User login
The Final Rule for 2022: What’s New and How Changes in the Medicare Physician Fee Schedule and Quality Payment Program Affect Dermatologists
On November 2, 2021, the Centers for Medicare & Medicaid Services (CMS) released its final rule for the 2022 Medicare Physician Fee Schedule (PFS) and the Quality Payment Program (QPP).1,2 These guidelines contain updates that will remarkably impact the field of medicine—and dermatology in particular—in 2022. This article will walk you through some of the updates most relevant to dermatology and how they may affect your practice.
Process for the Final Rule
The CMS releases an annual rule for the PFS and QPP. The interim rule generally is released over the summer with preliminary guidelines for the upcoming payment year. There is then a period of open comment where those affected by these changes, including physicians and medical associations, can submit comments to support what has been proposed or advocate for any changes. This input is then reviewed, and a final rule generally is published in the fall.
For this calendar year, the interim 2022 rule was released on July 13, 2021,3 and included many of guidelines that will be discussed in more detail in this article. Many associations that represent medicine overall and specifically dermatology, including the American Medical Association and the American Academy of Dermatology, submitted comments in response to these proposals.4,5
PFS Conversion Factor
The PFS conversion factor is updated annually to ensure budget neutrality in the setting of changes in relative value units. For 2022, the PFS conversion factor is $34.6062, representing a reduction of approximately $0.29 from the 2021 PFS conversion factor of $34.8931.6 This reduction does not take into account other payment adjustments due to legislative changes.
In combination, these changes previously were estimated to represent an overall payment cut of 10% or higher for dermatology, with those practitioners doing more procedural work or dermatopathology likely being impacted more heavily. However, with the passing of the Protecting Medicare and American Farmers from Sequester Cuts Act, it is estimated that the reductions in payment to dermatology will begin at 0.75% and reach 2.75% in the second half of the year with the phased-in reinstatement of the Medicare sequester.4,5,7
Clinical Labor Pricing Updates
Starting in 2022, the CMS will utilize updated wage rates from the US Bureau of Labor Statistics to revise clinical labor costs over a 4-year period. Clinical labor rates are important, as they are used to calculate practice expense within the PFS. These clinical labor rates were last updated in 2002.8 Median wage data, as opposed to mean data, from the US Bureau of Labor Statistics will be utilized to calculate the updated clinical labor rates.
A multiyear implementation plan was put into place by CMS due to multiple concerns, including that current wage rates are inadequate and may not reflect current labor rate information. Additionally, comments on this proposal voiced concern that updating the supply and equipment pricing without updating the clinical labor pricing could create distortions in the allocation of direct practice expense, which also factored into the implementation of a multiyear plan.8
It is anticipated that specialties that rely primarily on clinical labor will receive the largest increases in these rates and that specialties that rely primarily on supply or equipment items are anticipated to receive the largest reductions relative to other specialties. Dermatology is estimated to have a 0% change during the year 1 transition period; however, it will have an estimated 1% reduction in clinical labor pricing overall once the updates are completed.1 Pathology also is estimated to have a similar overall decrease during this transition period.
Evaluation and Management Visits
The biggest update in this area primarily is related to refining policies for split (shared) evaluation and management (E/M) visits and teaching physician activities. Split E/M visits are defined by the CMS as visits provided in the facility setting by a physician and nonphysician practitioner in the same group, with the visit billed by whomever provides the substantive portion of the visit. For 2022, the term substantive portion will be defined by the CMS as history, physical examination, medical decision-making, or more than half of the total time; for 2023, it will be defined as more than half of the total time spent.3 A split visit also can apply to an E/M visit provided in part by both a teaching physician and resident. Split visits can be reported for new or established patients. For proper reimbursement, the 2 practitioners who performed the services must be documented in the medical record, and the practitioner who provided the substantive portion must sign and date the encounter in the medical record. Additionally, the CMS has indicated the modifier FS must be included on the claim to indicate the split visit.9
For dermatologists who act as teaching physicians, it is important to note that many of the existing CMS policies for billing E/M services are still in place, specifically that if a resident participates in a service in a teaching setting, the teaching physician can bill for the service only if they are present for the key or critical portion of the service. A primary care exception does exist, in which teaching physicians at certain teaching hospital primary care centers can bill for some services performed independently by a resident without the physical presence of the teaching physician; however, this often is not applicable within dermatology.
With updated outpatient E/M guidelines, if time is being selected to bill, only the time that the teaching physician was present can be included to determine the overall E/M level.
Billing for Physician Assistant Services
Currently Medicare can only make payments to the employer or independent contractor of a physician assistant (PA); however, starting January 1, 2022, the CMS has authorized Medicare to make direct payments to PAs for qualifying professional services, in the same manner that nurse practitioners can currently bill. This also will allow PAs to incorporate as a group and bill Medicare for PA services. This stems from a congressional mandate within the Consolidated Appropriations Act of 2021.8 As a result, in states where PAs can practice independently, they can opt out of physician-led care teams and furnish services independently, including dermatologic services.
QPP Updates
Several changes were made to the Merit-Based Incentive Payment System (MIPS). Some of these changes include:
- Increase the MIPS performance threshold to 75 points from 60 points.
- Set the performance threshold at 89 points.
- Reduce the quality performance category weight from 40% to 30% of the final MIPS score.
- Increase the cost performance category weight from 20% to 30% of the final MIPS score.
- The extreme and uncontrollable circumstances application also has been extended to the end of 2022, allowing those remarkably impacted by the COVID-19 public health emergency to request for reweighting on any or all MIPS performance categories.
Cost Measures and MIPS Value Pathways
The melanoma resection cost measure will be implemented in 2022, representing the first dermatology cost measure, which will include the cost to Medicare over a 1-year period for all patient care for the excision of a melanoma. Although cost measures will be part of the MIPS value pathways (MVPs) reporting, dermatology currently is not part of the MVP; however, with the CMS moving forward with an initial set of MVPs that physicians can voluntarily report on in 2023, there is a possibility that dermatology will be asked to be part of the program in the future.10
Final Thoughts
There are many upcoming changes as part of the 2022 final rule, including to the conversion factor, E/M split visits, PA billing, and the QPP. Advocacy in these areas to the CMS and lawmakers, either directly or through dermatologic and other medical societies, is critical to help influence eventual recommendations.
- Medicare Program; CY 2022 payment policies under the Physician Fee Schedule and other changes to part B payment policies; Medicare Shared Savings Program requirements; provider enrollment regulation updates; and provider and supplier prepayment and post-payment medical review requirements. Fed Regist. 2021;86:64996-66031. To be codified at 42 CFR §403, §405, §410, §411, §414, §415, §423, §424, and §425. https://www.federalregister.gov/documents/2021/11/19/2021-23972/medicare-program-cy-2022-payment-policies-under-the-physician-fee-schedule-and-other-changes-to-part
- Centers for Medicare & Medicaid Services. CMS physician payment rule promotes greater access to telehealth services, diabetes prevention programs. Published November 2, 2021. Accessed January 10, 2022. https://www.cms.gov/newsroom/press-releases/cms-physician-payment-rule-promotes-greater-access-telehealth-services-diabetes-prevention-programs
- Centers for Medicare & Medicaid Services. Calendar year (CY) 2022 Medicare Physician Fee Schedule proposed rule. Published July 13, 2021. Accessed January 10, 2022. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2022-medicare-physician-fee-schedule-proposed-rule
- American Academy of Dermatology. Dermatology World Weekly. October 27, 2021. Accessed January 20, 2022. https://www.aad.org/dw/weekly
- O’Reilly KB. 2022 Medicare pay schedule confirms Congress needs to act. American Medical Association website. Published November 10, 2021. Accessed January 10, 2021. https://www.ama-assn.org/practice-management/medicare-medicaid/2022-medicare-pay-schedule-confirms-congress-needs-act
- History of Medicare conversion factors. American Medical Association website. Accessed January 19, 2022. https://www.ama-assn.org/system/files/2021-01/cf-history.pdf
- American Academy of Dermatology. Dermatology World Weekly. December 15, 2021. Accessed January 20, 2022. https://www.aad.org/dw/weekly
- American Medical Association. CY 2022 Medicare Physician Fee Schedule (PFS) and Quality Payment Program (QPP) final rule summary. Accessed January 10, 2021. https://www.ama-assn.org/system/files/2022-pfs-qpp-final-rule.pdf
- Centers for Medicare & Medicaid Services. January 2022 alpha-numeric HCPCS file. Updated December 20, 2021. Accessed January 20, 2022. https://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/HCPCS-Quarterly-Update
- CMS finalizes Medicare payments for 2022. American Academy of Dermatology website. NEED PUB DATE. Accessed January 20, 2022. https://www.aad.org/member/practice/mips/fee-schedule/2022-fee-schedule-final
On November 2, 2021, the Centers for Medicare & Medicaid Services (CMS) released its final rule for the 2022 Medicare Physician Fee Schedule (PFS) and the Quality Payment Program (QPP).1,2 These guidelines contain updates that will remarkably impact the field of medicine—and dermatology in particular—in 2022. This article will walk you through some of the updates most relevant to dermatology and how they may affect your practice.
Process for the Final Rule
The CMS releases an annual rule for the PFS and QPP. The interim rule generally is released over the summer with preliminary guidelines for the upcoming payment year. There is then a period of open comment where those affected by these changes, including physicians and medical associations, can submit comments to support what has been proposed or advocate for any changes. This input is then reviewed, and a final rule generally is published in the fall.
For this calendar year, the interim 2022 rule was released on July 13, 2021,3 and included many of guidelines that will be discussed in more detail in this article. Many associations that represent medicine overall and specifically dermatology, including the American Medical Association and the American Academy of Dermatology, submitted comments in response to these proposals.4,5
PFS Conversion Factor
The PFS conversion factor is updated annually to ensure budget neutrality in the setting of changes in relative value units. For 2022, the PFS conversion factor is $34.6062, representing a reduction of approximately $0.29 from the 2021 PFS conversion factor of $34.8931.6 This reduction does not take into account other payment adjustments due to legislative changes.
In combination, these changes previously were estimated to represent an overall payment cut of 10% or higher for dermatology, with those practitioners doing more procedural work or dermatopathology likely being impacted more heavily. However, with the passing of the Protecting Medicare and American Farmers from Sequester Cuts Act, it is estimated that the reductions in payment to dermatology will begin at 0.75% and reach 2.75% in the second half of the year with the phased-in reinstatement of the Medicare sequester.4,5,7
Clinical Labor Pricing Updates
Starting in 2022, the CMS will utilize updated wage rates from the US Bureau of Labor Statistics to revise clinical labor costs over a 4-year period. Clinical labor rates are important, as they are used to calculate practice expense within the PFS. These clinical labor rates were last updated in 2002.8 Median wage data, as opposed to mean data, from the US Bureau of Labor Statistics will be utilized to calculate the updated clinical labor rates.
A multiyear implementation plan was put into place by CMS due to multiple concerns, including that current wage rates are inadequate and may not reflect current labor rate information. Additionally, comments on this proposal voiced concern that updating the supply and equipment pricing without updating the clinical labor pricing could create distortions in the allocation of direct practice expense, which also factored into the implementation of a multiyear plan.8
It is anticipated that specialties that rely primarily on clinical labor will receive the largest increases in these rates and that specialties that rely primarily on supply or equipment items are anticipated to receive the largest reductions relative to other specialties. Dermatology is estimated to have a 0% change during the year 1 transition period; however, it will have an estimated 1% reduction in clinical labor pricing overall once the updates are completed.1 Pathology also is estimated to have a similar overall decrease during this transition period.
Evaluation and Management Visits
The biggest update in this area primarily is related to refining policies for split (shared) evaluation and management (E/M) visits and teaching physician activities. Split E/M visits are defined by the CMS as visits provided in the facility setting by a physician and nonphysician practitioner in the same group, with the visit billed by whomever provides the substantive portion of the visit. For 2022, the term substantive portion will be defined by the CMS as history, physical examination, medical decision-making, or more than half of the total time; for 2023, it will be defined as more than half of the total time spent.3 A split visit also can apply to an E/M visit provided in part by both a teaching physician and resident. Split visits can be reported for new or established patients. For proper reimbursement, the 2 practitioners who performed the services must be documented in the medical record, and the practitioner who provided the substantive portion must sign and date the encounter in the medical record. Additionally, the CMS has indicated the modifier FS must be included on the claim to indicate the split visit.9
For dermatologists who act as teaching physicians, it is important to note that many of the existing CMS policies for billing E/M services are still in place, specifically that if a resident participates in a service in a teaching setting, the teaching physician can bill for the service only if they are present for the key or critical portion of the service. A primary care exception does exist, in which teaching physicians at certain teaching hospital primary care centers can bill for some services performed independently by a resident without the physical presence of the teaching physician; however, this often is not applicable within dermatology.
With updated outpatient E/M guidelines, if time is being selected to bill, only the time that the teaching physician was present can be included to determine the overall E/M level.
Billing for Physician Assistant Services
Currently Medicare can only make payments to the employer or independent contractor of a physician assistant (PA); however, starting January 1, 2022, the CMS has authorized Medicare to make direct payments to PAs for qualifying professional services, in the same manner that nurse practitioners can currently bill. This also will allow PAs to incorporate as a group and bill Medicare for PA services. This stems from a congressional mandate within the Consolidated Appropriations Act of 2021.8 As a result, in states where PAs can practice independently, they can opt out of physician-led care teams and furnish services independently, including dermatologic services.
QPP Updates
Several changes were made to the Merit-Based Incentive Payment System (MIPS). Some of these changes include:
- Increase the MIPS performance threshold to 75 points from 60 points.
- Set the performance threshold at 89 points.
- Reduce the quality performance category weight from 40% to 30% of the final MIPS score.
- Increase the cost performance category weight from 20% to 30% of the final MIPS score.
- The extreme and uncontrollable circumstances application also has been extended to the end of 2022, allowing those remarkably impacted by the COVID-19 public health emergency to request for reweighting on any or all MIPS performance categories.
Cost Measures and MIPS Value Pathways
The melanoma resection cost measure will be implemented in 2022, representing the first dermatology cost measure, which will include the cost to Medicare over a 1-year period for all patient care for the excision of a melanoma. Although cost measures will be part of the MIPS value pathways (MVPs) reporting, dermatology currently is not part of the MVP; however, with the CMS moving forward with an initial set of MVPs that physicians can voluntarily report on in 2023, there is a possibility that dermatology will be asked to be part of the program in the future.10
Final Thoughts
There are many upcoming changes as part of the 2022 final rule, including to the conversion factor, E/M split visits, PA billing, and the QPP. Advocacy in these areas to the CMS and lawmakers, either directly or through dermatologic and other medical societies, is critical to help influence eventual recommendations.
On November 2, 2021, the Centers for Medicare & Medicaid Services (CMS) released its final rule for the 2022 Medicare Physician Fee Schedule (PFS) and the Quality Payment Program (QPP).1,2 These guidelines contain updates that will remarkably impact the field of medicine—and dermatology in particular—in 2022. This article will walk you through some of the updates most relevant to dermatology and how they may affect your practice.
Process for the Final Rule
The CMS releases an annual rule for the PFS and QPP. The interim rule generally is released over the summer with preliminary guidelines for the upcoming payment year. There is then a period of open comment where those affected by these changes, including physicians and medical associations, can submit comments to support what has been proposed or advocate for any changes. This input is then reviewed, and a final rule generally is published in the fall.
For this calendar year, the interim 2022 rule was released on July 13, 2021,3 and included many of guidelines that will be discussed in more detail in this article. Many associations that represent medicine overall and specifically dermatology, including the American Medical Association and the American Academy of Dermatology, submitted comments in response to these proposals.4,5
PFS Conversion Factor
The PFS conversion factor is updated annually to ensure budget neutrality in the setting of changes in relative value units. For 2022, the PFS conversion factor is $34.6062, representing a reduction of approximately $0.29 from the 2021 PFS conversion factor of $34.8931.6 This reduction does not take into account other payment adjustments due to legislative changes.
In combination, these changes previously were estimated to represent an overall payment cut of 10% or higher for dermatology, with those practitioners doing more procedural work or dermatopathology likely being impacted more heavily. However, with the passing of the Protecting Medicare and American Farmers from Sequester Cuts Act, it is estimated that the reductions in payment to dermatology will begin at 0.75% and reach 2.75% in the second half of the year with the phased-in reinstatement of the Medicare sequester.4,5,7
Clinical Labor Pricing Updates
Starting in 2022, the CMS will utilize updated wage rates from the US Bureau of Labor Statistics to revise clinical labor costs over a 4-year period. Clinical labor rates are important, as they are used to calculate practice expense within the PFS. These clinical labor rates were last updated in 2002.8 Median wage data, as opposed to mean data, from the US Bureau of Labor Statistics will be utilized to calculate the updated clinical labor rates.
A multiyear implementation plan was put into place by CMS due to multiple concerns, including that current wage rates are inadequate and may not reflect current labor rate information. Additionally, comments on this proposal voiced concern that updating the supply and equipment pricing without updating the clinical labor pricing could create distortions in the allocation of direct practice expense, which also factored into the implementation of a multiyear plan.8
It is anticipated that specialties that rely primarily on clinical labor will receive the largest increases in these rates and that specialties that rely primarily on supply or equipment items are anticipated to receive the largest reductions relative to other specialties. Dermatology is estimated to have a 0% change during the year 1 transition period; however, it will have an estimated 1% reduction in clinical labor pricing overall once the updates are completed.1 Pathology also is estimated to have a similar overall decrease during this transition period.
Evaluation and Management Visits
The biggest update in this area primarily is related to refining policies for split (shared) evaluation and management (E/M) visits and teaching physician activities. Split E/M visits are defined by the CMS as visits provided in the facility setting by a physician and nonphysician practitioner in the same group, with the visit billed by whomever provides the substantive portion of the visit. For 2022, the term substantive portion will be defined by the CMS as history, physical examination, medical decision-making, or more than half of the total time; for 2023, it will be defined as more than half of the total time spent.3 A split visit also can apply to an E/M visit provided in part by both a teaching physician and resident. Split visits can be reported for new or established patients. For proper reimbursement, the 2 practitioners who performed the services must be documented in the medical record, and the practitioner who provided the substantive portion must sign and date the encounter in the medical record. Additionally, the CMS has indicated the modifier FS must be included on the claim to indicate the split visit.9
For dermatologists who act as teaching physicians, it is important to note that many of the existing CMS policies for billing E/M services are still in place, specifically that if a resident participates in a service in a teaching setting, the teaching physician can bill for the service only if they are present for the key or critical portion of the service. A primary care exception does exist, in which teaching physicians at certain teaching hospital primary care centers can bill for some services performed independently by a resident without the physical presence of the teaching physician; however, this often is not applicable within dermatology.
With updated outpatient E/M guidelines, if time is being selected to bill, only the time that the teaching physician was present can be included to determine the overall E/M level.
Billing for Physician Assistant Services
Currently Medicare can only make payments to the employer or independent contractor of a physician assistant (PA); however, starting January 1, 2022, the CMS has authorized Medicare to make direct payments to PAs for qualifying professional services, in the same manner that nurse practitioners can currently bill. This also will allow PAs to incorporate as a group and bill Medicare for PA services. This stems from a congressional mandate within the Consolidated Appropriations Act of 2021.8 As a result, in states where PAs can practice independently, they can opt out of physician-led care teams and furnish services independently, including dermatologic services.
QPP Updates
Several changes were made to the Merit-Based Incentive Payment System (MIPS). Some of these changes include:
- Increase the MIPS performance threshold to 75 points from 60 points.
- Set the performance threshold at 89 points.
- Reduce the quality performance category weight from 40% to 30% of the final MIPS score.
- Increase the cost performance category weight from 20% to 30% of the final MIPS score.
- The extreme and uncontrollable circumstances application also has been extended to the end of 2022, allowing those remarkably impacted by the COVID-19 public health emergency to request for reweighting on any or all MIPS performance categories.
Cost Measures and MIPS Value Pathways
The melanoma resection cost measure will be implemented in 2022, representing the first dermatology cost measure, which will include the cost to Medicare over a 1-year period for all patient care for the excision of a melanoma. Although cost measures will be part of the MIPS value pathways (MVPs) reporting, dermatology currently is not part of the MVP; however, with the CMS moving forward with an initial set of MVPs that physicians can voluntarily report on in 2023, there is a possibility that dermatology will be asked to be part of the program in the future.10
Final Thoughts
There are many upcoming changes as part of the 2022 final rule, including to the conversion factor, E/M split visits, PA billing, and the QPP. Advocacy in these areas to the CMS and lawmakers, either directly or through dermatologic and other medical societies, is critical to help influence eventual recommendations.
- Medicare Program; CY 2022 payment policies under the Physician Fee Schedule and other changes to part B payment policies; Medicare Shared Savings Program requirements; provider enrollment regulation updates; and provider and supplier prepayment and post-payment medical review requirements. Fed Regist. 2021;86:64996-66031. To be codified at 42 CFR §403, §405, §410, §411, §414, §415, §423, §424, and §425. https://www.federalregister.gov/documents/2021/11/19/2021-23972/medicare-program-cy-2022-payment-policies-under-the-physician-fee-schedule-and-other-changes-to-part
- Centers for Medicare & Medicaid Services. CMS physician payment rule promotes greater access to telehealth services, diabetes prevention programs. Published November 2, 2021. Accessed January 10, 2022. https://www.cms.gov/newsroom/press-releases/cms-physician-payment-rule-promotes-greater-access-telehealth-services-diabetes-prevention-programs
- Centers for Medicare & Medicaid Services. Calendar year (CY) 2022 Medicare Physician Fee Schedule proposed rule. Published July 13, 2021. Accessed January 10, 2022. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2022-medicare-physician-fee-schedule-proposed-rule
- American Academy of Dermatology. Dermatology World Weekly. October 27, 2021. Accessed January 20, 2022. https://www.aad.org/dw/weekly
- O’Reilly KB. 2022 Medicare pay schedule confirms Congress needs to act. American Medical Association website. Published November 10, 2021. Accessed January 10, 2021. https://www.ama-assn.org/practice-management/medicare-medicaid/2022-medicare-pay-schedule-confirms-congress-needs-act
- History of Medicare conversion factors. American Medical Association website. Accessed January 19, 2022. https://www.ama-assn.org/system/files/2021-01/cf-history.pdf
- American Academy of Dermatology. Dermatology World Weekly. December 15, 2021. Accessed January 20, 2022. https://www.aad.org/dw/weekly
- American Medical Association. CY 2022 Medicare Physician Fee Schedule (PFS) and Quality Payment Program (QPP) final rule summary. Accessed January 10, 2021. https://www.ama-assn.org/system/files/2022-pfs-qpp-final-rule.pdf
- Centers for Medicare & Medicaid Services. January 2022 alpha-numeric HCPCS file. Updated December 20, 2021. Accessed January 20, 2022. https://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/HCPCS-Quarterly-Update
- CMS finalizes Medicare payments for 2022. American Academy of Dermatology website. NEED PUB DATE. Accessed January 20, 2022. https://www.aad.org/member/practice/mips/fee-schedule/2022-fee-schedule-final
- Medicare Program; CY 2022 payment policies under the Physician Fee Schedule and other changes to part B payment policies; Medicare Shared Savings Program requirements; provider enrollment regulation updates; and provider and supplier prepayment and post-payment medical review requirements. Fed Regist. 2021;86:64996-66031. To be codified at 42 CFR §403, §405, §410, §411, §414, §415, §423, §424, and §425. https://www.federalregister.gov/documents/2021/11/19/2021-23972/medicare-program-cy-2022-payment-policies-under-the-physician-fee-schedule-and-other-changes-to-part
- Centers for Medicare & Medicaid Services. CMS physician payment rule promotes greater access to telehealth services, diabetes prevention programs. Published November 2, 2021. Accessed January 10, 2022. https://www.cms.gov/newsroom/press-releases/cms-physician-payment-rule-promotes-greater-access-telehealth-services-diabetes-prevention-programs
- Centers for Medicare & Medicaid Services. Calendar year (CY) 2022 Medicare Physician Fee Schedule proposed rule. Published July 13, 2021. Accessed January 10, 2022. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2022-medicare-physician-fee-schedule-proposed-rule
- American Academy of Dermatology. Dermatology World Weekly. October 27, 2021. Accessed January 20, 2022. https://www.aad.org/dw/weekly
- O’Reilly KB. 2022 Medicare pay schedule confirms Congress needs to act. American Medical Association website. Published November 10, 2021. Accessed January 10, 2021. https://www.ama-assn.org/practice-management/medicare-medicaid/2022-medicare-pay-schedule-confirms-congress-needs-act
- History of Medicare conversion factors. American Medical Association website. Accessed January 19, 2022. https://www.ama-assn.org/system/files/2021-01/cf-history.pdf
- American Academy of Dermatology. Dermatology World Weekly. December 15, 2021. Accessed January 20, 2022. https://www.aad.org/dw/weekly
- American Medical Association. CY 2022 Medicare Physician Fee Schedule (PFS) and Quality Payment Program (QPP) final rule summary. Accessed January 10, 2021. https://www.ama-assn.org/system/files/2022-pfs-qpp-final-rule.pdf
- Centers for Medicare & Medicaid Services. January 2022 alpha-numeric HCPCS file. Updated December 20, 2021. Accessed January 20, 2022. https://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/HCPCS-Quarterly-Update
- CMS finalizes Medicare payments for 2022. American Academy of Dermatology website. NEED PUB DATE. Accessed January 20, 2022. https://www.aad.org/member/practice/mips/fee-schedule/2022-fee-schedule-final
Practice Points
- The Centers for Medicare & Medicaid Services (CMS) 2022 final rule contains multiple updates affecting the practice of dermatology.
- Adjustments to the conversion factor and legislative-level actions have led to changes in reimbursement for many procedures within dermatology and beyond.
- Other notable updates include refining the definition of split evaluation and management visits, clinical labor pricing, and billing for physician assistant services.
- Changes in the Merit-Based Incentive Payment System (MIPS), cost measures, and MIPS value pathways also will impact many dermatology practices.
Advocacy Update: Is Your Practice Equipped to Handle Looming Changes in Dermatopathology?
The proposed 2022 Medicare physician fee schedule and quality payment program (QPP) regulations were released on July 13, 2021.1 Final regulations are expected to be released on or around November 1, 2021, but they may be delayed. Multiple national medical organizations, including the College of American Pathologists (CAP), the American Society of Dermatopathology, the American Academy of Dermatology Association (AADA), and the American Medical Association (AMA) Physicians’ Grassroots Network all work together to engage with the Centers for Medicare & Medicaid Services (CMS) to influence these regulations. Stated advocacy priorities include protecting the value of dermatopathology services, mobilizing dermatopathologists for political action, ensuring dermatopathologists can participate in new payment models, strengthening the profession with advocacy on a state level, and conducting socioeconomic research. Is your practice aware and prepared to handle the changes coming in 2022?
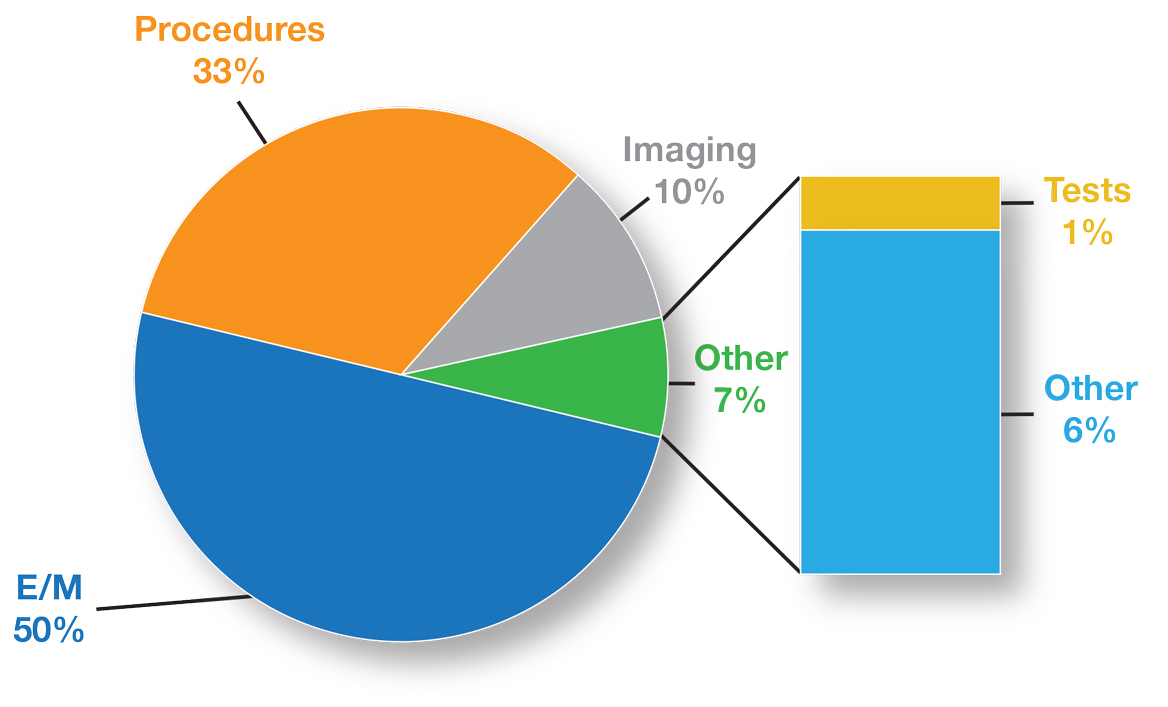
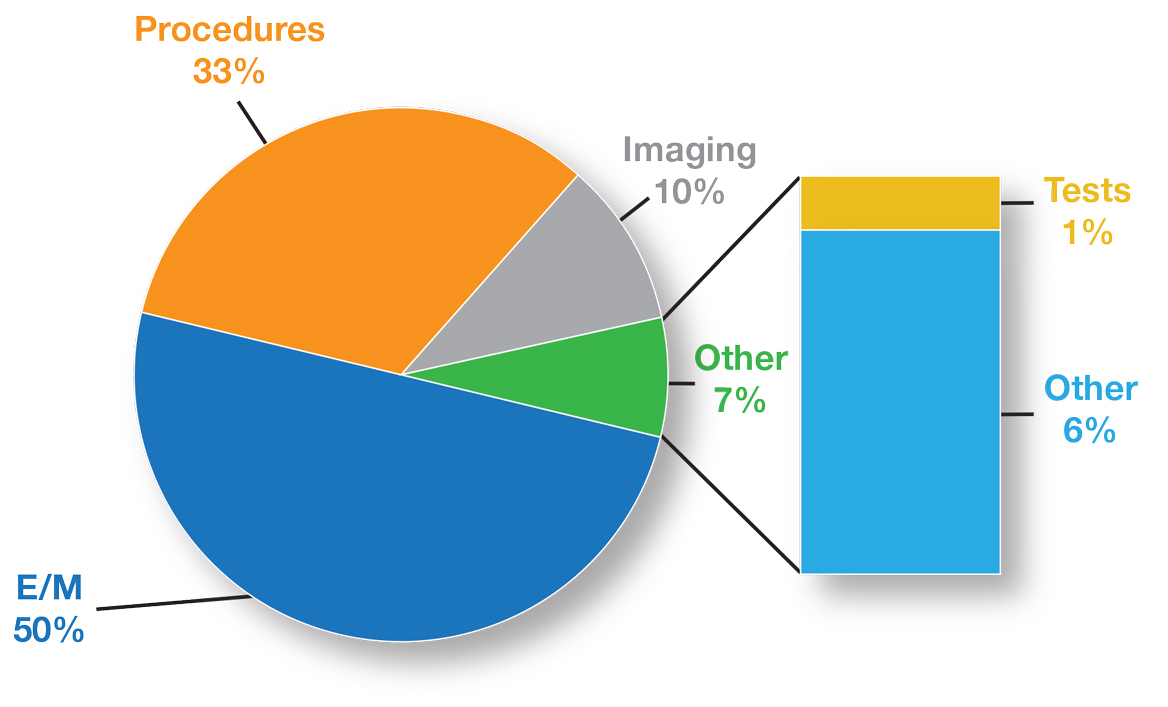
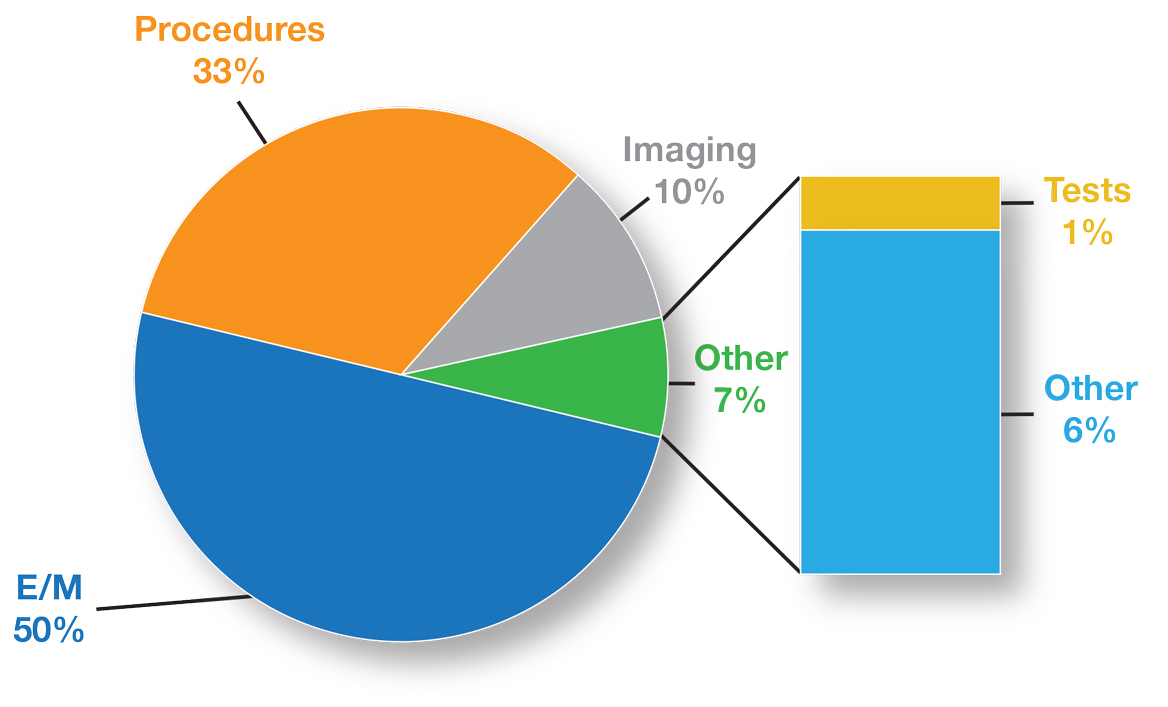
The recent revisions and revaluations of the outpatient evaluation and management (E/M) codes2 resulted in a considerable redistribution of Medicare dollars in 2021, negatively impacting dermatopathologists and other specialties and services due to budget neutrality required by law (Figure). Important steps were taken to mitigate the 2021 Medicare cuts for all non–office-based dermatopathology services (eg, pathology, surgical services, emergency department).1,3 Direct engagement by the CAP, American Society of Dermatopathology, and AADA, along with the AMA Physicians’ Grassroots Network resulted in legislative action on December 27, 2020, which directed Medicare to make a 3.75% positive adjustment to the 2021 physician payments. Additionally, the CMS updated the 2021 physician conversion factor to $34.8931, a 3.3% reduction from the 2020 conversion factor rather than $32.41, or a 10.20% decrease. The 2% payment adjustment (sequestration) through December 21, 2021, also was suspended, and Congress and the Biden administration mandated delayed implementation of the inherent complexity add-on code for E/M services (G2211) until 2024.1,3
Threat of Medicare Cuts in 2022
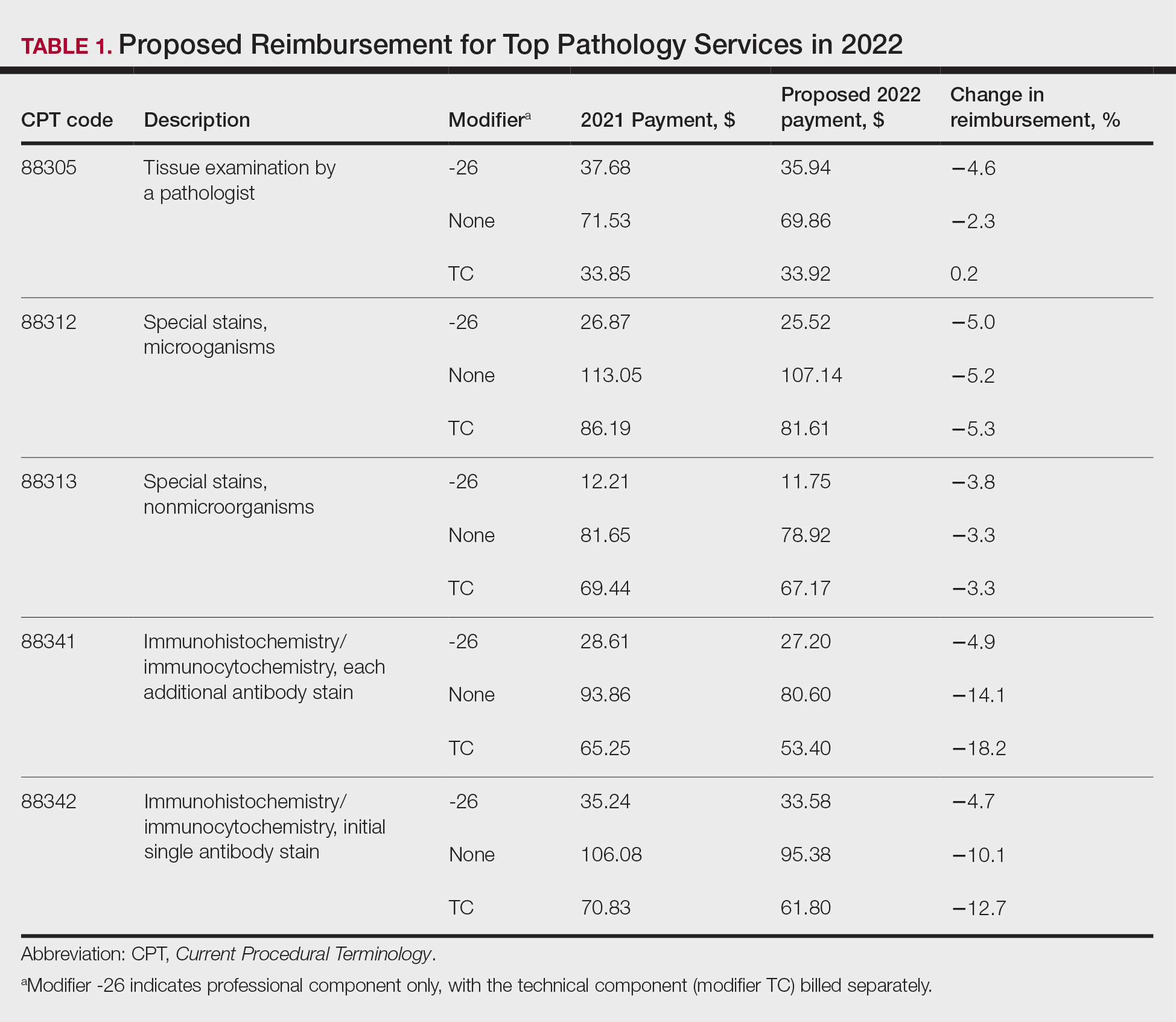
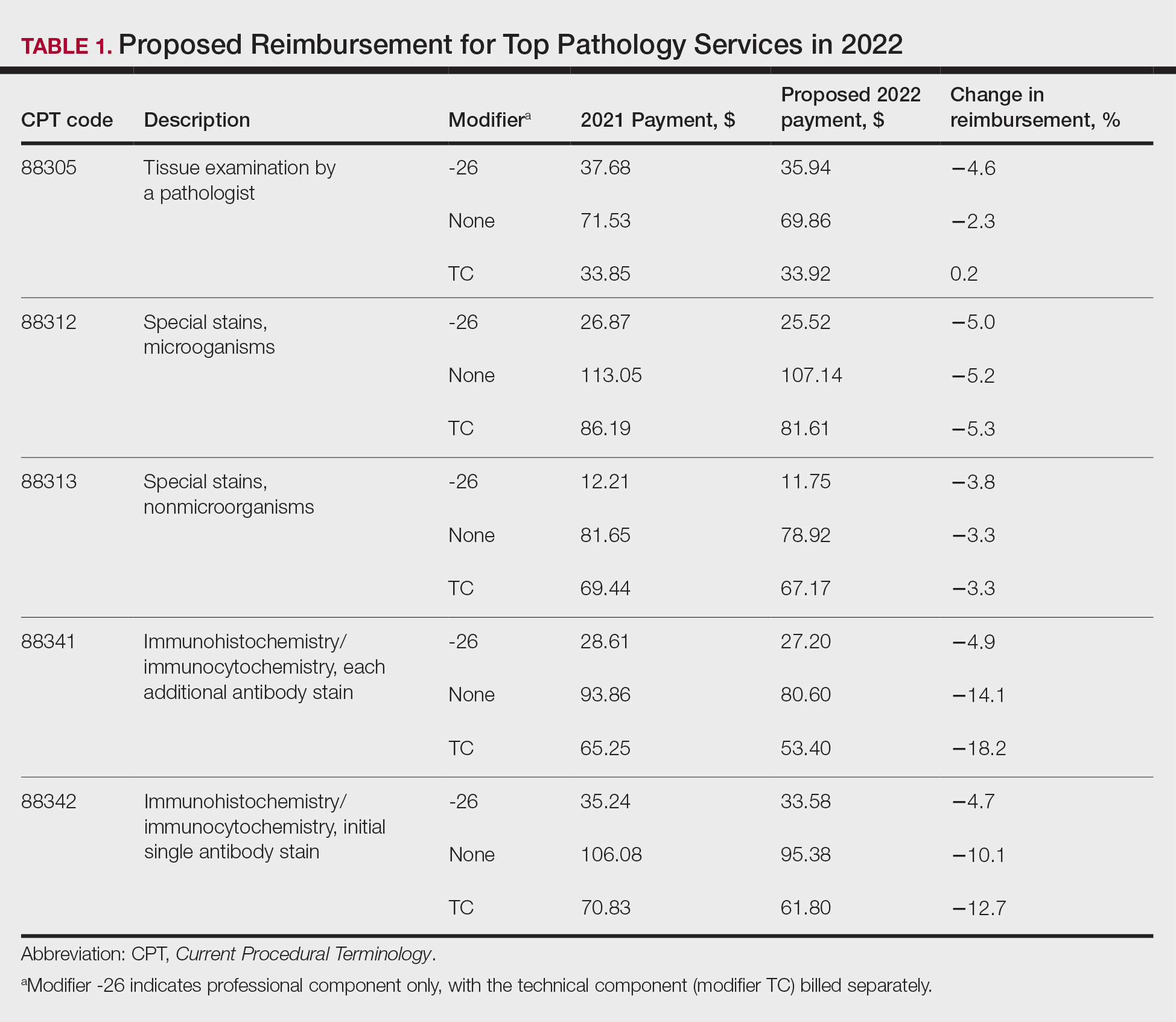
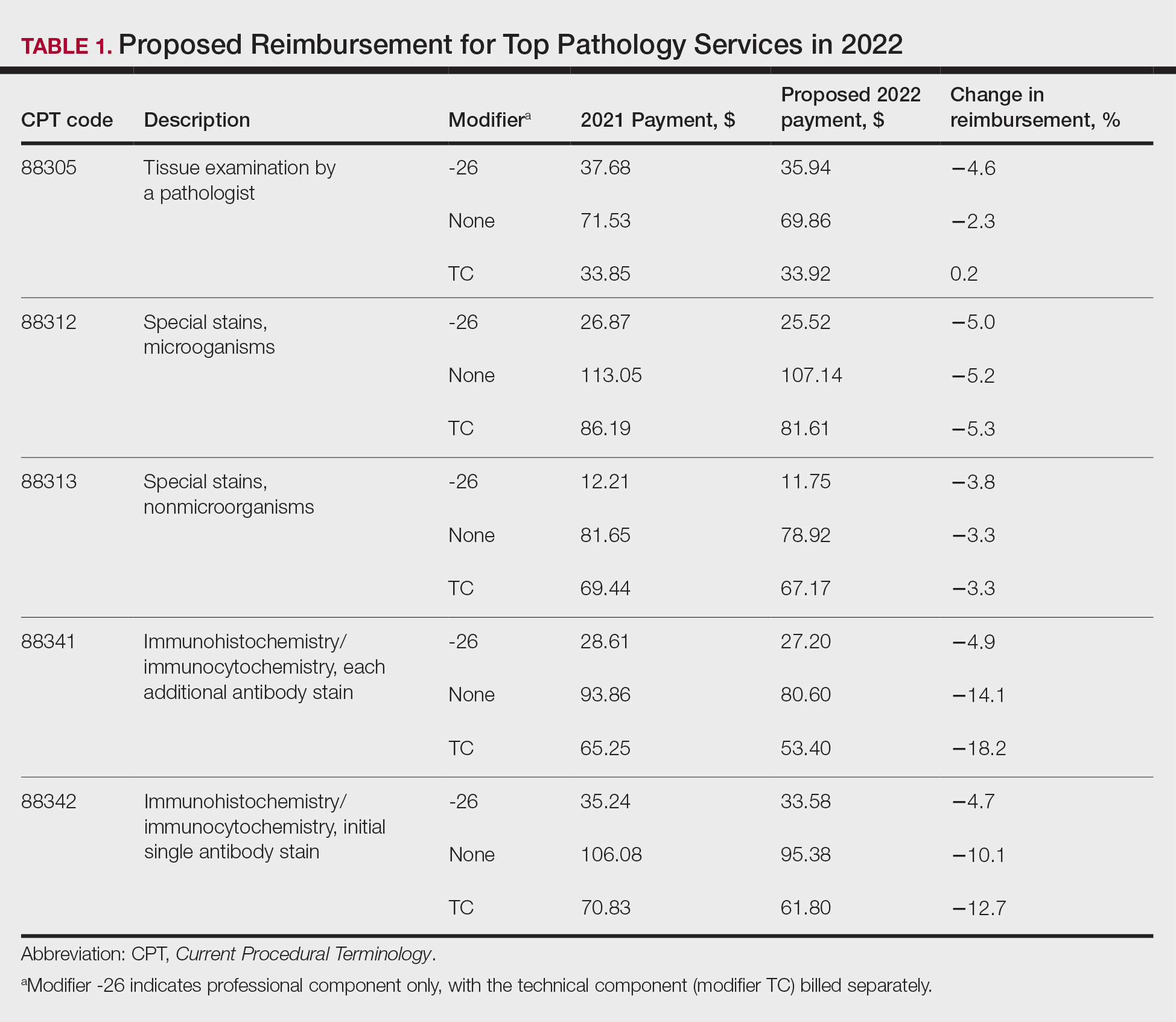
Based on dermatopathology utilization data, the overall impact on reimbursement for 2022 represents an approximately 5% decrease from 2021 dermatopathology payments (Table 1).1,4 This represents a 3.75% cut from revaluation of E/M services, and a 1% cut due to changes in practice expense pricing. The estimated change in reimbursement for independent laboratories is a 6% decrease. Advocacy groups have been working to mitigate the 2022 cuts by engaging with Congress and urging them to act before these changes go into effect next year. Keep in mind that approximately half of all pathology Current Procedural Terminology (CPT) codes have been targeted for evaluation by the CMS since 2006.1,4
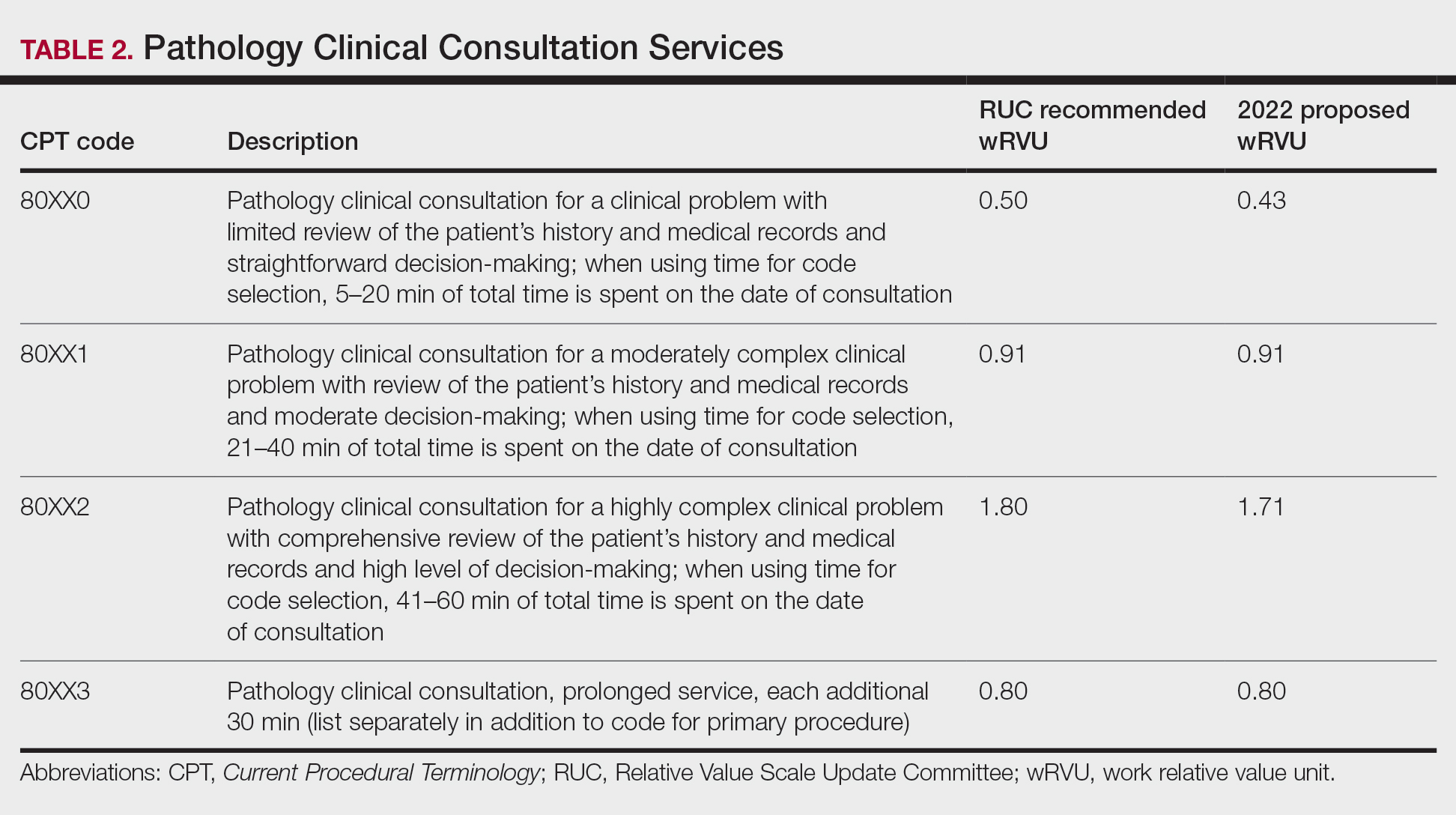
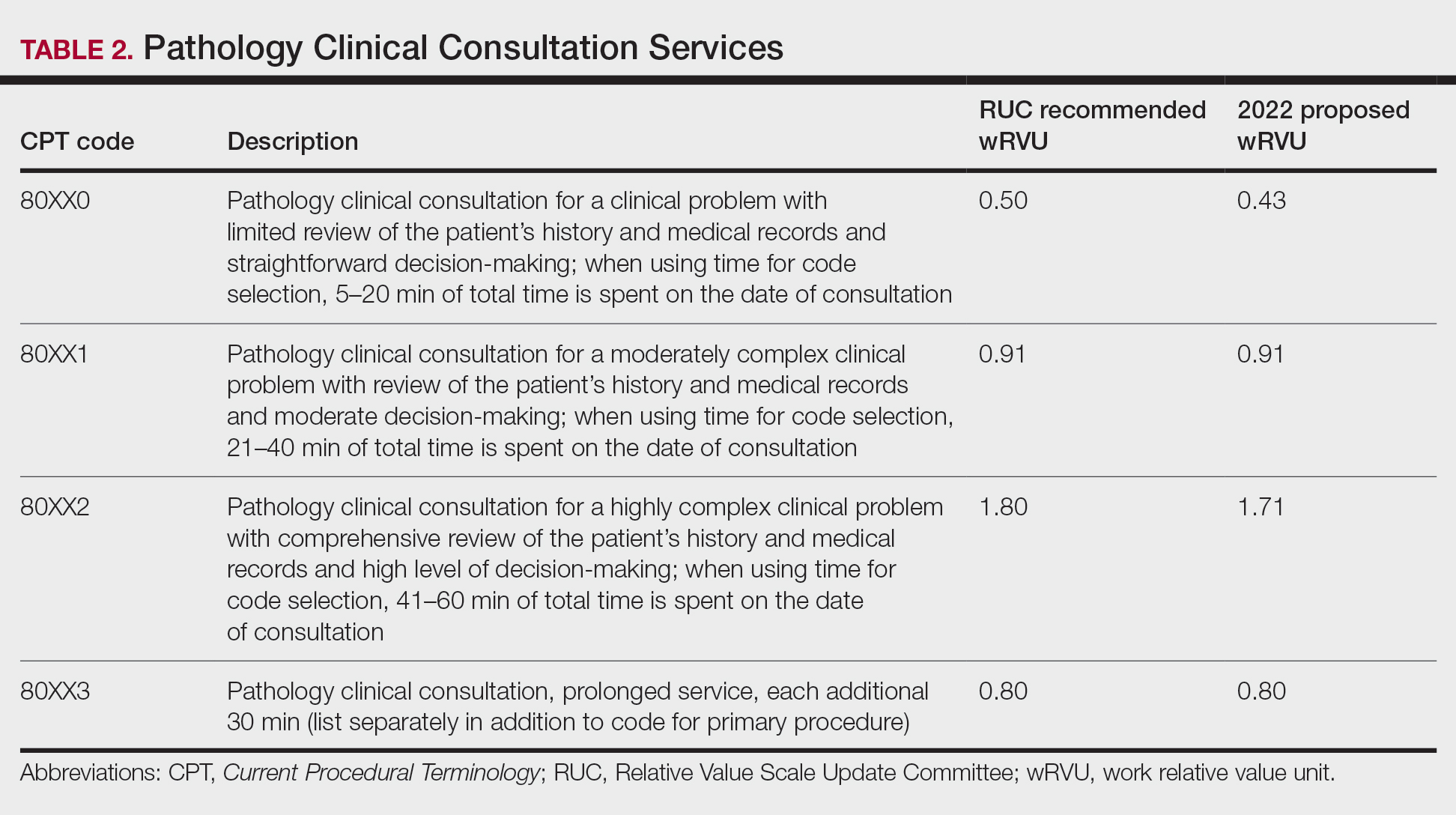
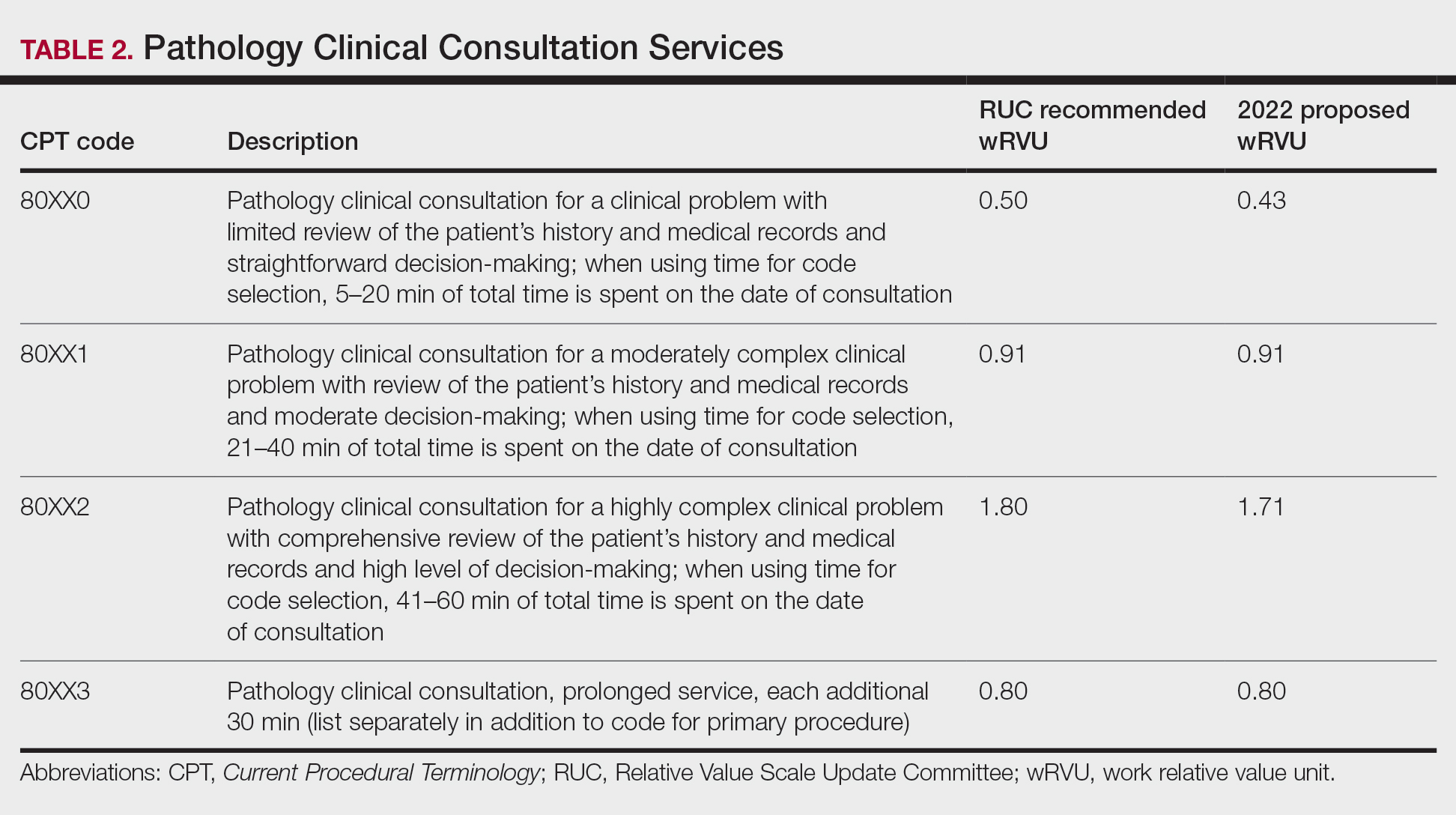
The current clinical pathology consultation services (CPT codes 80500 and 80502) previously were identified as potentially misvalued for review by the AMA Relative Value Scale Update Committee’s (RUC’s) relativity assessment workgroup.4 Consequently, the CAP worked with the AMA’s CPT Editorial Panel to delete codes 80500 and 80502, as well as to modernize and create the 4 new clinical pathology consultation codes: 80XX0, 80XX1, 80XX2, and 80XX3. Then the CAP worked with the RUC to develop physician work and practice expense values for the new clinical pathology consultation codes. Once the fee schedule is finalized, pathologists can begin using the new codes to bill these services in 2022 (Table 2).4
According to CPT, clinical pathology consultation services may be reported when the following criteria have been met: (1) the pathologist renders a clinical pathology consultation at the request of a physician or qualified health care professional at the same or another institution; (2) the pathology clinical consultation request relating to pathology and laboratory findings or other relevant clinical or diagnostic information requiring additional medical interpretative judgment is made; and (3) these codes are not reported in conjunction with codes 88321, 88323, and 88325.4
Proposed 2022 Medicare QPP Requirements
On July 13, 2021, the CMS also published its proposed 2022 QPP proposals that will take effect next year.4 According to the proposed regulation, nearly all dermatopathologists will be required to participate in Medicare’s QPP, either through advanced alternative payment models (APMs) or the Merit-based Incentive Payment System (MIPS). The CAP has long advocated for reducing MIPS reporting burdens for dermatopathologists. In this regulation, the CMS is proposing key program changes that move the program forward but also introduce additional complexities; for example, the CMS will move forward with a new participation pathway called MIPS Value Pathways (MVPs). The CMS proposed 7 specific MVPs that align with certain clinical topics; however, it will not implement these MVPs until the 2023 MIPS performance period.
In 2022, dermatopathologists who are eligible for MIPS will have to take action to avoid penalties that reduce future Medicare Part B payments for their services. Performance in MIPS in 2022 affects Medicare Part B payments in 2024 by an increase of 9% to a decrease of 9%.
In its proposed 2022 QPP regulations, the CMS proposed an increase of the performance threshold from 60 MIPS points to 75 MIPS points. It also proposed an increase of the exceptional Performance Threshold from 85 MIPS points to 89 MIPS points.
The CMS also proposed notable scoring changes for quality measures, including removing the 3-point floor for measures that can be scored against a benchmark. These measures would receive 1 to 10 points. Measures without a benchmark or that do not meet case requirements would earn 0 points, with an exception for small practices. The CMS also proposed removing bonus points for reporting additional outcomes and high-priority measures beyond the 1 that is required, as well as establishing a 5-point floor for the first 2 performance periods for new measures, which is in line with the CAP’s advocacy.
The Pathology Specialty Measure Set will remain the same as the 2021 set containing 6 quality measures, including the AADA-stewarded quality measure #440 (skin cancer: biopsy reporting time—pathologist to clinician). Although the CAP recognizes the importance of prompt turnaround of biopsy reports, it also is working with the CMS and the AADA to mitigate the operational challenges dermatopathologists encounter when using this measure.
Due to advocacy from the CAP, the CMS included a CAP-proposed improvement activity on implementation of a laboratory preparedness plan to support continued or expanded patient care during the COVID-19 pandemic or another public health emergency. This plan should address how the laboratory would maintain or expand access to improve beneficiary health outcomes and reduce health care disparities.
The CAP has actively worked with the CMS to demonstrate the need for more appropriate and alternative measures and improvement activities so that pathologists can more fully participate in MIPS.
Alternative Payment Models—For those dermatopathologists who practice in an APM, the proposed 2022 QPP makes minimal changes to the advanced APM track while adding transition time for accountable care organizations in the Medicare Shared Savings Program to report on certain quality measures and increasing flexibility related to the program’s quality performance standard.
Cures Act 2021: To Do No Harm
The 21st Century Cures Act (Cures Act) was signed into federal law in 2016. The Office of the National Coordinator for Health Information Technology (ONC) laid the groundwork for patients to have easier access to and control of their health information.5 The ONC’s final rule, which went into effect on April 5, 2021, requires that all providers make their office notes, laboratory results, and other diagnostic reports (including dermatopathology reports) available to patients as soon as the physician’s office receives an electronic copy. Penalty for noncompliance has not been determined.
There are information-blocking exceptions, but delaying access to a patient’s report so that a provider can review the result before the patient receives it is not considered an exception.6 The exceptions are situational and must be evaluated by the referring clinician or their employer. Documentation of the exception is critical. The specific facts and circumstances associated with your decision to use an exception will be important to include in your documentation. Information blocking necessary to prevent “harm” to a patient or another person requires a reasonable belief that the practice will substantially reduce the risk of harm.6
The AMA passed a resolution in June 2021 calling for changes to this rule to allow for a delay of pathology results, advocating to the Office for Civil Rights to revise the harm exception to include psychological distress.6 In August 2021, the AADA met with senior officials at the ONC also asking to revise its definition of harm, sharing examples of emotional strain that resulted from receiving results without clinical context.7 California enacted a law requiring a delay before a patient receives the result of a malignant diagnosis, giving the clinician time to contact the patient before they see their report.8
The Cures Act requirements are about patients accessing their health care information. Always consider what is best for the patient and ensure that your policies and procedures reflect this.5
Final Thoughts
It is important to learn and support advocacy priorities and efforts and to join forces to protect your practice. Physician advocacy is no longer an elective pursuit. We need to be involved and engaged through our medical societies to help patients, communities, and ourselves.
- Centers for Medicare & Medicaid Services. Calendar Year (CY) 2022 Medicare Physician Fee Schedule Proposed Rule. Published July 13, 2021. Accessed October 22, 2021. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2022-medicare-physician-fee-schedule-proposed-rule
- Healthcare spending and the Medicare program. Medicare Payment Advisory Commission; July 2020. Accessed October 25, 2021.http://www.medpac.gov/docs/default-source/data-book/july2020_databook_entirereport_sec.pdf
- Frieden J. 2021 Medicare fee schedule includes 10.2% cut in conversion factor. MedPage Today website. Published December 2, 2020. Accessed October 22, 2021. https://www.medpagetoday.com/practicemanagement/reimbursement/89970
- Advocacy. College of American Pathologists website. Accessed October 13, 2021. https://www.cap.org/advocacy
- ONC’s Cures Act Final Rule. The Office of the National Coordinator for Health Information Technology website. Accessed October 13, 2021. https://www.healthit.gov/curesrule/
- Nelson H. Delegates call AMA to advocate for provider info-blocking flexibility. Published June 18, 2021. Accessed October 13, 2021. https://ehrintelligence.com/news/delegates-call-ama-to-advocate-for-provider-info-blocking-flexibility
- Rosamilia LL. Immediate Pathology report release to patients—is the 21st Century Cures Act worse than the disease? American Academy of Dermatology website. Published August 25, 2021. Accessed October 22, 2021. https://www.aad.org/dw/dw-insights-and-inquiries/archive/2021/cures-act-immediate-pathology-report-release-to-patients
- Purington K, Alfreds ST, Pritts J, et al; The National Academy for State Health Policy. Electronic release of clinical laboratory results: a review of state and federal policy. Published January 2010. Accessed October 13, 2021. https://www.nashp.org/wp-content/uploads/2010/02/ElectronicLabResultsExchangePolicy.pdf
The proposed 2022 Medicare physician fee schedule and quality payment program (QPP) regulations were released on July 13, 2021.1 Final regulations are expected to be released on or around November 1, 2021, but they may be delayed. Multiple national medical organizations, including the College of American Pathologists (CAP), the American Society of Dermatopathology, the American Academy of Dermatology Association (AADA), and the American Medical Association (AMA) Physicians’ Grassroots Network all work together to engage with the Centers for Medicare & Medicaid Services (CMS) to influence these regulations. Stated advocacy priorities include protecting the value of dermatopathology services, mobilizing dermatopathologists for political action, ensuring dermatopathologists can participate in new payment models, strengthening the profession with advocacy on a state level, and conducting socioeconomic research. Is your practice aware and prepared to handle the changes coming in 2022?
The recent revisions and revaluations of the outpatient evaluation and management (E/M) codes2 resulted in a considerable redistribution of Medicare dollars in 2021, negatively impacting dermatopathologists and other specialties and services due to budget neutrality required by law (Figure). Important steps were taken to mitigate the 2021 Medicare cuts for all non–office-based dermatopathology services (eg, pathology, surgical services, emergency department).1,3 Direct engagement by the CAP, American Society of Dermatopathology, and AADA, along with the AMA Physicians’ Grassroots Network resulted in legislative action on December 27, 2020, which directed Medicare to make a 3.75% positive adjustment to the 2021 physician payments. Additionally, the CMS updated the 2021 physician conversion factor to $34.8931, a 3.3% reduction from the 2020 conversion factor rather than $32.41, or a 10.20% decrease. The 2% payment adjustment (sequestration) through December 21, 2021, also was suspended, and Congress and the Biden administration mandated delayed implementation of the inherent complexity add-on code for E/M services (G2211) until 2024.1,3
Threat of Medicare Cuts in 2022
Based on dermatopathology utilization data, the overall impact on reimbursement for 2022 represents an approximately 5% decrease from 2021 dermatopathology payments (Table 1).1,4 This represents a 3.75% cut from revaluation of E/M services, and a 1% cut due to changes in practice expense pricing. The estimated change in reimbursement for independent laboratories is a 6% decrease. Advocacy groups have been working to mitigate the 2022 cuts by engaging with Congress and urging them to act before these changes go into effect next year. Keep in mind that approximately half of all pathology Current Procedural Terminology (CPT) codes have been targeted for evaluation by the CMS since 2006.1,4
The current clinical pathology consultation services (CPT codes 80500 and 80502) previously were identified as potentially misvalued for review by the AMA Relative Value Scale Update Committee’s (RUC’s) relativity assessment workgroup.4 Consequently, the CAP worked with the AMA’s CPT Editorial Panel to delete codes 80500 and 80502, as well as to modernize and create the 4 new clinical pathology consultation codes: 80XX0, 80XX1, 80XX2, and 80XX3. Then the CAP worked with the RUC to develop physician work and practice expense values for the new clinical pathology consultation codes. Once the fee schedule is finalized, pathologists can begin using the new codes to bill these services in 2022 (Table 2).4
According to CPT, clinical pathology consultation services may be reported when the following criteria have been met: (1) the pathologist renders a clinical pathology consultation at the request of a physician or qualified health care professional at the same or another institution; (2) the pathology clinical consultation request relating to pathology and laboratory findings or other relevant clinical or diagnostic information requiring additional medical interpretative judgment is made; and (3) these codes are not reported in conjunction with codes 88321, 88323, and 88325.4
Proposed 2022 Medicare QPP Requirements
On July 13, 2021, the CMS also published its proposed 2022 QPP proposals that will take effect next year.4 According to the proposed regulation, nearly all dermatopathologists will be required to participate in Medicare’s QPP, either through advanced alternative payment models (APMs) or the Merit-based Incentive Payment System (MIPS). The CAP has long advocated for reducing MIPS reporting burdens for dermatopathologists. In this regulation, the CMS is proposing key program changes that move the program forward but also introduce additional complexities; for example, the CMS will move forward with a new participation pathway called MIPS Value Pathways (MVPs). The CMS proposed 7 specific MVPs that align with certain clinical topics; however, it will not implement these MVPs until the 2023 MIPS performance period.
In 2022, dermatopathologists who are eligible for MIPS will have to take action to avoid penalties that reduce future Medicare Part B payments for their services. Performance in MIPS in 2022 affects Medicare Part B payments in 2024 by an increase of 9% to a decrease of 9%.
In its proposed 2022 QPP regulations, the CMS proposed an increase of the performance threshold from 60 MIPS points to 75 MIPS points. It also proposed an increase of the exceptional Performance Threshold from 85 MIPS points to 89 MIPS points.
The CMS also proposed notable scoring changes for quality measures, including removing the 3-point floor for measures that can be scored against a benchmark. These measures would receive 1 to 10 points. Measures without a benchmark or that do not meet case requirements would earn 0 points, with an exception for small practices. The CMS also proposed removing bonus points for reporting additional outcomes and high-priority measures beyond the 1 that is required, as well as establishing a 5-point floor for the first 2 performance periods for new measures, which is in line with the CAP’s advocacy.
The Pathology Specialty Measure Set will remain the same as the 2021 set containing 6 quality measures, including the AADA-stewarded quality measure #440 (skin cancer: biopsy reporting time—pathologist to clinician). Although the CAP recognizes the importance of prompt turnaround of biopsy reports, it also is working with the CMS and the AADA to mitigate the operational challenges dermatopathologists encounter when using this measure.
Due to advocacy from the CAP, the CMS included a CAP-proposed improvement activity on implementation of a laboratory preparedness plan to support continued or expanded patient care during the COVID-19 pandemic or another public health emergency. This plan should address how the laboratory would maintain or expand access to improve beneficiary health outcomes and reduce health care disparities.
The CAP has actively worked with the CMS to demonstrate the need for more appropriate and alternative measures and improvement activities so that pathologists can more fully participate in MIPS.
Alternative Payment Models—For those dermatopathologists who practice in an APM, the proposed 2022 QPP makes minimal changes to the advanced APM track while adding transition time for accountable care organizations in the Medicare Shared Savings Program to report on certain quality measures and increasing flexibility related to the program’s quality performance standard.
Cures Act 2021: To Do No Harm
The 21st Century Cures Act (Cures Act) was signed into federal law in 2016. The Office of the National Coordinator for Health Information Technology (ONC) laid the groundwork for patients to have easier access to and control of their health information.5 The ONC’s final rule, which went into effect on April 5, 2021, requires that all providers make their office notes, laboratory results, and other diagnostic reports (including dermatopathology reports) available to patients as soon as the physician’s office receives an electronic copy. Penalty for noncompliance has not been determined.
There are information-blocking exceptions, but delaying access to a patient’s report so that a provider can review the result before the patient receives it is not considered an exception.6 The exceptions are situational and must be evaluated by the referring clinician or their employer. Documentation of the exception is critical. The specific facts and circumstances associated with your decision to use an exception will be important to include in your documentation. Information blocking necessary to prevent “harm” to a patient or another person requires a reasonable belief that the practice will substantially reduce the risk of harm.6
The AMA passed a resolution in June 2021 calling for changes to this rule to allow for a delay of pathology results, advocating to the Office for Civil Rights to revise the harm exception to include psychological distress.6 In August 2021, the AADA met with senior officials at the ONC also asking to revise its definition of harm, sharing examples of emotional strain that resulted from receiving results without clinical context.7 California enacted a law requiring a delay before a patient receives the result of a malignant diagnosis, giving the clinician time to contact the patient before they see their report.8
The Cures Act requirements are about patients accessing their health care information. Always consider what is best for the patient and ensure that your policies and procedures reflect this.5
Final Thoughts
It is important to learn and support advocacy priorities and efforts and to join forces to protect your practice. Physician advocacy is no longer an elective pursuit. We need to be involved and engaged through our medical societies to help patients, communities, and ourselves.
The proposed 2022 Medicare physician fee schedule and quality payment program (QPP) regulations were released on July 13, 2021.1 Final regulations are expected to be released on or around November 1, 2021, but they may be delayed. Multiple national medical organizations, including the College of American Pathologists (CAP), the American Society of Dermatopathology, the American Academy of Dermatology Association (AADA), and the American Medical Association (AMA) Physicians’ Grassroots Network all work together to engage with the Centers for Medicare & Medicaid Services (CMS) to influence these regulations. Stated advocacy priorities include protecting the value of dermatopathology services, mobilizing dermatopathologists for political action, ensuring dermatopathologists can participate in new payment models, strengthening the profession with advocacy on a state level, and conducting socioeconomic research. Is your practice aware and prepared to handle the changes coming in 2022?
The recent revisions and revaluations of the outpatient evaluation and management (E/M) codes2 resulted in a considerable redistribution of Medicare dollars in 2021, negatively impacting dermatopathologists and other specialties and services due to budget neutrality required by law (Figure). Important steps were taken to mitigate the 2021 Medicare cuts for all non–office-based dermatopathology services (eg, pathology, surgical services, emergency department).1,3 Direct engagement by the CAP, American Society of Dermatopathology, and AADA, along with the AMA Physicians’ Grassroots Network resulted in legislative action on December 27, 2020, which directed Medicare to make a 3.75% positive adjustment to the 2021 physician payments. Additionally, the CMS updated the 2021 physician conversion factor to $34.8931, a 3.3% reduction from the 2020 conversion factor rather than $32.41, or a 10.20% decrease. The 2% payment adjustment (sequestration) through December 21, 2021, also was suspended, and Congress and the Biden administration mandated delayed implementation of the inherent complexity add-on code for E/M services (G2211) until 2024.1,3
Threat of Medicare Cuts in 2022
Based on dermatopathology utilization data, the overall impact on reimbursement for 2022 represents an approximately 5% decrease from 2021 dermatopathology payments (Table 1).1,4 This represents a 3.75% cut from revaluation of E/M services, and a 1% cut due to changes in practice expense pricing. The estimated change in reimbursement for independent laboratories is a 6% decrease. Advocacy groups have been working to mitigate the 2022 cuts by engaging with Congress and urging them to act before these changes go into effect next year. Keep in mind that approximately half of all pathology Current Procedural Terminology (CPT) codes have been targeted for evaluation by the CMS since 2006.1,4
The current clinical pathology consultation services (CPT codes 80500 and 80502) previously were identified as potentially misvalued for review by the AMA Relative Value Scale Update Committee’s (RUC’s) relativity assessment workgroup.4 Consequently, the CAP worked with the AMA’s CPT Editorial Panel to delete codes 80500 and 80502, as well as to modernize and create the 4 new clinical pathology consultation codes: 80XX0, 80XX1, 80XX2, and 80XX3. Then the CAP worked with the RUC to develop physician work and practice expense values for the new clinical pathology consultation codes. Once the fee schedule is finalized, pathologists can begin using the new codes to bill these services in 2022 (Table 2).4
According to CPT, clinical pathology consultation services may be reported when the following criteria have been met: (1) the pathologist renders a clinical pathology consultation at the request of a physician or qualified health care professional at the same or another institution; (2) the pathology clinical consultation request relating to pathology and laboratory findings or other relevant clinical or diagnostic information requiring additional medical interpretative judgment is made; and (3) these codes are not reported in conjunction with codes 88321, 88323, and 88325.4
Proposed 2022 Medicare QPP Requirements
On July 13, 2021, the CMS also published its proposed 2022 QPP proposals that will take effect next year.4 According to the proposed regulation, nearly all dermatopathologists will be required to participate in Medicare’s QPP, either through advanced alternative payment models (APMs) or the Merit-based Incentive Payment System (MIPS). The CAP has long advocated for reducing MIPS reporting burdens for dermatopathologists. In this regulation, the CMS is proposing key program changes that move the program forward but also introduce additional complexities; for example, the CMS will move forward with a new participation pathway called MIPS Value Pathways (MVPs). The CMS proposed 7 specific MVPs that align with certain clinical topics; however, it will not implement these MVPs until the 2023 MIPS performance period.
In 2022, dermatopathologists who are eligible for MIPS will have to take action to avoid penalties that reduce future Medicare Part B payments for their services. Performance in MIPS in 2022 affects Medicare Part B payments in 2024 by an increase of 9% to a decrease of 9%.
In its proposed 2022 QPP regulations, the CMS proposed an increase of the performance threshold from 60 MIPS points to 75 MIPS points. It also proposed an increase of the exceptional Performance Threshold from 85 MIPS points to 89 MIPS points.
The CMS also proposed notable scoring changes for quality measures, including removing the 3-point floor for measures that can be scored against a benchmark. These measures would receive 1 to 10 points. Measures without a benchmark or that do not meet case requirements would earn 0 points, with an exception for small practices. The CMS also proposed removing bonus points for reporting additional outcomes and high-priority measures beyond the 1 that is required, as well as establishing a 5-point floor for the first 2 performance periods for new measures, which is in line with the CAP’s advocacy.
The Pathology Specialty Measure Set will remain the same as the 2021 set containing 6 quality measures, including the AADA-stewarded quality measure #440 (skin cancer: biopsy reporting time—pathologist to clinician). Although the CAP recognizes the importance of prompt turnaround of biopsy reports, it also is working with the CMS and the AADA to mitigate the operational challenges dermatopathologists encounter when using this measure.
Due to advocacy from the CAP, the CMS included a CAP-proposed improvement activity on implementation of a laboratory preparedness plan to support continued or expanded patient care during the COVID-19 pandemic or another public health emergency. This plan should address how the laboratory would maintain or expand access to improve beneficiary health outcomes and reduce health care disparities.
The CAP has actively worked with the CMS to demonstrate the need for more appropriate and alternative measures and improvement activities so that pathologists can more fully participate in MIPS.
Alternative Payment Models—For those dermatopathologists who practice in an APM, the proposed 2022 QPP makes minimal changes to the advanced APM track while adding transition time for accountable care organizations in the Medicare Shared Savings Program to report on certain quality measures and increasing flexibility related to the program’s quality performance standard.
Cures Act 2021: To Do No Harm
The 21st Century Cures Act (Cures Act) was signed into federal law in 2016. The Office of the National Coordinator for Health Information Technology (ONC) laid the groundwork for patients to have easier access to and control of their health information.5 The ONC’s final rule, which went into effect on April 5, 2021, requires that all providers make their office notes, laboratory results, and other diagnostic reports (including dermatopathology reports) available to patients as soon as the physician’s office receives an electronic copy. Penalty for noncompliance has not been determined.
There are information-blocking exceptions, but delaying access to a patient’s report so that a provider can review the result before the patient receives it is not considered an exception.6 The exceptions are situational and must be evaluated by the referring clinician or their employer. Documentation of the exception is critical. The specific facts and circumstances associated with your decision to use an exception will be important to include in your documentation. Information blocking necessary to prevent “harm” to a patient or another person requires a reasonable belief that the practice will substantially reduce the risk of harm.6
The AMA passed a resolution in June 2021 calling for changes to this rule to allow for a delay of pathology results, advocating to the Office for Civil Rights to revise the harm exception to include psychological distress.6 In August 2021, the AADA met with senior officials at the ONC also asking to revise its definition of harm, sharing examples of emotional strain that resulted from receiving results without clinical context.7 California enacted a law requiring a delay before a patient receives the result of a malignant diagnosis, giving the clinician time to contact the patient before they see their report.8
The Cures Act requirements are about patients accessing their health care information. Always consider what is best for the patient and ensure that your policies and procedures reflect this.5
Final Thoughts
It is important to learn and support advocacy priorities and efforts and to join forces to protect your practice. Physician advocacy is no longer an elective pursuit. We need to be involved and engaged through our medical societies to help patients, communities, and ourselves.
- Centers for Medicare & Medicaid Services. Calendar Year (CY) 2022 Medicare Physician Fee Schedule Proposed Rule. Published July 13, 2021. Accessed October 22, 2021. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2022-medicare-physician-fee-schedule-proposed-rule
- Healthcare spending and the Medicare program. Medicare Payment Advisory Commission; July 2020. Accessed October 25, 2021.http://www.medpac.gov/docs/default-source/data-book/july2020_databook_entirereport_sec.pdf
- Frieden J. 2021 Medicare fee schedule includes 10.2% cut in conversion factor. MedPage Today website. Published December 2, 2020. Accessed October 22, 2021. https://www.medpagetoday.com/practicemanagement/reimbursement/89970
- Advocacy. College of American Pathologists website. Accessed October 13, 2021. https://www.cap.org/advocacy
- ONC’s Cures Act Final Rule. The Office of the National Coordinator for Health Information Technology website. Accessed October 13, 2021. https://www.healthit.gov/curesrule/
- Nelson H. Delegates call AMA to advocate for provider info-blocking flexibility. Published June 18, 2021. Accessed October 13, 2021. https://ehrintelligence.com/news/delegates-call-ama-to-advocate-for-provider-info-blocking-flexibility
- Rosamilia LL. Immediate Pathology report release to patients—is the 21st Century Cures Act worse than the disease? American Academy of Dermatology website. Published August 25, 2021. Accessed October 22, 2021. https://www.aad.org/dw/dw-insights-and-inquiries/archive/2021/cures-act-immediate-pathology-report-release-to-patients
- Purington K, Alfreds ST, Pritts J, et al; The National Academy for State Health Policy. Electronic release of clinical laboratory results: a review of state and federal policy. Published January 2010. Accessed October 13, 2021. https://www.nashp.org/wp-content/uploads/2010/02/ElectronicLabResultsExchangePolicy.pdf
- Centers for Medicare & Medicaid Services. Calendar Year (CY) 2022 Medicare Physician Fee Schedule Proposed Rule. Published July 13, 2021. Accessed October 22, 2021. https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2022-medicare-physician-fee-schedule-proposed-rule
- Healthcare spending and the Medicare program. Medicare Payment Advisory Commission; July 2020. Accessed October 25, 2021.http://www.medpac.gov/docs/default-source/data-book/july2020_databook_entirereport_sec.pdf
- Frieden J. 2021 Medicare fee schedule includes 10.2% cut in conversion factor. MedPage Today website. Published December 2, 2020. Accessed October 22, 2021. https://www.medpagetoday.com/practicemanagement/reimbursement/89970
- Advocacy. College of American Pathologists website. Accessed October 13, 2021. https://www.cap.org/advocacy
- ONC’s Cures Act Final Rule. The Office of the National Coordinator for Health Information Technology website. Accessed October 13, 2021. https://www.healthit.gov/curesrule/
- Nelson H. Delegates call AMA to advocate for provider info-blocking flexibility. Published June 18, 2021. Accessed October 13, 2021. https://ehrintelligence.com/news/delegates-call-ama-to-advocate-for-provider-info-blocking-flexibility
- Rosamilia LL. Immediate Pathology report release to patients—is the 21st Century Cures Act worse than the disease? American Academy of Dermatology website. Published August 25, 2021. Accessed October 22, 2021. https://www.aad.org/dw/dw-insights-and-inquiries/archive/2021/cures-act-immediate-pathology-report-release-to-patients
- Purington K, Alfreds ST, Pritts J, et al; The National Academy for State Health Policy. Electronic release of clinical laboratory results: a review of state and federal policy. Published January 2010. Accessed October 13, 2021. https://www.nashp.org/wp-content/uploads/2010/02/ElectronicLabResultsExchangePolicy.pdf
Practice Points
- A proposed 2022 fee schedule negatively impacting dermatopathology practices has been published by the Centers for Medicare & Medicaid Services (CMS) in July 2021.
- New pathology consultation codes with new payment rates proposed by CMS can be used starting January 1, 2022.
- The 21st Century Cures Act Final Rule has information blocking provisions.
Modifier -25 and the New 2021 E/M Codes: Documentation of Separate and Distinct Just Got Easier
Insurers Target Modifier -25
Modifier -25 allows reporting of both a minor procedure (ie, one with a 0- or 10-day global period) and a separate and distinct evaluation and management (E/M) service on the same date of service.1 Because of the multicomplaint nature of dermatology, the ability to report a same-day procedure and an E/M service is critical for efficient, cost-effective, and patient-centered dermatologic care. However, it is well known that the use of modifier -25 has been under notable insurer scrutiny and is a common reason for medical record audits.2,3 Some insurers have responded to increased utilization of modifier -25 by cutting reimbursement for claims that include both a procedure and an E/M service or by denying one of the services altogether.4-6 The Centers for Medicare and Medicaid Services also have expressed concern about this coding combination with proposed cuts to reimbursement.7 Moreover, the Office of Inspector General has announced a work plan to investigate the frequent utilization of E/M codes and minor procedures by dermatologists.8 Clearly, modifier -25 is a continued target by insurers and regulators; therefore, dermatologists will want to make sure their coding and documentation meet all requirements and are updated for the new E/M codes for 2021.
The American Medical Association’s Current Procedural Terminology indicates that modifier -25 allows reporting of a “significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of a procedure or other service.”1 Given that dermatology patients typically present with multiple concerns, dermatologists commonly evaluate and treat numerous conditions during one visit. Understanding what constitutes a separately identifiable E/M service is critical to bill accurately and to pass insurer audits.
Global Surgical Package
To appropriately bill both a procedure and an E/M service, the physician must indicate that the patient’s condition required an E/M service above and beyond the usual work of the procedure. The compilation of evaluation and work included in the payment for a procedure is called the global surgical package.9 In general, the global surgical package includes local or topical anesthesia; the surgical service/procedure itself; immediate postoperative care, including dictating the operative note; meeting/discussing the patient’s procedure with family and other physicians; and writing orders for the patient. For minor procedures (ie, those with either 0- or 10-day global periods), the surgical package also includes same-day E/M services associated with the decision to perform surgery. An appropriate history and physical examination as well as a discussion of the differential diagnosis, treatment options, and risk and benefits of treatment are all included in the payment of a minor procedure itself. Therefore, an evaluation to discuss a patient’s condition or change in condition, alternatives to treatment, or next steps after a diagnosis related to a treatment or diagnostic procedure should not be separately reported. Moreover, the fact that the patient is new to the physician is not in itself sufficient to allow reporting of an E/M service with these minor procedures. For major procedures (ie, those with 90-day postoperative periods), the decision for surgery is excluded from the global surgical package.
2021 E/M Codes Simplify Documentation
The biggest coding change of 2021 was the new E/M codes.10 Prior to this year, the descriptors of E/M services recognized 7 components to define the levels of E/M services11: history and nature of the presenting problem; physical examination; medical decision-making (MDM); counseling; coordination of care; and time. Furthermore, history, physical examination, and MDM were all broken down into more granular elements that were summed to determine the level for each component; for example, the history of the presenting problem was defined as a chronological description of the development of the patient’s present illness, including the following elements: location, quality, severity, duration, timing, context, modifying factors, and associated signs and symptoms. Each of these categories would constitute bullet points to be summed to determine the level of history. Physical examination and MDM bullet points also would be summed to determine a proper coding level.11 Understandably, this coding scheme was complicated and burdensome to medical providers.
The redefinition of the E/M codes for 2021 substantially simplified the determination of coding level and documentation.10 The revisions to the E/M office visit code descriptors and documentation standards are now centered around how physicians think and take care of patients and not on mandatory standards and checking boxes. The main changes involve MDM as the prime determinant of the coding level. Elements of MDM affecting coding for an outpatient or office visit now include only 3 components: the number and complexity of problems addressed in the encounter, the amount or complexity of data to be reviewed and analyzed, and the risk of complications or morbidity of patient management. Gone are the requirements from the earlier criteria requiring so many bullet points for the history, physical examination, and MDM.
Dermatologists may ask, “How does the new E/M coding structure affect reporting and documenting an E/M and a procedure on the same day?” The answer is that the determination of separate and distinct is basically unchanged with the new E/M codes; however, the documentation requirements for modifier -25 using the new E/M codes are simplified.
As always, the key to determining whether a separate and distinct E/M service was provided and subsequently documented is to deconstruct the medical note. All evaluation services associated with the procedure—making a clinical diagnosis or differential diagnosis, decision to perform surgery, and discussion of alternative treatments—should be removed from one’s documentation as shown in the example below. If a complete E/M service still exists, then an E/M may be billed in addition to the procedure. Physical examination of the treatment area is included in the surgical package. With the prior E/M criteria, physical examination of the procedural area could not be used again as a bullet point to count for the E/M level. However, with the new 2021 coding requirements, the documentation of a separate MDM will be sufficient to meet criteria because documentation of physical examination is not a requirement.
Modifier -25 Examples
Let’s examine a typical dermatologist medical note. An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. The patient also complains of a growing tender lesion on the left elbow of 2 months’ duration. Physical examination reveals a linear vesicular eruption on the left wrist and a tender hyperkeratotic papule on the left elbow. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed. The decision is made to perform a tangential biopsy of the lesion on the left elbow because of the suspicion for malignancy. The biopsy is performed the same day.
This case clearly illustrates performance of an E/M service in the treatment of rhus dermatitis, which is separate and distinct from the biopsy procedure; however, in evaluating whether the case meets the documentation requirements for modifier -25, the information in the medical note inclusive to the procedure’s global surgical package, including history associated with establishing the diagnosis, physical examination of the procedure area(s), and discussion of treatment options, is eliminated, leaving the following notes: An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed.
Because the physical examination of the body part (left arm) is included in the procedure’s global surgical package, the examination of the left wrist cannot be used as coding support for the E/M service. This makes a difference for coding level in the prior E/M coding requirements, which required examination bullet points. However, with the 2021 E/M codes, documentation of physical examination bullet points is irrelevant to the coding level. Therefore, qualifying for a modifier -25 claim is more straightforward in this case with the new code set. Because bullet points are not integral to the 2021 E/M codes, qualifying and properly documenting for a higher level of service will likely be more common in dermatology.
Final Thoughts
Frequent use of modifier -25 is a critical part of a high-quality and cost-effective dermatology practice. Same-day performance of minor procedures and E/M services allows for more rapid and efficient diagnosis and treatment of various conditions as well as minimizing unnecessary office visits. The new E/M codes for 2021 actually make the documentation of a separate and distinct E/M service less complicated because the bullet point requirements associated with the old E/M codes have been eliminated. Understanding how the new E/M code descriptors affect modifier -25 reporting and clear documentation of separate, distinct, and medically necessary E/M services will be needed due to increased insurer scrutiny and audits.
- Current Procedural Terminology 2021, Professional Edition. American Medical Association; 2020.
- Rogers HW. Modifier −25 victory, but the battle is not over. Cutis. 2018;101:409-410.
- Rogers HW. One diagnosis and modifier −25: appropriate or audit target? Cutis. 2017;99:165-166.
- Update regarding E/M with modifier −25—professional. Anthem Blue Cross Blue Shield website. Published February 1, 2019. Accessed August 17, 2021. https://providernews.anthem.com/ohio/article/update-regarding-em-with-modifier-25-professional
- Payment policies—surgery. Harvard Pilgrim Health Care website. Updated May 2021. Accessed August 17, 2021. https://www.harvardpilgrim.org/provider/wp-content/uploads/sites/7/2020/07/H-6-Surgery-PM.pdf
- Modifier 25: frequently asked questions. Independence Blue Cross website. Updated September 25, 2017. Accessed August 17, 2021. https://provcomm.ibx.com/ibc/archive/pages/A86603B03881756B8525817E00768006.aspx
- Huang G. CMS 2019 fee schedule takes modifier 25 cuts, runs with them. Doctors Management website. Accessed August 17, 2021. https://www.doctors-management.com/cms-2019-feeschedule-modifier25/
- Dermatologist claims for evaluation and management services on the same day as minor surgical procedures. US Department of Health and Humans Services Office of Inspector General website. Accessed August 17, 2021. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000577.asp
- Global surgery booklet. Centers for Medicare and Medicaid Services website. Updated September 2018. Accessed August 17, 2021. https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/globallsurgery-icn907166.pdf
- American Medical Association. CPT® Evaluation and management (E/M)—office or other outpatient (99202-99215) and prolonged services (99354, 99355, 99356, 99417) code and guideline changes. Updated March 9, 2021. Accessed August 17, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
- 1997 documentation guidelines for evaluation and management services. Centers for Medicare and Medicaid Services website. Accessed August 17, 2021. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf
Insurers Target Modifier -25
Modifier -25 allows reporting of both a minor procedure (ie, one with a 0- or 10-day global period) and a separate and distinct evaluation and management (E/M) service on the same date of service.1 Because of the multicomplaint nature of dermatology, the ability to report a same-day procedure and an E/M service is critical for efficient, cost-effective, and patient-centered dermatologic care. However, it is well known that the use of modifier -25 has been under notable insurer scrutiny and is a common reason for medical record audits.2,3 Some insurers have responded to increased utilization of modifier -25 by cutting reimbursement for claims that include both a procedure and an E/M service or by denying one of the services altogether.4-6 The Centers for Medicare and Medicaid Services also have expressed concern about this coding combination with proposed cuts to reimbursement.7 Moreover, the Office of Inspector General has announced a work plan to investigate the frequent utilization of E/M codes and minor procedures by dermatologists.8 Clearly, modifier -25 is a continued target by insurers and regulators; therefore, dermatologists will want to make sure their coding and documentation meet all requirements and are updated for the new E/M codes for 2021.
The American Medical Association’s Current Procedural Terminology indicates that modifier -25 allows reporting of a “significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of a procedure or other service.”1 Given that dermatology patients typically present with multiple concerns, dermatologists commonly evaluate and treat numerous conditions during one visit. Understanding what constitutes a separately identifiable E/M service is critical to bill accurately and to pass insurer audits.
Global Surgical Package
To appropriately bill both a procedure and an E/M service, the physician must indicate that the patient’s condition required an E/M service above and beyond the usual work of the procedure. The compilation of evaluation and work included in the payment for a procedure is called the global surgical package.9 In general, the global surgical package includes local or topical anesthesia; the surgical service/procedure itself; immediate postoperative care, including dictating the operative note; meeting/discussing the patient’s procedure with family and other physicians; and writing orders for the patient. For minor procedures (ie, those with either 0- or 10-day global periods), the surgical package also includes same-day E/M services associated with the decision to perform surgery. An appropriate history and physical examination as well as a discussion of the differential diagnosis, treatment options, and risk and benefits of treatment are all included in the payment of a minor procedure itself. Therefore, an evaluation to discuss a patient’s condition or change in condition, alternatives to treatment, or next steps after a diagnosis related to a treatment or diagnostic procedure should not be separately reported. Moreover, the fact that the patient is new to the physician is not in itself sufficient to allow reporting of an E/M service with these minor procedures. For major procedures (ie, those with 90-day postoperative periods), the decision for surgery is excluded from the global surgical package.
2021 E/M Codes Simplify Documentation
The biggest coding change of 2021 was the new E/M codes.10 Prior to this year, the descriptors of E/M services recognized 7 components to define the levels of E/M services11: history and nature of the presenting problem; physical examination; medical decision-making (MDM); counseling; coordination of care; and time. Furthermore, history, physical examination, and MDM were all broken down into more granular elements that were summed to determine the level for each component; for example, the history of the presenting problem was defined as a chronological description of the development of the patient’s present illness, including the following elements: location, quality, severity, duration, timing, context, modifying factors, and associated signs and symptoms. Each of these categories would constitute bullet points to be summed to determine the level of history. Physical examination and MDM bullet points also would be summed to determine a proper coding level.11 Understandably, this coding scheme was complicated and burdensome to medical providers.
The redefinition of the E/M codes for 2021 substantially simplified the determination of coding level and documentation.10 The revisions to the E/M office visit code descriptors and documentation standards are now centered around how physicians think and take care of patients and not on mandatory standards and checking boxes. The main changes involve MDM as the prime determinant of the coding level. Elements of MDM affecting coding for an outpatient or office visit now include only 3 components: the number and complexity of problems addressed in the encounter, the amount or complexity of data to be reviewed and analyzed, and the risk of complications or morbidity of patient management. Gone are the requirements from the earlier criteria requiring so many bullet points for the history, physical examination, and MDM.
Dermatologists may ask, “How does the new E/M coding structure affect reporting and documenting an E/M and a procedure on the same day?” The answer is that the determination of separate and distinct is basically unchanged with the new E/M codes; however, the documentation requirements for modifier -25 using the new E/M codes are simplified.
As always, the key to determining whether a separate and distinct E/M service was provided and subsequently documented is to deconstruct the medical note. All evaluation services associated with the procedure—making a clinical diagnosis or differential diagnosis, decision to perform surgery, and discussion of alternative treatments—should be removed from one’s documentation as shown in the example below. If a complete E/M service still exists, then an E/M may be billed in addition to the procedure. Physical examination of the treatment area is included in the surgical package. With the prior E/M criteria, physical examination of the procedural area could not be used again as a bullet point to count for the E/M level. However, with the new 2021 coding requirements, the documentation of a separate MDM will be sufficient to meet criteria because documentation of physical examination is not a requirement.
Modifier -25 Examples
Let’s examine a typical dermatologist medical note. An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. The patient also complains of a growing tender lesion on the left elbow of 2 months’ duration. Physical examination reveals a linear vesicular eruption on the left wrist and a tender hyperkeratotic papule on the left elbow. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed. The decision is made to perform a tangential biopsy of the lesion on the left elbow because of the suspicion for malignancy. The biopsy is performed the same day.
This case clearly illustrates performance of an E/M service in the treatment of rhus dermatitis, which is separate and distinct from the biopsy procedure; however, in evaluating whether the case meets the documentation requirements for modifier -25, the information in the medical note inclusive to the procedure’s global surgical package, including history associated with establishing the diagnosis, physical examination of the procedure area(s), and discussion of treatment options, is eliminated, leaving the following notes: An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed.
Because the physical examination of the body part (left arm) is included in the procedure’s global surgical package, the examination of the left wrist cannot be used as coding support for the E/M service. This makes a difference for coding level in the prior E/M coding requirements, which required examination bullet points. However, with the 2021 E/M codes, documentation of physical examination bullet points is irrelevant to the coding level. Therefore, qualifying for a modifier -25 claim is more straightforward in this case with the new code set. Because bullet points are not integral to the 2021 E/M codes, qualifying and properly documenting for a higher level of service will likely be more common in dermatology.
Final Thoughts
Frequent use of modifier -25 is a critical part of a high-quality and cost-effective dermatology practice. Same-day performance of minor procedures and E/M services allows for more rapid and efficient diagnosis and treatment of various conditions as well as minimizing unnecessary office visits. The new E/M codes for 2021 actually make the documentation of a separate and distinct E/M service less complicated because the bullet point requirements associated with the old E/M codes have been eliminated. Understanding how the new E/M code descriptors affect modifier -25 reporting and clear documentation of separate, distinct, and medically necessary E/M services will be needed due to increased insurer scrutiny and audits.
Insurers Target Modifier -25
Modifier -25 allows reporting of both a minor procedure (ie, one with a 0- or 10-day global period) and a separate and distinct evaluation and management (E/M) service on the same date of service.1 Because of the multicomplaint nature of dermatology, the ability to report a same-day procedure and an E/M service is critical for efficient, cost-effective, and patient-centered dermatologic care. However, it is well known that the use of modifier -25 has been under notable insurer scrutiny and is a common reason for medical record audits.2,3 Some insurers have responded to increased utilization of modifier -25 by cutting reimbursement for claims that include both a procedure and an E/M service or by denying one of the services altogether.4-6 The Centers for Medicare and Medicaid Services also have expressed concern about this coding combination with proposed cuts to reimbursement.7 Moreover, the Office of Inspector General has announced a work plan to investigate the frequent utilization of E/M codes and minor procedures by dermatologists.8 Clearly, modifier -25 is a continued target by insurers and regulators; therefore, dermatologists will want to make sure their coding and documentation meet all requirements and are updated for the new E/M codes for 2021.
The American Medical Association’s Current Procedural Terminology indicates that modifier -25 allows reporting of a “significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of a procedure or other service.”1 Given that dermatology patients typically present with multiple concerns, dermatologists commonly evaluate and treat numerous conditions during one visit. Understanding what constitutes a separately identifiable E/M service is critical to bill accurately and to pass insurer audits.
Global Surgical Package
To appropriately bill both a procedure and an E/M service, the physician must indicate that the patient’s condition required an E/M service above and beyond the usual work of the procedure. The compilation of evaluation and work included in the payment for a procedure is called the global surgical package.9 In general, the global surgical package includes local or topical anesthesia; the surgical service/procedure itself; immediate postoperative care, including dictating the operative note; meeting/discussing the patient’s procedure with family and other physicians; and writing orders for the patient. For minor procedures (ie, those with either 0- or 10-day global periods), the surgical package also includes same-day E/M services associated with the decision to perform surgery. An appropriate history and physical examination as well as a discussion of the differential diagnosis, treatment options, and risk and benefits of treatment are all included in the payment of a minor procedure itself. Therefore, an evaluation to discuss a patient’s condition or change in condition, alternatives to treatment, or next steps after a diagnosis related to a treatment or diagnostic procedure should not be separately reported. Moreover, the fact that the patient is new to the physician is not in itself sufficient to allow reporting of an E/M service with these minor procedures. For major procedures (ie, those with 90-day postoperative periods), the decision for surgery is excluded from the global surgical package.
2021 E/M Codes Simplify Documentation
The biggest coding change of 2021 was the new E/M codes.10 Prior to this year, the descriptors of E/M services recognized 7 components to define the levels of E/M services11: history and nature of the presenting problem; physical examination; medical decision-making (MDM); counseling; coordination of care; and time. Furthermore, history, physical examination, and MDM were all broken down into more granular elements that were summed to determine the level for each component; for example, the history of the presenting problem was defined as a chronological description of the development of the patient’s present illness, including the following elements: location, quality, severity, duration, timing, context, modifying factors, and associated signs and symptoms. Each of these categories would constitute bullet points to be summed to determine the level of history. Physical examination and MDM bullet points also would be summed to determine a proper coding level.11 Understandably, this coding scheme was complicated and burdensome to medical providers.
The redefinition of the E/M codes for 2021 substantially simplified the determination of coding level and documentation.10 The revisions to the E/M office visit code descriptors and documentation standards are now centered around how physicians think and take care of patients and not on mandatory standards and checking boxes. The main changes involve MDM as the prime determinant of the coding level. Elements of MDM affecting coding for an outpatient or office visit now include only 3 components: the number and complexity of problems addressed in the encounter, the amount or complexity of data to be reviewed and analyzed, and the risk of complications or morbidity of patient management. Gone are the requirements from the earlier criteria requiring so many bullet points for the history, physical examination, and MDM.
Dermatologists may ask, “How does the new E/M coding structure affect reporting and documenting an E/M and a procedure on the same day?” The answer is that the determination of separate and distinct is basically unchanged with the new E/M codes; however, the documentation requirements for modifier -25 using the new E/M codes are simplified.
As always, the key to determining whether a separate and distinct E/M service was provided and subsequently documented is to deconstruct the medical note. All evaluation services associated with the procedure—making a clinical diagnosis or differential diagnosis, decision to perform surgery, and discussion of alternative treatments—should be removed from one’s documentation as shown in the example below. If a complete E/M service still exists, then an E/M may be billed in addition to the procedure. Physical examination of the treatment area is included in the surgical package. With the prior E/M criteria, physical examination of the procedural area could not be used again as a bullet point to count for the E/M level. However, with the new 2021 coding requirements, the documentation of a separate MDM will be sufficient to meet criteria because documentation of physical examination is not a requirement.
Modifier -25 Examples
Let’s examine a typical dermatologist medical note. An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. The patient also complains of a growing tender lesion on the left elbow of 2 months’ duration. Physical examination reveals a linear vesicular eruption on the left wrist and a tender hyperkeratotic papule on the left elbow. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed. The decision is made to perform a tangential biopsy of the lesion on the left elbow because of the suspicion for malignancy. The biopsy is performed the same day.
This case clearly illustrates performance of an E/M service in the treatment of rhus dermatitis, which is separate and distinct from the biopsy procedure; however, in evaluating whether the case meets the documentation requirements for modifier -25, the information in the medical note inclusive to the procedure’s global surgical package, including history associated with establishing the diagnosis, physical examination of the procedure area(s), and discussion of treatment options, is eliminated, leaving the following notes: An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed.
Because the physical examination of the body part (left arm) is included in the procedure’s global surgical package, the examination of the left wrist cannot be used as coding support for the E/M service. This makes a difference for coding level in the prior E/M coding requirements, which required examination bullet points. However, with the 2021 E/M codes, documentation of physical examination bullet points is irrelevant to the coding level. Therefore, qualifying for a modifier -25 claim is more straightforward in this case with the new code set. Because bullet points are not integral to the 2021 E/M codes, qualifying and properly documenting for a higher level of service will likely be more common in dermatology.
Final Thoughts
Frequent use of modifier -25 is a critical part of a high-quality and cost-effective dermatology practice. Same-day performance of minor procedures and E/M services allows for more rapid and efficient diagnosis and treatment of various conditions as well as minimizing unnecessary office visits. The new E/M codes for 2021 actually make the documentation of a separate and distinct E/M service less complicated because the bullet point requirements associated with the old E/M codes have been eliminated. Understanding how the new E/M code descriptors affect modifier -25 reporting and clear documentation of separate, distinct, and medically necessary E/M services will be needed due to increased insurer scrutiny and audits.
- Current Procedural Terminology 2021, Professional Edition. American Medical Association; 2020.
- Rogers HW. Modifier −25 victory, but the battle is not over. Cutis. 2018;101:409-410.
- Rogers HW. One diagnosis and modifier −25: appropriate or audit target? Cutis. 2017;99:165-166.
- Update regarding E/M with modifier −25—professional. Anthem Blue Cross Blue Shield website. Published February 1, 2019. Accessed August 17, 2021. https://providernews.anthem.com/ohio/article/update-regarding-em-with-modifier-25-professional
- Payment policies—surgery. Harvard Pilgrim Health Care website. Updated May 2021. Accessed August 17, 2021. https://www.harvardpilgrim.org/provider/wp-content/uploads/sites/7/2020/07/H-6-Surgery-PM.pdf
- Modifier 25: frequently asked questions. Independence Blue Cross website. Updated September 25, 2017. Accessed August 17, 2021. https://provcomm.ibx.com/ibc/archive/pages/A86603B03881756B8525817E00768006.aspx
- Huang G. CMS 2019 fee schedule takes modifier 25 cuts, runs with them. Doctors Management website. Accessed August 17, 2021. https://www.doctors-management.com/cms-2019-feeschedule-modifier25/
- Dermatologist claims for evaluation and management services on the same day as minor surgical procedures. US Department of Health and Humans Services Office of Inspector General website. Accessed August 17, 2021. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000577.asp
- Global surgery booklet. Centers for Medicare and Medicaid Services website. Updated September 2018. Accessed August 17, 2021. https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/globallsurgery-icn907166.pdf
- American Medical Association. CPT® Evaluation and management (E/M)—office or other outpatient (99202-99215) and prolonged services (99354, 99355, 99356, 99417) code and guideline changes. Updated March 9, 2021. Accessed August 17, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
- 1997 documentation guidelines for evaluation and management services. Centers for Medicare and Medicaid Services website. Accessed August 17, 2021. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf
- Current Procedural Terminology 2021, Professional Edition. American Medical Association; 2020.
- Rogers HW. Modifier −25 victory, but the battle is not over. Cutis. 2018;101:409-410.
- Rogers HW. One diagnosis and modifier −25: appropriate or audit target? Cutis. 2017;99:165-166.
- Update regarding E/M with modifier −25—professional. Anthem Blue Cross Blue Shield website. Published February 1, 2019. Accessed August 17, 2021. https://providernews.anthem.com/ohio/article/update-regarding-em-with-modifier-25-professional
- Payment policies—surgery. Harvard Pilgrim Health Care website. Updated May 2021. Accessed August 17, 2021. https://www.harvardpilgrim.org/provider/wp-content/uploads/sites/7/2020/07/H-6-Surgery-PM.pdf
- Modifier 25: frequently asked questions. Independence Blue Cross website. Updated September 25, 2017. Accessed August 17, 2021. https://provcomm.ibx.com/ibc/archive/pages/A86603B03881756B8525817E00768006.aspx
- Huang G. CMS 2019 fee schedule takes modifier 25 cuts, runs with them. Doctors Management website. Accessed August 17, 2021. https://www.doctors-management.com/cms-2019-feeschedule-modifier25/
- Dermatologist claims for evaluation and management services on the same day as minor surgical procedures. US Department of Health and Humans Services Office of Inspector General website. Accessed August 17, 2021. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000577.asp
- Global surgery booklet. Centers for Medicare and Medicaid Services website. Updated September 2018. Accessed August 17, 2021. https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/globallsurgery-icn907166.pdf
- American Medical Association. CPT® Evaluation and management (E/M)—office or other outpatient (99202-99215) and prolonged services (99354, 99355, 99356, 99417) code and guideline changes. Updated March 9, 2021. Accessed August 17, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
- 1997 documentation guidelines for evaluation and management services. Centers for Medicare and Medicaid Services website. Accessed August 17, 2021. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf
Practice Points
- Insurer scrutiny of same-day evaluation and management (E/M) and procedure services has increased, and dermatologists should be prepared for more frequent medical record reviews and audits.
- The new 2021 E/M codes actually reduce the hurdles for reporting a separate and distinct E/M service by eliminating the history and physical examination bullet points of the previous code set.
E/M Coding in 2021: The Times (and More) Are A-Changin’
Effective on January 1, 2021, the outpatient evaluation and management (E/M) codes underwent substantial changes, which were the culmination of multiple years of revision and surveying via the American Medical Association (AMA) Relative Value Scale Update Committee and Current Procedural Terminology (RUC-CPT) process to streamline definitions and promote consistency as well as to decrease the administrative burden for all specialties within the house of medicine.1 These updates represent a notable change from the previous documentation requirements for this oft used family of codes. Herein, we break down some of the highlights of the changes and how they may be applied for some commonly used dermatologic diagnoses.
Time Is Time Is Time
Prior to the 2021 revisions, a physician generally could only code for an E/M level by time for a face-to-face encounter dominated by counseling and/or care coordination. With the new updates, any encounter can be coded by total time spent by the physician with the patient1; however, clinical staff time is not included. There also are now clear guidelines of the time ranges corresponding to the level of E/M,1 as noted in Table 1.
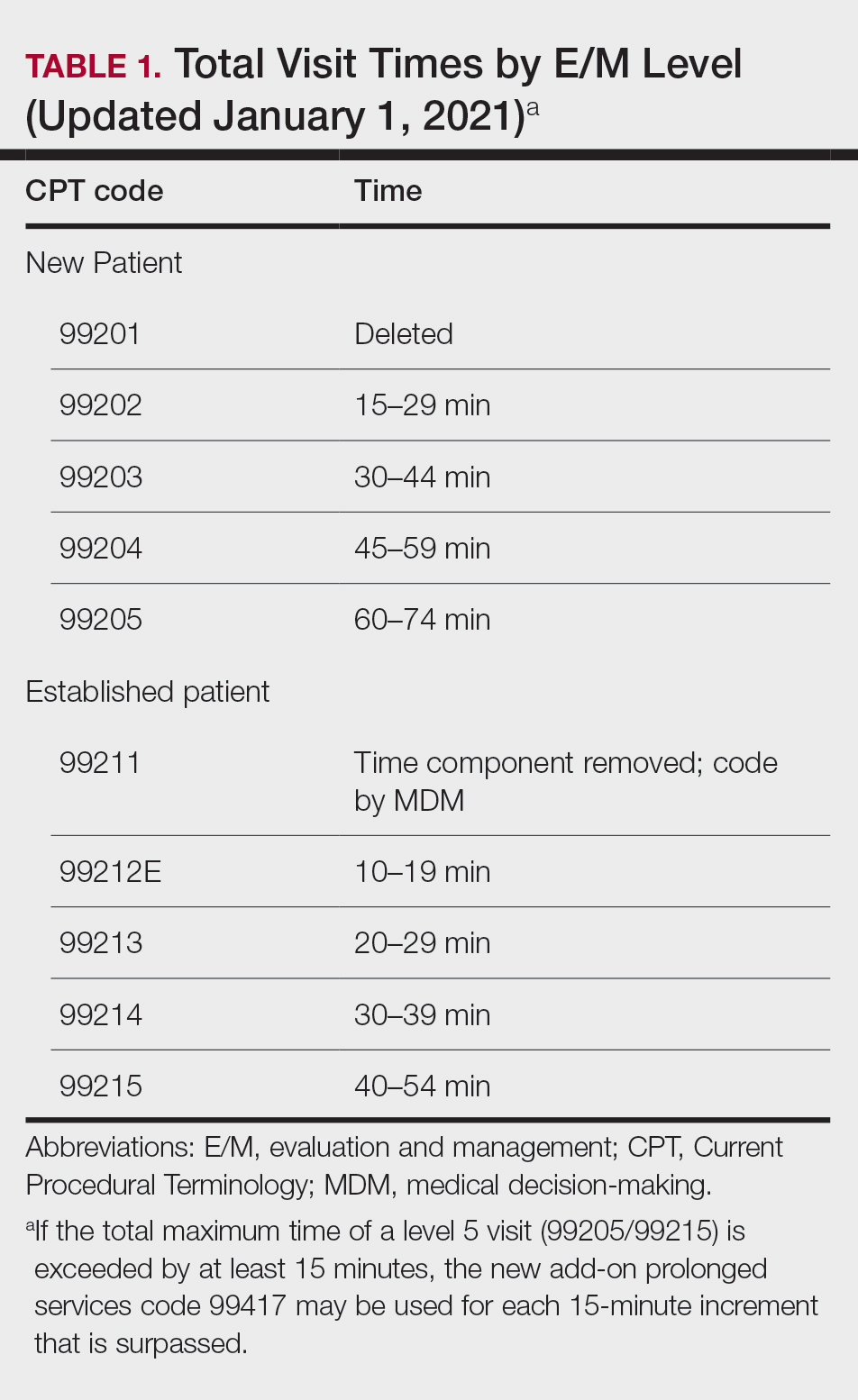
Importantly, time now includes not just face-to-face time with the patient but also any time on the date of the encounter that the physician is involved in the care of the patient when not reported with a separate code. This can include reviewing notes or data before or after the examination, care coordination, ordering laboratory tests, and providing any documentation related to the encounter. Importantly, this applies only when these activities are done on the date of the encounter.
If you work with a nurse practitioner or physician assistant (PA) who assists you and you are the one reporting the service, you cannot double-dip. For example, if your PA spends 10 minutes alone with a patient, you are in the room together for 5 minutes, the PA spends another 10 minutes alone with the patient afterward, and you do chart work for 10 minutes at the end of the day, the total time spent is 35 minutes, not 40 minutes, as you cannot count the time you and the PA spent together twice.
Decisions, Decisions
Evaluation and management coding also can be determined via the level of medical decision-making (MDM). Per the 2021 guidelines, MDM is comprised of 3 categories: (1) number and complexity of problems addressed at the encounter, (2) amount and/or complexity of data to be reviewed or analyzed, and (3) risk of complications and/or morbidity or mortality of patient management.1 To reach a certain overall E/M level, 2 of 3 categories must be met or exceeded. Let’s dive into each of these in a little more detail.
Number and Complexity of Problems Addressed at the Encounter
First, it is important to understand the definition of a problem addressed. Per AMA guidelines, this includes a disease, condition, illness, injury, symptom, sign, finding, complaint, or other matter addressed at the encounter that is evaluated or treated at the encounter by the physician. If the problem is referred to another provider without evaluation or consideration of treatment, it is not considered to be a problem addressed and cannot count toward this first category. An example could be a patient with a lump on the abdomen that you refer to plastic or general surgery for evaluation and treatment.
Once you have determined that you are addressing a problem, you will need to determine the level of complexity of the problem, as outlined in Table 2. Keep in mind that some entities and disease states in dermatology may fit the requirements of more than 1 level of complexity depending on the clinical situation, while there are many entities in dermatology that may not be perfectly captured by any of the levels described. In these situations, clinical judgement is required to determine where the problem would best fit. Importantly, whatever you decide, your documentation should support that decision.
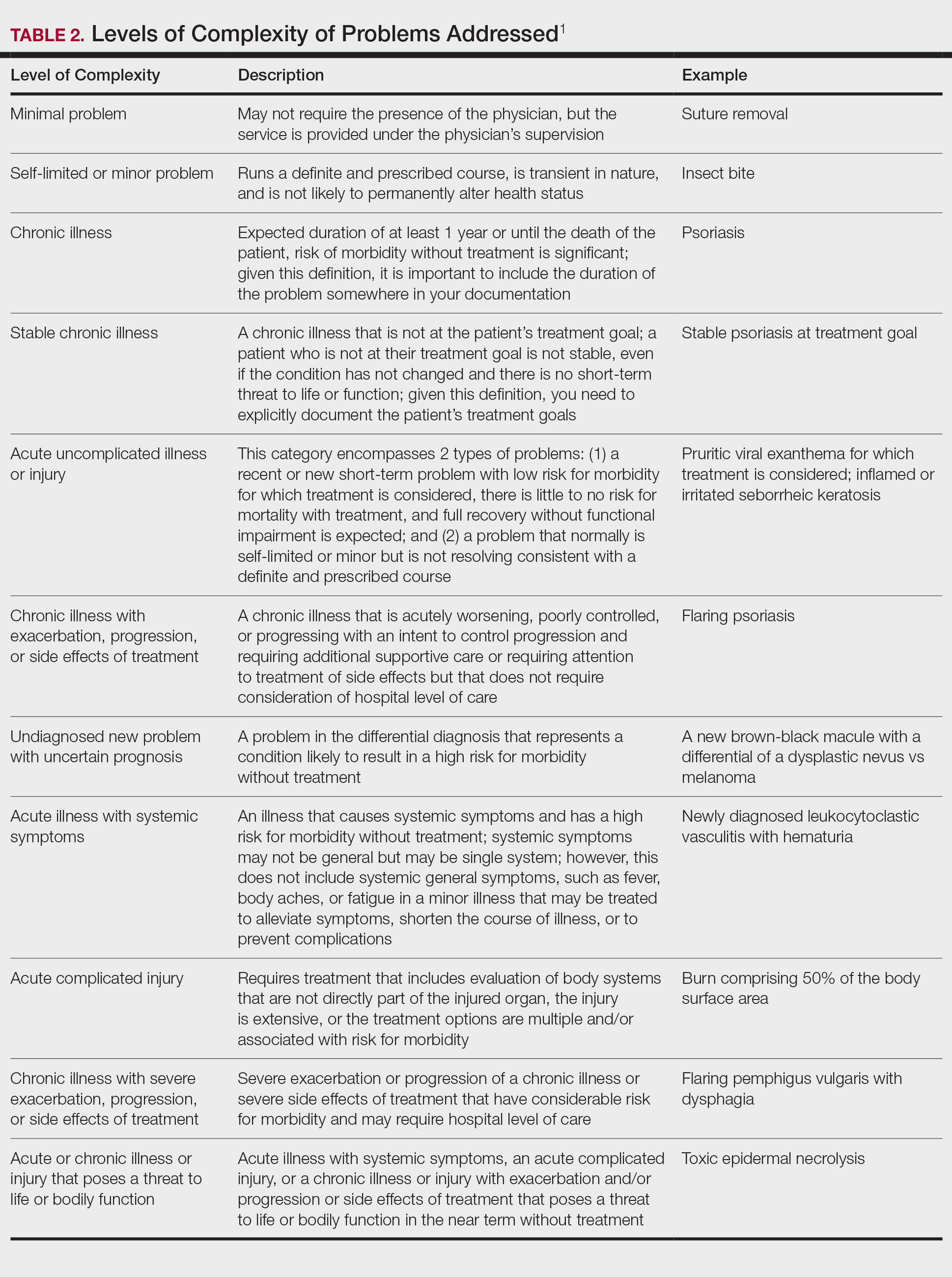
Amount and/or Complexity of Data to Be Reviewed and Analyzed
This category encompasses any external notes reviewed, unique laboratory tests or imaging ordered or reviewed, the need for an independent historian or discussion with external health care providers or appropriate sources, or independent interpretation of tests. Some high-yield definitions in this category are outlined in Table 3.
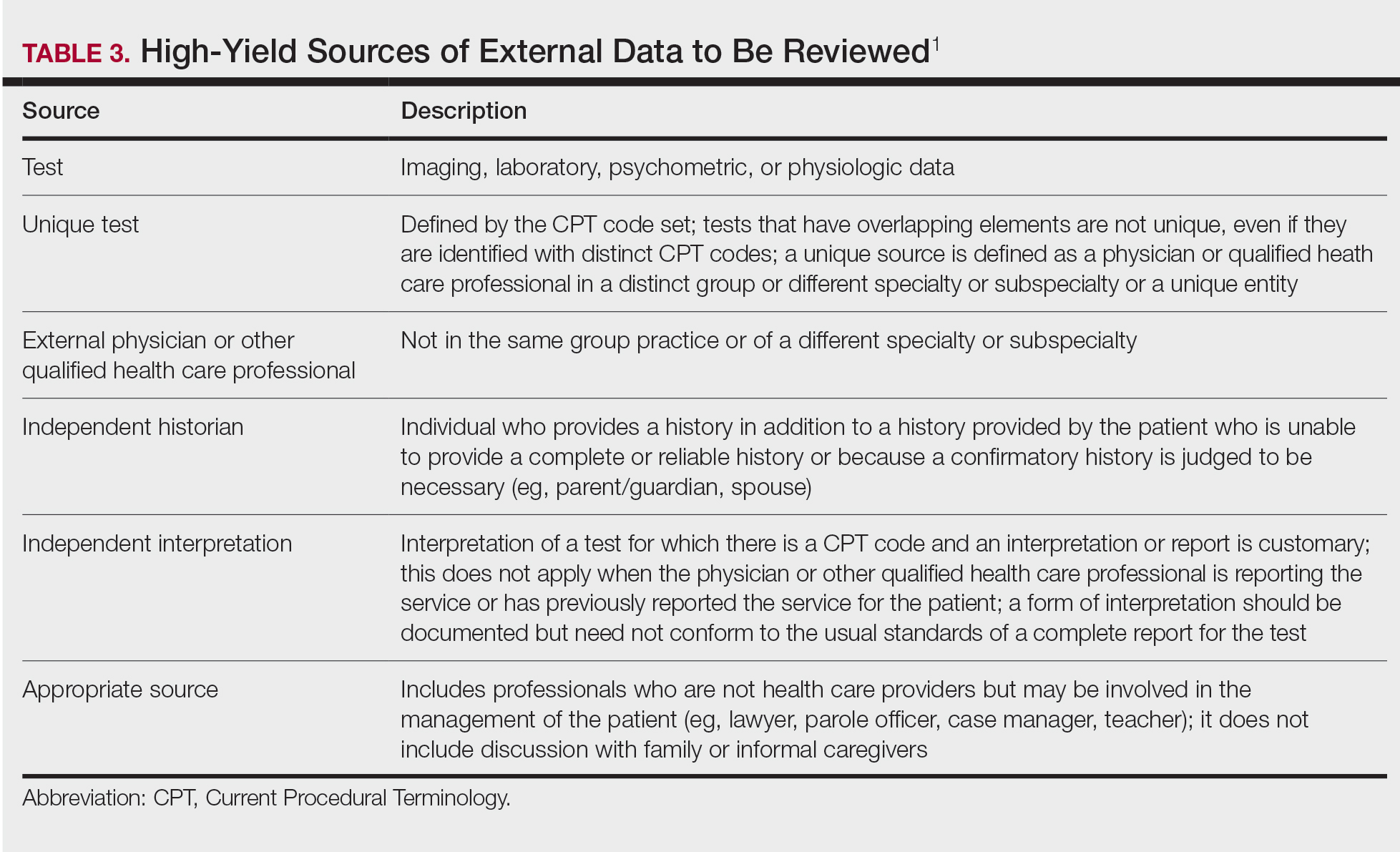
Risk of Complications and/or Morbidity or Mortality of Patient Management
In this category, risk relates to both the patient’s diagnosis and treatment(s). Importantly, for treatment and diagnostic options, these include both the options selected and those considered but not selected. Risk is defined as the probability and/or consequences of an event and is based on the usual behavior and thought processes of a physician in the same specialty. In other words, think of the risk as compared to risk in the setting of other dermatologists diagnosing and/or treating the same condition.
Social determinants of health also play a part in this category and are defined as economic and social conditions that influence the health of individuals and communities. Social determinants of health can be indicated by the specific corresponding International Statistical Classification of Diseases, Tenth Revision code and may need to be included in your billing according to specific institutional or carrier guidelines if they are a factor in your level of MDM.
For the purposes of MDM, risk is stratified into minimal, low, moderate, and high. Some examples for each level are outlined in Table 4.
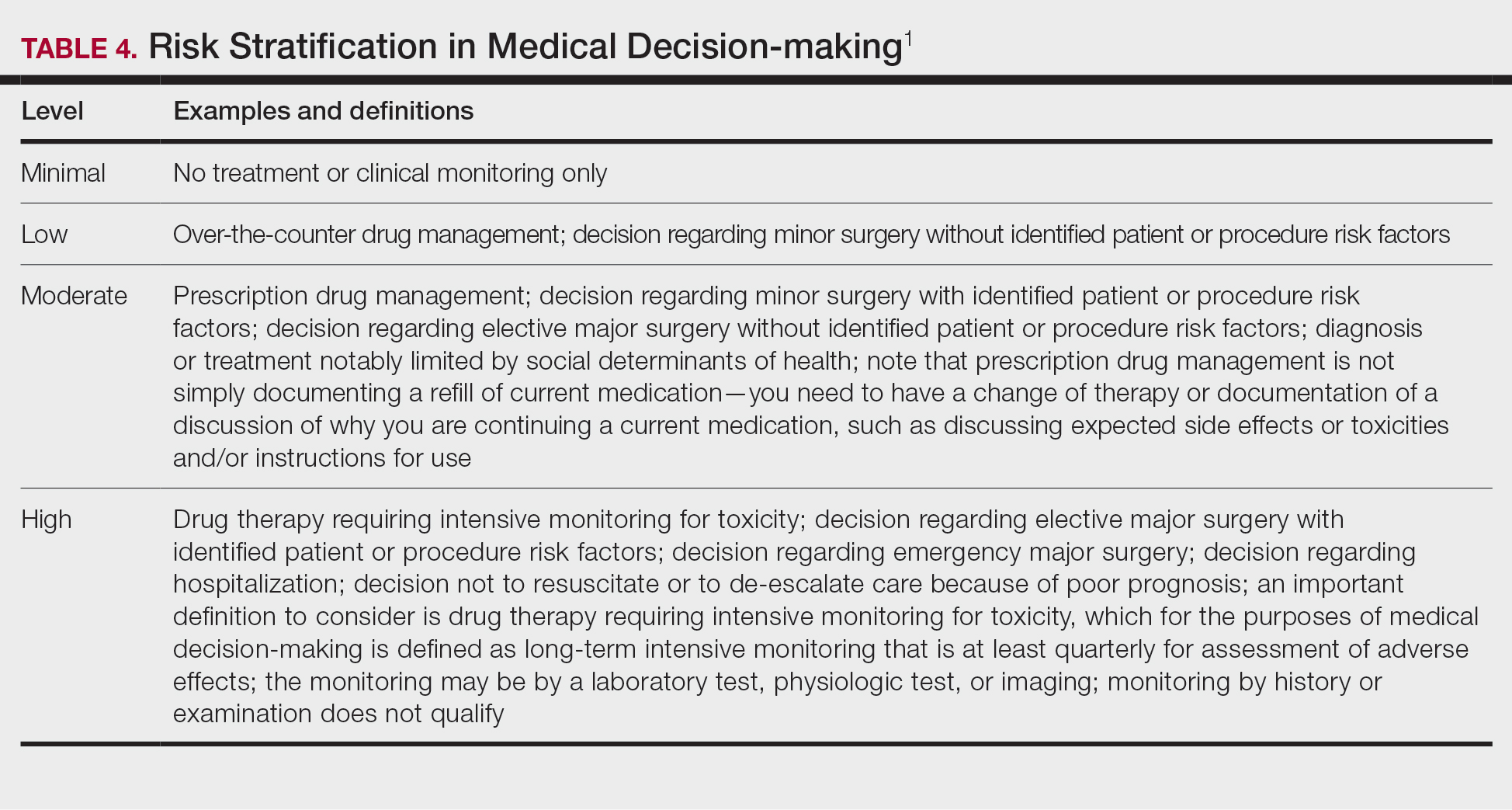
Putting It All Together
Once you have determined each of the above 3 categories, you can put them together into the MDM chart to ascertain the overall level of MDM. (The official AMA medical decision-making grid is available online [https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf]). Keep in mind that 2 of 3 columns in the table must be obtained in that level to reach an overall E/M level; for example, a visit that addresses 2 self-limited or minor problems (level 3) in which no data is reviewed (level 2) and involves prescribing a new medication (level 4), would be an overall level 3 visit.
Final Thoughts
The outpatient E/M guidelines have undergone substantial revisions; therefore, it is crucial to understand the updated definitions to ensure proper billing and documentation. History and physical examination documentation must be medically appropriate but are no longer used to determine overall E/M level; time and MDM are the sole options that can be used. Importantly, try to code as accurately as possible, documenting which problems were both noted and addressed. If you are unsure of a definition within the updated changes and MDM table, referencing the appropriate sources for guidance is recommended.
Although representing a considerable shift, the revaluation of this family of codes and the intended decrease in documentation burden has the ability to be a positive gain for dermatologists. Expect other code families to mirror these changes in the next few years.
- American Medical Association. CPT® Evaluation and management (E/M) office or other outpatient (99202-99215) and prolonged services (99354, 99355, 99356, 99417) code and guideline changes. Accessed May 14, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
Effective on January 1, 2021, the outpatient evaluation and management (E/M) codes underwent substantial changes, which were the culmination of multiple years of revision and surveying via the American Medical Association (AMA) Relative Value Scale Update Committee and Current Procedural Terminology (RUC-CPT) process to streamline definitions and promote consistency as well as to decrease the administrative burden for all specialties within the house of medicine.1 These updates represent a notable change from the previous documentation requirements for this oft used family of codes. Herein, we break down some of the highlights of the changes and how they may be applied for some commonly used dermatologic diagnoses.
Time Is Time Is Time
Prior to the 2021 revisions, a physician generally could only code for an E/M level by time for a face-to-face encounter dominated by counseling and/or care coordination. With the new updates, any encounter can be coded by total time spent by the physician with the patient1; however, clinical staff time is not included. There also are now clear guidelines of the time ranges corresponding to the level of E/M,1 as noted in Table 1.
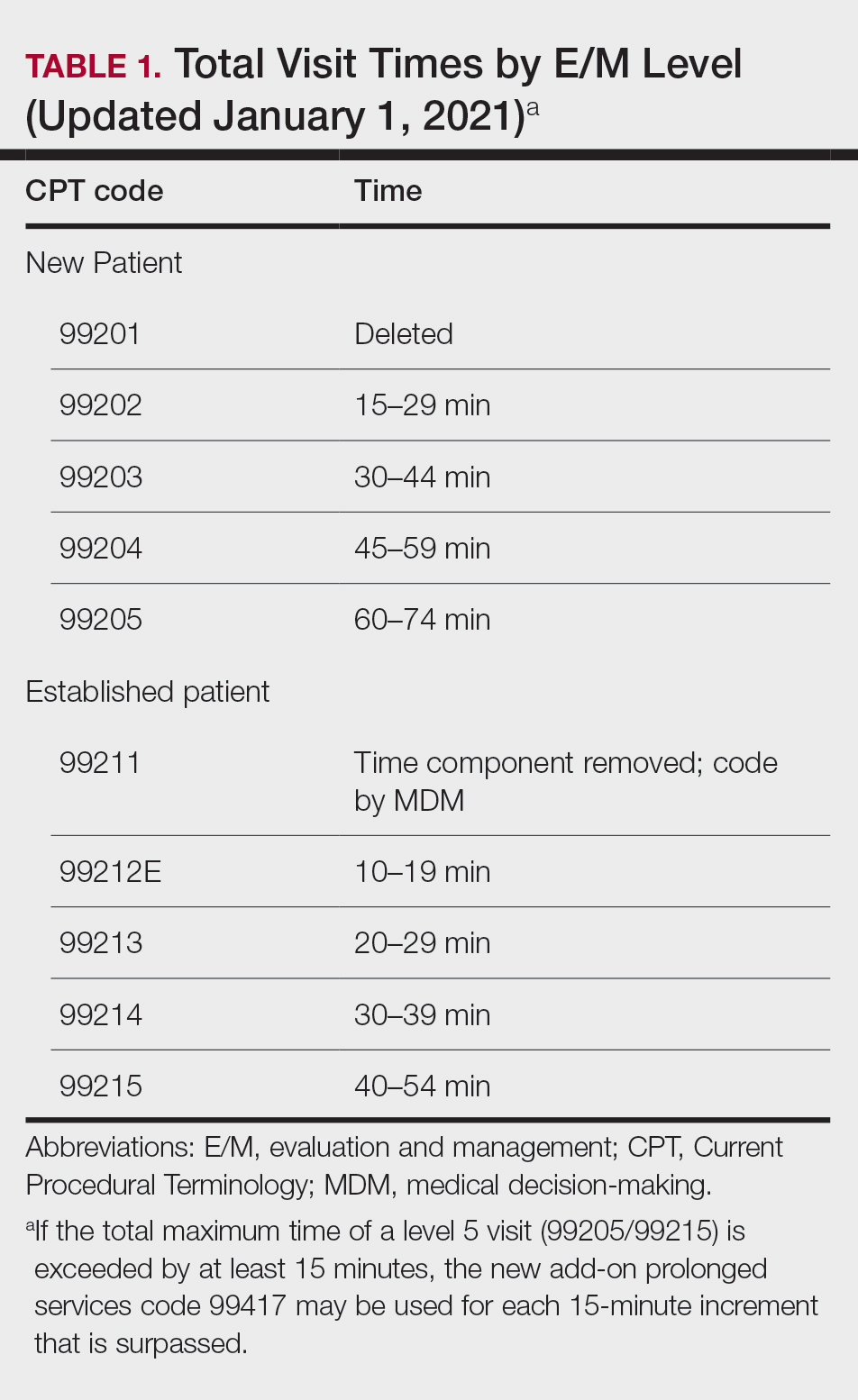
Importantly, time now includes not just face-to-face time with the patient but also any time on the date of the encounter that the physician is involved in the care of the patient when not reported with a separate code. This can include reviewing notes or data before or after the examination, care coordination, ordering laboratory tests, and providing any documentation related to the encounter. Importantly, this applies only when these activities are done on the date of the encounter.
If you work with a nurse practitioner or physician assistant (PA) who assists you and you are the one reporting the service, you cannot double-dip. For example, if your PA spends 10 minutes alone with a patient, you are in the room together for 5 minutes, the PA spends another 10 minutes alone with the patient afterward, and you do chart work for 10 minutes at the end of the day, the total time spent is 35 minutes, not 40 minutes, as you cannot count the time you and the PA spent together twice.
Decisions, Decisions
Evaluation and management coding also can be determined via the level of medical decision-making (MDM). Per the 2021 guidelines, MDM is comprised of 3 categories: (1) number and complexity of problems addressed at the encounter, (2) amount and/or complexity of data to be reviewed or analyzed, and (3) risk of complications and/or morbidity or mortality of patient management.1 To reach a certain overall E/M level, 2 of 3 categories must be met or exceeded. Let’s dive into each of these in a little more detail.
Number and Complexity of Problems Addressed at the Encounter
First, it is important to understand the definition of a problem addressed. Per AMA guidelines, this includes a disease, condition, illness, injury, symptom, sign, finding, complaint, or other matter addressed at the encounter that is evaluated or treated at the encounter by the physician. If the problem is referred to another provider without evaluation or consideration of treatment, it is not considered to be a problem addressed and cannot count toward this first category. An example could be a patient with a lump on the abdomen that you refer to plastic or general surgery for evaluation and treatment.
Once you have determined that you are addressing a problem, you will need to determine the level of complexity of the problem, as outlined in Table 2. Keep in mind that some entities and disease states in dermatology may fit the requirements of more than 1 level of complexity depending on the clinical situation, while there are many entities in dermatology that may not be perfectly captured by any of the levels described. In these situations, clinical judgement is required to determine where the problem would best fit. Importantly, whatever you decide, your documentation should support that decision.
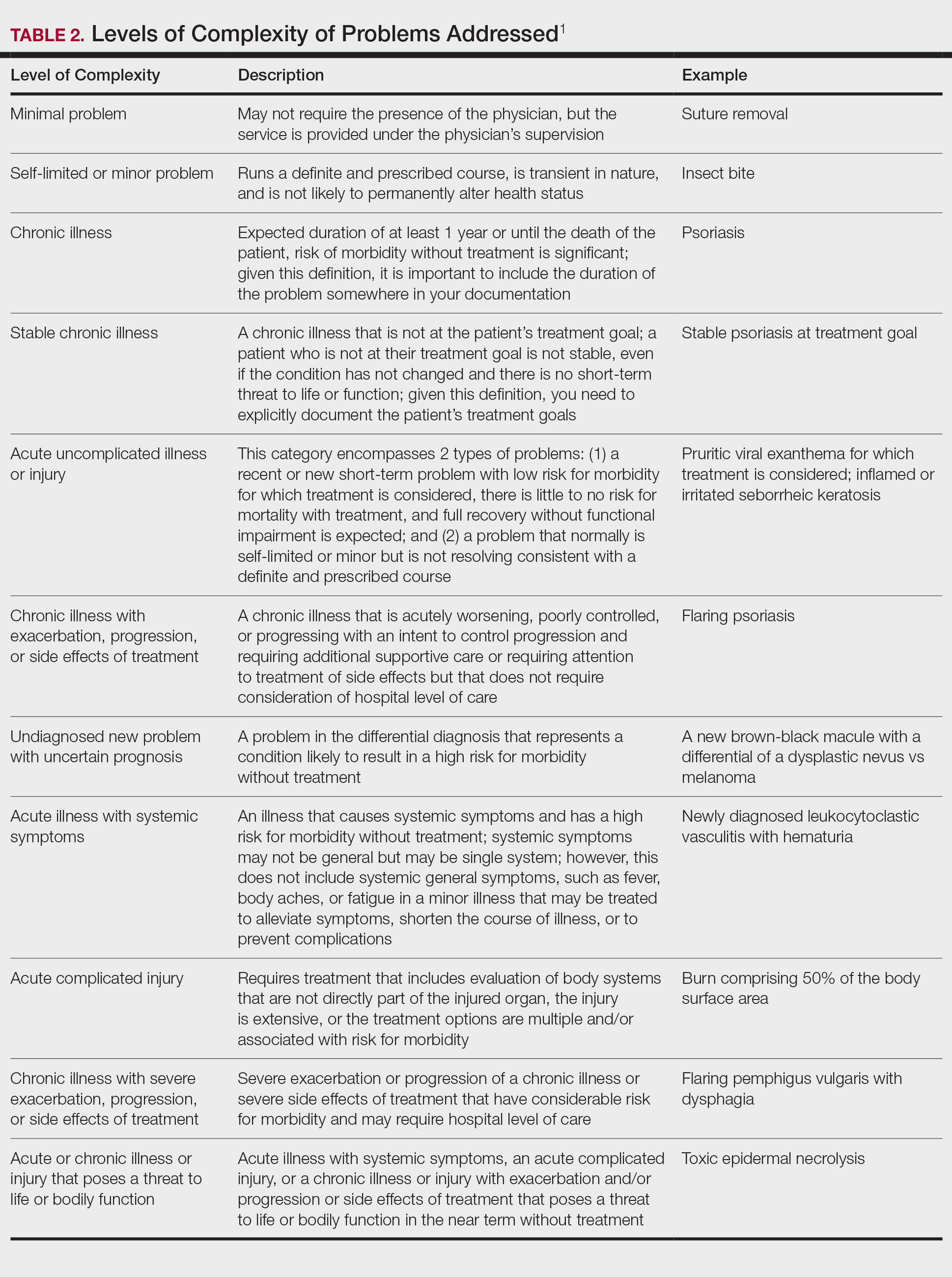
Amount and/or Complexity of Data to Be Reviewed and Analyzed
This category encompasses any external notes reviewed, unique laboratory tests or imaging ordered or reviewed, the need for an independent historian or discussion with external health care providers or appropriate sources, or independent interpretation of tests. Some high-yield definitions in this category are outlined in Table 3.
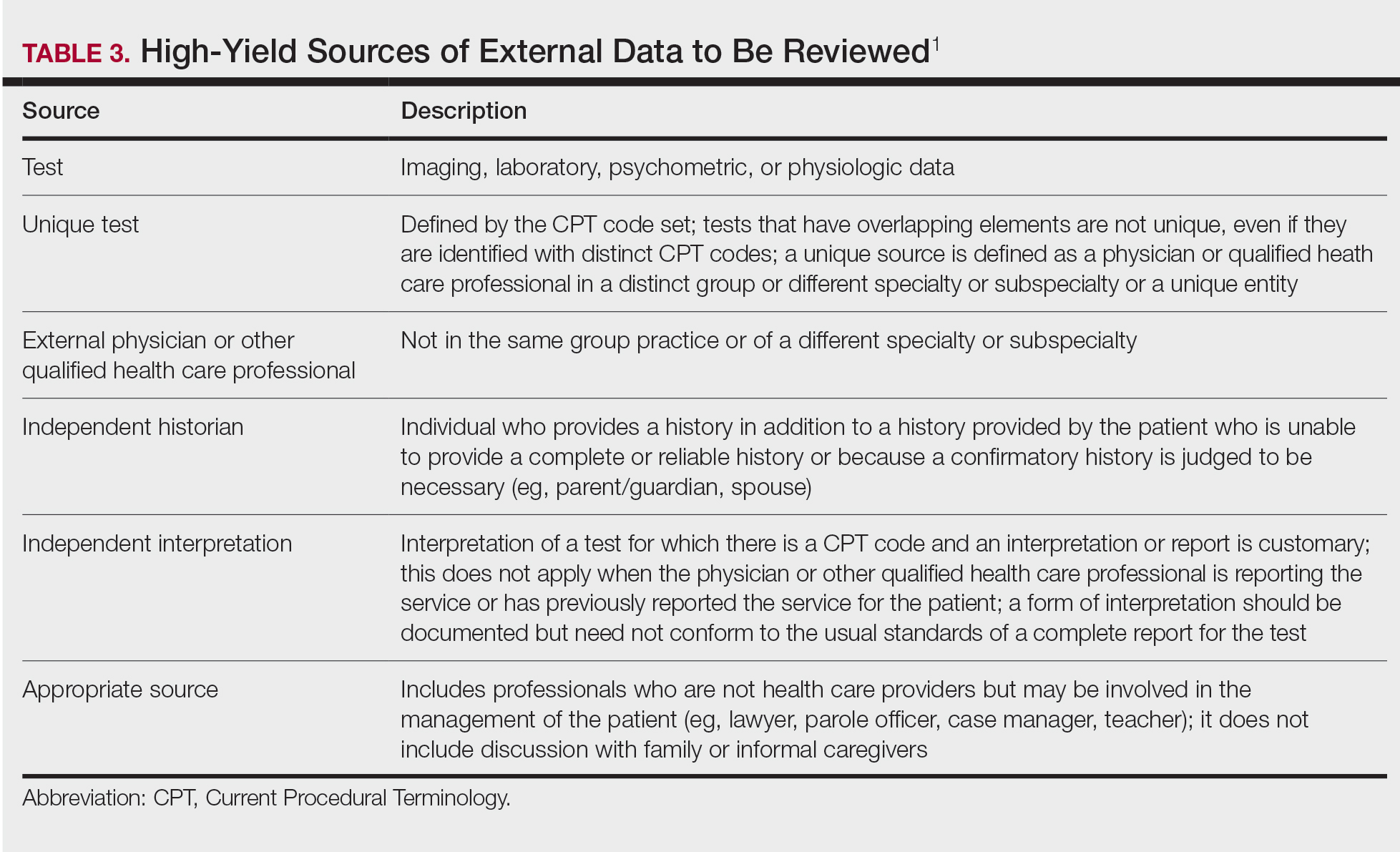
Risk of Complications and/or Morbidity or Mortality of Patient Management
In this category, risk relates to both the patient’s diagnosis and treatment(s). Importantly, for treatment and diagnostic options, these include both the options selected and those considered but not selected. Risk is defined as the probability and/or consequences of an event and is based on the usual behavior and thought processes of a physician in the same specialty. In other words, think of the risk as compared to risk in the setting of other dermatologists diagnosing and/or treating the same condition.
Social determinants of health also play a part in this category and are defined as economic and social conditions that influence the health of individuals and communities. Social determinants of health can be indicated by the specific corresponding International Statistical Classification of Diseases, Tenth Revision code and may need to be included in your billing according to specific institutional or carrier guidelines if they are a factor in your level of MDM.
For the purposes of MDM, risk is stratified into minimal, low, moderate, and high. Some examples for each level are outlined in Table 4.
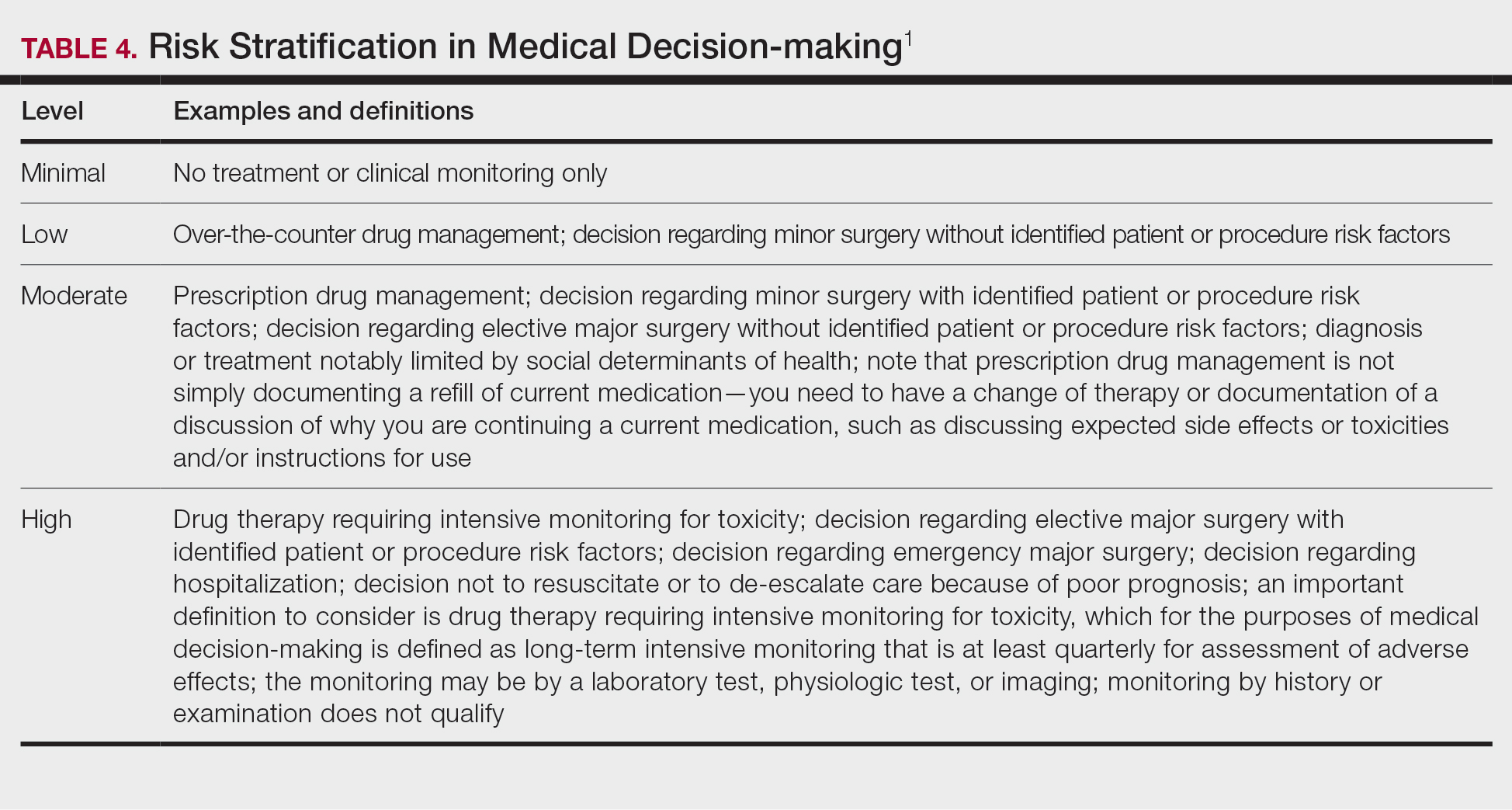
Putting It All Together
Once you have determined each of the above 3 categories, you can put them together into the MDM chart to ascertain the overall level of MDM. (The official AMA medical decision-making grid is available online [https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf]). Keep in mind that 2 of 3 columns in the table must be obtained in that level to reach an overall E/M level; for example, a visit that addresses 2 self-limited or minor problems (level 3) in which no data is reviewed (level 2) and involves prescribing a new medication (level 4), would be an overall level 3 visit.
Final Thoughts
The outpatient E/M guidelines have undergone substantial revisions; therefore, it is crucial to understand the updated definitions to ensure proper billing and documentation. History and physical examination documentation must be medically appropriate but are no longer used to determine overall E/M level; time and MDM are the sole options that can be used. Importantly, try to code as accurately as possible, documenting which problems were both noted and addressed. If you are unsure of a definition within the updated changes and MDM table, referencing the appropriate sources for guidance is recommended.
Although representing a considerable shift, the revaluation of this family of codes and the intended decrease in documentation burden has the ability to be a positive gain for dermatologists. Expect other code families to mirror these changes in the next few years.
Effective on January 1, 2021, the outpatient evaluation and management (E/M) codes underwent substantial changes, which were the culmination of multiple years of revision and surveying via the American Medical Association (AMA) Relative Value Scale Update Committee and Current Procedural Terminology (RUC-CPT) process to streamline definitions and promote consistency as well as to decrease the administrative burden for all specialties within the house of medicine.1 These updates represent a notable change from the previous documentation requirements for this oft used family of codes. Herein, we break down some of the highlights of the changes and how they may be applied for some commonly used dermatologic diagnoses.
Time Is Time Is Time
Prior to the 2021 revisions, a physician generally could only code for an E/M level by time for a face-to-face encounter dominated by counseling and/or care coordination. With the new updates, any encounter can be coded by total time spent by the physician with the patient1; however, clinical staff time is not included. There also are now clear guidelines of the time ranges corresponding to the level of E/M,1 as noted in Table 1.
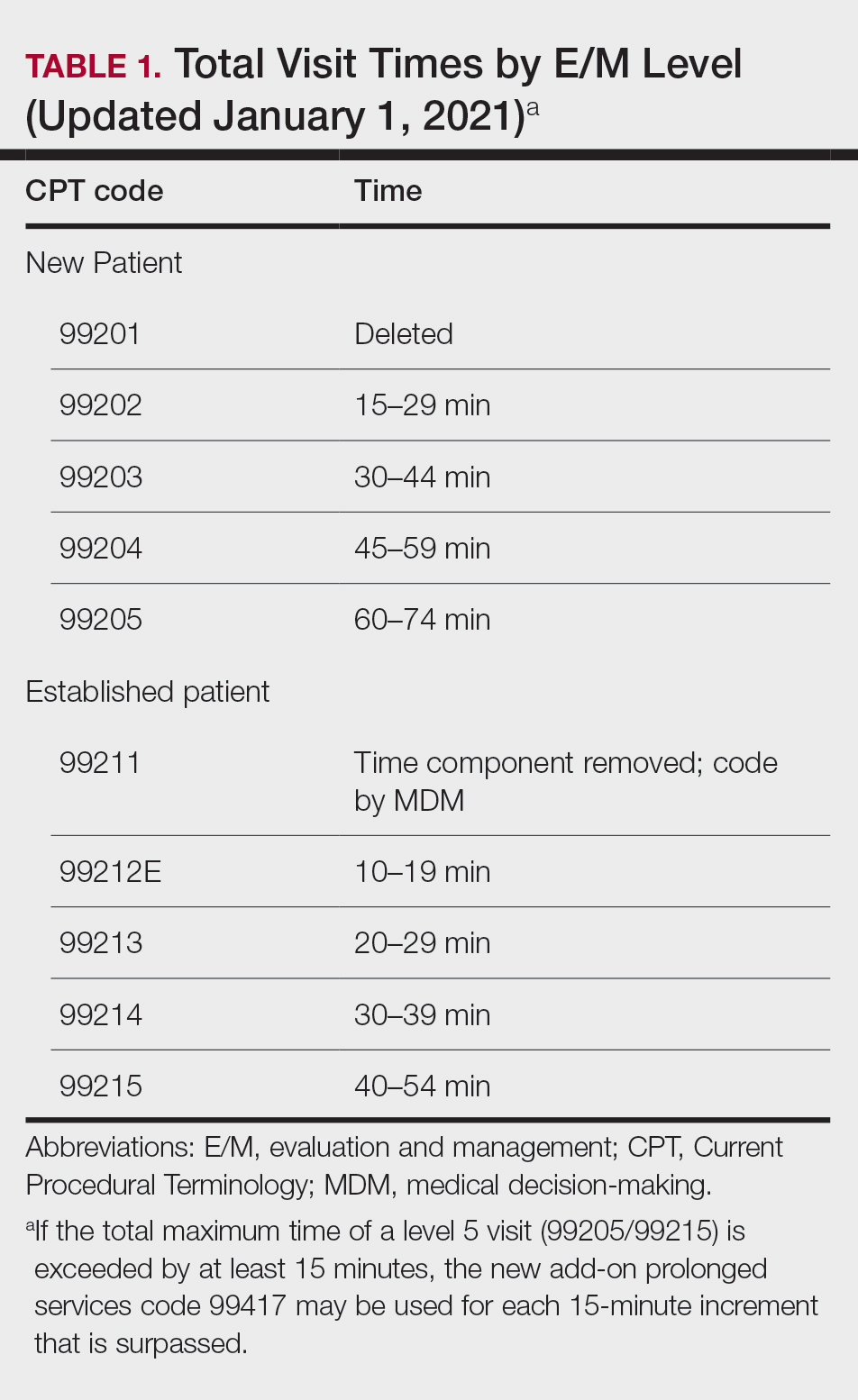
Importantly, time now includes not just face-to-face time with the patient but also any time on the date of the encounter that the physician is involved in the care of the patient when not reported with a separate code. This can include reviewing notes or data before or after the examination, care coordination, ordering laboratory tests, and providing any documentation related to the encounter. Importantly, this applies only when these activities are done on the date of the encounter.
If you work with a nurse practitioner or physician assistant (PA) who assists you and you are the one reporting the service, you cannot double-dip. For example, if your PA spends 10 minutes alone with a patient, you are in the room together for 5 minutes, the PA spends another 10 minutes alone with the patient afterward, and you do chart work for 10 minutes at the end of the day, the total time spent is 35 minutes, not 40 minutes, as you cannot count the time you and the PA spent together twice.
Decisions, Decisions
Evaluation and management coding also can be determined via the level of medical decision-making (MDM). Per the 2021 guidelines, MDM is comprised of 3 categories: (1) number and complexity of problems addressed at the encounter, (2) amount and/or complexity of data to be reviewed or analyzed, and (3) risk of complications and/or morbidity or mortality of patient management.1 To reach a certain overall E/M level, 2 of 3 categories must be met or exceeded. Let’s dive into each of these in a little more detail.
Number and Complexity of Problems Addressed at the Encounter
First, it is important to understand the definition of a problem addressed. Per AMA guidelines, this includes a disease, condition, illness, injury, symptom, sign, finding, complaint, or other matter addressed at the encounter that is evaluated or treated at the encounter by the physician. If the problem is referred to another provider without evaluation or consideration of treatment, it is not considered to be a problem addressed and cannot count toward this first category. An example could be a patient with a lump on the abdomen that you refer to plastic or general surgery for evaluation and treatment.
Once you have determined that you are addressing a problem, you will need to determine the level of complexity of the problem, as outlined in Table 2. Keep in mind that some entities and disease states in dermatology may fit the requirements of more than 1 level of complexity depending on the clinical situation, while there are many entities in dermatology that may not be perfectly captured by any of the levels described. In these situations, clinical judgement is required to determine where the problem would best fit. Importantly, whatever you decide, your documentation should support that decision.
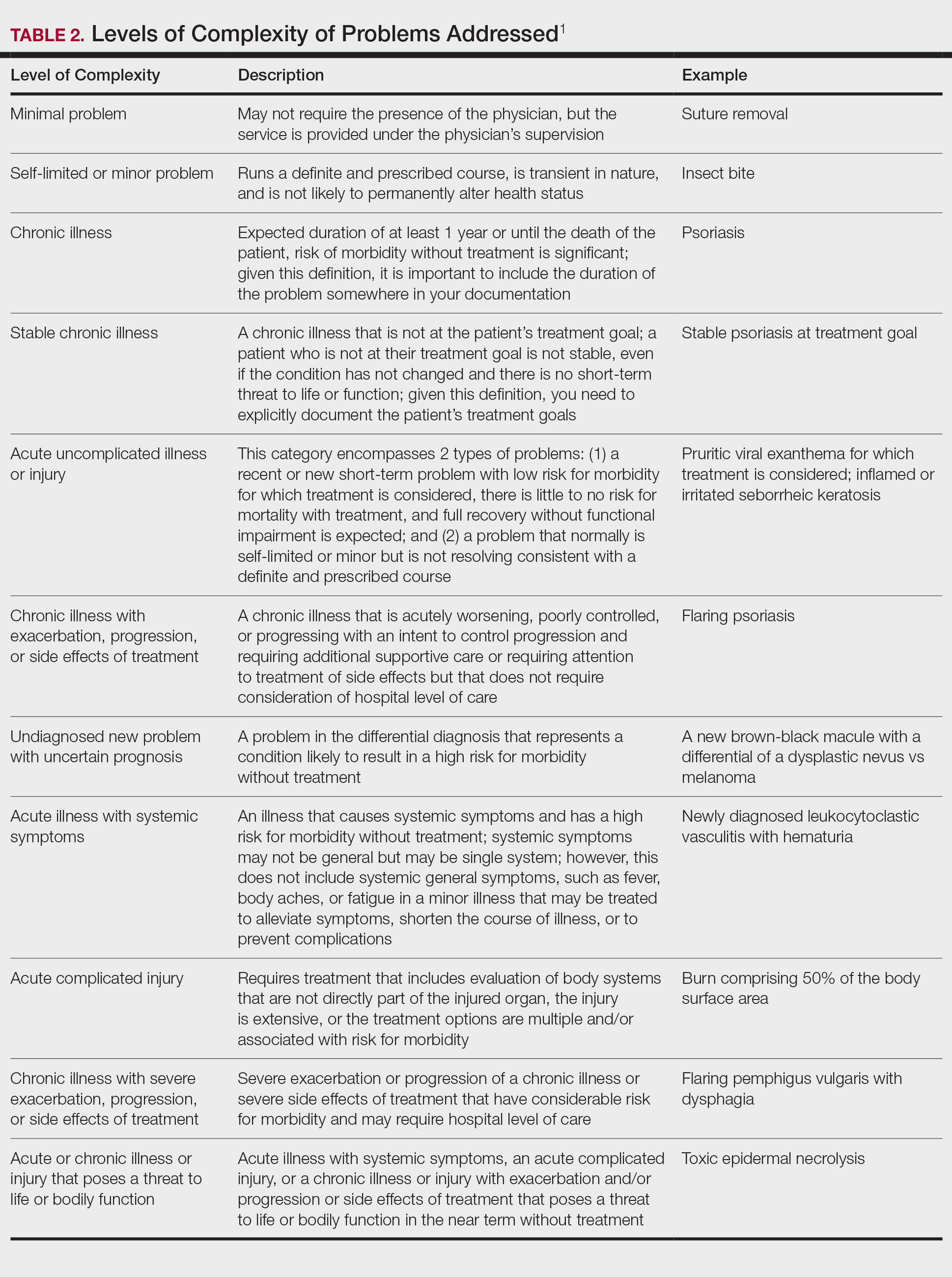
Amount and/or Complexity of Data to Be Reviewed and Analyzed
This category encompasses any external notes reviewed, unique laboratory tests or imaging ordered or reviewed, the need for an independent historian or discussion with external health care providers or appropriate sources, or independent interpretation of tests. Some high-yield definitions in this category are outlined in Table 3.
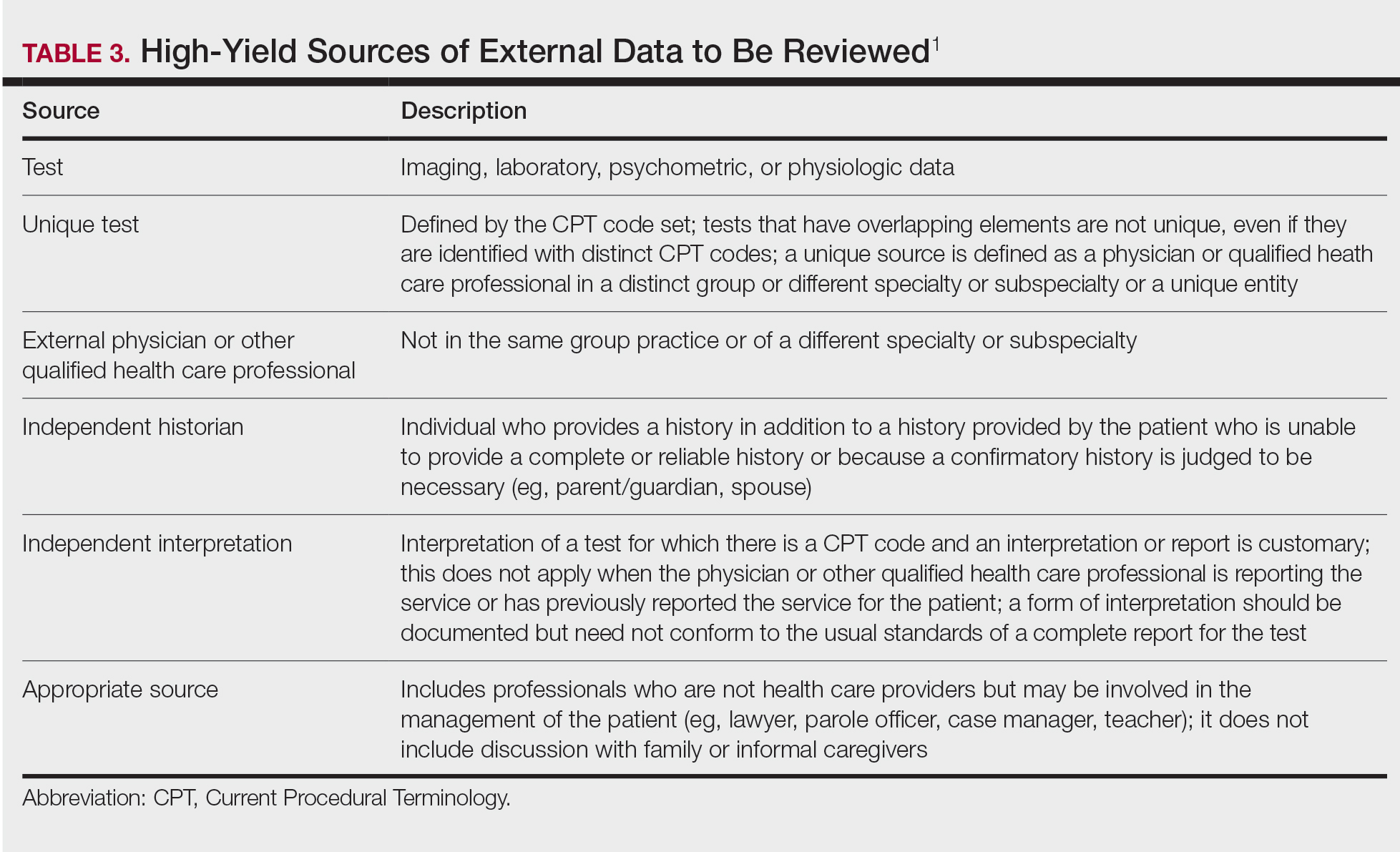
Risk of Complications and/or Morbidity or Mortality of Patient Management
In this category, risk relates to both the patient’s diagnosis and treatment(s). Importantly, for treatment and diagnostic options, these include both the options selected and those considered but not selected. Risk is defined as the probability and/or consequences of an event and is based on the usual behavior and thought processes of a physician in the same specialty. In other words, think of the risk as compared to risk in the setting of other dermatologists diagnosing and/or treating the same condition.
Social determinants of health also play a part in this category and are defined as economic and social conditions that influence the health of individuals and communities. Social determinants of health can be indicated by the specific corresponding International Statistical Classification of Diseases, Tenth Revision code and may need to be included in your billing according to specific institutional or carrier guidelines if they are a factor in your level of MDM.
For the purposes of MDM, risk is stratified into minimal, low, moderate, and high. Some examples for each level are outlined in Table 4.
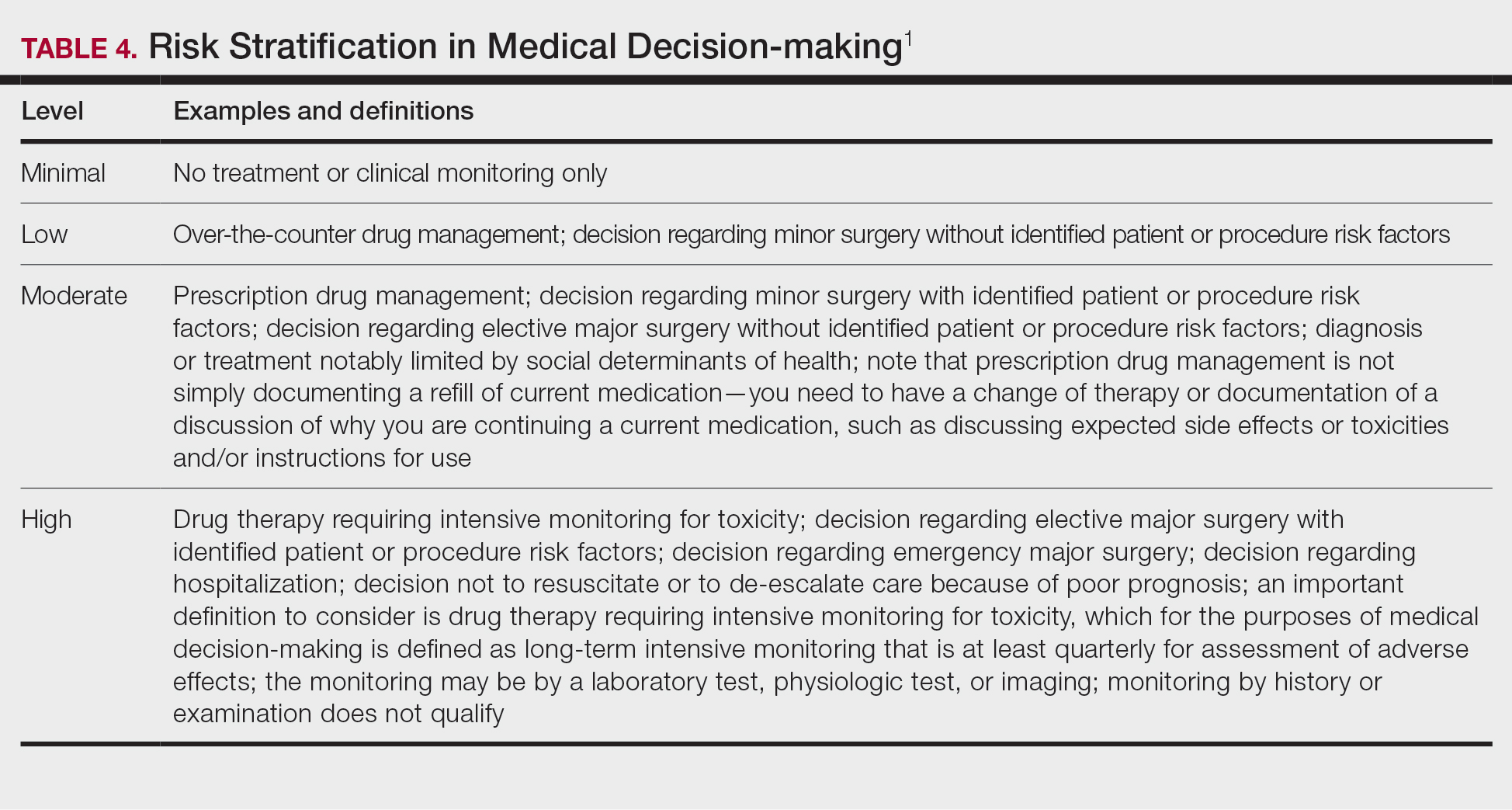
Putting It All Together
Once you have determined each of the above 3 categories, you can put them together into the MDM chart to ascertain the overall level of MDM. (The official AMA medical decision-making grid is available online [https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf]). Keep in mind that 2 of 3 columns in the table must be obtained in that level to reach an overall E/M level; for example, a visit that addresses 2 self-limited or minor problems (level 3) in which no data is reviewed (level 2) and involves prescribing a new medication (level 4), would be an overall level 3 visit.
Final Thoughts
The outpatient E/M guidelines have undergone substantial revisions; therefore, it is crucial to understand the updated definitions to ensure proper billing and documentation. History and physical examination documentation must be medically appropriate but are no longer used to determine overall E/M level; time and MDM are the sole options that can be used. Importantly, try to code as accurately as possible, documenting which problems were both noted and addressed. If you are unsure of a definition within the updated changes and MDM table, referencing the appropriate sources for guidance is recommended.
Although representing a considerable shift, the revaluation of this family of codes and the intended decrease in documentation burden has the ability to be a positive gain for dermatologists. Expect other code families to mirror these changes in the next few years.
- American Medical Association. CPT® Evaluation and management (E/M) office or other outpatient (99202-99215) and prolonged services (99354, 99355, 99356, 99417) code and guideline changes. Accessed May 14, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
- American Medical Association. CPT® Evaluation and management (E/M) office or other outpatient (99202-99215) and prolonged services (99354, 99355, 99356, 99417) code and guideline changes. Accessed May 14, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
Practice Points
- The outpatient evaluation and management (E/M) codes have undergone substantial changes that took effect January 1, 2021.
- Outpatient E/M visits are now coded based on time or level of medical decision-making (MDM).
- Time now includes all preservice, intraservice, and postservice time the physician spends with the patient on the date of the encounter.
- Many of the key definitions used in order to determine level of MDM have been streamlined and updated.
Practice Expense–Only Codes: No Physician Work, No Sweat
I have written previously about Current Procedural Terminology (CPT) procedure codes submitted on the same date of service as evaluation and management (E/M) services in the context of modifier -25.1 Billing same-day procedures and E/M services is under close scrutiny by insurers, and accurate and complete documentation is a must.2 An understanding of what aspects of evaluation are included in the global surgical package is critical in deciding whether a separate and distinct same-day evaluation was performed. In general, the decision to perform a procedure is included in the payment for the procedure itself, as is the examination of the body site in question, diagnosis of the medical condition, discussion of treatment options, and postoperative services related to the procedure. This is true for CPT codes that contain physician work, which constitute the majority of CPT codes reported by dermatologists.3
However, there is one set of codes where these principles do not apply: the practice expense (PE)–only codes, or no physician work codes. These codes are defined by CPT and the Relative Value Scale Update Committee (RUC) of the American Medical Association as containing no physician work. Their valuations are based only on staff/nursing time and the other aspects of direct and indirect practice costs included in providing the service, such as gauze, sutures, equipment, office rent, and utilities.4 Examples of PE-only codes include the nonphysician-performed photodynamic therapy code 96567; phototherapy codes 96900, 96910, and 96912; and patch testing and photopatch testing codes 95044, 95052, and 95056.
For PE-only codes, only the provision of the service by staff is included in the code reimbursement; there is no physician time or work built into these codes. Thus, neither the initial evaluation of the patient by the physician, the decision to perform the procedure, nor the evaluation of therapy effectiveness or side effects or interpretation of the results is included. Understanding that there is no physician involvement in PE-only codes is critical in deciding whether an E/M service should be billed on the same day as a PE-only code. To that end, although a physician does not actually have to personally evaluate the patient on the day of service to bill PE-only codes, the Centers for Medicare & Medicaid Services has indicated that a physician or qualified medical provider must be on premises.5 Billing for PE-only services when no provider is present will be interpreted as a false claim or fraudulent billing practice.
Because PE-only codes do not include physician work, an E/M service will be billed in addition to the treatment almost any time a same-day physician evaluation is performed. For example, if a patient presents with a changing mole that is evaluated on the same date of service as phototherapy for the treatment of psoriasis, that service is clearly reportable with an E/M code because the mole check is separate and distinct from the phototherapy treatment. A more common scenario is for the physician to see a patient with a rash consistent with an allergic contact dermatitis and the decision to perform same-day patch testing is made. In this circumstance, the E/M service is still reportable because the evaluation of the rash and the decision to perform patch testing are not included in this PE-only code.
Phototherapy typically is provided as a prolonged course of multiple treatments, and reporting of same-day E/M services during the course of therapy is common. Phototherapy must be monitored by the physician for clinical effectiveness, dose changes, and side effects, as well as to determine whether to continue therapy. A standard operating procedure should be created to document that the physician typically evaluates the patient’s progress at set intervals or as dictated by patient or staff concerns. Reporting an E/M service with every phototherapy session is not considered medically necessary. Moreover, a nurse evaluation of the patient prior to each phototherapy treatment, including questions on disease severity, how the patient did with the last treatment, and whether medications have changed, is included in the payment for the phototherapy codes. Only formal and medically necessary physician E/M services should be billed, not drive-by visits in which the physician pops in just to see how the patient is doing.
Final Thoughts
Practice expense–only codes include no payment for physician time or work but require the presence of a qualified health care provider on premises to bill. Medically necessary physician evaluations on the same day as PE-only services will typically result in both an E/M service and the procedure being reported. Understanding performance and documentation requirements of PE-only codes is critical for proper reimbursement for a dermatology practice.
- Rogers H. One diagnosis and modifier -25: appropriate or audit target? Cutis. 2017;99:165-166.
- Rogers H. Modifier -25 victory, but the battle is not over. Cutis. 2018;101:409-410.
- American Academy of Dermatology. Medicare update. Derm Coding Consult. March 2001;5:5-7. https://www.aad.org/File%20Library/Global%20navigation/Member%20tools%20and%20benefits/Publications/Derm%20Coding%20Consult%20archives/2001-spring.pdf.
- Current Procedural Terminology 2018, Professional Edition. Chicago, IL: American Medical Association; 2018.
- Determining who has the authority to bill. The Dermatologist. September 4, 2018. https://www.the-dermatologist.com/article/3006. Accessed October 25, 2018.
I have written previously about Current Procedural Terminology (CPT) procedure codes submitted on the same date of service as evaluation and management (E/M) services in the context of modifier -25.1 Billing same-day procedures and E/M services is under close scrutiny by insurers, and accurate and complete documentation is a must.2 An understanding of what aspects of evaluation are included in the global surgical package is critical in deciding whether a separate and distinct same-day evaluation was performed. In general, the decision to perform a procedure is included in the payment for the procedure itself, as is the examination of the body site in question, diagnosis of the medical condition, discussion of treatment options, and postoperative services related to the procedure. This is true for CPT codes that contain physician work, which constitute the majority of CPT codes reported by dermatologists.3
However, there is one set of codes where these principles do not apply: the practice expense (PE)–only codes, or no physician work codes. These codes are defined by CPT and the Relative Value Scale Update Committee (RUC) of the American Medical Association as containing no physician work. Their valuations are based only on staff/nursing time and the other aspects of direct and indirect practice costs included in providing the service, such as gauze, sutures, equipment, office rent, and utilities.4 Examples of PE-only codes include the nonphysician-performed photodynamic therapy code 96567; phototherapy codes 96900, 96910, and 96912; and patch testing and photopatch testing codes 95044, 95052, and 95056.
For PE-only codes, only the provision of the service by staff is included in the code reimbursement; there is no physician time or work built into these codes. Thus, neither the initial evaluation of the patient by the physician, the decision to perform the procedure, nor the evaluation of therapy effectiveness or side effects or interpretation of the results is included. Understanding that there is no physician involvement in PE-only codes is critical in deciding whether an E/M service should be billed on the same day as a PE-only code. To that end, although a physician does not actually have to personally evaluate the patient on the day of service to bill PE-only codes, the Centers for Medicare & Medicaid Services has indicated that a physician or qualified medical provider must be on premises.5 Billing for PE-only services when no provider is present will be interpreted as a false claim or fraudulent billing practice.
Because PE-only codes do not include physician work, an E/M service will be billed in addition to the treatment almost any time a same-day physician evaluation is performed. For example, if a patient presents with a changing mole that is evaluated on the same date of service as phototherapy for the treatment of psoriasis, that service is clearly reportable with an E/M code because the mole check is separate and distinct from the phototherapy treatment. A more common scenario is for the physician to see a patient with a rash consistent with an allergic contact dermatitis and the decision to perform same-day patch testing is made. In this circumstance, the E/M service is still reportable because the evaluation of the rash and the decision to perform patch testing are not included in this PE-only code.
Phototherapy typically is provided as a prolonged course of multiple treatments, and reporting of same-day E/M services during the course of therapy is common. Phototherapy must be monitored by the physician for clinical effectiveness, dose changes, and side effects, as well as to determine whether to continue therapy. A standard operating procedure should be created to document that the physician typically evaluates the patient’s progress at set intervals or as dictated by patient or staff concerns. Reporting an E/M service with every phototherapy session is not considered medically necessary. Moreover, a nurse evaluation of the patient prior to each phototherapy treatment, including questions on disease severity, how the patient did with the last treatment, and whether medications have changed, is included in the payment for the phototherapy codes. Only formal and medically necessary physician E/M services should be billed, not drive-by visits in which the physician pops in just to see how the patient is doing.
Final Thoughts
Practice expense–only codes include no payment for physician time or work but require the presence of a qualified health care provider on premises to bill. Medically necessary physician evaluations on the same day as PE-only services will typically result in both an E/M service and the procedure being reported. Understanding performance and documentation requirements of PE-only codes is critical for proper reimbursement for a dermatology practice.
I have written previously about Current Procedural Terminology (CPT) procedure codes submitted on the same date of service as evaluation and management (E/M) services in the context of modifier -25.1 Billing same-day procedures and E/M services is under close scrutiny by insurers, and accurate and complete documentation is a must.2 An understanding of what aspects of evaluation are included in the global surgical package is critical in deciding whether a separate and distinct same-day evaluation was performed. In general, the decision to perform a procedure is included in the payment for the procedure itself, as is the examination of the body site in question, diagnosis of the medical condition, discussion of treatment options, and postoperative services related to the procedure. This is true for CPT codes that contain physician work, which constitute the majority of CPT codes reported by dermatologists.3
However, there is one set of codes where these principles do not apply: the practice expense (PE)–only codes, or no physician work codes. These codes are defined by CPT and the Relative Value Scale Update Committee (RUC) of the American Medical Association as containing no physician work. Their valuations are based only on staff/nursing time and the other aspects of direct and indirect practice costs included in providing the service, such as gauze, sutures, equipment, office rent, and utilities.4 Examples of PE-only codes include the nonphysician-performed photodynamic therapy code 96567; phototherapy codes 96900, 96910, and 96912; and patch testing and photopatch testing codes 95044, 95052, and 95056.
For PE-only codes, only the provision of the service by staff is included in the code reimbursement; there is no physician time or work built into these codes. Thus, neither the initial evaluation of the patient by the physician, the decision to perform the procedure, nor the evaluation of therapy effectiveness or side effects or interpretation of the results is included. Understanding that there is no physician involvement in PE-only codes is critical in deciding whether an E/M service should be billed on the same day as a PE-only code. To that end, although a physician does not actually have to personally evaluate the patient on the day of service to bill PE-only codes, the Centers for Medicare & Medicaid Services has indicated that a physician or qualified medical provider must be on premises.5 Billing for PE-only services when no provider is present will be interpreted as a false claim or fraudulent billing practice.
Because PE-only codes do not include physician work, an E/M service will be billed in addition to the treatment almost any time a same-day physician evaluation is performed. For example, if a patient presents with a changing mole that is evaluated on the same date of service as phototherapy for the treatment of psoriasis, that service is clearly reportable with an E/M code because the mole check is separate and distinct from the phototherapy treatment. A more common scenario is for the physician to see a patient with a rash consistent with an allergic contact dermatitis and the decision to perform same-day patch testing is made. In this circumstance, the E/M service is still reportable because the evaluation of the rash and the decision to perform patch testing are not included in this PE-only code.
Phototherapy typically is provided as a prolonged course of multiple treatments, and reporting of same-day E/M services during the course of therapy is common. Phototherapy must be monitored by the physician for clinical effectiveness, dose changes, and side effects, as well as to determine whether to continue therapy. A standard operating procedure should be created to document that the physician typically evaluates the patient’s progress at set intervals or as dictated by patient or staff concerns. Reporting an E/M service with every phototherapy session is not considered medically necessary. Moreover, a nurse evaluation of the patient prior to each phototherapy treatment, including questions on disease severity, how the patient did with the last treatment, and whether medications have changed, is included in the payment for the phototherapy codes. Only formal and medically necessary physician E/M services should be billed, not drive-by visits in which the physician pops in just to see how the patient is doing.
Final Thoughts
Practice expense–only codes include no payment for physician time or work but require the presence of a qualified health care provider on premises to bill. Medically necessary physician evaluations on the same day as PE-only services will typically result in both an E/M service and the procedure being reported. Understanding performance and documentation requirements of PE-only codes is critical for proper reimbursement for a dermatology practice.
- Rogers H. One diagnosis and modifier -25: appropriate or audit target? Cutis. 2017;99:165-166.
- Rogers H. Modifier -25 victory, but the battle is not over. Cutis. 2018;101:409-410.
- American Academy of Dermatology. Medicare update. Derm Coding Consult. March 2001;5:5-7. https://www.aad.org/File%20Library/Global%20navigation/Member%20tools%20and%20benefits/Publications/Derm%20Coding%20Consult%20archives/2001-spring.pdf.
- Current Procedural Terminology 2018, Professional Edition. Chicago, IL: American Medical Association; 2018.
- Determining who has the authority to bill. The Dermatologist. September 4, 2018. https://www.the-dermatologist.com/article/3006. Accessed October 25, 2018.
- Rogers H. One diagnosis and modifier -25: appropriate or audit target? Cutis. 2017;99:165-166.
- Rogers H. Modifier -25 victory, but the battle is not over. Cutis. 2018;101:409-410.
- American Academy of Dermatology. Medicare update. Derm Coding Consult. March 2001;5:5-7. https://www.aad.org/File%20Library/Global%20navigation/Member%20tools%20and%20benefits/Publications/Derm%20Coding%20Consult%20archives/2001-spring.pdf.
- Current Procedural Terminology 2018, Professional Edition. Chicago, IL: American Medical Association; 2018.
- Determining who has the authority to bill. The Dermatologist. September 4, 2018. https://www.the-dermatologist.com/article/3006. Accessed October 25, 2018.
Practice Points
- Billing same-day procedures and evaluation and management services is under close scrutiny by insurers, and accurate and complete documentation is a must.
- For practice expense–only codes, only the provision of the service by staff is included in the code reimbursement; there is no physician time or work built into these codes.
- Practice expense–only codes require the presence of a qualified health care provider on premises to bill.
Modifier -25 Victory, But the Battle Is Not Over
On February 23, 2018, Anthem Insurance Companies, Inc, announced the reversal of its proposed policy to reduce reimbursement for evaluation and management (E/M) services billed using modifier -25.1 This win for physicians was the result of a broad-based, multipronged advocacy campaign, and the American Academy of Dermatology Association (AADA) was critical to this victory.
Dermatology Took the Lead in Opposing Policy That Would Reduce Reimbursement
Dermatology was the first to trumpet the dangers of modifier -25 reduction policies and explain why other specialty societies should care. The AADA took the lead in assembling a coalition of physician groups to oppose the proposed policy by sharing language for opposition letters and meeting talking points with many societies outside of dermatology as well as producing the first draft for the American Medical Association (AMA) House of Delegates’ resolution that spurred action against Anthem’s proposed policy.2 Members of the AADA attended numerous conference calls and in-person meetings with health insurance officials to urge them to reverse the policy and helped coordinate opposition from state and national specialty societies. The influence and advocacy of the AMA was critical in reversing the proposed policy, but dermatology started the opposition and organized the players to bring the fight against Anthem.
AADA Continues to Fight
Despite the victory against Anthem, challenges to fair reimbursement of modifier -25 claims are ongoing. Two insurers recently announced implementation of new modifier -25 reduction policies.3,4 Moreover, 4 other insurers have existing modifier -25 reduction policies in place.5-8 The AADA has engaged, and will continue engaging, each of these insurers with the message that the ability to perform procedures and distinct E/M services on the same day is integral to efficient, patient-centered care of dermatologic diseases. The AADA argues that insurers’ rationale (overlapping indirect practice expenses) for payment reduction is improper and that appropriately documented modifier -25 claims should be reimbursed at 100% of allowable charges.
In addition to the existing insurer policies affecting modifier -25, Anthem has announced that it plans to conduct audits of modifier -25 claims with recoupments of inappropriate charges.1 Some Medicare Administrative Contractors also have cited modifier -25 as an area of concern and issued guidelines for reporting modifier -25, which frequently precede audits.9 The AADA is concerned that if Anthem follows through with its aggressive audits to recoup money, which can result in substantial take-backs, and finds a high error rate in modifier -25 claims, it also may consider revisiting its reduction policy. Moreover, it is likely that other insurers will use failed modifier -25 audits as an excuse to continue, expand, or adopt modifier -25 reduction policies. It is clear that blanket reduction in payment is much easier and less expensive for insurers than auditing medical records and not paying those who abuse modifier -25. As long as insurers are under financial pressure, modifier -25 will be a tempting target for reducing health care costs.
How to Use Modifier -25 Correctly
In addition to opposing inappropriate reimbursement of modifier -25, the AADA is committed to educating its members and insurers on the correct use and documentation of modifier -25. In December 2017, Mollie A. MacCormack, MD (Nashua, New Hampshire), and I led an educational webinar on modifier -25 for more than 1100 attendees.10 We discussed the performance standards and documentation requirements of modifier -25. It was clear that dermatologists were interested not only in the correct coding of modifier -25 claims but also avoiding the consequences of audits.
My peers frequently ask, “What can we [dermatologists] do to prepare for potential modifier -25 audits?” My advice is always, “Physician audit thyself.” I recommend self-auditing to make sure you and your practice are in compliance with modifier -25 documentation requirements. In a March 2017 Cutis column on modifier -25, I discussed what constitutes separate and distinct E/M services and what is included in a procedure’s global surgical package.11 A self-audit is as simple as pulling 10 to 20 medical records in which a same-day procedure and E/M service were billed. Cross out any information in the note included in the procedure’s global surgical package including history associated with establishing the diagnosis, physical examination of the procedure area(s), and discussion of treatment options. If complete documentation for an E/M is still present after removing the procedure and associated evaluation, you have passed the self-audit. If not, consider changing your coding to better reflect the documentation in your records. In my experience, insurance auditors are not physicians and often are not even medical professionals. Clear documentation and clear existence of a separate, distinct, and medically necessary E/M service is needed to succeed in a modifier -25 audit.
Final Thoughts
Dermatologists should rejoice that Anthem decided to rescind its modifier -25 policy. If this policy had gone into effect, the modifier -25 reduction would likely have spread to most other insurers as industry standard. This victory certainly shows what can be accomplished when organized medicine works together. Your state dermatology and medical societies, national societies, and the AMA collaborated on a critical existential threat to cost-effective and efficient patient care and won. These organizations deserve your membership and support as well as your thanks; however, our celebration must be short-lived, as there still are other insurers with modifier -25 reductions in place, and audits have been promised. We must continue to focus on proper use and documentation of modifier -25. This effort will not only help dermatologists decrease the risk of large recoupments from audits but also help the AADA continue to oppose inappropriate payment policies.
- Anthem Insurance Companies, Inc. Network Update. April 2018. https://www11.anthem.com/provider/ct/f5/s1/t0/pw_g334020.pdf?refer=ahpprovider&state=ct. Accessed May 25, 2018.
- American Academy of Dermatology, American Society for Dermatologic Surgery Association, American College of Mohs Surgery, American Society of Dermatopathology, Society for Investigative Dermatology. Opposition to reduced payment for the 25 modifier. https://www.ama-assn.org/sites/default/files/media-browser/public/hod/i17-808.pdf. Accessed May 14, 2018.
- We’re changing the payment policy when evaluation and management services are billed with surgery. Blue Cross Blue Shield of Michigan website. https://www.bcbsm.com/newsletter/therecord/2018/record_0418/Record_0418u.shtml. Published April 2018. Accessed May 14, 2018.
- Centene Corporation. Payment policy: problem oriented visits billed with surgical procedures. https://www.superiorhealthplan.com/content/dam/centene/Superior/Provider/PDFs/Problem%20Oriented%20Visits%20Billed
%20with%20Surgical%20Procedures%20(Ambetter%20MMP
%20and%20Medicare%20Advantage%20Only).pdf. Accessed May 14, 2018. - Blue Cross Blue Shield of Rhode Island. Payment Policy: Coding and Payment Guidelines. August 16, 2016. https://www.bcbsri.com/sites/default/files/polices/Coding-and-Payment-Guidelines-Oct2016.pdf. Accessed May 9, 2018.
- Modifier payment policy. Tufts Health Plan website. https://tuftshealthplan.com/documents/providers/payment-policies/modifier-payment-policy. Updated November 2017. Accessed May 14, 2018.
- Harvard Pilgrim Health Care. Payment Policies: Evaluation and Management. February 2018. https://www.harvardpilgrim.org/pls/portal/docs/PAGE/PROVIDERS/MANUALS/PAYMENT%20POLICIES/H-2%20EVALUATION-MGT_02
0118.PDF. Accessed May 25, 2018. - Updates to the policies on modifier 25 reporting and reimbursement. Independence Blue Cross website. http://provcomm.ibx.com/ProvComm/ProvComm.nsf/4bcc623b93e226638525792c00575962/bbe9e72728cc01e285258167005c629d!OpenDocument. Published July 24, 2017. Accessed May 14, 2018.
- Centers for Medicare & Medicaid Services. Payment for evaluation and management services provided during global period of surgery. MLN Matters. May 19, 2006. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM5025.pdf. Accessed May 14, 2018.
- Audits on modifier 25 are coming—complimentary live webinar. American Academy of Dermatology website. https://store.aad.org/products/11928. Accessed May 9, 2018.
- Rogers HW. One diagnosis and modifier -25: appropriate or audit target? Cutis. 2017;99:165-166.
On February 23, 2018, Anthem Insurance Companies, Inc, announced the reversal of its proposed policy to reduce reimbursement for evaluation and management (E/M) services billed using modifier -25.1 This win for physicians was the result of a broad-based, multipronged advocacy campaign, and the American Academy of Dermatology Association (AADA) was critical to this victory.
Dermatology Took the Lead in Opposing Policy That Would Reduce Reimbursement
Dermatology was the first to trumpet the dangers of modifier -25 reduction policies and explain why other specialty societies should care. The AADA took the lead in assembling a coalition of physician groups to oppose the proposed policy by sharing language for opposition letters and meeting talking points with many societies outside of dermatology as well as producing the first draft for the American Medical Association (AMA) House of Delegates’ resolution that spurred action against Anthem’s proposed policy.2 Members of the AADA attended numerous conference calls and in-person meetings with health insurance officials to urge them to reverse the policy and helped coordinate opposition from state and national specialty societies. The influence and advocacy of the AMA was critical in reversing the proposed policy, but dermatology started the opposition and organized the players to bring the fight against Anthem.
AADA Continues to Fight
Despite the victory against Anthem, challenges to fair reimbursement of modifier -25 claims are ongoing. Two insurers recently announced implementation of new modifier -25 reduction policies.3,4 Moreover, 4 other insurers have existing modifier -25 reduction policies in place.5-8 The AADA has engaged, and will continue engaging, each of these insurers with the message that the ability to perform procedures and distinct E/M services on the same day is integral to efficient, patient-centered care of dermatologic diseases. The AADA argues that insurers’ rationale (overlapping indirect practice expenses) for payment reduction is improper and that appropriately documented modifier -25 claims should be reimbursed at 100% of allowable charges.
In addition to the existing insurer policies affecting modifier -25, Anthem has announced that it plans to conduct audits of modifier -25 claims with recoupments of inappropriate charges.1 Some Medicare Administrative Contractors also have cited modifier -25 as an area of concern and issued guidelines for reporting modifier -25, which frequently precede audits.9 The AADA is concerned that if Anthem follows through with its aggressive audits to recoup money, which can result in substantial take-backs, and finds a high error rate in modifier -25 claims, it also may consider revisiting its reduction policy. Moreover, it is likely that other insurers will use failed modifier -25 audits as an excuse to continue, expand, or adopt modifier -25 reduction policies. It is clear that blanket reduction in payment is much easier and less expensive for insurers than auditing medical records and not paying those who abuse modifier -25. As long as insurers are under financial pressure, modifier -25 will be a tempting target for reducing health care costs.
How to Use Modifier -25 Correctly
In addition to opposing inappropriate reimbursement of modifier -25, the AADA is committed to educating its members and insurers on the correct use and documentation of modifier -25. In December 2017, Mollie A. MacCormack, MD (Nashua, New Hampshire), and I led an educational webinar on modifier -25 for more than 1100 attendees.10 We discussed the performance standards and documentation requirements of modifier -25. It was clear that dermatologists were interested not only in the correct coding of modifier -25 claims but also avoiding the consequences of audits.
My peers frequently ask, “What can we [dermatologists] do to prepare for potential modifier -25 audits?” My advice is always, “Physician audit thyself.” I recommend self-auditing to make sure you and your practice are in compliance with modifier -25 documentation requirements. In a March 2017 Cutis column on modifier -25, I discussed what constitutes separate and distinct E/M services and what is included in a procedure’s global surgical package.11 A self-audit is as simple as pulling 10 to 20 medical records in which a same-day procedure and E/M service were billed. Cross out any information in the note included in the procedure’s global surgical package including history associated with establishing the diagnosis, physical examination of the procedure area(s), and discussion of treatment options. If complete documentation for an E/M is still present after removing the procedure and associated evaluation, you have passed the self-audit. If not, consider changing your coding to better reflect the documentation in your records. In my experience, insurance auditors are not physicians and often are not even medical professionals. Clear documentation and clear existence of a separate, distinct, and medically necessary E/M service is needed to succeed in a modifier -25 audit.
Final Thoughts
Dermatologists should rejoice that Anthem decided to rescind its modifier -25 policy. If this policy had gone into effect, the modifier -25 reduction would likely have spread to most other insurers as industry standard. This victory certainly shows what can be accomplished when organized medicine works together. Your state dermatology and medical societies, national societies, and the AMA collaborated on a critical existential threat to cost-effective and efficient patient care and won. These organizations deserve your membership and support as well as your thanks; however, our celebration must be short-lived, as there still are other insurers with modifier -25 reductions in place, and audits have been promised. We must continue to focus on proper use and documentation of modifier -25. This effort will not only help dermatologists decrease the risk of large recoupments from audits but also help the AADA continue to oppose inappropriate payment policies.
On February 23, 2018, Anthem Insurance Companies, Inc, announced the reversal of its proposed policy to reduce reimbursement for evaluation and management (E/M) services billed using modifier -25.1 This win for physicians was the result of a broad-based, multipronged advocacy campaign, and the American Academy of Dermatology Association (AADA) was critical to this victory.
Dermatology Took the Lead in Opposing Policy That Would Reduce Reimbursement
Dermatology was the first to trumpet the dangers of modifier -25 reduction policies and explain why other specialty societies should care. The AADA took the lead in assembling a coalition of physician groups to oppose the proposed policy by sharing language for opposition letters and meeting talking points with many societies outside of dermatology as well as producing the first draft for the American Medical Association (AMA) House of Delegates’ resolution that spurred action against Anthem’s proposed policy.2 Members of the AADA attended numerous conference calls and in-person meetings with health insurance officials to urge them to reverse the policy and helped coordinate opposition from state and national specialty societies. The influence and advocacy of the AMA was critical in reversing the proposed policy, but dermatology started the opposition and organized the players to bring the fight against Anthem.
AADA Continues to Fight
Despite the victory against Anthem, challenges to fair reimbursement of modifier -25 claims are ongoing. Two insurers recently announced implementation of new modifier -25 reduction policies.3,4 Moreover, 4 other insurers have existing modifier -25 reduction policies in place.5-8 The AADA has engaged, and will continue engaging, each of these insurers with the message that the ability to perform procedures and distinct E/M services on the same day is integral to efficient, patient-centered care of dermatologic diseases. The AADA argues that insurers’ rationale (overlapping indirect practice expenses) for payment reduction is improper and that appropriately documented modifier -25 claims should be reimbursed at 100% of allowable charges.
In addition to the existing insurer policies affecting modifier -25, Anthem has announced that it plans to conduct audits of modifier -25 claims with recoupments of inappropriate charges.1 Some Medicare Administrative Contractors also have cited modifier -25 as an area of concern and issued guidelines for reporting modifier -25, which frequently precede audits.9 The AADA is concerned that if Anthem follows through with its aggressive audits to recoup money, which can result in substantial take-backs, and finds a high error rate in modifier -25 claims, it also may consider revisiting its reduction policy. Moreover, it is likely that other insurers will use failed modifier -25 audits as an excuse to continue, expand, or adopt modifier -25 reduction policies. It is clear that blanket reduction in payment is much easier and less expensive for insurers than auditing medical records and not paying those who abuse modifier -25. As long as insurers are under financial pressure, modifier -25 will be a tempting target for reducing health care costs.
How to Use Modifier -25 Correctly
In addition to opposing inappropriate reimbursement of modifier -25, the AADA is committed to educating its members and insurers on the correct use and documentation of modifier -25. In December 2017, Mollie A. MacCormack, MD (Nashua, New Hampshire), and I led an educational webinar on modifier -25 for more than 1100 attendees.10 We discussed the performance standards and documentation requirements of modifier -25. It was clear that dermatologists were interested not only in the correct coding of modifier -25 claims but also avoiding the consequences of audits.
My peers frequently ask, “What can we [dermatologists] do to prepare for potential modifier -25 audits?” My advice is always, “Physician audit thyself.” I recommend self-auditing to make sure you and your practice are in compliance with modifier -25 documentation requirements. In a March 2017 Cutis column on modifier -25, I discussed what constitutes separate and distinct E/M services and what is included in a procedure’s global surgical package.11 A self-audit is as simple as pulling 10 to 20 medical records in which a same-day procedure and E/M service were billed. Cross out any information in the note included in the procedure’s global surgical package including history associated with establishing the diagnosis, physical examination of the procedure area(s), and discussion of treatment options. If complete documentation for an E/M is still present after removing the procedure and associated evaluation, you have passed the self-audit. If not, consider changing your coding to better reflect the documentation in your records. In my experience, insurance auditors are not physicians and often are not even medical professionals. Clear documentation and clear existence of a separate, distinct, and medically necessary E/M service is needed to succeed in a modifier -25 audit.
Final Thoughts
Dermatologists should rejoice that Anthem decided to rescind its modifier -25 policy. If this policy had gone into effect, the modifier -25 reduction would likely have spread to most other insurers as industry standard. This victory certainly shows what can be accomplished when organized medicine works together. Your state dermatology and medical societies, national societies, and the AMA collaborated on a critical existential threat to cost-effective and efficient patient care and won. These organizations deserve your membership and support as well as your thanks; however, our celebration must be short-lived, as there still are other insurers with modifier -25 reductions in place, and audits have been promised. We must continue to focus on proper use and documentation of modifier -25. This effort will not only help dermatologists decrease the risk of large recoupments from audits but also help the AADA continue to oppose inappropriate payment policies.
- Anthem Insurance Companies, Inc. Network Update. April 2018. https://www11.anthem.com/provider/ct/f5/s1/t0/pw_g334020.pdf?refer=ahpprovider&state=ct. Accessed May 25, 2018.
- American Academy of Dermatology, American Society for Dermatologic Surgery Association, American College of Mohs Surgery, American Society of Dermatopathology, Society for Investigative Dermatology. Opposition to reduced payment for the 25 modifier. https://www.ama-assn.org/sites/default/files/media-browser/public/hod/i17-808.pdf. Accessed May 14, 2018.
- We’re changing the payment policy when evaluation and management services are billed with surgery. Blue Cross Blue Shield of Michigan website. https://www.bcbsm.com/newsletter/therecord/2018/record_0418/Record_0418u.shtml. Published April 2018. Accessed May 14, 2018.
- Centene Corporation. Payment policy: problem oriented visits billed with surgical procedures. https://www.superiorhealthplan.com/content/dam/centene/Superior/Provider/PDFs/Problem%20Oriented%20Visits%20Billed
%20with%20Surgical%20Procedures%20(Ambetter%20MMP
%20and%20Medicare%20Advantage%20Only).pdf. Accessed May 14, 2018. - Blue Cross Blue Shield of Rhode Island. Payment Policy: Coding and Payment Guidelines. August 16, 2016. https://www.bcbsri.com/sites/default/files/polices/Coding-and-Payment-Guidelines-Oct2016.pdf. Accessed May 9, 2018.
- Modifier payment policy. Tufts Health Plan website. https://tuftshealthplan.com/documents/providers/payment-policies/modifier-payment-policy. Updated November 2017. Accessed May 14, 2018.
- Harvard Pilgrim Health Care. Payment Policies: Evaluation and Management. February 2018. https://www.harvardpilgrim.org/pls/portal/docs/PAGE/PROVIDERS/MANUALS/PAYMENT%20POLICIES/H-2%20EVALUATION-MGT_02
0118.PDF. Accessed May 25, 2018. - Updates to the policies on modifier 25 reporting and reimbursement. Independence Blue Cross website. http://provcomm.ibx.com/ProvComm/ProvComm.nsf/4bcc623b93e226638525792c00575962/bbe9e72728cc01e285258167005c629d!OpenDocument. Published July 24, 2017. Accessed May 14, 2018.
- Centers for Medicare & Medicaid Services. Payment for evaluation and management services provided during global period of surgery. MLN Matters. May 19, 2006. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM5025.pdf. Accessed May 14, 2018.
- Audits on modifier 25 are coming—complimentary live webinar. American Academy of Dermatology website. https://store.aad.org/products/11928. Accessed May 9, 2018.
- Rogers HW. One diagnosis and modifier -25: appropriate or audit target? Cutis. 2017;99:165-166.
- Anthem Insurance Companies, Inc. Network Update. April 2018. https://www11.anthem.com/provider/ct/f5/s1/t0/pw_g334020.pdf?refer=ahpprovider&state=ct. Accessed May 25, 2018.
- American Academy of Dermatology, American Society for Dermatologic Surgery Association, American College of Mohs Surgery, American Society of Dermatopathology, Society for Investigative Dermatology. Opposition to reduced payment for the 25 modifier. https://www.ama-assn.org/sites/default/files/media-browser/public/hod/i17-808.pdf. Accessed May 14, 2018.
- We’re changing the payment policy when evaluation and management services are billed with surgery. Blue Cross Blue Shield of Michigan website. https://www.bcbsm.com/newsletter/therecord/2018/record_0418/Record_0418u.shtml. Published April 2018. Accessed May 14, 2018.
- Centene Corporation. Payment policy: problem oriented visits billed with surgical procedures. https://www.superiorhealthplan.com/content/dam/centene/Superior/Provider/PDFs/Problem%20Oriented%20Visits%20Billed
%20with%20Surgical%20Procedures%20(Ambetter%20MMP
%20and%20Medicare%20Advantage%20Only).pdf. Accessed May 14, 2018. - Blue Cross Blue Shield of Rhode Island. Payment Policy: Coding and Payment Guidelines. August 16, 2016. https://www.bcbsri.com/sites/default/files/polices/Coding-and-Payment-Guidelines-Oct2016.pdf. Accessed May 9, 2018.
- Modifier payment policy. Tufts Health Plan website. https://tuftshealthplan.com/documents/providers/payment-policies/modifier-payment-policy. Updated November 2017. Accessed May 14, 2018.
- Harvard Pilgrim Health Care. Payment Policies: Evaluation and Management. February 2018. https://www.harvardpilgrim.org/pls/portal/docs/PAGE/PROVIDERS/MANUALS/PAYMENT%20POLICIES/H-2%20EVALUATION-MGT_02
0118.PDF. Accessed May 25, 2018. - Updates to the policies on modifier 25 reporting and reimbursement. Independence Blue Cross website. http://provcomm.ibx.com/ProvComm/ProvComm.nsf/4bcc623b93e226638525792c00575962/bbe9e72728cc01e285258167005c629d!OpenDocument. Published July 24, 2017. Accessed May 14, 2018.
- Centers for Medicare & Medicaid Services. Payment for evaluation and management services provided during global period of surgery. MLN Matters. May 19, 2006. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM5025.pdf. Accessed May 14, 2018.
- Audits on modifier 25 are coming—complimentary live webinar. American Academy of Dermatology website. https://store.aad.org/products/11928. Accessed May 9, 2018.
- Rogers HW. One diagnosis and modifier -25: appropriate or audit target? Cutis. 2017;99:165-166.
Practice Points
- Insurers are increasingly targeting modifier -25 for audits and payment reductions.
- Physicians should understand modifier -25 documentation requirements and self-audit to ensure compliance.
Let There Be Light: Update on Coding for Photodynamic Therapy and Lasers
Winter is the time when many religions celebrate a renewal of the year as the days begin to get longer. On January 1 of each year in the United States we celebrate the official activation of new and revised
Photodynamic Therapy
In 2004, a methyl aminolevulinate cream that was activated with a red light source was brought to market; however, after failing to gain a substantial market share, the product is no longer available in the United States. In May of 2016, a nanoemulsion gel formulation of aminolevulinic acid hydrochloride 10% was approved by the US Food and Drug Administration4 for use with a red light source. Unlike 5-aminolevulinic acid hydrochloride solution, which was approved for application with no prior debridement of the skin,5 the new gel formulation was meant to be applied after degreasing with an ethanol- or isopropanol-soaked cotton pad and removal of any scaling or crusts, followed by roughening of the lesion surfaces (with care taken to avoid bleeding).4 The product must be administered by a health care provider and is reported using CPT codes 96573 and 96574, which are new in 2018 and are discussed in more detail below. Effective January 1, 2018, the Healthcare Common Procedure Coding System supply code for the product is J7345 (aminolevulinic acid hydrochloride gel for topical administration, 10% gel, 10 mg).6 A single tube contains 200 mg, so when an entire tube is used (which is typical), 200 units must be reported. Partial tubes may be used in some patients and should be reported appropriately based on actual usage.
The development of new CPT codes for PDT revealed a middle ground in which many physicians, including myself, have applied the photosensitizing drug themselves instead of a nonphysician provider in order to use their professional judgment to ensure the entire treatment area was covered and also allow for multiple applications of the drug to lesions that in their opinion may have warranted greater dosing, which led to the creation of CPT code 96573. The revision and refinement from one code to 3 (96567, 96573, and 96574) also involved rewording of the preamble for all 3 codes so that the phrase “premalignant and/or malignant lesions” was simplified to “premalignant lesions.” This change was made so that if and when this therapeutic approach is refined enough to be used on malignant lesions, new codes can be created to distinguish between the work performed for both types of lesions.
The new PDT codes include 96573 (photodynamic therapy by external application of light to destroy premalignant lesions of the skin and adjacent mucosa with application and illumination/activation of photosensitizing drug[s] provided by a physician or other qualified healthcare professional, per day) and 96574 (debridement of premalignant hyperkeratotic lesion[s][ie, targeted curettage, abrasion] followed with photodynamic therapy by external application of light to destroy premalignant lesions of the skin and adjacent mucosa with application and illumination/activation of photosensitizing drug[s] provided by a physician or other qualified healthcare professional, per day). According to the 2018 CPT manual,2 these codes should be used to report nonsurgical treatment of cutaneous lesions using PDT (ie, external application of light to destroy premalignant lesions of the skin and adjacent mucosa by activation of photosensitizing drug). A treatment session is defined as an application of a photosensitizer to all lesions within an anatomic area (eg, face, scalp) with or without debridement of all premalignant hyperkeratotic lesions in that area followed by illumination and activation with an appropriate light source. Providers should not report codes for debridement (11000, 11001, 11004, 11005), lesion shaving (11300–11313), biopsy (11100, 11101), or lesion excision (11400–11471) within the treatment area on the same day that PDT is administered.2
With the inclusion of these new PDT codes, the older code 96567 (photodynamic therapy by external application of light to destroy premalignant lesions of the skin and adjacent mucosa with application and illumination/activation of photosensitive drug[s], per day)—which is the base or parent code of the set—should only be used for reporting PDT when a physician or other qualified health care professional is not directly involved in the delivery of the service. Code 96573 is an upgrade to 96567 to account for physician work, while code 96574 captures the extra work of disruption of the skin barrier by debridement.
The novelty here is that old codes often are replaced when new codes come along. The reader should be aware of the distinct differences, as the total value expressed in relative value units for code 96567 is lower than it was in 2017 (3.24 vs 3.80), while the 2 newer codes have higher values (codes 96573 and 96574, 5.37 and 6.92, respectively). Additionally, the reader should note that only one of the 3 codes can be used on a given anatomic area (ie, face and scalp) on a given day. In general, a single-dose package of either of the approved photosensitizing drugs can usually treat an entire anatomic area. The codes themselves are not reserved for specific anatomic areas, but the US Food and Drug Administration clearances are for only face and scalp for both drugs, so the use of more than 2 PDT codes on a given day might raise payer queries.
Whatever you do, be sure your documentation includes an explicit notation about who applied the photosensitizing drug and the technique used for debridement, if performed. Code 96574 explicitly refers to targeted curettage and abrasion but does not include other destructive modalities (eg, chemical peeling), which an auditor may or may not consider an acceptable method of debridement. Personally, I will not be using peels as a justifier for this code.
Lasers
Lasers have played a role in the treatment of severe scarring in wounded warriors and other patient populations.7 Until 2018, there were no CPT codes that allowed precise reporting of these therapies. We now have a series of tracking codes, which are not valued by the Specialty Society Relative Value Scale Update Committee process but are nonetheless reportable, for this valuable treatment.8
The base code for a new pair of codes for reporting fractional ablative laser treatment, which is modeled after the skin graft code series, is 0479T (fractional ablative laser fenestration of burn and traumatic scars for functional improvement; first 100 cm2 or part thereof, or 1% of body surface area of infants and children). The add-on code is 0480T (fractional ablative laser fenestration of burn and traumatic scars for functional improvement; each additional 100 cm2, or each additional 1% of body surface area of infants and children, or part thereof [list separately in addition to code for primary procedure]), which means the code can be reported multiple times in addition to a single unit of 0479T. The aggregate treatment area should only be reported once per day regardless of the number of passes of one or more lasers over the area that day, and codes 0479T and 0480T should not be reported with codes 0491T or 0492T, which are a new family of tracking codes used for ablative laser treatment of chronic open wounds. If the scars are excised in a full-thickness manner, the benign excision codes 11400 to 11446 should be used instead.
For laser treatment of open wounds, 0491T (ablative laser treatment, noncontact, full-field and fractional ablation, open wound, per day, total treatment surface area; first 20 cm2 or less) is the base code for this pair of codes, and 0492T (ablative laser treatment, noncontact, full-field and fractional ablation, open wound, per day, total treatment surface area; each additional 20 cm2, or part thereof [list separately in addition to code for primary procedure]) is the add-on code, similar to the 0479T and 00480T codes described above. Keep in mind that all 4 of these tracking codes do not have defined values, and payment is at the discretion of the payer. If utilization of the procedures increases along with the development of appropriate evidence-based literature to support it, it is possible these will be converted into standard category I CPT codes that will be valued and covered by payers.
Final Thoughts
For more details on the new codes for PDT and lasers, I would strongly suggest obtaining a copy of CPT Changes 2018: An Insider’s View (https://commerce.ama-assn.org/store/catalog/productDetail.jsp?product_id=prod2800018&navAction=push), as well as the 2018 CPT manual for those who are actively practicing. Members of the American Academy of Dermatology also can get the new CPT manual as part of the group’s Coding Value Pack (https://store.aad.org/products/11383) along with Principles of Documentation for Dermatology and 2018 Coding & Billing for Dermatology.
- Daniell MD, Hill JS. A history of photodynamic therapy. Aust N Z J Surg. 1991;61:340-348.
- Current Procedural Terminology 2018, Professional Edition. Chicago, IL: American Medical Association; 2018.
- HCPCS code J7308. HCPCS Complete Reference website. https://hcpcs.codes/j-codes/J7308/. Accessed March 1, 2018.
- Ameluz [package insert]. Wakefield, MA: Biofrontera Inc; 2017.
- Levulan Kerastick [package insert]. Wilmington, MA: Dusa Pharmaceuticals, Inc; 2010.
- Centers for Medicare & Medicaid Services. 2018 Table of drugs. CMS website. https://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/Downloads/2018-Table-of-Drugs.pdf. Updated February 15, 2018. Accessed February 21, 2018.
- Waibel JS, Rudnick A. Current trends and future considerations in scar treatment. Semin Cutan Med Surg. 2015;34:13-16.
- American Medical Association. CPT category III codes. AMA website. https://www.ama-assn.org/sites/default/files/media-browser/public/cpt/cpt-category3-codes-descriptors.pdf. Updated December 21, 2017. Accessed February 21, 2018.
Winter is the time when many religions celebrate a renewal of the year as the days begin to get longer. On January 1 of each year in the United States we celebrate the official activation of new and revised
Photodynamic Therapy
In 2004, a methyl aminolevulinate cream that was activated with a red light source was brought to market; however, after failing to gain a substantial market share, the product is no longer available in the United States. In May of 2016, a nanoemulsion gel formulation of aminolevulinic acid hydrochloride 10% was approved by the US Food and Drug Administration4 for use with a red light source. Unlike 5-aminolevulinic acid hydrochloride solution, which was approved for application with no prior debridement of the skin,5 the new gel formulation was meant to be applied after degreasing with an ethanol- or isopropanol-soaked cotton pad and removal of any scaling or crusts, followed by roughening of the lesion surfaces (with care taken to avoid bleeding).4 The product must be administered by a health care provider and is reported using CPT codes 96573 and 96574, which are new in 2018 and are discussed in more detail below. Effective January 1, 2018, the Healthcare Common Procedure Coding System supply code for the product is J7345 (aminolevulinic acid hydrochloride gel for topical administration, 10% gel, 10 mg).6 A single tube contains 200 mg, so when an entire tube is used (which is typical), 200 units must be reported. Partial tubes may be used in some patients and should be reported appropriately based on actual usage.
The development of new CPT codes for PDT revealed a middle ground in which many physicians, including myself, have applied the photosensitizing drug themselves instead of a nonphysician provider in order to use their professional judgment to ensure the entire treatment area was covered and also allow for multiple applications of the drug to lesions that in their opinion may have warranted greater dosing, which led to the creation of CPT code 96573. The revision and refinement from one code to 3 (96567, 96573, and 96574) also involved rewording of the preamble for all 3 codes so that the phrase “premalignant and/or malignant lesions” was simplified to “premalignant lesions.” This change was made so that if and when this therapeutic approach is refined enough to be used on malignant lesions, new codes can be created to distinguish between the work performed for both types of lesions.
The new PDT codes include 96573 (photodynamic therapy by external application of light to destroy premalignant lesions of the skin and adjacent mucosa with application and illumination/activation of photosensitizing drug[s] provided by a physician or other qualified healthcare professional, per day) and 96574 (debridement of premalignant hyperkeratotic lesion[s][ie, targeted curettage, abrasion] followed with photodynamic therapy by external application of light to destroy premalignant lesions of the skin and adjacent mucosa with application and illumination/activation of photosensitizing drug[s] provided by a physician or other qualified healthcare professional, per day). According to the 2018 CPT manual,2 these codes should be used to report nonsurgical treatment of cutaneous lesions using PDT (ie, external application of light to destroy premalignant lesions of the skin and adjacent mucosa by activation of photosensitizing drug). A treatment session is defined as an application of a photosensitizer to all lesions within an anatomic area (eg, face, scalp) with or without debridement of all premalignant hyperkeratotic lesions in that area followed by illumination and activation with an appropriate light source. Providers should not report codes for debridement (11000, 11001, 11004, 11005), lesion shaving (11300–11313), biopsy (11100, 11101), or lesion excision (11400–11471) within the treatment area on the same day that PDT is administered.2
With the inclusion of these new PDT codes, the older code 96567 (photodynamic therapy by external application of light to destroy premalignant lesions of the skin and adjacent mucosa with application and illumination/activation of photosensitive drug[s], per day)—which is the base or parent code of the set—should only be used for reporting PDT when a physician or other qualified health care professional is not directly involved in the delivery of the service. Code 96573 is an upgrade to 96567 to account for physician work, while code 96574 captures the extra work of disruption of the skin barrier by debridement.
The novelty here is that old codes often are replaced when new codes come along. The reader should be aware of the distinct differences, as the total value expressed in relative value units for code 96567 is lower than it was in 2017 (3.24 vs 3.80), while the 2 newer codes have higher values (codes 96573 and 96574, 5.37 and 6.92, respectively). Additionally, the reader should note that only one of the 3 codes can be used on a given anatomic area (ie, face and scalp) on a given day. In general, a single-dose package of either of the approved photosensitizing drugs can usually treat an entire anatomic area. The codes themselves are not reserved for specific anatomic areas, but the US Food and Drug Administration clearances are for only face and scalp for both drugs, so the use of more than 2 PDT codes on a given day might raise payer queries.
Whatever you do, be sure your documentation includes an explicit notation about who applied the photosensitizing drug and the technique used for debridement, if performed. Code 96574 explicitly refers to targeted curettage and abrasion but does not include other destructive modalities (eg, chemical peeling), which an auditor may or may not consider an acceptable method of debridement. Personally, I will not be using peels as a justifier for this code.
Lasers
Lasers have played a role in the treatment of severe scarring in wounded warriors and other patient populations.7 Until 2018, there were no CPT codes that allowed precise reporting of these therapies. We now have a series of tracking codes, which are not valued by the Specialty Society Relative Value Scale Update Committee process but are nonetheless reportable, for this valuable treatment.8
The base code for a new pair of codes for reporting fractional ablative laser treatment, which is modeled after the skin graft code series, is 0479T (fractional ablative laser fenestration of burn and traumatic scars for functional improvement; first 100 cm2 or part thereof, or 1% of body surface area of infants and children). The add-on code is 0480T (fractional ablative laser fenestration of burn and traumatic scars for functional improvement; each additional 100 cm2, or each additional 1% of body surface area of infants and children, or part thereof [list separately in addition to code for primary procedure]), which means the code can be reported multiple times in addition to a single unit of 0479T. The aggregate treatment area should only be reported once per day regardless of the number of passes of one or more lasers over the area that day, and codes 0479T and 0480T should not be reported with codes 0491T or 0492T, which are a new family of tracking codes used for ablative laser treatment of chronic open wounds. If the scars are excised in a full-thickness manner, the benign excision codes 11400 to 11446 should be used instead.
For laser treatment of open wounds, 0491T (ablative laser treatment, noncontact, full-field and fractional ablation, open wound, per day, total treatment surface area; first 20 cm2 or less) is the base code for this pair of codes, and 0492T (ablative laser treatment, noncontact, full-field and fractional ablation, open wound, per day, total treatment surface area; each additional 20 cm2, or part thereof [list separately in addition to code for primary procedure]) is the add-on code, similar to the 0479T and 00480T codes described above. Keep in mind that all 4 of these tracking codes do not have defined values, and payment is at the discretion of the payer. If utilization of the procedures increases along with the development of appropriate evidence-based literature to support it, it is possible these will be converted into standard category I CPT codes that will be valued and covered by payers.
Final Thoughts
For more details on the new codes for PDT and lasers, I would strongly suggest obtaining a copy of CPT Changes 2018: An Insider’s View (https://commerce.ama-assn.org/store/catalog/productDetail.jsp?product_id=prod2800018&navAction=push), as well as the 2018 CPT manual for those who are actively practicing. Members of the American Academy of Dermatology also can get the new CPT manual as part of the group’s Coding Value Pack (https://store.aad.org/products/11383) along with Principles of Documentation for Dermatology and 2018 Coding & Billing for Dermatology.
Winter is the time when many religions celebrate a renewal of the year as the days begin to get longer. On January 1 of each year in the United States we celebrate the official activation of new and revised
Photodynamic Therapy
In 2004, a methyl aminolevulinate cream that was activated with a red light source was brought to market; however, after failing to gain a substantial market share, the product is no longer available in the United States. In May of 2016, a nanoemulsion gel formulation of aminolevulinic acid hydrochloride 10% was approved by the US Food and Drug Administration4 for use with a red light source. Unlike 5-aminolevulinic acid hydrochloride solution, which was approved for application with no prior debridement of the skin,5 the new gel formulation was meant to be applied after degreasing with an ethanol- or isopropanol-soaked cotton pad and removal of any scaling or crusts, followed by roughening of the lesion surfaces (with care taken to avoid bleeding).4 The product must be administered by a health care provider and is reported using CPT codes 96573 and 96574, which are new in 2018 and are discussed in more detail below. Effective January 1, 2018, the Healthcare Common Procedure Coding System supply code for the product is J7345 (aminolevulinic acid hydrochloride gel for topical administration, 10% gel, 10 mg).6 A single tube contains 200 mg, so when an entire tube is used (which is typical), 200 units must be reported. Partial tubes may be used in some patients and should be reported appropriately based on actual usage.
The development of new CPT codes for PDT revealed a middle ground in which many physicians, including myself, have applied the photosensitizing drug themselves instead of a nonphysician provider in order to use their professional judgment to ensure the entire treatment area was covered and also allow for multiple applications of the drug to lesions that in their opinion may have warranted greater dosing, which led to the creation of CPT code 96573. The revision and refinement from one code to 3 (96567, 96573, and 96574) also involved rewording of the preamble for all 3 codes so that the phrase “premalignant and/or malignant lesions” was simplified to “premalignant lesions.” This change was made so that if and when this therapeutic approach is refined enough to be used on malignant lesions, new codes can be created to distinguish between the work performed for both types of lesions.
The new PDT codes include 96573 (photodynamic therapy by external application of light to destroy premalignant lesions of the skin and adjacent mucosa with application and illumination/activation of photosensitizing drug[s] provided by a physician or other qualified healthcare professional, per day) and 96574 (debridement of premalignant hyperkeratotic lesion[s][ie, targeted curettage, abrasion] followed with photodynamic therapy by external application of light to destroy premalignant lesions of the skin and adjacent mucosa with application and illumination/activation of photosensitizing drug[s] provided by a physician or other qualified healthcare professional, per day). According to the 2018 CPT manual,2 these codes should be used to report nonsurgical treatment of cutaneous lesions using PDT (ie, external application of light to destroy premalignant lesions of the skin and adjacent mucosa by activation of photosensitizing drug). A treatment session is defined as an application of a photosensitizer to all lesions within an anatomic area (eg, face, scalp) with or without debridement of all premalignant hyperkeratotic lesions in that area followed by illumination and activation with an appropriate light source. Providers should not report codes for debridement (11000, 11001, 11004, 11005), lesion shaving (11300–11313), biopsy (11100, 11101), or lesion excision (11400–11471) within the treatment area on the same day that PDT is administered.2
With the inclusion of these new PDT codes, the older code 96567 (photodynamic therapy by external application of light to destroy premalignant lesions of the skin and adjacent mucosa with application and illumination/activation of photosensitive drug[s], per day)—which is the base or parent code of the set—should only be used for reporting PDT when a physician or other qualified health care professional is not directly involved in the delivery of the service. Code 96573 is an upgrade to 96567 to account for physician work, while code 96574 captures the extra work of disruption of the skin barrier by debridement.
The novelty here is that old codes often are replaced when new codes come along. The reader should be aware of the distinct differences, as the total value expressed in relative value units for code 96567 is lower than it was in 2017 (3.24 vs 3.80), while the 2 newer codes have higher values (codes 96573 and 96574, 5.37 and 6.92, respectively). Additionally, the reader should note that only one of the 3 codes can be used on a given anatomic area (ie, face and scalp) on a given day. In general, a single-dose package of either of the approved photosensitizing drugs can usually treat an entire anatomic area. The codes themselves are not reserved for specific anatomic areas, but the US Food and Drug Administration clearances are for only face and scalp for both drugs, so the use of more than 2 PDT codes on a given day might raise payer queries.
Whatever you do, be sure your documentation includes an explicit notation about who applied the photosensitizing drug and the technique used for debridement, if performed. Code 96574 explicitly refers to targeted curettage and abrasion but does not include other destructive modalities (eg, chemical peeling), which an auditor may or may not consider an acceptable method of debridement. Personally, I will not be using peels as a justifier for this code.
Lasers
Lasers have played a role in the treatment of severe scarring in wounded warriors and other patient populations.7 Until 2018, there were no CPT codes that allowed precise reporting of these therapies. We now have a series of tracking codes, which are not valued by the Specialty Society Relative Value Scale Update Committee process but are nonetheless reportable, for this valuable treatment.8
The base code for a new pair of codes for reporting fractional ablative laser treatment, which is modeled after the skin graft code series, is 0479T (fractional ablative laser fenestration of burn and traumatic scars for functional improvement; first 100 cm2 or part thereof, or 1% of body surface area of infants and children). The add-on code is 0480T (fractional ablative laser fenestration of burn and traumatic scars for functional improvement; each additional 100 cm2, or each additional 1% of body surface area of infants and children, or part thereof [list separately in addition to code for primary procedure]), which means the code can be reported multiple times in addition to a single unit of 0479T. The aggregate treatment area should only be reported once per day regardless of the number of passes of one or more lasers over the area that day, and codes 0479T and 0480T should not be reported with codes 0491T or 0492T, which are a new family of tracking codes used for ablative laser treatment of chronic open wounds. If the scars are excised in a full-thickness manner, the benign excision codes 11400 to 11446 should be used instead.
For laser treatment of open wounds, 0491T (ablative laser treatment, noncontact, full-field and fractional ablation, open wound, per day, total treatment surface area; first 20 cm2 or less) is the base code for this pair of codes, and 0492T (ablative laser treatment, noncontact, full-field and fractional ablation, open wound, per day, total treatment surface area; each additional 20 cm2, or part thereof [list separately in addition to code for primary procedure]) is the add-on code, similar to the 0479T and 00480T codes described above. Keep in mind that all 4 of these tracking codes do not have defined values, and payment is at the discretion of the payer. If utilization of the procedures increases along with the development of appropriate evidence-based literature to support it, it is possible these will be converted into standard category I CPT codes that will be valued and covered by payers.
Final Thoughts
For more details on the new codes for PDT and lasers, I would strongly suggest obtaining a copy of CPT Changes 2018: An Insider’s View (https://commerce.ama-assn.org/store/catalog/productDetail.jsp?product_id=prod2800018&navAction=push), as well as the 2018 CPT manual for those who are actively practicing. Members of the American Academy of Dermatology also can get the new CPT manual as part of the group’s Coding Value Pack (https://store.aad.org/products/11383) along with Principles of Documentation for Dermatology and 2018 Coding & Billing for Dermatology.
- Daniell MD, Hill JS. A history of photodynamic therapy. Aust N Z J Surg. 1991;61:340-348.
- Current Procedural Terminology 2018, Professional Edition. Chicago, IL: American Medical Association; 2018.
- HCPCS code J7308. HCPCS Complete Reference website. https://hcpcs.codes/j-codes/J7308/. Accessed March 1, 2018.
- Ameluz [package insert]. Wakefield, MA: Biofrontera Inc; 2017.
- Levulan Kerastick [package insert]. Wilmington, MA: Dusa Pharmaceuticals, Inc; 2010.
- Centers for Medicare & Medicaid Services. 2018 Table of drugs. CMS website. https://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/Downloads/2018-Table-of-Drugs.pdf. Updated February 15, 2018. Accessed February 21, 2018.
- Waibel JS, Rudnick A. Current trends and future considerations in scar treatment. Semin Cutan Med Surg. 2015;34:13-16.
- American Medical Association. CPT category III codes. AMA website. https://www.ama-assn.org/sites/default/files/media-browser/public/cpt/cpt-category3-codes-descriptors.pdf. Updated December 21, 2017. Accessed February 21, 2018.
- Daniell MD, Hill JS. A history of photodynamic therapy. Aust N Z J Surg. 1991;61:340-348.
- Current Procedural Terminology 2018, Professional Edition. Chicago, IL: American Medical Association; 2018.
- HCPCS code J7308. HCPCS Complete Reference website. https://hcpcs.codes/j-codes/J7308/. Accessed March 1, 2018.
- Ameluz [package insert]. Wakefield, MA: Biofrontera Inc; 2017.
- Levulan Kerastick [package insert]. Wilmington, MA: Dusa Pharmaceuticals, Inc; 2010.
- Centers for Medicare & Medicaid Services. 2018 Table of drugs. CMS website. https://www.cms.gov/Medicare/Coding/HCPCSReleaseCodeSets/Downloads/2018-Table-of-Drugs.pdf. Updated February 15, 2018. Accessed February 21, 2018.
- Waibel JS, Rudnick A. Current trends and future considerations in scar treatment. Semin Cutan Med Surg. 2015;34:13-16.
- American Medical Association. CPT category III codes. AMA website. https://www.ama-assn.org/sites/default/files/media-browser/public/cpt/cpt-category3-codes-descriptors.pdf. Updated December 21, 2017. Accessed February 21, 2018.
Practice Points
- In 2018, there are new sets of codes for photodynamic therapy (PDT) and lasers that all dermatologists should be aware of.
- The Current Procedural Terminology (CPT) codes for PDT—96567, 96573, and 96574—can only be used once per patient per day, and only one of the 3 codes can be used on a given anatomic area (ie, face and scalp) on a given day.
- Until 2018, there were no CPT codes that allowed for precise reporting of laser therapies, but there now is a series of tracking codes that are not valued by the Specialty Society Relative Value Scale Update Committee process but are nonetheless reportable.
Acronymic Despair: MACRA, MIPS, and Me
The year is moving ahead, and we are in the first year with a new president and a new administration. There have been multiple attempts to defund, revoke, or otherwise eliminate the Patient Protection and Affordable Care Act. As a physician, you may be asking, “What should I be doing for MACRA (Medicare Access and CHIP Reauthorization Act of 2015) and MIPS (Merit-Based Incentive Payments System)?”
RELATED VIDEO: Update on Coding Changes: Report From the Mount Sinai Fall Symposium
What is MACRA?
Of course, there is no such thing as a free lunch. The less pleasant side of MACRA is the Quality Payment Program under which providers will be paid based on the quality and effectiveness of the care provided; physician assistants, nurse practitioners, clinical nurse specialists, and certified registered nurse anesthetists also will be under the new system in addition to physicians. We are to be paid based on value, not volume. Heady stuff. The devil, as always, is in the details, as the factors we will be measured against are diverse. Having an electronic medical record (EMR) can make capturing data for some of these measures a bit less onerous. If you do not have an EMR, the cost of transitioning to one, especially if you are a small solo practice or approaching the end of your career, may outweigh the benefits.
RELATED VIDEO: Update on Coding Changes: Report From the Mount Sinai Fall Symposium
What is MIPS?
A small group of providers, most likely those in large multispecialty groups or academic settings, will instead participate in advanced Alternative Payment Models that will provide a lump sum bonus payment of 5% of their Medicare charges from 2019 to 2024.
For those taking the more common MIPS pathway, beginning in 2019 you can see a penalty of up to 4% on your Medicare payments if you do nothing and a bonus of up to 4% if you do it all. This rate will increase to a 5% penalty or a reward of up to 5% in 2020, 7% in 2021, and 9% in 2022. The penalty is a result of nonparticipation, while complete participation might get you to the maximum bonus. Of course, the bonus pool is limited, and if everyone does it all, the bonus would be much less, assuming the program is not changed or eliminated by the current administration. At the time of writing this column, Senate Majority Leader Mitch McConnell (R-KY) has failed multiple times to pass a Patient Protection and Affordable Care Act repeal bill following rebellions in his own party.4
So what do you, dear colleague, need to do right now, or at least before the end of the calendar year? You could do it all and try to grab the brass ring 4% bonus for 2019, putting time, effort, and expense into going after what could be an elusive reward. Or you could simply avoid the penalty and go back to work knowing you have locked in normal payments (whatever that will be!) for 2019. We are both doing the latter, and so might you, especially if you have not done anything yet this year.
MIPS Made Merry
To learn what you need to do or can do, pay a visit to the Quality Payment Program website (https://qpp.cms.gov/) where you can look yourself up with your national provider identifier number and find out what system you are under. Unless you are part of a large enterprise, you are likely under MIPS, but it never hurts to check.
It will then give you the options for reporting as an individual or a group. Either way, you can send in quality data through your routine Medicare claims process, which is our suggested route; no registry, no EMR, just an extra line on a claim form. You can review the complete list of quality measures that are available on the Quality Payment Program website (https://qpp.cms.gov/mips/quality-measures). There are 271 measures to read through and ponder, but by now you already have a headache, so take the following advice:
- Filter with the “Data Submission Method” by checking off “Claims,” which gives you 74 choices.
- Filter further with the “Specialty Measure Set”by checking off “Dermatology,” which gives you 4 choices.
- The top choice and probably the easiest one to get your staff to help with is “Documentation of Current Medications in the Medical Record,” which if you click on it further identifies it as “Quality ID: 130,” the official name of this measure.
You can see the MIPS program information in all its bureaucratic glory on the Quality Payment Program website (https://qpp.cms.gov/resources/education); click on “Quality Measure Specifications” to download a 250 MB zip file that contains information on all the measures in detail. The Measure #130 (Documentation of Current Medications in the Medical Record) file indicates that the clinician must use a G code (G8427) to report that current medications have been documented. The measure reads: “Eligible clinician attests to documenting, updating or reviewing a patient’s current medications using all immediate resources available on the date of encounter. This list must include ALL known prescriptions, over-the counters, herbals, and vitamin/mineral/dietary (nutritional) supplements AND must contain the medications’ name, dosages, frequency and route of administration.”5
You likely already confirm current medications with patients in some form or other, so simply look at the list of medications and supplements with all their dosages, frequencies, and routes of administration and sign the sheet of paper your practice likely already uses as an extra way of confirming that you have reviewed it. You report code G8427 as you would any Current Procedural Terminology code and link it to any International Classification of Diseases, Tenth Revision, code in your claim along with any evaluation and management and/or procedure codes that you would otherwise report for that encounter.
Some clearinghouses will not accept $0 charges, so we recommend you place a $0.01 charge for G8427 and write it off later. Upon receiving your explanation of benefits, you should notice 2 remark codes relating to the G8427 line: CO-246 and N620. Both of these codes indicate that the Centers for Medicare & Medicaid Services acknowledge your quality submission. To avoid that 4% penalty in 2019, you only need to do it once, but doing it a few times until you get back an explanation of benefits acknowledging it may help you sleep better.
Conclusion
Although the future of the Patient Protection and Affordable Care Act is still unclear, one thing is for sure: MACRA and MIPS are here to stay. Avoid the 4% penalty in 2019 and take good care of your patients and, if eligible, make donations to the American Academy of Dermatology Association Political Action Committee (skinPAC). It is going to be a wild ride.
- MACRA: delivery system reform, Medicare payment reform. Centers for Medicare & Medicaid Services website. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html. Updated June 26, 2016. Accessed August 1, 2017.
- MACRA tools and resources. American Academy of Dermatology website. https://www.aad.org/practicecenter/coding-and-reimbursement/macra. Accessed August 1, 2017.
- Balanced Budget Act of 1997. Senate and House of Representatives of the United States of America. https://www.gpo.gov/fdsys/pkg/PLAW-105publ33/html/PLAW-105publ33.htm. Accessed August 1, 2017.
- Bruni F. The misery of Mitch McConnell. New York Times. June 28, 2017. https://www.nytimes.com/2017/06/28/opinion/mitch-mcconnell-health-care-misery.html. Accessed August 1, 2017.
- American Medical Association. Measure #130 (NQF 0419): Documentation of Current Medications in the Medical Record-National Quality Strategy Domain: Patient Safety. Published November 15, 2016. Accessed August 18, 2016.
The year is moving ahead, and we are in the first year with a new president and a new administration. There have been multiple attempts to defund, revoke, or otherwise eliminate the Patient Protection and Affordable Care Act. As a physician, you may be asking, “What should I be doing for MACRA (Medicare Access and CHIP Reauthorization Act of 2015) and MIPS (Merit-Based Incentive Payments System)?”
RELATED VIDEO: Update on Coding Changes: Report From the Mount Sinai Fall Symposium
What is MACRA?
Of course, there is no such thing as a free lunch. The less pleasant side of MACRA is the Quality Payment Program under which providers will be paid based on the quality and effectiveness of the care provided; physician assistants, nurse practitioners, clinical nurse specialists, and certified registered nurse anesthetists also will be under the new system in addition to physicians. We are to be paid based on value, not volume. Heady stuff. The devil, as always, is in the details, as the factors we will be measured against are diverse. Having an electronic medical record (EMR) can make capturing data for some of these measures a bit less onerous. If you do not have an EMR, the cost of transitioning to one, especially if you are a small solo practice or approaching the end of your career, may outweigh the benefits.
RELATED VIDEO: Update on Coding Changes: Report From the Mount Sinai Fall Symposium
What is MIPS?
A small group of providers, most likely those in large multispecialty groups or academic settings, will instead participate in advanced Alternative Payment Models that will provide a lump sum bonus payment of 5% of their Medicare charges from 2019 to 2024.
For those taking the more common MIPS pathway, beginning in 2019 you can see a penalty of up to 4% on your Medicare payments if you do nothing and a bonus of up to 4% if you do it all. This rate will increase to a 5% penalty or a reward of up to 5% in 2020, 7% in 2021, and 9% in 2022. The penalty is a result of nonparticipation, while complete participation might get you to the maximum bonus. Of course, the bonus pool is limited, and if everyone does it all, the bonus would be much less, assuming the program is not changed or eliminated by the current administration. At the time of writing this column, Senate Majority Leader Mitch McConnell (R-KY) has failed multiple times to pass a Patient Protection and Affordable Care Act repeal bill following rebellions in his own party.4
So what do you, dear colleague, need to do right now, or at least before the end of the calendar year? You could do it all and try to grab the brass ring 4% bonus for 2019, putting time, effort, and expense into going after what could be an elusive reward. Or you could simply avoid the penalty and go back to work knowing you have locked in normal payments (whatever that will be!) for 2019. We are both doing the latter, and so might you, especially if you have not done anything yet this year.
MIPS Made Merry
To learn what you need to do or can do, pay a visit to the Quality Payment Program website (https://qpp.cms.gov/) where you can look yourself up with your national provider identifier number and find out what system you are under. Unless you are part of a large enterprise, you are likely under MIPS, but it never hurts to check.
It will then give you the options for reporting as an individual or a group. Either way, you can send in quality data through your routine Medicare claims process, which is our suggested route; no registry, no EMR, just an extra line on a claim form. You can review the complete list of quality measures that are available on the Quality Payment Program website (https://qpp.cms.gov/mips/quality-measures). There are 271 measures to read through and ponder, but by now you already have a headache, so take the following advice:
- Filter with the “Data Submission Method” by checking off “Claims,” which gives you 74 choices.
- Filter further with the “Specialty Measure Set”by checking off “Dermatology,” which gives you 4 choices.
- The top choice and probably the easiest one to get your staff to help with is “Documentation of Current Medications in the Medical Record,” which if you click on it further identifies it as “Quality ID: 130,” the official name of this measure.
You can see the MIPS program information in all its bureaucratic glory on the Quality Payment Program website (https://qpp.cms.gov/resources/education); click on “Quality Measure Specifications” to download a 250 MB zip file that contains information on all the measures in detail. The Measure #130 (Documentation of Current Medications in the Medical Record) file indicates that the clinician must use a G code (G8427) to report that current medications have been documented. The measure reads: “Eligible clinician attests to documenting, updating or reviewing a patient’s current medications using all immediate resources available on the date of encounter. This list must include ALL known prescriptions, over-the counters, herbals, and vitamin/mineral/dietary (nutritional) supplements AND must contain the medications’ name, dosages, frequency and route of administration.”5
You likely already confirm current medications with patients in some form or other, so simply look at the list of medications and supplements with all their dosages, frequencies, and routes of administration and sign the sheet of paper your practice likely already uses as an extra way of confirming that you have reviewed it. You report code G8427 as you would any Current Procedural Terminology code and link it to any International Classification of Diseases, Tenth Revision, code in your claim along with any evaluation and management and/or procedure codes that you would otherwise report for that encounter.
Some clearinghouses will not accept $0 charges, so we recommend you place a $0.01 charge for G8427 and write it off later. Upon receiving your explanation of benefits, you should notice 2 remark codes relating to the G8427 line: CO-246 and N620. Both of these codes indicate that the Centers for Medicare & Medicaid Services acknowledge your quality submission. To avoid that 4% penalty in 2019, you only need to do it once, but doing it a few times until you get back an explanation of benefits acknowledging it may help you sleep better.
Conclusion
Although the future of the Patient Protection and Affordable Care Act is still unclear, one thing is for sure: MACRA and MIPS are here to stay. Avoid the 4% penalty in 2019 and take good care of your patients and, if eligible, make donations to the American Academy of Dermatology Association Political Action Committee (skinPAC). It is going to be a wild ride.
The year is moving ahead, and we are in the first year with a new president and a new administration. There have been multiple attempts to defund, revoke, or otherwise eliminate the Patient Protection and Affordable Care Act. As a physician, you may be asking, “What should I be doing for MACRA (Medicare Access and CHIP Reauthorization Act of 2015) and MIPS (Merit-Based Incentive Payments System)?”
RELATED VIDEO: Update on Coding Changes: Report From the Mount Sinai Fall Symposium
What is MACRA?
Of course, there is no such thing as a free lunch. The less pleasant side of MACRA is the Quality Payment Program under which providers will be paid based on the quality and effectiveness of the care provided; physician assistants, nurse practitioners, clinical nurse specialists, and certified registered nurse anesthetists also will be under the new system in addition to physicians. We are to be paid based on value, not volume. Heady stuff. The devil, as always, is in the details, as the factors we will be measured against are diverse. Having an electronic medical record (EMR) can make capturing data for some of these measures a bit less onerous. If you do not have an EMR, the cost of transitioning to one, especially if you are a small solo practice or approaching the end of your career, may outweigh the benefits.
RELATED VIDEO: Update on Coding Changes: Report From the Mount Sinai Fall Symposium
What is MIPS?
A small group of providers, most likely those in large multispecialty groups or academic settings, will instead participate in advanced Alternative Payment Models that will provide a lump sum bonus payment of 5% of their Medicare charges from 2019 to 2024.
For those taking the more common MIPS pathway, beginning in 2019 you can see a penalty of up to 4% on your Medicare payments if you do nothing and a bonus of up to 4% if you do it all. This rate will increase to a 5% penalty or a reward of up to 5% in 2020, 7% in 2021, and 9% in 2022. The penalty is a result of nonparticipation, while complete participation might get you to the maximum bonus. Of course, the bonus pool is limited, and if everyone does it all, the bonus would be much less, assuming the program is not changed or eliminated by the current administration. At the time of writing this column, Senate Majority Leader Mitch McConnell (R-KY) has failed multiple times to pass a Patient Protection and Affordable Care Act repeal bill following rebellions in his own party.4
So what do you, dear colleague, need to do right now, or at least before the end of the calendar year? You could do it all and try to grab the brass ring 4% bonus for 2019, putting time, effort, and expense into going after what could be an elusive reward. Or you could simply avoid the penalty and go back to work knowing you have locked in normal payments (whatever that will be!) for 2019. We are both doing the latter, and so might you, especially if you have not done anything yet this year.
MIPS Made Merry
To learn what you need to do or can do, pay a visit to the Quality Payment Program website (https://qpp.cms.gov/) where you can look yourself up with your national provider identifier number and find out what system you are under. Unless you are part of a large enterprise, you are likely under MIPS, but it never hurts to check.
It will then give you the options for reporting as an individual or a group. Either way, you can send in quality data through your routine Medicare claims process, which is our suggested route; no registry, no EMR, just an extra line on a claim form. You can review the complete list of quality measures that are available on the Quality Payment Program website (https://qpp.cms.gov/mips/quality-measures). There are 271 measures to read through and ponder, but by now you already have a headache, so take the following advice:
- Filter with the “Data Submission Method” by checking off “Claims,” which gives you 74 choices.
- Filter further with the “Specialty Measure Set”by checking off “Dermatology,” which gives you 4 choices.
- The top choice and probably the easiest one to get your staff to help with is “Documentation of Current Medications in the Medical Record,” which if you click on it further identifies it as “Quality ID: 130,” the official name of this measure.
You can see the MIPS program information in all its bureaucratic glory on the Quality Payment Program website (https://qpp.cms.gov/resources/education); click on “Quality Measure Specifications” to download a 250 MB zip file that contains information on all the measures in detail. The Measure #130 (Documentation of Current Medications in the Medical Record) file indicates that the clinician must use a G code (G8427) to report that current medications have been documented. The measure reads: “Eligible clinician attests to documenting, updating or reviewing a patient’s current medications using all immediate resources available on the date of encounter. This list must include ALL known prescriptions, over-the counters, herbals, and vitamin/mineral/dietary (nutritional) supplements AND must contain the medications’ name, dosages, frequency and route of administration.”5
You likely already confirm current medications with patients in some form or other, so simply look at the list of medications and supplements with all their dosages, frequencies, and routes of administration and sign the sheet of paper your practice likely already uses as an extra way of confirming that you have reviewed it. You report code G8427 as you would any Current Procedural Terminology code and link it to any International Classification of Diseases, Tenth Revision, code in your claim along with any evaluation and management and/or procedure codes that you would otherwise report for that encounter.
Some clearinghouses will not accept $0 charges, so we recommend you place a $0.01 charge for G8427 and write it off later. Upon receiving your explanation of benefits, you should notice 2 remark codes relating to the G8427 line: CO-246 and N620. Both of these codes indicate that the Centers for Medicare & Medicaid Services acknowledge your quality submission. To avoid that 4% penalty in 2019, you only need to do it once, but doing it a few times until you get back an explanation of benefits acknowledging it may help you sleep better.
Conclusion
Although the future of the Patient Protection and Affordable Care Act is still unclear, one thing is for sure: MACRA and MIPS are here to stay. Avoid the 4% penalty in 2019 and take good care of your patients and, if eligible, make donations to the American Academy of Dermatology Association Political Action Committee (skinPAC). It is going to be a wild ride.
- MACRA: delivery system reform, Medicare payment reform. Centers for Medicare & Medicaid Services website. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html. Updated June 26, 2016. Accessed August 1, 2017.
- MACRA tools and resources. American Academy of Dermatology website. https://www.aad.org/practicecenter/coding-and-reimbursement/macra. Accessed August 1, 2017.
- Balanced Budget Act of 1997. Senate and House of Representatives of the United States of America. https://www.gpo.gov/fdsys/pkg/PLAW-105publ33/html/PLAW-105publ33.htm. Accessed August 1, 2017.
- Bruni F. The misery of Mitch McConnell. New York Times. June 28, 2017. https://www.nytimes.com/2017/06/28/opinion/mitch-mcconnell-health-care-misery.html. Accessed August 1, 2017.
- American Medical Association. Measure #130 (NQF 0419): Documentation of Current Medications in the Medical Record-National Quality Strategy Domain: Patient Safety. Published November 15, 2016. Accessed August 18, 2016.
- MACRA: delivery system reform, Medicare payment reform. Centers for Medicare & Medicaid Services website. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html. Updated June 26, 2016. Accessed August 1, 2017.
- MACRA tools and resources. American Academy of Dermatology website. https://www.aad.org/practicecenter/coding-and-reimbursement/macra. Accessed August 1, 2017.
- Balanced Budget Act of 1997. Senate and House of Representatives of the United States of America. https://www.gpo.gov/fdsys/pkg/PLAW-105publ33/html/PLAW-105publ33.htm. Accessed August 1, 2017.
- Bruni F. The misery of Mitch McConnell. New York Times. June 28, 2017. https://www.nytimes.com/2017/06/28/opinion/mitch-mcconnell-health-care-misery.html. Accessed August 1, 2017.
- American Medical Association. Measure #130 (NQF 0419): Documentation of Current Medications in the Medical Record-National Quality Strategy Domain: Patient Safety. Published November 15, 2016. Accessed August 18, 2016.
Practice Points
- MACRA (Medicare Access and CHIP Reauthorization Act of 2015) and MIPS (Merit-Based Incentive Payments System) need not ruin your life this year.
- A single measure can eliminate your downside risk for 2019.
In-Office Diagnostic Needle Arthroscopy: Understanding the Potential Value for the US Healthcare System
Take-Home Points
- In-office diagnostic needle arthroscopy is a minimally invasive, rapid method for identification of intra-articular joint pathology.
- Cost savings of a significant value can be realized to both the patient and healthcare system via small-bore needle arthroscopy as opposed to MRI.
- Diagnostic needle arthroscopy can lead to quicker identification of pathology than MRI.
- Diagnostic needle arthroscopy can reduce the number of undue "formal" surgical diagnostic arthroscopies.
- Standardization of image quality of small bore arthroscopy may pose benefits to the variable quality of MRI.
Patient satisfaction and healthcare costs have taken a leading role in today’s health care market. Patient satisfaction, often categorized as the "patient experience," can be measured on numerous levels, such as access to healthcare professionals and diagnostic testing, wait time for appointments, and timely test results. Furthermore, patients’ having a full understanding of their pathology and treatment options may correlate with their overall satisfaction. Some metrics are subjective, but procedure costs are objective.
The algorithm for treating patients who present with knee or shoulder pathology to an orthopedic office involves taking a thorough history, performing a physical examination, and, in many cases, obtaining diagnostic imaging. After arriving at a diagnosis, the physician plans the patient’s treatment. In most cases in which magnetic resonance imaging (MRI) is required, the process can take 2 to 3 weeks.1
Surgical knee arthroscopy is one of the most common procedures in the United States.2,3 Worldwide, more than 2 million knee arthroscopies are performed yearly.4 For most procedures, the decision to treat is based on physical examination findings, and the diagnosis is confirmed with MRI. MRI has 86% sensitivity and 91% specificity for diagnosing ligamentous and meniscal tears.5 However, regular use of MRI has led to increased healthcare expenditures and a larger financial burden for patients, which can delay diagnosis.6
Since 2000, MRI use in the United States has risen significantly—by 10% over a 10-year period.7 According to a 2013 population analysis, 107 in 1000 US inhabitants had an MRI yearly.8
MRI costs vary widely because of several factors, including state/regional consideration, scanning in a hospital or an independent facility, and use of contrast and arthrography. In a 2017 study of the variation in noncontrast MRI costs at 71 hospitals and 26 independent facilities in Iowa, Westermann and colleagues9 found that, excluding radiologist interpretation fees, the mean MRI technical component cost to consumers was US $1874 (SD, $694; range, $500-$4000).
Patient factors may preclude use of MRI (Table).
Small-bore needle arthroscopy is a cost-effective alternative diagnostic tool with efficacy and accuracy similar to those of MRI and standard arthroscopy for intra-articular pathologies.6,11 The procedure is performed with a disposable handpiece equipped with an internal light source and optics; this handpiece attaches to a reusable tablet for ease of transportation and visualization (Figure 1).
In 2014, Voigt and colleagues6 reported a significant net healthcare system cost saving with use of a small-needle arthroscope for diagnostic testing. The saving was estimated at $115 million to $177 million for simple isolation of medial meniscus pathology—or, more specifically, for appropriate care after more accurate visualization with the diagnostic needle arthroscope coupled with a decrease in false positives compared with MRI use. Other factors include the economic impact of the patient’s lost work hours, often associated with the time off needed for the MRI and for the follow-up visit for review of results.
Methods
We retrospectively reviewed the patient charts for 200 in-office knee and shoulder diagnostic needle arthroscopies performed by 5 surgeons over a 12-month period and examined the costs. Medicare, Medicaid, worker’s compensation, self-pay, and motor vehicle cases were excluded to provide uniformity across commercial insurance payers. Only the reimbursement amounts for Current Procedural Terminology codes 29870 (diagnostic knee arthroscopy) and 29805 (diagnostic shoulder arthroscopy) were examined. Geographical differences in commercial payer reimbursements were considered. The 5 surgeons who submitted data for this study practice in different parts of the United States—the Northeast, the Mid-Atlantic, the Southeast, the Midwest, and the West Coast. Similarly, the costs of outpatient and inpatient MRI and MRA were reported by each physician based on regional rates. MRI reimbursement was considered only if the MRI magnet was 1.5 Tesla or stronger.
Results
We reviewed 200 (175 knee, 25 shoulder) in-office diagnostic needle arthroscopies of patients with commercial insurances. Average reimbursement was calculated across all commercial payers for both knee and shoulder arthroscopies (Figure 2).
For in-office diagnostic needle arthroscopy of the knee, average reimbursement was $628.92 (range, $340-$1391). For in-office diagnostic needle arthroscopy of the shoulder, average reimbursement was $492.38 (range, $471-$593). Outpatient MRI without contrast of the knee or shoulder averaged $1047 (range, $565-$2100) (Figure 3).
Discussion
Over the past decade, the combination of health and economics has often driven patient care and consumer demand. With rising deductibles and variations in secondary insurance carriers, patients often base healthcare decisions on their financial impact. Conversely, physicians are often in the difficult position of treating patients who are hesitant to obtain medical imaging out of financial concern. In addition, physicians and patients routinely are concerned about delays in care and timely reporting of test results. A patient’s ability to quickly obtain test results and start a course of definitive treatment may affect the patient’s perception of the overall healthcare experience with the physician, as has been noted in popular healthcare polls, such as Press-Ganey.13
Diagnostic needle arthroscopy performed in an office can yield a cost saving over MRI. Our review revealed in-office needle arthroscopy of the knee provided an average cost saving of $418.08 over standard MRI performed in an outpatient facility (Figure 3). That saving more than doubled, to $961.08, when MRI was performed in a hospital. Similarly, in-office needle arthroscopy of the shoulder provided an average cost saving of $554.62 over standard MRI. This saving also increased substantially, to $1097.62, over hospital MRI. An additional cost saving of $100 to $350 was found for knee or shoulder diagnostic needle arthroscopy over MRA.
Other factors affect the economic benefit of diagnostic needle arthroscopy over standard MRI. Having the procedure performed the same day as the presenting office visit can save the patient time and allow the physician to create a medical treatment plan sooner. In addition, the patient (and the insurance company) can save costs by avoiding a later office visit for review of MRI findings. Time spent going to MRI follow-up visits potentially can be analyzed as lost wages or as time lost from other segments of life. For the patient, this time can be defined as value hours. Last, there is a cost saving in avoiding nonoperative treatments in cases in which the initial definitive diagnosis would have called for surgical intervention. Accordingly, for patients who cannot undergo MRI, obtaining information on intra-articular pathology in the office may also decrease unnecessary "traditional" diagnostic arthroscopy in the operating room. Therefore, patients who do not require true formal arthroscopy to determine lack of pertinent intra-articular pathology can avoid unnecessary anesthesia, time off work, and associated healthcare expenses.
This study had several limitations. First, evaluating more cases would have increased the strength of the findings. Second, the large number of knee cases relative to shoulder cases may have been a by-product of the practice makeup of the surgeons rather than a matter of preference with this relatively new technology. However, the significant gap in cost savings between needle arthroscope and MRI cannot be discounted, and it provides a window on the potential cost savings the healthcare system can realize. Furthermore, analysis of payments made by the commercial payers in each state may have revealed a reimbursement fluctuation. The largest challenge in this study was the extreme variation in MRI costs. According to the literature, MRI of the upper or lower extremity ranges in cost from $500 to $4000.4 In addition, this cost is often negotiated between the patient and the MRI facility if the patient is willing to work outside insurance, which potentially can alter the overall average MRI cost.
The last points to consider are the reliability of users and the reproducibility of in-office diagnostic needle arthroscopy. Much as with true surgical arthroscopy and other diagnostic imaging practices, this procedure has a learning curve. We know that the number of successful diagnoses will increase with training and repetition, but so far there are no data on the number of procedures needed for proficiency. However, diagnostic needle arthroscopy images are of high quality and are static across users (Figures 5A, 5B). By contrast, the quality of MRI in the United States varies with the quality of the magnets used in individual facilities.
Conclusion
In-office diagnostic needle arthroscopy is a cost-effective and reproducible procedure with potential cost and quality-of-life benefits for commercial payers and patients. Although further study of long-term cost savings for the health care system is needed, significant value was realized in this 200-patient retrospective review. Minimum savings of $418 and $554.62 were realized for noncontrast knee and shoulder MRIs, respectively, in independent facilities. Those cost savings more than doubled in hospital-based facilities: $961.08 and $1097.62, respectively, for knee and shoulder noncontrast MRIs.
For More on In-office Arthroscopy...
Don’t miss Dr. Sean McMillan’s “Innovative Technique Update: In-Office Arthroscopy: My Technique and Results” at the upcoming Innovative Techniques® Knee, Hip, and Shoulder Course in Las Vegas. 29.5 CME/MOC available. Learn more
1. O’Donnell J. Trice Medical literature. #4-10-0032 Rev A.
2. Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93(11):994-1000.
3. Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Rep. 2009;(11):1-25.
4. Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ. 2017;(357):j1982.
5. Crawford R, Walley G, Bridgman S, Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;(84):5-23.
6. Voigt JD, Mosier M, Huber B. Diagnostic needle arthroscopy and the economics of improved diagnostic accuracy: a cost analysis. Appl Health Econ Health Policy. 2014;12(5):523-535.
7. Sharpe RE Jr, Levin DC, Parker L, Rao VM. The recent reversal of the growth trend in MRI: a harbinger of the future? J Am Coll Radiol. 2013;10(8):599-602.
8. Organisation for Economic Cooperation and Development (OECD). 46. Magnetic resonance imaging (MRI) exams, total per 1 000 population. OECD website. http://dx.doi.org/10.1787/mri-exam-total-table-2014-1-en. Published June 30, 2014. Accessed August 14, 2017.
9. Westermann RW, Schick C, Graves CM, Duchman KR, Weinstein SL. What does a shoulder MRI cost the consumer? Clin Orthop Relat Res. 2017;475(3):580-584.
10. Thakkar RS, Thakkar SC, Srikumaran U, McFarland EG, Fayad LM. Complications of rotator cuff surgery—the role of post-operative imaging in patient care. Br J Radiol. 2014;87(1039):20130630.
11. Gramas DA, Antounian FS, Peterfy CG, Genant HK, Lane NE. Assessment of needle arthroscopy, standard arthroscopy, physical examination, and magnetic resonance imaging in knee pain: a pilot study. J Clin Rheumatol. 1995;1(1):26-34.
12. McMillan S, Saini S, Alyea E, Ford EA. Office-based needle arthroscopy: a standardized diagnostic approach to the knee. Arthrosc Tech. 2017.
13. Keeping me waiting: medical practice wait times and patient satisfaction [white paper]. South Bend, IN: Press Ganey; 2010. https://helpandtraining.pressganey.com/Documents_secure/Medical%20Practices/White%20Papers/Keep_Me_Waiting.pdf. Published 2010. Accessed August 14, 2017.
Take-Home Points
- In-office diagnostic needle arthroscopy is a minimally invasive, rapid method for identification of intra-articular joint pathology.
- Cost savings of a significant value can be realized to both the patient and healthcare system via small-bore needle arthroscopy as opposed to MRI.
- Diagnostic needle arthroscopy can lead to quicker identification of pathology than MRI.
- Diagnostic needle arthroscopy can reduce the number of undue "formal" surgical diagnostic arthroscopies.
- Standardization of image quality of small bore arthroscopy may pose benefits to the variable quality of MRI.
Patient satisfaction and healthcare costs have taken a leading role in today’s health care market. Patient satisfaction, often categorized as the "patient experience," can be measured on numerous levels, such as access to healthcare professionals and diagnostic testing, wait time for appointments, and timely test results. Furthermore, patients’ having a full understanding of their pathology and treatment options may correlate with their overall satisfaction. Some metrics are subjective, but procedure costs are objective.
The algorithm for treating patients who present with knee or shoulder pathology to an orthopedic office involves taking a thorough history, performing a physical examination, and, in many cases, obtaining diagnostic imaging. After arriving at a diagnosis, the physician plans the patient’s treatment. In most cases in which magnetic resonance imaging (MRI) is required, the process can take 2 to 3 weeks.1
Surgical knee arthroscopy is one of the most common procedures in the United States.2,3 Worldwide, more than 2 million knee arthroscopies are performed yearly.4 For most procedures, the decision to treat is based on physical examination findings, and the diagnosis is confirmed with MRI. MRI has 86% sensitivity and 91% specificity for diagnosing ligamentous and meniscal tears.5 However, regular use of MRI has led to increased healthcare expenditures and a larger financial burden for patients, which can delay diagnosis.6
Since 2000, MRI use in the United States has risen significantly—by 10% over a 10-year period.7 According to a 2013 population analysis, 107 in 1000 US inhabitants had an MRI yearly.8
MRI costs vary widely because of several factors, including state/regional consideration, scanning in a hospital or an independent facility, and use of contrast and arthrography. In a 2017 study of the variation in noncontrast MRI costs at 71 hospitals and 26 independent facilities in Iowa, Westermann and colleagues9 found that, excluding radiologist interpretation fees, the mean MRI technical component cost to consumers was US $1874 (SD, $694; range, $500-$4000).
Patient factors may preclude use of MRI (Table).
Small-bore needle arthroscopy is a cost-effective alternative diagnostic tool with efficacy and accuracy similar to those of MRI and standard arthroscopy for intra-articular pathologies.6,11 The procedure is performed with a disposable handpiece equipped with an internal light source and optics; this handpiece attaches to a reusable tablet for ease of transportation and visualization (Figure 1).
In 2014, Voigt and colleagues6 reported a significant net healthcare system cost saving with use of a small-needle arthroscope for diagnostic testing. The saving was estimated at $115 million to $177 million for simple isolation of medial meniscus pathology—or, more specifically, for appropriate care after more accurate visualization with the diagnostic needle arthroscope coupled with a decrease in false positives compared with MRI use. Other factors include the economic impact of the patient’s lost work hours, often associated with the time off needed for the MRI and for the follow-up visit for review of results.
Methods
We retrospectively reviewed the patient charts for 200 in-office knee and shoulder diagnostic needle arthroscopies performed by 5 surgeons over a 12-month period and examined the costs. Medicare, Medicaid, worker’s compensation, self-pay, and motor vehicle cases were excluded to provide uniformity across commercial insurance payers. Only the reimbursement amounts for Current Procedural Terminology codes 29870 (diagnostic knee arthroscopy) and 29805 (diagnostic shoulder arthroscopy) were examined. Geographical differences in commercial payer reimbursements were considered. The 5 surgeons who submitted data for this study practice in different parts of the United States—the Northeast, the Mid-Atlantic, the Southeast, the Midwest, and the West Coast. Similarly, the costs of outpatient and inpatient MRI and MRA were reported by each physician based on regional rates. MRI reimbursement was considered only if the MRI magnet was 1.5 Tesla or stronger.
Results
We reviewed 200 (175 knee, 25 shoulder) in-office diagnostic needle arthroscopies of patients with commercial insurances. Average reimbursement was calculated across all commercial payers for both knee and shoulder arthroscopies (Figure 2).
For in-office diagnostic needle arthroscopy of the knee, average reimbursement was $628.92 (range, $340-$1391). For in-office diagnostic needle arthroscopy of the shoulder, average reimbursement was $492.38 (range, $471-$593). Outpatient MRI without contrast of the knee or shoulder averaged $1047 (range, $565-$2100) (Figure 3).
Discussion
Over the past decade, the combination of health and economics has often driven patient care and consumer demand. With rising deductibles and variations in secondary insurance carriers, patients often base healthcare decisions on their financial impact. Conversely, physicians are often in the difficult position of treating patients who are hesitant to obtain medical imaging out of financial concern. In addition, physicians and patients routinely are concerned about delays in care and timely reporting of test results. A patient’s ability to quickly obtain test results and start a course of definitive treatment may affect the patient’s perception of the overall healthcare experience with the physician, as has been noted in popular healthcare polls, such as Press-Ganey.13
Diagnostic needle arthroscopy performed in an office can yield a cost saving over MRI. Our review revealed in-office needle arthroscopy of the knee provided an average cost saving of $418.08 over standard MRI performed in an outpatient facility (Figure 3). That saving more than doubled, to $961.08, when MRI was performed in a hospital. Similarly, in-office needle arthroscopy of the shoulder provided an average cost saving of $554.62 over standard MRI. This saving also increased substantially, to $1097.62, over hospital MRI. An additional cost saving of $100 to $350 was found for knee or shoulder diagnostic needle arthroscopy over MRA.
Other factors affect the economic benefit of diagnostic needle arthroscopy over standard MRI. Having the procedure performed the same day as the presenting office visit can save the patient time and allow the physician to create a medical treatment plan sooner. In addition, the patient (and the insurance company) can save costs by avoiding a later office visit for review of MRI findings. Time spent going to MRI follow-up visits potentially can be analyzed as lost wages or as time lost from other segments of life. For the patient, this time can be defined as value hours. Last, there is a cost saving in avoiding nonoperative treatments in cases in which the initial definitive diagnosis would have called for surgical intervention. Accordingly, for patients who cannot undergo MRI, obtaining information on intra-articular pathology in the office may also decrease unnecessary "traditional" diagnostic arthroscopy in the operating room. Therefore, patients who do not require true formal arthroscopy to determine lack of pertinent intra-articular pathology can avoid unnecessary anesthesia, time off work, and associated healthcare expenses.
This study had several limitations. First, evaluating more cases would have increased the strength of the findings. Second, the large number of knee cases relative to shoulder cases may have been a by-product of the practice makeup of the surgeons rather than a matter of preference with this relatively new technology. However, the significant gap in cost savings between needle arthroscope and MRI cannot be discounted, and it provides a window on the potential cost savings the healthcare system can realize. Furthermore, analysis of payments made by the commercial payers in each state may have revealed a reimbursement fluctuation. The largest challenge in this study was the extreme variation in MRI costs. According to the literature, MRI of the upper or lower extremity ranges in cost from $500 to $4000.4 In addition, this cost is often negotiated between the patient and the MRI facility if the patient is willing to work outside insurance, which potentially can alter the overall average MRI cost.
The last points to consider are the reliability of users and the reproducibility of in-office diagnostic needle arthroscopy. Much as with true surgical arthroscopy and other diagnostic imaging practices, this procedure has a learning curve. We know that the number of successful diagnoses will increase with training and repetition, but so far there are no data on the number of procedures needed for proficiency. However, diagnostic needle arthroscopy images are of high quality and are static across users (Figures 5A, 5B). By contrast, the quality of MRI in the United States varies with the quality of the magnets used in individual facilities.
Conclusion
In-office diagnostic needle arthroscopy is a cost-effective and reproducible procedure with potential cost and quality-of-life benefits for commercial payers and patients. Although further study of long-term cost savings for the health care system is needed, significant value was realized in this 200-patient retrospective review. Minimum savings of $418 and $554.62 were realized for noncontrast knee and shoulder MRIs, respectively, in independent facilities. Those cost savings more than doubled in hospital-based facilities: $961.08 and $1097.62, respectively, for knee and shoulder noncontrast MRIs.
For More on In-office Arthroscopy...
Don’t miss Dr. Sean McMillan’s “Innovative Technique Update: In-Office Arthroscopy: My Technique and Results” at the upcoming Innovative Techniques® Knee, Hip, and Shoulder Course in Las Vegas. 29.5 CME/MOC available. Learn more
Take-Home Points
- In-office diagnostic needle arthroscopy is a minimally invasive, rapid method for identification of intra-articular joint pathology.
- Cost savings of a significant value can be realized to both the patient and healthcare system via small-bore needle arthroscopy as opposed to MRI.
- Diagnostic needle arthroscopy can lead to quicker identification of pathology than MRI.
- Diagnostic needle arthroscopy can reduce the number of undue "formal" surgical diagnostic arthroscopies.
- Standardization of image quality of small bore arthroscopy may pose benefits to the variable quality of MRI.
Patient satisfaction and healthcare costs have taken a leading role in today’s health care market. Patient satisfaction, often categorized as the "patient experience," can be measured on numerous levels, such as access to healthcare professionals and diagnostic testing, wait time for appointments, and timely test results. Furthermore, patients’ having a full understanding of their pathology and treatment options may correlate with their overall satisfaction. Some metrics are subjective, but procedure costs are objective.
The algorithm for treating patients who present with knee or shoulder pathology to an orthopedic office involves taking a thorough history, performing a physical examination, and, in many cases, obtaining diagnostic imaging. After arriving at a diagnosis, the physician plans the patient’s treatment. In most cases in which magnetic resonance imaging (MRI) is required, the process can take 2 to 3 weeks.1
Surgical knee arthroscopy is one of the most common procedures in the United States.2,3 Worldwide, more than 2 million knee arthroscopies are performed yearly.4 For most procedures, the decision to treat is based on physical examination findings, and the diagnosis is confirmed with MRI. MRI has 86% sensitivity and 91% specificity for diagnosing ligamentous and meniscal tears.5 However, regular use of MRI has led to increased healthcare expenditures and a larger financial burden for patients, which can delay diagnosis.6
Since 2000, MRI use in the United States has risen significantly—by 10% over a 10-year period.7 According to a 2013 population analysis, 107 in 1000 US inhabitants had an MRI yearly.8
MRI costs vary widely because of several factors, including state/regional consideration, scanning in a hospital or an independent facility, and use of contrast and arthrography. In a 2017 study of the variation in noncontrast MRI costs at 71 hospitals and 26 independent facilities in Iowa, Westermann and colleagues9 found that, excluding radiologist interpretation fees, the mean MRI technical component cost to consumers was US $1874 (SD, $694; range, $500-$4000).
Patient factors may preclude use of MRI (Table).
Small-bore needle arthroscopy is a cost-effective alternative diagnostic tool with efficacy and accuracy similar to those of MRI and standard arthroscopy for intra-articular pathologies.6,11 The procedure is performed with a disposable handpiece equipped with an internal light source and optics; this handpiece attaches to a reusable tablet for ease of transportation and visualization (Figure 1).
In 2014, Voigt and colleagues6 reported a significant net healthcare system cost saving with use of a small-needle arthroscope for diagnostic testing. The saving was estimated at $115 million to $177 million for simple isolation of medial meniscus pathology—or, more specifically, for appropriate care after more accurate visualization with the diagnostic needle arthroscope coupled with a decrease in false positives compared with MRI use. Other factors include the economic impact of the patient’s lost work hours, often associated with the time off needed for the MRI and for the follow-up visit for review of results.
Methods
We retrospectively reviewed the patient charts for 200 in-office knee and shoulder diagnostic needle arthroscopies performed by 5 surgeons over a 12-month period and examined the costs. Medicare, Medicaid, worker’s compensation, self-pay, and motor vehicle cases were excluded to provide uniformity across commercial insurance payers. Only the reimbursement amounts for Current Procedural Terminology codes 29870 (diagnostic knee arthroscopy) and 29805 (diagnostic shoulder arthroscopy) were examined. Geographical differences in commercial payer reimbursements were considered. The 5 surgeons who submitted data for this study practice in different parts of the United States—the Northeast, the Mid-Atlantic, the Southeast, the Midwest, and the West Coast. Similarly, the costs of outpatient and inpatient MRI and MRA were reported by each physician based on regional rates. MRI reimbursement was considered only if the MRI magnet was 1.5 Tesla or stronger.
Results
We reviewed 200 (175 knee, 25 shoulder) in-office diagnostic needle arthroscopies of patients with commercial insurances. Average reimbursement was calculated across all commercial payers for both knee and shoulder arthroscopies (Figure 2).
For in-office diagnostic needle arthroscopy of the knee, average reimbursement was $628.92 (range, $340-$1391). For in-office diagnostic needle arthroscopy of the shoulder, average reimbursement was $492.38 (range, $471-$593). Outpatient MRI without contrast of the knee or shoulder averaged $1047 (range, $565-$2100) (Figure 3).
Discussion
Over the past decade, the combination of health and economics has often driven patient care and consumer demand. With rising deductibles and variations in secondary insurance carriers, patients often base healthcare decisions on their financial impact. Conversely, physicians are often in the difficult position of treating patients who are hesitant to obtain medical imaging out of financial concern. In addition, physicians and patients routinely are concerned about delays in care and timely reporting of test results. A patient’s ability to quickly obtain test results and start a course of definitive treatment may affect the patient’s perception of the overall healthcare experience with the physician, as has been noted in popular healthcare polls, such as Press-Ganey.13
Diagnostic needle arthroscopy performed in an office can yield a cost saving over MRI. Our review revealed in-office needle arthroscopy of the knee provided an average cost saving of $418.08 over standard MRI performed in an outpatient facility (Figure 3). That saving more than doubled, to $961.08, when MRI was performed in a hospital. Similarly, in-office needle arthroscopy of the shoulder provided an average cost saving of $554.62 over standard MRI. This saving also increased substantially, to $1097.62, over hospital MRI. An additional cost saving of $100 to $350 was found for knee or shoulder diagnostic needle arthroscopy over MRA.
Other factors affect the economic benefit of diagnostic needle arthroscopy over standard MRI. Having the procedure performed the same day as the presenting office visit can save the patient time and allow the physician to create a medical treatment plan sooner. In addition, the patient (and the insurance company) can save costs by avoiding a later office visit for review of MRI findings. Time spent going to MRI follow-up visits potentially can be analyzed as lost wages or as time lost from other segments of life. For the patient, this time can be defined as value hours. Last, there is a cost saving in avoiding nonoperative treatments in cases in which the initial definitive diagnosis would have called for surgical intervention. Accordingly, for patients who cannot undergo MRI, obtaining information on intra-articular pathology in the office may also decrease unnecessary "traditional" diagnostic arthroscopy in the operating room. Therefore, patients who do not require true formal arthroscopy to determine lack of pertinent intra-articular pathology can avoid unnecessary anesthesia, time off work, and associated healthcare expenses.
This study had several limitations. First, evaluating more cases would have increased the strength of the findings. Second, the large number of knee cases relative to shoulder cases may have been a by-product of the practice makeup of the surgeons rather than a matter of preference with this relatively new technology. However, the significant gap in cost savings between needle arthroscope and MRI cannot be discounted, and it provides a window on the potential cost savings the healthcare system can realize. Furthermore, analysis of payments made by the commercial payers in each state may have revealed a reimbursement fluctuation. The largest challenge in this study was the extreme variation in MRI costs. According to the literature, MRI of the upper or lower extremity ranges in cost from $500 to $4000.4 In addition, this cost is often negotiated between the patient and the MRI facility if the patient is willing to work outside insurance, which potentially can alter the overall average MRI cost.
The last points to consider are the reliability of users and the reproducibility of in-office diagnostic needle arthroscopy. Much as with true surgical arthroscopy and other diagnostic imaging practices, this procedure has a learning curve. We know that the number of successful diagnoses will increase with training and repetition, but so far there are no data on the number of procedures needed for proficiency. However, diagnostic needle arthroscopy images are of high quality and are static across users (Figures 5A, 5B). By contrast, the quality of MRI in the United States varies with the quality of the magnets used in individual facilities.
Conclusion
In-office diagnostic needle arthroscopy is a cost-effective and reproducible procedure with potential cost and quality-of-life benefits for commercial payers and patients. Although further study of long-term cost savings for the health care system is needed, significant value was realized in this 200-patient retrospective review. Minimum savings of $418 and $554.62 were realized for noncontrast knee and shoulder MRIs, respectively, in independent facilities. Those cost savings more than doubled in hospital-based facilities: $961.08 and $1097.62, respectively, for knee and shoulder noncontrast MRIs.
For More on In-office Arthroscopy...
Don’t miss Dr. Sean McMillan’s “Innovative Technique Update: In-Office Arthroscopy: My Technique and Results” at the upcoming Innovative Techniques® Knee, Hip, and Shoulder Course in Las Vegas. 29.5 CME/MOC available. Learn more
1. O’Donnell J. Trice Medical literature. #4-10-0032 Rev A.
2. Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93(11):994-1000.
3. Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Rep. 2009;(11):1-25.
4. Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ. 2017;(357):j1982.
5. Crawford R, Walley G, Bridgman S, Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;(84):5-23.
6. Voigt JD, Mosier M, Huber B. Diagnostic needle arthroscopy and the economics of improved diagnostic accuracy: a cost analysis. Appl Health Econ Health Policy. 2014;12(5):523-535.
7. Sharpe RE Jr, Levin DC, Parker L, Rao VM. The recent reversal of the growth trend in MRI: a harbinger of the future? J Am Coll Radiol. 2013;10(8):599-602.
8. Organisation for Economic Cooperation and Development (OECD). 46. Magnetic resonance imaging (MRI) exams, total per 1 000 population. OECD website. http://dx.doi.org/10.1787/mri-exam-total-table-2014-1-en. Published June 30, 2014. Accessed August 14, 2017.
9. Westermann RW, Schick C, Graves CM, Duchman KR, Weinstein SL. What does a shoulder MRI cost the consumer? Clin Orthop Relat Res. 2017;475(3):580-584.
10. Thakkar RS, Thakkar SC, Srikumaran U, McFarland EG, Fayad LM. Complications of rotator cuff surgery—the role of post-operative imaging in patient care. Br J Radiol. 2014;87(1039):20130630.
11. Gramas DA, Antounian FS, Peterfy CG, Genant HK, Lane NE. Assessment of needle arthroscopy, standard arthroscopy, physical examination, and magnetic resonance imaging in knee pain: a pilot study. J Clin Rheumatol. 1995;1(1):26-34.
12. McMillan S, Saini S, Alyea E, Ford EA. Office-based needle arthroscopy: a standardized diagnostic approach to the knee. Arthrosc Tech. 2017.
13. Keeping me waiting: medical practice wait times and patient satisfaction [white paper]. South Bend, IN: Press Ganey; 2010. https://helpandtraining.pressganey.com/Documents_secure/Medical%20Practices/White%20Papers/Keep_Me_Waiting.pdf. Published 2010. Accessed August 14, 2017.
1. O’Donnell J. Trice Medical literature. #4-10-0032 Rev A.
2. Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93(11):994-1000.
3. Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Rep. 2009;(11):1-25.
4. Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ. 2017;(357):j1982.
5. Crawford R, Walley G, Bridgman S, Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;(84):5-23.
6. Voigt JD, Mosier M, Huber B. Diagnostic needle arthroscopy and the economics of improved diagnostic accuracy: a cost analysis. Appl Health Econ Health Policy. 2014;12(5):523-535.
7. Sharpe RE Jr, Levin DC, Parker L, Rao VM. The recent reversal of the growth trend in MRI: a harbinger of the future? J Am Coll Radiol. 2013;10(8):599-602.
8. Organisation for Economic Cooperation and Development (OECD). 46. Magnetic resonance imaging (MRI) exams, total per 1 000 population. OECD website. http://dx.doi.org/10.1787/mri-exam-total-table-2014-1-en. Published June 30, 2014. Accessed August 14, 2017.
9. Westermann RW, Schick C, Graves CM, Duchman KR, Weinstein SL. What does a shoulder MRI cost the consumer? Clin Orthop Relat Res. 2017;475(3):580-584.
10. Thakkar RS, Thakkar SC, Srikumaran U, McFarland EG, Fayad LM. Complications of rotator cuff surgery—the role of post-operative imaging in patient care. Br J Radiol. 2014;87(1039):20130630.
11. Gramas DA, Antounian FS, Peterfy CG, Genant HK, Lane NE. Assessment of needle arthroscopy, standard arthroscopy, physical examination, and magnetic resonance imaging in knee pain: a pilot study. J Clin Rheumatol. 1995;1(1):26-34.
12. McMillan S, Saini S, Alyea E, Ford EA. Office-based needle arthroscopy: a standardized diagnostic approach to the knee. Arthrosc Tech. 2017.
13. Keeping me waiting: medical practice wait times and patient satisfaction [white paper]. South Bend, IN: Press Ganey; 2010. https://helpandtraining.pressganey.com/Documents_secure/Medical%20Practices/White%20Papers/Keep_Me_Waiting.pdf. Published 2010. Accessed August 14, 2017.
Phototherapy Coding and Documentation in the Time of Biologics
In this era of biologics for psoriasis with ever-increasing effectiveness and safety as well as patients who have less and less time to visit the physician's office, it would seem that the days of in-office UV treatments would be numbered. However, rumors of the demise of phototherapy may be greatly exaggerated. Phototherapy is still one of the safest and most cost-effective treatments for psoriasis and other dermatoses.1 Its use often is a prerequisite for biologic therapy, and it may be the only therapeutic option for certain subsets of patients, such as children, pregnant women, and immunosuppressed patients. Moreover, narrowband UVB technology has breathed new life into phototherapy, with better efficacy and less long-term risk. Although the utilization of psoralen plus UVA (PUVA) light therapy has indeed decreased over the last 2 decades, the use of UVB therapies continues to increase dramatically.2
Phototherapy Codes
There are 4 chief Current Procedural Terminology (CPT) codes for reporting phototherapy services: (1) 96900: actinotherapy (UV light treatment); (2) 96910: photochemotherapy, tar, and UVB (Goeckerman treatment) or petrolatum and UVB; (3) 96912: photochemotherapy and PUVA; and (4) 96913: photochemotherapy (Goeckerman and/or PUVA) for severe photoresponsive dermatoses requiring at least 4 to 8 hours of care under direct supervision of the physician.3
There is lack of specificity of the CPT code descriptions for phototherapy. Moreover, insurer guidance for documentation for phototherapy is vague to nonexistent, and of course whenever the use of any medical service increases, insurer scrutiny is sure to follow. Therefore, it is not surprising that dermatology practices have reported that private insurers as well as Medicare are auditing medical records for phototherapy treatments.4 In fact, recently we have seen a Midwest private insurer demand payment from dermatologists for hundreds of 96910 phototherapy services, which the insurer asserted should have been coded as 96900 because topical therapies were not applied by the dermatology staff. The insurer did not just evaluate medical records but also contacted patients directly and asked how services had been provided. Clearly, more detailed guidance for dermatologists and insurers on documentation and performance standards for each phototherapy service is needed.
Existing coding guidance for phototherapy indicates that actinotherapy (96900) defines the basic service of treating a patient with a UV light unit.5 Actinotherapy does not involve application of topical medications while the patient is in the office.
In contrast, photochemotherapy (96910) implies addition of a chemo agent to phototherapy. Despite the somewhat nonspecific nature of the code descriptor, it is apparent that application of photoenhancing agents such as tar, petrolatum, or distillates of petrolatum meet the requirements of 96910. The Coder's Desk Reference for Procedures 2017 describes 96910 as "the physician uses photosensitizing chemicals and light rays to treat skin ailments."6 Application of light-enhancing topical products should occur within the office by either staff or the patient. In fact, examination of practice expense data from the Centers for Medicare & Medicaid Services indicated that the 96910 code includes payment for clinical staff time to apply topical products as well as the cost of the topical agent(s).7
The PUVA code 96912 is defined by the use of photosensitizing psoralen medication, which can be administered topically or orally, followed by UVA treatment. In my experience, PUVA has similar performance standards with in-office application of psoralen, if applicable. If application of topical photoenhancing products occurs outside the office, the requirements of photochemotherapy are not met, and 96900 should be reported.
The 96913 code defines prolonged phototherapy service with intensive topical therapy requirements and multiple phototherapy sessions per day.3 This code is rarely reported (average of fewer than 100 times in the Medicare population per year), and most insurers do not reimburse this service.
Protecting Yourself From an Audit
In my experience, review of private insurer audits of phototherapy services has yielded important lessons. First, having a written standard operating procedure in place regarding the performance of phototherapy services and how application of topicals will be handled has been helpful in audit defense. The other key to beating audits for phototherapy services is to have detailed documentation or a flowchart in the medical record regarding the topical agent and the light administration. The medical record should include what topical agent was applied, if any; whether the topical agent was applied in the office; where the topical product was applied; and who applied the topical product. Sometimes topical product application by a physician or staff is not feasible because of patient preference or the site of application. If the patient applied the topical, document that assistance was offered and refused, along with what type of UV light was used and the dosage. Inclusion of these elements in the medical record provides a clear picture of the delivery of the phototherapy service and will aid in responding to medical record audit.
Final Thoughts
Phototherapy is a critical treatment modality that continues to be utilized frequently in the expanding armamentarium of treatments for dermatoses. Phototherapy is performed almost exclusively by dermatologists and allows dermatologists to offer a unique level of care and value in the treatment of skin disease. Careful documentation, a written standard operating procedure, and adherence to proper performance standards will allow dermatologists to be compensated fairly for this important treatment modality and pass audits that are likely to occur.
- Lapolla W, Yentzer BA, Bagel J, et al. A review of phototherapy protocols for psoriasis treatment. J Am Acad Dermatol. 2011;64:936-949.
- Simpson GL, Yelverton CB, Rittenberg S, et al. Do utilization management controls for phototherapy increase the prescription of biologics? J Dermatolog Treat. 2006;17:359-361.
- Current Procedural Terminology 2017, Professional Edition. Chicago IL: American Medical Association; 2016.
- American Academy of Dermatology Association. Insurers review billing for photochemotherapy (CPT 96910). Derm Coding Consult. Spring 2009;13:4.
- American Academy of Dermatology Association. Coding Q&A's. Derm Coding Consult. Spring 2007;11:5, 7, 8.
- Coders' Desk Reference for Procedures 2017. Chicago, IL: Optum360; 2017.
- Relative Value Scale Update Committee Database. Chicago, IL: American Medical Association; 2016.
In this era of biologics for psoriasis with ever-increasing effectiveness and safety as well as patients who have less and less time to visit the physician's office, it would seem that the days of in-office UV treatments would be numbered. However, rumors of the demise of phototherapy may be greatly exaggerated. Phototherapy is still one of the safest and most cost-effective treatments for psoriasis and other dermatoses.1 Its use often is a prerequisite for biologic therapy, and it may be the only therapeutic option for certain subsets of patients, such as children, pregnant women, and immunosuppressed patients. Moreover, narrowband UVB technology has breathed new life into phototherapy, with better efficacy and less long-term risk. Although the utilization of psoralen plus UVA (PUVA) light therapy has indeed decreased over the last 2 decades, the use of UVB therapies continues to increase dramatically.2
Phototherapy Codes
There are 4 chief Current Procedural Terminology (CPT) codes for reporting phototherapy services: (1) 96900: actinotherapy (UV light treatment); (2) 96910: photochemotherapy, tar, and UVB (Goeckerman treatment) or petrolatum and UVB; (3) 96912: photochemotherapy and PUVA; and (4) 96913: photochemotherapy (Goeckerman and/or PUVA) for severe photoresponsive dermatoses requiring at least 4 to 8 hours of care under direct supervision of the physician.3
There is lack of specificity of the CPT code descriptions for phototherapy. Moreover, insurer guidance for documentation for phototherapy is vague to nonexistent, and of course whenever the use of any medical service increases, insurer scrutiny is sure to follow. Therefore, it is not surprising that dermatology practices have reported that private insurers as well as Medicare are auditing medical records for phototherapy treatments.4 In fact, recently we have seen a Midwest private insurer demand payment from dermatologists for hundreds of 96910 phototherapy services, which the insurer asserted should have been coded as 96900 because topical therapies were not applied by the dermatology staff. The insurer did not just evaluate medical records but also contacted patients directly and asked how services had been provided. Clearly, more detailed guidance for dermatologists and insurers on documentation and performance standards for each phototherapy service is needed.
Existing coding guidance for phototherapy indicates that actinotherapy (96900) defines the basic service of treating a patient with a UV light unit.5 Actinotherapy does not involve application of topical medications while the patient is in the office.
In contrast, photochemotherapy (96910) implies addition of a chemo agent to phototherapy. Despite the somewhat nonspecific nature of the code descriptor, it is apparent that application of photoenhancing agents such as tar, petrolatum, or distillates of petrolatum meet the requirements of 96910. The Coder's Desk Reference for Procedures 2017 describes 96910 as "the physician uses photosensitizing chemicals and light rays to treat skin ailments."6 Application of light-enhancing topical products should occur within the office by either staff or the patient. In fact, examination of practice expense data from the Centers for Medicare & Medicaid Services indicated that the 96910 code includes payment for clinical staff time to apply topical products as well as the cost of the topical agent(s).7
The PUVA code 96912 is defined by the use of photosensitizing psoralen medication, which can be administered topically or orally, followed by UVA treatment. In my experience, PUVA has similar performance standards with in-office application of psoralen, if applicable. If application of topical photoenhancing products occurs outside the office, the requirements of photochemotherapy are not met, and 96900 should be reported.
The 96913 code defines prolonged phototherapy service with intensive topical therapy requirements and multiple phototherapy sessions per day.3 This code is rarely reported (average of fewer than 100 times in the Medicare population per year), and most insurers do not reimburse this service.
Protecting Yourself From an Audit
In my experience, review of private insurer audits of phototherapy services has yielded important lessons. First, having a written standard operating procedure in place regarding the performance of phototherapy services and how application of topicals will be handled has been helpful in audit defense. The other key to beating audits for phototherapy services is to have detailed documentation or a flowchart in the medical record regarding the topical agent and the light administration. The medical record should include what topical agent was applied, if any; whether the topical agent was applied in the office; where the topical product was applied; and who applied the topical product. Sometimes topical product application by a physician or staff is not feasible because of patient preference or the site of application. If the patient applied the topical, document that assistance was offered and refused, along with what type of UV light was used and the dosage. Inclusion of these elements in the medical record provides a clear picture of the delivery of the phototherapy service and will aid in responding to medical record audit.
Final Thoughts
Phototherapy is a critical treatment modality that continues to be utilized frequently in the expanding armamentarium of treatments for dermatoses. Phototherapy is performed almost exclusively by dermatologists and allows dermatologists to offer a unique level of care and value in the treatment of skin disease. Careful documentation, a written standard operating procedure, and adherence to proper performance standards will allow dermatologists to be compensated fairly for this important treatment modality and pass audits that are likely to occur.
In this era of biologics for psoriasis with ever-increasing effectiveness and safety as well as patients who have less and less time to visit the physician's office, it would seem that the days of in-office UV treatments would be numbered. However, rumors of the demise of phototherapy may be greatly exaggerated. Phototherapy is still one of the safest and most cost-effective treatments for psoriasis and other dermatoses.1 Its use often is a prerequisite for biologic therapy, and it may be the only therapeutic option for certain subsets of patients, such as children, pregnant women, and immunosuppressed patients. Moreover, narrowband UVB technology has breathed new life into phototherapy, with better efficacy and less long-term risk. Although the utilization of psoralen plus UVA (PUVA) light therapy has indeed decreased over the last 2 decades, the use of UVB therapies continues to increase dramatically.2
Phototherapy Codes
There are 4 chief Current Procedural Terminology (CPT) codes for reporting phototherapy services: (1) 96900: actinotherapy (UV light treatment); (2) 96910: photochemotherapy, tar, and UVB (Goeckerman treatment) or petrolatum and UVB; (3) 96912: photochemotherapy and PUVA; and (4) 96913: photochemotherapy (Goeckerman and/or PUVA) for severe photoresponsive dermatoses requiring at least 4 to 8 hours of care under direct supervision of the physician.3
There is lack of specificity of the CPT code descriptions for phototherapy. Moreover, insurer guidance for documentation for phototherapy is vague to nonexistent, and of course whenever the use of any medical service increases, insurer scrutiny is sure to follow. Therefore, it is not surprising that dermatology practices have reported that private insurers as well as Medicare are auditing medical records for phototherapy treatments.4 In fact, recently we have seen a Midwest private insurer demand payment from dermatologists for hundreds of 96910 phototherapy services, which the insurer asserted should have been coded as 96900 because topical therapies were not applied by the dermatology staff. The insurer did not just evaluate medical records but also contacted patients directly and asked how services had been provided. Clearly, more detailed guidance for dermatologists and insurers on documentation and performance standards for each phototherapy service is needed.
Existing coding guidance for phototherapy indicates that actinotherapy (96900) defines the basic service of treating a patient with a UV light unit.5 Actinotherapy does not involve application of topical medications while the patient is in the office.
In contrast, photochemotherapy (96910) implies addition of a chemo agent to phototherapy. Despite the somewhat nonspecific nature of the code descriptor, it is apparent that application of photoenhancing agents such as tar, petrolatum, or distillates of petrolatum meet the requirements of 96910. The Coder's Desk Reference for Procedures 2017 describes 96910 as "the physician uses photosensitizing chemicals and light rays to treat skin ailments."6 Application of light-enhancing topical products should occur within the office by either staff or the patient. In fact, examination of practice expense data from the Centers for Medicare & Medicaid Services indicated that the 96910 code includes payment for clinical staff time to apply topical products as well as the cost of the topical agent(s).7
The PUVA code 96912 is defined by the use of photosensitizing psoralen medication, which can be administered topically or orally, followed by UVA treatment. In my experience, PUVA has similar performance standards with in-office application of psoralen, if applicable. If application of topical photoenhancing products occurs outside the office, the requirements of photochemotherapy are not met, and 96900 should be reported.
The 96913 code defines prolonged phototherapy service with intensive topical therapy requirements and multiple phototherapy sessions per day.3 This code is rarely reported (average of fewer than 100 times in the Medicare population per year), and most insurers do not reimburse this service.
Protecting Yourself From an Audit
In my experience, review of private insurer audits of phototherapy services has yielded important lessons. First, having a written standard operating procedure in place regarding the performance of phototherapy services and how application of topicals will be handled has been helpful in audit defense. The other key to beating audits for phototherapy services is to have detailed documentation or a flowchart in the medical record regarding the topical agent and the light administration. The medical record should include what topical agent was applied, if any; whether the topical agent was applied in the office; where the topical product was applied; and who applied the topical product. Sometimes topical product application by a physician or staff is not feasible because of patient preference or the site of application. If the patient applied the topical, document that assistance was offered and refused, along with what type of UV light was used and the dosage. Inclusion of these elements in the medical record provides a clear picture of the delivery of the phototherapy service and will aid in responding to medical record audit.
Final Thoughts
Phototherapy is a critical treatment modality that continues to be utilized frequently in the expanding armamentarium of treatments for dermatoses. Phototherapy is performed almost exclusively by dermatologists and allows dermatologists to offer a unique level of care and value in the treatment of skin disease. Careful documentation, a written standard operating procedure, and adherence to proper performance standards will allow dermatologists to be compensated fairly for this important treatment modality and pass audits that are likely to occur.
- Lapolla W, Yentzer BA, Bagel J, et al. A review of phototherapy protocols for psoriasis treatment. J Am Acad Dermatol. 2011;64:936-949.
- Simpson GL, Yelverton CB, Rittenberg S, et al. Do utilization management controls for phototherapy increase the prescription of biologics? J Dermatolog Treat. 2006;17:359-361.
- Current Procedural Terminology 2017, Professional Edition. Chicago IL: American Medical Association; 2016.
- American Academy of Dermatology Association. Insurers review billing for photochemotherapy (CPT 96910). Derm Coding Consult. Spring 2009;13:4.
- American Academy of Dermatology Association. Coding Q&A's. Derm Coding Consult. Spring 2007;11:5, 7, 8.
- Coders' Desk Reference for Procedures 2017. Chicago, IL: Optum360; 2017.
- Relative Value Scale Update Committee Database. Chicago, IL: American Medical Association; 2016.
- Lapolla W, Yentzer BA, Bagel J, et al. A review of phototherapy protocols for psoriasis treatment. J Am Acad Dermatol. 2011;64:936-949.
- Simpson GL, Yelverton CB, Rittenberg S, et al. Do utilization management controls for phototherapy increase the prescription of biologics? J Dermatolog Treat. 2006;17:359-361.
- Current Procedural Terminology 2017, Professional Edition. Chicago IL: American Medical Association; 2016.
- American Academy of Dermatology Association. Insurers review billing for photochemotherapy (CPT 96910). Derm Coding Consult. Spring 2009;13:4.
- American Academy of Dermatology Association. Coding Q&A's. Derm Coding Consult. Spring 2007;11:5, 7, 8.
- Coders' Desk Reference for Procedures 2017. Chicago, IL: Optum360; 2017.
- Relative Value Scale Update Committee Database. Chicago, IL: American Medical Association; 2016.