User login
Telehealth models of care for pediatric hospital medicine
PHM 2021 session
Let’s Go Virtual! Developing, Implementing, and Evaluating Telehealth Models of Care for Pediatric Hospital Medicine
Presenters
Brooke Geyer, DO; Christina Olson, MD; and Amy Willis, MD, FAAP
Session summary
Dr. Geyer, Dr. Olson, and Dr. Willis of the University of Colorado presented and facilitated a workshop discussing the role of telehealth in pediatric hospital medicine. Participants were given a brief introduction to the basics of telehealth practices before breaking up into small groups to explore the process of developing, implementing, and evaluating a telehealth model in a pediatric hospital. For each of these topics, the presenters led the breakout groups through a discussion of Colorado’s successful telehealth models, including virtual nocturnists, health system resource optimization, and virtual transitions of care, as well as addressed the participants’ questions unique to their telehealth experiences. The session emphasized the emerging role of telehealth in pediatric hospital medicine and that “telehealth is here to stay, and we have an opportunity to redesign health care forever.”
Key takeaways
- Telehealth is more than just synchronous virtual patient care, it encompasses asynchronous care, remote patient monitoring, education, policy, and more.
- Telehealth standards of care are the same as in-person care.
- Development and implementation of a telehealth model in pediatric hospital medicine is feasible with appropriate planning and conversations with key stakeholders.
- Evaluation and refinement of telehealth models is an iterative process that will take time, much like Plan-Do-Study-Act cycles in quality improvement work.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
PHM 2021 session
Let’s Go Virtual! Developing, Implementing, and Evaluating Telehealth Models of Care for Pediatric Hospital Medicine
Presenters
Brooke Geyer, DO; Christina Olson, MD; and Amy Willis, MD, FAAP
Session summary
Dr. Geyer, Dr. Olson, and Dr. Willis of the University of Colorado presented and facilitated a workshop discussing the role of telehealth in pediatric hospital medicine. Participants were given a brief introduction to the basics of telehealth practices before breaking up into small groups to explore the process of developing, implementing, and evaluating a telehealth model in a pediatric hospital. For each of these topics, the presenters led the breakout groups through a discussion of Colorado’s successful telehealth models, including virtual nocturnists, health system resource optimization, and virtual transitions of care, as well as addressed the participants’ questions unique to their telehealth experiences. The session emphasized the emerging role of telehealth in pediatric hospital medicine and that “telehealth is here to stay, and we have an opportunity to redesign health care forever.”
Key takeaways
- Telehealth is more than just synchronous virtual patient care, it encompasses asynchronous care, remote patient monitoring, education, policy, and more.
- Telehealth standards of care are the same as in-person care.
- Development and implementation of a telehealth model in pediatric hospital medicine is feasible with appropriate planning and conversations with key stakeholders.
- Evaluation and refinement of telehealth models is an iterative process that will take time, much like Plan-Do-Study-Act cycles in quality improvement work.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
PHM 2021 session
Let’s Go Virtual! Developing, Implementing, and Evaluating Telehealth Models of Care for Pediatric Hospital Medicine
Presenters
Brooke Geyer, DO; Christina Olson, MD; and Amy Willis, MD, FAAP
Session summary
Dr. Geyer, Dr. Olson, and Dr. Willis of the University of Colorado presented and facilitated a workshop discussing the role of telehealth in pediatric hospital medicine. Participants were given a brief introduction to the basics of telehealth practices before breaking up into small groups to explore the process of developing, implementing, and evaluating a telehealth model in a pediatric hospital. For each of these topics, the presenters led the breakout groups through a discussion of Colorado’s successful telehealth models, including virtual nocturnists, health system resource optimization, and virtual transitions of care, as well as addressed the participants’ questions unique to their telehealth experiences. The session emphasized the emerging role of telehealth in pediatric hospital medicine and that “telehealth is here to stay, and we have an opportunity to redesign health care forever.”
Key takeaways
- Telehealth is more than just synchronous virtual patient care, it encompasses asynchronous care, remote patient monitoring, education, policy, and more.
- Telehealth standards of care are the same as in-person care.
- Development and implementation of a telehealth model in pediatric hospital medicine is feasible with appropriate planning and conversations with key stakeholders.
- Evaluation and refinement of telehealth models is an iterative process that will take time, much like Plan-Do-Study-Act cycles in quality improvement work.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
Hospitalist movers and shakers – September 2021
Chi-Cheng Huang, MD, SFHM, was recently was named one of the Notable Asian/Pacific American Physicians in U.S. History by the American Board of Internal Medicine. May was Asian/Pacific American Heritage Month. Dr. Huang is the executive medical director and service line director of general medicine and hospital medicine within the Wake Forest Baptist Health System (Winston-Salem, N.C.) and associate professor at Wake Forest School of Medicine.
Dr. Huang is a board-certified hospitalist and pediatrician, and he is the founder of the Bolivian Children Project, a non-profit organization that focuses on sheltering street children in La Paz and other areas of Bolivia. Dr. Huang was inspired to start the project during a year sabbatical from medical school. He worked at an orphanage and cared for children who were victims of physical abuse. The Bolivian Children Project supports those children, and Dr. Huang’s book, When Invisible Children Sing, tells their story.
Joshua Lenchus, DO, RPh, SFHM, has been elected president of the Florida Medical Association. It is the first time in its history that the FMA will have a DO as its president. Dr. Lenchus is a hospitalist and chief medical officer at the Broward Health Medical Center in Fort Lauderdale, Fla.
Mark V. Williams, MD, MHM, will join Washington University School of Medicine and BJC HealthCare, both in St. Louis, as professor and chief for the Division of Hospital Medicine in October 2021. Dr. Williams is currently professor and director of the Center for Health Services Research at the University of Kentucky and chief quality officer at UK HealthCare, both in Lexington.
Dr. Williams was a founding member of the Society of Hospital Medicine, one of the first two elected members of the Board of SHM, its former president, founding editor of the Journal of Hospital Medicine, and principal investigator for Project BOOST. He established the first hospitalist program at a public hospital (Grady Memorial in Atlanta) in 1998, and later became the founding chief of the Division of Hospital Medicine in 2007 at Northwestern University School of Medicine in Chicago. At the University of Kentucky, he established the Center for Health Services Research and the Division of Hospital Medicine in 2014.
At Washington University, Dr. Williams will be tasked with translating the division of hospital medicine’s scholarly work, innovation, and research into practice improvement, focusing on developing new systems of health care delivery that are patient-centered, cost effective, and provide outstanding value.
Jordan Messler, MD, SFHM, has been named the new chief medical officer at Glytec (Waltham, Mass.), where he has worked as executive director of clinical practice since 2018. Dr. Messler will be tasked with leading strategy and product development while also supporting efforts in quality care, customer relations, and delivery of products.
Glytec provides insulin management software across the care continuum and is touted as the only cloud-based software provider of its kind. Dr. Messler’s background includes expertise in glycemic management. In addition, he still works as a hospitalist at Morton Plant Hospitalist Group (Clearwater, Fla.).
Dr. Messler is a senior fellow with SHM and is physician editor of SHM’s official blog The Hospital Leader.
Tiffani Maycock, DO, recently was named to the Board of Directors for the American Board of Family Medicine. Dr. Maycock is director of the Selma Family Medicine Residency Program at the University of Alabama at Birmingham, where she is an assistant professor in the department of family medicine.
Dr. Maycock helped create hospitalist services at Vaughan Regional Medical Center (Selma, Ala.) – Selma Family Medicine’s primary teaching site – and currently serves as its hospitalist director and on its Medical Executive Committee. She has worked at the facility since 2017.
Preetham Talari, MD, SFHM, has been named associate chief of quality safety for the Division of Hospital Medicine at the University of Kentucky’s UK HealthCare (Lexington, Ky.). Dr. Talari is an associate professor of internal medicine in the Division of Hospital Medicine at the UK College of Medicine.
Over the last decade, Dr. Talari’s work in quality, safety, and health care leadership has positioned him as a leader in several UK Healthcare committees and transformation projects. In his role as associate chief, Dr. Talari collaborates with hospital medicine directors, enterprise leadership, and medical education leadership to improve the system’s quality of care.
Dr. Talari is the president of the Kentucky chapter of SHM and is a member of SHM’s Hospital Quality and Patient Safety Committee.
Adrian Paraschiv, MD, FHM, is being recognized by Continental Who’s Who as a Trusted Internist and Hospitalist in the field of Medicine in acknowledgment of his commitment to providing quality health care services.
Dr. Paraschiv is a board-certified Internist at Garnet Health Medical Center in Middletown, N.Y. He also serves in an administrative capacity as the Garnet Health Doctors Hospitalist Division’s Associate Program Director. He is also the Director of Clinical Informatics. Dr. Paraschiv is certified as the Epic physician builder in analytics, information technology, and improved documentation.
DCH Health System (Tuscaloosa, Ala.) recently selected Capstone Health Services Foundation (Tuscaloosa) and IN Compass Health Inc. (Alpharetta, Ga.) as its joint hospitalist service provider for facilities in Northport and Tuscaloosa. Capstone will provide the physicians, while IN Compass will handle staffing management of the hospitalists, as well as day-to-day operations and calculating quality care metrics. The agreement is slated to begin on Oct. 1, 2021, at Northport Medical Center, and on Nov. 1, 2021, at DCH Regional Medical Center.
Capstone is an affiliate of the University of Alabama and oversees University Hospitalist Group, which currently provides hospitalists at DCH Regional Medical Center. Its partnership with IN Compass includes working together in recruiting and hiring physicians for both facilities.
UPMC Kane Medical Center (Kane, Pa.) recently announced the creation of a virtual telemedicine hospitalist program. UPMC Kane is partnering with the UPMC Center for Community Hospitalist Medicine to create this new mode of care.
Telehospitalists will care for UPMC Kane patients using advanced diagnostic technique and high-definition cameras. The physicians will bring expert service to Kane 24 hours per day utilizing physicians and specialists based in Pittsburgh. Those hospitalists will work with local nurse practitioners and support staff and deliver care to Kane patients.
Wake Forest Baptist Health (Winston-Salem, N.C.) has launched a Hospitalist at Home program with hopes of keeping patients safe while also reducing time they spend in the hospital. The telehealth initiative kicked into gear at the start of 2021 and considered the first of its kind in the region.
Patients who qualify for the program establish a plan before they leave the hospital. Wake Forest Baptist Health paramedics makes home visits and conducts care with a hospitalist reviewing the visit virtually. Those appointments continue until the patient does not require monitoring.
The impetus of creating the program was the COVID-19 pandemic, however, Wake Forest said it expects to care for between 75-100 patients through Hospitalist at Home at any one time.
Chi-Cheng Huang, MD, SFHM, was recently was named one of the Notable Asian/Pacific American Physicians in U.S. History by the American Board of Internal Medicine. May was Asian/Pacific American Heritage Month. Dr. Huang is the executive medical director and service line director of general medicine and hospital medicine within the Wake Forest Baptist Health System (Winston-Salem, N.C.) and associate professor at Wake Forest School of Medicine.
Dr. Huang is a board-certified hospitalist and pediatrician, and he is the founder of the Bolivian Children Project, a non-profit organization that focuses on sheltering street children in La Paz and other areas of Bolivia. Dr. Huang was inspired to start the project during a year sabbatical from medical school. He worked at an orphanage and cared for children who were victims of physical abuse. The Bolivian Children Project supports those children, and Dr. Huang’s book, When Invisible Children Sing, tells their story.
Joshua Lenchus, DO, RPh, SFHM, has been elected president of the Florida Medical Association. It is the first time in its history that the FMA will have a DO as its president. Dr. Lenchus is a hospitalist and chief medical officer at the Broward Health Medical Center in Fort Lauderdale, Fla.
Mark V. Williams, MD, MHM, will join Washington University School of Medicine and BJC HealthCare, both in St. Louis, as professor and chief for the Division of Hospital Medicine in October 2021. Dr. Williams is currently professor and director of the Center for Health Services Research at the University of Kentucky and chief quality officer at UK HealthCare, both in Lexington.
Dr. Williams was a founding member of the Society of Hospital Medicine, one of the first two elected members of the Board of SHM, its former president, founding editor of the Journal of Hospital Medicine, and principal investigator for Project BOOST. He established the first hospitalist program at a public hospital (Grady Memorial in Atlanta) in 1998, and later became the founding chief of the Division of Hospital Medicine in 2007 at Northwestern University School of Medicine in Chicago. At the University of Kentucky, he established the Center for Health Services Research and the Division of Hospital Medicine in 2014.
At Washington University, Dr. Williams will be tasked with translating the division of hospital medicine’s scholarly work, innovation, and research into practice improvement, focusing on developing new systems of health care delivery that are patient-centered, cost effective, and provide outstanding value.
Jordan Messler, MD, SFHM, has been named the new chief medical officer at Glytec (Waltham, Mass.), where he has worked as executive director of clinical practice since 2018. Dr. Messler will be tasked with leading strategy and product development while also supporting efforts in quality care, customer relations, and delivery of products.
Glytec provides insulin management software across the care continuum and is touted as the only cloud-based software provider of its kind. Dr. Messler’s background includes expertise in glycemic management. In addition, he still works as a hospitalist at Morton Plant Hospitalist Group (Clearwater, Fla.).
Dr. Messler is a senior fellow with SHM and is physician editor of SHM’s official blog The Hospital Leader.
Tiffani Maycock, DO, recently was named to the Board of Directors for the American Board of Family Medicine. Dr. Maycock is director of the Selma Family Medicine Residency Program at the University of Alabama at Birmingham, where she is an assistant professor in the department of family medicine.
Dr. Maycock helped create hospitalist services at Vaughan Regional Medical Center (Selma, Ala.) – Selma Family Medicine’s primary teaching site – and currently serves as its hospitalist director and on its Medical Executive Committee. She has worked at the facility since 2017.
Preetham Talari, MD, SFHM, has been named associate chief of quality safety for the Division of Hospital Medicine at the University of Kentucky’s UK HealthCare (Lexington, Ky.). Dr. Talari is an associate professor of internal medicine in the Division of Hospital Medicine at the UK College of Medicine.
Over the last decade, Dr. Talari’s work in quality, safety, and health care leadership has positioned him as a leader in several UK Healthcare committees and transformation projects. In his role as associate chief, Dr. Talari collaborates with hospital medicine directors, enterprise leadership, and medical education leadership to improve the system’s quality of care.
Dr. Talari is the president of the Kentucky chapter of SHM and is a member of SHM’s Hospital Quality and Patient Safety Committee.
Adrian Paraschiv, MD, FHM, is being recognized by Continental Who’s Who as a Trusted Internist and Hospitalist in the field of Medicine in acknowledgment of his commitment to providing quality health care services.
Dr. Paraschiv is a board-certified Internist at Garnet Health Medical Center in Middletown, N.Y. He also serves in an administrative capacity as the Garnet Health Doctors Hospitalist Division’s Associate Program Director. He is also the Director of Clinical Informatics. Dr. Paraschiv is certified as the Epic physician builder in analytics, information technology, and improved documentation.
DCH Health System (Tuscaloosa, Ala.) recently selected Capstone Health Services Foundation (Tuscaloosa) and IN Compass Health Inc. (Alpharetta, Ga.) as its joint hospitalist service provider for facilities in Northport and Tuscaloosa. Capstone will provide the physicians, while IN Compass will handle staffing management of the hospitalists, as well as day-to-day operations and calculating quality care metrics. The agreement is slated to begin on Oct. 1, 2021, at Northport Medical Center, and on Nov. 1, 2021, at DCH Regional Medical Center.
Capstone is an affiliate of the University of Alabama and oversees University Hospitalist Group, which currently provides hospitalists at DCH Regional Medical Center. Its partnership with IN Compass includes working together in recruiting and hiring physicians for both facilities.
UPMC Kane Medical Center (Kane, Pa.) recently announced the creation of a virtual telemedicine hospitalist program. UPMC Kane is partnering with the UPMC Center for Community Hospitalist Medicine to create this new mode of care.
Telehospitalists will care for UPMC Kane patients using advanced diagnostic technique and high-definition cameras. The physicians will bring expert service to Kane 24 hours per day utilizing physicians and specialists based in Pittsburgh. Those hospitalists will work with local nurse practitioners and support staff and deliver care to Kane patients.
Wake Forest Baptist Health (Winston-Salem, N.C.) has launched a Hospitalist at Home program with hopes of keeping patients safe while also reducing time they spend in the hospital. The telehealth initiative kicked into gear at the start of 2021 and considered the first of its kind in the region.
Patients who qualify for the program establish a plan before they leave the hospital. Wake Forest Baptist Health paramedics makes home visits and conducts care with a hospitalist reviewing the visit virtually. Those appointments continue until the patient does not require monitoring.
The impetus of creating the program was the COVID-19 pandemic, however, Wake Forest said it expects to care for between 75-100 patients through Hospitalist at Home at any one time.
Chi-Cheng Huang, MD, SFHM, was recently was named one of the Notable Asian/Pacific American Physicians in U.S. History by the American Board of Internal Medicine. May was Asian/Pacific American Heritage Month. Dr. Huang is the executive medical director and service line director of general medicine and hospital medicine within the Wake Forest Baptist Health System (Winston-Salem, N.C.) and associate professor at Wake Forest School of Medicine.
Dr. Huang is a board-certified hospitalist and pediatrician, and he is the founder of the Bolivian Children Project, a non-profit organization that focuses on sheltering street children in La Paz and other areas of Bolivia. Dr. Huang was inspired to start the project during a year sabbatical from medical school. He worked at an orphanage and cared for children who were victims of physical abuse. The Bolivian Children Project supports those children, and Dr. Huang’s book, When Invisible Children Sing, tells their story.
Joshua Lenchus, DO, RPh, SFHM, has been elected president of the Florida Medical Association. It is the first time in its history that the FMA will have a DO as its president. Dr. Lenchus is a hospitalist and chief medical officer at the Broward Health Medical Center in Fort Lauderdale, Fla.
Mark V. Williams, MD, MHM, will join Washington University School of Medicine and BJC HealthCare, both in St. Louis, as professor and chief for the Division of Hospital Medicine in October 2021. Dr. Williams is currently professor and director of the Center for Health Services Research at the University of Kentucky and chief quality officer at UK HealthCare, both in Lexington.
Dr. Williams was a founding member of the Society of Hospital Medicine, one of the first two elected members of the Board of SHM, its former president, founding editor of the Journal of Hospital Medicine, and principal investigator for Project BOOST. He established the first hospitalist program at a public hospital (Grady Memorial in Atlanta) in 1998, and later became the founding chief of the Division of Hospital Medicine in 2007 at Northwestern University School of Medicine in Chicago. At the University of Kentucky, he established the Center for Health Services Research and the Division of Hospital Medicine in 2014.
At Washington University, Dr. Williams will be tasked with translating the division of hospital medicine’s scholarly work, innovation, and research into practice improvement, focusing on developing new systems of health care delivery that are patient-centered, cost effective, and provide outstanding value.
Jordan Messler, MD, SFHM, has been named the new chief medical officer at Glytec (Waltham, Mass.), where he has worked as executive director of clinical practice since 2018. Dr. Messler will be tasked with leading strategy and product development while also supporting efforts in quality care, customer relations, and delivery of products.
Glytec provides insulin management software across the care continuum and is touted as the only cloud-based software provider of its kind. Dr. Messler’s background includes expertise in glycemic management. In addition, he still works as a hospitalist at Morton Plant Hospitalist Group (Clearwater, Fla.).
Dr. Messler is a senior fellow with SHM and is physician editor of SHM’s official blog The Hospital Leader.
Tiffani Maycock, DO, recently was named to the Board of Directors for the American Board of Family Medicine. Dr. Maycock is director of the Selma Family Medicine Residency Program at the University of Alabama at Birmingham, where she is an assistant professor in the department of family medicine.
Dr. Maycock helped create hospitalist services at Vaughan Regional Medical Center (Selma, Ala.) – Selma Family Medicine’s primary teaching site – and currently serves as its hospitalist director and on its Medical Executive Committee. She has worked at the facility since 2017.
Preetham Talari, MD, SFHM, has been named associate chief of quality safety for the Division of Hospital Medicine at the University of Kentucky’s UK HealthCare (Lexington, Ky.). Dr. Talari is an associate professor of internal medicine in the Division of Hospital Medicine at the UK College of Medicine.
Over the last decade, Dr. Talari’s work in quality, safety, and health care leadership has positioned him as a leader in several UK Healthcare committees and transformation projects. In his role as associate chief, Dr. Talari collaborates with hospital medicine directors, enterprise leadership, and medical education leadership to improve the system’s quality of care.
Dr. Talari is the president of the Kentucky chapter of SHM and is a member of SHM’s Hospital Quality and Patient Safety Committee.
Adrian Paraschiv, MD, FHM, is being recognized by Continental Who’s Who as a Trusted Internist and Hospitalist in the field of Medicine in acknowledgment of his commitment to providing quality health care services.
Dr. Paraschiv is a board-certified Internist at Garnet Health Medical Center in Middletown, N.Y. He also serves in an administrative capacity as the Garnet Health Doctors Hospitalist Division’s Associate Program Director. He is also the Director of Clinical Informatics. Dr. Paraschiv is certified as the Epic physician builder in analytics, information technology, and improved documentation.
DCH Health System (Tuscaloosa, Ala.) recently selected Capstone Health Services Foundation (Tuscaloosa) and IN Compass Health Inc. (Alpharetta, Ga.) as its joint hospitalist service provider for facilities in Northport and Tuscaloosa. Capstone will provide the physicians, while IN Compass will handle staffing management of the hospitalists, as well as day-to-day operations and calculating quality care metrics. The agreement is slated to begin on Oct. 1, 2021, at Northport Medical Center, and on Nov. 1, 2021, at DCH Regional Medical Center.
Capstone is an affiliate of the University of Alabama and oversees University Hospitalist Group, which currently provides hospitalists at DCH Regional Medical Center. Its partnership with IN Compass includes working together in recruiting and hiring physicians for both facilities.
UPMC Kane Medical Center (Kane, Pa.) recently announced the creation of a virtual telemedicine hospitalist program. UPMC Kane is partnering with the UPMC Center for Community Hospitalist Medicine to create this new mode of care.
Telehospitalists will care for UPMC Kane patients using advanced diagnostic technique and high-definition cameras. The physicians will bring expert service to Kane 24 hours per day utilizing physicians and specialists based in Pittsburgh. Those hospitalists will work with local nurse practitioners and support staff and deliver care to Kane patients.
Wake Forest Baptist Health (Winston-Salem, N.C.) has launched a Hospitalist at Home program with hopes of keeping patients safe while also reducing time they spend in the hospital. The telehealth initiative kicked into gear at the start of 2021 and considered the first of its kind in the region.
Patients who qualify for the program establish a plan before they leave the hospital. Wake Forest Baptist Health paramedics makes home visits and conducts care with a hospitalist reviewing the visit virtually. Those appointments continue until the patient does not require monitoring.
The impetus of creating the program was the COVID-19 pandemic, however, Wake Forest said it expects to care for between 75-100 patients through Hospitalist at Home at any one time.
POCUS in hospital pediatrics
PHM 2021 Session
Safe and (Ultra)sound: Why you should use POCUS in your Pediatric Practice
Presenter
Ria Dancel, MD, FAAP, FACP
Session summary
Dr. Ria Dancel and her colleagues from the University of North Carolina at Chapel Hill presented a broad overview of point-of-care ultrasound (POCUS) applications in the field of pediatric hospital medicine. They discussed its advantages and potential uses, ranging from common scenarios to critical care to procedural guidance. Using illustrative scenarios and interactive cases, she discussed the bedside applications to improve care of hospitalized children. The benefits and risks of radiography and POCUS were reviewed.
The session highlighted the use of POCUS in SSTI (skin and soft tissue infection) to help with differentiating cellulitis from abscesses. Use of POCUS for safer incision and drainages and making day-to-day changes in management was discussed. The ease and benefits of performing real-time lung ultrasound in different pathologies (like pneumonia, effusion, COVID-19) was presented. The speakers discussed the use of POCUS in emergency situations like hypotension and different types of shock. The use of ultrasound in common bedside procedures (bladder catheterization, lumbar ultrasound, peripheral IV placement) were also highlighted. Current literature and evidence were reviewed.
Key takeaways
- Pediatric POCUS is an extremely valuable bedside tool in pediatric hospital medicine.
- It can be used to guide clinical care for many conditions including SSTI, pneumonia, and shock.
- It can be used for procedural guidance for bladder catheterization, lumbar puncture, and intravenous access.
Dr. Patra is a pediatric hospitalist at West Virginia University Children’s Hospital, Morgantown, and associate professor at West Virginia University School of Medicine. He is interested in medical education, quality improvement and clinical research. He is a member of the Executive Council of the Pediatric Special Interest Group of the Society of Hospital Medicine.
PHM 2021 Session
Safe and (Ultra)sound: Why you should use POCUS in your Pediatric Practice
Presenter
Ria Dancel, MD, FAAP, FACP
Session summary
Dr. Ria Dancel and her colleagues from the University of North Carolina at Chapel Hill presented a broad overview of point-of-care ultrasound (POCUS) applications in the field of pediatric hospital medicine. They discussed its advantages and potential uses, ranging from common scenarios to critical care to procedural guidance. Using illustrative scenarios and interactive cases, she discussed the bedside applications to improve care of hospitalized children. The benefits and risks of radiography and POCUS were reviewed.
The session highlighted the use of POCUS in SSTI (skin and soft tissue infection) to help with differentiating cellulitis from abscesses. Use of POCUS for safer incision and drainages and making day-to-day changes in management was discussed. The ease and benefits of performing real-time lung ultrasound in different pathologies (like pneumonia, effusion, COVID-19) was presented. The speakers discussed the use of POCUS in emergency situations like hypotension and different types of shock. The use of ultrasound in common bedside procedures (bladder catheterization, lumbar ultrasound, peripheral IV placement) were also highlighted. Current literature and evidence were reviewed.
Key takeaways
- Pediatric POCUS is an extremely valuable bedside tool in pediatric hospital medicine.
- It can be used to guide clinical care for many conditions including SSTI, pneumonia, and shock.
- It can be used for procedural guidance for bladder catheterization, lumbar puncture, and intravenous access.
Dr. Patra is a pediatric hospitalist at West Virginia University Children’s Hospital, Morgantown, and associate professor at West Virginia University School of Medicine. He is interested in medical education, quality improvement and clinical research. He is a member of the Executive Council of the Pediatric Special Interest Group of the Society of Hospital Medicine.
PHM 2021 Session
Safe and (Ultra)sound: Why you should use POCUS in your Pediatric Practice
Presenter
Ria Dancel, MD, FAAP, FACP
Session summary
Dr. Ria Dancel and her colleagues from the University of North Carolina at Chapel Hill presented a broad overview of point-of-care ultrasound (POCUS) applications in the field of pediatric hospital medicine. They discussed its advantages and potential uses, ranging from common scenarios to critical care to procedural guidance. Using illustrative scenarios and interactive cases, she discussed the bedside applications to improve care of hospitalized children. The benefits and risks of radiography and POCUS were reviewed.
The session highlighted the use of POCUS in SSTI (skin and soft tissue infection) to help with differentiating cellulitis from abscesses. Use of POCUS for safer incision and drainages and making day-to-day changes in management was discussed. The ease and benefits of performing real-time lung ultrasound in different pathologies (like pneumonia, effusion, COVID-19) was presented. The speakers discussed the use of POCUS in emergency situations like hypotension and different types of shock. The use of ultrasound in common bedside procedures (bladder catheterization, lumbar ultrasound, peripheral IV placement) were also highlighted. Current literature and evidence were reviewed.
Key takeaways
- Pediatric POCUS is an extremely valuable bedside tool in pediatric hospital medicine.
- It can be used to guide clinical care for many conditions including SSTI, pneumonia, and shock.
- It can be used for procedural guidance for bladder catheterization, lumbar puncture, and intravenous access.
Dr. Patra is a pediatric hospitalist at West Virginia University Children’s Hospital, Morgantown, and associate professor at West Virginia University School of Medicine. He is interested in medical education, quality improvement and clinical research. He is a member of the Executive Council of the Pediatric Special Interest Group of the Society of Hospital Medicine.
New fellowship, no problem
Using growth mindset to tackle fellowship in a new program
Growth mindset is a well-established phenomenon in childhood education that is now starting to appear in health care education literature.1 This concept emphasizes the capacity of individuals to change and grow through experience and that an individual’s basic qualities can be cultivated through hard work, open-mindedness, and help from others.2
Growth mindset opposes the concept of fixed mindset, which implies intelligence or other personal traits are set in stone, unable to be fundamentally changed.2 Individuals with fixed mindsets are less adept at coping with perceived failures and critical feedback because they view these as attacks on their own abilities.2 This oftentimes leads these individuals to avoid potential challenges and feedback because of fear of being exposed as incompetent or feeling inadequate. Conversely, individuals with a growth mindset embrace challenges and failures as learning opportunities and identify feedback as a critical element of growth.2 These individuals maintain a sense of resilience in the face of adversity and strive to become lifelong learners.
As the field of pediatric hospital medicine (PHM) continues to rapidly evolve, so too does the landscape of PHM fellowships. New programs are opening at a torrid pace to accommodate the increasing demand of residents looking to enter the field with new subspecialty accreditation. Most first-year PHM fellows in established programs enter with a clear precedent to follow, set forth by fellows who have come before them. For PHM fellows in new programs, however, there is often no beaten path to follow.
Entering fellowship as a first-year PHM fellow in a new program and blazing one’s own trail can be intriguing and exhilarating given the unique opportunities available. However, the potential challenges for both fellows and program directors during this transition cannot be understated. The role of new PHM fellows within the institutional framework may initially be unclear to others, which can lead to ambiguous expectations and disruptions to normal workflows. Furthermore, assessing and evaluating new fellows may prove difficult as a result of these unclear expectations and general uncertainties. Using the growth mindset can help both PHM fellows and program directors take a deliberate approach to the challenges and uncertainty that may accompany the creation of a new fellowship program.
One of the challenges new PHM fellows may encounter lies within the structure of the care team. Resident and medical student learners may express consternation that the new fellow role may limit their own autonomy. In addition, finding the right balance of autonomy and supervision between the attending-fellow dyad may prove to be difficult. However, using the growth mindset may allow fellows to see the inherent benefits of this new role.
Fellows should seize the opportunity to discuss the nuances and differing approaches to difficult clinical questions, managing a team and interpersonal dynamics, and balancing clinical and nonclinical responsibilities with an experienced supervising clinician; issues that are often less pressing as a resident. The fellow role also affords the opportunity to more carefully observe different clinical styles of practice to subsequently shape one’s own preferred style.
Finally, fellows should employ a growth mindset to optimize clinical time by discussing expectations with involved stakeholders prior to rotations and explicitly identifying goals for feedback and improvement. Program directors can also help stakeholders including faculty, residency programs, medical schools, and other health care professionals on the clinical teams prepare for this transition by providing expectations for the fellow role and by soliciting questions and feedback before and after fellows begin.
One of the key tenets of the growth mindset is actively seeking out constructive feedback and learning from failures to grow and improve. This can be a particularly useful practice for fellows during the course of their scholarly pursuits in clinical research, quality improvement, and medical education. From initial stages of idea development through the final steps of manuscript submission and peer review, fellows will undoubtedly navigate a plethora of challenges and setbacks along the way. Program directors and other core faculty members can promote a growth mindset culture by honestly discussing their own challenges and failures in career endeavors in addition to giving thoughtful constructive feedback.
Fellows should routinely practice explicitly identifying knowledge and skills gaps that represent areas for potential improvement. But perhaps most importantly, fellows must strive to see all feedback and perceived failures not as personal affronts or as commentaries on personal abilities, but rather as opportunities to strengthen their scholarly products and gain valuable experience for future endeavors.
Not all learners will come equipped with a growth mindset. So, what can fellows and program directors in new programs do to develop this practice and mitigate some of the inevitable uncertainty? To begin, program directors should think about how to create cultures of growth and development as the fixed and growth mindsets are not just limited to individuals.3 Program directors can strive to augment this process by committing to solicit feedback for themselves and acknowledging their own vulnerabilities and perceived weaknesses.
Fellows must have early, honest discussions with program directors and other stakeholders about expectations and goals. Program directors should consider creating lists of “must meet” individuals within the institution that can help fellows begin to carve out their roles in the clinical, educational, and research realms. Deliberately crafting a mentorship team that will encourage a commitment to growth and improvement is critical. Seeking out growth feedback, particularly in areas that prove challenging, should become common practice for fellows from the onset.
Most importantly, fellows should reframe uncertainty as opportunity for growth and progression. Seeing oneself as a work in progress provides a new perspective that prioritizes learning and emphasizes improvement potential.
Embodying this approach requires patience and practice. Being part of a newly created fellowship represents an opportunity to learn from personal challenges rather than leaning on the precedent set by previous fellows. And although fellows will often face uncertainty as a part of the novelty within a new program, they can ultimately succeed by practicing the principles of Dweck’s Growth Mindset: embracing challenges and failure as learning experiences, seeking out feedback, and pursuing the opportunities among ambiguity.
Dr. Herchline is a pediatric hospitalist at Cincinnati Children’s Hospital Medical Center and recent fellow graduate of the Children’s Hospital of Philadelphia. During fellowship, he completed a master’s degree in medical education at the University of Pennsylvania. His academic interests include graduate medical education, interprofessional collaboration and teamwork, and quality improvement.
References
1. Klein J et al. A growth mindset approach to preparing trainees for medical error. BMJ Qual Saf. 2017 Sep;26(9):771-4. doi: 10.1136/bmjqs-2016-006416.
2. Dweck C. Mindset: The new psychology of success. New York: Ballantine Books; 2006.
3. Murphy MC, Dweck CS. A culture of genius: How an organization’s lay theory shapes people’s cognition, affect, and behavior. Pers Soc Psychol Bull. 2010 Mar;36(3):283-96. doi: 10.1177/0146167209347380.
Using growth mindset to tackle fellowship in a new program
Using growth mindset to tackle fellowship in a new program
Growth mindset is a well-established phenomenon in childhood education that is now starting to appear in health care education literature.1 This concept emphasizes the capacity of individuals to change and grow through experience and that an individual’s basic qualities can be cultivated through hard work, open-mindedness, and help from others.2
Growth mindset opposes the concept of fixed mindset, which implies intelligence or other personal traits are set in stone, unable to be fundamentally changed.2 Individuals with fixed mindsets are less adept at coping with perceived failures and critical feedback because they view these as attacks on their own abilities.2 This oftentimes leads these individuals to avoid potential challenges and feedback because of fear of being exposed as incompetent or feeling inadequate. Conversely, individuals with a growth mindset embrace challenges and failures as learning opportunities and identify feedback as a critical element of growth.2 These individuals maintain a sense of resilience in the face of adversity and strive to become lifelong learners.
As the field of pediatric hospital medicine (PHM) continues to rapidly evolve, so too does the landscape of PHM fellowships. New programs are opening at a torrid pace to accommodate the increasing demand of residents looking to enter the field with new subspecialty accreditation. Most first-year PHM fellows in established programs enter with a clear precedent to follow, set forth by fellows who have come before them. For PHM fellows in new programs, however, there is often no beaten path to follow.
Entering fellowship as a first-year PHM fellow in a new program and blazing one’s own trail can be intriguing and exhilarating given the unique opportunities available. However, the potential challenges for both fellows and program directors during this transition cannot be understated. The role of new PHM fellows within the institutional framework may initially be unclear to others, which can lead to ambiguous expectations and disruptions to normal workflows. Furthermore, assessing and evaluating new fellows may prove difficult as a result of these unclear expectations and general uncertainties. Using the growth mindset can help both PHM fellows and program directors take a deliberate approach to the challenges and uncertainty that may accompany the creation of a new fellowship program.
One of the challenges new PHM fellows may encounter lies within the structure of the care team. Resident and medical student learners may express consternation that the new fellow role may limit their own autonomy. In addition, finding the right balance of autonomy and supervision between the attending-fellow dyad may prove to be difficult. However, using the growth mindset may allow fellows to see the inherent benefits of this new role.
Fellows should seize the opportunity to discuss the nuances and differing approaches to difficult clinical questions, managing a team and interpersonal dynamics, and balancing clinical and nonclinical responsibilities with an experienced supervising clinician; issues that are often less pressing as a resident. The fellow role also affords the opportunity to more carefully observe different clinical styles of practice to subsequently shape one’s own preferred style.
Finally, fellows should employ a growth mindset to optimize clinical time by discussing expectations with involved stakeholders prior to rotations and explicitly identifying goals for feedback and improvement. Program directors can also help stakeholders including faculty, residency programs, medical schools, and other health care professionals on the clinical teams prepare for this transition by providing expectations for the fellow role and by soliciting questions and feedback before and after fellows begin.
One of the key tenets of the growth mindset is actively seeking out constructive feedback and learning from failures to grow and improve. This can be a particularly useful practice for fellows during the course of their scholarly pursuits in clinical research, quality improvement, and medical education. From initial stages of idea development through the final steps of manuscript submission and peer review, fellows will undoubtedly navigate a plethora of challenges and setbacks along the way. Program directors and other core faculty members can promote a growth mindset culture by honestly discussing their own challenges and failures in career endeavors in addition to giving thoughtful constructive feedback.
Fellows should routinely practice explicitly identifying knowledge and skills gaps that represent areas for potential improvement. But perhaps most importantly, fellows must strive to see all feedback and perceived failures not as personal affronts or as commentaries on personal abilities, but rather as opportunities to strengthen their scholarly products and gain valuable experience for future endeavors.
Not all learners will come equipped with a growth mindset. So, what can fellows and program directors in new programs do to develop this practice and mitigate some of the inevitable uncertainty? To begin, program directors should think about how to create cultures of growth and development as the fixed and growth mindsets are not just limited to individuals.3 Program directors can strive to augment this process by committing to solicit feedback for themselves and acknowledging their own vulnerabilities and perceived weaknesses.
Fellows must have early, honest discussions with program directors and other stakeholders about expectations and goals. Program directors should consider creating lists of “must meet” individuals within the institution that can help fellows begin to carve out their roles in the clinical, educational, and research realms. Deliberately crafting a mentorship team that will encourage a commitment to growth and improvement is critical. Seeking out growth feedback, particularly in areas that prove challenging, should become common practice for fellows from the onset.
Most importantly, fellows should reframe uncertainty as opportunity for growth and progression. Seeing oneself as a work in progress provides a new perspective that prioritizes learning and emphasizes improvement potential.
Embodying this approach requires patience and practice. Being part of a newly created fellowship represents an opportunity to learn from personal challenges rather than leaning on the precedent set by previous fellows. And although fellows will often face uncertainty as a part of the novelty within a new program, they can ultimately succeed by practicing the principles of Dweck’s Growth Mindset: embracing challenges and failure as learning experiences, seeking out feedback, and pursuing the opportunities among ambiguity.
Dr. Herchline is a pediatric hospitalist at Cincinnati Children’s Hospital Medical Center and recent fellow graduate of the Children’s Hospital of Philadelphia. During fellowship, he completed a master’s degree in medical education at the University of Pennsylvania. His academic interests include graduate medical education, interprofessional collaboration and teamwork, and quality improvement.
References
1. Klein J et al. A growth mindset approach to preparing trainees for medical error. BMJ Qual Saf. 2017 Sep;26(9):771-4. doi: 10.1136/bmjqs-2016-006416.
2. Dweck C. Mindset: The new psychology of success. New York: Ballantine Books; 2006.
3. Murphy MC, Dweck CS. A culture of genius: How an organization’s lay theory shapes people’s cognition, affect, and behavior. Pers Soc Psychol Bull. 2010 Mar;36(3):283-96. doi: 10.1177/0146167209347380.
Growth mindset is a well-established phenomenon in childhood education that is now starting to appear in health care education literature.1 This concept emphasizes the capacity of individuals to change and grow through experience and that an individual’s basic qualities can be cultivated through hard work, open-mindedness, and help from others.2
Growth mindset opposes the concept of fixed mindset, which implies intelligence or other personal traits are set in stone, unable to be fundamentally changed.2 Individuals with fixed mindsets are less adept at coping with perceived failures and critical feedback because they view these as attacks on their own abilities.2 This oftentimes leads these individuals to avoid potential challenges and feedback because of fear of being exposed as incompetent or feeling inadequate. Conversely, individuals with a growth mindset embrace challenges and failures as learning opportunities and identify feedback as a critical element of growth.2 These individuals maintain a sense of resilience in the face of adversity and strive to become lifelong learners.
As the field of pediatric hospital medicine (PHM) continues to rapidly evolve, so too does the landscape of PHM fellowships. New programs are opening at a torrid pace to accommodate the increasing demand of residents looking to enter the field with new subspecialty accreditation. Most first-year PHM fellows in established programs enter with a clear precedent to follow, set forth by fellows who have come before them. For PHM fellows in new programs, however, there is often no beaten path to follow.
Entering fellowship as a first-year PHM fellow in a new program and blazing one’s own trail can be intriguing and exhilarating given the unique opportunities available. However, the potential challenges for both fellows and program directors during this transition cannot be understated. The role of new PHM fellows within the institutional framework may initially be unclear to others, which can lead to ambiguous expectations and disruptions to normal workflows. Furthermore, assessing and evaluating new fellows may prove difficult as a result of these unclear expectations and general uncertainties. Using the growth mindset can help both PHM fellows and program directors take a deliberate approach to the challenges and uncertainty that may accompany the creation of a new fellowship program.
One of the challenges new PHM fellows may encounter lies within the structure of the care team. Resident and medical student learners may express consternation that the new fellow role may limit their own autonomy. In addition, finding the right balance of autonomy and supervision between the attending-fellow dyad may prove to be difficult. However, using the growth mindset may allow fellows to see the inherent benefits of this new role.
Fellows should seize the opportunity to discuss the nuances and differing approaches to difficult clinical questions, managing a team and interpersonal dynamics, and balancing clinical and nonclinical responsibilities with an experienced supervising clinician; issues that are often less pressing as a resident. The fellow role also affords the opportunity to more carefully observe different clinical styles of practice to subsequently shape one’s own preferred style.
Finally, fellows should employ a growth mindset to optimize clinical time by discussing expectations with involved stakeholders prior to rotations and explicitly identifying goals for feedback and improvement. Program directors can also help stakeholders including faculty, residency programs, medical schools, and other health care professionals on the clinical teams prepare for this transition by providing expectations for the fellow role and by soliciting questions and feedback before and after fellows begin.
One of the key tenets of the growth mindset is actively seeking out constructive feedback and learning from failures to grow and improve. This can be a particularly useful practice for fellows during the course of their scholarly pursuits in clinical research, quality improvement, and medical education. From initial stages of idea development through the final steps of manuscript submission and peer review, fellows will undoubtedly navigate a plethora of challenges and setbacks along the way. Program directors and other core faculty members can promote a growth mindset culture by honestly discussing their own challenges and failures in career endeavors in addition to giving thoughtful constructive feedback.
Fellows should routinely practice explicitly identifying knowledge and skills gaps that represent areas for potential improvement. But perhaps most importantly, fellows must strive to see all feedback and perceived failures not as personal affronts or as commentaries on personal abilities, but rather as opportunities to strengthen their scholarly products and gain valuable experience for future endeavors.
Not all learners will come equipped with a growth mindset. So, what can fellows and program directors in new programs do to develop this practice and mitigate some of the inevitable uncertainty? To begin, program directors should think about how to create cultures of growth and development as the fixed and growth mindsets are not just limited to individuals.3 Program directors can strive to augment this process by committing to solicit feedback for themselves and acknowledging their own vulnerabilities and perceived weaknesses.
Fellows must have early, honest discussions with program directors and other stakeholders about expectations and goals. Program directors should consider creating lists of “must meet” individuals within the institution that can help fellows begin to carve out their roles in the clinical, educational, and research realms. Deliberately crafting a mentorship team that will encourage a commitment to growth and improvement is critical. Seeking out growth feedback, particularly in areas that prove challenging, should become common practice for fellows from the onset.
Most importantly, fellows should reframe uncertainty as opportunity for growth and progression. Seeing oneself as a work in progress provides a new perspective that prioritizes learning and emphasizes improvement potential.
Embodying this approach requires patience and practice. Being part of a newly created fellowship represents an opportunity to learn from personal challenges rather than leaning on the precedent set by previous fellows. And although fellows will often face uncertainty as a part of the novelty within a new program, they can ultimately succeed by practicing the principles of Dweck’s Growth Mindset: embracing challenges and failure as learning experiences, seeking out feedback, and pursuing the opportunities among ambiguity.
Dr. Herchline is a pediatric hospitalist at Cincinnati Children’s Hospital Medical Center and recent fellow graduate of the Children’s Hospital of Philadelphia. During fellowship, he completed a master’s degree in medical education at the University of Pennsylvania. His academic interests include graduate medical education, interprofessional collaboration and teamwork, and quality improvement.
References
1. Klein J et al. A growth mindset approach to preparing trainees for medical error. BMJ Qual Saf. 2017 Sep;26(9):771-4. doi: 10.1136/bmjqs-2016-006416.
2. Dweck C. Mindset: The new psychology of success. New York: Ballantine Books; 2006.
3. Murphy MC, Dweck CS. A culture of genius: How an organization’s lay theory shapes people’s cognition, affect, and behavior. Pers Soc Psychol Bull. 2010 Mar;36(3):283-96. doi: 10.1177/0146167209347380.
Mean leadership
The differences between the mean and median of leadership data
Let me apologize for misleading all of you; this is not an article about malignant physician leaders; instead, it goes over the numbers and trends uncovered by the 2020 State of Hospital Medicine report (SoHM).1 The hospital medicine leader ends up doing many tasks like planning, growth, collaboration, finance, recruiting, scheduling, onboarding, coaching, and most near and dear to our hearts, putting out the fires and conflict resolution.
Ratio of leadership FTE to physician hospitalists FTE
If my pun has already put you off, you can avoid reading the rest of the piece and go to the 2020 SoHM to look at pages 52 (Table 3.7c), 121 (Table 4.7c), and 166 (Table 5.7c). It has a newly added table (3.7c), and it is phenomenal; it is the ratio of leadership FTE to physician hospitalists FTE. As an avid user of SoHM, I always ended up doing a makeshift calculation to “guesstimate” this number. Now that we have it calculated for us and the ultimate revelation lies in its narrow range across all groups. We might differ in the region, employment type, academics, teaching, or size, but this range is relatively narrow.
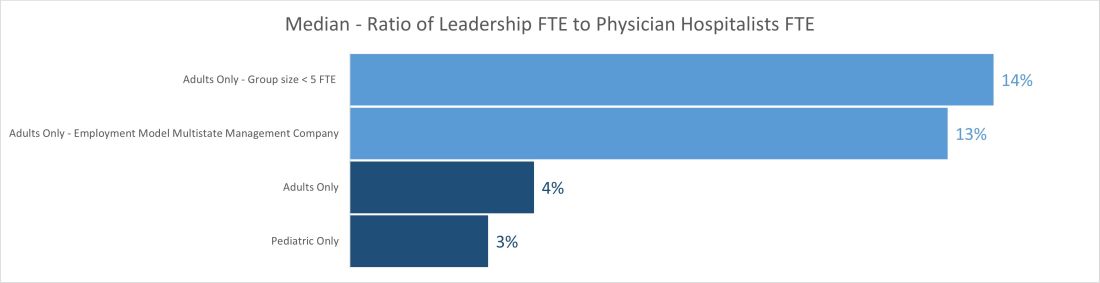
The median ratio of leadership FTE to total FTE lies between 2% and 5% in pediatric groups and between 3% and 6% for most adult groups. The only two outliers are on the adult side, with less than 5 FTE and multistate management companies. The higher median for the less than 5 FTE group size is understandable because of the small number of hospitalist FTEs that the leader’s time must be spread over. Even a small amount of dedicated leadership time will result in a high ratio of leader time to hospitalist clinical time if the group is very small. The multistate management company is probably a result of multiple layers of physician leadership (for example, regional medical directors) and travel-related time adjustments. Still, it raises the question of why the local leadership is not developed to decrease the leadership cost and better access.
Another helpful pattern is the decrease in standard deviation with the increase in group size. The hospital medicine leaders and CEOs of the hospital need to watch this number closely; any extremes on high or low side would be indicators for a deep dive in leadership structure and health.
Total number and total dedicated FTE for all physician leaders
Once we start seeing the differences between the mean and median of leadership data, we can see the median is relatively static while the mean has increased year after year and took a big jump in the 2020 SoHM. The chart below shows trends for the number of individuals in leadership positions (“Total No” and total FTEs allocated to leadership (“Total FTE”) over the last several surveys. The data is heavily skewed toward the right (positive); so, it makes sense to use the median in this case rather than mean. A few factors could explain the right skew of data.
- Large groups of 30 or more hospitalists are increasing, and so is their leadership need.
- There is more recognition of the need for dedicated leadership individuals and FTE.
- The leadership is getting less concentrated among just one or a few leaders.
- Outliers on the high side.
- Lower bounds of 0 or 0.1 FTE.
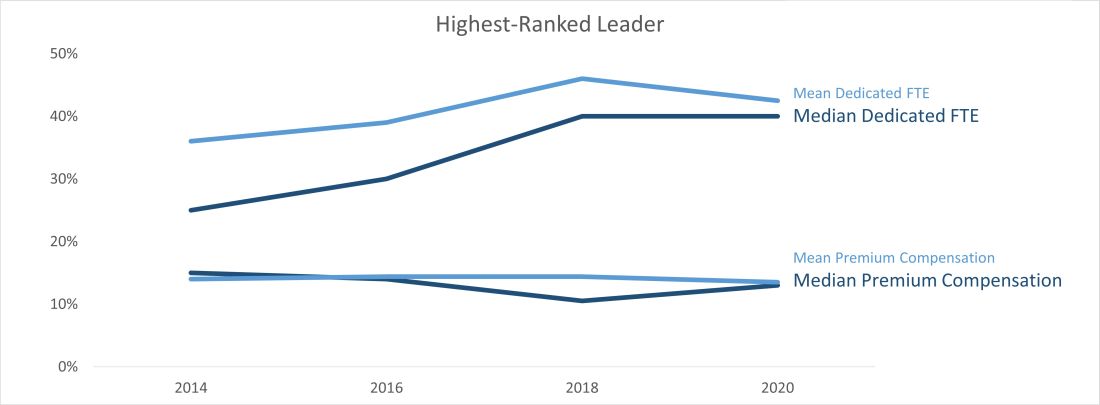
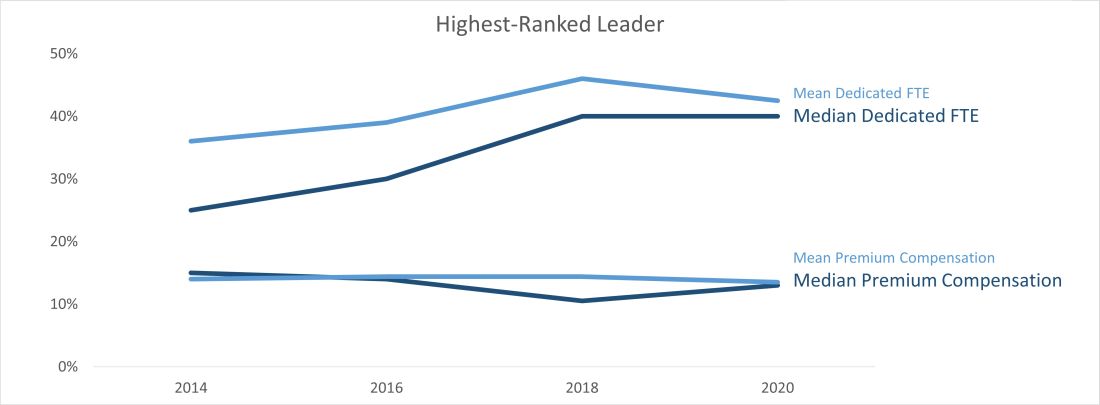
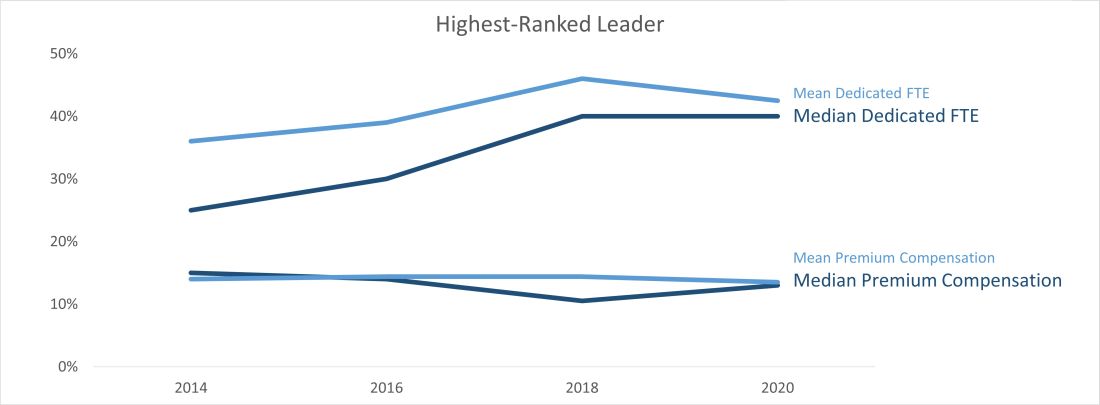
Highest-ranked leader dedicated FTE and premium compensation
Another pleasing trend is an increase in dedicated FTE for the highest-paid leader. Like any skill-set development, leadership requires the investment of deliberate practice, financial acumen, negotiation skills, and increased vulnerability. Time helps way more in developing these skill sets than money. SoHM trends show increase in dedicated FTE for the highest physician leader over the years and static premium compensation.
At last, we can say median leadership is always better than “mean” leadership in skewed data. Pun apart, every group needs leadership, and SoHM offers a nice window to the trends in leadership amongst many practice groups. It is a valuable resource for every group.
Dr. Chadha is chief of the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, practice analysis, and operation of the group. He is finishing his first tenure in the Practice Analysis Committee. He is often found spending a lot more than required time with spreadsheets and graphs.
Reference
1. 2020 State of Hospital Medicine. www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
The differences between the mean and median of leadership data
The differences between the mean and median of leadership data
Let me apologize for misleading all of you; this is not an article about malignant physician leaders; instead, it goes over the numbers and trends uncovered by the 2020 State of Hospital Medicine report (SoHM).1 The hospital medicine leader ends up doing many tasks like planning, growth, collaboration, finance, recruiting, scheduling, onboarding, coaching, and most near and dear to our hearts, putting out the fires and conflict resolution.
Ratio of leadership FTE to physician hospitalists FTE
If my pun has already put you off, you can avoid reading the rest of the piece and go to the 2020 SoHM to look at pages 52 (Table 3.7c), 121 (Table 4.7c), and 166 (Table 5.7c). It has a newly added table (3.7c), and it is phenomenal; it is the ratio of leadership FTE to physician hospitalists FTE. As an avid user of SoHM, I always ended up doing a makeshift calculation to “guesstimate” this number. Now that we have it calculated for us and the ultimate revelation lies in its narrow range across all groups. We might differ in the region, employment type, academics, teaching, or size, but this range is relatively narrow.
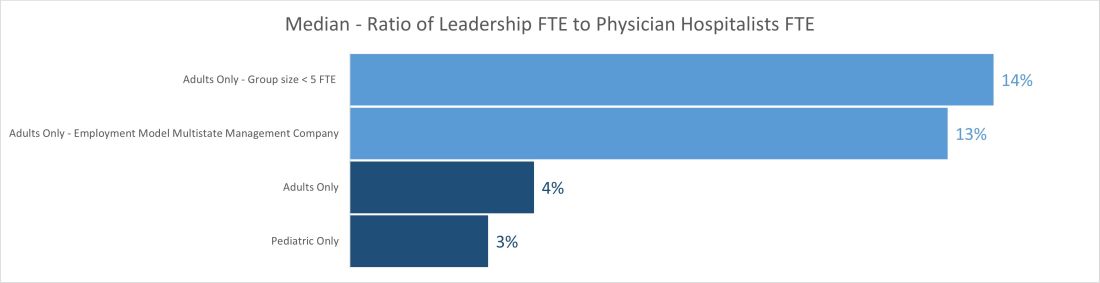
The median ratio of leadership FTE to total FTE lies between 2% and 5% in pediatric groups and between 3% and 6% for most adult groups. The only two outliers are on the adult side, with less than 5 FTE and multistate management companies. The higher median for the less than 5 FTE group size is understandable because of the small number of hospitalist FTEs that the leader’s time must be spread over. Even a small amount of dedicated leadership time will result in a high ratio of leader time to hospitalist clinical time if the group is very small. The multistate management company is probably a result of multiple layers of physician leadership (for example, regional medical directors) and travel-related time adjustments. Still, it raises the question of why the local leadership is not developed to decrease the leadership cost and better access.
Another helpful pattern is the decrease in standard deviation with the increase in group size. The hospital medicine leaders and CEOs of the hospital need to watch this number closely; any extremes on high or low side would be indicators for a deep dive in leadership structure and health.
Total number and total dedicated FTE for all physician leaders
Once we start seeing the differences between the mean and median of leadership data, we can see the median is relatively static while the mean has increased year after year and took a big jump in the 2020 SoHM. The chart below shows trends for the number of individuals in leadership positions (“Total No” and total FTEs allocated to leadership (“Total FTE”) over the last several surveys. The data is heavily skewed toward the right (positive); so, it makes sense to use the median in this case rather than mean. A few factors could explain the right skew of data.
- Large groups of 30 or more hospitalists are increasing, and so is their leadership need.
- There is more recognition of the need for dedicated leadership individuals and FTE.
- The leadership is getting less concentrated among just one or a few leaders.
- Outliers on the high side.
- Lower bounds of 0 or 0.1 FTE.
Highest-ranked leader dedicated FTE and premium compensation
Another pleasing trend is an increase in dedicated FTE for the highest-paid leader. Like any skill-set development, leadership requires the investment of deliberate practice, financial acumen, negotiation skills, and increased vulnerability. Time helps way more in developing these skill sets than money. SoHM trends show increase in dedicated FTE for the highest physician leader over the years and static premium compensation.
At last, we can say median leadership is always better than “mean” leadership in skewed data. Pun apart, every group needs leadership, and SoHM offers a nice window to the trends in leadership amongst many practice groups. It is a valuable resource for every group.
Dr. Chadha is chief of the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, practice analysis, and operation of the group. He is finishing his first tenure in the Practice Analysis Committee. He is often found spending a lot more than required time with spreadsheets and graphs.
Reference
1. 2020 State of Hospital Medicine. www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
Let me apologize for misleading all of you; this is not an article about malignant physician leaders; instead, it goes over the numbers and trends uncovered by the 2020 State of Hospital Medicine report (SoHM).1 The hospital medicine leader ends up doing many tasks like planning, growth, collaboration, finance, recruiting, scheduling, onboarding, coaching, and most near and dear to our hearts, putting out the fires and conflict resolution.
Ratio of leadership FTE to physician hospitalists FTE
If my pun has already put you off, you can avoid reading the rest of the piece and go to the 2020 SoHM to look at pages 52 (Table 3.7c), 121 (Table 4.7c), and 166 (Table 5.7c). It has a newly added table (3.7c), and it is phenomenal; it is the ratio of leadership FTE to physician hospitalists FTE. As an avid user of SoHM, I always ended up doing a makeshift calculation to “guesstimate” this number. Now that we have it calculated for us and the ultimate revelation lies in its narrow range across all groups. We might differ in the region, employment type, academics, teaching, or size, but this range is relatively narrow.
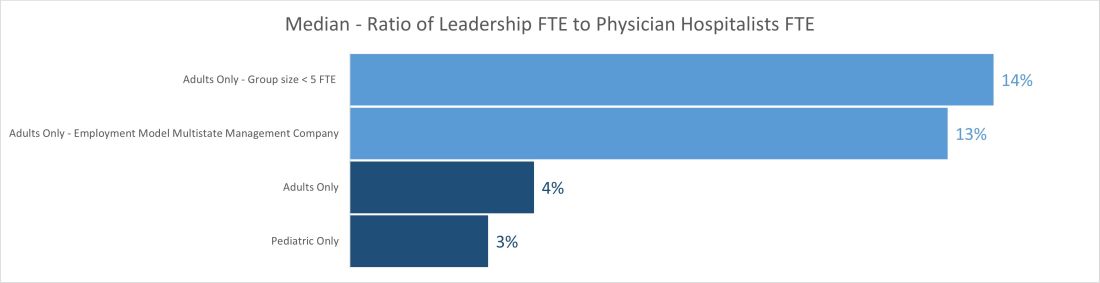
The median ratio of leadership FTE to total FTE lies between 2% and 5% in pediatric groups and between 3% and 6% for most adult groups. The only two outliers are on the adult side, with less than 5 FTE and multistate management companies. The higher median for the less than 5 FTE group size is understandable because of the small number of hospitalist FTEs that the leader’s time must be spread over. Even a small amount of dedicated leadership time will result in a high ratio of leader time to hospitalist clinical time if the group is very small. The multistate management company is probably a result of multiple layers of physician leadership (for example, regional medical directors) and travel-related time adjustments. Still, it raises the question of why the local leadership is not developed to decrease the leadership cost and better access.
Another helpful pattern is the decrease in standard deviation with the increase in group size. The hospital medicine leaders and CEOs of the hospital need to watch this number closely; any extremes on high or low side would be indicators for a deep dive in leadership structure and health.
Total number and total dedicated FTE for all physician leaders
Once we start seeing the differences between the mean and median of leadership data, we can see the median is relatively static while the mean has increased year after year and took a big jump in the 2020 SoHM. The chart below shows trends for the number of individuals in leadership positions (“Total No” and total FTEs allocated to leadership (“Total FTE”) over the last several surveys. The data is heavily skewed toward the right (positive); so, it makes sense to use the median in this case rather than mean. A few factors could explain the right skew of data.
- Large groups of 30 or more hospitalists are increasing, and so is their leadership need.
- There is more recognition of the need for dedicated leadership individuals and FTE.
- The leadership is getting less concentrated among just one or a few leaders.
- Outliers on the high side.
- Lower bounds of 0 or 0.1 FTE.
Highest-ranked leader dedicated FTE and premium compensation
Another pleasing trend is an increase in dedicated FTE for the highest-paid leader. Like any skill-set development, leadership requires the investment of deliberate practice, financial acumen, negotiation skills, and increased vulnerability. Time helps way more in developing these skill sets than money. SoHM trends show increase in dedicated FTE for the highest physician leader over the years and static premium compensation.
At last, we can say median leadership is always better than “mean” leadership in skewed data. Pun apart, every group needs leadership, and SoHM offers a nice window to the trends in leadership amongst many practice groups. It is a valuable resource for every group.
Dr. Chadha is chief of the division of hospital medicine at the University of Kentucky Healthcare, Lexington. He actively leads efforts of recruiting, practice analysis, and operation of the group. He is finishing his first tenure in the Practice Analysis Committee. He is often found spending a lot more than required time with spreadsheets and graphs.
Reference
1. 2020 State of Hospital Medicine. www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/
Should hospitalists use albumin to treat non-SBP infections in patients with cirrhosis?
Caution is advised in patients at risk of pulmonary edema
Case
A 56 year-old male with hypertension, alcohol use disorder, stage II chronic kidney disease, and biopsy-proven cirrhosis presents with fever and chills, pyuria, flank pain, and an acute kidney injury concerning for pyelonephritis. Is there a benefit in treating with albumin in addition to guideline-based antibiotics?
Brief overview of the issue
Albumin is a negatively charged human protein produced by the liver. Albumin comprises 50% of plasma protein and over 75% of plasma oncotic pressure.1 It was first used at Walter Reed Hospital in 1940 and subsequently for burn injuries after the attack on Pearl Harbor in 1941.2
Albumin serves several important physiologic functions including maintaining oncotic pressure, endothelial support, antioxidation, nitrogen oxide scavenging, and buffering and transport of solutes and drugs, including antibiotics. In cirrhosis, albumin is diluted due to sodium and water retention. There is increased redistribution, decreased synthesis by the liver, and impaired albumin molecule binding.3
For patients with liver disease, per the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD), albumin should be administered to prevent post paracentesis circulatory dysfunction after large volume paracentesis, to prevent renal failure and mortality in the setting of spontaneous bacterial peritonitis (SBP), and in the diagnosis and treatment of hepatorenal syndrome (HRS) type I to potentially improve mortality.4,5 Beyond these three guideline-based indications, other uses for albumin for patients with liver disease have been proposed, including treatment of hyponatremia, posttransplant fluid resuscitation, diuretic unresponsive ascites, and long-term management of cirrhosis. There has yet to be strong evidence supporting these additional indications. However, given the known benefits of albumin in patients with SBP, there has been recent research into treatment of non-SBP infections, including urinary tract infections.
Overview of the data
There have been three randomized controlled trials (RCTs) regarding albumin administration for the treatment of non-SBP infections for hospitalized patients with cirrhosis. All three trials randomized patients to a treatment arm of albumin and antibiotics versus a control group of antibiotics alone. The treatment protocol prescribed 20% albumin with 1.5 g/kg on day 1 and 1.0 g/kg on day 3. The most common infections studied were pneumonia and urinary tract infection. These RCTs found that albumin administration was associated with improved renal and/or circulatory function, but not with a reduction in mortality.

First, there was a single center RCT by Guevara et al. in 2012 of 110 patients with cirrhosis and infection based on SIRS criteria.6 The primary outcome was 90-day survival with secondary outcomes of renal failure development, renal function at days 3,7 and 14, and circulatory function measured by plasma renin, aldosterone, and norepinephrine. Renal function and circulatory function improved in the albumin group, but not mortality. In a multivariable regression analysis, albumin was statistically predictive of survival (hazard ratio of 0.294).
Second, there was a multicenter RCT by Thévenot et al. in 2015 of 193 patients.7 The primary outcome was 90-day renal failure and the secondary outcome was 90-day survival. Renal failure was chosen as the primary endpoint because of its association with survival in this patient population. The treatment group had delayed onset of renal failure, but no difference in the development of 90-day renal failure or 90-day mortality rate. Notably, eight patients (8.3%) in the albumin group developed pulmonary edema with two deaths. This led the oversight committee to prematurely terminate the study.
Third and most recently, there was a multicenter RCT by Fernández et al. in 2019 of 118 patients.8 The primary outcome was in-hospital mortality, with secondary outcomes of circulatory dysfunction measured by plasma renin concentration, systemic inflammation measured by plasma IL-6 and biomarkers, complications including acute-on-chronic liver failure (ACLF) and nosocomial bacterial infections, and 90-day mortality. Between the albumin and control group, there were no differences in in-hospital mortality (13.1% vs. 10.5%, P > .66), inflammation, circulatory dysfunction, or liver severity. However, a significantly higher proportion of patients in the albumin group had resolution of their ACLF (82.3% vs. 33.3%, P = .003) and a lower proportion developed nosocomial infections (6.6% vs. 24.6%, P = .007). A major weakness of this study was that patients in the albumin group had a higher combined rate of ACLF and kidney dysfunction (44.3% vs. 24.6%, P = .02).
Beyond these three randomized controlled trials, there was a study on the long-term administration of albumin for patients with cirrhosis and ascites. Patients who received twice weekly albumin infusions had a lower 2-year mortality rate and a reduction in the incidence of both SBP and non-SBP infections.9 Another long-term study of albumin administration found similar results with greater 18-month survival and fewer non-SBP infections.10 A trial looking at inflammation in patients without bacterial infections and in biobanked samples from cirrhotic patients with bacterial infections found that treatment with albumin reduced systemic inflammation.11
In summary, the three RCTs looked at comparable patients with cirrhosis and a non-SBP infection and all underwent similar treatment protocols with 20% albumin dosed at 1.5 g/kg on day 1 and 1.0 g/kg on day 3. All studies evaluated mortality in either the primary or secondary outcome, and none found significant differences in mortality between treatment and control groups. Each study also evaluated and found improvement in renal and/or circulatory function. Fernández et al. also found increased resolution of ACLF, fewer nosocomial infections, and reduction in some inflammatory markers. However, all studies had relatively small sample sizes that were underpowered to detect mortality differences. Furthermore, randomization did not lead to well-matched groups, with the treatment group patients in the Fernández study having higher rates of ACLF and kidney dysfunction.
The data suggest that albumin may be beneficial in improving renal and circulatory function. In select patients with ACLF and elevated serum creatinine, albumin treatment may be considered. There has been discussion about the use of albumin preferentially in patients with subdiaphragmatic bacterial infections, most related to increased risk of renal failure such as biliary and urinary tract infections.12 The authors of these studies also note that albumin may be more beneficial in patients with higher baseline creatinine. Caution is warranted for patients with impaired cardiac function or poor respiratory status given the possibility of pulmonary edema. Finally, the high cost of albumin in many medical centers is a major limitation of this treatment approach.
Application of data to our patient
Our patient has cirrhosis and is acutely presenting with pyelonephritis and acute kidney injury. He has no baseline pulmonary disease or oxygen requirement. His recent transthoracic echocardiogram is reviewed and he has no evidence of cardiac disease.
Because he has an elevated creatinine, an infectious process associated with progressive renal failure, and is not at an elevated baseline risk of developing pulmonary edema, albumin would be reasonable to administer at 1.5 g/kg on day 1 and 1.0 g/kg on day 3 of hospitalization.
Bottom line
In certain patients with cirrhosis and a non-SBP infection, the use of albumin to help improve renal and circulatory function is reasonable. There is no evidence that albumin will improve mortality and caution is warranted for patients at risk for pulmonary edema.
Dr. Rambachan is an academic hospital medicine fellow at the University of California, San Francisco.
References
1. Caironi P and Gattinoni L. The clinical use of albumin: the point of view of a specialist in intensive care. Blood Transfus. 2009;7(4):259-67. doi: 10.2450/2009.0002-09.
2. Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
3. Walayat S et al. Role of albumin in cirrhosis: from a hospitalist’s perspective. J Community Hosp Intern Med Perspect. 2017;7(1):8-14. 2017 Mar 31. doi: 10.1080/20009666.2017.1302704.
4. Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
5. European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [published correction appears in J Hepatol. 2018 Nov;69(5):1207]. J Hepatol. 2018 Aug;69(2):406-60. doi: 10.1016/j.jhep.2018.03.024.
6. Guevara M et al. Albumin for bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. A randomized, controlled study. J Hepatol. 2012 Oct;57(4):759-65. doi: 10.1016/j.jhep.2012.06.013.
7. Thévenot T et al. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol. 2015 Apr;62(4):822-30. doi: 10.1016/j.jhep.2014.11.017.
8. Fernández J et al. Efficacy of albumin treatment for patients with cirrhosis and infections unrelated to spontaneous bacterial peritonitis. Clin Gastroenterol Hepatol. 2020 Apr;18(4):963-73.e14. doi: 10.1016/j.c gh.2019.07.055.
9. Di Pascoli M et al. Long-term administration of human albumin improves survival in patients with cirrhosis and refractory ascites. Liver Int. 2019 Jan;39(1):98-105. doi: 10.1111/liv.13968.
10. Caraceni P et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial [published correction appears in Lancet. 2018 Aug 4;392(10145):386]. Lancet. 2018 June;391(10138):2417-29. doi: 10.1016/S0140-6736(18)30840-7.
11. Fernández J et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology. 2019 July;157(1):149-62. doi: 10.1053/j.gastro.2019.03.021.
12. Fasolato S et al. Renal failure and bacterial infections in patients with cirrhosis: Epidemiology and clinical features. Hepatology. 2007;45(1):223-9. doi: 10.1002/hep.21443.
Key points
- In patients with spontaneous bacterial peritonitis, hepatorenal syndrome, and for large volume paracentesis, albumin improves outcomes and is recommended by guidelines.
- In patients with cirrhosis and a non-SBP infection, there is some evidence that albumin may improve renal and circulatory function.
- Clinicians should be cautious about albumin use in patients at an elevated risk for development of pulmonary edema.
Quiz
Which of the following is not a guideline-recommended use of albumin for patients with cirrhosis?
A. Treatment of type 1 hepatorenal syndrome
B. Treatment of spontaneous bacterial peritonitis
C. To correct plasma albumin < 2.5 g/dL in nontransplant patients
D. Post large-volume paracentesis
The answer is C. Per the EASL and AASLD, A,B, and D are recommended. There is not strong evidence to support administering albumin to correct low plasma albumin.
Additional reading
- Bernardi M et al. Albumin in decompensated cirrhosis: new concepts and perspectives. Gut. 2020 June;69(6):1127-38. doi: 10.1136/gutjnl-2019-318843.
- Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
- Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019 June;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
Caution is advised in patients at risk of pulmonary edema
Caution is advised in patients at risk of pulmonary edema
Case
A 56 year-old male with hypertension, alcohol use disorder, stage II chronic kidney disease, and biopsy-proven cirrhosis presents with fever and chills, pyuria, flank pain, and an acute kidney injury concerning for pyelonephritis. Is there a benefit in treating with albumin in addition to guideline-based antibiotics?
Brief overview of the issue
Albumin is a negatively charged human protein produced by the liver. Albumin comprises 50% of plasma protein and over 75% of plasma oncotic pressure.1 It was first used at Walter Reed Hospital in 1940 and subsequently for burn injuries after the attack on Pearl Harbor in 1941.2
Albumin serves several important physiologic functions including maintaining oncotic pressure, endothelial support, antioxidation, nitrogen oxide scavenging, and buffering and transport of solutes and drugs, including antibiotics. In cirrhosis, albumin is diluted due to sodium and water retention. There is increased redistribution, decreased synthesis by the liver, and impaired albumin molecule binding.3
For patients with liver disease, per the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD), albumin should be administered to prevent post paracentesis circulatory dysfunction after large volume paracentesis, to prevent renal failure and mortality in the setting of spontaneous bacterial peritonitis (SBP), and in the diagnosis and treatment of hepatorenal syndrome (HRS) type I to potentially improve mortality.4,5 Beyond these three guideline-based indications, other uses for albumin for patients with liver disease have been proposed, including treatment of hyponatremia, posttransplant fluid resuscitation, diuretic unresponsive ascites, and long-term management of cirrhosis. There has yet to be strong evidence supporting these additional indications. However, given the known benefits of albumin in patients with SBP, there has been recent research into treatment of non-SBP infections, including urinary tract infections.
Overview of the data
There have been three randomized controlled trials (RCTs) regarding albumin administration for the treatment of non-SBP infections for hospitalized patients with cirrhosis. All three trials randomized patients to a treatment arm of albumin and antibiotics versus a control group of antibiotics alone. The treatment protocol prescribed 20% albumin with 1.5 g/kg on day 1 and 1.0 g/kg on day 3. The most common infections studied were pneumonia and urinary tract infection. These RCTs found that albumin administration was associated with improved renal and/or circulatory function, but not with a reduction in mortality.

First, there was a single center RCT by Guevara et al. in 2012 of 110 patients with cirrhosis and infection based on SIRS criteria.6 The primary outcome was 90-day survival with secondary outcomes of renal failure development, renal function at days 3,7 and 14, and circulatory function measured by plasma renin, aldosterone, and norepinephrine. Renal function and circulatory function improved in the albumin group, but not mortality. In a multivariable regression analysis, albumin was statistically predictive of survival (hazard ratio of 0.294).
Second, there was a multicenter RCT by Thévenot et al. in 2015 of 193 patients.7 The primary outcome was 90-day renal failure and the secondary outcome was 90-day survival. Renal failure was chosen as the primary endpoint because of its association with survival in this patient population. The treatment group had delayed onset of renal failure, but no difference in the development of 90-day renal failure or 90-day mortality rate. Notably, eight patients (8.3%) in the albumin group developed pulmonary edema with two deaths. This led the oversight committee to prematurely terminate the study.
Third and most recently, there was a multicenter RCT by Fernández et al. in 2019 of 118 patients.8 The primary outcome was in-hospital mortality, with secondary outcomes of circulatory dysfunction measured by plasma renin concentration, systemic inflammation measured by plasma IL-6 and biomarkers, complications including acute-on-chronic liver failure (ACLF) and nosocomial bacterial infections, and 90-day mortality. Between the albumin and control group, there were no differences in in-hospital mortality (13.1% vs. 10.5%, P > .66), inflammation, circulatory dysfunction, or liver severity. However, a significantly higher proportion of patients in the albumin group had resolution of their ACLF (82.3% vs. 33.3%, P = .003) and a lower proportion developed nosocomial infections (6.6% vs. 24.6%, P = .007). A major weakness of this study was that patients in the albumin group had a higher combined rate of ACLF and kidney dysfunction (44.3% vs. 24.6%, P = .02).
Beyond these three randomized controlled trials, there was a study on the long-term administration of albumin for patients with cirrhosis and ascites. Patients who received twice weekly albumin infusions had a lower 2-year mortality rate and a reduction in the incidence of both SBP and non-SBP infections.9 Another long-term study of albumin administration found similar results with greater 18-month survival and fewer non-SBP infections.10 A trial looking at inflammation in patients without bacterial infections and in biobanked samples from cirrhotic patients with bacterial infections found that treatment with albumin reduced systemic inflammation.11
In summary, the three RCTs looked at comparable patients with cirrhosis and a non-SBP infection and all underwent similar treatment protocols with 20% albumin dosed at 1.5 g/kg on day 1 and 1.0 g/kg on day 3. All studies evaluated mortality in either the primary or secondary outcome, and none found significant differences in mortality between treatment and control groups. Each study also evaluated and found improvement in renal and/or circulatory function. Fernández et al. also found increased resolution of ACLF, fewer nosocomial infections, and reduction in some inflammatory markers. However, all studies had relatively small sample sizes that were underpowered to detect mortality differences. Furthermore, randomization did not lead to well-matched groups, with the treatment group patients in the Fernández study having higher rates of ACLF and kidney dysfunction.
The data suggest that albumin may be beneficial in improving renal and circulatory function. In select patients with ACLF and elevated serum creatinine, albumin treatment may be considered. There has been discussion about the use of albumin preferentially in patients with subdiaphragmatic bacterial infections, most related to increased risk of renal failure such as biliary and urinary tract infections.12 The authors of these studies also note that albumin may be more beneficial in patients with higher baseline creatinine. Caution is warranted for patients with impaired cardiac function or poor respiratory status given the possibility of pulmonary edema. Finally, the high cost of albumin in many medical centers is a major limitation of this treatment approach.
Application of data to our patient
Our patient has cirrhosis and is acutely presenting with pyelonephritis and acute kidney injury. He has no baseline pulmonary disease or oxygen requirement. His recent transthoracic echocardiogram is reviewed and he has no evidence of cardiac disease.
Because he has an elevated creatinine, an infectious process associated with progressive renal failure, and is not at an elevated baseline risk of developing pulmonary edema, albumin would be reasonable to administer at 1.5 g/kg on day 1 and 1.0 g/kg on day 3 of hospitalization.
Bottom line
In certain patients with cirrhosis and a non-SBP infection, the use of albumin to help improve renal and circulatory function is reasonable. There is no evidence that albumin will improve mortality and caution is warranted for patients at risk for pulmonary edema.
Dr. Rambachan is an academic hospital medicine fellow at the University of California, San Francisco.
References
1. Caironi P and Gattinoni L. The clinical use of albumin: the point of view of a specialist in intensive care. Blood Transfus. 2009;7(4):259-67. doi: 10.2450/2009.0002-09.
2. Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
3. Walayat S et al. Role of albumin in cirrhosis: from a hospitalist’s perspective. J Community Hosp Intern Med Perspect. 2017;7(1):8-14. 2017 Mar 31. doi: 10.1080/20009666.2017.1302704.
4. Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
5. European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [published correction appears in J Hepatol. 2018 Nov;69(5):1207]. J Hepatol. 2018 Aug;69(2):406-60. doi: 10.1016/j.jhep.2018.03.024.
6. Guevara M et al. Albumin for bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. A randomized, controlled study. J Hepatol. 2012 Oct;57(4):759-65. doi: 10.1016/j.jhep.2012.06.013.
7. Thévenot T et al. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol. 2015 Apr;62(4):822-30. doi: 10.1016/j.jhep.2014.11.017.
8. Fernández J et al. Efficacy of albumin treatment for patients with cirrhosis and infections unrelated to spontaneous bacterial peritonitis. Clin Gastroenterol Hepatol. 2020 Apr;18(4):963-73.e14. doi: 10.1016/j.c gh.2019.07.055.
9. Di Pascoli M et al. Long-term administration of human albumin improves survival in patients with cirrhosis and refractory ascites. Liver Int. 2019 Jan;39(1):98-105. doi: 10.1111/liv.13968.
10. Caraceni P et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial [published correction appears in Lancet. 2018 Aug 4;392(10145):386]. Lancet. 2018 June;391(10138):2417-29. doi: 10.1016/S0140-6736(18)30840-7.
11. Fernández J et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology. 2019 July;157(1):149-62. doi: 10.1053/j.gastro.2019.03.021.
12. Fasolato S et al. Renal failure and bacterial infections in patients with cirrhosis: Epidemiology and clinical features. Hepatology. 2007;45(1):223-9. doi: 10.1002/hep.21443.
Key points
- In patients with spontaneous bacterial peritonitis, hepatorenal syndrome, and for large volume paracentesis, albumin improves outcomes and is recommended by guidelines.
- In patients with cirrhosis and a non-SBP infection, there is some evidence that albumin may improve renal and circulatory function.
- Clinicians should be cautious about albumin use in patients at an elevated risk for development of pulmonary edema.
Quiz
Which of the following is not a guideline-recommended use of albumin for patients with cirrhosis?
A. Treatment of type 1 hepatorenal syndrome
B. Treatment of spontaneous bacterial peritonitis
C. To correct plasma albumin < 2.5 g/dL in nontransplant patients
D. Post large-volume paracentesis
The answer is C. Per the EASL and AASLD, A,B, and D are recommended. There is not strong evidence to support administering albumin to correct low plasma albumin.
Additional reading
- Bernardi M et al. Albumin in decompensated cirrhosis: new concepts and perspectives. Gut. 2020 June;69(6):1127-38. doi: 10.1136/gutjnl-2019-318843.
- Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
- Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019 June;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
Case
A 56 year-old male with hypertension, alcohol use disorder, stage II chronic kidney disease, and biopsy-proven cirrhosis presents with fever and chills, pyuria, flank pain, and an acute kidney injury concerning for pyelonephritis. Is there a benefit in treating with albumin in addition to guideline-based antibiotics?
Brief overview of the issue
Albumin is a negatively charged human protein produced by the liver. Albumin comprises 50% of plasma protein and over 75% of plasma oncotic pressure.1 It was first used at Walter Reed Hospital in 1940 and subsequently for burn injuries after the attack on Pearl Harbor in 1941.2
Albumin serves several important physiologic functions including maintaining oncotic pressure, endothelial support, antioxidation, nitrogen oxide scavenging, and buffering and transport of solutes and drugs, including antibiotics. In cirrhosis, albumin is diluted due to sodium and water retention. There is increased redistribution, decreased synthesis by the liver, and impaired albumin molecule binding.3
For patients with liver disease, per the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD), albumin should be administered to prevent post paracentesis circulatory dysfunction after large volume paracentesis, to prevent renal failure and mortality in the setting of spontaneous bacterial peritonitis (SBP), and in the diagnosis and treatment of hepatorenal syndrome (HRS) type I to potentially improve mortality.4,5 Beyond these three guideline-based indications, other uses for albumin for patients with liver disease have been proposed, including treatment of hyponatremia, posttransplant fluid resuscitation, diuretic unresponsive ascites, and long-term management of cirrhosis. There has yet to be strong evidence supporting these additional indications. However, given the known benefits of albumin in patients with SBP, there has been recent research into treatment of non-SBP infections, including urinary tract infections.
Overview of the data
There have been three randomized controlled trials (RCTs) regarding albumin administration for the treatment of non-SBP infections for hospitalized patients with cirrhosis. All three trials randomized patients to a treatment arm of albumin and antibiotics versus a control group of antibiotics alone. The treatment protocol prescribed 20% albumin with 1.5 g/kg on day 1 and 1.0 g/kg on day 3. The most common infections studied were pneumonia and urinary tract infection. These RCTs found that albumin administration was associated with improved renal and/or circulatory function, but not with a reduction in mortality.

First, there was a single center RCT by Guevara et al. in 2012 of 110 patients with cirrhosis and infection based on SIRS criteria.6 The primary outcome was 90-day survival with secondary outcomes of renal failure development, renal function at days 3,7 and 14, and circulatory function measured by plasma renin, aldosterone, and norepinephrine. Renal function and circulatory function improved in the albumin group, but not mortality. In a multivariable regression analysis, albumin was statistically predictive of survival (hazard ratio of 0.294).
Second, there was a multicenter RCT by Thévenot et al. in 2015 of 193 patients.7 The primary outcome was 90-day renal failure and the secondary outcome was 90-day survival. Renal failure was chosen as the primary endpoint because of its association with survival in this patient population. The treatment group had delayed onset of renal failure, but no difference in the development of 90-day renal failure or 90-day mortality rate. Notably, eight patients (8.3%) in the albumin group developed pulmonary edema with two deaths. This led the oversight committee to prematurely terminate the study.
Third and most recently, there was a multicenter RCT by Fernández et al. in 2019 of 118 patients.8 The primary outcome was in-hospital mortality, with secondary outcomes of circulatory dysfunction measured by plasma renin concentration, systemic inflammation measured by plasma IL-6 and biomarkers, complications including acute-on-chronic liver failure (ACLF) and nosocomial bacterial infections, and 90-day mortality. Between the albumin and control group, there were no differences in in-hospital mortality (13.1% vs. 10.5%, P > .66), inflammation, circulatory dysfunction, or liver severity. However, a significantly higher proportion of patients in the albumin group had resolution of their ACLF (82.3% vs. 33.3%, P = .003) and a lower proportion developed nosocomial infections (6.6% vs. 24.6%, P = .007). A major weakness of this study was that patients in the albumin group had a higher combined rate of ACLF and kidney dysfunction (44.3% vs. 24.6%, P = .02).
Beyond these three randomized controlled trials, there was a study on the long-term administration of albumin for patients with cirrhosis and ascites. Patients who received twice weekly albumin infusions had a lower 2-year mortality rate and a reduction in the incidence of both SBP and non-SBP infections.9 Another long-term study of albumin administration found similar results with greater 18-month survival and fewer non-SBP infections.10 A trial looking at inflammation in patients without bacterial infections and in biobanked samples from cirrhotic patients with bacterial infections found that treatment with albumin reduced systemic inflammation.11
In summary, the three RCTs looked at comparable patients with cirrhosis and a non-SBP infection and all underwent similar treatment protocols with 20% albumin dosed at 1.5 g/kg on day 1 and 1.0 g/kg on day 3. All studies evaluated mortality in either the primary or secondary outcome, and none found significant differences in mortality between treatment and control groups. Each study also evaluated and found improvement in renal and/or circulatory function. Fernández et al. also found increased resolution of ACLF, fewer nosocomial infections, and reduction in some inflammatory markers. However, all studies had relatively small sample sizes that were underpowered to detect mortality differences. Furthermore, randomization did not lead to well-matched groups, with the treatment group patients in the Fernández study having higher rates of ACLF and kidney dysfunction.
The data suggest that albumin may be beneficial in improving renal and circulatory function. In select patients with ACLF and elevated serum creatinine, albumin treatment may be considered. There has been discussion about the use of albumin preferentially in patients with subdiaphragmatic bacterial infections, most related to increased risk of renal failure such as biliary and urinary tract infections.12 The authors of these studies also note that albumin may be more beneficial in patients with higher baseline creatinine. Caution is warranted for patients with impaired cardiac function or poor respiratory status given the possibility of pulmonary edema. Finally, the high cost of albumin in many medical centers is a major limitation of this treatment approach.
Application of data to our patient
Our patient has cirrhosis and is acutely presenting with pyelonephritis and acute kidney injury. He has no baseline pulmonary disease or oxygen requirement. His recent transthoracic echocardiogram is reviewed and he has no evidence of cardiac disease.
Because he has an elevated creatinine, an infectious process associated with progressive renal failure, and is not at an elevated baseline risk of developing pulmonary edema, albumin would be reasonable to administer at 1.5 g/kg on day 1 and 1.0 g/kg on day 3 of hospitalization.
Bottom line
In certain patients with cirrhosis and a non-SBP infection, the use of albumin to help improve renal and circulatory function is reasonable. There is no evidence that albumin will improve mortality and caution is warranted for patients at risk for pulmonary edema.
Dr. Rambachan is an academic hospital medicine fellow at the University of California, San Francisco.
References
1. Caironi P and Gattinoni L. The clinical use of albumin: the point of view of a specialist in intensive care. Blood Transfus. 2009;7(4):259-67. doi: 10.2450/2009.0002-09.
2. Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
3. Walayat S et al. Role of albumin in cirrhosis: from a hospitalist’s perspective. J Community Hosp Intern Med Perspect. 2017;7(1):8-14. 2017 Mar 31. doi: 10.1080/20009666.2017.1302704.
4. Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
5. European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [published correction appears in J Hepatol. 2018 Nov;69(5):1207]. J Hepatol. 2018 Aug;69(2):406-60. doi: 10.1016/j.jhep.2018.03.024.
6. Guevara M et al. Albumin for bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. A randomized, controlled study. J Hepatol. 2012 Oct;57(4):759-65. doi: 10.1016/j.jhep.2012.06.013.
7. Thévenot T et al. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol. 2015 Apr;62(4):822-30. doi: 10.1016/j.jhep.2014.11.017.
8. Fernández J et al. Efficacy of albumin treatment for patients with cirrhosis and infections unrelated to spontaneous bacterial peritonitis. Clin Gastroenterol Hepatol. 2020 Apr;18(4):963-73.e14. doi: 10.1016/j.c gh.2019.07.055.
9. Di Pascoli M et al. Long-term administration of human albumin improves survival in patients with cirrhosis and refractory ascites. Liver Int. 2019 Jan;39(1):98-105. doi: 10.1111/liv.13968.
10. Caraceni P et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial [published correction appears in Lancet. 2018 Aug 4;392(10145):386]. Lancet. 2018 June;391(10138):2417-29. doi: 10.1016/S0140-6736(18)30840-7.
11. Fernández J et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology. 2019 July;157(1):149-62. doi: 10.1053/j.gastro.2019.03.021.
12. Fasolato S et al. Renal failure and bacterial infections in patients with cirrhosis: Epidemiology and clinical features. Hepatology. 2007;45(1):223-9. doi: 10.1002/hep.21443.
Key points
- In patients with spontaneous bacterial peritonitis, hepatorenal syndrome, and for large volume paracentesis, albumin improves outcomes and is recommended by guidelines.
- In patients with cirrhosis and a non-SBP infection, there is some evidence that albumin may improve renal and circulatory function.
- Clinicians should be cautious about albumin use in patients at an elevated risk for development of pulmonary edema.
Quiz
Which of the following is not a guideline-recommended use of albumin for patients with cirrhosis?
A. Treatment of type 1 hepatorenal syndrome
B. Treatment of spontaneous bacterial peritonitis
C. To correct plasma albumin < 2.5 g/dL in nontransplant patients
D. Post large-volume paracentesis
The answer is C. Per the EASL and AASLD, A,B, and D are recommended. There is not strong evidence to support administering albumin to correct low plasma albumin.
Additional reading
- Bernardi M et al. Albumin in decompensated cirrhosis: new concepts and perspectives. Gut. 2020 June;69(6):1127-38. doi: 10.1136/gutjnl-2019-318843.
- Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
- Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019 June;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
Embedding diversity, equity, inclusion, and justice in hospital medicine
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 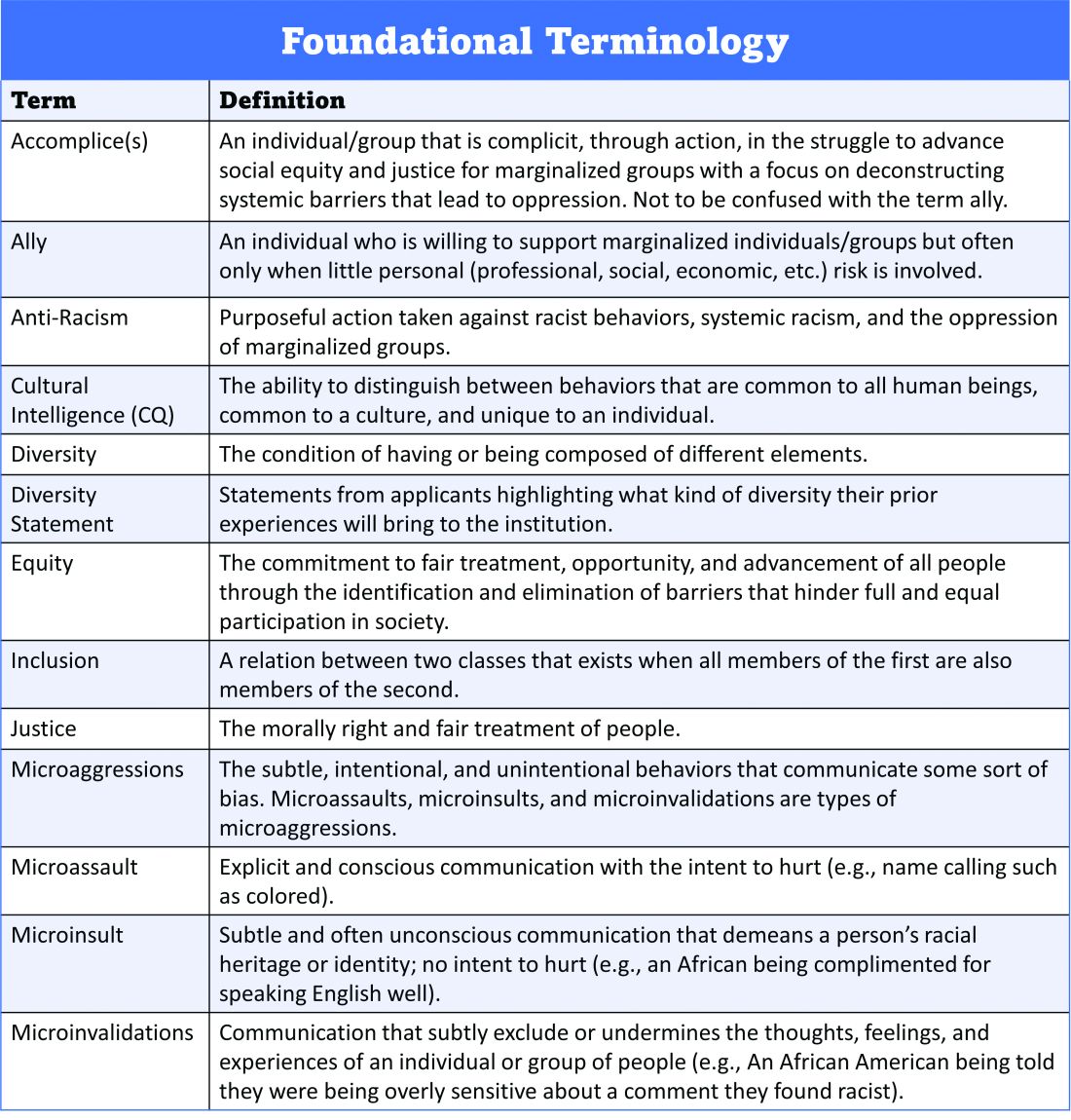
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 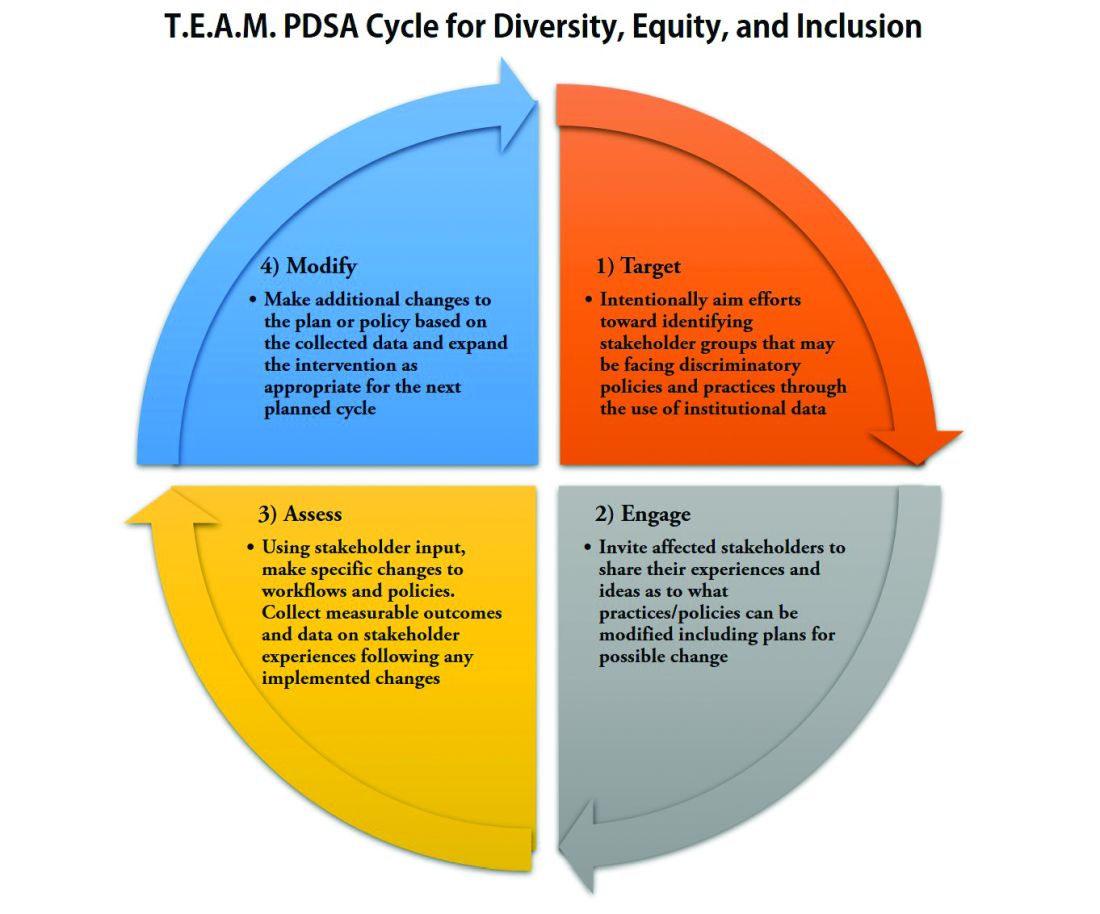
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
A road map for success
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 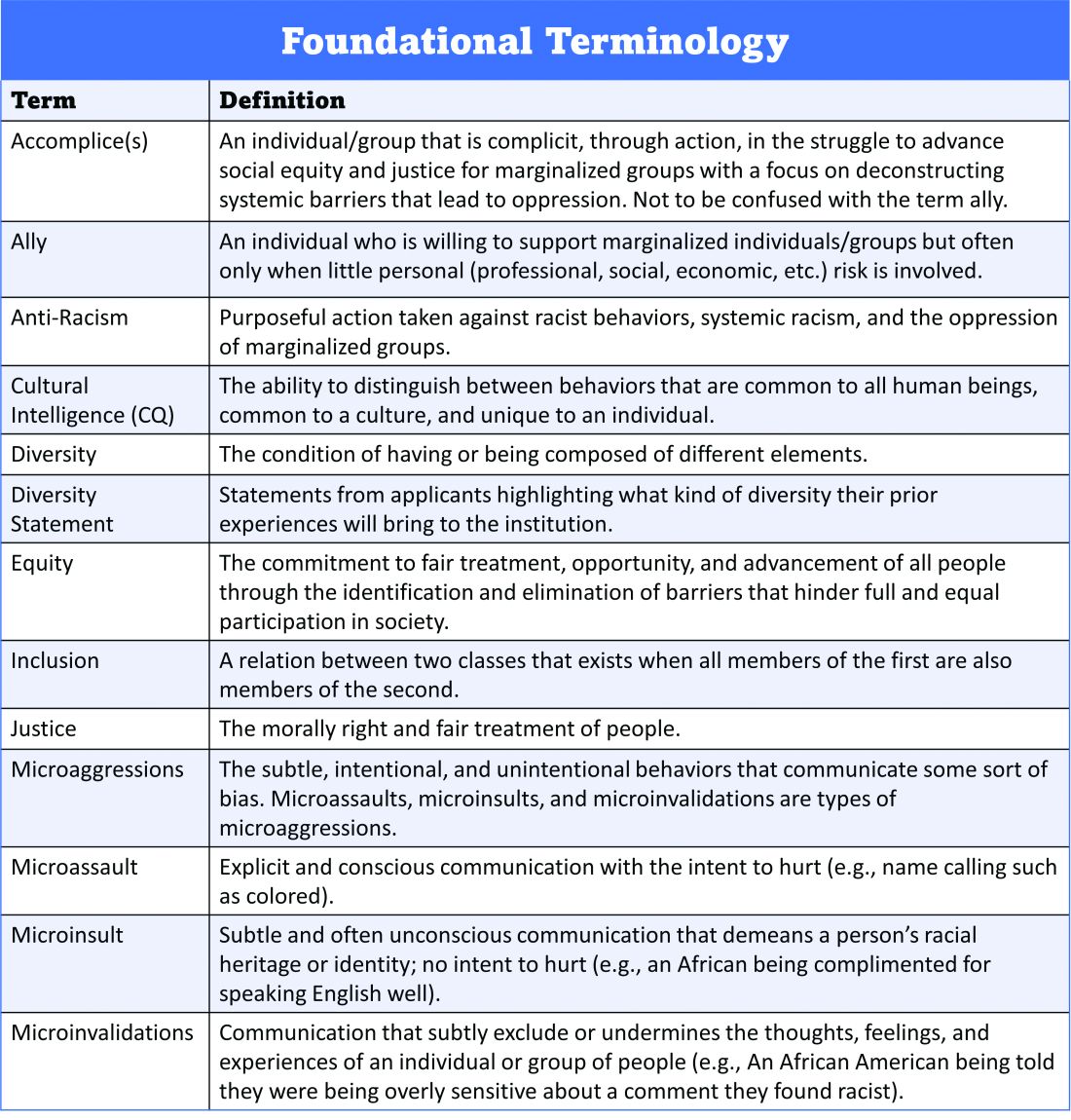
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 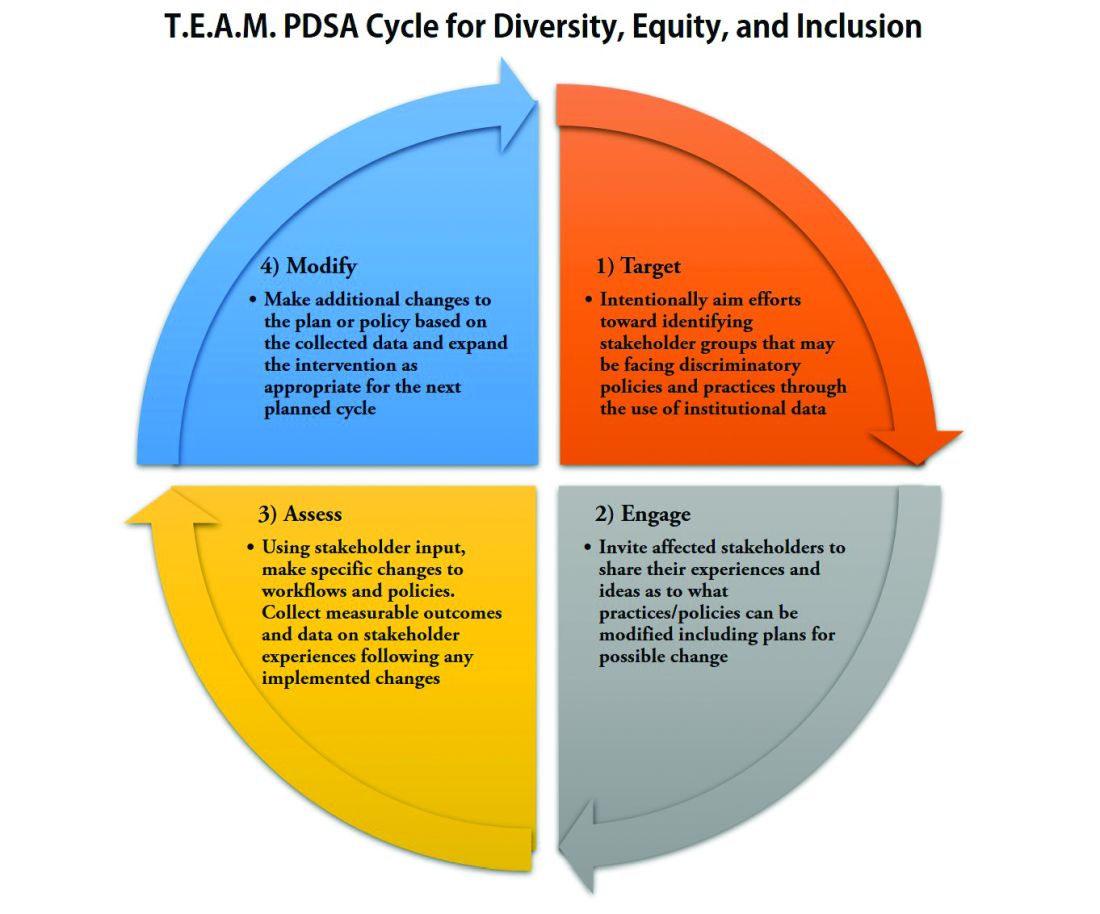
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 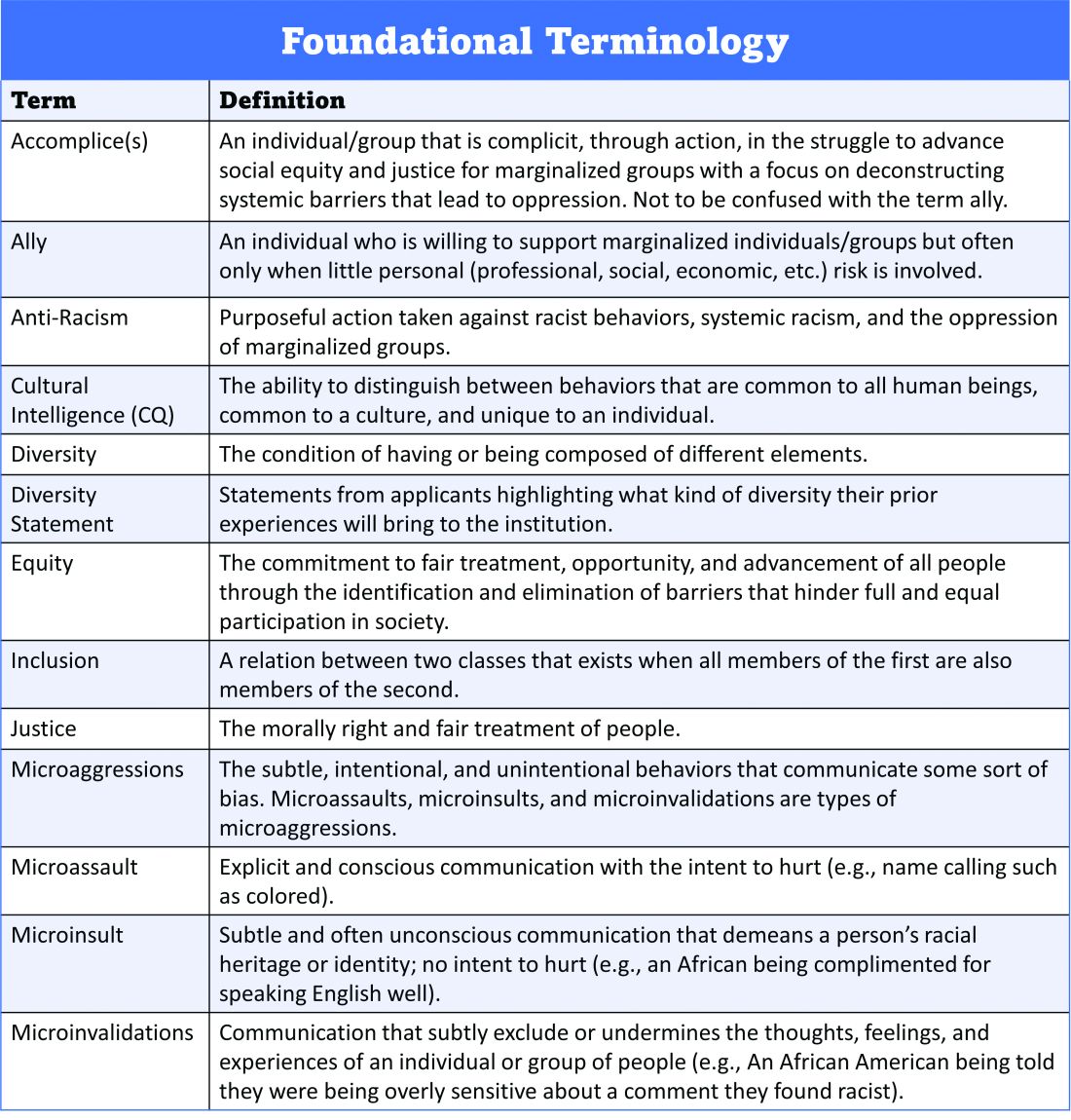
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 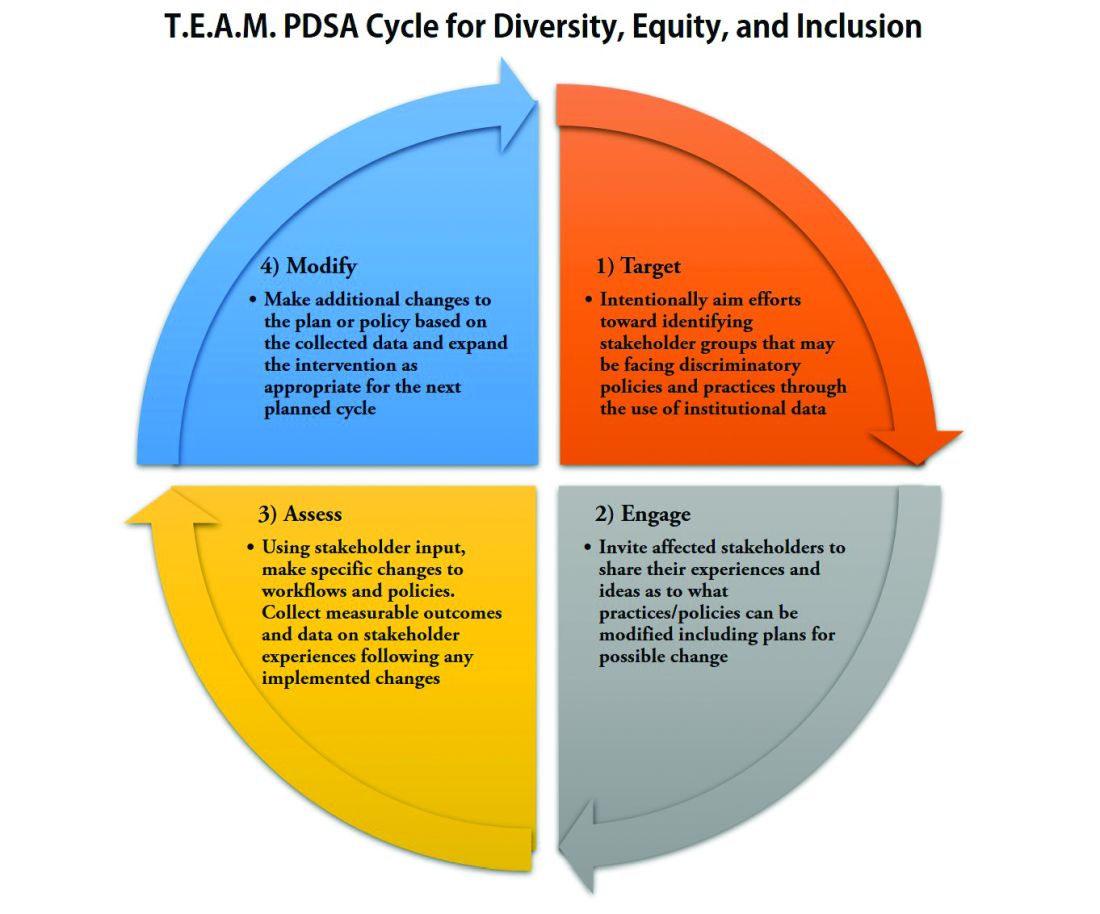
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
Navigating parenthood as pediatricians
PHM 2021 session
The Baby at Work or the Baby at Home: Navigating Parenthood as Pediatricians
Presenters
Jessica Gold, MD; Dana Foradori, MD, MEd; Nivedita Srinivas, MD; Honora Burnett, MD; Julie Pantaleoni, MD; and Barrett Fromme, MD, MHPE
Session summary
A group of physician-mothers from multiple academic children’s hospitals came together in a storytelling format to discuss topics relating to being a parent and pediatric hospitalist. Through short and poignant stories, the presenters shared their experiences and reviewed recent literature and policy changes relating to the topic. This mini-plenary focused on three themes:
1. Easing the transition back to work after the birth of a child.
2. Coping with the tension between being a parent and pediatrician.
3. The role that divisions, departments, and institutions can play in supporting parents and promoting workplace engagement.
The session concluded with a robust question-and-answer portion where participants built upon the themes above and shared their own experiences as pediatric hospitalist parents.
Key takeaways
- “Use your voice.” Physicians who are parents must continue having conversations about the challenging aspects of being a parent and hospitalist and advocate for the changes they would like to see.
- There will always be tension as a physician parent, but we can learn to embrace it while also learning how to ask for help, set boundaries, and share when we are struggling.
- There are numerous challenges for hospitalists who are parents because of poor parental leave policies in the United States, but this is slowly changing. For example, starting in July 2021, the ACGME mandated 6 weeks of parental leave during training without having to extend training.
- “You are not alone.” The presenters emphasized that their reason for hosting this session was to shed light on this topic and let all pediatric hospitalist parents know that they are not alone in this experience.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
PHM 2021 session
The Baby at Work or the Baby at Home: Navigating Parenthood as Pediatricians
Presenters
Jessica Gold, MD; Dana Foradori, MD, MEd; Nivedita Srinivas, MD; Honora Burnett, MD; Julie Pantaleoni, MD; and Barrett Fromme, MD, MHPE
Session summary
A group of physician-mothers from multiple academic children’s hospitals came together in a storytelling format to discuss topics relating to being a parent and pediatric hospitalist. Through short and poignant stories, the presenters shared their experiences and reviewed recent literature and policy changes relating to the topic. This mini-plenary focused on three themes:
1. Easing the transition back to work after the birth of a child.
2. Coping with the tension between being a parent and pediatrician.
3. The role that divisions, departments, and institutions can play in supporting parents and promoting workplace engagement.
The session concluded with a robust question-and-answer portion where participants built upon the themes above and shared their own experiences as pediatric hospitalist parents.
Key takeaways
- “Use your voice.” Physicians who are parents must continue having conversations about the challenging aspects of being a parent and hospitalist and advocate for the changes they would like to see.
- There will always be tension as a physician parent, but we can learn to embrace it while also learning how to ask for help, set boundaries, and share when we are struggling.
- There are numerous challenges for hospitalists who are parents because of poor parental leave policies in the United States, but this is slowly changing. For example, starting in July 2021, the ACGME mandated 6 weeks of parental leave during training without having to extend training.
- “You are not alone.” The presenters emphasized that their reason for hosting this session was to shed light on this topic and let all pediatric hospitalist parents know that they are not alone in this experience.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
PHM 2021 session
The Baby at Work or the Baby at Home: Navigating Parenthood as Pediatricians
Presenters
Jessica Gold, MD; Dana Foradori, MD, MEd; Nivedita Srinivas, MD; Honora Burnett, MD; Julie Pantaleoni, MD; and Barrett Fromme, MD, MHPE
Session summary
A group of physician-mothers from multiple academic children’s hospitals came together in a storytelling format to discuss topics relating to being a parent and pediatric hospitalist. Through short and poignant stories, the presenters shared their experiences and reviewed recent literature and policy changes relating to the topic. This mini-plenary focused on three themes:
1. Easing the transition back to work after the birth of a child.
2. Coping with the tension between being a parent and pediatrician.
3. The role that divisions, departments, and institutions can play in supporting parents and promoting workplace engagement.
The session concluded with a robust question-and-answer portion where participants built upon the themes above and shared their own experiences as pediatric hospitalist parents.
Key takeaways
- “Use your voice.” Physicians who are parents must continue having conversations about the challenging aspects of being a parent and hospitalist and advocate for the changes they would like to see.
- There will always be tension as a physician parent, but we can learn to embrace it while also learning how to ask for help, set boundaries, and share when we are struggling.
- There are numerous challenges for hospitalists who are parents because of poor parental leave policies in the United States, but this is slowly changing. For example, starting in July 2021, the ACGME mandated 6 weeks of parental leave during training without having to extend training.
- “You are not alone.” The presenters emphasized that their reason for hosting this session was to shed light on this topic and let all pediatric hospitalist parents know that they are not alone in this experience.
Dr. Scott is a second-year pediatric hospital medicine fellow at New York–Presbyterian Columbia/Cornell. Her academic interests are in curriculum development and evaluation in medical education with a focus on telemedicine.
Top 10 things to know about the AHA ACLS 2020 updates
Plus, how things differ in a COVID-19 cardiac arrest case
Top 10 things to know about the AHA ACLS 2020 updates1
1. There were no changes to the 2015 cardiac arrest algorithms.
2. The 2020 adult bradycardia algorithm increased the atropine dose to 1 mg (from 0.5-1 mg) but maintains the same frequency of dosing as every 3-5 minutes with max dose of 3 mg.
3. Epinephrine was reaffirmed. Specifically, give epinephrine as soon as possible in nonshockable rhythms (pulseless electrical activity and asystole). In shockable rhythms (ventricular fibrillation and pulseless ventricular tachycardia), the timing is less clear but it is reasonable to give the first dose after initial defibrillation attempts have failed. Currently the shockable rhythms algorithm has the first dose of epinephrine given after the second shock.
4. Giving medications intravenously is preferred over intraosseous (IO) cannulation because of some small observational studies that showed worsened outcomes with IO delivery. Try to get an IV if possible, but can still use IO if necessary. Central venous catheters are still not recommended during a code unless no other access can be obtained.
5. Double sequential defibrillation in refractory VF, which is the application of two sets of pads using two defibrillators to provide defibrillation either in rapid succession or at the same time, is not recommended because of lack of evidence.
6. It is reasonable to use physiological parameters such as arterial blood pressure or end-tidal CO2 (EtCO2) to monitor CPR quality. Goal EtCO2 is greater than 10 but ideally greater 20 mm Hg, so if you’re not reaching that ideal goal, push harder and/or faster! Of note, to use arterial blood pressure monitoring you must have an arterial line in place and to get adequate EtCO2 monitoring, the patient must be intubated with an EtCO2 monitor attached.
7. The need for intubation and the ideal timing are still unknown. The American Heart Association recommends either bag valve mask or an advanced airway.
8. In pregnant patients who develop cardiac arrest, focus on high-quality CPR and relief of aortocaval compression through left lateral uterine displacement while the patient is supine. This means that someone on the team stands on the left side of the patient and cups the uterus, pulling it up and leftward. Alternately, if standing on the right of the patient, push the uterus left and upward off of the maternal vessels.
9. AHA released new algorithms for opioid overdose given the current crisis. There is an absence of proven naloxone benefit in cardiac arrest so focus on standard resuscitative efforts and do not wait for effects of naloxone before initiating CPR. However, naloxone is still reasonable to give if overdose is suspected.
10. Clinicians should wait a minimum of 72 hours after return to normothermia before performing multimodal neuroprognostication. This allows for confounding factors (that is, meds) to hopefully be removed for improved accuracy.
Top 5 things that differ in a COVID-19+/PUI cardiac arrest case2
1. Don adequate personal protective equipment prior to entering the room. This might create a necessary delay in care.
2. Use a high-efficiency particulate air (HEPA) filter on all airway modalities.
3. Intubate as early as possible by someone highly experienced and place the patient on a ventilator with HEPA filter while undergoing resuscitation. This decreases aerosolization risk.
4. Use a mechanical CPR device if possible. This results in less people needed in the room.
5. If a patient is NOT intubated but is prone when they arrest, safely turn them supine and perform resuscitative effort. If a patient is intubated and prone when they arrest: If unable to safely turn them, place the pads in the AP position and perform compressions over T7-T10 vertebral bodies. Evidence for this is extremely limited but comes from a small pilot study which showed that reverse CPR generated a higher mean arterial pressure, compared with standard resuscitation.3
Dr. Allen is assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
References
1. Merchant RM et al. Part 1: Executive Summary: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020 Oct 21;142:S337-57. doi: 10.1161/CIR.0000000000000918.
2. Edelson DP et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19. 2020 Jun 23;141(25):e933-43. doi: 10.1161/CIRCULATIONAHA.120.047463.
3. Mazer SP et al. Reverse CPR: A pilot study of CPR in the prone position. Resuscitation. 2003 Jun;57(3):279-85. doi: 10.1016/s0300-9572(03)00037-6.
Plus, how things differ in a COVID-19 cardiac arrest case
Plus, how things differ in a COVID-19 cardiac arrest case
Top 10 things to know about the AHA ACLS 2020 updates1
1. There were no changes to the 2015 cardiac arrest algorithms.
2. The 2020 adult bradycardia algorithm increased the atropine dose to 1 mg (from 0.5-1 mg) but maintains the same frequency of dosing as every 3-5 minutes with max dose of 3 mg.
3. Epinephrine was reaffirmed. Specifically, give epinephrine as soon as possible in nonshockable rhythms (pulseless electrical activity and asystole). In shockable rhythms (ventricular fibrillation and pulseless ventricular tachycardia), the timing is less clear but it is reasonable to give the first dose after initial defibrillation attempts have failed. Currently the shockable rhythms algorithm has the first dose of epinephrine given after the second shock.
4. Giving medications intravenously is preferred over intraosseous (IO) cannulation because of some small observational studies that showed worsened outcomes with IO delivery. Try to get an IV if possible, but can still use IO if necessary. Central venous catheters are still not recommended during a code unless no other access can be obtained.
5. Double sequential defibrillation in refractory VF, which is the application of two sets of pads using two defibrillators to provide defibrillation either in rapid succession or at the same time, is not recommended because of lack of evidence.
6. It is reasonable to use physiological parameters such as arterial blood pressure or end-tidal CO2 (EtCO2) to monitor CPR quality. Goal EtCO2 is greater than 10 but ideally greater 20 mm Hg, so if you’re not reaching that ideal goal, push harder and/or faster! Of note, to use arterial blood pressure monitoring you must have an arterial line in place and to get adequate EtCO2 monitoring, the patient must be intubated with an EtCO2 monitor attached.
7. The need for intubation and the ideal timing are still unknown. The American Heart Association recommends either bag valve mask or an advanced airway.
8. In pregnant patients who develop cardiac arrest, focus on high-quality CPR and relief of aortocaval compression through left lateral uterine displacement while the patient is supine. This means that someone on the team stands on the left side of the patient and cups the uterus, pulling it up and leftward. Alternately, if standing on the right of the patient, push the uterus left and upward off of the maternal vessels.
9. AHA released new algorithms for opioid overdose given the current crisis. There is an absence of proven naloxone benefit in cardiac arrest so focus on standard resuscitative efforts and do not wait for effects of naloxone before initiating CPR. However, naloxone is still reasonable to give if overdose is suspected.
10. Clinicians should wait a minimum of 72 hours after return to normothermia before performing multimodal neuroprognostication. This allows for confounding factors (that is, meds) to hopefully be removed for improved accuracy.
Top 5 things that differ in a COVID-19+/PUI cardiac arrest case2
1. Don adequate personal protective equipment prior to entering the room. This might create a necessary delay in care.
2. Use a high-efficiency particulate air (HEPA) filter on all airway modalities.
3. Intubate as early as possible by someone highly experienced and place the patient on a ventilator with HEPA filter while undergoing resuscitation. This decreases aerosolization risk.
4. Use a mechanical CPR device if possible. This results in less people needed in the room.
5. If a patient is NOT intubated but is prone when they arrest, safely turn them supine and perform resuscitative effort. If a patient is intubated and prone when they arrest: If unable to safely turn them, place the pads in the AP position and perform compressions over T7-T10 vertebral bodies. Evidence for this is extremely limited but comes from a small pilot study which showed that reverse CPR generated a higher mean arterial pressure, compared with standard resuscitation.3
Dr. Allen is assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
References
1. Merchant RM et al. Part 1: Executive Summary: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020 Oct 21;142:S337-57. doi: 10.1161/CIR.0000000000000918.
2. Edelson DP et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19. 2020 Jun 23;141(25):e933-43. doi: 10.1161/CIRCULATIONAHA.120.047463.
3. Mazer SP et al. Reverse CPR: A pilot study of CPR in the prone position. Resuscitation. 2003 Jun;57(3):279-85. doi: 10.1016/s0300-9572(03)00037-6.
Top 10 things to know about the AHA ACLS 2020 updates1
1. There were no changes to the 2015 cardiac arrest algorithms.
2. The 2020 adult bradycardia algorithm increased the atropine dose to 1 mg (from 0.5-1 mg) but maintains the same frequency of dosing as every 3-5 minutes with max dose of 3 mg.
3. Epinephrine was reaffirmed. Specifically, give epinephrine as soon as possible in nonshockable rhythms (pulseless electrical activity and asystole). In shockable rhythms (ventricular fibrillation and pulseless ventricular tachycardia), the timing is less clear but it is reasonable to give the first dose after initial defibrillation attempts have failed. Currently the shockable rhythms algorithm has the first dose of epinephrine given after the second shock.
4. Giving medications intravenously is preferred over intraosseous (IO) cannulation because of some small observational studies that showed worsened outcomes with IO delivery. Try to get an IV if possible, but can still use IO if necessary. Central venous catheters are still not recommended during a code unless no other access can be obtained.
5. Double sequential defibrillation in refractory VF, which is the application of two sets of pads using two defibrillators to provide defibrillation either in rapid succession or at the same time, is not recommended because of lack of evidence.
6. It is reasonable to use physiological parameters such as arterial blood pressure or end-tidal CO2 (EtCO2) to monitor CPR quality. Goal EtCO2 is greater than 10 but ideally greater 20 mm Hg, so if you’re not reaching that ideal goal, push harder and/or faster! Of note, to use arterial blood pressure monitoring you must have an arterial line in place and to get adequate EtCO2 monitoring, the patient must be intubated with an EtCO2 monitor attached.
7. The need for intubation and the ideal timing are still unknown. The American Heart Association recommends either bag valve mask or an advanced airway.
8. In pregnant patients who develop cardiac arrest, focus on high-quality CPR and relief of aortocaval compression through left lateral uterine displacement while the patient is supine. This means that someone on the team stands on the left side of the patient and cups the uterus, pulling it up and leftward. Alternately, if standing on the right of the patient, push the uterus left and upward off of the maternal vessels.
9. AHA released new algorithms for opioid overdose given the current crisis. There is an absence of proven naloxone benefit in cardiac arrest so focus on standard resuscitative efforts and do not wait for effects of naloxone before initiating CPR. However, naloxone is still reasonable to give if overdose is suspected.
10. Clinicians should wait a minimum of 72 hours after return to normothermia before performing multimodal neuroprognostication. This allows for confounding factors (that is, meds) to hopefully be removed for improved accuracy.
Top 5 things that differ in a COVID-19+/PUI cardiac arrest case2
1. Don adequate personal protective equipment prior to entering the room. This might create a necessary delay in care.
2. Use a high-efficiency particulate air (HEPA) filter on all airway modalities.
3. Intubate as early as possible by someone highly experienced and place the patient on a ventilator with HEPA filter while undergoing resuscitation. This decreases aerosolization risk.
4. Use a mechanical CPR device if possible. This results in less people needed in the room.
5. If a patient is NOT intubated but is prone when they arrest, safely turn them supine and perform resuscitative effort. If a patient is intubated and prone when they arrest: If unable to safely turn them, place the pads in the AP position and perform compressions over T7-T10 vertebral bodies. Evidence for this is extremely limited but comes from a small pilot study which showed that reverse CPR generated a higher mean arterial pressure, compared with standard resuscitation.3
Dr. Allen is assistant professor of medicine in the division of hospital medicine at Emory University, Atlanta.
References
1. Merchant RM et al. Part 1: Executive Summary: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020 Oct 21;142:S337-57. doi: 10.1161/CIR.0000000000000918.
2. Edelson DP et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19. 2020 Jun 23;141(25):e933-43. doi: 10.1161/CIRCULATIONAHA.120.047463.
3. Mazer SP et al. Reverse CPR: A pilot study of CPR in the prone position. Resuscitation. 2003 Jun;57(3):279-85. doi: 10.1016/s0300-9572(03)00037-6.
Trio of awardees illustrate excellence in SHM chapters
2020 required resiliency, innovation
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
2020 required resiliency, innovation
2020 required resiliency, innovation
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”