User login
FIND: A framework for success as a first-year hospitalist
Congratulations! You’re about to start your first year as a hospitalist, and in many cases your first real job. Hospital medicine is an incredibly rewarding subspecialty, but the progression from resident to attending physician can be daunting. To facilitate this transition, we present FIND (Familiarity, Identity, Network, and Direction) – a novel, sequential framework for success as a first-year hospitalist. For each component, we provide a narrative overview and a summary bullet point for quick reference.
Familiarity
- Lay the foundation: Learn the ins and outs of your job, EMR, and team.
Familiarize yourself with your surroundings. Know where your patients are located, where you can document, where to find equipment for procedures, and how to reach information technology. Proactively set up the electronic medical record on your home computer and phone. Make sure to review your responsibilities, including your call schedule, your shifts, your assigned patient panel, when you can leave campus, and how people should contact you. Also, others should know your expectations of them, especially if you are working with trainees.
Maintain a file with all of your orientation materials, including phone numbers and emails of key personnel. Know who your people are – who can access your calendar, who you can call with a clinical question or to escalate care, who can assist you with billing, and who helps with the throughput of your patients in the hospital. Take time to review your benefits, including parental leave, insurance coverage, retirement planning, vacation time, and ancillary services like laundry for your white coat. Familiarizing yourself with these basics will provide comfort and lay the foundation for your first year.
Identity
- Perform self-reflection: Overcome imposter syndrome and invest in hobbies.
One of the fundamental realizations that will occur with your first hospitalist job is that you are the attending. You walk in with a vision of your first job; be prepared to be surprised. You have earned the privilege of deciding on patient plans, and you are no longer obligated to staff with a senior physician. This is both empowering and terrifying. In a way, it may oddly remind you of intern year. A new hospital, new EMR, new colleagues, and imposter syndrome will trick you into doubting your decisions.
How to battle it? Positive thinking. You do know the basics of inpatient medicine and you do have a support system to cheer you on. As part of imposter syndrome, you may feel pressured to focus solely on work. Yet, your first job as a hospitalist is finally an amazing opportunity to focus on you. What hobbies have you been neglecting: cooking, photography, reading, more time with family, a new pet? You have the power to schedule your off-weeks. Are you interested in academics? Reserve a portion of your time off to explore scholarship opportunities at your institution. Your first job as a hospitalist is a chance to develop your identity, both as a physician and as an individual.
Network
- Engage your support system: Communicate with nursing, administration, colleagues.
Networking, or building a web of mutually beneficial professional relationships, is imperative for long-term career success. Hospitalists should focus on developing their network across multiple departments, such as nursing, subspecialties, medical education, and hospital administration. Curating a broad network will increase your visibility within your organization, showcase your unique services, and demonstrate your value.
To make networking encounters impactful, express interest, actively listen, ask relevant questions, and seek areas of mutual benefit. It’s equally important to cultivate these new relationships after the initial encounter and to demonstrate how your skill set will aid colleagues in achieving their professional goals. Over time, as you establish your niche, deliberate networking with those who share similar interests can lead to a wealth of new experiences and opportunities. Intentionally mastering networking early in your career provides insight into different aspects of the hospital system, new perspectives on ideas, and access to valuable guidance from other professionals. Engaging in networking to establish your support system is an essential step towards success as a first-year hospitalist.
Direction
- Visualize your path: Find a mentor and develop a mission statement and career plan.
Once you’re familiar with your work environment, confident in your identity, and acquainted with your support network, you’re ready for the final step – direction. Hospital medicine offers many professional avenues and clarifying your career path is challenging when attempted alone. A mentor is the necessary catalyst to find direction and purpose.
Selecting and engaging with a mentor will bolster your professional advancement, academic productivity, and most importantly, career satisfaction.1 At its best, mentorship is a symbiotic relationship. Your mentor should inspire you, challenge you, and support your growth and emotional well-being. In turn, as the mentee, you should be proactive, establish expectations, and take responsibility for maintaining communication to ensure a successful relationship. As your career takes shape over time, you may require a mentorship team to fulfill your unique needs.
When you’ve established a relationship with your mentor, take time to develop 1-year and 5-year plans. Your 1-year plan should focus on a few “quick wins,” often projects or opportunities at your home institution. Small victories in your first year will boost your confidence, motivation, and sense of control. Your 5-year plan should delineate the steps necessary to make your first major career transition, such as from instructor to assistant professor. Working with your mentor to draft a career mission statement is a useful first step in this process. Beginning with the end in mind, will help you visualize your direction.2
We hope that the FIND framework will help you find your path to success as a first-year hospitalist.
Dr. Nelson is a hospitalist and instructor of medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, both in Boston. Dr. Ashford is assistant professor and program director, department of internal medicine/pediatrics, at the University of Nebraska Medical Center, Omaha. Dr. Rawal is clinical assistant professor of medicine at the University of Pittsburgh Medical Center. Dr. Crecelius is assistant professor of clinical medicine at Indiana University, Indianapolis. This article is sponsored by the SHM Physicians in Training committee, which submits quarterly content to the Hospitalist on topics relevant to trainees and early -career hospitalists.
References
1. Zerzan JT et al. Making the most of mentors: a guide for mentees. Acad Med. 2009;84:140-4. doi: 10.1097/ACM.0b013e3181906e8f.
2. Covey F. The seven habits of highly effective people. 25th anniversary edition. New York: Simon and Schuster, 2013.
Congratulations! You’re about to start your first year as a hospitalist, and in many cases your first real job. Hospital medicine is an incredibly rewarding subspecialty, but the progression from resident to attending physician can be daunting. To facilitate this transition, we present FIND (Familiarity, Identity, Network, and Direction) – a novel, sequential framework for success as a first-year hospitalist. For each component, we provide a narrative overview and a summary bullet point for quick reference.
Familiarity
- Lay the foundation: Learn the ins and outs of your job, EMR, and team.
Familiarize yourself with your surroundings. Know where your patients are located, where you can document, where to find equipment for procedures, and how to reach information technology. Proactively set up the electronic medical record on your home computer and phone. Make sure to review your responsibilities, including your call schedule, your shifts, your assigned patient panel, when you can leave campus, and how people should contact you. Also, others should know your expectations of them, especially if you are working with trainees.
Maintain a file with all of your orientation materials, including phone numbers and emails of key personnel. Know who your people are – who can access your calendar, who you can call with a clinical question or to escalate care, who can assist you with billing, and who helps with the throughput of your patients in the hospital. Take time to review your benefits, including parental leave, insurance coverage, retirement planning, vacation time, and ancillary services like laundry for your white coat. Familiarizing yourself with these basics will provide comfort and lay the foundation for your first year.
Identity
- Perform self-reflection: Overcome imposter syndrome and invest in hobbies.
One of the fundamental realizations that will occur with your first hospitalist job is that you are the attending. You walk in with a vision of your first job; be prepared to be surprised. You have earned the privilege of deciding on patient plans, and you are no longer obligated to staff with a senior physician. This is both empowering and terrifying. In a way, it may oddly remind you of intern year. A new hospital, new EMR, new colleagues, and imposter syndrome will trick you into doubting your decisions.
How to battle it? Positive thinking. You do know the basics of inpatient medicine and you do have a support system to cheer you on. As part of imposter syndrome, you may feel pressured to focus solely on work. Yet, your first job as a hospitalist is finally an amazing opportunity to focus on you. What hobbies have you been neglecting: cooking, photography, reading, more time with family, a new pet? You have the power to schedule your off-weeks. Are you interested in academics? Reserve a portion of your time off to explore scholarship opportunities at your institution. Your first job as a hospitalist is a chance to develop your identity, both as a physician and as an individual.
Network
- Engage your support system: Communicate with nursing, administration, colleagues.
Networking, or building a web of mutually beneficial professional relationships, is imperative for long-term career success. Hospitalists should focus on developing their network across multiple departments, such as nursing, subspecialties, medical education, and hospital administration. Curating a broad network will increase your visibility within your organization, showcase your unique services, and demonstrate your value.
To make networking encounters impactful, express interest, actively listen, ask relevant questions, and seek areas of mutual benefit. It’s equally important to cultivate these new relationships after the initial encounter and to demonstrate how your skill set will aid colleagues in achieving their professional goals. Over time, as you establish your niche, deliberate networking with those who share similar interests can lead to a wealth of new experiences and opportunities. Intentionally mastering networking early in your career provides insight into different aspects of the hospital system, new perspectives on ideas, and access to valuable guidance from other professionals. Engaging in networking to establish your support system is an essential step towards success as a first-year hospitalist.
Direction
- Visualize your path: Find a mentor and develop a mission statement and career plan.
Once you’re familiar with your work environment, confident in your identity, and acquainted with your support network, you’re ready for the final step – direction. Hospital medicine offers many professional avenues and clarifying your career path is challenging when attempted alone. A mentor is the necessary catalyst to find direction and purpose.
Selecting and engaging with a mentor will bolster your professional advancement, academic productivity, and most importantly, career satisfaction.1 At its best, mentorship is a symbiotic relationship. Your mentor should inspire you, challenge you, and support your growth and emotional well-being. In turn, as the mentee, you should be proactive, establish expectations, and take responsibility for maintaining communication to ensure a successful relationship. As your career takes shape over time, you may require a mentorship team to fulfill your unique needs.
When you’ve established a relationship with your mentor, take time to develop 1-year and 5-year plans. Your 1-year plan should focus on a few “quick wins,” often projects or opportunities at your home institution. Small victories in your first year will boost your confidence, motivation, and sense of control. Your 5-year plan should delineate the steps necessary to make your first major career transition, such as from instructor to assistant professor. Working with your mentor to draft a career mission statement is a useful first step in this process. Beginning with the end in mind, will help you visualize your direction.2
We hope that the FIND framework will help you find your path to success as a first-year hospitalist.
Dr. Nelson is a hospitalist and instructor of medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, both in Boston. Dr. Ashford is assistant professor and program director, department of internal medicine/pediatrics, at the University of Nebraska Medical Center, Omaha. Dr. Rawal is clinical assistant professor of medicine at the University of Pittsburgh Medical Center. Dr. Crecelius is assistant professor of clinical medicine at Indiana University, Indianapolis. This article is sponsored by the SHM Physicians in Training committee, which submits quarterly content to the Hospitalist on topics relevant to trainees and early -career hospitalists.
References
1. Zerzan JT et al. Making the most of mentors: a guide for mentees. Acad Med. 2009;84:140-4. doi: 10.1097/ACM.0b013e3181906e8f.
2. Covey F. The seven habits of highly effective people. 25th anniversary edition. New York: Simon and Schuster, 2013.
Congratulations! You’re about to start your first year as a hospitalist, and in many cases your first real job. Hospital medicine is an incredibly rewarding subspecialty, but the progression from resident to attending physician can be daunting. To facilitate this transition, we present FIND (Familiarity, Identity, Network, and Direction) – a novel, sequential framework for success as a first-year hospitalist. For each component, we provide a narrative overview and a summary bullet point for quick reference.
Familiarity
- Lay the foundation: Learn the ins and outs of your job, EMR, and team.
Familiarize yourself with your surroundings. Know where your patients are located, where you can document, where to find equipment for procedures, and how to reach information technology. Proactively set up the electronic medical record on your home computer and phone. Make sure to review your responsibilities, including your call schedule, your shifts, your assigned patient panel, when you can leave campus, and how people should contact you. Also, others should know your expectations of them, especially if you are working with trainees.
Maintain a file with all of your orientation materials, including phone numbers and emails of key personnel. Know who your people are – who can access your calendar, who you can call with a clinical question or to escalate care, who can assist you with billing, and who helps with the throughput of your patients in the hospital. Take time to review your benefits, including parental leave, insurance coverage, retirement planning, vacation time, and ancillary services like laundry for your white coat. Familiarizing yourself with these basics will provide comfort and lay the foundation for your first year.
Identity
- Perform self-reflection: Overcome imposter syndrome and invest in hobbies.
One of the fundamental realizations that will occur with your first hospitalist job is that you are the attending. You walk in with a vision of your first job; be prepared to be surprised. You have earned the privilege of deciding on patient plans, and you are no longer obligated to staff with a senior physician. This is both empowering and terrifying. In a way, it may oddly remind you of intern year. A new hospital, new EMR, new colleagues, and imposter syndrome will trick you into doubting your decisions.
How to battle it? Positive thinking. You do know the basics of inpatient medicine and you do have a support system to cheer you on. As part of imposter syndrome, you may feel pressured to focus solely on work. Yet, your first job as a hospitalist is finally an amazing opportunity to focus on you. What hobbies have you been neglecting: cooking, photography, reading, more time with family, a new pet? You have the power to schedule your off-weeks. Are you interested in academics? Reserve a portion of your time off to explore scholarship opportunities at your institution. Your first job as a hospitalist is a chance to develop your identity, both as a physician and as an individual.
Network
- Engage your support system: Communicate with nursing, administration, colleagues.
Networking, or building a web of mutually beneficial professional relationships, is imperative for long-term career success. Hospitalists should focus on developing their network across multiple departments, such as nursing, subspecialties, medical education, and hospital administration. Curating a broad network will increase your visibility within your organization, showcase your unique services, and demonstrate your value.
To make networking encounters impactful, express interest, actively listen, ask relevant questions, and seek areas of mutual benefit. It’s equally important to cultivate these new relationships after the initial encounter and to demonstrate how your skill set will aid colleagues in achieving their professional goals. Over time, as you establish your niche, deliberate networking with those who share similar interests can lead to a wealth of new experiences and opportunities. Intentionally mastering networking early in your career provides insight into different aspects of the hospital system, new perspectives on ideas, and access to valuable guidance from other professionals. Engaging in networking to establish your support system is an essential step towards success as a first-year hospitalist.
Direction
- Visualize your path: Find a mentor and develop a mission statement and career plan.
Once you’re familiar with your work environment, confident in your identity, and acquainted with your support network, you’re ready for the final step – direction. Hospital medicine offers many professional avenues and clarifying your career path is challenging when attempted alone. A mentor is the necessary catalyst to find direction and purpose.
Selecting and engaging with a mentor will bolster your professional advancement, academic productivity, and most importantly, career satisfaction.1 At its best, mentorship is a symbiotic relationship. Your mentor should inspire you, challenge you, and support your growth and emotional well-being. In turn, as the mentee, you should be proactive, establish expectations, and take responsibility for maintaining communication to ensure a successful relationship. As your career takes shape over time, you may require a mentorship team to fulfill your unique needs.
When you’ve established a relationship with your mentor, take time to develop 1-year and 5-year plans. Your 1-year plan should focus on a few “quick wins,” often projects or opportunities at your home institution. Small victories in your first year will boost your confidence, motivation, and sense of control. Your 5-year plan should delineate the steps necessary to make your first major career transition, such as from instructor to assistant professor. Working with your mentor to draft a career mission statement is a useful first step in this process. Beginning with the end in mind, will help you visualize your direction.2
We hope that the FIND framework will help you find your path to success as a first-year hospitalist.
Dr. Nelson is a hospitalist and instructor of medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, both in Boston. Dr. Ashford is assistant professor and program director, department of internal medicine/pediatrics, at the University of Nebraska Medical Center, Omaha. Dr. Rawal is clinical assistant professor of medicine at the University of Pittsburgh Medical Center. Dr. Crecelius is assistant professor of clinical medicine at Indiana University, Indianapolis. This article is sponsored by the SHM Physicians in Training committee, which submits quarterly content to the Hospitalist on topics relevant to trainees and early -career hospitalists.
References
1. Zerzan JT et al. Making the most of mentors: a guide for mentees. Acad Med. 2009;84:140-4. doi: 10.1097/ACM.0b013e3181906e8f.
2. Covey F. The seven habits of highly effective people. 25th anniversary edition. New York: Simon and Schuster, 2013.
High rates of work-related trauma, PTSD in intern physicians
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”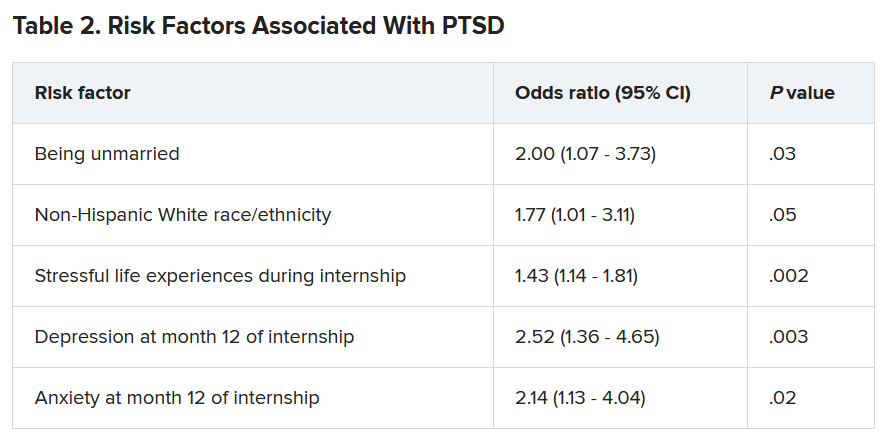
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”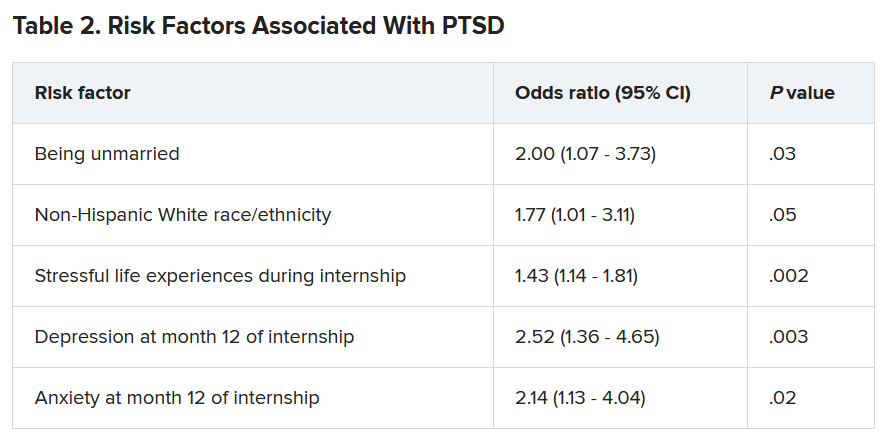
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”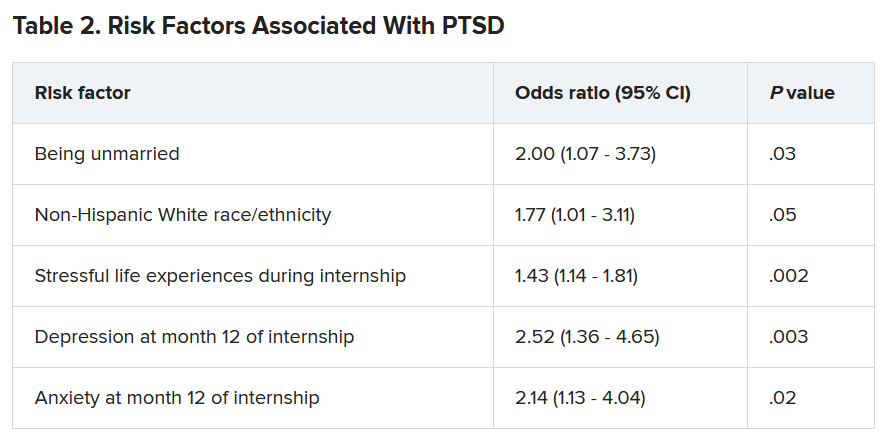
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Preparing pediatric hospital medicine fellows for leadership
Reflecting on a longitudinal leadership elective experience
The practice of pediatric hospital medicine (PHM) has been evolving and rapidly expanding over the last several decades. Not only has the scope of clinical practice matured and become more defined, but hospitalists now also have the responsibility to advance the performance of hospitals and health care systems. Pediatric hospitalists are increasingly incorporating medical education, research, high-value care, patient quality and safety initiatives, and process improvement into their careers.1 As a result, pediatric hospitalists are occupying a wider range of administrative and leadership positions within the health care system.
The field of PHM has highlighted the importance of leadership in the practice of hospital medicine by dedicating a chapter to “Leadership in Healthcare” in the PHM Core Competencies.1 The competencies define the expertise required of hospitalists and serve as guidance for the development of education, training, and career development series. Hospitalists may seek out opportunities for leadership training at an institutional or national level. Options may include advanced degrees, national conferences, division training seminars, or self-directed learning through reading or observational experiences. Unfortunately, all of these take time and motivation. As a result, hospitalists tend to pursue these opportunities only after they have already been appointed to leadership positions.
PHM fellowship is the optimal time to build a foundation of leadership skills. Over the course of a 2-year fellowship, fellows have a combined 16 weeks dedicated to educational activities beyond direct patient care.2 The Accreditation Council for Graduate Medical Education (ACGME) encourages educational innovation during this time, allowing programs to create unique opportunities for their fellows that will promote progress towards their ultimate career goals.3 This curricular framework provides the flexibility to integrate leadership training into fellowship training.
Many fellows are eager for leadership experiences and mentorship, myself included. As a pediatric chief resident, I was immersed in a diverse range of clinical, educational, research, and administrative responsibilities. I found myself in a leadership position with no prior education on how to manage people or team dynamics, make high-stress decisions on behalf of a group of people, or handle conflict. Although I learned new strategies on a daily basis, the experience showed me how much more I still had to learn in order to be a successful leader. This was one of the reasons I decided to pursue fellowship training. I think many PHM fellowship applicants feel similarly. They may have served in a leadership position in the past but feel underprepared to fulfill leadership positions in the next phase of their careers.
But despite this eagerness, evidence suggests that fellows do not feel that they receive as much management training as they need to start their careers. In a 2014 survey of PHM fellowship graduates, many held formal leadership positions within their institution (23/51) and within national organizations (6/51), despite having only five years of hospitalist experience on average (including time spent in fellowship). When asked about training needs, respondents identified “hospital program management” as an area where they wished they received more training during fellowship.4
Anyone who has gone through the PHM fellowship interview process can tell you that a common refrain of program directors is, “One of the goals of our program is to create future leaders in PHM.” This led me to wonder: how do fellowship programs prepare their fellows for future leadership positions?
I began my fellowship training at Nationwide Children’s Hospital in the summer of 2020. The program had just designed a longitudinal leadership elective, which the second-year fellow and I decided to pilot together. As I reflected on the first half of this academic year, I realized that it is unique experiences like this elective that make me thankful I pursued fellowship. I want to share with the hospitalist community the structure of the elective and why it has been particularly valuable with the hope that it will inspire similar opportunities for other fellows.
The program is semi-structured but allows the fellow and preceptors the flexibility to decide what activities would benefit that particular fellow. We attend a variety of administrative and committee meetings with each preceptor that expose us to the responsibilities of their positions, their leadership style in action, their approach to crisis management, and differences in divisional operations. On a monthly basis we meet with a preceptor to discuss a topic related to leadership. Examples of topics include how to run a more effective meeting, barriers to organizational change, leading in crisis, and the importance of mission, vision, values, and goals of organizations. The preceptor sends us articles or other learning materials they have found useful on the topic, and these serve as a starting point for our discussions. These discussions provide a point of reflection as we apply the day’s concept to our own prior experiences or to our observations during the elective.
The combination of learning experiences, discussions, and dedicated preceptorship has prepared me far better for future leadership than my past personal and observational experiences. I have summarized my top three reasons why this structure of leadership development is particularly valuable to me as a fellow.
First, the longitudinal structure of the elective allows us to learn from multiple preceptors over the course of the academic year. The preceptors include the current chief of hospital pediatrics at Nationwide Children’s Hospital; the division director of hospital medicine at the Ohio State University Wexner Medical Center; and the physician lead for hospital medicine at one of the satellite hospitals in the region. With faculty from the Department of Pediatrics and the Department of Internal Medicine-Pediatrics in these leadership positions, we have the unique ability to compare and contrast operational systems between the two different hospital systems.
Recently, we also had the opportunity to meet with both the chairman of the department of pediatrics and chief medical officer. All of these physician leaders hold a variety of administrative roles and have differing leadership philosophies, each providing useful insights. For instance, one leader ensures his team holds him accountable as the leader by always asking for honest feedback. He recommends telling those you work with to “never let me fail.” Another leader acknowledges that creating five-year plans can be daunting but encouraged us to still be intentional with our direction on a smaller scale by writing down goals for the year and sharing with a mentor. Ultimately, I came away with a wide variety of perspectives to reference as I go forward.
Second, the learning is contextualized. I can take concepts that I learn through reading and discussions and construct meaning based on observations from meetings or other encounters with different leaders. For example, after reviewing several articles on strategies to make meetings more effective, I started noticing what went well and what didn’t go well in every meeting I attended. I observed preceptors employing many of the strategies successfully with positive feedback. This included not only simple practices, such as setting an agenda to provide a compass for the conversation, but also more nuanced practices like controlling the meeting but not the conversation.
After reading about leadership styles I also found myself analyzing the qualities and strategies of leaders I encountered and reflecting on their approach, noticing what I could possibly interlace in my own practice. Several of the leaders I spoke with during the elective recommended paying attention to the actions of the ineffective bosses or mentors because they can teach you something too: how not to act. I even started applying this strategy to the popular television series The Office – Michael Scott, the regional manager of a fictional paper company, demonstrates some of the best and worst leadership skills in every episode. I am developing a repertoire of strategies to lead and motivate people.
Finally, the design allows for real-time application of new methods to my current practice. One particularly useful tool I have learned is Leader Standard Work, a systematic method to get leaders to maintain stability, problem solve, and drive continuous improvement within their organization.5 I have used elements of Leader Standard Work on a personal level to improve my time management skills and increase my productivity. For example, I reconceptualized my calendar as a standardized checklist and I organized it to allot more time to critical activities, such as my research and scholarly output, and less on administrative tasks. I am also implementing changes to how I prepare and run meetings, collaborate, and communicate with members of my research team.
Mastery requires practice and feedback, so applying concepts even on a small, personal scale shortly after learning them has been very valuable. Over the last several months I have often wished I had this type of structured leadership education during my year as a chief resident. I think I could have been more intentional in my decision-making, possibly being a stronger leader for the program. Now that I am transferring skills into practice right away, I am setting the stage for lasting changes in behavior that will hopefully benefit all those that I work with in the future.
Leadership development through a customizable longitudinal elective may be an effective way to prepare PHM fellow graduates for future leadership positions. Fellows can emerge with the skills and real-world practice to allow them to feel confident in future positions. However, leadership doesn’t end when we get the position. We must remember to continuously ask for feedback and build upon our experiences to evolve as leaders in PHM.
Dr. Westphal is a first-year pediatric hospital medicine fellow at Nationwide Children’s Hospital in Columbus, Ohio with an interest in improving the delivery of quality care for hospitalized infants.
References
1. Maniscalco, J, et al. The Pediatric Hospital Medicine Core Competencies: 2020 Revision. Introduction and Methodology (C). J Hosp Med. 2020;S1;E12-E17. doi: 10.12788/jhm.3391.
2. Jerardi KE, et al; Council of Pediatric Hospital Medicine Fellowship Directors. Development of a Curricular Framework for Pediatric Hospital Medicine Fellowships. Pediatrics. 2017 Jul;140(1):e20170698. doi: 10.1542/peds.2017-0698.
3. ACGME Program Requirements for Graduate Medical Education in Pediatric Hospital Medicine. 2020 Edition. Accessed 2021 Jan 14.
4. Oshimura, JM et al. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-7. doi: 10.1542/hpeds.2016-0031.
5. Murli, J. Standard Work for Lean Leaders: One of the Keys to Sustaining Performance Gains. Lean Institute Enterprise, Lean Institute Enterprise Inc. 4 Dec 2013. www.lean.org/common/display/?o=2493
Reflecting on a longitudinal leadership elective experience
Reflecting on a longitudinal leadership elective experience
The practice of pediatric hospital medicine (PHM) has been evolving and rapidly expanding over the last several decades. Not only has the scope of clinical practice matured and become more defined, but hospitalists now also have the responsibility to advance the performance of hospitals and health care systems. Pediatric hospitalists are increasingly incorporating medical education, research, high-value care, patient quality and safety initiatives, and process improvement into their careers.1 As a result, pediatric hospitalists are occupying a wider range of administrative and leadership positions within the health care system.
The field of PHM has highlighted the importance of leadership in the practice of hospital medicine by dedicating a chapter to “Leadership in Healthcare” in the PHM Core Competencies.1 The competencies define the expertise required of hospitalists and serve as guidance for the development of education, training, and career development series. Hospitalists may seek out opportunities for leadership training at an institutional or national level. Options may include advanced degrees, national conferences, division training seminars, or self-directed learning through reading or observational experiences. Unfortunately, all of these take time and motivation. As a result, hospitalists tend to pursue these opportunities only after they have already been appointed to leadership positions.
PHM fellowship is the optimal time to build a foundation of leadership skills. Over the course of a 2-year fellowship, fellows have a combined 16 weeks dedicated to educational activities beyond direct patient care.2 The Accreditation Council for Graduate Medical Education (ACGME) encourages educational innovation during this time, allowing programs to create unique opportunities for their fellows that will promote progress towards their ultimate career goals.3 This curricular framework provides the flexibility to integrate leadership training into fellowship training.
Many fellows are eager for leadership experiences and mentorship, myself included. As a pediatric chief resident, I was immersed in a diverse range of clinical, educational, research, and administrative responsibilities. I found myself in a leadership position with no prior education on how to manage people or team dynamics, make high-stress decisions on behalf of a group of people, or handle conflict. Although I learned new strategies on a daily basis, the experience showed me how much more I still had to learn in order to be a successful leader. This was one of the reasons I decided to pursue fellowship training. I think many PHM fellowship applicants feel similarly. They may have served in a leadership position in the past but feel underprepared to fulfill leadership positions in the next phase of their careers.
But despite this eagerness, evidence suggests that fellows do not feel that they receive as much management training as they need to start their careers. In a 2014 survey of PHM fellowship graduates, many held formal leadership positions within their institution (23/51) and within national organizations (6/51), despite having only five years of hospitalist experience on average (including time spent in fellowship). When asked about training needs, respondents identified “hospital program management” as an area where they wished they received more training during fellowship.4
Anyone who has gone through the PHM fellowship interview process can tell you that a common refrain of program directors is, “One of the goals of our program is to create future leaders in PHM.” This led me to wonder: how do fellowship programs prepare their fellows for future leadership positions?
I began my fellowship training at Nationwide Children’s Hospital in the summer of 2020. The program had just designed a longitudinal leadership elective, which the second-year fellow and I decided to pilot together. As I reflected on the first half of this academic year, I realized that it is unique experiences like this elective that make me thankful I pursued fellowship. I want to share with the hospitalist community the structure of the elective and why it has been particularly valuable with the hope that it will inspire similar opportunities for other fellows.
The program is semi-structured but allows the fellow and preceptors the flexibility to decide what activities would benefit that particular fellow. We attend a variety of administrative and committee meetings with each preceptor that expose us to the responsibilities of their positions, their leadership style in action, their approach to crisis management, and differences in divisional operations. On a monthly basis we meet with a preceptor to discuss a topic related to leadership. Examples of topics include how to run a more effective meeting, barriers to organizational change, leading in crisis, and the importance of mission, vision, values, and goals of organizations. The preceptor sends us articles or other learning materials they have found useful on the topic, and these serve as a starting point for our discussions. These discussions provide a point of reflection as we apply the day’s concept to our own prior experiences or to our observations during the elective.
The combination of learning experiences, discussions, and dedicated preceptorship has prepared me far better for future leadership than my past personal and observational experiences. I have summarized my top three reasons why this structure of leadership development is particularly valuable to me as a fellow.
First, the longitudinal structure of the elective allows us to learn from multiple preceptors over the course of the academic year. The preceptors include the current chief of hospital pediatrics at Nationwide Children’s Hospital; the division director of hospital medicine at the Ohio State University Wexner Medical Center; and the physician lead for hospital medicine at one of the satellite hospitals in the region. With faculty from the Department of Pediatrics and the Department of Internal Medicine-Pediatrics in these leadership positions, we have the unique ability to compare and contrast operational systems between the two different hospital systems.
Recently, we also had the opportunity to meet with both the chairman of the department of pediatrics and chief medical officer. All of these physician leaders hold a variety of administrative roles and have differing leadership philosophies, each providing useful insights. For instance, one leader ensures his team holds him accountable as the leader by always asking for honest feedback. He recommends telling those you work with to “never let me fail.” Another leader acknowledges that creating five-year plans can be daunting but encouraged us to still be intentional with our direction on a smaller scale by writing down goals for the year and sharing with a mentor. Ultimately, I came away with a wide variety of perspectives to reference as I go forward.
Second, the learning is contextualized. I can take concepts that I learn through reading and discussions and construct meaning based on observations from meetings or other encounters with different leaders. For example, after reviewing several articles on strategies to make meetings more effective, I started noticing what went well and what didn’t go well in every meeting I attended. I observed preceptors employing many of the strategies successfully with positive feedback. This included not only simple practices, such as setting an agenda to provide a compass for the conversation, but also more nuanced practices like controlling the meeting but not the conversation.
After reading about leadership styles I also found myself analyzing the qualities and strategies of leaders I encountered and reflecting on their approach, noticing what I could possibly interlace in my own practice. Several of the leaders I spoke with during the elective recommended paying attention to the actions of the ineffective bosses or mentors because they can teach you something too: how not to act. I even started applying this strategy to the popular television series The Office – Michael Scott, the regional manager of a fictional paper company, demonstrates some of the best and worst leadership skills in every episode. I am developing a repertoire of strategies to lead and motivate people.
Finally, the design allows for real-time application of new methods to my current practice. One particularly useful tool I have learned is Leader Standard Work, a systematic method to get leaders to maintain stability, problem solve, and drive continuous improvement within their organization.5 I have used elements of Leader Standard Work on a personal level to improve my time management skills and increase my productivity. For example, I reconceptualized my calendar as a standardized checklist and I organized it to allot more time to critical activities, such as my research and scholarly output, and less on administrative tasks. I am also implementing changes to how I prepare and run meetings, collaborate, and communicate with members of my research team.
Mastery requires practice and feedback, so applying concepts even on a small, personal scale shortly after learning them has been very valuable. Over the last several months I have often wished I had this type of structured leadership education during my year as a chief resident. I think I could have been more intentional in my decision-making, possibly being a stronger leader for the program. Now that I am transferring skills into practice right away, I am setting the stage for lasting changes in behavior that will hopefully benefit all those that I work with in the future.
Leadership development through a customizable longitudinal elective may be an effective way to prepare PHM fellow graduates for future leadership positions. Fellows can emerge with the skills and real-world practice to allow them to feel confident in future positions. However, leadership doesn’t end when we get the position. We must remember to continuously ask for feedback and build upon our experiences to evolve as leaders in PHM.
Dr. Westphal is a first-year pediatric hospital medicine fellow at Nationwide Children’s Hospital in Columbus, Ohio with an interest in improving the delivery of quality care for hospitalized infants.
References
1. Maniscalco, J, et al. The Pediatric Hospital Medicine Core Competencies: 2020 Revision. Introduction and Methodology (C). J Hosp Med. 2020;S1;E12-E17. doi: 10.12788/jhm.3391.
2. Jerardi KE, et al; Council of Pediatric Hospital Medicine Fellowship Directors. Development of a Curricular Framework for Pediatric Hospital Medicine Fellowships. Pediatrics. 2017 Jul;140(1):e20170698. doi: 10.1542/peds.2017-0698.
3. ACGME Program Requirements for Graduate Medical Education in Pediatric Hospital Medicine. 2020 Edition. Accessed 2021 Jan 14.
4. Oshimura, JM et al. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-7. doi: 10.1542/hpeds.2016-0031.
5. Murli, J. Standard Work for Lean Leaders: One of the Keys to Sustaining Performance Gains. Lean Institute Enterprise, Lean Institute Enterprise Inc. 4 Dec 2013. www.lean.org/common/display/?o=2493
The practice of pediatric hospital medicine (PHM) has been evolving and rapidly expanding over the last several decades. Not only has the scope of clinical practice matured and become more defined, but hospitalists now also have the responsibility to advance the performance of hospitals and health care systems. Pediatric hospitalists are increasingly incorporating medical education, research, high-value care, patient quality and safety initiatives, and process improvement into their careers.1 As a result, pediatric hospitalists are occupying a wider range of administrative and leadership positions within the health care system.
The field of PHM has highlighted the importance of leadership in the practice of hospital medicine by dedicating a chapter to “Leadership in Healthcare” in the PHM Core Competencies.1 The competencies define the expertise required of hospitalists and serve as guidance for the development of education, training, and career development series. Hospitalists may seek out opportunities for leadership training at an institutional or national level. Options may include advanced degrees, national conferences, division training seminars, or self-directed learning through reading or observational experiences. Unfortunately, all of these take time and motivation. As a result, hospitalists tend to pursue these opportunities only after they have already been appointed to leadership positions.
PHM fellowship is the optimal time to build a foundation of leadership skills. Over the course of a 2-year fellowship, fellows have a combined 16 weeks dedicated to educational activities beyond direct patient care.2 The Accreditation Council for Graduate Medical Education (ACGME) encourages educational innovation during this time, allowing programs to create unique opportunities for their fellows that will promote progress towards their ultimate career goals.3 This curricular framework provides the flexibility to integrate leadership training into fellowship training.
Many fellows are eager for leadership experiences and mentorship, myself included. As a pediatric chief resident, I was immersed in a diverse range of clinical, educational, research, and administrative responsibilities. I found myself in a leadership position with no prior education on how to manage people or team dynamics, make high-stress decisions on behalf of a group of people, or handle conflict. Although I learned new strategies on a daily basis, the experience showed me how much more I still had to learn in order to be a successful leader. This was one of the reasons I decided to pursue fellowship training. I think many PHM fellowship applicants feel similarly. They may have served in a leadership position in the past but feel underprepared to fulfill leadership positions in the next phase of their careers.
But despite this eagerness, evidence suggests that fellows do not feel that they receive as much management training as they need to start their careers. In a 2014 survey of PHM fellowship graduates, many held formal leadership positions within their institution (23/51) and within national organizations (6/51), despite having only five years of hospitalist experience on average (including time spent in fellowship). When asked about training needs, respondents identified “hospital program management” as an area where they wished they received more training during fellowship.4
Anyone who has gone through the PHM fellowship interview process can tell you that a common refrain of program directors is, “One of the goals of our program is to create future leaders in PHM.” This led me to wonder: how do fellowship programs prepare their fellows for future leadership positions?
I began my fellowship training at Nationwide Children’s Hospital in the summer of 2020. The program had just designed a longitudinal leadership elective, which the second-year fellow and I decided to pilot together. As I reflected on the first half of this academic year, I realized that it is unique experiences like this elective that make me thankful I pursued fellowship. I want to share with the hospitalist community the structure of the elective and why it has been particularly valuable with the hope that it will inspire similar opportunities for other fellows.
The program is semi-structured but allows the fellow and preceptors the flexibility to decide what activities would benefit that particular fellow. We attend a variety of administrative and committee meetings with each preceptor that expose us to the responsibilities of their positions, their leadership style in action, their approach to crisis management, and differences in divisional operations. On a monthly basis we meet with a preceptor to discuss a topic related to leadership. Examples of topics include how to run a more effective meeting, barriers to organizational change, leading in crisis, and the importance of mission, vision, values, and goals of organizations. The preceptor sends us articles or other learning materials they have found useful on the topic, and these serve as a starting point for our discussions. These discussions provide a point of reflection as we apply the day’s concept to our own prior experiences or to our observations during the elective.
The combination of learning experiences, discussions, and dedicated preceptorship has prepared me far better for future leadership than my past personal and observational experiences. I have summarized my top three reasons why this structure of leadership development is particularly valuable to me as a fellow.
First, the longitudinal structure of the elective allows us to learn from multiple preceptors over the course of the academic year. The preceptors include the current chief of hospital pediatrics at Nationwide Children’s Hospital; the division director of hospital medicine at the Ohio State University Wexner Medical Center; and the physician lead for hospital medicine at one of the satellite hospitals in the region. With faculty from the Department of Pediatrics and the Department of Internal Medicine-Pediatrics in these leadership positions, we have the unique ability to compare and contrast operational systems between the two different hospital systems.
Recently, we also had the opportunity to meet with both the chairman of the department of pediatrics and chief medical officer. All of these physician leaders hold a variety of administrative roles and have differing leadership philosophies, each providing useful insights. For instance, one leader ensures his team holds him accountable as the leader by always asking for honest feedback. He recommends telling those you work with to “never let me fail.” Another leader acknowledges that creating five-year plans can be daunting but encouraged us to still be intentional with our direction on a smaller scale by writing down goals for the year and sharing with a mentor. Ultimately, I came away with a wide variety of perspectives to reference as I go forward.
Second, the learning is contextualized. I can take concepts that I learn through reading and discussions and construct meaning based on observations from meetings or other encounters with different leaders. For example, after reviewing several articles on strategies to make meetings more effective, I started noticing what went well and what didn’t go well in every meeting I attended. I observed preceptors employing many of the strategies successfully with positive feedback. This included not only simple practices, such as setting an agenda to provide a compass for the conversation, but also more nuanced practices like controlling the meeting but not the conversation.
After reading about leadership styles I also found myself analyzing the qualities and strategies of leaders I encountered and reflecting on their approach, noticing what I could possibly interlace in my own practice. Several of the leaders I spoke with during the elective recommended paying attention to the actions of the ineffective bosses or mentors because they can teach you something too: how not to act. I even started applying this strategy to the popular television series The Office – Michael Scott, the regional manager of a fictional paper company, demonstrates some of the best and worst leadership skills in every episode. I am developing a repertoire of strategies to lead and motivate people.
Finally, the design allows for real-time application of new methods to my current practice. One particularly useful tool I have learned is Leader Standard Work, a systematic method to get leaders to maintain stability, problem solve, and drive continuous improvement within their organization.5 I have used elements of Leader Standard Work on a personal level to improve my time management skills and increase my productivity. For example, I reconceptualized my calendar as a standardized checklist and I organized it to allot more time to critical activities, such as my research and scholarly output, and less on administrative tasks. I am also implementing changes to how I prepare and run meetings, collaborate, and communicate with members of my research team.
Mastery requires practice and feedback, so applying concepts even on a small, personal scale shortly after learning them has been very valuable. Over the last several months I have often wished I had this type of structured leadership education during my year as a chief resident. I think I could have been more intentional in my decision-making, possibly being a stronger leader for the program. Now that I am transferring skills into practice right away, I am setting the stage for lasting changes in behavior that will hopefully benefit all those that I work with in the future.
Leadership development through a customizable longitudinal elective may be an effective way to prepare PHM fellow graduates for future leadership positions. Fellows can emerge with the skills and real-world practice to allow them to feel confident in future positions. However, leadership doesn’t end when we get the position. We must remember to continuously ask for feedback and build upon our experiences to evolve as leaders in PHM.
Dr. Westphal is a first-year pediatric hospital medicine fellow at Nationwide Children’s Hospital in Columbus, Ohio with an interest in improving the delivery of quality care for hospitalized infants.
References
1. Maniscalco, J, et al. The Pediatric Hospital Medicine Core Competencies: 2020 Revision. Introduction and Methodology (C). J Hosp Med. 2020;S1;E12-E17. doi: 10.12788/jhm.3391.
2. Jerardi KE, et al; Council of Pediatric Hospital Medicine Fellowship Directors. Development of a Curricular Framework for Pediatric Hospital Medicine Fellowships. Pediatrics. 2017 Jul;140(1):e20170698. doi: 10.1542/peds.2017-0698.
3. ACGME Program Requirements for Graduate Medical Education in Pediatric Hospital Medicine. 2020 Edition. Accessed 2021 Jan 14.
4. Oshimura, JM et al. Current roles and perceived needs of pediatric hospital medicine fellowship graduates. Hosp Pediatr. 2016;6(10):633-7. doi: 10.1542/hpeds.2016-0031.
5. Murli, J. Standard Work for Lean Leaders: One of the Keys to Sustaining Performance Gains. Lean Institute Enterprise, Lean Institute Enterprise Inc. 4 Dec 2013. www.lean.org/common/display/?o=2493
Hospital medicine leaders offer tips for gender equity
When Marisha Burden, MD, division head of hospital medicine at the University of Colorado at Denver, Aurora, would go to medical conferences, it seemed as if very few women were giving talks. She wondered if she could be wrong.
“I started doing my own assessments at every conference I would go to, just to make sure I wasn’t biased in my own belief system,” she said in a session at SHM Converge 2021, the annual conference of the Society of Hospital Medicine.
She wasn’t wrong.
In 2015, only 35% of all speakers at the SHM annual conference were women, and only 23% of the plenary speakers were women. In the years after that, when the society put out open calls for speakers, the numbers of women who spoke increased substantially, to 47% overall and 45% of plenary speakers.
The results – part of the SPEAK UP study Dr. Burden led in 2020 – show how gender disparity can be improved with a systematic process that is designed to improve it. The results of the study also showed that as the percentages of female speakers increased, the attendee ratings of the sessions did, too.
“You can do these things, and the quality of your conference doesn’t get negatively impacted – and in this case, actually improved,” Dr. Burden said.
That study marked progress toward leveling a traditionally uneven playing field when it comes to men and women in medicine, and the panelists in the session called on the field to use a variety of tools and strategies to continue toward something closer to equality.
Sara Spilseth, MD, MBA, chief of staff at Regions Hospital, in St. Paul, Minn., said it’s well established that although almost 50% of medical school students are women, the percentage shrinks each step from faculty to full professor to dean – of which only 16% are women. She referred to what’s known as the “leaky pipe.”
In what Dr. Spilseth said was one of her favorite studies, researchers in 2015 found that only 13% of clinical department leaders at the top 50 U.S. medical schools were women – they were outnumbered by the percentage of department leaders with mustaches, at 19%, even though mustaches are dwindling in popularity.
“Why does this exist? Why did we end up like this?” Part of the problem is a “respect gap,” she said, pointing to a study on the tendency of women to use the formal title of “doctor” when introducing male colleagues, whereas men who introduce women use that title less than half the time.
The COVID-19 pandemic has only made these disparities worse. Women are responsible for childcare much more frequently than men, Dr. Burden said, although the pandemic has brought caregiving duties to the forefront.
Dr. Spilseth said mentoring can help women navigate the workplace so as to help overcome these disparities. At Regions, the mentoring program is robust.
“Even before a new hire steps foot in the hospital, we have established them with a mentor,” she said. Sponsoring – the “ability of someone with political capital to use it to help colleagues” – can also help boost women’s careers, she said.
Her hospital also has a Women in Medicine Cooperative, which provides a way for women to talk about common struggles and to network.
Flexible work opportunities – working in transitional care units, being a physician advisor, and doing research – can all help boost a career as well, Dr. Spilseth said.
She said that at the University of Colorado, leaders set out to reach salary equity in a year and a half – and “it was a painful, painful process.” They found that different people held different beliefs about how people were paid, which led to a lot of unnecessary stress as they tried to construct a fairer system.
“On the back end of having done that, while it was a rough year and half, it has saved so much time – and I think built a culture of trust and transparency,” she said.
Recruiting in a more thoughtful way can also have a big impact, Dr. Spilseth said. The manner in which people are told about opportunities could exclude people without intending to.
“Are you casting a wide net?” she asked.
Adia Ross, MD, MHA, chief medical officer at Duke Regional Hospital, Durham, N.C., said that even in the face of obvious disparities, women can take steps on their own to boost their careers. She encouraged taking on “stretch assignments,” a project or task that is a bit beyond one’s current comfort level or level of experience or knowledge. “It can be a little scary, and sometimes there are bumps along the way,” she said.
All of these measures, though incremental, are the way to make bigger change, she said. “We want to take small steps but big strides forward.”
A version of this article first appeared on Medscape.com.
When Marisha Burden, MD, division head of hospital medicine at the University of Colorado at Denver, Aurora, would go to medical conferences, it seemed as if very few women were giving talks. She wondered if she could be wrong.
“I started doing my own assessments at every conference I would go to, just to make sure I wasn’t biased in my own belief system,” she said in a session at SHM Converge 2021, the annual conference of the Society of Hospital Medicine.
She wasn’t wrong.
In 2015, only 35% of all speakers at the SHM annual conference were women, and only 23% of the plenary speakers were women. In the years after that, when the society put out open calls for speakers, the numbers of women who spoke increased substantially, to 47% overall and 45% of plenary speakers.
The results – part of the SPEAK UP study Dr. Burden led in 2020 – show how gender disparity can be improved with a systematic process that is designed to improve it. The results of the study also showed that as the percentages of female speakers increased, the attendee ratings of the sessions did, too.
“You can do these things, and the quality of your conference doesn’t get negatively impacted – and in this case, actually improved,” Dr. Burden said.
That study marked progress toward leveling a traditionally uneven playing field when it comes to men and women in medicine, and the panelists in the session called on the field to use a variety of tools and strategies to continue toward something closer to equality.
Sara Spilseth, MD, MBA, chief of staff at Regions Hospital, in St. Paul, Minn., said it’s well established that although almost 50% of medical school students are women, the percentage shrinks each step from faculty to full professor to dean – of which only 16% are women. She referred to what’s known as the “leaky pipe.”
In what Dr. Spilseth said was one of her favorite studies, researchers in 2015 found that only 13% of clinical department leaders at the top 50 U.S. medical schools were women – they were outnumbered by the percentage of department leaders with mustaches, at 19%, even though mustaches are dwindling in popularity.
“Why does this exist? Why did we end up like this?” Part of the problem is a “respect gap,” she said, pointing to a study on the tendency of women to use the formal title of “doctor” when introducing male colleagues, whereas men who introduce women use that title less than half the time.
The COVID-19 pandemic has only made these disparities worse. Women are responsible for childcare much more frequently than men, Dr. Burden said, although the pandemic has brought caregiving duties to the forefront.
Dr. Spilseth said mentoring can help women navigate the workplace so as to help overcome these disparities. At Regions, the mentoring program is robust.
“Even before a new hire steps foot in the hospital, we have established them with a mentor,” she said. Sponsoring – the “ability of someone with political capital to use it to help colleagues” – can also help boost women’s careers, she said.
Her hospital also has a Women in Medicine Cooperative, which provides a way for women to talk about common struggles and to network.
Flexible work opportunities – working in transitional care units, being a physician advisor, and doing research – can all help boost a career as well, Dr. Spilseth said.
She said that at the University of Colorado, leaders set out to reach salary equity in a year and a half – and “it was a painful, painful process.” They found that different people held different beliefs about how people were paid, which led to a lot of unnecessary stress as they tried to construct a fairer system.
“On the back end of having done that, while it was a rough year and half, it has saved so much time – and I think built a culture of trust and transparency,” she said.
Recruiting in a more thoughtful way can also have a big impact, Dr. Spilseth said. The manner in which people are told about opportunities could exclude people without intending to.
“Are you casting a wide net?” she asked.
Adia Ross, MD, MHA, chief medical officer at Duke Regional Hospital, Durham, N.C., said that even in the face of obvious disparities, women can take steps on their own to boost their careers. She encouraged taking on “stretch assignments,” a project or task that is a bit beyond one’s current comfort level or level of experience or knowledge. “It can be a little scary, and sometimes there are bumps along the way,” she said.
All of these measures, though incremental, are the way to make bigger change, she said. “We want to take small steps but big strides forward.”
A version of this article first appeared on Medscape.com.
When Marisha Burden, MD, division head of hospital medicine at the University of Colorado at Denver, Aurora, would go to medical conferences, it seemed as if very few women were giving talks. She wondered if she could be wrong.
“I started doing my own assessments at every conference I would go to, just to make sure I wasn’t biased in my own belief system,” she said in a session at SHM Converge 2021, the annual conference of the Society of Hospital Medicine.
She wasn’t wrong.
In 2015, only 35% of all speakers at the SHM annual conference were women, and only 23% of the plenary speakers were women. In the years after that, when the society put out open calls for speakers, the numbers of women who spoke increased substantially, to 47% overall and 45% of plenary speakers.
The results – part of the SPEAK UP study Dr. Burden led in 2020 – show how gender disparity can be improved with a systematic process that is designed to improve it. The results of the study also showed that as the percentages of female speakers increased, the attendee ratings of the sessions did, too.
“You can do these things, and the quality of your conference doesn’t get negatively impacted – and in this case, actually improved,” Dr. Burden said.
That study marked progress toward leveling a traditionally uneven playing field when it comes to men and women in medicine, and the panelists in the session called on the field to use a variety of tools and strategies to continue toward something closer to equality.
Sara Spilseth, MD, MBA, chief of staff at Regions Hospital, in St. Paul, Minn., said it’s well established that although almost 50% of medical school students are women, the percentage shrinks each step from faculty to full professor to dean – of which only 16% are women. She referred to what’s known as the “leaky pipe.”
In what Dr. Spilseth said was one of her favorite studies, researchers in 2015 found that only 13% of clinical department leaders at the top 50 U.S. medical schools were women – they were outnumbered by the percentage of department leaders with mustaches, at 19%, even though mustaches are dwindling in popularity.
“Why does this exist? Why did we end up like this?” Part of the problem is a “respect gap,” she said, pointing to a study on the tendency of women to use the formal title of “doctor” when introducing male colleagues, whereas men who introduce women use that title less than half the time.
The COVID-19 pandemic has only made these disparities worse. Women are responsible for childcare much more frequently than men, Dr. Burden said, although the pandemic has brought caregiving duties to the forefront.
Dr. Spilseth said mentoring can help women navigate the workplace so as to help overcome these disparities. At Regions, the mentoring program is robust.
“Even before a new hire steps foot in the hospital, we have established them with a mentor,” she said. Sponsoring – the “ability of someone with political capital to use it to help colleagues” – can also help boost women’s careers, she said.
Her hospital also has a Women in Medicine Cooperative, which provides a way for women to talk about common struggles and to network.
Flexible work opportunities – working in transitional care units, being a physician advisor, and doing research – can all help boost a career as well, Dr. Spilseth said.
She said that at the University of Colorado, leaders set out to reach salary equity in a year and a half – and “it was a painful, painful process.” They found that different people held different beliefs about how people were paid, which led to a lot of unnecessary stress as they tried to construct a fairer system.
“On the back end of having done that, while it was a rough year and half, it has saved so much time – and I think built a culture of trust and transparency,” she said.
Recruiting in a more thoughtful way can also have a big impact, Dr. Spilseth said. The manner in which people are told about opportunities could exclude people without intending to.
“Are you casting a wide net?” she asked.
Adia Ross, MD, MHA, chief medical officer at Duke Regional Hospital, Durham, N.C., said that even in the face of obvious disparities, women can take steps on their own to boost their careers. She encouraged taking on “stretch assignments,” a project or task that is a bit beyond one’s current comfort level or level of experience or knowledge. “It can be a little scary, and sometimes there are bumps along the way,” she said.
All of these measures, though incremental, are the way to make bigger change, she said. “We want to take small steps but big strides forward.”
A version of this article first appeared on Medscape.com.
FROM SHM CONVERGE 2021
Visa worries intensify pandemic stress for immigrant hospitalist moms
The COVID-19 pandemic has been difficult for all hospitalists, especially those who are parents of young children. For hospitalist moms who are also immigrants working on temporary H1-B visas, this stress is exacerbated. Though each story is unique, the underlying themes are the same: Worries over visa renewals, the immigration process, family members back home, and the risk of illness, job loss, and deportation.
Supporting the family
Like all health care workers, Prasanna Palabindela, MD, a hospitalist at Jennie Stuart Health in Hopkinsville, Ky., has been worried about bringing COVID-19 home to her family, especially in the beginning. Her in-laws had just arrived from India for a visit in March 2020 when the pandemic began, everything was shut down, and her in-laws were forced to settle in for an unexpected months-long stay.
Along with her elderly in-laws, who also have chronic conditions, Dr. Palabindela had two small children to worry about – a then-5-month-old daughter and a 5-year-old son. “I was more worried about them than me,” she said. “I used to take showers before coming home and just do all precautions as much as I can. I’m glad that I did not bring COVID, so far, to the family.”
Once she could safely send her in-laws back to India, Dr. Palabindela began searching for a nanny. Daycare was out of the question because she didn’t want her children to be exposed to illness. After a long search, she found a nanny who could also help her son with virtual school. “It’s expensive, but still, my family and my family’s health is my priority,” she said.
Working on visas has caused multiple issues for Dr. Palabindela and her husband. After living in different states because of their jobs, her husband joined her in West Virginia for her residency and found a job there. When Dr. Palabindela took her current position, her husband had to quit his job in West Virginia and move with her to Kentucky for them to stay together. Unfortunately, he couldn’t find a good fit for work in Kentucky, so the couple decided to put him on her visa so they wouldn’t have to live apart.
Now Dr. Palabindela is the family’s sole breadwinner. “That means if something happens to me, I always worry what’s going to happen with my family because legally, my husband cannot work. Technically, everyone is deported back to home,” she said. Not being able to work is hard for her husband too. “It’s just so much stress in the family because he worked for 11 years,” said Dr. Palabindela.
Through all the upheavals, Dr. Palabindela has had support from all sides. Her husband has been the biggest source. “He’s my backbone. Every time, he supported me in each and every aspect,” she said. Her parents and her brothers check in on her constantly to make sure she’s staying safe. Even the chief at her hospital has played a significant role, going to bat for his physicians to ensure their safety.
Dr. Palabindela credits everyone who works with COVID-19 patients as heroes. “The nurses, the physicians, the housekeeping, respiratory therapist, speech therapist, physical therapy ... everybody has a role. Everybody is a hero,” she said. “Whoever is wearing a mask is a hero, too, because they are contributing to this community.”
Advocating for immigration reform
A lack of transparency and information in the beginning of the pandemic significantly contributed to anxiety, said Anuradha Amara, MD, MBBS, a hospitalist in Wilmington, Del. She felt that what was on the news and what was actually going on in the hospitals were quite different. Colleagues were getting sick, there wasn’t enough personal protective equipment, and planning went out the window. “It’s like a meteor hitting a place and then we start dealing with the aftermath, but we weren’t ready before,” Dr. Amara said. “We didn’t have a plan for a pandemic.”
Then there was the concern of either her or her husband, a cardiologist, getting sick and potentially losing their jobs and immigration status. “How am I going to go back to my country if I had to? What will happen to my family if I die? If I go on the ventilator? Those are the insecurities we found additional to the pandemic challenges we had,” Dr. Amara said.
Not being able to go see their family in India or have them come visit was difficult – “it was pretty bad up there,” said Dr. Amara. Fortunately, her family members in India remained safe, but there’s a very real uneasiness about returning should an emergency arise. “Should I go back and then take the risk of losing my job and losing my position and my kids are here, they’re going to school here. How do you decide that?” she asked.
One of the worst effects of her visa restrictions was not being able to help in New York when hospitals were so short-staffed, and the morgues were overflowing. “New York is 3 hours away from where I live, but I was in chains. I couldn’t help them because of these visa restrictions,” Dr. Amara said. During the emergency, the state allowed physicians from other states to practice without being licensed in New York, but immigrant physicians were not included. “Even if we wanted to, we couldn’t volunteer,” said Dr. Amara. “I have family in New York, and I was really worried. Out of compassion I wanted to help, but I couldn’t do anything.”
Before the pandemic, Dr. Amara joined in advocacy efforts for immigrant physicians through Physicians for American Healthcare Access (PAHA). “In uncertain times, like COVID, it gets worse that you’re challenged with everything on top of your health, your family, and you have to be worried about deportation,” she said. “We need to strengthen legislation. Nobody should suffer with immigration processes during an active pandemic or otherwise.”
In the United States, 28% of physicians are immigrants. Dr. Amara pointed out that these physicians go through years of expensive training with extensive background checks at every level, yet they’re classified as second preference (EB-2) workers. She believes that physicians as a group should be excluded from this category and allowed to automatically become citizens after 5 years of living in the United States and working in an underserved area.
There have been an estimated 15,000 unused green cards since 2005. And if Congress went back to 1992, there could be more than 220,000 previously unused green cards recaptured. These unused green cards are the basis behind bills H.R.2255 and S.1024, the Healthcare Workforce Resiliency Act, which has been championed by SHM and PAHA. “It will allow the frontline physicians, 15,000 of them, and 25,000 nurses, to obtain their permanent residency,” said Dr. Amara. “These are people who already applied for their permanent residencies and they’re still waiting.”
SHM has consistently advocated for the Act since it was first introduced, written multiple letters on the issue, and supported it both on and off Capitol Hill. The society says the legislation would be an “important first step toward addressing a critical shortage” in the U.S. health care system by “recognizing the vital role immigrant physicians and nurses are playing in the fight against COVID-19.”
Currently, SHM has a live action alert open for the reintroduced bill, and encourages members to contact their legislators and urge them to support the reintroduction of the Act by cosponsoring and working to pass the legislation
Dr. Amara encourages physicians to start engaging in advocacy efforts early. Though she didn’t begin participating until late in her career, she said being aware of and part of policies that affect medicine is important. If more physicians get involved, “there are so many things we can take care of,” said Dr. Amara. “The medical profession doesn’t have to be so difficult and so busy. There are ways we can make it better and I believe that. And obviously I’ll continue to work and advocate for the entire medical profession, their problems, their health and well-being, to prevent burnout.”
Making time for positivity and self-care
Sandhya Tagaram, MD, a hospitalist at UMass Memorial Medical Center in Worcester, Mass., and her husband, also a hospitalist physician, had only ever read about pandemics in books. They certainly never expected to be in the middle of one. “That was a totally different level of anxiety to work as frontline physicians with two kids under 5 years and families away back home in India,” she said.
Dr. Tagaram and her husband work opposite shifts so that one of them is always home with their two young children. “Our schedules became more challenging when the pandemic started. Between both of our schedules and with minimal childcare facilities, we managed to strike a decent work-family balance, although we experience less vacation time together. We are fortunate to have an understanding work group,” said Dr. Tagaram.
Even before COVID-19, Dr. Tagaram found working on the temporary work visa challenging. “I think the pandemic has exposed the layer of uncertainty associated with it,” she said. “It’s incredibly stressful to imagine any minor turbulence that could alter our family and work lives. As a frontline physician mom, I take pride in raising my kids and taking care of my patients. We want to serve our communities and at the same time secure our families.”
Not being able to visit family back home and travel is exceedingly difficult. Dr. Tagaram said it would be helpful if there was a separate permanent residence pathway for physicians because they play a critical role in public health and they have been an integral part of the COVID-19 pandemic response team. A separate pathway could help keep their families secure and enable them to give their best to their communities.
Amid all the anxiety, Dr. Tagaram said she and her husband realized they could not keep living with so much pressure. As parents and as physicians, they did not want their stress to leak out and affect their ability and commitment to care for their children or their patients. They decided they needed to figure out how to be positive and constructive.
“We try some daily fun activities with the kids after returning home from work,” said Dr. Tagaram. They also formed a bubble group with two other physician families so the children could interact safely. She said that it’s critical that physicians take time for themselves. “We have to cultivate a serious hobby that helps to rejuvenate and calm our busy minds,” said Dr. Tagaram.
She makes time every day to exercise and to read at least a few pages from a good book. She is also learning Carnatic music along with one of her daughters. And every month since March 2020, she has journaled about her work and what she learned so her daughters can read it someday. “These things keep me jazzed up,” she said.
The pandemic has highlighted the fact that we are all part of one global community. “Although we hail from different backgrounds, we learned that we do have some common goals of being kind and supportive to each other and to give back to our communities. Hopefully we will continue this spirit,” said Dr. Tagaram. As a physician mother, “I feel it’s a privilege and honor to take care of my family and my community.”
Soldiering on in the COVID-19 war
The uncertainty everyone felt at the beginning of the pandemic was “very, very scary,” said Mamtha Balla, MD, MPH, a hospitalist and clinical assistant professor in northwest Ohio. “Initially, I was so involved in it and I felt like it was like a war, a COVID-19 war, and we are soldiers in that and trying to protect and do whatever we can.”
She and her husband, a geriatrician also working on an H-1B visa, have worked hard not to bring the virus home to their 2-year-old daughter. Going into 2021, the past 2 years have been “the most hectic and emotionally draining – and physically exhausting – years of my life,” said Dr. Balla.
The COVID-19 vaccine has helped reduce some pressure, but Dr. Balla is still concerned about the high risk to health care workers and the new COVID-19 strains coming out. “We are really not sure what we are dealing with and how the COVID will calm,” she said. “It is pretty challenging being a health care worker because not only are you responsible for your patients at the end of the day, but you are also responsible for your families.”
Initially in the United States from India on a student visa in 2008, Dr. Balla was placed on an H-1B visa when she started her residency. It was during this time that her mother was diagnosed with cancer and went through surgeries and chemotherapy. “She was pretty ill,” recalled Dr. Balla.
Despite the situation, Dr. Balla was afraid to go stay with her mother in case her visa application was rejected, and she couldn’t complete her third year of education. “I opted not to go to India at that time because I did not want to take a chance,” Dr. Balla said. “I have tears in my eyes because those are not easy moments, to withhold from seeing your parents, or to be in any other emergency where you cannot travel. That especially puts us at a higher risk emotionally and physically.”
She has not seen her parents in 2½ years. Between the very real possibility of not being able to get her visa stamp and the unpredictability of how other countries are dealing with COVID-19, Dr. Balla feels it is impossible to even think of going to visit. “Even if I go, what if something happens where my visa gets stuck, or the visa office is not open?” she said. If she could not get back to the United States as planned, she would have patients left behind here.
Recently, Dr. Balla did travel to India and her passport stamp did not come on time, so her husband had to come back to the United States by himself. She had to wait for her stamp for a couple more weeks before she could leave and, in the meantime, had to make arrangements at her hospital. “It is so much trauma,” she said.
There’s also the worry she has about getting sick or disabled and not being able to work anymore, resulting in deportation. “Is that what we are doing for people who are working like soldiers? Are we really treating them the correct way?” Dr. Balla asked.
Dr. Balla considers all health care workers to be soldiers in the COVID-19 war. As such, she believes the government should step up to make sure they are supporting and helping these immigrant physician-soldiers who are so necessary. She applauds France’s recent decision to grant citizenship to its frontline immigrant health care workers and feels that the same should be done in the United States. She filed her green card application in 2012, but she is nowhere close to getting it. (The backlog for employment-based green cards is more than 900,000 now.)
As people putting their own and their family’s lives at risk to care for patients with COVID-19, Dr. Balla and her husband have talked about moving to another country or even back to India. “I am a taxpayer; I am a good human being working for the community and for the job. This is my 13th year here. If I am not eligible [for citizenship] still, then I am not sure what else I have to do to prove myself,” she said. “I am owning United States citizens as my people, so please own us and help us out in this difficult scenario.”
The COVID-19 pandemic has been difficult for all hospitalists, especially those who are parents of young children. For hospitalist moms who are also immigrants working on temporary H1-B visas, this stress is exacerbated. Though each story is unique, the underlying themes are the same: Worries over visa renewals, the immigration process, family members back home, and the risk of illness, job loss, and deportation.
Supporting the family
Like all health care workers, Prasanna Palabindela, MD, a hospitalist at Jennie Stuart Health in Hopkinsville, Ky., has been worried about bringing COVID-19 home to her family, especially in the beginning. Her in-laws had just arrived from India for a visit in March 2020 when the pandemic began, everything was shut down, and her in-laws were forced to settle in for an unexpected months-long stay.
Along with her elderly in-laws, who also have chronic conditions, Dr. Palabindela had two small children to worry about – a then-5-month-old daughter and a 5-year-old son. “I was more worried about them than me,” she said. “I used to take showers before coming home and just do all precautions as much as I can. I’m glad that I did not bring COVID, so far, to the family.”
Once she could safely send her in-laws back to India, Dr. Palabindela began searching for a nanny. Daycare was out of the question because she didn’t want her children to be exposed to illness. After a long search, she found a nanny who could also help her son with virtual school. “It’s expensive, but still, my family and my family’s health is my priority,” she said.
Working on visas has caused multiple issues for Dr. Palabindela and her husband. After living in different states because of their jobs, her husband joined her in West Virginia for her residency and found a job there. When Dr. Palabindela took her current position, her husband had to quit his job in West Virginia and move with her to Kentucky for them to stay together. Unfortunately, he couldn’t find a good fit for work in Kentucky, so the couple decided to put him on her visa so they wouldn’t have to live apart.
Now Dr. Palabindela is the family’s sole breadwinner. “That means if something happens to me, I always worry what’s going to happen with my family because legally, my husband cannot work. Technically, everyone is deported back to home,” she said. Not being able to work is hard for her husband too. “It’s just so much stress in the family because he worked for 11 years,” said Dr. Palabindela.
Through all the upheavals, Dr. Palabindela has had support from all sides. Her husband has been the biggest source. “He’s my backbone. Every time, he supported me in each and every aspect,” she said. Her parents and her brothers check in on her constantly to make sure she’s staying safe. Even the chief at her hospital has played a significant role, going to bat for his physicians to ensure their safety.
Dr. Palabindela credits everyone who works with COVID-19 patients as heroes. “The nurses, the physicians, the housekeeping, respiratory therapist, speech therapist, physical therapy ... everybody has a role. Everybody is a hero,” she said. “Whoever is wearing a mask is a hero, too, because they are contributing to this community.”
Advocating for immigration reform
A lack of transparency and information in the beginning of the pandemic significantly contributed to anxiety, said Anuradha Amara, MD, MBBS, a hospitalist in Wilmington, Del. She felt that what was on the news and what was actually going on in the hospitals were quite different. Colleagues were getting sick, there wasn’t enough personal protective equipment, and planning went out the window. “It’s like a meteor hitting a place and then we start dealing with the aftermath, but we weren’t ready before,” Dr. Amara said. “We didn’t have a plan for a pandemic.”
Then there was the concern of either her or her husband, a cardiologist, getting sick and potentially losing their jobs and immigration status. “How am I going to go back to my country if I had to? What will happen to my family if I die? If I go on the ventilator? Those are the insecurities we found additional to the pandemic challenges we had,” Dr. Amara said.
Not being able to go see their family in India or have them come visit was difficult – “it was pretty bad up there,” said Dr. Amara. Fortunately, her family members in India remained safe, but there’s a very real uneasiness about returning should an emergency arise. “Should I go back and then take the risk of losing my job and losing my position and my kids are here, they’re going to school here. How do you decide that?” she asked.
One of the worst effects of her visa restrictions was not being able to help in New York when hospitals were so short-staffed, and the morgues were overflowing. “New York is 3 hours away from where I live, but I was in chains. I couldn’t help them because of these visa restrictions,” Dr. Amara said. During the emergency, the state allowed physicians from other states to practice without being licensed in New York, but immigrant physicians were not included. “Even if we wanted to, we couldn’t volunteer,” said Dr. Amara. “I have family in New York, and I was really worried. Out of compassion I wanted to help, but I couldn’t do anything.”
Before the pandemic, Dr. Amara joined in advocacy efforts for immigrant physicians through Physicians for American Healthcare Access (PAHA). “In uncertain times, like COVID, it gets worse that you’re challenged with everything on top of your health, your family, and you have to be worried about deportation,” she said. “We need to strengthen legislation. Nobody should suffer with immigration processes during an active pandemic or otherwise.”
In the United States, 28% of physicians are immigrants. Dr. Amara pointed out that these physicians go through years of expensive training with extensive background checks at every level, yet they’re classified as second preference (EB-2) workers. She believes that physicians as a group should be excluded from this category and allowed to automatically become citizens after 5 years of living in the United States and working in an underserved area.
There have been an estimated 15,000 unused green cards since 2005. And if Congress went back to 1992, there could be more than 220,000 previously unused green cards recaptured. These unused green cards are the basis behind bills H.R.2255 and S.1024, the Healthcare Workforce Resiliency Act, which has been championed by SHM and PAHA. “It will allow the frontline physicians, 15,000 of them, and 25,000 nurses, to obtain their permanent residency,” said Dr. Amara. “These are people who already applied for their permanent residencies and they’re still waiting.”
SHM has consistently advocated for the Act since it was first introduced, written multiple letters on the issue, and supported it both on and off Capitol Hill. The society says the legislation would be an “important first step toward addressing a critical shortage” in the U.S. health care system by “recognizing the vital role immigrant physicians and nurses are playing in the fight against COVID-19.”
Currently, SHM has a live action alert open for the reintroduced bill, and encourages members to contact their legislators and urge them to support the reintroduction of the Act by cosponsoring and working to pass the legislation
Dr. Amara encourages physicians to start engaging in advocacy efforts early. Though she didn’t begin participating until late in her career, she said being aware of and part of policies that affect medicine is important. If more physicians get involved, “there are so many things we can take care of,” said Dr. Amara. “The medical profession doesn’t have to be so difficult and so busy. There are ways we can make it better and I believe that. And obviously I’ll continue to work and advocate for the entire medical profession, their problems, their health and well-being, to prevent burnout.”
Making time for positivity and self-care
Sandhya Tagaram, MD, a hospitalist at UMass Memorial Medical Center in Worcester, Mass., and her husband, also a hospitalist physician, had only ever read about pandemics in books. They certainly never expected to be in the middle of one. “That was a totally different level of anxiety to work as frontline physicians with two kids under 5 years and families away back home in India,” she said.
Dr. Tagaram and her husband work opposite shifts so that one of them is always home with their two young children. “Our schedules became more challenging when the pandemic started. Between both of our schedules and with minimal childcare facilities, we managed to strike a decent work-family balance, although we experience less vacation time together. We are fortunate to have an understanding work group,” said Dr. Tagaram.
Even before COVID-19, Dr. Tagaram found working on the temporary work visa challenging. “I think the pandemic has exposed the layer of uncertainty associated with it,” she said. “It’s incredibly stressful to imagine any minor turbulence that could alter our family and work lives. As a frontline physician mom, I take pride in raising my kids and taking care of my patients. We want to serve our communities and at the same time secure our families.”
Not being able to visit family back home and travel is exceedingly difficult. Dr. Tagaram said it would be helpful if there was a separate permanent residence pathway for physicians because they play a critical role in public health and they have been an integral part of the COVID-19 pandemic response team. A separate pathway could help keep their families secure and enable them to give their best to their communities.
Amid all the anxiety, Dr. Tagaram said she and her husband realized they could not keep living with so much pressure. As parents and as physicians, they did not want their stress to leak out and affect their ability and commitment to care for their children or their patients. They decided they needed to figure out how to be positive and constructive.
“We try some daily fun activities with the kids after returning home from work,” said Dr. Tagaram. They also formed a bubble group with two other physician families so the children could interact safely. She said that it’s critical that physicians take time for themselves. “We have to cultivate a serious hobby that helps to rejuvenate and calm our busy minds,” said Dr. Tagaram.
She makes time every day to exercise and to read at least a few pages from a good book. She is also learning Carnatic music along with one of her daughters. And every month since March 2020, she has journaled about her work and what she learned so her daughters can read it someday. “These things keep me jazzed up,” she said.
The pandemic has highlighted the fact that we are all part of one global community. “Although we hail from different backgrounds, we learned that we do have some common goals of being kind and supportive to each other and to give back to our communities. Hopefully we will continue this spirit,” said Dr. Tagaram. As a physician mother, “I feel it’s a privilege and honor to take care of my family and my community.”
Soldiering on in the COVID-19 war
The uncertainty everyone felt at the beginning of the pandemic was “very, very scary,” said Mamtha Balla, MD, MPH, a hospitalist and clinical assistant professor in northwest Ohio. “Initially, I was so involved in it and I felt like it was like a war, a COVID-19 war, and we are soldiers in that and trying to protect and do whatever we can.”
She and her husband, a geriatrician also working on an H-1B visa, have worked hard not to bring the virus home to their 2-year-old daughter. Going into 2021, the past 2 years have been “the most hectic and emotionally draining – and physically exhausting – years of my life,” said Dr. Balla.
The COVID-19 vaccine has helped reduce some pressure, but Dr. Balla is still concerned about the high risk to health care workers and the new COVID-19 strains coming out. “We are really not sure what we are dealing with and how the COVID will calm,” she said. “It is pretty challenging being a health care worker because not only are you responsible for your patients at the end of the day, but you are also responsible for your families.”
Initially in the United States from India on a student visa in 2008, Dr. Balla was placed on an H-1B visa when she started her residency. It was during this time that her mother was diagnosed with cancer and went through surgeries and chemotherapy. “She was pretty ill,” recalled Dr. Balla.
Despite the situation, Dr. Balla was afraid to go stay with her mother in case her visa application was rejected, and she couldn’t complete her third year of education. “I opted not to go to India at that time because I did not want to take a chance,” Dr. Balla said. “I have tears in my eyes because those are not easy moments, to withhold from seeing your parents, or to be in any other emergency where you cannot travel. That especially puts us at a higher risk emotionally and physically.”
She has not seen her parents in 2½ years. Between the very real possibility of not being able to get her visa stamp and the unpredictability of how other countries are dealing with COVID-19, Dr. Balla feels it is impossible to even think of going to visit. “Even if I go, what if something happens where my visa gets stuck, or the visa office is not open?” she said. If she could not get back to the United States as planned, she would have patients left behind here.
Recently, Dr. Balla did travel to India and her passport stamp did not come on time, so her husband had to come back to the United States by himself. She had to wait for her stamp for a couple more weeks before she could leave and, in the meantime, had to make arrangements at her hospital. “It is so much trauma,” she said.
There’s also the worry she has about getting sick or disabled and not being able to work anymore, resulting in deportation. “Is that what we are doing for people who are working like soldiers? Are we really treating them the correct way?” Dr. Balla asked.
Dr. Balla considers all health care workers to be soldiers in the COVID-19 war. As such, she believes the government should step up to make sure they are supporting and helping these immigrant physician-soldiers who are so necessary. She applauds France’s recent decision to grant citizenship to its frontline immigrant health care workers and feels that the same should be done in the United States. She filed her green card application in 2012, but she is nowhere close to getting it. (The backlog for employment-based green cards is more than 900,000 now.)
As people putting their own and their family’s lives at risk to care for patients with COVID-19, Dr. Balla and her husband have talked about moving to another country or even back to India. “I am a taxpayer; I am a good human being working for the community and for the job. This is my 13th year here. If I am not eligible [for citizenship] still, then I am not sure what else I have to do to prove myself,” she said. “I am owning United States citizens as my people, so please own us and help us out in this difficult scenario.”
The COVID-19 pandemic has been difficult for all hospitalists, especially those who are parents of young children. For hospitalist moms who are also immigrants working on temporary H1-B visas, this stress is exacerbated. Though each story is unique, the underlying themes are the same: Worries over visa renewals, the immigration process, family members back home, and the risk of illness, job loss, and deportation.
Supporting the family
Like all health care workers, Prasanna Palabindela, MD, a hospitalist at Jennie Stuart Health in Hopkinsville, Ky., has been worried about bringing COVID-19 home to her family, especially in the beginning. Her in-laws had just arrived from India for a visit in March 2020 when the pandemic began, everything was shut down, and her in-laws were forced to settle in for an unexpected months-long stay.
Along with her elderly in-laws, who also have chronic conditions, Dr. Palabindela had two small children to worry about – a then-5-month-old daughter and a 5-year-old son. “I was more worried about them than me,” she said. “I used to take showers before coming home and just do all precautions as much as I can. I’m glad that I did not bring COVID, so far, to the family.”
Once she could safely send her in-laws back to India, Dr. Palabindela began searching for a nanny. Daycare was out of the question because she didn’t want her children to be exposed to illness. After a long search, she found a nanny who could also help her son with virtual school. “It’s expensive, but still, my family and my family’s health is my priority,” she said.
Working on visas has caused multiple issues for Dr. Palabindela and her husband. After living in different states because of their jobs, her husband joined her in West Virginia for her residency and found a job there. When Dr. Palabindela took her current position, her husband had to quit his job in West Virginia and move with her to Kentucky for them to stay together. Unfortunately, he couldn’t find a good fit for work in Kentucky, so the couple decided to put him on her visa so they wouldn’t have to live apart.
Now Dr. Palabindela is the family’s sole breadwinner. “That means if something happens to me, I always worry what’s going to happen with my family because legally, my husband cannot work. Technically, everyone is deported back to home,” she said. Not being able to work is hard for her husband too. “It’s just so much stress in the family because he worked for 11 years,” said Dr. Palabindela.
Through all the upheavals, Dr. Palabindela has had support from all sides. Her husband has been the biggest source. “He’s my backbone. Every time, he supported me in each and every aspect,” she said. Her parents and her brothers check in on her constantly to make sure she’s staying safe. Even the chief at her hospital has played a significant role, going to bat for his physicians to ensure their safety.
Dr. Palabindela credits everyone who works with COVID-19 patients as heroes. “The nurses, the physicians, the housekeeping, respiratory therapist, speech therapist, physical therapy ... everybody has a role. Everybody is a hero,” she said. “Whoever is wearing a mask is a hero, too, because they are contributing to this community.”
Advocating for immigration reform
A lack of transparency and information in the beginning of the pandemic significantly contributed to anxiety, said Anuradha Amara, MD, MBBS, a hospitalist in Wilmington, Del. She felt that what was on the news and what was actually going on in the hospitals were quite different. Colleagues were getting sick, there wasn’t enough personal protective equipment, and planning went out the window. “It’s like a meteor hitting a place and then we start dealing with the aftermath, but we weren’t ready before,” Dr. Amara said. “We didn’t have a plan for a pandemic.”
Then there was the concern of either her or her husband, a cardiologist, getting sick and potentially losing their jobs and immigration status. “How am I going to go back to my country if I had to? What will happen to my family if I die? If I go on the ventilator? Those are the insecurities we found additional to the pandemic challenges we had,” Dr. Amara said.
Not being able to go see their family in India or have them come visit was difficult – “it was pretty bad up there,” said Dr. Amara. Fortunately, her family members in India remained safe, but there’s a very real uneasiness about returning should an emergency arise. “Should I go back and then take the risk of losing my job and losing my position and my kids are here, they’re going to school here. How do you decide that?” she asked.
One of the worst effects of her visa restrictions was not being able to help in New York when hospitals were so short-staffed, and the morgues were overflowing. “New York is 3 hours away from where I live, but I was in chains. I couldn’t help them because of these visa restrictions,” Dr. Amara said. During the emergency, the state allowed physicians from other states to practice without being licensed in New York, but immigrant physicians were not included. “Even if we wanted to, we couldn’t volunteer,” said Dr. Amara. “I have family in New York, and I was really worried. Out of compassion I wanted to help, but I couldn’t do anything.”
Before the pandemic, Dr. Amara joined in advocacy efforts for immigrant physicians through Physicians for American Healthcare Access (PAHA). “In uncertain times, like COVID, it gets worse that you’re challenged with everything on top of your health, your family, and you have to be worried about deportation,” she said. “We need to strengthen legislation. Nobody should suffer with immigration processes during an active pandemic or otherwise.”
In the United States, 28% of physicians are immigrants. Dr. Amara pointed out that these physicians go through years of expensive training with extensive background checks at every level, yet they’re classified as second preference (EB-2) workers. She believes that physicians as a group should be excluded from this category and allowed to automatically become citizens after 5 years of living in the United States and working in an underserved area.
There have been an estimated 15,000 unused green cards since 2005. And if Congress went back to 1992, there could be more than 220,000 previously unused green cards recaptured. These unused green cards are the basis behind bills H.R.2255 and S.1024, the Healthcare Workforce Resiliency Act, which has been championed by SHM and PAHA. “It will allow the frontline physicians, 15,000 of them, and 25,000 nurses, to obtain their permanent residency,” said Dr. Amara. “These are people who already applied for their permanent residencies and they’re still waiting.”
SHM has consistently advocated for the Act since it was first introduced, written multiple letters on the issue, and supported it both on and off Capitol Hill. The society says the legislation would be an “important first step toward addressing a critical shortage” in the U.S. health care system by “recognizing the vital role immigrant physicians and nurses are playing in the fight against COVID-19.”
Currently, SHM has a live action alert open for the reintroduced bill, and encourages members to contact their legislators and urge them to support the reintroduction of the Act by cosponsoring and working to pass the legislation
Dr. Amara encourages physicians to start engaging in advocacy efforts early. Though she didn’t begin participating until late in her career, she said being aware of and part of policies that affect medicine is important. If more physicians get involved, “there are so many things we can take care of,” said Dr. Amara. “The medical profession doesn’t have to be so difficult and so busy. There are ways we can make it better and I believe that. And obviously I’ll continue to work and advocate for the entire medical profession, their problems, their health and well-being, to prevent burnout.”
Making time for positivity and self-care
Sandhya Tagaram, MD, a hospitalist at UMass Memorial Medical Center in Worcester, Mass., and her husband, also a hospitalist physician, had only ever read about pandemics in books. They certainly never expected to be in the middle of one. “That was a totally different level of anxiety to work as frontline physicians with two kids under 5 years and families away back home in India,” she said.
Dr. Tagaram and her husband work opposite shifts so that one of them is always home with their two young children. “Our schedules became more challenging when the pandemic started. Between both of our schedules and with minimal childcare facilities, we managed to strike a decent work-family balance, although we experience less vacation time together. We are fortunate to have an understanding work group,” said Dr. Tagaram.
Even before COVID-19, Dr. Tagaram found working on the temporary work visa challenging. “I think the pandemic has exposed the layer of uncertainty associated with it,” she said. “It’s incredibly stressful to imagine any minor turbulence that could alter our family and work lives. As a frontline physician mom, I take pride in raising my kids and taking care of my patients. We want to serve our communities and at the same time secure our families.”
Not being able to visit family back home and travel is exceedingly difficult. Dr. Tagaram said it would be helpful if there was a separate permanent residence pathway for physicians because they play a critical role in public health and they have been an integral part of the COVID-19 pandemic response team. A separate pathway could help keep their families secure and enable them to give their best to their communities.
Amid all the anxiety, Dr. Tagaram said she and her husband realized they could not keep living with so much pressure. As parents and as physicians, they did not want their stress to leak out and affect their ability and commitment to care for their children or their patients. They decided they needed to figure out how to be positive and constructive.
“We try some daily fun activities with the kids after returning home from work,” said Dr. Tagaram. They also formed a bubble group with two other physician families so the children could interact safely. She said that it’s critical that physicians take time for themselves. “We have to cultivate a serious hobby that helps to rejuvenate and calm our busy minds,” said Dr. Tagaram.
She makes time every day to exercise and to read at least a few pages from a good book. She is also learning Carnatic music along with one of her daughters. And every month since March 2020, she has journaled about her work and what she learned so her daughters can read it someday. “These things keep me jazzed up,” she said.
The pandemic has highlighted the fact that we are all part of one global community. “Although we hail from different backgrounds, we learned that we do have some common goals of being kind and supportive to each other and to give back to our communities. Hopefully we will continue this spirit,” said Dr. Tagaram. As a physician mother, “I feel it’s a privilege and honor to take care of my family and my community.”
Soldiering on in the COVID-19 war
The uncertainty everyone felt at the beginning of the pandemic was “very, very scary,” said Mamtha Balla, MD, MPH, a hospitalist and clinical assistant professor in northwest Ohio. “Initially, I was so involved in it and I felt like it was like a war, a COVID-19 war, and we are soldiers in that and trying to protect and do whatever we can.”
She and her husband, a geriatrician also working on an H-1B visa, have worked hard not to bring the virus home to their 2-year-old daughter. Going into 2021, the past 2 years have been “the most hectic and emotionally draining – and physically exhausting – years of my life,” said Dr. Balla.
The COVID-19 vaccine has helped reduce some pressure, but Dr. Balla is still concerned about the high risk to health care workers and the new COVID-19 strains coming out. “We are really not sure what we are dealing with and how the COVID will calm,” she said. “It is pretty challenging being a health care worker because not only are you responsible for your patients at the end of the day, but you are also responsible for your families.”
Initially in the United States from India on a student visa in 2008, Dr. Balla was placed on an H-1B visa when she started her residency. It was during this time that her mother was diagnosed with cancer and went through surgeries and chemotherapy. “She was pretty ill,” recalled Dr. Balla.
Despite the situation, Dr. Balla was afraid to go stay with her mother in case her visa application was rejected, and she couldn’t complete her third year of education. “I opted not to go to India at that time because I did not want to take a chance,” Dr. Balla said. “I have tears in my eyes because those are not easy moments, to withhold from seeing your parents, or to be in any other emergency where you cannot travel. That especially puts us at a higher risk emotionally and physically.”
She has not seen her parents in 2½ years. Between the very real possibility of not being able to get her visa stamp and the unpredictability of how other countries are dealing with COVID-19, Dr. Balla feels it is impossible to even think of going to visit. “Even if I go, what if something happens where my visa gets stuck, or the visa office is not open?” she said. If she could not get back to the United States as planned, she would have patients left behind here.
Recently, Dr. Balla did travel to India and her passport stamp did not come on time, so her husband had to come back to the United States by himself. She had to wait for her stamp for a couple more weeks before she could leave and, in the meantime, had to make arrangements at her hospital. “It is so much trauma,” she said.
There’s also the worry she has about getting sick or disabled and not being able to work anymore, resulting in deportation. “Is that what we are doing for people who are working like soldiers? Are we really treating them the correct way?” Dr. Balla asked.
Dr. Balla considers all health care workers to be soldiers in the COVID-19 war. As such, she believes the government should step up to make sure they are supporting and helping these immigrant physician-soldiers who are so necessary. She applauds France’s recent decision to grant citizenship to its frontline immigrant health care workers and feels that the same should be done in the United States. She filed her green card application in 2012, but she is nowhere close to getting it. (The backlog for employment-based green cards is more than 900,000 now.)
As people putting their own and their family’s lives at risk to care for patients with COVID-19, Dr. Balla and her husband have talked about moving to another country or even back to India. “I am a taxpayer; I am a good human being working for the community and for the job. This is my 13th year here. If I am not eligible [for citizenship] still, then I am not sure what else I have to do to prove myself,” she said. “I am owning United States citizens as my people, so please own us and help us out in this difficult scenario.”
Hospitalist movers and shakers – May 2021
Rebecca Jaffe, MD, has been elevated to the permanent role of director of the division of hospital medicine at Thomas Jefferson University Hospital in Philadelphia. Dr. Jaffe has been the interim director since July 2020.
In the position, Dr. Jaffe will be responsible for leading an academic hospital medicine division that includes 36 faculty and 10 advanced-practice providers. She said her focus will be on developing physicians, advanced providers, and the inpatient practice model used while “educating the next generation of creative and compassionate clinicians.”
Dr. Jaffe is associate professor of medicine at Jefferson’s Sidney Kimmel Medical College and the hospital’s director of clinical learning environment improvement.
Christopher Freer, DO, recently was named the new senior vice president for emergency hospital medicine for RWJBarnabas Health (West Orange, N.J.). In a concurrent move, Maninder “Dolly” Abraham, MD, was named RWJBH’s chief of hospital medicine. The selections were made as RWJBH has become a direct employer for Envision Physician Services, a former hospital partner.
Dr. Freer has spent the past 5 years with RWJBH, where he has served as emergency services system director since 2015. He previously worked in leadership roles at Saint Barnabas Medical Center.
Dr. Abraham was previously medical director of Saint Barnabas’ hospitalist program, as well as a regional medical director with Envision during her 17 years of experience.
Sheetal Patel, MD, has been named the new regional medical director for Eagle Telemedicine (Cincinnati, Ohio), a physician-led company that provides telehospitalist services to hospitals around the country.
Dr. Patel will work closely with hospital administrators and medical directors to provide high-level telemedicine services, as well as devising processes and guidelines to guarantee streamlined care across Eagle’s facilities.
Dr. Patel has spent 4 years as a telehospitalist for Eagle, where she has been in charge of guiding on-site and remote staff members and providing training to new telehospitalists.
Timothy Crone, MD, MBA, has been elevated to the role of president of Cleveland Clinic Mercy Hospital (Canton, Ohio). The move comes as Cleveland Clinic recently added Mercy Medical Center as a full member of its health system.
Dr. Crone has served as chief medical officer at Cleveland Clinic Hillcrest Hospital in Cleveland since 2019. Previously, he was a medical director in enterprise business intelligence and analytics in medical operations at Cleveland Clinic’s main campus. He also was vice chairman of hospital medicine and has served as a staff hospitalist since 2010.
In addition to his role as president, Dr. Crone plans to work in patient care at Mercy Hospital.
Just prior to the start of 2021, Wake Forest Baptist Health (Winston-Salem, N.C.) established a “Hospitalist at Home” program with the goal of reducing the length of time patients spend in the hospital.
Hospitalist at Home was created as the COVID-19 pandemic threatened hospital capacity. Wakehealth’s innovative approach involves developing an at-home plan with each patient before they leave the facility. Patients include those with COVID-19 who are stable but require supplemental oxygen or have diseases that need intravenous medication administration.
At home, a Wakehealth paramedic visits the patient while a hospitalist communicates and reviews the patient’s care plan via smartphone, tablet, or computer. The visits continue until the patient’s hospital-related care is complete.
The Multicare Health System (Tacoma, Wash.) has bulked up its hospitalist program by partnering with nationwide, physician-led health care provider Sound Physicians. The goal is to provide health care management at a regional level instead of individually per hospital.
Sound Physicians, which already contracts to provide hospitalist services at two Multicare facilities in Washington, transitioned its services to three other facilities as of April 5, 2021.
Conemaugh Meyersdale Medical Center (Meyersdale, Pa.) has started a hospitalist program at its facility in Somerset County. The program will be led by nurse practitioners Zeke Feyock and Sarah Piscatello.
Rebecca Jaffe, MD, has been elevated to the permanent role of director of the division of hospital medicine at Thomas Jefferson University Hospital in Philadelphia. Dr. Jaffe has been the interim director since July 2020.
In the position, Dr. Jaffe will be responsible for leading an academic hospital medicine division that includes 36 faculty and 10 advanced-practice providers. She said her focus will be on developing physicians, advanced providers, and the inpatient practice model used while “educating the next generation of creative and compassionate clinicians.”
Dr. Jaffe is associate professor of medicine at Jefferson’s Sidney Kimmel Medical College and the hospital’s director of clinical learning environment improvement.
Christopher Freer, DO, recently was named the new senior vice president for emergency hospital medicine for RWJBarnabas Health (West Orange, N.J.). In a concurrent move, Maninder “Dolly” Abraham, MD, was named RWJBH’s chief of hospital medicine. The selections were made as RWJBH has become a direct employer for Envision Physician Services, a former hospital partner.
Dr. Freer has spent the past 5 years with RWJBH, where he has served as emergency services system director since 2015. He previously worked in leadership roles at Saint Barnabas Medical Center.
Dr. Abraham was previously medical director of Saint Barnabas’ hospitalist program, as well as a regional medical director with Envision during her 17 years of experience.
Sheetal Patel, MD, has been named the new regional medical director for Eagle Telemedicine (Cincinnati, Ohio), a physician-led company that provides telehospitalist services to hospitals around the country.
Dr. Patel will work closely with hospital administrators and medical directors to provide high-level telemedicine services, as well as devising processes and guidelines to guarantee streamlined care across Eagle’s facilities.
Dr. Patel has spent 4 years as a telehospitalist for Eagle, where she has been in charge of guiding on-site and remote staff members and providing training to new telehospitalists.
Timothy Crone, MD, MBA, has been elevated to the role of president of Cleveland Clinic Mercy Hospital (Canton, Ohio). The move comes as Cleveland Clinic recently added Mercy Medical Center as a full member of its health system.
Dr. Crone has served as chief medical officer at Cleveland Clinic Hillcrest Hospital in Cleveland since 2019. Previously, he was a medical director in enterprise business intelligence and analytics in medical operations at Cleveland Clinic’s main campus. He also was vice chairman of hospital medicine and has served as a staff hospitalist since 2010.
In addition to his role as president, Dr. Crone plans to work in patient care at Mercy Hospital.
Just prior to the start of 2021, Wake Forest Baptist Health (Winston-Salem, N.C.) established a “Hospitalist at Home” program with the goal of reducing the length of time patients spend in the hospital.
Hospitalist at Home was created as the COVID-19 pandemic threatened hospital capacity. Wakehealth’s innovative approach involves developing an at-home plan with each patient before they leave the facility. Patients include those with COVID-19 who are stable but require supplemental oxygen or have diseases that need intravenous medication administration.
At home, a Wakehealth paramedic visits the patient while a hospitalist communicates and reviews the patient’s care plan via smartphone, tablet, or computer. The visits continue until the patient’s hospital-related care is complete.
The Multicare Health System (Tacoma, Wash.) has bulked up its hospitalist program by partnering with nationwide, physician-led health care provider Sound Physicians. The goal is to provide health care management at a regional level instead of individually per hospital.
Sound Physicians, which already contracts to provide hospitalist services at two Multicare facilities in Washington, transitioned its services to three other facilities as of April 5, 2021.
Conemaugh Meyersdale Medical Center (Meyersdale, Pa.) has started a hospitalist program at its facility in Somerset County. The program will be led by nurse practitioners Zeke Feyock and Sarah Piscatello.
Rebecca Jaffe, MD, has been elevated to the permanent role of director of the division of hospital medicine at Thomas Jefferson University Hospital in Philadelphia. Dr. Jaffe has been the interim director since July 2020.
In the position, Dr. Jaffe will be responsible for leading an academic hospital medicine division that includes 36 faculty and 10 advanced-practice providers. She said her focus will be on developing physicians, advanced providers, and the inpatient practice model used while “educating the next generation of creative and compassionate clinicians.”
Dr. Jaffe is associate professor of medicine at Jefferson’s Sidney Kimmel Medical College and the hospital’s director of clinical learning environment improvement.
Christopher Freer, DO, recently was named the new senior vice president for emergency hospital medicine for RWJBarnabas Health (West Orange, N.J.). In a concurrent move, Maninder “Dolly” Abraham, MD, was named RWJBH’s chief of hospital medicine. The selections were made as RWJBH has become a direct employer for Envision Physician Services, a former hospital partner.
Dr. Freer has spent the past 5 years with RWJBH, where he has served as emergency services system director since 2015. He previously worked in leadership roles at Saint Barnabas Medical Center.
Dr. Abraham was previously medical director of Saint Barnabas’ hospitalist program, as well as a regional medical director with Envision during her 17 years of experience.
Sheetal Patel, MD, has been named the new regional medical director for Eagle Telemedicine (Cincinnati, Ohio), a physician-led company that provides telehospitalist services to hospitals around the country.
Dr. Patel will work closely with hospital administrators and medical directors to provide high-level telemedicine services, as well as devising processes and guidelines to guarantee streamlined care across Eagle’s facilities.
Dr. Patel has spent 4 years as a telehospitalist for Eagle, where she has been in charge of guiding on-site and remote staff members and providing training to new telehospitalists.
Timothy Crone, MD, MBA, has been elevated to the role of president of Cleveland Clinic Mercy Hospital (Canton, Ohio). The move comes as Cleveland Clinic recently added Mercy Medical Center as a full member of its health system.
Dr. Crone has served as chief medical officer at Cleveland Clinic Hillcrest Hospital in Cleveland since 2019. Previously, he was a medical director in enterprise business intelligence and analytics in medical operations at Cleveland Clinic’s main campus. He also was vice chairman of hospital medicine and has served as a staff hospitalist since 2010.
In addition to his role as president, Dr. Crone plans to work in patient care at Mercy Hospital.
Just prior to the start of 2021, Wake Forest Baptist Health (Winston-Salem, N.C.) established a “Hospitalist at Home” program with the goal of reducing the length of time patients spend in the hospital.
Hospitalist at Home was created as the COVID-19 pandemic threatened hospital capacity. Wakehealth’s innovative approach involves developing an at-home plan with each patient before they leave the facility. Patients include those with COVID-19 who are stable but require supplemental oxygen or have diseases that need intravenous medication administration.
At home, a Wakehealth paramedic visits the patient while a hospitalist communicates and reviews the patient’s care plan via smartphone, tablet, or computer. The visits continue until the patient’s hospital-related care is complete.
The Multicare Health System (Tacoma, Wash.) has bulked up its hospitalist program by partnering with nationwide, physician-led health care provider Sound Physicians. The goal is to provide health care management at a regional level instead of individually per hospital.
Sound Physicians, which already contracts to provide hospitalist services at two Multicare facilities in Washington, transitioned its services to three other facilities as of April 5, 2021.
Conemaugh Meyersdale Medical Center (Meyersdale, Pa.) has started a hospitalist program at its facility in Somerset County. The program will be led by nurse practitioners Zeke Feyock and Sarah Piscatello.
Pandemic experience taught lessons about clinician wellness
As a member of the Society of Hospital Medicine Wellbeing Task Force, Mark Rudolph, MD, SFHM, thought he understood a thing or two about resilience, but nothing could prepare him for the vulnerability he felt when his parents became infected with COVID-19 following a visit to New York City in March 2020 – which soon became an epicenter of disease outbreak.
“They were both quite ill but fortunately they recovered,” Dr. Rudolph, chief experience officer for Sound Physicians said during SHM Converge, the annual conference of the Society of Hospital Medicine. He had completed his residency training in New York, where he cared for patients following the 9/11 terrorist attacks, “so I had a lot of PTSD related to all that stuff,” he recalled. Then he started to worry about the clinicians who work for Sound Physicians, a multispecialty group with roots in hospital medicine. “I found it difficult knowing there was someone in the hospital somewhere taking care of our patients all day long, all night long,” he said. “I felt fearful for them.”
Other members of the SHM Wellbeing Task Force shared challenges they faced during the pandemic’s early stages, as well as lessons learned. Task force chair Sarah Richards, MD, said the COVID-19 pandemic brought on feelings of guilt after hearing from fellow hospitalists about the surge of cases they were caring for, or that their best friend or colleague died by suicide. “I felt a sense of guilt because I didn’t have a loved one get COVID or die from COVID,” said Dr. Richards, a hospitalist at the University of Nebraska Medical Center in Omaha. “I felt like the world was crumbling around me and I was still okay. That guilt was almost like a helplessness. I didn’t know how make it better. I didn’t know how to help people because the problem was so big, especially during the height of the pandemic. That was tough for me because I’m a helper. I think we go into this field wanting to help and I feel like we didn’t know how to help make things better.”
Sonia George, MD, recalled first hearing about COVID-19 as she was preparing to attend the 2020 SHM annual conference in San Diego, which was planned for April but was canceled amid the escalating health concerns. “That was difficult for me, because I wanted to travel more in 2020,” said Dr. George, a hospitalist at Long Island Jewish Medical Center in New Hyde Park, N.Y. “Traveling is something that I’ve been wanting to do ever since I finished residency, after all that training. I wanted to reward myself. What I have learned about myself is that I’ve learned to be more patient, to take every day as it is, to find some small moments of joy within each day and try to take that forward with me, and try to remember what I do have, and celebrate that a bit more every day.”
Over the past 14 months or so, Dr. Rudolph said that he grew to appreciate the importance of connecting with colleagues, “however short [the time] may be, where we can talk with one another, commiserate, discuss situations and experiences – whether virtually or in person. Those have been critical. If you add those all up, that’s what’s keeping us all going. At least it’s keeping me going.”
Dr. Richards echoed that sentiment. “The lesson I learned is that people really do want to share and to talk,” she said. “I can’t tell you how many times I told people about my [sense of] guilt and they would say things like, ‘Me, too!’ Knowing ‘it’s not just me’ made me feel so much better.”
During the course of the pandemic, the SHM Wellbeing Task Force created a one-page resource for clinicians known as the “Hospital Medicine COVID-19 Check-in Guide for Self & Peers,” which can be accessed here:. The three main recommended steps are to identify (“self-assess” to see if you are experiencing physical, emotional, cognitive, or behavioral stress); initiate (“reach out to your colleagues one-one-one or in small informal groups”); and intervene (“take action to make change or get help.”)
“Wellness and thriving are a team sport,” observed task force member Patrick Kneeland, MD, vice president of medical affairs at DispatchHealth, which provides hospital to home services. “It’s not an individual task to achieve. The team sport thing is complicated by gowns and masks and the lack of in-person meetings. You can’t even grab a cup of coffee with colleagues. That part has impacted most of us.” However, he said, he learned that clinicians can “double down on those small practices that form human connection” by using virtual communication platforms like Zoom. “For me, it’s been a great reminder [of] why presence with others matters, even if it’s in an unusual format, and how sharing our humanity across [communication] channels or through several layers of PPE is so critical.” Dr. Kneeland said.
None of the presenters reported having financial disclosures.
As a member of the Society of Hospital Medicine Wellbeing Task Force, Mark Rudolph, MD, SFHM, thought he understood a thing or two about resilience, but nothing could prepare him for the vulnerability he felt when his parents became infected with COVID-19 following a visit to New York City in March 2020 – which soon became an epicenter of disease outbreak.
“They were both quite ill but fortunately they recovered,” Dr. Rudolph, chief experience officer for Sound Physicians said during SHM Converge, the annual conference of the Society of Hospital Medicine. He had completed his residency training in New York, where he cared for patients following the 9/11 terrorist attacks, “so I had a lot of PTSD related to all that stuff,” he recalled. Then he started to worry about the clinicians who work for Sound Physicians, a multispecialty group with roots in hospital medicine. “I found it difficult knowing there was someone in the hospital somewhere taking care of our patients all day long, all night long,” he said. “I felt fearful for them.”
Other members of the SHM Wellbeing Task Force shared challenges they faced during the pandemic’s early stages, as well as lessons learned. Task force chair Sarah Richards, MD, said the COVID-19 pandemic brought on feelings of guilt after hearing from fellow hospitalists about the surge of cases they were caring for, or that their best friend or colleague died by suicide. “I felt a sense of guilt because I didn’t have a loved one get COVID or die from COVID,” said Dr. Richards, a hospitalist at the University of Nebraska Medical Center in Omaha. “I felt like the world was crumbling around me and I was still okay. That guilt was almost like a helplessness. I didn’t know how make it better. I didn’t know how to help people because the problem was so big, especially during the height of the pandemic. That was tough for me because I’m a helper. I think we go into this field wanting to help and I feel like we didn’t know how to help make things better.”
Sonia George, MD, recalled first hearing about COVID-19 as she was preparing to attend the 2020 SHM annual conference in San Diego, which was planned for April but was canceled amid the escalating health concerns. “That was difficult for me, because I wanted to travel more in 2020,” said Dr. George, a hospitalist at Long Island Jewish Medical Center in New Hyde Park, N.Y. “Traveling is something that I’ve been wanting to do ever since I finished residency, after all that training. I wanted to reward myself. What I have learned about myself is that I’ve learned to be more patient, to take every day as it is, to find some small moments of joy within each day and try to take that forward with me, and try to remember what I do have, and celebrate that a bit more every day.”
Over the past 14 months or so, Dr. Rudolph said that he grew to appreciate the importance of connecting with colleagues, “however short [the time] may be, where we can talk with one another, commiserate, discuss situations and experiences – whether virtually or in person. Those have been critical. If you add those all up, that’s what’s keeping us all going. At least it’s keeping me going.”
Dr. Richards echoed that sentiment. “The lesson I learned is that people really do want to share and to talk,” she said. “I can’t tell you how many times I told people about my [sense of] guilt and they would say things like, ‘Me, too!’ Knowing ‘it’s not just me’ made me feel so much better.”
During the course of the pandemic, the SHM Wellbeing Task Force created a one-page resource for clinicians known as the “Hospital Medicine COVID-19 Check-in Guide for Self & Peers,” which can be accessed here:. The three main recommended steps are to identify (“self-assess” to see if you are experiencing physical, emotional, cognitive, or behavioral stress); initiate (“reach out to your colleagues one-one-one or in small informal groups”); and intervene (“take action to make change or get help.”)
“Wellness and thriving are a team sport,” observed task force member Patrick Kneeland, MD, vice president of medical affairs at DispatchHealth, which provides hospital to home services. “It’s not an individual task to achieve. The team sport thing is complicated by gowns and masks and the lack of in-person meetings. You can’t even grab a cup of coffee with colleagues. That part has impacted most of us.” However, he said, he learned that clinicians can “double down on those small practices that form human connection” by using virtual communication platforms like Zoom. “For me, it’s been a great reminder [of] why presence with others matters, even if it’s in an unusual format, and how sharing our humanity across [communication] channels or through several layers of PPE is so critical.” Dr. Kneeland said.
None of the presenters reported having financial disclosures.
As a member of the Society of Hospital Medicine Wellbeing Task Force, Mark Rudolph, MD, SFHM, thought he understood a thing or two about resilience, but nothing could prepare him for the vulnerability he felt when his parents became infected with COVID-19 following a visit to New York City in March 2020 – which soon became an epicenter of disease outbreak.
“They were both quite ill but fortunately they recovered,” Dr. Rudolph, chief experience officer for Sound Physicians said during SHM Converge, the annual conference of the Society of Hospital Medicine. He had completed his residency training in New York, where he cared for patients following the 9/11 terrorist attacks, “so I had a lot of PTSD related to all that stuff,” he recalled. Then he started to worry about the clinicians who work for Sound Physicians, a multispecialty group with roots in hospital medicine. “I found it difficult knowing there was someone in the hospital somewhere taking care of our patients all day long, all night long,” he said. “I felt fearful for them.”
Other members of the SHM Wellbeing Task Force shared challenges they faced during the pandemic’s early stages, as well as lessons learned. Task force chair Sarah Richards, MD, said the COVID-19 pandemic brought on feelings of guilt after hearing from fellow hospitalists about the surge of cases they were caring for, or that their best friend or colleague died by suicide. “I felt a sense of guilt because I didn’t have a loved one get COVID or die from COVID,” said Dr. Richards, a hospitalist at the University of Nebraska Medical Center in Omaha. “I felt like the world was crumbling around me and I was still okay. That guilt was almost like a helplessness. I didn’t know how make it better. I didn’t know how to help people because the problem was so big, especially during the height of the pandemic. That was tough for me because I’m a helper. I think we go into this field wanting to help and I feel like we didn’t know how to help make things better.”
Sonia George, MD, recalled first hearing about COVID-19 as she was preparing to attend the 2020 SHM annual conference in San Diego, which was planned for April but was canceled amid the escalating health concerns. “That was difficult for me, because I wanted to travel more in 2020,” said Dr. George, a hospitalist at Long Island Jewish Medical Center in New Hyde Park, N.Y. “Traveling is something that I’ve been wanting to do ever since I finished residency, after all that training. I wanted to reward myself. What I have learned about myself is that I’ve learned to be more patient, to take every day as it is, to find some small moments of joy within each day and try to take that forward with me, and try to remember what I do have, and celebrate that a bit more every day.”
Over the past 14 months or so, Dr. Rudolph said that he grew to appreciate the importance of connecting with colleagues, “however short [the time] may be, where we can talk with one another, commiserate, discuss situations and experiences – whether virtually or in person. Those have been critical. If you add those all up, that’s what’s keeping us all going. At least it’s keeping me going.”
Dr. Richards echoed that sentiment. “The lesson I learned is that people really do want to share and to talk,” she said. “I can’t tell you how many times I told people about my [sense of] guilt and they would say things like, ‘Me, too!’ Knowing ‘it’s not just me’ made me feel so much better.”
During the course of the pandemic, the SHM Wellbeing Task Force created a one-page resource for clinicians known as the “Hospital Medicine COVID-19 Check-in Guide for Self & Peers,” which can be accessed here:. The three main recommended steps are to identify (“self-assess” to see if you are experiencing physical, emotional, cognitive, or behavioral stress); initiate (“reach out to your colleagues one-one-one or in small informal groups”); and intervene (“take action to make change or get help.”)
“Wellness and thriving are a team sport,” observed task force member Patrick Kneeland, MD, vice president of medical affairs at DispatchHealth, which provides hospital to home services. “It’s not an individual task to achieve. The team sport thing is complicated by gowns and masks and the lack of in-person meetings. You can’t even grab a cup of coffee with colleagues. That part has impacted most of us.” However, he said, he learned that clinicians can “double down on those small practices that form human connection” by using virtual communication platforms like Zoom. “For me, it’s been a great reminder [of] why presence with others matters, even if it’s in an unusual format, and how sharing our humanity across [communication] channels or through several layers of PPE is so critical.” Dr. Kneeland said.
None of the presenters reported having financial disclosures.
FROM SHM CONVERGE 2021
Mentor-mentee relationships in hospital medicine
Your mentor has been looking for someone to help lead a new project in your division, and tells you she’s been having a hard time finding someone – but that you would be great. The project isn’t something you are very interested in doing and you’re already swamped with other projects, but the mentor seems to need the help. What do you do?
Mentor-mentee relationships can be deeply beneficial, but the dynamics – in this situation and many others – can be complex. At SHM Converge, the annual conference of the Society of Hospital Medicine, panelists offered guidance on how best to navigate this terrain.
Vineet Arora, MD, MAPP, MHM, associate chief medical officer for clinical learning environment at the University of Chicago, suggested that, in the situation involving the mentor’s request to an uncertain mentee, the mentee should not give an immediate answer, but consider the pros and cons.
“It’s tough when it’s somebody who’s directly overseeing you,” she said. “If you’re really truly the best person, they’re going to want you in the job, and maybe they’ll make it work for you.” She said it would be important to find out why the mentor is having trouble finding someone, and suggested the mentee could find someone with whom to discuss it.
Calling mentoring a “team sport,” Dr. Arora described several types: the traditional mentor who helps many aspects of a mentee’s career, a “coach” who helps on a specific project or topic, a “sponsor” that can help elevate a mentee to a bigger opportunity, and a “connector” who can help a mentee begin new career relationships.
“Don’t invest in just one person,” she said. “Try to get that personal board of directors.”
She mentioned six things all mentors should do: Choose mentees carefully, establish a mentorship team, run a tight ship, head off rifts or resolve them, prepare for transitions when they take a new position and might have a new relationship with a mentee, and don’t commit “mentorship malpractice.”
Mentoring is a two-way street, with both people benefiting and learning, but mentoring can have its troubles, either through active, dysfunctional behavior that’s easy to spot, or passive behavior, such as the “bottleneck” problem when a mentor is too preoccupied with his or her own priorities to mentor well, the “country clubber” who mentors only for popularity and social capital but doesn’t do the work required, and the “world traveler” who is sought after but has little time for day-to-day mentoring.
Valerie Vaughan, MD, MSc, assistant professor of medicine at the University of Utah, described four “golden rules” of being a mentee. First, find a CAPE mentor (for capable, availability, projects of interest, and easy to get along with). Then, be respectful of a mentor’s time, communicate effectively, and be engaged and energizing.
“Mentors typically don’t get paid to mentor and so a lot of them are doing it because they find joy for doing it,” Dr. Vaughan said. “So as much as you can as a mentee, try to be the person who brings energy to the mentor-mentee relationship. It’s up to you to drive projects forward.”
Valerie Press, MD, MPH, SFHM, associate professor of medicine at the University of Chicago, offered tips for men who are mentoring women. She said that, while cross-gender mentorship is common and important, gender-based stereotypes and “unconscious assumptions” are alive and well. Women, she noted, have less access to mentorship and sponsorship, are paid less for the same work, and have high rates of attrition.
Male mentors have to meet the challenge of thinking outside of their own lived experience, combating stereotypes, and addressing these gender-based career disparities, she said.
She suggested that male mentors, for one thing, “rewrite gender scripts,” with comments such as, “This is a difficult situation, but I have confidence in you! What do you think your next move should be?” They should also “learn from each other on how to change the power dynamic,” and start and participate in conversations involving emotions, since they can be clues to what a mentee is experiencing.
When it comes to pushing for better policies, “be an upstander, not a bystander,” Dr. Press said.
“Use your organizational power and your social capital,” she said. “Use your voice to help make more equitable policies. Don’t just leave it to the women’s committee to come up with solutions to lack of lactation rooms, or paternity and maternity leave, or better daycare. These are family issues and everybody issues.”
Maylyn S. Martinez, MD, clinical associate professor of medicine at the University of Chicago, suggested that mentors for physicians from minority groups should resist the tendency to view their interests narrowly.
“Don’t assume that their interests are going to center on their gender or minority status – invite them to be on projects that have nothing to do with that,” she said. They should also not be encouraged to do projects that won’t help with career advancement any more than others would be encouraged to take on such projects.
“Be the solution,” she said. “Not the problem.”
Your mentor has been looking for someone to help lead a new project in your division, and tells you she’s been having a hard time finding someone – but that you would be great. The project isn’t something you are very interested in doing and you’re already swamped with other projects, but the mentor seems to need the help. What do you do?
Mentor-mentee relationships can be deeply beneficial, but the dynamics – in this situation and many others – can be complex. At SHM Converge, the annual conference of the Society of Hospital Medicine, panelists offered guidance on how best to navigate this terrain.
Vineet Arora, MD, MAPP, MHM, associate chief medical officer for clinical learning environment at the University of Chicago, suggested that, in the situation involving the mentor’s request to an uncertain mentee, the mentee should not give an immediate answer, but consider the pros and cons.
“It’s tough when it’s somebody who’s directly overseeing you,” she said. “If you’re really truly the best person, they’re going to want you in the job, and maybe they’ll make it work for you.” She said it would be important to find out why the mentor is having trouble finding someone, and suggested the mentee could find someone with whom to discuss it.
Calling mentoring a “team sport,” Dr. Arora described several types: the traditional mentor who helps many aspects of a mentee’s career, a “coach” who helps on a specific project or topic, a “sponsor” that can help elevate a mentee to a bigger opportunity, and a “connector” who can help a mentee begin new career relationships.
“Don’t invest in just one person,” she said. “Try to get that personal board of directors.”
She mentioned six things all mentors should do: Choose mentees carefully, establish a mentorship team, run a tight ship, head off rifts or resolve them, prepare for transitions when they take a new position and might have a new relationship with a mentee, and don’t commit “mentorship malpractice.”
Mentoring is a two-way street, with both people benefiting and learning, but mentoring can have its troubles, either through active, dysfunctional behavior that’s easy to spot, or passive behavior, such as the “bottleneck” problem when a mentor is too preoccupied with his or her own priorities to mentor well, the “country clubber” who mentors only for popularity and social capital but doesn’t do the work required, and the “world traveler” who is sought after but has little time for day-to-day mentoring.
Valerie Vaughan, MD, MSc, assistant professor of medicine at the University of Utah, described four “golden rules” of being a mentee. First, find a CAPE mentor (for capable, availability, projects of interest, and easy to get along with). Then, be respectful of a mentor’s time, communicate effectively, and be engaged and energizing.
“Mentors typically don’t get paid to mentor and so a lot of them are doing it because they find joy for doing it,” Dr. Vaughan said. “So as much as you can as a mentee, try to be the person who brings energy to the mentor-mentee relationship. It’s up to you to drive projects forward.”
Valerie Press, MD, MPH, SFHM, associate professor of medicine at the University of Chicago, offered tips for men who are mentoring women. She said that, while cross-gender mentorship is common and important, gender-based stereotypes and “unconscious assumptions” are alive and well. Women, she noted, have less access to mentorship and sponsorship, are paid less for the same work, and have high rates of attrition.
Male mentors have to meet the challenge of thinking outside of their own lived experience, combating stereotypes, and addressing these gender-based career disparities, she said.
She suggested that male mentors, for one thing, “rewrite gender scripts,” with comments such as, “This is a difficult situation, but I have confidence in you! What do you think your next move should be?” They should also “learn from each other on how to change the power dynamic,” and start and participate in conversations involving emotions, since they can be clues to what a mentee is experiencing.
When it comes to pushing for better policies, “be an upstander, not a bystander,” Dr. Press said.
“Use your organizational power and your social capital,” she said. “Use your voice to help make more equitable policies. Don’t just leave it to the women’s committee to come up with solutions to lack of lactation rooms, or paternity and maternity leave, or better daycare. These are family issues and everybody issues.”
Maylyn S. Martinez, MD, clinical associate professor of medicine at the University of Chicago, suggested that mentors for physicians from minority groups should resist the tendency to view their interests narrowly.
“Don’t assume that their interests are going to center on their gender or minority status – invite them to be on projects that have nothing to do with that,” she said. They should also not be encouraged to do projects that won’t help with career advancement any more than others would be encouraged to take on such projects.
“Be the solution,” she said. “Not the problem.”
Your mentor has been looking for someone to help lead a new project in your division, and tells you she’s been having a hard time finding someone – but that you would be great. The project isn’t something you are very interested in doing and you’re already swamped with other projects, but the mentor seems to need the help. What do you do?
Mentor-mentee relationships can be deeply beneficial, but the dynamics – in this situation and many others – can be complex. At SHM Converge, the annual conference of the Society of Hospital Medicine, panelists offered guidance on how best to navigate this terrain.
Vineet Arora, MD, MAPP, MHM, associate chief medical officer for clinical learning environment at the University of Chicago, suggested that, in the situation involving the mentor’s request to an uncertain mentee, the mentee should not give an immediate answer, but consider the pros and cons.
“It’s tough when it’s somebody who’s directly overseeing you,” she said. “If you’re really truly the best person, they’re going to want you in the job, and maybe they’ll make it work for you.” She said it would be important to find out why the mentor is having trouble finding someone, and suggested the mentee could find someone with whom to discuss it.
Calling mentoring a “team sport,” Dr. Arora described several types: the traditional mentor who helps many aspects of a mentee’s career, a “coach” who helps on a specific project or topic, a “sponsor” that can help elevate a mentee to a bigger opportunity, and a “connector” who can help a mentee begin new career relationships.
“Don’t invest in just one person,” she said. “Try to get that personal board of directors.”
She mentioned six things all mentors should do: Choose mentees carefully, establish a mentorship team, run a tight ship, head off rifts or resolve them, prepare for transitions when they take a new position and might have a new relationship with a mentee, and don’t commit “mentorship malpractice.”
Mentoring is a two-way street, with both people benefiting and learning, but mentoring can have its troubles, either through active, dysfunctional behavior that’s easy to spot, or passive behavior, such as the “bottleneck” problem when a mentor is too preoccupied with his or her own priorities to mentor well, the “country clubber” who mentors only for popularity and social capital but doesn’t do the work required, and the “world traveler” who is sought after but has little time for day-to-day mentoring.
Valerie Vaughan, MD, MSc, assistant professor of medicine at the University of Utah, described four “golden rules” of being a mentee. First, find a CAPE mentor (for capable, availability, projects of interest, and easy to get along with). Then, be respectful of a mentor’s time, communicate effectively, and be engaged and energizing.
“Mentors typically don’t get paid to mentor and so a lot of them are doing it because they find joy for doing it,” Dr. Vaughan said. “So as much as you can as a mentee, try to be the person who brings energy to the mentor-mentee relationship. It’s up to you to drive projects forward.”
Valerie Press, MD, MPH, SFHM, associate professor of medicine at the University of Chicago, offered tips for men who are mentoring women. She said that, while cross-gender mentorship is common and important, gender-based stereotypes and “unconscious assumptions” are alive and well. Women, she noted, have less access to mentorship and sponsorship, are paid less for the same work, and have high rates of attrition.
Male mentors have to meet the challenge of thinking outside of their own lived experience, combating stereotypes, and addressing these gender-based career disparities, she said.
She suggested that male mentors, for one thing, “rewrite gender scripts,” with comments such as, “This is a difficult situation, but I have confidence in you! What do you think your next move should be?” They should also “learn from each other on how to change the power dynamic,” and start and participate in conversations involving emotions, since they can be clues to what a mentee is experiencing.
When it comes to pushing for better policies, “be an upstander, not a bystander,” Dr. Press said.
“Use your organizational power and your social capital,” she said. “Use your voice to help make more equitable policies. Don’t just leave it to the women’s committee to come up with solutions to lack of lactation rooms, or paternity and maternity leave, or better daycare. These are family issues and everybody issues.”
Maylyn S. Martinez, MD, clinical associate professor of medicine at the University of Chicago, suggested that mentors for physicians from minority groups should resist the tendency to view their interests narrowly.
“Don’t assume that their interests are going to center on their gender or minority status – invite them to be on projects that have nothing to do with that,” she said. They should also not be encouraged to do projects that won’t help with career advancement any more than others would be encouraged to take on such projects.
“Be the solution,” she said. “Not the problem.”
FROM SHM CONVERGE 2021
SHM 2021 Awards of Excellence and Junior Investigator Awards
Clinical Leadership for Physicians
Christopher P. Bruti, MD, MPH
Dr. Christopher P. Bruti is the division chief of hospital medicine at Rush University and the program director of Rush’s combined Internal Medicine–Pediatrics Residency Program. He is an associate professor of internal medicine and pediatrics and practices as a hospitalist in both departments.
Dr. Bruti always rises to any challenge that comes his way with empathetic, organized, and insightful leadership. Dr. Bruti is known for his innovation in patient care and optimization practices in the hospital setting – from expanding and optimizing the nonteaching service and a high-functioning observation unit to geolocalization and reorganization of medical teams. While his reputation as a leader was well established before the pandemic hit, the way he rose to the many challenges over the past year has been truly remarkable. After he identified one of the first cases of COVID-19 in his hospital, Dr. Bruti’s leadership was evident. He ensured that his staff was wearing proper PPE, reorganized hospitalist staffing, coordinated onboarding of subspecialists, developed algorithms around testing, and created safety-driven patient transfer strategies.
He is a member of the Rush University Medical Center Medical Executive Committee and is the chair of its Medical Records Committee. He has been recognized by both Internal Medicine and Pediatrics clerkships multiple times for excellence in teaching.
Dr. Bruti became a member of SHM in 2014 and has been extremely active with the Chicago chapter. He has also served on the Quality Improvement and Pediatric Medicine Special Interest Groups.
Clinical Leadership for NPs & PAs
Krystle D. Apodaca, DNP, FHM
Dr. Krystle D. Apodaca is a nurse practitioner hospitalist at the University of New Mexico Hospital, where she is assistant professor of medicine within the university’s Clinician Education Track.
She was one of the first APPs welcomed into the UNM Hospital Medicine division and has been integral not only in the development of UNM’s APP program, but also its APP Hospital Medicine Fellowship, which she helped to cofound. She is a member of the UNM Hospital Medicine Executive Committee as well as its LGBTQ Collaborative.
She is known for her leadership within Project ECHO at UNM, a worldwide program focused on democratizing medical knowledge. She is the co–medical director of its National Nursing Home COVID-19 Safety and Medicaid Quality Improvement Hospitalization Avoidance efforts, both focused on improving nursing home practices. This program, in partnership with the Agency for Healthcare Research and Quality, UNM’s ECHO Institute, and the Institute for Healthcare Improvement, is now a national initiative dedicated to standardizing COVID-19 best practices at nursing homes across the country. To achieve its goals, more than 15,000 nursing homes have been certified and a community of more than 250 training centers has been built through Project ECHO.
Dr. Apodaca has been a member of SHM since 2015. She has been an active member of SHM’s NP/PA Special Interest Group since she joined and was appointed as the first APP president of SHM’s New Mexico chapter in April 2020. Under her leadership, the chapter achieved Gold and Platinum status as well as the Chapter of the Year Award. She is also a Fellow in Hospital Medicine.
Certificate of Leadership in Hospital Medicine
Mihir Patel, MD, MBA, MPH, CLHM, SFHM
The Certificate of Leadership in Hospital Medicine (CLHM) cultivates leadership skills in the context of specific hospital medicine challenges. This designation informs employers – or potential employers – with confidence that a candidate is equipped and ready to lead teams and grow an organization.
Dr. Mihir Patel serves as medical director of virtual medicine and a full-time hospitalist at Ballad Health in Johnson City, Tenn. He also works part time as a telehospitalist with Sound Physicians, covering multiple hospitals in California and Washington State. He has previously served in a number of administrative roles including medical director of hospitalist program, chief of staff, and director of medical informatics committee, in addition to working as hospitalist in both rural and urban hospitals. He is cofounder and president of the Blue Ridge Chapter of the Society of Hospital Medicine.
Dr. Mihir’s research and clinical interests focus on integration of telemedicine, electronic medical records, and principles of lean healthcare to reduce waste and cost of care while improving overall quality and safety.
Humanitarian Services
Eileen Barrett, MD, MPH, MACP, SFHM
Dr. Eileen Barrett is an internal medicine hospitalist at the University of New Mexico, where she also serves as associate professor of medicine and the director of Continuing Medical Education in the Office of Continuous Professional Learning.
In addition to current clinical and educational roles at UNM, Dr. Barrett has extensive leadership experience as the former director of Graduate Medical Education Wellness Initiatives, the current District 10 Chair of SHM, as chair of a multiorganizational Diversity Equity and Inclusion (DEI) Collaborative Task Force, and as a former regent of the American College of Physicians.
Her tremendous efforts in humanitarian services are reflected in her dedication to supporting communities in need. In 2015, Dr. Barrett traveled to Sierra Leone, where she served as an Ebola response clinician. There, she helped to develop safer care protocols, including initiating morning huddles, standardizing onboarding, and improving medication administration and documentation. These skills were developed while she worked for the Navajo Area Indian Health Service (including as an infection control consultant) for more than 9 years and in volunteering at the Myanmar-Thai border with refugees. Her work abroad helped support her training for directing UNM hospitalist COVID-19 Operations while also providing direct care.
Dr. Barrett has represented the specialty of hospital medicine both nationally and internationally. She has served on national committees and spoken from the perspective of an academic and community hospitalist leader on issues such as performance management, patient engagement, DEI, and professional fulfillment.
She has been a member of SHM since 2014 and has served as cochair of the three most recent Innovations Poster Competitions. Dr. Barrett is a former president of SHM’s New Mexico chapter where under her leadership the chapter received SHM’s Outstanding Chapter Award in 2018. She is a dedicated member of SHM’s Physicians in Training Committee and Chapter Support Committee. Dr. Barrett is an elected member of the Gold Humanism Honor Society, received a 2019 Exemplary Mentor Award from the American Medical Women’s Association, and is a Senior Fellow in Hospital Medicine.
Leadership for Practice Management
Leah Lleras, MS
Leah Lleras is the division administrator for the University of Colorado, Anschutz Medical Campus, and holds a Master of Science Management and Organization degree from the University of Colorado.
Her leadership as a practice manager is exemplified through her efforts in challenges of salary inequity. After joining the Division of Hospital Medicine in 2018, Ms. Lleras was successful in launching and achieving compensation equity and transparency across the department. She has demonstrated an incredible ability to collaborate with clinical leadership to marry the vision of clinical leaders with the administrative support required to turn a vision into a reality. During the COVID-19 pandemic, Ms. Lleras has been instrumental in ensuring that the division was prepared and supported to care for an influx of new patients. She did this by leading emergent onboarding of new practitioners, strategizing financial management of hazard pay for frontline clinicians, and creating a streamlined budget system during rapid change.
Ms. Lleras joined the Society in 2018 and has been an active member of the Rocky Mountain Chapter and the Hospital Medicine Administrator Special Interest Group.
Outstanding Service
Robert Zipper, MD, MMM, SFHM
Dr. Robert Zipper is a physician advisor and senior policy advisor for Sound Physicians, with more than 20 years of clinical experience as a hospital medicine leader.
He has a diverse background in quality and patient safety, hospitalist program design, and performance management. He began working as a hospitalist in 1999, in private practice. In 2006, he launched his career at Sound, where he began as a hospitalist but eventually managed Sound’s West Coast programs. In 2017, he was appointed Sound vice president of innovation technology. He later became Sound’s leader for healthcare policy, and now serves as a senior policy advisor for Sound, and physician advisor within the Advisory Services line.
Dr. Zipper has been a longtime supporter and advocate of SHM and the field of hospital medicine since joining in 2005. He attended his first Leadership Academy in 2006 and went on to serve as facilitator four times. His passion for SHM’s conferences is evident, as he has presented at three Annual Conferences alongside notable SHM leaders. He has been active in a variety of committees, including Quality and Safety, Leadership, and Performance Measurement and Reporting.
He is a member of the Society’s Public Policy Committee, and his insight has elevated hospital medicine both in the eyes of peer specialties and in discussions with the Centers for Medicare and Medicaid Services. Dr. Zipper has joined a number of calls with key Capitol Hill and CMS staff to help advocate for issues affecting hospital medicine. His ability to explain issues clearly and eloquently has helped stakeholders better understand the issues and move them forward on lawmakers’ agendas.
Research
S. Ryan Greysen, MD, MHS, SFHM
Dr. S. Ryan Greysen is chief of the Section of Hospital Medicine and associate professor at the University of Pennsylvania. He is the executive director for the Center for Evidence-based Practice (CEP) which serves all hospitals in the University of Pennsylvania Health System.
Dr. Greysen’s work comprises more than 80 peer-reviewed publications focused on improving outcomes of care for older adults during and after acute illness. Prior to arriving at Penn, he practiced at the University of California, San Francisco, where the impact of his work was extremely visible on the wards. He helped implement care pathways for an Acute Care for Elders (ACE) unit that uses evidence-based protocols and order sets to prevent functional decline and delirium of vulnerable seniors.
At Penn, he has continued to champion care for seniors and has supported other successful programs focused on vulnerable populations: SOAR (Supporting Older Adults at Risk), STEP (Supporting Transitions and Empowering Patients), and MED (Mental health Engagement navigation & Delivery).
During the COVID-19 pandemic, Dr. Greysen helped to accelerate the synthesis of emerging evidence through CEP and the Hospital Medicine Re-engineering Network (HOMERuN) to produce rapid evidence summaries in record speed. These reports have been broadly disseminated across other networks, such as AHRQ and the VA Evidence Synthesis Program.
Since joining the Society 10 years ago, Dr. Greysen has been an engaged member of SHM’s Greater Philadelphia Chapter and has held leadership roles on SHM’s Research Committee and the JHM Editorial Team as an associate editor. He has presented at multiple SHM annual conferences and is an ambassador of the specialty and of the importance of research in hospital medicine.
He is a Senior Fellow in Hospital Medicine.
Teaching
Grace C. Huang, MD
Dr. Grace C. Huang is an educator and hospitalist at Beth Israel Deaconess Medical Center and associate professor of medicine at Harvard Medical School who epitomizes commitment to education and lifelong learning.
Dr. Huang’s nationally recognized hospitalist expertise spans medical education and innovation, administrative management, and editorial leadership. She was among the early hospitalist pioneers who helped to transform how residents were trained to do procedures. Her early work led to the creation of one of the first procedure rotations for residents in the country – an RCT on central line simulation, the validation of a central line placement instrument, and a systematic review on procedural training for nonsurgeons.
Dr. Huang is vice chair for career development and mentoring in the department of medicine and oversees faculty development at the institutional level. She leads a Harvard Medical School–wide medical education fellowship for faculty and codirects the BIDMC Academy. On a broader scale, her efforts in the field have helped to catalyze the growth of computer-based simulation, define new standards for critical thinking education, and influence high-value care and invasive bedside procedure teaching approaches. Finally, she is editor-in-chief of MedEdPORTAL, an innovative journal of the Association of American Medical Colleges that publishes and disseminates educational resources.
Dr. Huang has been awarded the Gordon J. Strewler Mentoring of Resident Research Award in 2018, the Robert Stone Award for Excellence in Teaching Award, and most recently the A. Clifford Barger Excellence in Mentoring Award at Harvard Medical School, among many others. She is an editorial board member of Academic Medicine.
Dr. Huang joined SHM in 2010. Since then, she has been an engaged member of the Boston Chapter and has regularly participated in SHM’s annual conferences. She was also a member of SHM’s Practice Analysis Committee for 7 years.
Teamwork in Quality Improvement
Intermountain Healthcare
Intermountain Healthcare is a not-for-profit health system based in Salt Lake City serving the needs of patients primarily in Utah, Idaho, and Nevada. Intermountain recently reimagined its leadership structure with an integrated approach focused on developing and implementing common goals across its 23-hospital healthcare system, which was previously divided into regions. With key focus areas including communication, best practices, and goal setting, this structure has helped to combat former fragmentation struggles by creating an environment that provides a consistent high-level care experience regardless of the treatment center a patient selects.
With this reorganization came improved structure allowing for a unique team-based approach while still promoting clear communication lines across the 23 hospitals. This innovative Med/Surg Operations Lane allowed for flexible adaptation to the rapidly changing landscape of the COVID-19 pandemic. Intermountain Healthcare utilized its new framework to ensure crisis-ready operations by defining best practices through real-time literature review and teaming with ED, ICU, and Nursing to create COVID-19 workflows, order sets, and dashboards. Capacity issues were addressed with a variety of strategies: (1) daily systemwide huddles to facilitate load leveling between hospitals; (2) the use of telehealth for early discharges; and (3) remote patient monitoring and admission to the “Intermountain at Home” program, which preserved the ability to deliver critical surgical services.
This new value model clearly sets Intermountain apart from its peers.
Diversity
Lilia Cervantes, MD
Dr. Lilia Cervantes is associate professor in the department of medicine at Denver Health Medical Center and the University of Colorado, where she demonstrates an unparalleled commitment to diversity through her patient care, community service efforts, research, and health policy activism.
Following her internal medicine residency at the University of Colorado in 2008, Dr. Cervantes went on to obtain her master of science degree in clinical science, and became associate professor of medicine and a hospitalist at Denver Health Medical Center. In addition to her patient-centric roles at Denver Health, Dr. Cervantes has held a variety of roles in the health equity space. These include founding Denver Health Medical Center’s Health Equity Learning Series and the Healthcare Interest Program, a pre–health pipeline program for undergraduate students interested in a healthcare career.
Dr. Cervantes attributes her passion for becoming a physician to her background as a bilingual Latina who grew up in poverty. She says that her upbringing allows her to use this unique lens to connect with her diverse patient population and to advocate for marginalized communities and eliminate structural inequities.
Her experience with Hilda, an undocumented immigrant with kidney failure, was the catalyst for further research on marginalized patients without access to healthcare, which earned her interviews with NPR and CNN’s Chief Health Correspondent Dr. Sanjay Gupta. Her research and advocacy led to Colorado Medicaid’s expanding access to scheduled dialysis for undocumented immigrants with kidney failure. Upon announcement of the change, Dr. Cervantes was recognized as the driving force whose research informed the decision.
During the COVID-19 pandemic, Dr. Cervantes has worked diligently to launch research projects and create grant-funded programs to reduce the disproportionate burden of COVID-19 cases and deaths in the Latinx community in Denver. One of her studies centers on the Latinx community – through qualitative interviews of Latinx who had survived a COVID-19 hospitalization, Dr. Cervantes learned about the challenges faced during the pandemic. These findings informed local and national interventions to reduce COVID-19 in the Latinx community.
She has received numerous accolades, including the inaugural Outstanding Service to the Community in 2019 by Denver Health, the Florence Rena Sabin Award from the University of Colorado, and awards from the community – Health Equity Champion Award from the Center for Health Progress and the Unsung Heroine Award from the Latina First Foundation. She serves on several boards including two community-based organizations – the Center for Health Progress and Vuela for Health.
Dr. Cervantes has been an active member of SHM since 2009 and served as keynote speaker for the annual “Summit of the Rockies” Rocky Mountain Chapter SHM conference, “The role of advocacy: Moving the needle towards health equity.”
Junior Investigator Award
Matthew Pappas, MD, MPH, FHM
Dr. Matthew Pappas is a staff physician at the Cleveland Clinic, where he serves as assistant professor at the Lerner College of Medicine and Research Investigator at the Center for Value-Based Care Research.
Dr. Pappas completed his residency at the University of Michigan Health System and a postdoctoral fellowship with the VA Ann Arbor Healthcare System in 2016. Currently a hospitalist, he believes in addressing the tension between evidence-based and personal decisions, a fundamental hypothesis of his research career. As a Fellow, he created a model to predict the benefit of bridging anticoagulation for patients with atrial fibrillation. He sees his research mission as addressing the importance of these balanced decisions.
In 2019, Dr. Pappas secured a K08 award from the National Heart, Lung, and Blood Institute, and has turned his attention to preoperative cardiac testing and perioperative outcomes. He has published two manuscripts from this project, with a robust pipeline of others in progress.
He was recognized for his research by the Society of General Internal Medicine in 2018 with the Hamolsky Award for best abstract and had one of his research articles included in the Top 10 Articles of 2019 by the Journal of Hospital Medicine. Dr. Pappas has ongoing research support from the National Heart, Lung and Blood Institute.
He has been a member of SHM since 2015 and currently serves on the Perioperative Special Interest Group and Research Committee.
Clinical Leadership for Physicians
Christopher P. Bruti, MD, MPH
Dr. Christopher P. Bruti is the division chief of hospital medicine at Rush University and the program director of Rush’s combined Internal Medicine–Pediatrics Residency Program. He is an associate professor of internal medicine and pediatrics and practices as a hospitalist in both departments.
Dr. Bruti always rises to any challenge that comes his way with empathetic, organized, and insightful leadership. Dr. Bruti is known for his innovation in patient care and optimization practices in the hospital setting – from expanding and optimizing the nonteaching service and a high-functioning observation unit to geolocalization and reorganization of medical teams. While his reputation as a leader was well established before the pandemic hit, the way he rose to the many challenges over the past year has been truly remarkable. After he identified one of the first cases of COVID-19 in his hospital, Dr. Bruti’s leadership was evident. He ensured that his staff was wearing proper PPE, reorganized hospitalist staffing, coordinated onboarding of subspecialists, developed algorithms around testing, and created safety-driven patient transfer strategies.
He is a member of the Rush University Medical Center Medical Executive Committee and is the chair of its Medical Records Committee. He has been recognized by both Internal Medicine and Pediatrics clerkships multiple times for excellence in teaching.
Dr. Bruti became a member of SHM in 2014 and has been extremely active with the Chicago chapter. He has also served on the Quality Improvement and Pediatric Medicine Special Interest Groups.
Clinical Leadership for NPs & PAs
Krystle D. Apodaca, DNP, FHM
Dr. Krystle D. Apodaca is a nurse practitioner hospitalist at the University of New Mexico Hospital, where she is assistant professor of medicine within the university’s Clinician Education Track.
She was one of the first APPs welcomed into the UNM Hospital Medicine division and has been integral not only in the development of UNM’s APP program, but also its APP Hospital Medicine Fellowship, which she helped to cofound. She is a member of the UNM Hospital Medicine Executive Committee as well as its LGBTQ Collaborative.
She is known for her leadership within Project ECHO at UNM, a worldwide program focused on democratizing medical knowledge. She is the co–medical director of its National Nursing Home COVID-19 Safety and Medicaid Quality Improvement Hospitalization Avoidance efforts, both focused on improving nursing home practices. This program, in partnership with the Agency for Healthcare Research and Quality, UNM’s ECHO Institute, and the Institute for Healthcare Improvement, is now a national initiative dedicated to standardizing COVID-19 best practices at nursing homes across the country. To achieve its goals, more than 15,000 nursing homes have been certified and a community of more than 250 training centers has been built through Project ECHO.
Dr. Apodaca has been a member of SHM since 2015. She has been an active member of SHM’s NP/PA Special Interest Group since she joined and was appointed as the first APP president of SHM’s New Mexico chapter in April 2020. Under her leadership, the chapter achieved Gold and Platinum status as well as the Chapter of the Year Award. She is also a Fellow in Hospital Medicine.
Certificate of Leadership in Hospital Medicine
Mihir Patel, MD, MBA, MPH, CLHM, SFHM
The Certificate of Leadership in Hospital Medicine (CLHM) cultivates leadership skills in the context of specific hospital medicine challenges. This designation informs employers – or potential employers – with confidence that a candidate is equipped and ready to lead teams and grow an organization.
Dr. Mihir Patel serves as medical director of virtual medicine and a full-time hospitalist at Ballad Health in Johnson City, Tenn. He also works part time as a telehospitalist with Sound Physicians, covering multiple hospitals in California and Washington State. He has previously served in a number of administrative roles including medical director of hospitalist program, chief of staff, and director of medical informatics committee, in addition to working as hospitalist in both rural and urban hospitals. He is cofounder and president of the Blue Ridge Chapter of the Society of Hospital Medicine.
Dr. Mihir’s research and clinical interests focus on integration of telemedicine, electronic medical records, and principles of lean healthcare to reduce waste and cost of care while improving overall quality and safety.
Humanitarian Services
Eileen Barrett, MD, MPH, MACP, SFHM
Dr. Eileen Barrett is an internal medicine hospitalist at the University of New Mexico, where she also serves as associate professor of medicine and the director of Continuing Medical Education in the Office of Continuous Professional Learning.
In addition to current clinical and educational roles at UNM, Dr. Barrett has extensive leadership experience as the former director of Graduate Medical Education Wellness Initiatives, the current District 10 Chair of SHM, as chair of a multiorganizational Diversity Equity and Inclusion (DEI) Collaborative Task Force, and as a former regent of the American College of Physicians.
Her tremendous efforts in humanitarian services are reflected in her dedication to supporting communities in need. In 2015, Dr. Barrett traveled to Sierra Leone, where she served as an Ebola response clinician. There, she helped to develop safer care protocols, including initiating morning huddles, standardizing onboarding, and improving medication administration and documentation. These skills were developed while she worked for the Navajo Area Indian Health Service (including as an infection control consultant) for more than 9 years and in volunteering at the Myanmar-Thai border with refugees. Her work abroad helped support her training for directing UNM hospitalist COVID-19 Operations while also providing direct care.
Dr. Barrett has represented the specialty of hospital medicine both nationally and internationally. She has served on national committees and spoken from the perspective of an academic and community hospitalist leader on issues such as performance management, patient engagement, DEI, and professional fulfillment.
She has been a member of SHM since 2014 and has served as cochair of the three most recent Innovations Poster Competitions. Dr. Barrett is a former president of SHM’s New Mexico chapter where under her leadership the chapter received SHM’s Outstanding Chapter Award in 2018. She is a dedicated member of SHM’s Physicians in Training Committee and Chapter Support Committee. Dr. Barrett is an elected member of the Gold Humanism Honor Society, received a 2019 Exemplary Mentor Award from the American Medical Women’s Association, and is a Senior Fellow in Hospital Medicine.
Leadership for Practice Management
Leah Lleras, MS
Leah Lleras is the division administrator for the University of Colorado, Anschutz Medical Campus, and holds a Master of Science Management and Organization degree from the University of Colorado.
Her leadership as a practice manager is exemplified through her efforts in challenges of salary inequity. After joining the Division of Hospital Medicine in 2018, Ms. Lleras was successful in launching and achieving compensation equity and transparency across the department. She has demonstrated an incredible ability to collaborate with clinical leadership to marry the vision of clinical leaders with the administrative support required to turn a vision into a reality. During the COVID-19 pandemic, Ms. Lleras has been instrumental in ensuring that the division was prepared and supported to care for an influx of new patients. She did this by leading emergent onboarding of new practitioners, strategizing financial management of hazard pay for frontline clinicians, and creating a streamlined budget system during rapid change.
Ms. Lleras joined the Society in 2018 and has been an active member of the Rocky Mountain Chapter and the Hospital Medicine Administrator Special Interest Group.
Outstanding Service
Robert Zipper, MD, MMM, SFHM
Dr. Robert Zipper is a physician advisor and senior policy advisor for Sound Physicians, with more than 20 years of clinical experience as a hospital medicine leader.
He has a diverse background in quality and patient safety, hospitalist program design, and performance management. He began working as a hospitalist in 1999, in private practice. In 2006, he launched his career at Sound, where he began as a hospitalist but eventually managed Sound’s West Coast programs. In 2017, he was appointed Sound vice president of innovation technology. He later became Sound’s leader for healthcare policy, and now serves as a senior policy advisor for Sound, and physician advisor within the Advisory Services line.
Dr. Zipper has been a longtime supporter and advocate of SHM and the field of hospital medicine since joining in 2005. He attended his first Leadership Academy in 2006 and went on to serve as facilitator four times. His passion for SHM’s conferences is evident, as he has presented at three Annual Conferences alongside notable SHM leaders. He has been active in a variety of committees, including Quality and Safety, Leadership, and Performance Measurement and Reporting.
He is a member of the Society’s Public Policy Committee, and his insight has elevated hospital medicine both in the eyes of peer specialties and in discussions with the Centers for Medicare and Medicaid Services. Dr. Zipper has joined a number of calls with key Capitol Hill and CMS staff to help advocate for issues affecting hospital medicine. His ability to explain issues clearly and eloquently has helped stakeholders better understand the issues and move them forward on lawmakers’ agendas.
Research
S. Ryan Greysen, MD, MHS, SFHM
Dr. S. Ryan Greysen is chief of the Section of Hospital Medicine and associate professor at the University of Pennsylvania. He is the executive director for the Center for Evidence-based Practice (CEP) which serves all hospitals in the University of Pennsylvania Health System.
Dr. Greysen’s work comprises more than 80 peer-reviewed publications focused on improving outcomes of care for older adults during and after acute illness. Prior to arriving at Penn, he practiced at the University of California, San Francisco, where the impact of his work was extremely visible on the wards. He helped implement care pathways for an Acute Care for Elders (ACE) unit that uses evidence-based protocols and order sets to prevent functional decline and delirium of vulnerable seniors.
At Penn, he has continued to champion care for seniors and has supported other successful programs focused on vulnerable populations: SOAR (Supporting Older Adults at Risk), STEP (Supporting Transitions and Empowering Patients), and MED (Mental health Engagement navigation & Delivery).
During the COVID-19 pandemic, Dr. Greysen helped to accelerate the synthesis of emerging evidence through CEP and the Hospital Medicine Re-engineering Network (HOMERuN) to produce rapid evidence summaries in record speed. These reports have been broadly disseminated across other networks, such as AHRQ and the VA Evidence Synthesis Program.
Since joining the Society 10 years ago, Dr. Greysen has been an engaged member of SHM’s Greater Philadelphia Chapter and has held leadership roles on SHM’s Research Committee and the JHM Editorial Team as an associate editor. He has presented at multiple SHM annual conferences and is an ambassador of the specialty and of the importance of research in hospital medicine.
He is a Senior Fellow in Hospital Medicine.
Teaching
Grace C. Huang, MD
Dr. Grace C. Huang is an educator and hospitalist at Beth Israel Deaconess Medical Center and associate professor of medicine at Harvard Medical School who epitomizes commitment to education and lifelong learning.
Dr. Huang’s nationally recognized hospitalist expertise spans medical education and innovation, administrative management, and editorial leadership. She was among the early hospitalist pioneers who helped to transform how residents were trained to do procedures. Her early work led to the creation of one of the first procedure rotations for residents in the country – an RCT on central line simulation, the validation of a central line placement instrument, and a systematic review on procedural training for nonsurgeons.
Dr. Huang is vice chair for career development and mentoring in the department of medicine and oversees faculty development at the institutional level. She leads a Harvard Medical School–wide medical education fellowship for faculty and codirects the BIDMC Academy. On a broader scale, her efforts in the field have helped to catalyze the growth of computer-based simulation, define new standards for critical thinking education, and influence high-value care and invasive bedside procedure teaching approaches. Finally, she is editor-in-chief of MedEdPORTAL, an innovative journal of the Association of American Medical Colleges that publishes and disseminates educational resources.
Dr. Huang has been awarded the Gordon J. Strewler Mentoring of Resident Research Award in 2018, the Robert Stone Award for Excellence in Teaching Award, and most recently the A. Clifford Barger Excellence in Mentoring Award at Harvard Medical School, among many others. She is an editorial board member of Academic Medicine.
Dr. Huang joined SHM in 2010. Since then, she has been an engaged member of the Boston Chapter and has regularly participated in SHM’s annual conferences. She was also a member of SHM’s Practice Analysis Committee for 7 years.
Teamwork in Quality Improvement
Intermountain Healthcare
Intermountain Healthcare is a not-for-profit health system based in Salt Lake City serving the needs of patients primarily in Utah, Idaho, and Nevada. Intermountain recently reimagined its leadership structure with an integrated approach focused on developing and implementing common goals across its 23-hospital healthcare system, which was previously divided into regions. With key focus areas including communication, best practices, and goal setting, this structure has helped to combat former fragmentation struggles by creating an environment that provides a consistent high-level care experience regardless of the treatment center a patient selects.
With this reorganization came improved structure allowing for a unique team-based approach while still promoting clear communication lines across the 23 hospitals. This innovative Med/Surg Operations Lane allowed for flexible adaptation to the rapidly changing landscape of the COVID-19 pandemic. Intermountain Healthcare utilized its new framework to ensure crisis-ready operations by defining best practices through real-time literature review and teaming with ED, ICU, and Nursing to create COVID-19 workflows, order sets, and dashboards. Capacity issues were addressed with a variety of strategies: (1) daily systemwide huddles to facilitate load leveling between hospitals; (2) the use of telehealth for early discharges; and (3) remote patient monitoring and admission to the “Intermountain at Home” program, which preserved the ability to deliver critical surgical services.
This new value model clearly sets Intermountain apart from its peers.
Diversity
Lilia Cervantes, MD
Dr. Lilia Cervantes is associate professor in the department of medicine at Denver Health Medical Center and the University of Colorado, where she demonstrates an unparalleled commitment to diversity through her patient care, community service efforts, research, and health policy activism.
Following her internal medicine residency at the University of Colorado in 2008, Dr. Cervantes went on to obtain her master of science degree in clinical science, and became associate professor of medicine and a hospitalist at Denver Health Medical Center. In addition to her patient-centric roles at Denver Health, Dr. Cervantes has held a variety of roles in the health equity space. These include founding Denver Health Medical Center’s Health Equity Learning Series and the Healthcare Interest Program, a pre–health pipeline program for undergraduate students interested in a healthcare career.
Dr. Cervantes attributes her passion for becoming a physician to her background as a bilingual Latina who grew up in poverty. She says that her upbringing allows her to use this unique lens to connect with her diverse patient population and to advocate for marginalized communities and eliminate structural inequities.
Her experience with Hilda, an undocumented immigrant with kidney failure, was the catalyst for further research on marginalized patients without access to healthcare, which earned her interviews with NPR and CNN’s Chief Health Correspondent Dr. Sanjay Gupta. Her research and advocacy led to Colorado Medicaid’s expanding access to scheduled dialysis for undocumented immigrants with kidney failure. Upon announcement of the change, Dr. Cervantes was recognized as the driving force whose research informed the decision.
During the COVID-19 pandemic, Dr. Cervantes has worked diligently to launch research projects and create grant-funded programs to reduce the disproportionate burden of COVID-19 cases and deaths in the Latinx community in Denver. One of her studies centers on the Latinx community – through qualitative interviews of Latinx who had survived a COVID-19 hospitalization, Dr. Cervantes learned about the challenges faced during the pandemic. These findings informed local and national interventions to reduce COVID-19 in the Latinx community.
She has received numerous accolades, including the inaugural Outstanding Service to the Community in 2019 by Denver Health, the Florence Rena Sabin Award from the University of Colorado, and awards from the community – Health Equity Champion Award from the Center for Health Progress and the Unsung Heroine Award from the Latina First Foundation. She serves on several boards including two community-based organizations – the Center for Health Progress and Vuela for Health.
Dr. Cervantes has been an active member of SHM since 2009 and served as keynote speaker for the annual “Summit of the Rockies” Rocky Mountain Chapter SHM conference, “The role of advocacy: Moving the needle towards health equity.”
Junior Investigator Award
Matthew Pappas, MD, MPH, FHM
Dr. Matthew Pappas is a staff physician at the Cleveland Clinic, where he serves as assistant professor at the Lerner College of Medicine and Research Investigator at the Center for Value-Based Care Research.
Dr. Pappas completed his residency at the University of Michigan Health System and a postdoctoral fellowship with the VA Ann Arbor Healthcare System in 2016. Currently a hospitalist, he believes in addressing the tension between evidence-based and personal decisions, a fundamental hypothesis of his research career. As a Fellow, he created a model to predict the benefit of bridging anticoagulation for patients with atrial fibrillation. He sees his research mission as addressing the importance of these balanced decisions.
In 2019, Dr. Pappas secured a K08 award from the National Heart, Lung, and Blood Institute, and has turned his attention to preoperative cardiac testing and perioperative outcomes. He has published two manuscripts from this project, with a robust pipeline of others in progress.
He was recognized for his research by the Society of General Internal Medicine in 2018 with the Hamolsky Award for best abstract and had one of his research articles included in the Top 10 Articles of 2019 by the Journal of Hospital Medicine. Dr. Pappas has ongoing research support from the National Heart, Lung and Blood Institute.
He has been a member of SHM since 2015 and currently serves on the Perioperative Special Interest Group and Research Committee.
Clinical Leadership for Physicians
Christopher P. Bruti, MD, MPH
Dr. Christopher P. Bruti is the division chief of hospital medicine at Rush University and the program director of Rush’s combined Internal Medicine–Pediatrics Residency Program. He is an associate professor of internal medicine and pediatrics and practices as a hospitalist in both departments.
Dr. Bruti always rises to any challenge that comes his way with empathetic, organized, and insightful leadership. Dr. Bruti is known for his innovation in patient care and optimization practices in the hospital setting – from expanding and optimizing the nonteaching service and a high-functioning observation unit to geolocalization and reorganization of medical teams. While his reputation as a leader was well established before the pandemic hit, the way he rose to the many challenges over the past year has been truly remarkable. After he identified one of the first cases of COVID-19 in his hospital, Dr. Bruti’s leadership was evident. He ensured that his staff was wearing proper PPE, reorganized hospitalist staffing, coordinated onboarding of subspecialists, developed algorithms around testing, and created safety-driven patient transfer strategies.
He is a member of the Rush University Medical Center Medical Executive Committee and is the chair of its Medical Records Committee. He has been recognized by both Internal Medicine and Pediatrics clerkships multiple times for excellence in teaching.
Dr. Bruti became a member of SHM in 2014 and has been extremely active with the Chicago chapter. He has also served on the Quality Improvement and Pediatric Medicine Special Interest Groups.
Clinical Leadership for NPs & PAs
Krystle D. Apodaca, DNP, FHM
Dr. Krystle D. Apodaca is a nurse practitioner hospitalist at the University of New Mexico Hospital, where she is assistant professor of medicine within the university’s Clinician Education Track.
She was one of the first APPs welcomed into the UNM Hospital Medicine division and has been integral not only in the development of UNM’s APP program, but also its APP Hospital Medicine Fellowship, which she helped to cofound. She is a member of the UNM Hospital Medicine Executive Committee as well as its LGBTQ Collaborative.
She is known for her leadership within Project ECHO at UNM, a worldwide program focused on democratizing medical knowledge. She is the co–medical director of its National Nursing Home COVID-19 Safety and Medicaid Quality Improvement Hospitalization Avoidance efforts, both focused on improving nursing home practices. This program, in partnership with the Agency for Healthcare Research and Quality, UNM’s ECHO Institute, and the Institute for Healthcare Improvement, is now a national initiative dedicated to standardizing COVID-19 best practices at nursing homes across the country. To achieve its goals, more than 15,000 nursing homes have been certified and a community of more than 250 training centers has been built through Project ECHO.
Dr. Apodaca has been a member of SHM since 2015. She has been an active member of SHM’s NP/PA Special Interest Group since she joined and was appointed as the first APP president of SHM’s New Mexico chapter in April 2020. Under her leadership, the chapter achieved Gold and Platinum status as well as the Chapter of the Year Award. She is also a Fellow in Hospital Medicine.
Certificate of Leadership in Hospital Medicine
Mihir Patel, MD, MBA, MPH, CLHM, SFHM
The Certificate of Leadership in Hospital Medicine (CLHM) cultivates leadership skills in the context of specific hospital medicine challenges. This designation informs employers – or potential employers – with confidence that a candidate is equipped and ready to lead teams and grow an organization.
Dr. Mihir Patel serves as medical director of virtual medicine and a full-time hospitalist at Ballad Health in Johnson City, Tenn. He also works part time as a telehospitalist with Sound Physicians, covering multiple hospitals in California and Washington State. He has previously served in a number of administrative roles including medical director of hospitalist program, chief of staff, and director of medical informatics committee, in addition to working as hospitalist in both rural and urban hospitals. He is cofounder and president of the Blue Ridge Chapter of the Society of Hospital Medicine.
Dr. Mihir’s research and clinical interests focus on integration of telemedicine, electronic medical records, and principles of lean healthcare to reduce waste and cost of care while improving overall quality and safety.
Humanitarian Services
Eileen Barrett, MD, MPH, MACP, SFHM
Dr. Eileen Barrett is an internal medicine hospitalist at the University of New Mexico, where she also serves as associate professor of medicine and the director of Continuing Medical Education in the Office of Continuous Professional Learning.
In addition to current clinical and educational roles at UNM, Dr. Barrett has extensive leadership experience as the former director of Graduate Medical Education Wellness Initiatives, the current District 10 Chair of SHM, as chair of a multiorganizational Diversity Equity and Inclusion (DEI) Collaborative Task Force, and as a former regent of the American College of Physicians.
Her tremendous efforts in humanitarian services are reflected in her dedication to supporting communities in need. In 2015, Dr. Barrett traveled to Sierra Leone, where she served as an Ebola response clinician. There, she helped to develop safer care protocols, including initiating morning huddles, standardizing onboarding, and improving medication administration and documentation. These skills were developed while she worked for the Navajo Area Indian Health Service (including as an infection control consultant) for more than 9 years and in volunteering at the Myanmar-Thai border with refugees. Her work abroad helped support her training for directing UNM hospitalist COVID-19 Operations while also providing direct care.
Dr. Barrett has represented the specialty of hospital medicine both nationally and internationally. She has served on national committees and spoken from the perspective of an academic and community hospitalist leader on issues such as performance management, patient engagement, DEI, and professional fulfillment.
She has been a member of SHM since 2014 and has served as cochair of the three most recent Innovations Poster Competitions. Dr. Barrett is a former president of SHM’s New Mexico chapter where under her leadership the chapter received SHM’s Outstanding Chapter Award in 2018. She is a dedicated member of SHM’s Physicians in Training Committee and Chapter Support Committee. Dr. Barrett is an elected member of the Gold Humanism Honor Society, received a 2019 Exemplary Mentor Award from the American Medical Women’s Association, and is a Senior Fellow in Hospital Medicine.
Leadership for Practice Management
Leah Lleras, MS
Leah Lleras is the division administrator for the University of Colorado, Anschutz Medical Campus, and holds a Master of Science Management and Organization degree from the University of Colorado.
Her leadership as a practice manager is exemplified through her efforts in challenges of salary inequity. After joining the Division of Hospital Medicine in 2018, Ms. Lleras was successful in launching and achieving compensation equity and transparency across the department. She has demonstrated an incredible ability to collaborate with clinical leadership to marry the vision of clinical leaders with the administrative support required to turn a vision into a reality. During the COVID-19 pandemic, Ms. Lleras has been instrumental in ensuring that the division was prepared and supported to care for an influx of new patients. She did this by leading emergent onboarding of new practitioners, strategizing financial management of hazard pay for frontline clinicians, and creating a streamlined budget system during rapid change.
Ms. Lleras joined the Society in 2018 and has been an active member of the Rocky Mountain Chapter and the Hospital Medicine Administrator Special Interest Group.
Outstanding Service
Robert Zipper, MD, MMM, SFHM
Dr. Robert Zipper is a physician advisor and senior policy advisor for Sound Physicians, with more than 20 years of clinical experience as a hospital medicine leader.
He has a diverse background in quality and patient safety, hospitalist program design, and performance management. He began working as a hospitalist in 1999, in private practice. In 2006, he launched his career at Sound, where he began as a hospitalist but eventually managed Sound’s West Coast programs. In 2017, he was appointed Sound vice president of innovation technology. He later became Sound’s leader for healthcare policy, and now serves as a senior policy advisor for Sound, and physician advisor within the Advisory Services line.
Dr. Zipper has been a longtime supporter and advocate of SHM and the field of hospital medicine since joining in 2005. He attended his first Leadership Academy in 2006 and went on to serve as facilitator four times. His passion for SHM’s conferences is evident, as he has presented at three Annual Conferences alongside notable SHM leaders. He has been active in a variety of committees, including Quality and Safety, Leadership, and Performance Measurement and Reporting.
He is a member of the Society’s Public Policy Committee, and his insight has elevated hospital medicine both in the eyes of peer specialties and in discussions with the Centers for Medicare and Medicaid Services. Dr. Zipper has joined a number of calls with key Capitol Hill and CMS staff to help advocate for issues affecting hospital medicine. His ability to explain issues clearly and eloquently has helped stakeholders better understand the issues and move them forward on lawmakers’ agendas.
Research
S. Ryan Greysen, MD, MHS, SFHM
Dr. S. Ryan Greysen is chief of the Section of Hospital Medicine and associate professor at the University of Pennsylvania. He is the executive director for the Center for Evidence-based Practice (CEP) which serves all hospitals in the University of Pennsylvania Health System.
Dr. Greysen’s work comprises more than 80 peer-reviewed publications focused on improving outcomes of care for older adults during and after acute illness. Prior to arriving at Penn, he practiced at the University of California, San Francisco, where the impact of his work was extremely visible on the wards. He helped implement care pathways for an Acute Care for Elders (ACE) unit that uses evidence-based protocols and order sets to prevent functional decline and delirium of vulnerable seniors.
At Penn, he has continued to champion care for seniors and has supported other successful programs focused on vulnerable populations: SOAR (Supporting Older Adults at Risk), STEP (Supporting Transitions and Empowering Patients), and MED (Mental health Engagement navigation & Delivery).
During the COVID-19 pandemic, Dr. Greysen helped to accelerate the synthesis of emerging evidence through CEP and the Hospital Medicine Re-engineering Network (HOMERuN) to produce rapid evidence summaries in record speed. These reports have been broadly disseminated across other networks, such as AHRQ and the VA Evidence Synthesis Program.
Since joining the Society 10 years ago, Dr. Greysen has been an engaged member of SHM’s Greater Philadelphia Chapter and has held leadership roles on SHM’s Research Committee and the JHM Editorial Team as an associate editor. He has presented at multiple SHM annual conferences and is an ambassador of the specialty and of the importance of research in hospital medicine.
He is a Senior Fellow in Hospital Medicine.
Teaching
Grace C. Huang, MD
Dr. Grace C. Huang is an educator and hospitalist at Beth Israel Deaconess Medical Center and associate professor of medicine at Harvard Medical School who epitomizes commitment to education and lifelong learning.
Dr. Huang’s nationally recognized hospitalist expertise spans medical education and innovation, administrative management, and editorial leadership. She was among the early hospitalist pioneers who helped to transform how residents were trained to do procedures. Her early work led to the creation of one of the first procedure rotations for residents in the country – an RCT on central line simulation, the validation of a central line placement instrument, and a systematic review on procedural training for nonsurgeons.
Dr. Huang is vice chair for career development and mentoring in the department of medicine and oversees faculty development at the institutional level. She leads a Harvard Medical School–wide medical education fellowship for faculty and codirects the BIDMC Academy. On a broader scale, her efforts in the field have helped to catalyze the growth of computer-based simulation, define new standards for critical thinking education, and influence high-value care and invasive bedside procedure teaching approaches. Finally, she is editor-in-chief of MedEdPORTAL, an innovative journal of the Association of American Medical Colleges that publishes and disseminates educational resources.
Dr. Huang has been awarded the Gordon J. Strewler Mentoring of Resident Research Award in 2018, the Robert Stone Award for Excellence in Teaching Award, and most recently the A. Clifford Barger Excellence in Mentoring Award at Harvard Medical School, among many others. She is an editorial board member of Academic Medicine.
Dr. Huang joined SHM in 2010. Since then, she has been an engaged member of the Boston Chapter and has regularly participated in SHM’s annual conferences. She was also a member of SHM’s Practice Analysis Committee for 7 years.
Teamwork in Quality Improvement
Intermountain Healthcare
Intermountain Healthcare is a not-for-profit health system based in Salt Lake City serving the needs of patients primarily in Utah, Idaho, and Nevada. Intermountain recently reimagined its leadership structure with an integrated approach focused on developing and implementing common goals across its 23-hospital healthcare system, which was previously divided into regions. With key focus areas including communication, best practices, and goal setting, this structure has helped to combat former fragmentation struggles by creating an environment that provides a consistent high-level care experience regardless of the treatment center a patient selects.
With this reorganization came improved structure allowing for a unique team-based approach while still promoting clear communication lines across the 23 hospitals. This innovative Med/Surg Operations Lane allowed for flexible adaptation to the rapidly changing landscape of the COVID-19 pandemic. Intermountain Healthcare utilized its new framework to ensure crisis-ready operations by defining best practices through real-time literature review and teaming with ED, ICU, and Nursing to create COVID-19 workflows, order sets, and dashboards. Capacity issues were addressed with a variety of strategies: (1) daily systemwide huddles to facilitate load leveling between hospitals; (2) the use of telehealth for early discharges; and (3) remote patient monitoring and admission to the “Intermountain at Home” program, which preserved the ability to deliver critical surgical services.
This new value model clearly sets Intermountain apart from its peers.
Diversity
Lilia Cervantes, MD
Dr. Lilia Cervantes is associate professor in the department of medicine at Denver Health Medical Center and the University of Colorado, where she demonstrates an unparalleled commitment to diversity through her patient care, community service efforts, research, and health policy activism.
Following her internal medicine residency at the University of Colorado in 2008, Dr. Cervantes went on to obtain her master of science degree in clinical science, and became associate professor of medicine and a hospitalist at Denver Health Medical Center. In addition to her patient-centric roles at Denver Health, Dr. Cervantes has held a variety of roles in the health equity space. These include founding Denver Health Medical Center’s Health Equity Learning Series and the Healthcare Interest Program, a pre–health pipeline program for undergraduate students interested in a healthcare career.
Dr. Cervantes attributes her passion for becoming a physician to her background as a bilingual Latina who grew up in poverty. She says that her upbringing allows her to use this unique lens to connect with her diverse patient population and to advocate for marginalized communities and eliminate structural inequities.
Her experience with Hilda, an undocumented immigrant with kidney failure, was the catalyst for further research on marginalized patients without access to healthcare, which earned her interviews with NPR and CNN’s Chief Health Correspondent Dr. Sanjay Gupta. Her research and advocacy led to Colorado Medicaid’s expanding access to scheduled dialysis for undocumented immigrants with kidney failure. Upon announcement of the change, Dr. Cervantes was recognized as the driving force whose research informed the decision.
During the COVID-19 pandemic, Dr. Cervantes has worked diligently to launch research projects and create grant-funded programs to reduce the disproportionate burden of COVID-19 cases and deaths in the Latinx community in Denver. One of her studies centers on the Latinx community – through qualitative interviews of Latinx who had survived a COVID-19 hospitalization, Dr. Cervantes learned about the challenges faced during the pandemic. These findings informed local and national interventions to reduce COVID-19 in the Latinx community.
She has received numerous accolades, including the inaugural Outstanding Service to the Community in 2019 by Denver Health, the Florence Rena Sabin Award from the University of Colorado, and awards from the community – Health Equity Champion Award from the Center for Health Progress and the Unsung Heroine Award from the Latina First Foundation. She serves on several boards including two community-based organizations – the Center for Health Progress and Vuela for Health.
Dr. Cervantes has been an active member of SHM since 2009 and served as keynote speaker for the annual “Summit of the Rockies” Rocky Mountain Chapter SHM conference, “The role of advocacy: Moving the needle towards health equity.”
Junior Investigator Award
Matthew Pappas, MD, MPH, FHM
Dr. Matthew Pappas is a staff physician at the Cleveland Clinic, where he serves as assistant professor at the Lerner College of Medicine and Research Investigator at the Center for Value-Based Care Research.
Dr. Pappas completed his residency at the University of Michigan Health System and a postdoctoral fellowship with the VA Ann Arbor Healthcare System in 2016. Currently a hospitalist, he believes in addressing the tension between evidence-based and personal decisions, a fundamental hypothesis of his research career. As a Fellow, he created a model to predict the benefit of bridging anticoagulation for patients with atrial fibrillation. He sees his research mission as addressing the importance of these balanced decisions.
In 2019, Dr. Pappas secured a K08 award from the National Heart, Lung, and Blood Institute, and has turned his attention to preoperative cardiac testing and perioperative outcomes. He has published two manuscripts from this project, with a robust pipeline of others in progress.
He was recognized for his research by the Society of General Internal Medicine in 2018 with the Hamolsky Award for best abstract and had one of his research articles included in the Top 10 Articles of 2019 by the Journal of Hospital Medicine. Dr. Pappas has ongoing research support from the National Heart, Lung and Blood Institute.
He has been a member of SHM since 2015 and currently serves on the Perioperative Special Interest Group and Research Committee.
FROM SHM CONVERGE 2021
Wellness tips: How to build on failure
Converge 2021 session
Fall Down Seven Get Up Eight: Making Your Setbacks Count: Strategic Risk Taking, Maintaining Resilience, and Finding Success
Presenters
Marisha Burden, MD, and Flora Kisuule, MD, MPH, SFHM
Session summary
The speakers at this Converge session, in the “Wellness and Resilience” track, covered four major topics: strategic risk-taking, wrestling with failure, embracing constraints, and embracing institutional chaos. First, they began by relating a personal story about failure and discussed how reframing failure could help you learn how to “fail forward.” They outlined how building upon failures can lead to many benefits, such as gaining personal strength, gaining perspective, and seeing new possibilities. They also introduced three roadblocks to failing forward: Personalization, Pervasiveness, and Permanence.
Next, the speakers lead the attendees through an exercise called The Nine Dot Problem, the purpose of which was to illustrate how thinking outside the box can help you find solutions that you cannot otherwise see. They also discussed how thinking inside the box could have its own advantages in that it teaches us to embrace our limitations, which can open up our creativity. They expounded upon this by showing a TED talk about finding liberation in constraints. The speakers wrapped up the session relating the tale of David and Goliath, and explained how David used his own unique advantages to gain power over a seemingly insurmountable problem.
Key takeaways
- Failing forward helps you continue to push ahead and grow, and perspective can help you fail forward.
- When failing, beware the Three Ps.
- Reframe constraints and be sure to think both inside and outside of the box – embrace limitations as a way to inspire new thinking.
- When facing something bigger than you, play to your own advantages in order to succeed.
Ms. Panek is hospital medicine division administrator at the Johns Hopkins Bayview Medical Center, Baltimore.
Converge 2021 session
Fall Down Seven Get Up Eight: Making Your Setbacks Count: Strategic Risk Taking, Maintaining Resilience, and Finding Success
Presenters
Marisha Burden, MD, and Flora Kisuule, MD, MPH, SFHM
Session summary
The speakers at this Converge session, in the “Wellness and Resilience” track, covered four major topics: strategic risk-taking, wrestling with failure, embracing constraints, and embracing institutional chaos. First, they began by relating a personal story about failure and discussed how reframing failure could help you learn how to “fail forward.” They outlined how building upon failures can lead to many benefits, such as gaining personal strength, gaining perspective, and seeing new possibilities. They also introduced three roadblocks to failing forward: Personalization, Pervasiveness, and Permanence.
Next, the speakers lead the attendees through an exercise called The Nine Dot Problem, the purpose of which was to illustrate how thinking outside the box can help you find solutions that you cannot otherwise see. They also discussed how thinking inside the box could have its own advantages in that it teaches us to embrace our limitations, which can open up our creativity. They expounded upon this by showing a TED talk about finding liberation in constraints. The speakers wrapped up the session relating the tale of David and Goliath, and explained how David used his own unique advantages to gain power over a seemingly insurmountable problem.
Key takeaways
- Failing forward helps you continue to push ahead and grow, and perspective can help you fail forward.
- When failing, beware the Three Ps.
- Reframe constraints and be sure to think both inside and outside of the box – embrace limitations as a way to inspire new thinking.
- When facing something bigger than you, play to your own advantages in order to succeed.
Ms. Panek is hospital medicine division administrator at the Johns Hopkins Bayview Medical Center, Baltimore.
Converge 2021 session
Fall Down Seven Get Up Eight: Making Your Setbacks Count: Strategic Risk Taking, Maintaining Resilience, and Finding Success
Presenters
Marisha Burden, MD, and Flora Kisuule, MD, MPH, SFHM
Session summary
The speakers at this Converge session, in the “Wellness and Resilience” track, covered four major topics: strategic risk-taking, wrestling with failure, embracing constraints, and embracing institutional chaos. First, they began by relating a personal story about failure and discussed how reframing failure could help you learn how to “fail forward.” They outlined how building upon failures can lead to many benefits, such as gaining personal strength, gaining perspective, and seeing new possibilities. They also introduced three roadblocks to failing forward: Personalization, Pervasiveness, and Permanence.
Next, the speakers lead the attendees through an exercise called The Nine Dot Problem, the purpose of which was to illustrate how thinking outside the box can help you find solutions that you cannot otherwise see. They also discussed how thinking inside the box could have its own advantages in that it teaches us to embrace our limitations, which can open up our creativity. They expounded upon this by showing a TED talk about finding liberation in constraints. The speakers wrapped up the session relating the tale of David and Goliath, and explained how David used his own unique advantages to gain power over a seemingly insurmountable problem.
Key takeaways
- Failing forward helps you continue to push ahead and grow, and perspective can help you fail forward.
- When failing, beware the Three Ps.
- Reframe constraints and be sure to think both inside and outside of the box – embrace limitations as a way to inspire new thinking.
- When facing something bigger than you, play to your own advantages in order to succeed.
Ms. Panek is hospital medicine division administrator at the Johns Hopkins Bayview Medical Center, Baltimore.
FROM SHM CONVERGE 2021