User login
Happy National Hospitalist Day!
Hospitalists across the United States have been and continue to be a critical part of our nation’s response to COVID-19. On National Hospitalist Day, Thursday, March 4, 2021, the Society of Hospital Medicine invites you to celebrate the individuals and teams that make up the hospital medicine community.

On this special day, SHM encourages you to share your story, showcase your team’s efforts to improve patient care, express your pride for the specialty, or share how you are making a difference in your hospital and in the lives of patients.
Here are just a few of the ways you can celebrate:
- Register for our live roundtable, featuring Mark Shapiro, MD, hospitalist and host of the Explore the Space podcast, and four hospitalist panelists, on March 4 at 7 p.m. ET/4 p.m. PT.
- Download shareable graphics, posters, Zoom backgrounds, and coloring book pages
- Enter our social media photo contest and follow the #HowWeHospitalist hashtag across all platforms
- Read special hospitalist profiles in the Hospitalist, including: Eric E. Howell, MD, MHM; Grace Huang, MD; Bridget McGrath, PA-C, FHM; and Harry Cho, MD, SFHM
Thank you for all you do and continue to do for hospital medicine. We hope you take some time today to celebrate you and your colleagues, as well as your commendable contributions to health care and the future of the specialty.
To learn more about National Hospitalist Day, visit hospitalmedicine.org/hospitalistday.
Hospitalists across the United States have been and continue to be a critical part of our nation’s response to COVID-19. On National Hospitalist Day, Thursday, March 4, 2021, the Society of Hospital Medicine invites you to celebrate the individuals and teams that make up the hospital medicine community.

On this special day, SHM encourages you to share your story, showcase your team’s efforts to improve patient care, express your pride for the specialty, or share how you are making a difference in your hospital and in the lives of patients.
Here are just a few of the ways you can celebrate:
- Register for our live roundtable, featuring Mark Shapiro, MD, hospitalist and host of the Explore the Space podcast, and four hospitalist panelists, on March 4 at 7 p.m. ET/4 p.m. PT.
- Download shareable graphics, posters, Zoom backgrounds, and coloring book pages
- Enter our social media photo contest and follow the #HowWeHospitalist hashtag across all platforms
- Read special hospitalist profiles in the Hospitalist, including: Eric E. Howell, MD, MHM; Grace Huang, MD; Bridget McGrath, PA-C, FHM; and Harry Cho, MD, SFHM
Thank you for all you do and continue to do for hospital medicine. We hope you take some time today to celebrate you and your colleagues, as well as your commendable contributions to health care and the future of the specialty.
To learn more about National Hospitalist Day, visit hospitalmedicine.org/hospitalistday.
Hospitalists across the United States have been and continue to be a critical part of our nation’s response to COVID-19. On National Hospitalist Day, Thursday, March 4, 2021, the Society of Hospital Medicine invites you to celebrate the individuals and teams that make up the hospital medicine community.

On this special day, SHM encourages you to share your story, showcase your team’s efforts to improve patient care, express your pride for the specialty, or share how you are making a difference in your hospital and in the lives of patients.
Here are just a few of the ways you can celebrate:
- Register for our live roundtable, featuring Mark Shapiro, MD, hospitalist and host of the Explore the Space podcast, and four hospitalist panelists, on March 4 at 7 p.m. ET/4 p.m. PT.
- Download shareable graphics, posters, Zoom backgrounds, and coloring book pages
- Enter our social media photo contest and follow the #HowWeHospitalist hashtag across all platforms
- Read special hospitalist profiles in the Hospitalist, including: Eric E. Howell, MD, MHM; Grace Huang, MD; Bridget McGrath, PA-C, FHM; and Harry Cho, MD, SFHM
Thank you for all you do and continue to do for hospital medicine. We hope you take some time today to celebrate you and your colleagues, as well as your commendable contributions to health care and the future of the specialty.
To learn more about National Hospitalist Day, visit hospitalmedicine.org/hospitalistday.
A ‘hospitalist plus’: Grace C. Huang, MD
Editor’s note: This profile is part of SHM’s celebration of National Hospitalist Day on March 4. National Hospitalist Day occurs the first Thursday in March annually, and celebrates the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
Grace C. Huang, MD, is a hospitalist at Beth Israel Deaconess Medical Center and an associate professor of medicine at Harvard Medical School, both in Boston.
Dr. Huang currently serves as vice chair for career development and mentoring in the department of medicine at Beth Israel Deaconess as well as director of the Office of Academic Careers and Faculty Development, and codirector of the Beth Israel Deaconess Academy of Medical Educators. She is also director of the Rabkin Fellowship in Medical Education, a program for Harvard Medical School faculty designed to help develop the skills needed to launch or advance academic careers in medical education or academic leadership.
Additionally, Dr. Huang is the editor in chief of MedEdPORTAL, a MEDLINE-indexed, open-access journal of the Association of American Medical Colleges.
At what point in your training did you decide to practice hospital medicine, and what about it appealed to you?
I trained at a point in time where it was rare for people to aspire to go in to hospital medicine. It just wasn’t that common, and there were so few examples of what a career trajectory in hospital medicine would look like. So I don’t know that I actively chose to go into hospital medicine; I chose it because it was what I knew how to do, based on my residency experience.
But it is really easy and authentic for me now to share about what makes hospital medicine such a vibrant career choice. I’m doing a lot of things in my job other than hospital medicine, but when I am on service, it reminds me acutely what it means to stay connected to why I became a doctor. The practice of hospital medicine means to be there at the most intense time of many people’s lives, to shoulder the responsibility of knowing that what I say to my patients will be remembered forever, and to be challenged by some of medicine’s hardest problems.
Hospital medicine has a way of putting you at the nexus of individual, family, society, government, and planet. But it also means that, even while I am witness to disease, suffering, broken relationships, social injustice, and environmental issues, I get a privileged look at what it means to comfort, to identify what really matters to people, to understand what gives us dignity as human beings. Lastly, I always come back to the fact that working as a team has made my clinical job so much more enriching; it’s not trench warfare, but you do create bonds quickly with learners, colleagues, and other health professionals in such an intense, fast-paced environment.
What is your current role at Beth Israel Deaconess Medical Center?
At Beth Israel Deaconess, I’m holding four different jobs. It’s sometimes hard for me to keep track of them, but they all center on career and faculty development. I’m a vice chair for career development within the department of medicine, and I also have an institutional role for faculty development for clinicians, educators, and researchers. I provide academic promotion support for the faculty, provide ad hoc mentorship, and run professional development programming. I also direct a year-long medical education fellowship. On the side, I am the editor in chief for a medical education journal.
What are your favorite areas of clinical practice and research?
Being a generalist means I love a lot of areas of clinical practice. I’m not sure there’s a particular area that I enjoy more than others. I love teaching specific topics – antibiotics, pharmacology, direct oral anticoagulants, the microbiology of common infections. I love thinking about how the heart and kidney battle for dominance each day and being the mediator. I have a particular interest in high-value care and lab ordering (or the fact that we should do much less of it). I love complex diagnostic problems and mapping them out on paper for my team.
The research that I’ve been doing over the past 20 years has focused on how we train internists and internists-to-be to do bedside procedures. It stemmed from my own ineptitude in doing procedures, and it caused me to question the age-old approach we took in sticking needles into patients without standardized training, supervision, or safety measures.
I’ve been proud of the small role I’ve been able to play in influencing how residents are taught to do procedures, and now I’m working with others to focus on how we should teach procedures to hospitalists, who don’t do procedures on a regular basis, and aren’t under the same expectations for ongoing skill development.
What are the most challenging aspects of practicing hospital medicine, and what are the most rewarding?
The intensity is probably what’s hardest for me about hospital medicine. At this point in my career, if I’m on service for a week, it takes me just as long to recover. It’s the cognitive load of needing to keep track of details that can make a big difference, the rapidity at which patients can deteriorate, the need to change course in an instant because of new information, and wanting to be mentally present and available for my patients and my learners.
It’s also hard to see suffering up close and personal and to leave feeling helpless to change the course of severe illness or to optimize care within the constraints of the health care system. This is why I do – and have to – extract satisfaction from the smallest of wins and brief moments of connection. Like seeing a patient turn the corner after being on the brink. Or gaining trust from an initially upset family member. Getting a copy of the eulogy from the daughter of my patient. A phone call from a patient I cared for 18 months ago, thanking me for my care. Visiting patients in the hospital socially that I had gotten to know over the years.
How has COVID-19 impacted hospitalist practice, and what changes will outlast the pandemic?
What you read in the lay press has put a spotlight on hospital-based work. What has been shared resonates with my own experience – the loss of connection from visitor restrictions, the isolation patients experience when everyone is wearing personal protective equipment, the worsening of everything that was already hard to begin with, like health care disparities, mental health, access to community supports, financial challenges, the disproportionate burden on unpaid caregivers, etc.
After the pandemic is “over,” I hope that we will retain a sense of intentionality how we address limited resources, the importance of social connection, the structural racism that has disadvantaged patients and physicians of color.
How will hospital medicine as a field change in the next decade or 2?
The hospitalist model has already influenced other specialties, like ob.gyn., neurology, and cardiology, and I expect that to continue. Hospitalists have already become leaders at the highest levels, and we will see them in higher numbers throughout health care leadership.
Are there any particular mentors who have been influential in your journey as a hospitalist?
Because I’m one of the older hospitalists in my group, there were fewer mentors, other than my boss, Joe Li, MD, SFHM, [section chief in hospital medicine at Beth Israel Deaconess], who has been an amazing role model. I think also of my colleagues as peer mentors, who continue to push me to be a better doctor. Whether it means remaining curious during the physical exam, or inspiring me with their excitement about clinical cases.
Do you have any advice for students and residents interested in hospital medicine?
When I talk to trainees about career development as a hospitalist, I encourage them to think about what will make them a “Hospitalist Plus.” Whether that Plus is teaching, research, or leadership, being a hospitalist gives you an opportunity to extend your impact as a physician into related realm.
I look around at our hospital medicine group, and every person has their Plus. We have educators, quality improvement leaders, a health services researcher, a health policy expert, a textbook editor – everyone brings special expertise to the group. My Plus now is much bigger than my footprint as a hospitalist, but I would never have gotten here had I not chosen a career path that would allow me to explore the farthest reaches of my potential as a physician.
Editor’s note: This profile is part of SHM’s celebration of National Hospitalist Day on March 4. National Hospitalist Day occurs the first Thursday in March annually, and celebrates the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
Grace C. Huang, MD, is a hospitalist at Beth Israel Deaconess Medical Center and an associate professor of medicine at Harvard Medical School, both in Boston.
Dr. Huang currently serves as vice chair for career development and mentoring in the department of medicine at Beth Israel Deaconess as well as director of the Office of Academic Careers and Faculty Development, and codirector of the Beth Israel Deaconess Academy of Medical Educators. She is also director of the Rabkin Fellowship in Medical Education, a program for Harvard Medical School faculty designed to help develop the skills needed to launch or advance academic careers in medical education or academic leadership.
Additionally, Dr. Huang is the editor in chief of MedEdPORTAL, a MEDLINE-indexed, open-access journal of the Association of American Medical Colleges.
At what point in your training did you decide to practice hospital medicine, and what about it appealed to you?
I trained at a point in time where it was rare for people to aspire to go in to hospital medicine. It just wasn’t that common, and there were so few examples of what a career trajectory in hospital medicine would look like. So I don’t know that I actively chose to go into hospital medicine; I chose it because it was what I knew how to do, based on my residency experience.
But it is really easy and authentic for me now to share about what makes hospital medicine such a vibrant career choice. I’m doing a lot of things in my job other than hospital medicine, but when I am on service, it reminds me acutely what it means to stay connected to why I became a doctor. The practice of hospital medicine means to be there at the most intense time of many people’s lives, to shoulder the responsibility of knowing that what I say to my patients will be remembered forever, and to be challenged by some of medicine’s hardest problems.
Hospital medicine has a way of putting you at the nexus of individual, family, society, government, and planet. But it also means that, even while I am witness to disease, suffering, broken relationships, social injustice, and environmental issues, I get a privileged look at what it means to comfort, to identify what really matters to people, to understand what gives us dignity as human beings. Lastly, I always come back to the fact that working as a team has made my clinical job so much more enriching; it’s not trench warfare, but you do create bonds quickly with learners, colleagues, and other health professionals in such an intense, fast-paced environment.
What is your current role at Beth Israel Deaconess Medical Center?
At Beth Israel Deaconess, I’m holding four different jobs. It’s sometimes hard for me to keep track of them, but they all center on career and faculty development. I’m a vice chair for career development within the department of medicine, and I also have an institutional role for faculty development for clinicians, educators, and researchers. I provide academic promotion support for the faculty, provide ad hoc mentorship, and run professional development programming. I also direct a year-long medical education fellowship. On the side, I am the editor in chief for a medical education journal.
What are your favorite areas of clinical practice and research?
Being a generalist means I love a lot of areas of clinical practice. I’m not sure there’s a particular area that I enjoy more than others. I love teaching specific topics – antibiotics, pharmacology, direct oral anticoagulants, the microbiology of common infections. I love thinking about how the heart and kidney battle for dominance each day and being the mediator. I have a particular interest in high-value care and lab ordering (or the fact that we should do much less of it). I love complex diagnostic problems and mapping them out on paper for my team.
The research that I’ve been doing over the past 20 years has focused on how we train internists and internists-to-be to do bedside procedures. It stemmed from my own ineptitude in doing procedures, and it caused me to question the age-old approach we took in sticking needles into patients without standardized training, supervision, or safety measures.
I’ve been proud of the small role I’ve been able to play in influencing how residents are taught to do procedures, and now I’m working with others to focus on how we should teach procedures to hospitalists, who don’t do procedures on a regular basis, and aren’t under the same expectations for ongoing skill development.
What are the most challenging aspects of practicing hospital medicine, and what are the most rewarding?
The intensity is probably what’s hardest for me about hospital medicine. At this point in my career, if I’m on service for a week, it takes me just as long to recover. It’s the cognitive load of needing to keep track of details that can make a big difference, the rapidity at which patients can deteriorate, the need to change course in an instant because of new information, and wanting to be mentally present and available for my patients and my learners.
It’s also hard to see suffering up close and personal and to leave feeling helpless to change the course of severe illness or to optimize care within the constraints of the health care system. This is why I do – and have to – extract satisfaction from the smallest of wins and brief moments of connection. Like seeing a patient turn the corner after being on the brink. Or gaining trust from an initially upset family member. Getting a copy of the eulogy from the daughter of my patient. A phone call from a patient I cared for 18 months ago, thanking me for my care. Visiting patients in the hospital socially that I had gotten to know over the years.
How has COVID-19 impacted hospitalist practice, and what changes will outlast the pandemic?
What you read in the lay press has put a spotlight on hospital-based work. What has been shared resonates with my own experience – the loss of connection from visitor restrictions, the isolation patients experience when everyone is wearing personal protective equipment, the worsening of everything that was already hard to begin with, like health care disparities, mental health, access to community supports, financial challenges, the disproportionate burden on unpaid caregivers, etc.
After the pandemic is “over,” I hope that we will retain a sense of intentionality how we address limited resources, the importance of social connection, the structural racism that has disadvantaged patients and physicians of color.
How will hospital medicine as a field change in the next decade or 2?
The hospitalist model has already influenced other specialties, like ob.gyn., neurology, and cardiology, and I expect that to continue. Hospitalists have already become leaders at the highest levels, and we will see them in higher numbers throughout health care leadership.
Are there any particular mentors who have been influential in your journey as a hospitalist?
Because I’m one of the older hospitalists in my group, there were fewer mentors, other than my boss, Joe Li, MD, SFHM, [section chief in hospital medicine at Beth Israel Deaconess], who has been an amazing role model. I think also of my colleagues as peer mentors, who continue to push me to be a better doctor. Whether it means remaining curious during the physical exam, or inspiring me with their excitement about clinical cases.
Do you have any advice for students and residents interested in hospital medicine?
When I talk to trainees about career development as a hospitalist, I encourage them to think about what will make them a “Hospitalist Plus.” Whether that Plus is teaching, research, or leadership, being a hospitalist gives you an opportunity to extend your impact as a physician into related realm.
I look around at our hospital medicine group, and every person has their Plus. We have educators, quality improvement leaders, a health services researcher, a health policy expert, a textbook editor – everyone brings special expertise to the group. My Plus now is much bigger than my footprint as a hospitalist, but I would never have gotten here had I not chosen a career path that would allow me to explore the farthest reaches of my potential as a physician.
Editor’s note: This profile is part of SHM’s celebration of National Hospitalist Day on March 4. National Hospitalist Day occurs the first Thursday in March annually, and celebrates the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
Grace C. Huang, MD, is a hospitalist at Beth Israel Deaconess Medical Center and an associate professor of medicine at Harvard Medical School, both in Boston.
Dr. Huang currently serves as vice chair for career development and mentoring in the department of medicine at Beth Israel Deaconess as well as director of the Office of Academic Careers and Faculty Development, and codirector of the Beth Israel Deaconess Academy of Medical Educators. She is also director of the Rabkin Fellowship in Medical Education, a program for Harvard Medical School faculty designed to help develop the skills needed to launch or advance academic careers in medical education or academic leadership.
Additionally, Dr. Huang is the editor in chief of MedEdPORTAL, a MEDLINE-indexed, open-access journal of the Association of American Medical Colleges.
At what point in your training did you decide to practice hospital medicine, and what about it appealed to you?
I trained at a point in time where it was rare for people to aspire to go in to hospital medicine. It just wasn’t that common, and there were so few examples of what a career trajectory in hospital medicine would look like. So I don’t know that I actively chose to go into hospital medicine; I chose it because it was what I knew how to do, based on my residency experience.
But it is really easy and authentic for me now to share about what makes hospital medicine such a vibrant career choice. I’m doing a lot of things in my job other than hospital medicine, but when I am on service, it reminds me acutely what it means to stay connected to why I became a doctor. The practice of hospital medicine means to be there at the most intense time of many people’s lives, to shoulder the responsibility of knowing that what I say to my patients will be remembered forever, and to be challenged by some of medicine’s hardest problems.
Hospital medicine has a way of putting you at the nexus of individual, family, society, government, and planet. But it also means that, even while I am witness to disease, suffering, broken relationships, social injustice, and environmental issues, I get a privileged look at what it means to comfort, to identify what really matters to people, to understand what gives us dignity as human beings. Lastly, I always come back to the fact that working as a team has made my clinical job so much more enriching; it’s not trench warfare, but you do create bonds quickly with learners, colleagues, and other health professionals in such an intense, fast-paced environment.
What is your current role at Beth Israel Deaconess Medical Center?
At Beth Israel Deaconess, I’m holding four different jobs. It’s sometimes hard for me to keep track of them, but they all center on career and faculty development. I’m a vice chair for career development within the department of medicine, and I also have an institutional role for faculty development for clinicians, educators, and researchers. I provide academic promotion support for the faculty, provide ad hoc mentorship, and run professional development programming. I also direct a year-long medical education fellowship. On the side, I am the editor in chief for a medical education journal.
What are your favorite areas of clinical practice and research?
Being a generalist means I love a lot of areas of clinical practice. I’m not sure there’s a particular area that I enjoy more than others. I love teaching specific topics – antibiotics, pharmacology, direct oral anticoagulants, the microbiology of common infections. I love thinking about how the heart and kidney battle for dominance each day and being the mediator. I have a particular interest in high-value care and lab ordering (or the fact that we should do much less of it). I love complex diagnostic problems and mapping them out on paper for my team.
The research that I’ve been doing over the past 20 years has focused on how we train internists and internists-to-be to do bedside procedures. It stemmed from my own ineptitude in doing procedures, and it caused me to question the age-old approach we took in sticking needles into patients without standardized training, supervision, or safety measures.
I’ve been proud of the small role I’ve been able to play in influencing how residents are taught to do procedures, and now I’m working with others to focus on how we should teach procedures to hospitalists, who don’t do procedures on a regular basis, and aren’t under the same expectations for ongoing skill development.
What are the most challenging aspects of practicing hospital medicine, and what are the most rewarding?
The intensity is probably what’s hardest for me about hospital medicine. At this point in my career, if I’m on service for a week, it takes me just as long to recover. It’s the cognitive load of needing to keep track of details that can make a big difference, the rapidity at which patients can deteriorate, the need to change course in an instant because of new information, and wanting to be mentally present and available for my patients and my learners.
It’s also hard to see suffering up close and personal and to leave feeling helpless to change the course of severe illness or to optimize care within the constraints of the health care system. This is why I do – and have to – extract satisfaction from the smallest of wins and brief moments of connection. Like seeing a patient turn the corner after being on the brink. Or gaining trust from an initially upset family member. Getting a copy of the eulogy from the daughter of my patient. A phone call from a patient I cared for 18 months ago, thanking me for my care. Visiting patients in the hospital socially that I had gotten to know over the years.
How has COVID-19 impacted hospitalist practice, and what changes will outlast the pandemic?
What you read in the lay press has put a spotlight on hospital-based work. What has been shared resonates with my own experience – the loss of connection from visitor restrictions, the isolation patients experience when everyone is wearing personal protective equipment, the worsening of everything that was already hard to begin with, like health care disparities, mental health, access to community supports, financial challenges, the disproportionate burden on unpaid caregivers, etc.
After the pandemic is “over,” I hope that we will retain a sense of intentionality how we address limited resources, the importance of social connection, the structural racism that has disadvantaged patients and physicians of color.
How will hospital medicine as a field change in the next decade or 2?
The hospitalist model has already influenced other specialties, like ob.gyn., neurology, and cardiology, and I expect that to continue. Hospitalists have already become leaders at the highest levels, and we will see them in higher numbers throughout health care leadership.
Are there any particular mentors who have been influential in your journey as a hospitalist?
Because I’m one of the older hospitalists in my group, there were fewer mentors, other than my boss, Joe Li, MD, SFHM, [section chief in hospital medicine at Beth Israel Deaconess], who has been an amazing role model. I think also of my colleagues as peer mentors, who continue to push me to be a better doctor. Whether it means remaining curious during the physical exam, or inspiring me with their excitement about clinical cases.
Do you have any advice for students and residents interested in hospital medicine?
When I talk to trainees about career development as a hospitalist, I encourage them to think about what will make them a “Hospitalist Plus.” Whether that Plus is teaching, research, or leadership, being a hospitalist gives you an opportunity to extend your impact as a physician into related realm.
I look around at our hospital medicine group, and every person has their Plus. We have educators, quality improvement leaders, a health services researcher, a health policy expert, a textbook editor – everyone brings special expertise to the group. My Plus now is much bigger than my footprint as a hospitalist, but I would never have gotten here had I not chosen a career path that would allow me to explore the farthest reaches of my potential as a physician.
SHM CEO Eric Howell likes to fix things
Engineering provided a foundation for hospital medicine
Editor’s note: This profile is part of SHM’s celebration of National Hospitalist Day on March 4. National Hospitalist Day occurs the first Thursday in March annually, and celebrates the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
For Eric E. Howell, MD, MHM, CEO since July 2020 for the Society of Hospital Medicine, an undergraduate degree in electrical engineering and a lifelong proclivity for figuring out puzzles, solving problems, and taking things apart to see how they fit back together were building blocks for an exemplary career as a hospitalist, group administrator, and medical educator.
When he was growing up in historic Annapolis, Md., near the shores of Chesapeake Bay, things to put back together included remote control airplanes, small boat engines, and cars. As a hospitalist, his interest in solving problems and facility with numbers and systems led him to become an expert on quality improvement, transitions of care, and conflict management.
“One thing about engineering, you’re always having to fix things. It helps you learn to assess complex situations,” said Dr. Howell, who is 52. “It was helpful for me to bring an engineering approach into the hospital. One of my earliest successes was reengineering admissions processes to dramatically reduce the amount of time patients were spending in the emergency room before they could be admitted to the hospital.”
But his career path in hospital medicine came about by a lucky chance, following residency and a year as chief resident at Johns Hopkins Bayview Medical Center in Baltimore. “One of my duties as chief resident was taking care of hospitalized patients. I didn’t know it but I was becoming a de facto hospitalist,” he recalled.
At the time, he thought he might end up choosing to specialize in something like cardiology or critical care medicine, but in 2000 he was invited to join the new “non-house-staff” medical service at Bayview. Also called a general medicine inpatient service, it eventually evolved into the hospitalist service.
His residency program director, Roy Ziegelstein, MD, a cardiologist and now the vice dean of education at Johns Hopkins, created a job for him.
“I was one of the first four doctors hired. I thought I’d just do it for a year, but I loved inpatient work, so I stayed,” Dr. Howell said. “Roy mentored me for the next 20 years and helped me to become an above average hospitalist.”
Early on, Dr. Howell’s department chair, David Hellman, MD, who had worked at the University of California–San Francisco with hospital medicine pioneer Robert Wachter, MD, MHM, sent Dr. Howell to San Francisco to be mentored by Dr. Wachter, since there were few hospital mentors on the East Coast at that time.
“What I took away from that experience was how important it was to professionalize hospital medicine – in order to develop specialized expertise,” Dr. Howell recalled. “Dr. Wachter taught me that hospitalists need to have a professional focus. Quality improvement, systems-based improvement, and value all became part of that,” he said.
“Many people thought to be a hospitalist all you had to know was basic medicine. But it turns out medicine in the hospital is just as specialized as any other specialty. The hospital itself requires specialized knowledge that didn’t even exist 20 years ago.” Because of complicated disease states and clinical systems, hospitalists have to be better at navigating the software of today’s hospital.
New job opportunities
Dr. Howell describes his career path as a new job focus opening up every 5 years or so, redefining what he does and trying something new and exciting with better pay. His first was a focus on clinical hospital medicine and learning how to be a better doctor. Then in 2005 he began work as a teacher at Johns Hopkins School of Medicine. There he mastered the teaching of medical trainees, winning awards as an instructor, including SHM’s award for excellence in teaching.
In 2010 he again changed his focus to program building, leading the expansion of the hospitalist service for Bayview and three other hospitals in the Johns Hopkins system. Dr. Howell helped grow the service to nearly 200 clinicians while becoming skilled at operational and program development.
His fourth job incarnation, starting in 2015, was the obsessive pursuit of quality improvement, marshaling data to measure and improve clinical and other outcomes on the quality dashboard – mortality, length of stay, readmissions, rates of adverse events – and putting quality improvement strategies in place.
“Our mortality rates at Bayview were well below national standards. We came up with an amazing program. A lot of hospital medicine programs pursue improvement, but we really measured it. We benchmarked ourselves against other programs at Hopkins,” he said. “I set up a dedicated conference room, as many QI programs do. We called it True North, and each wall had a different QI focus, with updates on the reported metrics. Every other week we met there to talk about the metrics,” he said.
That experience led to working with SHM, which he had joined as a member early in his career and for which he had previously served as president. He became SHM’s quality improvement liaison and a co-principal investigator on Project BOOST (Better Outcomes for Older adults through Safe Transitions), SHM’s pioneering, national mentored-implementation model aimed at improving transitions of care from participating hospitals to reduce readmissions. “BOOST really established SHM’s reputation as a quality improvement-oriented organization. It was a stake in the ground for quality and led to SHM receiving the Joint Commission’s 2011 John M. Eisenberg Award for Innovation in Patient Safety and Quality,” he said.
Dr. Howell’s fifth career phase, medical society management, emerged when he was recruited to apply for the SHM chief executive position – held since its inception by retiring CEO Larry Wellikson, MD, MHM. Dr. Howell started work at SHM in the midst of the pandemic, spending much of his time working from home – especially when Philadelphia implemented stricter COVID-19 restrictions. Once pandemic restrictions are loosened, he expects to do a lot of traveling. But for now, the external-facing part of his job is mainly on Zoom.
Making the world a better place
Dr. Howell said he has held fast to three mottos in life, which have guided his career path as well as his personal life: (1) to make the world a better place; (2) to be ethical and transparent; and (3) to invest in people. His wife of 19 years, Heather Howell, an Annapolis realtor, says making the world a better place is what they taught their children, Mason, 18, who starts college at Rice University in fall 2021 with an interest in premed, and Anna, 16, a competitive sailor. “We always had a poster hanging in our house extolling that message,” Ms. Howell said.
Dr. Howell grew up in a nautical family, with many of his relatives working in the maritime business. His kids grew up on the water, learning to pilot a powerboat before driving a car, as he did. “We boat all the time on the bay” in his lobster boat, which he often works on to keep it seaworthy, Ms. Howell said.
“There’s nothing like taking care of hospitalized patients to make you feel you’re making the world a better place,” Dr. Howell observed. “Very often you can make a huge difference for the patients you do care for, and that is incredibly rewarding.” Although the demands of his SHM leadership position required relinquishing most of his responsibilities at Johns Hopkins, he continues to see patients and teach residents there 2-4 weeks a year on a teaching service.
“Why do I still see patients? I find it so rewarding. And I get to teach, which I love,” he said. “To be honest, I don’t think you truly need to see patients to be head of a professional medical society like SHM. Maybe someday I’ll give that up. But only if it’s necessary to make the society more successful.”
Half of Dr. Howell’s Society work now is planned and half is “putting out fires” – while learning members’ needs in real time. “Right now, we’re worried about burnout and PTSD, because frankly it’s stressful to take care of COVID patients. It’s scary for a lot of clinicians. I’m working with our members to make sure they have what they need to be clinically prepared, including resources to be more resilient professionally.”
Every step of his career, Dr. Howell said, has seemed like the best job he ever had. “Making the world a better place is still important to me. I tell SHM members that it’s important to know they are making a difference. What they’re doing is really important, especially with COVID, and it needs to be sustainable,” he said.
“SHM has such a powerful mission – it’s about making patient care better, and making hospitalists better clinicians. I know the Society is having a powerful impact, and that’s good enough for me. I’m into teams. Hospital medicine is a team sport, but so is SHM, interacting with its members, staff, and board.”
Initiating another new program
One of Dr. Howell’s last major projects for Hopkins was to launch and be chief medical officer for the Joint Commission–accredited Baltimore Civic Center Field Hospital for COVID-19 patients, opened in March 2020.
With a surge capacity of 250 beds, and a negative pressure ward set up in the center’s exhibit hall, it is jointly operated by the University of Maryland Medical System and Johns Hopkins Hospital. The field hospital’s mission has since expanded to include viral tests, infusions of monoclonal antibodies, and COVID-19 vaccinations.
Planning for a smooth transition, Dr. Howell brought Melinda E. Kantsiper, MD, director of clinical operations, Division of Hospital Medicine at Johns Hopkins Bayview, on board as associate medical officer, to eventually replace him as CMO after a few months working alongside him. “Eric brings that logical engineering eye to problem solving,” Dr. Kantsiper said.
“We wanted to build a very safe, high-quality hospital setting but had to do it very quickly. Watching him once again do what he does best, initiating a new program, building things carefully and thoughtfully, without being overly cautious, I could see his years of experience and good judgment about how hospitals run. He’s very logical but very caring. He’s also good at spotting young leaders and their talents.”
Some people have a knack for solving problems, added Dr. Ziegelstein, Dr. Howell’s mentor from his early days at Bayview. “Eric is different. He’s someone who’s able to identify gaps, problem areas, and vulnerabilities within an organization and then come up with a potential menu of solutions, think about which would be most likely to succeed, implement it, and assess the outcome. That’s the difference between a skilled manager and a true leader, and I’d say Eric had that ability while still in training,” Dr. Ziegelstein said.
“Eric understood early on not only what the field of hospital medicine could offer, he also understood how to catalyze change, without taking on too much change at one time,” Dr. Ziegelstein said. “He understood people’s sensibilities and concerns about this new service, and he catalyzed its growth through incremental change.”
Engineering provided a foundation for hospital medicine
Engineering provided a foundation for hospital medicine
Editor’s note: This profile is part of SHM’s celebration of National Hospitalist Day on March 4. National Hospitalist Day occurs the first Thursday in March annually, and celebrates the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
For Eric E. Howell, MD, MHM, CEO since July 2020 for the Society of Hospital Medicine, an undergraduate degree in electrical engineering and a lifelong proclivity for figuring out puzzles, solving problems, and taking things apart to see how they fit back together were building blocks for an exemplary career as a hospitalist, group administrator, and medical educator.
When he was growing up in historic Annapolis, Md., near the shores of Chesapeake Bay, things to put back together included remote control airplanes, small boat engines, and cars. As a hospitalist, his interest in solving problems and facility with numbers and systems led him to become an expert on quality improvement, transitions of care, and conflict management.
“One thing about engineering, you’re always having to fix things. It helps you learn to assess complex situations,” said Dr. Howell, who is 52. “It was helpful for me to bring an engineering approach into the hospital. One of my earliest successes was reengineering admissions processes to dramatically reduce the amount of time patients were spending in the emergency room before they could be admitted to the hospital.”
But his career path in hospital medicine came about by a lucky chance, following residency and a year as chief resident at Johns Hopkins Bayview Medical Center in Baltimore. “One of my duties as chief resident was taking care of hospitalized patients. I didn’t know it but I was becoming a de facto hospitalist,” he recalled.
At the time, he thought he might end up choosing to specialize in something like cardiology or critical care medicine, but in 2000 he was invited to join the new “non-house-staff” medical service at Bayview. Also called a general medicine inpatient service, it eventually evolved into the hospitalist service.
His residency program director, Roy Ziegelstein, MD, a cardiologist and now the vice dean of education at Johns Hopkins, created a job for him.
“I was one of the first four doctors hired. I thought I’d just do it for a year, but I loved inpatient work, so I stayed,” Dr. Howell said. “Roy mentored me for the next 20 years and helped me to become an above average hospitalist.”
Early on, Dr. Howell’s department chair, David Hellman, MD, who had worked at the University of California–San Francisco with hospital medicine pioneer Robert Wachter, MD, MHM, sent Dr. Howell to San Francisco to be mentored by Dr. Wachter, since there were few hospital mentors on the East Coast at that time.
“What I took away from that experience was how important it was to professionalize hospital medicine – in order to develop specialized expertise,” Dr. Howell recalled. “Dr. Wachter taught me that hospitalists need to have a professional focus. Quality improvement, systems-based improvement, and value all became part of that,” he said.
“Many people thought to be a hospitalist all you had to know was basic medicine. But it turns out medicine in the hospital is just as specialized as any other specialty. The hospital itself requires specialized knowledge that didn’t even exist 20 years ago.” Because of complicated disease states and clinical systems, hospitalists have to be better at navigating the software of today’s hospital.
New job opportunities
Dr. Howell describes his career path as a new job focus opening up every 5 years or so, redefining what he does and trying something new and exciting with better pay. His first was a focus on clinical hospital medicine and learning how to be a better doctor. Then in 2005 he began work as a teacher at Johns Hopkins School of Medicine. There he mastered the teaching of medical trainees, winning awards as an instructor, including SHM’s award for excellence in teaching.
In 2010 he again changed his focus to program building, leading the expansion of the hospitalist service for Bayview and three other hospitals in the Johns Hopkins system. Dr. Howell helped grow the service to nearly 200 clinicians while becoming skilled at operational and program development.
His fourth job incarnation, starting in 2015, was the obsessive pursuit of quality improvement, marshaling data to measure and improve clinical and other outcomes on the quality dashboard – mortality, length of stay, readmissions, rates of adverse events – and putting quality improvement strategies in place.
“Our mortality rates at Bayview were well below national standards. We came up with an amazing program. A lot of hospital medicine programs pursue improvement, but we really measured it. We benchmarked ourselves against other programs at Hopkins,” he said. “I set up a dedicated conference room, as many QI programs do. We called it True North, and each wall had a different QI focus, with updates on the reported metrics. Every other week we met there to talk about the metrics,” he said.
That experience led to working with SHM, which he had joined as a member early in his career and for which he had previously served as president. He became SHM’s quality improvement liaison and a co-principal investigator on Project BOOST (Better Outcomes for Older adults through Safe Transitions), SHM’s pioneering, national mentored-implementation model aimed at improving transitions of care from participating hospitals to reduce readmissions. “BOOST really established SHM’s reputation as a quality improvement-oriented organization. It was a stake in the ground for quality and led to SHM receiving the Joint Commission’s 2011 John M. Eisenberg Award for Innovation in Patient Safety and Quality,” he said.
Dr. Howell’s fifth career phase, medical society management, emerged when he was recruited to apply for the SHM chief executive position – held since its inception by retiring CEO Larry Wellikson, MD, MHM. Dr. Howell started work at SHM in the midst of the pandemic, spending much of his time working from home – especially when Philadelphia implemented stricter COVID-19 restrictions. Once pandemic restrictions are loosened, he expects to do a lot of traveling. But for now, the external-facing part of his job is mainly on Zoom.
Making the world a better place
Dr. Howell said he has held fast to three mottos in life, which have guided his career path as well as his personal life: (1) to make the world a better place; (2) to be ethical and transparent; and (3) to invest in people. His wife of 19 years, Heather Howell, an Annapolis realtor, says making the world a better place is what they taught their children, Mason, 18, who starts college at Rice University in fall 2021 with an interest in premed, and Anna, 16, a competitive sailor. “We always had a poster hanging in our house extolling that message,” Ms. Howell said.
Dr. Howell grew up in a nautical family, with many of his relatives working in the maritime business. His kids grew up on the water, learning to pilot a powerboat before driving a car, as he did. “We boat all the time on the bay” in his lobster boat, which he often works on to keep it seaworthy, Ms. Howell said.
“There’s nothing like taking care of hospitalized patients to make you feel you’re making the world a better place,” Dr. Howell observed. “Very often you can make a huge difference for the patients you do care for, and that is incredibly rewarding.” Although the demands of his SHM leadership position required relinquishing most of his responsibilities at Johns Hopkins, he continues to see patients and teach residents there 2-4 weeks a year on a teaching service.
“Why do I still see patients? I find it so rewarding. And I get to teach, which I love,” he said. “To be honest, I don’t think you truly need to see patients to be head of a professional medical society like SHM. Maybe someday I’ll give that up. But only if it’s necessary to make the society more successful.”
Half of Dr. Howell’s Society work now is planned and half is “putting out fires” – while learning members’ needs in real time. “Right now, we’re worried about burnout and PTSD, because frankly it’s stressful to take care of COVID patients. It’s scary for a lot of clinicians. I’m working with our members to make sure they have what they need to be clinically prepared, including resources to be more resilient professionally.”
Every step of his career, Dr. Howell said, has seemed like the best job he ever had. “Making the world a better place is still important to me. I tell SHM members that it’s important to know they are making a difference. What they’re doing is really important, especially with COVID, and it needs to be sustainable,” he said.
“SHM has such a powerful mission – it’s about making patient care better, and making hospitalists better clinicians. I know the Society is having a powerful impact, and that’s good enough for me. I’m into teams. Hospital medicine is a team sport, but so is SHM, interacting with its members, staff, and board.”
Initiating another new program
One of Dr. Howell’s last major projects for Hopkins was to launch and be chief medical officer for the Joint Commission–accredited Baltimore Civic Center Field Hospital for COVID-19 patients, opened in March 2020.
With a surge capacity of 250 beds, and a negative pressure ward set up in the center’s exhibit hall, it is jointly operated by the University of Maryland Medical System and Johns Hopkins Hospital. The field hospital’s mission has since expanded to include viral tests, infusions of monoclonal antibodies, and COVID-19 vaccinations.
Planning for a smooth transition, Dr. Howell brought Melinda E. Kantsiper, MD, director of clinical operations, Division of Hospital Medicine at Johns Hopkins Bayview, on board as associate medical officer, to eventually replace him as CMO after a few months working alongside him. “Eric brings that logical engineering eye to problem solving,” Dr. Kantsiper said.
“We wanted to build a very safe, high-quality hospital setting but had to do it very quickly. Watching him once again do what he does best, initiating a new program, building things carefully and thoughtfully, without being overly cautious, I could see his years of experience and good judgment about how hospitals run. He’s very logical but very caring. He’s also good at spotting young leaders and their talents.”
Some people have a knack for solving problems, added Dr. Ziegelstein, Dr. Howell’s mentor from his early days at Bayview. “Eric is different. He’s someone who’s able to identify gaps, problem areas, and vulnerabilities within an organization and then come up with a potential menu of solutions, think about which would be most likely to succeed, implement it, and assess the outcome. That’s the difference between a skilled manager and a true leader, and I’d say Eric had that ability while still in training,” Dr. Ziegelstein said.
“Eric understood early on not only what the field of hospital medicine could offer, he also understood how to catalyze change, without taking on too much change at one time,” Dr. Ziegelstein said. “He understood people’s sensibilities and concerns about this new service, and he catalyzed its growth through incremental change.”
Editor’s note: This profile is part of SHM’s celebration of National Hospitalist Day on March 4. National Hospitalist Day occurs the first Thursday in March annually, and celebrates the fastest growing specialty in modern medicine and hospitalists’ enduring contributions to the evolving health care landscape.
For Eric E. Howell, MD, MHM, CEO since July 2020 for the Society of Hospital Medicine, an undergraduate degree in electrical engineering and a lifelong proclivity for figuring out puzzles, solving problems, and taking things apart to see how they fit back together were building blocks for an exemplary career as a hospitalist, group administrator, and medical educator.
When he was growing up in historic Annapolis, Md., near the shores of Chesapeake Bay, things to put back together included remote control airplanes, small boat engines, and cars. As a hospitalist, his interest in solving problems and facility with numbers and systems led him to become an expert on quality improvement, transitions of care, and conflict management.
“One thing about engineering, you’re always having to fix things. It helps you learn to assess complex situations,” said Dr. Howell, who is 52. “It was helpful for me to bring an engineering approach into the hospital. One of my earliest successes was reengineering admissions processes to dramatically reduce the amount of time patients were spending in the emergency room before they could be admitted to the hospital.”
But his career path in hospital medicine came about by a lucky chance, following residency and a year as chief resident at Johns Hopkins Bayview Medical Center in Baltimore. “One of my duties as chief resident was taking care of hospitalized patients. I didn’t know it but I was becoming a de facto hospitalist,” he recalled.
At the time, he thought he might end up choosing to specialize in something like cardiology or critical care medicine, but in 2000 he was invited to join the new “non-house-staff” medical service at Bayview. Also called a general medicine inpatient service, it eventually evolved into the hospitalist service.
His residency program director, Roy Ziegelstein, MD, a cardiologist and now the vice dean of education at Johns Hopkins, created a job for him.
“I was one of the first four doctors hired. I thought I’d just do it for a year, but I loved inpatient work, so I stayed,” Dr. Howell said. “Roy mentored me for the next 20 years and helped me to become an above average hospitalist.”
Early on, Dr. Howell’s department chair, David Hellman, MD, who had worked at the University of California–San Francisco with hospital medicine pioneer Robert Wachter, MD, MHM, sent Dr. Howell to San Francisco to be mentored by Dr. Wachter, since there were few hospital mentors on the East Coast at that time.
“What I took away from that experience was how important it was to professionalize hospital medicine – in order to develop specialized expertise,” Dr. Howell recalled. “Dr. Wachter taught me that hospitalists need to have a professional focus. Quality improvement, systems-based improvement, and value all became part of that,” he said.
“Many people thought to be a hospitalist all you had to know was basic medicine. But it turns out medicine in the hospital is just as specialized as any other specialty. The hospital itself requires specialized knowledge that didn’t even exist 20 years ago.” Because of complicated disease states and clinical systems, hospitalists have to be better at navigating the software of today’s hospital.
New job opportunities
Dr. Howell describes his career path as a new job focus opening up every 5 years or so, redefining what he does and trying something new and exciting with better pay. His first was a focus on clinical hospital medicine and learning how to be a better doctor. Then in 2005 he began work as a teacher at Johns Hopkins School of Medicine. There he mastered the teaching of medical trainees, winning awards as an instructor, including SHM’s award for excellence in teaching.
In 2010 he again changed his focus to program building, leading the expansion of the hospitalist service for Bayview and three other hospitals in the Johns Hopkins system. Dr. Howell helped grow the service to nearly 200 clinicians while becoming skilled at operational and program development.
His fourth job incarnation, starting in 2015, was the obsessive pursuit of quality improvement, marshaling data to measure and improve clinical and other outcomes on the quality dashboard – mortality, length of stay, readmissions, rates of adverse events – and putting quality improvement strategies in place.
“Our mortality rates at Bayview were well below national standards. We came up with an amazing program. A lot of hospital medicine programs pursue improvement, but we really measured it. We benchmarked ourselves against other programs at Hopkins,” he said. “I set up a dedicated conference room, as many QI programs do. We called it True North, and each wall had a different QI focus, with updates on the reported metrics. Every other week we met there to talk about the metrics,” he said.
That experience led to working with SHM, which he had joined as a member early in his career and for which he had previously served as president. He became SHM’s quality improvement liaison and a co-principal investigator on Project BOOST (Better Outcomes for Older adults through Safe Transitions), SHM’s pioneering, national mentored-implementation model aimed at improving transitions of care from participating hospitals to reduce readmissions. “BOOST really established SHM’s reputation as a quality improvement-oriented organization. It was a stake in the ground for quality and led to SHM receiving the Joint Commission’s 2011 John M. Eisenberg Award for Innovation in Patient Safety and Quality,” he said.
Dr. Howell’s fifth career phase, medical society management, emerged when he was recruited to apply for the SHM chief executive position – held since its inception by retiring CEO Larry Wellikson, MD, MHM. Dr. Howell started work at SHM in the midst of the pandemic, spending much of his time working from home – especially when Philadelphia implemented stricter COVID-19 restrictions. Once pandemic restrictions are loosened, he expects to do a lot of traveling. But for now, the external-facing part of his job is mainly on Zoom.
Making the world a better place
Dr. Howell said he has held fast to three mottos in life, which have guided his career path as well as his personal life: (1) to make the world a better place; (2) to be ethical and transparent; and (3) to invest in people. His wife of 19 years, Heather Howell, an Annapolis realtor, says making the world a better place is what they taught their children, Mason, 18, who starts college at Rice University in fall 2021 with an interest in premed, and Anna, 16, a competitive sailor. “We always had a poster hanging in our house extolling that message,” Ms. Howell said.
Dr. Howell grew up in a nautical family, with many of his relatives working in the maritime business. His kids grew up on the water, learning to pilot a powerboat before driving a car, as he did. “We boat all the time on the bay” in his lobster boat, which he often works on to keep it seaworthy, Ms. Howell said.
“There’s nothing like taking care of hospitalized patients to make you feel you’re making the world a better place,” Dr. Howell observed. “Very often you can make a huge difference for the patients you do care for, and that is incredibly rewarding.” Although the demands of his SHM leadership position required relinquishing most of his responsibilities at Johns Hopkins, he continues to see patients and teach residents there 2-4 weeks a year on a teaching service.
“Why do I still see patients? I find it so rewarding. And I get to teach, which I love,” he said. “To be honest, I don’t think you truly need to see patients to be head of a professional medical society like SHM. Maybe someday I’ll give that up. But only if it’s necessary to make the society more successful.”
Half of Dr. Howell’s Society work now is planned and half is “putting out fires” – while learning members’ needs in real time. “Right now, we’re worried about burnout and PTSD, because frankly it’s stressful to take care of COVID patients. It’s scary for a lot of clinicians. I’m working with our members to make sure they have what they need to be clinically prepared, including resources to be more resilient professionally.”
Every step of his career, Dr. Howell said, has seemed like the best job he ever had. “Making the world a better place is still important to me. I tell SHM members that it’s important to know they are making a difference. What they’re doing is really important, especially with COVID, and it needs to be sustainable,” he said.
“SHM has such a powerful mission – it’s about making patient care better, and making hospitalists better clinicians. I know the Society is having a powerful impact, and that’s good enough for me. I’m into teams. Hospital medicine is a team sport, but so is SHM, interacting with its members, staff, and board.”
Initiating another new program
One of Dr. Howell’s last major projects for Hopkins was to launch and be chief medical officer for the Joint Commission–accredited Baltimore Civic Center Field Hospital for COVID-19 patients, opened in March 2020.
With a surge capacity of 250 beds, and a negative pressure ward set up in the center’s exhibit hall, it is jointly operated by the University of Maryland Medical System and Johns Hopkins Hospital. The field hospital’s mission has since expanded to include viral tests, infusions of monoclonal antibodies, and COVID-19 vaccinations.
Planning for a smooth transition, Dr. Howell brought Melinda E. Kantsiper, MD, director of clinical operations, Division of Hospital Medicine at Johns Hopkins Bayview, on board as associate medical officer, to eventually replace him as CMO after a few months working alongside him. “Eric brings that logical engineering eye to problem solving,” Dr. Kantsiper said.
“We wanted to build a very safe, high-quality hospital setting but had to do it very quickly. Watching him once again do what he does best, initiating a new program, building things carefully and thoughtfully, without being overly cautious, I could see his years of experience and good judgment about how hospitals run. He’s very logical but very caring. He’s also good at spotting young leaders and their talents.”
Some people have a knack for solving problems, added Dr. Ziegelstein, Dr. Howell’s mentor from his early days at Bayview. “Eric is different. He’s someone who’s able to identify gaps, problem areas, and vulnerabilities within an organization and then come up with a potential menu of solutions, think about which would be most likely to succeed, implement it, and assess the outcome. That’s the difference between a skilled manager and a true leader, and I’d say Eric had that ability while still in training,” Dr. Ziegelstein said.
“Eric understood early on not only what the field of hospital medicine could offer, he also understood how to catalyze change, without taking on too much change at one time,” Dr. Ziegelstein said. “He understood people’s sensibilities and concerns about this new service, and he catalyzed its growth through incremental change.”
Education and networking are driving forces behind Converge platform
As Jade Myers set out to help create the virtual platform for SHM Converge, she was aware, through surveys and other communication, that the top wish of members of the Society of Hospital Medicine was an extensive and interactive educational experience.
“People really wanted to get back to the in-person conference,” said Ms. Myers, SHM’s director of meetings. “While we couldn’t do that, we can provide the same caliber and as robust an experience from an educational perspective as we would for an in-person activity.”
That has required significant revamping of the virtual platform compared to the platform for last year’s annual conference. In 2020, there was only one session running live at a time. This year, there will be 12 sessions running at the same time. There will also be more opportunities for networking, as well as other features for enjoyment and a sense of calm.
Here are some features of the SHM Converge platform:
- A host segment to kick-start each day, with an introduction of the day’s sessions and events.
- Nine didactic educational sessions at any given time. These sessions will include a live chat for peer-to-peer engagement, as well as questions and answers throughout the session to continue the discussion between speakers and participants.
- Three workshops at any given time. These sessions – on topics such as communication, gender equity, and clinical guidelines – will provide an opportunity for dynamic small-group discussion.
- A scientific abstract poster competition and reception, with an e-gallery of about 700 posters, providing a networking opportunity and highlighting emerging scientific and clinical cases.
- Special Interest Forums, in the form of live, interactive Zoom conferences. There will be 25 forums, which are designed to build community and facilitate collaboration.
- A variety of games, including trivia and a word scramble.
- Personalized profiles with information such as “Hospitalist in Training,” or “Committee Member.” These will be visible to other attendees to make it easier for people to connect when they have something in common.
- Early- and Mid-Career Speed Mentorship, in which a mentor and mentee can interact one-on-one, with each mentee able to meet with two mentors, with pairings designed for the best mentorship experience.
- Sessions on wellness and resilience.
“People are kind of Zoom fatigued,” Ms. Myers said, “so we’re trying to meet their needs while also offering an opportunity for respite, because our attendees are on the front lines right now, and they’re dealing with all types of fatigue and challenging times.”
The annual conference was on target for a banner year in 2020 before the COVID-19 pandemic forced the cancellation of the in-person conference in San Diego, and SHM Converge is a product of planning that began then, as organizers started considering a virtual event.
“In 2020, we were slated to have the largest conference in person that we have ever had,” said Hayleigh Scott, SHM’s meeting projects manager. “San Diego was going to be our really big year.”
But attendance at last year’s virtual conference was a fraction of what was expected at the in-person conference. This year, that seems poised to improve. There will be many more offerings, with more than 125 AMA PRA Category 1 Credits™ and 45 Maintenance of Certification points possible, Ms. Myers said. Because attendees won’t have to worry about being in two places at once, it will be possible to secure more CME credits at SHM Converge than at any previous SHM annual conference, she said.
The volume of content will be a heavy load on SHM personnel. Last year, three society staff members were on hand at each session to make sure it ran smoothly and to answer questions. With 12 sessions running simultaneously this year, many more staff members will need to be involved. But that is not unfamiliar for the society during meeting week, Ms. Myers said.
“We’re going to need to pull from pretty much our entire staff in order to make this conference happen, which is exciting and daunting,” she said. “It’s always been an all-hands-on-deck program and this is going to be more similar to an in-person conference in that way.”
As Jade Myers set out to help create the virtual platform for SHM Converge, she was aware, through surveys and other communication, that the top wish of members of the Society of Hospital Medicine was an extensive and interactive educational experience.
“People really wanted to get back to the in-person conference,” said Ms. Myers, SHM’s director of meetings. “While we couldn’t do that, we can provide the same caliber and as robust an experience from an educational perspective as we would for an in-person activity.”
That has required significant revamping of the virtual platform compared to the platform for last year’s annual conference. In 2020, there was only one session running live at a time. This year, there will be 12 sessions running at the same time. There will also be more opportunities for networking, as well as other features for enjoyment and a sense of calm.
Here are some features of the SHM Converge platform:
- A host segment to kick-start each day, with an introduction of the day’s sessions and events.
- Nine didactic educational sessions at any given time. These sessions will include a live chat for peer-to-peer engagement, as well as questions and answers throughout the session to continue the discussion between speakers and participants.
- Three workshops at any given time. These sessions – on topics such as communication, gender equity, and clinical guidelines – will provide an opportunity for dynamic small-group discussion.
- A scientific abstract poster competition and reception, with an e-gallery of about 700 posters, providing a networking opportunity and highlighting emerging scientific and clinical cases.
- Special Interest Forums, in the form of live, interactive Zoom conferences. There will be 25 forums, which are designed to build community and facilitate collaboration.
- A variety of games, including trivia and a word scramble.
- Personalized profiles with information such as “Hospitalist in Training,” or “Committee Member.” These will be visible to other attendees to make it easier for people to connect when they have something in common.
- Early- and Mid-Career Speed Mentorship, in which a mentor and mentee can interact one-on-one, with each mentee able to meet with two mentors, with pairings designed for the best mentorship experience.
- Sessions on wellness and resilience.
“People are kind of Zoom fatigued,” Ms. Myers said, “so we’re trying to meet their needs while also offering an opportunity for respite, because our attendees are on the front lines right now, and they’re dealing with all types of fatigue and challenging times.”
The annual conference was on target for a banner year in 2020 before the COVID-19 pandemic forced the cancellation of the in-person conference in San Diego, and SHM Converge is a product of planning that began then, as organizers started considering a virtual event.
“In 2020, we were slated to have the largest conference in person that we have ever had,” said Hayleigh Scott, SHM’s meeting projects manager. “San Diego was going to be our really big year.”
But attendance at last year’s virtual conference was a fraction of what was expected at the in-person conference. This year, that seems poised to improve. There will be many more offerings, with more than 125 AMA PRA Category 1 Credits™ and 45 Maintenance of Certification points possible, Ms. Myers said. Because attendees won’t have to worry about being in two places at once, it will be possible to secure more CME credits at SHM Converge than at any previous SHM annual conference, she said.
The volume of content will be a heavy load on SHM personnel. Last year, three society staff members were on hand at each session to make sure it ran smoothly and to answer questions. With 12 sessions running simultaneously this year, many more staff members will need to be involved. But that is not unfamiliar for the society during meeting week, Ms. Myers said.
“We’re going to need to pull from pretty much our entire staff in order to make this conference happen, which is exciting and daunting,” she said. “It’s always been an all-hands-on-deck program and this is going to be more similar to an in-person conference in that way.”
As Jade Myers set out to help create the virtual platform for SHM Converge, she was aware, through surveys and other communication, that the top wish of members of the Society of Hospital Medicine was an extensive and interactive educational experience.
“People really wanted to get back to the in-person conference,” said Ms. Myers, SHM’s director of meetings. “While we couldn’t do that, we can provide the same caliber and as robust an experience from an educational perspective as we would for an in-person activity.”
That has required significant revamping of the virtual platform compared to the platform for last year’s annual conference. In 2020, there was only one session running live at a time. This year, there will be 12 sessions running at the same time. There will also be more opportunities for networking, as well as other features for enjoyment and a sense of calm.
Here are some features of the SHM Converge platform:
- A host segment to kick-start each day, with an introduction of the day’s sessions and events.
- Nine didactic educational sessions at any given time. These sessions will include a live chat for peer-to-peer engagement, as well as questions and answers throughout the session to continue the discussion between speakers and participants.
- Three workshops at any given time. These sessions – on topics such as communication, gender equity, and clinical guidelines – will provide an opportunity for dynamic small-group discussion.
- A scientific abstract poster competition and reception, with an e-gallery of about 700 posters, providing a networking opportunity and highlighting emerging scientific and clinical cases.
- Special Interest Forums, in the form of live, interactive Zoom conferences. There will be 25 forums, which are designed to build community and facilitate collaboration.
- A variety of games, including trivia and a word scramble.
- Personalized profiles with information such as “Hospitalist in Training,” or “Committee Member.” These will be visible to other attendees to make it easier for people to connect when they have something in common.
- Early- and Mid-Career Speed Mentorship, in which a mentor and mentee can interact one-on-one, with each mentee able to meet with two mentors, with pairings designed for the best mentorship experience.
- Sessions on wellness and resilience.
“People are kind of Zoom fatigued,” Ms. Myers said, “so we’re trying to meet their needs while also offering an opportunity for respite, because our attendees are on the front lines right now, and they’re dealing with all types of fatigue and challenging times.”
The annual conference was on target for a banner year in 2020 before the COVID-19 pandemic forced the cancellation of the in-person conference in San Diego, and SHM Converge is a product of planning that began then, as organizers started considering a virtual event.
“In 2020, we were slated to have the largest conference in person that we have ever had,” said Hayleigh Scott, SHM’s meeting projects manager. “San Diego was going to be our really big year.”
But attendance at last year’s virtual conference was a fraction of what was expected at the in-person conference. This year, that seems poised to improve. There will be many more offerings, with more than 125 AMA PRA Category 1 Credits™ and 45 Maintenance of Certification points possible, Ms. Myers said. Because attendees won’t have to worry about being in two places at once, it will be possible to secure more CME credits at SHM Converge than at any previous SHM annual conference, she said.
The volume of content will be a heavy load on SHM personnel. Last year, three society staff members were on hand at each session to make sure it ran smoothly and to answer questions. With 12 sessions running simultaneously this year, many more staff members will need to be involved. But that is not unfamiliar for the society during meeting week, Ms. Myers said.
“We’re going to need to pull from pretty much our entire staff in order to make this conference happen, which is exciting and daunting,” she said. “It’s always been an all-hands-on-deck program and this is going to be more similar to an in-person conference in that way.”
Immigrant hospitalists to share diverse experiences
Ingrid Pinzon, MD, FACP, was working as a medical assistant to a physician a decade ago when she heard the doctor prescribe ibuprofen to a woman who was in the latter stages of pregnancy. Dr. Pinzon was a doctor, having received her education and training in Colombia, but because she had emigrated to the United States and hadn’t yet completed her certification and training here, she was not recognized yet as an American physician.
But she knew that ibuprofen was not recommended during late-term pregnancy, and she was alarmed. She informed the physician of the mistake. The doctor headed to Google, Dr. Pinzon said, and called the patient to rescind the ibuprofen prescription. But she soon fired Dr. Pinzon, seemingly for having had the courage to speak up.
Dr. Pinzon, now medical director of care coordination at Emory Johns Creek Hospital in Atlanta, will describe her experience as an immigrant physician in the Society of Hospital Medicine Converge session: “A Walk in Our Shoes: Immigrant Physicians Sharing Their Stories.” She will be joined by Patricia O’Brien, MD, PhD, FAAP, a pediatric hospitalist in Tampa; Manpreet Malik, MD, a hospitalist at Emory University; and Benji Mathews, MD, SFHM, FACP, chief of hospital medicine at HealthPartners and associate professor at the University of Minnesota.
They will describe their struggles to find their way in the United States, along with the satisfaction of having hard work pay off with better lives for themselves and their families. And together, they’ll provide a variety of narratives that will show, contrary to how many Americans view immigrants, how the experiences of immigrants don’t follow the same path, but each one carves out a path of his or her own.
“The thrust of this is really storytelling, along with putting into context what we can do to help our hospitalist brothers and sisters who are immigrants, and shining the light on it,” Dr. O’Brien said.
Dr. Pinzon was working as a doctor for the Colombian government when she began receiving threats from soldiers in a guerrilla army, which didn’t agree with her alignment with the government. One day, a guerrilla soldier threatened her and her two daughters – aged 5 and 11 at the time – and accurately described her daughters’ whereabouts.
Less than a week later, she and her daughters flew from Bogota to the United States, never to return to Colombia.
“I dropped everything I had when I came here,” she said. An immigration attorney initially recommended that she marry an American man in order to stay in the United States. When Dr. Pinzon declined, they pursued political asylum, and she received it less than a year later.
For 3 years, she worked jobs as assistants in medical offices and in other jobs, well below her education level, as she guided her daughters through school and went through the U.S. medical certification process. She was besieged by doubt constantly, she said.
“I cried for 3 years in a row,” she said. “I wanted to go back to my country. I didn’t want to stay here.”
Finally, she did her medical residency between 2011 and 2014, and got a job with Emory. Her daughters are grown, and one is a doctor in general surgery residency. Dr. Pinzon said she is happy to care for patients, particularly those who are Spanish-speaking and struggle as she did. But she often encounters patients who don’t hide that they dislike her accent.
“I will mute the TV and I will say: ‘I have a strong accent and so I want to make sure communication is clear,’ ” she said. “We have to prove ourselves all of the time. I feel like I have to prove myself to my patients that I’m a good doctor all of the time.” American-born doctors, she added, “shouldn’t take for granted what they already have.”
Dr. O’Brien grew up in Ireland, but in the late 1980s, the country was in a serious recession, with unemployment close to 20%, and her father applied for residency in Canada and the United States. They were accepted in Canada first, and moved there in 1988. A few years later, her parents moved them to Florida.
“They knew in order for us to do well, we had to go abroad,” she said. Dr. O’Brien went to college, medical school and graduate school in Florida, and completed residency in Cincinnati. Feeling the tug of her birthplace, she moved back to Ireland and worked there for a couple years.
“I never really wanted to leave because it was my home,” she said. While there, she came to a new-found appreciation for the U.S. health care system. It’s true that, in Ireland, everyone is insured, but there long wait times – for example, up to 2 years for a sedated nonurgent MRI for a child. She once had to send a patient to Dublin in a taxi with a nurse because an ambulance was unavailable.
“After going back to Ireland, where – I honestly thought I was going to go back and settle there – I realized how visionary my parents were in moving us,” Dr. O’Brien said. “This system in the U.S., there are lot of things broken about it, but we have all the resources.”
She moved back to the United States in August 2016, during a period of anti-immigrant rhetoric.
Nonetheless, Dr. O’Brien said she is happy to be here despite the lack of tolerance she sees in a minority of the U.S. population.
“Have a bit of sensitivity toward your provider. Maybe they speak with an accent. Maybe they don’t speak English perfectly. Maybe they have a different skin color. But their intention is good and it’s to help you and improve your health,” she said.
Ingrid Pinzon, MD, FACP, was working as a medical assistant to a physician a decade ago when she heard the doctor prescribe ibuprofen to a woman who was in the latter stages of pregnancy. Dr. Pinzon was a doctor, having received her education and training in Colombia, but because she had emigrated to the United States and hadn’t yet completed her certification and training here, she was not recognized yet as an American physician.
But she knew that ibuprofen was not recommended during late-term pregnancy, and she was alarmed. She informed the physician of the mistake. The doctor headed to Google, Dr. Pinzon said, and called the patient to rescind the ibuprofen prescription. But she soon fired Dr. Pinzon, seemingly for having had the courage to speak up.
Dr. Pinzon, now medical director of care coordination at Emory Johns Creek Hospital in Atlanta, will describe her experience as an immigrant physician in the Society of Hospital Medicine Converge session: “A Walk in Our Shoes: Immigrant Physicians Sharing Their Stories.” She will be joined by Patricia O’Brien, MD, PhD, FAAP, a pediatric hospitalist in Tampa; Manpreet Malik, MD, a hospitalist at Emory University; and Benji Mathews, MD, SFHM, FACP, chief of hospital medicine at HealthPartners and associate professor at the University of Minnesota.
They will describe their struggles to find their way in the United States, along with the satisfaction of having hard work pay off with better lives for themselves and their families. And together, they’ll provide a variety of narratives that will show, contrary to how many Americans view immigrants, how the experiences of immigrants don’t follow the same path, but each one carves out a path of his or her own.
“The thrust of this is really storytelling, along with putting into context what we can do to help our hospitalist brothers and sisters who are immigrants, and shining the light on it,” Dr. O’Brien said.
Dr. Pinzon was working as a doctor for the Colombian government when she began receiving threats from soldiers in a guerrilla army, which didn’t agree with her alignment with the government. One day, a guerrilla soldier threatened her and her two daughters – aged 5 and 11 at the time – and accurately described her daughters’ whereabouts.
Less than a week later, she and her daughters flew from Bogota to the United States, never to return to Colombia.
“I dropped everything I had when I came here,” she said. An immigration attorney initially recommended that she marry an American man in order to stay in the United States. When Dr. Pinzon declined, they pursued political asylum, and she received it less than a year later.
For 3 years, she worked jobs as assistants in medical offices and in other jobs, well below her education level, as she guided her daughters through school and went through the U.S. medical certification process. She was besieged by doubt constantly, she said.
“I cried for 3 years in a row,” she said. “I wanted to go back to my country. I didn’t want to stay here.”
Finally, she did her medical residency between 2011 and 2014, and got a job with Emory. Her daughters are grown, and one is a doctor in general surgery residency. Dr. Pinzon said she is happy to care for patients, particularly those who are Spanish-speaking and struggle as she did. But she often encounters patients who don’t hide that they dislike her accent.
“I will mute the TV and I will say: ‘I have a strong accent and so I want to make sure communication is clear,’ ” she said. “We have to prove ourselves all of the time. I feel like I have to prove myself to my patients that I’m a good doctor all of the time.” American-born doctors, she added, “shouldn’t take for granted what they already have.”
Dr. O’Brien grew up in Ireland, but in the late 1980s, the country was in a serious recession, with unemployment close to 20%, and her father applied for residency in Canada and the United States. They were accepted in Canada first, and moved there in 1988. A few years later, her parents moved them to Florida.
“They knew in order for us to do well, we had to go abroad,” she said. Dr. O’Brien went to college, medical school and graduate school in Florida, and completed residency in Cincinnati. Feeling the tug of her birthplace, she moved back to Ireland and worked there for a couple years.
“I never really wanted to leave because it was my home,” she said. While there, she came to a new-found appreciation for the U.S. health care system. It’s true that, in Ireland, everyone is insured, but there long wait times – for example, up to 2 years for a sedated nonurgent MRI for a child. She once had to send a patient to Dublin in a taxi with a nurse because an ambulance was unavailable.
“After going back to Ireland, where – I honestly thought I was going to go back and settle there – I realized how visionary my parents were in moving us,” Dr. O’Brien said. “This system in the U.S., there are lot of things broken about it, but we have all the resources.”
She moved back to the United States in August 2016, during a period of anti-immigrant rhetoric.
Nonetheless, Dr. O’Brien said she is happy to be here despite the lack of tolerance she sees in a minority of the U.S. population.
“Have a bit of sensitivity toward your provider. Maybe they speak with an accent. Maybe they don’t speak English perfectly. Maybe they have a different skin color. But their intention is good and it’s to help you and improve your health,” she said.
Ingrid Pinzon, MD, FACP, was working as a medical assistant to a physician a decade ago when she heard the doctor prescribe ibuprofen to a woman who was in the latter stages of pregnancy. Dr. Pinzon was a doctor, having received her education and training in Colombia, but because she had emigrated to the United States and hadn’t yet completed her certification and training here, she was not recognized yet as an American physician.
But she knew that ibuprofen was not recommended during late-term pregnancy, and she was alarmed. She informed the physician of the mistake. The doctor headed to Google, Dr. Pinzon said, and called the patient to rescind the ibuprofen prescription. But she soon fired Dr. Pinzon, seemingly for having had the courage to speak up.
Dr. Pinzon, now medical director of care coordination at Emory Johns Creek Hospital in Atlanta, will describe her experience as an immigrant physician in the Society of Hospital Medicine Converge session: “A Walk in Our Shoes: Immigrant Physicians Sharing Their Stories.” She will be joined by Patricia O’Brien, MD, PhD, FAAP, a pediatric hospitalist in Tampa; Manpreet Malik, MD, a hospitalist at Emory University; and Benji Mathews, MD, SFHM, FACP, chief of hospital medicine at HealthPartners and associate professor at the University of Minnesota.
They will describe their struggles to find their way in the United States, along with the satisfaction of having hard work pay off with better lives for themselves and their families. And together, they’ll provide a variety of narratives that will show, contrary to how many Americans view immigrants, how the experiences of immigrants don’t follow the same path, but each one carves out a path of his or her own.
“The thrust of this is really storytelling, along with putting into context what we can do to help our hospitalist brothers and sisters who are immigrants, and shining the light on it,” Dr. O’Brien said.
Dr. Pinzon was working as a doctor for the Colombian government when she began receiving threats from soldiers in a guerrilla army, which didn’t agree with her alignment with the government. One day, a guerrilla soldier threatened her and her two daughters – aged 5 and 11 at the time – and accurately described her daughters’ whereabouts.
Less than a week later, she and her daughters flew from Bogota to the United States, never to return to Colombia.
“I dropped everything I had when I came here,” she said. An immigration attorney initially recommended that she marry an American man in order to stay in the United States. When Dr. Pinzon declined, they pursued political asylum, and she received it less than a year later.
For 3 years, she worked jobs as assistants in medical offices and in other jobs, well below her education level, as she guided her daughters through school and went through the U.S. medical certification process. She was besieged by doubt constantly, she said.
“I cried for 3 years in a row,” she said. “I wanted to go back to my country. I didn’t want to stay here.”
Finally, she did her medical residency between 2011 and 2014, and got a job with Emory. Her daughters are grown, and one is a doctor in general surgery residency. Dr. Pinzon said she is happy to care for patients, particularly those who are Spanish-speaking and struggle as she did. But she often encounters patients who don’t hide that they dislike her accent.
“I will mute the TV and I will say: ‘I have a strong accent and so I want to make sure communication is clear,’ ” she said. “We have to prove ourselves all of the time. I feel like I have to prove myself to my patients that I’m a good doctor all of the time.” American-born doctors, she added, “shouldn’t take for granted what they already have.”
Dr. O’Brien grew up in Ireland, but in the late 1980s, the country was in a serious recession, with unemployment close to 20%, and her father applied for residency in Canada and the United States. They were accepted in Canada first, and moved there in 1988. A few years later, her parents moved them to Florida.
“They knew in order for us to do well, we had to go abroad,” she said. Dr. O’Brien went to college, medical school and graduate school in Florida, and completed residency in Cincinnati. Feeling the tug of her birthplace, she moved back to Ireland and worked there for a couple years.
“I never really wanted to leave because it was my home,” she said. While there, she came to a new-found appreciation for the U.S. health care system. It’s true that, in Ireland, everyone is insured, but there long wait times – for example, up to 2 years for a sedated nonurgent MRI for a child. She once had to send a patient to Dublin in a taxi with a nurse because an ambulance was unavailable.
“After going back to Ireland, where – I honestly thought I was going to go back and settle there – I realized how visionary my parents were in moving us,” Dr. O’Brien said. “This system in the U.S., there are lot of things broken about it, but we have all the resources.”
She moved back to the United States in August 2016, during a period of anti-immigrant rhetoric.
Nonetheless, Dr. O’Brien said she is happy to be here despite the lack of tolerance she sees in a minority of the U.S. population.
“Have a bit of sensitivity toward your provider. Maybe they speak with an accent. Maybe they don’t speak English perfectly. Maybe they have a different skin color. But their intention is good and it’s to help you and improve your health,” she said.
Roots of physician burnout: It’s the work load
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
Work load, not personal vulnerability, may be at the root of the current physician burnout crisis, a recent study has concluded.
The cutting-edge research utilized cognitive theory and work load analysis to get at the source of burnout among practitioners. The findings indicate that, although some institutions continue to emphasize personal responsibility of physicians to address the issue, it may be the amount and structure of the work itself that triggers burnout in doctors.
“We evaluated the cognitive load of a clinical workday in a national sample of U.S. physicians and its relationship with burnout and professional satisfaction,” wrote Elizabeth Harry, MD, SFHM, a hospitalist at the University of Colorado at Denver, Aurora and coauthors. The results were reported in the Joint Commission Journal on Quality and Patient Safety.
The researchers investigated whether task load correlated with burnout scores in a large national study of U.S. physicians from October 2017 to March 2018.
As the delivery of health care becomes more complex, physicians are charged with ever-increasing amount of administrative and cognitive tasks. Recent evidence indicates that this growing complexity of work is tied to a greater risk of burnout in physicians, compared with workers in other fields. Cognitive load theory, pioneered by psychologist Jonathan Sweller, identified limitations in working memory that humans depend on to carry out cognitive tasks. Cognitive load refers to the amount of working memory used, which can be reduced in the presence of external emotional or physiological stressors. While a potential link between cognitive load and burnout may seem self-evident, the correlation between the cognitive load of physicians and burnout has not been evaluated in a large-scale study until recently.
Physician task load (PTL) was measured using the National Aeronautics and Space Administration Task Load Index (NASA-TLX), a validated questionnaire frequently used to evaluate the cognitive load of work environments, including health care environments. Four domains (perception of effort and mental, physical, and temporal demands) were used to calculate the total PTL score.
Burnout was evaluated using the Emotional Exhaustion and Depersonalization scales of the Maslach Burnout Inventory, a validated tool considered the gold standard for measurement.
The survey sample consisted of physicians of all specialties and was assembled using the American Medical Association Physician Masterfile, an almost complete record of all U.S. physicians independent of AMA membership. All responses were anonymous and participation was voluntary.
Results
Among 30,456 physicians who received the survey, 5,197 (17.1%) responded. In total, 5,276 physicians were included in the analysis.
The median age of respondents was 53 years, and 61.8% self-identified as male. Twenty-four specialties were identified: 23.8% were from a primary care discipline and internal medicine represented the largest respondent group (12.1%).
Almost half of respondents (49.7%) worked in private practice, and 44.8% had been in practice for 21 years or longer.
Overall, 44.0% had at least one symptom of burnout, 38.8% of participants scored in the high range for emotional exhaustion, and 27.4% scored in the high range for depersonalization. The mean score in task load dimension varied by specialty.
The mean PTL score was 260.9 (standard deviation, 71.4). The specialties with the highest PTL score were emergency medicine (369.8), urology (353.7), general surgery subspecialties (343.9), internal medicine subspecialties (342.2), and radiology (341.6).
Aside from specialty, PTL scores also varied by practice setting, gender, age, number of hours worked per week, number of nights on call per week, and years in practice.
The researchers observed a dose response relationship between PTL and risk of burnout. For every 40-point (10%) reduction in PTL, there was 33% lower odds of experiencing burnout (odds ratio, 0.67; 95% confidence interval, 0.65-0.70; P < .0001). Multivariable analyses also indicated that PTL was a significant predictor of burnout, independent of practice setting, specialty, age, gender, and hours worked.
Organizational strategies to reduce physician burnout
Coauthors of the study, Tait D. Shanafelt, MD, professor of medicine at Stanford (Calif.) University and Colin P. West, MD, PhD, of the Mayo Clinic in Rochester, Minn., are both experts on physician well-being and are passionate about finding new ways to reduce physician distress and improving health care delivery.
“Authentic efforts to address this problem must move beyond personal resilience,” Dr. Shanafelt said in an interview. “Organizations that fail to get serious about this issue are going to be left behind and struggle in the war for talent.
“Much like our efforts to improve quality, advancing clinician well-being requires organizations to make it a priority and establish the structure, process, and leadership to promote the desired outcomes,” said Dr. Shanafelt.
One potential strategy for improvement is appointing a chief wellness officer, a dedicated individual within the health care system that leads the organizational effort, explained Dr. Shanafelt. “Over 30 vanguard institutions across the United States have already taken this step.”
Dr. West, a coauthor of the study, explained that conducting an analysis of PTL is fairly straightforward for hospitals and individual institutions. “The NASA-TLX tool is widely available, free to use, and not overly complex, and it could be used to provide insight into physician effort and mental, physical, and temporal demand levels,” he said in an interview.
“Deeper evaluations could follow to identify specific potential solutions, particularly system-level approaches to alleviate PTL,” Dr. West explained. “In the short term, such analyses and solutions would have costs, but helping physicians work more optimally and with less chronic strain from excessive task load would save far more than these costs overall.”
Dr. West also noted that physician burnout is very expensive to a health care system, and strategies to promote physician well-being would be a prudent financial decision long term for health care organizations.
Dr. Harry, lead author of the study, agreed with Dr. West, noting that “quality improvement literature has demonstrated that improvements in inefficiencies that lead to increased demand in the workplace often has the benefit of reduced cost.
“Many studies have demonstrated the risk of turnover due to burnout and the significant cost of physician turn over,” she said in an interview. “This cost avoidance is well worth the investment in improved operations to minimize unnecessary task load.”
Dr. Harry also recommended the NASA-TLX tool as a free resource for health systems and organizations. She noted that future studies will further validate the reliability of the tool.
“At the core, we need to focus on system redesign at both the micro and the macro level,” Dr. Harry said. “Each health system will need to assess inefficiencies in their work flow, while regulatory bodies need to consider the downstream task load of mandates and reporting requirements, all of which contribute to more cognitive load.”
The study was supported by funding from the Stanford Medicine WellMD Center, the American Medical Association, and the Mayo Clinic department of medicine program on physician well-being. Coauthors Lotte N. Dyrbye, MD, and Dr. Shanafelt are coinventors of the Physician Well-being Index, Medical Student Well-Being Index, Nurse Well-Being, and Well-Being Index. Mayo Clinic holds the copyright to these instruments and has licensed them for external use. Dr. Dyrbye and Dr. Shanafelt receive a portion of any royalties paid to Mayo Clinic. All other authors reported no conflicts of interest.
FROM THE JOINT COMMISSION JOURNAL ON QUALITY AND PATIENT SAFETY
Back in session
Before the pandemic, the biggest parent-related challenge for Charlie Wray, DO, MS, a hospitalist and assistant clinical professor of medicine at the University of California, San Francisco, was “figuring out what I was going to pack in my kids’ lunches. Like most people, we were very much in our groove – we knew when my wife was going to leave work, and which day I’d pick up the kids,” Dr. Wray said. “I reflect back on that and think how easy it was.”
The old life – the one that seems so comparatively effortless – has been gone for close to a year now. And with the reopening of schools in the fall of 2020, hospitalists with school-age kids felt – and are still feeling – the strain in a variety of ways.
‘Podding up’
“The largest struggles that we have had involve dealing with the daily logistics of doing at-home learning,” said Dr. Wray, father to a 6-year-old and a 3-year-old. Dr. Wray and his wife are both physicians and have been juggling full work schedules with virtual school for their older child, who is not old enough to be autonomous. “For parents who have younger children who require one-on-one attention for the vast majority of their learning, that certainly takes more of a toll on your time, energy, and resources.”
Uncertainty has created anxiety about the future. “We have no idea what’s going to be happening next month. How do we plan for that? How do we allocate our time for that? That has been a real struggle for us, especially for a two-physician household where we are both considered front line and are both needing to be at the hospital or the clinic on a fairly regular basis,” he said.
Then there is the never-ending stress. Dr. Wray observed that physicians are used to operating under stress, especially at work. “What I think is gnawing at me, and probably a lot of other physicians out there, is you go home and that stress is still there. It’s really hard to escape it. And you wake up in the morning and it’s there, whereas in the past, you could have a nice day. There’s little separation between work and domestic life right now.”
Having to work later into the evening has eaten into time for himself and time with his wife too. “That’s another side effect of the pandemic – it not only takes your time during the day, it takes the time you used to have at night to relax.”
To manage these challenges, Dr. Wray said he and his wife regularly double check their schedules. The family has also created a pod – “I think ‘podded up’ is a verb now,” he laughed – with another family and hired a recent college graduate to help the kids with their virtual learning. “Is it as good as being at school and amongst friends and having an actual teacher there? Of course not. But I think it’s the best that we can do.”
Dr. Wray said his employers have been flexible and understanding regarding scheduling conflicts that parents can have. “It’s really difficult for us, so oftentimes I struggle to see how other people are pulling this off. We recognize how fortunate we are, so that’s something I never want to overlook.”
Dividing and conquering
The biggest prepandemic issue for Sridevi Alla, MD, a hospitalist at Baptist Memorial Health in Jackson, Miss., and mother to four children – a 10-year-old, 6-year-old, 2-year-old, and a 9-month-old – was finding a babysitter on the weekend to take her kids out somewhere to burn off energy.
That’s a noticeable departure from the current demand to be not just a parent, but a teacher and a counselor too, thanks to virtual school, noted Dr. Alla. “You are their everything now,” she said. “They don’t have friends. They don’t have any other atmosphere or learning environment to let out their energy, their emotions. You have become their world.”
The beginning of the pandemic was particularly stressful for Dr. Alla, who is in the United States on an H-1B visa. “It was totally worrisome because you’re putting yourself at risk with patients who have the coronavirus, despite not knowing what your future itself is going to be like or what your family’s future is going to be like if anything happens to you,” she said. “We are fortunate we have our jobs. A lot of my immigrant friends lost theirs in the middle of this and they’re still trying to find jobs.”
Dr. Alla’s first challenge was whether to send her older two children to school or keep them at home to do virtual learning. The lack of information from the schools at first did not help that process, but she and her husband ended up choosing virtual school, a decision they still occasionally question.
Next, they had to find child care, and not just someone who could look after the younger two kids – they needed someone with the ability to also help the older ones with their homework.
Though initially the family had help, their first nanny had to quit because her roommate contracted COVID. “After that, we didn’t have help and my husband decided to work from home,” said Dr. Alla. “As of now, we’re still looking for child care. And the main issues are the late hours and the hospitalist week-on, week-off schedule.”
“It’s extremely hard,” she reflected. “At home, there’s no line. A 2-year-old doesn’t understand office time or personal time.” Still, Dr. Alla and her husband are maintaining by dividing up responsibilities and making sure they are always planning ahead.
Maintaining a routine
The greatest challenge for Heather Nye, MD, PhD, a hospitalist and professor of clinical medicine at UCSF, has been “maintaining normalcy for the kids.” She mourns the loss of a normal childhood for her kids, however temporary. “Living with abandon, feeling like you’re invincible, going out there and breaking your arm, meeting people, not fearing the world – those are not things we can instill in them right now,” she said.
The mother of an eighth grader and a second grader, Dr. Nye said their school district did not communicate well about how school would proceed. The district ended up offering only virtual school, with no plans for even hybrid learning in the future, leaving parents scrambling to plan.
Dr. Nye lucked out when her youngest child was accepted for a slot at a day camp offered through a partnership between the YMCA and UCSF. However, her eighth grader did not do well with distance learning in the spring, so having that virtual school as the only option has been difficult.
“Neither of the kids are doing really well in school,” she said. Her older one is overwhelmed by all the disparate online platforms and her youngest is having a hard time adjusting to differences like using a virtual pen. “The learning itself without question has suffered. You wonder about evaluation and this whole cohort of children in what will probably be more or less a lost year.”
Routines are the backbone of the family’s survival. “I think one of the most important things for kids in any stage of development is having a routine and being comfortable with that routine because that creates a sense of wellbeing in this time of uncertainty,” Dr. Nye said.
Neither Dr. Nye nor her husband, a geriatrician, have cut back on their work, so they are balancing a full plate of activities with parenting. Though their family is managing, “there are streaks of days where we’re like: ‘Are we failing our children?’ I’m sure every parent out there is asking themselves: ‘Am I doing enough?’” But she said, “We’re very, very lucky. We got that [camp] slot, we have the money to pay for it, and we both have flexible jobs.”
Rallying resources
Avital O’Glasser, MD, a hospitalist and associate professor of medicine at Oregon Health and Science University, Portland, fervently wished she could clone herself when the pandemic first started. Not only were her kids suddenly thrown into online classes, but she was pulled in to create a new service line for the COVID response at her clinic.
“The number of times that I said I think I need a time turner from Harry Potter. ... I felt that nothing was getting done even close to adequately because we were cutting corners left and right,” she said.
Thankfully, things have simmered down and Dr. O’Glasser is now working from home 5 or 6 days a week while her husband, a lawyer, goes to his job. “I think stress is lower now, but that’s in large part because, by the end of June, I really had to just stop and acknowledge how stressed I was and do a dramatic realignment of what I was doing for myself in terms of mental health support and bandwidth,” she said. Part of that involved realizing that the family needed a homeschool nanny for their 10-year-old and 7-year-old. “It’s been a lifesaver,” said Dr. O’Glasser.
Though life is on more of an even keel now, stress pops up in unexpected ways. “My youngest has pretty intense separation anxiety from me. Even with getting attention all day from our homeschool nanny, the day after I’m out of the house at the hospital, he really clings to me,” Dr. O’Glasser said. There’s sibling rivalry too, in an attempt to get parental attention.
Setting boundaries between work and home was her biggest challenge prepandemic, and that has not changed. “You’re trying to find that happy balance between professional development and family,” Dr. O’Glasser said. “Where do I cut corners? Do I try to multitask but spread myself thin? How do I say no to things? When am I going to find time to do laundry? When am I disconnecting? I think that now it’s facets of the same conundrum, but just manifested in different ways.”
She emphasized that parents should go easy on themselves right now. “A lot of parenting rules went out the window. My kids have had more screen time…and the amount of junk food they eat right now? Celebrate the wins.” Dr. O’Glasser chuckled about how her definition of a “win” has changed. “The bar now is something that I may never have considered a win before. Just seize those small moments. If my 7-year-old needs to do reading at my feet while I’m finishing notes from the day before, that’s okay,” she said.
How hospitalist groups can help
All four hospitalists had ideas about how hospitalist groups can help parents with school-age kids during the pandemic.
Providing child care at health care systems gives employees additional support, said Dr. Alla. Some of her friends have been unable to find child care because they are physicians who care for COVID patients and people do not want the extra risk. “I think any institution should think about this option because it’s very beneficial for an employee, especially for the long hours.”
Dr. Wray said he saw a program that matches up a hospitalist who has kids with one who does not in a type of buddy system, and they check in with each other. Then, if the parent has something come up, the other hospitalist can fill in and the parent can “pay it back” at another time. “This doesn’t put all the impetus on the schedule or on a single individual but spreads the risk out a little more and gives parents a bit of a parachute to make them feel like the system is supporting them,” he said.
“I would encourage groups to reach appropriate accommodations that are equitable and that don’t create discord because they’re perceived as unfair,” said Dr. O’Glasser. For instance, giving child care stipends, but limiting them to care at a licensed facility when some people might need to pay for a homeschool tutor. “Some of the policies that I saw seem to leave out the elementary school lot. You can’t just lump all kids together.”
Dr. Nye thought group leaders should take unseen pressures into account when evaluating employee performance. “I think we’re going to need to shift our yardstick because we can’t do everything now,” she said. “I’m talking about the extra things that people do that they’re evaluated on at the end of the year like volunteering for more shifts, sitting on committees, the things that likely aren’t in their job description. We’re going to have times when people are filling every last minute for their families. Face it with kindness and understanding and know that, in future years, things are going to go back to normal.”
Before the pandemic, the biggest parent-related challenge for Charlie Wray, DO, MS, a hospitalist and assistant clinical professor of medicine at the University of California, San Francisco, was “figuring out what I was going to pack in my kids’ lunches. Like most people, we were very much in our groove – we knew when my wife was going to leave work, and which day I’d pick up the kids,” Dr. Wray said. “I reflect back on that and think how easy it was.”
The old life – the one that seems so comparatively effortless – has been gone for close to a year now. And with the reopening of schools in the fall of 2020, hospitalists with school-age kids felt – and are still feeling – the strain in a variety of ways.
‘Podding up’
“The largest struggles that we have had involve dealing with the daily logistics of doing at-home learning,” said Dr. Wray, father to a 6-year-old and a 3-year-old. Dr. Wray and his wife are both physicians and have been juggling full work schedules with virtual school for their older child, who is not old enough to be autonomous. “For parents who have younger children who require one-on-one attention for the vast majority of their learning, that certainly takes more of a toll on your time, energy, and resources.”
Uncertainty has created anxiety about the future. “We have no idea what’s going to be happening next month. How do we plan for that? How do we allocate our time for that? That has been a real struggle for us, especially for a two-physician household where we are both considered front line and are both needing to be at the hospital or the clinic on a fairly regular basis,” he said.
Then there is the never-ending stress. Dr. Wray observed that physicians are used to operating under stress, especially at work. “What I think is gnawing at me, and probably a lot of other physicians out there, is you go home and that stress is still there. It’s really hard to escape it. And you wake up in the morning and it’s there, whereas in the past, you could have a nice day. There’s little separation between work and domestic life right now.”
Having to work later into the evening has eaten into time for himself and time with his wife too. “That’s another side effect of the pandemic – it not only takes your time during the day, it takes the time you used to have at night to relax.”
To manage these challenges, Dr. Wray said he and his wife regularly double check their schedules. The family has also created a pod – “I think ‘podded up’ is a verb now,” he laughed – with another family and hired a recent college graduate to help the kids with their virtual learning. “Is it as good as being at school and amongst friends and having an actual teacher there? Of course not. But I think it’s the best that we can do.”
Dr. Wray said his employers have been flexible and understanding regarding scheduling conflicts that parents can have. “It’s really difficult for us, so oftentimes I struggle to see how other people are pulling this off. We recognize how fortunate we are, so that’s something I never want to overlook.”
Dividing and conquering
The biggest prepandemic issue for Sridevi Alla, MD, a hospitalist at Baptist Memorial Health in Jackson, Miss., and mother to four children – a 10-year-old, 6-year-old, 2-year-old, and a 9-month-old – was finding a babysitter on the weekend to take her kids out somewhere to burn off energy.
That’s a noticeable departure from the current demand to be not just a parent, but a teacher and a counselor too, thanks to virtual school, noted Dr. Alla. “You are their everything now,” she said. “They don’t have friends. They don’t have any other atmosphere or learning environment to let out their energy, their emotions. You have become their world.”
The beginning of the pandemic was particularly stressful for Dr. Alla, who is in the United States on an H-1B visa. “It was totally worrisome because you’re putting yourself at risk with patients who have the coronavirus, despite not knowing what your future itself is going to be like or what your family’s future is going to be like if anything happens to you,” she said. “We are fortunate we have our jobs. A lot of my immigrant friends lost theirs in the middle of this and they’re still trying to find jobs.”
Dr. Alla’s first challenge was whether to send her older two children to school or keep them at home to do virtual learning. The lack of information from the schools at first did not help that process, but she and her husband ended up choosing virtual school, a decision they still occasionally question.
Next, they had to find child care, and not just someone who could look after the younger two kids – they needed someone with the ability to also help the older ones with their homework.
Though initially the family had help, their first nanny had to quit because her roommate contracted COVID. “After that, we didn’t have help and my husband decided to work from home,” said Dr. Alla. “As of now, we’re still looking for child care. And the main issues are the late hours and the hospitalist week-on, week-off schedule.”
“It’s extremely hard,” she reflected. “At home, there’s no line. A 2-year-old doesn’t understand office time or personal time.” Still, Dr. Alla and her husband are maintaining by dividing up responsibilities and making sure they are always planning ahead.
Maintaining a routine
The greatest challenge for Heather Nye, MD, PhD, a hospitalist and professor of clinical medicine at UCSF, has been “maintaining normalcy for the kids.” She mourns the loss of a normal childhood for her kids, however temporary. “Living with abandon, feeling like you’re invincible, going out there and breaking your arm, meeting people, not fearing the world – those are not things we can instill in them right now,” she said.
The mother of an eighth grader and a second grader, Dr. Nye said their school district did not communicate well about how school would proceed. The district ended up offering only virtual school, with no plans for even hybrid learning in the future, leaving parents scrambling to plan.
Dr. Nye lucked out when her youngest child was accepted for a slot at a day camp offered through a partnership between the YMCA and UCSF. However, her eighth grader did not do well with distance learning in the spring, so having that virtual school as the only option has been difficult.
“Neither of the kids are doing really well in school,” she said. Her older one is overwhelmed by all the disparate online platforms and her youngest is having a hard time adjusting to differences like using a virtual pen. “The learning itself without question has suffered. You wonder about evaluation and this whole cohort of children in what will probably be more or less a lost year.”
Routines are the backbone of the family’s survival. “I think one of the most important things for kids in any stage of development is having a routine and being comfortable with that routine because that creates a sense of wellbeing in this time of uncertainty,” Dr. Nye said.
Neither Dr. Nye nor her husband, a geriatrician, have cut back on their work, so they are balancing a full plate of activities with parenting. Though their family is managing, “there are streaks of days where we’re like: ‘Are we failing our children?’ I’m sure every parent out there is asking themselves: ‘Am I doing enough?’” But she said, “We’re very, very lucky. We got that [camp] slot, we have the money to pay for it, and we both have flexible jobs.”
Rallying resources
Avital O’Glasser, MD, a hospitalist and associate professor of medicine at Oregon Health and Science University, Portland, fervently wished she could clone herself when the pandemic first started. Not only were her kids suddenly thrown into online classes, but she was pulled in to create a new service line for the COVID response at her clinic.
“The number of times that I said I think I need a time turner from Harry Potter. ... I felt that nothing was getting done even close to adequately because we were cutting corners left and right,” she said.
Thankfully, things have simmered down and Dr. O’Glasser is now working from home 5 or 6 days a week while her husband, a lawyer, goes to his job. “I think stress is lower now, but that’s in large part because, by the end of June, I really had to just stop and acknowledge how stressed I was and do a dramatic realignment of what I was doing for myself in terms of mental health support and bandwidth,” she said. Part of that involved realizing that the family needed a homeschool nanny for their 10-year-old and 7-year-old. “It’s been a lifesaver,” said Dr. O’Glasser.
Though life is on more of an even keel now, stress pops up in unexpected ways. “My youngest has pretty intense separation anxiety from me. Even with getting attention all day from our homeschool nanny, the day after I’m out of the house at the hospital, he really clings to me,” Dr. O’Glasser said. There’s sibling rivalry too, in an attempt to get parental attention.
Setting boundaries between work and home was her biggest challenge prepandemic, and that has not changed. “You’re trying to find that happy balance between professional development and family,” Dr. O’Glasser said. “Where do I cut corners? Do I try to multitask but spread myself thin? How do I say no to things? When am I going to find time to do laundry? When am I disconnecting? I think that now it’s facets of the same conundrum, but just manifested in different ways.”
She emphasized that parents should go easy on themselves right now. “A lot of parenting rules went out the window. My kids have had more screen time…and the amount of junk food they eat right now? Celebrate the wins.” Dr. O’Glasser chuckled about how her definition of a “win” has changed. “The bar now is something that I may never have considered a win before. Just seize those small moments. If my 7-year-old needs to do reading at my feet while I’m finishing notes from the day before, that’s okay,” she said.
How hospitalist groups can help
All four hospitalists had ideas about how hospitalist groups can help parents with school-age kids during the pandemic.
Providing child care at health care systems gives employees additional support, said Dr. Alla. Some of her friends have been unable to find child care because they are physicians who care for COVID patients and people do not want the extra risk. “I think any institution should think about this option because it’s very beneficial for an employee, especially for the long hours.”
Dr. Wray said he saw a program that matches up a hospitalist who has kids with one who does not in a type of buddy system, and they check in with each other. Then, if the parent has something come up, the other hospitalist can fill in and the parent can “pay it back” at another time. “This doesn’t put all the impetus on the schedule or on a single individual but spreads the risk out a little more and gives parents a bit of a parachute to make them feel like the system is supporting them,” he said.
“I would encourage groups to reach appropriate accommodations that are equitable and that don’t create discord because they’re perceived as unfair,” said Dr. O’Glasser. For instance, giving child care stipends, but limiting them to care at a licensed facility when some people might need to pay for a homeschool tutor. “Some of the policies that I saw seem to leave out the elementary school lot. You can’t just lump all kids together.”
Dr. Nye thought group leaders should take unseen pressures into account when evaluating employee performance. “I think we’re going to need to shift our yardstick because we can’t do everything now,” she said. “I’m talking about the extra things that people do that they’re evaluated on at the end of the year like volunteering for more shifts, sitting on committees, the things that likely aren’t in their job description. We’re going to have times when people are filling every last minute for their families. Face it with kindness and understanding and know that, in future years, things are going to go back to normal.”
Before the pandemic, the biggest parent-related challenge for Charlie Wray, DO, MS, a hospitalist and assistant clinical professor of medicine at the University of California, San Francisco, was “figuring out what I was going to pack in my kids’ lunches. Like most people, we were very much in our groove – we knew when my wife was going to leave work, and which day I’d pick up the kids,” Dr. Wray said. “I reflect back on that and think how easy it was.”
The old life – the one that seems so comparatively effortless – has been gone for close to a year now. And with the reopening of schools in the fall of 2020, hospitalists with school-age kids felt – and are still feeling – the strain in a variety of ways.
‘Podding up’
“The largest struggles that we have had involve dealing with the daily logistics of doing at-home learning,” said Dr. Wray, father to a 6-year-old and a 3-year-old. Dr. Wray and his wife are both physicians and have been juggling full work schedules with virtual school for their older child, who is not old enough to be autonomous. “For parents who have younger children who require one-on-one attention for the vast majority of their learning, that certainly takes more of a toll on your time, energy, and resources.”
Uncertainty has created anxiety about the future. “We have no idea what’s going to be happening next month. How do we plan for that? How do we allocate our time for that? That has been a real struggle for us, especially for a two-physician household where we are both considered front line and are both needing to be at the hospital or the clinic on a fairly regular basis,” he said.
Then there is the never-ending stress. Dr. Wray observed that physicians are used to operating under stress, especially at work. “What I think is gnawing at me, and probably a lot of other physicians out there, is you go home and that stress is still there. It’s really hard to escape it. And you wake up in the morning and it’s there, whereas in the past, you could have a nice day. There’s little separation between work and domestic life right now.”
Having to work later into the evening has eaten into time for himself and time with his wife too. “That’s another side effect of the pandemic – it not only takes your time during the day, it takes the time you used to have at night to relax.”
To manage these challenges, Dr. Wray said he and his wife regularly double check their schedules. The family has also created a pod – “I think ‘podded up’ is a verb now,” he laughed – with another family and hired a recent college graduate to help the kids with their virtual learning. “Is it as good as being at school and amongst friends and having an actual teacher there? Of course not. But I think it’s the best that we can do.”
Dr. Wray said his employers have been flexible and understanding regarding scheduling conflicts that parents can have. “It’s really difficult for us, so oftentimes I struggle to see how other people are pulling this off. We recognize how fortunate we are, so that’s something I never want to overlook.”
Dividing and conquering
The biggest prepandemic issue for Sridevi Alla, MD, a hospitalist at Baptist Memorial Health in Jackson, Miss., and mother to four children – a 10-year-old, 6-year-old, 2-year-old, and a 9-month-old – was finding a babysitter on the weekend to take her kids out somewhere to burn off energy.
That’s a noticeable departure from the current demand to be not just a parent, but a teacher and a counselor too, thanks to virtual school, noted Dr. Alla. “You are their everything now,” she said. “They don’t have friends. They don’t have any other atmosphere or learning environment to let out their energy, their emotions. You have become their world.”
The beginning of the pandemic was particularly stressful for Dr. Alla, who is in the United States on an H-1B visa. “It was totally worrisome because you’re putting yourself at risk with patients who have the coronavirus, despite not knowing what your future itself is going to be like or what your family’s future is going to be like if anything happens to you,” she said. “We are fortunate we have our jobs. A lot of my immigrant friends lost theirs in the middle of this and they’re still trying to find jobs.”
Dr. Alla’s first challenge was whether to send her older two children to school or keep them at home to do virtual learning. The lack of information from the schools at first did not help that process, but she and her husband ended up choosing virtual school, a decision they still occasionally question.
Next, they had to find child care, and not just someone who could look after the younger two kids – they needed someone with the ability to also help the older ones with their homework.
Though initially the family had help, their first nanny had to quit because her roommate contracted COVID. “After that, we didn’t have help and my husband decided to work from home,” said Dr. Alla. “As of now, we’re still looking for child care. And the main issues are the late hours and the hospitalist week-on, week-off schedule.”
“It’s extremely hard,” she reflected. “At home, there’s no line. A 2-year-old doesn’t understand office time or personal time.” Still, Dr. Alla and her husband are maintaining by dividing up responsibilities and making sure they are always planning ahead.
Maintaining a routine
The greatest challenge for Heather Nye, MD, PhD, a hospitalist and professor of clinical medicine at UCSF, has been “maintaining normalcy for the kids.” She mourns the loss of a normal childhood for her kids, however temporary. “Living with abandon, feeling like you’re invincible, going out there and breaking your arm, meeting people, not fearing the world – those are not things we can instill in them right now,” she said.
The mother of an eighth grader and a second grader, Dr. Nye said their school district did not communicate well about how school would proceed. The district ended up offering only virtual school, with no plans for even hybrid learning in the future, leaving parents scrambling to plan.
Dr. Nye lucked out when her youngest child was accepted for a slot at a day camp offered through a partnership between the YMCA and UCSF. However, her eighth grader did not do well with distance learning in the spring, so having that virtual school as the only option has been difficult.
“Neither of the kids are doing really well in school,” she said. Her older one is overwhelmed by all the disparate online platforms and her youngest is having a hard time adjusting to differences like using a virtual pen. “The learning itself without question has suffered. You wonder about evaluation and this whole cohort of children in what will probably be more or less a lost year.”
Routines are the backbone of the family’s survival. “I think one of the most important things for kids in any stage of development is having a routine and being comfortable with that routine because that creates a sense of wellbeing in this time of uncertainty,” Dr. Nye said.
Neither Dr. Nye nor her husband, a geriatrician, have cut back on their work, so they are balancing a full plate of activities with parenting. Though their family is managing, “there are streaks of days where we’re like: ‘Are we failing our children?’ I’m sure every parent out there is asking themselves: ‘Am I doing enough?’” But she said, “We’re very, very lucky. We got that [camp] slot, we have the money to pay for it, and we both have flexible jobs.”
Rallying resources
Avital O’Glasser, MD, a hospitalist and associate professor of medicine at Oregon Health and Science University, Portland, fervently wished she could clone herself when the pandemic first started. Not only were her kids suddenly thrown into online classes, but she was pulled in to create a new service line for the COVID response at her clinic.
“The number of times that I said I think I need a time turner from Harry Potter. ... I felt that nothing was getting done even close to adequately because we were cutting corners left and right,” she said.
Thankfully, things have simmered down and Dr. O’Glasser is now working from home 5 or 6 days a week while her husband, a lawyer, goes to his job. “I think stress is lower now, but that’s in large part because, by the end of June, I really had to just stop and acknowledge how stressed I was and do a dramatic realignment of what I was doing for myself in terms of mental health support and bandwidth,” she said. Part of that involved realizing that the family needed a homeschool nanny for their 10-year-old and 7-year-old. “It’s been a lifesaver,” said Dr. O’Glasser.
Though life is on more of an even keel now, stress pops up in unexpected ways. “My youngest has pretty intense separation anxiety from me. Even with getting attention all day from our homeschool nanny, the day after I’m out of the house at the hospital, he really clings to me,” Dr. O’Glasser said. There’s sibling rivalry too, in an attempt to get parental attention.
Setting boundaries between work and home was her biggest challenge prepandemic, and that has not changed. “You’re trying to find that happy balance between professional development and family,” Dr. O’Glasser said. “Where do I cut corners? Do I try to multitask but spread myself thin? How do I say no to things? When am I going to find time to do laundry? When am I disconnecting? I think that now it’s facets of the same conundrum, but just manifested in different ways.”
She emphasized that parents should go easy on themselves right now. “A lot of parenting rules went out the window. My kids have had more screen time…and the amount of junk food they eat right now? Celebrate the wins.” Dr. O’Glasser chuckled about how her definition of a “win” has changed. “The bar now is something that I may never have considered a win before. Just seize those small moments. If my 7-year-old needs to do reading at my feet while I’m finishing notes from the day before, that’s okay,” she said.
How hospitalist groups can help
All four hospitalists had ideas about how hospitalist groups can help parents with school-age kids during the pandemic.
Providing child care at health care systems gives employees additional support, said Dr. Alla. Some of her friends have been unable to find child care because they are physicians who care for COVID patients and people do not want the extra risk. “I think any institution should think about this option because it’s very beneficial for an employee, especially for the long hours.”
Dr. Wray said he saw a program that matches up a hospitalist who has kids with one who does not in a type of buddy system, and they check in with each other. Then, if the parent has something come up, the other hospitalist can fill in and the parent can “pay it back” at another time. “This doesn’t put all the impetus on the schedule or on a single individual but spreads the risk out a little more and gives parents a bit of a parachute to make them feel like the system is supporting them,” he said.
“I would encourage groups to reach appropriate accommodations that are equitable and that don’t create discord because they’re perceived as unfair,” said Dr. O’Glasser. For instance, giving child care stipends, but limiting them to care at a licensed facility when some people might need to pay for a homeschool tutor. “Some of the policies that I saw seem to leave out the elementary school lot. You can’t just lump all kids together.”
Dr. Nye thought group leaders should take unseen pressures into account when evaluating employee performance. “I think we’re going to need to shift our yardstick because we can’t do everything now,” she said. “I’m talking about the extra things that people do that they’re evaluated on at the end of the year like volunteering for more shifts, sitting on committees, the things that likely aren’t in their job description. We’re going to have times when people are filling every last minute for their families. Face it with kindness and understanding and know that, in future years, things are going to go back to normal.”
Key trends in hospitalist compensation from the 2020 SoHM Report
In a time of tremendous uncertainty, there is one trend that seems consistent year over year – the undisputed value of hospitalists. In the 2020 State of Hospital Medicine (SoHM) Report, the Society of Hospital Medicine partnered with the Medical Group Management Association (MGMA) to provide data on hospitalist compensation and productivity. The Report provides resounding evidence that hospitalists continue to be compensated at rising rates. This may be driven by both the continued demand-supply mismatch and a recognition of the overall value they generate rather than strictly the volume of their productivity.
In 2020, the median total compensation nationally for adult hospitalists (internal medicine and family medicine) was $307,633, representing an increase of over 6% from the 2018 Survey (see Figure 1). 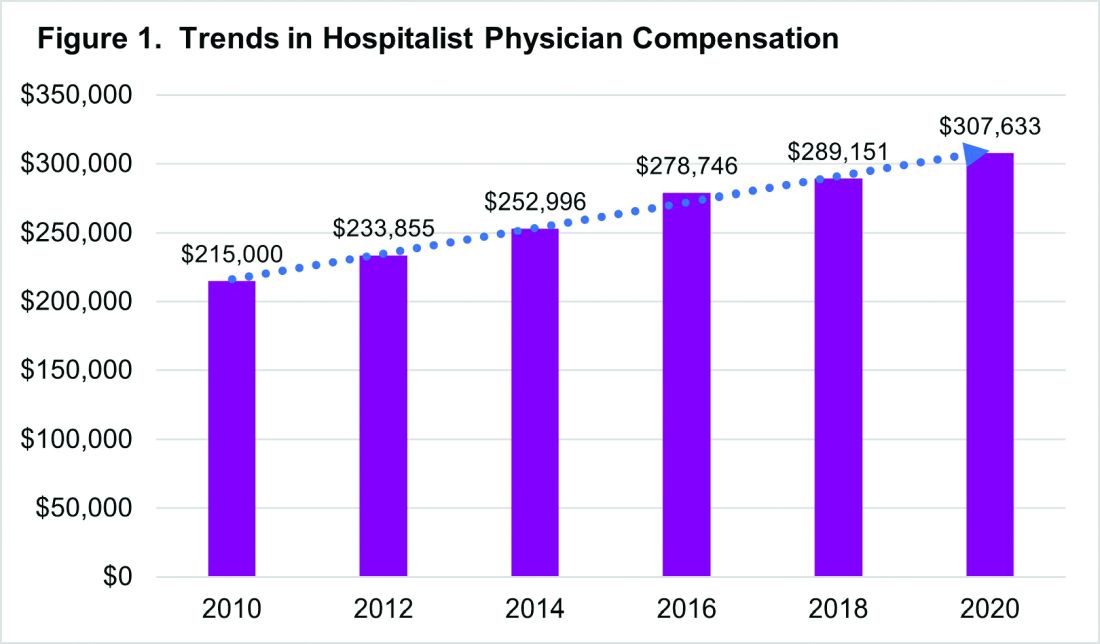
With significant regional variability in compensation across the country, hospitalists in the South continue to earn more than their colleagues in the East – a median compensation difference of about $33,000. However, absolute wage comparisons can be misleading without also considering regional variations in productivity as well.
Reviewing compensation per work relative value unit (wRVU) and per encounter offer additional insight for a more comprehensive assessment. When comparing regional compensation per wRVU, the 2020 Survey continues to show a trend toward hospitalists in the Midwest and West earning more per wRVU than their colleagues in other parts of the country ($78.13 per RVU in the Midwest, $78.95 per RVU in the West). More striking is how hospital medicine groups (HMGs) in the South garner lower compensation per RVU ($57.77) than those in the East ($67.54), even though their total compensation was much higher. This could reflect the gradual decline in compensation per wRVU that’s observed at higher productivity levels. While it’s typical for compensation to increase as productivity does, the rate of increase is generally to a lesser degree.
Like past SoHM Surveys, the 2020 Report revealed that academic and non-academic hospitalists are compensated similarly per wRVU (see Figure 2). 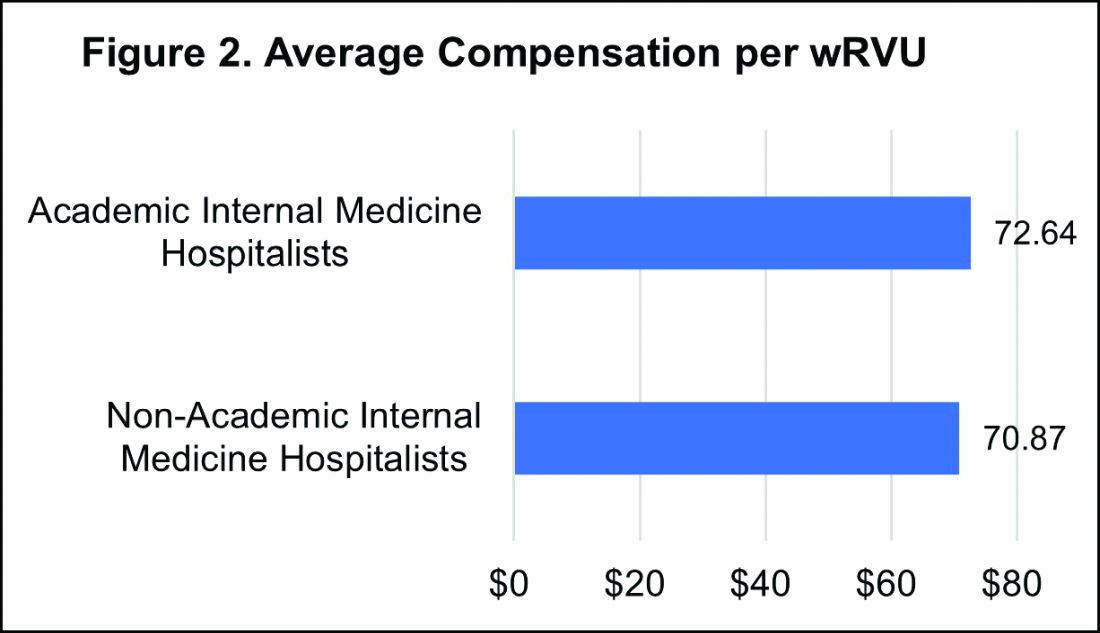
However, the total compensation continues to be lower for academic hospitalists, with a median compensation difference of approximately $70,000 compared to their non-academic colleagues. Some of this sizable variance is offset by the fact that academic HMGs receive more in employee benefits packages than non-academic groups – a difference in median value of $10,500. Ideally, academic hospitalist compensation models should appropriately reflect and value their work efforts toward the tripartite academic mission of clinical care, education, and research. It would be valuable for future surveys to define and measure academic production in order to develop national standards for compensation models that recognize these non-billable forms of productivity.
While it’s important to review compensation benchmarks to remain competitive, it’s difficult to put a price on some factors that many may consider more valuable – group culture, opportunities for professional growth, and schedules that afford better work-life integration. Indirect measures of such benefits include paid time off, paid sick days, CME allowances and time, and retirement benefits programs. In 2020, the median employer contribution to retirement plans was reported to be $13,955, with respondents in the Midwest receiving the highest retirement benefit of $33,771.
It’s encouraging to see that hospitalist compensation continues to rise compared to previous years, despite relatively flat trends in wRVUs and total patient encounters. Another continued trend over the past years is the rising amount of financial support per physician that hospitals or other organizations provide HMGs (see Figure 3). 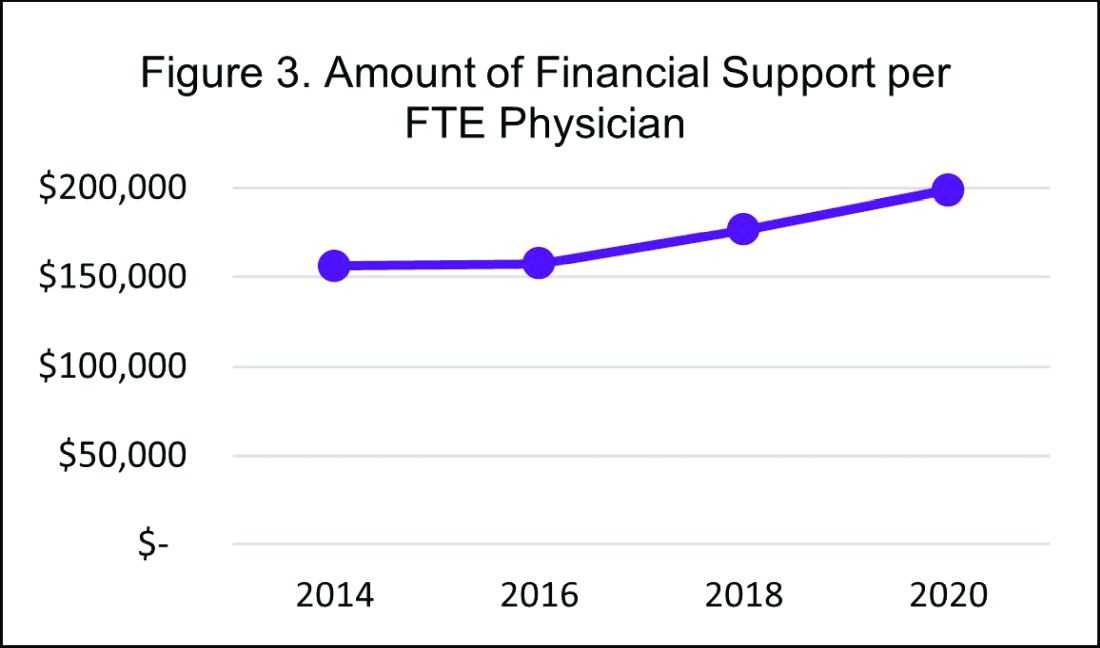
In 2020, the median financial support per FTE (full time equivalent) physician serving adult patients increased by 12% over 2018, to $198,750. Collectively these trends indicate hospitals are willing to compensate hospitalists for more than just their clinical volume.
There’s no doubt that the COVID-19 pandemic had some financial impact on hospital medicine groups in 2020. To assess this impact, SHM conducted a follow-up survey and compiled a COVID-19 Addendum to the SoHM Report. While 20.5% of HMG group respondents from the East reported providing hazard pay to clinicians caring for COVID-19 patients, nationally only 9.8% of groups said they offered this benefit. Of the 121 HMGs responding from across the country, 42% reported reductions in compensation, which included measures such as reductions in pay level and elimination or delays to bonus payments. The degree of reductions was not quantified, but fortunately the vast majority of these groups reported that these changes were likely to be temporary. To access all data in the 2020 SoHM Report and COVID-19 Addendum, visit hospitalmedicine.org/sohm to purchase your copy.
It’s certainly unclear what the future holds, but despite any transient changes observed during the COVID-19 pandemic, I believe that historical trends in hospitalist compensation will continue. If 2020 has taught us anything, it’s that hospitalists are essential, not only during an acute care crisis but for daily operations of any hospital.
Dr. Kurian is chief of the Division of Hospital Medicine at Northwell Health in New York. She is a member of SHM’s Practice Analysis Committee.
In a time of tremendous uncertainty, there is one trend that seems consistent year over year – the undisputed value of hospitalists. In the 2020 State of Hospital Medicine (SoHM) Report, the Society of Hospital Medicine partnered with the Medical Group Management Association (MGMA) to provide data on hospitalist compensation and productivity. The Report provides resounding evidence that hospitalists continue to be compensated at rising rates. This may be driven by both the continued demand-supply mismatch and a recognition of the overall value they generate rather than strictly the volume of their productivity.
In 2020, the median total compensation nationally for adult hospitalists (internal medicine and family medicine) was $307,633, representing an increase of over 6% from the 2018 Survey (see Figure 1). 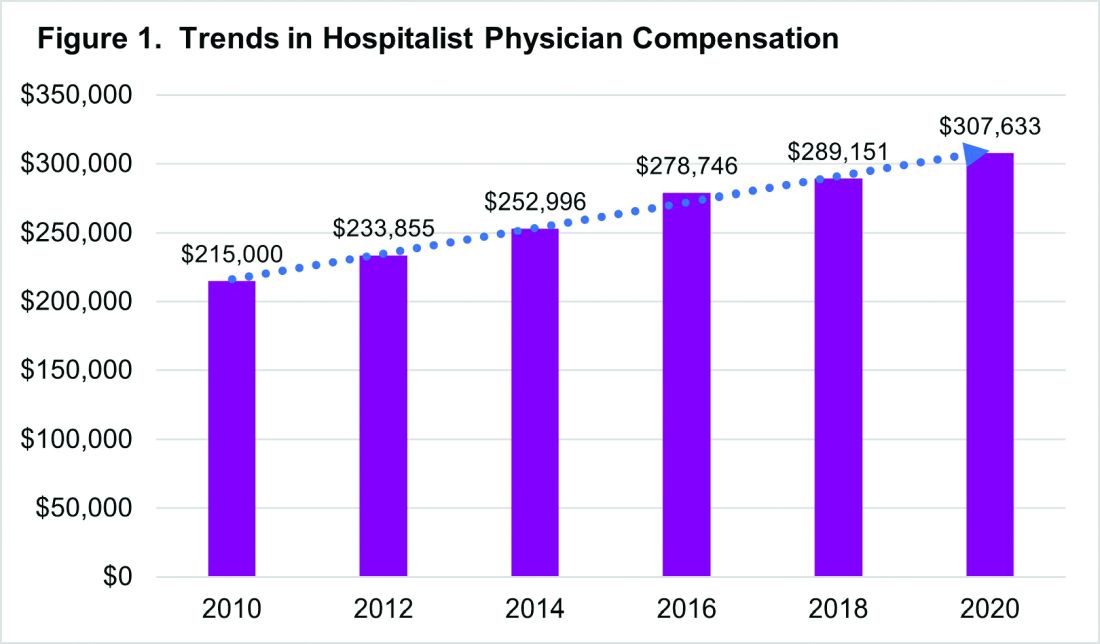
With significant regional variability in compensation across the country, hospitalists in the South continue to earn more than their colleagues in the East – a median compensation difference of about $33,000. However, absolute wage comparisons can be misleading without also considering regional variations in productivity as well.
Reviewing compensation per work relative value unit (wRVU) and per encounter offer additional insight for a more comprehensive assessment. When comparing regional compensation per wRVU, the 2020 Survey continues to show a trend toward hospitalists in the Midwest and West earning more per wRVU than their colleagues in other parts of the country ($78.13 per RVU in the Midwest, $78.95 per RVU in the West). More striking is how hospital medicine groups (HMGs) in the South garner lower compensation per RVU ($57.77) than those in the East ($67.54), even though their total compensation was much higher. This could reflect the gradual decline in compensation per wRVU that’s observed at higher productivity levels. While it’s typical for compensation to increase as productivity does, the rate of increase is generally to a lesser degree.
Like past SoHM Surveys, the 2020 Report revealed that academic and non-academic hospitalists are compensated similarly per wRVU (see Figure 2). 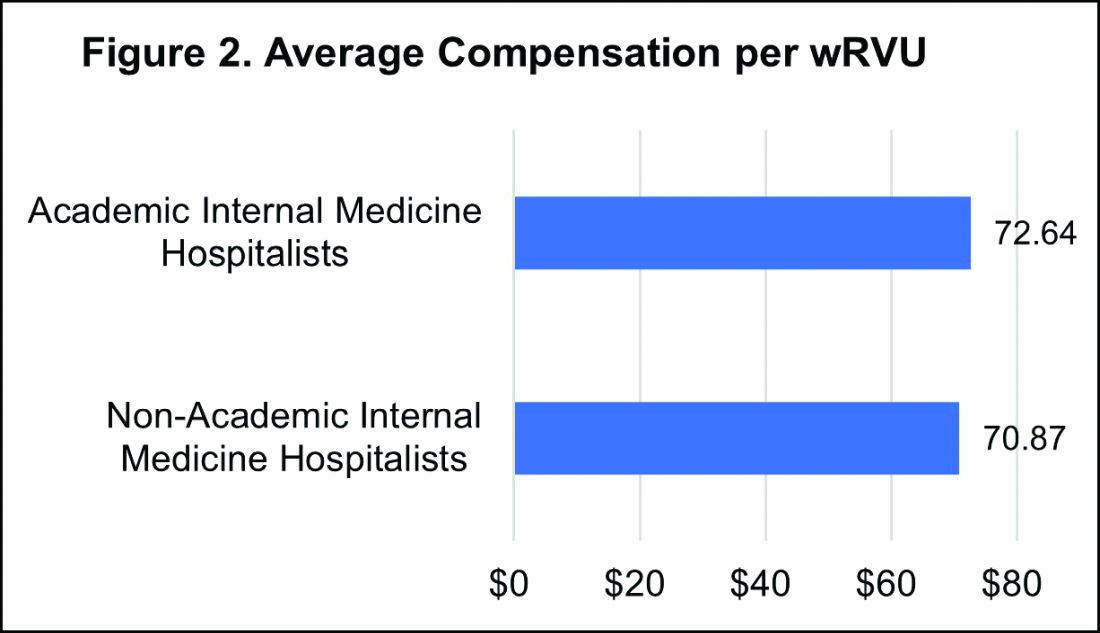
However, the total compensation continues to be lower for academic hospitalists, with a median compensation difference of approximately $70,000 compared to their non-academic colleagues. Some of this sizable variance is offset by the fact that academic HMGs receive more in employee benefits packages than non-academic groups – a difference in median value of $10,500. Ideally, academic hospitalist compensation models should appropriately reflect and value their work efforts toward the tripartite academic mission of clinical care, education, and research. It would be valuable for future surveys to define and measure academic production in order to develop national standards for compensation models that recognize these non-billable forms of productivity.
While it’s important to review compensation benchmarks to remain competitive, it’s difficult to put a price on some factors that many may consider more valuable – group culture, opportunities for professional growth, and schedules that afford better work-life integration. Indirect measures of such benefits include paid time off, paid sick days, CME allowances and time, and retirement benefits programs. In 2020, the median employer contribution to retirement plans was reported to be $13,955, with respondents in the Midwest receiving the highest retirement benefit of $33,771.
It’s encouraging to see that hospitalist compensation continues to rise compared to previous years, despite relatively flat trends in wRVUs and total patient encounters. Another continued trend over the past years is the rising amount of financial support per physician that hospitals or other organizations provide HMGs (see Figure 3). 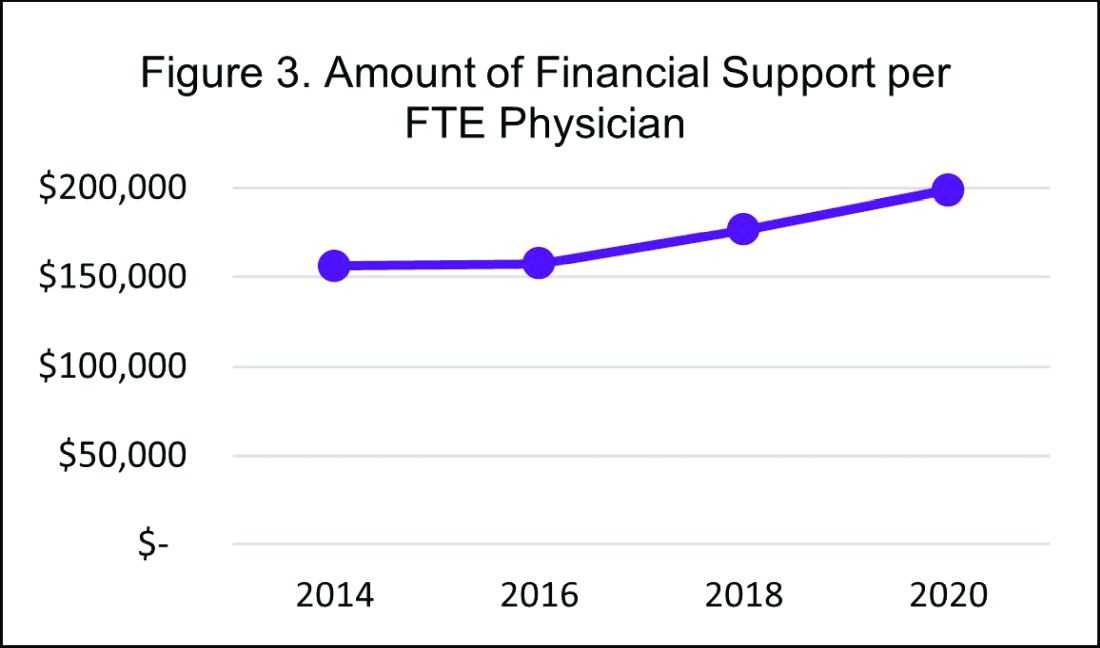
In 2020, the median financial support per FTE (full time equivalent) physician serving adult patients increased by 12% over 2018, to $198,750. Collectively these trends indicate hospitals are willing to compensate hospitalists for more than just their clinical volume.
There’s no doubt that the COVID-19 pandemic had some financial impact on hospital medicine groups in 2020. To assess this impact, SHM conducted a follow-up survey and compiled a COVID-19 Addendum to the SoHM Report. While 20.5% of HMG group respondents from the East reported providing hazard pay to clinicians caring for COVID-19 patients, nationally only 9.8% of groups said they offered this benefit. Of the 121 HMGs responding from across the country, 42% reported reductions in compensation, which included measures such as reductions in pay level and elimination or delays to bonus payments. The degree of reductions was not quantified, but fortunately the vast majority of these groups reported that these changes were likely to be temporary. To access all data in the 2020 SoHM Report and COVID-19 Addendum, visit hospitalmedicine.org/sohm to purchase your copy.
It’s certainly unclear what the future holds, but despite any transient changes observed during the COVID-19 pandemic, I believe that historical trends in hospitalist compensation will continue. If 2020 has taught us anything, it’s that hospitalists are essential, not only during an acute care crisis but for daily operations of any hospital.
Dr. Kurian is chief of the Division of Hospital Medicine at Northwell Health in New York. She is a member of SHM’s Practice Analysis Committee.
In a time of tremendous uncertainty, there is one trend that seems consistent year over year – the undisputed value of hospitalists. In the 2020 State of Hospital Medicine (SoHM) Report, the Society of Hospital Medicine partnered with the Medical Group Management Association (MGMA) to provide data on hospitalist compensation and productivity. The Report provides resounding evidence that hospitalists continue to be compensated at rising rates. This may be driven by both the continued demand-supply mismatch and a recognition of the overall value they generate rather than strictly the volume of their productivity.
In 2020, the median total compensation nationally for adult hospitalists (internal medicine and family medicine) was $307,633, representing an increase of over 6% from the 2018 Survey (see Figure 1). 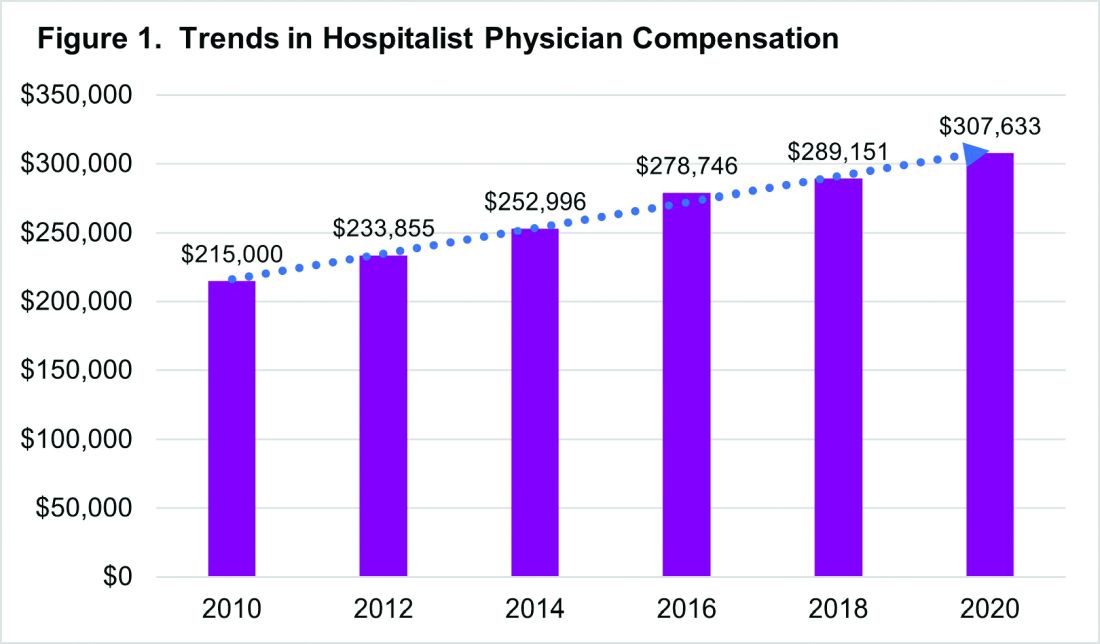
With significant regional variability in compensation across the country, hospitalists in the South continue to earn more than their colleagues in the East – a median compensation difference of about $33,000. However, absolute wage comparisons can be misleading without also considering regional variations in productivity as well.
Reviewing compensation per work relative value unit (wRVU) and per encounter offer additional insight for a more comprehensive assessment. When comparing regional compensation per wRVU, the 2020 Survey continues to show a trend toward hospitalists in the Midwest and West earning more per wRVU than their colleagues in other parts of the country ($78.13 per RVU in the Midwest, $78.95 per RVU in the West). More striking is how hospital medicine groups (HMGs) in the South garner lower compensation per RVU ($57.77) than those in the East ($67.54), even though their total compensation was much higher. This could reflect the gradual decline in compensation per wRVU that’s observed at higher productivity levels. While it’s typical for compensation to increase as productivity does, the rate of increase is generally to a lesser degree.
Like past SoHM Surveys, the 2020 Report revealed that academic and non-academic hospitalists are compensated similarly per wRVU (see Figure 2). 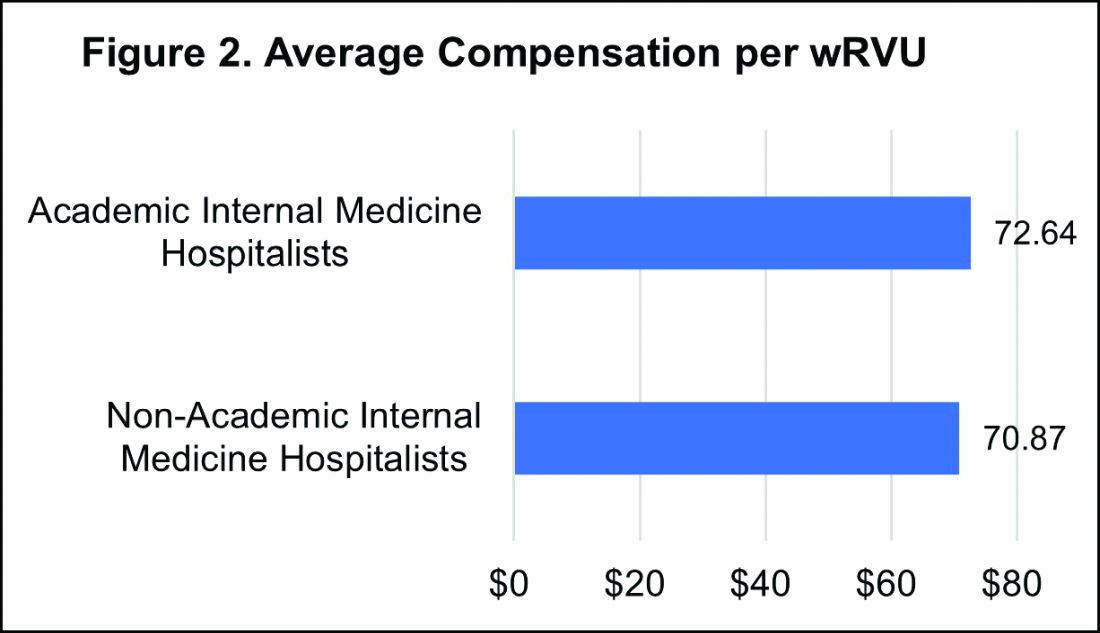
However, the total compensation continues to be lower for academic hospitalists, with a median compensation difference of approximately $70,000 compared to their non-academic colleagues. Some of this sizable variance is offset by the fact that academic HMGs receive more in employee benefits packages than non-academic groups – a difference in median value of $10,500. Ideally, academic hospitalist compensation models should appropriately reflect and value their work efforts toward the tripartite academic mission of clinical care, education, and research. It would be valuable for future surveys to define and measure academic production in order to develop national standards for compensation models that recognize these non-billable forms of productivity.
While it’s important to review compensation benchmarks to remain competitive, it’s difficult to put a price on some factors that many may consider more valuable – group culture, opportunities for professional growth, and schedules that afford better work-life integration. Indirect measures of such benefits include paid time off, paid sick days, CME allowances and time, and retirement benefits programs. In 2020, the median employer contribution to retirement plans was reported to be $13,955, with respondents in the Midwest receiving the highest retirement benefit of $33,771.
It’s encouraging to see that hospitalist compensation continues to rise compared to previous years, despite relatively flat trends in wRVUs and total patient encounters. Another continued trend over the past years is the rising amount of financial support per physician that hospitals or other organizations provide HMGs (see Figure 3). 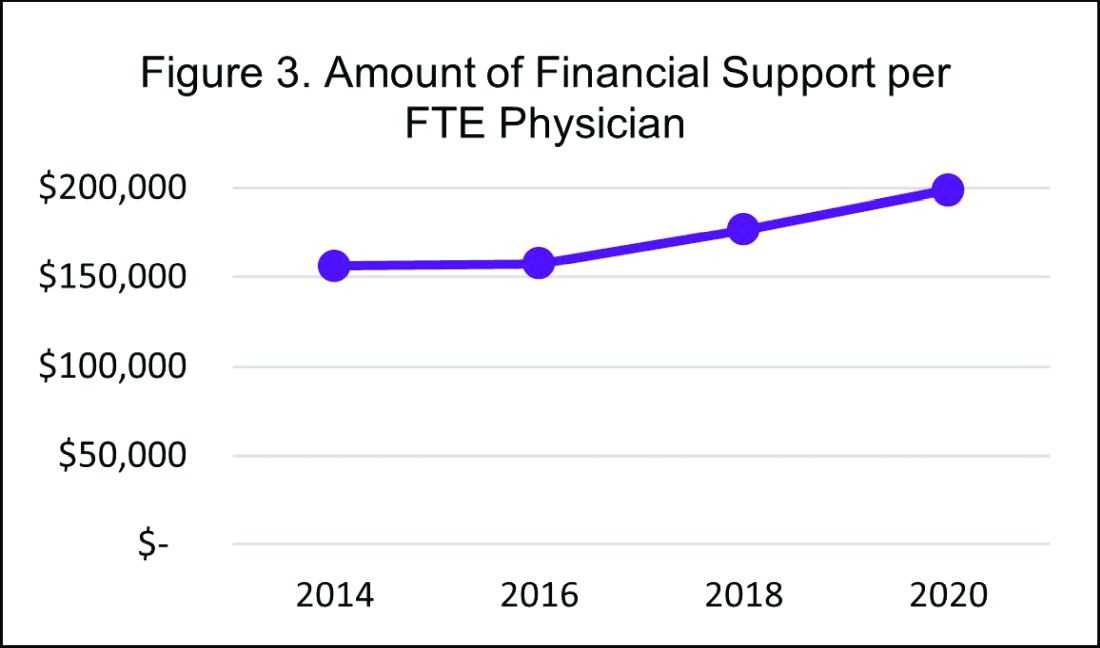
In 2020, the median financial support per FTE (full time equivalent) physician serving adult patients increased by 12% over 2018, to $198,750. Collectively these trends indicate hospitals are willing to compensate hospitalists for more than just their clinical volume.
There’s no doubt that the COVID-19 pandemic had some financial impact on hospital medicine groups in 2020. To assess this impact, SHM conducted a follow-up survey and compiled a COVID-19 Addendum to the SoHM Report. While 20.5% of HMG group respondents from the East reported providing hazard pay to clinicians caring for COVID-19 patients, nationally only 9.8% of groups said they offered this benefit. Of the 121 HMGs responding from across the country, 42% reported reductions in compensation, which included measures such as reductions in pay level and elimination or delays to bonus payments. The degree of reductions was not quantified, but fortunately the vast majority of these groups reported that these changes were likely to be temporary. To access all data in the 2020 SoHM Report and COVID-19 Addendum, visit hospitalmedicine.org/sohm to purchase your copy.
It’s certainly unclear what the future holds, but despite any transient changes observed during the COVID-19 pandemic, I believe that historical trends in hospitalist compensation will continue. If 2020 has taught us anything, it’s that hospitalists are essential, not only during an acute care crisis but for daily operations of any hospital.
Dr. Kurian is chief of the Division of Hospital Medicine at Northwell Health in New York. She is a member of SHM’s Practice Analysis Committee.
The journey from burnout to wellbeing
A check-in for you and your peers
COVID-19 did not discriminate when it came to the impact it imposed on our hospitalist community. As the nomenclature moves away from the negative connotations of ‘burnout’ to ‘wellbeing,’ the pandemic has taught us something important about being intentional about our personal health: we must secure our own oxygen masks before helping others.
In February 2020, the Society of Hospital Medicine’s Wellbeing Taskforce efforts quickly changed focus from addressing general wellbeing, to wellbeing during COVID-19. Our Taskforce was commissioned by SHM’s Board with a new charge: Address immediate and ongoing needs of well-being and resiliency support for hospitalists during the COVID-19 pandemic. In this essay, I will discuss how our SHM Wellbeing Taskforce approached the overall topic of wellbeing for hospitalists during the COVID-19 pandemic, including some of our Taskforce group experiences.
The Taskforce started with a framework to aide in cultivating open and authentic conversations within hospital medicine groups. Creating spaces for honest sharing around how providers are doing is a crucial first step to reducing stigma, building mutual support within a group, and elevating issues of wellbeing to the level where structural change can take place. The Taskforce established two objectives for normalizing and mitigating stressors we face as hospitalists during the COVID-19 pandemic:
- Provide a framework for hospitalists to take their own emotional pulse
- Provide an approach to reduce stigma of hospitalists who are suffering from pandemic stress
While a more typical approach to fix stress and burnout is using formal institutional interventions, we used the value and insight provided by SHM’s 7 Drivers of Burnout in Hospital Medicine to help guide the creation of SHM resources in addressing the severe emotional strain being felt across the country by hospitalists. The 7 Drivers support the idea that the social role peers and hospital leaders can make a crucial difference in mitigating stress and burnout. Two examples of social support come to mind from the Wellbeing Taskforce experience:
- Participate in your meetings. One example comes from a member of our group who had underestimated the “healing power” that our group meetings had provided to his psyche. The simple act of participating in our Taskforce meeting and being in the presence of our group had provided such a positive impact that he was better able to face the “death and misery” in his unit with a smile on his face.
- Share what is stressful. The second example of social support comes from an hour of Zoom-based facilitation meetings between the SHM’s Wellbeing Taskforce members and Chapter Leaders in late October. During our Taskforce debrief after the meeting, we came to realize the enormous burden of grief our peers were carrying as one hospitalist had lost a group colleague the previous week due to suicide. Our member who led this meeting was moved – as were we – at how this had impacted his small team, and he was reminded he was not alone.
To form meaningful relationships that foster support, there needs to be a space where people can safely come together at times that initially might feel awkward. After taking steps toward your peers, these conversations can become normalized and contribute to meaningful relationships, providing the opportunity for healthy exchanges on vulnerable topics like emotional and psychological wellbeing. A printable guide for this specific purpose (“HM COVID-19 Check-In Guide for Self and Peers”) was designed to help hospitalists move into safe and supportive conversations with each other. While it is difficult to place a value on the importance these types of conversations have on individual wellbeing, it is known that the quality of a positive work environment where people feel supported can moderate stress, morale, and depression. In other words, hospitalist groups can positively contribute to their social environment during stressful times by sharing meaningful and difficult experiences with one another.
Second, the Taskforce created a social media campaign to provide a public social space for sharing hospitalists’ COVID-19 experiences. We believed that sharing collective experiences with the theme of #YouAreNotAlone and a complementary social media campaign, SHM Cares, on SHM’s social media channels, would further connect the national hospitalist community and provide a different communication pathway to decrease a sense of isolation. This idea came from the second social support idea mentioned earlier to share what is stressful with others in a safe space. We understood that some hospitalists would be more comfortable sharing publicly their comments, photos, and videos in achieving a sense of hospitalist unity.
Using our shared experiences, we identified three pillars for the final structure of the HM COVID-19 Check-In Guide for Self and Peers:
- Pillar 1. Recognize your issues. Recall our oxygen mask metaphor and this is what we mean by recognizing symptoms of new stressors (e.g., sleeplessness, irritability, forgetfulness).
- Pillar 2. Know what to say. A simple open-ended question about how the other person is working through the pandemic is an easy way to start a connection. We learned from a mental health perspective that it is unlikely that you could say anything to make a situation worse by offering a listening ear.
- Pillar 3. Check in with others. Listen to others without trying to fix the person or the situation. When appropriate, offer humorous reflections without diminishing the problem. Be a partner and commit to check in regularly with the other person.
Cultivating human connections outside of your immediate peer group can be valuable and offer additional perspective to stressful situations. For instance, one of my roles as a hospitalist administrator has been offering support by regularly listening as my physicians ‘talk out’ their day confidentially for as long as they needed. Offering open conversation in a safe and confidential way can have a healing effect. As one of my former hospitalists used to say, if issues are not addressed, they will “ooze out somewhere else.”
The HM COVID-19 Check-In Guide for Self and Peers and the SHM Cares social media campaign was the result of the Taskforce’s collective observations to help others normalize the feeling that ‘it’s OK not to be OK.’ Using the pandemic as context, the 7 Drivers of Hospitalist Burnout reminded us that the increased burnout issues we face will require continued attention past the pandemic. The value in cultivating human connections has never been more important. The SHM Wellbeing Taskforce is committed to provide continued resources. Checking in with others and listening to peers are all part of a personal wellbeing and resilience strategy. On behalf of the SHM Wellbeing Taskforce, we hope the information in this article will highlight the importance of continued attention to personal wellbeing during and after the pandemic.
Dr. Robinson received her PhD in organizational learning, performance and change from Colorado State University in 2019. Her dissertation topic was exploring hospitalist burnout, engagement, and social support. She is administrative director of inpatient medicine at St. Mary’s Medical Center in Grand Junction, Colo., a part of SCL Health. She has volunteered in numerous SHM committees, and currently serves on the SHM Wellbeing Taskforce.
A check-in for you and your peers
A check-in for you and your peers
COVID-19 did not discriminate when it came to the impact it imposed on our hospitalist community. As the nomenclature moves away from the negative connotations of ‘burnout’ to ‘wellbeing,’ the pandemic has taught us something important about being intentional about our personal health: we must secure our own oxygen masks before helping others.
In February 2020, the Society of Hospital Medicine’s Wellbeing Taskforce efforts quickly changed focus from addressing general wellbeing, to wellbeing during COVID-19. Our Taskforce was commissioned by SHM’s Board with a new charge: Address immediate and ongoing needs of well-being and resiliency support for hospitalists during the COVID-19 pandemic. In this essay, I will discuss how our SHM Wellbeing Taskforce approached the overall topic of wellbeing for hospitalists during the COVID-19 pandemic, including some of our Taskforce group experiences.
The Taskforce started with a framework to aide in cultivating open and authentic conversations within hospital medicine groups. Creating spaces for honest sharing around how providers are doing is a crucial first step to reducing stigma, building mutual support within a group, and elevating issues of wellbeing to the level where structural change can take place. The Taskforce established two objectives for normalizing and mitigating stressors we face as hospitalists during the COVID-19 pandemic:
- Provide a framework for hospitalists to take their own emotional pulse
- Provide an approach to reduce stigma of hospitalists who are suffering from pandemic stress
While a more typical approach to fix stress and burnout is using formal institutional interventions, we used the value and insight provided by SHM’s 7 Drivers of Burnout in Hospital Medicine to help guide the creation of SHM resources in addressing the severe emotional strain being felt across the country by hospitalists. The 7 Drivers support the idea that the social role peers and hospital leaders can make a crucial difference in mitigating stress and burnout. Two examples of social support come to mind from the Wellbeing Taskforce experience:
- Participate in your meetings. One example comes from a member of our group who had underestimated the “healing power” that our group meetings had provided to his psyche. The simple act of participating in our Taskforce meeting and being in the presence of our group had provided such a positive impact that he was better able to face the “death and misery” in his unit with a smile on his face.
- Share what is stressful. The second example of social support comes from an hour of Zoom-based facilitation meetings between the SHM’s Wellbeing Taskforce members and Chapter Leaders in late October. During our Taskforce debrief after the meeting, we came to realize the enormous burden of grief our peers were carrying as one hospitalist had lost a group colleague the previous week due to suicide. Our member who led this meeting was moved – as were we – at how this had impacted his small team, and he was reminded he was not alone.
To form meaningful relationships that foster support, there needs to be a space where people can safely come together at times that initially might feel awkward. After taking steps toward your peers, these conversations can become normalized and contribute to meaningful relationships, providing the opportunity for healthy exchanges on vulnerable topics like emotional and psychological wellbeing. A printable guide for this specific purpose (“HM COVID-19 Check-In Guide for Self and Peers”) was designed to help hospitalists move into safe and supportive conversations with each other. While it is difficult to place a value on the importance these types of conversations have on individual wellbeing, it is known that the quality of a positive work environment where people feel supported can moderate stress, morale, and depression. In other words, hospitalist groups can positively contribute to their social environment during stressful times by sharing meaningful and difficult experiences with one another.
Second, the Taskforce created a social media campaign to provide a public social space for sharing hospitalists’ COVID-19 experiences. We believed that sharing collective experiences with the theme of #YouAreNotAlone and a complementary social media campaign, SHM Cares, on SHM’s social media channels, would further connect the national hospitalist community and provide a different communication pathway to decrease a sense of isolation. This idea came from the second social support idea mentioned earlier to share what is stressful with others in a safe space. We understood that some hospitalists would be more comfortable sharing publicly their comments, photos, and videos in achieving a sense of hospitalist unity.
Using our shared experiences, we identified three pillars for the final structure of the HM COVID-19 Check-In Guide for Self and Peers:
- Pillar 1. Recognize your issues. Recall our oxygen mask metaphor and this is what we mean by recognizing symptoms of new stressors (e.g., sleeplessness, irritability, forgetfulness).
- Pillar 2. Know what to say. A simple open-ended question about how the other person is working through the pandemic is an easy way to start a connection. We learned from a mental health perspective that it is unlikely that you could say anything to make a situation worse by offering a listening ear.
- Pillar 3. Check in with others. Listen to others without trying to fix the person or the situation. When appropriate, offer humorous reflections without diminishing the problem. Be a partner and commit to check in regularly with the other person.
Cultivating human connections outside of your immediate peer group can be valuable and offer additional perspective to stressful situations. For instance, one of my roles as a hospitalist administrator has been offering support by regularly listening as my physicians ‘talk out’ their day confidentially for as long as they needed. Offering open conversation in a safe and confidential way can have a healing effect. As one of my former hospitalists used to say, if issues are not addressed, they will “ooze out somewhere else.”
The HM COVID-19 Check-In Guide for Self and Peers and the SHM Cares social media campaign was the result of the Taskforce’s collective observations to help others normalize the feeling that ‘it’s OK not to be OK.’ Using the pandemic as context, the 7 Drivers of Hospitalist Burnout reminded us that the increased burnout issues we face will require continued attention past the pandemic. The value in cultivating human connections has never been more important. The SHM Wellbeing Taskforce is committed to provide continued resources. Checking in with others and listening to peers are all part of a personal wellbeing and resilience strategy. On behalf of the SHM Wellbeing Taskforce, we hope the information in this article will highlight the importance of continued attention to personal wellbeing during and after the pandemic.
Dr. Robinson received her PhD in organizational learning, performance and change from Colorado State University in 2019. Her dissertation topic was exploring hospitalist burnout, engagement, and social support. She is administrative director of inpatient medicine at St. Mary’s Medical Center in Grand Junction, Colo., a part of SCL Health. She has volunteered in numerous SHM committees, and currently serves on the SHM Wellbeing Taskforce.
COVID-19 did not discriminate when it came to the impact it imposed on our hospitalist community. As the nomenclature moves away from the negative connotations of ‘burnout’ to ‘wellbeing,’ the pandemic has taught us something important about being intentional about our personal health: we must secure our own oxygen masks before helping others.
In February 2020, the Society of Hospital Medicine’s Wellbeing Taskforce efforts quickly changed focus from addressing general wellbeing, to wellbeing during COVID-19. Our Taskforce was commissioned by SHM’s Board with a new charge: Address immediate and ongoing needs of well-being and resiliency support for hospitalists during the COVID-19 pandemic. In this essay, I will discuss how our SHM Wellbeing Taskforce approached the overall topic of wellbeing for hospitalists during the COVID-19 pandemic, including some of our Taskforce group experiences.
The Taskforce started with a framework to aide in cultivating open and authentic conversations within hospital medicine groups. Creating spaces for honest sharing around how providers are doing is a crucial first step to reducing stigma, building mutual support within a group, and elevating issues of wellbeing to the level where structural change can take place. The Taskforce established two objectives for normalizing and mitigating stressors we face as hospitalists during the COVID-19 pandemic:
- Provide a framework for hospitalists to take their own emotional pulse
- Provide an approach to reduce stigma of hospitalists who are suffering from pandemic stress
While a more typical approach to fix stress and burnout is using formal institutional interventions, we used the value and insight provided by SHM’s 7 Drivers of Burnout in Hospital Medicine to help guide the creation of SHM resources in addressing the severe emotional strain being felt across the country by hospitalists. The 7 Drivers support the idea that the social role peers and hospital leaders can make a crucial difference in mitigating stress and burnout. Two examples of social support come to mind from the Wellbeing Taskforce experience:
- Participate in your meetings. One example comes from a member of our group who had underestimated the “healing power” that our group meetings had provided to his psyche. The simple act of participating in our Taskforce meeting and being in the presence of our group had provided such a positive impact that he was better able to face the “death and misery” in his unit with a smile on his face.
- Share what is stressful. The second example of social support comes from an hour of Zoom-based facilitation meetings between the SHM’s Wellbeing Taskforce members and Chapter Leaders in late October. During our Taskforce debrief after the meeting, we came to realize the enormous burden of grief our peers were carrying as one hospitalist had lost a group colleague the previous week due to suicide. Our member who led this meeting was moved – as were we – at how this had impacted his small team, and he was reminded he was not alone.
To form meaningful relationships that foster support, there needs to be a space where people can safely come together at times that initially might feel awkward. After taking steps toward your peers, these conversations can become normalized and contribute to meaningful relationships, providing the opportunity for healthy exchanges on vulnerable topics like emotional and psychological wellbeing. A printable guide for this specific purpose (“HM COVID-19 Check-In Guide for Self and Peers”) was designed to help hospitalists move into safe and supportive conversations with each other. While it is difficult to place a value on the importance these types of conversations have on individual wellbeing, it is known that the quality of a positive work environment where people feel supported can moderate stress, morale, and depression. In other words, hospitalist groups can positively contribute to their social environment during stressful times by sharing meaningful and difficult experiences with one another.
Second, the Taskforce created a social media campaign to provide a public social space for sharing hospitalists’ COVID-19 experiences. We believed that sharing collective experiences with the theme of #YouAreNotAlone and a complementary social media campaign, SHM Cares, on SHM’s social media channels, would further connect the national hospitalist community and provide a different communication pathway to decrease a sense of isolation. This idea came from the second social support idea mentioned earlier to share what is stressful with others in a safe space. We understood that some hospitalists would be more comfortable sharing publicly their comments, photos, and videos in achieving a sense of hospitalist unity.
Using our shared experiences, we identified three pillars for the final structure of the HM COVID-19 Check-In Guide for Self and Peers:
- Pillar 1. Recognize your issues. Recall our oxygen mask metaphor and this is what we mean by recognizing symptoms of new stressors (e.g., sleeplessness, irritability, forgetfulness).
- Pillar 2. Know what to say. A simple open-ended question about how the other person is working through the pandemic is an easy way to start a connection. We learned from a mental health perspective that it is unlikely that you could say anything to make a situation worse by offering a listening ear.
- Pillar 3. Check in with others. Listen to others without trying to fix the person or the situation. When appropriate, offer humorous reflections without diminishing the problem. Be a partner and commit to check in regularly with the other person.
Cultivating human connections outside of your immediate peer group can be valuable and offer additional perspective to stressful situations. For instance, one of my roles as a hospitalist administrator has been offering support by regularly listening as my physicians ‘talk out’ their day confidentially for as long as they needed. Offering open conversation in a safe and confidential way can have a healing effect. As one of my former hospitalists used to say, if issues are not addressed, they will “ooze out somewhere else.”
The HM COVID-19 Check-In Guide for Self and Peers and the SHM Cares social media campaign was the result of the Taskforce’s collective observations to help others normalize the feeling that ‘it’s OK not to be OK.’ Using the pandemic as context, the 7 Drivers of Hospitalist Burnout reminded us that the increased burnout issues we face will require continued attention past the pandemic. The value in cultivating human connections has never been more important. The SHM Wellbeing Taskforce is committed to provide continued resources. Checking in with others and listening to peers are all part of a personal wellbeing and resilience strategy. On behalf of the SHM Wellbeing Taskforce, we hope the information in this article will highlight the importance of continued attention to personal wellbeing during and after the pandemic.
Dr. Robinson received her PhD in organizational learning, performance and change from Colorado State University in 2019. Her dissertation topic was exploring hospitalist burnout, engagement, and social support. She is administrative director of inpatient medicine at St. Mary’s Medical Center in Grand Junction, Colo., a part of SCL Health. She has volunteered in numerous SHM committees, and currently serves on the SHM Wellbeing Taskforce.
JHM Twitter chat sparks connections
Monthly social media event links editors, authors, and readers
Once upon a time, physicians wrote letters to peers and colleagues around the world, sharing their medical discoveries, theories, case reports, and questions; conferring on problems; and then waiting for return mail to bring a reply. And the science of medicine advanced at a glacial pace.
Today, communication in multiple mediums flows much faster, almost instantaneously, between many more physicians, regardless of distance, addressing a much greater complexity of medical topics and treatments. And one of the chief mediums for this rapid electronic conversation among doctors is Twitter, according to Charlie Wray, DO, MS, a hospitalist at the University of California, San Francisco.
Dr. Wray, associate editor and digital media editor for the Journal of Hospital Medicine, is one of the moderators of #JHMchat, a monthly get-together on Twitter for interested hospitalists to link up virtually; respond to questions posed by JHM editors and other moderators; exchange perspectives, experiences, and tips with their peers; and build professional relationships and personal friendships. Relationship building has become particularly important in the age of COVID-19, when opportunities to connect in person at events such as SHM’s annual conferences have been curtailed.
The online #JHMchat community began in 2015, shortly after Dr. Wray completed a hospitalist research fellowship at the University of Chicago. His fellowship mentor, Vineet Arora, MD, MAPP, MHM, associate chief medical officer for the clinical learning environment at University of Chicago Medicine, had noticed how other online medical communities were engaging in discussions around different topics.
“She thought it could be a great way for hospitalists to meet online and talk about the articles published in JHM,” Dr. Wray explained. “We were all getting into social media and learning how to moderate interactive discussions such as Twitter.”
The chat’s founders approached JHM’s then-editor Andrew Auerbach, MD, MHM, a hospitalist at UCSF, who agreed that it was a great idea. They asked Christopher Moriates, MD, author of a recently published paper on the advisability of nebulized bronchodilators for obstructive pulmonary symptoms and assistant dean for health care value at the University of Texas, Austin, to come on the chat and talk about his paper. Visiting Dr. Arora at the time, he joined her in her living room for the first chat on Oct. 12, 2015. Seventy-five participants posted 431 tweets, with a total of 2 million Twitter impressions, suggesting that they had tapped a latent need.
How the chat works
To participate in the JHM chats on Twitter, one needs to open an account on the platform (it’s free) and follow the Journal’s Twitter feed (@jhospmedicine). But that’s pretty much it, Dr. Wray said. The group convenes on a Monday evening each month for an hour, starting at 9 p.m. Eastern time. Upcoming chats and topics are announced on Twitter and at SHM’s website.
The chats have grown and evolved since 2015, shifting in focus given recent social upheavals over the pandemic and heated discussions about diversity, equity, and racial justice in medicine, he said. “When COVID hit, the journal’s editor – Dr. Samir Shah – recognized that we were in a unique moment with the pandemic. The journal took advantage of the opportunity to publish a lot more personal perspectives and viewpoints around COVID, along with a special issue devoted to social justice.”
Moderators for the chat typically choose three or four questions based on recently published articles or other relevant topics, such as racial inequities in health care or how to apply military principles to hospital medicine leadership. “We reach out to authors and tell them they can explain their articles to interested readers through the chat. I can’t think of a single one who said no. They see the opportunity to highlight their work and engage with readers who want to ask them questions,” Dr. Wray said.
The moderators’ questions are posed to stimulate participation, but another goal is to use that hour for networking. “It’s a powerful tool to allow SHM members to engage with each other,” he said. “Sometimes the chat has the feeling of trying to drink water from a fire hose – with the messages flashing past so quickly. But the key is not to try to respond to everything but rather to follow those threads that particularly interest you. We encourage you to engage, but it’s totally fine if you just sit back and observe. One thing we have done to make it a little more formal is to offer CME credits for participants.”
The chat welcomes hospitalists and nonhospitalists, nurse practitioners, physician assistants, academics, and nonacademics. “No matter how engaged you are with Twitter, if you have 10,000 followers or 10, we’ll amplify your voice,” he said. “We also have medical students participating and consider their perspectives valuable, too.”
Dr. Wray identified three main types of participants in the monthly chats. The first are regulars who come every month, rain or shine. Like the character Norm in the old television comedy “Cheers,” everybody knows their name. They become friends, sharing and reveling in each other’s accomplishments. “These are people who have multiple connections, personally and professionally, at a lot of different levels. I probably know a hundred or more people who I’ve primarily gotten to know online.”
A second and larger group might be drawn in because of an interest in a specific topic or article, but they’re also welcome to participate in the chat. And the third group may lurk in the background, following along but not commenting. The size of that third group is unknown, but metrics from SHM show a total of 796 participants posting 4,088 tweets during chats in 2020 (for an average of 132 participants and 681 tweets per chat). This adds up to a total of 34 million impressions across the platform for #JHMchat tweets for the year.
Creating community online
“Why do we do it? It’s difficult to read all of the relevant published articles and keep up to date,” said Dr. Arora, a medical educator whose job at Chicago Medicine is to improve the clinical learning environment for trainees and staff by aligning learning with the health system’s institutional quality, safety and value missions.
“Our idea was to bring together a kind of virtual journal club and have discussions around topics such as: how do you create a shared vision on rounds? How do you integrate that into clinical practice? How do we preserve work/life balance or address structural racism?” she said. Other topics have included work flow concerns, burnout, difficult conversations with patients, and career planning.
“The people we’re trying to reach are hospitalists – and they’re busy at the front lines of care. We also thought this was an interesting way to raise the journal’s profile and spark broader interest in the articles it publishes. But it’s really about creating community, with people who look forward to talking and connecting with each other each month through the chats,” Dr. Arora said. If they miss a chat, they feel they’ve missed important interactions.
“Many times when people log onto the chat, they give a status report on where they are at, such as ‘I’m home putting my kids to bed,’ or ‘I’m on call tonight,’ ” she added. “People are willing to engage with the medium because it’s easy to engage with. We can forget that physicians are like everyone else. They like to learn, but they want that learning to be fun.”
On Dec. 14, 2020, at 9 p.m. Eastern time, the first question for the monthly #JHMchat was posted: How will caring for COVID-19 patients this winter differ from caring for patients in the first wave? Given that another surge of hospitalized COVID patients is looming, participants posted that they feel familiar and more confident with effective clinical strategies for hospitalized COVID patients, having learned so much more about the virus. But they’re facing greater numbers of patients than in prior surges. “In March, we were in crisis, now we’re in complexity,” one noted.
Joining the moderators was the Pediatric Overflow Planning Contingency Response Network (POPCoRN), a group formed earlier this year to help mobilize pediatric medical capacity for COVID patients during pandemic surges (see “POPCoRN network mobilizes pediatric capacity during pandemic,” The Hospitalist, April 30, 2020). One of its questions involved the redeployment of physicians in response to COVID demands and what, for example, pediatric hospitalists need as resources and tools when they are reassigned to adult patients or to new roles in unfamiliar settings. A variety of educational resources were cited from POPCoRN, SHM, and ImproveDX, among others.
Defining medical communication
Another chat moderator is Angela Castellanos, MD, a pediatric hospitalist at Tufts Medical Center in Boston. Dr. Castellanos did a 1-year, full-time fellowship right after residency at the New England Journal of Medicine, participating hands-on as a member of the editorial team for the print and online editions of the venerable journal. She is now doing a digital media fellowship with JHM, a part-time commitment while holding down a full-time job as a hospitalist. She also puts together a Spanish language podcast covering primary care pediatric issues for parents and families.
“I’m interested in medical communication generally, as I try to figure out what that means,” she said. “I have continued to look for ways to be part of the social media community and to be more creative about it. The JHM fellowship came at a perfect time for me to learn to do more in digital media.”
COVID has created new opportunities for more immediate dialogue with colleagues – what are they seeing and what’s working in the absence of clinical trials, she explained. “That’s how we communicate, as a way to get information out fast, such as when hospitals began proning COVID patients to make it easier for them to breathe.”
Dr. Castellanos said she grew up with text messaging and social media and wants to continue to grow her skills in this area. “I think I developed some skills at NEJM, but the opportunity to see how they do things at another journal with a different mission was also valuable. I get to share the space with people in academic settings and leaders in my field. I tweet at them; they tweet at me. These two fellowships have given me unique insights and mentorships. I know I want to continue doing pediatric hospital medicine and to engage academically and learn how to do research.”
Twitter sometimes gets a bad reputation for hostile or incendiary posts, Dr. Wray noted. “If you look at social media writ large, it can sometimes seem like a dumpster fire.” But what has happened in the medical community and in most medical Twitter encounters is a more cordial approach to conversations. “People who work in medicine converse with each other, with room for respectful disagreements. We’re extra supportive of each other,” he said.
“I think if hospitalists are looking for a community of peers, to engage with them and network and to find colleagues in similar circumstances, the JHM chat is such a fantastic place,” Dr. Wray concluded. “Don’t just come once, come several times, meet people along the way. For me, one of the most beneficial ways to advance my career has been by connecting with people through the chat. It allows me to share my work and success with the hospitalist community, as well as highlighting my trainees’ and colleagues’ successes, and it has created opportunities I never would have expected for getting involved in other projects.”
Monthly social media event links editors, authors, and readers
Monthly social media event links editors, authors, and readers
Once upon a time, physicians wrote letters to peers and colleagues around the world, sharing their medical discoveries, theories, case reports, and questions; conferring on problems; and then waiting for return mail to bring a reply. And the science of medicine advanced at a glacial pace.
Today, communication in multiple mediums flows much faster, almost instantaneously, between many more physicians, regardless of distance, addressing a much greater complexity of medical topics and treatments. And one of the chief mediums for this rapid electronic conversation among doctors is Twitter, according to Charlie Wray, DO, MS, a hospitalist at the University of California, San Francisco.
Dr. Wray, associate editor and digital media editor for the Journal of Hospital Medicine, is one of the moderators of #JHMchat, a monthly get-together on Twitter for interested hospitalists to link up virtually; respond to questions posed by JHM editors and other moderators; exchange perspectives, experiences, and tips with their peers; and build professional relationships and personal friendships. Relationship building has become particularly important in the age of COVID-19, when opportunities to connect in person at events such as SHM’s annual conferences have been curtailed.
The online #JHMchat community began in 2015, shortly after Dr. Wray completed a hospitalist research fellowship at the University of Chicago. His fellowship mentor, Vineet Arora, MD, MAPP, MHM, associate chief medical officer for the clinical learning environment at University of Chicago Medicine, had noticed how other online medical communities were engaging in discussions around different topics.
“She thought it could be a great way for hospitalists to meet online and talk about the articles published in JHM,” Dr. Wray explained. “We were all getting into social media and learning how to moderate interactive discussions such as Twitter.”
The chat’s founders approached JHM’s then-editor Andrew Auerbach, MD, MHM, a hospitalist at UCSF, who agreed that it was a great idea. They asked Christopher Moriates, MD, author of a recently published paper on the advisability of nebulized bronchodilators for obstructive pulmonary symptoms and assistant dean for health care value at the University of Texas, Austin, to come on the chat and talk about his paper. Visiting Dr. Arora at the time, he joined her in her living room for the first chat on Oct. 12, 2015. Seventy-five participants posted 431 tweets, with a total of 2 million Twitter impressions, suggesting that they had tapped a latent need.
How the chat works
To participate in the JHM chats on Twitter, one needs to open an account on the platform (it’s free) and follow the Journal’s Twitter feed (@jhospmedicine). But that’s pretty much it, Dr. Wray said. The group convenes on a Monday evening each month for an hour, starting at 9 p.m. Eastern time. Upcoming chats and topics are announced on Twitter and at SHM’s website.
The chats have grown and evolved since 2015, shifting in focus given recent social upheavals over the pandemic and heated discussions about diversity, equity, and racial justice in medicine, he said. “When COVID hit, the journal’s editor – Dr. Samir Shah – recognized that we were in a unique moment with the pandemic. The journal took advantage of the opportunity to publish a lot more personal perspectives and viewpoints around COVID, along with a special issue devoted to social justice.”
Moderators for the chat typically choose three or four questions based on recently published articles or other relevant topics, such as racial inequities in health care or how to apply military principles to hospital medicine leadership. “We reach out to authors and tell them they can explain their articles to interested readers through the chat. I can’t think of a single one who said no. They see the opportunity to highlight their work and engage with readers who want to ask them questions,” Dr. Wray said.
The moderators’ questions are posed to stimulate participation, but another goal is to use that hour for networking. “It’s a powerful tool to allow SHM members to engage with each other,” he said. “Sometimes the chat has the feeling of trying to drink water from a fire hose – with the messages flashing past so quickly. But the key is not to try to respond to everything but rather to follow those threads that particularly interest you. We encourage you to engage, but it’s totally fine if you just sit back and observe. One thing we have done to make it a little more formal is to offer CME credits for participants.”
The chat welcomes hospitalists and nonhospitalists, nurse practitioners, physician assistants, academics, and nonacademics. “No matter how engaged you are with Twitter, if you have 10,000 followers or 10, we’ll amplify your voice,” he said. “We also have medical students participating and consider their perspectives valuable, too.”
Dr. Wray identified three main types of participants in the monthly chats. The first are regulars who come every month, rain or shine. Like the character Norm in the old television comedy “Cheers,” everybody knows their name. They become friends, sharing and reveling in each other’s accomplishments. “These are people who have multiple connections, personally and professionally, at a lot of different levels. I probably know a hundred or more people who I’ve primarily gotten to know online.”
A second and larger group might be drawn in because of an interest in a specific topic or article, but they’re also welcome to participate in the chat. And the third group may lurk in the background, following along but not commenting. The size of that third group is unknown, but metrics from SHM show a total of 796 participants posting 4,088 tweets during chats in 2020 (for an average of 132 participants and 681 tweets per chat). This adds up to a total of 34 million impressions across the platform for #JHMchat tweets for the year.
Creating community online
“Why do we do it? It’s difficult to read all of the relevant published articles and keep up to date,” said Dr. Arora, a medical educator whose job at Chicago Medicine is to improve the clinical learning environment for trainees and staff by aligning learning with the health system’s institutional quality, safety and value missions.
“Our idea was to bring together a kind of virtual journal club and have discussions around topics such as: how do you create a shared vision on rounds? How do you integrate that into clinical practice? How do we preserve work/life balance or address structural racism?” she said. Other topics have included work flow concerns, burnout, difficult conversations with patients, and career planning.
“The people we’re trying to reach are hospitalists – and they’re busy at the front lines of care. We also thought this was an interesting way to raise the journal’s profile and spark broader interest in the articles it publishes. But it’s really about creating community, with people who look forward to talking and connecting with each other each month through the chats,” Dr. Arora said. If they miss a chat, they feel they’ve missed important interactions.
“Many times when people log onto the chat, they give a status report on where they are at, such as ‘I’m home putting my kids to bed,’ or ‘I’m on call tonight,’ ” she added. “People are willing to engage with the medium because it’s easy to engage with. We can forget that physicians are like everyone else. They like to learn, but they want that learning to be fun.”
On Dec. 14, 2020, at 9 p.m. Eastern time, the first question for the monthly #JHMchat was posted: How will caring for COVID-19 patients this winter differ from caring for patients in the first wave? Given that another surge of hospitalized COVID patients is looming, participants posted that they feel familiar and more confident with effective clinical strategies for hospitalized COVID patients, having learned so much more about the virus. But they’re facing greater numbers of patients than in prior surges. “In March, we were in crisis, now we’re in complexity,” one noted.
Joining the moderators was the Pediatric Overflow Planning Contingency Response Network (POPCoRN), a group formed earlier this year to help mobilize pediatric medical capacity for COVID patients during pandemic surges (see “POPCoRN network mobilizes pediatric capacity during pandemic,” The Hospitalist, April 30, 2020). One of its questions involved the redeployment of physicians in response to COVID demands and what, for example, pediatric hospitalists need as resources and tools when they are reassigned to adult patients or to new roles in unfamiliar settings. A variety of educational resources were cited from POPCoRN, SHM, and ImproveDX, among others.
Defining medical communication
Another chat moderator is Angela Castellanos, MD, a pediatric hospitalist at Tufts Medical Center in Boston. Dr. Castellanos did a 1-year, full-time fellowship right after residency at the New England Journal of Medicine, participating hands-on as a member of the editorial team for the print and online editions of the venerable journal. She is now doing a digital media fellowship with JHM, a part-time commitment while holding down a full-time job as a hospitalist. She also puts together a Spanish language podcast covering primary care pediatric issues for parents and families.
“I’m interested in medical communication generally, as I try to figure out what that means,” she said. “I have continued to look for ways to be part of the social media community and to be more creative about it. The JHM fellowship came at a perfect time for me to learn to do more in digital media.”
COVID has created new opportunities for more immediate dialogue with colleagues – what are they seeing and what’s working in the absence of clinical trials, she explained. “That’s how we communicate, as a way to get information out fast, such as when hospitals began proning COVID patients to make it easier for them to breathe.”
Dr. Castellanos said she grew up with text messaging and social media and wants to continue to grow her skills in this area. “I think I developed some skills at NEJM, but the opportunity to see how they do things at another journal with a different mission was also valuable. I get to share the space with people in academic settings and leaders in my field. I tweet at them; they tweet at me. These two fellowships have given me unique insights and mentorships. I know I want to continue doing pediatric hospital medicine and to engage academically and learn how to do research.”
Twitter sometimes gets a bad reputation for hostile or incendiary posts, Dr. Wray noted. “If you look at social media writ large, it can sometimes seem like a dumpster fire.” But what has happened in the medical community and in most medical Twitter encounters is a more cordial approach to conversations. “People who work in medicine converse with each other, with room for respectful disagreements. We’re extra supportive of each other,” he said.
“I think if hospitalists are looking for a community of peers, to engage with them and network and to find colleagues in similar circumstances, the JHM chat is such a fantastic place,” Dr. Wray concluded. “Don’t just come once, come several times, meet people along the way. For me, one of the most beneficial ways to advance my career has been by connecting with people through the chat. It allows me to share my work and success with the hospitalist community, as well as highlighting my trainees’ and colleagues’ successes, and it has created opportunities I never would have expected for getting involved in other projects.”
Once upon a time, physicians wrote letters to peers and colleagues around the world, sharing their medical discoveries, theories, case reports, and questions; conferring on problems; and then waiting for return mail to bring a reply. And the science of medicine advanced at a glacial pace.
Today, communication in multiple mediums flows much faster, almost instantaneously, between many more physicians, regardless of distance, addressing a much greater complexity of medical topics and treatments. And one of the chief mediums for this rapid electronic conversation among doctors is Twitter, according to Charlie Wray, DO, MS, a hospitalist at the University of California, San Francisco.
Dr. Wray, associate editor and digital media editor for the Journal of Hospital Medicine, is one of the moderators of #JHMchat, a monthly get-together on Twitter for interested hospitalists to link up virtually; respond to questions posed by JHM editors and other moderators; exchange perspectives, experiences, and tips with their peers; and build professional relationships and personal friendships. Relationship building has become particularly important in the age of COVID-19, when opportunities to connect in person at events such as SHM’s annual conferences have been curtailed.
The online #JHMchat community began in 2015, shortly after Dr. Wray completed a hospitalist research fellowship at the University of Chicago. His fellowship mentor, Vineet Arora, MD, MAPP, MHM, associate chief medical officer for the clinical learning environment at University of Chicago Medicine, had noticed how other online medical communities were engaging in discussions around different topics.
“She thought it could be a great way for hospitalists to meet online and talk about the articles published in JHM,” Dr. Wray explained. “We were all getting into social media and learning how to moderate interactive discussions such as Twitter.”
The chat’s founders approached JHM’s then-editor Andrew Auerbach, MD, MHM, a hospitalist at UCSF, who agreed that it was a great idea. They asked Christopher Moriates, MD, author of a recently published paper on the advisability of nebulized bronchodilators for obstructive pulmonary symptoms and assistant dean for health care value at the University of Texas, Austin, to come on the chat and talk about his paper. Visiting Dr. Arora at the time, he joined her in her living room for the first chat on Oct. 12, 2015. Seventy-five participants posted 431 tweets, with a total of 2 million Twitter impressions, suggesting that they had tapped a latent need.
How the chat works
To participate in the JHM chats on Twitter, one needs to open an account on the platform (it’s free) and follow the Journal’s Twitter feed (@jhospmedicine). But that’s pretty much it, Dr. Wray said. The group convenes on a Monday evening each month for an hour, starting at 9 p.m. Eastern time. Upcoming chats and topics are announced on Twitter and at SHM’s website.
The chats have grown and evolved since 2015, shifting in focus given recent social upheavals over the pandemic and heated discussions about diversity, equity, and racial justice in medicine, he said. “When COVID hit, the journal’s editor – Dr. Samir Shah – recognized that we were in a unique moment with the pandemic. The journal took advantage of the opportunity to publish a lot more personal perspectives and viewpoints around COVID, along with a special issue devoted to social justice.”
Moderators for the chat typically choose three or four questions based on recently published articles or other relevant topics, such as racial inequities in health care or how to apply military principles to hospital medicine leadership. “We reach out to authors and tell them they can explain their articles to interested readers through the chat. I can’t think of a single one who said no. They see the opportunity to highlight their work and engage with readers who want to ask them questions,” Dr. Wray said.
The moderators’ questions are posed to stimulate participation, but another goal is to use that hour for networking. “It’s a powerful tool to allow SHM members to engage with each other,” he said. “Sometimes the chat has the feeling of trying to drink water from a fire hose – with the messages flashing past so quickly. But the key is not to try to respond to everything but rather to follow those threads that particularly interest you. We encourage you to engage, but it’s totally fine if you just sit back and observe. One thing we have done to make it a little more formal is to offer CME credits for participants.”
The chat welcomes hospitalists and nonhospitalists, nurse practitioners, physician assistants, academics, and nonacademics. “No matter how engaged you are with Twitter, if you have 10,000 followers or 10, we’ll amplify your voice,” he said. “We also have medical students participating and consider their perspectives valuable, too.”
Dr. Wray identified three main types of participants in the monthly chats. The first are regulars who come every month, rain or shine. Like the character Norm in the old television comedy “Cheers,” everybody knows their name. They become friends, sharing and reveling in each other’s accomplishments. “These are people who have multiple connections, personally and professionally, at a lot of different levels. I probably know a hundred or more people who I’ve primarily gotten to know online.”
A second and larger group might be drawn in because of an interest in a specific topic or article, but they’re also welcome to participate in the chat. And the third group may lurk in the background, following along but not commenting. The size of that third group is unknown, but metrics from SHM show a total of 796 participants posting 4,088 tweets during chats in 2020 (for an average of 132 participants and 681 tweets per chat). This adds up to a total of 34 million impressions across the platform for #JHMchat tweets for the year.
Creating community online
“Why do we do it? It’s difficult to read all of the relevant published articles and keep up to date,” said Dr. Arora, a medical educator whose job at Chicago Medicine is to improve the clinical learning environment for trainees and staff by aligning learning with the health system’s institutional quality, safety and value missions.
“Our idea was to bring together a kind of virtual journal club and have discussions around topics such as: how do you create a shared vision on rounds? How do you integrate that into clinical practice? How do we preserve work/life balance or address structural racism?” she said. Other topics have included work flow concerns, burnout, difficult conversations with patients, and career planning.
“The people we’re trying to reach are hospitalists – and they’re busy at the front lines of care. We also thought this was an interesting way to raise the journal’s profile and spark broader interest in the articles it publishes. But it’s really about creating community, with people who look forward to talking and connecting with each other each month through the chats,” Dr. Arora said. If they miss a chat, they feel they’ve missed important interactions.
“Many times when people log onto the chat, they give a status report on where they are at, such as ‘I’m home putting my kids to bed,’ or ‘I’m on call tonight,’ ” she added. “People are willing to engage with the medium because it’s easy to engage with. We can forget that physicians are like everyone else. They like to learn, but they want that learning to be fun.”
On Dec. 14, 2020, at 9 p.m. Eastern time, the first question for the monthly #JHMchat was posted: How will caring for COVID-19 patients this winter differ from caring for patients in the first wave? Given that another surge of hospitalized COVID patients is looming, participants posted that they feel familiar and more confident with effective clinical strategies for hospitalized COVID patients, having learned so much more about the virus. But they’re facing greater numbers of patients than in prior surges. “In March, we were in crisis, now we’re in complexity,” one noted.
Joining the moderators was the Pediatric Overflow Planning Contingency Response Network (POPCoRN), a group formed earlier this year to help mobilize pediatric medical capacity for COVID patients during pandemic surges (see “POPCoRN network mobilizes pediatric capacity during pandemic,” The Hospitalist, April 30, 2020). One of its questions involved the redeployment of physicians in response to COVID demands and what, for example, pediatric hospitalists need as resources and tools when they are reassigned to adult patients or to new roles in unfamiliar settings. A variety of educational resources were cited from POPCoRN, SHM, and ImproveDX, among others.
Defining medical communication
Another chat moderator is Angela Castellanos, MD, a pediatric hospitalist at Tufts Medical Center in Boston. Dr. Castellanos did a 1-year, full-time fellowship right after residency at the New England Journal of Medicine, participating hands-on as a member of the editorial team for the print and online editions of the venerable journal. She is now doing a digital media fellowship with JHM, a part-time commitment while holding down a full-time job as a hospitalist. She also puts together a Spanish language podcast covering primary care pediatric issues for parents and families.
“I’m interested in medical communication generally, as I try to figure out what that means,” she said. “I have continued to look for ways to be part of the social media community and to be more creative about it. The JHM fellowship came at a perfect time for me to learn to do more in digital media.”
COVID has created new opportunities for more immediate dialogue with colleagues – what are they seeing and what’s working in the absence of clinical trials, she explained. “That’s how we communicate, as a way to get information out fast, such as when hospitals began proning COVID patients to make it easier for them to breathe.”
Dr. Castellanos said she grew up with text messaging and social media and wants to continue to grow her skills in this area. “I think I developed some skills at NEJM, but the opportunity to see how they do things at another journal with a different mission was also valuable. I get to share the space with people in academic settings and leaders in my field. I tweet at them; they tweet at me. These two fellowships have given me unique insights and mentorships. I know I want to continue doing pediatric hospital medicine and to engage academically and learn how to do research.”
Twitter sometimes gets a bad reputation for hostile or incendiary posts, Dr. Wray noted. “If you look at social media writ large, it can sometimes seem like a dumpster fire.” But what has happened in the medical community and in most medical Twitter encounters is a more cordial approach to conversations. “People who work in medicine converse with each other, with room for respectful disagreements. We’re extra supportive of each other,” he said.
“I think if hospitalists are looking for a community of peers, to engage with them and network and to find colleagues in similar circumstances, the JHM chat is such a fantastic place,” Dr. Wray concluded. “Don’t just come once, come several times, meet people along the way. For me, one of the most beneficial ways to advance my career has been by connecting with people through the chat. It allows me to share my work and success with the hospitalist community, as well as highlighting my trainees’ and colleagues’ successes, and it has created opportunities I never would have expected for getting involved in other projects.”