User login
Social media and health information: Empowering or misleading?
The search engine giants, Dr. Google or Dr. Bing, are visited by most of our patients before seeking medical help. In 1976, medical student Tom Ferguson, MD, first coined the term e-Patient. It means a health consumer who uses the Internet to gather information about a medical condition for themselves or on behalf of family and friends and uses electronic communication tools to cope with medical conditions. Dr. Ferguson described e-Patients as “empowered medical consumers.”1
During the COVID-19 pandemic, social media and networking platforms – such as Facebook, Twitter, Instagram, Snapchat, YouTube, WhatsApp, online health support groups – are used increasingly by e-Patients to gather critical health information. Health care providers often take a conflicted stand on the use of social media. Though we want our patients to read about their illnesses and make informed choices, we often get frustrated by misdiagnoses, misinformation, and disinformation that comes with it.
According to a study investigating the differential diffusion of news stories distributed on Twitter from 2006 to 2017, fake news was considered more novel than true news, and people were more likely to share novel information.2 Bots accelerated the spread of true and fake news at the same rate, implying that fake news spreads more than the truth because humans, not robots, are more likely to spread it. Social media has promoted some of the best health campaigns, like public cancer awareness, the ALS Ice Bucket Challenge, World Heart Day, and others. At the same time, it has also provided a platform for antivaccination activists, dangerous and unproven alternative cancer therapies, weight loss pills, and nutrition plans.
According to a Pew Research Center survey, 72% of adult Internet users had searched online for information about a range of health issues of their own or for others in the past 12 months.3 A survey from 2019-2020 showed that those who relied on social media for news were among the least knowledgeable about key facts during the COVID-19 outbreak.4 About 74% of public posts about COVID-19 were linked to news organizations, while just 1% linked to health and science sites.5 While social media has emerged as one of the most significant health information sources, it famously has only a few safeguards in place against medical misinformation. Requiring responsibility and regulations for accurate or evidence-based information walks a thin line on infringing freedom of speech. Medical misinformation related to COVID-19 has become as contagious as the virus itself.
In February 2020, the World Health Organization warned that a massive ‘Infodemic’ had accompanied the COVID-19 outbreak, with an overabundance of information, some accurate and some not, making it difficult for people to find reliable sources and trustworthy information.6 The Black immunity myth, groups opposing vaccines, campaigns against 5G mobile phone networks, suggestions that SARS-CoV-2 was an engineered bioweapon, and online rumors leading to mob attacks in India and mass poisonings in Iran are some of the misleading health information that has circulated related to COVID-19.
In the Web 2.0 era, in which credible health information comes packaged with divisive and misleading information, social media’s full impact on health care, health outcomes, and mental health has yet to be explored. Social networks and media sharing networks have recently announced initiatives to stop misinformation and disinformation by fact-checking, flagging, issuing warnings, and deleting misinformation or misleading content. Providing links to more and correct information and partnering with health and science organizations can also encourage the spread of verifiable information.
While we have yet to see if social media safeguards are adequate, the medical community needs to proactively educate patients on the appropriate use of social media for health information, e-Health literacy, and media health literacy. Like health care providers evaluating scientific papers, we need to cultivate e-Patients’ ability to seek, evaluate, understand, and convey health information from electronic sources. Although the measurement and training tools for e-Health and media health literacy are still scarce, a good place to start could be to have simple conversations with patients. Encouraging patients to critically analyze online information, use credible social media sources, and recognizing the warnings, red flags, and links on unreliable information are some of the discussions worth considering. Equally important is to discourage patients from changing health behaviors or practices based on unverified social media resources and discussing the possible impact of medical misinformation.
A practical approach for e-Patients could be to ask the Five Ws, considered fundamental in information gathering: Who, What, Why, When, and Where.7,8
- Who runs the website? Examine the authors, sponsors, and sources. Federal agencies’ website addresses end in “.gov,” educational institutions maintain “.edu,” large professional or nonprofit organizations often use “.org,” and commercial websites use “.com.”
- What is offered, and What is the evidence? Does it provide unbelievable solutions or quick, miracle cures?
- Why was the site created? Is the mission or goal to inform, explain, or sell health or medical products? Check details on “About This Site” or “About Us.”
- When was the information written or the webpage last updated?
- Where are the privacy policies? Is your privacy protected?
The anonymity of sources, sponsors, financial interests, or the lack of medical credentials and reputable medical research, the use of testimonials as evidence, outdated or incomplete information, and emotional or exaggerated language should raise suspicion about the reliability of the information. Tools like the online tutorial and a checklist from the National Institute of Health’s National Library of Medicine can also be offered to e-Patients to learn how to evaluate health information online.9,10
Online health support groups widely used by patients can be an additional layer of support but can also be a source of misinformation. Since they have fewer gatekeepers than traditional face-to-face communication, keeping a check on the credibility of the information can be difficult. Support groups affiliated with local hospitals or national organizations, or those endorsed by well-known scientific societies, can be encouraged instead of less credible sources. Some online support groups, run by non–health care professionals but with experienced and reliable scientific panels, can be useful resources. However, patients must check for the credibility and reliability of the information.
Lastly, just as hospitalists take a social history of our patients, we could also ask for a “social media history” to understand patients’ sources of health information. We can then guide them toward more credible sources to make them truly empowered medical consumers.
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Nelson R. Informatics: Empowering ePatients to drive health care reform - part I. Online J Issues Nurs. 2016 Sep 13;21(3):9.
2. Vosoughi S et al. The spread of true and false news online. Science. 2012;359(6380):1146-51.
3. Fox S. The social life of health information. Pew Research Center: Fact Tank. 2014 Jan 15. Accessed 2020 Jul 31.
4. Mitchel A, Jurkowitz M, Oliphant JB, Shearer E. Americans Who Mainly Get Their News on Social Media Are Less Engaged, Less Knowledgeable. Pew Research Center: Journalism & Media. 2020 Jul 30. Accessed 2020 Jul 31.
5. Stocking G, Matsa KE, Khuzam M. As COVID-19 Emerged in U.S., Facebook Posts About It Appeared in a Wide Range of Public Pages, Groups Pew Research Center: Journalism & Media. 2020 Jun 24. Accessed 2020 Jul 31.
6. Munich Security Conference. World Health Organization. 2020 Feb 15. Accessed 2020 Jul 31.
7. Levin-Zamir D, Bertschi I. Media health literacy, eHealth literacy, and the role of the social environment in context. Int J Environ Res Public Health. 2018 Aug 3;15(8):1643.
8. Online Health Information: Is It Reliable? National Institute on Aging, National Institutes of Health. 2018 Oct 31. Accessed 2020 Aug 10.
9. How To Evaluate Health Information on the Internet: Questions and Answers. Office of Dietary Supplements, National Institutes of Health. 2011 Jun 24. Accessed 2020 Aug 10.
10. Evaluating Internet Health Information: A Tutorial From the National Library of Medicine. Medline Plus. 2020 Mar 6. Accessed 2020 Aug 10.
The search engine giants, Dr. Google or Dr. Bing, are visited by most of our patients before seeking medical help. In 1976, medical student Tom Ferguson, MD, first coined the term e-Patient. It means a health consumer who uses the Internet to gather information about a medical condition for themselves or on behalf of family and friends and uses electronic communication tools to cope with medical conditions. Dr. Ferguson described e-Patients as “empowered medical consumers.”1
During the COVID-19 pandemic, social media and networking platforms – such as Facebook, Twitter, Instagram, Snapchat, YouTube, WhatsApp, online health support groups – are used increasingly by e-Patients to gather critical health information. Health care providers often take a conflicted stand on the use of social media. Though we want our patients to read about their illnesses and make informed choices, we often get frustrated by misdiagnoses, misinformation, and disinformation that comes with it.
According to a study investigating the differential diffusion of news stories distributed on Twitter from 2006 to 2017, fake news was considered more novel than true news, and people were more likely to share novel information.2 Bots accelerated the spread of true and fake news at the same rate, implying that fake news spreads more than the truth because humans, not robots, are more likely to spread it. Social media has promoted some of the best health campaigns, like public cancer awareness, the ALS Ice Bucket Challenge, World Heart Day, and others. At the same time, it has also provided a platform for antivaccination activists, dangerous and unproven alternative cancer therapies, weight loss pills, and nutrition plans.
According to a Pew Research Center survey, 72% of adult Internet users had searched online for information about a range of health issues of their own or for others in the past 12 months.3 A survey from 2019-2020 showed that those who relied on social media for news were among the least knowledgeable about key facts during the COVID-19 outbreak.4 About 74% of public posts about COVID-19 were linked to news organizations, while just 1% linked to health and science sites.5 While social media has emerged as one of the most significant health information sources, it famously has only a few safeguards in place against medical misinformation. Requiring responsibility and regulations for accurate or evidence-based information walks a thin line on infringing freedom of speech. Medical misinformation related to COVID-19 has become as contagious as the virus itself.
In February 2020, the World Health Organization warned that a massive ‘Infodemic’ had accompanied the COVID-19 outbreak, with an overabundance of information, some accurate and some not, making it difficult for people to find reliable sources and trustworthy information.6 The Black immunity myth, groups opposing vaccines, campaigns against 5G mobile phone networks, suggestions that SARS-CoV-2 was an engineered bioweapon, and online rumors leading to mob attacks in India and mass poisonings in Iran are some of the misleading health information that has circulated related to COVID-19.
In the Web 2.0 era, in which credible health information comes packaged with divisive and misleading information, social media’s full impact on health care, health outcomes, and mental health has yet to be explored. Social networks and media sharing networks have recently announced initiatives to stop misinformation and disinformation by fact-checking, flagging, issuing warnings, and deleting misinformation or misleading content. Providing links to more and correct information and partnering with health and science organizations can also encourage the spread of verifiable information.
While we have yet to see if social media safeguards are adequate, the medical community needs to proactively educate patients on the appropriate use of social media for health information, e-Health literacy, and media health literacy. Like health care providers evaluating scientific papers, we need to cultivate e-Patients’ ability to seek, evaluate, understand, and convey health information from electronic sources. Although the measurement and training tools for e-Health and media health literacy are still scarce, a good place to start could be to have simple conversations with patients. Encouraging patients to critically analyze online information, use credible social media sources, and recognizing the warnings, red flags, and links on unreliable information are some of the discussions worth considering. Equally important is to discourage patients from changing health behaviors or practices based on unverified social media resources and discussing the possible impact of medical misinformation.
A practical approach for e-Patients could be to ask the Five Ws, considered fundamental in information gathering: Who, What, Why, When, and Where.7,8
- Who runs the website? Examine the authors, sponsors, and sources. Federal agencies’ website addresses end in “.gov,” educational institutions maintain “.edu,” large professional or nonprofit organizations often use “.org,” and commercial websites use “.com.”
- What is offered, and What is the evidence? Does it provide unbelievable solutions or quick, miracle cures?
- Why was the site created? Is the mission or goal to inform, explain, or sell health or medical products? Check details on “About This Site” or “About Us.”
- When was the information written or the webpage last updated?
- Where are the privacy policies? Is your privacy protected?
The anonymity of sources, sponsors, financial interests, or the lack of medical credentials and reputable medical research, the use of testimonials as evidence, outdated or incomplete information, and emotional or exaggerated language should raise suspicion about the reliability of the information. Tools like the online tutorial and a checklist from the National Institute of Health’s National Library of Medicine can also be offered to e-Patients to learn how to evaluate health information online.9,10
Online health support groups widely used by patients can be an additional layer of support but can also be a source of misinformation. Since they have fewer gatekeepers than traditional face-to-face communication, keeping a check on the credibility of the information can be difficult. Support groups affiliated with local hospitals or national organizations, or those endorsed by well-known scientific societies, can be encouraged instead of less credible sources. Some online support groups, run by non–health care professionals but with experienced and reliable scientific panels, can be useful resources. However, patients must check for the credibility and reliability of the information.
Lastly, just as hospitalists take a social history of our patients, we could also ask for a “social media history” to understand patients’ sources of health information. We can then guide them toward more credible sources to make them truly empowered medical consumers.
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Nelson R. Informatics: Empowering ePatients to drive health care reform - part I. Online J Issues Nurs. 2016 Sep 13;21(3):9.
2. Vosoughi S et al. The spread of true and false news online. Science. 2012;359(6380):1146-51.
3. Fox S. The social life of health information. Pew Research Center: Fact Tank. 2014 Jan 15. Accessed 2020 Jul 31.
4. Mitchel A, Jurkowitz M, Oliphant JB, Shearer E. Americans Who Mainly Get Their News on Social Media Are Less Engaged, Less Knowledgeable. Pew Research Center: Journalism & Media. 2020 Jul 30. Accessed 2020 Jul 31.
5. Stocking G, Matsa KE, Khuzam M. As COVID-19 Emerged in U.S., Facebook Posts About It Appeared in a Wide Range of Public Pages, Groups Pew Research Center: Journalism & Media. 2020 Jun 24. Accessed 2020 Jul 31.
6. Munich Security Conference. World Health Organization. 2020 Feb 15. Accessed 2020 Jul 31.
7. Levin-Zamir D, Bertschi I. Media health literacy, eHealth literacy, and the role of the social environment in context. Int J Environ Res Public Health. 2018 Aug 3;15(8):1643.
8. Online Health Information: Is It Reliable? National Institute on Aging, National Institutes of Health. 2018 Oct 31. Accessed 2020 Aug 10.
9. How To Evaluate Health Information on the Internet: Questions and Answers. Office of Dietary Supplements, National Institutes of Health. 2011 Jun 24. Accessed 2020 Aug 10.
10. Evaluating Internet Health Information: A Tutorial From the National Library of Medicine. Medline Plus. 2020 Mar 6. Accessed 2020 Aug 10.
The search engine giants, Dr. Google or Dr. Bing, are visited by most of our patients before seeking medical help. In 1976, medical student Tom Ferguson, MD, first coined the term e-Patient. It means a health consumer who uses the Internet to gather information about a medical condition for themselves or on behalf of family and friends and uses electronic communication tools to cope with medical conditions. Dr. Ferguson described e-Patients as “empowered medical consumers.”1
During the COVID-19 pandemic, social media and networking platforms – such as Facebook, Twitter, Instagram, Snapchat, YouTube, WhatsApp, online health support groups – are used increasingly by e-Patients to gather critical health information. Health care providers often take a conflicted stand on the use of social media. Though we want our patients to read about their illnesses and make informed choices, we often get frustrated by misdiagnoses, misinformation, and disinformation that comes with it.
According to a study investigating the differential diffusion of news stories distributed on Twitter from 2006 to 2017, fake news was considered more novel than true news, and people were more likely to share novel information.2 Bots accelerated the spread of true and fake news at the same rate, implying that fake news spreads more than the truth because humans, not robots, are more likely to spread it. Social media has promoted some of the best health campaigns, like public cancer awareness, the ALS Ice Bucket Challenge, World Heart Day, and others. At the same time, it has also provided a platform for antivaccination activists, dangerous and unproven alternative cancer therapies, weight loss pills, and nutrition plans.
According to a Pew Research Center survey, 72% of adult Internet users had searched online for information about a range of health issues of their own or for others in the past 12 months.3 A survey from 2019-2020 showed that those who relied on social media for news were among the least knowledgeable about key facts during the COVID-19 outbreak.4 About 74% of public posts about COVID-19 were linked to news organizations, while just 1% linked to health and science sites.5 While social media has emerged as one of the most significant health information sources, it famously has only a few safeguards in place against medical misinformation. Requiring responsibility and regulations for accurate or evidence-based information walks a thin line on infringing freedom of speech. Medical misinformation related to COVID-19 has become as contagious as the virus itself.
In February 2020, the World Health Organization warned that a massive ‘Infodemic’ had accompanied the COVID-19 outbreak, with an overabundance of information, some accurate and some not, making it difficult for people to find reliable sources and trustworthy information.6 The Black immunity myth, groups opposing vaccines, campaigns against 5G mobile phone networks, suggestions that SARS-CoV-2 was an engineered bioweapon, and online rumors leading to mob attacks in India and mass poisonings in Iran are some of the misleading health information that has circulated related to COVID-19.
In the Web 2.0 era, in which credible health information comes packaged with divisive and misleading information, social media’s full impact on health care, health outcomes, and mental health has yet to be explored. Social networks and media sharing networks have recently announced initiatives to stop misinformation and disinformation by fact-checking, flagging, issuing warnings, and deleting misinformation or misleading content. Providing links to more and correct information and partnering with health and science organizations can also encourage the spread of verifiable information.
While we have yet to see if social media safeguards are adequate, the medical community needs to proactively educate patients on the appropriate use of social media for health information, e-Health literacy, and media health literacy. Like health care providers evaluating scientific papers, we need to cultivate e-Patients’ ability to seek, evaluate, understand, and convey health information from electronic sources. Although the measurement and training tools for e-Health and media health literacy are still scarce, a good place to start could be to have simple conversations with patients. Encouraging patients to critically analyze online information, use credible social media sources, and recognizing the warnings, red flags, and links on unreliable information are some of the discussions worth considering. Equally important is to discourage patients from changing health behaviors or practices based on unverified social media resources and discussing the possible impact of medical misinformation.
A practical approach for e-Patients could be to ask the Five Ws, considered fundamental in information gathering: Who, What, Why, When, and Where.7,8
- Who runs the website? Examine the authors, sponsors, and sources. Federal agencies’ website addresses end in “.gov,” educational institutions maintain “.edu,” large professional or nonprofit organizations often use “.org,” and commercial websites use “.com.”
- What is offered, and What is the evidence? Does it provide unbelievable solutions or quick, miracle cures?
- Why was the site created? Is the mission or goal to inform, explain, or sell health or medical products? Check details on “About This Site” or “About Us.”
- When was the information written or the webpage last updated?
- Where are the privacy policies? Is your privacy protected?
The anonymity of sources, sponsors, financial interests, or the lack of medical credentials and reputable medical research, the use of testimonials as evidence, outdated or incomplete information, and emotional or exaggerated language should raise suspicion about the reliability of the information. Tools like the online tutorial and a checklist from the National Institute of Health’s National Library of Medicine can also be offered to e-Patients to learn how to evaluate health information online.9,10
Online health support groups widely used by patients can be an additional layer of support but can also be a source of misinformation. Since they have fewer gatekeepers than traditional face-to-face communication, keeping a check on the credibility of the information can be difficult. Support groups affiliated with local hospitals or national organizations, or those endorsed by well-known scientific societies, can be encouraged instead of less credible sources. Some online support groups, run by non–health care professionals but with experienced and reliable scientific panels, can be useful resources. However, patients must check for the credibility and reliability of the information.
Lastly, just as hospitalists take a social history of our patients, we could also ask for a “social media history” to understand patients’ sources of health information. We can then guide them toward more credible sources to make them truly empowered medical consumers.
Dr. Saigal is a hospitalist and clinical assistant professor of medicine in the division of hospital medicine at the Ohio State University Wexner Medical Center, Columbus.
References
1. Nelson R. Informatics: Empowering ePatients to drive health care reform - part I. Online J Issues Nurs. 2016 Sep 13;21(3):9.
2. Vosoughi S et al. The spread of true and false news online. Science. 2012;359(6380):1146-51.
3. Fox S. The social life of health information. Pew Research Center: Fact Tank. 2014 Jan 15. Accessed 2020 Jul 31.
4. Mitchel A, Jurkowitz M, Oliphant JB, Shearer E. Americans Who Mainly Get Their News on Social Media Are Less Engaged, Less Knowledgeable. Pew Research Center: Journalism & Media. 2020 Jul 30. Accessed 2020 Jul 31.
5. Stocking G, Matsa KE, Khuzam M. As COVID-19 Emerged in U.S., Facebook Posts About It Appeared in a Wide Range of Public Pages, Groups Pew Research Center: Journalism & Media. 2020 Jun 24. Accessed 2020 Jul 31.
6. Munich Security Conference. World Health Organization. 2020 Feb 15. Accessed 2020 Jul 31.
7. Levin-Zamir D, Bertschi I. Media health literacy, eHealth literacy, and the role of the social environment in context. Int J Environ Res Public Health. 2018 Aug 3;15(8):1643.
8. Online Health Information: Is It Reliable? National Institute on Aging, National Institutes of Health. 2018 Oct 31. Accessed 2020 Aug 10.
9. How To Evaluate Health Information on the Internet: Questions and Answers. Office of Dietary Supplements, National Institutes of Health. 2011 Jun 24. Accessed 2020 Aug 10.
10. Evaluating Internet Health Information: A Tutorial From the National Library of Medicine. Medline Plus. 2020 Mar 6. Accessed 2020 Aug 10.
The path to leadership
It was 6 a.m. on a rainy, cold Pacific Northwest morning as I walked from my apartment to the hospital, dodging puddles and dreaming of the mediocre-yet-hot physician-lounge coffee. Another long day full of clinical and administrative tasks awaited me.
I was 6 months’ pregnant with our first child and working my sixth 12-hour shift in a row. We had recently lost our medical director, and the C-suite had offered me the role. The day ahead seemed like an enormous mountain to climb.
I felt tired and more than a little overwhelmed. But I whispered to myself: “Today is going to be a fantastic day. I will not fail my team. I will not fail my patients!”
Physician leadership starts with a decision
The timing of this call to leadership had not been ideal. There’s probably never a perfect time to step into a medical director role. And my situation was no exception.
In addition to the baby on the way, my husband was traveling a lot for work. Also, the job of a medical director seemed a little daunting – especially to a young physician leading a team for the first time.
But I knew that leadership was my calling. While I didn’t yet have decades of experience, I had been selected as the chief resident in internal medicine, completed a nephrology fellowship, and mentored several medical students and residents along my career path.
I also knew that I was passionate about supporting my patients and hospitalist team. I’d previously served as associate medical director in charge of quality, readmission reduction, and patient experience. Having achieved the highest patient satisfaction scores on the team for 2 consecutive years, I was specially tasked to improve our team’s HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores.
These experiences taught me that coaching with positive reinforcement was in my blood. This gave me the courage to face my tallest mountain yet.
No one climbs a mountain alone
I also stepped into my new physician leadership role with amazing support. Our outgoing medical director had recommended me, and my entire team was rooting for me. My spouse was 100% behind the idea.
What’s more, I had received amazing feedback from patients throughout my 3 years at the hospital. I had papered an entire office wall with their thank-you notes. I even had a quilt that an 85-year-old patient’s wife made to thank me for my compassionate care.
As I weighed my decision, I realized that I had a higher calling to be a true advocate for my patients. I loved what I did. Each day, I resolved to bring my best and most authentic self for them – no matter how drained I felt.
My team and patients needed me now, not at some more convenient time down the road. A medical director job was the natural next step for me. And so, I resolved to climb the mountain.
Climbing through storms
Stepping into a medical director job forced me to grow into a completely new person. So maybe starting that role during pregnancy was a great metaphor!
Each day, there was immense pressure to perform, to deliver quality outcomes, and to simultaneously meet expectations of the C-suite as well as my hospitalist team. There was no room for failure, because too much was at stake.
Looking back today, I wouldn’t trade the experience for anything. The medical director role was one of the most gratifying experiences in my life, and I am truly thankful for it.
A leader’s role truly boils down to working tirelessly to collaborate with different care teams. It’s important to care not only about our patients but also about our fellow hospitalists. We can do this by truly leading by example – be it picking up extra shifts, covering holidays so team members can be with family, or coming in at 10 p.m. to round with your night team.
I was also able to bring a unique perspective to the hospital C-suite meetings as a woman, an immigrant, and a true “mama bear” – not only of my infant son but also of my team.
My first year as a medical director required more commitment and heart than I could have imagined. But all this hard work paid off when our hospitalist group received the coveted Best Team Award for most improved quality outcomes, financial performance, and patient experience.
The summit is the beginning
My first medical director job fueled my passion for patient satisfaction even further. I now serve as the director of patient experience for the more than 4,200 clinicians at Vituity. Together we care for more than 6.5 million lives a year across the country.
In 2019, I coached 300 physicians and hospital leaders on communication, collaboration, and service recovery skills, leading to significant improvement in their HCAHPS scores. I was delighted to receive the Vituity Distinguished Service Award for my contributions. It’s such an honor to be instrumental in impacting patient care at a larger scale.
This year, I was invited to serve as vice chair of the Society for Hospital Medicine’s patient experience committee and to join the executive board of the SHM San Francisco chapter. Together, we have created a COVID-19 patient communication resource and reached out to our hospitalists to provide them with a space to share their stories during this pandemic. I am so excited to share my knowledge and passion with clinicians across the country given the wide reach of Vituity & SHM!
Many hospitalists shy away from leadership roles. The mountain is tough to scale, but the view from the top is worth it. The key is to start, even if you don’t feel ready. I am here to tell you it can be done!
Dr. Mehta is a hospitalist and director of quality & performance and patient experience at Vituity in Emeryville, Calif. She is vice chair of the SHM patient experience committee and executive board member of the SHM San Francisco Bay Area chapter.
It was 6 a.m. on a rainy, cold Pacific Northwest morning as I walked from my apartment to the hospital, dodging puddles and dreaming of the mediocre-yet-hot physician-lounge coffee. Another long day full of clinical and administrative tasks awaited me.
I was 6 months’ pregnant with our first child and working my sixth 12-hour shift in a row. We had recently lost our medical director, and the C-suite had offered me the role. The day ahead seemed like an enormous mountain to climb.
I felt tired and more than a little overwhelmed. But I whispered to myself: “Today is going to be a fantastic day. I will not fail my team. I will not fail my patients!”
Physician leadership starts with a decision
The timing of this call to leadership had not been ideal. There’s probably never a perfect time to step into a medical director role. And my situation was no exception.
In addition to the baby on the way, my husband was traveling a lot for work. Also, the job of a medical director seemed a little daunting – especially to a young physician leading a team for the first time.
But I knew that leadership was my calling. While I didn’t yet have decades of experience, I had been selected as the chief resident in internal medicine, completed a nephrology fellowship, and mentored several medical students and residents along my career path.
I also knew that I was passionate about supporting my patients and hospitalist team. I’d previously served as associate medical director in charge of quality, readmission reduction, and patient experience. Having achieved the highest patient satisfaction scores on the team for 2 consecutive years, I was specially tasked to improve our team’s HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores.
These experiences taught me that coaching with positive reinforcement was in my blood. This gave me the courage to face my tallest mountain yet.
No one climbs a mountain alone
I also stepped into my new physician leadership role with amazing support. Our outgoing medical director had recommended me, and my entire team was rooting for me. My spouse was 100% behind the idea.
What’s more, I had received amazing feedback from patients throughout my 3 years at the hospital. I had papered an entire office wall with their thank-you notes. I even had a quilt that an 85-year-old patient’s wife made to thank me for my compassionate care.
As I weighed my decision, I realized that I had a higher calling to be a true advocate for my patients. I loved what I did. Each day, I resolved to bring my best and most authentic self for them – no matter how drained I felt.
My team and patients needed me now, not at some more convenient time down the road. A medical director job was the natural next step for me. And so, I resolved to climb the mountain.
Climbing through storms
Stepping into a medical director job forced me to grow into a completely new person. So maybe starting that role during pregnancy was a great metaphor!
Each day, there was immense pressure to perform, to deliver quality outcomes, and to simultaneously meet expectations of the C-suite as well as my hospitalist team. There was no room for failure, because too much was at stake.
Looking back today, I wouldn’t trade the experience for anything. The medical director role was one of the most gratifying experiences in my life, and I am truly thankful for it.
A leader’s role truly boils down to working tirelessly to collaborate with different care teams. It’s important to care not only about our patients but also about our fellow hospitalists. We can do this by truly leading by example – be it picking up extra shifts, covering holidays so team members can be with family, or coming in at 10 p.m. to round with your night team.
I was also able to bring a unique perspective to the hospital C-suite meetings as a woman, an immigrant, and a true “mama bear” – not only of my infant son but also of my team.
My first year as a medical director required more commitment and heart than I could have imagined. But all this hard work paid off when our hospitalist group received the coveted Best Team Award for most improved quality outcomes, financial performance, and patient experience.
The summit is the beginning
My first medical director job fueled my passion for patient satisfaction even further. I now serve as the director of patient experience for the more than 4,200 clinicians at Vituity. Together we care for more than 6.5 million lives a year across the country.
In 2019, I coached 300 physicians and hospital leaders on communication, collaboration, and service recovery skills, leading to significant improvement in their HCAHPS scores. I was delighted to receive the Vituity Distinguished Service Award for my contributions. It’s such an honor to be instrumental in impacting patient care at a larger scale.
This year, I was invited to serve as vice chair of the Society for Hospital Medicine’s patient experience committee and to join the executive board of the SHM San Francisco chapter. Together, we have created a COVID-19 patient communication resource and reached out to our hospitalists to provide them with a space to share their stories during this pandemic. I am so excited to share my knowledge and passion with clinicians across the country given the wide reach of Vituity & SHM!
Many hospitalists shy away from leadership roles. The mountain is tough to scale, but the view from the top is worth it. The key is to start, even if you don’t feel ready. I am here to tell you it can be done!
Dr. Mehta is a hospitalist and director of quality & performance and patient experience at Vituity in Emeryville, Calif. She is vice chair of the SHM patient experience committee and executive board member of the SHM San Francisco Bay Area chapter.
It was 6 a.m. on a rainy, cold Pacific Northwest morning as I walked from my apartment to the hospital, dodging puddles and dreaming of the mediocre-yet-hot physician-lounge coffee. Another long day full of clinical and administrative tasks awaited me.
I was 6 months’ pregnant with our first child and working my sixth 12-hour shift in a row. We had recently lost our medical director, and the C-suite had offered me the role. The day ahead seemed like an enormous mountain to climb.
I felt tired and more than a little overwhelmed. But I whispered to myself: “Today is going to be a fantastic day. I will not fail my team. I will not fail my patients!”
Physician leadership starts with a decision
The timing of this call to leadership had not been ideal. There’s probably never a perfect time to step into a medical director role. And my situation was no exception.
In addition to the baby on the way, my husband was traveling a lot for work. Also, the job of a medical director seemed a little daunting – especially to a young physician leading a team for the first time.
But I knew that leadership was my calling. While I didn’t yet have decades of experience, I had been selected as the chief resident in internal medicine, completed a nephrology fellowship, and mentored several medical students and residents along my career path.
I also knew that I was passionate about supporting my patients and hospitalist team. I’d previously served as associate medical director in charge of quality, readmission reduction, and patient experience. Having achieved the highest patient satisfaction scores on the team for 2 consecutive years, I was specially tasked to improve our team’s HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores.
These experiences taught me that coaching with positive reinforcement was in my blood. This gave me the courage to face my tallest mountain yet.
No one climbs a mountain alone
I also stepped into my new physician leadership role with amazing support. Our outgoing medical director had recommended me, and my entire team was rooting for me. My spouse was 100% behind the idea.
What’s more, I had received amazing feedback from patients throughout my 3 years at the hospital. I had papered an entire office wall with their thank-you notes. I even had a quilt that an 85-year-old patient’s wife made to thank me for my compassionate care.
As I weighed my decision, I realized that I had a higher calling to be a true advocate for my patients. I loved what I did. Each day, I resolved to bring my best and most authentic self for them – no matter how drained I felt.
My team and patients needed me now, not at some more convenient time down the road. A medical director job was the natural next step for me. And so, I resolved to climb the mountain.
Climbing through storms
Stepping into a medical director job forced me to grow into a completely new person. So maybe starting that role during pregnancy was a great metaphor!
Each day, there was immense pressure to perform, to deliver quality outcomes, and to simultaneously meet expectations of the C-suite as well as my hospitalist team. There was no room for failure, because too much was at stake.
Looking back today, I wouldn’t trade the experience for anything. The medical director role was one of the most gratifying experiences in my life, and I am truly thankful for it.
A leader’s role truly boils down to working tirelessly to collaborate with different care teams. It’s important to care not only about our patients but also about our fellow hospitalists. We can do this by truly leading by example – be it picking up extra shifts, covering holidays so team members can be with family, or coming in at 10 p.m. to round with your night team.
I was also able to bring a unique perspective to the hospital C-suite meetings as a woman, an immigrant, and a true “mama bear” – not only of my infant son but also of my team.
My first year as a medical director required more commitment and heart than I could have imagined. But all this hard work paid off when our hospitalist group received the coveted Best Team Award for most improved quality outcomes, financial performance, and patient experience.
The summit is the beginning
My first medical director job fueled my passion for patient satisfaction even further. I now serve as the director of patient experience for the more than 4,200 clinicians at Vituity. Together we care for more than 6.5 million lives a year across the country.
In 2019, I coached 300 physicians and hospital leaders on communication, collaboration, and service recovery skills, leading to significant improvement in their HCAHPS scores. I was delighted to receive the Vituity Distinguished Service Award for my contributions. It’s such an honor to be instrumental in impacting patient care at a larger scale.
This year, I was invited to serve as vice chair of the Society for Hospital Medicine’s patient experience committee and to join the executive board of the SHM San Francisco chapter. Together, we have created a COVID-19 patient communication resource and reached out to our hospitalists to provide them with a space to share their stories during this pandemic. I am so excited to share my knowledge and passion with clinicians across the country given the wide reach of Vituity & SHM!
Many hospitalists shy away from leadership roles. The mountain is tough to scale, but the view from the top is worth it. The key is to start, even if you don’t feel ready. I am here to tell you it can be done!
Dr. Mehta is a hospitalist and director of quality & performance and patient experience at Vituity in Emeryville, Calif. She is vice chair of the SHM patient experience committee and executive board member of the SHM San Francisco Bay Area chapter.
Defining excellence with Dr. Kimberly Manning
2020 SHM Award of Excellence winner: Diversity Leadership
Each year, the Society of Hospital Medicine celebrates the exemplary actions and successes of its members through the Awards of Excellence program. Nominations open every fall, providing the SHM community with the opportunity to nominate a peer, or themselves, to receive an esteemed award of excellence in an array of categories including Teaching, Outstanding Service in Hospital Medicine, Research, and so many others.
While the program and its Awards Committee review nominations with a predetermined set of criteria, excellence is not a ‘one-size-fits-all’ defined term.
Kimberly D. Manning, MD, FACP, FAAP, is a professor of medicine and associate vice chair of Diversity, Equity and Inclusion at the Emory University School of Medicine and a hospitalist at Grady Memorial Hospital, both in Atlanta. She believes that every single person contributes something uniquely meaningful, and that it is up to each person to decide how to use their influence to make an impact.
“To me, being excellent is about discovering your mission and pushing yourself to explore ways to be the best steward of that mission,” Dr. Manning said. “My mission is focused on serving underserved populations, humanizing patients, and amplifying voices of those who have traditionally been silenced.”
Dr. Manning has challenged herself to be the best steward of her evolving mission for equity, representation, and accessibility in medical education and health care innovation for many years. An active member of SHM for 14 years and an inspiring social impact–driven hospitalist of 20 years, Dr. Manning is known for her extensive work in the diversity, equity, and inclusion (DEI) space.
In 2020, Dr. Manning was nominated for and received SHM’s inaugural Excellence in Diversity Leadership Award by her peer and colleague, Dr. Daniel Dressler of Emory University School of Medicine.
She was honored for her commitment to improving the care of underrepresented patient populations, increasing awareness of DEI necessity, and building inclusive communities. In addition to these noteworthy achievements, she demonstrated scholarship on diversity, equity, and inclusion.
One way that Dr. Manning is fusing her love for diversity, equity, and inclusion with innovation is through her role as associate vice chair of the DEI department of Emory University’s School of Medicine. Within the department’s programs, resources and affinity groups, Dr. Manning leads a Virtual Visiting Clerkship Program for underrepresented medical students interested in pursuing a career in internal medicine.
“It includes coaching, mentorship, and diagnostic reasoning in an intimate and personal way,” she explained. “It makes me wish I were a medical student!”
In addition to her patient-centric and student-focused initiatives in Atlanta, Dr. Manning is an active contributor to SHM’s publications, including the Journal of Hospital Medicine and The Hospital Leader blog, in speaking out about racism in medicine, and other social inequities in health care. She even helped to lead a #JHMchat discussion on Twitter around these topics.
In fact, beyond being presented with the Diversity Leadership Award, she says that SHM and JHM have really demonstrated a strong commitment to diversity, equity, and inclusion.
“If you are a person with a lived experience or a person who is underrepresented in medicine, a lot of this work in diversity, equity, and inclusion never really had a name. It was called survival and looking out for each other,” Dr. Manning explained. “It’s exciting to be in this space now where there is focused, professional attention being given to something so important in our clinical and learning environments.”
SHM continues to reaffirm its longstanding commitment to diversity and inclusion and is dedicated to supporting and learning from its diverse member community. While SHM’s new Excellence in Diversity Leadership award is symbolic of a step in the right direction of change, Dr. Manning says that it is also an honor to be recognized for her areas of expertise and passion.
But that recognition moves far beyond this award. With so many more ways to connect with one another, Dr. Manning, a self-proclaimed optimist, says that one of the most exciting changes is centered on communication.
“For us to move the needle on anti-racism and representation, and to do more for our patients and colleagues, it must be a shared conversation. I feel particularly optimistic that I’m able to be more transparent than ever. I’m saying things to people whom I would have been too scared to say them to in the past.
“We’re hungry to grow and learn together,” she continued. “People are interacting in a more positive and constructive way. I’m so glad that we’re pushing diversity and you can see that a lot of people want to see us do better with this. We can continue to do better with this.”
SHM’s 2020-2021 Awards of Excellence nominations are now open with nine unique categories, including Excellence in Diversity, Equity, and Inclusion Leadership. If you have a peer or colleague in mind, like Dr. Manning, who has made exceptional contributions to DEI, or another important domain in hospital medicine, submit your nomination by Sept. 28, 2020.
“I have a feeling that this year has provided a lot of opportunity for people to emerge. The Committee is going to have a very, very tough job,” Dr. Manning said. “They are going to have some exciting nominations on their hands!”
Ms. Cowan is the marketing communications specialist at the Society of Hospital Medicine.
2020 SHM Award of Excellence winner: Diversity Leadership
2020 SHM Award of Excellence winner: Diversity Leadership
Each year, the Society of Hospital Medicine celebrates the exemplary actions and successes of its members through the Awards of Excellence program. Nominations open every fall, providing the SHM community with the opportunity to nominate a peer, or themselves, to receive an esteemed award of excellence in an array of categories including Teaching, Outstanding Service in Hospital Medicine, Research, and so many others.
While the program and its Awards Committee review nominations with a predetermined set of criteria, excellence is not a ‘one-size-fits-all’ defined term.
Kimberly D. Manning, MD, FACP, FAAP, is a professor of medicine and associate vice chair of Diversity, Equity and Inclusion at the Emory University School of Medicine and a hospitalist at Grady Memorial Hospital, both in Atlanta. She believes that every single person contributes something uniquely meaningful, and that it is up to each person to decide how to use their influence to make an impact.
“To me, being excellent is about discovering your mission and pushing yourself to explore ways to be the best steward of that mission,” Dr. Manning said. “My mission is focused on serving underserved populations, humanizing patients, and amplifying voices of those who have traditionally been silenced.”
Dr. Manning has challenged herself to be the best steward of her evolving mission for equity, representation, and accessibility in medical education and health care innovation for many years. An active member of SHM for 14 years and an inspiring social impact–driven hospitalist of 20 years, Dr. Manning is known for her extensive work in the diversity, equity, and inclusion (DEI) space.
In 2020, Dr. Manning was nominated for and received SHM’s inaugural Excellence in Diversity Leadership Award by her peer and colleague, Dr. Daniel Dressler of Emory University School of Medicine.
She was honored for her commitment to improving the care of underrepresented patient populations, increasing awareness of DEI necessity, and building inclusive communities. In addition to these noteworthy achievements, she demonstrated scholarship on diversity, equity, and inclusion.
One way that Dr. Manning is fusing her love for diversity, equity, and inclusion with innovation is through her role as associate vice chair of the DEI department of Emory University’s School of Medicine. Within the department’s programs, resources and affinity groups, Dr. Manning leads a Virtual Visiting Clerkship Program for underrepresented medical students interested in pursuing a career in internal medicine.
“It includes coaching, mentorship, and diagnostic reasoning in an intimate and personal way,” she explained. “It makes me wish I were a medical student!”
In addition to her patient-centric and student-focused initiatives in Atlanta, Dr. Manning is an active contributor to SHM’s publications, including the Journal of Hospital Medicine and The Hospital Leader blog, in speaking out about racism in medicine, and other social inequities in health care. She even helped to lead a #JHMchat discussion on Twitter around these topics.
In fact, beyond being presented with the Diversity Leadership Award, she says that SHM and JHM have really demonstrated a strong commitment to diversity, equity, and inclusion.
“If you are a person with a lived experience or a person who is underrepresented in medicine, a lot of this work in diversity, equity, and inclusion never really had a name. It was called survival and looking out for each other,” Dr. Manning explained. “It’s exciting to be in this space now where there is focused, professional attention being given to something so important in our clinical and learning environments.”
SHM continues to reaffirm its longstanding commitment to diversity and inclusion and is dedicated to supporting and learning from its diverse member community. While SHM’s new Excellence in Diversity Leadership award is symbolic of a step in the right direction of change, Dr. Manning says that it is also an honor to be recognized for her areas of expertise and passion.
But that recognition moves far beyond this award. With so many more ways to connect with one another, Dr. Manning, a self-proclaimed optimist, says that one of the most exciting changes is centered on communication.
“For us to move the needle on anti-racism and representation, and to do more for our patients and colleagues, it must be a shared conversation. I feel particularly optimistic that I’m able to be more transparent than ever. I’m saying things to people whom I would have been too scared to say them to in the past.
“We’re hungry to grow and learn together,” she continued. “People are interacting in a more positive and constructive way. I’m so glad that we’re pushing diversity and you can see that a lot of people want to see us do better with this. We can continue to do better with this.”
SHM’s 2020-2021 Awards of Excellence nominations are now open with nine unique categories, including Excellence in Diversity, Equity, and Inclusion Leadership. If you have a peer or colleague in mind, like Dr. Manning, who has made exceptional contributions to DEI, or another important domain in hospital medicine, submit your nomination by Sept. 28, 2020.
“I have a feeling that this year has provided a lot of opportunity for people to emerge. The Committee is going to have a very, very tough job,” Dr. Manning said. “They are going to have some exciting nominations on their hands!”
Ms. Cowan is the marketing communications specialist at the Society of Hospital Medicine.
Each year, the Society of Hospital Medicine celebrates the exemplary actions and successes of its members through the Awards of Excellence program. Nominations open every fall, providing the SHM community with the opportunity to nominate a peer, or themselves, to receive an esteemed award of excellence in an array of categories including Teaching, Outstanding Service in Hospital Medicine, Research, and so many others.
While the program and its Awards Committee review nominations with a predetermined set of criteria, excellence is not a ‘one-size-fits-all’ defined term.
Kimberly D. Manning, MD, FACP, FAAP, is a professor of medicine and associate vice chair of Diversity, Equity and Inclusion at the Emory University School of Medicine and a hospitalist at Grady Memorial Hospital, both in Atlanta. She believes that every single person contributes something uniquely meaningful, and that it is up to each person to decide how to use their influence to make an impact.
“To me, being excellent is about discovering your mission and pushing yourself to explore ways to be the best steward of that mission,” Dr. Manning said. “My mission is focused on serving underserved populations, humanizing patients, and amplifying voices of those who have traditionally been silenced.”
Dr. Manning has challenged herself to be the best steward of her evolving mission for equity, representation, and accessibility in medical education and health care innovation for many years. An active member of SHM for 14 years and an inspiring social impact–driven hospitalist of 20 years, Dr. Manning is known for her extensive work in the diversity, equity, and inclusion (DEI) space.
In 2020, Dr. Manning was nominated for and received SHM’s inaugural Excellence in Diversity Leadership Award by her peer and colleague, Dr. Daniel Dressler of Emory University School of Medicine.
She was honored for her commitment to improving the care of underrepresented patient populations, increasing awareness of DEI necessity, and building inclusive communities. In addition to these noteworthy achievements, she demonstrated scholarship on diversity, equity, and inclusion.
One way that Dr. Manning is fusing her love for diversity, equity, and inclusion with innovation is through her role as associate vice chair of the DEI department of Emory University’s School of Medicine. Within the department’s programs, resources and affinity groups, Dr. Manning leads a Virtual Visiting Clerkship Program for underrepresented medical students interested in pursuing a career in internal medicine.
“It includes coaching, mentorship, and diagnostic reasoning in an intimate and personal way,” she explained. “It makes me wish I were a medical student!”
In addition to her patient-centric and student-focused initiatives in Atlanta, Dr. Manning is an active contributor to SHM’s publications, including the Journal of Hospital Medicine and The Hospital Leader blog, in speaking out about racism in medicine, and other social inequities in health care. She even helped to lead a #JHMchat discussion on Twitter around these topics.
In fact, beyond being presented with the Diversity Leadership Award, she says that SHM and JHM have really demonstrated a strong commitment to diversity, equity, and inclusion.
“If you are a person with a lived experience or a person who is underrepresented in medicine, a lot of this work in diversity, equity, and inclusion never really had a name. It was called survival and looking out for each other,” Dr. Manning explained. “It’s exciting to be in this space now where there is focused, professional attention being given to something so important in our clinical and learning environments.”
SHM continues to reaffirm its longstanding commitment to diversity and inclusion and is dedicated to supporting and learning from its diverse member community. While SHM’s new Excellence in Diversity Leadership award is symbolic of a step in the right direction of change, Dr. Manning says that it is also an honor to be recognized for her areas of expertise and passion.
But that recognition moves far beyond this award. With so many more ways to connect with one another, Dr. Manning, a self-proclaimed optimist, says that one of the most exciting changes is centered on communication.
“For us to move the needle on anti-racism and representation, and to do more for our patients and colleagues, it must be a shared conversation. I feel particularly optimistic that I’m able to be more transparent than ever. I’m saying things to people whom I would have been too scared to say them to in the past.
“We’re hungry to grow and learn together,” she continued. “People are interacting in a more positive and constructive way. I’m so glad that we’re pushing diversity and you can see that a lot of people want to see us do better with this. We can continue to do better with this.”
SHM’s 2020-2021 Awards of Excellence nominations are now open with nine unique categories, including Excellence in Diversity, Equity, and Inclusion Leadership. If you have a peer or colleague in mind, like Dr. Manning, who has made exceptional contributions to DEI, or another important domain in hospital medicine, submit your nomination by Sept. 28, 2020.
“I have a feeling that this year has provided a lot of opportunity for people to emerge. The Committee is going to have a very, very tough job,” Dr. Manning said. “They are going to have some exciting nominations on their hands!”
Ms. Cowan is the marketing communications specialist at the Society of Hospital Medicine.
In a time of two pandemics, a recommitment to work together
Overwhelmed. As if we weren’t already overwhelmed. For decades, hospitalists have been on the forefront of improving acute care amidst a rapidly changing environment. These last few decades have seen tremendous advances in medicine, technology, safety culture, innovations in payment models, transformation in business models, and a rising tide of health care policy. There was never a year we didn’t face major change … and adapt to it. Then 2020 came upon us.
This year, we adapt to more than a score and 4 years’ worth of change.
The two pandemics that have come upon us are like tsunamis. And many of us are drowning. We know of threats of pandemics: influenza, Ebola, and the like. But SARS-CoV-2 is new and like no other. We live in fear and isolation, each and every day learning new information and debunking others. We also know of racial injustice and racism, implicit or explicit in our nation, whether we live it or just read of it. George Floyd’s death in my hometown marked another tsunami, a great realization in our nation, and a great unmasking of our denial.
Yet our country is not united.
Hospital medicine is not immune to this disunity. At a time that we are all treading water, staying afloat in our own hospitals and communities, confronting these issues beyond our immediate spheres of influence is overwhelming. We are impacted by these pandemics, personally and professionally. And admittedly, we can be both victim and perpetrator.
In the face of a novel infectious agent, medicine responded quickly and pushed us beyond our limits. We have developed new infection prevention guidelines. We worked creatively to solve PPE shortages. We fashioned new work flows and new care models. We accelerated telehealth applications. We expanded the boundaries on home-based programs and reached out to vulnerable elderly in congregate living – an isolation no older person should have to endure. We cared for our colleagues, neighbors, and family members who fell ill, some who recovered, and sadly, some who fell. We developed best-practice guidelines, research protocols, created new order sets, note templates, and documentation standards. We flexed into EDs, ICUs, and field hospitals. Amidst the turmoil, we took pay cuts and saw colleagues go on furlough. And still, we mentored leaders in our schools, churches, synagogues, mosques, and civic communities.
And just when we thought we could endure no more, on May 25, we witnessed a black man in Minneapolis killed by a policeman’s knee. The same knee that divided Americans when black American athletes knelt to protest the injustice their people have endured for centuries. A knee that has been confused for insolence, when it was meant for justice ... yes, justice, for all. So, in early June, around the nation in support of black lives we also knelt, for almost 9 minutes.
This was the third time I cried during the pandemics.
For many of us, structural racism in America had finally been unmasked. The nation protested and rioted for weeks, and some communities have continued. Indeed, these two pandemics are still surging.
Side by side COVID-19 case conferences we lay transparent data demonstrating health disparities that we have tolerated for so long. We have vowed to resource equity work, and we opened dialogue, not only with patients and communities of color, but also with colleagues of color – some ready and some not yet ready to share and relive the traumas of their past and their present.
And still, we are not united.
While we physically mask to prevent the spread of COVID-19, we must make efforts to unmask the truths of SARS-CoV-2, the failings of our health system, the richness of our communities of color, and the injustice in the fabric of our society. More importantly, we must work together to create solutions. While we have diverse interests and priorities, at SHM, we can find common ground with kindred spirits, enhance the role of our specialty, and advance the health of our patients.
Let’s not be mistaken. These pandemics add to a growing list of interwoven issues in our society. In 2018, I wrote a piece on the role of hospitalists in addressing rural health disparities.1 According to the Sheps Center for Health Services Research, 129 rural hospitals have closed since 2010, closures that have accelerated with the COVID-19 pandemic.2 More than ever, we must stand above our inner and outer conflicts and be united to promote the health of our nation during these pandemics, because “all policy is health policy.”3
Most SHM presidents and president-elects come in with a platform, a priority for the specialty and for the society. This year, the platform has chosen us. For 20 years, I have witnessed SHM be a workshop for our members to address the pressing needs of our specialty and our patients. In 2020, we’ve continued to see SHM as a workshop for our members and a tour de force addressing these pandemics, from just in time publications of research and perspectives in the Journal of Hospital Medicine, to webinars and open access education in the Learning Portal, to advocacy on Capitol Hill. All of that work has been informed by you and for you. While there is still so much to do, we need not be overwhelmed when we do it together.
A score and 4 years ago, Robert Wachter, MD, and Lee Goldman, MD, dubbed us “hospitalists.” A year later, our shared workshop was born. Through one name change and now our first CEO transition from Larry Wellikson, MD, to Eric Howell, MD, SHM will continue to be where hospitalists both adapt and shape our nation through solutions that put an end to these pandemics. Let’s recommit to this work together.
Dr. Siy is division medical director, hospital specialties, in the departments of hospital medicine and community senior and palliative care, at HealthPartners in Bloomington, Minn. He is president-elect of SHM.
Sources
1. Hardeman RR et al. Stolen Breaths. N Engl J Med. 2020 Jul 16;383:197-9.
2. Siy JC. Reviving Rural Health Care. The Hospitalist. 2018 Sep 24.
3. The Cecil G. Sheps Center For Health Services Research. Rural Hospital Closures. 2014. https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/
Overwhelmed. As if we weren’t already overwhelmed. For decades, hospitalists have been on the forefront of improving acute care amidst a rapidly changing environment. These last few decades have seen tremendous advances in medicine, technology, safety culture, innovations in payment models, transformation in business models, and a rising tide of health care policy. There was never a year we didn’t face major change … and adapt to it. Then 2020 came upon us.
This year, we adapt to more than a score and 4 years’ worth of change.
The two pandemics that have come upon us are like tsunamis. And many of us are drowning. We know of threats of pandemics: influenza, Ebola, and the like. But SARS-CoV-2 is new and like no other. We live in fear and isolation, each and every day learning new information and debunking others. We also know of racial injustice and racism, implicit or explicit in our nation, whether we live it or just read of it. George Floyd’s death in my hometown marked another tsunami, a great realization in our nation, and a great unmasking of our denial.
Yet our country is not united.
Hospital medicine is not immune to this disunity. At a time that we are all treading water, staying afloat in our own hospitals and communities, confronting these issues beyond our immediate spheres of influence is overwhelming. We are impacted by these pandemics, personally and professionally. And admittedly, we can be both victim and perpetrator.
In the face of a novel infectious agent, medicine responded quickly and pushed us beyond our limits. We have developed new infection prevention guidelines. We worked creatively to solve PPE shortages. We fashioned new work flows and new care models. We accelerated telehealth applications. We expanded the boundaries on home-based programs and reached out to vulnerable elderly in congregate living – an isolation no older person should have to endure. We cared for our colleagues, neighbors, and family members who fell ill, some who recovered, and sadly, some who fell. We developed best-practice guidelines, research protocols, created new order sets, note templates, and documentation standards. We flexed into EDs, ICUs, and field hospitals. Amidst the turmoil, we took pay cuts and saw colleagues go on furlough. And still, we mentored leaders in our schools, churches, synagogues, mosques, and civic communities.
And just when we thought we could endure no more, on May 25, we witnessed a black man in Minneapolis killed by a policeman’s knee. The same knee that divided Americans when black American athletes knelt to protest the injustice their people have endured for centuries. A knee that has been confused for insolence, when it was meant for justice ... yes, justice, for all. So, in early June, around the nation in support of black lives we also knelt, for almost 9 minutes.
This was the third time I cried during the pandemics.
For many of us, structural racism in America had finally been unmasked. The nation protested and rioted for weeks, and some communities have continued. Indeed, these two pandemics are still surging.
Side by side COVID-19 case conferences we lay transparent data demonstrating health disparities that we have tolerated for so long. We have vowed to resource equity work, and we opened dialogue, not only with patients and communities of color, but also with colleagues of color – some ready and some not yet ready to share and relive the traumas of their past and their present.
And still, we are not united.
While we physically mask to prevent the spread of COVID-19, we must make efforts to unmask the truths of SARS-CoV-2, the failings of our health system, the richness of our communities of color, and the injustice in the fabric of our society. More importantly, we must work together to create solutions. While we have diverse interests and priorities, at SHM, we can find common ground with kindred spirits, enhance the role of our specialty, and advance the health of our patients.
Let’s not be mistaken. These pandemics add to a growing list of interwoven issues in our society. In 2018, I wrote a piece on the role of hospitalists in addressing rural health disparities.1 According to the Sheps Center for Health Services Research, 129 rural hospitals have closed since 2010, closures that have accelerated with the COVID-19 pandemic.2 More than ever, we must stand above our inner and outer conflicts and be united to promote the health of our nation during these pandemics, because “all policy is health policy.”3
Most SHM presidents and president-elects come in with a platform, a priority for the specialty and for the society. This year, the platform has chosen us. For 20 years, I have witnessed SHM be a workshop for our members to address the pressing needs of our specialty and our patients. In 2020, we’ve continued to see SHM as a workshop for our members and a tour de force addressing these pandemics, from just in time publications of research and perspectives in the Journal of Hospital Medicine, to webinars and open access education in the Learning Portal, to advocacy on Capitol Hill. All of that work has been informed by you and for you. While there is still so much to do, we need not be overwhelmed when we do it together.
A score and 4 years ago, Robert Wachter, MD, and Lee Goldman, MD, dubbed us “hospitalists.” A year later, our shared workshop was born. Through one name change and now our first CEO transition from Larry Wellikson, MD, to Eric Howell, MD, SHM will continue to be where hospitalists both adapt and shape our nation through solutions that put an end to these pandemics. Let’s recommit to this work together.
Dr. Siy is division medical director, hospital specialties, in the departments of hospital medicine and community senior and palliative care, at HealthPartners in Bloomington, Minn. He is president-elect of SHM.
Sources
1. Hardeman RR et al. Stolen Breaths. N Engl J Med. 2020 Jul 16;383:197-9.
2. Siy JC. Reviving Rural Health Care. The Hospitalist. 2018 Sep 24.
3. The Cecil G. Sheps Center For Health Services Research. Rural Hospital Closures. 2014. https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/
Overwhelmed. As if we weren’t already overwhelmed. For decades, hospitalists have been on the forefront of improving acute care amidst a rapidly changing environment. These last few decades have seen tremendous advances in medicine, technology, safety culture, innovations in payment models, transformation in business models, and a rising tide of health care policy. There was never a year we didn’t face major change … and adapt to it. Then 2020 came upon us.
This year, we adapt to more than a score and 4 years’ worth of change.
The two pandemics that have come upon us are like tsunamis. And many of us are drowning. We know of threats of pandemics: influenza, Ebola, and the like. But SARS-CoV-2 is new and like no other. We live in fear and isolation, each and every day learning new information and debunking others. We also know of racial injustice and racism, implicit or explicit in our nation, whether we live it or just read of it. George Floyd’s death in my hometown marked another tsunami, a great realization in our nation, and a great unmasking of our denial.
Yet our country is not united.
Hospital medicine is not immune to this disunity. At a time that we are all treading water, staying afloat in our own hospitals and communities, confronting these issues beyond our immediate spheres of influence is overwhelming. We are impacted by these pandemics, personally and professionally. And admittedly, we can be both victim and perpetrator.
In the face of a novel infectious agent, medicine responded quickly and pushed us beyond our limits. We have developed new infection prevention guidelines. We worked creatively to solve PPE shortages. We fashioned new work flows and new care models. We accelerated telehealth applications. We expanded the boundaries on home-based programs and reached out to vulnerable elderly in congregate living – an isolation no older person should have to endure. We cared for our colleagues, neighbors, and family members who fell ill, some who recovered, and sadly, some who fell. We developed best-practice guidelines, research protocols, created new order sets, note templates, and documentation standards. We flexed into EDs, ICUs, and field hospitals. Amidst the turmoil, we took pay cuts and saw colleagues go on furlough. And still, we mentored leaders in our schools, churches, synagogues, mosques, and civic communities.
And just when we thought we could endure no more, on May 25, we witnessed a black man in Minneapolis killed by a policeman’s knee. The same knee that divided Americans when black American athletes knelt to protest the injustice their people have endured for centuries. A knee that has been confused for insolence, when it was meant for justice ... yes, justice, for all. So, in early June, around the nation in support of black lives we also knelt, for almost 9 minutes.
This was the third time I cried during the pandemics.
For many of us, structural racism in America had finally been unmasked. The nation protested and rioted for weeks, and some communities have continued. Indeed, these two pandemics are still surging.
Side by side COVID-19 case conferences we lay transparent data demonstrating health disparities that we have tolerated for so long. We have vowed to resource equity work, and we opened dialogue, not only with patients and communities of color, but also with colleagues of color – some ready and some not yet ready to share and relive the traumas of their past and their present.
And still, we are not united.
While we physically mask to prevent the spread of COVID-19, we must make efforts to unmask the truths of SARS-CoV-2, the failings of our health system, the richness of our communities of color, and the injustice in the fabric of our society. More importantly, we must work together to create solutions. While we have diverse interests and priorities, at SHM, we can find common ground with kindred spirits, enhance the role of our specialty, and advance the health of our patients.
Let’s not be mistaken. These pandemics add to a growing list of interwoven issues in our society. In 2018, I wrote a piece on the role of hospitalists in addressing rural health disparities.1 According to the Sheps Center for Health Services Research, 129 rural hospitals have closed since 2010, closures that have accelerated with the COVID-19 pandemic.2 More than ever, we must stand above our inner and outer conflicts and be united to promote the health of our nation during these pandemics, because “all policy is health policy.”3
Most SHM presidents and president-elects come in with a platform, a priority for the specialty and for the society. This year, the platform has chosen us. For 20 years, I have witnessed SHM be a workshop for our members to address the pressing needs of our specialty and our patients. In 2020, we’ve continued to see SHM as a workshop for our members and a tour de force addressing these pandemics, from just in time publications of research and perspectives in the Journal of Hospital Medicine, to webinars and open access education in the Learning Portal, to advocacy on Capitol Hill. All of that work has been informed by you and for you. While there is still so much to do, we need not be overwhelmed when we do it together.
A score and 4 years ago, Robert Wachter, MD, and Lee Goldman, MD, dubbed us “hospitalists.” A year later, our shared workshop was born. Through one name change and now our first CEO transition from Larry Wellikson, MD, to Eric Howell, MD, SHM will continue to be where hospitalists both adapt and shape our nation through solutions that put an end to these pandemics. Let’s recommit to this work together.
Dr. Siy is division medical director, hospital specialties, in the departments of hospital medicine and community senior and palliative care, at HealthPartners in Bloomington, Minn. He is president-elect of SHM.
Sources
1. Hardeman RR et al. Stolen Breaths. N Engl J Med. 2020 Jul 16;383:197-9.
2. Siy JC. Reviving Rural Health Care. The Hospitalist. 2018 Sep 24.
3. The Cecil G. Sheps Center For Health Services Research. Rural Hospital Closures. 2014. https://www.shepscenter.unc.edu/programs-projects/rural-health/rural-hospital-closures/
Hospitalist movers and shakers – September 2020
The American Board of Internal Medicine has named David Pizzimenti, DO, to its board of trustees. The appointment comes with a 3-year term.
Dr. Pizzimenti has been a practicing internist in Mississippi since 2005. He currently serves as associate medical officer of acute care at North Mississippi Medical Center, Tupelo, where he also directs the hospitalist program and the internal medicine residency program. Prior to joining NMMC, he managed the same role at Magnolia Regional Health Center (Corinth, Miss.).
Dr. Pizzimenti is an inducted member of the American College of Osteopathic Internist College of Fellows, as well as a certified wound care specialist.
Tommy Ibrahim, MD, FHM, recently was named the new president and CEO for Bassett Healthcare Network, replacing William Streck, who had served in the role from 1984 to 2014, and then on an interim basis since 2018.
Dr. Ibrahim comes to Bassett from Integris Health, the largest nonprofit health care system in Oklahoma, where he was executive vice president and chief physician executive. He started his career as a hospitalist before moving into administration, and is a fellow in hospital medicine as well as a fellow of the American College of Healthcare Executives.
Bassett Healthcare Network is based at Bassett Medical Center in Cooperstown, N.Y., and includes four hospitals and more than two dozen primary care centers in eight New York counties.
Russell Kerbel, MD, MBA, has been named medical director for sepsis prevention at the University of California, Los Angeles. Since his arrival at UCLA in 2014, Dr. Kerbel – a hospitalist by training – has worked to increase awareness and standardize sepsis treatment through his advocacy, interdepartmental collaboration, and informatics knowledge.
Joshua Lenchus, DO, RPh, SFHM, was installed as vice president of the Florida Medical Association during the all-virtual 2020 FMA annual meeting in August. Dr. Lenchus is a hospitalist and chief medical officer at the Broward Health Medical Center in Fort Lauderdale, Fla.
Christopher Carpenter, MD, has been elevated to chief of staff at Natividad, a 172-bed, county-owned hospital in Salinas, Calif. Dr. Carpenter has served Natividad for the past 4 years, holding the positions of chief hospitalist, chief of service for pediatrics, vice chief of staff, and most recently director of pediatric services.
Dr. Carpenter’s term as chief of staff is limited to 2 years, during which he said his goals include promoting diversity within the facility’s leadership.
Prior to arriving at Natividad, Dr. Carpenter was instructor of pediatrics at Harvard Medical School, Boston, as well as associate director of the Boston Children’s Hospital Pediatric Global Health Fellowship.
David Fagan, MD, recently was promoted to medical director at Mid-State Health Center (Plymouth, N.H.), where he has served for the past 10 years. The 30-year medical veteran began working in his new role in May 2020.
Previously, Dr. Fagan has served the facility as an internist and hospitalist, and he has been among the leaders at Mid-State in ensuring safety for patients and staff during the COVID-19 response.
The Carroll County Memorial Hospital (Carrolton, Mo.) recently announced its new hospitalist program, which officially began on June 1, 2020. CCMH officials said the focus of the hospitalists will be to maintain communication with primary care physicians once patients leave the hospital facility.
CCMH added three physicians to its staff to work in the hospitalist program: Reuben I. Thaker, MD; Samuel C. Evans, MD; and Charles C. Glendenning, DO.
NorthShore University HealthSystem (Evanston, Ill.) has agreed to purchase Northwest Community Healthcare, a single-hospital health system located in Arlington Heights, Ill. NCH will become a hospital hub for NorthShore in the northwest Chicago suburbs.
When the agreement is finalized, NorthShore’s stable of hospitals will rise to six in and around Chicago. The system also provides outpatient care, labwork, and pharmacy services.
The American Board of Internal Medicine has named David Pizzimenti, DO, to its board of trustees. The appointment comes with a 3-year term.
Dr. Pizzimenti has been a practicing internist in Mississippi since 2005. He currently serves as associate medical officer of acute care at North Mississippi Medical Center, Tupelo, where he also directs the hospitalist program and the internal medicine residency program. Prior to joining NMMC, he managed the same role at Magnolia Regional Health Center (Corinth, Miss.).
Dr. Pizzimenti is an inducted member of the American College of Osteopathic Internist College of Fellows, as well as a certified wound care specialist.
Tommy Ibrahim, MD, FHM, recently was named the new president and CEO for Bassett Healthcare Network, replacing William Streck, who had served in the role from 1984 to 2014, and then on an interim basis since 2018.
Dr. Ibrahim comes to Bassett from Integris Health, the largest nonprofit health care system in Oklahoma, where he was executive vice president and chief physician executive. He started his career as a hospitalist before moving into administration, and is a fellow in hospital medicine as well as a fellow of the American College of Healthcare Executives.
Bassett Healthcare Network is based at Bassett Medical Center in Cooperstown, N.Y., and includes four hospitals and more than two dozen primary care centers in eight New York counties.
Russell Kerbel, MD, MBA, has been named medical director for sepsis prevention at the University of California, Los Angeles. Since his arrival at UCLA in 2014, Dr. Kerbel – a hospitalist by training – has worked to increase awareness and standardize sepsis treatment through his advocacy, interdepartmental collaboration, and informatics knowledge.
Joshua Lenchus, DO, RPh, SFHM, was installed as vice president of the Florida Medical Association during the all-virtual 2020 FMA annual meeting in August. Dr. Lenchus is a hospitalist and chief medical officer at the Broward Health Medical Center in Fort Lauderdale, Fla.
Christopher Carpenter, MD, has been elevated to chief of staff at Natividad, a 172-bed, county-owned hospital in Salinas, Calif. Dr. Carpenter has served Natividad for the past 4 years, holding the positions of chief hospitalist, chief of service for pediatrics, vice chief of staff, and most recently director of pediatric services.
Dr. Carpenter’s term as chief of staff is limited to 2 years, during which he said his goals include promoting diversity within the facility’s leadership.
Prior to arriving at Natividad, Dr. Carpenter was instructor of pediatrics at Harvard Medical School, Boston, as well as associate director of the Boston Children’s Hospital Pediatric Global Health Fellowship.
David Fagan, MD, recently was promoted to medical director at Mid-State Health Center (Plymouth, N.H.), where he has served for the past 10 years. The 30-year medical veteran began working in his new role in May 2020.
Previously, Dr. Fagan has served the facility as an internist and hospitalist, and he has been among the leaders at Mid-State in ensuring safety for patients and staff during the COVID-19 response.
The Carroll County Memorial Hospital (Carrolton, Mo.) recently announced its new hospitalist program, which officially began on June 1, 2020. CCMH officials said the focus of the hospitalists will be to maintain communication with primary care physicians once patients leave the hospital facility.
CCMH added three physicians to its staff to work in the hospitalist program: Reuben I. Thaker, MD; Samuel C. Evans, MD; and Charles C. Glendenning, DO.
NorthShore University HealthSystem (Evanston, Ill.) has agreed to purchase Northwest Community Healthcare, a single-hospital health system located in Arlington Heights, Ill. NCH will become a hospital hub for NorthShore in the northwest Chicago suburbs.
When the agreement is finalized, NorthShore’s stable of hospitals will rise to six in and around Chicago. The system also provides outpatient care, labwork, and pharmacy services.
The American Board of Internal Medicine has named David Pizzimenti, DO, to its board of trustees. The appointment comes with a 3-year term.
Dr. Pizzimenti has been a practicing internist in Mississippi since 2005. He currently serves as associate medical officer of acute care at North Mississippi Medical Center, Tupelo, where he also directs the hospitalist program and the internal medicine residency program. Prior to joining NMMC, he managed the same role at Magnolia Regional Health Center (Corinth, Miss.).
Dr. Pizzimenti is an inducted member of the American College of Osteopathic Internist College of Fellows, as well as a certified wound care specialist.
Tommy Ibrahim, MD, FHM, recently was named the new president and CEO for Bassett Healthcare Network, replacing William Streck, who had served in the role from 1984 to 2014, and then on an interim basis since 2018.
Dr. Ibrahim comes to Bassett from Integris Health, the largest nonprofit health care system in Oklahoma, where he was executive vice president and chief physician executive. He started his career as a hospitalist before moving into administration, and is a fellow in hospital medicine as well as a fellow of the American College of Healthcare Executives.
Bassett Healthcare Network is based at Bassett Medical Center in Cooperstown, N.Y., and includes four hospitals and more than two dozen primary care centers in eight New York counties.
Russell Kerbel, MD, MBA, has been named medical director for sepsis prevention at the University of California, Los Angeles. Since his arrival at UCLA in 2014, Dr. Kerbel – a hospitalist by training – has worked to increase awareness and standardize sepsis treatment through his advocacy, interdepartmental collaboration, and informatics knowledge.
Joshua Lenchus, DO, RPh, SFHM, was installed as vice president of the Florida Medical Association during the all-virtual 2020 FMA annual meeting in August. Dr. Lenchus is a hospitalist and chief medical officer at the Broward Health Medical Center in Fort Lauderdale, Fla.
Christopher Carpenter, MD, has been elevated to chief of staff at Natividad, a 172-bed, county-owned hospital in Salinas, Calif. Dr. Carpenter has served Natividad for the past 4 years, holding the positions of chief hospitalist, chief of service for pediatrics, vice chief of staff, and most recently director of pediatric services.
Dr. Carpenter’s term as chief of staff is limited to 2 years, during which he said his goals include promoting diversity within the facility’s leadership.
Prior to arriving at Natividad, Dr. Carpenter was instructor of pediatrics at Harvard Medical School, Boston, as well as associate director of the Boston Children’s Hospital Pediatric Global Health Fellowship.
David Fagan, MD, recently was promoted to medical director at Mid-State Health Center (Plymouth, N.H.), where he has served for the past 10 years. The 30-year medical veteran began working in his new role in May 2020.
Previously, Dr. Fagan has served the facility as an internist and hospitalist, and he has been among the leaders at Mid-State in ensuring safety for patients and staff during the COVID-19 response.
The Carroll County Memorial Hospital (Carrolton, Mo.) recently announced its new hospitalist program, which officially began on June 1, 2020. CCMH officials said the focus of the hospitalists will be to maintain communication with primary care physicians once patients leave the hospital facility.
CCMH added three physicians to its staff to work in the hospitalist program: Reuben I. Thaker, MD; Samuel C. Evans, MD; and Charles C. Glendenning, DO.
NorthShore University HealthSystem (Evanston, Ill.) has agreed to purchase Northwest Community Healthcare, a single-hospital health system located in Arlington Heights, Ill. NCH will become a hospital hub for NorthShore in the northwest Chicago suburbs.
When the agreement is finalized, NorthShore’s stable of hospitals will rise to six in and around Chicago. The system also provides outpatient care, labwork, and pharmacy services.
Hospital medicine in a worldwide pandemic
SHM releases 2020 State of Hospital Medicine report
Every 2 years the Society of Hospital Medicine’s Practice Analysis Committee (PAC) surveys hospitalist groups nationwide on such key practice parameters as compensation, services provided, hours of work, and participation in leadership roles. Combined with compensation and productivity data on adult and pediatric hospitalists collected by the Medical Group Management Association, licensed to SHM for inclusion in this report, the State of Hospital Medicine (SoHM) report is the most authoritative and comprehensive source of information regarding contemporary hospitalist practice.
This year’s biannual report is based on survey responses submitted between Jan. 6 and Feb. 28, 2020, by 502 hospitalist group practices. That’s slightly fewer groups reporting data than for past surveys, but these groups were larger, on average, resulting in more full-time equivalents (FTEs) incorporated into the results, said PAC member Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants. A total of 19.7% of the reporting groups provided pediatric hospital medicine data only, a much larger proportion than in past years.
The report is slated for publication in September, and SHM members can purchase it at a discount in print or electronic versions. “Our sense is that a lot of the fundamental information in the report will not have changed that much from 2018,” Ms. Flores said. “But these results convey the state of the field prior to the world-altering impact of the COVID-19 pandemic on hospitals of all sizes and settings.” How the hospital business and the practice of hospitalist groups have been and will be impacted by the pandemic, obviously, aren’t reflected in the data.
“We are finalizing a supplemental survey to go out to members at the end of the summer, specifically asking how COVID has impacted their hospitalist groups,” Ms. Flores said. These COVID-19 supplemental results will be released after the main report, sometime around the end of September. But results from the main survey, showing consistency in a number of key parameters, indicate that hospitalists continue to have a large and essential role in the U.S. health care system.
The leadership offered by hospitalists in the U.S. health care system’s response to surges of COVID-19 patients in many hospitals only underscores their importance, Ms. Flores added. “Hospitalists have definitely proven their worth. Imagine what the pandemic would have been like for hospitals if our specialty hadn’t been well-positioned to respond.” Hospitalists also showed an ability to adapt quickly to crises on the ground. But financial pressures imposed by the pandemic, combined with other trends previously in play, suggest that demands to cut costs and do more with less will be relentless as the field – and the world – tries to pull out of the pandemic crisis.
Compensation trends
One of the most eagerly anticipated findings in the SoHM is compensation. The median compensation for all adult hospitalists at the beginning of 2020 was $307,633 (with an average of $317,640), higher in the Midwest and lower in the East. The average base rate share of hospitalist compensation was 81.3%, with 11.6% based on productivity and 7.1% for performance – scored on such measures as patient satisfaction; accuracy and/or timeliness of documentation, billing, and coding; clinical processes; early morning discharge orders and times; and readmissions rates. A total of 46.6% of responding groups said they anticipated an increase in budgeted FTEs in the next year, while 51.2% expected to stay the same.
Subsidies or financial support for hospitalist practices break down in different ways, but in 2020 the median figure for financial support provided per adult hospitalist FTE was $198,750 (average, $201,760). This suggests that hospitals continue to see hospitalists as valued partners in health care, with useful knowledge of how the various components of the health care system work, said Tresa McNeal, MD, a hospitalist at Baylor Scott & White Medical Center, Temple, Tex., and a member of the PAC.
Scope of practice
Scope of practice for the hospitalist model continues to evolve, with increased demand for comanagement roles as other medical specialties are less inclined to visit patients in the hospital. Surgical comanagement accounted for much of that growth, but there were significant rates of comanagement for neurology, gastrointestinal and liver medicine, cardiology, and palliative care.
“Comanagement is a broad term without a single clear definition,” Ms. Flores said. “But when I talk about it, I refer to a broader array of hospitalists interacting with specialists.” The hospitalist‘s role could be as a consultant, or taking responsibility for admitting and attending.
Other identified roles played by hospitalists in adult-only groups included providing care for patients in the ICU (59.6% of reporting groups); primary responsibility for observation/short stay units, rapid response teams or code blue/cardiac arrest teams; cross-coverage for patients admitted without a hospitalist; and performing procedures such as vascular access, lumbar puncture, paracentesis, and thoracentesis. The hospitalist role’s in the ICU likely increased in many hospitals confronting COVID surges, Ms. Flores said.
The median number of shifts performed per year by a full-time hospitalist physician was 182.0 (average, 182.3), with 12 hours as the most common average duration for a shift in a daytime schedule. The 7-days-on/7-days-off model remained the most popular way to schedule adult hospitalists, at the same rate as in 2018. Backup coverage is another important issue for hospitalist groups, with 52.6% reporting no formal backup system. For those with a backup system, the highest proportion paid no additional compensation to the physician for being on the on-call schedule, but additional compensation was paid if called into the hospital.
Presence of nocturnists was reported by 71.9% of responding groups, slightly down from 2018, but increasing with the size of the group. “We continue to see a trend for dedicated nocturnists,” said Dr. McNeal. Hospitals see the benefits from the presence of a nocturnist, reflected in pay differentials or requiring fewer full-time shifts from nocturnists. It’s more consistent, higher quality of care delivered by people who are dedicated to that role.
In other findings from the survey, turnover in adult hospitalist groups is 10.9%t, which is up from 2018 but down from 2016. Unit-based assignment, also known as geographical rounding, was utilized by 42.7% of responding adult groups, with likelihood increasing with the size of the group. Unfilled positions were reported by 73.5% of groups, with an average of 11.2% of positions unfilled at the time of the survey.
The use of telemedicine in the hospital setting is evolving, likely considerably accelerated of necessity by the pandemic. “Many of us are using telemedicine with COVID patients in order to decrease clinicians’ time in the room, and to find a way to use a work force that has to be on leave,” Dr. McNeal said.
Nurse practitioners and physician assistants
The role for nurse practitioners and physician assistants in adult hospital medicine groups continues to increase, with 83.3% of groups reporting the presence of PAs and NPs, up from 77% in 2018. NPs/PAs are more likely in multistate hospitalist groups or integrated delivery system practices in hospitals/health systems.
The most common billing model for their professional services is a combination of independent billing by the PA/NP where allowed and shared services billing under a supervisory physician’s provider number – although 8.1% of groups report that their NPs/PAs didn’t generally provide billable services or submit bills for payment.
NPs and PAs spend one-fifth of their time, on average, on nonbillable, value-added work, including dedicated cross-coverage shifts, scheduling, patient assignments, nonbillable clinical work such as glycemic control, and quality improvement and performance improvement activities. “This is one example of the changing skill mix for the hospitalist group, helping the practice become more efficient,” Ms. Flores said.
NPs and PAs provide valuable services, Dr. McNeal added. “But it also takes some investment in time and training for them to be able to practice at the top of their license. My own hospitalist group has a training program for newly hired NPs/PAs. Everyone goes through this orientation for around 6-10 weeks, largely in a shadowing role starting out, until they gradually adjust to more clinical autonomy.”
This onboarding includes real-time evaluations and self-evaluations, and opportunities for conversations with experienced clinicians, working from a list of 30 “bread-and-butter” topics in hospital medicine, she noted.
Pediatric hospital medicine
The 2020 SoHM report includes a greater representation for pediatric hospital medicine, with a 200% increase in the proportion of reporting hospitalist groups that only take care of children. Thus, the pediatric data are more robust – and helpful – than in prior year surveys, said Sandra Gage, MD, SFHM, a pediatric hospitalist at Phoenix Children’s Hospital. Dr. Gage headed up the PAC’s expanded pediatric data initiative, with targeted outreach to pediatric groups to encourage their participation. She also convened a task force to come up with pediatric-specific questions that were more pertinent and user friendly.
One of the important questions for pediatric hospitalists involves scheduling – including variations in length of shifts – which can vary dramatically in pediatric HM groups. “This year we reported by number of hours expected for a clinical FTE, which should be more useful for group leaders,” Dr. Gage said. The median number of hours required per FTE from pediatric hospitalists was fairly consistent at 1,800 per year, with minor variations based on region and academic status.
“I don’t know that there’s anything too surprising in most of the data,” she said, but noted that SHM will now have a better pediatric baseline going forward. The survey also asked how many pediatric hospitalists were board certified in the new subspecialty of pediatric hospital medicine under the program launched last year by the American Board of Pediatrics. Its first qualifying exam was in November 2019. The average was 26%, but the variation between academic and nonacademic programs was unexpected, Dr. Gage said.
Pediatric hospitalists come from a variety of professional specialties besides pediatrics. Nearly half of all programs had at least one med/peds provider, while a smaller number of programs had providers from family medicine, internal medicine, emergency medicine, or palliative care, she noted. Half of pediatric hospitalists reported joining their practice directly out of residency. About 26% of pediatric hospital medicine (PHM) physicians were described as part time, and 34.3% of pediatric groups had the presence of an NP or PA.
“I think PHM evolved a little later than for adult hospitalists, but it has clearly come into its own as a field,” Dr. Gage said. In the COVID-19 crisis, some pediatric hospitalists have been asked to care for adult patients, which necessitated a flurry of activity to refresh their medical knowledge. Where pediatric units existed within the walls of adult hospitals and were temporarily closed for COVID, it’s not clear how many will reopen – perhaps ever.
Long-term impacts of the crisis
Some of the hospitalist group leaders Ms. Flores has spoken with in recent months point out that, while New York and some other early COVID-19 hot spots experienced a tremendous surge of patients and hospital crowding in March and April 2020, other hospitals didn’t see anywhere near the impact.
“For some, there was nothing going on with COVID where they were,” she said. Elective surgeries were widely canceled, but with no corresponding increase of COVID admissions; and with fewer patients showing up in EDs, some physicians found themselves idled.
What will be the longer-term impact of COVID-19? How will it change hospital medicine? “I definitely think things are going to change,” Ms. Flores said, speculating that licensing boards could find a way to make it easier for physicians to practice across state lines in response to crises like the pandemic. “Do we need to think at the national level about what we can do to create more surge capacity, to move people when and where they need to go in a crisis? Are there things SHM could do to help?”
Ms. Flores expects more hospital closures than followed the 2008-2009 economic recession, which likely will further drive the trend toward mergers and acquisitions – both of hospitalist groups and of hospitals.
“From the point of view of hospitals, financial pressures will only get worse, pressing us to reinvent how hospitalists work and how that could be made more efficient,” she said. “I hear hospitals saying: ‘We can’t sustain current trends.’ Meanwhile, specialists are saying they need more help from hospitalists, and frontline hospitalists are saying they’re already working too hard. What will we do about burnout?”
These competing trends were all headed toward a perfect storm even before the epidemic hit, Ms. Flores said. “The response will require some innovations we haven’t yet conceived of. Incremental change won’t get us where we need to be. But the hospitalist’s role will be more essential than ever.”
The 2020 data show that a lot of things have been fairly steady for hospitalists, said Thomas Frederickson, MD, a member of SHM’s PAC and a specialist in hospital medicine at CHI Health in Omaha, Neb. But one concern about this stability is that, while hospitalist compensation continues to go up, workload and by extension productivity remain relatively flat. “That has been a trend over the past decade, and some of us find it hard to make sense of that.”
Dr. Frederickson, too, sees a need for disruptive innovation. “I just wish I knew what that will be.” Perhaps, just as hospitalists played a large role in the quality revolution in hospitals over the past decade, maybe in the next decade they will come to play a large role in the right-sizing of hospital care in health systems, he said.
One other important finding: the number of hospitalists per group who play roles as physician leaders has also increased, with an average of 3.2 physicians per group in a formal leadership role (median of 2). But currently, 73% of the highest-ranking leaders in hospitalist groups are male, and they are disproportionally white. As reported in Medscape in 2019, 40% of working hospitalists are women and only 36% of hospitalists overall self-identified as White.1
“When you think of the demographics of actual working hospitalists, we could say the field of hospital medicine could and should do better in creating opportunities for diversity in leadership roles,” Ms. Flores said.
Reference
1. Martin KL. Hospitalist Compensation Report for 2019. Medscape. 2019 Jun 5. https://www.medscape.com/slideshow/2019-compensation-hospitalist-6011429#3.
SHM releases 2020 State of Hospital Medicine report
SHM releases 2020 State of Hospital Medicine report
Every 2 years the Society of Hospital Medicine’s Practice Analysis Committee (PAC) surveys hospitalist groups nationwide on such key practice parameters as compensation, services provided, hours of work, and participation in leadership roles. Combined with compensation and productivity data on adult and pediatric hospitalists collected by the Medical Group Management Association, licensed to SHM for inclusion in this report, the State of Hospital Medicine (SoHM) report is the most authoritative and comprehensive source of information regarding contemporary hospitalist practice.
This year’s biannual report is based on survey responses submitted between Jan. 6 and Feb. 28, 2020, by 502 hospitalist group practices. That’s slightly fewer groups reporting data than for past surveys, but these groups were larger, on average, resulting in more full-time equivalents (FTEs) incorporated into the results, said PAC member Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants. A total of 19.7% of the reporting groups provided pediatric hospital medicine data only, a much larger proportion than in past years.
The report is slated for publication in September, and SHM members can purchase it at a discount in print or electronic versions. “Our sense is that a lot of the fundamental information in the report will not have changed that much from 2018,” Ms. Flores said. “But these results convey the state of the field prior to the world-altering impact of the COVID-19 pandemic on hospitals of all sizes and settings.” How the hospital business and the practice of hospitalist groups have been and will be impacted by the pandemic, obviously, aren’t reflected in the data.
“We are finalizing a supplemental survey to go out to members at the end of the summer, specifically asking how COVID has impacted their hospitalist groups,” Ms. Flores said. These COVID-19 supplemental results will be released after the main report, sometime around the end of September. But results from the main survey, showing consistency in a number of key parameters, indicate that hospitalists continue to have a large and essential role in the U.S. health care system.
The leadership offered by hospitalists in the U.S. health care system’s response to surges of COVID-19 patients in many hospitals only underscores their importance, Ms. Flores added. “Hospitalists have definitely proven their worth. Imagine what the pandemic would have been like for hospitals if our specialty hadn’t been well-positioned to respond.” Hospitalists also showed an ability to adapt quickly to crises on the ground. But financial pressures imposed by the pandemic, combined with other trends previously in play, suggest that demands to cut costs and do more with less will be relentless as the field – and the world – tries to pull out of the pandemic crisis.
Compensation trends
One of the most eagerly anticipated findings in the SoHM is compensation. The median compensation for all adult hospitalists at the beginning of 2020 was $307,633 (with an average of $317,640), higher in the Midwest and lower in the East. The average base rate share of hospitalist compensation was 81.3%, with 11.6% based on productivity and 7.1% for performance – scored on such measures as patient satisfaction; accuracy and/or timeliness of documentation, billing, and coding; clinical processes; early morning discharge orders and times; and readmissions rates. A total of 46.6% of responding groups said they anticipated an increase in budgeted FTEs in the next year, while 51.2% expected to stay the same.
Subsidies or financial support for hospitalist practices break down in different ways, but in 2020 the median figure for financial support provided per adult hospitalist FTE was $198,750 (average, $201,760). This suggests that hospitals continue to see hospitalists as valued partners in health care, with useful knowledge of how the various components of the health care system work, said Tresa McNeal, MD, a hospitalist at Baylor Scott & White Medical Center, Temple, Tex., and a member of the PAC.
Scope of practice
Scope of practice for the hospitalist model continues to evolve, with increased demand for comanagement roles as other medical specialties are less inclined to visit patients in the hospital. Surgical comanagement accounted for much of that growth, but there were significant rates of comanagement for neurology, gastrointestinal and liver medicine, cardiology, and palliative care.
“Comanagement is a broad term without a single clear definition,” Ms. Flores said. “But when I talk about it, I refer to a broader array of hospitalists interacting with specialists.” The hospitalist‘s role could be as a consultant, or taking responsibility for admitting and attending.
Other identified roles played by hospitalists in adult-only groups included providing care for patients in the ICU (59.6% of reporting groups); primary responsibility for observation/short stay units, rapid response teams or code blue/cardiac arrest teams; cross-coverage for patients admitted without a hospitalist; and performing procedures such as vascular access, lumbar puncture, paracentesis, and thoracentesis. The hospitalist role’s in the ICU likely increased in many hospitals confronting COVID surges, Ms. Flores said.
The median number of shifts performed per year by a full-time hospitalist physician was 182.0 (average, 182.3), with 12 hours as the most common average duration for a shift in a daytime schedule. The 7-days-on/7-days-off model remained the most popular way to schedule adult hospitalists, at the same rate as in 2018. Backup coverage is another important issue for hospitalist groups, with 52.6% reporting no formal backup system. For those with a backup system, the highest proportion paid no additional compensation to the physician for being on the on-call schedule, but additional compensation was paid if called into the hospital.
Presence of nocturnists was reported by 71.9% of responding groups, slightly down from 2018, but increasing with the size of the group. “We continue to see a trend for dedicated nocturnists,” said Dr. McNeal. Hospitals see the benefits from the presence of a nocturnist, reflected in pay differentials or requiring fewer full-time shifts from nocturnists. It’s more consistent, higher quality of care delivered by people who are dedicated to that role.
In other findings from the survey, turnover in adult hospitalist groups is 10.9%t, which is up from 2018 but down from 2016. Unit-based assignment, also known as geographical rounding, was utilized by 42.7% of responding adult groups, with likelihood increasing with the size of the group. Unfilled positions were reported by 73.5% of groups, with an average of 11.2% of positions unfilled at the time of the survey.
The use of telemedicine in the hospital setting is evolving, likely considerably accelerated of necessity by the pandemic. “Many of us are using telemedicine with COVID patients in order to decrease clinicians’ time in the room, and to find a way to use a work force that has to be on leave,” Dr. McNeal said.
Nurse practitioners and physician assistants
The role for nurse practitioners and physician assistants in adult hospital medicine groups continues to increase, with 83.3% of groups reporting the presence of PAs and NPs, up from 77% in 2018. NPs/PAs are more likely in multistate hospitalist groups or integrated delivery system practices in hospitals/health systems.
The most common billing model for their professional services is a combination of independent billing by the PA/NP where allowed and shared services billing under a supervisory physician’s provider number – although 8.1% of groups report that their NPs/PAs didn’t generally provide billable services or submit bills for payment.
NPs and PAs spend one-fifth of their time, on average, on nonbillable, value-added work, including dedicated cross-coverage shifts, scheduling, patient assignments, nonbillable clinical work such as glycemic control, and quality improvement and performance improvement activities. “This is one example of the changing skill mix for the hospitalist group, helping the practice become more efficient,” Ms. Flores said.
NPs and PAs provide valuable services, Dr. McNeal added. “But it also takes some investment in time and training for them to be able to practice at the top of their license. My own hospitalist group has a training program for newly hired NPs/PAs. Everyone goes through this orientation for around 6-10 weeks, largely in a shadowing role starting out, until they gradually adjust to more clinical autonomy.”
This onboarding includes real-time evaluations and self-evaluations, and opportunities for conversations with experienced clinicians, working from a list of 30 “bread-and-butter” topics in hospital medicine, she noted.
Pediatric hospital medicine
The 2020 SoHM report includes a greater representation for pediatric hospital medicine, with a 200% increase in the proportion of reporting hospitalist groups that only take care of children. Thus, the pediatric data are more robust – and helpful – than in prior year surveys, said Sandra Gage, MD, SFHM, a pediatric hospitalist at Phoenix Children’s Hospital. Dr. Gage headed up the PAC’s expanded pediatric data initiative, with targeted outreach to pediatric groups to encourage their participation. She also convened a task force to come up with pediatric-specific questions that were more pertinent and user friendly.
One of the important questions for pediatric hospitalists involves scheduling – including variations in length of shifts – which can vary dramatically in pediatric HM groups. “This year we reported by number of hours expected for a clinical FTE, which should be more useful for group leaders,” Dr. Gage said. The median number of hours required per FTE from pediatric hospitalists was fairly consistent at 1,800 per year, with minor variations based on region and academic status.
“I don’t know that there’s anything too surprising in most of the data,” she said, but noted that SHM will now have a better pediatric baseline going forward. The survey also asked how many pediatric hospitalists were board certified in the new subspecialty of pediatric hospital medicine under the program launched last year by the American Board of Pediatrics. Its first qualifying exam was in November 2019. The average was 26%, but the variation between academic and nonacademic programs was unexpected, Dr. Gage said.
Pediatric hospitalists come from a variety of professional specialties besides pediatrics. Nearly half of all programs had at least one med/peds provider, while a smaller number of programs had providers from family medicine, internal medicine, emergency medicine, or palliative care, she noted. Half of pediatric hospitalists reported joining their practice directly out of residency. About 26% of pediatric hospital medicine (PHM) physicians were described as part time, and 34.3% of pediatric groups had the presence of an NP or PA.
“I think PHM evolved a little later than for adult hospitalists, but it has clearly come into its own as a field,” Dr. Gage said. In the COVID-19 crisis, some pediatric hospitalists have been asked to care for adult patients, which necessitated a flurry of activity to refresh their medical knowledge. Where pediatric units existed within the walls of adult hospitals and were temporarily closed for COVID, it’s not clear how many will reopen – perhaps ever.
Long-term impacts of the crisis
Some of the hospitalist group leaders Ms. Flores has spoken with in recent months point out that, while New York and some other early COVID-19 hot spots experienced a tremendous surge of patients and hospital crowding in March and April 2020, other hospitals didn’t see anywhere near the impact.
“For some, there was nothing going on with COVID where they were,” she said. Elective surgeries were widely canceled, but with no corresponding increase of COVID admissions; and with fewer patients showing up in EDs, some physicians found themselves idled.
What will be the longer-term impact of COVID-19? How will it change hospital medicine? “I definitely think things are going to change,” Ms. Flores said, speculating that licensing boards could find a way to make it easier for physicians to practice across state lines in response to crises like the pandemic. “Do we need to think at the national level about what we can do to create more surge capacity, to move people when and where they need to go in a crisis? Are there things SHM could do to help?”
Ms. Flores expects more hospital closures than followed the 2008-2009 economic recession, which likely will further drive the trend toward mergers and acquisitions – both of hospitalist groups and of hospitals.
“From the point of view of hospitals, financial pressures will only get worse, pressing us to reinvent how hospitalists work and how that could be made more efficient,” she said. “I hear hospitals saying: ‘We can’t sustain current trends.’ Meanwhile, specialists are saying they need more help from hospitalists, and frontline hospitalists are saying they’re already working too hard. What will we do about burnout?”
These competing trends were all headed toward a perfect storm even before the epidemic hit, Ms. Flores said. “The response will require some innovations we haven’t yet conceived of. Incremental change won’t get us where we need to be. But the hospitalist’s role will be more essential than ever.”
The 2020 data show that a lot of things have been fairly steady for hospitalists, said Thomas Frederickson, MD, a member of SHM’s PAC and a specialist in hospital medicine at CHI Health in Omaha, Neb. But one concern about this stability is that, while hospitalist compensation continues to go up, workload and by extension productivity remain relatively flat. “That has been a trend over the past decade, and some of us find it hard to make sense of that.”
Dr. Frederickson, too, sees a need for disruptive innovation. “I just wish I knew what that will be.” Perhaps, just as hospitalists played a large role in the quality revolution in hospitals over the past decade, maybe in the next decade they will come to play a large role in the right-sizing of hospital care in health systems, he said.
One other important finding: the number of hospitalists per group who play roles as physician leaders has also increased, with an average of 3.2 physicians per group in a formal leadership role (median of 2). But currently, 73% of the highest-ranking leaders in hospitalist groups are male, and they are disproportionally white. As reported in Medscape in 2019, 40% of working hospitalists are women and only 36% of hospitalists overall self-identified as White.1
“When you think of the demographics of actual working hospitalists, we could say the field of hospital medicine could and should do better in creating opportunities for diversity in leadership roles,” Ms. Flores said.
Reference
1. Martin KL. Hospitalist Compensation Report for 2019. Medscape. 2019 Jun 5. https://www.medscape.com/slideshow/2019-compensation-hospitalist-6011429#3.
Every 2 years the Society of Hospital Medicine’s Practice Analysis Committee (PAC) surveys hospitalist groups nationwide on such key practice parameters as compensation, services provided, hours of work, and participation in leadership roles. Combined with compensation and productivity data on adult and pediatric hospitalists collected by the Medical Group Management Association, licensed to SHM for inclusion in this report, the State of Hospital Medicine (SoHM) report is the most authoritative and comprehensive source of information regarding contemporary hospitalist practice.
This year’s biannual report is based on survey responses submitted between Jan. 6 and Feb. 28, 2020, by 502 hospitalist group practices. That’s slightly fewer groups reporting data than for past surveys, but these groups were larger, on average, resulting in more full-time equivalents (FTEs) incorporated into the results, said PAC member Leslie Flores, MHA, SFHM, of Nelson Flores Hospital Medicine Consultants. A total of 19.7% of the reporting groups provided pediatric hospital medicine data only, a much larger proportion than in past years.
The report is slated for publication in September, and SHM members can purchase it at a discount in print or electronic versions. “Our sense is that a lot of the fundamental information in the report will not have changed that much from 2018,” Ms. Flores said. “But these results convey the state of the field prior to the world-altering impact of the COVID-19 pandemic on hospitals of all sizes and settings.” How the hospital business and the practice of hospitalist groups have been and will be impacted by the pandemic, obviously, aren’t reflected in the data.
“We are finalizing a supplemental survey to go out to members at the end of the summer, specifically asking how COVID has impacted their hospitalist groups,” Ms. Flores said. These COVID-19 supplemental results will be released after the main report, sometime around the end of September. But results from the main survey, showing consistency in a number of key parameters, indicate that hospitalists continue to have a large and essential role in the U.S. health care system.
The leadership offered by hospitalists in the U.S. health care system’s response to surges of COVID-19 patients in many hospitals only underscores their importance, Ms. Flores added. “Hospitalists have definitely proven their worth. Imagine what the pandemic would have been like for hospitals if our specialty hadn’t been well-positioned to respond.” Hospitalists also showed an ability to adapt quickly to crises on the ground. But financial pressures imposed by the pandemic, combined with other trends previously in play, suggest that demands to cut costs and do more with less will be relentless as the field – and the world – tries to pull out of the pandemic crisis.
Compensation trends
One of the most eagerly anticipated findings in the SoHM is compensation. The median compensation for all adult hospitalists at the beginning of 2020 was $307,633 (with an average of $317,640), higher in the Midwest and lower in the East. The average base rate share of hospitalist compensation was 81.3%, with 11.6% based on productivity and 7.1% for performance – scored on such measures as patient satisfaction; accuracy and/or timeliness of documentation, billing, and coding; clinical processes; early morning discharge orders and times; and readmissions rates. A total of 46.6% of responding groups said they anticipated an increase in budgeted FTEs in the next year, while 51.2% expected to stay the same.
Subsidies or financial support for hospitalist practices break down in different ways, but in 2020 the median figure for financial support provided per adult hospitalist FTE was $198,750 (average, $201,760). This suggests that hospitals continue to see hospitalists as valued partners in health care, with useful knowledge of how the various components of the health care system work, said Tresa McNeal, MD, a hospitalist at Baylor Scott & White Medical Center, Temple, Tex., and a member of the PAC.
Scope of practice
Scope of practice for the hospitalist model continues to evolve, with increased demand for comanagement roles as other medical specialties are less inclined to visit patients in the hospital. Surgical comanagement accounted for much of that growth, but there were significant rates of comanagement for neurology, gastrointestinal and liver medicine, cardiology, and palliative care.
“Comanagement is a broad term without a single clear definition,” Ms. Flores said. “But when I talk about it, I refer to a broader array of hospitalists interacting with specialists.” The hospitalist‘s role could be as a consultant, or taking responsibility for admitting and attending.
Other identified roles played by hospitalists in adult-only groups included providing care for patients in the ICU (59.6% of reporting groups); primary responsibility for observation/short stay units, rapid response teams or code blue/cardiac arrest teams; cross-coverage for patients admitted without a hospitalist; and performing procedures such as vascular access, lumbar puncture, paracentesis, and thoracentesis. The hospitalist role’s in the ICU likely increased in many hospitals confronting COVID surges, Ms. Flores said.
The median number of shifts performed per year by a full-time hospitalist physician was 182.0 (average, 182.3), with 12 hours as the most common average duration for a shift in a daytime schedule. The 7-days-on/7-days-off model remained the most popular way to schedule adult hospitalists, at the same rate as in 2018. Backup coverage is another important issue for hospitalist groups, with 52.6% reporting no formal backup system. For those with a backup system, the highest proportion paid no additional compensation to the physician for being on the on-call schedule, but additional compensation was paid if called into the hospital.
Presence of nocturnists was reported by 71.9% of responding groups, slightly down from 2018, but increasing with the size of the group. “We continue to see a trend for dedicated nocturnists,” said Dr. McNeal. Hospitals see the benefits from the presence of a nocturnist, reflected in pay differentials or requiring fewer full-time shifts from nocturnists. It’s more consistent, higher quality of care delivered by people who are dedicated to that role.
In other findings from the survey, turnover in adult hospitalist groups is 10.9%t, which is up from 2018 but down from 2016. Unit-based assignment, also known as geographical rounding, was utilized by 42.7% of responding adult groups, with likelihood increasing with the size of the group. Unfilled positions were reported by 73.5% of groups, with an average of 11.2% of positions unfilled at the time of the survey.
The use of telemedicine in the hospital setting is evolving, likely considerably accelerated of necessity by the pandemic. “Many of us are using telemedicine with COVID patients in order to decrease clinicians’ time in the room, and to find a way to use a work force that has to be on leave,” Dr. McNeal said.
Nurse practitioners and physician assistants
The role for nurse practitioners and physician assistants in adult hospital medicine groups continues to increase, with 83.3% of groups reporting the presence of PAs and NPs, up from 77% in 2018. NPs/PAs are more likely in multistate hospitalist groups or integrated delivery system practices in hospitals/health systems.
The most common billing model for their professional services is a combination of independent billing by the PA/NP where allowed and shared services billing under a supervisory physician’s provider number – although 8.1% of groups report that their NPs/PAs didn’t generally provide billable services or submit bills for payment.
NPs and PAs spend one-fifth of their time, on average, on nonbillable, value-added work, including dedicated cross-coverage shifts, scheduling, patient assignments, nonbillable clinical work such as glycemic control, and quality improvement and performance improvement activities. “This is one example of the changing skill mix for the hospitalist group, helping the practice become more efficient,” Ms. Flores said.
NPs and PAs provide valuable services, Dr. McNeal added. “But it also takes some investment in time and training for them to be able to practice at the top of their license. My own hospitalist group has a training program for newly hired NPs/PAs. Everyone goes through this orientation for around 6-10 weeks, largely in a shadowing role starting out, until they gradually adjust to more clinical autonomy.”
This onboarding includes real-time evaluations and self-evaluations, and opportunities for conversations with experienced clinicians, working from a list of 30 “bread-and-butter” topics in hospital medicine, she noted.
Pediatric hospital medicine
The 2020 SoHM report includes a greater representation for pediatric hospital medicine, with a 200% increase in the proportion of reporting hospitalist groups that only take care of children. Thus, the pediatric data are more robust – and helpful – than in prior year surveys, said Sandra Gage, MD, SFHM, a pediatric hospitalist at Phoenix Children’s Hospital. Dr. Gage headed up the PAC’s expanded pediatric data initiative, with targeted outreach to pediatric groups to encourage their participation. She also convened a task force to come up with pediatric-specific questions that were more pertinent and user friendly.
One of the important questions for pediatric hospitalists involves scheduling – including variations in length of shifts – which can vary dramatically in pediatric HM groups. “This year we reported by number of hours expected for a clinical FTE, which should be more useful for group leaders,” Dr. Gage said. The median number of hours required per FTE from pediatric hospitalists was fairly consistent at 1,800 per year, with minor variations based on region and academic status.
“I don’t know that there’s anything too surprising in most of the data,” she said, but noted that SHM will now have a better pediatric baseline going forward. The survey also asked how many pediatric hospitalists were board certified in the new subspecialty of pediatric hospital medicine under the program launched last year by the American Board of Pediatrics. Its first qualifying exam was in November 2019. The average was 26%, but the variation between academic and nonacademic programs was unexpected, Dr. Gage said.
Pediatric hospitalists come from a variety of professional specialties besides pediatrics. Nearly half of all programs had at least one med/peds provider, while a smaller number of programs had providers from family medicine, internal medicine, emergency medicine, or palliative care, she noted. Half of pediatric hospitalists reported joining their practice directly out of residency. About 26% of pediatric hospital medicine (PHM) physicians were described as part time, and 34.3% of pediatric groups had the presence of an NP or PA.
“I think PHM evolved a little later than for adult hospitalists, but it has clearly come into its own as a field,” Dr. Gage said. In the COVID-19 crisis, some pediatric hospitalists have been asked to care for adult patients, which necessitated a flurry of activity to refresh their medical knowledge. Where pediatric units existed within the walls of adult hospitals and were temporarily closed for COVID, it’s not clear how many will reopen – perhaps ever.
Long-term impacts of the crisis
Some of the hospitalist group leaders Ms. Flores has spoken with in recent months point out that, while New York and some other early COVID-19 hot spots experienced a tremendous surge of patients and hospital crowding in March and April 2020, other hospitals didn’t see anywhere near the impact.
“For some, there was nothing going on with COVID where they were,” she said. Elective surgeries were widely canceled, but with no corresponding increase of COVID admissions; and with fewer patients showing up in EDs, some physicians found themselves idled.
What will be the longer-term impact of COVID-19? How will it change hospital medicine? “I definitely think things are going to change,” Ms. Flores said, speculating that licensing boards could find a way to make it easier for physicians to practice across state lines in response to crises like the pandemic. “Do we need to think at the national level about what we can do to create more surge capacity, to move people when and where they need to go in a crisis? Are there things SHM could do to help?”
Ms. Flores expects more hospital closures than followed the 2008-2009 economic recession, which likely will further drive the trend toward mergers and acquisitions – both of hospitalist groups and of hospitals.
“From the point of view of hospitals, financial pressures will only get worse, pressing us to reinvent how hospitalists work and how that could be made more efficient,” she said. “I hear hospitals saying: ‘We can’t sustain current trends.’ Meanwhile, specialists are saying they need more help from hospitalists, and frontline hospitalists are saying they’re already working too hard. What will we do about burnout?”
These competing trends were all headed toward a perfect storm even before the epidemic hit, Ms. Flores said. “The response will require some innovations we haven’t yet conceived of. Incremental change won’t get us where we need to be. But the hospitalist’s role will be more essential than ever.”
The 2020 data show that a lot of things have been fairly steady for hospitalists, said Thomas Frederickson, MD, a member of SHM’s PAC and a specialist in hospital medicine at CHI Health in Omaha, Neb. But one concern about this stability is that, while hospitalist compensation continues to go up, workload and by extension productivity remain relatively flat. “That has been a trend over the past decade, and some of us find it hard to make sense of that.”
Dr. Frederickson, too, sees a need for disruptive innovation. “I just wish I knew what that will be.” Perhaps, just as hospitalists played a large role in the quality revolution in hospitals over the past decade, maybe in the next decade they will come to play a large role in the right-sizing of hospital care in health systems, he said.
One other important finding: the number of hospitalists per group who play roles as physician leaders has also increased, with an average of 3.2 physicians per group in a formal leadership role (median of 2). But currently, 73% of the highest-ranking leaders in hospitalist groups are male, and they are disproportionally white. As reported in Medscape in 2019, 40% of working hospitalists are women and only 36% of hospitalists overall self-identified as White.1
“When you think of the demographics of actual working hospitalists, we could say the field of hospital medicine could and should do better in creating opportunities for diversity in leadership roles,” Ms. Flores said.
Reference
1. Martin KL. Hospitalist Compensation Report for 2019. Medscape. 2019 Jun 5. https://www.medscape.com/slideshow/2019-compensation-hospitalist-6011429#3.
PHM20 Virtual: Impact of racism in medicine
Presenters
Michael Bryant, MD – Children’s Hospital of Los Angeles
Kimberly Manning, MD – Emory University, Atlanta
Kimberly Reynolds, MD – University of Miami
Samir Shah, MD, MSCE, MHM – Cincinnati Children’s Hospital
Ndidi Unaka, MD, MEd – Cincinnati Children’s Hospital
Moderator
Erin Shaughnessy, MD – Phoenix Children’s Hospital
Session summary
This session was devoted to a discussion about how pediatric hospital medicine (PHM) as a field can address racism in medicine. The structural inequity rooted in poverty, housing problems, and differential education represents the essential social determinant of health. No longer can pediatric hospitalists neglect or be in denial of the crucial role that race plays in propagating further inequalities in our society and at our workplace. Historically Black people were exploited in research and still are disproportionately affected when it comes to infant prematurity and mortality, asthma, pain treatments, and so on. The pediatric hospitalist must explore and understand the reasons behind nonadherence and noncompliance among Black patients and always seek to understand before criticizing.
Within learning environments, we must improve how to “autocorrect” and proactively work on our own biases. Dr. Bryant pointed out that each institution has the responsibility to build on the civil rights movement and seize the moment to create a robust response to the inequities manifested during the COVID-19 epidemic, as well as the events following the deaths of George Floyd, Breonna Taylor, Ahmoud Arbery, and many others. Dr. Shah called on the PHM community to take on that obligation by “stepping into the tension,” as Mark Shapiro, MD, has suggested in a conversation/podcast with Dr. Unaka.
As pediatric hospitalists, we will have to show up both individually and as constituents of institutions to address racism by specific projects looking at all data relevant for racism rather than race in quality and safety – thereby amplifying the voices of our Black patients and families, remarked Dr. Unaka. There was a brief reflection on the use of the word “allies” by Dr. Manning and Dr. Reynolds to remind the more than 200 session participants that a bidirectional framework of this process is crucial and that there is a clear need for a partnership to a common goal that should start by “a laydown of privilege of those who have it” to establish equal playing fields once and for all.
Dr. Bryant encouraged a deliberate and early thoughtful process to identify those with opportunities and help young Black people explore journeys in medicine and increase diversity among PHM faculty. Dr. Manning reminded the audience of the power that relationships have and hold in our lives, and not only those of mentors and mentees, but also relationships among all of us as humans. As with those simple situations in which we mess up and have to be able to admit it, apologize for it, and learn to move on, this requires also showing up as a mentee, articulating one’s needs, and learning to break the habits rooted in biases. Dr. Unaka warned against stereotypes and reminded us to look deeper and understand better all of our learners and their blind spots, as well as our own.
Key takeaways
- The field of PHM must recognize the role that race plays in propagating inequalities.
- Learning and mentorship environments have to be assessed for the safety of all learners and adjusted to correct (and autocorrect) as many biases as possible.
- Institutions must assume responsibilities to establish a conscious, robust response to injustice and racism in a timely and specific manner.
- Further research efforts must be made to address racism, rather than race.
- The PHM community must show up to create a new, healthy, and deliberate bidirectional framework to endorse and support diversity.
Dr. Giordano is assistant professor of pediatrics at Columbia University and a pediatric hospitalist at NewYork–Presbyterian Morgan Stanley Children’s Hospital, both in New York, with an interest in surgical comanagement. She serves on the Society of Hospital Medicine’s Pediatric Special Interest Group Executive Committee and is the chair of the Education Subcommittee. She is also an advisory board member for the New York/Westchester SHM Chapter.
Presenters
Michael Bryant, MD – Children’s Hospital of Los Angeles
Kimberly Manning, MD – Emory University, Atlanta
Kimberly Reynolds, MD – University of Miami
Samir Shah, MD, MSCE, MHM – Cincinnati Children’s Hospital
Ndidi Unaka, MD, MEd – Cincinnati Children’s Hospital
Moderator
Erin Shaughnessy, MD – Phoenix Children’s Hospital
Session summary
This session was devoted to a discussion about how pediatric hospital medicine (PHM) as a field can address racism in medicine. The structural inequity rooted in poverty, housing problems, and differential education represents the essential social determinant of health. No longer can pediatric hospitalists neglect or be in denial of the crucial role that race plays in propagating further inequalities in our society and at our workplace. Historically Black people were exploited in research and still are disproportionately affected when it comes to infant prematurity and mortality, asthma, pain treatments, and so on. The pediatric hospitalist must explore and understand the reasons behind nonadherence and noncompliance among Black patients and always seek to understand before criticizing.
Within learning environments, we must improve how to “autocorrect” and proactively work on our own biases. Dr. Bryant pointed out that each institution has the responsibility to build on the civil rights movement and seize the moment to create a robust response to the inequities manifested during the COVID-19 epidemic, as well as the events following the deaths of George Floyd, Breonna Taylor, Ahmoud Arbery, and many others. Dr. Shah called on the PHM community to take on that obligation by “stepping into the tension,” as Mark Shapiro, MD, has suggested in a conversation/podcast with Dr. Unaka.
As pediatric hospitalists, we will have to show up both individually and as constituents of institutions to address racism by specific projects looking at all data relevant for racism rather than race in quality and safety – thereby amplifying the voices of our Black patients and families, remarked Dr. Unaka. There was a brief reflection on the use of the word “allies” by Dr. Manning and Dr. Reynolds to remind the more than 200 session participants that a bidirectional framework of this process is crucial and that there is a clear need for a partnership to a common goal that should start by “a laydown of privilege of those who have it” to establish equal playing fields once and for all.
Dr. Bryant encouraged a deliberate and early thoughtful process to identify those with opportunities and help young Black people explore journeys in medicine and increase diversity among PHM faculty. Dr. Manning reminded the audience of the power that relationships have and hold in our lives, and not only those of mentors and mentees, but also relationships among all of us as humans. As with those simple situations in which we mess up and have to be able to admit it, apologize for it, and learn to move on, this requires also showing up as a mentee, articulating one’s needs, and learning to break the habits rooted in biases. Dr. Unaka warned against stereotypes and reminded us to look deeper and understand better all of our learners and their blind spots, as well as our own.
Key takeaways
- The field of PHM must recognize the role that race plays in propagating inequalities.
- Learning and mentorship environments have to be assessed for the safety of all learners and adjusted to correct (and autocorrect) as many biases as possible.
- Institutions must assume responsibilities to establish a conscious, robust response to injustice and racism in a timely and specific manner.
- Further research efforts must be made to address racism, rather than race.
- The PHM community must show up to create a new, healthy, and deliberate bidirectional framework to endorse and support diversity.
Dr. Giordano is assistant professor of pediatrics at Columbia University and a pediatric hospitalist at NewYork–Presbyterian Morgan Stanley Children’s Hospital, both in New York, with an interest in surgical comanagement. She serves on the Society of Hospital Medicine’s Pediatric Special Interest Group Executive Committee and is the chair of the Education Subcommittee. She is also an advisory board member for the New York/Westchester SHM Chapter.
Presenters
Michael Bryant, MD – Children’s Hospital of Los Angeles
Kimberly Manning, MD – Emory University, Atlanta
Kimberly Reynolds, MD – University of Miami
Samir Shah, MD, MSCE, MHM – Cincinnati Children’s Hospital
Ndidi Unaka, MD, MEd – Cincinnati Children’s Hospital
Moderator
Erin Shaughnessy, MD – Phoenix Children’s Hospital
Session summary
This session was devoted to a discussion about how pediatric hospital medicine (PHM) as a field can address racism in medicine. The structural inequity rooted in poverty, housing problems, and differential education represents the essential social determinant of health. No longer can pediatric hospitalists neglect or be in denial of the crucial role that race plays in propagating further inequalities in our society and at our workplace. Historically Black people were exploited in research and still are disproportionately affected when it comes to infant prematurity and mortality, asthma, pain treatments, and so on. The pediatric hospitalist must explore and understand the reasons behind nonadherence and noncompliance among Black patients and always seek to understand before criticizing.
Within learning environments, we must improve how to “autocorrect” and proactively work on our own biases. Dr. Bryant pointed out that each institution has the responsibility to build on the civil rights movement and seize the moment to create a robust response to the inequities manifested during the COVID-19 epidemic, as well as the events following the deaths of George Floyd, Breonna Taylor, Ahmoud Arbery, and many others. Dr. Shah called on the PHM community to take on that obligation by “stepping into the tension,” as Mark Shapiro, MD, has suggested in a conversation/podcast with Dr. Unaka.
As pediatric hospitalists, we will have to show up both individually and as constituents of institutions to address racism by specific projects looking at all data relevant for racism rather than race in quality and safety – thereby amplifying the voices of our Black patients and families, remarked Dr. Unaka. There was a brief reflection on the use of the word “allies” by Dr. Manning and Dr. Reynolds to remind the more than 200 session participants that a bidirectional framework of this process is crucial and that there is a clear need for a partnership to a common goal that should start by “a laydown of privilege of those who have it” to establish equal playing fields once and for all.
Dr. Bryant encouraged a deliberate and early thoughtful process to identify those with opportunities and help young Black people explore journeys in medicine and increase diversity among PHM faculty. Dr. Manning reminded the audience of the power that relationships have and hold in our lives, and not only those of mentors and mentees, but also relationships among all of us as humans. As with those simple situations in which we mess up and have to be able to admit it, apologize for it, and learn to move on, this requires also showing up as a mentee, articulating one’s needs, and learning to break the habits rooted in biases. Dr. Unaka warned against stereotypes and reminded us to look deeper and understand better all of our learners and their blind spots, as well as our own.
Key takeaways
- The field of PHM must recognize the role that race plays in propagating inequalities.
- Learning and mentorship environments have to be assessed for the safety of all learners and adjusted to correct (and autocorrect) as many biases as possible.
- Institutions must assume responsibilities to establish a conscious, robust response to injustice and racism in a timely and specific manner.
- Further research efforts must be made to address racism, rather than race.
- The PHM community must show up to create a new, healthy, and deliberate bidirectional framework to endorse and support diversity.
Dr. Giordano is assistant professor of pediatrics at Columbia University and a pediatric hospitalist at NewYork–Presbyterian Morgan Stanley Children’s Hospital, both in New York, with an interest in surgical comanagement. She serves on the Society of Hospital Medicine’s Pediatric Special Interest Group Executive Committee and is the chair of the Education Subcommittee. She is also an advisory board member for the New York/Westchester SHM Chapter.
NYC public hospitals rose to the demands of the COVID-19 crisis
Hospitalists at the center of the storm
New York City Health + Hospitals (NYCH+H), the country’s largest public health care system, encompasses 11 hospitals with 4,354 staffed acute beds during normal times. It serves as the safety net for 1.1 million of the 8.4 million residents of the most populous city in the United States, many of them uninsured, undocumented, covered by Medicaid, or otherwise disadvantaged.
At the very epicenter in the early days of the historic COVID-19 pandemic, NYCH+H transferred patients between its facilities, added medical and ICU beds by the hundreds, mobilized palliative care volunteers, harnessed telemedicine and a clinician hotline, and made other sweeping changes to ensure that the city’s public health system would be able to respond to demand at the peak of the surge. That peak hit in April, when an average of 9,000 new COVID-19 cases were being reported in the city every day.
Through it all, hospitalists have played critical roles in both planning for the system’s response and caring for severely ill COVID-19 patients. Their stories reflect both the unprecedented demands on the system and the dedication of frontline clinicians.
One of those, Carla Saladini-Aponte, MD, who just finished her residency in June 2019, found herself on the firing line in March 2020 as an attending physician at 457-bed NYCH+H/Jacobi Hospital in the Bronx. “I have experienced so much in my first year on the job, dealing with a disease that we’ve never seen before,” she said. “We didn’t grasp the extent of the COVID crisis in the beginning, so we were emotionally unprepared when it first hit.”
Starting on March 30, NYCH+H administration mobilized a centralized incident command structure to coordinate response systemwide to a rapidly changing situation.
Two weeks later Jacobi was a COVID-19 hospital, top to bottom, with its medical ICU beds increased from 12 to more than 100. By mid-April, Dr. Saladini-Aponte’s team, one of 11 medical teams in the hospital, had 26 patients, all of them with COVID-19. There was not a consensus in the early days on how to manage patients with severe respiratory distress. “But by the time the surge came, we had a better understanding of the scope of the situation,” she said.
Learning to be an attending
“They don’t teach you how to be an attending during residency,” Dr. Saladini-Aponte said. “At the beginning I wasn’t such a good teacher. I just wanted to prove myself and stay one step ahead of the residents. But as an academic hospitalist you have to listen to others. I learned to ask questions of the residents every morning, including how they were doing personally.”
Sometimes a visiting consultant would ask on the floor: “‘Where’s your attending?’” not recognizing Dr. Saladini-Aponte, fresh out of residency, filling that role. At times, she felt like a PGY-4 (postgraduate year 4). But she quickly grew into the attending role and was asked to be site coordinator for the mobilization of palliative medicine volunteers at Jacobi.
“We found ourselves having to make tough ethical decisions. Some patients, even if we provided a ventilator and maximum oxygen therapy, would still die. There were difficult discussions when we didn’t know if we had enough dialysis machines, or how to manage other limited resources. The hospital was saying: You decide, if there’s a high degree of certainty about the outcome. But we had never practiced medicine this way before,” she said.
“That’s why our hospital provided daily ethics meetings with our ethics council. There would be eight people sitting 6 feet apart in a conference room, all wearing masks. We’d talk about situations that were giving us trouble. Their role wasn’t to provide answers but to help us see the scope of the situation and the complexities,” she explained.
Dr. Saladini-Aponte said she has had many sleepless nights since the pandemic began. “Sometimes, I would come home from work and lie down on the floor and cry,” she said. “But we had so much support from volunteers helping our little hospitalist service of seven.” It was also important to keep up with the clinical information, and one of her coworkers created “cheat sheets” for the clinicians, regularly updated with the latest essential information on antibiotics, testing, and the like.
“At the peak, I was trying to read everything I could about the virus. I was just pulling myself in too many directions. I asked for help from my boyfriend to remind me not to log onto my computer when I came home from work,” she said. “One of my techniques for preventing burnout was just to avoid social media. I couldn’t deal with what was going on in the news. It just angered me. Even now, seeing people without masks makes me very uncomfortable.”
Organizing the crisis response
As chief value officer for NYCH+H, Hyung (Harry) Cho, MD, FACP, SFHM, typically focuses on issues of patient safety and overuse of medical treatments in the health system. But in the COVID-19 crisis, he found himself at the forefront of organizing its response. “We tried to provide support centrally and to standardize practice in how we test and treat,” he said.
“We were truly at the epicenter of the pandemic,” Dr. Cho said. “All of our hospitals had different experiences, and unique responses. But the system worked well.” Patients were transferred from the more overtaxed hospitals to Bellevue and other NYCH+H hospitals with spare beds. An emergency medical response structure was put in place, and every morning the system’s Tiger Team, with multidisciplinary personnel from administration, operations, logistics, and medical/technical specialists, would gather virtually to discuss needs across the system.
“It was a very open atmosphere and we asked people to report what was happening on the ground,” Dr. Cho said. “We started rapidly reviewing batches of 20 patients at a time for transfer in order to alleviate pressure in the most overtaxed ERs.”
NYCH+H also had to work through concerns about PPE, just like other U.S. hospitals. Treatment guidelines were changing by the day. Medical concerns were relayed at a rapid pace. Another priority was trying to limit unnecessary exposure for staff through a recommendation that only one clinician from a team would go into the room of an infected patient, unless another was absolutely needed.
The reality of public health
NYCH+H was created by the New York State Legislature in 1969 and rebranded in 2015. It includes a low- to no-cost health insurance plan called MetroPlus, along with outpatient centers, comprehensive case management, and social supports in the home.
“What people know about public health systems is that we typically are underresourced. That’s just the reality of public health,” Dr. Cho said. “We help the community, the underserved. The people who truly needed our help are also the ones who have been disproportionately affected by COVID-19. And that is where we really shine as a system.”
Dr. Cho lauded the performance of the health system’s frontline staff. “Watching them come together during the entire pandemic, and do their best every day, was truly inspiring,” he said. “But when they got to the peak, it really took an emotional toll on them.”
NYCH+H’s in-house staff support program, called Helping Healers Heal, was mobilized with specially trained teams at each of its 11 hospitals to provide peer-to-peer support, mental health expertise, and team-debriefing sessions to staff members following traumatic events. Support is provided both over the phone and in person on the floors, Dr. Cho said. “During the surge, everything was happening so quickly, there was no time to take a pause. Now, as we are able to catch our breath, that’s when they most need support.”
The hospitalists at NYCH+H hospitals intended to have goals-of-care conversations with all patients, but everyone was very busy – so having these conversations became harder and harder, Dr. Cho said. Recognizing limited staffing for the quadrupling of patients who needed palliative care at NYCH+H hospitals, he asked the medicine chairs about their palliative care needs and then used social media outreach to ask for help. The message went viral, attracting 413 volunteers from across the country. Sixty-seven telepalliative volunteers were put to work doing goals-of-care conversations remotely with inpatients and their families.1
Expediting transfers
For Ian Fagan, MD, a hospitalist and associate medical director for general internal medicine Inpatient Services at Bellevue Hospital in Manhattan, hospitalist shifts are a normal part of his job. But he had to give them up during the surge to focus on planning, management, and especially scheduling other doctors, with sufficient backups needed to cover last minute changes. Dr. Fagan did that by using the existing pool of hospitalist staff, physicians who were reassigned from other specialties, agency staff, military medical personnel, and volunteer doctors who flew in from around the country to help. He also worked 10- to 12-hour days for 36 consecutive days.
The impact of disparities in access to care in New York City was reflected in the greater demand for care in the hospitals in Brooklyn, Queens, and the Bronx. “With fewer patients and more hospital beds in Manhattan, we had the capacity to share our beds,” Dr. Fagan said. “It was so amazing to me how quickly we could move patients from one hospital to another. We started accepting up to 40 transfers a day. But hey, we were still really busy.”
Bellevue is the nation’s oldest public hospital. “We care for the homeless, for immigrants, and we don’t ask questions. That’s our mission. I’m so proud to work here, and so grateful,” Dr. Fagan said. “If someone is undocumented or without insurance, I will give them exactly the same care. We stepped up in a big way to care for people of New York, but we’ve always been there for them – and we were there for them during the COVID surge.”
The hospitals in the system also worked together in ways Dr. Fagan had never seen. “It helped to have a central command structure with a bird’s eye view from above the level of individual hospitals, to organize and see which hospitals could step up. It’s good to have the data to put it in perspective,” he said. The system also utilized a temporary low-acuity medical center set up by NYCH+H on Roosevelt Island, as well as field hospitals organized at the Jacob K. Javits Convention Center and the USTA Billie Jean King National Tennis Center.
“At Bellevue we tried to stay ready, with the ability to turn former hospital units that were being used as offices back to beds. We always had three units lined up that were fully ready to convert. For example, I was medical director of the preop clinic and one day they gave us 24 hours to pack everything and move out. Three days later, it was a 24-bed unit. We also built a more robust rapid response and code team,” he said.
“It was hard for me not to take hospitalist shifts, because my identity is being a doctor. I eventually came to terms with the importance of the role that I was doing every day. I felt I could protect my colleagues, and if they were having an emotional day, to give them the opportunity to talk to someone. I also did the onboarding, one-on-one, of the new doctors.”
As the crisis in New York City has ebbed, Dr. Fagan was recently able to again take a week of clinical service. “The first day back on the floor I felt that I had forgotten everything. But by the end of the day, I thought, ‘Okay, I do know how to do this, after all.’ Census is down here. It’s quiet. That’s good. We need it now,” he said.
“I think the hardest moment for me was when the head nurse on our trauma unit, Ernesto DeLeon, known to everybody here, died of COVID in our ICU in April,” Dr. Fagan said. When Mr. DeLeon died, 100 hospital personnel gathered in the halls outside the room to pay their respects. “There had been a palpable fear in our lives – and this showed us that the fear was real. Ernesto was the first person I knew well who died, who acquired COVID at work doing what we’re all doing. We haven’t lost any doctors yet, but when this nurse died, we allowed ourselves to realize that this is personal. In that moment, we needed to allow ourselves to be human.”
Joan Curcio, MD, associate director of medicine at Elmhurst Hospital, said Elmhurst was where the story started for New York City and for NYCH+H. “I trained here and have spent my entire career at this hospital. It came to feel like what a battleground must be like, with things coming at you from every direction,” she said. “It was overwhelming in ways I could not have foreseen. I had seen videos from Italy [an early COVID-19 epicenter], but until it happened here, it was just hard to process.”
Things started slowly, with a few patients with severe acute respiratory distress syndrome and a 5- to 7-day turnaround to get results of their viral infection tests. “By week 2, a greater number of patients from our clinics and testing sites were filtering through the emergency department. Then hundreds.”
The normal occupancy rate for the department of medicine at Elmhurst is 110-115%, which typically means full beds plus patients in the emergency department. “We started to grow to 160, then 180, and then a peak of 250% of occupancy. We took over a rehab surgery floor, then a 35-bed surgery and hospice floor, which went to full capacity just like that,” she said. The number of non–critical care service teams increased to 20, working with redeployed staff, volunteers, military, and agency personnel, while ICU beds increased from 20 to 105.
“We were dealing with a much higher acuity level and enduring emotional turmoil with families, trying to carve out time to call them after our shift was over,” Dr. Curcio explained. Elmhurst developed a call-in hotline and a daily call-out service for families. Technology was mobilized to provide video visits and new systems were designed for isolation and for PPE distribution and use.
“I just felt that I couldn’t get everything done. I felt continually overwhelmed, and it didn’t matter how much time I took. I never felt I was able to give enough to anybody in any area, which was hard to take,” Dr. Curcio said. “But I still felt a sense of purpose and that I was making a difference – thanks to lots of support from the central office.”
Patient volume at Elmhurst is now down, lower than Dr. Curcio has ever seen it. “One of the main issues right now, moving forward, is ‘how do we function in a post-crisis mode?’” she said. The process of transitioning back to non-COVID-19 care will be complex. “When we clear a floor and clean it to go back to being a cold [COVID-19-negative] unit, it’s a whole different level of cleaning that takes 7 days.”
One moment that was particularly jarring for Dr. Curcio occurred while she was giving a tour of the hospital to visiting military medical personnel. “We went into the emergency department and I turned around and looked into a shower room, which was full of body bags. They were all full.”
But the experience has also been inspiring. “People gave their all without complaint. We hospitalists, and all those recruited to act as hospitalists, essentially took responsibility for the COVID response,” she said. “This was, hopefully, the experience of a lifetime as a medical professional. I wouldn’t want to ever experience something as daunting as this again.”
Reference
1. Israilov S et al. National outreach of telepalliative medicine volunteers for a New York City safety net system COVID-19 pandemic response. J Pain Symptom Manag. 2020 May 29. doi: 10.1016/j.jpainsymman.2020.05.026.
Hospitalists at the center of the storm
Hospitalists at the center of the storm
New York City Health + Hospitals (NYCH+H), the country’s largest public health care system, encompasses 11 hospitals with 4,354 staffed acute beds during normal times. It serves as the safety net for 1.1 million of the 8.4 million residents of the most populous city in the United States, many of them uninsured, undocumented, covered by Medicaid, or otherwise disadvantaged.
At the very epicenter in the early days of the historic COVID-19 pandemic, NYCH+H transferred patients between its facilities, added medical and ICU beds by the hundreds, mobilized palliative care volunteers, harnessed telemedicine and a clinician hotline, and made other sweeping changes to ensure that the city’s public health system would be able to respond to demand at the peak of the surge. That peak hit in April, when an average of 9,000 new COVID-19 cases were being reported in the city every day.
Through it all, hospitalists have played critical roles in both planning for the system’s response and caring for severely ill COVID-19 patients. Their stories reflect both the unprecedented demands on the system and the dedication of frontline clinicians.
One of those, Carla Saladini-Aponte, MD, who just finished her residency in June 2019, found herself on the firing line in March 2020 as an attending physician at 457-bed NYCH+H/Jacobi Hospital in the Bronx. “I have experienced so much in my first year on the job, dealing with a disease that we’ve never seen before,” she said. “We didn’t grasp the extent of the COVID crisis in the beginning, so we were emotionally unprepared when it first hit.”
Starting on March 30, NYCH+H administration mobilized a centralized incident command structure to coordinate response systemwide to a rapidly changing situation.
Two weeks later Jacobi was a COVID-19 hospital, top to bottom, with its medical ICU beds increased from 12 to more than 100. By mid-April, Dr. Saladini-Aponte’s team, one of 11 medical teams in the hospital, had 26 patients, all of them with COVID-19. There was not a consensus in the early days on how to manage patients with severe respiratory distress. “But by the time the surge came, we had a better understanding of the scope of the situation,” she said.
Learning to be an attending
“They don’t teach you how to be an attending during residency,” Dr. Saladini-Aponte said. “At the beginning I wasn’t such a good teacher. I just wanted to prove myself and stay one step ahead of the residents. But as an academic hospitalist you have to listen to others. I learned to ask questions of the residents every morning, including how they were doing personally.”
Sometimes a visiting consultant would ask on the floor: “‘Where’s your attending?’” not recognizing Dr. Saladini-Aponte, fresh out of residency, filling that role. At times, she felt like a PGY-4 (postgraduate year 4). But she quickly grew into the attending role and was asked to be site coordinator for the mobilization of palliative medicine volunteers at Jacobi.
“We found ourselves having to make tough ethical decisions. Some patients, even if we provided a ventilator and maximum oxygen therapy, would still die. There were difficult discussions when we didn’t know if we had enough dialysis machines, or how to manage other limited resources. The hospital was saying: You decide, if there’s a high degree of certainty about the outcome. But we had never practiced medicine this way before,” she said.
“That’s why our hospital provided daily ethics meetings with our ethics council. There would be eight people sitting 6 feet apart in a conference room, all wearing masks. We’d talk about situations that were giving us trouble. Their role wasn’t to provide answers but to help us see the scope of the situation and the complexities,” she explained.
Dr. Saladini-Aponte said she has had many sleepless nights since the pandemic began. “Sometimes, I would come home from work and lie down on the floor and cry,” she said. “But we had so much support from volunteers helping our little hospitalist service of seven.” It was also important to keep up with the clinical information, and one of her coworkers created “cheat sheets” for the clinicians, regularly updated with the latest essential information on antibiotics, testing, and the like.
“At the peak, I was trying to read everything I could about the virus. I was just pulling myself in too many directions. I asked for help from my boyfriend to remind me not to log onto my computer when I came home from work,” she said. “One of my techniques for preventing burnout was just to avoid social media. I couldn’t deal with what was going on in the news. It just angered me. Even now, seeing people without masks makes me very uncomfortable.”
Organizing the crisis response
As chief value officer for NYCH+H, Hyung (Harry) Cho, MD, FACP, SFHM, typically focuses on issues of patient safety and overuse of medical treatments in the health system. But in the COVID-19 crisis, he found himself at the forefront of organizing its response. “We tried to provide support centrally and to standardize practice in how we test and treat,” he said.
“We were truly at the epicenter of the pandemic,” Dr. Cho said. “All of our hospitals had different experiences, and unique responses. But the system worked well.” Patients were transferred from the more overtaxed hospitals to Bellevue and other NYCH+H hospitals with spare beds. An emergency medical response structure was put in place, and every morning the system’s Tiger Team, with multidisciplinary personnel from administration, operations, logistics, and medical/technical specialists, would gather virtually to discuss needs across the system.
“It was a very open atmosphere and we asked people to report what was happening on the ground,” Dr. Cho said. “We started rapidly reviewing batches of 20 patients at a time for transfer in order to alleviate pressure in the most overtaxed ERs.”
NYCH+H also had to work through concerns about PPE, just like other U.S. hospitals. Treatment guidelines were changing by the day. Medical concerns were relayed at a rapid pace. Another priority was trying to limit unnecessary exposure for staff through a recommendation that only one clinician from a team would go into the room of an infected patient, unless another was absolutely needed.
The reality of public health
NYCH+H was created by the New York State Legislature in 1969 and rebranded in 2015. It includes a low- to no-cost health insurance plan called MetroPlus, along with outpatient centers, comprehensive case management, and social supports in the home.
“What people know about public health systems is that we typically are underresourced. That’s just the reality of public health,” Dr. Cho said. “We help the community, the underserved. The people who truly needed our help are also the ones who have been disproportionately affected by COVID-19. And that is where we really shine as a system.”
Dr. Cho lauded the performance of the health system’s frontline staff. “Watching them come together during the entire pandemic, and do their best every day, was truly inspiring,” he said. “But when they got to the peak, it really took an emotional toll on them.”
NYCH+H’s in-house staff support program, called Helping Healers Heal, was mobilized with specially trained teams at each of its 11 hospitals to provide peer-to-peer support, mental health expertise, and team-debriefing sessions to staff members following traumatic events. Support is provided both over the phone and in person on the floors, Dr. Cho said. “During the surge, everything was happening so quickly, there was no time to take a pause. Now, as we are able to catch our breath, that’s when they most need support.”
The hospitalists at NYCH+H hospitals intended to have goals-of-care conversations with all patients, but everyone was very busy – so having these conversations became harder and harder, Dr. Cho said. Recognizing limited staffing for the quadrupling of patients who needed palliative care at NYCH+H hospitals, he asked the medicine chairs about their palliative care needs and then used social media outreach to ask for help. The message went viral, attracting 413 volunteers from across the country. Sixty-seven telepalliative volunteers were put to work doing goals-of-care conversations remotely with inpatients and their families.1
Expediting transfers
For Ian Fagan, MD, a hospitalist and associate medical director for general internal medicine Inpatient Services at Bellevue Hospital in Manhattan, hospitalist shifts are a normal part of his job. But he had to give them up during the surge to focus on planning, management, and especially scheduling other doctors, with sufficient backups needed to cover last minute changes. Dr. Fagan did that by using the existing pool of hospitalist staff, physicians who were reassigned from other specialties, agency staff, military medical personnel, and volunteer doctors who flew in from around the country to help. He also worked 10- to 12-hour days for 36 consecutive days.
The impact of disparities in access to care in New York City was reflected in the greater demand for care in the hospitals in Brooklyn, Queens, and the Bronx. “With fewer patients and more hospital beds in Manhattan, we had the capacity to share our beds,” Dr. Fagan said. “It was so amazing to me how quickly we could move patients from one hospital to another. We started accepting up to 40 transfers a day. But hey, we were still really busy.”
Bellevue is the nation’s oldest public hospital. “We care for the homeless, for immigrants, and we don’t ask questions. That’s our mission. I’m so proud to work here, and so grateful,” Dr. Fagan said. “If someone is undocumented or without insurance, I will give them exactly the same care. We stepped up in a big way to care for people of New York, but we’ve always been there for them – and we were there for them during the COVID surge.”
The hospitals in the system also worked together in ways Dr. Fagan had never seen. “It helped to have a central command structure with a bird’s eye view from above the level of individual hospitals, to organize and see which hospitals could step up. It’s good to have the data to put it in perspective,” he said. The system also utilized a temporary low-acuity medical center set up by NYCH+H on Roosevelt Island, as well as field hospitals organized at the Jacob K. Javits Convention Center and the USTA Billie Jean King National Tennis Center.
“At Bellevue we tried to stay ready, with the ability to turn former hospital units that were being used as offices back to beds. We always had three units lined up that were fully ready to convert. For example, I was medical director of the preop clinic and one day they gave us 24 hours to pack everything and move out. Three days later, it was a 24-bed unit. We also built a more robust rapid response and code team,” he said.
“It was hard for me not to take hospitalist shifts, because my identity is being a doctor. I eventually came to terms with the importance of the role that I was doing every day. I felt I could protect my colleagues, and if they were having an emotional day, to give them the opportunity to talk to someone. I also did the onboarding, one-on-one, of the new doctors.”
As the crisis in New York City has ebbed, Dr. Fagan was recently able to again take a week of clinical service. “The first day back on the floor I felt that I had forgotten everything. But by the end of the day, I thought, ‘Okay, I do know how to do this, after all.’ Census is down here. It’s quiet. That’s good. We need it now,” he said.
“I think the hardest moment for me was when the head nurse on our trauma unit, Ernesto DeLeon, known to everybody here, died of COVID in our ICU in April,” Dr. Fagan said. When Mr. DeLeon died, 100 hospital personnel gathered in the halls outside the room to pay their respects. “There had been a palpable fear in our lives – and this showed us that the fear was real. Ernesto was the first person I knew well who died, who acquired COVID at work doing what we’re all doing. We haven’t lost any doctors yet, but when this nurse died, we allowed ourselves to realize that this is personal. In that moment, we needed to allow ourselves to be human.”
Joan Curcio, MD, associate director of medicine at Elmhurst Hospital, said Elmhurst was where the story started for New York City and for NYCH+H. “I trained here and have spent my entire career at this hospital. It came to feel like what a battleground must be like, with things coming at you from every direction,” she said. “It was overwhelming in ways I could not have foreseen. I had seen videos from Italy [an early COVID-19 epicenter], but until it happened here, it was just hard to process.”
Things started slowly, with a few patients with severe acute respiratory distress syndrome and a 5- to 7-day turnaround to get results of their viral infection tests. “By week 2, a greater number of patients from our clinics and testing sites were filtering through the emergency department. Then hundreds.”
The normal occupancy rate for the department of medicine at Elmhurst is 110-115%, which typically means full beds plus patients in the emergency department. “We started to grow to 160, then 180, and then a peak of 250% of occupancy. We took over a rehab surgery floor, then a 35-bed surgery and hospice floor, which went to full capacity just like that,” she said. The number of non–critical care service teams increased to 20, working with redeployed staff, volunteers, military, and agency personnel, while ICU beds increased from 20 to 105.
“We were dealing with a much higher acuity level and enduring emotional turmoil with families, trying to carve out time to call them after our shift was over,” Dr. Curcio explained. Elmhurst developed a call-in hotline and a daily call-out service for families. Technology was mobilized to provide video visits and new systems were designed for isolation and for PPE distribution and use.
“I just felt that I couldn’t get everything done. I felt continually overwhelmed, and it didn’t matter how much time I took. I never felt I was able to give enough to anybody in any area, which was hard to take,” Dr. Curcio said. “But I still felt a sense of purpose and that I was making a difference – thanks to lots of support from the central office.”
Patient volume at Elmhurst is now down, lower than Dr. Curcio has ever seen it. “One of the main issues right now, moving forward, is ‘how do we function in a post-crisis mode?’” she said. The process of transitioning back to non-COVID-19 care will be complex. “When we clear a floor and clean it to go back to being a cold [COVID-19-negative] unit, it’s a whole different level of cleaning that takes 7 days.”
One moment that was particularly jarring for Dr. Curcio occurred while she was giving a tour of the hospital to visiting military medical personnel. “We went into the emergency department and I turned around and looked into a shower room, which was full of body bags. They were all full.”
But the experience has also been inspiring. “People gave their all without complaint. We hospitalists, and all those recruited to act as hospitalists, essentially took responsibility for the COVID response,” she said. “This was, hopefully, the experience of a lifetime as a medical professional. I wouldn’t want to ever experience something as daunting as this again.”
Reference
1. Israilov S et al. National outreach of telepalliative medicine volunteers for a New York City safety net system COVID-19 pandemic response. J Pain Symptom Manag. 2020 May 29. doi: 10.1016/j.jpainsymman.2020.05.026.
New York City Health + Hospitals (NYCH+H), the country’s largest public health care system, encompasses 11 hospitals with 4,354 staffed acute beds during normal times. It serves as the safety net for 1.1 million of the 8.4 million residents of the most populous city in the United States, many of them uninsured, undocumented, covered by Medicaid, or otherwise disadvantaged.
At the very epicenter in the early days of the historic COVID-19 pandemic, NYCH+H transferred patients between its facilities, added medical and ICU beds by the hundreds, mobilized palliative care volunteers, harnessed telemedicine and a clinician hotline, and made other sweeping changes to ensure that the city’s public health system would be able to respond to demand at the peak of the surge. That peak hit in April, when an average of 9,000 new COVID-19 cases were being reported in the city every day.
Through it all, hospitalists have played critical roles in both planning for the system’s response and caring for severely ill COVID-19 patients. Their stories reflect both the unprecedented demands on the system and the dedication of frontline clinicians.
One of those, Carla Saladini-Aponte, MD, who just finished her residency in June 2019, found herself on the firing line in March 2020 as an attending physician at 457-bed NYCH+H/Jacobi Hospital in the Bronx. “I have experienced so much in my first year on the job, dealing with a disease that we’ve never seen before,” she said. “We didn’t grasp the extent of the COVID crisis in the beginning, so we were emotionally unprepared when it first hit.”
Starting on March 30, NYCH+H administration mobilized a centralized incident command structure to coordinate response systemwide to a rapidly changing situation.
Two weeks later Jacobi was a COVID-19 hospital, top to bottom, with its medical ICU beds increased from 12 to more than 100. By mid-April, Dr. Saladini-Aponte’s team, one of 11 medical teams in the hospital, had 26 patients, all of them with COVID-19. There was not a consensus in the early days on how to manage patients with severe respiratory distress. “But by the time the surge came, we had a better understanding of the scope of the situation,” she said.
Learning to be an attending
“They don’t teach you how to be an attending during residency,” Dr. Saladini-Aponte said. “At the beginning I wasn’t such a good teacher. I just wanted to prove myself and stay one step ahead of the residents. But as an academic hospitalist you have to listen to others. I learned to ask questions of the residents every morning, including how they were doing personally.”
Sometimes a visiting consultant would ask on the floor: “‘Where’s your attending?’” not recognizing Dr. Saladini-Aponte, fresh out of residency, filling that role. At times, she felt like a PGY-4 (postgraduate year 4). But she quickly grew into the attending role and was asked to be site coordinator for the mobilization of palliative medicine volunteers at Jacobi.
“We found ourselves having to make tough ethical decisions. Some patients, even if we provided a ventilator and maximum oxygen therapy, would still die. There were difficult discussions when we didn’t know if we had enough dialysis machines, or how to manage other limited resources. The hospital was saying: You decide, if there’s a high degree of certainty about the outcome. But we had never practiced medicine this way before,” she said.
“That’s why our hospital provided daily ethics meetings with our ethics council. There would be eight people sitting 6 feet apart in a conference room, all wearing masks. We’d talk about situations that were giving us trouble. Their role wasn’t to provide answers but to help us see the scope of the situation and the complexities,” she explained.
Dr. Saladini-Aponte said she has had many sleepless nights since the pandemic began. “Sometimes, I would come home from work and lie down on the floor and cry,” she said. “But we had so much support from volunteers helping our little hospitalist service of seven.” It was also important to keep up with the clinical information, and one of her coworkers created “cheat sheets” for the clinicians, regularly updated with the latest essential information on antibiotics, testing, and the like.
“At the peak, I was trying to read everything I could about the virus. I was just pulling myself in too many directions. I asked for help from my boyfriend to remind me not to log onto my computer when I came home from work,” she said. “One of my techniques for preventing burnout was just to avoid social media. I couldn’t deal with what was going on in the news. It just angered me. Even now, seeing people without masks makes me very uncomfortable.”
Organizing the crisis response
As chief value officer for NYCH+H, Hyung (Harry) Cho, MD, FACP, SFHM, typically focuses on issues of patient safety and overuse of medical treatments in the health system. But in the COVID-19 crisis, he found himself at the forefront of organizing its response. “We tried to provide support centrally and to standardize practice in how we test and treat,” he said.
“We were truly at the epicenter of the pandemic,” Dr. Cho said. “All of our hospitals had different experiences, and unique responses. But the system worked well.” Patients were transferred from the more overtaxed hospitals to Bellevue and other NYCH+H hospitals with spare beds. An emergency medical response structure was put in place, and every morning the system’s Tiger Team, with multidisciplinary personnel from administration, operations, logistics, and medical/technical specialists, would gather virtually to discuss needs across the system.
“It was a very open atmosphere and we asked people to report what was happening on the ground,” Dr. Cho said. “We started rapidly reviewing batches of 20 patients at a time for transfer in order to alleviate pressure in the most overtaxed ERs.”
NYCH+H also had to work through concerns about PPE, just like other U.S. hospitals. Treatment guidelines were changing by the day. Medical concerns were relayed at a rapid pace. Another priority was trying to limit unnecessary exposure for staff through a recommendation that only one clinician from a team would go into the room of an infected patient, unless another was absolutely needed.
The reality of public health
NYCH+H was created by the New York State Legislature in 1969 and rebranded in 2015. It includes a low- to no-cost health insurance plan called MetroPlus, along with outpatient centers, comprehensive case management, and social supports in the home.
“What people know about public health systems is that we typically are underresourced. That’s just the reality of public health,” Dr. Cho said. “We help the community, the underserved. The people who truly needed our help are also the ones who have been disproportionately affected by COVID-19. And that is where we really shine as a system.”
Dr. Cho lauded the performance of the health system’s frontline staff. “Watching them come together during the entire pandemic, and do their best every day, was truly inspiring,” he said. “But when they got to the peak, it really took an emotional toll on them.”
NYCH+H’s in-house staff support program, called Helping Healers Heal, was mobilized with specially trained teams at each of its 11 hospitals to provide peer-to-peer support, mental health expertise, and team-debriefing sessions to staff members following traumatic events. Support is provided both over the phone and in person on the floors, Dr. Cho said. “During the surge, everything was happening so quickly, there was no time to take a pause. Now, as we are able to catch our breath, that’s when they most need support.”
The hospitalists at NYCH+H hospitals intended to have goals-of-care conversations with all patients, but everyone was very busy – so having these conversations became harder and harder, Dr. Cho said. Recognizing limited staffing for the quadrupling of patients who needed palliative care at NYCH+H hospitals, he asked the medicine chairs about their palliative care needs and then used social media outreach to ask for help. The message went viral, attracting 413 volunteers from across the country. Sixty-seven telepalliative volunteers were put to work doing goals-of-care conversations remotely with inpatients and their families.1
Expediting transfers
For Ian Fagan, MD, a hospitalist and associate medical director for general internal medicine Inpatient Services at Bellevue Hospital in Manhattan, hospitalist shifts are a normal part of his job. But he had to give them up during the surge to focus on planning, management, and especially scheduling other doctors, with sufficient backups needed to cover last minute changes. Dr. Fagan did that by using the existing pool of hospitalist staff, physicians who were reassigned from other specialties, agency staff, military medical personnel, and volunteer doctors who flew in from around the country to help. He also worked 10- to 12-hour days for 36 consecutive days.
The impact of disparities in access to care in New York City was reflected in the greater demand for care in the hospitals in Brooklyn, Queens, and the Bronx. “With fewer patients and more hospital beds in Manhattan, we had the capacity to share our beds,” Dr. Fagan said. “It was so amazing to me how quickly we could move patients from one hospital to another. We started accepting up to 40 transfers a day. But hey, we were still really busy.”
Bellevue is the nation’s oldest public hospital. “We care for the homeless, for immigrants, and we don’t ask questions. That’s our mission. I’m so proud to work here, and so grateful,” Dr. Fagan said. “If someone is undocumented or without insurance, I will give them exactly the same care. We stepped up in a big way to care for people of New York, but we’ve always been there for them – and we were there for them during the COVID surge.”
The hospitals in the system also worked together in ways Dr. Fagan had never seen. “It helped to have a central command structure with a bird’s eye view from above the level of individual hospitals, to organize and see which hospitals could step up. It’s good to have the data to put it in perspective,” he said. The system also utilized a temporary low-acuity medical center set up by NYCH+H on Roosevelt Island, as well as field hospitals organized at the Jacob K. Javits Convention Center and the USTA Billie Jean King National Tennis Center.
“At Bellevue we tried to stay ready, with the ability to turn former hospital units that were being used as offices back to beds. We always had three units lined up that were fully ready to convert. For example, I was medical director of the preop clinic and one day they gave us 24 hours to pack everything and move out. Three days later, it was a 24-bed unit. We also built a more robust rapid response and code team,” he said.
“It was hard for me not to take hospitalist shifts, because my identity is being a doctor. I eventually came to terms with the importance of the role that I was doing every day. I felt I could protect my colleagues, and if they were having an emotional day, to give them the opportunity to talk to someone. I also did the onboarding, one-on-one, of the new doctors.”
As the crisis in New York City has ebbed, Dr. Fagan was recently able to again take a week of clinical service. “The first day back on the floor I felt that I had forgotten everything. But by the end of the day, I thought, ‘Okay, I do know how to do this, after all.’ Census is down here. It’s quiet. That’s good. We need it now,” he said.
“I think the hardest moment for me was when the head nurse on our trauma unit, Ernesto DeLeon, known to everybody here, died of COVID in our ICU in April,” Dr. Fagan said. When Mr. DeLeon died, 100 hospital personnel gathered in the halls outside the room to pay their respects. “There had been a palpable fear in our lives – and this showed us that the fear was real. Ernesto was the first person I knew well who died, who acquired COVID at work doing what we’re all doing. We haven’t lost any doctors yet, but when this nurse died, we allowed ourselves to realize that this is personal. In that moment, we needed to allow ourselves to be human.”
Joan Curcio, MD, associate director of medicine at Elmhurst Hospital, said Elmhurst was where the story started for New York City and for NYCH+H. “I trained here and have spent my entire career at this hospital. It came to feel like what a battleground must be like, with things coming at you from every direction,” she said. “It was overwhelming in ways I could not have foreseen. I had seen videos from Italy [an early COVID-19 epicenter], but until it happened here, it was just hard to process.”
Things started slowly, with a few patients with severe acute respiratory distress syndrome and a 5- to 7-day turnaround to get results of their viral infection tests. “By week 2, a greater number of patients from our clinics and testing sites were filtering through the emergency department. Then hundreds.”
The normal occupancy rate for the department of medicine at Elmhurst is 110-115%, which typically means full beds plus patients in the emergency department. “We started to grow to 160, then 180, and then a peak of 250% of occupancy. We took over a rehab surgery floor, then a 35-bed surgery and hospice floor, which went to full capacity just like that,” she said. The number of non–critical care service teams increased to 20, working with redeployed staff, volunteers, military, and agency personnel, while ICU beds increased from 20 to 105.
“We were dealing with a much higher acuity level and enduring emotional turmoil with families, trying to carve out time to call them after our shift was over,” Dr. Curcio explained. Elmhurst developed a call-in hotline and a daily call-out service for families. Technology was mobilized to provide video visits and new systems were designed for isolation and for PPE distribution and use.
“I just felt that I couldn’t get everything done. I felt continually overwhelmed, and it didn’t matter how much time I took. I never felt I was able to give enough to anybody in any area, which was hard to take,” Dr. Curcio said. “But I still felt a sense of purpose and that I was making a difference – thanks to lots of support from the central office.”
Patient volume at Elmhurst is now down, lower than Dr. Curcio has ever seen it. “One of the main issues right now, moving forward, is ‘how do we function in a post-crisis mode?’” she said. The process of transitioning back to non-COVID-19 care will be complex. “When we clear a floor and clean it to go back to being a cold [COVID-19-negative] unit, it’s a whole different level of cleaning that takes 7 days.”
One moment that was particularly jarring for Dr. Curcio occurred while she was giving a tour of the hospital to visiting military medical personnel. “We went into the emergency department and I turned around and looked into a shower room, which was full of body bags. They were all full.”
But the experience has also been inspiring. “People gave their all without complaint. We hospitalists, and all those recruited to act as hospitalists, essentially took responsibility for the COVID response,” she said. “This was, hopefully, the experience of a lifetime as a medical professional. I wouldn’t want to ever experience something as daunting as this again.”
Reference
1. Israilov S et al. National outreach of telepalliative medicine volunteers for a New York City safety net system COVID-19 pandemic response. J Pain Symptom Manag. 2020 May 29. doi: 10.1016/j.jpainsymman.2020.05.026.
Being a pediatric hospitalist during the COVID-19 pandemic
“Times of great calamity and confusion have been productive for the greatest minds. The purest ore is produced from the hottest furnace. The brightest thunderbolt is elicited from the darkest storm.” – Charles Caleb Colton
I walk inside the pediatric unit of our hospital, only to be welcomed by an eerie silence. There are a handful of nurses at the nursing station, faces covered with masks sitting 6 feet apart and quietly working on their computers. The resident work lounge also depicts a similar picture of emptiness. Just over a month ago, these halls were bustling with children, parents, consultants, and a host of ancillary staff. I recall times in which I was running around from one patient room to another talking to families and attending to patient needs. For the past 2 months I have often spent hours alone in my office waiting to see a patient. This is the new norm for many of us.
Across the board in hospitals, pediatric census has dropped since the start of the COVID-19 pandemic. Reasons for these are nonspecific but may include fear among parents of “exposure” to the virus by bringing their sick children to the hospital to get evaluated for other concerns. A few patients that we have seen in our hospital are sicker when they have arrived because their parents avoided seeking medical care earlier, plagued by the same fear. Social distancing and school closure have also limited the amount of infectious diseases going around, which are responsible for a bulk of pediatric admissions.
While many of us are still coming in to see the limited number of patients we have, we are not in the true sense frontline providers during this pandemic. There have been limited cases of COVID-19 in children, most of which – fortunately – present with mild symptoms. Although multisystem inflammatory syndrome in children (MIS-C) is a new disease that COVID-19 has brought us closer to, many of us have yet to see our first case because of its rarity.
I have read through the news daily in the past few months to find many adult provider physicians succumbing to COVID-19 and felt a pang of guilt. My social media is full of heartbreaking stories as adult hospitalists are having difficult conversations with families and supporting them through this unknown territory, often sacrificing their own safety. I feel so proud of them and my profession. My heart tells me, though, I personally may not be living up to the true calling I was expected to have as a physician.
As pediatric hospitalists, while we sit and wait for this pandemic to pass, we have been ruminating on and anxious about our future. As census drops, there is a financial strain that many of us are feeling. Job cuts and furloughing of health care workers in our surroundings leave us with a sense of insecurity and low morale. Many small inpatient pediatric units have had to be shut down temporarily either so they could be used for adult patients or because of lack of pediatric patients. Limiting staffing to avoid exposure and cohorting providers has also been a challenge.
A big question that has risen in these times is how to ensure productivity and stay useful while at the same time being prepared for the unknown that lies ahead. The economics of medicine is staring hard at our years of hard work, questioning the need for our specialty in the first place.
In smaller community settings, the closure of pediatric units has put an additional strain on the overall framework of the community, parents, and referring primary care providers. With the absence of local resources, children who have needed care have had to be transferred to bigger referral centers that are still taking care of pediatric patients. On one end of the spectrum there is concern for pediatric inpatient units not being productive enough for the hospital, but that coexists with a worry that, as we pass through this pandemic, we could see more hospitalizations for vaccine-preventable illnesses, child abuse/medical neglect, and respiratory syncytial virus plus COVID.
The question remains about how best to cope and use this time of uncertainty to be productive and prepare for the worst. A few solutions and suggestions are highlighted below.
- Helping adult providers: Many pediatric hospitalist colleagues in highly affected states have filled the increasing need for clinicians and taken care of adult patients. As pediatric units have closed, providers have continued to offer care where it is needed. Pediatric hospitalists have used this time to take urgent refresher courses in advanced cardiac life support and adult critical care. In states that are not as severely hit, many pediatric hospitalists have utilized this time to plan and prepare protocols for the future as information continues coming in regarding MIS-C and COVID-19 in pediatric patients.
- Use of telemedicine: With the ease in restrictions for use of telemedicine in many states, pediatric hospitalists can consider using it to restructure their staffing model whenever feasible. This can help in cohorting and allowing high risk and quarantined providers to work from home. This model simultaneously provides opportunities for pediatric hospitalists to continue providing their services, while at the same time decreasing financial burden on their institution.
- Reaching out to the community: Engaging with the community during these times can help ensure services and options remain available to our referral providers and patients for pediatric services. Information about COVID-19 can be widely disseminated. We can also play our part by continuing to encourage parents in our maximum capacity to obtain care for their children when needed and to not avoid the hospital because of fears of exposure.
- Supporting each other: There is no doubt that these times are unsettling for the pediatric hospitalist community, and the uncertainty that surrounds us can feel crippling. Strong team building is imperative in these times. While we may not be frequently meeting in work lounges and sharing meals, a good sense of support and camaraderie will go a long way in building morale for the future. Seeking mental health resources if needed is essential for us and should not be looked at with shame or guilt. This is something that many of us have never seen before, and it is okay to ask for help. Seeking help is and always will be a sign of strength.
Today, as I envision myself walking in the hospital on the other side of this pandemic I see a cheerful pediatric unit, smiling faces without masks, my 3-year-old patient cruising around the hallways in a toy car, our therapy dog walking around bringing joy to many, and many healthy patients feeling better and ready to go home. A time when we are not scared to hug each other, shake hands, or share emotion. When our teams are stronger and more well bonded. A time when parents are not scared to bring their sick children to the hospital. Will it be many months before this happens? I don’t know. But I do know that the children I take care of are known for their resilience. I will live up to them today by practicing the same.
Dr. Fatima is a pediatric hospitalist at Wesley Children’s Hospital and assistant professor of pediatrics at Kansas University School of Medicine, both in Wichita. Her research interests include medical errors, medical education, and high-value care.
“Times of great calamity and confusion have been productive for the greatest minds. The purest ore is produced from the hottest furnace. The brightest thunderbolt is elicited from the darkest storm.” – Charles Caleb Colton
I walk inside the pediatric unit of our hospital, only to be welcomed by an eerie silence. There are a handful of nurses at the nursing station, faces covered with masks sitting 6 feet apart and quietly working on their computers. The resident work lounge also depicts a similar picture of emptiness. Just over a month ago, these halls were bustling with children, parents, consultants, and a host of ancillary staff. I recall times in which I was running around from one patient room to another talking to families and attending to patient needs. For the past 2 months I have often spent hours alone in my office waiting to see a patient. This is the new norm for many of us.
Across the board in hospitals, pediatric census has dropped since the start of the COVID-19 pandemic. Reasons for these are nonspecific but may include fear among parents of “exposure” to the virus by bringing their sick children to the hospital to get evaluated for other concerns. A few patients that we have seen in our hospital are sicker when they have arrived because their parents avoided seeking medical care earlier, plagued by the same fear. Social distancing and school closure have also limited the amount of infectious diseases going around, which are responsible for a bulk of pediatric admissions.
While many of us are still coming in to see the limited number of patients we have, we are not in the true sense frontline providers during this pandemic. There have been limited cases of COVID-19 in children, most of which – fortunately – present with mild symptoms. Although multisystem inflammatory syndrome in children (MIS-C) is a new disease that COVID-19 has brought us closer to, many of us have yet to see our first case because of its rarity.
I have read through the news daily in the past few months to find many adult provider physicians succumbing to COVID-19 and felt a pang of guilt. My social media is full of heartbreaking stories as adult hospitalists are having difficult conversations with families and supporting them through this unknown territory, often sacrificing their own safety. I feel so proud of them and my profession. My heart tells me, though, I personally may not be living up to the true calling I was expected to have as a physician.
As pediatric hospitalists, while we sit and wait for this pandemic to pass, we have been ruminating on and anxious about our future. As census drops, there is a financial strain that many of us are feeling. Job cuts and furloughing of health care workers in our surroundings leave us with a sense of insecurity and low morale. Many small inpatient pediatric units have had to be shut down temporarily either so they could be used for adult patients or because of lack of pediatric patients. Limiting staffing to avoid exposure and cohorting providers has also been a challenge.
A big question that has risen in these times is how to ensure productivity and stay useful while at the same time being prepared for the unknown that lies ahead. The economics of medicine is staring hard at our years of hard work, questioning the need for our specialty in the first place.
In smaller community settings, the closure of pediatric units has put an additional strain on the overall framework of the community, parents, and referring primary care providers. With the absence of local resources, children who have needed care have had to be transferred to bigger referral centers that are still taking care of pediatric patients. On one end of the spectrum there is concern for pediatric inpatient units not being productive enough for the hospital, but that coexists with a worry that, as we pass through this pandemic, we could see more hospitalizations for vaccine-preventable illnesses, child abuse/medical neglect, and respiratory syncytial virus plus COVID.
The question remains about how best to cope and use this time of uncertainty to be productive and prepare for the worst. A few solutions and suggestions are highlighted below.
- Helping adult providers: Many pediatric hospitalist colleagues in highly affected states have filled the increasing need for clinicians and taken care of adult patients. As pediatric units have closed, providers have continued to offer care where it is needed. Pediatric hospitalists have used this time to take urgent refresher courses in advanced cardiac life support and adult critical care. In states that are not as severely hit, many pediatric hospitalists have utilized this time to plan and prepare protocols for the future as information continues coming in regarding MIS-C and COVID-19 in pediatric patients.
- Use of telemedicine: With the ease in restrictions for use of telemedicine in many states, pediatric hospitalists can consider using it to restructure their staffing model whenever feasible. This can help in cohorting and allowing high risk and quarantined providers to work from home. This model simultaneously provides opportunities for pediatric hospitalists to continue providing their services, while at the same time decreasing financial burden on their institution.
- Reaching out to the community: Engaging with the community during these times can help ensure services and options remain available to our referral providers and patients for pediatric services. Information about COVID-19 can be widely disseminated. We can also play our part by continuing to encourage parents in our maximum capacity to obtain care for their children when needed and to not avoid the hospital because of fears of exposure.
- Supporting each other: There is no doubt that these times are unsettling for the pediatric hospitalist community, and the uncertainty that surrounds us can feel crippling. Strong team building is imperative in these times. While we may not be frequently meeting in work lounges and sharing meals, a good sense of support and camaraderie will go a long way in building morale for the future. Seeking mental health resources if needed is essential for us and should not be looked at with shame or guilt. This is something that many of us have never seen before, and it is okay to ask for help. Seeking help is and always will be a sign of strength.
Today, as I envision myself walking in the hospital on the other side of this pandemic I see a cheerful pediatric unit, smiling faces without masks, my 3-year-old patient cruising around the hallways in a toy car, our therapy dog walking around bringing joy to many, and many healthy patients feeling better and ready to go home. A time when we are not scared to hug each other, shake hands, or share emotion. When our teams are stronger and more well bonded. A time when parents are not scared to bring their sick children to the hospital. Will it be many months before this happens? I don’t know. But I do know that the children I take care of are known for their resilience. I will live up to them today by practicing the same.
Dr. Fatima is a pediatric hospitalist at Wesley Children’s Hospital and assistant professor of pediatrics at Kansas University School of Medicine, both in Wichita. Her research interests include medical errors, medical education, and high-value care.
“Times of great calamity and confusion have been productive for the greatest minds. The purest ore is produced from the hottest furnace. The brightest thunderbolt is elicited from the darkest storm.” – Charles Caleb Colton
I walk inside the pediatric unit of our hospital, only to be welcomed by an eerie silence. There are a handful of nurses at the nursing station, faces covered with masks sitting 6 feet apart and quietly working on their computers. The resident work lounge also depicts a similar picture of emptiness. Just over a month ago, these halls were bustling with children, parents, consultants, and a host of ancillary staff. I recall times in which I was running around from one patient room to another talking to families and attending to patient needs. For the past 2 months I have often spent hours alone in my office waiting to see a patient. This is the new norm for many of us.
Across the board in hospitals, pediatric census has dropped since the start of the COVID-19 pandemic. Reasons for these are nonspecific but may include fear among parents of “exposure” to the virus by bringing their sick children to the hospital to get evaluated for other concerns. A few patients that we have seen in our hospital are sicker when they have arrived because their parents avoided seeking medical care earlier, plagued by the same fear. Social distancing and school closure have also limited the amount of infectious diseases going around, which are responsible for a bulk of pediatric admissions.
While many of us are still coming in to see the limited number of patients we have, we are not in the true sense frontline providers during this pandemic. There have been limited cases of COVID-19 in children, most of which – fortunately – present with mild symptoms. Although multisystem inflammatory syndrome in children (MIS-C) is a new disease that COVID-19 has brought us closer to, many of us have yet to see our first case because of its rarity.
I have read through the news daily in the past few months to find many adult provider physicians succumbing to COVID-19 and felt a pang of guilt. My social media is full of heartbreaking stories as adult hospitalists are having difficult conversations with families and supporting them through this unknown territory, often sacrificing their own safety. I feel so proud of them and my profession. My heart tells me, though, I personally may not be living up to the true calling I was expected to have as a physician.
As pediatric hospitalists, while we sit and wait for this pandemic to pass, we have been ruminating on and anxious about our future. As census drops, there is a financial strain that many of us are feeling. Job cuts and furloughing of health care workers in our surroundings leave us with a sense of insecurity and low morale. Many small inpatient pediatric units have had to be shut down temporarily either so they could be used for adult patients or because of lack of pediatric patients. Limiting staffing to avoid exposure and cohorting providers has also been a challenge.
A big question that has risen in these times is how to ensure productivity and stay useful while at the same time being prepared for the unknown that lies ahead. The economics of medicine is staring hard at our years of hard work, questioning the need for our specialty in the first place.
In smaller community settings, the closure of pediatric units has put an additional strain on the overall framework of the community, parents, and referring primary care providers. With the absence of local resources, children who have needed care have had to be transferred to bigger referral centers that are still taking care of pediatric patients. On one end of the spectrum there is concern for pediatric inpatient units not being productive enough for the hospital, but that coexists with a worry that, as we pass through this pandemic, we could see more hospitalizations for vaccine-preventable illnesses, child abuse/medical neglect, and respiratory syncytial virus plus COVID.
The question remains about how best to cope and use this time of uncertainty to be productive and prepare for the worst. A few solutions and suggestions are highlighted below.
- Helping adult providers: Many pediatric hospitalist colleagues in highly affected states have filled the increasing need for clinicians and taken care of adult patients. As pediatric units have closed, providers have continued to offer care where it is needed. Pediatric hospitalists have used this time to take urgent refresher courses in advanced cardiac life support and adult critical care. In states that are not as severely hit, many pediatric hospitalists have utilized this time to plan and prepare protocols for the future as information continues coming in regarding MIS-C and COVID-19 in pediatric patients.
- Use of telemedicine: With the ease in restrictions for use of telemedicine in many states, pediatric hospitalists can consider using it to restructure their staffing model whenever feasible. This can help in cohorting and allowing high risk and quarantined providers to work from home. This model simultaneously provides opportunities for pediatric hospitalists to continue providing their services, while at the same time decreasing financial burden on their institution.
- Reaching out to the community: Engaging with the community during these times can help ensure services and options remain available to our referral providers and patients for pediatric services. Information about COVID-19 can be widely disseminated. We can also play our part by continuing to encourage parents in our maximum capacity to obtain care for their children when needed and to not avoid the hospital because of fears of exposure.
- Supporting each other: There is no doubt that these times are unsettling for the pediatric hospitalist community, and the uncertainty that surrounds us can feel crippling. Strong team building is imperative in these times. While we may not be frequently meeting in work lounges and sharing meals, a good sense of support and camaraderie will go a long way in building morale for the future. Seeking mental health resources if needed is essential for us and should not be looked at with shame or guilt. This is something that many of us have never seen before, and it is okay to ask for help. Seeking help is and always will be a sign of strength.
Today, as I envision myself walking in the hospital on the other side of this pandemic I see a cheerful pediatric unit, smiling faces without masks, my 3-year-old patient cruising around the hallways in a toy car, our therapy dog walking around bringing joy to many, and many healthy patients feeling better and ready to go home. A time when we are not scared to hug each other, shake hands, or share emotion. When our teams are stronger and more well bonded. A time when parents are not scared to bring their sick children to the hospital. Will it be many months before this happens? I don’t know. But I do know that the children I take care of are known for their resilience. I will live up to them today by practicing the same.
Dr. Fatima is a pediatric hospitalist at Wesley Children’s Hospital and assistant professor of pediatrics at Kansas University School of Medicine, both in Wichita. Her research interests include medical errors, medical education, and high-value care.
Serum cortisol testing for suspected adrenal insufficiency
Evaluating the hospitalized adult patient
Case
A 45-year-old female with moderate persistent asthma is admitted for right lower extremity cellulitis. She has hyponatremia with a sodium of 129 mEq/L and reports a history of longstanding fatigue and lightheadedness on standing. An early morning serum cortisol was 10 mcg/dL, normal per the reference range for the laboratory. Has adrenal insufficiency been excluded in this patient?
Overview
Adrenal insufficiency (AI) is a clinical syndrome characterized by a deficiency of cortisol. Presentation may range from nonspecific symptoms such as fatigue, weight loss, and gastrointestinal concerns to a fulminant adrenal crisis with severe weakness and hypotension (Table 1). The diagnosis of AI is commonly delayed, negatively impacting patients’ quality of life and risking dangerous complications.1,2
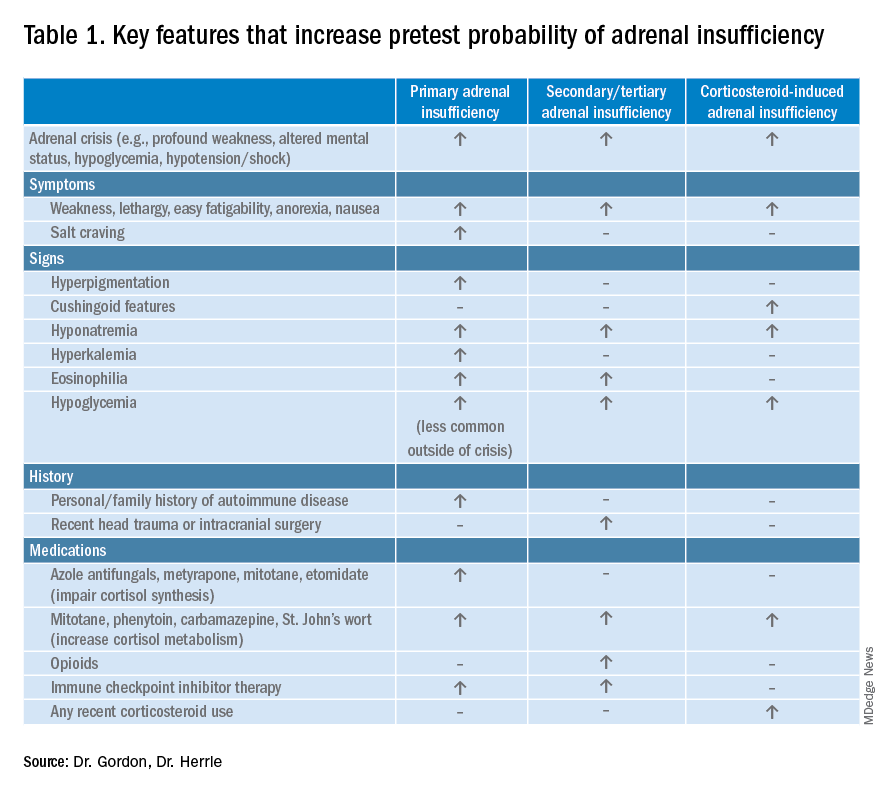
AI can occur due to diseases of the adrenal glands themselves (primary) or impairment of adrenocorticotropin (ACTH) secretion from the pituitary (secondary) or corticotropin-releasing hormone (CRH) secretion from the hypothalamus (tertiary). In the hospital setting, causes of primary AI may include autoimmune disease, infection, metastatic disease, hemorrhage, and adverse medication effects. Secondary and tertiary AI would be of particular concern for patients with traumatic brain injuries or pituitary surgery, but also are seen commonly as a result of adverse medication effects in the hospitalized patient, notably opioids and corticosteroids through suppression the hypothalamic-pituitary-adrenal (HPA) axis and immune checkpoint inhibitors via autoimmune hypophysitis.
Testing for AI in the hospitalized patient presents a host of challenges. Among these are the variability in presentation of different types of AI, high rates of exogenous corticosteroid use, the impact of critical illness on the HPA axis, medical illness altering protein binding of serum cortisol, interfering medications, the variation in assays used by laboratories, and the logistical challenges of obtaining appropriately timed phlebotomy.2,3
Cortisol testing
An intact HPA axis results in ACTH-dependent cortisol release from the adrenal glands. Cortisol secretion exhibits circadian rhythm, with the highest levels in the early morning (6 a.m. to 8 a.m.) and the lowest at night (12 a.m.). It also is pulsatile, which may explain the range of “normal” morning serum cortisol observed in a study of healthy volunteers.3 Note that serum cortisol is equivalent to plasma cortisol in current immunoassays, and will henceforth be called “cortisol” in this paper.3
There are instances when morning cortisol may strongly suggest a diagnosis of AI on its own. A meta-analysis found that morning cortisol of < 5 mcg/dL predicts AI and morning cortisol of > 13 mcg/dL ruled out AI.4 The Endocrine Society of America favors dynamic assessment of adrenal function for most patients.2
Historically, the gold standard for assessing dynamic adrenal function has been the insulin tolerance test (ITT), whereby cortisol is measured after inducing hypoglycemia to a blood glucose < 35 mg/dL. ITT is logistically difficult and poses some risk to the patient. The corticotropin (or cosyntropin) stimulation test (CST), in which a supraphysiologic dose of a synthetic ACTH analog is administered parenterally to a patient and resultant cortisol levels are measured, has been validated against the ITT and is generally preferred.5 CST is used to diagnose primary AI as well as chronic secondary and tertiary AI, given that longstanding lack of ACTH stimulation causes atrophy of the adrenal glands. The sensitivity for secondary and tertiary AI is likely lower than primary AI especially in acute onset of disease.6,7
In performance of the CST a baseline cortisol and ACTH are obtained, with subsequent cortisol testing at 30 and/or 60 minutes after administration of the ACTH analog (Figure 1). Currently, there is no consensus for which time point is preferred, but the 30-minute test is more sensitive for AI and the 60-minute test is more specific.2,7,8
CST is typically performed using a “standard high dose” of 250 mcg of the ACTH analog. There has been interest in the use of a “low-dose” 1 mcg test, which is closer to normal physiologic stimulation of the adrenal glands and may have better sensitivity for early secondary or partial AI. However, the 250-mcg dose is easier to prepare and has fewer technical pitfalls in administration as well as a lower risk for false positive testing. At this point the data do not compellingly favor the use of low-dose CST testing in general practice.2,3,7
Clinical decision making
Diagnostic evaluation should be guided by the likelihood of the disease (i.e., the pretest probability) (Figure 1). Begin with a review of the patient’s signs and symptoms, medical and family history, and medications with special consideration for opioids, exogenous steroids, and immune checkpoint inhibitors (Table 1).
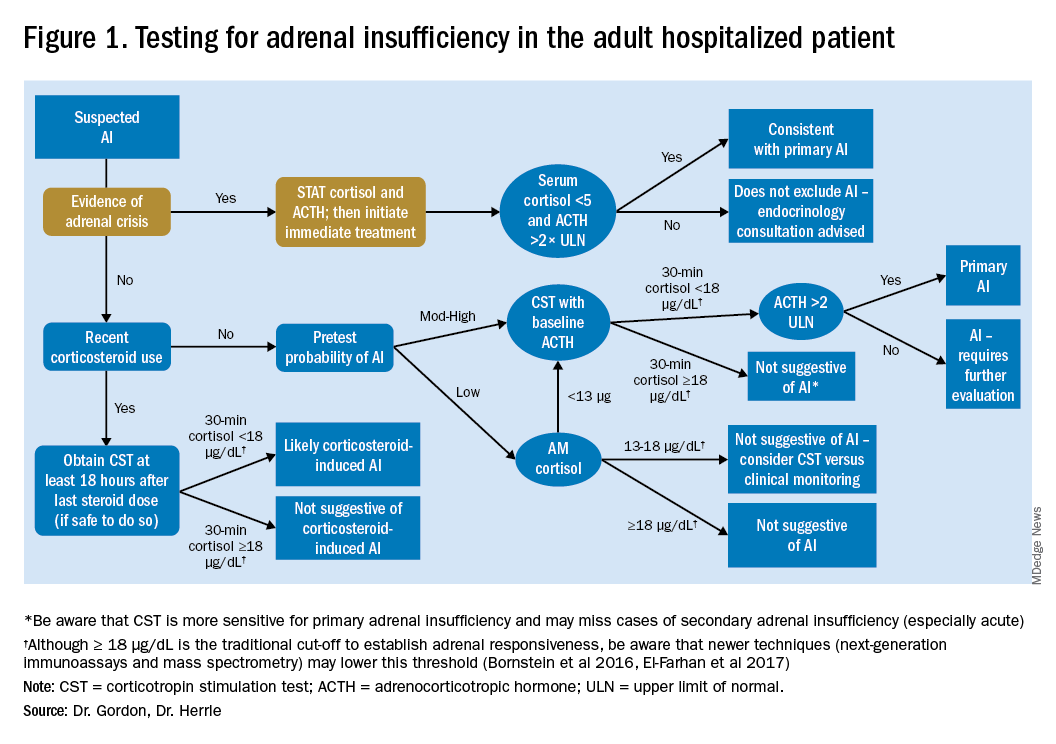
For patients with low pretest probability for AI, morning cortisol and ACTH is a reasonable first test (Figure 1). A cortisol value of 18 mcg/dL or greater does not support AI and no further testing is needed.2 Patients with morning cortisol of 13-18 mcg/dL could be followed clinically or could undergo further testing in the inpatient environment with CST, depending upon the clinical scenario.4 Patients with serum cortisol of <13 mcg/dL warrant CST.
For patients with moderate to high pretest probability for AI, we recommend initial testing with CST. While the results of high-dose CST are not necessarily impacted by time of day, if an a.m. cortisol has not yet been obtained and it is logistically feasible to do so, performing CST in the morning will provide the most useful data for clinical interpretation.
For patients presenting with possible adrenal crisis, it is essential not to delay treatment. In these patients, obtain a cortisol paired with ACTH and initiate treatment immediately. Further testing can be deferred until the time the patient is stable.2
Potential pitfalls
Interpreting cortisol requires awareness of multiple conditions that could directly impact the results.2,3 (Table 2).
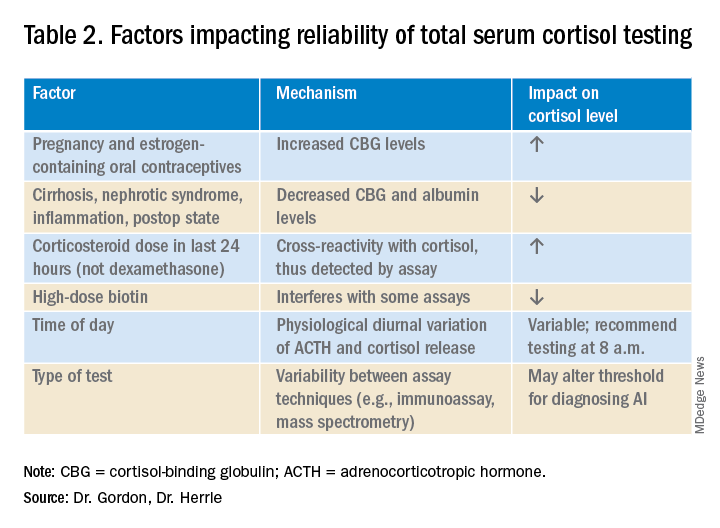
Currently available assays measure “total cortisol,” most of which is protein bound (cortisol-binding globulin as well as albumin). Therefore, conditions that lower serum protein (e.g., nephrotic syndrome, liver disease, inflammation) will lower the measured cortisol. Conversely, conditions that increase serum protein (e.g., estrogen excess in pregnancy and oral contraceptive use) will increase the measured cortisol.2,3
It is also important to recognize that existing immunoassay testing techniques informed the established cut-off for exclusion of AI at 18 mcg/dL. With newer immunoassays and emerging liquid chromatography/tandem mass spectrometry, this cut-off may be lowered; thus the assay should be confirmed with the performing laboratory. There is emerging evidence that serum or plasma free cortisol and salivary cortisol testing for AI may be useful in certain cases, but these techniques are not yet widespread or included in clinical practice guidelines.2,3,7
Population focus: Patients on exogenous steroids
Exogenous corticosteroids suppress the HPA axis via negative inhibition of CRH and ACTH release, often resulting in low endogenous cortisol levels which may or may not reflect true loss of adrenal function. In addition, many corticosteroids will be detected by standard serum cortisol tests that rely on immunoassays. For this reason, cortisol measurement and CST should be done at least 18-24 hours after the last dose of exogenous steroids.
Although the focus has been on higher doses and longer courses of steroids (e.g., chronic use of ≥ 5 mg prednisone daily, or ≥ 20 mg prednisone daily for > 3 weeks), there is increasing evidence that lower doses, shorter courses, and alternate routes (e.g., inhaled, intra-articular) can result in biochemical and clinical evidence of AI.9 Thus, a thorough history and exam should be obtained to determine all recent corticosteroid exposure and cushingoid features.
Application of the data to the case
To effectively assess the patient for adrenal insufficiency, we need additional information. First and foremost, is a description of the patient’s current clinical status. If she is demonstrating evidence of adrenal crisis, treatment should not be delayed for additional testing. If she is stable, a thorough history including use of corticosteroids by any route, pregnancy, oral contraceptives, recent surgery, and liver and kidney disease is essential.
Additional evaluation reveals the patient has been using her fluticasone inhaler daily. No other source of hyponatremia or lightheadedness is identified. The patient’s risk factors of corticosteroid use and unexplained hyponatremia with associated lightheadedness increase her pretest probability of AI and a single morning cortisol of 10 mcg/dL is insufficient to exclude adrenal insufficiency. The appropriate follow-up test is a standard high-dose cosyntropin stimulation test at least 18 hours after her last dose of fluticasone. A cortisol level > 18 mcg/dL at 30 minutes in the absence of other conditions that impact cortisol testing would not be suggestive of AI. A serum cortisol level of < 18 mcg/dL at 30 minutes would raise concern for abnormal adrenal reserve due to chronic corticosteroid therapy and would warrant referral to an endocrinologist.
Bottom line
An isolated serum cortisol is often insufficient to exclude adrenal insufficiency. Hospitalists should be aware of the many factors that impact the interpretation of this test.
Dr. Gordon is assistant professor of medicine at Tufts University, Boston, and a hospitalist at Maine Medical Center, Portland. She is the subspecialty education coordinator of inpatient medicine for the Internal Medicine Residency Program. Dr. Herrle is assistant professor of medicine at Tufts University and a hospitalist at Maine Medical Center. She is the associate director of medical student education for the department of internal medicine at MMC and a medical director for clinical informatics at MaineHealth.
References
1. Bleicken B et al. Delayed diagnosis of adrenal insufficiency is common: A cross-sectional study in 216 patients. Am J Med Sci. 2010;339(6):525-31. doi: 10.1097/MAJ.0b013e3181db6b7a.
2. Bornstein SR et al. Diagnosis and treatment of primary adrenal insufficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016 Feb;101(2):364-89.
3. El-Farhan N et al. Measuring cortisol in serum, urine and saliva – Are our assays good enough? Ann Clin Biochem. 2017 May;54(3):308-22. doi: 10.1177/0004563216687335.
4. Kazlauskaite R et al. Corticotropin tests for hypothalamic-pituitary-adrenal insufficiency: A metaanalysis. J Clin Endocrinol Metab. 2008;93:4245-53.
5. Wood JB et al. A rapid test of adrenocortical function. Lancet. 1965;191:243-5.
6. Singh Ospina N et al. ACTH stimulation tests for the diagnosis of adrenal insufficiency: systematic review and meta-analysis. J Clin Endocrinol Metab. 2016;101(2):427-34.
7. Burgos N et al. Pitfalls in the interpretation of the cosyntropin stimulation test for the diagnosis of adrenal insufficiency. Curr Opin Endocrinol Diabetes Obes. 2019;26(3):139-45.
8. Odom DC et al. A Single, post-ACTH cortisol measurement to screen for adrenal insufficiency in the hospitalized patient. J Hosp Med. 2018;13(8):526-30. doi: 10.12788/jhm.2928.
9. Broersen LHA et al. Adrenal insufficiency in corticosteroids use: Systematic review and meta-analysis. J Clin Endocrinol Metab. 2015;100(6): 2171-80.
Key points
• In general, random cortisol testing is of limited value and should be avoided.
• Serum cortisol testing in the hospitalized patient is impacted by a variety of patient and disease factors and should be interpreted carefully.
• For patients with low pretest probability of adrenal insufficiency, early morning serum cortisol testing may be sufficient to exclude the diagnosis.
• For patients with moderate to high pretest probability of adrenal insufficiency, standard high-dose (250 mcg) corticotropin stimulation testing is preferred.
Additional reading
Bornstein SR et al. Diagnosis and treatment of primary adrenal insufficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016 Feb;101(2):364-89.
Burgos N et al. Pitfalls in the interpretation of the cosyntropin stimulation test for the diagnosis of adrenal insufficiency. Curr Opin Endocrinol Diabetes Obes. 2019;26(3):139-45.
Quiz
An 82 y.o. woman with depression is admitted from her long-term care facility with worsening weakness and mild hypoglycemia. Her supine vital signs are stable, but she exhibits a drop in systolic blood pressure of 21 mm Hg upon standing. There is no evidence of infection by history, exam, or initial workup. She is not on chronic corticosteroids by any route.
What would be your initial workup for adrenal insufficiency?
A) Morning serum cortisol and ACTH
B) Insulin tolerance test
C) Corticotropin stimulation test
D) Would not test at this point
Answer: C. Although her symptom of weakness is nonspecific, her hypoglycemia and orthostatic hypotension are concerning enough that she would qualify as moderate to high pretest probability for AI. In this setting, one would acquire a basal serum total cortisol and ACTH then administer the standard high-dose corticotropin stimulation test (250 mcg) followed by repeat serum total cortisol at 30 or 60 minutes.
Evaluating the hospitalized adult patient
Evaluating the hospitalized adult patient
Case
A 45-year-old female with moderate persistent asthma is admitted for right lower extremity cellulitis. She has hyponatremia with a sodium of 129 mEq/L and reports a history of longstanding fatigue and lightheadedness on standing. An early morning serum cortisol was 10 mcg/dL, normal per the reference range for the laboratory. Has adrenal insufficiency been excluded in this patient?
Overview
Adrenal insufficiency (AI) is a clinical syndrome characterized by a deficiency of cortisol. Presentation may range from nonspecific symptoms such as fatigue, weight loss, and gastrointestinal concerns to a fulminant adrenal crisis with severe weakness and hypotension (Table 1). The diagnosis of AI is commonly delayed, negatively impacting patients’ quality of life and risking dangerous complications.1,2
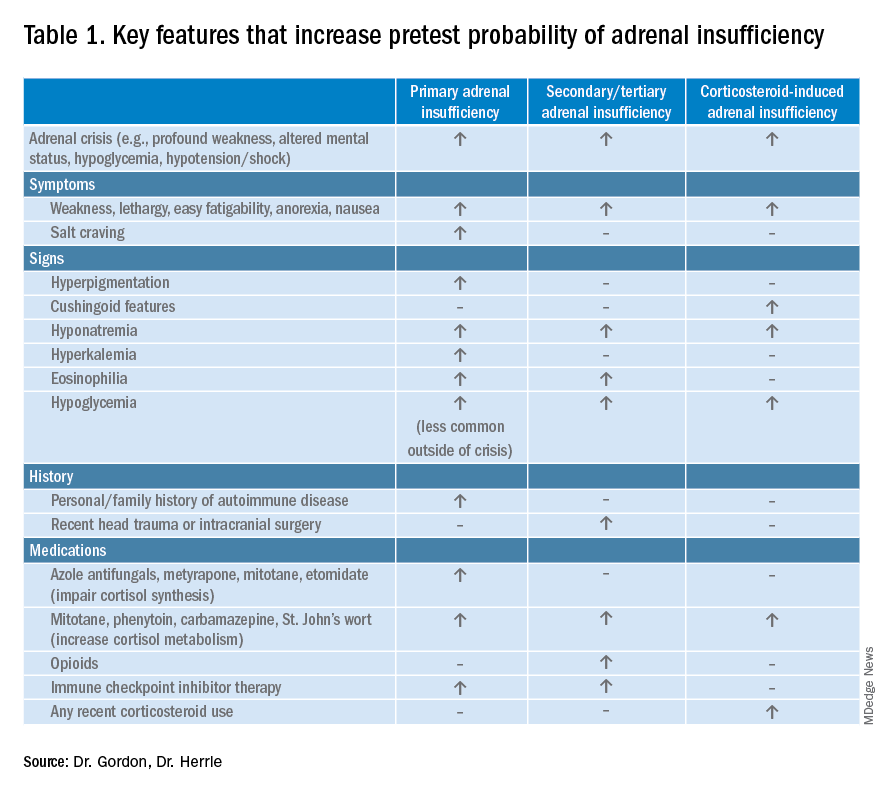
AI can occur due to diseases of the adrenal glands themselves (primary) or impairment of adrenocorticotropin (ACTH) secretion from the pituitary (secondary) or corticotropin-releasing hormone (CRH) secretion from the hypothalamus (tertiary). In the hospital setting, causes of primary AI may include autoimmune disease, infection, metastatic disease, hemorrhage, and adverse medication effects. Secondary and tertiary AI would be of particular concern for patients with traumatic brain injuries or pituitary surgery, but also are seen commonly as a result of adverse medication effects in the hospitalized patient, notably opioids and corticosteroids through suppression the hypothalamic-pituitary-adrenal (HPA) axis and immune checkpoint inhibitors via autoimmune hypophysitis.
Testing for AI in the hospitalized patient presents a host of challenges. Among these are the variability in presentation of different types of AI, high rates of exogenous corticosteroid use, the impact of critical illness on the HPA axis, medical illness altering protein binding of serum cortisol, interfering medications, the variation in assays used by laboratories, and the logistical challenges of obtaining appropriately timed phlebotomy.2,3
Cortisol testing
An intact HPA axis results in ACTH-dependent cortisol release from the adrenal glands. Cortisol secretion exhibits circadian rhythm, with the highest levels in the early morning (6 a.m. to 8 a.m.) and the lowest at night (12 a.m.). It also is pulsatile, which may explain the range of “normal” morning serum cortisol observed in a study of healthy volunteers.3 Note that serum cortisol is equivalent to plasma cortisol in current immunoassays, and will henceforth be called “cortisol” in this paper.3
There are instances when morning cortisol may strongly suggest a diagnosis of AI on its own. A meta-analysis found that morning cortisol of < 5 mcg/dL predicts AI and morning cortisol of > 13 mcg/dL ruled out AI.4 The Endocrine Society of America favors dynamic assessment of adrenal function for most patients.2
Historically, the gold standard for assessing dynamic adrenal function has been the insulin tolerance test (ITT), whereby cortisol is measured after inducing hypoglycemia to a blood glucose < 35 mg/dL. ITT is logistically difficult and poses some risk to the patient. The corticotropin (or cosyntropin) stimulation test (CST), in which a supraphysiologic dose of a synthetic ACTH analog is administered parenterally to a patient and resultant cortisol levels are measured, has been validated against the ITT and is generally preferred.5 CST is used to diagnose primary AI as well as chronic secondary and tertiary AI, given that longstanding lack of ACTH stimulation causes atrophy of the adrenal glands. The sensitivity for secondary and tertiary AI is likely lower than primary AI especially in acute onset of disease.6,7
In performance of the CST a baseline cortisol and ACTH are obtained, with subsequent cortisol testing at 30 and/or 60 minutes after administration of the ACTH analog (Figure 1). Currently, there is no consensus for which time point is preferred, but the 30-minute test is more sensitive for AI and the 60-minute test is more specific.2,7,8
CST is typically performed using a “standard high dose” of 250 mcg of the ACTH analog. There has been interest in the use of a “low-dose” 1 mcg test, which is closer to normal physiologic stimulation of the adrenal glands and may have better sensitivity for early secondary or partial AI. However, the 250-mcg dose is easier to prepare and has fewer technical pitfalls in administration as well as a lower risk for false positive testing. At this point the data do not compellingly favor the use of low-dose CST testing in general practice.2,3,7
Clinical decision making
Diagnostic evaluation should be guided by the likelihood of the disease (i.e., the pretest probability) (Figure 1). Begin with a review of the patient’s signs and symptoms, medical and family history, and medications with special consideration for opioids, exogenous steroids, and immune checkpoint inhibitors (Table 1).
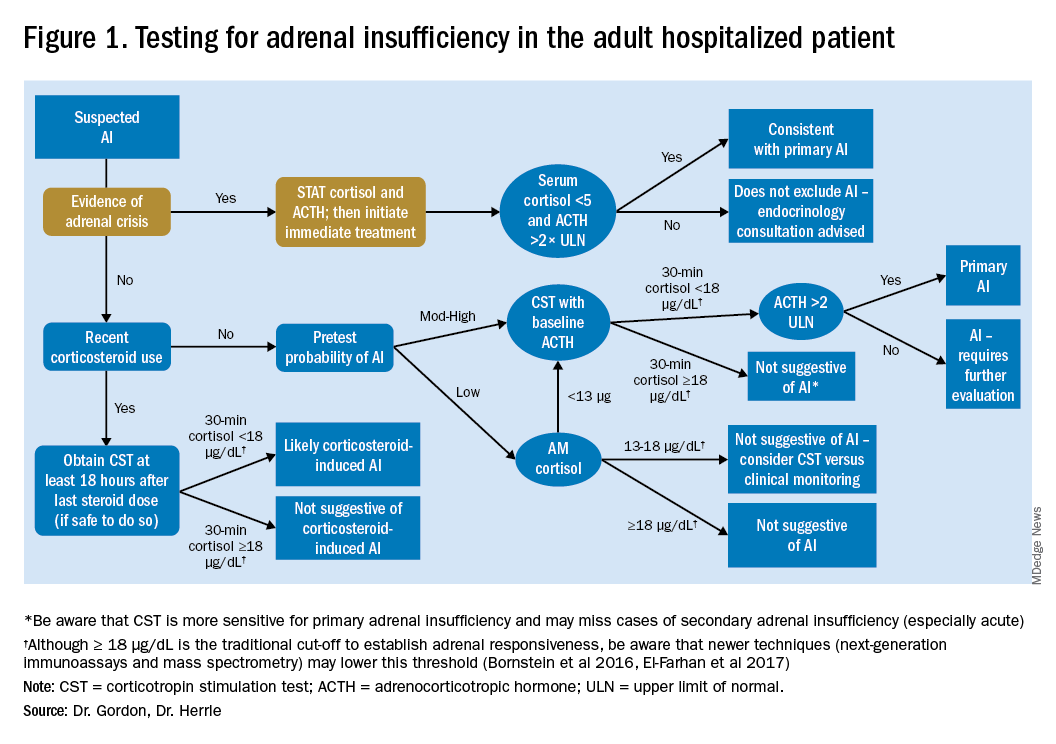
For patients with low pretest probability for AI, morning cortisol and ACTH is a reasonable first test (Figure 1). A cortisol value of 18 mcg/dL or greater does not support AI and no further testing is needed.2 Patients with morning cortisol of 13-18 mcg/dL could be followed clinically or could undergo further testing in the inpatient environment with CST, depending upon the clinical scenario.4 Patients with serum cortisol of <13 mcg/dL warrant CST.
For patients with moderate to high pretest probability for AI, we recommend initial testing with CST. While the results of high-dose CST are not necessarily impacted by time of day, if an a.m. cortisol has not yet been obtained and it is logistically feasible to do so, performing CST in the morning will provide the most useful data for clinical interpretation.
For patients presenting with possible adrenal crisis, it is essential not to delay treatment. In these patients, obtain a cortisol paired with ACTH and initiate treatment immediately. Further testing can be deferred until the time the patient is stable.2
Potential pitfalls
Interpreting cortisol requires awareness of multiple conditions that could directly impact the results.2,3 (Table 2).
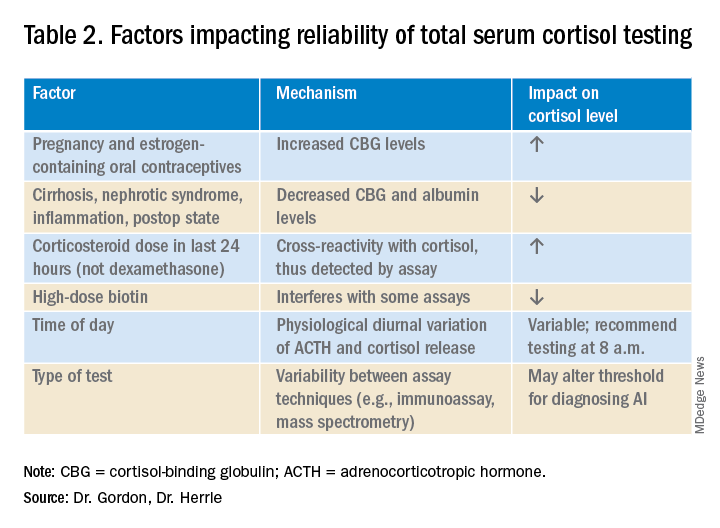
Currently available assays measure “total cortisol,” most of which is protein bound (cortisol-binding globulin as well as albumin). Therefore, conditions that lower serum protein (e.g., nephrotic syndrome, liver disease, inflammation) will lower the measured cortisol. Conversely, conditions that increase serum protein (e.g., estrogen excess in pregnancy and oral contraceptive use) will increase the measured cortisol.2,3
It is also important to recognize that existing immunoassay testing techniques informed the established cut-off for exclusion of AI at 18 mcg/dL. With newer immunoassays and emerging liquid chromatography/tandem mass spectrometry, this cut-off may be lowered; thus the assay should be confirmed with the performing laboratory. There is emerging evidence that serum or plasma free cortisol and salivary cortisol testing for AI may be useful in certain cases, but these techniques are not yet widespread or included in clinical practice guidelines.2,3,7
Population focus: Patients on exogenous steroids
Exogenous corticosteroids suppress the HPA axis via negative inhibition of CRH and ACTH release, often resulting in low endogenous cortisol levels which may or may not reflect true loss of adrenal function. In addition, many corticosteroids will be detected by standard serum cortisol tests that rely on immunoassays. For this reason, cortisol measurement and CST should be done at least 18-24 hours after the last dose of exogenous steroids.
Although the focus has been on higher doses and longer courses of steroids (e.g., chronic use of ≥ 5 mg prednisone daily, or ≥ 20 mg prednisone daily for > 3 weeks), there is increasing evidence that lower doses, shorter courses, and alternate routes (e.g., inhaled, intra-articular) can result in biochemical and clinical evidence of AI.9 Thus, a thorough history and exam should be obtained to determine all recent corticosteroid exposure and cushingoid features.
Application of the data to the case
To effectively assess the patient for adrenal insufficiency, we need additional information. First and foremost, is a description of the patient’s current clinical status. If she is demonstrating evidence of adrenal crisis, treatment should not be delayed for additional testing. If she is stable, a thorough history including use of corticosteroids by any route, pregnancy, oral contraceptives, recent surgery, and liver and kidney disease is essential.
Additional evaluation reveals the patient has been using her fluticasone inhaler daily. No other source of hyponatremia or lightheadedness is identified. The patient’s risk factors of corticosteroid use and unexplained hyponatremia with associated lightheadedness increase her pretest probability of AI and a single morning cortisol of 10 mcg/dL is insufficient to exclude adrenal insufficiency. The appropriate follow-up test is a standard high-dose cosyntropin stimulation test at least 18 hours after her last dose of fluticasone. A cortisol level > 18 mcg/dL at 30 minutes in the absence of other conditions that impact cortisol testing would not be suggestive of AI. A serum cortisol level of < 18 mcg/dL at 30 minutes would raise concern for abnormal adrenal reserve due to chronic corticosteroid therapy and would warrant referral to an endocrinologist.
Bottom line
An isolated serum cortisol is often insufficient to exclude adrenal insufficiency. Hospitalists should be aware of the many factors that impact the interpretation of this test.
Dr. Gordon is assistant professor of medicine at Tufts University, Boston, and a hospitalist at Maine Medical Center, Portland. She is the subspecialty education coordinator of inpatient medicine for the Internal Medicine Residency Program. Dr. Herrle is assistant professor of medicine at Tufts University and a hospitalist at Maine Medical Center. She is the associate director of medical student education for the department of internal medicine at MMC and a medical director for clinical informatics at MaineHealth.
References
1. Bleicken B et al. Delayed diagnosis of adrenal insufficiency is common: A cross-sectional study in 216 patients. Am J Med Sci. 2010;339(6):525-31. doi: 10.1097/MAJ.0b013e3181db6b7a.
2. Bornstein SR et al. Diagnosis and treatment of primary adrenal insufficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016 Feb;101(2):364-89.
3. El-Farhan N et al. Measuring cortisol in serum, urine and saliva – Are our assays good enough? Ann Clin Biochem. 2017 May;54(3):308-22. doi: 10.1177/0004563216687335.
4. Kazlauskaite R et al. Corticotropin tests for hypothalamic-pituitary-adrenal insufficiency: A metaanalysis. J Clin Endocrinol Metab. 2008;93:4245-53.
5. Wood JB et al. A rapid test of adrenocortical function. Lancet. 1965;191:243-5.
6. Singh Ospina N et al. ACTH stimulation tests for the diagnosis of adrenal insufficiency: systematic review and meta-analysis. J Clin Endocrinol Metab. 2016;101(2):427-34.
7. Burgos N et al. Pitfalls in the interpretation of the cosyntropin stimulation test for the diagnosis of adrenal insufficiency. Curr Opin Endocrinol Diabetes Obes. 2019;26(3):139-45.
8. Odom DC et al. A Single, post-ACTH cortisol measurement to screen for adrenal insufficiency in the hospitalized patient. J Hosp Med. 2018;13(8):526-30. doi: 10.12788/jhm.2928.
9. Broersen LHA et al. Adrenal insufficiency in corticosteroids use: Systematic review and meta-analysis. J Clin Endocrinol Metab. 2015;100(6): 2171-80.
Key points
• In general, random cortisol testing is of limited value and should be avoided.
• Serum cortisol testing in the hospitalized patient is impacted by a variety of patient and disease factors and should be interpreted carefully.
• For patients with low pretest probability of adrenal insufficiency, early morning serum cortisol testing may be sufficient to exclude the diagnosis.
• For patients with moderate to high pretest probability of adrenal insufficiency, standard high-dose (250 mcg) corticotropin stimulation testing is preferred.
Additional reading
Bornstein SR et al. Diagnosis and treatment of primary adrenal insufficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016 Feb;101(2):364-89.
Burgos N et al. Pitfalls in the interpretation of the cosyntropin stimulation test for the diagnosis of adrenal insufficiency. Curr Opin Endocrinol Diabetes Obes. 2019;26(3):139-45.
Quiz
An 82 y.o. woman with depression is admitted from her long-term care facility with worsening weakness and mild hypoglycemia. Her supine vital signs are stable, but she exhibits a drop in systolic blood pressure of 21 mm Hg upon standing. There is no evidence of infection by history, exam, or initial workup. She is not on chronic corticosteroids by any route.
What would be your initial workup for adrenal insufficiency?
A) Morning serum cortisol and ACTH
B) Insulin tolerance test
C) Corticotropin stimulation test
D) Would not test at this point
Answer: C. Although her symptom of weakness is nonspecific, her hypoglycemia and orthostatic hypotension are concerning enough that she would qualify as moderate to high pretest probability for AI. In this setting, one would acquire a basal serum total cortisol and ACTH then administer the standard high-dose corticotropin stimulation test (250 mcg) followed by repeat serum total cortisol at 30 or 60 minutes.
Case
A 45-year-old female with moderate persistent asthma is admitted for right lower extremity cellulitis. She has hyponatremia with a sodium of 129 mEq/L and reports a history of longstanding fatigue and lightheadedness on standing. An early morning serum cortisol was 10 mcg/dL, normal per the reference range for the laboratory. Has adrenal insufficiency been excluded in this patient?
Overview
Adrenal insufficiency (AI) is a clinical syndrome characterized by a deficiency of cortisol. Presentation may range from nonspecific symptoms such as fatigue, weight loss, and gastrointestinal concerns to a fulminant adrenal crisis with severe weakness and hypotension (Table 1). The diagnosis of AI is commonly delayed, negatively impacting patients’ quality of life and risking dangerous complications.1,2
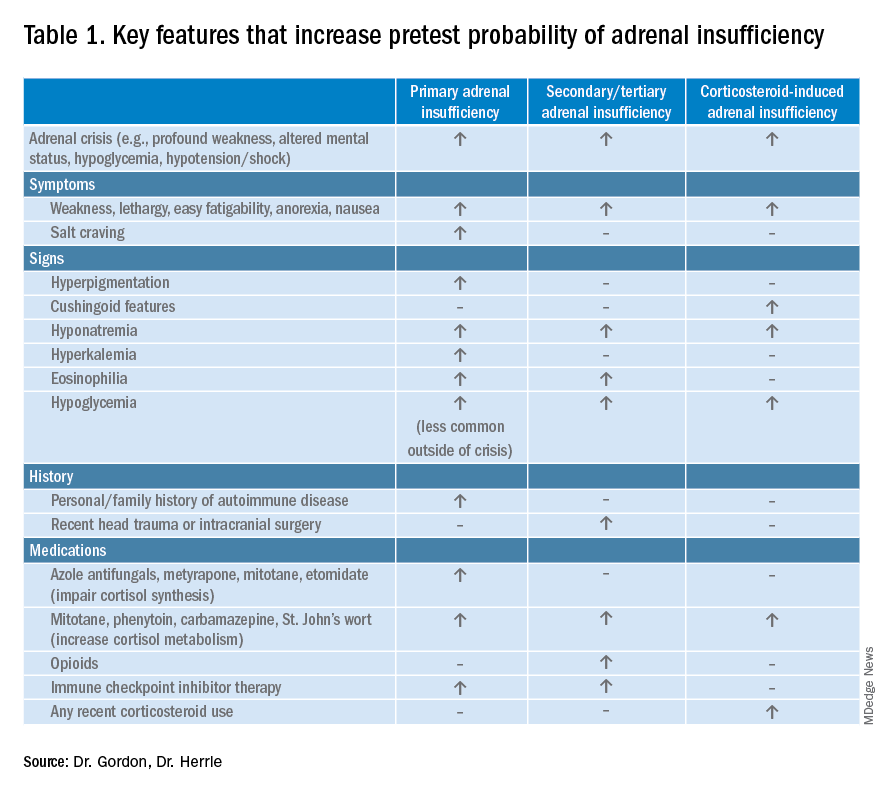
AI can occur due to diseases of the adrenal glands themselves (primary) or impairment of adrenocorticotropin (ACTH) secretion from the pituitary (secondary) or corticotropin-releasing hormone (CRH) secretion from the hypothalamus (tertiary). In the hospital setting, causes of primary AI may include autoimmune disease, infection, metastatic disease, hemorrhage, and adverse medication effects. Secondary and tertiary AI would be of particular concern for patients with traumatic brain injuries or pituitary surgery, but also are seen commonly as a result of adverse medication effects in the hospitalized patient, notably opioids and corticosteroids through suppression the hypothalamic-pituitary-adrenal (HPA) axis and immune checkpoint inhibitors via autoimmune hypophysitis.
Testing for AI in the hospitalized patient presents a host of challenges. Among these are the variability in presentation of different types of AI, high rates of exogenous corticosteroid use, the impact of critical illness on the HPA axis, medical illness altering protein binding of serum cortisol, interfering medications, the variation in assays used by laboratories, and the logistical challenges of obtaining appropriately timed phlebotomy.2,3
Cortisol testing
An intact HPA axis results in ACTH-dependent cortisol release from the adrenal glands. Cortisol secretion exhibits circadian rhythm, with the highest levels in the early morning (6 a.m. to 8 a.m.) and the lowest at night (12 a.m.). It also is pulsatile, which may explain the range of “normal” morning serum cortisol observed in a study of healthy volunteers.3 Note that serum cortisol is equivalent to plasma cortisol in current immunoassays, and will henceforth be called “cortisol” in this paper.3
There are instances when morning cortisol may strongly suggest a diagnosis of AI on its own. A meta-analysis found that morning cortisol of < 5 mcg/dL predicts AI and morning cortisol of > 13 mcg/dL ruled out AI.4 The Endocrine Society of America favors dynamic assessment of adrenal function for most patients.2
Historically, the gold standard for assessing dynamic adrenal function has been the insulin tolerance test (ITT), whereby cortisol is measured after inducing hypoglycemia to a blood glucose < 35 mg/dL. ITT is logistically difficult and poses some risk to the patient. The corticotropin (or cosyntropin) stimulation test (CST), in which a supraphysiologic dose of a synthetic ACTH analog is administered parenterally to a patient and resultant cortisol levels are measured, has been validated against the ITT and is generally preferred.5 CST is used to diagnose primary AI as well as chronic secondary and tertiary AI, given that longstanding lack of ACTH stimulation causes atrophy of the adrenal glands. The sensitivity for secondary and tertiary AI is likely lower than primary AI especially in acute onset of disease.6,7
In performance of the CST a baseline cortisol and ACTH are obtained, with subsequent cortisol testing at 30 and/or 60 minutes after administration of the ACTH analog (Figure 1). Currently, there is no consensus for which time point is preferred, but the 30-minute test is more sensitive for AI and the 60-minute test is more specific.2,7,8
CST is typically performed using a “standard high dose” of 250 mcg of the ACTH analog. There has been interest in the use of a “low-dose” 1 mcg test, which is closer to normal physiologic stimulation of the adrenal glands and may have better sensitivity for early secondary or partial AI. However, the 250-mcg dose is easier to prepare and has fewer technical pitfalls in administration as well as a lower risk for false positive testing. At this point the data do not compellingly favor the use of low-dose CST testing in general practice.2,3,7
Clinical decision making
Diagnostic evaluation should be guided by the likelihood of the disease (i.e., the pretest probability) (Figure 1). Begin with a review of the patient’s signs and symptoms, medical and family history, and medications with special consideration for opioids, exogenous steroids, and immune checkpoint inhibitors (Table 1).
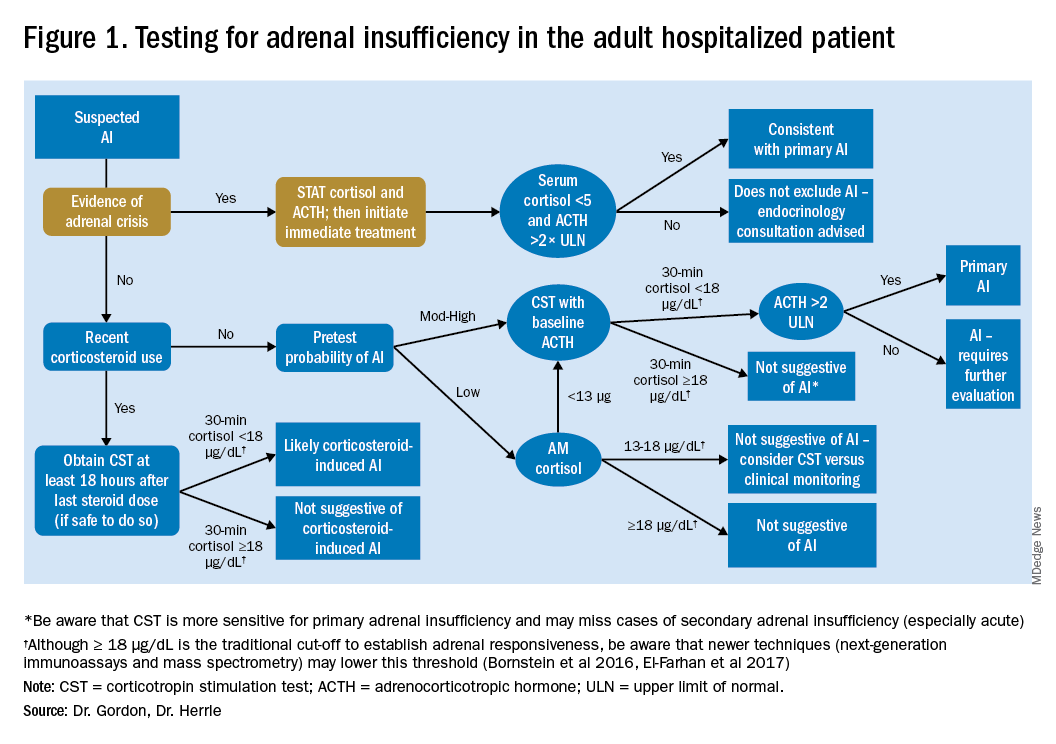
For patients with low pretest probability for AI, morning cortisol and ACTH is a reasonable first test (Figure 1). A cortisol value of 18 mcg/dL or greater does not support AI and no further testing is needed.2 Patients with morning cortisol of 13-18 mcg/dL could be followed clinically or could undergo further testing in the inpatient environment with CST, depending upon the clinical scenario.4 Patients with serum cortisol of <13 mcg/dL warrant CST.
For patients with moderate to high pretest probability for AI, we recommend initial testing with CST. While the results of high-dose CST are not necessarily impacted by time of day, if an a.m. cortisol has not yet been obtained and it is logistically feasible to do so, performing CST in the morning will provide the most useful data for clinical interpretation.
For patients presenting with possible adrenal crisis, it is essential not to delay treatment. In these patients, obtain a cortisol paired with ACTH and initiate treatment immediately. Further testing can be deferred until the time the patient is stable.2
Potential pitfalls
Interpreting cortisol requires awareness of multiple conditions that could directly impact the results.2,3 (Table 2).
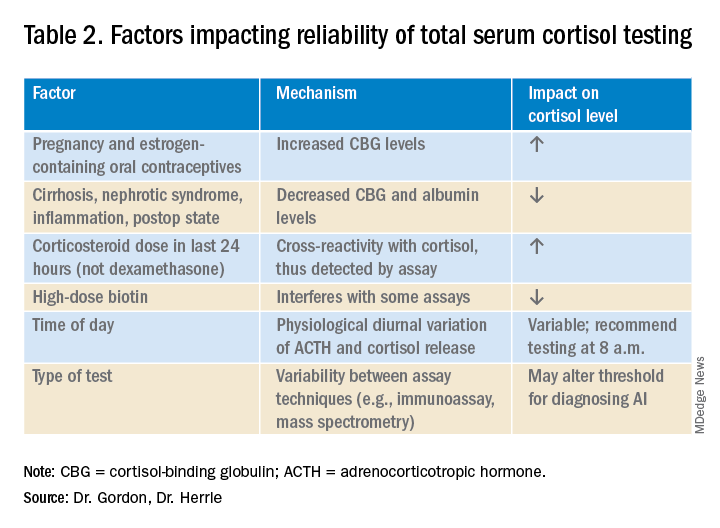
Currently available assays measure “total cortisol,” most of which is protein bound (cortisol-binding globulin as well as albumin). Therefore, conditions that lower serum protein (e.g., nephrotic syndrome, liver disease, inflammation) will lower the measured cortisol. Conversely, conditions that increase serum protein (e.g., estrogen excess in pregnancy and oral contraceptive use) will increase the measured cortisol.2,3
It is also important to recognize that existing immunoassay testing techniques informed the established cut-off for exclusion of AI at 18 mcg/dL. With newer immunoassays and emerging liquid chromatography/tandem mass spectrometry, this cut-off may be lowered; thus the assay should be confirmed with the performing laboratory. There is emerging evidence that serum or plasma free cortisol and salivary cortisol testing for AI may be useful in certain cases, but these techniques are not yet widespread or included in clinical practice guidelines.2,3,7
Population focus: Patients on exogenous steroids
Exogenous corticosteroids suppress the HPA axis via negative inhibition of CRH and ACTH release, often resulting in low endogenous cortisol levels which may or may not reflect true loss of adrenal function. In addition, many corticosteroids will be detected by standard serum cortisol tests that rely on immunoassays. For this reason, cortisol measurement and CST should be done at least 18-24 hours after the last dose of exogenous steroids.
Although the focus has been on higher doses and longer courses of steroids (e.g., chronic use of ≥ 5 mg prednisone daily, or ≥ 20 mg prednisone daily for > 3 weeks), there is increasing evidence that lower doses, shorter courses, and alternate routes (e.g., inhaled, intra-articular) can result in biochemical and clinical evidence of AI.9 Thus, a thorough history and exam should be obtained to determine all recent corticosteroid exposure and cushingoid features.
Application of the data to the case
To effectively assess the patient for adrenal insufficiency, we need additional information. First and foremost, is a description of the patient’s current clinical status. If she is demonstrating evidence of adrenal crisis, treatment should not be delayed for additional testing. If she is stable, a thorough history including use of corticosteroids by any route, pregnancy, oral contraceptives, recent surgery, and liver and kidney disease is essential.
Additional evaluation reveals the patient has been using her fluticasone inhaler daily. No other source of hyponatremia or lightheadedness is identified. The patient’s risk factors of corticosteroid use and unexplained hyponatremia with associated lightheadedness increase her pretest probability of AI and a single morning cortisol of 10 mcg/dL is insufficient to exclude adrenal insufficiency. The appropriate follow-up test is a standard high-dose cosyntropin stimulation test at least 18 hours after her last dose of fluticasone. A cortisol level > 18 mcg/dL at 30 minutes in the absence of other conditions that impact cortisol testing would not be suggestive of AI. A serum cortisol level of < 18 mcg/dL at 30 minutes would raise concern for abnormal adrenal reserve due to chronic corticosteroid therapy and would warrant referral to an endocrinologist.
Bottom line
An isolated serum cortisol is often insufficient to exclude adrenal insufficiency. Hospitalists should be aware of the many factors that impact the interpretation of this test.
Dr. Gordon is assistant professor of medicine at Tufts University, Boston, and a hospitalist at Maine Medical Center, Portland. She is the subspecialty education coordinator of inpatient medicine for the Internal Medicine Residency Program. Dr. Herrle is assistant professor of medicine at Tufts University and a hospitalist at Maine Medical Center. She is the associate director of medical student education for the department of internal medicine at MMC and a medical director for clinical informatics at MaineHealth.
References
1. Bleicken B et al. Delayed diagnosis of adrenal insufficiency is common: A cross-sectional study in 216 patients. Am J Med Sci. 2010;339(6):525-31. doi: 10.1097/MAJ.0b013e3181db6b7a.
2. Bornstein SR et al. Diagnosis and treatment of primary adrenal insufficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016 Feb;101(2):364-89.
3. El-Farhan N et al. Measuring cortisol in serum, urine and saliva – Are our assays good enough? Ann Clin Biochem. 2017 May;54(3):308-22. doi: 10.1177/0004563216687335.
4. Kazlauskaite R et al. Corticotropin tests for hypothalamic-pituitary-adrenal insufficiency: A metaanalysis. J Clin Endocrinol Metab. 2008;93:4245-53.
5. Wood JB et al. A rapid test of adrenocortical function. Lancet. 1965;191:243-5.
6. Singh Ospina N et al. ACTH stimulation tests for the diagnosis of adrenal insufficiency: systematic review and meta-analysis. J Clin Endocrinol Metab. 2016;101(2):427-34.
7. Burgos N et al. Pitfalls in the interpretation of the cosyntropin stimulation test for the diagnosis of adrenal insufficiency. Curr Opin Endocrinol Diabetes Obes. 2019;26(3):139-45.
8. Odom DC et al. A Single, post-ACTH cortisol measurement to screen for adrenal insufficiency in the hospitalized patient. J Hosp Med. 2018;13(8):526-30. doi: 10.12788/jhm.2928.
9. Broersen LHA et al. Adrenal insufficiency in corticosteroids use: Systematic review and meta-analysis. J Clin Endocrinol Metab. 2015;100(6): 2171-80.
Key points
• In general, random cortisol testing is of limited value and should be avoided.
• Serum cortisol testing in the hospitalized patient is impacted by a variety of patient and disease factors and should be interpreted carefully.
• For patients with low pretest probability of adrenal insufficiency, early morning serum cortisol testing may be sufficient to exclude the diagnosis.
• For patients with moderate to high pretest probability of adrenal insufficiency, standard high-dose (250 mcg) corticotropin stimulation testing is preferred.
Additional reading
Bornstein SR et al. Diagnosis and treatment of primary adrenal insufficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016 Feb;101(2):364-89.
Burgos N et al. Pitfalls in the interpretation of the cosyntropin stimulation test for the diagnosis of adrenal insufficiency. Curr Opin Endocrinol Diabetes Obes. 2019;26(3):139-45.
Quiz
An 82 y.o. woman with depression is admitted from her long-term care facility with worsening weakness and mild hypoglycemia. Her supine vital signs are stable, but she exhibits a drop in systolic blood pressure of 21 mm Hg upon standing. There is no evidence of infection by history, exam, or initial workup. She is not on chronic corticosteroids by any route.
What would be your initial workup for adrenal insufficiency?
A) Morning serum cortisol and ACTH
B) Insulin tolerance test
C) Corticotropin stimulation test
D) Would not test at this point
Answer: C. Although her symptom of weakness is nonspecific, her hypoglycemia and orthostatic hypotension are concerning enough that she would qualify as moderate to high pretest probability for AI. In this setting, one would acquire a basal serum total cortisol and ACTH then administer the standard high-dose corticotropin stimulation test (250 mcg) followed by repeat serum total cortisol at 30 or 60 minutes.