User login
Increasing racial diversity in hospital medicine’s leadership ranks
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
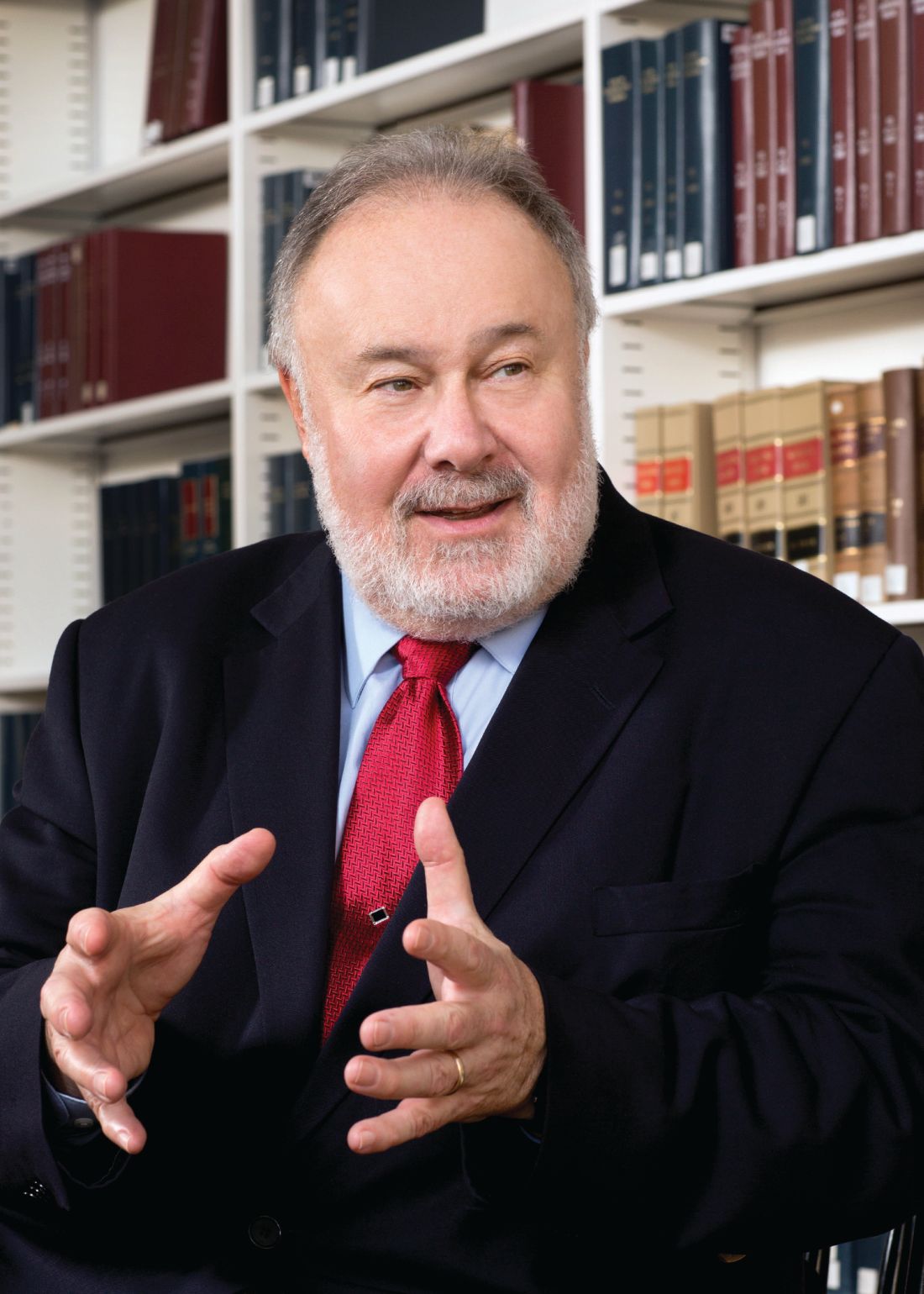
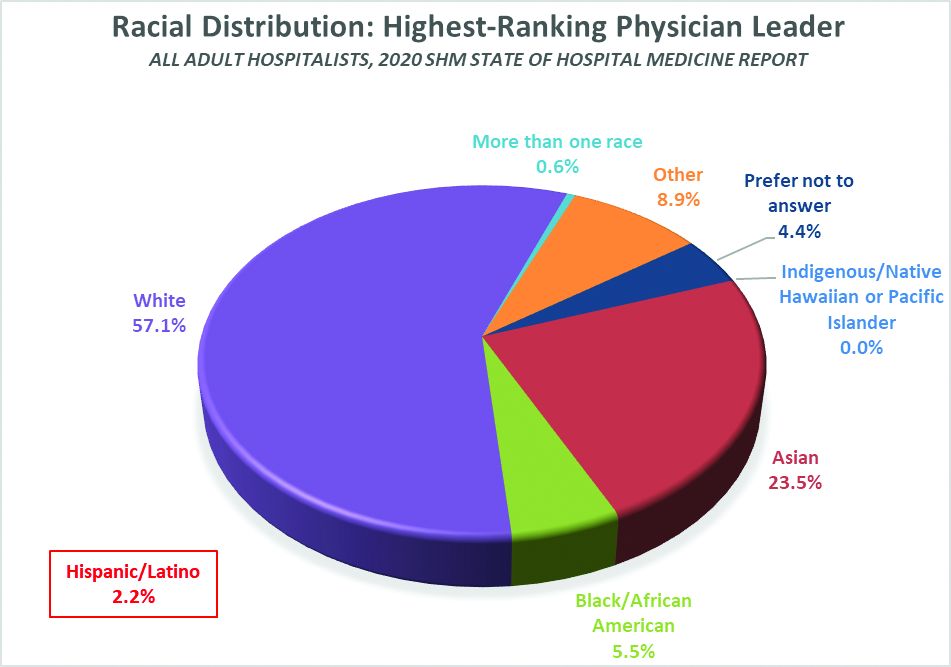
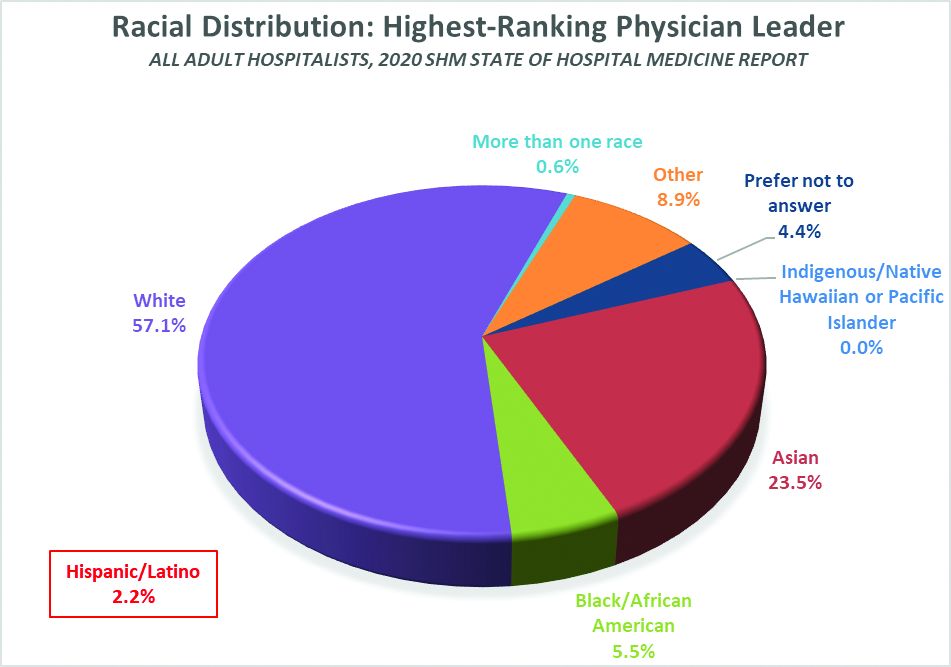
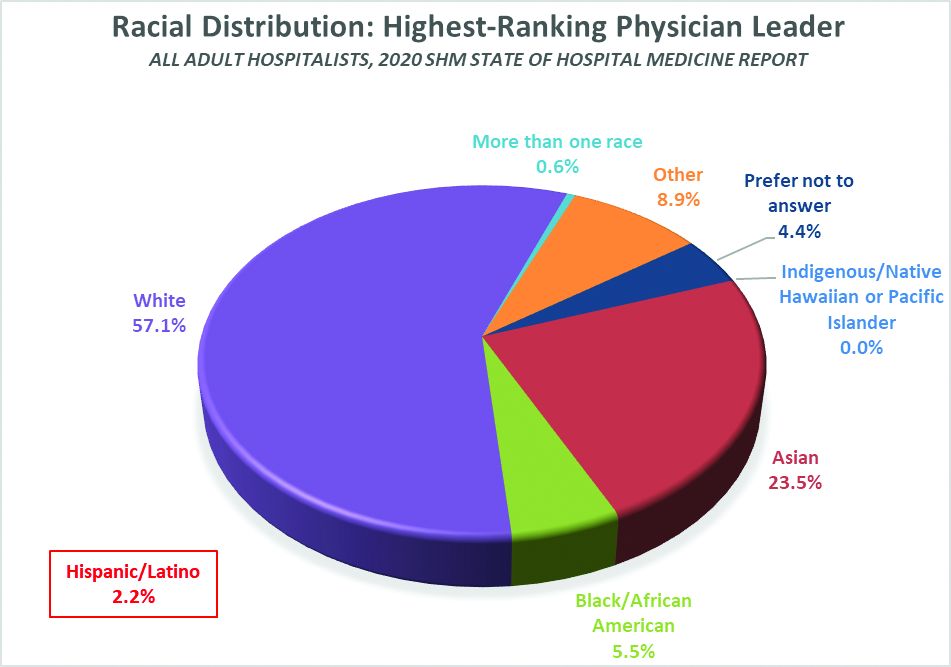
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Have you ever done something where you’re not quite sure why you did it at the time, but later on you realize it was part of some larger cosmic purpose, and you go, “Ahhh, now I understand…that’s why!”? Call it a fortuitous coincidence. Or a subconscious act of anticipation. Maybe a little push from God.
Last summer, as SHM’s Practice Analysis Committee was planning the State of Hospital Medicine survey for 2020, we received a request from SHM’s Diversity, Equity & Inclusion (DEI) Special Interest Group (SIG) to include a series of questions related to hospitalist gender, race and ethnic distribution in the new survey. We’ve generally resisted doing things like this because the SoHM is designed to capture data at the group level, not the individual level – and honestly, it’s as much as a lot of groups can do to tell us reliably how many FTEs they have, much less provide details about individual providers. In addition, the survey is already really long, and we are always looking for ways to make it shorter and easier for participants while still collecting the information report users care most about.
But we wanted to take the asks from the DEI SIG seriously, and as we considered their request, we realized that though it wasn’t practical to collect this information for individual hospital medicine group (HMG) members, we could collect it for group leaders. Little did we know last summer that issues of gender and racial diversity and equity would be so front-and-center right now, as we prepare to release the 2020 SoHM Report in early September. Ahhh, now I understand…that’s why – with the prompting of the DEI SIG – we so fortuitously chose to include those questions this year!
Here’s a sneak preview of what we learned. Among SoHM respondents, 57.1% reported that the highest-ranking leader in their HMG is White, and 23.5% of highest-ranking leaders are Asian. Only 5.5% of HMG leaders were Black/African American. Ethnicity was a separate question, and only 2.2% of HMG leaders were reported as Hispanic/Latino.
I have been profoundly moved by the wretched deaths of George Floyd and other people of color at the hands of police in recent months, and by the subsequent protests and our growing national reckoning over issues of racial equity and justice. In my efforts to understand more about race in America, I have been challenged by my friend Ryan Brown, MD, specialty medical director for hospital medicine with Atrium Health in Charlotte, N.C., and others to go beyond just learning about these issues. I want to use my voice to advocate for change, and my actions to participate in effecting change, within the context of my sphere of influence.
So, what does that have to do with the SoHM data on HMG leader demographics? Well, it’s clear that Black and brown people are woefully underrepresented in the ranks of hospital medicine leadership.
Unfortunately, we don’t have good information on racial diversity for hospitalists as a specialty, though I understand that SHM is working on plans to update membership profiles to begin collecting this information. In searching the Internet, I found a 2018 paper from the Journal of Health Care for the Poor and Underserved that studied racial and ethnic distribution of U.S. primary care physicians (doi: 10.1353/hpu.2018.0036). It reported that, in 2012, 7.8% of general internists were Black, along with 5.8% of family medicine/general practice physicians and 6.8% of pediatricians. A separate data set issued by the Association of American Medical Colleges reported that, in 2019, 6.4% of all actively practicing general internal medicine doctors were Black (5.5% of male IM physicians and 7.9% of female IM physicians). While this doesn’t mean hospitalists have the same racial and ethnic distribution, this is probably the best proxy we can come up with.
At first glance, having 5.5% of HMG leaders who are Black doesn’t seem terribly out of line with the reported range of 6.4 to 7.8% in the general population of internal medicine physicians (apologies to the family medicine and pediatric hospitalists reading this, but I’ll confine my discussion to internists for ease and brevity, since they represent the vast majority of the nation’s hospitalists). But do the math. It means Black hospitalists are likely underrepresented in HMG leadership ranks by something like 14% to 29% compared to their likely presence among hospitalists in general.
The real problem, of course, is that according the U.S. Census Bureau, 13.4% of the U.S. population is Black. So even if the racial distribution of HMG leaders catches up to the general hospitalist population, hospital medicine is still woefully underrepresenting the racial and ethnic distribution of our patient population.
The disconnect between the ethnic distribution of HMG leaders vs. hospitalists (based on general internal medicine distribution) is even more pronounced for Latinos. The JHCPU paper reported that, in 2012, 5.6% of general internists were Hispanic. The AAMC data set reported 5.8% of IM doctors were Hispanic/Latino. But only 2.2% of SoHM respondent HMGs reported a Hispanic/Latino leader, which means Latinos are underrepresented by somewhere around 61% or so relative to the likely hospitalist population, and by a whole lot more considering the fact that Latinos make up about 18.5% of the U.S. population.
I’m not saying that a White or Asian doctor can’t provide skilled, compassionate care to a Black or Latino patient, or vice-versa. It happens every day. I guess what I am saying is that we as a country and in the medical profession need to do a better job of creating pathways and promoting careers in medicine for people of color. A JAMA paper from 2019 reported that while the numbers and proportions of minority medical school matriculants has slowly been increasing from 2002 to 2017, the rate of increase was “slower than their age-matched counterparts in the U.S. population, resulting in increased underrepresentation” (doi:10.1001/jamanetworkopen.2019.10490). This means we’re falling behind, not catching up.
We need to make sure that people like Dr. Ryan Brown aren’t discouraged from pursuing medicine by teachers or school counselors because of their skin color or accent, or their gender or sexual orientation. And among those who become doctors, we need to promote hospital medicine as a desirable specialty for people of color and actively invite them in.
In my view, much of this starts with creating more and better paths to leadership within hospital medicine for people of color. Hospital medicine group leaders wield enormous – and increasing – influence, not only within their HMGs and within SHM, but within their institutions and health care systems. We need their voices and their influence to promote diversity within their groups, their institutions, within hospital medicine, and within medicine and the U.S. health care system more broadly.
The Society of Hospital Medicine is already taking steps to promote diversity, equity and inclusion. These include issuing a formal Diversity and Inclusion Statement, creating the DEI SIG, and the recent formation of a Board-designated DEI task force charged with making recommendations to promote DEI within SHM and in hospital medicine more broadly. But I want to challenge SHM to do more, particularly with regard to promoting diversity in leadership. Here are a few ideas to consider:
- Create and sponsor a mentoring program in which hospitalists volunteer to mentor minority junior high and high school students and help them prepare to pursue a career in medicine.
- Develop a formal, structured advocacy or collaboration effort with organizations like AAMC and the Accreditation Council for Graduate Medical Education designed to promote meaningful increases in the proportion of medical school students and residents who are people of color, and in the proportion who choose primary care – and ultimately, hospital medicine.
- Work hard to collect reliable racial, ethnic and gender information about SHM members and consider collaborating with MGMA to incorporate demographic questions into its survey tool for individual hospitalist compensation and productivity data. Challenge us on the Practice Analysis Committee who are responsible for the SoHM survey to continue surveying leadership demographics, and to consider how we can expand our collection of DEI information in 2022.
- Undertake a public relations campaign to highlight to health systems and other employers the under-representation of Black and Latino hospitalists in leadership positions, and to promote conscious efforts to increase those ranks.
- Create scholarships for hospitalists from underrepresented racial and ethnic groups to attend SHM-sponsored leadership development programs such as Leadership Academy, Academic Hospitalist Academy, and Quality and Safety Educators Academy, with the goal of increasing their ranks in positions of influence throughout healthcare. A scholarship program might even include raising funds to help minority hospitalists pursue Master’s-level programs such as an MBA, MHA, or MMM.
- Develop an educational track, mentoring program, or other support initiative for early-career hospitalist leaders and those interested in developing leadership skills, and ensure it gives specific attention to strategies for increasing the proportion of hospitalists of color in leadership positions.
- Review and revise existing SHM documents such as The Key Principles and Characteristics of an Effective Hospital Medicine Group, the Core Competencies in Hospital Medicine, and various white papers and position statements to ensure they address diversity, equity and inclusion – both with regard to the hospital medicine workforce and leadership, and with regard to patient care and eliminating health disparities.
I’m sure there are plenty of other similar actions we can take that I haven’t thought of. But we need to start the conversation about concrete steps our Society, and the medical specialty we represent, can take to foster real change. And then, we need to follow our words up with actions.
Ms. Flores is a partner at Nelson Flores Hospital Medicine Consultants in La Quinta, Calif. She serves on SHM’s Practice Analysis and Annual Conference Committees and helps to coordinate SHM’s biannual State of Hospital Medicine survey.
Hospitalists and unit-based assignments
What seems like a usual day to a seasoned hospitalist can be a daunting task for a new hospitalist. A routine day as a hospitalist begins with prerounding, organizing, familiarizing, and gathering data on the list of patients, and most importantly prioritizing the tasks for the day. I have experienced both traditional and unit-based rounding models, and the geographic (unit-based) rounding model stands out for me.
The push for geographic rounding comes from the need to achieve excellence in patient care, coordination with nursing staff, higher HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, better provider satisfaction, and efficiency in work flow and in documentation. The goal is typically to use this well-established tool to provide quality care to acutely ill patients admitted to the hospital, creating an environment of improved communication with the staff. It’s a “patient-centered care” model – if the patient wants to see a physician, it’s quicker to get to the patient and provides more visibility for the physician. These encounters result in improved patient-provider relationships, which in turn influences HCAHPS scores. Proximity encourages empathy, better work flow, and productivity.
The American health care system is intense and complex, and effective hospital medicine groups (HMGs) strive to provide quality care. Performance of an effective HMG is often scored on a “balanced score card.” The “balanced score” evaluates performance on domains such as clinical quality and safety, financial stability, HCAHPS, and operational effectiveness (length of stay and readmission rates). In my experience, effective unit-based rounding positively influences all the measures of the balanced score card.
Multidisciplinary roundings (MDRs) provide a platform where “the team” meets every morning to discuss the daily plan of care, everyone gets on the same page, and unit-based assignments facilitate hospitalist participation in MDRs. MDRs typically are a collaborative effort between care team members, such as a case manager, nurse, and hospitalist, physical therapist, and pharmacist. Each team member provides a precise input. Team members feel accountable and are better prepared for the day. It’s easier to develop a rapport with your patient when the same organized, comprehensive plan of care gets communicated to the patient.

It is important that each team member is prepared prior to the rounds. The total time for the rounds is often tightly controlled, as a fundamental concern is that MDRs can take up too much time. Use of a checklist or whiteboard during the unit-based rounds can improve efficiency. Midday MDRs are another gem in patient care, where the team proactively addresses early barriers in patient care and discharge plans for the next day.
The 2020 State of Hospital Medicine report highlights utilization of unit-based rounding, including breakdowns based on employment model. In groups serving adults patients only, 43% of university/medical school practices utilized unit-based assignments versus 48% for hospital-employed HMGs and only 32% for HMGs employed by multistate management companies. In HMGs that served pediatric patients only, 27% utilized unit-based assignments.
Undoubtedly geographic rounding has its own challenges. The pros and cons and the feasibility needs to be determined by each HMG. It’s often best to conduct the unit-based rounds on a few units and then roll it out to all the floors.
An important prerequisite to establishing a unit-based model for rounding is a detailed data analysis of total number of patients in various units to ensure there is adequate staffing. It must be practical to localize providers to different units, and complexity of various units can differ. At Lahey Hospital and Medical Center in Burlington, Mass., an efficient unit-based model has been achieved with complex units typically assigned two providers. Units including oncology and the progressive care unit can be a challenge, because of higher intensity and patient turnover.

Each unit is tagged to another unit in the same geographical area; these units are designated “sister pods.” The intention of these units is to strike a balance and level off patient load when needed. This process helps with standardization of the work between the providers. A big challenge of the unit-based model is to understand that it’s not always feasible to maintain consistency in patient assignments. Some patients can get transferred to a different unit due to limited telemetry and specialty units. At Lahey the provider manages their own patient as “patient drift” happens, in an attempt to maintain continuity of care.
The ultimate goal of unit-based assignments is to improve quality, financial, and operational metrics for the organization and take a deeper dive into provider and staff satisfaction. The simplest benefit for a hospitalist is to reduce travel time while rounding.
Education and teaching opportunities during the daily MDRs are still debatable. Another big step in this area may be a “resident-centered MDR” with the dual goals of improving both quality of care and resident education by focusing on evidence-based medicine.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
What seems like a usual day to a seasoned hospitalist can be a daunting task for a new hospitalist. A routine day as a hospitalist begins with prerounding, organizing, familiarizing, and gathering data on the list of patients, and most importantly prioritizing the tasks for the day. I have experienced both traditional and unit-based rounding models, and the geographic (unit-based) rounding model stands out for me.
The push for geographic rounding comes from the need to achieve excellence in patient care, coordination with nursing staff, higher HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, better provider satisfaction, and efficiency in work flow and in documentation. The goal is typically to use this well-established tool to provide quality care to acutely ill patients admitted to the hospital, creating an environment of improved communication with the staff. It’s a “patient-centered care” model – if the patient wants to see a physician, it’s quicker to get to the patient and provides more visibility for the physician. These encounters result in improved patient-provider relationships, which in turn influences HCAHPS scores. Proximity encourages empathy, better work flow, and productivity.
The American health care system is intense and complex, and effective hospital medicine groups (HMGs) strive to provide quality care. Performance of an effective HMG is often scored on a “balanced score card.” The “balanced score” evaluates performance on domains such as clinical quality and safety, financial stability, HCAHPS, and operational effectiveness (length of stay and readmission rates). In my experience, effective unit-based rounding positively influences all the measures of the balanced score card.
Multidisciplinary roundings (MDRs) provide a platform where “the team” meets every morning to discuss the daily plan of care, everyone gets on the same page, and unit-based assignments facilitate hospitalist participation in MDRs. MDRs typically are a collaborative effort between care team members, such as a case manager, nurse, and hospitalist, physical therapist, and pharmacist. Each team member provides a precise input. Team members feel accountable and are better prepared for the day. It’s easier to develop a rapport with your patient when the same organized, comprehensive plan of care gets communicated to the patient.

It is important that each team member is prepared prior to the rounds. The total time for the rounds is often tightly controlled, as a fundamental concern is that MDRs can take up too much time. Use of a checklist or whiteboard during the unit-based rounds can improve efficiency. Midday MDRs are another gem in patient care, where the team proactively addresses early barriers in patient care and discharge plans for the next day.
The 2020 State of Hospital Medicine report highlights utilization of unit-based rounding, including breakdowns based on employment model. In groups serving adults patients only, 43% of university/medical school practices utilized unit-based assignments versus 48% for hospital-employed HMGs and only 32% for HMGs employed by multistate management companies. In HMGs that served pediatric patients only, 27% utilized unit-based assignments.
Undoubtedly geographic rounding has its own challenges. The pros and cons and the feasibility needs to be determined by each HMG. It’s often best to conduct the unit-based rounds on a few units and then roll it out to all the floors.
An important prerequisite to establishing a unit-based model for rounding is a detailed data analysis of total number of patients in various units to ensure there is adequate staffing. It must be practical to localize providers to different units, and complexity of various units can differ. At Lahey Hospital and Medical Center in Burlington, Mass., an efficient unit-based model has been achieved with complex units typically assigned two providers. Units including oncology and the progressive care unit can be a challenge, because of higher intensity and patient turnover.

Each unit is tagged to another unit in the same geographical area; these units are designated “sister pods.” The intention of these units is to strike a balance and level off patient load when needed. This process helps with standardization of the work between the providers. A big challenge of the unit-based model is to understand that it’s not always feasible to maintain consistency in patient assignments. Some patients can get transferred to a different unit due to limited telemetry and specialty units. At Lahey the provider manages their own patient as “patient drift” happens, in an attempt to maintain continuity of care.
The ultimate goal of unit-based assignments is to improve quality, financial, and operational metrics for the organization and take a deeper dive into provider and staff satisfaction. The simplest benefit for a hospitalist is to reduce travel time while rounding.
Education and teaching opportunities during the daily MDRs are still debatable. Another big step in this area may be a “resident-centered MDR” with the dual goals of improving both quality of care and resident education by focusing on evidence-based medicine.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
What seems like a usual day to a seasoned hospitalist can be a daunting task for a new hospitalist. A routine day as a hospitalist begins with prerounding, organizing, familiarizing, and gathering data on the list of patients, and most importantly prioritizing the tasks for the day. I have experienced both traditional and unit-based rounding models, and the geographic (unit-based) rounding model stands out for me.
The push for geographic rounding comes from the need to achieve excellence in patient care, coordination with nursing staff, higher HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, better provider satisfaction, and efficiency in work flow and in documentation. The goal is typically to use this well-established tool to provide quality care to acutely ill patients admitted to the hospital, creating an environment of improved communication with the staff. It’s a “patient-centered care” model – if the patient wants to see a physician, it’s quicker to get to the patient and provides more visibility for the physician. These encounters result in improved patient-provider relationships, which in turn influences HCAHPS scores. Proximity encourages empathy, better work flow, and productivity.
The American health care system is intense and complex, and effective hospital medicine groups (HMGs) strive to provide quality care. Performance of an effective HMG is often scored on a “balanced score card.” The “balanced score” evaluates performance on domains such as clinical quality and safety, financial stability, HCAHPS, and operational effectiveness (length of stay and readmission rates). In my experience, effective unit-based rounding positively influences all the measures of the balanced score card.
Multidisciplinary roundings (MDRs) provide a platform where “the team” meets every morning to discuss the daily plan of care, everyone gets on the same page, and unit-based assignments facilitate hospitalist participation in MDRs. MDRs typically are a collaborative effort between care team members, such as a case manager, nurse, and hospitalist, physical therapist, and pharmacist. Each team member provides a precise input. Team members feel accountable and are better prepared for the day. It’s easier to develop a rapport with your patient when the same organized, comprehensive plan of care gets communicated to the patient.

It is important that each team member is prepared prior to the rounds. The total time for the rounds is often tightly controlled, as a fundamental concern is that MDRs can take up too much time. Use of a checklist or whiteboard during the unit-based rounds can improve efficiency. Midday MDRs are another gem in patient care, where the team proactively addresses early barriers in patient care and discharge plans for the next day.
The 2020 State of Hospital Medicine report highlights utilization of unit-based rounding, including breakdowns based on employment model. In groups serving adults patients only, 43% of university/medical school practices utilized unit-based assignments versus 48% for hospital-employed HMGs and only 32% for HMGs employed by multistate management companies. In HMGs that served pediatric patients only, 27% utilized unit-based assignments.
Undoubtedly geographic rounding has its own challenges. The pros and cons and the feasibility needs to be determined by each HMG. It’s often best to conduct the unit-based rounds on a few units and then roll it out to all the floors.
An important prerequisite to establishing a unit-based model for rounding is a detailed data analysis of total number of patients in various units to ensure there is adequate staffing. It must be practical to localize providers to different units, and complexity of various units can differ. At Lahey Hospital and Medical Center in Burlington, Mass., an efficient unit-based model has been achieved with complex units typically assigned two providers. Units including oncology and the progressive care unit can be a challenge, because of higher intensity and patient turnover.

Each unit is tagged to another unit in the same geographical area; these units are designated “sister pods.” The intention of these units is to strike a balance and level off patient load when needed. This process helps with standardization of the work between the providers. A big challenge of the unit-based model is to understand that it’s not always feasible to maintain consistency in patient assignments. Some patients can get transferred to a different unit due to limited telemetry and specialty units. At Lahey the provider manages their own patient as “patient drift” happens, in an attempt to maintain continuity of care.
The ultimate goal of unit-based assignments is to improve quality, financial, and operational metrics for the organization and take a deeper dive into provider and staff satisfaction. The simplest benefit for a hospitalist is to reduce travel time while rounding.
Education and teaching opportunities during the daily MDRs are still debatable. Another big step in this area may be a “resident-centered MDR” with the dual goals of improving both quality of care and resident education by focusing on evidence-based medicine.
Dr. Puri is a hospitalist at Lahey Hospital and Medical Center in Burlington, Mass.
SHM Chapter innovations: A provider exchange program
The SHM Annual Conference is more than an educational event. It also provides an opportunity to collaborate, network and create innovative ideas to improve the quality of inpatient care.
During the 2019 Annual Conference (HM19) – the last “in-person” Annual Conference before the COVID pandemic – SHM chapter leaders from the New Mexico chapter (Krystle Apodaca) and the Wiregrass chapter (Amith Skandhan), which covers the counties of Southern Alabama and the Panhandle of Florida, met during a networking event.
As we talked, we realized the unique differences and similarities our practice settings shared. We debated the role of clinician wellbeing, quality of medical education, and faculty development on individual hospital medicine group (HMG) practice styles.
Clinician well-being is the prerequisite to the Triple Aim of improving the health of populations, enhancing the patient experience, and reducing the cost of care. Engagement in local SHM chapter activities promotes the efficiency of practice, a culture of wellness, and personal resilience. Each HMG faces similar challenges but approaches to solving them vary. Professional challenges can affect the well-being of individual clinicians. During our discussion we realized that an interinstitutional exchange programs could provide a platform to exchange ideas and establish mentors.
The quality of medical education is directly linked to the quality of faculty development. Improving the quality of medical education requires a multifaceted approach by highly developed faculty. The complex factors affecting medical education and faculty development are further complicated by geographic location, patient characteristics, and professional growth opportunities.
Overcoming these obstacles requires an innovative and collaborative approach. Although faculty exchanges are common in academic medicine, they are not commonly attempted with HMGs. Hospitalists are responsible for a significant part of inpatient training for residents, medical students, and nurse practitioners/physician assistants (NPs/PAs) but their faculty training can vary based on location.
As a young specialty, hospital medicine is still evolving and incorporating NPs/PAs and physician hospitalists in varied practice models. Each HMG addresses common obstacles differently based on their culture and practice styles. As chapter leaders we determined that an exchange program would afford the opportunity for visiting faculty members to experience these differences.
We shared the idea of a chapter-level exchange with SHM’s Chapter Development Committee and obtained chapter development funds to execute the event. We also requested that an SHM national board member visit during the exchange to provide insight and feedback. We researched the characteristics of individual academic HMGs and structured a faculty exchange involving physicians and NPs/PAs. During the exchange program planning, the visiting faculty itinerary was tailored to a well-planned agenda for one week, with separate tracks for physicians and NPs/PAs, giving increased access to their individual peer practice styles. Additionally, the visiting faculty had meetings and discussions with the HMG and hospital leadership, to specifically address the visiting faculty’s institutional challenges.
The overall goal of the exchange program was to promote cross-institutional collaboration, increase engagement, improve medical education through faculty development and improve the quality of care. The focus of the exchange program was to share ideas and innovation, and learn the approaches to unique challenges at each institution. Out of this also grew collaboration and mentoring opportunities.
SHM’s New Mexico chapter is based in Albuquerque, a city in the desert Southwest with an ethnically diverse population of 545,000, The chapter leadership works at the University of New Mexico (UNM), a 553-bed medical center. UNM has a well-established internal medicine residency program, an academic hospitalist program, and an NP/PA fellowship program embedded within the hospital medicine department. At the time of the exchange, the HMG at UNM has 26 physicians and 9 NP/PA’s.
The SHM Wiregrass chapter is located in Dothan, Ala., a town of 80,000 near the Gulf of Mexico. Chapter leadership works at Southeast Health, a tertiary care facility with 420 beds, an affiliated medical school, and an internal medicine residency program. At the time of the exchange, the HMG at SEH has 28 physicians and 5 NP/PA’s.
These are two similarly sized hospital medicine programs, located in different geographic regions, and serving different populations. SHM board member Howard Epstein, MD, SFHM, vice president and chief medical officer of Presbyterian Healthcare Services in Albuquerque, participated on behalf of the Society when SEH faculty visited UNM. Kris Rehm, MD, SFHM, a pediatric hospitalist and the vice chair of outreach medicine at Vanderbilt University Medical Center, Nashville, came to Dothan during the faculty visit by UNM.
Two SEH faculty members, a physician and an NP, visited the University of New Mexico Hospital for one week. They participated as observers, rounding with the teams and meeting the UNM HMG leadership. The focus of the discussions included faculty education, a curriculum for quality improvement, and ways to address practice challenges. The SEH faculty also presented a QI project from their institution, and established collaborative relationships.
During the second part of the exchange, three UNM faculty members, including one physician and two NPs, visited SEH for one week. During the visit, they observed NP/PA hospitalist team models, discussed innovations, established mentoring relationships with leadership, and discussed QI projects at SEH. Additionally, the visiting UNM faculty participated in Women In Medicine events and participated as judges for a poster competition. They also had an opportunity to explore the rural landscape and visit the beach.
The evaluation process after the exchanges involved interviews, a survey, and the establishment of shared QI projects in mutual areas of challenge. The survey provided feedback, lessons learned from the exchange, and areas to be improved. Collaborative QI projects currently underway as a result of the exchange include paging etiquette, quality of sleep for hospitalized patients, and onboarding of NPs/PAs in HMGs.
This innovation changed our thinking as medical educators by addressing faculty development and medical education via clinician well-being. The physician and NP/PA Faculty Exchange program was an essential and meaningful innovation that resulted in increased SHM member engagement, crossinstitutional collaboration, networking, and mentorship.
This event created opportunities for faculty collaboration and expanded the professional network of participating institutions. The costs of the exchange were minimal given support from SHM. We believe that once the COVID pandemic has ended, this initiative has the potential to expand facilitated exchanges nationally and internationally, enhance faculty development, and improve medical education.
Dr. Apodaca is assistant professor and nurse practitioner hospitalist at the University of New Mexico. She serves as codirector of the UNM APP Hospital Medicine Fellowship and director of the APP Hospital Medicine Team. Dr. Skandhan is a hospitalist and member of the Core Faculty for the Internal Medicine Residency Program at Southeast Health (SEH), Dothan Ala., and an assistant professor at the Alabama College of Osteopathic Medicine. He serves as the medical director/physician liaison for the Clinical Documentation Program at SEH and also as the director for physician integration for Southeast Health Statera Network, an Accountable Care Organization.
The SHM Annual Conference is more than an educational event. It also provides an opportunity to collaborate, network and create innovative ideas to improve the quality of inpatient care.
During the 2019 Annual Conference (HM19) – the last “in-person” Annual Conference before the COVID pandemic – SHM chapter leaders from the New Mexico chapter (Krystle Apodaca) and the Wiregrass chapter (Amith Skandhan), which covers the counties of Southern Alabama and the Panhandle of Florida, met during a networking event.
As we talked, we realized the unique differences and similarities our practice settings shared. We debated the role of clinician wellbeing, quality of medical education, and faculty development on individual hospital medicine group (HMG) practice styles.
Clinician well-being is the prerequisite to the Triple Aim of improving the health of populations, enhancing the patient experience, and reducing the cost of care. Engagement in local SHM chapter activities promotes the efficiency of practice, a culture of wellness, and personal resilience. Each HMG faces similar challenges but approaches to solving them vary. Professional challenges can affect the well-being of individual clinicians. During our discussion we realized that an interinstitutional exchange programs could provide a platform to exchange ideas and establish mentors.
The quality of medical education is directly linked to the quality of faculty development. Improving the quality of medical education requires a multifaceted approach by highly developed faculty. The complex factors affecting medical education and faculty development are further complicated by geographic location, patient characteristics, and professional growth opportunities.
Overcoming these obstacles requires an innovative and collaborative approach. Although faculty exchanges are common in academic medicine, they are not commonly attempted with HMGs. Hospitalists are responsible for a significant part of inpatient training for residents, medical students, and nurse practitioners/physician assistants (NPs/PAs) but their faculty training can vary based on location.
As a young specialty, hospital medicine is still evolving and incorporating NPs/PAs and physician hospitalists in varied practice models. Each HMG addresses common obstacles differently based on their culture and practice styles. As chapter leaders we determined that an exchange program would afford the opportunity for visiting faculty members to experience these differences.
We shared the idea of a chapter-level exchange with SHM’s Chapter Development Committee and obtained chapter development funds to execute the event. We also requested that an SHM national board member visit during the exchange to provide insight and feedback. We researched the characteristics of individual academic HMGs and structured a faculty exchange involving physicians and NPs/PAs. During the exchange program planning, the visiting faculty itinerary was tailored to a well-planned agenda for one week, with separate tracks for physicians and NPs/PAs, giving increased access to their individual peer practice styles. Additionally, the visiting faculty had meetings and discussions with the HMG and hospital leadership, to specifically address the visiting faculty’s institutional challenges.
The overall goal of the exchange program was to promote cross-institutional collaboration, increase engagement, improve medical education through faculty development and improve the quality of care. The focus of the exchange program was to share ideas and innovation, and learn the approaches to unique challenges at each institution. Out of this also grew collaboration and mentoring opportunities.
SHM’s New Mexico chapter is based in Albuquerque, a city in the desert Southwest with an ethnically diverse population of 545,000, The chapter leadership works at the University of New Mexico (UNM), a 553-bed medical center. UNM has a well-established internal medicine residency program, an academic hospitalist program, and an NP/PA fellowship program embedded within the hospital medicine department. At the time of the exchange, the HMG at UNM has 26 physicians and 9 NP/PA’s.
The SHM Wiregrass chapter is located in Dothan, Ala., a town of 80,000 near the Gulf of Mexico. Chapter leadership works at Southeast Health, a tertiary care facility with 420 beds, an affiliated medical school, and an internal medicine residency program. At the time of the exchange, the HMG at SEH has 28 physicians and 5 NP/PA’s.
These are two similarly sized hospital medicine programs, located in different geographic regions, and serving different populations. SHM board member Howard Epstein, MD, SFHM, vice president and chief medical officer of Presbyterian Healthcare Services in Albuquerque, participated on behalf of the Society when SEH faculty visited UNM. Kris Rehm, MD, SFHM, a pediatric hospitalist and the vice chair of outreach medicine at Vanderbilt University Medical Center, Nashville, came to Dothan during the faculty visit by UNM.
Two SEH faculty members, a physician and an NP, visited the University of New Mexico Hospital for one week. They participated as observers, rounding with the teams and meeting the UNM HMG leadership. The focus of the discussions included faculty education, a curriculum for quality improvement, and ways to address practice challenges. The SEH faculty also presented a QI project from their institution, and established collaborative relationships.
During the second part of the exchange, three UNM faculty members, including one physician and two NPs, visited SEH for one week. During the visit, they observed NP/PA hospitalist team models, discussed innovations, established mentoring relationships with leadership, and discussed QI projects at SEH. Additionally, the visiting UNM faculty participated in Women In Medicine events and participated as judges for a poster competition. They also had an opportunity to explore the rural landscape and visit the beach.
The evaluation process after the exchanges involved interviews, a survey, and the establishment of shared QI projects in mutual areas of challenge. The survey provided feedback, lessons learned from the exchange, and areas to be improved. Collaborative QI projects currently underway as a result of the exchange include paging etiquette, quality of sleep for hospitalized patients, and onboarding of NPs/PAs in HMGs.
This innovation changed our thinking as medical educators by addressing faculty development and medical education via clinician well-being. The physician and NP/PA Faculty Exchange program was an essential and meaningful innovation that resulted in increased SHM member engagement, crossinstitutional collaboration, networking, and mentorship.
This event created opportunities for faculty collaboration and expanded the professional network of participating institutions. The costs of the exchange were minimal given support from SHM. We believe that once the COVID pandemic has ended, this initiative has the potential to expand facilitated exchanges nationally and internationally, enhance faculty development, and improve medical education.
Dr. Apodaca is assistant professor and nurse practitioner hospitalist at the University of New Mexico. She serves as codirector of the UNM APP Hospital Medicine Fellowship and director of the APP Hospital Medicine Team. Dr. Skandhan is a hospitalist and member of the Core Faculty for the Internal Medicine Residency Program at Southeast Health (SEH), Dothan Ala., and an assistant professor at the Alabama College of Osteopathic Medicine. He serves as the medical director/physician liaison for the Clinical Documentation Program at SEH and also as the director for physician integration for Southeast Health Statera Network, an Accountable Care Organization.
The SHM Annual Conference is more than an educational event. It also provides an opportunity to collaborate, network and create innovative ideas to improve the quality of inpatient care.
During the 2019 Annual Conference (HM19) – the last “in-person” Annual Conference before the COVID pandemic – SHM chapter leaders from the New Mexico chapter (Krystle Apodaca) and the Wiregrass chapter (Amith Skandhan), which covers the counties of Southern Alabama and the Panhandle of Florida, met during a networking event.
As we talked, we realized the unique differences and similarities our practice settings shared. We debated the role of clinician wellbeing, quality of medical education, and faculty development on individual hospital medicine group (HMG) practice styles.
Clinician well-being is the prerequisite to the Triple Aim of improving the health of populations, enhancing the patient experience, and reducing the cost of care. Engagement in local SHM chapter activities promotes the efficiency of practice, a culture of wellness, and personal resilience. Each HMG faces similar challenges but approaches to solving them vary. Professional challenges can affect the well-being of individual clinicians. During our discussion we realized that an interinstitutional exchange programs could provide a platform to exchange ideas and establish mentors.
The quality of medical education is directly linked to the quality of faculty development. Improving the quality of medical education requires a multifaceted approach by highly developed faculty. The complex factors affecting medical education and faculty development are further complicated by geographic location, patient characteristics, and professional growth opportunities.
Overcoming these obstacles requires an innovative and collaborative approach. Although faculty exchanges are common in academic medicine, they are not commonly attempted with HMGs. Hospitalists are responsible for a significant part of inpatient training for residents, medical students, and nurse practitioners/physician assistants (NPs/PAs) but their faculty training can vary based on location.
As a young specialty, hospital medicine is still evolving and incorporating NPs/PAs and physician hospitalists in varied practice models. Each HMG addresses common obstacles differently based on their culture and practice styles. As chapter leaders we determined that an exchange program would afford the opportunity for visiting faculty members to experience these differences.
We shared the idea of a chapter-level exchange with SHM’s Chapter Development Committee and obtained chapter development funds to execute the event. We also requested that an SHM national board member visit during the exchange to provide insight and feedback. We researched the characteristics of individual academic HMGs and structured a faculty exchange involving physicians and NPs/PAs. During the exchange program planning, the visiting faculty itinerary was tailored to a well-planned agenda for one week, with separate tracks for physicians and NPs/PAs, giving increased access to their individual peer practice styles. Additionally, the visiting faculty had meetings and discussions with the HMG and hospital leadership, to specifically address the visiting faculty’s institutional challenges.
The overall goal of the exchange program was to promote cross-institutional collaboration, increase engagement, improve medical education through faculty development and improve the quality of care. The focus of the exchange program was to share ideas and innovation, and learn the approaches to unique challenges at each institution. Out of this also grew collaboration and mentoring opportunities.
SHM’s New Mexico chapter is based in Albuquerque, a city in the desert Southwest with an ethnically diverse population of 545,000, The chapter leadership works at the University of New Mexico (UNM), a 553-bed medical center. UNM has a well-established internal medicine residency program, an academic hospitalist program, and an NP/PA fellowship program embedded within the hospital medicine department. At the time of the exchange, the HMG at UNM has 26 physicians and 9 NP/PA’s.
The SHM Wiregrass chapter is located in Dothan, Ala., a town of 80,000 near the Gulf of Mexico. Chapter leadership works at Southeast Health, a tertiary care facility with 420 beds, an affiliated medical school, and an internal medicine residency program. At the time of the exchange, the HMG at SEH has 28 physicians and 5 NP/PA’s.
These are two similarly sized hospital medicine programs, located in different geographic regions, and serving different populations. SHM board member Howard Epstein, MD, SFHM, vice president and chief medical officer of Presbyterian Healthcare Services in Albuquerque, participated on behalf of the Society when SEH faculty visited UNM. Kris Rehm, MD, SFHM, a pediatric hospitalist and the vice chair of outreach medicine at Vanderbilt University Medical Center, Nashville, came to Dothan during the faculty visit by UNM.
Two SEH faculty members, a physician and an NP, visited the University of New Mexico Hospital for one week. They participated as observers, rounding with the teams and meeting the UNM HMG leadership. The focus of the discussions included faculty education, a curriculum for quality improvement, and ways to address practice challenges. The SEH faculty also presented a QI project from their institution, and established collaborative relationships.
During the second part of the exchange, three UNM faculty members, including one physician and two NPs, visited SEH for one week. During the visit, they observed NP/PA hospitalist team models, discussed innovations, established mentoring relationships with leadership, and discussed QI projects at SEH. Additionally, the visiting UNM faculty participated in Women In Medicine events and participated as judges for a poster competition. They also had an opportunity to explore the rural landscape and visit the beach.
The evaluation process after the exchanges involved interviews, a survey, and the establishment of shared QI projects in mutual areas of challenge. The survey provided feedback, lessons learned from the exchange, and areas to be improved. Collaborative QI projects currently underway as a result of the exchange include paging etiquette, quality of sleep for hospitalized patients, and onboarding of NPs/PAs in HMGs.
This innovation changed our thinking as medical educators by addressing faculty development and medical education via clinician well-being. The physician and NP/PA Faculty Exchange program was an essential and meaningful innovation that resulted in increased SHM member engagement, crossinstitutional collaboration, networking, and mentorship.
This event created opportunities for faculty collaboration and expanded the professional network of participating institutions. The costs of the exchange were minimal given support from SHM. We believe that once the COVID pandemic has ended, this initiative has the potential to expand facilitated exchanges nationally and internationally, enhance faculty development, and improve medical education.
Dr. Apodaca is assistant professor and nurse practitioner hospitalist at the University of New Mexico. She serves as codirector of the UNM APP Hospital Medicine Fellowship and director of the APP Hospital Medicine Team. Dr. Skandhan is a hospitalist and member of the Core Faculty for the Internal Medicine Residency Program at Southeast Health (SEH), Dothan Ala., and an assistant professor at the Alabama College of Osteopathic Medicine. He serves as the medical director/physician liaison for the Clinical Documentation Program at SEH and also as the director for physician integration for Southeast Health Statera Network, an Accountable Care Organization.
Medicine and the meritocracy
Addressing systemic bias, gender inequity and discrimination
There are many challenges facing modern medicine today. Recent events have highlighted important issues affecting our society as a whole – systemic racism, sexism, and implicit bias. In medicine, we have seen a renewed focus on health equity, health disparities and the implicit systemic bias that affect those who work in the field. It is truly troubling that it has taken the continued loss of black lives to police brutality and a pandemic for this conversation to happen at every level in society.
Systemic bias is present throughout corporate America, and it is no different within the physician workforce. Overall, there has been gradual interest in promoting and teaching diversity. Institutions have been slowly creating policies and administrative positions focused on inclusion and diversity over the last decade. So has diversity training objectively increased representation and advancement of women and minority groups? Do traditionally marginalized groups have better access to health? And are women and people of color (POC) represented equally in leadership positions in medicine?
Clearly, the answers are not straightforward.
Diving into the data
A guilty pleasure of mine is to assess how diverse and inclusive an institution is by looking at the wall of pictures recognizing top leadership in hospitals. Despite women accounting for 47.9% of graduates from medical school in 2018-2019, I still see very few women or POC elevated to this level. Of the total women graduates, 22.6% were Asian, 8% were Black and 5.4% were Hispanic.
Being of Indian descent, I am a woman of color (albeit one who may not be as profoundly affected by racism in medicine as my less represented colleagues). It is especially rare for me to see someone I can identify with in the ranks of top leadership. I find encouragement in seeing any woman on any leadership board because to me, it means that there is hope. The literature seems to support this degree of disparity as well. For example, a recent analysis shows that presidential leadership in medical societies are predominantly held by men (82.6% male vs. 17.4% female). Other datasets demonstrate that only 15% of deans and interim deans are women and AAMC’s report shows that women account for only 18% of all department chairs.
Growing up, my parents fueled my interest to pursue medicine. They described it as a noble profession that rewarded true merit and dedication to the cause. However, those that have been traditionally elevated in medicine are men. If merit knows no gender, why does a gender gap exist? If merit is blind to race, why are minorities so poorly represented in the workforce (much less in leadership)? My view of the wall leaves me wondering about the role of both sexism and racism in medicine.
These visual representations of the medical culture reinforce the acceptable norms and values – white and masculine – in medicine. The feminist movement over the last several decades has increased awareness about the need for equality of the sexes. However, it was not until the concept of intersectionality was introduced by Black feminist Professor Kimberle Crenshaw, that feminism become a more inclusive term. Professor Crenshaw’s paper details how every individual has intersecting factors – race, gender, sexual identity, socioeconomic status – that create the sum of their experience be it privilege, oppression, or discrimination.
For example, a White woman has privileges that a woman of color does not. Among non-white women, race and sexual identity are confounding factors – a Black woman, a Black LGBTQ woman, and an Asian woman, for example, will not experience discrimination in the same way. The farther you deviate from the accepted norms and values, the harder it is for you to obtain support and achieve recognition.
Addressing the patriarchal structure and systemic bias in medicine
Why do patriarchal structures still exist in medicine? How do we resolve systemic bias? Addressing them in isolation – race or gender or sexual identity – is unlikely to create long-lasting change. For change to occur, organizations and individuals need to be intrinsically motivated. Creating awareness and challenging the status quo is the first step.
Over the last decade, implicit bias training and diversity training have become mandatory in various industries and states. Diversity training has grown to be a multi-billion-dollar industry that corporate America has embraced over the last several years. And yet, research shows that mandating such training may not be the most effective. To get results, organizations need to implement programs that “spark engagement, increase contact between different groups and draw on people’s desire to look good to others.”
Historically, the medical curriculum has not included a discourse on feminist theories and the advancement of women in medicine. Cultural competency training is typically offered on an annual basis once we are in the workforce, but in my experience, it focuses more on our interactions with patients and other health care colleagues, and less with regards to our physician peers and leadership. Is this enough to change deep rooted beliefs and traditions?
We can take our cue from non-medical organizations and consider changing this culture of no culture in medicine – introducing diversity task forces that hold departments accountable for recruiting and promoting women and minorities; employing diversity managers; voluntary training; cross-training to increase contact among different groups and mentoring programs that match senior leadership to women and POC. While some medical institutions have implemented some of these principles, changing century-old traditions will require embracing concepts of organizational change and every available effective tool.
Committing to change
Change is especially hard when the target outcome is not accurately quantifiable – even if you can measure attitudes, values, and beliefs, these are subject to reporting bias and tokenism. At the organizational level, change management involves employing a systematic approach to change organizational values, goals, policies, and processes.
Individual change, self-reflection, and personal growth are key components in changing culture. Reflexivity is being aware of your own values, norms, position, and power – an important concept to understand and apply in our everyday interactions. Believing that one’s class, gender, race and sexual orientation are irrelevant to their practice of medicine would not foster the change that we direly need in medicine. Rather, identifying how your own values and professional identity are shaped by your medical training, your organization and the broader cultural context are critically important to developing a greater empathic sense to motivate systemic change.
There has been valuable discussion on bottom-up changes to ensure women and POC have support, encouragement and a pathway to advance in an organization. Some of these include policy and process changes including providing flexible working conditions for women and sponsorship of women and minorities to help them navigate the barriers and microaggressions they encounter at work. While technical (policy) changes form the foundation for any organizational change, it is important to remember that the people side of change – the resistance that you encounter for any change effort in an organization – is equally important to address at the organizational level. A top-down approach is also vital to ensure that change is permanent in an organization and does not end when the individuals responsible for the change leave the organization.
Lewin’s three-stage change management model provides a framework for structural and organizational change in hospital systems. The three-stages of this model are: unfreezing, changing, and refreezing. Unfreezing is the process of determining what needs to change and obtaining leadership support. The actual change process involves getting people on board, empowering them to change and communicating with them frequently. Refreezing cements this change into the organization’s culture by providing support and training to sustain changes. Research has shown that Lewin’s change management model has applicability in the hospital setting.
Industry research in change management methodologies in the business sector has identified sponsorship by CEOs/senior management of an organization and having a structured implementation model for change management as two important factors for ensuring that change efforts are successful and sustainable.
This can be extrapolated to health care organizations – top leadership committed to changing the status quo should solidify organizational commitment by incorporating new attainable and measurable goals into their vision for the organization. Designing a phased implementation of change management methodologies should follow an open discussion to identify an organization’s weaknesses, strengths, capacity, and readiness for change. Lastly, helping busy professionals adapt to change requires innovative and continuous improvement strategies using formal, systematic tools for organization-wide strategic deployment.
Without a concrete commitment at the organizational level, programs such as diversity training may end up being band-aids on wounds that run deep.
I believe that the combination of both individual and organizational commitment to change systemic bias in medicine can be quite powerful. One without the other will fail to permanently change the system. The work to true equality – regardless of the intersecting factors of discrimination – starts with a commitment to change. We may all have different opportunities because of the inequality that is apparent in our systems today, but if we unite around the goal of a bias-free, merit-based equality, it gives us the strength we need to overcome challenges that we once thought insurmountable.
Each one of us is a leader in our own right. Speaking up for those with less power or opportunity than us and supporting talent and hard work solidifies medicine as a meritocracy. Even if the magnitude of change that we fight for may not be realized during our time in medical practice, our commitment to eradicate sexism, racism and discrimination will shape the future of medicine.
Just as our children are a legacy that we leave behind, our work in correcting bias in medicine will pave the path for a better future for the doctors of tomorrow. After all, when I think that my young daughter will be affected by what I do or do not do to address the discrimination, there is no better motivation for me to break down every barrier for her success.
Dr. Kanikkannan is a practicing hospitalist and assistant professor of medicine at Albany Medical College in Albany, NY. This article first appeared on The Hospital Leader, the official blog of SHM.
Addressing systemic bias, gender inequity and discrimination
Addressing systemic bias, gender inequity and discrimination
There are many challenges facing modern medicine today. Recent events have highlighted important issues affecting our society as a whole – systemic racism, sexism, and implicit bias. In medicine, we have seen a renewed focus on health equity, health disparities and the implicit systemic bias that affect those who work in the field. It is truly troubling that it has taken the continued loss of black lives to police brutality and a pandemic for this conversation to happen at every level in society.
Systemic bias is present throughout corporate America, and it is no different within the physician workforce. Overall, there has been gradual interest in promoting and teaching diversity. Institutions have been slowly creating policies and administrative positions focused on inclusion and diversity over the last decade. So has diversity training objectively increased representation and advancement of women and minority groups? Do traditionally marginalized groups have better access to health? And are women and people of color (POC) represented equally in leadership positions in medicine?
Clearly, the answers are not straightforward.
Diving into the data
A guilty pleasure of mine is to assess how diverse and inclusive an institution is by looking at the wall of pictures recognizing top leadership in hospitals. Despite women accounting for 47.9% of graduates from medical school in 2018-2019, I still see very few women or POC elevated to this level. Of the total women graduates, 22.6% were Asian, 8% were Black and 5.4% were Hispanic.
Being of Indian descent, I am a woman of color (albeit one who may not be as profoundly affected by racism in medicine as my less represented colleagues). It is especially rare for me to see someone I can identify with in the ranks of top leadership. I find encouragement in seeing any woman on any leadership board because to me, it means that there is hope. The literature seems to support this degree of disparity as well. For example, a recent analysis shows that presidential leadership in medical societies are predominantly held by men (82.6% male vs. 17.4% female). Other datasets demonstrate that only 15% of deans and interim deans are women and AAMC’s report shows that women account for only 18% of all department chairs.
Growing up, my parents fueled my interest to pursue medicine. They described it as a noble profession that rewarded true merit and dedication to the cause. However, those that have been traditionally elevated in medicine are men. If merit knows no gender, why does a gender gap exist? If merit is blind to race, why are minorities so poorly represented in the workforce (much less in leadership)? My view of the wall leaves me wondering about the role of both sexism and racism in medicine.
These visual representations of the medical culture reinforce the acceptable norms and values – white and masculine – in medicine. The feminist movement over the last several decades has increased awareness about the need for equality of the sexes. However, it was not until the concept of intersectionality was introduced by Black feminist Professor Kimberle Crenshaw, that feminism become a more inclusive term. Professor Crenshaw’s paper details how every individual has intersecting factors – race, gender, sexual identity, socioeconomic status – that create the sum of their experience be it privilege, oppression, or discrimination.
For example, a White woman has privileges that a woman of color does not. Among non-white women, race and sexual identity are confounding factors – a Black woman, a Black LGBTQ woman, and an Asian woman, for example, will not experience discrimination in the same way. The farther you deviate from the accepted norms and values, the harder it is for you to obtain support and achieve recognition.
Addressing the patriarchal structure and systemic bias in medicine
Why do patriarchal structures still exist in medicine? How do we resolve systemic bias? Addressing them in isolation – race or gender or sexual identity – is unlikely to create long-lasting change. For change to occur, organizations and individuals need to be intrinsically motivated. Creating awareness and challenging the status quo is the first step.
Over the last decade, implicit bias training and diversity training have become mandatory in various industries and states. Diversity training has grown to be a multi-billion-dollar industry that corporate America has embraced over the last several years. And yet, research shows that mandating such training may not be the most effective. To get results, organizations need to implement programs that “spark engagement, increase contact between different groups and draw on people’s desire to look good to others.”
Historically, the medical curriculum has not included a discourse on feminist theories and the advancement of women in medicine. Cultural competency training is typically offered on an annual basis once we are in the workforce, but in my experience, it focuses more on our interactions with patients and other health care colleagues, and less with regards to our physician peers and leadership. Is this enough to change deep rooted beliefs and traditions?
We can take our cue from non-medical organizations and consider changing this culture of no culture in medicine – introducing diversity task forces that hold departments accountable for recruiting and promoting women and minorities; employing diversity managers; voluntary training; cross-training to increase contact among different groups and mentoring programs that match senior leadership to women and POC. While some medical institutions have implemented some of these principles, changing century-old traditions will require embracing concepts of organizational change and every available effective tool.
Committing to change
Change is especially hard when the target outcome is not accurately quantifiable – even if you can measure attitudes, values, and beliefs, these are subject to reporting bias and tokenism. At the organizational level, change management involves employing a systematic approach to change organizational values, goals, policies, and processes.
Individual change, self-reflection, and personal growth are key components in changing culture. Reflexivity is being aware of your own values, norms, position, and power – an important concept to understand and apply in our everyday interactions. Believing that one’s class, gender, race and sexual orientation are irrelevant to their practice of medicine would not foster the change that we direly need in medicine. Rather, identifying how your own values and professional identity are shaped by your medical training, your organization and the broader cultural context are critically important to developing a greater empathic sense to motivate systemic change.
There has been valuable discussion on bottom-up changes to ensure women and POC have support, encouragement and a pathway to advance in an organization. Some of these include policy and process changes including providing flexible working conditions for women and sponsorship of women and minorities to help them navigate the barriers and microaggressions they encounter at work. While technical (policy) changes form the foundation for any organizational change, it is important to remember that the people side of change – the resistance that you encounter for any change effort in an organization – is equally important to address at the organizational level. A top-down approach is also vital to ensure that change is permanent in an organization and does not end when the individuals responsible for the change leave the organization.
Lewin’s three-stage change management model provides a framework for structural and organizational change in hospital systems. The three-stages of this model are: unfreezing, changing, and refreezing. Unfreezing is the process of determining what needs to change and obtaining leadership support. The actual change process involves getting people on board, empowering them to change and communicating with them frequently. Refreezing cements this change into the organization’s culture by providing support and training to sustain changes. Research has shown that Lewin’s change management model has applicability in the hospital setting.
Industry research in change management methodologies in the business sector has identified sponsorship by CEOs/senior management of an organization and having a structured implementation model for change management as two important factors for ensuring that change efforts are successful and sustainable.
This can be extrapolated to health care organizations – top leadership committed to changing the status quo should solidify organizational commitment by incorporating new attainable and measurable goals into their vision for the organization. Designing a phased implementation of change management methodologies should follow an open discussion to identify an organization’s weaknesses, strengths, capacity, and readiness for change. Lastly, helping busy professionals adapt to change requires innovative and continuous improvement strategies using formal, systematic tools for organization-wide strategic deployment.
Without a concrete commitment at the organizational level, programs such as diversity training may end up being band-aids on wounds that run deep.
I believe that the combination of both individual and organizational commitment to change systemic bias in medicine can be quite powerful. One without the other will fail to permanently change the system. The work to true equality – regardless of the intersecting factors of discrimination – starts with a commitment to change. We may all have different opportunities because of the inequality that is apparent in our systems today, but if we unite around the goal of a bias-free, merit-based equality, it gives us the strength we need to overcome challenges that we once thought insurmountable.
Each one of us is a leader in our own right. Speaking up for those with less power or opportunity than us and supporting talent and hard work solidifies medicine as a meritocracy. Even if the magnitude of change that we fight for may not be realized during our time in medical practice, our commitment to eradicate sexism, racism and discrimination will shape the future of medicine.
Just as our children are a legacy that we leave behind, our work in correcting bias in medicine will pave the path for a better future for the doctors of tomorrow. After all, when I think that my young daughter will be affected by what I do or do not do to address the discrimination, there is no better motivation for me to break down every barrier for her success.
Dr. Kanikkannan is a practicing hospitalist and assistant professor of medicine at Albany Medical College in Albany, NY. This article first appeared on The Hospital Leader, the official blog of SHM.
There are many challenges facing modern medicine today. Recent events have highlighted important issues affecting our society as a whole – systemic racism, sexism, and implicit bias. In medicine, we have seen a renewed focus on health equity, health disparities and the implicit systemic bias that affect those who work in the field. It is truly troubling that it has taken the continued loss of black lives to police brutality and a pandemic for this conversation to happen at every level in society.
Systemic bias is present throughout corporate America, and it is no different within the physician workforce. Overall, there has been gradual interest in promoting and teaching diversity. Institutions have been slowly creating policies and administrative positions focused on inclusion and diversity over the last decade. So has diversity training objectively increased representation and advancement of women and minority groups? Do traditionally marginalized groups have better access to health? And are women and people of color (POC) represented equally in leadership positions in medicine?
Clearly, the answers are not straightforward.
Diving into the data
A guilty pleasure of mine is to assess how diverse and inclusive an institution is by looking at the wall of pictures recognizing top leadership in hospitals. Despite women accounting for 47.9% of graduates from medical school in 2018-2019, I still see very few women or POC elevated to this level. Of the total women graduates, 22.6% were Asian, 8% were Black and 5.4% were Hispanic.
Being of Indian descent, I am a woman of color (albeit one who may not be as profoundly affected by racism in medicine as my less represented colleagues). It is especially rare for me to see someone I can identify with in the ranks of top leadership. I find encouragement in seeing any woman on any leadership board because to me, it means that there is hope. The literature seems to support this degree of disparity as well. For example, a recent analysis shows that presidential leadership in medical societies are predominantly held by men (82.6% male vs. 17.4% female). Other datasets demonstrate that only 15% of deans and interim deans are women and AAMC’s report shows that women account for only 18% of all department chairs.
Growing up, my parents fueled my interest to pursue medicine. They described it as a noble profession that rewarded true merit and dedication to the cause. However, those that have been traditionally elevated in medicine are men. If merit knows no gender, why does a gender gap exist? If merit is blind to race, why are minorities so poorly represented in the workforce (much less in leadership)? My view of the wall leaves me wondering about the role of both sexism and racism in medicine.
These visual representations of the medical culture reinforce the acceptable norms and values – white and masculine – in medicine. The feminist movement over the last several decades has increased awareness about the need for equality of the sexes. However, it was not until the concept of intersectionality was introduced by Black feminist Professor Kimberle Crenshaw, that feminism become a more inclusive term. Professor Crenshaw’s paper details how every individual has intersecting factors – race, gender, sexual identity, socioeconomic status – that create the sum of their experience be it privilege, oppression, or discrimination.
For example, a White woman has privileges that a woman of color does not. Among non-white women, race and sexual identity are confounding factors – a Black woman, a Black LGBTQ woman, and an Asian woman, for example, will not experience discrimination in the same way. The farther you deviate from the accepted norms and values, the harder it is for you to obtain support and achieve recognition.
Addressing the patriarchal structure and systemic bias in medicine
Why do patriarchal structures still exist in medicine? How do we resolve systemic bias? Addressing them in isolation – race or gender or sexual identity – is unlikely to create long-lasting change. For change to occur, organizations and individuals need to be intrinsically motivated. Creating awareness and challenging the status quo is the first step.
Over the last decade, implicit bias training and diversity training have become mandatory in various industries and states. Diversity training has grown to be a multi-billion-dollar industry that corporate America has embraced over the last several years. And yet, research shows that mandating such training may not be the most effective. To get results, organizations need to implement programs that “spark engagement, increase contact between different groups and draw on people’s desire to look good to others.”
Historically, the medical curriculum has not included a discourse on feminist theories and the advancement of women in medicine. Cultural competency training is typically offered on an annual basis once we are in the workforce, but in my experience, it focuses more on our interactions with patients and other health care colleagues, and less with regards to our physician peers and leadership. Is this enough to change deep rooted beliefs and traditions?
We can take our cue from non-medical organizations and consider changing this culture of no culture in medicine – introducing diversity task forces that hold departments accountable for recruiting and promoting women and minorities; employing diversity managers; voluntary training; cross-training to increase contact among different groups and mentoring programs that match senior leadership to women and POC. While some medical institutions have implemented some of these principles, changing century-old traditions will require embracing concepts of organizational change and every available effective tool.
Committing to change
Change is especially hard when the target outcome is not accurately quantifiable – even if you can measure attitudes, values, and beliefs, these are subject to reporting bias and tokenism. At the organizational level, change management involves employing a systematic approach to change organizational values, goals, policies, and processes.
Individual change, self-reflection, and personal growth are key components in changing culture. Reflexivity is being aware of your own values, norms, position, and power – an important concept to understand and apply in our everyday interactions. Believing that one’s class, gender, race and sexual orientation are irrelevant to their practice of medicine would not foster the change that we direly need in medicine. Rather, identifying how your own values and professional identity are shaped by your medical training, your organization and the broader cultural context are critically important to developing a greater empathic sense to motivate systemic change.
There has been valuable discussion on bottom-up changes to ensure women and POC have support, encouragement and a pathway to advance in an organization. Some of these include policy and process changes including providing flexible working conditions for women and sponsorship of women and minorities to help them navigate the barriers and microaggressions they encounter at work. While technical (policy) changes form the foundation for any organizational change, it is important to remember that the people side of change – the resistance that you encounter for any change effort in an organization – is equally important to address at the organizational level. A top-down approach is also vital to ensure that change is permanent in an organization and does not end when the individuals responsible for the change leave the organization.
Lewin’s three-stage change management model provides a framework for structural and organizational change in hospital systems. The three-stages of this model are: unfreezing, changing, and refreezing. Unfreezing is the process of determining what needs to change and obtaining leadership support. The actual change process involves getting people on board, empowering them to change and communicating with them frequently. Refreezing cements this change into the organization’s culture by providing support and training to sustain changes. Research has shown that Lewin’s change management model has applicability in the hospital setting.
Industry research in change management methodologies in the business sector has identified sponsorship by CEOs/senior management of an organization and having a structured implementation model for change management as two important factors for ensuring that change efforts are successful and sustainable.
This can be extrapolated to health care organizations – top leadership committed to changing the status quo should solidify organizational commitment by incorporating new attainable and measurable goals into their vision for the organization. Designing a phased implementation of change management methodologies should follow an open discussion to identify an organization’s weaknesses, strengths, capacity, and readiness for change. Lastly, helping busy professionals adapt to change requires innovative and continuous improvement strategies using formal, systematic tools for organization-wide strategic deployment.
Without a concrete commitment at the organizational level, programs such as diversity training may end up being band-aids on wounds that run deep.
I believe that the combination of both individual and organizational commitment to change systemic bias in medicine can be quite powerful. One without the other will fail to permanently change the system. The work to true equality – regardless of the intersecting factors of discrimination – starts with a commitment to change. We may all have different opportunities because of the inequality that is apparent in our systems today, but if we unite around the goal of a bias-free, merit-based equality, it gives us the strength we need to overcome challenges that we once thought insurmountable.
Each one of us is a leader in our own right. Speaking up for those with less power or opportunity than us and supporting talent and hard work solidifies medicine as a meritocracy. Even if the magnitude of change that we fight for may not be realized during our time in medical practice, our commitment to eradicate sexism, racism and discrimination will shape the future of medicine.
Just as our children are a legacy that we leave behind, our work in correcting bias in medicine will pave the path for a better future for the doctors of tomorrow. After all, when I think that my young daughter will be affected by what I do or do not do to address the discrimination, there is no better motivation for me to break down every barrier for her success.
Dr. Kanikkannan is a practicing hospitalist and assistant professor of medicine at Albany Medical College in Albany, NY. This article first appeared on The Hospital Leader, the official blog of SHM.
COVID-19 pandemic amplifies uncertainty for immigrant hospitalists
H1-B visa program needs improvement
Statistics tell the tale of immigrants in the American health care workforce in broad strokes. In an interview, though, one hospitalist shared the particulars of his professional and personal journey since arriving in the United States from India 15 years ago.
Mihir Patel, MD, MPH, FHM, came to the United States in 2005 to complete a Master’s in Public Health. Fifteen years later, he is still waiting for the green card that signifies U.S. permanent residency status. The paperwork for the application, he said, was completed in 2012. Since then, he’s been renewing his H-1B visa every three years, and he has no expectation that anything will change soon.
“If you are from India, which has a significant backlog of green cards – up to 50 years…you just wait forever,” he said. “Many people even die waiting for their green card to arrive.”
Arriving on a student visa, Dr. Patel completed his MPH in 2008 and began an internal medicine residency that same year, holding a J-1 visa for the 3 years of his US residency program.
“Post-residency, I started working in a rural hospital in an underserved area of northeast Tennessee as a hospitalist,” thus completing the 3 years of service in a rural underserved area that’s a requirement for J-1 visa holders, said Dr. Patel. “I loved this rural community hospital so much that I ended up staying there for 6 years. During my work at this rural hospital, I was able to enjoy the autonomy of managing a small ICU, doing both critical care procedures and management of intubated critical patients while working as a hospitalist,” he said. Dr. Patel served as chief of staff at the hospital for two years, and also served on the board of directors for his 400-physician medical group.
“I was a proud member of this rural community – Rogersville,” said Dr. Patel. Although he and his wife, who was completing her hospitalist residency, lived in Johnson City, Tenn., “I did not mind driving 120 miles round trip every day to go to my small-town hospital for 6 years,” he said.
Spending this time in rural Tennessee allowed Dr. Patel to finish the requirements necessary for the Physician National Interest Waiver and submit his application for permanent residency. The waiver, though, doesn’t give him priority status in the waiting list for permanent residency status.
After a stint in northern California to be closer to extended family, the pull of “beautiful northeast Tennesse and the rural community” was too strong, so Dr. Patel and his family moved back to Johnson City in 2018.
Now, Dr. Patel is a hospitalist at Ballad Health System in Johnson City. He is the corporate director of Ballad’s telemedicine program and is now also the medical director of the COVID-19 Strike Team. He co-founded and is president of the Blue Ridge Chapter of the Society of Hospital Medicine. Under another H-1B visa, Dr. Patel works part-time from home as a telehospitalist, covering six hospitals in 4 different states.
Even in ordinary circumstances, the H-1B visa comes with constraints. Although Dr. Patel’s 6-year old daughter was born in the U.S. and is a citizen, Dr. Patel and his wife have to reapply for their visas every 3 years. “If we travel outside the U.S., we have to get our visas stamped. We cannot change jobs easily due to fear of visa denial, especially with the recent political environment,” said Dr. Patel. “It feels like we are essential health care workers but non-essential immigrants.”
Having recently completed a physician executive MBA program, Dr. Patel said he’d like to start a business of his own using Lean health care principles and telemedicine to improve rural health care. “But while on an H-1B I cannot do anything outside my sponsored employment,” he said.
Ideally, health care organizations would have high flexibility in how and where staff are deployed when a surge of COVID-19 patients hits. Dr. Patel made the point that visa restrictions can make this much harder: “During this COVID crisis, this restriction can cause significant negative impact for small rural hospitals, where local physicians are quarantined and available physicians are on a visa who cannot legally work outside their primary facilities – even though they are willing to work,” he said. “One cannot even work using telemedicine in the same health system, if that is not specifically mentioned during H-1B petition filling. More than 15,000 physicians who are struck by the green card backlog are in the same situation all over U.S.,” he added.
These constraints, though, pale before the consequences of a worst-case pandemic scenario for an immigrant family, where the physician – the primary visa-holder – becomes disabled or dies. In this case, dependent family members must self-deport. “In addition, there would not be any disability or Social Security benefits for the physician or dependents, as they are not citizens or green card holders and they cannot legally stay in the US,” noted Dr. Patel. “Any hospitalist working during the COVID-19 pandemic can have this fate due to our high exposure risk.”
Reauthorizing the H1-B visa program
SHM has been advocating to improve the H1-B visa system for years, Dr. Patel said, The Fairness for High Skilled Immigrants Act passed the U.S. House of Representatives with bipartisan support, and the Society is advocating for its passage in the Senate.
The Fairness for High-Skilled Immigrants Act (S. 386) simplifies the employment-based immigration system by removing per-country caps, converting the employment-based immigration system into a “first-come, first serve” system that does not discriminate on country of origin. The act will also help alleviate the decades-long green card and permanent residency application backlogs.
Dr. Patel emphasized the importance of action by Congress to reauthorize the physician visa waiver program and expediting physician permanent residency. “This is a crisis and we are all physicians who are ready to serve, regardless of our country of origin. Please let us help this great nation by giving us freedom from visa restrictions and providing security for our families.
“During wartime, all frontline soldiers are naturalized and given citizenship by presidential mandate; this is more than war and we are not asking for citizenship – but at least give us a green card which we have already satisfied all requirements for. If not now, then when?” he asked.
H1-B visa program needs improvement
H1-B visa program needs improvement
Statistics tell the tale of immigrants in the American health care workforce in broad strokes. In an interview, though, one hospitalist shared the particulars of his professional and personal journey since arriving in the United States from India 15 years ago.
Mihir Patel, MD, MPH, FHM, came to the United States in 2005 to complete a Master’s in Public Health. Fifteen years later, he is still waiting for the green card that signifies U.S. permanent residency status. The paperwork for the application, he said, was completed in 2012. Since then, he’s been renewing his H-1B visa every three years, and he has no expectation that anything will change soon.
“If you are from India, which has a significant backlog of green cards – up to 50 years…you just wait forever,” he said. “Many people even die waiting for their green card to arrive.”
Arriving on a student visa, Dr. Patel completed his MPH in 2008 and began an internal medicine residency that same year, holding a J-1 visa for the 3 years of his US residency program.
“Post-residency, I started working in a rural hospital in an underserved area of northeast Tennessee as a hospitalist,” thus completing the 3 years of service in a rural underserved area that’s a requirement for J-1 visa holders, said Dr. Patel. “I loved this rural community hospital so much that I ended up staying there for 6 years. During my work at this rural hospital, I was able to enjoy the autonomy of managing a small ICU, doing both critical care procedures and management of intubated critical patients while working as a hospitalist,” he said. Dr. Patel served as chief of staff at the hospital for two years, and also served on the board of directors for his 400-physician medical group.
“I was a proud member of this rural community – Rogersville,” said Dr. Patel. Although he and his wife, who was completing her hospitalist residency, lived in Johnson City, Tenn., “I did not mind driving 120 miles round trip every day to go to my small-town hospital for 6 years,” he said.
Spending this time in rural Tennessee allowed Dr. Patel to finish the requirements necessary for the Physician National Interest Waiver and submit his application for permanent residency. The waiver, though, doesn’t give him priority status in the waiting list for permanent residency status.
After a stint in northern California to be closer to extended family, the pull of “beautiful northeast Tennesse and the rural community” was too strong, so Dr. Patel and his family moved back to Johnson City in 2018.
Now, Dr. Patel is a hospitalist at Ballad Health System in Johnson City. He is the corporate director of Ballad’s telemedicine program and is now also the medical director of the COVID-19 Strike Team. He co-founded and is president of the Blue Ridge Chapter of the Society of Hospital Medicine. Under another H-1B visa, Dr. Patel works part-time from home as a telehospitalist, covering six hospitals in 4 different states.
Even in ordinary circumstances, the H-1B visa comes with constraints. Although Dr. Patel’s 6-year old daughter was born in the U.S. and is a citizen, Dr. Patel and his wife have to reapply for their visas every 3 years. “If we travel outside the U.S., we have to get our visas stamped. We cannot change jobs easily due to fear of visa denial, especially with the recent political environment,” said Dr. Patel. “It feels like we are essential health care workers but non-essential immigrants.”
Having recently completed a physician executive MBA program, Dr. Patel said he’d like to start a business of his own using Lean health care principles and telemedicine to improve rural health care. “But while on an H-1B I cannot do anything outside my sponsored employment,” he said.
Ideally, health care organizations would have high flexibility in how and where staff are deployed when a surge of COVID-19 patients hits. Dr. Patel made the point that visa restrictions can make this much harder: “During this COVID crisis, this restriction can cause significant negative impact for small rural hospitals, where local physicians are quarantined and available physicians are on a visa who cannot legally work outside their primary facilities – even though they are willing to work,” he said. “One cannot even work using telemedicine in the same health system, if that is not specifically mentioned during H-1B petition filling. More than 15,000 physicians who are struck by the green card backlog are in the same situation all over U.S.,” he added.
These constraints, though, pale before the consequences of a worst-case pandemic scenario for an immigrant family, where the physician – the primary visa-holder – becomes disabled or dies. In this case, dependent family members must self-deport. “In addition, there would not be any disability or Social Security benefits for the physician or dependents, as they are not citizens or green card holders and they cannot legally stay in the US,” noted Dr. Patel. “Any hospitalist working during the COVID-19 pandemic can have this fate due to our high exposure risk.”
Reauthorizing the H1-B visa program
SHM has been advocating to improve the H1-B visa system for years, Dr. Patel said, The Fairness for High Skilled Immigrants Act passed the U.S. House of Representatives with bipartisan support, and the Society is advocating for its passage in the Senate.
The Fairness for High-Skilled Immigrants Act (S. 386) simplifies the employment-based immigration system by removing per-country caps, converting the employment-based immigration system into a “first-come, first serve” system that does not discriminate on country of origin. The act will also help alleviate the decades-long green card and permanent residency application backlogs.
Dr. Patel emphasized the importance of action by Congress to reauthorize the physician visa waiver program and expediting physician permanent residency. “This is a crisis and we are all physicians who are ready to serve, regardless of our country of origin. Please let us help this great nation by giving us freedom from visa restrictions and providing security for our families.
“During wartime, all frontline soldiers are naturalized and given citizenship by presidential mandate; this is more than war and we are not asking for citizenship – but at least give us a green card which we have already satisfied all requirements for. If not now, then when?” he asked.
Statistics tell the tale of immigrants in the American health care workforce in broad strokes. In an interview, though, one hospitalist shared the particulars of his professional and personal journey since arriving in the United States from India 15 years ago.
Mihir Patel, MD, MPH, FHM, came to the United States in 2005 to complete a Master’s in Public Health. Fifteen years later, he is still waiting for the green card that signifies U.S. permanent residency status. The paperwork for the application, he said, was completed in 2012. Since then, he’s been renewing his H-1B visa every three years, and he has no expectation that anything will change soon.
“If you are from India, which has a significant backlog of green cards – up to 50 years…you just wait forever,” he said. “Many people even die waiting for their green card to arrive.”
Arriving on a student visa, Dr. Patel completed his MPH in 2008 and began an internal medicine residency that same year, holding a J-1 visa for the 3 years of his US residency program.
“Post-residency, I started working in a rural hospital in an underserved area of northeast Tennessee as a hospitalist,” thus completing the 3 years of service in a rural underserved area that’s a requirement for J-1 visa holders, said Dr. Patel. “I loved this rural community hospital so much that I ended up staying there for 6 years. During my work at this rural hospital, I was able to enjoy the autonomy of managing a small ICU, doing both critical care procedures and management of intubated critical patients while working as a hospitalist,” he said. Dr. Patel served as chief of staff at the hospital for two years, and also served on the board of directors for his 400-physician medical group.
“I was a proud member of this rural community – Rogersville,” said Dr. Patel. Although he and his wife, who was completing her hospitalist residency, lived in Johnson City, Tenn., “I did not mind driving 120 miles round trip every day to go to my small-town hospital for 6 years,” he said.
Spending this time in rural Tennessee allowed Dr. Patel to finish the requirements necessary for the Physician National Interest Waiver and submit his application for permanent residency. The waiver, though, doesn’t give him priority status in the waiting list for permanent residency status.
After a stint in northern California to be closer to extended family, the pull of “beautiful northeast Tennesse and the rural community” was too strong, so Dr. Patel and his family moved back to Johnson City in 2018.
Now, Dr. Patel is a hospitalist at Ballad Health System in Johnson City. He is the corporate director of Ballad’s telemedicine program and is now also the medical director of the COVID-19 Strike Team. He co-founded and is president of the Blue Ridge Chapter of the Society of Hospital Medicine. Under another H-1B visa, Dr. Patel works part-time from home as a telehospitalist, covering six hospitals in 4 different states.
Even in ordinary circumstances, the H-1B visa comes with constraints. Although Dr. Patel’s 6-year old daughter was born in the U.S. and is a citizen, Dr. Patel and his wife have to reapply for their visas every 3 years. “If we travel outside the U.S., we have to get our visas stamped. We cannot change jobs easily due to fear of visa denial, especially with the recent political environment,” said Dr. Patel. “It feels like we are essential health care workers but non-essential immigrants.”
Having recently completed a physician executive MBA program, Dr. Patel said he’d like to start a business of his own using Lean health care principles and telemedicine to improve rural health care. “But while on an H-1B I cannot do anything outside my sponsored employment,” he said.
Ideally, health care organizations would have high flexibility in how and where staff are deployed when a surge of COVID-19 patients hits. Dr. Patel made the point that visa restrictions can make this much harder: “During this COVID crisis, this restriction can cause significant negative impact for small rural hospitals, where local physicians are quarantined and available physicians are on a visa who cannot legally work outside their primary facilities – even though they are willing to work,” he said. “One cannot even work using telemedicine in the same health system, if that is not specifically mentioned during H-1B petition filling. More than 15,000 physicians who are struck by the green card backlog are in the same situation all over U.S.,” he added.
These constraints, though, pale before the consequences of a worst-case pandemic scenario for an immigrant family, where the physician – the primary visa-holder – becomes disabled or dies. In this case, dependent family members must self-deport. “In addition, there would not be any disability or Social Security benefits for the physician or dependents, as they are not citizens or green card holders and they cannot legally stay in the US,” noted Dr. Patel. “Any hospitalist working during the COVID-19 pandemic can have this fate due to our high exposure risk.”
Reauthorizing the H1-B visa program
SHM has been advocating to improve the H1-B visa system for years, Dr. Patel said, The Fairness for High Skilled Immigrants Act passed the U.S. House of Representatives with bipartisan support, and the Society is advocating for its passage in the Senate.
The Fairness for High-Skilled Immigrants Act (S. 386) simplifies the employment-based immigration system by removing per-country caps, converting the employment-based immigration system into a “first-come, first serve” system that does not discriminate on country of origin. The act will also help alleviate the decades-long green card and permanent residency application backlogs.
Dr. Patel emphasized the importance of action by Congress to reauthorize the physician visa waiver program and expediting physician permanent residency. “This is a crisis and we are all physicians who are ready to serve, regardless of our country of origin. Please let us help this great nation by giving us freedom from visa restrictions and providing security for our families.
“During wartime, all frontline soldiers are naturalized and given citizenship by presidential mandate; this is more than war and we are not asking for citizenship – but at least give us a green card which we have already satisfied all requirements for. If not now, then when?” he asked.
Hospital leadership lessons in the era of COVID-19
The year 2020 has brought the COVID-19 pandemic and civil unrest and protests, which have resulted in unprecedented health care challenges to hospitals and clinics. The daunting prospect of a fall influenza season has hospital staff and administrators looking ahead to still greater challenges.
This year of crisis has put even greater emphasis on leadership in hospitals, as patients, clinicians, and staff look for direction in the face of uncertainty and stress. But hospital leaders often arrive at their positions unprepared for their roles, according to Leonard Marcus, PhD, director of the Program for Health Care Negotiation and Conflict Resolution at Harvard T.H. Chan School of Public Health, Boston.
“Many times what happens in medicine is that someone with the greatest technical skills or greatest clinical skills emerges to be leader of a department, or a group, or a hospital, without having really paid attention to how they can build their leadership skills,” Dr. Marcus said during the 2020 Society of Hospital Medicine Leadership Virtual Seminar, held online Sept. 16-17.
Over 2 days, Dr. Marcus discussed the complex environments faced by hospital leaders, and some of the tools and strategies that can be used to maintain calm, problem-solve, and chart a course ahead.
He emphasized that hospitals and medical systems are complex, nonlinear organizations, which could be swept up by change in the form of mergers, financial policies, patient surges due to local emergencies, or pandemics.
“Complexity has to be central to how you think about leadership. If you think you can control everything, that doesn’t work that well,” said Dr. Marcus.
Most think of leadership as hierarchical, with a boss on top and underlings below, though this is starting to change. Dr. Marcus suggested a different view. Instead of just “leading down” to those who report to them, leaders should consider “leading up” to their own bosses or oversight committees, and across to other departments or even beyond to interlinked organizations such as nursing homes.
“Being able to build that connectivity not only within your hospital, but beyond your hospital, lets you see the chain that goes through the experience of any patient. You are looking at the problem from a much wider lens. We call this meta-leadership,” Dr. Marcus said.
A key focus of meta-leadership is to create a culture where individuals are working together to help one another succeed. Leadership in hospitals is often dominated by egos, with individual leaders battling one another in a win-lose effort, and this gets in the way of incorporating different perspectives into problem-solving.
Dr. Marcus used an example from previous seminars in which he instructed participants to arm wrestle the person sitting next to them. The goal was to attain as many pins as possible in 30 seconds. About half would fight as hard as they could, and achieve a few victories. The other half worked cooperatively, letting one person win, then the other, so that they could have 30 or 40 wins each. Dr. Marcus told the story of a young nurse who was paired up with a much stronger surgeon. She let him win twice, and when he asked her why she wasn’t resisting, she took his arm and placed it in a winning position, then a losing position, and then a winning position again, and he instantly understood that the cooperative approach could be more effective. Why didn’t she just tell him? She told Dr. Marcus that she knew he wouldn’t take instruction, so she let him win and then demonstrated an alternative. “We nurses learned how to do that a long time ago,” she told Dr. Marcus.
The idea is collaborative problem-solving. “How do you orient people looking to you for leadership so that we’re in this together and we can accomplish a whole lot more in 30 seconds if we’re working together instead of always battling one another? If we’re always battling one another, we’re putting all of our effort into the contest,” said Dr. Marcus. This sort of approach is all the more important when facing the complexity experienced by hospital systems, especially during crises such as COVID-19.
A critical element of meta-leadership is emotional intelligence, which includes elements such as self-awareness, self-regulation, empathy, determining motivation of yourself and others, and the social skills to portray yourself as caring, open, and interested.
Emotional intelligence also can help recognize when you’ve entered survival mode in reaction to a crisis or incident, or something as simple as losing your car keys – what Dr. Marcus terms “going to the basement.” Responses revolve around freeze, fight, or flight. It’s helpful in the wake of a car accident, but not when trying to make managerial decisions or respond to a complex situation. It’s vital for leaders to quickly get themselves out of the basement, said Dr. Marcus, and that they help other members of the team get out as well.
He recommended protocols designed in advance, both to recognize when you’re in the basement, and to lift yourself out. Dr. Marcus uses a trigger script, telling himself “I can do this,” and then when he’s working with other people, “we can do this.” He also speaks slowly, measuring every word. Whatever you do, “it has to be a pivot you do to get yourself out of the basement,” he said. It can be helpful to predict the kinds of situations that send you “to the basement” to help recognize it when it has happened.
It’s very important not to lead, negotiate, or make important decisions while in the basement, according to Dr. Marcus. If one thinks about some of the things they’ve said to others while under duress, they are often some of the statements they regret most.
Practical leadership skills
On the second day of the Leadership Seminar, Dr. Marcus moved his focus to using leadership skills and techniques. One important technique is to incorporate multiple perspectives. He gave the example of an opaque cube with a cone inside it, with a window on the side and one on top. Viewers from the side see the cone in profile, and see it as a triangle. Viewers from the top see an aerial perspective that looks like the circular base of the cone. The two groups could argue about what’s inside the cube, but they can only identify the object if they work together.
“When dealing with complex reality, you oftentimes find there are different people with different perspectives on a problem. They may have different experiences of what the problem is, and what often happens is that people get into an adversarial fight. Looking at the problem from different perspectives actually allows a much richer and more comprehensive view,” said Dr. Marcus.
The metaphor comes from a study of the tragic events at the Twin Towers in Manhattan on Sept. 11, 2001. The New York Fire Department had a command center at the base of the building, while the police had a helicopter flying around the buildings. The helicopter could see the steel girders beginning to melt and predicted a collapse, and therefore ordered their personnel out of the buildings. But they were unable to convey that information to the firefighters, who continued to send personnel into the buildings. In all, 343 firefighters lost their lives. The police force lost 32.
To best understand a problem, a key element is the “unknown knowns.” That is, information that is available, that someone has, but is unknown to you. It takes some imagination to conceive of what “unknown knowns” might be out there, but it’s worth the effort to identify possible knowledge sources. It’s vital to seek out this information, because a common leadership mistake is to assume you know something when you really don’t.
“In many ways what you’re doing is looking for obstacles. It could be you don’t have access to the information, that it’s beyond some sort of curtain you need to overcome, or it could be people in your own department who have the information and they’re not sharing it with you,” Dr. Marcus said.
He outlined a tool called the POP-DOC loop, which is a 6-step exercise designed to analyze problems and implement solutions. Step 1 is Perceiving the situation, determining knowns and unknowns, and incorporating multiple perspectives, emotions, and politics. Step 2 is to Orient oneself: examine patterns and how they may replicate themselves as long as conditions don’t change. For example, during COVID-19, physicians have begun to learn how the virus transmits and how it affects the immune system. Step 3, based on those patterns is to make Predictions. With COVID-19, it’s predictable that people who assemble without wearing masks are vulnerable to transmission. Step 4 is to use the predictions to begin to make Decisions. Step 5 is to begin Operationalizing those decisions, and step 6 is to Communicate those decisions effectively.
Dr. Marcus emphasized that POP-DOC is not a one-time exercise. Once decisions have been made and implemented, if they aren’t having the planned effect, it’s important to incorporate the results of those actions and start right back at the beginning of the POP-DOC loop.
“The POP side of the loop is perceiving, analysis. You get out of the basement and understand the situation that surrounds you. On the DOC side, you lead down, lead up, lead across and lead beyond. You’re bringing people into the action to get things done,” Dr. Marcus said.
Another tool Dr. Marcus described, aimed at problem-solving and negotiation, is the “Walk in the Woods.” The idea is to bring two parties together to help each other succeed. The first step is Self-Interest, where both parties articulate their objectives, perspectives, and fears. The second step, Enlarged Interests, requires each party to list their points of agreement, and only then should they focus on and list their points of disagreement. During conflict, people tend to focus on their disagreements. The parties often find that they agree on more than they realize, and this can frame the disagreements as more manageable. The third step, Enlightened Interest, is a free thinking period where both parties come up with potential solutions that had not been previously considered. In step 4, Aligned Interests, the parties discuss some of those ideas that can be explored further.
The Walk in the Woods is applicable to a wide range of situations, and negotiation is central to being a leader. “Being a clinician is all about negotiating – with patients, family members, with other clinicians, with the institution,” Dr. Marcus said. “We all want the patient to have the best possible care, and in the course of those conversations if we can better understand people, have empathy, and if there are new ideas or ways we can individualize our care, let’s do it, and then at the end of the day combine our motivations so that we’re providing the best possible care.”
In the end, meta-leadership is about creating a culture where individuals strive to help each other succeed, said Dr. Marcus. “That’s the essence: involving people, making them part of the solution, and if it’s a solution they’ve created together, everyone wants to make that solution a success.”
For more information, see the book “You’re It,” coauthored by Dr. Marcus, and available on Amazon for $16.99 in hardback, or $3.99 in Kindle format.
The year 2020 has brought the COVID-19 pandemic and civil unrest and protests, which have resulted in unprecedented health care challenges to hospitals and clinics. The daunting prospect of a fall influenza season has hospital staff and administrators looking ahead to still greater challenges.
This year of crisis has put even greater emphasis on leadership in hospitals, as patients, clinicians, and staff look for direction in the face of uncertainty and stress. But hospital leaders often arrive at their positions unprepared for their roles, according to Leonard Marcus, PhD, director of the Program for Health Care Negotiation and Conflict Resolution at Harvard T.H. Chan School of Public Health, Boston.
“Many times what happens in medicine is that someone with the greatest technical skills or greatest clinical skills emerges to be leader of a department, or a group, or a hospital, without having really paid attention to how they can build their leadership skills,” Dr. Marcus said during the 2020 Society of Hospital Medicine Leadership Virtual Seminar, held online Sept. 16-17.
Over 2 days, Dr. Marcus discussed the complex environments faced by hospital leaders, and some of the tools and strategies that can be used to maintain calm, problem-solve, and chart a course ahead.
He emphasized that hospitals and medical systems are complex, nonlinear organizations, which could be swept up by change in the form of mergers, financial policies, patient surges due to local emergencies, or pandemics.
“Complexity has to be central to how you think about leadership. If you think you can control everything, that doesn’t work that well,” said Dr. Marcus.
Most think of leadership as hierarchical, with a boss on top and underlings below, though this is starting to change. Dr. Marcus suggested a different view. Instead of just “leading down” to those who report to them, leaders should consider “leading up” to their own bosses or oversight committees, and across to other departments or even beyond to interlinked organizations such as nursing homes.
“Being able to build that connectivity not only within your hospital, but beyond your hospital, lets you see the chain that goes through the experience of any patient. You are looking at the problem from a much wider lens. We call this meta-leadership,” Dr. Marcus said.
A key focus of meta-leadership is to create a culture where individuals are working together to help one another succeed. Leadership in hospitals is often dominated by egos, with individual leaders battling one another in a win-lose effort, and this gets in the way of incorporating different perspectives into problem-solving.
Dr. Marcus used an example from previous seminars in which he instructed participants to arm wrestle the person sitting next to them. The goal was to attain as many pins as possible in 30 seconds. About half would fight as hard as they could, and achieve a few victories. The other half worked cooperatively, letting one person win, then the other, so that they could have 30 or 40 wins each. Dr. Marcus told the story of a young nurse who was paired up with a much stronger surgeon. She let him win twice, and when he asked her why she wasn’t resisting, she took his arm and placed it in a winning position, then a losing position, and then a winning position again, and he instantly understood that the cooperative approach could be more effective. Why didn’t she just tell him? She told Dr. Marcus that she knew he wouldn’t take instruction, so she let him win and then demonstrated an alternative. “We nurses learned how to do that a long time ago,” she told Dr. Marcus.
The idea is collaborative problem-solving. “How do you orient people looking to you for leadership so that we’re in this together and we can accomplish a whole lot more in 30 seconds if we’re working together instead of always battling one another? If we’re always battling one another, we’re putting all of our effort into the contest,” said Dr. Marcus. This sort of approach is all the more important when facing the complexity experienced by hospital systems, especially during crises such as COVID-19.
A critical element of meta-leadership is emotional intelligence, which includes elements such as self-awareness, self-regulation, empathy, determining motivation of yourself and others, and the social skills to portray yourself as caring, open, and interested.
Emotional intelligence also can help recognize when you’ve entered survival mode in reaction to a crisis or incident, or something as simple as losing your car keys – what Dr. Marcus terms “going to the basement.” Responses revolve around freeze, fight, or flight. It’s helpful in the wake of a car accident, but not when trying to make managerial decisions or respond to a complex situation. It’s vital for leaders to quickly get themselves out of the basement, said Dr. Marcus, and that they help other members of the team get out as well.
He recommended protocols designed in advance, both to recognize when you’re in the basement, and to lift yourself out. Dr. Marcus uses a trigger script, telling himself “I can do this,” and then when he’s working with other people, “we can do this.” He also speaks slowly, measuring every word. Whatever you do, “it has to be a pivot you do to get yourself out of the basement,” he said. It can be helpful to predict the kinds of situations that send you “to the basement” to help recognize it when it has happened.
It’s very important not to lead, negotiate, or make important decisions while in the basement, according to Dr. Marcus. If one thinks about some of the things they’ve said to others while under duress, they are often some of the statements they regret most.
Practical leadership skills
On the second day of the Leadership Seminar, Dr. Marcus moved his focus to using leadership skills and techniques. One important technique is to incorporate multiple perspectives. He gave the example of an opaque cube with a cone inside it, with a window on the side and one on top. Viewers from the side see the cone in profile, and see it as a triangle. Viewers from the top see an aerial perspective that looks like the circular base of the cone. The two groups could argue about what’s inside the cube, but they can only identify the object if they work together.
“When dealing with complex reality, you oftentimes find there are different people with different perspectives on a problem. They may have different experiences of what the problem is, and what often happens is that people get into an adversarial fight. Looking at the problem from different perspectives actually allows a much richer and more comprehensive view,” said Dr. Marcus.
The metaphor comes from a study of the tragic events at the Twin Towers in Manhattan on Sept. 11, 2001. The New York Fire Department had a command center at the base of the building, while the police had a helicopter flying around the buildings. The helicopter could see the steel girders beginning to melt and predicted a collapse, and therefore ordered their personnel out of the buildings. But they were unable to convey that information to the firefighters, who continued to send personnel into the buildings. In all, 343 firefighters lost their lives. The police force lost 32.
To best understand a problem, a key element is the “unknown knowns.” That is, information that is available, that someone has, but is unknown to you. It takes some imagination to conceive of what “unknown knowns” might be out there, but it’s worth the effort to identify possible knowledge sources. It’s vital to seek out this information, because a common leadership mistake is to assume you know something when you really don’t.
“In many ways what you’re doing is looking for obstacles. It could be you don’t have access to the information, that it’s beyond some sort of curtain you need to overcome, or it could be people in your own department who have the information and they’re not sharing it with you,” Dr. Marcus said.
He outlined a tool called the POP-DOC loop, which is a 6-step exercise designed to analyze problems and implement solutions. Step 1 is Perceiving the situation, determining knowns and unknowns, and incorporating multiple perspectives, emotions, and politics. Step 2 is to Orient oneself: examine patterns and how they may replicate themselves as long as conditions don’t change. For example, during COVID-19, physicians have begun to learn how the virus transmits and how it affects the immune system. Step 3, based on those patterns is to make Predictions. With COVID-19, it’s predictable that people who assemble without wearing masks are vulnerable to transmission. Step 4 is to use the predictions to begin to make Decisions. Step 5 is to begin Operationalizing those decisions, and step 6 is to Communicate those decisions effectively.
Dr. Marcus emphasized that POP-DOC is not a one-time exercise. Once decisions have been made and implemented, if they aren’t having the planned effect, it’s important to incorporate the results of those actions and start right back at the beginning of the POP-DOC loop.
“The POP side of the loop is perceiving, analysis. You get out of the basement and understand the situation that surrounds you. On the DOC side, you lead down, lead up, lead across and lead beyond. You’re bringing people into the action to get things done,” Dr. Marcus said.
Another tool Dr. Marcus described, aimed at problem-solving and negotiation, is the “Walk in the Woods.” The idea is to bring two parties together to help each other succeed. The first step is Self-Interest, where both parties articulate their objectives, perspectives, and fears. The second step, Enlarged Interests, requires each party to list their points of agreement, and only then should they focus on and list their points of disagreement. During conflict, people tend to focus on their disagreements. The parties often find that they agree on more than they realize, and this can frame the disagreements as more manageable. The third step, Enlightened Interest, is a free thinking period where both parties come up with potential solutions that had not been previously considered. In step 4, Aligned Interests, the parties discuss some of those ideas that can be explored further.
The Walk in the Woods is applicable to a wide range of situations, and negotiation is central to being a leader. “Being a clinician is all about negotiating – with patients, family members, with other clinicians, with the institution,” Dr. Marcus said. “We all want the patient to have the best possible care, and in the course of those conversations if we can better understand people, have empathy, and if there are new ideas or ways we can individualize our care, let’s do it, and then at the end of the day combine our motivations so that we’re providing the best possible care.”
In the end, meta-leadership is about creating a culture where individuals strive to help each other succeed, said Dr. Marcus. “That’s the essence: involving people, making them part of the solution, and if it’s a solution they’ve created together, everyone wants to make that solution a success.”
For more information, see the book “You’re It,” coauthored by Dr. Marcus, and available on Amazon for $16.99 in hardback, or $3.99 in Kindle format.
The year 2020 has brought the COVID-19 pandemic and civil unrest and protests, which have resulted in unprecedented health care challenges to hospitals and clinics. The daunting prospect of a fall influenza season has hospital staff and administrators looking ahead to still greater challenges.
This year of crisis has put even greater emphasis on leadership in hospitals, as patients, clinicians, and staff look for direction in the face of uncertainty and stress. But hospital leaders often arrive at their positions unprepared for their roles, according to Leonard Marcus, PhD, director of the Program for Health Care Negotiation and Conflict Resolution at Harvard T.H. Chan School of Public Health, Boston.
“Many times what happens in medicine is that someone with the greatest technical skills or greatest clinical skills emerges to be leader of a department, or a group, or a hospital, without having really paid attention to how they can build their leadership skills,” Dr. Marcus said during the 2020 Society of Hospital Medicine Leadership Virtual Seminar, held online Sept. 16-17.
Over 2 days, Dr. Marcus discussed the complex environments faced by hospital leaders, and some of the tools and strategies that can be used to maintain calm, problem-solve, and chart a course ahead.
He emphasized that hospitals and medical systems are complex, nonlinear organizations, which could be swept up by change in the form of mergers, financial policies, patient surges due to local emergencies, or pandemics.
“Complexity has to be central to how you think about leadership. If you think you can control everything, that doesn’t work that well,” said Dr. Marcus.
Most think of leadership as hierarchical, with a boss on top and underlings below, though this is starting to change. Dr. Marcus suggested a different view. Instead of just “leading down” to those who report to them, leaders should consider “leading up” to their own bosses or oversight committees, and across to other departments or even beyond to interlinked organizations such as nursing homes.
“Being able to build that connectivity not only within your hospital, but beyond your hospital, lets you see the chain that goes through the experience of any patient. You are looking at the problem from a much wider lens. We call this meta-leadership,” Dr. Marcus said.
A key focus of meta-leadership is to create a culture where individuals are working together to help one another succeed. Leadership in hospitals is often dominated by egos, with individual leaders battling one another in a win-lose effort, and this gets in the way of incorporating different perspectives into problem-solving.
Dr. Marcus used an example from previous seminars in which he instructed participants to arm wrestle the person sitting next to them. The goal was to attain as many pins as possible in 30 seconds. About half would fight as hard as they could, and achieve a few victories. The other half worked cooperatively, letting one person win, then the other, so that they could have 30 or 40 wins each. Dr. Marcus told the story of a young nurse who was paired up with a much stronger surgeon. She let him win twice, and when he asked her why she wasn’t resisting, she took his arm and placed it in a winning position, then a losing position, and then a winning position again, and he instantly understood that the cooperative approach could be more effective. Why didn’t she just tell him? She told Dr. Marcus that she knew he wouldn’t take instruction, so she let him win and then demonstrated an alternative. “We nurses learned how to do that a long time ago,” she told Dr. Marcus.
The idea is collaborative problem-solving. “How do you orient people looking to you for leadership so that we’re in this together and we can accomplish a whole lot more in 30 seconds if we’re working together instead of always battling one another? If we’re always battling one another, we’re putting all of our effort into the contest,” said Dr. Marcus. This sort of approach is all the more important when facing the complexity experienced by hospital systems, especially during crises such as COVID-19.
A critical element of meta-leadership is emotional intelligence, which includes elements such as self-awareness, self-regulation, empathy, determining motivation of yourself and others, and the social skills to portray yourself as caring, open, and interested.
Emotional intelligence also can help recognize when you’ve entered survival mode in reaction to a crisis or incident, or something as simple as losing your car keys – what Dr. Marcus terms “going to the basement.” Responses revolve around freeze, fight, or flight. It’s helpful in the wake of a car accident, but not when trying to make managerial decisions or respond to a complex situation. It’s vital for leaders to quickly get themselves out of the basement, said Dr. Marcus, and that they help other members of the team get out as well.
He recommended protocols designed in advance, both to recognize when you’re in the basement, and to lift yourself out. Dr. Marcus uses a trigger script, telling himself “I can do this,” and then when he’s working with other people, “we can do this.” He also speaks slowly, measuring every word. Whatever you do, “it has to be a pivot you do to get yourself out of the basement,” he said. It can be helpful to predict the kinds of situations that send you “to the basement” to help recognize it when it has happened.
It’s very important not to lead, negotiate, or make important decisions while in the basement, according to Dr. Marcus. If one thinks about some of the things they’ve said to others while under duress, they are often some of the statements they regret most.
Practical leadership skills
On the second day of the Leadership Seminar, Dr. Marcus moved his focus to using leadership skills and techniques. One important technique is to incorporate multiple perspectives. He gave the example of an opaque cube with a cone inside it, with a window on the side and one on top. Viewers from the side see the cone in profile, and see it as a triangle. Viewers from the top see an aerial perspective that looks like the circular base of the cone. The two groups could argue about what’s inside the cube, but they can only identify the object if they work together.
“When dealing with complex reality, you oftentimes find there are different people with different perspectives on a problem. They may have different experiences of what the problem is, and what often happens is that people get into an adversarial fight. Looking at the problem from different perspectives actually allows a much richer and more comprehensive view,” said Dr. Marcus.
The metaphor comes from a study of the tragic events at the Twin Towers in Manhattan on Sept. 11, 2001. The New York Fire Department had a command center at the base of the building, while the police had a helicopter flying around the buildings. The helicopter could see the steel girders beginning to melt and predicted a collapse, and therefore ordered their personnel out of the buildings. But they were unable to convey that information to the firefighters, who continued to send personnel into the buildings. In all, 343 firefighters lost their lives. The police force lost 32.
To best understand a problem, a key element is the “unknown knowns.” That is, information that is available, that someone has, but is unknown to you. It takes some imagination to conceive of what “unknown knowns” might be out there, but it’s worth the effort to identify possible knowledge sources. It’s vital to seek out this information, because a common leadership mistake is to assume you know something when you really don’t.
“In many ways what you’re doing is looking for obstacles. It could be you don’t have access to the information, that it’s beyond some sort of curtain you need to overcome, or it could be people in your own department who have the information and they’re not sharing it with you,” Dr. Marcus said.
He outlined a tool called the POP-DOC loop, which is a 6-step exercise designed to analyze problems and implement solutions. Step 1 is Perceiving the situation, determining knowns and unknowns, and incorporating multiple perspectives, emotions, and politics. Step 2 is to Orient oneself: examine patterns and how they may replicate themselves as long as conditions don’t change. For example, during COVID-19, physicians have begun to learn how the virus transmits and how it affects the immune system. Step 3, based on those patterns is to make Predictions. With COVID-19, it’s predictable that people who assemble without wearing masks are vulnerable to transmission. Step 4 is to use the predictions to begin to make Decisions. Step 5 is to begin Operationalizing those decisions, and step 6 is to Communicate those decisions effectively.
Dr. Marcus emphasized that POP-DOC is not a one-time exercise. Once decisions have been made and implemented, if they aren’t having the planned effect, it’s important to incorporate the results of those actions and start right back at the beginning of the POP-DOC loop.
“The POP side of the loop is perceiving, analysis. You get out of the basement and understand the situation that surrounds you. On the DOC side, you lead down, lead up, lead across and lead beyond. You’re bringing people into the action to get things done,” Dr. Marcus said.
Another tool Dr. Marcus described, aimed at problem-solving and negotiation, is the “Walk in the Woods.” The idea is to bring two parties together to help each other succeed. The first step is Self-Interest, where both parties articulate their objectives, perspectives, and fears. The second step, Enlarged Interests, requires each party to list their points of agreement, and only then should they focus on and list their points of disagreement. During conflict, people tend to focus on their disagreements. The parties often find that they agree on more than they realize, and this can frame the disagreements as more manageable. The third step, Enlightened Interest, is a free thinking period where both parties come up with potential solutions that had not been previously considered. In step 4, Aligned Interests, the parties discuss some of those ideas that can be explored further.
The Walk in the Woods is applicable to a wide range of situations, and negotiation is central to being a leader. “Being a clinician is all about negotiating – with patients, family members, with other clinicians, with the institution,” Dr. Marcus said. “We all want the patient to have the best possible care, and in the course of those conversations if we can better understand people, have empathy, and if there are new ideas or ways we can individualize our care, let’s do it, and then at the end of the day combine our motivations so that we’re providing the best possible care.”
In the end, meta-leadership is about creating a culture where individuals strive to help each other succeed, said Dr. Marcus. “That’s the essence: involving people, making them part of the solution, and if it’s a solution they’ve created together, everyone wants to make that solution a success.”
For more information, see the book “You’re It,” coauthored by Dr. Marcus, and available on Amazon for $16.99 in hardback, or $3.99 in Kindle format.
FROM THE SHM LEADERSHIP SEMINAR
Hospital medicine, it’s time to vote
Whether physicians or advanced practice practitioners, we are the backbone of our nation’s network of acute care facilities, and on a daily basis, we see just about everything. We have valuable insight into how to improve our nation’s health care system, especially now, as our nation continues to battle COVID-19.
Our role, squarely on the front lines during this pandemic, has given us an important perspective that needs to be heard. We spend our days managing patients with complexity, coordinating with specialists and subspecialists, and advocating – at local, state, and national levels – so that our patients can more easily transition to their lives out of the hospital.
Our current polarized political climate makes it seem that individual voices will not make a difference. It is easy to feel frustrated and powerless. However, those in our specialty are actually in a perfect position to have an educated and influential say in how we move forward, not only about the immediate health crises, but also regarding future health care issues. That voice begins with voting.
Historically, physicians have had surprisingly low rates of voting. For example, a 2007 study found significantly lower rates of voting among physicians, compared with the general public.1 While physician voter turnout may have improved in the past decade, given the substantial changes in health care and the increasing amount of physician engagement in the public sphere, our participation should be greater still. Elected officials listen to, and follow up with, constituents who make their voices heard. Each of us can ensure that the health care policy priorities of our fast-growing specialty are addressed by mobilizing to the voting booth.
Candidates we elect shape our health care system for the future, directly impacting us and our patients. Cost, coverage, access to health care, the Centers for Medicare & Medicaid Services inpatient fee schedules, the ongoing pandemic response, surprise billing, use of telehealth, observation status, and the three-midnight rule are just a few of the issues most important to hospital medicine.
Therefore, we, the SHM Public Policy Committee, urge all of our colleagues, regardless of political sway, to make your voice heard this and every election henceforth. The first step is to register to vote, if you have not done so already.2 Next, exercise that privilege. Given the pandemic, this is not as simple a process as it has been in the past. Take the time to plan your approach to early voting, mail-in voting, or election day voting. Check your County Supervisor of Elections’ website for further information, including how to register, view candidate profiles, check your precinct, and request a mail-in ballot.
In addition to casting your vote, we encourage you to share your opinions and engage in dialogue about health care issues. Clinical fact can dispel rumor and misinformation, and daily experiences can personalize our patients’ health care stories and the impact laws and rules have on our ability to practice. We are part of a trusted profession and have a unique perspective; others need and want to hear it. They can only do that if we are part of the process. Arming yourself with information and voting are the first steps on the path of advocacy. Interpersonal advocacy can also be done on social media. For example, SHM has an active grassroots advocacy network on Twitter. Tag @SHMadvocacy in your tweets to share your thoughts with their network.
Finally, as advocates for our patients in health care, we can also help ensure their safety during this election, in particular regarding COVID-19. Some patients may not wish to engage us in politics, and we must respect their decision. Others may seek our counsel and we should provide it in an unbiased fashion. We can ask our patients if they have considered a safe voting plan, help patients review the alternatives to voting in person if desired, and inform those who wish to physically cast a vote on Election Day of how to mitigate the risk of in-person voting.
Every election is important and health care is front and center for a multitude of reasons. We who practice hospital medicine are integral to our communities and need to be more politically involved. This is our chance to share our voice through our vote, not just this year, but in future elections as well.
Ann Sheehy, MD, SFHM, is division chief of the Division of Hospital Medicine at the University of Wisconsin, Madison, and chair of the SHM Public Policy Committee. Other members of the SHM PPC include Marta Almli, MD; John Biebelhausen, MD; Robert Burke, MD, MS, FHM; George Cheely, MD; Hyung (Harry) Cho, MD, SFHM; Jennifer Cowart, MD, FHM; Suparna Dutta, MD, MS, MPH; Bradley Flansbaum, DO, MPH, MHM; Alain Folefack, MD; Rick Hilger MD SFHM; Melinda Johnson, MD; Sevan Karadolian, MD; Joshua D. Lenchus, DO, FACP, SFHM; Steve Phillipson, MD; Dahlia Rizk, DO; Kendall Rogers, MD, SFHM; Brett Stauffer, MD, MHS; Amit Vashist, MD, SFHM; Robert Zipper, MD, SFHM.
References
1. Grande D et al. Do doctors vote? J Gen Int Med. 2007 May;22(5):585-9.
2. How to register to vote, confirm or change your registration and get a voter registration card. https://www.usa.gov/voter-registration/.
Whether physicians or advanced practice practitioners, we are the backbone of our nation’s network of acute care facilities, and on a daily basis, we see just about everything. We have valuable insight into how to improve our nation’s health care system, especially now, as our nation continues to battle COVID-19.
Our role, squarely on the front lines during this pandemic, has given us an important perspective that needs to be heard. We spend our days managing patients with complexity, coordinating with specialists and subspecialists, and advocating – at local, state, and national levels – so that our patients can more easily transition to their lives out of the hospital.
Our current polarized political climate makes it seem that individual voices will not make a difference. It is easy to feel frustrated and powerless. However, those in our specialty are actually in a perfect position to have an educated and influential say in how we move forward, not only about the immediate health crises, but also regarding future health care issues. That voice begins with voting.
Historically, physicians have had surprisingly low rates of voting. For example, a 2007 study found significantly lower rates of voting among physicians, compared with the general public.1 While physician voter turnout may have improved in the past decade, given the substantial changes in health care and the increasing amount of physician engagement in the public sphere, our participation should be greater still. Elected officials listen to, and follow up with, constituents who make their voices heard. Each of us can ensure that the health care policy priorities of our fast-growing specialty are addressed by mobilizing to the voting booth.
Candidates we elect shape our health care system for the future, directly impacting us and our patients. Cost, coverage, access to health care, the Centers for Medicare & Medicaid Services inpatient fee schedules, the ongoing pandemic response, surprise billing, use of telehealth, observation status, and the three-midnight rule are just a few of the issues most important to hospital medicine.
Therefore, we, the SHM Public Policy Committee, urge all of our colleagues, regardless of political sway, to make your voice heard this and every election henceforth. The first step is to register to vote, if you have not done so already.2 Next, exercise that privilege. Given the pandemic, this is not as simple a process as it has been in the past. Take the time to plan your approach to early voting, mail-in voting, or election day voting. Check your County Supervisor of Elections’ website for further information, including how to register, view candidate profiles, check your precinct, and request a mail-in ballot.
In addition to casting your vote, we encourage you to share your opinions and engage in dialogue about health care issues. Clinical fact can dispel rumor and misinformation, and daily experiences can personalize our patients’ health care stories and the impact laws and rules have on our ability to practice. We are part of a trusted profession and have a unique perspective; others need and want to hear it. They can only do that if we are part of the process. Arming yourself with information and voting are the first steps on the path of advocacy. Interpersonal advocacy can also be done on social media. For example, SHM has an active grassroots advocacy network on Twitter. Tag @SHMadvocacy in your tweets to share your thoughts with their network.
Finally, as advocates for our patients in health care, we can also help ensure their safety during this election, in particular regarding COVID-19. Some patients may not wish to engage us in politics, and we must respect their decision. Others may seek our counsel and we should provide it in an unbiased fashion. We can ask our patients if they have considered a safe voting plan, help patients review the alternatives to voting in person if desired, and inform those who wish to physically cast a vote on Election Day of how to mitigate the risk of in-person voting.
Every election is important and health care is front and center for a multitude of reasons. We who practice hospital medicine are integral to our communities and need to be more politically involved. This is our chance to share our voice through our vote, not just this year, but in future elections as well.
Ann Sheehy, MD, SFHM, is division chief of the Division of Hospital Medicine at the University of Wisconsin, Madison, and chair of the SHM Public Policy Committee. Other members of the SHM PPC include Marta Almli, MD; John Biebelhausen, MD; Robert Burke, MD, MS, FHM; George Cheely, MD; Hyung (Harry) Cho, MD, SFHM; Jennifer Cowart, MD, FHM; Suparna Dutta, MD, MS, MPH; Bradley Flansbaum, DO, MPH, MHM; Alain Folefack, MD; Rick Hilger MD SFHM; Melinda Johnson, MD; Sevan Karadolian, MD; Joshua D. Lenchus, DO, FACP, SFHM; Steve Phillipson, MD; Dahlia Rizk, DO; Kendall Rogers, MD, SFHM; Brett Stauffer, MD, MHS; Amit Vashist, MD, SFHM; Robert Zipper, MD, SFHM.
References
1. Grande D et al. Do doctors vote? J Gen Int Med. 2007 May;22(5):585-9.
2. How to register to vote, confirm or change your registration and get a voter registration card. https://www.usa.gov/voter-registration/.
Whether physicians or advanced practice practitioners, we are the backbone of our nation’s network of acute care facilities, and on a daily basis, we see just about everything. We have valuable insight into how to improve our nation’s health care system, especially now, as our nation continues to battle COVID-19.
Our role, squarely on the front lines during this pandemic, has given us an important perspective that needs to be heard. We spend our days managing patients with complexity, coordinating with specialists and subspecialists, and advocating – at local, state, and national levels – so that our patients can more easily transition to their lives out of the hospital.
Our current polarized political climate makes it seem that individual voices will not make a difference. It is easy to feel frustrated and powerless. However, those in our specialty are actually in a perfect position to have an educated and influential say in how we move forward, not only about the immediate health crises, but also regarding future health care issues. That voice begins with voting.
Historically, physicians have had surprisingly low rates of voting. For example, a 2007 study found significantly lower rates of voting among physicians, compared with the general public.1 While physician voter turnout may have improved in the past decade, given the substantial changes in health care and the increasing amount of physician engagement in the public sphere, our participation should be greater still. Elected officials listen to, and follow up with, constituents who make their voices heard. Each of us can ensure that the health care policy priorities of our fast-growing specialty are addressed by mobilizing to the voting booth.
Candidates we elect shape our health care system for the future, directly impacting us and our patients. Cost, coverage, access to health care, the Centers for Medicare & Medicaid Services inpatient fee schedules, the ongoing pandemic response, surprise billing, use of telehealth, observation status, and the three-midnight rule are just a few of the issues most important to hospital medicine.
Therefore, we, the SHM Public Policy Committee, urge all of our colleagues, regardless of political sway, to make your voice heard this and every election henceforth. The first step is to register to vote, if you have not done so already.2 Next, exercise that privilege. Given the pandemic, this is not as simple a process as it has been in the past. Take the time to plan your approach to early voting, mail-in voting, or election day voting. Check your County Supervisor of Elections’ website for further information, including how to register, view candidate profiles, check your precinct, and request a mail-in ballot.
In addition to casting your vote, we encourage you to share your opinions and engage in dialogue about health care issues. Clinical fact can dispel rumor and misinformation, and daily experiences can personalize our patients’ health care stories and the impact laws and rules have on our ability to practice. We are part of a trusted profession and have a unique perspective; others need and want to hear it. They can only do that if we are part of the process. Arming yourself with information and voting are the first steps on the path of advocacy. Interpersonal advocacy can also be done on social media. For example, SHM has an active grassroots advocacy network on Twitter. Tag @SHMadvocacy in your tweets to share your thoughts with their network.
Finally, as advocates for our patients in health care, we can also help ensure their safety during this election, in particular regarding COVID-19. Some patients may not wish to engage us in politics, and we must respect their decision. Others may seek our counsel and we should provide it in an unbiased fashion. We can ask our patients if they have considered a safe voting plan, help patients review the alternatives to voting in person if desired, and inform those who wish to physically cast a vote on Election Day of how to mitigate the risk of in-person voting.
Every election is important and health care is front and center for a multitude of reasons. We who practice hospital medicine are integral to our communities and need to be more politically involved. This is our chance to share our voice through our vote, not just this year, but in future elections as well.
Ann Sheehy, MD, SFHM, is division chief of the Division of Hospital Medicine at the University of Wisconsin, Madison, and chair of the SHM Public Policy Committee. Other members of the SHM PPC include Marta Almli, MD; John Biebelhausen, MD; Robert Burke, MD, MS, FHM; George Cheely, MD; Hyung (Harry) Cho, MD, SFHM; Jennifer Cowart, MD, FHM; Suparna Dutta, MD, MS, MPH; Bradley Flansbaum, DO, MPH, MHM; Alain Folefack, MD; Rick Hilger MD SFHM; Melinda Johnson, MD; Sevan Karadolian, MD; Joshua D. Lenchus, DO, FACP, SFHM; Steve Phillipson, MD; Dahlia Rizk, DO; Kendall Rogers, MD, SFHM; Brett Stauffer, MD, MHS; Amit Vashist, MD, SFHM; Robert Zipper, MD, SFHM.
References
1. Grande D et al. Do doctors vote? J Gen Int Med. 2007 May;22(5):585-9.
2. How to register to vote, confirm or change your registration and get a voter registration card. https://www.usa.gov/voter-registration/.
2020 has been quite a year
I remember New Year’s Day 2020, full of hope and wonderment of what the year would bring. I was coming into the Society of Hospital Medicine as the incoming President, taking the 2020 reins in the organization’s 20th year. It would be a year of transitioning to a new CEO, reinvigorating our membership engagement efforts, and renewing a strategic plan for forward progress into the next decade. It would be a year chock full of travel, speaking engagements, and meetings with thousands of hospitalists around the globe.
What I didn’t know is that we would soon face the grim reality that the long-voiced concern of infectious disease experts and epidemiologists would come true. That our colleagues and friends and families would be infected, hospitalized, and die from this new disease, for which there were no good, effective treatments. That our ability to come together as a nation to implement basic infection control and epidemiologic practices would be fractured, uncoordinated, and ineffective. That within 6 months of the first case on U.S. soil, we would witness 5,270,000 people being infected from the disease, and 167,000 dying from it. And that the stunning toll of the disease would ripple into every nook and cranny of our society, from the economy to the fabric of our families and to the mental and physical health of all of our citizens.
However, what I couldn’t have known on this past New Year’s Day is how incredibly resilient and innovative our hospital medicine society and community would be to not only endure this new way of working and living, but also to find ways to improve upon how we care for all patients, despite COVID-19. What I couldn’t have known is how hospitalists would pivot to new arenas of care settings, including the EDs, ICUs, “COVID units,” and telehealth – flawlessly and seamlessly filling care gaps that would otherwise be catastrophically unfilled.
What I couldn’t have known is how we would be willing to come back into work, day after day, to care for our patients, despite the risks to ourselves and our families. What I couldn’t have known is how hospitalists would come together as a community to network and share knowledge in unprecedented ways, both humbly and proactively – knowing that we would not have all the answers but that we probably had better answers than most. What I couldn’t have known is that the SHM staff would pivot our entire SHM team away from previous “staple” offerings (e.g., live meetings) to virtual learning and network opportunities, which would be attended at rates higher than ever seen before, including live webinars, HMX exchanges, and e-learnings. What I couldn’t have known is that we would figure out, in a matter of weeks, what treatments were and were not effective for our patients and get those treatments to them despite the difficulties. And what I couldn’t have known is how much prouder I would be, more than ever before, to tell people: “I am a hospitalist.”
I took my son to the dentist recently, and when we were just about to leave, the dentist asked: “What do you do for a living?” and I stated: “I am a hospitalist.” He slowly breathed in and replied: “Oh … wow … you have really seen things …” Yes, we have.
So, is 2020 shaping up as expected? Absolutely not! But I am more inspired, humbled, and motivated than ever to proudly serve SHM with more energy and enthusiasm than I would have dreamed on New Year’s Day. And even if we can’t see each other in person (as we so naively planned), through virtual meetings (national, regional, and chapter), webinars, social media, and other listening modes, we will still be able to connect as a community and share ideas and issues as we muddle through the remainder of 2020 and beyond. We need each other more than ever before, and I am so proud to be a part of this SHM family.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is president of SHM.
I remember New Year’s Day 2020, full of hope and wonderment of what the year would bring. I was coming into the Society of Hospital Medicine as the incoming President, taking the 2020 reins in the organization’s 20th year. It would be a year of transitioning to a new CEO, reinvigorating our membership engagement efforts, and renewing a strategic plan for forward progress into the next decade. It would be a year chock full of travel, speaking engagements, and meetings with thousands of hospitalists around the globe.
What I didn’t know is that we would soon face the grim reality that the long-voiced concern of infectious disease experts and epidemiologists would come true. That our colleagues and friends and families would be infected, hospitalized, and die from this new disease, for which there were no good, effective treatments. That our ability to come together as a nation to implement basic infection control and epidemiologic practices would be fractured, uncoordinated, and ineffective. That within 6 months of the first case on U.S. soil, we would witness 5,270,000 people being infected from the disease, and 167,000 dying from it. And that the stunning toll of the disease would ripple into every nook and cranny of our society, from the economy to the fabric of our families and to the mental and physical health of all of our citizens.
However, what I couldn’t have known on this past New Year’s Day is how incredibly resilient and innovative our hospital medicine society and community would be to not only endure this new way of working and living, but also to find ways to improve upon how we care for all patients, despite COVID-19. What I couldn’t have known is how hospitalists would pivot to new arenas of care settings, including the EDs, ICUs, “COVID units,” and telehealth – flawlessly and seamlessly filling care gaps that would otherwise be catastrophically unfilled.
What I couldn’t have known is how we would be willing to come back into work, day after day, to care for our patients, despite the risks to ourselves and our families. What I couldn’t have known is how hospitalists would come together as a community to network and share knowledge in unprecedented ways, both humbly and proactively – knowing that we would not have all the answers but that we probably had better answers than most. What I couldn’t have known is that the SHM staff would pivot our entire SHM team away from previous “staple” offerings (e.g., live meetings) to virtual learning and network opportunities, which would be attended at rates higher than ever seen before, including live webinars, HMX exchanges, and e-learnings. What I couldn’t have known is that we would figure out, in a matter of weeks, what treatments were and were not effective for our patients and get those treatments to them despite the difficulties. And what I couldn’t have known is how much prouder I would be, more than ever before, to tell people: “I am a hospitalist.”
I took my son to the dentist recently, and when we were just about to leave, the dentist asked: “What do you do for a living?” and I stated: “I am a hospitalist.” He slowly breathed in and replied: “Oh … wow … you have really seen things …” Yes, we have.
So, is 2020 shaping up as expected? Absolutely not! But I am more inspired, humbled, and motivated than ever to proudly serve SHM with more energy and enthusiasm than I would have dreamed on New Year’s Day. And even if we can’t see each other in person (as we so naively planned), through virtual meetings (national, regional, and chapter), webinars, social media, and other listening modes, we will still be able to connect as a community and share ideas and issues as we muddle through the remainder of 2020 and beyond. We need each other more than ever before, and I am so proud to be a part of this SHM family.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is president of SHM.
I remember New Year’s Day 2020, full of hope and wonderment of what the year would bring. I was coming into the Society of Hospital Medicine as the incoming President, taking the 2020 reins in the organization’s 20th year. It would be a year of transitioning to a new CEO, reinvigorating our membership engagement efforts, and renewing a strategic plan for forward progress into the next decade. It would be a year chock full of travel, speaking engagements, and meetings with thousands of hospitalists around the globe.
What I didn’t know is that we would soon face the grim reality that the long-voiced concern of infectious disease experts and epidemiologists would come true. That our colleagues and friends and families would be infected, hospitalized, and die from this new disease, for which there were no good, effective treatments. That our ability to come together as a nation to implement basic infection control and epidemiologic practices would be fractured, uncoordinated, and ineffective. That within 6 months of the first case on U.S. soil, we would witness 5,270,000 people being infected from the disease, and 167,000 dying from it. And that the stunning toll of the disease would ripple into every nook and cranny of our society, from the economy to the fabric of our families and to the mental and physical health of all of our citizens.
However, what I couldn’t have known on this past New Year’s Day is how incredibly resilient and innovative our hospital medicine society and community would be to not only endure this new way of working and living, but also to find ways to improve upon how we care for all patients, despite COVID-19. What I couldn’t have known is how hospitalists would pivot to new arenas of care settings, including the EDs, ICUs, “COVID units,” and telehealth – flawlessly and seamlessly filling care gaps that would otherwise be catastrophically unfilled.
What I couldn’t have known is how we would be willing to come back into work, day after day, to care for our patients, despite the risks to ourselves and our families. What I couldn’t have known is how hospitalists would come together as a community to network and share knowledge in unprecedented ways, both humbly and proactively – knowing that we would not have all the answers but that we probably had better answers than most. What I couldn’t have known is that the SHM staff would pivot our entire SHM team away from previous “staple” offerings (e.g., live meetings) to virtual learning and network opportunities, which would be attended at rates higher than ever seen before, including live webinars, HMX exchanges, and e-learnings. What I couldn’t have known is that we would figure out, in a matter of weeks, what treatments were and were not effective for our patients and get those treatments to them despite the difficulties. And what I couldn’t have known is how much prouder I would be, more than ever before, to tell people: “I am a hospitalist.”
I took my son to the dentist recently, and when we were just about to leave, the dentist asked: “What do you do for a living?” and I stated: “I am a hospitalist.” He slowly breathed in and replied: “Oh … wow … you have really seen things …” Yes, we have.
So, is 2020 shaping up as expected? Absolutely not! But I am more inspired, humbled, and motivated than ever to proudly serve SHM with more energy and enthusiasm than I would have dreamed on New Year’s Day. And even if we can’t see each other in person (as we so naively planned), through virtual meetings (national, regional, and chapter), webinars, social media, and other listening modes, we will still be able to connect as a community and share ideas and issues as we muddle through the remainder of 2020 and beyond. We need each other more than ever before, and I am so proud to be a part of this SHM family.
Dr. Scheurer is chief quality officer and professor of medicine at the Medical University of South Carolina, Charleston. She is president of SHM.
The ally in the waiting room
Improving communication with patients’ loved ones
We think of a patient’s recovery happening in multiple locations – in a hospital room or a rehabilitation facility, for example. But many clinicians may not consider the opportunity to aid healing that lies in the waiting room.
The waiting room is where a patient’s loved ones often are and they, sometimes more than anyone, can unlock the path to a patient’s quicker recovery. Friends and family can offer encouragement, as they have an existing bond of trust that can help if a patient needs reinforcement to take their medications or follow other health care advice. But if loved ones are going to help patients, they need help from clinicians. Beyond being potential allies, they are also hurting, experiencing worry or confusion in a world of medical jargon.
The coronavirus changes the relationship of patients and their loved ones, as patients are often isolated or limited in the number of visitors they are allowed to see. A smartphone replaces the smiling faces of friends and relatives at their bedside, and a text is a poor substitute for a hug.
The Hospitalist asked some experienced hospitalists for insight on how best to communicate with patients’ loved ones to improve outcomes for all, medically and emotionally.
Team approach
“Patients feel isolated, terrified, and vulnerable but still need an advocate in the hospital, so daily communication with a patient’s loved one is important to give a sense that the patient is looked after,” said Kari Esbensen, MD, PhD, a hospitalist and palliative care expert at Emory University Hospital Midtown, Atlanta.
Glenn Rosenbluth, MD, a pediatric hospitalist and director, quality and safety programs, at the University of California, San Francisco, Benioff Children’s Hospital, agreed. He said that the most important thing is to communicate, period.
“We fall into this pattern of ‘out of sight, out of mind,’ ” he said. “We need to take the extra step to find out who a patient’s loved ones are. If it is a clinical visit, ask the patient, or maybe get the information from a caseworker, or just pay attention to who is dropping in to see the patient. Having a second person available to jot down notes, or having a handy list of questions – it all helps the patient. We forget that sometimes it can seem like a whirlwind for the patient when they are hurting. We have to remember that a loved one is important to a patient’s care team and we need to include them, empower them, and show that we want to hear their voices.”
Dr. Esbensen said it is critical to start off on the right foot when communicating with a patient’s loved one, especially during the current pandemic.
“With COVID-19, the most important thing is to speak honestly, to say hope for the best but prepare for the worst-case scenario,” Dr. Esbensen said. “We’ve seen that conditions can shift dramatically in short periods of time. The loved one needs to have a sense of the positive and negative possibilities. Families tend to lack understanding of the changes in the patient that are caused by COVID-19. The patient can come out of the hospital debilitated, very different than when they entered the hospital, and we need to warn people close to them about this. Unrealistic expectations need to be guarded against if a patient’s loved ones are going to help.”
Perhaps the best form of communication with a patient’s loved ones is an often-forgotten skill: listening.
“Get an idea from the patient’s loved ones of what the issues are, as well as their idea of what they think of the disease and how it spreads,” Dr. Esbensen said. “Sometimes they are right on target but sometimes there are misinterpretations and we need to help them understand it better. It’s not a ‘one-size-fits-all’ speech that we should give, but try to say, ‘tell me what you think is going on, what you think you’ve heard, and what you’re worried about,’ and learn what is most important to the patient. Start on those terms and adapt; this way you can correct and address what makes them most fearful, which can be different for each loved one. For some, the concern could be that they have children or other vulnerable people in the house. Finding out these other issues is important.”
Venkatrao Medarametla, MD, SFHM, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., emphasized that, in a time when hospitalists are being pulled in every direction, it is easy to lose your attention.
“It’s very important that family members know you’re present with them,” he said. “This can be an emotional time and they need empathy. It’s very easy for our list of tasks to get in the way of communicating, including with our body language.”
Dr. Medarametla said one of the reasons to communicate with patients’ loved ones is to calm them – a patient’s relatives or their friends may not be under your medical care, but they are still human beings.
“A lot of people just want information and want to be helpful, but we also need to realize that, while we are caring for many patients, this one person is the patient they are focused on,” said Laura Nell Hodo, MD, a pediatric hospitalist at Kravis Children’s Hospital at Mount Sinai in New York. “Don’t rush, and if you know that a patient’s loved one needs more time, make sure it can be found – if not then, at least later on the phone. Fifteen to 20 minutes may be what’s needed, and you can’t shortchange them.”
Dr. Hodo said that a patient’s loved ones often do not realize it is possible to receive phone calls from hospitalists. “We need to remind them that they can get in touch with us. We have to remember how helpless they can feel and how they want to understand what is happening in the hospital.”
For medical adherence issues, sometimes it is best to communicate with the patient and loved one at the same time, Dr. Hodo advised. “Whether it’s for medication or postdischarge exercises, if they both receive the information together it can reinforce adherence. But you also need to remember that the patient may only want a loved one told about certain things, or possibly nothing at all. We need to make sure we understand the patient’s wishes, regardless of whether we think a person close to them can be an ally or not.”
Dr. Esbensen also noted that a loved one can give hospitalists important clues to the emotional components of a patient’s care.
“I remember a patient whose wife told me how he worked in a garage, how he was strong and did not want people to think he was a weak guy just because of what was happening to him,” Dr. Esbensen said. “I didn’t know that he felt he might be perceived in this way. I mentioned to him how I learned he was a good mechanic and he perked up and felt seen in a different light. These things make a difference.”
But when is the best time to speak with a patient’s loved ones? Since much communication is done via phone during the pandemic, there are different philosophies.
“We had a debate among colleagues to see how each of us did it,” Dr. Esbensen said. “Some try to call after each patient encounter, while they are outside the room and it’s fresh in their mind, but others find it better to make the call after their rounds, to give the person their full attention. Most of the time I try to do it that way.”
She noted that, in the current environment, a phone call may be better than a face-to-face conversation with patients’ loved ones.
“We’re covered in so much gear to protect us from the coronavirus that it can feel like a great distance exists between us and the person with whom we’re speaking,” she said. “It’s strange, but the phone can make the conversation seem more relaxed and may get people to open up more.”
Even when they leave
All the hospitalists affirmed that loved ones can make a big difference for the patient through all aspects of care. Long after a patient returns home, the support of loved ones can have a profound impact in speeding healing and improving long-term outcomes.
Dr. Esbensen said COVID-19 and other serious illnesses can leave a patient needing support, and maybe a “push” when feeling low keeps them from adhering to medical advice.
“It’s not just in the hospital but after discharge,” she said. “A person offering support can really help patients throughout their journey, and much success in recovering from illness occurs after the transition home. Having the support of that one person a patient trusts can be critical.”
Dr. Hodo believes that the coronavirus pandemic could forever change the way hospitalists communicate with patients and their loved ones.
“I work in pediatrics and we know serious medical decisions can’t be made without guardians or parents,” she said. “But in adult medicine doctors may not automatically ask the patient about calling someone for input on decision-making. With COVID, you cannot assume a patient is on their own, because there are protocols keeping people from physically being present in the patient’s room. My experience from working in adult coronavirus units is that the thinking about the loved ones’ role in patient care – and communication with them – might just change. … At least, I hope so.”
Quick takeaways for hospitalists
- Get beyond personal protective equipment. A conversation with a patient’s loved one might be easier to achieve via phone, without all the protective gear in the way.
- Encourage adherence. Speaking with patients and loved ones together may be more effective. They may reach agreement quicker on how best to adhere to medical advice.
- Loved ones offer clues. They might give you a better sense of a patient’s worries, or help you to connect better with those in your care.
- Be present. You have a long to-do list but do not let empathy fall off it, even if you feel overwhelmed.
Improving communication with patients’ loved ones
Improving communication with patients’ loved ones
We think of a patient’s recovery happening in multiple locations – in a hospital room or a rehabilitation facility, for example. But many clinicians may not consider the opportunity to aid healing that lies in the waiting room.
The waiting room is where a patient’s loved ones often are and they, sometimes more than anyone, can unlock the path to a patient’s quicker recovery. Friends and family can offer encouragement, as they have an existing bond of trust that can help if a patient needs reinforcement to take their medications or follow other health care advice. But if loved ones are going to help patients, they need help from clinicians. Beyond being potential allies, they are also hurting, experiencing worry or confusion in a world of medical jargon.
The coronavirus changes the relationship of patients and their loved ones, as patients are often isolated or limited in the number of visitors they are allowed to see. A smartphone replaces the smiling faces of friends and relatives at their bedside, and a text is a poor substitute for a hug.
The Hospitalist asked some experienced hospitalists for insight on how best to communicate with patients’ loved ones to improve outcomes for all, medically and emotionally.
Team approach
“Patients feel isolated, terrified, and vulnerable but still need an advocate in the hospital, so daily communication with a patient’s loved one is important to give a sense that the patient is looked after,” said Kari Esbensen, MD, PhD, a hospitalist and palliative care expert at Emory University Hospital Midtown, Atlanta.
Glenn Rosenbluth, MD, a pediatric hospitalist and director, quality and safety programs, at the University of California, San Francisco, Benioff Children’s Hospital, agreed. He said that the most important thing is to communicate, period.
“We fall into this pattern of ‘out of sight, out of mind,’ ” he said. “We need to take the extra step to find out who a patient’s loved ones are. If it is a clinical visit, ask the patient, or maybe get the information from a caseworker, or just pay attention to who is dropping in to see the patient. Having a second person available to jot down notes, or having a handy list of questions – it all helps the patient. We forget that sometimes it can seem like a whirlwind for the patient when they are hurting. We have to remember that a loved one is important to a patient’s care team and we need to include them, empower them, and show that we want to hear their voices.”
Dr. Esbensen said it is critical to start off on the right foot when communicating with a patient’s loved one, especially during the current pandemic.
“With COVID-19, the most important thing is to speak honestly, to say hope for the best but prepare for the worst-case scenario,” Dr. Esbensen said. “We’ve seen that conditions can shift dramatically in short periods of time. The loved one needs to have a sense of the positive and negative possibilities. Families tend to lack understanding of the changes in the patient that are caused by COVID-19. The patient can come out of the hospital debilitated, very different than when they entered the hospital, and we need to warn people close to them about this. Unrealistic expectations need to be guarded against if a patient’s loved ones are going to help.”
Perhaps the best form of communication with a patient’s loved ones is an often-forgotten skill: listening.
“Get an idea from the patient’s loved ones of what the issues are, as well as their idea of what they think of the disease and how it spreads,” Dr. Esbensen said. “Sometimes they are right on target but sometimes there are misinterpretations and we need to help them understand it better. It’s not a ‘one-size-fits-all’ speech that we should give, but try to say, ‘tell me what you think is going on, what you think you’ve heard, and what you’re worried about,’ and learn what is most important to the patient. Start on those terms and adapt; this way you can correct and address what makes them most fearful, which can be different for each loved one. For some, the concern could be that they have children or other vulnerable people in the house. Finding out these other issues is important.”
Venkatrao Medarametla, MD, SFHM, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., emphasized that, in a time when hospitalists are being pulled in every direction, it is easy to lose your attention.
“It’s very important that family members know you’re present with them,” he said. “This can be an emotional time and they need empathy. It’s very easy for our list of tasks to get in the way of communicating, including with our body language.”
Dr. Medarametla said one of the reasons to communicate with patients’ loved ones is to calm them – a patient’s relatives or their friends may not be under your medical care, but they are still human beings.
“A lot of people just want information and want to be helpful, but we also need to realize that, while we are caring for many patients, this one person is the patient they are focused on,” said Laura Nell Hodo, MD, a pediatric hospitalist at Kravis Children’s Hospital at Mount Sinai in New York. “Don’t rush, and if you know that a patient’s loved one needs more time, make sure it can be found – if not then, at least later on the phone. Fifteen to 20 minutes may be what’s needed, and you can’t shortchange them.”
Dr. Hodo said that a patient’s loved ones often do not realize it is possible to receive phone calls from hospitalists. “We need to remind them that they can get in touch with us. We have to remember how helpless they can feel and how they want to understand what is happening in the hospital.”
For medical adherence issues, sometimes it is best to communicate with the patient and loved one at the same time, Dr. Hodo advised. “Whether it’s for medication or postdischarge exercises, if they both receive the information together it can reinforce adherence. But you also need to remember that the patient may only want a loved one told about certain things, or possibly nothing at all. We need to make sure we understand the patient’s wishes, regardless of whether we think a person close to them can be an ally or not.”
Dr. Esbensen also noted that a loved one can give hospitalists important clues to the emotional components of a patient’s care.
“I remember a patient whose wife told me how he worked in a garage, how he was strong and did not want people to think he was a weak guy just because of what was happening to him,” Dr. Esbensen said. “I didn’t know that he felt he might be perceived in this way. I mentioned to him how I learned he was a good mechanic and he perked up and felt seen in a different light. These things make a difference.”
But when is the best time to speak with a patient’s loved ones? Since much communication is done via phone during the pandemic, there are different philosophies.
“We had a debate among colleagues to see how each of us did it,” Dr. Esbensen said. “Some try to call after each patient encounter, while they are outside the room and it’s fresh in their mind, but others find it better to make the call after their rounds, to give the person their full attention. Most of the time I try to do it that way.”
She noted that, in the current environment, a phone call may be better than a face-to-face conversation with patients’ loved ones.
“We’re covered in so much gear to protect us from the coronavirus that it can feel like a great distance exists between us and the person with whom we’re speaking,” she said. “It’s strange, but the phone can make the conversation seem more relaxed and may get people to open up more.”
Even when they leave
All the hospitalists affirmed that loved ones can make a big difference for the patient through all aspects of care. Long after a patient returns home, the support of loved ones can have a profound impact in speeding healing and improving long-term outcomes.
Dr. Esbensen said COVID-19 and other serious illnesses can leave a patient needing support, and maybe a “push” when feeling low keeps them from adhering to medical advice.
“It’s not just in the hospital but after discharge,” she said. “A person offering support can really help patients throughout their journey, and much success in recovering from illness occurs after the transition home. Having the support of that one person a patient trusts can be critical.”
Dr. Hodo believes that the coronavirus pandemic could forever change the way hospitalists communicate with patients and their loved ones.
“I work in pediatrics and we know serious medical decisions can’t be made without guardians or parents,” she said. “But in adult medicine doctors may not automatically ask the patient about calling someone for input on decision-making. With COVID, you cannot assume a patient is on their own, because there are protocols keeping people from physically being present in the patient’s room. My experience from working in adult coronavirus units is that the thinking about the loved ones’ role in patient care – and communication with them – might just change. … At least, I hope so.”
Quick takeaways for hospitalists
- Get beyond personal protective equipment. A conversation with a patient’s loved one might be easier to achieve via phone, without all the protective gear in the way.
- Encourage adherence. Speaking with patients and loved ones together may be more effective. They may reach agreement quicker on how best to adhere to medical advice.
- Loved ones offer clues. They might give you a better sense of a patient’s worries, or help you to connect better with those in your care.
- Be present. You have a long to-do list but do not let empathy fall off it, even if you feel overwhelmed.
We think of a patient’s recovery happening in multiple locations – in a hospital room or a rehabilitation facility, for example. But many clinicians may not consider the opportunity to aid healing that lies in the waiting room.
The waiting room is where a patient’s loved ones often are and they, sometimes more than anyone, can unlock the path to a patient’s quicker recovery. Friends and family can offer encouragement, as they have an existing bond of trust that can help if a patient needs reinforcement to take their medications or follow other health care advice. But if loved ones are going to help patients, they need help from clinicians. Beyond being potential allies, they are also hurting, experiencing worry or confusion in a world of medical jargon.
The coronavirus changes the relationship of patients and their loved ones, as patients are often isolated or limited in the number of visitors they are allowed to see. A smartphone replaces the smiling faces of friends and relatives at their bedside, and a text is a poor substitute for a hug.
The Hospitalist asked some experienced hospitalists for insight on how best to communicate with patients’ loved ones to improve outcomes for all, medically and emotionally.
Team approach
“Patients feel isolated, terrified, and vulnerable but still need an advocate in the hospital, so daily communication with a patient’s loved one is important to give a sense that the patient is looked after,” said Kari Esbensen, MD, PhD, a hospitalist and palliative care expert at Emory University Hospital Midtown, Atlanta.
Glenn Rosenbluth, MD, a pediatric hospitalist and director, quality and safety programs, at the University of California, San Francisco, Benioff Children’s Hospital, agreed. He said that the most important thing is to communicate, period.
“We fall into this pattern of ‘out of sight, out of mind,’ ” he said. “We need to take the extra step to find out who a patient’s loved ones are. If it is a clinical visit, ask the patient, or maybe get the information from a caseworker, or just pay attention to who is dropping in to see the patient. Having a second person available to jot down notes, or having a handy list of questions – it all helps the patient. We forget that sometimes it can seem like a whirlwind for the patient when they are hurting. We have to remember that a loved one is important to a patient’s care team and we need to include them, empower them, and show that we want to hear their voices.”
Dr. Esbensen said it is critical to start off on the right foot when communicating with a patient’s loved one, especially during the current pandemic.
“With COVID-19, the most important thing is to speak honestly, to say hope for the best but prepare for the worst-case scenario,” Dr. Esbensen said. “We’ve seen that conditions can shift dramatically in short periods of time. The loved one needs to have a sense of the positive and negative possibilities. Families tend to lack understanding of the changes in the patient that are caused by COVID-19. The patient can come out of the hospital debilitated, very different than when they entered the hospital, and we need to warn people close to them about this. Unrealistic expectations need to be guarded against if a patient’s loved ones are going to help.”
Perhaps the best form of communication with a patient’s loved ones is an often-forgotten skill: listening.
“Get an idea from the patient’s loved ones of what the issues are, as well as their idea of what they think of the disease and how it spreads,” Dr. Esbensen said. “Sometimes they are right on target but sometimes there are misinterpretations and we need to help them understand it better. It’s not a ‘one-size-fits-all’ speech that we should give, but try to say, ‘tell me what you think is going on, what you think you’ve heard, and what you’re worried about,’ and learn what is most important to the patient. Start on those terms and adapt; this way you can correct and address what makes them most fearful, which can be different for each loved one. For some, the concern could be that they have children or other vulnerable people in the house. Finding out these other issues is important.”
Venkatrao Medarametla, MD, SFHM, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., emphasized that, in a time when hospitalists are being pulled in every direction, it is easy to lose your attention.
“It’s very important that family members know you’re present with them,” he said. “This can be an emotional time and they need empathy. It’s very easy for our list of tasks to get in the way of communicating, including with our body language.”
Dr. Medarametla said one of the reasons to communicate with patients’ loved ones is to calm them – a patient’s relatives or their friends may not be under your medical care, but they are still human beings.
“A lot of people just want information and want to be helpful, but we also need to realize that, while we are caring for many patients, this one person is the patient they are focused on,” said Laura Nell Hodo, MD, a pediatric hospitalist at Kravis Children’s Hospital at Mount Sinai in New York. “Don’t rush, and if you know that a patient’s loved one needs more time, make sure it can be found – if not then, at least later on the phone. Fifteen to 20 minutes may be what’s needed, and you can’t shortchange them.”
Dr. Hodo said that a patient’s loved ones often do not realize it is possible to receive phone calls from hospitalists. “We need to remind them that they can get in touch with us. We have to remember how helpless they can feel and how they want to understand what is happening in the hospital.”
For medical adherence issues, sometimes it is best to communicate with the patient and loved one at the same time, Dr. Hodo advised. “Whether it’s for medication or postdischarge exercises, if they both receive the information together it can reinforce adherence. But you also need to remember that the patient may only want a loved one told about certain things, or possibly nothing at all. We need to make sure we understand the patient’s wishes, regardless of whether we think a person close to them can be an ally or not.”
Dr. Esbensen also noted that a loved one can give hospitalists important clues to the emotional components of a patient’s care.
“I remember a patient whose wife told me how he worked in a garage, how he was strong and did not want people to think he was a weak guy just because of what was happening to him,” Dr. Esbensen said. “I didn’t know that he felt he might be perceived in this way. I mentioned to him how I learned he was a good mechanic and he perked up and felt seen in a different light. These things make a difference.”
But when is the best time to speak with a patient’s loved ones? Since much communication is done via phone during the pandemic, there are different philosophies.
“We had a debate among colleagues to see how each of us did it,” Dr. Esbensen said. “Some try to call after each patient encounter, while they are outside the room and it’s fresh in their mind, but others find it better to make the call after their rounds, to give the person their full attention. Most of the time I try to do it that way.”
She noted that, in the current environment, a phone call may be better than a face-to-face conversation with patients’ loved ones.
“We’re covered in so much gear to protect us from the coronavirus that it can feel like a great distance exists between us and the person with whom we’re speaking,” she said. “It’s strange, but the phone can make the conversation seem more relaxed and may get people to open up more.”
Even when they leave
All the hospitalists affirmed that loved ones can make a big difference for the patient through all aspects of care. Long after a patient returns home, the support of loved ones can have a profound impact in speeding healing and improving long-term outcomes.
Dr. Esbensen said COVID-19 and other serious illnesses can leave a patient needing support, and maybe a “push” when feeling low keeps them from adhering to medical advice.
“It’s not just in the hospital but after discharge,” she said. “A person offering support can really help patients throughout their journey, and much success in recovering from illness occurs after the transition home. Having the support of that one person a patient trusts can be critical.”
Dr. Hodo believes that the coronavirus pandemic could forever change the way hospitalists communicate with patients and their loved ones.
“I work in pediatrics and we know serious medical decisions can’t be made without guardians or parents,” she said. “But in adult medicine doctors may not automatically ask the patient about calling someone for input on decision-making. With COVID, you cannot assume a patient is on their own, because there are protocols keeping people from physically being present in the patient’s room. My experience from working in adult coronavirus units is that the thinking about the loved ones’ role in patient care – and communication with them – might just change. … At least, I hope so.”
Quick takeaways for hospitalists
- Get beyond personal protective equipment. A conversation with a patient’s loved one might be easier to achieve via phone, without all the protective gear in the way.
- Encourage adherence. Speaking with patients and loved ones together may be more effective. They may reach agreement quicker on how best to adhere to medical advice.
- Loved ones offer clues. They might give you a better sense of a patient’s worries, or help you to connect better with those in your care.
- Be present. You have a long to-do list but do not let empathy fall off it, even if you feel overwhelmed.
Physicians, make a plan to vote
In March 2020, following the announcement of the United States’ first death related to COVID-19, many physicians began using their voices to discuss the shortage of personal protective equipment (PPE). Many physicians, myself included, petitioned elected leaders at the community, state, and federal levels to address the PPE shortage.
Historically, physicians have advocated for improved public health. From seat belt laws in the 1980s and 1990s to the Affordable Care Act in the 2000s, physicians have testified at the community, state, and federal levels to advocate for the health and safety of our patients and the public. Yet while we have been making our voices heard, we are often silent at the ballot box.
In the 1996 and 2000 elections, physicians voted 9% less often than the general public, and compared with lawyers – professionals with similar educational attainment and finances – physicians voted 22% less often.1 It is unclear why physicians are less likely to vote. In a 2016 article, David Grande, MD, and Katrina Armstrong, MD, postulated that physicians may not vote because our work hours create barriers to visiting polls.2
Despite our lack of engagement at the ballot box, voting is important to improving our patients’ social determinants of health. In a recently published systematic review, the authors found several studies supporting the association between voting and social determinants of health. Their review found that, when large numbers of people from communities participated in voting, it translated into greater influence over determining who held political power in that community. Those with power introduced and supported policies responding to their constituents’ needs, ultimately influencing their constituents’ social determinants of health.3 By voting, we as physicians are helping to address the social determinants of health in our communities.
Many medical students have been doing their part to improve the social determinants of health in their communities by pledging to vote. In 2018, the American Medical Student Association launched their “Med Out the Vote” initiative prior to the election. The organization called on all health care providers and providers in training to pledge to vote in the election.4 They are continuing these efforts for the 2020 elections.
We should join our nation’s medical students by also pledging to vote. To begin, we can all Make A Plan To Vote. Each plan should include the following:
- Register to vote: In many states eligible voters can register online.
- Request an absentee ballot: Many states require registered voters to request absentee ballots online or by mail.
- Vote: Submit an absentee ballot prior to election or vote in-person on election day. Some counties allow voting early in person.
In practice, our plans will differ slightly because each state has its own election laws.
This election season let us ensure all physician voices are heard. Make A Plan To Vote for your patients and communities.
Dr. Kumar is the pediatric editor of The Hospitalist. She is clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University and a pediatric hospitalist at Cleveland Clinic Children’s.
References
1. Grande D et al. Do Doctors Vote? J Gen Intern Med. 2007 May;22(5):585-9.
2. Grande D, Armstrong K. Will Physicians Vote? Ann Intern Med. 2016;165:814-5.
3. Brown CL et al. Voting, health and interventions in healthcare settings: A scoping review. Public Health Rev. 2020 Jul. doi: 10.1186/s40985-020-00133-6.
4. American Medical Student Association. AMSA Launches Med Out the Vote Campaign, Call to Action. 2018 Jul 29. Accessed 2020 Sep 14. https://www.amsa.org/about/amsa-press-room/amsa-launches-med-out-the-vote-campaign-call-to-action/
In March 2020, following the announcement of the United States’ first death related to COVID-19, many physicians began using their voices to discuss the shortage of personal protective equipment (PPE). Many physicians, myself included, petitioned elected leaders at the community, state, and federal levels to address the PPE shortage.
Historically, physicians have advocated for improved public health. From seat belt laws in the 1980s and 1990s to the Affordable Care Act in the 2000s, physicians have testified at the community, state, and federal levels to advocate for the health and safety of our patients and the public. Yet while we have been making our voices heard, we are often silent at the ballot box.
In the 1996 and 2000 elections, physicians voted 9% less often than the general public, and compared with lawyers – professionals with similar educational attainment and finances – physicians voted 22% less often.1 It is unclear why physicians are less likely to vote. In a 2016 article, David Grande, MD, and Katrina Armstrong, MD, postulated that physicians may not vote because our work hours create barriers to visiting polls.2
Despite our lack of engagement at the ballot box, voting is important to improving our patients’ social determinants of health. In a recently published systematic review, the authors found several studies supporting the association between voting and social determinants of health. Their review found that, when large numbers of people from communities participated in voting, it translated into greater influence over determining who held political power in that community. Those with power introduced and supported policies responding to their constituents’ needs, ultimately influencing their constituents’ social determinants of health.3 By voting, we as physicians are helping to address the social determinants of health in our communities.
Many medical students have been doing their part to improve the social determinants of health in their communities by pledging to vote. In 2018, the American Medical Student Association launched their “Med Out the Vote” initiative prior to the election. The organization called on all health care providers and providers in training to pledge to vote in the election.4 They are continuing these efforts for the 2020 elections.
We should join our nation’s medical students by also pledging to vote. To begin, we can all Make A Plan To Vote. Each plan should include the following:
- Register to vote: In many states eligible voters can register online.
- Request an absentee ballot: Many states require registered voters to request absentee ballots online or by mail.
- Vote: Submit an absentee ballot prior to election or vote in-person on election day. Some counties allow voting early in person.
In practice, our plans will differ slightly because each state has its own election laws.
This election season let us ensure all physician voices are heard. Make A Plan To Vote for your patients and communities.
Dr. Kumar is the pediatric editor of The Hospitalist. She is clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University and a pediatric hospitalist at Cleveland Clinic Children’s.
References
1. Grande D et al. Do Doctors Vote? J Gen Intern Med. 2007 May;22(5):585-9.
2. Grande D, Armstrong K. Will Physicians Vote? Ann Intern Med. 2016;165:814-5.
3. Brown CL et al. Voting, health and interventions in healthcare settings: A scoping review. Public Health Rev. 2020 Jul. doi: 10.1186/s40985-020-00133-6.
4. American Medical Student Association. AMSA Launches Med Out the Vote Campaign, Call to Action. 2018 Jul 29. Accessed 2020 Sep 14. https://www.amsa.org/about/amsa-press-room/amsa-launches-med-out-the-vote-campaign-call-to-action/
In March 2020, following the announcement of the United States’ first death related to COVID-19, many physicians began using their voices to discuss the shortage of personal protective equipment (PPE). Many physicians, myself included, petitioned elected leaders at the community, state, and federal levels to address the PPE shortage.
Historically, physicians have advocated for improved public health. From seat belt laws in the 1980s and 1990s to the Affordable Care Act in the 2000s, physicians have testified at the community, state, and federal levels to advocate for the health and safety of our patients and the public. Yet while we have been making our voices heard, we are often silent at the ballot box.
In the 1996 and 2000 elections, physicians voted 9% less often than the general public, and compared with lawyers – professionals with similar educational attainment and finances – physicians voted 22% less often.1 It is unclear why physicians are less likely to vote. In a 2016 article, David Grande, MD, and Katrina Armstrong, MD, postulated that physicians may not vote because our work hours create barriers to visiting polls.2
Despite our lack of engagement at the ballot box, voting is important to improving our patients’ social determinants of health. In a recently published systematic review, the authors found several studies supporting the association between voting and social determinants of health. Their review found that, when large numbers of people from communities participated in voting, it translated into greater influence over determining who held political power in that community. Those with power introduced and supported policies responding to their constituents’ needs, ultimately influencing their constituents’ social determinants of health.3 By voting, we as physicians are helping to address the social determinants of health in our communities.
Many medical students have been doing their part to improve the social determinants of health in their communities by pledging to vote. In 2018, the American Medical Student Association launched their “Med Out the Vote” initiative prior to the election. The organization called on all health care providers and providers in training to pledge to vote in the election.4 They are continuing these efforts for the 2020 elections.
We should join our nation’s medical students by also pledging to vote. To begin, we can all Make A Plan To Vote. Each plan should include the following:
- Register to vote: In many states eligible voters can register online.
- Request an absentee ballot: Many states require registered voters to request absentee ballots online or by mail.
- Vote: Submit an absentee ballot prior to election or vote in-person on election day. Some counties allow voting early in person.
In practice, our plans will differ slightly because each state has its own election laws.
This election season let us ensure all physician voices are heard. Make A Plan To Vote for your patients and communities.
Dr. Kumar is the pediatric editor of The Hospitalist. She is clinical assistant professor of pediatrics at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University and a pediatric hospitalist at Cleveland Clinic Children’s.
References
1. Grande D et al. Do Doctors Vote? J Gen Intern Med. 2007 May;22(5):585-9.
2. Grande D, Armstrong K. Will Physicians Vote? Ann Intern Med. 2016;165:814-5.
3. Brown CL et al. Voting, health and interventions in healthcare settings: A scoping review. Public Health Rev. 2020 Jul. doi: 10.1186/s40985-020-00133-6.
4. American Medical Student Association. AMSA Launches Med Out the Vote Campaign, Call to Action. 2018 Jul 29. Accessed 2020 Sep 14. https://www.amsa.org/about/amsa-press-room/amsa-launches-med-out-the-vote-campaign-call-to-action/