. adults. Diabetes Care. 2001;24:1397-1402.
55. Decode Study Group. Glucose tolerance and cardiovascular mortality: comparison of fasting and 2-hour diagnostic criteria. Arch Intern Med. 2001;161:397-405.
56. Korytkowski M, Thomas A, Reid L, Tedesco MB, Gooding WE, Gerich J. Glimepiride improves both first and second phases of insulin secretion in type 2 diabetes. Diabetes Care. 2002;25:1607-1611.
57. Riddle MC. The underuse of insulin therapy in North America. Diabetes Metab Res Rev. 2002;18:S42-S49.
58. DeFronzo RA, Goodman AM. The Multicenter Metformin Study Group. Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. N Engl J Med. 1995;333:541-549.
59. Lin BJ, Wu HP, Huang HS, et al. Efficacy and tolerability of acarbose in Asian patients with type 2 diabetes inadequately controlled with diet and sulfonylureas. J Diabetes Complications. 2003;17:179-185.
Ottawa Ankle Rules accurately assess injuries and reduce reliance on radiographs
- If a patient does not exhibit any of the criteria of the Ottawa Ankle Rules, radiographs of the foot or ankle are unnecessary (SOR: A).
- Discuss the history, exam findings, and Ottawa Rules with patients. Evidence suggests that satisfaction with care does not depend on whether radiographs are ordered (SOR: B).
In the United States, most ankle injuries are evaluated radiographically, 1,2 even though only about 15% are found to involve fractures. 3 An estimated 6 million ankle radiographs are performed annually in the US and Canada, costing approximately $300 million dollars (US). The Ottawa Ankle Rules can significantly decrease the number of unnecessary ankle radiographs.
The rules are not a substitute for sound clinical judgment, but augment findings in the history and physical examination to help the clinician determine the appropriateness of ankle films. If the rules are met and radiographs are avoided, it is unlikely, especially with good communication and follow-up, that a patient will turn out to have a significant fracture. Moreover, discussing physical examination findings and the reasons for doing or not doing radiographs will enhance patient-physician communication. As we report in this article, patients’ satisfaction with care seems not to depend on whether x-ray films are ordered.
Applying the Ottawa Ankle Rules
To address the problem of low positive predictive value of ankle radiographs, Stiell and colleagues4 at the University of Ottawa and the Ontario Health Ministry developed a set of clinical parameters in the early 1990s to evaluate the need for ankle and midfoot radiographs. Their criteria were based on a multivariable data analysis involving a large number of clinical variables associated with ankle injuries. The resulting rules (Figure) have been shown to decrease the need for films by about 30%.4 If a patient does not exhibit any of the criteria, radiographs of the foot or ankle are not needed after trauma (strength of recommendation [SOR]: A).
FIGURE
Ottawa Ankle Rules for determining the need for radiographs Indications for ankle radiographs
Validation of the rules in different settings
A number of studies have tested the negative predictive value of the Ottawa Ankle Rules. A high negative predictive value implies that if the rules are followed, a fracture will not be missed. Most of these studies were conducted in emergency medicine, sports medicine, and orthopedic settings. In a follow-up study, Stiell and colleagues found a sensitivity of 1.0 (95% confidence interval, 0.95–1.0) for ankle fractures and mid-foot fractures. A positive result is a clinically significant fracture, described as one greater than 3 mm. Such avulsion type injuries are treated clinically like a sprain. In the Stiell study, all films were evaluated by radiologists. The authors estimated a decrease in ankle radiographs by 28% if the rules were followed.4
Emergency medicine. The sensitivity in this setting was also found to be 1.0, with a negative predictive value of 1.0 when used by physicians. This means that no fractures would be missed by using the rules. Specificity was only 0.19.3 In a multicenter Canadian trial, the results were similar. Over 12,000 adults were evaluated with the ankle rule at 8 teaching and community hospital emergency departments. This study found a significant decrease in the number of ankle radiographs ordered without an increase in the rate of fractures missed.5
Orthopedic surgery. In a study involving 153 military cadets at West Point, orthopedic surgeons also showed the sensitivity of these rules was 1.0, with no false negatives. The investigators estimated they could safely forego 40% of all ankle films and 79% of all midfoot films. In the 4 years of training at the Military Academy, an estimated 33% of all cadets suffer an ankle sprain, which speaks to the prevalence of this condition among young, active persons.4
Sports medicine. A prospective study in a university sports medicine clinic validated the use of the ankle rules in a population of 94 athletes. The investigators found a sensitivity of 1.0 for both ankle and midfoot injuries, and a reduction by 34% in the number of films ordered.7 In that study the authors comment on the value of these rules in the sports medicine venue, where the rate of ankle and midfoot fractures is low (less than 3%, as opposed to up to 20% in the emergency setting).8
Family medicine. Little research in family medicine discusses office use of the Ottawa Ankle Rules, but there is a need for a set of evidence-based protocols in evaluating acute ankle injuries. Before establishment of the ankle rules, family physicians used the clinical findings of (1) absence of tenderness on the dorsum of the foot, (2) lack of impaired weight bearing, (3) recentness of injury (more than 12 hours earlier), and (4) absence of additional injuries. Each of these findings had a negative predictive value of least 94%. While family physician researchers involved in one study did not establish a set of decision “rules,” they estimated that using these criteria could reduce unnecessary films by about 30%.9
Meta-analysis. To synthesize results from a large number of studies of the Ottawa Ankle Rules, a meta-analysis involving 27 studies including over 15,000 patients found that evidence supported the rules as an instrument for clinically excluding fractures of the ankle and midfoot. This analysis noted the sensitivity of 1.0 found in virtually every study and estimated that the Ottawa Ankle Rules would decrease the need for films by 30% to 40%.10
The Ottawa Ankle Rules and children
The original Ottawa Ankle Rules were applied strictly to adults, but they also have been studied considerably in the care of children. Pediatric studies have documented sensitivities ranging from 97% to 100% and specificities from 24% to 47%. All studies have shown significant decreases in unnecessary films and significant cost savings. The conclusion of all authors was that the Ottawa Ankle Rules are a cost-effective, highly sensitive test for evaluating acute ankle injuries in children. 11-14
However, researchers at the University of Colorado prospectively evaluated the use of Ottawa Ankle Rules in children aged <18 years. The previous studies had used the same criteria as used for adults, but because of the uncertainty of the long-term effects of Salter I (epiphyseal injury) or small (<3 mm) avulsion fractures in the pediatric population, those injuries were included in the fracture category. This brought the sensitivity down to 83%, with a negative predictive value of 93%. The authors suggested that the Ottawa Rules not be employed in the pediatric population.15 Clearly, more work needs to be done in order to clear them for use in children.
Using the rules reduces costs
Researchers analyzed the cost effectiveness of the rules in the US.16 Variables used to estimate savings included waiting time and lost productivity as well as the obvious medical and radiographic costs. Previous studies have indicated at least a 28% decrease in unneeded ankle films.4 By using this admittedly conservative reduction, it was estimated that the savings would range from $18 to $90 million annually (depending on payer mix involved). Even the smaller amount represents a significant cost savings.
Rule modifications could increase specificity
Because of the low specificity of the Ottawa Rules (a large number of false-positive results are still obtained), sports medicine physicians at the University of Buffalo determined that a modified set of ankle rules could increase specificity significantly. These rules, called the “Buffalo Rules,” kept most of the original rules but changed the original area of fibular tenderness from the posterior and inferior malleolar edges to the midline crest. Using this modification maintained the high sensitivity of the original rules and decreased the need for radiographs from 34% to over 50% (SOR: B).7
Patient satisfaction not dependent on films
While most radiographs done for acute ankle injuries are not helpful, many physicians believe patients expect them and will be dissatisfied or upset if films are not taken. A recent Canadian study evaluated the claim that patient preferences influenced physician test ordering and compliance with clinical guidelines. Specifically it looked at emergency department implementation of the Ottawa Ankle Rules and patient satisfaction.17
This study of almost 1000 patients, split between a population who received films and those who did not for an acute ankle or midfoot injury, indicated that patients who did not get radiographs were just as satisfied with their care as those that did. In the study, 76% of physicians supported the use of clinical guidelines, but 78% admitted that patient expectations influenced their decision making. These rules would likely be of great value where radiographic facilities are inconvenient or costly for patients.
Correspondence
Dr. Paul J. Nugent, 4411 Montgomery Rd, Suite 200, Cincinnati, Ohio 45212. E-mail: [email protected].
1. Dunlop MG, Beattie TF, White GK, Raab GM, Doull RI. Guidelines for selective radiologic assessment of inversion ankle injuries. BMJ (Clin Res Ed) 1986;293:603-605.
2. Vargish T, Clarke WR. The ankle injury: indication for selective use of X-rays. Injury 1983;14:507-512.
3. Pigman EC, Klug RK, Sanford S, Jolly BT. Evaluation of the Ottawa clinical decision rules for the use of radiography in acute ankle and midfoot injuries in the emergency department: an independent site assessment. Ann Emerg Med 1994;24:41-45.
4. Stiell IG, McKnight RD, Greenberg GH, et al. Implementation of the Ottawa Ankle Rules. JAMA 1994;271:827-832.
5. McBride KL. Validation of the Ottawa ankle rules. Experience at a community hospital. Can Fam Physician 1997;43:459-465.
6. Springer, Arciero RA, Tenuta JJ, Taylor DC. A prospective study of modified Ottawa ankle rule in a military population. Am J Sports Med 2000;28:864-868.
7. Leddy JL, Smolinski RJ, Lawrence J, Snyder JL, Priore RL. Prospective evaluation of the Ottawa ankle rules in a university sports medicine center. With a modification to increase specificity for identifying malleolar fractures. Am J Sports Med 1998;26:158-165.
8. Garrick JG. Epidemiological perspective. Clin Sports Med 1982;1:13-18.
9. Smith GF, Madlon-Kay DJ, Hunt V. Clinical inversion injuries in family practice offices. J Fam Pract 1993;37:345-348.
10. Bachmann LM, Kolb E, Koller MT, Steurer J, ter Riet G. Accuracy of Ottawa ankle rules to exclude fracture of the ankle and midfoot: systematic review. BMJ 2003;326:417.-
11. Chande VT. Decision rules for roentgenography of children with acute ankle injuries. Arch Pediatr Adolesc Med 1995;149:255-258.
12. Karpas A, Hennes H, Walsh-Kelly C. Utilization of the Ottawa ankle rules by nurses in a pediatric emergency department. Acad Emerg Med 2002;9:130-133.
13. Libetta C, Burke D, Brennan P, Yassa J. Validation of the Ottawa ankle rules in children. J Accid Emerg Med 1999;16:342-344.
14. Plint AC, Bulloch B, Osmond MH, et al. Validation of the Ottawa ankle rules in children with ankle injuries. Acad Emerg Med 1999;6:1005-1009.
15. Clark KD, Tanner S. Evaluation of the Ottawa ankle rules in children. Pedriatr Emerg Care 2003;19:73-78.
16. Anis AH, Stiell IG, Stewart DG, Laupacis A. Cost-effectiveness analysis of the Ottawa ankle rules. Ann Emerg Med 1995;26:422-428.
17. Wilson DE, Noseworthy TW, Rowe BH, Holroyd BR. Evaluation of patient satisfaction and outcomes after assessment for acute ankle injuries. Am J Emerg Med 2002;20:18-22.
- If a patient does not exhibit any of the criteria of the Ottawa Ankle Rules, radiographs of the foot or ankle are unnecessary (SOR: A).
- Discuss the history, exam findings, and Ottawa Rules with patients. Evidence suggests that satisfaction with care does not depend on whether radiographs are ordered (SOR: B).
In the United States, most ankle injuries are evaluated radiographically, 1,2 even though only about 15% are found to involve fractures. 3 An estimated 6 million ankle radiographs are performed annually in the US and Canada, costing approximately $300 million dollars (US). The Ottawa Ankle Rules can significantly decrease the number of unnecessary ankle radiographs.
The rules are not a substitute for sound clinical judgment, but augment findings in the history and physical examination to help the clinician determine the appropriateness of ankle films. If the rules are met and radiographs are avoided, it is unlikely, especially with good communication and follow-up, that a patient will turn out to have a significant fracture. Moreover, discussing physical examination findings and the reasons for doing or not doing radiographs will enhance patient-physician communication. As we report in this article, patients’ satisfaction with care seems not to depend on whether x-ray films are ordered.
Applying the Ottawa Ankle Rules
To address the problem of low positive predictive value of ankle radiographs, Stiell and colleagues4 at the University of Ottawa and the Ontario Health Ministry developed a set of clinical parameters in the early 1990s to evaluate the need for ankle and midfoot radiographs. Their criteria were based on a multivariable data analysis involving a large number of clinical variables associated with ankle injuries. The resulting rules (Figure) have been shown to decrease the need for films by about 30%.4 If a patient does not exhibit any of the criteria, radiographs of the foot or ankle are not needed after trauma (strength of recommendation [SOR]: A).
FIGURE
Ottawa Ankle Rules for determining the need for radiographs Indications for ankle radiographs
Validation of the rules in different settings
A number of studies have tested the negative predictive value of the Ottawa Ankle Rules. A high negative predictive value implies that if the rules are followed, a fracture will not be missed. Most of these studies were conducted in emergency medicine, sports medicine, and orthopedic settings. In a follow-up study, Stiell and colleagues found a sensitivity of 1.0 (95% confidence interval, 0.95–1.0) for ankle fractures and mid-foot fractures. A positive result is a clinically significant fracture, described as one greater than 3 mm. Such avulsion type injuries are treated clinically like a sprain. In the Stiell study, all films were evaluated by radiologists. The authors estimated a decrease in ankle radiographs by 28% if the rules were followed.4
Emergency medicine. The sensitivity in this setting was also found to be 1.0, with a negative predictive value of 1.0 when used by physicians. This means that no fractures would be missed by using the rules. Specificity was only 0.19.3 In a multicenter Canadian trial, the results were similar. Over 12,000 adults were evaluated with the ankle rule at 8 teaching and community hospital emergency departments. This study found a significant decrease in the number of ankle radiographs ordered without an increase in the rate of fractures missed.5
Orthopedic surgery. In a study involving 153 military cadets at West Point, orthopedic surgeons also showed the sensitivity of these rules was 1.0, with no false negatives. The investigators estimated they could safely forego 40% of all ankle films and 79% of all midfoot films. In the 4 years of training at the Military Academy, an estimated 33% of all cadets suffer an ankle sprain, which speaks to the prevalence of this condition among young, active persons.4
Sports medicine. A prospective study in a university sports medicine clinic validated the use of the ankle rules in a population of 94 athletes. The investigators found a sensitivity of 1.0 for both ankle and midfoot injuries, and a reduction by 34% in the number of films ordered.7 In that study the authors comment on the value of these rules in the sports medicine venue, where the rate of ankle and midfoot fractures is low (less than 3%, as opposed to up to 20% in the emergency setting).8
Family medicine. Little research in family medicine discusses office use of the Ottawa Ankle Rules, but there is a need for a set of evidence-based protocols in evaluating acute ankle injuries. Before establishment of the ankle rules, family physicians used the clinical findings of (1) absence of tenderness on the dorsum of the foot, (2) lack of impaired weight bearing, (3) recentness of injury (more than 12 hours earlier), and (4) absence of additional injuries. Each of these findings had a negative predictive value of least 94%. While family physician researchers involved in one study did not establish a set of decision “rules,” they estimated that using these criteria could reduce unnecessary films by about 30%.9
Meta-analysis. To synthesize results from a large number of studies of the Ottawa Ankle Rules, a meta-analysis involving 27 studies including over 15,000 patients found that evidence supported the rules as an instrument for clinically excluding fractures of the ankle and midfoot. This analysis noted the sensitivity of 1.0 found in virtually every study and estimated that the Ottawa Ankle Rules would decrease the need for films by 30% to 40%.10
The Ottawa Ankle Rules and children
The original Ottawa Ankle Rules were applied strictly to adults, but they also have been studied considerably in the care of children. Pediatric studies have documented sensitivities ranging from 97% to 100% and specificities from 24% to 47%. All studies have shown significant decreases in unnecessary films and significant cost savings. The conclusion of all authors was that the Ottawa Ankle Rules are a cost-effective, highly sensitive test for evaluating acute ankle injuries in children. 11-14
However, researchers at the University of Colorado prospectively evaluated the use of Ottawa Ankle Rules in children aged <18 years. The previous studies had used the same criteria as used for adults, but because of the uncertainty of the long-term effects of Salter I (epiphyseal injury) or small (<3 mm) avulsion fractures in the pediatric population, those injuries were included in the fracture category. This brought the sensitivity down to 83%, with a negative predictive value of 93%. The authors suggested that the Ottawa Rules not be employed in the pediatric population.15 Clearly, more work needs to be done in order to clear them for use in children.
Using the rules reduces costs
Researchers analyzed the cost effectiveness of the rules in the US.16 Variables used to estimate savings included waiting time and lost productivity as well as the obvious medical and radiographic costs. Previous studies have indicated at least a 28% decrease in unneeded ankle films.4 By using this admittedly conservative reduction, it was estimated that the savings would range from $18 to $90 million annually (depending on payer mix involved). Even the smaller amount represents a significant cost savings.
Rule modifications could increase specificity
Because of the low specificity of the Ottawa Rules (a large number of false-positive results are still obtained), sports medicine physicians at the University of Buffalo determined that a modified set of ankle rules could increase specificity significantly. These rules, called the “Buffalo Rules,” kept most of the original rules but changed the original area of fibular tenderness from the posterior and inferior malleolar edges to the midline crest. Using this modification maintained the high sensitivity of the original rules and decreased the need for radiographs from 34% to over 50% (SOR: B).7
Patient satisfaction not dependent on films
While most radiographs done for acute ankle injuries are not helpful, many physicians believe patients expect them and will be dissatisfied or upset if films are not taken. A recent Canadian study evaluated the claim that patient preferences influenced physician test ordering and compliance with clinical guidelines. Specifically it looked at emergency department implementation of the Ottawa Ankle Rules and patient satisfaction.17
This study of almost 1000 patients, split between a population who received films and those who did not for an acute ankle or midfoot injury, indicated that patients who did not get radiographs were just as satisfied with their care as those that did. In the study, 76% of physicians supported the use of clinical guidelines, but 78% admitted that patient expectations influenced their decision making. These rules would likely be of great value where radiographic facilities are inconvenient or costly for patients.
Correspondence
Dr. Paul J. Nugent, 4411 Montgomery Rd, Suite 200, Cincinnati, Ohio 45212. E-mail: [email protected].
- If a patient does not exhibit any of the criteria of the Ottawa Ankle Rules, radiographs of the foot or ankle are unnecessary (SOR: A).
- Discuss the history, exam findings, and Ottawa Rules with patients. Evidence suggests that satisfaction with care does not depend on whether radiographs are ordered (SOR: B).
In the United States, most ankle injuries are evaluated radiographically, 1,2 even though only about 15% are found to involve fractures. 3 An estimated 6 million ankle radiographs are performed annually in the US and Canada, costing approximately $300 million dollars (US). The Ottawa Ankle Rules can significantly decrease the number of unnecessary ankle radiographs.
The rules are not a substitute for sound clinical judgment, but augment findings in the history and physical examination to help the clinician determine the appropriateness of ankle films. If the rules are met and radiographs are avoided, it is unlikely, especially with good communication and follow-up, that a patient will turn out to have a significant fracture. Moreover, discussing physical examination findings and the reasons for doing or not doing radiographs will enhance patient-physician communication. As we report in this article, patients’ satisfaction with care seems not to depend on whether x-ray films are ordered.
Applying the Ottawa Ankle Rules
To address the problem of low positive predictive value of ankle radiographs, Stiell and colleagues4 at the University of Ottawa and the Ontario Health Ministry developed a set of clinical parameters in the early 1990s to evaluate the need for ankle and midfoot radiographs. Their criteria were based on a multivariable data analysis involving a large number of clinical variables associated with ankle injuries. The resulting rules (Figure) have been shown to decrease the need for films by about 30%.4 If a patient does not exhibit any of the criteria, radiographs of the foot or ankle are not needed after trauma (strength of recommendation [SOR]: A).
FIGURE
Ottawa Ankle Rules for determining the need for radiographs Indications for ankle radiographs
Validation of the rules in different settings
A number of studies have tested the negative predictive value of the Ottawa Ankle Rules. A high negative predictive value implies that if the rules are followed, a fracture will not be missed. Most of these studies were conducted in emergency medicine, sports medicine, and orthopedic settings. In a follow-up study, Stiell and colleagues found a sensitivity of 1.0 (95% confidence interval, 0.95–1.0) for ankle fractures and mid-foot fractures. A positive result is a clinically significant fracture, described as one greater than 3 mm. Such avulsion type injuries are treated clinically like a sprain. In the Stiell study, all films were evaluated by radiologists. The authors estimated a decrease in ankle radiographs by 28% if the rules were followed.4
Emergency medicine. The sensitivity in this setting was also found to be 1.0, with a negative predictive value of 1.0 when used by physicians. This means that no fractures would be missed by using the rules. Specificity was only 0.19.3 In a multicenter Canadian trial, the results were similar. Over 12,000 adults were evaluated with the ankle rule at 8 teaching and community hospital emergency departments. This study found a significant decrease in the number of ankle radiographs ordered without an increase in the rate of fractures missed.5
Orthopedic surgery. In a study involving 153 military cadets at West Point, orthopedic surgeons also showed the sensitivity of these rules was 1.0, with no false negatives. The investigators estimated they could safely forego 40% of all ankle films and 79% of all midfoot films. In the 4 years of training at the Military Academy, an estimated 33% of all cadets suffer an ankle sprain, which speaks to the prevalence of this condition among young, active persons.4
Sports medicine. A prospective study in a university sports medicine clinic validated the use of the ankle rules in a population of 94 athletes. The investigators found a sensitivity of 1.0 for both ankle and midfoot injuries, and a reduction by 34% in the number of films ordered.7 In that study the authors comment on the value of these rules in the sports medicine venue, where the rate of ankle and midfoot fractures is low (less than 3%, as opposed to up to 20% in the emergency setting).8
Family medicine. Little research in family medicine discusses office use of the Ottawa Ankle Rules, but there is a need for a set of evidence-based protocols in evaluating acute ankle injuries. Before establishment of the ankle rules, family physicians used the clinical findings of (1) absence of tenderness on the dorsum of the foot, (2) lack of impaired weight bearing, (3) recentness of injury (more than 12 hours earlier), and (4) absence of additional injuries. Each of these findings had a negative predictive value of least 94%. While family physician researchers involved in one study did not establish a set of decision “rules,” they estimated that using these criteria could reduce unnecessary films by about 30%.9
Meta-analysis. To synthesize results from a large number of studies of the Ottawa Ankle Rules, a meta-analysis involving 27 studies including over 15,000 patients found that evidence supported the rules as an instrument for clinically excluding fractures of the ankle and midfoot. This analysis noted the sensitivity of 1.0 found in virtually every study and estimated that the Ottawa Ankle Rules would decrease the need for films by 30% to 40%.10
The Ottawa Ankle Rules and children
The original Ottawa Ankle Rules were applied strictly to adults, but they also have been studied considerably in the care of children. Pediatric studies have documented sensitivities ranging from 97% to 100% and specificities from 24% to 47%. All studies have shown significant decreases in unnecessary films and significant cost savings. The conclusion of all authors was that the Ottawa Ankle Rules are a cost-effective, highly sensitive test for evaluating acute ankle injuries in children. 11-14
However, researchers at the University of Colorado prospectively evaluated the use of Ottawa Ankle Rules in children aged <18 years. The previous studies had used the same criteria as used for adults, but because of the uncertainty of the long-term effects of Salter I (epiphyseal injury) or small (<3 mm) avulsion fractures in the pediatric population, those injuries were included in the fracture category. This brought the sensitivity down to 83%, with a negative predictive value of 93%. The authors suggested that the Ottawa Rules not be employed in the pediatric population.15 Clearly, more work needs to be done in order to clear them for use in children.
Using the rules reduces costs
Researchers analyzed the cost effectiveness of the rules in the US.16 Variables used to estimate savings included waiting time and lost productivity as well as the obvious medical and radiographic costs. Previous studies have indicated at least a 28% decrease in unneeded ankle films.4 By using this admittedly conservative reduction, it was estimated that the savings would range from $18 to $90 million annually (depending on payer mix involved). Even the smaller amount represents a significant cost savings.
Rule modifications could increase specificity
Because of the low specificity of the Ottawa Rules (a large number of false-positive results are still obtained), sports medicine physicians at the University of Buffalo determined that a modified set of ankle rules could increase specificity significantly. These rules, called the “Buffalo Rules,” kept most of the original rules but changed the original area of fibular tenderness from the posterior and inferior malleolar edges to the midline crest. Using this modification maintained the high sensitivity of the original rules and decreased the need for radiographs from 34% to over 50% (SOR: B).7
Patient satisfaction not dependent on films
While most radiographs done for acute ankle injuries are not helpful, many physicians believe patients expect them and will be dissatisfied or upset if films are not taken. A recent Canadian study evaluated the claim that patient preferences influenced physician test ordering and compliance with clinical guidelines. Specifically it looked at emergency department implementation of the Ottawa Ankle Rules and patient satisfaction.17
This study of almost 1000 patients, split between a population who received films and those who did not for an acute ankle or midfoot injury, indicated that patients who did not get radiographs were just as satisfied with their care as those that did. In the study, 76% of physicians supported the use of clinical guidelines, but 78% admitted that patient expectations influenced their decision making. These rules would likely be of great value where radiographic facilities are inconvenient or costly for patients.
Correspondence
Dr. Paul J. Nugent, 4411 Montgomery Rd, Suite 200, Cincinnati, Ohio 45212. E-mail: [email protected].
1. Dunlop MG, Beattie TF, White GK, Raab GM, Doull RI. Guidelines for selective radiologic assessment of inversion ankle injuries. BMJ (Clin Res Ed) 1986;293:603-605.
2. Vargish T, Clarke WR. The ankle injury: indication for selective use of X-rays. Injury 1983;14:507-512.
3. Pigman EC, Klug RK, Sanford S, Jolly BT. Evaluation of the Ottawa clinical decision rules for the use of radiography in acute ankle and midfoot injuries in the emergency department: an independent site assessment. Ann Emerg Med 1994;24:41-45.
4. Stiell IG, McKnight RD, Greenberg GH, et al. Implementation of the Ottawa Ankle Rules. JAMA 1994;271:827-832.
5. McBride KL. Validation of the Ottawa ankle rules. Experience at a community hospital. Can Fam Physician 1997;43:459-465.
6. Springer, Arciero RA, Tenuta JJ, Taylor DC. A prospective study of modified Ottawa ankle rule in a military population. Am J Sports Med 2000;28:864-868.
7. Leddy JL, Smolinski RJ, Lawrence J, Snyder JL, Priore RL. Prospective evaluation of the Ottawa ankle rules in a university sports medicine center. With a modification to increase specificity for identifying malleolar fractures. Am J Sports Med 1998;26:158-165.
8. Garrick JG. Epidemiological perspective. Clin Sports Med 1982;1:13-18.
9. Smith GF, Madlon-Kay DJ, Hunt V. Clinical inversion injuries in family practice offices. J Fam Pract 1993;37:345-348.
10. Bachmann LM, Kolb E, Koller MT, Steurer J, ter Riet G. Accuracy of Ottawa ankle rules to exclude fracture of the ankle and midfoot: systematic review. BMJ 2003;326:417.-
11. Chande VT. Decision rules for roentgenography of children with acute ankle injuries. Arch Pediatr Adolesc Med 1995;149:255-258.
12. Karpas A, Hennes H, Walsh-Kelly C. Utilization of the Ottawa ankle rules by nurses in a pediatric emergency department. Acad Emerg Med 2002;9:130-133.
13. Libetta C, Burke D, Brennan P, Yassa J. Validation of the Ottawa ankle rules in children. J Accid Emerg Med 1999;16:342-344.
14. Plint AC, Bulloch B, Osmond MH, et al. Validation of the Ottawa ankle rules in children with ankle injuries. Acad Emerg Med 1999;6:1005-1009.
15. Clark KD, Tanner S. Evaluation of the Ottawa ankle rules in children. Pedriatr Emerg Care 2003;19:73-78.
16. Anis AH, Stiell IG, Stewart DG, Laupacis A. Cost-effectiveness analysis of the Ottawa ankle rules. Ann Emerg Med 1995;26:422-428.
17. Wilson DE, Noseworthy TW, Rowe BH, Holroyd BR. Evaluation of patient satisfaction and outcomes after assessment for acute ankle injuries. Am J Emerg Med 2002;20:18-22.
1. Dunlop MG, Beattie TF, White GK, Raab GM, Doull RI. Guidelines for selective radiologic assessment of inversion ankle injuries. BMJ (Clin Res Ed) 1986;293:603-605.
2. Vargish T, Clarke WR. The ankle injury: indication for selective use of X-rays. Injury 1983;14:507-512.
3. Pigman EC, Klug RK, Sanford S, Jolly BT. Evaluation of the Ottawa clinical decision rules for the use of radiography in acute ankle and midfoot injuries in the emergency department: an independent site assessment. Ann Emerg Med 1994;24:41-45.
4. Stiell IG, McKnight RD, Greenberg GH, et al. Implementation of the Ottawa Ankle Rules. JAMA 1994;271:827-832.
5. McBride KL. Validation of the Ottawa ankle rules. Experience at a community hospital. Can Fam Physician 1997;43:459-465.
6. Springer, Arciero RA, Tenuta JJ, Taylor DC. A prospective study of modified Ottawa ankle rule in a military population. Am J Sports Med 2000;28:864-868.
7. Leddy JL, Smolinski RJ, Lawrence J, Snyder JL, Priore RL. Prospective evaluation of the Ottawa ankle rules in a university sports medicine center. With a modification to increase specificity for identifying malleolar fractures. Am J Sports Med 1998;26:158-165.
8. Garrick JG. Epidemiological perspective. Clin Sports Med 1982;1:13-18.
9. Smith GF, Madlon-Kay DJ, Hunt V. Clinical inversion injuries in family practice offices. J Fam Pract 1993;37:345-348.
10. Bachmann LM, Kolb E, Koller MT, Steurer J, ter Riet G. Accuracy of Ottawa ankle rules to exclude fracture of the ankle and midfoot: systematic review. BMJ 2003;326:417.-
11. Chande VT. Decision rules for roentgenography of children with acute ankle injuries. Arch Pediatr Adolesc Med 1995;149:255-258.
12. Karpas A, Hennes H, Walsh-Kelly C. Utilization of the Ottawa ankle rules by nurses in a pediatric emergency department. Acad Emerg Med 2002;9:130-133.
13. Libetta C, Burke D, Brennan P, Yassa J. Validation of the Ottawa ankle rules in children. J Accid Emerg Med 1999;16:342-344.
14. Plint AC, Bulloch B, Osmond MH, et al. Validation of the Ottawa ankle rules in children with ankle injuries. Acad Emerg Med 1999;6:1005-1009.
15. Clark KD, Tanner S. Evaluation of the Ottawa ankle rules in children. Pedriatr Emerg Care 2003;19:73-78.
16. Anis AH, Stiell IG, Stewart DG, Laupacis A. Cost-effectiveness analysis of the Ottawa ankle rules. Ann Emerg Med 1995;26:422-428.
17. Wilson DE, Noseworthy TW, Rowe BH, Holroyd BR. Evaluation of patient satisfaction and outcomes after assessment for acute ankle injuries. Am J Emerg Med 2002;20:18-22.
Abnormal vaginal discharge: Using office diagnostic testing more effectively
- Accurate differential diagnosis for women complaining of abnormal vaginal discharge requires in-office diagnostic testing at minimum, and laboratory testing in selected cases.
- Test for Chlamydia trachomatis and Neisseria gonorrhea when signs of purulent cervicitis are present (SOR: B).
- In suspected vulvovaginal candidiasis, culture is recommended for patients with recurrent or persistent symptoms and a negative wet mount result (SOR:B); rapid slide latex agglutination testing is not better than microscopy for diagnosing VVC (SOR: B).
In primary care practice, abnormal vaginal discharge is a common complaint. Signs and symptoms of vaginitis—the most common gynecologic diagnosis in primary care1 —are not specific for any single underlying cause.2 Officebased diagnostic testing, which is underused,3 must be employed to ensure accurate diagnosis and effective treatment. (An article on treatment by the same authors will appear in next month’s issue of The journal of family practice.)
In a primary-care study,4 vulvovaginal symptoms including vaginal discharge were due to vulvovaginal candidiasis (VVC) in 27% of patients, bacterial vaginosis (BV) in 21%, trichomoniasis in 8%, Chlamydia trachomatis in 2%, Neisseria gonorrhea (GC) in 1%, and no infection in 34%. Several pathogens may coexist.2 VVC, BV, and trichomoniasis account for at least 90% of infectious vaginitis.5 This review will therefore focus heavily on these causes of vaginal discharge among women of reproductive age, including pregnant women.
Cervicitis and physiologic cervical discharge
Some women may interpret a physiologic increase in cervical mucous production as abnormal. It occurs cyclically prior to ovulation, is typically transparent and colorless, and may be more pronounced in women with an everted cervix.
Chlamydial infection
In the clinical examination of the cervix, 3 characteristics have been associated with chlamydial infection: yellow endocervical discharge, easily induced cervical bleeding, and opaque cervical discharge.6 All 3 findings are statistically significant and independently associated with chlamydial infection (odds ratios 2.8, 2.3, and 2.9, respectively). In the primary care study cited above, purulent cervical discharge was found in 6% of women, most commonly testing positive for Chlamydia, less often for GC.4
Trichomonas vaginalis may cause cervicitis as well as vaginitis. Mycoplasma genitalium has been proposed as an additional possible pathogen. It was identified in 7% of more than 700 women with mucopurulent cervical discharge seen in a STD clinic with otherwise negative cultures.7 With cervical discharge that appears to be purulent, testing is warranted as a minimum for Chlamydia and GC (SOR: B). Screening of asymptomatic women less than 26 years of age for Chlamydia is recommended by the US Preventive Services Task Force (SOR: A).
Bacterial Vaginosis
Bacterial vaginosis (BV) is neither an inflammatory condition nor an STD, but is a shift in vaginal flora from the normal condition in which lactobacilli predominate, to a polymicrobial flora in which gram-positive anaerobes predominate. In addition to annoying vaginal symptoms, BV is associated with increased risks of more serious conditions such as pelvic inflammatory disease (PID), postoperative infections, and pregnancyrelated complications including prematurity. It also increases the likelihood of acquiring HIV in women exposed to the virus.8,9
Two principal factors put women at risk for acquiring BV: douching and exposure to a new sexual partner, both of which are thought to disrupt the vaginal ecosystem.10
Relative benefits of diagnostic tests
A gold standard test has not been established for BV. In about 50% of asymptomatic women, culture results are positive for flora such as Gardnerella vaginalis.5 While Amsel’s criteria are often used as a reference and generally suffice for the evaluation of symptomatic women, the best candidate for a gold standard test is probably Gram stain assessment using Nugent’s criteria (described in this section).11 Lack of leukocytes in the vaginal fluid supports a diagnosis of BV. A finding of white blood cells in excess of the number of vaginal epithelial cells suggests an inflammatory process (SOR: C).12
Amsel’s criteria with wet mount. The diagnostic approach most commonly used in the office is Amsel’s criteria—homogenous discharge, positive whiff-amine test, pH >4.5, and clue cells found on wet-mount microscopy (see How to perform a wet mount ).13 Three of 4 criteria deemed positive is considered diagnostic. If Gram stain is used as the reference standard, then Amsel’s criteria have 70% sensitivity and 94% specificity for diagnosing BV.14 An analysis of the individual criteria follows. The positive and negative predictive values of each compared with the whole group as reference standard is displayed in Table 1 .
Homogenous discharge. A thin, homogenous, grayish discharge is traditionally associated with BV. However, it is not specific to BV, being found commonly also in women with culture results positive for VVC or no diagnosis of vaginitis.2,15 It is the criterion least likely to be consistent with the whole group, seen in about half of women BVpositive and over one third of women BV-negative using Amsel’s criteria as the reference standard. 15
To perform a wet-mount preparation correctly, dilute the vaginal discharge with 1 or 2 drops of 0.9% saline and place it on a slide. Examine the slide under lowand high-powered fields for vaginal squamous cells, white blood cells (WBCs), lactobacilli, clue cells, and trichomonads. An increased number of WBCs can be defined as >5–10 WBC/HPF or WBCs exceeding the number vaginal epithelial cells.
To prepare the potassium hydroxide (KOH) slide, place a generous amount of vaginal discharge on a slide with 10% KOH solution. Air- or flame-drying before examination under low-power microscopy may improve sensitivity. A positive KOH preparation will have hyphae, mycelial tangles, or spores.
Whiff test. The whiff test is performed by adding drops of 10% potassium hydroxide solution to the vaginal fluid. A positive result is a “fishy” amine odor. In a study16 of 100 women complaining of malodorous discharge, a positive whiff test was predictive of positive culture results for anaerobic flora such as Bacteroides sp. with sensitivity 67%, specificity 94%, and a positive predictive value of 95%. The whiff test was not positive in any of the 5 cases with positive culture results for G vaginalis in the absence of anaerobes. There were also 12 cases positive for anaerobes without G vaginalis.
pH >4.5. Since the abnormal flora of BV is consistently associated with a vaginal pH >4.5, a normal pH excludes a diagnosis of BV.17,18 The determination of pH in the narrow range around 4.5 is not accurate using standard nitrazine paper. Narrower-range test paper is available and more accurate. Examples include pH paper for 4.5 to 5.5 (Micro Essential Laboratory), FemExam pH and Amines Test Card (Litmus Concepts), pHem-ALERT: pH paper on a stick (Imagyn Gynecology). Cervical mucous, semen, and blood are alkaline and can interfere with pH testing. Estrogen production is also necessary to maintain an acidic environment. A pH of 3.8 to 4.5 is consistent with normal vaginal flora in premenopausal women with normal estrogen production.17
Clue cells. Clue cells are vaginal epithelial cells coated with coccobacilli giving an appearance as if coated with ground black pepper. Clue cells on wet mount preparation is considered the most accurate of Amsel’s diagnostic criteria for BV.19 On the other hand, office evaluation of the wet mount is considered by some authors to be unreliable due to dependence on the clinician’s microscopy skills and lack of a durable record of the patient sample.
Gram stain a more objective test. A Gram stain evaluation using Nugent’s criteria has been adopted as the gold standard test for research purposes, including studies of prematurity. The Gram-stained vaginal specimen is scored from 0 to 10 based on semi-quantitative assessment of 3 classes of morphotypes ( Table 2 ): large gram-positive rods (Lactobacilli), small gram-negative rods (Gardnerella and Bacteroides spp.), and small curved gram-variable rods (Mobiluncus spp.).11
Diagnosis of BV is typically made when the Nugent score is 7 or more, which appears qualitatively as dominant morphotypes other than Lactobacilli. Gram staining is more objective and reproducible compared with wet-mount examination, with a sensitivity of 93% and specificity of 70% if Amsel’s criteria are used as the gold standard.14 It is useful for the evaluation of asymptomatic women. It also provides a durable record of the patient specimen. Compared with Gram stain, Amsel’s criteria tend to underdiagnose cases. We can expect that if screening for BV in pregnancy becomes a recommendation, Gram staining in a clinical laboratory will be the recommended method of diagnosis.
Other diagnostic tests for BV. DNA testing for Gardnerella is accurate for detection, but it is not synonymous with a diagnosis of BV, as described.20 DNA testing is further described under “Differential Diagnosis.” Gram staining is more reliable than gas-liquid chromatography21 and an assay for proline aminopeptidase (a metabolic product of some of the bacteria associated with BV).22 Latex agglutination testing for vaginal lactoferrin is a nonspecific marker for leukocytes, and thus inflammation. It is of little clinical utility in the diagnosis of vaginal discharge.23
TABLE 1
Predictive values of Amsel’s criteria (using 3 of 4 positive as diagnostic reference standard)
| Diagnostic criterion | Predictive value (%) | |
|---|---|---|
| Positive | Negative | |
| Homogeneous thin discharge seen at introitus | 42 | 89 |
| pH >4.5 | 53 | 94 |
| Odor on alkalinization | 94 | 93 |
| Clue cells on wet mount | 90 | 99 |
| Source: Thomason et al 1990.15 | ||
TABLE 2
How to use Nugent’s Gram stain criteria to diagnose bacterial vaginosis
| Lactobacillus morphophytes | Gardnerella and Bacteroides spp. morphophytes | Curved gram-variable rods | Points |
|---|---|---|---|
| 4+ | 0 | 0 | 0 |
| 3+ | 1+ | 1+ or 2+ | 1 |
| 2+ | 2+ | 3+ or 4+ | 2 |
| 1+ | 3+ | 3 | |
| 0 | 4+ | 4 | |
| Review each of the first 3 columns in turn, assigning points at far right according to your exam findings. | |||
| Add the points for all 3 columns for a final sum. A score of 7 or higher indicates bacterial vaginosis. Source: Nugent et al 1991.11 | |||
Vulvovaginal Candidiasis
Candidiasis is the second most commonly diagnosed vaginitis in the United States. Some experts estimate that 75% of women will have a yeast infection at some point in life and 5% will have recurrent infections.24 However, 10% to 30% of asymptomatic women with normal flora have positive culture results for Candida.25-29 The proportion of symptomatic women with positive culture results is 20% to 40%.4,30,31 Complications of VVC are rare,32 though vulvar vestibulitis33 and chorioamnionitis in pregnancy32 have been reported.
Risk factors. Symptomatic yeast vaginitis has been associated with condom and diaphragm use, recent antibiotic use, receptive oral sex, oral contraceptive use, spermicide use, diabetes, and immunosuppression including AIDS.31,34-37 The associations with antibiotic use and oral contraceptives are not consistent.30,38 Although pregnancy has been postulated as a risk factor for symptomatic VVC, prevalence of yeast on culture in pregnant women is similar to that of nonpregnant women.30
Suggestive symptoms. Among women with a culture result positive for Candida, the most common symptom is pruritus or burning.28 Abnormal discharge is a complaint for most symptomatic women with VVC confirmed by culture.2 In addition, women may complain of a thick, odorless, cottage cheese–like discharge.39 A thick, curdled-appearing discharge points to a diagnosis of Candida because it is rarely present with BV or trichomoniasis. In one study,28 a thick curdled discharge had a positive predictive value of 84% for diagnosis of VVC by culture (SOR: B). However, a thin discharge does not rule out VVC; in another study, clinicians described discharge as thin in about half of women ultimately diagnosed with VVC by culture in another study (SOR: B).2 On exam, vulvar and vaginal erythema are often present but are not specific findings. The accuracy of the clinical exam for VVC is poor compared with culture (SOR: A).2,30
Pathogens. Candida albicans is present in 80% to 90% of patients with VVC.5,40 remainder have non-albicans species, including C glabrata and others.28 An increase to almost 20% of non-Candida species in a vaginitis clinic by the mid-1990’s may be related to increased use of imidazoles available over-the-counter.40,41 Wet mount results are typically negative in the presence of non-Candida VVC.28
Diagnosis of VVC
The gold standard test for diagnosis of VVC is culture. The potassium hydroxide (KOH) wet mount is only 40% to 75% sensitive.28,29,42,43 False-positive results are also observed with variable frequency.44 The pH of the discharge is usually not more than 5.0 with Candida albicans, but may be higher with non-albicans species such as C glabrata.45 Culture is recommended for patients with recurrent or persistent symptoms and a negative wet mount result (SOR: B).5,28,46 Rapid slide latex agglutination testing is not better than microscopy (SOR: B).42
Trichomoniasis
Trichomonas, a motile protozoan with 4 flagella, causes the third most common form of vaginitis in the United States and is more common in some developing countries. Trichomoniasis accounts for no more than 10% of all cases of vaginitis, and it appears to be decreasing since the introduction of metronidazole.47,48 It is classified as an STD, although transmission is possible by other means if the organism is protected from desiccation—for example, in dirty washcloths or towels and contaminated water. Nonsexual transmission is thought to be uncommon.
Trichomoniasis is associated with GC and Chlamydia infections, and, like them, has been associated with seroconversion to HIV-positive status.49 Trichomonads are identified in 30% to 80% of male sexual partners of infected women. In men, trichomoniasis most often is an asymptomatic carrier state.50 However, it is the cause of about 10% of cases of nongonococcal urethritis in men.51
Our knowledge of the epidemiology of abnormal vaginal discharge is limited. Studies of vaginitis may exclude patients with vaginal discharge due to cervicitis; studies performed in sexually transmitted disease clinics are not representative of primary care practice; women who do not complain of abnormal vaginal discharge may have positive cultures for Gardnerella vaginalis and Candida albicans; and self-treatment of presumed yeast vaginitis with antifungals available over-the-counter further limits our knowledge of the prevalence and causes of vaginal discharge.
Clinical presentations. Women with trichomoniasis have variable presentations ranging from an asymptomatic carrier state to a malodorous, purulent discharge with vulvovaginal erythema. Punctate hemorrhagic cervical lesions are considered pathognomonic of trichomoniasis, but are seen in only about 2% of cases (SOR: B).52
Diagnosis. Culture for trichomoniasis is the gold standard. Several culture media have been used, most commonly the Diamond medium. Recently introduced is a transport and culture medium for detection of Trichomonas (InPouch TV), which performs as well as Diamond medium (SOR: A).53-55 A DNA probe is also available and accurate (SOR: A).
Motile trichomonads are seen on wet preparation in only 50% to 80% of culture-positive cases (SOR: B).50,54,56 Polymorphonuclear leukocytes can be dominant on wet mount, making visualization of trichomonads more difficult. The pH of the vaginal fluid is usually basic.
Trichomonas reported with cervical cytology
Trichomonas may also be reported on Pap smears. A meta-analysis57 comparing the pooled sensitivities and specificities of wet mounts and cytology demonstrated low sensitivities of 68% and 58%, respectively, and high specificities, 99.9% and 97%, respectively (SOR: A).
However, since cytology carries a 3% false-positive rate, its results are not diagnostic of trichomoniasis in low-risk, asymptomatic women.50,57 Treatment may be prescribed empirically based on positive cytology results. However, if an asymptomatic woman were concerned about whether she really has an STD, a positive wet prep would confirm the diagnosis. A negative wet prep should be followed up with culture to reliably rule out disease (SOR: B).
Trichomoniasis in pregnancy
Screening for asymptomatic trichomoniasis in pregnancy has not been recommended. In fact, some evidence suggests that treatment of trichomoniasis in pregnancy is associated with poorer pregnancy outcomes including lower birth weight and more prematurity (SOR: B).58,59
Aerobic vaginitis
Aerobic vaginitis is a term proposed to describe purulent vaginal discharge with predominance of abnormal aerobic flora.60 Aerobic vaginitis, which may be severe, has been reported as the cause of 5% of cases in a series from a specialty vaginitis clinic.61 The usual predominant microorganisms are group B streptococci, Escherichia coli, and Staphylococcus aureus. It is likely that less severe cases of aerobic vaginitis are not recognized in the primary care setting and are treated as BV or resolve spontaneously (SOR: C). The case series referred to above also reported good therapeutic response to 2% topical clindamycin (SOR: C).61
Noninfectious Vaginitis
Noninfectious causes of vaginal discharge include physiologic, irritant and allergic, cytolytic vaginitis, desquamative inflammatory vaginitis, collagen vascular disease, and idiopathic vaginitis.
Irritant and allergic vaginitis may result from sensitivities to topical medications, the active or base ingredients of spermicidal products, douching solutions, and the latex of condoms or diaphragms. If a woman with persistent symptoms has been using such intravaginal products, she should stop (SOR: C).
Cytolytic vaginitis is characterized by overgrowth of lactobacilli and cytolysis of squamous cells, including presence of cytoplasmic fragments and intact cells with naked nuclei.62 The cause is uncertain but may include a reaction to intravaginal medications or other products such as tampons. It can be found in up to 5% of women with symptoms and signs of vaginitis.62,63 Symptoms often mimic VVC and may include a white, cheesy discharge. Vaginal pH ranges from 3.5 to 5.5. Recurrences during luteal phase of the menstrual cycle have been described.64 Intravaginal antifungals should be discontinued. Baking soda sitz baths or douches are often used, but clinical trial data to support this practice are lacking (SOR: C).
Noninfectious desquamative inflammatory vaginitis (DIV) has also been described.65 DIV is an uncommon vaginitis characterized by profuse purulent discharge with epithelial cell exfoliation. It may occur at any time during the reproductive years or after menopause. There is probably a heterogeneous group of causes of DIV. Some cases may correspond to a disorder within the spectrum of lichen planus.66 Treatment is usually difficult, though there may be some response to local or systemic corticosteroid therapy (SOR: C).65
Differential diagnosis
A comparison of physical examination findings an diagnostic test results for various etiologies of vaginitis is summarized in Table 3 . An algorithmic approach to the differential diagnosis of abnormal vaginal discharge is presented in the Figure . Diagnosis is complicated in that signs and symptoms do little to help differentiate among BV, VVC, and trichomoniasis. A study2 of 22 genitourinary symptoms and signs showed that none differentiated among the 3 infections. This lack of clear-cut differences in symptoms also makes self-diagnosis and telephone triage inaccurate.67,68
A DNA probe testing system (Affirm VP III Microbial ID Test) for differential diagnosis is available but expensive. It identifies Gardnerella, Trichomonas, and Candida albicans with a sensitivity of 90% to 95%.54,66 The analyzer costs approximately $10,000 and would typically be purchased by a laboratory. Individual test kits cost about $27.
TABLE 3
Comparative findings among causes of vaginitis
| Cause | Physical exam findings* | Gold standard test | pH | Leukocytes | Wet mount | Alternative test |
|---|---|---|---|---|---|---|
| Bacterial vaginosis | Variable | Gram stain | >4.5 | No | Clue cells | Amsel’s criteria |
| Aerobic vaginitis | Abundant purulent discharge | Culture | >4.5 | Yes | Cocci or coarse rods | |
| Candida vaginitis | Adherent white disch. (thrush) | Culture | 3.8–4.5 | ± | Pseudohyphae or budding yeast | DNA testing |
| Non-Candida yeast vaginitis | Variable | Culture | Any | ± | Usually negative | |
| Trichomoniasis | Variable, occ. strawberry spots on cervix | Culture | >4.5 | ± | Motile trichomonads | DNA testing |
| Cytolytic vaginitis | Profuse discharge, often cheesy | Cytology and negative culture | 3.5–5.5 | ± | Overgrowth of lactobacilli and squamous cell fragments | |
| Desquamative inflammatory vaginitis | Abundant purulent discharge | Parabasal epithelial cells and negative culture | >4.5 | Yes | ||
| Irritant and allergic vaginitis | Variable, often erythema | None | Any | ± | ||
| * Helpful when present. | ||||||
FIGURE
Sequence of office tests to evaluate abnormal vaginal discharge
Corresponding author
Linda French, MD, Associate Professor, Department of Family Practice, College of Human Medicine, Michigan State University, B101 Clinical Center, East Lansing, MI 48824. E-mail: [email protected].
1. National Center for Health Statistics. National Ambulatory Medicine Care Survey. Available at: www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm.
2. Schaaf VM, Perez-Stable EJ, Borchardt K. The limited value of symptoms and signs in the diagnosis of vaginal infections. Arch Intern Med 1990;150:1929-1933.
3. Wiesenfeld HC, Macio I. The infrequent use of officebased diagnostic tests for vaginitis. Am J Obstet Gynecol 1999;181:39-41.
4. Berg AO, Heidrich FE, Fihn SD, et al. Establishing the cause of genitourinary symptoms in women in a family practice. Comparison of clinical examination and comprehensive microbiology. JAMA 1984;251:620-625.
5. Sobel JD. Vaginitis. N Engl J Med 1997;337:1896-1903.
6. Sellors JW, Walter SD, Howard M. A new visual indicator of chlamydial cervicitis? Sex Transm Infect 2000;76:46-48.
7. Manhart LE, Critchlow CW, Holmes KK, et al. Mucopurulent cervicitis and Mycoplasma genitalium. J Infect Dis 2003;187:650-657.
8. Martin HL, Richardson BA, Nyange PM, et al. Vaginal lactobacilli, microbial flora, and risk of human immunodeficiency virus type 1 and sexually transmitted disease acquisition. J Infect Dis 1999;180:1863-1868.
9. Hillier SL. The vaginal microbial ecosystem and resistance to HIV. AIDS Res Hum Retroviruses 1998;14Suppl 1:S17-21.
10. Hawes SE, Hillier SL, Benedetti J, et al. Hydrogenperoxide-producing lactobacilli and acquisition of vaginal infections. J Infect Dis 1996;174:1058-1063.
11. Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. JClin Microbiol 1991;29:297-301.
12. Quan M. Vaginitis: meeting the clinical challenge. Clin Cornerstone 2000;3:36-47.
13. Amsel R, Totten PA, Spiegel CA, Chen KC, Eschenbach D, Holmes KK. Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med 1983;74:14-22.
14. Schwebke JR, Hillier SL, Sobel JD, McGregor JA, Sweet RL. Validity of the vaginal gram stain for the diagnosis of bacterial vaginosis. ObstetGynecol 1996;88:573-576.
15. Thomason JL, Gelbart SM, Anderson RJ, Walt AK, Osypowski PJ, Broekhuizen FF. Statistical evaluation of diagnostic criteria for bacterial vaginosis. Am J Obstet Gynecol. 1990;162:155-160.
16. Erkkola R, Jarvinen H, Terho P, Meurman O. Microbial flora in women showing symptoms of nonspecific vaginosis: applicability of KOH test for diagnosis. Scand J Infect Dis Suppl. 1983;40:59-63.
17. Caillouette JC, Sharp CF, Jr, Zimmerman GJ, Roy S. Vaginal pH as a marker for bacterial pathogens and menopausal status. Am J Obstet Gynecol. 1997;176:1270-1275discussion1275-1277.
18. Carr PL, Felsenstein D, Friedman RH. Evaluation and management of vaginitis. J Gen Intern Med 1998;13:335-346.
19. Eschenbach DA, Hillier S, Critchlow C, Stevens C, DeRouen T, Holmes KK. Diagnosis and clinical manifestations of bacterial vaginosis. Am J Obstet Gynecol 1988;158:819-828.
20. Sheiness D, Dix K, Watanabe S, Hillier SL. Highlevels of Gardnerella vaginalis detected with an oligonucleotide probe combined with elevated pH as a diagnostic indicator of bacterial vaginosis. J Clin Microbiol 1992;30:642-648.
21. Thomason JL, Gelbart SM, James JA, Edwards JM, Hamilton PR. Is analysis of vaginal secretions for volatile organic acids to detect bacterial vaginosis of any diagnostic value? Am J Obstet Gynecol. 1988;159:1509-1511.
22. Thomason JL, Gelbart SM, Wilcoski LM, Peterson AK, Jilly BJ, Hamilton PR. Proline aminopeptidase activity as a rapid diagnostic test to confirm bacterial vaginosis. Obstet Gynecol 1988;71:607-611.
23. Rein MF, Shih LM, Miller JR, Guerrant RL. Use of a lactoferrin assay in the differential diagnosis of female genital tract infections and implications for the pathophysiology of bacterial vaginosis. Sex Transm Dis 1996;23:517-521.
24. Monif GR. Classification and pathogenesis of vulvovaginal candidiasis. Am J Obstet Gynecol 1985;152:935-939.
25. Giraldo P, von Nowaskonski A, Gomes FA, Linhares I, Neves NA, Witkin SS. Vaginal colonization by Candida in asymptomatic women with and without a history of recurrent vulvovaginal candidiasis. Obstet Gynecol 2000;95:413-416.
26. Bergman JJ, Berg AO. How useful are symptoms in the diagnosis of Candida vaginitis? J Fam Pract 1983;16:509-511.
27. Bro F. Patients with vaginal discharge in general practice. Acta Obstet Gynecol Scand 1989;68:41-43.
28. Eckert LO, Hawes SE, Stevens CE, Koutsky LA, Eschenbach DA, Holmes KK. Vulvovaginal candidiasis: clinical manifestations, risk factors, management algorithm. Obstet Gynecol 1998;92:757-765.
29. Bertholf ME, Stafford MJ. Colonization of Candida albicans in vagina, rectum, and mouth. J Fam Pract 1983;16:919-924.
30. Reed BD, Huck W, Zazove P. Differentiation of Gardnerella vaginalis, Candida albicans, and Trichomonas vaginalis infections of the vagina. J Fam Pract 1989;28:673-680.
31. Bro F. The diagnosis of candida vaginitis in general practice. Scand J Prim Health Care 1989;7:19-22.
32. Cotch MF, Hillier SL, Gibbs RS, Eschenbach DA. Epidemiology and outcomes associated with moderate to heavy Candida colonization during pregnancy. Vaginal Infections and Prematurity Study Group. Am J Obstet Gynecol 1998;178:374-380.
33. Pagano R. Vulvar vestibulitis syndrome: an often unrecognized cause of dyspareunia. Aust N Z J Obstet Gynaecol 1999;39:79-83.
34. Foxman B. The epidemiology of vulvovaginal candidiasis: risk factors. Am J Public Health 1990;80:329-331.
35. Geiger AM, Foxman B. Risk factors for vulvovaginal candidiasis: a case-control study among university students. Epidemiology 1996;7:182-187.
36. Sobel JD, Faro S, Force RW, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol 1998;178:203-211.
37. Spinillo A, Capuzzo E, Acciano S, De Santolo A, Zara F. Effect of antibiotic use on the prevalence of symptomatic vulvovaginal candidiasis. Am J Obstet Gynecol 1999;180:14-17.
38. Davidson F, Oates JK. The pill does not cause ‘thrush’. Br J Obstet Gynaecol Dec 1985;92:1265-1266.
39. Abbott J. Clinical and microscopic diagnosis of vaginal yeast infection: a prospective analysis. Ann Emerg Med 1995;25:587-591.
40. Horowitz BJ, Giaquinta D, Ito S. Evolving pathogens in vulvovaginal candidiasis: implications for patient care. J Clin Pharmacol 1992;32:248-255.
41. Spinillo A, Capuzzo E, Gulminetti R, Marone P, Colonna L, Piazzi G. Prevalence of and risk factors for fungal vaginitis caused by non-albicans species. Am J Obstet Gynecol 1997;176:138-141.
42. Reed BD, Pierson CL. Evaluation of a latex agglutination test for the identification of Candida species in vaginal discharge. J Am Board Fam Pract 1992;5:375-380.
43. Ferris DG, Hendrich J, Payne PM, et al. Office laboratoAE_French.1004.final 9/20/04 3:18 PM Page 813 ry diagnosis of vaginitis. Clinician-performed tests compared with a rapid nucleic acid hybridization test. J Fam Pract 1995;41:575-581.
44. Bergman JJ, Berg AO, Schneeweiss R, Heidrich FE. Clinical comparison of microscopic and culture techniques in the diagnosis of Candida vaginitis. J Fam Pract 1984;18:549-552.
45. Sobel JD. Vulvovaginitis due to Candida glabrata. An emerging problem. Mycoses. 1998;41:Suppl 2:18-22.
46. Zdolsek B, Hellberg D, Froman G, Nilsson S, Mardh PA. Culture and wet smear microscopy in the diagnosis of low-symptomatic vulvovaginal candidosis. Eur J Obstet Gynecol Reprod Biol 1995;58:47-51.
47. Lossick JG, Kent HL. Trichomoniasis: trends in diagnosis and management. Am J Obstet Gynecol 1991;165:1217-1222.
48. Kent HL. Epidemiology of vaginitis. Am J Obstet Gynecol 1991;165:1168-1176.
49. Laga M, Manoka A, Kivuvu M, et al. Non-ulcerative sexually transmitted diseases as risk factors for HIV-1 transmission in women: results from a cohort study. AIDS 1993;7:95-102.
50. Krieger JN, Tam MR, Stevens CE, et al. Diagnosis of trichomoniasis. Comparison of conventional wet-mount examination with cytologic studies, cultures, and monoclonal antibody staining of direct specimens. JAMA 1988;259:1223-1227.
51. Krieger JN. Trichomoniasis in men: old issues and new data. Sex Transm Dis 1995;22:83-96.
52. Fouts AC, Kraus SJ. Trichomonas vaginalis: reevaluation of its clinical presentation and laboratory diagnosis. J Infect Dis 1980;141:137-143.
53. Ohlemeyer CL, Hornberger LL, Lynch DA, Swierkosz EM. Diagnosis of Trichomonas vaginalis in adolescent females: InPouch TV culture versus wet-mount microscopy. J Adolesc Health 1998;22:205-208.
54. Borchardt KA, Smith RF. An evaluation of an InPouch TV culture method for diagnosing Trichomonas vaginalis infection. Genitourin Med 1991;67:149-152.
55. Levi MH, Torres J, Pina C, Klein RS. Comparison of the InPouch TV culture system and Diamond’s modified medium for detection of Trichomonas vaginalis. J Clin Microbiol 1997;35:3308-3310.
56. DeMeo LR, Draper DL, McGregor JA, et al. Evaluation of a deoxyribonucleic acid probe for the detection of Trichomonas vaginalis in vaginal secretions. Am J Obstet Gynecol 1996;174:1339-1342.
57. Wiese W, Patel SR, Patel SC, Ohl CA, Estrada CA. A meta-analysis of the Papanicolaou smear and wet mount for the diagnosis of vaginal trichomoniasis. Am J Med 2000;108:301-308.
58. Klebanoff MA, Carey JC, Hauth JC, et al. Failure of metronidazole to prevent preterm delivery among pregnant women with asymptomatic Trichomonas vaginalis infection. N Engl J Med 2001;345:487-493.
59. Kigozi GG, Brahmbhatt H, Wabwire-Mangen F, et al. Treatment of Trichomonas in pregnancy and adverse outcomes of pregnancy: a subanalysis of a randomized trial in Rakai, Uganda. Am J Obstet Gynecol 2003;189:1398-1400.
60. Donder GG, Vereecken A, Bosmans E, Dekeersmaecker A, Salembier G, Spitz B. Definition of a type of abnormal vaginal flora that is distinct from bacterial vaginosis: aerobic vaginitis. Bjog 2002;109:34-43.
61. Sobel JD. Desquamative inflammatory vaginitis: a new subgroup of purulent vaginitis responsive to topical 2% clindamycin therapy. Am J Obstet Gynecol 1994;171:1215-1220.
62. Demirezen S. Cytolytic vaginosis: examination of 2947 vaginal smears. Cent Eur J Public Health 2003;11:23-24.
63. Wathne B, Holst E, Hovelius B, Mardh PA. Vaginal discharge—comparison of clinical, laboratory and microbiological findings. Acta Obstet Gynecol Scand 1994;73:802-808.
64. Secor RM. Cytolytic vaginosis: a common cause of cyclic vulvovaginitis. Nurse Pract Forum 1992;3:145-148.
65. Oates JK, Rowen D. Desquamative inflammatory vaginitis. A review. Genitourin Med 1990;66:275-279.
66. Pelisse M. The vulvo-vaginal-gingival syndrome. A new form of erosive lichen planus. Int J Dermatol 1989;28:381-384.
67. Ferris DG, Nyirjesy P, Sobel JD, Soper D, Pavletic A, Litaker MS. Over-the-counter antifungal drug misuse associated with patient-diagnosed vulvovaginal candidiasis. Obstet Gynecol 2002;99:419-425.
68. Allen-Davis JT, Beck A, Parker R, Ellis JL, Polley D. Assessment of vulvovaginal complaints: accuracy of telephone triage and in-office diagnosis. Obstet Gynecol 2002;99:18-22.
- Accurate differential diagnosis for women complaining of abnormal vaginal discharge requires in-office diagnostic testing at minimum, and laboratory testing in selected cases.
- Test for Chlamydia trachomatis and Neisseria gonorrhea when signs of purulent cervicitis are present (SOR: B).
- In suspected vulvovaginal candidiasis, culture is recommended for patients with recurrent or persistent symptoms and a negative wet mount result (SOR:B); rapid slide latex agglutination testing is not better than microscopy for diagnosing VVC (SOR: B).
In primary care practice, abnormal vaginal discharge is a common complaint. Signs and symptoms of vaginitis—the most common gynecologic diagnosis in primary care1 —are not specific for any single underlying cause.2 Officebased diagnostic testing, which is underused,3 must be employed to ensure accurate diagnosis and effective treatment. (An article on treatment by the same authors will appear in next month’s issue of The journal of family practice.)
In a primary-care study,4 vulvovaginal symptoms including vaginal discharge were due to vulvovaginal candidiasis (VVC) in 27% of patients, bacterial vaginosis (BV) in 21%, trichomoniasis in 8%, Chlamydia trachomatis in 2%, Neisseria gonorrhea (GC) in 1%, and no infection in 34%. Several pathogens may coexist.2 VVC, BV, and trichomoniasis account for at least 90% of infectious vaginitis.5 This review will therefore focus heavily on these causes of vaginal discharge among women of reproductive age, including pregnant women.
Cervicitis and physiologic cervical discharge
Some women may interpret a physiologic increase in cervical mucous production as abnormal. It occurs cyclically prior to ovulation, is typically transparent and colorless, and may be more pronounced in women with an everted cervix.
Chlamydial infection
In the clinical examination of the cervix, 3 characteristics have been associated with chlamydial infection: yellow endocervical discharge, easily induced cervical bleeding, and opaque cervical discharge.6 All 3 findings are statistically significant and independently associated with chlamydial infection (odds ratios 2.8, 2.3, and 2.9, respectively). In the primary care study cited above, purulent cervical discharge was found in 6% of women, most commonly testing positive for Chlamydia, less often for GC.4
Trichomonas vaginalis may cause cervicitis as well as vaginitis. Mycoplasma genitalium has been proposed as an additional possible pathogen. It was identified in 7% of more than 700 women with mucopurulent cervical discharge seen in a STD clinic with otherwise negative cultures.7 With cervical discharge that appears to be purulent, testing is warranted as a minimum for Chlamydia and GC (SOR: B). Screening of asymptomatic women less than 26 years of age for Chlamydia is recommended by the US Preventive Services Task Force (SOR: A).
Bacterial Vaginosis
Bacterial vaginosis (BV) is neither an inflammatory condition nor an STD, but is a shift in vaginal flora from the normal condition in which lactobacilli predominate, to a polymicrobial flora in which gram-positive anaerobes predominate. In addition to annoying vaginal symptoms, BV is associated with increased risks of more serious conditions such as pelvic inflammatory disease (PID), postoperative infections, and pregnancyrelated complications including prematurity. It also increases the likelihood of acquiring HIV in women exposed to the virus.8,9
Two principal factors put women at risk for acquiring BV: douching and exposure to a new sexual partner, both of which are thought to disrupt the vaginal ecosystem.10
Relative benefits of diagnostic tests
A gold standard test has not been established for BV. In about 50% of asymptomatic women, culture results are positive for flora such as Gardnerella vaginalis.5 While Amsel’s criteria are often used as a reference and generally suffice for the evaluation of symptomatic women, the best candidate for a gold standard test is probably Gram stain assessment using Nugent’s criteria (described in this section).11 Lack of leukocytes in the vaginal fluid supports a diagnosis of BV. A finding of white blood cells in excess of the number of vaginal epithelial cells suggests an inflammatory process (SOR: C).12
Amsel’s criteria with wet mount. The diagnostic approach most commonly used in the office is Amsel’s criteria—homogenous discharge, positive whiff-amine test, pH >4.5, and clue cells found on wet-mount microscopy (see How to perform a wet mount ).13 Three of 4 criteria deemed positive is considered diagnostic. If Gram stain is used as the reference standard, then Amsel’s criteria have 70% sensitivity and 94% specificity for diagnosing BV.14 An analysis of the individual criteria follows. The positive and negative predictive values of each compared with the whole group as reference standard is displayed in Table 1 .
Homogenous discharge. A thin, homogenous, grayish discharge is traditionally associated with BV. However, it is not specific to BV, being found commonly also in women with culture results positive for VVC or no diagnosis of vaginitis.2,15 It is the criterion least likely to be consistent with the whole group, seen in about half of women BVpositive and over one third of women BV-negative using Amsel’s criteria as the reference standard. 15
To perform a wet-mount preparation correctly, dilute the vaginal discharge with 1 or 2 drops of 0.9% saline and place it on a slide. Examine the slide under lowand high-powered fields for vaginal squamous cells, white blood cells (WBCs), lactobacilli, clue cells, and trichomonads. An increased number of WBCs can be defined as >5–10 WBC/HPF or WBCs exceeding the number vaginal epithelial cells.
To prepare the potassium hydroxide (KOH) slide, place a generous amount of vaginal discharge on a slide with 10% KOH solution. Air- or flame-drying before examination under low-power microscopy may improve sensitivity. A positive KOH preparation will have hyphae, mycelial tangles, or spores.
Whiff test. The whiff test is performed by adding drops of 10% potassium hydroxide solution to the vaginal fluid. A positive result is a “fishy” amine odor. In a study16 of 100 women complaining of malodorous discharge, a positive whiff test was predictive of positive culture results for anaerobic flora such as Bacteroides sp. with sensitivity 67%, specificity 94%, and a positive predictive value of 95%. The whiff test was not positive in any of the 5 cases with positive culture results for G vaginalis in the absence of anaerobes. There were also 12 cases positive for anaerobes without G vaginalis.
pH >4.5. Since the abnormal flora of BV is consistently associated with a vaginal pH >4.5, a normal pH excludes a diagnosis of BV.17,18 The determination of pH in the narrow range around 4.5 is not accurate using standard nitrazine paper. Narrower-range test paper is available and more accurate. Examples include pH paper for 4.5 to 5.5 (Micro Essential Laboratory), FemExam pH and Amines Test Card (Litmus Concepts), pHem-ALERT: pH paper on a stick (Imagyn Gynecology). Cervical mucous, semen, and blood are alkaline and can interfere with pH testing. Estrogen production is also necessary to maintain an acidic environment. A pH of 3.8 to 4.5 is consistent with normal vaginal flora in premenopausal women with normal estrogen production.17
Clue cells. Clue cells are vaginal epithelial cells coated with coccobacilli giving an appearance as if coated with ground black pepper. Clue cells on wet mount preparation is considered the most accurate of Amsel’s diagnostic criteria for BV.19 On the other hand, office evaluation of the wet mount is considered by some authors to be unreliable due to dependence on the clinician’s microscopy skills and lack of a durable record of the patient sample.
Gram stain a more objective test. A Gram stain evaluation using Nugent’s criteria has been adopted as the gold standard test for research purposes, including studies of prematurity. The Gram-stained vaginal specimen is scored from 0 to 10 based on semi-quantitative assessment of 3 classes of morphotypes ( Table 2 ): large gram-positive rods (Lactobacilli), small gram-negative rods (Gardnerella and Bacteroides spp.), and small curved gram-variable rods (Mobiluncus spp.).11
Diagnosis of BV is typically made when the Nugent score is 7 or more, which appears qualitatively as dominant morphotypes other than Lactobacilli. Gram staining is more objective and reproducible compared with wet-mount examination, with a sensitivity of 93% and specificity of 70% if Amsel’s criteria are used as the gold standard.14 It is useful for the evaluation of asymptomatic women. It also provides a durable record of the patient specimen. Compared with Gram stain, Amsel’s criteria tend to underdiagnose cases. We can expect that if screening for BV in pregnancy becomes a recommendation, Gram staining in a clinical laboratory will be the recommended method of diagnosis.
Other diagnostic tests for BV. DNA testing for Gardnerella is accurate for detection, but it is not synonymous with a diagnosis of BV, as described.20 DNA testing is further described under “Differential Diagnosis.” Gram staining is more reliable than gas-liquid chromatography21 and an assay for proline aminopeptidase (a metabolic product of some of the bacteria associated with BV).22 Latex agglutination testing for vaginal lactoferrin is a nonspecific marker for leukocytes, and thus inflammation. It is of little clinical utility in the diagnosis of vaginal discharge.23
TABLE 1
Predictive values of Amsel’s criteria (using 3 of 4 positive as diagnostic reference standard)
| Diagnostic criterion | Predictive value (%) | |
|---|---|---|
| Positive | Negative | |
| Homogeneous thin discharge seen at introitus | 42 | 89 |
| pH >4.5 | 53 | 94 |
| Odor on alkalinization | 94 | 93 |
| Clue cells on wet mount | 90 | 99 |
| Source: Thomason et al 1990.15 | ||
TABLE 2
How to use Nugent’s Gram stain criteria to diagnose bacterial vaginosis
| Lactobacillus morphophytes | Gardnerella and Bacteroides spp. morphophytes | Curved gram-variable rods | Points |
|---|---|---|---|
| 4+ | 0 | 0 | 0 |
| 3+ | 1+ | 1+ or 2+ | 1 |
| 2+ | 2+ | 3+ or 4+ | 2 |
| 1+ | 3+ | 3 | |
| 0 | 4+ | 4 | |
| Review each of the first 3 columns in turn, assigning points at far right according to your exam findings. | |||
| Add the points for all 3 columns for a final sum. A score of 7 or higher indicates bacterial vaginosis. Source: Nugent et al 1991.11 | |||
Vulvovaginal Candidiasis
Candidiasis is the second most commonly diagnosed vaginitis in the United States. Some experts estimate that 75% of women will have a yeast infection at some point in life and 5% will have recurrent infections.24 However, 10% to 30% of asymptomatic women with normal flora have positive culture results for Candida.25-29 The proportion of symptomatic women with positive culture results is 20% to 40%.4,30,31 Complications of VVC are rare,32 though vulvar vestibulitis33 and chorioamnionitis in pregnancy32 have been reported.
Risk factors. Symptomatic yeast vaginitis has been associated with condom and diaphragm use, recent antibiotic use, receptive oral sex, oral contraceptive use, spermicide use, diabetes, and immunosuppression including AIDS.31,34-37 The associations with antibiotic use and oral contraceptives are not consistent.30,38 Although pregnancy has been postulated as a risk factor for symptomatic VVC, prevalence of yeast on culture in pregnant women is similar to that of nonpregnant women.30
Suggestive symptoms. Among women with a culture result positive for Candida, the most common symptom is pruritus or burning.28 Abnormal discharge is a complaint for most symptomatic women with VVC confirmed by culture.2 In addition, women may complain of a thick, odorless, cottage cheese–like discharge.39 A thick, curdled-appearing discharge points to a diagnosis of Candida because it is rarely present with BV or trichomoniasis. In one study,28 a thick curdled discharge had a positive predictive value of 84% for diagnosis of VVC by culture (SOR: B). However, a thin discharge does not rule out VVC; in another study, clinicians described discharge as thin in about half of women ultimately diagnosed with VVC by culture in another study (SOR: B).2 On exam, vulvar and vaginal erythema are often present but are not specific findings. The accuracy of the clinical exam for VVC is poor compared with culture (SOR: A).2,30
Pathogens. Candida albicans is present in 80% to 90% of patients with VVC.5,40 remainder have non-albicans species, including C glabrata and others.28 An increase to almost 20% of non-Candida species in a vaginitis clinic by the mid-1990’s may be related to increased use of imidazoles available over-the-counter.40,41 Wet mount results are typically negative in the presence of non-Candida VVC.28
Diagnosis of VVC
The gold standard test for diagnosis of VVC is culture. The potassium hydroxide (KOH) wet mount is only 40% to 75% sensitive.28,29,42,43 False-positive results are also observed with variable frequency.44 The pH of the discharge is usually not more than 5.0 with Candida albicans, but may be higher with non-albicans species such as C glabrata.45 Culture is recommended for patients with recurrent or persistent symptoms and a negative wet mount result (SOR: B).5,28,46 Rapid slide latex agglutination testing is not better than microscopy (SOR: B).42
Trichomoniasis
Trichomonas, a motile protozoan with 4 flagella, causes the third most common form of vaginitis in the United States and is more common in some developing countries. Trichomoniasis accounts for no more than 10% of all cases of vaginitis, and it appears to be decreasing since the introduction of metronidazole.47,48 It is classified as an STD, although transmission is possible by other means if the organism is protected from desiccation—for example, in dirty washcloths or towels and contaminated water. Nonsexual transmission is thought to be uncommon.
Trichomoniasis is associated with GC and Chlamydia infections, and, like them, has been associated with seroconversion to HIV-positive status.49 Trichomonads are identified in 30% to 80% of male sexual partners of infected women. In men, trichomoniasis most often is an asymptomatic carrier state.50 However, it is the cause of about 10% of cases of nongonococcal urethritis in men.51
Our knowledge of the epidemiology of abnormal vaginal discharge is limited. Studies of vaginitis may exclude patients with vaginal discharge due to cervicitis; studies performed in sexually transmitted disease clinics are not representative of primary care practice; women who do not complain of abnormal vaginal discharge may have positive cultures for Gardnerella vaginalis and Candida albicans; and self-treatment of presumed yeast vaginitis with antifungals available over-the-counter further limits our knowledge of the prevalence and causes of vaginal discharge.
Clinical presentations. Women with trichomoniasis have variable presentations ranging from an asymptomatic carrier state to a malodorous, purulent discharge with vulvovaginal erythema. Punctate hemorrhagic cervical lesions are considered pathognomonic of trichomoniasis, but are seen in only about 2% of cases (SOR: B).52
Diagnosis. Culture for trichomoniasis is the gold standard. Several culture media have been used, most commonly the Diamond medium. Recently introduced is a transport and culture medium for detection of Trichomonas (InPouch TV), which performs as well as Diamond medium (SOR: A).53-55 A DNA probe is also available and accurate (SOR: A).
Motile trichomonads are seen on wet preparation in only 50% to 80% of culture-positive cases (SOR: B).50,54,56 Polymorphonuclear leukocytes can be dominant on wet mount, making visualization of trichomonads more difficult. The pH of the vaginal fluid is usually basic.
Trichomonas reported with cervical cytology
Trichomonas may also be reported on Pap smears. A meta-analysis57 comparing the pooled sensitivities and specificities of wet mounts and cytology demonstrated low sensitivities of 68% and 58%, respectively, and high specificities, 99.9% and 97%, respectively (SOR: A).
However, since cytology carries a 3% false-positive rate, its results are not diagnostic of trichomoniasis in low-risk, asymptomatic women.50,57 Treatment may be prescribed empirically based on positive cytology results. However, if an asymptomatic woman were concerned about whether she really has an STD, a positive wet prep would confirm the diagnosis. A negative wet prep should be followed up with culture to reliably rule out disease (SOR: B).
Trichomoniasis in pregnancy
Screening for asymptomatic trichomoniasis in pregnancy has not been recommended. In fact, some evidence suggests that treatment of trichomoniasis in pregnancy is associated with poorer pregnancy outcomes including lower birth weight and more prematurity (SOR: B).58,59
Aerobic vaginitis
Aerobic vaginitis is a term proposed to describe purulent vaginal discharge with predominance of abnormal aerobic flora.60 Aerobic vaginitis, which may be severe, has been reported as the cause of 5% of cases in a series from a specialty vaginitis clinic.61 The usual predominant microorganisms are group B streptococci, Escherichia coli, and Staphylococcus aureus. It is likely that less severe cases of aerobic vaginitis are not recognized in the primary care setting and are treated as BV or resolve spontaneously (SOR: C). The case series referred to above also reported good therapeutic response to 2% topical clindamycin (SOR: C).61
Noninfectious Vaginitis
Noninfectious causes of vaginal discharge include physiologic, irritant and allergic, cytolytic vaginitis, desquamative inflammatory vaginitis, collagen vascular disease, and idiopathic vaginitis.
Irritant and allergic vaginitis may result from sensitivities to topical medications, the active or base ingredients of spermicidal products, douching solutions, and the latex of condoms or diaphragms. If a woman with persistent symptoms has been using such intravaginal products, she should stop (SOR: C).
Cytolytic vaginitis is characterized by overgrowth of lactobacilli and cytolysis of squamous cells, including presence of cytoplasmic fragments and intact cells with naked nuclei.62 The cause is uncertain but may include a reaction to intravaginal medications or other products such as tampons. It can be found in up to 5% of women with symptoms and signs of vaginitis.62,63 Symptoms often mimic VVC and may include a white, cheesy discharge. Vaginal pH ranges from 3.5 to 5.5. Recurrences during luteal phase of the menstrual cycle have been described.64 Intravaginal antifungals should be discontinued. Baking soda sitz baths or douches are often used, but clinical trial data to support this practice are lacking (SOR: C).
Noninfectious desquamative inflammatory vaginitis (DIV) has also been described.65 DIV is an uncommon vaginitis characterized by profuse purulent discharge with epithelial cell exfoliation. It may occur at any time during the reproductive years or after menopause. There is probably a heterogeneous group of causes of DIV. Some cases may correspond to a disorder within the spectrum of lichen planus.66 Treatment is usually difficult, though there may be some response to local or systemic corticosteroid therapy (SOR: C).65
Differential diagnosis
A comparison of physical examination findings an diagnostic test results for various etiologies of vaginitis is summarized in Table 3 . An algorithmic approach to the differential diagnosis of abnormal vaginal discharge is presented in the Figure . Diagnosis is complicated in that signs and symptoms do little to help differentiate among BV, VVC, and trichomoniasis. A study2 of 22 genitourinary symptoms and signs showed that none differentiated among the 3 infections. This lack of clear-cut differences in symptoms also makes self-diagnosis and telephone triage inaccurate.67,68
A DNA probe testing system (Affirm VP III Microbial ID Test) for differential diagnosis is available but expensive. It identifies Gardnerella, Trichomonas, and Candida albicans with a sensitivity of 90% to 95%.54,66 The analyzer costs approximately $10,000 and would typically be purchased by a laboratory. Individual test kits cost about $27.
TABLE 3
Comparative findings among causes of vaginitis
| Cause | Physical exam findings* | Gold standard test | pH | Leukocytes | Wet mount | Alternative test |
|---|---|---|---|---|---|---|
| Bacterial vaginosis | Variable | Gram stain | >4.5 | No | Clue cells | Amsel’s criteria |
| Aerobic vaginitis | Abundant purulent discharge | Culture | >4.5 | Yes | Cocci or coarse rods | |
| Candida vaginitis | Adherent white disch. (thrush) | Culture | 3.8–4.5 | ± | Pseudohyphae or budding yeast | DNA testing |
| Non-Candida yeast vaginitis | Variable | Culture | Any | ± | Usually negative | |
| Trichomoniasis | Variable, occ. strawberry spots on cervix | Culture | >4.5 | ± | Motile trichomonads | DNA testing |
| Cytolytic vaginitis | Profuse discharge, often cheesy | Cytology and negative culture | 3.5–5.5 | ± | Overgrowth of lactobacilli and squamous cell fragments | |
| Desquamative inflammatory vaginitis | Abundant purulent discharge | Parabasal epithelial cells and negative culture | >4.5 | Yes | ||
| Irritant and allergic vaginitis | Variable, often erythema | None | Any | ± | ||
| * Helpful when present. | ||||||
FIGURE
Sequence of office tests to evaluate abnormal vaginal discharge
Corresponding author
Linda French, MD, Associate Professor, Department of Family Practice, College of Human Medicine, Michigan State University, B101 Clinical Center, East Lansing, MI 48824. E-mail: [email protected].
- Accurate differential diagnosis for women complaining of abnormal vaginal discharge requires in-office diagnostic testing at minimum, and laboratory testing in selected cases.
- Test for Chlamydia trachomatis and Neisseria gonorrhea when signs of purulent cervicitis are present (SOR: B).
- In suspected vulvovaginal candidiasis, culture is recommended for patients with recurrent or persistent symptoms and a negative wet mount result (SOR:B); rapid slide latex agglutination testing is not better than microscopy for diagnosing VVC (SOR: B).
In primary care practice, abnormal vaginal discharge is a common complaint. Signs and symptoms of vaginitis—the most common gynecologic diagnosis in primary care1 —are not specific for any single underlying cause.2 Officebased diagnostic testing, which is underused,3 must be employed to ensure accurate diagnosis and effective treatment. (An article on treatment by the same authors will appear in next month’s issue of The journal of family practice.)
In a primary-care study,4 vulvovaginal symptoms including vaginal discharge were due to vulvovaginal candidiasis (VVC) in 27% of patients, bacterial vaginosis (BV) in 21%, trichomoniasis in 8%, Chlamydia trachomatis in 2%, Neisseria gonorrhea (GC) in 1%, and no infection in 34%. Several pathogens may coexist.2 VVC, BV, and trichomoniasis account for at least 90% of infectious vaginitis.5 This review will therefore focus heavily on these causes of vaginal discharge among women of reproductive age, including pregnant women.
Cervicitis and physiologic cervical discharge
Some women may interpret a physiologic increase in cervical mucous production as abnormal. It occurs cyclically prior to ovulation, is typically transparent and colorless, and may be more pronounced in women with an everted cervix.
Chlamydial infection
In the clinical examination of the cervix, 3 characteristics have been associated with chlamydial infection: yellow endocervical discharge, easily induced cervical bleeding, and opaque cervical discharge.6 All 3 findings are statistically significant and independently associated with chlamydial infection (odds ratios 2.8, 2.3, and 2.9, respectively). In the primary care study cited above, purulent cervical discharge was found in 6% of women, most commonly testing positive for Chlamydia, less often for GC.4
Trichomonas vaginalis may cause cervicitis as well as vaginitis. Mycoplasma genitalium has been proposed as an additional possible pathogen. It was identified in 7% of more than 700 women with mucopurulent cervical discharge seen in a STD clinic with otherwise negative cultures.7 With cervical discharge that appears to be purulent, testing is warranted as a minimum for Chlamydia and GC (SOR: B). Screening of asymptomatic women less than 26 years of age for Chlamydia is recommended by the US Preventive Services Task Force (SOR: A).
Bacterial Vaginosis
Bacterial vaginosis (BV) is neither an inflammatory condition nor an STD, but is a shift in vaginal flora from the normal condition in which lactobacilli predominate, to a polymicrobial flora in which gram-positive anaerobes predominate. In addition to annoying vaginal symptoms, BV is associated with increased risks of more serious conditions such as pelvic inflammatory disease (PID), postoperative infections, and pregnancyrelated complications including prematurity. It also increases the likelihood of acquiring HIV in women exposed to the virus.8,9
Two principal factors put women at risk for acquiring BV: douching and exposure to a new sexual partner, both of which are thought to disrupt the vaginal ecosystem.10
Relative benefits of diagnostic tests
A gold standard test has not been established for BV. In about 50% of asymptomatic women, culture results are positive for flora such as Gardnerella vaginalis.5 While Amsel’s criteria are often used as a reference and generally suffice for the evaluation of symptomatic women, the best candidate for a gold standard test is probably Gram stain assessment using Nugent’s criteria (described in this section).11 Lack of leukocytes in the vaginal fluid supports a diagnosis of BV. A finding of white blood cells in excess of the number of vaginal epithelial cells suggests an inflammatory process (SOR: C).12
Amsel’s criteria with wet mount. The diagnostic approach most commonly used in the office is Amsel’s criteria—homogenous discharge, positive whiff-amine test, pH >4.5, and clue cells found on wet-mount microscopy (see How to perform a wet mount ).13 Three of 4 criteria deemed positive is considered diagnostic. If Gram stain is used as the reference standard, then Amsel’s criteria have 70% sensitivity and 94% specificity for diagnosing BV.14 An analysis of the individual criteria follows. The positive and negative predictive values of each compared with the whole group as reference standard is displayed in Table 1 .
Homogenous discharge. A thin, homogenous, grayish discharge is traditionally associated with BV. However, it is not specific to BV, being found commonly also in women with culture results positive for VVC or no diagnosis of vaginitis.2,15 It is the criterion least likely to be consistent with the whole group, seen in about half of women BVpositive and over one third of women BV-negative using Amsel’s criteria as the reference standard. 15
To perform a wet-mount preparation correctly, dilute the vaginal discharge with 1 or 2 drops of 0.9% saline and place it on a slide. Examine the slide under lowand high-powered fields for vaginal squamous cells, white blood cells (WBCs), lactobacilli, clue cells, and trichomonads. An increased number of WBCs can be defined as >5–10 WBC/HPF or WBCs exceeding the number vaginal epithelial cells.
To prepare the potassium hydroxide (KOH) slide, place a generous amount of vaginal discharge on a slide with 10% KOH solution. Air- or flame-drying before examination under low-power microscopy may improve sensitivity. A positive KOH preparation will have hyphae, mycelial tangles, or spores.
Whiff test. The whiff test is performed by adding drops of 10% potassium hydroxide solution to the vaginal fluid. A positive result is a “fishy” amine odor. In a study16 of 100 women complaining of malodorous discharge, a positive whiff test was predictive of positive culture results for anaerobic flora such as Bacteroides sp. with sensitivity 67%, specificity 94%, and a positive predictive value of 95%. The whiff test was not positive in any of the 5 cases with positive culture results for G vaginalis in the absence of anaerobes. There were also 12 cases positive for anaerobes without G vaginalis.
pH >4.5. Since the abnormal flora of BV is consistently associated with a vaginal pH >4.5, a normal pH excludes a diagnosis of BV.17,18 The determination of pH in the narrow range around 4.5 is not accurate using standard nitrazine paper. Narrower-range test paper is available and more accurate. Examples include pH paper for 4.5 to 5.5 (Micro Essential Laboratory), FemExam pH and Amines Test Card (Litmus Concepts), pHem-ALERT: pH paper on a stick (Imagyn Gynecology). Cervical mucous, semen, and blood are alkaline and can interfere with pH testing. Estrogen production is also necessary to maintain an acidic environment. A pH of 3.8 to 4.5 is consistent with normal vaginal flora in premenopausal women with normal estrogen production.17
Clue cells. Clue cells are vaginal epithelial cells coated with coccobacilli giving an appearance as if coated with ground black pepper. Clue cells on wet mount preparation is considered the most accurate of Amsel’s diagnostic criteria for BV.19 On the other hand, office evaluation of the wet mount is considered by some authors to be unreliable due to dependence on the clinician’s microscopy skills and lack of a durable record of the patient sample.
Gram stain a more objective test. A Gram stain evaluation using Nugent’s criteria has been adopted as the gold standard test for research purposes, including studies of prematurity. The Gram-stained vaginal specimen is scored from 0 to 10 based on semi-quantitative assessment of 3 classes of morphotypes ( Table 2 ): large gram-positive rods (Lactobacilli), small gram-negative rods (Gardnerella and Bacteroides spp.), and small curved gram-variable rods (Mobiluncus spp.).11
Diagnosis of BV is typically made when the Nugent score is 7 or more, which appears qualitatively as dominant morphotypes other than Lactobacilli. Gram staining is more objective and reproducible compared with wet-mount examination, with a sensitivity of 93% and specificity of 70% if Amsel’s criteria are used as the gold standard.14 It is useful for the evaluation of asymptomatic women. It also provides a durable record of the patient specimen. Compared with Gram stain, Amsel’s criteria tend to underdiagnose cases. We can expect that if screening for BV in pregnancy becomes a recommendation, Gram staining in a clinical laboratory will be the recommended method of diagnosis.
Other diagnostic tests for BV. DNA testing for Gardnerella is accurate for detection, but it is not synonymous with a diagnosis of BV, as described.20 DNA testing is further described under “Differential Diagnosis.” Gram staining is more reliable than gas-liquid chromatography21 and an assay for proline aminopeptidase (a metabolic product of some of the bacteria associated with BV).22 Latex agglutination testing for vaginal lactoferrin is a nonspecific marker for leukocytes, and thus inflammation. It is of little clinical utility in the diagnosis of vaginal discharge.23
TABLE 1
Predictive values of Amsel’s criteria (using 3 of 4 positive as diagnostic reference standard)
| Diagnostic criterion | Predictive value (%) | |
|---|---|---|
| Positive | Negative | |
| Homogeneous thin discharge seen at introitus | 42 | 89 |
| pH >4.5 | 53 | 94 |
| Odor on alkalinization | 94 | 93 |
| Clue cells on wet mount | 90 | 99 |
| Source: Thomason et al 1990.15 | ||
TABLE 2
How to use Nugent’s Gram stain criteria to diagnose bacterial vaginosis
| Lactobacillus morphophytes | Gardnerella and Bacteroides spp. morphophytes | Curved gram-variable rods | Points |
|---|---|---|---|
| 4+ | 0 | 0 | 0 |
| 3+ | 1+ | 1+ or 2+ | 1 |
| 2+ | 2+ | 3+ or 4+ | 2 |
| 1+ | 3+ | 3 | |
| 0 | 4+ | 4 | |
| Review each of the first 3 columns in turn, assigning points at far right according to your exam findings. | |||
| Add the points for all 3 columns for a final sum. A score of 7 or higher indicates bacterial vaginosis. Source: Nugent et al 1991.11 | |||
Vulvovaginal Candidiasis
Candidiasis is the second most commonly diagnosed vaginitis in the United States. Some experts estimate that 75% of women will have a yeast infection at some point in life and 5% will have recurrent infections.24 However, 10% to 30% of asymptomatic women with normal flora have positive culture results for Candida.25-29 The proportion of symptomatic women with positive culture results is 20% to 40%.4,30,31 Complications of VVC are rare,32 though vulvar vestibulitis33 and chorioamnionitis in pregnancy32 have been reported.
Risk factors. Symptomatic yeast vaginitis has been associated with condom and diaphragm use, recent antibiotic use, receptive oral sex, oral contraceptive use, spermicide use, diabetes, and immunosuppression including AIDS.31,34-37 The associations with antibiotic use and oral contraceptives are not consistent.30,38 Although pregnancy has been postulated as a risk factor for symptomatic VVC, prevalence of yeast on culture in pregnant women is similar to that of nonpregnant women.30
Suggestive symptoms. Among women with a culture result positive for Candida, the most common symptom is pruritus or burning.28 Abnormal discharge is a complaint for most symptomatic women with VVC confirmed by culture.2 In addition, women may complain of a thick, odorless, cottage cheese–like discharge.39 A thick, curdled-appearing discharge points to a diagnosis of Candida because it is rarely present with BV or trichomoniasis. In one study,28 a thick curdled discharge had a positive predictive value of 84% for diagnosis of VVC by culture (SOR: B). However, a thin discharge does not rule out VVC; in another study, clinicians described discharge as thin in about half of women ultimately diagnosed with VVC by culture in another study (SOR: B).2 On exam, vulvar and vaginal erythema are often present but are not specific findings. The accuracy of the clinical exam for VVC is poor compared with culture (SOR: A).2,30
Pathogens. Candida albicans is present in 80% to 90% of patients with VVC.5,40 remainder have non-albicans species, including C glabrata and others.28 An increase to almost 20% of non-Candida species in a vaginitis clinic by the mid-1990’s may be related to increased use of imidazoles available over-the-counter.40,41 Wet mount results are typically negative in the presence of non-Candida VVC.28
Diagnosis of VVC
The gold standard test for diagnosis of VVC is culture. The potassium hydroxide (KOH) wet mount is only 40% to 75% sensitive.28,29,42,43 False-positive results are also observed with variable frequency.44 The pH of the discharge is usually not more than 5.0 with Candida albicans, but may be higher with non-albicans species such as C glabrata.45 Culture is recommended for patients with recurrent or persistent symptoms and a negative wet mount result (SOR: B).5,28,46 Rapid slide latex agglutination testing is not better than microscopy (SOR: B).42
Trichomoniasis
Trichomonas, a motile protozoan with 4 flagella, causes the third most common form of vaginitis in the United States and is more common in some developing countries. Trichomoniasis accounts for no more than 10% of all cases of vaginitis, and it appears to be decreasing since the introduction of metronidazole.47,48 It is classified as an STD, although transmission is possible by other means if the organism is protected from desiccation—for example, in dirty washcloths or towels and contaminated water. Nonsexual transmission is thought to be uncommon.
Trichomoniasis is associated with GC and Chlamydia infections, and, like them, has been associated with seroconversion to HIV-positive status.49 Trichomonads are identified in 30% to 80% of male sexual partners of infected women. In men, trichomoniasis most often is an asymptomatic carrier state.50 However, it is the cause of about 10% of cases of nongonococcal urethritis in men.51
Our knowledge of the epidemiology of abnormal vaginal discharge is limited. Studies of vaginitis may exclude patients with vaginal discharge due to cervicitis; studies performed in sexually transmitted disease clinics are not representative of primary care practice; women who do not complain of abnormal vaginal discharge may have positive cultures for Gardnerella vaginalis and Candida albicans; and self-treatment of presumed yeast vaginitis with antifungals available over-the-counter further limits our knowledge of the prevalence and causes of vaginal discharge.
Clinical presentations. Women with trichomoniasis have variable presentations ranging from an asymptomatic carrier state to a malodorous, purulent discharge with vulvovaginal erythema. Punctate hemorrhagic cervical lesions are considered pathognomonic of trichomoniasis, but are seen in only about 2% of cases (SOR: B).52
Diagnosis. Culture for trichomoniasis is the gold standard. Several culture media have been used, most commonly the Diamond medium. Recently introduced is a transport and culture medium for detection of Trichomonas (InPouch TV), which performs as well as Diamond medium (SOR: A).53-55 A DNA probe is also available and accurate (SOR: A).
Motile trichomonads are seen on wet preparation in only 50% to 80% of culture-positive cases (SOR: B).50,54,56 Polymorphonuclear leukocytes can be dominant on wet mount, making visualization of trichomonads more difficult. The pH of the vaginal fluid is usually basic.
Trichomonas reported with cervical cytology
Trichomonas may also be reported on Pap smears. A meta-analysis57 comparing the pooled sensitivities and specificities of wet mounts and cytology demonstrated low sensitivities of 68% and 58%, respectively, and high specificities, 99.9% and 97%, respectively (SOR: A).
However, since cytology carries a 3% false-positive rate, its results are not diagnostic of trichomoniasis in low-risk, asymptomatic women.50,57 Treatment may be prescribed empirically based on positive cytology results. However, if an asymptomatic woman were concerned about whether she really has an STD, a positive wet prep would confirm the diagnosis. A negative wet prep should be followed up with culture to reliably rule out disease (SOR: B).
Trichomoniasis in pregnancy
Screening for asymptomatic trichomoniasis in pregnancy has not been recommended. In fact, some evidence suggests that treatment of trichomoniasis in pregnancy is associated with poorer pregnancy outcomes including lower birth weight and more prematurity (SOR: B).58,59
Aerobic vaginitis
Aerobic vaginitis is a term proposed to describe purulent vaginal discharge with predominance of abnormal aerobic flora.60 Aerobic vaginitis, which may be severe, has been reported as the cause of 5% of cases in a series from a specialty vaginitis clinic.61 The usual predominant microorganisms are group B streptococci, Escherichia coli, and Staphylococcus aureus. It is likely that less severe cases of aerobic vaginitis are not recognized in the primary care setting and are treated as BV or resolve spontaneously (SOR: C). The case series referred to above also reported good therapeutic response to 2% topical clindamycin (SOR: C).61
Noninfectious Vaginitis
Noninfectious causes of vaginal discharge include physiologic, irritant and allergic, cytolytic vaginitis, desquamative inflammatory vaginitis, collagen vascular disease, and idiopathic vaginitis.
Irritant and allergic vaginitis may result from sensitivities to topical medications, the active or base ingredients of spermicidal products, douching solutions, and the latex of condoms or diaphragms. If a woman with persistent symptoms has been using such intravaginal products, she should stop (SOR: C).
Cytolytic vaginitis is characterized by overgrowth of lactobacilli and cytolysis of squamous cells, including presence of cytoplasmic fragments and intact cells with naked nuclei.62 The cause is uncertain but may include a reaction to intravaginal medications or other products such as tampons. It can be found in up to 5% of women with symptoms and signs of vaginitis.62,63 Symptoms often mimic VVC and may include a white, cheesy discharge. Vaginal pH ranges from 3.5 to 5.5. Recurrences during luteal phase of the menstrual cycle have been described.64 Intravaginal antifungals should be discontinued. Baking soda sitz baths or douches are often used, but clinical trial data to support this practice are lacking (SOR: C).
Noninfectious desquamative inflammatory vaginitis (DIV) has also been described.65 DIV is an uncommon vaginitis characterized by profuse purulent discharge with epithelial cell exfoliation. It may occur at any time during the reproductive years or after menopause. There is probably a heterogeneous group of causes of DIV. Some cases may correspond to a disorder within the spectrum of lichen planus.66 Treatment is usually difficult, though there may be some response to local or systemic corticosteroid therapy (SOR: C).65
Differential diagnosis
A comparison of physical examination findings an diagnostic test results for various etiologies of vaginitis is summarized in Table 3 . An algorithmic approach to the differential diagnosis of abnormal vaginal discharge is presented in the Figure . Diagnosis is complicated in that signs and symptoms do little to help differentiate among BV, VVC, and trichomoniasis. A study2 of 22 genitourinary symptoms and signs showed that none differentiated among the 3 infections. This lack of clear-cut differences in symptoms also makes self-diagnosis and telephone triage inaccurate.67,68
A DNA probe testing system (Affirm VP III Microbial ID Test) for differential diagnosis is available but expensive. It identifies Gardnerella, Trichomonas, and Candida albicans with a sensitivity of 90% to 95%.54,66 The analyzer costs approximately $10,000 and would typically be purchased by a laboratory. Individual test kits cost about $27.
TABLE 3
Comparative findings among causes of vaginitis
| Cause | Physical exam findings* | Gold standard test | pH | Leukocytes | Wet mount | Alternative test |
|---|---|---|---|---|---|---|
| Bacterial vaginosis | Variable | Gram stain | >4.5 | No | Clue cells | Amsel’s criteria |
| Aerobic vaginitis | Abundant purulent discharge | Culture | >4.5 | Yes | Cocci or coarse rods | |
| Candida vaginitis | Adherent white disch. (thrush) | Culture | 3.8–4.5 | ± | Pseudohyphae or budding yeast | DNA testing |
| Non-Candida yeast vaginitis | Variable | Culture | Any | ± | Usually negative | |
| Trichomoniasis | Variable, occ. strawberry spots on cervix | Culture | >4.5 | ± | Motile trichomonads | DNA testing |
| Cytolytic vaginitis | Profuse discharge, often cheesy | Cytology and negative culture | 3.5–5.5 | ± | Overgrowth of lactobacilli and squamous cell fragments | |
| Desquamative inflammatory vaginitis | Abundant purulent discharge | Parabasal epithelial cells and negative culture | >4.5 | Yes | ||
| Irritant and allergic vaginitis | Variable, often erythema | None | Any | ± | ||
| * Helpful when present. | ||||||
FIGURE
Sequence of office tests to evaluate abnormal vaginal discharge
Corresponding author
Linda French, MD, Associate Professor, Department of Family Practice, College of Human Medicine, Michigan State University, B101 Clinical Center, East Lansing, MI 48824. E-mail: [email protected].
1. National Center for Health Statistics. National Ambulatory Medicine Care Survey. Available at: www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm.
2. Schaaf VM, Perez-Stable EJ, Borchardt K. The limited value of symptoms and signs in the diagnosis of vaginal infections. Arch Intern Med 1990;150:1929-1933.
3. Wiesenfeld HC, Macio I. The infrequent use of officebased diagnostic tests for vaginitis. Am J Obstet Gynecol 1999;181:39-41.
4. Berg AO, Heidrich FE, Fihn SD, et al. Establishing the cause of genitourinary symptoms in women in a family practice. Comparison of clinical examination and comprehensive microbiology. JAMA 1984;251:620-625.
5. Sobel JD. Vaginitis. N Engl J Med 1997;337:1896-1903.
6. Sellors JW, Walter SD, Howard M. A new visual indicator of chlamydial cervicitis? Sex Transm Infect 2000;76:46-48.
7. Manhart LE, Critchlow CW, Holmes KK, et al. Mucopurulent cervicitis and Mycoplasma genitalium. J Infect Dis 2003;187:650-657.
8. Martin HL, Richardson BA, Nyange PM, et al. Vaginal lactobacilli, microbial flora, and risk of human immunodeficiency virus type 1 and sexually transmitted disease acquisition. J Infect Dis 1999;180:1863-1868.
9. Hillier SL. The vaginal microbial ecosystem and resistance to HIV. AIDS Res Hum Retroviruses 1998;14Suppl 1:S17-21.
10. Hawes SE, Hillier SL, Benedetti J, et al. Hydrogenperoxide-producing lactobacilli and acquisition of vaginal infections. J Infect Dis 1996;174:1058-1063.
11. Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. JClin Microbiol 1991;29:297-301.
12. Quan M. Vaginitis: meeting the clinical challenge. Clin Cornerstone 2000;3:36-47.
13. Amsel R, Totten PA, Spiegel CA, Chen KC, Eschenbach D, Holmes KK. Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med 1983;74:14-22.
14. Schwebke JR, Hillier SL, Sobel JD, McGregor JA, Sweet RL. Validity of the vaginal gram stain for the diagnosis of bacterial vaginosis. ObstetGynecol 1996;88:573-576.
15. Thomason JL, Gelbart SM, Anderson RJ, Walt AK, Osypowski PJ, Broekhuizen FF. Statistical evaluation of diagnostic criteria for bacterial vaginosis. Am J Obstet Gynecol. 1990;162:155-160.
16. Erkkola R, Jarvinen H, Terho P, Meurman O. Microbial flora in women showing symptoms of nonspecific vaginosis: applicability of KOH test for diagnosis. Scand J Infect Dis Suppl. 1983;40:59-63.
17. Caillouette JC, Sharp CF, Jr, Zimmerman GJ, Roy S. Vaginal pH as a marker for bacterial pathogens and menopausal status. Am J Obstet Gynecol. 1997;176:1270-1275discussion1275-1277.
18. Carr PL, Felsenstein D, Friedman RH. Evaluation and management of vaginitis. J Gen Intern Med 1998;13:335-346.
19. Eschenbach DA, Hillier S, Critchlow C, Stevens C, DeRouen T, Holmes KK. Diagnosis and clinical manifestations of bacterial vaginosis. Am J Obstet Gynecol 1988;158:819-828.
20. Sheiness D, Dix K, Watanabe S, Hillier SL. Highlevels of Gardnerella vaginalis detected with an oligonucleotide probe combined with elevated pH as a diagnostic indicator of bacterial vaginosis. J Clin Microbiol 1992;30:642-648.
21. Thomason JL, Gelbart SM, James JA, Edwards JM, Hamilton PR. Is analysis of vaginal secretions for volatile organic acids to detect bacterial vaginosis of any diagnostic value? Am J Obstet Gynecol. 1988;159:1509-1511.
22. Thomason JL, Gelbart SM, Wilcoski LM, Peterson AK, Jilly BJ, Hamilton PR. Proline aminopeptidase activity as a rapid diagnostic test to confirm bacterial vaginosis. Obstet Gynecol 1988;71:607-611.
23. Rein MF, Shih LM, Miller JR, Guerrant RL. Use of a lactoferrin assay in the differential diagnosis of female genital tract infections and implications for the pathophysiology of bacterial vaginosis. Sex Transm Dis 1996;23:517-521.
24. Monif GR. Classification and pathogenesis of vulvovaginal candidiasis. Am J Obstet Gynecol 1985;152:935-939.
25. Giraldo P, von Nowaskonski A, Gomes FA, Linhares I, Neves NA, Witkin SS. Vaginal colonization by Candida in asymptomatic women with and without a history of recurrent vulvovaginal candidiasis. Obstet Gynecol 2000;95:413-416.
26. Bergman JJ, Berg AO. How useful are symptoms in the diagnosis of Candida vaginitis? J Fam Pract 1983;16:509-511.
27. Bro F. Patients with vaginal discharge in general practice. Acta Obstet Gynecol Scand 1989;68:41-43.
28. Eckert LO, Hawes SE, Stevens CE, Koutsky LA, Eschenbach DA, Holmes KK. Vulvovaginal candidiasis: clinical manifestations, risk factors, management algorithm. Obstet Gynecol 1998;92:757-765.
29. Bertholf ME, Stafford MJ. Colonization of Candida albicans in vagina, rectum, and mouth. J Fam Pract 1983;16:919-924.
30. Reed BD, Huck W, Zazove P. Differentiation of Gardnerella vaginalis, Candida albicans, and Trichomonas vaginalis infections of the vagina. J Fam Pract 1989;28:673-680.
31. Bro F. The diagnosis of candida vaginitis in general practice. Scand J Prim Health Care 1989;7:19-22.
32. Cotch MF, Hillier SL, Gibbs RS, Eschenbach DA. Epidemiology and outcomes associated with moderate to heavy Candida colonization during pregnancy. Vaginal Infections and Prematurity Study Group. Am J Obstet Gynecol 1998;178:374-380.
33. Pagano R. Vulvar vestibulitis syndrome: an often unrecognized cause of dyspareunia. Aust N Z J Obstet Gynaecol 1999;39:79-83.
34. Foxman B. The epidemiology of vulvovaginal candidiasis: risk factors. Am J Public Health 1990;80:329-331.
35. Geiger AM, Foxman B. Risk factors for vulvovaginal candidiasis: a case-control study among university students. Epidemiology 1996;7:182-187.
36. Sobel JD, Faro S, Force RW, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol 1998;178:203-211.
37. Spinillo A, Capuzzo E, Acciano S, De Santolo A, Zara F. Effect of antibiotic use on the prevalence of symptomatic vulvovaginal candidiasis. Am J Obstet Gynecol 1999;180:14-17.
38. Davidson F, Oates JK. The pill does not cause ‘thrush’. Br J Obstet Gynaecol Dec 1985;92:1265-1266.
39. Abbott J. Clinical and microscopic diagnosis of vaginal yeast infection: a prospective analysis. Ann Emerg Med 1995;25:587-591.
40. Horowitz BJ, Giaquinta D, Ito S. Evolving pathogens in vulvovaginal candidiasis: implications for patient care. J Clin Pharmacol 1992;32:248-255.
41. Spinillo A, Capuzzo E, Gulminetti R, Marone P, Colonna L, Piazzi G. Prevalence of and risk factors for fungal vaginitis caused by non-albicans species. Am J Obstet Gynecol 1997;176:138-141.
42. Reed BD, Pierson CL. Evaluation of a latex agglutination test for the identification of Candida species in vaginal discharge. J Am Board Fam Pract 1992;5:375-380.
43. Ferris DG, Hendrich J, Payne PM, et al. Office laboratoAE_French.1004.final 9/20/04 3:18 PM Page 813 ry diagnosis of vaginitis. Clinician-performed tests compared with a rapid nucleic acid hybridization test. J Fam Pract 1995;41:575-581.
44. Bergman JJ, Berg AO, Schneeweiss R, Heidrich FE. Clinical comparison of microscopic and culture techniques in the diagnosis of Candida vaginitis. J Fam Pract 1984;18:549-552.
45. Sobel JD. Vulvovaginitis due to Candida glabrata. An emerging problem. Mycoses. 1998;41:Suppl 2:18-22.
46. Zdolsek B, Hellberg D, Froman G, Nilsson S, Mardh PA. Culture and wet smear microscopy in the diagnosis of low-symptomatic vulvovaginal candidosis. Eur J Obstet Gynecol Reprod Biol 1995;58:47-51.
47. Lossick JG, Kent HL. Trichomoniasis: trends in diagnosis and management. Am J Obstet Gynecol 1991;165:1217-1222.
48. Kent HL. Epidemiology of vaginitis. Am J Obstet Gynecol 1991;165:1168-1176.
49. Laga M, Manoka A, Kivuvu M, et al. Non-ulcerative sexually transmitted diseases as risk factors for HIV-1 transmission in women: results from a cohort study. AIDS 1993;7:95-102.
50. Krieger JN, Tam MR, Stevens CE, et al. Diagnosis of trichomoniasis. Comparison of conventional wet-mount examination with cytologic studies, cultures, and monoclonal antibody staining of direct specimens. JAMA 1988;259:1223-1227.
51. Krieger JN. Trichomoniasis in men: old issues and new data. Sex Transm Dis 1995;22:83-96.
52. Fouts AC, Kraus SJ. Trichomonas vaginalis: reevaluation of its clinical presentation and laboratory diagnosis. J Infect Dis 1980;141:137-143.
53. Ohlemeyer CL, Hornberger LL, Lynch DA, Swierkosz EM. Diagnosis of Trichomonas vaginalis in adolescent females: InPouch TV culture versus wet-mount microscopy. J Adolesc Health 1998;22:205-208.
54. Borchardt KA, Smith RF. An evaluation of an InPouch TV culture method for diagnosing Trichomonas vaginalis infection. Genitourin Med 1991;67:149-152.
55. Levi MH, Torres J, Pina C, Klein RS. Comparison of the InPouch TV culture system and Diamond’s modified medium for detection of Trichomonas vaginalis. J Clin Microbiol 1997;35:3308-3310.
56. DeMeo LR, Draper DL, McGregor JA, et al. Evaluation of a deoxyribonucleic acid probe for the detection of Trichomonas vaginalis in vaginal secretions. Am J Obstet Gynecol 1996;174:1339-1342.
57. Wiese W, Patel SR, Patel SC, Ohl CA, Estrada CA. A meta-analysis of the Papanicolaou smear and wet mount for the diagnosis of vaginal trichomoniasis. Am J Med 2000;108:301-308.
58. Klebanoff MA, Carey JC, Hauth JC, et al. Failure of metronidazole to prevent preterm delivery among pregnant women with asymptomatic Trichomonas vaginalis infection. N Engl J Med 2001;345:487-493.
59. Kigozi GG, Brahmbhatt H, Wabwire-Mangen F, et al. Treatment of Trichomonas in pregnancy and adverse outcomes of pregnancy: a subanalysis of a randomized trial in Rakai, Uganda. Am J Obstet Gynecol 2003;189:1398-1400.
60. Donder GG, Vereecken A, Bosmans E, Dekeersmaecker A, Salembier G, Spitz B. Definition of a type of abnormal vaginal flora that is distinct from bacterial vaginosis: aerobic vaginitis. Bjog 2002;109:34-43.
61. Sobel JD. Desquamative inflammatory vaginitis: a new subgroup of purulent vaginitis responsive to topical 2% clindamycin therapy. Am J Obstet Gynecol 1994;171:1215-1220.
62. Demirezen S. Cytolytic vaginosis: examination of 2947 vaginal smears. Cent Eur J Public Health 2003;11:23-24.
63. Wathne B, Holst E, Hovelius B, Mardh PA. Vaginal discharge—comparison of clinical, laboratory and microbiological findings. Acta Obstet Gynecol Scand 1994;73:802-808.
64. Secor RM. Cytolytic vaginosis: a common cause of cyclic vulvovaginitis. Nurse Pract Forum 1992;3:145-148.
65. Oates JK, Rowen D. Desquamative inflammatory vaginitis. A review. Genitourin Med 1990;66:275-279.
66. Pelisse M. The vulvo-vaginal-gingival syndrome. A new form of erosive lichen planus. Int J Dermatol 1989;28:381-384.
67. Ferris DG, Nyirjesy P, Sobel JD, Soper D, Pavletic A, Litaker MS. Over-the-counter antifungal drug misuse associated with patient-diagnosed vulvovaginal candidiasis. Obstet Gynecol 2002;99:419-425.
68. Allen-Davis JT, Beck A, Parker R, Ellis JL, Polley D. Assessment of vulvovaginal complaints: accuracy of telephone triage and in-office diagnosis. Obstet Gynecol 2002;99:18-22.
1. National Center for Health Statistics. National Ambulatory Medicine Care Survey. Available at: www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm.
2. Schaaf VM, Perez-Stable EJ, Borchardt K. The limited value of symptoms and signs in the diagnosis of vaginal infections. Arch Intern Med 1990;150:1929-1933.
3. Wiesenfeld HC, Macio I. The infrequent use of officebased diagnostic tests for vaginitis. Am J Obstet Gynecol 1999;181:39-41.
4. Berg AO, Heidrich FE, Fihn SD, et al. Establishing the cause of genitourinary symptoms in women in a family practice. Comparison of clinical examination and comprehensive microbiology. JAMA 1984;251:620-625.
5. Sobel JD. Vaginitis. N Engl J Med 1997;337:1896-1903.
6. Sellors JW, Walter SD, Howard M. A new visual indicator of chlamydial cervicitis? Sex Transm Infect 2000;76:46-48.
7. Manhart LE, Critchlow CW, Holmes KK, et al. Mucopurulent cervicitis and Mycoplasma genitalium. J Infect Dis 2003;187:650-657.
8. Martin HL, Richardson BA, Nyange PM, et al. Vaginal lactobacilli, microbial flora, and risk of human immunodeficiency virus type 1 and sexually transmitted disease acquisition. J Infect Dis 1999;180:1863-1868.
9. Hillier SL. The vaginal microbial ecosystem and resistance to HIV. AIDS Res Hum Retroviruses 1998;14Suppl 1:S17-21.
10. Hawes SE, Hillier SL, Benedetti J, et al. Hydrogenperoxide-producing lactobacilli and acquisition of vaginal infections. J Infect Dis 1996;174:1058-1063.
11. Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. JClin Microbiol 1991;29:297-301.
12. Quan M. Vaginitis: meeting the clinical challenge. Clin Cornerstone 2000;3:36-47.
13. Amsel R, Totten PA, Spiegel CA, Chen KC, Eschenbach D, Holmes KK. Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med 1983;74:14-22.
14. Schwebke JR, Hillier SL, Sobel JD, McGregor JA, Sweet RL. Validity of the vaginal gram stain for the diagnosis of bacterial vaginosis. ObstetGynecol 1996;88:573-576.
15. Thomason JL, Gelbart SM, Anderson RJ, Walt AK, Osypowski PJ, Broekhuizen FF. Statistical evaluation of diagnostic criteria for bacterial vaginosis. Am J Obstet Gynecol. 1990;162:155-160.
16. Erkkola R, Jarvinen H, Terho P, Meurman O. Microbial flora in women showing symptoms of nonspecific vaginosis: applicability of KOH test for diagnosis. Scand J Infect Dis Suppl. 1983;40:59-63.
17. Caillouette JC, Sharp CF, Jr, Zimmerman GJ, Roy S. Vaginal pH as a marker for bacterial pathogens and menopausal status. Am J Obstet Gynecol. 1997;176:1270-1275discussion1275-1277.
18. Carr PL, Felsenstein D, Friedman RH. Evaluation and management of vaginitis. J Gen Intern Med 1998;13:335-346.
19. Eschenbach DA, Hillier S, Critchlow C, Stevens C, DeRouen T, Holmes KK. Diagnosis and clinical manifestations of bacterial vaginosis. Am J Obstet Gynecol 1988;158:819-828.
20. Sheiness D, Dix K, Watanabe S, Hillier SL. Highlevels of Gardnerella vaginalis detected with an oligonucleotide probe combined with elevated pH as a diagnostic indicator of bacterial vaginosis. J Clin Microbiol 1992;30:642-648.
21. Thomason JL, Gelbart SM, James JA, Edwards JM, Hamilton PR. Is analysis of vaginal secretions for volatile organic acids to detect bacterial vaginosis of any diagnostic value? Am J Obstet Gynecol. 1988;159:1509-1511.
22. Thomason JL, Gelbart SM, Wilcoski LM, Peterson AK, Jilly BJ, Hamilton PR. Proline aminopeptidase activity as a rapid diagnostic test to confirm bacterial vaginosis. Obstet Gynecol 1988;71:607-611.
23. Rein MF, Shih LM, Miller JR, Guerrant RL. Use of a lactoferrin assay in the differential diagnosis of female genital tract infections and implications for the pathophysiology of bacterial vaginosis. Sex Transm Dis 1996;23:517-521.
24. Monif GR. Classification and pathogenesis of vulvovaginal candidiasis. Am J Obstet Gynecol 1985;152:935-939.
25. Giraldo P, von Nowaskonski A, Gomes FA, Linhares I, Neves NA, Witkin SS. Vaginal colonization by Candida in asymptomatic women with and without a history of recurrent vulvovaginal candidiasis. Obstet Gynecol 2000;95:413-416.
26. Bergman JJ, Berg AO. How useful are symptoms in the diagnosis of Candida vaginitis? J Fam Pract 1983;16:509-511.
27. Bro F. Patients with vaginal discharge in general practice. Acta Obstet Gynecol Scand 1989;68:41-43.
28. Eckert LO, Hawes SE, Stevens CE, Koutsky LA, Eschenbach DA, Holmes KK. Vulvovaginal candidiasis: clinical manifestations, risk factors, management algorithm. Obstet Gynecol 1998;92:757-765.
29. Bertholf ME, Stafford MJ. Colonization of Candida albicans in vagina, rectum, and mouth. J Fam Pract 1983;16:919-924.
30. Reed BD, Huck W, Zazove P. Differentiation of Gardnerella vaginalis, Candida albicans, and Trichomonas vaginalis infections of the vagina. J Fam Pract 1989;28:673-680.
31. Bro F. The diagnosis of candida vaginitis in general practice. Scand J Prim Health Care 1989;7:19-22.
32. Cotch MF, Hillier SL, Gibbs RS, Eschenbach DA. Epidemiology and outcomes associated with moderate to heavy Candida colonization during pregnancy. Vaginal Infections and Prematurity Study Group. Am J Obstet Gynecol 1998;178:374-380.
33. Pagano R. Vulvar vestibulitis syndrome: an often unrecognized cause of dyspareunia. Aust N Z J Obstet Gynaecol 1999;39:79-83.
34. Foxman B. The epidemiology of vulvovaginal candidiasis: risk factors. Am J Public Health 1990;80:329-331.
35. Geiger AM, Foxman B. Risk factors for vulvovaginal candidiasis: a case-control study among university students. Epidemiology 1996;7:182-187.
36. Sobel JD, Faro S, Force RW, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol 1998;178:203-211.
37. Spinillo A, Capuzzo E, Acciano S, De Santolo A, Zara F. Effect of antibiotic use on the prevalence of symptomatic vulvovaginal candidiasis. Am J Obstet Gynecol 1999;180:14-17.
38. Davidson F, Oates JK. The pill does not cause ‘thrush’. Br J Obstet Gynaecol Dec 1985;92:1265-1266.
39. Abbott J. Clinical and microscopic diagnosis of vaginal yeast infection: a prospective analysis. Ann Emerg Med 1995;25:587-591.
40. Horowitz BJ, Giaquinta D, Ito S. Evolving pathogens in vulvovaginal candidiasis: implications for patient care. J Clin Pharmacol 1992;32:248-255.
41. Spinillo A, Capuzzo E, Gulminetti R, Marone P, Colonna L, Piazzi G. Prevalence of and risk factors for fungal vaginitis caused by non-albicans species. Am J Obstet Gynecol 1997;176:138-141.
42. Reed BD, Pierson CL. Evaluation of a latex agglutination test for the identification of Candida species in vaginal discharge. J Am Board Fam Pract 1992;5:375-380.
43. Ferris DG, Hendrich J, Payne PM, et al. Office laboratoAE_French.1004.final 9/20/04 3:18 PM Page 813 ry diagnosis of vaginitis. Clinician-performed tests compared with a rapid nucleic acid hybridization test. J Fam Pract 1995;41:575-581.
44. Bergman JJ, Berg AO, Schneeweiss R, Heidrich FE. Clinical comparison of microscopic and culture techniques in the diagnosis of Candida vaginitis. J Fam Pract 1984;18:549-552.
45. Sobel JD. Vulvovaginitis due to Candida glabrata. An emerging problem. Mycoses. 1998;41:Suppl 2:18-22.
46. Zdolsek B, Hellberg D, Froman G, Nilsson S, Mardh PA. Culture and wet smear microscopy in the diagnosis of low-symptomatic vulvovaginal candidosis. Eur J Obstet Gynecol Reprod Biol 1995;58:47-51.
47. Lossick JG, Kent HL. Trichomoniasis: trends in diagnosis and management. Am J Obstet Gynecol 1991;165:1217-1222.
48. Kent HL. Epidemiology of vaginitis. Am J Obstet Gynecol 1991;165:1168-1176.
49. Laga M, Manoka A, Kivuvu M, et al. Non-ulcerative sexually transmitted diseases as risk factors for HIV-1 transmission in women: results from a cohort study. AIDS 1993;7:95-102.
50. Krieger JN, Tam MR, Stevens CE, et al. Diagnosis of trichomoniasis. Comparison of conventional wet-mount examination with cytologic studies, cultures, and monoclonal antibody staining of direct specimens. JAMA 1988;259:1223-1227.
51. Krieger JN. Trichomoniasis in men: old issues and new data. Sex Transm Dis 1995;22:83-96.
52. Fouts AC, Kraus SJ. Trichomonas vaginalis: reevaluation of its clinical presentation and laboratory diagnosis. J Infect Dis 1980;141:137-143.
53. Ohlemeyer CL, Hornberger LL, Lynch DA, Swierkosz EM. Diagnosis of Trichomonas vaginalis in adolescent females: InPouch TV culture versus wet-mount microscopy. J Adolesc Health 1998;22:205-208.
54. Borchardt KA, Smith RF. An evaluation of an InPouch TV culture method for diagnosing Trichomonas vaginalis infection. Genitourin Med 1991;67:149-152.
55. Levi MH, Torres J, Pina C, Klein RS. Comparison of the InPouch TV culture system and Diamond’s modified medium for detection of Trichomonas vaginalis. J Clin Microbiol 1997;35:3308-3310.
56. DeMeo LR, Draper DL, McGregor JA, et al. Evaluation of a deoxyribonucleic acid probe for the detection of Trichomonas vaginalis in vaginal secretions. Am J Obstet Gynecol 1996;174:1339-1342.
57. Wiese W, Patel SR, Patel SC, Ohl CA, Estrada CA. A meta-analysis of the Papanicolaou smear and wet mount for the diagnosis of vaginal trichomoniasis. Am J Med 2000;108:301-308.
58. Klebanoff MA, Carey JC, Hauth JC, et al. Failure of metronidazole to prevent preterm delivery among pregnant women with asymptomatic Trichomonas vaginalis infection. N Engl J Med 2001;345:487-493.
59. Kigozi GG, Brahmbhatt H, Wabwire-Mangen F, et al. Treatment of Trichomonas in pregnancy and adverse outcomes of pregnancy: a subanalysis of a randomized trial in Rakai, Uganda. Am J Obstet Gynecol 2003;189:1398-1400.
60. Donder GG, Vereecken A, Bosmans E, Dekeersmaecker A, Salembier G, Spitz B. Definition of a type of abnormal vaginal flora that is distinct from bacterial vaginosis: aerobic vaginitis. Bjog 2002;109:34-43.
61. Sobel JD. Desquamative inflammatory vaginitis: a new subgroup of purulent vaginitis responsive to topical 2% clindamycin therapy. Am J Obstet Gynecol 1994;171:1215-1220.
62. Demirezen S. Cytolytic vaginosis: examination of 2947 vaginal smears. Cent Eur J Public Health 2003;11:23-24.
63. Wathne B, Holst E, Hovelius B, Mardh PA. Vaginal discharge—comparison of clinical, laboratory and microbiological findings. Acta Obstet Gynecol Scand 1994;73:802-808.
64. Secor RM. Cytolytic vaginosis: a common cause of cyclic vulvovaginitis. Nurse Pract Forum 1992;3:145-148.
65. Oates JK, Rowen D. Desquamative inflammatory vaginitis. A review. Genitourin Med 1990;66:275-279.
66. Pelisse M. The vulvo-vaginal-gingival syndrome. A new form of erosive lichen planus. Int J Dermatol 1989;28:381-384.
67. Ferris DG, Nyirjesy P, Sobel JD, Soper D, Pavletic A, Litaker MS. Over-the-counter antifungal drug misuse associated with patient-diagnosed vulvovaginal candidiasis. Obstet Gynecol 2002;99:419-425.
68. Allen-Davis JT, Beck A, Parker R, Ellis JL, Polley D. Assessment of vulvovaginal complaints: accuracy of telephone triage and in-office diagnosis. Obstet Gynecol 2002;99:18-22.
Resting injured limbs delays recovery: A systematic review
- Injured limbs are traditionally rested by splint or cast. This is undertaken both for palliation and also in the belief that resting improves recovery time, and reduces complications such as deformity, functional problems and long-term pain.
- Early mobilization decreases pain, swelling and stiffness, particularly in the short term, without longer-term cosmetic or radiologic deformity. (SOR: A)
- Patients usually (but not always) prefer early mobilization, and return to work earlier. (SOR: C)
- Rest may be overused for limbs injury, although the extent to which early mobilization should be adopted needs more research. (SOR: C)
- The scope of limb injuries explored with trials of mobilization also needs further research.
Objectives: Rest is commonly used as primary treatment, rather than just palliation, for injured limbs. We searched the literature for evidence of benefit or harm from immobilization or mobilization of acute limb injury in adults.
Data Sources: We systematically searched for and retrieved randomized controlled trials (RCTs) of mobilization or rest for treatment of acute limb injuries, in Medline (1966–2002), EMBASE, Web of Science, and the Cochrane library, in all languages.
Review Methods: We examined patient-centered outcomes (pain, swelling, and cost), functional outcomes (range of motion, days lost from work) and complications of treatment.
Results: Forty-nine trials of immobilization for soft tissue injuries and fractures of both upper and lower limbs were identified (3366 patients). All studies reported either no difference between rest and early mobilization protocols, or found in favor of early mobilization. Reported benefits of mobilization included earlier return to work; decreased pain, swelling, and stiffness; and a greater preserved range of joint motion. Early mobilization caused no increased complications, deformity or residual symptoms.
Conclusions: We should not assume any benefit for immobilization after acute upper or lower limb injuries in adults. Rest appears to be overused as a treatment. More trials are needed to identify optimal programs for early mobilization.
We know that bed rest generally is over-prescribed.1 But what about resting or immobilizing acutely injured limbs—from simple sprains to gunshot wounds? This specific application of rest is controversial.2-6
Theoretically, rest should reduce further tissue damage by limiting movement, decreasing pain and swelling, and lessening loss of fracture reduction.7-15 However, mobilization increases blood flow and so reduces muscle atrophy, disuse osteoporosis, adhesions, and joint stiffness.7-15
The first empirical trials to determine whether rest or mobilization would offer greater benefit were undertaken in the 1980s, using both human and animal models. Systematic reviews have looked at specific injuries: acute ankle sprains16; ankle ligament rupture17; isolated ulnar fracture18; metacarpal fractures19; collateral ankle ligament sprains20; and soft-tissue ankle injury.21 Each review independently suggests benefits for early mobilization.
However, most clinicians employ some period of enforced rest of injured limbs. For example, a survey of orthopedic surgeons in Denmark found early mobilization for ankle fractures is prescribed for only 6% of patients.22
We systematically reviewed the literature to find trials that compared rest with early mobilization in acute limb injuries.
Methods
Protocol and search strategy
We searched the literature to identify prospective randomized controlled trials (RCTs) comparing rest with mobilization for acute limb injuries, searching the Cochrane Controlled Trials Register and Systematic Reviews, Medline (1966–2002), EMBASE (Rehabilitation and Physical Therapy), and Web of Science, combined with the following terms:
- immobilis*, immobiliz*, mobilis*, mobiliz*,
injur*, fracture*, limb*, cast*, brace*, splint*,
leg*, arm*, wrist*, elbow*, joint*, *carpal*,
*tarsal*, knee*, ankle*, femur*, tibia*, fibula*,
colles*, ulna*, radi*, humer*, sprain*, soft tissue,
plaster slab, dislocat*
We accepted all publication languages and translated several papers. We found 445 potentially relevant papers by examining their titles or abstracts (Figure). Studies that did not fulfill our inclusion criteria were discarded.
We obtained full texts for 76 studies and undertook a prospective cited reference search in Web of Science for each study to identify more recent articles. A total of 187 papers were then evaluated further for duplicate data and inclusion criteria.
Trials that met our inclusion criteria:
- Were randomized and controlled
- Studied acute limb injuries
- Compared groups whose only treatment difference was mobilization (studies that compared surgery and immobilization against nonsurgical early mobilization were not included; studies with internal fixation were included only if internal fixation was applied to both groups)
- Had loss to follow-up of 20%, except where analysis was clearly intention to treat
- Studied populations not focussed solely on young children, (studies in which the given age range included a small number of patients as young as 11 or 12 years were accepted—in these studies the median age was much higher)
- adequately reported data collection and statistical analysis.
By these criteria, we excluded 138 studies (a list of which is available from the authors). Finally, 49 studies were included.
FIGURE
Literature search process, and methods by which randomized controlled trials (RCTs) were selected
Study methods quality and validity
Two authors independently scored the validity of each of the included 49 studies, meeting to discuss and resolve any disagreements. We relied on published data, without writing to authors to clarify or obtain information. Included studies were evaluated against 11 standard criteria.23 Each criterion was scored 0–2. However, the practical maximum possible score was 18 because it was impossible to blind patients or their caregivers to mobilization. We considered the quality of 16 studies scoring 11 to be high.
Results
Across the 49 eligible studies, the different interventions were well described and differentiated, and data collection methods were clearly explained. Duration of immobilization in a cast was described (if at all) from 10 days to 8 weeks. Mobilization strategies varied and included active exercise, orthoses, crutches, or bandages.
Study quality was poor in many respects: several did not include important demographic data (including age, sex, or the numbers randomized to control and experimental group). Most did not report data about the methods of randomization. Many studies used inadequate randomization methods, with only 5 reporting optimal methods. Loss to follow-up was addressed poorly (not described or intention-to-treat analysis was not used). Outcome assessment was not blinded (a serious shortcoming in view of the subjective assessment of some patient outcomes). Reporting of inclusion criteria was inadequate in a few studies.
Given these deficiencies, our discussion emphasizes conclusions supported by studies of high quality.
Reporting of the studies
We divided the 49 studies into 4 groups: lower-limb fractures, other lower-limb injuries, upper-limb fractures, and other upper-limb injuries (Table W, at www.jfponline.com). Each group was further divided into trials using some form of limb support (such as a brace, splint, or a short period of immobilization) or minimal or no support (bandage, crutches, or tape) in the early mobilization group.
Most studies used some form of dynamic treatment for the injured limb, with highest use in lowerlimb injuries (74%); 2 studies included both supported and unsupported mobilization.24-26 In studies of upper-limb fractures, support was used in 50%. In high-quality studies, 12 out of 16 studies used some support, but results were consistent with studies that did not. The smaller number of studies using minimal support makes comparison with supported mobilization difficult, but results suggest that supported mobilization may result in an earlier return to work or sport, whereas minimally supported patients achieved better composite scores and muscle strength. There was too much clinical heterogeneity to sensibly combine the results; however, we were interested to see whether mobilization was useful across a heterogeneous group of conditions.
Patient-centered outcomes
No study reported any significant improvement with rest on swelling and pain. To the contrary, 13 studies reported significant improvement with early mobilization compared with rest,16,17,27-37 and 9 studies reported enhanced patient satisfaction.16,30,36,38-43 High-quality studies that reported pain levels found no difference or favored early mobilization.25,26,30,31,39,44-51 This was significant in only 2 studies of lower-limb nonfractures.25,26,30 No study reported adverse patient opinion in an early mobilization regime,28,31,38,40,44-46,48,51-56 and patients appreciated their ability to use the affected limb.34,43,49
Functional outcomes
Ten studies measured global function, using composite scores including subjective and objective criteria—pain, stiffness, swelling, use of supports, and ability to climb stairs, play sport, work, and undertake activities of daily life (Table W). Seven studies reported significant improvements with early mobilization—after 6 months (6 studies),28,35,42,46,52,57 or 12 months (1 study).32 Four studies of high quality found significant benefit for early mobilization in composite scores, most of these for lower-limb fractures.46,47,52,54 Significantly more patients with acute ankle sprain, who were immobilized in a cast, sought medical and physiotherapy advice in the initial 3 weeks, compared with those mobilized early with a functional brace.50
Return to work and sport
Thirteen studies reported that early mobilization resulted in a significantly earlier return to work (about 30%–60% earlier),16,17,30,33,35,36,38-40,52,57-59 especially in lower-limb nonfracture injuries. In 1 study of ankle fractures, patients randomized to wear a cast reported better performance of daily activities at 6 weeks than those mobilized with crutches.28 Perhaps, this reflects practical difficulties associated with using crutches. Five studies of lower-limb injury reported an earlier return to sport,16,30,39,57,60 as did 3 studies of postoperative Achilles tendon repair30,39,60 and 2 of ankle ligament injury or sprains.16,57 Five studies reporting a significantly earlier return to work or sport were of high quality, as were all studies of lower limb injuries.25,26,30,39,46,52
Range of movement
Fourteen studies of upper- and lower-limb fractures reported significant improvements in range of movement. Significant differences in range of movement were typically observed within 13 weeks of the injury,12,27,29,34,38,42,45,46,49,52,61-64 although a few studies reported differences for longer periods. Similarly for lower-limb nonfractures, significantly better ranges of motion were found within short periods,25,33,37,39,43 and also after 12 months.30,39-41 Eleven studies reporting this outcome were of high quality,25,26,30,31,39,45,46,48-51,54 and 4 studies found significant benefit for early mobilization.25,26,30,46,49 The other 7 high-quality studies favored early mobilization, and 1 found no difference.45
Deformity and other complications
Four studies found early mobilization reduced deformity: for angular displacement61 and radial shortening32 in Colles’ fractures; displacement of metacarpal fractures58 and cosmetic deformity in radial fractures.42 Two studies were of high quality.30,65 Ten trials reported no changes in deformity, no loss of fracture reduction, or any other complications with early mobilization of fractures.28,31,45,48,50,59,62-64,66 In contrast, for Colles’ fractures, significantly greater dorsal angulation61 and significant increases in radial tilt and decreased radioulnar joint space49 were reported for mobilized wrists.
Patient preferences
Patients expressed preference for a brace following anterior cruciate ligament surgery because it helped reduce pain and swelling67; they expressed preference for a cast following surgery for ankle fracture because it improved ability to perform everyday activities.28
Patients with distal radius fractures preferred early treatment with a Tubigrip bandage and a back-slab instead of removable splints, which increased pain and decreased mobilization.53 Generally, patients with fractures preferred rigid support immediately after the injury. Some also expected to have a traditional cast applied after learning their injured wrist was fractured.53
Cost of treatment
Full economic evaluations were not usually satisfactorily undertaken in these clinical studies. The cost of early mobilization was more expensive than immobilization in some studies8,23 but cheaper in others.2,9,10,24,68 It is estimated that direct costs to the patient were lower for early mobilization because of the decreased loss of working time.10,44,68,69
Adherence and supervision
Ten studies excluded patients who were unable to understand the nature of the treatment; had dementia; existing joint disease; drug abuse; alcohol problems; or difficulty with walking aids.28,31,38-41,45,46,49,69 Thus, many researchers have assumed that early mobilization requires greater patient responsibility. Some researchers have recommended applying casts for patients deemed “uncooperative” or “unlikely to be compliant,” despite their positive findings for early mobilization.3,16
Although 10 trials employed physiotherapy or supervised mobilization sessions,25,26,28,29,40,41,46,65,70 11 studies relied on self-controlled mobilization.27,30,31,38,39,42,44,45,48,49,52 In addition, some interventions (eg, braces) intrinsically required more supervision with their removal and reapplication than others (eg, functional casts or semirigid bandages).
Discussion
Early mobilization seems to decrease pain, swelling, and stiffness—at least in the short-term—and patients generally prefer it to immobilization. It results in earlier return—to work and to a greater range of motion, which is most significant within the first 2 months of the injury and can be maintained for up to 12 months for nonfracture injuries. Early mobilization does not increase cosmetic or radiological deformity for stable fractures, and patients experience fewer complications and residual symptoms. However, early mobilization may place greater demands on patients and require higher levels of understanding and responsibility, therefore making it unsuitable for some patients.
This systematic review of all upper- and lower-limb injuries, including fractures, consistently found in favor of early mobilization over rest. We acknowledge that the range of injuries reviewed is very limited. However, the clear benefits of mobilization indicated by this review suggest we need research in a wider range of injuries.
Similarly, it would be naïve to assume mobilization is better than immobilization in all circumstances. Harm must occur at some level of increased activity. In addition we know that pain and discomfort are often experienced by patients who demand immobilization (a “palliative” form of management). Finding the ideal level and type of activity must be undertaken empirically. Therefore more quality clinical trials are required to determine and evaluate the best regimens for early mobilization.
Newer studies will probably find that mobilization can be employed more often (and perhaps more vigorously) than we now advise. The best evidence at hand suggests the medical profession generally errs too conservatively on the side of immobilization.
Acknowledgments
Charlotte Nash did the searches, assembled and analysed the tables and wrote the first draft. Charlotte Nash and Sharon Mickan assessed the quality of all included studies and edited drafts. Paul Glasziou and Chris Del Mar initiated the question and edited drafts. This work was supported in part by a scholarship awarded by the Centre for General Practice, The University of Queensland, and funded by the Australian Commonwealth Department of Health and Ageing through the Primary Health Care Research, Evaluation and Development Strategy.
Corresponding author
Professor Chris B. Del Mar, Centre for General Practice, Faculty Heath Science and Medicine, Bond University, Gold Coast, Queensland 4229, Australia. E-mail: [email protected].
1. Allen C, Glasziou P, Del Mar C. Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet. 1999;354:1229-1233.
2. Madhok R, Bhopal RS. Coping with an upper limb fracture? A study of the elderly. Public Health. 1992;106:19-28.
3. Salter RB. Motion versus rest: Why immobilize joints? J Bone Joint Surg Br. 1982;64B:251-254.
4. Safran MR, Zachazewski JE, Benedetti RS, Bartolozzi AR, Mandelbaum R. Lateral ankle sprains: a comprehensive review. Part 2: treatment and rehabilitation with an emphasis on the athlete. Med Sci Sports Exerc. 1999;31:S438-S447.
5. Willems C. Immediate active mobilization in the treatment of gunshot wounds of joints. Medical Record. 1919;95:953-962.
6. Dent JA. Continuous passive motion in hand rehabilitation. Prosthet Orthot Int 1993;17:130-135.
7. Pneumaticos SG, Noble PC, McGarvey WC, Mody DR, Trevino SG. The effects of early mobilization in the healing of Achilles tendon repair. Foot Ankle Int. 2000;21:551-557.
8. Gelberman RH, Menon J, Gonsalves M, Akeson WH. The effects of mobilisation on the vascularisation of healing flexor tendons in dogs. Clin Orthop. 1980;153:283-289.
9. Kannus P. Immobilisation or early mobilisation after an acute soft tissue injury. The Physician and Sportsmedicine. 2000;28:55-63.
10. Halikis MN, Manske PR, Kubota H, Aoki M. Effect of immobilization, immediate mobilization and delayed mobilization of the resistance to digital flexion using a tendon injury model. J Hand Surg [Am]. 1997;22A:464-472.
11. Romanelli DA, Almekinders LC, Mandelbaum BR. Achilles rupture in the athlete: Current science and treatment. Sports Medicine and Arthroscopy Review. 2000;8:377-386.
12. Stockle U, Konig B, Tempka A, Sudkamp NP. Cast immobilisation or vacuum stabilizing system? Unfallchirurg. 2000;103:215-219.
13. Viidik A. The effect of training on the tensile strength of isolated rabbit tendons. Scandinavian Journal of Plastic and Reconstructive Surgery. 1967;1:141-147.
14. Woo SL, Gelberman RH, Cobb NG, Amiel D, Lothringer K, Akeson WH. The importance of controlled passive mobilization on flexor tendon healing. A biomechanical study. Acta Orthop Scand. 1981;52:615-622.
15. Peacock E. Biological principles in the healing of long tendons. Surg Clin North Am. 1965;45:461-476.
16. Kerkhoffs GMMJ, Rowe BH, Assendelft WJJ, Kelly KD, Struijs PAA, Niek van Dijk C. Immobilisation for acute ankle sprain: a systematic review. Arch Orthop Trauma Surg. 2001;121:462-471.
17. Pijnenburg ACM, van Dijk CN, Bossuyt PMM, Marti RK. Treatment of ruptures of the lateral ankle ligaments: A meta-analysis. J Bone Joint Surg Am. 2000;82A:761-773.
18. Mackay D, Wood L, Rangan A. The treatment of isolated ulnar fractures in adults: a systematic review. Injury. 2000;31:565-570.
19. Prokop A, Kulus S, Helling HJ, Burger C, Rehm KE. Are there concepts in treatment of metacarpal fractures? Own results and a review of the literature of the last 12 years. Unfallchirurg. 1999;102:50-58.
20. Shrier I. Treatment of lateral collateral ligament sprains of the ankle: a critical appraisal of the literature. Clin J Sport Med. 1995;5:187-195.
21. Ogilvie-Harris DJ, Gilbart M. Treatment modalities for soft tissue injuries of the ankle: a critical review. Clin J Sport Med. 1995;5:175-186.
22. Hviid K, Harager K, Schantz K. Aftercare of malleolar fractures in Denmark. A questionnaire study. Ugeskr Læger. 2000;62:2747-2750.
23. Gillespie W, Gillespie L, Morton L. Cochrane Musculoskeletal Injuries Group. Cochrane Database 2002.
24. Sommer HM, Schreiber H. Early functional conservative therapy of fresh fibular capsular ligament rupture from the socioeconomic viewpoint. Sportverletzung Sportschaden. 1993;7:40-46.
25. Dettori JR. Early ankle mobilization, part I: The immediate effect on acute, lateral ankle sprains. A randomised clinical trial. Mil Med. 1994;159:15-20.
26. Dettori JR, Basmania CJ. Early ankle mobilization, part II: A one-year follow-up of acute, lateral ankle sprains. A randomized clinical trial. Mil Med. 1994;159:20-24.
27. Stuart PR, Brumby C, Smith SR. Comparative study of functional bracing and plaster cast treatment of stable lateral malleolar fractures. Injury. 1989;20:323-326.
28. van Laarhoven CJHM, Meeuwis JD, van der Werken C. Postoperative treatment of internally fixed ankle fractures. J Bone Joint Surg Br. 1996;78B:395-399.
29. Søndenaa K, Høigaard U, Smith D, Alho A. Immobilisation of operated ankle fractures. Acta Orthop Scand. 1986;57:59-61.
30. Cetti R, Henriksen LO, Jacobsen KS. A new treatment of ruptured Achilles tendons. Clin Orthop. 1994;308:155-165.
31. Dias JJ, Wray CC, Jones JM, Gregg PJ. The value of early mobilisation in the treatment of Colles’ fractures. J Bone Joint Surg Br. 1987;69B:463-467.
32. Abbaszadegan H, Conradi P, Jonsson U. Fixation not needed for undisplaced Colles’ fracture. Acta Orthop Scand. 1989;60:60-62.
33. Nyska M, Weisel Y, Halperin N, Mann G, Segal D. Controlled mobilization after acute ankle inversion injury. Journal of Sports Traumatology and Related Research. 1999;21:114-120.
34. McMahon PJ, Woods DA, Burge PD. Initial treatment of closed metacarpal fractures. J Hand Surg [Br]. 1994;19B:597-600.
35. Konradsen L, Hølmer P, Søndergaard L. Early mobilizing treatment for grade III ankle ligament injuries. Foot and Ankle. 1991;12:69-73.
36. Cetti R, Christensen SE, Corfitzen MT. Ruptured fibular ankle ligament: Plaster or Pliton brace? Br J Sports Med. 1984;18:104-109.
37. Eiff MP, Smith AT, Smith GE. Early mobilisation versus immobilisation in the treatment of lateral ankle sprains. Am J Sports Med. 1994;22:83-86.
38. Gebuhr P, Hölmich P, Ørsnes T, Soelberg M, Krasheninnikoff M, Kjersgaard AG. Isolated ulnar shaft fractures. J Bone Joint Surg Br. 1992;74B:757-759.
39. Mortensen NHM, Skov O, Jensen PE. Early motion of the ankle after operative treatment of a rupture of the Achilles tendon. J Bone Joint Surg Am. 1999;81A:983-990.
40. Buchgraber A, Pässler HH. Percutaneous repair of Achilles tendon rupture. Clin Orthop. 1997;341:113-122.
41. Saleh M, Marshall PD, Senior R, MacFarlane A. The Sheffield Splint for controlled early mobilisation after rupture of the calcaneal tendon. J Bone Joint Surg Br. 1992;74B:206-209.
42. Davis TRC, Buchanan JM. A controlled prospective study of early mobilization of minimally displaced fractures of the distal radial metaphysis. Injury. 1987;18:283-285.
43. Avci S, Sayli U. Comparison of the results of short-term rigid and semi-rigid cast immobilization for the treatment of grade 3 inversion injuries of the ankle. Injury. 1998;29:581-584.
44. Dogra AS, Rangan A. Early mobilisation versus immobilisation of surgically treated ankle fracture. Prospective randomised control trial. Injury. 1999;30:417-419.
45. Hedström M, Ahl T, Dalén N. Early postoperative ankle exercises: a study of postoperative lateral malleolar fractures. Clin Orthop. 1994;300:193-196.
46. Port AM, McVie JL, Naylor G, Kreibich DN. Comparison of two conservative methods of treating an isolated fracture of the lateral malleous. J Bone Joint Surg Br. 1996;78B:568-572.
47. Klein J, Rixen D, Albring T, Tiling T. Functional treatment with a pneumatic ankle brace versus cast immobilisation for recent rupture of the fibular ligament in the ankle. A randomised clinical trial. Unfallchirurg. 1991;94:99-104.
48. Allain J, le Guilloux P, Mouël SL, Goutallier D. Trans-styloid fixation of fractures of the distal radius: A prospective randomized comparison between 6- and 1-week postoperative immobilization in 60 fractures. Acta Orthop Scand. 1999;70:119-123.
49. Millett PJ, Rushton N. Early mobilization in the treatment of Colles’ fracture: a 3 year prospective study. Injury. 1995;26:671-675.
50. Stewart HD, Innes AR, Burke FD. Functional cast-bracing for Colles’ fractures. A comparison between cast-bracing and conventional plaster casts. J Bone Joint Surg Br. 1984;66B:749-753.
51. Unsworth-White J, Koka R, Churchill M, D’Arcy JC, James SE. The non-operative management of radial head fractures: a randomized trial of three treatments. Injury. 1994;25:165-167.
52. Egol KA, Dolan R, Koval KJ. Functional outcome of surgery for fractures of the ankle. J Bone Joint Surg Br. 2000;82:246-249.
53. Stoffelen D, Broos P. Minimally displaced distal radius fractures: do they need plaster treatment? J Trauma. 1998;44:503-505.
54. DiStasio AJ, Jaggears FR, DePasquale LV, Frassica FJ, Turen CH. Protected early motion versus cast immobilization in postoperative management of ankle fractures. Contemporary Orthopaedics. 1994;29:273-277.
55. Regis D, Montanari M, Magnan B, Spagnol S, Bragantini A. Dynamic orthopaedic brace in the treatment of ankle sprains. Foot Ankle Int. 1995;16:422-426.
56. Grønmark T, Johnsen O, Kogstad O. Rupture of the lateral ligaments of the ankle: a controlled clinical trial. Injury. 1980;11:215-218.
57. Eggert A, Gruber J, Darda L. Treatment of ankle joint injuries. Randomized study of postoperative therapy and early functional treatment. Unfallchirurg. 1986;89:316-320.
58. Konradsen L, Nielsen PT, Albrecht-Beste E. Functional treatment of metacarpal fractures. Acta Orthop Scand. 1990;61:531-534.
59. Broström L. Sprained ankles. V. Treatment and prognosis in recent ligament ruptures. Acta Chir Scand. 1966;132:537-550.
60. Kerkhoffs GMMJ, Struijs PAA, Raaymakers ELFB, Marti RK. Functional treatment after surgical repair of acute Achilles tendon rupture: wrap vs walking cast. Arch Orthop Trauma Surg. 2002;122:102-105.
61. Ferris BD, Thomas NP, Dewar ME, Simpson DA. Brace treatment of Colles’ fracture. Acta Orthop Scand. 1989;60:63-65.
62. Braakman M, Oderwald EE, Haentjens MHHJ. Functional taping of fractures of the 5th metacarpal results in a quicker recovery. Injury. 1998;29:5-9.
63. Tropp H, Norlin R. Ankle performance after ankle fracture: randomised study of early mobilization. Foot Ankle Int. 1995;16:79-83.
64. Kuokkanen HOM, Mulari-Karanen SK, Niskanen RO, Haapala JK, Korkala OL. Treatment of subcapital fractures of the fifth metacarpal bone: a prospective randomised comparison between functional treatment and reposition and splinting. Scand J Plast Recontr Surg Hand Surg. 1999;33:315-317.
65. Murty AN, El Zebdeh MY, Ireland J. Tibial tunnel enlargement following anterior cruciate reconstruction: does post-operative immobilisation make a difference? Knee. 2001;8:39-43.
66. McAuliffe TB, Hilliar KM, Coates CJ, Grange WJ. Early mobilisation of Colles’ fractures: a prospective trial. J Bone Joint Surg Br. 1987;69B:727-729.
67. Brandsson S, Faxén E, Kartus J, Eriksson BI, Karlsson J. Is a knee brace advantageous after anterior cruciate ligament surgery? Scand J Med Sci Sports. 2001;11:110-114.
68. Lind K. Konservativ behandling af laterale ligamentrupturer i fodleddet. Ugeskr Lger. 1984;146:4017-4019.
69. Rafai M, Largab A, Cohen D, Trafeh M. Pure posterior luxation of the elbow in adults: immobilization or early mobilization. A randomized prospective study of 50 cases. Chir Main. 1999;18:272-278.
70. Strickland JW, Glogovac SV. Digital function following flexor tendon repair in Zone II: A comparison of immobilization and controlled passive motion techniques. Journal of Hand Surgery. 1980;5:537-543.
71. Møller-Larsen F, Wethelund JO, Jurik AG, de Carvalho A, Lucht U. Comparison of three different treatments for ruptured lateral ankle ligaments. Acta Orthop Scand. 1988;59:564-566.
72. Caro D, Craft IL, Howells JB, Shaw PC. Diagnosis and treatment of injury of lateral ligament of the ankle joint. Lancet. 1964;2:720-723.
- Injured limbs are traditionally rested by splint or cast. This is undertaken both for palliation and also in the belief that resting improves recovery time, and reduces complications such as deformity, functional problems and long-term pain.
- Early mobilization decreases pain, swelling and stiffness, particularly in the short term, without longer-term cosmetic or radiologic deformity. (SOR: A)
- Patients usually (but not always) prefer early mobilization, and return to work earlier. (SOR: C)
- Rest may be overused for limbs injury, although the extent to which early mobilization should be adopted needs more research. (SOR: C)
- The scope of limb injuries explored with trials of mobilization also needs further research.
Objectives: Rest is commonly used as primary treatment, rather than just palliation, for injured limbs. We searched the literature for evidence of benefit or harm from immobilization or mobilization of acute limb injury in adults.
Data Sources: We systematically searched for and retrieved randomized controlled trials (RCTs) of mobilization or rest for treatment of acute limb injuries, in Medline (1966–2002), EMBASE, Web of Science, and the Cochrane library, in all languages.
Review Methods: We examined patient-centered outcomes (pain, swelling, and cost), functional outcomes (range of motion, days lost from work) and complications of treatment.
Results: Forty-nine trials of immobilization for soft tissue injuries and fractures of both upper and lower limbs were identified (3366 patients). All studies reported either no difference between rest and early mobilization protocols, or found in favor of early mobilization. Reported benefits of mobilization included earlier return to work; decreased pain, swelling, and stiffness; and a greater preserved range of joint motion. Early mobilization caused no increased complications, deformity or residual symptoms.
Conclusions: We should not assume any benefit for immobilization after acute upper or lower limb injuries in adults. Rest appears to be overused as a treatment. More trials are needed to identify optimal programs for early mobilization.
We know that bed rest generally is over-prescribed.1 But what about resting or immobilizing acutely injured limbs—from simple sprains to gunshot wounds? This specific application of rest is controversial.2-6
Theoretically, rest should reduce further tissue damage by limiting movement, decreasing pain and swelling, and lessening loss of fracture reduction.7-15 However, mobilization increases blood flow and so reduces muscle atrophy, disuse osteoporosis, adhesions, and joint stiffness.7-15
The first empirical trials to determine whether rest or mobilization would offer greater benefit were undertaken in the 1980s, using both human and animal models. Systematic reviews have looked at specific injuries: acute ankle sprains16; ankle ligament rupture17; isolated ulnar fracture18; metacarpal fractures19; collateral ankle ligament sprains20; and soft-tissue ankle injury.21 Each review independently suggests benefits for early mobilization.
However, most clinicians employ some period of enforced rest of injured limbs. For example, a survey of orthopedic surgeons in Denmark found early mobilization for ankle fractures is prescribed for only 6% of patients.22
We systematically reviewed the literature to find trials that compared rest with early mobilization in acute limb injuries.
Methods
Protocol and search strategy
We searched the literature to identify prospective randomized controlled trials (RCTs) comparing rest with mobilization for acute limb injuries, searching the Cochrane Controlled Trials Register and Systematic Reviews, Medline (1966–2002), EMBASE (Rehabilitation and Physical Therapy), and Web of Science, combined with the following terms:
- immobilis*, immobiliz*, mobilis*, mobiliz*,
injur*, fracture*, limb*, cast*, brace*, splint*,
leg*, arm*, wrist*, elbow*, joint*, *carpal*,
*tarsal*, knee*, ankle*, femur*, tibia*, fibula*,
colles*, ulna*, radi*, humer*, sprain*, soft tissue,
plaster slab, dislocat*
We accepted all publication languages and translated several papers. We found 445 potentially relevant papers by examining their titles or abstracts (Figure). Studies that did not fulfill our inclusion criteria were discarded.
We obtained full texts for 76 studies and undertook a prospective cited reference search in Web of Science for each study to identify more recent articles. A total of 187 papers were then evaluated further for duplicate data and inclusion criteria.
Trials that met our inclusion criteria:
- Were randomized and controlled
- Studied acute limb injuries
- Compared groups whose only treatment difference was mobilization (studies that compared surgery and immobilization against nonsurgical early mobilization were not included; studies with internal fixation were included only if internal fixation was applied to both groups)
- Had loss to follow-up of 20%, except where analysis was clearly intention to treat
- Studied populations not focussed solely on young children, (studies in which the given age range included a small number of patients as young as 11 or 12 years were accepted—in these studies the median age was much higher)
- adequately reported data collection and statistical analysis.
By these criteria, we excluded 138 studies (a list of which is available from the authors). Finally, 49 studies were included.
FIGURE
Literature search process, and methods by which randomized controlled trials (RCTs) were selected
Study methods quality and validity
Two authors independently scored the validity of each of the included 49 studies, meeting to discuss and resolve any disagreements. We relied on published data, without writing to authors to clarify or obtain information. Included studies were evaluated against 11 standard criteria.23 Each criterion was scored 0–2. However, the practical maximum possible score was 18 because it was impossible to blind patients or their caregivers to mobilization. We considered the quality of 16 studies scoring 11 to be high.
Results
Across the 49 eligible studies, the different interventions were well described and differentiated, and data collection methods were clearly explained. Duration of immobilization in a cast was described (if at all) from 10 days to 8 weeks. Mobilization strategies varied and included active exercise, orthoses, crutches, or bandages.
Study quality was poor in many respects: several did not include important demographic data (including age, sex, or the numbers randomized to control and experimental group). Most did not report data about the methods of randomization. Many studies used inadequate randomization methods, with only 5 reporting optimal methods. Loss to follow-up was addressed poorly (not described or intention-to-treat analysis was not used). Outcome assessment was not blinded (a serious shortcoming in view of the subjective assessment of some patient outcomes). Reporting of inclusion criteria was inadequate in a few studies.
Given these deficiencies, our discussion emphasizes conclusions supported by studies of high quality.
Reporting of the studies
We divided the 49 studies into 4 groups: lower-limb fractures, other lower-limb injuries, upper-limb fractures, and other upper-limb injuries (Table W, at www.jfponline.com). Each group was further divided into trials using some form of limb support (such as a brace, splint, or a short period of immobilization) or minimal or no support (bandage, crutches, or tape) in the early mobilization group.
Most studies used some form of dynamic treatment for the injured limb, with highest use in lowerlimb injuries (74%); 2 studies included both supported and unsupported mobilization.24-26 In studies of upper-limb fractures, support was used in 50%. In high-quality studies, 12 out of 16 studies used some support, but results were consistent with studies that did not. The smaller number of studies using minimal support makes comparison with supported mobilization difficult, but results suggest that supported mobilization may result in an earlier return to work or sport, whereas minimally supported patients achieved better composite scores and muscle strength. There was too much clinical heterogeneity to sensibly combine the results; however, we were interested to see whether mobilization was useful across a heterogeneous group of conditions.
Patient-centered outcomes
No study reported any significant improvement with rest on swelling and pain. To the contrary, 13 studies reported significant improvement with early mobilization compared with rest,16,17,27-37 and 9 studies reported enhanced patient satisfaction.16,30,36,38-43 High-quality studies that reported pain levels found no difference or favored early mobilization.25,26,30,31,39,44-51 This was significant in only 2 studies of lower-limb nonfractures.25,26,30 No study reported adverse patient opinion in an early mobilization regime,28,31,38,40,44-46,48,51-56 and patients appreciated their ability to use the affected limb.34,43,49
Functional outcomes
Ten studies measured global function, using composite scores including subjective and objective criteria—pain, stiffness, swelling, use of supports, and ability to climb stairs, play sport, work, and undertake activities of daily life (Table W). Seven studies reported significant improvements with early mobilization—after 6 months (6 studies),28,35,42,46,52,57 or 12 months (1 study).32 Four studies of high quality found significant benefit for early mobilization in composite scores, most of these for lower-limb fractures.46,47,52,54 Significantly more patients with acute ankle sprain, who were immobilized in a cast, sought medical and physiotherapy advice in the initial 3 weeks, compared with those mobilized early with a functional brace.50
Return to work and sport
Thirteen studies reported that early mobilization resulted in a significantly earlier return to work (about 30%–60% earlier),16,17,30,33,35,36,38-40,52,57-59 especially in lower-limb nonfracture injuries. In 1 study of ankle fractures, patients randomized to wear a cast reported better performance of daily activities at 6 weeks than those mobilized with crutches.28 Perhaps, this reflects practical difficulties associated with using crutches. Five studies of lower-limb injury reported an earlier return to sport,16,30,39,57,60 as did 3 studies of postoperative Achilles tendon repair30,39,60 and 2 of ankle ligament injury or sprains.16,57 Five studies reporting a significantly earlier return to work or sport were of high quality, as were all studies of lower limb injuries.25,26,30,39,46,52
Range of movement
Fourteen studies of upper- and lower-limb fractures reported significant improvements in range of movement. Significant differences in range of movement were typically observed within 13 weeks of the injury,12,27,29,34,38,42,45,46,49,52,61-64 although a few studies reported differences for longer periods. Similarly for lower-limb nonfractures, significantly better ranges of motion were found within short periods,25,33,37,39,43 and also after 12 months.30,39-41 Eleven studies reporting this outcome were of high quality,25,26,30,31,39,45,46,48-51,54 and 4 studies found significant benefit for early mobilization.25,26,30,46,49 The other 7 high-quality studies favored early mobilization, and 1 found no difference.45
Deformity and other complications
Four studies found early mobilization reduced deformity: for angular displacement61 and radial shortening32 in Colles’ fractures; displacement of metacarpal fractures58 and cosmetic deformity in radial fractures.42 Two studies were of high quality.30,65 Ten trials reported no changes in deformity, no loss of fracture reduction, or any other complications with early mobilization of fractures.28,31,45,48,50,59,62-64,66 In contrast, for Colles’ fractures, significantly greater dorsal angulation61 and significant increases in radial tilt and decreased radioulnar joint space49 were reported for mobilized wrists.
Patient preferences
Patients expressed preference for a brace following anterior cruciate ligament surgery because it helped reduce pain and swelling67; they expressed preference for a cast following surgery for ankle fracture because it improved ability to perform everyday activities.28
Patients with distal radius fractures preferred early treatment with a Tubigrip bandage and a back-slab instead of removable splints, which increased pain and decreased mobilization.53 Generally, patients with fractures preferred rigid support immediately after the injury. Some also expected to have a traditional cast applied after learning their injured wrist was fractured.53
Cost of treatment
Full economic evaluations were not usually satisfactorily undertaken in these clinical studies. The cost of early mobilization was more expensive than immobilization in some studies8,23 but cheaper in others.2,9,10,24,68 It is estimated that direct costs to the patient were lower for early mobilization because of the decreased loss of working time.10,44,68,69
Adherence and supervision
Ten studies excluded patients who were unable to understand the nature of the treatment; had dementia; existing joint disease; drug abuse; alcohol problems; or difficulty with walking aids.28,31,38-41,45,46,49,69 Thus, many researchers have assumed that early mobilization requires greater patient responsibility. Some researchers have recommended applying casts for patients deemed “uncooperative” or “unlikely to be compliant,” despite their positive findings for early mobilization.3,16
Although 10 trials employed physiotherapy or supervised mobilization sessions,25,26,28,29,40,41,46,65,70 11 studies relied on self-controlled mobilization.27,30,31,38,39,42,44,45,48,49,52 In addition, some interventions (eg, braces) intrinsically required more supervision with their removal and reapplication than others (eg, functional casts or semirigid bandages).
Discussion
Early mobilization seems to decrease pain, swelling, and stiffness—at least in the short-term—and patients generally prefer it to immobilization. It results in earlier return—to work and to a greater range of motion, which is most significant within the first 2 months of the injury and can be maintained for up to 12 months for nonfracture injuries. Early mobilization does not increase cosmetic or radiological deformity for stable fractures, and patients experience fewer complications and residual symptoms. However, early mobilization may place greater demands on patients and require higher levels of understanding and responsibility, therefore making it unsuitable for some patients.
This systematic review of all upper- and lower-limb injuries, including fractures, consistently found in favor of early mobilization over rest. We acknowledge that the range of injuries reviewed is very limited. However, the clear benefits of mobilization indicated by this review suggest we need research in a wider range of injuries.
Similarly, it would be naïve to assume mobilization is better than immobilization in all circumstances. Harm must occur at some level of increased activity. In addition we know that pain and discomfort are often experienced by patients who demand immobilization (a “palliative” form of management). Finding the ideal level and type of activity must be undertaken empirically. Therefore more quality clinical trials are required to determine and evaluate the best regimens for early mobilization.
Newer studies will probably find that mobilization can be employed more often (and perhaps more vigorously) than we now advise. The best evidence at hand suggests the medical profession generally errs too conservatively on the side of immobilization.
Acknowledgments
Charlotte Nash did the searches, assembled and analysed the tables and wrote the first draft. Charlotte Nash and Sharon Mickan assessed the quality of all included studies and edited drafts. Paul Glasziou and Chris Del Mar initiated the question and edited drafts. This work was supported in part by a scholarship awarded by the Centre for General Practice, The University of Queensland, and funded by the Australian Commonwealth Department of Health and Ageing through the Primary Health Care Research, Evaluation and Development Strategy.
Corresponding author
Professor Chris B. Del Mar, Centre for General Practice, Faculty Heath Science and Medicine, Bond University, Gold Coast, Queensland 4229, Australia. E-mail: [email protected].
- Injured limbs are traditionally rested by splint or cast. This is undertaken both for palliation and also in the belief that resting improves recovery time, and reduces complications such as deformity, functional problems and long-term pain.
- Early mobilization decreases pain, swelling and stiffness, particularly in the short term, without longer-term cosmetic or radiologic deformity. (SOR: A)
- Patients usually (but not always) prefer early mobilization, and return to work earlier. (SOR: C)
- Rest may be overused for limbs injury, although the extent to which early mobilization should be adopted needs more research. (SOR: C)
- The scope of limb injuries explored with trials of mobilization also needs further research.
Objectives: Rest is commonly used as primary treatment, rather than just palliation, for injured limbs. We searched the literature for evidence of benefit or harm from immobilization or mobilization of acute limb injury in adults.
Data Sources: We systematically searched for and retrieved randomized controlled trials (RCTs) of mobilization or rest for treatment of acute limb injuries, in Medline (1966–2002), EMBASE, Web of Science, and the Cochrane library, in all languages.
Review Methods: We examined patient-centered outcomes (pain, swelling, and cost), functional outcomes (range of motion, days lost from work) and complications of treatment.
Results: Forty-nine trials of immobilization for soft tissue injuries and fractures of both upper and lower limbs were identified (3366 patients). All studies reported either no difference between rest and early mobilization protocols, or found in favor of early mobilization. Reported benefits of mobilization included earlier return to work; decreased pain, swelling, and stiffness; and a greater preserved range of joint motion. Early mobilization caused no increased complications, deformity or residual symptoms.
Conclusions: We should not assume any benefit for immobilization after acute upper or lower limb injuries in adults. Rest appears to be overused as a treatment. More trials are needed to identify optimal programs for early mobilization.
We know that bed rest generally is over-prescribed.1 But what about resting or immobilizing acutely injured limbs—from simple sprains to gunshot wounds? This specific application of rest is controversial.2-6
Theoretically, rest should reduce further tissue damage by limiting movement, decreasing pain and swelling, and lessening loss of fracture reduction.7-15 However, mobilization increases blood flow and so reduces muscle atrophy, disuse osteoporosis, adhesions, and joint stiffness.7-15
The first empirical trials to determine whether rest or mobilization would offer greater benefit were undertaken in the 1980s, using both human and animal models. Systematic reviews have looked at specific injuries: acute ankle sprains16; ankle ligament rupture17; isolated ulnar fracture18; metacarpal fractures19; collateral ankle ligament sprains20; and soft-tissue ankle injury.21 Each review independently suggests benefits for early mobilization.
However, most clinicians employ some period of enforced rest of injured limbs. For example, a survey of orthopedic surgeons in Denmark found early mobilization for ankle fractures is prescribed for only 6% of patients.22
We systematically reviewed the literature to find trials that compared rest with early mobilization in acute limb injuries.
Methods
Protocol and search strategy
We searched the literature to identify prospective randomized controlled trials (RCTs) comparing rest with mobilization for acute limb injuries, searching the Cochrane Controlled Trials Register and Systematic Reviews, Medline (1966–2002), EMBASE (Rehabilitation and Physical Therapy), and Web of Science, combined with the following terms:
- immobilis*, immobiliz*, mobilis*, mobiliz*,
injur*, fracture*, limb*, cast*, brace*, splint*,
leg*, arm*, wrist*, elbow*, joint*, *carpal*,
*tarsal*, knee*, ankle*, femur*, tibia*, fibula*,
colles*, ulna*, radi*, humer*, sprain*, soft tissue,
plaster slab, dislocat*
We accepted all publication languages and translated several papers. We found 445 potentially relevant papers by examining their titles or abstracts (Figure). Studies that did not fulfill our inclusion criteria were discarded.
We obtained full texts for 76 studies and undertook a prospective cited reference search in Web of Science for each study to identify more recent articles. A total of 187 papers were then evaluated further for duplicate data and inclusion criteria.
Trials that met our inclusion criteria:
- Were randomized and controlled
- Studied acute limb injuries
- Compared groups whose only treatment difference was mobilization (studies that compared surgery and immobilization against nonsurgical early mobilization were not included; studies with internal fixation were included only if internal fixation was applied to both groups)
- Had loss to follow-up of 20%, except where analysis was clearly intention to treat
- Studied populations not focussed solely on young children, (studies in which the given age range included a small number of patients as young as 11 or 12 years were accepted—in these studies the median age was much higher)
- adequately reported data collection and statistical analysis.
By these criteria, we excluded 138 studies (a list of which is available from the authors). Finally, 49 studies were included.
FIGURE
Literature search process, and methods by which randomized controlled trials (RCTs) were selected
Study methods quality and validity
Two authors independently scored the validity of each of the included 49 studies, meeting to discuss and resolve any disagreements. We relied on published data, without writing to authors to clarify or obtain information. Included studies were evaluated against 11 standard criteria.23 Each criterion was scored 0–2. However, the practical maximum possible score was 18 because it was impossible to blind patients or their caregivers to mobilization. We considered the quality of 16 studies scoring 11 to be high.
Results
Across the 49 eligible studies, the different interventions were well described and differentiated, and data collection methods were clearly explained. Duration of immobilization in a cast was described (if at all) from 10 days to 8 weeks. Mobilization strategies varied and included active exercise, orthoses, crutches, or bandages.
Study quality was poor in many respects: several did not include important demographic data (including age, sex, or the numbers randomized to control and experimental group). Most did not report data about the methods of randomization. Many studies used inadequate randomization methods, with only 5 reporting optimal methods. Loss to follow-up was addressed poorly (not described or intention-to-treat analysis was not used). Outcome assessment was not blinded (a serious shortcoming in view of the subjective assessment of some patient outcomes). Reporting of inclusion criteria was inadequate in a few studies.
Given these deficiencies, our discussion emphasizes conclusions supported by studies of high quality.
Reporting of the studies
We divided the 49 studies into 4 groups: lower-limb fractures, other lower-limb injuries, upper-limb fractures, and other upper-limb injuries (Table W, at www.jfponline.com). Each group was further divided into trials using some form of limb support (such as a brace, splint, or a short period of immobilization) or minimal or no support (bandage, crutches, or tape) in the early mobilization group.
Most studies used some form of dynamic treatment for the injured limb, with highest use in lowerlimb injuries (74%); 2 studies included both supported and unsupported mobilization.24-26 In studies of upper-limb fractures, support was used in 50%. In high-quality studies, 12 out of 16 studies used some support, but results were consistent with studies that did not. The smaller number of studies using minimal support makes comparison with supported mobilization difficult, but results suggest that supported mobilization may result in an earlier return to work or sport, whereas minimally supported patients achieved better composite scores and muscle strength. There was too much clinical heterogeneity to sensibly combine the results; however, we were interested to see whether mobilization was useful across a heterogeneous group of conditions.
Patient-centered outcomes
No study reported any significant improvement with rest on swelling and pain. To the contrary, 13 studies reported significant improvement with early mobilization compared with rest,16,17,27-37 and 9 studies reported enhanced patient satisfaction.16,30,36,38-43 High-quality studies that reported pain levels found no difference or favored early mobilization.25,26,30,31,39,44-51 This was significant in only 2 studies of lower-limb nonfractures.25,26,30 No study reported adverse patient opinion in an early mobilization regime,28,31,38,40,44-46,48,51-56 and patients appreciated their ability to use the affected limb.34,43,49
Functional outcomes
Ten studies measured global function, using composite scores including subjective and objective criteria—pain, stiffness, swelling, use of supports, and ability to climb stairs, play sport, work, and undertake activities of daily life (Table W). Seven studies reported significant improvements with early mobilization—after 6 months (6 studies),28,35,42,46,52,57 or 12 months (1 study).32 Four studies of high quality found significant benefit for early mobilization in composite scores, most of these for lower-limb fractures.46,47,52,54 Significantly more patients with acute ankle sprain, who were immobilized in a cast, sought medical and physiotherapy advice in the initial 3 weeks, compared with those mobilized early with a functional brace.50
Return to work and sport
Thirteen studies reported that early mobilization resulted in a significantly earlier return to work (about 30%–60% earlier),16,17,30,33,35,36,38-40,52,57-59 especially in lower-limb nonfracture injuries. In 1 study of ankle fractures, patients randomized to wear a cast reported better performance of daily activities at 6 weeks than those mobilized with crutches.28 Perhaps, this reflects practical difficulties associated with using crutches. Five studies of lower-limb injury reported an earlier return to sport,16,30,39,57,60 as did 3 studies of postoperative Achilles tendon repair30,39,60 and 2 of ankle ligament injury or sprains.16,57 Five studies reporting a significantly earlier return to work or sport were of high quality, as were all studies of lower limb injuries.25,26,30,39,46,52
Range of movement
Fourteen studies of upper- and lower-limb fractures reported significant improvements in range of movement. Significant differences in range of movement were typically observed within 13 weeks of the injury,12,27,29,34,38,42,45,46,49,52,61-64 although a few studies reported differences for longer periods. Similarly for lower-limb nonfractures, significantly better ranges of motion were found within short periods,25,33,37,39,43 and also after 12 months.30,39-41 Eleven studies reporting this outcome were of high quality,25,26,30,31,39,45,46,48-51,54 and 4 studies found significant benefit for early mobilization.25,26,30,46,49 The other 7 high-quality studies favored early mobilization, and 1 found no difference.45
Deformity and other complications
Four studies found early mobilization reduced deformity: for angular displacement61 and radial shortening32 in Colles’ fractures; displacement of metacarpal fractures58 and cosmetic deformity in radial fractures.42 Two studies were of high quality.30,65 Ten trials reported no changes in deformity, no loss of fracture reduction, or any other complications with early mobilization of fractures.28,31,45,48,50,59,62-64,66 In contrast, for Colles’ fractures, significantly greater dorsal angulation61 and significant increases in radial tilt and decreased radioulnar joint space49 were reported for mobilized wrists.
Patient preferences
Patients expressed preference for a brace following anterior cruciate ligament surgery because it helped reduce pain and swelling67; they expressed preference for a cast following surgery for ankle fracture because it improved ability to perform everyday activities.28
Patients with distal radius fractures preferred early treatment with a Tubigrip bandage and a back-slab instead of removable splints, which increased pain and decreased mobilization.53 Generally, patients with fractures preferred rigid support immediately after the injury. Some also expected to have a traditional cast applied after learning their injured wrist was fractured.53
Cost of treatment
Full economic evaluations were not usually satisfactorily undertaken in these clinical studies. The cost of early mobilization was more expensive than immobilization in some studies8,23 but cheaper in others.2,9,10,24,68 It is estimated that direct costs to the patient were lower for early mobilization because of the decreased loss of working time.10,44,68,69
Adherence and supervision
Ten studies excluded patients who were unable to understand the nature of the treatment; had dementia; existing joint disease; drug abuse; alcohol problems; or difficulty with walking aids.28,31,38-41,45,46,49,69 Thus, many researchers have assumed that early mobilization requires greater patient responsibility. Some researchers have recommended applying casts for patients deemed “uncooperative” or “unlikely to be compliant,” despite their positive findings for early mobilization.3,16
Although 10 trials employed physiotherapy or supervised mobilization sessions,25,26,28,29,40,41,46,65,70 11 studies relied on self-controlled mobilization.27,30,31,38,39,42,44,45,48,49,52 In addition, some interventions (eg, braces) intrinsically required more supervision with their removal and reapplication than others (eg, functional casts or semirigid bandages).
Discussion
Early mobilization seems to decrease pain, swelling, and stiffness—at least in the short-term—and patients generally prefer it to immobilization. It results in earlier return—to work and to a greater range of motion, which is most significant within the first 2 months of the injury and can be maintained for up to 12 months for nonfracture injuries. Early mobilization does not increase cosmetic or radiological deformity for stable fractures, and patients experience fewer complications and residual symptoms. However, early mobilization may place greater demands on patients and require higher levels of understanding and responsibility, therefore making it unsuitable for some patients.
This systematic review of all upper- and lower-limb injuries, including fractures, consistently found in favor of early mobilization over rest. We acknowledge that the range of injuries reviewed is very limited. However, the clear benefits of mobilization indicated by this review suggest we need research in a wider range of injuries.
Similarly, it would be naïve to assume mobilization is better than immobilization in all circumstances. Harm must occur at some level of increased activity. In addition we know that pain and discomfort are often experienced by patients who demand immobilization (a “palliative” form of management). Finding the ideal level and type of activity must be undertaken empirically. Therefore more quality clinical trials are required to determine and evaluate the best regimens for early mobilization.
Newer studies will probably find that mobilization can be employed more often (and perhaps more vigorously) than we now advise. The best evidence at hand suggests the medical profession generally errs too conservatively on the side of immobilization.
Acknowledgments
Charlotte Nash did the searches, assembled and analysed the tables and wrote the first draft. Charlotte Nash and Sharon Mickan assessed the quality of all included studies and edited drafts. Paul Glasziou and Chris Del Mar initiated the question and edited drafts. This work was supported in part by a scholarship awarded by the Centre for General Practice, The University of Queensland, and funded by the Australian Commonwealth Department of Health and Ageing through the Primary Health Care Research, Evaluation and Development Strategy.
Corresponding author
Professor Chris B. Del Mar, Centre for General Practice, Faculty Heath Science and Medicine, Bond University, Gold Coast, Queensland 4229, Australia. E-mail: [email protected].
1. Allen C, Glasziou P, Del Mar C. Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet. 1999;354:1229-1233.
2. Madhok R, Bhopal RS. Coping with an upper limb fracture? A study of the elderly. Public Health. 1992;106:19-28.
3. Salter RB. Motion versus rest: Why immobilize joints? J Bone Joint Surg Br. 1982;64B:251-254.
4. Safran MR, Zachazewski JE, Benedetti RS, Bartolozzi AR, Mandelbaum R. Lateral ankle sprains: a comprehensive review. Part 2: treatment and rehabilitation with an emphasis on the athlete. Med Sci Sports Exerc. 1999;31:S438-S447.
5. Willems C. Immediate active mobilization in the treatment of gunshot wounds of joints. Medical Record. 1919;95:953-962.
6. Dent JA. Continuous passive motion in hand rehabilitation. Prosthet Orthot Int 1993;17:130-135.
7. Pneumaticos SG, Noble PC, McGarvey WC, Mody DR, Trevino SG. The effects of early mobilization in the healing of Achilles tendon repair. Foot Ankle Int. 2000;21:551-557.
8. Gelberman RH, Menon J, Gonsalves M, Akeson WH. The effects of mobilisation on the vascularisation of healing flexor tendons in dogs. Clin Orthop. 1980;153:283-289.
9. Kannus P. Immobilisation or early mobilisation after an acute soft tissue injury. The Physician and Sportsmedicine. 2000;28:55-63.
10. Halikis MN, Manske PR, Kubota H, Aoki M. Effect of immobilization, immediate mobilization and delayed mobilization of the resistance to digital flexion using a tendon injury model. J Hand Surg [Am]. 1997;22A:464-472.
11. Romanelli DA, Almekinders LC, Mandelbaum BR. Achilles rupture in the athlete: Current science and treatment. Sports Medicine and Arthroscopy Review. 2000;8:377-386.
12. Stockle U, Konig B, Tempka A, Sudkamp NP. Cast immobilisation or vacuum stabilizing system? Unfallchirurg. 2000;103:215-219.
13. Viidik A. The effect of training on the tensile strength of isolated rabbit tendons. Scandinavian Journal of Plastic and Reconstructive Surgery. 1967;1:141-147.
14. Woo SL, Gelberman RH, Cobb NG, Amiel D, Lothringer K, Akeson WH. The importance of controlled passive mobilization on flexor tendon healing. A biomechanical study. Acta Orthop Scand. 1981;52:615-622.
15. Peacock E. Biological principles in the healing of long tendons. Surg Clin North Am. 1965;45:461-476.
16. Kerkhoffs GMMJ, Rowe BH, Assendelft WJJ, Kelly KD, Struijs PAA, Niek van Dijk C. Immobilisation for acute ankle sprain: a systematic review. Arch Orthop Trauma Surg. 2001;121:462-471.
17. Pijnenburg ACM, van Dijk CN, Bossuyt PMM, Marti RK. Treatment of ruptures of the lateral ankle ligaments: A meta-analysis. J Bone Joint Surg Am. 2000;82A:761-773.
18. Mackay D, Wood L, Rangan A. The treatment of isolated ulnar fractures in adults: a systematic review. Injury. 2000;31:565-570.
19. Prokop A, Kulus S, Helling HJ, Burger C, Rehm KE. Are there concepts in treatment of metacarpal fractures? Own results and a review of the literature of the last 12 years. Unfallchirurg. 1999;102:50-58.
20. Shrier I. Treatment of lateral collateral ligament sprains of the ankle: a critical appraisal of the literature. Clin J Sport Med. 1995;5:187-195.
21. Ogilvie-Harris DJ, Gilbart M. Treatment modalities for soft tissue injuries of the ankle: a critical review. Clin J Sport Med. 1995;5:175-186.
22. Hviid K, Harager K, Schantz K. Aftercare of malleolar fractures in Denmark. A questionnaire study. Ugeskr Læger. 2000;62:2747-2750.
23. Gillespie W, Gillespie L, Morton L. Cochrane Musculoskeletal Injuries Group. Cochrane Database 2002.
24. Sommer HM, Schreiber H. Early functional conservative therapy of fresh fibular capsular ligament rupture from the socioeconomic viewpoint. Sportverletzung Sportschaden. 1993;7:40-46.
25. Dettori JR. Early ankle mobilization, part I: The immediate effect on acute, lateral ankle sprains. A randomised clinical trial. Mil Med. 1994;159:15-20.
26. Dettori JR, Basmania CJ. Early ankle mobilization, part II: A one-year follow-up of acute, lateral ankle sprains. A randomized clinical trial. Mil Med. 1994;159:20-24.
27. Stuart PR, Brumby C, Smith SR. Comparative study of functional bracing and plaster cast treatment of stable lateral malleolar fractures. Injury. 1989;20:323-326.
28. van Laarhoven CJHM, Meeuwis JD, van der Werken C. Postoperative treatment of internally fixed ankle fractures. J Bone Joint Surg Br. 1996;78B:395-399.
29. Søndenaa K, Høigaard U, Smith D, Alho A. Immobilisation of operated ankle fractures. Acta Orthop Scand. 1986;57:59-61.
30. Cetti R, Henriksen LO, Jacobsen KS. A new treatment of ruptured Achilles tendons. Clin Orthop. 1994;308:155-165.
31. Dias JJ, Wray CC, Jones JM, Gregg PJ. The value of early mobilisation in the treatment of Colles’ fractures. J Bone Joint Surg Br. 1987;69B:463-467.
32. Abbaszadegan H, Conradi P, Jonsson U. Fixation not needed for undisplaced Colles’ fracture. Acta Orthop Scand. 1989;60:60-62.
33. Nyska M, Weisel Y, Halperin N, Mann G, Segal D. Controlled mobilization after acute ankle inversion injury. Journal of Sports Traumatology and Related Research. 1999;21:114-120.
34. McMahon PJ, Woods DA, Burge PD. Initial treatment of closed metacarpal fractures. J Hand Surg [Br]. 1994;19B:597-600.
35. Konradsen L, Hølmer P, Søndergaard L. Early mobilizing treatment for grade III ankle ligament injuries. Foot and Ankle. 1991;12:69-73.
36. Cetti R, Christensen SE, Corfitzen MT. Ruptured fibular ankle ligament: Plaster or Pliton brace? Br J Sports Med. 1984;18:104-109.
37. Eiff MP, Smith AT, Smith GE. Early mobilisation versus immobilisation in the treatment of lateral ankle sprains. Am J Sports Med. 1994;22:83-86.
38. Gebuhr P, Hölmich P, Ørsnes T, Soelberg M, Krasheninnikoff M, Kjersgaard AG. Isolated ulnar shaft fractures. J Bone Joint Surg Br. 1992;74B:757-759.
39. Mortensen NHM, Skov O, Jensen PE. Early motion of the ankle after operative treatment of a rupture of the Achilles tendon. J Bone Joint Surg Am. 1999;81A:983-990.
40. Buchgraber A, Pässler HH. Percutaneous repair of Achilles tendon rupture. Clin Orthop. 1997;341:113-122.
41. Saleh M, Marshall PD, Senior R, MacFarlane A. The Sheffield Splint for controlled early mobilisation after rupture of the calcaneal tendon. J Bone Joint Surg Br. 1992;74B:206-209.
42. Davis TRC, Buchanan JM. A controlled prospective study of early mobilization of minimally displaced fractures of the distal radial metaphysis. Injury. 1987;18:283-285.
43. Avci S, Sayli U. Comparison of the results of short-term rigid and semi-rigid cast immobilization for the treatment of grade 3 inversion injuries of the ankle. Injury. 1998;29:581-584.
44. Dogra AS, Rangan A. Early mobilisation versus immobilisation of surgically treated ankle fracture. Prospective randomised control trial. Injury. 1999;30:417-419.
45. Hedström M, Ahl T, Dalén N. Early postoperative ankle exercises: a study of postoperative lateral malleolar fractures. Clin Orthop. 1994;300:193-196.
46. Port AM, McVie JL, Naylor G, Kreibich DN. Comparison of two conservative methods of treating an isolated fracture of the lateral malleous. J Bone Joint Surg Br. 1996;78B:568-572.
47. Klein J, Rixen D, Albring T, Tiling T. Functional treatment with a pneumatic ankle brace versus cast immobilisation for recent rupture of the fibular ligament in the ankle. A randomised clinical trial. Unfallchirurg. 1991;94:99-104.
48. Allain J, le Guilloux P, Mouël SL, Goutallier D. Trans-styloid fixation of fractures of the distal radius: A prospective randomized comparison between 6- and 1-week postoperative immobilization in 60 fractures. Acta Orthop Scand. 1999;70:119-123.
49. Millett PJ, Rushton N. Early mobilization in the treatment of Colles’ fracture: a 3 year prospective study. Injury. 1995;26:671-675.
50. Stewart HD, Innes AR, Burke FD. Functional cast-bracing for Colles’ fractures. A comparison between cast-bracing and conventional plaster casts. J Bone Joint Surg Br. 1984;66B:749-753.
51. Unsworth-White J, Koka R, Churchill M, D’Arcy JC, James SE. The non-operative management of radial head fractures: a randomized trial of three treatments. Injury. 1994;25:165-167.
52. Egol KA, Dolan R, Koval KJ. Functional outcome of surgery for fractures of the ankle. J Bone Joint Surg Br. 2000;82:246-249.
53. Stoffelen D, Broos P. Minimally displaced distal radius fractures: do they need plaster treatment? J Trauma. 1998;44:503-505.
54. DiStasio AJ, Jaggears FR, DePasquale LV, Frassica FJ, Turen CH. Protected early motion versus cast immobilization in postoperative management of ankle fractures. Contemporary Orthopaedics. 1994;29:273-277.
55. Regis D, Montanari M, Magnan B, Spagnol S, Bragantini A. Dynamic orthopaedic brace in the treatment of ankle sprains. Foot Ankle Int. 1995;16:422-426.
56. Grønmark T, Johnsen O, Kogstad O. Rupture of the lateral ligaments of the ankle: a controlled clinical trial. Injury. 1980;11:215-218.
57. Eggert A, Gruber J, Darda L. Treatment of ankle joint injuries. Randomized study of postoperative therapy and early functional treatment. Unfallchirurg. 1986;89:316-320.
58. Konradsen L, Nielsen PT, Albrecht-Beste E. Functional treatment of metacarpal fractures. Acta Orthop Scand. 1990;61:531-534.
59. Broström L. Sprained ankles. V. Treatment and prognosis in recent ligament ruptures. Acta Chir Scand. 1966;132:537-550.
60. Kerkhoffs GMMJ, Struijs PAA, Raaymakers ELFB, Marti RK. Functional treatment after surgical repair of acute Achilles tendon rupture: wrap vs walking cast. Arch Orthop Trauma Surg. 2002;122:102-105.
61. Ferris BD, Thomas NP, Dewar ME, Simpson DA. Brace treatment of Colles’ fracture. Acta Orthop Scand. 1989;60:63-65.
62. Braakman M, Oderwald EE, Haentjens MHHJ. Functional taping of fractures of the 5th metacarpal results in a quicker recovery. Injury. 1998;29:5-9.
63. Tropp H, Norlin R. Ankle performance after ankle fracture: randomised study of early mobilization. Foot Ankle Int. 1995;16:79-83.
64. Kuokkanen HOM, Mulari-Karanen SK, Niskanen RO, Haapala JK, Korkala OL. Treatment of subcapital fractures of the fifth metacarpal bone: a prospective randomised comparison between functional treatment and reposition and splinting. Scand J Plast Recontr Surg Hand Surg. 1999;33:315-317.
65. Murty AN, El Zebdeh MY, Ireland J. Tibial tunnel enlargement following anterior cruciate reconstruction: does post-operative immobilisation make a difference? Knee. 2001;8:39-43.
66. McAuliffe TB, Hilliar KM, Coates CJ, Grange WJ. Early mobilisation of Colles’ fractures: a prospective trial. J Bone Joint Surg Br. 1987;69B:727-729.
67. Brandsson S, Faxén E, Kartus J, Eriksson BI, Karlsson J. Is a knee brace advantageous after anterior cruciate ligament surgery? Scand J Med Sci Sports. 2001;11:110-114.
68. Lind K. Konservativ behandling af laterale ligamentrupturer i fodleddet. Ugeskr Lger. 1984;146:4017-4019.
69. Rafai M, Largab A, Cohen D, Trafeh M. Pure posterior luxation of the elbow in adults: immobilization or early mobilization. A randomized prospective study of 50 cases. Chir Main. 1999;18:272-278.
70. Strickland JW, Glogovac SV. Digital function following flexor tendon repair in Zone II: A comparison of immobilization and controlled passive motion techniques. Journal of Hand Surgery. 1980;5:537-543.
71. Møller-Larsen F, Wethelund JO, Jurik AG, de Carvalho A, Lucht U. Comparison of three different treatments for ruptured lateral ankle ligaments. Acta Orthop Scand. 1988;59:564-566.
72. Caro D, Craft IL, Howells JB, Shaw PC. Diagnosis and treatment of injury of lateral ligament of the ankle joint. Lancet. 1964;2:720-723.
1. Allen C, Glasziou P, Del Mar C. Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet. 1999;354:1229-1233.
2. Madhok R, Bhopal RS. Coping with an upper limb fracture? A study of the elderly. Public Health. 1992;106:19-28.
3. Salter RB. Motion versus rest: Why immobilize joints? J Bone Joint Surg Br. 1982;64B:251-254.
4. Safran MR, Zachazewski JE, Benedetti RS, Bartolozzi AR, Mandelbaum R. Lateral ankle sprains: a comprehensive review. Part 2: treatment and rehabilitation with an emphasis on the athlete. Med Sci Sports Exerc. 1999;31:S438-S447.
5. Willems C. Immediate active mobilization in the treatment of gunshot wounds of joints. Medical Record. 1919;95:953-962.
6. Dent JA. Continuous passive motion in hand rehabilitation. Prosthet Orthot Int 1993;17:130-135.
7. Pneumaticos SG, Noble PC, McGarvey WC, Mody DR, Trevino SG. The effects of early mobilization in the healing of Achilles tendon repair. Foot Ankle Int. 2000;21:551-557.
8. Gelberman RH, Menon J, Gonsalves M, Akeson WH. The effects of mobilisation on the vascularisation of healing flexor tendons in dogs. Clin Orthop. 1980;153:283-289.
9. Kannus P. Immobilisation or early mobilisation after an acute soft tissue injury. The Physician and Sportsmedicine. 2000;28:55-63.
10. Halikis MN, Manske PR, Kubota H, Aoki M. Effect of immobilization, immediate mobilization and delayed mobilization of the resistance to digital flexion using a tendon injury model. J Hand Surg [Am]. 1997;22A:464-472.
11. Romanelli DA, Almekinders LC, Mandelbaum BR. Achilles rupture in the athlete: Current science and treatment. Sports Medicine and Arthroscopy Review. 2000;8:377-386.
12. Stockle U, Konig B, Tempka A, Sudkamp NP. Cast immobilisation or vacuum stabilizing system? Unfallchirurg. 2000;103:215-219.
13. Viidik A. The effect of training on the tensile strength of isolated rabbit tendons. Scandinavian Journal of Plastic and Reconstructive Surgery. 1967;1:141-147.
14. Woo SL, Gelberman RH, Cobb NG, Amiel D, Lothringer K, Akeson WH. The importance of controlled passive mobilization on flexor tendon healing. A biomechanical study. Acta Orthop Scand. 1981;52:615-622.
15. Peacock E. Biological principles in the healing of long tendons. Surg Clin North Am. 1965;45:461-476.
16. Kerkhoffs GMMJ, Rowe BH, Assendelft WJJ, Kelly KD, Struijs PAA, Niek van Dijk C. Immobilisation for acute ankle sprain: a systematic review. Arch Orthop Trauma Surg. 2001;121:462-471.
17. Pijnenburg ACM, van Dijk CN, Bossuyt PMM, Marti RK. Treatment of ruptures of the lateral ankle ligaments: A meta-analysis. J Bone Joint Surg Am. 2000;82A:761-773.
18. Mackay D, Wood L, Rangan A. The treatment of isolated ulnar fractures in adults: a systematic review. Injury. 2000;31:565-570.
19. Prokop A, Kulus S, Helling HJ, Burger C, Rehm KE. Are there concepts in treatment of metacarpal fractures? Own results and a review of the literature of the last 12 years. Unfallchirurg. 1999;102:50-58.
20. Shrier I. Treatment of lateral collateral ligament sprains of the ankle: a critical appraisal of the literature. Clin J Sport Med. 1995;5:187-195.
21. Ogilvie-Harris DJ, Gilbart M. Treatment modalities for soft tissue injuries of the ankle: a critical review. Clin J Sport Med. 1995;5:175-186.
22. Hviid K, Harager K, Schantz K. Aftercare of malleolar fractures in Denmark. A questionnaire study. Ugeskr Læger. 2000;62:2747-2750.
23. Gillespie W, Gillespie L, Morton L. Cochrane Musculoskeletal Injuries Group. Cochrane Database 2002.
24. Sommer HM, Schreiber H. Early functional conservative therapy of fresh fibular capsular ligament rupture from the socioeconomic viewpoint. Sportverletzung Sportschaden. 1993;7:40-46.
25. Dettori JR. Early ankle mobilization, part I: The immediate effect on acute, lateral ankle sprains. A randomised clinical trial. Mil Med. 1994;159:15-20.
26. Dettori JR, Basmania CJ. Early ankle mobilization, part II: A one-year follow-up of acute, lateral ankle sprains. A randomized clinical trial. Mil Med. 1994;159:20-24.
27. Stuart PR, Brumby C, Smith SR. Comparative study of functional bracing and plaster cast treatment of stable lateral malleolar fractures. Injury. 1989;20:323-326.
28. van Laarhoven CJHM, Meeuwis JD, van der Werken C. Postoperative treatment of internally fixed ankle fractures. J Bone Joint Surg Br. 1996;78B:395-399.
29. Søndenaa K, Høigaard U, Smith D, Alho A. Immobilisation of operated ankle fractures. Acta Orthop Scand. 1986;57:59-61.
30. Cetti R, Henriksen LO, Jacobsen KS. A new treatment of ruptured Achilles tendons. Clin Orthop. 1994;308:155-165.
31. Dias JJ, Wray CC, Jones JM, Gregg PJ. The value of early mobilisation in the treatment of Colles’ fractures. J Bone Joint Surg Br. 1987;69B:463-467.
32. Abbaszadegan H, Conradi P, Jonsson U. Fixation not needed for undisplaced Colles’ fracture. Acta Orthop Scand. 1989;60:60-62.
33. Nyska M, Weisel Y, Halperin N, Mann G, Segal D. Controlled mobilization after acute ankle inversion injury. Journal of Sports Traumatology and Related Research. 1999;21:114-120.
34. McMahon PJ, Woods DA, Burge PD. Initial treatment of closed metacarpal fractures. J Hand Surg [Br]. 1994;19B:597-600.
35. Konradsen L, Hølmer P, Søndergaard L. Early mobilizing treatment for grade III ankle ligament injuries. Foot and Ankle. 1991;12:69-73.
36. Cetti R, Christensen SE, Corfitzen MT. Ruptured fibular ankle ligament: Plaster or Pliton brace? Br J Sports Med. 1984;18:104-109.
37. Eiff MP, Smith AT, Smith GE. Early mobilisation versus immobilisation in the treatment of lateral ankle sprains. Am J Sports Med. 1994;22:83-86.
38. Gebuhr P, Hölmich P, Ørsnes T, Soelberg M, Krasheninnikoff M, Kjersgaard AG. Isolated ulnar shaft fractures. J Bone Joint Surg Br. 1992;74B:757-759.
39. Mortensen NHM, Skov O, Jensen PE. Early motion of the ankle after operative treatment of a rupture of the Achilles tendon. J Bone Joint Surg Am. 1999;81A:983-990.
40. Buchgraber A, Pässler HH. Percutaneous repair of Achilles tendon rupture. Clin Orthop. 1997;341:113-122.
41. Saleh M, Marshall PD, Senior R, MacFarlane A. The Sheffield Splint for controlled early mobilisation after rupture of the calcaneal tendon. J Bone Joint Surg Br. 1992;74B:206-209.
42. Davis TRC, Buchanan JM. A controlled prospective study of early mobilization of minimally displaced fractures of the distal radial metaphysis. Injury. 1987;18:283-285.
43. Avci S, Sayli U. Comparison of the results of short-term rigid and semi-rigid cast immobilization for the treatment of grade 3 inversion injuries of the ankle. Injury. 1998;29:581-584.
44. Dogra AS, Rangan A. Early mobilisation versus immobilisation of surgically treated ankle fracture. Prospective randomised control trial. Injury. 1999;30:417-419.
45. Hedström M, Ahl T, Dalén N. Early postoperative ankle exercises: a study of postoperative lateral malleolar fractures. Clin Orthop. 1994;300:193-196.
46. Port AM, McVie JL, Naylor G, Kreibich DN. Comparison of two conservative methods of treating an isolated fracture of the lateral malleous. J Bone Joint Surg Br. 1996;78B:568-572.
47. Klein J, Rixen D, Albring T, Tiling T. Functional treatment with a pneumatic ankle brace versus cast immobilisation for recent rupture of the fibular ligament in the ankle. A randomised clinical trial. Unfallchirurg. 1991;94:99-104.
48. Allain J, le Guilloux P, Mouël SL, Goutallier D. Trans-styloid fixation of fractures of the distal radius: A prospective randomized comparison between 6- and 1-week postoperative immobilization in 60 fractures. Acta Orthop Scand. 1999;70:119-123.
49. Millett PJ, Rushton N. Early mobilization in the treatment of Colles’ fracture: a 3 year prospective study. Injury. 1995;26:671-675.
50. Stewart HD, Innes AR, Burke FD. Functional cast-bracing for Colles’ fractures. A comparison between cast-bracing and conventional plaster casts. J Bone Joint Surg Br. 1984;66B:749-753.
51. Unsworth-White J, Koka R, Churchill M, D’Arcy JC, James SE. The non-operative management of radial head fractures: a randomized trial of three treatments. Injury. 1994;25:165-167.
52. Egol KA, Dolan R, Koval KJ. Functional outcome of surgery for fractures of the ankle. J Bone Joint Surg Br. 2000;82:246-249.
53. Stoffelen D, Broos P. Minimally displaced distal radius fractures: do they need plaster treatment? J Trauma. 1998;44:503-505.
54. DiStasio AJ, Jaggears FR, DePasquale LV, Frassica FJ, Turen CH. Protected early motion versus cast immobilization in postoperative management of ankle fractures. Contemporary Orthopaedics. 1994;29:273-277.
55. Regis D, Montanari M, Magnan B, Spagnol S, Bragantini A. Dynamic orthopaedic brace in the treatment of ankle sprains. Foot Ankle Int. 1995;16:422-426.
56. Grønmark T, Johnsen O, Kogstad O. Rupture of the lateral ligaments of the ankle: a controlled clinical trial. Injury. 1980;11:215-218.
57. Eggert A, Gruber J, Darda L. Treatment of ankle joint injuries. Randomized study of postoperative therapy and early functional treatment. Unfallchirurg. 1986;89:316-320.
58. Konradsen L, Nielsen PT, Albrecht-Beste E. Functional treatment of metacarpal fractures. Acta Orthop Scand. 1990;61:531-534.
59. Broström L. Sprained ankles. V. Treatment and prognosis in recent ligament ruptures. Acta Chir Scand. 1966;132:537-550.
60. Kerkhoffs GMMJ, Struijs PAA, Raaymakers ELFB, Marti RK. Functional treatment after surgical repair of acute Achilles tendon rupture: wrap vs walking cast. Arch Orthop Trauma Surg. 2002;122:102-105.
61. Ferris BD, Thomas NP, Dewar ME, Simpson DA. Brace treatment of Colles’ fracture. Acta Orthop Scand. 1989;60:63-65.
62. Braakman M, Oderwald EE, Haentjens MHHJ. Functional taping of fractures of the 5th metacarpal results in a quicker recovery. Injury. 1998;29:5-9.
63. Tropp H, Norlin R. Ankle performance after ankle fracture: randomised study of early mobilization. Foot Ankle Int. 1995;16:79-83.
64. Kuokkanen HOM, Mulari-Karanen SK, Niskanen RO, Haapala JK, Korkala OL. Treatment of subcapital fractures of the fifth metacarpal bone: a prospective randomised comparison between functional treatment and reposition and splinting. Scand J Plast Recontr Surg Hand Surg. 1999;33:315-317.
65. Murty AN, El Zebdeh MY, Ireland J. Tibial tunnel enlargement following anterior cruciate reconstruction: does post-operative immobilisation make a difference? Knee. 2001;8:39-43.
66. McAuliffe TB, Hilliar KM, Coates CJ, Grange WJ. Early mobilisation of Colles’ fractures: a prospective trial. J Bone Joint Surg Br. 1987;69B:727-729.
67. Brandsson S, Faxén E, Kartus J, Eriksson BI, Karlsson J. Is a knee brace advantageous after anterior cruciate ligament surgery? Scand J Med Sci Sports. 2001;11:110-114.
68. Lind K. Konservativ behandling af laterale ligamentrupturer i fodleddet. Ugeskr Lger. 1984;146:4017-4019.
69. Rafai M, Largab A, Cohen D, Trafeh M. Pure posterior luxation of the elbow in adults: immobilization or early mobilization. A randomized prospective study of 50 cases. Chir Main. 1999;18:272-278.
70. Strickland JW, Glogovac SV. Digital function following flexor tendon repair in Zone II: A comparison of immobilization and controlled passive motion techniques. Journal of Hand Surgery. 1980;5:537-543.
71. Møller-Larsen F, Wethelund JO, Jurik AG, de Carvalho A, Lucht U. Comparison of three different treatments for ruptured lateral ankle ligaments. Acta Orthop Scand. 1988;59:564-566.
72. Caro D, Craft IL, Howells JB, Shaw PC. Diagnosis and treatment of injury of lateral ligament of the ankle joint. Lancet. 1964;2:720-723.
Changes in recommended treatments for mild and moderate asthma
- Every patient with persistent asthma, regardless of disease severity, should use a daily controller medication.
- Consider an inhaled corticosteroid (ICS) first when choosing controller medications for long-term treatment of mild, moderate, and severe persistent asthma in adults and children. Leukotriene modifiers, cromolyn, and nedocromil may be considered as alternative, not preferred, controller medications for patients with persistent asthma.
- Long-acting β2-adrenergic agonists should not be used as monotherapy.
- Long-term use of ICSs within labeled doses is safe for children in terms of growth, bone mineral density, and adrenal function; nonetheless, asthma should be monitored and ICS therapy stepped down to the lowest effective dose.
- Low-to medium-dose ICSs are not associated with the development of cataracts or glaucoma in children, but high cumulative lifetime doses may slightly increase the prevalence of cataracts in adults and elderly patients.
- ICSs are recommended for use in pregnant women with asthma; budesonide is the only ICS rated Pregnancy Category B.
Consider an adult with the following characteristics. To which disease severity would you assign this patient’s asthma?
- Forced expiratory volume in 1 second (FEV1) or peak expiratory flow (PEF) ≥80%
- PEF variability 20%–30%
- Daytime symptoms less than once a day
- Nighttime symptoms more than 1 night a week.
This patient is said to have moderate persistent asthma based on nighttime symptoms. An accurate classification of a patient’s asthma is the foundation for selecting an appropriate treatment strategy.
In 2002 the National Asthma Education and Prevention Program (NAEPP) updated select topics1from its 1997 Guidelines for the Diagnosis and Management of Asthma.2 These evidence-based revisions to the stepwise approach to asthma management were made following a systematic review of the literature (see Search function).
A comprehensive search of Medline and EMBASE databases was performed to identify controlled clinical studies relevant to each topic that were published (in English or foreign languages with English abstracts) from 1980 through August 2000. The search included studies published before 1980 if referenced in the post-1980 literature. Studies that did not include control groups were excluded, except for those reporting adverse effects of ICSs. Studies that met the study selection criteria established for each topic were included in a systematic review of the evidence. An expert panel reviewed the evidence, along with additional literature published since August 2000, and reached a consensus on whether the evidence supported 1997 guideline recommendations or indicated a need for revision. Writing committees were then assigned to developed position statements for each topic. The level of evidence for included studies was rated based on the system of Jadad and colleagues,3 where A = randomized controlled trials, rich body of data; B = randomized controlled trials, limited data; C = nonrandomized trials and observational studies; D = panel consensus judgment.
This article reviews the 2002 NAEPP recommendations for the use of controller medications for asthma, including:
- Relative effectiveness of inhaled corticosteroids (ICSs) versus other controller medications
- Safety of long-term ICS use in children
- Potential benefits of early ICS treatment.
We emphasize mild and moderate persistent asthma because the recommended treatments for these levels of severity have been most affected by the recent guideline changes. We also discuss a recent change by the US Food and Drug Administration (FDA) in its pregnancy category rating for an ICS.
2002 Stepwise approach to asthma management
New criteria for classifying asthma severity
The NAEPP classifies asthma severity according to symptoms and lung function in adults and children older than 5 years, and symptoms in children 5 years and younger.1 Persistent asthma is classified as mild, moderate, or severe according to the feature of greatest severity.
Asthma severity should be assigned according to symptoms before treatment.1 Because it is difficult to predict which infants and young children who wheeze with acute viral upper respiratory infection will go on to develop persistent asthma, new criteria have been detailed to help distinguish these children from those with transient wheeze (Table 1).1,4
TABLE 1
Criteria for children with intermittent wheeze
Infants and young children meeting these criteria should receive controller therapy for asthma:
|
AND presence of risk factors for development of persistent asthma:
|
Choosing pharmacologic treatment according to asthma classification
Quick-relief medications, which include the short-acting β2-agonists (SABAs), are taken as needed to promptly reverse acute airflow obstruction and relieve accompanying symptoms.2
Asthma controller medications (ie, ICSs, cromolyn sodium, long-acting β2-adrenergic-agonists [LABAs], leukotriene modifiers, nedocromil, and theophylline) are used daily to achieve and maintain long-term control of persistent asthma. All patients with persistent asthma, regardless of disease severity, should use a daily controller. Criteria for determining asthma severity and updated recommendations for the use of controller treatment in mild and moderate persistent asthma are presented in the Figure.3,5 Levels of evidence justifying NAEPP treatment recommendations are shown in Table 2.
For use in children. Asthma controller medications approved for use in children younger than 5 years include the fluticasone dry-powder inhalers (Flovent, Rotadisk, and Flovent Diskus), which are approved for children as young as 4 years (Flovent Diskus is not yet commercially available), and nebulized budesonide inhalation suspension (Pulmicort Respules), which is approved for children as young as 12 months.
The LABAs formoterol (Foradil) and salmeterol (Serevent Diskus) are approved for children as young as 5 and 4 years, respectively. Cromolyn sodium nebulizer solution is approved for children as young as 2 years, and theophylline is available for use at any age.
Based on safety and extrapolation of efficacy data in older patients, the oral granule formulation of the leukotriene receptor antagonist (LTRA) montelukast (Singulair) is approved for children as young as 1 year, and the chewable tablets are approved for children 2 to 5 years of age. Zafirlukast (Accolate) is approved for use in children 5 years and older.
New recommendations for mild persistent asthma. Recommendations for the treatment of mild and moderate persistent asthma have changed considerably from the 1997 guidelines. ICSs are now the preferred controller medications, based on greater efficacy. The updated guidelines no longer recommend an initial trial of cromolyn or nedocromil for the treatment of mild persistent asthma; these agents, along with the leukotriene modifiers and slow-release theophylline, are now considered alternatives to low-dose ICSs for adults and children older than 5 years with mild persistent disease (Figure).
According to the NAEPP update, daily low-dose ICS treatment also is preferred for the control of mild persistent asthma in preschool children. As in older children, cromolyn and nedocromil are no longer considered appropriate initial treatments for infants and children 5 years and younger. Cromolyn is considered an alternative controller, whereas nedocromil is no longer recommended for use.
New recommendations for moderate persistent asthma. For adults and children older than 5 years with moderate persistent asthma, revision to the guidelines involved recommendation of a low- to medium-dose ICS plus a LABA as the preferred controller treatment (Figure). Comparative low, medium, and high daily doses for ICSs are shown in Table 3 .1
For preschool children, preferred controller treatments for moderate persistent asthma include low-dose ICSs plus a LABA, or increasing ICSs within the medium-dose range (Figure). Recommendations for the use of LABAs as add-on therapy in this age group are based on extrapolation of data from older patients, since therapy with an ICS/LABA combination has not been adequately studied in children younger than 5 years. Four studies included in the NAEPP evaluation showed clear benefit of medium-dose ICSs in this age group, supporting the use of medium-dose ICSs as a preferred option.6-9 LABAs are not recommended for use without an ICS, and the only ICS/LABA combination product currently available has been FDA approved only for patients aged 12 years and older.
TABLE 2
Levels of evidence for NAEPP assessments*
| Medication | NAEPP assessment | SOR* |
|---|---|---|
| ICS | Preferred treatment for children of all ages with persistent asthma | A (A) |
| SABA | ICSs improve asthma control compared with as-needed SABAs | A (A) |
| Cromolyn/nedocromil | For use as alternative, not preferred, treatment of mild persistent asthma in children of all ages (cromolyn) or children >5 years of age (nedocromil) | A (A) |
| LABA | For use with ICSs as the preferred combination treatment for moderate and severe persistent asthma in children >5 years of age | A (A) |
| For use as a preferred option for combination treatment in children 5 years of age | B (B) | |
| Leukotriene modifier | For use as alternative, not preferred, treatment of mild persistent asthma and as ICS adjunct in moderate persistent asthma | B (B) |
| Theophylline | For use as an alternative ICS add-on in moderate or severe persistent asthma if serum concentrations are monitored | D (D) |
| Not considered an alternative controller for young children with mild persistent asthma due to potential adverse effects in infants with frequent febrile illnesses | ||
| *Highest level of evidence available is reported. Strengths of recommendation are based on the method of Jadad et al.3 Strength of evidence based on the Oxford Center for Evidence-Based Medicine5 is in parentheses. SOR, strength of recommendation; NAEPP, National Asthma Education and Prevention Program; ICS, inhaled corticosteroid; SABA, short-acting β2-adrenergic agonist; LABA, long-acting β2-adrenergic agonist. | ||
TABLE 3
Estimated comparative daily doses for inhaled corticosteroids*
| Drug | Low daily dose | Medium daily dose | High daily dose | |||
|---|---|---|---|---|---|---|
| Adult | Child† | Adult | Child† | Adult | Child† | |
| Beclomethasone CFC 42 or 84 μg/puff | 168–504 μg | 84–336 μg | 504–840 μg | 336–672 μg | >840 μg | >672 μg |
| Beclomethasone HFA 40 or 80 μg/puff | 80–240 μg | 80–160 μg | 240–480 μg | 160–320 μg | >480 μg | >320 μg |
| Budesonide DPI 200 μg/inhalation | 200–600 μg | 200–400 μg | 600–1200 μg | 400–800 μg | >1200 μg | >800 μg |
| Budesonide inhalation suspension for nebulization (child dose) | 0.5mg | 1.0 mg | 2.0 mg | |||
| Fluticasone MDI 44, 110, or 220 μg/puff | 88–264 μg | 88–176 μg | 264–660 μg | 176–440 μg | >660 μg | >440 μg |
| Fluticasone DPI 50, 100, or 250 μg/inhalation | 100–300 μg | 100–200 μg | 300–600 μg | 200–400 μg | >600 μg | >400 μg |
| Triamcinolone acetonide 100 μg/puff | 400–1000 μg | 400–800 μg | 1000–2000 μg | 800–1200 μg | >2000 μg | >1200 μg |
| *The most important determinant of appropriate dosing is the clinician’s judgment of the patient’s response to therapy. This updated comparative dose chart is based on review of recently published clinical trials involving more than 5000 patients and published reviews. Some doses may be outside package labeling, especially in the high-dose range. | ||||||
| †Children 12 years of age. | ||||||
| CFC, chlorofluorocarbon; HFA, hydrofluoroalkane; DPI, dry-powder inhaler; MDI, metered-dose inhaler. | ||||||
FIGURE
Updated National Asthma Education and Prevention Program recommendations for long-term controller treatment in mild and moderate persistent asthma
Topics in the management of asthma in children
Recognizing the need for continual appraisal of the benefits and risks of asthma medications in children, the NAEPP Expert Panel considered new studies comparing the effectiveness of ICS monotherapy with that of as-needed SABAs and other controllers used as monotherapy in children with mild or moderate persistent asthma. In addition, the safety of long-term ICS use in children was evaluated based on vertical growth, bone mineral density, ocular toxicity, and adrenal suppression.
Effectiveness of ICSs compared with other asthma medications
Short-acting β2-adrenergic agonists. Eight studies met the eligibility criteria for evaluating the effectiveness of ICSs versus as-needed SABAs.6,10-16 Six studies (4 involving budesonide) in children 5 years and older showed that ICSs improve lung function and symptoms and reduce the need for emergency intervention compared with as-needed SABAs.1 Among all studies included in the NAEPP update, the Childhood Asthma Management Program (CAMP) Research Group Study,9 a placebo-controlled study of inhaled budesonide and nedocromil, contributed the most evidence. Studies with children 5 years and younger are limited to 2 small studies enrolling a total of 69 children.6,15 Consistent with studies of older children, these studies indicate that ICSs improve asthma control compared with as-needed SABAs.1
Cromolyn and nedocromil. Despite well-established safety profiles, cromolyn and nedocromil are no longer recommended as first-line therapy for children, even those with mild disease. New recommendations reflect the greater effectiveness of inhaled budesonide compared with nedocromil demonstrated in the CAMP study,10 and the lack of apparent benefit of cromolyn as maintenance treatment in childhood asthma reported by Tasche and colleagues in a systematic review of the literature.17
In the CAMP study, children 5 to 12 years of age receiving inhaled budesonide showed greater reductions in symptoms and albuterol use, lower rates of hospitalization and urgent care visits, and less need for additional asthma therapy and oral prednisone compared with placebo over 4 to 6 years of treatment.10 The marginal effectiveness of nedocromil demonstrated in the CAMP study mirrored that of cromolyn reported in the review of 24 randomized placebo-controlled studies by Tasche and colleagues.1,17
For children 5 years and younger, the NAEPP Expert Panel took into account 1 randomized placebo-controlled study conducted with children 2 to 5 years of age; it showed improvements in lung function, symptoms, and bronchial hyperre-activity with inhaled budesonide.9 Support for the new NAEPP recommendations preferring ICSs for preschool children is found in a more recent open-label study18 that showed greater symptom improvement and significantly lower rates of asthma exacerbations, urgent care visits, and oral prednisone use with budesonide inhalation suspension, compared with cromolyn sodium nebulizer solution (Intal Nebulizer Solution) in children 2 to 6 years of age with persistent asthma.
Leukotriene modifiers. The LTRAs zafir-lukast and montelukast are approved for use in children. According to the NAEPP Expert Panel, studies have shown only modest improvements in lung function and other asthma control outcomes with LTRA monotherapy in children as young as 6 and 2 years, respectively.1 Because studies comparing ICSs with LTRAs in children are lacking, findings of greater overall efficacy of ICSs in adults with persistent asthma have been extrapolated for use with children; clear superiority of ICSs versus LTRAs in most outcomes has resulted in the recommendation for ICSs as the preferred treatment for mild persistent asthma in children.
Long-acting β2-adrenergic agonists. There is no role for LABAs as monotherapy in asthma. No studies have compared the effectiveness of ICS versus LABA monotherapy in children younger than 5 years, and studies in older children have shown greater effectiveness of inhaled beclomethasone versus salmeterol.14,19 In the study by Verberne and colleagues, salmeterol monotherapy was associated with deterioration in FEV1.19 In a more recent study that included patients as young as 16 years, a switch from ICS to LABA treatment was associated with a significant increase in treatment failures and exacerbations.20
Theophylline. Only 1 study has compared outcomes with low-dose ICSs versus theophylline in adults and children.21 Although limited, the data support greater effectiveness of ICSs based on symptoms, bronchial hyperresponsiveness, and the need for β2-adrenergic agonists and oral corticosteroids.1
Safety of long-term ICS use in children
Systemic corticosteroids have the potential to suppress growth over the long term.2 Short-term growth studies with ICSs show an average reduction in growth velocity of 1 cm per year during the first year of treatment, but the CAMP study showed that initial reductions in growth velocity with inhaled budesonide were not maintained over a 4- to 6-year treatment period.1,10
Although catch-up growth was not observed in the CAMP study, Agertoft and Pedersen reported no effect of long-term treatment with inhaled budesonide (mean 9.2 years) on final adult height.22 Based on these long-term prospective studies of budesonide, showing only a transient reduction in growth velocity and attainment of expected final adult height, and retrospective studies including inhaled beclomethasone, the Expert Panel concluded that the ICS class is safe regarding growth effects.
According to the NAEPP Expert Panel, clinical study data for children monitored for up to 6 years strongly suggest that ICSs are safe when used at recommended doses (strength of recommendation: A).1 The panel could not rule out a potential cumulative effect of ICS use on some conditions, (eg, osteoporosis, cataracts, glaucoma) in adulthood, as sufficient long-term data are not available.
The panel did conclude that low- to medium-dose ICSs (Table 3) appear to have no serious adverse effects on bone mineral density in children.
Likewise, low- to medium-dose ICS use was not associated with the development of cataracts or glaucoma in children, although the potential for high cumulative lifetime doses of ICSs to slightly increase the prevalence of cataracts in adults and elderly patients was noted.
Strong evidence also indicates that ICS effects on adrenal function are usually clinically insignificant at low to medium doses; however, certain individuals may be at higher risk for hypothalam-ic pituitary adrenal axis effects while using conventional ICS doses.1
Although ICSs are safe when used within labeled dosing, it is still preferable to maintain doses at the lowest effective dose. In general, treatment should be reviewed every 1 to 6 months and doses reduced in a stepwise fashion when possible.1 For children showing a favorable response to treatment, a step down in dose should be considered, but not more frequently than every 3 months. If children show no clear response to treatment within 4 to 6 weeks, consider an alternative treatment or diagnosis.1
Safety of long-term ICS use in pregnant women
Uncontrolled asthma during pregnancy is associated with an increased risk of perinatal complications. 23 Since the consequences of not using asthma controllers during pregnancy can be worse than those with using them, daily controller treatment is recommended for all pregnant women with persistent asthma. 23
The American College of Obstetricians and Gynecologists and the American College of Allergy, Asthma and Immunology previously recommended cromolyn as the treatment of choice for pregnant women with mild persistent asthma. ICSs were recommended for patients whose asthma was inadequately controlled with cromolyn. 24 Beclomethasone and budesonide were the ICSs of choice for pregnant women and those who might become pregnant, with a preference for budesonide when high-dose therapy was indicated.24
These recommendations predate the 2002 NAEPP recommendations for ICSs as preferred therapy in mild persistent asthma and the 2004 NAEPP recommendations for ICSs as the first-choice controller therapy for mild persistent asthma during pregnancy. 25 Among ICSs, one (inhaled budesonide) has an FDA Pregnancy Category B rating based on studies showing no risk in pregnant women. 26,27 All other ICSs are rated Pregnancy Category C.
Based on current evidence, it seems reasonable to consider whether budesonide should now be the preferred therapy for mild persistent asthma during pregnancy.
Effects of early treatment on asthma progression
The potential for early ICS intervention to prevent progression of mild or moderate persistent asthma was evaluated solely with data from children enrolled in the CAMP study. 10 The NAEPP Expert Panel concluded that CAMP study data do not support a progressive decline in lung function in children aged 5 to 12 years with mild or moderate persistent asthma, but do suggest that lung function decline is influenced by age of asthma onset.
According to the panel, CAMP data suggest that most deficits in lung function growth due to childhood asthma occur during the first 3 years of life. Preliminary results of the recent START study (Inhaled Steroid Treatment As Regular Therapy in Early Asthma), 28 conducted with 7165 corticosteroidnaïve patients 5 to 66 years of age with recent onset mild persistent asthma, did show a decline in lung function in patients with mild persistent disease.
Although improvements in prebronchodilator and postbronchodilator FEV1 were significant after 3 years of treatment with inhaled budes-onide, differences from placebo in both outcomes were greatest after the first year. When patients with mild persistent disease inhaled budesonide once daily in addition to normal treatment within 2 years of asthma onset,28 they enjoyed considerable protection from severe and life-threatening asthma exacerbations and overall greater asthma control.
- Budesonide • Pulmicort
- Rhinocort Cromolyn • Intal
- Fluticasone • Flovent
- Formoterol • Foradil
- Montelukast • Singulair
- Nedocromil • Tilade
- Salmeterol • Servent
- Triamcinolone acetonide • Azmacort
- Zafirlukast • Accolate
Corresponding author
Gregory J. Redding, MD, Children’s Hospital and Regional Medical Center, 4800 Sand Point Way, NE, Seattle, WA 98105-0371. E-mail: [email protected].
1. National Asthma Education and Prevention Program. Expert panel report: guidelines for the diagnosis and management of asthma. Update on selected topics–2002. J Allergy Clin Immunol 2002;110(5 suppl):S141-S219.
2. National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health; 1997. Publication 97;4051.-
3. Jadad AR, Moher M, Browman GP, Booker L, Sigouin C, Fuentes M, et al. Systematic reviews and meta-analyses on treatment of asthma: critical evaluation. BMJ 2000;320:537-540.
4. Castro-Rodríguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med 2000;162:1403-1406.
5. Oxford Centre for Evidence-based Medicine Levels of Evidence Available atwww.cebm.net/levels_faq.asp . Accessed January 8, 2004.
6. Connett GJ, Warde C, Wooler E, Lenney W. Use of budes-onide in severe asthmatics aged 1–3 years. Arch Dis Child 1993;69:351-355.
7. de Blic J, Delacourt C, Le Bourgeois M, Mahut B, Ostinelli J, Caswell C, et al. Efficacy of nebulized budesonide in treatment of severe infantile asthma: a double-blind study. J Allergy Clin Immunol 1996;98:14-20.
8. Bisgaard H, Gillies J, Groenewald M, Maden C, . for an International Study Group The effect of inhaled fluticas-one propionate in the treatment of young asthmatic children: a dose comparison study. Am J Respir Crit Care Med 1999;160:126-131.
9. Nielsen KG, Bisgaard H. The effect of inhaled budesonide on symptoms, lung function, and cold air and metha-choline responsiveness in 2- to 5-year–old asthmatic children. Am J Respir Crit Care Med 2000;162:1500-1506.
10. Childhood Asthma Management Program Research Group. Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med 2000;343:1054-1063.
11. Agertoft L, Pedersen S. Effects of long-term treatment with an inhaled corticosteroid on growth and pulmonary function in asthmatic children. Respir Med 1994;88:373-381.
12. Hoekstra MO, Grol MH, Bouman K, Stijnen T, Koëter GH, Kauffman HF, et al. Fluticasone propionate in children with moderate asthma. Am J Respir Crit Care Med 1996;154:1039-1044.
13. Jónasson G, Carlsen K-H, Blomqvist P. Clinical efficacy of low-dose inhaled budesonide once or twice daily in children with mild asthma not previously treated with steroids. Eur Respir J 1998;12:1099-1104.
14. Simons FER and the Canadian Beclomethasone Dipropionate-Salmeterol Xinafoate Study Group. A comparison of beclomethasone, salmeterol, and placebo in children with asthma. N Engl J Med 1997;337:1659-1665.
15. Storr J, Lenney CA, Lenney W. Nebulized beclomethasone dipropionate in preschool asthma. Arch Dis Child 1986;61:270-273.
16. Van Essen-Zandvliet EE, Hughes MD, Waalkens HJ, Duiverman EJ, Pocock SJ, Kerrebijn KF. and the Dutch Chronic Non-Specific Lung Disease Study Group Effects of 22 months of treatment with inhaled corticosteroids and/or beta-2-agonists on lung function, airway responsiveness, and symptoms in children with asthma. Am Rev Respir Dis 1992;146:547-554.
17. Tasche MJA, Uijen JHJM, Bernsen RMD, de Jongste JC, van der Wouden JC. Inhaled disodium cromoglycate (DSCG) as maintenance therapy in children with asthma: a systematic review. Thorax 2000;55:913-920.
18. Leflein JG, Szefler SJ, Murphy KR, Fitzpatrick S, Cruz-Rivera M, Miller CJ, et al. Nebulized budesonide inhalation suspension compared with cromolyn sodium nebulizer solution for asthma in young children: results of a randomized outcomes trial. Pediatrics 2002;109:866-872.
19. Verberne AAPH, Frost C, Duiverman EJ, Grol MH, Kerrebijn KF. and the Dutch Paediatric Asthma Study Group Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. Am J Respir Crit Care Med 1998;158:213-219.
20. Lazarus SC, Boushey HA, Fahy JV, Chinchilli VM, Lemanske RF Jr, Sorkness CA, , et al. for the Asthma Clinical Research Network of the National Heart Lung and Blood Institute. Long-acting 2-agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma: a randomized controlled trial. JAMA 2001;285:2583-2593.
21. Reed CE, Offord KP, Nelson HS, Li JT, Tinkelman DG. and the American Academy of Allergy, Asthma and Immunology Beclomethasone Dipropionate-Theophylline Study Group. Aerosol beclomethasone dipropionate spray compared with theophylline as primary treatment for chronic mild or moderate persistent asthma. J Allergy Clin Immunol 1998;101:14-23.
22. Agertoft L, Pedersen S. Effect of long-term treatment with inhaled budesonide on adult height in children with asthma. N Engl J Med 2000;343:1064-1069.
23. National Asthma Education Program (NAEP). Report of the Working Group on Asthma and Pregnancy: Management of Asthma during Pregnancy. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health, 1993. NIH Publication No. 96-141593.
24. American College of Obstetricians and Gynecologists (ACOG) and the American College of Allergy, Asthmaand Immunology (ACAAI). The use of newer asthma and allergy medications during pregnancy. Ann Allergy Asthma Immunol 2000;84:475-480.
25. National Asthma Education and Prevention Program. NAEPP Expert Panel Report. Managing Asthma During Pregnancy: Recommendations for Pharmacologic Treatment—Update 2004. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health. NIH Publication No. 04-5246. March 2004.
26. Källén B, Rydhstroem H, Äberg A. Congenital malformations after the use of inhaled budesonide in early pregnancy. Obstet Gynecol 1999;93:392-395.
27. Ericson A, Källén B. Use of drugs during pregnancy—unique Swedish registration method that can be improved. Information From the Swedish Medical Products Agency 1999;1:8-11.
28. Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen Y-Z, Ohlsson SV, et al. for the START Investigators Group. Early intervention with budesonide in mild persistent asthma. Lancet 2003;361:1071-1076.
- Every patient with persistent asthma, regardless of disease severity, should use a daily controller medication.
- Consider an inhaled corticosteroid (ICS) first when choosing controller medications for long-term treatment of mild, moderate, and severe persistent asthma in adults and children. Leukotriene modifiers, cromolyn, and nedocromil may be considered as alternative, not preferred, controller medications for patients with persistent asthma.
- Long-acting β2-adrenergic agonists should not be used as monotherapy.
- Long-term use of ICSs within labeled doses is safe for children in terms of growth, bone mineral density, and adrenal function; nonetheless, asthma should be monitored and ICS therapy stepped down to the lowest effective dose.
- Low-to medium-dose ICSs are not associated with the development of cataracts or glaucoma in children, but high cumulative lifetime doses may slightly increase the prevalence of cataracts in adults and elderly patients.
- ICSs are recommended for use in pregnant women with asthma; budesonide is the only ICS rated Pregnancy Category B.
Consider an adult with the following characteristics. To which disease severity would you assign this patient’s asthma?
- Forced expiratory volume in 1 second (FEV1) or peak expiratory flow (PEF) ≥80%
- PEF variability 20%–30%
- Daytime symptoms less than once a day
- Nighttime symptoms more than 1 night a week.
This patient is said to have moderate persistent asthma based on nighttime symptoms. An accurate classification of a patient’s asthma is the foundation for selecting an appropriate treatment strategy.
In 2002 the National Asthma Education and Prevention Program (NAEPP) updated select topics1from its 1997 Guidelines for the Diagnosis and Management of Asthma.2 These evidence-based revisions to the stepwise approach to asthma management were made following a systematic review of the literature (see Search function).
A comprehensive search of Medline and EMBASE databases was performed to identify controlled clinical studies relevant to each topic that were published (in English or foreign languages with English abstracts) from 1980 through August 2000. The search included studies published before 1980 if referenced in the post-1980 literature. Studies that did not include control groups were excluded, except for those reporting adverse effects of ICSs. Studies that met the study selection criteria established for each topic were included in a systematic review of the evidence. An expert panel reviewed the evidence, along with additional literature published since August 2000, and reached a consensus on whether the evidence supported 1997 guideline recommendations or indicated a need for revision. Writing committees were then assigned to developed position statements for each topic. The level of evidence for included studies was rated based on the system of Jadad and colleagues,3 where A = randomized controlled trials, rich body of data; B = randomized controlled trials, limited data; C = nonrandomized trials and observational studies; D = panel consensus judgment.
This article reviews the 2002 NAEPP recommendations for the use of controller medications for asthma, including:
- Relative effectiveness of inhaled corticosteroids (ICSs) versus other controller medications
- Safety of long-term ICS use in children
- Potential benefits of early ICS treatment.
We emphasize mild and moderate persistent asthma because the recommended treatments for these levels of severity have been most affected by the recent guideline changes. We also discuss a recent change by the US Food and Drug Administration (FDA) in its pregnancy category rating for an ICS.
2002 Stepwise approach to asthma management
New criteria for classifying asthma severity
The NAEPP classifies asthma severity according to symptoms and lung function in adults and children older than 5 years, and symptoms in children 5 years and younger.1 Persistent asthma is classified as mild, moderate, or severe according to the feature of greatest severity.
Asthma severity should be assigned according to symptoms before treatment.1 Because it is difficult to predict which infants and young children who wheeze with acute viral upper respiratory infection will go on to develop persistent asthma, new criteria have been detailed to help distinguish these children from those with transient wheeze (Table 1).1,4
TABLE 1
Criteria for children with intermittent wheeze
Infants and young children meeting these criteria should receive controller therapy for asthma:
|
AND presence of risk factors for development of persistent asthma:
|
Choosing pharmacologic treatment according to asthma classification
Quick-relief medications, which include the short-acting β2-agonists (SABAs), are taken as needed to promptly reverse acute airflow obstruction and relieve accompanying symptoms.2
Asthma controller medications (ie, ICSs, cromolyn sodium, long-acting β2-adrenergic-agonists [LABAs], leukotriene modifiers, nedocromil, and theophylline) are used daily to achieve and maintain long-term control of persistent asthma. All patients with persistent asthma, regardless of disease severity, should use a daily controller. Criteria for determining asthma severity and updated recommendations for the use of controller treatment in mild and moderate persistent asthma are presented in the Figure.3,5 Levels of evidence justifying NAEPP treatment recommendations are shown in Table 2.
For use in children. Asthma controller medications approved for use in children younger than 5 years include the fluticasone dry-powder inhalers (Flovent, Rotadisk, and Flovent Diskus), which are approved for children as young as 4 years (Flovent Diskus is not yet commercially available), and nebulized budesonide inhalation suspension (Pulmicort Respules), which is approved for children as young as 12 months.
The LABAs formoterol (Foradil) and salmeterol (Serevent Diskus) are approved for children as young as 5 and 4 years, respectively. Cromolyn sodium nebulizer solution is approved for children as young as 2 years, and theophylline is available for use at any age.
Based on safety and extrapolation of efficacy data in older patients, the oral granule formulation of the leukotriene receptor antagonist (LTRA) montelukast (Singulair) is approved for children as young as 1 year, and the chewable tablets are approved for children 2 to 5 years of age. Zafirlukast (Accolate) is approved for use in children 5 years and older.
New recommendations for mild persistent asthma. Recommendations for the treatment of mild and moderate persistent asthma have changed considerably from the 1997 guidelines. ICSs are now the preferred controller medications, based on greater efficacy. The updated guidelines no longer recommend an initial trial of cromolyn or nedocromil for the treatment of mild persistent asthma; these agents, along with the leukotriene modifiers and slow-release theophylline, are now considered alternatives to low-dose ICSs for adults and children older than 5 years with mild persistent disease (Figure).
According to the NAEPP update, daily low-dose ICS treatment also is preferred for the control of mild persistent asthma in preschool children. As in older children, cromolyn and nedocromil are no longer considered appropriate initial treatments for infants and children 5 years and younger. Cromolyn is considered an alternative controller, whereas nedocromil is no longer recommended for use.
New recommendations for moderate persistent asthma. For adults and children older than 5 years with moderate persistent asthma, revision to the guidelines involved recommendation of a low- to medium-dose ICS plus a LABA as the preferred controller treatment (Figure). Comparative low, medium, and high daily doses for ICSs are shown in Table 3 .1
For preschool children, preferred controller treatments for moderate persistent asthma include low-dose ICSs plus a LABA, or increasing ICSs within the medium-dose range (Figure). Recommendations for the use of LABAs as add-on therapy in this age group are based on extrapolation of data from older patients, since therapy with an ICS/LABA combination has not been adequately studied in children younger than 5 years. Four studies included in the NAEPP evaluation showed clear benefit of medium-dose ICSs in this age group, supporting the use of medium-dose ICSs as a preferred option.6-9 LABAs are not recommended for use without an ICS, and the only ICS/LABA combination product currently available has been FDA approved only for patients aged 12 years and older.
TABLE 2
Levels of evidence for NAEPP assessments*
| Medication | NAEPP assessment | SOR* |
|---|---|---|
| ICS | Preferred treatment for children of all ages with persistent asthma | A (A) |
| SABA | ICSs improve asthma control compared with as-needed SABAs | A (A) |
| Cromolyn/nedocromil | For use as alternative, not preferred, treatment of mild persistent asthma in children of all ages (cromolyn) or children >5 years of age (nedocromil) | A (A) |
| LABA | For use with ICSs as the preferred combination treatment for moderate and severe persistent asthma in children >5 years of age | A (A) |
| For use as a preferred option for combination treatment in children 5 years of age | B (B) | |
| Leukotriene modifier | For use as alternative, not preferred, treatment of mild persistent asthma and as ICS adjunct in moderate persistent asthma | B (B) |
| Theophylline | For use as an alternative ICS add-on in moderate or severe persistent asthma if serum concentrations are monitored | D (D) |
| Not considered an alternative controller for young children with mild persistent asthma due to potential adverse effects in infants with frequent febrile illnesses | ||
| *Highest level of evidence available is reported. Strengths of recommendation are based on the method of Jadad et al.3 Strength of evidence based on the Oxford Center for Evidence-Based Medicine5 is in parentheses. SOR, strength of recommendation; NAEPP, National Asthma Education and Prevention Program; ICS, inhaled corticosteroid; SABA, short-acting β2-adrenergic agonist; LABA, long-acting β2-adrenergic agonist. | ||
TABLE 3
Estimated comparative daily doses for inhaled corticosteroids*
| Drug | Low daily dose | Medium daily dose | High daily dose | |||
|---|---|---|---|---|---|---|
| Adult | Child† | Adult | Child† | Adult | Child† | |
| Beclomethasone CFC 42 or 84 μg/puff | 168–504 μg | 84–336 μg | 504–840 μg | 336–672 μg | >840 μg | >672 μg |
| Beclomethasone HFA 40 or 80 μg/puff | 80–240 μg | 80–160 μg | 240–480 μg | 160–320 μg | >480 μg | >320 μg |
| Budesonide DPI 200 μg/inhalation | 200–600 μg | 200–400 μg | 600–1200 μg | 400–800 μg | >1200 μg | >800 μg |
| Budesonide inhalation suspension for nebulization (child dose) | 0.5mg | 1.0 mg | 2.0 mg | |||
| Fluticasone MDI 44, 110, or 220 μg/puff | 88–264 μg | 88–176 μg | 264–660 μg | 176–440 μg | >660 μg | >440 μg |
| Fluticasone DPI 50, 100, or 250 μg/inhalation | 100–300 μg | 100–200 μg | 300–600 μg | 200–400 μg | >600 μg | >400 μg |
| Triamcinolone acetonide 100 μg/puff | 400–1000 μg | 400–800 μg | 1000–2000 μg | 800–1200 μg | >2000 μg | >1200 μg |
| *The most important determinant of appropriate dosing is the clinician’s judgment of the patient’s response to therapy. This updated comparative dose chart is based on review of recently published clinical trials involving more than 5000 patients and published reviews. Some doses may be outside package labeling, especially in the high-dose range. | ||||||
| †Children 12 years of age. | ||||||
| CFC, chlorofluorocarbon; HFA, hydrofluoroalkane; DPI, dry-powder inhaler; MDI, metered-dose inhaler. | ||||||
FIGURE
Updated National Asthma Education and Prevention Program recommendations for long-term controller treatment in mild and moderate persistent asthma
Topics in the management of asthma in children
Recognizing the need for continual appraisal of the benefits and risks of asthma medications in children, the NAEPP Expert Panel considered new studies comparing the effectiveness of ICS monotherapy with that of as-needed SABAs and other controllers used as monotherapy in children with mild or moderate persistent asthma. In addition, the safety of long-term ICS use in children was evaluated based on vertical growth, bone mineral density, ocular toxicity, and adrenal suppression.
Effectiveness of ICSs compared with other asthma medications
Short-acting β2-adrenergic agonists. Eight studies met the eligibility criteria for evaluating the effectiveness of ICSs versus as-needed SABAs.6,10-16 Six studies (4 involving budesonide) in children 5 years and older showed that ICSs improve lung function and symptoms and reduce the need for emergency intervention compared with as-needed SABAs.1 Among all studies included in the NAEPP update, the Childhood Asthma Management Program (CAMP) Research Group Study,9 a placebo-controlled study of inhaled budesonide and nedocromil, contributed the most evidence. Studies with children 5 years and younger are limited to 2 small studies enrolling a total of 69 children.6,15 Consistent with studies of older children, these studies indicate that ICSs improve asthma control compared with as-needed SABAs.1
Cromolyn and nedocromil. Despite well-established safety profiles, cromolyn and nedocromil are no longer recommended as first-line therapy for children, even those with mild disease. New recommendations reflect the greater effectiveness of inhaled budesonide compared with nedocromil demonstrated in the CAMP study,10 and the lack of apparent benefit of cromolyn as maintenance treatment in childhood asthma reported by Tasche and colleagues in a systematic review of the literature.17
In the CAMP study, children 5 to 12 years of age receiving inhaled budesonide showed greater reductions in symptoms and albuterol use, lower rates of hospitalization and urgent care visits, and less need for additional asthma therapy and oral prednisone compared with placebo over 4 to 6 years of treatment.10 The marginal effectiveness of nedocromil demonstrated in the CAMP study mirrored that of cromolyn reported in the review of 24 randomized placebo-controlled studies by Tasche and colleagues.1,17
For children 5 years and younger, the NAEPP Expert Panel took into account 1 randomized placebo-controlled study conducted with children 2 to 5 years of age; it showed improvements in lung function, symptoms, and bronchial hyperre-activity with inhaled budesonide.9 Support for the new NAEPP recommendations preferring ICSs for preschool children is found in a more recent open-label study18 that showed greater symptom improvement and significantly lower rates of asthma exacerbations, urgent care visits, and oral prednisone use with budesonide inhalation suspension, compared with cromolyn sodium nebulizer solution (Intal Nebulizer Solution) in children 2 to 6 years of age with persistent asthma.
Leukotriene modifiers. The LTRAs zafir-lukast and montelukast are approved for use in children. According to the NAEPP Expert Panel, studies have shown only modest improvements in lung function and other asthma control outcomes with LTRA monotherapy in children as young as 6 and 2 years, respectively.1 Because studies comparing ICSs with LTRAs in children are lacking, findings of greater overall efficacy of ICSs in adults with persistent asthma have been extrapolated for use with children; clear superiority of ICSs versus LTRAs in most outcomes has resulted in the recommendation for ICSs as the preferred treatment for mild persistent asthma in children.
Long-acting β2-adrenergic agonists. There is no role for LABAs as monotherapy in asthma. No studies have compared the effectiveness of ICS versus LABA monotherapy in children younger than 5 years, and studies in older children have shown greater effectiveness of inhaled beclomethasone versus salmeterol.14,19 In the study by Verberne and colleagues, salmeterol monotherapy was associated with deterioration in FEV1.19 In a more recent study that included patients as young as 16 years, a switch from ICS to LABA treatment was associated with a significant increase in treatment failures and exacerbations.20
Theophylline. Only 1 study has compared outcomes with low-dose ICSs versus theophylline in adults and children.21 Although limited, the data support greater effectiveness of ICSs based on symptoms, bronchial hyperresponsiveness, and the need for β2-adrenergic agonists and oral corticosteroids.1
Safety of long-term ICS use in children
Systemic corticosteroids have the potential to suppress growth over the long term.2 Short-term growth studies with ICSs show an average reduction in growth velocity of 1 cm per year during the first year of treatment, but the CAMP study showed that initial reductions in growth velocity with inhaled budesonide were not maintained over a 4- to 6-year treatment period.1,10
Although catch-up growth was not observed in the CAMP study, Agertoft and Pedersen reported no effect of long-term treatment with inhaled budesonide (mean 9.2 years) on final adult height.22 Based on these long-term prospective studies of budesonide, showing only a transient reduction in growth velocity and attainment of expected final adult height, and retrospective studies including inhaled beclomethasone, the Expert Panel concluded that the ICS class is safe regarding growth effects.
According to the NAEPP Expert Panel, clinical study data for children monitored for up to 6 years strongly suggest that ICSs are safe when used at recommended doses (strength of recommendation: A).1 The panel could not rule out a potential cumulative effect of ICS use on some conditions, (eg, osteoporosis, cataracts, glaucoma) in adulthood, as sufficient long-term data are not available.
The panel did conclude that low- to medium-dose ICSs (Table 3) appear to have no serious adverse effects on bone mineral density in children.
Likewise, low- to medium-dose ICS use was not associated with the development of cataracts or glaucoma in children, although the potential for high cumulative lifetime doses of ICSs to slightly increase the prevalence of cataracts in adults and elderly patients was noted.
Strong evidence also indicates that ICS effects on adrenal function are usually clinically insignificant at low to medium doses; however, certain individuals may be at higher risk for hypothalam-ic pituitary adrenal axis effects while using conventional ICS doses.1
Although ICSs are safe when used within labeled dosing, it is still preferable to maintain doses at the lowest effective dose. In general, treatment should be reviewed every 1 to 6 months and doses reduced in a stepwise fashion when possible.1 For children showing a favorable response to treatment, a step down in dose should be considered, but not more frequently than every 3 months. If children show no clear response to treatment within 4 to 6 weeks, consider an alternative treatment or diagnosis.1
Safety of long-term ICS use in pregnant women
Uncontrolled asthma during pregnancy is associated with an increased risk of perinatal complications. 23 Since the consequences of not using asthma controllers during pregnancy can be worse than those with using them, daily controller treatment is recommended for all pregnant women with persistent asthma. 23
The American College of Obstetricians and Gynecologists and the American College of Allergy, Asthma and Immunology previously recommended cromolyn as the treatment of choice for pregnant women with mild persistent asthma. ICSs were recommended for patients whose asthma was inadequately controlled with cromolyn. 24 Beclomethasone and budesonide were the ICSs of choice for pregnant women and those who might become pregnant, with a preference for budesonide when high-dose therapy was indicated.24
These recommendations predate the 2002 NAEPP recommendations for ICSs as preferred therapy in mild persistent asthma and the 2004 NAEPP recommendations for ICSs as the first-choice controller therapy for mild persistent asthma during pregnancy. 25 Among ICSs, one (inhaled budesonide) has an FDA Pregnancy Category B rating based on studies showing no risk in pregnant women. 26,27 All other ICSs are rated Pregnancy Category C.
Based on current evidence, it seems reasonable to consider whether budesonide should now be the preferred therapy for mild persistent asthma during pregnancy.
Effects of early treatment on asthma progression
The potential for early ICS intervention to prevent progression of mild or moderate persistent asthma was evaluated solely with data from children enrolled in the CAMP study. 10 The NAEPP Expert Panel concluded that CAMP study data do not support a progressive decline in lung function in children aged 5 to 12 years with mild or moderate persistent asthma, but do suggest that lung function decline is influenced by age of asthma onset.
According to the panel, CAMP data suggest that most deficits in lung function growth due to childhood asthma occur during the first 3 years of life. Preliminary results of the recent START study (Inhaled Steroid Treatment As Regular Therapy in Early Asthma), 28 conducted with 7165 corticosteroidnaïve patients 5 to 66 years of age with recent onset mild persistent asthma, did show a decline in lung function in patients with mild persistent disease.
Although improvements in prebronchodilator and postbronchodilator FEV1 were significant after 3 years of treatment with inhaled budes-onide, differences from placebo in both outcomes were greatest after the first year. When patients with mild persistent disease inhaled budesonide once daily in addition to normal treatment within 2 years of asthma onset,28 they enjoyed considerable protection from severe and life-threatening asthma exacerbations and overall greater asthma control.
- Budesonide • Pulmicort
- Rhinocort Cromolyn • Intal
- Fluticasone • Flovent
- Formoterol • Foradil
- Montelukast • Singulair
- Nedocromil • Tilade
- Salmeterol • Servent
- Triamcinolone acetonide • Azmacort
- Zafirlukast • Accolate
Corresponding author
Gregory J. Redding, MD, Children’s Hospital and Regional Medical Center, 4800 Sand Point Way, NE, Seattle, WA 98105-0371. E-mail: [email protected].
- Every patient with persistent asthma, regardless of disease severity, should use a daily controller medication.
- Consider an inhaled corticosteroid (ICS) first when choosing controller medications for long-term treatment of mild, moderate, and severe persistent asthma in adults and children. Leukotriene modifiers, cromolyn, and nedocromil may be considered as alternative, not preferred, controller medications for patients with persistent asthma.
- Long-acting β2-adrenergic agonists should not be used as monotherapy.
- Long-term use of ICSs within labeled doses is safe for children in terms of growth, bone mineral density, and adrenal function; nonetheless, asthma should be monitored and ICS therapy stepped down to the lowest effective dose.
- Low-to medium-dose ICSs are not associated with the development of cataracts or glaucoma in children, but high cumulative lifetime doses may slightly increase the prevalence of cataracts in adults and elderly patients.
- ICSs are recommended for use in pregnant women with asthma; budesonide is the only ICS rated Pregnancy Category B.
Consider an adult with the following characteristics. To which disease severity would you assign this patient’s asthma?
- Forced expiratory volume in 1 second (FEV1) or peak expiratory flow (PEF) ≥80%
- PEF variability 20%–30%
- Daytime symptoms less than once a day
- Nighttime symptoms more than 1 night a week.
This patient is said to have moderate persistent asthma based on nighttime symptoms. An accurate classification of a patient’s asthma is the foundation for selecting an appropriate treatment strategy.
In 2002 the National Asthma Education and Prevention Program (NAEPP) updated select topics1from its 1997 Guidelines for the Diagnosis and Management of Asthma.2 These evidence-based revisions to the stepwise approach to asthma management were made following a systematic review of the literature (see Search function).
A comprehensive search of Medline and EMBASE databases was performed to identify controlled clinical studies relevant to each topic that were published (in English or foreign languages with English abstracts) from 1980 through August 2000. The search included studies published before 1980 if referenced in the post-1980 literature. Studies that did not include control groups were excluded, except for those reporting adverse effects of ICSs. Studies that met the study selection criteria established for each topic were included in a systematic review of the evidence. An expert panel reviewed the evidence, along with additional literature published since August 2000, and reached a consensus on whether the evidence supported 1997 guideline recommendations or indicated a need for revision. Writing committees were then assigned to developed position statements for each topic. The level of evidence for included studies was rated based on the system of Jadad and colleagues,3 where A = randomized controlled trials, rich body of data; B = randomized controlled trials, limited data; C = nonrandomized trials and observational studies; D = panel consensus judgment.
This article reviews the 2002 NAEPP recommendations for the use of controller medications for asthma, including:
- Relative effectiveness of inhaled corticosteroids (ICSs) versus other controller medications
- Safety of long-term ICS use in children
- Potential benefits of early ICS treatment.
We emphasize mild and moderate persistent asthma because the recommended treatments for these levels of severity have been most affected by the recent guideline changes. We also discuss a recent change by the US Food and Drug Administration (FDA) in its pregnancy category rating for an ICS.
2002 Stepwise approach to asthma management
New criteria for classifying asthma severity
The NAEPP classifies asthma severity according to symptoms and lung function in adults and children older than 5 years, and symptoms in children 5 years and younger.1 Persistent asthma is classified as mild, moderate, or severe according to the feature of greatest severity.
Asthma severity should be assigned according to symptoms before treatment.1 Because it is difficult to predict which infants and young children who wheeze with acute viral upper respiratory infection will go on to develop persistent asthma, new criteria have been detailed to help distinguish these children from those with transient wheeze (Table 1).1,4
TABLE 1
Criteria for children with intermittent wheeze
Infants and young children meeting these criteria should receive controller therapy for asthma:
|
AND presence of risk factors for development of persistent asthma:
|
Choosing pharmacologic treatment according to asthma classification
Quick-relief medications, which include the short-acting β2-agonists (SABAs), are taken as needed to promptly reverse acute airflow obstruction and relieve accompanying symptoms.2
Asthma controller medications (ie, ICSs, cromolyn sodium, long-acting β2-adrenergic-agonists [LABAs], leukotriene modifiers, nedocromil, and theophylline) are used daily to achieve and maintain long-term control of persistent asthma. All patients with persistent asthma, regardless of disease severity, should use a daily controller. Criteria for determining asthma severity and updated recommendations for the use of controller treatment in mild and moderate persistent asthma are presented in the Figure.3,5 Levels of evidence justifying NAEPP treatment recommendations are shown in Table 2.
For use in children. Asthma controller medications approved for use in children younger than 5 years include the fluticasone dry-powder inhalers (Flovent, Rotadisk, and Flovent Diskus), which are approved for children as young as 4 years (Flovent Diskus is not yet commercially available), and nebulized budesonide inhalation suspension (Pulmicort Respules), which is approved for children as young as 12 months.
The LABAs formoterol (Foradil) and salmeterol (Serevent Diskus) are approved for children as young as 5 and 4 years, respectively. Cromolyn sodium nebulizer solution is approved for children as young as 2 years, and theophylline is available for use at any age.
Based on safety and extrapolation of efficacy data in older patients, the oral granule formulation of the leukotriene receptor antagonist (LTRA) montelukast (Singulair) is approved for children as young as 1 year, and the chewable tablets are approved for children 2 to 5 years of age. Zafirlukast (Accolate) is approved for use in children 5 years and older.
New recommendations for mild persistent asthma. Recommendations for the treatment of mild and moderate persistent asthma have changed considerably from the 1997 guidelines. ICSs are now the preferred controller medications, based on greater efficacy. The updated guidelines no longer recommend an initial trial of cromolyn or nedocromil for the treatment of mild persistent asthma; these agents, along with the leukotriene modifiers and slow-release theophylline, are now considered alternatives to low-dose ICSs for adults and children older than 5 years with mild persistent disease (Figure).
According to the NAEPP update, daily low-dose ICS treatment also is preferred for the control of mild persistent asthma in preschool children. As in older children, cromolyn and nedocromil are no longer considered appropriate initial treatments for infants and children 5 years and younger. Cromolyn is considered an alternative controller, whereas nedocromil is no longer recommended for use.
New recommendations for moderate persistent asthma. For adults and children older than 5 years with moderate persistent asthma, revision to the guidelines involved recommendation of a low- to medium-dose ICS plus a LABA as the preferred controller treatment (Figure). Comparative low, medium, and high daily doses for ICSs are shown in Table 3 .1
For preschool children, preferred controller treatments for moderate persistent asthma include low-dose ICSs plus a LABA, or increasing ICSs within the medium-dose range (Figure). Recommendations for the use of LABAs as add-on therapy in this age group are based on extrapolation of data from older patients, since therapy with an ICS/LABA combination has not been adequately studied in children younger than 5 years. Four studies included in the NAEPP evaluation showed clear benefit of medium-dose ICSs in this age group, supporting the use of medium-dose ICSs as a preferred option.6-9 LABAs are not recommended for use without an ICS, and the only ICS/LABA combination product currently available has been FDA approved only for patients aged 12 years and older.
TABLE 2
Levels of evidence for NAEPP assessments*
| Medication | NAEPP assessment | SOR* |
|---|---|---|
| ICS | Preferred treatment for children of all ages with persistent asthma | A (A) |
| SABA | ICSs improve asthma control compared with as-needed SABAs | A (A) |
| Cromolyn/nedocromil | For use as alternative, not preferred, treatment of mild persistent asthma in children of all ages (cromolyn) or children >5 years of age (nedocromil) | A (A) |
| LABA | For use with ICSs as the preferred combination treatment for moderate and severe persistent asthma in children >5 years of age | A (A) |
| For use as a preferred option for combination treatment in children 5 years of age | B (B) | |
| Leukotriene modifier | For use as alternative, not preferred, treatment of mild persistent asthma and as ICS adjunct in moderate persistent asthma | B (B) |
| Theophylline | For use as an alternative ICS add-on in moderate or severe persistent asthma if serum concentrations are monitored | D (D) |
| Not considered an alternative controller for young children with mild persistent asthma due to potential adverse effects in infants with frequent febrile illnesses | ||
| *Highest level of evidence available is reported. Strengths of recommendation are based on the method of Jadad et al.3 Strength of evidence based on the Oxford Center for Evidence-Based Medicine5 is in parentheses. SOR, strength of recommendation; NAEPP, National Asthma Education and Prevention Program; ICS, inhaled corticosteroid; SABA, short-acting β2-adrenergic agonist; LABA, long-acting β2-adrenergic agonist. | ||
TABLE 3
Estimated comparative daily doses for inhaled corticosteroids*
| Drug | Low daily dose | Medium daily dose | High daily dose | |||
|---|---|---|---|---|---|---|
| Adult | Child† | Adult | Child† | Adult | Child† | |
| Beclomethasone CFC 42 or 84 μg/puff | 168–504 μg | 84–336 μg | 504–840 μg | 336–672 μg | >840 μg | >672 μg |
| Beclomethasone HFA 40 or 80 μg/puff | 80–240 μg | 80–160 μg | 240–480 μg | 160–320 μg | >480 μg | >320 μg |
| Budesonide DPI 200 μg/inhalation | 200–600 μg | 200–400 μg | 600–1200 μg | 400–800 μg | >1200 μg | >800 μg |
| Budesonide inhalation suspension for nebulization (child dose) | 0.5mg | 1.0 mg | 2.0 mg | |||
| Fluticasone MDI 44, 110, or 220 μg/puff | 88–264 μg | 88–176 μg | 264–660 μg | 176–440 μg | >660 μg | >440 μg |
| Fluticasone DPI 50, 100, or 250 μg/inhalation | 100–300 μg | 100–200 μg | 300–600 μg | 200–400 μg | >600 μg | >400 μg |
| Triamcinolone acetonide 100 μg/puff | 400–1000 μg | 400–800 μg | 1000–2000 μg | 800–1200 μg | >2000 μg | >1200 μg |
| *The most important determinant of appropriate dosing is the clinician’s judgment of the patient’s response to therapy. This updated comparative dose chart is based on review of recently published clinical trials involving more than 5000 patients and published reviews. Some doses may be outside package labeling, especially in the high-dose range. | ||||||
| †Children 12 years of age. | ||||||
| CFC, chlorofluorocarbon; HFA, hydrofluoroalkane; DPI, dry-powder inhaler; MDI, metered-dose inhaler. | ||||||
FIGURE
Updated National Asthma Education and Prevention Program recommendations for long-term controller treatment in mild and moderate persistent asthma
Topics in the management of asthma in children
Recognizing the need for continual appraisal of the benefits and risks of asthma medications in children, the NAEPP Expert Panel considered new studies comparing the effectiveness of ICS monotherapy with that of as-needed SABAs and other controllers used as monotherapy in children with mild or moderate persistent asthma. In addition, the safety of long-term ICS use in children was evaluated based on vertical growth, bone mineral density, ocular toxicity, and adrenal suppression.
Effectiveness of ICSs compared with other asthma medications
Short-acting β2-adrenergic agonists. Eight studies met the eligibility criteria for evaluating the effectiveness of ICSs versus as-needed SABAs.6,10-16 Six studies (4 involving budesonide) in children 5 years and older showed that ICSs improve lung function and symptoms and reduce the need for emergency intervention compared with as-needed SABAs.1 Among all studies included in the NAEPP update, the Childhood Asthma Management Program (CAMP) Research Group Study,9 a placebo-controlled study of inhaled budesonide and nedocromil, contributed the most evidence. Studies with children 5 years and younger are limited to 2 small studies enrolling a total of 69 children.6,15 Consistent with studies of older children, these studies indicate that ICSs improve asthma control compared with as-needed SABAs.1
Cromolyn and nedocromil. Despite well-established safety profiles, cromolyn and nedocromil are no longer recommended as first-line therapy for children, even those with mild disease. New recommendations reflect the greater effectiveness of inhaled budesonide compared with nedocromil demonstrated in the CAMP study,10 and the lack of apparent benefit of cromolyn as maintenance treatment in childhood asthma reported by Tasche and colleagues in a systematic review of the literature.17
In the CAMP study, children 5 to 12 years of age receiving inhaled budesonide showed greater reductions in symptoms and albuterol use, lower rates of hospitalization and urgent care visits, and less need for additional asthma therapy and oral prednisone compared with placebo over 4 to 6 years of treatment.10 The marginal effectiveness of nedocromil demonstrated in the CAMP study mirrored that of cromolyn reported in the review of 24 randomized placebo-controlled studies by Tasche and colleagues.1,17
For children 5 years and younger, the NAEPP Expert Panel took into account 1 randomized placebo-controlled study conducted with children 2 to 5 years of age; it showed improvements in lung function, symptoms, and bronchial hyperre-activity with inhaled budesonide.9 Support for the new NAEPP recommendations preferring ICSs for preschool children is found in a more recent open-label study18 that showed greater symptom improvement and significantly lower rates of asthma exacerbations, urgent care visits, and oral prednisone use with budesonide inhalation suspension, compared with cromolyn sodium nebulizer solution (Intal Nebulizer Solution) in children 2 to 6 years of age with persistent asthma.
Leukotriene modifiers. The LTRAs zafir-lukast and montelukast are approved for use in children. According to the NAEPP Expert Panel, studies have shown only modest improvements in lung function and other asthma control outcomes with LTRA monotherapy in children as young as 6 and 2 years, respectively.1 Because studies comparing ICSs with LTRAs in children are lacking, findings of greater overall efficacy of ICSs in adults with persistent asthma have been extrapolated for use with children; clear superiority of ICSs versus LTRAs in most outcomes has resulted in the recommendation for ICSs as the preferred treatment for mild persistent asthma in children.
Long-acting β2-adrenergic agonists. There is no role for LABAs as monotherapy in asthma. No studies have compared the effectiveness of ICS versus LABA monotherapy in children younger than 5 years, and studies in older children have shown greater effectiveness of inhaled beclomethasone versus salmeterol.14,19 In the study by Verberne and colleagues, salmeterol monotherapy was associated with deterioration in FEV1.19 In a more recent study that included patients as young as 16 years, a switch from ICS to LABA treatment was associated with a significant increase in treatment failures and exacerbations.20
Theophylline. Only 1 study has compared outcomes with low-dose ICSs versus theophylline in adults and children.21 Although limited, the data support greater effectiveness of ICSs based on symptoms, bronchial hyperresponsiveness, and the need for β2-adrenergic agonists and oral corticosteroids.1
Safety of long-term ICS use in children
Systemic corticosteroids have the potential to suppress growth over the long term.2 Short-term growth studies with ICSs show an average reduction in growth velocity of 1 cm per year during the first year of treatment, but the CAMP study showed that initial reductions in growth velocity with inhaled budesonide were not maintained over a 4- to 6-year treatment period.1,10
Although catch-up growth was not observed in the CAMP study, Agertoft and Pedersen reported no effect of long-term treatment with inhaled budesonide (mean 9.2 years) on final adult height.22 Based on these long-term prospective studies of budesonide, showing only a transient reduction in growth velocity and attainment of expected final adult height, and retrospective studies including inhaled beclomethasone, the Expert Panel concluded that the ICS class is safe regarding growth effects.
According to the NAEPP Expert Panel, clinical study data for children monitored for up to 6 years strongly suggest that ICSs are safe when used at recommended doses (strength of recommendation: A).1 The panel could not rule out a potential cumulative effect of ICS use on some conditions, (eg, osteoporosis, cataracts, glaucoma) in adulthood, as sufficient long-term data are not available.
The panel did conclude that low- to medium-dose ICSs (Table 3) appear to have no serious adverse effects on bone mineral density in children.
Likewise, low- to medium-dose ICS use was not associated with the development of cataracts or glaucoma in children, although the potential for high cumulative lifetime doses of ICSs to slightly increase the prevalence of cataracts in adults and elderly patients was noted.
Strong evidence also indicates that ICS effects on adrenal function are usually clinically insignificant at low to medium doses; however, certain individuals may be at higher risk for hypothalam-ic pituitary adrenal axis effects while using conventional ICS doses.1
Although ICSs are safe when used within labeled dosing, it is still preferable to maintain doses at the lowest effective dose. In general, treatment should be reviewed every 1 to 6 months and doses reduced in a stepwise fashion when possible.1 For children showing a favorable response to treatment, a step down in dose should be considered, but not more frequently than every 3 months. If children show no clear response to treatment within 4 to 6 weeks, consider an alternative treatment or diagnosis.1
Safety of long-term ICS use in pregnant women
Uncontrolled asthma during pregnancy is associated with an increased risk of perinatal complications. 23 Since the consequences of not using asthma controllers during pregnancy can be worse than those with using them, daily controller treatment is recommended for all pregnant women with persistent asthma. 23
The American College of Obstetricians and Gynecologists and the American College of Allergy, Asthma and Immunology previously recommended cromolyn as the treatment of choice for pregnant women with mild persistent asthma. ICSs were recommended for patients whose asthma was inadequately controlled with cromolyn. 24 Beclomethasone and budesonide were the ICSs of choice for pregnant women and those who might become pregnant, with a preference for budesonide when high-dose therapy was indicated.24
These recommendations predate the 2002 NAEPP recommendations for ICSs as preferred therapy in mild persistent asthma and the 2004 NAEPP recommendations for ICSs as the first-choice controller therapy for mild persistent asthma during pregnancy. 25 Among ICSs, one (inhaled budesonide) has an FDA Pregnancy Category B rating based on studies showing no risk in pregnant women. 26,27 All other ICSs are rated Pregnancy Category C.
Based on current evidence, it seems reasonable to consider whether budesonide should now be the preferred therapy for mild persistent asthma during pregnancy.
Effects of early treatment on asthma progression
The potential for early ICS intervention to prevent progression of mild or moderate persistent asthma was evaluated solely with data from children enrolled in the CAMP study. 10 The NAEPP Expert Panel concluded that CAMP study data do not support a progressive decline in lung function in children aged 5 to 12 years with mild or moderate persistent asthma, but do suggest that lung function decline is influenced by age of asthma onset.
According to the panel, CAMP data suggest that most deficits in lung function growth due to childhood asthma occur during the first 3 years of life. Preliminary results of the recent START study (Inhaled Steroid Treatment As Regular Therapy in Early Asthma), 28 conducted with 7165 corticosteroidnaïve patients 5 to 66 years of age with recent onset mild persistent asthma, did show a decline in lung function in patients with mild persistent disease.
Although improvements in prebronchodilator and postbronchodilator FEV1 were significant after 3 years of treatment with inhaled budes-onide, differences from placebo in both outcomes were greatest after the first year. When patients with mild persistent disease inhaled budesonide once daily in addition to normal treatment within 2 years of asthma onset,28 they enjoyed considerable protection from severe and life-threatening asthma exacerbations and overall greater asthma control.
- Budesonide • Pulmicort
- Rhinocort Cromolyn • Intal
- Fluticasone • Flovent
- Formoterol • Foradil
- Montelukast • Singulair
- Nedocromil • Tilade
- Salmeterol • Servent
- Triamcinolone acetonide • Azmacort
- Zafirlukast • Accolate
Corresponding author
Gregory J. Redding, MD, Children’s Hospital and Regional Medical Center, 4800 Sand Point Way, NE, Seattle, WA 98105-0371. E-mail: [email protected].
1. National Asthma Education and Prevention Program. Expert panel report: guidelines for the diagnosis and management of asthma. Update on selected topics–2002. J Allergy Clin Immunol 2002;110(5 suppl):S141-S219.
2. National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health; 1997. Publication 97;4051.-
3. Jadad AR, Moher M, Browman GP, Booker L, Sigouin C, Fuentes M, et al. Systematic reviews and meta-analyses on treatment of asthma: critical evaluation. BMJ 2000;320:537-540.
4. Castro-Rodríguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med 2000;162:1403-1406.
5. Oxford Centre for Evidence-based Medicine Levels of Evidence Available atwww.cebm.net/levels_faq.asp . Accessed January 8, 2004.
6. Connett GJ, Warde C, Wooler E, Lenney W. Use of budes-onide in severe asthmatics aged 1–3 years. Arch Dis Child 1993;69:351-355.
7. de Blic J, Delacourt C, Le Bourgeois M, Mahut B, Ostinelli J, Caswell C, et al. Efficacy of nebulized budesonide in treatment of severe infantile asthma: a double-blind study. J Allergy Clin Immunol 1996;98:14-20.
8. Bisgaard H, Gillies J, Groenewald M, Maden C, . for an International Study Group The effect of inhaled fluticas-one propionate in the treatment of young asthmatic children: a dose comparison study. Am J Respir Crit Care Med 1999;160:126-131.
9. Nielsen KG, Bisgaard H. The effect of inhaled budesonide on symptoms, lung function, and cold air and metha-choline responsiveness in 2- to 5-year–old asthmatic children. Am J Respir Crit Care Med 2000;162:1500-1506.
10. Childhood Asthma Management Program Research Group. Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med 2000;343:1054-1063.
11. Agertoft L, Pedersen S. Effects of long-term treatment with an inhaled corticosteroid on growth and pulmonary function in asthmatic children. Respir Med 1994;88:373-381.
12. Hoekstra MO, Grol MH, Bouman K, Stijnen T, Koëter GH, Kauffman HF, et al. Fluticasone propionate in children with moderate asthma. Am J Respir Crit Care Med 1996;154:1039-1044.
13. Jónasson G, Carlsen K-H, Blomqvist P. Clinical efficacy of low-dose inhaled budesonide once or twice daily in children with mild asthma not previously treated with steroids. Eur Respir J 1998;12:1099-1104.
14. Simons FER and the Canadian Beclomethasone Dipropionate-Salmeterol Xinafoate Study Group. A comparison of beclomethasone, salmeterol, and placebo in children with asthma. N Engl J Med 1997;337:1659-1665.
15. Storr J, Lenney CA, Lenney W. Nebulized beclomethasone dipropionate in preschool asthma. Arch Dis Child 1986;61:270-273.
16. Van Essen-Zandvliet EE, Hughes MD, Waalkens HJ, Duiverman EJ, Pocock SJ, Kerrebijn KF. and the Dutch Chronic Non-Specific Lung Disease Study Group Effects of 22 months of treatment with inhaled corticosteroids and/or beta-2-agonists on lung function, airway responsiveness, and symptoms in children with asthma. Am Rev Respir Dis 1992;146:547-554.
17. Tasche MJA, Uijen JHJM, Bernsen RMD, de Jongste JC, van der Wouden JC. Inhaled disodium cromoglycate (DSCG) as maintenance therapy in children with asthma: a systematic review. Thorax 2000;55:913-920.
18. Leflein JG, Szefler SJ, Murphy KR, Fitzpatrick S, Cruz-Rivera M, Miller CJ, et al. Nebulized budesonide inhalation suspension compared with cromolyn sodium nebulizer solution for asthma in young children: results of a randomized outcomes trial. Pediatrics 2002;109:866-872.
19. Verberne AAPH, Frost C, Duiverman EJ, Grol MH, Kerrebijn KF. and the Dutch Paediatric Asthma Study Group Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. Am J Respir Crit Care Med 1998;158:213-219.
20. Lazarus SC, Boushey HA, Fahy JV, Chinchilli VM, Lemanske RF Jr, Sorkness CA, , et al. for the Asthma Clinical Research Network of the National Heart Lung and Blood Institute. Long-acting 2-agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma: a randomized controlled trial. JAMA 2001;285:2583-2593.
21. Reed CE, Offord KP, Nelson HS, Li JT, Tinkelman DG. and the American Academy of Allergy, Asthma and Immunology Beclomethasone Dipropionate-Theophylline Study Group. Aerosol beclomethasone dipropionate spray compared with theophylline as primary treatment for chronic mild or moderate persistent asthma. J Allergy Clin Immunol 1998;101:14-23.
22. Agertoft L, Pedersen S. Effect of long-term treatment with inhaled budesonide on adult height in children with asthma. N Engl J Med 2000;343:1064-1069.
23. National Asthma Education Program (NAEP). Report of the Working Group on Asthma and Pregnancy: Management of Asthma during Pregnancy. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health, 1993. NIH Publication No. 96-141593.
24. American College of Obstetricians and Gynecologists (ACOG) and the American College of Allergy, Asthmaand Immunology (ACAAI). The use of newer asthma and allergy medications during pregnancy. Ann Allergy Asthma Immunol 2000;84:475-480.
25. National Asthma Education and Prevention Program. NAEPP Expert Panel Report. Managing Asthma During Pregnancy: Recommendations for Pharmacologic Treatment—Update 2004. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health. NIH Publication No. 04-5246. March 2004.
26. Källén B, Rydhstroem H, Äberg A. Congenital malformations after the use of inhaled budesonide in early pregnancy. Obstet Gynecol 1999;93:392-395.
27. Ericson A, Källén B. Use of drugs during pregnancy—unique Swedish registration method that can be improved. Information From the Swedish Medical Products Agency 1999;1:8-11.
28. Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen Y-Z, Ohlsson SV, et al. for the START Investigators Group. Early intervention with budesonide in mild persistent asthma. Lancet 2003;361:1071-1076.
1. National Asthma Education and Prevention Program. Expert panel report: guidelines for the diagnosis and management of asthma. Update on selected topics–2002. J Allergy Clin Immunol 2002;110(5 suppl):S141-S219.
2. National Asthma Education and Prevention Program Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health; 1997. Publication 97;4051.-
3. Jadad AR, Moher M, Browman GP, Booker L, Sigouin C, Fuentes M, et al. Systematic reviews and meta-analyses on treatment of asthma: critical evaluation. BMJ 2000;320:537-540.
4. Castro-Rodríguez JA, Holberg CJ, Wright AL, Martinez FD. A clinical index to define risk of asthma in young children with recurrent wheezing. Am J Respir Crit Care Med 2000;162:1403-1406.
5. Oxford Centre for Evidence-based Medicine Levels of Evidence Available atwww.cebm.net/levels_faq.asp . Accessed January 8, 2004.
6. Connett GJ, Warde C, Wooler E, Lenney W. Use of budes-onide in severe asthmatics aged 1–3 years. Arch Dis Child 1993;69:351-355.
7. de Blic J, Delacourt C, Le Bourgeois M, Mahut B, Ostinelli J, Caswell C, et al. Efficacy of nebulized budesonide in treatment of severe infantile asthma: a double-blind study. J Allergy Clin Immunol 1996;98:14-20.
8. Bisgaard H, Gillies J, Groenewald M, Maden C, . for an International Study Group The effect of inhaled fluticas-one propionate in the treatment of young asthmatic children: a dose comparison study. Am J Respir Crit Care Med 1999;160:126-131.
9. Nielsen KG, Bisgaard H. The effect of inhaled budesonide on symptoms, lung function, and cold air and metha-choline responsiveness in 2- to 5-year–old asthmatic children. Am J Respir Crit Care Med 2000;162:1500-1506.
10. Childhood Asthma Management Program Research Group. Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med 2000;343:1054-1063.
11. Agertoft L, Pedersen S. Effects of long-term treatment with an inhaled corticosteroid on growth and pulmonary function in asthmatic children. Respir Med 1994;88:373-381.
12. Hoekstra MO, Grol MH, Bouman K, Stijnen T, Koëter GH, Kauffman HF, et al. Fluticasone propionate in children with moderate asthma. Am J Respir Crit Care Med 1996;154:1039-1044.
13. Jónasson G, Carlsen K-H, Blomqvist P. Clinical efficacy of low-dose inhaled budesonide once or twice daily in children with mild asthma not previously treated with steroids. Eur Respir J 1998;12:1099-1104.
14. Simons FER and the Canadian Beclomethasone Dipropionate-Salmeterol Xinafoate Study Group. A comparison of beclomethasone, salmeterol, and placebo in children with asthma. N Engl J Med 1997;337:1659-1665.
15. Storr J, Lenney CA, Lenney W. Nebulized beclomethasone dipropionate in preschool asthma. Arch Dis Child 1986;61:270-273.
16. Van Essen-Zandvliet EE, Hughes MD, Waalkens HJ, Duiverman EJ, Pocock SJ, Kerrebijn KF. and the Dutch Chronic Non-Specific Lung Disease Study Group Effects of 22 months of treatment with inhaled corticosteroids and/or beta-2-agonists on lung function, airway responsiveness, and symptoms in children with asthma. Am Rev Respir Dis 1992;146:547-554.
17. Tasche MJA, Uijen JHJM, Bernsen RMD, de Jongste JC, van der Wouden JC. Inhaled disodium cromoglycate (DSCG) as maintenance therapy in children with asthma: a systematic review. Thorax 2000;55:913-920.
18. Leflein JG, Szefler SJ, Murphy KR, Fitzpatrick S, Cruz-Rivera M, Miller CJ, et al. Nebulized budesonide inhalation suspension compared with cromolyn sodium nebulizer solution for asthma in young children: results of a randomized outcomes trial. Pediatrics 2002;109:866-872.
19. Verberne AAPH, Frost C, Duiverman EJ, Grol MH, Kerrebijn KF. and the Dutch Paediatric Asthma Study Group Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. Am J Respir Crit Care Med 1998;158:213-219.
20. Lazarus SC, Boushey HA, Fahy JV, Chinchilli VM, Lemanske RF Jr, Sorkness CA, , et al. for the Asthma Clinical Research Network of the National Heart Lung and Blood Institute. Long-acting 2-agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma: a randomized controlled trial. JAMA 2001;285:2583-2593.
21. Reed CE, Offord KP, Nelson HS, Li JT, Tinkelman DG. and the American Academy of Allergy, Asthma and Immunology Beclomethasone Dipropionate-Theophylline Study Group. Aerosol beclomethasone dipropionate spray compared with theophylline as primary treatment for chronic mild or moderate persistent asthma. J Allergy Clin Immunol 1998;101:14-23.
22. Agertoft L, Pedersen S. Effect of long-term treatment with inhaled budesonide on adult height in children with asthma. N Engl J Med 2000;343:1064-1069.
23. National Asthma Education Program (NAEP). Report of the Working Group on Asthma and Pregnancy: Management of Asthma during Pregnancy. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health, 1993. NIH Publication No. 96-141593.
24. American College of Obstetricians and Gynecologists (ACOG) and the American College of Allergy, Asthmaand Immunology (ACAAI). The use of newer asthma and allergy medications during pregnancy. Ann Allergy Asthma Immunol 2000;84:475-480.
25. National Asthma Education and Prevention Program. NAEPP Expert Panel Report. Managing Asthma During Pregnancy: Recommendations for Pharmacologic Treatment—Update 2004. Bethesda, Md: National Heart, Lung, and Blood Institute; National Institutes of Health. NIH Publication No. 04-5246. March 2004.
26. Källén B, Rydhstroem H, Äberg A. Congenital malformations after the use of inhaled budesonide in early pregnancy. Obstet Gynecol 1999;93:392-395.
27. Ericson A, Källén B. Use of drugs during pregnancy—unique Swedish registration method that can be improved. Information From the Swedish Medical Products Agency 1999;1:8-11.
28. Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen Y-Z, Ohlsson SV, et al. for the START Investigators Group. Early intervention with budesonide in mild persistent asthma. Lancet 2003;361:1071-1076.
Allowing spirituality into the healing process
- Research indicates spirituality and religion are a core aspect of life, and patients want physicians to address issues of spirituality in the context of medical care (C).
- Studies of the effect of patients’ faith on disease outcomes have shown reduced hypertension, better lipid profiles and lower cholesterol levels, and improved immune function (C).
- An appropriate model for addressing patients’ spiritual concerns should include active-listening skills, identification of spiritual/emotional issues, effective referrals to “spiritual specialists,” and ongoing communication about this aspect of the healing process (C).
- Remember, it is all about the patient’s spirituality, not the caregiver’s, and about supporting the patient’s spiritual beliefs (unless clearly pathologic) (C).
Most people have a strong awareness of themselves as spiritual beings. For many, their spirituality profoundly impacts, and is impacted by, illness. A review of studies in which spiritual factors are included suggests spirituality influences the process of healing significantly, either positively or negatively. A healthy spirituality can aid in prevention, improve outcomes, and facilitate coping, and should be supported and encouraged. A negative spirituality can hinder the process of healing and should be addressed.
This article considers means by which physicians may enable patients to express their spiritual concerns and find support for them, without stepping over professional boundaries or imposing personal views on those of patients.
Patients’ regard of spirituality and medical care
According to a myriad surveys, most Americans consider spirituality and religion a significant part of who they are.1,2 Although definitions and expressions vary, in general spirituality is defined as a search for what is sacred or holy in life, coupled with a transcendent (greater than self) relationship with God or a higher power or universal energy.3 Religion is seen as focusing more on prescribed beliefs, rituals, and practices as well as social institutional features,4 and on the undertaking of a spiritual search using specific means or methods (ie, rituals or behaviors) within an identifiable group.
Research in the field indicates that spirituality and religion are seen as a core aspect of life, and patients want physicians to address issues of spirituality in the context of medical care.5,6 A public survey done in 1996 by USA Weekend showed that 63% of patients believe doctors should ask about spirituality issues, but only 10% have actually been asked.2 In another study, 77% of patients surveyed said physicians should consider patients’ spiritual needs, and 37% wanted physicians to discuss religious beliefs with them more frequently.7
Intertwining of medicine and spirituality
The relationship of the discipline of medicine with the world of spirituality has been long and varied. The beginning of medicine was deeply imbedded in spirituality with spiritual leaders being some of the earliest “healers.”
A chasm forms
With the advent of the scientific revolution and the emergence of the scientific method in the late 1500s, the relationship between spirituality and science changed dramatically. Since this new experimental method could not be readily or confidently applied to God, or to one’s experiences with God, religion/spirituality was excluded from the realm of science and a chasm emerged between the 2 realms.
The chasm widened given the religious community’s tendency to reject many of the discoveries generated by the scientific method. Distrust, even dislike, of the spiritual by the medical community became widespread. Mandel, in The Psychobiology of Consciousness, calls spirituality a “temporal lobe dysfunction.”8 Perhaps more telling was the use of spirituality in the glossary of technical terms in Diagnostic and Statistical Manual of Mental Disorders, revised 3rd edition (DSM-III-R).9 In that document, all allusions to spirituality were illustrations of psychopathology; 22.2% of all the negative illustrations in the glossary had religious content, while none had sexual, ethnic, racial, or cultural content.
This negativity was exacerbated by an ever-increasing emphasis on the science of medicine, reflecting the exponential growth of scientific knowledge relevant to medical practice, the public’s demand for technologically sophisticated medical care, and an increased emphasis on tools such as evidence-based medicine. Medical practice became centered on the task of choosing treatments proven effective through rigorous study. Aspects of the “art of medicine” that had not undergone rigid empirical evaluation were considered suspect and deemed unworthy of inclusion in medical practice.
Spanning the chasm
However, a new interest in the integration of medicine and spirituality has emerged. One reflection of this interest is the discussion of the topic in both popular and professional journals. A search by Oregon Health and Science University faculty in 1999 of a large public library database of popular magazines using the key words “spirituality and health” revealed only 25 articles from 1990 to 1994, but over 100 articles from 1995 to 1999.
A similar movement can be seen in the medical literature. A search of MedLine using the keyword “spirituality” produced 52 articles from 1960 to 1990, 90 from 1991 to 1995, and almost 200 from 1996 to 1999. A more recent search produced 554 citations from January 2000 to April 2003.
What outcomes research has shown about spirituality
Much of the focus in this area has been on what research can reveal regarding the impact of spirituality on health. The late David Larson, MD, MSPH, of the International Center for the Integration of Health and Spirituality (ICIHS) and his collaborators extensively reviewed journals and identified large numbers of studies that included spiritual indicators. They found a strong trend toward identifying spirituality as a positive factor for coping with illness, preventing illness, and aiding treatment.3,10
Harold G. Koenig of Duke University continued the effort and recently published a Handbook of Religion and Health.11 This work systematically reviewed and rated around 1600 studies related to the relationships between religion and a variety of mental and physical health conditions, starting with the earliest identified studies through 2000. The research can be broken down into 3 major categories: religion and mental health, religion and physical disorders, and religion and the use of health services. A smaller number of studies focus on research issues, spiritual development, and implications for health and religious professionals ( Table 1).
Although most studies in English have focused on “Western faiths” such as Roman Catholicism, Orthodoxy, mainline and fundamentalist Protestantism, Pentecostalism, Jehovah’s Witnesses, Judaism, and Mormonism, studies have also looked at such faiths as Baha’i, Hare Krishna, Islam, Sikhism, and Hinduism.12,13 In some cases, especially in the area of mental health (depression and psychoses), the type of religious affiliation did seem to be a factor in outcomes, both positive and negative.11
Studies have also included a variety of cultures and nations. Thirty-nine different countries are specifically listed as study locals, with many other studies listing the “world” as the local. Many studies contrast nations, cultures, or faith systems. In some cases these differences were significant, with one study focused on suicide showing opposite results depending on culture.14
Religion and mental health. Studies have looked at the impact of religion or spirituality on well-being, self-esteem, depression and suicide, as well as alcohol and drug use and abuse. Religious or spiritual people, especially those who are regularly involved with a community of faith, experience depression less often than others, are less likely to abuse drugs or alcohol, cope with life-issues and illness more effectively, and are less likely to commit suicide.11
Religion and physical disorders. Studies have focused specifically on the effect of faith on heart disease, hypertension, cerebrovascular disease, immune system dysfunctions, and cancer. Other studies have looked at broader issues such as pain and mortality.11 Results have shown reduced hypertension,15,16 better lipid profiles,17,18 improved immune function,19,20 and lower cholesterol levels21 ( Table 2).
A recent article in American Psychologist notes there is more evidence that religion or spirituality impedes recovery than it improves recovery.21 However, the evidence cited by the article was connected to religious struggle or to negative coping (eg, “I feel God has abandoned me”). This is not surprising, and it underscores the need to support positive religious coping and to help patients move beyond negative religious coping.
Religion and use of health services. Studies looking at the use of health services focus on such matters as screening services22 and compliance.23 One of the interesting factors here is the role of religion in noncompliance. The refusal of Jehovah’s Witnesses to receive blood products has been a highly visible example. But other issues—more subtle, but nevertheless critical—emerge when one examines the literature; these include noncompliance due to a belief that a higher power “caused” the illness, or that illness is the result of “sinful” behavior.24
In general, research shows the impact of religion and spirituality is positive. Although a person’s spirituality sometimes is pathological, and spiritual beliefs can create health issues, an overwhelming number of studies show a positive benefit. Of those studies reviewed by Koenig et al,11 where the impact of spirituality could be classified as positive, negative, no association, complex, or mixed, 70% showed a positive impact (68% a strong positive with P<.05) while only 5% showed a negative impact. The studies show spirituality and religion benefit patients by helping prevent illness, increasing the ability to cope, and improving outcomes.
TABLE 1
Areas of spirituality research to date
| Major focus | Subtopics | Earliest publication | Number of publications |
|---|---|---|---|
| Mental health | Religious coping, hope and optimism, purpose/meaning in life, self-esteem, bereavement, social support, depression, suicide, assisted suicide/euthanasia, anxiety, schizophrenia/psychosis, alcohol use/abuse, drug use/abuse, delinquency/crime, marital instability, personality, general mental health | 1932 | 1075 |
| Physical health | Heart disease, hypertension, cerebrovascular disease, immune system, cancer risk, mortality, functional disability, pain and somatic symptoms, health behaviors, miscellaneous | 1902 | 455 |
| Use of health services | General medical services, mental health services, disease prevention, health responsibility, compliance | 1960 | 53 |
| Clinical implications and applications | Health professionals, religious professionals | 1973 | 131 |
| Research | Measurement | 1967 | 40 |
| Miscellaneous | Religious beliefs/behaviors, religious/faith development, religious conversion, spiritual/faith healing, prayer, death and dying, religious harm | 1902 | 171 |
TABLE 2
Propositions regarding the effect of spirituality on physical outcomes
| Proposition Studies | Rating* #-Letter |
|---|---|
| Religious coping aids stress management | |
| Ellison, CG, Taylor RJ. Turning to prayer: Social and situational antecedents of religious coping among African Americans. Rev Religious Research 1996; 38:111–131. | 8/NA |
| Pargament KI, Smith BW, Koenig HG, et al. Patterns of positive and negative religious 8/NA coping with major life stressors. J Scientific Study Religion 1998; 37(4):710–724. | 8/NA |
| Spirituality/religious affiliation prevents substance abuse | |
| Bell R, Wechsler H, Johnston LD. Correlates of college student marijuana use: Results of a US national survey. Addiction 1997; 92:571–581. | 9/NA |
| Religious practices/spirituality decreases the incidence of depression | |
| Idler EL, Kasl S. Religion, disability, depression, and the timing of death. Am J Sociology 1992; 97:1052–1079. | 10/NA |
| Kennedy GJ, Kelman HR, Thomas C, et al. The relation of religious preference 10/NA and practice to depressive symptoms among 1,855 older adults. J Gerontol 1996; 51B:301–308. | 10/NA |
| Religious practice/spirituality lowers suicide rates | |
| Neeleman J, Halpern D, Leon D. Tolerance of suicide, religion, and suicide rates: An ecological and individual study in 19 Western countries. Psychol Med 1997; 27(5):1165–1171. | 10/NA |
| Religious practice/spirituality prevents hypertension/lowers blood pressure | |
| Steffen PR, Hinderliter AL, Blumenthal JA, et al. Religious coping, ethnicity, and ambulatory blood pressure. Psychosomatic Med 2001; 63:523–530. | 7–A/B |
| Koenig, HG, George LK, Hays, JC, et al. The relationships between religious activities 9 A/B and blood pressure in older adults. International J Psych Med 1998; 28:189–213. | 7–A/B |
| Religious practice/spirituality is related to better lipid profiles | |
| Friedlander Y, Kark JD, Stein Y. Religious observance and plasma lipids and lipoproteins among 17 year old Jewish residents of Jerusalem. Prevent Med 1987; 16:70–79. | 8-B |
| Religious practice/spirituality is associated with better immune function | |
| Woods TE, Antoni MH, Ironson GH, et al. Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. J Psychosomatic Research 1999; 46:165–176. | 7-B |
| Koenig HG, Cohen JH, George LK, et al. Attendance at religious services, interleukin-6, 8-A/B and other biological parameters of immune function in older adults, International J Psych Med 1997; 27:233–250. | 7-B |
| Religious practice/spirituality is related to lower cholesterol | |
| Patel, C, Marmot MG, Terry DJ, et al. Trial of relaxation in reducing coronary risk: Four year follow up. Brit Med J 1985; 290:1103–1106 | NA/A |
| Attendance at church services leads to longer life | |
| Koenig JG, Hays JC, Larson DB, et al. Does religious attendance prolong survival? A six-year follow-up study of 3,968 older adults. J Gerontology Series A: Biologic Sci Med Sci 1999; 54A:M370–M376. | 9-A |
| *Ratings Systems: Koenig/Miller | |
| Number = Rating system from Koenig et al. Handbook of Religion and Health. Scale of 1–10 (1=poor, 10=excellent). Based on overall study design, sampling method, quality of religious measure, quality of statistical analysis, interpretation of results, and discussion in the context of existing literature). Methodology validated by outside reviewers. | |
| Letter = Rating system from Miller WR, Thoresen CE, Spirituality, Religion and Health: An Emerging Research Field. A = Methodologically Sound B= Methodologically Sound with at least one methodological limitation. | |
| NA = not rated by this system | |
Barriers and issues
In spite of the evidence showing religion and spirituality to be positive health factors, there are still reasons to be cautious. Many obvious concerns have been expressed by physicians in recent surveys.25,26 More than 50% of physicians surveyed by Ellis and colleagues26 listed such factors as time, lack of training in taking a spiritual history, and a concern about projecting their own beliefs onto patients as barriers to discussing spiritual issues.
Recently a group of articles strongly challenged the entire premise of integration. Richard P. Sloan and his associates, in the “Sounding Board” section of the New England Journal of Medicine, said they are “troubled by the uncritical embrace of this trend….”27 They cite a number of reasons to be wary of this integration:
- Studies suggesting a relationship between spirituality and health are flawed.
- The unique nature of the patient/physician relationship causes physician assumptions and beliefs to have undue influence.
- Physicians have no expertise in spiritual matters.
- Most patients do not truly want to discuss spiritual issues, and interest does not necessarily justify the incorporation of religious matters.
- The integration of spirituality into practice is an attempt to use religion that trivializes a deep and complex reality.
A similar article in the Lancet echoed these concerns.28 Again, the empirical evidence is challenged. Added to that concern is a variety of ethical issues. The first ethical issue relates to boundaries. The authors insist “when doctors depart from areas of established expertise to promote a nonmedical agenda, they abuse their status as professionals.” The second issue involves the ethics of “taking into account” spiritual issues versus “‘taking them on’ as the objects of interventions.” A third ethical problem focuses on the possibility that physicians might actually do harm to patients by linking health status and spirituality.28
It is fair to say these cautions are worthy of serious consideration and need to be addressed by any responsible model of integration. Certainly there is a need for added research on this subject. Koenig et al,11 for example, in rating the research done on the subject, rate only 18.5% of the studies a 10, 9, or 8 on a scale of 1 to 10 (10=excellent) and assert “we have only scratched the surface in acquiring knowledge about the influences of religion on health, the influences of health on religion, and the mechanisms by which these effects occur.” A review of studies attempting to link religiosity to physiological processes notes that the results are “suggestive,” but that additional research is needed that combines both stronger research methodology with more representative populations.29 Even proponents of integration are aware of the difficulties related to boundaries.30
Providers with an interest in the integration of medicine and spirituality are thus left with a dilemma. On the one hand there appear to be some very good reasons for integration: patient need and desire, the respect such an approach illustrates for the whole person, and strong clues that it does aid with coping, prevention, and recovery. On the other hand, there appear to be very real dangers with integration: a potential violation of boundaries, lack of training, lack of time, and potential misuse of the spiritual.
A model for integration
An appropriate response seems to be finding a model that encourages physicians to treat the patient as a whole person, addressing not only physical, but also social, emotional, and spiritual issues. This model should provide the physician with the ability to identify patients who are struggling with such issues, and the tools for addressing them in an appropriate manner. But this model should take into account the serious issues of time, boundaries, and respect for the deep and complex nature of spiritual and emotional issues.
In general the model should have the following components:
- Good active-listening skills and other tools that encourage the patient to share safely and freely about such issues, providing new self-awareness on the part of the patient, and in some cases spiritual relief.
- Identification of spiritual/emotional issues.
- Appropriate and effective referral of the patient to a “spiritual specialist,” one trained to deal with spiritual issues in a longer term, deeper manner.
- Ongoing communication with the patient and their specialist about this aspect of the person’s healing process.
The first step involves simply asking specific questions to develop a basic understanding of the patients’ spiritual culture. Various sets of questions have been developed to aid practitioners with this task.31-33 It is also a matter of practicing what many have called the “art of medicine.” It is being patient centered and entering into a true dialogue with patients that involves active-listening skills. Active listening is important, because most patients will not make direct statements regarding their feelings or issues. Usually their deep spiritual turmoil is expressed indirectly through body language, tone of voice, stories, and other subtle expressions. True dialogue allows physicians to pick up the clues patients are sending regarding spiritual issues, and to help their patients come to a clear awareness of those issues for themselves.
Once the discussion has begun, it is important to include some element of assessment. A hospital chaplain has developed an assessment tool that he uses to think about the spiritual health of those he visits and to structure his interventions with those patients.34 At Oregon Health and Science University we have adapted his approach by encouraging physicians to develop a set of 5 to 8 paired terms, such as anger and acceptance, which they believe reflect important spiritual issues (Table 3). Using these terms, a continuum is developed that can be used to help assess patients from a spiritual perspective.
A physician can use this continuum to think about the patient and to develop ideas for intervention. First, the physician places an “X” on each continuum of the chart, noting his or her perception of how the patient is functioning.
Second, the physician evaluates that position. Is this a logical place for the patient to be at this place, in this time? Severe anger might be appropriate when one first receives news of a terminal illness. It may not be as appropriate 6 months later.
Third, the physician picks the issue(s) they believe should be addressed through intervention. If a person is feeling helpless, what might be done to help them feel more empowered? The physician can ask what he or she can do. This is likely to be somewhat limited due to training, time, and other issues. The physician can also seek collaboration. Who can be brought into the healing mix, who might become a partner in helping healing happen?
In some cases it will be clear that the patient is spiritual, and that spirituality is a very positive factor in the effort to find wholeness. What these patients need is support, an affirmation that what they are doing is working. They need permission to bring their spirituality into the exam and treatment space as a powerful resource for wellness.35,36 If, for example, a patient is coping well and is maintaining a sense of purpose in the face of a debilitating illness, they should be commended for that, and the coping mechanisms that support that stance should be reinforced.
TABLE 3
Emotional continuums used in spiritual assessment
| Curse ↔ Blessing |
| Dread ↔ Courage |
| Alone ↔ Connected |
| Abandoned ↔ Supported |
| Anger ↔ Acceptance |
| Despair ↔ Hope |
| Meaninglessness ↔ Purpose |
| Helplessness ↔ Empowerment |
Collaborative intervention
Collaboration begins with the patient. The physician must be clear that this is all about the patient’s spirituality (not their own) and support the spiritual beliefs of the patient, working within the framework of those beliefs (unless clearly pathological). But there are many others who can be brought into the therapeutic process. Providers can collaborate with “spiritual specialists,” such as the patient’s spiritual leader or the hospital chaplains. Other collaborators may include social workers, mental health specialists, or even a group of some sort. Research suggests social support is a key factor that leads to improved outcomes.11
Many options are available for intervention. Connecting the patient with a religious leader or “spiritual specialist” is often very appropriate. In hospital settings, chaplains are a good place to begin. In a community-based setting, the patient’s own spiritual leader or, if the patient is not affiliated with any specific group, a spiritual specialist who is willing to work from the patient’s perspective is often the most viable option. Support groups, study groups, worship experiences all can be a part of this strategy. The use of literature and tapes, prayer (best done with a religious professional if possible) are relatively easy responses to spiritual distress. Appointments with various professional “healers” such as social workers and psychologists may also be helpful, and in some cases necessary.
Follow-up is also critical in working with patients. To bring up such sensitive issues as spiritual matters, and then not show a continued interest in them would be detrimental. The physician should return to the issue(s) in following visits, until it is clear that the patient is moving toward resolution, or until the patient indicates they would like to drop the issue. Communication should continue to take place, if possible, between the physician and others working with the patient. Ongoing dialogue with chaplains, religious leaders, therapists, and others should take place.
Pursuing, not avoiding, integration
We are still early in the process of studying and understanding the complex relationship between spirituality and health. Much more research needs to be done to clarify the benefits and dispel the myths. What is it about spirituality and religious practice that benefits patients? Is it, as some have suggested, merely a matter of lifestyle or compliance? Or is there something deeper and more profound involved? When is religious or spiritual coping positive, and when is it negative?
A continued research agenda focusing on the impact of spirituality on health is needed. There is also a need to look at viable assessment tools, as well as appropriate interventions. Perhaps the issue of intervention is the most difficult challenge. What is appropriate? What can be done given time constraints, the need for boundaries, and limited training? Most research to date has focused on the existing spirituality of patients. Research that looks at the impact of practical spiritual interventions, such as spiritual listening, referral to a spiritual specialist, or prayer is needed to move integration to a new stage.
Careful attention to such issues can move us forward in the task of providing effective and humane care to patients. This task is increasingly important in today’s medical environment. As theologian Martin E. Marty notes, “The modern biomedical enterprise—with its threefold work of knowledge acquisition, technology development, and care delivery—urgently needs the guiding visions and values embodied in the faith traditions. When technological momentum or economic necessity alone guides the health care enterprise, the sustaining impulses of respect, meaning and purpose often fall aside.”37
The process of learning how to integrate medicine and spirituality is not an easy one, nor will it be accomplished without struggle. But it is a process vitally important for modern medicine. The issue truly is one of caring, both when cure is possible, and when it is not. It is a matter of focusing on part of what makes us truly human, and supporting a healing process that often transcends the biomedical agenda.
Correspondence
Stephen P. Kliewer, DMin, Department of Family Medicine, Oregon Health and Science University, 3181 SW Sam Jackson Park Road, Portland, OR 97201. E-mail: [email protected].
1. Gallup G, Jr, Lindsay DM. Surveying the Religious Landscape: Trends in US Beliefs. Harrisburg, Pa: Morehouse; 1999:21.
2. McNichol T. (1996) The new faith in medicine. USA Weekend, April:5-7,4-5.
3. Larson DB, Swyers JP, McCullough ME. Scientific Research on Spirituality and Health: A Consensus Report. Rockville, Md: National Institute for Healthcare Research; 1997.
4. Zinnbauer BJ, Pargament KI, Cole B, et al. Religion and spirituality: Unfuzzying the fuzzy. J Scientific Study Religion 1998;36:549-564.
5. Ehman JW, Ott BB, Short TH. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med 1999;159:1803-1806.
6. Daaleman TP, Nease DE, Jr. Patient attitudes regarding physician inquiry into spiritual and religious issues. J Fam Pract 1994;39:564-568.
7. King DE, Bushwick B. Beliefs and attitudes of hospital inpatients about faith healing and prayer. J Fam Pract 1994;39:349-352.
8. Mandel AJ. Toward a psychobiology of transcendence: God in the brain. In RJ Davidson and JM Davidson, eds: The Psychobiology of Consciousness. New York, NY: Plenum; 1980;379-479.
9. American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed, rev (DSM-III-R). Washington, DC: American Psychiatric Press; 1987.
10. Miller WR, ed. Integrating Spirituality into Treatment. Washington, DC: American Psychological Association; 1999:3.
11. Koenig HG, McCullough ME, Larson DB. Handbook of Religion and Health. Oxford: Oxford University Press; 2001.
12. Gupta R, Prakash H, Gupta VP, Gupta KD. Prevalence and determinants of coronary heart disease in a rural population of India. J Clin Epidemiol 1997;50:203-209.
13. Gopinath N, Chadha S, Jain P, Shekhawat S, Tandon R. An epidemiological study of coronary heart disease in different ethnic groups in a Delhi urban population. J Assoc Physicians India 1995;43:30-33.
14. Zhang J, Jin S. Determinants of suicide ideation: A comparison of Chinese and American college students. Adolescence 1996;31:451-467.
15. Koenig HG, George LK, Hays JC, Larson DB, Cohen HJ, Blazer DG. The relationships between religious activities and blood pressure in older adults. Int J Psychiatry Med 1998;28:189-213.
16. Steffen PR, Hinderliter AL, Blumenthal JA, Sherwood A. Religious coping, ethnicity, and ambulatory blood pressure. Psychosomatic Medicine 2001;63:523-530.
17. Friedlander Y, Kark JD, Kaufmann NA, Stein Y. Coronary heart disease risk factors among religious groups in a Jewish population sample in Jerusalem. Am J Clin Nutrition 1985;42:511-521.
18. Friedlander Y, Kark JD, Stein Y. Religious observance and plasma lipids and lipoproteins among 17 year old Jewish residents of Jerusalem. Preventive Medicine 1987;16:70-79.
19. Koenig HG, Cohen JH, George LK, Hayes JC, Larson DB, Blazer DG. Attendance at religious services, interleukin-6, and other biological parameters of immune function in older adults. Int J Psychiatry Med 1987;27:233-250.
20. Woods TE, Antoni MH, Ironson GH, Kling DW. Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. J Psychosomatic Research 1999;46:165-176.
21. Powell L, Shahabi L, Thoresen CE. Religion and spirituality: linkages to physical health. Am Psychol 2003;58:36-52.
22. Naguib SM, Geiser PB, Comstock GW. Responses to a program of screening for cervical cancer. Public Health Reports 1968;83:990-998.
23. O’Brien ME. Religious faith and adjustment to long-term hemodialysis. J Religion Faith 1982;21:68-80.
24. Foulks EF, Persons JB, Merkel RL. The effect of patients’ beliefs about their illness on compliance in psychotherapy. Am J Psychiatry 1986;143:340-344.
25. Graigie F, Hobbs R, III. Spiritual perspectives and practices of family physicians with an expressed interest in spirituality. Fam Med 1999;31:578-585.
26. Ellis M, Vinson D, Ewigman B. Addressing spiritual concerns with patients: family physicians attitudes and practices. J Fam Pract 1999;48:105-109.
27. Sloan RP, Bagiella E, VandeCreek L, et al. Should physicians prescribe religious activities? N Engl J Med 2000;342:913-916Sounding Board.
28. Sloan RP, Bagiella E, Powell T. Religion spirituality, and medicine. Lancet 1999;343:664-667.
29. Seeman TE, Dubin LF, Seeman M. Religiosity/spirituality and health: a critical review of the evidence for biological pathways. Am Psychologist 2003;58:53-63.
30. Post SG, Puchalski CM, Larson DB. Physicians and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med 2000;132:578-583.
31. Maugans TA. The spiritual history. Arch Fam Med 1996;5:11-16.
32. Puchalski CM, Romer AL. Taking a spiritual history allows clinicians to understand patients more fully. J Palliative Med 2000;3:129-137.
33. Anandarajah G, Hight E. Spirituality and medical practice: using the HOPE questions as a practical tool for spiritual assessment. Am Fam Physician 2001;63:81-89.
34. Hodges S. Spiritual screening: the starting place for intentional pastoral care. Chaplaincy Today 1999;15:30-39.
35. Dewald PA. Psychotherapy: A Dynamic Approach. New York, NY: Basic Books; 1971;105:127.-
36. Clinebell H. Growth Counseling. Nashville, Tenn: Abingdon; 1979;96-97.
37. Numbers RL, Amundsen DW. Caring and Curing: Health and Medicine in the Western Religious Traditions. Baltimore, Md: Johns Hopkins University Press; 1998:viii.
- Research indicates spirituality and religion are a core aspect of life, and patients want physicians to address issues of spirituality in the context of medical care (C).
- Studies of the effect of patients’ faith on disease outcomes have shown reduced hypertension, better lipid profiles and lower cholesterol levels, and improved immune function (C).
- An appropriate model for addressing patients’ spiritual concerns should include active-listening skills, identification of spiritual/emotional issues, effective referrals to “spiritual specialists,” and ongoing communication about this aspect of the healing process (C).
- Remember, it is all about the patient’s spirituality, not the caregiver’s, and about supporting the patient’s spiritual beliefs (unless clearly pathologic) (C).
Most people have a strong awareness of themselves as spiritual beings. For many, their spirituality profoundly impacts, and is impacted by, illness. A review of studies in which spiritual factors are included suggests spirituality influences the process of healing significantly, either positively or negatively. A healthy spirituality can aid in prevention, improve outcomes, and facilitate coping, and should be supported and encouraged. A negative spirituality can hinder the process of healing and should be addressed.
This article considers means by which physicians may enable patients to express their spiritual concerns and find support for them, without stepping over professional boundaries or imposing personal views on those of patients.
Patients’ regard of spirituality and medical care
According to a myriad surveys, most Americans consider spirituality and religion a significant part of who they are.1,2 Although definitions and expressions vary, in general spirituality is defined as a search for what is sacred or holy in life, coupled with a transcendent (greater than self) relationship with God or a higher power or universal energy.3 Religion is seen as focusing more on prescribed beliefs, rituals, and practices as well as social institutional features,4 and on the undertaking of a spiritual search using specific means or methods (ie, rituals or behaviors) within an identifiable group.
Research in the field indicates that spirituality and religion are seen as a core aspect of life, and patients want physicians to address issues of spirituality in the context of medical care.5,6 A public survey done in 1996 by USA Weekend showed that 63% of patients believe doctors should ask about spirituality issues, but only 10% have actually been asked.2 In another study, 77% of patients surveyed said physicians should consider patients’ spiritual needs, and 37% wanted physicians to discuss religious beliefs with them more frequently.7
Intertwining of medicine and spirituality
The relationship of the discipline of medicine with the world of spirituality has been long and varied. The beginning of medicine was deeply imbedded in spirituality with spiritual leaders being some of the earliest “healers.”
A chasm forms
With the advent of the scientific revolution and the emergence of the scientific method in the late 1500s, the relationship between spirituality and science changed dramatically. Since this new experimental method could not be readily or confidently applied to God, or to one’s experiences with God, religion/spirituality was excluded from the realm of science and a chasm emerged between the 2 realms.
The chasm widened given the religious community’s tendency to reject many of the discoveries generated by the scientific method. Distrust, even dislike, of the spiritual by the medical community became widespread. Mandel, in The Psychobiology of Consciousness, calls spirituality a “temporal lobe dysfunction.”8 Perhaps more telling was the use of spirituality in the glossary of technical terms in Diagnostic and Statistical Manual of Mental Disorders, revised 3rd edition (DSM-III-R).9 In that document, all allusions to spirituality were illustrations of psychopathology; 22.2% of all the negative illustrations in the glossary had religious content, while none had sexual, ethnic, racial, or cultural content.
This negativity was exacerbated by an ever-increasing emphasis on the science of medicine, reflecting the exponential growth of scientific knowledge relevant to medical practice, the public’s demand for technologically sophisticated medical care, and an increased emphasis on tools such as evidence-based medicine. Medical practice became centered on the task of choosing treatments proven effective through rigorous study. Aspects of the “art of medicine” that had not undergone rigid empirical evaluation were considered suspect and deemed unworthy of inclusion in medical practice.
Spanning the chasm
However, a new interest in the integration of medicine and spirituality has emerged. One reflection of this interest is the discussion of the topic in both popular and professional journals. A search by Oregon Health and Science University faculty in 1999 of a large public library database of popular magazines using the key words “spirituality and health” revealed only 25 articles from 1990 to 1994, but over 100 articles from 1995 to 1999.
A similar movement can be seen in the medical literature. A search of MedLine using the keyword “spirituality” produced 52 articles from 1960 to 1990, 90 from 1991 to 1995, and almost 200 from 1996 to 1999. A more recent search produced 554 citations from January 2000 to April 2003.
What outcomes research has shown about spirituality
Much of the focus in this area has been on what research can reveal regarding the impact of spirituality on health. The late David Larson, MD, MSPH, of the International Center for the Integration of Health and Spirituality (ICIHS) and his collaborators extensively reviewed journals and identified large numbers of studies that included spiritual indicators. They found a strong trend toward identifying spirituality as a positive factor for coping with illness, preventing illness, and aiding treatment.3,10
Harold G. Koenig of Duke University continued the effort and recently published a Handbook of Religion and Health.11 This work systematically reviewed and rated around 1600 studies related to the relationships between religion and a variety of mental and physical health conditions, starting with the earliest identified studies through 2000. The research can be broken down into 3 major categories: religion and mental health, religion and physical disorders, and religion and the use of health services. A smaller number of studies focus on research issues, spiritual development, and implications for health and religious professionals ( Table 1).
Although most studies in English have focused on “Western faiths” such as Roman Catholicism, Orthodoxy, mainline and fundamentalist Protestantism, Pentecostalism, Jehovah’s Witnesses, Judaism, and Mormonism, studies have also looked at such faiths as Baha’i, Hare Krishna, Islam, Sikhism, and Hinduism.12,13 In some cases, especially in the area of mental health (depression and psychoses), the type of religious affiliation did seem to be a factor in outcomes, both positive and negative.11
Studies have also included a variety of cultures and nations. Thirty-nine different countries are specifically listed as study locals, with many other studies listing the “world” as the local. Many studies contrast nations, cultures, or faith systems. In some cases these differences were significant, with one study focused on suicide showing opposite results depending on culture.14
Religion and mental health. Studies have looked at the impact of religion or spirituality on well-being, self-esteem, depression and suicide, as well as alcohol and drug use and abuse. Religious or spiritual people, especially those who are regularly involved with a community of faith, experience depression less often than others, are less likely to abuse drugs or alcohol, cope with life-issues and illness more effectively, and are less likely to commit suicide.11
Religion and physical disorders. Studies have focused specifically on the effect of faith on heart disease, hypertension, cerebrovascular disease, immune system dysfunctions, and cancer. Other studies have looked at broader issues such as pain and mortality.11 Results have shown reduced hypertension,15,16 better lipid profiles,17,18 improved immune function,19,20 and lower cholesterol levels21 ( Table 2).
A recent article in American Psychologist notes there is more evidence that religion or spirituality impedes recovery than it improves recovery.21 However, the evidence cited by the article was connected to religious struggle or to negative coping (eg, “I feel God has abandoned me”). This is not surprising, and it underscores the need to support positive religious coping and to help patients move beyond negative religious coping.
Religion and use of health services. Studies looking at the use of health services focus on such matters as screening services22 and compliance.23 One of the interesting factors here is the role of religion in noncompliance. The refusal of Jehovah’s Witnesses to receive blood products has been a highly visible example. But other issues—more subtle, but nevertheless critical—emerge when one examines the literature; these include noncompliance due to a belief that a higher power “caused” the illness, or that illness is the result of “sinful” behavior.24
In general, research shows the impact of religion and spirituality is positive. Although a person’s spirituality sometimes is pathological, and spiritual beliefs can create health issues, an overwhelming number of studies show a positive benefit. Of those studies reviewed by Koenig et al,11 where the impact of spirituality could be classified as positive, negative, no association, complex, or mixed, 70% showed a positive impact (68% a strong positive with P<.05) while only 5% showed a negative impact. The studies show spirituality and religion benefit patients by helping prevent illness, increasing the ability to cope, and improving outcomes.
TABLE 1
Areas of spirituality research to date
| Major focus | Subtopics | Earliest publication | Number of publications |
|---|---|---|---|
| Mental health | Religious coping, hope and optimism, purpose/meaning in life, self-esteem, bereavement, social support, depression, suicide, assisted suicide/euthanasia, anxiety, schizophrenia/psychosis, alcohol use/abuse, drug use/abuse, delinquency/crime, marital instability, personality, general mental health | 1932 | 1075 |
| Physical health | Heart disease, hypertension, cerebrovascular disease, immune system, cancer risk, mortality, functional disability, pain and somatic symptoms, health behaviors, miscellaneous | 1902 | 455 |
| Use of health services | General medical services, mental health services, disease prevention, health responsibility, compliance | 1960 | 53 |
| Clinical implications and applications | Health professionals, religious professionals | 1973 | 131 |
| Research | Measurement | 1967 | 40 |
| Miscellaneous | Religious beliefs/behaviors, religious/faith development, religious conversion, spiritual/faith healing, prayer, death and dying, religious harm | 1902 | 171 |
TABLE 2
Propositions regarding the effect of spirituality on physical outcomes
| Proposition Studies | Rating* #-Letter |
|---|---|
| Religious coping aids stress management | |
| Ellison, CG, Taylor RJ. Turning to prayer: Social and situational antecedents of religious coping among African Americans. Rev Religious Research 1996; 38:111–131. | 8/NA |
| Pargament KI, Smith BW, Koenig HG, et al. Patterns of positive and negative religious 8/NA coping with major life stressors. J Scientific Study Religion 1998; 37(4):710–724. | 8/NA |
| Spirituality/religious affiliation prevents substance abuse | |
| Bell R, Wechsler H, Johnston LD. Correlates of college student marijuana use: Results of a US national survey. Addiction 1997; 92:571–581. | 9/NA |
| Religious practices/spirituality decreases the incidence of depression | |
| Idler EL, Kasl S. Religion, disability, depression, and the timing of death. Am J Sociology 1992; 97:1052–1079. | 10/NA |
| Kennedy GJ, Kelman HR, Thomas C, et al. The relation of religious preference 10/NA and practice to depressive symptoms among 1,855 older adults. J Gerontol 1996; 51B:301–308. | 10/NA |
| Religious practice/spirituality lowers suicide rates | |
| Neeleman J, Halpern D, Leon D. Tolerance of suicide, religion, and suicide rates: An ecological and individual study in 19 Western countries. Psychol Med 1997; 27(5):1165–1171. | 10/NA |
| Religious practice/spirituality prevents hypertension/lowers blood pressure | |
| Steffen PR, Hinderliter AL, Blumenthal JA, et al. Religious coping, ethnicity, and ambulatory blood pressure. Psychosomatic Med 2001; 63:523–530. | 7–A/B |
| Koenig, HG, George LK, Hays, JC, et al. The relationships between religious activities 9 A/B and blood pressure in older adults. International J Psych Med 1998; 28:189–213. | 7–A/B |
| Religious practice/spirituality is related to better lipid profiles | |
| Friedlander Y, Kark JD, Stein Y. Religious observance and plasma lipids and lipoproteins among 17 year old Jewish residents of Jerusalem. Prevent Med 1987; 16:70–79. | 8-B |
| Religious practice/spirituality is associated with better immune function | |
| Woods TE, Antoni MH, Ironson GH, et al. Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. J Psychosomatic Research 1999; 46:165–176. | 7-B |
| Koenig HG, Cohen JH, George LK, et al. Attendance at religious services, interleukin-6, 8-A/B and other biological parameters of immune function in older adults, International J Psych Med 1997; 27:233–250. | 7-B |
| Religious practice/spirituality is related to lower cholesterol | |
| Patel, C, Marmot MG, Terry DJ, et al. Trial of relaxation in reducing coronary risk: Four year follow up. Brit Med J 1985; 290:1103–1106 | NA/A |
| Attendance at church services leads to longer life | |
| Koenig JG, Hays JC, Larson DB, et al. Does religious attendance prolong survival? A six-year follow-up study of 3,968 older adults. J Gerontology Series A: Biologic Sci Med Sci 1999; 54A:M370–M376. | 9-A |
| *Ratings Systems: Koenig/Miller | |
| Number = Rating system from Koenig et al. Handbook of Religion and Health. Scale of 1–10 (1=poor, 10=excellent). Based on overall study design, sampling method, quality of religious measure, quality of statistical analysis, interpretation of results, and discussion in the context of existing literature). Methodology validated by outside reviewers. | |
| Letter = Rating system from Miller WR, Thoresen CE, Spirituality, Religion and Health: An Emerging Research Field. A = Methodologically Sound B= Methodologically Sound with at least one methodological limitation. | |
| NA = not rated by this system | |
Barriers and issues
In spite of the evidence showing religion and spirituality to be positive health factors, there are still reasons to be cautious. Many obvious concerns have been expressed by physicians in recent surveys.25,26 More than 50% of physicians surveyed by Ellis and colleagues26 listed such factors as time, lack of training in taking a spiritual history, and a concern about projecting their own beliefs onto patients as barriers to discussing spiritual issues.
Recently a group of articles strongly challenged the entire premise of integration. Richard P. Sloan and his associates, in the “Sounding Board” section of the New England Journal of Medicine, said they are “troubled by the uncritical embrace of this trend….”27 They cite a number of reasons to be wary of this integration:
- Studies suggesting a relationship between spirituality and health are flawed.
- The unique nature of the patient/physician relationship causes physician assumptions and beliefs to have undue influence.
- Physicians have no expertise in spiritual matters.
- Most patients do not truly want to discuss spiritual issues, and interest does not necessarily justify the incorporation of religious matters.
- The integration of spirituality into practice is an attempt to use religion that trivializes a deep and complex reality.
A similar article in the Lancet echoed these concerns.28 Again, the empirical evidence is challenged. Added to that concern is a variety of ethical issues. The first ethical issue relates to boundaries. The authors insist “when doctors depart from areas of established expertise to promote a nonmedical agenda, they abuse their status as professionals.” The second issue involves the ethics of “taking into account” spiritual issues versus “‘taking them on’ as the objects of interventions.” A third ethical problem focuses on the possibility that physicians might actually do harm to patients by linking health status and spirituality.28
It is fair to say these cautions are worthy of serious consideration and need to be addressed by any responsible model of integration. Certainly there is a need for added research on this subject. Koenig et al,11 for example, in rating the research done on the subject, rate only 18.5% of the studies a 10, 9, or 8 on a scale of 1 to 10 (10=excellent) and assert “we have only scratched the surface in acquiring knowledge about the influences of religion on health, the influences of health on religion, and the mechanisms by which these effects occur.” A review of studies attempting to link religiosity to physiological processes notes that the results are “suggestive,” but that additional research is needed that combines both stronger research methodology with more representative populations.29 Even proponents of integration are aware of the difficulties related to boundaries.30
Providers with an interest in the integration of medicine and spirituality are thus left with a dilemma. On the one hand there appear to be some very good reasons for integration: patient need and desire, the respect such an approach illustrates for the whole person, and strong clues that it does aid with coping, prevention, and recovery. On the other hand, there appear to be very real dangers with integration: a potential violation of boundaries, lack of training, lack of time, and potential misuse of the spiritual.
A model for integration
An appropriate response seems to be finding a model that encourages physicians to treat the patient as a whole person, addressing not only physical, but also social, emotional, and spiritual issues. This model should provide the physician with the ability to identify patients who are struggling with such issues, and the tools for addressing them in an appropriate manner. But this model should take into account the serious issues of time, boundaries, and respect for the deep and complex nature of spiritual and emotional issues.
In general the model should have the following components:
- Good active-listening skills and other tools that encourage the patient to share safely and freely about such issues, providing new self-awareness on the part of the patient, and in some cases spiritual relief.
- Identification of spiritual/emotional issues.
- Appropriate and effective referral of the patient to a “spiritual specialist,” one trained to deal with spiritual issues in a longer term, deeper manner.
- Ongoing communication with the patient and their specialist about this aspect of the person’s healing process.
The first step involves simply asking specific questions to develop a basic understanding of the patients’ spiritual culture. Various sets of questions have been developed to aid practitioners with this task.31-33 It is also a matter of practicing what many have called the “art of medicine.” It is being patient centered and entering into a true dialogue with patients that involves active-listening skills. Active listening is important, because most patients will not make direct statements regarding their feelings or issues. Usually their deep spiritual turmoil is expressed indirectly through body language, tone of voice, stories, and other subtle expressions. True dialogue allows physicians to pick up the clues patients are sending regarding spiritual issues, and to help their patients come to a clear awareness of those issues for themselves.
Once the discussion has begun, it is important to include some element of assessment. A hospital chaplain has developed an assessment tool that he uses to think about the spiritual health of those he visits and to structure his interventions with those patients.34 At Oregon Health and Science University we have adapted his approach by encouraging physicians to develop a set of 5 to 8 paired terms, such as anger and acceptance, which they believe reflect important spiritual issues (Table 3). Using these terms, a continuum is developed that can be used to help assess patients from a spiritual perspective.
A physician can use this continuum to think about the patient and to develop ideas for intervention. First, the physician places an “X” on each continuum of the chart, noting his or her perception of how the patient is functioning.
Second, the physician evaluates that position. Is this a logical place for the patient to be at this place, in this time? Severe anger might be appropriate when one first receives news of a terminal illness. It may not be as appropriate 6 months later.
Third, the physician picks the issue(s) they believe should be addressed through intervention. If a person is feeling helpless, what might be done to help them feel more empowered? The physician can ask what he or she can do. This is likely to be somewhat limited due to training, time, and other issues. The physician can also seek collaboration. Who can be brought into the healing mix, who might become a partner in helping healing happen?
In some cases it will be clear that the patient is spiritual, and that spirituality is a very positive factor in the effort to find wholeness. What these patients need is support, an affirmation that what they are doing is working. They need permission to bring their spirituality into the exam and treatment space as a powerful resource for wellness.35,36 If, for example, a patient is coping well and is maintaining a sense of purpose in the face of a debilitating illness, they should be commended for that, and the coping mechanisms that support that stance should be reinforced.
TABLE 3
Emotional continuums used in spiritual assessment
| Curse ↔ Blessing |
| Dread ↔ Courage |
| Alone ↔ Connected |
| Abandoned ↔ Supported |
| Anger ↔ Acceptance |
| Despair ↔ Hope |
| Meaninglessness ↔ Purpose |
| Helplessness ↔ Empowerment |
Collaborative intervention
Collaboration begins with the patient. The physician must be clear that this is all about the patient’s spirituality (not their own) and support the spiritual beliefs of the patient, working within the framework of those beliefs (unless clearly pathological). But there are many others who can be brought into the therapeutic process. Providers can collaborate with “spiritual specialists,” such as the patient’s spiritual leader or the hospital chaplains. Other collaborators may include social workers, mental health specialists, or even a group of some sort. Research suggests social support is a key factor that leads to improved outcomes.11
Many options are available for intervention. Connecting the patient with a religious leader or “spiritual specialist” is often very appropriate. In hospital settings, chaplains are a good place to begin. In a community-based setting, the patient’s own spiritual leader or, if the patient is not affiliated with any specific group, a spiritual specialist who is willing to work from the patient’s perspective is often the most viable option. Support groups, study groups, worship experiences all can be a part of this strategy. The use of literature and tapes, prayer (best done with a religious professional if possible) are relatively easy responses to spiritual distress. Appointments with various professional “healers” such as social workers and psychologists may also be helpful, and in some cases necessary.
Follow-up is also critical in working with patients. To bring up such sensitive issues as spiritual matters, and then not show a continued interest in them would be detrimental. The physician should return to the issue(s) in following visits, until it is clear that the patient is moving toward resolution, or until the patient indicates they would like to drop the issue. Communication should continue to take place, if possible, between the physician and others working with the patient. Ongoing dialogue with chaplains, religious leaders, therapists, and others should take place.
Pursuing, not avoiding, integration
We are still early in the process of studying and understanding the complex relationship between spirituality and health. Much more research needs to be done to clarify the benefits and dispel the myths. What is it about spirituality and religious practice that benefits patients? Is it, as some have suggested, merely a matter of lifestyle or compliance? Or is there something deeper and more profound involved? When is religious or spiritual coping positive, and when is it negative?
A continued research agenda focusing on the impact of spirituality on health is needed. There is also a need to look at viable assessment tools, as well as appropriate interventions. Perhaps the issue of intervention is the most difficult challenge. What is appropriate? What can be done given time constraints, the need for boundaries, and limited training? Most research to date has focused on the existing spirituality of patients. Research that looks at the impact of practical spiritual interventions, such as spiritual listening, referral to a spiritual specialist, or prayer is needed to move integration to a new stage.
Careful attention to such issues can move us forward in the task of providing effective and humane care to patients. This task is increasingly important in today’s medical environment. As theologian Martin E. Marty notes, “The modern biomedical enterprise—with its threefold work of knowledge acquisition, technology development, and care delivery—urgently needs the guiding visions and values embodied in the faith traditions. When technological momentum or economic necessity alone guides the health care enterprise, the sustaining impulses of respect, meaning and purpose often fall aside.”37
The process of learning how to integrate medicine and spirituality is not an easy one, nor will it be accomplished without struggle. But it is a process vitally important for modern medicine. The issue truly is one of caring, both when cure is possible, and when it is not. It is a matter of focusing on part of what makes us truly human, and supporting a healing process that often transcends the biomedical agenda.
Correspondence
Stephen P. Kliewer, DMin, Department of Family Medicine, Oregon Health and Science University, 3181 SW Sam Jackson Park Road, Portland, OR 97201. E-mail: [email protected].
- Research indicates spirituality and religion are a core aspect of life, and patients want physicians to address issues of spirituality in the context of medical care (C).
- Studies of the effect of patients’ faith on disease outcomes have shown reduced hypertension, better lipid profiles and lower cholesterol levels, and improved immune function (C).
- An appropriate model for addressing patients’ spiritual concerns should include active-listening skills, identification of spiritual/emotional issues, effective referrals to “spiritual specialists,” and ongoing communication about this aspect of the healing process (C).
- Remember, it is all about the patient’s spirituality, not the caregiver’s, and about supporting the patient’s spiritual beliefs (unless clearly pathologic) (C).
Most people have a strong awareness of themselves as spiritual beings. For many, their spirituality profoundly impacts, and is impacted by, illness. A review of studies in which spiritual factors are included suggests spirituality influences the process of healing significantly, either positively or negatively. A healthy spirituality can aid in prevention, improve outcomes, and facilitate coping, and should be supported and encouraged. A negative spirituality can hinder the process of healing and should be addressed.
This article considers means by which physicians may enable patients to express their spiritual concerns and find support for them, without stepping over professional boundaries or imposing personal views on those of patients.
Patients’ regard of spirituality and medical care
According to a myriad surveys, most Americans consider spirituality and religion a significant part of who they are.1,2 Although definitions and expressions vary, in general spirituality is defined as a search for what is sacred or holy in life, coupled with a transcendent (greater than self) relationship with God or a higher power or universal energy.3 Religion is seen as focusing more on prescribed beliefs, rituals, and practices as well as social institutional features,4 and on the undertaking of a spiritual search using specific means or methods (ie, rituals or behaviors) within an identifiable group.
Research in the field indicates that spirituality and religion are seen as a core aspect of life, and patients want physicians to address issues of spirituality in the context of medical care.5,6 A public survey done in 1996 by USA Weekend showed that 63% of patients believe doctors should ask about spirituality issues, but only 10% have actually been asked.2 In another study, 77% of patients surveyed said physicians should consider patients’ spiritual needs, and 37% wanted physicians to discuss religious beliefs with them more frequently.7
Intertwining of medicine and spirituality
The relationship of the discipline of medicine with the world of spirituality has been long and varied. The beginning of medicine was deeply imbedded in spirituality with spiritual leaders being some of the earliest “healers.”
A chasm forms
With the advent of the scientific revolution and the emergence of the scientific method in the late 1500s, the relationship between spirituality and science changed dramatically. Since this new experimental method could not be readily or confidently applied to God, or to one’s experiences with God, religion/spirituality was excluded from the realm of science and a chasm emerged between the 2 realms.
The chasm widened given the religious community’s tendency to reject many of the discoveries generated by the scientific method. Distrust, even dislike, of the spiritual by the medical community became widespread. Mandel, in The Psychobiology of Consciousness, calls spirituality a “temporal lobe dysfunction.”8 Perhaps more telling was the use of spirituality in the glossary of technical terms in Diagnostic and Statistical Manual of Mental Disorders, revised 3rd edition (DSM-III-R).9 In that document, all allusions to spirituality were illustrations of psychopathology; 22.2% of all the negative illustrations in the glossary had religious content, while none had sexual, ethnic, racial, or cultural content.
This negativity was exacerbated by an ever-increasing emphasis on the science of medicine, reflecting the exponential growth of scientific knowledge relevant to medical practice, the public’s demand for technologically sophisticated medical care, and an increased emphasis on tools such as evidence-based medicine. Medical practice became centered on the task of choosing treatments proven effective through rigorous study. Aspects of the “art of medicine” that had not undergone rigid empirical evaluation were considered suspect and deemed unworthy of inclusion in medical practice.
Spanning the chasm
However, a new interest in the integration of medicine and spirituality has emerged. One reflection of this interest is the discussion of the topic in both popular and professional journals. A search by Oregon Health and Science University faculty in 1999 of a large public library database of popular magazines using the key words “spirituality and health” revealed only 25 articles from 1990 to 1994, but over 100 articles from 1995 to 1999.
A similar movement can be seen in the medical literature. A search of MedLine using the keyword “spirituality” produced 52 articles from 1960 to 1990, 90 from 1991 to 1995, and almost 200 from 1996 to 1999. A more recent search produced 554 citations from January 2000 to April 2003.
What outcomes research has shown about spirituality
Much of the focus in this area has been on what research can reveal regarding the impact of spirituality on health. The late David Larson, MD, MSPH, of the International Center for the Integration of Health and Spirituality (ICIHS) and his collaborators extensively reviewed journals and identified large numbers of studies that included spiritual indicators. They found a strong trend toward identifying spirituality as a positive factor for coping with illness, preventing illness, and aiding treatment.3,10
Harold G. Koenig of Duke University continued the effort and recently published a Handbook of Religion and Health.11 This work systematically reviewed and rated around 1600 studies related to the relationships between religion and a variety of mental and physical health conditions, starting with the earliest identified studies through 2000. The research can be broken down into 3 major categories: religion and mental health, religion and physical disorders, and religion and the use of health services. A smaller number of studies focus on research issues, spiritual development, and implications for health and religious professionals ( Table 1).
Although most studies in English have focused on “Western faiths” such as Roman Catholicism, Orthodoxy, mainline and fundamentalist Protestantism, Pentecostalism, Jehovah’s Witnesses, Judaism, and Mormonism, studies have also looked at such faiths as Baha’i, Hare Krishna, Islam, Sikhism, and Hinduism.12,13 In some cases, especially in the area of mental health (depression and psychoses), the type of religious affiliation did seem to be a factor in outcomes, both positive and negative.11
Studies have also included a variety of cultures and nations. Thirty-nine different countries are specifically listed as study locals, with many other studies listing the “world” as the local. Many studies contrast nations, cultures, or faith systems. In some cases these differences were significant, with one study focused on suicide showing opposite results depending on culture.14
Religion and mental health. Studies have looked at the impact of religion or spirituality on well-being, self-esteem, depression and suicide, as well as alcohol and drug use and abuse. Religious or spiritual people, especially those who are regularly involved with a community of faith, experience depression less often than others, are less likely to abuse drugs or alcohol, cope with life-issues and illness more effectively, and are less likely to commit suicide.11
Religion and physical disorders. Studies have focused specifically on the effect of faith on heart disease, hypertension, cerebrovascular disease, immune system dysfunctions, and cancer. Other studies have looked at broader issues such as pain and mortality.11 Results have shown reduced hypertension,15,16 better lipid profiles,17,18 improved immune function,19,20 and lower cholesterol levels21 ( Table 2).
A recent article in American Psychologist notes there is more evidence that religion or spirituality impedes recovery than it improves recovery.21 However, the evidence cited by the article was connected to religious struggle or to negative coping (eg, “I feel God has abandoned me”). This is not surprising, and it underscores the need to support positive religious coping and to help patients move beyond negative religious coping.
Religion and use of health services. Studies looking at the use of health services focus on such matters as screening services22 and compliance.23 One of the interesting factors here is the role of religion in noncompliance. The refusal of Jehovah’s Witnesses to receive blood products has been a highly visible example. But other issues—more subtle, but nevertheless critical—emerge when one examines the literature; these include noncompliance due to a belief that a higher power “caused” the illness, or that illness is the result of “sinful” behavior.24
In general, research shows the impact of religion and spirituality is positive. Although a person’s spirituality sometimes is pathological, and spiritual beliefs can create health issues, an overwhelming number of studies show a positive benefit. Of those studies reviewed by Koenig et al,11 where the impact of spirituality could be classified as positive, negative, no association, complex, or mixed, 70% showed a positive impact (68% a strong positive with P<.05) while only 5% showed a negative impact. The studies show spirituality and religion benefit patients by helping prevent illness, increasing the ability to cope, and improving outcomes.
TABLE 1
Areas of spirituality research to date
| Major focus | Subtopics | Earliest publication | Number of publications |
|---|---|---|---|
| Mental health | Religious coping, hope and optimism, purpose/meaning in life, self-esteem, bereavement, social support, depression, suicide, assisted suicide/euthanasia, anxiety, schizophrenia/psychosis, alcohol use/abuse, drug use/abuse, delinquency/crime, marital instability, personality, general mental health | 1932 | 1075 |
| Physical health | Heart disease, hypertension, cerebrovascular disease, immune system, cancer risk, mortality, functional disability, pain and somatic symptoms, health behaviors, miscellaneous | 1902 | 455 |
| Use of health services | General medical services, mental health services, disease prevention, health responsibility, compliance | 1960 | 53 |
| Clinical implications and applications | Health professionals, religious professionals | 1973 | 131 |
| Research | Measurement | 1967 | 40 |
| Miscellaneous | Religious beliefs/behaviors, religious/faith development, religious conversion, spiritual/faith healing, prayer, death and dying, religious harm | 1902 | 171 |
TABLE 2
Propositions regarding the effect of spirituality on physical outcomes
| Proposition Studies | Rating* #-Letter |
|---|---|
| Religious coping aids stress management | |
| Ellison, CG, Taylor RJ. Turning to prayer: Social and situational antecedents of religious coping among African Americans. Rev Religious Research 1996; 38:111–131. | 8/NA |
| Pargament KI, Smith BW, Koenig HG, et al. Patterns of positive and negative religious 8/NA coping with major life stressors. J Scientific Study Religion 1998; 37(4):710–724. | 8/NA |
| Spirituality/religious affiliation prevents substance abuse | |
| Bell R, Wechsler H, Johnston LD. Correlates of college student marijuana use: Results of a US national survey. Addiction 1997; 92:571–581. | 9/NA |
| Religious practices/spirituality decreases the incidence of depression | |
| Idler EL, Kasl S. Religion, disability, depression, and the timing of death. Am J Sociology 1992; 97:1052–1079. | 10/NA |
| Kennedy GJ, Kelman HR, Thomas C, et al. The relation of religious preference 10/NA and practice to depressive symptoms among 1,855 older adults. J Gerontol 1996; 51B:301–308. | 10/NA |
| Religious practice/spirituality lowers suicide rates | |
| Neeleman J, Halpern D, Leon D. Tolerance of suicide, religion, and suicide rates: An ecological and individual study in 19 Western countries. Psychol Med 1997; 27(5):1165–1171. | 10/NA |
| Religious practice/spirituality prevents hypertension/lowers blood pressure | |
| Steffen PR, Hinderliter AL, Blumenthal JA, et al. Religious coping, ethnicity, and ambulatory blood pressure. Psychosomatic Med 2001; 63:523–530. | 7–A/B |
| Koenig, HG, George LK, Hays, JC, et al. The relationships between religious activities 9 A/B and blood pressure in older adults. International J Psych Med 1998; 28:189–213. | 7–A/B |
| Religious practice/spirituality is related to better lipid profiles | |
| Friedlander Y, Kark JD, Stein Y. Religious observance and plasma lipids and lipoproteins among 17 year old Jewish residents of Jerusalem. Prevent Med 1987; 16:70–79. | 8-B |
| Religious practice/spirituality is associated with better immune function | |
| Woods TE, Antoni MH, Ironson GH, et al. Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. J Psychosomatic Research 1999; 46:165–176. | 7-B |
| Koenig HG, Cohen JH, George LK, et al. Attendance at religious services, interleukin-6, 8-A/B and other biological parameters of immune function in older adults, International J Psych Med 1997; 27:233–250. | 7-B |
| Religious practice/spirituality is related to lower cholesterol | |
| Patel, C, Marmot MG, Terry DJ, et al. Trial of relaxation in reducing coronary risk: Four year follow up. Brit Med J 1985; 290:1103–1106 | NA/A |
| Attendance at church services leads to longer life | |
| Koenig JG, Hays JC, Larson DB, et al. Does religious attendance prolong survival? A six-year follow-up study of 3,968 older adults. J Gerontology Series A: Biologic Sci Med Sci 1999; 54A:M370–M376. | 9-A |
| *Ratings Systems: Koenig/Miller | |
| Number = Rating system from Koenig et al. Handbook of Religion and Health. Scale of 1–10 (1=poor, 10=excellent). Based on overall study design, sampling method, quality of religious measure, quality of statistical analysis, interpretation of results, and discussion in the context of existing literature). Methodology validated by outside reviewers. | |
| Letter = Rating system from Miller WR, Thoresen CE, Spirituality, Religion and Health: An Emerging Research Field. A = Methodologically Sound B= Methodologically Sound with at least one methodological limitation. | |
| NA = not rated by this system | |
Barriers and issues
In spite of the evidence showing religion and spirituality to be positive health factors, there are still reasons to be cautious. Many obvious concerns have been expressed by physicians in recent surveys.25,26 More than 50% of physicians surveyed by Ellis and colleagues26 listed such factors as time, lack of training in taking a spiritual history, and a concern about projecting their own beliefs onto patients as barriers to discussing spiritual issues.
Recently a group of articles strongly challenged the entire premise of integration. Richard P. Sloan and his associates, in the “Sounding Board” section of the New England Journal of Medicine, said they are “troubled by the uncritical embrace of this trend….”27 They cite a number of reasons to be wary of this integration:
- Studies suggesting a relationship between spirituality and health are flawed.
- The unique nature of the patient/physician relationship causes physician assumptions and beliefs to have undue influence.
- Physicians have no expertise in spiritual matters.
- Most patients do not truly want to discuss spiritual issues, and interest does not necessarily justify the incorporation of religious matters.
- The integration of spirituality into practice is an attempt to use religion that trivializes a deep and complex reality.
A similar article in the Lancet echoed these concerns.28 Again, the empirical evidence is challenged. Added to that concern is a variety of ethical issues. The first ethical issue relates to boundaries. The authors insist “when doctors depart from areas of established expertise to promote a nonmedical agenda, they abuse their status as professionals.” The second issue involves the ethics of “taking into account” spiritual issues versus “‘taking them on’ as the objects of interventions.” A third ethical problem focuses on the possibility that physicians might actually do harm to patients by linking health status and spirituality.28
It is fair to say these cautions are worthy of serious consideration and need to be addressed by any responsible model of integration. Certainly there is a need for added research on this subject. Koenig et al,11 for example, in rating the research done on the subject, rate only 18.5% of the studies a 10, 9, or 8 on a scale of 1 to 10 (10=excellent) and assert “we have only scratched the surface in acquiring knowledge about the influences of religion on health, the influences of health on religion, and the mechanisms by which these effects occur.” A review of studies attempting to link religiosity to physiological processes notes that the results are “suggestive,” but that additional research is needed that combines both stronger research methodology with more representative populations.29 Even proponents of integration are aware of the difficulties related to boundaries.30
Providers with an interest in the integration of medicine and spirituality are thus left with a dilemma. On the one hand there appear to be some very good reasons for integration: patient need and desire, the respect such an approach illustrates for the whole person, and strong clues that it does aid with coping, prevention, and recovery. On the other hand, there appear to be very real dangers with integration: a potential violation of boundaries, lack of training, lack of time, and potential misuse of the spiritual.
A model for integration
An appropriate response seems to be finding a model that encourages physicians to treat the patient as a whole person, addressing not only physical, but also social, emotional, and spiritual issues. This model should provide the physician with the ability to identify patients who are struggling with such issues, and the tools for addressing them in an appropriate manner. But this model should take into account the serious issues of time, boundaries, and respect for the deep and complex nature of spiritual and emotional issues.
In general the model should have the following components:
- Good active-listening skills and other tools that encourage the patient to share safely and freely about such issues, providing new self-awareness on the part of the patient, and in some cases spiritual relief.
- Identification of spiritual/emotional issues.
- Appropriate and effective referral of the patient to a “spiritual specialist,” one trained to deal with spiritual issues in a longer term, deeper manner.
- Ongoing communication with the patient and their specialist about this aspect of the person’s healing process.
The first step involves simply asking specific questions to develop a basic understanding of the patients’ spiritual culture. Various sets of questions have been developed to aid practitioners with this task.31-33 It is also a matter of practicing what many have called the “art of medicine.” It is being patient centered and entering into a true dialogue with patients that involves active-listening skills. Active listening is important, because most patients will not make direct statements regarding their feelings or issues. Usually their deep spiritual turmoil is expressed indirectly through body language, tone of voice, stories, and other subtle expressions. True dialogue allows physicians to pick up the clues patients are sending regarding spiritual issues, and to help their patients come to a clear awareness of those issues for themselves.
Once the discussion has begun, it is important to include some element of assessment. A hospital chaplain has developed an assessment tool that he uses to think about the spiritual health of those he visits and to structure his interventions with those patients.34 At Oregon Health and Science University we have adapted his approach by encouraging physicians to develop a set of 5 to 8 paired terms, such as anger and acceptance, which they believe reflect important spiritual issues (Table 3). Using these terms, a continuum is developed that can be used to help assess patients from a spiritual perspective.
A physician can use this continuum to think about the patient and to develop ideas for intervention. First, the physician places an “X” on each continuum of the chart, noting his or her perception of how the patient is functioning.
Second, the physician evaluates that position. Is this a logical place for the patient to be at this place, in this time? Severe anger might be appropriate when one first receives news of a terminal illness. It may not be as appropriate 6 months later.
Third, the physician picks the issue(s) they believe should be addressed through intervention. If a person is feeling helpless, what might be done to help them feel more empowered? The physician can ask what he or she can do. This is likely to be somewhat limited due to training, time, and other issues. The physician can also seek collaboration. Who can be brought into the healing mix, who might become a partner in helping healing happen?
In some cases it will be clear that the patient is spiritual, and that spirituality is a very positive factor in the effort to find wholeness. What these patients need is support, an affirmation that what they are doing is working. They need permission to bring their spirituality into the exam and treatment space as a powerful resource for wellness.35,36 If, for example, a patient is coping well and is maintaining a sense of purpose in the face of a debilitating illness, they should be commended for that, and the coping mechanisms that support that stance should be reinforced.
TABLE 3
Emotional continuums used in spiritual assessment
| Curse ↔ Blessing |
| Dread ↔ Courage |
| Alone ↔ Connected |
| Abandoned ↔ Supported |
| Anger ↔ Acceptance |
| Despair ↔ Hope |
| Meaninglessness ↔ Purpose |
| Helplessness ↔ Empowerment |
Collaborative intervention
Collaboration begins with the patient. The physician must be clear that this is all about the patient’s spirituality (not their own) and support the spiritual beliefs of the patient, working within the framework of those beliefs (unless clearly pathological). But there are many others who can be brought into the therapeutic process. Providers can collaborate with “spiritual specialists,” such as the patient’s spiritual leader or the hospital chaplains. Other collaborators may include social workers, mental health specialists, or even a group of some sort. Research suggests social support is a key factor that leads to improved outcomes.11
Many options are available for intervention. Connecting the patient with a religious leader or “spiritual specialist” is often very appropriate. In hospital settings, chaplains are a good place to begin. In a community-based setting, the patient’s own spiritual leader or, if the patient is not affiliated with any specific group, a spiritual specialist who is willing to work from the patient’s perspective is often the most viable option. Support groups, study groups, worship experiences all can be a part of this strategy. The use of literature and tapes, prayer (best done with a religious professional if possible) are relatively easy responses to spiritual distress. Appointments with various professional “healers” such as social workers and psychologists may also be helpful, and in some cases necessary.
Follow-up is also critical in working with patients. To bring up such sensitive issues as spiritual matters, and then not show a continued interest in them would be detrimental. The physician should return to the issue(s) in following visits, until it is clear that the patient is moving toward resolution, or until the patient indicates they would like to drop the issue. Communication should continue to take place, if possible, between the physician and others working with the patient. Ongoing dialogue with chaplains, religious leaders, therapists, and others should take place.
Pursuing, not avoiding, integration
We are still early in the process of studying and understanding the complex relationship between spirituality and health. Much more research needs to be done to clarify the benefits and dispel the myths. What is it about spirituality and religious practice that benefits patients? Is it, as some have suggested, merely a matter of lifestyle or compliance? Or is there something deeper and more profound involved? When is religious or spiritual coping positive, and when is it negative?
A continued research agenda focusing on the impact of spirituality on health is needed. There is also a need to look at viable assessment tools, as well as appropriate interventions. Perhaps the issue of intervention is the most difficult challenge. What is appropriate? What can be done given time constraints, the need for boundaries, and limited training? Most research to date has focused on the existing spirituality of patients. Research that looks at the impact of practical spiritual interventions, such as spiritual listening, referral to a spiritual specialist, or prayer is needed to move integration to a new stage.
Careful attention to such issues can move us forward in the task of providing effective and humane care to patients. This task is increasingly important in today’s medical environment. As theologian Martin E. Marty notes, “The modern biomedical enterprise—with its threefold work of knowledge acquisition, technology development, and care delivery—urgently needs the guiding visions and values embodied in the faith traditions. When technological momentum or economic necessity alone guides the health care enterprise, the sustaining impulses of respect, meaning and purpose often fall aside.”37
The process of learning how to integrate medicine and spirituality is not an easy one, nor will it be accomplished without struggle. But it is a process vitally important for modern medicine. The issue truly is one of caring, both when cure is possible, and when it is not. It is a matter of focusing on part of what makes us truly human, and supporting a healing process that often transcends the biomedical agenda.
Correspondence
Stephen P. Kliewer, DMin, Department of Family Medicine, Oregon Health and Science University, 3181 SW Sam Jackson Park Road, Portland, OR 97201. E-mail: [email protected].
1. Gallup G, Jr, Lindsay DM. Surveying the Religious Landscape: Trends in US Beliefs. Harrisburg, Pa: Morehouse; 1999:21.
2. McNichol T. (1996) The new faith in medicine. USA Weekend, April:5-7,4-5.
3. Larson DB, Swyers JP, McCullough ME. Scientific Research on Spirituality and Health: A Consensus Report. Rockville, Md: National Institute for Healthcare Research; 1997.
4. Zinnbauer BJ, Pargament KI, Cole B, et al. Religion and spirituality: Unfuzzying the fuzzy. J Scientific Study Religion 1998;36:549-564.
5. Ehman JW, Ott BB, Short TH. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med 1999;159:1803-1806.
6. Daaleman TP, Nease DE, Jr. Patient attitudes regarding physician inquiry into spiritual and religious issues. J Fam Pract 1994;39:564-568.
7. King DE, Bushwick B. Beliefs and attitudes of hospital inpatients about faith healing and prayer. J Fam Pract 1994;39:349-352.
8. Mandel AJ. Toward a psychobiology of transcendence: God in the brain. In RJ Davidson and JM Davidson, eds: The Psychobiology of Consciousness. New York, NY: Plenum; 1980;379-479.
9. American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed, rev (DSM-III-R). Washington, DC: American Psychiatric Press; 1987.
10. Miller WR, ed. Integrating Spirituality into Treatment. Washington, DC: American Psychological Association; 1999:3.
11. Koenig HG, McCullough ME, Larson DB. Handbook of Religion and Health. Oxford: Oxford University Press; 2001.
12. Gupta R, Prakash H, Gupta VP, Gupta KD. Prevalence and determinants of coronary heart disease in a rural population of India. J Clin Epidemiol 1997;50:203-209.
13. Gopinath N, Chadha S, Jain P, Shekhawat S, Tandon R. An epidemiological study of coronary heart disease in different ethnic groups in a Delhi urban population. J Assoc Physicians India 1995;43:30-33.
14. Zhang J, Jin S. Determinants of suicide ideation: A comparison of Chinese and American college students. Adolescence 1996;31:451-467.
15. Koenig HG, George LK, Hays JC, Larson DB, Cohen HJ, Blazer DG. The relationships between religious activities and blood pressure in older adults. Int J Psychiatry Med 1998;28:189-213.
16. Steffen PR, Hinderliter AL, Blumenthal JA, Sherwood A. Religious coping, ethnicity, and ambulatory blood pressure. Psychosomatic Medicine 2001;63:523-530.
17. Friedlander Y, Kark JD, Kaufmann NA, Stein Y. Coronary heart disease risk factors among religious groups in a Jewish population sample in Jerusalem. Am J Clin Nutrition 1985;42:511-521.
18. Friedlander Y, Kark JD, Stein Y. Religious observance and plasma lipids and lipoproteins among 17 year old Jewish residents of Jerusalem. Preventive Medicine 1987;16:70-79.
19. Koenig HG, Cohen JH, George LK, Hayes JC, Larson DB, Blazer DG. Attendance at religious services, interleukin-6, and other biological parameters of immune function in older adults. Int J Psychiatry Med 1987;27:233-250.
20. Woods TE, Antoni MH, Ironson GH, Kling DW. Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. J Psychosomatic Research 1999;46:165-176.
21. Powell L, Shahabi L, Thoresen CE. Religion and spirituality: linkages to physical health. Am Psychol 2003;58:36-52.
22. Naguib SM, Geiser PB, Comstock GW. Responses to a program of screening for cervical cancer. Public Health Reports 1968;83:990-998.
23. O’Brien ME. Religious faith and adjustment to long-term hemodialysis. J Religion Faith 1982;21:68-80.
24. Foulks EF, Persons JB, Merkel RL. The effect of patients’ beliefs about their illness on compliance in psychotherapy. Am J Psychiatry 1986;143:340-344.
25. Graigie F, Hobbs R, III. Spiritual perspectives and practices of family physicians with an expressed interest in spirituality. Fam Med 1999;31:578-585.
26. Ellis M, Vinson D, Ewigman B. Addressing spiritual concerns with patients: family physicians attitudes and practices. J Fam Pract 1999;48:105-109.
27. Sloan RP, Bagiella E, VandeCreek L, et al. Should physicians prescribe religious activities? N Engl J Med 2000;342:913-916Sounding Board.
28. Sloan RP, Bagiella E, Powell T. Religion spirituality, and medicine. Lancet 1999;343:664-667.
29. Seeman TE, Dubin LF, Seeman M. Religiosity/spirituality and health: a critical review of the evidence for biological pathways. Am Psychologist 2003;58:53-63.
30. Post SG, Puchalski CM, Larson DB. Physicians and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med 2000;132:578-583.
31. Maugans TA. The spiritual history. Arch Fam Med 1996;5:11-16.
32. Puchalski CM, Romer AL. Taking a spiritual history allows clinicians to understand patients more fully. J Palliative Med 2000;3:129-137.
33. Anandarajah G, Hight E. Spirituality and medical practice: using the HOPE questions as a practical tool for spiritual assessment. Am Fam Physician 2001;63:81-89.
34. Hodges S. Spiritual screening: the starting place for intentional pastoral care. Chaplaincy Today 1999;15:30-39.
35. Dewald PA. Psychotherapy: A Dynamic Approach. New York, NY: Basic Books; 1971;105:127.-
36. Clinebell H. Growth Counseling. Nashville, Tenn: Abingdon; 1979;96-97.
37. Numbers RL, Amundsen DW. Caring and Curing: Health and Medicine in the Western Religious Traditions. Baltimore, Md: Johns Hopkins University Press; 1998:viii.
1. Gallup G, Jr, Lindsay DM. Surveying the Religious Landscape: Trends in US Beliefs. Harrisburg, Pa: Morehouse; 1999:21.
2. McNichol T. (1996) The new faith in medicine. USA Weekend, April:5-7,4-5.
3. Larson DB, Swyers JP, McCullough ME. Scientific Research on Spirituality and Health: A Consensus Report. Rockville, Md: National Institute for Healthcare Research; 1997.
4. Zinnbauer BJ, Pargament KI, Cole B, et al. Religion and spirituality: Unfuzzying the fuzzy. J Scientific Study Religion 1998;36:549-564.
5. Ehman JW, Ott BB, Short TH. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med 1999;159:1803-1806.
6. Daaleman TP, Nease DE, Jr. Patient attitudes regarding physician inquiry into spiritual and religious issues. J Fam Pract 1994;39:564-568.
7. King DE, Bushwick B. Beliefs and attitudes of hospital inpatients about faith healing and prayer. J Fam Pract 1994;39:349-352.
8. Mandel AJ. Toward a psychobiology of transcendence: God in the brain. In RJ Davidson and JM Davidson, eds: The Psychobiology of Consciousness. New York, NY: Plenum; 1980;379-479.
9. American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed, rev (DSM-III-R). Washington, DC: American Psychiatric Press; 1987.
10. Miller WR, ed. Integrating Spirituality into Treatment. Washington, DC: American Psychological Association; 1999:3.
11. Koenig HG, McCullough ME, Larson DB. Handbook of Religion and Health. Oxford: Oxford University Press; 2001.
12. Gupta R, Prakash H, Gupta VP, Gupta KD. Prevalence and determinants of coronary heart disease in a rural population of India. J Clin Epidemiol 1997;50:203-209.
13. Gopinath N, Chadha S, Jain P, Shekhawat S, Tandon R. An epidemiological study of coronary heart disease in different ethnic groups in a Delhi urban population. J Assoc Physicians India 1995;43:30-33.
14. Zhang J, Jin S. Determinants of suicide ideation: A comparison of Chinese and American college students. Adolescence 1996;31:451-467.
15. Koenig HG, George LK, Hays JC, Larson DB, Cohen HJ, Blazer DG. The relationships between religious activities and blood pressure in older adults. Int J Psychiatry Med 1998;28:189-213.
16. Steffen PR, Hinderliter AL, Blumenthal JA, Sherwood A. Religious coping, ethnicity, and ambulatory blood pressure. Psychosomatic Medicine 2001;63:523-530.
17. Friedlander Y, Kark JD, Kaufmann NA, Stein Y. Coronary heart disease risk factors among religious groups in a Jewish population sample in Jerusalem. Am J Clin Nutrition 1985;42:511-521.
18. Friedlander Y, Kark JD, Stein Y. Religious observance and plasma lipids and lipoproteins among 17 year old Jewish residents of Jerusalem. Preventive Medicine 1987;16:70-79.
19. Koenig HG, Cohen JH, George LK, Hayes JC, Larson DB, Blazer DG. Attendance at religious services, interleukin-6, and other biological parameters of immune function in older adults. Int J Psychiatry Med 1987;27:233-250.
20. Woods TE, Antoni MH, Ironson GH, Kling DW. Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. J Psychosomatic Research 1999;46:165-176.
21. Powell L, Shahabi L, Thoresen CE. Religion and spirituality: linkages to physical health. Am Psychol 2003;58:36-52.
22. Naguib SM, Geiser PB, Comstock GW. Responses to a program of screening for cervical cancer. Public Health Reports 1968;83:990-998.
23. O’Brien ME. Religious faith and adjustment to long-term hemodialysis. J Religion Faith 1982;21:68-80.
24. Foulks EF, Persons JB, Merkel RL. The effect of patients’ beliefs about their illness on compliance in psychotherapy. Am J Psychiatry 1986;143:340-344.
25. Graigie F, Hobbs R, III. Spiritual perspectives and practices of family physicians with an expressed interest in spirituality. Fam Med 1999;31:578-585.
26. Ellis M, Vinson D, Ewigman B. Addressing spiritual concerns with patients: family physicians attitudes and practices. J Fam Pract 1999;48:105-109.
27. Sloan RP, Bagiella E, VandeCreek L, et al. Should physicians prescribe religious activities? N Engl J Med 2000;342:913-916Sounding Board.
28. Sloan RP, Bagiella E, Powell T. Religion spirituality, and medicine. Lancet 1999;343:664-667.
29. Seeman TE, Dubin LF, Seeman M. Religiosity/spirituality and health: a critical review of the evidence for biological pathways. Am Psychologist 2003;58:53-63.
30. Post SG, Puchalski CM, Larson DB. Physicians and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med 2000;132:578-583.
31. Maugans TA. The spiritual history. Arch Fam Med 1996;5:11-16.
32. Puchalski CM, Romer AL. Taking a spiritual history allows clinicians to understand patients more fully. J Palliative Med 2000;3:129-137.
33. Anandarajah G, Hight E. Spirituality and medical practice: using the HOPE questions as a practical tool for spiritual assessment. Am Fam Physician 2001;63:81-89.
34. Hodges S. Spiritual screening: the starting place for intentional pastoral care. Chaplaincy Today 1999;15:30-39.
35. Dewald PA. Psychotherapy: A Dynamic Approach. New York, NY: Basic Books; 1971;105:127.-
36. Clinebell H. Growth Counseling. Nashville, Tenn: Abingdon; 1979;96-97.
37. Numbers RL, Amundsen DW. Caring and Curing: Health and Medicine in the Western Religious Traditions. Baltimore, Md: Johns Hopkins University Press; 1998:viii.
Is religious devotion relevant to the doctor-patient relationship?
- For the faithful, a secularist approach to “generic religion” is of little value; the value of religious belief lies precisely in its particularity (C).
- For the devout, no dimension of life is unaffected by religious beliefs (C).
- Even when physician and patient speak from religiously discordant perspectives, the physician can compassionately and sensitively engage the patient on the patient’s terms, rather than forcing the patient to address difficult questions within a foreign moral framework (C).
- An enriched dialectic will enable sensitive and appropriate care for religiously devout patients, ensuring that their concerns are addressed more than superficially (C).
As I walked toward the elevators at the end of a her bed, staring blankly into the hall. Like many on the oncology floor, she had lost her hair. I waved at her. She nodded. I took a few steps into her room. long call night, I saw a patient sitting on the edge of
I introduced myself; she told me her name—Julie. I asked Julie how she was feeling. “I’m trying to make a decision,” she said, choking back emotion. She explained she was trying to decide whether to allow placement of a permanent chest tube to drain her recurrent pleural effusion.
“I don’t know if I can take it any more,” Julie said. “I’ve been through too much.” She knew she was dying and was reluctant to endure another painful procedure.
As a medical student, I could not offer her advice. But I hoped my presence would be a comfort. We talked about her life, her work, her interests, and her family (she was alone in the city). As we talked, she reminisced, joked, and cried about the experiences that had enriched her life. On my way out, I told her that I would be praying for her—and she broke into tears. “Can you pray with me?” she asked.
A changing landscape
For years, the medical profession has witnessed a growing interest in all things spiritual. A recent increase in scholarly attention to spirituality in medicine reflects the larger trend in the culture. (“Principles to make a spiritual assessment work in your practice,”) Yet this renewed interest in faith is not without caveats.
Scientific misunderstanding of faith
Empirical studies of the salutary effects of faith on everything from the immune system to recovery from surgery has, not surprisingly, elevated religion’s effects over its claims, contributing to widespread support of what theologians Shuman and Meador call a “generic religion." (“Allowing spirituality into the healing process,”)
Spirituality ignored diminishes medical encounter
Suffering has a way of pointing patients toward the transcendent, and the discussions that accompany this inner process require a vocabulary beyond that of physiology and pathology. The artificial neutrality of enforced secularism inevitably leads to a discussion that is conceptually impoverished, lacking the language to address the existential questions of suffering in ways that are meaningful to the patient. By honestly sharing their own experiences and perspectives, and sensitively inquiring about the patient’s worldview, physicians can raise the level of discussion and create a powerful experience of shared humanity.
This enriched dialectic will enable sensitive and appropriate care for religiously devout patients, ensuring that their concerns are addressed more than superficially. In this way, the clinical encounter will be defined neither by the bland commendation of a generic religion for its salutary effects, nor by the enforced secularism of modernity, but by the contextualization of a patient’s illness against the particularities of her life commitments. When a Muslim with diabetes inquires about fasting during Ramadan, when a Catholic grandfather speaks of divine healing of his cancer, and when a Buddhist teenager explains the role that ulcerative colitis has played in her spiritual development, the relationship between physician and patient will deepen, transforming the medical encounter into an “interhuman event.”23
Ackowledgments
We are indebted to Daniel Hall for his careful review of this manuscript and to Bobbie Sweitzer for her thoughtful critique of these ideas.
Corresponding author
Peter P. Moschovis, 1700 E. 56th St., #3010, Chicago, IL 60637. E-mail:[email protected]
1. Weaver AJ, Flannelly KJ, Oppenheimer JE. Religion, spirituality, and chaplains in the biomedical literature: 1965–2000. Int J Psychiatry Med 2003;33:155-161.
2. Puchalski CM, Larson DB. Developing curricula in spirituality and medicine. Acad Med 1998;73:970-974.
3. Brokaw JJ, Tunnicliff G, Raess BU, Saxon DW. The teaching of complementary and alternative medicine in U.S. medical schools: a survey of course directors. Acad Med 2002;77:876-881.
4. Shuman JJ, Meador KG. Heal Thyself: Spirituality, Medicine, and the Distortion of Christianity. New York, NY: Oxford University Press; 2002.
5. Benson Herbert. Timeless Healing: The Power of Biology of Belief. New York, NY: Scribners; 1996.
6. Gorsuch RL, Mcpherson SE. Intrinsic-Extrinsic Measurement, I/E-Revised and Single-Item Scales. J Sci Study Relig 1989;28:348-354.
7. Allport GW. The Individual and His Religion. New York, NY: MacMillian 1962.
8. Allport GW, Ross J. Personal religious orientation and prejudice. J Pers Soc Psychol 1967;5:447-457.
9. Scheurich N. Reconsidering spirituality and medicine. Acad Med 2003;78:356-360.
10. Ehman JW, Ott BB, Short TH, Ciampa RC, Hansen Flaschen J. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med 1999;159:1803-1806.
11. King DE, Bushwick B. Beliefs and attitudes of hospital inpatients about faith healing and prayer. J Fam Pract 1994;39:349-352.
12. MacLean CD, Susi B, Phifer N, et al. Patient preference for physician discussion and practice of spirituality. J Gen Intern Med 2003;18:38-43.
13. Sloan RP, Bagiella E, VandeCreek L, et al. Should physicians prescribe religious activities? N Engl J Med 2000;342:1913-1916.
14. Post SG, Puchalski CM, Larson DB. Physicians and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med 2000;132:578-583.
15. Lawrence RJ. The witches’ brew of spirituality and medicine. Ann Behav Med 2002;24:74-76.
16. Lo B, Ruston D, Kates LW, et al. Discussing religious and spiritual issues at the end of life: a practical guide for physicians. JAMA 2002;287:749-754.
17. Fish SE. The Trouble With Principle. Cambridge, Mass: Harvard University Press; 1999.
18. Hall DE, Koenig HG, Meador KG. Conceptualizing “religion”: How language shapes and constrains knowledge in the study of religion and health. Perspect Biol Med 2004;In press.
19. Hall DE, Curlin F. Can physicians’ care be neutral regarding religion? Acad Med 2004;in press.
20. MacIntyre A. After Virtue A Study in Moral Theory. 2nd ed Notre Dame, Ind: University of Notre Dame Press; 1984.
21. MacIntyre A. Whose Justice, Which Rationality? Notre Dame, Ind: University of Notre Dame Press; 1988.
22. Plantinga A, Wolsterstorff N. Faith and Rationality: Reason and Belief in God. Notre Dame, Ind: University of Notre Dame Press; 1984.
23. Pellegrino E, Thomasma D. A Philosophical Basis of Medical Practice. New York, NY: Oxford University Press; 1981.
- For the faithful, a secularist approach to “generic religion” is of little value; the value of religious belief lies precisely in its particularity (C).
- For the devout, no dimension of life is unaffected by religious beliefs (C).
- Even when physician and patient speak from religiously discordant perspectives, the physician can compassionately and sensitively engage the patient on the patient’s terms, rather than forcing the patient to address difficult questions within a foreign moral framework (C).
- An enriched dialectic will enable sensitive and appropriate care for religiously devout patients, ensuring that their concerns are addressed more than superficially (C).
As I walked toward the elevators at the end of a her bed, staring blankly into the hall. Like many on the oncology floor, she had lost her hair. I waved at her. She nodded. I took a few steps into her room. long call night, I saw a patient sitting on the edge of
I introduced myself; she told me her name—Julie. I asked Julie how she was feeling. “I’m trying to make a decision,” she said, choking back emotion. She explained she was trying to decide whether to allow placement of a permanent chest tube to drain her recurrent pleural effusion.
“I don’t know if I can take it any more,” Julie said. “I’ve been through too much.” She knew she was dying and was reluctant to endure another painful procedure.
As a medical student, I could not offer her advice. But I hoped my presence would be a comfort. We talked about her life, her work, her interests, and her family (she was alone in the city). As we talked, she reminisced, joked, and cried about the experiences that had enriched her life. On my way out, I told her that I would be praying for her—and she broke into tears. “Can you pray with me?” she asked.
A changing landscape
For years, the medical profession has witnessed a growing interest in all things spiritual. A recent increase in scholarly attention to spirituality in medicine reflects the larger trend in the culture. (“Principles to make a spiritual assessment work in your practice,”) Yet this renewed interest in faith is not without caveats.
Scientific misunderstanding of faith
Empirical studies of the salutary effects of faith on everything from the immune system to recovery from surgery has, not surprisingly, elevated religion’s effects over its claims, contributing to widespread support of what theologians Shuman and Meador call a “generic religion." (“Allowing spirituality into the healing process,”)
Spirituality ignored diminishes medical encounter
Suffering has a way of pointing patients toward the transcendent, and the discussions that accompany this inner process require a vocabulary beyond that of physiology and pathology. The artificial neutrality of enforced secularism inevitably leads to a discussion that is conceptually impoverished, lacking the language to address the existential questions of suffering in ways that are meaningful to the patient. By honestly sharing their own experiences and perspectives, and sensitively inquiring about the patient’s worldview, physicians can raise the level of discussion and create a powerful experience of shared humanity.
This enriched dialectic will enable sensitive and appropriate care for religiously devout patients, ensuring that their concerns are addressed more than superficially. In this way, the clinical encounter will be defined neither by the bland commendation of a generic religion for its salutary effects, nor by the enforced secularism of modernity, but by the contextualization of a patient’s illness against the particularities of her life commitments. When a Muslim with diabetes inquires about fasting during Ramadan, when a Catholic grandfather speaks of divine healing of his cancer, and when a Buddhist teenager explains the role that ulcerative colitis has played in her spiritual development, the relationship between physician and patient will deepen, transforming the medical encounter into an “interhuman event.”23
Ackowledgments
We are indebted to Daniel Hall for his careful review of this manuscript and to Bobbie Sweitzer for her thoughtful critique of these ideas.
Corresponding author
Peter P. Moschovis, 1700 E. 56th St., #3010, Chicago, IL 60637. E-mail:[email protected]
- For the faithful, a secularist approach to “generic religion” is of little value; the value of religious belief lies precisely in its particularity (C).
- For the devout, no dimension of life is unaffected by religious beliefs (C).
- Even when physician and patient speak from religiously discordant perspectives, the physician can compassionately and sensitively engage the patient on the patient’s terms, rather than forcing the patient to address difficult questions within a foreign moral framework (C).
- An enriched dialectic will enable sensitive and appropriate care for religiously devout patients, ensuring that their concerns are addressed more than superficially (C).
As I walked toward the elevators at the end of a her bed, staring blankly into the hall. Like many on the oncology floor, she had lost her hair. I waved at her. She nodded. I took a few steps into her room. long call night, I saw a patient sitting on the edge of
I introduced myself; she told me her name—Julie. I asked Julie how she was feeling. “I’m trying to make a decision,” she said, choking back emotion. She explained she was trying to decide whether to allow placement of a permanent chest tube to drain her recurrent pleural effusion.
“I don’t know if I can take it any more,” Julie said. “I’ve been through too much.” She knew she was dying and was reluctant to endure another painful procedure.
As a medical student, I could not offer her advice. But I hoped my presence would be a comfort. We talked about her life, her work, her interests, and her family (she was alone in the city). As we talked, she reminisced, joked, and cried about the experiences that had enriched her life. On my way out, I told her that I would be praying for her—and she broke into tears. “Can you pray with me?” she asked.
A changing landscape
For years, the medical profession has witnessed a growing interest in all things spiritual. A recent increase in scholarly attention to spirituality in medicine reflects the larger trend in the culture. (“Principles to make a spiritual assessment work in your practice,”) Yet this renewed interest in faith is not without caveats.
Scientific misunderstanding of faith
Empirical studies of the salutary effects of faith on everything from the immune system to recovery from surgery has, not surprisingly, elevated religion’s effects over its claims, contributing to widespread support of what theologians Shuman and Meador call a “generic religion." (“Allowing spirituality into the healing process,”)
Spirituality ignored diminishes medical encounter
Suffering has a way of pointing patients toward the transcendent, and the discussions that accompany this inner process require a vocabulary beyond that of physiology and pathology. The artificial neutrality of enforced secularism inevitably leads to a discussion that is conceptually impoverished, lacking the language to address the existential questions of suffering in ways that are meaningful to the patient. By honestly sharing their own experiences and perspectives, and sensitively inquiring about the patient’s worldview, physicians can raise the level of discussion and create a powerful experience of shared humanity.
This enriched dialectic will enable sensitive and appropriate care for religiously devout patients, ensuring that their concerns are addressed more than superficially. In this way, the clinical encounter will be defined neither by the bland commendation of a generic religion for its salutary effects, nor by the enforced secularism of modernity, but by the contextualization of a patient’s illness against the particularities of her life commitments. When a Muslim with diabetes inquires about fasting during Ramadan, when a Catholic grandfather speaks of divine healing of his cancer, and when a Buddhist teenager explains the role that ulcerative colitis has played in her spiritual development, the relationship between physician and patient will deepen, transforming the medical encounter into an “interhuman event.”23
Ackowledgments
We are indebted to Daniel Hall for his careful review of this manuscript and to Bobbie Sweitzer for her thoughtful critique of these ideas.
Corresponding author
Peter P. Moschovis, 1700 E. 56th St., #3010, Chicago, IL 60637. E-mail:[email protected]
1. Weaver AJ, Flannelly KJ, Oppenheimer JE. Religion, spirituality, and chaplains in the biomedical literature: 1965–2000. Int J Psychiatry Med 2003;33:155-161.
2. Puchalski CM, Larson DB. Developing curricula in spirituality and medicine. Acad Med 1998;73:970-974.
3. Brokaw JJ, Tunnicliff G, Raess BU, Saxon DW. The teaching of complementary and alternative medicine in U.S. medical schools: a survey of course directors. Acad Med 2002;77:876-881.
4. Shuman JJ, Meador KG. Heal Thyself: Spirituality, Medicine, and the Distortion of Christianity. New York, NY: Oxford University Press; 2002.
5. Benson Herbert. Timeless Healing: The Power of Biology of Belief. New York, NY: Scribners; 1996.
6. Gorsuch RL, Mcpherson SE. Intrinsic-Extrinsic Measurement, I/E-Revised and Single-Item Scales. J Sci Study Relig 1989;28:348-354.
7. Allport GW. The Individual and His Religion. New York, NY: MacMillian 1962.
8. Allport GW, Ross J. Personal religious orientation and prejudice. J Pers Soc Psychol 1967;5:447-457.
9. Scheurich N. Reconsidering spirituality and medicine. Acad Med 2003;78:356-360.
10. Ehman JW, Ott BB, Short TH, Ciampa RC, Hansen Flaschen J. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med 1999;159:1803-1806.
11. King DE, Bushwick B. Beliefs and attitudes of hospital inpatients about faith healing and prayer. J Fam Pract 1994;39:349-352.
12. MacLean CD, Susi B, Phifer N, et al. Patient preference for physician discussion and practice of spirituality. J Gen Intern Med 2003;18:38-43.
13. Sloan RP, Bagiella E, VandeCreek L, et al. Should physicians prescribe religious activities? N Engl J Med 2000;342:1913-1916.
14. Post SG, Puchalski CM, Larson DB. Physicians and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med 2000;132:578-583.
15. Lawrence RJ. The witches’ brew of spirituality and medicine. Ann Behav Med 2002;24:74-76.
16. Lo B, Ruston D, Kates LW, et al. Discussing religious and spiritual issues at the end of life: a practical guide for physicians. JAMA 2002;287:749-754.
17. Fish SE. The Trouble With Principle. Cambridge, Mass: Harvard University Press; 1999.
18. Hall DE, Koenig HG, Meador KG. Conceptualizing “religion”: How language shapes and constrains knowledge in the study of religion and health. Perspect Biol Med 2004;In press.
19. Hall DE, Curlin F. Can physicians’ care be neutral regarding religion? Acad Med 2004;in press.
20. MacIntyre A. After Virtue A Study in Moral Theory. 2nd ed Notre Dame, Ind: University of Notre Dame Press; 1984.
21. MacIntyre A. Whose Justice, Which Rationality? Notre Dame, Ind: University of Notre Dame Press; 1988.
22. Plantinga A, Wolsterstorff N. Faith and Rationality: Reason and Belief in God. Notre Dame, Ind: University of Notre Dame Press; 1984.
23. Pellegrino E, Thomasma D. A Philosophical Basis of Medical Practice. New York, NY: Oxford University Press; 1981.
1. Weaver AJ, Flannelly KJ, Oppenheimer JE. Religion, spirituality, and chaplains in the biomedical literature: 1965–2000. Int J Psychiatry Med 2003;33:155-161.
2. Puchalski CM, Larson DB. Developing curricula in spirituality and medicine. Acad Med 1998;73:970-974.
3. Brokaw JJ, Tunnicliff G, Raess BU, Saxon DW. The teaching of complementary and alternative medicine in U.S. medical schools: a survey of course directors. Acad Med 2002;77:876-881.
4. Shuman JJ, Meador KG. Heal Thyself: Spirituality, Medicine, and the Distortion of Christianity. New York, NY: Oxford University Press; 2002.
5. Benson Herbert. Timeless Healing: The Power of Biology of Belief. New York, NY: Scribners; 1996.
6. Gorsuch RL, Mcpherson SE. Intrinsic-Extrinsic Measurement, I/E-Revised and Single-Item Scales. J Sci Study Relig 1989;28:348-354.
7. Allport GW. The Individual and His Religion. New York, NY: MacMillian 1962.
8. Allport GW, Ross J. Personal religious orientation and prejudice. J Pers Soc Psychol 1967;5:447-457.
9. Scheurich N. Reconsidering spirituality and medicine. Acad Med 2003;78:356-360.
10. Ehman JW, Ott BB, Short TH, Ciampa RC, Hansen Flaschen J. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med 1999;159:1803-1806.
11. King DE, Bushwick B. Beliefs and attitudes of hospital inpatients about faith healing and prayer. J Fam Pract 1994;39:349-352.
12. MacLean CD, Susi B, Phifer N, et al. Patient preference for physician discussion and practice of spirituality. J Gen Intern Med 2003;18:38-43.
13. Sloan RP, Bagiella E, VandeCreek L, et al. Should physicians prescribe religious activities? N Engl J Med 2000;342:1913-1916.
14. Post SG, Puchalski CM, Larson DB. Physicians and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med 2000;132:578-583.
15. Lawrence RJ. The witches’ brew of spirituality and medicine. Ann Behav Med 2002;24:74-76.
16. Lo B, Ruston D, Kates LW, et al. Discussing religious and spiritual issues at the end of life: a practical guide for physicians. JAMA 2002;287:749-754.
17. Fish SE. The Trouble With Principle. Cambridge, Mass: Harvard University Press; 1999.
18. Hall DE, Koenig HG, Meador KG. Conceptualizing “religion”: How language shapes and constrains knowledge in the study of religion and health. Perspect Biol Med 2004;In press.
19. Hall DE, Curlin F. Can physicians’ care be neutral regarding religion? Acad Med 2004;in press.
20. MacIntyre A. After Virtue A Study in Moral Theory. 2nd ed Notre Dame, Ind: University of Notre Dame Press; 1984.
21. MacIntyre A. Whose Justice, Which Rationality? Notre Dame, Ind: University of Notre Dame Press; 1988.
22. Plantinga A, Wolsterstorff N. Faith and Rationality: Reason and Belief in God. Notre Dame, Ind: University of Notre Dame Press; 1984.
23. Pellegrino E, Thomasma D. A Philosophical Basis of Medical Practice. New York, NY: Oxford University Press; 1981.
Principles to make a spiritual assessment work in your practice
- Consider the research showing that spiritual faith is an ally to health and positive health behaviors, and that many patients rely on their spiritual beliefs in times of illness (C).
- Regardless of personal ethic, physicians need a set of principles to guide decisions concerning the appropriateness of addressing spiritual issues when such issues arise in the clinical setting (C).
- The EBQT (Evidence-Belief-Quality Care-Time) paradigm provides a natural set of principles for consistent clinical decision-making regarding spiritual or alternative adjuncts to medical therapy (C).
In recent years, physicians have been encouraged to assess their patient’s spiritual sources of strength or stress when taking a medical history. However, the decision to act on such information can be ethically complex. Physicians may feel apprehensive about delving into spiritual issues in clinical practice without clear ethical guidelines as to which actions may, or may not, be taken in response to information gained from such an inquiry. This paper introduces the EBQT paradigm, a set of 4 principles designed to guide physicians who wish to address clinically relevant spiritual issues in their practice.
Need for guidelines
The contribution of a patient’s personal faith to the success or failure of medical care has long been a subject of interest to physicians. Sir William Osler, contrasting the beneficial and harmful effects of various expressions of faith, called it “an essential factor in the practice of medicine.”1 Research highlights both the beneficial aspects of a patient’s spiritual faith,2-7 and the harmful effects of religious struggle in regard to illness8 or lack of strength and comfort from religion.10
Due to the potential relevance of spiritual beliefs and practices, many authors9-13 recommend that physicians include a brief spiritual assessment when taking a patient’s medical history. A decision to act on such information, however, can prove ethically complex. Should physicians have a referral relationship with local clergy? Is it ethical to pray with patients who make such a request? Can a physician express support for faith-based activities? When is it appropriate to confront a patient’s harmful religious beliefs?
Some authors argue against addressing spiritual issues, calling the activity premature and ethically questionable.14 Others acknowledge a connection between spiritual faith and health, yet do not agree on the extent to which physicians should address spiritual issues.15 We elect not to discuss the details of each point of view here, but do emphasize that, despite holding divergent viewpoints, authors seem to agree that guidelines for behavior are lacking. Richard Sloan and colleagues conclude their critique by stating “between the extremes of rejecting the idea that religion and faith can bring comfort to some people coping with illness and endorsing the view that physicians should actively promote religious activity among patients lies a vast uncharted territory in which guidelines for appropriate behavior are needed urgently.”16
This paper introduces such guidelines in the form of what we call the EBQT Paradigm. With the principles of this paradigm, physicians may personally evaluate or openly debate the ethics of certain spiritual adjuncts to therapy using consistent parameters on which to base their conclusions. Previous authors have developed principles for accommodating the religious beliefs of patients.17 Others have provided recommendations for the discussion of spiritual issues with patients.18 However, guidelines for acting on a patient’s spiritual history were not found in a Medline search of the medical literature, including articles and letters from peer-reviewed publications from the last 15 years that refer to or assess the clinical relevance of spirituality, prayer, clergy, religion, or faith.
The EBQT paradigm for spiritual assessment
The EBQT paradigm (Table 1) involves 4 principles: Evidence, Belief, Quality Care, and Time. Used in concert with a spiritual assessment, these principles provide an ethical model with which physicians may evaluate the benefit or harm in addressing spiritual sources of strength or stress in the clinical setting.
TABLE 1
EBQT Paradigm: 4 principles for determining appropriateness of religious/spiritual prescriptive recommendations
| Evidence |
| Does sufficient evidence of good quality exist to recommend this spiritual adjunct to therapy for this patient? |
| Belief |
| Does sufficient congruence exist between the patient’s belief, the physician’s belief, and relevance of therapy? |
| Quality care |
| Will this recommendation improve the quality of care for this patient? |
| Time |
| Can this recommendation be made and implemented within the time constraints of the clinical encounter, respecting the time committed to other patients? |
Principle of evidence
Before considering a spiritual adjunct to therapy, evaluate the evidence that supports a therapeutic advantage to such action. Two questions must be answered: 1) does sufficient evidence exist to recommend the action, and 2) what is the quality of that evidence?
One might logically question whether evidence exists at all to support a physician addressing spiritual issues. Several authors have thoroughly reviewed the evidence for a connection between spiritual commitment and health outcomes.19-21 It is not our intent to repeat their effort here. However, in reviewing their findings, we were struck by the varying quality of evidence found in the medical literature. In some cases, spiritually related actions are supported by abundant evidence; other spiritual practices lack sufficient data for recommendation in the clinical setting. As empirical evidence accumulates, physicians will be increasingly able to discern the therapeutic benefit of certain faith-based practices. Evidence alone, however, does not establish an ethical imperative to address a patient’s spiritual or faith-based practices. The physician’s belief, medical and patient values, and available time must also be taken into account.
Principle of belief
Belief in a given therapy, by both the patient and the physician, is a major part of successful doctor-patient interactions. Researchers recognize that a caregiver’s belief or disbelief in a given therapy can significantly alter a patient’s response to treatment; otherwise there would be no need to double-blind studies.
The principle of belief, illustrated in Figure 1, states a spiritual adjunct to therapy is maximally beneficial when congruence exists between the patient’s belief, the caregiver’s belief, and the relevance of that shared belief to therapy. Conversely, a spiritual adjunct to treatment is less appropriate when the principle of belief is violated by caregiver incongruence, patient incongruence, incongruence of therapy, or extreme incongruence of the caregiver, patient, and therapy.
FIGURE 1
Congruence of belief
Spiritual adjuncts to therapy are maximally beneficial when congruence exists between the patient’s belief (PT), the caregiver’s belief (CG), and the relevance of that shared belief to therapy (Tx).
A physician may respectfully observe and document the faith-based practices of a patient without supporting or criticizing these practices. Encouraging or integrating the patient’s faith-based practices into therapy, however, requires a personal judgment concerning how the patient’s beliefs and those of the caregiver are relevant to a medical condition. Even in cases of incongruence, using this model may lead to serendipitous therapeutic options as a caregiver and patient work together to find common ground for relevant recommendations.
Principle of quality care
The principle of quality care states that a patient’s spiritual beliefs are most appropriately incorporated into therapy when and if doing so improves the quality of care received by the patient.
A popular definition characterizes quality care as the “degree to which health services for individuals and populations increase the likelihood of desired health outcomes....”22 Many definitions of quality care share this narrow focus on health outcomes. However, patients may more broadly define quality of care by including the degree to which personal values are preserved. A comprehensive definition of quality care, illustrated in Figure 2, takes into account both desired health outcomes and the patient’s values.
Complete care occurs when medical goals are achieved and the patient’s values are preserved.
Accommodative care occurs when medical treatment is adjusted for the sake of a patient’s values, as when a patient declines vaccination or other therapies for religious reasons.
Compulsory care describes forced medical therapy without preservation of the patient’s values. This type of care may result from conflicts between religious beliefs and medical standards leading to a patient being treated against his or her will. The adverse effects of compulsory care can be minimized by a thorough patient history that includes questions concerning personal beliefs that may conflict with standard treatment.
Deficient care, defined as failure to achieve medical goals while also violating patient values, can result from poor medical management, patient non-adherence, or lack of communication.
During any clinical encounter, the caregiver’s ultimate goal should be to provide complete care. Accommodative care and compulsory care may be necessary at times, but deficient care should always be avoided.
FIGURE 2
Criteria for defining quality of care
Principle of time
Research underscores the commonly recognized relation between longer consultations and general satisfaction among patients.23,24 Yet time is too often a clinical luxury. Primary care physicians report lack of time as a barrier to providing a variety of potentially beneficial preventive services, including basic counsel on health issues,25-26 despite evidence that brief physician advice can lead to changes in a patient’s health behaviors.27 Similarly, family physicians28 report lack of time as the number one barrier to discussions of spiritual issues.
Generally, preventive health counseling in a primary care setting increases the length of time with a patient anywhere from 2.5 to 3.8 minutes.26,29 Time like this must be taken into account when weighing the importance of addressing spiritual issues with one patient against the time committed to other patients.
The principle of time states that addressing spiritual issues with patients who wish to do so is most appropriate when these issues can be entertained and any actions completed within the time constraints of clinical practice.
Lack of time should not be used routinely as an excuse to withhold care. Though spiritual matters, like other lifestyle issues, take time to address, the time invested may prove beneficial in the long run and management will require less time during follow up if core issues are addressed early and possibly incorporated into therapy.
The principle of time allows the caregiver to evaluate the feasibility of addressing clinically-relevant spiritual issues given a limited amount of time.
Applying the principles
Together, the principles of evidence, belief, quality care, and time serve as ethical precepts for guiding an appropriate response to information gained from a patient’s spiritual history. The scale shown in Table 2, and applied to the following cases, illustrates how these principles might be used in the clinical setting. The scale differentiates between appropriate, potential, and inappropriate recommendations according to the number of principles upheld by each recommendation. While admittedly pragmatic and far from comprehensive, this scale allows for the consistent clinical application of an otherwise theoretical model.
TABLE 2
Using the 4 EBQT principles to determine the usefulness of an action in the physician-patient encounter
| Number of EBQT principles upheld to treatment | Appropriateness of adjunct |
|---|---|
| All 4 | APPROPRIATE recommendation: potentially useful to physicians when a patient’s history warrants such action. Likely ethical. |
| 2 or 3 | POTENTIAL recommendation: action is limited to special circumstances and may not be useful to all physicians, even if warranted by the patient’s history. |
| 0 or 1 | INAPPROPRIATE recommendation: unlikely to be useful in the clinical physician-patient encounter. Risks being unethical. |
Case 1
A physician who maintains a relationship with local clergy is treating a 55-year-old woman with diabetes who has end-stage renal disease. The patient is distraught over lifestyle changes necessitated by dialysis. A spiritual assessment reveals the patient finds strength in her religious faith, actively participates in a local church, and speaks well of the pastoral staff.
Is referral to clergy an appropriate recommendation for addressing the patient’s social and personal issues?
Principle of evidence [+]: Evidence suggests a beneficial role for clergy in facilitating the use of in-home and community-based health services.30 Additionally, a chaplain or minister who knows the patient would be able to ensure she has access and transportation to congregational activities, such as worship or support groups. Religious involvement is associated with better disability outcomes31 and lower use of hospital services32 by medically ill older adults. In contrast, lack of religious participation33 and absence of strength and comfort in religion4 are associated with higher mortality.
Finally, clergy may help facilitate the use of private religious activities, such as prayer or devotional reading, which appear to promote lower blood pressure,34 survival advantage,3 and a reduction in cognitive symptoms of depression.35 The latter finding is particularly relevant to this patient whose intrinsic religious beliefs, according to research, statistically and independently predict a faster remission from depression related to the medical illness.36
Principle of belief [+]: Upheld by physician, patient, and therapy congruence. The physician maintains a referral relationship with local clergy, the patient expresses trust in her pastoral staff, and spiritual support from a trusted pastoral counselor, minister, or chaplain is relevant to the patient’s therapy.
Principle of quality care [+]: Referral promotes a more complete care, advancing medical goals, such as adherence to a renal treatment protocol, in a way that reinforces the patient’s values.
Principle of time [+]: The recommendation can actually save time in a busy practice, assuming an existing relationship with qualified local clergy.
The referral to clergy in this setting upholds all 4 principles and may be considered appropriate.
Case 2
A 25-year-old man with cystic fibrosis is admitted to a private religious hospital for an exacerbation of his illness. The patient’s spiritual history reveals a distant belief in a supreme being, but no formal faith or religious practice.
Can a religiously devout physician recommend religious attendance or devotional reading given this patient’s spiritual history?
Principle of evidence [–]: Some patients may rely on religious activities as a positive means of coping with chronic illness; however, no evidence suggests an advantage for beginning religious activities or attendance for mere health benefits.
Principle of belief [–]: The suggestion violates the principle of belief due to physician-patient incongruence.
Principle of quality care [–]: The recommendation does not acknowledge the patient’s values and would fail to advance medical goals, thereby increasing the risk of compulsory, or worse, deficient care.
Principle of time [+/–]: Whether the principle of time is violated depends on the amount of time allotted to make and implement such a recommendation.
Since only 1, if any, of the principles is upheld in this clinical scenario, the recommendation is considered inappropriate.
Even when faced with a scenario like this, the perceptive physician will gain insight into how a patient copes with illness by taking a spiritual history. Simply asking the question, “What do you rely on in times of illness?” may help identify adjuncts to therapy that will be useful and more appropriate in a patient’s care.
Benefits of the EBQT paradigm
The EBQT paradigm was designed to help health-care providers regardless of their personal belief. Physicians with divergent points of view may use the 4 principles to come to similar, if not identical, conclusions on whether support of a patient’s spiritual practices is warranted. And, as illustrated in case 2, the paradigm allows recognition of inappropriate spiritually-based recommendations.
The cases discussed relate to organized religious practices, because it is in this arena we find the most controversy over physicians’ involvement with patients’ spiritual beliefs. However, we recognize that patients may seek spiritual sources of strength outside organized religion. The 4 principles are also helpful when encountering less formal and less controversial practices of spirituality as found in art, music, relaxation techniques, support groups, gardening, writing, etc. Furthermore, the principles are beneficial for evaluating the appropriateness of certain forms of alternative medicine—acupuncture, hypnosis, homeopathic or naturopathic therapies—regardless of whether these therapies are spiritual in nature.
Of course, conscience trumps all other principles. Caregivers should not compromise their own values. Nor should a patient be put into a potentially compromising position concerning his or her spiritual beliefs. Providing optimum care while avoiding such conflicts requires discernment. We find the EBQT paradigm, used with a careful spiritual assessment, provides helpful guidance in this regard.
Acknowledgments
The authors would like to acknowledge Ken Mueller, PhD, clinical psychologist in Anchorage, AK, and Dan Stockstill, PhD, professor of Bible and Religion, Harding University, for their thoughtful contribution to the development of the EBQT paradigm and the formation of this article. Disclosure: Robert T. Lawrence has served as a Christian minister since 1989. He completed medical school at the University of Washington School of Medicine and is currently a resident at the Greenwood Family Practice Residency in Greenwood, SC.
Corresponding author
Robert T. Lawrence, MD, MEd., 110 Firethorn Rd, Greenwood, SC 29649. E-mail: [email protected].
1. Osler W. The faith that heals. BMJ 1910;June 18:1470-1472.
2. Matthews D, McCullough M, Larson D, Koenig H, Sawyers J, Milano M. Religious commitment and health status: a review of the research and implications for family medicine. Arch Fam Med 1998;7:118-124.
3. Helm H, Hays J, Flint E, Koenig H, Blazer D. Does private religious activity prolong survival? A six-year follow-up study of 3,851 older adults. J Gerontol A Biol Sci Med Sci 2000;55:M400-M405.
4. Oxman T, Freeman D, Manheimer E. Lack of social participation or religious strength and comfort as risk factors for death after cardiac surgery in the elderly. Psychosom Med 1995;57:5-15.
5. Koenig H, Cohen H, George L, Hays J, Larson D, Blazer D. Attendance at religious services, interleukin-6, and other biological parameters of immune function in older adults. Int J Psychiatry Med 1997;27:233-250.
6. Woods T, Antoni M, Ironson G, Kling D. Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. J Psychosom Res 1999;46:165-176.
7. Koenig H, George L, Meador K, Blazer D, Ford S. Religious practices and alcoholism in a southern adult population. Hosp Community Psychiatry 1994;45:225-231.
8. Pargament K, Koenig H, Tarakeshwar N, Hahn J. Religious struggle as a predictor of mortality among medically ill elderly patients. Arch Intern Med 2001;161:1881-1885.
9. Anandarajah G, Hight E. Spirituality and medical practice: using the HOPE questions as a practical tool for spiritual assessment. Am Fam Physician 2001;63:81-88.
10. Post S, Puchalski C, Larson D. Physicians and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med 2000;132:578-583.
11. Maugans T, Wadland W. Religion and family medicine: a survey of physicians and patients. J Fam Pract 1991;32:210-213.
12. Ehman J, Ott B, Short T, Ciampa R, Hansen-Flaschen J. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med 1999;159:1803-1806.
13. Block S. Psychological considerations, growth, and transcendence at the end of life. JAMA 2001;285:2898-2905.
14. Sloan R, Bagiella E, VandeCreek L, et al. Should physicians prescribe religious activities? N Engl J Med 2000;342:1913-1916.
15. Koenig G, Idler E, Kasl S, et al. Religion, spirituality, and medicine: a rebuttal to skeptics. Int J Psychiatry Med 1999;29:123-131.
16. Sloan R, Bagiella E, Powell T. Religion, spirituality, and medicine. Lancet 1999;353:664-667.
17. Buryska J. Assessing the Ethical weight of cultural, religious and spiritual claims in the clinical context. J Med Ethics 2001;27:118-122.
18. Lo B, Ruston D, Kates L, Arnold R, Cohen C, Faber-Langendoen K, et al. Discussing religious and spiritual issues at the end of life. a practical guide for physicians. JAMA 2002;287:749-754.
19. Matthews D, McCullough M, Larson D, Koenig H, Swyers J, Milano M. Religious commitment and health status: a review of the research and implications for family medicine. Arch Fam Med 1998;7:118-124.
20. Mueller P, Plevak D, Rummans T. Religious involvement, spirituality, and medicine: implications for clinical practice. Mayo Clin Proc 2001;76:1225-1235.
21. Levin J, Puchalski C. Religion and spirituality in medicine: research and education. JAMA 1997;278:792-793.
22. Blumenthal D. Quality of health care, part 1: quality of care—what is it? N Engl J Med 1996;335:891-894.
23. Shum C, Humphreys A, Wheeler D, Cochrane M, Skoda S, Clement S. Nurse management of patients with minor illnesses in general practice: multicentre, randomised controlled trial. BMJ 2000;320:1038-1043.
24. Venning P, Durie A, Roland M, Roberts C, Leese B. Randomised controlled trial comparing cost effectiveness of general practitioners and nurse practitioners in primary care. BMJ 2000;320:1048-1053.
25. Jaen C, Stange K, Nutting P. Competing demands of primary care: a model for the delivery of clinical preventive services. J Fam Pract 1994;38:166-171.
26. Goodwin M, Flocke S, Borawski E, Zyzanski S, Stange K. Direct observation of health-habit counseling of adolescents. Arch Ped Ado Med 1999;153:367-373.
27. Fleming M, Manwell L, Barry K, Adams W, Stauffacher E. Brief physician advice for alcohol problems in older adults: a randomized community-based trial. J Fam Pract 1999;48:378-384.
28. Ellis M, Vinson D, Ewigman B. Addressing spiritual concerns of patients. J Fam Pract 1999;48:105-109.
29. Merenstein D, Green L, Fryer G, Dovey S. Shortchanging adolescents: room for improvement in preventive care by physicians. Fam Med 2001;33:120-123.
30. Schoenberg N, Campbell K, Johnson M. Physicians and clergy as facilitators of formal services for older adults. J Aging Soc Policy 1999;11(1):9-26.
31. Idler E, Kasl S. Religion among disabled and nondisabled persons ii: attendance at religious services as a predictor of the course of disability. J Gerontol B Psychol Sci Soc Sci 1997;52:S306-S316.
32. Koenig H, Larson D. Use of hospital services, religious attendance, and religious affiliation. South Med J 1998;91:925-932.
33. Strawbridge W, Cohen R, Shema S, Kaplan G. Frequent attendance at religious services and mortality over 28 years. Am J Pub Health 1997;87:957-968.
34. Koenig H, George L, Hays J, Larson D, Cohen H, Blazer D. The relationship between religious activities and blood pressure in older adults. Int J Psychiatry Med 1998;28:189-213.
35. Koenig H, Cohen H, Blazer D, Kudler H, Drishnan K, Sibert T. Religious coping and cognitive symptoms of depression in elderly medical patients. Psychosomatics 1995;36(4):369-375.
36. Koenig H, George L, Peterson B. Religiosity and remission of depression in medically ill older adults. Am J Psychiatry 1998;155:536-542.
- Consider the research showing that spiritual faith is an ally to health and positive health behaviors, and that many patients rely on their spiritual beliefs in times of illness (C).
- Regardless of personal ethic, physicians need a set of principles to guide decisions concerning the appropriateness of addressing spiritual issues when such issues arise in the clinical setting (C).
- The EBQT (Evidence-Belief-Quality Care-Time) paradigm provides a natural set of principles for consistent clinical decision-making regarding spiritual or alternative adjuncts to medical therapy (C).
In recent years, physicians have been encouraged to assess their patient’s spiritual sources of strength or stress when taking a medical history. However, the decision to act on such information can be ethically complex. Physicians may feel apprehensive about delving into spiritual issues in clinical practice without clear ethical guidelines as to which actions may, or may not, be taken in response to information gained from such an inquiry. This paper introduces the EBQT paradigm, a set of 4 principles designed to guide physicians who wish to address clinically relevant spiritual issues in their practice.
Need for guidelines
The contribution of a patient’s personal faith to the success or failure of medical care has long been a subject of interest to physicians. Sir William Osler, contrasting the beneficial and harmful effects of various expressions of faith, called it “an essential factor in the practice of medicine.”1 Research highlights both the beneficial aspects of a patient’s spiritual faith,2-7 and the harmful effects of religious struggle in regard to illness8 or lack of strength and comfort from religion.10
Due to the potential relevance of spiritual beliefs and practices, many authors9-13 recommend that physicians include a brief spiritual assessment when taking a patient’s medical history. A decision to act on such information, however, can prove ethically complex. Should physicians have a referral relationship with local clergy? Is it ethical to pray with patients who make such a request? Can a physician express support for faith-based activities? When is it appropriate to confront a patient’s harmful religious beliefs?
Some authors argue against addressing spiritual issues, calling the activity premature and ethically questionable.14 Others acknowledge a connection between spiritual faith and health, yet do not agree on the extent to which physicians should address spiritual issues.15 We elect not to discuss the details of each point of view here, but do emphasize that, despite holding divergent viewpoints, authors seem to agree that guidelines for behavior are lacking. Richard Sloan and colleagues conclude their critique by stating “between the extremes of rejecting the idea that religion and faith can bring comfort to some people coping with illness and endorsing the view that physicians should actively promote religious activity among patients lies a vast uncharted territory in which guidelines for appropriate behavior are needed urgently.”16
This paper introduces such guidelines in the form of what we call the EBQT Paradigm. With the principles of this paradigm, physicians may personally evaluate or openly debate the ethics of certain spiritual adjuncts to therapy using consistent parameters on which to base their conclusions. Previous authors have developed principles for accommodating the religious beliefs of patients.17 Others have provided recommendations for the discussion of spiritual issues with patients.18 However, guidelines for acting on a patient’s spiritual history were not found in a Medline search of the medical literature, including articles and letters from peer-reviewed publications from the last 15 years that refer to or assess the clinical relevance of spirituality, prayer, clergy, religion, or faith.
The EBQT paradigm for spiritual assessment
The EBQT paradigm (Table 1) involves 4 principles: Evidence, Belief, Quality Care, and Time. Used in concert with a spiritual assessment, these principles provide an ethical model with which physicians may evaluate the benefit or harm in addressing spiritual sources of strength or stress in the clinical setting.
TABLE 1
EBQT Paradigm: 4 principles for determining appropriateness of religious/spiritual prescriptive recommendations
| Evidence |
| Does sufficient evidence of good quality exist to recommend this spiritual adjunct to therapy for this patient? |
| Belief |
| Does sufficient congruence exist between the patient’s belief, the physician’s belief, and relevance of therapy? |
| Quality care |
| Will this recommendation improve the quality of care for this patient? |
| Time |
| Can this recommendation be made and implemented within the time constraints of the clinical encounter, respecting the time committed to other patients? |
Principle of evidence
Before considering a spiritual adjunct to therapy, evaluate the evidence that supports a therapeutic advantage to such action. Two questions must be answered: 1) does sufficient evidence exist to recommend the action, and 2) what is the quality of that evidence?
One might logically question whether evidence exists at all to support a physician addressing spiritual issues. Several authors have thoroughly reviewed the evidence for a connection between spiritual commitment and health outcomes.19-21 It is not our intent to repeat their effort here. However, in reviewing their findings, we were struck by the varying quality of evidence found in the medical literature. In some cases, spiritually related actions are supported by abundant evidence; other spiritual practices lack sufficient data for recommendation in the clinical setting. As empirical evidence accumulates, physicians will be increasingly able to discern the therapeutic benefit of certain faith-based practices. Evidence alone, however, does not establish an ethical imperative to address a patient’s spiritual or faith-based practices. The physician’s belief, medical and patient values, and available time must also be taken into account.
Principle of belief
Belief in a given therapy, by both the patient and the physician, is a major part of successful doctor-patient interactions. Researchers recognize that a caregiver’s belief or disbelief in a given therapy can significantly alter a patient’s response to treatment; otherwise there would be no need to double-blind studies.
The principle of belief, illustrated in Figure 1, states a spiritual adjunct to therapy is maximally beneficial when congruence exists between the patient’s belief, the caregiver’s belief, and the relevance of that shared belief to therapy. Conversely, a spiritual adjunct to treatment is less appropriate when the principle of belief is violated by caregiver incongruence, patient incongruence, incongruence of therapy, or extreme incongruence of the caregiver, patient, and therapy.
FIGURE 1
Congruence of belief
Spiritual adjuncts to therapy are maximally beneficial when congruence exists between the patient’s belief (PT), the caregiver’s belief (CG), and the relevance of that shared belief to therapy (Tx).
A physician may respectfully observe and document the faith-based practices of a patient without supporting or criticizing these practices. Encouraging or integrating the patient’s faith-based practices into therapy, however, requires a personal judgment concerning how the patient’s beliefs and those of the caregiver are relevant to a medical condition. Even in cases of incongruence, using this model may lead to serendipitous therapeutic options as a caregiver and patient work together to find common ground for relevant recommendations.
Principle of quality care
The principle of quality care states that a patient’s spiritual beliefs are most appropriately incorporated into therapy when and if doing so improves the quality of care received by the patient.
A popular definition characterizes quality care as the “degree to which health services for individuals and populations increase the likelihood of desired health outcomes....”22 Many definitions of quality care share this narrow focus on health outcomes. However, patients may more broadly define quality of care by including the degree to which personal values are preserved. A comprehensive definition of quality care, illustrated in Figure 2, takes into account both desired health outcomes and the patient’s values.
Complete care occurs when medical goals are achieved and the patient’s values are preserved.
Accommodative care occurs when medical treatment is adjusted for the sake of a patient’s values, as when a patient declines vaccination or other therapies for religious reasons.
Compulsory care describes forced medical therapy without preservation of the patient’s values. This type of care may result from conflicts between religious beliefs and medical standards leading to a patient being treated against his or her will. The adverse effects of compulsory care can be minimized by a thorough patient history that includes questions concerning personal beliefs that may conflict with standard treatment.
Deficient care, defined as failure to achieve medical goals while also violating patient values, can result from poor medical management, patient non-adherence, or lack of communication.
During any clinical encounter, the caregiver’s ultimate goal should be to provide complete care. Accommodative care and compulsory care may be necessary at times, but deficient care should always be avoided.
FIGURE 2
Criteria for defining quality of care
Principle of time
Research underscores the commonly recognized relation between longer consultations and general satisfaction among patients.23,24 Yet time is too often a clinical luxury. Primary care physicians report lack of time as a barrier to providing a variety of potentially beneficial preventive services, including basic counsel on health issues,25-26 despite evidence that brief physician advice can lead to changes in a patient’s health behaviors.27 Similarly, family physicians28 report lack of time as the number one barrier to discussions of spiritual issues.
Generally, preventive health counseling in a primary care setting increases the length of time with a patient anywhere from 2.5 to 3.8 minutes.26,29 Time like this must be taken into account when weighing the importance of addressing spiritual issues with one patient against the time committed to other patients.
The principle of time states that addressing spiritual issues with patients who wish to do so is most appropriate when these issues can be entertained and any actions completed within the time constraints of clinical practice.
Lack of time should not be used routinely as an excuse to withhold care. Though spiritual matters, like other lifestyle issues, take time to address, the time invested may prove beneficial in the long run and management will require less time during follow up if core issues are addressed early and possibly incorporated into therapy.
The principle of time allows the caregiver to evaluate the feasibility of addressing clinically-relevant spiritual issues given a limited amount of time.
Applying the principles
Together, the principles of evidence, belief, quality care, and time serve as ethical precepts for guiding an appropriate response to information gained from a patient’s spiritual history. The scale shown in Table 2, and applied to the following cases, illustrates how these principles might be used in the clinical setting. The scale differentiates between appropriate, potential, and inappropriate recommendations according to the number of principles upheld by each recommendation. While admittedly pragmatic and far from comprehensive, this scale allows for the consistent clinical application of an otherwise theoretical model.
TABLE 2
Using the 4 EBQT principles to determine the usefulness of an action in the physician-patient encounter
| Number of EBQT principles upheld to treatment | Appropriateness of adjunct |
|---|---|
| All 4 | APPROPRIATE recommendation: potentially useful to physicians when a patient’s history warrants such action. Likely ethical. |
| 2 or 3 | POTENTIAL recommendation: action is limited to special circumstances and may not be useful to all physicians, even if warranted by the patient’s history. |
| 0 or 1 | INAPPROPRIATE recommendation: unlikely to be useful in the clinical physician-patient encounter. Risks being unethical. |
Case 1
A physician who maintains a relationship with local clergy is treating a 55-year-old woman with diabetes who has end-stage renal disease. The patient is distraught over lifestyle changes necessitated by dialysis. A spiritual assessment reveals the patient finds strength in her religious faith, actively participates in a local church, and speaks well of the pastoral staff.
Is referral to clergy an appropriate recommendation for addressing the patient’s social and personal issues?
Principle of evidence [+]: Evidence suggests a beneficial role for clergy in facilitating the use of in-home and community-based health services.30 Additionally, a chaplain or minister who knows the patient would be able to ensure she has access and transportation to congregational activities, such as worship or support groups. Religious involvement is associated with better disability outcomes31 and lower use of hospital services32 by medically ill older adults. In contrast, lack of religious participation33 and absence of strength and comfort in religion4 are associated with higher mortality.
Finally, clergy may help facilitate the use of private religious activities, such as prayer or devotional reading, which appear to promote lower blood pressure,34 survival advantage,3 and a reduction in cognitive symptoms of depression.35 The latter finding is particularly relevant to this patient whose intrinsic religious beliefs, according to research, statistically and independently predict a faster remission from depression related to the medical illness.36
Principle of belief [+]: Upheld by physician, patient, and therapy congruence. The physician maintains a referral relationship with local clergy, the patient expresses trust in her pastoral staff, and spiritual support from a trusted pastoral counselor, minister, or chaplain is relevant to the patient’s therapy.
Principle of quality care [+]: Referral promotes a more complete care, advancing medical goals, such as adherence to a renal treatment protocol, in a way that reinforces the patient’s values.
Principle of time [+]: The recommendation can actually save time in a busy practice, assuming an existing relationship with qualified local clergy.
The referral to clergy in this setting upholds all 4 principles and may be considered appropriate.
Case 2
A 25-year-old man with cystic fibrosis is admitted to a private religious hospital for an exacerbation of his illness. The patient’s spiritual history reveals a distant belief in a supreme being, but no formal faith or religious practice.
Can a religiously devout physician recommend religious attendance or devotional reading given this patient’s spiritual history?
Principle of evidence [–]: Some patients may rely on religious activities as a positive means of coping with chronic illness; however, no evidence suggests an advantage for beginning religious activities or attendance for mere health benefits.
Principle of belief [–]: The suggestion violates the principle of belief due to physician-patient incongruence.
Principle of quality care [–]: The recommendation does not acknowledge the patient’s values and would fail to advance medical goals, thereby increasing the risk of compulsory, or worse, deficient care.
Principle of time [+/–]: Whether the principle of time is violated depends on the amount of time allotted to make and implement such a recommendation.
Since only 1, if any, of the principles is upheld in this clinical scenario, the recommendation is considered inappropriate.
Even when faced with a scenario like this, the perceptive physician will gain insight into how a patient copes with illness by taking a spiritual history. Simply asking the question, “What do you rely on in times of illness?” may help identify adjuncts to therapy that will be useful and more appropriate in a patient’s care.
Benefits of the EBQT paradigm
The EBQT paradigm was designed to help health-care providers regardless of their personal belief. Physicians with divergent points of view may use the 4 principles to come to similar, if not identical, conclusions on whether support of a patient’s spiritual practices is warranted. And, as illustrated in case 2, the paradigm allows recognition of inappropriate spiritually-based recommendations.
The cases discussed relate to organized religious practices, because it is in this arena we find the most controversy over physicians’ involvement with patients’ spiritual beliefs. However, we recognize that patients may seek spiritual sources of strength outside organized religion. The 4 principles are also helpful when encountering less formal and less controversial practices of spirituality as found in art, music, relaxation techniques, support groups, gardening, writing, etc. Furthermore, the principles are beneficial for evaluating the appropriateness of certain forms of alternative medicine—acupuncture, hypnosis, homeopathic or naturopathic therapies—regardless of whether these therapies are spiritual in nature.
Of course, conscience trumps all other principles. Caregivers should not compromise their own values. Nor should a patient be put into a potentially compromising position concerning his or her spiritual beliefs. Providing optimum care while avoiding such conflicts requires discernment. We find the EBQT paradigm, used with a careful spiritual assessment, provides helpful guidance in this regard.
Acknowledgments
The authors would like to acknowledge Ken Mueller, PhD, clinical psychologist in Anchorage, AK, and Dan Stockstill, PhD, professor of Bible and Religion, Harding University, for their thoughtful contribution to the development of the EBQT paradigm and the formation of this article. Disclosure: Robert T. Lawrence has served as a Christian minister since 1989. He completed medical school at the University of Washington School of Medicine and is currently a resident at the Greenwood Family Practice Residency in Greenwood, SC.
Corresponding author
Robert T. Lawrence, MD, MEd., 110 Firethorn Rd, Greenwood, SC 29649. E-mail: [email protected].
- Consider the research showing that spiritual faith is an ally to health and positive health behaviors, and that many patients rely on their spiritual beliefs in times of illness (C).
- Regardless of personal ethic, physicians need a set of principles to guide decisions concerning the appropriateness of addressing spiritual issues when such issues arise in the clinical setting (C).
- The EBQT (Evidence-Belief-Quality Care-Time) paradigm provides a natural set of principles for consistent clinical decision-making regarding spiritual or alternative adjuncts to medical therapy (C).
In recent years, physicians have been encouraged to assess their patient’s spiritual sources of strength or stress when taking a medical history. However, the decision to act on such information can be ethically complex. Physicians may feel apprehensive about delving into spiritual issues in clinical practice without clear ethical guidelines as to which actions may, or may not, be taken in response to information gained from such an inquiry. This paper introduces the EBQT paradigm, a set of 4 principles designed to guide physicians who wish to address clinically relevant spiritual issues in their practice.
Need for guidelines
The contribution of a patient’s personal faith to the success or failure of medical care has long been a subject of interest to physicians. Sir William Osler, contrasting the beneficial and harmful effects of various expressions of faith, called it “an essential factor in the practice of medicine.”1 Research highlights both the beneficial aspects of a patient’s spiritual faith,2-7 and the harmful effects of religious struggle in regard to illness8 or lack of strength and comfort from religion.10
Due to the potential relevance of spiritual beliefs and practices, many authors9-13 recommend that physicians include a brief spiritual assessment when taking a patient’s medical history. A decision to act on such information, however, can prove ethically complex. Should physicians have a referral relationship with local clergy? Is it ethical to pray with patients who make such a request? Can a physician express support for faith-based activities? When is it appropriate to confront a patient’s harmful religious beliefs?
Some authors argue against addressing spiritual issues, calling the activity premature and ethically questionable.14 Others acknowledge a connection between spiritual faith and health, yet do not agree on the extent to which physicians should address spiritual issues.15 We elect not to discuss the details of each point of view here, but do emphasize that, despite holding divergent viewpoints, authors seem to agree that guidelines for behavior are lacking. Richard Sloan and colleagues conclude their critique by stating “between the extremes of rejecting the idea that religion and faith can bring comfort to some people coping with illness and endorsing the view that physicians should actively promote religious activity among patients lies a vast uncharted territory in which guidelines for appropriate behavior are needed urgently.”16
This paper introduces such guidelines in the form of what we call the EBQT Paradigm. With the principles of this paradigm, physicians may personally evaluate or openly debate the ethics of certain spiritual adjuncts to therapy using consistent parameters on which to base their conclusions. Previous authors have developed principles for accommodating the religious beliefs of patients.17 Others have provided recommendations for the discussion of spiritual issues with patients.18 However, guidelines for acting on a patient’s spiritual history were not found in a Medline search of the medical literature, including articles and letters from peer-reviewed publications from the last 15 years that refer to or assess the clinical relevance of spirituality, prayer, clergy, religion, or faith.
The EBQT paradigm for spiritual assessment
The EBQT paradigm (Table 1) involves 4 principles: Evidence, Belief, Quality Care, and Time. Used in concert with a spiritual assessment, these principles provide an ethical model with which physicians may evaluate the benefit or harm in addressing spiritual sources of strength or stress in the clinical setting.
TABLE 1
EBQT Paradigm: 4 principles for determining appropriateness of religious/spiritual prescriptive recommendations
| Evidence |
| Does sufficient evidence of good quality exist to recommend this spiritual adjunct to therapy for this patient? |
| Belief |
| Does sufficient congruence exist between the patient’s belief, the physician’s belief, and relevance of therapy? |
| Quality care |
| Will this recommendation improve the quality of care for this patient? |
| Time |
| Can this recommendation be made and implemented within the time constraints of the clinical encounter, respecting the time committed to other patients? |
Principle of evidence
Before considering a spiritual adjunct to therapy, evaluate the evidence that supports a therapeutic advantage to such action. Two questions must be answered: 1) does sufficient evidence exist to recommend the action, and 2) what is the quality of that evidence?
One might logically question whether evidence exists at all to support a physician addressing spiritual issues. Several authors have thoroughly reviewed the evidence for a connection between spiritual commitment and health outcomes.19-21 It is not our intent to repeat their effort here. However, in reviewing their findings, we were struck by the varying quality of evidence found in the medical literature. In some cases, spiritually related actions are supported by abundant evidence; other spiritual practices lack sufficient data for recommendation in the clinical setting. As empirical evidence accumulates, physicians will be increasingly able to discern the therapeutic benefit of certain faith-based practices. Evidence alone, however, does not establish an ethical imperative to address a patient’s spiritual or faith-based practices. The physician’s belief, medical and patient values, and available time must also be taken into account.
Principle of belief
Belief in a given therapy, by both the patient and the physician, is a major part of successful doctor-patient interactions. Researchers recognize that a caregiver’s belief or disbelief in a given therapy can significantly alter a patient’s response to treatment; otherwise there would be no need to double-blind studies.
The principle of belief, illustrated in Figure 1, states a spiritual adjunct to therapy is maximally beneficial when congruence exists between the patient’s belief, the caregiver’s belief, and the relevance of that shared belief to therapy. Conversely, a spiritual adjunct to treatment is less appropriate when the principle of belief is violated by caregiver incongruence, patient incongruence, incongruence of therapy, or extreme incongruence of the caregiver, patient, and therapy.
FIGURE 1
Congruence of belief
Spiritual adjuncts to therapy are maximally beneficial when congruence exists between the patient’s belief (PT), the caregiver’s belief (CG), and the relevance of that shared belief to therapy (Tx).
A physician may respectfully observe and document the faith-based practices of a patient without supporting or criticizing these practices. Encouraging or integrating the patient’s faith-based practices into therapy, however, requires a personal judgment concerning how the patient’s beliefs and those of the caregiver are relevant to a medical condition. Even in cases of incongruence, using this model may lead to serendipitous therapeutic options as a caregiver and patient work together to find common ground for relevant recommendations.
Principle of quality care
The principle of quality care states that a patient’s spiritual beliefs are most appropriately incorporated into therapy when and if doing so improves the quality of care received by the patient.
A popular definition characterizes quality care as the “degree to which health services for individuals and populations increase the likelihood of desired health outcomes....”22 Many definitions of quality care share this narrow focus on health outcomes. However, patients may more broadly define quality of care by including the degree to which personal values are preserved. A comprehensive definition of quality care, illustrated in Figure 2, takes into account both desired health outcomes and the patient’s values.
Complete care occurs when medical goals are achieved and the patient’s values are preserved.
Accommodative care occurs when medical treatment is adjusted for the sake of a patient’s values, as when a patient declines vaccination or other therapies for religious reasons.
Compulsory care describes forced medical therapy without preservation of the patient’s values. This type of care may result from conflicts between religious beliefs and medical standards leading to a patient being treated against his or her will. The adverse effects of compulsory care can be minimized by a thorough patient history that includes questions concerning personal beliefs that may conflict with standard treatment.
Deficient care, defined as failure to achieve medical goals while also violating patient values, can result from poor medical management, patient non-adherence, or lack of communication.
During any clinical encounter, the caregiver’s ultimate goal should be to provide complete care. Accommodative care and compulsory care may be necessary at times, but deficient care should always be avoided.
FIGURE 2
Criteria for defining quality of care
Principle of time
Research underscores the commonly recognized relation between longer consultations and general satisfaction among patients.23,24 Yet time is too often a clinical luxury. Primary care physicians report lack of time as a barrier to providing a variety of potentially beneficial preventive services, including basic counsel on health issues,25-26 despite evidence that brief physician advice can lead to changes in a patient’s health behaviors.27 Similarly, family physicians28 report lack of time as the number one barrier to discussions of spiritual issues.
Generally, preventive health counseling in a primary care setting increases the length of time with a patient anywhere from 2.5 to 3.8 minutes.26,29 Time like this must be taken into account when weighing the importance of addressing spiritual issues with one patient against the time committed to other patients.
The principle of time states that addressing spiritual issues with patients who wish to do so is most appropriate when these issues can be entertained and any actions completed within the time constraints of clinical practice.
Lack of time should not be used routinely as an excuse to withhold care. Though spiritual matters, like other lifestyle issues, take time to address, the time invested may prove beneficial in the long run and management will require less time during follow up if core issues are addressed early and possibly incorporated into therapy.
The principle of time allows the caregiver to evaluate the feasibility of addressing clinically-relevant spiritual issues given a limited amount of time.
Applying the principles
Together, the principles of evidence, belief, quality care, and time serve as ethical precepts for guiding an appropriate response to information gained from a patient’s spiritual history. The scale shown in Table 2, and applied to the following cases, illustrates how these principles might be used in the clinical setting. The scale differentiates between appropriate, potential, and inappropriate recommendations according to the number of principles upheld by each recommendation. While admittedly pragmatic and far from comprehensive, this scale allows for the consistent clinical application of an otherwise theoretical model.
TABLE 2
Using the 4 EBQT principles to determine the usefulness of an action in the physician-patient encounter
| Number of EBQT principles upheld to treatment | Appropriateness of adjunct |
|---|---|
| All 4 | APPROPRIATE recommendation: potentially useful to physicians when a patient’s history warrants such action. Likely ethical. |
| 2 or 3 | POTENTIAL recommendation: action is limited to special circumstances and may not be useful to all physicians, even if warranted by the patient’s history. |
| 0 or 1 | INAPPROPRIATE recommendation: unlikely to be useful in the clinical physician-patient encounter. Risks being unethical. |
Case 1
A physician who maintains a relationship with local clergy is treating a 55-year-old woman with diabetes who has end-stage renal disease. The patient is distraught over lifestyle changes necessitated by dialysis. A spiritual assessment reveals the patient finds strength in her religious faith, actively participates in a local church, and speaks well of the pastoral staff.
Is referral to clergy an appropriate recommendation for addressing the patient’s social and personal issues?
Principle of evidence [+]: Evidence suggests a beneficial role for clergy in facilitating the use of in-home and community-based health services.30 Additionally, a chaplain or minister who knows the patient would be able to ensure she has access and transportation to congregational activities, such as worship or support groups. Religious involvement is associated with better disability outcomes31 and lower use of hospital services32 by medically ill older adults. In contrast, lack of religious participation33 and absence of strength and comfort in religion4 are associated with higher mortality.
Finally, clergy may help facilitate the use of private religious activities, such as prayer or devotional reading, which appear to promote lower blood pressure,34 survival advantage,3 and a reduction in cognitive symptoms of depression.35 The latter finding is particularly relevant to this patient whose intrinsic religious beliefs, according to research, statistically and independently predict a faster remission from depression related to the medical illness.36
Principle of belief [+]: Upheld by physician, patient, and therapy congruence. The physician maintains a referral relationship with local clergy, the patient expresses trust in her pastoral staff, and spiritual support from a trusted pastoral counselor, minister, or chaplain is relevant to the patient’s therapy.
Principle of quality care [+]: Referral promotes a more complete care, advancing medical goals, such as adherence to a renal treatment protocol, in a way that reinforces the patient’s values.
Principle of time [+]: The recommendation can actually save time in a busy practice, assuming an existing relationship with qualified local clergy.
The referral to clergy in this setting upholds all 4 principles and may be considered appropriate.
Case 2
A 25-year-old man with cystic fibrosis is admitted to a private religious hospital for an exacerbation of his illness. The patient’s spiritual history reveals a distant belief in a supreme being, but no formal faith or religious practice.
Can a religiously devout physician recommend religious attendance or devotional reading given this patient’s spiritual history?
Principle of evidence [–]: Some patients may rely on religious activities as a positive means of coping with chronic illness; however, no evidence suggests an advantage for beginning religious activities or attendance for mere health benefits.
Principle of belief [–]: The suggestion violates the principle of belief due to physician-patient incongruence.
Principle of quality care [–]: The recommendation does not acknowledge the patient’s values and would fail to advance medical goals, thereby increasing the risk of compulsory, or worse, deficient care.
Principle of time [+/–]: Whether the principle of time is violated depends on the amount of time allotted to make and implement such a recommendation.
Since only 1, if any, of the principles is upheld in this clinical scenario, the recommendation is considered inappropriate.
Even when faced with a scenario like this, the perceptive physician will gain insight into how a patient copes with illness by taking a spiritual history. Simply asking the question, “What do you rely on in times of illness?” may help identify adjuncts to therapy that will be useful and more appropriate in a patient’s care.
Benefits of the EBQT paradigm
The EBQT paradigm was designed to help health-care providers regardless of their personal belief. Physicians with divergent points of view may use the 4 principles to come to similar, if not identical, conclusions on whether support of a patient’s spiritual practices is warranted. And, as illustrated in case 2, the paradigm allows recognition of inappropriate spiritually-based recommendations.
The cases discussed relate to organized religious practices, because it is in this arena we find the most controversy over physicians’ involvement with patients’ spiritual beliefs. However, we recognize that patients may seek spiritual sources of strength outside organized religion. The 4 principles are also helpful when encountering less formal and less controversial practices of spirituality as found in art, music, relaxation techniques, support groups, gardening, writing, etc. Furthermore, the principles are beneficial for evaluating the appropriateness of certain forms of alternative medicine—acupuncture, hypnosis, homeopathic or naturopathic therapies—regardless of whether these therapies are spiritual in nature.
Of course, conscience trumps all other principles. Caregivers should not compromise their own values. Nor should a patient be put into a potentially compromising position concerning his or her spiritual beliefs. Providing optimum care while avoiding such conflicts requires discernment. We find the EBQT paradigm, used with a careful spiritual assessment, provides helpful guidance in this regard.
Acknowledgments
The authors would like to acknowledge Ken Mueller, PhD, clinical psychologist in Anchorage, AK, and Dan Stockstill, PhD, professor of Bible and Religion, Harding University, for their thoughtful contribution to the development of the EBQT paradigm and the formation of this article. Disclosure: Robert T. Lawrence has served as a Christian minister since 1989. He completed medical school at the University of Washington School of Medicine and is currently a resident at the Greenwood Family Practice Residency in Greenwood, SC.
Corresponding author
Robert T. Lawrence, MD, MEd., 110 Firethorn Rd, Greenwood, SC 29649. E-mail: [email protected].
1. Osler W. The faith that heals. BMJ 1910;June 18:1470-1472.
2. Matthews D, McCullough M, Larson D, Koenig H, Sawyers J, Milano M. Religious commitment and health status: a review of the research and implications for family medicine. Arch Fam Med 1998;7:118-124.
3. Helm H, Hays J, Flint E, Koenig H, Blazer D. Does private religious activity prolong survival? A six-year follow-up study of 3,851 older adults. J Gerontol A Biol Sci Med Sci 2000;55:M400-M405.
4. Oxman T, Freeman D, Manheimer E. Lack of social participation or religious strength and comfort as risk factors for death after cardiac surgery in the elderly. Psychosom Med 1995;57:5-15.
5. Koenig H, Cohen H, George L, Hays J, Larson D, Blazer D. Attendance at religious services, interleukin-6, and other biological parameters of immune function in older adults. Int J Psychiatry Med 1997;27:233-250.
6. Woods T, Antoni M, Ironson G, Kling D. Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. J Psychosom Res 1999;46:165-176.
7. Koenig H, George L, Meador K, Blazer D, Ford S. Religious practices and alcoholism in a southern adult population. Hosp Community Psychiatry 1994;45:225-231.
8. Pargament K, Koenig H, Tarakeshwar N, Hahn J. Religious struggle as a predictor of mortality among medically ill elderly patients. Arch Intern Med 2001;161:1881-1885.
9. Anandarajah G, Hight E. Spirituality and medical practice: using the HOPE questions as a practical tool for spiritual assessment. Am Fam Physician 2001;63:81-88.
10. Post S, Puchalski C, Larson D. Physicians and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med 2000;132:578-583.
11. Maugans T, Wadland W. Religion and family medicine: a survey of physicians and patients. J Fam Pract 1991;32:210-213.
12. Ehman J, Ott B, Short T, Ciampa R, Hansen-Flaschen J. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med 1999;159:1803-1806.
13. Block S. Psychological considerations, growth, and transcendence at the end of life. JAMA 2001;285:2898-2905.
14. Sloan R, Bagiella E, VandeCreek L, et al. Should physicians prescribe religious activities? N Engl J Med 2000;342:1913-1916.
15. Koenig G, Idler E, Kasl S, et al. Religion, spirituality, and medicine: a rebuttal to skeptics. Int J Psychiatry Med 1999;29:123-131.
16. Sloan R, Bagiella E, Powell T. Religion, spirituality, and medicine. Lancet 1999;353:664-667.
17. Buryska J. Assessing the Ethical weight of cultural, religious and spiritual claims in the clinical context. J Med Ethics 2001;27:118-122.
18. Lo B, Ruston D, Kates L, Arnold R, Cohen C, Faber-Langendoen K, et al. Discussing religious and spiritual issues at the end of life. a practical guide for physicians. JAMA 2002;287:749-754.
19. Matthews D, McCullough M, Larson D, Koenig H, Swyers J, Milano M. Religious commitment and health status: a review of the research and implications for family medicine. Arch Fam Med 1998;7:118-124.
20. Mueller P, Plevak D, Rummans T. Religious involvement, spirituality, and medicine: implications for clinical practice. Mayo Clin Proc 2001;76:1225-1235.
21. Levin J, Puchalski C. Religion and spirituality in medicine: research and education. JAMA 1997;278:792-793.
22. Blumenthal D. Quality of health care, part 1: quality of care—what is it? N Engl J Med 1996;335:891-894.
23. Shum C, Humphreys A, Wheeler D, Cochrane M, Skoda S, Clement S. Nurse management of patients with minor illnesses in general practice: multicentre, randomised controlled trial. BMJ 2000;320:1038-1043.
24. Venning P, Durie A, Roland M, Roberts C, Leese B. Randomised controlled trial comparing cost effectiveness of general practitioners and nurse practitioners in primary care. BMJ 2000;320:1048-1053.
25. Jaen C, Stange K, Nutting P. Competing demands of primary care: a model for the delivery of clinical preventive services. J Fam Pract 1994;38:166-171.
26. Goodwin M, Flocke S, Borawski E, Zyzanski S, Stange K. Direct observation of health-habit counseling of adolescents. Arch Ped Ado Med 1999;153:367-373.
27. Fleming M, Manwell L, Barry K, Adams W, Stauffacher E. Brief physician advice for alcohol problems in older adults: a randomized community-based trial. J Fam Pract 1999;48:378-384.
28. Ellis M, Vinson D, Ewigman B. Addressing spiritual concerns of patients. J Fam Pract 1999;48:105-109.
29. Merenstein D, Green L, Fryer G, Dovey S. Shortchanging adolescents: room for improvement in preventive care by physicians. Fam Med 2001;33:120-123.
30. Schoenberg N, Campbell K, Johnson M. Physicians and clergy as facilitators of formal services for older adults. J Aging Soc Policy 1999;11(1):9-26.
31. Idler E, Kasl S. Religion among disabled and nondisabled persons ii: attendance at religious services as a predictor of the course of disability. J Gerontol B Psychol Sci Soc Sci 1997;52:S306-S316.
32. Koenig H, Larson D. Use of hospital services, religious attendance, and religious affiliation. South Med J 1998;91:925-932.
33. Strawbridge W, Cohen R, Shema S, Kaplan G. Frequent attendance at religious services and mortality over 28 years. Am J Pub Health 1997;87:957-968.
34. Koenig H, George L, Hays J, Larson D, Cohen H, Blazer D. The relationship between religious activities and blood pressure in older adults. Int J Psychiatry Med 1998;28:189-213.
35. Koenig H, Cohen H, Blazer D, Kudler H, Drishnan K, Sibert T. Religious coping and cognitive symptoms of depression in elderly medical patients. Psychosomatics 1995;36(4):369-375.
36. Koenig H, George L, Peterson B. Religiosity and remission of depression in medically ill older adults. Am J Psychiatry 1998;155:536-542.
1. Osler W. The faith that heals. BMJ 1910;June 18:1470-1472.
2. Matthews D, McCullough M, Larson D, Koenig H, Sawyers J, Milano M. Religious commitment and health status: a review of the research and implications for family medicine. Arch Fam Med 1998;7:118-124.
3. Helm H, Hays J, Flint E, Koenig H, Blazer D. Does private religious activity prolong survival? A six-year follow-up study of 3,851 older adults. J Gerontol A Biol Sci Med Sci 2000;55:M400-M405.
4. Oxman T, Freeman D, Manheimer E. Lack of social participation or religious strength and comfort as risk factors for death after cardiac surgery in the elderly. Psychosom Med 1995;57:5-15.
5. Koenig H, Cohen H, George L, Hays J, Larson D, Blazer D. Attendance at religious services, interleukin-6, and other biological parameters of immune function in older adults. Int J Psychiatry Med 1997;27:233-250.
6. Woods T, Antoni M, Ironson G, Kling D. Religiosity is associated with affective and immune status in symptomatic HIV-infected gay men. J Psychosom Res 1999;46:165-176.
7. Koenig H, George L, Meador K, Blazer D, Ford S. Religious practices and alcoholism in a southern adult population. Hosp Community Psychiatry 1994;45:225-231.
8. Pargament K, Koenig H, Tarakeshwar N, Hahn J. Religious struggle as a predictor of mortality among medically ill elderly patients. Arch Intern Med 2001;161:1881-1885.
9. Anandarajah G, Hight E. Spirituality and medical practice: using the HOPE questions as a practical tool for spiritual assessment. Am Fam Physician 2001;63:81-88.
10. Post S, Puchalski C, Larson D. Physicians and patient spirituality: professional boundaries, competency, and ethics. Ann Intern Med 2000;132:578-583.
11. Maugans T, Wadland W. Religion and family medicine: a survey of physicians and patients. J Fam Pract 1991;32:210-213.
12. Ehman J, Ott B, Short T, Ciampa R, Hansen-Flaschen J. Do patients want physicians to inquire about their spiritual or religious beliefs if they become gravely ill? Arch Intern Med 1999;159:1803-1806.
13. Block S. Psychological considerations, growth, and transcendence at the end of life. JAMA 2001;285:2898-2905.
14. Sloan R, Bagiella E, VandeCreek L, et al. Should physicians prescribe religious activities? N Engl J Med 2000;342:1913-1916.
15. Koenig G, Idler E, Kasl S, et al. Religion, spirituality, and medicine: a rebuttal to skeptics. Int J Psychiatry Med 1999;29:123-131.
16. Sloan R, Bagiella E, Powell T. Religion, spirituality, and medicine. Lancet 1999;353:664-667.
17. Buryska J. Assessing the Ethical weight of cultural, religious and spiritual claims in the clinical context. J Med Ethics 2001;27:118-122.
18. Lo B, Ruston D, Kates L, Arnold R, Cohen C, Faber-Langendoen K, et al. Discussing religious and spiritual issues at the end of life. a practical guide for physicians. JAMA 2002;287:749-754.
19. Matthews D, McCullough M, Larson D, Koenig H, Swyers J, Milano M. Religious commitment and health status: a review of the research and implications for family medicine. Arch Fam Med 1998;7:118-124.
20. Mueller P, Plevak D, Rummans T. Religious involvement, spirituality, and medicine: implications for clinical practice. Mayo Clin Proc 2001;76:1225-1235.
21. Levin J, Puchalski C. Religion and spirituality in medicine: research and education. JAMA 1997;278:792-793.
22. Blumenthal D. Quality of health care, part 1: quality of care—what is it? N Engl J Med 1996;335:891-894.
23. Shum C, Humphreys A, Wheeler D, Cochrane M, Skoda S, Clement S. Nurse management of patients with minor illnesses in general practice: multicentre, randomised controlled trial. BMJ 2000;320:1038-1043.
24. Venning P, Durie A, Roland M, Roberts C, Leese B. Randomised controlled trial comparing cost effectiveness of general practitioners and nurse practitioners in primary care. BMJ 2000;320:1048-1053.
25. Jaen C, Stange K, Nutting P. Competing demands of primary care: a model for the delivery of clinical preventive services. J Fam Pract 1994;38:166-171.
26. Goodwin M, Flocke S, Borawski E, Zyzanski S, Stange K. Direct observation of health-habit counseling of adolescents. Arch Ped Ado Med 1999;153:367-373.
27. Fleming M, Manwell L, Barry K, Adams W, Stauffacher E. Brief physician advice for alcohol problems in older adults: a randomized community-based trial. J Fam Pract 1999;48:378-384.
28. Ellis M, Vinson D, Ewigman B. Addressing spiritual concerns of patients. J Fam Pract 1999;48:105-109.
29. Merenstein D, Green L, Fryer G, Dovey S. Shortchanging adolescents: room for improvement in preventive care by physicians. Fam Med 2001;33:120-123.
30. Schoenberg N, Campbell K, Johnson M. Physicians and clergy as facilitators of formal services for older adults. J Aging Soc Policy 1999;11(1):9-26.
31. Idler E, Kasl S. Religion among disabled and nondisabled persons ii: attendance at religious services as a predictor of the course of disability. J Gerontol B Psychol Sci Soc Sci 1997;52:S306-S316.
32. Koenig H, Larson D. Use of hospital services, religious attendance, and religious affiliation. South Med J 1998;91:925-932.
33. Strawbridge W, Cohen R, Shema S, Kaplan G. Frequent attendance at religious services and mortality over 28 years. Am J Pub Health 1997;87:957-968.
34. Koenig H, George L, Hays J, Larson D, Cohen H, Blazer D. The relationship between religious activities and blood pressure in older adults. Int J Psychiatry Med 1998;28:189-213.
35. Koenig H, Cohen H, Blazer D, Kudler H, Drishnan K, Sibert T. Religious coping and cognitive symptoms of depression in elderly medical patients. Psychosomatics 1995;36(4):369-375.
36. Koenig H, George L, Peterson B. Religiosity and remission of depression in medically ill older adults. Am J Psychiatry 1998;155:536-542.
3 Regimens for alcohol withdrawal and detoxification
- Patients with mild to moderate alcohol withdrawal symptoms and no serious psychiatric or medical comorbidities can be safely treated in the outpatient setting (SOR:A).
- Patients with moderate withdrawal should receive pharmacotherapy to treat their symptoms and reduce their risk of seizures and delirium tremens during outpatient detoxification (SOR:A).
- Benzodiazepines are the treatment of choice for alcohol withdrawal (SOR:A).
- ln healthy individuals with mild-to-moderate alcohol withdrawal, carbamazepine has many advantages making it a first-line treatment for properly selected patients (SOR:A).
In our small community hospital—with limited financial and medical resources—we have designed and implemented an outpatient alcohol detoxification clinical practice guideline to provide cost-effective, evidence-based medical care to our patients, in support of their alcohol treatment.
Those patients with mild-to-moderate alcohol withdrawal symptoms and no serious psychiatric or medical comorbidities can be safely treated in the outpatient setting. Patients with history of severe withdrawal symptoms, seizures or delirium tremens, comorbid serious psychiatric or medical illnesses, or lack of reliable support network should be considered for detoxification in the inpatient setting.
The problem of alcohol withdrawal
Up to 71% of individuals presenting for alcohol detoxification manifest significant symptoms of alcohol withdrawal.4 Alcohol withdrawal is a clinical syndrome that affects people accustomed to regular alcohol intake who either decrease their alcohol consumption or stop drinking completely.
Physiology
Alcohol enhances gamma-aminobutyric acid’s (GABA) inhibitory effects on signal-receiving neurons, thereby lowering neuronal activity, leading to an increase in excitatory glutamate receptors. Over time, tolerance occurs as GABA receptors become less responsive to neurotransmitters, and more alcohol is required to produce the same inhibitory effect. When alcohol is removed acutely, the number of excitatory glutamate receptors remains, but without the suppressive GABA effect.5 This situation leads to the signs and symptoms of alcohol withdrawal.
Symptoms
Noticeable alcohol withdrawal symptoms may appear within hours of cessation or decreasing alcohol intake. The most common symptoms include tremor, craving for alcohol, insomnia, vivid dreams, anxiety, hypervigilance, agitation, irritability, loss of appetite, nausea, vomiting, headache, and sweating.5 Even without treatment, most of these relatively benign symptoms resolve within hours to days.
More concerning are hallucinations, delirium tremens (DTs), and seizures. Transient auditory or visual hallucinations may occur within the first 2 days of decreasing or discontinuing alcohol consumption, and can be separate from DTs. DTs, which present within 2 to 4 days of the last drink (and can last up to 3 to 4 days), are characterized by disorientation, persistent visual and auditory hallucinations, agitation and tremulousness, and autonomic signs resulting from the activation of stress-related hormones. These signs include tachycardia, hypertension, and fevers.
DTs are much more serious than the “alcohol shakes”—5% of patients who experience DTs die from metabolic complications.6 The occurrence of DTs is 5.3 times higher in men than in women;7 however, women may exhibit fewer autonomic symptoms, making DTs in women more difficult to diagnose.6
Grand mal seizures can occur in up to 25% of alcoholics undergoing withdrawal.4 If alcohol-related seizures do occur, they generally do so within 1 day of cessation of alcohol intake, but can occur up to 5 days later.
Risk factors for prolonged or complicated alcohol withdrawal include duration of alcohol consumption, the number of lifetime prior detoxifications, prior seizures, prior episodes of DTs, and current intense craving for alcohol.6-10
Before treatment: assess and stabilize
Initial assessment of the patient
Before initiating treatment for alcohol withdrawal, perform a thorough assessment of the patient’s medical condition. This evaluation should include an assessment of coexisting medical and psychiatric conditions, the severity of previous withdrawal symptoms, and the risk factors for withdrawal complications. The initial symptoms of alcohol withdrawal are not specific and may mimic other serious disease conditions; therefore, the initial assessment should exclude potentially serious medical and psychiatric comorbidities.
Initially, assessment of common alcohol-related medical problems should be conducted. These complications include gastritis, gastrointestinal bleeding, liver disease, cardiomyopathy, pancreatitis, neurological impairment, electrolyte imbalances, and nutritional deficiencies. A physical examination should be performed to assess for arrhythmias, congestive heart failure, hepatic or pancreatic disease, infectious conditions, bleeding, and nervous system impairment.
Initial alcohol level and urine drug screen should be assessed, as recent high levels of alcohol intake and substance abuse place the patient at higher risk for complications. Unstable mood disorders—delirium, psychosis, severe depression, suicidal or homicidal ideation—while potentially difficult to assess during intoxication, need to be considered and ruled out.
Stabilize the patient
After initial assessment, vital signs (eg, heart rate, blood pressure, and temperature) should be stabilized while fluid, electrolyte, and nutritional disturbances are corrected. Some patients undergoing alcohol withdrawal may require intravenous fluids to correct severe dehydration resulting from vomiting, diarrhea, sweating, and fever.
Alcoholics are often deficient in electrolytes or minerals, including thiamine, folate, and magnesium (although replacing magnesium makes no difference in clinically meaningful outcomes) (level of evidence [LOE]: 1, double-blind randomized controlled trial).11 All patients being treated for alcohol withdrawal should be given 100 mg of thiamine immediately and daily (LOE: 3; insufficient evidence from randomized controlled trials to guide clinicians in the dose, frequency, route, or duration of thiamine treatment for prophylaxis against or treatment of WKS due to alcohol abuse).4 Thiamine should be given before glucose containing fluids, to avoid the risk of precipitating Wernicke syndrome (LOE: 3).12
Assess the severity of the withdrawal
Once a diagnosis of alcohol withdrawal is made, complete an assessment of the severity of withdrawal and the risk of complications. The best validated tool is the Clinical Institute Withdrawal Assessment for Alcohol-Revised (CIWA-Ar) symptom scale (Figure 1).10 This instrument rates 10 withdrawal features; it takes only a few minutes to administer and may be repeated when re-evaluation is necessary. CIWA-Ar scores of ≤8 are suggestive of mild withdrawal symptoms, while those ≥15 confer an increased risk for confusion and seizures.
CIWA-Ar is reliable, brief, uncomplicated, and clinically useful scale that can also be used to monitor response to treatment. It offers an increase in efficiency over the original CIWA-A scale, while retaining clinical usefulness, validity, and reliability. It can be incorporated into the usual clinical care of patients undergoing alcohol withdrawal and into clinical drug trials of alcohol withdrawal (strength of recommendation [SOR]=A].5,13
Pharmacotherapy
Patients experiencing more serious withdrawal (with CIWA-Ar scores >8) should receive pharmacotherapy to treat their symptoms and reduce their risk of seizures and DTs (SOR=A).14
Benzodiazepines
Benzodiazepines are the mainstay of treatment in alcohol withdrawal (number needed to treat [NNT]=17; data from large meta-analysis of 6 prospective, placebo-controlled trials) (SOR=A).10,14,16 Like alcohol, these agents magnify GABA’s effect on the brain. Benzodiazepines are cross-tolerant with alcohol; during withdrawal from 1 agent, the other may serve as a substitute. Benzodiazepines also reduce the incidence of DTs and seizures (Table 1).5,14
The problem. In our small community hospital, prior to the development of a clinical practice guideline, admissions for “inpatient alcohol detoxification” were among our top 5, with a select few patients making multiple, repeat visits. Additionally, we had no standardized, consistent strategy for initial emergency room evaluation; frequent early discharges against medical advice; multiple readmissions; infrequent and inconsistent entry into our outpatient Alcohol and Substance Abuse Program; and no existing process for primary care outpatient follow-up. We found ourselves in a situation where we were essentially enabling our patients in a destructive behavior. With no formal policy or guidelines, physicians tended to follow the path of least resistance: repeated short-stay admissions with limited therapeutic benefit.
The process. Our initial goal was to develop a standardized policy in an attempt to minimize the number of admissions of mild-to-moderate, uncomplicated alcohol withdrawal patients. Many of our patients are at low risk for serious complications, and we hoped to triage such individuals to an outpatient treatment setting. To organize the thought process, a flowchart was developed and refined. By incorporating current evidence, a clinical practice guideline was developed.
Evidence-based algorithm. We developed an evidence-based algorithm, Outpatient Treatment for Alcohol Detoxification (Figure 2), which uses a gradually tapering regimen, and allows providers to prescribe the medication they feel most appropriate given the clinical situation.
Results. In the 12 months since implementation of our clinical practice guideline, total alcohol-related admission decreased from 4 to 5 per month to only 1 during the entire period; furthermore, no patients treated with our guidelines were subsequently hospitalized for complications of alcohol withdrawal.
The most commonly used benzodiazepines are diazepam (Valium), chlordiazepoxide (Librium), and lorazepam (Ativan). All appear to be equally efficacious in treating alcohol withdrawal symptoms (LOE: 1; randomized controlled trial).
Longer-acting agents, such as chlordiazepoxide or diazepam, contribute to an overall smoother withdrawal course with lessened breakthrough or rebound symptoms, but they may also lead to excess sedation for patients with hepatic dysfunction.17-20 Shorter-acting benzodiazepines, such as oxazepam (Serax), may result in greater discomfort and more discharges against medical advice, because alcohol withdrawal symptoms tend to recur when serum benzodiazepine levels drop.
TABLE 1
Pharmacologic treatment of alcohol withdrawal
| Medication | Comments | LOE |
|---|---|---|
| Benzodiazepines | Remain drug of choice for acute alcohol withdrawal14 | A |
| Highly significant decrease in seizures and delirium | ||
| Risk reduction 7.72 seizures/100 patients, 4.9 DTs/100 patients20 | ||
| Some abuse potential | ||
| Carbamazepine | Well-documented anticonvulsant activity; prevents seizures from alcohol Withdrawal | A |
| No abuse potential | ||
| Especially good for those with multiple previously treated withdrawals22 | ||
| Relative risk of first drink after withdrawal in benzodiazepine group over 3 times higher than carbamazepine22 | ||
| If carbamazepine-treated patients relapse, they drink less than benzodiazepine-treated patients [absolute risk reduction=4]22 | ||
| Valproic acid | Significantly affects the course of acute alcohol withdrawal and reduces need for treatment with a benzodiazepine [absolute risk reduction=4]24 | A |
| Use limited by side effects which mimic alcohol withdrawal | ||
| Wide therapeutic range makes unintentional overdose uncommon |
FIGURE 2
Guiding a patient through alcohol detoxification
Anticonvulsants
Attractive alternatives to benzodiazepines include the anticonvulsants carbamazepine (Tegretol) and valproic acid (Depakote).
Carbamazepine. Carbamazepine has been used successfully for many years in Europe,21 but has not been used widely in the US due to the safety, efficacy, and familiarity of benzodiazepines (Table 1). The use of anticonvulsants, however, has several advantages. They are not as sedating as benzodiazepines and do not have the abuse potential, making them particularly useful in the outpatient setting.
The use of anticonvulsant medication decreases the possibility of seizures, one of the more serious complications of alcohol withdrawal (NNT=36) (LOE: 1, 2 double-blind randomized controlled trials). The brain cell kindling-like phenomenon—in which repeated episodes of alcohol withdrawal is associated with increasing severity of withdrawal—is decreased with the anticonvulsant carbamazepine.14
In a double-blind controlled trial comparing carbamazepine with oxazepam, carbamazepine was shown to be superior in ameliorating global psychological distress and reducing aggression and anxiety.21 Stuppaeck et al showed that for alcohol withdrawal longer than 5 days, carbamazepine was statistically superior (P<.05) to oxazepam in reduction of CIWA scores.22,23 Carbamazepine is also superior to benzodiazepines in preventing rebound withdrawal symptoms and reducing post-treatment drinking, especially in those with a history of multiple repeated withdrawals (SOR=A).22 It has been shown that patients treated with carbamazepine were less likely to have a first drink following detoxification, and if they did drink, they drank less. This difference was especially evident for those patients with a history of multiple withdrawal attempts.22
A limitation of carbamazepine use, however, is its interaction with multiple medications that undergo hepatic oxidative metabolism, making it less useful in older patients or those with multiple medical problems. In summary, in generally healthy individuals with mild-to-moderate alcohol withdrawal, carbamazepine is just as efficacious as benzodiazepines, but has many advantages making it the drug of choice for properly selected patients (SOR=A).21-23
Valproic acid. Another widely used anticonvulsant, valproic acid, significantly affects the course of alcohol withdrawal and reduces the need for treatment with a benzodiazepine (LOE: 1).24 Two double-blind, randomized studies showed that patients treated with valproic acid for 4 to 7 days had fewer seizures, dropped out less frequently, had less severe withdrawal symptoms, and require less oxazepam than those treated with placebo or carbamazepine.24,25
Although effective, valproic acid use may be limited by side effects—somnolence, gastrointestinal disturbances, confusion, and tremor—that mimic the symptoms of alcohol withdrawal, making it difficult to assess improvement.
Other types of medications
Alpha-adrenergic agonists,24,30, beta-blockers,31,33 and calcium channel blockers34,35 have been used to control symptoms of acute alcohol withdrawal, but have demonstrated little efficacy in prevention of seizures or DTs (LOE: 1).5,36
Treatment regimens
The acceptable medication regimens for treating alcohol withdrawal are the gradually tapering dose approach, the fixed-schedule approach, and the symptom-triggered approach. The first 2 regimens are appropriate for the pharmacological treatment of outpatient alcohol detoxification.
Gradually tapering regimen. With the gradual-dosing plan, patients receive medication according to a predetermined dosing schedule for several days as the medication is gradually discontinued (Table 2).
Fixed-schedule regimen. In the fixed-schedule dosing regimen, the patient receives a fixed dose of medication every 6 hours for 2 to 3 days regardless of severity of symptoms.
Symptom-triggered regimen. For the symptom-triggered approach, the patient’s CIWA-Ar score is determined hourly or bihourly and the medication is administered only when the score is elevated. Typically, benzodiazepines are used in a symptom-triggered regimen, although either benzodiazepines or anticonvulsants may be used in a fixed-schedule plan.
The main advantage to the symptom-triggered approach is that much less medication is used to achieve the same withdrawal state (LOE: 1).37-39 The symptom-triggered approach has also shown a possible decrease in DTs and may lead to less oversedation.38,39
We favor a symptom-based approach whenever adequate periodic assessment of CIWA-Ar can be performed, such as in an inpatient setting. For those patients who require pharmacological treatment during outpatient detoxification (CIWA-Ar score 8–15), we prefer the gradually tapering or fixed dosing plan, to provide a margin of safety, simplify the dosing schedule, and maximize compliance (SOR: C, expert opinion).14
TABLE 2
Outpatient treatment for alcohol detoxification
| Thiamine – 100 mg orally per day (for 5 days) |
| Consider folate (1 mg) and multiple vitamin injection |
| One of the following regimens: |
| 3-day supply (only) of the following: Chlordiazepoxide |
| 50–100 mg every 6 hours for 4 doses, then |
| 25–50 mg every 6 hours for 8 doses |
| Diazepam |
| 10–20 mg every 6 hours for 4 doses, then |
| 5–10 mg every 6 hours for 8 doses |
| Lorazepam |
| 2–4 mg every 6 hours for 4 doses, then |
| 1–2 mg every 6 hours for 8 doses (consider this choice if significant hepatic dysfunction) |
| Carbamazepine (Tegretol) —5-day supply |
| 200 mg 4 times on day 1, |
| 200 mg 3 times on day 2, |
| 200 mg 2 times on day 3, |
| 200 mg daily for 2 more days (5 days total) |
Inpatient vs outpatient treatment
Most patients undergoing alcohol withdrawal may be treated safely in either an inpatient or out-patient setting (SOR=A).40 Treatment professionals should assess whether inpatient or outpatient treatment would contribute more therapeutically to an alcoholic’s recovery process.41
Patients with severe alcohol withdrawal symptoms (CIWA-Ar ≥15), previous history of DTs or seizures, or those with serious psychiatric or medical comorbidities should be considered for detoxification in an inpatient setting (SOR=B) (Table 3).10,42 The main advantage of inpatient detoxification is the availability of constant medical care, supervision, and treatment of serious complications.
A major disadvantage is the high cost of inpatient treatment. Hayashida and colleagues found inpatient treatment to be significantly more costly than outpatient treatment ($3,319–$3,665 vs $175–$388).43 Additionally, while inpatient care may temporarily relieve people from the social stressors that contribute to their alcohol problem, repeated inpatient detoxification may not provide an overall therapeutic benefit.
Most alcohol treatment programs find that <10% of patients need admission to an inpatient unit for treatment of withdrawal symptoms.44 For patients with mild-to-moderate alcohol withdrawal symptoms (CIWA-Ar <15), and no serious psychiatric or medical comorbidities, outpatient detoxification has been shown to be as safe and effective as inpatient detoxification (SOR=A).40 Additionally, most patients in an outpatient setting experience greater social support, and maintain the freedom to continue working or maintaining day-to-day activities with fewer disruptions, and incur fewer treatment costs.41 When assessing a patient for suitability for outpatient detoxification, it is important to ascertain motivation to stay sober, ability to return for daily nursing checks, and presence of a supportive observer at home.
TABLE 3
Criteria for inpatient alcohol detoxification
| Consider transfer for inpatient detoxification if the patient: |
|---|
|
Corresponding author
Chad Asplund, MD, 5663 Marshall Road, Fort Belvoir, VA 22060. E-mail: [email protected].
1. Angell M, Kassirer JP. Alcohol and other drugs–toward a more rational and consistent policy. N Engl J Med 1994;331:537-539.
2. Harwood H. Updating Estimates of the Economic Costs of Alcohol Abuse in the United States: Estimates, Update Methods, and Data. Report prepared by The Lewin Group for the National Institute on Alcohol Abuse and Alcoholism, 2000.
3. Whitmore CC, Yi H, Chen CM, et al. Surveillance Report #58: Trends in Alcohol-Related Morbidity Among Short-Stay Community Hospital Discharges, United States, 1979–99. Bethesda, Md: National Institute on Alcohol Abuse and Alcoholism, Division of Biometry and Epidemiology, 2002.
4. Myrick H, Anton RF. Treatment of alcohol withdrawal. Alcohol Health Res World 1998;22:38-43.
5. Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World 1998;22:5-12.
6. Trevisan LA, Boutros N, Petrakas IL, et al. Complications of alcohol withdrawal pathophysiologic insights. Alcohol Health Res World 1998;22:61-66.
7. Dvirskii AA. The role of genetic factors in the manifestation of delirium tremens [in Russian]. Zh Nevrol Psikhiatr Im S S Korsakova 1999;99:48-50.
8. Fiellin DA, O’Connor PG, Holmboe ES, Horwitz RI. Risk for delirium tremens in patients with alcohol withdrawal syndrome. Subst Abus 2002;23:83-94.
9. Saunders JB, Janca A. Delirium tremens: its aetiology, natural history and treatment. Curr Opin Psychiatry 2000;13:629-633.
10. Foy A, Kay J, Taylor A. The course of alcohol withdrawal in a general hospital. QJM 1997;90:253-261.
11. Wilson A, Vulcano B. A double-blind placebo-controlled trial of magnesium sulfate in the ethanol withdrawal syndrome. Alcohol Clin Exp Res 1984;8:542-545.
12. Victor M, Adams RD. The effect of alcohol on the nervous system. In: Metabolic and toxic diseases of the nervous system. Research publications of the Association for Research in Nervous and Mental Disease. Baltimore, Md: Williams and Wilkins, 1952.
13. Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: The revised Clinical Institute Withdrawal Assessment for Alcohol scale (CIWA-Ar). Br J Addict 1989;84:1353-1357.
14. Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA 1997;278:144-151.
15. Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Diagnosis and management of acute alcohol withdrawal. CMAJ 1999;160:675-680.
16. Shaw JM, Kolesar GS, Sellers EM, Kaplan HL, Sandor P. Development of optimal tactics for alcohol withdrawal. I. Assessment and effectiveness of supportive care. J Clin Psychopharmacol 1981;1:382-387.
17. Myrick H, Anton RF. Clinical management of alcohol withdrawal. CNS Spectrums 2000;5:22-23.
18. Hill A, Williams D. Hazards associated with the use of benzodiazepines in alcohol detoxification. J Subst Abuse Treat 1993;10:449-451.
19. Ritson B, Chick J. Comparison of two benzodiazepines in the treatment of alcohol withdrawal; effects on symptoms and cognitive recovery. Drug Alcohol Depend 1986;18:329-334.
20. Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Meta-analysis of benzodiazepine use in the treatment of acute alcohol withdrawal. CMAJ 1999;160:649-655.
21. Malcolm R, Ballenger JC, Sturgis ET, Anton R. Double-blind controlled trial comparing carbamazepine to oxazepam treatment of alcohol withdrawal. Am J Psychiatry 1989;146:617-621.
22. Malcolm R, Myrick H, Roberts J, et al. The effects of carbamazepine and lorazepam on single versus multiple previous alcohol withdrawals in an outpatient randomized trial. J Gen Intern Med 2002;17:349-355.
23. Stuppaeck CH, Pycha R, Miller C, Whitworth AB, Oberbauer H, Fleischhacker WW. Carbamazepine versus oxazepam in the treatment of alcohol withdrawal: a double-blind study. Alcohol # Alcoholism 1992;27:153-158.
24. Reoux JP, Saxon AJ, Malte CA, Baer JS, Sloan KL. Divalproex sodium in alcohol withdrawal: a randomized double-blind placebo-controlled clinical trial. Alcohol Clin Exp Res 2001;25:1324-1329.
25. Malcolm R, Myrick H, Brady KT, Ballenger JC. Update on anticonvulsants for the treatment of alcohol withdrawal. Am J Addict 2001;10(Suppl):16-23.
26. Bjorkqvist SE. Clonidine in alcohol withdrawal. Acta Psychiatr Scand 1975;52:256-263.
27. Wilkins AJ, Jenkins WJ, Steiner JA. Efficacy of clonidine in treatment of alcohol withdrawal state. Psychopharmacology (Berl) 1983;81:78-80.
28. Manhem P, Nilsson LH, Moberg AL, Wadstein J, Hokfelt B. Alcohol withdrawal: effects of clonidine treatment on sympathetic activity, the renin-aldosterone system, and clinical symptoms. Alcohol Clin Exp Res 1985;9:238-243.
29. Baumgartner GR, Rowen RC. Clonidine vs. chlordiazepoxide in the management of acute alcohol withdrawal syndrome. Arch Int Med 1987;147:1223-1226.
30. Robinson BJ, Robinson GM, Maling TJ, Johnson RH. Is clonidine useful in the treatment of alcohol withdrawal? Alchol Clin Exp Res 1989;13:95-98.
31. Worner TM. Propranolol versus diazepam in the management of the alcohol withdrawal syndrome: double-blind controlled trial. Am J Drug Alcohol Abuse 1994;20:115-124.
32. Horwitz RI, Gottlieb LD, Kraus ML. The efficacy of atenolol in the outpatient management of the alcohol withdrawal syndrome. Results of a randomized clinical trial. Arch Intern Med 1989;149:1089-1093.
33. Kraus ML, Gottlieb LD, Horwitz RI, et al. Randomized clinical trial of atenolol in patients with alcohol withdrawal. N Engl J Med 1985;313:905-909.
34. Banger M, Benkert O, Roschke J, et al. Nimodipine in acute alcohol withdrawal state. J Psychiatr Res 1992;26:117-123.
35. Altamura AC, Regazzetti MG, Porta M. Nimodipine in human alcohol withdrawal syndrome—an open study. Eur Neuropsychopharmacol 1990;1:37-40.
36. Saitz R, O’Malley SS. Pharmacotherapies of alcohol abuse. Withdrawal and treatment. Med Clin North Am 1997;81:881-907.
37. Reoux JP, Miller K. Routine hospital alcohol detoxification practice compared with symptom triggered management with an Objective Withdrawal Scale (CIWA-Ar). Am J Addict 2000;9:135-144.
38. Daeppen JB, Gache P, Landry U, et al. Symptom-triggered versus fixed-schedule doses of benzodiazepines for alcohol withdrawal: a randomized treatment trial. Arch Intern Med 2002;162:1117-1121.
39. Saitz R, Mayo-Smith MF, Roberts MS, Redmond HA, Bernard DR, Calkins DR. Individualized treatment for alcohol withdrawal: a randomized double-blind controlled trial. JAMA 1994;272:519-523.
40. Mattick RP, Jarvis T. In-patient setting and long duration for the treatment of alcohol dependence: out-patient care is as good. Drug Alcohol Rev 1994;13:127-135.
41. Hayashida M. An overview of outpatient and inpatient detoxification. Alcohol Health Res World 1998;22:44-46.
42. Booth BM, Blow FC, Ludke RL, Ross RL. Utilization of inpatient services for alcohol detoxification. J Men Health Adm 1996;23:366-374.
43. Hayashida M, Alterman AI, McLellan AT, et al. Comparative effectiveness and costs of inpatient and outpatient detoxification of patients with mild-to-moderate alcohol withdrawal syndrome. N Engl J Med 1989;320:358-365.
44. Abbott PJ, Quinn D, Knox L. Ambulatory medical detoxification for alcohol. Am J Drug Alcohol Abuse 1995;21:549-563.
- Patients with mild to moderate alcohol withdrawal symptoms and no serious psychiatric or medical comorbidities can be safely treated in the outpatient setting (SOR:A).
- Patients with moderate withdrawal should receive pharmacotherapy to treat their symptoms and reduce their risk of seizures and delirium tremens during outpatient detoxification (SOR:A).
- Benzodiazepines are the treatment of choice for alcohol withdrawal (SOR:A).
- ln healthy individuals with mild-to-moderate alcohol withdrawal, carbamazepine has many advantages making it a first-line treatment for properly selected patients (SOR:A).
In our small community hospital—with limited financial and medical resources—we have designed and implemented an outpatient alcohol detoxification clinical practice guideline to provide cost-effective, evidence-based medical care to our patients, in support of their alcohol treatment.
Those patients with mild-to-moderate alcohol withdrawal symptoms and no serious psychiatric or medical comorbidities can be safely treated in the outpatient setting. Patients with history of severe withdrawal symptoms, seizures or delirium tremens, comorbid serious psychiatric or medical illnesses, or lack of reliable support network should be considered for detoxification in the inpatient setting.
The problem of alcohol withdrawal
Up to 71% of individuals presenting for alcohol detoxification manifest significant symptoms of alcohol withdrawal.4 Alcohol withdrawal is a clinical syndrome that affects people accustomed to regular alcohol intake who either decrease their alcohol consumption or stop drinking completely.
Physiology
Alcohol enhances gamma-aminobutyric acid’s (GABA) inhibitory effects on signal-receiving neurons, thereby lowering neuronal activity, leading to an increase in excitatory glutamate receptors. Over time, tolerance occurs as GABA receptors become less responsive to neurotransmitters, and more alcohol is required to produce the same inhibitory effect. When alcohol is removed acutely, the number of excitatory glutamate receptors remains, but without the suppressive GABA effect.5 This situation leads to the signs and symptoms of alcohol withdrawal.
Symptoms
Noticeable alcohol withdrawal symptoms may appear within hours of cessation or decreasing alcohol intake. The most common symptoms include tremor, craving for alcohol, insomnia, vivid dreams, anxiety, hypervigilance, agitation, irritability, loss of appetite, nausea, vomiting, headache, and sweating.5 Even without treatment, most of these relatively benign symptoms resolve within hours to days.
More concerning are hallucinations, delirium tremens (DTs), and seizures. Transient auditory or visual hallucinations may occur within the first 2 days of decreasing or discontinuing alcohol consumption, and can be separate from DTs. DTs, which present within 2 to 4 days of the last drink (and can last up to 3 to 4 days), are characterized by disorientation, persistent visual and auditory hallucinations, agitation and tremulousness, and autonomic signs resulting from the activation of stress-related hormones. These signs include tachycardia, hypertension, and fevers.
DTs are much more serious than the “alcohol shakes”—5% of patients who experience DTs die from metabolic complications.6 The occurrence of DTs is 5.3 times higher in men than in women;7 however, women may exhibit fewer autonomic symptoms, making DTs in women more difficult to diagnose.6
Grand mal seizures can occur in up to 25% of alcoholics undergoing withdrawal.4 If alcohol-related seizures do occur, they generally do so within 1 day of cessation of alcohol intake, but can occur up to 5 days later.
Risk factors for prolonged or complicated alcohol withdrawal include duration of alcohol consumption, the number of lifetime prior detoxifications, prior seizures, prior episodes of DTs, and current intense craving for alcohol.6-10
Before treatment: assess and stabilize
Initial assessment of the patient
Before initiating treatment for alcohol withdrawal, perform a thorough assessment of the patient’s medical condition. This evaluation should include an assessment of coexisting medical and psychiatric conditions, the severity of previous withdrawal symptoms, and the risk factors for withdrawal complications. The initial symptoms of alcohol withdrawal are not specific and may mimic other serious disease conditions; therefore, the initial assessment should exclude potentially serious medical and psychiatric comorbidities.
Initially, assessment of common alcohol-related medical problems should be conducted. These complications include gastritis, gastrointestinal bleeding, liver disease, cardiomyopathy, pancreatitis, neurological impairment, electrolyte imbalances, and nutritional deficiencies. A physical examination should be performed to assess for arrhythmias, congestive heart failure, hepatic or pancreatic disease, infectious conditions, bleeding, and nervous system impairment.
Initial alcohol level and urine drug screen should be assessed, as recent high levels of alcohol intake and substance abuse place the patient at higher risk for complications. Unstable mood disorders—delirium, psychosis, severe depression, suicidal or homicidal ideation—while potentially difficult to assess during intoxication, need to be considered and ruled out.
Stabilize the patient
After initial assessment, vital signs (eg, heart rate, blood pressure, and temperature) should be stabilized while fluid, electrolyte, and nutritional disturbances are corrected. Some patients undergoing alcohol withdrawal may require intravenous fluids to correct severe dehydration resulting from vomiting, diarrhea, sweating, and fever.
Alcoholics are often deficient in electrolytes or minerals, including thiamine, folate, and magnesium (although replacing magnesium makes no difference in clinically meaningful outcomes) (level of evidence [LOE]: 1, double-blind randomized controlled trial).11 All patients being treated for alcohol withdrawal should be given 100 mg of thiamine immediately and daily (LOE: 3; insufficient evidence from randomized controlled trials to guide clinicians in the dose, frequency, route, or duration of thiamine treatment for prophylaxis against or treatment of WKS due to alcohol abuse).4 Thiamine should be given before glucose containing fluids, to avoid the risk of precipitating Wernicke syndrome (LOE: 3).12
Assess the severity of the withdrawal
Once a diagnosis of alcohol withdrawal is made, complete an assessment of the severity of withdrawal and the risk of complications. The best validated tool is the Clinical Institute Withdrawal Assessment for Alcohol-Revised (CIWA-Ar) symptom scale (Figure 1).10 This instrument rates 10 withdrawal features; it takes only a few minutes to administer and may be repeated when re-evaluation is necessary. CIWA-Ar scores of ≤8 are suggestive of mild withdrawal symptoms, while those ≥15 confer an increased risk for confusion and seizures.
CIWA-Ar is reliable, brief, uncomplicated, and clinically useful scale that can also be used to monitor response to treatment. It offers an increase in efficiency over the original CIWA-A scale, while retaining clinical usefulness, validity, and reliability. It can be incorporated into the usual clinical care of patients undergoing alcohol withdrawal and into clinical drug trials of alcohol withdrawal (strength of recommendation [SOR]=A].5,13
Pharmacotherapy
Patients experiencing more serious withdrawal (with CIWA-Ar scores >8) should receive pharmacotherapy to treat their symptoms and reduce their risk of seizures and DTs (SOR=A).14
Benzodiazepines
Benzodiazepines are the mainstay of treatment in alcohol withdrawal (number needed to treat [NNT]=17; data from large meta-analysis of 6 prospective, placebo-controlled trials) (SOR=A).10,14,16 Like alcohol, these agents magnify GABA’s effect on the brain. Benzodiazepines are cross-tolerant with alcohol; during withdrawal from 1 agent, the other may serve as a substitute. Benzodiazepines also reduce the incidence of DTs and seizures (Table 1).5,14
The problem. In our small community hospital, prior to the development of a clinical practice guideline, admissions for “inpatient alcohol detoxification” were among our top 5, with a select few patients making multiple, repeat visits. Additionally, we had no standardized, consistent strategy for initial emergency room evaluation; frequent early discharges against medical advice; multiple readmissions; infrequent and inconsistent entry into our outpatient Alcohol and Substance Abuse Program; and no existing process for primary care outpatient follow-up. We found ourselves in a situation where we were essentially enabling our patients in a destructive behavior. With no formal policy or guidelines, physicians tended to follow the path of least resistance: repeated short-stay admissions with limited therapeutic benefit.
The process. Our initial goal was to develop a standardized policy in an attempt to minimize the number of admissions of mild-to-moderate, uncomplicated alcohol withdrawal patients. Many of our patients are at low risk for serious complications, and we hoped to triage such individuals to an outpatient treatment setting. To organize the thought process, a flowchart was developed and refined. By incorporating current evidence, a clinical practice guideline was developed.
Evidence-based algorithm. We developed an evidence-based algorithm, Outpatient Treatment for Alcohol Detoxification (Figure 2), which uses a gradually tapering regimen, and allows providers to prescribe the medication they feel most appropriate given the clinical situation.
Results. In the 12 months since implementation of our clinical practice guideline, total alcohol-related admission decreased from 4 to 5 per month to only 1 during the entire period; furthermore, no patients treated with our guidelines were subsequently hospitalized for complications of alcohol withdrawal.
The most commonly used benzodiazepines are diazepam (Valium), chlordiazepoxide (Librium), and lorazepam (Ativan). All appear to be equally efficacious in treating alcohol withdrawal symptoms (LOE: 1; randomized controlled trial).
Longer-acting agents, such as chlordiazepoxide or diazepam, contribute to an overall smoother withdrawal course with lessened breakthrough or rebound symptoms, but they may also lead to excess sedation for patients with hepatic dysfunction.17-20 Shorter-acting benzodiazepines, such as oxazepam (Serax), may result in greater discomfort and more discharges against medical advice, because alcohol withdrawal symptoms tend to recur when serum benzodiazepine levels drop.
TABLE 1
Pharmacologic treatment of alcohol withdrawal
| Medication | Comments | LOE |
|---|---|---|
| Benzodiazepines | Remain drug of choice for acute alcohol withdrawal14 | A |
| Highly significant decrease in seizures and delirium | ||
| Risk reduction 7.72 seizures/100 patients, 4.9 DTs/100 patients20 | ||
| Some abuse potential | ||
| Carbamazepine | Well-documented anticonvulsant activity; prevents seizures from alcohol Withdrawal | A |
| No abuse potential | ||
| Especially good for those with multiple previously treated withdrawals22 | ||
| Relative risk of first drink after withdrawal in benzodiazepine group over 3 times higher than carbamazepine22 | ||
| If carbamazepine-treated patients relapse, they drink less than benzodiazepine-treated patients [absolute risk reduction=4]22 | ||
| Valproic acid | Significantly affects the course of acute alcohol withdrawal and reduces need for treatment with a benzodiazepine [absolute risk reduction=4]24 | A |
| Use limited by side effects which mimic alcohol withdrawal | ||
| Wide therapeutic range makes unintentional overdose uncommon |
FIGURE 2
Guiding a patient through alcohol detoxification
Anticonvulsants
Attractive alternatives to benzodiazepines include the anticonvulsants carbamazepine (Tegretol) and valproic acid (Depakote).
Carbamazepine. Carbamazepine has been used successfully for many years in Europe,21 but has not been used widely in the US due to the safety, efficacy, and familiarity of benzodiazepines (Table 1). The use of anticonvulsants, however, has several advantages. They are not as sedating as benzodiazepines and do not have the abuse potential, making them particularly useful in the outpatient setting.
The use of anticonvulsant medication decreases the possibility of seizures, one of the more serious complications of alcohol withdrawal (NNT=36) (LOE: 1, 2 double-blind randomized controlled trials). The brain cell kindling-like phenomenon—in which repeated episodes of alcohol withdrawal is associated with increasing severity of withdrawal—is decreased with the anticonvulsant carbamazepine.14
In a double-blind controlled trial comparing carbamazepine with oxazepam, carbamazepine was shown to be superior in ameliorating global psychological distress and reducing aggression and anxiety.21 Stuppaeck et al showed that for alcohol withdrawal longer than 5 days, carbamazepine was statistically superior (P<.05) to oxazepam in reduction of CIWA scores.22,23 Carbamazepine is also superior to benzodiazepines in preventing rebound withdrawal symptoms and reducing post-treatment drinking, especially in those with a history of multiple repeated withdrawals (SOR=A).22 It has been shown that patients treated with carbamazepine were less likely to have a first drink following detoxification, and if they did drink, they drank less. This difference was especially evident for those patients with a history of multiple withdrawal attempts.22
A limitation of carbamazepine use, however, is its interaction with multiple medications that undergo hepatic oxidative metabolism, making it less useful in older patients or those with multiple medical problems. In summary, in generally healthy individuals with mild-to-moderate alcohol withdrawal, carbamazepine is just as efficacious as benzodiazepines, but has many advantages making it the drug of choice for properly selected patients (SOR=A).21-23
Valproic acid. Another widely used anticonvulsant, valproic acid, significantly affects the course of alcohol withdrawal and reduces the need for treatment with a benzodiazepine (LOE: 1).24 Two double-blind, randomized studies showed that patients treated with valproic acid for 4 to 7 days had fewer seizures, dropped out less frequently, had less severe withdrawal symptoms, and require less oxazepam than those treated with placebo or carbamazepine.24,25
Although effective, valproic acid use may be limited by side effects—somnolence, gastrointestinal disturbances, confusion, and tremor—that mimic the symptoms of alcohol withdrawal, making it difficult to assess improvement.
Other types of medications
Alpha-adrenergic agonists,24,30, beta-blockers,31,33 and calcium channel blockers34,35 have been used to control symptoms of acute alcohol withdrawal, but have demonstrated little efficacy in prevention of seizures or DTs (LOE: 1).5,36
Treatment regimens
The acceptable medication regimens for treating alcohol withdrawal are the gradually tapering dose approach, the fixed-schedule approach, and the symptom-triggered approach. The first 2 regimens are appropriate for the pharmacological treatment of outpatient alcohol detoxification.
Gradually tapering regimen. With the gradual-dosing plan, patients receive medication according to a predetermined dosing schedule for several days as the medication is gradually discontinued (Table 2).
Fixed-schedule regimen. In the fixed-schedule dosing regimen, the patient receives a fixed dose of medication every 6 hours for 2 to 3 days regardless of severity of symptoms.
Symptom-triggered regimen. For the symptom-triggered approach, the patient’s CIWA-Ar score is determined hourly or bihourly and the medication is administered only when the score is elevated. Typically, benzodiazepines are used in a symptom-triggered regimen, although either benzodiazepines or anticonvulsants may be used in a fixed-schedule plan.
The main advantage to the symptom-triggered approach is that much less medication is used to achieve the same withdrawal state (LOE: 1).37-39 The symptom-triggered approach has also shown a possible decrease in DTs and may lead to less oversedation.38,39
We favor a symptom-based approach whenever adequate periodic assessment of CIWA-Ar can be performed, such as in an inpatient setting. For those patients who require pharmacological treatment during outpatient detoxification (CIWA-Ar score 8–15), we prefer the gradually tapering or fixed dosing plan, to provide a margin of safety, simplify the dosing schedule, and maximize compliance (SOR: C, expert opinion).14
TABLE 2
Outpatient treatment for alcohol detoxification
| Thiamine – 100 mg orally per day (for 5 days) |
| Consider folate (1 mg) and multiple vitamin injection |
| One of the following regimens: |
| 3-day supply (only) of the following: Chlordiazepoxide |
| 50–100 mg every 6 hours for 4 doses, then |
| 25–50 mg every 6 hours for 8 doses |
| Diazepam |
| 10–20 mg every 6 hours for 4 doses, then |
| 5–10 mg every 6 hours for 8 doses |
| Lorazepam |
| 2–4 mg every 6 hours for 4 doses, then |
| 1–2 mg every 6 hours for 8 doses (consider this choice if significant hepatic dysfunction) |
| Carbamazepine (Tegretol) —5-day supply |
| 200 mg 4 times on day 1, |
| 200 mg 3 times on day 2, |
| 200 mg 2 times on day 3, |
| 200 mg daily for 2 more days (5 days total) |
Inpatient vs outpatient treatment
Most patients undergoing alcohol withdrawal may be treated safely in either an inpatient or out-patient setting (SOR=A).40 Treatment professionals should assess whether inpatient or outpatient treatment would contribute more therapeutically to an alcoholic’s recovery process.41
Patients with severe alcohol withdrawal symptoms (CIWA-Ar ≥15), previous history of DTs or seizures, or those with serious psychiatric or medical comorbidities should be considered for detoxification in an inpatient setting (SOR=B) (Table 3).10,42 The main advantage of inpatient detoxification is the availability of constant medical care, supervision, and treatment of serious complications.
A major disadvantage is the high cost of inpatient treatment. Hayashida and colleagues found inpatient treatment to be significantly more costly than outpatient treatment ($3,319–$3,665 vs $175–$388).43 Additionally, while inpatient care may temporarily relieve people from the social stressors that contribute to their alcohol problem, repeated inpatient detoxification may not provide an overall therapeutic benefit.
Most alcohol treatment programs find that <10% of patients need admission to an inpatient unit for treatment of withdrawal symptoms.44 For patients with mild-to-moderate alcohol withdrawal symptoms (CIWA-Ar <15), and no serious psychiatric or medical comorbidities, outpatient detoxification has been shown to be as safe and effective as inpatient detoxification (SOR=A).40 Additionally, most patients in an outpatient setting experience greater social support, and maintain the freedom to continue working or maintaining day-to-day activities with fewer disruptions, and incur fewer treatment costs.41 When assessing a patient for suitability for outpatient detoxification, it is important to ascertain motivation to stay sober, ability to return for daily nursing checks, and presence of a supportive observer at home.
TABLE 3
Criteria for inpatient alcohol detoxification
| Consider transfer for inpatient detoxification if the patient: |
|---|
|
Corresponding author
Chad Asplund, MD, 5663 Marshall Road, Fort Belvoir, VA 22060. E-mail: [email protected].
- Patients with mild to moderate alcohol withdrawal symptoms and no serious psychiatric or medical comorbidities can be safely treated in the outpatient setting (SOR:A).
- Patients with moderate withdrawal should receive pharmacotherapy to treat their symptoms and reduce their risk of seizures and delirium tremens during outpatient detoxification (SOR:A).
- Benzodiazepines are the treatment of choice for alcohol withdrawal (SOR:A).
- ln healthy individuals with mild-to-moderate alcohol withdrawal, carbamazepine has many advantages making it a first-line treatment for properly selected patients (SOR:A).
In our small community hospital—with limited financial and medical resources—we have designed and implemented an outpatient alcohol detoxification clinical practice guideline to provide cost-effective, evidence-based medical care to our patients, in support of their alcohol treatment.
Those patients with mild-to-moderate alcohol withdrawal symptoms and no serious psychiatric or medical comorbidities can be safely treated in the outpatient setting. Patients with history of severe withdrawal symptoms, seizures or delirium tremens, comorbid serious psychiatric or medical illnesses, or lack of reliable support network should be considered for detoxification in the inpatient setting.
The problem of alcohol withdrawal
Up to 71% of individuals presenting for alcohol detoxification manifest significant symptoms of alcohol withdrawal.4 Alcohol withdrawal is a clinical syndrome that affects people accustomed to regular alcohol intake who either decrease their alcohol consumption or stop drinking completely.
Physiology
Alcohol enhances gamma-aminobutyric acid’s (GABA) inhibitory effects on signal-receiving neurons, thereby lowering neuronal activity, leading to an increase in excitatory glutamate receptors. Over time, tolerance occurs as GABA receptors become less responsive to neurotransmitters, and more alcohol is required to produce the same inhibitory effect. When alcohol is removed acutely, the number of excitatory glutamate receptors remains, but without the suppressive GABA effect.5 This situation leads to the signs and symptoms of alcohol withdrawal.
Symptoms
Noticeable alcohol withdrawal symptoms may appear within hours of cessation or decreasing alcohol intake. The most common symptoms include tremor, craving for alcohol, insomnia, vivid dreams, anxiety, hypervigilance, agitation, irritability, loss of appetite, nausea, vomiting, headache, and sweating.5 Even without treatment, most of these relatively benign symptoms resolve within hours to days.
More concerning are hallucinations, delirium tremens (DTs), and seizures. Transient auditory or visual hallucinations may occur within the first 2 days of decreasing or discontinuing alcohol consumption, and can be separate from DTs. DTs, which present within 2 to 4 days of the last drink (and can last up to 3 to 4 days), are characterized by disorientation, persistent visual and auditory hallucinations, agitation and tremulousness, and autonomic signs resulting from the activation of stress-related hormones. These signs include tachycardia, hypertension, and fevers.
DTs are much more serious than the “alcohol shakes”—5% of patients who experience DTs die from metabolic complications.6 The occurrence of DTs is 5.3 times higher in men than in women;7 however, women may exhibit fewer autonomic symptoms, making DTs in women more difficult to diagnose.6
Grand mal seizures can occur in up to 25% of alcoholics undergoing withdrawal.4 If alcohol-related seizures do occur, they generally do so within 1 day of cessation of alcohol intake, but can occur up to 5 days later.
Risk factors for prolonged or complicated alcohol withdrawal include duration of alcohol consumption, the number of lifetime prior detoxifications, prior seizures, prior episodes of DTs, and current intense craving for alcohol.6-10
Before treatment: assess and stabilize
Initial assessment of the patient
Before initiating treatment for alcohol withdrawal, perform a thorough assessment of the patient’s medical condition. This evaluation should include an assessment of coexisting medical and psychiatric conditions, the severity of previous withdrawal symptoms, and the risk factors for withdrawal complications. The initial symptoms of alcohol withdrawal are not specific and may mimic other serious disease conditions; therefore, the initial assessment should exclude potentially serious medical and psychiatric comorbidities.
Initially, assessment of common alcohol-related medical problems should be conducted. These complications include gastritis, gastrointestinal bleeding, liver disease, cardiomyopathy, pancreatitis, neurological impairment, electrolyte imbalances, and nutritional deficiencies. A physical examination should be performed to assess for arrhythmias, congestive heart failure, hepatic or pancreatic disease, infectious conditions, bleeding, and nervous system impairment.
Initial alcohol level and urine drug screen should be assessed, as recent high levels of alcohol intake and substance abuse place the patient at higher risk for complications. Unstable mood disorders—delirium, psychosis, severe depression, suicidal or homicidal ideation—while potentially difficult to assess during intoxication, need to be considered and ruled out.
Stabilize the patient
After initial assessment, vital signs (eg, heart rate, blood pressure, and temperature) should be stabilized while fluid, electrolyte, and nutritional disturbances are corrected. Some patients undergoing alcohol withdrawal may require intravenous fluids to correct severe dehydration resulting from vomiting, diarrhea, sweating, and fever.
Alcoholics are often deficient in electrolytes or minerals, including thiamine, folate, and magnesium (although replacing magnesium makes no difference in clinically meaningful outcomes) (level of evidence [LOE]: 1, double-blind randomized controlled trial).11 All patients being treated for alcohol withdrawal should be given 100 mg of thiamine immediately and daily (LOE: 3; insufficient evidence from randomized controlled trials to guide clinicians in the dose, frequency, route, or duration of thiamine treatment for prophylaxis against or treatment of WKS due to alcohol abuse).4 Thiamine should be given before glucose containing fluids, to avoid the risk of precipitating Wernicke syndrome (LOE: 3).12
Assess the severity of the withdrawal
Once a diagnosis of alcohol withdrawal is made, complete an assessment of the severity of withdrawal and the risk of complications. The best validated tool is the Clinical Institute Withdrawal Assessment for Alcohol-Revised (CIWA-Ar) symptom scale (Figure 1).10 This instrument rates 10 withdrawal features; it takes only a few minutes to administer and may be repeated when re-evaluation is necessary. CIWA-Ar scores of ≤8 are suggestive of mild withdrawal symptoms, while those ≥15 confer an increased risk for confusion and seizures.
CIWA-Ar is reliable, brief, uncomplicated, and clinically useful scale that can also be used to monitor response to treatment. It offers an increase in efficiency over the original CIWA-A scale, while retaining clinical usefulness, validity, and reliability. It can be incorporated into the usual clinical care of patients undergoing alcohol withdrawal and into clinical drug trials of alcohol withdrawal (strength of recommendation [SOR]=A].5,13
Pharmacotherapy
Patients experiencing more serious withdrawal (with CIWA-Ar scores >8) should receive pharmacotherapy to treat their symptoms and reduce their risk of seizures and DTs (SOR=A).14
Benzodiazepines
Benzodiazepines are the mainstay of treatment in alcohol withdrawal (number needed to treat [NNT]=17; data from large meta-analysis of 6 prospective, placebo-controlled trials) (SOR=A).10,14,16 Like alcohol, these agents magnify GABA’s effect on the brain. Benzodiazepines are cross-tolerant with alcohol; during withdrawal from 1 agent, the other may serve as a substitute. Benzodiazepines also reduce the incidence of DTs and seizures (Table 1).5,14
The problem. In our small community hospital, prior to the development of a clinical practice guideline, admissions for “inpatient alcohol detoxification” were among our top 5, with a select few patients making multiple, repeat visits. Additionally, we had no standardized, consistent strategy for initial emergency room evaluation; frequent early discharges against medical advice; multiple readmissions; infrequent and inconsistent entry into our outpatient Alcohol and Substance Abuse Program; and no existing process for primary care outpatient follow-up. We found ourselves in a situation where we were essentially enabling our patients in a destructive behavior. With no formal policy or guidelines, physicians tended to follow the path of least resistance: repeated short-stay admissions with limited therapeutic benefit.
The process. Our initial goal was to develop a standardized policy in an attempt to minimize the number of admissions of mild-to-moderate, uncomplicated alcohol withdrawal patients. Many of our patients are at low risk for serious complications, and we hoped to triage such individuals to an outpatient treatment setting. To organize the thought process, a flowchart was developed and refined. By incorporating current evidence, a clinical practice guideline was developed.
Evidence-based algorithm. We developed an evidence-based algorithm, Outpatient Treatment for Alcohol Detoxification (Figure 2), which uses a gradually tapering regimen, and allows providers to prescribe the medication they feel most appropriate given the clinical situation.
Results. In the 12 months since implementation of our clinical practice guideline, total alcohol-related admission decreased from 4 to 5 per month to only 1 during the entire period; furthermore, no patients treated with our guidelines were subsequently hospitalized for complications of alcohol withdrawal.
The most commonly used benzodiazepines are diazepam (Valium), chlordiazepoxide (Librium), and lorazepam (Ativan). All appear to be equally efficacious in treating alcohol withdrawal symptoms (LOE: 1; randomized controlled trial).
Longer-acting agents, such as chlordiazepoxide or diazepam, contribute to an overall smoother withdrawal course with lessened breakthrough or rebound symptoms, but they may also lead to excess sedation for patients with hepatic dysfunction.17-20 Shorter-acting benzodiazepines, such as oxazepam (Serax), may result in greater discomfort and more discharges against medical advice, because alcohol withdrawal symptoms tend to recur when serum benzodiazepine levels drop.
TABLE 1
Pharmacologic treatment of alcohol withdrawal
| Medication | Comments | LOE |
|---|---|---|
| Benzodiazepines | Remain drug of choice for acute alcohol withdrawal14 | A |
| Highly significant decrease in seizures and delirium | ||
| Risk reduction 7.72 seizures/100 patients, 4.9 DTs/100 patients20 | ||
| Some abuse potential | ||
| Carbamazepine | Well-documented anticonvulsant activity; prevents seizures from alcohol Withdrawal | A |
| No abuse potential | ||
| Especially good for those with multiple previously treated withdrawals22 | ||
| Relative risk of first drink after withdrawal in benzodiazepine group over 3 times higher than carbamazepine22 | ||
| If carbamazepine-treated patients relapse, they drink less than benzodiazepine-treated patients [absolute risk reduction=4]22 | ||
| Valproic acid | Significantly affects the course of acute alcohol withdrawal and reduces need for treatment with a benzodiazepine [absolute risk reduction=4]24 | A |
| Use limited by side effects which mimic alcohol withdrawal | ||
| Wide therapeutic range makes unintentional overdose uncommon |
FIGURE 2
Guiding a patient through alcohol detoxification
Anticonvulsants
Attractive alternatives to benzodiazepines include the anticonvulsants carbamazepine (Tegretol) and valproic acid (Depakote).
Carbamazepine. Carbamazepine has been used successfully for many years in Europe,21 but has not been used widely in the US due to the safety, efficacy, and familiarity of benzodiazepines (Table 1). The use of anticonvulsants, however, has several advantages. They are not as sedating as benzodiazepines and do not have the abuse potential, making them particularly useful in the outpatient setting.
The use of anticonvulsant medication decreases the possibility of seizures, one of the more serious complications of alcohol withdrawal (NNT=36) (LOE: 1, 2 double-blind randomized controlled trials). The brain cell kindling-like phenomenon—in which repeated episodes of alcohol withdrawal is associated with increasing severity of withdrawal—is decreased with the anticonvulsant carbamazepine.14
In a double-blind controlled trial comparing carbamazepine with oxazepam, carbamazepine was shown to be superior in ameliorating global psychological distress and reducing aggression and anxiety.21 Stuppaeck et al showed that for alcohol withdrawal longer than 5 days, carbamazepine was statistically superior (P<.05) to oxazepam in reduction of CIWA scores.22,23 Carbamazepine is also superior to benzodiazepines in preventing rebound withdrawal symptoms and reducing post-treatment drinking, especially in those with a history of multiple repeated withdrawals (SOR=A).22 It has been shown that patients treated with carbamazepine were less likely to have a first drink following detoxification, and if they did drink, they drank less. This difference was especially evident for those patients with a history of multiple withdrawal attempts.22
A limitation of carbamazepine use, however, is its interaction with multiple medications that undergo hepatic oxidative metabolism, making it less useful in older patients or those with multiple medical problems. In summary, in generally healthy individuals with mild-to-moderate alcohol withdrawal, carbamazepine is just as efficacious as benzodiazepines, but has many advantages making it the drug of choice for properly selected patients (SOR=A).21-23
Valproic acid. Another widely used anticonvulsant, valproic acid, significantly affects the course of alcohol withdrawal and reduces the need for treatment with a benzodiazepine (LOE: 1).24 Two double-blind, randomized studies showed that patients treated with valproic acid for 4 to 7 days had fewer seizures, dropped out less frequently, had less severe withdrawal symptoms, and require less oxazepam than those treated with placebo or carbamazepine.24,25
Although effective, valproic acid use may be limited by side effects—somnolence, gastrointestinal disturbances, confusion, and tremor—that mimic the symptoms of alcohol withdrawal, making it difficult to assess improvement.
Other types of medications
Alpha-adrenergic agonists,24,30, beta-blockers,31,33 and calcium channel blockers34,35 have been used to control symptoms of acute alcohol withdrawal, but have demonstrated little efficacy in prevention of seizures or DTs (LOE: 1).5,36
Treatment regimens
The acceptable medication regimens for treating alcohol withdrawal are the gradually tapering dose approach, the fixed-schedule approach, and the symptom-triggered approach. The first 2 regimens are appropriate for the pharmacological treatment of outpatient alcohol detoxification.
Gradually tapering regimen. With the gradual-dosing plan, patients receive medication according to a predetermined dosing schedule for several days as the medication is gradually discontinued (Table 2).
Fixed-schedule regimen. In the fixed-schedule dosing regimen, the patient receives a fixed dose of medication every 6 hours for 2 to 3 days regardless of severity of symptoms.
Symptom-triggered regimen. For the symptom-triggered approach, the patient’s CIWA-Ar score is determined hourly or bihourly and the medication is administered only when the score is elevated. Typically, benzodiazepines are used in a symptom-triggered regimen, although either benzodiazepines or anticonvulsants may be used in a fixed-schedule plan.
The main advantage to the symptom-triggered approach is that much less medication is used to achieve the same withdrawal state (LOE: 1).37-39 The symptom-triggered approach has also shown a possible decrease in DTs and may lead to less oversedation.38,39
We favor a symptom-based approach whenever adequate periodic assessment of CIWA-Ar can be performed, such as in an inpatient setting. For those patients who require pharmacological treatment during outpatient detoxification (CIWA-Ar score 8–15), we prefer the gradually tapering or fixed dosing plan, to provide a margin of safety, simplify the dosing schedule, and maximize compliance (SOR: C, expert opinion).14
TABLE 2
Outpatient treatment for alcohol detoxification
| Thiamine – 100 mg orally per day (for 5 days) |
| Consider folate (1 mg) and multiple vitamin injection |
| One of the following regimens: |
| 3-day supply (only) of the following: Chlordiazepoxide |
| 50–100 mg every 6 hours for 4 doses, then |
| 25–50 mg every 6 hours for 8 doses |
| Diazepam |
| 10–20 mg every 6 hours for 4 doses, then |
| 5–10 mg every 6 hours for 8 doses |
| Lorazepam |
| 2–4 mg every 6 hours for 4 doses, then |
| 1–2 mg every 6 hours for 8 doses (consider this choice if significant hepatic dysfunction) |
| Carbamazepine (Tegretol) —5-day supply |
| 200 mg 4 times on day 1, |
| 200 mg 3 times on day 2, |
| 200 mg 2 times on day 3, |
| 200 mg daily for 2 more days (5 days total) |
Inpatient vs outpatient treatment
Most patients undergoing alcohol withdrawal may be treated safely in either an inpatient or out-patient setting (SOR=A).40 Treatment professionals should assess whether inpatient or outpatient treatment would contribute more therapeutically to an alcoholic’s recovery process.41
Patients with severe alcohol withdrawal symptoms (CIWA-Ar ≥15), previous history of DTs or seizures, or those with serious psychiatric or medical comorbidities should be considered for detoxification in an inpatient setting (SOR=B) (Table 3).10,42 The main advantage of inpatient detoxification is the availability of constant medical care, supervision, and treatment of serious complications.
A major disadvantage is the high cost of inpatient treatment. Hayashida and colleagues found inpatient treatment to be significantly more costly than outpatient treatment ($3,319–$3,665 vs $175–$388).43 Additionally, while inpatient care may temporarily relieve people from the social stressors that contribute to their alcohol problem, repeated inpatient detoxification may not provide an overall therapeutic benefit.
Most alcohol treatment programs find that <10% of patients need admission to an inpatient unit for treatment of withdrawal symptoms.44 For patients with mild-to-moderate alcohol withdrawal symptoms (CIWA-Ar <15), and no serious psychiatric or medical comorbidities, outpatient detoxification has been shown to be as safe and effective as inpatient detoxification (SOR=A).40 Additionally, most patients in an outpatient setting experience greater social support, and maintain the freedom to continue working or maintaining day-to-day activities with fewer disruptions, and incur fewer treatment costs.41 When assessing a patient for suitability for outpatient detoxification, it is important to ascertain motivation to stay sober, ability to return for daily nursing checks, and presence of a supportive observer at home.
TABLE 3
Criteria for inpatient alcohol detoxification
| Consider transfer for inpatient detoxification if the patient: |
|---|
|
Corresponding author
Chad Asplund, MD, 5663 Marshall Road, Fort Belvoir, VA 22060. E-mail: [email protected].
1. Angell M, Kassirer JP. Alcohol and other drugs–toward a more rational and consistent policy. N Engl J Med 1994;331:537-539.
2. Harwood H. Updating Estimates of the Economic Costs of Alcohol Abuse in the United States: Estimates, Update Methods, and Data. Report prepared by The Lewin Group for the National Institute on Alcohol Abuse and Alcoholism, 2000.
3. Whitmore CC, Yi H, Chen CM, et al. Surveillance Report #58: Trends in Alcohol-Related Morbidity Among Short-Stay Community Hospital Discharges, United States, 1979–99. Bethesda, Md: National Institute on Alcohol Abuse and Alcoholism, Division of Biometry and Epidemiology, 2002.
4. Myrick H, Anton RF. Treatment of alcohol withdrawal. Alcohol Health Res World 1998;22:38-43.
5. Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World 1998;22:5-12.
6. Trevisan LA, Boutros N, Petrakas IL, et al. Complications of alcohol withdrawal pathophysiologic insights. Alcohol Health Res World 1998;22:61-66.
7. Dvirskii AA. The role of genetic factors in the manifestation of delirium tremens [in Russian]. Zh Nevrol Psikhiatr Im S S Korsakova 1999;99:48-50.
8. Fiellin DA, O’Connor PG, Holmboe ES, Horwitz RI. Risk for delirium tremens in patients with alcohol withdrawal syndrome. Subst Abus 2002;23:83-94.
9. Saunders JB, Janca A. Delirium tremens: its aetiology, natural history and treatment. Curr Opin Psychiatry 2000;13:629-633.
10. Foy A, Kay J, Taylor A. The course of alcohol withdrawal in a general hospital. QJM 1997;90:253-261.
11. Wilson A, Vulcano B. A double-blind placebo-controlled trial of magnesium sulfate in the ethanol withdrawal syndrome. Alcohol Clin Exp Res 1984;8:542-545.
12. Victor M, Adams RD. The effect of alcohol on the nervous system. In: Metabolic and toxic diseases of the nervous system. Research publications of the Association for Research in Nervous and Mental Disease. Baltimore, Md: Williams and Wilkins, 1952.
13. Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: The revised Clinical Institute Withdrawal Assessment for Alcohol scale (CIWA-Ar). Br J Addict 1989;84:1353-1357.
14. Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA 1997;278:144-151.
15. Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Diagnosis and management of acute alcohol withdrawal. CMAJ 1999;160:675-680.
16. Shaw JM, Kolesar GS, Sellers EM, Kaplan HL, Sandor P. Development of optimal tactics for alcohol withdrawal. I. Assessment and effectiveness of supportive care. J Clin Psychopharmacol 1981;1:382-387.
17. Myrick H, Anton RF. Clinical management of alcohol withdrawal. CNS Spectrums 2000;5:22-23.
18. Hill A, Williams D. Hazards associated with the use of benzodiazepines in alcohol detoxification. J Subst Abuse Treat 1993;10:449-451.
19. Ritson B, Chick J. Comparison of two benzodiazepines in the treatment of alcohol withdrawal; effects on symptoms and cognitive recovery. Drug Alcohol Depend 1986;18:329-334.
20. Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Meta-analysis of benzodiazepine use in the treatment of acute alcohol withdrawal. CMAJ 1999;160:649-655.
21. Malcolm R, Ballenger JC, Sturgis ET, Anton R. Double-blind controlled trial comparing carbamazepine to oxazepam treatment of alcohol withdrawal. Am J Psychiatry 1989;146:617-621.
22. Malcolm R, Myrick H, Roberts J, et al. The effects of carbamazepine and lorazepam on single versus multiple previous alcohol withdrawals in an outpatient randomized trial. J Gen Intern Med 2002;17:349-355.
23. Stuppaeck CH, Pycha R, Miller C, Whitworth AB, Oberbauer H, Fleischhacker WW. Carbamazepine versus oxazepam in the treatment of alcohol withdrawal: a double-blind study. Alcohol # Alcoholism 1992;27:153-158.
24. Reoux JP, Saxon AJ, Malte CA, Baer JS, Sloan KL. Divalproex sodium in alcohol withdrawal: a randomized double-blind placebo-controlled clinical trial. Alcohol Clin Exp Res 2001;25:1324-1329.
25. Malcolm R, Myrick H, Brady KT, Ballenger JC. Update on anticonvulsants for the treatment of alcohol withdrawal. Am J Addict 2001;10(Suppl):16-23.
26. Bjorkqvist SE. Clonidine in alcohol withdrawal. Acta Psychiatr Scand 1975;52:256-263.
27. Wilkins AJ, Jenkins WJ, Steiner JA. Efficacy of clonidine in treatment of alcohol withdrawal state. Psychopharmacology (Berl) 1983;81:78-80.
28. Manhem P, Nilsson LH, Moberg AL, Wadstein J, Hokfelt B. Alcohol withdrawal: effects of clonidine treatment on sympathetic activity, the renin-aldosterone system, and clinical symptoms. Alcohol Clin Exp Res 1985;9:238-243.
29. Baumgartner GR, Rowen RC. Clonidine vs. chlordiazepoxide in the management of acute alcohol withdrawal syndrome. Arch Int Med 1987;147:1223-1226.
30. Robinson BJ, Robinson GM, Maling TJ, Johnson RH. Is clonidine useful in the treatment of alcohol withdrawal? Alchol Clin Exp Res 1989;13:95-98.
31. Worner TM. Propranolol versus diazepam in the management of the alcohol withdrawal syndrome: double-blind controlled trial. Am J Drug Alcohol Abuse 1994;20:115-124.
32. Horwitz RI, Gottlieb LD, Kraus ML. The efficacy of atenolol in the outpatient management of the alcohol withdrawal syndrome. Results of a randomized clinical trial. Arch Intern Med 1989;149:1089-1093.
33. Kraus ML, Gottlieb LD, Horwitz RI, et al. Randomized clinical trial of atenolol in patients with alcohol withdrawal. N Engl J Med 1985;313:905-909.
34. Banger M, Benkert O, Roschke J, et al. Nimodipine in acute alcohol withdrawal state. J Psychiatr Res 1992;26:117-123.
35. Altamura AC, Regazzetti MG, Porta M. Nimodipine in human alcohol withdrawal syndrome—an open study. Eur Neuropsychopharmacol 1990;1:37-40.
36. Saitz R, O’Malley SS. Pharmacotherapies of alcohol abuse. Withdrawal and treatment. Med Clin North Am 1997;81:881-907.
37. Reoux JP, Miller K. Routine hospital alcohol detoxification practice compared with symptom triggered management with an Objective Withdrawal Scale (CIWA-Ar). Am J Addict 2000;9:135-144.
38. Daeppen JB, Gache P, Landry U, et al. Symptom-triggered versus fixed-schedule doses of benzodiazepines for alcohol withdrawal: a randomized treatment trial. Arch Intern Med 2002;162:1117-1121.
39. Saitz R, Mayo-Smith MF, Roberts MS, Redmond HA, Bernard DR, Calkins DR. Individualized treatment for alcohol withdrawal: a randomized double-blind controlled trial. JAMA 1994;272:519-523.
40. Mattick RP, Jarvis T. In-patient setting and long duration for the treatment of alcohol dependence: out-patient care is as good. Drug Alcohol Rev 1994;13:127-135.
41. Hayashida M. An overview of outpatient and inpatient detoxification. Alcohol Health Res World 1998;22:44-46.
42. Booth BM, Blow FC, Ludke RL, Ross RL. Utilization of inpatient services for alcohol detoxification. J Men Health Adm 1996;23:366-374.
43. Hayashida M, Alterman AI, McLellan AT, et al. Comparative effectiveness and costs of inpatient and outpatient detoxification of patients with mild-to-moderate alcohol withdrawal syndrome. N Engl J Med 1989;320:358-365.
44. Abbott PJ, Quinn D, Knox L. Ambulatory medical detoxification for alcohol. Am J Drug Alcohol Abuse 1995;21:549-563.
1. Angell M, Kassirer JP. Alcohol and other drugs–toward a more rational and consistent policy. N Engl J Med 1994;331:537-539.
2. Harwood H. Updating Estimates of the Economic Costs of Alcohol Abuse in the United States: Estimates, Update Methods, and Data. Report prepared by The Lewin Group for the National Institute on Alcohol Abuse and Alcoholism, 2000.
3. Whitmore CC, Yi H, Chen CM, et al. Surveillance Report #58: Trends in Alcohol-Related Morbidity Among Short-Stay Community Hospital Discharges, United States, 1979–99. Bethesda, Md: National Institute on Alcohol Abuse and Alcoholism, Division of Biometry and Epidemiology, 2002.
4. Myrick H, Anton RF. Treatment of alcohol withdrawal. Alcohol Health Res World 1998;22:38-43.
5. Saitz R. Introduction to alcohol withdrawal. Alcohol Health Res World 1998;22:5-12.
6. Trevisan LA, Boutros N, Petrakas IL, et al. Complications of alcohol withdrawal pathophysiologic insights. Alcohol Health Res World 1998;22:61-66.
7. Dvirskii AA. The role of genetic factors in the manifestation of delirium tremens [in Russian]. Zh Nevrol Psikhiatr Im S S Korsakova 1999;99:48-50.
8. Fiellin DA, O’Connor PG, Holmboe ES, Horwitz RI. Risk for delirium tremens in patients with alcohol withdrawal syndrome. Subst Abus 2002;23:83-94.
9. Saunders JB, Janca A. Delirium tremens: its aetiology, natural history and treatment. Curr Opin Psychiatry 2000;13:629-633.
10. Foy A, Kay J, Taylor A. The course of alcohol withdrawal in a general hospital. QJM 1997;90:253-261.
11. Wilson A, Vulcano B. A double-blind placebo-controlled trial of magnesium sulfate in the ethanol withdrawal syndrome. Alcohol Clin Exp Res 1984;8:542-545.
12. Victor M, Adams RD. The effect of alcohol on the nervous system. In: Metabolic and toxic diseases of the nervous system. Research publications of the Association for Research in Nervous and Mental Disease. Baltimore, Md: Williams and Wilkins, 1952.
13. Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: The revised Clinical Institute Withdrawal Assessment for Alcohol scale (CIWA-Ar). Br J Addict 1989;84:1353-1357.
14. Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA 1997;278:144-151.
15. Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Diagnosis and management of acute alcohol withdrawal. CMAJ 1999;160:675-680.
16. Shaw JM, Kolesar GS, Sellers EM, Kaplan HL, Sandor P. Development of optimal tactics for alcohol withdrawal. I. Assessment and effectiveness of supportive care. J Clin Psychopharmacol 1981;1:382-387.
17. Myrick H, Anton RF. Clinical management of alcohol withdrawal. CNS Spectrums 2000;5:22-23.
18. Hill A, Williams D. Hazards associated with the use of benzodiazepines in alcohol detoxification. J Subst Abuse Treat 1993;10:449-451.
19. Ritson B, Chick J. Comparison of two benzodiazepines in the treatment of alcohol withdrawal; effects on symptoms and cognitive recovery. Drug Alcohol Depend 1986;18:329-334.
20. Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Meta-analysis of benzodiazepine use in the treatment of acute alcohol withdrawal. CMAJ 1999;160:649-655.
21. Malcolm R, Ballenger JC, Sturgis ET, Anton R. Double-blind controlled trial comparing carbamazepine to oxazepam treatment of alcohol withdrawal. Am J Psychiatry 1989;146:617-621.
22. Malcolm R, Myrick H, Roberts J, et al. The effects of carbamazepine and lorazepam on single versus multiple previous alcohol withdrawals in an outpatient randomized trial. J Gen Intern Med 2002;17:349-355.
23. Stuppaeck CH, Pycha R, Miller C, Whitworth AB, Oberbauer H, Fleischhacker WW. Carbamazepine versus oxazepam in the treatment of alcohol withdrawal: a double-blind study. Alcohol # Alcoholism 1992;27:153-158.
24. Reoux JP, Saxon AJ, Malte CA, Baer JS, Sloan KL. Divalproex sodium in alcohol withdrawal: a randomized double-blind placebo-controlled clinical trial. Alcohol Clin Exp Res 2001;25:1324-1329.
25. Malcolm R, Myrick H, Brady KT, Ballenger JC. Update on anticonvulsants for the treatment of alcohol withdrawal. Am J Addict 2001;10(Suppl):16-23.
26. Bjorkqvist SE. Clonidine in alcohol withdrawal. Acta Psychiatr Scand 1975;52:256-263.
27. Wilkins AJ, Jenkins WJ, Steiner JA. Efficacy of clonidine in treatment of alcohol withdrawal state. Psychopharmacology (Berl) 1983;81:78-80.
28. Manhem P, Nilsson LH, Moberg AL, Wadstein J, Hokfelt B. Alcohol withdrawal: effects of clonidine treatment on sympathetic activity, the renin-aldosterone system, and clinical symptoms. Alcohol Clin Exp Res 1985;9:238-243.
29. Baumgartner GR, Rowen RC. Clonidine vs. chlordiazepoxide in the management of acute alcohol withdrawal syndrome. Arch Int Med 1987;147:1223-1226.
30. Robinson BJ, Robinson GM, Maling TJ, Johnson RH. Is clonidine useful in the treatment of alcohol withdrawal? Alchol Clin Exp Res 1989;13:95-98.
31. Worner TM. Propranolol versus diazepam in the management of the alcohol withdrawal syndrome: double-blind controlled trial. Am J Drug Alcohol Abuse 1994;20:115-124.
32. Horwitz RI, Gottlieb LD, Kraus ML. The efficacy of atenolol in the outpatient management of the alcohol withdrawal syndrome. Results of a randomized clinical trial. Arch Intern Med 1989;149:1089-1093.
33. Kraus ML, Gottlieb LD, Horwitz RI, et al. Randomized clinical trial of atenolol in patients with alcohol withdrawal. N Engl J Med 1985;313:905-909.
34. Banger M, Benkert O, Roschke J, et al. Nimodipine in acute alcohol withdrawal state. J Psychiatr Res 1992;26:117-123.
35. Altamura AC, Regazzetti MG, Porta M. Nimodipine in human alcohol withdrawal syndrome—an open study. Eur Neuropsychopharmacol 1990;1:37-40.
36. Saitz R, O’Malley SS. Pharmacotherapies of alcohol abuse. Withdrawal and treatment. Med Clin North Am 1997;81:881-907.
37. Reoux JP, Miller K. Routine hospital alcohol detoxification practice compared with symptom triggered management with an Objective Withdrawal Scale (CIWA-Ar). Am J Addict 2000;9:135-144.
38. Daeppen JB, Gache P, Landry U, et al. Symptom-triggered versus fixed-schedule doses of benzodiazepines for alcohol withdrawal: a randomized treatment trial. Arch Intern Med 2002;162:1117-1121.
39. Saitz R, Mayo-Smith MF, Roberts MS, Redmond HA, Bernard DR, Calkins DR. Individualized treatment for alcohol withdrawal: a randomized double-blind controlled trial. JAMA 1994;272:519-523.
40. Mattick RP, Jarvis T. In-patient setting and long duration for the treatment of alcohol dependence: out-patient care is as good. Drug Alcohol Rev 1994;13:127-135.
41. Hayashida M. An overview of outpatient and inpatient detoxification. Alcohol Health Res World 1998;22:44-46.
42. Booth BM, Blow FC, Ludke RL, Ross RL. Utilization of inpatient services for alcohol detoxification. J Men Health Adm 1996;23:366-374.
43. Hayashida M, Alterman AI, McLellan AT, et al. Comparative effectiveness and costs of inpatient and outpatient detoxification of patients with mild-to-moderate alcohol withdrawal syndrome. N Engl J Med 1989;320:358-365.
44. Abbott PJ, Quinn D, Knox L. Ambulatory medical detoxification for alcohol. Am J Drug Alcohol Abuse 1995;21:549-563.
Tinnitus: Questions to reveal the cause, answers to provide relief
- If no treatable cause of tinnitus is found, assess the severity of tinnitus, secondary problems (such as depression, anxiety, and insomnia), and implement tinnitus management strategies (SOR:B).
- Acoustic therapy is effective for tinnitus management (SOR:B).
- All patients should wear hearing protection when they are exposed to loud sounds such as a gas lawnmower, leaf blower, power tools, or gunfire (SOR:A).
- Successful management of insomnia, anxiety or depression will decrease the severity of tinnitus for most patients (SOR:B).
Tinnitus—the perception of sound that does not have an external source—can be constant or intermittent and perceived as ringing, buzzing, hissing, sizzling, roaring, chirping, or other sounds.
Acute tinnitus, which can last days or weeks, may be caused by ear infection, medications, head or neck injury, excessive sound exposure, earwax, and changes in blood pressure or metabolism. With appropriate evaluation, such underlying conditions usually can be identified and treated, often with resultant resolution of tinnitus.
Chronic tinnitus (persistence for 6 months or more) can also result from these conditions and is more likely to occur in people who have hearing loss.1 (See Prevalence of tinnitus.) Even though a true “cure” for most cases of chronic tinnitus is not available, patients can obtain relief from the symptom with assistance from clinicians who are familiar with tinnitus management strategies.
Seidman and Jacobson2 estimated that 40 million people in the United States experience chronic tinnitus. The prevalence of tinnitus increases with age: 27% of males and 15% of females aged 45 years or older experience the symptom.3
Tinnitus is rare in children who have normal hearing.4 However, the prevalence of tinnitus in children with severe or profound hearing loss has been reported as 33%5 or 64%.6 More males than females experience tinnitus because men traditionally have had a greater amount of noise exposure in military service, in the workplace, and during recreational activities. Consequently, hearing loss and tinnitus are both more prevalent among men aged 45 years or older compared with women in the same age group.3
Damage depends on intensity, length of exposure
Tinnitus is most commonly caused by exposure to excessively loud sounds such as gunfire, power tools, machinery, or music. Ringing in the ears occurs because of damage to stereocilia, microscopic appendages attached to the apical ends of hair cells in the cochlea.
Moderate sounds (80 decibels sound pressure level [dB SPL] or lower) normally cause stereocilia to make tiny movements, triggering the releaseof neurotransmitter molecules from the basal ends of hair cells that activate auditory neurons in the eighth cranial nerve.
Excessive sound exposure (85 dB SPL or louder) causes stereocilia to bend more than they should. People then perceive high-pitched ringing tinnitus because hair cells that respond to higher-frequency sounds are located at the base of the cochlea and are the first to be damaged by loud noise.
If the damage is modest and infrequent, stereocilia can recover, returning to their normal function in a few minutes or hours. The patient’s hearing will be restored and the tinnitus will stop. However, repeated exposure to hazardous sounds eventually causes irreparable damage to stereocilia and hair cells, resulting in permanent sensorineural hearing loss and possibly chronic tinnitus.
In addition to noise exposure, any condition that causes hearing loss or damages the auditory system can contribute to the generation of tinnitus (Table). Imaging studies using functional magnetic resonance imaging7 or positron-emission tomography8-9 demonstrated that the perception of chronic tinnitus usually occurs as a result of hyperactivity within central auditory areas of the human brain, especially the auditory cortex. As portions of the auditory system degenerate during the aging process or acquire damage from noise exposure, disease, and accidents, the natural balance of central auditory excitation vs inhibition is disrupted. In patients who hear tinnitus, excitatory pathways within the auditory system are active when they shouldn’t be: in quiet environments. This gives patients the perception of tinnitus sounds.
TABLE
Causes of subjective tinnitus
| Presbycusis: hearing loss due to aging |
| Prolonged noise exposure: Noise-induced hearing loss |
| Acoustic trauma: one-time exposure to high intensity sound |
| Otosclerosis: abnormal accumulation of calcium on middle ear ossicles or cochlea |
| Infections: bacterial, viral, fungal |
| Autoimmune hearing loss |
| Meniere’s disease or endolymphatic hydrops: abnormally high inner ear pressure |
| Neoplasms: for example, acoustic neuroma or cholesteatoma |
| Genetic predisposition |
Ototoxicity
|
Vascular
|
Metabolic
|
| Head or neck injury |
Objective tinnitus
Objective tinnitus—which can be heard also by people in proximity to the patient’s ear—can be caused by vascular abnormalities (congenital arteriovenous fistula, acquired arteriovenous shunt, glomus jugulare, high-riding carotid artery, carotid stenosis, persistent stapedial artery, dehiscent jugular bulb or a vascular loop such as anterior inferior communicating artery [AICA] or posterior inferior communicating artery [PICA] compressing the auditory nerve) or mechanical disorders (abnormally patent Eustachian tube, palatal myoclonus, temporo-mandibular joint disorder, or stapedial muscle spasticity).10 However, objective tinnitus is rare, accounting for <1% of all cases. The vast majority of tinnitus cases are subjective—sounds are perceived only by the patient.
Patient evaluation
Figure 1 is an algorithm that outlines steps in the evaluation and management of patients who experience tinnitus. The first step is to collect as much information as possible about the patient and his condition.
FIGURE 1
Evaluation and management of tinnitus
Tinnitus history
Determine the duration of tinnitus and whether circumstances such as upper respiratory infection, otalgia, noise exposure, head trauma, sudden hearing loss, or vertigo occurred at the time of tinnitus onset. Ask the patient to describe the tinnitus: Is it intermittent or constant? High- or low-pitched? Unilateral or bilateral? Pulsatile or steady?
Unilateral tinnitus and hearing loss provide preliminary evidence for acoustic neuroma or cerebrovascular accident. High-pitched tinnitus is usually associated with high-frequency hearing loss caused by presbycusis (hearing impairment in the aged) or excessive noise exposure. Low-pitched roaring tinnitus is sometimes associated with low-frequency hearing loss exhibited by patients with Meniere’s disease. Pulsatile tinnitus, especially if synchronous with the patient’s pulse, can indicate vascular abnormalities.
Ask the patient if fatigue, stress, noise exposure, or any medications exacerbate the tinnitus. Also ask if masking sounds (such as water running in the shower), medications, or any other factors provide relief from tinnitus. This information can be used to formulate a tinnitus management program.
Assess the severity of the patient’s tinnitus using an instrument such as the Tinnitus Severity Index (Figure 2).11 A score of 36 or higher indicates bothersome tinnitus (level of evidence [LOE]: 2).12 Higher scores indicate that patients perceive their tinnitus to be a significant, even debilitating problem.
FIGURE 2
Tinnitus Severity Index
Hearing history
If possible, determine the presence and type of hearing loss (congenital, sudden, sensorineural, conductive, or mixed). Note the patient’s history of ear infections, surgeries, noise exposure (occupational or recreational), otalgia, otorrhea, and vertigo or other balance problems. Ask whether immediate family members have experienced hearing loss or tinnitus.
Health history
Look particularly for conditions that can contribute to hearing loss and tinnitus, such as hypertension, hypothyroidism, diabetes mellitus, arteriosclerosis, and autoimmune disorders (eg, lupus or rheumatoid arthritis). Also consider ototoxic medications, such as aminoglycoside antibiotics, cisplatin, furosemide, valproic acid, and high doses of quinine-containing compounds. When possible, patients with hearing loss or tinnitus should be given alternative medications free from ototoxicity.
Excessive use of alcohol, caffeine, and aspirin or other nonsteroidal anti-inflammatory drugs can exacerbate tinnitus for some patients. However, moderate use of these products is often possible.
Psychosocial history
Inquire about the patient’s marital and occupational status. Unemployed patients living alone often perceive tinnitus to be more severe than do employed patients who have supportive social networks. Also ask about any history of insomnia, anxiety, depression, obsessive-compulsive disorder, or psychosis. A questionnaire such as the abbreviated Beck Depression Inventory13 can be used to assess the presence and severity of depression.
Physical exam and testing
Patient evaluation should include the following physical examinations and tests.
Otolaryngologic/head and neck exam. Otoscopic examination can detect infections such as otitis media, which will usually be accompanied by complaints of ear pain or fullness, and possibly hearing loss in combination with tinnitus. Otoscopy can also detect impacted earwax (cerumen), which can occlude the ear canal or cause immobilization of the tympanic membrane, resulting in conductive hearing loss, tinnitus, and a feeling of fullness in the ear. Symptoms usually resolve when the earwax is removed.
If the tinnitus is synchronous with the patient’s pulse, it suggests a vascular contribution for the symptom. Auscultation of blood vessels in the neck can reveal venous hums or other types of bruits audible to the patient. Venous hum can be diagnosed by temporarily blocking blood flow through the jugular vein on the side where tinnitus is perceived.
Neurologic exam. A complete neurologic exam should include the Romberg test, Dix-Hallpike maneuver (if the patient experiences vertigo), gait testing, and cranial nerve function tests.
Audiologic testing. Audiologic tests should include pure tone air and bone conduction thresholds, speech discrimination testing, tympanometry, and most comfortable loudness (MCL) and uncomfortable loudness level (UCL) tests. Tympanometry is used to assess middle-ear function. Abnormal tympanograms and significant differences between air and bone conduction thresholds can indicate otitis media, otosclerosis, or cholesteatoma.
MCL and UCL tests are used to assess the dynamic range of patients’ hearing. Patients with UCLs that are only 5 to 20 dBs above their MCLs have a reduced dynamic range of hearing that can be caused by recruitment or hyperacusis. The audiometer can also be used to match the tinnitus for pitch and loudness and to test the effects of masking sounds on the patient’s tinnitus.
Additional evaluations. Results of patient examinations and history collection might warrant additional evaluations. For example, asymmetrical hearing loss (15 dB or greater asymmetry at 2 or more consecutive test frequencies) and unilateral tinnitus can indicate a retrocochlear lesion such as acoustic neuroma (also known as vestibular schwannoma).
One test for retrocochlear pathology is the auditory brainstem response (ABR). In this test, clicks are presented through earphones while scalp electrodes record brain responses to the sounds. Abnormal ABR waveforms can indicate retrocochlear lesion (such as acoustic neuroma) as a possible cause of ipsilateral hearing loss and tinnitus. If positive ABR results are obtained, MRI evaluation of the cerebellopontine angle with contrast material (such as gadolinium) should be performed.
Low-pitched roaring, ringing, or hissing tinnitus; hearing loss, which may be temporary or permanent; vertigo; and a feeling of pressure or fullness in the ear can indicate endolymphatic hydrops or Meniere’s disease. Symptoms usually occur in the form of “attacks” that increase in frequency during the first few years of the disease, then decrease in frequency as hearing thresholds stabilize. Electrocochleography testing is one way to diagnose endolymphatic hydrops. Patients who exhibit vestibular disorders should undergo electronystagmography testing to assess the severity and characteristics of their symptoms.
Pulsatile tinnitus associated with abnormalities of blood vessels in the neck can be evaluated with sonography, conventional angiography, or magnetic resonance angiography. Conditions such as a dehiscent jugular bulb or stenosis of carotid arteries can sometimes be treated surgically. However, many forms of pulsatile tinnitus are not caused by these conditions. Pulsatile tinnitus is often a consequence of hearing loss, arteriosclerosis, or weight loss or weight gain. These physiologic changes can cause patients to hear blood pulsing or “swishing” in vessels—sounds they did not perceive previously. Surgery is not recommended for most cases of pulsatile tinnitus.
Sudden hearing loss, especially if bilateral, might indicate autoimmune inner ear disease. Diagnostic tests include the Western blot immunoassay.
Treatment of active disease processes
Many contributors to tinnitus can be treated surgically or with medication.
Otitis media. Successful treatment of the infection with oral antibiotics usually resolves all auditory symptoms.
Allergies, sinus congestion, or infection. When inflammation subsides, tinnitus associated with these conditions usually resolves.
Otosclerosis. Abnormal accumulations of calcium on middle-ear ossicles (especially the stapes) or the cochlea can result in slowly progressing conductive or sensorineural hearing loss, tinnitus, and vestibular disturbances. Stapedectomy surgery—including implantation of ossicular prostheses—is often successful for advanced cases associated with significant hearing loss. Hearing aids also benefit some patients.
Meniere’s disease or other forms of endolymphatic hydrops. Meniere’s disease, characterized by abnormally high fluid pressure within the cochlea, has an estimated prevalence of 1% in the US.14 Management includes meclizine, antiemetics and diuretics, and a low-sodium diet.15 If patients do not respond to meclizine, diazepam can be prescribed to reduce the severity of vertigo attacks. Surgical intervention—including installation of an endolymphatic shunt, labyrinthectomy, or vestibular neurectomy16—or transtympanic injections of gentamicin17 are options in severe cases.
Autoimmune inner ear disease. This disease has an estimated prevalence of 0.1% in the US.18 Symptoms include sudden hearing loss in one ear that usually progresses to the second ear. Patients may also feel fullness in the ear and experience vertigo as well as ringing, hissing, or roaring tinnitus. Most patients with autoimmune inner ear disease respond to initial treatment with oral prednisone.
Auditory neoplasms. Growths such as acoustic neuroma or cholesteatoma can cause tinnitus. Acoustic neuroma (or vestibular schwannoma) is a benign neoplasm that arises from the vestibular division of the eighth cranial nerve. Symptoms include unilateral hearing loss, tinnitus, and vestibular disturbances. Surgical resection or radiation treatment of the tumor can resolve these symptoms, especially if the neoplasm is detected while it is small.
Cholesteatoma is a benign epithelial cell mass that grows in the middle-ear cavity. Over time, cholesteatomas can enlarge and destroy middleear ossicles. Hearing loss, tinnitus, dizziness, and facial muscle paralysis can result from continued cholesteatoma growth. Early detection and surgical resection of auditory neoplasms can reduce the likelihood of residual symptoms.
Hyper- or hypotension. Of these two disorders, hypertension is more likely to contribute to tinnitus. Maintenance of blood pressure within the optimum range can decrease or resolve tinnitus for some patients.
Metabolic disorders. Disorders such as diabetes mellitus, hyperthyroidism, or hypothyroidism can contribute to tinnitus. Successful management of these conditions can reduce or resolve the patient’s tinnitus.
Managing persistent tinnitus
Successful treatment of the disorders discussed can resolve or reduce tinnitus. However, if tinnitus continues to bother the patient after other diseases have been treated, shift the clinical focus from treatment to management of the symptom. At this point, the clinician should do 1 of 2 things: 1) spend the time necessary to help the patient manage tinnitus using strategies described in the following sections of this article; or 2) refer the patient to a comprehensive tinnitus management program with experienced personnel who are willing and able to spend a substantial amount of time with each patient.
Like other neurologic symptoms, tinnitus can be considered chronic if it persists for 6 months or more. Approximately 90% of cases of chronic tinnitus are associated with some degree of sensorineural hearing loss.19 Because sensorineural hearing loss is irreversible, most cases of chronic tinnitus cannot be “cured.” Duckro et al20 wrote: “As with chronic pain, the treatment of chronic tinnitus is more accurately described in terms of management rather than cure.”
The goal of management is not necessarily to mask or remove the patient’s perception of tinnitus. In many cases, this is not possible. Successful management enables patients to pay less attention to their tinnitus. An effective management program helps patients to understand and gain control over their tinnitus, rather than allowing it to control them. The ultimate goal is to reduce the severity of tinnitus. Clinicians should strive to help patients progress to where tinnitus is no longer a negative factor in their lives.
Establishing tinnitus severity
Only 25% of people who experience chronic tinnitus consider the symptom to be a significant problem.2 These are the patients most likely to seek treatment. If a patient is not bothered by tinnitus and no active disease processes are detected, no treatments are necessary. The clinician should reassure such patients that tinnitus is a harmless perception of sound and does not usually portend more serious medical conditions.
What differentiates the majority of people not bothered by tinnitus from the minority who perceive it as a significant, even debilitating problem? Is it the matched loudness, pitch, or other qualities of the sound(s) they hear? Several studies have concluded that tinnitus severity is not correlated with any of these psychoacoustic parameters.21-23
Tinnitus severity can be defined and quantified several ways: by how much or how often a patient is bothered by tinnitus; by how much or how often tinnitus detracts from the patient’s enjoyment of life; or by how disabling patients perceive their tinnitus to be. Instruments such as the Tinnitus Severity Index11 can be used to assess tinnitus severity (Figure 2).
Tinnitus management strategies
Once underlying conditions have been treated or ruled out, reassure and counsel patients regarding factors that could exacerbate or improve their condition. If patients understand their tinnitus is nothing more than a perception of sound, they will be better able to pay less attention to it. This process of patient education and counseling helps to “demystify” the symptom of tinnitus and encourages patients to view their tinnitus with a more realistic perspective.
The severity of tinnitus is often associated with problems such as insomnia,24 anxiety,25 and depression.26 Such issues can form a vicious circle, with each one exacerbating the others.23 Tinnitus is not always the starting point of this cycle—many patients experience depression, insomnia, or anxiety before tinnitus. Medication or psychotherapy will often reduce the severity of these symptoms and associated tinnitus (LOE: 2).27-28
Because each patient has a unique medical, psychological, and social history, management programs should be individualized. In fact, the most successful tinnitus management programs employ multimodal strategies designed to address the specific needs of each patient (LOE: 2).27,29
Recommendations should be formulated and explained to the patient: appropriate acoustic therapy; use of hearing protection (all patients should wear earplugs or ear muffs when they are exposed to excessively loud sounds [LOE: 1]);30 and strategies for management of insomnia, anxiety, or depression. As appropriate, provide patients with referral and contact information for physical or psychiatric evaluations, psychological counseling, and other recommended services or products.
Acoustic therapy
Patients should add pleasant sounds (music, relaxation CDs, or a tabletop sound machine) to any environment that is too quiet, and listen to them through speakers or headphones. Patients who experience chronic insomnia because of tinnitus may find relief in using a tabletop sound machine in combination with a pillow embedded with speakers (such as the Sound Pillow, distributed by Phoenix Productions, San Antonio, TX).
Patients with normal or nearly normal hearing might benefit from in-the-ear sound generators (such as those manufactured by General Hearing Instruments, Harahan, LA) that produce a broad-band sound to muffle or mask the tinnitus.31 Significant, aidable hearing loss can often be lessened with hearing aids or combination instruments (hearing aid and sound generator in one unit). Hearing aids not only improve communication ability, the devices can also reduce the perception of tinnitus.32
Follow-up
Encourage patients to ask questions about recommended tinnitus management procedures and to report their progress. Reassess patients at 1 month. If necessary, recommendations can be modified to facilitate patient improvement. Follow-up questionnaires can be mailed to patients 6 and 12 months after their initial appointment to assess the effectiveness of the tinnitus management program.
A customized combination of recommendations is effective for many patients with chronic and bothersome tinnitus (LOE: 2),27 but the process can be very time consuming. For a certain number of patients with severe tinnitus, only a comprehensive management program can help them to improve their condition.
Corresponding author
Robert L. Folmer, PhD, OHSU Tinnitus Clinic, Mail Code NRC04, Oregon Health & Science University, 3181 SW Sam Jackson Park Road, Portland, OR 97239. E-mail: [email protected].
1. Schleuning A. Medical aspects of tinnitus. In: Vernon JA, ed. Tinnitus Treatment and Relief. Boston, Mass: Allyn and Bacon; 1998;20-27.
2. Seidman MD, Jacobson GP. Update on tinnitus. Otolaryngol Clin N Amer 1996;29:455-465.
3. Adams PF, Hendershot GE, Marano MA. Current estimates from the National Health Interview Survey, 1996. Hyattsville, Md: National Center for Health Statistics, 1999.
4. Stouffer JL, Tyler RS, Booth JC, Buckrell B. Tinnitus in normal-hearing and hearing-impaired children. In: Aran J-M, Dauman R, eds. Tinnitus 91: Proceedings of the Fourth International Tinnitus Seminar. Amsterdam: Kugler Publications 1992;255-258.
5. Drukier GS. The prevalence and characteristics of tinnitus with profound sensori-neural hearing impairment. Amer Ann Deaf 1989;134:260-264.
6. Graham J. Paediatric tinnitus. J Laryngol Otol 1981;95(Suppl):117-120.
7. Levine RA, Benson RR, Talavage TM, Melcher JR, Rosen BR. Functional magnetic resonance imaging and tinnitus: preliminary results. Abstr Assoc Res Otolaryngol 1997;20:65.-
8. Arnold W, Bartenstein P, Oestreicher E, Romer W, Schwaiger M. Focal metabolic activation in the predominant left auditory cortex in patients suffering from tinnitus: a PET study with [18F]deoxyglucose. ORL J Otorhinolaryngol Relat Spec 1996;58:195-199.
9. Lockwood AH, Salvi RJ, Coad ML, Towsley ML, Wach DS, Murphy BW. The functional neuroanatomy of tinnitus: evidence for limbic system links and neuroplasticity. Neurology 1998;50:114-120.
10. Ciocon JO, Amede F, Lechtenberg C, Astor F. Tinnitus: a stepwise workup to quiet the noise within. Geriatrics 1995;50:18-25.
11. Meikle MB, Griest SE, Stewart BJ, Press LS. Measuring the negative impact of tinnitus: a brief severity index. Abstr Assoc Res Otolaryngol 1995;167.-
12. Folmer RL, Stevenson EA, Tran A. Factors associated with long-term improvements in tinnitus severity. In Patuzzi R, ed: Proceedings of the Seventh International Tinnitus Seminar. Crawley: University of Western Australia; 2002;115-123.
13. Beck AT, Beck RW. Screening depressed patients in family practice: a rapid technic. Postgrad Medicine 1972;52:81-85.
14. daCosta SS, deSousa LC, Piza MR. Meniere’s Disease: overview, epidemiology, and natural history. Otolaryngol Clin N Amer 2002;35:455-495.
15. Thai-Van H, Bounaix MJ, Fraysse B. Meniere’s disease: pathophysiology and treatment. Drugs 2001;61:1089-1102.
16. Hillman TA, Chen DA, Arriaga MA. Vestibular nerve section versus intratympanic gentamicin for Meniere’s disease. Laryngoscope 2004;114:216-222.
17. Diamond C, Hornig JD, Liu R, O’Connell DA. Systematic review of intratympanic gentamicin in Meniere’s disease. J Otolaryngol 2003;32:351-361.
18. Hain TC. Autoimmune inner ear disease. American Hearing Research Foundation Web site. March 23, 2002. Available at www.american-hearing.org/name/autoimmune.html. Accessed on May 15, 2004.
19. Meikle MB. Electronic access to tinnitus data: The Oregon Tinnitus Data Archive. Otolaryngol Head Neck Surg 1997;117:698-700.
20. Duckro PN, Pollard CA, Bray HD, Scheiter L. Comprehensive behavioral management of complex tinnitus: a case illustration. Biofeedback and Self-Regulation 1984;9:459-469.
21. Meikle MB, Vernon J, Johnson RM. The perceived severity of tinnitus. Otolaryngol Head Neck Surg 1984;92:689-696.
22. van Veen ED, Jacobs JB, Bensing JM. Assessment of distress associated with tinnitus. J Laryngol Otol 1998;112:258-263.
23. Folmer RL, Griest SE, Martin WH. Chronic tinnitus as phantom auditory pain. Otolaryngol Head Neck Surg 2001;124:394-400.
24. Folmer RL, Griest SE. Tinnitus and insomnia. Am J Otolaryngol 2000;21:287-293.
25. Attias J, Shemesh Z, Bleich A, Solomon Z, Bar-Or G, Alster J, Sohmer H. Psychological profile of help-seeking and non-help-seeking tinnitus patients. Scand Audiol 1995;24:13-18.
26. Folmer RL, Griest SE, Meikle MB, Martin WH. Tinnitus severity, loudness and depression. Otolaryngol Head Neck Surg 1999;121:48-51.
27. Folmer R. Long-term reductions in tinnitus severity. BMC Ear Nose and Throat Disorders 2002;2:3.-Available at: www.biomedcentral.com/1472-6815/2/3.
28. Folmer RL, Shi YB. SSRI use by tinnitus patients: interactions between depression and tinnitus severity ENT J 2004;83:107-117.
29. Sullivan M, Katon W, Russo J, Dobie R, Sakai C. Coping and marital support as correlates of tinnitus disability. Gen Hosp Psychiatry 1994;16:259-266.
30. Lusk SL. Preventing noise-induced hearing loss. Nurs Clin North Amer 2002;37:257-262.
31. Henry JA, Schechter MA, Nagler SM, Fausti SA. Comparison of tinnitus masking and tinnitus retraining therapy. J Amer Acad Audiol 2002;13:559-581.
32. Surr RK, Montgomery AA, Mueller HG. Effect of amplification on tinnitus among new hearing aid users. Ear and Hearing 1985;6:71-75.
- If no treatable cause of tinnitus is found, assess the severity of tinnitus, secondary problems (such as depression, anxiety, and insomnia), and implement tinnitus management strategies (SOR:B).
- Acoustic therapy is effective for tinnitus management (SOR:B).
- All patients should wear hearing protection when they are exposed to loud sounds such as a gas lawnmower, leaf blower, power tools, or gunfire (SOR:A).
- Successful management of insomnia, anxiety or depression will decrease the severity of tinnitus for most patients (SOR:B).
Tinnitus—the perception of sound that does not have an external source—can be constant or intermittent and perceived as ringing, buzzing, hissing, sizzling, roaring, chirping, or other sounds.
Acute tinnitus, which can last days or weeks, may be caused by ear infection, medications, head or neck injury, excessive sound exposure, earwax, and changes in blood pressure or metabolism. With appropriate evaluation, such underlying conditions usually can be identified and treated, often with resultant resolution of tinnitus.
Chronic tinnitus (persistence for 6 months or more) can also result from these conditions and is more likely to occur in people who have hearing loss.1 (See Prevalence of tinnitus.) Even though a true “cure” for most cases of chronic tinnitus is not available, patients can obtain relief from the symptom with assistance from clinicians who are familiar with tinnitus management strategies.
Seidman and Jacobson2 estimated that 40 million people in the United States experience chronic tinnitus. The prevalence of tinnitus increases with age: 27% of males and 15% of females aged 45 years or older experience the symptom.3
Tinnitus is rare in children who have normal hearing.4 However, the prevalence of tinnitus in children with severe or profound hearing loss has been reported as 33%5 or 64%.6 More males than females experience tinnitus because men traditionally have had a greater amount of noise exposure in military service, in the workplace, and during recreational activities. Consequently, hearing loss and tinnitus are both more prevalent among men aged 45 years or older compared with women in the same age group.3
Damage depends on intensity, length of exposure
Tinnitus is most commonly caused by exposure to excessively loud sounds such as gunfire, power tools, machinery, or music. Ringing in the ears occurs because of damage to stereocilia, microscopic appendages attached to the apical ends of hair cells in the cochlea.
Moderate sounds (80 decibels sound pressure level [dB SPL] or lower) normally cause stereocilia to make tiny movements, triggering the releaseof neurotransmitter molecules from the basal ends of hair cells that activate auditory neurons in the eighth cranial nerve.
Excessive sound exposure (85 dB SPL or louder) causes stereocilia to bend more than they should. People then perceive high-pitched ringing tinnitus because hair cells that respond to higher-frequency sounds are located at the base of the cochlea and are the first to be damaged by loud noise.
If the damage is modest and infrequent, stereocilia can recover, returning to their normal function in a few minutes or hours. The patient’s hearing will be restored and the tinnitus will stop. However, repeated exposure to hazardous sounds eventually causes irreparable damage to stereocilia and hair cells, resulting in permanent sensorineural hearing loss and possibly chronic tinnitus.
In addition to noise exposure, any condition that causes hearing loss or damages the auditory system can contribute to the generation of tinnitus (Table). Imaging studies using functional magnetic resonance imaging7 or positron-emission tomography8-9 demonstrated that the perception of chronic tinnitus usually occurs as a result of hyperactivity within central auditory areas of the human brain, especially the auditory cortex. As portions of the auditory system degenerate during the aging process or acquire damage from noise exposure, disease, and accidents, the natural balance of central auditory excitation vs inhibition is disrupted. In patients who hear tinnitus, excitatory pathways within the auditory system are active when they shouldn’t be: in quiet environments. This gives patients the perception of tinnitus sounds.
TABLE
Causes of subjective tinnitus
| Presbycusis: hearing loss due to aging |
| Prolonged noise exposure: Noise-induced hearing loss |
| Acoustic trauma: one-time exposure to high intensity sound |
| Otosclerosis: abnormal accumulation of calcium on middle ear ossicles or cochlea |
| Infections: bacterial, viral, fungal |
| Autoimmune hearing loss |
| Meniere’s disease or endolymphatic hydrops: abnormally high inner ear pressure |
| Neoplasms: for example, acoustic neuroma or cholesteatoma |
| Genetic predisposition |
Ototoxicity
|
Vascular
|
Metabolic
|
| Head or neck injury |
Objective tinnitus
Objective tinnitus—which can be heard also by people in proximity to the patient’s ear—can be caused by vascular abnormalities (congenital arteriovenous fistula, acquired arteriovenous shunt, glomus jugulare, high-riding carotid artery, carotid stenosis, persistent stapedial artery, dehiscent jugular bulb or a vascular loop such as anterior inferior communicating artery [AICA] or posterior inferior communicating artery [PICA] compressing the auditory nerve) or mechanical disorders (abnormally patent Eustachian tube, palatal myoclonus, temporo-mandibular joint disorder, or stapedial muscle spasticity).10 However, objective tinnitus is rare, accounting for <1% of all cases. The vast majority of tinnitus cases are subjective—sounds are perceived only by the patient.
Patient evaluation
Figure 1 is an algorithm that outlines steps in the evaluation and management of patients who experience tinnitus. The first step is to collect as much information as possible about the patient and his condition.
FIGURE 1
Evaluation and management of tinnitus
Tinnitus history
Determine the duration of tinnitus and whether circumstances such as upper respiratory infection, otalgia, noise exposure, head trauma, sudden hearing loss, or vertigo occurred at the time of tinnitus onset. Ask the patient to describe the tinnitus: Is it intermittent or constant? High- or low-pitched? Unilateral or bilateral? Pulsatile or steady?
Unilateral tinnitus and hearing loss provide preliminary evidence for acoustic neuroma or cerebrovascular accident. High-pitched tinnitus is usually associated with high-frequency hearing loss caused by presbycusis (hearing impairment in the aged) or excessive noise exposure. Low-pitched roaring tinnitus is sometimes associated with low-frequency hearing loss exhibited by patients with Meniere’s disease. Pulsatile tinnitus, especially if synchronous with the patient’s pulse, can indicate vascular abnormalities.
Ask the patient if fatigue, stress, noise exposure, or any medications exacerbate the tinnitus. Also ask if masking sounds (such as water running in the shower), medications, or any other factors provide relief from tinnitus. This information can be used to formulate a tinnitus management program.
Assess the severity of the patient’s tinnitus using an instrument such as the Tinnitus Severity Index (Figure 2).11 A score of 36 or higher indicates bothersome tinnitus (level of evidence [LOE]: 2).12 Higher scores indicate that patients perceive their tinnitus to be a significant, even debilitating problem.
FIGURE 2
Tinnitus Severity Index
Hearing history
If possible, determine the presence and type of hearing loss (congenital, sudden, sensorineural, conductive, or mixed). Note the patient’s history of ear infections, surgeries, noise exposure (occupational or recreational), otalgia, otorrhea, and vertigo or other balance problems. Ask whether immediate family members have experienced hearing loss or tinnitus.
Health history
Look particularly for conditions that can contribute to hearing loss and tinnitus, such as hypertension, hypothyroidism, diabetes mellitus, arteriosclerosis, and autoimmune disorders (eg, lupus or rheumatoid arthritis). Also consider ototoxic medications, such as aminoglycoside antibiotics, cisplatin, furosemide, valproic acid, and high doses of quinine-containing compounds. When possible, patients with hearing loss or tinnitus should be given alternative medications free from ototoxicity.
Excessive use of alcohol, caffeine, and aspirin or other nonsteroidal anti-inflammatory drugs can exacerbate tinnitus for some patients. However, moderate use of these products is often possible.
Psychosocial history
Inquire about the patient’s marital and occupational status. Unemployed patients living alone often perceive tinnitus to be more severe than do employed patients who have supportive social networks. Also ask about any history of insomnia, anxiety, depression, obsessive-compulsive disorder, or psychosis. A questionnaire such as the abbreviated Beck Depression Inventory13 can be used to assess the presence and severity of depression.
Physical exam and testing
Patient evaluation should include the following physical examinations and tests.
Otolaryngologic/head and neck exam. Otoscopic examination can detect infections such as otitis media, which will usually be accompanied by complaints of ear pain or fullness, and possibly hearing loss in combination with tinnitus. Otoscopy can also detect impacted earwax (cerumen), which can occlude the ear canal or cause immobilization of the tympanic membrane, resulting in conductive hearing loss, tinnitus, and a feeling of fullness in the ear. Symptoms usually resolve when the earwax is removed.
If the tinnitus is synchronous with the patient’s pulse, it suggests a vascular contribution for the symptom. Auscultation of blood vessels in the neck can reveal venous hums or other types of bruits audible to the patient. Venous hum can be diagnosed by temporarily blocking blood flow through the jugular vein on the side where tinnitus is perceived.
Neurologic exam. A complete neurologic exam should include the Romberg test, Dix-Hallpike maneuver (if the patient experiences vertigo), gait testing, and cranial nerve function tests.
Audiologic testing. Audiologic tests should include pure tone air and bone conduction thresholds, speech discrimination testing, tympanometry, and most comfortable loudness (MCL) and uncomfortable loudness level (UCL) tests. Tympanometry is used to assess middle-ear function. Abnormal tympanograms and significant differences between air and bone conduction thresholds can indicate otitis media, otosclerosis, or cholesteatoma.
MCL and UCL tests are used to assess the dynamic range of patients’ hearing. Patients with UCLs that are only 5 to 20 dBs above their MCLs have a reduced dynamic range of hearing that can be caused by recruitment or hyperacusis. The audiometer can also be used to match the tinnitus for pitch and loudness and to test the effects of masking sounds on the patient’s tinnitus.
Additional evaluations. Results of patient examinations and history collection might warrant additional evaluations. For example, asymmetrical hearing loss (15 dB or greater asymmetry at 2 or more consecutive test frequencies) and unilateral tinnitus can indicate a retrocochlear lesion such as acoustic neuroma (also known as vestibular schwannoma).
One test for retrocochlear pathology is the auditory brainstem response (ABR). In this test, clicks are presented through earphones while scalp electrodes record brain responses to the sounds. Abnormal ABR waveforms can indicate retrocochlear lesion (such as acoustic neuroma) as a possible cause of ipsilateral hearing loss and tinnitus. If positive ABR results are obtained, MRI evaluation of the cerebellopontine angle with contrast material (such as gadolinium) should be performed.
Low-pitched roaring, ringing, or hissing tinnitus; hearing loss, which may be temporary or permanent; vertigo; and a feeling of pressure or fullness in the ear can indicate endolymphatic hydrops or Meniere’s disease. Symptoms usually occur in the form of “attacks” that increase in frequency during the first few years of the disease, then decrease in frequency as hearing thresholds stabilize. Electrocochleography testing is one way to diagnose endolymphatic hydrops. Patients who exhibit vestibular disorders should undergo electronystagmography testing to assess the severity and characteristics of their symptoms.
Pulsatile tinnitus associated with abnormalities of blood vessels in the neck can be evaluated with sonography, conventional angiography, or magnetic resonance angiography. Conditions such as a dehiscent jugular bulb or stenosis of carotid arteries can sometimes be treated surgically. However, many forms of pulsatile tinnitus are not caused by these conditions. Pulsatile tinnitus is often a consequence of hearing loss, arteriosclerosis, or weight loss or weight gain. These physiologic changes can cause patients to hear blood pulsing or “swishing” in vessels—sounds they did not perceive previously. Surgery is not recommended for most cases of pulsatile tinnitus.
Sudden hearing loss, especially if bilateral, might indicate autoimmune inner ear disease. Diagnostic tests include the Western blot immunoassay.
Treatment of active disease processes
Many contributors to tinnitus can be treated surgically or with medication.
Otitis media. Successful treatment of the infection with oral antibiotics usually resolves all auditory symptoms.
Allergies, sinus congestion, or infection. When inflammation subsides, tinnitus associated with these conditions usually resolves.
Otosclerosis. Abnormal accumulations of calcium on middle-ear ossicles (especially the stapes) or the cochlea can result in slowly progressing conductive or sensorineural hearing loss, tinnitus, and vestibular disturbances. Stapedectomy surgery—including implantation of ossicular prostheses—is often successful for advanced cases associated with significant hearing loss. Hearing aids also benefit some patients.
Meniere’s disease or other forms of endolymphatic hydrops. Meniere’s disease, characterized by abnormally high fluid pressure within the cochlea, has an estimated prevalence of 1% in the US.14 Management includes meclizine, antiemetics and diuretics, and a low-sodium diet.15 If patients do not respond to meclizine, diazepam can be prescribed to reduce the severity of vertigo attacks. Surgical intervention—including installation of an endolymphatic shunt, labyrinthectomy, or vestibular neurectomy16—or transtympanic injections of gentamicin17 are options in severe cases.
Autoimmune inner ear disease. This disease has an estimated prevalence of 0.1% in the US.18 Symptoms include sudden hearing loss in one ear that usually progresses to the second ear. Patients may also feel fullness in the ear and experience vertigo as well as ringing, hissing, or roaring tinnitus. Most patients with autoimmune inner ear disease respond to initial treatment with oral prednisone.
Auditory neoplasms. Growths such as acoustic neuroma or cholesteatoma can cause tinnitus. Acoustic neuroma (or vestibular schwannoma) is a benign neoplasm that arises from the vestibular division of the eighth cranial nerve. Symptoms include unilateral hearing loss, tinnitus, and vestibular disturbances. Surgical resection or radiation treatment of the tumor can resolve these symptoms, especially if the neoplasm is detected while it is small.
Cholesteatoma is a benign epithelial cell mass that grows in the middle-ear cavity. Over time, cholesteatomas can enlarge and destroy middleear ossicles. Hearing loss, tinnitus, dizziness, and facial muscle paralysis can result from continued cholesteatoma growth. Early detection and surgical resection of auditory neoplasms can reduce the likelihood of residual symptoms.
Hyper- or hypotension. Of these two disorders, hypertension is more likely to contribute to tinnitus. Maintenance of blood pressure within the optimum range can decrease or resolve tinnitus for some patients.
Metabolic disorders. Disorders such as diabetes mellitus, hyperthyroidism, or hypothyroidism can contribute to tinnitus. Successful management of these conditions can reduce or resolve the patient’s tinnitus.
Managing persistent tinnitus
Successful treatment of the disorders discussed can resolve or reduce tinnitus. However, if tinnitus continues to bother the patient after other diseases have been treated, shift the clinical focus from treatment to management of the symptom. At this point, the clinician should do 1 of 2 things: 1) spend the time necessary to help the patient manage tinnitus using strategies described in the following sections of this article; or 2) refer the patient to a comprehensive tinnitus management program with experienced personnel who are willing and able to spend a substantial amount of time with each patient.
Like other neurologic symptoms, tinnitus can be considered chronic if it persists for 6 months or more. Approximately 90% of cases of chronic tinnitus are associated with some degree of sensorineural hearing loss.19 Because sensorineural hearing loss is irreversible, most cases of chronic tinnitus cannot be “cured.” Duckro et al20 wrote: “As with chronic pain, the treatment of chronic tinnitus is more accurately described in terms of management rather than cure.”
The goal of management is not necessarily to mask or remove the patient’s perception of tinnitus. In many cases, this is not possible. Successful management enables patients to pay less attention to their tinnitus. An effective management program helps patients to understand and gain control over their tinnitus, rather than allowing it to control them. The ultimate goal is to reduce the severity of tinnitus. Clinicians should strive to help patients progress to where tinnitus is no longer a negative factor in their lives.
Establishing tinnitus severity
Only 25% of people who experience chronic tinnitus consider the symptom to be a significant problem.2 These are the patients most likely to seek treatment. If a patient is not bothered by tinnitus and no active disease processes are detected, no treatments are necessary. The clinician should reassure such patients that tinnitus is a harmless perception of sound and does not usually portend more serious medical conditions.
What differentiates the majority of people not bothered by tinnitus from the minority who perceive it as a significant, even debilitating problem? Is it the matched loudness, pitch, or other qualities of the sound(s) they hear? Several studies have concluded that tinnitus severity is not correlated with any of these psychoacoustic parameters.21-23
Tinnitus severity can be defined and quantified several ways: by how much or how often a patient is bothered by tinnitus; by how much or how often tinnitus detracts from the patient’s enjoyment of life; or by how disabling patients perceive their tinnitus to be. Instruments such as the Tinnitus Severity Index11 can be used to assess tinnitus severity (Figure 2).
Tinnitus management strategies
Once underlying conditions have been treated or ruled out, reassure and counsel patients regarding factors that could exacerbate or improve their condition. If patients understand their tinnitus is nothing more than a perception of sound, they will be better able to pay less attention to it. This process of patient education and counseling helps to “demystify” the symptom of tinnitus and encourages patients to view their tinnitus with a more realistic perspective.
The severity of tinnitus is often associated with problems such as insomnia,24 anxiety,25 and depression.26 Such issues can form a vicious circle, with each one exacerbating the others.23 Tinnitus is not always the starting point of this cycle—many patients experience depression, insomnia, or anxiety before tinnitus. Medication or psychotherapy will often reduce the severity of these symptoms and associated tinnitus (LOE: 2).27-28
Because each patient has a unique medical, psychological, and social history, management programs should be individualized. In fact, the most successful tinnitus management programs employ multimodal strategies designed to address the specific needs of each patient (LOE: 2).27,29
Recommendations should be formulated and explained to the patient: appropriate acoustic therapy; use of hearing protection (all patients should wear earplugs or ear muffs when they are exposed to excessively loud sounds [LOE: 1]);30 and strategies for management of insomnia, anxiety, or depression. As appropriate, provide patients with referral and contact information for physical or psychiatric evaluations, psychological counseling, and other recommended services or products.
Acoustic therapy
Patients should add pleasant sounds (music, relaxation CDs, or a tabletop sound machine) to any environment that is too quiet, and listen to them through speakers or headphones. Patients who experience chronic insomnia because of tinnitus may find relief in using a tabletop sound machine in combination with a pillow embedded with speakers (such as the Sound Pillow, distributed by Phoenix Productions, San Antonio, TX).
Patients with normal or nearly normal hearing might benefit from in-the-ear sound generators (such as those manufactured by General Hearing Instruments, Harahan, LA) that produce a broad-band sound to muffle or mask the tinnitus.31 Significant, aidable hearing loss can often be lessened with hearing aids or combination instruments (hearing aid and sound generator in one unit). Hearing aids not only improve communication ability, the devices can also reduce the perception of tinnitus.32
Follow-up
Encourage patients to ask questions about recommended tinnitus management procedures and to report their progress. Reassess patients at 1 month. If necessary, recommendations can be modified to facilitate patient improvement. Follow-up questionnaires can be mailed to patients 6 and 12 months after their initial appointment to assess the effectiveness of the tinnitus management program.
A customized combination of recommendations is effective for many patients with chronic and bothersome tinnitus (LOE: 2),27 but the process can be very time consuming. For a certain number of patients with severe tinnitus, only a comprehensive management program can help them to improve their condition.
Corresponding author
Robert L. Folmer, PhD, OHSU Tinnitus Clinic, Mail Code NRC04, Oregon Health & Science University, 3181 SW Sam Jackson Park Road, Portland, OR 97239. E-mail: [email protected].
- If no treatable cause of tinnitus is found, assess the severity of tinnitus, secondary problems (such as depression, anxiety, and insomnia), and implement tinnitus management strategies (SOR:B).
- Acoustic therapy is effective for tinnitus management (SOR:B).
- All patients should wear hearing protection when they are exposed to loud sounds such as a gas lawnmower, leaf blower, power tools, or gunfire (SOR:A).
- Successful management of insomnia, anxiety or depression will decrease the severity of tinnitus for most patients (SOR:B).
Tinnitus—the perception of sound that does not have an external source—can be constant or intermittent and perceived as ringing, buzzing, hissing, sizzling, roaring, chirping, or other sounds.
Acute tinnitus, which can last days or weeks, may be caused by ear infection, medications, head or neck injury, excessive sound exposure, earwax, and changes in blood pressure or metabolism. With appropriate evaluation, such underlying conditions usually can be identified and treated, often with resultant resolution of tinnitus.
Chronic tinnitus (persistence for 6 months or more) can also result from these conditions and is more likely to occur in people who have hearing loss.1 (See Prevalence of tinnitus.) Even though a true “cure” for most cases of chronic tinnitus is not available, patients can obtain relief from the symptom with assistance from clinicians who are familiar with tinnitus management strategies.
Seidman and Jacobson2 estimated that 40 million people in the United States experience chronic tinnitus. The prevalence of tinnitus increases with age: 27% of males and 15% of females aged 45 years or older experience the symptom.3
Tinnitus is rare in children who have normal hearing.4 However, the prevalence of tinnitus in children with severe or profound hearing loss has been reported as 33%5 or 64%.6 More males than females experience tinnitus because men traditionally have had a greater amount of noise exposure in military service, in the workplace, and during recreational activities. Consequently, hearing loss and tinnitus are both more prevalent among men aged 45 years or older compared with women in the same age group.3
Damage depends on intensity, length of exposure
Tinnitus is most commonly caused by exposure to excessively loud sounds such as gunfire, power tools, machinery, or music. Ringing in the ears occurs because of damage to stereocilia, microscopic appendages attached to the apical ends of hair cells in the cochlea.
Moderate sounds (80 decibels sound pressure level [dB SPL] or lower) normally cause stereocilia to make tiny movements, triggering the releaseof neurotransmitter molecules from the basal ends of hair cells that activate auditory neurons in the eighth cranial nerve.
Excessive sound exposure (85 dB SPL or louder) causes stereocilia to bend more than they should. People then perceive high-pitched ringing tinnitus because hair cells that respond to higher-frequency sounds are located at the base of the cochlea and are the first to be damaged by loud noise.
If the damage is modest and infrequent, stereocilia can recover, returning to their normal function in a few minutes or hours. The patient’s hearing will be restored and the tinnitus will stop. However, repeated exposure to hazardous sounds eventually causes irreparable damage to stereocilia and hair cells, resulting in permanent sensorineural hearing loss and possibly chronic tinnitus.
In addition to noise exposure, any condition that causes hearing loss or damages the auditory system can contribute to the generation of tinnitus (Table). Imaging studies using functional magnetic resonance imaging7 or positron-emission tomography8-9 demonstrated that the perception of chronic tinnitus usually occurs as a result of hyperactivity within central auditory areas of the human brain, especially the auditory cortex. As portions of the auditory system degenerate during the aging process or acquire damage from noise exposure, disease, and accidents, the natural balance of central auditory excitation vs inhibition is disrupted. In patients who hear tinnitus, excitatory pathways within the auditory system are active when they shouldn’t be: in quiet environments. This gives patients the perception of tinnitus sounds.
TABLE
Causes of subjective tinnitus
| Presbycusis: hearing loss due to aging |
| Prolonged noise exposure: Noise-induced hearing loss |
| Acoustic trauma: one-time exposure to high intensity sound |
| Otosclerosis: abnormal accumulation of calcium on middle ear ossicles or cochlea |
| Infections: bacterial, viral, fungal |
| Autoimmune hearing loss |
| Meniere’s disease or endolymphatic hydrops: abnormally high inner ear pressure |
| Neoplasms: for example, acoustic neuroma or cholesteatoma |
| Genetic predisposition |
Ototoxicity
|
Vascular
|
Metabolic
|
| Head or neck injury |
Objective tinnitus
Objective tinnitus—which can be heard also by people in proximity to the patient’s ear—can be caused by vascular abnormalities (congenital arteriovenous fistula, acquired arteriovenous shunt, glomus jugulare, high-riding carotid artery, carotid stenosis, persistent stapedial artery, dehiscent jugular bulb or a vascular loop such as anterior inferior communicating artery [AICA] or posterior inferior communicating artery [PICA] compressing the auditory nerve) or mechanical disorders (abnormally patent Eustachian tube, palatal myoclonus, temporo-mandibular joint disorder, or stapedial muscle spasticity).10 However, objective tinnitus is rare, accounting for <1% of all cases. The vast majority of tinnitus cases are subjective—sounds are perceived only by the patient.
Patient evaluation
Figure 1 is an algorithm that outlines steps in the evaluation and management of patients who experience tinnitus. The first step is to collect as much information as possible about the patient and his condition.
FIGURE 1
Evaluation and management of tinnitus
Tinnitus history
Determine the duration of tinnitus and whether circumstances such as upper respiratory infection, otalgia, noise exposure, head trauma, sudden hearing loss, or vertigo occurred at the time of tinnitus onset. Ask the patient to describe the tinnitus: Is it intermittent or constant? High- or low-pitched? Unilateral or bilateral? Pulsatile or steady?
Unilateral tinnitus and hearing loss provide preliminary evidence for acoustic neuroma or cerebrovascular accident. High-pitched tinnitus is usually associated with high-frequency hearing loss caused by presbycusis (hearing impairment in the aged) or excessive noise exposure. Low-pitched roaring tinnitus is sometimes associated with low-frequency hearing loss exhibited by patients with Meniere’s disease. Pulsatile tinnitus, especially if synchronous with the patient’s pulse, can indicate vascular abnormalities.
Ask the patient if fatigue, stress, noise exposure, or any medications exacerbate the tinnitus. Also ask if masking sounds (such as water running in the shower), medications, or any other factors provide relief from tinnitus. This information can be used to formulate a tinnitus management program.
Assess the severity of the patient’s tinnitus using an instrument such as the Tinnitus Severity Index (Figure 2).11 A score of 36 or higher indicates bothersome tinnitus (level of evidence [LOE]: 2).12 Higher scores indicate that patients perceive their tinnitus to be a significant, even debilitating problem.
FIGURE 2
Tinnitus Severity Index
Hearing history
If possible, determine the presence and type of hearing loss (congenital, sudden, sensorineural, conductive, or mixed). Note the patient’s history of ear infections, surgeries, noise exposure (occupational or recreational), otalgia, otorrhea, and vertigo or other balance problems. Ask whether immediate family members have experienced hearing loss or tinnitus.
Health history
Look particularly for conditions that can contribute to hearing loss and tinnitus, such as hypertension, hypothyroidism, diabetes mellitus, arteriosclerosis, and autoimmune disorders (eg, lupus or rheumatoid arthritis). Also consider ototoxic medications, such as aminoglycoside antibiotics, cisplatin, furosemide, valproic acid, and high doses of quinine-containing compounds. When possible, patients with hearing loss or tinnitus should be given alternative medications free from ototoxicity.
Excessive use of alcohol, caffeine, and aspirin or other nonsteroidal anti-inflammatory drugs can exacerbate tinnitus for some patients. However, moderate use of these products is often possible.
Psychosocial history
Inquire about the patient’s marital and occupational status. Unemployed patients living alone often perceive tinnitus to be more severe than do employed patients who have supportive social networks. Also ask about any history of insomnia, anxiety, depression, obsessive-compulsive disorder, or psychosis. A questionnaire such as the abbreviated Beck Depression Inventory13 can be used to assess the presence and severity of depression.
Physical exam and testing
Patient evaluation should include the following physical examinations and tests.
Otolaryngologic/head and neck exam. Otoscopic examination can detect infections such as otitis media, which will usually be accompanied by complaints of ear pain or fullness, and possibly hearing loss in combination with tinnitus. Otoscopy can also detect impacted earwax (cerumen), which can occlude the ear canal or cause immobilization of the tympanic membrane, resulting in conductive hearing loss, tinnitus, and a feeling of fullness in the ear. Symptoms usually resolve when the earwax is removed.
If the tinnitus is synchronous with the patient’s pulse, it suggests a vascular contribution for the symptom. Auscultation of blood vessels in the neck can reveal venous hums or other types of bruits audible to the patient. Venous hum can be diagnosed by temporarily blocking blood flow through the jugular vein on the side where tinnitus is perceived.
Neurologic exam. A complete neurologic exam should include the Romberg test, Dix-Hallpike maneuver (if the patient experiences vertigo), gait testing, and cranial nerve function tests.
Audiologic testing. Audiologic tests should include pure tone air and bone conduction thresholds, speech discrimination testing, tympanometry, and most comfortable loudness (MCL) and uncomfortable loudness level (UCL) tests. Tympanometry is used to assess middle-ear function. Abnormal tympanograms and significant differences between air and bone conduction thresholds can indicate otitis media, otosclerosis, or cholesteatoma.
MCL and UCL tests are used to assess the dynamic range of patients’ hearing. Patients with UCLs that are only 5 to 20 dBs above their MCLs have a reduced dynamic range of hearing that can be caused by recruitment or hyperacusis. The audiometer can also be used to match the tinnitus for pitch and loudness and to test the effects of masking sounds on the patient’s tinnitus.
Additional evaluations. Results of patient examinations and history collection might warrant additional evaluations. For example, asymmetrical hearing loss (15 dB or greater asymmetry at 2 or more consecutive test frequencies) and unilateral tinnitus can indicate a retrocochlear lesion such as acoustic neuroma (also known as vestibular schwannoma).
One test for retrocochlear pathology is the auditory brainstem response (ABR). In this test, clicks are presented through earphones while scalp electrodes record brain responses to the sounds. Abnormal ABR waveforms can indicate retrocochlear lesion (such as acoustic neuroma) as a possible cause of ipsilateral hearing loss and tinnitus. If positive ABR results are obtained, MRI evaluation of the cerebellopontine angle with contrast material (such as gadolinium) should be performed.
Low-pitched roaring, ringing, or hissing tinnitus; hearing loss, which may be temporary or permanent; vertigo; and a feeling of pressure or fullness in the ear can indicate endolymphatic hydrops or Meniere’s disease. Symptoms usually occur in the form of “attacks” that increase in frequency during the first few years of the disease, then decrease in frequency as hearing thresholds stabilize. Electrocochleography testing is one way to diagnose endolymphatic hydrops. Patients who exhibit vestibular disorders should undergo electronystagmography testing to assess the severity and characteristics of their symptoms.
Pulsatile tinnitus associated with abnormalities of blood vessels in the neck can be evaluated with sonography, conventional angiography, or magnetic resonance angiography. Conditions such as a dehiscent jugular bulb or stenosis of carotid arteries can sometimes be treated surgically. However, many forms of pulsatile tinnitus are not caused by these conditions. Pulsatile tinnitus is often a consequence of hearing loss, arteriosclerosis, or weight loss or weight gain. These physiologic changes can cause patients to hear blood pulsing or “swishing” in vessels—sounds they did not perceive previously. Surgery is not recommended for most cases of pulsatile tinnitus.
Sudden hearing loss, especially if bilateral, might indicate autoimmune inner ear disease. Diagnostic tests include the Western blot immunoassay.
Treatment of active disease processes
Many contributors to tinnitus can be treated surgically or with medication.
Otitis media. Successful treatment of the infection with oral antibiotics usually resolves all auditory symptoms.
Allergies, sinus congestion, or infection. When inflammation subsides, tinnitus associated with these conditions usually resolves.
Otosclerosis. Abnormal accumulations of calcium on middle-ear ossicles (especially the stapes) or the cochlea can result in slowly progressing conductive or sensorineural hearing loss, tinnitus, and vestibular disturbances. Stapedectomy surgery—including implantation of ossicular prostheses—is often successful for advanced cases associated with significant hearing loss. Hearing aids also benefit some patients.
Meniere’s disease or other forms of endolymphatic hydrops. Meniere’s disease, characterized by abnormally high fluid pressure within the cochlea, has an estimated prevalence of 1% in the US.14 Management includes meclizine, antiemetics and diuretics, and a low-sodium diet.15 If patients do not respond to meclizine, diazepam can be prescribed to reduce the severity of vertigo attacks. Surgical intervention—including installation of an endolymphatic shunt, labyrinthectomy, or vestibular neurectomy16—or transtympanic injections of gentamicin17 are options in severe cases.
Autoimmune inner ear disease. This disease has an estimated prevalence of 0.1% in the US.18 Symptoms include sudden hearing loss in one ear that usually progresses to the second ear. Patients may also feel fullness in the ear and experience vertigo as well as ringing, hissing, or roaring tinnitus. Most patients with autoimmune inner ear disease respond to initial treatment with oral prednisone.
Auditory neoplasms. Growths such as acoustic neuroma or cholesteatoma can cause tinnitus. Acoustic neuroma (or vestibular schwannoma) is a benign neoplasm that arises from the vestibular division of the eighth cranial nerve. Symptoms include unilateral hearing loss, tinnitus, and vestibular disturbances. Surgical resection or radiation treatment of the tumor can resolve these symptoms, especially if the neoplasm is detected while it is small.
Cholesteatoma is a benign epithelial cell mass that grows in the middle-ear cavity. Over time, cholesteatomas can enlarge and destroy middleear ossicles. Hearing loss, tinnitus, dizziness, and facial muscle paralysis can result from continued cholesteatoma growth. Early detection and surgical resection of auditory neoplasms can reduce the likelihood of residual symptoms.
Hyper- or hypotension. Of these two disorders, hypertension is more likely to contribute to tinnitus. Maintenance of blood pressure within the optimum range can decrease or resolve tinnitus for some patients.
Metabolic disorders. Disorders such as diabetes mellitus, hyperthyroidism, or hypothyroidism can contribute to tinnitus. Successful management of these conditions can reduce or resolve the patient’s tinnitus.
Managing persistent tinnitus
Successful treatment of the disorders discussed can resolve or reduce tinnitus. However, if tinnitus continues to bother the patient after other diseases have been treated, shift the clinical focus from treatment to management of the symptom. At this point, the clinician should do 1 of 2 things: 1) spend the time necessary to help the patient manage tinnitus using strategies described in the following sections of this article; or 2) refer the patient to a comprehensive tinnitus management program with experienced personnel who are willing and able to spend a substantial amount of time with each patient.
Like other neurologic symptoms, tinnitus can be considered chronic if it persists for 6 months or more. Approximately 90% of cases of chronic tinnitus are associated with some degree of sensorineural hearing loss.19 Because sensorineural hearing loss is irreversible, most cases of chronic tinnitus cannot be “cured.” Duckro et al20 wrote: “As with chronic pain, the treatment of chronic tinnitus is more accurately described in terms of management rather than cure.”
The goal of management is not necessarily to mask or remove the patient’s perception of tinnitus. In many cases, this is not possible. Successful management enables patients to pay less attention to their tinnitus. An effective management program helps patients to understand and gain control over their tinnitus, rather than allowing it to control them. The ultimate goal is to reduce the severity of tinnitus. Clinicians should strive to help patients progress to where tinnitus is no longer a negative factor in their lives.
Establishing tinnitus severity
Only 25% of people who experience chronic tinnitus consider the symptom to be a significant problem.2 These are the patients most likely to seek treatment. If a patient is not bothered by tinnitus and no active disease processes are detected, no treatments are necessary. The clinician should reassure such patients that tinnitus is a harmless perception of sound and does not usually portend more serious medical conditions.
What differentiates the majority of people not bothered by tinnitus from the minority who perceive it as a significant, even debilitating problem? Is it the matched loudness, pitch, or other qualities of the sound(s) they hear? Several studies have concluded that tinnitus severity is not correlated with any of these psychoacoustic parameters.21-23
Tinnitus severity can be defined and quantified several ways: by how much or how often a patient is bothered by tinnitus; by how much or how often tinnitus detracts from the patient’s enjoyment of life; or by how disabling patients perceive their tinnitus to be. Instruments such as the Tinnitus Severity Index11 can be used to assess tinnitus severity (Figure 2).
Tinnitus management strategies
Once underlying conditions have been treated or ruled out, reassure and counsel patients regarding factors that could exacerbate or improve their condition. If patients understand their tinnitus is nothing more than a perception of sound, they will be better able to pay less attention to it. This process of patient education and counseling helps to “demystify” the symptom of tinnitus and encourages patients to view their tinnitus with a more realistic perspective.
The severity of tinnitus is often associated with problems such as insomnia,24 anxiety,25 and depression.26 Such issues can form a vicious circle, with each one exacerbating the others.23 Tinnitus is not always the starting point of this cycle—many patients experience depression, insomnia, or anxiety before tinnitus. Medication or psychotherapy will often reduce the severity of these symptoms and associated tinnitus (LOE: 2).27-28
Because each patient has a unique medical, psychological, and social history, management programs should be individualized. In fact, the most successful tinnitus management programs employ multimodal strategies designed to address the specific needs of each patient (LOE: 2).27,29
Recommendations should be formulated and explained to the patient: appropriate acoustic therapy; use of hearing protection (all patients should wear earplugs or ear muffs when they are exposed to excessively loud sounds [LOE: 1]);30 and strategies for management of insomnia, anxiety, or depression. As appropriate, provide patients with referral and contact information for physical or psychiatric evaluations, psychological counseling, and other recommended services or products.
Acoustic therapy
Patients should add pleasant sounds (music, relaxation CDs, or a tabletop sound machine) to any environment that is too quiet, and listen to them through speakers or headphones. Patients who experience chronic insomnia because of tinnitus may find relief in using a tabletop sound machine in combination with a pillow embedded with speakers (such as the Sound Pillow, distributed by Phoenix Productions, San Antonio, TX).
Patients with normal or nearly normal hearing might benefit from in-the-ear sound generators (such as those manufactured by General Hearing Instruments, Harahan, LA) that produce a broad-band sound to muffle or mask the tinnitus.31 Significant, aidable hearing loss can often be lessened with hearing aids or combination instruments (hearing aid and sound generator in one unit). Hearing aids not only improve communication ability, the devices can also reduce the perception of tinnitus.32
Follow-up
Encourage patients to ask questions about recommended tinnitus management procedures and to report their progress. Reassess patients at 1 month. If necessary, recommendations can be modified to facilitate patient improvement. Follow-up questionnaires can be mailed to patients 6 and 12 months after their initial appointment to assess the effectiveness of the tinnitus management program.
A customized combination of recommendations is effective for many patients with chronic and bothersome tinnitus (LOE: 2),27 but the process can be very time consuming. For a certain number of patients with severe tinnitus, only a comprehensive management program can help them to improve their condition.
Corresponding author
Robert L. Folmer, PhD, OHSU Tinnitus Clinic, Mail Code NRC04, Oregon Health & Science University, 3181 SW Sam Jackson Park Road, Portland, OR 97239. E-mail: [email protected].
1. Schleuning A. Medical aspects of tinnitus. In: Vernon JA, ed. Tinnitus Treatment and Relief. Boston, Mass: Allyn and Bacon; 1998;20-27.
2. Seidman MD, Jacobson GP. Update on tinnitus. Otolaryngol Clin N Amer 1996;29:455-465.
3. Adams PF, Hendershot GE, Marano MA. Current estimates from the National Health Interview Survey, 1996. Hyattsville, Md: National Center for Health Statistics, 1999.
4. Stouffer JL, Tyler RS, Booth JC, Buckrell B. Tinnitus in normal-hearing and hearing-impaired children. In: Aran J-M, Dauman R, eds. Tinnitus 91: Proceedings of the Fourth International Tinnitus Seminar. Amsterdam: Kugler Publications 1992;255-258.
5. Drukier GS. The prevalence and characteristics of tinnitus with profound sensori-neural hearing impairment. Amer Ann Deaf 1989;134:260-264.
6. Graham J. Paediatric tinnitus. J Laryngol Otol 1981;95(Suppl):117-120.
7. Levine RA, Benson RR, Talavage TM, Melcher JR, Rosen BR. Functional magnetic resonance imaging and tinnitus: preliminary results. Abstr Assoc Res Otolaryngol 1997;20:65.-
8. Arnold W, Bartenstein P, Oestreicher E, Romer W, Schwaiger M. Focal metabolic activation in the predominant left auditory cortex in patients suffering from tinnitus: a PET study with [18F]deoxyglucose. ORL J Otorhinolaryngol Relat Spec 1996;58:195-199.
9. Lockwood AH, Salvi RJ, Coad ML, Towsley ML, Wach DS, Murphy BW. The functional neuroanatomy of tinnitus: evidence for limbic system links and neuroplasticity. Neurology 1998;50:114-120.
10. Ciocon JO, Amede F, Lechtenberg C, Astor F. Tinnitus: a stepwise workup to quiet the noise within. Geriatrics 1995;50:18-25.
11. Meikle MB, Griest SE, Stewart BJ, Press LS. Measuring the negative impact of tinnitus: a brief severity index. Abstr Assoc Res Otolaryngol 1995;167.-
12. Folmer RL, Stevenson EA, Tran A. Factors associated with long-term improvements in tinnitus severity. In Patuzzi R, ed: Proceedings of the Seventh International Tinnitus Seminar. Crawley: University of Western Australia; 2002;115-123.
13. Beck AT, Beck RW. Screening depressed patients in family practice: a rapid technic. Postgrad Medicine 1972;52:81-85.
14. daCosta SS, deSousa LC, Piza MR. Meniere’s Disease: overview, epidemiology, and natural history. Otolaryngol Clin N Amer 2002;35:455-495.
15. Thai-Van H, Bounaix MJ, Fraysse B. Meniere’s disease: pathophysiology and treatment. Drugs 2001;61:1089-1102.
16. Hillman TA, Chen DA, Arriaga MA. Vestibular nerve section versus intratympanic gentamicin for Meniere’s disease. Laryngoscope 2004;114:216-222.
17. Diamond C, Hornig JD, Liu R, O’Connell DA. Systematic review of intratympanic gentamicin in Meniere’s disease. J Otolaryngol 2003;32:351-361.
18. Hain TC. Autoimmune inner ear disease. American Hearing Research Foundation Web site. March 23, 2002. Available at www.american-hearing.org/name/autoimmune.html. Accessed on May 15, 2004.
19. Meikle MB. Electronic access to tinnitus data: The Oregon Tinnitus Data Archive. Otolaryngol Head Neck Surg 1997;117:698-700.
20. Duckro PN, Pollard CA, Bray HD, Scheiter L. Comprehensive behavioral management of complex tinnitus: a case illustration. Biofeedback and Self-Regulation 1984;9:459-469.
21. Meikle MB, Vernon J, Johnson RM. The perceived severity of tinnitus. Otolaryngol Head Neck Surg 1984;92:689-696.
22. van Veen ED, Jacobs JB, Bensing JM. Assessment of distress associated with tinnitus. J Laryngol Otol 1998;112:258-263.
23. Folmer RL, Griest SE, Martin WH. Chronic tinnitus as phantom auditory pain. Otolaryngol Head Neck Surg 2001;124:394-400.
24. Folmer RL, Griest SE. Tinnitus and insomnia. Am J Otolaryngol 2000;21:287-293.
25. Attias J, Shemesh Z, Bleich A, Solomon Z, Bar-Or G, Alster J, Sohmer H. Psychological profile of help-seeking and non-help-seeking tinnitus patients. Scand Audiol 1995;24:13-18.
26. Folmer RL, Griest SE, Meikle MB, Martin WH. Tinnitus severity, loudness and depression. Otolaryngol Head Neck Surg 1999;121:48-51.
27. Folmer R. Long-term reductions in tinnitus severity. BMC Ear Nose and Throat Disorders 2002;2:3.-Available at: www.biomedcentral.com/1472-6815/2/3.
28. Folmer RL, Shi YB. SSRI use by tinnitus patients: interactions between depression and tinnitus severity ENT J 2004;83:107-117.
29. Sullivan M, Katon W, Russo J, Dobie R, Sakai C. Coping and marital support as correlates of tinnitus disability. Gen Hosp Psychiatry 1994;16:259-266.
30. Lusk SL. Preventing noise-induced hearing loss. Nurs Clin North Amer 2002;37:257-262.
31. Henry JA, Schechter MA, Nagler SM, Fausti SA. Comparison of tinnitus masking and tinnitus retraining therapy. J Amer Acad Audiol 2002;13:559-581.
32. Surr RK, Montgomery AA, Mueller HG. Effect of amplification on tinnitus among new hearing aid users. Ear and Hearing 1985;6:71-75.
1. Schleuning A. Medical aspects of tinnitus. In: Vernon JA, ed. Tinnitus Treatment and Relief. Boston, Mass: Allyn and Bacon; 1998;20-27.
2. Seidman MD, Jacobson GP. Update on tinnitus. Otolaryngol Clin N Amer 1996;29:455-465.
3. Adams PF, Hendershot GE, Marano MA. Current estimates from the National Health Interview Survey, 1996. Hyattsville, Md: National Center for Health Statistics, 1999.
4. Stouffer JL, Tyler RS, Booth JC, Buckrell B. Tinnitus in normal-hearing and hearing-impaired children. In: Aran J-M, Dauman R, eds. Tinnitus 91: Proceedings of the Fourth International Tinnitus Seminar. Amsterdam: Kugler Publications 1992;255-258.
5. Drukier GS. The prevalence and characteristics of tinnitus with profound sensori-neural hearing impairment. Amer Ann Deaf 1989;134:260-264.
6. Graham J. Paediatric tinnitus. J Laryngol Otol 1981;95(Suppl):117-120.
7. Levine RA, Benson RR, Talavage TM, Melcher JR, Rosen BR. Functional magnetic resonance imaging and tinnitus: preliminary results. Abstr Assoc Res Otolaryngol 1997;20:65.-
8. Arnold W, Bartenstein P, Oestreicher E, Romer W, Schwaiger M. Focal metabolic activation in the predominant left auditory cortex in patients suffering from tinnitus: a PET study with [18F]deoxyglucose. ORL J Otorhinolaryngol Relat Spec 1996;58:195-199.
9. Lockwood AH, Salvi RJ, Coad ML, Towsley ML, Wach DS, Murphy BW. The functional neuroanatomy of tinnitus: evidence for limbic system links and neuroplasticity. Neurology 1998;50:114-120.
10. Ciocon JO, Amede F, Lechtenberg C, Astor F. Tinnitus: a stepwise workup to quiet the noise within. Geriatrics 1995;50:18-25.
11. Meikle MB, Griest SE, Stewart BJ, Press LS. Measuring the negative impact of tinnitus: a brief severity index. Abstr Assoc Res Otolaryngol 1995;167.-
12. Folmer RL, Stevenson EA, Tran A. Factors associated with long-term improvements in tinnitus severity. In Patuzzi R, ed: Proceedings of the Seventh International Tinnitus Seminar. Crawley: University of Western Australia; 2002;115-123.
13. Beck AT, Beck RW. Screening depressed patients in family practice: a rapid technic. Postgrad Medicine 1972;52:81-85.
14. daCosta SS, deSousa LC, Piza MR. Meniere’s Disease: overview, epidemiology, and natural history. Otolaryngol Clin N Amer 2002;35:455-495.
15. Thai-Van H, Bounaix MJ, Fraysse B. Meniere’s disease: pathophysiology and treatment. Drugs 2001;61:1089-1102.
16. Hillman TA, Chen DA, Arriaga MA. Vestibular nerve section versus intratympanic gentamicin for Meniere’s disease. Laryngoscope 2004;114:216-222.
17. Diamond C, Hornig JD, Liu R, O’Connell DA. Systematic review of intratympanic gentamicin in Meniere’s disease. J Otolaryngol 2003;32:351-361.
18. Hain TC. Autoimmune inner ear disease. American Hearing Research Foundation Web site. March 23, 2002. Available at www.american-hearing.org/name/autoimmune.html. Accessed on May 15, 2004.
19. Meikle MB. Electronic access to tinnitus data: The Oregon Tinnitus Data Archive. Otolaryngol Head Neck Surg 1997;117:698-700.
20. Duckro PN, Pollard CA, Bray HD, Scheiter L. Comprehensive behavioral management of complex tinnitus: a case illustration. Biofeedback and Self-Regulation 1984;9:459-469.
21. Meikle MB, Vernon J, Johnson RM. The perceived severity of tinnitus. Otolaryngol Head Neck Surg 1984;92:689-696.
22. van Veen ED, Jacobs JB, Bensing JM. Assessment of distress associated with tinnitus. J Laryngol Otol 1998;112:258-263.
23. Folmer RL, Griest SE, Martin WH. Chronic tinnitus as phantom auditory pain. Otolaryngol Head Neck Surg 2001;124:394-400.
24. Folmer RL, Griest SE. Tinnitus and insomnia. Am J Otolaryngol 2000;21:287-293.
25. Attias J, Shemesh Z, Bleich A, Solomon Z, Bar-Or G, Alster J, Sohmer H. Psychological profile of help-seeking and non-help-seeking tinnitus patients. Scand Audiol 1995;24:13-18.
26. Folmer RL, Griest SE, Meikle MB, Martin WH. Tinnitus severity, loudness and depression. Otolaryngol Head Neck Surg 1999;121:48-51.
27. Folmer R. Long-term reductions in tinnitus severity. BMC Ear Nose and Throat Disorders 2002;2:3.-Available at: www.biomedcentral.com/1472-6815/2/3.
28. Folmer RL, Shi YB. SSRI use by tinnitus patients: interactions between depression and tinnitus severity ENT J 2004;83:107-117.
29. Sullivan M, Katon W, Russo J, Dobie R, Sakai C. Coping and marital support as correlates of tinnitus disability. Gen Hosp Psychiatry 1994;16:259-266.
30. Lusk SL. Preventing noise-induced hearing loss. Nurs Clin North Amer 2002;37:257-262.
31. Henry JA, Schechter MA, Nagler SM, Fausti SA. Comparison of tinnitus masking and tinnitus retraining therapy. J Amer Acad Audiol 2002;13:559-581.
32. Surr RK, Montgomery AA, Mueller HG. Effect of amplification on tinnitus among new hearing aid users. Ear and Hearing 1985;6:71-75.