User login
Colorism can lead to intrafamily conflict
The color hue of a person’s skin is the most obvious criteria for society to judge a person and has always been deeply rooted in racism. Discrimination based on skin color is called colorism and is usually meted out by members of the same race and in the same family. The general belief is that someone with a lighter complexion is more beautiful, intelligent, or valuable than someone with a darker complexion. The term colorism can be widely applied in our assessment of conflict within families and society. The following case example gives guidance for psychiatrists faced with a family where colorism fuels family conflict.
Meeting the family
The Jaspers, a Black family, arrive at the psychiatrist’s office. They come in and look around before they choose their seats. Dr. Sally watches who sits next to whom and how they organize themselves in the office. After brief introductions, Mr. Jaspers begins, explaining why they are there.
“We are always fighting. We need this to stop. She, my wife, contradicts me all the time. Our kids are getting frustrated, and Bruce is acting out in school. He got in a fight again last week.”
Everyone looks at Bruce. He is darker skinned than the other siblings and carries all the African features in a family that favors the lighter end of the color spectrum. He sits next to his mother who leans into him. Mrs. Jaspers speaks next.
“Bruce gets picked on in school.”
Mr. Jaspers responds, “Well, if you didn’t run in there all the time and take him out, maybe he would learn how to deal with it better!”
“But they are mistreating him,” Mrs. Jaspers says.
The other children look away and play with their phones. Dr. Sally wonders whether this is a pattern: The parents fighting about how to deal with Bruce and his difficulties in the world – and the other siblings getting ignored and not included.
Dr. Sally asks Mrs. Jaspers for more details. She tells a narrative that is a strong thread in this family’s story.
“As you can see, Bruce is darker than the rest of our children. When we see the rest of our family, they all comment on what good skin and light coloring and good hair the other children have. Bruce just sits there. He is always being left out. He doesn’t speak up for himself. Maybe they think he can’t hear them, but I know he does and it affects him. They say the others are more intelligent, but I don’t think that is true. Bruce just gets picked on in school and he doesn’t feel like he matters. He doesn’t say anything, so maybe people think he doesn’t care, but I know he does.”
Dr. Sally turns to Bruce, who is still sitting silently next to his mother, his head down.
“Bruce, what do you have to say?”
Bruce shrugs his shoulders. His siblings still do not want to be drawn in and are otherwise occupied.
At this point, Dr. Sally might be thinking that she could see Bruce alone to assess his depression/self-esteem and maybe find ways to try to build him up. She does not want this to be an opportunity wasted. The goal is to work with the family to get Bruce where he needs to be faster and help the whole family.
Dr. Sally presses on. “Mr. Jaspers, what is your opinion?”
“She babies him. She treats him differently from the other kids. She is driving a wedge between him and his siblings. We fight about it all the time. She is driving a wedge between us, too.”
Mrs. Jaspers jumps in: “But you don’t know what it is like! When I was the only Black person in math class, I got picked on all the time! It made me self-conscious, and I couldn’t do my work. “
The other siblings look up briefly then back down at their devices. Dr. Sally asks them as a group:
“Can I ask you a question as a family? Can I ask the children a question?” They look up again. “Is this what goes on at home?” They all nod but offer no details.
Dr. Sally asks the oldest: “How does this affect your relationship with Bruce?”
They all look back and forth at each other. There is another long silence.
“See!” says Mr. Jaspers! “You can't protect him forever, and you are just ostracizing him from the rest of us! “
“But, but, he, he needs to learn different things. He is different. He faces different struggles. The police will stop him more. I am afraid for him.” Mrs. Jaspers starts to cry.
“You can’t protect him forever,” says her husband, gently reaching over to her.
Bruce has psychologically disappeared from the room, hiding behind his mother, who is now the largest and neediest presence in the room. Mr. Jaspers looks at Dr. Sally helplessly.
Dr. Sally asks the important question to the whole family.
“How do you all think this should work? If you don’t think Mrs. Jaspers is right, what do you think should be the way forward?”
This question is the turning point and indicates that Dr. Sally sees that the solution lies in how the family wants to manage things.
“I believe that your whole family has the answers, that you all have thought through this situation much more deeply and for much longer than I have. I am just hearing about it, and I am White and don’t have this experience. I have faith in your family, that with an opportunity to openly discuss this issue, that this knot can be unraveled. It does not mean that there are not more knots to unravel. For today, how to help you all help Bruce, is the work."
Dr. Sally talks to everyone but finishes up by looking at Mr. Jaspers, who has indicated that Bruce is part of the family and should not be treated differently from the other children.
Sean, the oldest sibling, now pipes up: “Bruce gets everything he wants. Mum spoils him; she always takes his side if there are arguments. Bruce knows this, and he steals our stuff because he knows he will get away with it.”
Bruce is quiet and leans in more to his mother. Dr. Sally motions to the mother not to speak.
“Is this true, Bruce?” Silence speaks that the answer is yes. The disparities in the family are aired for a while longer.
“Mrs. Jaspers, it is now your turn to respond.”
“Bruce is darker and faces more challenges than the others; he needs more protection and to know that he is loved.”
“Your family seems to think otherwise. They seem to think that your protection, while admirable, needs to be tempered to allow him to grow into a man who can stand on his own feet.”
Dr. Sally guides the family as a whole to a place where they can agree on the problem. The problem is now framed as a mother who cares too much and is too protective of Bruce but now her love and care need to be tempered. As a mother, she feels that it is her duty to protect her most vulnerable son. The family knows that Bruce will face more social scrutiny than the others, that he will have more internal struggles with self-worth than the others. How can the family help?
This conceptualization causes the family to look searchingly at one another. It is nothing they haven’t thought about privately, but this is the first time they are together thinking about it.
Dr. Sally says that she can help by providing time and space for them to wok through this together. They all agree to come back the following week with some thoughts about moving forward.
Offering perspective on colorism
In her book “Facing the Black Shadow,” couples and family therapist Marlene F. Watson, PhD, discusses colorism.
“African Americans still have a tough time talking about slavery – the origin of colorism. Seriously, what can we really expect to change without acknowledging and challenging the psychological residuals of slavery in our families and communities? What doesn’t get resolved in one generation is passed on to the next so our issues from slavery go from one generation to the next.”
Dr. Watson continues: “Confronting the secret about skin color in our families and communities is necessary for all Black girls to feel lovable, worthy, and deserving of care and for all Black boys to feel their value lies within them, not a dark, light, bright, near-white or White woman. African Americans need to get that preferring light over dark or dark over light is problematic for all of us. Skin color preferences in the African American community follow society’s racial hierarchy. African Americans as a group are at the bottom in the larger society and dark-skinned African Americans are at the bottom in the Black community.”
and patterns about skin color. Her advice is to ask each family member, from oldest to youngest, to identify the spoken and unspoken skin color beliefs he or she experiences in the family. Ask about skin color beliefs from outside that affect family members, and what each person thinks the family could do to stop promoting the “less than/better than” mentality that is often present with skin color assignment.
Thank you to Lynette Ramsingh Barros, who collaborated on creating the case.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest.
The color hue of a person’s skin is the most obvious criteria for society to judge a person and has always been deeply rooted in racism. Discrimination based on skin color is called colorism and is usually meted out by members of the same race and in the same family. The general belief is that someone with a lighter complexion is more beautiful, intelligent, or valuable than someone with a darker complexion. The term colorism can be widely applied in our assessment of conflict within families and society. The following case example gives guidance for psychiatrists faced with a family where colorism fuels family conflict.
Meeting the family
The Jaspers, a Black family, arrive at the psychiatrist’s office. They come in and look around before they choose their seats. Dr. Sally watches who sits next to whom and how they organize themselves in the office. After brief introductions, Mr. Jaspers begins, explaining why they are there.
“We are always fighting. We need this to stop. She, my wife, contradicts me all the time. Our kids are getting frustrated, and Bruce is acting out in school. He got in a fight again last week.”
Everyone looks at Bruce. He is darker skinned than the other siblings and carries all the African features in a family that favors the lighter end of the color spectrum. He sits next to his mother who leans into him. Mrs. Jaspers speaks next.
“Bruce gets picked on in school.”
Mr. Jaspers responds, “Well, if you didn’t run in there all the time and take him out, maybe he would learn how to deal with it better!”
“But they are mistreating him,” Mrs. Jaspers says.
The other children look away and play with their phones. Dr. Sally wonders whether this is a pattern: The parents fighting about how to deal with Bruce and his difficulties in the world – and the other siblings getting ignored and not included.
Dr. Sally asks Mrs. Jaspers for more details. She tells a narrative that is a strong thread in this family’s story.
“As you can see, Bruce is darker than the rest of our children. When we see the rest of our family, they all comment on what good skin and light coloring and good hair the other children have. Bruce just sits there. He is always being left out. He doesn’t speak up for himself. Maybe they think he can’t hear them, but I know he does and it affects him. They say the others are more intelligent, but I don’t think that is true. Bruce just gets picked on in school and he doesn’t feel like he matters. He doesn’t say anything, so maybe people think he doesn’t care, but I know he does.”
Dr. Sally turns to Bruce, who is still sitting silently next to his mother, his head down.
“Bruce, what do you have to say?”
Bruce shrugs his shoulders. His siblings still do not want to be drawn in and are otherwise occupied.
At this point, Dr. Sally might be thinking that she could see Bruce alone to assess his depression/self-esteem and maybe find ways to try to build him up. She does not want this to be an opportunity wasted. The goal is to work with the family to get Bruce where he needs to be faster and help the whole family.
Dr. Sally presses on. “Mr. Jaspers, what is your opinion?”
“She babies him. She treats him differently from the other kids. She is driving a wedge between him and his siblings. We fight about it all the time. She is driving a wedge between us, too.”
Mrs. Jaspers jumps in: “But you don’t know what it is like! When I was the only Black person in math class, I got picked on all the time! It made me self-conscious, and I couldn’t do my work. “
The other siblings look up briefly then back down at their devices. Dr. Sally asks them as a group:
“Can I ask you a question as a family? Can I ask the children a question?” They look up again. “Is this what goes on at home?” They all nod but offer no details.
Dr. Sally asks the oldest: “How does this affect your relationship with Bruce?”
They all look back and forth at each other. There is another long silence.
“See!” says Mr. Jaspers! “You can't protect him forever, and you are just ostracizing him from the rest of us! “
“But, but, he, he needs to learn different things. He is different. He faces different struggles. The police will stop him more. I am afraid for him.” Mrs. Jaspers starts to cry.
“You can’t protect him forever,” says her husband, gently reaching over to her.
Bruce has psychologically disappeared from the room, hiding behind his mother, who is now the largest and neediest presence in the room. Mr. Jaspers looks at Dr. Sally helplessly.
Dr. Sally asks the important question to the whole family.
“How do you all think this should work? If you don’t think Mrs. Jaspers is right, what do you think should be the way forward?”
This question is the turning point and indicates that Dr. Sally sees that the solution lies in how the family wants to manage things.
“I believe that your whole family has the answers, that you all have thought through this situation much more deeply and for much longer than I have. I am just hearing about it, and I am White and don’t have this experience. I have faith in your family, that with an opportunity to openly discuss this issue, that this knot can be unraveled. It does not mean that there are not more knots to unravel. For today, how to help you all help Bruce, is the work."
Dr. Sally talks to everyone but finishes up by looking at Mr. Jaspers, who has indicated that Bruce is part of the family and should not be treated differently from the other children.
Sean, the oldest sibling, now pipes up: “Bruce gets everything he wants. Mum spoils him; she always takes his side if there are arguments. Bruce knows this, and he steals our stuff because he knows he will get away with it.”
Bruce is quiet and leans in more to his mother. Dr. Sally motions to the mother not to speak.
“Is this true, Bruce?” Silence speaks that the answer is yes. The disparities in the family are aired for a while longer.
“Mrs. Jaspers, it is now your turn to respond.”
“Bruce is darker and faces more challenges than the others; he needs more protection and to know that he is loved.”
“Your family seems to think otherwise. They seem to think that your protection, while admirable, needs to be tempered to allow him to grow into a man who can stand on his own feet.”
Dr. Sally guides the family as a whole to a place where they can agree on the problem. The problem is now framed as a mother who cares too much and is too protective of Bruce but now her love and care need to be tempered. As a mother, she feels that it is her duty to protect her most vulnerable son. The family knows that Bruce will face more social scrutiny than the others, that he will have more internal struggles with self-worth than the others. How can the family help?
This conceptualization causes the family to look searchingly at one another. It is nothing they haven’t thought about privately, but this is the first time they are together thinking about it.
Dr. Sally says that she can help by providing time and space for them to wok through this together. They all agree to come back the following week with some thoughts about moving forward.
Offering perspective on colorism
In her book “Facing the Black Shadow,” couples and family therapist Marlene F. Watson, PhD, discusses colorism.
“African Americans still have a tough time talking about slavery – the origin of colorism. Seriously, what can we really expect to change without acknowledging and challenging the psychological residuals of slavery in our families and communities? What doesn’t get resolved in one generation is passed on to the next so our issues from slavery go from one generation to the next.”
Dr. Watson continues: “Confronting the secret about skin color in our families and communities is necessary for all Black girls to feel lovable, worthy, and deserving of care and for all Black boys to feel their value lies within them, not a dark, light, bright, near-white or White woman. African Americans need to get that preferring light over dark or dark over light is problematic for all of us. Skin color preferences in the African American community follow society’s racial hierarchy. African Americans as a group are at the bottom in the larger society and dark-skinned African Americans are at the bottom in the Black community.”
and patterns about skin color. Her advice is to ask each family member, from oldest to youngest, to identify the spoken and unspoken skin color beliefs he or she experiences in the family. Ask about skin color beliefs from outside that affect family members, and what each person thinks the family could do to stop promoting the “less than/better than” mentality that is often present with skin color assignment.
Thank you to Lynette Ramsingh Barros, who collaborated on creating the case.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest.
The color hue of a person’s skin is the most obvious criteria for society to judge a person and has always been deeply rooted in racism. Discrimination based on skin color is called colorism and is usually meted out by members of the same race and in the same family. The general belief is that someone with a lighter complexion is more beautiful, intelligent, or valuable than someone with a darker complexion. The term colorism can be widely applied in our assessment of conflict within families and society. The following case example gives guidance for psychiatrists faced with a family where colorism fuels family conflict.
Meeting the family
The Jaspers, a Black family, arrive at the psychiatrist’s office. They come in and look around before they choose their seats. Dr. Sally watches who sits next to whom and how they organize themselves in the office. After brief introductions, Mr. Jaspers begins, explaining why they are there.
“We are always fighting. We need this to stop. She, my wife, contradicts me all the time. Our kids are getting frustrated, and Bruce is acting out in school. He got in a fight again last week.”
Everyone looks at Bruce. He is darker skinned than the other siblings and carries all the African features in a family that favors the lighter end of the color spectrum. He sits next to his mother who leans into him. Mrs. Jaspers speaks next.
“Bruce gets picked on in school.”
Mr. Jaspers responds, “Well, if you didn’t run in there all the time and take him out, maybe he would learn how to deal with it better!”
“But they are mistreating him,” Mrs. Jaspers says.
The other children look away and play with their phones. Dr. Sally wonders whether this is a pattern: The parents fighting about how to deal with Bruce and his difficulties in the world – and the other siblings getting ignored and not included.
Dr. Sally asks Mrs. Jaspers for more details. She tells a narrative that is a strong thread in this family’s story.
“As you can see, Bruce is darker than the rest of our children. When we see the rest of our family, they all comment on what good skin and light coloring and good hair the other children have. Bruce just sits there. He is always being left out. He doesn’t speak up for himself. Maybe they think he can’t hear them, but I know he does and it affects him. They say the others are more intelligent, but I don’t think that is true. Bruce just gets picked on in school and he doesn’t feel like he matters. He doesn’t say anything, so maybe people think he doesn’t care, but I know he does.”
Dr. Sally turns to Bruce, who is still sitting silently next to his mother, his head down.
“Bruce, what do you have to say?”
Bruce shrugs his shoulders. His siblings still do not want to be drawn in and are otherwise occupied.
At this point, Dr. Sally might be thinking that she could see Bruce alone to assess his depression/self-esteem and maybe find ways to try to build him up. She does not want this to be an opportunity wasted. The goal is to work with the family to get Bruce where he needs to be faster and help the whole family.
Dr. Sally presses on. “Mr. Jaspers, what is your opinion?”
“She babies him. She treats him differently from the other kids. She is driving a wedge between him and his siblings. We fight about it all the time. She is driving a wedge between us, too.”
Mrs. Jaspers jumps in: “But you don’t know what it is like! When I was the only Black person in math class, I got picked on all the time! It made me self-conscious, and I couldn’t do my work. “
The other siblings look up briefly then back down at their devices. Dr. Sally asks them as a group:
“Can I ask you a question as a family? Can I ask the children a question?” They look up again. “Is this what goes on at home?” They all nod but offer no details.
Dr. Sally asks the oldest: “How does this affect your relationship with Bruce?”
They all look back and forth at each other. There is another long silence.
“See!” says Mr. Jaspers! “You can't protect him forever, and you are just ostracizing him from the rest of us! “
“But, but, he, he needs to learn different things. He is different. He faces different struggles. The police will stop him more. I am afraid for him.” Mrs. Jaspers starts to cry.
“You can’t protect him forever,” says her husband, gently reaching over to her.
Bruce has psychologically disappeared from the room, hiding behind his mother, who is now the largest and neediest presence in the room. Mr. Jaspers looks at Dr. Sally helplessly.
Dr. Sally asks the important question to the whole family.
“How do you all think this should work? If you don’t think Mrs. Jaspers is right, what do you think should be the way forward?”
This question is the turning point and indicates that Dr. Sally sees that the solution lies in how the family wants to manage things.
“I believe that your whole family has the answers, that you all have thought through this situation much more deeply and for much longer than I have. I am just hearing about it, and I am White and don’t have this experience. I have faith in your family, that with an opportunity to openly discuss this issue, that this knot can be unraveled. It does not mean that there are not more knots to unravel. For today, how to help you all help Bruce, is the work."
Dr. Sally talks to everyone but finishes up by looking at Mr. Jaspers, who has indicated that Bruce is part of the family and should not be treated differently from the other children.
Sean, the oldest sibling, now pipes up: “Bruce gets everything he wants. Mum spoils him; she always takes his side if there are arguments. Bruce knows this, and he steals our stuff because he knows he will get away with it.”
Bruce is quiet and leans in more to his mother. Dr. Sally motions to the mother not to speak.
“Is this true, Bruce?” Silence speaks that the answer is yes. The disparities in the family are aired for a while longer.
“Mrs. Jaspers, it is now your turn to respond.”
“Bruce is darker and faces more challenges than the others; he needs more protection and to know that he is loved.”
“Your family seems to think otherwise. They seem to think that your protection, while admirable, needs to be tempered to allow him to grow into a man who can stand on his own feet.”
Dr. Sally guides the family as a whole to a place where they can agree on the problem. The problem is now framed as a mother who cares too much and is too protective of Bruce but now her love and care need to be tempered. As a mother, she feels that it is her duty to protect her most vulnerable son. The family knows that Bruce will face more social scrutiny than the others, that he will have more internal struggles with self-worth than the others. How can the family help?
This conceptualization causes the family to look searchingly at one another. It is nothing they haven’t thought about privately, but this is the first time they are together thinking about it.
Dr. Sally says that she can help by providing time and space for them to wok through this together. They all agree to come back the following week with some thoughts about moving forward.
Offering perspective on colorism
In her book “Facing the Black Shadow,” couples and family therapist Marlene F. Watson, PhD, discusses colorism.
“African Americans still have a tough time talking about slavery – the origin of colorism. Seriously, what can we really expect to change without acknowledging and challenging the psychological residuals of slavery in our families and communities? What doesn’t get resolved in one generation is passed on to the next so our issues from slavery go from one generation to the next.”
Dr. Watson continues: “Confronting the secret about skin color in our families and communities is necessary for all Black girls to feel lovable, worthy, and deserving of care and for all Black boys to feel their value lies within them, not a dark, light, bright, near-white or White woman. African Americans need to get that preferring light over dark or dark over light is problematic for all of us. Skin color preferences in the African American community follow society’s racial hierarchy. African Americans as a group are at the bottom in the larger society and dark-skinned African Americans are at the bottom in the Black community.”
and patterns about skin color. Her advice is to ask each family member, from oldest to youngest, to identify the spoken and unspoken skin color beliefs he or she experiences in the family. Ask about skin color beliefs from outside that affect family members, and what each person thinks the family could do to stop promoting the “less than/better than” mentality that is often present with skin color assignment.
Thank you to Lynette Ramsingh Barros, who collaborated on creating the case.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest.
The transitions of COVID-19
When I was preparing for the recent birth of my baby, I anticipated a period of transition for myself. As a reproductive psychiatrist, I have treated many women during the perinatal and postpartum periods, and have a unique appreciation for the life changes that accompany birth. What I did not expect, however, was the world transitioning with me.
“The new normal” is an economic phrase that describes the COVID-19 era. The pandemic has engendered economic instability, collapsed industries, challenged health care systems, and has led to many deaths worldwide. The COVID-19 pandemic also has been associated with overall increases in anxiety and depression.1 Emerging research suggests that frontline medical workers are especially at risk for developing psychological distress.2
COVID-19 has also created immense challenges for families. Because of concern for the spread of the virus, schools have been suspended, older grandparents isolated, and many parents continue to work remotely. For families in psychiatric care, this time has also been a time of change. Telepsychiatry might be more accessible, but the transition has been an adjustment for patients and clinicians.
As psychiatrists, how do we best treat families during this time? What are some ways to support our psychiatric colleagues? How do we ensure our own emotional well-being amid the tremendous changes occurring around us?
Background of interpersonal psychotherapy
Interpersonal psychotherapy (IPT) is a form of psychotherapy designed to treat depression following periods of transition. Its main goals include improving interpersonal connection and reducing psychological distress. Originally developed in the 1970s by Gerald Klerman, MD; Myrna Weissman, PhD; and Eugene Paykel, MD, IPT is a structured, time-limited form of psychotherapy.3
Conceptualizing depression as a treatable illness, Pim Cuijpers, PhD, and associates summarized the division of IPT into three phases.4 The initial phase involves history taking, forming an alliance, and choosing an interpersonal focus for treatment. The middle phase focuses on applying interpersonal problem-specific therapeutic techniques. The concluding phase of treatment involves consolidation of gains as well as formulating contingency plans for relapse of symptoms. Over the course of treatment, an IPT clinician focuses on life transitions and emphasizes that isolation and antagonistic relationships increase an individual’s vulnerability for a depressive episode.3
Randomized, controlled trials support IPT’s efficacy as a treatment for depression. Research also suggests it can possibly prevent the development of depression.4 Although IPT initially was designed as an individual form of psychotherapy, it has been adapted to both family and group contexts.5,6 IPT is also an empirically valid form of psychotherapy for postpartum depression.7
Interpersonal psychotherapy for families
Given IPT’s role for treating depression following times of transition, clinicians should consider adapting interpersonal psychotherapy to family treatment during this time. Addressing social isolation, managing complex family relationships, and monitoring the family’s overall emotional health should be prioritized. Families under quarantine or who are grieving the death of family members may especially benefit from improved interpersonal connection. Consistent with the IPT model, contingency plans for the family should also be explored to prepare for potential future waves of the pandemic.
In addition to supporting and strengthening families, psychiatrists can use IPT themes to identify positive changes for families tied to COVID-19. Despite its difficulties, the stay-at-home order provided some families a unique chance to slow down and adapt a more relaxed routine. Busy families were suddenly given the opportunity to spend more time with one another. Although many older grandparents were isolated, creative uses of technology provided a chance for grandparents to remain an integral part of family life. Psychiatrists can assist families in transitioning back to previous schedules, while also exploring ways to incorporate the positive changes gained during this time.
Interpersonal psychotherapy for psychiatrists
An interpersonal focus could also be helpful for clinicians to adapt to changes in psychiatric practice. Many clinicians have been thrust into telepsychiatry practice, some with little to no preparation. Because of the trauma associated with frontline work, some psychiatrists have expanded their patient panel to treat physician colleagues. For consult-liaison psychiatrists, the possible neuropsychiatric effects of COVID-19 are new symptoms to consider when evaluating patients in a medical hospital setting.8 Fundamentally, modern day psychiatrists have never encountered a pandemic nor attempted to treat its psychological implications. Prioritizing seeking support from colleagues and caring for one’s personal relationships are helpful tools for clinicians to maintain their own emotional health during this challenging period.
Personal reflection
When I reflect on my baby’s recent birth, I recognize the importance of interpersonal relationships. COVID-19 developed shortly after I gave birth, during the initial haze of the newborn period. Initially, I felt overwhelmed by the many transitions and emotions that were occurring simultaneously. However, as I began to prioritize socialization for myself and my family (albeit creatively at times while socially distancing), I witnessed its positive effects on my emotional well-being and recognized its value in managing times of transition.
Using IPT for families, colleagues, and ourselves
As general psychiatrists, there are several ways to utilize IPT-related themes during this time:
- Connect with families: Although families may recognize they are struggling emotionally, some may find it difficult to navigate the sea of mental health resources. This is particularly true when a family’s financial situation is also stressed. Reaching out to local religious services and community medical resources or inquiring about the mental health of other family members are ways for psychiatrists to engage more families in mental health treatment.
- Reach out to colleagues: Psychiatrists are not immune to developing psychiatric disorders,and it is important to support each other.9 This is also an unusual time when psychiatrists are treating symptoms in patients that they themselves may be also experiencing. Supporting help groups and hot lines, reaching out to colleagues who appear to be struggling and addressing interpersonal conflicts within one’s practice are crucial practices for psychiatrists during this time.
- Explore within ourselves: Evaluating our own interpersonal relationships as well as areas for improvement are critical skills to maintain our own emotional well-being. Setting aside time to connect with friends in a nonclinical setting and prioritizing our family connections are helpful tools. In addition, exploring our reactions to past life transitions could improve our own level of insight into our response to COVID-19.
Conclusion
Conceptualizing COVID-19 as a period of transition and using IPT themes are helpful tools to mitigate the potential adverse psychological effects of COVID-19 on families. Similarly, they can also be helpful in supporting our colleagues and helping ourselves cope during this difficult period.
References
1. Qiu J et al. Gen Psychiatr. 2020 Mar 6;33(2):e100213.
2. Gautam M et al. Psychosomatics. 2020 Apr 20. doi: 10.1016/j.psym.2020.04.009.
3. Markowitz JC, Weissman MM. Clin Psychol Psychother. 2012 Mar-Apr;19(2):99-105.
4. Cuijpers P et al. Am J Psychiatry. 2016 Jul;173(7):680-7.
5. Dietz LJ et al. J Am Acad Child Adolesc Psychiatry. 2015 Mar;54(3):191-9.
6. Verdeli H et al. Child Adolesc Psychiatr Clin N Am. 2008 Jul;17(3):605-24.
7. Stuart S. Clin Psychol Psychother. 2012 Mar-Apr;19(2):134-40.
8. Rogers JP et al. Lancet Psychiatry. 2020 Jul;7(7):611-27.
9. Korkeila JA et al. Scand J Public Health. 2003;31(2):85-91.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care. Dr. Reinstein has no conflicts of interest. Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
When I was preparing for the recent birth of my baby, I anticipated a period of transition for myself. As a reproductive psychiatrist, I have treated many women during the perinatal and postpartum periods, and have a unique appreciation for the life changes that accompany birth. What I did not expect, however, was the world transitioning with me.
“The new normal” is an economic phrase that describes the COVID-19 era. The pandemic has engendered economic instability, collapsed industries, challenged health care systems, and has led to many deaths worldwide. The COVID-19 pandemic also has been associated with overall increases in anxiety and depression.1 Emerging research suggests that frontline medical workers are especially at risk for developing psychological distress.2
COVID-19 has also created immense challenges for families. Because of concern for the spread of the virus, schools have been suspended, older grandparents isolated, and many parents continue to work remotely. For families in psychiatric care, this time has also been a time of change. Telepsychiatry might be more accessible, but the transition has been an adjustment for patients and clinicians.
As psychiatrists, how do we best treat families during this time? What are some ways to support our psychiatric colleagues? How do we ensure our own emotional well-being amid the tremendous changes occurring around us?
Background of interpersonal psychotherapy
Interpersonal psychotherapy (IPT) is a form of psychotherapy designed to treat depression following periods of transition. Its main goals include improving interpersonal connection and reducing psychological distress. Originally developed in the 1970s by Gerald Klerman, MD; Myrna Weissman, PhD; and Eugene Paykel, MD, IPT is a structured, time-limited form of psychotherapy.3
Conceptualizing depression as a treatable illness, Pim Cuijpers, PhD, and associates summarized the division of IPT into three phases.4 The initial phase involves history taking, forming an alliance, and choosing an interpersonal focus for treatment. The middle phase focuses on applying interpersonal problem-specific therapeutic techniques. The concluding phase of treatment involves consolidation of gains as well as formulating contingency plans for relapse of symptoms. Over the course of treatment, an IPT clinician focuses on life transitions and emphasizes that isolation and antagonistic relationships increase an individual’s vulnerability for a depressive episode.3
Randomized, controlled trials support IPT’s efficacy as a treatment for depression. Research also suggests it can possibly prevent the development of depression.4 Although IPT initially was designed as an individual form of psychotherapy, it has been adapted to both family and group contexts.5,6 IPT is also an empirically valid form of psychotherapy for postpartum depression.7
Interpersonal psychotherapy for families
Given IPT’s role for treating depression following times of transition, clinicians should consider adapting interpersonal psychotherapy to family treatment during this time. Addressing social isolation, managing complex family relationships, and monitoring the family’s overall emotional health should be prioritized. Families under quarantine or who are grieving the death of family members may especially benefit from improved interpersonal connection. Consistent with the IPT model, contingency plans for the family should also be explored to prepare for potential future waves of the pandemic.
In addition to supporting and strengthening families, psychiatrists can use IPT themes to identify positive changes for families tied to COVID-19. Despite its difficulties, the stay-at-home order provided some families a unique chance to slow down and adapt a more relaxed routine. Busy families were suddenly given the opportunity to spend more time with one another. Although many older grandparents were isolated, creative uses of technology provided a chance for grandparents to remain an integral part of family life. Psychiatrists can assist families in transitioning back to previous schedules, while also exploring ways to incorporate the positive changes gained during this time.
Interpersonal psychotherapy for psychiatrists
An interpersonal focus could also be helpful for clinicians to adapt to changes in psychiatric practice. Many clinicians have been thrust into telepsychiatry practice, some with little to no preparation. Because of the trauma associated with frontline work, some psychiatrists have expanded their patient panel to treat physician colleagues. For consult-liaison psychiatrists, the possible neuropsychiatric effects of COVID-19 are new symptoms to consider when evaluating patients in a medical hospital setting.8 Fundamentally, modern day psychiatrists have never encountered a pandemic nor attempted to treat its psychological implications. Prioritizing seeking support from colleagues and caring for one’s personal relationships are helpful tools for clinicians to maintain their own emotional health during this challenging period.
Personal reflection
When I reflect on my baby’s recent birth, I recognize the importance of interpersonal relationships. COVID-19 developed shortly after I gave birth, during the initial haze of the newborn period. Initially, I felt overwhelmed by the many transitions and emotions that were occurring simultaneously. However, as I began to prioritize socialization for myself and my family (albeit creatively at times while socially distancing), I witnessed its positive effects on my emotional well-being and recognized its value in managing times of transition.
Using IPT for families, colleagues, and ourselves
As general psychiatrists, there are several ways to utilize IPT-related themes during this time:
- Connect with families: Although families may recognize they are struggling emotionally, some may find it difficult to navigate the sea of mental health resources. This is particularly true when a family’s financial situation is also stressed. Reaching out to local religious services and community medical resources or inquiring about the mental health of other family members are ways for psychiatrists to engage more families in mental health treatment.
- Reach out to colleagues: Psychiatrists are not immune to developing psychiatric disorders,and it is important to support each other.9 This is also an unusual time when psychiatrists are treating symptoms in patients that they themselves may be also experiencing. Supporting help groups and hot lines, reaching out to colleagues who appear to be struggling and addressing interpersonal conflicts within one’s practice are crucial practices for psychiatrists during this time.
- Explore within ourselves: Evaluating our own interpersonal relationships as well as areas for improvement are critical skills to maintain our own emotional well-being. Setting aside time to connect with friends in a nonclinical setting and prioritizing our family connections are helpful tools. In addition, exploring our reactions to past life transitions could improve our own level of insight into our response to COVID-19.
Conclusion
Conceptualizing COVID-19 as a period of transition and using IPT themes are helpful tools to mitigate the potential adverse psychological effects of COVID-19 on families. Similarly, they can also be helpful in supporting our colleagues and helping ourselves cope during this difficult period.
References
1. Qiu J et al. Gen Psychiatr. 2020 Mar 6;33(2):e100213.
2. Gautam M et al. Psychosomatics. 2020 Apr 20. doi: 10.1016/j.psym.2020.04.009.
3. Markowitz JC, Weissman MM. Clin Psychol Psychother. 2012 Mar-Apr;19(2):99-105.
4. Cuijpers P et al. Am J Psychiatry. 2016 Jul;173(7):680-7.
5. Dietz LJ et al. J Am Acad Child Adolesc Psychiatry. 2015 Mar;54(3):191-9.
6. Verdeli H et al. Child Adolesc Psychiatr Clin N Am. 2008 Jul;17(3):605-24.
7. Stuart S. Clin Psychol Psychother. 2012 Mar-Apr;19(2):134-40.
8. Rogers JP et al. Lancet Psychiatry. 2020 Jul;7(7):611-27.
9. Korkeila JA et al. Scand J Public Health. 2003;31(2):85-91.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care. Dr. Reinstein has no conflicts of interest. Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
When I was preparing for the recent birth of my baby, I anticipated a period of transition for myself. As a reproductive psychiatrist, I have treated many women during the perinatal and postpartum periods, and have a unique appreciation for the life changes that accompany birth. What I did not expect, however, was the world transitioning with me.
“The new normal” is an economic phrase that describes the COVID-19 era. The pandemic has engendered economic instability, collapsed industries, challenged health care systems, and has led to many deaths worldwide. The COVID-19 pandemic also has been associated with overall increases in anxiety and depression.1 Emerging research suggests that frontline medical workers are especially at risk for developing psychological distress.2
COVID-19 has also created immense challenges for families. Because of concern for the spread of the virus, schools have been suspended, older grandparents isolated, and many parents continue to work remotely. For families in psychiatric care, this time has also been a time of change. Telepsychiatry might be more accessible, but the transition has been an adjustment for patients and clinicians.
As psychiatrists, how do we best treat families during this time? What are some ways to support our psychiatric colleagues? How do we ensure our own emotional well-being amid the tremendous changes occurring around us?
Background of interpersonal psychotherapy
Interpersonal psychotherapy (IPT) is a form of psychotherapy designed to treat depression following periods of transition. Its main goals include improving interpersonal connection and reducing psychological distress. Originally developed in the 1970s by Gerald Klerman, MD; Myrna Weissman, PhD; and Eugene Paykel, MD, IPT is a structured, time-limited form of psychotherapy.3
Conceptualizing depression as a treatable illness, Pim Cuijpers, PhD, and associates summarized the division of IPT into three phases.4 The initial phase involves history taking, forming an alliance, and choosing an interpersonal focus for treatment. The middle phase focuses on applying interpersonal problem-specific therapeutic techniques. The concluding phase of treatment involves consolidation of gains as well as formulating contingency plans for relapse of symptoms. Over the course of treatment, an IPT clinician focuses on life transitions and emphasizes that isolation and antagonistic relationships increase an individual’s vulnerability for a depressive episode.3
Randomized, controlled trials support IPT’s efficacy as a treatment for depression. Research also suggests it can possibly prevent the development of depression.4 Although IPT initially was designed as an individual form of psychotherapy, it has been adapted to both family and group contexts.5,6 IPT is also an empirically valid form of psychotherapy for postpartum depression.7
Interpersonal psychotherapy for families
Given IPT’s role for treating depression following times of transition, clinicians should consider adapting interpersonal psychotherapy to family treatment during this time. Addressing social isolation, managing complex family relationships, and monitoring the family’s overall emotional health should be prioritized. Families under quarantine or who are grieving the death of family members may especially benefit from improved interpersonal connection. Consistent with the IPT model, contingency plans for the family should also be explored to prepare for potential future waves of the pandemic.
In addition to supporting and strengthening families, psychiatrists can use IPT themes to identify positive changes for families tied to COVID-19. Despite its difficulties, the stay-at-home order provided some families a unique chance to slow down and adapt a more relaxed routine. Busy families were suddenly given the opportunity to spend more time with one another. Although many older grandparents were isolated, creative uses of technology provided a chance for grandparents to remain an integral part of family life. Psychiatrists can assist families in transitioning back to previous schedules, while also exploring ways to incorporate the positive changes gained during this time.
Interpersonal psychotherapy for psychiatrists
An interpersonal focus could also be helpful for clinicians to adapt to changes in psychiatric practice. Many clinicians have been thrust into telepsychiatry practice, some with little to no preparation. Because of the trauma associated with frontline work, some psychiatrists have expanded their patient panel to treat physician colleagues. For consult-liaison psychiatrists, the possible neuropsychiatric effects of COVID-19 are new symptoms to consider when evaluating patients in a medical hospital setting.8 Fundamentally, modern day psychiatrists have never encountered a pandemic nor attempted to treat its psychological implications. Prioritizing seeking support from colleagues and caring for one’s personal relationships are helpful tools for clinicians to maintain their own emotional health during this challenging period.
Personal reflection
When I reflect on my baby’s recent birth, I recognize the importance of interpersonal relationships. COVID-19 developed shortly after I gave birth, during the initial haze of the newborn period. Initially, I felt overwhelmed by the many transitions and emotions that were occurring simultaneously. However, as I began to prioritize socialization for myself and my family (albeit creatively at times while socially distancing), I witnessed its positive effects on my emotional well-being and recognized its value in managing times of transition.
Using IPT for families, colleagues, and ourselves
As general psychiatrists, there are several ways to utilize IPT-related themes during this time:
- Connect with families: Although families may recognize they are struggling emotionally, some may find it difficult to navigate the sea of mental health resources. This is particularly true when a family’s financial situation is also stressed. Reaching out to local religious services and community medical resources or inquiring about the mental health of other family members are ways for psychiatrists to engage more families in mental health treatment.
- Reach out to colleagues: Psychiatrists are not immune to developing psychiatric disorders,and it is important to support each other.9 This is also an unusual time when psychiatrists are treating symptoms in patients that they themselves may be also experiencing. Supporting help groups and hot lines, reaching out to colleagues who appear to be struggling and addressing interpersonal conflicts within one’s practice are crucial practices for psychiatrists during this time.
- Explore within ourselves: Evaluating our own interpersonal relationships as well as areas for improvement are critical skills to maintain our own emotional well-being. Setting aside time to connect with friends in a nonclinical setting and prioritizing our family connections are helpful tools. In addition, exploring our reactions to past life transitions could improve our own level of insight into our response to COVID-19.
Conclusion
Conceptualizing COVID-19 as a period of transition and using IPT themes are helpful tools to mitigate the potential adverse psychological effects of COVID-19 on families. Similarly, they can also be helpful in supporting our colleagues and helping ourselves cope during this difficult period.
References
1. Qiu J et al. Gen Psychiatr. 2020 Mar 6;33(2):e100213.
2. Gautam M et al. Psychosomatics. 2020 Apr 20. doi: 10.1016/j.psym.2020.04.009.
3. Markowitz JC, Weissman MM. Clin Psychol Psychother. 2012 Mar-Apr;19(2):99-105.
4. Cuijpers P et al. Am J Psychiatry. 2016 Jul;173(7):680-7.
5. Dietz LJ et al. J Am Acad Child Adolesc Psychiatry. 2015 Mar;54(3):191-9.
6. Verdeli H et al. Child Adolesc Psychiatr Clin N Am. 2008 Jul;17(3):605-24.
7. Stuart S. Clin Psychol Psychother. 2012 Mar-Apr;19(2):134-40.
8. Rogers JP et al. Lancet Psychiatry. 2020 Jul;7(7):611-27.
9. Korkeila JA et al. Scand J Public Health. 2003;31(2):85-91.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care. Dr. Reinstein has no conflicts of interest. Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
Helping families understand internalized racism
Ms. Jones brings her 15-year-old daughter, Angela, to the resident clinic. Angela is becoming increasingly anxious, withdrawn, and difficult to manage. As part of the initial interview, the resident, Dr. Sota, asks about the sociocultural background of the family. Ms. Jones is African American and recently began a relationship with a white man. Her daughter, Angela, is biracial; her biological father is white and has moved out of state with little ongoing contact with Angela and her mother.
At interview, Angela expresses a lot of anger at her mother, her biological father, and her new “stepfather.” Ms. Jones says: “I do not want Angela growing up as an ‘angry black woman.’ ” When asked for an explanation, she stated that she doesn’t want her daughter to be stereotyped, to be perceived as an angry black person. “She needs to fit in with our new life. She has lots of opportunities if only she would take them.”
Dr. Sota recognizes that Angela’s struggle, and perhaps also the struggle of Ms. Jones, has a component of internalized racism. How should Dr. Sota proceed? Dr. Sota puts herself in Angela’s shoes: How does Angela see herself? Angela has light brown skin, and
The term internalized racism (IR) first appeared in the 1980s. IR was compared to the oppression of black people in the 1800s: “The slavery that captures the mind and incarcerates the motivation, perception, aspiration, and identity in a web of anti-self images, generating a personal and collective self destruction, is more cruel than the shackles on the wrists and ankles.”1 According to Susanne Lipsky,2 IR “in African Americans manifests as internalizing stereotypes, mistrusting the self and other Blacks, and narrows one’s view of authentic Black culture.”
IR refers to the internalization and acceptance of the dominant white culture’s actions and beliefs, while rejecting one’s own cultural background. There is a long history of negative cultural representations of African Americans in popular American culture, and IR has a detrimental impact on the emotional well-being of African Americans.3
IR is associated with poorer metabolic health4 and psychological distress, depression and anxiety,5-8 and decreased self-esteem.9 However, protective processes can reduce one’s response to risk and can be developed through the psychotherapeutic relationship.
Interventions at an individual, family, or community levels
Angela: Tell me about yourself: What type of person are you? How do you identify? How do you feel about yourself/your appearance/your language?
Tell me about your friends/family? What interests do you have?
“Tell me more” questions can reveal conflicted feelings, etc., even if Angela does not answer. A good therapist can talk about IR; even if Angela does not bring it up, it is important for the therapist to find language suitable for the age of the patient.
Dr. Sota has some luck with Angela, who nods her head but says little. Dr. Sota then turns to Ms. Jones and asks whether she can answer these questions, too, and rephrases the questions for an adult. Interviewing parents in the presence of their children gives Dr. Sota and Angela an idea of what is permitted to talk about in the family.
A therapist can also note other permissions in the family: How do Angela and her mother use language? Do they claim or reject words and phrases such as “angry black woman” and choose, instead, to use language to “fit in” with the dominant white culture?
Dr. Sota notices that Ms. Jones presents herself as keen to fit in with her new future husband’s life. She wants Angela to do likewise. Dr. Sota notices that Angela vacillates between wanting to claim her black identity and having to navigate what that means in this family (not a good thing) – and wanting to assimilate into white culture. Her peers fall into two separate groups: a set of black friends and a set of white friends. Her mother prefers that she see her white friends, mistrusting her black friends.
Dr. Sota’s supervisor suggests that she introduce IR more forcefully because this seems to be a major course of conflict for Angela and encourage a frank discussion between mother and daughter. Dr. Sota starts the next session in the following way: “I noticed last week that the way you each identify yourselves is quite different. Ms. Jones, you want Angela to ‘fit in’ and perhaps just embrace white culture, whereas Angela, perhaps you vacillate between a white identity and a black identity?”
The following questions can help Dr. Sota elicit IR:
- What information about yourself would you like others to know – about your heritage, country of origin, family, class background, and so on?
- What makes you proud about being a member of this group, and what do you love about other members of this group?
- What has been hard about being a member of this group, and what don’t you like about others in this group?
- What were your early life experiences with people in this group? How were you treated? How did you feel about others in your group when you were young?
At a community level, family workshops support positive cultural identities that strengthen family functioning and reducing behavioral health risks. In a study of 575 urban American Indian (AI) families from diverse tribal backgrounds, the AI families who participated in such a workshop had significant increases in their ethnic identity, improved sense of spirituality, and a more positive cultural identification. The workshops provided culturally adaptive parenting interventions.10
IR is a serious determinant of both physical and mental health. Assessment of IR can be done using rating scales, such as the Nadanolitization Scale11 or the Internalized Racial Oppression Scale.12 IR also can also be assessed using a more formalized interview guide, such as the DSM-5 Cultural Formulation Interview (CFI).13 This 16-question interview guide helps behavioral health providers better understand the way service users and their social networks (e.g., families, friends) understand what is happening to them and why, as well as the barriers they experience, such as racism, discrimination, stigma, and financial stressors.
Individuals’ cultures and experiences have a profound impact on their understanding of their symptoms and their engagement in care. The American Psychiatric Association considers it to be part of mental health providers’ duty of care to engage all individuals in culturally relevant conversations about their past experiences and care expectations. More relevant, I submit that you cannot treat someone without having made this inquiry. A cultural assessment improves understanding but also shifts power relationships between providers and patients. The DSM-5 CFI and training guides are widely available and provide additional information for those who want to improve their cultural literacy.
Conclusion
Internalized racism is the component of racism that is the most difficult to discern. Psychiatrists and mental health professionals are uniquely poised to address IR, and any subsequent internal conflict and identity difficulties. Each program, office, and clinic can easily find the resources to do this through the APA. If you would like help providing education, contact me at [email protected].
References
1. Akbar N. J Black Studies. 1984. doi: 10.11771002193478401400401.
2. Lipsky S. Internalized Racism. Seattle: Rational Island Publishers, 1987.
3. Williams DR and Mohammed SA. Am Behav Sci. 2013 May 8. doi: 10.1177/00027642134873340.
4. DeLilly CR and Flaskerud JH. Issues Ment Health Nurs. 2012 Nov;33(11):804-11.
5. Molina KM and James D. Group Process Intergroup Relat. 2016 Jul;19(4):439-61.
6. Szymanski D and Obiri O. Couns Psychologist. 2011;39(3):438-62.
7. Carter RT et al. J Multicul Couns Dev. 2017 Oct 5;45(4):232-59.
8. Mouzon DM and McLean JS. Ethn Health. 2017 Feb;22(1):36-48.
9. Szymanski DM and Gupta A. J Couns Psychol. 2009;56(1):110-18.
10. Kulis SS et al. Cultural Diversity and Ethnic Minority Psychol. 2019. doi: 10.1037/cpd000315.
11. Taylor J and Grundy C. “Measuring black internalization of white stereotypes about African Americans: The Nadanolization Scale.” In: Jones RL, ed. Handbook of Tests and Measurements of Black Populations. Hampton, Va.: Cobb & Henry, 1996.
12. Bailey T-K M et al. J Couns Psychol. 2011 Oct;58(4):481-93.
13. American Psychiatric Association. Cultural Formulation Interview. DSM-5. American Psychiatric Association Publishing: Arlington, Va. 2013.
Various aspects about the case described above have been changed to protect the clinician’s and patients’ identities. Thanks to the following individuals for their contributions to this article: Suzanne Huberty, MD, and Shiona Heru, JD.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose.
Ms. Jones brings her 15-year-old daughter, Angela, to the resident clinic. Angela is becoming increasingly anxious, withdrawn, and difficult to manage. As part of the initial interview, the resident, Dr. Sota, asks about the sociocultural background of the family. Ms. Jones is African American and recently began a relationship with a white man. Her daughter, Angela, is biracial; her biological father is white and has moved out of state with little ongoing contact with Angela and her mother.
At interview, Angela expresses a lot of anger at her mother, her biological father, and her new “stepfather.” Ms. Jones says: “I do not want Angela growing up as an ‘angry black woman.’ ” When asked for an explanation, she stated that she doesn’t want her daughter to be stereotyped, to be perceived as an angry black person. “She needs to fit in with our new life. She has lots of opportunities if only she would take them.”
Dr. Sota recognizes that Angela’s struggle, and perhaps also the struggle of Ms. Jones, has a component of internalized racism. How should Dr. Sota proceed? Dr. Sota puts herself in Angela’s shoes: How does Angela see herself? Angela has light brown skin, and
The term internalized racism (IR) first appeared in the 1980s. IR was compared to the oppression of black people in the 1800s: “The slavery that captures the mind and incarcerates the motivation, perception, aspiration, and identity in a web of anti-self images, generating a personal and collective self destruction, is more cruel than the shackles on the wrists and ankles.”1 According to Susanne Lipsky,2 IR “in African Americans manifests as internalizing stereotypes, mistrusting the self and other Blacks, and narrows one’s view of authentic Black culture.”
IR refers to the internalization and acceptance of the dominant white culture’s actions and beliefs, while rejecting one’s own cultural background. There is a long history of negative cultural representations of African Americans in popular American culture, and IR has a detrimental impact on the emotional well-being of African Americans.3
IR is associated with poorer metabolic health4 and psychological distress, depression and anxiety,5-8 and decreased self-esteem.9 However, protective processes can reduce one’s response to risk and can be developed through the psychotherapeutic relationship.
Interventions at an individual, family, or community levels
Angela: Tell me about yourself: What type of person are you? How do you identify? How do you feel about yourself/your appearance/your language?
Tell me about your friends/family? What interests do you have?
“Tell me more” questions can reveal conflicted feelings, etc., even if Angela does not answer. A good therapist can talk about IR; even if Angela does not bring it up, it is important for the therapist to find language suitable for the age of the patient.
Dr. Sota has some luck with Angela, who nods her head but says little. Dr. Sota then turns to Ms. Jones and asks whether she can answer these questions, too, and rephrases the questions for an adult. Interviewing parents in the presence of their children gives Dr. Sota and Angela an idea of what is permitted to talk about in the family.
A therapist can also note other permissions in the family: How do Angela and her mother use language? Do they claim or reject words and phrases such as “angry black woman” and choose, instead, to use language to “fit in” with the dominant white culture?
Dr. Sota notices that Ms. Jones presents herself as keen to fit in with her new future husband’s life. She wants Angela to do likewise. Dr. Sota notices that Angela vacillates between wanting to claim her black identity and having to navigate what that means in this family (not a good thing) – and wanting to assimilate into white culture. Her peers fall into two separate groups: a set of black friends and a set of white friends. Her mother prefers that she see her white friends, mistrusting her black friends.
Dr. Sota’s supervisor suggests that she introduce IR more forcefully because this seems to be a major course of conflict for Angela and encourage a frank discussion between mother and daughter. Dr. Sota starts the next session in the following way: “I noticed last week that the way you each identify yourselves is quite different. Ms. Jones, you want Angela to ‘fit in’ and perhaps just embrace white culture, whereas Angela, perhaps you vacillate between a white identity and a black identity?”
The following questions can help Dr. Sota elicit IR:
- What information about yourself would you like others to know – about your heritage, country of origin, family, class background, and so on?
- What makes you proud about being a member of this group, and what do you love about other members of this group?
- What has been hard about being a member of this group, and what don’t you like about others in this group?
- What were your early life experiences with people in this group? How were you treated? How did you feel about others in your group when you were young?
At a community level, family workshops support positive cultural identities that strengthen family functioning and reducing behavioral health risks. In a study of 575 urban American Indian (AI) families from diverse tribal backgrounds, the AI families who participated in such a workshop had significant increases in their ethnic identity, improved sense of spirituality, and a more positive cultural identification. The workshops provided culturally adaptive parenting interventions.10
IR is a serious determinant of both physical and mental health. Assessment of IR can be done using rating scales, such as the Nadanolitization Scale11 or the Internalized Racial Oppression Scale.12 IR also can also be assessed using a more formalized interview guide, such as the DSM-5 Cultural Formulation Interview (CFI).13 This 16-question interview guide helps behavioral health providers better understand the way service users and their social networks (e.g., families, friends) understand what is happening to them and why, as well as the barriers they experience, such as racism, discrimination, stigma, and financial stressors.
Individuals’ cultures and experiences have a profound impact on their understanding of their symptoms and their engagement in care. The American Psychiatric Association considers it to be part of mental health providers’ duty of care to engage all individuals in culturally relevant conversations about their past experiences and care expectations. More relevant, I submit that you cannot treat someone without having made this inquiry. A cultural assessment improves understanding but also shifts power relationships between providers and patients. The DSM-5 CFI and training guides are widely available and provide additional information for those who want to improve their cultural literacy.
Conclusion
Internalized racism is the component of racism that is the most difficult to discern. Psychiatrists and mental health professionals are uniquely poised to address IR, and any subsequent internal conflict and identity difficulties. Each program, office, and clinic can easily find the resources to do this through the APA. If you would like help providing education, contact me at [email protected].
References
1. Akbar N. J Black Studies. 1984. doi: 10.11771002193478401400401.
2. Lipsky S. Internalized Racism. Seattle: Rational Island Publishers, 1987.
3. Williams DR and Mohammed SA. Am Behav Sci. 2013 May 8. doi: 10.1177/00027642134873340.
4. DeLilly CR and Flaskerud JH. Issues Ment Health Nurs. 2012 Nov;33(11):804-11.
5. Molina KM and James D. Group Process Intergroup Relat. 2016 Jul;19(4):439-61.
6. Szymanski D and Obiri O. Couns Psychologist. 2011;39(3):438-62.
7. Carter RT et al. J Multicul Couns Dev. 2017 Oct 5;45(4):232-59.
8. Mouzon DM and McLean JS. Ethn Health. 2017 Feb;22(1):36-48.
9. Szymanski DM and Gupta A. J Couns Psychol. 2009;56(1):110-18.
10. Kulis SS et al. Cultural Diversity and Ethnic Minority Psychol. 2019. doi: 10.1037/cpd000315.
11. Taylor J and Grundy C. “Measuring black internalization of white stereotypes about African Americans: The Nadanolization Scale.” In: Jones RL, ed. Handbook of Tests and Measurements of Black Populations. Hampton, Va.: Cobb & Henry, 1996.
12. Bailey T-K M et al. J Couns Psychol. 2011 Oct;58(4):481-93.
13. American Psychiatric Association. Cultural Formulation Interview. DSM-5. American Psychiatric Association Publishing: Arlington, Va. 2013.
Various aspects about the case described above have been changed to protect the clinician’s and patients’ identities. Thanks to the following individuals for their contributions to this article: Suzanne Huberty, MD, and Shiona Heru, JD.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose.
Ms. Jones brings her 15-year-old daughter, Angela, to the resident clinic. Angela is becoming increasingly anxious, withdrawn, and difficult to manage. As part of the initial interview, the resident, Dr. Sota, asks about the sociocultural background of the family. Ms. Jones is African American and recently began a relationship with a white man. Her daughter, Angela, is biracial; her biological father is white and has moved out of state with little ongoing contact with Angela and her mother.
At interview, Angela expresses a lot of anger at her mother, her biological father, and her new “stepfather.” Ms. Jones says: “I do not want Angela growing up as an ‘angry black woman.’ ” When asked for an explanation, she stated that she doesn’t want her daughter to be stereotyped, to be perceived as an angry black person. “She needs to fit in with our new life. She has lots of opportunities if only she would take them.”
Dr. Sota recognizes that Angela’s struggle, and perhaps also the struggle of Ms. Jones, has a component of internalized racism. How should Dr. Sota proceed? Dr. Sota puts herself in Angela’s shoes: How does Angela see herself? Angela has light brown skin, and
The term internalized racism (IR) first appeared in the 1980s. IR was compared to the oppression of black people in the 1800s: “The slavery that captures the mind and incarcerates the motivation, perception, aspiration, and identity in a web of anti-self images, generating a personal and collective self destruction, is more cruel than the shackles on the wrists and ankles.”1 According to Susanne Lipsky,2 IR “in African Americans manifests as internalizing stereotypes, mistrusting the self and other Blacks, and narrows one’s view of authentic Black culture.”
IR refers to the internalization and acceptance of the dominant white culture’s actions and beliefs, while rejecting one’s own cultural background. There is a long history of negative cultural representations of African Americans in popular American culture, and IR has a detrimental impact on the emotional well-being of African Americans.3
IR is associated with poorer metabolic health4 and psychological distress, depression and anxiety,5-8 and decreased self-esteem.9 However, protective processes can reduce one’s response to risk and can be developed through the psychotherapeutic relationship.
Interventions at an individual, family, or community levels
Angela: Tell me about yourself: What type of person are you? How do you identify? How do you feel about yourself/your appearance/your language?
Tell me about your friends/family? What interests do you have?
“Tell me more” questions can reveal conflicted feelings, etc., even if Angela does not answer. A good therapist can talk about IR; even if Angela does not bring it up, it is important for the therapist to find language suitable for the age of the patient.
Dr. Sota has some luck with Angela, who nods her head but says little. Dr. Sota then turns to Ms. Jones and asks whether she can answer these questions, too, and rephrases the questions for an adult. Interviewing parents in the presence of their children gives Dr. Sota and Angela an idea of what is permitted to talk about in the family.
A therapist can also note other permissions in the family: How do Angela and her mother use language? Do they claim or reject words and phrases such as “angry black woman” and choose, instead, to use language to “fit in” with the dominant white culture?
Dr. Sota notices that Ms. Jones presents herself as keen to fit in with her new future husband’s life. She wants Angela to do likewise. Dr. Sota notices that Angela vacillates between wanting to claim her black identity and having to navigate what that means in this family (not a good thing) – and wanting to assimilate into white culture. Her peers fall into two separate groups: a set of black friends and a set of white friends. Her mother prefers that she see her white friends, mistrusting her black friends.
Dr. Sota’s supervisor suggests that she introduce IR more forcefully because this seems to be a major course of conflict for Angela and encourage a frank discussion between mother and daughter. Dr. Sota starts the next session in the following way: “I noticed last week that the way you each identify yourselves is quite different. Ms. Jones, you want Angela to ‘fit in’ and perhaps just embrace white culture, whereas Angela, perhaps you vacillate between a white identity and a black identity?”
The following questions can help Dr. Sota elicit IR:
- What information about yourself would you like others to know – about your heritage, country of origin, family, class background, and so on?
- What makes you proud about being a member of this group, and what do you love about other members of this group?
- What has been hard about being a member of this group, and what don’t you like about others in this group?
- What were your early life experiences with people in this group? How were you treated? How did you feel about others in your group when you were young?
At a community level, family workshops support positive cultural identities that strengthen family functioning and reducing behavioral health risks. In a study of 575 urban American Indian (AI) families from diverse tribal backgrounds, the AI families who participated in such a workshop had significant increases in their ethnic identity, improved sense of spirituality, and a more positive cultural identification. The workshops provided culturally adaptive parenting interventions.10
IR is a serious determinant of both physical and mental health. Assessment of IR can be done using rating scales, such as the Nadanolitization Scale11 or the Internalized Racial Oppression Scale.12 IR also can also be assessed using a more formalized interview guide, such as the DSM-5 Cultural Formulation Interview (CFI).13 This 16-question interview guide helps behavioral health providers better understand the way service users and their social networks (e.g., families, friends) understand what is happening to them and why, as well as the barriers they experience, such as racism, discrimination, stigma, and financial stressors.
Individuals’ cultures and experiences have a profound impact on their understanding of their symptoms and their engagement in care. The American Psychiatric Association considers it to be part of mental health providers’ duty of care to engage all individuals in culturally relevant conversations about their past experiences and care expectations. More relevant, I submit that you cannot treat someone without having made this inquiry. A cultural assessment improves understanding but also shifts power relationships between providers and patients. The DSM-5 CFI and training guides are widely available and provide additional information for those who want to improve their cultural literacy.
Conclusion
Internalized racism is the component of racism that is the most difficult to discern. Psychiatrists and mental health professionals are uniquely poised to address IR, and any subsequent internal conflict and identity difficulties. Each program, office, and clinic can easily find the resources to do this through the APA. If you would like help providing education, contact me at [email protected].
References
1. Akbar N. J Black Studies. 1984. doi: 10.11771002193478401400401.
2. Lipsky S. Internalized Racism. Seattle: Rational Island Publishers, 1987.
3. Williams DR and Mohammed SA. Am Behav Sci. 2013 May 8. doi: 10.1177/00027642134873340.
4. DeLilly CR and Flaskerud JH. Issues Ment Health Nurs. 2012 Nov;33(11):804-11.
5. Molina KM and James D. Group Process Intergroup Relat. 2016 Jul;19(4):439-61.
6. Szymanski D and Obiri O. Couns Psychologist. 2011;39(3):438-62.
7. Carter RT et al. J Multicul Couns Dev. 2017 Oct 5;45(4):232-59.
8. Mouzon DM and McLean JS. Ethn Health. 2017 Feb;22(1):36-48.
9. Szymanski DM and Gupta A. J Couns Psychol. 2009;56(1):110-18.
10. Kulis SS et al. Cultural Diversity and Ethnic Minority Psychol. 2019. doi: 10.1037/cpd000315.
11. Taylor J and Grundy C. “Measuring black internalization of white stereotypes about African Americans: The Nadanolization Scale.” In: Jones RL, ed. Handbook of Tests and Measurements of Black Populations. Hampton, Va.: Cobb & Henry, 1996.
12. Bailey T-K M et al. J Couns Psychol. 2011 Oct;58(4):481-93.
13. American Psychiatric Association. Cultural Formulation Interview. DSM-5. American Psychiatric Association Publishing: Arlington, Va. 2013.
Various aspects about the case described above have been changed to protect the clinician’s and patients’ identities. Thanks to the following individuals for their contributions to this article: Suzanne Huberty, MD, and Shiona Heru, JD.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose.
Steven, Linda, and predictive processing
Steven, a 45-year-old engineer, and Linda, a 40-year-old data processor, have been married for 12 years and have a 10-year-old child. In 2018, Steven was fired from his job after he exploded at his boss, who he felt had gone out of his way to humiliate Steven.
He was having difficulty finding a new job. Linda had to pick up extra hours at work and became annoyed with Steven. “What do you do all day? Why can’t you finish all these half-done house projects? What is the matter with you?” Linda felt that he was only half-heartedly looking for a new job and wondered whether he preferred letting her be the breadwinner and the boss.
Steven agreed to seek individual therapy to assuage his wife’s concerns. After several sessions, Steven realized that his father had criticized him in a way similar to the way his wife did, and that this was similar to his perception of his former boss. He began to discuss his parents’ backgrounds to try to understand their behavior. Steven began to change his behavior, looking for work more seriously and finishing up home projects. However, Linda did not accept that these changes were “real” and continued to berate him. She stated that he was doing this only temporarily to appease his therapist. Steven tried to explain why he had changed, with descriptions of his father’s behavior toward him. Months went by, and despite securing an interview for a job and having finished the projects at home, Linda remained steadfast in denying his change. Steven and Linda were referred to couples therapy.
In the first session, Steven complained that Linda had to have everything done exactly her way, and he opined that she liked to be the dominant force in the relationship. Linda countered with: “One time on TV there was this woman complaining about the glass ceiling.” Meanwhile, he said things such as “women seem to think that men work because they like to work.” She countered: “I think he got himself fired on purpose!”
Predictive models
Linda had formed a mental model of her husband based on her experience of his repetitive behavior over the 15 years that they had known each other. She had long ago decided that she needed to nag him to get him to do anything productive. This had occurred early in their relationship, and it was her fixed belief about her husband.
Steven entered their relationship believing that Linda would be critical of him, regardless of what he did. This belief was not a conscious belief, more of an expectation based on his prior relationship with his father. He ignored her nagging until it became so persistent than he would eventually do what she asked. When Steven began to resolve his anger toward his father more effectively, he became less begrudging of others and more self-motivated. Linda’s continued nagging made Steven wonder whether it was “worth it” to make self-improvement changes, as Linda did not appreciate his efforts to change.
When we get to “know someone” in a coupled relationship, our experience of the other person falls into predictive patterns. We expect the “usual” responses from them: We “know” how they will respond. This predictability makes it easy for us to understand the other person, so that we do not have to continually analyze and reanalyze each utterance or behavior as a new experience.
Steven’s predictive model of Linda reflects his predictive model of the other as indicative of the fact that he will be always berated. He, at some level, expects others to berate him. Linda prefers to maintain her current model of her husband and believe that his changes are not real, rather than do the work of changing her internal model – work that she does not think is necessary. In their couples therapy, predictive modeling “explains” how Linda and Steven use their internal models of each other to direct their interactions.
Couples therapy helps them describe the change they both want. As Linda approaches Steven, her internal model must now change to incorporate his new interactional style. Of course, she will be suspicious that he might “relapse.” But understanding that he desires to interact with her in this new way, and that she actually would prefer to stop nagging him, helps her to develop a new model of interaction with him.
Relational theories are numerous: Why add one more?
Predictive processing is a paradigm shift in psychiatry. This shift moves psychiatry away from psychodynamic explanations of behavior to explanations that are brain based. Psychodynamic explanations are how our prior experiences in the world get played out in the current world. Predictive processing explains how the brain incorporates the dynamics of child rearing and prior relational interactions into internal models that we use to reduce the work of repeatedly reinterpreting people’s behavior.
The historical explanations that create internal models are interesting, especially to Steven, who felt there was a connection between his prior experiences and his current experiences. Acknowledging the psychodynamic cause is helpful, but it is the how of relational change that is the work of couples therapy.
The positives of predictive modeling
or built a certain way or that the other person lacks the will to change. A neuroscience-based visualization of our internal models of other people helps us more neutrally describe the iterative process that occurs. Other systemic family models use their own languages to achieve the same end, but as Carlos E. Sluzki, MD, opines: We need to update our models to keep up with the times!
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose. The case, which was changed to protect patients’ confidentiality, was provided by David M. Allen, MD, professor of psychiatry emeritus at the University of Tennessee Health Science Center, Memphis. Dr. Allen is author of three books, “Coping with Critical, Demanding, and Dysfunctional Parents” (New Harbinger Publications, 2018); “How Dysfunctional Families Spur Mental Disorders” (Praeger, 2010); and “Psychotherapy with Borderline Patients: An Integrated Approach” (Lawrence Erlbaum Associates, 2003).
References
Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
Sluzki CE. Fam Process. 2007;46(2):173-84.
Steven, a 45-year-old engineer, and Linda, a 40-year-old data processor, have been married for 12 years and have a 10-year-old child. In 2018, Steven was fired from his job after he exploded at his boss, who he felt had gone out of his way to humiliate Steven.
He was having difficulty finding a new job. Linda had to pick up extra hours at work and became annoyed with Steven. “What do you do all day? Why can’t you finish all these half-done house projects? What is the matter with you?” Linda felt that he was only half-heartedly looking for a new job and wondered whether he preferred letting her be the breadwinner and the boss.
Steven agreed to seek individual therapy to assuage his wife’s concerns. After several sessions, Steven realized that his father had criticized him in a way similar to the way his wife did, and that this was similar to his perception of his former boss. He began to discuss his parents’ backgrounds to try to understand their behavior. Steven began to change his behavior, looking for work more seriously and finishing up home projects. However, Linda did not accept that these changes were “real” and continued to berate him. She stated that he was doing this only temporarily to appease his therapist. Steven tried to explain why he had changed, with descriptions of his father’s behavior toward him. Months went by, and despite securing an interview for a job and having finished the projects at home, Linda remained steadfast in denying his change. Steven and Linda were referred to couples therapy.
In the first session, Steven complained that Linda had to have everything done exactly her way, and he opined that she liked to be the dominant force in the relationship. Linda countered with: “One time on TV there was this woman complaining about the glass ceiling.” Meanwhile, he said things such as “women seem to think that men work because they like to work.” She countered: “I think he got himself fired on purpose!”
Predictive models
Linda had formed a mental model of her husband based on her experience of his repetitive behavior over the 15 years that they had known each other. She had long ago decided that she needed to nag him to get him to do anything productive. This had occurred early in their relationship, and it was her fixed belief about her husband.
Steven entered their relationship believing that Linda would be critical of him, regardless of what he did. This belief was not a conscious belief, more of an expectation based on his prior relationship with his father. He ignored her nagging until it became so persistent than he would eventually do what she asked. When Steven began to resolve his anger toward his father more effectively, he became less begrudging of others and more self-motivated. Linda’s continued nagging made Steven wonder whether it was “worth it” to make self-improvement changes, as Linda did not appreciate his efforts to change.
When we get to “know someone” in a coupled relationship, our experience of the other person falls into predictive patterns. We expect the “usual” responses from them: We “know” how they will respond. This predictability makes it easy for us to understand the other person, so that we do not have to continually analyze and reanalyze each utterance or behavior as a new experience.
Steven’s predictive model of Linda reflects his predictive model of the other as indicative of the fact that he will be always berated. He, at some level, expects others to berate him. Linda prefers to maintain her current model of her husband and believe that his changes are not real, rather than do the work of changing her internal model – work that she does not think is necessary. In their couples therapy, predictive modeling “explains” how Linda and Steven use their internal models of each other to direct their interactions.
Couples therapy helps them describe the change they both want. As Linda approaches Steven, her internal model must now change to incorporate his new interactional style. Of course, she will be suspicious that he might “relapse.” But understanding that he desires to interact with her in this new way, and that she actually would prefer to stop nagging him, helps her to develop a new model of interaction with him.
Relational theories are numerous: Why add one more?
Predictive processing is a paradigm shift in psychiatry. This shift moves psychiatry away from psychodynamic explanations of behavior to explanations that are brain based. Psychodynamic explanations are how our prior experiences in the world get played out in the current world. Predictive processing explains how the brain incorporates the dynamics of child rearing and prior relational interactions into internal models that we use to reduce the work of repeatedly reinterpreting people’s behavior.
The historical explanations that create internal models are interesting, especially to Steven, who felt there was a connection between his prior experiences and his current experiences. Acknowledging the psychodynamic cause is helpful, but it is the how of relational change that is the work of couples therapy.
The positives of predictive modeling
or built a certain way or that the other person lacks the will to change. A neuroscience-based visualization of our internal models of other people helps us more neutrally describe the iterative process that occurs. Other systemic family models use their own languages to achieve the same end, but as Carlos E. Sluzki, MD, opines: We need to update our models to keep up with the times!
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose. The case, which was changed to protect patients’ confidentiality, was provided by David M. Allen, MD, professor of psychiatry emeritus at the University of Tennessee Health Science Center, Memphis. Dr. Allen is author of three books, “Coping with Critical, Demanding, and Dysfunctional Parents” (New Harbinger Publications, 2018); “How Dysfunctional Families Spur Mental Disorders” (Praeger, 2010); and “Psychotherapy with Borderline Patients: An Integrated Approach” (Lawrence Erlbaum Associates, 2003).
References
Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
Sluzki CE. Fam Process. 2007;46(2):173-84.
Steven, a 45-year-old engineer, and Linda, a 40-year-old data processor, have been married for 12 years and have a 10-year-old child. In 2018, Steven was fired from his job after he exploded at his boss, who he felt had gone out of his way to humiliate Steven.
He was having difficulty finding a new job. Linda had to pick up extra hours at work and became annoyed with Steven. “What do you do all day? Why can’t you finish all these half-done house projects? What is the matter with you?” Linda felt that he was only half-heartedly looking for a new job and wondered whether he preferred letting her be the breadwinner and the boss.
Steven agreed to seek individual therapy to assuage his wife’s concerns. After several sessions, Steven realized that his father had criticized him in a way similar to the way his wife did, and that this was similar to his perception of his former boss. He began to discuss his parents’ backgrounds to try to understand their behavior. Steven began to change his behavior, looking for work more seriously and finishing up home projects. However, Linda did not accept that these changes were “real” and continued to berate him. She stated that he was doing this only temporarily to appease his therapist. Steven tried to explain why he had changed, with descriptions of his father’s behavior toward him. Months went by, and despite securing an interview for a job and having finished the projects at home, Linda remained steadfast in denying his change. Steven and Linda were referred to couples therapy.
In the first session, Steven complained that Linda had to have everything done exactly her way, and he opined that she liked to be the dominant force in the relationship. Linda countered with: “One time on TV there was this woman complaining about the glass ceiling.” Meanwhile, he said things such as “women seem to think that men work because they like to work.” She countered: “I think he got himself fired on purpose!”
Predictive models
Linda had formed a mental model of her husband based on her experience of his repetitive behavior over the 15 years that they had known each other. She had long ago decided that she needed to nag him to get him to do anything productive. This had occurred early in their relationship, and it was her fixed belief about her husband.
Steven entered their relationship believing that Linda would be critical of him, regardless of what he did. This belief was not a conscious belief, more of an expectation based on his prior relationship with his father. He ignored her nagging until it became so persistent than he would eventually do what she asked. When Steven began to resolve his anger toward his father more effectively, he became less begrudging of others and more self-motivated. Linda’s continued nagging made Steven wonder whether it was “worth it” to make self-improvement changes, as Linda did not appreciate his efforts to change.
When we get to “know someone” in a coupled relationship, our experience of the other person falls into predictive patterns. We expect the “usual” responses from them: We “know” how they will respond. This predictability makes it easy for us to understand the other person, so that we do not have to continually analyze and reanalyze each utterance or behavior as a new experience.
Steven’s predictive model of Linda reflects his predictive model of the other as indicative of the fact that he will be always berated. He, at some level, expects others to berate him. Linda prefers to maintain her current model of her husband and believe that his changes are not real, rather than do the work of changing her internal model – work that she does not think is necessary. In their couples therapy, predictive modeling “explains” how Linda and Steven use their internal models of each other to direct their interactions.
Couples therapy helps them describe the change they both want. As Linda approaches Steven, her internal model must now change to incorporate his new interactional style. Of course, she will be suspicious that he might “relapse.” But understanding that he desires to interact with her in this new way, and that she actually would prefer to stop nagging him, helps her to develop a new model of interaction with him.
Relational theories are numerous: Why add one more?
Predictive processing is a paradigm shift in psychiatry. This shift moves psychiatry away from psychodynamic explanations of behavior to explanations that are brain based. Psychodynamic explanations are how our prior experiences in the world get played out in the current world. Predictive processing explains how the brain incorporates the dynamics of child rearing and prior relational interactions into internal models that we use to reduce the work of repeatedly reinterpreting people’s behavior.
The historical explanations that create internal models are interesting, especially to Steven, who felt there was a connection between his prior experiences and his current experiences. Acknowledging the psychodynamic cause is helpful, but it is the how of relational change that is the work of couples therapy.
The positives of predictive modeling
or built a certain way or that the other person lacks the will to change. A neuroscience-based visualization of our internal models of other people helps us more neutrally describe the iterative process that occurs. Other systemic family models use their own languages to achieve the same end, but as Carlos E. Sluzki, MD, opines: We need to update our models to keep up with the times!
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose. The case, which was changed to protect patients’ confidentiality, was provided by David M. Allen, MD, professor of psychiatry emeritus at the University of Tennessee Health Science Center, Memphis. Dr. Allen is author of three books, “Coping with Critical, Demanding, and Dysfunctional Parents” (New Harbinger Publications, 2018); “How Dysfunctional Families Spur Mental Disorders” (Praeger, 2010); and “Psychotherapy with Borderline Patients: An Integrated Approach” (Lawrence Erlbaum Associates, 2003).
References
Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
Sluzki CE. Fam Process. 2007;46(2):173-84.
John Bowlby and Heinz Kohut, meet Karl Friston
Attachment theory and object relations theory, meet neuroscience
The bonding process between individuals is essential to human life as we know it. The depth and strength of emotional bonds that we develop with other individuals are among the cardinal aspects of being human.
The strengths of the bonds that we form with others often are the most enduring aspects of our lives and can stretch back in time to include family members and friends who are no longer alive. The brain processes and neurochemicals involved in the bonding process are related to psychological processes using Bayesian theory. Abnormalities in attachment are described in terms of abnormal predictive models.
John Bowlby MD, and colleagues developed a psychological theory of early childhood attachment that shows the impact of different childhood experiences.1 Over many decades, they conducted painstaking observations, trials, and retrials that elucidated specific types of attachment that reflect the child’s internal representations of the parent.
Dr. Bowlby described the mental representations of attachment as “the internal working models of expectations” about the maternal-child relationship. This internal model guides the child’s behaviors, attitudes, and expectations, and is constantly being revised and expanded as the child matures in order to adapt to increasingly complex relationships. More current research has shown that adults who have experienced extreme early childhood adversity develop odd or deficient descriptions of primary attachment relationships, now refined into a low-coherence CC category.2 These children experience attachments that are characterized by feelings of emptiness, inconsistency, and fragmentation.
Object relations theory was created by Heinz Kohut, MD, to explain our internal models of others in psychoanalytic language.3 Dr. Kohut expands the concept of transference describing three new transferential relationships: mirroring, idealized, and twinship transferences. A mirroring transference describes the psychological mechanism whereby “the other” serves as a mirror that reflects back to the person a sense of self-worth and value. A mirroring transference uses the affirming and positive responses of others so that a person then can see positive traits within themselves. The idealizing transference refers to a person’s need for “another” who will make them feel calm and comfortable. The other is idealized as somebody who is calm and soothing when the person cannot provide that on their own. The twinship/alter ego transference occurs when a person feels a sense of likeness with “an other.” These advances in psychoanalytic theory advance our understanding of how we internalize aspects of other people and use these internalizations in our own development.
The neuroscience of attachment was revealed in the study of the children abandoned in Romanian orphanages before the 1989 revolution. These children were placed in orphanages that lacked adequate staff, and they were subjected to profound psychosocial neglect. In the Bucharest Early Intervention Project, the effects of neglect were seen in children aged less than 30-96 months, in EEG data.4 Abnormalities were found in two aberrantly connected brain networks: a hyperconnected parieto-occipital network and a hypoconnected network between left temporal and distributed bilateral regions. This study provides the first evidence of the adverse effects of early psychosocial neglect on the wiring of the developing brain.
Neurochemistry has suggested the impact of oxytocin on the promotion of attachment. Oxytocin has been called the “cuddle hormone,” as it is stimulated in mothers to promote bonding with their infant. Many studies have examined the introduction of intranasal oxytocin increases bonding and trust with others, but recent meta-analyses challenge those findings.5,6 Nevertheless, the process of bonding and attachment is thought to engage the mesocorticolimbic, nigrostriatal dopaminergic, and oxytocinergic systems. Tops and colleagues proposed that oxytocin facilitates a shift from ventral striatal “novelty processing” toward dorsal striatal “familiarity processing.”7 This shift to familiarity is thought to create secure internal working models. In addition, brain activity in specific regions, such as the right caudate, is correlated with romantic love.8 In summary, specific pathways and neurotransmitters underlie the emotional process of bonding and attachment.
However, it is Karl Friston, MD, who suggests a model of brain functioning that describes how we actually process our experiences of the world.9 Dr. Friston uses Bayesian modeling to describe how we interact and understand our world, describing the way we process information. Dr. Friston states that the process of inference that we use to discern our world is a process that uses Bayes’ theorem to update the probability for a specific hypothesis about our world. As more evidence or information becomes available, we update our internal models of the world. Predictive modeling is the term used in Bayesian terms to describe this process of continuous revision of our internal model of the world. Any new sensory input is compared to our current internal model, and if they do not match, our internal model of the world is updated and revised. Dr. Friston states: “As surprise is resolved, Bayesian model evidence is increased. This means that every living organism behaves as if it is a little statistician, analyzing its sensory data in exactly the same way that scientists evaluate the evidence for their hypotheses about how experimental data were caused. In this view, minimizing surprise is, literally, the search for evidence for one’s own existence.” This process of predictive modeling also can be applied to our internal models of other people, meaning that our internal model of another person is an iterative process that changes as the other person changes.
When our experience of the world and others fall into predictive patterns, we expect the “usual” responses from our world and from the people in it. This predictive processing makes it easier for us to understand our world, so that we do not have to continually analyze and reanalyze each event as a new experience. For example, a young child examines the waves as they crash on the shore. For a while, he will watch the waves but soon begins to recognize that there is a predictable pattern. With each ocean he visits, he will examine wave action and soon develop an internal model of what happens when the water reaches the shore. Similarly, when a young child has a secure and loving parent, he will expect security and love in his future relationships. On the other hand, the child who has been subjected to abuse and neglect has an internal working model of the other as nonreciprocal and perhaps irrelevant to their well-being. They will, therefore, have extreme difficulty in understanding the purpose or value of relationships. Their predictive model of the other reflects a lack of input in the case of neglect, or perverted input in the case of abuse. Their internal predictive model will require a great deal of therapeutic healthy inputs to be able to evolve to allow a healthy relationship with the other. This is the work of therapy.
When thinking about relationships, predictive processing makes clinical sense. In a committed partnership, each partner has a predictive model of their partner’s response to events/speech utterances/emotional displays. The prediction of the partner’s response is based on prior experience. This predictive model reduces the need to repeatedly reinterpret the partner’s actions. The partner is understood through an internal predictive model. When one partner changes their behavior, the other partner experiences the world/environment as disrupted or different. The couple, through an iterative process, can incorporate change and grow together. If the patient has an internalized model of a loving relationship, then they are more likely to find a partner who resonates with this internalized model. Using predictive modeling, we can understand how two people with their own internal models of each other interact. As one person approaches the other person, each internal model of the other person finds a “fit” with the behaviors of the other person. When a child with emotional deprivation approaches the other, the child perceives the other person in a way that fits with their prior experience of deprivation. It is an easy fit that requires little internal work, and the patient falls into a familiar relational pattern. This model of predictive processing explains why people repeatedly fall into similar familiar relationships: They recognize the relationship patterns. There is less predictive processing required, less emotional and cognitive work, and therefore less adjustment.
Psychotherapy helps patients by improving their understanding of the link between prior and current experience. Each piece of behavior is analyzed and compared with the patient’s internal model of the event. What neuroscience now provides is a deeper scientific understanding of this process.
In summary, the processes of attachment and bonding occur through oxytocin-mediated caudate–dorsal striatum pathways. Bayesian predictive modeling describes the processes by which our internal models of others are shaped and refined, and underscores the work of our psychotherapies. Neuroscience is beginning to delineate the “where” and “how” of attachment and bonding, thus advancing our understanding of the attachment process and giving us a new language to describe the work of psychotherapy.
References
1. Bowlby J. “A Secure Base: Parent-Child Attachment and Healthy Human Development.” New York: Basic Books, 1988.
2. Speranza AM et al. Attach Hum Dev. 2017 Dec;19(6):613-34.
3. Kohut H. “How Does Analysis Cure?” Chicago: University of Chicago Press, 1984.
4. Stamoulis C et al. J Neurophysiol. 2017 Oct 1;118(4):2275-88.
5. Leng G and Ludwig M.Biol Psychiatry. 2016 Feb 1;79(3):243-50.
6. Leppanen J et al. Neurosci Biobehav Rev. 2017 Jul;78:125-44.
7. Tops M et al. Pharmacol Biochem Behav. 2014 Apr;119:39-48.
8. Acevedo BP et al. Soc Cogn Affect Neurosci. 2012 Feb;7(2):145-59.
9. Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
Attachment theory and object relations theory, meet neuroscience
Attachment theory and object relations theory, meet neuroscience
The bonding process between individuals is essential to human life as we know it. The depth and strength of emotional bonds that we develop with other individuals are among the cardinal aspects of being human.
The strengths of the bonds that we form with others often are the most enduring aspects of our lives and can stretch back in time to include family members and friends who are no longer alive. The brain processes and neurochemicals involved in the bonding process are related to psychological processes using Bayesian theory. Abnormalities in attachment are described in terms of abnormal predictive models.
John Bowlby MD, and colleagues developed a psychological theory of early childhood attachment that shows the impact of different childhood experiences.1 Over many decades, they conducted painstaking observations, trials, and retrials that elucidated specific types of attachment that reflect the child’s internal representations of the parent.
Dr. Bowlby described the mental representations of attachment as “the internal working models of expectations” about the maternal-child relationship. This internal model guides the child’s behaviors, attitudes, and expectations, and is constantly being revised and expanded as the child matures in order to adapt to increasingly complex relationships. More current research has shown that adults who have experienced extreme early childhood adversity develop odd or deficient descriptions of primary attachment relationships, now refined into a low-coherence CC category.2 These children experience attachments that are characterized by feelings of emptiness, inconsistency, and fragmentation.
Object relations theory was created by Heinz Kohut, MD, to explain our internal models of others in psychoanalytic language.3 Dr. Kohut expands the concept of transference describing three new transferential relationships: mirroring, idealized, and twinship transferences. A mirroring transference describes the psychological mechanism whereby “the other” serves as a mirror that reflects back to the person a sense of self-worth and value. A mirroring transference uses the affirming and positive responses of others so that a person then can see positive traits within themselves. The idealizing transference refers to a person’s need for “another” who will make them feel calm and comfortable. The other is idealized as somebody who is calm and soothing when the person cannot provide that on their own. The twinship/alter ego transference occurs when a person feels a sense of likeness with “an other.” These advances in psychoanalytic theory advance our understanding of how we internalize aspects of other people and use these internalizations in our own development.
The neuroscience of attachment was revealed in the study of the children abandoned in Romanian orphanages before the 1989 revolution. These children were placed in orphanages that lacked adequate staff, and they were subjected to profound psychosocial neglect. In the Bucharest Early Intervention Project, the effects of neglect were seen in children aged less than 30-96 months, in EEG data.4 Abnormalities were found in two aberrantly connected brain networks: a hyperconnected parieto-occipital network and a hypoconnected network between left temporal and distributed bilateral regions. This study provides the first evidence of the adverse effects of early psychosocial neglect on the wiring of the developing brain.
Neurochemistry has suggested the impact of oxytocin on the promotion of attachment. Oxytocin has been called the “cuddle hormone,” as it is stimulated in mothers to promote bonding with their infant. Many studies have examined the introduction of intranasal oxytocin increases bonding and trust with others, but recent meta-analyses challenge those findings.5,6 Nevertheless, the process of bonding and attachment is thought to engage the mesocorticolimbic, nigrostriatal dopaminergic, and oxytocinergic systems. Tops and colleagues proposed that oxytocin facilitates a shift from ventral striatal “novelty processing” toward dorsal striatal “familiarity processing.”7 This shift to familiarity is thought to create secure internal working models. In addition, brain activity in specific regions, such as the right caudate, is correlated with romantic love.8 In summary, specific pathways and neurotransmitters underlie the emotional process of bonding and attachment.
However, it is Karl Friston, MD, who suggests a model of brain functioning that describes how we actually process our experiences of the world.9 Dr. Friston uses Bayesian modeling to describe how we interact and understand our world, describing the way we process information. Dr. Friston states that the process of inference that we use to discern our world is a process that uses Bayes’ theorem to update the probability for a specific hypothesis about our world. As more evidence or information becomes available, we update our internal models of the world. Predictive modeling is the term used in Bayesian terms to describe this process of continuous revision of our internal model of the world. Any new sensory input is compared to our current internal model, and if they do not match, our internal model of the world is updated and revised. Dr. Friston states: “As surprise is resolved, Bayesian model evidence is increased. This means that every living organism behaves as if it is a little statistician, analyzing its sensory data in exactly the same way that scientists evaluate the evidence for their hypotheses about how experimental data were caused. In this view, minimizing surprise is, literally, the search for evidence for one’s own existence.” This process of predictive modeling also can be applied to our internal models of other people, meaning that our internal model of another person is an iterative process that changes as the other person changes.
When our experience of the world and others fall into predictive patterns, we expect the “usual” responses from our world and from the people in it. This predictive processing makes it easier for us to understand our world, so that we do not have to continually analyze and reanalyze each event as a new experience. For example, a young child examines the waves as they crash on the shore. For a while, he will watch the waves but soon begins to recognize that there is a predictable pattern. With each ocean he visits, he will examine wave action and soon develop an internal model of what happens when the water reaches the shore. Similarly, when a young child has a secure and loving parent, he will expect security and love in his future relationships. On the other hand, the child who has been subjected to abuse and neglect has an internal working model of the other as nonreciprocal and perhaps irrelevant to their well-being. They will, therefore, have extreme difficulty in understanding the purpose or value of relationships. Their predictive model of the other reflects a lack of input in the case of neglect, or perverted input in the case of abuse. Their internal predictive model will require a great deal of therapeutic healthy inputs to be able to evolve to allow a healthy relationship with the other. This is the work of therapy.
When thinking about relationships, predictive processing makes clinical sense. In a committed partnership, each partner has a predictive model of their partner’s response to events/speech utterances/emotional displays. The prediction of the partner’s response is based on prior experience. This predictive model reduces the need to repeatedly reinterpret the partner’s actions. The partner is understood through an internal predictive model. When one partner changes their behavior, the other partner experiences the world/environment as disrupted or different. The couple, through an iterative process, can incorporate change and grow together. If the patient has an internalized model of a loving relationship, then they are more likely to find a partner who resonates with this internalized model. Using predictive modeling, we can understand how two people with their own internal models of each other interact. As one person approaches the other person, each internal model of the other person finds a “fit” with the behaviors of the other person. When a child with emotional deprivation approaches the other, the child perceives the other person in a way that fits with their prior experience of deprivation. It is an easy fit that requires little internal work, and the patient falls into a familiar relational pattern. This model of predictive processing explains why people repeatedly fall into similar familiar relationships: They recognize the relationship patterns. There is less predictive processing required, less emotional and cognitive work, and therefore less adjustment.
Psychotherapy helps patients by improving their understanding of the link between prior and current experience. Each piece of behavior is analyzed and compared with the patient’s internal model of the event. What neuroscience now provides is a deeper scientific understanding of this process.
In summary, the processes of attachment and bonding occur through oxytocin-mediated caudate–dorsal striatum pathways. Bayesian predictive modeling describes the processes by which our internal models of others are shaped and refined, and underscores the work of our psychotherapies. Neuroscience is beginning to delineate the “where” and “how” of attachment and bonding, thus advancing our understanding of the attachment process and giving us a new language to describe the work of psychotherapy.
References
1. Bowlby J. “A Secure Base: Parent-Child Attachment and Healthy Human Development.” New York: Basic Books, 1988.
2. Speranza AM et al. Attach Hum Dev. 2017 Dec;19(6):613-34.
3. Kohut H. “How Does Analysis Cure?” Chicago: University of Chicago Press, 1984.
4. Stamoulis C et al. J Neurophysiol. 2017 Oct 1;118(4):2275-88.
5. Leng G and Ludwig M.Biol Psychiatry. 2016 Feb 1;79(3):243-50.
6. Leppanen J et al. Neurosci Biobehav Rev. 2017 Jul;78:125-44.
7. Tops M et al. Pharmacol Biochem Behav. 2014 Apr;119:39-48.
8. Acevedo BP et al. Soc Cogn Affect Neurosci. 2012 Feb;7(2):145-59.
9. Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
The bonding process between individuals is essential to human life as we know it. The depth and strength of emotional bonds that we develop with other individuals are among the cardinal aspects of being human.
The strengths of the bonds that we form with others often are the most enduring aspects of our lives and can stretch back in time to include family members and friends who are no longer alive. The brain processes and neurochemicals involved in the bonding process are related to psychological processes using Bayesian theory. Abnormalities in attachment are described in terms of abnormal predictive models.
John Bowlby MD, and colleagues developed a psychological theory of early childhood attachment that shows the impact of different childhood experiences.1 Over many decades, they conducted painstaking observations, trials, and retrials that elucidated specific types of attachment that reflect the child’s internal representations of the parent.
Dr. Bowlby described the mental representations of attachment as “the internal working models of expectations” about the maternal-child relationship. This internal model guides the child’s behaviors, attitudes, and expectations, and is constantly being revised and expanded as the child matures in order to adapt to increasingly complex relationships. More current research has shown that adults who have experienced extreme early childhood adversity develop odd or deficient descriptions of primary attachment relationships, now refined into a low-coherence CC category.2 These children experience attachments that are characterized by feelings of emptiness, inconsistency, and fragmentation.
Object relations theory was created by Heinz Kohut, MD, to explain our internal models of others in psychoanalytic language.3 Dr. Kohut expands the concept of transference describing three new transferential relationships: mirroring, idealized, and twinship transferences. A mirroring transference describes the psychological mechanism whereby “the other” serves as a mirror that reflects back to the person a sense of self-worth and value. A mirroring transference uses the affirming and positive responses of others so that a person then can see positive traits within themselves. The idealizing transference refers to a person’s need for “another” who will make them feel calm and comfortable. The other is idealized as somebody who is calm and soothing when the person cannot provide that on their own. The twinship/alter ego transference occurs when a person feels a sense of likeness with “an other.” These advances in psychoanalytic theory advance our understanding of how we internalize aspects of other people and use these internalizations in our own development.
The neuroscience of attachment was revealed in the study of the children abandoned in Romanian orphanages before the 1989 revolution. These children were placed in orphanages that lacked adequate staff, and they were subjected to profound psychosocial neglect. In the Bucharest Early Intervention Project, the effects of neglect were seen in children aged less than 30-96 months, in EEG data.4 Abnormalities were found in two aberrantly connected brain networks: a hyperconnected parieto-occipital network and a hypoconnected network between left temporal and distributed bilateral regions. This study provides the first evidence of the adverse effects of early psychosocial neglect on the wiring of the developing brain.
Neurochemistry has suggested the impact of oxytocin on the promotion of attachment. Oxytocin has been called the “cuddle hormone,” as it is stimulated in mothers to promote bonding with their infant. Many studies have examined the introduction of intranasal oxytocin increases bonding and trust with others, but recent meta-analyses challenge those findings.5,6 Nevertheless, the process of bonding and attachment is thought to engage the mesocorticolimbic, nigrostriatal dopaminergic, and oxytocinergic systems. Tops and colleagues proposed that oxytocin facilitates a shift from ventral striatal “novelty processing” toward dorsal striatal “familiarity processing.”7 This shift to familiarity is thought to create secure internal working models. In addition, brain activity in specific regions, such as the right caudate, is correlated with romantic love.8 In summary, specific pathways and neurotransmitters underlie the emotional process of bonding and attachment.
However, it is Karl Friston, MD, who suggests a model of brain functioning that describes how we actually process our experiences of the world.9 Dr. Friston uses Bayesian modeling to describe how we interact and understand our world, describing the way we process information. Dr. Friston states that the process of inference that we use to discern our world is a process that uses Bayes’ theorem to update the probability for a specific hypothesis about our world. As more evidence or information becomes available, we update our internal models of the world. Predictive modeling is the term used in Bayesian terms to describe this process of continuous revision of our internal model of the world. Any new sensory input is compared to our current internal model, and if they do not match, our internal model of the world is updated and revised. Dr. Friston states: “As surprise is resolved, Bayesian model evidence is increased. This means that every living organism behaves as if it is a little statistician, analyzing its sensory data in exactly the same way that scientists evaluate the evidence for their hypotheses about how experimental data were caused. In this view, minimizing surprise is, literally, the search for evidence for one’s own existence.” This process of predictive modeling also can be applied to our internal models of other people, meaning that our internal model of another person is an iterative process that changes as the other person changes.
When our experience of the world and others fall into predictive patterns, we expect the “usual” responses from our world and from the people in it. This predictive processing makes it easier for us to understand our world, so that we do not have to continually analyze and reanalyze each event as a new experience. For example, a young child examines the waves as they crash on the shore. For a while, he will watch the waves but soon begins to recognize that there is a predictable pattern. With each ocean he visits, he will examine wave action and soon develop an internal model of what happens when the water reaches the shore. Similarly, when a young child has a secure and loving parent, he will expect security and love in his future relationships. On the other hand, the child who has been subjected to abuse and neglect has an internal working model of the other as nonreciprocal and perhaps irrelevant to their well-being. They will, therefore, have extreme difficulty in understanding the purpose or value of relationships. Their predictive model of the other reflects a lack of input in the case of neglect, or perverted input in the case of abuse. Their internal predictive model will require a great deal of therapeutic healthy inputs to be able to evolve to allow a healthy relationship with the other. This is the work of therapy.
When thinking about relationships, predictive processing makes clinical sense. In a committed partnership, each partner has a predictive model of their partner’s response to events/speech utterances/emotional displays. The prediction of the partner’s response is based on prior experience. This predictive model reduces the need to repeatedly reinterpret the partner’s actions. The partner is understood through an internal predictive model. When one partner changes their behavior, the other partner experiences the world/environment as disrupted or different. The couple, through an iterative process, can incorporate change and grow together. If the patient has an internalized model of a loving relationship, then they are more likely to find a partner who resonates with this internalized model. Using predictive modeling, we can understand how two people with their own internal models of each other interact. As one person approaches the other person, each internal model of the other person finds a “fit” with the behaviors of the other person. When a child with emotional deprivation approaches the other, the child perceives the other person in a way that fits with their prior experience of deprivation. It is an easy fit that requires little internal work, and the patient falls into a familiar relational pattern. This model of predictive processing explains why people repeatedly fall into similar familiar relationships: They recognize the relationship patterns. There is less predictive processing required, less emotional and cognitive work, and therefore less adjustment.
Psychotherapy helps patients by improving their understanding of the link between prior and current experience. Each piece of behavior is analyzed and compared with the patient’s internal model of the event. What neuroscience now provides is a deeper scientific understanding of this process.
In summary, the processes of attachment and bonding occur through oxytocin-mediated caudate–dorsal striatum pathways. Bayesian predictive modeling describes the processes by which our internal models of others are shaped and refined, and underscores the work of our psychotherapies. Neuroscience is beginning to delineate the “where” and “how” of attachment and bonding, thus advancing our understanding of the attachment process and giving us a new language to describe the work of psychotherapy.
References
1. Bowlby J. “A Secure Base: Parent-Child Attachment and Healthy Human Development.” New York: Basic Books, 1988.
2. Speranza AM et al. Attach Hum Dev. 2017 Dec;19(6):613-34.
3. Kohut H. “How Does Analysis Cure?” Chicago: University of Chicago Press, 1984.
4. Stamoulis C et al. J Neurophysiol. 2017 Oct 1;118(4):2275-88.
5. Leng G and Ludwig M.Biol Psychiatry. 2016 Feb 1;79(3):243-50.
6. Leppanen J et al. Neurosci Biobehav Rev. 2017 Jul;78:125-44.
7. Tops M et al. Pharmacol Biochem Behav. 2014 Apr;119:39-48.
8. Acevedo BP et al. Soc Cogn Affect Neurosci. 2012 Feb;7(2):145-59.
9. Friston K. Entropy (Basel). 2012 Nov;14(11):2100-21.
Helping patients find balance between self and other
Cultural considerations require careful assessments on therapists’ part
This column is dedicated to the late Carl C. Bell, MD.
When we work with patients and their families from cultures that are not the culture in which we ourselves were raised, we think more deeply about this balance. In this column, I offer a simple but solid framework for this inquiry.
The first family therapist to crystallize the dialectic between the self and its relationship to others was Murray Bowen, MD. He believed that the differentiation of self from the family was the major task of human development. Dr. Bowen worked in a time when vilification of the “other” was common practice in individual psychotherapies and the goal of individual psychotherapy was the development of a healthy sense of self rather than repairing or developing relationships.
When faced with patients from cultures that are unfamiliar to us, we are less confident about how to assess the balance between self and other. In many cultures, marriages are based on social class and perceived social opportunities and are arranged by the respective families. If you come from a collectivist culture, where the focus is on the belief that the group is more important than the individual, the focus is more on self in relation to a group, belonging to a group, and participating in a group than self-striving. This is most evident in the role of women in many families (as well as in other organizations), in which women shoulder the responsibility for keeping families functional and together.
American culture is focused on serious self-striving. From kindergarten, children are expected to excel and to become the best self that they can be – regardless of the toll this takes on relationships. Self-expression and self-actualization frequently are considered the pinnacle of a life’s achievement. Relationships may take a backseat, often being transitory or utilitarian. This leads to switching relationships, peer groups, and friends – and a strong emphasis on cultivating work relationships.
Exploring Dr. Bowen’s theories
Dr. Bowen posited that the family relational pull affects individual development in a negative way. Despite this, his model is considered one of the most comprehensive explanations for the development of psychological problems from a systemic, relational, and multigenerational perspective.1 He identified the basic self (B-self), which strives for differentiation in contrast to the false/pseudo/relational self (R-self), which strives to meet group or family norms.
Dr. Bowen was the oldest of three and grew up in a small town in Tennessee. His father was the mayor of the town and owned several properties, including the funeral home. Following medical training, Dr. Bowen served during World War II. He accepted a fellowship in surgery at the Mayo Clinic in Rochester, Minn., but his wartime experiences resulted in a change of interest to psychiatry. Dr. Bowen trained at the Menninger Clinic in Topeka, Kan., and in 1954 became the first director of the family division at the National Institute of Mental Health. He and his colleagues studied the families of patients with schizophrenia. They described eight fundamental concepts that supported the important aspects of individual growth. When he moved to Georgetown University in Washington, he developed the Bowen Family Systems Theory.2
Dr. Bowen’s eight concepts
1. Nuclear Family Emotional Process
2. Differentiation of self
3. Triangles
4. Emotional cutoff
5. Family projection process
6. Multigenerational transmission process
7. Sibling position
8. Societal Emotional Process
According to Dr. Bowen, the B-self makes decisions on facts, principles, and intrinsic motivation and decides what they are willing to do/not willing to do based on their own internal ethics. On the other hand, the R-self goes along with everybody else, even when the person internally disagrees. He considered the R-self as wanting acceptance in relationship, possibly changing beliefs to find approval, and striving to be liked. Carmen Knudson-Martin, PhD,3 explored the relationship between the B-self and the R-self and suggested that they exist along two dimensions, both of which are important. My contention is that the R-self is undertheorized and deserves much more exploration.
Developmental psychologists and psychiatrists have focused on understanding the process of psychological maturation of the individual throughout life. However, there is little study of the development of a healthy relationship between self and other. We have, instead, gathered examples and descriptors of the pathological examples of the “other.” We can readily call out enmeshment, the manipulations of the borderline personality disordered, the cold withholding mother – to name the most vilified. What do we know about the healthy R-self?
Measuring the relational self
We have understood the R-self mostly through the study of pathological relationships. For example, pathological parenting has been shown to “result” in individual pathology and as a factor in the development of psychiatric illness. The measurement of the relationship between patient and family member/partner is aimed at elucidating pathology. The supreme example is emotional overinvolvement (EOI).
EOI is an integral part of the construct called expressed emotion and is often measured using the Camberwell Family Interview.4 High EOI has been identified routinely as predictive of worsening of psychiatric illness.5 However, exceptions are found (when you look for them)! In African American families, for example, high EOI is predictive of better outcomes in patients with schizophrenia.6 Jill M. Hooley, DPhil, also has identified that patients with borderline personality disorders do better in families with high EOI.7
A shorter equivalent research tool is the 5-minute speech sample (FMSS). The FMSS analyses 5 minutes of the speech of a parent/family member who is asked to describe the identified patient. EOI is identified by expressions of excessive worry or concern, self-sacrifice, or exaggerated praise. In a study of 223 child-mother dyads, 56.5% of which were Hispanic, use of the FMSS found high EOI predicted externalizing behaviors.8
More recently, psychiatry has sought to identify and measure positive factors, such as family warmth. In Puerto Rican children, high parental warmth was found to be protective against psychiatric disorders.9 In a study of Burmese migrant families from 20 communities in Thailand (513 caregivers and 479 patients with schizophrenia, aged 7-15 years), families were randomized to a waitlist or a 12-week family intervention that promoted warmth.10 The family intervention resulted in increased parental warmth and affection and increased family well-being.
Applying the theories to practice
An adolescent, Jan, does not speak when her mother is in the room. Jan has a small B-self, and her mother has a large B-self. Not only does Jan have to develop a strong B, but she also has to change how she is in relation – she has to change her R-self. For Jan, individual therapy supports the development of a stronger B-self. Working with the patient and her mother, the balance between both B-selves and the joined R-self can be reworked. In essence, the therapist encourages Jan to speak and helps the mother keep her own counsel. This is a situation in which the individual and family intervention are best implemented by the same therapist.
Systemic family therapy, a specific type of family intervention, focuses on how all the R-selves in a family work together as a unit called the family, or F-self. The F-self also has its own family history, as relationship patterns are transmitted and played out through families and play out through subsequent generations. A new type of family therapy called family constellation therapy (FCT) focuses on the F-self as a collection of ancestral selves. This resonates strongly with families who have experienced significant trauma, such as war and Holocaust survivors. FCT is popular in collectivist cultures, where there is a strong belief in the power and influence of ancestors and where the self is understood as an “assemblage of ancestral relationships that often creates problems in the present day.”11 Dr. Bowen recognized this multigenerational pattern as one of his eight fundamental principles.
The patients whom we see often have failing or fractured relationships. They might be stuck in dysfunctional transactional patterns with intimate partners, or they might fail to find a suitable intimate partner. We recognize relational dysfunction such as “codependency,” “symbiosis,” and “enmeshment.” We recognize too much distance, identifying family cutoffs. We still have a long way to go before clinical practice incorporates the importance of assessment and development of healthy relationships in a deep way. A typical question heard across all clinics: Is your partner/family supportive? Not much else is asked in regard to relationships, unless the answer is no. We have yet to develop a good set of inquiring questions that focus on the assessment of healthy relationships.
What can the therapist do to help the patient manage this continual dialectic? The therapist can ask the questions: How important is your B-self versus your R-self? What is the balance between your B-self and your R-self? What do you know about your family or F-self? Is your F-self important to you?
References
1. Nichols MP and Davis S. Family Therapy: Concepts & Methods, 8th ed. (Boston: Allyn & Bacon, 2008).
2. The Bowen Center for the Study of the Family.
3. Knudson-Martin C. Fam J. 1996 Jul 1. doi: 1066480796043002.
4. Leff J and Vaughn C. Expressed Emotion in Families. (New York: The Guilford Press, 1985).
5. Breitborde NJK et al. J Nerv Ment Dis. 2013 Oct;201(10):833-40.
6. Gurak K and de Mamani AW. Fam Process. 2017;56(2):476-86.
7. Hooley JM et al. J Clin Psychiatry. 2010 Aug;71(8):1017-24.
8. Khafi TY et al. J Fam Psychol. 2015 Aug;29(4):585-94.
9. Santesteban-Echarr et al. J Psychiatr Res. 2017 Apr;87:30-6.
10. Puffer ES et al. PLoS One. 2017 Mar 28;12(3):e0172611.
11. Pritzker SE and WL Duncan. Cult Med Psychiatry. 2019 Sep;43(3):468-95.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of Working With Families in Family Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals (New York: Routledge, 2013). She has no conflicts of interest.
Cultural considerations require careful assessments on therapists’ part
Cultural considerations require careful assessments on therapists’ part
This column is dedicated to the late Carl C. Bell, MD.
When we work with patients and their families from cultures that are not the culture in which we ourselves were raised, we think more deeply about this balance. In this column, I offer a simple but solid framework for this inquiry.
The first family therapist to crystallize the dialectic between the self and its relationship to others was Murray Bowen, MD. He believed that the differentiation of self from the family was the major task of human development. Dr. Bowen worked in a time when vilification of the “other” was common practice in individual psychotherapies and the goal of individual psychotherapy was the development of a healthy sense of self rather than repairing or developing relationships.
When faced with patients from cultures that are unfamiliar to us, we are less confident about how to assess the balance between self and other. In many cultures, marriages are based on social class and perceived social opportunities and are arranged by the respective families. If you come from a collectivist culture, where the focus is on the belief that the group is more important than the individual, the focus is more on self in relation to a group, belonging to a group, and participating in a group than self-striving. This is most evident in the role of women in many families (as well as in other organizations), in which women shoulder the responsibility for keeping families functional and together.
American culture is focused on serious self-striving. From kindergarten, children are expected to excel and to become the best self that they can be – regardless of the toll this takes on relationships. Self-expression and self-actualization frequently are considered the pinnacle of a life’s achievement. Relationships may take a backseat, often being transitory or utilitarian. This leads to switching relationships, peer groups, and friends – and a strong emphasis on cultivating work relationships.
Exploring Dr. Bowen’s theories
Dr. Bowen posited that the family relational pull affects individual development in a negative way. Despite this, his model is considered one of the most comprehensive explanations for the development of psychological problems from a systemic, relational, and multigenerational perspective.1 He identified the basic self (B-self), which strives for differentiation in contrast to the false/pseudo/relational self (R-self), which strives to meet group or family norms.
Dr. Bowen was the oldest of three and grew up in a small town in Tennessee. His father was the mayor of the town and owned several properties, including the funeral home. Following medical training, Dr. Bowen served during World War II. He accepted a fellowship in surgery at the Mayo Clinic in Rochester, Minn., but his wartime experiences resulted in a change of interest to psychiatry. Dr. Bowen trained at the Menninger Clinic in Topeka, Kan., and in 1954 became the first director of the family division at the National Institute of Mental Health. He and his colleagues studied the families of patients with schizophrenia. They described eight fundamental concepts that supported the important aspects of individual growth. When he moved to Georgetown University in Washington, he developed the Bowen Family Systems Theory.2
Dr. Bowen’s eight concepts
1. Nuclear Family Emotional Process
2. Differentiation of self
3. Triangles
4. Emotional cutoff
5. Family projection process
6. Multigenerational transmission process
7. Sibling position
8. Societal Emotional Process
According to Dr. Bowen, the B-self makes decisions on facts, principles, and intrinsic motivation and decides what they are willing to do/not willing to do based on their own internal ethics. On the other hand, the R-self goes along with everybody else, even when the person internally disagrees. He considered the R-self as wanting acceptance in relationship, possibly changing beliefs to find approval, and striving to be liked. Carmen Knudson-Martin, PhD,3 explored the relationship between the B-self and the R-self and suggested that they exist along two dimensions, both of which are important. My contention is that the R-self is undertheorized and deserves much more exploration.
Developmental psychologists and psychiatrists have focused on understanding the process of psychological maturation of the individual throughout life. However, there is little study of the development of a healthy relationship between self and other. We have, instead, gathered examples and descriptors of the pathological examples of the “other.” We can readily call out enmeshment, the manipulations of the borderline personality disordered, the cold withholding mother – to name the most vilified. What do we know about the healthy R-self?
Measuring the relational self
We have understood the R-self mostly through the study of pathological relationships. For example, pathological parenting has been shown to “result” in individual pathology and as a factor in the development of psychiatric illness. The measurement of the relationship between patient and family member/partner is aimed at elucidating pathology. The supreme example is emotional overinvolvement (EOI).
EOI is an integral part of the construct called expressed emotion and is often measured using the Camberwell Family Interview.4 High EOI has been identified routinely as predictive of worsening of psychiatric illness.5 However, exceptions are found (when you look for them)! In African American families, for example, high EOI is predictive of better outcomes in patients with schizophrenia.6 Jill M. Hooley, DPhil, also has identified that patients with borderline personality disorders do better in families with high EOI.7
A shorter equivalent research tool is the 5-minute speech sample (FMSS). The FMSS analyses 5 minutes of the speech of a parent/family member who is asked to describe the identified patient. EOI is identified by expressions of excessive worry or concern, self-sacrifice, or exaggerated praise. In a study of 223 child-mother dyads, 56.5% of which were Hispanic, use of the FMSS found high EOI predicted externalizing behaviors.8
More recently, psychiatry has sought to identify and measure positive factors, such as family warmth. In Puerto Rican children, high parental warmth was found to be protective against psychiatric disorders.9 In a study of Burmese migrant families from 20 communities in Thailand (513 caregivers and 479 patients with schizophrenia, aged 7-15 years), families were randomized to a waitlist or a 12-week family intervention that promoted warmth.10 The family intervention resulted in increased parental warmth and affection and increased family well-being.
Applying the theories to practice
An adolescent, Jan, does not speak when her mother is in the room. Jan has a small B-self, and her mother has a large B-self. Not only does Jan have to develop a strong B, but she also has to change how she is in relation – she has to change her R-self. For Jan, individual therapy supports the development of a stronger B-self. Working with the patient and her mother, the balance between both B-selves and the joined R-self can be reworked. In essence, the therapist encourages Jan to speak and helps the mother keep her own counsel. This is a situation in which the individual and family intervention are best implemented by the same therapist.
Systemic family therapy, a specific type of family intervention, focuses on how all the R-selves in a family work together as a unit called the family, or F-self. The F-self also has its own family history, as relationship patterns are transmitted and played out through families and play out through subsequent generations. A new type of family therapy called family constellation therapy (FCT) focuses on the F-self as a collection of ancestral selves. This resonates strongly with families who have experienced significant trauma, such as war and Holocaust survivors. FCT is popular in collectivist cultures, where there is a strong belief in the power and influence of ancestors and where the self is understood as an “assemblage of ancestral relationships that often creates problems in the present day.”11 Dr. Bowen recognized this multigenerational pattern as one of his eight fundamental principles.
The patients whom we see often have failing or fractured relationships. They might be stuck in dysfunctional transactional patterns with intimate partners, or they might fail to find a suitable intimate partner. We recognize relational dysfunction such as “codependency,” “symbiosis,” and “enmeshment.” We recognize too much distance, identifying family cutoffs. We still have a long way to go before clinical practice incorporates the importance of assessment and development of healthy relationships in a deep way. A typical question heard across all clinics: Is your partner/family supportive? Not much else is asked in regard to relationships, unless the answer is no. We have yet to develop a good set of inquiring questions that focus on the assessment of healthy relationships.
What can the therapist do to help the patient manage this continual dialectic? The therapist can ask the questions: How important is your B-self versus your R-self? What is the balance between your B-self and your R-self? What do you know about your family or F-self? Is your F-self important to you?
References
1. Nichols MP and Davis S. Family Therapy: Concepts & Methods, 8th ed. (Boston: Allyn & Bacon, 2008).
2. The Bowen Center for the Study of the Family.
3. Knudson-Martin C. Fam J. 1996 Jul 1. doi: 1066480796043002.
4. Leff J and Vaughn C. Expressed Emotion in Families. (New York: The Guilford Press, 1985).
5. Breitborde NJK et al. J Nerv Ment Dis. 2013 Oct;201(10):833-40.
6. Gurak K and de Mamani AW. Fam Process. 2017;56(2):476-86.
7. Hooley JM et al. J Clin Psychiatry. 2010 Aug;71(8):1017-24.
8. Khafi TY et al. J Fam Psychol. 2015 Aug;29(4):585-94.
9. Santesteban-Echarr et al. J Psychiatr Res. 2017 Apr;87:30-6.
10. Puffer ES et al. PLoS One. 2017 Mar 28;12(3):e0172611.
11. Pritzker SE and WL Duncan. Cult Med Psychiatry. 2019 Sep;43(3):468-95.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of Working With Families in Family Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals (New York: Routledge, 2013). She has no conflicts of interest.
This column is dedicated to the late Carl C. Bell, MD.
When we work with patients and their families from cultures that are not the culture in which we ourselves were raised, we think more deeply about this balance. In this column, I offer a simple but solid framework for this inquiry.
The first family therapist to crystallize the dialectic between the self and its relationship to others was Murray Bowen, MD. He believed that the differentiation of self from the family was the major task of human development. Dr. Bowen worked in a time when vilification of the “other” was common practice in individual psychotherapies and the goal of individual psychotherapy was the development of a healthy sense of self rather than repairing or developing relationships.
When faced with patients from cultures that are unfamiliar to us, we are less confident about how to assess the balance between self and other. In many cultures, marriages are based on social class and perceived social opportunities and are arranged by the respective families. If you come from a collectivist culture, where the focus is on the belief that the group is more important than the individual, the focus is more on self in relation to a group, belonging to a group, and participating in a group than self-striving. This is most evident in the role of women in many families (as well as in other organizations), in which women shoulder the responsibility for keeping families functional and together.
American culture is focused on serious self-striving. From kindergarten, children are expected to excel and to become the best self that they can be – regardless of the toll this takes on relationships. Self-expression and self-actualization frequently are considered the pinnacle of a life’s achievement. Relationships may take a backseat, often being transitory or utilitarian. This leads to switching relationships, peer groups, and friends – and a strong emphasis on cultivating work relationships.
Exploring Dr. Bowen’s theories
Dr. Bowen posited that the family relational pull affects individual development in a negative way. Despite this, his model is considered one of the most comprehensive explanations for the development of psychological problems from a systemic, relational, and multigenerational perspective.1 He identified the basic self (B-self), which strives for differentiation in contrast to the false/pseudo/relational self (R-self), which strives to meet group or family norms.
Dr. Bowen was the oldest of three and grew up in a small town in Tennessee. His father was the mayor of the town and owned several properties, including the funeral home. Following medical training, Dr. Bowen served during World War II. He accepted a fellowship in surgery at the Mayo Clinic in Rochester, Minn., but his wartime experiences resulted in a change of interest to psychiatry. Dr. Bowen trained at the Menninger Clinic in Topeka, Kan., and in 1954 became the first director of the family division at the National Institute of Mental Health. He and his colleagues studied the families of patients with schizophrenia. They described eight fundamental concepts that supported the important aspects of individual growth. When he moved to Georgetown University in Washington, he developed the Bowen Family Systems Theory.2
Dr. Bowen’s eight concepts
1. Nuclear Family Emotional Process
2. Differentiation of self
3. Triangles
4. Emotional cutoff
5. Family projection process
6. Multigenerational transmission process
7. Sibling position
8. Societal Emotional Process
According to Dr. Bowen, the B-self makes decisions on facts, principles, and intrinsic motivation and decides what they are willing to do/not willing to do based on their own internal ethics. On the other hand, the R-self goes along with everybody else, even when the person internally disagrees. He considered the R-self as wanting acceptance in relationship, possibly changing beliefs to find approval, and striving to be liked. Carmen Knudson-Martin, PhD,3 explored the relationship between the B-self and the R-self and suggested that they exist along two dimensions, both of which are important. My contention is that the R-self is undertheorized and deserves much more exploration.
Developmental psychologists and psychiatrists have focused on understanding the process of psychological maturation of the individual throughout life. However, there is little study of the development of a healthy relationship between self and other. We have, instead, gathered examples and descriptors of the pathological examples of the “other.” We can readily call out enmeshment, the manipulations of the borderline personality disordered, the cold withholding mother – to name the most vilified. What do we know about the healthy R-self?
Measuring the relational self
We have understood the R-self mostly through the study of pathological relationships. For example, pathological parenting has been shown to “result” in individual pathology and as a factor in the development of psychiatric illness. The measurement of the relationship between patient and family member/partner is aimed at elucidating pathology. The supreme example is emotional overinvolvement (EOI).
EOI is an integral part of the construct called expressed emotion and is often measured using the Camberwell Family Interview.4 High EOI has been identified routinely as predictive of worsening of psychiatric illness.5 However, exceptions are found (when you look for them)! In African American families, for example, high EOI is predictive of better outcomes in patients with schizophrenia.6 Jill M. Hooley, DPhil, also has identified that patients with borderline personality disorders do better in families with high EOI.7
A shorter equivalent research tool is the 5-minute speech sample (FMSS). The FMSS analyses 5 minutes of the speech of a parent/family member who is asked to describe the identified patient. EOI is identified by expressions of excessive worry or concern, self-sacrifice, or exaggerated praise. In a study of 223 child-mother dyads, 56.5% of which were Hispanic, use of the FMSS found high EOI predicted externalizing behaviors.8
More recently, psychiatry has sought to identify and measure positive factors, such as family warmth. In Puerto Rican children, high parental warmth was found to be protective against psychiatric disorders.9 In a study of Burmese migrant families from 20 communities in Thailand (513 caregivers and 479 patients with schizophrenia, aged 7-15 years), families were randomized to a waitlist or a 12-week family intervention that promoted warmth.10 The family intervention resulted in increased parental warmth and affection and increased family well-being.
Applying the theories to practice
An adolescent, Jan, does not speak when her mother is in the room. Jan has a small B-self, and her mother has a large B-self. Not only does Jan have to develop a strong B, but she also has to change how she is in relation – she has to change her R-self. For Jan, individual therapy supports the development of a stronger B-self. Working with the patient and her mother, the balance between both B-selves and the joined R-self can be reworked. In essence, the therapist encourages Jan to speak and helps the mother keep her own counsel. This is a situation in which the individual and family intervention are best implemented by the same therapist.
Systemic family therapy, a specific type of family intervention, focuses on how all the R-selves in a family work together as a unit called the family, or F-self. The F-self also has its own family history, as relationship patterns are transmitted and played out through families and play out through subsequent generations. A new type of family therapy called family constellation therapy (FCT) focuses on the F-self as a collection of ancestral selves. This resonates strongly with families who have experienced significant trauma, such as war and Holocaust survivors. FCT is popular in collectivist cultures, where there is a strong belief in the power and influence of ancestors and where the self is understood as an “assemblage of ancestral relationships that often creates problems in the present day.”11 Dr. Bowen recognized this multigenerational pattern as one of his eight fundamental principles.
The patients whom we see often have failing or fractured relationships. They might be stuck in dysfunctional transactional patterns with intimate partners, or they might fail to find a suitable intimate partner. We recognize relational dysfunction such as “codependency,” “symbiosis,” and “enmeshment.” We recognize too much distance, identifying family cutoffs. We still have a long way to go before clinical practice incorporates the importance of assessment and development of healthy relationships in a deep way. A typical question heard across all clinics: Is your partner/family supportive? Not much else is asked in regard to relationships, unless the answer is no. We have yet to develop a good set of inquiring questions that focus on the assessment of healthy relationships.
What can the therapist do to help the patient manage this continual dialectic? The therapist can ask the questions: How important is your B-self versus your R-self? What is the balance between your B-self and your R-self? What do you know about your family or F-self? Is your F-self important to you?
References
1. Nichols MP and Davis S. Family Therapy: Concepts & Methods, 8th ed. (Boston: Allyn & Bacon, 2008).
2. The Bowen Center for the Study of the Family.
3. Knudson-Martin C. Fam J. 1996 Jul 1. doi: 1066480796043002.
4. Leff J and Vaughn C. Expressed Emotion in Families. (New York: The Guilford Press, 1985).
5. Breitborde NJK et al. J Nerv Ment Dis. 2013 Oct;201(10):833-40.
6. Gurak K and de Mamani AW. Fam Process. 2017;56(2):476-86.
7. Hooley JM et al. J Clin Psychiatry. 2010 Aug;71(8):1017-24.
8. Khafi TY et al. J Fam Psychol. 2015 Aug;29(4):585-94.
9. Santesteban-Echarr et al. J Psychiatr Res. 2017 Apr;87:30-6.
10. Puffer ES et al. PLoS One. 2017 Mar 28;12(3):e0172611.
11. Pritzker SE and WL Duncan. Cult Med Psychiatry. 2019 Sep;43(3):468-95.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of Working With Families in Family Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals (New York: Routledge, 2013). She has no conflicts of interest.
‘The birth of a mother is a complex process’
Softening the blow to women and families of severe perinatal, postpartum psychiatric disorders
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
“But this was not what I expected!” That’s a statement I have heard from countless new mothers.
Women often envision pregnancy and the postpartum period as a time of pure joy. The glow of an expectant woman and the excitement of the arrival of a new baby masks the reality that many women struggle emotionally when transitioning to motherhood. Like the birth of a child, the birth of a mother is a complex process. Upholding the myth that all women seamlessly transform into mothers can have devastating effects and hinder access to mental health care.
As a psychiatrist working on a women’s inpatient unit with a perinatal program, I treat women at times of crisis. What may have begun as mild anxiety or depression sometimes quickly spirals into severe psychiatric illness. The sheer force of these severe perinatal and postpartum psychiatric disorders often leaves women and families shocked and confused, wondering what happened to their crumbled dreams of early motherhood.
What must general psychiatrists know about perinatal and postpartum psychiatric disorders? Why is maternal mental health so important? What are the barriers to treatment for these women? How can general psychiatrists best support and treat these new mothers and their families?
What data show
Maternal depression is now known to be one of the most common complications of pregnancy. Studies have suggested that about 11% of women experience depression during pregnancy1 and approximately 17% of women are depressed in the postpartum period.2 Perinatal generalized anxiety disorder has been shown to have a prevalence of 8.5%-10.5% during pregnancy with a wider variance post partum.3 Approximately 3% of women in the general community develop PTSD symptoms following childbirth.4 Research suggests that about 2% of women develop obsessive-compulsive disorder symptoms in the postpartum period.5 Postpartum psychosis, a rare but potentially devastating illness, occurs after 0.1%-0.2% of births.6
Importance of maternal mental health
There is a growing body of literature supporting both obstetric and pediatric adverse outcomes related to untreated psychiatric illness. Untreated maternal depression has been associated with obstetric complications, such as preterm delivery, preeclampsia, low birth weight, as well as the child’s developing cognitive function.7 Anxiety during pregnancy has been associated with both a shorter gestational period and adverse implications for fetal neurodevelopment.
These adverse effects were found to be even more potent in “pregnancy anxiety,” or anxiety specifically focused on the pregnancy, the birth experience, and the transition to motherhood.8 The psychotic symptoms occurring during postpartum psychosis can jeopardize the lives of both a woman and her child and carries a 4% risk of infanticide.9 Although there are limited data about the long-term effects of postpartum obsessive-compulsive disorders and PTSD, it is reasonable to assume that they might carry negative long-term implications for the mother and possibly her child.
Barriers to treatment
Despite the significant rates of mental illness, pregnant and new mothers often face barriers to receiving treatment. Many psychiatrists are hesitant to prescribe psychiatric medication to pregnant women because of concerns about teratogenic potential of psychiatric medications; similar concerns exist for newborn babies when prescribing medications to lactating mothers. In addition, the field of reproductive psychiatry is evolving at a rapid pace, making it difficult for busy psychiatrists to keep up with the ever-growing literature.
Also, it is hard to imagine a population that has more barriers to attending outpatient appointments. For many new mothers, the exhaustion and all-consuming work involved with taking care of a newborn are insurmountable barriers to obtaining mental health care. In addition, despite the awareness that new mothers often are more emotional, families can be slow to recognize the developing severity of a psychiatric illness during the peripartum and postpartum periods.
Supporting and treating new mothers
As general psychiatrists, there are several ways to directly help these women.
1. Expect the expected. Even in women with no prior psychiatric history, a significant percentage of expectant and postpartum women will develop acute psychiatric symptoms. Learn about the different presentations and treatments of perinatal and postpartum psychiatric disorders. For example, a woman might have thoughts of harming her baby in both postpartum psychosis and obsessive-compulsive disorder. However, the acuity and treatment of these two conditions drastically differ.
2. Learn more about psychiatric medications. Several apps and websites are available to psychiatrists to learn about the safety profile of psychiatric medications, such as Reprotox.org, mothertobaby.org, lactmed, and womensmentalhealth.org. Many medications are considered to be relatively safe during pregnancy and breastfeeding. It is important for psychiatrists to appreciate the risks when choosing not to prescribe to pregnant and postpartum women. Sometimes a known risk of a specific medication may be preferable to the unknown risk of leaving a woman susceptible to a severe psychiatric decompensation.
3. Involve all members of the family. A mother’s mental health has significant implications for the entire family. Psychoeducation for the family as well as frequent family sessions are key tools when treating this population. In addition, prescribing to pregnant women provides the opportunity for a psychiatrist to refine skills in joint decision making; it is crucial to involve both a patient and her spouse when discussing psychiatric medications.
4. Provide ready access and collaborate care. It is important to understand the potential rapid onset of psychiatric symptoms during the pregnancy and postpartum period. Psychiatrists should be prepared to collaborate care with other specialties. It is important to establish relationships with community psychotherapists specializing in maternal mental health, pediatricians, as well as obstetricians.
5. Learn when to seek a higher level of care. Although many women with perinatal and postpartum psychiatric symptoms can be managed as outpatients, women at times need a higher level of care. Similar to general psychiatry, women who are acutely suicidal or homicidal or have a sudden onset of psychotic and manic symptoms all should be evaluated immediately for inpatient hospitalization. Women with less severe symptoms but who require a higher level of care than typically offered in standard outpatient treatment should be candidates for partial hospitalization programs.
General intensive programs usually can accommodate these women, but it is ideal to refer this population to perinatal intensive programs. Postpartum Support International (postpartum.net) lists the nationwide inpatient and partial perinatal programs as well as regional and local services. An example of inpatient perinatal care is the women’s unit at Zucker Hillside Hospital (Northwell Health System, Glen Oaks, N.Y.), which houses an inpatient perinatal program. As a psychiatrist on the unit, I treat acute symptoms such as depression, anxiety, psychosis, mania, and catatonia that occur during the perinatal and postpartum periods. Given the severity of symptoms, I use a wide range of psychiatric medications with the possibility of electroconvulsive therapy when indicated. Psychotherapy staff on the unit offer specialized perinatal, mothers, and dialectical behavioral therapy groups. Breast pumps are available for women who wish to breastfeed. Accommodations are made for babies and children to visit their mother when clinically appropriate. Once discharged, women often are referred to Zucker Hillside’s own perinatal outpatient clinic for continued treatment. Similar models exist in select inpatient units as well as an increasing number of partial programs across the United States.
Conclusion
Psychiatric care for pregnant and new mothers can be challenging, but it is also immensely rewarding. Restoring a mother’s mental health usually leads to increased emotional stability for her entire family. Given the prevalence of maternal mental health disorders, psychiatrists in nearly every setting will encounter this population of women. With dedicated time devoted to reviewing the literature and learning about local resources, psychiatrists can feel comfortable treating women throughout the childbearing experience.
References
1. J Affect Disord. 2017 Sep;219:86-92.
2. J Psychiatr Res. 2018 Sep;104:235-48.
3. J Womens Health. (Larchmt). 2015 Sep;24(9):762-70.
4. Clin Psychol Rev. 2014 Jul;34(5):389-401.
5. Compr Psychiatry. 2009 Nov-Dec;50(6):503-9.
6. Int Rev Psychiatry. 2003 Aug;15(3):231-42.
7. Clin Obstet Gynecol. 2018 Sep;61(3):533-43.
8. Curr Opinion Psychiatry. 2012 Mar;25(2):141-8.
9. Am J Psychiatry. 2009 Apr;166(4):405-8.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine, New York, after graduating from the Albert Einstein College of Medicine and Yeshiva University, New York, with a BA in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Softening the blow to women and families of severe perinatal, postpartum psychiatric disorders
Softening the blow to women and families of severe perinatal, postpartum psychiatric disorders
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
“But this was not what I expected!” That’s a statement I have heard from countless new mothers.
Women often envision pregnancy and the postpartum period as a time of pure joy. The glow of an expectant woman and the excitement of the arrival of a new baby masks the reality that many women struggle emotionally when transitioning to motherhood. Like the birth of a child, the birth of a mother is a complex process. Upholding the myth that all women seamlessly transform into mothers can have devastating effects and hinder access to mental health care.
As a psychiatrist working on a women’s inpatient unit with a perinatal program, I treat women at times of crisis. What may have begun as mild anxiety or depression sometimes quickly spirals into severe psychiatric illness. The sheer force of these severe perinatal and postpartum psychiatric disorders often leaves women and families shocked and confused, wondering what happened to their crumbled dreams of early motherhood.
What must general psychiatrists know about perinatal and postpartum psychiatric disorders? Why is maternal mental health so important? What are the barriers to treatment for these women? How can general psychiatrists best support and treat these new mothers and their families?
What data show
Maternal depression is now known to be one of the most common complications of pregnancy. Studies have suggested that about 11% of women experience depression during pregnancy1 and approximately 17% of women are depressed in the postpartum period.2 Perinatal generalized anxiety disorder has been shown to have a prevalence of 8.5%-10.5% during pregnancy with a wider variance post partum.3 Approximately 3% of women in the general community develop PTSD symptoms following childbirth.4 Research suggests that about 2% of women develop obsessive-compulsive disorder symptoms in the postpartum period.5 Postpartum psychosis, a rare but potentially devastating illness, occurs after 0.1%-0.2% of births.6
Importance of maternal mental health
There is a growing body of literature supporting both obstetric and pediatric adverse outcomes related to untreated psychiatric illness. Untreated maternal depression has been associated with obstetric complications, such as preterm delivery, preeclampsia, low birth weight, as well as the child’s developing cognitive function.7 Anxiety during pregnancy has been associated with both a shorter gestational period and adverse implications for fetal neurodevelopment.
These adverse effects were found to be even more potent in “pregnancy anxiety,” or anxiety specifically focused on the pregnancy, the birth experience, and the transition to motherhood.8 The psychotic symptoms occurring during postpartum psychosis can jeopardize the lives of both a woman and her child and carries a 4% risk of infanticide.9 Although there are limited data about the long-term effects of postpartum obsessive-compulsive disorders and PTSD, it is reasonable to assume that they might carry negative long-term implications for the mother and possibly her child.
Barriers to treatment
Despite the significant rates of mental illness, pregnant and new mothers often face barriers to receiving treatment. Many psychiatrists are hesitant to prescribe psychiatric medication to pregnant women because of concerns about teratogenic potential of psychiatric medications; similar concerns exist for newborn babies when prescribing medications to lactating mothers. In addition, the field of reproductive psychiatry is evolving at a rapid pace, making it difficult for busy psychiatrists to keep up with the ever-growing literature.
Also, it is hard to imagine a population that has more barriers to attending outpatient appointments. For many new mothers, the exhaustion and all-consuming work involved with taking care of a newborn are insurmountable barriers to obtaining mental health care. In addition, despite the awareness that new mothers often are more emotional, families can be slow to recognize the developing severity of a psychiatric illness during the peripartum and postpartum periods.
Supporting and treating new mothers
As general psychiatrists, there are several ways to directly help these women.
1. Expect the expected. Even in women with no prior psychiatric history, a significant percentage of expectant and postpartum women will develop acute psychiatric symptoms. Learn about the different presentations and treatments of perinatal and postpartum psychiatric disorders. For example, a woman might have thoughts of harming her baby in both postpartum psychosis and obsessive-compulsive disorder. However, the acuity and treatment of these two conditions drastically differ.
2. Learn more about psychiatric medications. Several apps and websites are available to psychiatrists to learn about the safety profile of psychiatric medications, such as Reprotox.org, mothertobaby.org, lactmed, and womensmentalhealth.org. Many medications are considered to be relatively safe during pregnancy and breastfeeding. It is important for psychiatrists to appreciate the risks when choosing not to prescribe to pregnant and postpartum women. Sometimes a known risk of a specific medication may be preferable to the unknown risk of leaving a woman susceptible to a severe psychiatric decompensation.
3. Involve all members of the family. A mother’s mental health has significant implications for the entire family. Psychoeducation for the family as well as frequent family sessions are key tools when treating this population. In addition, prescribing to pregnant women provides the opportunity for a psychiatrist to refine skills in joint decision making; it is crucial to involve both a patient and her spouse when discussing psychiatric medications.
4. Provide ready access and collaborate care. It is important to understand the potential rapid onset of psychiatric symptoms during the pregnancy and postpartum period. Psychiatrists should be prepared to collaborate care with other specialties. It is important to establish relationships with community psychotherapists specializing in maternal mental health, pediatricians, as well as obstetricians.
5. Learn when to seek a higher level of care. Although many women with perinatal and postpartum psychiatric symptoms can be managed as outpatients, women at times need a higher level of care. Similar to general psychiatry, women who are acutely suicidal or homicidal or have a sudden onset of psychotic and manic symptoms all should be evaluated immediately for inpatient hospitalization. Women with less severe symptoms but who require a higher level of care than typically offered in standard outpatient treatment should be candidates for partial hospitalization programs.
General intensive programs usually can accommodate these women, but it is ideal to refer this population to perinatal intensive programs. Postpartum Support International (postpartum.net) lists the nationwide inpatient and partial perinatal programs as well as regional and local services. An example of inpatient perinatal care is the women’s unit at Zucker Hillside Hospital (Northwell Health System, Glen Oaks, N.Y.), which houses an inpatient perinatal program. As a psychiatrist on the unit, I treat acute symptoms such as depression, anxiety, psychosis, mania, and catatonia that occur during the perinatal and postpartum periods. Given the severity of symptoms, I use a wide range of psychiatric medications with the possibility of electroconvulsive therapy when indicated. Psychotherapy staff on the unit offer specialized perinatal, mothers, and dialectical behavioral therapy groups. Breast pumps are available for women who wish to breastfeed. Accommodations are made for babies and children to visit their mother when clinically appropriate. Once discharged, women often are referred to Zucker Hillside’s own perinatal outpatient clinic for continued treatment. Similar models exist in select inpatient units as well as an increasing number of partial programs across the United States.
Conclusion
Psychiatric care for pregnant and new mothers can be challenging, but it is also immensely rewarding. Restoring a mother’s mental health usually leads to increased emotional stability for her entire family. Given the prevalence of maternal mental health disorders, psychiatrists in nearly every setting will encounter this population of women. With dedicated time devoted to reviewing the literature and learning about local resources, psychiatrists can feel comfortable treating women throughout the childbearing experience.
References
1. J Affect Disord. 2017 Sep;219:86-92.
2. J Psychiatr Res. 2018 Sep;104:235-48.
3. J Womens Health. (Larchmt). 2015 Sep;24(9):762-70.
4. Clin Psychol Rev. 2014 Jul;34(5):389-401.
5. Compr Psychiatry. 2009 Nov-Dec;50(6):503-9.
6. Int Rev Psychiatry. 2003 Aug;15(3):231-42.
7. Clin Obstet Gynecol. 2018 Sep;61(3):533-43.
8. Curr Opinion Psychiatry. 2012 Mar;25(2):141-8.
9. Am J Psychiatry. 2009 Apr;166(4):405-8.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine, New York, after graduating from the Albert Einstein College of Medicine and Yeshiva University, New York, with a BA in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
“But this was not what I expected!” That’s a statement I have heard from countless new mothers.
Women often envision pregnancy and the postpartum period as a time of pure joy. The glow of an expectant woman and the excitement of the arrival of a new baby masks the reality that many women struggle emotionally when transitioning to motherhood. Like the birth of a child, the birth of a mother is a complex process. Upholding the myth that all women seamlessly transform into mothers can have devastating effects and hinder access to mental health care.
As a psychiatrist working on a women’s inpatient unit with a perinatal program, I treat women at times of crisis. What may have begun as mild anxiety or depression sometimes quickly spirals into severe psychiatric illness. The sheer force of these severe perinatal and postpartum psychiatric disorders often leaves women and families shocked and confused, wondering what happened to their crumbled dreams of early motherhood.
What must general psychiatrists know about perinatal and postpartum psychiatric disorders? Why is maternal mental health so important? What are the barriers to treatment for these women? How can general psychiatrists best support and treat these new mothers and their families?
What data show
Maternal depression is now known to be one of the most common complications of pregnancy. Studies have suggested that about 11% of women experience depression during pregnancy1 and approximately 17% of women are depressed in the postpartum period.2 Perinatal generalized anxiety disorder has been shown to have a prevalence of 8.5%-10.5% during pregnancy with a wider variance post partum.3 Approximately 3% of women in the general community develop PTSD symptoms following childbirth.4 Research suggests that about 2% of women develop obsessive-compulsive disorder symptoms in the postpartum period.5 Postpartum psychosis, a rare but potentially devastating illness, occurs after 0.1%-0.2% of births.6
Importance of maternal mental health
There is a growing body of literature supporting both obstetric and pediatric adverse outcomes related to untreated psychiatric illness. Untreated maternal depression has been associated with obstetric complications, such as preterm delivery, preeclampsia, low birth weight, as well as the child’s developing cognitive function.7 Anxiety during pregnancy has been associated with both a shorter gestational period and adverse implications for fetal neurodevelopment.
These adverse effects were found to be even more potent in “pregnancy anxiety,” or anxiety specifically focused on the pregnancy, the birth experience, and the transition to motherhood.8 The psychotic symptoms occurring during postpartum psychosis can jeopardize the lives of both a woman and her child and carries a 4% risk of infanticide.9 Although there are limited data about the long-term effects of postpartum obsessive-compulsive disorders and PTSD, it is reasonable to assume that they might carry negative long-term implications for the mother and possibly her child.
Barriers to treatment
Despite the significant rates of mental illness, pregnant and new mothers often face barriers to receiving treatment. Many psychiatrists are hesitant to prescribe psychiatric medication to pregnant women because of concerns about teratogenic potential of psychiatric medications; similar concerns exist for newborn babies when prescribing medications to lactating mothers. In addition, the field of reproductive psychiatry is evolving at a rapid pace, making it difficult for busy psychiatrists to keep up with the ever-growing literature.
Also, it is hard to imagine a population that has more barriers to attending outpatient appointments. For many new mothers, the exhaustion and all-consuming work involved with taking care of a newborn are insurmountable barriers to obtaining mental health care. In addition, despite the awareness that new mothers often are more emotional, families can be slow to recognize the developing severity of a psychiatric illness during the peripartum and postpartum periods.
Supporting and treating new mothers
As general psychiatrists, there are several ways to directly help these women.
1. Expect the expected. Even in women with no prior psychiatric history, a significant percentage of expectant and postpartum women will develop acute psychiatric symptoms. Learn about the different presentations and treatments of perinatal and postpartum psychiatric disorders. For example, a woman might have thoughts of harming her baby in both postpartum psychosis and obsessive-compulsive disorder. However, the acuity and treatment of these two conditions drastically differ.
2. Learn more about psychiatric medications. Several apps and websites are available to psychiatrists to learn about the safety profile of psychiatric medications, such as Reprotox.org, mothertobaby.org, lactmed, and womensmentalhealth.org. Many medications are considered to be relatively safe during pregnancy and breastfeeding. It is important for psychiatrists to appreciate the risks when choosing not to prescribe to pregnant and postpartum women. Sometimes a known risk of a specific medication may be preferable to the unknown risk of leaving a woman susceptible to a severe psychiatric decompensation.
3. Involve all members of the family. A mother’s mental health has significant implications for the entire family. Psychoeducation for the family as well as frequent family sessions are key tools when treating this population. In addition, prescribing to pregnant women provides the opportunity for a psychiatrist to refine skills in joint decision making; it is crucial to involve both a patient and her spouse when discussing psychiatric medications.
4. Provide ready access and collaborate care. It is important to understand the potential rapid onset of psychiatric symptoms during the pregnancy and postpartum period. Psychiatrists should be prepared to collaborate care with other specialties. It is important to establish relationships with community psychotherapists specializing in maternal mental health, pediatricians, as well as obstetricians.
5. Learn when to seek a higher level of care. Although many women with perinatal and postpartum psychiatric symptoms can be managed as outpatients, women at times need a higher level of care. Similar to general psychiatry, women who are acutely suicidal or homicidal or have a sudden onset of psychotic and manic symptoms all should be evaluated immediately for inpatient hospitalization. Women with less severe symptoms but who require a higher level of care than typically offered in standard outpatient treatment should be candidates for partial hospitalization programs.
General intensive programs usually can accommodate these women, but it is ideal to refer this population to perinatal intensive programs. Postpartum Support International (postpartum.net) lists the nationwide inpatient and partial perinatal programs as well as regional and local services. An example of inpatient perinatal care is the women’s unit at Zucker Hillside Hospital (Northwell Health System, Glen Oaks, N.Y.), which houses an inpatient perinatal program. As a psychiatrist on the unit, I treat acute symptoms such as depression, anxiety, psychosis, mania, and catatonia that occur during the perinatal and postpartum periods. Given the severity of symptoms, I use a wide range of psychiatric medications with the possibility of electroconvulsive therapy when indicated. Psychotherapy staff on the unit offer specialized perinatal, mothers, and dialectical behavioral therapy groups. Breast pumps are available for women who wish to breastfeed. Accommodations are made for babies and children to visit their mother when clinically appropriate. Once discharged, women often are referred to Zucker Hillside’s own perinatal outpatient clinic for continued treatment. Similar models exist in select inpatient units as well as an increasing number of partial programs across the United States.
Conclusion
Psychiatric care for pregnant and new mothers can be challenging, but it is also immensely rewarding. Restoring a mother’s mental health usually leads to increased emotional stability for her entire family. Given the prevalence of maternal mental health disorders, psychiatrists in nearly every setting will encounter this population of women. With dedicated time devoted to reviewing the literature and learning about local resources, psychiatrists can feel comfortable treating women throughout the childbearing experience.
References
1. J Affect Disord. 2017 Sep;219:86-92.
2. J Psychiatr Res. 2018 Sep;104:235-48.
3. J Womens Health. (Larchmt). 2015 Sep;24(9):762-70.
4. Clin Psychol Rev. 2014 Jul;34(5):389-401.
5. Compr Psychiatry. 2009 Nov-Dec;50(6):503-9.
6. Int Rev Psychiatry. 2003 Aug;15(3):231-42.
7. Clin Obstet Gynecol. 2018 Sep;61(3):533-43.
8. Curr Opinion Psychiatry. 2012 Mar;25(2):141-8.
9. Am J Psychiatry. 2009 Apr;166(4):405-8.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine, New York, after graduating from the Albert Einstein College of Medicine and Yeshiva University, New York, with a BA in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Family separations and the intergenerational transmission of trauma
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
Growing up, I was always intrigued by the strong emotions that even the mildest separation evoked within me. As a psychiatrist, I now believe that these emotions were related to my family’s difficulty with separation, a concept likely transmitted from my grandmother’s sudden separation as a child.
The political circumstances of the “Kindertransport” and the recent family separation at the southern U.S. border differ, but the Kindertransport is a model for studying the effects of forced parent-child separation and its intergenerational transmission. As a rescue operation that took place immediately before World War II, the Kindertransport was the emigration of approximately 10,000 German Jewish children from Germany and Nazi-occupied countries to England. Even though they were not literally forced, the parents involved were compelled to separate from their children to give their children a chance to survive.
In a recent letter1 published in The New York Times, Eva Yachnes, herself a Kindertransport participant, reflected on the current situation at the southern U.S. border. She alluded to the lifelong effects of her own separation at the age of 6 when emigrating from Vienna to Germany. Personally, as a granddaughter of a Kindertransport participant, I am particularly concerned about the intergenerational transmission of the trauma of family separation.
Since early May 2018, more than 2,000 children have been forcibly separated from their parents after illegally crossing the border. As part of a “zero tolerance policy,” the separation was characterized by the Trump administration as a deterrent to illegal border crossings. Although many Americans are horrified by the news reports about family separation, psychiatrists in particular have expressed concern about this trauma. The American Psychiatric Association issued a statement2 warning that “any forced separation is highly stressful for children and can cause lifelong trauma.” Several weeks later, the APA joined several other mental health organizations in a letter3 calling for the immediate end of enforcement of those policies. In that letter, the organizations said forced separations can cause “an increased risk of ... mental illnesses such as depression, anxiety, and posttraumatic stress disorder.”
What must psychiatrists understand about the impact of childhood trauma? How can psychiatrists approach treatment of children separated from their parents? Are there ways to minimize the risk for intergenerational impact of this trauma?
What do we know?
Childhood trauma is influenced by multiple factors and can be expressed in several ways. According to research,4 the age of the child at the time of traumatic event, the frequency of traumatic experiences, and the degree to which the child’s caretakers were involved in the trauma are factors that influence the extent of psychological damage. This research also suggests that childhood trauma is associated with emotional dysregulation, aggression against self and others, difficulties in attention and dissociation, medical problems, and difficulty with navigating adult interpersonal relationships.
When viewed through the lens of attachment theory, the forced separation of a child from its caretakers is a potent form of childhood trauma. Joanna E. Chambers, MD, summarizes and explains John Bowlby’s attachment theory as a neurobiological system originating from an infant’s connection to the primary caretaker. This connection becomes a lifelong model for all subsequent relationships.
Any traumatic disruptions in the development of this system puts the child at risk of developing “insecure attachment.” This insecure attachment can lead to lifelong emotional problems for the child, affecting the quality of subsequent marital relationships, relationships to children, and the development of personality disorders.
In addition, it correlates to the development of psychiatric illnesses, specifically depression and anxiety. There is also a plausible biological basis for attachment theory. Both oxytocin, a hormone released in human bonding, and social interaction itself have been shown to decrease cortisol levels. Elevated cortisol has been found to negatively affect infant brain development, Dr. Chambers argued.5
Given those significant effects of childhood trauma, it is understandable that there exists a concept of “intergenerational transmission of trauma.” Originating from studies of Holocaust survivors and their descendants, researchers Amy Lehrner, PhD, and Rachel Yehuda, PhD, conceptualize intergenerational transmission of trauma as the intergenerational impact of prenatal PTSD.6 This impact is expressed as a predisposition in the offspring of Holocaust survivors to developing PTSD, difficulties in individuation and separation, higher rates of mood and anxiety disorders, and higher rates of physical health issues.
Although they are complex and clearly multidetermined, Dr. Yehuda and Dr. Lehrner also summarize plausible biological theories for the intergenerational transmission of trauma. Epigenetic differences in the hypothalamic-pituitary-adrenal axis, circadian rhythm, urinary and plasma cortisol levels, glucocorticoid sensitivity, and regulation of the glucocorticoid receptor gene all have been found in Holocaust offspring with parental PTSD, in contrast to offspring without parental PTSD.6
What can we as psychiatrists do?
We are uniquely equipped to take several concrete steps to help mitigate the effects of these traumatic events. Among them, we can:
- Provide opportunities for the child and the family to process their experience. This can be profoundly healing and can help minimize the devastating psychological effects of this separation.
- Become acquainted with the concept of intergenerational transmission of resilience.
- Work with trauma survivors to develop their own personal narratives and cultural rituals surrounding the trauma.6
- Encourage second- and third-generation descendants to engage in artistic expression of the trauma, visit places of importance to their parents, and engage in social and political activism. These are all expressions of resilience in the offspring of trauma victims.6
In summary, recent U.S. political events have caused thousands of children to be forcibly separated from their parents. Those separations are traumatic and can have lifelong psychological implications for the children and their offspring. It is important to provide quality mental health treatment to these children with a specific focus on treating PTSD and processing the traumatic experience. Psychological treatment can help mitigate the effects of the traumatic separation and create a sense of resiliency.
References
1. New York Times. June 20, 2018. “My separation trauma.”
2. American Psychiatric Association statement, May 30, 2018.
3. Letter to the departments of Justice, Health & Human Services, and Homeland Security, June 20, 2018.
4. Child Adolesc Psychiatric Clin N Am. 2003;(12.2):293-318.
5. Psychodynamic Psychiatry. 2017 Dec;45(4):542-63.
6. Psychological Trauma: Theory, Research, Practice, and Policy. 2018 Jan;10(1):22-9.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital of the Northwell Health System, Glen Oaks, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine after graduating from the Albert Einstein College of Medicine and Yeshiva University with a B.A. in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
Growing up, I was always intrigued by the strong emotions that even the mildest separation evoked within me. As a psychiatrist, I now believe that these emotions were related to my family’s difficulty with separation, a concept likely transmitted from my grandmother’s sudden separation as a child.
The political circumstances of the “Kindertransport” and the recent family separation at the southern U.S. border differ, but the Kindertransport is a model for studying the effects of forced parent-child separation and its intergenerational transmission. As a rescue operation that took place immediately before World War II, the Kindertransport was the emigration of approximately 10,000 German Jewish children from Germany and Nazi-occupied countries to England. Even though they were not literally forced, the parents involved were compelled to separate from their children to give their children a chance to survive.
In a recent letter1 published in The New York Times, Eva Yachnes, herself a Kindertransport participant, reflected on the current situation at the southern U.S. border. She alluded to the lifelong effects of her own separation at the age of 6 when emigrating from Vienna to Germany. Personally, as a granddaughter of a Kindertransport participant, I am particularly concerned about the intergenerational transmission of the trauma of family separation.
Since early May 2018, more than 2,000 children have been forcibly separated from their parents after illegally crossing the border. As part of a “zero tolerance policy,” the separation was characterized by the Trump administration as a deterrent to illegal border crossings. Although many Americans are horrified by the news reports about family separation, psychiatrists in particular have expressed concern about this trauma. The American Psychiatric Association issued a statement2 warning that “any forced separation is highly stressful for children and can cause lifelong trauma.” Several weeks later, the APA joined several other mental health organizations in a letter3 calling for the immediate end of enforcement of those policies. In that letter, the organizations said forced separations can cause “an increased risk of ... mental illnesses such as depression, anxiety, and posttraumatic stress disorder.”
What must psychiatrists understand about the impact of childhood trauma? How can psychiatrists approach treatment of children separated from their parents? Are there ways to minimize the risk for intergenerational impact of this trauma?
What do we know?
Childhood trauma is influenced by multiple factors and can be expressed in several ways. According to research,4 the age of the child at the time of traumatic event, the frequency of traumatic experiences, and the degree to which the child’s caretakers were involved in the trauma are factors that influence the extent of psychological damage. This research also suggests that childhood trauma is associated with emotional dysregulation, aggression against self and others, difficulties in attention and dissociation, medical problems, and difficulty with navigating adult interpersonal relationships.
When viewed through the lens of attachment theory, the forced separation of a child from its caretakers is a potent form of childhood trauma. Joanna E. Chambers, MD, summarizes and explains John Bowlby’s attachment theory as a neurobiological system originating from an infant’s connection to the primary caretaker. This connection becomes a lifelong model for all subsequent relationships.
Any traumatic disruptions in the development of this system puts the child at risk of developing “insecure attachment.” This insecure attachment can lead to lifelong emotional problems for the child, affecting the quality of subsequent marital relationships, relationships to children, and the development of personality disorders.
In addition, it correlates to the development of psychiatric illnesses, specifically depression and anxiety. There is also a plausible biological basis for attachment theory. Both oxytocin, a hormone released in human bonding, and social interaction itself have been shown to decrease cortisol levels. Elevated cortisol has been found to negatively affect infant brain development, Dr. Chambers argued.5
Given those significant effects of childhood trauma, it is understandable that there exists a concept of “intergenerational transmission of trauma.” Originating from studies of Holocaust survivors and their descendants, researchers Amy Lehrner, PhD, and Rachel Yehuda, PhD, conceptualize intergenerational transmission of trauma as the intergenerational impact of prenatal PTSD.6 This impact is expressed as a predisposition in the offspring of Holocaust survivors to developing PTSD, difficulties in individuation and separation, higher rates of mood and anxiety disorders, and higher rates of physical health issues.
Although they are complex and clearly multidetermined, Dr. Yehuda and Dr. Lehrner also summarize plausible biological theories for the intergenerational transmission of trauma. Epigenetic differences in the hypothalamic-pituitary-adrenal axis, circadian rhythm, urinary and plasma cortisol levels, glucocorticoid sensitivity, and regulation of the glucocorticoid receptor gene all have been found in Holocaust offspring with parental PTSD, in contrast to offspring without parental PTSD.6
What can we as psychiatrists do?
We are uniquely equipped to take several concrete steps to help mitigate the effects of these traumatic events. Among them, we can:
- Provide opportunities for the child and the family to process their experience. This can be profoundly healing and can help minimize the devastating psychological effects of this separation.
- Become acquainted with the concept of intergenerational transmission of resilience.
- Work with trauma survivors to develop their own personal narratives and cultural rituals surrounding the trauma.6
- Encourage second- and third-generation descendants to engage in artistic expression of the trauma, visit places of importance to their parents, and engage in social and political activism. These are all expressions of resilience in the offspring of trauma victims.6
In summary, recent U.S. political events have caused thousands of children to be forcibly separated from their parents. Those separations are traumatic and can have lifelong psychological implications for the children and their offspring. It is important to provide quality mental health treatment to these children with a specific focus on treating PTSD and processing the traumatic experience. Psychological treatment can help mitigate the effects of the traumatic separation and create a sense of resiliency.
References
1. New York Times. June 20, 2018. “My separation trauma.”
2. American Psychiatric Association statement, May 30, 2018.
3. Letter to the departments of Justice, Health & Human Services, and Homeland Security, June 20, 2018.
4. Child Adolesc Psychiatric Clin N Am. 2003;(12.2):293-318.
5. Psychodynamic Psychiatry. 2017 Dec;45(4):542-63.
6. Psychological Trauma: Theory, Research, Practice, and Policy. 2018 Jan;10(1):22-9.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital of the Northwell Health System, Glen Oaks, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine after graduating from the Albert Einstein College of Medicine and Yeshiva University with a B.A. in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
Growing up, I was always intrigued by the strong emotions that even the mildest separation evoked within me. As a psychiatrist, I now believe that these emotions were related to my family’s difficulty with separation, a concept likely transmitted from my grandmother’s sudden separation as a child.
The political circumstances of the “Kindertransport” and the recent family separation at the southern U.S. border differ, but the Kindertransport is a model for studying the effects of forced parent-child separation and its intergenerational transmission. As a rescue operation that took place immediately before World War II, the Kindertransport was the emigration of approximately 10,000 German Jewish children from Germany and Nazi-occupied countries to England. Even though they were not literally forced, the parents involved were compelled to separate from their children to give their children a chance to survive.
In a recent letter1 published in The New York Times, Eva Yachnes, herself a Kindertransport participant, reflected on the current situation at the southern U.S. border. She alluded to the lifelong effects of her own separation at the age of 6 when emigrating from Vienna to Germany. Personally, as a granddaughter of a Kindertransport participant, I am particularly concerned about the intergenerational transmission of the trauma of family separation.
Since early May 2018, more than 2,000 children have been forcibly separated from their parents after illegally crossing the border. As part of a “zero tolerance policy,” the separation was characterized by the Trump administration as a deterrent to illegal border crossings. Although many Americans are horrified by the news reports about family separation, psychiatrists in particular have expressed concern about this trauma. The American Psychiatric Association issued a statement2 warning that “any forced separation is highly stressful for children and can cause lifelong trauma.” Several weeks later, the APA joined several other mental health organizations in a letter3 calling for the immediate end of enforcement of those policies. In that letter, the organizations said forced separations can cause “an increased risk of ... mental illnesses such as depression, anxiety, and posttraumatic stress disorder.”
What must psychiatrists understand about the impact of childhood trauma? How can psychiatrists approach treatment of children separated from their parents? Are there ways to minimize the risk for intergenerational impact of this trauma?
What do we know?
Childhood trauma is influenced by multiple factors and can be expressed in several ways. According to research,4 the age of the child at the time of traumatic event, the frequency of traumatic experiences, and the degree to which the child’s caretakers were involved in the trauma are factors that influence the extent of psychological damage. This research also suggests that childhood trauma is associated with emotional dysregulation, aggression against self and others, difficulties in attention and dissociation, medical problems, and difficulty with navigating adult interpersonal relationships.
When viewed through the lens of attachment theory, the forced separation of a child from its caretakers is a potent form of childhood trauma. Joanna E. Chambers, MD, summarizes and explains John Bowlby’s attachment theory as a neurobiological system originating from an infant’s connection to the primary caretaker. This connection becomes a lifelong model for all subsequent relationships.
Any traumatic disruptions in the development of this system puts the child at risk of developing “insecure attachment.” This insecure attachment can lead to lifelong emotional problems for the child, affecting the quality of subsequent marital relationships, relationships to children, and the development of personality disorders.
In addition, it correlates to the development of psychiatric illnesses, specifically depression and anxiety. There is also a plausible biological basis for attachment theory. Both oxytocin, a hormone released in human bonding, and social interaction itself have been shown to decrease cortisol levels. Elevated cortisol has been found to negatively affect infant brain development, Dr. Chambers argued.5
Given those significant effects of childhood trauma, it is understandable that there exists a concept of “intergenerational transmission of trauma.” Originating from studies of Holocaust survivors and their descendants, researchers Amy Lehrner, PhD, and Rachel Yehuda, PhD, conceptualize intergenerational transmission of trauma as the intergenerational impact of prenatal PTSD.6 This impact is expressed as a predisposition in the offspring of Holocaust survivors to developing PTSD, difficulties in individuation and separation, higher rates of mood and anxiety disorders, and higher rates of physical health issues.
Although they are complex and clearly multidetermined, Dr. Yehuda and Dr. Lehrner also summarize plausible biological theories for the intergenerational transmission of trauma. Epigenetic differences in the hypothalamic-pituitary-adrenal axis, circadian rhythm, urinary and plasma cortisol levels, glucocorticoid sensitivity, and regulation of the glucocorticoid receptor gene all have been found in Holocaust offspring with parental PTSD, in contrast to offspring without parental PTSD.6
What can we as psychiatrists do?
We are uniquely equipped to take several concrete steps to help mitigate the effects of these traumatic events. Among them, we can:
- Provide opportunities for the child and the family to process their experience. This can be profoundly healing and can help minimize the devastating psychological effects of this separation.
- Become acquainted with the concept of intergenerational transmission of resilience.
- Work with trauma survivors to develop their own personal narratives and cultural rituals surrounding the trauma.6
- Encourage second- and third-generation descendants to engage in artistic expression of the trauma, visit places of importance to their parents, and engage in social and political activism. These are all expressions of resilience in the offspring of trauma victims.6
In summary, recent U.S. political events have caused thousands of children to be forcibly separated from their parents. Those separations are traumatic and can have lifelong psychological implications for the children and their offspring. It is important to provide quality mental health treatment to these children with a specific focus on treating PTSD and processing the traumatic experience. Psychological treatment can help mitigate the effects of the traumatic separation and create a sense of resiliency.
References
1. New York Times. June 20, 2018. “My separation trauma.”
2. American Psychiatric Association statement, May 30, 2018.
3. Letter to the departments of Justice, Health & Human Services, and Homeland Security, June 20, 2018.
4. Child Adolesc Psychiatric Clin N Am. 2003;(12.2):293-318.
5. Psychodynamic Psychiatry. 2017 Dec;45(4):542-63.
6. Psychological Trauma: Theory, Research, Practice, and Policy. 2018 Jan;10(1):22-9.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital of the Northwell Health System, Glen Oaks, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine after graduating from the Albert Einstein College of Medicine and Yeshiva University with a B.A. in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Families are essential partners in treating substance use disorders
Addiction used to be considered a moral failing, and the family was blamed for keeping the relative with addictions sick, through behaviors labeled “codependency” and “enabling.” The opioid epidemic can take credit for putting a serious dent in these destructive and stigmatizing notions. When psychiatrists actively include families as educated treatment partners, fatalities are less likely, and the havoc created by addiction on families is mitigated.
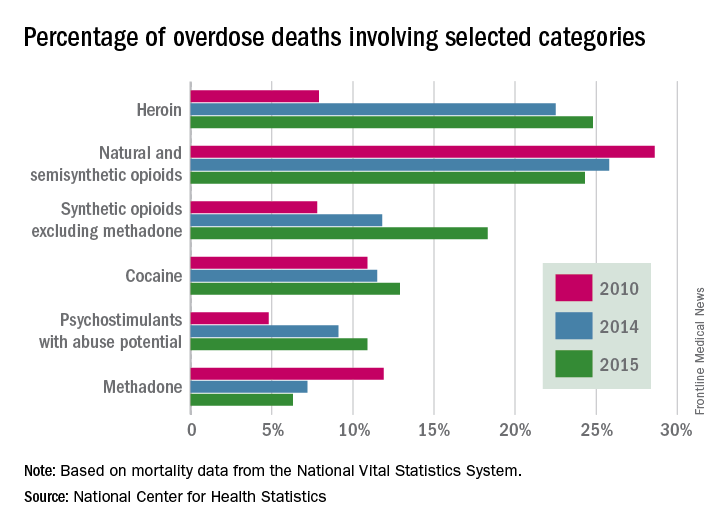
Genes and addiction
What causes addiction? Statistics show that Native Americans fare the worst of all minority groups, with death by opiates in whites and Native Americans double or triple the rates of African Americans and Latinos. Reasons put forward for Native American deaths are their vulnerability related to systemic racism, intergenerational trauma, and lack of access to health care. These “reasons” are well known to contribute to poor overall health status of impoverished communities.
Among impoverished white communities, the Monongahela Valley of Pennsylvania has been studied by Katherine McLean, PhD, as an example of postindustrial decay (Int J Drug Policy. 2016;[29]:19-26). Once a global center of steel production, the exodus of jobs, residents, and businesses since the early 1980s is thought to contribute to the high numbers of opioid deaths. A qualitative study of the people with addiction in the deteriorating mill city of McKeesport, Pa., characterized a risk environment hidden behind closed doors, and populated by unprepared, ambivalent overdose “assistants.” These people are “co-drug” users who themselves are reluctant to step forward because of fear of getting in trouble. The participants described the hopelessness and lack of opportunity as driving the use of heroin, with many stating that jobs and community reinvestment are needed to reduce fatalities. This certainly resonates with the Native American experience.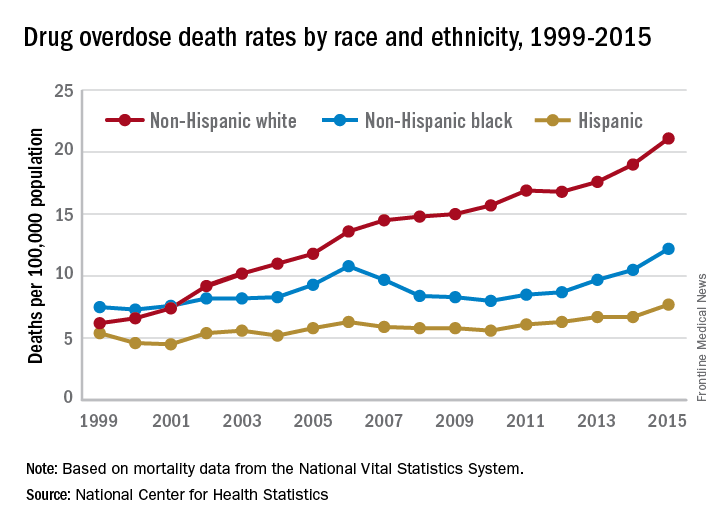
People with the AA variant of OXTR also have been shown to have less secure adult attachment and more social anxiety (World J Biol Psychiatry. 2016;17[1]:76-83). Comparing people with OXTR variants, the AA genotype was associated with a perceived negative social environment and significantly increased PTSD symptoms, whereas the GG genotype was protective.
However, for many decades, psychological theories about the defects of individuals and their moral failing have prevailed. In the family, aspersions have been cast on the family’s deficits in terms of setting limits and their enabling behaviors, mostly focusing on wives and mothers. The social mantra has been that since not all people get addicted, the strong resist and the weak succumb. Psychiatry has focused on providing psychotherapy to correct the personal deficits of the weak and addicted and, from a family perspective, on correcting negative personality traits in the caregivers, classified as codependency.
Roots of codependency
The concept of codependency began as a grassroots idea in the 1960s to describe family members, usually wives or mothers, who were deemed excessive in their caring for their husband or son with addiction. The term was used to describe women who had an overresponsibility for relationships, rather than a responsibility to self. Support groups for codependency, such as Co-Dependents Anonymous, Al-Anon/Alateen, Nar-Anon, and Adult Children of Alcoholics, based on the 12-step program model of Alcoholics Anonymous, were established. Codependents were negatively labeled as rescuers, supporters, and confidantes of their family member with substance use disorder. These helpers were described as dependent on the other person’s poor functioning to satisfy their own emotional needs.
In these early descriptions, there was a lack of discussion about possible deeper family dynamics: Inequality in financial independence of each partner, the desire for family stability focusing on the welfare of children, the real possibility that disrupting a relationship might result in violence if the woman was more assertive. Women were blamed for trying to love their spouse out of the addiction. One aspect of codependency is self-sacrifice, which used to be considered an important trait of the good wife but became a negative trait in the 1960s. Recovery from codependence was considered achieved when the wife or mother expressed healthy self-assertiveness. Some scholars did state, however, that they believed that codependency was not a negative trait, but rather a healthy personality trait taken to excess. In most studies, women with high codependency ratings have tended to be unemployed and with lower educations. Their behavior had been considered worthy of a DSM inclusion as a personality disorder, but luckily, this was thwarted.
A family is forced to make some accounting when an individual develops a substance use disorder. If the family tries to maintain equilibrium and keeps things as stable as possible for the sake of maintaining the family unit or the stability of the lives of the children, accommodation will be required. Accommodation minimizes the impact of the addiction: the sober spouse stepping up to complete the roles of the ill relative and in all ways reducing the impact of dysfunction on the family. If you swap out the illness and consider the ill family member as having cancer or respiratory distress, then you reframe the spouse’s “codependence” as the behavior of a caring spouse.
This long preamble is intended to illustrate how little family dynamics have to do with the etiology of addiction. Addiction is a chronic neurobiological disease, and like all diseases, individuals, and couples and families have the option of learning to cope well. We, as psychiatrists, must move away from blaming people (usually women who have less-than-optimal coping skills) and consider how best to engage partners and families in optimal programs.*
Families can benefit from specialist treatment and thus contribute to the recovery process. One example is a telepsychiatry program that aimed to improve family coping skills to cope with relatives who have substance use disorders. The Tele-intervention Model and Monitoring of Families of Drug Users is based on motivational interviewing and stages of change. Families were randomized into the intervention group (n = 163) or the usual treatment (n = 162). After 6 months of follow-up, the family members of the telepsychiatry group were twice as likely to modify their behavior (odds ratio; 2.08; 95% confidence interval, 1.18-3.65) (J Sub Use Misuse. 2017 Jan 28;52[2]:164-74). This model was organized so that each of nine calls had a specific goal to stimulate the family members in their process of change.
Family change and engagement also can occur through Alanon (Subst Use Misuse. 2015; 50[1]:62-71) and the use of the Arise program of Judith Landau, MD, (Landau J et al. Am J Drug Alcohol Abuse. 2000;26[3]:379-98).
In summary, the family can be engaged in treatment and can develop family coping skills to support their relative with this chronic neurobiological disease.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.
*Updated on January 12, 2018.
Addiction used to be considered a moral failing, and the family was blamed for keeping the relative with addictions sick, through behaviors labeled “codependency” and “enabling.” The opioid epidemic can take credit for putting a serious dent in these destructive and stigmatizing notions. When psychiatrists actively include families as educated treatment partners, fatalities are less likely, and the havoc created by addiction on families is mitigated.
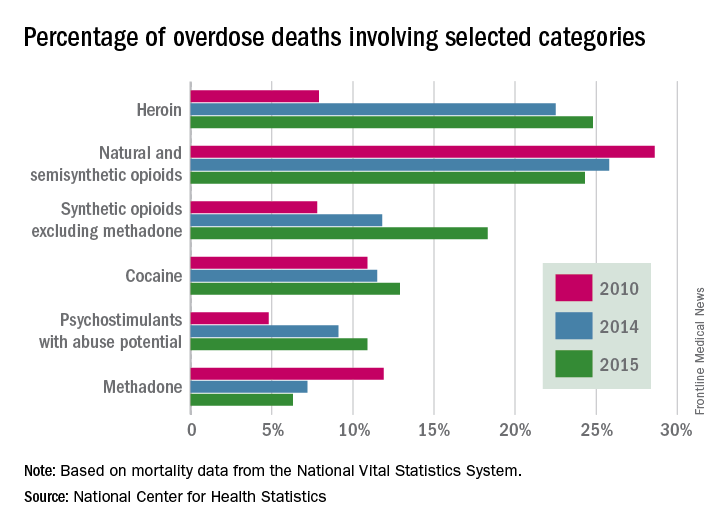
Genes and addiction
What causes addiction? Statistics show that Native Americans fare the worst of all minority groups, with death by opiates in whites and Native Americans double or triple the rates of African Americans and Latinos. Reasons put forward for Native American deaths are their vulnerability related to systemic racism, intergenerational trauma, and lack of access to health care. These “reasons” are well known to contribute to poor overall health status of impoverished communities.
Among impoverished white communities, the Monongahela Valley of Pennsylvania has been studied by Katherine McLean, PhD, as an example of postindustrial decay (Int J Drug Policy. 2016;[29]:19-26). Once a global center of steel production, the exodus of jobs, residents, and businesses since the early 1980s is thought to contribute to the high numbers of opioid deaths. A qualitative study of the people with addiction in the deteriorating mill city of McKeesport, Pa., characterized a risk environment hidden behind closed doors, and populated by unprepared, ambivalent overdose “assistants.” These people are “co-drug” users who themselves are reluctant to step forward because of fear of getting in trouble. The participants described the hopelessness and lack of opportunity as driving the use of heroin, with many stating that jobs and community reinvestment are needed to reduce fatalities. This certainly resonates with the Native American experience.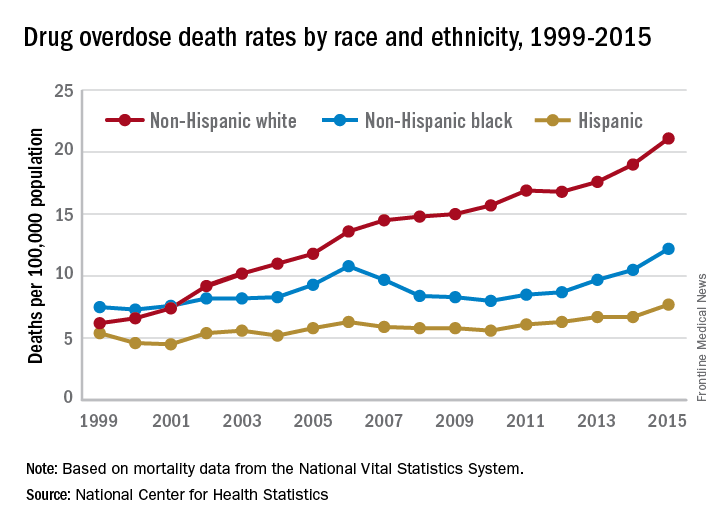
People with the AA variant of OXTR also have been shown to have less secure adult attachment and more social anxiety (World J Biol Psychiatry. 2016;17[1]:76-83). Comparing people with OXTR variants, the AA genotype was associated with a perceived negative social environment and significantly increased PTSD symptoms, whereas the GG genotype was protective.
However, for many decades, psychological theories about the defects of individuals and their moral failing have prevailed. In the family, aspersions have been cast on the family’s deficits in terms of setting limits and their enabling behaviors, mostly focusing on wives and mothers. The social mantra has been that since not all people get addicted, the strong resist and the weak succumb. Psychiatry has focused on providing psychotherapy to correct the personal deficits of the weak and addicted and, from a family perspective, on correcting negative personality traits in the caregivers, classified as codependency.
Roots of codependency
The concept of codependency began as a grassroots idea in the 1960s to describe family members, usually wives or mothers, who were deemed excessive in their caring for their husband or son with addiction. The term was used to describe women who had an overresponsibility for relationships, rather than a responsibility to self. Support groups for codependency, such as Co-Dependents Anonymous, Al-Anon/Alateen, Nar-Anon, and Adult Children of Alcoholics, based on the 12-step program model of Alcoholics Anonymous, were established. Codependents were negatively labeled as rescuers, supporters, and confidantes of their family member with substance use disorder. These helpers were described as dependent on the other person’s poor functioning to satisfy their own emotional needs.
In these early descriptions, there was a lack of discussion about possible deeper family dynamics: Inequality in financial independence of each partner, the desire for family stability focusing on the welfare of children, the real possibility that disrupting a relationship might result in violence if the woman was more assertive. Women were blamed for trying to love their spouse out of the addiction. One aspect of codependency is self-sacrifice, which used to be considered an important trait of the good wife but became a negative trait in the 1960s. Recovery from codependence was considered achieved when the wife or mother expressed healthy self-assertiveness. Some scholars did state, however, that they believed that codependency was not a negative trait, but rather a healthy personality trait taken to excess. In most studies, women with high codependency ratings have tended to be unemployed and with lower educations. Their behavior had been considered worthy of a DSM inclusion as a personality disorder, but luckily, this was thwarted.
A family is forced to make some accounting when an individual develops a substance use disorder. If the family tries to maintain equilibrium and keeps things as stable as possible for the sake of maintaining the family unit or the stability of the lives of the children, accommodation will be required. Accommodation minimizes the impact of the addiction: the sober spouse stepping up to complete the roles of the ill relative and in all ways reducing the impact of dysfunction on the family. If you swap out the illness and consider the ill family member as having cancer or respiratory distress, then you reframe the spouse’s “codependence” as the behavior of a caring spouse.
This long preamble is intended to illustrate how little family dynamics have to do with the etiology of addiction. Addiction is a chronic neurobiological disease, and like all diseases, individuals, and couples and families have the option of learning to cope well. We, as psychiatrists, must move away from blaming people (usually women who have less-than-optimal coping skills) and consider how best to engage partners and families in optimal programs.*
Families can benefit from specialist treatment and thus contribute to the recovery process. One example is a telepsychiatry program that aimed to improve family coping skills to cope with relatives who have substance use disorders. The Tele-intervention Model and Monitoring of Families of Drug Users is based on motivational interviewing and stages of change. Families were randomized into the intervention group (n = 163) or the usual treatment (n = 162). After 6 months of follow-up, the family members of the telepsychiatry group were twice as likely to modify their behavior (odds ratio; 2.08; 95% confidence interval, 1.18-3.65) (J Sub Use Misuse. 2017 Jan 28;52[2]:164-74). This model was organized so that each of nine calls had a specific goal to stimulate the family members in their process of change.
Family change and engagement also can occur through Alanon (Subst Use Misuse. 2015; 50[1]:62-71) and the use of the Arise program of Judith Landau, MD, (Landau J et al. Am J Drug Alcohol Abuse. 2000;26[3]:379-98).
In summary, the family can be engaged in treatment and can develop family coping skills to support their relative with this chronic neurobiological disease.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.
*Updated on January 12, 2018.
Addiction used to be considered a moral failing, and the family was blamed for keeping the relative with addictions sick, through behaviors labeled “codependency” and “enabling.” The opioid epidemic can take credit for putting a serious dent in these destructive and stigmatizing notions. When psychiatrists actively include families as educated treatment partners, fatalities are less likely, and the havoc created by addiction on families is mitigated.
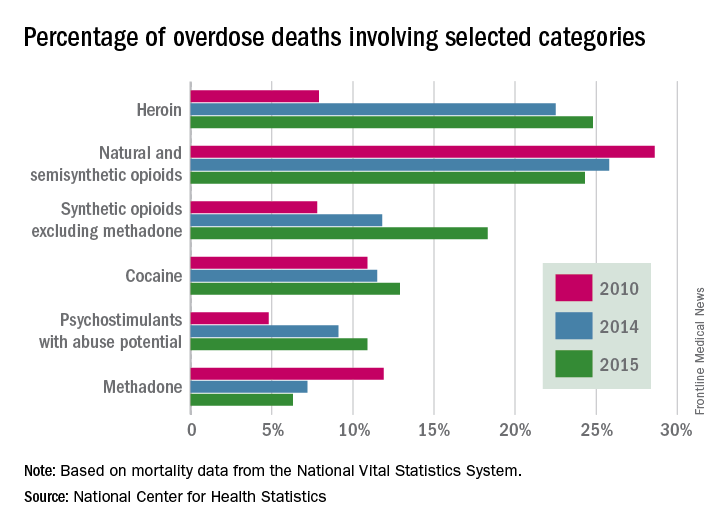
Genes and addiction
What causes addiction? Statistics show that Native Americans fare the worst of all minority groups, with death by opiates in whites and Native Americans double or triple the rates of African Americans and Latinos. Reasons put forward for Native American deaths are their vulnerability related to systemic racism, intergenerational trauma, and lack of access to health care. These “reasons” are well known to contribute to poor overall health status of impoverished communities.
Among impoverished white communities, the Monongahela Valley of Pennsylvania has been studied by Katherine McLean, PhD, as an example of postindustrial decay (Int J Drug Policy. 2016;[29]:19-26). Once a global center of steel production, the exodus of jobs, residents, and businesses since the early 1980s is thought to contribute to the high numbers of opioid deaths. A qualitative study of the people with addiction in the deteriorating mill city of McKeesport, Pa., characterized a risk environment hidden behind closed doors, and populated by unprepared, ambivalent overdose “assistants.” These people are “co-drug” users who themselves are reluctant to step forward because of fear of getting in trouble. The participants described the hopelessness and lack of opportunity as driving the use of heroin, with many stating that jobs and community reinvestment are needed to reduce fatalities. This certainly resonates with the Native American experience.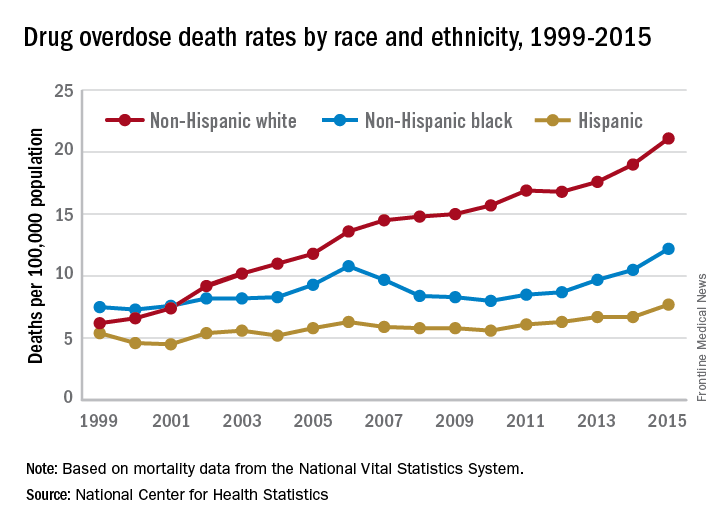
People with the AA variant of OXTR also have been shown to have less secure adult attachment and more social anxiety (World J Biol Psychiatry. 2016;17[1]:76-83). Comparing people with OXTR variants, the AA genotype was associated with a perceived negative social environment and significantly increased PTSD symptoms, whereas the GG genotype was protective.
However, for many decades, psychological theories about the defects of individuals and their moral failing have prevailed. In the family, aspersions have been cast on the family’s deficits in terms of setting limits and their enabling behaviors, mostly focusing on wives and mothers. The social mantra has been that since not all people get addicted, the strong resist and the weak succumb. Psychiatry has focused on providing psychotherapy to correct the personal deficits of the weak and addicted and, from a family perspective, on correcting negative personality traits in the caregivers, classified as codependency.
Roots of codependency
The concept of codependency began as a grassroots idea in the 1960s to describe family members, usually wives or mothers, who were deemed excessive in their caring for their husband or son with addiction. The term was used to describe women who had an overresponsibility for relationships, rather than a responsibility to self. Support groups for codependency, such as Co-Dependents Anonymous, Al-Anon/Alateen, Nar-Anon, and Adult Children of Alcoholics, based on the 12-step program model of Alcoholics Anonymous, were established. Codependents were negatively labeled as rescuers, supporters, and confidantes of their family member with substance use disorder. These helpers were described as dependent on the other person’s poor functioning to satisfy their own emotional needs.
In these early descriptions, there was a lack of discussion about possible deeper family dynamics: Inequality in financial independence of each partner, the desire for family stability focusing on the welfare of children, the real possibility that disrupting a relationship might result in violence if the woman was more assertive. Women were blamed for trying to love their spouse out of the addiction. One aspect of codependency is self-sacrifice, which used to be considered an important trait of the good wife but became a negative trait in the 1960s. Recovery from codependence was considered achieved when the wife or mother expressed healthy self-assertiveness. Some scholars did state, however, that they believed that codependency was not a negative trait, but rather a healthy personality trait taken to excess. In most studies, women with high codependency ratings have tended to be unemployed and with lower educations. Their behavior had been considered worthy of a DSM inclusion as a personality disorder, but luckily, this was thwarted.
A family is forced to make some accounting when an individual develops a substance use disorder. If the family tries to maintain equilibrium and keeps things as stable as possible for the sake of maintaining the family unit or the stability of the lives of the children, accommodation will be required. Accommodation minimizes the impact of the addiction: the sober spouse stepping up to complete the roles of the ill relative and in all ways reducing the impact of dysfunction on the family. If you swap out the illness and consider the ill family member as having cancer or respiratory distress, then you reframe the spouse’s “codependence” as the behavior of a caring spouse.
This long preamble is intended to illustrate how little family dynamics have to do with the etiology of addiction. Addiction is a chronic neurobiological disease, and like all diseases, individuals, and couples and families have the option of learning to cope well. We, as psychiatrists, must move away from blaming people (usually women who have less-than-optimal coping skills) and consider how best to engage partners and families in optimal programs.*
Families can benefit from specialist treatment and thus contribute to the recovery process. One example is a telepsychiatry program that aimed to improve family coping skills to cope with relatives who have substance use disorders. The Tele-intervention Model and Monitoring of Families of Drug Users is based on motivational interviewing and stages of change. Families were randomized into the intervention group (n = 163) or the usual treatment (n = 162). After 6 months of follow-up, the family members of the telepsychiatry group were twice as likely to modify their behavior (odds ratio; 2.08; 95% confidence interval, 1.18-3.65) (J Sub Use Misuse. 2017 Jan 28;52[2]:164-74). This model was organized so that each of nine calls had a specific goal to stimulate the family members in their process of change.
Family change and engagement also can occur through Alanon (Subst Use Misuse. 2015; 50[1]:62-71) and the use of the Arise program of Judith Landau, MD, (Landau J et al. Am J Drug Alcohol Abuse. 2000;26[3]:379-98).
In summary, the family can be engaged in treatment and can develop family coping skills to support their relative with this chronic neurobiological disease.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.
*Updated on January 12, 2018.
Changing the dance
I supervise the family clinic in the outpatient psychiatry resident-run clinic. The Suttons are a typical couple, encountered by the new resident, whom I will call Dr. Suraj. Initially, Dr. Suraj is enthusiastic in his meeting with the Suttons, but soon enters into a conundrum and brings the case to supervision. The couple has an intricate inexplicable dance, leaving the resident baffled. Let’s review the case. (I have changed several key details to protect the couple’s confidentiality.)
Ms. Sutton presents with complaints of “depression,” and slowly, it becomes clear that her complaints center on her spouse’s deficiencies. “He doesn’t understand me; he doesn’t know what it is like being depressed.”
Other complaints follow; some are practical, such as: “He doesn’t help around the house.” Ms. Sutton’s complaints mostly reflect her perception that either her spouse does not care for her adequately, he has lost interest in her, or he is fundamentally unable to respond adequately to her needs. “He says bad things to me, like ‘Just get over it,’ or ‘Don’t make such a fuss about things.’ ”
After three further sessions of listening to her complaints, and a general lack of response to prior and current medications, Dr. Suraj decides that Mr. Sutton needs to come in. Dr. Suraj follows what he has been taught so far: Get a history from the partner to validate symptoms, functioning, and quality of life. Mostly, the session goes as predicted, ending with Dr. Suraj’s attempt to educate Mr. Sutton about the signs and symptoms of depression. It doesn’t come out right, because the impression that Mr. Sutton gets is that Dr. Suraj is siding with his wife. This seems to make things worse, as Mr. Sutton then complains to his wife that “The doctor doesn’t know what he’s talking about,” “is too young to understand,” or a myriad of other put-downs. Ms. Sutton, of course, tells Dr. Suraj about all of this, following it up with “Don’t worry Doc; you are doing a great job.” Other comments are more in the way of commentary: “I told my husband what you said last week, and he disagrees with you.”
Dr. Suraj realizes that “something is amiss;” the case is stuck, and worse, he is stuck in the middle. The general impression, says Dr. Suraj, “is of a woman who feels victimized, neglected, or overlooked, but somehow, she has the power. She presents as the victim but also is the victimizer. He seems to be the victimizer and tormenter, but all in all, just as much the victim of her torments! I do not know how to think about this couple: They seem stuck, unhappily but inexorably stuck together in perpetuity.” Can anything be done to change this relationship?
Dr. Suraj’s uncensored thoughts: Perhaps they should break up or at least stop complaining. What is it that makes people keep complaining about their relationships? Either they accept it or they leave.
Initial areas of focus
Interpersonal violence. The archetypal extreme is that of an abusive relationship, where the victim is subjected to domestic violence. As I wrote in Advances in Psychiatric Treatment, many relationships where violence is present are bidirectional (2007;13[5]:376-83). Couples may not voice this concern for fear of the spouse being turned over to the police. I usually include a question such as: “How many times do your arguments include pushing or shoving or things like that?”
Asking about income, specifically, who controls the finances and how money is spent, clarifies whether one person feels that he or she has no option but to stay in the relationship.
If intimate partner violence (IPV) exists, there are typical protocols for helping the victim leave. When IPV is not a consideration, the resident wonders about the Suttons, when the victim and abuser change or share roles. Why do they keep up this struggle if they are unhappy?
Life expectations. Many couples do not discuss their expectations or what they imagine will happen when they get married. There may be unspoken fantasies such as “I always assumed that you would retire at 65, and we would go traveling together.” People may change their minds, or life circumstances change so that expectations and fantasies about their life together can no longer be sustained. Are there goals that have changed? Are there dependent relatives that prevent marital goals from being achieved? Is there a lack of agreement about what are important life goals?
Change! One spouse may try to make the other person change, according to his or her preferences. In the psychiatrist’s office, this can take the form of pathologizing: He just wasn’t brought up to talk about feelings, meaning he needs to talk about feelings. We hear questions such as: “Can you take him on in therapy?”; “He doesn’t listen ... can you check him for hearing loss?”; “She doesn’t remember what I said: Can you check her for dementia?” These complaints may come up at the beginning of a relationship or later in life, for example, after retirement when the couple is home together for extended periods of time. Is the expectation that each person should be able to fulfill the partner’s every wish and desire? Be all things? That is a tough order.
The Suttons report that change is the main thing they want from each other. After a full family assessment, it is clear that roles are evenly and acceptably shared; they have no differences in family rules; they both enjoy the same hobbies, care for each other, and work together to solve family crises. However, they cannot accept each other the way they are. When the children were young, she said: “I was too busy to get depressed.” Mr. Sutton states that she now wants him to be attentive to her but he is too tired after a lifetime of work, and anyway, she is so whiny he does not want to be around her. So they bicker back and forth, neither giving an inch.
Useful theories
A. Dr. Gottman’s typology. John Gottman, PhD, categorizes couples into five types: Conflict-Avoiding, Validating, Volatile, Hostile, and Hostile-Detached. The three happy couple types (Conflict-Avoiding, Validating, and Volatile) are very different from one another, and each type has its own benefits and risks. Of the two unhappy couple types, hostile couples stayed unhappily married. He derived this categorization from observations of couples in his lab (https://www.gottman.com).
Conflict-Avoiding: Conflict avoiders minimize persuasion attempts and instead emphasize their areas of common ground. They avoid conflict, avoid expressing what they need from one another, and congratulate their relationship for being generally happy. Conflict-avoiding couples balance independence and interdependence. They have clear boundaries, and are separate people with separate interests. They can be connected and caring in areas of overlap where they are interdependent. While they are minimally emotionally expressive, they maintain a ratio of positive-to-negative affect around 5 to 1. Their interaction is good enough for them.
Validating: The interaction of these couples is characterized by ease and calm. They are somewhat expressive but mostly neutral. They are intermediate between avoiders and the volatile couples. They put a lot of emphasis on supporting and understanding their partner’s point of view, and are often empathetic about their partner’s feelings. They will confront their differences, but only on some topics and not on others. They can become highly competitive on some issues, which can turn into a power struggle, but they usually calm down and compromise. The ratio of positive-to-negative comments is 5 to 1.
Volatile: Volatile couples are intensely emotional. During a conflict discussion, they begin persuasion immediately, and they debate with laughter and humor. They are not disrespectful or insulting. Their positive-to-negative comments ratio is 5 to 1. Anger and feelings of insecurity are expressed, but not contempt. They have no clear boundaries around their individual worlds. While they argue about their roles, they emphasize connection and honesty in their communication.
Hostile: Hostile couples are like validators, except there are high levels of defensiveness on the part of both partners. In Dr. Gottman’s lab, the husband was usually the validator and the wife was the avoider.
Hostile-Detached: These couples are like two armies engaged in a standoff. They snipe at one another during conflict, although the air is one of emotional detachment and resignation. In Dr. Gottman’s lab, usually there was a validator husband with a volatile wife. Escalating conflict will occur between two validators, but then one of them will back down. But the volatile will not let the validator withdraw. Dr. Gottman notes that there is a superiority involved in the woman: that the man needs to be taught the right way to be. The woman does not see the need to change.
B. The approach/avoidance dance
The approach/avoidance dance is based on the motivation of each person (Psychol Sci. 2008 Oct 19;[10]:1030-6). A partner with approach goals focuses on attaining positive outcomes, such as intimacy and growth. A partner with avoidance goals focuses away from negative outcomes, such as conflict and rejection (Educational Psychologist. 1999;34:169-89). For example, in a discussion about child care, a husband who has strong approach goals may be concerned with wanting the discussion to go smoothly and wanting both partners to be happy with the outcome. In contrast, a husband with strong avoidance goals may be more concerned with avoiding conflict about child care and preventing both partners from being unhappy with the outcome. People who are not motivated by approach goals are not particularly interested in pursuing positive experiences in their relationships, such as bonding, intimacy, or fun activities. In contrast, people who are motivated by avoidance goals are interested in avoiding negative experiences, such as conflict, betrayal, or rejection by a romantic partner.
C. Attachment
Both of the previously discussed theories have attachment theory at their core, and are organized around anxiety and avoidance. The anxiety would be tied to concern that the partner may not be available or supportive in times of need, and the avoidance piece would be tied to worry that the partner cannot be fully trusted (Fam Process. 2002 Fall;41[3]:546-50). A low score on both of these indices means a secure attachment style. For unhappy couples with cemented attachments, there is no thought that one would leave. They are bound together in unhappiness (Current Opin Psychol. 2017 Feb;13:60-4).
Nice guy husband/borderline wife relationship or hysterical wife/obsessive-compulsive husband: These relationship can be explained using an attachment framework. This male personality type truly enjoys giving and often finds that he needs nothing more in return than a feeling of being appreciated.
D. Emotionally focused therapy
Sue Johnson, EdD, has an evidence-based couples therapy called emotionally focused couples and family therapy. She would interpret the Suttons as a couple caught in a dance of negativity. The goal of therapy is to help couples let down defenses enough to be vulnerable and then to help them express emotional needs to each other. Dr. Johnson helps each person meet the emotional needs of the other. (See http://drsuejohnson.com/)
E. The game of struggle for power and control
In most relationships, there is a minimizer and a maximizer. The minimizer is more subdued within the relationship, while the maximizer is more evocative. When this turns into a game of “Who has the power,” then minimizing and maximizing turns into submission and dominance. Typically, the minimizer becomes dominant, and the maximizer becomes submissive. One partner can become parentalized and the other infantilized. Most often, the maximizer, being more emotional, tends to become infantilized and submissive for fear of angering or disappointing his or her partner. The minimizer, being more contained, tends to gather the power in the relationship, whether by intention or default, and, in this way, becomes parentalized.
Is this power struggle similar to the developmental challenges faced by toddlers? Being in a growth-supporting relationship means that the relationship helps people develop a more mature interpersonal relationship. It is this notion that supports the theory that people at the same developmental level find each other compatible, as they both face the same challenges in life.
So what happened to the Suttons? The resident referred the patient to the outpatient couples therapist, who treated them for six sessions. The assessment revealed that they had played this dance for decades, but it had intensified after Mr. Sutton retired and was available as a daily target for Ms. Sutton’s unhappiness with the way that life had treated her. The mutual negative impact of their interactions was ameliorated to some extent, by helping the couple develop individual interests. They moved from being hostile-detached to conflict-avoiding. The Suttons moved from waltzing to circle dancing.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.
I supervise the family clinic in the outpatient psychiatry resident-run clinic. The Suttons are a typical couple, encountered by the new resident, whom I will call Dr. Suraj. Initially, Dr. Suraj is enthusiastic in his meeting with the Suttons, but soon enters into a conundrum and brings the case to supervision. The couple has an intricate inexplicable dance, leaving the resident baffled. Let’s review the case. (I have changed several key details to protect the couple’s confidentiality.)
Ms. Sutton presents with complaints of “depression,” and slowly, it becomes clear that her complaints center on her spouse’s deficiencies. “He doesn’t understand me; he doesn’t know what it is like being depressed.”
Other complaints follow; some are practical, such as: “He doesn’t help around the house.” Ms. Sutton’s complaints mostly reflect her perception that either her spouse does not care for her adequately, he has lost interest in her, or he is fundamentally unable to respond adequately to her needs. “He says bad things to me, like ‘Just get over it,’ or ‘Don’t make such a fuss about things.’ ”
After three further sessions of listening to her complaints, and a general lack of response to prior and current medications, Dr. Suraj decides that Mr. Sutton needs to come in. Dr. Suraj follows what he has been taught so far: Get a history from the partner to validate symptoms, functioning, and quality of life. Mostly, the session goes as predicted, ending with Dr. Suraj’s attempt to educate Mr. Sutton about the signs and symptoms of depression. It doesn’t come out right, because the impression that Mr. Sutton gets is that Dr. Suraj is siding with his wife. This seems to make things worse, as Mr. Sutton then complains to his wife that “The doctor doesn’t know what he’s talking about,” “is too young to understand,” or a myriad of other put-downs. Ms. Sutton, of course, tells Dr. Suraj about all of this, following it up with “Don’t worry Doc; you are doing a great job.” Other comments are more in the way of commentary: “I told my husband what you said last week, and he disagrees with you.”
Dr. Suraj realizes that “something is amiss;” the case is stuck, and worse, he is stuck in the middle. The general impression, says Dr. Suraj, “is of a woman who feels victimized, neglected, or overlooked, but somehow, she has the power. She presents as the victim but also is the victimizer. He seems to be the victimizer and tormenter, but all in all, just as much the victim of her torments! I do not know how to think about this couple: They seem stuck, unhappily but inexorably stuck together in perpetuity.” Can anything be done to change this relationship?
Dr. Suraj’s uncensored thoughts: Perhaps they should break up or at least stop complaining. What is it that makes people keep complaining about their relationships? Either they accept it or they leave.
Initial areas of focus
Interpersonal violence. The archetypal extreme is that of an abusive relationship, where the victim is subjected to domestic violence. As I wrote in Advances in Psychiatric Treatment, many relationships where violence is present are bidirectional (2007;13[5]:376-83). Couples may not voice this concern for fear of the spouse being turned over to the police. I usually include a question such as: “How many times do your arguments include pushing or shoving or things like that?”
Asking about income, specifically, who controls the finances and how money is spent, clarifies whether one person feels that he or she has no option but to stay in the relationship.
If intimate partner violence (IPV) exists, there are typical protocols for helping the victim leave. When IPV is not a consideration, the resident wonders about the Suttons, when the victim and abuser change or share roles. Why do they keep up this struggle if they are unhappy?
Life expectations. Many couples do not discuss their expectations or what they imagine will happen when they get married. There may be unspoken fantasies such as “I always assumed that you would retire at 65, and we would go traveling together.” People may change their minds, or life circumstances change so that expectations and fantasies about their life together can no longer be sustained. Are there goals that have changed? Are there dependent relatives that prevent marital goals from being achieved? Is there a lack of agreement about what are important life goals?
Change! One spouse may try to make the other person change, according to his or her preferences. In the psychiatrist’s office, this can take the form of pathologizing: He just wasn’t brought up to talk about feelings, meaning he needs to talk about feelings. We hear questions such as: “Can you take him on in therapy?”; “He doesn’t listen ... can you check him for hearing loss?”; “She doesn’t remember what I said: Can you check her for dementia?” These complaints may come up at the beginning of a relationship or later in life, for example, after retirement when the couple is home together for extended periods of time. Is the expectation that each person should be able to fulfill the partner’s every wish and desire? Be all things? That is a tough order.
The Suttons report that change is the main thing they want from each other. After a full family assessment, it is clear that roles are evenly and acceptably shared; they have no differences in family rules; they both enjoy the same hobbies, care for each other, and work together to solve family crises. However, they cannot accept each other the way they are. When the children were young, she said: “I was too busy to get depressed.” Mr. Sutton states that she now wants him to be attentive to her but he is too tired after a lifetime of work, and anyway, she is so whiny he does not want to be around her. So they bicker back and forth, neither giving an inch.
Useful theories
A. Dr. Gottman’s typology. John Gottman, PhD, categorizes couples into five types: Conflict-Avoiding, Validating, Volatile, Hostile, and Hostile-Detached. The three happy couple types (Conflict-Avoiding, Validating, and Volatile) are very different from one another, and each type has its own benefits and risks. Of the two unhappy couple types, hostile couples stayed unhappily married. He derived this categorization from observations of couples in his lab (https://www.gottman.com).
Conflict-Avoiding: Conflict avoiders minimize persuasion attempts and instead emphasize their areas of common ground. They avoid conflict, avoid expressing what they need from one another, and congratulate their relationship for being generally happy. Conflict-avoiding couples balance independence and interdependence. They have clear boundaries, and are separate people with separate interests. They can be connected and caring in areas of overlap where they are interdependent. While they are minimally emotionally expressive, they maintain a ratio of positive-to-negative affect around 5 to 1. Their interaction is good enough for them.
Validating: The interaction of these couples is characterized by ease and calm. They are somewhat expressive but mostly neutral. They are intermediate between avoiders and the volatile couples. They put a lot of emphasis on supporting and understanding their partner’s point of view, and are often empathetic about their partner’s feelings. They will confront their differences, but only on some topics and not on others. They can become highly competitive on some issues, which can turn into a power struggle, but they usually calm down and compromise. The ratio of positive-to-negative comments is 5 to 1.
Volatile: Volatile couples are intensely emotional. During a conflict discussion, they begin persuasion immediately, and they debate with laughter and humor. They are not disrespectful or insulting. Their positive-to-negative comments ratio is 5 to 1. Anger and feelings of insecurity are expressed, but not contempt. They have no clear boundaries around their individual worlds. While they argue about their roles, they emphasize connection and honesty in their communication.
Hostile: Hostile couples are like validators, except there are high levels of defensiveness on the part of both partners. In Dr. Gottman’s lab, the husband was usually the validator and the wife was the avoider.
Hostile-Detached: These couples are like two armies engaged in a standoff. They snipe at one another during conflict, although the air is one of emotional detachment and resignation. In Dr. Gottman’s lab, usually there was a validator husband with a volatile wife. Escalating conflict will occur between two validators, but then one of them will back down. But the volatile will not let the validator withdraw. Dr. Gottman notes that there is a superiority involved in the woman: that the man needs to be taught the right way to be. The woman does not see the need to change.
B. The approach/avoidance dance
The approach/avoidance dance is based on the motivation of each person (Psychol Sci. 2008 Oct 19;[10]:1030-6). A partner with approach goals focuses on attaining positive outcomes, such as intimacy and growth. A partner with avoidance goals focuses away from negative outcomes, such as conflict and rejection (Educational Psychologist. 1999;34:169-89). For example, in a discussion about child care, a husband who has strong approach goals may be concerned with wanting the discussion to go smoothly and wanting both partners to be happy with the outcome. In contrast, a husband with strong avoidance goals may be more concerned with avoiding conflict about child care and preventing both partners from being unhappy with the outcome. People who are not motivated by approach goals are not particularly interested in pursuing positive experiences in their relationships, such as bonding, intimacy, or fun activities. In contrast, people who are motivated by avoidance goals are interested in avoiding negative experiences, such as conflict, betrayal, or rejection by a romantic partner.
C. Attachment
Both of the previously discussed theories have attachment theory at their core, and are organized around anxiety and avoidance. The anxiety would be tied to concern that the partner may not be available or supportive in times of need, and the avoidance piece would be tied to worry that the partner cannot be fully trusted (Fam Process. 2002 Fall;41[3]:546-50). A low score on both of these indices means a secure attachment style. For unhappy couples with cemented attachments, there is no thought that one would leave. They are bound together in unhappiness (Current Opin Psychol. 2017 Feb;13:60-4).
Nice guy husband/borderline wife relationship or hysterical wife/obsessive-compulsive husband: These relationship can be explained using an attachment framework. This male personality type truly enjoys giving and often finds that he needs nothing more in return than a feeling of being appreciated.
D. Emotionally focused therapy
Sue Johnson, EdD, has an evidence-based couples therapy called emotionally focused couples and family therapy. She would interpret the Suttons as a couple caught in a dance of negativity. The goal of therapy is to help couples let down defenses enough to be vulnerable and then to help them express emotional needs to each other. Dr. Johnson helps each person meet the emotional needs of the other. (See http://drsuejohnson.com/)
E. The game of struggle for power and control
In most relationships, there is a minimizer and a maximizer. The minimizer is more subdued within the relationship, while the maximizer is more evocative. When this turns into a game of “Who has the power,” then minimizing and maximizing turns into submission and dominance. Typically, the minimizer becomes dominant, and the maximizer becomes submissive. One partner can become parentalized and the other infantilized. Most often, the maximizer, being more emotional, tends to become infantilized and submissive for fear of angering or disappointing his or her partner. The minimizer, being more contained, tends to gather the power in the relationship, whether by intention or default, and, in this way, becomes parentalized.
Is this power struggle similar to the developmental challenges faced by toddlers? Being in a growth-supporting relationship means that the relationship helps people develop a more mature interpersonal relationship. It is this notion that supports the theory that people at the same developmental level find each other compatible, as they both face the same challenges in life.
So what happened to the Suttons? The resident referred the patient to the outpatient couples therapist, who treated them for six sessions. The assessment revealed that they had played this dance for decades, but it had intensified after Mr. Sutton retired and was available as a daily target for Ms. Sutton’s unhappiness with the way that life had treated her. The mutual negative impact of their interactions was ameliorated to some extent, by helping the couple develop individual interests. They moved from being hostile-detached to conflict-avoiding. The Suttons moved from waltzing to circle dancing.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.
I supervise the family clinic in the outpatient psychiatry resident-run clinic. The Suttons are a typical couple, encountered by the new resident, whom I will call Dr. Suraj. Initially, Dr. Suraj is enthusiastic in his meeting with the Suttons, but soon enters into a conundrum and brings the case to supervision. The couple has an intricate inexplicable dance, leaving the resident baffled. Let’s review the case. (I have changed several key details to protect the couple’s confidentiality.)
Ms. Sutton presents with complaints of “depression,” and slowly, it becomes clear that her complaints center on her spouse’s deficiencies. “He doesn’t understand me; he doesn’t know what it is like being depressed.”
Other complaints follow; some are practical, such as: “He doesn’t help around the house.” Ms. Sutton’s complaints mostly reflect her perception that either her spouse does not care for her adequately, he has lost interest in her, or he is fundamentally unable to respond adequately to her needs. “He says bad things to me, like ‘Just get over it,’ or ‘Don’t make such a fuss about things.’ ”
After three further sessions of listening to her complaints, and a general lack of response to prior and current medications, Dr. Suraj decides that Mr. Sutton needs to come in. Dr. Suraj follows what he has been taught so far: Get a history from the partner to validate symptoms, functioning, and quality of life. Mostly, the session goes as predicted, ending with Dr. Suraj’s attempt to educate Mr. Sutton about the signs and symptoms of depression. It doesn’t come out right, because the impression that Mr. Sutton gets is that Dr. Suraj is siding with his wife. This seems to make things worse, as Mr. Sutton then complains to his wife that “The doctor doesn’t know what he’s talking about,” “is too young to understand,” or a myriad of other put-downs. Ms. Sutton, of course, tells Dr. Suraj about all of this, following it up with “Don’t worry Doc; you are doing a great job.” Other comments are more in the way of commentary: “I told my husband what you said last week, and he disagrees with you.”
Dr. Suraj realizes that “something is amiss;” the case is stuck, and worse, he is stuck in the middle. The general impression, says Dr. Suraj, “is of a woman who feels victimized, neglected, or overlooked, but somehow, she has the power. She presents as the victim but also is the victimizer. He seems to be the victimizer and tormenter, but all in all, just as much the victim of her torments! I do not know how to think about this couple: They seem stuck, unhappily but inexorably stuck together in perpetuity.” Can anything be done to change this relationship?
Dr. Suraj’s uncensored thoughts: Perhaps they should break up or at least stop complaining. What is it that makes people keep complaining about their relationships? Either they accept it or they leave.
Initial areas of focus
Interpersonal violence. The archetypal extreme is that of an abusive relationship, where the victim is subjected to domestic violence. As I wrote in Advances in Psychiatric Treatment, many relationships where violence is present are bidirectional (2007;13[5]:376-83). Couples may not voice this concern for fear of the spouse being turned over to the police. I usually include a question such as: “How many times do your arguments include pushing or shoving or things like that?”
Asking about income, specifically, who controls the finances and how money is spent, clarifies whether one person feels that he or she has no option but to stay in the relationship.
If intimate partner violence (IPV) exists, there are typical protocols for helping the victim leave. When IPV is not a consideration, the resident wonders about the Suttons, when the victim and abuser change or share roles. Why do they keep up this struggle if they are unhappy?
Life expectations. Many couples do not discuss their expectations or what they imagine will happen when they get married. There may be unspoken fantasies such as “I always assumed that you would retire at 65, and we would go traveling together.” People may change their minds, or life circumstances change so that expectations and fantasies about their life together can no longer be sustained. Are there goals that have changed? Are there dependent relatives that prevent marital goals from being achieved? Is there a lack of agreement about what are important life goals?
Change! One spouse may try to make the other person change, according to his or her preferences. In the psychiatrist’s office, this can take the form of pathologizing: He just wasn’t brought up to talk about feelings, meaning he needs to talk about feelings. We hear questions such as: “Can you take him on in therapy?”; “He doesn’t listen ... can you check him for hearing loss?”; “She doesn’t remember what I said: Can you check her for dementia?” These complaints may come up at the beginning of a relationship or later in life, for example, after retirement when the couple is home together for extended periods of time. Is the expectation that each person should be able to fulfill the partner’s every wish and desire? Be all things? That is a tough order.
The Suttons report that change is the main thing they want from each other. After a full family assessment, it is clear that roles are evenly and acceptably shared; they have no differences in family rules; they both enjoy the same hobbies, care for each other, and work together to solve family crises. However, they cannot accept each other the way they are. When the children were young, she said: “I was too busy to get depressed.” Mr. Sutton states that she now wants him to be attentive to her but he is too tired after a lifetime of work, and anyway, she is so whiny he does not want to be around her. So they bicker back and forth, neither giving an inch.
Useful theories
A. Dr. Gottman’s typology. John Gottman, PhD, categorizes couples into five types: Conflict-Avoiding, Validating, Volatile, Hostile, and Hostile-Detached. The three happy couple types (Conflict-Avoiding, Validating, and Volatile) are very different from one another, and each type has its own benefits and risks. Of the two unhappy couple types, hostile couples stayed unhappily married. He derived this categorization from observations of couples in his lab (https://www.gottman.com).
Conflict-Avoiding: Conflict avoiders minimize persuasion attempts and instead emphasize their areas of common ground. They avoid conflict, avoid expressing what they need from one another, and congratulate their relationship for being generally happy. Conflict-avoiding couples balance independence and interdependence. They have clear boundaries, and are separate people with separate interests. They can be connected and caring in areas of overlap where they are interdependent. While they are minimally emotionally expressive, they maintain a ratio of positive-to-negative affect around 5 to 1. Their interaction is good enough for them.
Validating: The interaction of these couples is characterized by ease and calm. They are somewhat expressive but mostly neutral. They are intermediate between avoiders and the volatile couples. They put a lot of emphasis on supporting and understanding their partner’s point of view, and are often empathetic about their partner’s feelings. They will confront their differences, but only on some topics and not on others. They can become highly competitive on some issues, which can turn into a power struggle, but they usually calm down and compromise. The ratio of positive-to-negative comments is 5 to 1.
Volatile: Volatile couples are intensely emotional. During a conflict discussion, they begin persuasion immediately, and they debate with laughter and humor. They are not disrespectful or insulting. Their positive-to-negative comments ratio is 5 to 1. Anger and feelings of insecurity are expressed, but not contempt. They have no clear boundaries around their individual worlds. While they argue about their roles, they emphasize connection and honesty in their communication.
Hostile: Hostile couples are like validators, except there are high levels of defensiveness on the part of both partners. In Dr. Gottman’s lab, the husband was usually the validator and the wife was the avoider.
Hostile-Detached: These couples are like two armies engaged in a standoff. They snipe at one another during conflict, although the air is one of emotional detachment and resignation. In Dr. Gottman’s lab, usually there was a validator husband with a volatile wife. Escalating conflict will occur between two validators, but then one of them will back down. But the volatile will not let the validator withdraw. Dr. Gottman notes that there is a superiority involved in the woman: that the man needs to be taught the right way to be. The woman does not see the need to change.
B. The approach/avoidance dance
The approach/avoidance dance is based on the motivation of each person (Psychol Sci. 2008 Oct 19;[10]:1030-6). A partner with approach goals focuses on attaining positive outcomes, such as intimacy and growth. A partner with avoidance goals focuses away from negative outcomes, such as conflict and rejection (Educational Psychologist. 1999;34:169-89). For example, in a discussion about child care, a husband who has strong approach goals may be concerned with wanting the discussion to go smoothly and wanting both partners to be happy with the outcome. In contrast, a husband with strong avoidance goals may be more concerned with avoiding conflict about child care and preventing both partners from being unhappy with the outcome. People who are not motivated by approach goals are not particularly interested in pursuing positive experiences in their relationships, such as bonding, intimacy, or fun activities. In contrast, people who are motivated by avoidance goals are interested in avoiding negative experiences, such as conflict, betrayal, or rejection by a romantic partner.
C. Attachment
Both of the previously discussed theories have attachment theory at their core, and are organized around anxiety and avoidance. The anxiety would be tied to concern that the partner may not be available or supportive in times of need, and the avoidance piece would be tied to worry that the partner cannot be fully trusted (Fam Process. 2002 Fall;41[3]:546-50). A low score on both of these indices means a secure attachment style. For unhappy couples with cemented attachments, there is no thought that one would leave. They are bound together in unhappiness (Current Opin Psychol. 2017 Feb;13:60-4).
Nice guy husband/borderline wife relationship or hysterical wife/obsessive-compulsive husband: These relationship can be explained using an attachment framework. This male personality type truly enjoys giving and often finds that he needs nothing more in return than a feeling of being appreciated.
D. Emotionally focused therapy
Sue Johnson, EdD, has an evidence-based couples therapy called emotionally focused couples and family therapy. She would interpret the Suttons as a couple caught in a dance of negativity. The goal of therapy is to help couples let down defenses enough to be vulnerable and then to help them express emotional needs to each other. Dr. Johnson helps each person meet the emotional needs of the other. (See http://drsuejohnson.com/)
E. The game of struggle for power and control
In most relationships, there is a minimizer and a maximizer. The minimizer is more subdued within the relationship, while the maximizer is more evocative. When this turns into a game of “Who has the power,” then minimizing and maximizing turns into submission and dominance. Typically, the minimizer becomes dominant, and the maximizer becomes submissive. One partner can become parentalized and the other infantilized. Most often, the maximizer, being more emotional, tends to become infantilized and submissive for fear of angering or disappointing his or her partner. The minimizer, being more contained, tends to gather the power in the relationship, whether by intention or default, and, in this way, becomes parentalized.
Is this power struggle similar to the developmental challenges faced by toddlers? Being in a growth-supporting relationship means that the relationship helps people develop a more mature interpersonal relationship. It is this notion that supports the theory that people at the same developmental level find each other compatible, as they both face the same challenges in life.
So what happened to the Suttons? The resident referred the patient to the outpatient couples therapist, who treated them for six sessions. The assessment revealed that they had played this dance for decades, but it had intensified after Mr. Sutton retired and was available as a daily target for Ms. Sutton’s unhappiness with the way that life had treated her. The mutual negative impact of their interactions was ameliorated to some extent, by helping the couple develop individual interests. They moved from being hostile-detached to conflict-avoiding. The Suttons moved from waltzing to circle dancing.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.











