User login
Salary, Staffing Issues Common Sticking Points Between Hospitalists, Hospital Administrators
A Rough Patch
I was the medical director of a hospitalist group in the Southeast that had been hospital-owned for eight years and grew to more than 20 full-time providers. New hospital administrators took over and, faced with staffing and compensation issues, outsourced the program. Within a year, all but one of the HMG employees (physicians, nurse practitioners, and physician assistants) resigned. As expected, the exodus put a strain on the program, patient care, and community. After a shakeup in administration, the management company pulled out. The hospital now runs the HM program. Is this occurrence just an outlier or are thes kind of situations becoming common to our field?
—Dr. Nore-grets
Dr. Hospitalist responds:
While I’m saddened at the disruption of so many lives (hospital executives, physicians, advanced practice providers, other clinical staff, and patients), I must say I’m not surprised by the outcome. Hospital medicine continues to be a rapidly growing specialty; approximately 70% of all hospitals in the U.S. have a hospitalist program. It’s only 17 years old, and as with all adolescents still finding their way, disputes are common.
Like most good stories, there are usually two sides. Hospitals have a board to satisfy, large numbers of employees (professional and non-professional), varying revenue streams to contend with, and an annual budget. There are many different groups vying for a larger slice of the pie—and the pie is only so big. No matter how we see it, some administrators believe physicians are overpaid and are not hard workers. There may not be much empathy for the docs, who work "only 182 days a year," asking for more time off, paid vacations, smaller patient loads, and more money.
Physicians see their student loans stretched out for 30 years, hospitals on building sprees, heavy patient loads, complex administrative tasks, and a lack of appreciation for the myriad intangible and non-billable services they render every day. Not being able to take a paid vacation like most workers in this country seems unfair to many. Even though most hospitalists still work 12-hour shifts, we resist being labeled "shift workers" because of the negative and non-professional inference.
It appears your hospitalist group had concerns about staffing and pay, and instead of effectively dealing with their concerns, the hospital’s administrators decided to outsource the program. While most national firms that hire hospitalists are well intentioned, they (like most hospitals) are driven by profit and sometimes bring in transient and inexperienced physicians. The eight-year-old group, while still relatively young, likely had members who had established both personal and professional relationships with many of the physicians and other clinical staff. These relationships, when built on trust, mutual respect, and competence, are the foundation of good clinical care. It is no surprise they were not able to adequately replace the clinicians who resigned.
The issues of pay and staffing are common points of contention among hospitalist and hospital administrators. The mode of compensation most often used is based on hospitalist productivity and is heavily subsidized by the hospital. While this model has served us well, the passage of the Affordable Care Act will change how healthcare systems are reimbursed. There will likely be many instances of bundled payments tied to inpatient care, but also an opportunity for hospitalists to further expand their roles into improving the quality of care and efficiency of delivery. The formation of accountable care organizations will offer even more opportunities for physician leadership and organizational assistance. The more hospitalists become imbedded in and invaluable to the hospital, the less likely we are placed on the chopping block when budget cuts happen or leadership changes (as in your case).
Until the reimbursement model changes, both groups need to understand the other’s position and use some basis for comparative analysis. I find the information from SHM surveys serves as a good basis to initiate discussion and allows for transparency. As in any negotiation, a shared sense of responsibility, goodwill, and commitment is necessary to find a just solution.
Because HM continues its rapid growth and hospitalists are in such high demand, many in the group are not tolerant of what they perceive as unfair treatment or pay. The principles of supply and demand economics are at work and have so far benefitted hospitalists well. We must balance our desire for just pay and fair staffing models with our responsibility as clinicians to care for the injured and heal the sick.
A Rough Patch
I was the medical director of a hospitalist group in the Southeast that had been hospital-owned for eight years and grew to more than 20 full-time providers. New hospital administrators took over and, faced with staffing and compensation issues, outsourced the program. Within a year, all but one of the HMG employees (physicians, nurse practitioners, and physician assistants) resigned. As expected, the exodus put a strain on the program, patient care, and community. After a shakeup in administration, the management company pulled out. The hospital now runs the HM program. Is this occurrence just an outlier or are thes kind of situations becoming common to our field?
—Dr. Nore-grets
Dr. Hospitalist responds:
While I’m saddened at the disruption of so many lives (hospital executives, physicians, advanced practice providers, other clinical staff, and patients), I must say I’m not surprised by the outcome. Hospital medicine continues to be a rapidly growing specialty; approximately 70% of all hospitals in the U.S. have a hospitalist program. It’s only 17 years old, and as with all adolescents still finding their way, disputes are common.
Like most good stories, there are usually two sides. Hospitals have a board to satisfy, large numbers of employees (professional and non-professional), varying revenue streams to contend with, and an annual budget. There are many different groups vying for a larger slice of the pie—and the pie is only so big. No matter how we see it, some administrators believe physicians are overpaid and are not hard workers. There may not be much empathy for the docs, who work "only 182 days a year," asking for more time off, paid vacations, smaller patient loads, and more money.
Physicians see their student loans stretched out for 30 years, hospitals on building sprees, heavy patient loads, complex administrative tasks, and a lack of appreciation for the myriad intangible and non-billable services they render every day. Not being able to take a paid vacation like most workers in this country seems unfair to many. Even though most hospitalists still work 12-hour shifts, we resist being labeled "shift workers" because of the negative and non-professional inference.
It appears your hospitalist group had concerns about staffing and pay, and instead of effectively dealing with their concerns, the hospital’s administrators decided to outsource the program. While most national firms that hire hospitalists are well intentioned, they (like most hospitals) are driven by profit and sometimes bring in transient and inexperienced physicians. The eight-year-old group, while still relatively young, likely had members who had established both personal and professional relationships with many of the physicians and other clinical staff. These relationships, when built on trust, mutual respect, and competence, are the foundation of good clinical care. It is no surprise they were not able to adequately replace the clinicians who resigned.
The issues of pay and staffing are common points of contention among hospitalist and hospital administrators. The mode of compensation most often used is based on hospitalist productivity and is heavily subsidized by the hospital. While this model has served us well, the passage of the Affordable Care Act will change how healthcare systems are reimbursed. There will likely be many instances of bundled payments tied to inpatient care, but also an opportunity for hospitalists to further expand their roles into improving the quality of care and efficiency of delivery. The formation of accountable care organizations will offer even more opportunities for physician leadership and organizational assistance. The more hospitalists become imbedded in and invaluable to the hospital, the less likely we are placed on the chopping block when budget cuts happen or leadership changes (as in your case).
Until the reimbursement model changes, both groups need to understand the other’s position and use some basis for comparative analysis. I find the information from SHM surveys serves as a good basis to initiate discussion and allows for transparency. As in any negotiation, a shared sense of responsibility, goodwill, and commitment is necessary to find a just solution.
Because HM continues its rapid growth and hospitalists are in such high demand, many in the group are not tolerant of what they perceive as unfair treatment or pay. The principles of supply and demand economics are at work and have so far benefitted hospitalists well. We must balance our desire for just pay and fair staffing models with our responsibility as clinicians to care for the injured and heal the sick.
A Rough Patch
I was the medical director of a hospitalist group in the Southeast that had been hospital-owned for eight years and grew to more than 20 full-time providers. New hospital administrators took over and, faced with staffing and compensation issues, outsourced the program. Within a year, all but one of the HMG employees (physicians, nurse practitioners, and physician assistants) resigned. As expected, the exodus put a strain on the program, patient care, and community. After a shakeup in administration, the management company pulled out. The hospital now runs the HM program. Is this occurrence just an outlier or are thes kind of situations becoming common to our field?
—Dr. Nore-grets
Dr. Hospitalist responds:
While I’m saddened at the disruption of so many lives (hospital executives, physicians, advanced practice providers, other clinical staff, and patients), I must say I’m not surprised by the outcome. Hospital medicine continues to be a rapidly growing specialty; approximately 70% of all hospitals in the U.S. have a hospitalist program. It’s only 17 years old, and as with all adolescents still finding their way, disputes are common.
Like most good stories, there are usually two sides. Hospitals have a board to satisfy, large numbers of employees (professional and non-professional), varying revenue streams to contend with, and an annual budget. There are many different groups vying for a larger slice of the pie—and the pie is only so big. No matter how we see it, some administrators believe physicians are overpaid and are not hard workers. There may not be much empathy for the docs, who work "only 182 days a year," asking for more time off, paid vacations, smaller patient loads, and more money.
Physicians see their student loans stretched out for 30 years, hospitals on building sprees, heavy patient loads, complex administrative tasks, and a lack of appreciation for the myriad intangible and non-billable services they render every day. Not being able to take a paid vacation like most workers in this country seems unfair to many. Even though most hospitalists still work 12-hour shifts, we resist being labeled "shift workers" because of the negative and non-professional inference.
It appears your hospitalist group had concerns about staffing and pay, and instead of effectively dealing with their concerns, the hospital’s administrators decided to outsource the program. While most national firms that hire hospitalists are well intentioned, they (like most hospitals) are driven by profit and sometimes bring in transient and inexperienced physicians. The eight-year-old group, while still relatively young, likely had members who had established both personal and professional relationships with many of the physicians and other clinical staff. These relationships, when built on trust, mutual respect, and competence, are the foundation of good clinical care. It is no surprise they were not able to adequately replace the clinicians who resigned.
The issues of pay and staffing are common points of contention among hospitalist and hospital administrators. The mode of compensation most often used is based on hospitalist productivity and is heavily subsidized by the hospital. While this model has served us well, the passage of the Affordable Care Act will change how healthcare systems are reimbursed. There will likely be many instances of bundled payments tied to inpatient care, but also an opportunity for hospitalists to further expand their roles into improving the quality of care and efficiency of delivery. The formation of accountable care organizations will offer even more opportunities for physician leadership and organizational assistance. The more hospitalists become imbedded in and invaluable to the hospital, the less likely we are placed on the chopping block when budget cuts happen or leadership changes (as in your case).
Until the reimbursement model changes, both groups need to understand the other’s position and use some basis for comparative analysis. I find the information from SHM surveys serves as a good basis to initiate discussion and allows for transparency. As in any negotiation, a shared sense of responsibility, goodwill, and commitment is necessary to find a just solution.
Because HM continues its rapid growth and hospitalists are in such high demand, many in the group are not tolerant of what they perceive as unfair treatment or pay. The principles of supply and demand economics are at work and have so far benefitted hospitalists well. We must balance our desire for just pay and fair staffing models with our responsibility as clinicians to care for the injured and heal the sick.
Four Hospitalists Retrace Path to C-Suite Executive Ranks

Dr. Steve Narang
CEO, Banner Health’s Good Samaritan Medical Center, Phoenix
Path to the C-suite: Medical school at Northwestern University; residency at Johns Hopkins; pediatric hospitalist at Children’s Hospital of New Orleans; medical director of Pediatric Hospitalists of Louisiana; master’s in healthcare management from Harvard; chief medical officer at Banner Health’s Cardon Children’s Medical Center
As a resident at Johns Hopkins in pediatrics, Dr. Narang wasn’t always pleased by what he saw—too many process errors and patient safety gaps, and too much waste. Healthcare resources were not being spent in the right way, he discovered.
“I was struck by [the fact] that we spent a lot of our resources in publishing more articles about what’s new, and what the coolest drug is,” he says. “I saw very little of that [relating to] what does this mean in terms of value?”
He became a hospitalist because he saw it as a role in which he could “really touch everything” if he chose to do so and work within the system to improve it.
“The hospital could use a partner,” he says. “One of the biggest challenges we have in healthcare is hospitals and physicians are often not working together to add value, and they’re subtracting from value, and they’re competing with each other.”
If doctors make the effort to learn the management aspects of working in a hospital, they can put themselves in a great position to take on big leadership roles, Dr. Narang says. He says hospitals are seeing the value in having physicians in those roles.
“If you can find the right leader and it happens to be a physician, if it happens to be a physician who can speak that language—and find a sweet spot for independent physicians, employed physicians, and hospitalists to deliver value, which we have to now I think it’s the best way to go,” he says. “I think you’re going to see a trend moving forward to this as more physicians become more interested in this track.” —TC
Being a hospitalist was a key strength of my background. Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
—Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix

Dr. Brian Harte
President, South Pointe Hospital, Warrenville Heights, Ohio
Path to the C-suite: Resident at University of California San Francisco; private practice hospitalist in Marin County, near San Francisco; hospitalist at Cleveland Clinic; program director of hospital medicine at Cleveland Clinic’s Euclid Hospital; chief operating officer at Cleveland Clinic’s Hillcrest Hospital For about two hours a day, Dr. Harte makes his way through South Pointe Hospital—to see and to be seen. Before he started doing this as president of the hospital, he underestimated how important it was to stay visible to everyone—nurses, doctors, housekeeping, and so on.
“The impression that makes surprised me,” he says.
He’ll ask what people need to do their jobs better. He’ll also pop into patients’ rooms, introduce himself, and ask how their experiences have been. Then he takes that feedback and incorporates it into his planning.
Dr. Harte says he likes to have an “open and transparent” relationship with physicians and lists his credibility, both as a physician and a person, as a top attribute for a leader. For those embarking on leadership roles in a hospital, he says it’s a must to have a “strong mentor that you can go to.”
He also says a supportive environment is critical.
“You must work in an organization that is a resource to help you succeed, because when you move out of the purely clinical or clinical administrative jobs like division chair, department chair, program director, even CMO or VPMA [vice president of medical affairs], those are doctor jobs,” he says. “When you really become a doctor doing administrative work, unless it’s in your background and in your skill set, I think it’s important to work in an organization that is going to support you in your continued growth.
“Because these are jobs that I think you grow into.” —TC
I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment. You have pockets of enormous expertise that sometimes function like silos. Being a hospitalist actually trains you well for those things.
—Brian Harte, MD, SFHM, president, South Pointe Hospital, Warrenville Heights, Ohio, SHM board member

Dr. Nasim Afsar
Associate Chief Medical Officer, UCLA Hospitals, Los Angeles
Path to the C-suite: Residency at UCLA; advanced training program in quality improvement at Intermountain Healthcare Dr. Afsar wasn’t aiming for a top administrative job in a hospital. But, during her time spent working as a hospitalist, she started noticing trouble within the system. Eventually, she wanted to try to solve problems in a way that would have a ripple effect. Inspired, she ventured into quality improvement.
“I’m very passionate about helping the patient in front of me, whether it’s helping them get better or helping them during a really challenging time of their life,” she says. “But there’s something about feeling that the improvements that you make will not just impact the person in front of you, but the thousands of patients that come after them.”
Part of her job is instilling in other healthcare providers the sense that they themselves are agents of change. One big difference in her administrative job and clinical work is how to gauge success.
“The job is a lot harder than it seems. In our clinical world, I know what constitutes a good job. I know that when I’m on service, I get up early in the morning, I come in, I pre-round on my patients extensively, I read up on a couple of different things, I go out onto the wards with my team,” she explains. “This type of leadership role, I think, is more challenging. Initiatives that you do to improve care in one area could have detrimental or challenging impacts on another set of stakeholders or care area. You’re constantly navigating the system.” —TC
By nature when you’re a hospitalist, you are a problem solver. You don’t shy away from problems that you don’t understand.
—Nasim Afsar, MD, SFHM, associate chief medical officer, UCLA Hospitals, Los Angeles, SHM board member

Dr. Patrick Torcson
Chief Integration Officer, St. Tammany Parish Hospital, Covington, La.
Path to the C-Suite: Residency at Ochsner Clinic in New Orleans; private internist; director of hospital medicine at St. Tammany Parish Hospital Dr. Torcson recently became his hospital’s first chief integration officer, a job in which he promotes clinical quality and service quality using information technology.
But it was never about a promotion, he says.
“It’s really been more about just trying to provide quality care and make contributions to fixing a broken healthcare system,” he says. “Staying focused on that personal journey has really brought me to where I am.”
A good leader within a hospital is a “systems-level thinker,” not one focusing on a specific agenda. And, prioritizing important items is crucial to success, he notes.
“We all have a limited amount of energy. If you can pick three to five things that are really important and prioritize them and they turn out to be important, that’s going to facilitate your success,” he says.
He can’t emphasize “clinical credibility” enough. That’s where it all begins, he says.
“Your leadership is facilitated if you’re seen as someone that takes good care of your patients,” being the doctor that other doctors would want themselves and their families to go to. “That’s huge.”
Also, he says, running out and getting a master’s degree in business management and then applying for positions around the country is probably not the best approach to seeking out leadership positions, he says.
“I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something,” he points out. “Leadership is home-grown, and you work your way up.” —TC
I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something. Leadership is home-grown, and you work your way up.
—Patrick Torcson, MD, MMM, FACP, SFHM, vice president and chief integration officer, St. Tammany Parish Hospital, Covington, La., SHM board member

Dr. Steve Narang
CEO, Banner Health’s Good Samaritan Medical Center, Phoenix
Path to the C-suite: Medical school at Northwestern University; residency at Johns Hopkins; pediatric hospitalist at Children’s Hospital of New Orleans; medical director of Pediatric Hospitalists of Louisiana; master’s in healthcare management from Harvard; chief medical officer at Banner Health’s Cardon Children’s Medical Center
As a resident at Johns Hopkins in pediatrics, Dr. Narang wasn’t always pleased by what he saw—too many process errors and patient safety gaps, and too much waste. Healthcare resources were not being spent in the right way, he discovered.
“I was struck by [the fact] that we spent a lot of our resources in publishing more articles about what’s new, and what the coolest drug is,” he says. “I saw very little of that [relating to] what does this mean in terms of value?”
He became a hospitalist because he saw it as a role in which he could “really touch everything” if he chose to do so and work within the system to improve it.
“The hospital could use a partner,” he says. “One of the biggest challenges we have in healthcare is hospitals and physicians are often not working together to add value, and they’re subtracting from value, and they’re competing with each other.”
If doctors make the effort to learn the management aspects of working in a hospital, they can put themselves in a great position to take on big leadership roles, Dr. Narang says. He says hospitals are seeing the value in having physicians in those roles.
“If you can find the right leader and it happens to be a physician, if it happens to be a physician who can speak that language—and find a sweet spot for independent physicians, employed physicians, and hospitalists to deliver value, which we have to now I think it’s the best way to go,” he says. “I think you’re going to see a trend moving forward to this as more physicians become more interested in this track.” —TC
Being a hospitalist was a key strength of my background. Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
—Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix

Dr. Brian Harte
President, South Pointe Hospital, Warrenville Heights, Ohio
Path to the C-suite: Resident at University of California San Francisco; private practice hospitalist in Marin County, near San Francisco; hospitalist at Cleveland Clinic; program director of hospital medicine at Cleveland Clinic’s Euclid Hospital; chief operating officer at Cleveland Clinic’s Hillcrest Hospital For about two hours a day, Dr. Harte makes his way through South Pointe Hospital—to see and to be seen. Before he started doing this as president of the hospital, he underestimated how important it was to stay visible to everyone—nurses, doctors, housekeeping, and so on.
“The impression that makes surprised me,” he says.
He’ll ask what people need to do their jobs better. He’ll also pop into patients’ rooms, introduce himself, and ask how their experiences have been. Then he takes that feedback and incorporates it into his planning.
Dr. Harte says he likes to have an “open and transparent” relationship with physicians and lists his credibility, both as a physician and a person, as a top attribute for a leader. For those embarking on leadership roles in a hospital, he says it’s a must to have a “strong mentor that you can go to.”
He also says a supportive environment is critical.
“You must work in an organization that is a resource to help you succeed, because when you move out of the purely clinical or clinical administrative jobs like division chair, department chair, program director, even CMO or VPMA [vice president of medical affairs], those are doctor jobs,” he says. “When you really become a doctor doing administrative work, unless it’s in your background and in your skill set, I think it’s important to work in an organization that is going to support you in your continued growth.
“Because these are jobs that I think you grow into.” —TC
I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment. You have pockets of enormous expertise that sometimes function like silos. Being a hospitalist actually trains you well for those things.
—Brian Harte, MD, SFHM, president, South Pointe Hospital, Warrenville Heights, Ohio, SHM board member

Dr. Nasim Afsar
Associate Chief Medical Officer, UCLA Hospitals, Los Angeles
Path to the C-suite: Residency at UCLA; advanced training program in quality improvement at Intermountain Healthcare Dr. Afsar wasn’t aiming for a top administrative job in a hospital. But, during her time spent working as a hospitalist, she started noticing trouble within the system. Eventually, she wanted to try to solve problems in a way that would have a ripple effect. Inspired, she ventured into quality improvement.
“I’m very passionate about helping the patient in front of me, whether it’s helping them get better or helping them during a really challenging time of their life,” she says. “But there’s something about feeling that the improvements that you make will not just impact the person in front of you, but the thousands of patients that come after them.”
Part of her job is instilling in other healthcare providers the sense that they themselves are agents of change. One big difference in her administrative job and clinical work is how to gauge success.
“The job is a lot harder than it seems. In our clinical world, I know what constitutes a good job. I know that when I’m on service, I get up early in the morning, I come in, I pre-round on my patients extensively, I read up on a couple of different things, I go out onto the wards with my team,” she explains. “This type of leadership role, I think, is more challenging. Initiatives that you do to improve care in one area could have detrimental or challenging impacts on another set of stakeholders or care area. You’re constantly navigating the system.” —TC
By nature when you’re a hospitalist, you are a problem solver. You don’t shy away from problems that you don’t understand.
—Nasim Afsar, MD, SFHM, associate chief medical officer, UCLA Hospitals, Los Angeles, SHM board member

Dr. Patrick Torcson
Chief Integration Officer, St. Tammany Parish Hospital, Covington, La.
Path to the C-Suite: Residency at Ochsner Clinic in New Orleans; private internist; director of hospital medicine at St. Tammany Parish Hospital Dr. Torcson recently became his hospital’s first chief integration officer, a job in which he promotes clinical quality and service quality using information technology.
But it was never about a promotion, he says.
“It’s really been more about just trying to provide quality care and make contributions to fixing a broken healthcare system,” he says. “Staying focused on that personal journey has really brought me to where I am.”
A good leader within a hospital is a “systems-level thinker,” not one focusing on a specific agenda. And, prioritizing important items is crucial to success, he notes.
“We all have a limited amount of energy. If you can pick three to five things that are really important and prioritize them and they turn out to be important, that’s going to facilitate your success,” he says.
He can’t emphasize “clinical credibility” enough. That’s where it all begins, he says.
“Your leadership is facilitated if you’re seen as someone that takes good care of your patients,” being the doctor that other doctors would want themselves and their families to go to. “That’s huge.”
Also, he says, running out and getting a master’s degree in business management and then applying for positions around the country is probably not the best approach to seeking out leadership positions, he says.
“I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something,” he points out. “Leadership is home-grown, and you work your way up.” —TC
I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something. Leadership is home-grown, and you work your way up.
—Patrick Torcson, MD, MMM, FACP, SFHM, vice president and chief integration officer, St. Tammany Parish Hospital, Covington, La., SHM board member

Dr. Steve Narang
CEO, Banner Health’s Good Samaritan Medical Center, Phoenix
Path to the C-suite: Medical school at Northwestern University; residency at Johns Hopkins; pediatric hospitalist at Children’s Hospital of New Orleans; medical director of Pediatric Hospitalists of Louisiana; master’s in healthcare management from Harvard; chief medical officer at Banner Health’s Cardon Children’s Medical Center
As a resident at Johns Hopkins in pediatrics, Dr. Narang wasn’t always pleased by what he saw—too many process errors and patient safety gaps, and too much waste. Healthcare resources were not being spent in the right way, he discovered.
“I was struck by [the fact] that we spent a lot of our resources in publishing more articles about what’s new, and what the coolest drug is,” he says. “I saw very little of that [relating to] what does this mean in terms of value?”
He became a hospitalist because he saw it as a role in which he could “really touch everything” if he chose to do so and work within the system to improve it.
“The hospital could use a partner,” he says. “One of the biggest challenges we have in healthcare is hospitals and physicians are often not working together to add value, and they’re subtracting from value, and they’re competing with each other.”
If doctors make the effort to learn the management aspects of working in a hospital, they can put themselves in a great position to take on big leadership roles, Dr. Narang says. He says hospitals are seeing the value in having physicians in those roles.
“If you can find the right leader and it happens to be a physician, if it happens to be a physician who can speak that language—and find a sweet spot for independent physicians, employed physicians, and hospitalists to deliver value, which we have to now I think it’s the best way to go,” he says. “I think you’re going to see a trend moving forward to this as more physicians become more interested in this track.” —TC
Being a hospitalist was a key strength of my background. Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
—Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix

Dr. Brian Harte
President, South Pointe Hospital, Warrenville Heights, Ohio
Path to the C-suite: Resident at University of California San Francisco; private practice hospitalist in Marin County, near San Francisco; hospitalist at Cleveland Clinic; program director of hospital medicine at Cleveland Clinic’s Euclid Hospital; chief operating officer at Cleveland Clinic’s Hillcrest Hospital For about two hours a day, Dr. Harte makes his way through South Pointe Hospital—to see and to be seen. Before he started doing this as president of the hospital, he underestimated how important it was to stay visible to everyone—nurses, doctors, housekeeping, and so on.
“The impression that makes surprised me,” he says.
He’ll ask what people need to do their jobs better. He’ll also pop into patients’ rooms, introduce himself, and ask how their experiences have been. Then he takes that feedback and incorporates it into his planning.
Dr. Harte says he likes to have an “open and transparent” relationship with physicians and lists his credibility, both as a physician and a person, as a top attribute for a leader. For those embarking on leadership roles in a hospital, he says it’s a must to have a “strong mentor that you can go to.”
He also says a supportive environment is critical.
“You must work in an organization that is a resource to help you succeed, because when you move out of the purely clinical or clinical administrative jobs like division chair, department chair, program director, even CMO or VPMA [vice president of medical affairs], those are doctor jobs,” he says. “When you really become a doctor doing administrative work, unless it’s in your background and in your skill set, I think it’s important to work in an organization that is going to support you in your continued growth.
“Because these are jobs that I think you grow into.” —TC
I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment. You have pockets of enormous expertise that sometimes function like silos. Being a hospitalist actually trains you well for those things.
—Brian Harte, MD, SFHM, president, South Pointe Hospital, Warrenville Heights, Ohio, SHM board member

Dr. Nasim Afsar
Associate Chief Medical Officer, UCLA Hospitals, Los Angeles
Path to the C-suite: Residency at UCLA; advanced training program in quality improvement at Intermountain Healthcare Dr. Afsar wasn’t aiming for a top administrative job in a hospital. But, during her time spent working as a hospitalist, she started noticing trouble within the system. Eventually, she wanted to try to solve problems in a way that would have a ripple effect. Inspired, she ventured into quality improvement.
“I’m very passionate about helping the patient in front of me, whether it’s helping them get better or helping them during a really challenging time of their life,” she says. “But there’s something about feeling that the improvements that you make will not just impact the person in front of you, but the thousands of patients that come after them.”
Part of her job is instilling in other healthcare providers the sense that they themselves are agents of change. One big difference in her administrative job and clinical work is how to gauge success.
“The job is a lot harder than it seems. In our clinical world, I know what constitutes a good job. I know that when I’m on service, I get up early in the morning, I come in, I pre-round on my patients extensively, I read up on a couple of different things, I go out onto the wards with my team,” she explains. “This type of leadership role, I think, is more challenging. Initiatives that you do to improve care in one area could have detrimental or challenging impacts on another set of stakeholders or care area. You’re constantly navigating the system.” —TC
By nature when you’re a hospitalist, you are a problem solver. You don’t shy away from problems that you don’t understand.
—Nasim Afsar, MD, SFHM, associate chief medical officer, UCLA Hospitals, Los Angeles, SHM board member

Dr. Patrick Torcson
Chief Integration Officer, St. Tammany Parish Hospital, Covington, La.
Path to the C-Suite: Residency at Ochsner Clinic in New Orleans; private internist; director of hospital medicine at St. Tammany Parish Hospital Dr. Torcson recently became his hospital’s first chief integration officer, a job in which he promotes clinical quality and service quality using information technology.
But it was never about a promotion, he says.
“It’s really been more about just trying to provide quality care and make contributions to fixing a broken healthcare system,” he says. “Staying focused on that personal journey has really brought me to where I am.”
A good leader within a hospital is a “systems-level thinker,” not one focusing on a specific agenda. And, prioritizing important items is crucial to success, he notes.
“We all have a limited amount of energy. If you can pick three to five things that are really important and prioritize them and they turn out to be important, that’s going to facilitate your success,” he says.
He can’t emphasize “clinical credibility” enough. That’s where it all begins, he says.
“Your leadership is facilitated if you’re seen as someone that takes good care of your patients,” being the doctor that other doctors would want themselves and their families to go to. “That’s huge.”
Also, he says, running out and getting a master’s degree in business management and then applying for positions around the country is probably not the best approach to seeking out leadership positions, he says.
“I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something,” he points out. “Leadership is home-grown, and you work your way up.” —TC
I don’t think many people are put in a position where you’re just asked to pull a sword out of a stone and you’re suddenly chief of something. Leadership is home-grown, and you work your way up.
—Patrick Torcson, MD, MMM, FACP, SFHM, vice president and chief integration officer, St. Tammany Parish Hospital, Covington, La., SHM board member
Hospital Medicine Group Leaders Need Not Work Clinical Shifts to Achieve Respect
Hospitalist Group Leaders Need Not Work Clinical Shifts to Achieve Respect
The “Survey Insights” article by Dr. Rachel Lovins (“Physician Practice Leaders,” November 2013) makes excellent points about the importance of leadership in hospital medicine groups but perpetuates a fallacy that undercuts the effectiveness of physician leaders. Dr. Lovins states that hospitalist leaders need to work as clinical hospitalists to achieve respect. Consider the example of professional sports, where athletes are highly skilled and earn more than doctors, but the concept of a player/coach has essentially disappeared. The difference is that athletes understand that they are playing on a team that needs a cohesive vision to succeed. They value the insights of a coach who can watch their performance from the sidelines and help them improve, even though that person’s own playing skills may have been undistinguished.
Dr. Lovins states that hospitalist leaders need to experience firsthand the frustrations of hospital practice. Would it not be better to replace anecdotal evidence with systematic communication and analysis of experiences from the entire group? The demand by physicians that their leaders be active clinicians is really a way to ensure that those individuals are unable to secure the time and perspective needed to become effective coaches, and it encroaches upon the autonomy of the individuals.
HM cannot achieve its potential until it develops leaders who can move beyond the level of chief resident and engage meaningfully with the concerns of senior hospital leaders to drive the performance of their teams. Hospitalists must understand that they are part of an organization that will be led by persons with different skill sets than those required to diagnose and treat disease.
—Richard Rohr, MD, SFHM, team leader, United Health Group, Broomall, Pa.
Hospitalist Group Leaders Need Not Work Clinical Shifts to Achieve Respect
The “Survey Insights” article by Dr. Rachel Lovins (“Physician Practice Leaders,” November 2013) makes excellent points about the importance of leadership in hospital medicine groups but perpetuates a fallacy that undercuts the effectiveness of physician leaders. Dr. Lovins states that hospitalist leaders need to work as clinical hospitalists to achieve respect. Consider the example of professional sports, where athletes are highly skilled and earn more than doctors, but the concept of a player/coach has essentially disappeared. The difference is that athletes understand that they are playing on a team that needs a cohesive vision to succeed. They value the insights of a coach who can watch their performance from the sidelines and help them improve, even though that person’s own playing skills may have been undistinguished.
Dr. Lovins states that hospitalist leaders need to experience firsthand the frustrations of hospital practice. Would it not be better to replace anecdotal evidence with systematic communication and analysis of experiences from the entire group? The demand by physicians that their leaders be active clinicians is really a way to ensure that those individuals are unable to secure the time and perspective needed to become effective coaches, and it encroaches upon the autonomy of the individuals.
HM cannot achieve its potential until it develops leaders who can move beyond the level of chief resident and engage meaningfully with the concerns of senior hospital leaders to drive the performance of their teams. Hospitalists must understand that they are part of an organization that will be led by persons with different skill sets than those required to diagnose and treat disease.
—Richard Rohr, MD, SFHM, team leader, United Health Group, Broomall, Pa.
Hospitalist Group Leaders Need Not Work Clinical Shifts to Achieve Respect
The “Survey Insights” article by Dr. Rachel Lovins (“Physician Practice Leaders,” November 2013) makes excellent points about the importance of leadership in hospital medicine groups but perpetuates a fallacy that undercuts the effectiveness of physician leaders. Dr. Lovins states that hospitalist leaders need to work as clinical hospitalists to achieve respect. Consider the example of professional sports, where athletes are highly skilled and earn more than doctors, but the concept of a player/coach has essentially disappeared. The difference is that athletes understand that they are playing on a team that needs a cohesive vision to succeed. They value the insights of a coach who can watch their performance from the sidelines and help them improve, even though that person’s own playing skills may have been undistinguished.
Dr. Lovins states that hospitalist leaders need to experience firsthand the frustrations of hospital practice. Would it not be better to replace anecdotal evidence with systematic communication and analysis of experiences from the entire group? The demand by physicians that their leaders be active clinicians is really a way to ensure that those individuals are unable to secure the time and perspective needed to become effective coaches, and it encroaches upon the autonomy of the individuals.
HM cannot achieve its potential until it develops leaders who can move beyond the level of chief resident and engage meaningfully with the concerns of senior hospital leaders to drive the performance of their teams. Hospitalists must understand that they are part of an organization that will be led by persons with different skill sets than those required to diagnose and treat disease.
—Richard Rohr, MD, SFHM, team leader, United Health Group, Broomall, Pa.
Hospitalists’ Skill Sets, Work Experience Perfect for Hospitals' C-Suite Positions
Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix, was attending a leadership summit where all of Banner’s top officials were gathered. It was his third day in his new job.
Banner’s President, Peter Fine, gave a presentation in the future of healthcare and asked for questions. Dr. Narang stepped up to the microphone, asked a question, and made remarks about how the organization needed to ready itself for the changing landscape. Kathy Bollinger, president of the Arizona West Region of Banner, was struck by those remarks. Less than two years later, she made Dr. Narang the CEO at Arizona’s largest teaching hospital, Good Samaritan Medical Center.
His hospitalist background was an important ingredient in the kind of leader Dr. Narang has become, she says.
“The correlation is that hospitalists are leading teams; they are quarterbacking care,” Bollinger adds. “A good hospitalist brings the team together.”
Physicians with a background in hospital medicine are no strangers to C-suite level positions at hospitals. In April, Brian Harte, MD, SFHM, was named president of South Pointe Hospital in Warrenville Heights, Ohio, a center within the Cleveland Clinic system. In January, Patrick Cawley, MD, MBA, MHM, a former SHM president, was named CEO at the Medical University of South Carolina Medical Center in Charleston.
Other recent C-suite arrivals include Nasim Afsar, MD, SFHM, an SHM board member who is associate CMO at UCLA Hospitals in Los Angeles, and Patrick Torcson, MD, MMM, FACP, SFHM, another SHM board member, vice president, and chief integration officer at St. Tammany Parish Hospital in Covington, La.
Although their paths to the C-suite have differed, each agrees that their experience in hospital medicine gave them the knowledge of the system that was required to begin an ascent to the highest levels of leadership. Just as important, or maybe more so, their exposure to the inner workings of a hospital awakened within them a desire to see the system function better. And the necessity of working with all types of healthcare providers within the complicated hospital setting helped them recognize—or at least get others to recognize—their potential for leadership, and helped hone the teamwork skills that are vital in top administrative roles.
They also say that, when they were starting out, they never aspired to high leadership positions. Rather, it was simply following their own interests that ultimately led them there.
By the time Dr. Narang stepped up to the microphone that day in Phoenix, he had more than a dozen years under his belt working as a hospitalist for a children’s hospital and as part of a group that created a pediatric hospitalist company in Louisiana.
And that work helped lay the foundation for him, he says.
“Being a hospitalist was a key strength of my background,” Dr. Narang explains. “Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
“At the end of the day, it’s about leadership. And I learned that from day one as a hospitalist.”
His confidence and sense of the big picture were not lost on Bollinger that day at the leadership summit.
“I thought that took a fair amount of courage,” she says, “on Day 3, to stand up to the mic and have [a] specific conversation with the president of the company. In my mind, he was very enlightened. His comments were very enlightened.”
Firm Foundation
Robert Zipper, MD, MMM, SFHM, chair of SHM’s Leadership Committee, and CMO of Sound Physicians’ West Region, says it’s probably not realistic for a hospitalist to vault up immediately to a chief executive officer position. Pursuing lower-level leadership roles would be a good starting point for hospitalists with C-suite aspirations, he says.
“For those just starting out, I would recommend that they seek out opportunities to lead or be a part of managing change in their hospitals. The right opportunities should feel like a bit of a stretch, but not overwhelming. This might be work in quality, medical staff leadership, etc.,” Dr. Zipper says.
For hospitalists with leadership experience, CMO and vice president of medical affairs have the closest translation, he adds. He also says jobs like chief informatics officer and roles in quality improvement are highly suitable for hospitalists.
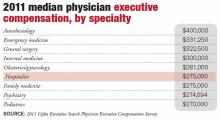
According to the 2011 Cejka Executive Search Physician Executive Compensation Survey, a survey of the American College of Physician Executives’ membership of physicians in management, the median salary of physicians in CEO positions was $393,152. That figure was $343,334 for CMO and $307,500 for chief quality and patient safety officer. The median for all physician executive positions was $305,000. Compensation was typically higher in academic medical centers and lower for hospitals and multi-specialty groups.
Hospitalists in executive positions had a 2011 median income of $275,000, according to the survey.
The survey also showed a wide range of compensation, typically dependent on the size of the institution. Some hospitalist leaders with more than 75% of their full-time-equivalent hours worked clinically “might actually take a small pay cut to make a move,” Dr. Zipper says.
Natural Progression
The hospitalist executives interviewed, for the most part, were emphatic that C-suite level leadership was not something that they imagined for themselves when they began their medical careers.
“In 2007, I could never imagine doing anything less than 100 percent clinical hospitalist work,” UCLA Hospitals’ Dr. Afsar says. “But once I started working and doing my hospitalist job day in and day out, I realized that there were many aspects of our care where I knew we could do better.”
Dr. Harte, president of South Pointe Hospital in Cleveland, says he never really thought about hospital administration as a career ambition. But, “opportunities presented themselves.”
Dr. Torcson says he was so firmly disinterested in administrative positions that when he was asked to join the Medical Executive Committee at his hospital, his first thought was “no way … I’m a doctor, not an administrator.” But after talking to some senior colleagues about it, they reminded him that he was basically obliged to say “yes.” And it ended up being a crucial component in his ascent through the ranks.
Dr. Narang imagined having a career that impacted value fairly early on, after making observations during his pediatric residency. But even he was surprised when he got the call to be CEO, after less than two years on the job.
Now, in retrospect, they all see their years working as a rank-and-file hospitalist as formative.
As a leader in a hospital, you have to be good at recruiting physicians, retaining them and developing them professionally, Dr. Harte says. That requires having clinical credibility, being a decent mentor, being a good role model, and “wearing your integrity on your sleeve.”
“I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment,” Dr. Harte notes. “You have pockets of enormous expertise that sometimes function like silos.
“Being a hospitalist actually trains you well for those things. By nature of what we do, we tend to be folks who do multi-disciplinary rounds. We can sit around a table or walk rounds with nurses, case managers, physical therapists, respiratory therapists, and the like, and actually develop a plan of care that recognizes the expertise of the other individuals within that group. That is a very good incubator for that kind of thinking.”
Hospital leaders also have to know how everything works together within the hospital.
“Hospital medicine has this overlap with that domain as it is,” Dr. Harte continues. “We work in hospitals. It is not such a stretch then, to think that we could be running a hospital.”
Golden Opportunity
Dr. Torcson says the opportunities to lead in the hospital setting abound. A former internist, he says hospitalists are primed to “improve quality and service at the hospital level because of the system-based approach to hospital care.”
Dealing with incomplete information and uncertainty are important challenges for hospital leaders, something Dr. Afsar says are daily hurdles for hospitalists.
“By nature when you’re a hospitalist, you are a problem solver,” she says. “You don’t shy away from problems that you don’t understand.”
That problem-solver outlook is what prompted Neil Martin, MD, chief of neurosurgery at UCLA, to ask Dr. Afsar to join a quality improvement program within the department—first as a participant and then as its leader.
“She was always one of the most active and vocal and solution-oriented people on the committees that I was participating in,” Dr. Martin says. “She was not the kind of person who would describe all of the problems and leave it at that. But, rather, [she] would help identify problems and then propose solutions and then help follow through to implement solutions.”
Hospitalist C-suiters describe days dominated by meetings with executive teams, staff, and individual physicians or groups. Meetings are a necessity, as executives are tasked with crafting a vision, constantly assessing progress, and refining the approach when necessary.
Continuing at least some clinical work is important, Dr. Harte says. It depends on the organization, but he says he sees benefits that help him in his administrative duties.
“It changes the dynamic of the interaction with some of the naysayers on the medical staff,” he says. “That’s still something that I enjoy doing. I think it’s important for me, it’s important for the credibility of my job, and particularly for the organization that I work at.”
A lot of C-suiters sought out formal training in administrative areas—though not necessarily an MBA—once they realized they had an interest in administration.
Dr. Torcson says getting a master’s in medical management degree was “absolutely invaluable.”
“It was obvious to me that I had some needs to develop some additional competencies and capabilities, a different skill set than I gained in medical school and residency,” he says. “The same skill set that makes one a successful or quality physician isn’t necessarily the same skill set that you need to be an effective manager or administrator.”
Dr. Afsar completed an advanced quality improvement training program at Intermountain Healthcare, and Dr. Narang received a master’s in healthcare management from Harvard.
Dr. Harte, who does not have an advanced management degree, says that at some institutions, such as Cleveland Clinic, you can learn on the job the non-clinical areas needed to be a top leader in a hospital, including finance and strategy.
Dr. Zipper says a related degree can be a big leg up.
“If one is specifically looking to enter the C-suite, an advanced business or management degree will make that barrier a lot lower,” he says. Whether that degree is a master’s in business administration, healthcare administration, medical management, or a similar degree doesn’t seem to matter much, he adds.
When she was looking for a new CEO for Good Samaritan Medical Center, Bollinger says that she preferred to hire a physician. That candidate, she says, had to have certain leadership qualities, including the ability to create a suitable vision, curiosity, an “executive presence,” and a “tolerance of ambiguity.”
As it turns out, the value of having a physician CEO has been “probably three times what I anticipated,” she says.
If you’re a hospitalist and have an interest in rising up the leadership ladder, getting involved and getting exposure to areas of interest is where it begins.
“I would say go for it,” Dr. Afsar says. “Raising your hand and being willing to take on responsibility are kind of the first steps in getting involved. I think it’s just as much making sure that you’re the right fit for that type of work, as it is to excel and do well. Not everyone, I think, will thrive and enjoy this type of work. So I think having the opportunity to get exposed to it and see if it’s something that you enjoy is a critical piece.”
Tom Collins is a freelance writer in Florida.
Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix, was attending a leadership summit where all of Banner’s top officials were gathered. It was his third day in his new job.
Banner’s President, Peter Fine, gave a presentation in the future of healthcare and asked for questions. Dr. Narang stepped up to the microphone, asked a question, and made remarks about how the organization needed to ready itself for the changing landscape. Kathy Bollinger, president of the Arizona West Region of Banner, was struck by those remarks. Less than two years later, she made Dr. Narang the CEO at Arizona’s largest teaching hospital, Good Samaritan Medical Center.
His hospitalist background was an important ingredient in the kind of leader Dr. Narang has become, she says.
“The correlation is that hospitalists are leading teams; they are quarterbacking care,” Bollinger adds. “A good hospitalist brings the team together.”
Physicians with a background in hospital medicine are no strangers to C-suite level positions at hospitals. In April, Brian Harte, MD, SFHM, was named president of South Pointe Hospital in Warrenville Heights, Ohio, a center within the Cleveland Clinic system. In January, Patrick Cawley, MD, MBA, MHM, a former SHM president, was named CEO at the Medical University of South Carolina Medical Center in Charleston.
Other recent C-suite arrivals include Nasim Afsar, MD, SFHM, an SHM board member who is associate CMO at UCLA Hospitals in Los Angeles, and Patrick Torcson, MD, MMM, FACP, SFHM, another SHM board member, vice president, and chief integration officer at St. Tammany Parish Hospital in Covington, La.
Although their paths to the C-suite have differed, each agrees that their experience in hospital medicine gave them the knowledge of the system that was required to begin an ascent to the highest levels of leadership. Just as important, or maybe more so, their exposure to the inner workings of a hospital awakened within them a desire to see the system function better. And the necessity of working with all types of healthcare providers within the complicated hospital setting helped them recognize—or at least get others to recognize—their potential for leadership, and helped hone the teamwork skills that are vital in top administrative roles.
They also say that, when they were starting out, they never aspired to high leadership positions. Rather, it was simply following their own interests that ultimately led them there.
By the time Dr. Narang stepped up to the microphone that day in Phoenix, he had more than a dozen years under his belt working as a hospitalist for a children’s hospital and as part of a group that created a pediatric hospitalist company in Louisiana.
And that work helped lay the foundation for him, he says.
“Being a hospitalist was a key strength of my background,” Dr. Narang explains. “Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
“At the end of the day, it’s about leadership. And I learned that from day one as a hospitalist.”
His confidence and sense of the big picture were not lost on Bollinger that day at the leadership summit.
“I thought that took a fair amount of courage,” she says, “on Day 3, to stand up to the mic and have [a] specific conversation with the president of the company. In my mind, he was very enlightened. His comments were very enlightened.”
Firm Foundation
Robert Zipper, MD, MMM, SFHM, chair of SHM’s Leadership Committee, and CMO of Sound Physicians’ West Region, says it’s probably not realistic for a hospitalist to vault up immediately to a chief executive officer position. Pursuing lower-level leadership roles would be a good starting point for hospitalists with C-suite aspirations, he says.
“For those just starting out, I would recommend that they seek out opportunities to lead or be a part of managing change in their hospitals. The right opportunities should feel like a bit of a stretch, but not overwhelming. This might be work in quality, medical staff leadership, etc.,” Dr. Zipper says.
For hospitalists with leadership experience, CMO and vice president of medical affairs have the closest translation, he adds. He also says jobs like chief informatics officer and roles in quality improvement are highly suitable for hospitalists.
According to the 2011 Cejka Executive Search Physician Executive Compensation Survey, a survey of the American College of Physician Executives’ membership of physicians in management, the median salary of physicians in CEO positions was $393,152. That figure was $343,334 for CMO and $307,500 for chief quality and patient safety officer. The median for all physician executive positions was $305,000. Compensation was typically higher in academic medical centers and lower for hospitals and multi-specialty groups.
Hospitalists in executive positions had a 2011 median income of $275,000, according to the survey.
The survey also showed a wide range of compensation, typically dependent on the size of the institution. Some hospitalist leaders with more than 75% of their full-time-equivalent hours worked clinically “might actually take a small pay cut to make a move,” Dr. Zipper says.
Natural Progression
The hospitalist executives interviewed, for the most part, were emphatic that C-suite level leadership was not something that they imagined for themselves when they began their medical careers.
“In 2007, I could never imagine doing anything less than 100 percent clinical hospitalist work,” UCLA Hospitals’ Dr. Afsar says. “But once I started working and doing my hospitalist job day in and day out, I realized that there were many aspects of our care where I knew we could do better.”
Dr. Harte, president of South Pointe Hospital in Cleveland, says he never really thought about hospital administration as a career ambition. But, “opportunities presented themselves.”
Dr. Torcson says he was so firmly disinterested in administrative positions that when he was asked to join the Medical Executive Committee at his hospital, his first thought was “no way … I’m a doctor, not an administrator.” But after talking to some senior colleagues about it, they reminded him that he was basically obliged to say “yes.” And it ended up being a crucial component in his ascent through the ranks.
Dr. Narang imagined having a career that impacted value fairly early on, after making observations during his pediatric residency. But even he was surprised when he got the call to be CEO, after less than two years on the job.
Now, in retrospect, they all see their years working as a rank-and-file hospitalist as formative.
As a leader in a hospital, you have to be good at recruiting physicians, retaining them and developing them professionally, Dr. Harte says. That requires having clinical credibility, being a decent mentor, being a good role model, and “wearing your integrity on your sleeve.”
“I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment,” Dr. Harte notes. “You have pockets of enormous expertise that sometimes function like silos.
“Being a hospitalist actually trains you well for those things. By nature of what we do, we tend to be folks who do multi-disciplinary rounds. We can sit around a table or walk rounds with nurses, case managers, physical therapists, respiratory therapists, and the like, and actually develop a plan of care that recognizes the expertise of the other individuals within that group. That is a very good incubator for that kind of thinking.”
Hospital leaders also have to know how everything works together within the hospital.
“Hospital medicine has this overlap with that domain as it is,” Dr. Harte continues. “We work in hospitals. It is not such a stretch then, to think that we could be running a hospital.”
Golden Opportunity
Dr. Torcson says the opportunities to lead in the hospital setting abound. A former internist, he says hospitalists are primed to “improve quality and service at the hospital level because of the system-based approach to hospital care.”
Dealing with incomplete information and uncertainty are important challenges for hospital leaders, something Dr. Afsar says are daily hurdles for hospitalists.
“By nature when you’re a hospitalist, you are a problem solver,” she says. “You don’t shy away from problems that you don’t understand.”
That problem-solver outlook is what prompted Neil Martin, MD, chief of neurosurgery at UCLA, to ask Dr. Afsar to join a quality improvement program within the department—first as a participant and then as its leader.
“She was always one of the most active and vocal and solution-oriented people on the committees that I was participating in,” Dr. Martin says. “She was not the kind of person who would describe all of the problems and leave it at that. But, rather, [she] would help identify problems and then propose solutions and then help follow through to implement solutions.”
Hospitalist C-suiters describe days dominated by meetings with executive teams, staff, and individual physicians or groups. Meetings are a necessity, as executives are tasked with crafting a vision, constantly assessing progress, and refining the approach when necessary.
Continuing at least some clinical work is important, Dr. Harte says. It depends on the organization, but he says he sees benefits that help him in his administrative duties.
“It changes the dynamic of the interaction with some of the naysayers on the medical staff,” he says. “That’s still something that I enjoy doing. I think it’s important for me, it’s important for the credibility of my job, and particularly for the organization that I work at.”
A lot of C-suiters sought out formal training in administrative areas—though not necessarily an MBA—once they realized they had an interest in administration.
Dr. Torcson says getting a master’s in medical management degree was “absolutely invaluable.”
“It was obvious to me that I had some needs to develop some additional competencies and capabilities, a different skill set than I gained in medical school and residency,” he says. “The same skill set that makes one a successful or quality physician isn’t necessarily the same skill set that you need to be an effective manager or administrator.”
Dr. Afsar completed an advanced quality improvement training program at Intermountain Healthcare, and Dr. Narang received a master’s in healthcare management from Harvard.
Dr. Harte, who does not have an advanced management degree, says that at some institutions, such as Cleveland Clinic, you can learn on the job the non-clinical areas needed to be a top leader in a hospital, including finance and strategy.
Dr. Zipper says a related degree can be a big leg up.
“If one is specifically looking to enter the C-suite, an advanced business or management degree will make that barrier a lot lower,” he says. Whether that degree is a master’s in business administration, healthcare administration, medical management, or a similar degree doesn’t seem to matter much, he adds.
When she was looking for a new CEO for Good Samaritan Medical Center, Bollinger says that she preferred to hire a physician. That candidate, she says, had to have certain leadership qualities, including the ability to create a suitable vision, curiosity, an “executive presence,” and a “tolerance of ambiguity.”
As it turns out, the value of having a physician CEO has been “probably three times what I anticipated,” she says.
If you’re a hospitalist and have an interest in rising up the leadership ladder, getting involved and getting exposure to areas of interest is where it begins.
“I would say go for it,” Dr. Afsar says. “Raising your hand and being willing to take on responsibility are kind of the first steps in getting involved. I think it’s just as much making sure that you’re the right fit for that type of work, as it is to excel and do well. Not everyone, I think, will thrive and enjoy this type of work. So I think having the opportunity to get exposed to it and see if it’s something that you enjoy is a critical piece.”
Tom Collins is a freelance writer in Florida.
Steve Narang, MD, a pediatrician, hospitalist, and the then-CMO at Banner Health’s Cardon Children’s Medical Center in Phoenix, was attending a leadership summit where all of Banner’s top officials were gathered. It was his third day in his new job.
Banner’s President, Peter Fine, gave a presentation in the future of healthcare and asked for questions. Dr. Narang stepped up to the microphone, asked a question, and made remarks about how the organization needed to ready itself for the changing landscape. Kathy Bollinger, president of the Arizona West Region of Banner, was struck by those remarks. Less than two years later, she made Dr. Narang the CEO at Arizona’s largest teaching hospital, Good Samaritan Medical Center.
His hospitalist background was an important ingredient in the kind of leader Dr. Narang has become, she says.
“The correlation is that hospitalists are leading teams; they are quarterbacking care,” Bollinger adds. “A good hospitalist brings the team together.”
Physicians with a background in hospital medicine are no strangers to C-suite level positions at hospitals. In April, Brian Harte, MD, SFHM, was named president of South Pointe Hospital in Warrenville Heights, Ohio, a center within the Cleveland Clinic system. In January, Patrick Cawley, MD, MBA, MHM, a former SHM president, was named CEO at the Medical University of South Carolina Medical Center in Charleston.
Other recent C-suite arrivals include Nasim Afsar, MD, SFHM, an SHM board member who is associate CMO at UCLA Hospitals in Los Angeles, and Patrick Torcson, MD, MMM, FACP, SFHM, another SHM board member, vice president, and chief integration officer at St. Tammany Parish Hospital in Covington, La.
Although their paths to the C-suite have differed, each agrees that their experience in hospital medicine gave them the knowledge of the system that was required to begin an ascent to the highest levels of leadership. Just as important, or maybe more so, their exposure to the inner workings of a hospital awakened within them a desire to see the system function better. And the necessity of working with all types of healthcare providers within the complicated hospital setting helped them recognize—or at least get others to recognize—their potential for leadership, and helped hone the teamwork skills that are vital in top administrative roles.
They also say that, when they were starting out, they never aspired to high leadership positions. Rather, it was simply following their own interests that ultimately led them there.
By the time Dr. Narang stepped up to the microphone that day in Phoenix, he had more than a dozen years under his belt working as a hospitalist for a children’s hospital and as part of a group that created a pediatric hospitalist company in Louisiana.
And that work helped lay the foundation for him, he says.
“Being a hospitalist was a key strength of my background,” Dr. Narang explains. “Hospitalists are so well-positioned…to get truly at the intersection of operations and find value in a complex puzzle. Hospitalists are able to do that.
“At the end of the day, it’s about leadership. And I learned that from day one as a hospitalist.”
His confidence and sense of the big picture were not lost on Bollinger that day at the leadership summit.
“I thought that took a fair amount of courage,” she says, “on Day 3, to stand up to the mic and have [a] specific conversation with the president of the company. In my mind, he was very enlightened. His comments were very enlightened.”
Firm Foundation
Robert Zipper, MD, MMM, SFHM, chair of SHM’s Leadership Committee, and CMO of Sound Physicians’ West Region, says it’s probably not realistic for a hospitalist to vault up immediately to a chief executive officer position. Pursuing lower-level leadership roles would be a good starting point for hospitalists with C-suite aspirations, he says.
“For those just starting out, I would recommend that they seek out opportunities to lead or be a part of managing change in their hospitals. The right opportunities should feel like a bit of a stretch, but not overwhelming. This might be work in quality, medical staff leadership, etc.,” Dr. Zipper says.
For hospitalists with leadership experience, CMO and vice president of medical affairs have the closest translation, he adds. He also says jobs like chief informatics officer and roles in quality improvement are highly suitable for hospitalists.
According to the 2011 Cejka Executive Search Physician Executive Compensation Survey, a survey of the American College of Physician Executives’ membership of physicians in management, the median salary of physicians in CEO positions was $393,152. That figure was $343,334 for CMO and $307,500 for chief quality and patient safety officer. The median for all physician executive positions was $305,000. Compensation was typically higher in academic medical centers and lower for hospitals and multi-specialty groups.
Hospitalists in executive positions had a 2011 median income of $275,000, according to the survey.
The survey also showed a wide range of compensation, typically dependent on the size of the institution. Some hospitalist leaders with more than 75% of their full-time-equivalent hours worked clinically “might actually take a small pay cut to make a move,” Dr. Zipper says.
Natural Progression
The hospitalist executives interviewed, for the most part, were emphatic that C-suite level leadership was not something that they imagined for themselves when they began their medical careers.
“In 2007, I could never imagine doing anything less than 100 percent clinical hospitalist work,” UCLA Hospitals’ Dr. Afsar says. “But once I started working and doing my hospitalist job day in and day out, I realized that there were many aspects of our care where I knew we could do better.”
Dr. Harte, president of South Pointe Hospital in Cleveland, says he never really thought about hospital administration as a career ambition. But, “opportunities presented themselves.”
Dr. Torcson says he was so firmly disinterested in administrative positions that when he was asked to join the Medical Executive Committee at his hospital, his first thought was “no way … I’m a doctor, not an administrator.” But after talking to some senior colleagues about it, they reminded him that he was basically obliged to say “yes.” And it ended up being a crucial component in his ascent through the ranks.
Dr. Narang imagined having a career that impacted value fairly early on, after making observations during his pediatric residency. But even he was surprised when he got the call to be CEO, after less than two years on the job.
Now, in retrospect, they all see their years working as a rank-and-file hospitalist as formative.
As a leader in a hospital, you have to be good at recruiting physicians, retaining them and developing them professionally, Dr. Harte says. That requires having clinical credibility, being a decent mentor, being a good role model, and “wearing your integrity on your sleeve.”
“I think one of the things that makes hospitalists fairly natural fits for the hospital leadership positions is that a hospital is a very complicated environment,” Dr. Harte notes. “You have pockets of enormous expertise that sometimes function like silos.
“Being a hospitalist actually trains you well for those things. By nature of what we do, we tend to be folks who do multi-disciplinary rounds. We can sit around a table or walk rounds with nurses, case managers, physical therapists, respiratory therapists, and the like, and actually develop a plan of care that recognizes the expertise of the other individuals within that group. That is a very good incubator for that kind of thinking.”
Hospital leaders also have to know how everything works together within the hospital.
“Hospital medicine has this overlap with that domain as it is,” Dr. Harte continues. “We work in hospitals. It is not such a stretch then, to think that we could be running a hospital.”
Golden Opportunity
Dr. Torcson says the opportunities to lead in the hospital setting abound. A former internist, he says hospitalists are primed to “improve quality and service at the hospital level because of the system-based approach to hospital care.”
Dealing with incomplete information and uncertainty are important challenges for hospital leaders, something Dr. Afsar says are daily hurdles for hospitalists.
“By nature when you’re a hospitalist, you are a problem solver,” she says. “You don’t shy away from problems that you don’t understand.”
That problem-solver outlook is what prompted Neil Martin, MD, chief of neurosurgery at UCLA, to ask Dr. Afsar to join a quality improvement program within the department—first as a participant and then as its leader.
“She was always one of the most active and vocal and solution-oriented people on the committees that I was participating in,” Dr. Martin says. “She was not the kind of person who would describe all of the problems and leave it at that. But, rather, [she] would help identify problems and then propose solutions and then help follow through to implement solutions.”
Hospitalist C-suiters describe days dominated by meetings with executive teams, staff, and individual physicians or groups. Meetings are a necessity, as executives are tasked with crafting a vision, constantly assessing progress, and refining the approach when necessary.
Continuing at least some clinical work is important, Dr. Harte says. It depends on the organization, but he says he sees benefits that help him in his administrative duties.
“It changes the dynamic of the interaction with some of the naysayers on the medical staff,” he says. “That’s still something that I enjoy doing. I think it’s important for me, it’s important for the credibility of my job, and particularly for the organization that I work at.”
A lot of C-suiters sought out formal training in administrative areas—though not necessarily an MBA—once they realized they had an interest in administration.
Dr. Torcson says getting a master’s in medical management degree was “absolutely invaluable.”
“It was obvious to me that I had some needs to develop some additional competencies and capabilities, a different skill set than I gained in medical school and residency,” he says. “The same skill set that makes one a successful or quality physician isn’t necessarily the same skill set that you need to be an effective manager or administrator.”
Dr. Afsar completed an advanced quality improvement training program at Intermountain Healthcare, and Dr. Narang received a master’s in healthcare management from Harvard.
Dr. Harte, who does not have an advanced management degree, says that at some institutions, such as Cleveland Clinic, you can learn on the job the non-clinical areas needed to be a top leader in a hospital, including finance and strategy.
Dr. Zipper says a related degree can be a big leg up.
“If one is specifically looking to enter the C-suite, an advanced business or management degree will make that barrier a lot lower,” he says. Whether that degree is a master’s in business administration, healthcare administration, medical management, or a similar degree doesn’t seem to matter much, he adds.
When she was looking for a new CEO for Good Samaritan Medical Center, Bollinger says that she preferred to hire a physician. That candidate, she says, had to have certain leadership qualities, including the ability to create a suitable vision, curiosity, an “executive presence,” and a “tolerance of ambiguity.”
As it turns out, the value of having a physician CEO has been “probably three times what I anticipated,” she says.
If you’re a hospitalist and have an interest in rising up the leadership ladder, getting involved and getting exposure to areas of interest is where it begins.
“I would say go for it,” Dr. Afsar says. “Raising your hand and being willing to take on responsibility are kind of the first steps in getting involved. I think it’s just as much making sure that you’re the right fit for that type of work, as it is to excel and do well. Not everyone, I think, will thrive and enjoy this type of work. So I think having the opportunity to get exposed to it and see if it’s something that you enjoy is a critical piece.”
Tom Collins is a freelance writer in Florida.
Using the Internet in your practice. Part 2: Generating new patients using social media
With this article, we intend to illustrate the value of having a social media presence and how you can use social media to attract new patients. One of us (NHB) has been using social media to promote his medical practice for 3 years and can be found on the first page of Google search results for several of the medical conditions he treats. As a result of these high search rankings, he is able to generate two to four new patient visits every day.
You can achieve the same results using the techniques described in this article. You certainly can buy banner ads and buy traffic to your page, but we want to show you how to get on the first page of Google using the natural, organic method.
PUSH VS PULL
Social media can be used in different ways to build your practice. What you employ depends on what you want to accomplish and the time and energy you want to devote to each of these social media opportunities.
By its very definition, social media is social engagement—and what is known as a “pull” technology. There are two ways to share your information with people on the Internet:
- “Pull” Web site surfers to your information
- “Push” your information to them.
Push occurs when you initiate the process by placing your information in front of the Web site surfer. They get it or see it because of the actions you have taken. Sending e-mails is one way to push information to your target audience, or potential patients, to your practice. Another way to push your Web site and its contents is to get listed on the first page of search engine results. You want to “push” your Web site in plain view of the person who has typed in keywords or keyword phrases that relate to your practice (ie, “OBGYN” plus “<your city>,” “tubal ligation” plus “<your city>,” or “loss of urine” plus “<your zip code>.” Push techniques are the best way to market your services and offer the best return on your marketing investment.
Using social media, you are able to “pull” your audience of potential patients to you and your practice. In other words, your target market of potential patients has to take the time and make the effort to type in your Web site address in order to come to you. The information or message you have on your social media sites has to be strong enough and of sufficient compelling interest that patients want to come to read what you have to say. Web surfers are looking for online relationships for information sharing. It is this interaction with your potential patients that makes social media unique. Using this pull technology, you have the opportunity to interact and develop a relationship with a patient before she picks up the phone to make an appointment, before she comes to the office to see you eyeball to eyeball.
FACEBOOK AND HOW IT RELATES TO YOUR PRACTICE
Originally, Facebook was developed as a way for people to see what was going on in each other’s lives, a method to stay in contact with one another. In the beginning, it was friends, family members, or groups of like-minded individuals frequenting each other’s Facebook pages. Typically, they would keep tabs on who was having a party or post pictures of their kids for family members to see.
Facebook has evolved. Today, companies, businesses, and, yes, medical practices are trying to “pull” more Web site visitors to their Facebook pages. To do this, they hold contests with prizes; offer great content, coupons, and videos; and provide special offers to get Web surfers to their site. Large companies and large group practices like the Mayo Clinic, Cleveland Clinic, and MD Anderson Cancer Center, have whole social media departments that post regularly, respond to comments left on their pages, and answer questions posted by those who “like” their page or site.
Individual practicing clinicians, and most smaller ObGyn practices, do not have the budget for a social media team. They also don’t have the time or the training to write effective copy that is so compelling that Web surfers are drawn or “pulled” to their Facebook page. The reality is, your patients expect you to have a Facebook page, and they expect you to have quality information that is helpful and relevant to their well-being. But, the question remains…
Related article: Four pillars of a successful practice: 1. Keep your current patients happy Neal H. Baum, MD (Practice Management, March 2013)
Can Facebook generate new patients?
You and your practice certainly can place a lot of information and pictures on Facebook, and potential patients can leave comments or ask questions easily. You can start a dialog with a patient without providing medical advice and motivate her to see that you are providing medical value before the doctor–patient relationship is established. Still, does a Facebook page generate new patients? It depends on the information you post and how you use Facebook to acquire new patients.
For instance, your practice is probably restricted to a local area—a few zip codes surrounding your office and hospital—which means you really only want patients who are in your area to visit your practice’s Facebook page because those are the only ones who are likely to call and make an appointment. Unless you are highly specialized in a particular field, such as fistula repair, robotic surgery, or the treatment of mesh complications, the Facebook surfer from New York isn’t likely to hop on a plane to come to your practice on the West Coast for gynecologic or obstetric care.
Related article: Four pillars of a successful practice: 2. Attract new patients Neal H. Baum, MD (Practice Management, May 2013)
On the surface, it appears that it is impossible to compete with larger practices and hospitals that have more dedicated staff to draw prospective patients to a practice through Facebook. However, the real, overarching challenge is to improve your Web site rankings on the major search engines, to be on the first page of Google, Bing, and Yahoo search results. And what we do know is that Google has placed a high value on Web site rankings through social media sites like Facebook, Twitter, and YouTube—that is, of course, as long as your Facebook page provides content that has keywords relevant to your target market and the content on your page links back to your Web site.
Therefore, it is not necessary to devote an inordinate amount of time to your social media presence to obtain results. You will, on the other hand, get more visitors to your Web site if it is found on the first page of search engine results because of your Facebook posts. Of course, if your Web site is not set up properly for easy visitor navigation and visitor conversion, you may not be able to obtain the desired result of gaining new patients even if they do find your site. You need to have a Web site with marketing and patient conversion systems built into it; don’t overlook the layout of your Web site. For more on this issue, see Part 1 of this series.
Related article: Using the Internet in your practice. Part 1: Why social media are important and how to get started Neal H. Baum, MD, and Ron Romano (Practice Management, February 2014)
YOUTUBE VIDEOS AND YOUR PRACTICE
YouTube has become a significant search engine for virtually every product and service you offer your patients. There are millions of videos on YouTube, and you can search topics simply by typing in any topic that your patients might be interested in, from birth control to cancer.
There are five ways your practice can benefit from a video posted on YouTube:
- Web site traffic driver. To achieve this “pull,” you must label your posted video correctly, with keyword phrases that are relevant to the type of patient or conditions you are looking for, and offer a description that would make a viewer want to see the video. You also must provide a link back to your Web site, which increases your chances of gaining a new patient from YouTube.
- Boost your search engine optimization. Google places a high-ranking factor on videos posted to YouTube that are keyword-relevant.
- A video library can position you as an expert in the field. You can create your own YouTube channel and keep adding videos. One of us (NHB) has more than
70 medical videos on his YouTube channel. If someone views one of these videos, they will have immediate access to the rest of the video collection even though they may be labelled with other keywords. This further positions you as the knowledgeable expert in your field. - Video embedding capability. Any video you have posted to YouTube can be placed on your Web site, in a format that keeps the viewer on your site. This means the viewer has less of a chance of getting distracted with other video offerings and landing on someone else’s Web site.
- Free video storage. Because you have stored the video on YouTube, you are not using the resources on your Web site when someone, or several people, view the video at the same time.
Getting started with YouTube
Making a video can be easier than you think. First, a video can simply be a PowerPoint presentation. Studies have demonstrated that it is more about the content of the video than a physician being in front of a camera. There are lots of Web sites you can use to record a presentation; one of the most popular and easy to use is http://www.GoToWebinar.com. There are computer programs that make it easy to record and then simply upload the recording to YouTube. Cam Studio (http://camstudio.org) is a free open-source program available that has a lot of flexibility for editing audio and video files, and it is easy to use. Camtasia (http://www.techsmith.com/camtasia.html) is a popular program that costs about $300 and has a lot of features for advanced editing. Camtasia also has a simple navigation system for the nontechnical person.
Content is key. You can select a few frequently asked questions (FAQs) that your patients regularly ask and simply record yourself giving the answers. Take a look at what is new, relevant, or controversial in regard to the procedures you perform. Or just look at all the pages on your Web site that have the procedures and services you provide and make a video on those topics. The ideal video is 3 to 5 minutes in length.
ATTRACTING PATIENTS VIA TWITTER
The most amazing example of social media and building a fan base is Twitter. Here’s a question: Who are the people that have the biggest following on Twitter? The answer: Celebrities, rock stars, and athletes. As a society, we are obsessed with these groups and want to know their every thought, what they like, what they had for lunch, what they think, and who they think about.
Now how, as a practicing ObGyn, do you expect to build a base of Web site surfers who want to know your every thought on urinary incontinence? The harsh reality is, if you think you are going to get new patients by making posts on Twitter of 140 characters or less every day, you will be disappointed.
However, the return from using Twitter is, similar to Facebook and YouTube, related to the fact that Twitter is one of the top accessed Web sites in the world. Linking your own content from such a Web site increases the search placement of your content when a potential patient performs a general Google search.
ARE SOCIAL MEDIA EFFECTIVE?
The effective use of social media can result in attracting new patients every day to your practice—if you post quality information on a regular basis that is helpful to your existing patients and especially to potential new patients. Overall, social media can help you get new patients through search engine rankings. Even if you don’t want to do any work on your social media sites, you can hire companies that will do it for you.
However, the return from using Twitter is, similar to Facebook and YouTube, related to the fact that Twitter is one of the top accessed Web sites in the world. Linking your own content from such a Web site increases the search placement of your content when a potential patient performs a general Google search.
The bottom line
There will be many ObGyns who will read this article, throw up their hands and say, “Makes sense, but this is over my head.” Because it sounds so technical, many clinicians will just ignore social media and hope it goes away. If your plans for the next 5 years include practicing medicine, we don’t recommend that you take that approach. The Internet and social media are the “places” in which patients of today are searching for their doctors. Trust us—potential new patients are no longer using the Yellow Pages.
The patients of tomorrow will be increasingly technologically sophisticated, and these social media techniques will continue to evolve. Don’t get left behind. And don’t let your competitors dominate one of the most important sources of new patients you have, along with patient referrals and physician referrals. Jump into this world yourself, and you will be richly rewarded. The social media train is leaving the station, and we hope that we have shown you how to hitch a ride. See you online!
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
With this article, we intend to illustrate the value of having a social media presence and how you can use social media to attract new patients. One of us (NHB) has been using social media to promote his medical practice for 3 years and can be found on the first page of Google search results for several of the medical conditions he treats. As a result of these high search rankings, he is able to generate two to four new patient visits every day.
You can achieve the same results using the techniques described in this article. You certainly can buy banner ads and buy traffic to your page, but we want to show you how to get on the first page of Google using the natural, organic method.
PUSH VS PULL
Social media can be used in different ways to build your practice. What you employ depends on what you want to accomplish and the time and energy you want to devote to each of these social media opportunities.
By its very definition, social media is social engagement—and what is known as a “pull” technology. There are two ways to share your information with people on the Internet:
- “Pull” Web site surfers to your information
- “Push” your information to them.
Push occurs when you initiate the process by placing your information in front of the Web site surfer. They get it or see it because of the actions you have taken. Sending e-mails is one way to push information to your target audience, or potential patients, to your practice. Another way to push your Web site and its contents is to get listed on the first page of search engine results. You want to “push” your Web site in plain view of the person who has typed in keywords or keyword phrases that relate to your practice (ie, “OBGYN” plus “<your city>,” “tubal ligation” plus “<your city>,” or “loss of urine” plus “<your zip code>.” Push techniques are the best way to market your services and offer the best return on your marketing investment.
Using social media, you are able to “pull” your audience of potential patients to you and your practice. In other words, your target market of potential patients has to take the time and make the effort to type in your Web site address in order to come to you. The information or message you have on your social media sites has to be strong enough and of sufficient compelling interest that patients want to come to read what you have to say. Web surfers are looking for online relationships for information sharing. It is this interaction with your potential patients that makes social media unique. Using this pull technology, you have the opportunity to interact and develop a relationship with a patient before she picks up the phone to make an appointment, before she comes to the office to see you eyeball to eyeball.
FACEBOOK AND HOW IT RELATES TO YOUR PRACTICE
Originally, Facebook was developed as a way for people to see what was going on in each other’s lives, a method to stay in contact with one another. In the beginning, it was friends, family members, or groups of like-minded individuals frequenting each other’s Facebook pages. Typically, they would keep tabs on who was having a party or post pictures of their kids for family members to see.
Facebook has evolved. Today, companies, businesses, and, yes, medical practices are trying to “pull” more Web site visitors to their Facebook pages. To do this, they hold contests with prizes; offer great content, coupons, and videos; and provide special offers to get Web surfers to their site. Large companies and large group practices like the Mayo Clinic, Cleveland Clinic, and MD Anderson Cancer Center, have whole social media departments that post regularly, respond to comments left on their pages, and answer questions posted by those who “like” their page or site.
Individual practicing clinicians, and most smaller ObGyn practices, do not have the budget for a social media team. They also don’t have the time or the training to write effective copy that is so compelling that Web surfers are drawn or “pulled” to their Facebook page. The reality is, your patients expect you to have a Facebook page, and they expect you to have quality information that is helpful and relevant to their well-being. But, the question remains…
Related article: Four pillars of a successful practice: 1. Keep your current patients happy Neal H. Baum, MD (Practice Management, March 2013)
Can Facebook generate new patients?
You and your practice certainly can place a lot of information and pictures on Facebook, and potential patients can leave comments or ask questions easily. You can start a dialog with a patient without providing medical advice and motivate her to see that you are providing medical value before the doctor–patient relationship is established. Still, does a Facebook page generate new patients? It depends on the information you post and how you use Facebook to acquire new patients.
For instance, your practice is probably restricted to a local area—a few zip codes surrounding your office and hospital—which means you really only want patients who are in your area to visit your practice’s Facebook page because those are the only ones who are likely to call and make an appointment. Unless you are highly specialized in a particular field, such as fistula repair, robotic surgery, or the treatment of mesh complications, the Facebook surfer from New York isn’t likely to hop on a plane to come to your practice on the West Coast for gynecologic or obstetric care.
Related article: Four pillars of a successful practice: 2. Attract new patients Neal H. Baum, MD (Practice Management, May 2013)
On the surface, it appears that it is impossible to compete with larger practices and hospitals that have more dedicated staff to draw prospective patients to a practice through Facebook. However, the real, overarching challenge is to improve your Web site rankings on the major search engines, to be on the first page of Google, Bing, and Yahoo search results. And what we do know is that Google has placed a high value on Web site rankings through social media sites like Facebook, Twitter, and YouTube—that is, of course, as long as your Facebook page provides content that has keywords relevant to your target market and the content on your page links back to your Web site.
Therefore, it is not necessary to devote an inordinate amount of time to your social media presence to obtain results. You will, on the other hand, get more visitors to your Web site if it is found on the first page of search engine results because of your Facebook posts. Of course, if your Web site is not set up properly for easy visitor navigation and visitor conversion, you may not be able to obtain the desired result of gaining new patients even if they do find your site. You need to have a Web site with marketing and patient conversion systems built into it; don’t overlook the layout of your Web site. For more on this issue, see Part 1 of this series.
Related article: Using the Internet in your practice. Part 1: Why social media are important and how to get started Neal H. Baum, MD, and Ron Romano (Practice Management, February 2014)
YOUTUBE VIDEOS AND YOUR PRACTICE
YouTube has become a significant search engine for virtually every product and service you offer your patients. There are millions of videos on YouTube, and you can search topics simply by typing in any topic that your patients might be interested in, from birth control to cancer.
There are five ways your practice can benefit from a video posted on YouTube:
- Web site traffic driver. To achieve this “pull,” you must label your posted video correctly, with keyword phrases that are relevant to the type of patient or conditions you are looking for, and offer a description that would make a viewer want to see the video. You also must provide a link back to your Web site, which increases your chances of gaining a new patient from YouTube.
- Boost your search engine optimization. Google places a high-ranking factor on videos posted to YouTube that are keyword-relevant.
- A video library can position you as an expert in the field. You can create your own YouTube channel and keep adding videos. One of us (NHB) has more than
70 medical videos on his YouTube channel. If someone views one of these videos, they will have immediate access to the rest of the video collection even though they may be labelled with other keywords. This further positions you as the knowledgeable expert in your field. - Video embedding capability. Any video you have posted to YouTube can be placed on your Web site, in a format that keeps the viewer on your site. This means the viewer has less of a chance of getting distracted with other video offerings and landing on someone else’s Web site.
- Free video storage. Because you have stored the video on YouTube, you are not using the resources on your Web site when someone, or several people, view the video at the same time.
Getting started with YouTube
Making a video can be easier than you think. First, a video can simply be a PowerPoint presentation. Studies have demonstrated that it is more about the content of the video than a physician being in front of a camera. There are lots of Web sites you can use to record a presentation; one of the most popular and easy to use is http://www.GoToWebinar.com. There are computer programs that make it easy to record and then simply upload the recording to YouTube. Cam Studio (http://camstudio.org) is a free open-source program available that has a lot of flexibility for editing audio and video files, and it is easy to use. Camtasia (http://www.techsmith.com/camtasia.html) is a popular program that costs about $300 and has a lot of features for advanced editing. Camtasia also has a simple navigation system for the nontechnical person.
Content is key. You can select a few frequently asked questions (FAQs) that your patients regularly ask and simply record yourself giving the answers. Take a look at what is new, relevant, or controversial in regard to the procedures you perform. Or just look at all the pages on your Web site that have the procedures and services you provide and make a video on those topics. The ideal video is 3 to 5 minutes in length.
ATTRACTING PATIENTS VIA TWITTER
The most amazing example of social media and building a fan base is Twitter. Here’s a question: Who are the people that have the biggest following on Twitter? The answer: Celebrities, rock stars, and athletes. As a society, we are obsessed with these groups and want to know their every thought, what they like, what they had for lunch, what they think, and who they think about.
Now how, as a practicing ObGyn, do you expect to build a base of Web site surfers who want to know your every thought on urinary incontinence? The harsh reality is, if you think you are going to get new patients by making posts on Twitter of 140 characters or less every day, you will be disappointed.
However, the return from using Twitter is, similar to Facebook and YouTube, related to the fact that Twitter is one of the top accessed Web sites in the world. Linking your own content from such a Web site increases the search placement of your content when a potential patient performs a general Google search.
ARE SOCIAL MEDIA EFFECTIVE?
The effective use of social media can result in attracting new patients every day to your practice—if you post quality information on a regular basis that is helpful to your existing patients and especially to potential new patients. Overall, social media can help you get new patients through search engine rankings. Even if you don’t want to do any work on your social media sites, you can hire companies that will do it for you.
However, the return from using Twitter is, similar to Facebook and YouTube, related to the fact that Twitter is one of the top accessed Web sites in the world. Linking your own content from such a Web site increases the search placement of your content when a potential patient performs a general Google search.
The bottom line
There will be many ObGyns who will read this article, throw up their hands and say, “Makes sense, but this is over my head.” Because it sounds so technical, many clinicians will just ignore social media and hope it goes away. If your plans for the next 5 years include practicing medicine, we don’t recommend that you take that approach. The Internet and social media are the “places” in which patients of today are searching for their doctors. Trust us—potential new patients are no longer using the Yellow Pages.
The patients of tomorrow will be increasingly technologically sophisticated, and these social media techniques will continue to evolve. Don’t get left behind. And don’t let your competitors dominate one of the most important sources of new patients you have, along with patient referrals and physician referrals. Jump into this world yourself, and you will be richly rewarded. The social media train is leaving the station, and we hope that we have shown you how to hitch a ride. See you online!
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
With this article, we intend to illustrate the value of having a social media presence and how you can use social media to attract new patients. One of us (NHB) has been using social media to promote his medical practice for 3 years and can be found on the first page of Google search results for several of the medical conditions he treats. As a result of these high search rankings, he is able to generate two to four new patient visits every day.
You can achieve the same results using the techniques described in this article. You certainly can buy banner ads and buy traffic to your page, but we want to show you how to get on the first page of Google using the natural, organic method.
PUSH VS PULL
Social media can be used in different ways to build your practice. What you employ depends on what you want to accomplish and the time and energy you want to devote to each of these social media opportunities.
By its very definition, social media is social engagement—and what is known as a “pull” technology. There are two ways to share your information with people on the Internet:
- “Pull” Web site surfers to your information
- “Push” your information to them.
Push occurs when you initiate the process by placing your information in front of the Web site surfer. They get it or see it because of the actions you have taken. Sending e-mails is one way to push information to your target audience, or potential patients, to your practice. Another way to push your Web site and its contents is to get listed on the first page of search engine results. You want to “push” your Web site in plain view of the person who has typed in keywords or keyword phrases that relate to your practice (ie, “OBGYN” plus “<your city>,” “tubal ligation” plus “<your city>,” or “loss of urine” plus “<your zip code>.” Push techniques are the best way to market your services and offer the best return on your marketing investment.
Using social media, you are able to “pull” your audience of potential patients to you and your practice. In other words, your target market of potential patients has to take the time and make the effort to type in your Web site address in order to come to you. The information or message you have on your social media sites has to be strong enough and of sufficient compelling interest that patients want to come to read what you have to say. Web surfers are looking for online relationships for information sharing. It is this interaction with your potential patients that makes social media unique. Using this pull technology, you have the opportunity to interact and develop a relationship with a patient before she picks up the phone to make an appointment, before she comes to the office to see you eyeball to eyeball.
FACEBOOK AND HOW IT RELATES TO YOUR PRACTICE
Originally, Facebook was developed as a way for people to see what was going on in each other’s lives, a method to stay in contact with one another. In the beginning, it was friends, family members, or groups of like-minded individuals frequenting each other’s Facebook pages. Typically, they would keep tabs on who was having a party or post pictures of their kids for family members to see.
Facebook has evolved. Today, companies, businesses, and, yes, medical practices are trying to “pull” more Web site visitors to their Facebook pages. To do this, they hold contests with prizes; offer great content, coupons, and videos; and provide special offers to get Web surfers to their site. Large companies and large group practices like the Mayo Clinic, Cleveland Clinic, and MD Anderson Cancer Center, have whole social media departments that post regularly, respond to comments left on their pages, and answer questions posted by those who “like” their page or site.
Individual practicing clinicians, and most smaller ObGyn practices, do not have the budget for a social media team. They also don’t have the time or the training to write effective copy that is so compelling that Web surfers are drawn or “pulled” to their Facebook page. The reality is, your patients expect you to have a Facebook page, and they expect you to have quality information that is helpful and relevant to their well-being. But, the question remains…
Related article: Four pillars of a successful practice: 1. Keep your current patients happy Neal H. Baum, MD (Practice Management, March 2013)
Can Facebook generate new patients?
You and your practice certainly can place a lot of information and pictures on Facebook, and potential patients can leave comments or ask questions easily. You can start a dialog with a patient without providing medical advice and motivate her to see that you are providing medical value before the doctor–patient relationship is established. Still, does a Facebook page generate new patients? It depends on the information you post and how you use Facebook to acquire new patients.
For instance, your practice is probably restricted to a local area—a few zip codes surrounding your office and hospital—which means you really only want patients who are in your area to visit your practice’s Facebook page because those are the only ones who are likely to call and make an appointment. Unless you are highly specialized in a particular field, such as fistula repair, robotic surgery, or the treatment of mesh complications, the Facebook surfer from New York isn’t likely to hop on a plane to come to your practice on the West Coast for gynecologic or obstetric care.
Related article: Four pillars of a successful practice: 2. Attract new patients Neal H. Baum, MD (Practice Management, May 2013)
On the surface, it appears that it is impossible to compete with larger practices and hospitals that have more dedicated staff to draw prospective patients to a practice through Facebook. However, the real, overarching challenge is to improve your Web site rankings on the major search engines, to be on the first page of Google, Bing, and Yahoo search results. And what we do know is that Google has placed a high value on Web site rankings through social media sites like Facebook, Twitter, and YouTube—that is, of course, as long as your Facebook page provides content that has keywords relevant to your target market and the content on your page links back to your Web site.
Therefore, it is not necessary to devote an inordinate amount of time to your social media presence to obtain results. You will, on the other hand, get more visitors to your Web site if it is found on the first page of search engine results because of your Facebook posts. Of course, if your Web site is not set up properly for easy visitor navigation and visitor conversion, you may not be able to obtain the desired result of gaining new patients even if they do find your site. You need to have a Web site with marketing and patient conversion systems built into it; don’t overlook the layout of your Web site. For more on this issue, see Part 1 of this series.
Related article: Using the Internet in your practice. Part 1: Why social media are important and how to get started Neal H. Baum, MD, and Ron Romano (Practice Management, February 2014)
YOUTUBE VIDEOS AND YOUR PRACTICE
YouTube has become a significant search engine for virtually every product and service you offer your patients. There are millions of videos on YouTube, and you can search topics simply by typing in any topic that your patients might be interested in, from birth control to cancer.
There are five ways your practice can benefit from a video posted on YouTube:
- Web site traffic driver. To achieve this “pull,” you must label your posted video correctly, with keyword phrases that are relevant to the type of patient or conditions you are looking for, and offer a description that would make a viewer want to see the video. You also must provide a link back to your Web site, which increases your chances of gaining a new patient from YouTube.
- Boost your search engine optimization. Google places a high-ranking factor on videos posted to YouTube that are keyword-relevant.
- A video library can position you as an expert in the field. You can create your own YouTube channel and keep adding videos. One of us (NHB) has more than
70 medical videos on his YouTube channel. If someone views one of these videos, they will have immediate access to the rest of the video collection even though they may be labelled with other keywords. This further positions you as the knowledgeable expert in your field. - Video embedding capability. Any video you have posted to YouTube can be placed on your Web site, in a format that keeps the viewer on your site. This means the viewer has less of a chance of getting distracted with other video offerings and landing on someone else’s Web site.
- Free video storage. Because you have stored the video on YouTube, you are not using the resources on your Web site when someone, or several people, view the video at the same time.
Getting started with YouTube
Making a video can be easier than you think. First, a video can simply be a PowerPoint presentation. Studies have demonstrated that it is more about the content of the video than a physician being in front of a camera. There are lots of Web sites you can use to record a presentation; one of the most popular and easy to use is http://www.GoToWebinar.com. There are computer programs that make it easy to record and then simply upload the recording to YouTube. Cam Studio (http://camstudio.org) is a free open-source program available that has a lot of flexibility for editing audio and video files, and it is easy to use. Camtasia (http://www.techsmith.com/camtasia.html) is a popular program that costs about $300 and has a lot of features for advanced editing. Camtasia also has a simple navigation system for the nontechnical person.
Content is key. You can select a few frequently asked questions (FAQs) that your patients regularly ask and simply record yourself giving the answers. Take a look at what is new, relevant, or controversial in regard to the procedures you perform. Or just look at all the pages on your Web site that have the procedures and services you provide and make a video on those topics. The ideal video is 3 to 5 minutes in length.
ATTRACTING PATIENTS VIA TWITTER
The most amazing example of social media and building a fan base is Twitter. Here’s a question: Who are the people that have the biggest following on Twitter? The answer: Celebrities, rock stars, and athletes. As a society, we are obsessed with these groups and want to know their every thought, what they like, what they had for lunch, what they think, and who they think about.
Now how, as a practicing ObGyn, do you expect to build a base of Web site surfers who want to know your every thought on urinary incontinence? The harsh reality is, if you think you are going to get new patients by making posts on Twitter of 140 characters or less every day, you will be disappointed.
However, the return from using Twitter is, similar to Facebook and YouTube, related to the fact that Twitter is one of the top accessed Web sites in the world. Linking your own content from such a Web site increases the search placement of your content when a potential patient performs a general Google search.
ARE SOCIAL MEDIA EFFECTIVE?
The effective use of social media can result in attracting new patients every day to your practice—if you post quality information on a regular basis that is helpful to your existing patients and especially to potential new patients. Overall, social media can help you get new patients through search engine rankings. Even if you don’t want to do any work on your social media sites, you can hire companies that will do it for you.
However, the return from using Twitter is, similar to Facebook and YouTube, related to the fact that Twitter is one of the top accessed Web sites in the world. Linking your own content from such a Web site increases the search placement of your content when a potential patient performs a general Google search.
The bottom line
There will be many ObGyns who will read this article, throw up their hands and say, “Makes sense, but this is over my head.” Because it sounds so technical, many clinicians will just ignore social media and hope it goes away. If your plans for the next 5 years include practicing medicine, we don’t recommend that you take that approach. The Internet and social media are the “places” in which patients of today are searching for their doctors. Trust us—potential new patients are no longer using the Yellow Pages.
The patients of tomorrow will be increasingly technologically sophisticated, and these social media techniques will continue to evolve. Don’t get left behind. And don’t let your competitors dominate one of the most important sources of new patients you have, along with patient referrals and physician referrals. Jump into this world yourself, and you will be richly rewarded. The social media train is leaving the station, and we hope that we have shown you how to hitch a ride. See you online!
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
THE SERIES: USING THE INTERNET IN YOUR PRACTICE
Part 1: Why social media are important and how to get started (February 2014)
Part 3: Search engine optimization
Part 4: Online reputation management
(Look for Parts 3 and 4 in 2014)
UTI, then massive hemorrhage
UTI, THEN MASSIVE HEMORRHAGE
A woman in her 60s was hospitalized with a urinary tract infection (UTI). She was treated with antibiotics and intravenous (IV) fluids but developed deep vein thrombosis (DVT) at the IV site. Enoxaparin sodium was ordered to treat the clot. After 3 days, she suffered a massive abdominal hemorrhage. When she woke from resuscitation, her weight had doubled. She developed a methicillin-resistant Staphylococcus aureus (MRSA) infection, then Clostridium difficile infection due to antibiotics, plus bedsores. Multiple surgeries left her with an abdominal wall defect that cannot be repaired, and a permanent hernia. She was hospitalized for 75 days.
PATIENT’S CLAIM The hemorrhage was caused when enoxaparin was given at 1.5 times the proper dosage because the patient’s weight was overestimated by 50%. Excessive blood, plasma, and fluids caused her weight to double after resuscitation. Her intestines were forced out of her abdominal cavity by the hemorrhage. A permanent hernia, visible underneath her skin, causes pain.
DEFENDANTS’ DEFENSE The patient’s preexisting diabetes, heart condition, high cholesterol levels, and orthopedic issues impacted her condition. She was not compliant in managing her diabetes, causing many of the current problems.
VERDICT A $9.3 million Connecticut verdict was returned.
Related article: Update: Pelvic floor dysfunction Autumn L. Edenfield, MD, and Cindy L. Amundsen, MD (October 2012)
CESAREAN DELAYED UNNECESSARILY
At 37 weeks’ gestation, a mother reported decreased fetal movement. When the biophysical profile test scored 8/8 and the fetal heart rate was reassuring, the attending ObGyn discharged the patient. However, it was the middle of the night, and the nurse kept the mother in the emergency department (ED). At 8:30 am, the fetus began to show signs of fetal distress. Three ObGyns agreed to monitor labor, although one physician wanted delivery to occur that morning.
The next morning, a second biophysical profile scored 2/8, but the on-call ObGyn misunderstood the score as 6/8 and scheduled cesarean delivery for noon. Two hours after the second biophysical profile, the fetal heart rate crashed. A nurse called the ObGyn, who began an emergency cesarean 15 minutes later. The baby, born lifeless, was resuscitated. The child suffered permanent brain damage, and has cerebral palsy, severe cognitive deficits and speech deficits, and walks with an abnormal gait.
PARENTS’ CLAIM A physician did not see the patient for 24 hours, once the decision was made to monitor the mother, even though the fetal heart rate continued to decline. A biophysical profile test score of 2/8 indicates the need for immediate delivery. An earlier cesarean delivery could have reduced the child’s injuries.
DEFENDANTS’ DEFENSE After a settlement was reached with the hospital, the trial continued against the delivering ObGyn. He claimed that decreased fetal movement indicated that the brain injury had occurred 1 to 4 days before the mother came to the ED. The technician had manipulated the mother’s abdomen to wake the fetus before starting the first biophysical profile, which invalidated the score. The nurse miscommunicated the score of the second biophysical profile.
VERDICT A gross $29.8 million Illinois verdict was returned that included a $1.65 million settlement with the hospital.
WAS FACILITY ADEQUATELY STAFFED AFTER HURRICANE IKE?
A mother was admitted to a hospital for induction of labor in September 2008. After birth, the child was found to have cerebral palsy.
PARENTS’ CLAIM The mother should have been sent to another facility before delivery was induced because the hospital was short-staffed and low on resources due to Hurricane Ike. Too much oxytocin was used to induce contractions, which led to a lack of oxygen for the fetus. All prenatal testing had shown a healthy fetus. A cesarean delivery should have occurred when fetal distress was noted.
DEFENDANTS’ DEFENSE The mother had gastric bypass surgery 8 months before she became pregnant, and smoked during pregnancy, which accounted for the infant’s injuries. Treatment during labor and delivery was appropriate. Hospital staffing and resources were adequate.
VERDICT A $6.5 million Texas settlement was reached.
PLACENTA ACCRETA; MOTHER DIES
A 33-year-old woman became pregnant with her second child. A variety of conditions caused this to be high-risk pregnancy, so she saw a maternal-fetal medicine (MFM) specialist 2 months before delivery. The MFM reported that his examination and the ultrasonography (US) results were normal.
The ObGyn who provided prenatal care and delivered her first child scheduled cesarean delivery. During the procedure, the ObGyn noticed a 3- to 4-inch lesion where the placenta had penetrated the uterus. When the placenta was removed, the patient began to hemorrhage and a hysterectomy was performed. The hemorrhage created blood clots that led to gangrene in the patient’s extremities. She died 5 days after giving birth.
ESTATE’S CLAIM Both the MFM and the ObGyn failed to recognize placenta accreta on US prior to delivery. The ObGyn should have performed US prior to beginning cesarean delivery. The hospital’s protocols were not followed: the ObGyn should have stopped the procedure and called for extra surgical assistance and additional blood when he encountered placenta accreta, and again when the patient began to hemorrhage. Placenta accreta does not have to be fatal if detected and managed properly.
DEFENDANTS’ DEFENSE There was no negligence; the patient was treated properly.
VERDICT A $15.5 million Illinois verdict was returned against both physicians and the medical center.
Related article: Is the risk of placenta accreta in a subsequent pregnancy higher after emergent primary cesarean or after elective primary cesarean? Yinka Oyelese, MD (Examining the Evidence, December 2013)
ANTICONVULSANT AND MIGRAINE MEDS TAKEN DURING PREGNANCY
A woman was prescribed topiramate (Topamax) for migraine headaches and hand tremors during the first trimester of her pregnancy in 2007. With a history of seizures, she also took several anticonvulsants throughout her pregnancy. Her child was diagnosed with right unilateral cleft lip (cheiloschisis) in utero. The condition had not been surgically corrected at the time of trial.
PARENTS’ CLAIM The use of topiramate caused the child’s cleft lip. Janssen Pharmaceuticals, the manufacturer of Topamax, knew about the risk of birth defects associated with the drug in 2007, but failed to provide adequate warnings.
DEFENDANTS’ DEFENSE The mother received at least two warnings from her physician regarding the potential risks of anticonvulsant and antiepileptic drugs and the importance of not becoming pregnant while taking the medications. An action against the physician was barred by the applicable statute of limitations. The mother had taken topiramate prescribed to her mother for a time; such actions should release Janssen from liability.
VERDICT A $11 million Pennsylvania verdict was returned.
PID MASKS ECTOPIC PREGNANCY
A woman in her 40s became pregnant. On the first two prenatal diagnostic imaging studies, the ObGyn saw an intrauterine pregnancy. He later realized that the pregnancy was ectopic after beta human chorionic gonadotrophin (beta-hCG) blood levels were abnormal. During surgery to terminate the pregnancy, he found he had to perform a total hysterectomy because the patient had extensive pelvic inflammatory disease (PID) caused by a long history of sexually transmitted disease.
PATIENT’S CLAIM If the ectopic pregnancy had been diagnosed earlier, one of her ovaries could have been preserved, saving her from the symptoms of surgical menopause.
PHYSICIAN’S DEFENSE PID had caused the ovaries, numerous fibroid tumors, and the uterus to fuse into one mass. That was why the first two imaging studies appeared to show an intrauterine pregnancy. It was not possible to diagnose the extent of the problem until surgery. The patient did not have a true ectopic pregnancy.
The patient’s difficulties occurred during a 2-week time period in which she had one visit with him and another visit to an ED where two other physicians examined her and missed the diagnosis.
VERDICT A Michigan defense verdict was returned.
ILIAC ARTERY INJURED DURING LAPAROSCOPIC SURGERY; PATIENT DIES
A 40-year-old woman underwent laparoscopic gynecologic surgery performed by her ObGyn. During the procedure, the patient’s left internal iliac artery was punctured, but the injury was not recognized at the time. She was discharged the same day. The next morning, she went into hypovolemic shock due to internal bleeding. She was taken to the ED, where she died.
ESTATE’S CLAIM The ObGyn, anesthesiologist, and hospital staff were negligent in their postoperative care. The anesthesiologist prescribed pain medication that masked the injury; the patient was discharged from the postanesthesia unit too early and without proper examination. The nursing staff did not react to the patient’s reports of abdominal pain, nor did they properly assess her condition prior to discharge. The ObGyn failed to return a phone call the evening after the procedure.
DEFENDANTS’ DEFENSE The ObGyn settled before trial. The anesthesiologist and hospital denied negligence: care was proper and followed all protocols.
VERDICT A confidential California settlement was reached with the ObGyn. A defense verdict was returned for the anesthesiologist and hospital.
Related article: Anatomy for the laparoscopic surgeon Emad Mikhail, MD; Lauren Scott, MD; Stuart Hart, MD, MS (April 2014)
GENETIC TESTING MISSED A KEY DIAGNOSIS
A 40-year-old woman underwent genetic testing after she became pregnant. She was assured that there were no abnormalities that would impact her child.
The baby was born with Wolf-Hirschhorn syndrome, characterized by facial deformities, intellectual disabilities, delayed growth, and seizures. The child is nonverbal, deaf, and blind. She uses a feeding tube and requires 24-hour care.
PARENTS’ CLAIM The genetic testing was improperly conducted. The mother would have had an abortion if she’d known that the child was so disabled.
DEFENDANTS’ DEFENSE Settlements were mediated.
VERDICT A $6.15 million New Jersey settlement was reached on behalf of the hospital and two laboratory technicians, and a $1 million settlement was reached with the director of the genetic laboratory.
HEAT INJURY TO COLON: ABSCESSES, PERITONITIS
A 43-year-old patient had a history of symptomatic uterine fibroids and infertility. Her ObGyn performed a hysteroscopy because he suspected endometriosis, but found none. He then successfully removed a large uterine fibroid during laparoscopic myomectomy. The patient was discharged the same day.
Two days later, the patient developed abdominal pain, nausea, and fever. She went to the ED and was taken into emergency surgery after a CT scan showed free air and fluid in her abdomen. She suffered multiple abscesses and peritonitis.
PATIENT’S CLAIM The ObGyn was negligent in performing the surgery: the sigmoid colon sustained a thermal injury, which caused the abscesses and peritonitis.
PHYSICIAN’S DEFENSE There was no evidence of thermal injury during the original operation; heat damage can and does occur in the absence of negligence. The patient’s previously unknown diverticulitis contributed to the development of the recurrent abscesses and peritonitis.
VERDICT A Florida defense verdict was returned.
RUPTURED UTERUS IS UNDETECTED
During labor and delivery, a declining fetal heart rate was observed, but there was an hour’s delay before cesarean delivery was started. The child suffered a hypoxic brain injury. He has spastic quadriplegia, cannot speak, and requires a respirator and feeding tube.
PARENTS’ CLAIM The mother suffered a ruptured uterus during labor that was not recognized by the ObGyn or nursing staff.
DEFENDANTS’ DEFENSE A settlement was reached during trial.
VERDICT A $7.5 million New Jersey settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Tell us what you think!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!
UTI, THEN MASSIVE HEMORRHAGE
A woman in her 60s was hospitalized with a urinary tract infection (UTI). She was treated with antibiotics and intravenous (IV) fluids but developed deep vein thrombosis (DVT) at the IV site. Enoxaparin sodium was ordered to treat the clot. After 3 days, she suffered a massive abdominal hemorrhage. When she woke from resuscitation, her weight had doubled. She developed a methicillin-resistant Staphylococcus aureus (MRSA) infection, then Clostridium difficile infection due to antibiotics, plus bedsores. Multiple surgeries left her with an abdominal wall defect that cannot be repaired, and a permanent hernia. She was hospitalized for 75 days.
PATIENT’S CLAIM The hemorrhage was caused when enoxaparin was given at 1.5 times the proper dosage because the patient’s weight was overestimated by 50%. Excessive blood, plasma, and fluids caused her weight to double after resuscitation. Her intestines were forced out of her abdominal cavity by the hemorrhage. A permanent hernia, visible underneath her skin, causes pain.
DEFENDANTS’ DEFENSE The patient’s preexisting diabetes, heart condition, high cholesterol levels, and orthopedic issues impacted her condition. She was not compliant in managing her diabetes, causing many of the current problems.
VERDICT A $9.3 million Connecticut verdict was returned.
Related article: Update: Pelvic floor dysfunction Autumn L. Edenfield, MD, and Cindy L. Amundsen, MD (October 2012)
CESAREAN DELAYED UNNECESSARILY
At 37 weeks’ gestation, a mother reported decreased fetal movement. When the biophysical profile test scored 8/8 and the fetal heart rate was reassuring, the attending ObGyn discharged the patient. However, it was the middle of the night, and the nurse kept the mother in the emergency department (ED). At 8:30 am, the fetus began to show signs of fetal distress. Three ObGyns agreed to monitor labor, although one physician wanted delivery to occur that morning.
The next morning, a second biophysical profile scored 2/8, but the on-call ObGyn misunderstood the score as 6/8 and scheduled cesarean delivery for noon. Two hours after the second biophysical profile, the fetal heart rate crashed. A nurse called the ObGyn, who began an emergency cesarean 15 minutes later. The baby, born lifeless, was resuscitated. The child suffered permanent brain damage, and has cerebral palsy, severe cognitive deficits and speech deficits, and walks with an abnormal gait.
PARENTS’ CLAIM A physician did not see the patient for 24 hours, once the decision was made to monitor the mother, even though the fetal heart rate continued to decline. A biophysical profile test score of 2/8 indicates the need for immediate delivery. An earlier cesarean delivery could have reduced the child’s injuries.
DEFENDANTS’ DEFENSE After a settlement was reached with the hospital, the trial continued against the delivering ObGyn. He claimed that decreased fetal movement indicated that the brain injury had occurred 1 to 4 days before the mother came to the ED. The technician had manipulated the mother’s abdomen to wake the fetus before starting the first biophysical profile, which invalidated the score. The nurse miscommunicated the score of the second biophysical profile.
VERDICT A gross $29.8 million Illinois verdict was returned that included a $1.65 million settlement with the hospital.
WAS FACILITY ADEQUATELY STAFFED AFTER HURRICANE IKE?
A mother was admitted to a hospital for induction of labor in September 2008. After birth, the child was found to have cerebral palsy.
PARENTS’ CLAIM The mother should have been sent to another facility before delivery was induced because the hospital was short-staffed and low on resources due to Hurricane Ike. Too much oxytocin was used to induce contractions, which led to a lack of oxygen for the fetus. All prenatal testing had shown a healthy fetus. A cesarean delivery should have occurred when fetal distress was noted.
DEFENDANTS’ DEFENSE The mother had gastric bypass surgery 8 months before she became pregnant, and smoked during pregnancy, which accounted for the infant’s injuries. Treatment during labor and delivery was appropriate. Hospital staffing and resources were adequate.
VERDICT A $6.5 million Texas settlement was reached.
PLACENTA ACCRETA; MOTHER DIES
A 33-year-old woman became pregnant with her second child. A variety of conditions caused this to be high-risk pregnancy, so she saw a maternal-fetal medicine (MFM) specialist 2 months before delivery. The MFM reported that his examination and the ultrasonography (US) results were normal.
The ObGyn who provided prenatal care and delivered her first child scheduled cesarean delivery. During the procedure, the ObGyn noticed a 3- to 4-inch lesion where the placenta had penetrated the uterus. When the placenta was removed, the patient began to hemorrhage and a hysterectomy was performed. The hemorrhage created blood clots that led to gangrene in the patient’s extremities. She died 5 days after giving birth.
ESTATE’S CLAIM Both the MFM and the ObGyn failed to recognize placenta accreta on US prior to delivery. The ObGyn should have performed US prior to beginning cesarean delivery. The hospital’s protocols were not followed: the ObGyn should have stopped the procedure and called for extra surgical assistance and additional blood when he encountered placenta accreta, and again when the patient began to hemorrhage. Placenta accreta does not have to be fatal if detected and managed properly.
DEFENDANTS’ DEFENSE There was no negligence; the patient was treated properly.
VERDICT A $15.5 million Illinois verdict was returned against both physicians and the medical center.
Related article: Is the risk of placenta accreta in a subsequent pregnancy higher after emergent primary cesarean or after elective primary cesarean? Yinka Oyelese, MD (Examining the Evidence, December 2013)
ANTICONVULSANT AND MIGRAINE MEDS TAKEN DURING PREGNANCY
A woman was prescribed topiramate (Topamax) for migraine headaches and hand tremors during the first trimester of her pregnancy in 2007. With a history of seizures, she also took several anticonvulsants throughout her pregnancy. Her child was diagnosed with right unilateral cleft lip (cheiloschisis) in utero. The condition had not been surgically corrected at the time of trial.
PARENTS’ CLAIM The use of topiramate caused the child’s cleft lip. Janssen Pharmaceuticals, the manufacturer of Topamax, knew about the risk of birth defects associated with the drug in 2007, but failed to provide adequate warnings.
DEFENDANTS’ DEFENSE The mother received at least two warnings from her physician regarding the potential risks of anticonvulsant and antiepileptic drugs and the importance of not becoming pregnant while taking the medications. An action against the physician was barred by the applicable statute of limitations. The mother had taken topiramate prescribed to her mother for a time; such actions should release Janssen from liability.
VERDICT A $11 million Pennsylvania verdict was returned.
PID MASKS ECTOPIC PREGNANCY
A woman in her 40s became pregnant. On the first two prenatal diagnostic imaging studies, the ObGyn saw an intrauterine pregnancy. He later realized that the pregnancy was ectopic after beta human chorionic gonadotrophin (beta-hCG) blood levels were abnormal. During surgery to terminate the pregnancy, he found he had to perform a total hysterectomy because the patient had extensive pelvic inflammatory disease (PID) caused by a long history of sexually transmitted disease.
PATIENT’S CLAIM If the ectopic pregnancy had been diagnosed earlier, one of her ovaries could have been preserved, saving her from the symptoms of surgical menopause.
PHYSICIAN’S DEFENSE PID had caused the ovaries, numerous fibroid tumors, and the uterus to fuse into one mass. That was why the first two imaging studies appeared to show an intrauterine pregnancy. It was not possible to diagnose the extent of the problem until surgery. The patient did not have a true ectopic pregnancy.
The patient’s difficulties occurred during a 2-week time period in which she had one visit with him and another visit to an ED where two other physicians examined her and missed the diagnosis.
VERDICT A Michigan defense verdict was returned.
ILIAC ARTERY INJURED DURING LAPAROSCOPIC SURGERY; PATIENT DIES
A 40-year-old woman underwent laparoscopic gynecologic surgery performed by her ObGyn. During the procedure, the patient’s left internal iliac artery was punctured, but the injury was not recognized at the time. She was discharged the same day. The next morning, she went into hypovolemic shock due to internal bleeding. She was taken to the ED, where she died.
ESTATE’S CLAIM The ObGyn, anesthesiologist, and hospital staff were negligent in their postoperative care. The anesthesiologist prescribed pain medication that masked the injury; the patient was discharged from the postanesthesia unit too early and without proper examination. The nursing staff did not react to the patient’s reports of abdominal pain, nor did they properly assess her condition prior to discharge. The ObGyn failed to return a phone call the evening after the procedure.
DEFENDANTS’ DEFENSE The ObGyn settled before trial. The anesthesiologist and hospital denied negligence: care was proper and followed all protocols.
VERDICT A confidential California settlement was reached with the ObGyn. A defense verdict was returned for the anesthesiologist and hospital.
Related article: Anatomy for the laparoscopic surgeon Emad Mikhail, MD; Lauren Scott, MD; Stuart Hart, MD, MS (April 2014)
GENETIC TESTING MISSED A KEY DIAGNOSIS
A 40-year-old woman underwent genetic testing after she became pregnant. She was assured that there were no abnormalities that would impact her child.
The baby was born with Wolf-Hirschhorn syndrome, characterized by facial deformities, intellectual disabilities, delayed growth, and seizures. The child is nonverbal, deaf, and blind. She uses a feeding tube and requires 24-hour care.
PARENTS’ CLAIM The genetic testing was improperly conducted. The mother would have had an abortion if she’d known that the child was so disabled.
DEFENDANTS’ DEFENSE Settlements were mediated.
VERDICT A $6.15 million New Jersey settlement was reached on behalf of the hospital and two laboratory technicians, and a $1 million settlement was reached with the director of the genetic laboratory.
HEAT INJURY TO COLON: ABSCESSES, PERITONITIS
A 43-year-old patient had a history of symptomatic uterine fibroids and infertility. Her ObGyn performed a hysteroscopy because he suspected endometriosis, but found none. He then successfully removed a large uterine fibroid during laparoscopic myomectomy. The patient was discharged the same day.
Two days later, the patient developed abdominal pain, nausea, and fever. She went to the ED and was taken into emergency surgery after a CT scan showed free air and fluid in her abdomen. She suffered multiple abscesses and peritonitis.
PATIENT’S CLAIM The ObGyn was negligent in performing the surgery: the sigmoid colon sustained a thermal injury, which caused the abscesses and peritonitis.
PHYSICIAN’S DEFENSE There was no evidence of thermal injury during the original operation; heat damage can and does occur in the absence of negligence. The patient’s previously unknown diverticulitis contributed to the development of the recurrent abscesses and peritonitis.
VERDICT A Florida defense verdict was returned.
RUPTURED UTERUS IS UNDETECTED
During labor and delivery, a declining fetal heart rate was observed, but there was an hour’s delay before cesarean delivery was started. The child suffered a hypoxic brain injury. He has spastic quadriplegia, cannot speak, and requires a respirator and feeding tube.
PARENTS’ CLAIM The mother suffered a ruptured uterus during labor that was not recognized by the ObGyn or nursing staff.
DEFENDANTS’ DEFENSE A settlement was reached during trial.
VERDICT A $7.5 million New Jersey settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Tell us what you think!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!
UTI, THEN MASSIVE HEMORRHAGE
A woman in her 60s was hospitalized with a urinary tract infection (UTI). She was treated with antibiotics and intravenous (IV) fluids but developed deep vein thrombosis (DVT) at the IV site. Enoxaparin sodium was ordered to treat the clot. After 3 days, she suffered a massive abdominal hemorrhage. When she woke from resuscitation, her weight had doubled. She developed a methicillin-resistant Staphylococcus aureus (MRSA) infection, then Clostridium difficile infection due to antibiotics, plus bedsores. Multiple surgeries left her with an abdominal wall defect that cannot be repaired, and a permanent hernia. She was hospitalized for 75 days.
PATIENT’S CLAIM The hemorrhage was caused when enoxaparin was given at 1.5 times the proper dosage because the patient’s weight was overestimated by 50%. Excessive blood, plasma, and fluids caused her weight to double after resuscitation. Her intestines were forced out of her abdominal cavity by the hemorrhage. A permanent hernia, visible underneath her skin, causes pain.
DEFENDANTS’ DEFENSE The patient’s preexisting diabetes, heart condition, high cholesterol levels, and orthopedic issues impacted her condition. She was not compliant in managing her diabetes, causing many of the current problems.
VERDICT A $9.3 million Connecticut verdict was returned.
Related article: Update: Pelvic floor dysfunction Autumn L. Edenfield, MD, and Cindy L. Amundsen, MD (October 2012)
CESAREAN DELAYED UNNECESSARILY
At 37 weeks’ gestation, a mother reported decreased fetal movement. When the biophysical profile test scored 8/8 and the fetal heart rate was reassuring, the attending ObGyn discharged the patient. However, it was the middle of the night, and the nurse kept the mother in the emergency department (ED). At 8:30 am, the fetus began to show signs of fetal distress. Three ObGyns agreed to monitor labor, although one physician wanted delivery to occur that morning.
The next morning, a second biophysical profile scored 2/8, but the on-call ObGyn misunderstood the score as 6/8 and scheduled cesarean delivery for noon. Two hours after the second biophysical profile, the fetal heart rate crashed. A nurse called the ObGyn, who began an emergency cesarean 15 minutes later. The baby, born lifeless, was resuscitated. The child suffered permanent brain damage, and has cerebral palsy, severe cognitive deficits and speech deficits, and walks with an abnormal gait.
PARENTS’ CLAIM A physician did not see the patient for 24 hours, once the decision was made to monitor the mother, even though the fetal heart rate continued to decline. A biophysical profile test score of 2/8 indicates the need for immediate delivery. An earlier cesarean delivery could have reduced the child’s injuries.
DEFENDANTS’ DEFENSE After a settlement was reached with the hospital, the trial continued against the delivering ObGyn. He claimed that decreased fetal movement indicated that the brain injury had occurred 1 to 4 days before the mother came to the ED. The technician had manipulated the mother’s abdomen to wake the fetus before starting the first biophysical profile, which invalidated the score. The nurse miscommunicated the score of the second biophysical profile.
VERDICT A gross $29.8 million Illinois verdict was returned that included a $1.65 million settlement with the hospital.
WAS FACILITY ADEQUATELY STAFFED AFTER HURRICANE IKE?
A mother was admitted to a hospital for induction of labor in September 2008. After birth, the child was found to have cerebral palsy.
PARENTS’ CLAIM The mother should have been sent to another facility before delivery was induced because the hospital was short-staffed and low on resources due to Hurricane Ike. Too much oxytocin was used to induce contractions, which led to a lack of oxygen for the fetus. All prenatal testing had shown a healthy fetus. A cesarean delivery should have occurred when fetal distress was noted.
DEFENDANTS’ DEFENSE The mother had gastric bypass surgery 8 months before she became pregnant, and smoked during pregnancy, which accounted for the infant’s injuries. Treatment during labor and delivery was appropriate. Hospital staffing and resources were adequate.
VERDICT A $6.5 million Texas settlement was reached.
PLACENTA ACCRETA; MOTHER DIES
A 33-year-old woman became pregnant with her second child. A variety of conditions caused this to be high-risk pregnancy, so she saw a maternal-fetal medicine (MFM) specialist 2 months before delivery. The MFM reported that his examination and the ultrasonography (US) results were normal.
The ObGyn who provided prenatal care and delivered her first child scheduled cesarean delivery. During the procedure, the ObGyn noticed a 3- to 4-inch lesion where the placenta had penetrated the uterus. When the placenta was removed, the patient began to hemorrhage and a hysterectomy was performed. The hemorrhage created blood clots that led to gangrene in the patient’s extremities. She died 5 days after giving birth.
ESTATE’S CLAIM Both the MFM and the ObGyn failed to recognize placenta accreta on US prior to delivery. The ObGyn should have performed US prior to beginning cesarean delivery. The hospital’s protocols were not followed: the ObGyn should have stopped the procedure and called for extra surgical assistance and additional blood when he encountered placenta accreta, and again when the patient began to hemorrhage. Placenta accreta does not have to be fatal if detected and managed properly.
DEFENDANTS’ DEFENSE There was no negligence; the patient was treated properly.
VERDICT A $15.5 million Illinois verdict was returned against both physicians and the medical center.
Related article: Is the risk of placenta accreta in a subsequent pregnancy higher after emergent primary cesarean or after elective primary cesarean? Yinka Oyelese, MD (Examining the Evidence, December 2013)
ANTICONVULSANT AND MIGRAINE MEDS TAKEN DURING PREGNANCY
A woman was prescribed topiramate (Topamax) for migraine headaches and hand tremors during the first trimester of her pregnancy in 2007. With a history of seizures, she also took several anticonvulsants throughout her pregnancy. Her child was diagnosed with right unilateral cleft lip (cheiloschisis) in utero. The condition had not been surgically corrected at the time of trial.
PARENTS’ CLAIM The use of topiramate caused the child’s cleft lip. Janssen Pharmaceuticals, the manufacturer of Topamax, knew about the risk of birth defects associated with the drug in 2007, but failed to provide adequate warnings.
DEFENDANTS’ DEFENSE The mother received at least two warnings from her physician regarding the potential risks of anticonvulsant and antiepileptic drugs and the importance of not becoming pregnant while taking the medications. An action against the physician was barred by the applicable statute of limitations. The mother had taken topiramate prescribed to her mother for a time; such actions should release Janssen from liability.
VERDICT A $11 million Pennsylvania verdict was returned.
PID MASKS ECTOPIC PREGNANCY
A woman in her 40s became pregnant. On the first two prenatal diagnostic imaging studies, the ObGyn saw an intrauterine pregnancy. He later realized that the pregnancy was ectopic after beta human chorionic gonadotrophin (beta-hCG) blood levels were abnormal. During surgery to terminate the pregnancy, he found he had to perform a total hysterectomy because the patient had extensive pelvic inflammatory disease (PID) caused by a long history of sexually transmitted disease.
PATIENT’S CLAIM If the ectopic pregnancy had been diagnosed earlier, one of her ovaries could have been preserved, saving her from the symptoms of surgical menopause.
PHYSICIAN’S DEFENSE PID had caused the ovaries, numerous fibroid tumors, and the uterus to fuse into one mass. That was why the first two imaging studies appeared to show an intrauterine pregnancy. It was not possible to diagnose the extent of the problem until surgery. The patient did not have a true ectopic pregnancy.
The patient’s difficulties occurred during a 2-week time period in which she had one visit with him and another visit to an ED where two other physicians examined her and missed the diagnosis.
VERDICT A Michigan defense verdict was returned.
ILIAC ARTERY INJURED DURING LAPAROSCOPIC SURGERY; PATIENT DIES
A 40-year-old woman underwent laparoscopic gynecologic surgery performed by her ObGyn. During the procedure, the patient’s left internal iliac artery was punctured, but the injury was not recognized at the time. She was discharged the same day. The next morning, she went into hypovolemic shock due to internal bleeding. She was taken to the ED, where she died.
ESTATE’S CLAIM The ObGyn, anesthesiologist, and hospital staff were negligent in their postoperative care. The anesthesiologist prescribed pain medication that masked the injury; the patient was discharged from the postanesthesia unit too early and without proper examination. The nursing staff did not react to the patient’s reports of abdominal pain, nor did they properly assess her condition prior to discharge. The ObGyn failed to return a phone call the evening after the procedure.
DEFENDANTS’ DEFENSE The ObGyn settled before trial. The anesthesiologist and hospital denied negligence: care was proper and followed all protocols.
VERDICT A confidential California settlement was reached with the ObGyn. A defense verdict was returned for the anesthesiologist and hospital.
Related article: Anatomy for the laparoscopic surgeon Emad Mikhail, MD; Lauren Scott, MD; Stuart Hart, MD, MS (April 2014)
GENETIC TESTING MISSED A KEY DIAGNOSIS
A 40-year-old woman underwent genetic testing after she became pregnant. She was assured that there were no abnormalities that would impact her child.
The baby was born with Wolf-Hirschhorn syndrome, characterized by facial deformities, intellectual disabilities, delayed growth, and seizures. The child is nonverbal, deaf, and blind. She uses a feeding tube and requires 24-hour care.
PARENTS’ CLAIM The genetic testing was improperly conducted. The mother would have had an abortion if she’d known that the child was so disabled.
DEFENDANTS’ DEFENSE Settlements were mediated.
VERDICT A $6.15 million New Jersey settlement was reached on behalf of the hospital and two laboratory technicians, and a $1 million settlement was reached with the director of the genetic laboratory.
HEAT INJURY TO COLON: ABSCESSES, PERITONITIS
A 43-year-old patient had a history of symptomatic uterine fibroids and infertility. Her ObGyn performed a hysteroscopy because he suspected endometriosis, but found none. He then successfully removed a large uterine fibroid during laparoscopic myomectomy. The patient was discharged the same day.
Two days later, the patient developed abdominal pain, nausea, and fever. She went to the ED and was taken into emergency surgery after a CT scan showed free air and fluid in her abdomen. She suffered multiple abscesses and peritonitis.
PATIENT’S CLAIM The ObGyn was negligent in performing the surgery: the sigmoid colon sustained a thermal injury, which caused the abscesses and peritonitis.
PHYSICIAN’S DEFENSE There was no evidence of thermal injury during the original operation; heat damage can and does occur in the absence of negligence. The patient’s previously unknown diverticulitis contributed to the development of the recurrent abscesses and peritonitis.
VERDICT A Florida defense verdict was returned.
RUPTURED UTERUS IS UNDETECTED
During labor and delivery, a declining fetal heart rate was observed, but there was an hour’s delay before cesarean delivery was started. The child suffered a hypoxic brain injury. He has spastic quadriplegia, cannot speak, and requires a respirator and feeding tube.
PARENTS’ CLAIM The mother suffered a ruptured uterus during labor that was not recognized by the ObGyn or nursing staff.
DEFENDANTS’ DEFENSE A settlement was reached during trial.
VERDICT A $7.5 million New Jersey settlement was reached.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Tell us what you think!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state.
Stay in touch! Your feedback is important to us!
Liability and casualty insurance claims
The current discussion of the transition to ICD-10 and other health insurance reforms has overshadowed the broader issue of dealing with other types of insurance claims. We buy casualty and liability insurance hoping we will never need it; but when we do, it’s important to get it right, and your extensive experience in coping with health insurance claims can be put to good use in such situations.
Prompt filing is just as important with a casualty or liability claim as it is with a health claim. All insurance policies have a filing deadline, which varies with different policies and states. But just because you file promptly does not mean you have to settle on a payment right away.
Most insurers want a quick resolution as much as you do, but if you allow yourself to be rushed, you could end up with a smaller settlement than you deserve.
If you’re a regular reader of this column, you’re familiar with my first rule of dealing with health insurers: Everything is negotiable. And it’s no different with casualty insurers. Regardless of what adjusters tell you, the initial amount offered is never engraved in stone.
Adjusters are evaluated on the basis of how much money they "save" on claims; so their initial number will usually be low – often too low.
Just as with health insurance claims, there are multiple "gray areas" in casualty policies that can be negotiated. In the case of a burglary or storm or fire damage in your office, for example, reasonable expenses will vary considerably for repair of damaged medical equipment and replacement of equipment that was destroyed, or for rental of alternate office space while a damaged office is being repaired.
Other negotiable costs are moving expenses, storage of damaged and undamaged equipment, and depreciation on specific items. And as we all know from our health insurance experience, injuries are particularly fertile areas for negotiation.
Another adjuster’s trick, which you may have already encountered with a damaged car, is to steer you to certain repair shops and contractors that give the insurer prenegotiated prices for their work, but may offer inferior parts and service. Most policies do not require that you accept the insurer’s choice of contractors. Insist on having work done by people you know and trust. Almost always, you are entitled to the same kind and quality of materials you had before the disaster.
Do your own research on the value of lost and damaged items; the more documentation you have, the less likely an adjuster is to question your claim. Just as with health insurance coding, preparation pays off.
Document your losses very specifically. Adjusters often attempt to group material losses nonselectively, just as health insurers sometimes attempt to "bundle" your services. For example, if a certain cabinet contained medical supplies, try to be very specific about the supplies it contained. That way, you can assign value to individual items, rather than allowing the insurance company to estimate a lump sum.
After the trauma of a burglary, fire, or flood, you may overlook some damage. As many victims of hurricanes and other natural disasters have learned, damage that is not immediately apparent can add up to a significant amount of money later. Another thing your insurer may not tell you is even after you arrive at a settlement, you can still file another claim if you discover additional losses.
It is usually not wise to rely solely on your insurance agent in such situations, because an agent’s loyalty resides primarily with the insurance company, not the claimant. Retaining a lawyer is often a good idea, if only to review paperwork and help you value your losses. It will cost comparatively little, and is usually money well spent. In addition, you will probably need a lawyer for representation if you have a large or complicated case, and certainly if you suspect that the insurance company is not dealing with you fairly.
A less expensive alternative to a lawyer may be a public insurance adjuster. Public adjusters are professionals who work for policyholders, not insurers. They inspect the loss site, analyze the damages, assemble claim support data, review your coverage, determine replacement costs, and strive to maximize your settlement in the same way the insurer’s adjuster will try to minimize it. You can find more information and a list of public adjusters in your area on the website of the National Association of Public Insurance Adjusters.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
The current discussion of the transition to ICD-10 and other health insurance reforms has overshadowed the broader issue of dealing with other types of insurance claims. We buy casualty and liability insurance hoping we will never need it; but when we do, it’s important to get it right, and your extensive experience in coping with health insurance claims can be put to good use in such situations.
Prompt filing is just as important with a casualty or liability claim as it is with a health claim. All insurance policies have a filing deadline, which varies with different policies and states. But just because you file promptly does not mean you have to settle on a payment right away.
Most insurers want a quick resolution as much as you do, but if you allow yourself to be rushed, you could end up with a smaller settlement than you deserve.
If you’re a regular reader of this column, you’re familiar with my first rule of dealing with health insurers: Everything is negotiable. And it’s no different with casualty insurers. Regardless of what adjusters tell you, the initial amount offered is never engraved in stone.
Adjusters are evaluated on the basis of how much money they "save" on claims; so their initial number will usually be low – often too low.
Just as with health insurance claims, there are multiple "gray areas" in casualty policies that can be negotiated. In the case of a burglary or storm or fire damage in your office, for example, reasonable expenses will vary considerably for repair of damaged medical equipment and replacement of equipment that was destroyed, or for rental of alternate office space while a damaged office is being repaired.
Other negotiable costs are moving expenses, storage of damaged and undamaged equipment, and depreciation on specific items. And as we all know from our health insurance experience, injuries are particularly fertile areas for negotiation.
Another adjuster’s trick, which you may have already encountered with a damaged car, is to steer you to certain repair shops and contractors that give the insurer prenegotiated prices for their work, but may offer inferior parts and service. Most policies do not require that you accept the insurer’s choice of contractors. Insist on having work done by people you know and trust. Almost always, you are entitled to the same kind and quality of materials you had before the disaster.
Do your own research on the value of lost and damaged items; the more documentation you have, the less likely an adjuster is to question your claim. Just as with health insurance coding, preparation pays off.
Document your losses very specifically. Adjusters often attempt to group material losses nonselectively, just as health insurers sometimes attempt to "bundle" your services. For example, if a certain cabinet contained medical supplies, try to be very specific about the supplies it contained. That way, you can assign value to individual items, rather than allowing the insurance company to estimate a lump sum.
After the trauma of a burglary, fire, or flood, you may overlook some damage. As many victims of hurricanes and other natural disasters have learned, damage that is not immediately apparent can add up to a significant amount of money later. Another thing your insurer may not tell you is even after you arrive at a settlement, you can still file another claim if you discover additional losses.
It is usually not wise to rely solely on your insurance agent in such situations, because an agent’s loyalty resides primarily with the insurance company, not the claimant. Retaining a lawyer is often a good idea, if only to review paperwork and help you value your losses. It will cost comparatively little, and is usually money well spent. In addition, you will probably need a lawyer for representation if you have a large or complicated case, and certainly if you suspect that the insurance company is not dealing with you fairly.
A less expensive alternative to a lawyer may be a public insurance adjuster. Public adjusters are professionals who work for policyholders, not insurers. They inspect the loss site, analyze the damages, assemble claim support data, review your coverage, determine replacement costs, and strive to maximize your settlement in the same way the insurer’s adjuster will try to minimize it. You can find more information and a list of public adjusters in your area on the website of the National Association of Public Insurance Adjusters.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
The current discussion of the transition to ICD-10 and other health insurance reforms has overshadowed the broader issue of dealing with other types of insurance claims. We buy casualty and liability insurance hoping we will never need it; but when we do, it’s important to get it right, and your extensive experience in coping with health insurance claims can be put to good use in such situations.
Prompt filing is just as important with a casualty or liability claim as it is with a health claim. All insurance policies have a filing deadline, which varies with different policies and states. But just because you file promptly does not mean you have to settle on a payment right away.
Most insurers want a quick resolution as much as you do, but if you allow yourself to be rushed, you could end up with a smaller settlement than you deserve.
If you’re a regular reader of this column, you’re familiar with my first rule of dealing with health insurers: Everything is negotiable. And it’s no different with casualty insurers. Regardless of what adjusters tell you, the initial amount offered is never engraved in stone.
Adjusters are evaluated on the basis of how much money they "save" on claims; so their initial number will usually be low – often too low.
Just as with health insurance claims, there are multiple "gray areas" in casualty policies that can be negotiated. In the case of a burglary or storm or fire damage in your office, for example, reasonable expenses will vary considerably for repair of damaged medical equipment and replacement of equipment that was destroyed, or for rental of alternate office space while a damaged office is being repaired.
Other negotiable costs are moving expenses, storage of damaged and undamaged equipment, and depreciation on specific items. And as we all know from our health insurance experience, injuries are particularly fertile areas for negotiation.
Another adjuster’s trick, which you may have already encountered with a damaged car, is to steer you to certain repair shops and contractors that give the insurer prenegotiated prices for their work, but may offer inferior parts and service. Most policies do not require that you accept the insurer’s choice of contractors. Insist on having work done by people you know and trust. Almost always, you are entitled to the same kind and quality of materials you had before the disaster.
Do your own research on the value of lost and damaged items; the more documentation you have, the less likely an adjuster is to question your claim. Just as with health insurance coding, preparation pays off.
Document your losses very specifically. Adjusters often attempt to group material losses nonselectively, just as health insurers sometimes attempt to "bundle" your services. For example, if a certain cabinet contained medical supplies, try to be very specific about the supplies it contained. That way, you can assign value to individual items, rather than allowing the insurance company to estimate a lump sum.
After the trauma of a burglary, fire, or flood, you may overlook some damage. As many victims of hurricanes and other natural disasters have learned, damage that is not immediately apparent can add up to a significant amount of money later. Another thing your insurer may not tell you is even after you arrive at a settlement, you can still file another claim if you discover additional losses.
It is usually not wise to rely solely on your insurance agent in such situations, because an agent’s loyalty resides primarily with the insurance company, not the claimant. Retaining a lawyer is often a good idea, if only to review paperwork and help you value your losses. It will cost comparatively little, and is usually money well spent. In addition, you will probably need a lawyer for representation if you have a large or complicated case, and certainly if you suspect that the insurance company is not dealing with you fairly.
A less expensive alternative to a lawyer may be a public insurance adjuster. Public adjusters are professionals who work for policyholders, not insurers. They inspect the loss site, analyze the damages, assemble claim support data, review your coverage, determine replacement costs, and strive to maximize your settlement in the same way the insurer’s adjuster will try to minimize it. You can find more information and a list of public adjusters in your area on the website of the National Association of Public Insurance Adjusters.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
Use Online Coding Discussion Tools With Caution
Single accreditation for MDs and DOs by 2020
For the first time, allopathic and osteopathic residency and fellowship programs will be accredited through a single body.
By June 30, 2020, the American Osteopathic Association (AOA) will stop offering accreditation to osteopathic graduate medical education programs. Instead, the Accreditation Council for Graduate Medical Education (ACGME) will assume responsibility for accrediting all graduate medical education programs in the United States under a single system.
The plan, which was announced jointly by the AOA, the ACGME, and the American Association of Colleges of Osteopathic Medicine (AACOM) on Feb. 26, gives AOA-accredited programs 5 years to transition to the new system. From July 1, 2015, to June 30, 2020, osteopathic programs can apply for and receive ACGME recognition and accreditation.
"This uniform path of preparation for practice ensures that the evaluation of and accountability for the competency of all resident physicians – MDs and DOs – will be consistent across all programs," said Dr. Thomas Nasca, chief executive officer of the ACGME. "A single accreditation system provides the opportunity to introduce and consistently evaluate new physician competencies that are needed to meet patient needs and the health care delivery challenges facing the U.S. over the next decade."
But osteopathic training programs will still retain their unique focus, said Dr. Norman E. Vinn, AOA president.
Under the plan, the AOA and the AACOM will join the ACGME as member organizations and will nominate individuals to serve on the ACGME board of directors. Two new osteopathic review committees will be created to set standards for the graduate medical education programs that seek osteopathic recognition.
"This is an opportunity to both reinforce and proliferate our principles," Dr. Vinn said.
Creating a single accreditation pathway is also expected to be more efficient for programs and trainees. Under the plan, MD and DO graduates who meet the prerequisite competencies can access any graduate medical education program or transfer from one accredited program to another without being required to repeat parts of their training. And institutions will not need to sponsor "dually accredited" or "parallel-accredited" allopathic and osteopathic medical residency programs.
Both the American Medical Association (AMA) and the Association of American Medical Colleges (AAMC) praised the move to a unified accreditation system.
"As the system develops, we expect that it will continue to raise the quality of graduate medical education for new physicians, ensuring a consistently high-quality health care workforce for the future," said Dr. Darrell G. Kirch, president and CEO of the AAMC. "The growing collaboration between the allopathic and osteopathic physician communities will only serve to improve patient care for all Americans."
OnTwitter @maryellenny
For the first time, allopathic and osteopathic residency and fellowship programs will be accredited through a single body.
By June 30, 2020, the American Osteopathic Association (AOA) will stop offering accreditation to osteopathic graduate medical education programs. Instead, the Accreditation Council for Graduate Medical Education (ACGME) will assume responsibility for accrediting all graduate medical education programs in the United States under a single system.
The plan, which was announced jointly by the AOA, the ACGME, and the American Association of Colleges of Osteopathic Medicine (AACOM) on Feb. 26, gives AOA-accredited programs 5 years to transition to the new system. From July 1, 2015, to June 30, 2020, osteopathic programs can apply for and receive ACGME recognition and accreditation.
"This uniform path of preparation for practice ensures that the evaluation of and accountability for the competency of all resident physicians – MDs and DOs – will be consistent across all programs," said Dr. Thomas Nasca, chief executive officer of the ACGME. "A single accreditation system provides the opportunity to introduce and consistently evaluate new physician competencies that are needed to meet patient needs and the health care delivery challenges facing the U.S. over the next decade."
But osteopathic training programs will still retain their unique focus, said Dr. Norman E. Vinn, AOA president.
Under the plan, the AOA and the AACOM will join the ACGME as member organizations and will nominate individuals to serve on the ACGME board of directors. Two new osteopathic review committees will be created to set standards for the graduate medical education programs that seek osteopathic recognition.
"This is an opportunity to both reinforce and proliferate our principles," Dr. Vinn said.
Creating a single accreditation pathway is also expected to be more efficient for programs and trainees. Under the plan, MD and DO graduates who meet the prerequisite competencies can access any graduate medical education program or transfer from one accredited program to another without being required to repeat parts of their training. And institutions will not need to sponsor "dually accredited" or "parallel-accredited" allopathic and osteopathic medical residency programs.
Both the American Medical Association (AMA) and the Association of American Medical Colleges (AAMC) praised the move to a unified accreditation system.
"As the system develops, we expect that it will continue to raise the quality of graduate medical education for new physicians, ensuring a consistently high-quality health care workforce for the future," said Dr. Darrell G. Kirch, president and CEO of the AAMC. "The growing collaboration between the allopathic and osteopathic physician communities will only serve to improve patient care for all Americans."
OnTwitter @maryellenny
For the first time, allopathic and osteopathic residency and fellowship programs will be accredited through a single body.
By June 30, 2020, the American Osteopathic Association (AOA) will stop offering accreditation to osteopathic graduate medical education programs. Instead, the Accreditation Council for Graduate Medical Education (ACGME) will assume responsibility for accrediting all graduate medical education programs in the United States under a single system.
The plan, which was announced jointly by the AOA, the ACGME, and the American Association of Colleges of Osteopathic Medicine (AACOM) on Feb. 26, gives AOA-accredited programs 5 years to transition to the new system. From July 1, 2015, to June 30, 2020, osteopathic programs can apply for and receive ACGME recognition and accreditation.
"This uniform path of preparation for practice ensures that the evaluation of and accountability for the competency of all resident physicians – MDs and DOs – will be consistent across all programs," said Dr. Thomas Nasca, chief executive officer of the ACGME. "A single accreditation system provides the opportunity to introduce and consistently evaluate new physician competencies that are needed to meet patient needs and the health care delivery challenges facing the U.S. over the next decade."
But osteopathic training programs will still retain their unique focus, said Dr. Norman E. Vinn, AOA president.
Under the plan, the AOA and the AACOM will join the ACGME as member organizations and will nominate individuals to serve on the ACGME board of directors. Two new osteopathic review committees will be created to set standards for the graduate medical education programs that seek osteopathic recognition.
"This is an opportunity to both reinforce and proliferate our principles," Dr. Vinn said.
Creating a single accreditation pathway is also expected to be more efficient for programs and trainees. Under the plan, MD and DO graduates who meet the prerequisite competencies can access any graduate medical education program or transfer from one accredited program to another without being required to repeat parts of their training. And institutions will not need to sponsor "dually accredited" or "parallel-accredited" allopathic and osteopathic medical residency programs.
Both the American Medical Association (AMA) and the Association of American Medical Colleges (AAMC) praised the move to a unified accreditation system.
"As the system develops, we expect that it will continue to raise the quality of graduate medical education for new physicians, ensuring a consistently high-quality health care workforce for the future," said Dr. Darrell G. Kirch, president and CEO of the AAMC. "The growing collaboration between the allopathic and osteopathic physician communities will only serve to improve patient care for all Americans."
OnTwitter @maryellenny
Placenta fails to deliver: Mother dies of hemorrhage
PLACENTA FAILS TO DELIVER: MOTHER DIES OF HEMORRHAGE
After a 38-year-old woman gave birth, the placenta did not deliver. The ObGyn was unable remove the entire placenta and the mother began to hemorrhage. After an hour, the patient was given a blood transfusion. She could not be stabilized and died.
ESTATE’S CLAIM The ObGyn was negligent. He failed to remove the entire placenta and did not treat the hemorrhage in a timely manner. The hospital staff was negligent in failing to properly address the massive hemorrhage. A prompt transfusion would have saved the woman’s life, but the anesthesiologist who had to approve the procedure could not be located. Other procedures, including a hysterectomy, could have saved the mother’s life.
DEFENDANTS’ DEFENSE The ObGyn claimed that incomplete delivery of the placenta and postpartum hemorrhage are known complications of a delivery. The hospital claimed that the staff had acted appropriately and that it was not responsible for the actions of the anesthesiologist, an independent contractor. The anesthesiologist denied negligence.
VERDICT A $2 million New York settlement was reached that included $200,000 from the hospital and $1.8 million from the physicians’ insurers.
Related Article: Postpartum hemorrhage: 11 critical questions, answered by an expert Haywood L. Brown, MD (January 2011)
DECREASED FETAL MOVEMENT OVERLOOKED; SEVERE INJURY TO BABY
At her 39th-week prenatal visit at a clinic, the mother reported decreased fetal movement. Acoustic stimulation of the fetus was attempted twice without response. The fetal heart-rate monitor identified a normal heart rate without variability or accelerations. The mother was taken by wheelchair to the hospital next door. A note explaining the nonreassuring findings allegedly accompanied her.
The mother waited to be admitted. When a fetal heart-rate monitor was connected 30 minutes after admission, results were still nonreassuring.
A resident examined the mother 45 minutes later. He called the attending ObGyn, and they decided to postpone cesarean delivery because the mother had eaten breakfast.
When the fetal heart rate crashed 4 hours later, a second-year resident began emergency cesarean delivery. The ObGyn, who had never examined the patient, observed some of the procedure in the OR.
The baby was born with catastrophic brain damage, and has spastic quadriplegia cerebral palsy, feeding problems, and significant cognitive and developmental delays.
PARENTS’ CLAIM A cesarean delivery should have been performed immediately after the mother’s admission. Even if the cesarean had been begun 15 to 20 minutes earlier, the injury could have been avoided. The ObGyn never examined the mother nor did he participate in the cesarean delivery.
DEFENDANTS’ DEFENSE The ObGyn and hospital denied negligence. The note was not attached to the patient’s chart. At trial, the ObGyn admitted that a delivery 15 to 20 minutes earlier might have avoided the injury.
VERDICT A $33,591,900 Tennessee verdict was returned.
WOMAN BECOMES PREGNANT AFTER TUBAL LIGATION
A 32-year-old woman requested sterilization after the birth of her third child. A Falope ring tubal ligation procedure was performed by a gynecologist in April 2006. During surgery, the device used by the gynecologist ejected 2 silastic bands on the right side instead of one.
The patient learned she was pregnant in March 2007. Her high-risk pregnancy ended with cesarean delivery in September 2007. The delivering ObGyn found the patient’s right fallopian tube in its natural, unscarred state. A silastic band was applied to the right ovarian ligament, not the right fallopian tube.
PATIENT’S CLAIM The gynecologist banded the ovarian ligament instead of the fallopian tube.
PHYSICIAN’S DEFENSE The procedure was properly performed. The rings initially enclosed the fallopian tube and ovarian ligament, but the top ring subsequently migrated off the structures, allowing the fallopian tube to slip out of the attachment. Failure to sterilize is a known risk of the procedure.
VERDICT An Illinois defense verdict was returned.
ABORTION ATTEMPTED BUT PREGNANCY IS ECTOPIC
A 14-year-old patient went to a clinic for elective abortion at 8 weeks’ gestation. Ultrasonography (US) prior to the procedure showed an intrauterine pregnancy. After dilating the cervix, the ObGyn inserted a semi-rigid vacuum aspiration curette to suction the uterine contents, but received nothing. A second US confirmed an intrauterine pregnancy. The ObGyn was able to locate the pregnancy and indent the gestational sac with 3 different dilators and the curette. The pregnancy decreased in size on US after the suction was applied. However, the patient’s vital signs dropped dramatically, and she was rushed to the hospital. During emergency surgery, severe pelvic adhesive disease complicated the ability to stop the hemorrhage. Four physicians concurred that supracervical hysterectomy was needed to save the patient’s life. Postoperative pathology identified a cornual or interstitial ectopic pregnancy.
PATIENT’S CLAIM The ObGyn failed to heed several warning signs of ectopic pregnancy. Further testing should have been done before the second round of vacuum. If ectopic pregnancy had been discovered earlier, the patient could have undergone surgery that would have preserved her uterus and allowed her to bear children. The ObGyn tore the uterus multiple times when he turned on the suction, causing massive hemorrhage.
PHYSICIAN’S DEFENSE Ultrasonography clearly showed an intrauterine pregnancy. There was nothing to cause suspicion that the pregnancy was ectopic. She might be able to have a child through surrogacy.
VERDICT A $950,000 Illinois verdict was returned.
Related Article: Is the hCG discriminatory zone a reliable indicator of intrauterine or ectopic pregnancy? Andrew M. Kaunitz, MD (Examining the Evidence, February 2012)
MACROSOMIC FETUS: MOTHER AND BABY BOTH INJURED
When prenatal ultrasonography indicated the fetal weight was 10 lbs, the patient and her mother expressed concern over delivery of such a large baby. The ObGyn reassured them that it would not be a problem.
Four days later, the mother went into labor. She was 9-cm dilated 4.5 hours later, but only progressed to 9.5 cm over the next 7 hours. She was told to begin to push, but, after 2 hours, birth had not occurred. The ObGyn used forceps to deliver the head 45 minutes later. Shoulder dystocia was encountered and there was a 3.5-minute delivery delay. The baby suffered oxygen deprivation and the mother experienced a 4th-degree perineal tear.
After the NICU team resuscitated the baby, she was transferred to another hospital, where she underwent “head cooling” in an attempt to mitigate her injuries. The child has mild cerebral palsy, with right hemiparesis, speech delay, and additional neurologic injuries.
PARENTS' CLAIM Cesarean delivery was unnecessarily delayed. The ObGyn was negligent in not performing an emergency cesarean delivery after 2 hours of pushing was not effective. The ObGyn never suggested a cesarean delivery, it was not noted in the chart, and no one else present at the time remembered the option being offered.
PHYSICIAN’S DEFENSE There was nothing during labor to contraindicate a vaginal birth. The ObGyn claimed that he offered a cesarean delivery after 2 hours of pushing. The baby’s blood gas reading at delivery was normal. Any brain injuries to the baby were from resuscitation.
VERDICT A $4,080,500 Pennsylvania verdict was returned.
Related Articles:
When macrosomia is suspected at term, does induction of labor lower the risk of cesarean delivery? Jennifer T. Ahn, MD (Examining the Evidence, May 2012)
Develop and use a checklist for 3rd- and 4th-degree perinatal lacerations Robert L. Barbieri, MD (Editorial, August 2013)
BOWEL INJURY DURING CESAREAN DELIVERY
During cesarean delivery, the mother suffered a bowel injury that led to infection and several abdominal abscesses. She required two procedures for drain placement plus two additional operations.
PATIENT’S CLAIM The ObGyn was negligent in how he performed the cesarean delivery and for not treating the injury and subsequent infection in a timely manner. The abscesses took 3 years to resolve; additional procedures left scarring and aggravated a spinal injury.
PHYSICIAN’S DEFENSE Bowel perforation is a known complication of cesarean delivery. It probably occurred during manipulation of the uterus in an area that was not visible.
VERDICT A $750,000 New Jersey verdict was returned.
Related Article: How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy Michael Baggish, MD (Surgical Technique, October 2012)
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
TELL US WHAT YOU THINK!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter and in a future issue.
Send your letter to: [email protected] Please include the city and state in which you practice.
Stay in touch! Your feedback is important to us!
PLACENTA FAILS TO DELIVER: MOTHER DIES OF HEMORRHAGE
After a 38-year-old woman gave birth, the placenta did not deliver. The ObGyn was unable remove the entire placenta and the mother began to hemorrhage. After an hour, the patient was given a blood transfusion. She could not be stabilized and died.
ESTATE’S CLAIM The ObGyn was negligent. He failed to remove the entire placenta and did not treat the hemorrhage in a timely manner. The hospital staff was negligent in failing to properly address the massive hemorrhage. A prompt transfusion would have saved the woman’s life, but the anesthesiologist who had to approve the procedure could not be located. Other procedures, including a hysterectomy, could have saved the mother’s life.
DEFENDANTS’ DEFENSE The ObGyn claimed that incomplete delivery of the placenta and postpartum hemorrhage are known complications of a delivery. The hospital claimed that the staff had acted appropriately and that it was not responsible for the actions of the anesthesiologist, an independent contractor. The anesthesiologist denied negligence.
VERDICT A $2 million New York settlement was reached that included $200,000 from the hospital and $1.8 million from the physicians’ insurers.
Related Article: Postpartum hemorrhage: 11 critical questions, answered by an expert Haywood L. Brown, MD (January 2011)
DECREASED FETAL MOVEMENT OVERLOOKED; SEVERE INJURY TO BABY
At her 39th-week prenatal visit at a clinic, the mother reported decreased fetal movement. Acoustic stimulation of the fetus was attempted twice without response. The fetal heart-rate monitor identified a normal heart rate without variability or accelerations. The mother was taken by wheelchair to the hospital next door. A note explaining the nonreassuring findings allegedly accompanied her.
The mother waited to be admitted. When a fetal heart-rate monitor was connected 30 minutes after admission, results were still nonreassuring.
A resident examined the mother 45 minutes later. He called the attending ObGyn, and they decided to postpone cesarean delivery because the mother had eaten breakfast.
When the fetal heart rate crashed 4 hours later, a second-year resident began emergency cesarean delivery. The ObGyn, who had never examined the patient, observed some of the procedure in the OR.
The baby was born with catastrophic brain damage, and has spastic quadriplegia cerebral palsy, feeding problems, and significant cognitive and developmental delays.
PARENTS’ CLAIM A cesarean delivery should have been performed immediately after the mother’s admission. Even if the cesarean had been begun 15 to 20 minutes earlier, the injury could have been avoided. The ObGyn never examined the mother nor did he participate in the cesarean delivery.
DEFENDANTS’ DEFENSE The ObGyn and hospital denied negligence. The note was not attached to the patient’s chart. At trial, the ObGyn admitted that a delivery 15 to 20 minutes earlier might have avoided the injury.
VERDICT A $33,591,900 Tennessee verdict was returned.
WOMAN BECOMES PREGNANT AFTER TUBAL LIGATION
A 32-year-old woman requested sterilization after the birth of her third child. A Falope ring tubal ligation procedure was performed by a gynecologist in April 2006. During surgery, the device used by the gynecologist ejected 2 silastic bands on the right side instead of one.
The patient learned she was pregnant in March 2007. Her high-risk pregnancy ended with cesarean delivery in September 2007. The delivering ObGyn found the patient’s right fallopian tube in its natural, unscarred state. A silastic band was applied to the right ovarian ligament, not the right fallopian tube.
PATIENT’S CLAIM The gynecologist banded the ovarian ligament instead of the fallopian tube.
PHYSICIAN’S DEFENSE The procedure was properly performed. The rings initially enclosed the fallopian tube and ovarian ligament, but the top ring subsequently migrated off the structures, allowing the fallopian tube to slip out of the attachment. Failure to sterilize is a known risk of the procedure.
VERDICT An Illinois defense verdict was returned.
ABORTION ATTEMPTED BUT PREGNANCY IS ECTOPIC
A 14-year-old patient went to a clinic for elective abortion at 8 weeks’ gestation. Ultrasonography (US) prior to the procedure showed an intrauterine pregnancy. After dilating the cervix, the ObGyn inserted a semi-rigid vacuum aspiration curette to suction the uterine contents, but received nothing. A second US confirmed an intrauterine pregnancy. The ObGyn was able to locate the pregnancy and indent the gestational sac with 3 different dilators and the curette. The pregnancy decreased in size on US after the suction was applied. However, the patient’s vital signs dropped dramatically, and she was rushed to the hospital. During emergency surgery, severe pelvic adhesive disease complicated the ability to stop the hemorrhage. Four physicians concurred that supracervical hysterectomy was needed to save the patient’s life. Postoperative pathology identified a cornual or interstitial ectopic pregnancy.
PATIENT’S CLAIM The ObGyn failed to heed several warning signs of ectopic pregnancy. Further testing should have been done before the second round of vacuum. If ectopic pregnancy had been discovered earlier, the patient could have undergone surgery that would have preserved her uterus and allowed her to bear children. The ObGyn tore the uterus multiple times when he turned on the suction, causing massive hemorrhage.
PHYSICIAN’S DEFENSE Ultrasonography clearly showed an intrauterine pregnancy. There was nothing to cause suspicion that the pregnancy was ectopic. She might be able to have a child through surrogacy.
VERDICT A $950,000 Illinois verdict was returned.
Related Article: Is the hCG discriminatory zone a reliable indicator of intrauterine or ectopic pregnancy? Andrew M. Kaunitz, MD (Examining the Evidence, February 2012)
MACROSOMIC FETUS: MOTHER AND BABY BOTH INJURED
When prenatal ultrasonography indicated the fetal weight was 10 lbs, the patient and her mother expressed concern over delivery of such a large baby. The ObGyn reassured them that it would not be a problem.
Four days later, the mother went into labor. She was 9-cm dilated 4.5 hours later, but only progressed to 9.5 cm over the next 7 hours. She was told to begin to push, but, after 2 hours, birth had not occurred. The ObGyn used forceps to deliver the head 45 minutes later. Shoulder dystocia was encountered and there was a 3.5-minute delivery delay. The baby suffered oxygen deprivation and the mother experienced a 4th-degree perineal tear.
After the NICU team resuscitated the baby, she was transferred to another hospital, where she underwent “head cooling” in an attempt to mitigate her injuries. The child has mild cerebral palsy, with right hemiparesis, speech delay, and additional neurologic injuries.
PARENTS' CLAIM Cesarean delivery was unnecessarily delayed. The ObGyn was negligent in not performing an emergency cesarean delivery after 2 hours of pushing was not effective. The ObGyn never suggested a cesarean delivery, it was not noted in the chart, and no one else present at the time remembered the option being offered.
PHYSICIAN’S DEFENSE There was nothing during labor to contraindicate a vaginal birth. The ObGyn claimed that he offered a cesarean delivery after 2 hours of pushing. The baby’s blood gas reading at delivery was normal. Any brain injuries to the baby were from resuscitation.
VERDICT A $4,080,500 Pennsylvania verdict was returned.
Related Articles:
When macrosomia is suspected at term, does induction of labor lower the risk of cesarean delivery? Jennifer T. Ahn, MD (Examining the Evidence, May 2012)
Develop and use a checklist for 3rd- and 4th-degree perinatal lacerations Robert L. Barbieri, MD (Editorial, August 2013)
BOWEL INJURY DURING CESAREAN DELIVERY
During cesarean delivery, the mother suffered a bowel injury that led to infection and several abdominal abscesses. She required two procedures for drain placement plus two additional operations.
PATIENT’S CLAIM The ObGyn was negligent in how he performed the cesarean delivery and for not treating the injury and subsequent infection in a timely manner. The abscesses took 3 years to resolve; additional procedures left scarring and aggravated a spinal injury.
PHYSICIAN’S DEFENSE Bowel perforation is a known complication of cesarean delivery. It probably occurred during manipulation of the uterus in an area that was not visible.
VERDICT A $750,000 New Jersey verdict was returned.
Related Article: How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy Michael Baggish, MD (Surgical Technique, October 2012)
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
TELL US WHAT YOU THINK!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter and in a future issue.
Send your letter to: [email protected] Please include the city and state in which you practice.
Stay in touch! Your feedback is important to us!
PLACENTA FAILS TO DELIVER: MOTHER DIES OF HEMORRHAGE
After a 38-year-old woman gave birth, the placenta did not deliver. The ObGyn was unable remove the entire placenta and the mother began to hemorrhage. After an hour, the patient was given a blood transfusion. She could not be stabilized and died.
ESTATE’S CLAIM The ObGyn was negligent. He failed to remove the entire placenta and did not treat the hemorrhage in a timely manner. The hospital staff was negligent in failing to properly address the massive hemorrhage. A prompt transfusion would have saved the woman’s life, but the anesthesiologist who had to approve the procedure could not be located. Other procedures, including a hysterectomy, could have saved the mother’s life.
DEFENDANTS’ DEFENSE The ObGyn claimed that incomplete delivery of the placenta and postpartum hemorrhage are known complications of a delivery. The hospital claimed that the staff had acted appropriately and that it was not responsible for the actions of the anesthesiologist, an independent contractor. The anesthesiologist denied negligence.
VERDICT A $2 million New York settlement was reached that included $200,000 from the hospital and $1.8 million from the physicians’ insurers.
Related Article: Postpartum hemorrhage: 11 critical questions, answered by an expert Haywood L. Brown, MD (January 2011)
DECREASED FETAL MOVEMENT OVERLOOKED; SEVERE INJURY TO BABY
At her 39th-week prenatal visit at a clinic, the mother reported decreased fetal movement. Acoustic stimulation of the fetus was attempted twice without response. The fetal heart-rate monitor identified a normal heart rate without variability or accelerations. The mother was taken by wheelchair to the hospital next door. A note explaining the nonreassuring findings allegedly accompanied her.
The mother waited to be admitted. When a fetal heart-rate monitor was connected 30 minutes after admission, results were still nonreassuring.
A resident examined the mother 45 minutes later. He called the attending ObGyn, and they decided to postpone cesarean delivery because the mother had eaten breakfast.
When the fetal heart rate crashed 4 hours later, a second-year resident began emergency cesarean delivery. The ObGyn, who had never examined the patient, observed some of the procedure in the OR.
The baby was born with catastrophic brain damage, and has spastic quadriplegia cerebral palsy, feeding problems, and significant cognitive and developmental delays.
PARENTS’ CLAIM A cesarean delivery should have been performed immediately after the mother’s admission. Even if the cesarean had been begun 15 to 20 minutes earlier, the injury could have been avoided. The ObGyn never examined the mother nor did he participate in the cesarean delivery.
DEFENDANTS’ DEFENSE The ObGyn and hospital denied negligence. The note was not attached to the patient’s chart. At trial, the ObGyn admitted that a delivery 15 to 20 minutes earlier might have avoided the injury.
VERDICT A $33,591,900 Tennessee verdict was returned.
WOMAN BECOMES PREGNANT AFTER TUBAL LIGATION
A 32-year-old woman requested sterilization after the birth of her third child. A Falope ring tubal ligation procedure was performed by a gynecologist in April 2006. During surgery, the device used by the gynecologist ejected 2 silastic bands on the right side instead of one.
The patient learned she was pregnant in March 2007. Her high-risk pregnancy ended with cesarean delivery in September 2007. The delivering ObGyn found the patient’s right fallopian tube in its natural, unscarred state. A silastic band was applied to the right ovarian ligament, not the right fallopian tube.
PATIENT’S CLAIM The gynecologist banded the ovarian ligament instead of the fallopian tube.
PHYSICIAN’S DEFENSE The procedure was properly performed. The rings initially enclosed the fallopian tube and ovarian ligament, but the top ring subsequently migrated off the structures, allowing the fallopian tube to slip out of the attachment. Failure to sterilize is a known risk of the procedure.
VERDICT An Illinois defense verdict was returned.
ABORTION ATTEMPTED BUT PREGNANCY IS ECTOPIC
A 14-year-old patient went to a clinic for elective abortion at 8 weeks’ gestation. Ultrasonography (US) prior to the procedure showed an intrauterine pregnancy. After dilating the cervix, the ObGyn inserted a semi-rigid vacuum aspiration curette to suction the uterine contents, but received nothing. A second US confirmed an intrauterine pregnancy. The ObGyn was able to locate the pregnancy and indent the gestational sac with 3 different dilators and the curette. The pregnancy decreased in size on US after the suction was applied. However, the patient’s vital signs dropped dramatically, and she was rushed to the hospital. During emergency surgery, severe pelvic adhesive disease complicated the ability to stop the hemorrhage. Four physicians concurred that supracervical hysterectomy was needed to save the patient’s life. Postoperative pathology identified a cornual or interstitial ectopic pregnancy.
PATIENT’S CLAIM The ObGyn failed to heed several warning signs of ectopic pregnancy. Further testing should have been done before the second round of vacuum. If ectopic pregnancy had been discovered earlier, the patient could have undergone surgery that would have preserved her uterus and allowed her to bear children. The ObGyn tore the uterus multiple times when he turned on the suction, causing massive hemorrhage.
PHYSICIAN’S DEFENSE Ultrasonography clearly showed an intrauterine pregnancy. There was nothing to cause suspicion that the pregnancy was ectopic. She might be able to have a child through surrogacy.
VERDICT A $950,000 Illinois verdict was returned.
Related Article: Is the hCG discriminatory zone a reliable indicator of intrauterine or ectopic pregnancy? Andrew M. Kaunitz, MD (Examining the Evidence, February 2012)
MACROSOMIC FETUS: MOTHER AND BABY BOTH INJURED
When prenatal ultrasonography indicated the fetal weight was 10 lbs, the patient and her mother expressed concern over delivery of such a large baby. The ObGyn reassured them that it would not be a problem.
Four days later, the mother went into labor. She was 9-cm dilated 4.5 hours later, but only progressed to 9.5 cm over the next 7 hours. She was told to begin to push, but, after 2 hours, birth had not occurred. The ObGyn used forceps to deliver the head 45 minutes later. Shoulder dystocia was encountered and there was a 3.5-minute delivery delay. The baby suffered oxygen deprivation and the mother experienced a 4th-degree perineal tear.
After the NICU team resuscitated the baby, she was transferred to another hospital, where she underwent “head cooling” in an attempt to mitigate her injuries. The child has mild cerebral palsy, with right hemiparesis, speech delay, and additional neurologic injuries.
PARENTS' CLAIM Cesarean delivery was unnecessarily delayed. The ObGyn was negligent in not performing an emergency cesarean delivery after 2 hours of pushing was not effective. The ObGyn never suggested a cesarean delivery, it was not noted in the chart, and no one else present at the time remembered the option being offered.
PHYSICIAN’S DEFENSE There was nothing during labor to contraindicate a vaginal birth. The ObGyn claimed that he offered a cesarean delivery after 2 hours of pushing. The baby’s blood gas reading at delivery was normal. Any brain injuries to the baby were from resuscitation.
VERDICT A $4,080,500 Pennsylvania verdict was returned.
Related Articles:
When macrosomia is suspected at term, does induction of labor lower the risk of cesarean delivery? Jennifer T. Ahn, MD (Examining the Evidence, May 2012)
Develop and use a checklist for 3rd- and 4th-degree perinatal lacerations Robert L. Barbieri, MD (Editorial, August 2013)
BOWEL INJURY DURING CESAREAN DELIVERY
During cesarean delivery, the mother suffered a bowel injury that led to infection and several abdominal abscesses. She required two procedures for drain placement plus two additional operations.
PATIENT’S CLAIM The ObGyn was negligent in how he performed the cesarean delivery and for not treating the injury and subsequent infection in a timely manner. The abscesses took 3 years to resolve; additional procedures left scarring and aggravated a spinal injury.
PHYSICIAN’S DEFENSE Bowel perforation is a known complication of cesarean delivery. It probably occurred during manipulation of the uterus in an area that was not visible.
VERDICT A $750,000 New Jersey verdict was returned.
Related Article: How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy Michael Baggish, MD (Surgical Technique, October 2012)
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
TELL US WHAT YOU THINK!
Share your thoughts on this article or on any topic relevant to ObGyns and women’s health practitioners. Tell us which topics you’d like to see covered in future issues, and what challenges you face in daily practice. We will consider publishing your letter and in a future issue.
Send your letter to: [email protected] Please include the city and state in which you practice.
Stay in touch! Your feedback is important to us!