User login
Echocardiography in AMI not associated with improved outcomes
Background: Guidelines recommend that patients with AMI undergo universal echocardiography for the assessment of cardiac structure and ejection fraction, despite modest diagnostic yield.
Study design: Retrospective cohort.
Setting: 397 U.S. hospitals contributing to the Premier Healthcare Informatics inpatient database.
Synopsis: ICD-9 codes were used to identify 98,999 hospitalizations with a discharge diagnosis of AMI. Of these, 70.4% had at least one transthoracic echocardiogram performed. Patients who underwent echocardiogram were more likely than patients without an echocardiogram to have heart failure, pulmonary disease, and intensive care unit stays and require interventions such as noninvasive and invasive ventilation, vasopressors, balloon pumps, and inotropic agents.
Risk-standardized echocardiography rates varied significantly across hospitals, ranging from a median of 54% in the lowest quartile to 83% in the highest quartile. The authors found that use of echocardiography was most strongly associated with the hospital, more so than individual patient factors. In adjusted analyses, no difference was seen in inpatient mortality (odds ratio, 1.02; 95% CI, 0.88-1.99) or 3-month readmission (OR, 1.01; 95% CI, 0.93-1.10), but slightly longer mean length of stay (0.23 days; 95% CI, 0.04-0.41; P = .01) and higher mean costs ($3,164; 95% CI, $1,843-$4,485; P < .001) were found in patients treated at hospitals with the highest quartile of echocardiography use, compared with those in the lowest quartile.
Limitations include lack of information about long-term clinical outcomes, inability to adjust for ejection fraction levels, and reliance on administrative data for AMI and procedure codes.
Bottom line: In a cohort of patients with AMI, higher rates of hospital echocardiography use did not appear to be associated with better clinical outcomes but were associated with longer length of stay and greater hospital costs.
Citation: Pack QR et al. Association between inpatient echocardiography use and outcomes in adult patients with acute myocardial infarction. JAMA Intern Med. 2019 Jun 17. doi: 10.1001/jamainternmed.2019.1051.
Dr. Liu is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: Guidelines recommend that patients with AMI undergo universal echocardiography for the assessment of cardiac structure and ejection fraction, despite modest diagnostic yield.
Study design: Retrospective cohort.
Setting: 397 U.S. hospitals contributing to the Premier Healthcare Informatics inpatient database.
Synopsis: ICD-9 codes were used to identify 98,999 hospitalizations with a discharge diagnosis of AMI. Of these, 70.4% had at least one transthoracic echocardiogram performed. Patients who underwent echocardiogram were more likely than patients without an echocardiogram to have heart failure, pulmonary disease, and intensive care unit stays and require interventions such as noninvasive and invasive ventilation, vasopressors, balloon pumps, and inotropic agents.
Risk-standardized echocardiography rates varied significantly across hospitals, ranging from a median of 54% in the lowest quartile to 83% in the highest quartile. The authors found that use of echocardiography was most strongly associated with the hospital, more so than individual patient factors. In adjusted analyses, no difference was seen in inpatient mortality (odds ratio, 1.02; 95% CI, 0.88-1.99) or 3-month readmission (OR, 1.01; 95% CI, 0.93-1.10), but slightly longer mean length of stay (0.23 days; 95% CI, 0.04-0.41; P = .01) and higher mean costs ($3,164; 95% CI, $1,843-$4,485; P < .001) were found in patients treated at hospitals with the highest quartile of echocardiography use, compared with those in the lowest quartile.
Limitations include lack of information about long-term clinical outcomes, inability to adjust for ejection fraction levels, and reliance on administrative data for AMI and procedure codes.
Bottom line: In a cohort of patients with AMI, higher rates of hospital echocardiography use did not appear to be associated with better clinical outcomes but were associated with longer length of stay and greater hospital costs.
Citation: Pack QR et al. Association between inpatient echocardiography use and outcomes in adult patients with acute myocardial infarction. JAMA Intern Med. 2019 Jun 17. doi: 10.1001/jamainternmed.2019.1051.
Dr. Liu is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: Guidelines recommend that patients with AMI undergo universal echocardiography for the assessment of cardiac structure and ejection fraction, despite modest diagnostic yield.
Study design: Retrospective cohort.
Setting: 397 U.S. hospitals contributing to the Premier Healthcare Informatics inpatient database.
Synopsis: ICD-9 codes were used to identify 98,999 hospitalizations with a discharge diagnosis of AMI. Of these, 70.4% had at least one transthoracic echocardiogram performed. Patients who underwent echocardiogram were more likely than patients without an echocardiogram to have heart failure, pulmonary disease, and intensive care unit stays and require interventions such as noninvasive and invasive ventilation, vasopressors, balloon pumps, and inotropic agents.
Risk-standardized echocardiography rates varied significantly across hospitals, ranging from a median of 54% in the lowest quartile to 83% in the highest quartile. The authors found that use of echocardiography was most strongly associated with the hospital, more so than individual patient factors. In adjusted analyses, no difference was seen in inpatient mortality (odds ratio, 1.02; 95% CI, 0.88-1.99) or 3-month readmission (OR, 1.01; 95% CI, 0.93-1.10), but slightly longer mean length of stay (0.23 days; 95% CI, 0.04-0.41; P = .01) and higher mean costs ($3,164; 95% CI, $1,843-$4,485; P < .001) were found in patients treated at hospitals with the highest quartile of echocardiography use, compared with those in the lowest quartile.
Limitations include lack of information about long-term clinical outcomes, inability to adjust for ejection fraction levels, and reliance on administrative data for AMI and procedure codes.
Bottom line: In a cohort of patients with AMI, higher rates of hospital echocardiography use did not appear to be associated with better clinical outcomes but were associated with longer length of stay and greater hospital costs.
Citation: Pack QR et al. Association between inpatient echocardiography use and outcomes in adult patients with acute myocardial infarction. JAMA Intern Med. 2019 Jun 17. doi: 10.1001/jamainternmed.2019.1051.
Dr. Liu is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Surgery for adhesive small-bowel obstruction linked with lower risk of recurrence
Background: Guidelines recommend nonoperative monitoring for aSBO; however, long-term association of operative versus nonoperative management and aSBO recurrence is poorly understood.
Study design: Longitudinal, retrospective cohort.
Setting: Hospitals in Ontario.
Synopsis: Administrative data for 2005-2014 was used to identify 27,904 adults hospitalized for an initial episode of aSBO who did not have known inflammatory bowel disease, history of radiotherapy, malignancy, ileus, impaction, or anatomical obstruction. Approximately 22% of patients were managed surgically during the index admission. Patients were followed for a median of 3.6 years. Overall, 19.6% of patients experienced at least one admission for recurrence of aSBO during the study period. With each recurrence, the probability of subsequent recurrence increased, the time between episodes decreased, and the probability of being treated surgically decreased.
Patients were then matched into operative (n = 6,160) and nonoperative (n = 6,160) cohorts based on a propensity score which incorporated comorbidity burden, age, gender, and socioeconomic status. Patients who underwent operative management during their index admission for aSBO had a lower overall risk of recurrence compared to patients managed nonoperatively (13.0% vs. 21.3%; P less than .001). Operative intervention was associated with lower hazards of recurrence even when accounting for death. Additionally, surgical intervention after any episode was associated with a significantly lower risk of recurrence, compared with nonoperative management.
Bottom line: Contrary to surgical dogma, surgical intervention is associated with reduced risk of recurrent aSBO in patients without complicating factors. Hospitalists should consider recurrence risk when managing these patients nonoperatively.
Citation: Behman R et al. Association of surgical intervention for adhesive small-bowel obstruction with the risk of recurrence. JAMA Surg. 2019 May 1;154(5):413-20.
Dr. Liu is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: Guidelines recommend nonoperative monitoring for aSBO; however, long-term association of operative versus nonoperative management and aSBO recurrence is poorly understood.
Study design: Longitudinal, retrospective cohort.
Setting: Hospitals in Ontario.
Synopsis: Administrative data for 2005-2014 was used to identify 27,904 adults hospitalized for an initial episode of aSBO who did not have known inflammatory bowel disease, history of radiotherapy, malignancy, ileus, impaction, or anatomical obstruction. Approximately 22% of patients were managed surgically during the index admission. Patients were followed for a median of 3.6 years. Overall, 19.6% of patients experienced at least one admission for recurrence of aSBO during the study period. With each recurrence, the probability of subsequent recurrence increased, the time between episodes decreased, and the probability of being treated surgically decreased.
Patients were then matched into operative (n = 6,160) and nonoperative (n = 6,160) cohorts based on a propensity score which incorporated comorbidity burden, age, gender, and socioeconomic status. Patients who underwent operative management during their index admission for aSBO had a lower overall risk of recurrence compared to patients managed nonoperatively (13.0% vs. 21.3%; P less than .001). Operative intervention was associated with lower hazards of recurrence even when accounting for death. Additionally, surgical intervention after any episode was associated with a significantly lower risk of recurrence, compared with nonoperative management.
Bottom line: Contrary to surgical dogma, surgical intervention is associated with reduced risk of recurrent aSBO in patients without complicating factors. Hospitalists should consider recurrence risk when managing these patients nonoperatively.
Citation: Behman R et al. Association of surgical intervention for adhesive small-bowel obstruction with the risk of recurrence. JAMA Surg. 2019 May 1;154(5):413-20.
Dr. Liu is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: Guidelines recommend nonoperative monitoring for aSBO; however, long-term association of operative versus nonoperative management and aSBO recurrence is poorly understood.
Study design: Longitudinal, retrospective cohort.
Setting: Hospitals in Ontario.
Synopsis: Administrative data for 2005-2014 was used to identify 27,904 adults hospitalized for an initial episode of aSBO who did not have known inflammatory bowel disease, history of radiotherapy, malignancy, ileus, impaction, or anatomical obstruction. Approximately 22% of patients were managed surgically during the index admission. Patients were followed for a median of 3.6 years. Overall, 19.6% of patients experienced at least one admission for recurrence of aSBO during the study period. With each recurrence, the probability of subsequent recurrence increased, the time between episodes decreased, and the probability of being treated surgically decreased.
Patients were then matched into operative (n = 6,160) and nonoperative (n = 6,160) cohorts based on a propensity score which incorporated comorbidity burden, age, gender, and socioeconomic status. Patients who underwent operative management during their index admission for aSBO had a lower overall risk of recurrence compared to patients managed nonoperatively (13.0% vs. 21.3%; P less than .001). Operative intervention was associated with lower hazards of recurrence even when accounting for death. Additionally, surgical intervention after any episode was associated with a significantly lower risk of recurrence, compared with nonoperative management.
Bottom line: Contrary to surgical dogma, surgical intervention is associated with reduced risk of recurrent aSBO in patients without complicating factors. Hospitalists should consider recurrence risk when managing these patients nonoperatively.
Citation: Behman R et al. Association of surgical intervention for adhesive small-bowel obstruction with the risk of recurrence. JAMA Surg. 2019 May 1;154(5):413-20.
Dr. Liu is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
The authority/accountability balance
Evaluating your career trajectory
I have had the pleasure of working on the Society of Hospital Medicine’s signature Leadership Academies since 2010, and I enjoy working with hospital medicine leaders from around the country every year. I started as a hospital medicine leader in 2000 and served during the unprecedented growth of the field when it was “the most rapidly growing specialty in the history of medicine.”
Most businesses dream of having a year of double-digit growth; my department grew an average of 15% annually for more than 10 years. These unique experiences have taught me many lessons and afforded me the opportunity to watch many stars of hospital medicine rise, as well as to learn from several less-scrupulous leaders about the darker side of hospital politics.
One of the lessons I learned the hard way about hospital politics is striking the “Authority/Accountability balance” in your career. I shared this perspective at the SHM annual conference in 2018, at speaking engagements on the West Coast, and with my leadership group at the academies. I am sharing it with you because the feedback I have received has been very positive.
The Authority/Accountability balance is a tool for evaluating your current career trajectory and measuring if it is set up for success or failure. The essence is that your Authority and Accountability need to be balanced for you to be successful in your career, regardless of your station. Everybody from the hospitalist fresh out of residency to the CEO needs to have Authority and Accountability in balance to be successful. And as you use the tool to measure your own potential for success or failure, learn to apply it to those who report to you.
I believe the rising tide lifts all boats and the success of your subordinates, through mentoring and support, will add to your success. There is another, more cynical view of subordinates that can be identified using the Authority/Accountability balance, which I will address.
Authority
In this construct, “Authority” has a much broader meaning than just the ability to tell people what to do. The ability to tell people what to do is important but not sufficient for success in hospital politics.
Financial resources are essential for a successful Authority/Accountability balance – not only the hardware such as computers, telephones, pagers, and so on, but also clerical support, technical support, and analytic support so that you are getting high-quality data on the performance of the members of your hospital medicine group (HMG). These “soft” resources (clerical, technical, and analytical) are often overlooked as needs that HMG leaders must advocate for; I speak with many HMG leaders who remain under-resourced with “soft” assets. However, being appropriately resourced in these areas can be transformational for a group. Hospitalists don’t like doing clerical work, and if you don’t like a menial job assigned to you, you probably won’t do it very well. Having an unlicensed person dedicated to these clerical activities not only will cost less, but will ensure the job is done better.
Reporting structure is critically important, often overlooked, and historically misaligned in HMGs. When hospital medicine was starting in the late 1990s and early 2000s, rapidly growing hospitalist groups were typically led by young, early-career physicians who had chosen hospital medicine as a career. The problem was that they often lacked the seniority and connections at the executive level to advocate for their HMG. All too often the hospitalist group was tucked in under another department or division which, in turn, reported HMG updates and issues to the board of directors and the CEO.
A common reporting structure in the early days was that a senior member of the medical staff, or group, had once worked in the hospital and therefore “understood” the issues and challenges that the hospitalists were facing. It was up to this physician with seniority and connections to advocate for the hospitalists as they saw fit. The problem was that the hospital landscape was, and is, constantly evolving in innumerable ways. These “once removed” reporting structures for HMGs failed to get the required information on the rapidly changing, and evolving, hospitalist landscape to the desks of executives who had the financial and structural control to address the challenges that the hospitalists in the trenches were facing.
Numerous HMGs failed in the early days of hospital medicine because of this type of misaligned reporting structure. This is a lesson that should not be forgotten: Make sure your HMG leader has a seat at the table where executive decisions are made, including but not limited to the board of directors. To be in balance, you have to be “in the room where it happens.”
Accountability
The outcomes that you are responsible for need to be explicit, appropriately resourced with Authority, and clearly spelled out in your job description. Your job description is a document you should know, own, and revisit regularly with whomever you report to, in order to ensure success.
Once you have the Authority side of the equation appropriately resourced, setting outcomes that are a stretch, but still realistic and achievable within the scope of your position, is critical to your success. It is good to think about short-, medium-, and long-term goals, especially if you are in a leadership role. For example, one expectation you will have, regardless of your station, is that you keep up on your email and answer your phone. These are short-term goals that will often be included in your job description. However, taking on a new hospital contract and making sure that it has 24/7 hospitalist coverage, that all the hospitalists are meeting the geometric mean length of stay, and that all the physicians are having 15 encounters per day doesn’t happen immediately. Long-term goals, such as taking on a new hospital contract, are the big-picture stuff that can make or break the career of an HMG leader. Long-term goals also need to be delineated in the job description, along with specific time stamps and the resources you need to accomplish big ticket items – which are spelled out in the Authority side (that is, physician recruiter, secretary, background checks, and so on).
One of the classic misuses of Accountability is the “Fall Guy” scenario. The Fall Guy scenario is often used by cynical hospital and medical group executives to expand their influence while limiting their liability. In the Fall Guy scenario, the executive is surrounded with junior partners who are underpowered with Authority, and then the executive makes decisions for which the junior partners are Accountable. This allows the senior executive to make risky decisions on behalf of the hospital or medical group without the liability of being held accountable when the decision-making process fails. When the risky, and often ill-informed, decision fails, the junior partner who lacked the Authority to make the decision – but held the Accountability for it – becomes the Fall Guy for the failed endeavor. This is a critical outcome that the Authority/Accountability balance can help you avoid, if you use it wisely and properly.
If you find yourself in the Fall Guy position, it is time for a change. The Authority, the Accountability, or both need to change so that they are in better balance. Or your employer needs to change. Changing employers is an outcome worth avoiding, if at all possible. I have scrutinized thousands of resumes in my career, and frequent job changes always wave a red flag to prospective employers. However, changing jobs remains a crucial option if you are being set up for failure when Authority and Accountability are out of balance.
If you are unable to negotiate for the balance that will allow you to be successful with your current group, remember that HMG leaders are a prized commodity and in short supply. Leaving a group that has been your career is hard, but it is better to leave than stay in a position where you are set up for failure as the Fall Guy. Further, the most effective time to expand your Authority is when you are negotiating the terms of a new position. Changing positions is the nuclear option. However, it is better than becoming the Fall Guy, and a change can create opportunities that will accelerate your career and influence, if done right.
When I talk about Authority/Accountability balance, I always counter the Fall Guy with an ignominious historical figure: General George B. McClellan. General McClellan was the commander of the Army of the Potomac during the early years of the American Civil War. General McClellan had the industrial might of the Union north at his beck and call, as well as extraordinary resources for recruiting and retaining soldiers for his army. At every encounter with General Robert E. Lee’s Army of Northern Virginia, General McClellan outnumbered them, sometimes by more than two to one. Yet General McClellan was outfoxed repeatedly for the same reason: He failed to take decisive action.
Every time that McClellan failed, he blamed insufficient resources and told President Lincoln that he needed more troops and more equipment to be successful. In summary, while the Fall Guy scenario needs to be avoided, once you are adequately resourced, success requires taking decisive and strategic action, or you will suffer as did General McClellan. Failing to act when you are appropriately resourced can be just as damaging to your career and credibility as allowing yourself to become the Fall Guy.
Job description
Everybody has somebody that they report to, no matter how high up on the executive ladder they have climbed. Even the CEO must report to the board of directors. And that reporting structure usually involves periodic formal reviews. Your formal review is a good time to go over your job description, note what is relevant, remove what is irrelevant, and add new elements that have evolved in importance since your last review.
Job descriptions take many forms, but they always include a list of qualifications. If you have the job, you have the qualifications, so that is not likely to change. You may become more qualified for a higher-level position, but that is an entirely different discussion. I like to think of a well-written job description as including short-term and long-term goals. Short-term goals are usually the daily stuff that keeps operations running smoothly but garners little attention. Examples would include staying current on your emails, answering your phone, organizing meetings, and regularly attending various committees. Even some of these short-term goals can and will change over time. I always enjoyed quality oversight in my department, but as the department and my responsibilities grew, I realized I couldn’t do everything that I wanted to do. I needed to focus on the things only I could do and delegate those things that could be done by someone else, even though I wanted to continue doing them myself. I created a position for a clinical quality officer, and quality oversight moved off of my job description.
Long-term goals are the aspirational items, such as increasing market share, decreasing readmissions, improving patient satisfaction, and the like. Effective leaders are often focused on these aspirational, long-term goals, but they still must effectively execute their short-term goals. Stephen Covey outlines the dilemma with the “time management matrix” in his seminal work “The 7 Habits of Highly Effective People.” An in-depth discussion is beyond the scope of this article, but the time management matrix places tasks into one of four categories based on urgency and importance, and provides strategies for staying up on short-term goals while continually moving long-term goals forward.If you show up at your review with a list of accomplishments as well as an understanding of how the “time management matrix” affects your responsibilities, your boss will be impressed. It is also worth mentioning that Covey’s first habit is “Proactivity.” He uses the term Proactivity in a much more nuanced form than we typically think of, however. Simply put, Proactivity is the opposite of Reactivity, and it is another invaluable tool for success with those long-term goals that will help you make a name for yourself.
When you show up for your review, be it annual, biannual, or other, be prepared. Not only should you bring your job description and recommendations for how it should be adapted in the changing environment, but also bring examples of your accomplishments since the last review.
I talk with leaders frequently who are hardworking and diligent and hate bragging about their achievements; I get that. At the same time, if you don’t inform your superiors about your successes, there is no guarantee that they will hear about them or understand them in the appropriate context. Bragging about how great you are in the physician’s lounge is annoying; telling your boss about your accomplishments since the last review is critical to maintaining the momentum of past accomplishments. If you are not willing to toot your own horn, there is a very good chance that your horn will remain silent. I don’t think self-promotion comes easily to anyone, and it has to be done with a degree of humility and sensitivity; but it has to be done, so prepare for it.
Look out for yourself and others
We talk about teamwork and collaboration as hospitalists, and SHM is always underscoring the importance of teamwork and highlighting examples of successful teamwork in its many conferences and publications. Most hospital executives are focused on their own careers, however, and many have no reservations about damaging your career (your brand) if they think it will promote theirs. You have to look out for yourself and size up every leadership position you get into.
Physicians can expect their careers to last decades. The average hospital CEO has a tenure of less than 3.5 years, however, and when a new CEO is hired, almost half of chief financial, chief operating, and chief information officers are fired within 9 months. You may be focused on the long-term success of your organization as you plan your career, but many hospital administrators are interested only in short-term gains. It is similar to some members of Congress who are interested only in what they need to do now to win the next election and not in the long-term needs of the country. You should understand this disconnect when dealing with hospital executives, and how you and your credibility can become cannon fodder in their quest for short-term self-preservation.
You have to look out for and take care of yourself as you promote your group. With a better understanding of the Authority/Accountability balance, you have new tools to assess your chances of success and to advocate for yourself so that you and your group can be successful.
Despite my cynicism toward executives in the medical field, I personally advocate for supporting the career development of those around you and advise against furthering your career at the expense of others. Many unscrupulous executives will use this approach, surrounding themselves with Fall Guys, but my experience shows that this is not a sustainable strategy for success. It can lead to short-term gains, but eventually the piper must be paid. Moreover, the most successful medical executives and leaders that I have encountered have been those who genuinely cared about their subordinates, looked out for them, and selflessly promoted their careers.
In the age of social media, tearing others down seems to be the fastest way to get more “likes.” However, I strongly believe that you can’t build up your group, and our profession, just by tearing people down. Lending a helping hand may bring you less attention in the short term, but such action raises your stature, creates loyalty, and leads to sustainable success for the long run.
Dr. McIlraith is the founding chairman of the Hospital Medicine Department at Mercy Medical Group in Sacramento, Calif. He received the SHM Award for Outstanding Service in Hospital Medicine in 2016 and is currently a member of the SHM Practice Management and Awards Committees, as well as the SHM Critical Care Task Force.
Sources
Quinn R. HM Turns 20: A look at the evolution of hospital medicine. The Hospitalist. 2016 August. https://www.the-hospitalist.org/hospitalist/article/121525/hm-turns-20-look-evolution-hospital-medicine
Stephen R. Covey. The 7 Habits of Highly Effective People: Powerful Lessons in Personal Change. Simon & Schuster. 1989.
10 Statistics on CEO Turnover, Recruitment. Becker’s Hospital Review. 2020. https://www.beckershospitalreview.com/hospital-management-administration/10-statistics-on-ceo-turnover-recruitment.html
Evaluating your career trajectory
Evaluating your career trajectory
I have had the pleasure of working on the Society of Hospital Medicine’s signature Leadership Academies since 2010, and I enjoy working with hospital medicine leaders from around the country every year. I started as a hospital medicine leader in 2000 and served during the unprecedented growth of the field when it was “the most rapidly growing specialty in the history of medicine.”
Most businesses dream of having a year of double-digit growth; my department grew an average of 15% annually for more than 10 years. These unique experiences have taught me many lessons and afforded me the opportunity to watch many stars of hospital medicine rise, as well as to learn from several less-scrupulous leaders about the darker side of hospital politics.
One of the lessons I learned the hard way about hospital politics is striking the “Authority/Accountability balance” in your career. I shared this perspective at the SHM annual conference in 2018, at speaking engagements on the West Coast, and with my leadership group at the academies. I am sharing it with you because the feedback I have received has been very positive.
The Authority/Accountability balance is a tool for evaluating your current career trajectory and measuring if it is set up for success or failure. The essence is that your Authority and Accountability need to be balanced for you to be successful in your career, regardless of your station. Everybody from the hospitalist fresh out of residency to the CEO needs to have Authority and Accountability in balance to be successful. And as you use the tool to measure your own potential for success or failure, learn to apply it to those who report to you.
I believe the rising tide lifts all boats and the success of your subordinates, through mentoring and support, will add to your success. There is another, more cynical view of subordinates that can be identified using the Authority/Accountability balance, which I will address.
Authority
In this construct, “Authority” has a much broader meaning than just the ability to tell people what to do. The ability to tell people what to do is important but not sufficient for success in hospital politics.
Financial resources are essential for a successful Authority/Accountability balance – not only the hardware such as computers, telephones, pagers, and so on, but also clerical support, technical support, and analytic support so that you are getting high-quality data on the performance of the members of your hospital medicine group (HMG). These “soft” resources (clerical, technical, and analytical) are often overlooked as needs that HMG leaders must advocate for; I speak with many HMG leaders who remain under-resourced with “soft” assets. However, being appropriately resourced in these areas can be transformational for a group. Hospitalists don’t like doing clerical work, and if you don’t like a menial job assigned to you, you probably won’t do it very well. Having an unlicensed person dedicated to these clerical activities not only will cost less, but will ensure the job is done better.
Reporting structure is critically important, often overlooked, and historically misaligned in HMGs. When hospital medicine was starting in the late 1990s and early 2000s, rapidly growing hospitalist groups were typically led by young, early-career physicians who had chosen hospital medicine as a career. The problem was that they often lacked the seniority and connections at the executive level to advocate for their HMG. All too often the hospitalist group was tucked in under another department or division which, in turn, reported HMG updates and issues to the board of directors and the CEO.
A common reporting structure in the early days was that a senior member of the medical staff, or group, had once worked in the hospital and therefore “understood” the issues and challenges that the hospitalists were facing. It was up to this physician with seniority and connections to advocate for the hospitalists as they saw fit. The problem was that the hospital landscape was, and is, constantly evolving in innumerable ways. These “once removed” reporting structures for HMGs failed to get the required information on the rapidly changing, and evolving, hospitalist landscape to the desks of executives who had the financial and structural control to address the challenges that the hospitalists in the trenches were facing.
Numerous HMGs failed in the early days of hospital medicine because of this type of misaligned reporting structure. This is a lesson that should not be forgotten: Make sure your HMG leader has a seat at the table where executive decisions are made, including but not limited to the board of directors. To be in balance, you have to be “in the room where it happens.”
Accountability
The outcomes that you are responsible for need to be explicit, appropriately resourced with Authority, and clearly spelled out in your job description. Your job description is a document you should know, own, and revisit regularly with whomever you report to, in order to ensure success.
Once you have the Authority side of the equation appropriately resourced, setting outcomes that are a stretch, but still realistic and achievable within the scope of your position, is critical to your success. It is good to think about short-, medium-, and long-term goals, especially if you are in a leadership role. For example, one expectation you will have, regardless of your station, is that you keep up on your email and answer your phone. These are short-term goals that will often be included in your job description. However, taking on a new hospital contract and making sure that it has 24/7 hospitalist coverage, that all the hospitalists are meeting the geometric mean length of stay, and that all the physicians are having 15 encounters per day doesn’t happen immediately. Long-term goals, such as taking on a new hospital contract, are the big-picture stuff that can make or break the career of an HMG leader. Long-term goals also need to be delineated in the job description, along with specific time stamps and the resources you need to accomplish big ticket items – which are spelled out in the Authority side (that is, physician recruiter, secretary, background checks, and so on).
One of the classic misuses of Accountability is the “Fall Guy” scenario. The Fall Guy scenario is often used by cynical hospital and medical group executives to expand their influence while limiting their liability. In the Fall Guy scenario, the executive is surrounded with junior partners who are underpowered with Authority, and then the executive makes decisions for which the junior partners are Accountable. This allows the senior executive to make risky decisions on behalf of the hospital or medical group without the liability of being held accountable when the decision-making process fails. When the risky, and often ill-informed, decision fails, the junior partner who lacked the Authority to make the decision – but held the Accountability for it – becomes the Fall Guy for the failed endeavor. This is a critical outcome that the Authority/Accountability balance can help you avoid, if you use it wisely and properly.
If you find yourself in the Fall Guy position, it is time for a change. The Authority, the Accountability, or both need to change so that they are in better balance. Or your employer needs to change. Changing employers is an outcome worth avoiding, if at all possible. I have scrutinized thousands of resumes in my career, and frequent job changes always wave a red flag to prospective employers. However, changing jobs remains a crucial option if you are being set up for failure when Authority and Accountability are out of balance.
If you are unable to negotiate for the balance that will allow you to be successful with your current group, remember that HMG leaders are a prized commodity and in short supply. Leaving a group that has been your career is hard, but it is better to leave than stay in a position where you are set up for failure as the Fall Guy. Further, the most effective time to expand your Authority is when you are negotiating the terms of a new position. Changing positions is the nuclear option. However, it is better than becoming the Fall Guy, and a change can create opportunities that will accelerate your career and influence, if done right.
When I talk about Authority/Accountability balance, I always counter the Fall Guy with an ignominious historical figure: General George B. McClellan. General McClellan was the commander of the Army of the Potomac during the early years of the American Civil War. General McClellan had the industrial might of the Union north at his beck and call, as well as extraordinary resources for recruiting and retaining soldiers for his army. At every encounter with General Robert E. Lee’s Army of Northern Virginia, General McClellan outnumbered them, sometimes by more than two to one. Yet General McClellan was outfoxed repeatedly for the same reason: He failed to take decisive action.
Every time that McClellan failed, he blamed insufficient resources and told President Lincoln that he needed more troops and more equipment to be successful. In summary, while the Fall Guy scenario needs to be avoided, once you are adequately resourced, success requires taking decisive and strategic action, or you will suffer as did General McClellan. Failing to act when you are appropriately resourced can be just as damaging to your career and credibility as allowing yourself to become the Fall Guy.
Job description
Everybody has somebody that they report to, no matter how high up on the executive ladder they have climbed. Even the CEO must report to the board of directors. And that reporting structure usually involves periodic formal reviews. Your formal review is a good time to go over your job description, note what is relevant, remove what is irrelevant, and add new elements that have evolved in importance since your last review.
Job descriptions take many forms, but they always include a list of qualifications. If you have the job, you have the qualifications, so that is not likely to change. You may become more qualified for a higher-level position, but that is an entirely different discussion. I like to think of a well-written job description as including short-term and long-term goals. Short-term goals are usually the daily stuff that keeps operations running smoothly but garners little attention. Examples would include staying current on your emails, answering your phone, organizing meetings, and regularly attending various committees. Even some of these short-term goals can and will change over time. I always enjoyed quality oversight in my department, but as the department and my responsibilities grew, I realized I couldn’t do everything that I wanted to do. I needed to focus on the things only I could do and delegate those things that could be done by someone else, even though I wanted to continue doing them myself. I created a position for a clinical quality officer, and quality oversight moved off of my job description.
Long-term goals are the aspirational items, such as increasing market share, decreasing readmissions, improving patient satisfaction, and the like. Effective leaders are often focused on these aspirational, long-term goals, but they still must effectively execute their short-term goals. Stephen Covey outlines the dilemma with the “time management matrix” in his seminal work “The 7 Habits of Highly Effective People.” An in-depth discussion is beyond the scope of this article, but the time management matrix places tasks into one of four categories based on urgency and importance, and provides strategies for staying up on short-term goals while continually moving long-term goals forward.If you show up at your review with a list of accomplishments as well as an understanding of how the “time management matrix” affects your responsibilities, your boss will be impressed. It is also worth mentioning that Covey’s first habit is “Proactivity.” He uses the term Proactivity in a much more nuanced form than we typically think of, however. Simply put, Proactivity is the opposite of Reactivity, and it is another invaluable tool for success with those long-term goals that will help you make a name for yourself.
When you show up for your review, be it annual, biannual, or other, be prepared. Not only should you bring your job description and recommendations for how it should be adapted in the changing environment, but also bring examples of your accomplishments since the last review.
I talk with leaders frequently who are hardworking and diligent and hate bragging about their achievements; I get that. At the same time, if you don’t inform your superiors about your successes, there is no guarantee that they will hear about them or understand them in the appropriate context. Bragging about how great you are in the physician’s lounge is annoying; telling your boss about your accomplishments since the last review is critical to maintaining the momentum of past accomplishments. If you are not willing to toot your own horn, there is a very good chance that your horn will remain silent. I don’t think self-promotion comes easily to anyone, and it has to be done with a degree of humility and sensitivity; but it has to be done, so prepare for it.
Look out for yourself and others
We talk about teamwork and collaboration as hospitalists, and SHM is always underscoring the importance of teamwork and highlighting examples of successful teamwork in its many conferences and publications. Most hospital executives are focused on their own careers, however, and many have no reservations about damaging your career (your brand) if they think it will promote theirs. You have to look out for yourself and size up every leadership position you get into.
Physicians can expect their careers to last decades. The average hospital CEO has a tenure of less than 3.5 years, however, and when a new CEO is hired, almost half of chief financial, chief operating, and chief information officers are fired within 9 months. You may be focused on the long-term success of your organization as you plan your career, but many hospital administrators are interested only in short-term gains. It is similar to some members of Congress who are interested only in what they need to do now to win the next election and not in the long-term needs of the country. You should understand this disconnect when dealing with hospital executives, and how you and your credibility can become cannon fodder in their quest for short-term self-preservation.
You have to look out for and take care of yourself as you promote your group. With a better understanding of the Authority/Accountability balance, you have new tools to assess your chances of success and to advocate for yourself so that you and your group can be successful.
Despite my cynicism toward executives in the medical field, I personally advocate for supporting the career development of those around you and advise against furthering your career at the expense of others. Many unscrupulous executives will use this approach, surrounding themselves with Fall Guys, but my experience shows that this is not a sustainable strategy for success. It can lead to short-term gains, but eventually the piper must be paid. Moreover, the most successful medical executives and leaders that I have encountered have been those who genuinely cared about their subordinates, looked out for them, and selflessly promoted their careers.
In the age of social media, tearing others down seems to be the fastest way to get more “likes.” However, I strongly believe that you can’t build up your group, and our profession, just by tearing people down. Lending a helping hand may bring you less attention in the short term, but such action raises your stature, creates loyalty, and leads to sustainable success for the long run.
Dr. McIlraith is the founding chairman of the Hospital Medicine Department at Mercy Medical Group in Sacramento, Calif. He received the SHM Award for Outstanding Service in Hospital Medicine in 2016 and is currently a member of the SHM Practice Management and Awards Committees, as well as the SHM Critical Care Task Force.
Sources
Quinn R. HM Turns 20: A look at the evolution of hospital medicine. The Hospitalist. 2016 August. https://www.the-hospitalist.org/hospitalist/article/121525/hm-turns-20-look-evolution-hospital-medicine
Stephen R. Covey. The 7 Habits of Highly Effective People: Powerful Lessons in Personal Change. Simon & Schuster. 1989.
10 Statistics on CEO Turnover, Recruitment. Becker’s Hospital Review. 2020. https://www.beckershospitalreview.com/hospital-management-administration/10-statistics-on-ceo-turnover-recruitment.html
I have had the pleasure of working on the Society of Hospital Medicine’s signature Leadership Academies since 2010, and I enjoy working with hospital medicine leaders from around the country every year. I started as a hospital medicine leader in 2000 and served during the unprecedented growth of the field when it was “the most rapidly growing specialty in the history of medicine.”
Most businesses dream of having a year of double-digit growth; my department grew an average of 15% annually for more than 10 years. These unique experiences have taught me many lessons and afforded me the opportunity to watch many stars of hospital medicine rise, as well as to learn from several less-scrupulous leaders about the darker side of hospital politics.
One of the lessons I learned the hard way about hospital politics is striking the “Authority/Accountability balance” in your career. I shared this perspective at the SHM annual conference in 2018, at speaking engagements on the West Coast, and with my leadership group at the academies. I am sharing it with you because the feedback I have received has been very positive.
The Authority/Accountability balance is a tool for evaluating your current career trajectory and measuring if it is set up for success or failure. The essence is that your Authority and Accountability need to be balanced for you to be successful in your career, regardless of your station. Everybody from the hospitalist fresh out of residency to the CEO needs to have Authority and Accountability in balance to be successful. And as you use the tool to measure your own potential for success or failure, learn to apply it to those who report to you.
I believe the rising tide lifts all boats and the success of your subordinates, through mentoring and support, will add to your success. There is another, more cynical view of subordinates that can be identified using the Authority/Accountability balance, which I will address.
Authority
In this construct, “Authority” has a much broader meaning than just the ability to tell people what to do. The ability to tell people what to do is important but not sufficient for success in hospital politics.
Financial resources are essential for a successful Authority/Accountability balance – not only the hardware such as computers, telephones, pagers, and so on, but also clerical support, technical support, and analytic support so that you are getting high-quality data on the performance of the members of your hospital medicine group (HMG). These “soft” resources (clerical, technical, and analytical) are often overlooked as needs that HMG leaders must advocate for; I speak with many HMG leaders who remain under-resourced with “soft” assets. However, being appropriately resourced in these areas can be transformational for a group. Hospitalists don’t like doing clerical work, and if you don’t like a menial job assigned to you, you probably won’t do it very well. Having an unlicensed person dedicated to these clerical activities not only will cost less, but will ensure the job is done better.
Reporting structure is critically important, often overlooked, and historically misaligned in HMGs. When hospital medicine was starting in the late 1990s and early 2000s, rapidly growing hospitalist groups were typically led by young, early-career physicians who had chosen hospital medicine as a career. The problem was that they often lacked the seniority and connections at the executive level to advocate for their HMG. All too often the hospitalist group was tucked in under another department or division which, in turn, reported HMG updates and issues to the board of directors and the CEO.
A common reporting structure in the early days was that a senior member of the medical staff, or group, had once worked in the hospital and therefore “understood” the issues and challenges that the hospitalists were facing. It was up to this physician with seniority and connections to advocate for the hospitalists as they saw fit. The problem was that the hospital landscape was, and is, constantly evolving in innumerable ways. These “once removed” reporting structures for HMGs failed to get the required information on the rapidly changing, and evolving, hospitalist landscape to the desks of executives who had the financial and structural control to address the challenges that the hospitalists in the trenches were facing.
Numerous HMGs failed in the early days of hospital medicine because of this type of misaligned reporting structure. This is a lesson that should not be forgotten: Make sure your HMG leader has a seat at the table where executive decisions are made, including but not limited to the board of directors. To be in balance, you have to be “in the room where it happens.”
Accountability
The outcomes that you are responsible for need to be explicit, appropriately resourced with Authority, and clearly spelled out in your job description. Your job description is a document you should know, own, and revisit regularly with whomever you report to, in order to ensure success.
Once you have the Authority side of the equation appropriately resourced, setting outcomes that are a stretch, but still realistic and achievable within the scope of your position, is critical to your success. It is good to think about short-, medium-, and long-term goals, especially if you are in a leadership role. For example, one expectation you will have, regardless of your station, is that you keep up on your email and answer your phone. These are short-term goals that will often be included in your job description. However, taking on a new hospital contract and making sure that it has 24/7 hospitalist coverage, that all the hospitalists are meeting the geometric mean length of stay, and that all the physicians are having 15 encounters per day doesn’t happen immediately. Long-term goals, such as taking on a new hospital contract, are the big-picture stuff that can make or break the career of an HMG leader. Long-term goals also need to be delineated in the job description, along with specific time stamps and the resources you need to accomplish big ticket items – which are spelled out in the Authority side (that is, physician recruiter, secretary, background checks, and so on).
One of the classic misuses of Accountability is the “Fall Guy” scenario. The Fall Guy scenario is often used by cynical hospital and medical group executives to expand their influence while limiting their liability. In the Fall Guy scenario, the executive is surrounded with junior partners who are underpowered with Authority, and then the executive makes decisions for which the junior partners are Accountable. This allows the senior executive to make risky decisions on behalf of the hospital or medical group without the liability of being held accountable when the decision-making process fails. When the risky, and often ill-informed, decision fails, the junior partner who lacked the Authority to make the decision – but held the Accountability for it – becomes the Fall Guy for the failed endeavor. This is a critical outcome that the Authority/Accountability balance can help you avoid, if you use it wisely and properly.
If you find yourself in the Fall Guy position, it is time for a change. The Authority, the Accountability, or both need to change so that they are in better balance. Or your employer needs to change. Changing employers is an outcome worth avoiding, if at all possible. I have scrutinized thousands of resumes in my career, and frequent job changes always wave a red flag to prospective employers. However, changing jobs remains a crucial option if you are being set up for failure when Authority and Accountability are out of balance.
If you are unable to negotiate for the balance that will allow you to be successful with your current group, remember that HMG leaders are a prized commodity and in short supply. Leaving a group that has been your career is hard, but it is better to leave than stay in a position where you are set up for failure as the Fall Guy. Further, the most effective time to expand your Authority is when you are negotiating the terms of a new position. Changing positions is the nuclear option. However, it is better than becoming the Fall Guy, and a change can create opportunities that will accelerate your career and influence, if done right.
When I talk about Authority/Accountability balance, I always counter the Fall Guy with an ignominious historical figure: General George B. McClellan. General McClellan was the commander of the Army of the Potomac during the early years of the American Civil War. General McClellan had the industrial might of the Union north at his beck and call, as well as extraordinary resources for recruiting and retaining soldiers for his army. At every encounter with General Robert E. Lee’s Army of Northern Virginia, General McClellan outnumbered them, sometimes by more than two to one. Yet General McClellan was outfoxed repeatedly for the same reason: He failed to take decisive action.
Every time that McClellan failed, he blamed insufficient resources and told President Lincoln that he needed more troops and more equipment to be successful. In summary, while the Fall Guy scenario needs to be avoided, once you are adequately resourced, success requires taking decisive and strategic action, or you will suffer as did General McClellan. Failing to act when you are appropriately resourced can be just as damaging to your career and credibility as allowing yourself to become the Fall Guy.
Job description
Everybody has somebody that they report to, no matter how high up on the executive ladder they have climbed. Even the CEO must report to the board of directors. And that reporting structure usually involves periodic formal reviews. Your formal review is a good time to go over your job description, note what is relevant, remove what is irrelevant, and add new elements that have evolved in importance since your last review.
Job descriptions take many forms, but they always include a list of qualifications. If you have the job, you have the qualifications, so that is not likely to change. You may become more qualified for a higher-level position, but that is an entirely different discussion. I like to think of a well-written job description as including short-term and long-term goals. Short-term goals are usually the daily stuff that keeps operations running smoothly but garners little attention. Examples would include staying current on your emails, answering your phone, organizing meetings, and regularly attending various committees. Even some of these short-term goals can and will change over time. I always enjoyed quality oversight in my department, but as the department and my responsibilities grew, I realized I couldn’t do everything that I wanted to do. I needed to focus on the things only I could do and delegate those things that could be done by someone else, even though I wanted to continue doing them myself. I created a position for a clinical quality officer, and quality oversight moved off of my job description.
Long-term goals are the aspirational items, such as increasing market share, decreasing readmissions, improving patient satisfaction, and the like. Effective leaders are often focused on these aspirational, long-term goals, but they still must effectively execute their short-term goals. Stephen Covey outlines the dilemma with the “time management matrix” in his seminal work “The 7 Habits of Highly Effective People.” An in-depth discussion is beyond the scope of this article, but the time management matrix places tasks into one of four categories based on urgency and importance, and provides strategies for staying up on short-term goals while continually moving long-term goals forward.If you show up at your review with a list of accomplishments as well as an understanding of how the “time management matrix” affects your responsibilities, your boss will be impressed. It is also worth mentioning that Covey’s first habit is “Proactivity.” He uses the term Proactivity in a much more nuanced form than we typically think of, however. Simply put, Proactivity is the opposite of Reactivity, and it is another invaluable tool for success with those long-term goals that will help you make a name for yourself.
When you show up for your review, be it annual, biannual, or other, be prepared. Not only should you bring your job description and recommendations for how it should be adapted in the changing environment, but also bring examples of your accomplishments since the last review.
I talk with leaders frequently who are hardworking and diligent and hate bragging about their achievements; I get that. At the same time, if you don’t inform your superiors about your successes, there is no guarantee that they will hear about them or understand them in the appropriate context. Bragging about how great you are in the physician’s lounge is annoying; telling your boss about your accomplishments since the last review is critical to maintaining the momentum of past accomplishments. If you are not willing to toot your own horn, there is a very good chance that your horn will remain silent. I don’t think self-promotion comes easily to anyone, and it has to be done with a degree of humility and sensitivity; but it has to be done, so prepare for it.
Look out for yourself and others
We talk about teamwork and collaboration as hospitalists, and SHM is always underscoring the importance of teamwork and highlighting examples of successful teamwork in its many conferences and publications. Most hospital executives are focused on their own careers, however, and many have no reservations about damaging your career (your brand) if they think it will promote theirs. You have to look out for yourself and size up every leadership position you get into.
Physicians can expect their careers to last decades. The average hospital CEO has a tenure of less than 3.5 years, however, and when a new CEO is hired, almost half of chief financial, chief operating, and chief information officers are fired within 9 months. You may be focused on the long-term success of your organization as you plan your career, but many hospital administrators are interested only in short-term gains. It is similar to some members of Congress who are interested only in what they need to do now to win the next election and not in the long-term needs of the country. You should understand this disconnect when dealing with hospital executives, and how you and your credibility can become cannon fodder in their quest for short-term self-preservation.
You have to look out for and take care of yourself as you promote your group. With a better understanding of the Authority/Accountability balance, you have new tools to assess your chances of success and to advocate for yourself so that you and your group can be successful.
Despite my cynicism toward executives in the medical field, I personally advocate for supporting the career development of those around you and advise against furthering your career at the expense of others. Many unscrupulous executives will use this approach, surrounding themselves with Fall Guys, but my experience shows that this is not a sustainable strategy for success. It can lead to short-term gains, but eventually the piper must be paid. Moreover, the most successful medical executives and leaders that I have encountered have been those who genuinely cared about their subordinates, looked out for them, and selflessly promoted their careers.
In the age of social media, tearing others down seems to be the fastest way to get more “likes.” However, I strongly believe that you can’t build up your group, and our profession, just by tearing people down. Lending a helping hand may bring you less attention in the short term, but such action raises your stature, creates loyalty, and leads to sustainable success for the long run.
Dr. McIlraith is the founding chairman of the Hospital Medicine Department at Mercy Medical Group in Sacramento, Calif. He received the SHM Award for Outstanding Service in Hospital Medicine in 2016 and is currently a member of the SHM Practice Management and Awards Committees, as well as the SHM Critical Care Task Force.
Sources
Quinn R. HM Turns 20: A look at the evolution of hospital medicine. The Hospitalist. 2016 August. https://www.the-hospitalist.org/hospitalist/article/121525/hm-turns-20-look-evolution-hospital-medicine
Stephen R. Covey. The 7 Habits of Highly Effective People: Powerful Lessons in Personal Change. Simon & Schuster. 1989.
10 Statistics on CEO Turnover, Recruitment. Becker’s Hospital Review. 2020. https://www.beckershospitalreview.com/hospital-management-administration/10-statistics-on-ceo-turnover-recruitment.html
Inpatient opioid administration associated with postdischarge opioid use
Background: Efforts to reduce and monitor high-risk opioid prescribing have largely focused on outpatient prescribing with less empiric evaluation of inpatient administration. Little is known about the association of inpatient opioid administration and postdischarge opioid use.
Study design: Retrospective cohort.
Setting: 12 community and academic hospitals in Pennsylvania.
Synopsis: With electronic health record data from 2010-2014 to evaluate 148,068 opioid-naive patients aged 18 years and older, this study showed a relationship between inpatient opioid administration, specific patterns of inpatient opioid administration, and postdischarge opioid use. Specifically, inpatient opioid administration was associated with a 3.0% increase (95% CI, 2.8%-3.2%) in opioid use at 90 days post discharge. Additionally, inpatient opioid administration within 12 hours of hospital discharge was associated with a 3.6% increase (95% CI, 3.3%-3.9%) in opioid use at 90 days post discharge.
This observational study is prone to potential unmeasured confounders negating any clear causation. Rather, hospitalists should be aware of the increasing focus on inpatient opioid administration as it relates to outpatient opioid use, especially in the setting of the current opioid crisis.
Bottom line: Inpatient opioid administration and administration patterns are associated with 90-day postdischarge opioid use in opioid-naive patients.
Citation: Donohue JM et al. Patterns of opioid administration among opioid-naive inpatients and associations with postdischarge opioid use. Ann Intern Med. 2019 Jun 18:171(2):81-90.
Dr. Ledford is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: Efforts to reduce and monitor high-risk opioid prescribing have largely focused on outpatient prescribing with less empiric evaluation of inpatient administration. Little is known about the association of inpatient opioid administration and postdischarge opioid use.
Study design: Retrospective cohort.
Setting: 12 community and academic hospitals in Pennsylvania.
Synopsis: With electronic health record data from 2010-2014 to evaluate 148,068 opioid-naive patients aged 18 years and older, this study showed a relationship between inpatient opioid administration, specific patterns of inpatient opioid administration, and postdischarge opioid use. Specifically, inpatient opioid administration was associated with a 3.0% increase (95% CI, 2.8%-3.2%) in opioid use at 90 days post discharge. Additionally, inpatient opioid administration within 12 hours of hospital discharge was associated with a 3.6% increase (95% CI, 3.3%-3.9%) in opioid use at 90 days post discharge.
This observational study is prone to potential unmeasured confounders negating any clear causation. Rather, hospitalists should be aware of the increasing focus on inpatient opioid administration as it relates to outpatient opioid use, especially in the setting of the current opioid crisis.
Bottom line: Inpatient opioid administration and administration patterns are associated with 90-day postdischarge opioid use in opioid-naive patients.
Citation: Donohue JM et al. Patterns of opioid administration among opioid-naive inpatients and associations with postdischarge opioid use. Ann Intern Med. 2019 Jun 18:171(2):81-90.
Dr. Ledford is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: Efforts to reduce and monitor high-risk opioid prescribing have largely focused on outpatient prescribing with less empiric evaluation of inpatient administration. Little is known about the association of inpatient opioid administration and postdischarge opioid use.
Study design: Retrospective cohort.
Setting: 12 community and academic hospitals in Pennsylvania.
Synopsis: With electronic health record data from 2010-2014 to evaluate 148,068 opioid-naive patients aged 18 years and older, this study showed a relationship between inpatient opioid administration, specific patterns of inpatient opioid administration, and postdischarge opioid use. Specifically, inpatient opioid administration was associated with a 3.0% increase (95% CI, 2.8%-3.2%) in opioid use at 90 days post discharge. Additionally, inpatient opioid administration within 12 hours of hospital discharge was associated with a 3.6% increase (95% CI, 3.3%-3.9%) in opioid use at 90 days post discharge.
This observational study is prone to potential unmeasured confounders negating any clear causation. Rather, hospitalists should be aware of the increasing focus on inpatient opioid administration as it relates to outpatient opioid use, especially in the setting of the current opioid crisis.
Bottom line: Inpatient opioid administration and administration patterns are associated with 90-day postdischarge opioid use in opioid-naive patients.
Citation: Donohue JM et al. Patterns of opioid administration among opioid-naive inpatients and associations with postdischarge opioid use. Ann Intern Med. 2019 Jun 18:171(2):81-90.
Dr. Ledford is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
PPI use associated with all-cause and cause-specific mortality
Background: PPI use has previously been associated with an increased risk of acute kidney injury, Clostridium difficile infection, osteoporosis, dementia, and all-cause mortality. An estimation of the level of mortality risk, as well as cause-specific mortality risk, may better inform decisions about prescribing PPIs.
Study design: Longitudinal observational cohort.
Setting: Department of Veterans Affairs.
Synopsis: Using a cohort of veterans newly prescribed acid suppression therapy in 2002-2004, 157,625 new PPI users were compared with 56,842 new H2 receptor–blocker users. Over the following 10 years, a specific cause of death was determined using national death index data. In that period, 37.3% of patients died, with PPI use associated with 45.2 excess deaths per 1,000 patients (95% confidence interval, 28.2-61.4). There were significant associations with the following specific causes of death: circulatory system diseases (17.5 excess deaths per 1,000 patients, 95% CI, 5.5-28.8), neoplasms (12.9; 95% CI, 1.2-24.3), genitourinary system diseases including chronic kidney disease (6.3; 95% CI, 1.6-7.0), and infectious/parasitic diseases (4.2; 95% CI, 3.2-9.2).
Limitations include the observational study design and potential for confounding variables not accounted for by the researchers. There is also a question of broader applicability given the VA patient population. Nevertheless, this study adds to growing evidence regarding risks associated with PPI use. Clinicians should consider prescribing PPIs only for indications and durations where it is known to offer benefit in order minimize risk of adverse events.
Bottom line: PPI use is associated with an excess risk of death, particularly death caused by cardiovascular disease, malignancy, genitourinary diseases, and infection.
CITATION: Xie Y et al. Estimates of all-cause mortality and cause specific mortality associated with proton pump inhibitors among US veterans: Cohort study. BMJ. 2019 May 29;365:l1580.
Dr. Kruse is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: PPI use has previously been associated with an increased risk of acute kidney injury, Clostridium difficile infection, osteoporosis, dementia, and all-cause mortality. An estimation of the level of mortality risk, as well as cause-specific mortality risk, may better inform decisions about prescribing PPIs.
Study design: Longitudinal observational cohort.
Setting: Department of Veterans Affairs.
Synopsis: Using a cohort of veterans newly prescribed acid suppression therapy in 2002-2004, 157,625 new PPI users were compared with 56,842 new H2 receptor–blocker users. Over the following 10 years, a specific cause of death was determined using national death index data. In that period, 37.3% of patients died, with PPI use associated with 45.2 excess deaths per 1,000 patients (95% confidence interval, 28.2-61.4). There were significant associations with the following specific causes of death: circulatory system diseases (17.5 excess deaths per 1,000 patients, 95% CI, 5.5-28.8), neoplasms (12.9; 95% CI, 1.2-24.3), genitourinary system diseases including chronic kidney disease (6.3; 95% CI, 1.6-7.0), and infectious/parasitic diseases (4.2; 95% CI, 3.2-9.2).
Limitations include the observational study design and potential for confounding variables not accounted for by the researchers. There is also a question of broader applicability given the VA patient population. Nevertheless, this study adds to growing evidence regarding risks associated with PPI use. Clinicians should consider prescribing PPIs only for indications and durations where it is known to offer benefit in order minimize risk of adverse events.
Bottom line: PPI use is associated with an excess risk of death, particularly death caused by cardiovascular disease, malignancy, genitourinary diseases, and infection.
CITATION: Xie Y et al. Estimates of all-cause mortality and cause specific mortality associated with proton pump inhibitors among US veterans: Cohort study. BMJ. 2019 May 29;365:l1580.
Dr. Kruse is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: PPI use has previously been associated with an increased risk of acute kidney injury, Clostridium difficile infection, osteoporosis, dementia, and all-cause mortality. An estimation of the level of mortality risk, as well as cause-specific mortality risk, may better inform decisions about prescribing PPIs.
Study design: Longitudinal observational cohort.
Setting: Department of Veterans Affairs.
Synopsis: Using a cohort of veterans newly prescribed acid suppression therapy in 2002-2004, 157,625 new PPI users were compared with 56,842 new H2 receptor–blocker users. Over the following 10 years, a specific cause of death was determined using national death index data. In that period, 37.3% of patients died, with PPI use associated with 45.2 excess deaths per 1,000 patients (95% confidence interval, 28.2-61.4). There were significant associations with the following specific causes of death: circulatory system diseases (17.5 excess deaths per 1,000 patients, 95% CI, 5.5-28.8), neoplasms (12.9; 95% CI, 1.2-24.3), genitourinary system diseases including chronic kidney disease (6.3; 95% CI, 1.6-7.0), and infectious/parasitic diseases (4.2; 95% CI, 3.2-9.2).
Limitations include the observational study design and potential for confounding variables not accounted for by the researchers. There is also a question of broader applicability given the VA patient population. Nevertheless, this study adds to growing evidence regarding risks associated with PPI use. Clinicians should consider prescribing PPIs only for indications and durations where it is known to offer benefit in order minimize risk of adverse events.
Bottom line: PPI use is associated with an excess risk of death, particularly death caused by cardiovascular disease, malignancy, genitourinary diseases, and infection.
CITATION: Xie Y et al. Estimates of all-cause mortality and cause specific mortality associated with proton pump inhibitors among US veterans: Cohort study. BMJ. 2019 May 29;365:l1580.
Dr. Kruse is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
PICC lines often used inappropriately in advanced CKD patients
Background: PICC insertion is associated with risk for venous thrombosis and stenosis. National guidelines recommend avoiding PICC lines in patients with CKD stage 3b (glomerular filtration rate less than 45 mL/min per 1.73 m2) in order to preserve venous integrity for future creation of arteriovenous fistula, which is the ideal vascular access for hemodialysis.
Study design: Prospective cohort.
Setting: 52 hospitals in Michigan.
Synopsis: Data obtained from inpatients within the Michigan Hospital Medicine Safety Consortium between 2013 and 2016 showed that, of 20,545 total PICCs placed, 23% were placed in patients with a glomerular filtration rate less than 45 mL/min per 1.73 m2, and 3.2% were placed in those receiving dialysis. PICC placement in advanced CKD was more common in the ICU than in the ward setting, and placement more frequently utilized multilumen instead of single-lumen catheters. PICC-related complications were not more common in advanced CKD but were more often seen in the ICU and with multilumen PICCs. About one-quarter of PICCs were used for durations of less than 5 days.
The study is limited by lack of data in a subset of patients who had no documented GFR (2.7%) or missing covariate data (2.7%). The inability to ascertain other clinical information, such as nephrology approval of PICC, functional AV fistula or other hemodialysis access, or PICC complications after discharge further limit the findings.
Hospitalists should first decide if a PICC line is truly indicated, and if so, carefully weigh the risks and benefits of PICC placement in patients with advanced CKD.
Bottom line: PICC placement is common and often inappropriate in hospitalized patients with advanced CKD.
Citation: Paje D et al. Use of peripherally inserted central catheters in patients with advanced chronic kidney disease A prospective cohort study. Ann Intern Med. 2019 Jun 4;171:10-8.
Dr. Hageman is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: PICC insertion is associated with risk for venous thrombosis and stenosis. National guidelines recommend avoiding PICC lines in patients with CKD stage 3b (glomerular filtration rate less than 45 mL/min per 1.73 m2) in order to preserve venous integrity for future creation of arteriovenous fistula, which is the ideal vascular access for hemodialysis.
Study design: Prospective cohort.
Setting: 52 hospitals in Michigan.
Synopsis: Data obtained from inpatients within the Michigan Hospital Medicine Safety Consortium between 2013 and 2016 showed that, of 20,545 total PICCs placed, 23% were placed in patients with a glomerular filtration rate less than 45 mL/min per 1.73 m2, and 3.2% were placed in those receiving dialysis. PICC placement in advanced CKD was more common in the ICU than in the ward setting, and placement more frequently utilized multilumen instead of single-lumen catheters. PICC-related complications were not more common in advanced CKD but were more often seen in the ICU and with multilumen PICCs. About one-quarter of PICCs were used for durations of less than 5 days.
The study is limited by lack of data in a subset of patients who had no documented GFR (2.7%) or missing covariate data (2.7%). The inability to ascertain other clinical information, such as nephrology approval of PICC, functional AV fistula or other hemodialysis access, or PICC complications after discharge further limit the findings.
Hospitalists should first decide if a PICC line is truly indicated, and if so, carefully weigh the risks and benefits of PICC placement in patients with advanced CKD.
Bottom line: PICC placement is common and often inappropriate in hospitalized patients with advanced CKD.
Citation: Paje D et al. Use of peripherally inserted central catheters in patients with advanced chronic kidney disease A prospective cohort study. Ann Intern Med. 2019 Jun 4;171:10-8.
Dr. Hageman is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: PICC insertion is associated with risk for venous thrombosis and stenosis. National guidelines recommend avoiding PICC lines in patients with CKD stage 3b (glomerular filtration rate less than 45 mL/min per 1.73 m2) in order to preserve venous integrity for future creation of arteriovenous fistula, which is the ideal vascular access for hemodialysis.
Study design: Prospective cohort.
Setting: 52 hospitals in Michigan.
Synopsis: Data obtained from inpatients within the Michigan Hospital Medicine Safety Consortium between 2013 and 2016 showed that, of 20,545 total PICCs placed, 23% were placed in patients with a glomerular filtration rate less than 45 mL/min per 1.73 m2, and 3.2% were placed in those receiving dialysis. PICC placement in advanced CKD was more common in the ICU than in the ward setting, and placement more frequently utilized multilumen instead of single-lumen catheters. PICC-related complications were not more common in advanced CKD but were more often seen in the ICU and with multilumen PICCs. About one-quarter of PICCs were used for durations of less than 5 days.
The study is limited by lack of data in a subset of patients who had no documented GFR (2.7%) or missing covariate data (2.7%). The inability to ascertain other clinical information, such as nephrology approval of PICC, functional AV fistula or other hemodialysis access, or PICC complications after discharge further limit the findings.
Hospitalists should first decide if a PICC line is truly indicated, and if so, carefully weigh the risks and benefits of PICC placement in patients with advanced CKD.
Bottom line: PICC placement is common and often inappropriate in hospitalized patients with advanced CKD.
Citation: Paje D et al. Use of peripherally inserted central catheters in patients with advanced chronic kidney disease A prospective cohort study. Ann Intern Med. 2019 Jun 4;171:10-8.
Dr. Hageman is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
How do you manage common inpatient oncologic emergencies?
Three routinely encountered emergencies in the inpatient setting
In 2016, there were an estimated 15,338,988 people living with cancer in the United States.1 As such, it is important that hospitalists be proficient in managing oncologic emergencies that can arise during the natural history of cancer or from its treatment. This article will review three emergencies that are routinely encountered in the inpatient setting: malignant spinal cord compression (MSCC), hypercalcemia of malignancy (HCM), and febrile neutropenia (FN).
Case
Mr. Williams is a 56-year-old man with newly diagnosed metastatic prostate cancer, diabetes mellitus, peptic ulcer disease, and hypertension. He is admitted with back pain and lower extremity weakness worsening over 2 weeks. He denies loss of sensation or bowel and bladder incontinence and can walk. MRI confirms cord compression at T10. What initial and subsequent steroid doses would be of most benefit to administer?
Malignant spinal cord compression
Treatment of MSCC usually aims to preserve function rather than reverse established deficits. MSCC from epidural tumor metastasis develops in 5%-14% of all cancer cases,2 with back pain as the most common symptom. Nearly 60%-85% of patients have weakness at the time of diagnosis,3 and unfortunately, nearly two-thirds of patients will be nonambulatory at presentation.
While timely steroid administration in addition to definitive treatment may maintain ambulatory capacity at 1 year after therapy,4 there is no consensus on the optimal loading and maintenance dose and duration of steroids.
Overview of the data
Although there are no formal guidelines on optimal steroid dosing for MSCC, it is common practice for dexamethasone to be initially dosed at 10 mg followed by 4 mg every 4-6 hours.5 The use of higher doses of dexamethasone may result in improvement in neurologic deficits, but has higher risks for toxicity and is not universally supported in the literature.
A study conducted by Vecht and colleagues demonstrated few differences between initial high-dose and low-dose dexamethasone.6 Intravenous administration of either 10 mg or 100 mg dexamethasone, both followed by total 16 mg of dexamethasone orally per day, showed no significant difference in mobility or survival between the groups.
In a prospective study by Heimdal and colleagues that evaluated the relationship between dexamethasone dose and toxicity, higher doses of steroids had no meaningful impact on neurological symptoms and resulted in more severe side effects.7 Patients were either given 96-mg IV loading dose, gradually tapered over 2 weeks, or enrolled in the low-dose group in which they received 4-mg IV dexamethasone four times per day with a taper over 2 weeks. The high-dose group experienced side effects in 28.6% of patients, with 14.3% experiencing serious side effects. Meanwhile, 7.9% of the low-dose group exhibited some side effects, with none experiencing serious adverse effects.The high-dose group did not experience a significant increase in mobility (57.1 vs. 57.9%).
Key takeaways
Dexamthasone 10-mg oral or IV followed by 4 mg every 4-6 hours until definitive treatment is started is associated with improved neurologic outcomes and minimal adverse side effects. Higher doses of steroids are unlikely to offer more benefit. In patients with paraplegia or autonomic dysfunction, the ability to restore neurologic function is reduced and the burdens of steroid treatment may outweigh its benefits.5
Case continued
Mr. Williams completed treatment for MSCC but was still complaining of extreme lethargy and noticed an increase in thirst and no bowel movement in 5 days. His serum calcium was 14 mg/dL.
Hypercalcemia of malignancy
HCM is the most common paraneoplastic syndrome, observed in nearly 30% of patients with advanced cancer. It is a poor prognostic indicator, and approximately half of all patients with HCM will die within 30 days.8 Cancer is the most common reason for hypercalcemia in the inpatient setting9 and is most often associated with multiple myeloma, non–small cell lung cancer, breast cancer, renal cell carcinoma, non-Hodgkins lymphoma, and leukemia.
Hypercalcemia most often presents with cognitive changes and lethargy, anorexia, nausea, constipation, polyuria and polydipsia, and renal failure. Bradycardia and shortened QT interval are seen more with severe hypercalcemia.
Management of hypercalcemia of malignancy
Management of HCM depends on corrected calcium or ionized calcium levels, chronicity, degree of symptoms, and presence of renal failure. In general, mild asymptomatic hypercalcemia can be managed with outpatient care. Serum calcium greater than 14 mg/dL should be treated regardless of symptoms (Table 1).
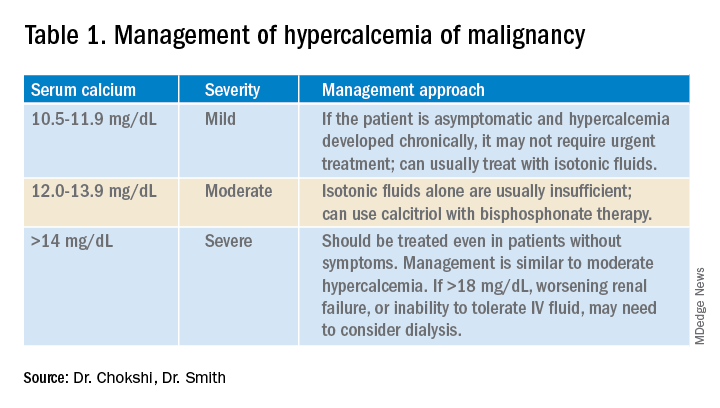
For mild to moderate HCM, management involves saline administration to achieve euvolemia and calcitonin, which has temporizing effects. Early administration of IV bisphosphonates for moderate to severe HCM is beneficial because onset of action is 24-48 hours. Furosemide for management of HCM has fallen out of favor unless the patient develops hypervolemia. Denosumab has been Food and Drug Administration–approved for HCM refractory to bisphosphonate therapy and can manage HCM in 64% of patients who did not respond adequately to bisphosphonate therapy.10 Because it can be used in advanced renal failure without dose adjustment, it is first-line therapy in this population, although the risk for hypocalcemia is increased in renal failure. For patients with serum calcium greater than 18 mg/dL, worsening renal failure, or inability to tolerate IV fluids, dialysis with a low-calcium bath should be considered (Table 2).
Zoledronic acid versus pamidronate
A single dose of zoledronic acid normalizes the serum calcium concentration in 88% of patients, compared with 70% of those who received pamidronate, in a pooled analysis of two phase 3 trials.11 The median duration of normocalcemia was longer for those receiving zoledronic acid (32-43 days vs. 18 days). The efficacy of the 4-mg and 8-mg zoledronic acid doses were similar, but the 4-mg dose was recommended because of renal toxicity and increased mortality associated with the higher dose.Despite this data, many specialists maintain that pamidronate, which is less expensive, is of similar clinical efficacy to ZA.12
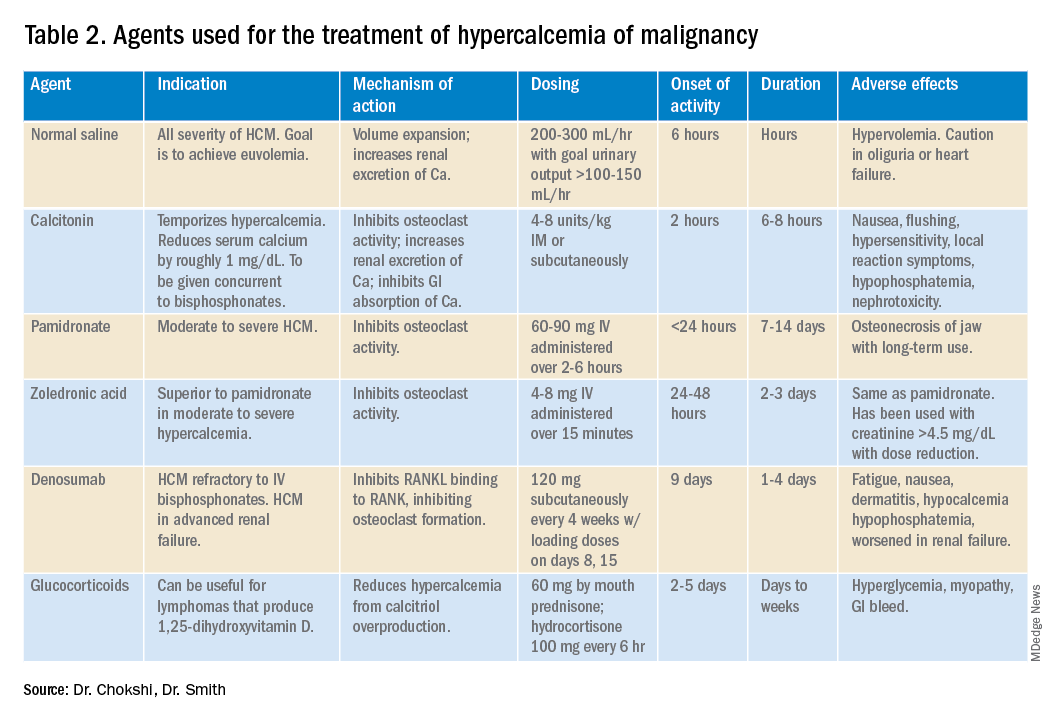
Key takeaways
Management of HCM should be determined by the severity of the calcium level. The mainstay of treatment includes hydration with normal saline, calcitonin ,and bisphosphonate therapy; zoledronic acid is preferred over pamidronate. For patients refractory to bisphosphonates or patients with renal insufficiency, denosumab should be used.
Case continued: Febrile neutropenia
Febrile neutropenia is defined as a single oral temperature of 100.9° F or a temperature of 100.4° F sustained over a 1-hour period in a patient with absolute neutrophil count (ANC) less than 1,000 cells/mL or ANC expected to decrease to less than 500 cells/mL within a 48-hour period.13 Up to 30% of patients with solid tumors develop febrile neutropenia after chemotherapy, and nearly 80% of patients with hematologic malignancy or after hematopoietic stem cell therapy (HSCT) experience it.
Even though an infectious etiology is identified in only 30%-40% of cases, all patients with febrile neutropenia should initially receive at least empiric gram-negative coverage. The mortality rate is nearly 70% in neutropenic patients who do not receive empiric antibiotics and is reduced to 4%-20% with antibiotics.14
Risk stratification for febrile neutropenia and early discharge
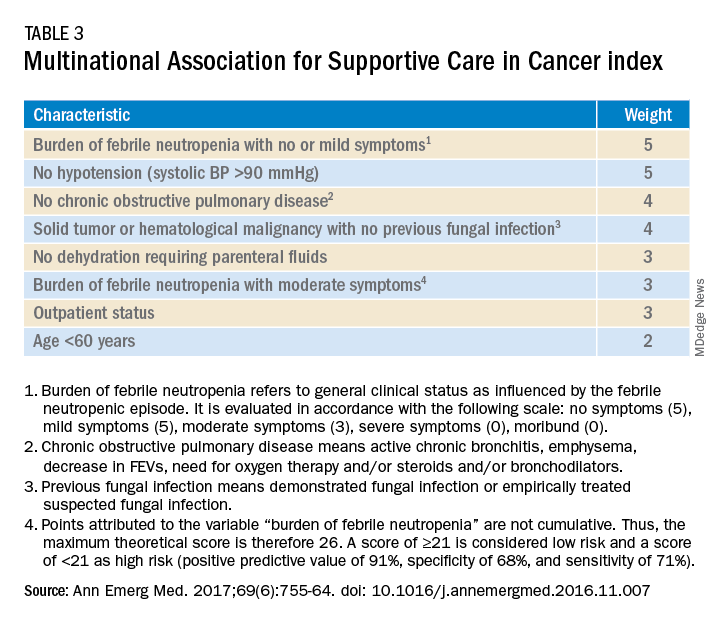
Talcott’s Rules, the Multinational Association for Supportive Care in Cancer (MASCC) score, and the Clinical Index of Stable Febrile Neutropenia (CISNE) are validated tools to determine low-risk febrile neutropenia patients (Tables 3 and 4). The Infectious Diseases Society of America guidelines validated the use of MASCC in 2002 but found that CISNE had better performance than other tools. Coyne and colleagues conducted a retrospective cohort study to assess these two risk stratification tools in the ED and found that the CISNE was 98.3% specific for identifying adverse outcomes, whereas the MASCC was 54.2% specific.15
A study by Talcott and colleagues used Talcott’s Rules to identify low-risk febrile neutropenia patients, who were randomized to early discharge with home intravenous antibiotics versus continued inpatient management. There were no significant differences in the primary outcomes, defined as any change in clinical status requiring medical evaluation.16 Another study suggested that discharge after 24 hours based on clinical stability with outpatient oral antibiotics were noninferior to standard inpatient and intravenous antibiotic therapy.17 A Cochrane review in 2013 of 22 randomized controlled trials determined that oral antibiotics were an acceptable treatment for low-risk patients.18
Key takeaways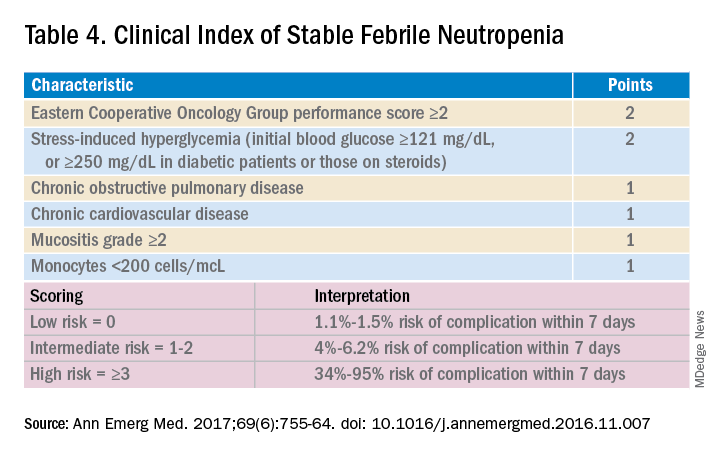
Though the MASCC is highly sensitive in identifying low-risk febrile neutropenia patients, it should be used with clinical caution because up to 11% of patients characterized as low risk developed severe complications.19 If a low-risk patient with solid tumor malignancy has adequate home support, lives within an hour of the hospital, and has access to follow-up within 72 hours, oral antibiotics and early discharge can be considered.
Dr. Chokshi is assistant professor in the division of hospital medicine at Mount Sinai Hospital, New York. Dr. Smith is associate professor in the division of hematology/oncology at Mount Sinai Hospital.
QUIZ
Mrs. Smith is a 64-year-old woman with endometrial cancer with temperature of 100.4° F at home. She takes no antibiotics, has no other medical history, and was sent in from clinic and admitted for further management. She feels well, and preliminary infectious workup is negative. She has been afebrile for more than 24 hours, and her ANC is 600 cells/mL.
Her son’s soccer game is tomorrow, and she would like to be present. Her family is involved in her care. Under what conditions can she be discharged?
A. She should not be discharged until full course of empiric intravenous antibiotics is completed.
B. Consider discharge in another 24 hours if she remains afebrile.
C. Discharge if low risk by MASCC or CISNE, with oral doses of levofloxacin or moxifloxacin or oral ciprofloxacin and amoxicillin/clavulanic acid.
Answer: C. The patient has a solid tumor malignancy, is low risk by both MASCC and CISNE, and can most likely be discharged if she is clinically stable or improved. A 7-day course of antibiotics is recommended with close follow-up.
References
1. SEER. Cancer of Any Site - Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/all.html. Accessed 2019 Jul 17.
2. Kwok Y et al. Clinical Approach to Metastatic Epidural Spinal Cord Compression. Hematol Oncol Clin North Am. 2006;20(6):1297-305.
3. Helweg-Larsen S et al. Prognostic factors in metastatic spinal cord compression: a prospective study using multivariate analysis of variables influencing survival and gait function in 153 patients. Int J Radiat Oncol Biol Phys. 2000;46(5):1163-9.
4. Sørensen P et al. Effect of high-dose dexamethasone in carcinomatous metastatic spinal cord compression treated with radiotherapy: A randomised trial. Eur J Cancer. 1994;30(1):22-7.
5. Skeoch G et al. Corticosteroid treatment for metastatic spinal cord compression: A review. Global Spine J. 2017;7(3):272-9.
6. Vecht C et al. Initial bolus of conventional versus high-dose dexamethasone in metastatic spinal cord compression. Neurology. 1989;39(9):1255-7.
7. Heimdal K et al. High incidence of serious side effects of high-dose dexamethasone treatment in patients with epidural spinal cord compression. J Neurooncol. 1992;12(2):141-4.
8. Ralston S et al. Cancer-associated hypercalcemia: Morbidity and mortality. Clinical experience in 126 treated patients. Ann Intern Med. 1990;112(7):499-504.
9. Lindner G et al. Hypercalcemia in the ED: Prevalence, etiology, and outcome. Am J Emerg Med. 2013;31(4):657-60.
10. Hu M et al. Denosumab for patients with persistent or relapsed hypercalcemia of malignancy despite recent bisphosphonate treatment. J Natl Cancer Inst. 2013;105(18):1417-20.
11. Major P et al. Zoledronic acid is superior to pamidronate in the treatment of hypercalcemia of malignancy: A pooled analysis of two randomized, controlled clinical trials. J Clin Oncol. 2001;19(2):558-67.
12. Stewart A. Clinical practice. Hypercalcemia associated with cancer. N Engl J Med. 2005;352(4):373-9.
13. Freifeld A et al. Executive summary: Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52(4):427-31.
14. Baden L et al. Prevention and treatment of cancer-related infections, version 2.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2016;14(7):882-913.
15. Coyne C et al. Application of the MASCC and CISNE risk-stratification scores to identify low-risk febrile neutropenic patients in the emergency department. Ann Emerg Med. 2017;69(6):755-64.
16. Talcott J et al. Safety of early discharge for low-risk patients with febrile neutropenia: a multicenter randomized controlled trial. J Clin Oncol. 2011;29(30):3977-83.
17. Innes H et al. Oral antibiotics with early hospital discharge compared with in-patient intravenous antibiotics for low-risk febrile neutropenia in patients with cancer: A prospective randomised controlled single centre study. Br J Cancer. 2003;89(1):43-9.
18. Vidal L, et al. Oral versus intravenous antibiotic treatment for febrile neutropenia in cancer patients. Cochrane Database Syst. Rev. 2013.
19. Taplitz RA et al. Outpatient management of fever and neutropenia in adults treated for malignancy: American Society of Clinical Oncology and Infectious Diseases Society of America clinical practice guideline update. J Clin Oncol. 2018;36(14):1443-53.
Three routinely encountered emergencies in the inpatient setting
Three routinely encountered emergencies in the inpatient setting
In 2016, there were an estimated 15,338,988 people living with cancer in the United States.1 As such, it is important that hospitalists be proficient in managing oncologic emergencies that can arise during the natural history of cancer or from its treatment. This article will review three emergencies that are routinely encountered in the inpatient setting: malignant spinal cord compression (MSCC), hypercalcemia of malignancy (HCM), and febrile neutropenia (FN).
Case
Mr. Williams is a 56-year-old man with newly diagnosed metastatic prostate cancer, diabetes mellitus, peptic ulcer disease, and hypertension. He is admitted with back pain and lower extremity weakness worsening over 2 weeks. He denies loss of sensation or bowel and bladder incontinence and can walk. MRI confirms cord compression at T10. What initial and subsequent steroid doses would be of most benefit to administer?
Malignant spinal cord compression
Treatment of MSCC usually aims to preserve function rather than reverse established deficits. MSCC from epidural tumor metastasis develops in 5%-14% of all cancer cases,2 with back pain as the most common symptom. Nearly 60%-85% of patients have weakness at the time of diagnosis,3 and unfortunately, nearly two-thirds of patients will be nonambulatory at presentation.
While timely steroid administration in addition to definitive treatment may maintain ambulatory capacity at 1 year after therapy,4 there is no consensus on the optimal loading and maintenance dose and duration of steroids.
Overview of the data
Although there are no formal guidelines on optimal steroid dosing for MSCC, it is common practice for dexamethasone to be initially dosed at 10 mg followed by 4 mg every 4-6 hours.5 The use of higher doses of dexamethasone may result in improvement in neurologic deficits, but has higher risks for toxicity and is not universally supported in the literature.
A study conducted by Vecht and colleagues demonstrated few differences between initial high-dose and low-dose dexamethasone.6 Intravenous administration of either 10 mg or 100 mg dexamethasone, both followed by total 16 mg of dexamethasone orally per day, showed no significant difference in mobility or survival between the groups.
In a prospective study by Heimdal and colleagues that evaluated the relationship between dexamethasone dose and toxicity, higher doses of steroids had no meaningful impact on neurological symptoms and resulted in more severe side effects.7 Patients were either given 96-mg IV loading dose, gradually tapered over 2 weeks, or enrolled in the low-dose group in which they received 4-mg IV dexamethasone four times per day with a taper over 2 weeks. The high-dose group experienced side effects in 28.6% of patients, with 14.3% experiencing serious side effects. Meanwhile, 7.9% of the low-dose group exhibited some side effects, with none experiencing serious adverse effects.The high-dose group did not experience a significant increase in mobility (57.1 vs. 57.9%).
Key takeaways
Dexamthasone 10-mg oral or IV followed by 4 mg every 4-6 hours until definitive treatment is started is associated with improved neurologic outcomes and minimal adverse side effects. Higher doses of steroids are unlikely to offer more benefit. In patients with paraplegia or autonomic dysfunction, the ability to restore neurologic function is reduced and the burdens of steroid treatment may outweigh its benefits.5
Case continued
Mr. Williams completed treatment for MSCC but was still complaining of extreme lethargy and noticed an increase in thirst and no bowel movement in 5 days. His serum calcium was 14 mg/dL.
Hypercalcemia of malignancy
HCM is the most common paraneoplastic syndrome, observed in nearly 30% of patients with advanced cancer. It is a poor prognostic indicator, and approximately half of all patients with HCM will die within 30 days.8 Cancer is the most common reason for hypercalcemia in the inpatient setting9 and is most often associated with multiple myeloma, non–small cell lung cancer, breast cancer, renal cell carcinoma, non-Hodgkins lymphoma, and leukemia.
Hypercalcemia most often presents with cognitive changes and lethargy, anorexia, nausea, constipation, polyuria and polydipsia, and renal failure. Bradycardia and shortened QT interval are seen more with severe hypercalcemia.
Management of hypercalcemia of malignancy
Management of HCM depends on corrected calcium or ionized calcium levels, chronicity, degree of symptoms, and presence of renal failure. In general, mild asymptomatic hypercalcemia can be managed with outpatient care. Serum calcium greater than 14 mg/dL should be treated regardless of symptoms (Table 1).
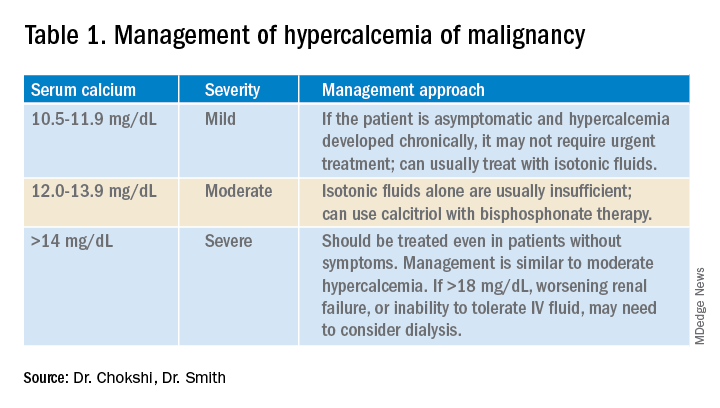
For mild to moderate HCM, management involves saline administration to achieve euvolemia and calcitonin, which has temporizing effects. Early administration of IV bisphosphonates for moderate to severe HCM is beneficial because onset of action is 24-48 hours. Furosemide for management of HCM has fallen out of favor unless the patient develops hypervolemia. Denosumab has been Food and Drug Administration–approved for HCM refractory to bisphosphonate therapy and can manage HCM in 64% of patients who did not respond adequately to bisphosphonate therapy.10 Because it can be used in advanced renal failure without dose adjustment, it is first-line therapy in this population, although the risk for hypocalcemia is increased in renal failure. For patients with serum calcium greater than 18 mg/dL, worsening renal failure, or inability to tolerate IV fluids, dialysis with a low-calcium bath should be considered (Table 2).
Zoledronic acid versus pamidronate
A single dose of zoledronic acid normalizes the serum calcium concentration in 88% of patients, compared with 70% of those who received pamidronate, in a pooled analysis of two phase 3 trials.11 The median duration of normocalcemia was longer for those receiving zoledronic acid (32-43 days vs. 18 days). The efficacy of the 4-mg and 8-mg zoledronic acid doses were similar, but the 4-mg dose was recommended because of renal toxicity and increased mortality associated with the higher dose.Despite this data, many specialists maintain that pamidronate, which is less expensive, is of similar clinical efficacy to ZA.12
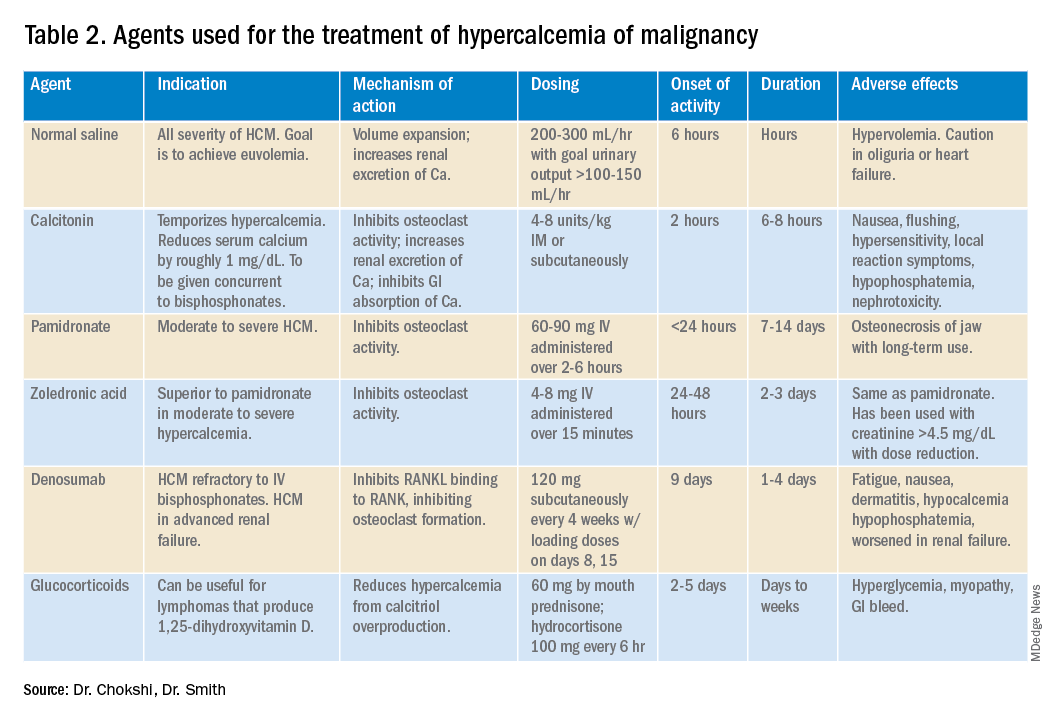
Key takeaways
Management of HCM should be determined by the severity of the calcium level. The mainstay of treatment includes hydration with normal saline, calcitonin ,and bisphosphonate therapy; zoledronic acid is preferred over pamidronate. For patients refractory to bisphosphonates or patients with renal insufficiency, denosumab should be used.
Case continued: Febrile neutropenia
Febrile neutropenia is defined as a single oral temperature of 100.9° F or a temperature of 100.4° F sustained over a 1-hour period in a patient with absolute neutrophil count (ANC) less than 1,000 cells/mL or ANC expected to decrease to less than 500 cells/mL within a 48-hour period.13 Up to 30% of patients with solid tumors develop febrile neutropenia after chemotherapy, and nearly 80% of patients with hematologic malignancy or after hematopoietic stem cell therapy (HSCT) experience it.
Even though an infectious etiology is identified in only 30%-40% of cases, all patients with febrile neutropenia should initially receive at least empiric gram-negative coverage. The mortality rate is nearly 70% in neutropenic patients who do not receive empiric antibiotics and is reduced to 4%-20% with antibiotics.14
Risk stratification for febrile neutropenia and early discharge
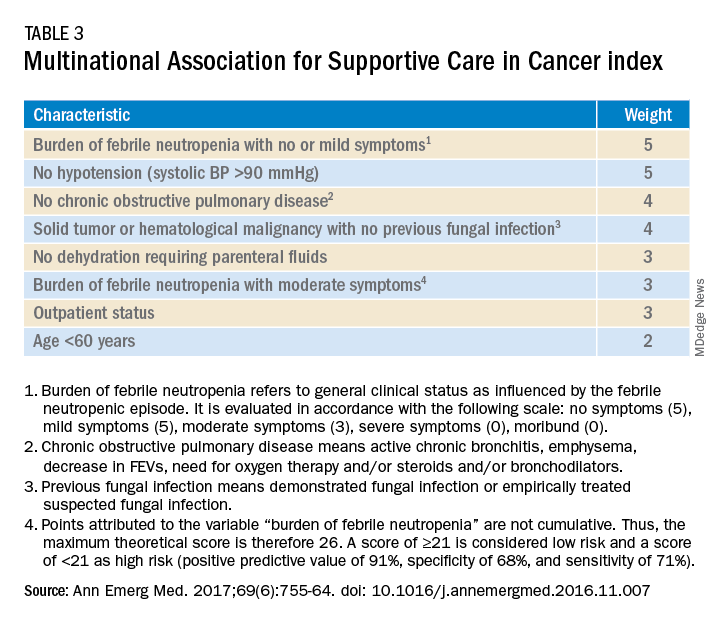
Talcott’s Rules, the Multinational Association for Supportive Care in Cancer (MASCC) score, and the Clinical Index of Stable Febrile Neutropenia (CISNE) are validated tools to determine low-risk febrile neutropenia patients (Tables 3 and 4). The Infectious Diseases Society of America guidelines validated the use of MASCC in 2002 but found that CISNE had better performance than other tools. Coyne and colleagues conducted a retrospective cohort study to assess these two risk stratification tools in the ED and found that the CISNE was 98.3% specific for identifying adverse outcomes, whereas the MASCC was 54.2% specific.15
A study by Talcott and colleagues used Talcott’s Rules to identify low-risk febrile neutropenia patients, who were randomized to early discharge with home intravenous antibiotics versus continued inpatient management. There were no significant differences in the primary outcomes, defined as any change in clinical status requiring medical evaluation.16 Another study suggested that discharge after 24 hours based on clinical stability with outpatient oral antibiotics were noninferior to standard inpatient and intravenous antibiotic therapy.17 A Cochrane review in 2013 of 22 randomized controlled trials determined that oral antibiotics were an acceptable treatment for low-risk patients.18
Key takeaways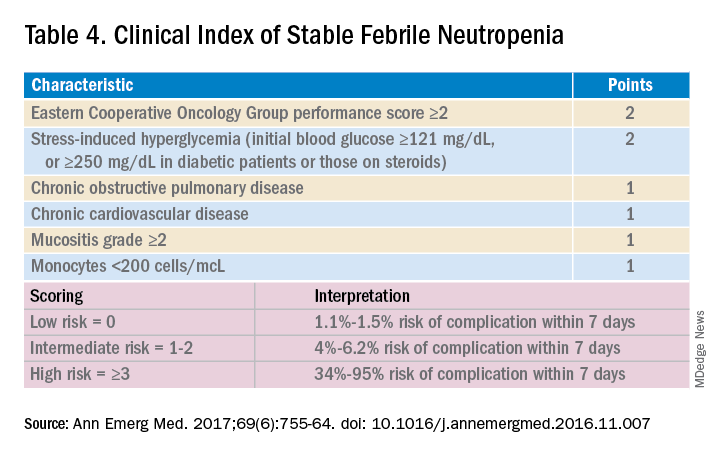
Though the MASCC is highly sensitive in identifying low-risk febrile neutropenia patients, it should be used with clinical caution because up to 11% of patients characterized as low risk developed severe complications.19 If a low-risk patient with solid tumor malignancy has adequate home support, lives within an hour of the hospital, and has access to follow-up within 72 hours, oral antibiotics and early discharge can be considered.
Dr. Chokshi is assistant professor in the division of hospital medicine at Mount Sinai Hospital, New York. Dr. Smith is associate professor in the division of hematology/oncology at Mount Sinai Hospital.
QUIZ
Mrs. Smith is a 64-year-old woman with endometrial cancer with temperature of 100.4° F at home. She takes no antibiotics, has no other medical history, and was sent in from clinic and admitted for further management. She feels well, and preliminary infectious workup is negative. She has been afebrile for more than 24 hours, and her ANC is 600 cells/mL.
Her son’s soccer game is tomorrow, and she would like to be present. Her family is involved in her care. Under what conditions can she be discharged?
A. She should not be discharged until full course of empiric intravenous antibiotics is completed.
B. Consider discharge in another 24 hours if she remains afebrile.
C. Discharge if low risk by MASCC or CISNE, with oral doses of levofloxacin or moxifloxacin or oral ciprofloxacin and amoxicillin/clavulanic acid.
Answer: C. The patient has a solid tumor malignancy, is low risk by both MASCC and CISNE, and can most likely be discharged if she is clinically stable or improved. A 7-day course of antibiotics is recommended with close follow-up.
References
1. SEER. Cancer of Any Site - Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/all.html. Accessed 2019 Jul 17.
2. Kwok Y et al. Clinical Approach to Metastatic Epidural Spinal Cord Compression. Hematol Oncol Clin North Am. 2006;20(6):1297-305.
3. Helweg-Larsen S et al. Prognostic factors in metastatic spinal cord compression: a prospective study using multivariate analysis of variables influencing survival and gait function in 153 patients. Int J Radiat Oncol Biol Phys. 2000;46(5):1163-9.
4. Sørensen P et al. Effect of high-dose dexamethasone in carcinomatous metastatic spinal cord compression treated with radiotherapy: A randomised trial. Eur J Cancer. 1994;30(1):22-7.
5. Skeoch G et al. Corticosteroid treatment for metastatic spinal cord compression: A review. Global Spine J. 2017;7(3):272-9.
6. Vecht C et al. Initial bolus of conventional versus high-dose dexamethasone in metastatic spinal cord compression. Neurology. 1989;39(9):1255-7.
7. Heimdal K et al. High incidence of serious side effects of high-dose dexamethasone treatment in patients with epidural spinal cord compression. J Neurooncol. 1992;12(2):141-4.
8. Ralston S et al. Cancer-associated hypercalcemia: Morbidity and mortality. Clinical experience in 126 treated patients. Ann Intern Med. 1990;112(7):499-504.
9. Lindner G et al. Hypercalcemia in the ED: Prevalence, etiology, and outcome. Am J Emerg Med. 2013;31(4):657-60.
10. Hu M et al. Denosumab for patients with persistent or relapsed hypercalcemia of malignancy despite recent bisphosphonate treatment. J Natl Cancer Inst. 2013;105(18):1417-20.
11. Major P et al. Zoledronic acid is superior to pamidronate in the treatment of hypercalcemia of malignancy: A pooled analysis of two randomized, controlled clinical trials. J Clin Oncol. 2001;19(2):558-67.
12. Stewart A. Clinical practice. Hypercalcemia associated with cancer. N Engl J Med. 2005;352(4):373-9.
13. Freifeld A et al. Executive summary: Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52(4):427-31.
14. Baden L et al. Prevention and treatment of cancer-related infections, version 2.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2016;14(7):882-913.
15. Coyne C et al. Application of the MASCC and CISNE risk-stratification scores to identify low-risk febrile neutropenic patients in the emergency department. Ann Emerg Med. 2017;69(6):755-64.
16. Talcott J et al. Safety of early discharge for low-risk patients with febrile neutropenia: a multicenter randomized controlled trial. J Clin Oncol. 2011;29(30):3977-83.
17. Innes H et al. Oral antibiotics with early hospital discharge compared with in-patient intravenous antibiotics for low-risk febrile neutropenia in patients with cancer: A prospective randomised controlled single centre study. Br J Cancer. 2003;89(1):43-9.
18. Vidal L, et al. Oral versus intravenous antibiotic treatment for febrile neutropenia in cancer patients. Cochrane Database Syst. Rev. 2013.
19. Taplitz RA et al. Outpatient management of fever and neutropenia in adults treated for malignancy: American Society of Clinical Oncology and Infectious Diseases Society of America clinical practice guideline update. J Clin Oncol. 2018;36(14):1443-53.
In 2016, there were an estimated 15,338,988 people living with cancer in the United States.1 As such, it is important that hospitalists be proficient in managing oncologic emergencies that can arise during the natural history of cancer or from its treatment. This article will review three emergencies that are routinely encountered in the inpatient setting: malignant spinal cord compression (MSCC), hypercalcemia of malignancy (HCM), and febrile neutropenia (FN).
Case
Mr. Williams is a 56-year-old man with newly diagnosed metastatic prostate cancer, diabetes mellitus, peptic ulcer disease, and hypertension. He is admitted with back pain and lower extremity weakness worsening over 2 weeks. He denies loss of sensation or bowel and bladder incontinence and can walk. MRI confirms cord compression at T10. What initial and subsequent steroid doses would be of most benefit to administer?
Malignant spinal cord compression
Treatment of MSCC usually aims to preserve function rather than reverse established deficits. MSCC from epidural tumor metastasis develops in 5%-14% of all cancer cases,2 with back pain as the most common symptom. Nearly 60%-85% of patients have weakness at the time of diagnosis,3 and unfortunately, nearly two-thirds of patients will be nonambulatory at presentation.
While timely steroid administration in addition to definitive treatment may maintain ambulatory capacity at 1 year after therapy,4 there is no consensus on the optimal loading and maintenance dose and duration of steroids.
Overview of the data
Although there are no formal guidelines on optimal steroid dosing for MSCC, it is common practice for dexamethasone to be initially dosed at 10 mg followed by 4 mg every 4-6 hours.5 The use of higher doses of dexamethasone may result in improvement in neurologic deficits, but has higher risks for toxicity and is not universally supported in the literature.
A study conducted by Vecht and colleagues demonstrated few differences between initial high-dose and low-dose dexamethasone.6 Intravenous administration of either 10 mg or 100 mg dexamethasone, both followed by total 16 mg of dexamethasone orally per day, showed no significant difference in mobility or survival between the groups.
In a prospective study by Heimdal and colleagues that evaluated the relationship between dexamethasone dose and toxicity, higher doses of steroids had no meaningful impact on neurological symptoms and resulted in more severe side effects.7 Patients were either given 96-mg IV loading dose, gradually tapered over 2 weeks, or enrolled in the low-dose group in which they received 4-mg IV dexamethasone four times per day with a taper over 2 weeks. The high-dose group experienced side effects in 28.6% of patients, with 14.3% experiencing serious side effects. Meanwhile, 7.9% of the low-dose group exhibited some side effects, with none experiencing serious adverse effects.The high-dose group did not experience a significant increase in mobility (57.1 vs. 57.9%).
Key takeaways
Dexamthasone 10-mg oral or IV followed by 4 mg every 4-6 hours until definitive treatment is started is associated with improved neurologic outcomes and minimal adverse side effects. Higher doses of steroids are unlikely to offer more benefit. In patients with paraplegia or autonomic dysfunction, the ability to restore neurologic function is reduced and the burdens of steroid treatment may outweigh its benefits.5
Case continued
Mr. Williams completed treatment for MSCC but was still complaining of extreme lethargy and noticed an increase in thirst and no bowel movement in 5 days. His serum calcium was 14 mg/dL.
Hypercalcemia of malignancy
HCM is the most common paraneoplastic syndrome, observed in nearly 30% of patients with advanced cancer. It is a poor prognostic indicator, and approximately half of all patients with HCM will die within 30 days.8 Cancer is the most common reason for hypercalcemia in the inpatient setting9 and is most often associated with multiple myeloma, non–small cell lung cancer, breast cancer, renal cell carcinoma, non-Hodgkins lymphoma, and leukemia.
Hypercalcemia most often presents with cognitive changes and lethargy, anorexia, nausea, constipation, polyuria and polydipsia, and renal failure. Bradycardia and shortened QT interval are seen more with severe hypercalcemia.
Management of hypercalcemia of malignancy
Management of HCM depends on corrected calcium or ionized calcium levels, chronicity, degree of symptoms, and presence of renal failure. In general, mild asymptomatic hypercalcemia can be managed with outpatient care. Serum calcium greater than 14 mg/dL should be treated regardless of symptoms (Table 1).
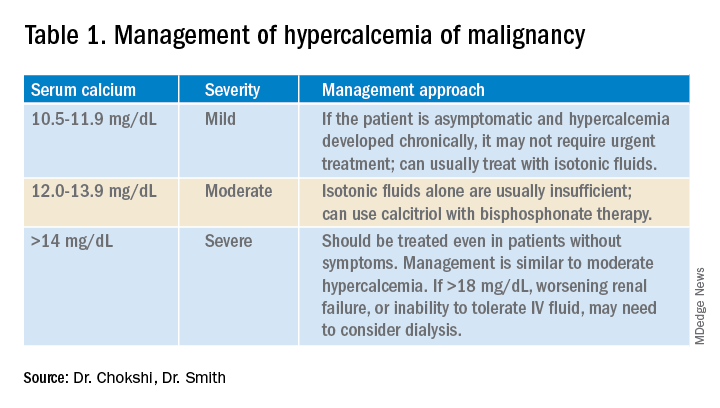
For mild to moderate HCM, management involves saline administration to achieve euvolemia and calcitonin, which has temporizing effects. Early administration of IV bisphosphonates for moderate to severe HCM is beneficial because onset of action is 24-48 hours. Furosemide for management of HCM has fallen out of favor unless the patient develops hypervolemia. Denosumab has been Food and Drug Administration–approved for HCM refractory to bisphosphonate therapy and can manage HCM in 64% of patients who did not respond adequately to bisphosphonate therapy.10 Because it can be used in advanced renal failure without dose adjustment, it is first-line therapy in this population, although the risk for hypocalcemia is increased in renal failure. For patients with serum calcium greater than 18 mg/dL, worsening renal failure, or inability to tolerate IV fluids, dialysis with a low-calcium bath should be considered (Table 2).
Zoledronic acid versus pamidronate
A single dose of zoledronic acid normalizes the serum calcium concentration in 88% of patients, compared with 70% of those who received pamidronate, in a pooled analysis of two phase 3 trials.11 The median duration of normocalcemia was longer for those receiving zoledronic acid (32-43 days vs. 18 days). The efficacy of the 4-mg and 8-mg zoledronic acid doses were similar, but the 4-mg dose was recommended because of renal toxicity and increased mortality associated with the higher dose.Despite this data, many specialists maintain that pamidronate, which is less expensive, is of similar clinical efficacy to ZA.12
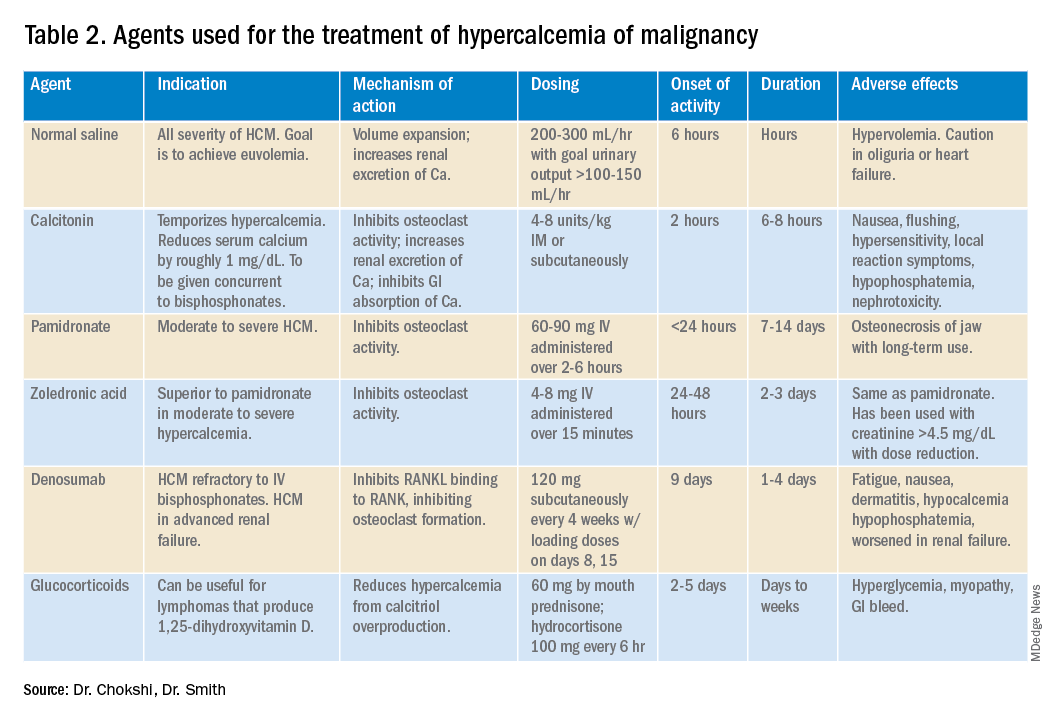
Key takeaways
Management of HCM should be determined by the severity of the calcium level. The mainstay of treatment includes hydration with normal saline, calcitonin ,and bisphosphonate therapy; zoledronic acid is preferred over pamidronate. For patients refractory to bisphosphonates or patients with renal insufficiency, denosumab should be used.
Case continued: Febrile neutropenia
Febrile neutropenia is defined as a single oral temperature of 100.9° F or a temperature of 100.4° F sustained over a 1-hour period in a patient with absolute neutrophil count (ANC) less than 1,000 cells/mL or ANC expected to decrease to less than 500 cells/mL within a 48-hour period.13 Up to 30% of patients with solid tumors develop febrile neutropenia after chemotherapy, and nearly 80% of patients with hematologic malignancy or after hematopoietic stem cell therapy (HSCT) experience it.
Even though an infectious etiology is identified in only 30%-40% of cases, all patients with febrile neutropenia should initially receive at least empiric gram-negative coverage. The mortality rate is nearly 70% in neutropenic patients who do not receive empiric antibiotics and is reduced to 4%-20% with antibiotics.14
Risk stratification for febrile neutropenia and early discharge
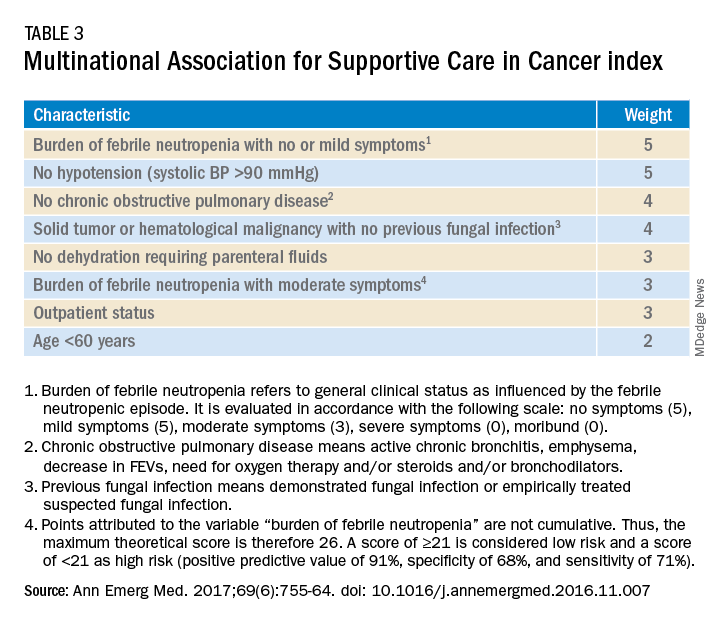
Talcott’s Rules, the Multinational Association for Supportive Care in Cancer (MASCC) score, and the Clinical Index of Stable Febrile Neutropenia (CISNE) are validated tools to determine low-risk febrile neutropenia patients (Tables 3 and 4). The Infectious Diseases Society of America guidelines validated the use of MASCC in 2002 but found that CISNE had better performance than other tools. Coyne and colleagues conducted a retrospective cohort study to assess these two risk stratification tools in the ED and found that the CISNE was 98.3% specific for identifying adverse outcomes, whereas the MASCC was 54.2% specific.15
A study by Talcott and colleagues used Talcott’s Rules to identify low-risk febrile neutropenia patients, who were randomized to early discharge with home intravenous antibiotics versus continued inpatient management. There were no significant differences in the primary outcomes, defined as any change in clinical status requiring medical evaluation.16 Another study suggested that discharge after 24 hours based on clinical stability with outpatient oral antibiotics were noninferior to standard inpatient and intravenous antibiotic therapy.17 A Cochrane review in 2013 of 22 randomized controlled trials determined that oral antibiotics were an acceptable treatment for low-risk patients.18
Key takeaways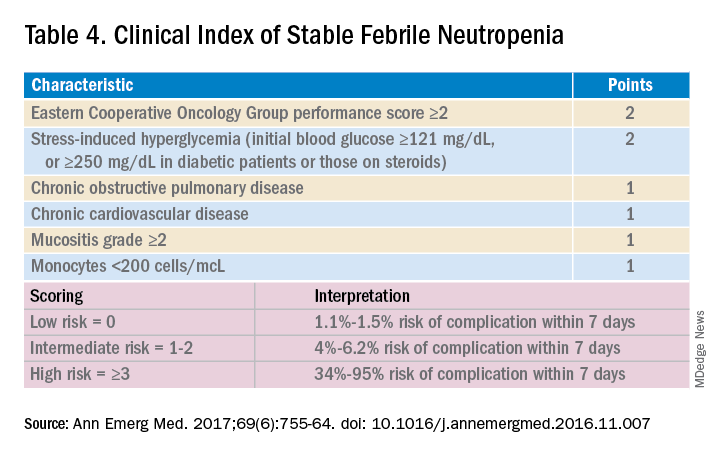
Though the MASCC is highly sensitive in identifying low-risk febrile neutropenia patients, it should be used with clinical caution because up to 11% of patients characterized as low risk developed severe complications.19 If a low-risk patient with solid tumor malignancy has adequate home support, lives within an hour of the hospital, and has access to follow-up within 72 hours, oral antibiotics and early discharge can be considered.
Dr. Chokshi is assistant professor in the division of hospital medicine at Mount Sinai Hospital, New York. Dr. Smith is associate professor in the division of hematology/oncology at Mount Sinai Hospital.
QUIZ
Mrs. Smith is a 64-year-old woman with endometrial cancer with temperature of 100.4° F at home. She takes no antibiotics, has no other medical history, and was sent in from clinic and admitted for further management. She feels well, and preliminary infectious workup is negative. She has been afebrile for more than 24 hours, and her ANC is 600 cells/mL.
Her son’s soccer game is tomorrow, and she would like to be present. Her family is involved in her care. Under what conditions can she be discharged?
A. She should not be discharged until full course of empiric intravenous antibiotics is completed.
B. Consider discharge in another 24 hours if she remains afebrile.
C. Discharge if low risk by MASCC or CISNE, with oral doses of levofloxacin or moxifloxacin or oral ciprofloxacin and amoxicillin/clavulanic acid.
Answer: C. The patient has a solid tumor malignancy, is low risk by both MASCC and CISNE, and can most likely be discharged if she is clinically stable or improved. A 7-day course of antibiotics is recommended with close follow-up.
References
1. SEER. Cancer of Any Site - Cancer Stat Facts. https://seer.cancer.gov/statfacts/html/all.html. Accessed 2019 Jul 17.
2. Kwok Y et al. Clinical Approach to Metastatic Epidural Spinal Cord Compression. Hematol Oncol Clin North Am. 2006;20(6):1297-305.
3. Helweg-Larsen S et al. Prognostic factors in metastatic spinal cord compression: a prospective study using multivariate analysis of variables influencing survival and gait function in 153 patients. Int J Radiat Oncol Biol Phys. 2000;46(5):1163-9.
4. Sørensen P et al. Effect of high-dose dexamethasone in carcinomatous metastatic spinal cord compression treated with radiotherapy: A randomised trial. Eur J Cancer. 1994;30(1):22-7.
5. Skeoch G et al. Corticosteroid treatment for metastatic spinal cord compression: A review. Global Spine J. 2017;7(3):272-9.
6. Vecht C et al. Initial bolus of conventional versus high-dose dexamethasone in metastatic spinal cord compression. Neurology. 1989;39(9):1255-7.
7. Heimdal K et al. High incidence of serious side effects of high-dose dexamethasone treatment in patients with epidural spinal cord compression. J Neurooncol. 1992;12(2):141-4.
8. Ralston S et al. Cancer-associated hypercalcemia: Morbidity and mortality. Clinical experience in 126 treated patients. Ann Intern Med. 1990;112(7):499-504.
9. Lindner G et al. Hypercalcemia in the ED: Prevalence, etiology, and outcome. Am J Emerg Med. 2013;31(4):657-60.
10. Hu M et al. Denosumab for patients with persistent or relapsed hypercalcemia of malignancy despite recent bisphosphonate treatment. J Natl Cancer Inst. 2013;105(18):1417-20.
11. Major P et al. Zoledronic acid is superior to pamidronate in the treatment of hypercalcemia of malignancy: A pooled analysis of two randomized, controlled clinical trials. J Clin Oncol. 2001;19(2):558-67.
12. Stewart A. Clinical practice. Hypercalcemia associated with cancer. N Engl J Med. 2005;352(4):373-9.
13. Freifeld A et al. Executive summary: Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2011;52(4):427-31.
14. Baden L et al. Prevention and treatment of cancer-related infections, version 2.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2016;14(7):882-913.
15. Coyne C et al. Application of the MASCC and CISNE risk-stratification scores to identify low-risk febrile neutropenic patients in the emergency department. Ann Emerg Med. 2017;69(6):755-64.
16. Talcott J et al. Safety of early discharge for low-risk patients with febrile neutropenia: a multicenter randomized controlled trial. J Clin Oncol. 2011;29(30):3977-83.
17. Innes H et al. Oral antibiotics with early hospital discharge compared with in-patient intravenous antibiotics for low-risk febrile neutropenia in patients with cancer: A prospective randomised controlled single centre study. Br J Cancer. 2003;89(1):43-9.
18. Vidal L, et al. Oral versus intravenous antibiotic treatment for febrile neutropenia in cancer patients. Cochrane Database Syst. Rev. 2013.
19. Taplitz RA et al. Outpatient management of fever and neutropenia in adults treated for malignancy: American Society of Clinical Oncology and Infectious Diseases Society of America clinical practice guideline update. J Clin Oncol. 2018;36(14):1443-53.
No mortality benefit after intensive glucose control once Hb A1c curves equalize
Background: A previous study reported that a median of 5.6 years of intensive versus standard glucose lowering in veterans with type 2 diabetes resulted in significantly reduced risk of major cardiovascular events after 10 years of combined intervention and observational follow-up.
Study design: Prospective cohort.
Setting: Veterans Affairs Healthcare System.
Synopsis: In the original trial, 1,791 veterans were randomly assigned to receive either intensive or standard glucose control therapy. After conclusion of that study, 1,655 participants were followed using central databases, and 1,391 also provided data via surveys and chart review. Initially the difference in the glycated hemoglobin (Hb A1c) curves between the two groups averaged 1.5%, but it declined to 0.2%-0.3% 3 years after the trial ended. The median Hb A1c then stabilized to 8% in both groups.
Over a period of 15 years of combined intervention and posttrial follow-up, the risks of major cardiovascular events or death were not lower in the intensive-therapy group (hazard ratio for composite outcome, 0.91; 95% confidence interval, 0.78-1.06; P = .23; HR for death, 1.02; 95% CI, 0.88-1.18). The risk of major cardiovascular disease outcomes was reduced during the approximately 10-year interval of separation of the Hb A1c curves (HR, 0.83; 95% CI, 0.70-0.99), but it did not persist after equalization of Hb A1c levels (HR, 1.26; 95% CI, 0.90-1.75). Limitations include the observational study design, the study population of mostly older men, and reliance on administrative data for outcomes.
Bottom line: More than 5 years of intensive glucose lowering, compared with standard therapy, did not show significantly lower risks of cardiovascular events or mortality once the glycated hemoglobin curves equalized during follow-up in years 11-15.
Citation: Reaven PD et al. Intensive glucose control in patients with type 2 diabetes – 15-year follow-up. New Engl J Med. 2019 Jun 6;380(23):2215-24.
Dr. Burke is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: A previous study reported that a median of 5.6 years of intensive versus standard glucose lowering in veterans with type 2 diabetes resulted in significantly reduced risk of major cardiovascular events after 10 years of combined intervention and observational follow-up.
Study design: Prospective cohort.
Setting: Veterans Affairs Healthcare System.
Synopsis: In the original trial, 1,791 veterans were randomly assigned to receive either intensive or standard glucose control therapy. After conclusion of that study, 1,655 participants were followed using central databases, and 1,391 also provided data via surveys and chart review. Initially the difference in the glycated hemoglobin (Hb A1c) curves between the two groups averaged 1.5%, but it declined to 0.2%-0.3% 3 years after the trial ended. The median Hb A1c then stabilized to 8% in both groups.
Over a period of 15 years of combined intervention and posttrial follow-up, the risks of major cardiovascular events or death were not lower in the intensive-therapy group (hazard ratio for composite outcome, 0.91; 95% confidence interval, 0.78-1.06; P = .23; HR for death, 1.02; 95% CI, 0.88-1.18). The risk of major cardiovascular disease outcomes was reduced during the approximately 10-year interval of separation of the Hb A1c curves (HR, 0.83; 95% CI, 0.70-0.99), but it did not persist after equalization of Hb A1c levels (HR, 1.26; 95% CI, 0.90-1.75). Limitations include the observational study design, the study population of mostly older men, and reliance on administrative data for outcomes.
Bottom line: More than 5 years of intensive glucose lowering, compared with standard therapy, did not show significantly lower risks of cardiovascular events or mortality once the glycated hemoglobin curves equalized during follow-up in years 11-15.
Citation: Reaven PD et al. Intensive glucose control in patients with type 2 diabetes – 15-year follow-up. New Engl J Med. 2019 Jun 6;380(23):2215-24.
Dr. Burke is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: A previous study reported that a median of 5.6 years of intensive versus standard glucose lowering in veterans with type 2 diabetes resulted in significantly reduced risk of major cardiovascular events after 10 years of combined intervention and observational follow-up.
Study design: Prospective cohort.
Setting: Veterans Affairs Healthcare System.
Synopsis: In the original trial, 1,791 veterans were randomly assigned to receive either intensive or standard glucose control therapy. After conclusion of that study, 1,655 participants were followed using central databases, and 1,391 also provided data via surveys and chart review. Initially the difference in the glycated hemoglobin (Hb A1c) curves between the two groups averaged 1.5%, but it declined to 0.2%-0.3% 3 years after the trial ended. The median Hb A1c then stabilized to 8% in both groups.
Over a period of 15 years of combined intervention and posttrial follow-up, the risks of major cardiovascular events or death were not lower in the intensive-therapy group (hazard ratio for composite outcome, 0.91; 95% confidence interval, 0.78-1.06; P = .23; HR for death, 1.02; 95% CI, 0.88-1.18). The risk of major cardiovascular disease outcomes was reduced during the approximately 10-year interval of separation of the Hb A1c curves (HR, 0.83; 95% CI, 0.70-0.99), but it did not persist after equalization of Hb A1c levels (HR, 1.26; 95% CI, 0.90-1.75). Limitations include the observational study design, the study population of mostly older men, and reliance on administrative data for outcomes.
Bottom line: More than 5 years of intensive glucose lowering, compared with standard therapy, did not show significantly lower risks of cardiovascular events or mortality once the glycated hemoglobin curves equalized during follow-up in years 11-15.
Citation: Reaven PD et al. Intensive glucose control in patients with type 2 diabetes – 15-year follow-up. New Engl J Med. 2019 Jun 6;380(23):2215-24.
Dr. Burke is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Establishing a strong and lasting mentor/mentee relationship
I. Finding a mentor
Case
You are a 27-year-old first-year resident who is seeking mentorship. You are halfway through the year and are thinking about your goals and future. You have a general interest in hematology/oncology but have limited experience and would like to gain more experience with clinically relevant scholarship. However, you do not know anyone in the field and are not sure who to ask for guidance.
Stage 1: Seeking the right mentor
Start first with your area of interest and then look broadly. In this case the resident is interested in heme/onc. The first place to look is on the heme/onc department website or in the faculty directory. It can be helpful to look at what the potential mentor has published recently and/or look at a version of their CV on the faculty directory or website. This can help determine how productive they are and help assess whether you share similar interests, and whether they have worked with many learners in the past.
It is also important to do some background work and ask around about potential mentors. Often resident colleagues and fellows have a good sense of current projects and which faculty work well with learners. Lastly, it is important to also look at non–heme/onc physicians as there may be internal medicine physicians or surgeons who are doing hematology or oncology research that more align with your interests.
After you have assessed whether you think this person would be a strong mentor for you, it is time to reach out. People are flattered to be asked and part of their promotion criteria is their ability to mentor. Do not assume that a potential mentor is too busy! Let him or her make that decision. Remember the worst a mentor can say is “no.” Even if they do not have time or the need for a mentee at the present time, they generally will offer some assistance or direction on who to ask.
Start with a straightforward, but pleasant email. Waiting up to 2 weeks for a response is reasonable. If after 2 weeks you have not received word, feel free to reach out again asking politely if he or she would be willing to work with you. Do not be afraid to ask bluntly for their guidance and mentorship and have a specific project or area of research that you would like their assistance with.
II. Optimizing the mentor/mentee relationship
Case continued
Success! Your email was received with interest by a hematologist who has done several projects, comes highly recommended by other residents, and worked with students and residents in the past. The project involves anticoagulation on the inpatient service. You are set to meet with her next month.
Stage 2: Establishing expectations and goals
Now comes the hard work in establishing an excellent mentor/mentee relationship. Before you meet with your mentor, brainstorm first. What do you want out of the relationship? A publication? Career advice? Attaining a fellowship position? You should feel empowered in knowing that you as the mentee are in the driver seat, but this relationship should be mutually beneficial. Consider basing the relationship and initial discussions on these key questions:
1. My goals
- What are my goals? It is okay not to know but be ready to communicate some information to your mentor.
- Remember to also ask your mentor what their goals are for you as well.
2. Outcome
- What type of outcome are both you and your mentor looking for from the relationship?
3. Expectations
- What mentorship expectations do you have?
- What are your mentor’s expectations of you?
Once you feel you have a sense of what you are looking for out of the relationship, it is important to communicate this with the mentor to establish congruent expectations of one another. For example, think about asking your mentor if the two of you can establish a mentor/mentee contract. This is a written document that can be found online and establishes a mutual agreement of roles, responsibilities, and expectations of one another for the relationship. It can further help to open a line for honest and consistent feedback. This can also give you a formalized endpoint and agreed upon scope for the mentoring relationship. Having a check-in preestablished in a contract reduces any potentially awkward conversations about redefining the relationship down the road. (For example, what if our case resident decides to pursue GI? It could happen.)
Stage 3: Establishing a common goal
After you have determined the goals and expectations of the relationship together (remember, this is a relationship), it is time to start exploring possible projects and establishing goals for those projects. Having a quality improvement or research project will determine a common goal to work towards and help establish and define the relationship.
Once you have delineated broadly what the project(s) should be, develop smaller SMART (specific, measurable, achievable, relevant, time-bound) goals to move the project forward. These goals determine stopping points for evaluation and feedback, which further establish the relationship and keep the project(s) progressing. For example, one goal could be to write the first draft of the proposal for your quality improvement project within 3 weeks.
Stage 4: Continued communication
With any project it is important to stay on the same page as your mentor and be clear to establish “who is doing what by when.” Do not expect accountability to be the mentor’s job. Remember that you are in the driver’s seat and that you should propose how often you need to meet and what those meetings look like by developing an agenda. You can have an open discussion and allow your mentor to help determine a reasonable timeline. Remember, the more you communicate your goals, the better your mentor will be able to address them.
One pro tip is to always exceed your mentor’s expectations – if you think you need 2 weeks to complete a task, ask for 3-4 weeks. This gives you extra padding in case of unforeseen circumstances and makes you look like a “rockstar” if you hit a deadline 1-2 weeks earlier than planned.
III. Ending and/or redefining the relationship
Case continued
You are now a senior resident who’s published multiple articles in the past year, and have completed an anticoagulation project for inpatients with pulmonary emboli. You look back on your experience and what stands out is the extent of your gratitude and appreciation for your incredible mentor. Not only do you feel that your mentor has guided you in your career and with your scholarship, but you feel that he or she has shaped your character and talent set. At this point your mentor is both a teacher and guide, but now also a friend. While you feel there is always more that you can learn from her, you are ready to explore new interests. How do you effectively end or redefine this relationship?
Stage 5: Redefining your mentoring relationship
First, go back to the expectations or contract established early in the relationship. The check-in is a key time in the relationship to reevaluate goals and priorities. At this point you may decide to amicably end the relationship or project, or move on to a new project with a change in your role. For example, the quality improvement project may change to research, or you as the mentee have a change in focus (e.g., change in specialty or scholarly focus).
In summary, the interaction between you and your mentor should be a relationship. And the keys to a great relationship are:
1. Establish clear expectations from the beginning. This clarifies the relationship and helps the mentee and mentor to become more successful.
2. Maintain clear and open communication throughout the relationship.3. Define your goals and discuss them with your mentor early. (Have we mentioned the importance of goals enough?) After all, your goal is the reason you started pursuing this relationship in the first place.
In clinical training having guidance can greatly enhance your experience and direct your future career in unexpected ways. We hope that using these tools will guide you towards forging a strong mentor/mentee relationship.
Dr. Zimmerberg-Helms is a resident physician at the University of New Mexico, Albuquerque. Dr. Rendon is an attending hospitalist at the University of New Mexico.
I. Finding a mentor
Case
You are a 27-year-old first-year resident who is seeking mentorship. You are halfway through the year and are thinking about your goals and future. You have a general interest in hematology/oncology but have limited experience and would like to gain more experience with clinically relevant scholarship. However, you do not know anyone in the field and are not sure who to ask for guidance.
Stage 1: Seeking the right mentor
Start first with your area of interest and then look broadly. In this case the resident is interested in heme/onc. The first place to look is on the heme/onc department website or in the faculty directory. It can be helpful to look at what the potential mentor has published recently and/or look at a version of their CV on the faculty directory or website. This can help determine how productive they are and help assess whether you share similar interests, and whether they have worked with many learners in the past.
It is also important to do some background work and ask around about potential mentors. Often resident colleagues and fellows have a good sense of current projects and which faculty work well with learners. Lastly, it is important to also look at non–heme/onc physicians as there may be internal medicine physicians or surgeons who are doing hematology or oncology research that more align with your interests.
After you have assessed whether you think this person would be a strong mentor for you, it is time to reach out. People are flattered to be asked and part of their promotion criteria is their ability to mentor. Do not assume that a potential mentor is too busy! Let him or her make that decision. Remember the worst a mentor can say is “no.” Even if they do not have time or the need for a mentee at the present time, they generally will offer some assistance or direction on who to ask.
Start with a straightforward, but pleasant email. Waiting up to 2 weeks for a response is reasonable. If after 2 weeks you have not received word, feel free to reach out again asking politely if he or she would be willing to work with you. Do not be afraid to ask bluntly for their guidance and mentorship and have a specific project or area of research that you would like their assistance with.
II. Optimizing the mentor/mentee relationship
Case continued
Success! Your email was received with interest by a hematologist who has done several projects, comes highly recommended by other residents, and worked with students and residents in the past. The project involves anticoagulation on the inpatient service. You are set to meet with her next month.
Stage 2: Establishing expectations and goals
Now comes the hard work in establishing an excellent mentor/mentee relationship. Before you meet with your mentor, brainstorm first. What do you want out of the relationship? A publication? Career advice? Attaining a fellowship position? You should feel empowered in knowing that you as the mentee are in the driver seat, but this relationship should be mutually beneficial. Consider basing the relationship and initial discussions on these key questions:
1. My goals
- What are my goals? It is okay not to know but be ready to communicate some information to your mentor.
- Remember to also ask your mentor what their goals are for you as well.
2. Outcome
- What type of outcome are both you and your mentor looking for from the relationship?
3. Expectations
- What mentorship expectations do you have?
- What are your mentor’s expectations of you?
Once you feel you have a sense of what you are looking for out of the relationship, it is important to communicate this with the mentor to establish congruent expectations of one another. For example, think about asking your mentor if the two of you can establish a mentor/mentee contract. This is a written document that can be found online and establishes a mutual agreement of roles, responsibilities, and expectations of one another for the relationship. It can further help to open a line for honest and consistent feedback. This can also give you a formalized endpoint and agreed upon scope for the mentoring relationship. Having a check-in preestablished in a contract reduces any potentially awkward conversations about redefining the relationship down the road. (For example, what if our case resident decides to pursue GI? It could happen.)
Stage 3: Establishing a common goal
After you have determined the goals and expectations of the relationship together (remember, this is a relationship), it is time to start exploring possible projects and establishing goals for those projects. Having a quality improvement or research project will determine a common goal to work towards and help establish and define the relationship.
Once you have delineated broadly what the project(s) should be, develop smaller SMART (specific, measurable, achievable, relevant, time-bound) goals to move the project forward. These goals determine stopping points for evaluation and feedback, which further establish the relationship and keep the project(s) progressing. For example, one goal could be to write the first draft of the proposal for your quality improvement project within 3 weeks.
Stage 4: Continued communication
With any project it is important to stay on the same page as your mentor and be clear to establish “who is doing what by when.” Do not expect accountability to be the mentor’s job. Remember that you are in the driver’s seat and that you should propose how often you need to meet and what those meetings look like by developing an agenda. You can have an open discussion and allow your mentor to help determine a reasonable timeline. Remember, the more you communicate your goals, the better your mentor will be able to address them.
One pro tip is to always exceed your mentor’s expectations – if you think you need 2 weeks to complete a task, ask for 3-4 weeks. This gives you extra padding in case of unforeseen circumstances and makes you look like a “rockstar” if you hit a deadline 1-2 weeks earlier than planned.
III. Ending and/or redefining the relationship
Case continued
You are now a senior resident who’s published multiple articles in the past year, and have completed an anticoagulation project for inpatients with pulmonary emboli. You look back on your experience and what stands out is the extent of your gratitude and appreciation for your incredible mentor. Not only do you feel that your mentor has guided you in your career and with your scholarship, but you feel that he or she has shaped your character and talent set. At this point your mentor is both a teacher and guide, but now also a friend. While you feel there is always more that you can learn from her, you are ready to explore new interests. How do you effectively end or redefine this relationship?
Stage 5: Redefining your mentoring relationship
First, go back to the expectations or contract established early in the relationship. The check-in is a key time in the relationship to reevaluate goals and priorities. At this point you may decide to amicably end the relationship or project, or move on to a new project with a change in your role. For example, the quality improvement project may change to research, or you as the mentee have a change in focus (e.g., change in specialty or scholarly focus).
In summary, the interaction between you and your mentor should be a relationship. And the keys to a great relationship are:
1. Establish clear expectations from the beginning. This clarifies the relationship and helps the mentee and mentor to become more successful.
2. Maintain clear and open communication throughout the relationship.3. Define your goals and discuss them with your mentor early. (Have we mentioned the importance of goals enough?) After all, your goal is the reason you started pursuing this relationship in the first place.
In clinical training having guidance can greatly enhance your experience and direct your future career in unexpected ways. We hope that using these tools will guide you towards forging a strong mentor/mentee relationship.
Dr. Zimmerberg-Helms is a resident physician at the University of New Mexico, Albuquerque. Dr. Rendon is an attending hospitalist at the University of New Mexico.
I. Finding a mentor
Case
You are a 27-year-old first-year resident who is seeking mentorship. You are halfway through the year and are thinking about your goals and future. You have a general interest in hematology/oncology but have limited experience and would like to gain more experience with clinically relevant scholarship. However, you do not know anyone in the field and are not sure who to ask for guidance.
Stage 1: Seeking the right mentor
Start first with your area of interest and then look broadly. In this case the resident is interested in heme/onc. The first place to look is on the heme/onc department website or in the faculty directory. It can be helpful to look at what the potential mentor has published recently and/or look at a version of their CV on the faculty directory or website. This can help determine how productive they are and help assess whether you share similar interests, and whether they have worked with many learners in the past.
It is also important to do some background work and ask around about potential mentors. Often resident colleagues and fellows have a good sense of current projects and which faculty work well with learners. Lastly, it is important to also look at non–heme/onc physicians as there may be internal medicine physicians or surgeons who are doing hematology or oncology research that more align with your interests.
After you have assessed whether you think this person would be a strong mentor for you, it is time to reach out. People are flattered to be asked and part of their promotion criteria is their ability to mentor. Do not assume that a potential mentor is too busy! Let him or her make that decision. Remember the worst a mentor can say is “no.” Even if they do not have time or the need for a mentee at the present time, they generally will offer some assistance or direction on who to ask.
Start with a straightforward, but pleasant email. Waiting up to 2 weeks for a response is reasonable. If after 2 weeks you have not received word, feel free to reach out again asking politely if he or she would be willing to work with you. Do not be afraid to ask bluntly for their guidance and mentorship and have a specific project or area of research that you would like their assistance with.
II. Optimizing the mentor/mentee relationship
Case continued
Success! Your email was received with interest by a hematologist who has done several projects, comes highly recommended by other residents, and worked with students and residents in the past. The project involves anticoagulation on the inpatient service. You are set to meet with her next month.
Stage 2: Establishing expectations and goals
Now comes the hard work in establishing an excellent mentor/mentee relationship. Before you meet with your mentor, brainstorm first. What do you want out of the relationship? A publication? Career advice? Attaining a fellowship position? You should feel empowered in knowing that you as the mentee are in the driver seat, but this relationship should be mutually beneficial. Consider basing the relationship and initial discussions on these key questions:
1. My goals
- What are my goals? It is okay not to know but be ready to communicate some information to your mentor.
- Remember to also ask your mentor what their goals are for you as well.
2. Outcome
- What type of outcome are both you and your mentor looking for from the relationship?
3. Expectations
- What mentorship expectations do you have?
- What are your mentor’s expectations of you?
Once you feel you have a sense of what you are looking for out of the relationship, it is important to communicate this with the mentor to establish congruent expectations of one another. For example, think about asking your mentor if the two of you can establish a mentor/mentee contract. This is a written document that can be found online and establishes a mutual agreement of roles, responsibilities, and expectations of one another for the relationship. It can further help to open a line for honest and consistent feedback. This can also give you a formalized endpoint and agreed upon scope for the mentoring relationship. Having a check-in preestablished in a contract reduces any potentially awkward conversations about redefining the relationship down the road. (For example, what if our case resident decides to pursue GI? It could happen.)
Stage 3: Establishing a common goal
After you have determined the goals and expectations of the relationship together (remember, this is a relationship), it is time to start exploring possible projects and establishing goals for those projects. Having a quality improvement or research project will determine a common goal to work towards and help establish and define the relationship.
Once you have delineated broadly what the project(s) should be, develop smaller SMART (specific, measurable, achievable, relevant, time-bound) goals to move the project forward. These goals determine stopping points for evaluation and feedback, which further establish the relationship and keep the project(s) progressing. For example, one goal could be to write the first draft of the proposal for your quality improvement project within 3 weeks.
Stage 4: Continued communication
With any project it is important to stay on the same page as your mentor and be clear to establish “who is doing what by when.” Do not expect accountability to be the mentor’s job. Remember that you are in the driver’s seat and that you should propose how often you need to meet and what those meetings look like by developing an agenda. You can have an open discussion and allow your mentor to help determine a reasonable timeline. Remember, the more you communicate your goals, the better your mentor will be able to address them.
One pro tip is to always exceed your mentor’s expectations – if you think you need 2 weeks to complete a task, ask for 3-4 weeks. This gives you extra padding in case of unforeseen circumstances and makes you look like a “rockstar” if you hit a deadline 1-2 weeks earlier than planned.
III. Ending and/or redefining the relationship
Case continued
You are now a senior resident who’s published multiple articles in the past year, and have completed an anticoagulation project for inpatients with pulmonary emboli. You look back on your experience and what stands out is the extent of your gratitude and appreciation for your incredible mentor. Not only do you feel that your mentor has guided you in your career and with your scholarship, but you feel that he or she has shaped your character and talent set. At this point your mentor is both a teacher and guide, but now also a friend. While you feel there is always more that you can learn from her, you are ready to explore new interests. How do you effectively end or redefine this relationship?
Stage 5: Redefining your mentoring relationship
First, go back to the expectations or contract established early in the relationship. The check-in is a key time in the relationship to reevaluate goals and priorities. At this point you may decide to amicably end the relationship or project, or move on to a new project with a change in your role. For example, the quality improvement project may change to research, or you as the mentee have a change in focus (e.g., change in specialty or scholarly focus).
In summary, the interaction between you and your mentor should be a relationship. And the keys to a great relationship are:
1. Establish clear expectations from the beginning. This clarifies the relationship and helps the mentee and mentor to become more successful.
2. Maintain clear and open communication throughout the relationship.3. Define your goals and discuss them with your mentor early. (Have we mentioned the importance of goals enough?) After all, your goal is the reason you started pursuing this relationship in the first place.
In clinical training having guidance can greatly enhance your experience and direct your future career in unexpected ways. We hope that using these tools will guide you towards forging a strong mentor/mentee relationship.
Dr. Zimmerberg-Helms is a resident physician at the University of New Mexico, Albuquerque. Dr. Rendon is an attending hospitalist at the University of New Mexico.
SHM announces 2021 virtual annual conference: SHM Converge
The Society of Hospital Medicine has announced its virtual annual conference for 2021: SHM Converge. Formerly known as Hospital Medicine 2021, SHM Converge will take place virtually from May 3-7, 2021, and will offer a fully digital experience with the same education, professional development, and networking hospitalists have come to expect from SHM’s annual conference.
“This year, COVID-19 has challenged us to embrace change and to innovate to better serve our hospital medicine community,” said Danielle Scheurer, MD, MSCR, SFHM, president of SHM’s board of directors. “In that spirit, not only are we introducing an exciting new brand for the SHM annual conference, we are unveiling a reimagined experience for attendees, complete with sessions highlighting the latest research, best practices and innovations in the field.”
The SHM Converge schedule features 20 educational tracks, including the addition of four new tracks to support hospital medicine professionals in some of the most relevant topics affecting health care: diagnostic safety; diversity, equity, and inclusion; leadership; and wellness and resilience
Attendees will also have the option to follow many of the most popular tracks from previous SHM annual conferences, including Rapid Fire, Clinical Updates, and High-Value Care, among others. In many sessions, speakers will present the latest data and information available about COVID-19’s impact on the practice of hospital medicine. Precourses will be held on May 3.
SHM Converge will also offer additional professional development opportunities, including the Research, Innovations, and Clinical Vignettes scientific abstract competition and a speed mentoring session. Networking will be an integral component of SHM Converge. Attendees will be able to choose from more than 20 Special Interest forums, live Q&A sessions and networking events through the interactive conference platform.
“While SHM Converge may look a bit different than the SHM annual conference we are accustomed to, I am confident the content will be among the best we have ever offered, spanning a broad range of clinical topics and issues affecting hospitalists and their patients,” said Daniel Steinberg, MD, SFHM, course director for SHM Converge. “This virtual experience will unite hospitalists from around the globe and connect them with renowned faculty members and thought leaders in hospital medicine – as well as with their hospitalist colleagues they look forward to reconnecting with each year.”
Keynote speaker announcements are forthcoming.
Registration for SHM Converge opens in November 2020. Learn more at shmconverge.org.
Members of the media can obtain press passes beginning in November 2020 by contacting [email protected].
The Society of Hospital Medicine has announced its virtual annual conference for 2021: SHM Converge. Formerly known as Hospital Medicine 2021, SHM Converge will take place virtually from May 3-7, 2021, and will offer a fully digital experience with the same education, professional development, and networking hospitalists have come to expect from SHM’s annual conference.
“This year, COVID-19 has challenged us to embrace change and to innovate to better serve our hospital medicine community,” said Danielle Scheurer, MD, MSCR, SFHM, president of SHM’s board of directors. “In that spirit, not only are we introducing an exciting new brand for the SHM annual conference, we are unveiling a reimagined experience for attendees, complete with sessions highlighting the latest research, best practices and innovations in the field.”
The SHM Converge schedule features 20 educational tracks, including the addition of four new tracks to support hospital medicine professionals in some of the most relevant topics affecting health care: diagnostic safety; diversity, equity, and inclusion; leadership; and wellness and resilience
Attendees will also have the option to follow many of the most popular tracks from previous SHM annual conferences, including Rapid Fire, Clinical Updates, and High-Value Care, among others. In many sessions, speakers will present the latest data and information available about COVID-19’s impact on the practice of hospital medicine. Precourses will be held on May 3.
SHM Converge will also offer additional professional development opportunities, including the Research, Innovations, and Clinical Vignettes scientific abstract competition and a speed mentoring session. Networking will be an integral component of SHM Converge. Attendees will be able to choose from more than 20 Special Interest forums, live Q&A sessions and networking events through the interactive conference platform.
“While SHM Converge may look a bit different than the SHM annual conference we are accustomed to, I am confident the content will be among the best we have ever offered, spanning a broad range of clinical topics and issues affecting hospitalists and their patients,” said Daniel Steinberg, MD, SFHM, course director for SHM Converge. “This virtual experience will unite hospitalists from around the globe and connect them with renowned faculty members and thought leaders in hospital medicine – as well as with their hospitalist colleagues they look forward to reconnecting with each year.”
Keynote speaker announcements are forthcoming.
Registration for SHM Converge opens in November 2020. Learn more at shmconverge.org.
Members of the media can obtain press passes beginning in November 2020 by contacting [email protected].
The Society of Hospital Medicine has announced its virtual annual conference for 2021: SHM Converge. Formerly known as Hospital Medicine 2021, SHM Converge will take place virtually from May 3-7, 2021, and will offer a fully digital experience with the same education, professional development, and networking hospitalists have come to expect from SHM’s annual conference.
“This year, COVID-19 has challenged us to embrace change and to innovate to better serve our hospital medicine community,” said Danielle Scheurer, MD, MSCR, SFHM, president of SHM’s board of directors. “In that spirit, not only are we introducing an exciting new brand for the SHM annual conference, we are unveiling a reimagined experience for attendees, complete with sessions highlighting the latest research, best practices and innovations in the field.”
The SHM Converge schedule features 20 educational tracks, including the addition of four new tracks to support hospital medicine professionals in some of the most relevant topics affecting health care: diagnostic safety; diversity, equity, and inclusion; leadership; and wellness and resilience
Attendees will also have the option to follow many of the most popular tracks from previous SHM annual conferences, including Rapid Fire, Clinical Updates, and High-Value Care, among others. In many sessions, speakers will present the latest data and information available about COVID-19’s impact on the practice of hospital medicine. Precourses will be held on May 3.
SHM Converge will also offer additional professional development opportunities, including the Research, Innovations, and Clinical Vignettes scientific abstract competition and a speed mentoring session. Networking will be an integral component of SHM Converge. Attendees will be able to choose from more than 20 Special Interest forums, live Q&A sessions and networking events through the interactive conference platform.
“While SHM Converge may look a bit different than the SHM annual conference we are accustomed to, I am confident the content will be among the best we have ever offered, spanning a broad range of clinical topics and issues affecting hospitalists and their patients,” said Daniel Steinberg, MD, SFHM, course director for SHM Converge. “This virtual experience will unite hospitalists from around the globe and connect them with renowned faculty members and thought leaders in hospital medicine – as well as with their hospitalist colleagues they look forward to reconnecting with each year.”
Keynote speaker announcements are forthcoming.
Registration for SHM Converge opens in November 2020. Learn more at shmconverge.org.
Members of the media can obtain press passes beginning in November 2020 by contacting [email protected].