User login
Doctors of Virtue and Vice: The Best and Worst of Federal Practice in 2023
Regular readers of Federal Practitioner may recall that I have had a tradition of dedicating the last column of the year to an ethics rendition of the popular trope of the annual best and worst. This year we will examine the stories of 2 military physicians through the lens of virtue ethics. Aristotle (384-322
Virtue ethics is among the oldest of ethical theories, and Aristotle articulates this school of thought in his work Nicomachean Ethics.2 It is a good fit for Federal Practitioner as it has been constructively applied to the moral development of both military3 and medical professionals.4
Here is a Reader’s Digest version of virtue theory with apologizes to all the real philosophers out there. There are different ways to categorize ethical theories. One approach is to distinguish them based on the aspects of primary interest. Consequentialist ethics theories are concerned with the outcomes of actions. Deontologic theories emphasize the intention of the moral agent. In contrast, virtue ethics theories focus on the character of a person. The virtuous individual is one who has practiced the habits of moral excellence and embodies the good life. They are honored as heroes and revered as saints; they are the exemplars we imitate in our aspirations.3
The epigraph sums up one of Aristotle’s central philosophical doctrines: the close relationship of ethics and politics.1 Personal virtue is intelligible only in the context of community and aim, and the goal of virtue is to contribute to human happiness.5 War, whether in ancient Greece or modern Europe, is among the forces most inimical to human flourishing. The current war in Ukraine that has united much of the Western world in opposition to tyranny has divided the 2 physicians in our story along the normative lines of virtue ethics.
The doctor of virtue: Michael Siclari, MD. A 71-year-old US Department of Veterans Affairs physician, Siclari had previously served in the military as a National Guard physician during Operation Enduring Freedom (2001-2014) in Afghanistan. He decided to serve again in Ukraine. Siclari expressed his reasons for going to Ukraine in the language of what Aristotle thought was among the highest virtues: justice. “In retrospect, as I think about why I wanted to go to Ukraine, I think it’s more of a sense that I thought an injustice was happening.”7
Echoing the great Rabbi Hillel, Siclari saw the Russian invasion of Ukraine as a personal call to use his experience and training as a trauma and emergency medicine physician to help the Ukrainian people. “If not me, then who?” Siclari demonstrated another virtue: generosity in taking 10 days of personal leave in August 2022 to make the trip to Ukraine, hoping to work in a combat zone tending to wounded soldiers as he had in Afghanistan. When due to logistics he instead was assigned to care for refugees and assist with evacuations from the battlefield, he humbly and compassionately cared for those in his charge. Even now, back home, he speaks to audiences of health care professionals encouraging them to consider similar acts of altruism.5
Virtue for Aristotle is technically defined as the mean between 2 extremes of disposition or temperament. The virtue of courage is found in the moral middle ground between the deficiency of bravery that is cowardice and the vice of excess of reckless abandon. The former person fears too much and the latter too little and both thus exhibit vicious behavior.
The doctor of vice: James Lee Henry. Henry is a major and internal medicine physician in the United States Army stationed at Fort Bragg, headquarters of the US Army Special Operations Command. Along with his wife Anna Gabrielian, a civilian anesthesiologist, he was charged in September with conspiring to divulge the protected health information of American military and government employees to the Russian government.8 According to the Grand Jury indictment, Henry delivered into the hands of an undercover Federal Bureau of Investigation (FBI) agent, the medical records of a US Army officer, Department of Defense employee, and the spouses of 3 Army veterans, 2 of whom were deceased.9 In a gross twisting of virtue language, Gabrielian explained her motivation for the couple’s espionage in terms of sacrifice and loyalty. In an antipode of Siclari’s service, Henry purportedly wanted to join the Russian army but did not have the requisite combat experience. For his part, Henry’s abysmal defense of his betrayal of his country and his oath speaks for itself, if the United States were to declare war on Russia, Henry told the FBI agent, “at that point, I’ll have some ethical issues I have to work through.”8
We become virtuous people through imitating the example of those who have perfected the habits of moral excellence. During 2022, 2 federal practitioners responded to the challenge of war: one displayed the zenith of virtue, the other exhibited the nadir of vice. Seldom does a single year present us with such clear choices of who and how we want to be in 2023. American culture has so trivialized New Year’s resolutions that they are no longer substantive enough for the weight of the profound question of what constitutes the good life. Rather let us make a commitment in keeping with such morally serious matters. All of us live as mixed creatures, drawn to virtue and prone to vice. May we all strive this coming year to help each other meet the high bar another great man of virtue Abraham Lincoln set in his first inaugural address, to be the “better angels of our natures.”10
1. Aristotle. Politics. Book I, 1253.a31.
2. The Ethics of Aristotle. Aristotle. The Nicomachean Ethics. Thompson JAK, trans. Penguin Books; 1953.
3. Schonfeld TL, Hester DM. Brief introduction to ethics and ethical theory. In: Schonfeld TL, Hester DM, eds. Guidance for Healthcare Ethics Committees. 2nd ed. Cambridge University Press; 2022:11-19.
4. Olsthoorn P. Military Ethics and Virtues: An Interdisciplinary Approach for the 21st Century. Routledge; 2010.
5. Pellegrino ED, Thomasma DC. The Virtues in Medical Practice. Oxford University Press; 1993.
6. Edward Clayton. Aristotle Politics. In: Internet Encyclopedia of Philosophy. Accessed November 28, 2022. https://iep.utm.edu/aristotle-politics
7. Tippets R. A VA doctor’s calling to help in Ukraine. VA News. October 23, 2022. Accessed November 28, 2022. https://news.va.gov/109957/a-va-doctors-calling-to-help-in-ukraine
8. Lybrand H. US Army doctor and anesthesiologist charged with conspiring to US military records to the Russian government. CNN Politics, September 29, 2022. Accessed November 28, 2022 https://www.cnn.com/2022/09/29/politics/us-army-doctor-anesthesiologist-russian-government-medical-records
9. United States v Anna Gabrielian and James Lee Henry, (SD Md 2022). Accessed November 28, 2022. https://www.documentcloud.org/documents/23106067-gabrielian-and-henry-indictment
10. Lincoln A. First Inaugural Address of Abraham Lincoln. Accessed November 28, 2022. https://avalon.law.yale.edu/19th_century/lincoln1.asp
Regular readers of Federal Practitioner may recall that I have had a tradition of dedicating the last column of the year to an ethics rendition of the popular trope of the annual best and worst. This year we will examine the stories of 2 military physicians through the lens of virtue ethics. Aristotle (384-322
Virtue ethics is among the oldest of ethical theories, and Aristotle articulates this school of thought in his work Nicomachean Ethics.2 It is a good fit for Federal Practitioner as it has been constructively applied to the moral development of both military3 and medical professionals.4
Here is a Reader’s Digest version of virtue theory with apologizes to all the real philosophers out there. There are different ways to categorize ethical theories. One approach is to distinguish them based on the aspects of primary interest. Consequentialist ethics theories are concerned with the outcomes of actions. Deontologic theories emphasize the intention of the moral agent. In contrast, virtue ethics theories focus on the character of a person. The virtuous individual is one who has practiced the habits of moral excellence and embodies the good life. They are honored as heroes and revered as saints; they are the exemplars we imitate in our aspirations.3
The epigraph sums up one of Aristotle’s central philosophical doctrines: the close relationship of ethics and politics.1 Personal virtue is intelligible only in the context of community and aim, and the goal of virtue is to contribute to human happiness.5 War, whether in ancient Greece or modern Europe, is among the forces most inimical to human flourishing. The current war in Ukraine that has united much of the Western world in opposition to tyranny has divided the 2 physicians in our story along the normative lines of virtue ethics.
The doctor of virtue: Michael Siclari, MD. A 71-year-old US Department of Veterans Affairs physician, Siclari had previously served in the military as a National Guard physician during Operation Enduring Freedom (2001-2014) in Afghanistan. He decided to serve again in Ukraine. Siclari expressed his reasons for going to Ukraine in the language of what Aristotle thought was among the highest virtues: justice. “In retrospect, as I think about why I wanted to go to Ukraine, I think it’s more of a sense that I thought an injustice was happening.”7
Echoing the great Rabbi Hillel, Siclari saw the Russian invasion of Ukraine as a personal call to use his experience and training as a trauma and emergency medicine physician to help the Ukrainian people. “If not me, then who?” Siclari demonstrated another virtue: generosity in taking 10 days of personal leave in August 2022 to make the trip to Ukraine, hoping to work in a combat zone tending to wounded soldiers as he had in Afghanistan. When due to logistics he instead was assigned to care for refugees and assist with evacuations from the battlefield, he humbly and compassionately cared for those in his charge. Even now, back home, he speaks to audiences of health care professionals encouraging them to consider similar acts of altruism.5
Virtue for Aristotle is technically defined as the mean between 2 extremes of disposition or temperament. The virtue of courage is found in the moral middle ground between the deficiency of bravery that is cowardice and the vice of excess of reckless abandon. The former person fears too much and the latter too little and both thus exhibit vicious behavior.
The doctor of vice: James Lee Henry. Henry is a major and internal medicine physician in the United States Army stationed at Fort Bragg, headquarters of the US Army Special Operations Command. Along with his wife Anna Gabrielian, a civilian anesthesiologist, he was charged in September with conspiring to divulge the protected health information of American military and government employees to the Russian government.8 According to the Grand Jury indictment, Henry delivered into the hands of an undercover Federal Bureau of Investigation (FBI) agent, the medical records of a US Army officer, Department of Defense employee, and the spouses of 3 Army veterans, 2 of whom were deceased.9 In a gross twisting of virtue language, Gabrielian explained her motivation for the couple’s espionage in terms of sacrifice and loyalty. In an antipode of Siclari’s service, Henry purportedly wanted to join the Russian army but did not have the requisite combat experience. For his part, Henry’s abysmal defense of his betrayal of his country and his oath speaks for itself, if the United States were to declare war on Russia, Henry told the FBI agent, “at that point, I’ll have some ethical issues I have to work through.”8
We become virtuous people through imitating the example of those who have perfected the habits of moral excellence. During 2022, 2 federal practitioners responded to the challenge of war: one displayed the zenith of virtue, the other exhibited the nadir of vice. Seldom does a single year present us with such clear choices of who and how we want to be in 2023. American culture has so trivialized New Year’s resolutions that they are no longer substantive enough for the weight of the profound question of what constitutes the good life. Rather let us make a commitment in keeping with such morally serious matters. All of us live as mixed creatures, drawn to virtue and prone to vice. May we all strive this coming year to help each other meet the high bar another great man of virtue Abraham Lincoln set in his first inaugural address, to be the “better angels of our natures.”10
Regular readers of Federal Practitioner may recall that I have had a tradition of dedicating the last column of the year to an ethics rendition of the popular trope of the annual best and worst. This year we will examine the stories of 2 military physicians through the lens of virtue ethics. Aristotle (384-322
Virtue ethics is among the oldest of ethical theories, and Aristotle articulates this school of thought in his work Nicomachean Ethics.2 It is a good fit for Federal Practitioner as it has been constructively applied to the moral development of both military3 and medical professionals.4
Here is a Reader’s Digest version of virtue theory with apologizes to all the real philosophers out there. There are different ways to categorize ethical theories. One approach is to distinguish them based on the aspects of primary interest. Consequentialist ethics theories are concerned with the outcomes of actions. Deontologic theories emphasize the intention of the moral agent. In contrast, virtue ethics theories focus on the character of a person. The virtuous individual is one who has practiced the habits of moral excellence and embodies the good life. They are honored as heroes and revered as saints; they are the exemplars we imitate in our aspirations.3
The epigraph sums up one of Aristotle’s central philosophical doctrines: the close relationship of ethics and politics.1 Personal virtue is intelligible only in the context of community and aim, and the goal of virtue is to contribute to human happiness.5 War, whether in ancient Greece or modern Europe, is among the forces most inimical to human flourishing. The current war in Ukraine that has united much of the Western world in opposition to tyranny has divided the 2 physicians in our story along the normative lines of virtue ethics.
The doctor of virtue: Michael Siclari, MD. A 71-year-old US Department of Veterans Affairs physician, Siclari had previously served in the military as a National Guard physician during Operation Enduring Freedom (2001-2014) in Afghanistan. He decided to serve again in Ukraine. Siclari expressed his reasons for going to Ukraine in the language of what Aristotle thought was among the highest virtues: justice. “In retrospect, as I think about why I wanted to go to Ukraine, I think it’s more of a sense that I thought an injustice was happening.”7
Echoing the great Rabbi Hillel, Siclari saw the Russian invasion of Ukraine as a personal call to use his experience and training as a trauma and emergency medicine physician to help the Ukrainian people. “If not me, then who?” Siclari demonstrated another virtue: generosity in taking 10 days of personal leave in August 2022 to make the trip to Ukraine, hoping to work in a combat zone tending to wounded soldiers as he had in Afghanistan. When due to logistics he instead was assigned to care for refugees and assist with evacuations from the battlefield, he humbly and compassionately cared for those in his charge. Even now, back home, he speaks to audiences of health care professionals encouraging them to consider similar acts of altruism.5
Virtue for Aristotle is technically defined as the mean between 2 extremes of disposition or temperament. The virtue of courage is found in the moral middle ground between the deficiency of bravery that is cowardice and the vice of excess of reckless abandon. The former person fears too much and the latter too little and both thus exhibit vicious behavior.
The doctor of vice: James Lee Henry. Henry is a major and internal medicine physician in the United States Army stationed at Fort Bragg, headquarters of the US Army Special Operations Command. Along with his wife Anna Gabrielian, a civilian anesthesiologist, he was charged in September with conspiring to divulge the protected health information of American military and government employees to the Russian government.8 According to the Grand Jury indictment, Henry delivered into the hands of an undercover Federal Bureau of Investigation (FBI) agent, the medical records of a US Army officer, Department of Defense employee, and the spouses of 3 Army veterans, 2 of whom were deceased.9 In a gross twisting of virtue language, Gabrielian explained her motivation for the couple’s espionage in terms of sacrifice and loyalty. In an antipode of Siclari’s service, Henry purportedly wanted to join the Russian army but did not have the requisite combat experience. For his part, Henry’s abysmal defense of his betrayal of his country and his oath speaks for itself, if the United States were to declare war on Russia, Henry told the FBI agent, “at that point, I’ll have some ethical issues I have to work through.”8
We become virtuous people through imitating the example of those who have perfected the habits of moral excellence. During 2022, 2 federal practitioners responded to the challenge of war: one displayed the zenith of virtue, the other exhibited the nadir of vice. Seldom does a single year present us with such clear choices of who and how we want to be in 2023. American culture has so trivialized New Year’s resolutions that they are no longer substantive enough for the weight of the profound question of what constitutes the good life. Rather let us make a commitment in keeping with such morally serious matters. All of us live as mixed creatures, drawn to virtue and prone to vice. May we all strive this coming year to help each other meet the high bar another great man of virtue Abraham Lincoln set in his first inaugural address, to be the “better angels of our natures.”10
1. Aristotle. Politics. Book I, 1253.a31.
2. The Ethics of Aristotle. Aristotle. The Nicomachean Ethics. Thompson JAK, trans. Penguin Books; 1953.
3. Schonfeld TL, Hester DM. Brief introduction to ethics and ethical theory. In: Schonfeld TL, Hester DM, eds. Guidance for Healthcare Ethics Committees. 2nd ed. Cambridge University Press; 2022:11-19.
4. Olsthoorn P. Military Ethics and Virtues: An Interdisciplinary Approach for the 21st Century. Routledge; 2010.
5. Pellegrino ED, Thomasma DC. The Virtues in Medical Practice. Oxford University Press; 1993.
6. Edward Clayton. Aristotle Politics. In: Internet Encyclopedia of Philosophy. Accessed November 28, 2022. https://iep.utm.edu/aristotle-politics
7. Tippets R. A VA doctor’s calling to help in Ukraine. VA News. October 23, 2022. Accessed November 28, 2022. https://news.va.gov/109957/a-va-doctors-calling-to-help-in-ukraine
8. Lybrand H. US Army doctor and anesthesiologist charged with conspiring to US military records to the Russian government. CNN Politics, September 29, 2022. Accessed November 28, 2022 https://www.cnn.com/2022/09/29/politics/us-army-doctor-anesthesiologist-russian-government-medical-records
9. United States v Anna Gabrielian and James Lee Henry, (SD Md 2022). Accessed November 28, 2022. https://www.documentcloud.org/documents/23106067-gabrielian-and-henry-indictment
10. Lincoln A. First Inaugural Address of Abraham Lincoln. Accessed November 28, 2022. https://avalon.law.yale.edu/19th_century/lincoln1.asp
1. Aristotle. Politics. Book I, 1253.a31.
2. The Ethics of Aristotle. Aristotle. The Nicomachean Ethics. Thompson JAK, trans. Penguin Books; 1953.
3. Schonfeld TL, Hester DM. Brief introduction to ethics and ethical theory. In: Schonfeld TL, Hester DM, eds. Guidance for Healthcare Ethics Committees. 2nd ed. Cambridge University Press; 2022:11-19.
4. Olsthoorn P. Military Ethics and Virtues: An Interdisciplinary Approach for the 21st Century. Routledge; 2010.
5. Pellegrino ED, Thomasma DC. The Virtues in Medical Practice. Oxford University Press; 1993.
6. Edward Clayton. Aristotle Politics. In: Internet Encyclopedia of Philosophy. Accessed November 28, 2022. https://iep.utm.edu/aristotle-politics
7. Tippets R. A VA doctor’s calling to help in Ukraine. VA News. October 23, 2022. Accessed November 28, 2022. https://news.va.gov/109957/a-va-doctors-calling-to-help-in-ukraine
8. Lybrand H. US Army doctor and anesthesiologist charged with conspiring to US military records to the Russian government. CNN Politics, September 29, 2022. Accessed November 28, 2022 https://www.cnn.com/2022/09/29/politics/us-army-doctor-anesthesiologist-russian-government-medical-records
9. United States v Anna Gabrielian and James Lee Henry, (SD Md 2022). Accessed November 28, 2022. https://www.documentcloud.org/documents/23106067-gabrielian-and-henry-indictment
10. Lincoln A. First Inaugural Address of Abraham Lincoln. Accessed November 28, 2022. https://avalon.law.yale.edu/19th_century/lincoln1.asp
The Long Arc of Justice for Veteran Benefits
This Veterans Day we honor the passing of the largest expansion of veterans benefits and services in history. On August 10, 2022, President Biden signed the Sergeant First Class Heath Robinson Honoring our Promise to Address Comprehensive Toxics (PACT) Act. This act was named for a combat medic who died of a rare form of lung cancer believed to be the result of a toxic military exposure. His widow was present during the President's State of the Union address that urged Congress to pass the legislation.2
Like all other congressional bills and government regulations, the PACT Act is complex in its details and still a work in progress. Simply put, the PACT Act expands and/or extends enrollment for a group of previously ineligible veterans. Eligibility will no longer require that veterans demonstrate a service-connected disability due to toxic exposure, including those from burn pits. This has long been a barrier for many veterans seeking benefits and not just related to toxic exposures. Logistical barriers and documentary losses have prevented many service members from establishing a clean chain of evidence for the injuries or illnesses they sustained while in uniform.
The new process is a massive step forward by the US Department of Veterans Affairs (VA) to establish high standards of procedural justice for settling beneficiary claims. The PACT Act removes the burden from the shoulders of the veteran and places it squarely on the VA to demonstrate that > 20 different medical conditions--primarily cancers and respiratory illnesses--are linked to toxic exposure. The VA must establish that exposure occurred to cohorts of service members in specific theaters and time frames. A veteran who served in that area and period and has one of the indexed illnesses is presumed to have been exposed in the line of duty.3,4
As a result, the VA instituted a new screening process to determine that toxic military exposures (a) led to illness; and (b) both exposure and illness are connected to service. According to the VA, the new process is evidence based, transparent, and allows the VA to fast-track policy decisions related to exposures. The PACT Act includes a provision intended to promote sustained implementation and prevent the program from succumbing as so many new initiatives have to inadequate adoption. VA is required to deploy its considerable internal research capacity to collaborate with external partners in and outside government to study military members with toxic exposures.4
Congress had initially proposed that the provisions of the PACT ACT would take effect in 2026, providing time to ramp up the process. The White House and VA telescoped that time line so veterans can begin now to apply for benefits that they could foreseeably receive in 2023. However, a long-standing problem for the VA has been unfunded agency or congressional mandates. These have often end in undermining the legislative intention or policy purpose of the program undermining their legislative intention or policy purpose through staffing shortages, leading to lack of or delayed access. The PACT Act promises to eschew the infamous Phoenix problem by providing increased personnel, training infrastructure, and technology resources for both the Veterans Benefit Administration and the Veterans Health Administration. Ironically, many seasoned VA observers expect the PACT expansion will lead to even larger backlogs of claims as hundreds of newly eligible veterans are added to the extant rolls of those seeking benefits.5
An estimated 1 in 5 veterans may be entitled to PACT benefits. The PACT Act is the latest of a long uneven movement toward distributive justice for veteran benefits and services. It is fitting in the month of Veterans Day 2022 to trace that trajectory. Congress first passed veteran benefits legislation in 1917, focused on soldiers with disabilities. This resulted in a massive investment in building hospitals. Ironically, part of the impetus for VA health care was an earlier toxic military exposure. World War I service members suffered from the detrimental effects of mustard gas among other chemical byproducts. In 1924, VA benefits and services underwent a momentous opening to include individuals with non-service-connected disabilities. Four years later, the VA tent became even bigger, welcoming women, National Guard, and militia members to receive care under its auspices.6
The PACT Act is a fitting memorial for Veterans Day as an increasingly divided country presents a unified response to veterans and their survivors exposed to a variety of toxins across multiple wars. The PACT Act was hard won with veterans and their advocates having to fight years of political bickering, government abdication of accountability, and scientific sparring before this bipartisan legislation passed.7 It covers Vietnam War veterans with several conditions due to Agent Orange exposure; Gulf War and post-9/11 veterans with cancer and respiratory conditions; and the service members deployed to Afghanistan and Iraq afflicted with illnesses due to the smoke of burn pits and other toxins.
As many areas of the country roll back LGBTQ+ rights to health care and social services, the VA has emerged as a leader in the movement for diversity and inclusion. VA Secretary McDonough provided a pathway to VA eligibility for other than honorably discharged veterans, including those LGBTQ+ persons discharged under Don't Ask, Don't Tell.8 Lest we take this new inclusivity for granted, we should never forget that this journey toward equity for the military and VA has been long, slow, and uneven. There are many difficult miles yet to travel if we are to achieve liberty and justice for veteran members of racial minorities, women, and other marginalized populations. Even the PACT Act does not cover all putative exposures to toxins.9 Yet it is a significant step closer to fulfilling the motto of the VA LGBTQ+ program: to serve all who served.10
- Parker T. Of justice and the conscience. In: Ten Sermons of Religion. Crosby, Nichols and Company; 1853:66-85.
- The White House. Fact sheet: President Biden signs the PACT Act and delivers on his promise to America's veterans. August 9, 2022. Accessed October 24, 2022. https://www.whitehouse.gov/briefing-room/statements-releases/2022/08/10/fact-sheet-president-biden-signs-the-pact-act-and-delivers-on-his-promise-to-americas-veterans
- Shane L. Vets can apply for all PACT benefits now after VA speeds up law. Military Times. September 1, 2022. Accessed October 24, 2022. https://www.militarytimes.com/news/burn-pits/2022/09/01/vets-can-apply-for-all-pact-act-benefits-now-after-va-speeds-up-law
- US Department of Veterans Affairs. The PACT Act and your VA benefits. Updated September 28, 2022. Accessed October 24, 2022. https://www.va.gov/resources/the-pact-act-and-your-va-benefits
- Wentling N. Discharged LGBTQ+ veterans now eligible for benefits under new guidance issued by VA. Stars & Stripes. September 20, 2021. Accessed October 24, 2022. https://www.stripes.com/veterans/2021-09-20/veterans-affairs-dont-ask-dont-tell-benefits-lgbt-discharges-2956761.html
- US Department of Veterans Affairs, VA History Office. History--Department of Veterans Affairs (VA). Updated May 27, 2021. Accessed October 24, 2022. https://www.va.gov/HISTORY/VA_History/Overview.asp
- Atkins D, Kilbourne A, Lipson L. Health equity research in the Veterans Health Administration: we've come far but aren't there yet. Am J Public Health. 2014;104(suppl 4):S525-S526. doi:10.2105/AJPH.2014.302216
- Stack MK. The soldiers came home sick. The government denied it was responsible. New York Times. Updated January 16, 2022. Accessed October 24, 2022. https://www.nytimes.com/2022/01/11/magazine/military-burn-pits.html
- Namaz A, Sagalyn D. VA secretary discusses health care overhaul helping veterans exposed to toxic burn pits. PBS NewsHour. September 1, 2022. Accessed October 24, 2022. https://www.pbs.org/newshour/show/va-secretary-discusses-health-care-overhaul-helping-veterans-exposed-to-toxic-burn-pits
- US Department of Veterans Affairs, Patient Care Services. VHA LGBTQ+ health program. Updated September 13, 2022. Accessed October 31, 2022. https://www.patientcare.va.gov/lgbt
This Veterans Day we honor the passing of the largest expansion of veterans benefits and services in history. On August 10, 2022, President Biden signed the Sergeant First Class Heath Robinson Honoring our Promise to Address Comprehensive Toxics (PACT) Act. This act was named for a combat medic who died of a rare form of lung cancer believed to be the result of a toxic military exposure. His widow was present during the President's State of the Union address that urged Congress to pass the legislation.2
Like all other congressional bills and government regulations, the PACT Act is complex in its details and still a work in progress. Simply put, the PACT Act expands and/or extends enrollment for a group of previously ineligible veterans. Eligibility will no longer require that veterans demonstrate a service-connected disability due to toxic exposure, including those from burn pits. This has long been a barrier for many veterans seeking benefits and not just related to toxic exposures. Logistical barriers and documentary losses have prevented many service members from establishing a clean chain of evidence for the injuries or illnesses they sustained while in uniform.
The new process is a massive step forward by the US Department of Veterans Affairs (VA) to establish high standards of procedural justice for settling beneficiary claims. The PACT Act removes the burden from the shoulders of the veteran and places it squarely on the VA to demonstrate that > 20 different medical conditions--primarily cancers and respiratory illnesses--are linked to toxic exposure. The VA must establish that exposure occurred to cohorts of service members in specific theaters and time frames. A veteran who served in that area and period and has one of the indexed illnesses is presumed to have been exposed in the line of duty.3,4
As a result, the VA instituted a new screening process to determine that toxic military exposures (a) led to illness; and (b) both exposure and illness are connected to service. According to the VA, the new process is evidence based, transparent, and allows the VA to fast-track policy decisions related to exposures. The PACT Act includes a provision intended to promote sustained implementation and prevent the program from succumbing as so many new initiatives have to inadequate adoption. VA is required to deploy its considerable internal research capacity to collaborate with external partners in and outside government to study military members with toxic exposures.4
Congress had initially proposed that the provisions of the PACT ACT would take effect in 2026, providing time to ramp up the process. The White House and VA telescoped that time line so veterans can begin now to apply for benefits that they could foreseeably receive in 2023. However, a long-standing problem for the VA has been unfunded agency or congressional mandates. These have often end in undermining the legislative intention or policy purpose of the program undermining their legislative intention or policy purpose through staffing shortages, leading to lack of or delayed access. The PACT Act promises to eschew the infamous Phoenix problem by providing increased personnel, training infrastructure, and technology resources for both the Veterans Benefit Administration and the Veterans Health Administration. Ironically, many seasoned VA observers expect the PACT expansion will lead to even larger backlogs of claims as hundreds of newly eligible veterans are added to the extant rolls of those seeking benefits.5
An estimated 1 in 5 veterans may be entitled to PACT benefits. The PACT Act is the latest of a long uneven movement toward distributive justice for veteran benefits and services. It is fitting in the month of Veterans Day 2022 to trace that trajectory. Congress first passed veteran benefits legislation in 1917, focused on soldiers with disabilities. This resulted in a massive investment in building hospitals. Ironically, part of the impetus for VA health care was an earlier toxic military exposure. World War I service members suffered from the detrimental effects of mustard gas among other chemical byproducts. In 1924, VA benefits and services underwent a momentous opening to include individuals with non-service-connected disabilities. Four years later, the VA tent became even bigger, welcoming women, National Guard, and militia members to receive care under its auspices.6
The PACT Act is a fitting memorial for Veterans Day as an increasingly divided country presents a unified response to veterans and their survivors exposed to a variety of toxins across multiple wars. The PACT Act was hard won with veterans and their advocates having to fight years of political bickering, government abdication of accountability, and scientific sparring before this bipartisan legislation passed.7 It covers Vietnam War veterans with several conditions due to Agent Orange exposure; Gulf War and post-9/11 veterans with cancer and respiratory conditions; and the service members deployed to Afghanistan and Iraq afflicted with illnesses due to the smoke of burn pits and other toxins.
As many areas of the country roll back LGBTQ+ rights to health care and social services, the VA has emerged as a leader in the movement for diversity and inclusion. VA Secretary McDonough provided a pathway to VA eligibility for other than honorably discharged veterans, including those LGBTQ+ persons discharged under Don't Ask, Don't Tell.8 Lest we take this new inclusivity for granted, we should never forget that this journey toward equity for the military and VA has been long, slow, and uneven. There are many difficult miles yet to travel if we are to achieve liberty and justice for veteran members of racial minorities, women, and other marginalized populations. Even the PACT Act does not cover all putative exposures to toxins.9 Yet it is a significant step closer to fulfilling the motto of the VA LGBTQ+ program: to serve all who served.10
This Veterans Day we honor the passing of the largest expansion of veterans benefits and services in history. On August 10, 2022, President Biden signed the Sergeant First Class Heath Robinson Honoring our Promise to Address Comprehensive Toxics (PACT) Act. This act was named for a combat medic who died of a rare form of lung cancer believed to be the result of a toxic military exposure. His widow was present during the President's State of the Union address that urged Congress to pass the legislation.2
Like all other congressional bills and government regulations, the PACT Act is complex in its details and still a work in progress. Simply put, the PACT Act expands and/or extends enrollment for a group of previously ineligible veterans. Eligibility will no longer require that veterans demonstrate a service-connected disability due to toxic exposure, including those from burn pits. This has long been a barrier for many veterans seeking benefits and not just related to toxic exposures. Logistical barriers and documentary losses have prevented many service members from establishing a clean chain of evidence for the injuries or illnesses they sustained while in uniform.
The new process is a massive step forward by the US Department of Veterans Affairs (VA) to establish high standards of procedural justice for settling beneficiary claims. The PACT Act removes the burden from the shoulders of the veteran and places it squarely on the VA to demonstrate that > 20 different medical conditions--primarily cancers and respiratory illnesses--are linked to toxic exposure. The VA must establish that exposure occurred to cohorts of service members in specific theaters and time frames. A veteran who served in that area and period and has one of the indexed illnesses is presumed to have been exposed in the line of duty.3,4
As a result, the VA instituted a new screening process to determine that toxic military exposures (a) led to illness; and (b) both exposure and illness are connected to service. According to the VA, the new process is evidence based, transparent, and allows the VA to fast-track policy decisions related to exposures. The PACT Act includes a provision intended to promote sustained implementation and prevent the program from succumbing as so many new initiatives have to inadequate adoption. VA is required to deploy its considerable internal research capacity to collaborate with external partners in and outside government to study military members with toxic exposures.4
Congress had initially proposed that the provisions of the PACT ACT would take effect in 2026, providing time to ramp up the process. The White House and VA telescoped that time line so veterans can begin now to apply for benefits that they could foreseeably receive in 2023. However, a long-standing problem for the VA has been unfunded agency or congressional mandates. These have often end in undermining the legislative intention or policy purpose of the program undermining their legislative intention or policy purpose through staffing shortages, leading to lack of or delayed access. The PACT Act promises to eschew the infamous Phoenix problem by providing increased personnel, training infrastructure, and technology resources for both the Veterans Benefit Administration and the Veterans Health Administration. Ironically, many seasoned VA observers expect the PACT expansion will lead to even larger backlogs of claims as hundreds of newly eligible veterans are added to the extant rolls of those seeking benefits.5
An estimated 1 in 5 veterans may be entitled to PACT benefits. The PACT Act is the latest of a long uneven movement toward distributive justice for veteran benefits and services. It is fitting in the month of Veterans Day 2022 to trace that trajectory. Congress first passed veteran benefits legislation in 1917, focused on soldiers with disabilities. This resulted in a massive investment in building hospitals. Ironically, part of the impetus for VA health care was an earlier toxic military exposure. World War I service members suffered from the detrimental effects of mustard gas among other chemical byproducts. In 1924, VA benefits and services underwent a momentous opening to include individuals with non-service-connected disabilities. Four years later, the VA tent became even bigger, welcoming women, National Guard, and militia members to receive care under its auspices.6
The PACT Act is a fitting memorial for Veterans Day as an increasingly divided country presents a unified response to veterans and their survivors exposed to a variety of toxins across multiple wars. The PACT Act was hard won with veterans and their advocates having to fight years of political bickering, government abdication of accountability, and scientific sparring before this bipartisan legislation passed.7 It covers Vietnam War veterans with several conditions due to Agent Orange exposure; Gulf War and post-9/11 veterans with cancer and respiratory conditions; and the service members deployed to Afghanistan and Iraq afflicted with illnesses due to the smoke of burn pits and other toxins.
As many areas of the country roll back LGBTQ+ rights to health care and social services, the VA has emerged as a leader in the movement for diversity and inclusion. VA Secretary McDonough provided a pathway to VA eligibility for other than honorably discharged veterans, including those LGBTQ+ persons discharged under Don't Ask, Don't Tell.8 Lest we take this new inclusivity for granted, we should never forget that this journey toward equity for the military and VA has been long, slow, and uneven. There are many difficult miles yet to travel if we are to achieve liberty and justice for veteran members of racial minorities, women, and other marginalized populations. Even the PACT Act does not cover all putative exposures to toxins.9 Yet it is a significant step closer to fulfilling the motto of the VA LGBTQ+ program: to serve all who served.10
- Parker T. Of justice and the conscience. In: Ten Sermons of Religion. Crosby, Nichols and Company; 1853:66-85.
- The White House. Fact sheet: President Biden signs the PACT Act and delivers on his promise to America's veterans. August 9, 2022. Accessed October 24, 2022. https://www.whitehouse.gov/briefing-room/statements-releases/2022/08/10/fact-sheet-president-biden-signs-the-pact-act-and-delivers-on-his-promise-to-americas-veterans
- Shane L. Vets can apply for all PACT benefits now after VA speeds up law. Military Times. September 1, 2022. Accessed October 24, 2022. https://www.militarytimes.com/news/burn-pits/2022/09/01/vets-can-apply-for-all-pact-act-benefits-now-after-va-speeds-up-law
- US Department of Veterans Affairs. The PACT Act and your VA benefits. Updated September 28, 2022. Accessed October 24, 2022. https://www.va.gov/resources/the-pact-act-and-your-va-benefits
- Wentling N. Discharged LGBTQ+ veterans now eligible for benefits under new guidance issued by VA. Stars & Stripes. September 20, 2021. Accessed October 24, 2022. https://www.stripes.com/veterans/2021-09-20/veterans-affairs-dont-ask-dont-tell-benefits-lgbt-discharges-2956761.html
- US Department of Veterans Affairs, VA History Office. History--Department of Veterans Affairs (VA). Updated May 27, 2021. Accessed October 24, 2022. https://www.va.gov/HISTORY/VA_History/Overview.asp
- Atkins D, Kilbourne A, Lipson L. Health equity research in the Veterans Health Administration: we've come far but aren't there yet. Am J Public Health. 2014;104(suppl 4):S525-S526. doi:10.2105/AJPH.2014.302216
- Stack MK. The soldiers came home sick. The government denied it was responsible. New York Times. Updated January 16, 2022. Accessed October 24, 2022. https://www.nytimes.com/2022/01/11/magazine/military-burn-pits.html
- Namaz A, Sagalyn D. VA secretary discusses health care overhaul helping veterans exposed to toxic burn pits. PBS NewsHour. September 1, 2022. Accessed October 24, 2022. https://www.pbs.org/newshour/show/va-secretary-discusses-health-care-overhaul-helping-veterans-exposed-to-toxic-burn-pits
- US Department of Veterans Affairs, Patient Care Services. VHA LGBTQ+ health program. Updated September 13, 2022. Accessed October 31, 2022. https://www.patientcare.va.gov/lgbt
- Parker T. Of justice and the conscience. In: Ten Sermons of Religion. Crosby, Nichols and Company; 1853:66-85.
- The White House. Fact sheet: President Biden signs the PACT Act and delivers on his promise to America's veterans. August 9, 2022. Accessed October 24, 2022. https://www.whitehouse.gov/briefing-room/statements-releases/2022/08/10/fact-sheet-president-biden-signs-the-pact-act-and-delivers-on-his-promise-to-americas-veterans
- Shane L. Vets can apply for all PACT benefits now after VA speeds up law. Military Times. September 1, 2022. Accessed October 24, 2022. https://www.militarytimes.com/news/burn-pits/2022/09/01/vets-can-apply-for-all-pact-act-benefits-now-after-va-speeds-up-law
- US Department of Veterans Affairs. The PACT Act and your VA benefits. Updated September 28, 2022. Accessed October 24, 2022. https://www.va.gov/resources/the-pact-act-and-your-va-benefits
- Wentling N. Discharged LGBTQ+ veterans now eligible for benefits under new guidance issued by VA. Stars & Stripes. September 20, 2021. Accessed October 24, 2022. https://www.stripes.com/veterans/2021-09-20/veterans-affairs-dont-ask-dont-tell-benefits-lgbt-discharges-2956761.html
- US Department of Veterans Affairs, VA History Office. History--Department of Veterans Affairs (VA). Updated May 27, 2021. Accessed October 24, 2022. https://www.va.gov/HISTORY/VA_History/Overview.asp
- Atkins D, Kilbourne A, Lipson L. Health equity research in the Veterans Health Administration: we've come far but aren't there yet. Am J Public Health. 2014;104(suppl 4):S525-S526. doi:10.2105/AJPH.2014.302216
- Stack MK. The soldiers came home sick. The government denied it was responsible. New York Times. Updated January 16, 2022. Accessed October 24, 2022. https://www.nytimes.com/2022/01/11/magazine/military-burn-pits.html
- Namaz A, Sagalyn D. VA secretary discusses health care overhaul helping veterans exposed to toxic burn pits. PBS NewsHour. September 1, 2022. Accessed October 24, 2022. https://www.pbs.org/newshour/show/va-secretary-discusses-health-care-overhaul-helping-veterans-exposed-to-toxic-burn-pits
- US Department of Veterans Affairs, Patient Care Services. VHA LGBTQ+ health program. Updated September 13, 2022. Accessed October 31, 2022. https://www.patientcare.va.gov/lgbt
Medicaid Expansion and Veterans’ Reliance on the VA for Depression Care
The US Department of Veterans Affairs (VA) is the largest integrated health care system in the United States, providing care for more than 9 million veterans.1 With veterans experiencing mental health conditions like posttraumatic stress disorder (PTSD), substance use disorders, and other serious mental illnesses (SMI) at higher rates compared with the general population, the VA plays an important role in the provision of mental health services.2-5 Since the implementation of its Mental Health Strategic Plan in 2004, the VA has overseen the development of a wide array of mental health programs geared toward the complex needs of veterans. Research has demonstrated VA care outperforming Medicaid-reimbursed services in terms of the percentage of veterans filling antidepressants for at least 12 weeks after initiation of treatment for major depressive disorder (MDD), as well as posthospitalization follow-up.6
Eligible veterans enrolled in the VA often also seek non-VA care. Medicaid covers nearly 10% of all nonelderly veterans, and of these veterans, 39% rely solely on Medicaid for health care access.7 Today, Medicaid is the largest payer for mental health services in the US, providing coverage for approximately 27% of Americans who have SMI and helping fulfill unmet mental health needs.8,9 Understanding which of these systems veterans choose to use, and under which circumstances, is essential in guiding the allocation of limited health care resources.10
Beyond Medicaid, alternatives to VA care may include TRICARE, Medicare, Indian Health Services, and employer-based or self-purchased private insurance. While these options potentially increase convenience, choice, and access to health care practitioners (HCPs) and services not available at local VA systems, cross-system utilization with poor integration may cause care coordination and continuity problems, such as medication mismanagement and opioid overdose, unnecessary duplicate utilization, and possible increased mortality.11-15 As recent national legislative changes, such as the Patient Protection and Affordable Care Act (ACA), Veterans Access, Choice and Accountability Act, and the VA MISSION Act, continue to shift the health care landscape for veterans, questions surrounding how veterans are changing their health care use become significant.16,17
Here, we approach the impacts of Medicaid expansion on veterans’ reliance on the VA for mental health services with a unique lens. We leverage a difference-in-difference design to study 2 historical Medicaid expansions in Arizona (AZ) and New York (NY), which extended eligibility to childless adults in 2001. Prior Medicaid dual-eligible mental health research investigated reliance shifts during the immediate postenrollment year in a subset of veterans newly enrolled in Medicaid.18 However, this study took place in a period of relative policy stability. In contrast, we investigate the potential effects of a broad policy shift by analyzing state-level changes in veterans’ reliance over 6 years after a statewide Medicaid expansion. We match expansion states with demographically similar nonexpansion states to account for unobserved trends and confounding effects. Prior studies have used this method to evaluate post-Medicaid expansion mortality changes and changes in veteran dual enrollment and hospitalizations.10,19 While a study of ACA Medicaid expansion states would be ideal, Medicaid data from most states were only available through 2014 at the time of this analysis. Our study offers a quasi-experimental framework leveraging longitudinal data that can be applied as more post-ACA data become available.
Given the rising incidence of suicide among veterans, understanding care-seeking behaviors for depression among veterans is important as it is the most common psychiatric condition found in those who died by suicide.20,21 Furthermore, depression may be useful as a clinical proxy for mental health policy impacts, given that the Patient Health Questionnaire-9 (PHQ-9) screening tool is well validated and increasingly research accessible, and it is a chronic condition responsive to both well-managed pharmacologic treatment and psychotherapeutic interventions.22,23
In this study, we quantify the change in care-seeking behavior for depression among veterans after Medicaid expansion, using a quasi-experimental design. We hypothesize that new access to Medicaid would be associated with a shift away from using VA services for depression. Given the income-dependent eligibility requirements of Medicaid, we also hypothesize that veterans who qualified for VA coverage due to low income, determined by a regional means test (Priority group 5, “income-eligible”), would be more likely to shift care compared with those whose serviced-connected conditions related to their military service (Priority groups 1-4, “service-connected”) provide VA access.
Methods
To investigate the relative changes in veterans’ reliance on the VA for depression care after the 2001 NY and AZ Medicaid expansions We used a retrospective, difference-in-difference analysis. Our comparison pairings, based on prior demographic analyses were as follows: NY with Pennsylvania(PA); AZ with New Mexico and Nevada (NM/NV).19 The time frame of our analysis was 1999 to 2006, with pre- and postexpansion periods defined as 1999 to 2000 and 2001 to 2006, respectively.
Data
We included veterans aged 18 to 64 years, seeking care for depression from 1999 to 2006, who were also VA-enrolled and residing in our states of interest. We counted veterans as enrolled in Medicaid if they were enrolled at least 1 month in a given year.
Using similar methods like those used in prior studies, we selected patients with encounters documenting depression as the primary outpatient or inpatient diagnosis using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: 296.2x for a single episode of major depressive disorder, 296.3x for a recurrent episode of MDD, 300.4 for dysthymia, and 311.0 for depression not otherwise specified.18,24 We used data from the Medicaid Analytic eXtract files (MAX) for Medicaid data and the VA Corporate Data Warehouse (CDW) for VA data. We chose 1999 as the first study year because it was the earliest year MAX data were available.
Our final sample included 1833 person-years pre-expansion and 7157 postexpansion in our inpatient analysis, as well as 31,767 person-years pre-expansion and 130,382 postexpansion in our outpatient analysis.
Outcomes and Variables
Our primary outcomes were comparative shifts in VA reliance between expansion and nonexpansion states after Medicaid expansion for both inpatient and outpatient depression care. For each year of study, we calculated a veteran’s VA reliance by aggregating the number of days with depression-related encounters at the VA and dividing by the total number of days with a VA or Medicaid depression-related encounters for the year. To provide context to these shifts in VA reliance, we further analyzed the changes in the proportion of annual VA-Medicaid dual users and annual per capita utilization of depression care across the VA and Medicaid.
We conducted subanalyses by income-eligible and service-connected veterans and adjusted our models for age, non-White race, sex, distances to the nearest inpatient and outpatient VA facilities, and VA Relative Risk Score, which is a measure of disease burden and clinical complexity validated specifically for veterans.25
Statistical Analysis
We used fractional logistic regression to model the adjusted effect of Medicaid expansion on VA reliance for depression care. In parallel, we leveraged ordered logit regression and negative binomial regression models to examine the proportion of VA-Medicaid dual users and the per capita utilization of Medicaid and VA depression care, respectively. To estimate the difference-in-difference effects, we used the interaction term of 2 categorical variables—expansion vs nonexpansion states and pre- vs postexpansion status—as the independent variable. We then calculated the average marginal effects with 95% CIs to estimate the differences in outcomes between expansion and nonexpansion states from pre- to postexpansion periods, as well as year-by-year shifts as a robustness check. We conducted these analyses using Stata MP, version 15.
Results
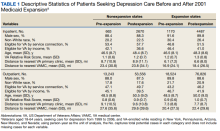
Baseline and postexpansion characteristics
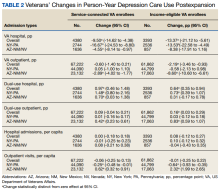
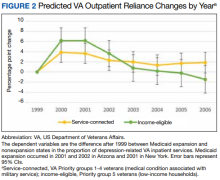
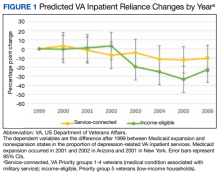
VA Reliance
Overall, we observed postexpansion decreases in VA reliance for depression care
At the state level, reliance on the VA for inpatient depression care in NY decreased by 13.53 pp (95% CI, -22.58 to -4.49) for income-eligible veterans and 16.67 pp (95% CI, -24.53 to -8.80) for service-connected veterans. No relative differences were observed in the outpatient comparisons for both income-eligible (-0.58 pp; 95% CI, -2.13 to 0.98) and service-connected (0.05 pp; 95% CI, -1.00 to 1.10) veterans. In AZ, Medicaid expansion was associated with decreased VA reliance for outpatient depression care among income-eligible veterans (-8.60 pp; 95% CI, -10.60 to -6.61), greater than that for service-connected veterans (-2.89 pp; 95% CI, -4.02 to -1.77). This decrease in VA reliance was significant in the inpatient context only for service-connected veterans (-4.55 pp; 95% CI, -8.14 to -0.97), not income-eligible veterans (-8.38 pp; 95% CI, -17.91 to 1.16).
By applying the aggregate pp changes toward the postexpansion number of visits across both expansion and nonexpansion states, we found that expansion of Medicaid across all our study states would have resulted in 996 fewer hospitalizations and 10,109 fewer outpatient visits for depression at VA in the postexpansion period vs if no states had chosen to expand Medicaid.
Dual Use/Per Capita Utilization
Overall, Medicaid expansion was associated with greater dual use for inpatient depression care—a 0.97-pp (95% CI, 0.46 to 1.48) increase among service-connected veterans and a 0.64-pp (95% CI, 0.35 to 0.94) increase among income-eligible veterans.
At the state level, NY similarly showed increases in dual use among both service-connected (1.48 pp; 95% CI, 0.80 to 2.16) and income-eligible veterans (0.73 pp; 95% CI, 0.39 to 1.07) after Medicaid expansion. However, dual use in AZ increased significantly only among service-connected veterans (0.70 pp; 95% CI, 0.03 to 1.38), not income-eligible veterans (0.31 pp; 95% CI, -0.17 to 0.78).
Among outpatient visits, Medicaid expansion was associated with increased dual use only for income-eligible veterans (0.16 pp; 95% CI, 0.03-0.29), and not service-connected veterans (0.09 pp; 95% CI, -0.04 to 0.21). State-level analyses showed that Medicaid expansion in NY was not associated with changes in dual use for either service-connected (0.01 pp; 95% CI, -0.16 to 0.17) or income-eligible veterans (0.03 pp; 95% CI, -0.12 to 0.18), while expansion in AZ was associated with increases in dual use among both service-connected (0.42 pp; 95% CI, 0.23 to 0.61) and income-eligible veterans (0.83 pp; 95% CI, 0.59 to 1.07).
Concerning per capita utilization of depression care after Medicaid expansion, analyses showed no detectable changes for either inpatient or outpatient services, among both service-connected and income-eligible veterans. However, while this pattern held at the state level among hospitalizations, outpatient visit results showed divergent trends between AZ and NY. In NY, Medicaid expansion was associated with decreased per capita utilization of outpatient depression care among both service-connected (-0.25 visits annually; 95% CI, -0.48 to -0.01) and income-eligible veterans (-0.64 visits annually; 95% CI, -0.93 to -0.35). In AZ, Medicaid expansion was associated with increased per capita utilization of outpatient depression care among both service-connected (0.62 visits annually; 95% CI, 0.32-0.91) and income-eligible veterans (2.32 visits annually; 95% CI, 1.99-2.65).
Discussion
Our study quantified changes in depression-related health care utilization after Medicaid expansions in NY and AZ in 2001. Overall, the balance of evidence indicated that Medicaid expansion was associated with decreased reliance on the VA for depression-related services. There was an exception: income-eligible veterans in AZ did not shift their hospital care away from the VA in a statistically discernible way, although the point estimate was lower. More broadly, these findings concerning veterans’ reliance varied not only in inpatient vs outpatient services and income- vs service-connected eligibility, but also in the state-level contexts of veteran dual users and per capita utilization.
Given that the overall per capita utilization of depression care was unchanged from pre- to postexpansion periods, one might interpret the decreases in VA reliance and increases in Medicaid-VA dual users as a substitution effect from VA care to non-VA care. This could be plausible for hospitalizations where state-level analyses showed similarly stable levels of per capita utilization. However, state-level trends in our outpatient utilization analysis, especially with a substantial 2.32 pp increase in annual per capita visits among income-eligible veterans in AZ, leave open the possibility that in some cases veterans may be complementing VA care with Medicaid-reimbursed services.
The causes underlying these differences in reliance shifts between NY and AZ are likely also influenced by the policy contexts of their respective Medicaid expansions. For example, in 1999, NY passed Kendra’s Law, which established a procedure for obtaining court orders for assisted outpatient mental health treatment for individuals deemed unlikely to survive safely in the community.26 A reasonable inference is that there was less unfulfilled outpatient mental health need in NY under the existing accessibility provisioned by Kendra’s Law. In addition, while both states extended coverage to childless adults under 100% of the Federal Poverty level (FPL), the AZ Medicaid expansion was via a voters’ initiative and extended family coverage to 200% FPL vs 150% FPL for families in NY. Given that the AZ Medicaid expansion enjoyed both broader public participation and generosity in terms of eligibility, its uptake and therefore effect size may have been larger than in NY for nonacute outpatient care.
Our findings contribute to the growing body of literature surrounding the changes in health care utilization after Medicaid expansion, specifically for a newly dual-eligible population of veterans seeking mental health services for depression. While prior research concerning Medicare dual-enrolled veterans has shown high reliance on the VA for both mental health diagnoses and services, scholars have established the association of Medicaid enrollment with decreased VA reliance.27-29 Our analysis is the first to investigate state-level effects of Medicaid expansion on VA reliance for a single mental health condition using a natural experimental framework. We focus on a population that includes a large portion of veterans who are newly Medicaid-eligible due to a sweeping policy change and use demographically matched nonexpansion states to draw comparisons in VA reliance for depression care. Our findings of Medicaid expansion–associated decreases in VA reliance for depression care complement prior literature that describe Medicaid enrollment–associated decreases in VA reliance for overall mental health care.
Implications
From a systems-level perspective, the implications of shifting services away from the VA are complex and incompletely understood. The VA lacks interoperability with the electronic health records (EHRs) used by Medicaid clinicians. Consequently, significant issues of service duplication and incomplete clinical data exist for veterans seeking treatment outside of the VA system, posing health care quality and safety concerns.30 On one hand, Medicaid access is associated with increased health care utilization attributed to filling unmet needs for Medicare dual enrollees, as well as increased prescription filling for psychiatric medications.31,32 Furthermore, the only randomized control trial of Medicaid expansion to date was associated with a 9-pp decrease in positive screening rates for depression among those who received access at around 2 years postexpansion.33 On the other hand, the VA has developed a mental health system tailored to the particular needs of veterans, and health care practitioners at the VA have significantly greater rates of military cultural competency compared to those in nonmilitary settings (70% vs 24% in the TRICARE network and 8% among those with no military or TRICARE affiliation).34 Compared to individuals seeking mental health services with private insurance plans, veterans were about twice as likely to receive appropriate treatment for schizophrenia and depression at the VA.35 These documented strengths of VA mental health care may together help explain the small absolute number of visits that were associated with shifts away from VA overall after Medicaid expansion.
Finally, it is worth considering extrinsic factors that influence utilization among newly dual-eligible veterans. For example, hospitalizations are less likely to be planned than outpatient services, translating to a greater importance of proximity to a nearby medical facility than a veteran’s preference of where to seek care. In the same vein, major VA medical centers are fewer and more distant on average than VA outpatient clinics, therefore reducing the advantage of a Medicaid-reimbursed outpatient clinic in terms of distance.36 These realities may partially explain the proportionally larger shifts away from the VA for hospitalizations compared to outpatient care for depression.
Limitations and Future Directions
Our results should be interpreted within methodological and data limitations. With only 2 states in our sample, NY demonstrably skewed overall results, contributing 1.7 to 3 times more observations than AZ across subanalyses—a challenge also cited by Sommers and colleagues.19 Our veteran groupings were also unable to distinguish those veterans classified as service-connected who may also have qualified by income-eligible criteria (which would tend to understate the size of results) and those veterans who gained and then lost Medicaid coverage in a given year. Our study also faces limitations in generalizability and establishing causality. First, we included only 2 historical state Medicaid expansions, compared with the 38 states and Washington, DC, that have now expanded Medicaid to date under the ACA. Just in the 2 states from our study, we noted significant heterogeneity in the shifts associated with Medicaid expansion, which makes extrapolating specific trends difficult. Differences in underlying health care resources, legislation, and other external factors may limit the applicability of Medicaid expansion in the era of the ACA, as well as the Veterans Choice and MISSION acts. Second, while we leveraged a difference-in-difference analysis using demographically matched, neighboring comparison states, our findings are nevertheless drawn from observational data obviating causality. VA data for other sources of coverage such as private insurance are limited and not included in our study, and MAX datasets vary by quality across states, translating to potential gaps in our study cohort.28
Moving forward, our study demonstrates the potential for applying a natural experimental approach to studying dual-eligible veterans at the interface of Medicaid expansion. We focused on changes in VA reliance for the specific condition of depression and, in doing so, invite further inquiry into the impact of state mental health policy on outcomes more proximate to veterans’ outcomes. Clinical indicators, such as rates of antidepressant filling, utilization and duration of psychotherapy, and PHQ-9 scores, can similarly be investigated by natural experimental design. While current limits of administrative data and the siloing of EHRs may pose barriers to some of these avenues of research, multidisciplinary methodologies and data querying innovations such as natural language processing algorithms for clinical notes hold exciting opportunities to bridge the gap between policy and clinical efficacy.
Conclusions
This study applied a difference-in-difference analysis and found that Medicaid expansion is associated with decreases in VA reliance for both inpatient and outpatient services for depression. As additional data are generated from the Medicaid expansions of the ACA, similarly robust methods should be applied to further explore the impacts associated with such policy shifts and open the door to a better understanding of implications at the clinical level.
Acknowledgments
We acknowledge the efforts of Janine Wong, who proofread and formatted the manuscript.
1. US Department of Veterans Affairs, Veterans Health Administration. About VA. 2019. Updated September 27, 2022. Accessed September 29, 2022. https://www.va.gov/health/
2. Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry. 2010;44(1):4-19. doi:10.3109/00048670903393597
3. Lan CW, Fiellin DA, Barry DT, et al. The epidemiology of substance use disorders in US veterans: a systematic review and analysis of assessment methods. Am J Addict. 2016;25(1):7-24. doi:10.1111/ajad.12319
4. Grant BF, Saha TD, June Ruan W, et al. Epidemiology of DSM-5 drug use disorder results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiat. 2016;73(1):39-47. doi:10.1001/jamapsychiatry.015.2132
5. Pemberton MR, Forman-Hoffman VL, Lipari RN, Ashley OS, Heller DC, Williams MR. Prevalence of past year substance use and mental illness by veteran status in a nationally representative sample. CBHSQ Data Review. Published November 9, 2016. Accessed October 6, 2022. https://www.samhsa.gov/data/report/prevalence-past-year-substance-use-and-mental-illness-veteran-status-nationally
6. Watkins KE, Pincus HA, Smith B, et al. Veterans Health Administration Mental Health Program Evaluation: Capstone Report. 2011. Accessed September 29, 2022. https://www.rand.org/pubs/technical_reports/TR956.html
7. Henry J. Kaiser Family Foundation. Medicaid’s role in covering veterans. June 29, 2017. Accessed September 29, 2022. https://www.kff.org/infographic/medicaids-role-in-covering-veterans
8. Substance Abuse and Mental Health Services Administration. Results from the 2016 National Survey on Drug Use and Health: detailed tables. September 7, 2017. Accessed September 29, 2022. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf
9. Wen H, Druss BG, Cummings JR. Effect of Medicaid expansions on health insurance coverage and access to care among low-income adults with behavioral health conditions. Health Serv Res. 2015;50:1787-1809. doi:10.1111/1475-6773.12411
10. O’Mahen PN, Petersen LA. Effects of state-level Medicaid expansion on Veterans Health Administration dual enrollment and utilization: potential implications for future coverage expansions. Med Care. 2020;58(6):526-533. doi:10.1097/MLR.0000000000001327
11. Ono SS, Dziak KM, Wittrock SM, et al. Treating dual-use patients across two health care systems: a qualitative study. Fed Pract. 2015;32(8):32-37.
12. Weeks WB, Mahar PJ, Wright SM. Utilization of VA and Medicare services by Medicare-eligible veterans: the impact of additional access points in a rural setting. J Healthc Manag. 2005;50(2):95-106.
13. Gellad WF, Thorpe JM, Zhao X, et al. Impact of dual use of Department of Veterans Affairs and Medicare part d drug benefits on potentially unsafe opioid use. Am J Public Health. 2018;108(2):248-255. doi:10.2105/AJPH.2017.304174
14. Coughlin SS, Young L. A review of dual health care system use by veterans with cardiometabolic disease. J Hosp Manag Health Policy. 2018;2:39. doi:10.21037/jhmhp.2018.07.05
15. Radomski TR, Zhao X, Thorpe CT, et al. The impact of medication-based risk adjustment on the association between veteran health outcomes and dual health system use. J Gen Intern Med. 2017;32(9):967-973. doi:10.1007/s11606-017-4064-4
16. Kullgren JT, Fagerlin A, Kerr EA. Completing the MISSION: a blueprint for helping veterans make the most of new choices. J Gen Intern Med. 2020;35(5):1567-1570. doi:10.1007/s11606-019-05404-w
17. VA MISSION Act of 2018, 38 USC §101 (2018). https://www.govinfo.gov/app/details/USCODE-2018-title38/USCODE-2018-title38-partI-chap1-sec101
18. Vanneman ME, Phibbs CS, Dally SK, Trivedi AN, Yoon J. The impact of Medicaid enrollment on Veterans Health Administration enrollees’ behavioral health services use. Health Serv Res. 2018;53(suppl 3):5238-5259. doi:10.1111/1475-6773.13062
19. Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012;367(11):1025-1034. doi:10.1056/NEJMsa1202099
20. US Department of Veterans Affairs Office of Mental Health. 2019 national veteran suicide prevention annual report. 2019. Accessed September 29, 2022. https://www.mentalhealth.va.gov/docs/data-sheets/2019/2019_National_Veteran_Suicide_Prevention_Annual_Report_508.pdf
21. Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147(1-3):17-28. doi:10.1016/j.jad.2013.01.004
22. Adekkanattu P, Sholle ET, DeFerio J, Pathak J, Johnson SB, Campion TR Jr. Ascertaining depression severity by extracting Patient Health Questionnaire-9 (PHQ-9) scores from clinical notes. AMIA Annu Symp Proc. 2018;2018:147-156.
23. DeRubeis RJ, Siegle GJ, Hollon SD. Cognitive therapy versus medication for depression: treatment outcomes and neural mechanisms. Nat Rev Neurosci. 2008;9(10):788-796. doi:10.1038/nrn2345
24. Cully JA, Zimmer M, Khan MM, Petersen LA. Quality of depression care and its impact on health service use and mortality among veterans. Psychiatr Serv. 2008;59(12):1399-1405. doi:10.1176/ps.2008.59.12.1399
25. Byrne MM, Kuebeler M, Pietz K, Petersen LA. Effect of using information from only one system for dually eligible health care users. Med Care. 2006;44(8):768-773. doi:10.1097/01.mlr.0000218786.44722.14
26. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396. doi:10.1176/appi.ps.201400537
27. Petersen LA, Byrne MM, Daw CN, Hasche J, Reis B, Pietz K. Relationship between clinical conditions and use of Veterans Affairs health care among Medicare-enrolled veterans. Health Serv Res. 2010;45(3):762-791. doi:10.1111/j.1475-6773.2010.01107.x
28. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Use of Veterans Affairs and Medicaid services for dually enrolled veterans. Health Serv Res. 2018;53(3):1539-1561. doi:10.1111/1475-6773.12727
29. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Veterans’ reliance on VA care by type of service and distance to VA for nonelderly VA-Medicaid dual enrollees. Med Care. 2019;57(3):225-229. doi:10.1097/MLR.0000000000001066
30. Gaglioti A, Cozad A, Wittrock S, et al. Non-VA primary care providers’ perspectives on comanagement for rural veterans. Mil Med. 2014;179(11):1236-1243. doi:10.7205/MILMED-D-13-00342
31. Moon S, Shin J. Health care utilization among Medicare-Medicaid dual eligibles: a count data analysis. BMC Public Health. 2006;6(1):88. doi:10.1186/1471-2458-6-88
32. Henry J. Kaiser Family Foundation. Facilitating access to mental health services: a look at Medicaid, private insurance, and the uninsured. November 27, 2017. Accessed September 29, 2022. https://www.kff.org/medicaid/fact-sheet/facilitating-access-to-mental-health-services-a-look-at-medicaid-private-insurance-and-the-uninsured
33. Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment - effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713-1722. doi:10.1056/NEJMsa1212321
34. Tanielian T, Farris C, Batka C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. 2014. Accessed September 29, 2022. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf
35. Kizer KW, Dudley RA. Extreme makeover: transformation of the Veterans Health Care System. Annu Rev Public Health. 2009;30(1):313-339. doi:10.1146/annurev.publhealth.29.020907.090940
36. Brennan KJ. Kendra’s Law: final report on the status of assisted outpatient treatment, appendix 2. 2002. Accessed September 29, 2022. https://omh.ny.gov/omhweb/kendra_web/finalreport/appendix2.htm
The US Department of Veterans Affairs (VA) is the largest integrated health care system in the United States, providing care for more than 9 million veterans.1 With veterans experiencing mental health conditions like posttraumatic stress disorder (PTSD), substance use disorders, and other serious mental illnesses (SMI) at higher rates compared with the general population, the VA plays an important role in the provision of mental health services.2-5 Since the implementation of its Mental Health Strategic Plan in 2004, the VA has overseen the development of a wide array of mental health programs geared toward the complex needs of veterans. Research has demonstrated VA care outperforming Medicaid-reimbursed services in terms of the percentage of veterans filling antidepressants for at least 12 weeks after initiation of treatment for major depressive disorder (MDD), as well as posthospitalization follow-up.6
Eligible veterans enrolled in the VA often also seek non-VA care. Medicaid covers nearly 10% of all nonelderly veterans, and of these veterans, 39% rely solely on Medicaid for health care access.7 Today, Medicaid is the largest payer for mental health services in the US, providing coverage for approximately 27% of Americans who have SMI and helping fulfill unmet mental health needs.8,9 Understanding which of these systems veterans choose to use, and under which circumstances, is essential in guiding the allocation of limited health care resources.10
Beyond Medicaid, alternatives to VA care may include TRICARE, Medicare, Indian Health Services, and employer-based or self-purchased private insurance. While these options potentially increase convenience, choice, and access to health care practitioners (HCPs) and services not available at local VA systems, cross-system utilization with poor integration may cause care coordination and continuity problems, such as medication mismanagement and opioid overdose, unnecessary duplicate utilization, and possible increased mortality.11-15 As recent national legislative changes, such as the Patient Protection and Affordable Care Act (ACA), Veterans Access, Choice and Accountability Act, and the VA MISSION Act, continue to shift the health care landscape for veterans, questions surrounding how veterans are changing their health care use become significant.16,17
Here, we approach the impacts of Medicaid expansion on veterans’ reliance on the VA for mental health services with a unique lens. We leverage a difference-in-difference design to study 2 historical Medicaid expansions in Arizona (AZ) and New York (NY), which extended eligibility to childless adults in 2001. Prior Medicaid dual-eligible mental health research investigated reliance shifts during the immediate postenrollment year in a subset of veterans newly enrolled in Medicaid.18 However, this study took place in a period of relative policy stability. In contrast, we investigate the potential effects of a broad policy shift by analyzing state-level changes in veterans’ reliance over 6 years after a statewide Medicaid expansion. We match expansion states with demographically similar nonexpansion states to account for unobserved trends and confounding effects. Prior studies have used this method to evaluate post-Medicaid expansion mortality changes and changes in veteran dual enrollment and hospitalizations.10,19 While a study of ACA Medicaid expansion states would be ideal, Medicaid data from most states were only available through 2014 at the time of this analysis. Our study offers a quasi-experimental framework leveraging longitudinal data that can be applied as more post-ACA data become available.
Given the rising incidence of suicide among veterans, understanding care-seeking behaviors for depression among veterans is important as it is the most common psychiatric condition found in those who died by suicide.20,21 Furthermore, depression may be useful as a clinical proxy for mental health policy impacts, given that the Patient Health Questionnaire-9 (PHQ-9) screening tool is well validated and increasingly research accessible, and it is a chronic condition responsive to both well-managed pharmacologic treatment and psychotherapeutic interventions.22,23
In this study, we quantify the change in care-seeking behavior for depression among veterans after Medicaid expansion, using a quasi-experimental design. We hypothesize that new access to Medicaid would be associated with a shift away from using VA services for depression. Given the income-dependent eligibility requirements of Medicaid, we also hypothesize that veterans who qualified for VA coverage due to low income, determined by a regional means test (Priority group 5, “income-eligible”), would be more likely to shift care compared with those whose serviced-connected conditions related to their military service (Priority groups 1-4, “service-connected”) provide VA access.
Methods
To investigate the relative changes in veterans’ reliance on the VA for depression care after the 2001 NY and AZ Medicaid expansions We used a retrospective, difference-in-difference analysis. Our comparison pairings, based on prior demographic analyses were as follows: NY with Pennsylvania(PA); AZ with New Mexico and Nevada (NM/NV).19 The time frame of our analysis was 1999 to 2006, with pre- and postexpansion periods defined as 1999 to 2000 and 2001 to 2006, respectively.
Data
We included veterans aged 18 to 64 years, seeking care for depression from 1999 to 2006, who were also VA-enrolled and residing in our states of interest. We counted veterans as enrolled in Medicaid if they were enrolled at least 1 month in a given year.
Using similar methods like those used in prior studies, we selected patients with encounters documenting depression as the primary outpatient or inpatient diagnosis using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: 296.2x for a single episode of major depressive disorder, 296.3x for a recurrent episode of MDD, 300.4 for dysthymia, and 311.0 for depression not otherwise specified.18,24 We used data from the Medicaid Analytic eXtract files (MAX) for Medicaid data and the VA Corporate Data Warehouse (CDW) for VA data. We chose 1999 as the first study year because it was the earliest year MAX data were available.
Our final sample included 1833 person-years pre-expansion and 7157 postexpansion in our inpatient analysis, as well as 31,767 person-years pre-expansion and 130,382 postexpansion in our outpatient analysis.
Outcomes and Variables
Our primary outcomes were comparative shifts in VA reliance between expansion and nonexpansion states after Medicaid expansion for both inpatient and outpatient depression care. For each year of study, we calculated a veteran’s VA reliance by aggregating the number of days with depression-related encounters at the VA and dividing by the total number of days with a VA or Medicaid depression-related encounters for the year. To provide context to these shifts in VA reliance, we further analyzed the changes in the proportion of annual VA-Medicaid dual users and annual per capita utilization of depression care across the VA and Medicaid.
We conducted subanalyses by income-eligible and service-connected veterans and adjusted our models for age, non-White race, sex, distances to the nearest inpatient and outpatient VA facilities, and VA Relative Risk Score, which is a measure of disease burden and clinical complexity validated specifically for veterans.25
Statistical Analysis
We used fractional logistic regression to model the adjusted effect of Medicaid expansion on VA reliance for depression care. In parallel, we leveraged ordered logit regression and negative binomial regression models to examine the proportion of VA-Medicaid dual users and the per capita utilization of Medicaid and VA depression care, respectively. To estimate the difference-in-difference effects, we used the interaction term of 2 categorical variables—expansion vs nonexpansion states and pre- vs postexpansion status—as the independent variable. We then calculated the average marginal effects with 95% CIs to estimate the differences in outcomes between expansion and nonexpansion states from pre- to postexpansion periods, as well as year-by-year shifts as a robustness check. We conducted these analyses using Stata MP, version 15.
Results
Baseline and postexpansion characteristics
VA Reliance
Overall, we observed postexpansion decreases in VA reliance for depression care
At the state level, reliance on the VA for inpatient depression care in NY decreased by 13.53 pp (95% CI, -22.58 to -4.49) for income-eligible veterans and 16.67 pp (95% CI, -24.53 to -8.80) for service-connected veterans. No relative differences were observed in the outpatient comparisons for both income-eligible (-0.58 pp; 95% CI, -2.13 to 0.98) and service-connected (0.05 pp; 95% CI, -1.00 to 1.10) veterans. In AZ, Medicaid expansion was associated with decreased VA reliance for outpatient depression care among income-eligible veterans (-8.60 pp; 95% CI, -10.60 to -6.61), greater than that for service-connected veterans (-2.89 pp; 95% CI, -4.02 to -1.77). This decrease in VA reliance was significant in the inpatient context only for service-connected veterans (-4.55 pp; 95% CI, -8.14 to -0.97), not income-eligible veterans (-8.38 pp; 95% CI, -17.91 to 1.16).
By applying the aggregate pp changes toward the postexpansion number of visits across both expansion and nonexpansion states, we found that expansion of Medicaid across all our study states would have resulted in 996 fewer hospitalizations and 10,109 fewer outpatient visits for depression at VA in the postexpansion period vs if no states had chosen to expand Medicaid.
Dual Use/Per Capita Utilization
Overall, Medicaid expansion was associated with greater dual use for inpatient depression care—a 0.97-pp (95% CI, 0.46 to 1.48) increase among service-connected veterans and a 0.64-pp (95% CI, 0.35 to 0.94) increase among income-eligible veterans.
At the state level, NY similarly showed increases in dual use among both service-connected (1.48 pp; 95% CI, 0.80 to 2.16) and income-eligible veterans (0.73 pp; 95% CI, 0.39 to 1.07) after Medicaid expansion. However, dual use in AZ increased significantly only among service-connected veterans (0.70 pp; 95% CI, 0.03 to 1.38), not income-eligible veterans (0.31 pp; 95% CI, -0.17 to 0.78).
Among outpatient visits, Medicaid expansion was associated with increased dual use only for income-eligible veterans (0.16 pp; 95% CI, 0.03-0.29), and not service-connected veterans (0.09 pp; 95% CI, -0.04 to 0.21). State-level analyses showed that Medicaid expansion in NY was not associated with changes in dual use for either service-connected (0.01 pp; 95% CI, -0.16 to 0.17) or income-eligible veterans (0.03 pp; 95% CI, -0.12 to 0.18), while expansion in AZ was associated with increases in dual use among both service-connected (0.42 pp; 95% CI, 0.23 to 0.61) and income-eligible veterans (0.83 pp; 95% CI, 0.59 to 1.07).
Concerning per capita utilization of depression care after Medicaid expansion, analyses showed no detectable changes for either inpatient or outpatient services, among both service-connected and income-eligible veterans. However, while this pattern held at the state level among hospitalizations, outpatient visit results showed divergent trends between AZ and NY. In NY, Medicaid expansion was associated with decreased per capita utilization of outpatient depression care among both service-connected (-0.25 visits annually; 95% CI, -0.48 to -0.01) and income-eligible veterans (-0.64 visits annually; 95% CI, -0.93 to -0.35). In AZ, Medicaid expansion was associated with increased per capita utilization of outpatient depression care among both service-connected (0.62 visits annually; 95% CI, 0.32-0.91) and income-eligible veterans (2.32 visits annually; 95% CI, 1.99-2.65).
Discussion
Our study quantified changes in depression-related health care utilization after Medicaid expansions in NY and AZ in 2001. Overall, the balance of evidence indicated that Medicaid expansion was associated with decreased reliance on the VA for depression-related services. There was an exception: income-eligible veterans in AZ did not shift their hospital care away from the VA in a statistically discernible way, although the point estimate was lower. More broadly, these findings concerning veterans’ reliance varied not only in inpatient vs outpatient services and income- vs service-connected eligibility, but also in the state-level contexts of veteran dual users and per capita utilization.
Given that the overall per capita utilization of depression care was unchanged from pre- to postexpansion periods, one might interpret the decreases in VA reliance and increases in Medicaid-VA dual users as a substitution effect from VA care to non-VA care. This could be plausible for hospitalizations where state-level analyses showed similarly stable levels of per capita utilization. However, state-level trends in our outpatient utilization analysis, especially with a substantial 2.32 pp increase in annual per capita visits among income-eligible veterans in AZ, leave open the possibility that in some cases veterans may be complementing VA care with Medicaid-reimbursed services.
The causes underlying these differences in reliance shifts between NY and AZ are likely also influenced by the policy contexts of their respective Medicaid expansions. For example, in 1999, NY passed Kendra’s Law, which established a procedure for obtaining court orders for assisted outpatient mental health treatment for individuals deemed unlikely to survive safely in the community.26 A reasonable inference is that there was less unfulfilled outpatient mental health need in NY under the existing accessibility provisioned by Kendra’s Law. In addition, while both states extended coverage to childless adults under 100% of the Federal Poverty level (FPL), the AZ Medicaid expansion was via a voters’ initiative and extended family coverage to 200% FPL vs 150% FPL for families in NY. Given that the AZ Medicaid expansion enjoyed both broader public participation and generosity in terms of eligibility, its uptake and therefore effect size may have been larger than in NY for nonacute outpatient care.
Our findings contribute to the growing body of literature surrounding the changes in health care utilization after Medicaid expansion, specifically for a newly dual-eligible population of veterans seeking mental health services for depression. While prior research concerning Medicare dual-enrolled veterans has shown high reliance on the VA for both mental health diagnoses and services, scholars have established the association of Medicaid enrollment with decreased VA reliance.27-29 Our analysis is the first to investigate state-level effects of Medicaid expansion on VA reliance for a single mental health condition using a natural experimental framework. We focus on a population that includes a large portion of veterans who are newly Medicaid-eligible due to a sweeping policy change and use demographically matched nonexpansion states to draw comparisons in VA reliance for depression care. Our findings of Medicaid expansion–associated decreases in VA reliance for depression care complement prior literature that describe Medicaid enrollment–associated decreases in VA reliance for overall mental health care.
Implications
From a systems-level perspective, the implications of shifting services away from the VA are complex and incompletely understood. The VA lacks interoperability with the electronic health records (EHRs) used by Medicaid clinicians. Consequently, significant issues of service duplication and incomplete clinical data exist for veterans seeking treatment outside of the VA system, posing health care quality and safety concerns.30 On one hand, Medicaid access is associated with increased health care utilization attributed to filling unmet needs for Medicare dual enrollees, as well as increased prescription filling for psychiatric medications.31,32 Furthermore, the only randomized control trial of Medicaid expansion to date was associated with a 9-pp decrease in positive screening rates for depression among those who received access at around 2 years postexpansion.33 On the other hand, the VA has developed a mental health system tailored to the particular needs of veterans, and health care practitioners at the VA have significantly greater rates of military cultural competency compared to those in nonmilitary settings (70% vs 24% in the TRICARE network and 8% among those with no military or TRICARE affiliation).34 Compared to individuals seeking mental health services with private insurance plans, veterans were about twice as likely to receive appropriate treatment for schizophrenia and depression at the VA.35 These documented strengths of VA mental health care may together help explain the small absolute number of visits that were associated with shifts away from VA overall after Medicaid expansion.
Finally, it is worth considering extrinsic factors that influence utilization among newly dual-eligible veterans. For example, hospitalizations are less likely to be planned than outpatient services, translating to a greater importance of proximity to a nearby medical facility than a veteran’s preference of where to seek care. In the same vein, major VA medical centers are fewer and more distant on average than VA outpatient clinics, therefore reducing the advantage of a Medicaid-reimbursed outpatient clinic in terms of distance.36 These realities may partially explain the proportionally larger shifts away from the VA for hospitalizations compared to outpatient care for depression.
Limitations and Future Directions
Our results should be interpreted within methodological and data limitations. With only 2 states in our sample, NY demonstrably skewed overall results, contributing 1.7 to 3 times more observations than AZ across subanalyses—a challenge also cited by Sommers and colleagues.19 Our veteran groupings were also unable to distinguish those veterans classified as service-connected who may also have qualified by income-eligible criteria (which would tend to understate the size of results) and those veterans who gained and then lost Medicaid coverage in a given year. Our study also faces limitations in generalizability and establishing causality. First, we included only 2 historical state Medicaid expansions, compared with the 38 states and Washington, DC, that have now expanded Medicaid to date under the ACA. Just in the 2 states from our study, we noted significant heterogeneity in the shifts associated with Medicaid expansion, which makes extrapolating specific trends difficult. Differences in underlying health care resources, legislation, and other external factors may limit the applicability of Medicaid expansion in the era of the ACA, as well as the Veterans Choice and MISSION acts. Second, while we leveraged a difference-in-difference analysis using demographically matched, neighboring comparison states, our findings are nevertheless drawn from observational data obviating causality. VA data for other sources of coverage such as private insurance are limited and not included in our study, and MAX datasets vary by quality across states, translating to potential gaps in our study cohort.28
Moving forward, our study demonstrates the potential for applying a natural experimental approach to studying dual-eligible veterans at the interface of Medicaid expansion. We focused on changes in VA reliance for the specific condition of depression and, in doing so, invite further inquiry into the impact of state mental health policy on outcomes more proximate to veterans’ outcomes. Clinical indicators, such as rates of antidepressant filling, utilization and duration of psychotherapy, and PHQ-9 scores, can similarly be investigated by natural experimental design. While current limits of administrative data and the siloing of EHRs may pose barriers to some of these avenues of research, multidisciplinary methodologies and data querying innovations such as natural language processing algorithms for clinical notes hold exciting opportunities to bridge the gap between policy and clinical efficacy.
Conclusions
This study applied a difference-in-difference analysis and found that Medicaid expansion is associated with decreases in VA reliance for both inpatient and outpatient services for depression. As additional data are generated from the Medicaid expansions of the ACA, similarly robust methods should be applied to further explore the impacts associated with such policy shifts and open the door to a better understanding of implications at the clinical level.
Acknowledgments
We acknowledge the efforts of Janine Wong, who proofread and formatted the manuscript.
The US Department of Veterans Affairs (VA) is the largest integrated health care system in the United States, providing care for more than 9 million veterans.1 With veterans experiencing mental health conditions like posttraumatic stress disorder (PTSD), substance use disorders, and other serious mental illnesses (SMI) at higher rates compared with the general population, the VA plays an important role in the provision of mental health services.2-5 Since the implementation of its Mental Health Strategic Plan in 2004, the VA has overseen the development of a wide array of mental health programs geared toward the complex needs of veterans. Research has demonstrated VA care outperforming Medicaid-reimbursed services in terms of the percentage of veterans filling antidepressants for at least 12 weeks after initiation of treatment for major depressive disorder (MDD), as well as posthospitalization follow-up.6
Eligible veterans enrolled in the VA often also seek non-VA care. Medicaid covers nearly 10% of all nonelderly veterans, and of these veterans, 39% rely solely on Medicaid for health care access.7 Today, Medicaid is the largest payer for mental health services in the US, providing coverage for approximately 27% of Americans who have SMI and helping fulfill unmet mental health needs.8,9 Understanding which of these systems veterans choose to use, and under which circumstances, is essential in guiding the allocation of limited health care resources.10
Beyond Medicaid, alternatives to VA care may include TRICARE, Medicare, Indian Health Services, and employer-based or self-purchased private insurance. While these options potentially increase convenience, choice, and access to health care practitioners (HCPs) and services not available at local VA systems, cross-system utilization with poor integration may cause care coordination and continuity problems, such as medication mismanagement and opioid overdose, unnecessary duplicate utilization, and possible increased mortality.11-15 As recent national legislative changes, such as the Patient Protection and Affordable Care Act (ACA), Veterans Access, Choice and Accountability Act, and the VA MISSION Act, continue to shift the health care landscape for veterans, questions surrounding how veterans are changing their health care use become significant.16,17
Here, we approach the impacts of Medicaid expansion on veterans’ reliance on the VA for mental health services with a unique lens. We leverage a difference-in-difference design to study 2 historical Medicaid expansions in Arizona (AZ) and New York (NY), which extended eligibility to childless adults in 2001. Prior Medicaid dual-eligible mental health research investigated reliance shifts during the immediate postenrollment year in a subset of veterans newly enrolled in Medicaid.18 However, this study took place in a period of relative policy stability. In contrast, we investigate the potential effects of a broad policy shift by analyzing state-level changes in veterans’ reliance over 6 years after a statewide Medicaid expansion. We match expansion states with demographically similar nonexpansion states to account for unobserved trends and confounding effects. Prior studies have used this method to evaluate post-Medicaid expansion mortality changes and changes in veteran dual enrollment and hospitalizations.10,19 While a study of ACA Medicaid expansion states would be ideal, Medicaid data from most states were only available through 2014 at the time of this analysis. Our study offers a quasi-experimental framework leveraging longitudinal data that can be applied as more post-ACA data become available.
Given the rising incidence of suicide among veterans, understanding care-seeking behaviors for depression among veterans is important as it is the most common psychiatric condition found in those who died by suicide.20,21 Furthermore, depression may be useful as a clinical proxy for mental health policy impacts, given that the Patient Health Questionnaire-9 (PHQ-9) screening tool is well validated and increasingly research accessible, and it is a chronic condition responsive to both well-managed pharmacologic treatment and psychotherapeutic interventions.22,23
In this study, we quantify the change in care-seeking behavior for depression among veterans after Medicaid expansion, using a quasi-experimental design. We hypothesize that new access to Medicaid would be associated with a shift away from using VA services for depression. Given the income-dependent eligibility requirements of Medicaid, we also hypothesize that veterans who qualified for VA coverage due to low income, determined by a regional means test (Priority group 5, “income-eligible”), would be more likely to shift care compared with those whose serviced-connected conditions related to their military service (Priority groups 1-4, “service-connected”) provide VA access.
Methods
To investigate the relative changes in veterans’ reliance on the VA for depression care after the 2001 NY and AZ Medicaid expansions We used a retrospective, difference-in-difference analysis. Our comparison pairings, based on prior demographic analyses were as follows: NY with Pennsylvania(PA); AZ with New Mexico and Nevada (NM/NV).19 The time frame of our analysis was 1999 to 2006, with pre- and postexpansion periods defined as 1999 to 2000 and 2001 to 2006, respectively.
Data
We included veterans aged 18 to 64 years, seeking care for depression from 1999 to 2006, who were also VA-enrolled and residing in our states of interest. We counted veterans as enrolled in Medicaid if they were enrolled at least 1 month in a given year.
Using similar methods like those used in prior studies, we selected patients with encounters documenting depression as the primary outpatient or inpatient diagnosis using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: 296.2x for a single episode of major depressive disorder, 296.3x for a recurrent episode of MDD, 300.4 for dysthymia, and 311.0 for depression not otherwise specified.18,24 We used data from the Medicaid Analytic eXtract files (MAX) for Medicaid data and the VA Corporate Data Warehouse (CDW) for VA data. We chose 1999 as the first study year because it was the earliest year MAX data were available.
Our final sample included 1833 person-years pre-expansion and 7157 postexpansion in our inpatient analysis, as well as 31,767 person-years pre-expansion and 130,382 postexpansion in our outpatient analysis.
Outcomes and Variables
Our primary outcomes were comparative shifts in VA reliance between expansion and nonexpansion states after Medicaid expansion for both inpatient and outpatient depression care. For each year of study, we calculated a veteran’s VA reliance by aggregating the number of days with depression-related encounters at the VA and dividing by the total number of days with a VA or Medicaid depression-related encounters for the year. To provide context to these shifts in VA reliance, we further analyzed the changes in the proportion of annual VA-Medicaid dual users and annual per capita utilization of depression care across the VA and Medicaid.
We conducted subanalyses by income-eligible and service-connected veterans and adjusted our models for age, non-White race, sex, distances to the nearest inpatient and outpatient VA facilities, and VA Relative Risk Score, which is a measure of disease burden and clinical complexity validated specifically for veterans.25
Statistical Analysis
We used fractional logistic regression to model the adjusted effect of Medicaid expansion on VA reliance for depression care. In parallel, we leveraged ordered logit regression and negative binomial regression models to examine the proportion of VA-Medicaid dual users and the per capita utilization of Medicaid and VA depression care, respectively. To estimate the difference-in-difference effects, we used the interaction term of 2 categorical variables—expansion vs nonexpansion states and pre- vs postexpansion status—as the independent variable. We then calculated the average marginal effects with 95% CIs to estimate the differences in outcomes between expansion and nonexpansion states from pre- to postexpansion periods, as well as year-by-year shifts as a robustness check. We conducted these analyses using Stata MP, version 15.
Results
Baseline and postexpansion characteristics
VA Reliance
Overall, we observed postexpansion decreases in VA reliance for depression care
At the state level, reliance on the VA for inpatient depression care in NY decreased by 13.53 pp (95% CI, -22.58 to -4.49) for income-eligible veterans and 16.67 pp (95% CI, -24.53 to -8.80) for service-connected veterans. No relative differences were observed in the outpatient comparisons for both income-eligible (-0.58 pp; 95% CI, -2.13 to 0.98) and service-connected (0.05 pp; 95% CI, -1.00 to 1.10) veterans. In AZ, Medicaid expansion was associated with decreased VA reliance for outpatient depression care among income-eligible veterans (-8.60 pp; 95% CI, -10.60 to -6.61), greater than that for service-connected veterans (-2.89 pp; 95% CI, -4.02 to -1.77). This decrease in VA reliance was significant in the inpatient context only for service-connected veterans (-4.55 pp; 95% CI, -8.14 to -0.97), not income-eligible veterans (-8.38 pp; 95% CI, -17.91 to 1.16).
By applying the aggregate pp changes toward the postexpansion number of visits across both expansion and nonexpansion states, we found that expansion of Medicaid across all our study states would have resulted in 996 fewer hospitalizations and 10,109 fewer outpatient visits for depression at VA in the postexpansion period vs if no states had chosen to expand Medicaid.
Dual Use/Per Capita Utilization
Overall, Medicaid expansion was associated with greater dual use for inpatient depression care—a 0.97-pp (95% CI, 0.46 to 1.48) increase among service-connected veterans and a 0.64-pp (95% CI, 0.35 to 0.94) increase among income-eligible veterans.
At the state level, NY similarly showed increases in dual use among both service-connected (1.48 pp; 95% CI, 0.80 to 2.16) and income-eligible veterans (0.73 pp; 95% CI, 0.39 to 1.07) after Medicaid expansion. However, dual use in AZ increased significantly only among service-connected veterans (0.70 pp; 95% CI, 0.03 to 1.38), not income-eligible veterans (0.31 pp; 95% CI, -0.17 to 0.78).
Among outpatient visits, Medicaid expansion was associated with increased dual use only for income-eligible veterans (0.16 pp; 95% CI, 0.03-0.29), and not service-connected veterans (0.09 pp; 95% CI, -0.04 to 0.21). State-level analyses showed that Medicaid expansion in NY was not associated with changes in dual use for either service-connected (0.01 pp; 95% CI, -0.16 to 0.17) or income-eligible veterans (0.03 pp; 95% CI, -0.12 to 0.18), while expansion in AZ was associated with increases in dual use among both service-connected (0.42 pp; 95% CI, 0.23 to 0.61) and income-eligible veterans (0.83 pp; 95% CI, 0.59 to 1.07).
Concerning per capita utilization of depression care after Medicaid expansion, analyses showed no detectable changes for either inpatient or outpatient services, among both service-connected and income-eligible veterans. However, while this pattern held at the state level among hospitalizations, outpatient visit results showed divergent trends between AZ and NY. In NY, Medicaid expansion was associated with decreased per capita utilization of outpatient depression care among both service-connected (-0.25 visits annually; 95% CI, -0.48 to -0.01) and income-eligible veterans (-0.64 visits annually; 95% CI, -0.93 to -0.35). In AZ, Medicaid expansion was associated with increased per capita utilization of outpatient depression care among both service-connected (0.62 visits annually; 95% CI, 0.32-0.91) and income-eligible veterans (2.32 visits annually; 95% CI, 1.99-2.65).
Discussion
Our study quantified changes in depression-related health care utilization after Medicaid expansions in NY and AZ in 2001. Overall, the balance of evidence indicated that Medicaid expansion was associated with decreased reliance on the VA for depression-related services. There was an exception: income-eligible veterans in AZ did not shift their hospital care away from the VA in a statistically discernible way, although the point estimate was lower. More broadly, these findings concerning veterans’ reliance varied not only in inpatient vs outpatient services and income- vs service-connected eligibility, but also in the state-level contexts of veteran dual users and per capita utilization.
Given that the overall per capita utilization of depression care was unchanged from pre- to postexpansion periods, one might interpret the decreases in VA reliance and increases in Medicaid-VA dual users as a substitution effect from VA care to non-VA care. This could be plausible for hospitalizations where state-level analyses showed similarly stable levels of per capita utilization. However, state-level trends in our outpatient utilization analysis, especially with a substantial 2.32 pp increase in annual per capita visits among income-eligible veterans in AZ, leave open the possibility that in some cases veterans may be complementing VA care with Medicaid-reimbursed services.
The causes underlying these differences in reliance shifts between NY and AZ are likely also influenced by the policy contexts of their respective Medicaid expansions. For example, in 1999, NY passed Kendra’s Law, which established a procedure for obtaining court orders for assisted outpatient mental health treatment for individuals deemed unlikely to survive safely in the community.26 A reasonable inference is that there was less unfulfilled outpatient mental health need in NY under the existing accessibility provisioned by Kendra’s Law. In addition, while both states extended coverage to childless adults under 100% of the Federal Poverty level (FPL), the AZ Medicaid expansion was via a voters’ initiative and extended family coverage to 200% FPL vs 150% FPL for families in NY. Given that the AZ Medicaid expansion enjoyed both broader public participation and generosity in terms of eligibility, its uptake and therefore effect size may have been larger than in NY for nonacute outpatient care.
Our findings contribute to the growing body of literature surrounding the changes in health care utilization after Medicaid expansion, specifically for a newly dual-eligible population of veterans seeking mental health services for depression. While prior research concerning Medicare dual-enrolled veterans has shown high reliance on the VA for both mental health diagnoses and services, scholars have established the association of Medicaid enrollment with decreased VA reliance.27-29 Our analysis is the first to investigate state-level effects of Medicaid expansion on VA reliance for a single mental health condition using a natural experimental framework. We focus on a population that includes a large portion of veterans who are newly Medicaid-eligible due to a sweeping policy change and use demographically matched nonexpansion states to draw comparisons in VA reliance for depression care. Our findings of Medicaid expansion–associated decreases in VA reliance for depression care complement prior literature that describe Medicaid enrollment–associated decreases in VA reliance for overall mental health care.
Implications
From a systems-level perspective, the implications of shifting services away from the VA are complex and incompletely understood. The VA lacks interoperability with the electronic health records (EHRs) used by Medicaid clinicians. Consequently, significant issues of service duplication and incomplete clinical data exist for veterans seeking treatment outside of the VA system, posing health care quality and safety concerns.30 On one hand, Medicaid access is associated with increased health care utilization attributed to filling unmet needs for Medicare dual enrollees, as well as increased prescription filling for psychiatric medications.31,32 Furthermore, the only randomized control trial of Medicaid expansion to date was associated with a 9-pp decrease in positive screening rates for depression among those who received access at around 2 years postexpansion.33 On the other hand, the VA has developed a mental health system tailored to the particular needs of veterans, and health care practitioners at the VA have significantly greater rates of military cultural competency compared to those in nonmilitary settings (70% vs 24% in the TRICARE network and 8% among those with no military or TRICARE affiliation).34 Compared to individuals seeking mental health services with private insurance plans, veterans were about twice as likely to receive appropriate treatment for schizophrenia and depression at the VA.35 These documented strengths of VA mental health care may together help explain the small absolute number of visits that were associated with shifts away from VA overall after Medicaid expansion.
Finally, it is worth considering extrinsic factors that influence utilization among newly dual-eligible veterans. For example, hospitalizations are less likely to be planned than outpatient services, translating to a greater importance of proximity to a nearby medical facility than a veteran’s preference of where to seek care. In the same vein, major VA medical centers are fewer and more distant on average than VA outpatient clinics, therefore reducing the advantage of a Medicaid-reimbursed outpatient clinic in terms of distance.36 These realities may partially explain the proportionally larger shifts away from the VA for hospitalizations compared to outpatient care for depression.
Limitations and Future Directions
Our results should be interpreted within methodological and data limitations. With only 2 states in our sample, NY demonstrably skewed overall results, contributing 1.7 to 3 times more observations than AZ across subanalyses—a challenge also cited by Sommers and colleagues.19 Our veteran groupings were also unable to distinguish those veterans classified as service-connected who may also have qualified by income-eligible criteria (which would tend to understate the size of results) and those veterans who gained and then lost Medicaid coverage in a given year. Our study also faces limitations in generalizability and establishing causality. First, we included only 2 historical state Medicaid expansions, compared with the 38 states and Washington, DC, that have now expanded Medicaid to date under the ACA. Just in the 2 states from our study, we noted significant heterogeneity in the shifts associated with Medicaid expansion, which makes extrapolating specific trends difficult. Differences in underlying health care resources, legislation, and other external factors may limit the applicability of Medicaid expansion in the era of the ACA, as well as the Veterans Choice and MISSION acts. Second, while we leveraged a difference-in-difference analysis using demographically matched, neighboring comparison states, our findings are nevertheless drawn from observational data obviating causality. VA data for other sources of coverage such as private insurance are limited and not included in our study, and MAX datasets vary by quality across states, translating to potential gaps in our study cohort.28
Moving forward, our study demonstrates the potential for applying a natural experimental approach to studying dual-eligible veterans at the interface of Medicaid expansion. We focused on changes in VA reliance for the specific condition of depression and, in doing so, invite further inquiry into the impact of state mental health policy on outcomes more proximate to veterans’ outcomes. Clinical indicators, such as rates of antidepressant filling, utilization and duration of psychotherapy, and PHQ-9 scores, can similarly be investigated by natural experimental design. While current limits of administrative data and the siloing of EHRs may pose barriers to some of these avenues of research, multidisciplinary methodologies and data querying innovations such as natural language processing algorithms for clinical notes hold exciting opportunities to bridge the gap between policy and clinical efficacy.
Conclusions
This study applied a difference-in-difference analysis and found that Medicaid expansion is associated with decreases in VA reliance for both inpatient and outpatient services for depression. As additional data are generated from the Medicaid expansions of the ACA, similarly robust methods should be applied to further explore the impacts associated with such policy shifts and open the door to a better understanding of implications at the clinical level.
Acknowledgments
We acknowledge the efforts of Janine Wong, who proofread and formatted the manuscript.
1. US Department of Veterans Affairs, Veterans Health Administration. About VA. 2019. Updated September 27, 2022. Accessed September 29, 2022. https://www.va.gov/health/
2. Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry. 2010;44(1):4-19. doi:10.3109/00048670903393597
3. Lan CW, Fiellin DA, Barry DT, et al. The epidemiology of substance use disorders in US veterans: a systematic review and analysis of assessment methods. Am J Addict. 2016;25(1):7-24. doi:10.1111/ajad.12319
4. Grant BF, Saha TD, June Ruan W, et al. Epidemiology of DSM-5 drug use disorder results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiat. 2016;73(1):39-47. doi:10.1001/jamapsychiatry.015.2132
5. Pemberton MR, Forman-Hoffman VL, Lipari RN, Ashley OS, Heller DC, Williams MR. Prevalence of past year substance use and mental illness by veteran status in a nationally representative sample. CBHSQ Data Review. Published November 9, 2016. Accessed October 6, 2022. https://www.samhsa.gov/data/report/prevalence-past-year-substance-use-and-mental-illness-veteran-status-nationally
6. Watkins KE, Pincus HA, Smith B, et al. Veterans Health Administration Mental Health Program Evaluation: Capstone Report. 2011. Accessed September 29, 2022. https://www.rand.org/pubs/technical_reports/TR956.html
7. Henry J. Kaiser Family Foundation. Medicaid’s role in covering veterans. June 29, 2017. Accessed September 29, 2022. https://www.kff.org/infographic/medicaids-role-in-covering-veterans
8. Substance Abuse and Mental Health Services Administration. Results from the 2016 National Survey on Drug Use and Health: detailed tables. September 7, 2017. Accessed September 29, 2022. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf
9. Wen H, Druss BG, Cummings JR. Effect of Medicaid expansions on health insurance coverage and access to care among low-income adults with behavioral health conditions. Health Serv Res. 2015;50:1787-1809. doi:10.1111/1475-6773.12411
10. O’Mahen PN, Petersen LA. Effects of state-level Medicaid expansion on Veterans Health Administration dual enrollment and utilization: potential implications for future coverage expansions. Med Care. 2020;58(6):526-533. doi:10.1097/MLR.0000000000001327
11. Ono SS, Dziak KM, Wittrock SM, et al. Treating dual-use patients across two health care systems: a qualitative study. Fed Pract. 2015;32(8):32-37.
12. Weeks WB, Mahar PJ, Wright SM. Utilization of VA and Medicare services by Medicare-eligible veterans: the impact of additional access points in a rural setting. J Healthc Manag. 2005;50(2):95-106.
13. Gellad WF, Thorpe JM, Zhao X, et al. Impact of dual use of Department of Veterans Affairs and Medicare part d drug benefits on potentially unsafe opioid use. Am J Public Health. 2018;108(2):248-255. doi:10.2105/AJPH.2017.304174
14. Coughlin SS, Young L. A review of dual health care system use by veterans with cardiometabolic disease. J Hosp Manag Health Policy. 2018;2:39. doi:10.21037/jhmhp.2018.07.05
15. Radomski TR, Zhao X, Thorpe CT, et al. The impact of medication-based risk adjustment on the association between veteran health outcomes and dual health system use. J Gen Intern Med. 2017;32(9):967-973. doi:10.1007/s11606-017-4064-4
16. Kullgren JT, Fagerlin A, Kerr EA. Completing the MISSION: a blueprint for helping veterans make the most of new choices. J Gen Intern Med. 2020;35(5):1567-1570. doi:10.1007/s11606-019-05404-w
17. VA MISSION Act of 2018, 38 USC §101 (2018). https://www.govinfo.gov/app/details/USCODE-2018-title38/USCODE-2018-title38-partI-chap1-sec101
18. Vanneman ME, Phibbs CS, Dally SK, Trivedi AN, Yoon J. The impact of Medicaid enrollment on Veterans Health Administration enrollees’ behavioral health services use. Health Serv Res. 2018;53(suppl 3):5238-5259. doi:10.1111/1475-6773.13062
19. Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012;367(11):1025-1034. doi:10.1056/NEJMsa1202099
20. US Department of Veterans Affairs Office of Mental Health. 2019 national veteran suicide prevention annual report. 2019. Accessed September 29, 2022. https://www.mentalhealth.va.gov/docs/data-sheets/2019/2019_National_Veteran_Suicide_Prevention_Annual_Report_508.pdf
21. Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147(1-3):17-28. doi:10.1016/j.jad.2013.01.004
22. Adekkanattu P, Sholle ET, DeFerio J, Pathak J, Johnson SB, Campion TR Jr. Ascertaining depression severity by extracting Patient Health Questionnaire-9 (PHQ-9) scores from clinical notes. AMIA Annu Symp Proc. 2018;2018:147-156.
23. DeRubeis RJ, Siegle GJ, Hollon SD. Cognitive therapy versus medication for depression: treatment outcomes and neural mechanisms. Nat Rev Neurosci. 2008;9(10):788-796. doi:10.1038/nrn2345
24. Cully JA, Zimmer M, Khan MM, Petersen LA. Quality of depression care and its impact on health service use and mortality among veterans. Psychiatr Serv. 2008;59(12):1399-1405. doi:10.1176/ps.2008.59.12.1399
25. Byrne MM, Kuebeler M, Pietz K, Petersen LA. Effect of using information from only one system for dually eligible health care users. Med Care. 2006;44(8):768-773. doi:10.1097/01.mlr.0000218786.44722.14
26. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396. doi:10.1176/appi.ps.201400537
27. Petersen LA, Byrne MM, Daw CN, Hasche J, Reis B, Pietz K. Relationship between clinical conditions and use of Veterans Affairs health care among Medicare-enrolled veterans. Health Serv Res. 2010;45(3):762-791. doi:10.1111/j.1475-6773.2010.01107.x
28. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Use of Veterans Affairs and Medicaid services for dually enrolled veterans. Health Serv Res. 2018;53(3):1539-1561. doi:10.1111/1475-6773.12727
29. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Veterans’ reliance on VA care by type of service and distance to VA for nonelderly VA-Medicaid dual enrollees. Med Care. 2019;57(3):225-229. doi:10.1097/MLR.0000000000001066
30. Gaglioti A, Cozad A, Wittrock S, et al. Non-VA primary care providers’ perspectives on comanagement for rural veterans. Mil Med. 2014;179(11):1236-1243. doi:10.7205/MILMED-D-13-00342
31. Moon S, Shin J. Health care utilization among Medicare-Medicaid dual eligibles: a count data analysis. BMC Public Health. 2006;6(1):88. doi:10.1186/1471-2458-6-88
32. Henry J. Kaiser Family Foundation. Facilitating access to mental health services: a look at Medicaid, private insurance, and the uninsured. November 27, 2017. Accessed September 29, 2022. https://www.kff.org/medicaid/fact-sheet/facilitating-access-to-mental-health-services-a-look-at-medicaid-private-insurance-and-the-uninsured
33. Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment - effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713-1722. doi:10.1056/NEJMsa1212321
34. Tanielian T, Farris C, Batka C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. 2014. Accessed September 29, 2022. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf
35. Kizer KW, Dudley RA. Extreme makeover: transformation of the Veterans Health Care System. Annu Rev Public Health. 2009;30(1):313-339. doi:10.1146/annurev.publhealth.29.020907.090940
36. Brennan KJ. Kendra’s Law: final report on the status of assisted outpatient treatment, appendix 2. 2002. Accessed September 29, 2022. https://omh.ny.gov/omhweb/kendra_web/finalreport/appendix2.htm
1. US Department of Veterans Affairs, Veterans Health Administration. About VA. 2019. Updated September 27, 2022. Accessed September 29, 2022. https://www.va.gov/health/
2. Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry. 2010;44(1):4-19. doi:10.3109/00048670903393597
3. Lan CW, Fiellin DA, Barry DT, et al. The epidemiology of substance use disorders in US veterans: a systematic review and analysis of assessment methods. Am J Addict. 2016;25(1):7-24. doi:10.1111/ajad.12319
4. Grant BF, Saha TD, June Ruan W, et al. Epidemiology of DSM-5 drug use disorder results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiat. 2016;73(1):39-47. doi:10.1001/jamapsychiatry.015.2132
5. Pemberton MR, Forman-Hoffman VL, Lipari RN, Ashley OS, Heller DC, Williams MR. Prevalence of past year substance use and mental illness by veteran status in a nationally representative sample. CBHSQ Data Review. Published November 9, 2016. Accessed October 6, 2022. https://www.samhsa.gov/data/report/prevalence-past-year-substance-use-and-mental-illness-veteran-status-nationally
6. Watkins KE, Pincus HA, Smith B, et al. Veterans Health Administration Mental Health Program Evaluation: Capstone Report. 2011. Accessed September 29, 2022. https://www.rand.org/pubs/technical_reports/TR956.html
7. Henry J. Kaiser Family Foundation. Medicaid’s role in covering veterans. June 29, 2017. Accessed September 29, 2022. https://www.kff.org/infographic/medicaids-role-in-covering-veterans
8. Substance Abuse and Mental Health Services Administration. Results from the 2016 National Survey on Drug Use and Health: detailed tables. September 7, 2017. Accessed September 29, 2022. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf
9. Wen H, Druss BG, Cummings JR. Effect of Medicaid expansions on health insurance coverage and access to care among low-income adults with behavioral health conditions. Health Serv Res. 2015;50:1787-1809. doi:10.1111/1475-6773.12411
10. O’Mahen PN, Petersen LA. Effects of state-level Medicaid expansion on Veterans Health Administration dual enrollment and utilization: potential implications for future coverage expansions. Med Care. 2020;58(6):526-533. doi:10.1097/MLR.0000000000001327
11. Ono SS, Dziak KM, Wittrock SM, et al. Treating dual-use patients across two health care systems: a qualitative study. Fed Pract. 2015;32(8):32-37.
12. Weeks WB, Mahar PJ, Wright SM. Utilization of VA and Medicare services by Medicare-eligible veterans: the impact of additional access points in a rural setting. J Healthc Manag. 2005;50(2):95-106.
13. Gellad WF, Thorpe JM, Zhao X, et al. Impact of dual use of Department of Veterans Affairs and Medicare part d drug benefits on potentially unsafe opioid use. Am J Public Health. 2018;108(2):248-255. doi:10.2105/AJPH.2017.304174
14. Coughlin SS, Young L. A review of dual health care system use by veterans with cardiometabolic disease. J Hosp Manag Health Policy. 2018;2:39. doi:10.21037/jhmhp.2018.07.05
15. Radomski TR, Zhao X, Thorpe CT, et al. The impact of medication-based risk adjustment on the association between veteran health outcomes and dual health system use. J Gen Intern Med. 2017;32(9):967-973. doi:10.1007/s11606-017-4064-4
16. Kullgren JT, Fagerlin A, Kerr EA. Completing the MISSION: a blueprint for helping veterans make the most of new choices. J Gen Intern Med. 2020;35(5):1567-1570. doi:10.1007/s11606-019-05404-w
17. VA MISSION Act of 2018, 38 USC §101 (2018). https://www.govinfo.gov/app/details/USCODE-2018-title38/USCODE-2018-title38-partI-chap1-sec101
18. Vanneman ME, Phibbs CS, Dally SK, Trivedi AN, Yoon J. The impact of Medicaid enrollment on Veterans Health Administration enrollees’ behavioral health services use. Health Serv Res. 2018;53(suppl 3):5238-5259. doi:10.1111/1475-6773.13062
19. Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012;367(11):1025-1034. doi:10.1056/NEJMsa1202099
20. US Department of Veterans Affairs Office of Mental Health. 2019 national veteran suicide prevention annual report. 2019. Accessed September 29, 2022. https://www.mentalhealth.va.gov/docs/data-sheets/2019/2019_National_Veteran_Suicide_Prevention_Annual_Report_508.pdf
21. Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147(1-3):17-28. doi:10.1016/j.jad.2013.01.004
22. Adekkanattu P, Sholle ET, DeFerio J, Pathak J, Johnson SB, Campion TR Jr. Ascertaining depression severity by extracting Patient Health Questionnaire-9 (PHQ-9) scores from clinical notes. AMIA Annu Symp Proc. 2018;2018:147-156.
23. DeRubeis RJ, Siegle GJ, Hollon SD. Cognitive therapy versus medication for depression: treatment outcomes and neural mechanisms. Nat Rev Neurosci. 2008;9(10):788-796. doi:10.1038/nrn2345
24. Cully JA, Zimmer M, Khan MM, Petersen LA. Quality of depression care and its impact on health service use and mortality among veterans. Psychiatr Serv. 2008;59(12):1399-1405. doi:10.1176/ps.2008.59.12.1399
25. Byrne MM, Kuebeler M, Pietz K, Petersen LA. Effect of using information from only one system for dually eligible health care users. Med Care. 2006;44(8):768-773. doi:10.1097/01.mlr.0000218786.44722.14
26. Watkins KE, Smith B, Akincigil A, et al. The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatr Serv. 2016;67(4):391-396. doi:10.1176/appi.ps.201400537
27. Petersen LA, Byrne MM, Daw CN, Hasche J, Reis B, Pietz K. Relationship between clinical conditions and use of Veterans Affairs health care among Medicare-enrolled veterans. Health Serv Res. 2010;45(3):762-791. doi:10.1111/j.1475-6773.2010.01107.x
28. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Use of Veterans Affairs and Medicaid services for dually enrolled veterans. Health Serv Res. 2018;53(3):1539-1561. doi:10.1111/1475-6773.12727
29. Yoon J, Vanneman ME, Dally SK, Trivedi AN, Phibbs Ciaran S. Veterans’ reliance on VA care by type of service and distance to VA for nonelderly VA-Medicaid dual enrollees. Med Care. 2019;57(3):225-229. doi:10.1097/MLR.0000000000001066
30. Gaglioti A, Cozad A, Wittrock S, et al. Non-VA primary care providers’ perspectives on comanagement for rural veterans. Mil Med. 2014;179(11):1236-1243. doi:10.7205/MILMED-D-13-00342
31. Moon S, Shin J. Health care utilization among Medicare-Medicaid dual eligibles: a count data analysis. BMC Public Health. 2006;6(1):88. doi:10.1186/1471-2458-6-88
32. Henry J. Kaiser Family Foundation. Facilitating access to mental health services: a look at Medicaid, private insurance, and the uninsured. November 27, 2017. Accessed September 29, 2022. https://www.kff.org/medicaid/fact-sheet/facilitating-access-to-mental-health-services-a-look-at-medicaid-private-insurance-and-the-uninsured
33. Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment - effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713-1722. doi:10.1056/NEJMsa1212321
34. Tanielian T, Farris C, Batka C, et al. Ready to serve: community-based provider capacity to deliver culturally competent, quality mental health care to veterans and their families. 2014. Accessed September 29, 2022. https://www.rand.org/content/dam/rand/pubs/research_reports/RR800/RR806/RAND_RR806.pdf
35. Kizer KW, Dudley RA. Extreme makeover: transformation of the Veterans Health Care System. Annu Rev Public Health. 2009;30(1):313-339. doi:10.1146/annurev.publhealth.29.020907.090940
36. Brennan KJ. Kendra’s Law: final report on the status of assisted outpatient treatment, appendix 2. 2002. Accessed September 29, 2022. https://omh.ny.gov/omhweb/kendra_web/finalreport/appendix2.htm
Black Veterans Less Likely to Get COVID-Specific Treatments at VAMCs
Black veterans hospitalized with COVID-19 were less likely to be treated with evidence-based treatments, in a study conducted in 130 US Department of Veterans Affairs (VA) medical centers between March 1, 2020, and February 28, 2022.
The study involved 12,135 Black veterans and 40,717 White veterans. Most patients hospitalized during period 1 (March-September 2020) were Black veterans and the proportion of White patients increased over time. The latter 3 periods, which included the Delta- and Omicron-predominant periods, saw the most admissions.
Controlling for the site of treatment, Black patients were equally likely to be admitted to the intensive care unit (40% vs 43%). However, they were less likely to receive steroids, remdesivir, or immunomodulatory drugs.
The researchers say their data confirm other findings from 41 US health care systems participating in the National Patient-Centered Clinical Research Network (PCORNet), which found lower use of monoclonal antibody treatment for COVID infection for patients who identified as Asian, Black, Hispanic, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, or multiple races.
The researchers did not observe consistent differences in clinical outcomes between Black and White patients. After adjusting for demographics, chronic health conditions, severity of acute illness, and receipt of COVID-19–specific treatments, there was no association of Black race with hospital mortality or 30-day readmission. Black and White patients had a similar burden of preexisting health conditions. Of 38,782 patients discharged, 14% were readmitted within 30 days; the median time to readmission for both groups was 9 days.
Differences in care were partially explained by within- and between-hospital differences, the researchers say. They also cite research that demonstrated a poorer quality of care for hospitals with higher monthly COVID-19 discharges and hospital size.
The study results contradict the assumptions that differences in inpatient treatment by race and ethnicity may be due to differences in clinical indications for medication use based on age and comorbidities, such as chronic kidney or liver disease, the researchers say. For one thing, the VA issued a systemwide COVID-19 response plan that included specific treatment guidelines and distribution plans. But they also point to recent reports that have suggested that occult hypoxemia not detected by pulse oximetry occurs “far more often in Black patients than White patients,” which could result in delayed or missed opportunities to treat patients with COVID-19.
Black veterans hospitalized with COVID-19 were less likely to be treated with evidence-based treatments, in a study conducted in 130 US Department of Veterans Affairs (VA) medical centers between March 1, 2020, and February 28, 2022.
The study involved 12,135 Black veterans and 40,717 White veterans. Most patients hospitalized during period 1 (March-September 2020) were Black veterans and the proportion of White patients increased over time. The latter 3 periods, which included the Delta- and Omicron-predominant periods, saw the most admissions.
Controlling for the site of treatment, Black patients were equally likely to be admitted to the intensive care unit (40% vs 43%). However, they were less likely to receive steroids, remdesivir, or immunomodulatory drugs.
The researchers say their data confirm other findings from 41 US health care systems participating in the National Patient-Centered Clinical Research Network (PCORNet), which found lower use of monoclonal antibody treatment for COVID infection for patients who identified as Asian, Black, Hispanic, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, or multiple races.
The researchers did not observe consistent differences in clinical outcomes between Black and White patients. After adjusting for demographics, chronic health conditions, severity of acute illness, and receipt of COVID-19–specific treatments, there was no association of Black race with hospital mortality or 30-day readmission. Black and White patients had a similar burden of preexisting health conditions. Of 38,782 patients discharged, 14% were readmitted within 30 days; the median time to readmission for both groups was 9 days.
Differences in care were partially explained by within- and between-hospital differences, the researchers say. They also cite research that demonstrated a poorer quality of care for hospitals with higher monthly COVID-19 discharges and hospital size.
The study results contradict the assumptions that differences in inpatient treatment by race and ethnicity may be due to differences in clinical indications for medication use based on age and comorbidities, such as chronic kidney or liver disease, the researchers say. For one thing, the VA issued a systemwide COVID-19 response plan that included specific treatment guidelines and distribution plans. But they also point to recent reports that have suggested that occult hypoxemia not detected by pulse oximetry occurs “far more often in Black patients than White patients,” which could result in delayed or missed opportunities to treat patients with COVID-19.
Black veterans hospitalized with COVID-19 were less likely to be treated with evidence-based treatments, in a study conducted in 130 US Department of Veterans Affairs (VA) medical centers between March 1, 2020, and February 28, 2022.
The study involved 12,135 Black veterans and 40,717 White veterans. Most patients hospitalized during period 1 (March-September 2020) were Black veterans and the proportion of White patients increased over time. The latter 3 periods, which included the Delta- and Omicron-predominant periods, saw the most admissions.
Controlling for the site of treatment, Black patients were equally likely to be admitted to the intensive care unit (40% vs 43%). However, they were less likely to receive steroids, remdesivir, or immunomodulatory drugs.
The researchers say their data confirm other findings from 41 US health care systems participating in the National Patient-Centered Clinical Research Network (PCORNet), which found lower use of monoclonal antibody treatment for COVID infection for patients who identified as Asian, Black, Hispanic, American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, or multiple races.
The researchers did not observe consistent differences in clinical outcomes between Black and White patients. After adjusting for demographics, chronic health conditions, severity of acute illness, and receipt of COVID-19–specific treatments, there was no association of Black race with hospital mortality or 30-day readmission. Black and White patients had a similar burden of preexisting health conditions. Of 38,782 patients discharged, 14% were readmitted within 30 days; the median time to readmission for both groups was 9 days.
Differences in care were partially explained by within- and between-hospital differences, the researchers say. They also cite research that demonstrated a poorer quality of care for hospitals with higher monthly COVID-19 discharges and hospital size.
The study results contradict the assumptions that differences in inpatient treatment by race and ethnicity may be due to differences in clinical indications for medication use based on age and comorbidities, such as chronic kidney or liver disease, the researchers say. For one thing, the VA issued a systemwide COVID-19 response plan that included specific treatment guidelines and distribution plans. But they also point to recent reports that have suggested that occult hypoxemia not detected by pulse oximetry occurs “far more often in Black patients than White patients,” which could result in delayed or missed opportunities to treat patients with COVID-19.
VA Delays EHR Rollout—Again
The US Department of Veterans Affairs (VA) is pushing further deployments of the system to June 2023 “to address challenges” and make sure it’s functioning optimally.
Among the challenges: Safety concerns “voluminous enough and prevalent enough” to prompt the VA to disclose to 41,500 veterans enrolled in Washington, Idaho, Oregon, Montana, and Ohio that their care “may have been impacted as a result of the system’s deployment as it is currently configured,” VA Undersecretary for Health Shereef Elnahal said in a news conference.
The plan was to launch in the first quarter of 2023 in Western Washington, Michigan, and Ohio. But in a recent release, the VA said an investigation had found several technical and system issues, such as latency and slowness, and problems with patient scheduling, referrals, medication management, and other types of medical orders. During this “assess and address” period, the VA says, it will correct outstanding issues—especially those that may have patient safety implications—before restarting deployments at other VA medical centers.
“Right now, the Oracle Cerner [EHR] system is not delivering for veterans or VA health care providers—and we are holding Oracle Cerner and ourselves accountable to get this right,” said VA Deputy Secretary Donald Remy, who has oversight over the EHR program. “We are delaying all future deployments of the new EHR while we fully assess performance and address every concern. Veterans and clinicians deserve a seamless, modernized health record system, and we will not rest until they get it.”
The modernized EHR, intended to replace the Veterans Health Information Systems and Technology Architecture (VistA), has been plagued by problems from the very first launch in October 2020 at Mann-Grandstaff VA Medical Center and associated clinics in the Northwest. Deputy Inspector David Case, of the Office of Inspector General (OIG), reported to the House Committee on Veterans’ Affairs on oversight between 2020 and July 2021. Among other things, the OIG identified problems with the infrastructure and with users’ experiences. Clinical and administrative staff at Mann-Grandstaff and a Columbus clinic shared their frustration with OIG personnel about the “significant system and process limitations that raised concerns about the continuity of and prompt access to quality patient care.”
For example, according to an OIG report from July 2022, the new EHR sent thousands of orders for medical care to an “undetectable location, or unknown queue” instead of the intended location. The mis-delivery caused 149 patient harm events.
On October 11, the VA confirmed to The Spokesman-Review, a Spokane-based newspaper, that a patient had died at the VA clinic in Columbus. The death was attributed to the patient not receiving medication due to incorrect information. The incident is being treated as a potential “sentinel event.”
Elnahal, who met with employees in September at the Columbus clinic where the Oracle Cerner system was launched in April, said he found that the highly complex system made it hard for clinicians to perform routine tasks, such as ordering tests or follow-up appointments. Delays in follow-ups—including a yearlong delay in treatment for a veteran ultimately diagnosed with terminal cancer—were the main cause of the cases of harm cited in the July OIG report.
The veterans who received the letter about the potential impact on their health care “got caught up in this phenomenon of commands not getting where they need to go,” Elnahal said in a news conference in September.
Senator Patty Murray (D-WA), a senior member of the Veterans Affairs Committee, has been consistently pressing the VA to do something about the EHR system’s flaws. “It’s painfully clear,” she said in a statement, “we need to stop this program until the VA can fix these serious issues before they hurt anyone else.”
After finding more than 200 orders in the unknown queue in May 2022, the OIG said, it “has concerns with the effectiveness of Cerner’s plan to mitigate the safety risk.” While executing its “assess and address” plan, the VA will continue to focus on the 5 facilities where the new system has been deployed. “Sometimes, you’re not presented with options to immediately resolve the safety concerns that are in front of you,” Elnahal told reporters. “It is simply the case that the best option in front of us to resolve these patient safety concerns is to work with Oracle Cerner over the next several months to resolve the Cerner system issues at the sites where it exists. We know that this is possible, because other health systems have gone through this journey before, and I think we can do it.”
Veterans who believe their care may have been affected can call a dedicated call center at 800.319.9446. A VA health care team will follow up within 5 days.
The US Department of Veterans Affairs (VA) is pushing further deployments of the system to June 2023 “to address challenges” and make sure it’s functioning optimally.
Among the challenges: Safety concerns “voluminous enough and prevalent enough” to prompt the VA to disclose to 41,500 veterans enrolled in Washington, Idaho, Oregon, Montana, and Ohio that their care “may have been impacted as a result of the system’s deployment as it is currently configured,” VA Undersecretary for Health Shereef Elnahal said in a news conference.
The plan was to launch in the first quarter of 2023 in Western Washington, Michigan, and Ohio. But in a recent release, the VA said an investigation had found several technical and system issues, such as latency and slowness, and problems with patient scheduling, referrals, medication management, and other types of medical orders. During this “assess and address” period, the VA says, it will correct outstanding issues—especially those that may have patient safety implications—before restarting deployments at other VA medical centers.
“Right now, the Oracle Cerner [EHR] system is not delivering for veterans or VA health care providers—and we are holding Oracle Cerner and ourselves accountable to get this right,” said VA Deputy Secretary Donald Remy, who has oversight over the EHR program. “We are delaying all future deployments of the new EHR while we fully assess performance and address every concern. Veterans and clinicians deserve a seamless, modernized health record system, and we will not rest until they get it.”
The modernized EHR, intended to replace the Veterans Health Information Systems and Technology Architecture (VistA), has been plagued by problems from the very first launch in October 2020 at Mann-Grandstaff VA Medical Center and associated clinics in the Northwest. Deputy Inspector David Case, of the Office of Inspector General (OIG), reported to the House Committee on Veterans’ Affairs on oversight between 2020 and July 2021. Among other things, the OIG identified problems with the infrastructure and with users’ experiences. Clinical and administrative staff at Mann-Grandstaff and a Columbus clinic shared their frustration with OIG personnel about the “significant system and process limitations that raised concerns about the continuity of and prompt access to quality patient care.”
For example, according to an OIG report from July 2022, the new EHR sent thousands of orders for medical care to an “undetectable location, or unknown queue” instead of the intended location. The mis-delivery caused 149 patient harm events.
On October 11, the VA confirmed to The Spokesman-Review, a Spokane-based newspaper, that a patient had died at the VA clinic in Columbus. The death was attributed to the patient not receiving medication due to incorrect information. The incident is being treated as a potential “sentinel event.”
Elnahal, who met with employees in September at the Columbus clinic where the Oracle Cerner system was launched in April, said he found that the highly complex system made it hard for clinicians to perform routine tasks, such as ordering tests or follow-up appointments. Delays in follow-ups—including a yearlong delay in treatment for a veteran ultimately diagnosed with terminal cancer—were the main cause of the cases of harm cited in the July OIG report.
The veterans who received the letter about the potential impact on their health care “got caught up in this phenomenon of commands not getting where they need to go,” Elnahal said in a news conference in September.
Senator Patty Murray (D-WA), a senior member of the Veterans Affairs Committee, has been consistently pressing the VA to do something about the EHR system’s flaws. “It’s painfully clear,” she said in a statement, “we need to stop this program until the VA can fix these serious issues before they hurt anyone else.”
After finding more than 200 orders in the unknown queue in May 2022, the OIG said, it “has concerns with the effectiveness of Cerner’s plan to mitigate the safety risk.” While executing its “assess and address” plan, the VA will continue to focus on the 5 facilities where the new system has been deployed. “Sometimes, you’re not presented with options to immediately resolve the safety concerns that are in front of you,” Elnahal told reporters. “It is simply the case that the best option in front of us to resolve these patient safety concerns is to work with Oracle Cerner over the next several months to resolve the Cerner system issues at the sites where it exists. We know that this is possible, because other health systems have gone through this journey before, and I think we can do it.”
Veterans who believe their care may have been affected can call a dedicated call center at 800.319.9446. A VA health care team will follow up within 5 days.
The US Department of Veterans Affairs (VA) is pushing further deployments of the system to June 2023 “to address challenges” and make sure it’s functioning optimally.
Among the challenges: Safety concerns “voluminous enough and prevalent enough” to prompt the VA to disclose to 41,500 veterans enrolled in Washington, Idaho, Oregon, Montana, and Ohio that their care “may have been impacted as a result of the system’s deployment as it is currently configured,” VA Undersecretary for Health Shereef Elnahal said in a news conference.
The plan was to launch in the first quarter of 2023 in Western Washington, Michigan, and Ohio. But in a recent release, the VA said an investigation had found several technical and system issues, such as latency and slowness, and problems with patient scheduling, referrals, medication management, and other types of medical orders. During this “assess and address” period, the VA says, it will correct outstanding issues—especially those that may have patient safety implications—before restarting deployments at other VA medical centers.
“Right now, the Oracle Cerner [EHR] system is not delivering for veterans or VA health care providers—and we are holding Oracle Cerner and ourselves accountable to get this right,” said VA Deputy Secretary Donald Remy, who has oversight over the EHR program. “We are delaying all future deployments of the new EHR while we fully assess performance and address every concern. Veterans and clinicians deserve a seamless, modernized health record system, and we will not rest until they get it.”
The modernized EHR, intended to replace the Veterans Health Information Systems and Technology Architecture (VistA), has been plagued by problems from the very first launch in October 2020 at Mann-Grandstaff VA Medical Center and associated clinics in the Northwest. Deputy Inspector David Case, of the Office of Inspector General (OIG), reported to the House Committee on Veterans’ Affairs on oversight between 2020 and July 2021. Among other things, the OIG identified problems with the infrastructure and with users’ experiences. Clinical and administrative staff at Mann-Grandstaff and a Columbus clinic shared their frustration with OIG personnel about the “significant system and process limitations that raised concerns about the continuity of and prompt access to quality patient care.”
For example, according to an OIG report from July 2022, the new EHR sent thousands of orders for medical care to an “undetectable location, or unknown queue” instead of the intended location. The mis-delivery caused 149 patient harm events.
On October 11, the VA confirmed to The Spokesman-Review, a Spokane-based newspaper, that a patient had died at the VA clinic in Columbus. The death was attributed to the patient not receiving medication due to incorrect information. The incident is being treated as a potential “sentinel event.”
Elnahal, who met with employees in September at the Columbus clinic where the Oracle Cerner system was launched in April, said he found that the highly complex system made it hard for clinicians to perform routine tasks, such as ordering tests or follow-up appointments. Delays in follow-ups—including a yearlong delay in treatment for a veteran ultimately diagnosed with terminal cancer—were the main cause of the cases of harm cited in the July OIG report.
The veterans who received the letter about the potential impact on their health care “got caught up in this phenomenon of commands not getting where they need to go,” Elnahal said in a news conference in September.
Senator Patty Murray (D-WA), a senior member of the Veterans Affairs Committee, has been consistently pressing the VA to do something about the EHR system’s flaws. “It’s painfully clear,” she said in a statement, “we need to stop this program until the VA can fix these serious issues before they hurt anyone else.”
After finding more than 200 orders in the unknown queue in May 2022, the OIG said, it “has concerns with the effectiveness of Cerner’s plan to mitigate the safety risk.” While executing its “assess and address” plan, the VA will continue to focus on the 5 facilities where the new system has been deployed. “Sometimes, you’re not presented with options to immediately resolve the safety concerns that are in front of you,” Elnahal told reporters. “It is simply the case that the best option in front of us to resolve these patient safety concerns is to work with Oracle Cerner over the next several months to resolve the Cerner system issues at the sites where it exists. We know that this is possible, because other health systems have gone through this journey before, and I think we can do it.”
Veterans who believe their care may have been affected can call a dedicated call center at 800.319.9446. A VA health care team will follow up within 5 days.
DoD will cover travel expenses for abortion care
Some 80,000 active-duty women are stationed in states with abortion restrictions or bans. That’s 40% of active-duty service women in the continental United States, according to research sponsored by the US Department of Defense (DoD) and released in September. Nearly all (95%) are of reproductive age. Annually, an estimated 2573 to 4126 women have an abortion, but just a handful of those are done at military treatment facilities. Moreover, roughly 275,000 DoD civilians also live in states with a full ban or extreme restrictions on access to abortion. Of those, more than 81,000 are women. Nearly 43% have no access to abortion or drastically abridged access.
The recent Supreme Court ruling in Dobbs v Jackson Women’s Health Organization has created uncertainty for those women and their families, and potential legal and financial risk for the health care practitioners who would provide reproductive care, Defense Secretary Lloyd Austin said in an October 20, 2022 memo.
Therefore, he has directed the DoD to take “all appropriate action… as soon as possible to ensure that our service members and their families can access reproductive health care and our health care providers can operate effectively.”
Among the actions he has approved: Paying for travel to reproductive health care—essentially, making it more feasible for members to cross state lines. Service members, he noted in the memo, are often required to travel or move to meet staffing, operational, and training requirements. The “practical effects,” he said, are that significant numbers of service members and their families “may be forced to travel greater distances, take more time off from work, and pay more out-of-pocket expenses to receive reproductive health care.”
Those effects, Austin said, “qualify as unusual, extraordinary, hardship, or emergency circumstances for service members and their dependents and will interfere with our ability to recruit, retain, and maintain the readiness of a highly qualified force.”
Women, who comprise 17% of the active-duty force, are the fastest-growing subpopulation in the military. For the past several years, according to the DoD research report, the military services have been “deliberately recruiting women”—who perform essential duties in every sector: health care and electrical and mechanical equipment repair, for example.
“The full effects of Dobbs on military readiness are yet to be known,” the report says, but it notes several potential problems: Women may not join the service knowing that they could end up in a state with restrictions. If already serving, they may leave. In some states, women face criminal prosecution.
The long arm of Dobbs reaches far into the future, too. For instance, if unintended pregnancies are carried to term, the DoD will need to provide care to women during pregnancy, delivery, and the postpartum period—and the family will need to care for the child. Looking only at women in states with restricted access or bans, the DoD estimates the number of unintended pregnancies annually would be 2800 among civilian employees and between 4400 and 4700 among active-duty service women.
Men are also directly affected: More than 40% of male service members are married to a civilian woman who is a TRICARE dependent, 20% of active-duty service women are married to a fellow service member, and active-duty service men might be responsible for pregnancies among women who are not DoD dependents but who might be unable to get an abortion, the DoD report notes.
Austin has directed the DoD to create a uniform policy that allows for appropriate administrative absence, to establish travel and transportation allowances, and to amend any applicable travel regulations to facilitate official travel to access noncovered reproductive health care that is unavailable within the local area of the service member’s permanent duty station.
So that health care practitioners do not have to face criminal or civil liability or risk losing their licenses, Austin directed the DoD to develop a program to reimburse applicable fees, as appropriate and consistent with applicable federal law, for DoD health care practitioners who wish to become licensed in a state other than that in which they are currently licensed. He also directed the DoD to develop a program to support DoD practitioners who are subject to adverse action, including indemnification of any verdict, judgment, or other monetary award consistent with applicable law.
“Our greatest strength is our people,” Austin wrote. “There is no higher priority than taking care of our people, and ensuring their health and well-being.” He directed that the actions outlined in the memorandum “be executed as soon as possible.”
Some 80,000 active-duty women are stationed in states with abortion restrictions or bans. That’s 40% of active-duty service women in the continental United States, according to research sponsored by the US Department of Defense (DoD) and released in September. Nearly all (95%) are of reproductive age. Annually, an estimated 2573 to 4126 women have an abortion, but just a handful of those are done at military treatment facilities. Moreover, roughly 275,000 DoD civilians also live in states with a full ban or extreme restrictions on access to abortion. Of those, more than 81,000 are women. Nearly 43% have no access to abortion or drastically abridged access.
The recent Supreme Court ruling in Dobbs v Jackson Women’s Health Organization has created uncertainty for those women and their families, and potential legal and financial risk for the health care practitioners who would provide reproductive care, Defense Secretary Lloyd Austin said in an October 20, 2022 memo.
Therefore, he has directed the DoD to take “all appropriate action… as soon as possible to ensure that our service members and their families can access reproductive health care and our health care providers can operate effectively.”
Among the actions he has approved: Paying for travel to reproductive health care—essentially, making it more feasible for members to cross state lines. Service members, he noted in the memo, are often required to travel or move to meet staffing, operational, and training requirements. The “practical effects,” he said, are that significant numbers of service members and their families “may be forced to travel greater distances, take more time off from work, and pay more out-of-pocket expenses to receive reproductive health care.”
Those effects, Austin said, “qualify as unusual, extraordinary, hardship, or emergency circumstances for service members and their dependents and will interfere with our ability to recruit, retain, and maintain the readiness of a highly qualified force.”
Women, who comprise 17% of the active-duty force, are the fastest-growing subpopulation in the military. For the past several years, according to the DoD research report, the military services have been “deliberately recruiting women”—who perform essential duties in every sector: health care and electrical and mechanical equipment repair, for example.
“The full effects of Dobbs on military readiness are yet to be known,” the report says, but it notes several potential problems: Women may not join the service knowing that they could end up in a state with restrictions. If already serving, they may leave. In some states, women face criminal prosecution.
The long arm of Dobbs reaches far into the future, too. For instance, if unintended pregnancies are carried to term, the DoD will need to provide care to women during pregnancy, delivery, and the postpartum period—and the family will need to care for the child. Looking only at women in states with restricted access or bans, the DoD estimates the number of unintended pregnancies annually would be 2800 among civilian employees and between 4400 and 4700 among active-duty service women.
Men are also directly affected: More than 40% of male service members are married to a civilian woman who is a TRICARE dependent, 20% of active-duty service women are married to a fellow service member, and active-duty service men might be responsible for pregnancies among women who are not DoD dependents but who might be unable to get an abortion, the DoD report notes.
Austin has directed the DoD to create a uniform policy that allows for appropriate administrative absence, to establish travel and transportation allowances, and to amend any applicable travel regulations to facilitate official travel to access noncovered reproductive health care that is unavailable within the local area of the service member’s permanent duty station.
So that health care practitioners do not have to face criminal or civil liability or risk losing their licenses, Austin directed the DoD to develop a program to reimburse applicable fees, as appropriate and consistent with applicable federal law, for DoD health care practitioners who wish to become licensed in a state other than that in which they are currently licensed. He also directed the DoD to develop a program to support DoD practitioners who are subject to adverse action, including indemnification of any verdict, judgment, or other monetary award consistent with applicable law.
“Our greatest strength is our people,” Austin wrote. “There is no higher priority than taking care of our people, and ensuring their health and well-being.” He directed that the actions outlined in the memorandum “be executed as soon as possible.”
Some 80,000 active-duty women are stationed in states with abortion restrictions or bans. That’s 40% of active-duty service women in the continental United States, according to research sponsored by the US Department of Defense (DoD) and released in September. Nearly all (95%) are of reproductive age. Annually, an estimated 2573 to 4126 women have an abortion, but just a handful of those are done at military treatment facilities. Moreover, roughly 275,000 DoD civilians also live in states with a full ban or extreme restrictions on access to abortion. Of those, more than 81,000 are women. Nearly 43% have no access to abortion or drastically abridged access.
The recent Supreme Court ruling in Dobbs v Jackson Women’s Health Organization has created uncertainty for those women and their families, and potential legal and financial risk for the health care practitioners who would provide reproductive care, Defense Secretary Lloyd Austin said in an October 20, 2022 memo.
Therefore, he has directed the DoD to take “all appropriate action… as soon as possible to ensure that our service members and their families can access reproductive health care and our health care providers can operate effectively.”
Among the actions he has approved: Paying for travel to reproductive health care—essentially, making it more feasible for members to cross state lines. Service members, he noted in the memo, are often required to travel or move to meet staffing, operational, and training requirements. The “practical effects,” he said, are that significant numbers of service members and their families “may be forced to travel greater distances, take more time off from work, and pay more out-of-pocket expenses to receive reproductive health care.”
Those effects, Austin said, “qualify as unusual, extraordinary, hardship, or emergency circumstances for service members and their dependents and will interfere with our ability to recruit, retain, and maintain the readiness of a highly qualified force.”
Women, who comprise 17% of the active-duty force, are the fastest-growing subpopulation in the military. For the past several years, according to the DoD research report, the military services have been “deliberately recruiting women”—who perform essential duties in every sector: health care and electrical and mechanical equipment repair, for example.
“The full effects of Dobbs on military readiness are yet to be known,” the report says, but it notes several potential problems: Women may not join the service knowing that they could end up in a state with restrictions. If already serving, they may leave. In some states, women face criminal prosecution.
The long arm of Dobbs reaches far into the future, too. For instance, if unintended pregnancies are carried to term, the DoD will need to provide care to women during pregnancy, delivery, and the postpartum period—and the family will need to care for the child. Looking only at women in states with restricted access or bans, the DoD estimates the number of unintended pregnancies annually would be 2800 among civilian employees and between 4400 and 4700 among active-duty service women.
Men are also directly affected: More than 40% of male service members are married to a civilian woman who is a TRICARE dependent, 20% of active-duty service women are married to a fellow service member, and active-duty service men might be responsible for pregnancies among women who are not DoD dependents but who might be unable to get an abortion, the DoD report notes.
Austin has directed the DoD to create a uniform policy that allows for appropriate administrative absence, to establish travel and transportation allowances, and to amend any applicable travel regulations to facilitate official travel to access noncovered reproductive health care that is unavailable within the local area of the service member’s permanent duty station.
So that health care practitioners do not have to face criminal or civil liability or risk losing their licenses, Austin directed the DoD to develop a program to reimburse applicable fees, as appropriate and consistent with applicable federal law, for DoD health care practitioners who wish to become licensed in a state other than that in which they are currently licensed. He also directed the DoD to develop a program to support DoD practitioners who are subject to adverse action, including indemnification of any verdict, judgment, or other monetary award consistent with applicable law.
“Our greatest strength is our people,” Austin wrote. “There is no higher priority than taking care of our people, and ensuring their health and well-being.” He directed that the actions outlined in the memorandum “be executed as soon as possible.”
VA Fast-Tracks Hiring to Address Critical Shortages
In an intensive push to fill acute workforce shortages, the US Department of Veterans Affairs (VA) is holding a “national onboarding surge event” the week of November 14. The goal is to get people who have already said yes to a job in the VA on that job more quickly. Every VA facility has been asked to submit a list of the highest-priority candidates, regardless of the position.
One of the most pressing reasons for getting more workers into the pipeline faster is that more and more veterans are entering VA care. As of October 1, tens of thousands of veterans will be eligible for VA health care, thanks to the Sergeant First Class Heath Robinson Honoring our Promise to Address Comprehensive Toxics Act of 2022 (PACT Act), passed in August, which expanded benefits for post-9/11 service members with illnesses due to toxic exposures.
Another reason is the need to fill the gaps left by attrition. In an October 19 press briefing, VA Undersecretary for Health Shereef Elnahal said the agency needs to hire about 52,000 employees per year just to keep up with the rate of health care professionals (HCPs) leaving the agency. At a September breakfast meeting with the Defense Writers Group, VA Secretary Denis McDonough said July 2022 marked the first month this year that the VA hired more nurses than it lost to retirement. He said the VA needs to hire 45,000 nurses over the next 3 years to keep up with attrition and growing demand for veteran care.
“We have to do a better job on hiring,” McDonough said. Streamlining the process is a major goal. Hiring rules loosened during the pandemic have since tightened back up. He pointed out that in many cases, the VA takes 90 to 100 days to onboard candidates and called the long-drawn-out process “being dragged through a bureaucratic morass.” During that time, he said, “They’re not being paid, they’re filling out paperwork… That’s disastrous.” In his press briefing, Elnahal said “we lose folks after we’ve made the selection” because the process is so long.
Moreover, the agency has a critical shortage not only of HCPs but the human resources professionals needed to fast-track the hirees’ progress. McDonough called it a “supply chain issue.” “We have the lowest ratio of human resource professionals per employee in the federal government by a long shot.” Partly, he said, because “a lot of our people end up hired away to other federal agencies.”
McDonough said the VA is also interested in transitioning more active-duty service members with in-demand skills, certifications, and talent into the VA workforce. “Cross-walking active duty into VA service much more aggressively,” he said, is another way to “grow that supply of ready, deployable, trained personnel.” The PACT Act gives the VA new incentives to entice workers, such as expanded recruitment, retention bonuses, and student loan repayment. The VA already provides training to about 1500 nurse and nurse residency programs across the VA, McDonough said but has plans for expanding to 5 times its current scope. He also addressed the question of a looming physician shortage: “Roughly 7 in 10 doctors in the United States will have had some portion of their training in a VA facility. We have to maintain that training function going forward.” The VA trains doctors, he added, “better than anybody else.”
The onboarding event will serve as a “national signal that we take this priority very seriously,” Elnahal said. “This will be not only a chance to have a step function improvement in the number of folks on board, which is an urgent priority, but to also set the groundwork for the more longitudinal work that we will need to do to improve the hiring process.”
Bulking up the workforce, he said, is “still far and away among our first priorities. Because if we don’t get our hospitals and facility staffed, it’s going to be a really hard effort to make process on the other priorities.”
In an intensive push to fill acute workforce shortages, the US Department of Veterans Affairs (VA) is holding a “national onboarding surge event” the week of November 14. The goal is to get people who have already said yes to a job in the VA on that job more quickly. Every VA facility has been asked to submit a list of the highest-priority candidates, regardless of the position.
One of the most pressing reasons for getting more workers into the pipeline faster is that more and more veterans are entering VA care. As of October 1, tens of thousands of veterans will be eligible for VA health care, thanks to the Sergeant First Class Heath Robinson Honoring our Promise to Address Comprehensive Toxics Act of 2022 (PACT Act), passed in August, which expanded benefits for post-9/11 service members with illnesses due to toxic exposures.
Another reason is the need to fill the gaps left by attrition. In an October 19 press briefing, VA Undersecretary for Health Shereef Elnahal said the agency needs to hire about 52,000 employees per year just to keep up with the rate of health care professionals (HCPs) leaving the agency. At a September breakfast meeting with the Defense Writers Group, VA Secretary Denis McDonough said July 2022 marked the first month this year that the VA hired more nurses than it lost to retirement. He said the VA needs to hire 45,000 nurses over the next 3 years to keep up with attrition and growing demand for veteran care.
“We have to do a better job on hiring,” McDonough said. Streamlining the process is a major goal. Hiring rules loosened during the pandemic have since tightened back up. He pointed out that in many cases, the VA takes 90 to 100 days to onboard candidates and called the long-drawn-out process “being dragged through a bureaucratic morass.” During that time, he said, “They’re not being paid, they’re filling out paperwork… That’s disastrous.” In his press briefing, Elnahal said “we lose folks after we’ve made the selection” because the process is so long.
Moreover, the agency has a critical shortage not only of HCPs but the human resources professionals needed to fast-track the hirees’ progress. McDonough called it a “supply chain issue.” “We have the lowest ratio of human resource professionals per employee in the federal government by a long shot.” Partly, he said, because “a lot of our people end up hired away to other federal agencies.”
McDonough said the VA is also interested in transitioning more active-duty service members with in-demand skills, certifications, and talent into the VA workforce. “Cross-walking active duty into VA service much more aggressively,” he said, is another way to “grow that supply of ready, deployable, trained personnel.” The PACT Act gives the VA new incentives to entice workers, such as expanded recruitment, retention bonuses, and student loan repayment. The VA already provides training to about 1500 nurse and nurse residency programs across the VA, McDonough said but has plans for expanding to 5 times its current scope. He also addressed the question of a looming physician shortage: “Roughly 7 in 10 doctors in the United States will have had some portion of their training in a VA facility. We have to maintain that training function going forward.” The VA trains doctors, he added, “better than anybody else.”
The onboarding event will serve as a “national signal that we take this priority very seriously,” Elnahal said. “This will be not only a chance to have a step function improvement in the number of folks on board, which is an urgent priority, but to also set the groundwork for the more longitudinal work that we will need to do to improve the hiring process.”
Bulking up the workforce, he said, is “still far and away among our first priorities. Because if we don’t get our hospitals and facility staffed, it’s going to be a really hard effort to make process on the other priorities.”
In an intensive push to fill acute workforce shortages, the US Department of Veterans Affairs (VA) is holding a “national onboarding surge event” the week of November 14. The goal is to get people who have already said yes to a job in the VA on that job more quickly. Every VA facility has been asked to submit a list of the highest-priority candidates, regardless of the position.
One of the most pressing reasons for getting more workers into the pipeline faster is that more and more veterans are entering VA care. As of October 1, tens of thousands of veterans will be eligible for VA health care, thanks to the Sergeant First Class Heath Robinson Honoring our Promise to Address Comprehensive Toxics Act of 2022 (PACT Act), passed in August, which expanded benefits for post-9/11 service members with illnesses due to toxic exposures.
Another reason is the need to fill the gaps left by attrition. In an October 19 press briefing, VA Undersecretary for Health Shereef Elnahal said the agency needs to hire about 52,000 employees per year just to keep up with the rate of health care professionals (HCPs) leaving the agency. At a September breakfast meeting with the Defense Writers Group, VA Secretary Denis McDonough said July 2022 marked the first month this year that the VA hired more nurses than it lost to retirement. He said the VA needs to hire 45,000 nurses over the next 3 years to keep up with attrition and growing demand for veteran care.
“We have to do a better job on hiring,” McDonough said. Streamlining the process is a major goal. Hiring rules loosened during the pandemic have since tightened back up. He pointed out that in many cases, the VA takes 90 to 100 days to onboard candidates and called the long-drawn-out process “being dragged through a bureaucratic morass.” During that time, he said, “They’re not being paid, they’re filling out paperwork… That’s disastrous.” In his press briefing, Elnahal said “we lose folks after we’ve made the selection” because the process is so long.
Moreover, the agency has a critical shortage not only of HCPs but the human resources professionals needed to fast-track the hirees’ progress. McDonough called it a “supply chain issue.” “We have the lowest ratio of human resource professionals per employee in the federal government by a long shot.” Partly, he said, because “a lot of our people end up hired away to other federal agencies.”
McDonough said the VA is also interested in transitioning more active-duty service members with in-demand skills, certifications, and talent into the VA workforce. “Cross-walking active duty into VA service much more aggressively,” he said, is another way to “grow that supply of ready, deployable, trained personnel.” The PACT Act gives the VA new incentives to entice workers, such as expanded recruitment, retention bonuses, and student loan repayment. The VA already provides training to about 1500 nurse and nurse residency programs across the VA, McDonough said but has plans for expanding to 5 times its current scope. He also addressed the question of a looming physician shortage: “Roughly 7 in 10 doctors in the United States will have had some portion of their training in a VA facility. We have to maintain that training function going forward.” The VA trains doctors, he added, “better than anybody else.”
The onboarding event will serve as a “national signal that we take this priority very seriously,” Elnahal said. “This will be not only a chance to have a step function improvement in the number of folks on board, which is an urgent priority, but to also set the groundwork for the more longitudinal work that we will need to do to improve the hiring process.”
Bulking up the workforce, he said, is “still far and away among our first priorities. Because if we don’t get our hospitals and facility staffed, it’s going to be a really hard effort to make process on the other priorities.”
VA Gets it Right on Suicide
For years, the US Department of Veterans Affairs (VA) has painstakingly labored to track, research, and address veteran suicide. Their exceptional work was dealt an unwarranted blow a month ago with the publication of an incomplete report entitled Operation Deep Dive (OpDD). The $3.9 million study from America’s Warrior Partnership (AWP) examined death data of former service members in 8 states between 2014 and 2018. The interim report criticized the VA for minimizing the extent of veteran suicide, asserting, “former service members take their own lives each year at a rate approximately 2.4 times greater than previously reported by the VA.”
The sensational results were accepted at face value and immediately garnered negative nationwide headlines, with lawmakers, media outlets, and veterans rushing to impugn the VA. Senate Committee on Veterans’ Affairs Ranking Republican Member Jerry Moran of Kansas opined, “The disparity between the numbers of veteran suicides reported by the VA and [OpDD] is concerning. We need an honest assessment of the scope of the problem.” A U.S. Medicine headline stated “VA undercounted thousands of veteran suicides. [OpDD] posited daily suicide rate is 240% higher.” Fox News declared, “Veterans committing suicide at rate 2 times higher than VA data show: study,” as did Military Times, “Veterans suicide rate may be double federal estimates, study suggests.”
Disturbingly, those who echoed AWP’s claims got the story backward. It’s AWP, not VA, whose suicide data and conclusions are faulty.
For starters, the VA data encompasses veterans across all 50 states, the District of Columbia, Puerto Rico, and the US Virgin Islands. In contrast, AWP inferred national veteran suicide figures based on partial, skewed data. As delineated by researchers in an in-press Military Medicine letter to the Editor, 7 of the 8 states sampled (Alabama, Florida, Maine, Massachusetts, Michigan, Minnesota, Montana, and Oregon) had suicide rates above the national average for the years under investigation. This factor alone overinflates AWP’s purported suicide numbers.
Additionally, AWP altered the definition of “taking one’s life” and then misapplied that designation. Conventionally, the term refers to suicide, but AWP used it to also include nonnatural deaths assessed by coroners and medical examiners as accidental or undetermined. Two examples of this self-injury mortality (SIM) are opioid overdoses and single-driver car crash deaths. AWP added suicides and SIMs to derive a total number of veterans who took their life and falsely contrasted that aggregate against the VA count of suicides. That’s like comparing the whole category of fruit to the subcategory of apples.
AWP should be applauded for drawing attention to and accounting for accidental and undetermined deaths. However, the standard protocol is to consider SIMs distinctly from suicides. Among the many reasons for precise labeling is so that grieving family members aren’t mistakenly informed that their loved one died by suicide. VA conveys the rate of veteran overdose deaths in separate reports, for example, the Veteran Drug Overdose Mortality, 2010-2019 publication. Those numbers were ignored in AWP’s calculations.
AWP was neglectful in another way. The second phase of the project—a deep examination of community-level factors preceding suicides and nonnatural deaths—began in 2019. This information was collected and analyzed through sociocultural death investigation (SDI) interviews of 3 to 4 family members, friends, and colleagues of the deceased. SDIs consisted of 19 factors, such as history of the veteran’s mental health problems, social connectedness, finances, group memberships, and access to firearms. However, the interim report omitted the preliminary analysis of these factors, which AWP stated would be made available this year.
OpDD conclusions were so unfounded that AWP’s analytic research partner, the University of Alabama, distanced itself from the interim report. “We were not consulted on the released figures,” Dr. Karl Hamner, the University of Alabama principal investigator on the study, told me. “We did not make any conclusions and we don’t endorse the reported findings about national rates or numbers per day. Nor did we make any statements about the VA’s data.”
As it happens, the VA’s 2022 National Veteran Suicide Prevention Annual Report was issued the same week as the OpDD report. VA found that veteran suicides decreased by 9.7% over the last 2 years, nearly twice the decrease for nonveterans. Yet, in a contemporaneous hearing of the House Committee on Veterans’ Affairs, AWP’s President and CEO Jim Lorraine testified that the progress preventing veteran suicide was “a disgrace” and “a failure.” He misattributed that it was VA (not AWP) that “must be more open and transparent about their data.”
Unsupported denigration of the VA tarnishes its reputation, undermining veterans’ trust in the health care system and increasing barriers to seeking needed services. More broadly, it fortifies those forces who wish to redirect allocations away from VA and towards non-VA veterans’ entities like AWP. The media and other stakeholders must take a lesson about getting the story straight before reflexively amplifying false accusations about the VA. Veterans deserve better.
For years, the US Department of Veterans Affairs (VA) has painstakingly labored to track, research, and address veteran suicide. Their exceptional work was dealt an unwarranted blow a month ago with the publication of an incomplete report entitled Operation Deep Dive (OpDD). The $3.9 million study from America’s Warrior Partnership (AWP) examined death data of former service members in 8 states between 2014 and 2018. The interim report criticized the VA for minimizing the extent of veteran suicide, asserting, “former service members take their own lives each year at a rate approximately 2.4 times greater than previously reported by the VA.”
The sensational results were accepted at face value and immediately garnered negative nationwide headlines, with lawmakers, media outlets, and veterans rushing to impugn the VA. Senate Committee on Veterans’ Affairs Ranking Republican Member Jerry Moran of Kansas opined, “The disparity between the numbers of veteran suicides reported by the VA and [OpDD] is concerning. We need an honest assessment of the scope of the problem.” A U.S. Medicine headline stated “VA undercounted thousands of veteran suicides. [OpDD] posited daily suicide rate is 240% higher.” Fox News declared, “Veterans committing suicide at rate 2 times higher than VA data show: study,” as did Military Times, “Veterans suicide rate may be double federal estimates, study suggests.”
Disturbingly, those who echoed AWP’s claims got the story backward. It’s AWP, not VA, whose suicide data and conclusions are faulty.
For starters, the VA data encompasses veterans across all 50 states, the District of Columbia, Puerto Rico, and the US Virgin Islands. In contrast, AWP inferred national veteran suicide figures based on partial, skewed data. As delineated by researchers in an in-press Military Medicine letter to the Editor, 7 of the 8 states sampled (Alabama, Florida, Maine, Massachusetts, Michigan, Minnesota, Montana, and Oregon) had suicide rates above the national average for the years under investigation. This factor alone overinflates AWP’s purported suicide numbers.
Additionally, AWP altered the definition of “taking one’s life” and then misapplied that designation. Conventionally, the term refers to suicide, but AWP used it to also include nonnatural deaths assessed by coroners and medical examiners as accidental or undetermined. Two examples of this self-injury mortality (SIM) are opioid overdoses and single-driver car crash deaths. AWP added suicides and SIMs to derive a total number of veterans who took their life and falsely contrasted that aggregate against the VA count of suicides. That’s like comparing the whole category of fruit to the subcategory of apples.
AWP should be applauded for drawing attention to and accounting for accidental and undetermined deaths. However, the standard protocol is to consider SIMs distinctly from suicides. Among the many reasons for precise labeling is so that grieving family members aren’t mistakenly informed that their loved one died by suicide. VA conveys the rate of veteran overdose deaths in separate reports, for example, the Veteran Drug Overdose Mortality, 2010-2019 publication. Those numbers were ignored in AWP’s calculations.
AWP was neglectful in another way. The second phase of the project—a deep examination of community-level factors preceding suicides and nonnatural deaths—began in 2019. This information was collected and analyzed through sociocultural death investigation (SDI) interviews of 3 to 4 family members, friends, and colleagues of the deceased. SDIs consisted of 19 factors, such as history of the veteran’s mental health problems, social connectedness, finances, group memberships, and access to firearms. However, the interim report omitted the preliminary analysis of these factors, which AWP stated would be made available this year.
OpDD conclusions were so unfounded that AWP’s analytic research partner, the University of Alabama, distanced itself from the interim report. “We were not consulted on the released figures,” Dr. Karl Hamner, the University of Alabama principal investigator on the study, told me. “We did not make any conclusions and we don’t endorse the reported findings about national rates or numbers per day. Nor did we make any statements about the VA’s data.”
As it happens, the VA’s 2022 National Veteran Suicide Prevention Annual Report was issued the same week as the OpDD report. VA found that veteran suicides decreased by 9.7% over the last 2 years, nearly twice the decrease for nonveterans. Yet, in a contemporaneous hearing of the House Committee on Veterans’ Affairs, AWP’s President and CEO Jim Lorraine testified that the progress preventing veteran suicide was “a disgrace” and “a failure.” He misattributed that it was VA (not AWP) that “must be more open and transparent about their data.”
Unsupported denigration of the VA tarnishes its reputation, undermining veterans’ trust in the health care system and increasing barriers to seeking needed services. More broadly, it fortifies those forces who wish to redirect allocations away from VA and towards non-VA veterans’ entities like AWP. The media and other stakeholders must take a lesson about getting the story straight before reflexively amplifying false accusations about the VA. Veterans deserve better.
For years, the US Department of Veterans Affairs (VA) has painstakingly labored to track, research, and address veteran suicide. Their exceptional work was dealt an unwarranted blow a month ago with the publication of an incomplete report entitled Operation Deep Dive (OpDD). The $3.9 million study from America’s Warrior Partnership (AWP) examined death data of former service members in 8 states between 2014 and 2018. The interim report criticized the VA for minimizing the extent of veteran suicide, asserting, “former service members take their own lives each year at a rate approximately 2.4 times greater than previously reported by the VA.”
The sensational results were accepted at face value and immediately garnered negative nationwide headlines, with lawmakers, media outlets, and veterans rushing to impugn the VA. Senate Committee on Veterans’ Affairs Ranking Republican Member Jerry Moran of Kansas opined, “The disparity between the numbers of veteran suicides reported by the VA and [OpDD] is concerning. We need an honest assessment of the scope of the problem.” A U.S. Medicine headline stated “VA undercounted thousands of veteran suicides. [OpDD] posited daily suicide rate is 240% higher.” Fox News declared, “Veterans committing suicide at rate 2 times higher than VA data show: study,” as did Military Times, “Veterans suicide rate may be double federal estimates, study suggests.”
Disturbingly, those who echoed AWP’s claims got the story backward. It’s AWP, not VA, whose suicide data and conclusions are faulty.
For starters, the VA data encompasses veterans across all 50 states, the District of Columbia, Puerto Rico, and the US Virgin Islands. In contrast, AWP inferred national veteran suicide figures based on partial, skewed data. As delineated by researchers in an in-press Military Medicine letter to the Editor, 7 of the 8 states sampled (Alabama, Florida, Maine, Massachusetts, Michigan, Minnesota, Montana, and Oregon) had suicide rates above the national average for the years under investigation. This factor alone overinflates AWP’s purported suicide numbers.
Additionally, AWP altered the definition of “taking one’s life” and then misapplied that designation. Conventionally, the term refers to suicide, but AWP used it to also include nonnatural deaths assessed by coroners and medical examiners as accidental or undetermined. Two examples of this self-injury mortality (SIM) are opioid overdoses and single-driver car crash deaths. AWP added suicides and SIMs to derive a total number of veterans who took their life and falsely contrasted that aggregate against the VA count of suicides. That’s like comparing the whole category of fruit to the subcategory of apples.
AWP should be applauded for drawing attention to and accounting for accidental and undetermined deaths. However, the standard protocol is to consider SIMs distinctly from suicides. Among the many reasons for precise labeling is so that grieving family members aren’t mistakenly informed that their loved one died by suicide. VA conveys the rate of veteran overdose deaths in separate reports, for example, the Veteran Drug Overdose Mortality, 2010-2019 publication. Those numbers were ignored in AWP’s calculations.
AWP was neglectful in another way. The second phase of the project—a deep examination of community-level factors preceding suicides and nonnatural deaths—began in 2019. This information was collected and analyzed through sociocultural death investigation (SDI) interviews of 3 to 4 family members, friends, and colleagues of the deceased. SDIs consisted of 19 factors, such as history of the veteran’s mental health problems, social connectedness, finances, group memberships, and access to firearms. However, the interim report omitted the preliminary analysis of these factors, which AWP stated would be made available this year.
OpDD conclusions were so unfounded that AWP’s analytic research partner, the University of Alabama, distanced itself from the interim report. “We were not consulted on the released figures,” Dr. Karl Hamner, the University of Alabama principal investigator on the study, told me. “We did not make any conclusions and we don’t endorse the reported findings about national rates or numbers per day. Nor did we make any statements about the VA’s data.”
As it happens, the VA’s 2022 National Veteran Suicide Prevention Annual Report was issued the same week as the OpDD report. VA found that veteran suicides decreased by 9.7% over the last 2 years, nearly twice the decrease for nonveterans. Yet, in a contemporaneous hearing of the House Committee on Veterans’ Affairs, AWP’s President and CEO Jim Lorraine testified that the progress preventing veteran suicide was “a disgrace” and “a failure.” He misattributed that it was VA (not AWP) that “must be more open and transparent about their data.”
Unsupported denigration of the VA tarnishes its reputation, undermining veterans’ trust in the health care system and increasing barriers to seeking needed services. More broadly, it fortifies those forces who wish to redirect allocations away from VA and towards non-VA veterans’ entities like AWP. The media and other stakeholders must take a lesson about getting the story straight before reflexively amplifying false accusations about the VA. Veterans deserve better.
Blind to Problems: How VA’s Electronic Record System Shuts Out Visually Impaired Patients
Sarah Sheffield, a nurse practitioner at a Veterans Affairs clinic in Eugene, Oregon, had a problem. Her patients — mostly in their 70s and beyond — couldn’t read computer screens. It’s not an unusual problem for older people, which is why you might think Oracle Cerner, the developers of the agency’s new digital health record system, would have anticipated it.
But they didn’t.
Federal law requires government resources to be accessible to patients with disabilities. But patients can’t easily enlarge the text. “They all learned to get strong reading glasses and magnifying glasses,” said Sheffield, who retired in early October.
The difficulties are everyday reminders of a dire reality for patients in the VA system. More than a million patients are blind or have low vision. They rely on software to access prescriptions or send messages to their doctors. But often the technology fails them. Either the screens don’t allow users to zoom in on the text, or screen-reader software that translates text to speech isn’t compatible.
“None of the systems are accessible” to these patients, said Donald Overton, executive director of the Blinded Veterans Association.
Patients often struggle even to log into websites or enter basic information needed to check in for hospital visits, Overton said: “We find our community stops trying, checks out, and disengages. They become dependent on other individuals; they give up independence.”
Now, the developing VA medical record system, already bloated by outsize costs, has been delayed until June 2023. So far, the project has threatened to exacerbate those issues.
While users in general have been affected by numerous incidents of downtime, delayed care, and missing information, barriers to access are particularly acute for blind and low-vision users — whether patients or workers within the health system. At least one Oregon-based employee has been offered aid — a helper assigned to read and click buttons — to navigate the system.
Over 1,000 Section 508 complaints are in a backlog to be assessed, or assigned to Oracle Cerner to fix, Veterans Affairs spokesperson Terrence Hayes confirmed. That section is part of federal law guaranteeing people with disabilities access to government technology.
Hayes said the problems described by these complaints don’t prevent employees and patients with disabilities from using the system. The complaints — 469 of which have been assigned to Oracle Cerner to fix, he said — mean that users’ disabilities make it more difficult, to the point of requiring mitigation.
The project is under new management with big promises. North Kansas City, Missouri-based developer Cerner, which originally landed the VA contract, was recently taken over by database technology giant Oracle, which plans to overhaul the software, company executive Mike Sicilia said during a September Senate hearing. “We intend to rewrite” the system, he said. “We have found nothing that can’t be addressed in relatively short order.”
But that will happen under continued scrutiny. Rep. Mark Takano (D-Calif.), chair of the House Veterans Affairs Committee, said his panel would continue to oversee the department’s compliance with accessibility standards. “Whether they work for VA or receive health care and benefits, the needs of veterans must be addressed by companies that want to work with the VA,” he said.
Takano, along with fellow Democrats Sens. Bob Casey of Pennsylvania and Jon Tester of Montana, sent a letter Oct. 7 to VA Secretary Denis McDonough noting the significant gaps in the agency’s systems, and urging VA to engage with all disabled veterans, not merely those who are blind.
VA was alerted early and often that Cerner’s software posed problems for blind- and low-vision users, interviews and a review of records show. As early as 2015, when the Department of Defense and VA were exploring purchasing new systems, the National Federation of the Blind submitted letters to both departments, and Cerner, expressing concerns that the product would be unusable for clinicians and patients.
Alerts also came from inside VA. “We pointed out to Cerner that their system was really dependent on vision and that it was a major problem. The icons are really, really small,” said Dr. Art Wallace, a VA anesthesiologist who participated in one of the agency’s user groups to provide input for the eventual design of the system.
The Cerner system, he told the agency and KHN, is user-unfriendly. On the clinician side, it requires multiple high-resolution monitors to display a patient’s entire record, and VA facilities don’t always enjoy that wealth of equipment. “It would be very hard for visually impaired people, or normal people wearing bifocals, to use,” he concluded.
Before the software was rolled out, the system also failed a test with an employee working with a team at Oregon’s White City VA Medical Center devoted to helping blind patients develop skills and independence, said Carolyn Schwab, president of the American Federation of Government Employees Local 1042.
In the testing, the system didn’t work with adaptive equipment, like text-to-speech software, she said. Despite receiving these complaints about the system, VA and Cerner “implemented it anyway.” Recently, when a regional AFGE president asked VA why they used the software — despite the federal mandates — he received no response, Schwab said.
Some within the company also thought there would be struggles. Two former Cerner employees said the standard medical record system was getting long in the tooth when VA signed an agreement to purchase and customize the product.
Because it was built on old code, the software was difficult to patch when problems were discovered, the employees said. What’s more, according to the employees, Cerner took a doggedly incremental approach to fixing errors. If someone complained about a malfunctioning button on a page filled with other potholes, the company would fix just that button — not the whole page, the employees said.
VA spokesperson Hayes denied the claims, saying the developer and department try to address problems holistically. Cerner did not respond to multiple requests for comment.
Accessibility errors are as present in private sector medical record systems as public. Cerner patched up a bug with the Safari web browser’s rendering of its patient portal when the Massachusetts Institute of Technology’s student clinic threatened legal action, the former employees said. (“MIT Medical does not, as a general practice, discuss individual vendor contracts or services,” said spokesperson David Tytell.)
Legal threats — with hospital systems and medical record systems routinely facing lawsuits — are the most obvious symptom of a lack of accessibility within the U.S. health care system.
Deep inaccessibility plagues the burgeoning telehealth sector. A recent survey from the American Federation for the Blind found that 57% of respondents struggled to use providers’ proprietary telehealth platforms. Some resorted to FaceTime. Many said they were unable to log in or couldn’t read information transmitted through chat sidebars.
Existing federal regulations could, in theory, be used to enforce higher standards of accessibility in health technology. The Department of Health and Human Services Office for Civil Rights issued guidance during the pandemic on making telehealth technologies easier to use for patients with disabilities. And other agencies could start leaning on hospitals, because they are recipients of government dollars or federal vendors, to make sure their offerings work for such patients.
That might not happen. These regulations could prove toothless, advocates warn. While there are several laws on the books, the advocates argue that enforcement and tougher regulations have not been forthcoming. “The concern from stakeholders is: Are you going to slow-walk this again?” said Joe Nahra, director of government relations at Powers Law, a Washington, D.C., law firm.
Building in accessibility has historically benefited all users. Voice assistance technology was originally developed to help blind- and low-vision users before winning widespread popularity with gadgets like Siri and Alexa.
Disability advocates believe vendors often push technology ahead without properly considering the impact on the people who will rely on it. “In the rush to be the first one, they put accessibility on the back burner,” said Eve Hill, a disability rights attorney with Brown, Goldstein & Levy, a civil rights law firm.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Sarah Sheffield, a nurse practitioner at a Veterans Affairs clinic in Eugene, Oregon, had a problem. Her patients — mostly in their 70s and beyond — couldn’t read computer screens. It’s not an unusual problem for older people, which is why you might think Oracle Cerner, the developers of the agency’s new digital health record system, would have anticipated it.
But they didn’t.
Federal law requires government resources to be accessible to patients with disabilities. But patients can’t easily enlarge the text. “They all learned to get strong reading glasses and magnifying glasses,” said Sheffield, who retired in early October.
The difficulties are everyday reminders of a dire reality for patients in the VA system. More than a million patients are blind or have low vision. They rely on software to access prescriptions or send messages to their doctors. But often the technology fails them. Either the screens don’t allow users to zoom in on the text, or screen-reader software that translates text to speech isn’t compatible.
“None of the systems are accessible” to these patients, said Donald Overton, executive director of the Blinded Veterans Association.
Patients often struggle even to log into websites or enter basic information needed to check in for hospital visits, Overton said: “We find our community stops trying, checks out, and disengages. They become dependent on other individuals; they give up independence.”
Now, the developing VA medical record system, already bloated by outsize costs, has been delayed until June 2023. So far, the project has threatened to exacerbate those issues.
While users in general have been affected by numerous incidents of downtime, delayed care, and missing information, barriers to access are particularly acute for blind and low-vision users — whether patients or workers within the health system. At least one Oregon-based employee has been offered aid — a helper assigned to read and click buttons — to navigate the system.
Over 1,000 Section 508 complaints are in a backlog to be assessed, or assigned to Oracle Cerner to fix, Veterans Affairs spokesperson Terrence Hayes confirmed. That section is part of federal law guaranteeing people with disabilities access to government technology.
Hayes said the problems described by these complaints don’t prevent employees and patients with disabilities from using the system. The complaints — 469 of which have been assigned to Oracle Cerner to fix, he said — mean that users’ disabilities make it more difficult, to the point of requiring mitigation.
The project is under new management with big promises. North Kansas City, Missouri-based developer Cerner, which originally landed the VA contract, was recently taken over by database technology giant Oracle, which plans to overhaul the software, company executive Mike Sicilia said during a September Senate hearing. “We intend to rewrite” the system, he said. “We have found nothing that can’t be addressed in relatively short order.”
But that will happen under continued scrutiny. Rep. Mark Takano (D-Calif.), chair of the House Veterans Affairs Committee, said his panel would continue to oversee the department’s compliance with accessibility standards. “Whether they work for VA or receive health care and benefits, the needs of veterans must be addressed by companies that want to work with the VA,” he said.
Takano, along with fellow Democrats Sens. Bob Casey of Pennsylvania and Jon Tester of Montana, sent a letter Oct. 7 to VA Secretary Denis McDonough noting the significant gaps in the agency’s systems, and urging VA to engage with all disabled veterans, not merely those who are blind.
VA was alerted early and often that Cerner’s software posed problems for blind- and low-vision users, interviews and a review of records show. As early as 2015, when the Department of Defense and VA were exploring purchasing new systems, the National Federation of the Blind submitted letters to both departments, and Cerner, expressing concerns that the product would be unusable for clinicians and patients.
Alerts also came from inside VA. “We pointed out to Cerner that their system was really dependent on vision and that it was a major problem. The icons are really, really small,” said Dr. Art Wallace, a VA anesthesiologist who participated in one of the agency’s user groups to provide input for the eventual design of the system.
The Cerner system, he told the agency and KHN, is user-unfriendly. On the clinician side, it requires multiple high-resolution monitors to display a patient’s entire record, and VA facilities don’t always enjoy that wealth of equipment. “It would be very hard for visually impaired people, or normal people wearing bifocals, to use,” he concluded.
Before the software was rolled out, the system also failed a test with an employee working with a team at Oregon’s White City VA Medical Center devoted to helping blind patients develop skills and independence, said Carolyn Schwab, president of the American Federation of Government Employees Local 1042.
In the testing, the system didn’t work with adaptive equipment, like text-to-speech software, she said. Despite receiving these complaints about the system, VA and Cerner “implemented it anyway.” Recently, when a regional AFGE president asked VA why they used the software — despite the federal mandates — he received no response, Schwab said.
Some within the company also thought there would be struggles. Two former Cerner employees said the standard medical record system was getting long in the tooth when VA signed an agreement to purchase and customize the product.
Because it was built on old code, the software was difficult to patch when problems were discovered, the employees said. What’s more, according to the employees, Cerner took a doggedly incremental approach to fixing errors. If someone complained about a malfunctioning button on a page filled with other potholes, the company would fix just that button — not the whole page, the employees said.
VA spokesperson Hayes denied the claims, saying the developer and department try to address problems holistically. Cerner did not respond to multiple requests for comment.
Accessibility errors are as present in private sector medical record systems as public. Cerner patched up a bug with the Safari web browser’s rendering of its patient portal when the Massachusetts Institute of Technology’s student clinic threatened legal action, the former employees said. (“MIT Medical does not, as a general practice, discuss individual vendor contracts or services,” said spokesperson David Tytell.)
Legal threats — with hospital systems and medical record systems routinely facing lawsuits — are the most obvious symptom of a lack of accessibility within the U.S. health care system.
Deep inaccessibility plagues the burgeoning telehealth sector. A recent survey from the American Federation for the Blind found that 57% of respondents struggled to use providers’ proprietary telehealth platforms. Some resorted to FaceTime. Many said they were unable to log in or couldn’t read information transmitted through chat sidebars.
Existing federal regulations could, in theory, be used to enforce higher standards of accessibility in health technology. The Department of Health and Human Services Office for Civil Rights issued guidance during the pandemic on making telehealth technologies easier to use for patients with disabilities. And other agencies could start leaning on hospitals, because they are recipients of government dollars or federal vendors, to make sure their offerings work for such patients.
That might not happen. These regulations could prove toothless, advocates warn. While there are several laws on the books, the advocates argue that enforcement and tougher regulations have not been forthcoming. “The concern from stakeholders is: Are you going to slow-walk this again?” said Joe Nahra, director of government relations at Powers Law, a Washington, D.C., law firm.
Building in accessibility has historically benefited all users. Voice assistance technology was originally developed to help blind- and low-vision users before winning widespread popularity with gadgets like Siri and Alexa.
Disability advocates believe vendors often push technology ahead without properly considering the impact on the people who will rely on it. “In the rush to be the first one, they put accessibility on the back burner,” said Eve Hill, a disability rights attorney with Brown, Goldstein & Levy, a civil rights law firm.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Sarah Sheffield, a nurse practitioner at a Veterans Affairs clinic in Eugene, Oregon, had a problem. Her patients — mostly in their 70s and beyond — couldn’t read computer screens. It’s not an unusual problem for older people, which is why you might think Oracle Cerner, the developers of the agency’s new digital health record system, would have anticipated it.
But they didn’t.
Federal law requires government resources to be accessible to patients with disabilities. But patients can’t easily enlarge the text. “They all learned to get strong reading glasses and magnifying glasses,” said Sheffield, who retired in early October.
The difficulties are everyday reminders of a dire reality for patients in the VA system. More than a million patients are blind or have low vision. They rely on software to access prescriptions or send messages to their doctors. But often the technology fails them. Either the screens don’t allow users to zoom in on the text, or screen-reader software that translates text to speech isn’t compatible.
“None of the systems are accessible” to these patients, said Donald Overton, executive director of the Blinded Veterans Association.
Patients often struggle even to log into websites or enter basic information needed to check in for hospital visits, Overton said: “We find our community stops trying, checks out, and disengages. They become dependent on other individuals; they give up independence.”
Now, the developing VA medical record system, already bloated by outsize costs, has been delayed until June 2023. So far, the project has threatened to exacerbate those issues.
While users in general have been affected by numerous incidents of downtime, delayed care, and missing information, barriers to access are particularly acute for blind and low-vision users — whether patients or workers within the health system. At least one Oregon-based employee has been offered aid — a helper assigned to read and click buttons — to navigate the system.
Over 1,000 Section 508 complaints are in a backlog to be assessed, or assigned to Oracle Cerner to fix, Veterans Affairs spokesperson Terrence Hayes confirmed. That section is part of federal law guaranteeing people with disabilities access to government technology.
Hayes said the problems described by these complaints don’t prevent employees and patients with disabilities from using the system. The complaints — 469 of which have been assigned to Oracle Cerner to fix, he said — mean that users’ disabilities make it more difficult, to the point of requiring mitigation.
The project is under new management with big promises. North Kansas City, Missouri-based developer Cerner, which originally landed the VA contract, was recently taken over by database technology giant Oracle, which plans to overhaul the software, company executive Mike Sicilia said during a September Senate hearing. “We intend to rewrite” the system, he said. “We have found nothing that can’t be addressed in relatively short order.”
But that will happen under continued scrutiny. Rep. Mark Takano (D-Calif.), chair of the House Veterans Affairs Committee, said his panel would continue to oversee the department’s compliance with accessibility standards. “Whether they work for VA or receive health care and benefits, the needs of veterans must be addressed by companies that want to work with the VA,” he said.
Takano, along with fellow Democrats Sens. Bob Casey of Pennsylvania and Jon Tester of Montana, sent a letter Oct. 7 to VA Secretary Denis McDonough noting the significant gaps in the agency’s systems, and urging VA to engage with all disabled veterans, not merely those who are blind.
VA was alerted early and often that Cerner’s software posed problems for blind- and low-vision users, interviews and a review of records show. As early as 2015, when the Department of Defense and VA were exploring purchasing new systems, the National Federation of the Blind submitted letters to both departments, and Cerner, expressing concerns that the product would be unusable for clinicians and patients.
Alerts also came from inside VA. “We pointed out to Cerner that their system was really dependent on vision and that it was a major problem. The icons are really, really small,” said Dr. Art Wallace, a VA anesthesiologist who participated in one of the agency’s user groups to provide input for the eventual design of the system.
The Cerner system, he told the agency and KHN, is user-unfriendly. On the clinician side, it requires multiple high-resolution monitors to display a patient’s entire record, and VA facilities don’t always enjoy that wealth of equipment. “It would be very hard for visually impaired people, or normal people wearing bifocals, to use,” he concluded.
Before the software was rolled out, the system also failed a test with an employee working with a team at Oregon’s White City VA Medical Center devoted to helping blind patients develop skills and independence, said Carolyn Schwab, president of the American Federation of Government Employees Local 1042.
In the testing, the system didn’t work with adaptive equipment, like text-to-speech software, she said. Despite receiving these complaints about the system, VA and Cerner “implemented it anyway.” Recently, when a regional AFGE president asked VA why they used the software — despite the federal mandates — he received no response, Schwab said.
Some within the company also thought there would be struggles. Two former Cerner employees said the standard medical record system was getting long in the tooth when VA signed an agreement to purchase and customize the product.
Because it was built on old code, the software was difficult to patch when problems were discovered, the employees said. What’s more, according to the employees, Cerner took a doggedly incremental approach to fixing errors. If someone complained about a malfunctioning button on a page filled with other potholes, the company would fix just that button — not the whole page, the employees said.
VA spokesperson Hayes denied the claims, saying the developer and department try to address problems holistically. Cerner did not respond to multiple requests for comment.
Accessibility errors are as present in private sector medical record systems as public. Cerner patched up a bug with the Safari web browser’s rendering of its patient portal when the Massachusetts Institute of Technology’s student clinic threatened legal action, the former employees said. (“MIT Medical does not, as a general practice, discuss individual vendor contracts or services,” said spokesperson David Tytell.)
Legal threats — with hospital systems and medical record systems routinely facing lawsuits — are the most obvious symptom of a lack of accessibility within the U.S. health care system.
Deep inaccessibility plagues the burgeoning telehealth sector. A recent survey from the American Federation for the Blind found that 57% of respondents struggled to use providers’ proprietary telehealth platforms. Some resorted to FaceTime. Many said they were unable to log in or couldn’t read information transmitted through chat sidebars.
Existing federal regulations could, in theory, be used to enforce higher standards of accessibility in health technology. The Department of Health and Human Services Office for Civil Rights issued guidance during the pandemic on making telehealth technologies easier to use for patients with disabilities. And other agencies could start leaning on hospitals, because they are recipients of government dollars or federal vendors, to make sure their offerings work for such patients.
That might not happen. These regulations could prove toothless, advocates warn. While there are several laws on the books, the advocates argue that enforcement and tougher regulations have not been forthcoming. “The concern from stakeholders is: Are you going to slow-walk this again?” said Joe Nahra, director of government relations at Powers Law, a Washington, D.C., law firm.
Building in accessibility has historically benefited all users. Voice assistance technology was originally developed to help blind- and low-vision users before winning widespread popularity with gadgets like Siri and Alexa.
Disability advocates believe vendors often push technology ahead without properly considering the impact on the people who will rely on it. “In the rush to be the first one, they put accessibility on the back burner,” said Eve Hill, a disability rights attorney with Brown, Goldstein & Levy, a civil rights law firm.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Roselyn Tso confirmed to head Indian Health Service
It took 609 days, but the US Senate has finally (unanimously) confirmed President Biden’s choice to head the Indian Health Service (IHS: Roselyn Tso.)
President Biden nominated Tso in March 2022, and she was formally sworn in on September 27, 2022. The long-awaited confirmation filled a space that hadn’t had a permanent director since Michael Weahkee, a Pueblo of Zuni citizen, stepped down in 2021. In the interim, Elizabeth Fowler, of the Comanche Nation, served as acting director.
Tso’s resume includes almost 40 years of professional experience working at all levels of the IHS. Before taking over as IHS director, she led the IHS Navajo area, the largest IHS regional area, managing more than 4000 employees and a budget of nearly $1 billion.
She also brings “decades of lived experience as a member of the Navajo Nation,” she said in a 40-minute Senate hearing with the US Senate Committee on Indian Affairs in May.
The first Navajo Nation citizen to head the IHS (and only the second woman to do so), Tso introduced herself in Navajo: Deeschii’nii (Start of the Red Streak People) and born for Hashk’aa hadzohi (Yucca Fruit Strung Out). “This is a historic achievement for all of our Navajo people and tribal nations across the country,” Navajo Nation President Jonathan Nez said. “To have one of our own Navajo members in the highest position with IHS is remarkable.”
Tso spoke of having to “navigate the services provided by the Agency for myself, family, and friends.” Her personal and professional backgrounds, she said, help her understand how patients experience the system and how that can be improved. “The health care provided at IHS is critical for those we serve. I understand this not just because I work there,” she said. “My family relies on IHS. My friends rely on IHS. I rely on the IHS.”
The long lacuna in confirming a permanent IHS director left the Native peoples particularly vulnerable—when the COVID-19 pandemic essentially worsened the existing problems they faced, such as diabetes mellitus and cancer. Life expectancy for Native people fell by more than 6 years between 2019 and 2021, to 65 years, compared with the US average of 76 years.
Without a full-time IHS leader, the National Council of Urban Indian Health said in a statement, tribal nations and other Native health care providers struggled to raise and address the issues they were facing amid the pandemic. “Since the resignation of Rear Admiral Weahkee, there have been countless requests from Indian Country calling on Congress and the Administration to nominate a new IHS director to address the growing health disparities experienced by AI/ANs.”
Tso laid out her priorities in her May testimony: creating a more unified health care system using the latest technology to develop centralized systems; improving accountability, transparency, and patient safety; addressing workforce needs and challenges, improving recruitment and retention.
Meeting her goals, she noted, would take “strong partnerships and communication with our Tribal partners…. Each tribe has unique needs, and those needs cannot be met if you do not understand them.”
Last year, President Joseph R. Biden asked Congress to significantly increase IHS funding, but his proposal was cut to $400 million. “For years, IHS has been funded at a rate that is far below its level of need, and the results of this historical neglect can be seen in the disparities in health outcomes for AI/AN people,” William Smith, Valdez Native Tribe, Chairman of the National Indian Health Board (NIHB), wrote to the Senate Committee on Indian Affairs, on the topic of the next IHS director. “Perhaps one of the greatest challenges facing the [Indian, tribal and urban] system is the chronic and severe underfunding and budgetary instability for health care and public health services infrastructure and delivery. Since its creation in 1955, IHS has been chronically underfunded, with annual appropriations never exceeding 50% of demonstrated need. This underfunding has contributed to substandard investment in health delivery systems, some of the worst health disparities among any US population and a severe lack of public health infrastructure and services for our people. At the start of the COVID-19 pandemic these vulnerabilities were starkly exposed and while Congress moved decisively to invest into Tribal health and public health, the new Director must work to maintain these one-time investments.”
Stacy Bohlen, NIHB chief executive, told The Oklahoman that tribal leaders will look to Tso to press Congress for more money and to secure mandatory full funding for IHS—in contrast with the current annual appropriations, where Congress includes IHS in much larger budget bills. “When those bills stall, so does the money tribal clinics need to pay employees and suppliers,” making it hard to recruit and retain employees. “In the Indian Health System,” Bohlen says, “we simply can’t afford that kind of vulnerability.”
Securing advance appropriations and, ultimately, full mandatory funding for IHS, Smith wrote in his letter to the Senate committee, “fulfills the commitment made to our people generations ago and breaks down the systemic healthcare funding inequities the federal government tolerates for Tribes.”
Tso emphasized her intent to “improve the physical, mental, social, and spiritual health and well-being of all American Indians and Alaskan Natives served by the Agency.” Tso “understands the healthcare needs that many first people of this country deal with,” President Nez said. “Her work ethic, value system and approach to problem solving demonstrates the resilience of Indigenous peoples and the commitment to combat the systemic inequities that impact tribal nations.”
It took 609 days, but the US Senate has finally (unanimously) confirmed President Biden’s choice to head the Indian Health Service (IHS: Roselyn Tso.)
President Biden nominated Tso in March 2022, and she was formally sworn in on September 27, 2022. The long-awaited confirmation filled a space that hadn’t had a permanent director since Michael Weahkee, a Pueblo of Zuni citizen, stepped down in 2021. In the interim, Elizabeth Fowler, of the Comanche Nation, served as acting director.
Tso’s resume includes almost 40 years of professional experience working at all levels of the IHS. Before taking over as IHS director, she led the IHS Navajo area, the largest IHS regional area, managing more than 4000 employees and a budget of nearly $1 billion.
She also brings “decades of lived experience as a member of the Navajo Nation,” she said in a 40-minute Senate hearing with the US Senate Committee on Indian Affairs in May.
The first Navajo Nation citizen to head the IHS (and only the second woman to do so), Tso introduced herself in Navajo: Deeschii’nii (Start of the Red Streak People) and born for Hashk’aa hadzohi (Yucca Fruit Strung Out). “This is a historic achievement for all of our Navajo people and tribal nations across the country,” Navajo Nation President Jonathan Nez said. “To have one of our own Navajo members in the highest position with IHS is remarkable.”
Tso spoke of having to “navigate the services provided by the Agency for myself, family, and friends.” Her personal and professional backgrounds, she said, help her understand how patients experience the system and how that can be improved. “The health care provided at IHS is critical for those we serve. I understand this not just because I work there,” she said. “My family relies on IHS. My friends rely on IHS. I rely on the IHS.”
The long lacuna in confirming a permanent IHS director left the Native peoples particularly vulnerable—when the COVID-19 pandemic essentially worsened the existing problems they faced, such as diabetes mellitus and cancer. Life expectancy for Native people fell by more than 6 years between 2019 and 2021, to 65 years, compared with the US average of 76 years.
Without a full-time IHS leader, the National Council of Urban Indian Health said in a statement, tribal nations and other Native health care providers struggled to raise and address the issues they were facing amid the pandemic. “Since the resignation of Rear Admiral Weahkee, there have been countless requests from Indian Country calling on Congress and the Administration to nominate a new IHS director to address the growing health disparities experienced by AI/ANs.”
Tso laid out her priorities in her May testimony: creating a more unified health care system using the latest technology to develop centralized systems; improving accountability, transparency, and patient safety; addressing workforce needs and challenges, improving recruitment and retention.
Meeting her goals, she noted, would take “strong partnerships and communication with our Tribal partners…. Each tribe has unique needs, and those needs cannot be met if you do not understand them.”
Last year, President Joseph R. Biden asked Congress to significantly increase IHS funding, but his proposal was cut to $400 million. “For years, IHS has been funded at a rate that is far below its level of need, and the results of this historical neglect can be seen in the disparities in health outcomes for AI/AN people,” William Smith, Valdez Native Tribe, Chairman of the National Indian Health Board (NIHB), wrote to the Senate Committee on Indian Affairs, on the topic of the next IHS director. “Perhaps one of the greatest challenges facing the [Indian, tribal and urban] system is the chronic and severe underfunding and budgetary instability for health care and public health services infrastructure and delivery. Since its creation in 1955, IHS has been chronically underfunded, with annual appropriations never exceeding 50% of demonstrated need. This underfunding has contributed to substandard investment in health delivery systems, some of the worst health disparities among any US population and a severe lack of public health infrastructure and services for our people. At the start of the COVID-19 pandemic these vulnerabilities were starkly exposed and while Congress moved decisively to invest into Tribal health and public health, the new Director must work to maintain these one-time investments.”
Stacy Bohlen, NIHB chief executive, told The Oklahoman that tribal leaders will look to Tso to press Congress for more money and to secure mandatory full funding for IHS—in contrast with the current annual appropriations, where Congress includes IHS in much larger budget bills. “When those bills stall, so does the money tribal clinics need to pay employees and suppliers,” making it hard to recruit and retain employees. “In the Indian Health System,” Bohlen says, “we simply can’t afford that kind of vulnerability.”
Securing advance appropriations and, ultimately, full mandatory funding for IHS, Smith wrote in his letter to the Senate committee, “fulfills the commitment made to our people generations ago and breaks down the systemic healthcare funding inequities the federal government tolerates for Tribes.”
Tso emphasized her intent to “improve the physical, mental, social, and spiritual health and well-being of all American Indians and Alaskan Natives served by the Agency.” Tso “understands the healthcare needs that many first people of this country deal with,” President Nez said. “Her work ethic, value system and approach to problem solving demonstrates the resilience of Indigenous peoples and the commitment to combat the systemic inequities that impact tribal nations.”
It took 609 days, but the US Senate has finally (unanimously) confirmed President Biden’s choice to head the Indian Health Service (IHS: Roselyn Tso.)
President Biden nominated Tso in March 2022, and she was formally sworn in on September 27, 2022. The long-awaited confirmation filled a space that hadn’t had a permanent director since Michael Weahkee, a Pueblo of Zuni citizen, stepped down in 2021. In the interim, Elizabeth Fowler, of the Comanche Nation, served as acting director.
Tso’s resume includes almost 40 years of professional experience working at all levels of the IHS. Before taking over as IHS director, she led the IHS Navajo area, the largest IHS regional area, managing more than 4000 employees and a budget of nearly $1 billion.
She also brings “decades of lived experience as a member of the Navajo Nation,” she said in a 40-minute Senate hearing with the US Senate Committee on Indian Affairs in May.
The first Navajo Nation citizen to head the IHS (and only the second woman to do so), Tso introduced herself in Navajo: Deeschii’nii (Start of the Red Streak People) and born for Hashk’aa hadzohi (Yucca Fruit Strung Out). “This is a historic achievement for all of our Navajo people and tribal nations across the country,” Navajo Nation President Jonathan Nez said. “To have one of our own Navajo members in the highest position with IHS is remarkable.”
Tso spoke of having to “navigate the services provided by the Agency for myself, family, and friends.” Her personal and professional backgrounds, she said, help her understand how patients experience the system and how that can be improved. “The health care provided at IHS is critical for those we serve. I understand this not just because I work there,” she said. “My family relies on IHS. My friends rely on IHS. I rely on the IHS.”
The long lacuna in confirming a permanent IHS director left the Native peoples particularly vulnerable—when the COVID-19 pandemic essentially worsened the existing problems they faced, such as diabetes mellitus and cancer. Life expectancy for Native people fell by more than 6 years between 2019 and 2021, to 65 years, compared with the US average of 76 years.
Without a full-time IHS leader, the National Council of Urban Indian Health said in a statement, tribal nations and other Native health care providers struggled to raise and address the issues they were facing amid the pandemic. “Since the resignation of Rear Admiral Weahkee, there have been countless requests from Indian Country calling on Congress and the Administration to nominate a new IHS director to address the growing health disparities experienced by AI/ANs.”
Tso laid out her priorities in her May testimony: creating a more unified health care system using the latest technology to develop centralized systems; improving accountability, transparency, and patient safety; addressing workforce needs and challenges, improving recruitment and retention.
Meeting her goals, she noted, would take “strong partnerships and communication with our Tribal partners…. Each tribe has unique needs, and those needs cannot be met if you do not understand them.”
Last year, President Joseph R. Biden asked Congress to significantly increase IHS funding, but his proposal was cut to $400 million. “For years, IHS has been funded at a rate that is far below its level of need, and the results of this historical neglect can be seen in the disparities in health outcomes for AI/AN people,” William Smith, Valdez Native Tribe, Chairman of the National Indian Health Board (NIHB), wrote to the Senate Committee on Indian Affairs, on the topic of the next IHS director. “Perhaps one of the greatest challenges facing the [Indian, tribal and urban] system is the chronic and severe underfunding and budgetary instability for health care and public health services infrastructure and delivery. Since its creation in 1955, IHS has been chronically underfunded, with annual appropriations never exceeding 50% of demonstrated need. This underfunding has contributed to substandard investment in health delivery systems, some of the worst health disparities among any US population and a severe lack of public health infrastructure and services for our people. At the start of the COVID-19 pandemic these vulnerabilities were starkly exposed and while Congress moved decisively to invest into Tribal health and public health, the new Director must work to maintain these one-time investments.”
Stacy Bohlen, NIHB chief executive, told The Oklahoman that tribal leaders will look to Tso to press Congress for more money and to secure mandatory full funding for IHS—in contrast with the current annual appropriations, where Congress includes IHS in much larger budget bills. “When those bills stall, so does the money tribal clinics need to pay employees and suppliers,” making it hard to recruit and retain employees. “In the Indian Health System,” Bohlen says, “we simply can’t afford that kind of vulnerability.”
Securing advance appropriations and, ultimately, full mandatory funding for IHS, Smith wrote in his letter to the Senate committee, “fulfills the commitment made to our people generations ago and breaks down the systemic healthcare funding inequities the federal government tolerates for Tribes.”
Tso emphasized her intent to “improve the physical, mental, social, and spiritual health and well-being of all American Indians and Alaskan Natives served by the Agency.” Tso “understands the healthcare needs that many first people of this country deal with,” President Nez said. “Her work ethic, value system and approach to problem solving demonstrates the resilience of Indigenous peoples and the commitment to combat the systemic inequities that impact tribal nations.”