User login
Survey Insights: Better Understand CPT Coding Intensity
Many of the practice-management-related questions we field from members here at SHM are about documentation and coding issues; members are looking for ways to benchmark their group’s coding performance against other similar groups. One helpful metric reported in the SHM/MGMA State of Hospital Medicine report is the ratio of work-RVUs to total encounters, which I refer to as “coding intensity.”
Median coding intensity for adult medicine hospitalists in the 2011 report was 1.90, up slightly from 2010 levels.
The most obvious factor that influences coding intensity is the distribution of CPT codes within specific evaluation and management code sets, such as inpatient admissions (99221-99223) or follow-up visits (99231-99233). Other considerations include the degree to which hospitalists provide high-wRVU services, such as critical care or procedures, the ratio of inpatient vs. observation patients, and the group’s average length of stay.
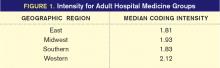
One interesting finding was that coding intensity varies greatly by geographic region (see Figure 1, right).
What’s going on out there in the Western states? Are those folks receiving different training than the rest of us? Or are they just mavericks, more interested in generating professional fee revenues than hospitalists elsewhere are? It’s hard to say. One big factor is that length of stay (LOS) tends to be shorter in the West than in other parts of the country. That means the typical Western hospitalist will have a larger proportion of high-wRVU value admission and discharge codes relative to their proportion of low-wRVU value subsequent visit codes.
This isn’t the whole story, though. Hospitalists in the West actually did report a significantly more aggressive code distribution for all three CPT code sets for which data were collected (inpatient admissions, subsequent visits, and discharges). And hospitalists in the South, where LOS tends to be longer, also reported the least aggressive code distributions.
Unfortunately, we don’t have a lot of clues as to why these differences exist. We don’t know, for example, whether more hospitalists in the West work in the ICU or perform more procedures compared to other parts of the country. One possibility suggested by report data is that hospitalists in Western states have the highest average proportion of their total compensation allocated to productivity incentives. Hospitalists in the East have the lowest proportion of their compensation based on productivity. So productivity-based compensation might cause hospitalists to care a lot more about doing a good job with documentation and CPT coding.
Other interesting findings include the fact that hospitalists employed by multistate hospitalist-management companies had the lowest median coding intensity, while hospitalists employed by private hospitalist-only groups had the highest coding intensity. And, perhaps not surprisingly, the small proportion of practices that did not receive any financial support had a higher average coding intensity than practices receiving financial support.
While there are no clear answers about variations in CPT coding intensity among hospitalist practices, the State of Hospital Medicine report does offer some intriguing pointers, along with a variety of useful benchmarks about hospitalist CPT coding practices. And stay tuned: The new report, due out in August, will offer even more ways of looking at coding intensity and CPT code distribution.
Leslie Flores, SHM senior advisor
Many of the practice-management-related questions we field from members here at SHM are about documentation and coding issues; members are looking for ways to benchmark their group’s coding performance against other similar groups. One helpful metric reported in the SHM/MGMA State of Hospital Medicine report is the ratio of work-RVUs to total encounters, which I refer to as “coding intensity.”
Median coding intensity for adult medicine hospitalists in the 2011 report was 1.90, up slightly from 2010 levels.
The most obvious factor that influences coding intensity is the distribution of CPT codes within specific evaluation and management code sets, such as inpatient admissions (99221-99223) or follow-up visits (99231-99233). Other considerations include the degree to which hospitalists provide high-wRVU services, such as critical care or procedures, the ratio of inpatient vs. observation patients, and the group’s average length of stay.
One interesting finding was that coding intensity varies greatly by geographic region (see Figure 1, right).
What’s going on out there in the Western states? Are those folks receiving different training than the rest of us? Or are they just mavericks, more interested in generating professional fee revenues than hospitalists elsewhere are? It’s hard to say. One big factor is that length of stay (LOS) tends to be shorter in the West than in other parts of the country. That means the typical Western hospitalist will have a larger proportion of high-wRVU value admission and discharge codes relative to their proportion of low-wRVU value subsequent visit codes.
This isn’t the whole story, though. Hospitalists in the West actually did report a significantly more aggressive code distribution for all three CPT code sets for which data were collected (inpatient admissions, subsequent visits, and discharges). And hospitalists in the South, where LOS tends to be longer, also reported the least aggressive code distributions.
Unfortunately, we don’t have a lot of clues as to why these differences exist. We don’t know, for example, whether more hospitalists in the West work in the ICU or perform more procedures compared to other parts of the country. One possibility suggested by report data is that hospitalists in Western states have the highest average proportion of their total compensation allocated to productivity incentives. Hospitalists in the East have the lowest proportion of their compensation based on productivity. So productivity-based compensation might cause hospitalists to care a lot more about doing a good job with documentation and CPT coding.
Other interesting findings include the fact that hospitalists employed by multistate hospitalist-management companies had the lowest median coding intensity, while hospitalists employed by private hospitalist-only groups had the highest coding intensity. And, perhaps not surprisingly, the small proportion of practices that did not receive any financial support had a higher average coding intensity than practices receiving financial support.
While there are no clear answers about variations in CPT coding intensity among hospitalist practices, the State of Hospital Medicine report does offer some intriguing pointers, along with a variety of useful benchmarks about hospitalist CPT coding practices. And stay tuned: The new report, due out in August, will offer even more ways of looking at coding intensity and CPT code distribution.
Leslie Flores, SHM senior advisor
Many of the practice-management-related questions we field from members here at SHM are about documentation and coding issues; members are looking for ways to benchmark their group’s coding performance against other similar groups. One helpful metric reported in the SHM/MGMA State of Hospital Medicine report is the ratio of work-RVUs to total encounters, which I refer to as “coding intensity.”
Median coding intensity for adult medicine hospitalists in the 2011 report was 1.90, up slightly from 2010 levels.
The most obvious factor that influences coding intensity is the distribution of CPT codes within specific evaluation and management code sets, such as inpatient admissions (99221-99223) or follow-up visits (99231-99233). Other considerations include the degree to which hospitalists provide high-wRVU services, such as critical care or procedures, the ratio of inpatient vs. observation patients, and the group’s average length of stay.
One interesting finding was that coding intensity varies greatly by geographic region (see Figure 1, right).
What’s going on out there in the Western states? Are those folks receiving different training than the rest of us? Or are they just mavericks, more interested in generating professional fee revenues than hospitalists elsewhere are? It’s hard to say. One big factor is that length of stay (LOS) tends to be shorter in the West than in other parts of the country. That means the typical Western hospitalist will have a larger proportion of high-wRVU value admission and discharge codes relative to their proportion of low-wRVU value subsequent visit codes.
This isn’t the whole story, though. Hospitalists in the West actually did report a significantly more aggressive code distribution for all three CPT code sets for which data were collected (inpatient admissions, subsequent visits, and discharges). And hospitalists in the South, where LOS tends to be longer, also reported the least aggressive code distributions.
Unfortunately, we don’t have a lot of clues as to why these differences exist. We don’t know, for example, whether more hospitalists in the West work in the ICU or perform more procedures compared to other parts of the country. One possibility suggested by report data is that hospitalists in Western states have the highest average proportion of their total compensation allocated to productivity incentives. Hospitalists in the East have the lowest proportion of their compensation based on productivity. So productivity-based compensation might cause hospitalists to care a lot more about doing a good job with documentation and CPT coding.
Other interesting findings include the fact that hospitalists employed by multistate hospitalist-management companies had the lowest median coding intensity, while hospitalists employed by private hospitalist-only groups had the highest coding intensity. And, perhaps not surprisingly, the small proportion of practices that did not receive any financial support had a higher average coding intensity than practices receiving financial support.
While there are no clear answers about variations in CPT coding intensity among hospitalist practices, the State of Hospital Medicine report does offer some intriguing pointers, along with a variety of useful benchmarks about hospitalist CPT coding practices. And stay tuned: The new report, due out in August, will offer even more ways of looking at coding intensity and CPT code distribution.
Leslie Flores, SHM senior advisor
Established Performance Metrics Help CMS Expand Its Value-Based Purchasing Program

—Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships, National Quality Forum, former CMS adviser
No longer content to be a passive purchaser of healthcare services, the Centers for Medicare & Medicaid Services (CMS) is becoming a savvier shopper, holding providers increasingly accountable for the quality and efficiency of the care they deliver. With its value-based purchasing (VPB) program for hospitals already in place, now it’s the physicians’ turn.
CMS is marching toward a value-based payment modifier program that will adjust physician reimbursement based on the relative quality and efficiency of care that physicians provide to Medicare fee-for-service patients. The program will begin January 2015 and will extend to all physicians in 2017. Like the hospital VBP program, it will be budget-neutral—meaning that payment will increase for some physicians but decrease for others.
The coming months mark a pivotal period for physicians as CMS tweaks its accountability apparatus in ways that will determine how reimbursement will rise and fall, for whom, and for what.
Menu of Metrics
In crafting the payment modifier program, CMS can tap performance metrics from several of its existing programs, including the Physician Quality Reporting System (PQRS), the soon-to-be-expanded Physician Compare website (www.medicare.gov/find-a-doctor/provider-search.aspx), and the Physician Feedback Program.
“These agendas are part of a continuum, and of equal importance, in the evolution toward physician value-based purchasing,” says Patrick J. Torcson, MD, MMM, FACP, SFHM, chair of SHM’s Performance Measurement and Reporting Committee, and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
PQRS began as a voluntary “pay for reporting” system that gave physicians a modest financial bonus (currently 0.5% of allowable Medicare charges) for submitting quality data (left). The Affordable Care Act (ACA) has since authorized CMS to penalize physicians who do not participate—1.5% of allowable Medicare charges beginning in 2015, and 2% in 2016.
The Physician Compare website, launched at the end of 2010, currently contains such rudimentary information as education, gender, and whether a physician is enrolled in Medicare and satisfactorily reports data to the PQRS. But as of January, the site will begin reporting some PQRS data, as well as other metrics.
CMS’ Physician Feedback Program provides quality and cost information to physicians in an effort to encourage them to improve the care they provide and its efficiency. CMS recently combined the program with its value-based payment modifier program as it moves toward physician reimbursement that it says will reward “value rather than volume.” The program, currently being piloted in Iowa, Nebraska, Kansas, and Missouri, issues to physicians confidential quality and resource use reports (QRURs) that compare their performance to peer groups in similar specialties by tracking PQRS results, Healthcare Effectiveness Data and Information Set (HEDIS) measures, and per-capita cost data and preventable hospital admission rates for various medical conditions. CMS will roll out the program nationwide next year.
Metrics Lack Relevance
Developing performance measures that capture the most relevant activities of physicians across many different specialties with equal validity is notoriously difficult—something that CMS acknowledges.1
Assigning the right patient to the right physician (i.e. figuring out who contributed what care, in what proportion, to which patient) also is fraught with complications, especially in the inpatient care setting, where a patient is likely to see many different physicians during a hospitalization.
SHM president Shaun Frost, MD, SFHM, highlighted these challenges in a letter sent in May to acting CMS administrator Marilyn B. Tavenner in which he pointed to dramatic data deficiencies in the initial round of QRURs sent to Physician Feedback Program participants that included hospitalists in Iowa, Nebraska, Kansas and Missouri. Because hospitalists were categorized as general internal-medicine physicians in the reports, their per-capita cost of care was dramatically higher (73% higher, in one case study) than the average cost of all internal-medicine physicians. No allowance was made for distinguishing the outpatient-oriented practice of a general internist from the inherently more expensive inpatient-focused hospitalist practice.
In the case study reviewed by SHM, the hospitalist’s patients saw, on average, 28 different physicians over the course of a year, during which the hospitalist contributed to the care of many patients but did not direct the care of any one of them—facts that clearly highlight the difficulty of assigning responsibility and accountability for a patient’s care when comparing physician performance.
“Based on the measurement used in the QRUR, it seems likely that a hospitalist would be severely disadvantaged with the introduction of a value-based modifier based on the present QRUR methodology,” Dr. Frost wrote.
SHM is similarly critical of the PQRS measures, which Dr. Torcson says lack relevance to hospitalist practices. “We want to be defined as HM physicians with our own unique measures of quality and cost,” he says. “Our results will look very different from those of an internist with a primarily outpatient practice.”
Dr. Torcson notes that SHM is an active participant in providing feedback during CMS rule proposals and has offered to work with the CMS on further refining the measures. For example, SHM proposed adding additional measures related to care transitions, given their particular relevance to hospitalist practices.
Rule-Changing Reform
The disruptive innovation of CMS’ healthcare reform agenda might wind up being a game-changer that dramatically affects the contours of all provider performance reporting and incentive systems, redefining the issues of physician accountability and patient assignment.
“We’re going to need to figure out how to restructure our measurement systems to match our evolving healthcare delivery and payment systems,” says Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships for the National Quality Forum and former CMS adviser to the VBP program. Healthcare quality reporting should focus more on measures that cut across care contexts and assess whether the care provided truly made a difference for patients—metrics such as health improvement, return to functional status, level of patient involvement in the management of their care, provider team coordination, and other patient needs and preferences, Dr. Valuck believes.
“We need to be focused more on measures that encourage joint responsibility and cooperation among providers, and are important to patients across hospital, post-acute, and ambulatory settings, rather than those that are compartmentalized to one setting or relevant only to specific diseases or subspecialties,” Dr. Valuck says.
Such measure sets, while still retaining some disease- and physician-specific metrics, ideally would be complementary with families of related measures at the community, state, and national levels, Dr. Valuck says. “Such a multidimensional framework can begin to tell a meaningful story about what’s happening to the patient, and how well our system is delivering the right care,” he adds.
Dr. Torcson says HM has a pioneering role to play in this evolution, and he notes that SHM has proposed that CMS harmonize measures that align hospital-based physician activities (e.g. hospital medicine, emergency medicine, anesthesia, radiology) with hospital-level performance agendas so that physicians practicing together in the hospital setting can report on measures that are relevant to both.
Christopher Guadagnino is a freelance medical writer in Philadelphia.
Reference
- Centers for Medicare & Medicaid Services. Physician Quality Reporting System Town Hall Meeting. Available at: http://www.usqualitymeasures.org/shared/content/C4M_PQRS_transcript.pdf. Accessed July 3, 2012.

—Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships, National Quality Forum, former CMS adviser
No longer content to be a passive purchaser of healthcare services, the Centers for Medicare & Medicaid Services (CMS) is becoming a savvier shopper, holding providers increasingly accountable for the quality and efficiency of the care they deliver. With its value-based purchasing (VPB) program for hospitals already in place, now it’s the physicians’ turn.
CMS is marching toward a value-based payment modifier program that will adjust physician reimbursement based on the relative quality and efficiency of care that physicians provide to Medicare fee-for-service patients. The program will begin January 2015 and will extend to all physicians in 2017. Like the hospital VBP program, it will be budget-neutral—meaning that payment will increase for some physicians but decrease for others.
The coming months mark a pivotal period for physicians as CMS tweaks its accountability apparatus in ways that will determine how reimbursement will rise and fall, for whom, and for what.
Menu of Metrics
In crafting the payment modifier program, CMS can tap performance metrics from several of its existing programs, including the Physician Quality Reporting System (PQRS), the soon-to-be-expanded Physician Compare website (www.medicare.gov/find-a-doctor/provider-search.aspx), and the Physician Feedback Program.
“These agendas are part of a continuum, and of equal importance, in the evolution toward physician value-based purchasing,” says Patrick J. Torcson, MD, MMM, FACP, SFHM, chair of SHM’s Performance Measurement and Reporting Committee, and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
PQRS began as a voluntary “pay for reporting” system that gave physicians a modest financial bonus (currently 0.5% of allowable Medicare charges) for submitting quality data (left). The Affordable Care Act (ACA) has since authorized CMS to penalize physicians who do not participate—1.5% of allowable Medicare charges beginning in 2015, and 2% in 2016.
The Physician Compare website, launched at the end of 2010, currently contains such rudimentary information as education, gender, and whether a physician is enrolled in Medicare and satisfactorily reports data to the PQRS. But as of January, the site will begin reporting some PQRS data, as well as other metrics.
CMS’ Physician Feedback Program provides quality and cost information to physicians in an effort to encourage them to improve the care they provide and its efficiency. CMS recently combined the program with its value-based payment modifier program as it moves toward physician reimbursement that it says will reward “value rather than volume.” The program, currently being piloted in Iowa, Nebraska, Kansas, and Missouri, issues to physicians confidential quality and resource use reports (QRURs) that compare their performance to peer groups in similar specialties by tracking PQRS results, Healthcare Effectiveness Data and Information Set (HEDIS) measures, and per-capita cost data and preventable hospital admission rates for various medical conditions. CMS will roll out the program nationwide next year.
Metrics Lack Relevance
Developing performance measures that capture the most relevant activities of physicians across many different specialties with equal validity is notoriously difficult—something that CMS acknowledges.1
Assigning the right patient to the right physician (i.e. figuring out who contributed what care, in what proportion, to which patient) also is fraught with complications, especially in the inpatient care setting, where a patient is likely to see many different physicians during a hospitalization.
SHM president Shaun Frost, MD, SFHM, highlighted these challenges in a letter sent in May to acting CMS administrator Marilyn B. Tavenner in which he pointed to dramatic data deficiencies in the initial round of QRURs sent to Physician Feedback Program participants that included hospitalists in Iowa, Nebraska, Kansas and Missouri. Because hospitalists were categorized as general internal-medicine physicians in the reports, their per-capita cost of care was dramatically higher (73% higher, in one case study) than the average cost of all internal-medicine physicians. No allowance was made for distinguishing the outpatient-oriented practice of a general internist from the inherently more expensive inpatient-focused hospitalist practice.
In the case study reviewed by SHM, the hospitalist’s patients saw, on average, 28 different physicians over the course of a year, during which the hospitalist contributed to the care of many patients but did not direct the care of any one of them—facts that clearly highlight the difficulty of assigning responsibility and accountability for a patient’s care when comparing physician performance.
“Based on the measurement used in the QRUR, it seems likely that a hospitalist would be severely disadvantaged with the introduction of a value-based modifier based on the present QRUR methodology,” Dr. Frost wrote.
SHM is similarly critical of the PQRS measures, which Dr. Torcson says lack relevance to hospitalist practices. “We want to be defined as HM physicians with our own unique measures of quality and cost,” he says. “Our results will look very different from those of an internist with a primarily outpatient practice.”
Dr. Torcson notes that SHM is an active participant in providing feedback during CMS rule proposals and has offered to work with the CMS on further refining the measures. For example, SHM proposed adding additional measures related to care transitions, given their particular relevance to hospitalist practices.
Rule-Changing Reform
The disruptive innovation of CMS’ healthcare reform agenda might wind up being a game-changer that dramatically affects the contours of all provider performance reporting and incentive systems, redefining the issues of physician accountability and patient assignment.
“We’re going to need to figure out how to restructure our measurement systems to match our evolving healthcare delivery and payment systems,” says Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships for the National Quality Forum and former CMS adviser to the VBP program. Healthcare quality reporting should focus more on measures that cut across care contexts and assess whether the care provided truly made a difference for patients—metrics such as health improvement, return to functional status, level of patient involvement in the management of their care, provider team coordination, and other patient needs and preferences, Dr. Valuck believes.
“We need to be focused more on measures that encourage joint responsibility and cooperation among providers, and are important to patients across hospital, post-acute, and ambulatory settings, rather than those that are compartmentalized to one setting or relevant only to specific diseases or subspecialties,” Dr. Valuck says.
Such measure sets, while still retaining some disease- and physician-specific metrics, ideally would be complementary with families of related measures at the community, state, and national levels, Dr. Valuck says. “Such a multidimensional framework can begin to tell a meaningful story about what’s happening to the patient, and how well our system is delivering the right care,” he adds.
Dr. Torcson says HM has a pioneering role to play in this evolution, and he notes that SHM has proposed that CMS harmonize measures that align hospital-based physician activities (e.g. hospital medicine, emergency medicine, anesthesia, radiology) with hospital-level performance agendas so that physicians practicing together in the hospital setting can report on measures that are relevant to both.
Christopher Guadagnino is a freelance medical writer in Philadelphia.
Reference
- Centers for Medicare & Medicaid Services. Physician Quality Reporting System Town Hall Meeting. Available at: http://www.usqualitymeasures.org/shared/content/C4M_PQRS_transcript.pdf. Accessed July 3, 2012.

—Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships, National Quality Forum, former CMS adviser
No longer content to be a passive purchaser of healthcare services, the Centers for Medicare & Medicaid Services (CMS) is becoming a savvier shopper, holding providers increasingly accountable for the quality and efficiency of the care they deliver. With its value-based purchasing (VPB) program for hospitals already in place, now it’s the physicians’ turn.
CMS is marching toward a value-based payment modifier program that will adjust physician reimbursement based on the relative quality and efficiency of care that physicians provide to Medicare fee-for-service patients. The program will begin January 2015 and will extend to all physicians in 2017. Like the hospital VBP program, it will be budget-neutral—meaning that payment will increase for some physicians but decrease for others.
The coming months mark a pivotal period for physicians as CMS tweaks its accountability apparatus in ways that will determine how reimbursement will rise and fall, for whom, and for what.
Menu of Metrics
In crafting the payment modifier program, CMS can tap performance metrics from several of its existing programs, including the Physician Quality Reporting System (PQRS), the soon-to-be-expanded Physician Compare website (www.medicare.gov/find-a-doctor/provider-search.aspx), and the Physician Feedback Program.
“These agendas are part of a continuum, and of equal importance, in the evolution toward physician value-based purchasing,” says Patrick J. Torcson, MD, MMM, FACP, SFHM, chair of SHM’s Performance Measurement and Reporting Committee, and director of hospital medicine at St. Tammany Parish Hospital in Covington, La.
PQRS began as a voluntary “pay for reporting” system that gave physicians a modest financial bonus (currently 0.5% of allowable Medicare charges) for submitting quality data (left). The Affordable Care Act (ACA) has since authorized CMS to penalize physicians who do not participate—1.5% of allowable Medicare charges beginning in 2015, and 2% in 2016.
The Physician Compare website, launched at the end of 2010, currently contains such rudimentary information as education, gender, and whether a physician is enrolled in Medicare and satisfactorily reports data to the PQRS. But as of January, the site will begin reporting some PQRS data, as well as other metrics.
CMS’ Physician Feedback Program provides quality and cost information to physicians in an effort to encourage them to improve the care they provide and its efficiency. CMS recently combined the program with its value-based payment modifier program as it moves toward physician reimbursement that it says will reward “value rather than volume.” The program, currently being piloted in Iowa, Nebraska, Kansas, and Missouri, issues to physicians confidential quality and resource use reports (QRURs) that compare their performance to peer groups in similar specialties by tracking PQRS results, Healthcare Effectiveness Data and Information Set (HEDIS) measures, and per-capita cost data and preventable hospital admission rates for various medical conditions. CMS will roll out the program nationwide next year.
Metrics Lack Relevance
Developing performance measures that capture the most relevant activities of physicians across many different specialties with equal validity is notoriously difficult—something that CMS acknowledges.1
Assigning the right patient to the right physician (i.e. figuring out who contributed what care, in what proportion, to which patient) also is fraught with complications, especially in the inpatient care setting, where a patient is likely to see many different physicians during a hospitalization.
SHM president Shaun Frost, MD, SFHM, highlighted these challenges in a letter sent in May to acting CMS administrator Marilyn B. Tavenner in which he pointed to dramatic data deficiencies in the initial round of QRURs sent to Physician Feedback Program participants that included hospitalists in Iowa, Nebraska, Kansas and Missouri. Because hospitalists were categorized as general internal-medicine physicians in the reports, their per-capita cost of care was dramatically higher (73% higher, in one case study) than the average cost of all internal-medicine physicians. No allowance was made for distinguishing the outpatient-oriented practice of a general internist from the inherently more expensive inpatient-focused hospitalist practice.
In the case study reviewed by SHM, the hospitalist’s patients saw, on average, 28 different physicians over the course of a year, during which the hospitalist contributed to the care of many patients but did not direct the care of any one of them—facts that clearly highlight the difficulty of assigning responsibility and accountability for a patient’s care when comparing physician performance.
“Based on the measurement used in the QRUR, it seems likely that a hospitalist would be severely disadvantaged with the introduction of a value-based modifier based on the present QRUR methodology,” Dr. Frost wrote.
SHM is similarly critical of the PQRS measures, which Dr. Torcson says lack relevance to hospitalist practices. “We want to be defined as HM physicians with our own unique measures of quality and cost,” he says. “Our results will look very different from those of an internist with a primarily outpatient practice.”
Dr. Torcson notes that SHM is an active participant in providing feedback during CMS rule proposals and has offered to work with the CMS on further refining the measures. For example, SHM proposed adding additional measures related to care transitions, given their particular relevance to hospitalist practices.
Rule-Changing Reform
The disruptive innovation of CMS’ healthcare reform agenda might wind up being a game-changer that dramatically affects the contours of all provider performance reporting and incentive systems, redefining the issues of physician accountability and patient assignment.
“We’re going to need to figure out how to restructure our measurement systems to match our evolving healthcare delivery and payment systems,” says Thomas B. Valuck, MD, JD, senior vice president of strategic partnerships for the National Quality Forum and former CMS adviser to the VBP program. Healthcare quality reporting should focus more on measures that cut across care contexts and assess whether the care provided truly made a difference for patients—metrics such as health improvement, return to functional status, level of patient involvement in the management of their care, provider team coordination, and other patient needs and preferences, Dr. Valuck believes.
“We need to be focused more on measures that encourage joint responsibility and cooperation among providers, and are important to patients across hospital, post-acute, and ambulatory settings, rather than those that are compartmentalized to one setting or relevant only to specific diseases or subspecialties,” Dr. Valuck says.
Such measure sets, while still retaining some disease- and physician-specific metrics, ideally would be complementary with families of related measures at the community, state, and national levels, Dr. Valuck says. “Such a multidimensional framework can begin to tell a meaningful story about what’s happening to the patient, and how well our system is delivering the right care,” he adds.
Dr. Torcson says HM has a pioneering role to play in this evolution, and he notes that SHM has proposed that CMS harmonize measures that align hospital-based physician activities (e.g. hospital medicine, emergency medicine, anesthesia, radiology) with hospital-level performance agendas so that physicians practicing together in the hospital setting can report on measures that are relevant to both.
Christopher Guadagnino is a freelance medical writer in Philadelphia.
Reference
- Centers for Medicare & Medicaid Services. Physician Quality Reporting System Town Hall Meeting. Available at: http://www.usqualitymeasures.org/shared/content/C4M_PQRS_transcript.pdf. Accessed July 3, 2012.
Know Surgical Package Requirements before Billing Postoperative Care
Hospitalists often are involved in the postoperative care of the surgical patient. However, HM is emerging in the admitting/attending role for procedural patients. Confusion can arise as to the nature of the hospitalist service, and whether it is deemed billable. Knowing the surgical package requirements can help hospitalists consider the issues.
Global Surgical Package Period1
Surgical procedures, categorized as major or minor surgery, are reimbursed for pre-, intra-, and postoperative care. Postoperative care varies according to the procedure’s assigned global period, which designates zero, 10, or 90 postoperative days. (Physicians can review the global period for any given CPT code in the Medicare Physician Fee Schedule, available at www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.)
Services classified with “XXX” do not have the global period concept. “ZZZ” services denote an “add-on” procedure code that must always be reported with a primary procedure code and assumes the global period assigned to the primary procedure performed.
Major surgery allocates a 90-day global period in which the surgeon is responsible for all related surgical care one day before surgery through 90 postoperative days with no additional charge. Minor surgery, including endoscopy, appoints a zero-day or 10-day postoperative period. The zero-day global period encompasses only services provided on the surgical day, whereas 10-day global periods include services on the surgical day through 10 postoperative days.
Global Surgical Package Components2
The global surgical package comprises a host of responsibilities that include standard facility requirements of filling out all necessary paperwork involved in surgical cases (e.g. preoperative H&P, operative consent forms, preoperative orders). Additionally, the surgeon’s packaged payment includes (at no extra charge):
- Preoperative visits after making the decision for surgery beginning one day prior to surgery;
- All additional postoperative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Postoperative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Postoperative pain management provided by the surgeon.
- Examples of services that are not included in the global surgical package, (i.e. are separately billable and may require an appropriate modifier) are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care (i.e. a formal agreement in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record);
- Postoperative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the postoperative period that do not result in repeat operations or treatment for complications;
- Treatment for postoperative complications that requires a return trip to the operating room (OR), catheterization lab or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical-care services (CPT codes 99291 and 99292) unrelated to the surgery where a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon.
Classification of “Surgeon”
For billing purposes, the “surgeon” is a qualified physician who can perform “surgical” services within their scope of practice. All physicians with the same specialty designation in the same group practice as the “surgeon” (i.e. reporting services under the same tax identification number) are considered a single entity and must adhere to the global period billing rules initiated by the “surgeon.”
Alternately, physicians with different specialty designations in the same group practice (e.g. a hospitalist and a cardiologist in a multispecialty group who report services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed-upon) transfer of care did not occur.
Medical Necessity
With the growth of HM programs and the admission/attending role expansion, involvement in surgical cases comes under scrutiny for medical necessity. Admitting a patient who has active medical conditions (e.g. hypertension, diabetes, emphysema) is reasonable and necessary because the patient has a well-defined need for medical management by the hospitalist. Participation in the care of these patients is separately billable from the surgeon’s global period package.
Alternatively, a hospitalist might be required to admit and follow surgical patients who have no other identifiable chronic or acute conditions aside from the surgical problem. In these cases, hospitalist involvement may satisfy facility policy (quality of care, risk reduction, etc.) and administrative functions (discharge services or coordination of care) rather than active clinical management. This “medical management” will not be considered “medically necessary” by the payor, and may be denied as incidental to the surgeon’s perioperative services. Erroneous payment can occur, which will result in refund requests, as payors do not want to pay twice for duplicate services. Hospitalists can attempt to negotiate other terms with facilities to account for the unpaid time and effort directed toward these types of cases.
Consider the Case
A patient with numerous medical comorbidities is admitted to the hospitalist service for stabilization prior to surgery, which will occur the next day. The hospitalist can report the appropriate admission code (99221-99223) without need for modifiers because the hospitalist is the attending of record and in a different specialty group. If a private insurer denies the claim as inclusive to the surgical service, the hospitalist can appeal with notes and a cover letter, along with the Medicare guidelines for global surgical package. The hospitalist may continue to provide postoperative daily care, as needed, to manage the patient’s chronic conditions, and report each service as subsequent hospital care (99231-99233) without modifier until the day of discharge (99238-99239). Again, if a payor issues a denial (inclusive to surgery), appealing with notes might be necessary.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 40. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed May 5, 2012.
- Centers for Medicare & Medicaid Services. ICD-10: HHS proposes one-year delay of ICD-10 compliance date. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Medicare/Coding/ICD10/index.html?redirect=/ICD10. Accessed May 5, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
Hospitalists often are involved in the postoperative care of the surgical patient. However, HM is emerging in the admitting/attending role for procedural patients. Confusion can arise as to the nature of the hospitalist service, and whether it is deemed billable. Knowing the surgical package requirements can help hospitalists consider the issues.
Global Surgical Package Period1
Surgical procedures, categorized as major or minor surgery, are reimbursed for pre-, intra-, and postoperative care. Postoperative care varies according to the procedure’s assigned global period, which designates zero, 10, or 90 postoperative days. (Physicians can review the global period for any given CPT code in the Medicare Physician Fee Schedule, available at www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.)
Services classified with “XXX” do not have the global period concept. “ZZZ” services denote an “add-on” procedure code that must always be reported with a primary procedure code and assumes the global period assigned to the primary procedure performed.
Major surgery allocates a 90-day global period in which the surgeon is responsible for all related surgical care one day before surgery through 90 postoperative days with no additional charge. Minor surgery, including endoscopy, appoints a zero-day or 10-day postoperative period. The zero-day global period encompasses only services provided on the surgical day, whereas 10-day global periods include services on the surgical day through 10 postoperative days.
Global Surgical Package Components2
The global surgical package comprises a host of responsibilities that include standard facility requirements of filling out all necessary paperwork involved in surgical cases (e.g. preoperative H&P, operative consent forms, preoperative orders). Additionally, the surgeon’s packaged payment includes (at no extra charge):
- Preoperative visits after making the decision for surgery beginning one day prior to surgery;
- All additional postoperative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Postoperative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Postoperative pain management provided by the surgeon.
- Examples of services that are not included in the global surgical package, (i.e. are separately billable and may require an appropriate modifier) are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care (i.e. a formal agreement in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record);
- Postoperative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the postoperative period that do not result in repeat operations or treatment for complications;
- Treatment for postoperative complications that requires a return trip to the operating room (OR), catheterization lab or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical-care services (CPT codes 99291 and 99292) unrelated to the surgery where a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon.
Classification of “Surgeon”
For billing purposes, the “surgeon” is a qualified physician who can perform “surgical” services within their scope of practice. All physicians with the same specialty designation in the same group practice as the “surgeon” (i.e. reporting services under the same tax identification number) are considered a single entity and must adhere to the global period billing rules initiated by the “surgeon.”
Alternately, physicians with different specialty designations in the same group practice (e.g. a hospitalist and a cardiologist in a multispecialty group who report services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed-upon) transfer of care did not occur.
Medical Necessity
With the growth of HM programs and the admission/attending role expansion, involvement in surgical cases comes under scrutiny for medical necessity. Admitting a patient who has active medical conditions (e.g. hypertension, diabetes, emphysema) is reasonable and necessary because the patient has a well-defined need for medical management by the hospitalist. Participation in the care of these patients is separately billable from the surgeon’s global period package.
Alternatively, a hospitalist might be required to admit and follow surgical patients who have no other identifiable chronic or acute conditions aside from the surgical problem. In these cases, hospitalist involvement may satisfy facility policy (quality of care, risk reduction, etc.) and administrative functions (discharge services or coordination of care) rather than active clinical management. This “medical management” will not be considered “medically necessary” by the payor, and may be denied as incidental to the surgeon’s perioperative services. Erroneous payment can occur, which will result in refund requests, as payors do not want to pay twice for duplicate services. Hospitalists can attempt to negotiate other terms with facilities to account for the unpaid time and effort directed toward these types of cases.
Consider the Case
A patient with numerous medical comorbidities is admitted to the hospitalist service for stabilization prior to surgery, which will occur the next day. The hospitalist can report the appropriate admission code (99221-99223) without need for modifiers because the hospitalist is the attending of record and in a different specialty group. If a private insurer denies the claim as inclusive to the surgical service, the hospitalist can appeal with notes and a cover letter, along with the Medicare guidelines for global surgical package. The hospitalist may continue to provide postoperative daily care, as needed, to manage the patient’s chronic conditions, and report each service as subsequent hospital care (99231-99233) without modifier until the day of discharge (99238-99239). Again, if a payor issues a denial (inclusive to surgery), appealing with notes might be necessary.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 40. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed May 5, 2012.
- Centers for Medicare & Medicaid Services. ICD-10: HHS proposes one-year delay of ICD-10 compliance date. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Medicare/Coding/ICD10/index.html?redirect=/ICD10. Accessed May 5, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
Hospitalists often are involved in the postoperative care of the surgical patient. However, HM is emerging in the admitting/attending role for procedural patients. Confusion can arise as to the nature of the hospitalist service, and whether it is deemed billable. Knowing the surgical package requirements can help hospitalists consider the issues.
Global Surgical Package Period1
Surgical procedures, categorized as major or minor surgery, are reimbursed for pre-, intra-, and postoperative care. Postoperative care varies according to the procedure’s assigned global period, which designates zero, 10, or 90 postoperative days. (Physicians can review the global period for any given CPT code in the Medicare Physician Fee Schedule, available at www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.)
Services classified with “XXX” do not have the global period concept. “ZZZ” services denote an “add-on” procedure code that must always be reported with a primary procedure code and assumes the global period assigned to the primary procedure performed.
Major surgery allocates a 90-day global period in which the surgeon is responsible for all related surgical care one day before surgery through 90 postoperative days with no additional charge. Minor surgery, including endoscopy, appoints a zero-day or 10-day postoperative period. The zero-day global period encompasses only services provided on the surgical day, whereas 10-day global periods include services on the surgical day through 10 postoperative days.
Global Surgical Package Components2
The global surgical package comprises a host of responsibilities that include standard facility requirements of filling out all necessary paperwork involved in surgical cases (e.g. preoperative H&P, operative consent forms, preoperative orders). Additionally, the surgeon’s packaged payment includes (at no extra charge):
- Preoperative visits after making the decision for surgery beginning one day prior to surgery;
- All additional postoperative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Postoperative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Postoperative pain management provided by the surgeon.
- Examples of services that are not included in the global surgical package, (i.e. are separately billable and may require an appropriate modifier) are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care (i.e. a formal agreement in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record);
- Postoperative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the postoperative period that do not result in repeat operations or treatment for complications;
- Treatment for postoperative complications that requires a return trip to the operating room (OR), catheterization lab or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical-care services (CPT codes 99291 and 99292) unrelated to the surgery where a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon.
Classification of “Surgeon”
For billing purposes, the “surgeon” is a qualified physician who can perform “surgical” services within their scope of practice. All physicians with the same specialty designation in the same group practice as the “surgeon” (i.e. reporting services under the same tax identification number) are considered a single entity and must adhere to the global period billing rules initiated by the “surgeon.”
Alternately, physicians with different specialty designations in the same group practice (e.g. a hospitalist and a cardiologist in a multispecialty group who report services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed-upon) transfer of care did not occur.
Medical Necessity
With the growth of HM programs and the admission/attending role expansion, involvement in surgical cases comes under scrutiny for medical necessity. Admitting a patient who has active medical conditions (e.g. hypertension, diabetes, emphysema) is reasonable and necessary because the patient has a well-defined need for medical management by the hospitalist. Participation in the care of these patients is separately billable from the surgeon’s global period package.
Alternatively, a hospitalist might be required to admit and follow surgical patients who have no other identifiable chronic or acute conditions aside from the surgical problem. In these cases, hospitalist involvement may satisfy facility policy (quality of care, risk reduction, etc.) and administrative functions (discharge services or coordination of care) rather than active clinical management. This “medical management” will not be considered “medically necessary” by the payor, and may be denied as incidental to the surgeon’s perioperative services. Erroneous payment can occur, which will result in refund requests, as payors do not want to pay twice for duplicate services. Hospitalists can attempt to negotiate other terms with facilities to account for the unpaid time and effort directed toward these types of cases.
Consider the Case
A patient with numerous medical comorbidities is admitted to the hospitalist service for stabilization prior to surgery, which will occur the next day. The hospitalist can report the appropriate admission code (99221-99223) without need for modifiers because the hospitalist is the attending of record and in a different specialty group. If a private insurer denies the claim as inclusive to the surgical service, the hospitalist can appeal with notes and a cover letter, along with the Medicare guidelines for global surgical package. The hospitalist may continue to provide postoperative daily care, as needed, to manage the patient’s chronic conditions, and report each service as subsequent hospital care (99231-99233) without modifier until the day of discharge (99238-99239). Again, if a payor issues a denial (inclusive to surgery), appealing with notes might be necessary.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 40. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed May 5, 2012.
- Centers for Medicare & Medicaid Services. ICD-10: HHS proposes one-year delay of ICD-10 compliance date. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Medicare/Coding/ICD10/index.html?redirect=/ICD10. Accessed May 5, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
Should Pediatric HM Pursue Subspecialty Certification, Required Fellowship Training?
PRO
A powerful tool, subspecialty certification should be adopted—and soon
There are many different ways for pediatric hospital medicine to evolve and gain recognition. Board certification with required fellowship training is the most well-known method. For adult hospitalists, recognition of Focused Practice in Hospital Medicine (FPHM) has been established. Residency programs are becoming more innovative, creating additional tracks to provide accelerated fellowship education. What path should be chosen for the future of pediatric hospital medicine?
The decision could be compared to purchasing a cellphone. Simple flip phones are sufficient for making phone calls, just as a graduating pediatrics resident might care for routine inpatients. But the smartphone, like the fellowship/subspecialty certification route, provides advantages that could be worth the additional costs.
You can tell a lot about a person by looking at their cellphone. It often reveals personality traits, professions, and behavioral tendencies. Similarly, administrators, colleagues, and other payors might make assumptions based on fellowship/subspecialty certification status. Pediatric hospitalists should be considered experts in the field of clinical HM, hospital-based research, quality improvement (QI), inpatient procedures, and administrative leadership. Fellowship directors have begun discussing how to standardize these content areas. Subspecialty certification after such training will provide a powerful tool for hospitalists to navigate potentially complex clinical scenarios, hospital bureaucracies and/or academic hierarchies. Fellowship training will add a more concrete identity and standards of quality to our subspecialty.
Smartphones are “smart” because they bring convenience and efficiency. The same can be said about fellowship training. Residency training no longer addresses all the needs of a practicing hospitalist. Although one can attend workshops on QI or research and learn hospital administration, all while on the job, many young hospitalists struggle to adapt quickly early in their career; they might fail to thrive. Fellowship programs would provide a learner-centered environment and protected time to accomplish these goals. Certification would help ensure that trainees have the knowledge and competencies needed for the job. This process, designed to create a well-prepared hospitalist work force, should lead to better advancement within the field, which would mean more hospitalists in meaningful leadership roles and improved quality of hospital care.
The cost of a cellphone and its monthly plan must be taken into account when choosing what purchase. Similarly, the benefits of additional education and recognition must be measured against the costs of additional training. For most, the benefits of well-trained hospitalists outweigh the costs in the long run. Concerns of alienating those without board certification or limiting the work force likely are unfounded. The majority of EDs are staffed by general emergency medicine physicians who do not have pediatric emergency medicine certification—and they all see children, and provide referrals to dedicated children’s facilities when needed. Similarly, community hospital wards can choose to follow suit, depending on their needs.
Fellowship training and subspecialty board certification offer numerous benefits that likely outweigh the costs of a new “plan.” We don’t want just anyone on call; we want a future full of smart hospitalists who are leading practitioners of QI, education, and scholarship.
Dr. Chen is assistant professor in the department of pediatrics at the University of Texas Southwestern in Dallas.
CON
One-size-fits-all approach is not what pediatric hospitalists need
According to Freed et al in the Journal of Hospital Medicine, the central goals of a fellowship in pediatric HM include “advanced training in the clinical care of hospitalized patients, quality improvement (QI), and hospital administration.”1 To determine if certification within pediatric hospital medicine should require a fellowship, it is necessary to decide if there are additional skills beyond those obtained during a pediatric residency that are required for practice as a pediatric hospitalist.
Pediatric residencies are designed to provide residents with the skills to practice in the field of general pediatrics. According to Accreditation Council for Graduate Medical Education (ACGME) standards, just 40% of a resident’s training is required to be in the outpatient setting. There is the expectation that at the end of three years, a resident is capable of spending 95% of their practice in the primary-care setting despite spending less than half of their training in outpatient medicine.
Having a greater focus on inpatient medicine during residency provides a knowledge base that is adequate to start an HM career. As intended, the amount of training dedicated to inpatient and outpatient care in a pediatric residency program is adequate to achieve the skills that make them capable of practicing both inpatient and outpatient care.
Although Freed stated the goal of advanced training, it is unclear what specialized body of knowledge would be gained during a fellowship. The need for advanced clinical training is a concept that is a careerlong, neverending endeavor. Even if this were the reason to require a fellowship, how long is long enough to have mastered clinical care?
One year? Two years? 35 years? If more than half of a three-year residency is not enough time to provide residents the education and training to care for hospitalized inpatients, we should not require more training; we should fix our current training system.
Administrative experience and training in QI and research are important skills that can help advance a hospitalist’s career. It is important to recognize that because these skills are not required for all pediatric hospitalist positions, it would be unnecessary for all hospitalists to attain these skills in a fellowship. In addition, for those interested in administration or research, there are many other ways to attain those skills, including the APA educational scholars program or obtaining a master’s degree in medical education. The added benefit of these avenues for additional skills is that they can be completed throughout a career as a pediatric hospitalist.
As pediatric hospital medicine is a field in its early stages, it is important to consider all options for certification. While fellowship training has been the path for many subspecialties within pediatrics, HM will be better served by recognizing the need to remain inclusive. The positions within HM are broad, and the training should be individualized for the skills each physician requires.
Dr. Eagle is a hospitalist in the general medicine service at The Joseph M. Sanzari Children’s Hospital at Hackensack University Medical Center in New Jersey.
Reference
- Freed G, Dunham K. Characteristics of pediatric hospital medicine fellowships and training programs. J Hosp Med. 2009;4(3):157-163.
PRO
A powerful tool, subspecialty certification should be adopted—and soon
There are many different ways for pediatric hospital medicine to evolve and gain recognition. Board certification with required fellowship training is the most well-known method. For adult hospitalists, recognition of Focused Practice in Hospital Medicine (FPHM) has been established. Residency programs are becoming more innovative, creating additional tracks to provide accelerated fellowship education. What path should be chosen for the future of pediatric hospital medicine?
The decision could be compared to purchasing a cellphone. Simple flip phones are sufficient for making phone calls, just as a graduating pediatrics resident might care for routine inpatients. But the smartphone, like the fellowship/subspecialty certification route, provides advantages that could be worth the additional costs.
You can tell a lot about a person by looking at their cellphone. It often reveals personality traits, professions, and behavioral tendencies. Similarly, administrators, colleagues, and other payors might make assumptions based on fellowship/subspecialty certification status. Pediatric hospitalists should be considered experts in the field of clinical HM, hospital-based research, quality improvement (QI), inpatient procedures, and administrative leadership. Fellowship directors have begun discussing how to standardize these content areas. Subspecialty certification after such training will provide a powerful tool for hospitalists to navigate potentially complex clinical scenarios, hospital bureaucracies and/or academic hierarchies. Fellowship training will add a more concrete identity and standards of quality to our subspecialty.
Smartphones are “smart” because they bring convenience and efficiency. The same can be said about fellowship training. Residency training no longer addresses all the needs of a practicing hospitalist. Although one can attend workshops on QI or research and learn hospital administration, all while on the job, many young hospitalists struggle to adapt quickly early in their career; they might fail to thrive. Fellowship programs would provide a learner-centered environment and protected time to accomplish these goals. Certification would help ensure that trainees have the knowledge and competencies needed for the job. This process, designed to create a well-prepared hospitalist work force, should lead to better advancement within the field, which would mean more hospitalists in meaningful leadership roles and improved quality of hospital care.
The cost of a cellphone and its monthly plan must be taken into account when choosing what purchase. Similarly, the benefits of additional education and recognition must be measured against the costs of additional training. For most, the benefits of well-trained hospitalists outweigh the costs in the long run. Concerns of alienating those without board certification or limiting the work force likely are unfounded. The majority of EDs are staffed by general emergency medicine physicians who do not have pediatric emergency medicine certification—and they all see children, and provide referrals to dedicated children’s facilities when needed. Similarly, community hospital wards can choose to follow suit, depending on their needs.
Fellowship training and subspecialty board certification offer numerous benefits that likely outweigh the costs of a new “plan.” We don’t want just anyone on call; we want a future full of smart hospitalists who are leading practitioners of QI, education, and scholarship.
Dr. Chen is assistant professor in the department of pediatrics at the University of Texas Southwestern in Dallas.
CON
One-size-fits-all approach is not what pediatric hospitalists need
According to Freed et al in the Journal of Hospital Medicine, the central goals of a fellowship in pediatric HM include “advanced training in the clinical care of hospitalized patients, quality improvement (QI), and hospital administration.”1 To determine if certification within pediatric hospital medicine should require a fellowship, it is necessary to decide if there are additional skills beyond those obtained during a pediatric residency that are required for practice as a pediatric hospitalist.
Pediatric residencies are designed to provide residents with the skills to practice in the field of general pediatrics. According to Accreditation Council for Graduate Medical Education (ACGME) standards, just 40% of a resident’s training is required to be in the outpatient setting. There is the expectation that at the end of three years, a resident is capable of spending 95% of their practice in the primary-care setting despite spending less than half of their training in outpatient medicine.
Having a greater focus on inpatient medicine during residency provides a knowledge base that is adequate to start an HM career. As intended, the amount of training dedicated to inpatient and outpatient care in a pediatric residency program is adequate to achieve the skills that make them capable of practicing both inpatient and outpatient care.
Although Freed stated the goal of advanced training, it is unclear what specialized body of knowledge would be gained during a fellowship. The need for advanced clinical training is a concept that is a careerlong, neverending endeavor. Even if this were the reason to require a fellowship, how long is long enough to have mastered clinical care?
One year? Two years? 35 years? If more than half of a three-year residency is not enough time to provide residents the education and training to care for hospitalized inpatients, we should not require more training; we should fix our current training system.
Administrative experience and training in QI and research are important skills that can help advance a hospitalist’s career. It is important to recognize that because these skills are not required for all pediatric hospitalist positions, it would be unnecessary for all hospitalists to attain these skills in a fellowship. In addition, for those interested in administration or research, there are many other ways to attain those skills, including the APA educational scholars program or obtaining a master’s degree in medical education. The added benefit of these avenues for additional skills is that they can be completed throughout a career as a pediatric hospitalist.
As pediatric hospital medicine is a field in its early stages, it is important to consider all options for certification. While fellowship training has been the path for many subspecialties within pediatrics, HM will be better served by recognizing the need to remain inclusive. The positions within HM are broad, and the training should be individualized for the skills each physician requires.
Dr. Eagle is a hospitalist in the general medicine service at The Joseph M. Sanzari Children’s Hospital at Hackensack University Medical Center in New Jersey.
Reference
- Freed G, Dunham K. Characteristics of pediatric hospital medicine fellowships and training programs. J Hosp Med. 2009;4(3):157-163.
PRO
A powerful tool, subspecialty certification should be adopted—and soon
There are many different ways for pediatric hospital medicine to evolve and gain recognition. Board certification with required fellowship training is the most well-known method. For adult hospitalists, recognition of Focused Practice in Hospital Medicine (FPHM) has been established. Residency programs are becoming more innovative, creating additional tracks to provide accelerated fellowship education. What path should be chosen for the future of pediatric hospital medicine?
The decision could be compared to purchasing a cellphone. Simple flip phones are sufficient for making phone calls, just as a graduating pediatrics resident might care for routine inpatients. But the smartphone, like the fellowship/subspecialty certification route, provides advantages that could be worth the additional costs.
You can tell a lot about a person by looking at their cellphone. It often reveals personality traits, professions, and behavioral tendencies. Similarly, administrators, colleagues, and other payors might make assumptions based on fellowship/subspecialty certification status. Pediatric hospitalists should be considered experts in the field of clinical HM, hospital-based research, quality improvement (QI), inpatient procedures, and administrative leadership. Fellowship directors have begun discussing how to standardize these content areas. Subspecialty certification after such training will provide a powerful tool for hospitalists to navigate potentially complex clinical scenarios, hospital bureaucracies and/or academic hierarchies. Fellowship training will add a more concrete identity and standards of quality to our subspecialty.
Smartphones are “smart” because they bring convenience and efficiency. The same can be said about fellowship training. Residency training no longer addresses all the needs of a practicing hospitalist. Although one can attend workshops on QI or research and learn hospital administration, all while on the job, many young hospitalists struggle to adapt quickly early in their career; they might fail to thrive. Fellowship programs would provide a learner-centered environment and protected time to accomplish these goals. Certification would help ensure that trainees have the knowledge and competencies needed for the job. This process, designed to create a well-prepared hospitalist work force, should lead to better advancement within the field, which would mean more hospitalists in meaningful leadership roles and improved quality of hospital care.
The cost of a cellphone and its monthly plan must be taken into account when choosing what purchase. Similarly, the benefits of additional education and recognition must be measured against the costs of additional training. For most, the benefits of well-trained hospitalists outweigh the costs in the long run. Concerns of alienating those without board certification or limiting the work force likely are unfounded. The majority of EDs are staffed by general emergency medicine physicians who do not have pediatric emergency medicine certification—and they all see children, and provide referrals to dedicated children’s facilities when needed. Similarly, community hospital wards can choose to follow suit, depending on their needs.
Fellowship training and subspecialty board certification offer numerous benefits that likely outweigh the costs of a new “plan.” We don’t want just anyone on call; we want a future full of smart hospitalists who are leading practitioners of QI, education, and scholarship.
Dr. Chen is assistant professor in the department of pediatrics at the University of Texas Southwestern in Dallas.
CON
One-size-fits-all approach is not what pediatric hospitalists need
According to Freed et al in the Journal of Hospital Medicine, the central goals of a fellowship in pediatric HM include “advanced training in the clinical care of hospitalized patients, quality improvement (QI), and hospital administration.”1 To determine if certification within pediatric hospital medicine should require a fellowship, it is necessary to decide if there are additional skills beyond those obtained during a pediatric residency that are required for practice as a pediatric hospitalist.
Pediatric residencies are designed to provide residents with the skills to practice in the field of general pediatrics. According to Accreditation Council for Graduate Medical Education (ACGME) standards, just 40% of a resident’s training is required to be in the outpatient setting. There is the expectation that at the end of three years, a resident is capable of spending 95% of their practice in the primary-care setting despite spending less than half of their training in outpatient medicine.
Having a greater focus on inpatient medicine during residency provides a knowledge base that is adequate to start an HM career. As intended, the amount of training dedicated to inpatient and outpatient care in a pediatric residency program is adequate to achieve the skills that make them capable of practicing both inpatient and outpatient care.
Although Freed stated the goal of advanced training, it is unclear what specialized body of knowledge would be gained during a fellowship. The need for advanced clinical training is a concept that is a careerlong, neverending endeavor. Even if this were the reason to require a fellowship, how long is long enough to have mastered clinical care?
One year? Two years? 35 years? If more than half of a three-year residency is not enough time to provide residents the education and training to care for hospitalized inpatients, we should not require more training; we should fix our current training system.
Administrative experience and training in QI and research are important skills that can help advance a hospitalist’s career. It is important to recognize that because these skills are not required for all pediatric hospitalist positions, it would be unnecessary for all hospitalists to attain these skills in a fellowship. In addition, for those interested in administration or research, there are many other ways to attain those skills, including the APA educational scholars program or obtaining a master’s degree in medical education. The added benefit of these avenues for additional skills is that they can be completed throughout a career as a pediatric hospitalist.
As pediatric hospital medicine is a field in its early stages, it is important to consider all options for certification. While fellowship training has been the path for many subspecialties within pediatrics, HM will be better served by recognizing the need to remain inclusive. The positions within HM are broad, and the training should be individualized for the skills each physician requires.
Dr. Eagle is a hospitalist in the general medicine service at The Joseph M. Sanzari Children’s Hospital at Hackensack University Medical Center in New Jersey.
Reference
- Freed G, Dunham K. Characteristics of pediatric hospital medicine fellowships and training programs. J Hosp Med. 2009;4(3):157-163.
Demographics Correlate with Physician Web Technology Use
A new study in the Journal of the American Medical Informatics Association offers demographic predictors of physicians and their usage of web-based communication technologies.1 Younger, male doctors who have privileges at a teaching hospital were better predictors of the use of various technologies during the previous six months than were practice-based characteristics, such as specialty, setting, years in practice, or number of patients treated. Communication strategies tallied included using portable devices to access the Internet, visiting social networking websites, communicating by email with patients, listening to podcasts, or writing blog posts.
Lead author Crystale Purvis Cooper, PhD, a researcher at the Soltera Center for Cancer Prevention and Control in Tucson, Ariz., and colleagues drew upon 2009 data from 1,750 physicians in DocStyles, an annual survey of physicians and other health professionals conducted by communications firm Porter Novelli.
References
A new study in the Journal of the American Medical Informatics Association offers demographic predictors of physicians and their usage of web-based communication technologies.1 Younger, male doctors who have privileges at a teaching hospital were better predictors of the use of various technologies during the previous six months than were practice-based characteristics, such as specialty, setting, years in practice, or number of patients treated. Communication strategies tallied included using portable devices to access the Internet, visiting social networking websites, communicating by email with patients, listening to podcasts, or writing blog posts.
Lead author Crystale Purvis Cooper, PhD, a researcher at the Soltera Center for Cancer Prevention and Control in Tucson, Ariz., and colleagues drew upon 2009 data from 1,750 physicians in DocStyles, an annual survey of physicians and other health professionals conducted by communications firm Porter Novelli.
References
A new study in the Journal of the American Medical Informatics Association offers demographic predictors of physicians and their usage of web-based communication technologies.1 Younger, male doctors who have privileges at a teaching hospital were better predictors of the use of various technologies during the previous six months than were practice-based characteristics, such as specialty, setting, years in practice, or number of patients treated. Communication strategies tallied included using portable devices to access the Internet, visiting social networking websites, communicating by email with patients, listening to podcasts, or writing blog posts.
Lead author Crystale Purvis Cooper, PhD, a researcher at the Soltera Center for Cancer Prevention and Control in Tucson, Ariz., and colleagues drew upon 2009 data from 1,750 physicians in DocStyles, an annual survey of physicians and other health professionals conducted by communications firm Porter Novelli.
References
Hospitalist-Run Observation Unit Demonstrates Financial Viability
A hospital observation unit run by hospitalists rather than the more typical model led by ED physicians can be financially viable, suggests an abstract presented at HM12 in April in San Diego. One such unit generated $915,000 in facility fee charges, and during a three-month audit posted net revenue of $49,000; the unit also reduced patients’ length of stay (LOS) on observation status by 25%, according to lead author Mary Maher, MD, a hospitalist at Denver Health Medical Center.1
Previously, Denver Health’s ED had informally operated a small observation unit, primarily for patients with such diagnoses as low-risk chest pain. But due to increasing numbers of observation admissions and the need to manage their flow through the typically full safety-net teaching hospital, the hospitalist department was asked in 2011 to develop a new, hospitalist-run unit, Dr. Maher explains.
In its first six months of operation, the five-bed observation unit cared for 648 patients, with 12% admitted to the hospital. A single hospitalist and mid-level practitioner cover each shift, with additional responsibilities for managing patient flow and new hospital admissions. Dr. Maher says specialized nursing staffers are now familiar with the hospital’s admission criteria and care pathways for common diagnoses. A typical observation patient has chest pain and a history of coronary artery disease but negative clinical markers. Other common diagnoses, with established clinical pathways and discharge criteria, include asthma, syncope, COPD, and gastrointestinal illness.
“Hospitalists are primed to take care of patients who are in this observation status,” Dr. Maher says. “They are a little more complex than patients typically seen in emergency department units. The challenge for hospitalists is to understand the hospital’s admission guidelines and to work collaboratively with utilization management staff.”
Denver Health uses the Milliman Care Guidelines to guide inpatient admissions, but these can be difficult to translate into clinical practice and require some study by physicians, she adds.2 For more information about the poster and the unit, email [email protected].
References
- Maher M, Mascolo M, Mancini D, et al. Creation of a financially viable hospitalist-run observation unit in a safety net hospital. Paper presented at Hospital Medicine 2012, April 1-4, 2012, San Diego.
- Milliman Inc. Milliman Care Guidelines. Milliman Inc. website. Available at: http://www.milliman.com/expertise/healthcare/products-tools/milliman-care-guidelines/. Accessed July 8, 2012.
A hospital observation unit run by hospitalists rather than the more typical model led by ED physicians can be financially viable, suggests an abstract presented at HM12 in April in San Diego. One such unit generated $915,000 in facility fee charges, and during a three-month audit posted net revenue of $49,000; the unit also reduced patients’ length of stay (LOS) on observation status by 25%, according to lead author Mary Maher, MD, a hospitalist at Denver Health Medical Center.1
Previously, Denver Health’s ED had informally operated a small observation unit, primarily for patients with such diagnoses as low-risk chest pain. But due to increasing numbers of observation admissions and the need to manage their flow through the typically full safety-net teaching hospital, the hospitalist department was asked in 2011 to develop a new, hospitalist-run unit, Dr. Maher explains.
In its first six months of operation, the five-bed observation unit cared for 648 patients, with 12% admitted to the hospital. A single hospitalist and mid-level practitioner cover each shift, with additional responsibilities for managing patient flow and new hospital admissions. Dr. Maher says specialized nursing staffers are now familiar with the hospital’s admission criteria and care pathways for common diagnoses. A typical observation patient has chest pain and a history of coronary artery disease but negative clinical markers. Other common diagnoses, with established clinical pathways and discharge criteria, include asthma, syncope, COPD, and gastrointestinal illness.
“Hospitalists are primed to take care of patients who are in this observation status,” Dr. Maher says. “They are a little more complex than patients typically seen in emergency department units. The challenge for hospitalists is to understand the hospital’s admission guidelines and to work collaboratively with utilization management staff.”
Denver Health uses the Milliman Care Guidelines to guide inpatient admissions, but these can be difficult to translate into clinical practice and require some study by physicians, she adds.2 For more information about the poster and the unit, email [email protected].
References
- Maher M, Mascolo M, Mancini D, et al. Creation of a financially viable hospitalist-run observation unit in a safety net hospital. Paper presented at Hospital Medicine 2012, April 1-4, 2012, San Diego.
- Milliman Inc. Milliman Care Guidelines. Milliman Inc. website. Available at: http://www.milliman.com/expertise/healthcare/products-tools/milliman-care-guidelines/. Accessed July 8, 2012.
A hospital observation unit run by hospitalists rather than the more typical model led by ED physicians can be financially viable, suggests an abstract presented at HM12 in April in San Diego. One such unit generated $915,000 in facility fee charges, and during a three-month audit posted net revenue of $49,000; the unit also reduced patients’ length of stay (LOS) on observation status by 25%, according to lead author Mary Maher, MD, a hospitalist at Denver Health Medical Center.1
Previously, Denver Health’s ED had informally operated a small observation unit, primarily for patients with such diagnoses as low-risk chest pain. But due to increasing numbers of observation admissions and the need to manage their flow through the typically full safety-net teaching hospital, the hospitalist department was asked in 2011 to develop a new, hospitalist-run unit, Dr. Maher explains.
In its first six months of operation, the five-bed observation unit cared for 648 patients, with 12% admitted to the hospital. A single hospitalist and mid-level practitioner cover each shift, with additional responsibilities for managing patient flow and new hospital admissions. Dr. Maher says specialized nursing staffers are now familiar with the hospital’s admission criteria and care pathways for common diagnoses. A typical observation patient has chest pain and a history of coronary artery disease but negative clinical markers. Other common diagnoses, with established clinical pathways and discharge criteria, include asthma, syncope, COPD, and gastrointestinal illness.
“Hospitalists are primed to take care of patients who are in this observation status,” Dr. Maher says. “They are a little more complex than patients typically seen in emergency department units. The challenge for hospitalists is to understand the hospital’s admission guidelines and to work collaboratively with utilization management staff.”
Denver Health uses the Milliman Care Guidelines to guide inpatient admissions, but these can be difficult to translate into clinical practice and require some study by physicians, she adds.2 For more information about the poster and the unit, email [email protected].
References
- Maher M, Mascolo M, Mancini D, et al. Creation of a financially viable hospitalist-run observation unit in a safety net hospital. Paper presented at Hospital Medicine 2012, April 1-4, 2012, San Diego.
- Milliman Inc. Milliman Care Guidelines. Milliman Inc. website. Available at: http://www.milliman.com/expertise/healthcare/products-tools/milliman-care-guidelines/. Accessed July 8, 2012.
Win Whitcomb: Spotlight on Medical Necessity
EDITOR’S NOTE: An incorrect version of Win Whitcomb’s “On the Horizon” column was published in the July issue of The Hospitalist. We deeply regret the error. The correct version of Dr. Whitcomb’s column appears this month, with proper attribution given to hospitalist Brad Flansbaum, DO, SFHM, who contributed to the column.
Assigning the appropriate status to patients (“inpatient” or “observation”) has emerged as a front-and-center issue for hospitalists. Also known as “medical necessity,” many HM groups have been called upon to help solve the “status” problem for their institutions. With nearly 1 in 5 hospitalized patients on observation status in U.S. hospitals, appropriately assigning status is now a dominant, system-level challenge for hospitalists.
This month, we asked two experts to shed light on the nature of this beast, with a focus on the impact on the patient. Brad Flansbaum, DO, SFHM, hospitalist at Lenox Hill Hospital in New York City, and Patrick Conway, MD, FAAP, MSC, SFHM, chief medical officer at the Centers for Medicare & Medicaid Services (CMS), were kind enough to participate in the interview. We start with Dr. Flansbaum.
Dr. Whitcomb: It appears that patients are caught in the middle of the observation status challenge, at least as it relates to footing the bill. Explain the patient perspective of being unwittingly placed on observation status.
Dr. Flansbaum: Recall your last credit card statement. On it is the hotel charge from your last out-of-town CME excursion. Below the total charge, which you were expecting, is a separate line item for a $75 “recreational fee.” You call the hotel, and they inform you that, because you used the hotel gym and pool—accessed with your room key, they levied the fee. No signs, alerts, or postings denoted the policy, so you expected inclusive use of the facilities as a price of your visit. Capture the emotion of the moment, when you see that bill, feel your heart race, and think to yourself, “Get me the manager!”
WW: Why has assigning appropriate status captured the attention of hospitals?
BF: Out of vigilance for penalties and fraud from recovery audit contractor (RAC) investigations, as well attentiveness to unnecessary readmissions, hospitals increasingly are categorizing patients under observation, rather than inpatient, status to avoid conflict with regulators. Beneficiaries are in the crosshairs because of this designation change, and much in the same way of our hotel charge, our patients experience sticker shock when they receive their bill. It is leading to confusion among providers and consternation within the Medicare recipient community.
WW: Why is there so much confusion around appropriate patient status?
BF: The dilemma stems from Medicare payment, and the key distinction between inpatient coverage (Part A) and outpatient coverage, including pharmaceuticals (Parts B and D). When a patient receives their discharge notification—without an “official” inpatient designation, sometimes staying greater than 24 to 48 hours in the ED or in a specially defined observation unit, beneficiary charges are different. This could result in discrete—and sometimes jolting—enrollee copayments and deductibles for drugs and services.
WW: I’ve heard observation status is having a big, adverse impact on patients who go to skilled nursing facilities. Why?
BF: If a patient requires a skilled nursing facility stay (the “three-day stay” inpatient requirement), Medicare will not pay because the patient never registered “official” hospital time. Patients and caregivers are not prepared for the unexpected bills, and consequently, tempers are rising. The rules for Medicare Advantage enrollees (Part C—commercial payers receive a fixed sum from CMS, and oversee parts A, B, and D for an individual beneficiary), which comprise 25% of the program, differ from conventional Medicare. However, commercial plans often shadow traditional, fee-for-service in their policies and, consequently, no exemplar of success in this realm exits.
WW: Why is the number of patients on observation status growing?
BF: Hospitals have significantly increased both the number of their observation stays, as well as their hourly lengths (>48 hours). Because the definition of “observation status” is vague, and even the one- to two-day window is inflating, hospitals and hospitalists often are navigating without a compass. Again, fear of fraud and penalty places hospitals and, indirectly, hospitalists—who often make judgments on admission grade—in a precarious position.
The responsibility of hospitals to notify beneficiaries of their status hinges on this murky determination milieu, which may change in real time during the stay, and makes for an unsatisfactory standard. Understandably, CMS is attempting to rectify this quandary, taking into account a hospital’s need to clarify its billing and designation practices, as well as the beneficiaries’ desire to obtain clear guidance on their responsibilities both during and after the stay. Hospitalists, of course, want direction on coding, along with an understanding of the impact their decisions will have on patients and subspecialty colleagues.
Let’s now bring in Dr. Conway, a pediatric hospitalist. I thank Dr. Flansbaum, who formulated the following questions.
BF/WW: Is it tenable to keep the current system in place? Would it help to require payors and providers to inform beneficiaries of inpatient versus observation status at time zero in a more rigorous, yet to-be-determined manner?
Dr. Conway: Current regulations only require CMS to inform beneficiaries when they are admitted as an inpatient and not when they are an outpatient receiving observation services. There are important implications for beneficiary coverage post-hospital stay, coverage of self-administered drugs, and beneficiary coinsurance from this distinction. As a hospitalist, I think it is best to inform the patient of their status, especially if it has the potential to impact beneficiary liability, including coverage of post-acute care. CMS prepared a pamphlet in 2009, “Are You a Hospital Inpatient or Outpatient? If You Have Medicare, Ask,” to educate beneficiaries on this issue. (Download a PDF of the pamphlet at www.medicare.gov/Publications/Pubs/pdf/11435.pdf.)
BF/WW: Due to the nature of how hospital care is changing, are admission decisions potentially becoming too conflicted an endeavor for inpatient caregivers?
PC: We want admission decisions to be based on clinical considerations. The decision to admit a patient should be based on the clinical judgment of the primary-care, emergency medicine, and/or HM clinician.
BF/WW: Before the U.S. healthcare system matures to a more full-out, integrated model with internalized risk, can you envision any near-term code changes that might simplify the difficulties all parties are facing, in a budget-neutral fashion?
PC: CMS is currently investigating options to clarify when it is appropriate to admit the patient as an inpatient versus keeping the patient as an outpatient receiving observation services. We understand that this issue is of concern to hospitals, hospitalists, and patients, and we are considering carefully how to simplify the rules in a way that best meets the needs of patients and providers without increasing costs to the system.
With growing attention to observation status coming from patients and provider groups (the AMA is requesting that CMS revise its coverage rules), we will no doubt be hearing more about this going forward.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
EDITOR’S NOTE: An incorrect version of Win Whitcomb’s “On the Horizon” column was published in the July issue of The Hospitalist. We deeply regret the error. The correct version of Dr. Whitcomb’s column appears this month, with proper attribution given to hospitalist Brad Flansbaum, DO, SFHM, who contributed to the column.
Assigning the appropriate status to patients (“inpatient” or “observation”) has emerged as a front-and-center issue for hospitalists. Also known as “medical necessity,” many HM groups have been called upon to help solve the “status” problem for their institutions. With nearly 1 in 5 hospitalized patients on observation status in U.S. hospitals, appropriately assigning status is now a dominant, system-level challenge for hospitalists.
This month, we asked two experts to shed light on the nature of this beast, with a focus on the impact on the patient. Brad Flansbaum, DO, SFHM, hospitalist at Lenox Hill Hospital in New York City, and Patrick Conway, MD, FAAP, MSC, SFHM, chief medical officer at the Centers for Medicare & Medicaid Services (CMS), were kind enough to participate in the interview. We start with Dr. Flansbaum.
Dr. Whitcomb: It appears that patients are caught in the middle of the observation status challenge, at least as it relates to footing the bill. Explain the patient perspective of being unwittingly placed on observation status.
Dr. Flansbaum: Recall your last credit card statement. On it is the hotel charge from your last out-of-town CME excursion. Below the total charge, which you were expecting, is a separate line item for a $75 “recreational fee.” You call the hotel, and they inform you that, because you used the hotel gym and pool—accessed with your room key, they levied the fee. No signs, alerts, or postings denoted the policy, so you expected inclusive use of the facilities as a price of your visit. Capture the emotion of the moment, when you see that bill, feel your heart race, and think to yourself, “Get me the manager!”
WW: Why has assigning appropriate status captured the attention of hospitals?
BF: Out of vigilance for penalties and fraud from recovery audit contractor (RAC) investigations, as well attentiveness to unnecessary readmissions, hospitals increasingly are categorizing patients under observation, rather than inpatient, status to avoid conflict with regulators. Beneficiaries are in the crosshairs because of this designation change, and much in the same way of our hotel charge, our patients experience sticker shock when they receive their bill. It is leading to confusion among providers and consternation within the Medicare recipient community.
WW: Why is there so much confusion around appropriate patient status?
BF: The dilemma stems from Medicare payment, and the key distinction between inpatient coverage (Part A) and outpatient coverage, including pharmaceuticals (Parts B and D). When a patient receives their discharge notification—without an “official” inpatient designation, sometimes staying greater than 24 to 48 hours in the ED or in a specially defined observation unit, beneficiary charges are different. This could result in discrete—and sometimes jolting—enrollee copayments and deductibles for drugs and services.
WW: I’ve heard observation status is having a big, adverse impact on patients who go to skilled nursing facilities. Why?
BF: If a patient requires a skilled nursing facility stay (the “three-day stay” inpatient requirement), Medicare will not pay because the patient never registered “official” hospital time. Patients and caregivers are not prepared for the unexpected bills, and consequently, tempers are rising. The rules for Medicare Advantage enrollees (Part C—commercial payers receive a fixed sum from CMS, and oversee parts A, B, and D for an individual beneficiary), which comprise 25% of the program, differ from conventional Medicare. However, commercial plans often shadow traditional, fee-for-service in their policies and, consequently, no exemplar of success in this realm exits.
WW: Why is the number of patients on observation status growing?
BF: Hospitals have significantly increased both the number of their observation stays, as well as their hourly lengths (>48 hours). Because the definition of “observation status” is vague, and even the one- to two-day window is inflating, hospitals and hospitalists often are navigating without a compass. Again, fear of fraud and penalty places hospitals and, indirectly, hospitalists—who often make judgments on admission grade—in a precarious position.
The responsibility of hospitals to notify beneficiaries of their status hinges on this murky determination milieu, which may change in real time during the stay, and makes for an unsatisfactory standard. Understandably, CMS is attempting to rectify this quandary, taking into account a hospital’s need to clarify its billing and designation practices, as well as the beneficiaries’ desire to obtain clear guidance on their responsibilities both during and after the stay. Hospitalists, of course, want direction on coding, along with an understanding of the impact their decisions will have on patients and subspecialty colleagues.
Let’s now bring in Dr. Conway, a pediatric hospitalist. I thank Dr. Flansbaum, who formulated the following questions.
BF/WW: Is it tenable to keep the current system in place? Would it help to require payors and providers to inform beneficiaries of inpatient versus observation status at time zero in a more rigorous, yet to-be-determined manner?
Dr. Conway: Current regulations only require CMS to inform beneficiaries when they are admitted as an inpatient and not when they are an outpatient receiving observation services. There are important implications for beneficiary coverage post-hospital stay, coverage of self-administered drugs, and beneficiary coinsurance from this distinction. As a hospitalist, I think it is best to inform the patient of their status, especially if it has the potential to impact beneficiary liability, including coverage of post-acute care. CMS prepared a pamphlet in 2009, “Are You a Hospital Inpatient or Outpatient? If You Have Medicare, Ask,” to educate beneficiaries on this issue. (Download a PDF of the pamphlet at www.medicare.gov/Publications/Pubs/pdf/11435.pdf.)
BF/WW: Due to the nature of how hospital care is changing, are admission decisions potentially becoming too conflicted an endeavor for inpatient caregivers?
PC: We want admission decisions to be based on clinical considerations. The decision to admit a patient should be based on the clinical judgment of the primary-care, emergency medicine, and/or HM clinician.
BF/WW: Before the U.S. healthcare system matures to a more full-out, integrated model with internalized risk, can you envision any near-term code changes that might simplify the difficulties all parties are facing, in a budget-neutral fashion?
PC: CMS is currently investigating options to clarify when it is appropriate to admit the patient as an inpatient versus keeping the patient as an outpatient receiving observation services. We understand that this issue is of concern to hospitals, hospitalists, and patients, and we are considering carefully how to simplify the rules in a way that best meets the needs of patients and providers without increasing costs to the system.
With growing attention to observation status coming from patients and provider groups (the AMA is requesting that CMS revise its coverage rules), we will no doubt be hearing more about this going forward.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
EDITOR’S NOTE: An incorrect version of Win Whitcomb’s “On the Horizon” column was published in the July issue of The Hospitalist. We deeply regret the error. The correct version of Dr. Whitcomb’s column appears this month, with proper attribution given to hospitalist Brad Flansbaum, DO, SFHM, who contributed to the column.
Assigning the appropriate status to patients (“inpatient” or “observation”) has emerged as a front-and-center issue for hospitalists. Also known as “medical necessity,” many HM groups have been called upon to help solve the “status” problem for their institutions. With nearly 1 in 5 hospitalized patients on observation status in U.S. hospitals, appropriately assigning status is now a dominant, system-level challenge for hospitalists.
This month, we asked two experts to shed light on the nature of this beast, with a focus on the impact on the patient. Brad Flansbaum, DO, SFHM, hospitalist at Lenox Hill Hospital in New York City, and Patrick Conway, MD, FAAP, MSC, SFHM, chief medical officer at the Centers for Medicare & Medicaid Services (CMS), were kind enough to participate in the interview. We start with Dr. Flansbaum.
Dr. Whitcomb: It appears that patients are caught in the middle of the observation status challenge, at least as it relates to footing the bill. Explain the patient perspective of being unwittingly placed on observation status.
Dr. Flansbaum: Recall your last credit card statement. On it is the hotel charge from your last out-of-town CME excursion. Below the total charge, which you were expecting, is a separate line item for a $75 “recreational fee.” You call the hotel, and they inform you that, because you used the hotel gym and pool—accessed with your room key, they levied the fee. No signs, alerts, or postings denoted the policy, so you expected inclusive use of the facilities as a price of your visit. Capture the emotion of the moment, when you see that bill, feel your heart race, and think to yourself, “Get me the manager!”
WW: Why has assigning appropriate status captured the attention of hospitals?
BF: Out of vigilance for penalties and fraud from recovery audit contractor (RAC) investigations, as well attentiveness to unnecessary readmissions, hospitals increasingly are categorizing patients under observation, rather than inpatient, status to avoid conflict with regulators. Beneficiaries are in the crosshairs because of this designation change, and much in the same way of our hotel charge, our patients experience sticker shock when they receive their bill. It is leading to confusion among providers and consternation within the Medicare recipient community.
WW: Why is there so much confusion around appropriate patient status?
BF: The dilemma stems from Medicare payment, and the key distinction between inpatient coverage (Part A) and outpatient coverage, including pharmaceuticals (Parts B and D). When a patient receives their discharge notification—without an “official” inpatient designation, sometimes staying greater than 24 to 48 hours in the ED or in a specially defined observation unit, beneficiary charges are different. This could result in discrete—and sometimes jolting—enrollee copayments and deductibles for drugs and services.
WW: I’ve heard observation status is having a big, adverse impact on patients who go to skilled nursing facilities. Why?
BF: If a patient requires a skilled nursing facility stay (the “three-day stay” inpatient requirement), Medicare will not pay because the patient never registered “official” hospital time. Patients and caregivers are not prepared for the unexpected bills, and consequently, tempers are rising. The rules for Medicare Advantage enrollees (Part C—commercial payers receive a fixed sum from CMS, and oversee parts A, B, and D for an individual beneficiary), which comprise 25% of the program, differ from conventional Medicare. However, commercial plans often shadow traditional, fee-for-service in their policies and, consequently, no exemplar of success in this realm exits.
WW: Why is the number of patients on observation status growing?
BF: Hospitals have significantly increased both the number of their observation stays, as well as their hourly lengths (>48 hours). Because the definition of “observation status” is vague, and even the one- to two-day window is inflating, hospitals and hospitalists often are navigating without a compass. Again, fear of fraud and penalty places hospitals and, indirectly, hospitalists—who often make judgments on admission grade—in a precarious position.
The responsibility of hospitals to notify beneficiaries of their status hinges on this murky determination milieu, which may change in real time during the stay, and makes for an unsatisfactory standard. Understandably, CMS is attempting to rectify this quandary, taking into account a hospital’s need to clarify its billing and designation practices, as well as the beneficiaries’ desire to obtain clear guidance on their responsibilities both during and after the stay. Hospitalists, of course, want direction on coding, along with an understanding of the impact their decisions will have on patients and subspecialty colleagues.
Let’s now bring in Dr. Conway, a pediatric hospitalist. I thank Dr. Flansbaum, who formulated the following questions.
BF/WW: Is it tenable to keep the current system in place? Would it help to require payors and providers to inform beneficiaries of inpatient versus observation status at time zero in a more rigorous, yet to-be-determined manner?
Dr. Conway: Current regulations only require CMS to inform beneficiaries when they are admitted as an inpatient and not when they are an outpatient receiving observation services. There are important implications for beneficiary coverage post-hospital stay, coverage of self-administered drugs, and beneficiary coinsurance from this distinction. As a hospitalist, I think it is best to inform the patient of their status, especially if it has the potential to impact beneficiary liability, including coverage of post-acute care. CMS prepared a pamphlet in 2009, “Are You a Hospital Inpatient or Outpatient? If You Have Medicare, Ask,” to educate beneficiaries on this issue. (Download a PDF of the pamphlet at www.medicare.gov/Publications/Pubs/pdf/11435.pdf.)
BF/WW: Due to the nature of how hospital care is changing, are admission decisions potentially becoming too conflicted an endeavor for inpatient caregivers?
PC: We want admission decisions to be based on clinical considerations. The decision to admit a patient should be based on the clinical judgment of the primary-care, emergency medicine, and/or HM clinician.
BF/WW: Before the U.S. healthcare system matures to a more full-out, integrated model with internalized risk, can you envision any near-term code changes that might simplify the difficulties all parties are facing, in a budget-neutral fashion?
PC: CMS is currently investigating options to clarify when it is appropriate to admit the patient as an inpatient versus keeping the patient as an outpatient receiving observation services. We understand that this issue is of concern to hospitals, hospitalists, and patients, and we are considering carefully how to simplify the rules in a way that best meets the needs of patients and providers without increasing costs to the system.
With growing attention to observation status coming from patients and provider groups (the AMA is requesting that CMS revise its coverage rules), we will no doubt be hearing more about this going forward.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at [email protected].
Southern California Hospitals Find BOOST Tools Helpful
When Harbor UCLA Medical Center, a teaching hospital in Torrance, Calif., and a major safety-net facility for Los Angeles County, looked at its 30-day readmissions data, it found that readmissions for heart failure patients had increased by about 25% in just one year.
“We parsed the data and said we’re going have to sort this out,” explains Charles McKay, MD, a cardiologist at the hospital. “Then the opportunity to join Project BOOST came along. It’s been helpful to have their tools, mentors, and the whole collaborative experience.”
Harbor UCLA is one of seven Southern California hospitals participating in the yearlong Readmissions Reduction Collaborative, co-sponsored by SHM and the Hospital Association of Southern California (HASC). The hospitals convened in early June in Montebello, Calif., to report results from their quality initiatives. Four of the hospitals reported reductions in readmissions ranging from 24% to 55%. The other three were slower in implementing their quality processes and are just now starting to see results, executives said.
Project BOOST is a national quality initiative created by SHM to improve hospital discharges and care transitions while reducing readmissions—a growing focus for hospitals and health policy makers. About 100 participating sites across the country have benefited from BOOST’s expert mentoring and collaboration, as well as access to such tools as the “teachback” communication techniques and the “8Ps” comprehensive patient risk assessment.
Harbor UCLA’s multidisciplinary readmissions team, with Dr. McKay as its physician champion, zeroed in on heart failure and developed a Cardiovascular Open Access Rapid Evaluation (CORE) service, which he describes as a sort of observation or clinical decisions unit aimed at relieving pressure on the ED. Open 7 a.m. to 7 p.m., the CORE service coordinates medical interventions—stress tests and trips to the cardiac catheter lab, for example—for patients who have not been admitted to the hospital.
The team also focuses on discharged patients who return to the hospital within 72 hours, before the hospital could place post-discharge follow-up phone calls. Many of these patients could not be reached after they left the hospital.
“These are the patients where the system has failed,” Dr. McKay says. “But you could flip it over and say they are our biggest opportunity. That’s where BOOST comes in, to talk about interventions during hospitalization, implementing teachback, streamlining the coordination of care.”
BOOST aims to accelerate the quality-improvement (QI) process, identifying readmission risks and making them a higher priority for nurses and doctors to mobilize resources in the discharge process. “That’s where BOOST shone at our institution,” Dr. McKay says, “and where we still have a lot to learn.”
Harbor UCLA also brought a home healthcare representative onto the team, engaged a discharge advocate, and referred appropriate patients to a heart failure disease management registry. Over the year of the collaborative, it posted a 5.5% decrease in readmissions of heart failure patients.
Hospitalists do not have prominent roles at most HASC readmissions sites; traditional hospitalist services are less common in Southern California hospitals, in part due to the prevalence of independent practice associations (IPAs), which act as intermediaries between physicians and health plans in the region, explains Z. Joseph Wanski, MD, FACE, medical director of the public L.A. Care Health Plan, which co-sponsored the readmissions collaborative. “The IPA is in charge of its members’ hospital and post-hospital care,” he says.
Dr. Wanski, a practicing endocrinologist and a hospitalist at California Hospital Medical Center in Los Angeles, says L.A. Care is now testing the use of hospitalists at some of its contracted acute-care facilities.
In many cases, readmissions involve avoidable costs, as well as reduce patient satisfaction. “If they do not get rehospitalized, patients are happier, their caretakers are happier, and I feel the quality of their care is better,” Dr. Wanski says. “If you can keep the person well at home, make sure they take their medications, hopefully not go back to the ER, and get on with their lives—all those things together are why we’re supporting this collaborative.”
But hospitalists, especially in larger groups, potentially have the leverage to negotiate access to services and the care coordination needed to reduce hospital costs and preventable readmissions, Dr. McKay notes. “In 2012, hospitalists are key, and we need to find a way to make readmission reduction part of their job description, so that they can direct that,” he says.
—Z. Joseph Wanski, MD, FACE, medical director, L.A. Care Health Plan, endocrinologist/hospitalist, California Hospital Medical Center, Los Angeles
At Valley Presbyterian Hospital in Van Nuys, which employs three part-time hospitalists who also maintain busy office practices, “the hospitalists have been very cooperative with our project,” reports Adriana Quintero, MSW, the hospital’s full-time Project BOOST facilitator. “They see a lot of our patients in their offices.” The physicians have agreed to carve out time to see, within seven days, discharge patients going home without scheduled appointments with their primary-care physicians (PCPs).
“We find that many of our discharged patients do not call their primary-care physicians for post-discharge appointments” and decline the hospital team’s offers for help—which makes it important for the discharge coordinator to follow up as soon as possible after the patient goes home, Quintero says.
At the collaborative congress in early June, team member Alice Gunderson reported results for Saint Francis Hospital in Lynwood. Gunderson, who sits on the hospital’s quality and safety board, has been a volunteer patient family advocate (PFA) for the past year and a half; she was inspired by her own experience as a family caregiver for her husband and mother, both of whom were Saint Francis patients. Gunderson challenged those in the audience to bring a PFA from their own hospital to the next BOOST meeting.
“From my point of view, wherever healthcare goes, the patient is becoming more educated, with all of the communication technology that is out there, and claiming that empowerment,” Gunderson says. “We must all work together, not in separate silos, for the best outcomes, and we can all learn from one another.”
Larry Beresford is a freelance writer in Oakland, Calif.
When Harbor UCLA Medical Center, a teaching hospital in Torrance, Calif., and a major safety-net facility for Los Angeles County, looked at its 30-day readmissions data, it found that readmissions for heart failure patients had increased by about 25% in just one year.
“We parsed the data and said we’re going have to sort this out,” explains Charles McKay, MD, a cardiologist at the hospital. “Then the opportunity to join Project BOOST came along. It’s been helpful to have their tools, mentors, and the whole collaborative experience.”
Harbor UCLA is one of seven Southern California hospitals participating in the yearlong Readmissions Reduction Collaborative, co-sponsored by SHM and the Hospital Association of Southern California (HASC). The hospitals convened in early June in Montebello, Calif., to report results from their quality initiatives. Four of the hospitals reported reductions in readmissions ranging from 24% to 55%. The other three were slower in implementing their quality processes and are just now starting to see results, executives said.
Project BOOST is a national quality initiative created by SHM to improve hospital discharges and care transitions while reducing readmissions—a growing focus for hospitals and health policy makers. About 100 participating sites across the country have benefited from BOOST’s expert mentoring and collaboration, as well as access to such tools as the “teachback” communication techniques and the “8Ps” comprehensive patient risk assessment.
Harbor UCLA’s multidisciplinary readmissions team, with Dr. McKay as its physician champion, zeroed in on heart failure and developed a Cardiovascular Open Access Rapid Evaluation (CORE) service, which he describes as a sort of observation or clinical decisions unit aimed at relieving pressure on the ED. Open 7 a.m. to 7 p.m., the CORE service coordinates medical interventions—stress tests and trips to the cardiac catheter lab, for example—for patients who have not been admitted to the hospital.
The team also focuses on discharged patients who return to the hospital within 72 hours, before the hospital could place post-discharge follow-up phone calls. Many of these patients could not be reached after they left the hospital.
“These are the patients where the system has failed,” Dr. McKay says. “But you could flip it over and say they are our biggest opportunity. That’s where BOOST comes in, to talk about interventions during hospitalization, implementing teachback, streamlining the coordination of care.”
BOOST aims to accelerate the quality-improvement (QI) process, identifying readmission risks and making them a higher priority for nurses and doctors to mobilize resources in the discharge process. “That’s where BOOST shone at our institution,” Dr. McKay says, “and where we still have a lot to learn.”
Harbor UCLA also brought a home healthcare representative onto the team, engaged a discharge advocate, and referred appropriate patients to a heart failure disease management registry. Over the year of the collaborative, it posted a 5.5% decrease in readmissions of heart failure patients.
Hospitalists do not have prominent roles at most HASC readmissions sites; traditional hospitalist services are less common in Southern California hospitals, in part due to the prevalence of independent practice associations (IPAs), which act as intermediaries between physicians and health plans in the region, explains Z. Joseph Wanski, MD, FACE, medical director of the public L.A. Care Health Plan, which co-sponsored the readmissions collaborative. “The IPA is in charge of its members’ hospital and post-hospital care,” he says.
Dr. Wanski, a practicing endocrinologist and a hospitalist at California Hospital Medical Center in Los Angeles, says L.A. Care is now testing the use of hospitalists at some of its contracted acute-care facilities.
In many cases, readmissions involve avoidable costs, as well as reduce patient satisfaction. “If they do not get rehospitalized, patients are happier, their caretakers are happier, and I feel the quality of their care is better,” Dr. Wanski says. “If you can keep the person well at home, make sure they take their medications, hopefully not go back to the ER, and get on with their lives—all those things together are why we’re supporting this collaborative.”
But hospitalists, especially in larger groups, potentially have the leverage to negotiate access to services and the care coordination needed to reduce hospital costs and preventable readmissions, Dr. McKay notes. “In 2012, hospitalists are key, and we need to find a way to make readmission reduction part of their job description, so that they can direct that,” he says.
—Z. Joseph Wanski, MD, FACE, medical director, L.A. Care Health Plan, endocrinologist/hospitalist, California Hospital Medical Center, Los Angeles
At Valley Presbyterian Hospital in Van Nuys, which employs three part-time hospitalists who also maintain busy office practices, “the hospitalists have been very cooperative with our project,” reports Adriana Quintero, MSW, the hospital’s full-time Project BOOST facilitator. “They see a lot of our patients in their offices.” The physicians have agreed to carve out time to see, within seven days, discharge patients going home without scheduled appointments with their primary-care physicians (PCPs).
“We find that many of our discharged patients do not call their primary-care physicians for post-discharge appointments” and decline the hospital team’s offers for help—which makes it important for the discharge coordinator to follow up as soon as possible after the patient goes home, Quintero says.
At the collaborative congress in early June, team member Alice Gunderson reported results for Saint Francis Hospital in Lynwood. Gunderson, who sits on the hospital’s quality and safety board, has been a volunteer patient family advocate (PFA) for the past year and a half; she was inspired by her own experience as a family caregiver for her husband and mother, both of whom were Saint Francis patients. Gunderson challenged those in the audience to bring a PFA from their own hospital to the next BOOST meeting.
“From my point of view, wherever healthcare goes, the patient is becoming more educated, with all of the communication technology that is out there, and claiming that empowerment,” Gunderson says. “We must all work together, not in separate silos, for the best outcomes, and we can all learn from one another.”
Larry Beresford is a freelance writer in Oakland, Calif.
When Harbor UCLA Medical Center, a teaching hospital in Torrance, Calif., and a major safety-net facility for Los Angeles County, looked at its 30-day readmissions data, it found that readmissions for heart failure patients had increased by about 25% in just one year.
“We parsed the data and said we’re going have to sort this out,” explains Charles McKay, MD, a cardiologist at the hospital. “Then the opportunity to join Project BOOST came along. It’s been helpful to have their tools, mentors, and the whole collaborative experience.”
Harbor UCLA is one of seven Southern California hospitals participating in the yearlong Readmissions Reduction Collaborative, co-sponsored by SHM and the Hospital Association of Southern California (HASC). The hospitals convened in early June in Montebello, Calif., to report results from their quality initiatives. Four of the hospitals reported reductions in readmissions ranging from 24% to 55%. The other three were slower in implementing their quality processes and are just now starting to see results, executives said.
Project BOOST is a national quality initiative created by SHM to improve hospital discharges and care transitions while reducing readmissions—a growing focus for hospitals and health policy makers. About 100 participating sites across the country have benefited from BOOST’s expert mentoring and collaboration, as well as access to such tools as the “teachback” communication techniques and the “8Ps” comprehensive patient risk assessment.
Harbor UCLA’s multidisciplinary readmissions team, with Dr. McKay as its physician champion, zeroed in on heart failure and developed a Cardiovascular Open Access Rapid Evaluation (CORE) service, which he describes as a sort of observation or clinical decisions unit aimed at relieving pressure on the ED. Open 7 a.m. to 7 p.m., the CORE service coordinates medical interventions—stress tests and trips to the cardiac catheter lab, for example—for patients who have not been admitted to the hospital.
The team also focuses on discharged patients who return to the hospital within 72 hours, before the hospital could place post-discharge follow-up phone calls. Many of these patients could not be reached after they left the hospital.
“These are the patients where the system has failed,” Dr. McKay says. “But you could flip it over and say they are our biggest opportunity. That’s where BOOST comes in, to talk about interventions during hospitalization, implementing teachback, streamlining the coordination of care.”
BOOST aims to accelerate the quality-improvement (QI) process, identifying readmission risks and making them a higher priority for nurses and doctors to mobilize resources in the discharge process. “That’s where BOOST shone at our institution,” Dr. McKay says, “and where we still have a lot to learn.”
Harbor UCLA also brought a home healthcare representative onto the team, engaged a discharge advocate, and referred appropriate patients to a heart failure disease management registry. Over the year of the collaborative, it posted a 5.5% decrease in readmissions of heart failure patients.
Hospitalists do not have prominent roles at most HASC readmissions sites; traditional hospitalist services are less common in Southern California hospitals, in part due to the prevalence of independent practice associations (IPAs), which act as intermediaries between physicians and health plans in the region, explains Z. Joseph Wanski, MD, FACE, medical director of the public L.A. Care Health Plan, which co-sponsored the readmissions collaborative. “The IPA is in charge of its members’ hospital and post-hospital care,” he says.
Dr. Wanski, a practicing endocrinologist and a hospitalist at California Hospital Medical Center in Los Angeles, says L.A. Care is now testing the use of hospitalists at some of its contracted acute-care facilities.
In many cases, readmissions involve avoidable costs, as well as reduce patient satisfaction. “If they do not get rehospitalized, patients are happier, their caretakers are happier, and I feel the quality of their care is better,” Dr. Wanski says. “If you can keep the person well at home, make sure they take their medications, hopefully not go back to the ER, and get on with their lives—all those things together are why we’re supporting this collaborative.”
But hospitalists, especially in larger groups, potentially have the leverage to negotiate access to services and the care coordination needed to reduce hospital costs and preventable readmissions, Dr. McKay notes. “In 2012, hospitalists are key, and we need to find a way to make readmission reduction part of their job description, so that they can direct that,” he says.
—Z. Joseph Wanski, MD, FACE, medical director, L.A. Care Health Plan, endocrinologist/hospitalist, California Hospital Medical Center, Los Angeles
At Valley Presbyterian Hospital in Van Nuys, which employs three part-time hospitalists who also maintain busy office practices, “the hospitalists have been very cooperative with our project,” reports Adriana Quintero, MSW, the hospital’s full-time Project BOOST facilitator. “They see a lot of our patients in their offices.” The physicians have agreed to carve out time to see, within seven days, discharge patients going home without scheduled appointments with their primary-care physicians (PCPs).
“We find that many of our discharged patients do not call their primary-care physicians for post-discharge appointments” and decline the hospital team’s offers for help—which makes it important for the discharge coordinator to follow up as soon as possible after the patient goes home, Quintero says.
At the collaborative congress in early June, team member Alice Gunderson reported results for Saint Francis Hospital in Lynwood. Gunderson, who sits on the hospital’s quality and safety board, has been a volunteer patient family advocate (PFA) for the past year and a half; she was inspired by her own experience as a family caregiver for her husband and mother, both of whom were Saint Francis patients. Gunderson challenged those in the audience to bring a PFA from their own hospital to the next BOOST meeting.
“From my point of view, wherever healthcare goes, the patient is becoming more educated, with all of the communication technology that is out there, and claiming that empowerment,” Gunderson says. “We must all work together, not in separate silos, for the best outcomes, and we can all learn from one another.”
Larry Beresford is a freelance writer in Oakland, Calif.
John Nelson: Admit Resolution
Editor’s note: Second in a two-part series.
I used last month’s column to frame the issue of disagreement between doctors over who should admit a particular patient, as well as discuss the value of good social connections to reduce the chance that divergent opinions lead to outright conflict. This month, I’ll review another worthwhile strategy—one that could be a definitive solution to these disagreements but often falls short of that goal in practice.
Service Agreements, or “Compacts,” between Physician Groups
If, at your hospital, there are reasonably frequent cases of divergent opinions regarding whether an ED admission or transfer from elsewhere should be admitted by a hospitalist or doctor in another specialty, why not meet in advance to decide this? Many hospitalist groups have held meetings with doctors in other specialties and now have a collection of agreements outlining scenarios, such as:
- ESRD patients: Hospitalist admits for non-dialysis issues (pneumonia, diabetic issues, etc.); nephrologist admits for urgent dialysis issues (K+>6.3, pH<7.3, etc.).
- Cardiology: Hospitalist admits CHF and non-ST elevation chest pain; cardiologist admits STEMI.
- General surgery: Hospitalist admits ileus, pseudo obstruction, and SBO due to adhesions; general surgery admits bowel obstruction in “virgin abdomen,” volvulus, and any obstruction thought to require urgent surgery.
To be clear, I’m not suggesting the above guidelines are evidence-based or are the right ones for your institution. I just made these up, so yours might differ significantly. I just want to provide a sense of the kinds of issues these agreements typically cover. The comanagement section of the SHM website has several documents regarding hospitalist-orthopedic service agreements.
The Negotiation Process
It’s tempting for the lead hospitalist to just have a hallway chat with a spokesperson from the other specialty, then email a draft agreement, exchange a few messages until both parties are satisfied, then email a copy of the final document to all the doctors in both groups. This might work for some simple service agreements, but for any area with significant ambiguity or disagreements (or potential for disagreements), one or more in-person meetings are usually necessary. Ideally, several doctors in both groups will attend these meetings.
Much work could be done in advance of the first meeting, including surveying other practices to see how they decide which group admits the same kinds of patents, gathering any relevant published research, and possibly drafting a “straw man” proposed agreement. When meeting in person, the doctors will have a chance to explain their points of view, needs, and concerns, and gain a greater appreciation of the way “the other guy” sees things. An important purpose of the in-person meeting is to “look the other guy in the eye” to know if he or she really is committed to following through.
Remember that written agreements like these might become an issue in malpractice suits, so you might want to have them reviewed first by risk managers. You might also write them as guidelines rather than rigid protocols that don’t allow variations.
Maximize Effectiveness
Ideally, every doctor involved in the agreement should document their approval with a signature and date. My experience is that this doesn’t happen at most places, but if there is concern about whether everyone will comply, signing the document will probably help at least a little.
The completed agreements should be provided to all doctors in both groups, the ED, affected hospital nursing units, and others. Any new doctor should get a copy of all such agreements that might be relevant. And, most important, it should be made available electronically so that it is easy to find at any time. Some agreements cover uncommon events, and the doctors on duty might not remember what the agreement said and will need ready access to it.
Most service agreements should be reviewed and updated every two or three years or as needed. If there is confusion or controversy around a particular agreement, or if disagreements about which doctor does the admission are common despite the agreement, then an in-person meeting between the physician groups should be scheduled to revise or update it.
Keep Your Fingers Crossed
If it sounds like a lot of work to develop and maintain these agreements, it is. But they’re worth every bit of that work if they reduce confusion or discord. Sadly, for several reasons, they rarely prove so effective.
One doctor might think the agreement applies, but the other doctor says this patient is an exception and the agreement doesn’t apply. It is impossible to write an agreement that addresses all possible scenarios, so a doctor can argue that any particular patient falls outside the agreement because of things like comorbidities, which service admitted the patient last time (many agreements will have defined “bounce back” intervals), which primary-care physician (PCP) the patient sees, etc.
Even if there is no dispute about whether the agreement covers a particular patient, many doctors simply don’t feel obligated to uphold the agreement. Such a doctor might tell the ED doctor: “Yep, I signed the agreement, but only as a way to get the meeting over with. I was never in favor of it and just can’t admit the patient. Call the other guy to admit.” So in spite of all the work done to create a reasonable agreement, some doctors might feel entitled to ignore it when it suits them.
Compliance Is Critical
Sadly, my take is that despite the tremendous hoped-for benefits that service agreements might provide, poor compliance means they rarely achieve their potential. Even so, they are usually worth the time and effort to create them if it leads doctors in the two specialties to schedule time away from patient care to listen to the other group’s point of view and discuss how best to handle particular types of patients. In some cases, it will be the first time the two groups of doctors have set aside time to talk about the work they do together; that alone can have significant value.
Tom Lorence, MD, a Kaiser hospitalist in Portland, Ore., who is chief of hospital medicine for Northwest Permanente, developed more than 20 service agreements with many different specialties at his institution. He has found that they are worth the effort, and that they helped allay hospitalists’ feeling of being “dumped on.”
He also told me a rule that probably applies to all such agreements in any setting: The tie goes to the hospitalist—that is, when there is reasonable uncertainty or disagreement about which group should admit a patient, it is nearly always the hospitalist who will do so.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
Editor’s note: Second in a two-part series.
I used last month’s column to frame the issue of disagreement between doctors over who should admit a particular patient, as well as discuss the value of good social connections to reduce the chance that divergent opinions lead to outright conflict. This month, I’ll review another worthwhile strategy—one that could be a definitive solution to these disagreements but often falls short of that goal in practice.
Service Agreements, or “Compacts,” between Physician Groups
If, at your hospital, there are reasonably frequent cases of divergent opinions regarding whether an ED admission or transfer from elsewhere should be admitted by a hospitalist or doctor in another specialty, why not meet in advance to decide this? Many hospitalist groups have held meetings with doctors in other specialties and now have a collection of agreements outlining scenarios, such as:
- ESRD patients: Hospitalist admits for non-dialysis issues (pneumonia, diabetic issues, etc.); nephrologist admits for urgent dialysis issues (K+>6.3, pH<7.3, etc.).
- Cardiology: Hospitalist admits CHF and non-ST elevation chest pain; cardiologist admits STEMI.
- General surgery: Hospitalist admits ileus, pseudo obstruction, and SBO due to adhesions; general surgery admits bowel obstruction in “virgin abdomen,” volvulus, and any obstruction thought to require urgent surgery.
To be clear, I’m not suggesting the above guidelines are evidence-based or are the right ones for your institution. I just made these up, so yours might differ significantly. I just want to provide a sense of the kinds of issues these agreements typically cover. The comanagement section of the SHM website has several documents regarding hospitalist-orthopedic service agreements.
The Negotiation Process
It’s tempting for the lead hospitalist to just have a hallway chat with a spokesperson from the other specialty, then email a draft agreement, exchange a few messages until both parties are satisfied, then email a copy of the final document to all the doctors in both groups. This might work for some simple service agreements, but for any area with significant ambiguity or disagreements (or potential for disagreements), one or more in-person meetings are usually necessary. Ideally, several doctors in both groups will attend these meetings.
Much work could be done in advance of the first meeting, including surveying other practices to see how they decide which group admits the same kinds of patents, gathering any relevant published research, and possibly drafting a “straw man” proposed agreement. When meeting in person, the doctors will have a chance to explain their points of view, needs, and concerns, and gain a greater appreciation of the way “the other guy” sees things. An important purpose of the in-person meeting is to “look the other guy in the eye” to know if he or she really is committed to following through.
Remember that written agreements like these might become an issue in malpractice suits, so you might want to have them reviewed first by risk managers. You might also write them as guidelines rather than rigid protocols that don’t allow variations.
Maximize Effectiveness
Ideally, every doctor involved in the agreement should document their approval with a signature and date. My experience is that this doesn’t happen at most places, but if there is concern about whether everyone will comply, signing the document will probably help at least a little.
The completed agreements should be provided to all doctors in both groups, the ED, affected hospital nursing units, and others. Any new doctor should get a copy of all such agreements that might be relevant. And, most important, it should be made available electronically so that it is easy to find at any time. Some agreements cover uncommon events, and the doctors on duty might not remember what the agreement said and will need ready access to it.
Most service agreements should be reviewed and updated every two or three years or as needed. If there is confusion or controversy around a particular agreement, or if disagreements about which doctor does the admission are common despite the agreement, then an in-person meeting between the physician groups should be scheduled to revise or update it.
Keep Your Fingers Crossed
If it sounds like a lot of work to develop and maintain these agreements, it is. But they’re worth every bit of that work if they reduce confusion or discord. Sadly, for several reasons, they rarely prove so effective.
One doctor might think the agreement applies, but the other doctor says this patient is an exception and the agreement doesn’t apply. It is impossible to write an agreement that addresses all possible scenarios, so a doctor can argue that any particular patient falls outside the agreement because of things like comorbidities, which service admitted the patient last time (many agreements will have defined “bounce back” intervals), which primary-care physician (PCP) the patient sees, etc.
Even if there is no dispute about whether the agreement covers a particular patient, many doctors simply don’t feel obligated to uphold the agreement. Such a doctor might tell the ED doctor: “Yep, I signed the agreement, but only as a way to get the meeting over with. I was never in favor of it and just can’t admit the patient. Call the other guy to admit.” So in spite of all the work done to create a reasonable agreement, some doctors might feel entitled to ignore it when it suits them.
Compliance Is Critical
Sadly, my take is that despite the tremendous hoped-for benefits that service agreements might provide, poor compliance means they rarely achieve their potential. Even so, they are usually worth the time and effort to create them if it leads doctors in the two specialties to schedule time away from patient care to listen to the other group’s point of view and discuss how best to handle particular types of patients. In some cases, it will be the first time the two groups of doctors have set aside time to talk about the work they do together; that alone can have significant value.
Tom Lorence, MD, a Kaiser hospitalist in Portland, Ore., who is chief of hospital medicine for Northwest Permanente, developed more than 20 service agreements with many different specialties at his institution. He has found that they are worth the effort, and that they helped allay hospitalists’ feeling of being “dumped on.”
He also told me a rule that probably applies to all such agreements in any setting: The tie goes to the hospitalist—that is, when there is reasonable uncertainty or disagreement about which group should admit a patient, it is nearly always the hospitalist who will do so.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
Editor’s note: Second in a two-part series.
I used last month’s column to frame the issue of disagreement between doctors over who should admit a particular patient, as well as discuss the value of good social connections to reduce the chance that divergent opinions lead to outright conflict. This month, I’ll review another worthwhile strategy—one that could be a definitive solution to these disagreements but often falls short of that goal in practice.
Service Agreements, or “Compacts,” between Physician Groups
If, at your hospital, there are reasonably frequent cases of divergent opinions regarding whether an ED admission or transfer from elsewhere should be admitted by a hospitalist or doctor in another specialty, why not meet in advance to decide this? Many hospitalist groups have held meetings with doctors in other specialties and now have a collection of agreements outlining scenarios, such as:
- ESRD patients: Hospitalist admits for non-dialysis issues (pneumonia, diabetic issues, etc.); nephrologist admits for urgent dialysis issues (K+>6.3, pH<7.3, etc.).
- Cardiology: Hospitalist admits CHF and non-ST elevation chest pain; cardiologist admits STEMI.
- General surgery: Hospitalist admits ileus, pseudo obstruction, and SBO due to adhesions; general surgery admits bowel obstruction in “virgin abdomen,” volvulus, and any obstruction thought to require urgent surgery.
To be clear, I’m not suggesting the above guidelines are evidence-based or are the right ones for your institution. I just made these up, so yours might differ significantly. I just want to provide a sense of the kinds of issues these agreements typically cover. The comanagement section of the SHM website has several documents regarding hospitalist-orthopedic service agreements.
The Negotiation Process
It’s tempting for the lead hospitalist to just have a hallway chat with a spokesperson from the other specialty, then email a draft agreement, exchange a few messages until both parties are satisfied, then email a copy of the final document to all the doctors in both groups. This might work for some simple service agreements, but for any area with significant ambiguity or disagreements (or potential for disagreements), one or more in-person meetings are usually necessary. Ideally, several doctors in both groups will attend these meetings.
Much work could be done in advance of the first meeting, including surveying other practices to see how they decide which group admits the same kinds of patents, gathering any relevant published research, and possibly drafting a “straw man” proposed agreement. When meeting in person, the doctors will have a chance to explain their points of view, needs, and concerns, and gain a greater appreciation of the way “the other guy” sees things. An important purpose of the in-person meeting is to “look the other guy in the eye” to know if he or she really is committed to following through.
Remember that written agreements like these might become an issue in malpractice suits, so you might want to have them reviewed first by risk managers. You might also write them as guidelines rather than rigid protocols that don’t allow variations.
Maximize Effectiveness
Ideally, every doctor involved in the agreement should document their approval with a signature and date. My experience is that this doesn’t happen at most places, but if there is concern about whether everyone will comply, signing the document will probably help at least a little.
The completed agreements should be provided to all doctors in both groups, the ED, affected hospital nursing units, and others. Any new doctor should get a copy of all such agreements that might be relevant. And, most important, it should be made available electronically so that it is easy to find at any time. Some agreements cover uncommon events, and the doctors on duty might not remember what the agreement said and will need ready access to it.
Most service agreements should be reviewed and updated every two or three years or as needed. If there is confusion or controversy around a particular agreement, or if disagreements about which doctor does the admission are common despite the agreement, then an in-person meeting between the physician groups should be scheduled to revise or update it.
Keep Your Fingers Crossed
If it sounds like a lot of work to develop and maintain these agreements, it is. But they’re worth every bit of that work if they reduce confusion or discord. Sadly, for several reasons, they rarely prove so effective.
One doctor might think the agreement applies, but the other doctor says this patient is an exception and the agreement doesn’t apply. It is impossible to write an agreement that addresses all possible scenarios, so a doctor can argue that any particular patient falls outside the agreement because of things like comorbidities, which service admitted the patient last time (many agreements will have defined “bounce back” intervals), which primary-care physician (PCP) the patient sees, etc.
Even if there is no dispute about whether the agreement covers a particular patient, many doctors simply don’t feel obligated to uphold the agreement. Such a doctor might tell the ED doctor: “Yep, I signed the agreement, but only as a way to get the meeting over with. I was never in favor of it and just can’t admit the patient. Call the other guy to admit.” So in spite of all the work done to create a reasonable agreement, some doctors might feel entitled to ignore it when it suits them.
Compliance Is Critical
Sadly, my take is that despite the tremendous hoped-for benefits that service agreements might provide, poor compliance means they rarely achieve their potential. Even so, they are usually worth the time and effort to create them if it leads doctors in the two specialties to schedule time away from patient care to listen to the other group’s point of view and discuss how best to handle particular types of patients. In some cases, it will be the first time the two groups of doctors have set aside time to talk about the work they do together; that alone can have significant value.
Tom Lorence, MD, a Kaiser hospitalist in Portland, Ore., who is chief of hospital medicine for Northwest Permanente, developed more than 20 service agreements with many different specialties at his institution. He has found that they are worth the effort, and that they helped allay hospitalists’ feeling of being “dumped on.”
He also told me a rule that probably applies to all such agreements in any setting: The tie goes to the hospitalist—that is, when there is reasonable uncertainty or disagreement about which group should admit a patient, it is nearly always the hospitalist who will do so.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM’s “Best Practices in Managing a Hospital Medicine Program” course.
Physician Payment Systems Remain Constant
I would like to know where payment for the service of hospitalists fits into the insurance/Medicare payment system. Are hospitalists considered employees of the hospital and, therefore, billed through the hospital system? Are they considered independent doctors and, therefore, do their own direct billing? Do they, in general, accept assignment of benefits from you for your insurance/Medicare? Do they sign contracts with insurance/Medicare to participate in their plans?
Carole L. Hughes
Dr. Hospitalist responds:
For the sake of argument, let’s say that Carole is on the outside looking in—meaning she’s not a healthcare practitioner, but a consumer. It might seem a bit strange to wonder where all these “hospitalists” come from, and who pays for them. Let’s walk through a few scenarios as outlined here.
Are hospitalists considered employees of the hospital? They certainly could be directly employed by the hospital, but it’s just as likely they could be contracted with the hospital for certain services, such as taking ED call for unassigned patients. It’s also entirely possible that the hospitalist has no direct financial relationship with the hospital at all. In this case, a hospitalist is taking cases that are referred from other physicians and for which there is a coverage agreement. The most common situation is a primary-care physician group that is looking for a hospitalist to care for their patients in the hospital. This is usually a handshake agreement, with no money involved.
Do hospitalists do their own direct billing to the insurers? As for this part of the question, it’s time to separate “hospital services” from “hospitalist services.” Hospital services are billed under Medicare Part A, while physician services are billed under Medicare Part B, meaning that even if a physician is employed directly by the hospital, that physician’s professional services are still billed and paid separate from any hospital charges (for things like the bed, supplies, and nursing). Because Medicare sets the ground rules, other insurances typically follow suit. Payment applies similarly to the contracted hospitalists and independent hospitalists.
Do hospitalists have to be credentialed with the insurers? Yes. Whether it is Medicare or Cigna or United, each individual physician must be credentialed with the payors to receive payment. Medicare credentialing for physicians is pretty universal, given that most of our patients have this as their primary insurance. Without it, there is no payment from Medicare to the physician. Many groups or hospitals won’t even let their physicians begin seeing patients until that paperwork is approved. Due to timely filing rules, you can’t just start to see patients and hope to get paid later. And there’s no negotiating with the government—whatever Medicare pays in a region for a specific service is the payment the physician receives.
For the private insurers, it’s generally easier to receive payment if you are credentialed, but I’ve seen a few physician groups negotiate payments without agreeing to a flat contracted rate. I don’t recommend this setup, as the patient can often get caught in the middle with a rather hefty bill. Still, there is some room for negotiation on the private insurer payment rates.
In summary, whether a hospitalist is employed by the hospital, contracted, or truly independent, they all bill Medicare and the insurers for their professional fees. Medicare payments won’t vary, but private insurance payments can. It’s certainly a challenging payment system to understand, from either the provider or the patient point of view.
I would like to know where payment for the service of hospitalists fits into the insurance/Medicare payment system. Are hospitalists considered employees of the hospital and, therefore, billed through the hospital system? Are they considered independent doctors and, therefore, do their own direct billing? Do they, in general, accept assignment of benefits from you for your insurance/Medicare? Do they sign contracts with insurance/Medicare to participate in their plans?
Carole L. Hughes
Dr. Hospitalist responds:
For the sake of argument, let’s say that Carole is on the outside looking in—meaning she’s not a healthcare practitioner, but a consumer. It might seem a bit strange to wonder where all these “hospitalists” come from, and who pays for them. Let’s walk through a few scenarios as outlined here.
Are hospitalists considered employees of the hospital? They certainly could be directly employed by the hospital, but it’s just as likely they could be contracted with the hospital for certain services, such as taking ED call for unassigned patients. It’s also entirely possible that the hospitalist has no direct financial relationship with the hospital at all. In this case, a hospitalist is taking cases that are referred from other physicians and for which there is a coverage agreement. The most common situation is a primary-care physician group that is looking for a hospitalist to care for their patients in the hospital. This is usually a handshake agreement, with no money involved.
Do hospitalists do their own direct billing to the insurers? As for this part of the question, it’s time to separate “hospital services” from “hospitalist services.” Hospital services are billed under Medicare Part A, while physician services are billed under Medicare Part B, meaning that even if a physician is employed directly by the hospital, that physician’s professional services are still billed and paid separate from any hospital charges (for things like the bed, supplies, and nursing). Because Medicare sets the ground rules, other insurances typically follow suit. Payment applies similarly to the contracted hospitalists and independent hospitalists.
Do hospitalists have to be credentialed with the insurers? Yes. Whether it is Medicare or Cigna or United, each individual physician must be credentialed with the payors to receive payment. Medicare credentialing for physicians is pretty universal, given that most of our patients have this as their primary insurance. Without it, there is no payment from Medicare to the physician. Many groups or hospitals won’t even let their physicians begin seeing patients until that paperwork is approved. Due to timely filing rules, you can’t just start to see patients and hope to get paid later. And there’s no negotiating with the government—whatever Medicare pays in a region for a specific service is the payment the physician receives.
For the private insurers, it’s generally easier to receive payment if you are credentialed, but I’ve seen a few physician groups negotiate payments without agreeing to a flat contracted rate. I don’t recommend this setup, as the patient can often get caught in the middle with a rather hefty bill. Still, there is some room for negotiation on the private insurer payment rates.
In summary, whether a hospitalist is employed by the hospital, contracted, or truly independent, they all bill Medicare and the insurers for their professional fees. Medicare payments won’t vary, but private insurance payments can. It’s certainly a challenging payment system to understand, from either the provider or the patient point of view.
I would like to know where payment for the service of hospitalists fits into the insurance/Medicare payment system. Are hospitalists considered employees of the hospital and, therefore, billed through the hospital system? Are they considered independent doctors and, therefore, do their own direct billing? Do they, in general, accept assignment of benefits from you for your insurance/Medicare? Do they sign contracts with insurance/Medicare to participate in their plans?
Carole L. Hughes
Dr. Hospitalist responds:
For the sake of argument, let’s say that Carole is on the outside looking in—meaning she’s not a healthcare practitioner, but a consumer. It might seem a bit strange to wonder where all these “hospitalists” come from, and who pays for them. Let’s walk through a few scenarios as outlined here.
Are hospitalists considered employees of the hospital? They certainly could be directly employed by the hospital, but it’s just as likely they could be contracted with the hospital for certain services, such as taking ED call for unassigned patients. It’s also entirely possible that the hospitalist has no direct financial relationship with the hospital at all. In this case, a hospitalist is taking cases that are referred from other physicians and for which there is a coverage agreement. The most common situation is a primary-care physician group that is looking for a hospitalist to care for their patients in the hospital. This is usually a handshake agreement, with no money involved.
Do hospitalists do their own direct billing to the insurers? As for this part of the question, it’s time to separate “hospital services” from “hospitalist services.” Hospital services are billed under Medicare Part A, while physician services are billed under Medicare Part B, meaning that even if a physician is employed directly by the hospital, that physician’s professional services are still billed and paid separate from any hospital charges (for things like the bed, supplies, and nursing). Because Medicare sets the ground rules, other insurances typically follow suit. Payment applies similarly to the contracted hospitalists and independent hospitalists.
Do hospitalists have to be credentialed with the insurers? Yes. Whether it is Medicare or Cigna or United, each individual physician must be credentialed with the payors to receive payment. Medicare credentialing for physicians is pretty universal, given that most of our patients have this as their primary insurance. Without it, there is no payment from Medicare to the physician. Many groups or hospitals won’t even let their physicians begin seeing patients until that paperwork is approved. Due to timely filing rules, you can’t just start to see patients and hope to get paid later. And there’s no negotiating with the government—whatever Medicare pays in a region for a specific service is the payment the physician receives.
For the private insurers, it’s generally easier to receive payment if you are credentialed, but I’ve seen a few physician groups negotiate payments without agreeing to a flat contracted rate. I don’t recommend this setup, as the patient can often get caught in the middle with a rather hefty bill. Still, there is some room for negotiation on the private insurer payment rates.
In summary, whether a hospitalist is employed by the hospital, contracted, or truly independent, they all bill Medicare and the insurers for their professional fees. Medicare payments won’t vary, but private insurance payments can. It’s certainly a challenging payment system to understand, from either the provider or the patient point of view.