User login
ICD-10 – The time is now
If you have been paying attention at all, you are aware that the International Classification of Diseases, 10th Revision (ICD-10) will be implemented later this year. So why – if you’re like most of the physicians I’ve talked with recently – have you done little or nothing about it? Since the launch is more than 6 months away, why am I telling you (and I am) that this is a very bad idea?
Because there is much to do before the deadline arrives. On Sept. 30, you will be using ICD-9 codes, and the next day you will have to begin using ICD-10. There is no transition period; all ICD-9–coded claims will be rejected from Oct. 1 forward, and no ICD-10 codes can be used before that date. Failure to prepare will be an unmitigated disaster for your practice’s cash flow.
The Centers for Medicare & Medicaid Services has already rejected a request from medical organizations for another 1-year delay (in addition to the one granted last year), so further extensions are highly unlikely. So you’ll need to be ready if you expect to be paid come October.
First, you will need to decide which parts of your coding and billing systems, and electronic health record (EHR, if you have one) need to be upgraded, how you will do it, and what it will cost. Then, you must get familiar with the new system.
Coders and billers will need the most training on the new methodology, but physicians and other providers also must learn how the new codes are different from the old ones. In general, the biggest differences are in level of documentation and specificity, but there are many brand-new codes as well.
I suggest that you start by identifying your 20 or 30 most-used diagnosis codes and then study in detail the differences between the ICD-9 and ICD-10 versions of them. Once you have mastered those, you can go on to other, less-used codes. Take as much time as you need to do this; remember, everything changes abruptly on Oct. 1, and you will have to get it right the first time.
Be sure to cross-train your coders and other staff members. If a crucial employee quits in the middle of September, you don’t want to have to start from square one. Also, ask your employees to plan their vacations well in advance – and not during the last 3 months of the year. This will not be a good time for the office to run short staffed.
Next, I suggest that you contact all of your third-party payers, billing services, and clearinghouses. Start with the payers responsible for the majority of your claims. Be aggressive; ask them how, exactly, they are preparing for the changeover, and stay in continuous contact with them. Unfortunately, many of these organizations are as behind as most medical practices in their preparations.
Many payers and clearinghouses (including CMS) will be staging "test runs," during which you will be able to submit "practice claims" using the new system. Payers will determine whether your ICD-10 code is in the right place and in the right format, whether the code you’ve used is appropriate, and whether the claim would have been accepted, rejected, or held pending additional information. You will have to do this for each payer, because each will have different coding policies; those policies have not yet been released, and in some cases, have not even been developed.
The CMS will run its first testing opportunity in March; you can register for it, or for future tests, through your local Medicare Administrative Contractor (MAC) website.
You can use these testing opportunities to test your internal system as well, ensuring that everything works smoothly from the time you code a claim until payment is received. Select commonly used ICD-9 claims and practice coding them in ICD-10. The American Academy of Dermatology offers a nice ICD-9/ICD-10 "crosswalk," along with other training aids, at its website.
Even the best laid plans can go awry, so it would be prudent to put aside a cash reserve, or secure a line of credit, to cover expenses during the first few months of the transition, in case the payment machinery falters and large numbers of claims go unpaid. For the same reason, consider postponing major capital investments from mid-year until early 2015.
You may have heard that ICD-10 is only a transition system; that ICD-11 will be following closely on its heels, only a year or 2 later. Many of the experts that I’ve spoken with feel that this highly unlikely, and I agree. So don’t feel that you are wasting your time adjusting to ICD-10; in all probability, we will be using it a lot longer than CMS is expecting.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
If you have been paying attention at all, you are aware that the International Classification of Diseases, 10th Revision (ICD-10) will be implemented later this year. So why – if you’re like most of the physicians I’ve talked with recently – have you done little or nothing about it? Since the launch is more than 6 months away, why am I telling you (and I am) that this is a very bad idea?
Because there is much to do before the deadline arrives. On Sept. 30, you will be using ICD-9 codes, and the next day you will have to begin using ICD-10. There is no transition period; all ICD-9–coded claims will be rejected from Oct. 1 forward, and no ICD-10 codes can be used before that date. Failure to prepare will be an unmitigated disaster for your practice’s cash flow.
The Centers for Medicare & Medicaid Services has already rejected a request from medical organizations for another 1-year delay (in addition to the one granted last year), so further extensions are highly unlikely. So you’ll need to be ready if you expect to be paid come October.
First, you will need to decide which parts of your coding and billing systems, and electronic health record (EHR, if you have one) need to be upgraded, how you will do it, and what it will cost. Then, you must get familiar with the new system.
Coders and billers will need the most training on the new methodology, but physicians and other providers also must learn how the new codes are different from the old ones. In general, the biggest differences are in level of documentation and specificity, but there are many brand-new codes as well.
I suggest that you start by identifying your 20 or 30 most-used diagnosis codes and then study in detail the differences between the ICD-9 and ICD-10 versions of them. Once you have mastered those, you can go on to other, less-used codes. Take as much time as you need to do this; remember, everything changes abruptly on Oct. 1, and you will have to get it right the first time.
Be sure to cross-train your coders and other staff members. If a crucial employee quits in the middle of September, you don’t want to have to start from square one. Also, ask your employees to plan their vacations well in advance – and not during the last 3 months of the year. This will not be a good time for the office to run short staffed.
Next, I suggest that you contact all of your third-party payers, billing services, and clearinghouses. Start with the payers responsible for the majority of your claims. Be aggressive; ask them how, exactly, they are preparing for the changeover, and stay in continuous contact with them. Unfortunately, many of these organizations are as behind as most medical practices in their preparations.
Many payers and clearinghouses (including CMS) will be staging "test runs," during which you will be able to submit "practice claims" using the new system. Payers will determine whether your ICD-10 code is in the right place and in the right format, whether the code you’ve used is appropriate, and whether the claim would have been accepted, rejected, or held pending additional information. You will have to do this for each payer, because each will have different coding policies; those policies have not yet been released, and in some cases, have not even been developed.
The CMS will run its first testing opportunity in March; you can register for it, or for future tests, through your local Medicare Administrative Contractor (MAC) website.
You can use these testing opportunities to test your internal system as well, ensuring that everything works smoothly from the time you code a claim until payment is received. Select commonly used ICD-9 claims and practice coding them in ICD-10. The American Academy of Dermatology offers a nice ICD-9/ICD-10 "crosswalk," along with other training aids, at its website.
Even the best laid plans can go awry, so it would be prudent to put aside a cash reserve, or secure a line of credit, to cover expenses during the first few months of the transition, in case the payment machinery falters and large numbers of claims go unpaid. For the same reason, consider postponing major capital investments from mid-year until early 2015.
You may have heard that ICD-10 is only a transition system; that ICD-11 will be following closely on its heels, only a year or 2 later. Many of the experts that I’ve spoken with feel that this highly unlikely, and I agree. So don’t feel that you are wasting your time adjusting to ICD-10; in all probability, we will be using it a lot longer than CMS is expecting.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
If you have been paying attention at all, you are aware that the International Classification of Diseases, 10th Revision (ICD-10) will be implemented later this year. So why – if you’re like most of the physicians I’ve talked with recently – have you done little or nothing about it? Since the launch is more than 6 months away, why am I telling you (and I am) that this is a very bad idea?
Because there is much to do before the deadline arrives. On Sept. 30, you will be using ICD-9 codes, and the next day you will have to begin using ICD-10. There is no transition period; all ICD-9–coded claims will be rejected from Oct. 1 forward, and no ICD-10 codes can be used before that date. Failure to prepare will be an unmitigated disaster for your practice’s cash flow.
The Centers for Medicare & Medicaid Services has already rejected a request from medical organizations for another 1-year delay (in addition to the one granted last year), so further extensions are highly unlikely. So you’ll need to be ready if you expect to be paid come October.
First, you will need to decide which parts of your coding and billing systems, and electronic health record (EHR, if you have one) need to be upgraded, how you will do it, and what it will cost. Then, you must get familiar with the new system.
Coders and billers will need the most training on the new methodology, but physicians and other providers also must learn how the new codes are different from the old ones. In general, the biggest differences are in level of documentation and specificity, but there are many brand-new codes as well.
I suggest that you start by identifying your 20 or 30 most-used diagnosis codes and then study in detail the differences between the ICD-9 and ICD-10 versions of them. Once you have mastered those, you can go on to other, less-used codes. Take as much time as you need to do this; remember, everything changes abruptly on Oct. 1, and you will have to get it right the first time.
Be sure to cross-train your coders and other staff members. If a crucial employee quits in the middle of September, you don’t want to have to start from square one. Also, ask your employees to plan their vacations well in advance – and not during the last 3 months of the year. This will not be a good time for the office to run short staffed.
Next, I suggest that you contact all of your third-party payers, billing services, and clearinghouses. Start with the payers responsible for the majority of your claims. Be aggressive; ask them how, exactly, they are preparing for the changeover, and stay in continuous contact with them. Unfortunately, many of these organizations are as behind as most medical practices in their preparations.
Many payers and clearinghouses (including CMS) will be staging "test runs," during which you will be able to submit "practice claims" using the new system. Payers will determine whether your ICD-10 code is in the right place and in the right format, whether the code you’ve used is appropriate, and whether the claim would have been accepted, rejected, or held pending additional information. You will have to do this for each payer, because each will have different coding policies; those policies have not yet been released, and in some cases, have not even been developed.
The CMS will run its first testing opportunity in March; you can register for it, or for future tests, through your local Medicare Administrative Contractor (MAC) website.
You can use these testing opportunities to test your internal system as well, ensuring that everything works smoothly from the time you code a claim until payment is received. Select commonly used ICD-9 claims and practice coding them in ICD-10. The American Academy of Dermatology offers a nice ICD-9/ICD-10 "crosswalk," along with other training aids, at its website.
Even the best laid plans can go awry, so it would be prudent to put aside a cash reserve, or secure a line of credit, to cover expenses during the first few months of the transition, in case the payment machinery falters and large numbers of claims go unpaid. For the same reason, consider postponing major capital investments from mid-year until early 2015.
You may have heard that ICD-10 is only a transition system; that ICD-11 will be following closely on its heels, only a year or 2 later. Many of the experts that I’ve spoken with feel that this highly unlikely, and I agree. So don’t feel that you are wasting your time adjusting to ICD-10; in all probability, we will be using it a lot longer than CMS is expecting.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
Shift from Productivity to Value-Based Compensation Gains Momentum
At the 2011 SHM annual meeting in Dallas, I served on an expert panel that reviewed the latest hospitalist survey data. Included in this review were the latest compensation and productivity figures. As the session concluded, I was satisfied that the panel had discussed important information in an accessible way; however, the keynote speaker who followed us to address an entirely different topic began his talk by pointing out that the data we had reviewed, including things like wRVUs, would very soon have little to do with compensation for any physician, regardless of specialty. He implied, quite persuasively, that we were pretty old school to be talking about wRVUs and compensation based on productivity; everyone should be prepared for and embrace compensation based on value, not production.
I hear a similar sentiment reasonably often. And I agree, but I think many make the mistake of oversimplifying the issue.
Physician Value-Based Payment
Measurement of physician performance using costs, quality, and outcomes has already begun and will influence Medicare payments to doctors beginning in 2015 for large groups (>100 providers with any mix of specialties billing under the same tax ID number) and in 2017 for smaller groups.
If Medicare is moving away from payment based on wRVUs, likely followed soon by other payors, then hospitalist compensation should do the same. But I don’t think that changes the potential role of compensation based on productivity.
Compensation Should Include Performance and Productivity Metrics
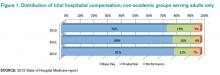
Survey data show a move from an essentially fixed annual compensation early in our field to an inclusion of components tied to performance several years before the introduction of the Physician Value-Based Payment Modifier program. Data from SHM’s 2010, 2011, and 2012 State of Hospital Medicine reports (www.hospitalmedicine.org/survey) show that a small, but probably increasing, part of compensation has been tied to performance on things like patient satisfaction and core measures (see “Distribution of Total Hospitalist Compensation,” below). Note that the percentages in the chart refer to the fraction of total compensation dollars allocated to each domain and not the portion of hospitalists who have compensation tied to each domain.
Over the same three years, the percentage of compensation tied to productivity has been decreasing overall, while “private groups are more likely to pay a higher proportion of compensation based on productivity, and hospital-employed groups are more likely to pay a higher proportion of compensation based on performance.”
Matching Performance Compensation to Medicare’s Value-Based Modifier
It makes sense for physician compensation to generally mirror Medicare and other payor professional fee reimbursement formulas. But, in that regard, hospitalists are ahead of the market already, because the portion of dollars allocated to performance (value) in hospitalist compensation plans already exceeds the 2% or less portion of Medicare reimbursement that is influenced by performance.
Medicare will steadily increase the portion of reimbursement allocated to performance (value) and decrease the part tied solely to wRVUs. So it makes sense that hospitalist compensation plans should do the same. Who knows, within the next 5-10 years, hospitalists, and potentially doctors in all specialties, might see 20% to 50% of their compensation tied to performance. I think that might be a good thing, as long as we can come up with effective measures of performance and value—not an easy thing to do in any business or industry.
Future Role of Productivity Compensation
I don’t think all the talk about value-based reimbursement means we should abandon the idea of connecting a portion of compensation to productivity. The first two practice management columns I wrote for The Hospitalist appeared in May 2006 (www.the-hospitalist.org/details/article/252413/The_Sweet_Spot.html) and June 2006 (www.the-hospitalist.org/details/article/246297.html) and recommended tying a meaningful portion of compensation to individual hospitalist productivity, and I think it still makes sense to do so.
Source: 2012 State of Hospital Medicine report
In any business or industry, financial performance is connected to the amount of product produced and its value. In the future, both metrics will determine reimbursement for even the highest performing healthcare providers. The new emphasis on value won’t ever make it unnecessary to produce at a reasonable level.
Unquestionably, there are many high-performing hospitalist practices with little or no productivity component in the compensation formula. So it isn’t an absolute sine qua non for success. But I think many practices dismiss it as a viable option when it might solve problems and liberate individuals in the group to exercise some autonomy in finding their own sweet spot between workload and compensation.
It will be interesting to see if future surveys show that the portion of dollars tied to hospitalist productivity continues to decrease, despite what I see as its potential benefits.

At the 2011 SHM annual meeting in Dallas, I served on an expert panel that reviewed the latest hospitalist survey data. Included in this review were the latest compensation and productivity figures. As the session concluded, I was satisfied that the panel had discussed important information in an accessible way; however, the keynote speaker who followed us to address an entirely different topic began his talk by pointing out that the data we had reviewed, including things like wRVUs, would very soon have little to do with compensation for any physician, regardless of specialty. He implied, quite persuasively, that we were pretty old school to be talking about wRVUs and compensation based on productivity; everyone should be prepared for and embrace compensation based on value, not production.
I hear a similar sentiment reasonably often. And I agree, but I think many make the mistake of oversimplifying the issue.
Physician Value-Based Payment
Measurement of physician performance using costs, quality, and outcomes has already begun and will influence Medicare payments to doctors beginning in 2015 for large groups (>100 providers with any mix of specialties billing under the same tax ID number) and in 2017 for smaller groups.
If Medicare is moving away from payment based on wRVUs, likely followed soon by other payors, then hospitalist compensation should do the same. But I don’t think that changes the potential role of compensation based on productivity.
Compensation Should Include Performance and Productivity Metrics
Survey data show a move from an essentially fixed annual compensation early in our field to an inclusion of components tied to performance several years before the introduction of the Physician Value-Based Payment Modifier program. Data from SHM’s 2010, 2011, and 2012 State of Hospital Medicine reports (www.hospitalmedicine.org/survey) show that a small, but probably increasing, part of compensation has been tied to performance on things like patient satisfaction and core measures (see “Distribution of Total Hospitalist Compensation,” below). Note that the percentages in the chart refer to the fraction of total compensation dollars allocated to each domain and not the portion of hospitalists who have compensation tied to each domain.
Over the same three years, the percentage of compensation tied to productivity has been decreasing overall, while “private groups are more likely to pay a higher proportion of compensation based on productivity, and hospital-employed groups are more likely to pay a higher proportion of compensation based on performance.”
Matching Performance Compensation to Medicare’s Value-Based Modifier
It makes sense for physician compensation to generally mirror Medicare and other payor professional fee reimbursement formulas. But, in that regard, hospitalists are ahead of the market already, because the portion of dollars allocated to performance (value) in hospitalist compensation plans already exceeds the 2% or less portion of Medicare reimbursement that is influenced by performance.
Medicare will steadily increase the portion of reimbursement allocated to performance (value) and decrease the part tied solely to wRVUs. So it makes sense that hospitalist compensation plans should do the same. Who knows, within the next 5-10 years, hospitalists, and potentially doctors in all specialties, might see 20% to 50% of their compensation tied to performance. I think that might be a good thing, as long as we can come up with effective measures of performance and value—not an easy thing to do in any business or industry.
Future Role of Productivity Compensation
I don’t think all the talk about value-based reimbursement means we should abandon the idea of connecting a portion of compensation to productivity. The first two practice management columns I wrote for The Hospitalist appeared in May 2006 (www.the-hospitalist.org/details/article/252413/The_Sweet_Spot.html) and June 2006 (www.the-hospitalist.org/details/article/246297.html) and recommended tying a meaningful portion of compensation to individual hospitalist productivity, and I think it still makes sense to do so.
Source: 2012 State of Hospital Medicine report
In any business or industry, financial performance is connected to the amount of product produced and its value. In the future, both metrics will determine reimbursement for even the highest performing healthcare providers. The new emphasis on value won’t ever make it unnecessary to produce at a reasonable level.
Unquestionably, there are many high-performing hospitalist practices with little or no productivity component in the compensation formula. So it isn’t an absolute sine qua non for success. But I think many practices dismiss it as a viable option when it might solve problems and liberate individuals in the group to exercise some autonomy in finding their own sweet spot between workload and compensation.
It will be interesting to see if future surveys show that the portion of dollars tied to hospitalist productivity continues to decrease, despite what I see as its potential benefits.

At the 2011 SHM annual meeting in Dallas, I served on an expert panel that reviewed the latest hospitalist survey data. Included in this review were the latest compensation and productivity figures. As the session concluded, I was satisfied that the panel had discussed important information in an accessible way; however, the keynote speaker who followed us to address an entirely different topic began his talk by pointing out that the data we had reviewed, including things like wRVUs, would very soon have little to do with compensation for any physician, regardless of specialty. He implied, quite persuasively, that we were pretty old school to be talking about wRVUs and compensation based on productivity; everyone should be prepared for and embrace compensation based on value, not production.
I hear a similar sentiment reasonably often. And I agree, but I think many make the mistake of oversimplifying the issue.
Physician Value-Based Payment
Measurement of physician performance using costs, quality, and outcomes has already begun and will influence Medicare payments to doctors beginning in 2015 for large groups (>100 providers with any mix of specialties billing under the same tax ID number) and in 2017 for smaller groups.
If Medicare is moving away from payment based on wRVUs, likely followed soon by other payors, then hospitalist compensation should do the same. But I don’t think that changes the potential role of compensation based on productivity.
Compensation Should Include Performance and Productivity Metrics
Survey data show a move from an essentially fixed annual compensation early in our field to an inclusion of components tied to performance several years before the introduction of the Physician Value-Based Payment Modifier program. Data from SHM’s 2010, 2011, and 2012 State of Hospital Medicine reports (www.hospitalmedicine.org/survey) show that a small, but probably increasing, part of compensation has been tied to performance on things like patient satisfaction and core measures (see “Distribution of Total Hospitalist Compensation,” below). Note that the percentages in the chart refer to the fraction of total compensation dollars allocated to each domain and not the portion of hospitalists who have compensation tied to each domain.
Over the same three years, the percentage of compensation tied to productivity has been decreasing overall, while “private groups are more likely to pay a higher proportion of compensation based on productivity, and hospital-employed groups are more likely to pay a higher proportion of compensation based on performance.”
Matching Performance Compensation to Medicare’s Value-Based Modifier
It makes sense for physician compensation to generally mirror Medicare and other payor professional fee reimbursement formulas. But, in that regard, hospitalists are ahead of the market already, because the portion of dollars allocated to performance (value) in hospitalist compensation plans already exceeds the 2% or less portion of Medicare reimbursement that is influenced by performance.
Medicare will steadily increase the portion of reimbursement allocated to performance (value) and decrease the part tied solely to wRVUs. So it makes sense that hospitalist compensation plans should do the same. Who knows, within the next 5-10 years, hospitalists, and potentially doctors in all specialties, might see 20% to 50% of their compensation tied to performance. I think that might be a good thing, as long as we can come up with effective measures of performance and value—not an easy thing to do in any business or industry.
Future Role of Productivity Compensation
I don’t think all the talk about value-based reimbursement means we should abandon the idea of connecting a portion of compensation to productivity. The first two practice management columns I wrote for The Hospitalist appeared in May 2006 (www.the-hospitalist.org/details/article/252413/The_Sweet_Spot.html) and June 2006 (www.the-hospitalist.org/details/article/246297.html) and recommended tying a meaningful portion of compensation to individual hospitalist productivity, and I think it still makes sense to do so.
Source: 2012 State of Hospital Medicine report
In any business or industry, financial performance is connected to the amount of product produced and its value. In the future, both metrics will determine reimbursement for even the highest performing healthcare providers. The new emphasis on value won’t ever make it unnecessary to produce at a reasonable level.
Unquestionably, there are many high-performing hospitalist practices with little or no productivity component in the compensation formula. So it isn’t an absolute sine qua non for success. But I think many practices dismiss it as a viable option when it might solve problems and liberate individuals in the group to exercise some autonomy in finding their own sweet spot between workload and compensation.
It will be interesting to see if future surveys show that the portion of dollars tied to hospitalist productivity continues to decrease, despite what I see as its potential benefits.

Using the Internet in your practice. Part 1: Why social media are important and how to get started
Let’s rewind to the year 2000, the dawning of a new millennium. It was then that many physicians decided the time was ripe to establish a Web presence. It wasn’t that difficult, after all: Just take the practice’s three-color, trifold brochure and convert it into a Web-site template. A teenager could do it—and many did, sometimes guided by a college student in computer sciences.
These early implementers were confident that they could cruise into the 21st Century with this new technology. They had no idea how much the Internet would change…or how fast…but their basic impulse was a wise one, to harness the power of the Internet for the good of their patients and their practices.
In this four-part series, we focus on the rapidly expanding utilization of the Internet for health-related purposes. In Part 1, we focus on why it’s important to address the Web, particularly social media, and we zoom in on creating a blog for your practice. In Part 2, our focus will be the “big three”: Facebook, Twitter, and YouTube. We will take up search engine optimization and online reputation management in Parts 3 and 4, respectively.
WHY IS THE INTERNET IMPORTANT?
It isn’t uncommon for patients to arrive in their doctor’s office with a stack of pages downloaded from the Internet that describe their disease state or tests they are about to undergo. Many patients also are beginning to expect to interact with their physicians through Web sites, blogs, and Facebook and Twitter accounts.
Related Article: Why (and how) you should encourage your patients' search for health information on the Web Jennifer Gunter, MD (December 2011)
In fact, so much of health care is moving online that many physicians assume that everybody uses the Internet. The most recent data from the Pew Internet & American Life Project indicate that, in the United States, one in three adults have gone online to find out more about a medical condition, and 59% of all adults use the Internet to search for health information (TABLE 1).1,2 Eight in 10 people who regularly use the Internet look online for health information, making it the third most popular online pursuit tracked by the Pew project, after reading and sending email and using a search engine.
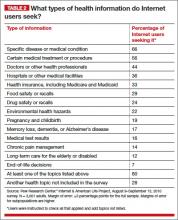
What types of health information do US adults look for online? Most people (66%) who use the Web to search for health information look for information on a specific disease or medical problem (see TABLE 2 for a list of other common health topics).3
The Pew Research Center also found that some demographic groups are more likely than others to seek health information online. They include:
- adults who have provided unpaid care to a parent, child, friend, or other loved one in the past 12 months
- women
- white adults
- adults aged 18 to 49 years
- adults with at least some college education
- adults in higher-income households.1
Check out the QUICK POLL on the OBG Management home page. To give your answer and see how other physicians have responded, Click Here.
WHAT ARE SOCIAL MEDIA AND WHY DO WE NEED THEM?
Social media encompass Web sites and other online communication applications used for social networking. Three of the most widely used media are Facebook, Twitter, and YouTube.
When someone once asked hockey great Wayne Gretzky about his sport strategy, he replied: “I don’t skate to where the puck is or where the puck has been; I skate to where the puck is going to be.” Social media are where the puck (ie, our patients) are going to be today and tomorrow.
If we review other media launches, we discover that it took nearly 40 years for radio to attract 50 million listeners, and 13 years for television to reach 50 million viewers. But it took only 4 years for the Internet to achieve 50 million users. Facebook alone reached 100 million users in just 9 months!
Just a decade ago, the Mayo Clinic relied on standard marketing techniques using radio, TV, and print media to attract new patients. Today, the Mayo Clinic makes use of Facebook, Twitter, YouTube, podcasts, and blogging. The Mayo Clinic even has developed a Center for Social Media to focus on the use of social media for its centers in Rochester, Minnesota; Jacksonville, Florida; and Phoenix, Arizona. If something is good for the Mayo Clinic, it has to be OK for the rest of us.
Social media also make it possible for smaller practices to compete with much larger practices that have huge marketing budgets. With very little expense, small practices—even solo practices—can develop a social media presence that can rival those of larger competitors.
HOW TO GET STARTED
There are four major social media programs to consider: Facebook, Twitter, YouTube, and blogging. We suggest that ObGyns who are ready to develop a social media presence begin with blogging, the focus of this article. We will cover Facebook, Twitter, and YouTube in Part 2 of this series.
Blogging is the easiest way to enter the world of social media. It’s free, can be accomplished reasonably quickly, and allows you to communicate with existing patients and attract new patients to your practice.
What is a blog? A blog is a Web site that is maintained with regular entries (posts) that invite comments from readers. Blogging allows feedback from people who visit your site and offers you the opportunity to respond to their comments. This creates a dialogue between you, your existing patients, and potential patients that is hard to achieve on an ordinary Web site.
The only expense for a blog is the cost of your time. There are several sites that will host your blog:
- WordPress.com offers free traffic stats, anti-spam features, search engine optimization, and more. Its platform is used by many popular blogs, including Forbes, Flickr, and CNN.
- Blogger.com (powered by Google) offers a user-friendly interface and smooth integration with the blogger’s Google account
- Blog.com provides the same basic features as other blog-hosting platforms, including free templates, but it charges a fee to keep ads off your site
- MovableType.com is a high-end hosting platform that charges a fee for its use
- LiveJournal.com provides its basic service at no charge but, like Blog.com, charges a fee to keep ads off your site.
We prefer WordPress.com because it was recommended in The Social Media Bible. WordPress.com offers tutorials that help you create a blog, enter content, and publish your material. You can access them at http://learn.wordpress.com.
We suggest that you develop your blog by incorporating a “hook” or other enticement to capture readers’ attention, keep your message relevant to their lives, and link the blog to your Web site so readers can find solutions to their medical problems.
Social media experts agree that regular posting is the key to success, particularly in regard to blogging. Commit to posting at least weekly. Visitors are more likely to return to your blog when they can count on regular updates.
Related Article: To blog or not to blog? What's the answer for you and your practice? Jennifer Gunter, MD (August 2011)
How to tell your story
One way to start your post is by offering a startling statistic or analogy. For example, if you are writing about breast cancer, you might begin by observing that more than 1,000 women under age 40 died of the disease in 2013—or that only lung cancer causes more cancer deaths in women.
Humor is another way to engage readers. We have found that people are attracted to funny anecdotes and stories. For example, when Dr. Baum is writing about erectile dysfunction, he might tell a story about arriving at a hotel and finding only 32 cents in his pocket to tip the bellman. When he offered the young bellman a copy of his new book, Impotence: It’s Reversible, the bellman replied, “Dr. Baum, if it’s all right with you, I’d just like to have the 32 cents.” In a blog post about this exchange, Dr. Baum might explain that the article is intended to give readers a little more than 32 cents’ worth of information about erectile dysfunction. The post would carry on from there.
Another option is to relate a compelling story about a recent patient (without using her name) that describes how you identified a problem, made a diagnosis, and resolved the patient’s complaint.
At the end of each blog post, we recommend that you invite readers to submit open-ended questions and comments. This motivates them to respond and starts a dialogue between your practice and potential new patients. Also include a call to action, preferably with a link from your blog to your Web site, inviting readers to visit your site or contact your practice to become a patient.
Most comments on your blog are likely to be positive, or to consist of requests for clarification or specific information. And most blog-hosting platforms allow you to review comments before they are published to your blog site. Any unnecessarily harsh or abusive comments can simply be rejected.
Once you have created a blog and begun to post regularly, we recommend that you check traffic to the site using the built-in analytics available through most hosting platforms. The traffic stats give you information on the number of visitors you have, how long they are spending at your blog, and how many are connecting to your main Web site. You can use this valuable information to identify what is working and tweak your blog posts accordingly.
Catchy titles make a difference
Strive to create titles that will capture the attention of your readers. People often decide whether or not to read a blog post on the basis of its title alone. Think of an effective title as a billboard. Drivers are speeding down the highway and have only 3 or 4 seconds to read the billboard and decide whether they will visit the restaurant, buy the product, or call for more information. The same holds true for titles on your blogs.
For example, Dr. Baum once titled a blog post “Urinary incontinence: Diagnosis and treatment.” It drew few readers. When he changed the title to “Urinary incontinence: You don’t have to depend on Depends,” nearly 1,000 readers commented on the post. Same article, different title.
Four pillars of a successful practice: 2. Attract new patients Neil H. Baum, MD (Four-part series, May 2013)
Pay attention to your practice Web site
We mentioned getting visitors from your blog site to your practice’s Web site. Once they arrive, two strategies are vital:
- visitor navigation
- patient-conversion systems.
Visitor navigation. The visitor comes to your Web site to get information that provides a solution to her problem. Once she lands on your site, you have less than 10 seconds to engage her; otherwise, she’ll leave instantly with the click of the mouse. Make it easy for her to find what she is looking for. For example, are the procedures and treatments you offer listed prominently so that the visitor can see them immediately and click on the link she wants? How about adding an icon, at the top right on every page, that says: “Schedule an appointment” or “Schedule a consultation.” The words you use (and their placement) are critically important if you want the visitor to become a patient!
Related Article: My #1 strategy for retaining patients Neil H. Baum, MD (Audiocast, March 2013)
Patient-conversion systems. Many Web sites are designed by people other than marketers. Even many Web-design companies focus on the look of the site rather than its main purpose: to convert visitors to patients.
If you want to get a Web-site visitor to schedule an appointment, your phone number should be clearly visible (along with the “Schedule an appointment” icon) on every page above the fold. “Above the fold” simply means that the visitor does not have to scroll down the page to see it. Believe it or not, many fancy Web sites fail to put these items in plain view!
And because you want to position yourself as a trusted authority in your field, patient testimonials are an important feature to include on your home page. And keep the information simple—stay away from technical jargon that the visitor will not understand.
Capture the visitor’s email address and use an auto-responder to follow up. You can get the visitor’s email address by offering something of value, such as a complimentary medical guide to a common condition. Once you have her email address, you have a way to stay in touch with the prospective patient and build a relationship of trust and confidence in your ability to solve her problem.
BOTTOM LINE: SOCIAL MEDIA ARE WORTH THE EFFORT
Social media marketing is a tool that most medical practices will be considering in the near future. A blog is a social media tool that can educate and inform existing patients and attract new ones to your practice. It is inexpensive, effective, and well worth the time and effort required to create a presence.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]
- Fox S, Duggan M. Health Online 2013: Summary of Findings. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2013/Health-online/Summary-of-Findings.aspx. Published January 15, 2013. Accessed January 9, 2014.
- Fox S. Health Topics: Health Information is a Popular Pursuit Online. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2011/HealthTopics/Part-1.aspx. Published February 1, 2011. Accessed January 9, 2014.
- Fox S. Health Topics: Eight in Ten Adult Internet Users Look for Information Online. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2011/Social-Life-of-Health-Info/Part-2/Section-1.aspx. Published May 12, 2011. Accessed January 9, 2014.
Let’s rewind to the year 2000, the dawning of a new millennium. It was then that many physicians decided the time was ripe to establish a Web presence. It wasn’t that difficult, after all: Just take the practice’s three-color, trifold brochure and convert it into a Web-site template. A teenager could do it—and many did, sometimes guided by a college student in computer sciences.
These early implementers were confident that they could cruise into the 21st Century with this new technology. They had no idea how much the Internet would change…or how fast…but their basic impulse was a wise one, to harness the power of the Internet for the good of their patients and their practices.
In this four-part series, we focus on the rapidly expanding utilization of the Internet for health-related purposes. In Part 1, we focus on why it’s important to address the Web, particularly social media, and we zoom in on creating a blog for your practice. In Part 2, our focus will be the “big three”: Facebook, Twitter, and YouTube. We will take up search engine optimization and online reputation management in Parts 3 and 4, respectively.
WHY IS THE INTERNET IMPORTANT?
It isn’t uncommon for patients to arrive in their doctor’s office with a stack of pages downloaded from the Internet that describe their disease state or tests they are about to undergo. Many patients also are beginning to expect to interact with their physicians through Web sites, blogs, and Facebook and Twitter accounts.
Related Article: Why (and how) you should encourage your patients' search for health information on the Web Jennifer Gunter, MD (December 2011)
In fact, so much of health care is moving online that many physicians assume that everybody uses the Internet. The most recent data from the Pew Internet & American Life Project indicate that, in the United States, one in three adults have gone online to find out more about a medical condition, and 59% of all adults use the Internet to search for health information (TABLE 1).1,2 Eight in 10 people who regularly use the Internet look online for health information, making it the third most popular online pursuit tracked by the Pew project, after reading and sending email and using a search engine.
What types of health information do US adults look for online? Most people (66%) who use the Web to search for health information look for information on a specific disease or medical problem (see TABLE 2 for a list of other common health topics).3
The Pew Research Center also found that some demographic groups are more likely than others to seek health information online. They include:
- adults who have provided unpaid care to a parent, child, friend, or other loved one in the past 12 months
- women
- white adults
- adults aged 18 to 49 years
- adults with at least some college education
- adults in higher-income households.1
Check out the QUICK POLL on the OBG Management home page. To give your answer and see how other physicians have responded, Click Here.
WHAT ARE SOCIAL MEDIA AND WHY DO WE NEED THEM?
Social media encompass Web sites and other online communication applications used for social networking. Three of the most widely used media are Facebook, Twitter, and YouTube.
When someone once asked hockey great Wayne Gretzky about his sport strategy, he replied: “I don’t skate to where the puck is or where the puck has been; I skate to where the puck is going to be.” Social media are where the puck (ie, our patients) are going to be today and tomorrow.
If we review other media launches, we discover that it took nearly 40 years for radio to attract 50 million listeners, and 13 years for television to reach 50 million viewers. But it took only 4 years for the Internet to achieve 50 million users. Facebook alone reached 100 million users in just 9 months!
Just a decade ago, the Mayo Clinic relied on standard marketing techniques using radio, TV, and print media to attract new patients. Today, the Mayo Clinic makes use of Facebook, Twitter, YouTube, podcasts, and blogging. The Mayo Clinic even has developed a Center for Social Media to focus on the use of social media for its centers in Rochester, Minnesota; Jacksonville, Florida; and Phoenix, Arizona. If something is good for the Mayo Clinic, it has to be OK for the rest of us.
Social media also make it possible for smaller practices to compete with much larger practices that have huge marketing budgets. With very little expense, small practices—even solo practices—can develop a social media presence that can rival those of larger competitors.
HOW TO GET STARTED
There are four major social media programs to consider: Facebook, Twitter, YouTube, and blogging. We suggest that ObGyns who are ready to develop a social media presence begin with blogging, the focus of this article. We will cover Facebook, Twitter, and YouTube in Part 2 of this series.
Blogging is the easiest way to enter the world of social media. It’s free, can be accomplished reasonably quickly, and allows you to communicate with existing patients and attract new patients to your practice.
What is a blog? A blog is a Web site that is maintained with regular entries (posts) that invite comments from readers. Blogging allows feedback from people who visit your site and offers you the opportunity to respond to their comments. This creates a dialogue between you, your existing patients, and potential patients that is hard to achieve on an ordinary Web site.
The only expense for a blog is the cost of your time. There are several sites that will host your blog:
- WordPress.com offers free traffic stats, anti-spam features, search engine optimization, and more. Its platform is used by many popular blogs, including Forbes, Flickr, and CNN.
- Blogger.com (powered by Google) offers a user-friendly interface and smooth integration with the blogger’s Google account
- Blog.com provides the same basic features as other blog-hosting platforms, including free templates, but it charges a fee to keep ads off your site
- MovableType.com is a high-end hosting platform that charges a fee for its use
- LiveJournal.com provides its basic service at no charge but, like Blog.com, charges a fee to keep ads off your site.
We prefer WordPress.com because it was recommended in The Social Media Bible. WordPress.com offers tutorials that help you create a blog, enter content, and publish your material. You can access them at http://learn.wordpress.com.
We suggest that you develop your blog by incorporating a “hook” or other enticement to capture readers’ attention, keep your message relevant to their lives, and link the blog to your Web site so readers can find solutions to their medical problems.
Social media experts agree that regular posting is the key to success, particularly in regard to blogging. Commit to posting at least weekly. Visitors are more likely to return to your blog when they can count on regular updates.
Related Article: To blog or not to blog? What's the answer for you and your practice? Jennifer Gunter, MD (August 2011)
How to tell your story
One way to start your post is by offering a startling statistic or analogy. For example, if you are writing about breast cancer, you might begin by observing that more than 1,000 women under age 40 died of the disease in 2013—or that only lung cancer causes more cancer deaths in women.
Humor is another way to engage readers. We have found that people are attracted to funny anecdotes and stories. For example, when Dr. Baum is writing about erectile dysfunction, he might tell a story about arriving at a hotel and finding only 32 cents in his pocket to tip the bellman. When he offered the young bellman a copy of his new book, Impotence: It’s Reversible, the bellman replied, “Dr. Baum, if it’s all right with you, I’d just like to have the 32 cents.” In a blog post about this exchange, Dr. Baum might explain that the article is intended to give readers a little more than 32 cents’ worth of information about erectile dysfunction. The post would carry on from there.
Another option is to relate a compelling story about a recent patient (without using her name) that describes how you identified a problem, made a diagnosis, and resolved the patient’s complaint.
At the end of each blog post, we recommend that you invite readers to submit open-ended questions and comments. This motivates them to respond and starts a dialogue between your practice and potential new patients. Also include a call to action, preferably with a link from your blog to your Web site, inviting readers to visit your site or contact your practice to become a patient.
Most comments on your blog are likely to be positive, or to consist of requests for clarification or specific information. And most blog-hosting platforms allow you to review comments before they are published to your blog site. Any unnecessarily harsh or abusive comments can simply be rejected.
Once you have created a blog and begun to post regularly, we recommend that you check traffic to the site using the built-in analytics available through most hosting platforms. The traffic stats give you information on the number of visitors you have, how long they are spending at your blog, and how many are connecting to your main Web site. You can use this valuable information to identify what is working and tweak your blog posts accordingly.
Catchy titles make a difference
Strive to create titles that will capture the attention of your readers. People often decide whether or not to read a blog post on the basis of its title alone. Think of an effective title as a billboard. Drivers are speeding down the highway and have only 3 or 4 seconds to read the billboard and decide whether they will visit the restaurant, buy the product, or call for more information. The same holds true for titles on your blogs.
For example, Dr. Baum once titled a blog post “Urinary incontinence: Diagnosis and treatment.” It drew few readers. When he changed the title to “Urinary incontinence: You don’t have to depend on Depends,” nearly 1,000 readers commented on the post. Same article, different title.
Four pillars of a successful practice: 2. Attract new patients Neil H. Baum, MD (Four-part series, May 2013)
Pay attention to your practice Web site
We mentioned getting visitors from your blog site to your practice’s Web site. Once they arrive, two strategies are vital:
- visitor navigation
- patient-conversion systems.
Visitor navigation. The visitor comes to your Web site to get information that provides a solution to her problem. Once she lands on your site, you have less than 10 seconds to engage her; otherwise, she’ll leave instantly with the click of the mouse. Make it easy for her to find what she is looking for. For example, are the procedures and treatments you offer listed prominently so that the visitor can see them immediately and click on the link she wants? How about adding an icon, at the top right on every page, that says: “Schedule an appointment” or “Schedule a consultation.” The words you use (and their placement) are critically important if you want the visitor to become a patient!
Related Article: My #1 strategy for retaining patients Neil H. Baum, MD (Audiocast, March 2013)
Patient-conversion systems. Many Web sites are designed by people other than marketers. Even many Web-design companies focus on the look of the site rather than its main purpose: to convert visitors to patients.
If you want to get a Web-site visitor to schedule an appointment, your phone number should be clearly visible (along with the “Schedule an appointment” icon) on every page above the fold. “Above the fold” simply means that the visitor does not have to scroll down the page to see it. Believe it or not, many fancy Web sites fail to put these items in plain view!
And because you want to position yourself as a trusted authority in your field, patient testimonials are an important feature to include on your home page. And keep the information simple—stay away from technical jargon that the visitor will not understand.
Capture the visitor’s email address and use an auto-responder to follow up. You can get the visitor’s email address by offering something of value, such as a complimentary medical guide to a common condition. Once you have her email address, you have a way to stay in touch with the prospective patient and build a relationship of trust and confidence in your ability to solve her problem.
BOTTOM LINE: SOCIAL MEDIA ARE WORTH THE EFFORT
Social media marketing is a tool that most medical practices will be considering in the near future. A blog is a social media tool that can educate and inform existing patients and attract new ones to your practice. It is inexpensive, effective, and well worth the time and effort required to create a presence.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]
Let’s rewind to the year 2000, the dawning of a new millennium. It was then that many physicians decided the time was ripe to establish a Web presence. It wasn’t that difficult, after all: Just take the practice’s three-color, trifold brochure and convert it into a Web-site template. A teenager could do it—and many did, sometimes guided by a college student in computer sciences.
These early implementers were confident that they could cruise into the 21st Century with this new technology. They had no idea how much the Internet would change…or how fast…but their basic impulse was a wise one, to harness the power of the Internet for the good of their patients and their practices.
In this four-part series, we focus on the rapidly expanding utilization of the Internet for health-related purposes. In Part 1, we focus on why it’s important to address the Web, particularly social media, and we zoom in on creating a blog for your practice. In Part 2, our focus will be the “big three”: Facebook, Twitter, and YouTube. We will take up search engine optimization and online reputation management in Parts 3 and 4, respectively.
WHY IS THE INTERNET IMPORTANT?
It isn’t uncommon for patients to arrive in their doctor’s office with a stack of pages downloaded from the Internet that describe their disease state or tests they are about to undergo. Many patients also are beginning to expect to interact with their physicians through Web sites, blogs, and Facebook and Twitter accounts.
Related Article: Why (and how) you should encourage your patients' search for health information on the Web Jennifer Gunter, MD (December 2011)
In fact, so much of health care is moving online that many physicians assume that everybody uses the Internet. The most recent data from the Pew Internet & American Life Project indicate that, in the United States, one in three adults have gone online to find out more about a medical condition, and 59% of all adults use the Internet to search for health information (TABLE 1).1,2 Eight in 10 people who regularly use the Internet look online for health information, making it the third most popular online pursuit tracked by the Pew project, after reading and sending email and using a search engine.
What types of health information do US adults look for online? Most people (66%) who use the Web to search for health information look for information on a specific disease or medical problem (see TABLE 2 for a list of other common health topics).3
The Pew Research Center also found that some demographic groups are more likely than others to seek health information online. They include:
- adults who have provided unpaid care to a parent, child, friend, or other loved one in the past 12 months
- women
- white adults
- adults aged 18 to 49 years
- adults with at least some college education
- adults in higher-income households.1
Check out the QUICK POLL on the OBG Management home page. To give your answer and see how other physicians have responded, Click Here.
WHAT ARE SOCIAL MEDIA AND WHY DO WE NEED THEM?
Social media encompass Web sites and other online communication applications used for social networking. Three of the most widely used media are Facebook, Twitter, and YouTube.
When someone once asked hockey great Wayne Gretzky about his sport strategy, he replied: “I don’t skate to where the puck is or where the puck has been; I skate to where the puck is going to be.” Social media are where the puck (ie, our patients) are going to be today and tomorrow.
If we review other media launches, we discover that it took nearly 40 years for radio to attract 50 million listeners, and 13 years for television to reach 50 million viewers. But it took only 4 years for the Internet to achieve 50 million users. Facebook alone reached 100 million users in just 9 months!
Just a decade ago, the Mayo Clinic relied on standard marketing techniques using radio, TV, and print media to attract new patients. Today, the Mayo Clinic makes use of Facebook, Twitter, YouTube, podcasts, and blogging. The Mayo Clinic even has developed a Center for Social Media to focus on the use of social media for its centers in Rochester, Minnesota; Jacksonville, Florida; and Phoenix, Arizona. If something is good for the Mayo Clinic, it has to be OK for the rest of us.
Social media also make it possible for smaller practices to compete with much larger practices that have huge marketing budgets. With very little expense, small practices—even solo practices—can develop a social media presence that can rival those of larger competitors.
HOW TO GET STARTED
There are four major social media programs to consider: Facebook, Twitter, YouTube, and blogging. We suggest that ObGyns who are ready to develop a social media presence begin with blogging, the focus of this article. We will cover Facebook, Twitter, and YouTube in Part 2 of this series.
Blogging is the easiest way to enter the world of social media. It’s free, can be accomplished reasonably quickly, and allows you to communicate with existing patients and attract new patients to your practice.
What is a blog? A blog is a Web site that is maintained with regular entries (posts) that invite comments from readers. Blogging allows feedback from people who visit your site and offers you the opportunity to respond to their comments. This creates a dialogue between you, your existing patients, and potential patients that is hard to achieve on an ordinary Web site.
The only expense for a blog is the cost of your time. There are several sites that will host your blog:
- WordPress.com offers free traffic stats, anti-spam features, search engine optimization, and more. Its platform is used by many popular blogs, including Forbes, Flickr, and CNN.
- Blogger.com (powered by Google) offers a user-friendly interface and smooth integration with the blogger’s Google account
- Blog.com provides the same basic features as other blog-hosting platforms, including free templates, but it charges a fee to keep ads off your site
- MovableType.com is a high-end hosting platform that charges a fee for its use
- LiveJournal.com provides its basic service at no charge but, like Blog.com, charges a fee to keep ads off your site.
We prefer WordPress.com because it was recommended in The Social Media Bible. WordPress.com offers tutorials that help you create a blog, enter content, and publish your material. You can access them at http://learn.wordpress.com.
We suggest that you develop your blog by incorporating a “hook” or other enticement to capture readers’ attention, keep your message relevant to their lives, and link the blog to your Web site so readers can find solutions to their medical problems.
Social media experts agree that regular posting is the key to success, particularly in regard to blogging. Commit to posting at least weekly. Visitors are more likely to return to your blog when they can count on regular updates.
Related Article: To blog or not to blog? What's the answer for you and your practice? Jennifer Gunter, MD (August 2011)
How to tell your story
One way to start your post is by offering a startling statistic or analogy. For example, if you are writing about breast cancer, you might begin by observing that more than 1,000 women under age 40 died of the disease in 2013—or that only lung cancer causes more cancer deaths in women.
Humor is another way to engage readers. We have found that people are attracted to funny anecdotes and stories. For example, when Dr. Baum is writing about erectile dysfunction, he might tell a story about arriving at a hotel and finding only 32 cents in his pocket to tip the bellman. When he offered the young bellman a copy of his new book, Impotence: It’s Reversible, the bellman replied, “Dr. Baum, if it’s all right with you, I’d just like to have the 32 cents.” In a blog post about this exchange, Dr. Baum might explain that the article is intended to give readers a little more than 32 cents’ worth of information about erectile dysfunction. The post would carry on from there.
Another option is to relate a compelling story about a recent patient (without using her name) that describes how you identified a problem, made a diagnosis, and resolved the patient’s complaint.
At the end of each blog post, we recommend that you invite readers to submit open-ended questions and comments. This motivates them to respond and starts a dialogue between your practice and potential new patients. Also include a call to action, preferably with a link from your blog to your Web site, inviting readers to visit your site or contact your practice to become a patient.
Most comments on your blog are likely to be positive, or to consist of requests for clarification or specific information. And most blog-hosting platforms allow you to review comments before they are published to your blog site. Any unnecessarily harsh or abusive comments can simply be rejected.
Once you have created a blog and begun to post regularly, we recommend that you check traffic to the site using the built-in analytics available through most hosting platforms. The traffic stats give you information on the number of visitors you have, how long they are spending at your blog, and how many are connecting to your main Web site. You can use this valuable information to identify what is working and tweak your blog posts accordingly.
Catchy titles make a difference
Strive to create titles that will capture the attention of your readers. People often decide whether or not to read a blog post on the basis of its title alone. Think of an effective title as a billboard. Drivers are speeding down the highway and have only 3 or 4 seconds to read the billboard and decide whether they will visit the restaurant, buy the product, or call for more information. The same holds true for titles on your blogs.
For example, Dr. Baum once titled a blog post “Urinary incontinence: Diagnosis and treatment.” It drew few readers. When he changed the title to “Urinary incontinence: You don’t have to depend on Depends,” nearly 1,000 readers commented on the post. Same article, different title.
Four pillars of a successful practice: 2. Attract new patients Neil H. Baum, MD (Four-part series, May 2013)
Pay attention to your practice Web site
We mentioned getting visitors from your blog site to your practice’s Web site. Once they arrive, two strategies are vital:
- visitor navigation
- patient-conversion systems.
Visitor navigation. The visitor comes to your Web site to get information that provides a solution to her problem. Once she lands on your site, you have less than 10 seconds to engage her; otherwise, she’ll leave instantly with the click of the mouse. Make it easy for her to find what she is looking for. For example, are the procedures and treatments you offer listed prominently so that the visitor can see them immediately and click on the link she wants? How about adding an icon, at the top right on every page, that says: “Schedule an appointment” or “Schedule a consultation.” The words you use (and their placement) are critically important if you want the visitor to become a patient!
Related Article: My #1 strategy for retaining patients Neil H. Baum, MD (Audiocast, March 2013)
Patient-conversion systems. Many Web sites are designed by people other than marketers. Even many Web-design companies focus on the look of the site rather than its main purpose: to convert visitors to patients.
If you want to get a Web-site visitor to schedule an appointment, your phone number should be clearly visible (along with the “Schedule an appointment” icon) on every page above the fold. “Above the fold” simply means that the visitor does not have to scroll down the page to see it. Believe it or not, many fancy Web sites fail to put these items in plain view!
And because you want to position yourself as a trusted authority in your field, patient testimonials are an important feature to include on your home page. And keep the information simple—stay away from technical jargon that the visitor will not understand.
Capture the visitor’s email address and use an auto-responder to follow up. You can get the visitor’s email address by offering something of value, such as a complimentary medical guide to a common condition. Once you have her email address, you have a way to stay in touch with the prospective patient and build a relationship of trust and confidence in your ability to solve her problem.
BOTTOM LINE: SOCIAL MEDIA ARE WORTH THE EFFORT
Social media marketing is a tool that most medical practices will be considering in the near future. A blog is a social media tool that can educate and inform existing patients and attract new ones to your practice. It is inexpensive, effective, and well worth the time and effort required to create a presence.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]
- Fox S, Duggan M. Health Online 2013: Summary of Findings. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2013/Health-online/Summary-of-Findings.aspx. Published January 15, 2013. Accessed January 9, 2014.
- Fox S. Health Topics: Health Information is a Popular Pursuit Online. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2011/HealthTopics/Part-1.aspx. Published February 1, 2011. Accessed January 9, 2014.
- Fox S. Health Topics: Eight in Ten Adult Internet Users Look for Information Online. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2011/Social-Life-of-Health-Info/Part-2/Section-1.aspx. Published May 12, 2011. Accessed January 9, 2014.
- Fox S, Duggan M. Health Online 2013: Summary of Findings. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2013/Health-online/Summary-of-Findings.aspx. Published January 15, 2013. Accessed January 9, 2014.
- Fox S. Health Topics: Health Information is a Popular Pursuit Online. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2011/HealthTopics/Part-1.aspx. Published February 1, 2011. Accessed January 9, 2014.
- Fox S. Health Topics: Eight in Ten Adult Internet Users Look for Information Online. Pew Internet & American Life Project. http://www.pewinternet.org/Reports/2011/Social-Life-of-Health-Info/Part-2/Section-1.aspx. Published May 12, 2011. Accessed January 9, 2014.
THE SERIES: USING THE INTERNET IN YOUR PRACTICE
Part 2: Generating new patients using social media (April 2014)
Part 3: Search engine optimization
Part 4: Online reputation management
(Look for Parts 2 through 4 in 2014)
Should you communicate with patients online?
A lot of mythology regarding the new Health Insurance Portability and Accountability Act rules (which I discussed in detail a few months ago) continues to circulate. One of the biggest myths is that e-mail communication with patients is now forbidden, so let’s debunk that one right now.
Here is a statement lifted verbatim from the official HIPAA web site (FAQ section):
"Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.
"If the provider feels the patient may not be aware of the possible risks of using unencrypted e-mail, or has concerns about potential liability, the provider can alert the patient of those risks, and let the patient decide whether to continue e-mail communications."
Okay, so it’s permissible – but is it a good idea? Aside from the obvious privacy issues, many physicians balk at taking on one more unreimbursed demand on their time. While no one denies that these concerns are real, there also are real benefits to be gained from properly managed online communication – among them increased practice efficiency, and increased quality of care and satisfaction for patients.
I started giving one of my e-mail addresses to selected patients several years ago as an experiment, hoping to take some pressure off of our overloaded telephone system. The patients were grateful for simplified and more direct access, and I appreciated the decrease in phone messages and interruptions while I was seeing patients. I also noticed a decrease in those frustrating, unnecessary office visits – you know, "The rash is completely gone, but you told me to come back ..."
In general, I have found that the advantages for everyone involved (not least my nurses and receptionists) far outweigh the problems. And now, newer technologies such as encryption, web-based messaging, and integrated online communication should go a long way toward assuaging privacy concerns.
Encryption software is now inexpensive, readily available, and easily added to most e-mail systems. Packages are available from companies such as EMC, Hilgraeve, Kryptiq, Proofpoint, Axway, and ZixCorp, among many others. (As always, I have no financial interest in any company mentioned in this column.)
Rather than simply encrypting their e-mail, increasing numbers of physicians are opting for the route taken by most online banking and shopping sites: a secure website. Patients sign onto it and send a message to your office. Physicians or staffers are notified in their regular e-mail of messages on the website, and then they post a reply to the patient on the site that can only be accessed by the patient. The patient is notified of the practice’s reply in his or her regular e-mail. Web-based messaging services can be incorporated into existing practice sites or can stand on their own. Medfusion, MyDocOnline, and RelayHealth are among the many vendors that offer secure cloud-based messaging services.
A big advantage of using such a service is that you’re partnering with a vendor who has to stay on top of HIPAA and other privacy requirements. Another is the option of using electronic forms, or templates. Templates ensure that patients’ messages include the information needed to process prescription refill requests, or to adequately describe their problems and provide some clinical assessment data for the physician or nurse. They also can be designed to triage messages to the front- and back-office staff, so that time is not wasted bouncing messages around the office until the proper responder is found.
Many electronic health record systems now allow you to integrate a web-based messaging system. Advantages here include the ability to view the patient’s medical record from home or anywhere else before answering the communication, and the fact that all messages automatically become a part of the patient’s record. Electronic health record vendors that provide this type of system include Allscripts, CompuGroup Medical, Cerner, Epic, GE Medical Systems, NextGen, McKesson, and Siemens.
As with any cloud-based service, insist on multiple layers of security, uninterruptible power sources, instant switchover to backup hardware in the event of a crash, and frequent, reliable backups.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
A lot of mythology regarding the new Health Insurance Portability and Accountability Act rules (which I discussed in detail a few months ago) continues to circulate. One of the biggest myths is that e-mail communication with patients is now forbidden, so let’s debunk that one right now.
Here is a statement lifted verbatim from the official HIPAA web site (FAQ section):
"Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.
"If the provider feels the patient may not be aware of the possible risks of using unencrypted e-mail, or has concerns about potential liability, the provider can alert the patient of those risks, and let the patient decide whether to continue e-mail communications."
Okay, so it’s permissible – but is it a good idea? Aside from the obvious privacy issues, many physicians balk at taking on one more unreimbursed demand on their time. While no one denies that these concerns are real, there also are real benefits to be gained from properly managed online communication – among them increased practice efficiency, and increased quality of care and satisfaction for patients.
I started giving one of my e-mail addresses to selected patients several years ago as an experiment, hoping to take some pressure off of our overloaded telephone system. The patients were grateful for simplified and more direct access, and I appreciated the decrease in phone messages and interruptions while I was seeing patients. I also noticed a decrease in those frustrating, unnecessary office visits – you know, "The rash is completely gone, but you told me to come back ..."
In general, I have found that the advantages for everyone involved (not least my nurses and receptionists) far outweigh the problems. And now, newer technologies such as encryption, web-based messaging, and integrated online communication should go a long way toward assuaging privacy concerns.
Encryption software is now inexpensive, readily available, and easily added to most e-mail systems. Packages are available from companies such as EMC, Hilgraeve, Kryptiq, Proofpoint, Axway, and ZixCorp, among many others. (As always, I have no financial interest in any company mentioned in this column.)
Rather than simply encrypting their e-mail, increasing numbers of physicians are opting for the route taken by most online banking and shopping sites: a secure website. Patients sign onto it and send a message to your office. Physicians or staffers are notified in their regular e-mail of messages on the website, and then they post a reply to the patient on the site that can only be accessed by the patient. The patient is notified of the practice’s reply in his or her regular e-mail. Web-based messaging services can be incorporated into existing practice sites or can stand on their own. Medfusion, MyDocOnline, and RelayHealth are among the many vendors that offer secure cloud-based messaging services.
A big advantage of using such a service is that you’re partnering with a vendor who has to stay on top of HIPAA and other privacy requirements. Another is the option of using electronic forms, or templates. Templates ensure that patients’ messages include the information needed to process prescription refill requests, or to adequately describe their problems and provide some clinical assessment data for the physician or nurse. They also can be designed to triage messages to the front- and back-office staff, so that time is not wasted bouncing messages around the office until the proper responder is found.
Many electronic health record systems now allow you to integrate a web-based messaging system. Advantages here include the ability to view the patient’s medical record from home or anywhere else before answering the communication, and the fact that all messages automatically become a part of the patient’s record. Electronic health record vendors that provide this type of system include Allscripts, CompuGroup Medical, Cerner, Epic, GE Medical Systems, NextGen, McKesson, and Siemens.
As with any cloud-based service, insist on multiple layers of security, uninterruptible power sources, instant switchover to backup hardware in the event of a crash, and frequent, reliable backups.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
A lot of mythology regarding the new Health Insurance Portability and Accountability Act rules (which I discussed in detail a few months ago) continues to circulate. One of the biggest myths is that e-mail communication with patients is now forbidden, so let’s debunk that one right now.
Here is a statement lifted verbatim from the official HIPAA web site (FAQ section):
"Patients may initiate communications with a provider using e-mail. If this situation occurs, the health care provider can assume (unless the patient has explicitly stated otherwise) that e-mail communications are acceptable to the individual.
"If the provider feels the patient may not be aware of the possible risks of using unencrypted e-mail, or has concerns about potential liability, the provider can alert the patient of those risks, and let the patient decide whether to continue e-mail communications."
Okay, so it’s permissible – but is it a good idea? Aside from the obvious privacy issues, many physicians balk at taking on one more unreimbursed demand on their time. While no one denies that these concerns are real, there also are real benefits to be gained from properly managed online communication – among them increased practice efficiency, and increased quality of care and satisfaction for patients.
I started giving one of my e-mail addresses to selected patients several years ago as an experiment, hoping to take some pressure off of our overloaded telephone system. The patients were grateful for simplified and more direct access, and I appreciated the decrease in phone messages and interruptions while I was seeing patients. I also noticed a decrease in those frustrating, unnecessary office visits – you know, "The rash is completely gone, but you told me to come back ..."
In general, I have found that the advantages for everyone involved (not least my nurses and receptionists) far outweigh the problems. And now, newer technologies such as encryption, web-based messaging, and integrated online communication should go a long way toward assuaging privacy concerns.
Encryption software is now inexpensive, readily available, and easily added to most e-mail systems. Packages are available from companies such as EMC, Hilgraeve, Kryptiq, Proofpoint, Axway, and ZixCorp, among many others. (As always, I have no financial interest in any company mentioned in this column.)
Rather than simply encrypting their e-mail, increasing numbers of physicians are opting for the route taken by most online banking and shopping sites: a secure website. Patients sign onto it and send a message to your office. Physicians or staffers are notified in their regular e-mail of messages on the website, and then they post a reply to the patient on the site that can only be accessed by the patient. The patient is notified of the practice’s reply in his or her regular e-mail. Web-based messaging services can be incorporated into existing practice sites or can stand on their own. Medfusion, MyDocOnline, and RelayHealth are among the many vendors that offer secure cloud-based messaging services.
A big advantage of using such a service is that you’re partnering with a vendor who has to stay on top of HIPAA and other privacy requirements. Another is the option of using electronic forms, or templates. Templates ensure that patients’ messages include the information needed to process prescription refill requests, or to adequately describe their problems and provide some clinical assessment data for the physician or nurse. They also can be designed to triage messages to the front- and back-office staff, so that time is not wasted bouncing messages around the office until the proper responder is found.
Many electronic health record systems now allow you to integrate a web-based messaging system. Advantages here include the ability to view the patient’s medical record from home or anywhere else before answering the communication, and the fact that all messages automatically become a part of the patient’s record. Electronic health record vendors that provide this type of system include Allscripts, CompuGroup Medical, Cerner, Epic, GE Medical Systems, NextGen, McKesson, and Siemens.
As with any cloud-based service, insist on multiple layers of security, uninterruptible power sources, instant switchover to backup hardware in the event of a crash, and frequent, reliable backups.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
As the Affordable Care Act comes of age, a look behind the headlines
The Affordable Care Act (ACA) faced—and failed—an important test on October 1, 2013, when open enrollment began in the new health-care marketplaces. Plenty has been written about Web site crashes, technical glitches, and what seems to be general mismanagement of this crucial aspect of implementation.
Let’s look behind the headlines to see which aspects of the ACA are working, and which aren’t, and why.
KNOWING THE FACTS CAN HELP YOU HELP YOUR PATIENTS
ObGyns are scientists. As a scientist, you know the importance of facts. In your research and clinical care, you seek out and rely on scientific facts and evidence. You leave aside unsubstantiated thinking.
It’s imperative that we take the same approach with this subject. Far too many misleading and unsubstantiated claims and headlines are crowding out reliable factual information, seriously hindering physicians’ ability to understand this important health-care system change and respond to it appropriately on behalf of patients. As much as we all love Facebook, for example, it may not be the most accurate source of information on the ACA.
Plenty of reliable, factual, unbiased sources of information about the ACA exist, such as “Understanding Obamacare, Politico’s Guide to the Affordable Care Act” (http://www.politico.com/obamacare-guide/). Other helpful sources of ACA outreach and enrollment information:
HealthCare.gov is the federal government’s main portal for information on the Affordable Care Act. A Spanish version of this site can be accessed at www.CuidadoDeSalud.gov.
“FAQ: What you need to know about the new online marketplaces” features questions and answers from Kaiser Health News at http://www.kaiserhealthnews.org/stories/2013/september/17/marketplace-faq-insurance-exchange-obamacare-aca.aspx.
“Fact sheets: Why the Affordable Care Act matters for women” offers links to summaries of ACA provisions; information on health care for pregnant, low-income and older women; preventive care; and more from the National Partnership for Women and Families at http://go.nationalpartnership.org/site/PageServer?pagename=issues_health_reform_anniversary.
Webinars, speakers, FAQs, and more from Doctors for America at http://www.drsforamerica.org/take-action/get-people-covered.
Reports, blog posts, and links to information on enrollment from Enroll America at www.enrollamerica.org.
An informative video on coverage decisions from the Kaiser Family Foundation at http://kff.org/health-reform/video/youtoons-obamacare-video/.
A REVIEW OF THE CHANGES UNDER ACA
Let’s start with one key fact: The ACA offers a lot of good for women’s health care. Many of these improvements hinge on individuals’ ability to enroll in private health insurance policies sold in the marketplaces.
Each state’s marketplace is similar to the system used by the Federal Employees Health Benefits Program (FEHBP), the insurance marketplace used nationwide by federal employees, including members of Congress. Private plans, such as Blue Cross Blue Shield, Aetna, and United Healthcare, offer health insurance on the FEHBP marketplace to the millions of federal employees each year.
In state marketplaces, private health insurers will offer plans to potentially millions of previously under- or uninsured individuals and families. In exchange for access to this huge new group of consumers, private insurers must abide by a number of important consumer protections in order to be eligible to sell their policies in a state marketplace:
Insurers must agree to abide by the 80/20 rule. Under this game-changer, insurers agree to return the actuarial value of 80% of an enrollee’s premium to health care, keeping only a maximum of 20% for profits and other non-health-care categories.
Insurers must agree to cover 10 essential benefits, including maternity care.
Insurers must agree to cover key preventive services, without copays or deductibles, helping our patients stay healthy.
Insurers must abide by significant insurance protections. They can’t, for example, deny a woman coverage because she has a preexisting condition, was once the victim of domestic violence, or once had a cesarean delivery.
Essential benefits and preventive services
All private health insurance plans sold in the state marketplaces must cover the 10 essential health benefits:
ambulatory patient services
emergency services
hospitalization
maternity and newborn care
mental health and substance use disorder services, including behavioral health treatment
prescription drugs
rehabilitative and habilitative services and devices
laboratory services
preventive and wellness services and chronic disease management
pediatric services, including oral and vision care.
These insurers also must cover—with no charge to the patient—preventive services:
well-woman visits (one or more)
all FDA-approved contraceptive methods and contraception counseling
gestational diabetes screening
mammograms
Pap tests
HIV and other sexually transmitted infection screening and counseling
breastfeeding support, supplies, and counseling
domestic violence screening and counseling.
Related Article: Your age-based guide to comprehensive well-woman care Robert L. Barbieri, MD (October 2012)
In addition, private insurers must offer additional preventive services, although they can charge copays for them:
anemia screening on a routine basis for pregnant women
screening for urinary tract or other infection for pregnant women
counseling about genetic testing for a BRCA mutation for women at higher risk
counseling about chemoprevention of breast cancer for women at higher risk
cervical cancer screening for sexually active women
folic acid supplementation for women who may become pregnant
osteoporosis screening for women over age 60, depending on risk factors
screening for Rh incompatibility for all pregnant women and follow-up testing for women at higher risk
tobacco use screening and interventions for all women, and expanded counseling for pregnant users of tobacco.
An end to preexisting-condition exclusions and other harmful practices
Insurers offering plans in the state marketplaces also must abide by important insurance reforms:
They must eliminate exclusions for preexisting conditions. Insurers cannot deny individuals coverage because they already have a condition that requires medical care, including pregnancy. Before this ACA rule, private insurers often rejected applicants who needed care, as well as those who accessed health care in the past. Insurers regularly denied coverage to women who had had a cesarean delivery or had once been a victim of domestic violence.
They cannot charge women more than men for the same coverage. Before the ACA, women seeking health-care coverage often faced higher premiums than men for identical coverage. This made private coverage less affordable for our patients.
They cannot impose a 9-month waiting period. (Need I say more?)
They must eliminate any annual lifetime limits on coverage. Insurers selling policies in the marketplaces cannot end coverage after a certain dollar amount has been reached, a common practice before the ACA. This change is good news for you and your patients. A patient needing long or expensive care won’t lose coverage when the cost of her care hits an arbitrary ceiling.
They cannot rescind coverage unless fraud is proven. Before the ACA, private health insurers would often drop an individual if he or she started racking up high health-care costs. Patients in the middle of expensive cancer treatments, for example, would find themselves suddenly without health insurance. This won’t happen for policies sold in marketplaces unless the patient lied on her enrollment forms or failed to keep up her premium payments.
What these changes mean, in real numbers
These protections are critically important to your ability to care for your patients. Here’s what they mean in real life:
Health-care coverage for about 10,000 insured women is no longer subject to an annual lifetime coverage limit.
Private insurers can’t drop coverage, a change that will affect about 5.5 million insured women.
Insurance companies cannot deny coverage for preexisting conditions, which will help insure about 100,000 women.
Each state marketplace offers four types of plans, the idea being to help people compare policies side by side. All plans sold in the marketplaces must abide by the consumer protections I just reviewed. Each tier is differentiated by the average percentage of an enrollee’s health-care expenses paid by the insurer. The more an enrollee agrees to pay out of pocket, the lower his or her premium.
The tiers are:
Bronze – The insurer covers 60% of health-care costs, and the insured covers 40%. This tier offers the cheapest premiums.
Silver – The insurer covers 70% of costs.
Gold – The insurer covers 80% of costs.
Platinum – The insurer covers 90% of costs.
WHAT WENT WRONG
If everything had gone according to plan, women’s access to health insurance would have increased dramatically nationwide, including in the dark blue states in FIGURE 1 (Map 1)—states that rank lowest in access to care. You’ll notice that many of the states that are dark blue in Map 1 shift to light blue in Map 2. Take a careful look at those dark blue states and see what colors they are in the next two maps (FIGURES 1 and 2). Hint: There’s a pattern.
Problem 1 – Strains on Healthcare.gov
When the ACA was signed into law, most states were expected to build and run their own online marketplaces. The federal government offered to run a state exchange if a state didn’t. Few ACA engineers anticipated that the federal government would have to run the marketplaces in more than half the states—politics-fueled decisions in many states. Now you can see that many of the states that are dark blue in Map 1 are gray in Map 3 (FIGURE 2). Many states whose populations have the greatest need left it to the federal government to run the marketplaces.
Data indicate that state-run marketplaces are doing pretty well—a fact not often caught in frenzied headlines. If we look at the percentage of the target population actually enrolled in marketplace insurance plans during the first month, we see that the lowest state marketplace enrollment was in Washington State, with 30% of its target population enrolled. The highest target-population enrollment was achieved in Connecticut, with 191%.
Compare these numbers to the rates of target-population enrollment in states with marketplaces run by the federal government, which range from 3% to 20% (FIGURE 2). During the first month, federal and state-run marketplaces together enrolled 106,000 individuals into new coverage, 21% of the national target.
The news media have focused on the federal online enrollment debacle. Easier enrollment options are available to people who live in federally run marketplace states, including direct enrollment. Strongly supported by America’s health insurance industry, direct enrollment lets potential enrollees purchase coverage directly from insurance companies participating in the marketplaces.
Problem 2: People lost their current coverage
This is a problem worth exploring—one that affects people who previously bought insurance on the individual insurance market. This is the market that offers people comparatively limited coverage, usually with no maternity care coverage, for comparatively high premiums.
So why are these individuals losing coverage?
They are losing coverage because, as of January 2014, new individual plans must abide by the 80/20 rule, abide by insurance protections, and cover 10 essential services with no cost sharing.
You may recall that, in August 2009, Americans were demanding that they be able to keep the health-care coverage they currently had, and President Barack Obama promised that they would be able to. Consequently, health insurance policies in effect before March 2010, when the ACA was signed into law, were exempted—“grandfathered”—from most ACA requirements. If people liked their old policies, they could keep them.
Grandfathered plans are exempt from:
the requirement to cover the 10 essential health benefits
the requirement that plans must provide preventive services with no patient cost sharing
state or federal review of insurance premium increases of 10% or more for non-group and small business plans
a rule allowing consumers to appeal denials of claims to a third-party reviewer.
Most ACA requirements apply to new policies—those offered after March 2010 and those that have been changed significantly by the insurance companies. Some examples of changes in coverage that would cause a plan to lose grandfathering include:
the elimination of benefits to diagnose or treat a particular condition
an increase in the up-front deductible patients must pay before coverage kicks in by more than the cumulative growth in medical inflation since March 2010 plus 15%
a reduction in the share of the premium that the employer pays by more than 5% since March 2010.
How many people are we talking about? Not the 40% of Americans who have employer-based coverage or the 20% of Americans on Medicare, Medicaid, or Tricare. This provision affects about 5% of the insured, as many as 15 million people—many with plans that offer little coverage for high premiums.
The ACA intention was that many people previously covered in the individual insurance market would find better and cheaper coverage in their state marketplaces. That may be a good option for people in states that have chosen to run their own marketplaces, and a good option for people in other states, too, as federal online enrollment issues get fixed.
Problem 3: Medicaid expansion became a state option
When the US Supreme Court upheld the constitutionality of the ACA’s individual mandate, it also effectively turned the ACA Medicaid expansion into a state option.
Think of the Medicaid expansion as Medicaid Part 2. Regular Medicaid remains largely unchanged, with the same eligibility rules and coverage requirements.
The ACA included a provision under which every state would add a new part to its Medicaid program. Beginning in 2014, this part—the expansion—would cover individuals in each state with incomes under 138% of the federal poverty line—about $32,000 for a family of four in 2014. Medicaid expansion coverage is based only on income eligibility, a major change for women, many of whom currently qualify for Medicaid only if they’re pregnant.
Who would pay for the new coverage?
In 2014, 2015, and 2016, the federal government pays 100% of the cost of care for Medicaid expansion. From 2017 to 2020, the federal share gradually drops to 90%.
Medicaid expansion is an integral part of reducing the number of uninsured under the ACA and is expected to reduce the uninsured rate by almost 30% if adopted by every state. Medicaid expansion plus the ACA marketplaces were expected to cut our uninsured rate almost in half.
FIGURE 3 shows how states responded when the Supreme Court effectively converted the Medicaid expansion into an option, leaving us, again, with coverage gaps. Many of the states that have opted not to expand Medicaid are the same states that declined to operate their own state marketplaces, the same states with highest percentages of the uninsured.
The ACA has many interdependent parts. Make the Medicaid expansion a state option, and you end up with higher than expected rates of uninsured. Trigger big changes in the individual market when there are still bugs in the system, and people are left in the lurch.
Related Article: ACOG to legislators: Partnership, not interference Lucia DiVenere, MA (April 2013)
What’s happening now
As this article is going to press, enrollment in the marketplaces is getting easier, with Web site fixes and useful alternatives to Web-based enrollment. Small changes are being made to some deadlines to help people who have gotten stuck in the process. We’ll likely continue to see steps forward and back over the next many months.
Two things remain important:
We need to stick with the facts. If you see something in the news that seems too crazy to be real, your hunch may be right.
Your patients can benefit significantly from the ACA. An ACOG Fellow recently told me about one of his patients who has a severe health condition, no insurance, and needs expensive treatment. The ACA, with its marketplace rules outlawing exclusions for preexisting conditions and offering premium assistance, may be a lifesaver to her. But first she needs to enroll.
As your patients’ trusted physician, you can help point them in the right direction, possibly toward coverage that they never had before.
That’s good for all of us.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]
The Affordable Care Act (ACA) faced—and failed—an important test on October 1, 2013, when open enrollment began in the new health-care marketplaces. Plenty has been written about Web site crashes, technical glitches, and what seems to be general mismanagement of this crucial aspect of implementation.
Let’s look behind the headlines to see which aspects of the ACA are working, and which aren’t, and why.
KNOWING THE FACTS CAN HELP YOU HELP YOUR PATIENTS
ObGyns are scientists. As a scientist, you know the importance of facts. In your research and clinical care, you seek out and rely on scientific facts and evidence. You leave aside unsubstantiated thinking.
It’s imperative that we take the same approach with this subject. Far too many misleading and unsubstantiated claims and headlines are crowding out reliable factual information, seriously hindering physicians’ ability to understand this important health-care system change and respond to it appropriately on behalf of patients. As much as we all love Facebook, for example, it may not be the most accurate source of information on the ACA.
Plenty of reliable, factual, unbiased sources of information about the ACA exist, such as “Understanding Obamacare, Politico’s Guide to the Affordable Care Act” (http://www.politico.com/obamacare-guide/). Other helpful sources of ACA outreach and enrollment information:
HealthCare.gov is the federal government’s main portal for information on the Affordable Care Act. A Spanish version of this site can be accessed at www.CuidadoDeSalud.gov.
“FAQ: What you need to know about the new online marketplaces” features questions and answers from Kaiser Health News at http://www.kaiserhealthnews.org/stories/2013/september/17/marketplace-faq-insurance-exchange-obamacare-aca.aspx.
“Fact sheets: Why the Affordable Care Act matters for women” offers links to summaries of ACA provisions; information on health care for pregnant, low-income and older women; preventive care; and more from the National Partnership for Women and Families at http://go.nationalpartnership.org/site/PageServer?pagename=issues_health_reform_anniversary.
Webinars, speakers, FAQs, and more from Doctors for America at http://www.drsforamerica.org/take-action/get-people-covered.
Reports, blog posts, and links to information on enrollment from Enroll America at www.enrollamerica.org.
An informative video on coverage decisions from the Kaiser Family Foundation at http://kff.org/health-reform/video/youtoons-obamacare-video/.
A REVIEW OF THE CHANGES UNDER ACA
Let’s start with one key fact: The ACA offers a lot of good for women’s health care. Many of these improvements hinge on individuals’ ability to enroll in private health insurance policies sold in the marketplaces.
Each state’s marketplace is similar to the system used by the Federal Employees Health Benefits Program (FEHBP), the insurance marketplace used nationwide by federal employees, including members of Congress. Private plans, such as Blue Cross Blue Shield, Aetna, and United Healthcare, offer health insurance on the FEHBP marketplace to the millions of federal employees each year.
In state marketplaces, private health insurers will offer plans to potentially millions of previously under- or uninsured individuals and families. In exchange for access to this huge new group of consumers, private insurers must abide by a number of important consumer protections in order to be eligible to sell their policies in a state marketplace:
Insurers must agree to abide by the 80/20 rule. Under this game-changer, insurers agree to return the actuarial value of 80% of an enrollee’s premium to health care, keeping only a maximum of 20% for profits and other non-health-care categories.
Insurers must agree to cover 10 essential benefits, including maternity care.
Insurers must agree to cover key preventive services, without copays or deductibles, helping our patients stay healthy.
Insurers must abide by significant insurance protections. They can’t, for example, deny a woman coverage because she has a preexisting condition, was once the victim of domestic violence, or once had a cesarean delivery.
Essential benefits and preventive services
All private health insurance plans sold in the state marketplaces must cover the 10 essential health benefits:
ambulatory patient services
emergency services
hospitalization
maternity and newborn care
mental health and substance use disorder services, including behavioral health treatment
prescription drugs
rehabilitative and habilitative services and devices
laboratory services
preventive and wellness services and chronic disease management
pediatric services, including oral and vision care.
These insurers also must cover—with no charge to the patient—preventive services:
well-woman visits (one or more)
all FDA-approved contraceptive methods and contraception counseling
gestational diabetes screening
mammograms
Pap tests
HIV and other sexually transmitted infection screening and counseling
breastfeeding support, supplies, and counseling
domestic violence screening and counseling.
Related Article: Your age-based guide to comprehensive well-woman care Robert L. Barbieri, MD (October 2012)
In addition, private insurers must offer additional preventive services, although they can charge copays for them:
anemia screening on a routine basis for pregnant women
screening for urinary tract or other infection for pregnant women
counseling about genetic testing for a BRCA mutation for women at higher risk
counseling about chemoprevention of breast cancer for women at higher risk
cervical cancer screening for sexually active women
folic acid supplementation for women who may become pregnant
osteoporosis screening for women over age 60, depending on risk factors
screening for Rh incompatibility for all pregnant women and follow-up testing for women at higher risk
tobacco use screening and interventions for all women, and expanded counseling for pregnant users of tobacco.
An end to preexisting-condition exclusions and other harmful practices
Insurers offering plans in the state marketplaces also must abide by important insurance reforms:
They must eliminate exclusions for preexisting conditions. Insurers cannot deny individuals coverage because they already have a condition that requires medical care, including pregnancy. Before this ACA rule, private insurers often rejected applicants who needed care, as well as those who accessed health care in the past. Insurers regularly denied coverage to women who had had a cesarean delivery or had once been a victim of domestic violence.
They cannot charge women more than men for the same coverage. Before the ACA, women seeking health-care coverage often faced higher premiums than men for identical coverage. This made private coverage less affordable for our patients.
They cannot impose a 9-month waiting period. (Need I say more?)
They must eliminate any annual lifetime limits on coverage. Insurers selling policies in the marketplaces cannot end coverage after a certain dollar amount has been reached, a common practice before the ACA. This change is good news for you and your patients. A patient needing long or expensive care won’t lose coverage when the cost of her care hits an arbitrary ceiling.
They cannot rescind coverage unless fraud is proven. Before the ACA, private health insurers would often drop an individual if he or she started racking up high health-care costs. Patients in the middle of expensive cancer treatments, for example, would find themselves suddenly without health insurance. This won’t happen for policies sold in marketplaces unless the patient lied on her enrollment forms or failed to keep up her premium payments.
What these changes mean, in real numbers
These protections are critically important to your ability to care for your patients. Here’s what they mean in real life:
Health-care coverage for about 10,000 insured women is no longer subject to an annual lifetime coverage limit.
Private insurers can’t drop coverage, a change that will affect about 5.5 million insured women.
Insurance companies cannot deny coverage for preexisting conditions, which will help insure about 100,000 women.
Each state marketplace offers four types of plans, the idea being to help people compare policies side by side. All plans sold in the marketplaces must abide by the consumer protections I just reviewed. Each tier is differentiated by the average percentage of an enrollee’s health-care expenses paid by the insurer. The more an enrollee agrees to pay out of pocket, the lower his or her premium.
The tiers are:
Bronze – The insurer covers 60% of health-care costs, and the insured covers 40%. This tier offers the cheapest premiums.
Silver – The insurer covers 70% of costs.
Gold – The insurer covers 80% of costs.
Platinum – The insurer covers 90% of costs.
WHAT WENT WRONG
If everything had gone according to plan, women’s access to health insurance would have increased dramatically nationwide, including in the dark blue states in FIGURE 1 (Map 1)—states that rank lowest in access to care. You’ll notice that many of the states that are dark blue in Map 1 shift to light blue in Map 2. Take a careful look at those dark blue states and see what colors they are in the next two maps (FIGURES 1 and 2). Hint: There’s a pattern.
Problem 1 – Strains on Healthcare.gov
When the ACA was signed into law, most states were expected to build and run their own online marketplaces. The federal government offered to run a state exchange if a state didn’t. Few ACA engineers anticipated that the federal government would have to run the marketplaces in more than half the states—politics-fueled decisions in many states. Now you can see that many of the states that are dark blue in Map 1 are gray in Map 3 (FIGURE 2). Many states whose populations have the greatest need left it to the federal government to run the marketplaces.
Data indicate that state-run marketplaces are doing pretty well—a fact not often caught in frenzied headlines. If we look at the percentage of the target population actually enrolled in marketplace insurance plans during the first month, we see that the lowest state marketplace enrollment was in Washington State, with 30% of its target population enrolled. The highest target-population enrollment was achieved in Connecticut, with 191%.
Compare these numbers to the rates of target-population enrollment in states with marketplaces run by the federal government, which range from 3% to 20% (FIGURE 2). During the first month, federal and state-run marketplaces together enrolled 106,000 individuals into new coverage, 21% of the national target.
The news media have focused on the federal online enrollment debacle. Easier enrollment options are available to people who live in federally run marketplace states, including direct enrollment. Strongly supported by America’s health insurance industry, direct enrollment lets potential enrollees purchase coverage directly from insurance companies participating in the marketplaces.
Problem 2: People lost their current coverage
This is a problem worth exploring—one that affects people who previously bought insurance on the individual insurance market. This is the market that offers people comparatively limited coverage, usually with no maternity care coverage, for comparatively high premiums.
So why are these individuals losing coverage?
They are losing coverage because, as of January 2014, new individual plans must abide by the 80/20 rule, abide by insurance protections, and cover 10 essential services with no cost sharing.
You may recall that, in August 2009, Americans were demanding that they be able to keep the health-care coverage they currently had, and President Barack Obama promised that they would be able to. Consequently, health insurance policies in effect before March 2010, when the ACA was signed into law, were exempted—“grandfathered”—from most ACA requirements. If people liked their old policies, they could keep them.
Grandfathered plans are exempt from:
the requirement to cover the 10 essential health benefits
the requirement that plans must provide preventive services with no patient cost sharing
state or federal review of insurance premium increases of 10% or more for non-group and small business plans
a rule allowing consumers to appeal denials of claims to a third-party reviewer.
Most ACA requirements apply to new policies—those offered after March 2010 and those that have been changed significantly by the insurance companies. Some examples of changes in coverage that would cause a plan to lose grandfathering include:
the elimination of benefits to diagnose or treat a particular condition
an increase in the up-front deductible patients must pay before coverage kicks in by more than the cumulative growth in medical inflation since March 2010 plus 15%
a reduction in the share of the premium that the employer pays by more than 5% since March 2010.
How many people are we talking about? Not the 40% of Americans who have employer-based coverage or the 20% of Americans on Medicare, Medicaid, or Tricare. This provision affects about 5% of the insured, as many as 15 million people—many with plans that offer little coverage for high premiums.
The ACA intention was that many people previously covered in the individual insurance market would find better and cheaper coverage in their state marketplaces. That may be a good option for people in states that have chosen to run their own marketplaces, and a good option for people in other states, too, as federal online enrollment issues get fixed.
Problem 3: Medicaid expansion became a state option
When the US Supreme Court upheld the constitutionality of the ACA’s individual mandate, it also effectively turned the ACA Medicaid expansion into a state option.
Think of the Medicaid expansion as Medicaid Part 2. Regular Medicaid remains largely unchanged, with the same eligibility rules and coverage requirements.
The ACA included a provision under which every state would add a new part to its Medicaid program. Beginning in 2014, this part—the expansion—would cover individuals in each state with incomes under 138% of the federal poverty line—about $32,000 for a family of four in 2014. Medicaid expansion coverage is based only on income eligibility, a major change for women, many of whom currently qualify for Medicaid only if they’re pregnant.
Who would pay for the new coverage?
In 2014, 2015, and 2016, the federal government pays 100% of the cost of care for Medicaid expansion. From 2017 to 2020, the federal share gradually drops to 90%.
Medicaid expansion is an integral part of reducing the number of uninsured under the ACA and is expected to reduce the uninsured rate by almost 30% if adopted by every state. Medicaid expansion plus the ACA marketplaces were expected to cut our uninsured rate almost in half.
FIGURE 3 shows how states responded when the Supreme Court effectively converted the Medicaid expansion into an option, leaving us, again, with coverage gaps. Many of the states that have opted not to expand Medicaid are the same states that declined to operate their own state marketplaces, the same states with highest percentages of the uninsured.
The ACA has many interdependent parts. Make the Medicaid expansion a state option, and you end up with higher than expected rates of uninsured. Trigger big changes in the individual market when there are still bugs in the system, and people are left in the lurch.
Related Article: ACOG to legislators: Partnership, not interference Lucia DiVenere, MA (April 2013)
What’s happening now
As this article is going to press, enrollment in the marketplaces is getting easier, with Web site fixes and useful alternatives to Web-based enrollment. Small changes are being made to some deadlines to help people who have gotten stuck in the process. We’ll likely continue to see steps forward and back over the next many months.
Two things remain important:
We need to stick with the facts. If you see something in the news that seems too crazy to be real, your hunch may be right.
Your patients can benefit significantly from the ACA. An ACOG Fellow recently told me about one of his patients who has a severe health condition, no insurance, and needs expensive treatment. The ACA, with its marketplace rules outlawing exclusions for preexisting conditions and offering premium assistance, may be a lifesaver to her. But first she needs to enroll.
As your patients’ trusted physician, you can help point them in the right direction, possibly toward coverage that they never had before.
That’s good for all of us.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]
The Affordable Care Act (ACA) faced—and failed—an important test on October 1, 2013, when open enrollment began in the new health-care marketplaces. Plenty has been written about Web site crashes, technical glitches, and what seems to be general mismanagement of this crucial aspect of implementation.
Let’s look behind the headlines to see which aspects of the ACA are working, and which aren’t, and why.
KNOWING THE FACTS CAN HELP YOU HELP YOUR PATIENTS
ObGyns are scientists. As a scientist, you know the importance of facts. In your research and clinical care, you seek out and rely on scientific facts and evidence. You leave aside unsubstantiated thinking.
It’s imperative that we take the same approach with this subject. Far too many misleading and unsubstantiated claims and headlines are crowding out reliable factual information, seriously hindering physicians’ ability to understand this important health-care system change and respond to it appropriately on behalf of patients. As much as we all love Facebook, for example, it may not be the most accurate source of information on the ACA.
Plenty of reliable, factual, unbiased sources of information about the ACA exist, such as “Understanding Obamacare, Politico’s Guide to the Affordable Care Act” (http://www.politico.com/obamacare-guide/). Other helpful sources of ACA outreach and enrollment information:
HealthCare.gov is the federal government’s main portal for information on the Affordable Care Act. A Spanish version of this site can be accessed at www.CuidadoDeSalud.gov.
“FAQ: What you need to know about the new online marketplaces” features questions and answers from Kaiser Health News at http://www.kaiserhealthnews.org/stories/2013/september/17/marketplace-faq-insurance-exchange-obamacare-aca.aspx.
“Fact sheets: Why the Affordable Care Act matters for women” offers links to summaries of ACA provisions; information on health care for pregnant, low-income and older women; preventive care; and more from the National Partnership for Women and Families at http://go.nationalpartnership.org/site/PageServer?pagename=issues_health_reform_anniversary.
Webinars, speakers, FAQs, and more from Doctors for America at http://www.drsforamerica.org/take-action/get-people-covered.
Reports, blog posts, and links to information on enrollment from Enroll America at www.enrollamerica.org.
An informative video on coverage decisions from the Kaiser Family Foundation at http://kff.org/health-reform/video/youtoons-obamacare-video/.
A REVIEW OF THE CHANGES UNDER ACA
Let’s start with one key fact: The ACA offers a lot of good for women’s health care. Many of these improvements hinge on individuals’ ability to enroll in private health insurance policies sold in the marketplaces.
Each state’s marketplace is similar to the system used by the Federal Employees Health Benefits Program (FEHBP), the insurance marketplace used nationwide by federal employees, including members of Congress. Private plans, such as Blue Cross Blue Shield, Aetna, and United Healthcare, offer health insurance on the FEHBP marketplace to the millions of federal employees each year.
In state marketplaces, private health insurers will offer plans to potentially millions of previously under- or uninsured individuals and families. In exchange for access to this huge new group of consumers, private insurers must abide by a number of important consumer protections in order to be eligible to sell their policies in a state marketplace:
Insurers must agree to abide by the 80/20 rule. Under this game-changer, insurers agree to return the actuarial value of 80% of an enrollee’s premium to health care, keeping only a maximum of 20% for profits and other non-health-care categories.
Insurers must agree to cover 10 essential benefits, including maternity care.
Insurers must agree to cover key preventive services, without copays or deductibles, helping our patients stay healthy.
Insurers must abide by significant insurance protections. They can’t, for example, deny a woman coverage because she has a preexisting condition, was once the victim of domestic violence, or once had a cesarean delivery.
Essential benefits and preventive services
All private health insurance plans sold in the state marketplaces must cover the 10 essential health benefits:
ambulatory patient services
emergency services
hospitalization
maternity and newborn care
mental health and substance use disorder services, including behavioral health treatment
prescription drugs
rehabilitative and habilitative services and devices
laboratory services
preventive and wellness services and chronic disease management
pediatric services, including oral and vision care.
These insurers also must cover—with no charge to the patient—preventive services:
well-woman visits (one or more)
all FDA-approved contraceptive methods and contraception counseling
gestational diabetes screening
mammograms
Pap tests
HIV and other sexually transmitted infection screening and counseling
breastfeeding support, supplies, and counseling
domestic violence screening and counseling.
Related Article: Your age-based guide to comprehensive well-woman care Robert L. Barbieri, MD (October 2012)
In addition, private insurers must offer additional preventive services, although they can charge copays for them:
anemia screening on a routine basis for pregnant women
screening for urinary tract or other infection for pregnant women
counseling about genetic testing for a BRCA mutation for women at higher risk
counseling about chemoprevention of breast cancer for women at higher risk
cervical cancer screening for sexually active women
folic acid supplementation for women who may become pregnant
osteoporosis screening for women over age 60, depending on risk factors
screening for Rh incompatibility for all pregnant women and follow-up testing for women at higher risk
tobacco use screening and interventions for all women, and expanded counseling for pregnant users of tobacco.
An end to preexisting-condition exclusions and other harmful practices
Insurers offering plans in the state marketplaces also must abide by important insurance reforms:
They must eliminate exclusions for preexisting conditions. Insurers cannot deny individuals coverage because they already have a condition that requires medical care, including pregnancy. Before this ACA rule, private insurers often rejected applicants who needed care, as well as those who accessed health care in the past. Insurers regularly denied coverage to women who had had a cesarean delivery or had once been a victim of domestic violence.
They cannot charge women more than men for the same coverage. Before the ACA, women seeking health-care coverage often faced higher premiums than men for identical coverage. This made private coverage less affordable for our patients.
They cannot impose a 9-month waiting period. (Need I say more?)
They must eliminate any annual lifetime limits on coverage. Insurers selling policies in the marketplaces cannot end coverage after a certain dollar amount has been reached, a common practice before the ACA. This change is good news for you and your patients. A patient needing long or expensive care won’t lose coverage when the cost of her care hits an arbitrary ceiling.
They cannot rescind coverage unless fraud is proven. Before the ACA, private health insurers would often drop an individual if he or she started racking up high health-care costs. Patients in the middle of expensive cancer treatments, for example, would find themselves suddenly without health insurance. This won’t happen for policies sold in marketplaces unless the patient lied on her enrollment forms or failed to keep up her premium payments.
What these changes mean, in real numbers
These protections are critically important to your ability to care for your patients. Here’s what they mean in real life:
Health-care coverage for about 10,000 insured women is no longer subject to an annual lifetime coverage limit.
Private insurers can’t drop coverage, a change that will affect about 5.5 million insured women.
Insurance companies cannot deny coverage for preexisting conditions, which will help insure about 100,000 women.
Each state marketplace offers four types of plans, the idea being to help people compare policies side by side. All plans sold in the marketplaces must abide by the consumer protections I just reviewed. Each tier is differentiated by the average percentage of an enrollee’s health-care expenses paid by the insurer. The more an enrollee agrees to pay out of pocket, the lower his or her premium.
The tiers are:
Bronze – The insurer covers 60% of health-care costs, and the insured covers 40%. This tier offers the cheapest premiums.
Silver – The insurer covers 70% of costs.
Gold – The insurer covers 80% of costs.
Platinum – The insurer covers 90% of costs.
WHAT WENT WRONG
If everything had gone according to plan, women’s access to health insurance would have increased dramatically nationwide, including in the dark blue states in FIGURE 1 (Map 1)—states that rank lowest in access to care. You’ll notice that many of the states that are dark blue in Map 1 shift to light blue in Map 2. Take a careful look at those dark blue states and see what colors they are in the next two maps (FIGURES 1 and 2). Hint: There’s a pattern.
Problem 1 – Strains on Healthcare.gov
When the ACA was signed into law, most states were expected to build and run their own online marketplaces. The federal government offered to run a state exchange if a state didn’t. Few ACA engineers anticipated that the federal government would have to run the marketplaces in more than half the states—politics-fueled decisions in many states. Now you can see that many of the states that are dark blue in Map 1 are gray in Map 3 (FIGURE 2). Many states whose populations have the greatest need left it to the federal government to run the marketplaces.
Data indicate that state-run marketplaces are doing pretty well—a fact not often caught in frenzied headlines. If we look at the percentage of the target population actually enrolled in marketplace insurance plans during the first month, we see that the lowest state marketplace enrollment was in Washington State, with 30% of its target population enrolled. The highest target-population enrollment was achieved in Connecticut, with 191%.
Compare these numbers to the rates of target-population enrollment in states with marketplaces run by the federal government, which range from 3% to 20% (FIGURE 2). During the first month, federal and state-run marketplaces together enrolled 106,000 individuals into new coverage, 21% of the national target.
The news media have focused on the federal online enrollment debacle. Easier enrollment options are available to people who live in federally run marketplace states, including direct enrollment. Strongly supported by America’s health insurance industry, direct enrollment lets potential enrollees purchase coverage directly from insurance companies participating in the marketplaces.
Problem 2: People lost their current coverage
This is a problem worth exploring—one that affects people who previously bought insurance on the individual insurance market. This is the market that offers people comparatively limited coverage, usually with no maternity care coverage, for comparatively high premiums.
So why are these individuals losing coverage?
They are losing coverage because, as of January 2014, new individual plans must abide by the 80/20 rule, abide by insurance protections, and cover 10 essential services with no cost sharing.
You may recall that, in August 2009, Americans were demanding that they be able to keep the health-care coverage they currently had, and President Barack Obama promised that they would be able to. Consequently, health insurance policies in effect before March 2010, when the ACA was signed into law, were exempted—“grandfathered”—from most ACA requirements. If people liked their old policies, they could keep them.
Grandfathered plans are exempt from:
the requirement to cover the 10 essential health benefits
the requirement that plans must provide preventive services with no patient cost sharing
state or federal review of insurance premium increases of 10% or more for non-group and small business plans
a rule allowing consumers to appeal denials of claims to a third-party reviewer.
Most ACA requirements apply to new policies—those offered after March 2010 and those that have been changed significantly by the insurance companies. Some examples of changes in coverage that would cause a plan to lose grandfathering include:
the elimination of benefits to diagnose or treat a particular condition
an increase in the up-front deductible patients must pay before coverage kicks in by more than the cumulative growth in medical inflation since March 2010 plus 15%
a reduction in the share of the premium that the employer pays by more than 5% since March 2010.
How many people are we talking about? Not the 40% of Americans who have employer-based coverage or the 20% of Americans on Medicare, Medicaid, or Tricare. This provision affects about 5% of the insured, as many as 15 million people—many with plans that offer little coverage for high premiums.
The ACA intention was that many people previously covered in the individual insurance market would find better and cheaper coverage in their state marketplaces. That may be a good option for people in states that have chosen to run their own marketplaces, and a good option for people in other states, too, as federal online enrollment issues get fixed.
Problem 3: Medicaid expansion became a state option
When the US Supreme Court upheld the constitutionality of the ACA’s individual mandate, it also effectively turned the ACA Medicaid expansion into a state option.
Think of the Medicaid expansion as Medicaid Part 2. Regular Medicaid remains largely unchanged, with the same eligibility rules and coverage requirements.
The ACA included a provision under which every state would add a new part to its Medicaid program. Beginning in 2014, this part—the expansion—would cover individuals in each state with incomes under 138% of the federal poverty line—about $32,000 for a family of four in 2014. Medicaid expansion coverage is based only on income eligibility, a major change for women, many of whom currently qualify for Medicaid only if they’re pregnant.
Who would pay for the new coverage?
In 2014, 2015, and 2016, the federal government pays 100% of the cost of care for Medicaid expansion. From 2017 to 2020, the federal share gradually drops to 90%.
Medicaid expansion is an integral part of reducing the number of uninsured under the ACA and is expected to reduce the uninsured rate by almost 30% if adopted by every state. Medicaid expansion plus the ACA marketplaces were expected to cut our uninsured rate almost in half.
FIGURE 3 shows how states responded when the Supreme Court effectively converted the Medicaid expansion into an option, leaving us, again, with coverage gaps. Many of the states that have opted not to expand Medicaid are the same states that declined to operate their own state marketplaces, the same states with highest percentages of the uninsured.
The ACA has many interdependent parts. Make the Medicaid expansion a state option, and you end up with higher than expected rates of uninsured. Trigger big changes in the individual market when there are still bugs in the system, and people are left in the lurch.
Related Article: ACOG to legislators: Partnership, not interference Lucia DiVenere, MA (April 2013)
What’s happening now
As this article is going to press, enrollment in the marketplaces is getting easier, with Web site fixes and useful alternatives to Web-based enrollment. Small changes are being made to some deadlines to help people who have gotten stuck in the process. We’ll likely continue to see steps forward and back over the next many months.
Two things remain important:
We need to stick with the facts. If you see something in the news that seems too crazy to be real, your hunch may be right.
Your patients can benefit significantly from the ACA. An ACOG Fellow recently told me about one of his patients who has a severe health condition, no insurance, and needs expensive treatment. The ACA, with its marketplace rules outlawing exclusions for preexisting conditions and offering premium assistance, may be a lifesaver to her. But first she needs to enroll.
As your patients’ trusted physician, you can help point them in the right direction, possibly toward coverage that they never had before.
That’s good for all of us.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected]
Promises, promises
For many, the making and breaking of New Year’s resolutions have become a humorless cliché. Still, the beginning of a new year is as good a time as any for reflection and inspiration; and if you restrict your fix-it list to a few realistic promises that can actually be kept, resolution time does not have to remain an exercise in futility.
I can’t presume to know what needs improving in your practice, but I do know the issues I get the most questions about. Perhaps the following Top Ten list will inspire you to create a realistic list of your own.
1. Do a HIPAA risk assessment. The new HIPAA rules are now in effect, as I discussed a few months ago. Is your office up to speed? Review every procedure that involves confidential information; make sure there are no violations. Penalties for carelessness are much stiffer now.
2. Encrypt your mobile devices. This is a subset of item 1. The biggest HIPAA vulnerability in many practices is laptops and tablets that carry confidential patient information; losing one could be a disaster. Encryption software is cheap and readily available, and a lost or stolen mobile device will probably not be treated as a HIPAA breach if it is properly encrypted.
3. Reduce your accounts receivable by keeping a credit card number on file for each patient, and charging patient-owed balances as they come in. A series of my past columns in the archives at edermatologynews.com explains exactly how to do it. Every hotel in the world does this, and you should too.
4. Review your coding habits. For example, are you billing for 99213 each and every time your evaluation and treatment meet the criteria for that code? If not, you’re leaving money on the table; and that will become a more and more significant issue if reimbursements tighten up in the next few years – as they almost surely will.
5. Clear your "horizontal file cabinet." That’s the mess on your desk, all the paperwork you never seem to get to (probably because you’re tweeting or answering e-mail). Set aside an hour or two and get it all done. You’ll find some interesting stuff in there. Then, for every piece of paper that arrives on your desk from now on, follow the DDD Rule: Do it, Delegate it, or Destroy it. Don’t start a new mess.
6. Keep a closer eye on your office finances. Most physicians delegate the bookkeeping, and that’s fine. But ignoring the financial side creates an atmosphere that facilitates embezzlement. Set aside a few hours each month to review the books personally. And make sure your employees know you’re doing it.
7. Make sure your long-range financial planning is on track. This is another task physicians tend to "set and forget," but the Great Recession was an eye-opener for many of us. Once a year, sit down with your accountant and planner and make sure your investments are well diversified and all other aspects of your finances – budgets, credit ratings, insurance coverage, tax situations, college savings, estate plans, and retirement accounts – are in the best shape possible. Now would be a good time.
8. Back up your data. Now is also an excellent time to verify that the information on your office and personal computers is being backed up – locally and online – on a regular schedule. Don’t wait until something crashes.
9. Take more vacations. Remember Eastern’s First Law: Your last words will not be, "I wish I had spent more time in the office." This is the year to start spending more time enjoying your life, your friends and family, and the world. As John Lennon said, "Life is what happens to you while you’re busy making other plans."
10. Look at yourself. A private practice lives or dies on the personalities of its physicians, and your staff copies your personality and style. Take a hard, honest look at yourself. Identify your negative personality traits and work to eliminate them. If you have any difficulty finding the things that need changing ... ask your spouse. He or she will be happy to outline them for you in great detail.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
For many, the making and breaking of New Year’s resolutions have become a humorless cliché. Still, the beginning of a new year is as good a time as any for reflection and inspiration; and if you restrict your fix-it list to a few realistic promises that can actually be kept, resolution time does not have to remain an exercise in futility.
I can’t presume to know what needs improving in your practice, but I do know the issues I get the most questions about. Perhaps the following Top Ten list will inspire you to create a realistic list of your own.
1. Do a HIPAA risk assessment. The new HIPAA rules are now in effect, as I discussed a few months ago. Is your office up to speed? Review every procedure that involves confidential information; make sure there are no violations. Penalties for carelessness are much stiffer now.
2. Encrypt your mobile devices. This is a subset of item 1. The biggest HIPAA vulnerability in many practices is laptops and tablets that carry confidential patient information; losing one could be a disaster. Encryption software is cheap and readily available, and a lost or stolen mobile device will probably not be treated as a HIPAA breach if it is properly encrypted.
3. Reduce your accounts receivable by keeping a credit card number on file for each patient, and charging patient-owed balances as they come in. A series of my past columns in the archives at edermatologynews.com explains exactly how to do it. Every hotel in the world does this, and you should too.
4. Review your coding habits. For example, are you billing for 99213 each and every time your evaluation and treatment meet the criteria for that code? If not, you’re leaving money on the table; and that will become a more and more significant issue if reimbursements tighten up in the next few years – as they almost surely will.
5. Clear your "horizontal file cabinet." That’s the mess on your desk, all the paperwork you never seem to get to (probably because you’re tweeting or answering e-mail). Set aside an hour or two and get it all done. You’ll find some interesting stuff in there. Then, for every piece of paper that arrives on your desk from now on, follow the DDD Rule: Do it, Delegate it, or Destroy it. Don’t start a new mess.
6. Keep a closer eye on your office finances. Most physicians delegate the bookkeeping, and that’s fine. But ignoring the financial side creates an atmosphere that facilitates embezzlement. Set aside a few hours each month to review the books personally. And make sure your employees know you’re doing it.
7. Make sure your long-range financial planning is on track. This is another task physicians tend to "set and forget," but the Great Recession was an eye-opener for many of us. Once a year, sit down with your accountant and planner and make sure your investments are well diversified and all other aspects of your finances – budgets, credit ratings, insurance coverage, tax situations, college savings, estate plans, and retirement accounts – are in the best shape possible. Now would be a good time.
8. Back up your data. Now is also an excellent time to verify that the information on your office and personal computers is being backed up – locally and online – on a regular schedule. Don’t wait until something crashes.
9. Take more vacations. Remember Eastern’s First Law: Your last words will not be, "I wish I had spent more time in the office." This is the year to start spending more time enjoying your life, your friends and family, and the world. As John Lennon said, "Life is what happens to you while you’re busy making other plans."
10. Look at yourself. A private practice lives or dies on the personalities of its physicians, and your staff copies your personality and style. Take a hard, honest look at yourself. Identify your negative personality traits and work to eliminate them. If you have any difficulty finding the things that need changing ... ask your spouse. He or she will be happy to outline them for you in great detail.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
For many, the making and breaking of New Year’s resolutions have become a humorless cliché. Still, the beginning of a new year is as good a time as any for reflection and inspiration; and if you restrict your fix-it list to a few realistic promises that can actually be kept, resolution time does not have to remain an exercise in futility.
I can’t presume to know what needs improving in your practice, but I do know the issues I get the most questions about. Perhaps the following Top Ten list will inspire you to create a realistic list of your own.
1. Do a HIPAA risk assessment. The new HIPAA rules are now in effect, as I discussed a few months ago. Is your office up to speed? Review every procedure that involves confidential information; make sure there are no violations. Penalties for carelessness are much stiffer now.
2. Encrypt your mobile devices. This is a subset of item 1. The biggest HIPAA vulnerability in many practices is laptops and tablets that carry confidential patient information; losing one could be a disaster. Encryption software is cheap and readily available, and a lost or stolen mobile device will probably not be treated as a HIPAA breach if it is properly encrypted.
3. Reduce your accounts receivable by keeping a credit card number on file for each patient, and charging patient-owed balances as they come in. A series of my past columns in the archives at edermatologynews.com explains exactly how to do it. Every hotel in the world does this, and you should too.
4. Review your coding habits. For example, are you billing for 99213 each and every time your evaluation and treatment meet the criteria for that code? If not, you’re leaving money on the table; and that will become a more and more significant issue if reimbursements tighten up in the next few years – as they almost surely will.
5. Clear your "horizontal file cabinet." That’s the mess on your desk, all the paperwork you never seem to get to (probably because you’re tweeting or answering e-mail). Set aside an hour or two and get it all done. You’ll find some interesting stuff in there. Then, for every piece of paper that arrives on your desk from now on, follow the DDD Rule: Do it, Delegate it, or Destroy it. Don’t start a new mess.
6. Keep a closer eye on your office finances. Most physicians delegate the bookkeeping, and that’s fine. But ignoring the financial side creates an atmosphere that facilitates embezzlement. Set aside a few hours each month to review the books personally. And make sure your employees know you’re doing it.
7. Make sure your long-range financial planning is on track. This is another task physicians tend to "set and forget," but the Great Recession was an eye-opener for many of us. Once a year, sit down with your accountant and planner and make sure your investments are well diversified and all other aspects of your finances – budgets, credit ratings, insurance coverage, tax situations, college savings, estate plans, and retirement accounts – are in the best shape possible. Now would be a good time.
8. Back up your data. Now is also an excellent time to verify that the information on your office and personal computers is being backed up – locally and online – on a regular schedule. Don’t wait until something crashes.
9. Take more vacations. Remember Eastern’s First Law: Your last words will not be, "I wish I had spent more time in the office." This is the year to start spending more time enjoying your life, your friends and family, and the world. As John Lennon said, "Life is what happens to you while you’re busy making other plans."
10. Look at yourself. A private practice lives or dies on the personalities of its physicians, and your staff copies your personality and style. Take a hard, honest look at yourself. Identify your negative personality traits and work to eliminate them. If you have any difficulty finding the things that need changing ... ask your spouse. He or she will be happy to outline them for you in great detail.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
How to Get Organized and Be Fearless About ICD-10
What To Do When the Hospitalist Group Leader Refuses to See Patients
My hospitalist group, which has nine employees, is hospital-employed in a small Midwest town. We use the traditional seven-on and seven-off rotation and hire locum tenens to fill schedule gaps, as we have a couple of MDs who recently left the group. A few of us are concerned because our “boss,” who controls the schedule, does not put himself in rotation regularly. Instead, he puts locum or part-timers on the schedule, even on weeks when he is available. We all know that the hospital is paying him extra to take care of administrative work, and that it costs more for the hospital to pay part-time/locums. In your experience, is this a common occurrence? Should we be upset? Lastly, should we bring this issue to administration, because many of us think that they are not aware this is happening.
–Mismatched in the Midwest
Dr. Hospitalist responds:
Opinions vary when it comes to the amount of clinical time hospitalist leaders should devote to their groups. As we have become more involved in the administrative aspects of the hospital, there are increasing demands placed on directors. Along with increased administrative demands comes the desire of many of these physician-leaders to remain adept in the practice of hospital medicine. Without a strong clinical connection and familiarity with what the others experience day to day, the group leader risks losing credibility and whatever leverage the title might offer.
Many groups have devised formulas based on the number of members in the group to help them derive a “fair” amount of administrative time to allow the director. For example, for every five full-time equivalents (FTEs) on staff, the director receives 0.1 FTE in admin time; so, for a group of 25 members, the director would get 0.5 admin time. The remainder of time would be clinical, but again, how that clinical time is managed is also highly variable.
This seems like a reasonable formula to me, because those with larger programs will have larger hospitals, more people to manage, and more personalities to deal with. The potential rewards and job satisfaction are also greater. (Another potential scheduling issue: Does the group leader “fall right into” the rotation or only work the services with light census or teaching services in an academic institution?)
Some groups that work the traditional seven-on/seven-off schedule have allowed the hospitalist physician-leader to work Monday through Friday and carry a smaller census (10-12). This allows the leader to be in the hospital during those critical times when most administrative duties are fulfilled, while also allowing for a mechanism to place overflow patients on those high census days—as long as it is a rare occurrence. He or she should also occasionally work all the different shifts (nocturnist, admitter, teams, and so on) to best understand the group’s opportunities for improvement and its challenges.
There are likely as many iterations of how to devise a fair division of time as there are hospitalist groups, but, most importantly, the days of getting someone to volunteer to be a hospitalist director without some form of compensation are long gone. In most programs, the job has become much more complex.
Many believe it is a conflict of interest for the group leader to prepare the schedule. There is too much room for perceived favoritism or mistreatment by the members when the schedule doesn’t work in everyone’s favor (which it never will). There are proprietary programs on the market that allow for easy and reliable scheduling; they also remove the potential for bias. In a group as small as yours, an astute administrative assistant or associate director can be entrusted with the schedule.
With regard to speaking up, you say a “few” in your group are concerned, so I assume more than one but still a small number of your group has expressed some dissatisfaction. There may be other members with similar sentiments, so it is important to have a discussion with all the group members and solicit their opinions. Instead of approaching the administrators with your concerns, I suggest you and your colleagues have an open and candid discussion with your group leader. After the discussion, if you still remain dissatisfied with the director’s level of clinical involvement, you are left with several choices:
- Approach hospital administration and see if they approve of how your director is carrying out his clinical responsibilities. Be prepared for the director to find out.
- Continue to do your job and let this issue rest.
- Start looking for another job. If the situation really bothers you, I favor the latter!
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to [email protected].
My hospitalist group, which has nine employees, is hospital-employed in a small Midwest town. We use the traditional seven-on and seven-off rotation and hire locum tenens to fill schedule gaps, as we have a couple of MDs who recently left the group. A few of us are concerned because our “boss,” who controls the schedule, does not put himself in rotation regularly. Instead, he puts locum or part-timers on the schedule, even on weeks when he is available. We all know that the hospital is paying him extra to take care of administrative work, and that it costs more for the hospital to pay part-time/locums. In your experience, is this a common occurrence? Should we be upset? Lastly, should we bring this issue to administration, because many of us think that they are not aware this is happening.
–Mismatched in the Midwest
Dr. Hospitalist responds:
Opinions vary when it comes to the amount of clinical time hospitalist leaders should devote to their groups. As we have become more involved in the administrative aspects of the hospital, there are increasing demands placed on directors. Along with increased administrative demands comes the desire of many of these physician-leaders to remain adept in the practice of hospital medicine. Without a strong clinical connection and familiarity with what the others experience day to day, the group leader risks losing credibility and whatever leverage the title might offer.
Many groups have devised formulas based on the number of members in the group to help them derive a “fair” amount of administrative time to allow the director. For example, for every five full-time equivalents (FTEs) on staff, the director receives 0.1 FTE in admin time; so, for a group of 25 members, the director would get 0.5 admin time. The remainder of time would be clinical, but again, how that clinical time is managed is also highly variable.
This seems like a reasonable formula to me, because those with larger programs will have larger hospitals, more people to manage, and more personalities to deal with. The potential rewards and job satisfaction are also greater. (Another potential scheduling issue: Does the group leader “fall right into” the rotation or only work the services with light census or teaching services in an academic institution?)
Some groups that work the traditional seven-on/seven-off schedule have allowed the hospitalist physician-leader to work Monday through Friday and carry a smaller census (10-12). This allows the leader to be in the hospital during those critical times when most administrative duties are fulfilled, while also allowing for a mechanism to place overflow patients on those high census days—as long as it is a rare occurrence. He or she should also occasionally work all the different shifts (nocturnist, admitter, teams, and so on) to best understand the group’s opportunities for improvement and its challenges.
There are likely as many iterations of how to devise a fair division of time as there are hospitalist groups, but, most importantly, the days of getting someone to volunteer to be a hospitalist director without some form of compensation are long gone. In most programs, the job has become much more complex.
Many believe it is a conflict of interest for the group leader to prepare the schedule. There is too much room for perceived favoritism or mistreatment by the members when the schedule doesn’t work in everyone’s favor (which it never will). There are proprietary programs on the market that allow for easy and reliable scheduling; they also remove the potential for bias. In a group as small as yours, an astute administrative assistant or associate director can be entrusted with the schedule.
With regard to speaking up, you say a “few” in your group are concerned, so I assume more than one but still a small number of your group has expressed some dissatisfaction. There may be other members with similar sentiments, so it is important to have a discussion with all the group members and solicit their opinions. Instead of approaching the administrators with your concerns, I suggest you and your colleagues have an open and candid discussion with your group leader. After the discussion, if you still remain dissatisfied with the director’s level of clinical involvement, you are left with several choices:
- Approach hospital administration and see if they approve of how your director is carrying out his clinical responsibilities. Be prepared for the director to find out.
- Continue to do your job and let this issue rest.
- Start looking for another job. If the situation really bothers you, I favor the latter!
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to [email protected].
My hospitalist group, which has nine employees, is hospital-employed in a small Midwest town. We use the traditional seven-on and seven-off rotation and hire locum tenens to fill schedule gaps, as we have a couple of MDs who recently left the group. A few of us are concerned because our “boss,” who controls the schedule, does not put himself in rotation regularly. Instead, he puts locum or part-timers on the schedule, even on weeks when he is available. We all know that the hospital is paying him extra to take care of administrative work, and that it costs more for the hospital to pay part-time/locums. In your experience, is this a common occurrence? Should we be upset? Lastly, should we bring this issue to administration, because many of us think that they are not aware this is happening.
–Mismatched in the Midwest
Dr. Hospitalist responds:
Opinions vary when it comes to the amount of clinical time hospitalist leaders should devote to their groups. As we have become more involved in the administrative aspects of the hospital, there are increasing demands placed on directors. Along with increased administrative demands comes the desire of many of these physician-leaders to remain adept in the practice of hospital medicine. Without a strong clinical connection and familiarity with what the others experience day to day, the group leader risks losing credibility and whatever leverage the title might offer.
Many groups have devised formulas based on the number of members in the group to help them derive a “fair” amount of administrative time to allow the director. For example, for every five full-time equivalents (FTEs) on staff, the director receives 0.1 FTE in admin time; so, for a group of 25 members, the director would get 0.5 admin time. The remainder of time would be clinical, but again, how that clinical time is managed is also highly variable.
This seems like a reasonable formula to me, because those with larger programs will have larger hospitals, more people to manage, and more personalities to deal with. The potential rewards and job satisfaction are also greater. (Another potential scheduling issue: Does the group leader “fall right into” the rotation or only work the services with light census or teaching services in an academic institution?)
Some groups that work the traditional seven-on/seven-off schedule have allowed the hospitalist physician-leader to work Monday through Friday and carry a smaller census (10-12). This allows the leader to be in the hospital during those critical times when most administrative duties are fulfilled, while also allowing for a mechanism to place overflow patients on those high census days—as long as it is a rare occurrence. He or she should also occasionally work all the different shifts (nocturnist, admitter, teams, and so on) to best understand the group’s opportunities for improvement and its challenges.
There are likely as many iterations of how to devise a fair division of time as there are hospitalist groups, but, most importantly, the days of getting someone to volunteer to be a hospitalist director without some form of compensation are long gone. In most programs, the job has become much more complex.
Many believe it is a conflict of interest for the group leader to prepare the schedule. There is too much room for perceived favoritism or mistreatment by the members when the schedule doesn’t work in everyone’s favor (which it never will). There are proprietary programs on the market that allow for easy and reliable scheduling; they also remove the potential for bias. In a group as small as yours, an astute administrative assistant or associate director can be entrusted with the schedule.
With regard to speaking up, you say a “few” in your group are concerned, so I assume more than one but still a small number of your group has expressed some dissatisfaction. There may be other members with similar sentiments, so it is important to have a discussion with all the group members and solicit their opinions. Instead of approaching the administrators with your concerns, I suggest you and your colleagues have an open and candid discussion with your group leader. After the discussion, if you still remain dissatisfied with the director’s level of clinical involvement, you are left with several choices:
- Approach hospital administration and see if they approve of how your director is carrying out his clinical responsibilities. Be prepared for the director to find out.
- Continue to do your job and let this issue rest.
- Start looking for another job. If the situation really bothers you, I favor the latter!
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to [email protected].
Workflow Interruptions Threaten Patient Safety, Hospitalists' Job Satisfaction
When I visit hospitalist programs, one of the things I am most interested in learning about is the degree to which the hospitalists enjoy their work and why. On a recent visit, in my usual meeting with the hospitalist group, we talked a lot about what it is like to be a hospitalist. When I asked them what the greatest threat to their job satisfaction was, there was a chorus of consistency in their answers: interruptions. The hospitalists were deeply frustrated by minute-to-minute intrusions into their workflow. The emergency department, nurses, pharmacy, the admitting department, the lab, radiology—you name it, everyone wants a piece of them.
Constant interruptions are a career satisfaction issue for hospitalists. But for patients, the interruptions represent a safety and quality of care issue. Why?
The Myth of Multi-tasking
Some of us take pride in our ability to multi-task. Others freely admit they aren’t very good at it. In any case, we know through cognitive psychology that the brain cannot multi-task, at least in the realm of conscious work. (The brain, of course, carries out basic, life-sustaining functions while we are doing other work cognitively.) The brain is actually a “sequential processor,” and multi-tasking actually is “task-switching.” Those of us who “multi-task” well are able to switch tasks easily and effectively.
But, task switching comes at a cost. When we switch tasks, we are prone to errors in the performance of those tasks. Two psychologists, Rogers and Monsell, demonstrated this in a study that looked at error rates when subjects performed tasks involving numerical or letter manipulations.1 The tasks involved classifying either the digit member of a pair of characters as even/odd or the letter member as consonant/vowel. When subjects performed the tasks while switching among multiple tasks, the error rate was fourfold the rate with no task switching (see Figure 1).1 These findings have been replicated since the original study. Further, there is now well-developed literature devoted to interruptions and patient safety.
It Takes Time
We also know that switching between tasks takes time. Why? Because changing one’s attention from one subject to another involves neurologic processes that are not instantaneous. In a simulated driving study comparing mean reaction times between intoxicated subjects (blood alcohol 0.08%) and those talking on a cell phone, Strayer and Drews found the mean time to brake onset was significantly slower in the cell phone group than in the drunk driving group, presumably because cell phone users had to switch tasks.2
How Can We Tame Interruptions?
I submit that we need to be realistic about our ability to control the number of interruptions hospitalists experience in a given workday. One approach is to identify “high stakes moments” that are protected from excessive interruptions. Taking an example from aviation, airplane takeoffs and landings are “no interruption” zones, meaning that no needless talking or tasking is allowed in the cockpit during these tasks. Potential “no interruption” zones in hospital medicine might include times when hospitalists are developing an assessment and plan, engaged in complex decision-making, or performing medication reconciliation.
But is it realistic to think that we can cordon off hospitalists during these tasks?
Another approach is to establish practices that may decrease interruptions. Interruptions likely are reduced by:
- Having unit-based hospitalist staffing;
- Holding multidisciplinary rounds;
- Training nurses to batch pages;
- Conducting structured evening and night rounds on all nursing units for non-urgent matters; and
- Developing paging “levels” so that a receiving physician knows if a call back is needed and, if so, if it is urgent or not.
In talking to hospitalists who cite interruptions as job dissatisfiers, it occurs to me that anything that erodes career engagement also threatens patient safety. If we could figure out how to control interruptions, we would kill two birds with one stone.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
When I visit hospitalist programs, one of the things I am most interested in learning about is the degree to which the hospitalists enjoy their work and why. On a recent visit, in my usual meeting with the hospitalist group, we talked a lot about what it is like to be a hospitalist. When I asked them what the greatest threat to their job satisfaction was, there was a chorus of consistency in their answers: interruptions. The hospitalists were deeply frustrated by minute-to-minute intrusions into their workflow. The emergency department, nurses, pharmacy, the admitting department, the lab, radiology—you name it, everyone wants a piece of them.
Constant interruptions are a career satisfaction issue for hospitalists. But for patients, the interruptions represent a safety and quality of care issue. Why?
The Myth of Multi-tasking
Some of us take pride in our ability to multi-task. Others freely admit they aren’t very good at it. In any case, we know through cognitive psychology that the brain cannot multi-task, at least in the realm of conscious work. (The brain, of course, carries out basic, life-sustaining functions while we are doing other work cognitively.) The brain is actually a “sequential processor,” and multi-tasking actually is “task-switching.” Those of us who “multi-task” well are able to switch tasks easily and effectively.
But, task switching comes at a cost. When we switch tasks, we are prone to errors in the performance of those tasks. Two psychologists, Rogers and Monsell, demonstrated this in a study that looked at error rates when subjects performed tasks involving numerical or letter manipulations.1 The tasks involved classifying either the digit member of a pair of characters as even/odd or the letter member as consonant/vowel. When subjects performed the tasks while switching among multiple tasks, the error rate was fourfold the rate with no task switching (see Figure 1).1 These findings have been replicated since the original study. Further, there is now well-developed literature devoted to interruptions and patient safety.
It Takes Time
We also know that switching between tasks takes time. Why? Because changing one’s attention from one subject to another involves neurologic processes that are not instantaneous. In a simulated driving study comparing mean reaction times between intoxicated subjects (blood alcohol 0.08%) and those talking on a cell phone, Strayer and Drews found the mean time to brake onset was significantly slower in the cell phone group than in the drunk driving group, presumably because cell phone users had to switch tasks.2
How Can We Tame Interruptions?
I submit that we need to be realistic about our ability to control the number of interruptions hospitalists experience in a given workday. One approach is to identify “high stakes moments” that are protected from excessive interruptions. Taking an example from aviation, airplane takeoffs and landings are “no interruption” zones, meaning that no needless talking or tasking is allowed in the cockpit during these tasks. Potential “no interruption” zones in hospital medicine might include times when hospitalists are developing an assessment and plan, engaged in complex decision-making, or performing medication reconciliation.
But is it realistic to think that we can cordon off hospitalists during these tasks?
Another approach is to establish practices that may decrease interruptions. Interruptions likely are reduced by:
- Having unit-based hospitalist staffing;
- Holding multidisciplinary rounds;
- Training nurses to batch pages;
- Conducting structured evening and night rounds on all nursing units for non-urgent matters; and
- Developing paging “levels” so that a receiving physician knows if a call back is needed and, if so, if it is urgent or not.
In talking to hospitalists who cite interruptions as job dissatisfiers, it occurs to me that anything that erodes career engagement also threatens patient safety. If we could figure out how to control interruptions, we would kill two birds with one stone.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
When I visit hospitalist programs, one of the things I am most interested in learning about is the degree to which the hospitalists enjoy their work and why. On a recent visit, in my usual meeting with the hospitalist group, we talked a lot about what it is like to be a hospitalist. When I asked them what the greatest threat to their job satisfaction was, there was a chorus of consistency in their answers: interruptions. The hospitalists were deeply frustrated by minute-to-minute intrusions into their workflow. The emergency department, nurses, pharmacy, the admitting department, the lab, radiology—you name it, everyone wants a piece of them.
Constant interruptions are a career satisfaction issue for hospitalists. But for patients, the interruptions represent a safety and quality of care issue. Why?
The Myth of Multi-tasking
Some of us take pride in our ability to multi-task. Others freely admit they aren’t very good at it. In any case, we know through cognitive psychology that the brain cannot multi-task, at least in the realm of conscious work. (The brain, of course, carries out basic, life-sustaining functions while we are doing other work cognitively.) The brain is actually a “sequential processor,” and multi-tasking actually is “task-switching.” Those of us who “multi-task” well are able to switch tasks easily and effectively.
But, task switching comes at a cost. When we switch tasks, we are prone to errors in the performance of those tasks. Two psychologists, Rogers and Monsell, demonstrated this in a study that looked at error rates when subjects performed tasks involving numerical or letter manipulations.1 The tasks involved classifying either the digit member of a pair of characters as even/odd or the letter member as consonant/vowel. When subjects performed the tasks while switching among multiple tasks, the error rate was fourfold the rate with no task switching (see Figure 1).1 These findings have been replicated since the original study. Further, there is now well-developed literature devoted to interruptions and patient safety.
It Takes Time
We also know that switching between tasks takes time. Why? Because changing one’s attention from one subject to another involves neurologic processes that are not instantaneous. In a simulated driving study comparing mean reaction times between intoxicated subjects (blood alcohol 0.08%) and those talking on a cell phone, Strayer and Drews found the mean time to brake onset was significantly slower in the cell phone group than in the drunk driving group, presumably because cell phone users had to switch tasks.2
How Can We Tame Interruptions?
I submit that we need to be realistic about our ability to control the number of interruptions hospitalists experience in a given workday. One approach is to identify “high stakes moments” that are protected from excessive interruptions. Taking an example from aviation, airplane takeoffs and landings are “no interruption” zones, meaning that no needless talking or tasking is allowed in the cockpit during these tasks. Potential “no interruption” zones in hospital medicine might include times when hospitalists are developing an assessment and plan, engaged in complex decision-making, or performing medication reconciliation.
But is it realistic to think that we can cordon off hospitalists during these tasks?
Another approach is to establish practices that may decrease interruptions. Interruptions likely are reduced by:
- Having unit-based hospitalist staffing;
- Holding multidisciplinary rounds;
- Training nurses to batch pages;
- Conducting structured evening and night rounds on all nursing units for non-urgent matters; and
- Developing paging “levels” so that a receiving physician knows if a call back is needed and, if so, if it is urgent or not.
In talking to hospitalists who cite interruptions as job dissatisfiers, it occurs to me that anything that erodes career engagement also threatens patient safety. If we could figure out how to control interruptions, we would kill two birds with one stone.
Dr. Whitcomb is Chief Medical Officer of Remedy Partners. He is co-founder and past president of SHM. Email him at [email protected].
References
Society of Hospital Medicine (SHM) Epitomizes Professional Diversity
I just got back from a trip to SHM headquarters in Philadelphia, and all I can say is “wow.” I was visiting there for a meeting with the staff, many SHM members and committee leaders, and the SHM board of directors. The first day we all went into a big, modern, beautiful room at SHM headquarters—there must have been more than 100 people—and we went around the room and introduced ourselves. The diversity of the staff that support our society, and the diversity of the members there, was truly breathtaking. What I saw was a microcosm of our society and our specialty.
Looking around the room, it was easy to see some aspects of our diverse organization: both genders and a variety of ethnicities and age groups were well represented. These traditional measures of diversity are critical to a healthy environment, in my opinion, and the data bear out the idea that a diverse workforce can reduce turnover and be more creative and qualified.1,2 Our diversity is not an accident. It is part of a larger, deliberate strategy by SHM to be “the home” for healthcare professionals who provide hospital-based patient care. SHM embraces diversity, whether it’s skin deep or deeply cognitive.
Although we are continually working to enrich the traditional aspects of diversity, we are also very hard at work to make SHM a place of professional diversity.
Open and Inclusive
Over the past several years, SHM has worked hard to be openly inclusive. Many of the committees and sections within the society have been developed specifically to embrace important aspects of hospital medicine that have special or common interests, characteristics, or needs. Examples include the international section, med-peds section, administrators’ committee, and the nurse practitioner and physician assistant committee. These venues allow individuals under a Big Tent to find others with similar interests or training, so that they can address unique aspects of hospital medicine as it relates directly to them. SHM’s virtual world is following our committee and section structure, which has some of the most actively growing HMXchange communities coming from the “administrators” community and the “NP/PA” community.
SHM has put its money where its mouth is, dedicating significant resources for educational programs that will help benefit professionals with a variety of backgrounds. Some are focused on the special needs of our diverse physician population, including the Academic Hospitalist Academy, the Quality and Safety Educators Academy, and the Pediatric Hospital Medicine annual meeting (through a partnership with the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association). Other events are focused specifically on helping our non-physician colleagues, like the boot camp that is presented in collaboration with the American Academy of Physician Assistants and American Association of Nurse Practitioners. The SHM Leadership Academies attract a venerable alphabet soup of professional designations, including many MDs and DOs, of course, but also increasing numbers of PAs and NPs, a growing number of administrators, and now even a few ED and OB docs! Now that’s a Big Tent.
My understanding is that these events are always popular and often sold out.
Maybe the most powerful evidence that our Big Tent philosophy is working is found in the relationships SHM has forged with other hospital-based specialties, like obstetrics, neurology, and surgery. The president of the Society of OB/GYN Hospitalists (societyofobgynhospitalists.com) has attended the SHM annual meeting and at least one of the Leadership Academies. Although “traditional” hospitalists like me may not be able to help in the OR or birthing suite, we have a lot of experience in quality improvement, leadership, and, of course, addressing the needs of a new and growing professional segment. The emergence and growth of these “specialty hospitalists” offers a unique opportunity for traditional hospitalists to partner with our subspecialty colleagues in a new way, so that together we can continue to improve patient care within the hospital across multiple disciplines.
What’s Ahead?
Based on the data I recently saw while at SHM headquarters, the Big Tent philosophy is a measurable success. Membership for NPs, PAs, and administrators is growing, with nearly 200 new members in those categories combined. Incredibly, we have ED physicians joining our organization—albeit, at a number dwarfed by internists—and the relationships with the specialty hospitalists are moving forward in a meaningful way. Looking at committees and committee chairs, there is plenty of ethnic, professional, and gender diversity.
What does all of this focus outside of internal medicine and physician groups mean for us internists? Will we be left behind? Fret not. Physicians make up more than 85% of our 12,000-plus members, with internists outnumbering—by a huge number—all of the other segments of our society combined. There is no Big Tent so large that physicians, or even internists, will ever be in jeopardy. We occupy plenty of space under this Big Tent and still have lots of room to spare for our colleagues. In welcoming others, we all strengthen our own standing, by elevating the entire field.
As a terrific mentor once said, a rising tide floats all boats. And the way to raise the tide of hospital medicine can be through partnerships whose gravity is a strong pull on the hospital medicine tide, as the moon pulls the ocean’s tides.
One area in which our society plans to place more effort in expanding the Big Tent is with trainees. Students and housestaff are one of the smallest groups in our organization, with the smallest growth. Those statistics are cause for concern. The need for future hospitalist growth, both in numbers and skill set, makes attracting this segment of paramount importance, in my view.
Fortunately, SHM is developing a strategy to make our society a valuable home to trainees. I have touched on those strategies previously, including a Physicians in Training Committee, free membership for students, $100 memberships for housestaff, and our “1,000 Challenge” to recruit 1,000 students and housestaff in the coming months.
In Sum
I am a firm believer in professional and personal diversity. I am proud to work in a society that also embraces this philosophy, places real value on it, and works hard to be inclusive. So, the next time you meet an NP, PA, student, or even a hospital-based OB physician, bring them under the SHM Big Tent, and encourage them to join us in making the hospital world a better place. They, we, and our patients will be better off for it.
Dr. Howell is president of SHM, chief of the division of hospital medicine at Johns Hopkins Bayview in Baltimore, and spends a significant part of his time and research on hospital operations. Email questions or comments to [email protected].
References
- Egan ME. Global diversity and inclusion: Fostering innovation through a diverse workforce. Forbes Insights. Forbes website. Available at: http://images.forbes.com/forbesinsights/StudyPDFs/Innovation_Through_Diversity.pdf. Accessed October 23, 2013.
- Kerby S, Burns C. The top 10 economic facts of diversity in the workplace. Center for American Progress website. Available at: http://www.americanprogress.org/issues/labor/news/2012/07/12/11900/the-top-10-economic-facts-of-diversity-in-the-workplace. Accessed October 23, 2013.
I just got back from a trip to SHM headquarters in Philadelphia, and all I can say is “wow.” I was visiting there for a meeting with the staff, many SHM members and committee leaders, and the SHM board of directors. The first day we all went into a big, modern, beautiful room at SHM headquarters—there must have been more than 100 people—and we went around the room and introduced ourselves. The diversity of the staff that support our society, and the diversity of the members there, was truly breathtaking. What I saw was a microcosm of our society and our specialty.
Looking around the room, it was easy to see some aspects of our diverse organization: both genders and a variety of ethnicities and age groups were well represented. These traditional measures of diversity are critical to a healthy environment, in my opinion, and the data bear out the idea that a diverse workforce can reduce turnover and be more creative and qualified.1,2 Our diversity is not an accident. It is part of a larger, deliberate strategy by SHM to be “the home” for healthcare professionals who provide hospital-based patient care. SHM embraces diversity, whether it’s skin deep or deeply cognitive.
Although we are continually working to enrich the traditional aspects of diversity, we are also very hard at work to make SHM a place of professional diversity.
Open and Inclusive
Over the past several years, SHM has worked hard to be openly inclusive. Many of the committees and sections within the society have been developed specifically to embrace important aspects of hospital medicine that have special or common interests, characteristics, or needs. Examples include the international section, med-peds section, administrators’ committee, and the nurse practitioner and physician assistant committee. These venues allow individuals under a Big Tent to find others with similar interests or training, so that they can address unique aspects of hospital medicine as it relates directly to them. SHM’s virtual world is following our committee and section structure, which has some of the most actively growing HMXchange communities coming from the “administrators” community and the “NP/PA” community.
SHM has put its money where its mouth is, dedicating significant resources for educational programs that will help benefit professionals with a variety of backgrounds. Some are focused on the special needs of our diverse physician population, including the Academic Hospitalist Academy, the Quality and Safety Educators Academy, and the Pediatric Hospital Medicine annual meeting (through a partnership with the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association). Other events are focused specifically on helping our non-physician colleagues, like the boot camp that is presented in collaboration with the American Academy of Physician Assistants and American Association of Nurse Practitioners. The SHM Leadership Academies attract a venerable alphabet soup of professional designations, including many MDs and DOs, of course, but also increasing numbers of PAs and NPs, a growing number of administrators, and now even a few ED and OB docs! Now that’s a Big Tent.
My understanding is that these events are always popular and often sold out.
Maybe the most powerful evidence that our Big Tent philosophy is working is found in the relationships SHM has forged with other hospital-based specialties, like obstetrics, neurology, and surgery. The president of the Society of OB/GYN Hospitalists (societyofobgynhospitalists.com) has attended the SHM annual meeting and at least one of the Leadership Academies. Although “traditional” hospitalists like me may not be able to help in the OR or birthing suite, we have a lot of experience in quality improvement, leadership, and, of course, addressing the needs of a new and growing professional segment. The emergence and growth of these “specialty hospitalists” offers a unique opportunity for traditional hospitalists to partner with our subspecialty colleagues in a new way, so that together we can continue to improve patient care within the hospital across multiple disciplines.
What’s Ahead?
Based on the data I recently saw while at SHM headquarters, the Big Tent philosophy is a measurable success. Membership for NPs, PAs, and administrators is growing, with nearly 200 new members in those categories combined. Incredibly, we have ED physicians joining our organization—albeit, at a number dwarfed by internists—and the relationships with the specialty hospitalists are moving forward in a meaningful way. Looking at committees and committee chairs, there is plenty of ethnic, professional, and gender diversity.
What does all of this focus outside of internal medicine and physician groups mean for us internists? Will we be left behind? Fret not. Physicians make up more than 85% of our 12,000-plus members, with internists outnumbering—by a huge number—all of the other segments of our society combined. There is no Big Tent so large that physicians, or even internists, will ever be in jeopardy. We occupy plenty of space under this Big Tent and still have lots of room to spare for our colleagues. In welcoming others, we all strengthen our own standing, by elevating the entire field.
As a terrific mentor once said, a rising tide floats all boats. And the way to raise the tide of hospital medicine can be through partnerships whose gravity is a strong pull on the hospital medicine tide, as the moon pulls the ocean’s tides.
One area in which our society plans to place more effort in expanding the Big Tent is with trainees. Students and housestaff are one of the smallest groups in our organization, with the smallest growth. Those statistics are cause for concern. The need for future hospitalist growth, both in numbers and skill set, makes attracting this segment of paramount importance, in my view.
Fortunately, SHM is developing a strategy to make our society a valuable home to trainees. I have touched on those strategies previously, including a Physicians in Training Committee, free membership for students, $100 memberships for housestaff, and our “1,000 Challenge” to recruit 1,000 students and housestaff in the coming months.
In Sum
I am a firm believer in professional and personal diversity. I am proud to work in a society that also embraces this philosophy, places real value on it, and works hard to be inclusive. So, the next time you meet an NP, PA, student, or even a hospital-based OB physician, bring them under the SHM Big Tent, and encourage them to join us in making the hospital world a better place. They, we, and our patients will be better off for it.
Dr. Howell is president of SHM, chief of the division of hospital medicine at Johns Hopkins Bayview in Baltimore, and spends a significant part of his time and research on hospital operations. Email questions or comments to [email protected].
References
- Egan ME. Global diversity and inclusion: Fostering innovation through a diverse workforce. Forbes Insights. Forbes website. Available at: http://images.forbes.com/forbesinsights/StudyPDFs/Innovation_Through_Diversity.pdf. Accessed October 23, 2013.
- Kerby S, Burns C. The top 10 economic facts of diversity in the workplace. Center for American Progress website. Available at: http://www.americanprogress.org/issues/labor/news/2012/07/12/11900/the-top-10-economic-facts-of-diversity-in-the-workplace. Accessed October 23, 2013.
I just got back from a trip to SHM headquarters in Philadelphia, and all I can say is “wow.” I was visiting there for a meeting with the staff, many SHM members and committee leaders, and the SHM board of directors. The first day we all went into a big, modern, beautiful room at SHM headquarters—there must have been more than 100 people—and we went around the room and introduced ourselves. The diversity of the staff that support our society, and the diversity of the members there, was truly breathtaking. What I saw was a microcosm of our society and our specialty.
Looking around the room, it was easy to see some aspects of our diverse organization: both genders and a variety of ethnicities and age groups were well represented. These traditional measures of diversity are critical to a healthy environment, in my opinion, and the data bear out the idea that a diverse workforce can reduce turnover and be more creative and qualified.1,2 Our diversity is not an accident. It is part of a larger, deliberate strategy by SHM to be “the home” for healthcare professionals who provide hospital-based patient care. SHM embraces diversity, whether it’s skin deep or deeply cognitive.
Although we are continually working to enrich the traditional aspects of diversity, we are also very hard at work to make SHM a place of professional diversity.
Open and Inclusive
Over the past several years, SHM has worked hard to be openly inclusive. Many of the committees and sections within the society have been developed specifically to embrace important aspects of hospital medicine that have special or common interests, characteristics, or needs. Examples include the international section, med-peds section, administrators’ committee, and the nurse practitioner and physician assistant committee. These venues allow individuals under a Big Tent to find others with similar interests or training, so that they can address unique aspects of hospital medicine as it relates directly to them. SHM’s virtual world is following our committee and section structure, which has some of the most actively growing HMXchange communities coming from the “administrators” community and the “NP/PA” community.
SHM has put its money where its mouth is, dedicating significant resources for educational programs that will help benefit professionals with a variety of backgrounds. Some are focused on the special needs of our diverse physician population, including the Academic Hospitalist Academy, the Quality and Safety Educators Academy, and the Pediatric Hospital Medicine annual meeting (through a partnership with the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association). Other events are focused specifically on helping our non-physician colleagues, like the boot camp that is presented in collaboration with the American Academy of Physician Assistants and American Association of Nurse Practitioners. The SHM Leadership Academies attract a venerable alphabet soup of professional designations, including many MDs and DOs, of course, but also increasing numbers of PAs and NPs, a growing number of administrators, and now even a few ED and OB docs! Now that’s a Big Tent.
My understanding is that these events are always popular and often sold out.
Maybe the most powerful evidence that our Big Tent philosophy is working is found in the relationships SHM has forged with other hospital-based specialties, like obstetrics, neurology, and surgery. The president of the Society of OB/GYN Hospitalists (societyofobgynhospitalists.com) has attended the SHM annual meeting and at least one of the Leadership Academies. Although “traditional” hospitalists like me may not be able to help in the OR or birthing suite, we have a lot of experience in quality improvement, leadership, and, of course, addressing the needs of a new and growing professional segment. The emergence and growth of these “specialty hospitalists” offers a unique opportunity for traditional hospitalists to partner with our subspecialty colleagues in a new way, so that together we can continue to improve patient care within the hospital across multiple disciplines.
What’s Ahead?
Based on the data I recently saw while at SHM headquarters, the Big Tent philosophy is a measurable success. Membership for NPs, PAs, and administrators is growing, with nearly 200 new members in those categories combined. Incredibly, we have ED physicians joining our organization—albeit, at a number dwarfed by internists—and the relationships with the specialty hospitalists are moving forward in a meaningful way. Looking at committees and committee chairs, there is plenty of ethnic, professional, and gender diversity.
What does all of this focus outside of internal medicine and physician groups mean for us internists? Will we be left behind? Fret not. Physicians make up more than 85% of our 12,000-plus members, with internists outnumbering—by a huge number—all of the other segments of our society combined. There is no Big Tent so large that physicians, or even internists, will ever be in jeopardy. We occupy plenty of space under this Big Tent and still have lots of room to spare for our colleagues. In welcoming others, we all strengthen our own standing, by elevating the entire field.
As a terrific mentor once said, a rising tide floats all boats. And the way to raise the tide of hospital medicine can be through partnerships whose gravity is a strong pull on the hospital medicine tide, as the moon pulls the ocean’s tides.
One area in which our society plans to place more effort in expanding the Big Tent is with trainees. Students and housestaff are one of the smallest groups in our organization, with the smallest growth. Those statistics are cause for concern. The need for future hospitalist growth, both in numbers and skill set, makes attracting this segment of paramount importance, in my view.
Fortunately, SHM is developing a strategy to make our society a valuable home to trainees. I have touched on those strategies previously, including a Physicians in Training Committee, free membership for students, $100 memberships for housestaff, and our “1,000 Challenge” to recruit 1,000 students and housestaff in the coming months.
In Sum
I am a firm believer in professional and personal diversity. I am proud to work in a society that also embraces this philosophy, places real value on it, and works hard to be inclusive. So, the next time you meet an NP, PA, student, or even a hospital-based OB physician, bring them under the SHM Big Tent, and encourage them to join us in making the hospital world a better place. They, we, and our patients will be better off for it.
Dr. Howell is president of SHM, chief of the division of hospital medicine at Johns Hopkins Bayview in Baltimore, and spends a significant part of his time and research on hospital operations. Email questions or comments to [email protected].
References
- Egan ME. Global diversity and inclusion: Fostering innovation through a diverse workforce. Forbes Insights. Forbes website. Available at: http://images.forbes.com/forbesinsights/StudyPDFs/Innovation_Through_Diversity.pdf. Accessed October 23, 2013.
- Kerby S, Burns C. The top 10 economic facts of diversity in the workplace. Center for American Progress website. Available at: http://www.americanprogress.org/issues/labor/news/2012/07/12/11900/the-top-10-economic-facts-of-diversity-in-the-workplace. Accessed October 23, 2013.