User login
Reengineering your office to be perfect for your patients
Independent of the Affordable Care Act or any upcoming changes in health care, the focus of an ObGyn practice remains paramount: the patient comes first.
The “recipe” for creating patient satisfaction and service excellence is predicated upon the mission of your practice and creating a shared vision with your employees. An action plan that is created and “visited/revisited”on a regular basis will serve to keep all abreast of the latest information to enhance the quality of patient care. It goes without saying, the ObGyn must first “lead by example” and always strive for satisfied patients who will tell their friends about your practice.
Start with the right tools
To organize a practice well, you need the right tools, which ideally include mission and vision statements and an action plan with goals and objectives.
Mission statement
A mission statement can be developed by the ObGyn(s) in your office or in concert with your staff. It should include:
- the “here and now” focus on the current approach to patient care
- why the practice exists (Develop a brief description of your practice, including the desired patient population.)
- the products and services offered and why and how those services are provided.
Here is an example of a mission statement for an ObGyn practice: “Our mission is to provide excellent, exceptional, personalized care for women of all ages in a warm and friendly environment. We incorporate leading-edge technology in our practice and continue to be a leader in obstetrics and gynecology.”
Vision statement
A vision statement should be developed in concert with your staff. It should include:
- the “then and there” focus on the historic perspective of your practice
- the ObGyn(s) and staff vision of the future
- what the ObGyn(s) and staff want to create.
The vision statement should energize and excite your personnel, create a shared and meaningful purpose, inspire passion and interest, and convey the values you want to share in your practice.
Here is an example of a vision statement for an ObGyn practice: “We aim to become the premier obstetrics and gynecology pro-vider to residents of (location) community.”
Action plan: Setting goals
To succeed, an ObGyn practice needs to:
- develop targets and challenges reflecting periodic (quarterly) meetings with staff and new entity development in the practice
- establish benchmarks and measurable parameters (How do you compare with other local practices? Set criteria/metrics to assess your progress.)
- ensure that the objectives support the goals (Develop goals and objectives over a defined period of time.)
- revisit the goals (Have they have been met? Do they need revision?)
Goals and objectives are essential for the continued health of your practice. This is all predicated upon developing a competitive advantage and then maintaining it.
Read about how to make a positive first impression on a new patient.
Is the environment welcoming?
When we examine a practice from the patient’s point of view, a good starting place is with the front desk. Have you looked at your front desk “from the outside in?” In one sense, this is the showcase of your practice.
Related article:
Four pillars of a successful practice: 2. Attract new patients
The first impression: Appointment scheduling
The first impression a patient receives about your practice occurs when she attempts to set up an appointment. Perhaps you might ask someone to call in to schedule an appointment. Is the caller immediately put on hold? Are your personnel courteous on the phone? Can she be seen quickly if she has a problem? How long is the wait for an annual exam? A test run can be very revealing.
Walk in the front door
When a patient walks in the door, does the physical office space radiate a friendly, relaxed atmosphere? Walk through the waiting room, then consultation and exam rooms as if you are a patient seeing it for the first time. Have you created an environment in which patients sense a well-organized office and the esprit de corps of the personnel? Does it look and smell fresh and clean? This all sends a loud and clear positive message about your practice.1–3
Here are some suggestions for making a waiting room more inviting:
- Provide a seating arrangement that is “patient centered.” For example, semi- circular arrangements allow easy viewing of any monitors in the waiting room.
- WiFi is a great addition. Post several signs with the user name and password.
- Offer computers for patients to use to complete registration
- Set up a fish tank. If well-maintained, it can be soothing to many people.
- Display medical information pamphlets, even if they are rarely taken.
- Provide a big screen television that offers information about your practice, including personnel and procedures.
Streaming ads for physician offices are available. One platform, Outcome Health (https://www.outcomehealth.com), provides flat-screen TVs and tablets that show patient education videos.4 Another vendor, Patient Point (http://patientpoint.com), offers waiting room networks, editorials, and other communications designed to support “the goals of improving healthcare.”5 Other available media include channel news and music programming to relax patients.6
Wait times. A patient’s perceived wait time and the actual wait time are often quite different. How long she waits to see the ObGyn is “numero uno” with regard to patient satisfaction and can be a key source of annoyance, irritability, stress, and anger.
Does someone inform waiting patients that the ObGyn is running late? Does staff at the front desk or perhaps your medical assistant inquire, “Can I get you anything? The doctor is running late,” or “Dr. Jones has just finished delivering a baby. He’ll be here in 10 minutes. He’ll see you first.”
Consultation and exam rooms
Suggestions to develop a relaxing environment in your consultation and exam rooms are7:
- decorate the walls with soft, pastel colors
- use “spa aesthetics” to create a colorful atmosphere with appropriate lighting, artwork, and modern furnishings
- present a few magazines neatly and update them periodically
- stock and appropriately maintain the patients rooms with medical supplies
- remember, “Subjects perceive people more positively in beautiful rooms than in ugly rooms.”5
Read about how to keep your patients satisfied and your business stable.
Set the lead example
The need for open and supportive communication between you and your office staff cannot be overly emphasized. An ideal office staff member understands and shares in the vision, is aware of stated goals and objectives, is responsive to patient needs, and wants to create a win-win environment.
Frequently discuss your expectations with your staff. Expect them to be responsive, courteous, competent, have good communication skills, and be influenced by the appearance of the physical environ-ment. Provide support and educational tools to help them successfully perform their work.
Related article:
Four pillars of a successful practice: 1. Keep your current patients happy
Discover your patients’ vision of customer service
Formal measurement of patient satisfaction began with Professor Irwin Press at the University of Notre Dame. Rod Ganey, a sociologist and statistician, then developed the Press Ganey Patient Satisfaction Survey. These points earlier conveyed by Maslow and Mintz8 addressed the “effects of esthetic surroundings.” Color and art proved to be preferences in an esthetically pleasing environment. Additional historical information has been provided by Siegrist, who addressed “the patient experience.”9 He cites the myth that patients do not fill out satisfaction surveys. Indeed they do. Patient satisfaction is not a personality contest but rather a reflection of the health care provider’s investment of time and effort to offer patient-centered care. Siegrist also notes that the patient’s family plays a key role in how a patient perceives her experience with her health care professional.9
The federal government has been actively involved in assessing patient satisfaction in the hospital setting since 2002. This is reflected in the Centers for Medicare and Medicaid Services, the Agency for Healthcare Research and Quality, and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys. The HCAHPS is a 27-question survey randomly administered to adult inpatients after discharge.10–12
The following metrics are often included in patient satisfaction surveys9,10:
- rating of hospital care from 0 (lowest) to 10 (highest)
- percentage of patients who would recommend a practice to family and friends
- number of patients who say their health care providers always communicate well
- the number of patients who report that the office is always clean and friendly.
Use of search engines focused on health care patient surveys can provide a number of options for clinicians to use in their practice.
Tips on patient satisfaction
Several interesting tips from the busi-ness world can be applied to an ObGyn’s practice14:
- You will only hear from 4% of unhappy customers.
- One dissatisfied customer tells 9.
- 95% of customers with resolved issues will do business with you again.
- If a problem is not addressed, that patient will tell 10 others.
- Resolve the problem and 5 people will know about it.
- It costs 5 times as much effort to gain 1 new customer.
- Loyal customers in 1 area of service are good prospects for other (new) services.
Related article:
Using the Internet in your practice. Part 2: Generating new patients using social media
Tell stories about good, satisfied patients
Sharing the stories of satisfied patients motivates others to consider coming to your practice. To develop these stories, offer a “suggestion box” where patients can leave compliments or comments about their experiences. Ask patients to record their positive reviews (be sure to obtain written consent before recording and publishing). Show the videos on the big-screen TVs in your waiting room and include patient reviews (written, audio, and video) on your website.15
Related article:
Four pillars of a successful practice: 4. Motivate your staff
Reevaluate periodically
Encouraging team spirit makes good business sense. Offer staff members bonuses for coming up with improved processes. Provide educational programs for staff on patient care, technology, etc. If a difficult experience occurs, discuss it openly with staff members without accusing, asking them for suggestions to improve the situation.16
To assess the monetary value of your practice, you need to know what contributes to your profit margin and overhead. What investments are the most profitable? Then monitor each segment of the office practice.
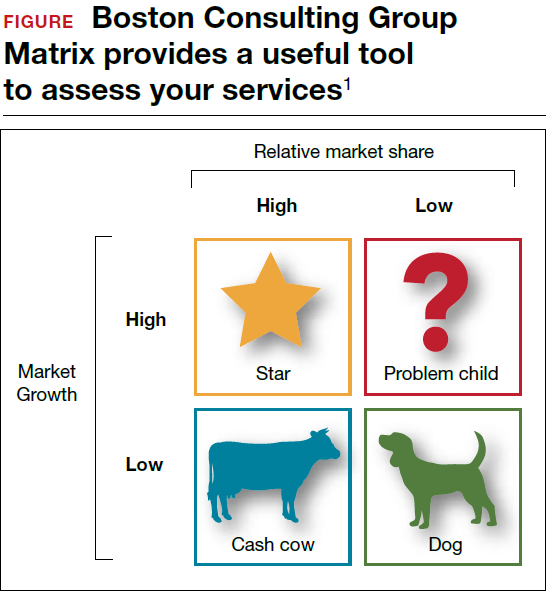
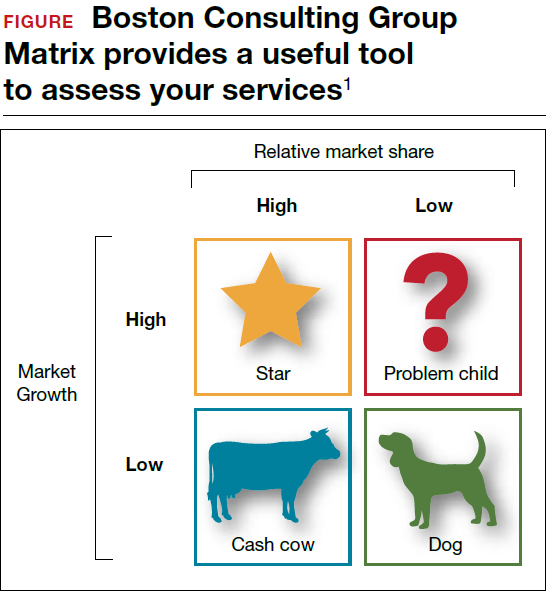
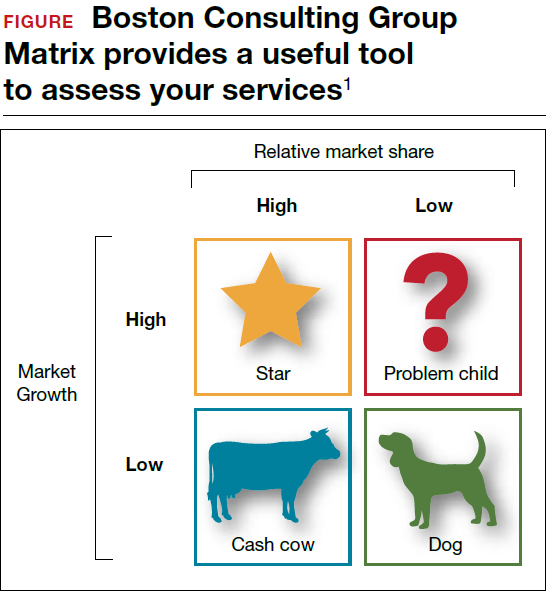
Should you proceed with a purchase? Should you take on a new hire? Let's look at one excellent model from the Boston Consulting Group (FIGURE) that provides insight into "low and high performance" aspects of business or practice.1
In the matrix, Stars use large amounts of cash and are leaders in cash generation. Stars lead to development of a Cash Cow, which are entities that generate profits and cash with low investment prerequisites. Dogs are segments of product and service line(s) that should be carefully reevaluated. A decision must be made to liquidate if the problem cannot be corrected. Question Marks have the worst cash characteristics of all and are associated with high demands and low profit margin(s).1
SWOT analysis
A SWOT analysis is most helpful when assessing a practice in real time. The basic tenets are2:
Strengths:
- prestigious reputation
- technological expertise
Weaknesses:
- antiquated computer system
- lack of experience in specific areas
Opportunities:
- growing market demand for a specific product or procedure
- provision of unique services
Threats:
- changing demographics
- competitive practices
- changes in health care third-party payers.
The American College of Obstetricians and Gynecologists (ACOG) has developed an "ACOG Medical Home Toolkit" to allow ObGyns to assess how significant the changes regarding payers will be to their practice. Sections include the patient/practice partnership support; clinical care information; community resources; care delivery management; performance measurement and improvement; and payment and finance.3 The toolkit is available for download from the ACOG website.
References
- Morrison A, Wensley R. Boxing up or boxed in? A short history of the Boston Consulting Group Share/Growth Matrix. J Market Manag. 1993;7(2):105-129. http://www.tandfonline.com/doi/abs/10.1080/0267257X.1991.9964145.
- Klasko SK, Toub DB. It's not a plan without a business plan. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:36-37.
- American Congress of Obstetricians and Gynecologists. ACOG Medical Home Toolkit. https://www.acog.org/About-ACOG/ACOG-Departments/Practice-Management-and-Managed-Care/ACOG-Medical-Home-Toolkit. Accessed August 14, 2017.
Bottom line
Ensuring that your patients have an outstanding experience is a smart business strategy. A unified approach that includes team members’ involvement to create a patient-centered environment will provide a quality experience and encourage patients to recommend your ObGyn practice to others.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Ulrich RS. Evidence-based environmental design for improving medical outcomes: Paper Delivered at a Conference Entitled Healing by Design: Building for Health Care in the 21st Century. Montreal: McGill University Health Centre; 2000. http://www.brikbase.org/sites/default/files/Evidence%20Based%20Environmental%20Design%20for%20Improving%20Medical.pdf. Accessed August 15, 2017.
- Becker F, Douglass S. The ecology of the patient visit: physical attractiveness, waiting times and perceived quality of care. J Ambul Care Manag. 2008;31(2):128–141.
- Becker F, Sweeney B, Parsons K. Ambulatory facility design and patients’ perceptions of healthcare quality. HERD. 2008;1(4):35–54.
- Outcome Health Website. https://www.outcomehealth.com/. Accessed August 14, 2017.
- Mazer SE. The waiting room: Where suffering begins. Healing Healthcare Systems website. http://www.healinghealth.com/waiting-room-suffering-begins/. Published November 7, 2014. Accessed August 14, 2017.
- Patient Point Programs Website. http://patientpoint.com/. Accessed August 14, 2017.
- Almquist J, Kelly C, Bromberg J, Bryant S, Christianson T, Montori V. Consultation room design and the clinical encounter: the space and interaction randomized trial. Health Environ Res Design. 2009;3(1):41–78.
- Maslow A, Mintz N. Effects of esthetic surroundings: I. Initial effects of three esthetic conditions upon perceiving “energy” and “well-being” in faces. J Psychology. 1956;41(2):247–254.
- Siegrist RB. The patient experience. In: Sanfilippo JS, Bieber E, Javich D, Siegrist R, eds. MBA for Healthcare. New York, NY: Oxford Press;2016:227–236.
- Press I. Patient satisfaction: Understanding and managing the experience of care. 2nd ed. Chicago, IL: Health Administration Press; 2005:66–78.
- Piper L, Tallman E. Hospital consumer assessment of healthcare providers and systems: An ethical leadership dilemma to satisfy patients. Health Care Manag (Frederick). 2016;35(2):151–155.
- Giordano L, Elliott M, Goldstein E, Lehrman W, Spencer P. Development, implementation and public reporting of HCAHPS survey. Med Care Res Rev. 2010;67(1):27–37.
- Jones KE. Helping the health profession help others: Applying business principles to the medical world. University of Tennessee, Knoxville Honors Thesis Projects. http://trace.tennessee.edu/cgi/viewcontent.cgi?article=1560&context=utk_chanhonoproj. Published 2002. Accessed August 14, 2017.
- Baum N. Marketing your practice: ethically, effectively and economically. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:123–154.
- Baum NH. Four pillars of a successful practice: 1. Keep your current patients happy. OBG Manag. 2013;25(3):49–56.
- Baum NH. Four pillars of a successful practice: 4. Motivate your staff. OBG Manag. 2013;25(8):29–33.
Independent of the Affordable Care Act or any upcoming changes in health care, the focus of an ObGyn practice remains paramount: the patient comes first.
The “recipe” for creating patient satisfaction and service excellence is predicated upon the mission of your practice and creating a shared vision with your employees. An action plan that is created and “visited/revisited”on a regular basis will serve to keep all abreast of the latest information to enhance the quality of patient care. It goes without saying, the ObGyn must first “lead by example” and always strive for satisfied patients who will tell their friends about your practice.
Start with the right tools
To organize a practice well, you need the right tools, which ideally include mission and vision statements and an action plan with goals and objectives.
Mission statement
A mission statement can be developed by the ObGyn(s) in your office or in concert with your staff. It should include:
- the “here and now” focus on the current approach to patient care
- why the practice exists (Develop a brief description of your practice, including the desired patient population.)
- the products and services offered and why and how those services are provided.
Here is an example of a mission statement for an ObGyn practice: “Our mission is to provide excellent, exceptional, personalized care for women of all ages in a warm and friendly environment. We incorporate leading-edge technology in our practice and continue to be a leader in obstetrics and gynecology.”
Vision statement
A vision statement should be developed in concert with your staff. It should include:
- the “then and there” focus on the historic perspective of your practice
- the ObGyn(s) and staff vision of the future
- what the ObGyn(s) and staff want to create.
The vision statement should energize and excite your personnel, create a shared and meaningful purpose, inspire passion and interest, and convey the values you want to share in your practice.
Here is an example of a vision statement for an ObGyn practice: “We aim to become the premier obstetrics and gynecology pro-vider to residents of (location) community.”
Action plan: Setting goals
To succeed, an ObGyn practice needs to:
- develop targets and challenges reflecting periodic (quarterly) meetings with staff and new entity development in the practice
- establish benchmarks and measurable parameters (How do you compare with other local practices? Set criteria/metrics to assess your progress.)
- ensure that the objectives support the goals (Develop goals and objectives over a defined period of time.)
- revisit the goals (Have they have been met? Do they need revision?)
Goals and objectives are essential for the continued health of your practice. This is all predicated upon developing a competitive advantage and then maintaining it.
Read about how to make a positive first impression on a new patient.
Is the environment welcoming?
When we examine a practice from the patient’s point of view, a good starting place is with the front desk. Have you looked at your front desk “from the outside in?” In one sense, this is the showcase of your practice.
Related article:
Four pillars of a successful practice: 2. Attract new patients
The first impression: Appointment scheduling
The first impression a patient receives about your practice occurs when she attempts to set up an appointment. Perhaps you might ask someone to call in to schedule an appointment. Is the caller immediately put on hold? Are your personnel courteous on the phone? Can she be seen quickly if she has a problem? How long is the wait for an annual exam? A test run can be very revealing.
Walk in the front door
When a patient walks in the door, does the physical office space radiate a friendly, relaxed atmosphere? Walk through the waiting room, then consultation and exam rooms as if you are a patient seeing it for the first time. Have you created an environment in which patients sense a well-organized office and the esprit de corps of the personnel? Does it look and smell fresh and clean? This all sends a loud and clear positive message about your practice.1–3
Here are some suggestions for making a waiting room more inviting:
- Provide a seating arrangement that is “patient centered.” For example, semi- circular arrangements allow easy viewing of any monitors in the waiting room.
- WiFi is a great addition. Post several signs with the user name and password.
- Offer computers for patients to use to complete registration
- Set up a fish tank. If well-maintained, it can be soothing to many people.
- Display medical information pamphlets, even if they are rarely taken.
- Provide a big screen television that offers information about your practice, including personnel and procedures.
Streaming ads for physician offices are available. One platform, Outcome Health (https://www.outcomehealth.com), provides flat-screen TVs and tablets that show patient education videos.4 Another vendor, Patient Point (http://patientpoint.com), offers waiting room networks, editorials, and other communications designed to support “the goals of improving healthcare.”5 Other available media include channel news and music programming to relax patients.6
Wait times. A patient’s perceived wait time and the actual wait time are often quite different. How long she waits to see the ObGyn is “numero uno” with regard to patient satisfaction and can be a key source of annoyance, irritability, stress, and anger.
Does someone inform waiting patients that the ObGyn is running late? Does staff at the front desk or perhaps your medical assistant inquire, “Can I get you anything? The doctor is running late,” or “Dr. Jones has just finished delivering a baby. He’ll be here in 10 minutes. He’ll see you first.”
Consultation and exam rooms
Suggestions to develop a relaxing environment in your consultation and exam rooms are7:
- decorate the walls with soft, pastel colors
- use “spa aesthetics” to create a colorful atmosphere with appropriate lighting, artwork, and modern furnishings
- present a few magazines neatly and update them periodically
- stock and appropriately maintain the patients rooms with medical supplies
- remember, “Subjects perceive people more positively in beautiful rooms than in ugly rooms.”5
Read about how to keep your patients satisfied and your business stable.
Set the lead example
The need for open and supportive communication between you and your office staff cannot be overly emphasized. An ideal office staff member understands and shares in the vision, is aware of stated goals and objectives, is responsive to patient needs, and wants to create a win-win environment.
Frequently discuss your expectations with your staff. Expect them to be responsive, courteous, competent, have good communication skills, and be influenced by the appearance of the physical environ-ment. Provide support and educational tools to help them successfully perform their work.
Related article:
Four pillars of a successful practice: 1. Keep your current patients happy
Discover your patients’ vision of customer service
Formal measurement of patient satisfaction began with Professor Irwin Press at the University of Notre Dame. Rod Ganey, a sociologist and statistician, then developed the Press Ganey Patient Satisfaction Survey. These points earlier conveyed by Maslow and Mintz8 addressed the “effects of esthetic surroundings.” Color and art proved to be preferences in an esthetically pleasing environment. Additional historical information has been provided by Siegrist, who addressed “the patient experience.”9 He cites the myth that patients do not fill out satisfaction surveys. Indeed they do. Patient satisfaction is not a personality contest but rather a reflection of the health care provider’s investment of time and effort to offer patient-centered care. Siegrist also notes that the patient’s family plays a key role in how a patient perceives her experience with her health care professional.9
The federal government has been actively involved in assessing patient satisfaction in the hospital setting since 2002. This is reflected in the Centers for Medicare and Medicaid Services, the Agency for Healthcare Research and Quality, and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys. The HCAHPS is a 27-question survey randomly administered to adult inpatients after discharge.10–12
The following metrics are often included in patient satisfaction surveys9,10:
- rating of hospital care from 0 (lowest) to 10 (highest)
- percentage of patients who would recommend a practice to family and friends
- number of patients who say their health care providers always communicate well
- the number of patients who report that the office is always clean and friendly.
Use of search engines focused on health care patient surveys can provide a number of options for clinicians to use in their practice.
Tips on patient satisfaction
Several interesting tips from the busi-ness world can be applied to an ObGyn’s practice14:
- You will only hear from 4% of unhappy customers.
- One dissatisfied customer tells 9.
- 95% of customers with resolved issues will do business with you again.
- If a problem is not addressed, that patient will tell 10 others.
- Resolve the problem and 5 people will know about it.
- It costs 5 times as much effort to gain 1 new customer.
- Loyal customers in 1 area of service are good prospects for other (new) services.
Related article:
Using the Internet in your practice. Part 2: Generating new patients using social media
Tell stories about good, satisfied patients
Sharing the stories of satisfied patients motivates others to consider coming to your practice. To develop these stories, offer a “suggestion box” where patients can leave compliments or comments about their experiences. Ask patients to record their positive reviews (be sure to obtain written consent before recording and publishing). Show the videos on the big-screen TVs in your waiting room and include patient reviews (written, audio, and video) on your website.15
Related article:
Four pillars of a successful practice: 4. Motivate your staff
Reevaluate periodically
Encouraging team spirit makes good business sense. Offer staff members bonuses for coming up with improved processes. Provide educational programs for staff on patient care, technology, etc. If a difficult experience occurs, discuss it openly with staff members without accusing, asking them for suggestions to improve the situation.16
To assess the monetary value of your practice, you need to know what contributes to your profit margin and overhead. What investments are the most profitable? Then monitor each segment of the office practice.
Should you proceed with a purchase? Should you take on a new hire? Let's look at one excellent model from the Boston Consulting Group (FIGURE) that provides insight into "low and high performance" aspects of business or practice.1
In the matrix, Stars use large amounts of cash and are leaders in cash generation. Stars lead to development of a Cash Cow, which are entities that generate profits and cash with low investment prerequisites. Dogs are segments of product and service line(s) that should be carefully reevaluated. A decision must be made to liquidate if the problem cannot be corrected. Question Marks have the worst cash characteristics of all and are associated with high demands and low profit margin(s).1
SWOT analysis
A SWOT analysis is most helpful when assessing a practice in real time. The basic tenets are2:
Strengths:
- prestigious reputation
- technological expertise
Weaknesses:
- antiquated computer system
- lack of experience in specific areas
Opportunities:
- growing market demand for a specific product or procedure
- provision of unique services
Threats:
- changing demographics
- competitive practices
- changes in health care third-party payers.
The American College of Obstetricians and Gynecologists (ACOG) has developed an "ACOG Medical Home Toolkit" to allow ObGyns to assess how significant the changes regarding payers will be to their practice. Sections include the patient/practice partnership support; clinical care information; community resources; care delivery management; performance measurement and improvement; and payment and finance.3 The toolkit is available for download from the ACOG website.
References
- Morrison A, Wensley R. Boxing up or boxed in? A short history of the Boston Consulting Group Share/Growth Matrix. J Market Manag. 1993;7(2):105-129. http://www.tandfonline.com/doi/abs/10.1080/0267257X.1991.9964145.
- Klasko SK, Toub DB. It's not a plan without a business plan. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:36-37.
- American Congress of Obstetricians and Gynecologists. ACOG Medical Home Toolkit. https://www.acog.org/About-ACOG/ACOG-Departments/Practice-Management-and-Managed-Care/ACOG-Medical-Home-Toolkit. Accessed August 14, 2017.
Bottom line
Ensuring that your patients have an outstanding experience is a smart business strategy. A unified approach that includes team members’ involvement to create a patient-centered environment will provide a quality experience and encourage patients to recommend your ObGyn practice to others.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Independent of the Affordable Care Act or any upcoming changes in health care, the focus of an ObGyn practice remains paramount: the patient comes first.
The “recipe” for creating patient satisfaction and service excellence is predicated upon the mission of your practice and creating a shared vision with your employees. An action plan that is created and “visited/revisited”on a regular basis will serve to keep all abreast of the latest information to enhance the quality of patient care. It goes without saying, the ObGyn must first “lead by example” and always strive for satisfied patients who will tell their friends about your practice.
Start with the right tools
To organize a practice well, you need the right tools, which ideally include mission and vision statements and an action plan with goals and objectives.
Mission statement
A mission statement can be developed by the ObGyn(s) in your office or in concert with your staff. It should include:
- the “here and now” focus on the current approach to patient care
- why the practice exists (Develop a brief description of your practice, including the desired patient population.)
- the products and services offered and why and how those services are provided.
Here is an example of a mission statement for an ObGyn practice: “Our mission is to provide excellent, exceptional, personalized care for women of all ages in a warm and friendly environment. We incorporate leading-edge technology in our practice and continue to be a leader in obstetrics and gynecology.”
Vision statement
A vision statement should be developed in concert with your staff. It should include:
- the “then and there” focus on the historic perspective of your practice
- the ObGyn(s) and staff vision of the future
- what the ObGyn(s) and staff want to create.
The vision statement should energize and excite your personnel, create a shared and meaningful purpose, inspire passion and interest, and convey the values you want to share in your practice.
Here is an example of a vision statement for an ObGyn practice: “We aim to become the premier obstetrics and gynecology pro-vider to residents of (location) community.”
Action plan: Setting goals
To succeed, an ObGyn practice needs to:
- develop targets and challenges reflecting periodic (quarterly) meetings with staff and new entity development in the practice
- establish benchmarks and measurable parameters (How do you compare with other local practices? Set criteria/metrics to assess your progress.)
- ensure that the objectives support the goals (Develop goals and objectives over a defined period of time.)
- revisit the goals (Have they have been met? Do they need revision?)
Goals and objectives are essential for the continued health of your practice. This is all predicated upon developing a competitive advantage and then maintaining it.
Read about how to make a positive first impression on a new patient.
Is the environment welcoming?
When we examine a practice from the patient’s point of view, a good starting place is with the front desk. Have you looked at your front desk “from the outside in?” In one sense, this is the showcase of your practice.
Related article:
Four pillars of a successful practice: 2. Attract new patients
The first impression: Appointment scheduling
The first impression a patient receives about your practice occurs when she attempts to set up an appointment. Perhaps you might ask someone to call in to schedule an appointment. Is the caller immediately put on hold? Are your personnel courteous on the phone? Can she be seen quickly if she has a problem? How long is the wait for an annual exam? A test run can be very revealing.
Walk in the front door
When a patient walks in the door, does the physical office space radiate a friendly, relaxed atmosphere? Walk through the waiting room, then consultation and exam rooms as if you are a patient seeing it for the first time. Have you created an environment in which patients sense a well-organized office and the esprit de corps of the personnel? Does it look and smell fresh and clean? This all sends a loud and clear positive message about your practice.1–3
Here are some suggestions for making a waiting room more inviting:
- Provide a seating arrangement that is “patient centered.” For example, semi- circular arrangements allow easy viewing of any monitors in the waiting room.
- WiFi is a great addition. Post several signs with the user name and password.
- Offer computers for patients to use to complete registration
- Set up a fish tank. If well-maintained, it can be soothing to many people.
- Display medical information pamphlets, even if they are rarely taken.
- Provide a big screen television that offers information about your practice, including personnel and procedures.
Streaming ads for physician offices are available. One platform, Outcome Health (https://www.outcomehealth.com), provides flat-screen TVs and tablets that show patient education videos.4 Another vendor, Patient Point (http://patientpoint.com), offers waiting room networks, editorials, and other communications designed to support “the goals of improving healthcare.”5 Other available media include channel news and music programming to relax patients.6
Wait times. A patient’s perceived wait time and the actual wait time are often quite different. How long she waits to see the ObGyn is “numero uno” with regard to patient satisfaction and can be a key source of annoyance, irritability, stress, and anger.
Does someone inform waiting patients that the ObGyn is running late? Does staff at the front desk or perhaps your medical assistant inquire, “Can I get you anything? The doctor is running late,” or “Dr. Jones has just finished delivering a baby. He’ll be here in 10 minutes. He’ll see you first.”
Consultation and exam rooms
Suggestions to develop a relaxing environment in your consultation and exam rooms are7:
- decorate the walls with soft, pastel colors
- use “spa aesthetics” to create a colorful atmosphere with appropriate lighting, artwork, and modern furnishings
- present a few magazines neatly and update them periodically
- stock and appropriately maintain the patients rooms with medical supplies
- remember, “Subjects perceive people more positively in beautiful rooms than in ugly rooms.”5
Read about how to keep your patients satisfied and your business stable.
Set the lead example
The need for open and supportive communication between you and your office staff cannot be overly emphasized. An ideal office staff member understands and shares in the vision, is aware of stated goals and objectives, is responsive to patient needs, and wants to create a win-win environment.
Frequently discuss your expectations with your staff. Expect them to be responsive, courteous, competent, have good communication skills, and be influenced by the appearance of the physical environ-ment. Provide support and educational tools to help them successfully perform their work.
Related article:
Four pillars of a successful practice: 1. Keep your current patients happy
Discover your patients’ vision of customer service
Formal measurement of patient satisfaction began with Professor Irwin Press at the University of Notre Dame. Rod Ganey, a sociologist and statistician, then developed the Press Ganey Patient Satisfaction Survey. These points earlier conveyed by Maslow and Mintz8 addressed the “effects of esthetic surroundings.” Color and art proved to be preferences in an esthetically pleasing environment. Additional historical information has been provided by Siegrist, who addressed “the patient experience.”9 He cites the myth that patients do not fill out satisfaction surveys. Indeed they do. Patient satisfaction is not a personality contest but rather a reflection of the health care provider’s investment of time and effort to offer patient-centered care. Siegrist also notes that the patient’s family plays a key role in how a patient perceives her experience with her health care professional.9
The federal government has been actively involved in assessing patient satisfaction in the hospital setting since 2002. This is reflected in the Centers for Medicare and Medicaid Services, the Agency for Healthcare Research and Quality, and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys. The HCAHPS is a 27-question survey randomly administered to adult inpatients after discharge.10–12
The following metrics are often included in patient satisfaction surveys9,10:
- rating of hospital care from 0 (lowest) to 10 (highest)
- percentage of patients who would recommend a practice to family and friends
- number of patients who say their health care providers always communicate well
- the number of patients who report that the office is always clean and friendly.
Use of search engines focused on health care patient surveys can provide a number of options for clinicians to use in their practice.
Tips on patient satisfaction
Several interesting tips from the busi-ness world can be applied to an ObGyn’s practice14:
- You will only hear from 4% of unhappy customers.
- One dissatisfied customer tells 9.
- 95% of customers with resolved issues will do business with you again.
- If a problem is not addressed, that patient will tell 10 others.
- Resolve the problem and 5 people will know about it.
- It costs 5 times as much effort to gain 1 new customer.
- Loyal customers in 1 area of service are good prospects for other (new) services.
Related article:
Using the Internet in your practice. Part 2: Generating new patients using social media
Tell stories about good, satisfied patients
Sharing the stories of satisfied patients motivates others to consider coming to your practice. To develop these stories, offer a “suggestion box” where patients can leave compliments or comments about their experiences. Ask patients to record their positive reviews (be sure to obtain written consent before recording and publishing). Show the videos on the big-screen TVs in your waiting room and include patient reviews (written, audio, and video) on your website.15
Related article:
Four pillars of a successful practice: 4. Motivate your staff
Reevaluate periodically
Encouraging team spirit makes good business sense. Offer staff members bonuses for coming up with improved processes. Provide educational programs for staff on patient care, technology, etc. If a difficult experience occurs, discuss it openly with staff members without accusing, asking them for suggestions to improve the situation.16
To assess the monetary value of your practice, you need to know what contributes to your profit margin and overhead. What investments are the most profitable? Then monitor each segment of the office practice.
Should you proceed with a purchase? Should you take on a new hire? Let's look at one excellent model from the Boston Consulting Group (FIGURE) that provides insight into "low and high performance" aspects of business or practice.1
In the matrix, Stars use large amounts of cash and are leaders in cash generation. Stars lead to development of a Cash Cow, which are entities that generate profits and cash with low investment prerequisites. Dogs are segments of product and service line(s) that should be carefully reevaluated. A decision must be made to liquidate if the problem cannot be corrected. Question Marks have the worst cash characteristics of all and are associated with high demands and low profit margin(s).1
SWOT analysis
A SWOT analysis is most helpful when assessing a practice in real time. The basic tenets are2:
Strengths:
- prestigious reputation
- technological expertise
Weaknesses:
- antiquated computer system
- lack of experience in specific areas
Opportunities:
- growing market demand for a specific product or procedure
- provision of unique services
Threats:
- changing demographics
- competitive practices
- changes in health care third-party payers.
The American College of Obstetricians and Gynecologists (ACOG) has developed an "ACOG Medical Home Toolkit" to allow ObGyns to assess how significant the changes regarding payers will be to their practice. Sections include the patient/practice partnership support; clinical care information; community resources; care delivery management; performance measurement and improvement; and payment and finance.3 The toolkit is available for download from the ACOG website.
References
- Morrison A, Wensley R. Boxing up or boxed in? A short history of the Boston Consulting Group Share/Growth Matrix. J Market Manag. 1993;7(2):105-129. http://www.tandfonline.com/doi/abs/10.1080/0267257X.1991.9964145.
- Klasko SK, Toub DB. It's not a plan without a business plan. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:36-37.
- American Congress of Obstetricians and Gynecologists. ACOG Medical Home Toolkit. https://www.acog.org/About-ACOG/ACOG-Departments/Practice-Management-and-Managed-Care/ACOG-Medical-Home-Toolkit. Accessed August 14, 2017.
Bottom line
Ensuring that your patients have an outstanding experience is a smart business strategy. A unified approach that includes team members’ involvement to create a patient-centered environment will provide a quality experience and encourage patients to recommend your ObGyn practice to others.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Ulrich RS. Evidence-based environmental design for improving medical outcomes: Paper Delivered at a Conference Entitled Healing by Design: Building for Health Care in the 21st Century. Montreal: McGill University Health Centre; 2000. http://www.brikbase.org/sites/default/files/Evidence%20Based%20Environmental%20Design%20for%20Improving%20Medical.pdf. Accessed August 15, 2017.
- Becker F, Douglass S. The ecology of the patient visit: physical attractiveness, waiting times and perceived quality of care. J Ambul Care Manag. 2008;31(2):128–141.
- Becker F, Sweeney B, Parsons K. Ambulatory facility design and patients’ perceptions of healthcare quality. HERD. 2008;1(4):35–54.
- Outcome Health Website. https://www.outcomehealth.com/. Accessed August 14, 2017.
- Mazer SE. The waiting room: Where suffering begins. Healing Healthcare Systems website. http://www.healinghealth.com/waiting-room-suffering-begins/. Published November 7, 2014. Accessed August 14, 2017.
- Patient Point Programs Website. http://patientpoint.com/. Accessed August 14, 2017.
- Almquist J, Kelly C, Bromberg J, Bryant S, Christianson T, Montori V. Consultation room design and the clinical encounter: the space and interaction randomized trial. Health Environ Res Design. 2009;3(1):41–78.
- Maslow A, Mintz N. Effects of esthetic surroundings: I. Initial effects of three esthetic conditions upon perceiving “energy” and “well-being” in faces. J Psychology. 1956;41(2):247–254.
- Siegrist RB. The patient experience. In: Sanfilippo JS, Bieber E, Javich D, Siegrist R, eds. MBA for Healthcare. New York, NY: Oxford Press;2016:227–236.
- Press I. Patient satisfaction: Understanding and managing the experience of care. 2nd ed. Chicago, IL: Health Administration Press; 2005:66–78.
- Piper L, Tallman E. Hospital consumer assessment of healthcare providers and systems: An ethical leadership dilemma to satisfy patients. Health Care Manag (Frederick). 2016;35(2):151–155.
- Giordano L, Elliott M, Goldstein E, Lehrman W, Spencer P. Development, implementation and public reporting of HCAHPS survey. Med Care Res Rev. 2010;67(1):27–37.
- Jones KE. Helping the health profession help others: Applying business principles to the medical world. University of Tennessee, Knoxville Honors Thesis Projects. http://trace.tennessee.edu/cgi/viewcontent.cgi?article=1560&context=utk_chanhonoproj. Published 2002. Accessed August 14, 2017.
- Baum N. Marketing your practice: ethically, effectively and economically. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:123–154.
- Baum NH. Four pillars of a successful practice: 1. Keep your current patients happy. OBG Manag. 2013;25(3):49–56.
- Baum NH. Four pillars of a successful practice: 4. Motivate your staff. OBG Manag. 2013;25(8):29–33.
- Ulrich RS. Evidence-based environmental design for improving medical outcomes: Paper Delivered at a Conference Entitled Healing by Design: Building for Health Care in the 21st Century. Montreal: McGill University Health Centre; 2000. http://www.brikbase.org/sites/default/files/Evidence%20Based%20Environmental%20Design%20for%20Improving%20Medical.pdf. Accessed August 15, 2017.
- Becker F, Douglass S. The ecology of the patient visit: physical attractiveness, waiting times and perceived quality of care. J Ambul Care Manag. 2008;31(2):128–141.
- Becker F, Sweeney B, Parsons K. Ambulatory facility design and patients’ perceptions of healthcare quality. HERD. 2008;1(4):35–54.
- Outcome Health Website. https://www.outcomehealth.com/. Accessed August 14, 2017.
- Mazer SE. The waiting room: Where suffering begins. Healing Healthcare Systems website. http://www.healinghealth.com/waiting-room-suffering-begins/. Published November 7, 2014. Accessed August 14, 2017.
- Patient Point Programs Website. http://patientpoint.com/. Accessed August 14, 2017.
- Almquist J, Kelly C, Bromberg J, Bryant S, Christianson T, Montori V. Consultation room design and the clinical encounter: the space and interaction randomized trial. Health Environ Res Design. 2009;3(1):41–78.
- Maslow A, Mintz N. Effects of esthetic surroundings: I. Initial effects of three esthetic conditions upon perceiving “energy” and “well-being” in faces. J Psychology. 1956;41(2):247–254.
- Siegrist RB. The patient experience. In: Sanfilippo JS, Bieber E, Javich D, Siegrist R, eds. MBA for Healthcare. New York, NY: Oxford Press;2016:227–236.
- Press I. Patient satisfaction: Understanding and managing the experience of care. 2nd ed. Chicago, IL: Health Administration Press; 2005:66–78.
- Piper L, Tallman E. Hospital consumer assessment of healthcare providers and systems: An ethical leadership dilemma to satisfy patients. Health Care Manag (Frederick). 2016;35(2):151–155.
- Giordano L, Elliott M, Goldstein E, Lehrman W, Spencer P. Development, implementation and public reporting of HCAHPS survey. Med Care Res Rev. 2010;67(1):27–37.
- Jones KE. Helping the health profession help others: Applying business principles to the medical world. University of Tennessee, Knoxville Honors Thesis Projects. http://trace.tennessee.edu/cgi/viewcontent.cgi?article=1560&context=utk_chanhonoproj. Published 2002. Accessed August 14, 2017.
- Baum N. Marketing your practice: ethically, effectively and economically. In: Sanfilippo JS, Nolan TE, Whiteside BH, eds. MBA Handbook for Healthcare Professionals. New York, NY: Parthenon Publishing Group; 2002:123–154.
- Baum NH. Four pillars of a successful practice: 1. Keep your current patients happy. OBG Manag. 2013;25(3):49–56.
- Baum NH. Four pillars of a successful practice: 4. Motivate your staff. OBG Manag. 2013;25(8):29–33.
Do you answer patient emails?
Recently I received a lengthy email from a woman who claimed to have once been a patient, though her name did not come up in my EHR system. She asked numerous questions about a self-diagnosed skin disorder.
I was undecided on how to reply – or even whether to reply at all – so I queried several dozen dermatology colleagues around the country, as well as a few physician friends and acquaintances in other specialties.
Responses varied all over the map – from “I never answer patient emails” to “What harm could it do, she’s better off getting correct answers from you than incorrect answers from some ‘advocacy’ web site” – and everything in between. I decided to look at what has been published on the subject.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/do-you-answer-patient-emails-take-our-poll?iframe=1"}]It turns out that as early as 1998, a group of investigators asked this same question and designed a study to address it (JAMA. 1998 Oct 21;280[15]:1333-5). Posing as a fictitious patient, they sent emails to random dermatologists describing an acute dermatological problem, tallied the responses they received, and followed up with a questionnaire to responders and nonresponders alike.
As with my informal survey, the authors found what they termed “a striking lack of consensus” on how to deal with this situation: 50% responded to the fictitious patient’s email; of those, 31% refused to give advice without seeing the patient, but 59% offered a diagnosis, and a third of that group went on to provide specific advice about therapy. In response to the questionnaire, 28% said that they tended not to answer any patient emails, 24% said they usually replied with a standard message, and 24% said they answered each request individually. The authors concluded that “standards for physician response to unsolicited patient e-mail are needed.”
Indeed. But my own unscientific survey suggests that, almost 20 years later, there is still nothing resembling a consensus on this issue. In the interim, several groups, including the American Medical Informatics Association, Medem, and the American Medical Association have proposed guidelines; but none have been generally accepted. Until such time as that happens, it seems prudent for each individual practice to adopt its own. For ideas, take a look at the proposals from the groups I mentioned, plus any others you can find. When you’re done, consider running your list past your lawyer to make sure you haven’t forgotten anything, and that there are no unique requirements in your state.
Your guidelines may be very simple (if you decide never to answer any queries) or very complex, depending on your situation and personal philosophy; but all guidelines should cover such issues as authentication of correspondents, informed consent, licensing jurisdiction (if you receive e-mails from states in which you are not licensed), and of course, confidentiality.
Contrary to popular belief, the Health Insurance Portability and Accountability Act (HIPAA) does not prohibit email communication with patients, nor does it require that it be encrypted. The HIPAA website specifically says, “Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.”
Still, if you are not comfortable with unencrypted communication, encryption software can be added to your practice’s email system. Enli, Sigaba, Tumbleweed, Zix, and many other vendors sell encryption packages. (As always, I have no financial interest in any product or enterprise mentioned in this column.)
Another option is web-based messaging: Patients enter your website and send a message using an electronic template that you design. A designated staffer will be notified by regular email when messages are received, and can post a reply on a page that can only be accessed by the patient. Besides enhancing privacy and security, you can state your guidelines in plain English to preclude any misunderstanding of what you will and will not address online.
Web-based messaging services can be freestanding or incorporated into existing secure web sites. Medfusion and RelayHealth are among the leading vendors of secure messaging services.
And now, I’m writing my guidelines.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Recently I received a lengthy email from a woman who claimed to have once been a patient, though her name did not come up in my EHR system. She asked numerous questions about a self-diagnosed skin disorder.
I was undecided on how to reply – or even whether to reply at all – so I queried several dozen dermatology colleagues around the country, as well as a few physician friends and acquaintances in other specialties.
Responses varied all over the map – from “I never answer patient emails” to “What harm could it do, she’s better off getting correct answers from you than incorrect answers from some ‘advocacy’ web site” – and everything in between. I decided to look at what has been published on the subject.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/do-you-answer-patient-emails-take-our-poll?iframe=1"}]It turns out that as early as 1998, a group of investigators asked this same question and designed a study to address it (JAMA. 1998 Oct 21;280[15]:1333-5). Posing as a fictitious patient, they sent emails to random dermatologists describing an acute dermatological problem, tallied the responses they received, and followed up with a questionnaire to responders and nonresponders alike.
As with my informal survey, the authors found what they termed “a striking lack of consensus” on how to deal with this situation: 50% responded to the fictitious patient’s email; of those, 31% refused to give advice without seeing the patient, but 59% offered a diagnosis, and a third of that group went on to provide specific advice about therapy. In response to the questionnaire, 28% said that they tended not to answer any patient emails, 24% said they usually replied with a standard message, and 24% said they answered each request individually. The authors concluded that “standards for physician response to unsolicited patient e-mail are needed.”
Indeed. But my own unscientific survey suggests that, almost 20 years later, there is still nothing resembling a consensus on this issue. In the interim, several groups, including the American Medical Informatics Association, Medem, and the American Medical Association have proposed guidelines; but none have been generally accepted. Until such time as that happens, it seems prudent for each individual practice to adopt its own. For ideas, take a look at the proposals from the groups I mentioned, plus any others you can find. When you’re done, consider running your list past your lawyer to make sure you haven’t forgotten anything, and that there are no unique requirements in your state.
Your guidelines may be very simple (if you decide never to answer any queries) or very complex, depending on your situation and personal philosophy; but all guidelines should cover such issues as authentication of correspondents, informed consent, licensing jurisdiction (if you receive e-mails from states in which you are not licensed), and of course, confidentiality.
Contrary to popular belief, the Health Insurance Portability and Accountability Act (HIPAA) does not prohibit email communication with patients, nor does it require that it be encrypted. The HIPAA website specifically says, “Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.”
Still, if you are not comfortable with unencrypted communication, encryption software can be added to your practice’s email system. Enli, Sigaba, Tumbleweed, Zix, and many other vendors sell encryption packages. (As always, I have no financial interest in any product or enterprise mentioned in this column.)
Another option is web-based messaging: Patients enter your website and send a message using an electronic template that you design. A designated staffer will be notified by regular email when messages are received, and can post a reply on a page that can only be accessed by the patient. Besides enhancing privacy and security, you can state your guidelines in plain English to preclude any misunderstanding of what you will and will not address online.
Web-based messaging services can be freestanding or incorporated into existing secure web sites. Medfusion and RelayHealth are among the leading vendors of secure messaging services.
And now, I’m writing my guidelines.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Recently I received a lengthy email from a woman who claimed to have once been a patient, though her name did not come up in my EHR system. She asked numerous questions about a self-diagnosed skin disorder.
I was undecided on how to reply – or even whether to reply at all – so I queried several dozen dermatology colleagues around the country, as well as a few physician friends and acquaintances in other specialties.
Responses varied all over the map – from “I never answer patient emails” to “What harm could it do, she’s better off getting correct answers from you than incorrect answers from some ‘advocacy’ web site” – and everything in between. I decided to look at what has been published on the subject.
[polldaddy:{"method":"iframe","type":"survey","src":"//newspolls2017.polldaddy.com/s/do-you-answer-patient-emails-take-our-poll?iframe=1"}]It turns out that as early as 1998, a group of investigators asked this same question and designed a study to address it (JAMA. 1998 Oct 21;280[15]:1333-5). Posing as a fictitious patient, they sent emails to random dermatologists describing an acute dermatological problem, tallied the responses they received, and followed up with a questionnaire to responders and nonresponders alike.
As with my informal survey, the authors found what they termed “a striking lack of consensus” on how to deal with this situation: 50% responded to the fictitious patient’s email; of those, 31% refused to give advice without seeing the patient, but 59% offered a diagnosis, and a third of that group went on to provide specific advice about therapy. In response to the questionnaire, 28% said that they tended not to answer any patient emails, 24% said they usually replied with a standard message, and 24% said they answered each request individually. The authors concluded that “standards for physician response to unsolicited patient e-mail are needed.”
Indeed. But my own unscientific survey suggests that, almost 20 years later, there is still nothing resembling a consensus on this issue. In the interim, several groups, including the American Medical Informatics Association, Medem, and the American Medical Association have proposed guidelines; but none have been generally accepted. Until such time as that happens, it seems prudent for each individual practice to adopt its own. For ideas, take a look at the proposals from the groups I mentioned, plus any others you can find. When you’re done, consider running your list past your lawyer to make sure you haven’t forgotten anything, and that there are no unique requirements in your state.
Your guidelines may be very simple (if you decide never to answer any queries) or very complex, depending on your situation and personal philosophy; but all guidelines should cover such issues as authentication of correspondents, informed consent, licensing jurisdiction (if you receive e-mails from states in which you are not licensed), and of course, confidentiality.
Contrary to popular belief, the Health Insurance Portability and Accountability Act (HIPAA) does not prohibit email communication with patients, nor does it require that it be encrypted. The HIPAA website specifically says, “Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.”
Still, if you are not comfortable with unencrypted communication, encryption software can be added to your practice’s email system. Enli, Sigaba, Tumbleweed, Zix, and many other vendors sell encryption packages. (As always, I have no financial interest in any product or enterprise mentioned in this column.)
Another option is web-based messaging: Patients enter your website and send a message using an electronic template that you design. A designated staffer will be notified by regular email when messages are received, and can post a reply on a page that can only be accessed by the patient. Besides enhancing privacy and security, you can state your guidelines in plain English to preclude any misunderstanding of what you will and will not address online.
Web-based messaging services can be freestanding or incorporated into existing secure web sites. Medfusion and RelayHealth are among the leading vendors of secure messaging services.
And now, I’m writing my guidelines.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
ICD-10-CM code changes: What's new for 2018
The list of new and revised International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes has been published, with changes becoming effective on October 1, 2017. This year, you can look forward to minimal code changes for gynecologic conditions. The biggest change in this category is the addition of codes that describe a lump in the breast according to which breast and the location on the breast, as well as the addition of a code for prophylactic removal of the fallopian tubes. The codes related to obstetrics will have more extensive changes. You will find revisions to the codes for ectopic pregnancy, a new set of codes for addressing an abnormal fetal heart rate during the antepartum period, and, most welcome of all, an expansion of the single code for antenatal testing to 17 very specific codes.
Gynecologic code changes
The single code N63, Unspecified lump in breast, has been expanded to include codes for both the right and the left breast. Code N63 therefore will be considered invalid after October 1, 2018. Expanded codes include:
- N63.0, Unspecified lump in unspecified breast
- N63.1, Unspecified lump in the right breast
- N63.10, Unspecified lump in the right breast, unspecified quadrant
- N63.11, Unspecified lump in the right breast, upper outer quadrant
- N63.12, Unspecified lump in the right breast, upper inner quadrant
- N63.13, Unspecified lump in the right breast, lower outer quadrant
- N63.14, Unspecified lump in the right breast, lower inner quadrant
- N63.2, Unspecified lump in the left breast
- N63.20, Unspecified lump in the left breast, unspecified quadrant
- N63.21, Unspecified lump in the left breast, upper outer quadrant
- N63.22, Unspecified lump in the left breast, upper inner quadrant
- N63.23, Unspecified lump in the left breast, lower outer quadrant
- N63.24, Unspecified lump in the left breast, lower inner quadrant
- N63.3, Unspecified lump in axillary tail
- N63.31, Unspecified lump in axillary tail of the right breast
- N63.32, Unspecified lump in axillary tail of the left breast
- N63.4, Unspecified lump in breast, subareolar
- N63.41, Unspecified lump in right breast, subareolar
- N63.42, Unspecified lump in left breast, subareolar
Other changes to gynecologic codes
There has been a minor change to the description for code Z31.5, Encounter for genetic counseling. It now is described as "Encounter for procreative genetic counseling."
The code Z40.02, Encounter for prophylactic removal of ovary(s), now refers to one or more ovaries without distinction of right or left, and a new code has been added for removal of the fallopian tube(s), Z40.03, Encounter for prophylactic removal of fallopian tube(s).
The inclusion term "endometriosis of the thorax" has been added to code N80.8, Other endometriosis.
The inclusion term "premenstrual dysphoric disorder" has been deleted from code N94.3, Premenstrual tension syndrome. If the patient has been diagnosed with this condition, the code F32.81, Premenstrual dysphoric disorder, should be reported, as this is considered a mental health issue.
The "excludes 1" note under code Z87.41, Personal history of dysplasia of the female genital tract, has been revised. The codes for personal history of intraepithelial neoplasia III that may not be reported with this code are Z86.001 and Z86.008.
Obstetric code changes
The ectopic pregnancy codes have been revised to include references to the right or left structure affected, which means the codes change from 5 digits to 6 digits in length, and the codes O00.10, O00.11, O00.20, and O00.21 will no longer be valid.
- O00.1, Tubal pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.101, Right tubal pregnancy without intrauterine pregnancy
- O00.102, Left tubal pregnancy without intrauterine pregnancy
- O00.109, Unspecified tubal pregnancy without intrauterine pregnancy
- O00.11, Tubal pregnancy with intrauterine pregnancy
- O00.111, Right tubal pregnancy with intrauterine pregnancy
- O00.112, Left tubal pregnancy with intrauterine pregnancy
- O00.119, Unspecified tubal pregnancy with intrauterine pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.2, Ovarian pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
- O00.201, Right ovarian pregnancy without intrauterine pregnancy
- O00.202, Left ovarian pregnancy without intrauterine pregnancy
- O00.209, Unspecified ovarian pregnancy without intrauterine pregnancy
- O00.21, Ovarian pregnancy with intrauterine pregnancy
- O00.211, Right ovarian pregnancy with intrauterine pregnancy
- O00.212, Left ovarian pregnancy with intrauterine pregnancy
- O00.219, Unspecified ovarian pregnancy with intrauterine pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
New codes for fetal heart rate abnormalities
New codes have been added to report a fetal heart rate or rhythm abnormality during the antepartum period. Until now, there only has been a code that addresses this issue during labor and delivery, O76, Abnormality in fetal heart rate and rhythm complicating labor and delivery.
- O36.83, Maternal care for abnormalities of the fetal heart rate or rhythm
- O36.831, Maternal care for abnormalities of the fetal heart rate or rhythm, first trimester
- O36.832, Maternal care for abnormalities of the fetal heart rate or rhythm, second trimester
- O36.833, Maternal care for abnormalities of the fetal heart rate or rhythm, third trimester
- O36.839, Maternal care for abnormalities of the fetal heart rate or rhythm, unspecified trimester
Several codes redefined
ICD-10 has corrected an "excludes" note error for the code O99.1, Other diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism complicating pregnancy, childbirth, and the puerperium. In 2017, any hemorrhage with coagulation defects defined in code category O45.- or codes O46.0-, O67.0, or O72.3 could be reported with O99.1. This set of codes has now been redefined as an "excludes 1" note, which means that they may not be reported with O99.1 since they are considered inclusive.
More specific codes added for antenatal screening
Great news for those awaiting a more specific code for antenatal screening: The code Z36 has been expanded to more closely match the codes that were available in ICD-9-CM, but it goes beyond the basic list in that codes have been added for things like nonvisualization of anatomic structures on a previous scan and screening for cervical length and fetal lung maturity. Be sure to pay attention to the excludes notes and other inclusive terms.
- Z36, Encounter for antenatal screening of mother (Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.)
Includes: Encounter for placental sample (taken vaginally)
Excludes 2: O28.-, Abnormal findings on antenatal screening of mother
- Z36.5, Encounter for antenatal screening for isoimmunization
- Z36.4, Encounter for antenatal screening for fetal growth retardation
Intrauterine growth restriction (IUGR)/small-for-dates - Z36.3, Encounter for antenatal screening for malformations
Screening for a suspected anomaly - Z36.2, Encounter for other antenatal screening follow-up
Nonvisualized anatomy on a previous scan - Z36.1, Encounter for antenatal screening for raised alpha-fetoprotein level
Encounter for antenatal screening for elevated maternal serum alpha-fetoprotein level - Z36.0, Encounter for antenatal screening for chromosomal anomalies
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.8A, Encounter for antenatal screening for other genetic defects
- Z36.89, Encounter for other specified antenatal screening
- Z36.88, Encounter for antenatal screening for fetal macrosomia
Screening for large-for-dates - Z36.87, Encounter for antenatal screening for uncertain dates
- Z36.86, Encounter for antenatal screening for cervical length
Screening for risk of preterm labor - Z36.85, Encounter for antenatal screening for Streptococcus B
- Z36.84, Encounter for antenatal screening for fetal lung maturity
- Z36.83, Encounter for fetal screening for congenital cardiac abnormalities
- Z36.82, Encounter for antenatal screening for nuchal translucency
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.9, Encounter for antenatal screening, unspecified
Code changes for abortion and complications
The code range for use with Z3A, weeks of gestation, has changed from O00-O9A to O09-O9A to reflect the guideline change last year to remove the requirement to use this code with any code that describes pregnancy with an abortive outcome (codes O00-O08).
In addition, if a patient has retained products of conception (POC) after either a spontaneous or elective abortion, report the "without complication" code for the retained POC (O03.4, Incomplete spontaneous abortion without complication, or O07.4, Failed attempted termination of pregnancy without complication). If any other complication occurred in addition to the retained POC, use the code for that particular complication and not O03.4 or O07.4.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The list of new and revised International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes has been published, with changes becoming effective on October 1, 2017. This year, you can look forward to minimal code changes for gynecologic conditions. The biggest change in this category is the addition of codes that describe a lump in the breast according to which breast and the location on the breast, as well as the addition of a code for prophylactic removal of the fallopian tubes. The codes related to obstetrics will have more extensive changes. You will find revisions to the codes for ectopic pregnancy, a new set of codes for addressing an abnormal fetal heart rate during the antepartum period, and, most welcome of all, an expansion of the single code for antenatal testing to 17 very specific codes.
Gynecologic code changes
The single code N63, Unspecified lump in breast, has been expanded to include codes for both the right and the left breast. Code N63 therefore will be considered invalid after October 1, 2018. Expanded codes include:
- N63.0, Unspecified lump in unspecified breast
- N63.1, Unspecified lump in the right breast
- N63.10, Unspecified lump in the right breast, unspecified quadrant
- N63.11, Unspecified lump in the right breast, upper outer quadrant
- N63.12, Unspecified lump in the right breast, upper inner quadrant
- N63.13, Unspecified lump in the right breast, lower outer quadrant
- N63.14, Unspecified lump in the right breast, lower inner quadrant
- N63.2, Unspecified lump in the left breast
- N63.20, Unspecified lump in the left breast, unspecified quadrant
- N63.21, Unspecified lump in the left breast, upper outer quadrant
- N63.22, Unspecified lump in the left breast, upper inner quadrant
- N63.23, Unspecified lump in the left breast, lower outer quadrant
- N63.24, Unspecified lump in the left breast, lower inner quadrant
- N63.3, Unspecified lump in axillary tail
- N63.31, Unspecified lump in axillary tail of the right breast
- N63.32, Unspecified lump in axillary tail of the left breast
- N63.4, Unspecified lump in breast, subareolar
- N63.41, Unspecified lump in right breast, subareolar
- N63.42, Unspecified lump in left breast, subareolar
Other changes to gynecologic codes
There has been a minor change to the description for code Z31.5, Encounter for genetic counseling. It now is described as "Encounter for procreative genetic counseling."
The code Z40.02, Encounter for prophylactic removal of ovary(s), now refers to one or more ovaries without distinction of right or left, and a new code has been added for removal of the fallopian tube(s), Z40.03, Encounter for prophylactic removal of fallopian tube(s).
The inclusion term "endometriosis of the thorax" has been added to code N80.8, Other endometriosis.
The inclusion term "premenstrual dysphoric disorder" has been deleted from code N94.3, Premenstrual tension syndrome. If the patient has been diagnosed with this condition, the code F32.81, Premenstrual dysphoric disorder, should be reported, as this is considered a mental health issue.
The "excludes 1" note under code Z87.41, Personal history of dysplasia of the female genital tract, has been revised. The codes for personal history of intraepithelial neoplasia III that may not be reported with this code are Z86.001 and Z86.008.
Obstetric code changes
The ectopic pregnancy codes have been revised to include references to the right or left structure affected, which means the codes change from 5 digits to 6 digits in length, and the codes O00.10, O00.11, O00.20, and O00.21 will no longer be valid.
- O00.1, Tubal pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.101, Right tubal pregnancy without intrauterine pregnancy
- O00.102, Left tubal pregnancy without intrauterine pregnancy
- O00.109, Unspecified tubal pregnancy without intrauterine pregnancy
- O00.11, Tubal pregnancy with intrauterine pregnancy
- O00.111, Right tubal pregnancy with intrauterine pregnancy
- O00.112, Left tubal pregnancy with intrauterine pregnancy
- O00.119, Unspecified tubal pregnancy with intrauterine pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.2, Ovarian pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
- O00.201, Right ovarian pregnancy without intrauterine pregnancy
- O00.202, Left ovarian pregnancy without intrauterine pregnancy
- O00.209, Unspecified ovarian pregnancy without intrauterine pregnancy
- O00.21, Ovarian pregnancy with intrauterine pregnancy
- O00.211, Right ovarian pregnancy with intrauterine pregnancy
- O00.212, Left ovarian pregnancy with intrauterine pregnancy
- O00.219, Unspecified ovarian pregnancy with intrauterine pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
New codes for fetal heart rate abnormalities
New codes have been added to report a fetal heart rate or rhythm abnormality during the antepartum period. Until now, there only has been a code that addresses this issue during labor and delivery, O76, Abnormality in fetal heart rate and rhythm complicating labor and delivery.
- O36.83, Maternal care for abnormalities of the fetal heart rate or rhythm
- O36.831, Maternal care for abnormalities of the fetal heart rate or rhythm, first trimester
- O36.832, Maternal care for abnormalities of the fetal heart rate or rhythm, second trimester
- O36.833, Maternal care for abnormalities of the fetal heart rate or rhythm, third trimester
- O36.839, Maternal care for abnormalities of the fetal heart rate or rhythm, unspecified trimester
Several codes redefined
ICD-10 has corrected an "excludes" note error for the code O99.1, Other diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism complicating pregnancy, childbirth, and the puerperium. In 2017, any hemorrhage with coagulation defects defined in code category O45.- or codes O46.0-, O67.0, or O72.3 could be reported with O99.1. This set of codes has now been redefined as an "excludes 1" note, which means that they may not be reported with O99.1 since they are considered inclusive.
More specific codes added for antenatal screening
Great news for those awaiting a more specific code for antenatal screening: The code Z36 has been expanded to more closely match the codes that were available in ICD-9-CM, but it goes beyond the basic list in that codes have been added for things like nonvisualization of anatomic structures on a previous scan and screening for cervical length and fetal lung maturity. Be sure to pay attention to the excludes notes and other inclusive terms.
- Z36, Encounter for antenatal screening of mother (Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.)
Includes: Encounter for placental sample (taken vaginally)
Excludes 2: O28.-, Abnormal findings on antenatal screening of mother
- Z36.5, Encounter for antenatal screening for isoimmunization
- Z36.4, Encounter for antenatal screening for fetal growth retardation
Intrauterine growth restriction (IUGR)/small-for-dates - Z36.3, Encounter for antenatal screening for malformations
Screening for a suspected anomaly - Z36.2, Encounter for other antenatal screening follow-up
Nonvisualized anatomy on a previous scan - Z36.1, Encounter for antenatal screening for raised alpha-fetoprotein level
Encounter for antenatal screening for elevated maternal serum alpha-fetoprotein level - Z36.0, Encounter for antenatal screening for chromosomal anomalies
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.8A, Encounter for antenatal screening for other genetic defects
- Z36.89, Encounter for other specified antenatal screening
- Z36.88, Encounter for antenatal screening for fetal macrosomia
Screening for large-for-dates - Z36.87, Encounter for antenatal screening for uncertain dates
- Z36.86, Encounter for antenatal screening for cervical length
Screening for risk of preterm labor - Z36.85, Encounter for antenatal screening for Streptococcus B
- Z36.84, Encounter for antenatal screening for fetal lung maturity
- Z36.83, Encounter for fetal screening for congenital cardiac abnormalities
- Z36.82, Encounter for antenatal screening for nuchal translucency
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.9, Encounter for antenatal screening, unspecified
Code changes for abortion and complications
The code range for use with Z3A, weeks of gestation, has changed from O00-O9A to O09-O9A to reflect the guideline change last year to remove the requirement to use this code with any code that describes pregnancy with an abortive outcome (codes O00-O08).
In addition, if a patient has retained products of conception (POC) after either a spontaneous or elective abortion, report the "without complication" code for the retained POC (O03.4, Incomplete spontaneous abortion without complication, or O07.4, Failed attempted termination of pregnancy without complication). If any other complication occurred in addition to the retained POC, use the code for that particular complication and not O03.4 or O07.4.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The list of new and revised International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes has been published, with changes becoming effective on October 1, 2017. This year, you can look forward to minimal code changes for gynecologic conditions. The biggest change in this category is the addition of codes that describe a lump in the breast according to which breast and the location on the breast, as well as the addition of a code for prophylactic removal of the fallopian tubes. The codes related to obstetrics will have more extensive changes. You will find revisions to the codes for ectopic pregnancy, a new set of codes for addressing an abnormal fetal heart rate during the antepartum period, and, most welcome of all, an expansion of the single code for antenatal testing to 17 very specific codes.
Gynecologic code changes
The single code N63, Unspecified lump in breast, has been expanded to include codes for both the right and the left breast. Code N63 therefore will be considered invalid after October 1, 2018. Expanded codes include:
- N63.0, Unspecified lump in unspecified breast
- N63.1, Unspecified lump in the right breast
- N63.10, Unspecified lump in the right breast, unspecified quadrant
- N63.11, Unspecified lump in the right breast, upper outer quadrant
- N63.12, Unspecified lump in the right breast, upper inner quadrant
- N63.13, Unspecified lump in the right breast, lower outer quadrant
- N63.14, Unspecified lump in the right breast, lower inner quadrant
- N63.2, Unspecified lump in the left breast
- N63.20, Unspecified lump in the left breast, unspecified quadrant
- N63.21, Unspecified lump in the left breast, upper outer quadrant
- N63.22, Unspecified lump in the left breast, upper inner quadrant
- N63.23, Unspecified lump in the left breast, lower outer quadrant
- N63.24, Unspecified lump in the left breast, lower inner quadrant
- N63.3, Unspecified lump in axillary tail
- N63.31, Unspecified lump in axillary tail of the right breast
- N63.32, Unspecified lump in axillary tail of the left breast
- N63.4, Unspecified lump in breast, subareolar
- N63.41, Unspecified lump in right breast, subareolar
- N63.42, Unspecified lump in left breast, subareolar
Other changes to gynecologic codes
There has been a minor change to the description for code Z31.5, Encounter for genetic counseling. It now is described as "Encounter for procreative genetic counseling."
The code Z40.02, Encounter for prophylactic removal of ovary(s), now refers to one or more ovaries without distinction of right or left, and a new code has been added for removal of the fallopian tube(s), Z40.03, Encounter for prophylactic removal of fallopian tube(s).
The inclusion term "endometriosis of the thorax" has been added to code N80.8, Other endometriosis.
The inclusion term "premenstrual dysphoric disorder" has been deleted from code N94.3, Premenstrual tension syndrome. If the patient has been diagnosed with this condition, the code F32.81, Premenstrual dysphoric disorder, should be reported, as this is considered a mental health issue.
The "excludes 1" note under code Z87.41, Personal history of dysplasia of the female genital tract, has been revised. The codes for personal history of intraepithelial neoplasia III that may not be reported with this code are Z86.001 and Z86.008.
Obstetric code changes
The ectopic pregnancy codes have been revised to include references to the right or left structure affected, which means the codes change from 5 digits to 6 digits in length, and the codes O00.10, O00.11, O00.20, and O00.21 will no longer be valid.
- O00.1, Tubal pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.101, Right tubal pregnancy without intrauterine pregnancy
- O00.102, Left tubal pregnancy without intrauterine pregnancy
- O00.109, Unspecified tubal pregnancy without intrauterine pregnancy
- O00.11, Tubal pregnancy with intrauterine pregnancy
- O00.111, Right tubal pregnancy with intrauterine pregnancy
- O00.112, Left tubal pregnancy with intrauterine pregnancy
- O00.119, Unspecified tubal pregnancy with intrauterine pregnancy
- O00.10, Tubal pregnancy without intrauterine pregnancy
- O00.2, Ovarian pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
- O00.201, Right ovarian pregnancy without intrauterine pregnancy
- O00.202, Left ovarian pregnancy without intrauterine pregnancy
- O00.209, Unspecified ovarian pregnancy without intrauterine pregnancy
- O00.21, Ovarian pregnancy with intrauterine pregnancy
- O00.211, Right ovarian pregnancy with intrauterine pregnancy
- O00.212, Left ovarian pregnancy with intrauterine pregnancy
- O00.219, Unspecified ovarian pregnancy with intrauterine pregnancy
- O00.20, Ovarian pregnancy without intrauterine pregnancy
New codes for fetal heart rate abnormalities
New codes have been added to report a fetal heart rate or rhythm abnormality during the antepartum period. Until now, there only has been a code that addresses this issue during labor and delivery, O76, Abnormality in fetal heart rate and rhythm complicating labor and delivery.
- O36.83, Maternal care for abnormalities of the fetal heart rate or rhythm
- O36.831, Maternal care for abnormalities of the fetal heart rate or rhythm, first trimester
- O36.832, Maternal care for abnormalities of the fetal heart rate or rhythm, second trimester
- O36.833, Maternal care for abnormalities of the fetal heart rate or rhythm, third trimester
- O36.839, Maternal care for abnormalities of the fetal heart rate or rhythm, unspecified trimester
Several codes redefined
ICD-10 has corrected an "excludes" note error for the code O99.1, Other diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism complicating pregnancy, childbirth, and the puerperium. In 2017, any hemorrhage with coagulation defects defined in code category O45.- or codes O46.0-, O67.0, or O72.3 could be reported with O99.1. This set of codes has now been redefined as an "excludes 1" note, which means that they may not be reported with O99.1 since they are considered inclusive.
More specific codes added for antenatal screening
Great news for those awaiting a more specific code for antenatal screening: The code Z36 has been expanded to more closely match the codes that were available in ICD-9-CM, but it goes beyond the basic list in that codes have been added for things like nonvisualization of anatomic structures on a previous scan and screening for cervical length and fetal lung maturity. Be sure to pay attention to the excludes notes and other inclusive terms.
- Z36, Encounter for antenatal screening of mother (Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.)
Includes: Encounter for placental sample (taken vaginally)
Excludes 2: O28.-, Abnormal findings on antenatal screening of mother
- Z36.5, Encounter for antenatal screening for isoimmunization
- Z36.4, Encounter for antenatal screening for fetal growth retardation
Intrauterine growth restriction (IUGR)/small-for-dates - Z36.3, Encounter for antenatal screening for malformations
Screening for a suspected anomaly - Z36.2, Encounter for other antenatal screening follow-up
Nonvisualized anatomy on a previous scan - Z36.1, Encounter for antenatal screening for raised alpha-fetoprotein level
Encounter for antenatal screening for elevated maternal serum alpha-fetoprotein level - Z36.0, Encounter for antenatal screening for chromosomal anomalies
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.8A, Encounter for antenatal screening for other genetic defects
- Z36.89, Encounter for other specified antenatal screening
- Z36.88, Encounter for antenatal screening for fetal macrosomia
Screening for large-for-dates - Z36.87, Encounter for antenatal screening for uncertain dates
- Z36.86, Encounter for antenatal screening for cervical length
Screening for risk of preterm labor - Z36.85, Encounter for antenatal screening for Streptococcus B
- Z36.84, Encounter for antenatal screening for fetal lung maturity
- Z36.83, Encounter for fetal screening for congenital cardiac abnormalities
- Z36.82, Encounter for antenatal screening for nuchal translucency
- Z36.81, Encounter for antenatal screening for hydrops fetalis
- Z36.9, Encounter for antenatal screening, unspecified
Code changes for abortion and complications
The code range for use with Z3A, weeks of gestation, has changed from O00-O9A to O09-O9A to reflect the guideline change last year to remove the requirement to use this code with any code that describes pregnancy with an abortive outcome (codes O00-O08).
In addition, if a patient has retained products of conception (POC) after either a spontaneous or elective abortion, report the "without complication" code for the retained POC (O03.4, Incomplete spontaneous abortion without complication, or O07.4, Failed attempted termination of pregnancy without complication). If any other complication occurred in addition to the retained POC, use the code for that particular complication and not O03.4 or O07.4.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Surgical catastrophe: Offering a lifeline to the second victim
CASE A surgeon's story of patient loss
It was a Wednesday morning and Ms. M was my first case of the day. I knew her well, having delivered her 2 children. Now she had a 7-cm complex cyst on her right ovary, she was in pain, and she was possibly experiencing ovarian torsion. My resident took care of the paperwork, I met the patient in preop, answered her few questions, and reassured her husband that I would call him as soon as surgery was over. She was rolled to the operating room.
When I entered the OR, Ms. M was under general anesthesia, draped, and placed on the operating table in the usual position. I made a 5-mm incision at the umbilicus and inserted the trocar under direct visualization. There was blood and the camera became blurry. I removed the camera to clean it, and the anesthesiologist alerted me that there was sudden hypotension. I reinserted the camera and saw blood in the abdomen. I feared the worst—major vessel injury. I requested a scalpel and made a midline skin sub–umbilical incision, entered the peritoneal cavity, and observed blood everywhere. The massive transfusion protocol was activated and vascular surgery was called in. I could not find the source of the bleeding. Using a laparotomy towel I applied pressure on the aorta. The vascular surgeon arrived and pushed my resident away. He identified the source of the bleeding: The right common iliac artery was injured.
The patient coded, the anesthesiologist initiated CPR, bleeding continued, blood was being transfused, and after 20 long minutes of CPR the lifeless body of my patient could not hold any more. She was pronounced dead on the table.
At that moment, there were multiple victims: Ms. M lying on the surgical table; her family members, who did not know what was happening; and the surgical team members, who were looking at each other in denial and feeling that we had failed this patient, hoping that we would wake up from this nightmare.
Defining patient harm
Many patients experience harm each year because of an adverse medical event or preventable medical error.1 A 2013 report revealed that 210,000 to 440,000 deaths occur each year in the United States related to preventable patient harm.2 Although this fact is deeply disturbing, it is well known that modern health care is a high-risk industry.
Medical errors vary in terms of the degree of potential or actual damage. A “near miss” is any event that could have resulted in adverse consequences but did not (for example, an incorrect drug or dose ordered but not administered). On the other hand, an “adverse event” describes an error that resulted in some degree of patient harm or suffering.3
Related article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
For each patient who dies because of a medical error or a surgical complication, whether preventable or not, many clinicians are involved in the unfolding of the case. These events have a profound impact on well-intentioned, competent, and caring physicians, and they elicit intense emotional responses.4 When a patient experiences an unexpected adverse surgical outcome, the surgeons involved in their care may become “second victims.” They may feel that they have failed the patient and they second-guess their surgical skills and knowledge base; some express concern about their reputation and perhaps career choice.
Psychological responses. It is importantto understand this process to ensure a healthy recovery. Psychological responses to an adverse medical event include guilt; distress, anxiety, and fear; frustration and anger; feelings of insufficiency; and long-standing suffering. Clinicians who experienced an adverse medical event have reported additional psychological as well as physical symptoms in the aftermath of the event (TABLE 1).5
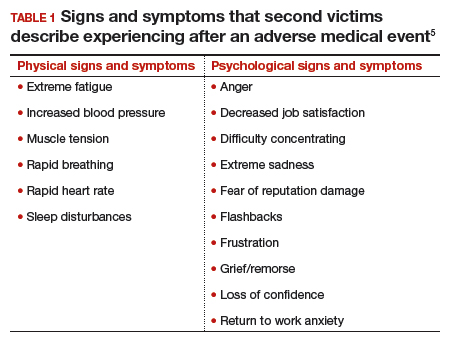
Risk factors. Certain factors are associated with a greater emotional impact of an adverse medical event, including6:
- severity of the harm or leaving permanent sequelae
- death of a healthy patient or a child (for example, from a motor vehicle accident)
- self-blame for the error
- unexpected patient death (for example, a catastrophic complication after a relatively benign procedure)
- physicians-in-training responsible for the patient
- first death under a clinician’s watch.
While most research in the field of medical error focuses on systems or process improvement, it is important not to neglect the individual and personal aspects of the clinicians involved in the event. The health care system must include care for our injured colleagues, the so-called second victims.
Read about the steps to recovery for the second victim.
Steps in recovery for the second victim
Based on a semistructured interview of 31 physicians involved in adverse events, Scott and colleagues described the following 6 stages of healing5:
Chaos and accident response. Immediately after the event, the physician feels a sense of confusion, panic, and denial. How can this be happening to me? The physician is frequently distracted, immersed in self-reflection.
Intrusive reflections. This is a period of self-questioning. Thoughts of the event and different possible scenarios dominate the physician’s mind. What if I had done this or that?
Restoring personal integrity. During this phase, the physician seeks support from individuals with whom trusted relationships exist, such as colleagues, peers, close friends, and family members. Advice from a colleague who has your same level of expertise is precious. The second victim often fears that friends and family will not be understanding.
Enduring the inquisition. Root cause analysis and in-depth case review is an important part of the quality improvement process after an adverse event. A debriefing or departmental morbidity and mortality conference can trigger emotions and increase the sense of shame, guilt, and self-doubt. The second victim starts to wonder about repercussions that may affect job security, licensure, and future litigation.
Obtaining emotional first aid. At this stage, the second victim begins to heal, but it is important to obtain external help from a colleague, mentor, counselor, department chair, or loved ones. Many physicians express concerns about not knowing who is a “safe person” to trust in this situation. Often, second victims perceive that their loved ones just do not understand their professional life or should be protected from this situation.
Moving on. There is an urge to move forward with life and simply put the event behind. This is difficult, however. A second victim may follow one of these paths:
- drop out—stop practicing clinical medicine
- survive—maintain the same career but with significant residual emotional burden from the event
- thrive—make something good out of the unfortunate clinical experience.
Related article:
TRUST: How to build a support net for ObGyns affected by a medical error
All these programs offer immediate help to any clinician in psychological distress. They provide confidentiality, and the individual is reassured that he or she can safely use the service without further consequences (TABLE 2).10
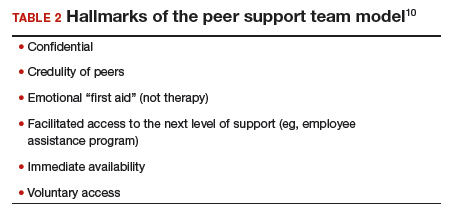
The normal human response to an adverse medical event can lead to significant psychological consequences, long-term emotional incapacity, impaired performance of clinical care, and feelings of guilt, fear, isolation, or even suicide. At some point during his or her career, almost every physician will be involved in a serious adverse medical event and is at risk of experiencing strong emotional reactions. Health care facilities should have a support system in place to help clinicians cope with these stressful circumstances.
Use these 5 strategies to facilitate recovery
- Be determined. No matter how bad you feel about the event, you need to get up and moving.
- Avoid isolation. Get outside and interact with people. Avoid long periods in isolation. Bring your team together and talk about the event.
- Sleep well. Most symptoms of posttraumatic stress disorder occur at night. If you have trouble falling asleep or you wake up in the middle of the night with nightmares related to the event, attempt to regulate your body’s sleep schedule. Seek professional help if needed.
- Avoid negative coping habits. Sometimes people turn to alcohol, cigarettes, food, or drugs to cope. Although these strategies may help in the short term, they will do more harm than good over time.
- Enroll in activities that provide positive distraction. While the mind focuses on the traumatic event (this is normal), you need to get busy with such positive distractions as sports, going to the movies, and engaging in outdoor activities. Do things that you enjoy.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kohn L. To err is human: an interview with the Institute of Medicine's Linda Kohn. Jt Comm J Qual Improv. 2000;26(4):227-234.
- James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf. 2013;9(3):122-128.
- Harrison R, Lawton R, Perlo J, Gardner P, Armitage G, Shapiro J. Emotion and coping in the aftermath of medical error: a cross-country exploration. J Patient Saf. 2015;11(1):28-35.
- Chan ST, Khong PC, Wang W. Psychological responses, coping and supporting needs of healthcare professionals as second victims. Int Nurs Rev. 2017;64(2):242-262.
- Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider "second victim" after adverse patient events. Qual Saf Health Care. 2009;18(5):325-330.
- Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33(8):467-476.
- Shapiro J, Galowitz P. Peer support for clinicians: a programmatic approach. Acad Med. 2016;91(9):1200-1204.
- Edrees H, Connors C, Paine L, Norvell M, Taylor H, Wu AW. Implementing the RISE second victim support programme at the Johns Hopkins Hospital: a case study. BMJ Open. 2016;6(9):e011708.
- Johnson B. Code lavender: initiating holistic rapid response at the Cleveland Clinic. Beginnings. 2014;34(2):10-11.
- van Pelt F. Peer support: healthcare professionals supporting each other after adverse medical events. Qual Saf Health Care. 2008;17(4):249-252.
CASE A surgeon's story of patient loss
It was a Wednesday morning and Ms. M was my first case of the day. I knew her well, having delivered her 2 children. Now she had a 7-cm complex cyst on her right ovary, she was in pain, and she was possibly experiencing ovarian torsion. My resident took care of the paperwork, I met the patient in preop, answered her few questions, and reassured her husband that I would call him as soon as surgery was over. She was rolled to the operating room.
When I entered the OR, Ms. M was under general anesthesia, draped, and placed on the operating table in the usual position. I made a 5-mm incision at the umbilicus and inserted the trocar under direct visualization. There was blood and the camera became blurry. I removed the camera to clean it, and the anesthesiologist alerted me that there was sudden hypotension. I reinserted the camera and saw blood in the abdomen. I feared the worst—major vessel injury. I requested a scalpel and made a midline skin sub–umbilical incision, entered the peritoneal cavity, and observed blood everywhere. The massive transfusion protocol was activated and vascular surgery was called in. I could not find the source of the bleeding. Using a laparotomy towel I applied pressure on the aorta. The vascular surgeon arrived and pushed my resident away. He identified the source of the bleeding: The right common iliac artery was injured.
The patient coded, the anesthesiologist initiated CPR, bleeding continued, blood was being transfused, and after 20 long minutes of CPR the lifeless body of my patient could not hold any more. She was pronounced dead on the table.
At that moment, there were multiple victims: Ms. M lying on the surgical table; her family members, who did not know what was happening; and the surgical team members, who were looking at each other in denial and feeling that we had failed this patient, hoping that we would wake up from this nightmare.
Defining patient harm
Many patients experience harm each year because of an adverse medical event or preventable medical error.1 A 2013 report revealed that 210,000 to 440,000 deaths occur each year in the United States related to preventable patient harm.2 Although this fact is deeply disturbing, it is well known that modern health care is a high-risk industry.
Medical errors vary in terms of the degree of potential or actual damage. A “near miss” is any event that could have resulted in adverse consequences but did not (for example, an incorrect drug or dose ordered but not administered). On the other hand, an “adverse event” describes an error that resulted in some degree of patient harm or suffering.3
Related article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
For each patient who dies because of a medical error or a surgical complication, whether preventable or not, many clinicians are involved in the unfolding of the case. These events have a profound impact on well-intentioned, competent, and caring physicians, and they elicit intense emotional responses.4 When a patient experiences an unexpected adverse surgical outcome, the surgeons involved in their care may become “second victims.” They may feel that they have failed the patient and they second-guess their surgical skills and knowledge base; some express concern about their reputation and perhaps career choice.
Psychological responses. It is importantto understand this process to ensure a healthy recovery. Psychological responses to an adverse medical event include guilt; distress, anxiety, and fear; frustration and anger; feelings of insufficiency; and long-standing suffering. Clinicians who experienced an adverse medical event have reported additional psychological as well as physical symptoms in the aftermath of the event (TABLE 1).5
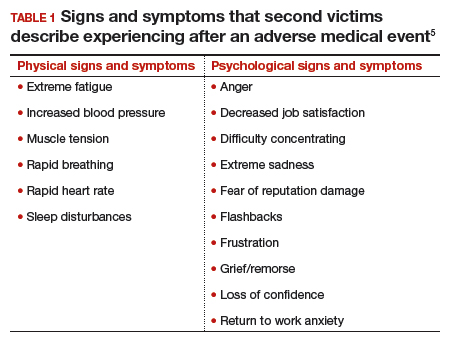
Risk factors. Certain factors are associated with a greater emotional impact of an adverse medical event, including6:
- severity of the harm or leaving permanent sequelae
- death of a healthy patient or a child (for example, from a motor vehicle accident)
- self-blame for the error
- unexpected patient death (for example, a catastrophic complication after a relatively benign procedure)
- physicians-in-training responsible for the patient
- first death under a clinician’s watch.
While most research in the field of medical error focuses on systems or process improvement, it is important not to neglect the individual and personal aspects of the clinicians involved in the event. The health care system must include care for our injured colleagues, the so-called second victims.
Read about the steps to recovery for the second victim.
Steps in recovery for the second victim
Based on a semistructured interview of 31 physicians involved in adverse events, Scott and colleagues described the following 6 stages of healing5:
Chaos and accident response. Immediately after the event, the physician feels a sense of confusion, panic, and denial. How can this be happening to me? The physician is frequently distracted, immersed in self-reflection.
Intrusive reflections. This is a period of self-questioning. Thoughts of the event and different possible scenarios dominate the physician’s mind. What if I had done this or that?
Restoring personal integrity. During this phase, the physician seeks support from individuals with whom trusted relationships exist, such as colleagues, peers, close friends, and family members. Advice from a colleague who has your same level of expertise is precious. The second victim often fears that friends and family will not be understanding.
Enduring the inquisition. Root cause analysis and in-depth case review is an important part of the quality improvement process after an adverse event. A debriefing or departmental morbidity and mortality conference can trigger emotions and increase the sense of shame, guilt, and self-doubt. The second victim starts to wonder about repercussions that may affect job security, licensure, and future litigation.
Obtaining emotional first aid. At this stage, the second victim begins to heal, but it is important to obtain external help from a colleague, mentor, counselor, department chair, or loved ones. Many physicians express concerns about not knowing who is a “safe person” to trust in this situation. Often, second victims perceive that their loved ones just do not understand their professional life or should be protected from this situation.
Moving on. There is an urge to move forward with life and simply put the event behind. This is difficult, however. A second victim may follow one of these paths:
- drop out—stop practicing clinical medicine
- survive—maintain the same career but with significant residual emotional burden from the event
- thrive—make something good out of the unfortunate clinical experience.
Related article:
TRUST: How to build a support net for ObGyns affected by a medical error
All these programs offer immediate help to any clinician in psychological distress. They provide confidentiality, and the individual is reassured that he or she can safely use the service without further consequences (TABLE 2).10
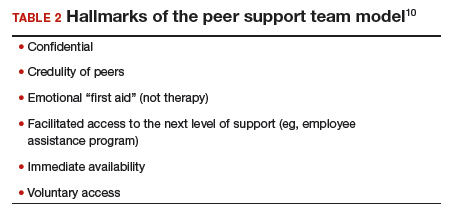
The normal human response to an adverse medical event can lead to significant psychological consequences, long-term emotional incapacity, impaired performance of clinical care, and feelings of guilt, fear, isolation, or even suicide. At some point during his or her career, almost every physician will be involved in a serious adverse medical event and is at risk of experiencing strong emotional reactions. Health care facilities should have a support system in place to help clinicians cope with these stressful circumstances.
Use these 5 strategies to facilitate recovery
- Be determined. No matter how bad you feel about the event, you need to get up and moving.
- Avoid isolation. Get outside and interact with people. Avoid long periods in isolation. Bring your team together and talk about the event.
- Sleep well. Most symptoms of posttraumatic stress disorder occur at night. If you have trouble falling asleep or you wake up in the middle of the night with nightmares related to the event, attempt to regulate your body’s sleep schedule. Seek professional help if needed.
- Avoid negative coping habits. Sometimes people turn to alcohol, cigarettes, food, or drugs to cope. Although these strategies may help in the short term, they will do more harm than good over time.
- Enroll in activities that provide positive distraction. While the mind focuses on the traumatic event (this is normal), you need to get busy with such positive distractions as sports, going to the movies, and engaging in outdoor activities. Do things that you enjoy.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
CASE A surgeon's story of patient loss
It was a Wednesday morning and Ms. M was my first case of the day. I knew her well, having delivered her 2 children. Now she had a 7-cm complex cyst on her right ovary, she was in pain, and she was possibly experiencing ovarian torsion. My resident took care of the paperwork, I met the patient in preop, answered her few questions, and reassured her husband that I would call him as soon as surgery was over. She was rolled to the operating room.
When I entered the OR, Ms. M was under general anesthesia, draped, and placed on the operating table in the usual position. I made a 5-mm incision at the umbilicus and inserted the trocar under direct visualization. There was blood and the camera became blurry. I removed the camera to clean it, and the anesthesiologist alerted me that there was sudden hypotension. I reinserted the camera and saw blood in the abdomen. I feared the worst—major vessel injury. I requested a scalpel and made a midline skin sub–umbilical incision, entered the peritoneal cavity, and observed blood everywhere. The massive transfusion protocol was activated and vascular surgery was called in. I could not find the source of the bleeding. Using a laparotomy towel I applied pressure on the aorta. The vascular surgeon arrived and pushed my resident away. He identified the source of the bleeding: The right common iliac artery was injured.
The patient coded, the anesthesiologist initiated CPR, bleeding continued, blood was being transfused, and after 20 long minutes of CPR the lifeless body of my patient could not hold any more. She was pronounced dead on the table.
At that moment, there were multiple victims: Ms. M lying on the surgical table; her family members, who did not know what was happening; and the surgical team members, who were looking at each other in denial and feeling that we had failed this patient, hoping that we would wake up from this nightmare.
Defining patient harm
Many patients experience harm each year because of an adverse medical event or preventable medical error.1 A 2013 report revealed that 210,000 to 440,000 deaths occur each year in the United States related to preventable patient harm.2 Although this fact is deeply disturbing, it is well known that modern health care is a high-risk industry.
Medical errors vary in terms of the degree of potential or actual damage. A “near miss” is any event that could have resulted in adverse consequences but did not (for example, an incorrect drug or dose ordered but not administered). On the other hand, an “adverse event” describes an error that resulted in some degree of patient harm or suffering.3
Related article:
Medical errors: Meeting ethical obligations and reducing liability with proper communication
For each patient who dies because of a medical error or a surgical complication, whether preventable or not, many clinicians are involved in the unfolding of the case. These events have a profound impact on well-intentioned, competent, and caring physicians, and they elicit intense emotional responses.4 When a patient experiences an unexpected adverse surgical outcome, the surgeons involved in their care may become “second victims.” They may feel that they have failed the patient and they second-guess their surgical skills and knowledge base; some express concern about their reputation and perhaps career choice.
Psychological responses. It is importantto understand this process to ensure a healthy recovery. Psychological responses to an adverse medical event include guilt; distress, anxiety, and fear; frustration and anger; feelings of insufficiency; and long-standing suffering. Clinicians who experienced an adverse medical event have reported additional psychological as well as physical symptoms in the aftermath of the event (TABLE 1).5
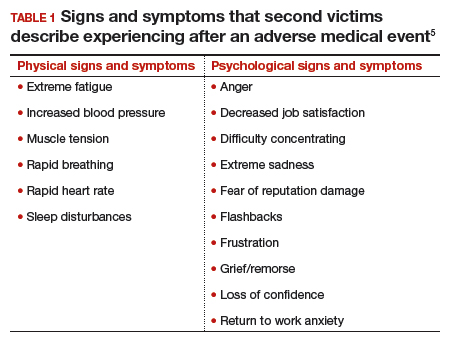
Risk factors. Certain factors are associated with a greater emotional impact of an adverse medical event, including6:
- severity of the harm or leaving permanent sequelae
- death of a healthy patient or a child (for example, from a motor vehicle accident)
- self-blame for the error
- unexpected patient death (for example, a catastrophic complication after a relatively benign procedure)
- physicians-in-training responsible for the patient
- first death under a clinician’s watch.
While most research in the field of medical error focuses on systems or process improvement, it is important not to neglect the individual and personal aspects of the clinicians involved in the event. The health care system must include care for our injured colleagues, the so-called second victims.
Read about the steps to recovery for the second victim.
Steps in recovery for the second victim
Based on a semistructured interview of 31 physicians involved in adverse events, Scott and colleagues described the following 6 stages of healing5:
Chaos and accident response. Immediately after the event, the physician feels a sense of confusion, panic, and denial. How can this be happening to me? The physician is frequently distracted, immersed in self-reflection.
Intrusive reflections. This is a period of self-questioning. Thoughts of the event and different possible scenarios dominate the physician’s mind. What if I had done this or that?
Restoring personal integrity. During this phase, the physician seeks support from individuals with whom trusted relationships exist, such as colleagues, peers, close friends, and family members. Advice from a colleague who has your same level of expertise is precious. The second victim often fears that friends and family will not be understanding.
Enduring the inquisition. Root cause analysis and in-depth case review is an important part of the quality improvement process after an adverse event. A debriefing or departmental morbidity and mortality conference can trigger emotions and increase the sense of shame, guilt, and self-doubt. The second victim starts to wonder about repercussions that may affect job security, licensure, and future litigation.
Obtaining emotional first aid. At this stage, the second victim begins to heal, but it is important to obtain external help from a colleague, mentor, counselor, department chair, or loved ones. Many physicians express concerns about not knowing who is a “safe person” to trust in this situation. Often, second victims perceive that their loved ones just do not understand their professional life or should be protected from this situation.
Moving on. There is an urge to move forward with life and simply put the event behind. This is difficult, however. A second victim may follow one of these paths:
- drop out—stop practicing clinical medicine
- survive—maintain the same career but with significant residual emotional burden from the event
- thrive—make something good out of the unfortunate clinical experience.
Related article:
TRUST: How to build a support net for ObGyns affected by a medical error
All these programs offer immediate help to any clinician in psychological distress. They provide confidentiality, and the individual is reassured that he or she can safely use the service without further consequences (TABLE 2).10
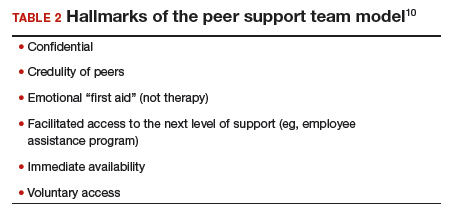
The normal human response to an adverse medical event can lead to significant psychological consequences, long-term emotional incapacity, impaired performance of clinical care, and feelings of guilt, fear, isolation, or even suicide. At some point during his or her career, almost every physician will be involved in a serious adverse medical event and is at risk of experiencing strong emotional reactions. Health care facilities should have a support system in place to help clinicians cope with these stressful circumstances.
Use these 5 strategies to facilitate recovery
- Be determined. No matter how bad you feel about the event, you need to get up and moving.
- Avoid isolation. Get outside and interact with people. Avoid long periods in isolation. Bring your team together and talk about the event.
- Sleep well. Most symptoms of posttraumatic stress disorder occur at night. If you have trouble falling asleep or you wake up in the middle of the night with nightmares related to the event, attempt to regulate your body’s sleep schedule. Seek professional help if needed.
- Avoid negative coping habits. Sometimes people turn to alcohol, cigarettes, food, or drugs to cope. Although these strategies may help in the short term, they will do more harm than good over time.
- Enroll in activities that provide positive distraction. While the mind focuses on the traumatic event (this is normal), you need to get busy with such positive distractions as sports, going to the movies, and engaging in outdoor activities. Do things that you enjoy.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Kohn L. To err is human: an interview with the Institute of Medicine's Linda Kohn. Jt Comm J Qual Improv. 2000;26(4):227-234.
- James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf. 2013;9(3):122-128.
- Harrison R, Lawton R, Perlo J, Gardner P, Armitage G, Shapiro J. Emotion and coping in the aftermath of medical error: a cross-country exploration. J Patient Saf. 2015;11(1):28-35.
- Chan ST, Khong PC, Wang W. Psychological responses, coping and supporting needs of healthcare professionals as second victims. Int Nurs Rev. 2017;64(2):242-262.
- Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider "second victim" after adverse patient events. Qual Saf Health Care. 2009;18(5):325-330.
- Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33(8):467-476.
- Shapiro J, Galowitz P. Peer support for clinicians: a programmatic approach. Acad Med. 2016;91(9):1200-1204.
- Edrees H, Connors C, Paine L, Norvell M, Taylor H, Wu AW. Implementing the RISE second victim support programme at the Johns Hopkins Hospital: a case study. BMJ Open. 2016;6(9):e011708.
- Johnson B. Code lavender: initiating holistic rapid response at the Cleveland Clinic. Beginnings. 2014;34(2):10-11.
- van Pelt F. Peer support: healthcare professionals supporting each other after adverse medical events. Qual Saf Health Care. 2008;17(4):249-252.
- Kohn L. To err is human: an interview with the Institute of Medicine's Linda Kohn. Jt Comm J Qual Improv. 2000;26(4):227-234.
- James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf. 2013;9(3):122-128.
- Harrison R, Lawton R, Perlo J, Gardner P, Armitage G, Shapiro J. Emotion and coping in the aftermath of medical error: a cross-country exploration. J Patient Saf. 2015;11(1):28-35.
- Chan ST, Khong PC, Wang W. Psychological responses, coping and supporting needs of healthcare professionals as second victims. Int Nurs Rev. 2017;64(2):242-262.
- Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider "second victim" after adverse patient events. Qual Saf Health Care. 2009;18(5):325-330.
- Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007;33(8):467-476.
- Shapiro J, Galowitz P. Peer support for clinicians: a programmatic approach. Acad Med. 2016;91(9):1200-1204.
- Edrees H, Connors C, Paine L, Norvell M, Taylor H, Wu AW. Implementing the RISE second victim support programme at the Johns Hopkins Hospital: a case study. BMJ Open. 2016;6(9):e011708.
- Johnson B. Code lavender: initiating holistic rapid response at the Cleveland Clinic. Beginnings. 2014;34(2):10-11.
- van Pelt F. Peer support: healthcare professionals supporting each other after adverse medical events. Qual Saf Health Care. 2008;17(4):249-252.
Fast Tracks
- A "near miss" is any event that could have resulted in adverse consequences but did not. An "adverse event" describes an error that resulted in some degree of patient harm or suffering.
- At some point in his or her career, almost every physician will be involved in a serious adverse medical event and is at risk of experiencing strong emotional reactions
Create an effective social media campaign to market your practice: Here’s how
Developing an effective social media marketing campaign can expand your practice to bring you more of the type of patient you want to treat. Although ObGyns are often not trained in marketing, we can bring our practices to the attention of women who need our services with a few simple processes.
The American Marketing Association defines marketing as “the activity, set of institutions, and processes for creating, communicating, delivering, and exchanging offerings that have value for customers, clients, partners, and society at large.”1 Social media is described as various forms of online and mobile electronic communication with user-generated content.2 Social media marketing is the application of traditional marketing strategies to a social media platform. Delivering an effective social media marketing campaign requires focused targeting of a particular community to match the needs of those patients with the value of services and products your practice provides.
By communicating and connecting with the spoken and unspoken needs and desires of potential patients, you will generate greater enthusiasm for your medical services. Social media marketing benefits include: accessibility, low cost, the ability to build brand recognition and social capital, and the availability of analytics that provide large amounts of data to measure the effectiveness of the campaign.3
Though social media is pervasive, the medical community has not rapidly embraced it for marketing.4,5 Creating a social media strategy, rather than randomly or impulsively posting on social media, allows for more effective marketing. The discussion here focuses on Facebook, which has 2 billion monthly users,6 but these strategies and tactics can be applied to any social media platform, including YouTube, Instagram, and Twitter.7
Use Facebook to create a business page
Your medical practice needs to have a Facebook account and a Facebook page, separate from your personal account. A business-related Facebook page is similar to a personal Facebook profile except that pages are designed for organizations, brands, businesses, and public figures to share photos, stories, and events with the public.
If you do not have a Facebook account, you can create a new account and profile at http://www.facebook.com. After creating a profile, click on the “create a Facebook page” link. Follow the instructions and select the page category you would like to create; most physicians would select the “Company,” “Organization,” or “Institution” category. Next, follow the instructions to complete the registration.8 Once your Facebook page is created, build an audience asking others to “like” your page. Start posting content and use hashtags in your posts to make them discoverable to others (ie, #fibroids #noscar #singlesitesurgery).9
Related article:
Using the Internet in your practice. Part 2: Generating new patients using social media
One benefit to having a practice-based Facebook page is the automated visible analytics that come with the page, which are not available for personal profiles. When you write a post or upload a photo or video, Facebook provides the demographics of those engaged with your posts plus analytics on that post, including the number of people who viewed the post, clicked on a photo, and viewed the video for more than 3 seconds.
Read how to get patients interested in your practice
Develop a social media marketing strategy
There are several key factors to consider when planning a strategy. First, know the mission of your organization and the specific service, value, or benefit you would like to provide to the targeted community.8
Segment, target, and position (STP)
It is tempting to try to reach out to all women because your ObGyn practice entails pre‑natal care, family planning, and gynecologic surgery, but by narrowing your target audience, your campaign will be better focused. A very specific target audience can reduce the costs for “boosting” (paid promotion of your posts on Facebook to a chosen audience based on demographics, interests, and behaviors) your posts and improve your return on investment (ROI).
Create different marketing campaigns, but focus on one at a time. Decide on the ideal patient you want to serve in your practice. The more detailed and focused you are about the demographics and type of medical needs to be served, the better you can target this patient.10
Segment. Divide the communities you are considering into different segments. For instance, even though you may do obstetrics and gynecologic surgery, consider breaking up the campaign to focus on 1 specific group, such as those interested in fibroid management.
Target. Identify the kinds of communities where you might find this patient. For example, if you want to focus on laparoscopic hysterectomies or myomectomies, start looking on Facebook for groups, pages, or website discussion boards or blogs that discuss abnormal uterine bleeding or fibroids and follow those pages.
Also, think about what other characteristics are associated with these ideal patients. For example, you might narrow it down to perimenopausal women with fibroids. A potential targeted group could be 40- to 50-year-old women who participate in yoga or running who have concerns about fibroids interfering in their active lifestyle. Perhaps this type of patient would want a minimally invasive surgical approach. A holistic health activist might be interested in nonsurgical management of fibroids.
Position. Once you have identified the specific community to target, position your practice within the community with the value proposition you are offering. For example, as an ObGyn who is focused on surgery, your position might be that your practice will provide the best experience for those medical services, with specific counseling to patients about resuming their active lifestyle.
Related article:
Four pillars of a successful practice: 2. Attract new patients
Get your potential patient to “raise her hand.” In the campaign, you are not trying to convince everyone up front to schedule an appointment from one post. First, try to get people who may be interested in your service(s) to “raise their hands.” Once your target market has expressed interest, either by their likes of your post, likes of your page, or other engagement, reach out to them with links for more information, such as free fibroid surgery education materials located on your website. On your website, create an opt-in page asking them to register their email address; once you have a compiled email list, send out monthly newsletters on your practice.11
Read how to guide patients to your office
Understand that marketing is a process
Think of marketing as an overall process in which you are guiding potential patients to come to your office. Your campaign has several steps; recognize that just one post will not make a huge difference. Use Facebook analytics to measure cost per engagement to calculate your return on investment and the campaign’s effectiveness, and revise as necessary.
Rather than just considering social media as a soap box to advertise your practice, break up the marketing process into 3 units: the before unit, the during unit, and the after unit.11 The word “unit” denotes the service, benefit, or product you are providing.
The before unit refers to the initial marketing that identifies potential patients—initially getting them to raise their hands and ultimately building an audience. (Once a potential patient provides her email address, you can send her a monthly newsletter or updates about your practice to continue the engagement.) Statistics show that an ObGyn needs to have 7 contacts, on average, with a patient over 18 months to “penetrate” her consciousness in a given market.12 Of course if there is an urgent or emergent need to see a physician, that timeline would be much shorter.

The during unit occurs when the patient comes to your practice and service is being provided. Since you know what she is coming for, you can create informational packets focused on her particular needs, perhaps about different management options for fibroids.
The after unit includes following up with the patient in some automated way. For those being treated for fibroids, it may be a reminder email that discusses the value of follow-up ultrasonography or the various kinds of surgical interventions for fibroids.
In order to continue your campaign, it is helpful to have a designated social media manager who will continue the social media posts and engagement.
When creating the posts, consider developing prescheduled assets (posts that are already produced with photos or links to articles), which can be done through Facebook or Hootsuite (http://www.hootsuite.com).
Manage the risks of social media interaction
There are risks associated with social media. Some things to consider are:
- Policy. Develop a policy for your practice; if you work for an institution, align your policy with the institution’s.
- Postings. Supervise content being posted. Never allow social media to be placed by someone without supervision. Either you should do this or assign a manager to be accountable to check on social media interactions so that any inappropriate comments can be addressed immediately.
- Privacy. Never mention patients’ private health information or use the platform to publicly engage with a patient or future patient about their care. Do not post any references to patients or their photos without written consent.
- Images. Use photographs and other images properly: obtain releases and obey copyright laws.
Related article:
Your patients are talking: Isn’t it time you take responsibility for your online reputation?
Bottom line
Social media is a powerful platform. Combined with good marketing strategies, social media campaigns can have a significant impact on expanding your practice to offer the kind of medical services you want to provide.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Definition of Marketing. American Marketing Association website. https://www.ama.org/AboutAMA/Pages/Definition-of-Marketing.aspx. Published July 2013. Accessed August 8, 2017.
- Kaplan AH, Haenlein M. Users of the world, unite! The challenges and opportunities of social media. Business Horiz. 2010;53(1):59–68.
- Lin KY, Lu HP. Intention to continue using Facebook fan pages from the perspective of social capital theory. Cyberpsychol Behav Soc Netw. 2011;14(10):565–570.
- Hawn C. Take two aspirin and tweet me in the morning: how Twitter, Facebook, and other social media are reshaping health care. Health Aff (Millwood). 2009;28(2):361–368.
- Wheeler CK, Said H, Prucz R, Rodrich RJ, Mathes DW. Social media in plastic surgery practices: emerging trends in North America. Aesthet Surg J. 2011;31(4):435–441.
- Nowak M, Spiller G. Two billion people coming together on Facebook. Facebook Newsroom. https://newsroom.fb.com/news/2017/06/two-billion-people-coming-together-on-facebook/. Published June 27, 2017. Accessed August 8, 2017.
- Adamson A. No contest: Twitter and Facebook can both play a role in branding. Forbes. http://www.forbes.com/2009/05/06/twitter-facebook-branding-leadership-cmo-network-adamson.html. Published May 6, 2009. Accessed August 8, 2017.
- Kim DS. Harness social media, enhance your practice. Contemp Obstet Gynecol. 2012;57(7):40–42,44–46.
- Wolf J. Social Media: Master, Manipulate, And Dominate Social Media Marketing Facebook, Twitter, YouTube, Instagram And LinkedIn. Createspace Independent Publishing Platform; 2015:129–143.
- Kotler PT, Keller KL. Marketing Management. 12th ed. Upper Saddle River, NJ: Prentice Hall; 2006:239–268.
- Jackson DP. Sunday marketing matinee: I love marketing live–Before, during, and after unit thinking. http://ilovemarketing.com/sunday-marketing-matineei-love-marketing-live-before-during-and-after-unit-thinking/. Accessed July 24, 2017.
- Payne D. How many contacts does it take before someone buys your product? Business Insider website. http://www.businessinsider.com/how-many-contacts-does-it-take-before-someone-buys-your-product-2011-7. Published July 12, 2011. Accessed August 8, 2017.
Developing an effective social media marketing campaign can expand your practice to bring you more of the type of patient you want to treat. Although ObGyns are often not trained in marketing, we can bring our practices to the attention of women who need our services with a few simple processes.
The American Marketing Association defines marketing as “the activity, set of institutions, and processes for creating, communicating, delivering, and exchanging offerings that have value for customers, clients, partners, and society at large.”1 Social media is described as various forms of online and mobile electronic communication with user-generated content.2 Social media marketing is the application of traditional marketing strategies to a social media platform. Delivering an effective social media marketing campaign requires focused targeting of a particular community to match the needs of those patients with the value of services and products your practice provides.
By communicating and connecting with the spoken and unspoken needs and desires of potential patients, you will generate greater enthusiasm for your medical services. Social media marketing benefits include: accessibility, low cost, the ability to build brand recognition and social capital, and the availability of analytics that provide large amounts of data to measure the effectiveness of the campaign.3
Though social media is pervasive, the medical community has not rapidly embraced it for marketing.4,5 Creating a social media strategy, rather than randomly or impulsively posting on social media, allows for more effective marketing. The discussion here focuses on Facebook, which has 2 billion monthly users,6 but these strategies and tactics can be applied to any social media platform, including YouTube, Instagram, and Twitter.7
Use Facebook to create a business page
Your medical practice needs to have a Facebook account and a Facebook page, separate from your personal account. A business-related Facebook page is similar to a personal Facebook profile except that pages are designed for organizations, brands, businesses, and public figures to share photos, stories, and events with the public.
If you do not have a Facebook account, you can create a new account and profile at http://www.facebook.com. After creating a profile, click on the “create a Facebook page” link. Follow the instructions and select the page category you would like to create; most physicians would select the “Company,” “Organization,” or “Institution” category. Next, follow the instructions to complete the registration.8 Once your Facebook page is created, build an audience asking others to “like” your page. Start posting content and use hashtags in your posts to make them discoverable to others (ie, #fibroids #noscar #singlesitesurgery).9
Related article:
Using the Internet in your practice. Part 2: Generating new patients using social media
One benefit to having a practice-based Facebook page is the automated visible analytics that come with the page, which are not available for personal profiles. When you write a post or upload a photo or video, Facebook provides the demographics of those engaged with your posts plus analytics on that post, including the number of people who viewed the post, clicked on a photo, and viewed the video for more than 3 seconds.
Read how to get patients interested in your practice
Develop a social media marketing strategy
There are several key factors to consider when planning a strategy. First, know the mission of your organization and the specific service, value, or benefit you would like to provide to the targeted community.8
Segment, target, and position (STP)
It is tempting to try to reach out to all women because your ObGyn practice entails pre‑natal care, family planning, and gynecologic surgery, but by narrowing your target audience, your campaign will be better focused. A very specific target audience can reduce the costs for “boosting” (paid promotion of your posts on Facebook to a chosen audience based on demographics, interests, and behaviors) your posts and improve your return on investment (ROI).
Create different marketing campaigns, but focus on one at a time. Decide on the ideal patient you want to serve in your practice. The more detailed and focused you are about the demographics and type of medical needs to be served, the better you can target this patient.10
Segment. Divide the communities you are considering into different segments. For instance, even though you may do obstetrics and gynecologic surgery, consider breaking up the campaign to focus on 1 specific group, such as those interested in fibroid management.
Target. Identify the kinds of communities where you might find this patient. For example, if you want to focus on laparoscopic hysterectomies or myomectomies, start looking on Facebook for groups, pages, or website discussion boards or blogs that discuss abnormal uterine bleeding or fibroids and follow those pages.
Also, think about what other characteristics are associated with these ideal patients. For example, you might narrow it down to perimenopausal women with fibroids. A potential targeted group could be 40- to 50-year-old women who participate in yoga or running who have concerns about fibroids interfering in their active lifestyle. Perhaps this type of patient would want a minimally invasive surgical approach. A holistic health activist might be interested in nonsurgical management of fibroids.
Position. Once you have identified the specific community to target, position your practice within the community with the value proposition you are offering. For example, as an ObGyn who is focused on surgery, your position might be that your practice will provide the best experience for those medical services, with specific counseling to patients about resuming their active lifestyle.
Related article:
Four pillars of a successful practice: 2. Attract new patients
Get your potential patient to “raise her hand.” In the campaign, you are not trying to convince everyone up front to schedule an appointment from one post. First, try to get people who may be interested in your service(s) to “raise their hands.” Once your target market has expressed interest, either by their likes of your post, likes of your page, or other engagement, reach out to them with links for more information, such as free fibroid surgery education materials located on your website. On your website, create an opt-in page asking them to register their email address; once you have a compiled email list, send out monthly newsletters on your practice.11
Read how to guide patients to your office
Understand that marketing is a process
Think of marketing as an overall process in which you are guiding potential patients to come to your office. Your campaign has several steps; recognize that just one post will not make a huge difference. Use Facebook analytics to measure cost per engagement to calculate your return on investment and the campaign’s effectiveness, and revise as necessary.
Rather than just considering social media as a soap box to advertise your practice, break up the marketing process into 3 units: the before unit, the during unit, and the after unit.11 The word “unit” denotes the service, benefit, or product you are providing.
The before unit refers to the initial marketing that identifies potential patients—initially getting them to raise their hands and ultimately building an audience. (Once a potential patient provides her email address, you can send her a monthly newsletter or updates about your practice to continue the engagement.) Statistics show that an ObGyn needs to have 7 contacts, on average, with a patient over 18 months to “penetrate” her consciousness in a given market.12 Of course if there is an urgent or emergent need to see a physician, that timeline would be much shorter.

The during unit occurs when the patient comes to your practice and service is being provided. Since you know what she is coming for, you can create informational packets focused on her particular needs, perhaps about different management options for fibroids.
The after unit includes following up with the patient in some automated way. For those being treated for fibroids, it may be a reminder email that discusses the value of follow-up ultrasonography or the various kinds of surgical interventions for fibroids.
In order to continue your campaign, it is helpful to have a designated social media manager who will continue the social media posts and engagement.
When creating the posts, consider developing prescheduled assets (posts that are already produced with photos or links to articles), which can be done through Facebook or Hootsuite (http://www.hootsuite.com).
Manage the risks of social media interaction
There are risks associated with social media. Some things to consider are:
- Policy. Develop a policy for your practice; if you work for an institution, align your policy with the institution’s.
- Postings. Supervise content being posted. Never allow social media to be placed by someone without supervision. Either you should do this or assign a manager to be accountable to check on social media interactions so that any inappropriate comments can be addressed immediately.
- Privacy. Never mention patients’ private health information or use the platform to publicly engage with a patient or future patient about their care. Do not post any references to patients or their photos without written consent.
- Images. Use photographs and other images properly: obtain releases and obey copyright laws.
Related article:
Your patients are talking: Isn’t it time you take responsibility for your online reputation?
Bottom line
Social media is a powerful platform. Combined with good marketing strategies, social media campaigns can have a significant impact on expanding your practice to offer the kind of medical services you want to provide.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Developing an effective social media marketing campaign can expand your practice to bring you more of the type of patient you want to treat. Although ObGyns are often not trained in marketing, we can bring our practices to the attention of women who need our services with a few simple processes.
The American Marketing Association defines marketing as “the activity, set of institutions, and processes for creating, communicating, delivering, and exchanging offerings that have value for customers, clients, partners, and society at large.”1 Social media is described as various forms of online and mobile electronic communication with user-generated content.2 Social media marketing is the application of traditional marketing strategies to a social media platform. Delivering an effective social media marketing campaign requires focused targeting of a particular community to match the needs of those patients with the value of services and products your practice provides.
By communicating and connecting with the spoken and unspoken needs and desires of potential patients, you will generate greater enthusiasm for your medical services. Social media marketing benefits include: accessibility, low cost, the ability to build brand recognition and social capital, and the availability of analytics that provide large amounts of data to measure the effectiveness of the campaign.3
Though social media is pervasive, the medical community has not rapidly embraced it for marketing.4,5 Creating a social media strategy, rather than randomly or impulsively posting on social media, allows for more effective marketing. The discussion here focuses on Facebook, which has 2 billion monthly users,6 but these strategies and tactics can be applied to any social media platform, including YouTube, Instagram, and Twitter.7
Use Facebook to create a business page
Your medical practice needs to have a Facebook account and a Facebook page, separate from your personal account. A business-related Facebook page is similar to a personal Facebook profile except that pages are designed for organizations, brands, businesses, and public figures to share photos, stories, and events with the public.
If you do not have a Facebook account, you can create a new account and profile at http://www.facebook.com. After creating a profile, click on the “create a Facebook page” link. Follow the instructions and select the page category you would like to create; most physicians would select the “Company,” “Organization,” or “Institution” category. Next, follow the instructions to complete the registration.8 Once your Facebook page is created, build an audience asking others to “like” your page. Start posting content and use hashtags in your posts to make them discoverable to others (ie, #fibroids #noscar #singlesitesurgery).9
Related article:
Using the Internet in your practice. Part 2: Generating new patients using social media
One benefit to having a practice-based Facebook page is the automated visible analytics that come with the page, which are not available for personal profiles. When you write a post or upload a photo or video, Facebook provides the demographics of those engaged with your posts plus analytics on that post, including the number of people who viewed the post, clicked on a photo, and viewed the video for more than 3 seconds.
Read how to get patients interested in your practice
Develop a social media marketing strategy
There are several key factors to consider when planning a strategy. First, know the mission of your organization and the specific service, value, or benefit you would like to provide to the targeted community.8
Segment, target, and position (STP)
It is tempting to try to reach out to all women because your ObGyn practice entails pre‑natal care, family planning, and gynecologic surgery, but by narrowing your target audience, your campaign will be better focused. A very specific target audience can reduce the costs for “boosting” (paid promotion of your posts on Facebook to a chosen audience based on demographics, interests, and behaviors) your posts and improve your return on investment (ROI).
Create different marketing campaigns, but focus on one at a time. Decide on the ideal patient you want to serve in your practice. The more detailed and focused you are about the demographics and type of medical needs to be served, the better you can target this patient.10
Segment. Divide the communities you are considering into different segments. For instance, even though you may do obstetrics and gynecologic surgery, consider breaking up the campaign to focus on 1 specific group, such as those interested in fibroid management.
Target. Identify the kinds of communities where you might find this patient. For example, if you want to focus on laparoscopic hysterectomies or myomectomies, start looking on Facebook for groups, pages, or website discussion boards or blogs that discuss abnormal uterine bleeding or fibroids and follow those pages.
Also, think about what other characteristics are associated with these ideal patients. For example, you might narrow it down to perimenopausal women with fibroids. A potential targeted group could be 40- to 50-year-old women who participate in yoga or running who have concerns about fibroids interfering in their active lifestyle. Perhaps this type of patient would want a minimally invasive surgical approach. A holistic health activist might be interested in nonsurgical management of fibroids.
Position. Once you have identified the specific community to target, position your practice within the community with the value proposition you are offering. For example, as an ObGyn who is focused on surgery, your position might be that your practice will provide the best experience for those medical services, with specific counseling to patients about resuming their active lifestyle.
Related article:
Four pillars of a successful practice: 2. Attract new patients
Get your potential patient to “raise her hand.” In the campaign, you are not trying to convince everyone up front to schedule an appointment from one post. First, try to get people who may be interested in your service(s) to “raise their hands.” Once your target market has expressed interest, either by their likes of your post, likes of your page, or other engagement, reach out to them with links for more information, such as free fibroid surgery education materials located on your website. On your website, create an opt-in page asking them to register their email address; once you have a compiled email list, send out monthly newsletters on your practice.11
Read how to guide patients to your office
Understand that marketing is a process
Think of marketing as an overall process in which you are guiding potential patients to come to your office. Your campaign has several steps; recognize that just one post will not make a huge difference. Use Facebook analytics to measure cost per engagement to calculate your return on investment and the campaign’s effectiveness, and revise as necessary.
Rather than just considering social media as a soap box to advertise your practice, break up the marketing process into 3 units: the before unit, the during unit, and the after unit.11 The word “unit” denotes the service, benefit, or product you are providing.
The before unit refers to the initial marketing that identifies potential patients—initially getting them to raise their hands and ultimately building an audience. (Once a potential patient provides her email address, you can send her a monthly newsletter or updates about your practice to continue the engagement.) Statistics show that an ObGyn needs to have 7 contacts, on average, with a patient over 18 months to “penetrate” her consciousness in a given market.12 Of course if there is an urgent or emergent need to see a physician, that timeline would be much shorter.

The during unit occurs when the patient comes to your practice and service is being provided. Since you know what she is coming for, you can create informational packets focused on her particular needs, perhaps about different management options for fibroids.
The after unit includes following up with the patient in some automated way. For those being treated for fibroids, it may be a reminder email that discusses the value of follow-up ultrasonography or the various kinds of surgical interventions for fibroids.
In order to continue your campaign, it is helpful to have a designated social media manager who will continue the social media posts and engagement.
When creating the posts, consider developing prescheduled assets (posts that are already produced with photos or links to articles), which can be done through Facebook or Hootsuite (http://www.hootsuite.com).
Manage the risks of social media interaction
There are risks associated with social media. Some things to consider are:
- Policy. Develop a policy for your practice; if you work for an institution, align your policy with the institution’s.
- Postings. Supervise content being posted. Never allow social media to be placed by someone without supervision. Either you should do this or assign a manager to be accountable to check on social media interactions so that any inappropriate comments can be addressed immediately.
- Privacy. Never mention patients’ private health information or use the platform to publicly engage with a patient or future patient about their care. Do not post any references to patients or their photos without written consent.
- Images. Use photographs and other images properly: obtain releases and obey copyright laws.
Related article:
Your patients are talking: Isn’t it time you take responsibility for your online reputation?
Bottom line
Social media is a powerful platform. Combined with good marketing strategies, social media campaigns can have a significant impact on expanding your practice to offer the kind of medical services you want to provide.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Definition of Marketing. American Marketing Association website. https://www.ama.org/AboutAMA/Pages/Definition-of-Marketing.aspx. Published July 2013. Accessed August 8, 2017.
- Kaplan AH, Haenlein M. Users of the world, unite! The challenges and opportunities of social media. Business Horiz. 2010;53(1):59–68.
- Lin KY, Lu HP. Intention to continue using Facebook fan pages from the perspective of social capital theory. Cyberpsychol Behav Soc Netw. 2011;14(10):565–570.
- Hawn C. Take two aspirin and tweet me in the morning: how Twitter, Facebook, and other social media are reshaping health care. Health Aff (Millwood). 2009;28(2):361–368.
- Wheeler CK, Said H, Prucz R, Rodrich RJ, Mathes DW. Social media in plastic surgery practices: emerging trends in North America. Aesthet Surg J. 2011;31(4):435–441.
- Nowak M, Spiller G. Two billion people coming together on Facebook. Facebook Newsroom. https://newsroom.fb.com/news/2017/06/two-billion-people-coming-together-on-facebook/. Published June 27, 2017. Accessed August 8, 2017.
- Adamson A. No contest: Twitter and Facebook can both play a role in branding. Forbes. http://www.forbes.com/2009/05/06/twitter-facebook-branding-leadership-cmo-network-adamson.html. Published May 6, 2009. Accessed August 8, 2017.
- Kim DS. Harness social media, enhance your practice. Contemp Obstet Gynecol. 2012;57(7):40–42,44–46.
- Wolf J. Social Media: Master, Manipulate, And Dominate Social Media Marketing Facebook, Twitter, YouTube, Instagram And LinkedIn. Createspace Independent Publishing Platform; 2015:129–143.
- Kotler PT, Keller KL. Marketing Management. 12th ed. Upper Saddle River, NJ: Prentice Hall; 2006:239–268.
- Jackson DP. Sunday marketing matinee: I love marketing live–Before, during, and after unit thinking. http://ilovemarketing.com/sunday-marketing-matineei-love-marketing-live-before-during-and-after-unit-thinking/. Accessed July 24, 2017.
- Payne D. How many contacts does it take before someone buys your product? Business Insider website. http://www.businessinsider.com/how-many-contacts-does-it-take-before-someone-buys-your-product-2011-7. Published July 12, 2011. Accessed August 8, 2017.
- Definition of Marketing. American Marketing Association website. https://www.ama.org/AboutAMA/Pages/Definition-of-Marketing.aspx. Published July 2013. Accessed August 8, 2017.
- Kaplan AH, Haenlein M. Users of the world, unite! The challenges and opportunities of social media. Business Horiz. 2010;53(1):59–68.
- Lin KY, Lu HP. Intention to continue using Facebook fan pages from the perspective of social capital theory. Cyberpsychol Behav Soc Netw. 2011;14(10):565–570.
- Hawn C. Take two aspirin and tweet me in the morning: how Twitter, Facebook, and other social media are reshaping health care. Health Aff (Millwood). 2009;28(2):361–368.
- Wheeler CK, Said H, Prucz R, Rodrich RJ, Mathes DW. Social media in plastic surgery practices: emerging trends in North America. Aesthet Surg J. 2011;31(4):435–441.
- Nowak M, Spiller G. Two billion people coming together on Facebook. Facebook Newsroom. https://newsroom.fb.com/news/2017/06/two-billion-people-coming-together-on-facebook/. Published June 27, 2017. Accessed August 8, 2017.
- Adamson A. No contest: Twitter and Facebook can both play a role in branding. Forbes. http://www.forbes.com/2009/05/06/twitter-facebook-branding-leadership-cmo-network-adamson.html. Published May 6, 2009. Accessed August 8, 2017.
- Kim DS. Harness social media, enhance your practice. Contemp Obstet Gynecol. 2012;57(7):40–42,44–46.
- Wolf J. Social Media: Master, Manipulate, And Dominate Social Media Marketing Facebook, Twitter, YouTube, Instagram And LinkedIn. Createspace Independent Publishing Platform; 2015:129–143.
- Kotler PT, Keller KL. Marketing Management. 12th ed. Upper Saddle River, NJ: Prentice Hall; 2006:239–268.
- Jackson DP. Sunday marketing matinee: I love marketing live–Before, during, and after unit thinking. http://ilovemarketing.com/sunday-marketing-matineei-love-marketing-live-before-during-and-after-unit-thinking/. Accessed July 24, 2017.
- Payne D. How many contacts does it take before someone buys your product? Business Insider website. http://www.businessinsider.com/how-many-contacts-does-it-take-before-someone-buys-your-product-2011-7. Published July 12, 2011. Accessed August 8, 2017.
Fast Tracks
- Open a business Facebook page, compile an email list from those who like your postings, and send out useful information and updates on your practice
- Develop an office policy for social media, supervise postings, ensure patient privacy, and obey copyright laws
Be alert for embezzlement
I can almost hear you saying it now: “Here’s a column I can skip! Embezzlement has never been a problem in this office.” Unfortunately, theft from within is way more common in medical offices than most of us suppose – and it often occurs in full view of physicians who are convinced that it cannot happen to them. Most embezzlers are not particularly skillful, nor very good at covering their tracks. But their transgressions can go undetected for years, simply because no one is watching.
A friend’s experience was all too typical: His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since she also balanced the checkbook, she got away with it for a long time. “It wasn’t at all clever,” he told me, “and I’m embarrassed to admit that it happened to me.” Is it happening to you, too? You won’t know unless you look.
Detecting fraud is an inexact science; there is no textbook approach that one can follow, but a few simple measures will uncover or prevent a large percentage of dishonest behavior:
• Hire honest employees. Check applicants’ references; find out if they are really as good as they look on paper. And for a few dollars, you can screen prospective employees on one of several public information websites to see if they have a criminal record, or have been sued (or are suing others). My columns on hiring and background checks can be found at http://www.mdedge.com/edermatologynews/managing-your-practice.
• Minimize opportunities for dishonesty. Theft and embezzlement are usually products of opportunity; there are many ways to minimize those opportunities. No one person should be in charge of the entire bookkeeping process. The person who enters charges should be different from the one who enters payments. The employee who writes the checks should not balance the checkbook, and so on. Internal audits should be done on a regular basis, and all employees should know that. Your accountant can help with this.
• Reconcile receipts and cash daily. The most common form of embezzlement is simply taking cash out of the till. In a typical scenario, a patient pays a $15 copay in cash; the receptionist records the payment as $5 and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the receipts and the cash daily.
• Insist on separate accounting duties. Another common scam – the one to which my friend fell victim – is false invoices: You think you are paying for supplies and services, but the money is going to an employee. Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
• Verify expense reports. False expense reports are another common form of fraud. When an employee asks for reimbursement of expenses, make sure they are real.
• Safeguard your computers. A major downside of computerization is the facilitation of embezzlement. Data are usually concentrated in one place, accounts can be accessed from remote workstations or off-premises servers, and a paper trail is often eliminated. Your computer vendor should be aware of this, and should have safeguards built into your system. Ask about them. If they aren’t there, ask why.
• Look for “red flags.” Do you have an employee who refuses to take vacations, because someone else will have to look at the books? Does someone insist on approving or entering expenses that are another employee’s responsibility, “just to be nice”? Is an employee suddenly living beyond his or her means?
• Consider bonding your employees. Dishonesty bonds are relatively inexpensive, and you will be assured of some measure of recovery should your safeguards fail. In addition, the mere knowledge that your staff is bonded will frighten off many dishonest applicants.
• Keep in mind that office personnel are not the only ones susceptible to temptation. A colleague recently told me about a per diem physician in his employ who conspired with a receptionist to keep fees collected for cosmetic neurotoxin and filler procedures “off the books,” then split the proceeds among themselves.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
I can almost hear you saying it now: “Here’s a column I can skip! Embezzlement has never been a problem in this office.” Unfortunately, theft from within is way more common in medical offices than most of us suppose – and it often occurs in full view of physicians who are convinced that it cannot happen to them. Most embezzlers are not particularly skillful, nor very good at covering their tracks. But their transgressions can go undetected for years, simply because no one is watching.
A friend’s experience was all too typical: His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since she also balanced the checkbook, she got away with it for a long time. “It wasn’t at all clever,” he told me, “and I’m embarrassed to admit that it happened to me.” Is it happening to you, too? You won’t know unless you look.
Detecting fraud is an inexact science; there is no textbook approach that one can follow, but a few simple measures will uncover or prevent a large percentage of dishonest behavior:
• Hire honest employees. Check applicants’ references; find out if they are really as good as they look on paper. And for a few dollars, you can screen prospective employees on one of several public information websites to see if they have a criminal record, or have been sued (or are suing others). My columns on hiring and background checks can be found at http://www.mdedge.com/edermatologynews/managing-your-practice.
• Minimize opportunities for dishonesty. Theft and embezzlement are usually products of opportunity; there are many ways to minimize those opportunities. No one person should be in charge of the entire bookkeeping process. The person who enters charges should be different from the one who enters payments. The employee who writes the checks should not balance the checkbook, and so on. Internal audits should be done on a regular basis, and all employees should know that. Your accountant can help with this.
• Reconcile receipts and cash daily. The most common form of embezzlement is simply taking cash out of the till. In a typical scenario, a patient pays a $15 copay in cash; the receptionist records the payment as $5 and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the receipts and the cash daily.
• Insist on separate accounting duties. Another common scam – the one to which my friend fell victim – is false invoices: You think you are paying for supplies and services, but the money is going to an employee. Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
• Verify expense reports. False expense reports are another common form of fraud. When an employee asks for reimbursement of expenses, make sure they are real.
• Safeguard your computers. A major downside of computerization is the facilitation of embezzlement. Data are usually concentrated in one place, accounts can be accessed from remote workstations or off-premises servers, and a paper trail is often eliminated. Your computer vendor should be aware of this, and should have safeguards built into your system. Ask about them. If they aren’t there, ask why.
• Look for “red flags.” Do you have an employee who refuses to take vacations, because someone else will have to look at the books? Does someone insist on approving or entering expenses that are another employee’s responsibility, “just to be nice”? Is an employee suddenly living beyond his or her means?
• Consider bonding your employees. Dishonesty bonds are relatively inexpensive, and you will be assured of some measure of recovery should your safeguards fail. In addition, the mere knowledge that your staff is bonded will frighten off many dishonest applicants.
• Keep in mind that office personnel are not the only ones susceptible to temptation. A colleague recently told me about a per diem physician in his employ who conspired with a receptionist to keep fees collected for cosmetic neurotoxin and filler procedures “off the books,” then split the proceeds among themselves.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
I can almost hear you saying it now: “Here’s a column I can skip! Embezzlement has never been a problem in this office.” Unfortunately, theft from within is way more common in medical offices than most of us suppose – and it often occurs in full view of physicians who are convinced that it cannot happen to them. Most embezzlers are not particularly skillful, nor very good at covering their tracks. But their transgressions can go undetected for years, simply because no one is watching.
A friend’s experience was all too typical: His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since she also balanced the checkbook, she got away with it for a long time. “It wasn’t at all clever,” he told me, “and I’m embarrassed to admit that it happened to me.” Is it happening to you, too? You won’t know unless you look.
Detecting fraud is an inexact science; there is no textbook approach that one can follow, but a few simple measures will uncover or prevent a large percentage of dishonest behavior:
• Hire honest employees. Check applicants’ references; find out if they are really as good as they look on paper. And for a few dollars, you can screen prospective employees on one of several public information websites to see if they have a criminal record, or have been sued (or are suing others). My columns on hiring and background checks can be found at http://www.mdedge.com/edermatologynews/managing-your-practice.
• Minimize opportunities for dishonesty. Theft and embezzlement are usually products of opportunity; there are many ways to minimize those opportunities. No one person should be in charge of the entire bookkeeping process. The person who enters charges should be different from the one who enters payments. The employee who writes the checks should not balance the checkbook, and so on. Internal audits should be done on a regular basis, and all employees should know that. Your accountant can help with this.
• Reconcile receipts and cash daily. The most common form of embezzlement is simply taking cash out of the till. In a typical scenario, a patient pays a $15 copay in cash; the receptionist records the payment as $5 and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the receipts and the cash daily.
• Insist on separate accounting duties. Another common scam – the one to which my friend fell victim – is false invoices: You think you are paying for supplies and services, but the money is going to an employee. Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
• Verify expense reports. False expense reports are another common form of fraud. When an employee asks for reimbursement of expenses, make sure they are real.
• Safeguard your computers. A major downside of computerization is the facilitation of embezzlement. Data are usually concentrated in one place, accounts can be accessed from remote workstations or off-premises servers, and a paper trail is often eliminated. Your computer vendor should be aware of this, and should have safeguards built into your system. Ask about them. If they aren’t there, ask why.
• Look for “red flags.” Do you have an employee who refuses to take vacations, because someone else will have to look at the books? Does someone insist on approving or entering expenses that are another employee’s responsibility, “just to be nice”? Is an employee suddenly living beyond his or her means?
• Consider bonding your employees. Dishonesty bonds are relatively inexpensive, and you will be assured of some measure of recovery should your safeguards fail. In addition, the mere knowledge that your staff is bonded will frighten off many dishonest applicants.
• Keep in mind that office personnel are not the only ones susceptible to temptation. A colleague recently told me about a per diem physician in his employ who conspired with a receptionist to keep fees collected for cosmetic neurotoxin and filler procedures “off the books,” then split the proceeds among themselves.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]
Landmark women’s health care remains law of the land
Starting in 2010 with the Patient Protection and Affordable Care Act (ACA), our patients have had insurance that provides maternity care coverage, no-deductible or copay contraceptives, and access to breast cancer screening. They also have been protected from predatory insurance practices—such as preexisting condition exclusions, arbitrary rescission, and annual or lifetime coverage limits—which had previously and regularly been used to deny coverage. These landmark protections apply to all our patients, regardless of where they live, how much they earn, who their employers are, and which insurance plan they use. They have become part of the fabric of our society.
Between 2008 and 2010, members of the American College of Obstetricians and Gynecologists (ACOG) worked hard to define and help enact these provisions, which we considered the women’s piece of the health care reform puzzle. We also worked with a broad community of clinicians to try to make sure reform would benefit them too. That effort did not go as well, and ACOG ultimately did not endorse the ACA.
Early ACA troubles, misguided solutions
Since the ACA was signed into law 7 years ago, insurers have raised premiums and deductibles and narrowed their provider networks—putting needed care out of the reach of many patients. In addition, skyrocketing prescription drug prices have driven health care costs even higher. Against this backdrop, Congress in 2017 started trying to pass bills that would undo the ACA.
ACOG and our medical colleague organizations stepped up. We brought many ideas to House and Senate Republicans and Democrats and sought opportunities to work with them to improve the ACA for our physicians and patients. Unfortunately, the statute was so polarizing that few in Congress wanted to amend or revise it; most wanted it repealed or left as is.
Throughout these proceedings, ACOG remained committed to ensuring that no one with health insurance coverage would lose it and that Congress would not turn back the clock on women’s health. As long as these 2 principles were assured, we would work with anyone on improving health insurance.
Path to a better way
We delivered our message repeatedly. ACOG President Haywood Brown, MD, often accompanied by his American College of Physicians, American Academy of Pediatrics, American Academy of Family Physicians, American Psychiatric Association, and American Osteopathic Association counterparts, attended high-level meetings with Congressional Republicans and Democrats. Dr. Brown also led fly-ins of our members. In addition, ACOG Past President Tom Gellhaus, MD, together with all 600 ObGyns at the 2017 ACOG Congressional Leadership Conference, spoke out.
Somehow, though, the proposed bills kept getting worse—more patients would be losing coverage, and women’s health protections would be stripped away—and Congress was not seeking or including physician input. None at all.
The ACOG teleconference
In response, ACOG set up a member teleconference headed by Dr. Brown, Dr. Gellhaus, Incoming President Lisa Hollier, MD, Past President and ObGyn PAC Chair Mark DeFrancesco, MD, and Executive Vice President and CEO Hal Lawrence, MD. Discussing our concerns, we focused on the Senate’s Better Care Reconciliation Act (BCRA) and its potential impact on maternity care coverage, preexisting condition coverage, Medicaid, Planned Parenthood (PP), and the opioid epidemic.
BCRA
Dr. Brown led off the teleconference with this assessment: “Without a doubt, the BCRA would not result in better care for our patients. This legislation would pull the rug out from under women and families. The nonpartisan Congressional Budget Office estimated that 22 million Americans, more than half of them women, would lose coverage. More than $770 billion would be cut from Medicaid, the program that covers nearly half of all births nationwide as well as primary and preventive care for low-income patients.”
Coverage for maternity care and preexisting conditions
Dr. Gellhaus discussed how the BCRA would gut maternity care coverage and hurt patients with preexisting conditions. Under this bill, states would be able to drop the requirement for such coverage, thereby creating an enormous hole in patient care. He asked an important question: “If your state opted out and allowed private insurers not to offer maternity care or preventive care, what would this mean for your patients?”
His answer: “It would take us back to a time when only 9 states required insurers cover maternity care, and when only 12% of plans included such coverage; a time when patients had to buy expensive riders, sometimes with 12-month waiting periods, if they wanted maternity coverage; a time when expecting families faced thousands of dollars in out-of-pocket costs. Do we want to go back to that time? It is also important to note that roughly half of all pregnancies are unplanned. Pregnancy should not leave patients fearing bankruptcy and unable to afford the full range of prenatal and postnatal care.
“States that opt out of covering preventive care would discontinue no-copay coverage for women’s preventive services, including contraception. Fifty-five million American women currently have this coverage, and as a result the country’s unintended pregnancy rate is at a 30-year low, and its teen pregnancy rate the lowest in recorded history. We cannot go back.”
Medicaid
Dr. Hollier pointed out that the BCRA would cut $772 billion from Medicaid, ending the program as we know it and shifting costs to states. “This section alone would devastate our patients in every state,” she said.
ACOG is a strong supporter of Medicaid expansion, which increased access to primary and preventive care, including contraception, for low-income women who otherwise would not see a physician until they became pregnant. Thirty-two states and the District of Columbia expanded their Medicaid programs, and other states have expressed interest in doing the same.
Medicaid expansion was a major factor in the almost 50% decrease in the rate of uninsured women since 2010. The BCRA would roll back coverage for essential health benefits beginning in 2020 and end federal expansion funding by 2023.
Dr. Hollier continued, “Regular Medicaid would be threatened, too. The Senate bill would limit, for the first time ever, federal funding for Medicaid services per beneficiary. This would jeopardize the ability of the United States to respond to disasters and public health crises and pose a threat to health care coverage and benefits for tens of millions of Americans.”
“Given that nearly half of US births are covered by Medicaid, cutting this program would have a huge impact on our practices and on our patients with high-risk and expensive pregnancies. What happens when a low-income pregnant patient with hypertension, gestational diabetes, or preeclampsia reaches her Medicaid cap? What happens to a patient with an opioid use disorder or a patient who may have been exposed to the Zika virus? In all likelihood, physicians would have to continue providing care, regardless of coverage, or states would have to reduce physician payments to fill the gap in federal funding. I am sure you are as horrified as I am by these scenarios,” said Dr. Hollier.
Planned Parenthood
Dr. DeFrancesco discussed the threat to PP. First, he explained what defunding the organization would mean. “Planned Parenthood does not just receive a check from the government each year. Like other qualified providers, like us, PP health centers receive federal reimbursement for primary and preventive services provided to patients with Medicaid coverage. Fifty-four percent of these centers are located in rural and medically underserved communities.”
The BCRA would exclude PP health centers from the Medicaid program, which means Medicaid patients would be denied primary and preventive care at these centers. Within the first year, up to 1 million women would find their access to care restricted. In addition, about half of all PP centers would have to close, and most would not reopen. Dr. DeFrancesco asked, “How would this move help our patients? It wouldn’t.”
Two examples shed light on the situation. First, when PP was excluded from a Texas program serving low-income patients, the number of women using the most effective birth control methods decreased by 35%, and the number of Medicaid-covered births increased by 27%. Second, when public health funding cuts forced many Indiana clinics to close, rural areas of the state experienced one of the fastest and largest HIV outbreaks ever to occur in the United States.
Dr. DeFrancesco said, “Excluding Planned Parenthood from the Medicaid program interferes with the patient–physician relationship and sets a dangerous precedent of targeting qualified providers for political purposes.”
Opioid epidemic
Dr. Brown indicated that the BCRA would cripple attempts to address our very serious national opioid epidemic. The $2 billion the bill would allocate for opioid use disorder treatment for 1 year would replace funding lost by Medicaid and would pay for only a fraction of what is needed. Dr. Brown called this measure a “token, not a commitment, and a big step back in the progress we have made to address this public health crisis.”
The Hippocratic oath
While preparing for the teleconference, I kept thinking about the Hippocratic oath and our deep obligation to our patients. Every physician I know goes beyond the exam room to care for patients. We lose sleep not only when we get up to deliver babies, but when we worry about the ailing mother of four we saw yesterday, or the scared teenager who missed last week’s appointment. We care for our patients because it is the right thing to do, and it is our calling. Well, this year, our patients needed us more than ever. We had to step up, speak out, do everything we could to stop BCRA from passing. The stakes could not have been higher.
The vote, and the road ahead
The morning after Senators Collins, Murkowski, and McCain joined Senate Democrats to end the bill, Dr. Brown wrote the following to ACOG members and the US Congress:
“This was a battle we simply had to win to protect our patients. Thanks to your tireless advocacy, landmark women’s health care protections remain law, and millions of our patients will continue to get the care they need. And our work continues. The ACA is not perfect and needs major reform. ACOG is ready, willing, and able to work with Republicans and Democrats in the US House and Senate to reform the law, through an open and collaborative process. We hope it is clear to everyone in Congress that physicians must be part of the conversation and the solution.”
Starting in 2010 with the Patient Protection and Affordable Care Act (ACA), our patients have had insurance that provides maternity care coverage, no-deductible or copay contraceptives, and access to breast cancer screening. They also have been protected from predatory insurance practices—such as preexisting condition exclusions, arbitrary rescission, and annual or lifetime coverage limits—which had previously and regularly been used to deny coverage. These landmark protections apply to all our patients, regardless of where they live, how much they earn, who their employers are, and which insurance plan they use. They have become part of the fabric of our society.
Between 2008 and 2010, members of the American College of Obstetricians and Gynecologists (ACOG) worked hard to define and help enact these provisions, which we considered the women’s piece of the health care reform puzzle. We also worked with a broad community of clinicians to try to make sure reform would benefit them too. That effort did not go as well, and ACOG ultimately did not endorse the ACA.
Early ACA troubles, misguided solutions
Since the ACA was signed into law 7 years ago, insurers have raised premiums and deductibles and narrowed their provider networks—putting needed care out of the reach of many patients. In addition, skyrocketing prescription drug prices have driven health care costs even higher. Against this backdrop, Congress in 2017 started trying to pass bills that would undo the ACA.
ACOG and our medical colleague organizations stepped up. We brought many ideas to House and Senate Republicans and Democrats and sought opportunities to work with them to improve the ACA for our physicians and patients. Unfortunately, the statute was so polarizing that few in Congress wanted to amend or revise it; most wanted it repealed or left as is.
Throughout these proceedings, ACOG remained committed to ensuring that no one with health insurance coverage would lose it and that Congress would not turn back the clock on women’s health. As long as these 2 principles were assured, we would work with anyone on improving health insurance.
Path to a better way
We delivered our message repeatedly. ACOG President Haywood Brown, MD, often accompanied by his American College of Physicians, American Academy of Pediatrics, American Academy of Family Physicians, American Psychiatric Association, and American Osteopathic Association counterparts, attended high-level meetings with Congressional Republicans and Democrats. Dr. Brown also led fly-ins of our members. In addition, ACOG Past President Tom Gellhaus, MD, together with all 600 ObGyns at the 2017 ACOG Congressional Leadership Conference, spoke out.
Somehow, though, the proposed bills kept getting worse—more patients would be losing coverage, and women’s health protections would be stripped away—and Congress was not seeking or including physician input. None at all.
The ACOG teleconference
In response, ACOG set up a member teleconference headed by Dr. Brown, Dr. Gellhaus, Incoming President Lisa Hollier, MD, Past President and ObGyn PAC Chair Mark DeFrancesco, MD, and Executive Vice President and CEO Hal Lawrence, MD. Discussing our concerns, we focused on the Senate’s Better Care Reconciliation Act (BCRA) and its potential impact on maternity care coverage, preexisting condition coverage, Medicaid, Planned Parenthood (PP), and the opioid epidemic.
BCRA
Dr. Brown led off the teleconference with this assessment: “Without a doubt, the BCRA would not result in better care for our patients. This legislation would pull the rug out from under women and families. The nonpartisan Congressional Budget Office estimated that 22 million Americans, more than half of them women, would lose coverage. More than $770 billion would be cut from Medicaid, the program that covers nearly half of all births nationwide as well as primary and preventive care for low-income patients.”
Coverage for maternity care and preexisting conditions
Dr. Gellhaus discussed how the BCRA would gut maternity care coverage and hurt patients with preexisting conditions. Under this bill, states would be able to drop the requirement for such coverage, thereby creating an enormous hole in patient care. He asked an important question: “If your state opted out and allowed private insurers not to offer maternity care or preventive care, what would this mean for your patients?”
His answer: “It would take us back to a time when only 9 states required insurers cover maternity care, and when only 12% of plans included such coverage; a time when patients had to buy expensive riders, sometimes with 12-month waiting periods, if they wanted maternity coverage; a time when expecting families faced thousands of dollars in out-of-pocket costs. Do we want to go back to that time? It is also important to note that roughly half of all pregnancies are unplanned. Pregnancy should not leave patients fearing bankruptcy and unable to afford the full range of prenatal and postnatal care.
“States that opt out of covering preventive care would discontinue no-copay coverage for women’s preventive services, including contraception. Fifty-five million American women currently have this coverage, and as a result the country’s unintended pregnancy rate is at a 30-year low, and its teen pregnancy rate the lowest in recorded history. We cannot go back.”
Medicaid
Dr. Hollier pointed out that the BCRA would cut $772 billion from Medicaid, ending the program as we know it and shifting costs to states. “This section alone would devastate our patients in every state,” she said.
ACOG is a strong supporter of Medicaid expansion, which increased access to primary and preventive care, including contraception, for low-income women who otherwise would not see a physician until they became pregnant. Thirty-two states and the District of Columbia expanded their Medicaid programs, and other states have expressed interest in doing the same.
Medicaid expansion was a major factor in the almost 50% decrease in the rate of uninsured women since 2010. The BCRA would roll back coverage for essential health benefits beginning in 2020 and end federal expansion funding by 2023.
Dr. Hollier continued, “Regular Medicaid would be threatened, too. The Senate bill would limit, for the first time ever, federal funding for Medicaid services per beneficiary. This would jeopardize the ability of the United States to respond to disasters and public health crises and pose a threat to health care coverage and benefits for tens of millions of Americans.”
“Given that nearly half of US births are covered by Medicaid, cutting this program would have a huge impact on our practices and on our patients with high-risk and expensive pregnancies. What happens when a low-income pregnant patient with hypertension, gestational diabetes, or preeclampsia reaches her Medicaid cap? What happens to a patient with an opioid use disorder or a patient who may have been exposed to the Zika virus? In all likelihood, physicians would have to continue providing care, regardless of coverage, or states would have to reduce physician payments to fill the gap in federal funding. I am sure you are as horrified as I am by these scenarios,” said Dr. Hollier.
Planned Parenthood
Dr. DeFrancesco discussed the threat to PP. First, he explained what defunding the organization would mean. “Planned Parenthood does not just receive a check from the government each year. Like other qualified providers, like us, PP health centers receive federal reimbursement for primary and preventive services provided to patients with Medicaid coverage. Fifty-four percent of these centers are located in rural and medically underserved communities.”
The BCRA would exclude PP health centers from the Medicaid program, which means Medicaid patients would be denied primary and preventive care at these centers. Within the first year, up to 1 million women would find their access to care restricted. In addition, about half of all PP centers would have to close, and most would not reopen. Dr. DeFrancesco asked, “How would this move help our patients? It wouldn’t.”
Two examples shed light on the situation. First, when PP was excluded from a Texas program serving low-income patients, the number of women using the most effective birth control methods decreased by 35%, and the number of Medicaid-covered births increased by 27%. Second, when public health funding cuts forced many Indiana clinics to close, rural areas of the state experienced one of the fastest and largest HIV outbreaks ever to occur in the United States.
Dr. DeFrancesco said, “Excluding Planned Parenthood from the Medicaid program interferes with the patient–physician relationship and sets a dangerous precedent of targeting qualified providers for political purposes.”
Opioid epidemic
Dr. Brown indicated that the BCRA would cripple attempts to address our very serious national opioid epidemic. The $2 billion the bill would allocate for opioid use disorder treatment for 1 year would replace funding lost by Medicaid and would pay for only a fraction of what is needed. Dr. Brown called this measure a “token, not a commitment, and a big step back in the progress we have made to address this public health crisis.”
The Hippocratic oath
While preparing for the teleconference, I kept thinking about the Hippocratic oath and our deep obligation to our patients. Every physician I know goes beyond the exam room to care for patients. We lose sleep not only when we get up to deliver babies, but when we worry about the ailing mother of four we saw yesterday, or the scared teenager who missed last week’s appointment. We care for our patients because it is the right thing to do, and it is our calling. Well, this year, our patients needed us more than ever. We had to step up, speak out, do everything we could to stop BCRA from passing. The stakes could not have been higher.
The vote, and the road ahead
The morning after Senators Collins, Murkowski, and McCain joined Senate Democrats to end the bill, Dr. Brown wrote the following to ACOG members and the US Congress:
“This was a battle we simply had to win to protect our patients. Thanks to your tireless advocacy, landmark women’s health care protections remain law, and millions of our patients will continue to get the care they need. And our work continues. The ACA is not perfect and needs major reform. ACOG is ready, willing, and able to work with Republicans and Democrats in the US House and Senate to reform the law, through an open and collaborative process. We hope it is clear to everyone in Congress that physicians must be part of the conversation and the solution.”
Starting in 2010 with the Patient Protection and Affordable Care Act (ACA), our patients have had insurance that provides maternity care coverage, no-deductible or copay contraceptives, and access to breast cancer screening. They also have been protected from predatory insurance practices—such as preexisting condition exclusions, arbitrary rescission, and annual or lifetime coverage limits—which had previously and regularly been used to deny coverage. These landmark protections apply to all our patients, regardless of where they live, how much they earn, who their employers are, and which insurance plan they use. They have become part of the fabric of our society.
Between 2008 and 2010, members of the American College of Obstetricians and Gynecologists (ACOG) worked hard to define and help enact these provisions, which we considered the women’s piece of the health care reform puzzle. We also worked with a broad community of clinicians to try to make sure reform would benefit them too. That effort did not go as well, and ACOG ultimately did not endorse the ACA.
Early ACA troubles, misguided solutions
Since the ACA was signed into law 7 years ago, insurers have raised premiums and deductibles and narrowed their provider networks—putting needed care out of the reach of many patients. In addition, skyrocketing prescription drug prices have driven health care costs even higher. Against this backdrop, Congress in 2017 started trying to pass bills that would undo the ACA.
ACOG and our medical colleague organizations stepped up. We brought many ideas to House and Senate Republicans and Democrats and sought opportunities to work with them to improve the ACA for our physicians and patients. Unfortunately, the statute was so polarizing that few in Congress wanted to amend or revise it; most wanted it repealed or left as is.
Throughout these proceedings, ACOG remained committed to ensuring that no one with health insurance coverage would lose it and that Congress would not turn back the clock on women’s health. As long as these 2 principles were assured, we would work with anyone on improving health insurance.
Path to a better way
We delivered our message repeatedly. ACOG President Haywood Brown, MD, often accompanied by his American College of Physicians, American Academy of Pediatrics, American Academy of Family Physicians, American Psychiatric Association, and American Osteopathic Association counterparts, attended high-level meetings with Congressional Republicans and Democrats. Dr. Brown also led fly-ins of our members. In addition, ACOG Past President Tom Gellhaus, MD, together with all 600 ObGyns at the 2017 ACOG Congressional Leadership Conference, spoke out.
Somehow, though, the proposed bills kept getting worse—more patients would be losing coverage, and women’s health protections would be stripped away—and Congress was not seeking or including physician input. None at all.
The ACOG teleconference
In response, ACOG set up a member teleconference headed by Dr. Brown, Dr. Gellhaus, Incoming President Lisa Hollier, MD, Past President and ObGyn PAC Chair Mark DeFrancesco, MD, and Executive Vice President and CEO Hal Lawrence, MD. Discussing our concerns, we focused on the Senate’s Better Care Reconciliation Act (BCRA) and its potential impact on maternity care coverage, preexisting condition coverage, Medicaid, Planned Parenthood (PP), and the opioid epidemic.
BCRA
Dr. Brown led off the teleconference with this assessment: “Without a doubt, the BCRA would not result in better care for our patients. This legislation would pull the rug out from under women and families. The nonpartisan Congressional Budget Office estimated that 22 million Americans, more than half of them women, would lose coverage. More than $770 billion would be cut from Medicaid, the program that covers nearly half of all births nationwide as well as primary and preventive care for low-income patients.”
Coverage for maternity care and preexisting conditions
Dr. Gellhaus discussed how the BCRA would gut maternity care coverage and hurt patients with preexisting conditions. Under this bill, states would be able to drop the requirement for such coverage, thereby creating an enormous hole in patient care. He asked an important question: “If your state opted out and allowed private insurers not to offer maternity care or preventive care, what would this mean for your patients?”
His answer: “It would take us back to a time when only 9 states required insurers cover maternity care, and when only 12% of plans included such coverage; a time when patients had to buy expensive riders, sometimes with 12-month waiting periods, if they wanted maternity coverage; a time when expecting families faced thousands of dollars in out-of-pocket costs. Do we want to go back to that time? It is also important to note that roughly half of all pregnancies are unplanned. Pregnancy should not leave patients fearing bankruptcy and unable to afford the full range of prenatal and postnatal care.
“States that opt out of covering preventive care would discontinue no-copay coverage for women’s preventive services, including contraception. Fifty-five million American women currently have this coverage, and as a result the country’s unintended pregnancy rate is at a 30-year low, and its teen pregnancy rate the lowest in recorded history. We cannot go back.”
Medicaid
Dr. Hollier pointed out that the BCRA would cut $772 billion from Medicaid, ending the program as we know it and shifting costs to states. “This section alone would devastate our patients in every state,” she said.
ACOG is a strong supporter of Medicaid expansion, which increased access to primary and preventive care, including contraception, for low-income women who otherwise would not see a physician until they became pregnant. Thirty-two states and the District of Columbia expanded their Medicaid programs, and other states have expressed interest in doing the same.
Medicaid expansion was a major factor in the almost 50% decrease in the rate of uninsured women since 2010. The BCRA would roll back coverage for essential health benefits beginning in 2020 and end federal expansion funding by 2023.
Dr. Hollier continued, “Regular Medicaid would be threatened, too. The Senate bill would limit, for the first time ever, federal funding for Medicaid services per beneficiary. This would jeopardize the ability of the United States to respond to disasters and public health crises and pose a threat to health care coverage and benefits for tens of millions of Americans.”
“Given that nearly half of US births are covered by Medicaid, cutting this program would have a huge impact on our practices and on our patients with high-risk and expensive pregnancies. What happens when a low-income pregnant patient with hypertension, gestational diabetes, or preeclampsia reaches her Medicaid cap? What happens to a patient with an opioid use disorder or a patient who may have been exposed to the Zika virus? In all likelihood, physicians would have to continue providing care, regardless of coverage, or states would have to reduce physician payments to fill the gap in federal funding. I am sure you are as horrified as I am by these scenarios,” said Dr. Hollier.
Planned Parenthood
Dr. DeFrancesco discussed the threat to PP. First, he explained what defunding the organization would mean. “Planned Parenthood does not just receive a check from the government each year. Like other qualified providers, like us, PP health centers receive federal reimbursement for primary and preventive services provided to patients with Medicaid coverage. Fifty-four percent of these centers are located in rural and medically underserved communities.”
The BCRA would exclude PP health centers from the Medicaid program, which means Medicaid patients would be denied primary and preventive care at these centers. Within the first year, up to 1 million women would find their access to care restricted. In addition, about half of all PP centers would have to close, and most would not reopen. Dr. DeFrancesco asked, “How would this move help our patients? It wouldn’t.”
Two examples shed light on the situation. First, when PP was excluded from a Texas program serving low-income patients, the number of women using the most effective birth control methods decreased by 35%, and the number of Medicaid-covered births increased by 27%. Second, when public health funding cuts forced many Indiana clinics to close, rural areas of the state experienced one of the fastest and largest HIV outbreaks ever to occur in the United States.
Dr. DeFrancesco said, “Excluding Planned Parenthood from the Medicaid program interferes with the patient–physician relationship and sets a dangerous precedent of targeting qualified providers for political purposes.”
Opioid epidemic
Dr. Brown indicated that the BCRA would cripple attempts to address our very serious national opioid epidemic. The $2 billion the bill would allocate for opioid use disorder treatment for 1 year would replace funding lost by Medicaid and would pay for only a fraction of what is needed. Dr. Brown called this measure a “token, not a commitment, and a big step back in the progress we have made to address this public health crisis.”
The Hippocratic oath
While preparing for the teleconference, I kept thinking about the Hippocratic oath and our deep obligation to our patients. Every physician I know goes beyond the exam room to care for patients. We lose sleep not only when we get up to deliver babies, but when we worry about the ailing mother of four we saw yesterday, or the scared teenager who missed last week’s appointment. We care for our patients because it is the right thing to do, and it is our calling. Well, this year, our patients needed us more than ever. We had to step up, speak out, do everything we could to stop BCRA from passing. The stakes could not have been higher.
The vote, and the road ahead
The morning after Senators Collins, Murkowski, and McCain joined Senate Democrats to end the bill, Dr. Brown wrote the following to ACOG members and the US Congress:
“This was a battle we simply had to win to protect our patients. Thanks to your tireless advocacy, landmark women’s health care protections remain law, and millions of our patients will continue to get the care they need. And our work continues. The ACA is not perfect and needs major reform. ACOG is ready, willing, and able to work with Republicans and Democrats in the US House and Senate to reform the law, through an open and collaborative process. We hope it is clear to everyone in Congress that physicians must be part of the conversation and the solution.”