User login
Hospital Medicine Groups Must Determine Tolerance Levels for Workload, Night Work
Dear Dr. Hospitalist:
Our group is considering hiring another nocturnist. This may reduce the number of shifts that hospitalists will be able to work per month—we have some who work 20 or more shifts per month. While the vast majority of hospitalists would welcome a nocturnist in order to decrease the number of night shifts required, some who work a lot of shifts are concerned that their income will be affected since there won’t necessarily be any day shifts available to compensate for the decrease in night shifts.
I am wondering if there is a maximum number of shifts per month that a hospitalist should not exceed. We work 12-hour shifts. In other words, is there a tipping point when too many shifts starts to negatively impact the quality of work, increase length of stay, decrease patient satisfaction, and lead to physician burnout? Are there any studies or data to look at this question?
Your feedback is very much appreciated.
–Donna Ting, MD, MPH
Dr. Hospitalist responds:
Although many jobs (i.e. air-traffic controllers, truck drivers) use hours worked as a gauge of operator fatigue, physicians traditionally have not used these criteria to judge one’s ability to be effective. That being said, we all know of occasions when we were physically and/or mentally exhausted and not performing at our best.
Multiple studies have shown that physicians tend to work an average of 60 hours a week. Of course, this does not take into consideration the typical hospitalist, who still tends to work 12-hour shifts on a seven-on/seven-off schedule, although there is a trend away from this type of block scheduling. A recent study also showed that physicians in practice less than five years were more likely to work hours in agreement with the 2003 Accreditation Council for Graduate Medical Education (ACGME) duty-hour regulations for physicians in training. The authors speculated that this was due to this group having trained under the new ACGME guidelines and being of Generation X, whose members tend to favor more work-life balance than their predecessors.
Several studies have examined physician work hours in relationship to fatigue and patient safety. Volp et al examined two large studies and found no change in mortality among Medicare patients for the first two years after implementation of the ACGME duty-hour regulations. However, they did find that mortality decreased for four common medical conditions in a VA hospital. Fletcher et al performed a systematic review and found no conclusive evidence that the decreased resident work hours had any affect on patient safety.
This is what I would have expected: inconclusive data. Most studies of this type are surveys, which have well-known limitations. Each of us has our own individual stamina, tolerance for fatigue, and desire for work-life balance. We intuitively know that most individuals are not at their best when tired or stressed, but to capture the true effect of these variables on patient satisfaction, morbidity, mortality, and other clinical metrics will be very difficult.
There are several ways I would approach a group that is contemplating another nocturnist. Because most hospitalists don’t want to work nights, the group members who feel their moonlighting income would be affected should commit to covering a certain portion or all of the available nights. If only some of the nights are covered, then you can hire a part-time nocturnist.
This is easier than you might imagine, as my very large hospitalist group has four nocturnists and none work a full FTE. I think three to four extra shifts a month are reasonable on a routine basis. We have, however, allowed physicians who wanted to have a month off to work seven extra days the months before and after to get their desired time off. We would not allow that to occur on a regular basis.
Ultimately, your group has to decide its own tolerance for fatigue and burnout, and have some mechanism to monitor the quality of work. After all, we owe it to our patients to not place their safety in jeopardy.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to [email protected].
Dear Dr. Hospitalist:
Our group is considering hiring another nocturnist. This may reduce the number of shifts that hospitalists will be able to work per month—we have some who work 20 or more shifts per month. While the vast majority of hospitalists would welcome a nocturnist in order to decrease the number of night shifts required, some who work a lot of shifts are concerned that their income will be affected since there won’t necessarily be any day shifts available to compensate for the decrease in night shifts.
I am wondering if there is a maximum number of shifts per month that a hospitalist should not exceed. We work 12-hour shifts. In other words, is there a tipping point when too many shifts starts to negatively impact the quality of work, increase length of stay, decrease patient satisfaction, and lead to physician burnout? Are there any studies or data to look at this question?
Your feedback is very much appreciated.
–Donna Ting, MD, MPH
Dr. Hospitalist responds:
Although many jobs (i.e. air-traffic controllers, truck drivers) use hours worked as a gauge of operator fatigue, physicians traditionally have not used these criteria to judge one’s ability to be effective. That being said, we all know of occasions when we were physically and/or mentally exhausted and not performing at our best.
Multiple studies have shown that physicians tend to work an average of 60 hours a week. Of course, this does not take into consideration the typical hospitalist, who still tends to work 12-hour shifts on a seven-on/seven-off schedule, although there is a trend away from this type of block scheduling. A recent study also showed that physicians in practice less than five years were more likely to work hours in agreement with the 2003 Accreditation Council for Graduate Medical Education (ACGME) duty-hour regulations for physicians in training. The authors speculated that this was due to this group having trained under the new ACGME guidelines and being of Generation X, whose members tend to favor more work-life balance than their predecessors.
Several studies have examined physician work hours in relationship to fatigue and patient safety. Volp et al examined two large studies and found no change in mortality among Medicare patients for the first two years after implementation of the ACGME duty-hour regulations. However, they did find that mortality decreased for four common medical conditions in a VA hospital. Fletcher et al performed a systematic review and found no conclusive evidence that the decreased resident work hours had any affect on patient safety.
This is what I would have expected: inconclusive data. Most studies of this type are surveys, which have well-known limitations. Each of us has our own individual stamina, tolerance for fatigue, and desire for work-life balance. We intuitively know that most individuals are not at their best when tired or stressed, but to capture the true effect of these variables on patient satisfaction, morbidity, mortality, and other clinical metrics will be very difficult.
There are several ways I would approach a group that is contemplating another nocturnist. Because most hospitalists don’t want to work nights, the group members who feel their moonlighting income would be affected should commit to covering a certain portion or all of the available nights. If only some of the nights are covered, then you can hire a part-time nocturnist.
This is easier than you might imagine, as my very large hospitalist group has four nocturnists and none work a full FTE. I think three to four extra shifts a month are reasonable on a routine basis. We have, however, allowed physicians who wanted to have a month off to work seven extra days the months before and after to get their desired time off. We would not allow that to occur on a regular basis.
Ultimately, your group has to decide its own tolerance for fatigue and burnout, and have some mechanism to monitor the quality of work. After all, we owe it to our patients to not place their safety in jeopardy.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to [email protected].
Dear Dr. Hospitalist:
Our group is considering hiring another nocturnist. This may reduce the number of shifts that hospitalists will be able to work per month—we have some who work 20 or more shifts per month. While the vast majority of hospitalists would welcome a nocturnist in order to decrease the number of night shifts required, some who work a lot of shifts are concerned that their income will be affected since there won’t necessarily be any day shifts available to compensate for the decrease in night shifts.
I am wondering if there is a maximum number of shifts per month that a hospitalist should not exceed. We work 12-hour shifts. In other words, is there a tipping point when too many shifts starts to negatively impact the quality of work, increase length of stay, decrease patient satisfaction, and lead to physician burnout? Are there any studies or data to look at this question?
Your feedback is very much appreciated.
–Donna Ting, MD, MPH
Dr. Hospitalist responds:
Although many jobs (i.e. air-traffic controllers, truck drivers) use hours worked as a gauge of operator fatigue, physicians traditionally have not used these criteria to judge one’s ability to be effective. That being said, we all know of occasions when we were physically and/or mentally exhausted and not performing at our best.
Multiple studies have shown that physicians tend to work an average of 60 hours a week. Of course, this does not take into consideration the typical hospitalist, who still tends to work 12-hour shifts on a seven-on/seven-off schedule, although there is a trend away from this type of block scheduling. A recent study also showed that physicians in practice less than five years were more likely to work hours in agreement with the 2003 Accreditation Council for Graduate Medical Education (ACGME) duty-hour regulations for physicians in training. The authors speculated that this was due to this group having trained under the new ACGME guidelines and being of Generation X, whose members tend to favor more work-life balance than their predecessors.
Several studies have examined physician work hours in relationship to fatigue and patient safety. Volp et al examined two large studies and found no change in mortality among Medicare patients for the first two years after implementation of the ACGME duty-hour regulations. However, they did find that mortality decreased for four common medical conditions in a VA hospital. Fletcher et al performed a systematic review and found no conclusive evidence that the decreased resident work hours had any affect on patient safety.
This is what I would have expected: inconclusive data. Most studies of this type are surveys, which have well-known limitations. Each of us has our own individual stamina, tolerance for fatigue, and desire for work-life balance. We intuitively know that most individuals are not at their best when tired or stressed, but to capture the true effect of these variables on patient satisfaction, morbidity, mortality, and other clinical metrics will be very difficult.
There are several ways I would approach a group that is contemplating another nocturnist. Because most hospitalists don’t want to work nights, the group members who feel their moonlighting income would be affected should commit to covering a certain portion or all of the available nights. If only some of the nights are covered, then you can hire a part-time nocturnist.
This is easier than you might imagine, as my very large hospitalist group has four nocturnists and none work a full FTE. I think three to four extra shifts a month are reasonable on a routine basis. We have, however, allowed physicians who wanted to have a month off to work seven extra days the months before and after to get their desired time off. We would not allow that to occur on a regular basis.
Ultimately, your group has to decide its own tolerance for fatigue and burnout, and have some mechanism to monitor the quality of work. After all, we owe it to our patients to not place their safety in jeopardy.
Do you have a problem or concern that you’d like Dr. Hospitalist to address? Email your questions to [email protected].
Bowel perforation causes woman’s death: $1.5M verdict
A 46-year-old woman underwent laparoscopic supracervical hysterectomy to remove her uterus but preserve her cervix. Postsurgically, she had difficulty breathing deeply and reported abdominal pain. The nurses and on-call physician reassured her that she was experiencing “gas pains” due to insufflation. After same-day discharge, she stayed in a motel room to avoid a second-floor bedroom at home.
She called the gynecologist’s office the following day to report continued pain and severe hot flashes and sweats. The gynecologist instructed his nurse to advise the patient to stop taking her birth control pill (ethinyl estradiol/norethindrone, Microgestin) and “to ride out” the hot flashes.
The woman was found dead in her motel room the next morning. An autopsy revealed a perforated small intestine with leakage into the abdominal cavity causing sepsis, multi-organ failure, and death.
ESTATE’S CLAIM The gynecologist reviewed the medical records and found an error in the operative report, but he made no addendum or late entry to correct the operative report. His defense counsel instructed him to draft a letter clarifying the surgery; this clarification was given to defense experts. The description of the procedure in the clarification was different from what was described in the medical records. For example, the clarification reported making 4 incisions for 4 trocars; the operative report indicated using 3 trocars. The pathologist and 2 nurses who treated the patient after surgery confirmed that there were 3 trocar incisions. The pathologist found no tissue necrosis at or around the perforation site, indicating that the perforation likely occurred during surgery.
PHYSICIAN’S DEFENSE Bowel perforation is a known complication of the procedure. The perforation was not present at the time of surgery because leakage of bowel content would have been obvious.
VERDICT A $1.5 million Virginia settlement was reached.
Retained products of conception after D&C
When sonography indicated that a 30-year-old woman was pregnant, she decided to abort the pregnancy and was given mifepristone.
Another sonogram 5 weeks later showed retained products of conception within the uterus. An ObGyn performed dilation and curettage (D&C) at an outpatient clinic. Because he believed the cannula did not remove everything, he used a curette to scrape the uterus. After the patient was dizzy, hypotensive, and in pain for 4 hours, an ambulance transported her to a hospital. Perforations of the uterus and sigmoid colon were discovered and repaired during emergency surgery. The patient has a large scar on her abdomen.
PATIENT'S CLAIM The ObGyn did not perform the D&C properly and perforated the uterus and colon. An earlier response to symptoms could have prevented repair surgery. Damage to the uterus may now preclude her from having a successful pregnancy.
DEFENDANTS’ DEFENSE The ObGyn argued that the aborted pregnancy was ectopic; spontaneous rupture caused the perforations.
VERDICT A $340,000 New York settlement was reached with the ObGyn. By the time of trial, the clinic had closed.
Wrong-site biopsy; records altered
A 40-year-old woman underwent excisional breast biopsy. The wrong lump was removed and the woman had to have another procedure.
PATIENT'S CLAIM The hospital’s nursing staff failed to properly mark the operative site. The breast surgeon did not confirm that the markings were correct. The surgeon altered the written operative report after the surgery to conceal negligence.
DEFENDANTS’ DEFENSE The nurses properly marked the biopsy site, but the surgeon chose another route. The surgeon edited the original report to reflect events that occurred during surgery that had not been included in the original dictation. The added material gave justification for performing the procedure at a different site than originally intended.
VERDICT A $15,500 Connecticut verdict was returned.
Second twin has CP and brain damage: $10M settlement
A woman gave birth to twins at an Army hospital. The first twin was delivered without complications. The second twin developed a prolapsed cord during delivery of the first twin. A resident and the attending physician allowed the mother to continue with vaginal delivery. The heart-rate monitor showed fetal distress, but the medical staff did not respond. After an hour, another physician was consulted, and he ordered immediate delivery. The attending physician decided to continue with vaginal delivery using forceps, but it took 15 minutes to locate forceps in the hospital. The infant suffered severe brain damage and cerebral palsy. She will require 24-hour nursing care for life, including treatment of a tracheostomy.
PARENTS' CLAIM The physicians were negligent for not reacting to non-reassuring monitor strips and for allowing the vaginal delivery to continue. An emergency cesarean delivery should have been performed.
DEFENDANTS’ DEFENSE The case was settled before trial.
VERDICT A $10 million North Carolina settlement was reached for past medical bills and future care.
Faulty biopsies: breast cancer diagnosis missed
In September 2006, a 40-year-old woman underwent breast sonography. A radiologist, Dr. A, reported finding a mass and a smaller nodule in the right breast, and recommended a biopsy of each area. Two weeks later, a second radiologist, Dr. B, biopsied the larger of the two areas and diagnosed a hyalinized fibroadenoma. He did not biopsy the smaller growth, but reported it as a benign nodule. He recommended more frequent screenings. The patient was referred to a surgeon, who determined that she should be seen in 6 months.
In June 2007, the patient underwent right-breast sonography that revealed cysts and three nodules. The surgeon recommended a biopsy, but the biopsy was performed on only two of three nodules. A third radiologist, Dr. C, determined that the nodules were all benign.
In November 2007, when the patient reported a painful lump in her right breast, her gynecologist ordered mammography, which revealed lesions. A biopsy revealed that one lesion was stage III invasive ductal carcinoma. The patient underwent extensive treatment, including a mastectomy, lymphadenectomy, chemotherapy, and radiation therapy, and prophylactic surgical reduction of the left breast.
PATIENT'S CLAIM The cancer should have been diagnosed in September 2006. Prompt treatment would have decreased the progression of the disease. The September 2006 biopsy should have included both lumps, as recommended by Dr. A.
DEFENDANTS’ DEFENSE There was no indication of cancer in September 2006. Reasonable follow-up care was given.
VERDICT A New York defense verdict was returned.
Tumor not found during surgery; BSO performed
A 41-year-old woman underwent surgery to remove a pelvic tumor in November 2004. The gynecologist was unable to locate the tumor during surgery. He performed bilateral salpingo-oophorectomy (BSO) because of a visual diagnosis of endometriosis. In August 2005, the patient underwent surgical removal of the tumor by another surgeon. She was hospitalized for several weeks and suffered a large scar that required additional surgery.
PATIENT'S CLAIM BSO was unnecessary, and caused early menopause, with vaginal atrophy and dryness, depression, fatigue, insomnia, loss of hair, and other symptoms.
The patient claimed lack of informed consent. From Ecuador, the patient’s command of English was not sufficient for her to completely understand the consent form; an interpreter should have been provided.
DEFENDANTS’ DEFENSE BSO did not cause a significant acceleration of the onset of menopause. It was necessary to treat the endometriosis.
The patient signed a consent form that included BSO. The patient did not indicate that she did not understand the language on the form; had she asked, an interpreter would have been provided.
VERDICT A $750,000 New York settlement was reached with the gynecologist and medical center.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
A 46-year-old woman underwent laparoscopic supracervical hysterectomy to remove her uterus but preserve her cervix. Postsurgically, she had difficulty breathing deeply and reported abdominal pain. The nurses and on-call physician reassured her that she was experiencing “gas pains” due to insufflation. After same-day discharge, she stayed in a motel room to avoid a second-floor bedroom at home.
She called the gynecologist’s office the following day to report continued pain and severe hot flashes and sweats. The gynecologist instructed his nurse to advise the patient to stop taking her birth control pill (ethinyl estradiol/norethindrone, Microgestin) and “to ride out” the hot flashes.
The woman was found dead in her motel room the next morning. An autopsy revealed a perforated small intestine with leakage into the abdominal cavity causing sepsis, multi-organ failure, and death.
ESTATE’S CLAIM The gynecologist reviewed the medical records and found an error in the operative report, but he made no addendum or late entry to correct the operative report. His defense counsel instructed him to draft a letter clarifying the surgery; this clarification was given to defense experts. The description of the procedure in the clarification was different from what was described in the medical records. For example, the clarification reported making 4 incisions for 4 trocars; the operative report indicated using 3 trocars. The pathologist and 2 nurses who treated the patient after surgery confirmed that there were 3 trocar incisions. The pathologist found no tissue necrosis at or around the perforation site, indicating that the perforation likely occurred during surgery.
PHYSICIAN’S DEFENSE Bowel perforation is a known complication of the procedure. The perforation was not present at the time of surgery because leakage of bowel content would have been obvious.
VERDICT A $1.5 million Virginia settlement was reached.
Retained products of conception after D&C
When sonography indicated that a 30-year-old woman was pregnant, she decided to abort the pregnancy and was given mifepristone.
Another sonogram 5 weeks later showed retained products of conception within the uterus. An ObGyn performed dilation and curettage (D&C) at an outpatient clinic. Because he believed the cannula did not remove everything, he used a curette to scrape the uterus. After the patient was dizzy, hypotensive, and in pain for 4 hours, an ambulance transported her to a hospital. Perforations of the uterus and sigmoid colon were discovered and repaired during emergency surgery. The patient has a large scar on her abdomen.
PATIENT'S CLAIM The ObGyn did not perform the D&C properly and perforated the uterus and colon. An earlier response to symptoms could have prevented repair surgery. Damage to the uterus may now preclude her from having a successful pregnancy.
DEFENDANTS’ DEFENSE The ObGyn argued that the aborted pregnancy was ectopic; spontaneous rupture caused the perforations.
VERDICT A $340,000 New York settlement was reached with the ObGyn. By the time of trial, the clinic had closed.
Wrong-site biopsy; records altered
A 40-year-old woman underwent excisional breast biopsy. The wrong lump was removed and the woman had to have another procedure.
PATIENT'S CLAIM The hospital’s nursing staff failed to properly mark the operative site. The breast surgeon did not confirm that the markings were correct. The surgeon altered the written operative report after the surgery to conceal negligence.
DEFENDANTS’ DEFENSE The nurses properly marked the biopsy site, but the surgeon chose another route. The surgeon edited the original report to reflect events that occurred during surgery that had not been included in the original dictation. The added material gave justification for performing the procedure at a different site than originally intended.
VERDICT A $15,500 Connecticut verdict was returned.
Second twin has CP and brain damage: $10M settlement
A woman gave birth to twins at an Army hospital. The first twin was delivered without complications. The second twin developed a prolapsed cord during delivery of the first twin. A resident and the attending physician allowed the mother to continue with vaginal delivery. The heart-rate monitor showed fetal distress, but the medical staff did not respond. After an hour, another physician was consulted, and he ordered immediate delivery. The attending physician decided to continue with vaginal delivery using forceps, but it took 15 minutes to locate forceps in the hospital. The infant suffered severe brain damage and cerebral palsy. She will require 24-hour nursing care for life, including treatment of a tracheostomy.
PARENTS' CLAIM The physicians were negligent for not reacting to non-reassuring monitor strips and for allowing the vaginal delivery to continue. An emergency cesarean delivery should have been performed.
DEFENDANTS’ DEFENSE The case was settled before trial.
VERDICT A $10 million North Carolina settlement was reached for past medical bills and future care.
Faulty biopsies: breast cancer diagnosis missed
In September 2006, a 40-year-old woman underwent breast sonography. A radiologist, Dr. A, reported finding a mass and a smaller nodule in the right breast, and recommended a biopsy of each area. Two weeks later, a second radiologist, Dr. B, biopsied the larger of the two areas and diagnosed a hyalinized fibroadenoma. He did not biopsy the smaller growth, but reported it as a benign nodule. He recommended more frequent screenings. The patient was referred to a surgeon, who determined that she should be seen in 6 months.
In June 2007, the patient underwent right-breast sonography that revealed cysts and three nodules. The surgeon recommended a biopsy, but the biopsy was performed on only two of three nodules. A third radiologist, Dr. C, determined that the nodules were all benign.
In November 2007, when the patient reported a painful lump in her right breast, her gynecologist ordered mammography, which revealed lesions. A biopsy revealed that one lesion was stage III invasive ductal carcinoma. The patient underwent extensive treatment, including a mastectomy, lymphadenectomy, chemotherapy, and radiation therapy, and prophylactic surgical reduction of the left breast.
PATIENT'S CLAIM The cancer should have been diagnosed in September 2006. Prompt treatment would have decreased the progression of the disease. The September 2006 biopsy should have included both lumps, as recommended by Dr. A.
DEFENDANTS’ DEFENSE There was no indication of cancer in September 2006. Reasonable follow-up care was given.
VERDICT A New York defense verdict was returned.
Tumor not found during surgery; BSO performed
A 41-year-old woman underwent surgery to remove a pelvic tumor in November 2004. The gynecologist was unable to locate the tumor during surgery. He performed bilateral salpingo-oophorectomy (BSO) because of a visual diagnosis of endometriosis. In August 2005, the patient underwent surgical removal of the tumor by another surgeon. She was hospitalized for several weeks and suffered a large scar that required additional surgery.
PATIENT'S CLAIM BSO was unnecessary, and caused early menopause, with vaginal atrophy and dryness, depression, fatigue, insomnia, loss of hair, and other symptoms.
The patient claimed lack of informed consent. From Ecuador, the patient’s command of English was not sufficient for her to completely understand the consent form; an interpreter should have been provided.
DEFENDANTS’ DEFENSE BSO did not cause a significant acceleration of the onset of menopause. It was necessary to treat the endometriosis.
The patient signed a consent form that included BSO. The patient did not indicate that she did not understand the language on the form; had she asked, an interpreter would have been provided.
VERDICT A $750,000 New York settlement was reached with the gynecologist and medical center.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
A 46-year-old woman underwent laparoscopic supracervical hysterectomy to remove her uterus but preserve her cervix. Postsurgically, she had difficulty breathing deeply and reported abdominal pain. The nurses and on-call physician reassured her that she was experiencing “gas pains” due to insufflation. After same-day discharge, she stayed in a motel room to avoid a second-floor bedroom at home.
She called the gynecologist’s office the following day to report continued pain and severe hot flashes and sweats. The gynecologist instructed his nurse to advise the patient to stop taking her birth control pill (ethinyl estradiol/norethindrone, Microgestin) and “to ride out” the hot flashes.
The woman was found dead in her motel room the next morning. An autopsy revealed a perforated small intestine with leakage into the abdominal cavity causing sepsis, multi-organ failure, and death.
ESTATE’S CLAIM The gynecologist reviewed the medical records and found an error in the operative report, but he made no addendum or late entry to correct the operative report. His defense counsel instructed him to draft a letter clarifying the surgery; this clarification was given to defense experts. The description of the procedure in the clarification was different from what was described in the medical records. For example, the clarification reported making 4 incisions for 4 trocars; the operative report indicated using 3 trocars. The pathologist and 2 nurses who treated the patient after surgery confirmed that there were 3 trocar incisions. The pathologist found no tissue necrosis at or around the perforation site, indicating that the perforation likely occurred during surgery.
PHYSICIAN’S DEFENSE Bowel perforation is a known complication of the procedure. The perforation was not present at the time of surgery because leakage of bowel content would have been obvious.
VERDICT A $1.5 million Virginia settlement was reached.
Retained products of conception after D&C
When sonography indicated that a 30-year-old woman was pregnant, she decided to abort the pregnancy and was given mifepristone.
Another sonogram 5 weeks later showed retained products of conception within the uterus. An ObGyn performed dilation and curettage (D&C) at an outpatient clinic. Because he believed the cannula did not remove everything, he used a curette to scrape the uterus. After the patient was dizzy, hypotensive, and in pain for 4 hours, an ambulance transported her to a hospital. Perforations of the uterus and sigmoid colon were discovered and repaired during emergency surgery. The patient has a large scar on her abdomen.
PATIENT'S CLAIM The ObGyn did not perform the D&C properly and perforated the uterus and colon. An earlier response to symptoms could have prevented repair surgery. Damage to the uterus may now preclude her from having a successful pregnancy.
DEFENDANTS’ DEFENSE The ObGyn argued that the aborted pregnancy was ectopic; spontaneous rupture caused the perforations.
VERDICT A $340,000 New York settlement was reached with the ObGyn. By the time of trial, the clinic had closed.
Wrong-site biopsy; records altered
A 40-year-old woman underwent excisional breast biopsy. The wrong lump was removed and the woman had to have another procedure.
PATIENT'S CLAIM The hospital’s nursing staff failed to properly mark the operative site. The breast surgeon did not confirm that the markings were correct. The surgeon altered the written operative report after the surgery to conceal negligence.
DEFENDANTS’ DEFENSE The nurses properly marked the biopsy site, but the surgeon chose another route. The surgeon edited the original report to reflect events that occurred during surgery that had not been included in the original dictation. The added material gave justification for performing the procedure at a different site than originally intended.
VERDICT A $15,500 Connecticut verdict was returned.
Second twin has CP and brain damage: $10M settlement
A woman gave birth to twins at an Army hospital. The first twin was delivered without complications. The second twin developed a prolapsed cord during delivery of the first twin. A resident and the attending physician allowed the mother to continue with vaginal delivery. The heart-rate monitor showed fetal distress, but the medical staff did not respond. After an hour, another physician was consulted, and he ordered immediate delivery. The attending physician decided to continue with vaginal delivery using forceps, but it took 15 minutes to locate forceps in the hospital. The infant suffered severe brain damage and cerebral palsy. She will require 24-hour nursing care for life, including treatment of a tracheostomy.
PARENTS' CLAIM The physicians were negligent for not reacting to non-reassuring monitor strips and for allowing the vaginal delivery to continue. An emergency cesarean delivery should have been performed.
DEFENDANTS’ DEFENSE The case was settled before trial.
VERDICT A $10 million North Carolina settlement was reached for past medical bills and future care.
Faulty biopsies: breast cancer diagnosis missed
In September 2006, a 40-year-old woman underwent breast sonography. A radiologist, Dr. A, reported finding a mass and a smaller nodule in the right breast, and recommended a biopsy of each area. Two weeks later, a second radiologist, Dr. B, biopsied the larger of the two areas and diagnosed a hyalinized fibroadenoma. He did not biopsy the smaller growth, but reported it as a benign nodule. He recommended more frequent screenings. The patient was referred to a surgeon, who determined that she should be seen in 6 months.
In June 2007, the patient underwent right-breast sonography that revealed cysts and three nodules. The surgeon recommended a biopsy, but the biopsy was performed on only two of three nodules. A third radiologist, Dr. C, determined that the nodules were all benign.
In November 2007, when the patient reported a painful lump in her right breast, her gynecologist ordered mammography, which revealed lesions. A biopsy revealed that one lesion was stage III invasive ductal carcinoma. The patient underwent extensive treatment, including a mastectomy, lymphadenectomy, chemotherapy, and radiation therapy, and prophylactic surgical reduction of the left breast.
PATIENT'S CLAIM The cancer should have been diagnosed in September 2006. Prompt treatment would have decreased the progression of the disease. The September 2006 biopsy should have included both lumps, as recommended by Dr. A.
DEFENDANTS’ DEFENSE There was no indication of cancer in September 2006. Reasonable follow-up care was given.
VERDICT A New York defense verdict was returned.
Tumor not found during surgery; BSO performed
A 41-year-old woman underwent surgery to remove a pelvic tumor in November 2004. The gynecologist was unable to locate the tumor during surgery. He performed bilateral salpingo-oophorectomy (BSO) because of a visual diagnosis of endometriosis. In August 2005, the patient underwent surgical removal of the tumor by another surgeon. She was hospitalized for several weeks and suffered a large scar that required additional surgery.
PATIENT'S CLAIM BSO was unnecessary, and caused early menopause, with vaginal atrophy and dryness, depression, fatigue, insomnia, loss of hair, and other symptoms.
The patient claimed lack of informed consent. From Ecuador, the patient’s command of English was not sufficient for her to completely understand the consent form; an interpreter should have been provided.
DEFENDANTS’ DEFENSE BSO did not cause a significant acceleration of the onset of menopause. It was necessary to treat the endometriosis.
The patient signed a consent form that included BSO. The patient did not indicate that she did not understand the language on the form; had she asked, an interpreter would have been provided.
VERDICT A $750,000 New York settlement was reached with the gynecologist and medical center.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Four pillars of a successful practice: 4. Motivate your staff
READ THE REST OF THE SERIES
Pillar 1: Keep your current patients happy (March 2013)
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 2: Attract new patients (May 2013)
Pillar 3: Obtain and maintain physician referrals (June 2013)
The success of any medical practice and any marketing program begins and ends with the staff. You can gain new patients, forge excellent relationships with referring physicians, and maintain a plentiful number of existing patients—but if you don’t have a staff that is excited, enthusiastic, and knowledgeable when answering the telephone and managing patients, your marketing plan will be ineffective, and you will be disappointed in your practice.
In this article, I review the importance of motivating employees by providing measurable, written goals in the form of a succinct, effective mission statement and policy manual. I also offer practical strategies to inspire your employees by sharing the power, vision, and rewards.
Start with your mission statement
Nearly every successful practice and every successful business has a well-defined vision, mission, goal, or objective. The mission statement should spell out the purpose of the practice and the methods of achieving it. It serves as the road map, providing direction to all members of the staff, doctors included.
The mission statement for my practice is:
We are committed to:
- excellence
- providing the best urologic health care for our patients
- persistent and consistent attention to the little details because they make a big difference.
Develop a policy manual
Every practice should have a manual that contains its rules and regulations. Ideally, this manual should also serve as a guide for any new or temporary employee who comes to work in the office.
The manual should cover job descriptions, the dress code, hours of operation, the division of office responsibilities, vacation and sick days, and emergency telephone numbers.
In my practice, we summarize our policy manual with this expectation:
Dr. Baum’s policy manual statement:
Rule #1— The patient is always right.
Rule #2— If you think the patient is wrong, reread rule #1.
ALL OTHER POLICIES ARE NULL AND VOID.
We post the mission statement in prominent places throughout the office (the reception area and most of the examination rooms, our Web site, and on a large banner in the employee lounge) to remind us and our patients of our dedication to excellent customer service.
Whenever a mistake or problem occurs, the first question we ask each other is, “Did we adhere to the mission statement and the policy statement?” Usually, we discover that we did not. We use the mission statement and the policy statement to refocus us on our number one priority: our patients.
10 LOW-COST WAYS TO MOTIVATE STAFF
A well-motivated staff creates an effective team environment. Most enlightened businesses have discovered that team management leads to increased output and productivity. Your employees want to be valued as human beings and individuals, not just as workers. The more you include them in the process of running the office, the more invested they become in helping to improve the way it works.
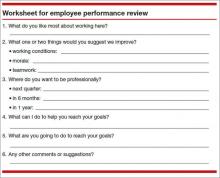
1. Review staff performance regularly
Employees like to know where they stand and how they can improve performance on the job. Motivated staff members appreciate feedback on their progress—or, even, their lack of it. The best way to furnish this important feedback is by conducting periodic performance reviews.
I suggest that you meet with your employees on a scheduled basis every 3 to 4 months. Give each employee a worksheet before the scheduled review (see Worksheet below), and then go over her responses during the review. You can learn a lot about what motivates her during this process.
I always end each performance review on a positive note, by telling the employee how great an asset she is to the practice. I document these meetings in the employee’s file.
2. Encourage continuing education
Just as physicians need continuing medical education to stay up to date, your staff members require continuing motivational experiences. Encourage your staff to participate in continuing education courses and support their efforts financially—you’ll get a favorable return on your investment.
I suggest that you offer to pay the fees for any seminars and classes your employees take. You may want to suggest courses in computers, social media, marketing, or any other subject area that will help the practice grow and prosper.
To make these educational experiences even more effective, ask employees to share what they have learned with other staff members. This can be done at a staff meeting. Simply ask the employee who attended a seminar or a course to share the information with the rest of the staff by briefly reviewing the course or describing what he learned and how it applies to the practice.
3. Empower your staff
Office management is complicated. Few ObGyns have a thorough understanding of all business aspects of a medical practice. Most successful ObGyns have learned to delegate the responsibility of running the office and to empower their employees to take control and assume responsibility for their decisions and actions.
In my practice, I empower any employee to make financial decisions up to a limit of $200 without consulting me. For instance, if the office needs a new telephone answering machine, I expect my employees to consider which features we need, check the machines that are available, and compare prices at the local electronics outlet, office supply store, and online retailers to find the best machine at the lowest price.
The take-home message: More than ever before, ObGyns should do what we are best trained to do—diagnose and treat diseases. Very few ObGyns are experts on fax machines. Don’t waste time on activities that your staff members can do.
4. Promote a positive mental attitude
As Ralph Waldo Emerson once said, “Nothing great was ever achieved without enthusiasm.” This is also true of the practice of medicine. When the doctor has a positive mental attitude, employees are motivated by the example. When a doctor is easily irritable and carries problems from home to the office and takes her frustration out on the staff, the employees will, in turn, take it out on the patients.
I have an attitude that employees are on stage. The moment they walk in the door in the morning, they have to leave all other problems and concerns behind them. They need to believe that they are responsible for making sure that each patient has a positive experience with the office at every contact point. That includes the telephone, the receptionist who welcomes patients to the practice, the nurse taking the patient into the exam room, the billing clerk who handles the patient’s bill, and, yes, the doctor, too! We all contribute to the patient’s experience, and we all need to have a positive attitude.
5. Recognize achievement
Nothing is more motivating for an employee than for the doctor to recognize his achievements and accomplishments. When an employee improves in job performance, tell him directly. You will satisfy that employee’s need for self-esteem, improve his confidence, and help him fulfill the need for self-esteem from fellow employees.
6. Show your staff that you care
Your employees need to know that you care about them not just as workers but as individuals with their own personal lives. When one of my employees is sick, or one of her family members is ill, I call her at home to check on her and make sure that she has access to adequate medical care. If someone gets sick in the office, I call another medical office and get the employee seen immediately.
7. Catch your employees doing things right
My philosophy is to praise in public, pan in private. When I catch an employee doing something right, I send a thank-you note to her home address, making sure that it arrives on a Saturday. I hope the employee will show my note to family and friends. I use a specially created card or a “thanks a million” check (a non-negotiable replication of a check that is made out to the employee and says, “Thanks a million,” with my name signed at the bottom).
You will be amazed at how appreciative the employee is that you not only recognized her superior service but took the time to put your recognition in writing.
8. Reward your staff for saving money
If a staff member comes up with an idea that saves the practice money, give her a bonus. For example, in my practice, the 15-year-old autoclave broke down. When I tried to get parts, I was informed that the machine is no longer made. The nurse in our office took the autoclave to the hospital’s biomedical engineering department, where workers installed a $30 part that saved me from buying a new $2,000 machine. The nurse deserved to be rewarded for that, so I gave her a $50 check on the spot.
I try to motivate my staff not just to earn more money for the practice but to reduce expenses, so I pay them when they identify and design money-saving ideas.
9. Involve your employees in decision making
Ask your employees for advice. Then make sure you follow it. Your staff members are on the front line; they want the office routine to go well. Include them in the decision-making process, whether the task is writing a mission statement or policy manual, determining a change in procedures, implementing an electronic health record, or meeting new job candidates. By including them, you make them feel like part of the team.
10. Have fun!
Surprise is the spice of life. Whenever you can provide an unexpected perk for your staff, you can be sure the gesture will be appreciated. For example, during a week in which two of my employees were unable to work (due to vacation and illness), the rest of us had to take up the slack. Despite being short-handed, we were able to function at regular speed and capacity without affecting the quality of care. I was so impressed by the extra effort that I arranged for a massage therapist to visit our practice at the end of the week and give everyone a 15- to 20-minute massage. It was my way of saying, “Thank you.”
THE BOTTOM LINE
Encourage team spirit. It makes good business sense. When your employees have a personal investment in problem-solving and decision-making, they will go the extra mile for your patients and your practice.
This is the last article in this four-part series on promoting your practice and increasing productivity. I hope you have identified the four pillars of success for your practice—and that I have helped you understand the importance of all four pillars. They represent the strength and stability of a successful ObGyn practice.
READ THE REST OF THE SERIES
Pillar 1: Keep your current patients happy (March 2013)
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 2: Attract new patients (May 2013)
Pillar 3: Obtain and maintain physician referrals (June 2013)
The success of any medical practice and any marketing program begins and ends with the staff. You can gain new patients, forge excellent relationships with referring physicians, and maintain a plentiful number of existing patients—but if you don’t have a staff that is excited, enthusiastic, and knowledgeable when answering the telephone and managing patients, your marketing plan will be ineffective, and you will be disappointed in your practice.
In this article, I review the importance of motivating employees by providing measurable, written goals in the form of a succinct, effective mission statement and policy manual. I also offer practical strategies to inspire your employees by sharing the power, vision, and rewards.
Start with your mission statement
Nearly every successful practice and every successful business has a well-defined vision, mission, goal, or objective. The mission statement should spell out the purpose of the practice and the methods of achieving it. It serves as the road map, providing direction to all members of the staff, doctors included.
The mission statement for my practice is:
We are committed to:
- excellence
- providing the best urologic health care for our patients
- persistent and consistent attention to the little details because they make a big difference.
Develop a policy manual
Every practice should have a manual that contains its rules and regulations. Ideally, this manual should also serve as a guide for any new or temporary employee who comes to work in the office.
The manual should cover job descriptions, the dress code, hours of operation, the division of office responsibilities, vacation and sick days, and emergency telephone numbers.
In my practice, we summarize our policy manual with this expectation:
Dr. Baum’s policy manual statement:
Rule #1— The patient is always right.
Rule #2— If you think the patient is wrong, reread rule #1.
ALL OTHER POLICIES ARE NULL AND VOID.
We post the mission statement in prominent places throughout the office (the reception area and most of the examination rooms, our Web site, and on a large banner in the employee lounge) to remind us and our patients of our dedication to excellent customer service.
Whenever a mistake or problem occurs, the first question we ask each other is, “Did we adhere to the mission statement and the policy statement?” Usually, we discover that we did not. We use the mission statement and the policy statement to refocus us on our number one priority: our patients.
10 LOW-COST WAYS TO MOTIVATE STAFF
A well-motivated staff creates an effective team environment. Most enlightened businesses have discovered that team management leads to increased output and productivity. Your employees want to be valued as human beings and individuals, not just as workers. The more you include them in the process of running the office, the more invested they become in helping to improve the way it works.
1. Review staff performance regularly
Employees like to know where they stand and how they can improve performance on the job. Motivated staff members appreciate feedback on their progress—or, even, their lack of it. The best way to furnish this important feedback is by conducting periodic performance reviews.
I suggest that you meet with your employees on a scheduled basis every 3 to 4 months. Give each employee a worksheet before the scheduled review (see Worksheet below), and then go over her responses during the review. You can learn a lot about what motivates her during this process.
I always end each performance review on a positive note, by telling the employee how great an asset she is to the practice. I document these meetings in the employee’s file.
2. Encourage continuing education
Just as physicians need continuing medical education to stay up to date, your staff members require continuing motivational experiences. Encourage your staff to participate in continuing education courses and support their efforts financially—you’ll get a favorable return on your investment.
I suggest that you offer to pay the fees for any seminars and classes your employees take. You may want to suggest courses in computers, social media, marketing, or any other subject area that will help the practice grow and prosper.
To make these educational experiences even more effective, ask employees to share what they have learned with other staff members. This can be done at a staff meeting. Simply ask the employee who attended a seminar or a course to share the information with the rest of the staff by briefly reviewing the course or describing what he learned and how it applies to the practice.
3. Empower your staff
Office management is complicated. Few ObGyns have a thorough understanding of all business aspects of a medical practice. Most successful ObGyns have learned to delegate the responsibility of running the office and to empower their employees to take control and assume responsibility for their decisions and actions.
In my practice, I empower any employee to make financial decisions up to a limit of $200 without consulting me. For instance, if the office needs a new telephone answering machine, I expect my employees to consider which features we need, check the machines that are available, and compare prices at the local electronics outlet, office supply store, and online retailers to find the best machine at the lowest price.
The take-home message: More than ever before, ObGyns should do what we are best trained to do—diagnose and treat diseases. Very few ObGyns are experts on fax machines. Don’t waste time on activities that your staff members can do.
4. Promote a positive mental attitude
As Ralph Waldo Emerson once said, “Nothing great was ever achieved without enthusiasm.” This is also true of the practice of medicine. When the doctor has a positive mental attitude, employees are motivated by the example. When a doctor is easily irritable and carries problems from home to the office and takes her frustration out on the staff, the employees will, in turn, take it out on the patients.
I have an attitude that employees are on stage. The moment they walk in the door in the morning, they have to leave all other problems and concerns behind them. They need to believe that they are responsible for making sure that each patient has a positive experience with the office at every contact point. That includes the telephone, the receptionist who welcomes patients to the practice, the nurse taking the patient into the exam room, the billing clerk who handles the patient’s bill, and, yes, the doctor, too! We all contribute to the patient’s experience, and we all need to have a positive attitude.
5. Recognize achievement
Nothing is more motivating for an employee than for the doctor to recognize his achievements and accomplishments. When an employee improves in job performance, tell him directly. You will satisfy that employee’s need for self-esteem, improve his confidence, and help him fulfill the need for self-esteem from fellow employees.
6. Show your staff that you care
Your employees need to know that you care about them not just as workers but as individuals with their own personal lives. When one of my employees is sick, or one of her family members is ill, I call her at home to check on her and make sure that she has access to adequate medical care. If someone gets sick in the office, I call another medical office and get the employee seen immediately.
7. Catch your employees doing things right
My philosophy is to praise in public, pan in private. When I catch an employee doing something right, I send a thank-you note to her home address, making sure that it arrives on a Saturday. I hope the employee will show my note to family and friends. I use a specially created card or a “thanks a million” check (a non-negotiable replication of a check that is made out to the employee and says, “Thanks a million,” with my name signed at the bottom).
You will be amazed at how appreciative the employee is that you not only recognized her superior service but took the time to put your recognition in writing.
8. Reward your staff for saving money
If a staff member comes up with an idea that saves the practice money, give her a bonus. For example, in my practice, the 15-year-old autoclave broke down. When I tried to get parts, I was informed that the machine is no longer made. The nurse in our office took the autoclave to the hospital’s biomedical engineering department, where workers installed a $30 part that saved me from buying a new $2,000 machine. The nurse deserved to be rewarded for that, so I gave her a $50 check on the spot.
I try to motivate my staff not just to earn more money for the practice but to reduce expenses, so I pay them when they identify and design money-saving ideas.
9. Involve your employees in decision making
Ask your employees for advice. Then make sure you follow it. Your staff members are on the front line; they want the office routine to go well. Include them in the decision-making process, whether the task is writing a mission statement or policy manual, determining a change in procedures, implementing an electronic health record, or meeting new job candidates. By including them, you make them feel like part of the team.
10. Have fun!
Surprise is the spice of life. Whenever you can provide an unexpected perk for your staff, you can be sure the gesture will be appreciated. For example, during a week in which two of my employees were unable to work (due to vacation and illness), the rest of us had to take up the slack. Despite being short-handed, we were able to function at regular speed and capacity without affecting the quality of care. I was so impressed by the extra effort that I arranged for a massage therapist to visit our practice at the end of the week and give everyone a 15- to 20-minute massage. It was my way of saying, “Thank you.”
THE BOTTOM LINE
Encourage team spirit. It makes good business sense. When your employees have a personal investment in problem-solving and decision-making, they will go the extra mile for your patients and your practice.
This is the last article in this four-part series on promoting your practice and increasing productivity. I hope you have identified the four pillars of success for your practice—and that I have helped you understand the importance of all four pillars. They represent the strength and stability of a successful ObGyn practice.
READ THE REST OF THE SERIES
Pillar 1: Keep your current patients happy (March 2013)
Dr. Baum describes his number one strategy to retain patients (Audiocast, March 2013)
Pillar 2: Attract new patients (May 2013)
Pillar 3: Obtain and maintain physician referrals (June 2013)
The success of any medical practice and any marketing program begins and ends with the staff. You can gain new patients, forge excellent relationships with referring physicians, and maintain a plentiful number of existing patients—but if you don’t have a staff that is excited, enthusiastic, and knowledgeable when answering the telephone and managing patients, your marketing plan will be ineffective, and you will be disappointed in your practice.
In this article, I review the importance of motivating employees by providing measurable, written goals in the form of a succinct, effective mission statement and policy manual. I also offer practical strategies to inspire your employees by sharing the power, vision, and rewards.
Start with your mission statement
Nearly every successful practice and every successful business has a well-defined vision, mission, goal, or objective. The mission statement should spell out the purpose of the practice and the methods of achieving it. It serves as the road map, providing direction to all members of the staff, doctors included.
The mission statement for my practice is:
We are committed to:
- excellence
- providing the best urologic health care for our patients
- persistent and consistent attention to the little details because they make a big difference.
Develop a policy manual
Every practice should have a manual that contains its rules and regulations. Ideally, this manual should also serve as a guide for any new or temporary employee who comes to work in the office.
The manual should cover job descriptions, the dress code, hours of operation, the division of office responsibilities, vacation and sick days, and emergency telephone numbers.
In my practice, we summarize our policy manual with this expectation:
Dr. Baum’s policy manual statement:
Rule #1— The patient is always right.
Rule #2— If you think the patient is wrong, reread rule #1.
ALL OTHER POLICIES ARE NULL AND VOID.
We post the mission statement in prominent places throughout the office (the reception area and most of the examination rooms, our Web site, and on a large banner in the employee lounge) to remind us and our patients of our dedication to excellent customer service.
Whenever a mistake or problem occurs, the first question we ask each other is, “Did we adhere to the mission statement and the policy statement?” Usually, we discover that we did not. We use the mission statement and the policy statement to refocus us on our number one priority: our patients.
10 LOW-COST WAYS TO MOTIVATE STAFF
A well-motivated staff creates an effective team environment. Most enlightened businesses have discovered that team management leads to increased output and productivity. Your employees want to be valued as human beings and individuals, not just as workers. The more you include them in the process of running the office, the more invested they become in helping to improve the way it works.
1. Review staff performance regularly
Employees like to know where they stand and how they can improve performance on the job. Motivated staff members appreciate feedback on their progress—or, even, their lack of it. The best way to furnish this important feedback is by conducting periodic performance reviews.
I suggest that you meet with your employees on a scheduled basis every 3 to 4 months. Give each employee a worksheet before the scheduled review (see Worksheet below), and then go over her responses during the review. You can learn a lot about what motivates her during this process.
I always end each performance review on a positive note, by telling the employee how great an asset she is to the practice. I document these meetings in the employee’s file.
2. Encourage continuing education
Just as physicians need continuing medical education to stay up to date, your staff members require continuing motivational experiences. Encourage your staff to participate in continuing education courses and support their efforts financially—you’ll get a favorable return on your investment.
I suggest that you offer to pay the fees for any seminars and classes your employees take. You may want to suggest courses in computers, social media, marketing, or any other subject area that will help the practice grow and prosper.
To make these educational experiences even more effective, ask employees to share what they have learned with other staff members. This can be done at a staff meeting. Simply ask the employee who attended a seminar or a course to share the information with the rest of the staff by briefly reviewing the course or describing what he learned and how it applies to the practice.
3. Empower your staff
Office management is complicated. Few ObGyns have a thorough understanding of all business aspects of a medical practice. Most successful ObGyns have learned to delegate the responsibility of running the office and to empower their employees to take control and assume responsibility for their decisions and actions.
In my practice, I empower any employee to make financial decisions up to a limit of $200 without consulting me. For instance, if the office needs a new telephone answering machine, I expect my employees to consider which features we need, check the machines that are available, and compare prices at the local electronics outlet, office supply store, and online retailers to find the best machine at the lowest price.
The take-home message: More than ever before, ObGyns should do what we are best trained to do—diagnose and treat diseases. Very few ObGyns are experts on fax machines. Don’t waste time on activities that your staff members can do.
4. Promote a positive mental attitude
As Ralph Waldo Emerson once said, “Nothing great was ever achieved without enthusiasm.” This is also true of the practice of medicine. When the doctor has a positive mental attitude, employees are motivated by the example. When a doctor is easily irritable and carries problems from home to the office and takes her frustration out on the staff, the employees will, in turn, take it out on the patients.
I have an attitude that employees are on stage. The moment they walk in the door in the morning, they have to leave all other problems and concerns behind them. They need to believe that they are responsible for making sure that each patient has a positive experience with the office at every contact point. That includes the telephone, the receptionist who welcomes patients to the practice, the nurse taking the patient into the exam room, the billing clerk who handles the patient’s bill, and, yes, the doctor, too! We all contribute to the patient’s experience, and we all need to have a positive attitude.
5. Recognize achievement
Nothing is more motivating for an employee than for the doctor to recognize his achievements and accomplishments. When an employee improves in job performance, tell him directly. You will satisfy that employee’s need for self-esteem, improve his confidence, and help him fulfill the need for self-esteem from fellow employees.
6. Show your staff that you care
Your employees need to know that you care about them not just as workers but as individuals with their own personal lives. When one of my employees is sick, or one of her family members is ill, I call her at home to check on her and make sure that she has access to adequate medical care. If someone gets sick in the office, I call another medical office and get the employee seen immediately.
7. Catch your employees doing things right
My philosophy is to praise in public, pan in private. When I catch an employee doing something right, I send a thank-you note to her home address, making sure that it arrives on a Saturday. I hope the employee will show my note to family and friends. I use a specially created card or a “thanks a million” check (a non-negotiable replication of a check that is made out to the employee and says, “Thanks a million,” with my name signed at the bottom).
You will be amazed at how appreciative the employee is that you not only recognized her superior service but took the time to put your recognition in writing.
8. Reward your staff for saving money
If a staff member comes up with an idea that saves the practice money, give her a bonus. For example, in my practice, the 15-year-old autoclave broke down. When I tried to get parts, I was informed that the machine is no longer made. The nurse in our office took the autoclave to the hospital’s biomedical engineering department, where workers installed a $30 part that saved me from buying a new $2,000 machine. The nurse deserved to be rewarded for that, so I gave her a $50 check on the spot.
I try to motivate my staff not just to earn more money for the practice but to reduce expenses, so I pay them when they identify and design money-saving ideas.
9. Involve your employees in decision making
Ask your employees for advice. Then make sure you follow it. Your staff members are on the front line; they want the office routine to go well. Include them in the decision-making process, whether the task is writing a mission statement or policy manual, determining a change in procedures, implementing an electronic health record, or meeting new job candidates. By including them, you make them feel like part of the team.
10. Have fun!
Surprise is the spice of life. Whenever you can provide an unexpected perk for your staff, you can be sure the gesture will be appreciated. For example, during a week in which two of my employees were unable to work (due to vacation and illness), the rest of us had to take up the slack. Despite being short-handed, we were able to function at regular speed and capacity without affecting the quality of care. I was so impressed by the extra effort that I arranged for a massage therapist to visit our practice at the end of the week and give everyone a 15- to 20-minute massage. It was my way of saying, “Thank you.”
THE BOTTOM LINE
Encourage team spirit. It makes good business sense. When your employees have a personal investment in problem-solving and decision-making, they will go the extra mile for your patients and your practice.
This is the last article in this four-part series on promoting your practice and increasing productivity. I hope you have identified the four pillars of success for your practice—and that I have helped you understand the importance of all four pillars. They represent the strength and stability of a successful ObGyn practice.
Premature baby is severely handicapped: $21M verdict
AT 31 2/7 WEEKS' GESTATION, a woman was admitted to the hospital for hypertension. A maternal-fetal medicine specialist determined that a vaginal delivery was reasonable as long as the mother and fetus remained clinically stable; a cesarean delivery would be required if the status changed. An ObGyn and nurse midwife took over the mother’s care. Before dinoprostone and oxytocin were administered the next morning, a second ObGyn conducted a vaginal exam and found the mother’s cervix to be 4-cm dilated. After noon, the fetal heart rate became nonreassuring, with late and prolonged variable decelerations. The baby was born shortly after 5:00 pm with the umbilical cord wrapped around his neck. He was pale, lifeless, and had Apgar scores of 4 and 7 at 1 and 5 minutes, respectively. He required initial positive pressure ventilation due to bradycardia and poor respiratory effort.
The boy has cerebral palsy; although not cognitively impaired, he is severely physically handicapped. He has had several operations because one leg is shorter than the other. He has 65% function of his arms, making it impossible for him to complete normal, daily tasks by himself.
PARENTS' CLAIM A cesarean delivery should have been performed 3 hours earlier.
DEFENDANT' DEFENSE Fetal heart-rate monitoring was reassuring during the last 40 minutes of labor. An Apgar score of 7 at 5 minutes is normal. Blood gases taken at birth were normal (7.3 pH). Ultrasonography of the baby’s head at age 3 days showed normal findings. Problems were not evident on the head ultrasound until the child was 2 weeks of age, showing that the injury occurred after birth and was due to prematurity. Defendants included both ObGyns, the midwife, and the hospital.
VERDICT A $21 million Maryland verdict was returned, including $1 million in noneconomic damages that was reduced to $650,000 under the state cap.
PHYSICIAN APOLOGIZED: DIDN'T READ BIOPSY REPORT BEFORE SURGERY
A 34-YEAR-OLD WOMAN with a family history of breast cancer found a lump in her left breast. After fine-needle aspiration, a general surgeon diagnosed cancer and performed a double mastectomy.
At the first postoperative visit, the surgeon told the patient that she did not have breast cancer, and that the fine-needle aspiration results were negative. The surgeon apologized for never looking at the biopsy report prior to surgery, and admitted that is she had seen the report, she would have cancelled surgery.
PATIENT'S CLAIM The surgeon was negligent in performing bilateral mastectomies without first reading biopsy results.
PHYSICIAN'S DEFENSE The case was settled before trial.
VERDICT Michigan case evaluation delivered an award of $542,000, which both parties accepted.
CYSTOSCOPY BLAMED FOR URETERAL OBSTRUCTION, POOR KIDNEY FUNCTION
WHEN A 59-YEAR-OLD WOMAN underwent gynecologic surgery that included a cystoscopy, her uterers were functioning normally. During the following month, the ObGyn performed several follow-up examinations. A year later, the patient's right ureter was completely obstructed. The obstruction was repaired, but the patient lost function in her right kidney. She must take a drug to improve kidney function for the rest of her life.
PATIENT'S CLAIM The obstruction was caused by ligation that occurred during cystoscopy. The ObGyn should have diagnosed the obstruction during the weeks following surgery.
PHYSICIAN'S DEFENSE The cystoscopy was properly performed. The patient had not reported any symptoms after the procedure that suggested the presence of an obstruction. The obstruction gradually developed and could not have been diagnosed earlier.
VERDICT A New York defense verdict was returned.
INFERIOR VENA CAVA DAMAGED DURING ROBOTIC HYSTERECTOMY
A HYSTERECTOMY AND SALPINGO-OOPHORECTOMY were performed on a 64-year-old woman using the da Vinci Surgical System. The gynecologist also removed a cancerous endometrial mass and dissected the periaortic lymph nodes. When the gynecologist used the robot to lift a lymph fat pad, the inferior vena cava was injured and the patient lost 3 L of blood. After converting the laparotomy, a vascular surgeon implanted an artificial graft to repair the inferior vena cava. The patient fully recovered.
PATIENT'S CLAIM The gynecologist did not perform robotic surgery properly, and the patient was not told of all of the risks associated with robotic surgery. Due to the uncertainty regarding the graft's effectiveness, the patient developed posttraumatic stress disorder.
PHYSICIAN'S DEFENSE The vascular injury was a known risk associated with the procedure. The vena cava was not lacerated or transected: perforator veins that joined the lymph fat pad were unintentionally pulled out. The injury was most likely due to the application of pressure, not laceration by the surgical instrument.
VERDICT A $300,000 New York settlement was reached.
READ: The robot is gaining ground in gynecologic surgery. Should you be using it? A roundtable discussion with Arnold P. Advincula, MD; Cheryl B. Iglesia, MD; Rosanne M. Kho, MD; Jamal Mourad, DO; Marie Fidela R. Paraiso, MD; and Jason D. Wright, MD (April 2013)
FETAL DISTRESS CAUSED BRAIN INJURY: $13.9M
DURING THE LAST 2 HOURS OF LABOR, the mother was febrile, the baby's heart rate rose to over 160 bpm, and fetal monitoring indicated fetal distress. Oxytocin was administered to hasten delivery, but the mother's uterus became hyperstimulated. After nearly 17 hours of labor, the child was born without respirations. A video of the vaginal birth shows that the child was blue and unresponsive. The baby was resuscitated, and was subsequently found to have cerebral palsy, epilepsy, and mental retardation. At the time of trial, the 10-year-old had the mental capacity of a 3-year-old.
PARENTS' CLAIM The child suffered brain injury due to hypoxic ischemic encephalopathy. A cesarean delivery should have been performed as soon as fetal distress was evident. The doctors and nurses misread the baseline heart rate, and did not react when the baby did not recover well from the mother's contractions. Brain imaging did not show damage caused by infection or meningitis.
PHYSICIAN'S DEFENSE The girl's condition was caused by an infection or meningitis.
VERDICT A confidential settlement was reached with the midwife before the trial. The ObGyn was dismissed because he was never alerted to any problem by the labor and delivery team. A $13.9 million Georgia verdict was returned against the hospital system.
UTERINE ARTERY INJURED DURING CESAREAN DELIVERY
AFTER A SCHEDULED CESAREAN delivery, the 29-year-old mother had low blood pressure and an altered state of consciousness When she returned to the OR several hours later, her ObGyn found a uterine artery hematoma and laceration. After the laceration was clamped and sutured, uterine atony was noted and an emergency hysterectomy was performed
PATIENT'S CLAIM The mother was no longer able to bear children. The ObGyn was negligent in lacerating the uterine artery, failing to recognize the laceration during cesarean surgery, failing to properly monitor the patient after surgery, and failing to repair the artery in a timely manner. The patient's low blood pressure and altered state of consciousness should have been an indication that she had severe blood loss. The hospital's nursing staff failed to properly check her vital signs after surgery, and failed to report the abnormalities in blood pressure and consciousness to the ObGyn.
DEFENDANTS' DEFENSE The ObGyn claimed that a uterine laceration is a known risk of cesarean delivery; it can occur in the absence of negligence. The hospital also denied negligence.
VERDICT A Texas defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.versictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
AT 31 2/7 WEEKS' GESTATION, a woman was admitted to the hospital for hypertension. A maternal-fetal medicine specialist determined that a vaginal delivery was reasonable as long as the mother and fetus remained clinically stable; a cesarean delivery would be required if the status changed. An ObGyn and nurse midwife took over the mother’s care. Before dinoprostone and oxytocin were administered the next morning, a second ObGyn conducted a vaginal exam and found the mother’s cervix to be 4-cm dilated. After noon, the fetal heart rate became nonreassuring, with late and prolonged variable decelerations. The baby was born shortly after 5:00 pm with the umbilical cord wrapped around his neck. He was pale, lifeless, and had Apgar scores of 4 and 7 at 1 and 5 minutes, respectively. He required initial positive pressure ventilation due to bradycardia and poor respiratory effort.
The boy has cerebral palsy; although not cognitively impaired, he is severely physically handicapped. He has had several operations because one leg is shorter than the other. He has 65% function of his arms, making it impossible for him to complete normal, daily tasks by himself.
PARENTS' CLAIM A cesarean delivery should have been performed 3 hours earlier.
DEFENDANT' DEFENSE Fetal heart-rate monitoring was reassuring during the last 40 minutes of labor. An Apgar score of 7 at 5 minutes is normal. Blood gases taken at birth were normal (7.3 pH). Ultrasonography of the baby’s head at age 3 days showed normal findings. Problems were not evident on the head ultrasound until the child was 2 weeks of age, showing that the injury occurred after birth and was due to prematurity. Defendants included both ObGyns, the midwife, and the hospital.
VERDICT A $21 million Maryland verdict was returned, including $1 million in noneconomic damages that was reduced to $650,000 under the state cap.
PHYSICIAN APOLOGIZED: DIDN'T READ BIOPSY REPORT BEFORE SURGERY
A 34-YEAR-OLD WOMAN with a family history of breast cancer found a lump in her left breast. After fine-needle aspiration, a general surgeon diagnosed cancer and performed a double mastectomy.
At the first postoperative visit, the surgeon told the patient that she did not have breast cancer, and that the fine-needle aspiration results were negative. The surgeon apologized for never looking at the biopsy report prior to surgery, and admitted that is she had seen the report, she would have cancelled surgery.
PATIENT'S CLAIM The surgeon was negligent in performing bilateral mastectomies without first reading biopsy results.
PHYSICIAN'S DEFENSE The case was settled before trial.
VERDICT Michigan case evaluation delivered an award of $542,000, which both parties accepted.
CYSTOSCOPY BLAMED FOR URETERAL OBSTRUCTION, POOR KIDNEY FUNCTION
WHEN A 59-YEAR-OLD WOMAN underwent gynecologic surgery that included a cystoscopy, her uterers were functioning normally. During the following month, the ObGyn performed several follow-up examinations. A year later, the patient's right ureter was completely obstructed. The obstruction was repaired, but the patient lost function in her right kidney. She must take a drug to improve kidney function for the rest of her life.
PATIENT'S CLAIM The obstruction was caused by ligation that occurred during cystoscopy. The ObGyn should have diagnosed the obstruction during the weeks following surgery.
PHYSICIAN'S DEFENSE The cystoscopy was properly performed. The patient had not reported any symptoms after the procedure that suggested the presence of an obstruction. The obstruction gradually developed and could not have been diagnosed earlier.
VERDICT A New York defense verdict was returned.
INFERIOR VENA CAVA DAMAGED DURING ROBOTIC HYSTERECTOMY
A HYSTERECTOMY AND SALPINGO-OOPHORECTOMY were performed on a 64-year-old woman using the da Vinci Surgical System. The gynecologist also removed a cancerous endometrial mass and dissected the periaortic lymph nodes. When the gynecologist used the robot to lift a lymph fat pad, the inferior vena cava was injured and the patient lost 3 L of blood. After converting the laparotomy, a vascular surgeon implanted an artificial graft to repair the inferior vena cava. The patient fully recovered.
PATIENT'S CLAIM The gynecologist did not perform robotic surgery properly, and the patient was not told of all of the risks associated with robotic surgery. Due to the uncertainty regarding the graft's effectiveness, the patient developed posttraumatic stress disorder.
PHYSICIAN'S DEFENSE The vascular injury was a known risk associated with the procedure. The vena cava was not lacerated or transected: perforator veins that joined the lymph fat pad were unintentionally pulled out. The injury was most likely due to the application of pressure, not laceration by the surgical instrument.
VERDICT A $300,000 New York settlement was reached.
READ: The robot is gaining ground in gynecologic surgery. Should you be using it? A roundtable discussion with Arnold P. Advincula, MD; Cheryl B. Iglesia, MD; Rosanne M. Kho, MD; Jamal Mourad, DO; Marie Fidela R. Paraiso, MD; and Jason D. Wright, MD (April 2013)
FETAL DISTRESS CAUSED BRAIN INJURY: $13.9M
DURING THE LAST 2 HOURS OF LABOR, the mother was febrile, the baby's heart rate rose to over 160 bpm, and fetal monitoring indicated fetal distress. Oxytocin was administered to hasten delivery, but the mother's uterus became hyperstimulated. After nearly 17 hours of labor, the child was born without respirations. A video of the vaginal birth shows that the child was blue and unresponsive. The baby was resuscitated, and was subsequently found to have cerebral palsy, epilepsy, and mental retardation. At the time of trial, the 10-year-old had the mental capacity of a 3-year-old.
PARENTS' CLAIM The child suffered brain injury due to hypoxic ischemic encephalopathy. A cesarean delivery should have been performed as soon as fetal distress was evident. The doctors and nurses misread the baseline heart rate, and did not react when the baby did not recover well from the mother's contractions. Brain imaging did not show damage caused by infection or meningitis.
PHYSICIAN'S DEFENSE The girl's condition was caused by an infection or meningitis.
VERDICT A confidential settlement was reached with the midwife before the trial. The ObGyn was dismissed because he was never alerted to any problem by the labor and delivery team. A $13.9 million Georgia verdict was returned against the hospital system.
UTERINE ARTERY INJURED DURING CESAREAN DELIVERY
AFTER A SCHEDULED CESAREAN delivery, the 29-year-old mother had low blood pressure and an altered state of consciousness When she returned to the OR several hours later, her ObGyn found a uterine artery hematoma and laceration. After the laceration was clamped and sutured, uterine atony was noted and an emergency hysterectomy was performed
PATIENT'S CLAIM The mother was no longer able to bear children. The ObGyn was negligent in lacerating the uterine artery, failing to recognize the laceration during cesarean surgery, failing to properly monitor the patient after surgery, and failing to repair the artery in a timely manner. The patient's low blood pressure and altered state of consciousness should have been an indication that she had severe blood loss. The hospital's nursing staff failed to properly check her vital signs after surgery, and failed to report the abnormalities in blood pressure and consciousness to the ObGyn.
DEFENDANTS' DEFENSE The ObGyn claimed that a uterine laceration is a known risk of cesarean delivery; it can occur in the absence of negligence. The hospital also denied negligence.
VERDICT A Texas defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.versictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
AT 31 2/7 WEEKS' GESTATION, a woman was admitted to the hospital for hypertension. A maternal-fetal medicine specialist determined that a vaginal delivery was reasonable as long as the mother and fetus remained clinically stable; a cesarean delivery would be required if the status changed. An ObGyn and nurse midwife took over the mother’s care. Before dinoprostone and oxytocin were administered the next morning, a second ObGyn conducted a vaginal exam and found the mother’s cervix to be 4-cm dilated. After noon, the fetal heart rate became nonreassuring, with late and prolonged variable decelerations. The baby was born shortly after 5:00 pm with the umbilical cord wrapped around his neck. He was pale, lifeless, and had Apgar scores of 4 and 7 at 1 and 5 minutes, respectively. He required initial positive pressure ventilation due to bradycardia and poor respiratory effort.
The boy has cerebral palsy; although not cognitively impaired, he is severely physically handicapped. He has had several operations because one leg is shorter than the other. He has 65% function of his arms, making it impossible for him to complete normal, daily tasks by himself.
PARENTS' CLAIM A cesarean delivery should have been performed 3 hours earlier.
DEFENDANT' DEFENSE Fetal heart-rate monitoring was reassuring during the last 40 minutes of labor. An Apgar score of 7 at 5 minutes is normal. Blood gases taken at birth were normal (7.3 pH). Ultrasonography of the baby’s head at age 3 days showed normal findings. Problems were not evident on the head ultrasound until the child was 2 weeks of age, showing that the injury occurred after birth and was due to prematurity. Defendants included both ObGyns, the midwife, and the hospital.
VERDICT A $21 million Maryland verdict was returned, including $1 million in noneconomic damages that was reduced to $650,000 under the state cap.
PHYSICIAN APOLOGIZED: DIDN'T READ BIOPSY REPORT BEFORE SURGERY
A 34-YEAR-OLD WOMAN with a family history of breast cancer found a lump in her left breast. After fine-needle aspiration, a general surgeon diagnosed cancer and performed a double mastectomy.
At the first postoperative visit, the surgeon told the patient that she did not have breast cancer, and that the fine-needle aspiration results were negative. The surgeon apologized for never looking at the biopsy report prior to surgery, and admitted that is she had seen the report, she would have cancelled surgery.
PATIENT'S CLAIM The surgeon was negligent in performing bilateral mastectomies without first reading biopsy results.
PHYSICIAN'S DEFENSE The case was settled before trial.
VERDICT Michigan case evaluation delivered an award of $542,000, which both parties accepted.
CYSTOSCOPY BLAMED FOR URETERAL OBSTRUCTION, POOR KIDNEY FUNCTION
WHEN A 59-YEAR-OLD WOMAN underwent gynecologic surgery that included a cystoscopy, her uterers were functioning normally. During the following month, the ObGyn performed several follow-up examinations. A year later, the patient's right ureter was completely obstructed. The obstruction was repaired, but the patient lost function in her right kidney. She must take a drug to improve kidney function for the rest of her life.
PATIENT'S CLAIM The obstruction was caused by ligation that occurred during cystoscopy. The ObGyn should have diagnosed the obstruction during the weeks following surgery.
PHYSICIAN'S DEFENSE The cystoscopy was properly performed. The patient had not reported any symptoms after the procedure that suggested the presence of an obstruction. The obstruction gradually developed and could not have been diagnosed earlier.
VERDICT A New York defense verdict was returned.
INFERIOR VENA CAVA DAMAGED DURING ROBOTIC HYSTERECTOMY
A HYSTERECTOMY AND SALPINGO-OOPHORECTOMY were performed on a 64-year-old woman using the da Vinci Surgical System. The gynecologist also removed a cancerous endometrial mass and dissected the periaortic lymph nodes. When the gynecologist used the robot to lift a lymph fat pad, the inferior vena cava was injured and the patient lost 3 L of blood. After converting the laparotomy, a vascular surgeon implanted an artificial graft to repair the inferior vena cava. The patient fully recovered.
PATIENT'S CLAIM The gynecologist did not perform robotic surgery properly, and the patient was not told of all of the risks associated with robotic surgery. Due to the uncertainty regarding the graft's effectiveness, the patient developed posttraumatic stress disorder.
PHYSICIAN'S DEFENSE The vascular injury was a known risk associated with the procedure. The vena cava was not lacerated or transected: perforator veins that joined the lymph fat pad were unintentionally pulled out. The injury was most likely due to the application of pressure, not laceration by the surgical instrument.
VERDICT A $300,000 New York settlement was reached.
READ: The robot is gaining ground in gynecologic surgery. Should you be using it? A roundtable discussion with Arnold P. Advincula, MD; Cheryl B. Iglesia, MD; Rosanne M. Kho, MD; Jamal Mourad, DO; Marie Fidela R. Paraiso, MD; and Jason D. Wright, MD (April 2013)
FETAL DISTRESS CAUSED BRAIN INJURY: $13.9M
DURING THE LAST 2 HOURS OF LABOR, the mother was febrile, the baby's heart rate rose to over 160 bpm, and fetal monitoring indicated fetal distress. Oxytocin was administered to hasten delivery, but the mother's uterus became hyperstimulated. After nearly 17 hours of labor, the child was born without respirations. A video of the vaginal birth shows that the child was blue and unresponsive. The baby was resuscitated, and was subsequently found to have cerebral palsy, epilepsy, and mental retardation. At the time of trial, the 10-year-old had the mental capacity of a 3-year-old.
PARENTS' CLAIM The child suffered brain injury due to hypoxic ischemic encephalopathy. A cesarean delivery should have been performed as soon as fetal distress was evident. The doctors and nurses misread the baseline heart rate, and did not react when the baby did not recover well from the mother's contractions. Brain imaging did not show damage caused by infection or meningitis.
PHYSICIAN'S DEFENSE The girl's condition was caused by an infection or meningitis.
VERDICT A confidential settlement was reached with the midwife before the trial. The ObGyn was dismissed because he was never alerted to any problem by the labor and delivery team. A $13.9 million Georgia verdict was returned against the hospital system.
UTERINE ARTERY INJURED DURING CESAREAN DELIVERY
AFTER A SCHEDULED CESAREAN delivery, the 29-year-old mother had low blood pressure and an altered state of consciousness When she returned to the OR several hours later, her ObGyn found a uterine artery hematoma and laceration. After the laceration was clamped and sutured, uterine atony was noted and an emergency hysterectomy was performed
PATIENT'S CLAIM The mother was no longer able to bear children. The ObGyn was negligent in lacerating the uterine artery, failing to recognize the laceration during cesarean surgery, failing to properly monitor the patient after surgery, and failing to repair the artery in a timely manner. The patient's low blood pressure and altered state of consciousness should have been an indication that she had severe blood loss. The hospital's nursing staff failed to properly check her vital signs after surgery, and failed to report the abnormalities in blood pressure and consciousness to the ObGyn.
DEFENDANTS' DEFENSE The ObGyn claimed that a uterine laceration is a known risk of cesarean delivery; it can occur in the absence of negligence. The hospital also denied negligence.
VERDICT A Texas defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.versictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
The Sunshine Act
This month, yet another new bureaucracy unfolds: Under the Physician Payment Sunshine Act – part of the Affordable Care Act – manufacturers of drugs, devices, and biological and medical supplies covered by federal health care programs are now required to begin reporting financial interactions with physicians and teaching hospitals to the Centers for Medicare and Medicaid Services.
Ownership or investment interests in the manufacturers by physicians and their family members also must be disclosed. Most of the data will be published online by September 2014.
In addition to reporting the type of financial exchange and the dollar amount, manufacturers are required to report the reason for the interaction, including consulting, food, ownership or investment interest, direct compensation for speakers at education programs (whether or not they are accredited or certified), and research. There are exclusions, including drug samples intended for distribution to patients. Medical students and residents are excluded entirely. You will be allowed to review your data and seek corrections before it is published; and you will have an additional 2 years to pursue corrections.
Compensation for conducting clinical trials will be reported, but not posted on the website until the product receives Food and Drug Administration approval, or until 4 years after the payment, whichever is earlier. Payments for trials involving a new indication for an approved drug will be posted immediately.
So what will be the likely effects on research, industry-sponsored meetings, meals provided by drug reps, and the like? The short answer is that no one knows. Much will depend on how the information is reported, and how patients interpret the data that they see – if they take notice at all.
Sunshine laws are already in effect in six states – California, Colorado, Massachusetts, Minnesota, Vermont, and West Virginia – and the District of Columbia. (Maine repealed its law in 2011.) Observers disagree on their impact. Data from Maine and West Virginia showed no significant changes in prescribing patterns after the laws took effect, according to a 2012 article in Archives of Internal Medicine (now JAMA Internal Medicine).
Evidence indicates that physicians have already decreased their industry interaction on their own: About a quarter of all private practices now refuse to see pharmaceutical reps; most medical schools prohibit samples, gifts, and on-site meals, and many prohibit on-site interaction of any kind between reps and residents.
How the disclosure legislation translates into physician-patient interaction remains equally unclear. Do patients think less of doctors who accept the occasional industry-sponsored lunch for their employees? Do they think more of doctors who conduct industry-sponsored clinical research? There are no objective data, so far as I know.
My guess – based on no evidence but 30 years of experience – is that attorneys, activists, and the occasional reporter will data-mine the website, but few patients will ever bother to visit. Nevertheless, you should prepare now to ensure the accuracy of anything posted about you when the database launches next year. Mark your calendar; the data must be reported to the CMS by March 31 annually, so you will need to set aside time each April or May to review it. If you have many or complex industry relationships, you should probably contact each of the manufacturers in January or February and ask to see the data before they are submitted. Then review the information again once the CMS gets it, to be sure nothing was changed. Maintaining accurate financial records has always been important, but it will be even more so now, to effectively dispute any inconsistencies.
If you don’t see drug reps or give sponsored talks, don’t assume that you won’t be on the website. Check anyway; you might be indirectly involved in compensation that you were not aware of, or you may have been reported in error.
Pharmaceutical companies face stiff penalties if they do not comply with the Sunshine Act. Those that fail to report can be fined up to $150,000 annually, and those fines can rise to $1 million for those that intentionally fail to report. This means that the information will be disclosed. If you have any financial relationships with the pharmaceutical industry, you will need to anticipate the implications of the increased scrutiny that may (or may not) result.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J.
This month, yet another new bureaucracy unfolds: Under the Physician Payment Sunshine Act – part of the Affordable Care Act – manufacturers of drugs, devices, and biological and medical supplies covered by federal health care programs are now required to begin reporting financial interactions with physicians and teaching hospitals to the Centers for Medicare and Medicaid Services.
Ownership or investment interests in the manufacturers by physicians and their family members also must be disclosed. Most of the data will be published online by September 2014.
In addition to reporting the type of financial exchange and the dollar amount, manufacturers are required to report the reason for the interaction, including consulting, food, ownership or investment interest, direct compensation for speakers at education programs (whether or not they are accredited or certified), and research. There are exclusions, including drug samples intended for distribution to patients. Medical students and residents are excluded entirely. You will be allowed to review your data and seek corrections before it is published; and you will have an additional 2 years to pursue corrections.
Compensation for conducting clinical trials will be reported, but not posted on the website until the product receives Food and Drug Administration approval, or until 4 years after the payment, whichever is earlier. Payments for trials involving a new indication for an approved drug will be posted immediately.
So what will be the likely effects on research, industry-sponsored meetings, meals provided by drug reps, and the like? The short answer is that no one knows. Much will depend on how the information is reported, and how patients interpret the data that they see – if they take notice at all.
Sunshine laws are already in effect in six states – California, Colorado, Massachusetts, Minnesota, Vermont, and West Virginia – and the District of Columbia. (Maine repealed its law in 2011.) Observers disagree on their impact. Data from Maine and West Virginia showed no significant changes in prescribing patterns after the laws took effect, according to a 2012 article in Archives of Internal Medicine (now JAMA Internal Medicine).
Evidence indicates that physicians have already decreased their industry interaction on their own: About a quarter of all private practices now refuse to see pharmaceutical reps; most medical schools prohibit samples, gifts, and on-site meals, and many prohibit on-site interaction of any kind between reps and residents.
How the disclosure legislation translates into physician-patient interaction remains equally unclear. Do patients think less of doctors who accept the occasional industry-sponsored lunch for their employees? Do they think more of doctors who conduct industry-sponsored clinical research? There are no objective data, so far as I know.
My guess – based on no evidence but 30 years of experience – is that attorneys, activists, and the occasional reporter will data-mine the website, but few patients will ever bother to visit. Nevertheless, you should prepare now to ensure the accuracy of anything posted about you when the database launches next year. Mark your calendar; the data must be reported to the CMS by March 31 annually, so you will need to set aside time each April or May to review it. If you have many or complex industry relationships, you should probably contact each of the manufacturers in January or February and ask to see the data before they are submitted. Then review the information again once the CMS gets it, to be sure nothing was changed. Maintaining accurate financial records has always been important, but it will be even more so now, to effectively dispute any inconsistencies.
If you don’t see drug reps or give sponsored talks, don’t assume that you won’t be on the website. Check anyway; you might be indirectly involved in compensation that you were not aware of, or you may have been reported in error.
Pharmaceutical companies face stiff penalties if they do not comply with the Sunshine Act. Those that fail to report can be fined up to $150,000 annually, and those fines can rise to $1 million for those that intentionally fail to report. This means that the information will be disclosed. If you have any financial relationships with the pharmaceutical industry, you will need to anticipate the implications of the increased scrutiny that may (or may not) result.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J.
This month, yet another new bureaucracy unfolds: Under the Physician Payment Sunshine Act – part of the Affordable Care Act – manufacturers of drugs, devices, and biological and medical supplies covered by federal health care programs are now required to begin reporting financial interactions with physicians and teaching hospitals to the Centers for Medicare and Medicaid Services.
Ownership or investment interests in the manufacturers by physicians and their family members also must be disclosed. Most of the data will be published online by September 2014.
In addition to reporting the type of financial exchange and the dollar amount, manufacturers are required to report the reason for the interaction, including consulting, food, ownership or investment interest, direct compensation for speakers at education programs (whether or not they are accredited or certified), and research. There are exclusions, including drug samples intended for distribution to patients. Medical students and residents are excluded entirely. You will be allowed to review your data and seek corrections before it is published; and you will have an additional 2 years to pursue corrections.
Compensation for conducting clinical trials will be reported, but not posted on the website until the product receives Food and Drug Administration approval, or until 4 years after the payment, whichever is earlier. Payments for trials involving a new indication for an approved drug will be posted immediately.
So what will be the likely effects on research, industry-sponsored meetings, meals provided by drug reps, and the like? The short answer is that no one knows. Much will depend on how the information is reported, and how patients interpret the data that they see – if they take notice at all.
Sunshine laws are already in effect in six states – California, Colorado, Massachusetts, Minnesota, Vermont, and West Virginia – and the District of Columbia. (Maine repealed its law in 2011.) Observers disagree on their impact. Data from Maine and West Virginia showed no significant changes in prescribing patterns after the laws took effect, according to a 2012 article in Archives of Internal Medicine (now JAMA Internal Medicine).
Evidence indicates that physicians have already decreased their industry interaction on their own: About a quarter of all private practices now refuse to see pharmaceutical reps; most medical schools prohibit samples, gifts, and on-site meals, and many prohibit on-site interaction of any kind between reps and residents.
How the disclosure legislation translates into physician-patient interaction remains equally unclear. Do patients think less of doctors who accept the occasional industry-sponsored lunch for their employees? Do they think more of doctors who conduct industry-sponsored clinical research? There are no objective data, so far as I know.
My guess – based on no evidence but 30 years of experience – is that attorneys, activists, and the occasional reporter will data-mine the website, but few patients will ever bother to visit. Nevertheless, you should prepare now to ensure the accuracy of anything posted about you when the database launches next year. Mark your calendar; the data must be reported to the CMS by March 31 annually, so you will need to set aside time each April or May to review it. If you have many or complex industry relationships, you should probably contact each of the manufacturers in January or February and ask to see the data before they are submitted. Then review the information again once the CMS gets it, to be sure nothing was changed. Maintaining accurate financial records has always been important, but it will be even more so now, to effectively dispute any inconsistencies.
If you don’t see drug reps or give sponsored talks, don’t assume that you won’t be on the website. Check anyway; you might be indirectly involved in compensation that you were not aware of, or you may have been reported in error.
Pharmaceutical companies face stiff penalties if they do not comply with the Sunshine Act. Those that fail to report can be fined up to $150,000 annually, and those fines can rise to $1 million for those that intentionally fail to report. This means that the information will be disclosed. If you have any financial relationships with the pharmaceutical industry, you will need to anticipate the implications of the increased scrutiny that may (or may not) result.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J.
The Affordable Care Act and the drive for electronic health records: Are small practices being squeezed?
Two years ago, I zeroed in on the pressures straining small ObGyn practices in an article entitled, “Is private ObGyn practice on its way out?”1 The pressures haven’t eased in the interim. Today, small practices are still feeling squeezed to keep up with the many demands of modern specialty care. The push for electronic health records (EHRs), in particular, can profoundly affect physicians in private practice.
In this article, I outline some of the challenges facing small practices when they set out to implement EHRs, as well as the potential benefits they stand to gain a little farther down the road. Before we begin, however, let’s look at the latest trends in ObGyn practice, as they are related, in part, to the need to implement EHRs.
The exodus from private practice continues
A 2012 Accenture Physicians Alignment Survey shows an accelerating increase in physician employment. In 2000, 57% of all physicians were in independent practice; by the end of 2013, only 36% of physicians are projected to remain independent.2
The ObGyn specialty is a clear part of this trend, with both seasoned and incoming physicians finding hospital or other employment an attractive alternative to private practice. Fully one-third of ObGyn residents entering practice today sign hospital employment contracts. ObGyns who have made the switch from private to hospital practice, or who have become ObGyn hospitalists, often point to the difficulties of maintaining a solvent private practice, especially given the push toward EHRs and increasing regulatory and administrative burdens, as justification for their move.
The main reasons for the shift to employment. Top concerns influencing physicians’ decisions to opt for employment include:
- business expenses (87%)
- the dominance of managed care (61%)
- the requirement for EHRs (53%)
- the need to maintain and manage staff (53%)
- the increasing number of patients needed to break even (39%).2
A 2008 socioeconomic survey from ACOG revealed that 23.6% of ObGyn practices are solo practices, and 27.1% are single-specialty group practices. Many ObGyns—especially those in solo or small practices—are hesitant to make the large capital investment that is necessary to adopt EHRs.
EHRs offer benefits—and real costs
The system-wide benefits of health information technology (HIT), including EHRs, are many. Insurers stand to save money by reducing unnecessary tests, and patients will benefit from better coordination of their care and fewer medical errors. But these advantages don’t necessarily translate into savings or revenue for physician practices. Instead, physicians face payment cuts from Medicare and private insurance.
Although there’s wide agreement that HIT can improve quality of care and reduce health-care costs, fewer than one-quarter (22%) of office-based physicians had adopted EHRs by 2009. We know the main reasons why:
- upfront cost and maintenance expense
- uncertain return on investment
- fragmented business model in a high proportion of small and solo practices
- changing and inconsistent information technology (IT) systems.
What can a practice expect to fork over?
In 2011, the Agency for Healthcare Research and Quality (AHRQ) found that the “real-life” cost of implementing EHRs “in an average five-physician primary care practice, operating within a large physician network committed to network-wide implementation of electronic health records, is about $162,000, with an additional $85,500 in maintenance expenses during the first year.”3
These figures include an average of 134 hours needed per physician to prepare to use EHRs during patient visits.3
Fleming and colleagues investigated the cost associated with implementing EHRs within 26 primary care practices in Texas. They found the cost to be $32,409 per physician through the first 60 days after the EHR system was launched, with one-time costs for hardware of $25,000 per practice and an additional $7,000 per physician for personal computers, printers, and scanners. The annual cost of software and maintenance was approximately $17,100 per physician.4
Why physicians should hold out for the return on their investment
Despite these considerable expenses, EHRs hold promise over the long term. The Medical Group Management Association reported, through a 2009 survey of about 1,300 primary care and specialty practice members using EHRs, that efficiency gains from the elimination of paper charts, as well as transcription savings, better charge capturing, and reduced billing errors, resulted in a median revenue increase of $49,916 per full-time physician after operating costs.
After 5 years of EHR use, practices reported a median operating margin 10.1% higher than that of practices in the first year of EHR use.5
Trends in the adoption of EHRs
Private practice. An article in Health Affairs showed that, by 2011, only one in six office-based physicians was using an EHR system robust enough to approach “meaningful use”—that is, the use of EHRs to measurably improve the quality of health care.6 These robust systems offered physicians the ability to record information on patient demographics, view laboratory and imaging results, maintain patients’ problem lists, compile clinical notes, and manage prescription ordering. EHR adoption lagged among non−primary care physicians, physicians aged 55 and older, and physicians in small (1–2 providers) practices and physician-owned practices.6 (ObGyns were considered primary care providers in this survey.)
“Big” practice. By comparison, in 2011, 99% of physicians in health maintenance organizations, or HMOs, and 73% in academic health centers and other hospitals used EHR systems.6 The number of physicians in these practice settings is small but growing.
In 2011, only 17% of physicians were in large practices of 10 or more physicians; 40% were in practices of one or two physicians.6
Primary care. These practices lead others in the adoption of EHRs, in part because of federal assistance, including a nationwide system of regional HIT assistance centers established by the Health Information Technology for Economic and Clinical Health (HITECH) Act to help providers located in rural areas participate in the Centers for Medicare and Medicaid Services (CMS) programs in EHR. The goal of these programs is to provide HIT support to at least 100,000 primary care providers, including ObGyns, by 2014.
The numbers cited in the Health Affairs article largely mirror data developed by other research organizations, including the Deloitte Center for Health Solutions.6
The EHR incentive
The drive for EHRs started long before the Affordable Care Act (ACA) was passed in 2010. The US Congress took a first stab at encouraging the health-care community to embrace HIT in 1996, when it passed the Health Insurance Portability and Accountability Act (HIPAA). HIPAA created an electronic data interchange that health plans, health-care clearinghouses, and certain health-care providers, including pharmacists, are required to use for electronic transactions, including:
- claims and encounter information
- payment and remittance advice
- claims status
- eligibility
- enrollment and disenrollment
- referrals and authorizations
- coordination of benefits
- premium payment.
Congress stepped up its game in 2009, when it offered higher Medicare and Medicaid payments to physicians who adopt and “meaningfully use” EHRs. The HITECH Act included $30 billion in new Medicare and Medicaid incentive payments—as much as $44,000 under Medicare and $63,750 under Medicaid—as well as $500 million for states to develop health information exchanges.
The Act also established a government-led process for certification of electronic health records through a $35 billion appropriation for the Office of the National Coordinator for Health IT, housed in CMS.
Other programs designed to encourage use of EHRs
Other federal programs include the Physician Quality Reporting System (PQRS), which, when created in 2006, was a voluntary physician electronic reporting program. Under the ACA, however, it has become a mandate. Starting in 2015, Medicare payments will be reduced for nonparticipating physicians.
The Electronic Prescribing (eRx) Incentive Program, created in 2008 under the Medicare Improvements for Patients and Providers Act, provides incentives for eligible physicians who e-prescribe Medicare Part D medications through a qualified system. This program converted to a penalty program last year for physicians who don’t use eRx.
Grants were also provided under the HITECH Act to fund an HIT infrastructure and low-interest HIT loans. The AHRQ has awarded $300 million in federal grant money to more than 200 projects in 48 states to promote access to and encourage HIT adoption. Over $150 million in Medicaid transformation grants have been awarded to three states and territories for HIT in the Medicaid program under the 2005 Deficit Reduction Act.
The ACA carried these initiatives even further by establishing uniform standards that HIT systems must meet, including:
- automatic reconciliation of electronic fund transfers and HIPAA payment and remittance
- improved claims payment process
- consistent methods of health plan enrollment and claim edits
- simplified and improved routing of health-care transactions
- electronic claims attachments.
Clearly, a lot of effort and taxpayer dollars have been dedicated to drive efficient use of HIT and EHRs in the hopes that they can:
- help make sense of our increasingly fragmented health-care system
- improve patient safety
- increase efficiency
- reduce paperwork
- reduce unnecessary tests
- better coordinate patient care.
To see which providers are cashing in on the government’s incentives for EHRs, see “Some physicians are more likely to seek incentives for meaningful use of EHRs” on page 37.
The long view
HIT and EHRs are here to stay. Products are maturing and improving. Acceptance by large and small practices has gained traction. Are small practices being squeezed? No doubt.
In 2011, I urged all ObGyns—especially those in private practice—to read an article written by President Barack Obama’s health-reform deputies on how physicians can be successful under the ACA.1 It reads, in part:
To realize the full benefits of the Affordable Care Act, physicians will need to embrace rather than resist change. The economic forces put in motion by the Act are likely to lead to vertical organization of providers and accelerate physician employment by hospitals and aggregation into larger physician groups. The most successful physicians will be those who most effectively collaborate with other providers to improve outcomes, care productivity, and patient experience.7
1. DiVenere L, Yates J. Is private ObGyn practice on its way out? OBG Manage. 2011;23(10):42–54.
2. More US doctors leaving private practice due to rising costs and technology mandates, Accenture report finds [news release]. Arlington, Virginia: Accenture Newsroom; October 31, 2012. http://newsroom.accenture.com/news/more-us-doctors-leaving-private-practice-due-to-rising-costs-and-technology-mandates-accenture-report-finds.htm. Accessed June 5, 2013.
3. Study identifies costs of implementing electronic health records in network of physician practices: Research Activities October 2011, No. 374. Rockville, MD: Agency for Healthcare Research and Quality. http://www.ahrq.gov/news/newsletters/research-activities/oct11/1011RA15.html. Accessed June 5, 2013.
5. MGMA survey: Medical groups with EHRs report better financial performance than practices with paper medical records [news release]. New Orleans, Louisiana: Medical Group Management Association; October 25, 2010. http://www.mgma.com/press/default.aspx?id=39824. Accessed June 6, 2013.
8. US Government Accountability Office. Electronic Health Records: Number and Characteristics of Providers Awarded Medicaid Incentive Payments for 2011. GAO-13-146R. December 13, 2012. http://www.gao.gov/products/GAO-13-146R. Accessed June 6, 2013.
9. US Government Accountability Office. Electronic Health Records: Number and Characteristics of Providers Awarded Medicare Incentive Payments for 2011. GAO-12-778R. July 26, 2012. http://www.gao.gov/products/GAO-12-778R. Accessed June 6, 2013.
10. US Department of Health and Human Services. Doctors’ and hospitals’ use of health IT more than doubles since 2012 [news release]. Washington, DC: HHS.gov; May 22, 2013. http://www.hhs.gov/news/press/2013pres/05/20130522a.html. Accessed June 6, 2013.
Two years ago, I zeroed in on the pressures straining small ObGyn practices in an article entitled, “Is private ObGyn practice on its way out?”1 The pressures haven’t eased in the interim. Today, small practices are still feeling squeezed to keep up with the many demands of modern specialty care. The push for electronic health records (EHRs), in particular, can profoundly affect physicians in private practice.
In this article, I outline some of the challenges facing small practices when they set out to implement EHRs, as well as the potential benefits they stand to gain a little farther down the road. Before we begin, however, let’s look at the latest trends in ObGyn practice, as they are related, in part, to the need to implement EHRs.
The exodus from private practice continues
A 2012 Accenture Physicians Alignment Survey shows an accelerating increase in physician employment. In 2000, 57% of all physicians were in independent practice; by the end of 2013, only 36% of physicians are projected to remain independent.2
The ObGyn specialty is a clear part of this trend, with both seasoned and incoming physicians finding hospital or other employment an attractive alternative to private practice. Fully one-third of ObGyn residents entering practice today sign hospital employment contracts. ObGyns who have made the switch from private to hospital practice, or who have become ObGyn hospitalists, often point to the difficulties of maintaining a solvent private practice, especially given the push toward EHRs and increasing regulatory and administrative burdens, as justification for their move.
The main reasons for the shift to employment. Top concerns influencing physicians’ decisions to opt for employment include:
- business expenses (87%)
- the dominance of managed care (61%)
- the requirement for EHRs (53%)
- the need to maintain and manage staff (53%)
- the increasing number of patients needed to break even (39%).2
A 2008 socioeconomic survey from ACOG revealed that 23.6% of ObGyn practices are solo practices, and 27.1% are single-specialty group practices. Many ObGyns—especially those in solo or small practices—are hesitant to make the large capital investment that is necessary to adopt EHRs.
EHRs offer benefits—and real costs
The system-wide benefits of health information technology (HIT), including EHRs, are many. Insurers stand to save money by reducing unnecessary tests, and patients will benefit from better coordination of their care and fewer medical errors. But these advantages don’t necessarily translate into savings or revenue for physician practices. Instead, physicians face payment cuts from Medicare and private insurance.
Although there’s wide agreement that HIT can improve quality of care and reduce health-care costs, fewer than one-quarter (22%) of office-based physicians had adopted EHRs by 2009. We know the main reasons why:
- upfront cost and maintenance expense
- uncertain return on investment
- fragmented business model in a high proportion of small and solo practices
- changing and inconsistent information technology (IT) systems.
What can a practice expect to fork over?
In 2011, the Agency for Healthcare Research and Quality (AHRQ) found that the “real-life” cost of implementing EHRs “in an average five-physician primary care practice, operating within a large physician network committed to network-wide implementation of electronic health records, is about $162,000, with an additional $85,500 in maintenance expenses during the first year.”3
These figures include an average of 134 hours needed per physician to prepare to use EHRs during patient visits.3
Fleming and colleagues investigated the cost associated with implementing EHRs within 26 primary care practices in Texas. They found the cost to be $32,409 per physician through the first 60 days after the EHR system was launched, with one-time costs for hardware of $25,000 per practice and an additional $7,000 per physician for personal computers, printers, and scanners. The annual cost of software and maintenance was approximately $17,100 per physician.4
Why physicians should hold out for the return on their investment
Despite these considerable expenses, EHRs hold promise over the long term. The Medical Group Management Association reported, through a 2009 survey of about 1,300 primary care and specialty practice members using EHRs, that efficiency gains from the elimination of paper charts, as well as transcription savings, better charge capturing, and reduced billing errors, resulted in a median revenue increase of $49,916 per full-time physician after operating costs.
After 5 years of EHR use, practices reported a median operating margin 10.1% higher than that of practices in the first year of EHR use.5
Trends in the adoption of EHRs
Private practice. An article in Health Affairs showed that, by 2011, only one in six office-based physicians was using an EHR system robust enough to approach “meaningful use”—that is, the use of EHRs to measurably improve the quality of health care.6 These robust systems offered physicians the ability to record information on patient demographics, view laboratory and imaging results, maintain patients’ problem lists, compile clinical notes, and manage prescription ordering. EHR adoption lagged among non−primary care physicians, physicians aged 55 and older, and physicians in small (1–2 providers) practices and physician-owned practices.6 (ObGyns were considered primary care providers in this survey.)
“Big” practice. By comparison, in 2011, 99% of physicians in health maintenance organizations, or HMOs, and 73% in academic health centers and other hospitals used EHR systems.6 The number of physicians in these practice settings is small but growing.
In 2011, only 17% of physicians were in large practices of 10 or more physicians; 40% were in practices of one or two physicians.6
Primary care. These practices lead others in the adoption of EHRs, in part because of federal assistance, including a nationwide system of regional HIT assistance centers established by the Health Information Technology for Economic and Clinical Health (HITECH) Act to help providers located in rural areas participate in the Centers for Medicare and Medicaid Services (CMS) programs in EHR. The goal of these programs is to provide HIT support to at least 100,000 primary care providers, including ObGyns, by 2014.
The numbers cited in the Health Affairs article largely mirror data developed by other research organizations, including the Deloitte Center for Health Solutions.6
The EHR incentive
The drive for EHRs started long before the Affordable Care Act (ACA) was passed in 2010. The US Congress took a first stab at encouraging the health-care community to embrace HIT in 1996, when it passed the Health Insurance Portability and Accountability Act (HIPAA). HIPAA created an electronic data interchange that health plans, health-care clearinghouses, and certain health-care providers, including pharmacists, are required to use for electronic transactions, including:
- claims and encounter information
- payment and remittance advice
- claims status
- eligibility
- enrollment and disenrollment
- referrals and authorizations
- coordination of benefits
- premium payment.
Congress stepped up its game in 2009, when it offered higher Medicare and Medicaid payments to physicians who adopt and “meaningfully use” EHRs. The HITECH Act included $30 billion in new Medicare and Medicaid incentive payments—as much as $44,000 under Medicare and $63,750 under Medicaid—as well as $500 million for states to develop health information exchanges.
The Act also established a government-led process for certification of electronic health records through a $35 billion appropriation for the Office of the National Coordinator for Health IT, housed in CMS.
Other programs designed to encourage use of EHRs
Other federal programs include the Physician Quality Reporting System (PQRS), which, when created in 2006, was a voluntary physician electronic reporting program. Under the ACA, however, it has become a mandate. Starting in 2015, Medicare payments will be reduced for nonparticipating physicians.
The Electronic Prescribing (eRx) Incentive Program, created in 2008 under the Medicare Improvements for Patients and Providers Act, provides incentives for eligible physicians who e-prescribe Medicare Part D medications through a qualified system. This program converted to a penalty program last year for physicians who don’t use eRx.
Grants were also provided under the HITECH Act to fund an HIT infrastructure and low-interest HIT loans. The AHRQ has awarded $300 million in federal grant money to more than 200 projects in 48 states to promote access to and encourage HIT adoption. Over $150 million in Medicaid transformation grants have been awarded to three states and territories for HIT in the Medicaid program under the 2005 Deficit Reduction Act.
The ACA carried these initiatives even further by establishing uniform standards that HIT systems must meet, including:
- automatic reconciliation of electronic fund transfers and HIPAA payment and remittance
- improved claims payment process
- consistent methods of health plan enrollment and claim edits
- simplified and improved routing of health-care transactions
- electronic claims attachments.
Clearly, a lot of effort and taxpayer dollars have been dedicated to drive efficient use of HIT and EHRs in the hopes that they can:
- help make sense of our increasingly fragmented health-care system
- improve patient safety
- increase efficiency
- reduce paperwork
- reduce unnecessary tests
- better coordinate patient care.
To see which providers are cashing in on the government’s incentives for EHRs, see “Some physicians are more likely to seek incentives for meaningful use of EHRs” on page 37.
The long view
HIT and EHRs are here to stay. Products are maturing and improving. Acceptance by large and small practices has gained traction. Are small practices being squeezed? No doubt.
In 2011, I urged all ObGyns—especially those in private practice—to read an article written by President Barack Obama’s health-reform deputies on how physicians can be successful under the ACA.1 It reads, in part:
To realize the full benefits of the Affordable Care Act, physicians will need to embrace rather than resist change. The economic forces put in motion by the Act are likely to lead to vertical organization of providers and accelerate physician employment by hospitals and aggregation into larger physician groups. The most successful physicians will be those who most effectively collaborate with other providers to improve outcomes, care productivity, and patient experience.7
Two years ago, I zeroed in on the pressures straining small ObGyn practices in an article entitled, “Is private ObGyn practice on its way out?”1 The pressures haven’t eased in the interim. Today, small practices are still feeling squeezed to keep up with the many demands of modern specialty care. The push for electronic health records (EHRs), in particular, can profoundly affect physicians in private practice.
In this article, I outline some of the challenges facing small practices when they set out to implement EHRs, as well as the potential benefits they stand to gain a little farther down the road. Before we begin, however, let’s look at the latest trends in ObGyn practice, as they are related, in part, to the need to implement EHRs.
The exodus from private practice continues
A 2012 Accenture Physicians Alignment Survey shows an accelerating increase in physician employment. In 2000, 57% of all physicians were in independent practice; by the end of 2013, only 36% of physicians are projected to remain independent.2
The ObGyn specialty is a clear part of this trend, with both seasoned and incoming physicians finding hospital or other employment an attractive alternative to private practice. Fully one-third of ObGyn residents entering practice today sign hospital employment contracts. ObGyns who have made the switch from private to hospital practice, or who have become ObGyn hospitalists, often point to the difficulties of maintaining a solvent private practice, especially given the push toward EHRs and increasing regulatory and administrative burdens, as justification for their move.
The main reasons for the shift to employment. Top concerns influencing physicians’ decisions to opt for employment include:
- business expenses (87%)
- the dominance of managed care (61%)
- the requirement for EHRs (53%)
- the need to maintain and manage staff (53%)
- the increasing number of patients needed to break even (39%).2
A 2008 socioeconomic survey from ACOG revealed that 23.6% of ObGyn practices are solo practices, and 27.1% are single-specialty group practices. Many ObGyns—especially those in solo or small practices—are hesitant to make the large capital investment that is necessary to adopt EHRs.
EHRs offer benefits—and real costs
The system-wide benefits of health information technology (HIT), including EHRs, are many. Insurers stand to save money by reducing unnecessary tests, and patients will benefit from better coordination of their care and fewer medical errors. But these advantages don’t necessarily translate into savings or revenue for physician practices. Instead, physicians face payment cuts from Medicare and private insurance.
Although there’s wide agreement that HIT can improve quality of care and reduce health-care costs, fewer than one-quarter (22%) of office-based physicians had adopted EHRs by 2009. We know the main reasons why:
- upfront cost and maintenance expense
- uncertain return on investment
- fragmented business model in a high proportion of small and solo practices
- changing and inconsistent information technology (IT) systems.
What can a practice expect to fork over?
In 2011, the Agency for Healthcare Research and Quality (AHRQ) found that the “real-life” cost of implementing EHRs “in an average five-physician primary care practice, operating within a large physician network committed to network-wide implementation of electronic health records, is about $162,000, with an additional $85,500 in maintenance expenses during the first year.”3
These figures include an average of 134 hours needed per physician to prepare to use EHRs during patient visits.3
Fleming and colleagues investigated the cost associated with implementing EHRs within 26 primary care practices in Texas. They found the cost to be $32,409 per physician through the first 60 days after the EHR system was launched, with one-time costs for hardware of $25,000 per practice and an additional $7,000 per physician for personal computers, printers, and scanners. The annual cost of software and maintenance was approximately $17,100 per physician.4
Why physicians should hold out for the return on their investment
Despite these considerable expenses, EHRs hold promise over the long term. The Medical Group Management Association reported, through a 2009 survey of about 1,300 primary care and specialty practice members using EHRs, that efficiency gains from the elimination of paper charts, as well as transcription savings, better charge capturing, and reduced billing errors, resulted in a median revenue increase of $49,916 per full-time physician after operating costs.
After 5 years of EHR use, practices reported a median operating margin 10.1% higher than that of practices in the first year of EHR use.5
Trends in the adoption of EHRs
Private practice. An article in Health Affairs showed that, by 2011, only one in six office-based physicians was using an EHR system robust enough to approach “meaningful use”—that is, the use of EHRs to measurably improve the quality of health care.6 These robust systems offered physicians the ability to record information on patient demographics, view laboratory and imaging results, maintain patients’ problem lists, compile clinical notes, and manage prescription ordering. EHR adoption lagged among non−primary care physicians, physicians aged 55 and older, and physicians in small (1–2 providers) practices and physician-owned practices.6 (ObGyns were considered primary care providers in this survey.)
“Big” practice. By comparison, in 2011, 99% of physicians in health maintenance organizations, or HMOs, and 73% in academic health centers and other hospitals used EHR systems.6 The number of physicians in these practice settings is small but growing.
In 2011, only 17% of physicians were in large practices of 10 or more physicians; 40% were in practices of one or two physicians.6
Primary care. These practices lead others in the adoption of EHRs, in part because of federal assistance, including a nationwide system of regional HIT assistance centers established by the Health Information Technology for Economic and Clinical Health (HITECH) Act to help providers located in rural areas participate in the Centers for Medicare and Medicaid Services (CMS) programs in EHR. The goal of these programs is to provide HIT support to at least 100,000 primary care providers, including ObGyns, by 2014.
The numbers cited in the Health Affairs article largely mirror data developed by other research organizations, including the Deloitte Center for Health Solutions.6
The EHR incentive
The drive for EHRs started long before the Affordable Care Act (ACA) was passed in 2010. The US Congress took a first stab at encouraging the health-care community to embrace HIT in 1996, when it passed the Health Insurance Portability and Accountability Act (HIPAA). HIPAA created an electronic data interchange that health plans, health-care clearinghouses, and certain health-care providers, including pharmacists, are required to use for electronic transactions, including:
- claims and encounter information
- payment and remittance advice
- claims status
- eligibility
- enrollment and disenrollment
- referrals and authorizations
- coordination of benefits
- premium payment.
Congress stepped up its game in 2009, when it offered higher Medicare and Medicaid payments to physicians who adopt and “meaningfully use” EHRs. The HITECH Act included $30 billion in new Medicare and Medicaid incentive payments—as much as $44,000 under Medicare and $63,750 under Medicaid—as well as $500 million for states to develop health information exchanges.
The Act also established a government-led process for certification of electronic health records through a $35 billion appropriation for the Office of the National Coordinator for Health IT, housed in CMS.
Other programs designed to encourage use of EHRs
Other federal programs include the Physician Quality Reporting System (PQRS), which, when created in 2006, was a voluntary physician electronic reporting program. Under the ACA, however, it has become a mandate. Starting in 2015, Medicare payments will be reduced for nonparticipating physicians.
The Electronic Prescribing (eRx) Incentive Program, created in 2008 under the Medicare Improvements for Patients and Providers Act, provides incentives for eligible physicians who e-prescribe Medicare Part D medications through a qualified system. This program converted to a penalty program last year for physicians who don’t use eRx.
Grants were also provided under the HITECH Act to fund an HIT infrastructure and low-interest HIT loans. The AHRQ has awarded $300 million in federal grant money to more than 200 projects in 48 states to promote access to and encourage HIT adoption. Over $150 million in Medicaid transformation grants have been awarded to three states and territories for HIT in the Medicaid program under the 2005 Deficit Reduction Act.
The ACA carried these initiatives even further by establishing uniform standards that HIT systems must meet, including:
- automatic reconciliation of electronic fund transfers and HIPAA payment and remittance
- improved claims payment process
- consistent methods of health plan enrollment and claim edits
- simplified and improved routing of health-care transactions
- electronic claims attachments.
Clearly, a lot of effort and taxpayer dollars have been dedicated to drive efficient use of HIT and EHRs in the hopes that they can:
- help make sense of our increasingly fragmented health-care system
- improve patient safety
- increase efficiency
- reduce paperwork
- reduce unnecessary tests
- better coordinate patient care.
To see which providers are cashing in on the government’s incentives for EHRs, see “Some physicians are more likely to seek incentives for meaningful use of EHRs” on page 37.
The long view
HIT and EHRs are here to stay. Products are maturing and improving. Acceptance by large and small practices has gained traction. Are small practices being squeezed? No doubt.
In 2011, I urged all ObGyns—especially those in private practice—to read an article written by President Barack Obama’s health-reform deputies on how physicians can be successful under the ACA.1 It reads, in part:
To realize the full benefits of the Affordable Care Act, physicians will need to embrace rather than resist change. The economic forces put in motion by the Act are likely to lead to vertical organization of providers and accelerate physician employment by hospitals and aggregation into larger physician groups. The most successful physicians will be those who most effectively collaborate with other providers to improve outcomes, care productivity, and patient experience.7
1. DiVenere L, Yates J. Is private ObGyn practice on its way out? OBG Manage. 2011;23(10):42–54.
2. More US doctors leaving private practice due to rising costs and technology mandates, Accenture report finds [news release]. Arlington, Virginia: Accenture Newsroom; October 31, 2012. http://newsroom.accenture.com/news/more-us-doctors-leaving-private-practice-due-to-rising-costs-and-technology-mandates-accenture-report-finds.htm. Accessed June 5, 2013.
3. Study identifies costs of implementing electronic health records in network of physician practices: Research Activities October 2011, No. 374. Rockville, MD: Agency for Healthcare Research and Quality. http://www.ahrq.gov/news/newsletters/research-activities/oct11/1011RA15.html. Accessed June 5, 2013.
5. MGMA survey: Medical groups with EHRs report better financial performance than practices with paper medical records [news release]. New Orleans, Louisiana: Medical Group Management Association; October 25, 2010. http://www.mgma.com/press/default.aspx?id=39824. Accessed June 6, 2013.
8. US Government Accountability Office. Electronic Health Records: Number and Characteristics of Providers Awarded Medicaid Incentive Payments for 2011. GAO-13-146R. December 13, 2012. http://www.gao.gov/products/GAO-13-146R. Accessed June 6, 2013.
9. US Government Accountability Office. Electronic Health Records: Number and Characteristics of Providers Awarded Medicare Incentive Payments for 2011. GAO-12-778R. July 26, 2012. http://www.gao.gov/products/GAO-12-778R. Accessed June 6, 2013.
10. US Department of Health and Human Services. Doctors’ and hospitals’ use of health IT more than doubles since 2012 [news release]. Washington, DC: HHS.gov; May 22, 2013. http://www.hhs.gov/news/press/2013pres/05/20130522a.html. Accessed June 6, 2013.
1. DiVenere L, Yates J. Is private ObGyn practice on its way out? OBG Manage. 2011;23(10):42–54.
2. More US doctors leaving private practice due to rising costs and technology mandates, Accenture report finds [news release]. Arlington, Virginia: Accenture Newsroom; October 31, 2012. http://newsroom.accenture.com/news/more-us-doctors-leaving-private-practice-due-to-rising-costs-and-technology-mandates-accenture-report-finds.htm. Accessed June 5, 2013.
3. Study identifies costs of implementing electronic health records in network of physician practices: Research Activities October 2011, No. 374. Rockville, MD: Agency for Healthcare Research and Quality. http://www.ahrq.gov/news/newsletters/research-activities/oct11/1011RA15.html. Accessed June 5, 2013.
5. MGMA survey: Medical groups with EHRs report better financial performance than practices with paper medical records [news release]. New Orleans, Louisiana: Medical Group Management Association; October 25, 2010. http://www.mgma.com/press/default.aspx?id=39824. Accessed June 6, 2013.
8. US Government Accountability Office. Electronic Health Records: Number and Characteristics of Providers Awarded Medicaid Incentive Payments for 2011. GAO-13-146R. December 13, 2012. http://www.gao.gov/products/GAO-13-146R. Accessed June 6, 2013.
9. US Government Accountability Office. Electronic Health Records: Number and Characteristics of Providers Awarded Medicare Incentive Payments for 2011. GAO-12-778R. July 26, 2012. http://www.gao.gov/products/GAO-12-778R. Accessed June 6, 2013.
10. US Department of Health and Human Services. Doctors’ and hospitals’ use of health IT more than doubles since 2012 [news release]. Washington, DC: HHS.gov; May 22, 2013. http://www.hhs.gov/news/press/2013pres/05/20130522a.html. Accessed June 6, 2013.
Mean income for ObGyns increased in 2012
ObGyns’ 2012 mean income was $242,000, up from a mean of $220,000 in 2011, although almost half (45%) of ObGyns reported their 2012 income to be the same as their 2011 income. In 2012, about 25% of ObGyns reported earnings of $300,000 or more, and 10% said they earn less than $100,000.1 The newest salary data are based on Medscape’s 2013 Compensation Report, a survey of 21,878 US physicians across 25 specialties.
Forty-three percent of ObGyns were satisfied with their 2012 compensation levels; 48% of all physicians were satisfied.1,2
Other Findings
Men still make more than women. In 2012, male ObGyns reported earning 14% more than female ObGyns. This pay gap is smaller for ObGyns than for all physicians, however; overall, male physicians earn 30% more than females. One contributing factor to the closer pay gap for ObGyns is that there are fewer women in the higher-paying specialties, such as orthopedics (only 9% of orthopedic respondents were female). Response rates also matter: of those who responded to the overall Medscape poll, 31% were female; of the ObGyn respondents, 43% were female.1,2
ObGyn compensation varies by region. Highest earnings were found in the South Central region (mean: $250,000 in 2012); lowest earnings were found in the Northeast (mean: $213,000).1
Work setting counts. When ranked by job setting, in 2012, ObGyns employed by health-care organizations were the top earners (mean income: $272,000). This figure rose considerably from the 2011 mean of $239,000. Additional mean earnings of ObGyns ranked by work setting in 2012 were1:
single-specialty (office-based) group practices: $264,000
multispecialty (office-based) group practices: $252,000
hospitals: $216,000
academic: $212,000
solo practices (office-based): $208,000
outpatient clinics: $206,000.
When ranked by work situation, partners beat all other situations at $268,000 (mean). Employed ObGyns earned more than owners of solo practices (mean: $241,000 vs $204,000, respectively). Independent contractors came in the lowest at $198,000 (mean).1
Satisfaction with career choice and practice setting showed a slight dip from 2011. When all physicians were asked if they would choose medicine again, 53% would do so in 2012, versus 55% in 2011. Among the ObGyns who said they would choose medicine again, 37% said they would choose the same specialty (the same as in 2011). In 2012, 18% of ObGyns said they would choose the same practice setting, compared with 23% in 2011.1,2
What’s most rewarding? In 2012, 42% of ObGyns ranked their relationships with patients as the most satisfying part of their job, compared with 31% of all physicians. While 34% of all physicians said that being good at the practice of medicine was their primary reward, 28% of ObGyns listed that first.1,2
FINDINGS ON HOW YOU MAKE AND DISCUSS MONEY
Where does your income come from? In the 2011 report, only 4% of ObGyns either participated in or planned to join an accountable care organization (ACO). In 2012, that figure jumped to 25%. Only 1% of ObGyns opted for concierge medical practices in 2012 and 2011, and only 3% chose cash-only practices in 2012 and 2011.1,2
What about Medicare and Medicaid? More physicians were concerned with the potential for reduced Medicare reimbursement in 2012 than in 2011. The current report indicated that 15% of ObGyns plan to stop taking new Medicare or Medicaid patients, 3% plan to stop seeing current Medicare or Medicaid patients, and 28% are undecided. However, 53% of ObGyns are not conflicted and will continue to see current patients and take on new Medicare and Medicaid patients. In 2012, 59% of all physicians planned to treat new Medicare and Medicaid patients.1,2
What about insurance company payments? Practice management experts often recommend that physicians review their annual payments from insurers and drop those who pay the worst or create the most trouble. In 2012, 26% of ObGyns reported that they already do that or are planning to take that advice. However, 29% will keep all insurers because they feel that even poor payers still represent income. About 15% felt that dropping insurers was inappropriate behavior.1
Do you provide ancillary services? When asked if they would offer additional medical services to increase income, 21% of ObGyns said yes. Nineteen percent of all physicians said they had begun to do that.1,2
Do you discuss cost with your patients? In larger practices and hospital settings, treatment costs are often discussed by a staff member responsible for billing and payment, rather than by the physician. As physicians move toward these larger organizations, the trend is becoming more apparent1:
In 2011, 41% of ObGyns reported that they regularly discuss the cost of services with their patients; 48% said they occasionally discuss cost if the patient brings it up (89% total).
In 2012, 35% of ObGyns said they regularly discuss cost with their patients; 41% said they occasionally discuss cost (76% total).
In 2011, 84% of all physicians either regularly or occasionally discussed the cost of treatment with patients. In 2012, 68% of all physicians regularly discussed cost of treatment (30%) or did so if the patient asked (38%), and 6% reported that it was inappropriate to discuss cost with patients.1,2
Findings on how you spend your time
How many hours do you work? The number of hours in a workweek remained approximately the same for the last 2 years: in 2012, 11% of ObGyns worked 41–45 h/w; 13% worked 46–50 h/w; 4% worked 51–55 h/w; and 9% worked 56–60 h/w. Approximately 20% of ObGyns reported working less than 30 h/w.1
How much time do you spend with patients? In 2012, most ObGyns spent 16 minutes or less per patient visit. Thirty percent of ObGyns spent 13–16 minutes with a patient, and another 30% spent less than 13 minutes. Some indicated longer patient visits—17% saw patients for 21 minutes or more.1
Demographics of the survey
Respondents to the Medscape survey totaled 21,878 US physicians and ranged in age from 28 years to older than 70; 66% were aged 40 to 64 years; 31% were female; 69% were male; and 89% were board certified.
Of the overall survey respondents, 5% (n = 1094) were ObGyns. Of these respondents, 71% were aged 40 to 64; 43% were female; 57% were male; and 92% were board certified.1,2
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Medscape News. Physician Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/public. Accessed June 30, 2013.
ObGyns’ 2012 mean income was $242,000, up from a mean of $220,000 in 2011, although almost half (45%) of ObGyns reported their 2012 income to be the same as their 2011 income. In 2012, about 25% of ObGyns reported earnings of $300,000 or more, and 10% said they earn less than $100,000.1 The newest salary data are based on Medscape’s 2013 Compensation Report, a survey of 21,878 US physicians across 25 specialties.
Forty-three percent of ObGyns were satisfied with their 2012 compensation levels; 48% of all physicians were satisfied.1,2
Other Findings
Men still make more than women. In 2012, male ObGyns reported earning 14% more than female ObGyns. This pay gap is smaller for ObGyns than for all physicians, however; overall, male physicians earn 30% more than females. One contributing factor to the closer pay gap for ObGyns is that there are fewer women in the higher-paying specialties, such as orthopedics (only 9% of orthopedic respondents were female). Response rates also matter: of those who responded to the overall Medscape poll, 31% were female; of the ObGyn respondents, 43% were female.1,2
ObGyn compensation varies by region. Highest earnings were found in the South Central region (mean: $250,000 in 2012); lowest earnings were found in the Northeast (mean: $213,000).1
Work setting counts. When ranked by job setting, in 2012, ObGyns employed by health-care organizations were the top earners (mean income: $272,000). This figure rose considerably from the 2011 mean of $239,000. Additional mean earnings of ObGyns ranked by work setting in 2012 were1:
single-specialty (office-based) group practices: $264,000
multispecialty (office-based) group practices: $252,000
hospitals: $216,000
academic: $212,000
solo practices (office-based): $208,000
outpatient clinics: $206,000.
When ranked by work situation, partners beat all other situations at $268,000 (mean). Employed ObGyns earned more than owners of solo practices (mean: $241,000 vs $204,000, respectively). Independent contractors came in the lowest at $198,000 (mean).1
Satisfaction with career choice and practice setting showed a slight dip from 2011. When all physicians were asked if they would choose medicine again, 53% would do so in 2012, versus 55% in 2011. Among the ObGyns who said they would choose medicine again, 37% said they would choose the same specialty (the same as in 2011). In 2012, 18% of ObGyns said they would choose the same practice setting, compared with 23% in 2011.1,2
What’s most rewarding? In 2012, 42% of ObGyns ranked their relationships with patients as the most satisfying part of their job, compared with 31% of all physicians. While 34% of all physicians said that being good at the practice of medicine was their primary reward, 28% of ObGyns listed that first.1,2
FINDINGS ON HOW YOU MAKE AND DISCUSS MONEY
Where does your income come from? In the 2011 report, only 4% of ObGyns either participated in or planned to join an accountable care organization (ACO). In 2012, that figure jumped to 25%. Only 1% of ObGyns opted for concierge medical practices in 2012 and 2011, and only 3% chose cash-only practices in 2012 and 2011.1,2
What about Medicare and Medicaid? More physicians were concerned with the potential for reduced Medicare reimbursement in 2012 than in 2011. The current report indicated that 15% of ObGyns plan to stop taking new Medicare or Medicaid patients, 3% plan to stop seeing current Medicare or Medicaid patients, and 28% are undecided. However, 53% of ObGyns are not conflicted and will continue to see current patients and take on new Medicare and Medicaid patients. In 2012, 59% of all physicians planned to treat new Medicare and Medicaid patients.1,2
What about insurance company payments? Practice management experts often recommend that physicians review their annual payments from insurers and drop those who pay the worst or create the most trouble. In 2012, 26% of ObGyns reported that they already do that or are planning to take that advice. However, 29% will keep all insurers because they feel that even poor payers still represent income. About 15% felt that dropping insurers was inappropriate behavior.1
Do you provide ancillary services? When asked if they would offer additional medical services to increase income, 21% of ObGyns said yes. Nineteen percent of all physicians said they had begun to do that.1,2
Do you discuss cost with your patients? In larger practices and hospital settings, treatment costs are often discussed by a staff member responsible for billing and payment, rather than by the physician. As physicians move toward these larger organizations, the trend is becoming more apparent1:
In 2011, 41% of ObGyns reported that they regularly discuss the cost of services with their patients; 48% said they occasionally discuss cost if the patient brings it up (89% total).
In 2012, 35% of ObGyns said they regularly discuss cost with their patients; 41% said they occasionally discuss cost (76% total).
In 2011, 84% of all physicians either regularly or occasionally discussed the cost of treatment with patients. In 2012, 68% of all physicians regularly discussed cost of treatment (30%) or did so if the patient asked (38%), and 6% reported that it was inappropriate to discuss cost with patients.1,2
Findings on how you spend your time
How many hours do you work? The number of hours in a workweek remained approximately the same for the last 2 years: in 2012, 11% of ObGyns worked 41–45 h/w; 13% worked 46–50 h/w; 4% worked 51–55 h/w; and 9% worked 56–60 h/w. Approximately 20% of ObGyns reported working less than 30 h/w.1
How much time do you spend with patients? In 2012, most ObGyns spent 16 minutes or less per patient visit. Thirty percent of ObGyns spent 13–16 minutes with a patient, and another 30% spent less than 13 minutes. Some indicated longer patient visits—17% saw patients for 21 minutes or more.1
Demographics of the survey
Respondents to the Medscape survey totaled 21,878 US physicians and ranged in age from 28 years to older than 70; 66% were aged 40 to 64 years; 31% were female; 69% were male; and 89% were board certified.
Of the overall survey respondents, 5% (n = 1094) were ObGyns. Of these respondents, 71% were aged 40 to 64; 43% were female; 57% were male; and 92% were board certified.1,2
ObGyns’ 2012 mean income was $242,000, up from a mean of $220,000 in 2011, although almost half (45%) of ObGyns reported their 2012 income to be the same as their 2011 income. In 2012, about 25% of ObGyns reported earnings of $300,000 or more, and 10% said they earn less than $100,000.1 The newest salary data are based on Medscape’s 2013 Compensation Report, a survey of 21,878 US physicians across 25 specialties.
Forty-three percent of ObGyns were satisfied with their 2012 compensation levels; 48% of all physicians were satisfied.1,2
Other Findings
Men still make more than women. In 2012, male ObGyns reported earning 14% more than female ObGyns. This pay gap is smaller for ObGyns than for all physicians, however; overall, male physicians earn 30% more than females. One contributing factor to the closer pay gap for ObGyns is that there are fewer women in the higher-paying specialties, such as orthopedics (only 9% of orthopedic respondents were female). Response rates also matter: of those who responded to the overall Medscape poll, 31% were female; of the ObGyn respondents, 43% were female.1,2
ObGyn compensation varies by region. Highest earnings were found in the South Central region (mean: $250,000 in 2012); lowest earnings were found in the Northeast (mean: $213,000).1
Work setting counts. When ranked by job setting, in 2012, ObGyns employed by health-care organizations were the top earners (mean income: $272,000). This figure rose considerably from the 2011 mean of $239,000. Additional mean earnings of ObGyns ranked by work setting in 2012 were1:
single-specialty (office-based) group practices: $264,000
multispecialty (office-based) group practices: $252,000
hospitals: $216,000
academic: $212,000
solo practices (office-based): $208,000
outpatient clinics: $206,000.
When ranked by work situation, partners beat all other situations at $268,000 (mean). Employed ObGyns earned more than owners of solo practices (mean: $241,000 vs $204,000, respectively). Independent contractors came in the lowest at $198,000 (mean).1
Satisfaction with career choice and practice setting showed a slight dip from 2011. When all physicians were asked if they would choose medicine again, 53% would do so in 2012, versus 55% in 2011. Among the ObGyns who said they would choose medicine again, 37% said they would choose the same specialty (the same as in 2011). In 2012, 18% of ObGyns said they would choose the same practice setting, compared with 23% in 2011.1,2
What’s most rewarding? In 2012, 42% of ObGyns ranked their relationships with patients as the most satisfying part of their job, compared with 31% of all physicians. While 34% of all physicians said that being good at the practice of medicine was their primary reward, 28% of ObGyns listed that first.1,2
FINDINGS ON HOW YOU MAKE AND DISCUSS MONEY
Where does your income come from? In the 2011 report, only 4% of ObGyns either participated in or planned to join an accountable care organization (ACO). In 2012, that figure jumped to 25%. Only 1% of ObGyns opted for concierge medical practices in 2012 and 2011, and only 3% chose cash-only practices in 2012 and 2011.1,2
What about Medicare and Medicaid? More physicians were concerned with the potential for reduced Medicare reimbursement in 2012 than in 2011. The current report indicated that 15% of ObGyns plan to stop taking new Medicare or Medicaid patients, 3% plan to stop seeing current Medicare or Medicaid patients, and 28% are undecided. However, 53% of ObGyns are not conflicted and will continue to see current patients and take on new Medicare and Medicaid patients. In 2012, 59% of all physicians planned to treat new Medicare and Medicaid patients.1,2
What about insurance company payments? Practice management experts often recommend that physicians review their annual payments from insurers and drop those who pay the worst or create the most trouble. In 2012, 26% of ObGyns reported that they already do that or are planning to take that advice. However, 29% will keep all insurers because they feel that even poor payers still represent income. About 15% felt that dropping insurers was inappropriate behavior.1
Do you provide ancillary services? When asked if they would offer additional medical services to increase income, 21% of ObGyns said yes. Nineteen percent of all physicians said they had begun to do that.1,2
Do you discuss cost with your patients? In larger practices and hospital settings, treatment costs are often discussed by a staff member responsible for billing and payment, rather than by the physician. As physicians move toward these larger organizations, the trend is becoming more apparent1:
In 2011, 41% of ObGyns reported that they regularly discuss the cost of services with their patients; 48% said they occasionally discuss cost if the patient brings it up (89% total).
In 2012, 35% of ObGyns said they regularly discuss cost with their patients; 41% said they occasionally discuss cost (76% total).
In 2011, 84% of all physicians either regularly or occasionally discussed the cost of treatment with patients. In 2012, 68% of all physicians regularly discussed cost of treatment (30%) or did so if the patient asked (38%), and 6% reported that it was inappropriate to discuss cost with patients.1,2
Findings on how you spend your time
How many hours do you work? The number of hours in a workweek remained approximately the same for the last 2 years: in 2012, 11% of ObGyns worked 41–45 h/w; 13% worked 46–50 h/w; 4% worked 51–55 h/w; and 9% worked 56–60 h/w. Approximately 20% of ObGyns reported working less than 30 h/w.1
How much time do you spend with patients? In 2012, most ObGyns spent 16 minutes or less per patient visit. Thirty percent of ObGyns spent 13–16 minutes with a patient, and another 30% spent less than 13 minutes. Some indicated longer patient visits—17% saw patients for 21 minutes or more.1
Demographics of the survey
Respondents to the Medscape survey totaled 21,878 US physicians and ranged in age from 28 years to older than 70; 66% were aged 40 to 64 years; 31% were female; 69% were male; and 89% were board certified.
Of the overall survey respondents, 5% (n = 1094) were ObGyns. Of these respondents, 71% were aged 40 to 64; 43% were female; 57% were male; and 92% were board certified.1,2
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Medscape News. Physician Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/public. Accessed June 30, 2013.
- Medscape News. Ob/Gyn Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/womenshealth. Accessed June 30, 2013.
- Medscape News. Physician Compensation Report 2013. Medscape Today Web site. http://www.medscape.com/features/slideshow/compensation/2013/public. Accessed June 30, 2013.
Should have used other dystocia maneuvers first
gb
AN OBGYN ENCOUNTERED SHOULDER DYSTOCIA. He used fundal pressure and downward lateral traction to free the baby’s shoulder. The child has a brachial plexus injury of the right shoulder, including nerve avulsion, a fractured clavicle, and permanent disfigurement. She underwent surgery; physical and occupational therapy will continue.
PARENTS' CLAIM The standard sequence of maneuvers should have been attempted before fundal pressure and lateral traction were used—the baby was sufficiently oxygenated to allow time for these maneuvers. Excessive lateral traction caused the injury.
DEFENDANTS' DEFENSE The injuries occurred in utero before or while the fetus progressed down the birth canal, and were due to the maternal forces of labor.
VERDICT A $3,070,000 Michigan verdict was returned against the hospital, ObGyn, and ObGyn group.
WHAT IS THE STANDARD SEQUENCE OF MANEUVERS FOR SHOULDER DYSTOCIA?
Read Dr. Robert L. Barbieri’s May Editorial, You are the second responder to a shoulder dystocia emergency. What do you do first? and Dr. Ronald T. Burkman’s March Stop/Start article, Stop all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Meconium aspiration leads to brain injury
LATE IN HER PREGNANCY, a woman went to the emergency department (ED) with hypertension; she was discharged the same day. She saw her ObGyns, Dr. A and Dr. B, three times in the next 2 weeks. A day after her last visit, she returned to the ED in active labor. Dr. B assumed her care. Fetal monitoring indicated a nonreassuring heart rate with decelerations. Dr. B administered oxytocin and labor continued.
The baby was born by cesarean delivery after 25 minutes of fetal bradycardia. She was covered in meconium, with a low heart rate and irregular, labored respirations. The baby was transferred to another hospital, where she was treated for pulmonary hypertension, meconium aspiration, and seizures. The child is totally disabled, and will require constant care for life.
PARENTS' CLAIM The mother’s hypertension was not properly treated. Dr. B and the nurse waited too long to perform a cesarean delivery.
DEFENDANTS' DEFENSE Proper prenatal care was provided. There was no reason for additional testing; fetal heart tones at the mother’s last office visit were reactive. There were no clinical signs of a hematoma or cord varix during office visits. An unpredictable, unpreventable umbilical cord hematoma caused ischemia and hypoxia, and the subsequent brain injury. Meconium had been in the amniotic fluid for at least 10 hours due to the ischemic/hypoxic episode. The hematoma formed between her last office visit and when the mother came to the hospital the next day.
VERDICT Settlements were reached with Dr. A and the hospital. An Arkansas defense verdict was returned for Dr. B and the nurse.
14 months' recovery after mass removed
A GYNECOLOGIC ONCOLOGIST operated on a woman in her 50s to remove a large, noncancerous pelvic mass. The patient, discharged on postoperative day 2, was readmitted the next day with a fever (temperature, 103ºF), nausea, vomiting, and abdominal pain. Four days later, the oncologist repaired a perforated bowel and created an ileostomy. Other procedures were needed to drain abscesses and repair fistulas, and resect a large portion of colon due to continuing infection. Treatment lasted 14 months.
PATIENT'S CLAIM The gynecologic oncologist was negligent in failing to timely diagnose and treat the bowel perforation. Earlier repair would have curtailed development of the abscesses and fistulae.
PHYSICIAN'S DEFENSE Any complications the patient experienced were unrelated to any delay in treatment.
VERDICT A $612,237 Michigan verdict was returned.
Colon perforated during abdominal access
WHEN A MORBIDLY OBESE 37-YEAR-OLD WOMAN reported chronic pelvic pain, her gynecologist suspected endometriosis. Conservative treatment failed and the gynecologist offered laparoscopic hysterectomy.
After abdominal insufflation was unsuccessfully attempted twice using a Veress needle, the gynecologist entered the abdomen with a Visiport optical trocar, and continued the procedure. The gynecologist inspected the abdomen before closing but found no injuries.
The patient did not do well after surgery. CT scan detected a bowel perforation on postoperative day 6. During exploratory laparotomy, a through-and-through “bayonet” colon perforation was repaired. Because of the extensive infection, the patient’s surgical wound was left open and several “washouts” were performed; the wound was closed several weeks later. The patient also underwent two adhesiolysis procedures.
PATIENT'S CLAIM Access to the abdomen was not properly performed and caused colon perforation. The injury should have been found and treated earlier.
PHYSICIAN'S DEFENSE The case was settled before trial.
VERDICT A $750,000 Virginia settlement was reached.
READ How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy, by Michael Baggish, MD (Surgical Techniques, October 2012) What caused this C. diff infection after hysterectomy?
AFTER A HYSTERECTOMY, a 42-year-old woman developed a persistent fever and increased white blood cell count. The gynecologist prescribed ciprofloxacin for a urinary tract infection, and discharged the patient from the hospital on postoperative day 4. She returned to the gynecologist’s office with severe abdominal pain and vomiting 4 days after discharge. The gynecologist prescribed an antacid and told her to continue taking ciprofloxacin.
The patient was taken to the ED by ambulance 3 days later. Testing revealed a Clostridium dificule (C. diff) infection. During emergency surgery, a large portion of her colon was resected, and a colostomy was performed. The colostomy was reversed 6 months later. The patient developed an incisional hernia and has abdominal scarring.
PATIENT'S CLAIM Prophylactic antibiotics should have been prescribed before surgery.
Two possible scenarios were presented: 1) A bowel injury occurred during surgery, and ciprofloxacin likely worsened the infection caused by the bowel injury; or 2) ciprofloxacin triggered the C. diff infection that caused leaking colon perforations and subsequent peritonitis.
The colon perforations could have been avoided if the gynecologist had diagnosed and treated the C. diff infection in a timely manner.
PHYSICIAN'S DEFENSE The patient’s symptoms did not suggest a C. diff infection; testing was not necessary. Ciprofloxacin might have allowed the proliferation of the C. diff infection, but the use of the drug was not negligent. The infection was not preventable and could not have been diagnosed earlier.
VERDICT A $776,000 New York verdict was returned.
Brain injury and cerebral palsy: When did this occur?
DURING LABOR AND DELIVERY, there were periods when the fetal heart-rate tracings were nonreassuring with variable decelerations and fetal tachycardia; some variables were severe. The child suffered anoxic encephalopathy that caused neurologic injury and cerebral palsy.
PARENTS' CLAIM The infant suffered numerous hypoxic incidents before cesarean delivery was performed. An earlier cesarean delivery could have prevented the injury.
PHYSICIAN'S DEFENSE The newborn had a normal blood cord gas level of 7.2 pH and Apgar scores of 9 and 10, at 1 and 5 minutes, respectively. Fetal heart-rate tracings did not show evidence of fetal hypoxia. The brain injury likely occurred prior to the onset of labor and was possibly related to a viral encephalopathy.
VERDICT A Virginia defense verdict was returned. These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
gb
AN OBGYN ENCOUNTERED SHOULDER DYSTOCIA. He used fundal pressure and downward lateral traction to free the baby’s shoulder. The child has a brachial plexus injury of the right shoulder, including nerve avulsion, a fractured clavicle, and permanent disfigurement. She underwent surgery; physical and occupational therapy will continue.
PARENTS' CLAIM The standard sequence of maneuvers should have been attempted before fundal pressure and lateral traction were used—the baby was sufficiently oxygenated to allow time for these maneuvers. Excessive lateral traction caused the injury.
DEFENDANTS' DEFENSE The injuries occurred in utero before or while the fetus progressed down the birth canal, and were due to the maternal forces of labor.
VERDICT A $3,070,000 Michigan verdict was returned against the hospital, ObGyn, and ObGyn group.
WHAT IS THE STANDARD SEQUENCE OF MANEUVERS FOR SHOULDER DYSTOCIA?
Read Dr. Robert L. Barbieri’s May Editorial, You are the second responder to a shoulder dystocia emergency. What do you do first? and Dr. Ronald T. Burkman’s March Stop/Start article, Stop all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Meconium aspiration leads to brain injury
LATE IN HER PREGNANCY, a woman went to the emergency department (ED) with hypertension; she was discharged the same day. She saw her ObGyns, Dr. A and Dr. B, three times in the next 2 weeks. A day after her last visit, she returned to the ED in active labor. Dr. B assumed her care. Fetal monitoring indicated a nonreassuring heart rate with decelerations. Dr. B administered oxytocin and labor continued.
The baby was born by cesarean delivery after 25 minutes of fetal bradycardia. She was covered in meconium, with a low heart rate and irregular, labored respirations. The baby was transferred to another hospital, where she was treated for pulmonary hypertension, meconium aspiration, and seizures. The child is totally disabled, and will require constant care for life.
PARENTS' CLAIM The mother’s hypertension was not properly treated. Dr. B and the nurse waited too long to perform a cesarean delivery.
DEFENDANTS' DEFENSE Proper prenatal care was provided. There was no reason for additional testing; fetal heart tones at the mother’s last office visit were reactive. There were no clinical signs of a hematoma or cord varix during office visits. An unpredictable, unpreventable umbilical cord hematoma caused ischemia and hypoxia, and the subsequent brain injury. Meconium had been in the amniotic fluid for at least 10 hours due to the ischemic/hypoxic episode. The hematoma formed between her last office visit and when the mother came to the hospital the next day.
VERDICT Settlements were reached with Dr. A and the hospital. An Arkansas defense verdict was returned for Dr. B and the nurse.
14 months' recovery after mass removed
A GYNECOLOGIC ONCOLOGIST operated on a woman in her 50s to remove a large, noncancerous pelvic mass. The patient, discharged on postoperative day 2, was readmitted the next day with a fever (temperature, 103ºF), nausea, vomiting, and abdominal pain. Four days later, the oncologist repaired a perforated bowel and created an ileostomy. Other procedures were needed to drain abscesses and repair fistulas, and resect a large portion of colon due to continuing infection. Treatment lasted 14 months.
PATIENT'S CLAIM The gynecologic oncologist was negligent in failing to timely diagnose and treat the bowel perforation. Earlier repair would have curtailed development of the abscesses and fistulae.
PHYSICIAN'S DEFENSE Any complications the patient experienced were unrelated to any delay in treatment.
VERDICT A $612,237 Michigan verdict was returned.
Colon perforated during abdominal access
WHEN A MORBIDLY OBESE 37-YEAR-OLD WOMAN reported chronic pelvic pain, her gynecologist suspected endometriosis. Conservative treatment failed and the gynecologist offered laparoscopic hysterectomy.
After abdominal insufflation was unsuccessfully attempted twice using a Veress needle, the gynecologist entered the abdomen with a Visiport optical trocar, and continued the procedure. The gynecologist inspected the abdomen before closing but found no injuries.
The patient did not do well after surgery. CT scan detected a bowel perforation on postoperative day 6. During exploratory laparotomy, a through-and-through “bayonet” colon perforation was repaired. Because of the extensive infection, the patient’s surgical wound was left open and several “washouts” were performed; the wound was closed several weeks later. The patient also underwent two adhesiolysis procedures.
PATIENT'S CLAIM Access to the abdomen was not properly performed and caused colon perforation. The injury should have been found and treated earlier.
PHYSICIAN'S DEFENSE The case was settled before trial.
VERDICT A $750,000 Virginia settlement was reached.
READ How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy, by Michael Baggish, MD (Surgical Techniques, October 2012) What caused this C. diff infection after hysterectomy?
AFTER A HYSTERECTOMY, a 42-year-old woman developed a persistent fever and increased white blood cell count. The gynecologist prescribed ciprofloxacin for a urinary tract infection, and discharged the patient from the hospital on postoperative day 4. She returned to the gynecologist’s office with severe abdominal pain and vomiting 4 days after discharge. The gynecologist prescribed an antacid and told her to continue taking ciprofloxacin.
The patient was taken to the ED by ambulance 3 days later. Testing revealed a Clostridium dificule (C. diff) infection. During emergency surgery, a large portion of her colon was resected, and a colostomy was performed. The colostomy was reversed 6 months later. The patient developed an incisional hernia and has abdominal scarring.
PATIENT'S CLAIM Prophylactic antibiotics should have been prescribed before surgery.
Two possible scenarios were presented: 1) A bowel injury occurred during surgery, and ciprofloxacin likely worsened the infection caused by the bowel injury; or 2) ciprofloxacin triggered the C. diff infection that caused leaking colon perforations and subsequent peritonitis.
The colon perforations could have been avoided if the gynecologist had diagnosed and treated the C. diff infection in a timely manner.
PHYSICIAN'S DEFENSE The patient’s symptoms did not suggest a C. diff infection; testing was not necessary. Ciprofloxacin might have allowed the proliferation of the C. diff infection, but the use of the drug was not negligent. The infection was not preventable and could not have been diagnosed earlier.
VERDICT A $776,000 New York verdict was returned.
Brain injury and cerebral palsy: When did this occur?
DURING LABOR AND DELIVERY, there were periods when the fetal heart-rate tracings were nonreassuring with variable decelerations and fetal tachycardia; some variables were severe. The child suffered anoxic encephalopathy that caused neurologic injury and cerebral palsy.
PARENTS' CLAIM The infant suffered numerous hypoxic incidents before cesarean delivery was performed. An earlier cesarean delivery could have prevented the injury.
PHYSICIAN'S DEFENSE The newborn had a normal blood cord gas level of 7.2 pH and Apgar scores of 9 and 10, at 1 and 5 minutes, respectively. Fetal heart-rate tracings did not show evidence of fetal hypoxia. The brain injury likely occurred prior to the onset of labor and was possibly related to a viral encephalopathy.
VERDICT A Virginia defense verdict was returned. These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
gb
AN OBGYN ENCOUNTERED SHOULDER DYSTOCIA. He used fundal pressure and downward lateral traction to free the baby’s shoulder. The child has a brachial plexus injury of the right shoulder, including nerve avulsion, a fractured clavicle, and permanent disfigurement. She underwent surgery; physical and occupational therapy will continue.
PARENTS' CLAIM The standard sequence of maneuvers should have been attempted before fundal pressure and lateral traction were used—the baby was sufficiently oxygenated to allow time for these maneuvers. Excessive lateral traction caused the injury.
DEFENDANTS' DEFENSE The injuries occurred in utero before or while the fetus progressed down the birth canal, and were due to the maternal forces of labor.
VERDICT A $3,070,000 Michigan verdict was returned against the hospital, ObGyn, and ObGyn group.
WHAT IS THE STANDARD SEQUENCE OF MANEUVERS FOR SHOULDER DYSTOCIA?
Read Dr. Robert L. Barbieri’s May Editorial, You are the second responder to a shoulder dystocia emergency. What do you do first? and Dr. Ronald T. Burkman’s March Stop/Start article, Stop all activities that may lead to further shoulder impaction when you suspect possible shoulder dystocia Meconium aspiration leads to brain injury
LATE IN HER PREGNANCY, a woman went to the emergency department (ED) with hypertension; she was discharged the same day. She saw her ObGyns, Dr. A and Dr. B, three times in the next 2 weeks. A day after her last visit, she returned to the ED in active labor. Dr. B assumed her care. Fetal monitoring indicated a nonreassuring heart rate with decelerations. Dr. B administered oxytocin and labor continued.
The baby was born by cesarean delivery after 25 minutes of fetal bradycardia. She was covered in meconium, with a low heart rate and irregular, labored respirations. The baby was transferred to another hospital, where she was treated for pulmonary hypertension, meconium aspiration, and seizures. The child is totally disabled, and will require constant care for life.
PARENTS' CLAIM The mother’s hypertension was not properly treated. Dr. B and the nurse waited too long to perform a cesarean delivery.
DEFENDANTS' DEFENSE Proper prenatal care was provided. There was no reason for additional testing; fetal heart tones at the mother’s last office visit were reactive. There were no clinical signs of a hematoma or cord varix during office visits. An unpredictable, unpreventable umbilical cord hematoma caused ischemia and hypoxia, and the subsequent brain injury. Meconium had been in the amniotic fluid for at least 10 hours due to the ischemic/hypoxic episode. The hematoma formed between her last office visit and when the mother came to the hospital the next day.
VERDICT Settlements were reached with Dr. A and the hospital. An Arkansas defense verdict was returned for Dr. B and the nurse.
14 months' recovery after mass removed
A GYNECOLOGIC ONCOLOGIST operated on a woman in her 50s to remove a large, noncancerous pelvic mass. The patient, discharged on postoperative day 2, was readmitted the next day with a fever (temperature, 103ºF), nausea, vomiting, and abdominal pain. Four days later, the oncologist repaired a perforated bowel and created an ileostomy. Other procedures were needed to drain abscesses and repair fistulas, and resect a large portion of colon due to continuing infection. Treatment lasted 14 months.
PATIENT'S CLAIM The gynecologic oncologist was negligent in failing to timely diagnose and treat the bowel perforation. Earlier repair would have curtailed development of the abscesses and fistulae.
PHYSICIAN'S DEFENSE Any complications the patient experienced were unrelated to any delay in treatment.
VERDICT A $612,237 Michigan verdict was returned.
Colon perforated during abdominal access
WHEN A MORBIDLY OBESE 37-YEAR-OLD WOMAN reported chronic pelvic pain, her gynecologist suspected endometriosis. Conservative treatment failed and the gynecologist offered laparoscopic hysterectomy.
After abdominal insufflation was unsuccessfully attempted twice using a Veress needle, the gynecologist entered the abdomen with a Visiport optical trocar, and continued the procedure. The gynecologist inspected the abdomen before closing but found no injuries.
The patient did not do well after surgery. CT scan detected a bowel perforation on postoperative day 6. During exploratory laparotomy, a through-and-through “bayonet” colon perforation was repaired. Because of the extensive infection, the patient’s surgical wound was left open and several “washouts” were performed; the wound was closed several weeks later. The patient also underwent two adhesiolysis procedures.
PATIENT'S CLAIM Access to the abdomen was not properly performed and caused colon perforation. The injury should have been found and treated earlier.
PHYSICIAN'S DEFENSE The case was settled before trial.
VERDICT A $750,000 Virginia settlement was reached.
READ How to avoid intestinal and urinary tract injuries during gynecologic laparoscopy, by Michael Baggish, MD (Surgical Techniques, October 2012) What caused this C. diff infection after hysterectomy?
AFTER A HYSTERECTOMY, a 42-year-old woman developed a persistent fever and increased white blood cell count. The gynecologist prescribed ciprofloxacin for a urinary tract infection, and discharged the patient from the hospital on postoperative day 4. She returned to the gynecologist’s office with severe abdominal pain and vomiting 4 days after discharge. The gynecologist prescribed an antacid and told her to continue taking ciprofloxacin.
The patient was taken to the ED by ambulance 3 days later. Testing revealed a Clostridium dificule (C. diff) infection. During emergency surgery, a large portion of her colon was resected, and a colostomy was performed. The colostomy was reversed 6 months later. The patient developed an incisional hernia and has abdominal scarring.
PATIENT'S CLAIM Prophylactic antibiotics should have been prescribed before surgery.
Two possible scenarios were presented: 1) A bowel injury occurred during surgery, and ciprofloxacin likely worsened the infection caused by the bowel injury; or 2) ciprofloxacin triggered the C. diff infection that caused leaking colon perforations and subsequent peritonitis.
The colon perforations could have been avoided if the gynecologist had diagnosed and treated the C. diff infection in a timely manner.
PHYSICIAN'S DEFENSE The patient’s symptoms did not suggest a C. diff infection; testing was not necessary. Ciprofloxacin might have allowed the proliferation of the C. diff infection, but the use of the drug was not negligent. The infection was not preventable and could not have been diagnosed earlier.
VERDICT A $776,000 New York verdict was returned.
Brain injury and cerebral palsy: When did this occur?
DURING LABOR AND DELIVERY, there were periods when the fetal heart-rate tracings were nonreassuring with variable decelerations and fetal tachycardia; some variables were severe. The child suffered anoxic encephalopathy that caused neurologic injury and cerebral palsy.
PARENTS' CLAIM The infant suffered numerous hypoxic incidents before cesarean delivery was performed. An earlier cesarean delivery could have prevented the injury.
PHYSICIAN'S DEFENSE The newborn had a normal blood cord gas level of 7.2 pH and Apgar scores of 9 and 10, at 1 and 5 minutes, respectively. Fetal heart-rate tracings did not show evidence of fetal hypoxia. The brain injury likely occurred prior to the onset of labor and was possibly related to a viral encephalopathy.
VERDICT A Virginia defense verdict was returned. These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
Duty-Hour Reforms Reduce Work Hours with No Impact on Resident, Patient Outcomes
Clinical question: What are the effects of the 2011 resident duty-hour requirements on first-year residents’ well-being and patient safety?
Background: In an effort to reduce adverse consequences associated with extended shift length and sleep deprivation, the Accreditation Council for Graduate Medical Education (ACGME) released a new set of duty-hour requirements effective July 2011. To date, little is known about the effects of the 2011 reforms on resident and patient outcomes.
Study design: Prospective, longitudinal cohort with pre-post analysis.
Setting: Residency programs from university- and community-based medical centers.
Synopsis: Fifty-one residency programs from 10 university-based and four community-based GME institutions were included. Incoming interns during the 2009, 2010, and 2011 academic years were invited to participate, and 58% (n=2,323) agreed to take part. Participants completed online surveys two months before starting their first residency (intern) year and at three, six, nine, and 12 months of internship. Questions addressed work hours, sleep, medical errors, depressive symptoms, and subjective well-being.
No significant differences in baseline findings were found between the pre-implementation cohort (interns entering in 2009 and 2010) and the post-implementation cohort (interns starting in 2011, following the new duty-hour requirements). Interns in the post-implementation cohort worked fewer hours than those in the pre-implementation cohort (mean hours per week 64.3 vs. 67.0, P<0.001). There were no significant changes in reported hours of sleep, depressive symptom score, or well-being score between the pre- and post-implementation cohorts. The percentage of respondents who reported committing a serious medical error increased in the post-implementation group (23.3% vs. 19.9%, P=0.007).
Limitations include the self-reported nature of the responses and the modest participation rate. The authors concluded that although the 2011 reforms decreased the total number of hours worked, additional strategies could be needed to achieve the desired effects on intern well-being and patient safety.
Bottom line: Following implementation of the 2011 ACGME duty-hour reforms, interns from diverse specialties and institutions experienced reductions in self-reported work hours, without any associated improvements in sleep, depressive symptoms, or well-being and with an increase in reported medical errors.
Citation: Sen S, Kranzler HR, Didwania AK, et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med. 2013;173(8):657-662.
Clinical question: What are the effects of the 2011 resident duty-hour requirements on first-year residents’ well-being and patient safety?
Background: In an effort to reduce adverse consequences associated with extended shift length and sleep deprivation, the Accreditation Council for Graduate Medical Education (ACGME) released a new set of duty-hour requirements effective July 2011. To date, little is known about the effects of the 2011 reforms on resident and patient outcomes.
Study design: Prospective, longitudinal cohort with pre-post analysis.
Setting: Residency programs from university- and community-based medical centers.
Synopsis: Fifty-one residency programs from 10 university-based and four community-based GME institutions were included. Incoming interns during the 2009, 2010, and 2011 academic years were invited to participate, and 58% (n=2,323) agreed to take part. Participants completed online surveys two months before starting their first residency (intern) year and at three, six, nine, and 12 months of internship. Questions addressed work hours, sleep, medical errors, depressive symptoms, and subjective well-being.
No significant differences in baseline findings were found between the pre-implementation cohort (interns entering in 2009 and 2010) and the post-implementation cohort (interns starting in 2011, following the new duty-hour requirements). Interns in the post-implementation cohort worked fewer hours than those in the pre-implementation cohort (mean hours per week 64.3 vs. 67.0, P<0.001). There were no significant changes in reported hours of sleep, depressive symptom score, or well-being score between the pre- and post-implementation cohorts. The percentage of respondents who reported committing a serious medical error increased in the post-implementation group (23.3% vs. 19.9%, P=0.007).
Limitations include the self-reported nature of the responses and the modest participation rate. The authors concluded that although the 2011 reforms decreased the total number of hours worked, additional strategies could be needed to achieve the desired effects on intern well-being and patient safety.
Bottom line: Following implementation of the 2011 ACGME duty-hour reforms, interns from diverse specialties and institutions experienced reductions in self-reported work hours, without any associated improvements in sleep, depressive symptoms, or well-being and with an increase in reported medical errors.
Citation: Sen S, Kranzler HR, Didwania AK, et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med. 2013;173(8):657-662.
Clinical question: What are the effects of the 2011 resident duty-hour requirements on first-year residents’ well-being and patient safety?
Background: In an effort to reduce adverse consequences associated with extended shift length and sleep deprivation, the Accreditation Council for Graduate Medical Education (ACGME) released a new set of duty-hour requirements effective July 2011. To date, little is known about the effects of the 2011 reforms on resident and patient outcomes.
Study design: Prospective, longitudinal cohort with pre-post analysis.
Setting: Residency programs from university- and community-based medical centers.
Synopsis: Fifty-one residency programs from 10 university-based and four community-based GME institutions were included. Incoming interns during the 2009, 2010, and 2011 academic years were invited to participate, and 58% (n=2,323) agreed to take part. Participants completed online surveys two months before starting their first residency (intern) year and at three, six, nine, and 12 months of internship. Questions addressed work hours, sleep, medical errors, depressive symptoms, and subjective well-being.
No significant differences in baseline findings were found between the pre-implementation cohort (interns entering in 2009 and 2010) and the post-implementation cohort (interns starting in 2011, following the new duty-hour requirements). Interns in the post-implementation cohort worked fewer hours than those in the pre-implementation cohort (mean hours per week 64.3 vs. 67.0, P<0.001). There were no significant changes in reported hours of sleep, depressive symptom score, or well-being score between the pre- and post-implementation cohorts. The percentage of respondents who reported committing a serious medical error increased in the post-implementation group (23.3% vs. 19.9%, P=0.007).
Limitations include the self-reported nature of the responses and the modest participation rate. The authors concluded that although the 2011 reforms decreased the total number of hours worked, additional strategies could be needed to achieve the desired effects on intern well-being and patient safety.
Bottom line: Following implementation of the 2011 ACGME duty-hour reforms, interns from diverse specialties and institutions experienced reductions in self-reported work hours, without any associated improvements in sleep, depressive symptoms, or well-being and with an increase in reported medical errors.
Citation: Sen S, Kranzler HR, Didwania AK, et al. Effects of the 2011 duty hour reforms on interns and their patients: a prospective longitudinal cohort study. JAMA Intern Med. 2013;173(8):657-662.
Direct Provider Communication Not Associated with 30-Day Readmissions
Clinical question: How often do inpatient providers report direct communication with outpatient providers, and how is direct communication associated with 30-day readmissions?
Background: Studies have demonstrated that adverse events and errors occurring after hospital discharge can result from poor provider communication between the inpatient and outpatient setting.
Study design: Prospective cohort.
Setting: Johns Hopkins Hospital, Baltimore.
Synopsis: The presence or absence of direct communication between inpatient and outpatient healthcare providers was captured from a required field in an electronic discharge worksheet completed by the discharging physician. Of 6,635 hospitalizations studied, successful direct communication was reported in 36.7% of cases. Predictors of successful direct communication included patients cared for by hospitalists without house staff (OR 1.81, 95% CI 1.59-2.08), high expected 30-day readmission rate (OR 1.18, 95% CI 1.10-1.28), and insurance by Medicare (OR 1.35, 95% CI 1.16-1.56) and private insurance companies (OR 1.35, 95% CI 1.18-1.56). In adjusted analyses, direct communication between the inpatient and outpatient providers was not associated with 30-day readmissions (OR 1.08, 95% CI 0.92-1.26).
There were several limitations in this study. Only the primary team was surveyed; thus, it is not known if consulting providers might have contacted the outpatient providers. Only readmissions to the same medical center were studied, and therefore it is not known if patients were readmitted to other facilities. Additionally, information regarding discharge communication was self-reported, which might have introduced bias.
Bottom line: Self-reported direct communication between inpatient and outpatient providers occurred infrequently and was not associated with 30-day same-hospital readmission.
Citation: Oduyebo I, Lehmann C, Pollack C, et al. Association of self-reported hospital discharge handoffs with 30-day readmissions. JAMA Intern Med. 2013;173:624-629.
Clinical question: How often do inpatient providers report direct communication with outpatient providers, and how is direct communication associated with 30-day readmissions?
Background: Studies have demonstrated that adverse events and errors occurring after hospital discharge can result from poor provider communication between the inpatient and outpatient setting.
Study design: Prospective cohort.
Setting: Johns Hopkins Hospital, Baltimore.
Synopsis: The presence or absence of direct communication between inpatient and outpatient healthcare providers was captured from a required field in an electronic discharge worksheet completed by the discharging physician. Of 6,635 hospitalizations studied, successful direct communication was reported in 36.7% of cases. Predictors of successful direct communication included patients cared for by hospitalists without house staff (OR 1.81, 95% CI 1.59-2.08), high expected 30-day readmission rate (OR 1.18, 95% CI 1.10-1.28), and insurance by Medicare (OR 1.35, 95% CI 1.16-1.56) and private insurance companies (OR 1.35, 95% CI 1.18-1.56). In adjusted analyses, direct communication between the inpatient and outpatient providers was not associated with 30-day readmissions (OR 1.08, 95% CI 0.92-1.26).
There were several limitations in this study. Only the primary team was surveyed; thus, it is not known if consulting providers might have contacted the outpatient providers. Only readmissions to the same medical center were studied, and therefore it is not known if patients were readmitted to other facilities. Additionally, information regarding discharge communication was self-reported, which might have introduced bias.
Bottom line: Self-reported direct communication between inpatient and outpatient providers occurred infrequently and was not associated with 30-day same-hospital readmission.
Citation: Oduyebo I, Lehmann C, Pollack C, et al. Association of self-reported hospital discharge handoffs with 30-day readmissions. JAMA Intern Med. 2013;173:624-629.
Clinical question: How often do inpatient providers report direct communication with outpatient providers, and how is direct communication associated with 30-day readmissions?
Background: Studies have demonstrated that adverse events and errors occurring after hospital discharge can result from poor provider communication between the inpatient and outpatient setting.
Study design: Prospective cohort.
Setting: Johns Hopkins Hospital, Baltimore.
Synopsis: The presence or absence of direct communication between inpatient and outpatient healthcare providers was captured from a required field in an electronic discharge worksheet completed by the discharging physician. Of 6,635 hospitalizations studied, successful direct communication was reported in 36.7% of cases. Predictors of successful direct communication included patients cared for by hospitalists without house staff (OR 1.81, 95% CI 1.59-2.08), high expected 30-day readmission rate (OR 1.18, 95% CI 1.10-1.28), and insurance by Medicare (OR 1.35, 95% CI 1.16-1.56) and private insurance companies (OR 1.35, 95% CI 1.18-1.56). In adjusted analyses, direct communication between the inpatient and outpatient providers was not associated with 30-day readmissions (OR 1.08, 95% CI 0.92-1.26).
There were several limitations in this study. Only the primary team was surveyed; thus, it is not known if consulting providers might have contacted the outpatient providers. Only readmissions to the same medical center were studied, and therefore it is not known if patients were readmitted to other facilities. Additionally, information regarding discharge communication was self-reported, which might have introduced bias.
Bottom line: Self-reported direct communication between inpatient and outpatient providers occurred infrequently and was not associated with 30-day same-hospital readmission.
Citation: Oduyebo I, Lehmann C, Pollack C, et al. Association of self-reported hospital discharge handoffs with 30-day readmissions. JAMA Intern Med. 2013;173:624-629.