User login
ObGyns’ choice of practice environment is a big deal
ObGyns are mindfully choosing their practice environments. The trend, as reported by the American College of Obstetricians and Gynecologists (ACOG),1 shows movement from private practice to employment: an increasing number of ObGyns have joined large practices and are employed. Overall, fewer than half of US physicians owned their medical practice in 2016, reported the American Medical Association (AMA).2 This is the first time that the majority of physicians are not practice owners.
Although employed ObGyns earn 9% less than self-employed ObGyns, ($276,000 vs $300,000, respectively), trading a higher salary for less time spent on administrative tasks seems to be worth the pay cut, reports Medscape. Employed ObGyns reported receiving additional benefits that might not have been available to self-employed ObGyns: professional liability coverage, employer-subsidized health and dental insurance, paid time off, and a retirement plan with employer match.3
What matters to ObGyns when choosing a practice setting?
Several decisions about practice setting need to be made at the beginning and throughout a career, among them the type of practice, desired salary, work-life balance, (the latter 2 may be influenced by practice type), and location.
Type of practice
“Patients benefit when physicians practice in settings they find professionally and personally rewarding,” said AMA President Andrew W. Gurman, MD. “The AMA is committed to helping physicians navigate their practice options and offers innovative strategies and resources to ensure physicians in all practice sizes and setting can thrive in the changing health environment.”2
More and more, that environment is a practice wholly owned by physicians. The AMA reports that in 2016, 55.8% of physicians worked in such a practice (including physicians who have an ownership stake in the practice, those who are employed by the practice, and those who are independent contractors).2 An approximate 13.8% of physicians worked at practices with more than 50 physicians in 2016. The majority (57.8%), however, practiced in groups with 10 or fewer physicians. The most common practice type was the single-specialty group (42.8%), followed by the multispecialty group practice (24.6%).2
Paying physicians a salary instead of compensating them based on volume may improve physician satisfaction—it removes the need to deal with complex fee-for-service systems, say Ian Larkin, PhD, and George Loewenstein, PhD. In fee-for-service payment arrangements, physicians may be encouraged to order more tests and procedures because doing so may increase income. A better strategy, say Larkin and Loewenstein, is to switch to a straight salary system. Known for their quality of care and comparatively low costs, the Mayo Clinic, Cleveland Clinic, and Kaiser Permanente have successfully implemented this payment system.4
Related article:
ObGyn salaries jumped in the last year
Desired salary
The mean income for ObGyns rose by 3% in 2016 over 2015 ($286,000 compared with $277,000), according to Medscape.5 This jump follows a gradual increase over the last few years ($249,000 in 2014; $243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1,5,6
The highest earnings among all physicians were orthopedists ($489,000), plastic surgeons ($440,000), and cardiologists ($410,000). Pediatricians were the lowest paid physicians at $202,000.3
Fair compensation. Fewer than half (48%) of ObGyns who completed the Medscape survey felt they were fairly compensated in 2016, and 41% of those who were dissatisfied with their compensation believed they deserved to be earning between 11% and 25% more. When asked if they would still choose medicine, 72% of ObGyns answered affirmatively. Of those who would choose medicine again, 76% would choose obstetrics and gynecology once more.3
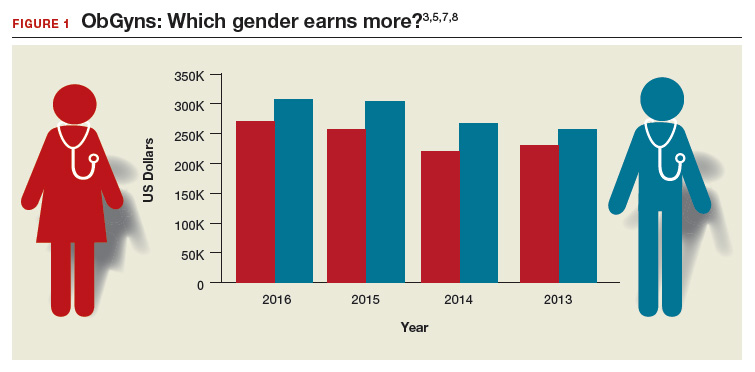
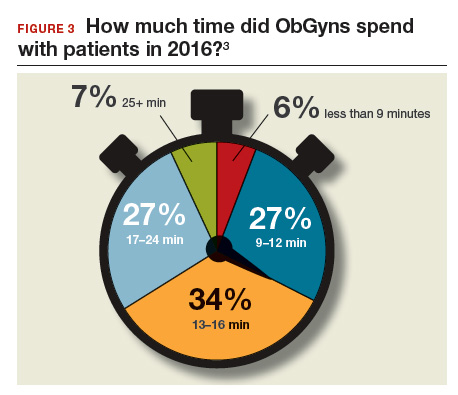
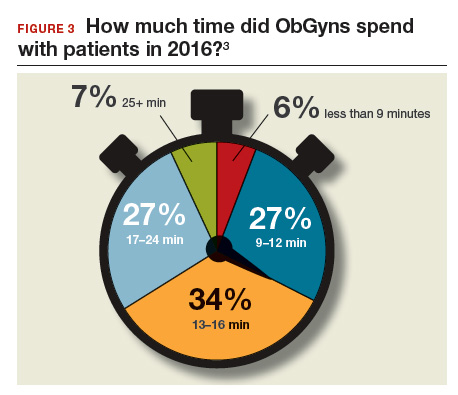
Gender differences. As in years past, full-time male ObGyns reported higher earnings (13%) than female ObGyns ($306,000 vs $270,000, respectively; (FIGURE 1).3,5,7,8
Among ObGyns who responded to the 2017 Medscape survey, 14% of women and 10% of men indicated that they work part-time.3 Last year, 13% of female ObGyns reported part-time employment versus 16% of male ObGyns.6
Among the ObGyns who answered the 2017 survey, there was a gender gap in participation related to race. Although more men than women responded to the survey, more women than men ObGyns among black/African American (women, 78%), Asian (women, 69%), and white/Caucasian (women, 53%) groups responded. Men outweighed women only among Hispanic/Latino ObGyns (60%) who answered the survey.3
Read about work-life balance, job satisfaction, and burnout
Work-life balance
ACOG predicts that mid-career and younger ObGyns will focus on work-life balance issues. Practice sites (ambulatory, hospital, or a combination) that offer part-time schedules or extra time for nonprofessional matters are becoming the most desirable to these practitioners.1
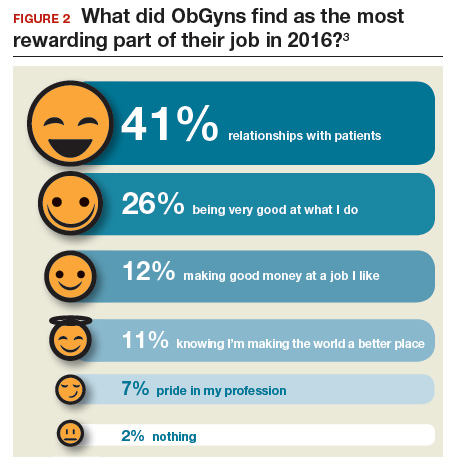
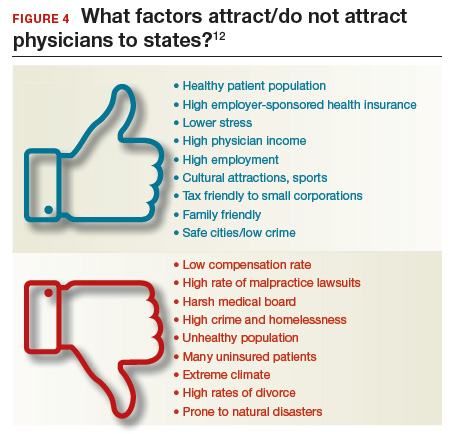
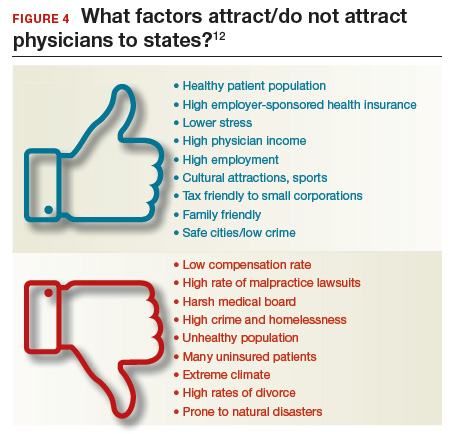
What satisfies and dissatisfies ObGyns? ObGyns reported to Medscape that their relationships with patients (41% of respondents) was the most rewarding part of their job (FIGURE 2).3
There are many job aspects that dissatisfy ObGyns, including1,3,9:
- too many bureaucratic tasks
- the short time allotted for each patient office visit
- electronic health records (EHR) and increased computerization
- not feeling appreciated or properly compensated
- spending too many hours at work
- the impact of regulatory changes on clinical practice.
Bureaucratic tasks remain a primary cause for burnout among all physicians.10 This year, 56% of all physicians reported spending 10 hours or more per week on paperwork and administrative tasks, up from 35% in the 2014 report. More than half (54%) of ObGyns reported spending 10 hours or more on paperwork.3 For every hour of face-to-face patient time, physicians spent nearly 2 additional hours on their EHR and administration tasks.9
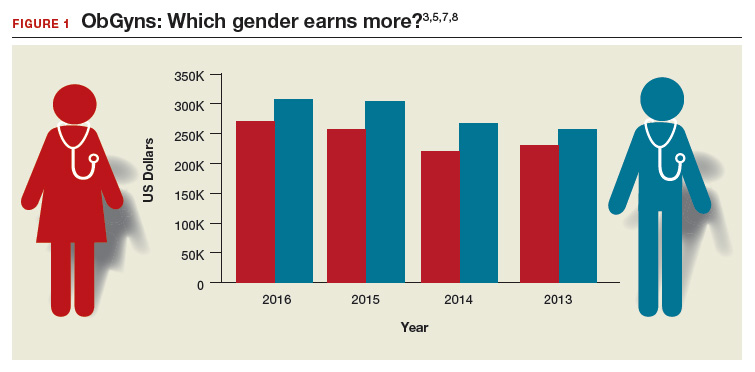
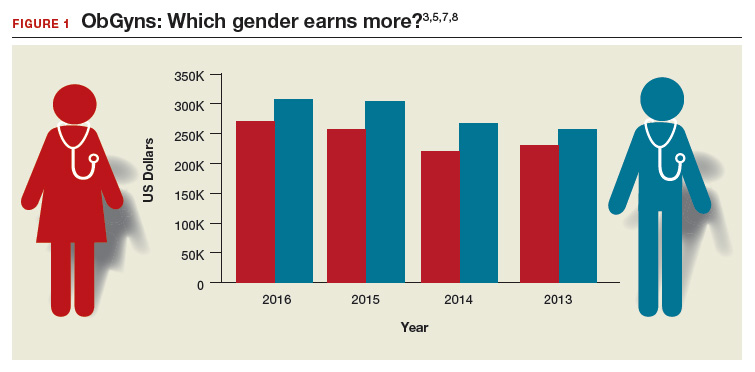
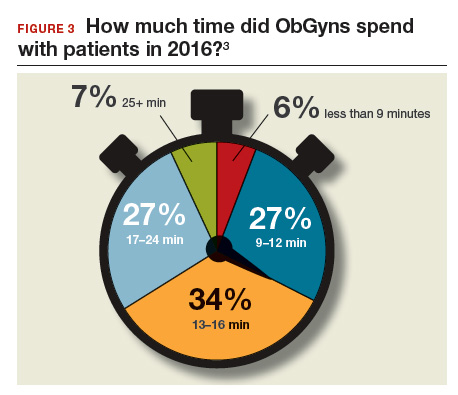
Time with patients. Medscape reported that 38% of ObGyns spent more than 45 hours per week with patients (FIGURE 3).
ACOG notes that ObGyns are increasingly referring patients to subspecialists, which frustrates patients and increases their costs.1
ObGyns rank high in burnout rates. Burnout rates for physicians are twice that of other working adults.1 ObGyns rank second (56%) in burn out (Emergency Medicine, 59%).10 When Medscape survey respondents were asked to grade their burnout level from 1 to 7 (1 = “It does not interfere with my life;” 7 = “It is so severe that I am thinking of leaving medicine altogether”), ObGyns ranked their burnout level at 4.3.10 Female physicians reported a higher percentage of burnout than their male colleagues (55% vs 45%, respectively).10 An estimated 40% to 75% of ObGyns experienced some level of burnout.1
According to ACOG, the specialty is included among the “noncontrollable” lifestyle specialties, especially for those aged 50 years or younger. Many Millennials (born 1980 to 2000) do not view their work and professional achievement as central to their lives; ObGyns aged younger than 35 years want to work fewer hours per week compared with their older colleagues, says ACOG. However, when this option is unavailable, an increasing number of Millennials report lowered job satisfaction.1
Related article:
What can administrators and ObGyns do together to reduce physician burnout?
Mindfulness about quality of life. The relationship of burnout to quality of life issues is gaining in awareness. In a recent
“We need to stop blaming individuals and treat physician burnout as a system issue…If it affects half our physicians, it is indirectly affecting half our patients,” notes Tait Shanafelt, MD, a hematologist and physician-burnout researcher at the Mayo Clinic.9 He says that burnout relates to a physician’s “professional spirit of life, and it primarily affects individuals whose work involves an intense interaction with people.”9
The Mayo Clinic in Minneapolis, Minnesota, has taken a lead in developing a space for their physicians to “reset” by offering a room where health professionals can retreat if they need a moment to recover from a traumatic event.9
Read about what factors attract ObGyns to specific locations
Location, location, location
Specific areas of the country are more attractive for their higher compensation rates. The highest average compensation was reported by ObGyns in the North Central area ($339,000), West ($301,000), and Great Lakes ($297,000) regions, while the lowest compensation rates were found in the Northwest ($260,000), Southwest ($268,000), and South Central ($275,000) areas.3
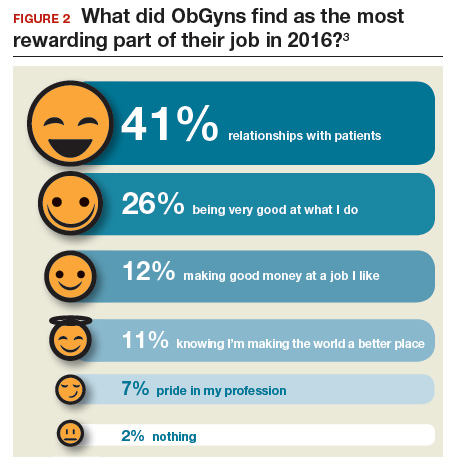
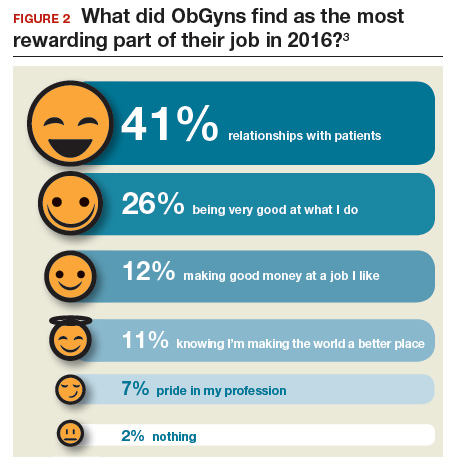
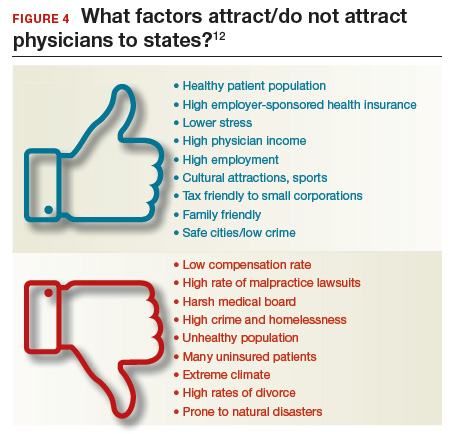
Key factors, such as healthy patient populations, higher rates of health insurance coverage, and lower stress levels attract physicians (FIGURE 4). Minnesota ranked the #1 best place to practice because it has the 4th healthiest population, 2nd highest rate of employer-sponsored health insurance, the 17th lowest number of malpractice lawsuits, and a medical board that is the 3rd least harsh in the nation.12 Unfortunate situations such as the highest malpractice rates per capita, least healthy population, 8th lowest rate of employer-sponsored health insurance, and the 9th lowest compensation rate for physicians make Louisiana the worst place to practice in 2017.12
Supply and demand creates substantial geographic imbalances in the number of ObGyns in the United States. ACOG pro-jects that the need for ObGyns will increase nationally by 6% in the next 10 years, although demand will vary geographically from a 27% increase in Nevada to an 11% decrease in West Virginia.1 Especially vulnerable states (Arizona, Washington, Utah, Idaho) currently have an insufficient supply of ObGyns and are projected to see an increased future demand. Florida, Texas, North Carolina, and Nevada will be at risk, according to ACOG, because the adult female population is expected to increase.1
2017 Medscape survey demographics
The Medscape Compensation Report 2017 is a based on the responses of 19,270 physicians across 27+ specialties, 5% of whom were ObGyns. Data were collected in an online survey conducted from December 20, 2016, to March 7, 2017.3
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- American Congress of Obstetricians and Gynecologists. The Obstetrician-Gynecologist Workforce in the United States: Facts, Figures, and Implications, 2017. https://www.acog.org/Resources-And-Publications/The-Ob-Gyn-Workforce/The-Obstetrician-Gynecologist-Workforce-in-the-United-States. Accessed June 7, 2017.
- Murphy B. For the first time, physician practice owners are not the majority. AMA Wire. https://wire.ama-assn.org/practice-management/first-time-physician-practice-owners-are-not-majority?utm_source=BulletinHealthCare&utm_medium=email&utm_term=060117&utm_content=general&utm_campaign=article_alert-morning_rounds_daily. Published May 31, 2017. Accessed June 7, 2017.
- Grisham S. Medscape Ob/Gyn Compensation Report 2017. Medscape Website. http://www.medscape.com/slideshow/compensation-2017-ob-gyn-6008576. Published April 12, 2017. Accessed June 7, 2017.
- Larkin I, Loewenstein G. Business model—Related conflict of interests in medicine: Problems and potential solutions. JAMA. 2017;317(17):1745–1746.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 7, 2017.
- Reale D, Christie K. ObGyn salaries jumped in the last year. OBG Manag. 2016;28(7):25–27, 30, 37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2015. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed July 24, 2017.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed July 24, 2017.
- Parks T. AMA burnout by specialty. AMA Wire. https://wire.ama-assn.org/life-career/report-reveals-severity-burnout-specialty. Published January 31, 2017. Accessed June 7, 2017.
- Peckham C. Medscape Lifestyle Report 2017: Race and Ethnicity, Bias and Burnout. Medscape Website. http://www.medscape.com/features/slideshow/lifestyle/2017/overview#page=1. Published January 11, 2017. Accessed June 7, 2017.
- DiVenere L. ObGyn burnout: ACOG takes aim. OBG Manag. 2016;28(9):25,30,32,33.
- Page L. Best and Worst Places to Practice 2017. Medscape Website. http://www.medscape.com/slideshow/best-places-to-practice-2017-6008688?src=wnl_physrep_170510_mscpmrk_bestplaces2017&impID=1345406&faf. Published May 10, 2017. Accessed June 7, 2017.
ObGyns are mindfully choosing their practice environments. The trend, as reported by the American College of Obstetricians and Gynecologists (ACOG),1 shows movement from private practice to employment: an increasing number of ObGyns have joined large practices and are employed. Overall, fewer than half of US physicians owned their medical practice in 2016, reported the American Medical Association (AMA).2 This is the first time that the majority of physicians are not practice owners.
Although employed ObGyns earn 9% less than self-employed ObGyns, ($276,000 vs $300,000, respectively), trading a higher salary for less time spent on administrative tasks seems to be worth the pay cut, reports Medscape. Employed ObGyns reported receiving additional benefits that might not have been available to self-employed ObGyns: professional liability coverage, employer-subsidized health and dental insurance, paid time off, and a retirement plan with employer match.3
What matters to ObGyns when choosing a practice setting?
Several decisions about practice setting need to be made at the beginning and throughout a career, among them the type of practice, desired salary, work-life balance, (the latter 2 may be influenced by practice type), and location.
Type of practice
“Patients benefit when physicians practice in settings they find professionally and personally rewarding,” said AMA President Andrew W. Gurman, MD. “The AMA is committed to helping physicians navigate their practice options and offers innovative strategies and resources to ensure physicians in all practice sizes and setting can thrive in the changing health environment.”2
More and more, that environment is a practice wholly owned by physicians. The AMA reports that in 2016, 55.8% of physicians worked in such a practice (including physicians who have an ownership stake in the practice, those who are employed by the practice, and those who are independent contractors).2 An approximate 13.8% of physicians worked at practices with more than 50 physicians in 2016. The majority (57.8%), however, practiced in groups with 10 or fewer physicians. The most common practice type was the single-specialty group (42.8%), followed by the multispecialty group practice (24.6%).2
Paying physicians a salary instead of compensating them based on volume may improve physician satisfaction—it removes the need to deal with complex fee-for-service systems, say Ian Larkin, PhD, and George Loewenstein, PhD. In fee-for-service payment arrangements, physicians may be encouraged to order more tests and procedures because doing so may increase income. A better strategy, say Larkin and Loewenstein, is to switch to a straight salary system. Known for their quality of care and comparatively low costs, the Mayo Clinic, Cleveland Clinic, and Kaiser Permanente have successfully implemented this payment system.4
Related article:
ObGyn salaries jumped in the last year
Desired salary
The mean income for ObGyns rose by 3% in 2016 over 2015 ($286,000 compared with $277,000), according to Medscape.5 This jump follows a gradual increase over the last few years ($249,000 in 2014; $243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1,5,6
The highest earnings among all physicians were orthopedists ($489,000), plastic surgeons ($440,000), and cardiologists ($410,000). Pediatricians were the lowest paid physicians at $202,000.3
Fair compensation. Fewer than half (48%) of ObGyns who completed the Medscape survey felt they were fairly compensated in 2016, and 41% of those who were dissatisfied with their compensation believed they deserved to be earning between 11% and 25% more. When asked if they would still choose medicine, 72% of ObGyns answered affirmatively. Of those who would choose medicine again, 76% would choose obstetrics and gynecology once more.3
Gender differences. As in years past, full-time male ObGyns reported higher earnings (13%) than female ObGyns ($306,000 vs $270,000, respectively; (FIGURE 1).3,5,7,8
Among ObGyns who responded to the 2017 Medscape survey, 14% of women and 10% of men indicated that they work part-time.3 Last year, 13% of female ObGyns reported part-time employment versus 16% of male ObGyns.6
Among the ObGyns who answered the 2017 survey, there was a gender gap in participation related to race. Although more men than women responded to the survey, more women than men ObGyns among black/African American (women, 78%), Asian (women, 69%), and white/Caucasian (women, 53%) groups responded. Men outweighed women only among Hispanic/Latino ObGyns (60%) who answered the survey.3
Read about work-life balance, job satisfaction, and burnout
Work-life balance
ACOG predicts that mid-career and younger ObGyns will focus on work-life balance issues. Practice sites (ambulatory, hospital, or a combination) that offer part-time schedules or extra time for nonprofessional matters are becoming the most desirable to these practitioners.1
What satisfies and dissatisfies ObGyns? ObGyns reported to Medscape that their relationships with patients (41% of respondents) was the most rewarding part of their job (FIGURE 2).3
There are many job aspects that dissatisfy ObGyns, including1,3,9:
- too many bureaucratic tasks
- the short time allotted for each patient office visit
- electronic health records (EHR) and increased computerization
- not feeling appreciated or properly compensated
- spending too many hours at work
- the impact of regulatory changes on clinical practice.
Bureaucratic tasks remain a primary cause for burnout among all physicians.10 This year, 56% of all physicians reported spending 10 hours or more per week on paperwork and administrative tasks, up from 35% in the 2014 report. More than half (54%) of ObGyns reported spending 10 hours or more on paperwork.3 For every hour of face-to-face patient time, physicians spent nearly 2 additional hours on their EHR and administration tasks.9
Time with patients. Medscape reported that 38% of ObGyns spent more than 45 hours per week with patients (FIGURE 3).
ACOG notes that ObGyns are increasingly referring patients to subspecialists, which frustrates patients and increases their costs.1
ObGyns rank high in burnout rates. Burnout rates for physicians are twice that of other working adults.1 ObGyns rank second (56%) in burn out (Emergency Medicine, 59%).10 When Medscape survey respondents were asked to grade their burnout level from 1 to 7 (1 = “It does not interfere with my life;” 7 = “It is so severe that I am thinking of leaving medicine altogether”), ObGyns ranked their burnout level at 4.3.10 Female physicians reported a higher percentage of burnout than their male colleagues (55% vs 45%, respectively).10 An estimated 40% to 75% of ObGyns experienced some level of burnout.1
According to ACOG, the specialty is included among the “noncontrollable” lifestyle specialties, especially for those aged 50 years or younger. Many Millennials (born 1980 to 2000) do not view their work and professional achievement as central to their lives; ObGyns aged younger than 35 years want to work fewer hours per week compared with their older colleagues, says ACOG. However, when this option is unavailable, an increasing number of Millennials report lowered job satisfaction.1
Related article:
What can administrators and ObGyns do together to reduce physician burnout?
Mindfulness about quality of life. The relationship of burnout to quality of life issues is gaining in awareness. In a recent
“We need to stop blaming individuals and treat physician burnout as a system issue…If it affects half our physicians, it is indirectly affecting half our patients,” notes Tait Shanafelt, MD, a hematologist and physician-burnout researcher at the Mayo Clinic.9 He says that burnout relates to a physician’s “professional spirit of life, and it primarily affects individuals whose work involves an intense interaction with people.”9
The Mayo Clinic in Minneapolis, Minnesota, has taken a lead in developing a space for their physicians to “reset” by offering a room where health professionals can retreat if they need a moment to recover from a traumatic event.9
Read about what factors attract ObGyns to specific locations
Location, location, location
Specific areas of the country are more attractive for their higher compensation rates. The highest average compensation was reported by ObGyns in the North Central area ($339,000), West ($301,000), and Great Lakes ($297,000) regions, while the lowest compensation rates were found in the Northwest ($260,000), Southwest ($268,000), and South Central ($275,000) areas.3
Key factors, such as healthy patient populations, higher rates of health insurance coverage, and lower stress levels attract physicians (FIGURE 4). Minnesota ranked the #1 best place to practice because it has the 4th healthiest population, 2nd highest rate of employer-sponsored health insurance, the 17th lowest number of malpractice lawsuits, and a medical board that is the 3rd least harsh in the nation.12 Unfortunate situations such as the highest malpractice rates per capita, least healthy population, 8th lowest rate of employer-sponsored health insurance, and the 9th lowest compensation rate for physicians make Louisiana the worst place to practice in 2017.12
Supply and demand creates substantial geographic imbalances in the number of ObGyns in the United States. ACOG pro-jects that the need for ObGyns will increase nationally by 6% in the next 10 years, although demand will vary geographically from a 27% increase in Nevada to an 11% decrease in West Virginia.1 Especially vulnerable states (Arizona, Washington, Utah, Idaho) currently have an insufficient supply of ObGyns and are projected to see an increased future demand. Florida, Texas, North Carolina, and Nevada will be at risk, according to ACOG, because the adult female population is expected to increase.1
2017 Medscape survey demographics
The Medscape Compensation Report 2017 is a based on the responses of 19,270 physicians across 27+ specialties, 5% of whom were ObGyns. Data were collected in an online survey conducted from December 20, 2016, to March 7, 2017.3
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
ObGyns are mindfully choosing their practice environments. The trend, as reported by the American College of Obstetricians and Gynecologists (ACOG),1 shows movement from private practice to employment: an increasing number of ObGyns have joined large practices and are employed. Overall, fewer than half of US physicians owned their medical practice in 2016, reported the American Medical Association (AMA).2 This is the first time that the majority of physicians are not practice owners.
Although employed ObGyns earn 9% less than self-employed ObGyns, ($276,000 vs $300,000, respectively), trading a higher salary for less time spent on administrative tasks seems to be worth the pay cut, reports Medscape. Employed ObGyns reported receiving additional benefits that might not have been available to self-employed ObGyns: professional liability coverage, employer-subsidized health and dental insurance, paid time off, and a retirement plan with employer match.3
What matters to ObGyns when choosing a practice setting?
Several decisions about practice setting need to be made at the beginning and throughout a career, among them the type of practice, desired salary, work-life balance, (the latter 2 may be influenced by practice type), and location.
Type of practice
“Patients benefit when physicians practice in settings they find professionally and personally rewarding,” said AMA President Andrew W. Gurman, MD. “The AMA is committed to helping physicians navigate their practice options and offers innovative strategies and resources to ensure physicians in all practice sizes and setting can thrive in the changing health environment.”2
More and more, that environment is a practice wholly owned by physicians. The AMA reports that in 2016, 55.8% of physicians worked in such a practice (including physicians who have an ownership stake in the practice, those who are employed by the practice, and those who are independent contractors).2 An approximate 13.8% of physicians worked at practices with more than 50 physicians in 2016. The majority (57.8%), however, practiced in groups with 10 or fewer physicians. The most common practice type was the single-specialty group (42.8%), followed by the multispecialty group practice (24.6%).2
Paying physicians a salary instead of compensating them based on volume may improve physician satisfaction—it removes the need to deal with complex fee-for-service systems, say Ian Larkin, PhD, and George Loewenstein, PhD. In fee-for-service payment arrangements, physicians may be encouraged to order more tests and procedures because doing so may increase income. A better strategy, say Larkin and Loewenstein, is to switch to a straight salary system. Known for their quality of care and comparatively low costs, the Mayo Clinic, Cleveland Clinic, and Kaiser Permanente have successfully implemented this payment system.4
Related article:
ObGyn salaries jumped in the last year
Desired salary
The mean income for ObGyns rose by 3% in 2016 over 2015 ($286,000 compared with $277,000), according to Medscape.5 This jump follows a gradual increase over the last few years ($249,000 in 2014; $243,000 in 2013; $242,000 in 2012; $220,000 in 2011).1,5,6
The highest earnings among all physicians were orthopedists ($489,000), plastic surgeons ($440,000), and cardiologists ($410,000). Pediatricians were the lowest paid physicians at $202,000.3
Fair compensation. Fewer than half (48%) of ObGyns who completed the Medscape survey felt they were fairly compensated in 2016, and 41% of those who were dissatisfied with their compensation believed they deserved to be earning between 11% and 25% more. When asked if they would still choose medicine, 72% of ObGyns answered affirmatively. Of those who would choose medicine again, 76% would choose obstetrics and gynecology once more.3
Gender differences. As in years past, full-time male ObGyns reported higher earnings (13%) than female ObGyns ($306,000 vs $270,000, respectively; (FIGURE 1).3,5,7,8
Among ObGyns who responded to the 2017 Medscape survey, 14% of women and 10% of men indicated that they work part-time.3 Last year, 13% of female ObGyns reported part-time employment versus 16% of male ObGyns.6
Among the ObGyns who answered the 2017 survey, there was a gender gap in participation related to race. Although more men than women responded to the survey, more women than men ObGyns among black/African American (women, 78%), Asian (women, 69%), and white/Caucasian (women, 53%) groups responded. Men outweighed women only among Hispanic/Latino ObGyns (60%) who answered the survey.3
Read about work-life balance, job satisfaction, and burnout
Work-life balance
ACOG predicts that mid-career and younger ObGyns will focus on work-life balance issues. Practice sites (ambulatory, hospital, or a combination) that offer part-time schedules or extra time for nonprofessional matters are becoming the most desirable to these practitioners.1
What satisfies and dissatisfies ObGyns? ObGyns reported to Medscape that their relationships with patients (41% of respondents) was the most rewarding part of their job (FIGURE 2).3
There are many job aspects that dissatisfy ObGyns, including1,3,9:
- too many bureaucratic tasks
- the short time allotted for each patient office visit
- electronic health records (EHR) and increased computerization
- not feeling appreciated or properly compensated
- spending too many hours at work
- the impact of regulatory changes on clinical practice.
Bureaucratic tasks remain a primary cause for burnout among all physicians.10 This year, 56% of all physicians reported spending 10 hours or more per week on paperwork and administrative tasks, up from 35% in the 2014 report. More than half (54%) of ObGyns reported spending 10 hours or more on paperwork.3 For every hour of face-to-face patient time, physicians spent nearly 2 additional hours on their EHR and administration tasks.9
Time with patients. Medscape reported that 38% of ObGyns spent more than 45 hours per week with patients (FIGURE 3).
ACOG notes that ObGyns are increasingly referring patients to subspecialists, which frustrates patients and increases their costs.1
ObGyns rank high in burnout rates. Burnout rates for physicians are twice that of other working adults.1 ObGyns rank second (56%) in burn out (Emergency Medicine, 59%).10 When Medscape survey respondents were asked to grade their burnout level from 1 to 7 (1 = “It does not interfere with my life;” 7 = “It is so severe that I am thinking of leaving medicine altogether”), ObGyns ranked their burnout level at 4.3.10 Female physicians reported a higher percentage of burnout than their male colleagues (55% vs 45%, respectively).10 An estimated 40% to 75% of ObGyns experienced some level of burnout.1
According to ACOG, the specialty is included among the “noncontrollable” lifestyle specialties, especially for those aged 50 years or younger. Many Millennials (born 1980 to 2000) do not view their work and professional achievement as central to their lives; ObGyns aged younger than 35 years want to work fewer hours per week compared with their older colleagues, says ACOG. However, when this option is unavailable, an increasing number of Millennials report lowered job satisfaction.1
Related article:
What can administrators and ObGyns do together to reduce physician burnout?
Mindfulness about quality of life. The relationship of burnout to quality of life issues is gaining in awareness. In a recent
“We need to stop blaming individuals and treat physician burnout as a system issue…If it affects half our physicians, it is indirectly affecting half our patients,” notes Tait Shanafelt, MD, a hematologist and physician-burnout researcher at the Mayo Clinic.9 He says that burnout relates to a physician’s “professional spirit of life, and it primarily affects individuals whose work involves an intense interaction with people.”9
The Mayo Clinic in Minneapolis, Minnesota, has taken a lead in developing a space for their physicians to “reset” by offering a room where health professionals can retreat if they need a moment to recover from a traumatic event.9
Read about what factors attract ObGyns to specific locations
Location, location, location
Specific areas of the country are more attractive for their higher compensation rates. The highest average compensation was reported by ObGyns in the North Central area ($339,000), West ($301,000), and Great Lakes ($297,000) regions, while the lowest compensation rates were found in the Northwest ($260,000), Southwest ($268,000), and South Central ($275,000) areas.3
Key factors, such as healthy patient populations, higher rates of health insurance coverage, and lower stress levels attract physicians (FIGURE 4). Minnesota ranked the #1 best place to practice because it has the 4th healthiest population, 2nd highest rate of employer-sponsored health insurance, the 17th lowest number of malpractice lawsuits, and a medical board that is the 3rd least harsh in the nation.12 Unfortunate situations such as the highest malpractice rates per capita, least healthy population, 8th lowest rate of employer-sponsored health insurance, and the 9th lowest compensation rate for physicians make Louisiana the worst place to practice in 2017.12
Supply and demand creates substantial geographic imbalances in the number of ObGyns in the United States. ACOG pro-jects that the need for ObGyns will increase nationally by 6% in the next 10 years, although demand will vary geographically from a 27% increase in Nevada to an 11% decrease in West Virginia.1 Especially vulnerable states (Arizona, Washington, Utah, Idaho) currently have an insufficient supply of ObGyns and are projected to see an increased future demand. Florida, Texas, North Carolina, and Nevada will be at risk, according to ACOG, because the adult female population is expected to increase.1
2017 Medscape survey demographics
The Medscape Compensation Report 2017 is a based on the responses of 19,270 physicians across 27+ specialties, 5% of whom were ObGyns. Data were collected in an online survey conducted from December 20, 2016, to March 7, 2017.3
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- American Congress of Obstetricians and Gynecologists. The Obstetrician-Gynecologist Workforce in the United States: Facts, Figures, and Implications, 2017. https://www.acog.org/Resources-And-Publications/The-Ob-Gyn-Workforce/The-Obstetrician-Gynecologist-Workforce-in-the-United-States. Accessed June 7, 2017.
- Murphy B. For the first time, physician practice owners are not the majority. AMA Wire. https://wire.ama-assn.org/practice-management/first-time-physician-practice-owners-are-not-majority?utm_source=BulletinHealthCare&utm_medium=email&utm_term=060117&utm_content=general&utm_campaign=article_alert-morning_rounds_daily. Published May 31, 2017. Accessed June 7, 2017.
- Grisham S. Medscape Ob/Gyn Compensation Report 2017. Medscape Website. http://www.medscape.com/slideshow/compensation-2017-ob-gyn-6008576. Published April 12, 2017. Accessed June 7, 2017.
- Larkin I, Loewenstein G. Business model—Related conflict of interests in medicine: Problems and potential solutions. JAMA. 2017;317(17):1745–1746.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 7, 2017.
- Reale D, Christie K. ObGyn salaries jumped in the last year. OBG Manag. 2016;28(7):25–27, 30, 37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2015. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed July 24, 2017.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed July 24, 2017.
- Parks T. AMA burnout by specialty. AMA Wire. https://wire.ama-assn.org/life-career/report-reveals-severity-burnout-specialty. Published January 31, 2017. Accessed June 7, 2017.
- Peckham C. Medscape Lifestyle Report 2017: Race and Ethnicity, Bias and Burnout. Medscape Website. http://www.medscape.com/features/slideshow/lifestyle/2017/overview#page=1. Published January 11, 2017. Accessed June 7, 2017.
- DiVenere L. ObGyn burnout: ACOG takes aim. OBG Manag. 2016;28(9):25,30,32,33.
- Page L. Best and Worst Places to Practice 2017. Medscape Website. http://www.medscape.com/slideshow/best-places-to-practice-2017-6008688?src=wnl_physrep_170510_mscpmrk_bestplaces2017&impID=1345406&faf. Published May 10, 2017. Accessed June 7, 2017.
- American Congress of Obstetricians and Gynecologists. The Obstetrician-Gynecologist Workforce in the United States: Facts, Figures, and Implications, 2017. https://www.acog.org/Resources-And-Publications/The-Ob-Gyn-Workforce/The-Obstetrician-Gynecologist-Workforce-in-the-United-States. Accessed June 7, 2017.
- Murphy B. For the first time, physician practice owners are not the majority. AMA Wire. https://wire.ama-assn.org/practice-management/first-time-physician-practice-owners-are-not-majority?utm_source=BulletinHealthCare&utm_medium=email&utm_term=060117&utm_content=general&utm_campaign=article_alert-morning_rounds_daily. Published May 31, 2017. Accessed June 7, 2017.
- Grisham S. Medscape Ob/Gyn Compensation Report 2017. Medscape Website. http://www.medscape.com/slideshow/compensation-2017-ob-gyn-6008576. Published April 12, 2017. Accessed June 7, 2017.
- Larkin I, Loewenstein G. Business model—Related conflict of interests in medicine: Problems and potential solutions. JAMA. 2017;317(17):1745–1746.
- Peckham C. Medscape Ob/Gyn Compensation Report 2016. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2016/womenshealth. Published April 1, 2016. Accessed June 7, 2017.
- Reale D, Christie K. ObGyn salaries jumped in the last year. OBG Manag. 2016;28(7):25–27, 30, 37.
- Peckham C. Medscape Ob/Gyn Compensation Report 2015. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2015/womenshealth. Published April 21, 2015. Accessed July 24, 2017.
- Peckham C. Medscape Ob/Gyn Compensation Report 2014. Medscape Website. http://www.medscape.com/features/slideshow/compensation/2014/womenshealth. Published April 14, 2014. Accessed July 24, 2017.
- Parks T. AMA burnout by specialty. AMA Wire. https://wire.ama-assn.org/life-career/report-reveals-severity-burnout-specialty. Published January 31, 2017. Accessed June 7, 2017.
- Peckham C. Medscape Lifestyle Report 2017: Race and Ethnicity, Bias and Burnout. Medscape Website. http://www.medscape.com/features/slideshow/lifestyle/2017/overview#page=1. Published January 11, 2017. Accessed June 7, 2017.
- DiVenere L. ObGyn burnout: ACOG takes aim. OBG Manag. 2016;28(9):25,30,32,33.
- Page L. Best and Worst Places to Practice 2017. Medscape Website. http://www.medscape.com/slideshow/best-places-to-practice-2017-6008688?src=wnl_physrep_170510_mscpmrk_bestplaces2017&impID=1345406&faf. Published May 10, 2017. Accessed June 7, 2017.
How to sell your ObGyn practice
For ObGyns, 2 intensely stressful career milestones are the day you start your practice and the day you decide to put it up for sale.
One of us, Dr. Baum, started a practice in 1976. At that time, many clinicians seemed to work right up until the day they died—in mid-examination or with scalpel in hand! Today, clinicians seriously contemplate leaving an active practice at age 55, 60, or, more traditionally, 65.
ObGyns in group practice, even those with only 1 or 2 partners, presumably have in place a well-thought-out and properly drafted contract with buyout and phase-down provisions. For members of a group practice, it is imperative to critically review and discuss contractual arrangements periodically and decide if they make sense as much now as they did at the start. ObGyns who continually revisit their contracts probably have an exit strategy that is fairly self-executing and effective and that will provide the seller with a seamless transition to retirement.
A solo ObGyn who is selling a practice has 3 basic options: find a successor physician, sell to a hospital or to a larger group, or close the practice.
Related article:
ObGyns’ choice of practice environment is a big deal
Preparing your practice for sale
Regardless of who will take over your practice, you need to prepare for its transition.
The most important aspect of selling your practice is knowing its finances and ensuring that they are in order. Any serious buyer will ask to examine your books, see how you are running the business, and assess its vitality and potential growth. Simply, a buyer will want to know where your revenue comes from and where it goes.
Your practice will be attractive to a buyer if it shows a stable or growing revenue base, an attractive payer mix, reasonable overhead, and personal income that is steady if not increasing. If your earning capacity is low or declining, you will need to explain why.
Timing is key
We strongly recommend beginning the process 3 to 5 years before your intended exit.
By starting early, up to 5 years in advance, you can maximize the likelihood that your practice will retain all or most of its value. Moreover, you can use the long lead time to thoroughly explore all available options and find a committed buyer.
Selling a practice can be a complicated affair, and many ObGyns do not have the requisite skills. So much of the success in selling depends on the specifics of the practice, the physician, and the market (the hospital and physician environment).
Identifying potential buyers
Other ObGyns. Recruiting an ObGyn to take over your practice seems to be the best option but can prove very difficult in today’s environment. Many younger clinicians are either joining large groups or becoming hospital employees.
Other physician groups. While working your way down your list of potential buyers, you should also be quietly, subtly, and tactfully assessing other practices, even your competitors, to see if any are candidates for merging with and/or acquiring yours and all your charts, records, and referring physicians.
Hospitals. In today’s health care environment, in which more than half of clinicians are becoming hospital employees, selling to your associated hospital may be a viable option.
Your practice is probably contributing millions of dollars in income to that hospital each year, and of course the hospital would like to maintain this revenue stream. You should consider talking to the hospital’s CEO or medical director.
Hospitals also know that, if you leave and the market cannot absorb the resulting increase in demand for care, patients may go elsewhere, to a competing hospital or outside the community. Rather than lose your market share, a hospital may consider the obvious solution: recruit a replacement ObGyn for your practice.
Your goal here is to negotiate an agreement in which your hospital will recruit a replacement ObGyn, provide financial support, and transition your practice to that ObGyn over a specified period.
The hospital could acquire your practice and either employ you during the transition or provide recruiting support and an income guarantee to help your practice pay the new physician’s salary. Whether to sell or remain independent is often driven by the needs and desires of the recruit. As the vast majority of clinicians coming out of training are seeking employment, in most cases the agreement will require a sale.
Selling to a hospital a few years before your retirement can be a plus. You might find employment a welcome respite from the daunting responsibility of managing your own practice. Life can become much less stressful as you introduce and transition your patients to the new ObGyn. You will be working less, taking fewer calls, and maintaining or even increasing your income, all without the burden of managing the practice.
Read about determining your practice’s value
Putting a monetary value on your practice
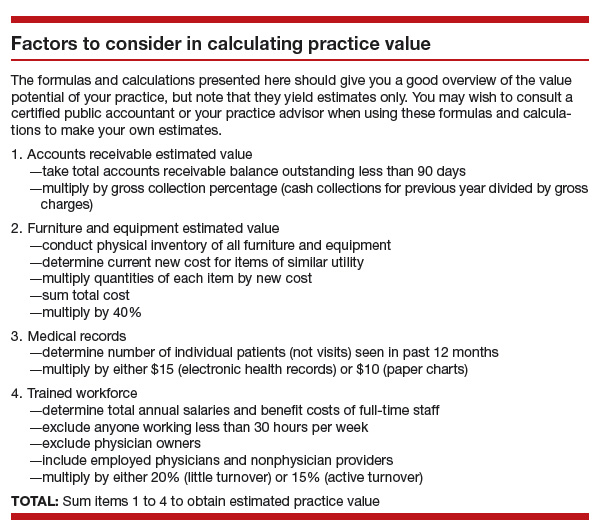
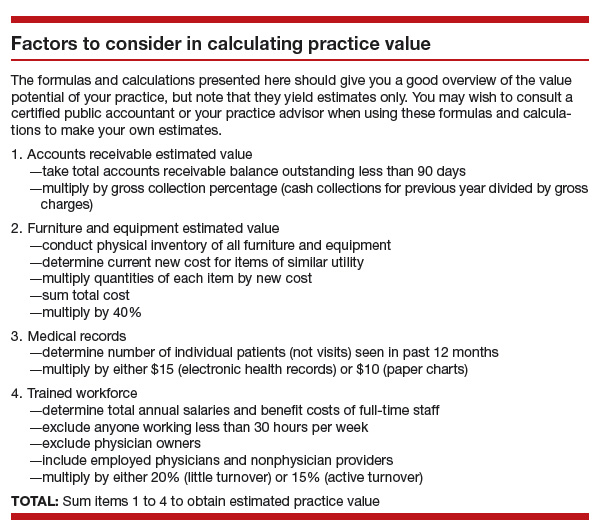
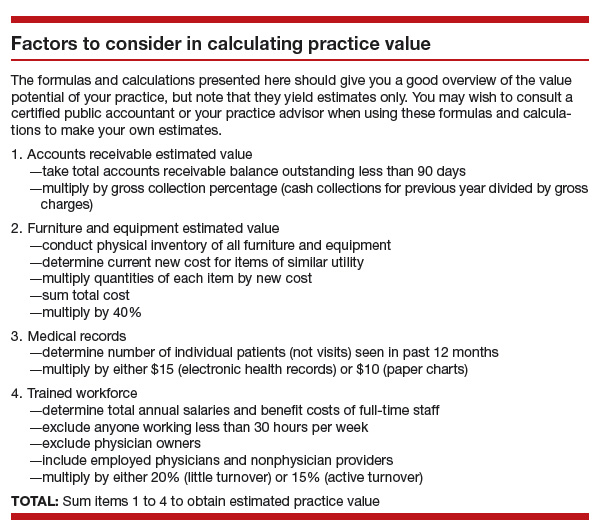
After deciding to sell your practice, you need to determine its value. Buying a practice may be the largest financial transaction a young ObGyn will ever make. For a retiring physician, valuation of a practice may reflect a career’s worth of “sweat equity.”
What is your practice worth?
All ObGyns believe their practice is worth far more than any young ObGyn or hospital is willing to pay for it. After all, you have spent a medical lifetime creating, building, and nurturing your practice. You have cared for several thousand patients, who have been loyal and may want to stay with the practice under its new ObGyn. So, how does a retiring physician put a value on his or her practice and then “cast the net” to the marketplace? How do you find a buyer who will pay the asking price and then help the practice make the transition from seller to buyer and continue to serve their patients?
The buyer’s perspective on value. In a pure sense, the value of any asset is what a potential buyer is willing to pay. From a value standpoint, the price that potential buyers are willing to pay varies by the specifics of the situation, regardless of what a valuation or practice appraisal might indicate.
For example, once your plan to retire becomes known, why would a young ObGyn agree to pay X dollars for all your medical records? After all, the potential buyer knows that your existing patients and your referral base will need to seek care from another ObGyn after you leave, and they will likely stay with the practice if they feel they will be treated well by the new clinician.
A hospital may take a similar tack but more often will be willing to pay fair market value for your practice. Hospitals, however, cannot legally pay more than fair market value as determined by an independent appraiser.
Related article:
Four pillars of a successful practice: 1. Keep your current patients happy
Valuation methods
The valuation of any business generally is approached in terms of market, assets, and income.
The market approach usually is taken only with regard to office real estate. Given the lack of reliable and comparable sales information, this approach is seldom used in the valuation of medical practices. If you own your office real estate, a real estate appraiser will establish its fair market value.
In the assets approach, the individual assets of a medical practice are valued on the basis of their current market values. These assets are either tangible or intangible.
Tangible assets can be seen and touched. Furniture, equipment, and office real estate are examples.
The fair market value of used furniture and equipment is most often determined by replacement cost. The value of these items is limited. Usually it starts at 50% of the cost of buying new furniture or equipment of the same utility. From there, the value is lowered on the basis of the age and condition of the items.
Often, the market value of major ObGyn office equipment, such as a DXA (dual-energy x-ray absorptiometry) scanner, is based on similar items for sale or recently sold in the used secondary equipment market.
Tangible assets may include accounts receivable (A/R). A/R represents uncollected payment for work performed. Most buyers want to avoid paying for A/R and assuming the risk of collections. Generally, you should expect to retain your A/R and pay a small or nominal fee to have the buyer handle the collections after you have retired.
Intangible assets are not physical. Examples include the physician’s name, phone number, reputation, referral base, trained staff, and medical records—in other words, what gets patients to keep coming back. Most physicians value these goodwill or “blue-sky” assets highly. Today, unfortunately, most sellers are unable to reap any financial benefit from their intangible assets.
The income approach is based on the premise that the value of any business is in the income it generates for its owner. In simple terms, value in the income approach is a multiple of the cash the business generates after expenses.
Read important keys to transitioning the practice
Transitioning the practice: Role of the seller and the buyer
First and very important is the contract agreement regarding the overlap period, when both the exiting ObGyn and the new ObGyn are at the practice. We suggest making the overlap a minimum of 6 months and a maximum of 1 year. During this period, the exiting physician can introduce the incoming physician to the patients. A face-to-face introduction can amount to an endorsement, which can ease a patient’s mind and help her decide to take on the new ObGyn and philosophy rather than search elsewhere for obstetric and gynecologic care. The new ObGyn also can use the overlap period to become familiar and comfortable with the staff and learn the process for physician and staff management of case flow, from scheduling and examination to insurance and patient follow-up.
We suggest that the exiting ObGyn send a farewell/welcome letter to patients and referring physicians. The letter should state the exiting ObGyn’s intention to leave (or retire from) the practice and should introduce the ObGyn who will be taking over.
The exiting ObGyn should also take the new ObGyn to meet the physicians who have been providing referrals over the years. We suggest visiting each referring physician’s office to make the introduction. Another good way to introduce a new ObGyn to referring physicians and other professionals—endocrinologists, cardiologists, nurses, pharmaceutical representatives—is to host an open house at your practice. Invite the staff members of the referring physicians as well, since they can be invaluable in making referrals.
We recommend that the exiting ObGyn spend the money to update all the practice’s stationery, brochures, and print materials and ensure they look professional. Note that it is not acceptable to place the new ObGyn’s name under the exiting ObGyn’s name. If the practice has a website, introduce the new physician there and make any necessary updates regarding office hours and accepted insurance plans.
If the exiting ObGyn’s practice lacks a robust Internet and social media presence, the new ObGyn should establish one. We recommend setting up an interactive website that patients can use to make appointments and pay bills. The website should have an email component that can be used to ask questions, raise concerns, and get answers. We also recommend opening Facebook, YouTube, and Twitter accounts for the practice and being active on these social media.
In our experience, smoothly transitioning practices can achieve patient retention rates as high as 90% to 95%. For practices without a plan, however, these rates may be as low as 50%, or worse. Therefore, work out a plan in advance, and include the steps described here, so that on arrival the new ObGyn can hit the ground running.
Acquiring a successful medical practice is doable and offers many advantages, such as autonomy and the ability to make business decisions affecting the practice. Despite all the changes happening in health care, we still think this is the best way to go.
Related article:
Four pillars of a successful practice: 4. Motivate your staff
Bottom line
Selling an ObGyn practice can be a daunting process. However, deciding to sell your practice, performing the valuation, and ensuring a smooth transition are part and parcel of making the transfer a success, equitable for both the buyer and the seller.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
For ObGyns, 2 intensely stressful career milestones are the day you start your practice and the day you decide to put it up for sale.
One of us, Dr. Baum, started a practice in 1976. At that time, many clinicians seemed to work right up until the day they died—in mid-examination or with scalpel in hand! Today, clinicians seriously contemplate leaving an active practice at age 55, 60, or, more traditionally, 65.
ObGyns in group practice, even those with only 1 or 2 partners, presumably have in place a well-thought-out and properly drafted contract with buyout and phase-down provisions. For members of a group practice, it is imperative to critically review and discuss contractual arrangements periodically and decide if they make sense as much now as they did at the start. ObGyns who continually revisit their contracts probably have an exit strategy that is fairly self-executing and effective and that will provide the seller with a seamless transition to retirement.
A solo ObGyn who is selling a practice has 3 basic options: find a successor physician, sell to a hospital or to a larger group, or close the practice.
Related article:
ObGyns’ choice of practice environment is a big deal
Preparing your practice for sale
Regardless of who will take over your practice, you need to prepare for its transition.
The most important aspect of selling your practice is knowing its finances and ensuring that they are in order. Any serious buyer will ask to examine your books, see how you are running the business, and assess its vitality and potential growth. Simply, a buyer will want to know where your revenue comes from and where it goes.
Your practice will be attractive to a buyer if it shows a stable or growing revenue base, an attractive payer mix, reasonable overhead, and personal income that is steady if not increasing. If your earning capacity is low or declining, you will need to explain why.
Timing is key
We strongly recommend beginning the process 3 to 5 years before your intended exit.
By starting early, up to 5 years in advance, you can maximize the likelihood that your practice will retain all or most of its value. Moreover, you can use the long lead time to thoroughly explore all available options and find a committed buyer.
Selling a practice can be a complicated affair, and many ObGyns do not have the requisite skills. So much of the success in selling depends on the specifics of the practice, the physician, and the market (the hospital and physician environment).
Identifying potential buyers
Other ObGyns. Recruiting an ObGyn to take over your practice seems to be the best option but can prove very difficult in today’s environment. Many younger clinicians are either joining large groups or becoming hospital employees.
Other physician groups. While working your way down your list of potential buyers, you should also be quietly, subtly, and tactfully assessing other practices, even your competitors, to see if any are candidates for merging with and/or acquiring yours and all your charts, records, and referring physicians.
Hospitals. In today’s health care environment, in which more than half of clinicians are becoming hospital employees, selling to your associated hospital may be a viable option.
Your practice is probably contributing millions of dollars in income to that hospital each year, and of course the hospital would like to maintain this revenue stream. You should consider talking to the hospital’s CEO or medical director.
Hospitals also know that, if you leave and the market cannot absorb the resulting increase in demand for care, patients may go elsewhere, to a competing hospital or outside the community. Rather than lose your market share, a hospital may consider the obvious solution: recruit a replacement ObGyn for your practice.
Your goal here is to negotiate an agreement in which your hospital will recruit a replacement ObGyn, provide financial support, and transition your practice to that ObGyn over a specified period.
The hospital could acquire your practice and either employ you during the transition or provide recruiting support and an income guarantee to help your practice pay the new physician’s salary. Whether to sell or remain independent is often driven by the needs and desires of the recruit. As the vast majority of clinicians coming out of training are seeking employment, in most cases the agreement will require a sale.
Selling to a hospital a few years before your retirement can be a plus. You might find employment a welcome respite from the daunting responsibility of managing your own practice. Life can become much less stressful as you introduce and transition your patients to the new ObGyn. You will be working less, taking fewer calls, and maintaining or even increasing your income, all without the burden of managing the practice.
Read about determining your practice’s value
Putting a monetary value on your practice
After deciding to sell your practice, you need to determine its value. Buying a practice may be the largest financial transaction a young ObGyn will ever make. For a retiring physician, valuation of a practice may reflect a career’s worth of “sweat equity.”
What is your practice worth?
All ObGyns believe their practice is worth far more than any young ObGyn or hospital is willing to pay for it. After all, you have spent a medical lifetime creating, building, and nurturing your practice. You have cared for several thousand patients, who have been loyal and may want to stay with the practice under its new ObGyn. So, how does a retiring physician put a value on his or her practice and then “cast the net” to the marketplace? How do you find a buyer who will pay the asking price and then help the practice make the transition from seller to buyer and continue to serve their patients?
The buyer’s perspective on value. In a pure sense, the value of any asset is what a potential buyer is willing to pay. From a value standpoint, the price that potential buyers are willing to pay varies by the specifics of the situation, regardless of what a valuation or practice appraisal might indicate.
For example, once your plan to retire becomes known, why would a young ObGyn agree to pay X dollars for all your medical records? After all, the potential buyer knows that your existing patients and your referral base will need to seek care from another ObGyn after you leave, and they will likely stay with the practice if they feel they will be treated well by the new clinician.
A hospital may take a similar tack but more often will be willing to pay fair market value for your practice. Hospitals, however, cannot legally pay more than fair market value as determined by an independent appraiser.
Related article:
Four pillars of a successful practice: 1. Keep your current patients happy
Valuation methods
The valuation of any business generally is approached in terms of market, assets, and income.
The market approach usually is taken only with regard to office real estate. Given the lack of reliable and comparable sales information, this approach is seldom used in the valuation of medical practices. If you own your office real estate, a real estate appraiser will establish its fair market value.
In the assets approach, the individual assets of a medical practice are valued on the basis of their current market values. These assets are either tangible or intangible.
Tangible assets can be seen and touched. Furniture, equipment, and office real estate are examples.
The fair market value of used furniture and equipment is most often determined by replacement cost. The value of these items is limited. Usually it starts at 50% of the cost of buying new furniture or equipment of the same utility. From there, the value is lowered on the basis of the age and condition of the items.
Often, the market value of major ObGyn office equipment, such as a DXA (dual-energy x-ray absorptiometry) scanner, is based on similar items for sale or recently sold in the used secondary equipment market.
Tangible assets may include accounts receivable (A/R). A/R represents uncollected payment for work performed. Most buyers want to avoid paying for A/R and assuming the risk of collections. Generally, you should expect to retain your A/R and pay a small or nominal fee to have the buyer handle the collections after you have retired.
Intangible assets are not physical. Examples include the physician’s name, phone number, reputation, referral base, trained staff, and medical records—in other words, what gets patients to keep coming back. Most physicians value these goodwill or “blue-sky” assets highly. Today, unfortunately, most sellers are unable to reap any financial benefit from their intangible assets.
The income approach is based on the premise that the value of any business is in the income it generates for its owner. In simple terms, value in the income approach is a multiple of the cash the business generates after expenses.
Read important keys to transitioning the practice
Transitioning the practice: Role of the seller and the buyer
First and very important is the contract agreement regarding the overlap period, when both the exiting ObGyn and the new ObGyn are at the practice. We suggest making the overlap a minimum of 6 months and a maximum of 1 year. During this period, the exiting physician can introduce the incoming physician to the patients. A face-to-face introduction can amount to an endorsement, which can ease a patient’s mind and help her decide to take on the new ObGyn and philosophy rather than search elsewhere for obstetric and gynecologic care. The new ObGyn also can use the overlap period to become familiar and comfortable with the staff and learn the process for physician and staff management of case flow, from scheduling and examination to insurance and patient follow-up.
We suggest that the exiting ObGyn send a farewell/welcome letter to patients and referring physicians. The letter should state the exiting ObGyn’s intention to leave (or retire from) the practice and should introduce the ObGyn who will be taking over.
The exiting ObGyn should also take the new ObGyn to meet the physicians who have been providing referrals over the years. We suggest visiting each referring physician’s office to make the introduction. Another good way to introduce a new ObGyn to referring physicians and other professionals—endocrinologists, cardiologists, nurses, pharmaceutical representatives—is to host an open house at your practice. Invite the staff members of the referring physicians as well, since they can be invaluable in making referrals.
We recommend that the exiting ObGyn spend the money to update all the practice’s stationery, brochures, and print materials and ensure they look professional. Note that it is not acceptable to place the new ObGyn’s name under the exiting ObGyn’s name. If the practice has a website, introduce the new physician there and make any necessary updates regarding office hours and accepted insurance plans.
If the exiting ObGyn’s practice lacks a robust Internet and social media presence, the new ObGyn should establish one. We recommend setting up an interactive website that patients can use to make appointments and pay bills. The website should have an email component that can be used to ask questions, raise concerns, and get answers. We also recommend opening Facebook, YouTube, and Twitter accounts for the practice and being active on these social media.
In our experience, smoothly transitioning practices can achieve patient retention rates as high as 90% to 95%. For practices without a plan, however, these rates may be as low as 50%, or worse. Therefore, work out a plan in advance, and include the steps described here, so that on arrival the new ObGyn can hit the ground running.
Acquiring a successful medical practice is doable and offers many advantages, such as autonomy and the ability to make business decisions affecting the practice. Despite all the changes happening in health care, we still think this is the best way to go.
Related article:
Four pillars of a successful practice: 4. Motivate your staff
Bottom line
Selling an ObGyn practice can be a daunting process. However, deciding to sell your practice, performing the valuation, and ensuring a smooth transition are part and parcel of making the transfer a success, equitable for both the buyer and the seller.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
For ObGyns, 2 intensely stressful career milestones are the day you start your practice and the day you decide to put it up for sale.
One of us, Dr. Baum, started a practice in 1976. At that time, many clinicians seemed to work right up until the day they died—in mid-examination or with scalpel in hand! Today, clinicians seriously contemplate leaving an active practice at age 55, 60, or, more traditionally, 65.
ObGyns in group practice, even those with only 1 or 2 partners, presumably have in place a well-thought-out and properly drafted contract with buyout and phase-down provisions. For members of a group practice, it is imperative to critically review and discuss contractual arrangements periodically and decide if they make sense as much now as they did at the start. ObGyns who continually revisit their contracts probably have an exit strategy that is fairly self-executing and effective and that will provide the seller with a seamless transition to retirement.
A solo ObGyn who is selling a practice has 3 basic options: find a successor physician, sell to a hospital or to a larger group, or close the practice.
Related article:
ObGyns’ choice of practice environment is a big deal
Preparing your practice for sale
Regardless of who will take over your practice, you need to prepare for its transition.
The most important aspect of selling your practice is knowing its finances and ensuring that they are in order. Any serious buyer will ask to examine your books, see how you are running the business, and assess its vitality and potential growth. Simply, a buyer will want to know where your revenue comes from and where it goes.
Your practice will be attractive to a buyer if it shows a stable or growing revenue base, an attractive payer mix, reasonable overhead, and personal income that is steady if not increasing. If your earning capacity is low or declining, you will need to explain why.
Timing is key
We strongly recommend beginning the process 3 to 5 years before your intended exit.
By starting early, up to 5 years in advance, you can maximize the likelihood that your practice will retain all or most of its value. Moreover, you can use the long lead time to thoroughly explore all available options and find a committed buyer.
Selling a practice can be a complicated affair, and many ObGyns do not have the requisite skills. So much of the success in selling depends on the specifics of the practice, the physician, and the market (the hospital and physician environment).
Identifying potential buyers
Other ObGyns. Recruiting an ObGyn to take over your practice seems to be the best option but can prove very difficult in today’s environment. Many younger clinicians are either joining large groups or becoming hospital employees.
Other physician groups. While working your way down your list of potential buyers, you should also be quietly, subtly, and tactfully assessing other practices, even your competitors, to see if any are candidates for merging with and/or acquiring yours and all your charts, records, and referring physicians.
Hospitals. In today’s health care environment, in which more than half of clinicians are becoming hospital employees, selling to your associated hospital may be a viable option.
Your practice is probably contributing millions of dollars in income to that hospital each year, and of course the hospital would like to maintain this revenue stream. You should consider talking to the hospital’s CEO or medical director.
Hospitals also know that, if you leave and the market cannot absorb the resulting increase in demand for care, patients may go elsewhere, to a competing hospital or outside the community. Rather than lose your market share, a hospital may consider the obvious solution: recruit a replacement ObGyn for your practice.
Your goal here is to negotiate an agreement in which your hospital will recruit a replacement ObGyn, provide financial support, and transition your practice to that ObGyn over a specified period.
The hospital could acquire your practice and either employ you during the transition or provide recruiting support and an income guarantee to help your practice pay the new physician’s salary. Whether to sell or remain independent is often driven by the needs and desires of the recruit. As the vast majority of clinicians coming out of training are seeking employment, in most cases the agreement will require a sale.
Selling to a hospital a few years before your retirement can be a plus. You might find employment a welcome respite from the daunting responsibility of managing your own practice. Life can become much less stressful as you introduce and transition your patients to the new ObGyn. You will be working less, taking fewer calls, and maintaining or even increasing your income, all without the burden of managing the practice.
Read about determining your practice’s value
Putting a monetary value on your practice
After deciding to sell your practice, you need to determine its value. Buying a practice may be the largest financial transaction a young ObGyn will ever make. For a retiring physician, valuation of a practice may reflect a career’s worth of “sweat equity.”
What is your practice worth?
All ObGyns believe their practice is worth far more than any young ObGyn or hospital is willing to pay for it. After all, you have spent a medical lifetime creating, building, and nurturing your practice. You have cared for several thousand patients, who have been loyal and may want to stay with the practice under its new ObGyn. So, how does a retiring physician put a value on his or her practice and then “cast the net” to the marketplace? How do you find a buyer who will pay the asking price and then help the practice make the transition from seller to buyer and continue to serve their patients?
The buyer’s perspective on value. In a pure sense, the value of any asset is what a potential buyer is willing to pay. From a value standpoint, the price that potential buyers are willing to pay varies by the specifics of the situation, regardless of what a valuation or practice appraisal might indicate.
For example, once your plan to retire becomes known, why would a young ObGyn agree to pay X dollars for all your medical records? After all, the potential buyer knows that your existing patients and your referral base will need to seek care from another ObGyn after you leave, and they will likely stay with the practice if they feel they will be treated well by the new clinician.
A hospital may take a similar tack but more often will be willing to pay fair market value for your practice. Hospitals, however, cannot legally pay more than fair market value as determined by an independent appraiser.
Related article:
Four pillars of a successful practice: 1. Keep your current patients happy
Valuation methods
The valuation of any business generally is approached in terms of market, assets, and income.
The market approach usually is taken only with regard to office real estate. Given the lack of reliable and comparable sales information, this approach is seldom used in the valuation of medical practices. If you own your office real estate, a real estate appraiser will establish its fair market value.
In the assets approach, the individual assets of a medical practice are valued on the basis of their current market values. These assets are either tangible or intangible.
Tangible assets can be seen and touched. Furniture, equipment, and office real estate are examples.
The fair market value of used furniture and equipment is most often determined by replacement cost. The value of these items is limited. Usually it starts at 50% of the cost of buying new furniture or equipment of the same utility. From there, the value is lowered on the basis of the age and condition of the items.
Often, the market value of major ObGyn office equipment, such as a DXA (dual-energy x-ray absorptiometry) scanner, is based on similar items for sale or recently sold in the used secondary equipment market.
Tangible assets may include accounts receivable (A/R). A/R represents uncollected payment for work performed. Most buyers want to avoid paying for A/R and assuming the risk of collections. Generally, you should expect to retain your A/R and pay a small or nominal fee to have the buyer handle the collections after you have retired.
Intangible assets are not physical. Examples include the physician’s name, phone number, reputation, referral base, trained staff, and medical records—in other words, what gets patients to keep coming back. Most physicians value these goodwill or “blue-sky” assets highly. Today, unfortunately, most sellers are unable to reap any financial benefit from their intangible assets.
The income approach is based on the premise that the value of any business is in the income it generates for its owner. In simple terms, value in the income approach is a multiple of the cash the business generates after expenses.
Read important keys to transitioning the practice
Transitioning the practice: Role of the seller and the buyer
First and very important is the contract agreement regarding the overlap period, when both the exiting ObGyn and the new ObGyn are at the practice. We suggest making the overlap a minimum of 6 months and a maximum of 1 year. During this period, the exiting physician can introduce the incoming physician to the patients. A face-to-face introduction can amount to an endorsement, which can ease a patient’s mind and help her decide to take on the new ObGyn and philosophy rather than search elsewhere for obstetric and gynecologic care. The new ObGyn also can use the overlap period to become familiar and comfortable with the staff and learn the process for physician and staff management of case flow, from scheduling and examination to insurance and patient follow-up.
We suggest that the exiting ObGyn send a farewell/welcome letter to patients and referring physicians. The letter should state the exiting ObGyn’s intention to leave (or retire from) the practice and should introduce the ObGyn who will be taking over.
The exiting ObGyn should also take the new ObGyn to meet the physicians who have been providing referrals over the years. We suggest visiting each referring physician’s office to make the introduction. Another good way to introduce a new ObGyn to referring physicians and other professionals—endocrinologists, cardiologists, nurses, pharmaceutical representatives—is to host an open house at your practice. Invite the staff members of the referring physicians as well, since they can be invaluable in making referrals.
We recommend that the exiting ObGyn spend the money to update all the practice’s stationery, brochures, and print materials and ensure they look professional. Note that it is not acceptable to place the new ObGyn’s name under the exiting ObGyn’s name. If the practice has a website, introduce the new physician there and make any necessary updates regarding office hours and accepted insurance plans.
If the exiting ObGyn’s practice lacks a robust Internet and social media presence, the new ObGyn should establish one. We recommend setting up an interactive website that patients can use to make appointments and pay bills. The website should have an email component that can be used to ask questions, raise concerns, and get answers. We also recommend opening Facebook, YouTube, and Twitter accounts for the practice and being active on these social media.
In our experience, smoothly transitioning practices can achieve patient retention rates as high as 90% to 95%. For practices without a plan, however, these rates may be as low as 50%, or worse. Therefore, work out a plan in advance, and include the steps described here, so that on arrival the new ObGyn can hit the ground running.
Acquiring a successful medical practice is doable and offers many advantages, such as autonomy and the ability to make business decisions affecting the practice. Despite all the changes happening in health care, we still think this is the best way to go.
Related article:
Four pillars of a successful practice: 4. Motivate your staff
Bottom line
Selling an ObGyn practice can be a daunting process. However, deciding to sell your practice, performing the valuation, and ensuring a smooth transition are part and parcel of making the transfer a success, equitable for both the buyer and the seller.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
IN THIS ARTICLE
Six Steps to Reduce Taxes on Investments: Minimizing What You Pay in a Tough Environment
Orthopedic physicians in the highest income tax brackets may have been presented with an unpleasant surprise in recent years when they learned of their investment tax liability. A prolonged period of strong domestic stock performance from 2009 to 2016, combined with the implementation of The American Taxpayer Relief Act of 2012, may have resulted in significantly higher taxes for many of you.
The top ordinary income tax rates increased by 24% when including the Net Investment Income surtax, while the top capital gains rate was increased by more than 58%. Writing a large check to the Internal Revenue Service serves as a harsh reminder that tax planning requires attention throughout the year, and is not a technique you can properly manage a few weeks before an April 15 deadline.
Proper tax planning became more critical as we moved into an era of higher taxes. A multi-year bull market for domestic stocks has caused many traditional investment vehicles to hold large amounts of unrealized gains, which can become realized gains if you are not careful. Most major equity indices took a breath in 2015 and finished the year in the red, which created a planning opportunity for astute investors and their advisors. Stocks in the US and emerging market countries quickly bounced back in 2016; however, European stocks struggled and continue to trade well below peak levels reached nearly a decade ago. Investors who missed the opportunity to offset gains of the prior 2 years may have an opportunity to reduce their tax bill in 2017.
In this article, we will provide you with 6 suggestions that could save you thousands of dollars in investment taxes over the next several years.
1. Account Registration Matters: A common mistake investors make is the failure to implement a tax diversification strategy. Brokerage accounts, Roth IRAs, and qualified plans are subject to various forms of taxation. It is important to utilize the tax advantages of these tools to ensure they work for you in the most productive manner possible. A properly integrated approach is critical during your accumulation phase. Further, it is just as important when you enter the distribution period of your investment life cycle (ie, retirement).
Master Limited Partnerships offer a potentially advantageous income stream for a brokerage account, while it is generally preferable for qualified accounts to own high yield bonds and corporate debt, as they are taxed at ordinary income rates. There are countless additional examples we could discuss, but the lesson is simple: it is important to review the pieces of your plan with an advisor who will consider both tax diversification and security diversification as they relate to your specific circumstances.
2. Consider Owning Municipal Bonds in Taxable Accounts: Most municipal bonds are exempt from federal taxation. Certain issues may also be exempt from state and local taxes. If you are in the highest federal tax bracket, you may be paying tax on investment income at a rate of 43.4%. Under these circumstances, a municipal bond yielding 3% will provide a superior after tax return in comparison to a corporate bond yielding 5% in an individual or joint registration, a pass-through LLC, or in many trust accounts. Therefore, it is important in many circumstances to make certain your long-term plan utilizes the advantages of owning certain municipal bonds in taxable accounts.
3. Be Cognizant of Holding Periods: Long-term capital gains rates are much more favorable than short-term rates. Holding a security for a period of 12 months presents an opportunity to save nearly 20% on the taxation of your appreciated position. For example, an initial investment of $50,000 which grows to $100,000 represents a $50,000 unrealized gain. If an investor in the highest tax bracket simply delays liquidation of the position (assuming the security price does not change) the tax savings in this scenario would be $9,800. Although an awareness of the holding period of a security would appear to be a basic principal of investing, many mutual funds and managed accounts are not designed for tax sensitivity. High income investors should be aware that the average client of most advisors is not in the highest federal tax bracket. Therefore, it is generally advantageous to seek the advice of a financial professional with experience executing an appropriate exit strategy that is aware of holding periods.
4. Proactively Realize Losses to Offset Gains: As mentioned in the opening paragraphs of the article, 2015 presented investors with an opportunity to realize losses in domestic stocks for the first time in 4 years. Clients with a diversified portfolio may still have an opportunity to offset gains in domestic stocks by selling foreign equities. One benefit of diversifying across asset classes is that if the portfolio is structured properly, the securities typically will not move in tandem. This divergence of returns among asset classes not only reduces portfolio volatility, but it creates a tax planning opportunity. Domestic equities experienced tremendous appreciation over a 5-year period through 2014; however, international stocks, commodities, and multiple fixed income investments experienced down years. Astute advisors were presented with the opportunity to save clients thousands of dollars in taxes by performing strategic tax swaps prior to year-end. It is important to understand the rules relating to wash sales when executing such tactics. The laws are confusing, and if a mistake is made your loss could be disallowed. Make certain your advisor is well-versed in utilizing tax offsets.
5. Think Twice About Gifting Cash: This is not to discourage your charitable intentions. Quite the opposite is true. However, a successful investor can occasionally find themselves in a precarious position. You may have allocated 5% of your portfolio to a growth stock with significant upside. Several years have passed, the security has experienced explosive growth, and it now represents 15% of your investable assets. Suddenly your portfolio has a concentrated position with significant gains, and the level of risk is no longer consistent with your long-term objectives. The sound practice of rebalancing your portfolio then becomes very costly, because liquidation of the stock could create a taxable event that may negatively impact your net return.
By planning ahead of time, you may be able to gift a portion of the appreciated security to a charitable organization able to accept this type of donation. The value of your gift can be replaced with the cash you originally intended to donate to the charitable organization and, in this scenario, your cash will create a new cost basis. The charity can liquidate the stock without paying tax, and you have removed a future tax liability from your portfolio. Implementing the aforementioned gifting strategy offers the potential to save thousands of dollars in taxes over the life of your portfolio.
6. Understand your Mutual Fund’s Tax Cost Ratio: The technical detail behind a mutual fund’s tax cost ratio is beyond the scope of this article. Our intent is to simply bring this topic to your attention. Tax cost ratio represents the percentage of an investor’s assets that are lost to taxes. Mutual funds avoid double taxation, provided they pay at least 90% of net investment income and realized capital gains to shareholders at the end of the calendar year. But all mutual funds are not created equally, and proper research will allow you to identify funds that are tax efficient.
A well-managed mutual fund will add diversification to a portfolio while creating the opportunity to outperform asset classes with inefficient markets. You do need to be aware of funds with excessive turnover. An understanding of when a fund pays its capital gains distributions is a critical component of successful investing. A poorly timed fund purchase can result in acquiring another investor’s tax liability. It is not unusual for an investor to experience a negative return in a calendar year, yet find himself on the receiving end of a capital gains distribution. Understanding the tax cost ratios of the funds that make up portions of your investment plan will enable you to take advantage of the many benefits of owning mutual funds.
The above steps are by no means the only tax strategies experienced advisors can execute on behalf of their clients. This article highlights several strategies you should discuss with your advisor to determine if implementation is appropriate for your unique portfolio and overall financial situation. Successful investing requires discipline that extends beyond proper security selection. While gross returns are important and should not be ignored, the percentage return you see on your statements does not tell the full story.
In today’s tax environment, successful investors must choose an advisor who will help them look beyond portfolio earnings and focus on strategic after-tax asset growth.
To receive a free hardcopy of Wealth Protection Planning for Orthopaedic Surgeons, please call 877-656-4362. Visit www.ojmbookstore.com and enter promotional code AJO30 for a free ebook download of Wealth Protection Planning or one of our other ebooks for your Kindle or iPad.
Orthopedic physicians in the highest income tax brackets may have been presented with an unpleasant surprise in recent years when they learned of their investment tax liability. A prolonged period of strong domestic stock performance from 2009 to 2016, combined with the implementation of The American Taxpayer Relief Act of 2012, may have resulted in significantly higher taxes for many of you.
The top ordinary income tax rates increased by 24% when including the Net Investment Income surtax, while the top capital gains rate was increased by more than 58%. Writing a large check to the Internal Revenue Service serves as a harsh reminder that tax planning requires attention throughout the year, and is not a technique you can properly manage a few weeks before an April 15 deadline.
Proper tax planning became more critical as we moved into an era of higher taxes. A multi-year bull market for domestic stocks has caused many traditional investment vehicles to hold large amounts of unrealized gains, which can become realized gains if you are not careful. Most major equity indices took a breath in 2015 and finished the year in the red, which created a planning opportunity for astute investors and their advisors. Stocks in the US and emerging market countries quickly bounced back in 2016; however, European stocks struggled and continue to trade well below peak levels reached nearly a decade ago. Investors who missed the opportunity to offset gains of the prior 2 years may have an opportunity to reduce their tax bill in 2017.
In this article, we will provide you with 6 suggestions that could save you thousands of dollars in investment taxes over the next several years.
1. Account Registration Matters: A common mistake investors make is the failure to implement a tax diversification strategy. Brokerage accounts, Roth IRAs, and qualified plans are subject to various forms of taxation. It is important to utilize the tax advantages of these tools to ensure they work for you in the most productive manner possible. A properly integrated approach is critical during your accumulation phase. Further, it is just as important when you enter the distribution period of your investment life cycle (ie, retirement).
Master Limited Partnerships offer a potentially advantageous income stream for a brokerage account, while it is generally preferable for qualified accounts to own high yield bonds and corporate debt, as they are taxed at ordinary income rates. There are countless additional examples we could discuss, but the lesson is simple: it is important to review the pieces of your plan with an advisor who will consider both tax diversification and security diversification as they relate to your specific circumstances.
2. Consider Owning Municipal Bonds in Taxable Accounts: Most municipal bonds are exempt from federal taxation. Certain issues may also be exempt from state and local taxes. If you are in the highest federal tax bracket, you may be paying tax on investment income at a rate of 43.4%. Under these circumstances, a municipal bond yielding 3% will provide a superior after tax return in comparison to a corporate bond yielding 5% in an individual or joint registration, a pass-through LLC, or in many trust accounts. Therefore, it is important in many circumstances to make certain your long-term plan utilizes the advantages of owning certain municipal bonds in taxable accounts.
3. Be Cognizant of Holding Periods: Long-term capital gains rates are much more favorable than short-term rates. Holding a security for a period of 12 months presents an opportunity to save nearly 20% on the taxation of your appreciated position. For example, an initial investment of $50,000 which grows to $100,000 represents a $50,000 unrealized gain. If an investor in the highest tax bracket simply delays liquidation of the position (assuming the security price does not change) the tax savings in this scenario would be $9,800. Although an awareness of the holding period of a security would appear to be a basic principal of investing, many mutual funds and managed accounts are not designed for tax sensitivity. High income investors should be aware that the average client of most advisors is not in the highest federal tax bracket. Therefore, it is generally advantageous to seek the advice of a financial professional with experience executing an appropriate exit strategy that is aware of holding periods.
4. Proactively Realize Losses to Offset Gains: As mentioned in the opening paragraphs of the article, 2015 presented investors with an opportunity to realize losses in domestic stocks for the first time in 4 years. Clients with a diversified portfolio may still have an opportunity to offset gains in domestic stocks by selling foreign equities. One benefit of diversifying across asset classes is that if the portfolio is structured properly, the securities typically will not move in tandem. This divergence of returns among asset classes not only reduces portfolio volatility, but it creates a tax planning opportunity. Domestic equities experienced tremendous appreciation over a 5-year period through 2014; however, international stocks, commodities, and multiple fixed income investments experienced down years. Astute advisors were presented with the opportunity to save clients thousands of dollars in taxes by performing strategic tax swaps prior to year-end. It is important to understand the rules relating to wash sales when executing such tactics. The laws are confusing, and if a mistake is made your loss could be disallowed. Make certain your advisor is well-versed in utilizing tax offsets.
5. Think Twice About Gifting Cash: This is not to discourage your charitable intentions. Quite the opposite is true. However, a successful investor can occasionally find themselves in a precarious position. You may have allocated 5% of your portfolio to a growth stock with significant upside. Several years have passed, the security has experienced explosive growth, and it now represents 15% of your investable assets. Suddenly your portfolio has a concentrated position with significant gains, and the level of risk is no longer consistent with your long-term objectives. The sound practice of rebalancing your portfolio then becomes very costly, because liquidation of the stock could create a taxable event that may negatively impact your net return.
By planning ahead of time, you may be able to gift a portion of the appreciated security to a charitable organization able to accept this type of donation. The value of your gift can be replaced with the cash you originally intended to donate to the charitable organization and, in this scenario, your cash will create a new cost basis. The charity can liquidate the stock without paying tax, and you have removed a future tax liability from your portfolio. Implementing the aforementioned gifting strategy offers the potential to save thousands of dollars in taxes over the life of your portfolio.
6. Understand your Mutual Fund’s Tax Cost Ratio: The technical detail behind a mutual fund’s tax cost ratio is beyond the scope of this article. Our intent is to simply bring this topic to your attention. Tax cost ratio represents the percentage of an investor’s assets that are lost to taxes. Mutual funds avoid double taxation, provided they pay at least 90% of net investment income and realized capital gains to shareholders at the end of the calendar year. But all mutual funds are not created equally, and proper research will allow you to identify funds that are tax efficient.
A well-managed mutual fund will add diversification to a portfolio while creating the opportunity to outperform asset classes with inefficient markets. You do need to be aware of funds with excessive turnover. An understanding of when a fund pays its capital gains distributions is a critical component of successful investing. A poorly timed fund purchase can result in acquiring another investor’s tax liability. It is not unusual for an investor to experience a negative return in a calendar year, yet find himself on the receiving end of a capital gains distribution. Understanding the tax cost ratios of the funds that make up portions of your investment plan will enable you to take advantage of the many benefits of owning mutual funds.
The above steps are by no means the only tax strategies experienced advisors can execute on behalf of their clients. This article highlights several strategies you should discuss with your advisor to determine if implementation is appropriate for your unique portfolio and overall financial situation. Successful investing requires discipline that extends beyond proper security selection. While gross returns are important and should not be ignored, the percentage return you see on your statements does not tell the full story.
In today’s tax environment, successful investors must choose an advisor who will help them look beyond portfolio earnings and focus on strategic after-tax asset growth.
To receive a free hardcopy of Wealth Protection Planning for Orthopaedic Surgeons, please call 877-656-4362. Visit www.ojmbookstore.com and enter promotional code AJO30 for a free ebook download of Wealth Protection Planning or one of our other ebooks for your Kindle or iPad.
Orthopedic physicians in the highest income tax brackets may have been presented with an unpleasant surprise in recent years when they learned of their investment tax liability. A prolonged period of strong domestic stock performance from 2009 to 2016, combined with the implementation of The American Taxpayer Relief Act of 2012, may have resulted in significantly higher taxes for many of you.
The top ordinary income tax rates increased by 24% when including the Net Investment Income surtax, while the top capital gains rate was increased by more than 58%. Writing a large check to the Internal Revenue Service serves as a harsh reminder that tax planning requires attention throughout the year, and is not a technique you can properly manage a few weeks before an April 15 deadline.
Proper tax planning became more critical as we moved into an era of higher taxes. A multi-year bull market for domestic stocks has caused many traditional investment vehicles to hold large amounts of unrealized gains, which can become realized gains if you are not careful. Most major equity indices took a breath in 2015 and finished the year in the red, which created a planning opportunity for astute investors and their advisors. Stocks in the US and emerging market countries quickly bounced back in 2016; however, European stocks struggled and continue to trade well below peak levels reached nearly a decade ago. Investors who missed the opportunity to offset gains of the prior 2 years may have an opportunity to reduce their tax bill in 2017.
In this article, we will provide you with 6 suggestions that could save you thousands of dollars in investment taxes over the next several years.
1. Account Registration Matters: A common mistake investors make is the failure to implement a tax diversification strategy. Brokerage accounts, Roth IRAs, and qualified plans are subject to various forms of taxation. It is important to utilize the tax advantages of these tools to ensure they work for you in the most productive manner possible. A properly integrated approach is critical during your accumulation phase. Further, it is just as important when you enter the distribution period of your investment life cycle (ie, retirement).
Master Limited Partnerships offer a potentially advantageous income stream for a brokerage account, while it is generally preferable for qualified accounts to own high yield bonds and corporate debt, as they are taxed at ordinary income rates. There are countless additional examples we could discuss, but the lesson is simple: it is important to review the pieces of your plan with an advisor who will consider both tax diversification and security diversification as they relate to your specific circumstances.
2. Consider Owning Municipal Bonds in Taxable Accounts: Most municipal bonds are exempt from federal taxation. Certain issues may also be exempt from state and local taxes. If you are in the highest federal tax bracket, you may be paying tax on investment income at a rate of 43.4%. Under these circumstances, a municipal bond yielding 3% will provide a superior after tax return in comparison to a corporate bond yielding 5% in an individual or joint registration, a pass-through LLC, or in many trust accounts. Therefore, it is important in many circumstances to make certain your long-term plan utilizes the advantages of owning certain municipal bonds in taxable accounts.
3. Be Cognizant of Holding Periods: Long-term capital gains rates are much more favorable than short-term rates. Holding a security for a period of 12 months presents an opportunity to save nearly 20% on the taxation of your appreciated position. For example, an initial investment of $50,000 which grows to $100,000 represents a $50,000 unrealized gain. If an investor in the highest tax bracket simply delays liquidation of the position (assuming the security price does not change) the tax savings in this scenario would be $9,800. Although an awareness of the holding period of a security would appear to be a basic principal of investing, many mutual funds and managed accounts are not designed for tax sensitivity. High income investors should be aware that the average client of most advisors is not in the highest federal tax bracket. Therefore, it is generally advantageous to seek the advice of a financial professional with experience executing an appropriate exit strategy that is aware of holding periods.
4. Proactively Realize Losses to Offset Gains: As mentioned in the opening paragraphs of the article, 2015 presented investors with an opportunity to realize losses in domestic stocks for the first time in 4 years. Clients with a diversified portfolio may still have an opportunity to offset gains in domestic stocks by selling foreign equities. One benefit of diversifying across asset classes is that if the portfolio is structured properly, the securities typically will not move in tandem. This divergence of returns among asset classes not only reduces portfolio volatility, but it creates a tax planning opportunity. Domestic equities experienced tremendous appreciation over a 5-year period through 2014; however, international stocks, commodities, and multiple fixed income investments experienced down years. Astute advisors were presented with the opportunity to save clients thousands of dollars in taxes by performing strategic tax swaps prior to year-end. It is important to understand the rules relating to wash sales when executing such tactics. The laws are confusing, and if a mistake is made your loss could be disallowed. Make certain your advisor is well-versed in utilizing tax offsets.
5. Think Twice About Gifting Cash: This is not to discourage your charitable intentions. Quite the opposite is true. However, a successful investor can occasionally find themselves in a precarious position. You may have allocated 5% of your portfolio to a growth stock with significant upside. Several years have passed, the security has experienced explosive growth, and it now represents 15% of your investable assets. Suddenly your portfolio has a concentrated position with significant gains, and the level of risk is no longer consistent with your long-term objectives. The sound practice of rebalancing your portfolio then becomes very costly, because liquidation of the stock could create a taxable event that may negatively impact your net return.
By planning ahead of time, you may be able to gift a portion of the appreciated security to a charitable organization able to accept this type of donation. The value of your gift can be replaced with the cash you originally intended to donate to the charitable organization and, in this scenario, your cash will create a new cost basis. The charity can liquidate the stock without paying tax, and you have removed a future tax liability from your portfolio. Implementing the aforementioned gifting strategy offers the potential to save thousands of dollars in taxes over the life of your portfolio.
6. Understand your Mutual Fund’s Tax Cost Ratio: The technical detail behind a mutual fund’s tax cost ratio is beyond the scope of this article. Our intent is to simply bring this topic to your attention. Tax cost ratio represents the percentage of an investor’s assets that are lost to taxes. Mutual funds avoid double taxation, provided they pay at least 90% of net investment income and realized capital gains to shareholders at the end of the calendar year. But all mutual funds are not created equally, and proper research will allow you to identify funds that are tax efficient.
A well-managed mutual fund will add diversification to a portfolio while creating the opportunity to outperform asset classes with inefficient markets. You do need to be aware of funds with excessive turnover. An understanding of when a fund pays its capital gains distributions is a critical component of successful investing. A poorly timed fund purchase can result in acquiring another investor’s tax liability. It is not unusual for an investor to experience a negative return in a calendar year, yet find himself on the receiving end of a capital gains distribution. Understanding the tax cost ratios of the funds that make up portions of your investment plan will enable you to take advantage of the many benefits of owning mutual funds.
The above steps are by no means the only tax strategies experienced advisors can execute on behalf of their clients. This article highlights several strategies you should discuss with your advisor to determine if implementation is appropriate for your unique portfolio and overall financial situation. Successful investing requires discipline that extends beyond proper security selection. While gross returns are important and should not be ignored, the percentage return you see on your statements does not tell the full story.
In today’s tax environment, successful investors must choose an advisor who will help them look beyond portfolio earnings and focus on strategic after-tax asset growth.
To receive a free hardcopy of Wealth Protection Planning for Orthopaedic Surgeons, please call 877-656-4362. Visit www.ojmbookstore.com and enter promotional code AJO30 for a free ebook download of Wealth Protection Planning or one of our other ebooks for your Kindle or iPad.
Firing
Last month’s column on good hiring practices, which stressed the importance of replacing marginal employees with excellent ones, triggered an interesting round of discussion. “Isn’t it true,” asked one contributor, “that most physicians tolerate marginal employees because it’s less painful than firing them?”
Indeed it is. Firing someone is never easy, and it is particularly tough on physicians. Sometimes, however, it is unavoidable if you want to preserve the efficiency and morale of your other employees, as well as your own.
Before you do it, however, be sure that you have legitimate grounds, and assemble as much documentation as you can. Record all terminatable transgressions in the employee’s permanent record, and document all verbal and written warnings. This is essential. You must be prepared to prove that your reasons for termination were legal.
Former employees will sometimes charge that any of a number of their civil rights was violated. For example, federal law prohibits you from firing anyone because of race, gender, national origin, disability, religion, or age (if the employee is over 40). You cannot fire a woman because she is pregnant or recently gave birth. Other illegal reasons include assertion of antidiscrimination rights, refusal to take a lie detector test, and report of OSHA violations.
You also can’t terminate someone for refusing to commit an illegal act, such as filing false insurance claims, or for exercising a legal right, such as voting or participating in a political demonstration. You cannot fire an alcohol abuser unless he or she is caught drinking at work, but many forms of illegal drug use are legitimate cause for termination. Other laws may apply, depending on where you live. When in doubt, contact your state labor department or fair employment office.
If a fired employee alleges that he or she was fired for any of these illegal reasons and you do not have convincing documentation to counter the charge, you may find yourself defending your actions in court. If you anticipate such problems, you can ask the employee to sign a waver of future litigation in exchange for a concession from you – such as extra severance pay or a promise not to contest an unemployment application. Also, consider adding employment practices liability insurance (EPLI) to your umbrella policy, since lawsuits are always a possibility despite all efforts to prevent them.
Once you have all your legal ducks in a row, don’t procrastinate. Get it over with first thing on Monday morning. If you wait until Friday afternoon (as many do), you will worry about the dreaded task all week long, and the fired employee will stew about it all weekend.
Explain the performance you have expected, the steps you have taken to help correct the problems you have seen, and the fact that the problems persist. Try to limit the conversation to a minute or two, have the final paycheck ready, and make it clear that the decision has already been made, so begging and pleading will not change anything.
I’ve been asked to share exactly what I say, so, for what it’s worth: “I have called you in to discuss a difficult issue. You know that we have not been happy with your performance. We are still not happy with it, despite all the discussions we have had, and we feel that you can do better elsewhere. So, today, we will part company, and I wish you the best of luck in your future endeavors. Here is your severance check. I hope there are no hard feelings.”
There will, of course, be hard feelings, but that cannot be helped. The point is to be quick, firm, and decisive. Get it over with and allow everyone to move on.
Be sure to get all your office keys back – or change the locks if you cannot. Back up all important computer files, and change all your passwords. Most employees know more of them than you would ever suspect.
Finally, call the staff together and explain what you have done. They should hear the real story from you, not some distorted version via the rumor mill. You don’t have to explain your reasoning or divulge every detail, but do explain how the termination will affect everyone else. Responsibilities will need to be shifted until a replacement can be hired, and all employees should understand that.
If you are asked in the future to give a reference or write a letter of recommendation for the terminated employee, be sure that everything you say is truthful and well documented.
Last month’s column on good hiring practices, which stressed the importance of replacing marginal employees with excellent ones, triggered an interesting round of discussion. “Isn’t it true,” asked one contributor, “that most physicians tolerate marginal employees because it’s less painful than firing them?”
Indeed it is. Firing someone is never easy, and it is particularly tough on physicians. Sometimes, however, it is unavoidable if you want to preserve the efficiency and morale of your other employees, as well as your own.
Before you do it, however, be sure that you have legitimate grounds, and assemble as much documentation as you can. Record all terminatable transgressions in the employee’s permanent record, and document all verbal and written warnings. This is essential. You must be prepared to prove that your reasons for termination were legal.
Former employees will sometimes charge that any of a number of their civil rights was violated. For example, federal law prohibits you from firing anyone because of race, gender, national origin, disability, religion, or age (if the employee is over 40). You cannot fire a woman because she is pregnant or recently gave birth. Other illegal reasons include assertion of antidiscrimination rights, refusal to take a lie detector test, and report of OSHA violations.
You also can’t terminate someone for refusing to commit an illegal act, such as filing false insurance claims, or for exercising a legal right, such as voting or participating in a political demonstration. You cannot fire an alcohol abuser unless he or she is caught drinking at work, but many forms of illegal drug use are legitimate cause for termination. Other laws may apply, depending on where you live. When in doubt, contact your state labor department or fair employment office.
If a fired employee alleges that he or she was fired for any of these illegal reasons and you do not have convincing documentation to counter the charge, you may find yourself defending your actions in court. If you anticipate such problems, you can ask the employee to sign a waver of future litigation in exchange for a concession from you – such as extra severance pay or a promise not to contest an unemployment application. Also, consider adding employment practices liability insurance (EPLI) to your umbrella policy, since lawsuits are always a possibility despite all efforts to prevent them.
Once you have all your legal ducks in a row, don’t procrastinate. Get it over with first thing on Monday morning. If you wait until Friday afternoon (as many do), you will worry about the dreaded task all week long, and the fired employee will stew about it all weekend.
Explain the performance you have expected, the steps you have taken to help correct the problems you have seen, and the fact that the problems persist. Try to limit the conversation to a minute or two, have the final paycheck ready, and make it clear that the decision has already been made, so begging and pleading will not change anything.
I’ve been asked to share exactly what I say, so, for what it’s worth: “I have called you in to discuss a difficult issue. You know that we have not been happy with your performance. We are still not happy with it, despite all the discussions we have had, and we feel that you can do better elsewhere. So, today, we will part company, and I wish you the best of luck in your future endeavors. Here is your severance check. I hope there are no hard feelings.”
There will, of course, be hard feelings, but that cannot be helped. The point is to be quick, firm, and decisive. Get it over with and allow everyone to move on.
Be sure to get all your office keys back – or change the locks if you cannot. Back up all important computer files, and change all your passwords. Most employees know more of them than you would ever suspect.
Finally, call the staff together and explain what you have done. They should hear the real story from you, not some distorted version via the rumor mill. You don’t have to explain your reasoning or divulge every detail, but do explain how the termination will affect everyone else. Responsibilities will need to be shifted until a replacement can be hired, and all employees should understand that.
If you are asked in the future to give a reference or write a letter of recommendation for the terminated employee, be sure that everything you say is truthful and well documented.
Last month’s column on good hiring practices, which stressed the importance of replacing marginal employees with excellent ones, triggered an interesting round of discussion. “Isn’t it true,” asked one contributor, “that most physicians tolerate marginal employees because it’s less painful than firing them?”
Indeed it is. Firing someone is never easy, and it is particularly tough on physicians. Sometimes, however, it is unavoidable if you want to preserve the efficiency and morale of your other employees, as well as your own.
Before you do it, however, be sure that you have legitimate grounds, and assemble as much documentation as you can. Record all terminatable transgressions in the employee’s permanent record, and document all verbal and written warnings. This is essential. You must be prepared to prove that your reasons for termination were legal.
Former employees will sometimes charge that any of a number of their civil rights was violated. For example, federal law prohibits you from firing anyone because of race, gender, national origin, disability, religion, or age (if the employee is over 40). You cannot fire a woman because she is pregnant or recently gave birth. Other illegal reasons include assertion of antidiscrimination rights, refusal to take a lie detector test, and report of OSHA violations.
You also can’t terminate someone for refusing to commit an illegal act, such as filing false insurance claims, or for exercising a legal right, such as voting or participating in a political demonstration. You cannot fire an alcohol abuser unless he or she is caught drinking at work, but many forms of illegal drug use are legitimate cause for termination. Other laws may apply, depending on where you live. When in doubt, contact your state labor department or fair employment office.
If a fired employee alleges that he or she was fired for any of these illegal reasons and you do not have convincing documentation to counter the charge, you may find yourself defending your actions in court. If you anticipate such problems, you can ask the employee to sign a waver of future litigation in exchange for a concession from you – such as extra severance pay or a promise not to contest an unemployment application. Also, consider adding employment practices liability insurance (EPLI) to your umbrella policy, since lawsuits are always a possibility despite all efforts to prevent them.
Once you have all your legal ducks in a row, don’t procrastinate. Get it over with first thing on Monday morning. If you wait until Friday afternoon (as many do), you will worry about the dreaded task all week long, and the fired employee will stew about it all weekend.
Explain the performance you have expected, the steps you have taken to help correct the problems you have seen, and the fact that the problems persist. Try to limit the conversation to a minute or two, have the final paycheck ready, and make it clear that the decision has already been made, so begging and pleading will not change anything.
I’ve been asked to share exactly what I say, so, for what it’s worth: “I have called you in to discuss a difficult issue. You know that we have not been happy with your performance. We are still not happy with it, despite all the discussions we have had, and we feel that you can do better elsewhere. So, today, we will part company, and I wish you the best of luck in your future endeavors. Here is your severance check. I hope there are no hard feelings.”
There will, of course, be hard feelings, but that cannot be helped. The point is to be quick, firm, and decisive. Get it over with and allow everyone to move on.
Be sure to get all your office keys back – or change the locks if you cannot. Back up all important computer files, and change all your passwords. Most employees know more of them than you would ever suspect.
Finally, call the staff together and explain what you have done. They should hear the real story from you, not some distorted version via the rumor mill. You don’t have to explain your reasoning or divulge every detail, but do explain how the termination will affect everyone else. Responsibilities will need to be shifted until a replacement can be hired, and all employees should understand that.
If you are asked in the future to give a reference or write a letter of recommendation for the terminated employee, be sure that everything you say is truthful and well documented.
In-office hysteroscopy procedures: Reimbursement jumps 237%
As it does annually, the Centers for Medicare & Medicaid Services (CMS) has announced changes to the resource-based relative value scale (RBRVS) physician payment system. This system is not static, and each year the CMS identifies codes to review that appear to be either overvalued or undervalued. While the CMS leads this process, the American Medical Association (AMA), working in conjunction with national medical specialty societies, provides annual recommended updates and changes to the CMS via its AMA/Specialty Society RVS Update Committee (RUC).
RVUs defined
Relative value units (RVUs), assigned to most codes found in the AMA’s Current Procedural Terminology (CPT) book, are calculated based on 3 elements: physician work, practice expense, and malpractice cost. For Medicare reimbursement purposes, these elements are adjusted by the current geographic index, and this adjusted RVU is then multiplied by the Medicare calculated annual conversion factor (in fiscal year 2017, that amount is $35.8887) to determine the final allowable for any given provider.
Commercial payers who use the RBRVS system for reimbursement usually calculate their own conversion factors, which they may or may not publish. Such calculation can be based on a percentage increase over the Medicare rate or other factors.
In-office hysteroscopy procedure reimbursement increases
This year, some notable increases and decreases in the practice expense element will impact payment to ObGyn practices. The best news is that for practices in which clinicians have been removing polyps or performing endometrial sampling or a full dilation and curettage (D & C) using a hysteroscope in the office, practice expense reimbursement now will improve dramatically. The practice expense RVU for CPT code 58558, Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy, with or without D & C, has been increased more than 450% in this setting, with an increase from 6.11 in 2016 to 33.82 as of January 2, 2017, which reduces to a 237% increase when the change to the total RVU is calculated.
More new-found income. The only other procedure showing at least a 10% increase in reimbursement in the office setting is the professional component for the ultrasonic guidance for aspiration of ova.
When your reimbursements will decrease
Unfortunately, reimbursement has also been decreased for some CPT code procedures. The urodynamic study code 51784, Electromyography studies (EMG) of anal or urethral sphincter, other than needle, any technique, has decreased in RVU value by about 64%. This is due to cutting by half the physician work, practice expense, and malpractice cost RVU elements. Although hit with a somewhat smaller decrease, code 58562, Hysteroscopy, surgical; with removal of impacted foreign body, also suffered a decrease in all 3 RVU elements in the office setting, amounting to about a 19% decrease.
In the facility setting, the RVU for the code for vaginoplasty has been increased by 10%, but 11 procedures have lost between 11% and 19% of their previous RVU levels in this setting, and more than half are for hysteroscopic procedures. The complete list of codes that have incurred at least a 10% RVU change in 2017 are listed in TABLES 1 and 2 according to place of service.
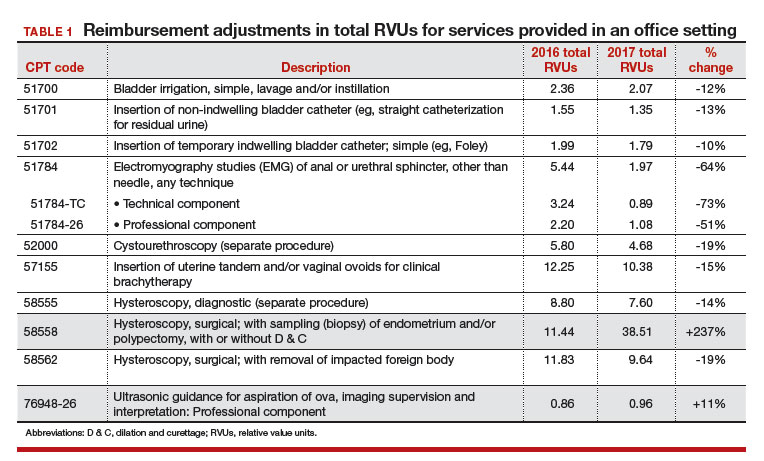
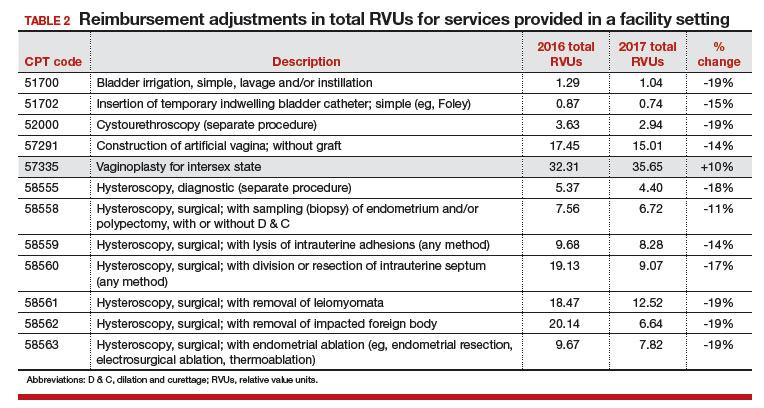
Related article:
GYN coding changes to note for your maximized reimbursement
What’s up next for review and possible adjustment
Finally, as a reminder to all providers, the CMS has identified 3 procedure codes that are potentially misvalued due to their being reported more than 50% of the time with an evaluation and management (E/M) service. These codes represent 0-day procedures and will be evaluated during 2017:
- 57150, Irrigation of vagina and/or application of medicament for treatment of bacterial, parasitic, or fungoid disease
- 57160, Fitting and insertion of pessary or other intravaginal support device
- 58100, Endometrial sampling (biopsy) with or without endocervical sampling (biopsy), without cervical dilation, any method (separate procedure).
The CMS has made it clear that all 0-day procedure codes include evaluation services on the date of service, including the decision to do the procedure. If the CMS examination of data finds that the documentation does not support a separate and significant E/M service at the time of the procedure, the agency will consider adjusting the physician work component. All providers should therefore examine their reporting of an E/M service with 0-day procedures to ensure that the documentation clearly supports doing so.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
As it does annually, the Centers for Medicare & Medicaid Services (CMS) has announced changes to the resource-based relative value scale (RBRVS) physician payment system. This system is not static, and each year the CMS identifies codes to review that appear to be either overvalued or undervalued. While the CMS leads this process, the American Medical Association (AMA), working in conjunction with national medical specialty societies, provides annual recommended updates and changes to the CMS via its AMA/Specialty Society RVS Update Committee (RUC).
RVUs defined
Relative value units (RVUs), assigned to most codes found in the AMA’s Current Procedural Terminology (CPT) book, are calculated based on 3 elements: physician work, practice expense, and malpractice cost. For Medicare reimbursement purposes, these elements are adjusted by the current geographic index, and this adjusted RVU is then multiplied by the Medicare calculated annual conversion factor (in fiscal year 2017, that amount is $35.8887) to determine the final allowable for any given provider.
Commercial payers who use the RBRVS system for reimbursement usually calculate their own conversion factors, which they may or may not publish. Such calculation can be based on a percentage increase over the Medicare rate or other factors.
In-office hysteroscopy procedure reimbursement increases
This year, some notable increases and decreases in the practice expense element will impact payment to ObGyn practices. The best news is that for practices in which clinicians have been removing polyps or performing endometrial sampling or a full dilation and curettage (D & C) using a hysteroscope in the office, practice expense reimbursement now will improve dramatically. The practice expense RVU for CPT code 58558, Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy, with or without D & C, has been increased more than 450% in this setting, with an increase from 6.11 in 2016 to 33.82 as of January 2, 2017, which reduces to a 237% increase when the change to the total RVU is calculated.
More new-found income. The only other procedure showing at least a 10% increase in reimbursement in the office setting is the professional component for the ultrasonic guidance for aspiration of ova.
When your reimbursements will decrease
Unfortunately, reimbursement has also been decreased for some CPT code procedures. The urodynamic study code 51784, Electromyography studies (EMG) of anal or urethral sphincter, other than needle, any technique, has decreased in RVU value by about 64%. This is due to cutting by half the physician work, practice expense, and malpractice cost RVU elements. Although hit with a somewhat smaller decrease, code 58562, Hysteroscopy, surgical; with removal of impacted foreign body, also suffered a decrease in all 3 RVU elements in the office setting, amounting to about a 19% decrease.
In the facility setting, the RVU for the code for vaginoplasty has been increased by 10%, but 11 procedures have lost between 11% and 19% of their previous RVU levels in this setting, and more than half are for hysteroscopic procedures. The complete list of codes that have incurred at least a 10% RVU change in 2017 are listed in TABLES 1 and 2 according to place of service.
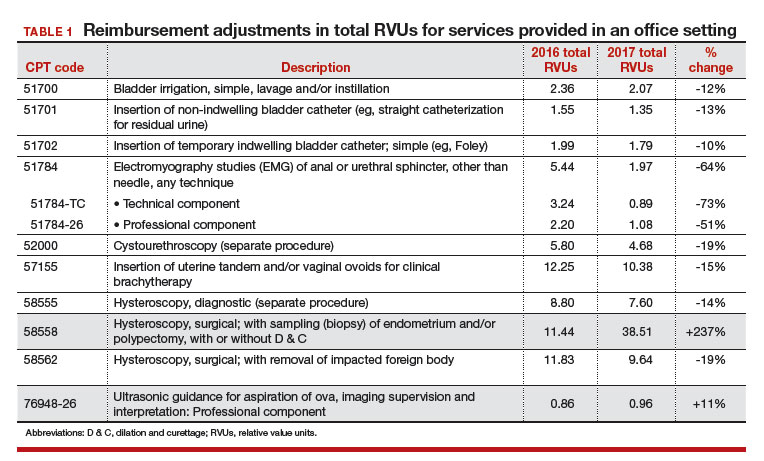
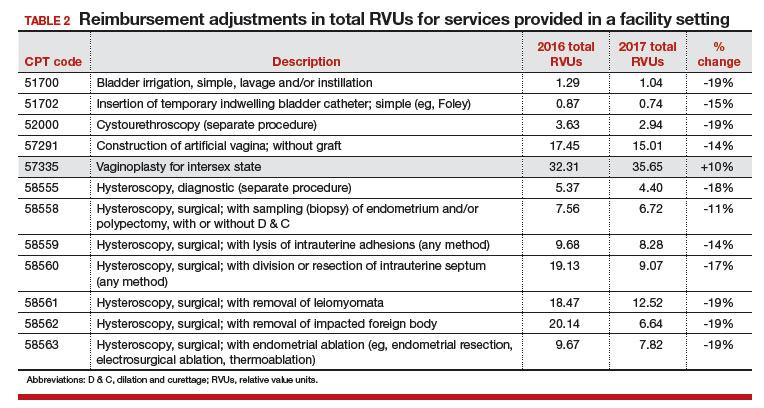
Related article:
GYN coding changes to note for your maximized reimbursement
What’s up next for review and possible adjustment
Finally, as a reminder to all providers, the CMS has identified 3 procedure codes that are potentially misvalued due to their being reported more than 50% of the time with an evaluation and management (E/M) service. These codes represent 0-day procedures and will be evaluated during 2017:
- 57150, Irrigation of vagina and/or application of medicament for treatment of bacterial, parasitic, or fungoid disease
- 57160, Fitting and insertion of pessary or other intravaginal support device
- 58100, Endometrial sampling (biopsy) with or without endocervical sampling (biopsy), without cervical dilation, any method (separate procedure).
The CMS has made it clear that all 0-day procedure codes include evaluation services on the date of service, including the decision to do the procedure. If the CMS examination of data finds that the documentation does not support a separate and significant E/M service at the time of the procedure, the agency will consider adjusting the physician work component. All providers should therefore examine their reporting of an E/M service with 0-day procedures to ensure that the documentation clearly supports doing so.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
As it does annually, the Centers for Medicare & Medicaid Services (CMS) has announced changes to the resource-based relative value scale (RBRVS) physician payment system. This system is not static, and each year the CMS identifies codes to review that appear to be either overvalued or undervalued. While the CMS leads this process, the American Medical Association (AMA), working in conjunction with national medical specialty societies, provides annual recommended updates and changes to the CMS via its AMA/Specialty Society RVS Update Committee (RUC).
RVUs defined
Relative value units (RVUs), assigned to most codes found in the AMA’s Current Procedural Terminology (CPT) book, are calculated based on 3 elements: physician work, practice expense, and malpractice cost. For Medicare reimbursement purposes, these elements are adjusted by the current geographic index, and this adjusted RVU is then multiplied by the Medicare calculated annual conversion factor (in fiscal year 2017, that amount is $35.8887) to determine the final allowable for any given provider.
Commercial payers who use the RBRVS system for reimbursement usually calculate their own conversion factors, which they may or may not publish. Such calculation can be based on a percentage increase over the Medicare rate or other factors.
In-office hysteroscopy procedure reimbursement increases
This year, some notable increases and decreases in the practice expense element will impact payment to ObGyn practices. The best news is that for practices in which clinicians have been removing polyps or performing endometrial sampling or a full dilation and curettage (D & C) using a hysteroscope in the office, practice expense reimbursement now will improve dramatically. The practice expense RVU for CPT code 58558, Hysteroscopy, surgical; with sampling (biopsy) of endometrium and/or polypectomy, with or without D & C, has been increased more than 450% in this setting, with an increase from 6.11 in 2016 to 33.82 as of January 2, 2017, which reduces to a 237% increase when the change to the total RVU is calculated.
More new-found income. The only other procedure showing at least a 10% increase in reimbursement in the office setting is the professional component for the ultrasonic guidance for aspiration of ova.
When your reimbursements will decrease
Unfortunately, reimbursement has also been decreased for some CPT code procedures. The urodynamic study code 51784, Electromyography studies (EMG) of anal or urethral sphincter, other than needle, any technique, has decreased in RVU value by about 64%. This is due to cutting by half the physician work, practice expense, and malpractice cost RVU elements. Although hit with a somewhat smaller decrease, code 58562, Hysteroscopy, surgical; with removal of impacted foreign body, also suffered a decrease in all 3 RVU elements in the office setting, amounting to about a 19% decrease.
In the facility setting, the RVU for the code for vaginoplasty has been increased by 10%, but 11 procedures have lost between 11% and 19% of their previous RVU levels in this setting, and more than half are for hysteroscopic procedures. The complete list of codes that have incurred at least a 10% RVU change in 2017 are listed in TABLES 1 and 2 according to place of service.
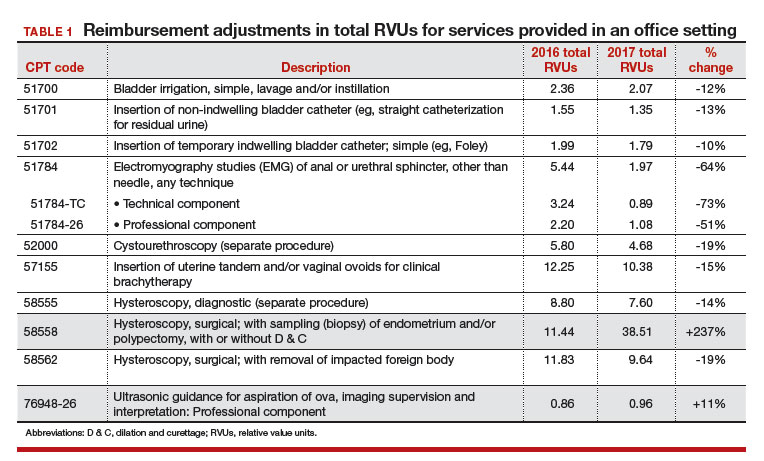
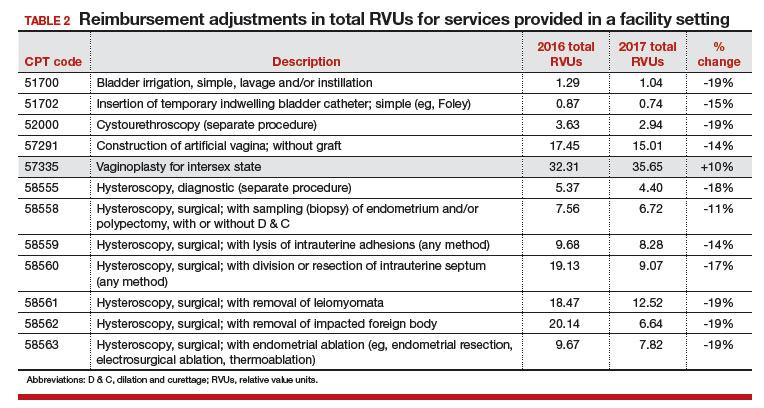
Related article:
GYN coding changes to note for your maximized reimbursement
What’s up next for review and possible adjustment
Finally, as a reminder to all providers, the CMS has identified 3 procedure codes that are potentially misvalued due to their being reported more than 50% of the time with an evaluation and management (E/M) service. These codes represent 0-day procedures and will be evaluated during 2017:
- 57150, Irrigation of vagina and/or application of medicament for treatment of bacterial, parasitic, or fungoid disease
- 57160, Fitting and insertion of pessary or other intravaginal support device
- 58100, Endometrial sampling (biopsy) with or without endocervical sampling (biopsy), without cervical dilation, any method (separate procedure).
The CMS has made it clear that all 0-day procedure codes include evaluation services on the date of service, including the decision to do the procedure. If the CMS examination of data finds that the documentation does not support a separate and significant E/M service at the time of the procedure, the agency will consider adjusting the physician work component. All providers should therefore examine their reporting of an E/M service with 0-day procedures to ensure that the documentation clearly supports doing so.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
IN THIS ARTICLE
- Relative value scale changes
- In-office servicesreimbursement
- In-facility servicesreimbursement
Hiring the right employees
Many of the personnel questions I receive concern the dreaded “marginal employee” – a person who has never done anything truly heinous to merit firing but also hasn’t done anything special to merit continued employment. I always advise getting rid of such people and then changing the hiring criteria that all too often result in poor hires.
Most bad hires come about because employers do not have a clear vision of the kind of employee they want. Many office manuals do not contain detailed job descriptions. If you don’t know exactly what you are looking for, your entire selection process will be inadequate from initial screening of applicants through assessments of their skills and personalities. Many physicians compound the problem with poor interview techniques and inadequate checking of references.
Once you have a clear job description in mind (and in print), take all the time you need to find the best possible match for it. This is not a place to cut corners. Screen your candidates carefully, and avoid lowering your expectations. This is the point at which it might be tempting to settle for a marginal candidate just to get the process over with.
It is also sometimes tempting to hire the candidate that you have the “best feeling” about, even though he or she is a poor match for the job, and then try to mold the job to that person. Every doctor knows that hunches are no substitute for hard data.
Be alert for red flags in resumes: significant time gaps between jobs, positions at companies that are no longer in business or are otherwise impossible to verify, job titles that don’t make sense given the applicant’s qualifications.
Background checks are a dicey subject, but publicly available information can be found, cheap or free, on multiple web sites created for that purpose. Be sure to tell applicants that you will be verifying facts in their resumes. It’s usually wise to get their written consent to do so.
Many employers skip the essential step of calling references, and many applicants know that. Some old bosses will be reluctant to tell you anything substantive, so I always ask, “Would you hire this person again?” You can interpret a lot from the answer – or lack of one.
Interviews often get short shrift as well. Many doctors tend to do all the talking. As I’ve observed numerous times, listening is not our strong suit, as a general rule. The purpose of an interview is to allow you to size up the prospective employee, not to deliver a lecture on the sterling attributes of your office. Important interview topics include educational background, skills, experience, and unrelated job history.
By law, you cannot ask an applicant’s age, date of birth, gender, creed, color, religion, or national origin. Other forbidden subjects include disabilities, marital status, military record, number of children (or who cares for them), addiction history, citizenship, criminal record, psychiatric history, absenteeism, or workman’s compensation.
However, there are acceptable alternatives to some of those questions. You can ask if applicants have ever gone by another name (for your background check), for example. You can ask if they are legally authorized to work in this country and whether they will be physically able to perform the duties specified in the job description. While past addictions are off limits, you do have a right to know about current addictions to illegal substances.
Once you have hired people whose skills and personalities best fit your needs, train them well. Then, give them the opportunity to succeed. “The best executive,” wrote Theodore Roosevelt, “is one who has sense enough to pick good people to do what he [or she] wants done and self-restraint enough to keep from meddling with them while they do it.” ”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Many of the personnel questions I receive concern the dreaded “marginal employee” – a person who has never done anything truly heinous to merit firing but also hasn’t done anything special to merit continued employment. I always advise getting rid of such people and then changing the hiring criteria that all too often result in poor hires.
Most bad hires come about because employers do not have a clear vision of the kind of employee they want. Many office manuals do not contain detailed job descriptions. If you don’t know exactly what you are looking for, your entire selection process will be inadequate from initial screening of applicants through assessments of their skills and personalities. Many physicians compound the problem with poor interview techniques and inadequate checking of references.
Once you have a clear job description in mind (and in print), take all the time you need to find the best possible match for it. This is not a place to cut corners. Screen your candidates carefully, and avoid lowering your expectations. This is the point at which it might be tempting to settle for a marginal candidate just to get the process over with.
It is also sometimes tempting to hire the candidate that you have the “best feeling” about, even though he or she is a poor match for the job, and then try to mold the job to that person. Every doctor knows that hunches are no substitute for hard data.
Be alert for red flags in resumes: significant time gaps between jobs, positions at companies that are no longer in business or are otherwise impossible to verify, job titles that don’t make sense given the applicant’s qualifications.
Background checks are a dicey subject, but publicly available information can be found, cheap or free, on multiple web sites created for that purpose. Be sure to tell applicants that you will be verifying facts in their resumes. It’s usually wise to get their written consent to do so.
Many employers skip the essential step of calling references, and many applicants know that. Some old bosses will be reluctant to tell you anything substantive, so I always ask, “Would you hire this person again?” You can interpret a lot from the answer – or lack of one.
Interviews often get short shrift as well. Many doctors tend to do all the talking. As I’ve observed numerous times, listening is not our strong suit, as a general rule. The purpose of an interview is to allow you to size up the prospective employee, not to deliver a lecture on the sterling attributes of your office. Important interview topics include educational background, skills, experience, and unrelated job history.
By law, you cannot ask an applicant’s age, date of birth, gender, creed, color, religion, or national origin. Other forbidden subjects include disabilities, marital status, military record, number of children (or who cares for them), addiction history, citizenship, criminal record, psychiatric history, absenteeism, or workman’s compensation.
However, there are acceptable alternatives to some of those questions. You can ask if applicants have ever gone by another name (for your background check), for example. You can ask if they are legally authorized to work in this country and whether they will be physically able to perform the duties specified in the job description. While past addictions are off limits, you do have a right to know about current addictions to illegal substances.
Once you have hired people whose skills and personalities best fit your needs, train them well. Then, give them the opportunity to succeed. “The best executive,” wrote Theodore Roosevelt, “is one who has sense enough to pick good people to do what he [or she] wants done and self-restraint enough to keep from meddling with them while they do it.” ”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Many of the personnel questions I receive concern the dreaded “marginal employee” – a person who has never done anything truly heinous to merit firing but also hasn’t done anything special to merit continued employment. I always advise getting rid of such people and then changing the hiring criteria that all too often result in poor hires.
Most bad hires come about because employers do not have a clear vision of the kind of employee they want. Many office manuals do not contain detailed job descriptions. If you don’t know exactly what you are looking for, your entire selection process will be inadequate from initial screening of applicants through assessments of their skills and personalities. Many physicians compound the problem with poor interview techniques and inadequate checking of references.
Once you have a clear job description in mind (and in print), take all the time you need to find the best possible match for it. This is not a place to cut corners. Screen your candidates carefully, and avoid lowering your expectations. This is the point at which it might be tempting to settle for a marginal candidate just to get the process over with.
It is also sometimes tempting to hire the candidate that you have the “best feeling” about, even though he or she is a poor match for the job, and then try to mold the job to that person. Every doctor knows that hunches are no substitute for hard data.
Be alert for red flags in resumes: significant time gaps between jobs, positions at companies that are no longer in business or are otherwise impossible to verify, job titles that don’t make sense given the applicant’s qualifications.
Background checks are a dicey subject, but publicly available information can be found, cheap or free, on multiple web sites created for that purpose. Be sure to tell applicants that you will be verifying facts in their resumes. It’s usually wise to get their written consent to do so.
Many employers skip the essential step of calling references, and many applicants know that. Some old bosses will be reluctant to tell you anything substantive, so I always ask, “Would you hire this person again?” You can interpret a lot from the answer – or lack of one.
Interviews often get short shrift as well. Many doctors tend to do all the talking. As I’ve observed numerous times, listening is not our strong suit, as a general rule. The purpose of an interview is to allow you to size up the prospective employee, not to deliver a lecture on the sterling attributes of your office. Important interview topics include educational background, skills, experience, and unrelated job history.
By law, you cannot ask an applicant’s age, date of birth, gender, creed, color, religion, or national origin. Other forbidden subjects include disabilities, marital status, military record, number of children (or who cares for them), addiction history, citizenship, criminal record, psychiatric history, absenteeism, or workman’s compensation.
However, there are acceptable alternatives to some of those questions. You can ask if applicants have ever gone by another name (for your background check), for example. You can ask if they are legally authorized to work in this country and whether they will be physically able to perform the duties specified in the job description. While past addictions are off limits, you do have a right to know about current addictions to illegal substances.
Once you have hired people whose skills and personalities best fit your needs, train them well. Then, give them the opportunity to succeed. “The best executive,” wrote Theodore Roosevelt, “is one who has sense enough to pick good people to do what he [or she] wants done and self-restraint enough to keep from meddling with them while they do it.” ”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
No-shows
Of all the headaches inherent in a private medical practice, few are more frustrating than patients who make appointments and then fail to keep them.
No-shows are a problem for all physicians but especially for dermatologists. In one study, the no-show rate in dermatology offices averaged 10% – almost double the average for medical offices as a whole.
Why the higher rate? One reason is a lag between appointment and visit. Many dermatologists are booked well in advance, so, by the time the appointment arrives, some patients’ complaints will have resolved spontaneously, while other patients will have found other offices willing to see them sooner. Another reason is lack of insurance coverage. Studies have shown that the no-show rate is highest when the patient is paying out-of-pocket for the visit.
Whatever the reasons, no-shows are an economic and medicolegal liability. It is worth the considerable effort it often takes to minimize them.
Deal with simple forgetfulness by calling your patients the day before to remind them of their appointments. Reasonably-priced phone software is available from a variety of vendors to automate this process. You could also hire a teenager to do it after school each day.
Whenever possible, use cell phone numbers for reminder calls. Patients often aren’t home during the day, and many don’t listen to their messages when they come in. Patients who have moved will often have a new home phone number, but their cell phone numbers will be the same.
Decrease the wait for new appointments. Keep some slots open each week for new patients, who will often “shop around” for a faster appointment while they’re waiting for an appointment they already have elsewhere.
If your no-shows are incorrigible, consider charging them. One increasingly popular mechanism is a fee ($20 seems to be popular) that must be paid at the time of the next appointment before being seen. Some patients will respond to that by never showing up again. Fine. You need to reserve your appointment slots for patients who plan to keep them. Those more contrite will pay and, hopefully, learn their lesson. Give your receptionists the power to override the charge since there are, obviously, legitimate reasons for missing an appointment.
One physician in my area told me he seldom actually collects the fee, which is okay with him. “After all,” he said, “the purpose is not to generate income. It’s to encourage patients to keep their appointments.”
If you go this route, be sure to post notices in your office and on your website clearly delineating your policy. Emphasize that it is not a service fee and cannot be billed to insurance. Remind patients about it during reminder calls. If you have a high no-show rate for cosmetic and other noninsurance procedures, consider collecting a nonrefundable deposit in advance.
Above all, seek to maximize the strength of your physician-patient relationships. Try not to shuttle patients between different physicians or PAs, and make it clear that you are genuinely concerned about their health. Impress upon them the crucial role they play in their own care, which includes keeping all their appointments.
In our office, significant no-shows (for example, a patient with a melanoma who misses the visit for re-excision) receive a phone call and a certified letter, and their records go into a special file for close follow-up by the nursing staff.
All missed appointments should be documented in the patient’s record – it’s important clinical and medicolegal information. A second missed appointment should prompt a written warning that measures will be taken if it happens again. Make sure to spell out what those measures are, and stick to them. Habitual no-shows should be dismissed from your practice. You cannot afford them.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Of all the headaches inherent in a private medical practice, few are more frustrating than patients who make appointments and then fail to keep them.
No-shows are a problem for all physicians but especially for dermatologists. In one study, the no-show rate in dermatology offices averaged 10% – almost double the average for medical offices as a whole.
Why the higher rate? One reason is a lag between appointment and visit. Many dermatologists are booked well in advance, so, by the time the appointment arrives, some patients’ complaints will have resolved spontaneously, while other patients will have found other offices willing to see them sooner. Another reason is lack of insurance coverage. Studies have shown that the no-show rate is highest when the patient is paying out-of-pocket for the visit.
Whatever the reasons, no-shows are an economic and medicolegal liability. It is worth the considerable effort it often takes to minimize them.
Deal with simple forgetfulness by calling your patients the day before to remind them of their appointments. Reasonably-priced phone software is available from a variety of vendors to automate this process. You could also hire a teenager to do it after school each day.
Whenever possible, use cell phone numbers for reminder calls. Patients often aren’t home during the day, and many don’t listen to their messages when they come in. Patients who have moved will often have a new home phone number, but their cell phone numbers will be the same.
Decrease the wait for new appointments. Keep some slots open each week for new patients, who will often “shop around” for a faster appointment while they’re waiting for an appointment they already have elsewhere.
If your no-shows are incorrigible, consider charging them. One increasingly popular mechanism is a fee ($20 seems to be popular) that must be paid at the time of the next appointment before being seen. Some patients will respond to that by never showing up again. Fine. You need to reserve your appointment slots for patients who plan to keep them. Those more contrite will pay and, hopefully, learn their lesson. Give your receptionists the power to override the charge since there are, obviously, legitimate reasons for missing an appointment.
One physician in my area told me he seldom actually collects the fee, which is okay with him. “After all,” he said, “the purpose is not to generate income. It’s to encourage patients to keep their appointments.”
If you go this route, be sure to post notices in your office and on your website clearly delineating your policy. Emphasize that it is not a service fee and cannot be billed to insurance. Remind patients about it during reminder calls. If you have a high no-show rate for cosmetic and other noninsurance procedures, consider collecting a nonrefundable deposit in advance.
Above all, seek to maximize the strength of your physician-patient relationships. Try not to shuttle patients between different physicians or PAs, and make it clear that you are genuinely concerned about their health. Impress upon them the crucial role they play in their own care, which includes keeping all their appointments.
In our office, significant no-shows (for example, a patient with a melanoma who misses the visit for re-excision) receive a phone call and a certified letter, and their records go into a special file for close follow-up by the nursing staff.
All missed appointments should be documented in the patient’s record – it’s important clinical and medicolegal information. A second missed appointment should prompt a written warning that measures will be taken if it happens again. Make sure to spell out what those measures are, and stick to them. Habitual no-shows should be dismissed from your practice. You cannot afford them.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Of all the headaches inherent in a private medical practice, few are more frustrating than patients who make appointments and then fail to keep them.
No-shows are a problem for all physicians but especially for dermatologists. In one study, the no-show rate in dermatology offices averaged 10% – almost double the average for medical offices as a whole.
Why the higher rate? One reason is a lag between appointment and visit. Many dermatologists are booked well in advance, so, by the time the appointment arrives, some patients’ complaints will have resolved spontaneously, while other patients will have found other offices willing to see them sooner. Another reason is lack of insurance coverage. Studies have shown that the no-show rate is highest when the patient is paying out-of-pocket for the visit.
Whatever the reasons, no-shows are an economic and medicolegal liability. It is worth the considerable effort it often takes to minimize them.
Deal with simple forgetfulness by calling your patients the day before to remind them of their appointments. Reasonably-priced phone software is available from a variety of vendors to automate this process. You could also hire a teenager to do it after school each day.
Whenever possible, use cell phone numbers for reminder calls. Patients often aren’t home during the day, and many don’t listen to their messages when they come in. Patients who have moved will often have a new home phone number, but their cell phone numbers will be the same.
Decrease the wait for new appointments. Keep some slots open each week for new patients, who will often “shop around” for a faster appointment while they’re waiting for an appointment they already have elsewhere.
If your no-shows are incorrigible, consider charging them. One increasingly popular mechanism is a fee ($20 seems to be popular) that must be paid at the time of the next appointment before being seen. Some patients will respond to that by never showing up again. Fine. You need to reserve your appointment slots for patients who plan to keep them. Those more contrite will pay and, hopefully, learn their lesson. Give your receptionists the power to override the charge since there are, obviously, legitimate reasons for missing an appointment.
One physician in my area told me he seldom actually collects the fee, which is okay with him. “After all,” he said, “the purpose is not to generate income. It’s to encourage patients to keep their appointments.”
If you go this route, be sure to post notices in your office and on your website clearly delineating your policy. Emphasize that it is not a service fee and cannot be billed to insurance. Remind patients about it during reminder calls. If you have a high no-show rate for cosmetic and other noninsurance procedures, consider collecting a nonrefundable deposit in advance.
Above all, seek to maximize the strength of your physician-patient relationships. Try not to shuttle patients between different physicians or PAs, and make it clear that you are genuinely concerned about their health. Impress upon them the crucial role they play in their own care, which includes keeping all their appointments.
In our office, significant no-shows (for example, a patient with a melanoma who misses the visit for re-excision) receive a phone call and a certified letter, and their records go into a special file for close follow-up by the nursing staff.
All missed appointments should be documented in the patient’s record – it’s important clinical and medicolegal information. A second missed appointment should prompt a written warning that measures will be taken if it happens again. Make sure to spell out what those measures are, and stick to them. Habitual no-shows should be dismissed from your practice. You cannot afford them.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Don’t forget HIPAA
In the struggle to understand and comply with new regulations, it’s easy to neglect older ones. Recently, I suggested reviewing your practice for potential Occupational Safety and Health Administration violations, which can be far more costly than anything MACRA has in store.
The same goes for HIPAA since HIPAA violations can be just as costly, in view of renewed governmental enforcement and some disturbing trends in completely unrelated government agencies.
Your most basic review should be a yearly examination of every part of your office where patient information is handled to identify potential violations. Examples discovered in my office included computers at our front desk whose screens were visible to patients checking in or out; laptops that were left on counters overnight; emails between staff involving patients or their care; and documents slated for shredding that remained in a “to shred” bin for days. All of these issues were easily solved at minimal cost – respectively, screen protectors, locking all laptops after hours, new email rules, and eliminating the “to shred” bin, forcing immediate shredding of all sensitive documents. Make sure you correct any problems you find before the OCR auditors come calling. You can compare your office’s compliance status against the recommendations listed on the OCR website.
Where safeguarding protected health information is concerned, you must now assume the worst-case scenario: Previously, when protected health information was compromised, you would have to notify the affected patients (and the government) only if there was a “significant risk of financial or reputational harm.” But now, any incident involving patient records is assumed to be a breach, and must be reported. Failure to do so could subject your practice to significant fines.
The biggest vulnerability in most practices is probably mobile devices carrying patient data; and that’s where the disturbing new trend comes in: Governments, both foreign and domestic, have developed an interest in the personal data on your devices. Travelers, including American citizens, now are being pressured into giving Customs and Border Protection officers access to their cellphones and laptops at airports.
As a physician, you can invoke HIPAA in such situations, since your devices likely contain patient data in some form. But rules may vary depending on where you are traveling to or from, and officials in other countries are not bound by U.S. HIPAA constraints.
So, how do you protect patients’ (and your personal) information from invasive searches? First, encrypt all of your data; encryption software is cheap, readily available, and easy to use. (I recently posted a list of inexpensive encryption applications on the website.) Desktop apps such as BitLocker or Apple’s FileVault let you encrypt your entire hard drive, requiring a password for decryption. (As always, I have no financial interest in anything I mention here.) To avoid surrendering the password, write it down and give it to a friend, then contact that person after crossing the border. It is easier to say you didn’t memorize it, as opposed to refusing to provide it – and nobody can compel you to reveal a password you don’t know.
Experts also recommend disabling the fingerprint sensor on your smartphone; customs officials have successfully used warrants to compel people to unlock their cellphones with a fingerprint. Because of your right to remain silent, it would be difficult (but not impossible) for them to force you to share your phone’s passcode.
A better alternative, in my view, is to travel with devices that have never contained any of your patient or personal data in the first place. Invest in a cheap phone and computer to use only when you are abroad; you don’t want your nice equipment lost or stolen, anyway. A budget Android phone that works with foreign SIM cards can be had for about $100; basic laptops run $500 or less.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
In the struggle to understand and comply with new regulations, it’s easy to neglect older ones. Recently, I suggested reviewing your practice for potential Occupational Safety and Health Administration violations, which can be far more costly than anything MACRA has in store.
The same goes for HIPAA since HIPAA violations can be just as costly, in view of renewed governmental enforcement and some disturbing trends in completely unrelated government agencies.
Your most basic review should be a yearly examination of every part of your office where patient information is handled to identify potential violations. Examples discovered in my office included computers at our front desk whose screens were visible to patients checking in or out; laptops that were left on counters overnight; emails between staff involving patients or their care; and documents slated for shredding that remained in a “to shred” bin for days. All of these issues were easily solved at minimal cost – respectively, screen protectors, locking all laptops after hours, new email rules, and eliminating the “to shred” bin, forcing immediate shredding of all sensitive documents. Make sure you correct any problems you find before the OCR auditors come calling. You can compare your office’s compliance status against the recommendations listed on the OCR website.
Where safeguarding protected health information is concerned, you must now assume the worst-case scenario: Previously, when protected health information was compromised, you would have to notify the affected patients (and the government) only if there was a “significant risk of financial or reputational harm.” But now, any incident involving patient records is assumed to be a breach, and must be reported. Failure to do so could subject your practice to significant fines.
The biggest vulnerability in most practices is probably mobile devices carrying patient data; and that’s where the disturbing new trend comes in: Governments, both foreign and domestic, have developed an interest in the personal data on your devices. Travelers, including American citizens, now are being pressured into giving Customs and Border Protection officers access to their cellphones and laptops at airports.
As a physician, you can invoke HIPAA in such situations, since your devices likely contain patient data in some form. But rules may vary depending on where you are traveling to or from, and officials in other countries are not bound by U.S. HIPAA constraints.
So, how do you protect patients’ (and your personal) information from invasive searches? First, encrypt all of your data; encryption software is cheap, readily available, and easy to use. (I recently posted a list of inexpensive encryption applications on the website.) Desktop apps such as BitLocker or Apple’s FileVault let you encrypt your entire hard drive, requiring a password for decryption. (As always, I have no financial interest in anything I mention here.) To avoid surrendering the password, write it down and give it to a friend, then contact that person after crossing the border. It is easier to say you didn’t memorize it, as opposed to refusing to provide it – and nobody can compel you to reveal a password you don’t know.
Experts also recommend disabling the fingerprint sensor on your smartphone; customs officials have successfully used warrants to compel people to unlock their cellphones with a fingerprint. Because of your right to remain silent, it would be difficult (but not impossible) for them to force you to share your phone’s passcode.
A better alternative, in my view, is to travel with devices that have never contained any of your patient or personal data in the first place. Invest in a cheap phone and computer to use only when you are abroad; you don’t want your nice equipment lost or stolen, anyway. A budget Android phone that works with foreign SIM cards can be had for about $100; basic laptops run $500 or less.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
In the struggle to understand and comply with new regulations, it’s easy to neglect older ones. Recently, I suggested reviewing your practice for potential Occupational Safety and Health Administration violations, which can be far more costly than anything MACRA has in store.
The same goes for HIPAA since HIPAA violations can be just as costly, in view of renewed governmental enforcement and some disturbing trends in completely unrelated government agencies.
Your most basic review should be a yearly examination of every part of your office where patient information is handled to identify potential violations. Examples discovered in my office included computers at our front desk whose screens were visible to patients checking in or out; laptops that were left on counters overnight; emails between staff involving patients or their care; and documents slated for shredding that remained in a “to shred” bin for days. All of these issues were easily solved at minimal cost – respectively, screen protectors, locking all laptops after hours, new email rules, and eliminating the “to shred” bin, forcing immediate shredding of all sensitive documents. Make sure you correct any problems you find before the OCR auditors come calling. You can compare your office’s compliance status against the recommendations listed on the OCR website.
Where safeguarding protected health information is concerned, you must now assume the worst-case scenario: Previously, when protected health information was compromised, you would have to notify the affected patients (and the government) only if there was a “significant risk of financial or reputational harm.” But now, any incident involving patient records is assumed to be a breach, and must be reported. Failure to do so could subject your practice to significant fines.
The biggest vulnerability in most practices is probably mobile devices carrying patient data; and that’s where the disturbing new trend comes in: Governments, both foreign and domestic, have developed an interest in the personal data on your devices. Travelers, including American citizens, now are being pressured into giving Customs and Border Protection officers access to their cellphones and laptops at airports.
As a physician, you can invoke HIPAA in such situations, since your devices likely contain patient data in some form. But rules may vary depending on where you are traveling to or from, and officials in other countries are not bound by U.S. HIPAA constraints.
So, how do you protect patients’ (and your personal) information from invasive searches? First, encrypt all of your data; encryption software is cheap, readily available, and easy to use. (I recently posted a list of inexpensive encryption applications on the website.) Desktop apps such as BitLocker or Apple’s FileVault let you encrypt your entire hard drive, requiring a password for decryption. (As always, I have no financial interest in anything I mention here.) To avoid surrendering the password, write it down and give it to a friend, then contact that person after crossing the border. It is easier to say you didn’t memorize it, as opposed to refusing to provide it – and nobody can compel you to reveal a password you don’t know.
Experts also recommend disabling the fingerprint sensor on your smartphone; customs officials have successfully used warrants to compel people to unlock their cellphones with a fingerprint. Because of your right to remain silent, it would be difficult (but not impossible) for them to force you to share your phone’s passcode.
A better alternative, in my view, is to travel with devices that have never contained any of your patient or personal data in the first place. Invest in a cheap phone and computer to use only when you are abroad; you don’t want your nice equipment lost or stolen, anyway. A budget Android phone that works with foreign SIM cards can be had for about $100; basic laptops run $500 or less.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].