User login
Trichomonas: Clinical Analysis of a Highly Prevalent and Misdiagnosed Infection
Chronic Pain Perspectives - September 2012
Managing chronic pain in older adults: 6 steps to overcoming medication barriers
Sickle cell disease: Gaining control over the pain
Treating herpes zoster and postherpetic neuralgia: An evidence-based approach
Managing chronic pain in older adults: 6 steps to overcoming medication barriers
Dr. Reid is a consultant to sanofi aventis. Dr. Ayres and Mr. Warmington reported no potential conflict of interest relevant to this article.
Managing chronic pain in an older adult can be a complicated task, with risks for adverse effects, under- or overmedication, and nonadherence. Pain can be alleviated in many cases, however, if you address potential complications and barriers to effective treatment when prescribing analgesic medications.
Pain is a part of daily life for many older adults
As many as 50% of community-dwelling older adults experience a chronic pain disorder, defined as pain on most days for at least 3 consecutive months.1 Prevalence rates are typically higher (49%-84%) among residents of long-term care facilities.2 Untreated chronic pain can lead to health consequences such as depression, decreased ability to socialize, impaired ambulation, impaired sleep, increased falls, malnutrition, and decreased quality of life.1,3 Among older women, pain is the most common reported cause of impairment in activities of daily living.4
Arthritis and arthritis-related diseases (such as back pain) are common causes of chronic pain in older adults.5 Other causes include neuropathies, vertebral compression fractures, cancer and cancer treatments, and advanced chronic diseases such as end-stage heart, lung, and kidney disease.6-10
Substantial literature documents that chronic pain is underdetected and undertreated with advancing age11,12 and strongly supports efforts to improve pain care in later life. Treatment guidelines recommend a multimodal approach, including evidence-based nonpharmacologic treatments such as cognitive-behavioral therapy, exercise, and physical therapy.1 At the same time, pharmacotherapies remain the primary treatment used by physicians,13 and studies indicate that older people use analgesics frequently:
- When 551 older black and non-Hispanic white adults with osteoarthritis were interviewed, more than 80% of each group reported regular use of prescription and over-the-counter (OTC) analgesic medications.14
- In a cross-sectional study of 272 community-dwelling older adults with chronic pain from diverse causes, 59% reported routine use of an analgesic medication.15
The following 6 steps can improve the likelihood of a successful analgesic trial when managing chronic pain in people ages 65 and older. They take into account barriers you are likely to encounter, including polypharmacy, multimorbidity, cognitive and sensory impairment, sociodemographic factors, specific health beliefs about pain and pain treatments, and age-related physiologic changes.
TABLE
Refine your approach to chronic pain in older patients with these 6 steps
| 1. Conduct a comprehensive pain history | Assess pain location and intensity, and ask how pain limits activity. What treatments have been tried? What worked best? Any intolerable adverse effects? |
| 2. Review the problem list | Obtain a full medication list (OTC and supplements) to identify potential interactions. What chronic conditions (kidney or liver disease, movement disorders, neurologic problems) might worsen with analgesic medication or operate as a contraindication? Which drugs or comorbidities might affect treatment choices? |
| 3. Establish treatment goals | Address potential unrealistic expectations (eg, complete relief of pain or no benefit from treatment). The patient’s goals might differ from yours; come to a mutual decision about the most important outcomes. |
| 4. Identify barriers to therapy | Be aware of how cognitive or sensory impairment, sociodemographic factors, or health beliefs may limit medication adherence. Elicit the patient’s concerns about medications and discuss openly. Include the caregiver, as needed, when discussing treatments and monitoring outcomes. |
| 5. Start low and go slow when initiating analgesia | Avoid “start low and stay low,” which can contribute to undertreatment. If treatment goals are not met and the patient is tolerating therapy, advancing the dose is reasonable before trying another intervention. |
| 6. Assess for effects and outcomes | Make certain that the patient (or caregiver) understands what adverse effects might occur, and create a plan to address them. Establish how often and when communication should occur. Encourage telephone calls and/or e-mail to communicate questions or concerns. |
| OTC, over the counter | |
Step 1. Conduct a comprehensive pain history
The first step in pain management is to perform a comprehensive pain assessment. Without a proper pain assessment, it will be difficult to effectively treat and monitor response to treatment. Whichever pain scale you decide to use, it is important to use the same pain scale consistently each time a pain assessment takes place.3 The numeric rating scale and verbal descriptor scales (or pain thermometer) are widely used and have been shown to be preferred in the older adult population.3,16 The numeric rating scale asks a patient to rate his or her pain on a scale of 0 to 10, with 0 being no pain and 10 being the most severe pain imaginable. The verbal descriptor scale is a measure of pain intensity on a vertical scale (typically a thermometer) from “no pain” to “excruciating.”3
Recommendations. In addition to assessing the intensity of the pain using a pain assessment tool, it is important to determine certain characteristics of the pain. What is the location and quality of the pain? Ask patients how the pain limits them. What prior treatments have been tried and failed? What has worked the best? What treatment/coping strategies are they using now? Have they had any intolerable adverse effects from specific treatments? Reliable predictors of treatment response require further definition,17 but a successful trial of a given analgesic in the past is often a good indicator of what might work again.
Step 2. Review the patient’s problem list
Use of multiple medications. Polypharmacy—with 5 or more being a typical threshold criterion—is common in people ages 65 and older and frequently complicates the pharmacologic management of chronic pain.16,18 Complications most often occur as a result of drug-drug interactions.
Multiple coexisting chronic conditions. Multimorbidity is common in older adults with chronic pain. Consider co-occurring diabetes, hypertension, and osteoporosis when initiating any trial of a pain medication. Nonsteroidal anti-inflammatory drugs (NSAIDs) can be effective in treating pain syndromes, but their use can be hazardous in older individuals, particularly those with coexisting hypertension, cardiovascular disease, history of peptic ulcer disease or gastropathy, or impaired renal function. NSAID use has been implicated as a cause of approximately one-quarter of all hospitalizations related to drug adverse effects among adults over age 65.1
NSAIDs can be effective in treating pain syndromes, but their use can be hazardous in older patients with hypertension, peptic ulcer disease, or impaired renal function.
The geriatric syndrome of frailty is defined by deficits in physiologic reserve and decreased resistance to multiple stressors.19 Risk of fracture is a particular concern of clinicians, older patients, and their caregivers. Opioids are the analgesic medications most often associated with increased fracture risk. In a recent analysis of Medicare claims data, opioid users were found to have a significantly increased fracture risk compared with users of nonselective NSAIDs.20 Mechanisms underlying this association include opioid-associated cognitive dysfunction and worsening gait/balance function.
Recommendations. Obtain a full list of the patient’s medications, including all OTC and complementary preparations. Also consider chronic kidney problems, liver disease, movement disorders, and neurologic problems when selecting a pharmacologic agent. Consider what chronic conditions might be made worse by an analgesic trial or would operate as a contraindication to starting a specific pain medication. Establish which medications or comorbidities might modify your treatment choices.
Step 3. Establish the patient’s treatment goals
We recommend shared decision-making when planning treatment and monitoring outcomes for older adults with chronic pain. Use your patient’s reports of the experience of pain— including pain intensity and how pain affects daily functioning1 —and identify his or her treatment goals, which might differ from yours. You may be aiming for the best pain relief possible, but your patient might be focused on practical issues such as increased mobility or ability to socialize. By talking openly, you can reach consensus and agree upon realistic treatment goals.
This approach can improve patients’ outcomes and satisfaction with treatment; it also has been shown to improve physician satisfaction when treating patients with chronic pain.21 In a recent qualitative study, older individuals varied in how much they wanted to participate in making decisions and being a “source of control” in their pain treatment. 22 Some patients—particularly those ages 80 and older—prefer to have their physicians make treatment decisions for them, whereas others embrace active participation. Regardless of how much older individuals wish to share in treatment decisions, they all value being listened to and understood by their physicians.21
Recommendations. The patient’s goals and expectations for treatment may or may not be the same as yours. Before starting a medication trial, address potential unrealistic expectations such as complete relief of pain or a belief that treatment is not likely to help. Come to a mutual decision as to what constitutes the most important outcomes, and you will then be able to monitor and assess treatment success.
Step 4. Identify barriers to initiating and adhering to therapy
Cognitive impairment is a strong risk factor for undertreatment of pain. It can lead to underreporting of pain by patients or difficulty for clinicians in assessing treatment response from those who are unable to communicate pain effectively. A study of nursing home residents found that only 56% of those with cognitive impairment received pain medications, compared with 80% of those with intact cognition.23 Older patients with cognitive deficits and memory loss also may take analgesic medications inappropriately or forget when/if they took them, increasing the risk of undertreatment or overdosing.
Fifty-six percent of nursing home residents with cognitive impairment received pain medications vs 80% of those with intact cognition.
Sensory impairment. Patients with visual deficits may have difficulty reading prescription bottle labels and information sheets. Those with auditory deficits may have trouble hearing, communicating, and understanding treatment instructions during a busy clinical encounter.
Sociodemographic factors. Many older adults live alone and have limited social support to encourage medication adherence.24 Some have significant caregiving responsibilities of their own (such as a spouse in poor health), which can lead to stress and inconsistent use of prescribed medications.25 Some older adults can’t afford the costs of certain pain medications and may take less than the prescribed amount.
Many older adults lack the necessary skills to read and process basic health care information, including understanding pill bottle instructions, information that appears in patient handouts, and clinicians’ instructions about possible adverse effects.26,27 Low health literacy can lead to problems with medication adherence (taking too much or too little of an analgesic medication) and associated complications.
Health beliefs. Many older adults believe chronic pain is a natural part of aging; in one study, this was true of 61% of approximately 700 primary care patients with osteoarthritis pain.28 Some older adults believe pain only gets worse over time,28 and others believe treatment for pain is not likely to provide any meaningful benefit.29,30 Beliefs such as these can lead to stoicism or acceptance of the status quo.31
Older adults also may endorse beliefs about pain medications that are likely to decrease their willingness to engage in, or adhere to, recommended pharmacologic interventions. Some use pain medicines sparingly because they fear addiction or dependence.32,33 Caregivers—often a spouse or adult child—also may express fears about the possibility of addiction.32 Finally, some older adults believe that using prescription analgesic medications invariably results in adverse effects;32 those who endorse this belief report minimizing medication use except when the pain is “very bad.”34
Recommendations. Elicit concerns patients may have about using analgesic medications and discuss them openly. Although not all barriers (such as economic issues) are modifiable, most (such as beliefs that pain medications are addictive) can be successfully addressed through patient education.
If other social support, such as a family member or caregiver in the home, could positively affect analgesic engagement/adherence, include these facilitators when discussing treatment decisions and in monitoring for medication effectiveness and adverse effects.
Step 5. Start low and go slow when initiating analgesia
Advancing age is associated with increased sensitivity to the anticholinergic effects of many commonly prescribed and OTC medications, including NSAIDs and opioids.35 Increasing the anticholinergic load can lead to cognitive impairments, including confusion, which can be particularly troublesome for older adults.1
Changes in pharmacokinetics (what the body does to the drug in terms of altering absorption, distribution, metabolism and excretion) and pharmacodynamics (what the drug does to the body in the form of adverse effects) occur as a function of advancing age. 1 Body fat increases by 20% to 40% on average, which increases the volume of distribution for fat-soluble medications.16 Hepatic and renal clearance decrease, leading to an increased half-life and decreased excretion of medications cleared by the liver or kidneys. Age-associated changes in gastrointestinal (GI) absorption and function include slower GI transit times and the possibility of increased opioid-related constipation from dysmotility problems.1
As a result of these physiologic changes, advancing age is associated with a greater incidence of drug-related adverse effects. Even so, individuals within the older population are highly heterogeneous, and no geriatric-specific dosing guidelines exist for prescribing pain medications to older adults.
Recommendations. We recommend the adage “start low and go slow” when initiating an analgesic trial for an older patient with chronic pain. This does not mean you should “start low and stay low,” which can contribute to undertreatment.36 If treatment goals are not being met and the patient is tolerating the therapy, advancing the dose is reasonable before moving on to another intervention.
We recommend that you “start low and go slow” but this does not mean that you should “start low and stay low.”
Step 6. Assess for effects and outcomes outside the office
Adverse effects are a primary reason older adults discontinue an analgesic trial.37 Make certain the patient (or caregiver, as appropriate) understands what adverse effects might occur, and create a plan to address them if they do.
Recommendations. Because many older people are reluctant to communicate with their physicians outside of an office visit, establish how often and when communication should occur. Telephone calls and/or e-mail are practical tools for patients to communicate questions or concerns to you, and you can enhance treatment outcomes with timely replies. In the near future, mobile health technologies may play a key role in monitoring for adverse effects and communicating positive treatment outcomes.
1. American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57:1331-1346.
2. Won AB, Lapane KL, Vallow S, et al. Persistent nonmalignant pain and analgesic prescribing patterns in elderly nursing home residents. J Am Geriatr Soc. 2004;52:867-874.
3. Gagliese L, Melzack R. Chronic pain in elderly people. Pain. 1997;70:3-14.
4. Leveille SG, Fried L, Guralnik JM. Disabling symptoms: what do older women report? J Gen Intern Med. 2002;17:766-773.
5. Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778-799.
6. Schmader KE. Epidemiology and impact on quality of life of postherpetic neuralgia and painful diabetic neuropathy. Clin J Pain. 2002;18:350-354.
7. Rao A, Cohen HJ. Symptom management in the elderly cancer patient: fatigue, pain, and depression. J Natl Cancer Inst Monogr. 2004;32:150-157.
8. Potter J, Hami F, Bryan T, et al. Symptoms in 400 patients referred to palliative care services: prevalence and patterns. Palliat Med. 2003;17:310-314.
9. Walke LM, Byers AL, Tinetti ME, et al. Range and severity of symptoms over time among older adults with chronic obstructive pulmonary disease and heart failure. Arch Intern Med. 2007;167:2503-2508.
10. Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31:58-69.
11. Landi F, Onder G, Cesari M, et al. Pain management in frail, community-living elderly patients. Arch Intern Med. 2001;161:2721-2724.
12. Institute of Medicine of the National Academies. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. June 29, 2011. Available at: http://www.iom.edu/Reports/2011/Relieving-Pain-in-America-A-Blueprint-for-Transforming-Prevention-Care-Education-Research.aspx. Accessed June 27, 2012.
13. Sarzi-Puttini P, Cimmino MA, Scarpa R, et al. Do physicians treat symptomatic osteoarthritis patients properly? Results of the AMICA experience. Semin Arthritis Rheum. 2005;35(suppl 1):38-42.
14. Silverman M, Nutini J, Musa D, et al. Daily temporal self-care responses to osteoarthritis symptoms by older African Americans and whites. J Cross Cult Gerontol. 2008;23:319-337.
15. Barry LC, Gill TM, Kerns RD, et al. Identification of pain-reduction strategies used by community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 2005;60:1569-1575.
16. Fine PG. Treatment guidelines for the pharmacological management of pain in older persons. Pain Med. 2012;13(suppl 2):S57-S66.
17. Reid MC, Bennett DA, Chen WG, et al. Improving the pharmacologic management of pain in older adults: identifying the research gaps and methods to address them. Pain Med. 2011;12:1336-1357.
18. Slone Epidemiology Center at Boston University. Patterns of medication use in the United States 2006: a report from the Slone Survey. Available at: http://www.bu.edu/slone/SloneSurvey/AnnualRpt/SloneSurveyWebReport2006.pdf. Accessed June 27, 2012.
19. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146-M156.
20. Solomon DH, Rassen JA, Glynn RJ, et al. The comparative safety of analgesics in older adults with arthritis. Arch Intern Med. 2010;170:1968-1976.
21. Sullivan MD, Leigh J, Gaster B. Brief report: training internists in shared decision making about chronic opioid treatment for noncancer pain. J Gen Intern Med. 2006;21:360-362.
22. Teh CF, Karp JF, Kleinman A, et al. Older people’s experiences of patient-centered treatment for chronic pain: a qualitative study. Pain Med. 2009;10:521-530.
23. Reynolds KS, Hanson LC, DeVellis RF, et al. Disparities in pain management between cognitively intact and cognitively impaired nursing home residents. J Pain Symptom Manage. 2008;35:388-396.
24. Elliott RA. Poor adherence to medication in adults with rheumatoid arthritis: reasons and solutions. Dis Manage Health Outcomes. 2008;16:13-29.
25. Cardenas-Valladolid J, Martin-Madrazo C, Salinero-Fort MA, et al. Prevalence of adherence to treatment in homebound elderly people in primary health care: a descriptive cross-sectional, multicentre study. Drugs Aging. 2010;27:641-651.
26. Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475-482.
27. Gazmararian JA, Baker DW, Williams MV, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545-551.
28. Appelt CJ, Burant CJ, Siminoff LA, et al. Arthritis-specific health beliefs related to aging among older male patients with knee and/or hip osteoarthritis. J Gerontol A Biol Sci Med Sci. 2007;62:184-190.
29. Weiner DK, Rudy TE. Attitudinal barriers to effective treatment of persistent pain in nursing home residents. J Am Geriatr Soc. 2002;50:2035-2040.
30. Yates P, Dewar A, Fentiman B. Pain: the views of elderly people living in long-term residential care settings. J Adv Nurs. 1995;21:667-674.
31. Cornally N, McCarthy G. Chronic pain: the help-seeking behavior, attitudes, and beliefs of older adults living in the community. Pain Manage Nurs. 2011;12:206-217.
32. Spitz A, Moore AA, Papaleontiou M, et al. Primary care providers’ perspective on prescribing opioids to older adults with chronic non-cancer pain: a qualitative study. BMC Geriatrics. 2011;11:35.-
33. Chia LR, Schlenk EA, Dunbar-Jacob J. Effect of personal and cultural beliefs on medication adherence in the elderly. Drugs Aging. 2006;23:191-202.
34. Sale J, Gignac M, Hawker G. How “bad” does the pain have to be? A qualitative study examining adherence to pain medication in older adults with osteoarthritis. Arthritis Rheum. 2006;55:272-278.
35. Rudolph JL, Salow MJ, Angelini MC, et al. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008;168:508-513.
36. Hanlon JT, Backonja M, Weiner D, et al. Evolving pharmacological management of persistent pain in older persons. Pain Med. 2009;10:959-961.
37. Reid MC, Henderson CR, Jr, Papaleontiou M, et al. Characteristics of older adults receiving opioids in primary care: treatment duration and outcomes. Pain Med. 2010;11:1063-1071.
Sickle cell disease: Gaining control over the pain
Treating herpes zoster and postherpetic neuralgia: An evidence-based approach
Managing chronic pain in older adults: 6 steps to overcoming medication barriers
Dr. Reid is a consultant to sanofi aventis. Dr. Ayres and Mr. Warmington reported no potential conflict of interest relevant to this article.
Managing chronic pain in an older adult can be a complicated task, with risks for adverse effects, under- or overmedication, and nonadherence. Pain can be alleviated in many cases, however, if you address potential complications and barriers to effective treatment when prescribing analgesic medications.
Pain is a part of daily life for many older adults
As many as 50% of community-dwelling older adults experience a chronic pain disorder, defined as pain on most days for at least 3 consecutive months.1 Prevalence rates are typically higher (49%-84%) among residents of long-term care facilities.2 Untreated chronic pain can lead to health consequences such as depression, decreased ability to socialize, impaired ambulation, impaired sleep, increased falls, malnutrition, and decreased quality of life.1,3 Among older women, pain is the most common reported cause of impairment in activities of daily living.4
Arthritis and arthritis-related diseases (such as back pain) are common causes of chronic pain in older adults.5 Other causes include neuropathies, vertebral compression fractures, cancer and cancer treatments, and advanced chronic diseases such as end-stage heart, lung, and kidney disease.6-10
Substantial literature documents that chronic pain is underdetected and undertreated with advancing age11,12 and strongly supports efforts to improve pain care in later life. Treatment guidelines recommend a multimodal approach, including evidence-based nonpharmacologic treatments such as cognitive-behavioral therapy, exercise, and physical therapy.1 At the same time, pharmacotherapies remain the primary treatment used by physicians,13 and studies indicate that older people use analgesics frequently:
- When 551 older black and non-Hispanic white adults with osteoarthritis were interviewed, more than 80% of each group reported regular use of prescription and over-the-counter (OTC) analgesic medications.14
- In a cross-sectional study of 272 community-dwelling older adults with chronic pain from diverse causes, 59% reported routine use of an analgesic medication.15
The following 6 steps can improve the likelihood of a successful analgesic trial when managing chronic pain in people ages 65 and older. They take into account barriers you are likely to encounter, including polypharmacy, multimorbidity, cognitive and sensory impairment, sociodemographic factors, specific health beliefs about pain and pain treatments, and age-related physiologic changes.
TABLE
Refine your approach to chronic pain in older patients with these 6 steps
| 1. Conduct a comprehensive pain history | Assess pain location and intensity, and ask how pain limits activity. What treatments have been tried? What worked best? Any intolerable adverse effects? |
| 2. Review the problem list | Obtain a full medication list (OTC and supplements) to identify potential interactions. What chronic conditions (kidney or liver disease, movement disorders, neurologic problems) might worsen with analgesic medication or operate as a contraindication? Which drugs or comorbidities might affect treatment choices? |
| 3. Establish treatment goals | Address potential unrealistic expectations (eg, complete relief of pain or no benefit from treatment). The patient’s goals might differ from yours; come to a mutual decision about the most important outcomes. |
| 4. Identify barriers to therapy | Be aware of how cognitive or sensory impairment, sociodemographic factors, or health beliefs may limit medication adherence. Elicit the patient’s concerns about medications and discuss openly. Include the caregiver, as needed, when discussing treatments and monitoring outcomes. |
| 5. Start low and go slow when initiating analgesia | Avoid “start low and stay low,” which can contribute to undertreatment. If treatment goals are not met and the patient is tolerating therapy, advancing the dose is reasonable before trying another intervention. |
| 6. Assess for effects and outcomes | Make certain that the patient (or caregiver) understands what adverse effects might occur, and create a plan to address them. Establish how often and when communication should occur. Encourage telephone calls and/or e-mail to communicate questions or concerns. |
| OTC, over the counter | |
Step 1. Conduct a comprehensive pain history
The first step in pain management is to perform a comprehensive pain assessment. Without a proper pain assessment, it will be difficult to effectively treat and monitor response to treatment. Whichever pain scale you decide to use, it is important to use the same pain scale consistently each time a pain assessment takes place.3 The numeric rating scale and verbal descriptor scales (or pain thermometer) are widely used and have been shown to be preferred in the older adult population.3,16 The numeric rating scale asks a patient to rate his or her pain on a scale of 0 to 10, with 0 being no pain and 10 being the most severe pain imaginable. The verbal descriptor scale is a measure of pain intensity on a vertical scale (typically a thermometer) from “no pain” to “excruciating.”3
Recommendations. In addition to assessing the intensity of the pain using a pain assessment tool, it is important to determine certain characteristics of the pain. What is the location and quality of the pain? Ask patients how the pain limits them. What prior treatments have been tried and failed? What has worked the best? What treatment/coping strategies are they using now? Have they had any intolerable adverse effects from specific treatments? Reliable predictors of treatment response require further definition,17 but a successful trial of a given analgesic in the past is often a good indicator of what might work again.
Step 2. Review the patient’s problem list
Use of multiple medications. Polypharmacy—with 5 or more being a typical threshold criterion—is common in people ages 65 and older and frequently complicates the pharmacologic management of chronic pain.16,18 Complications most often occur as a result of drug-drug interactions.
Multiple coexisting chronic conditions. Multimorbidity is common in older adults with chronic pain. Consider co-occurring diabetes, hypertension, and osteoporosis when initiating any trial of a pain medication. Nonsteroidal anti-inflammatory drugs (NSAIDs) can be effective in treating pain syndromes, but their use can be hazardous in older individuals, particularly those with coexisting hypertension, cardiovascular disease, history of peptic ulcer disease or gastropathy, or impaired renal function. NSAID use has been implicated as a cause of approximately one-quarter of all hospitalizations related to drug adverse effects among adults over age 65.1
NSAIDs can be effective in treating pain syndromes, but their use can be hazardous in older patients with hypertension, peptic ulcer disease, or impaired renal function.
The geriatric syndrome of frailty is defined by deficits in physiologic reserve and decreased resistance to multiple stressors.19 Risk of fracture is a particular concern of clinicians, older patients, and their caregivers. Opioids are the analgesic medications most often associated with increased fracture risk. In a recent analysis of Medicare claims data, opioid users were found to have a significantly increased fracture risk compared with users of nonselective NSAIDs.20 Mechanisms underlying this association include opioid-associated cognitive dysfunction and worsening gait/balance function.
Recommendations. Obtain a full list of the patient’s medications, including all OTC and complementary preparations. Also consider chronic kidney problems, liver disease, movement disorders, and neurologic problems when selecting a pharmacologic agent. Consider what chronic conditions might be made worse by an analgesic trial or would operate as a contraindication to starting a specific pain medication. Establish which medications or comorbidities might modify your treatment choices.
Step 3. Establish the patient’s treatment goals
We recommend shared decision-making when planning treatment and monitoring outcomes for older adults with chronic pain. Use your patient’s reports of the experience of pain— including pain intensity and how pain affects daily functioning1 —and identify his or her treatment goals, which might differ from yours. You may be aiming for the best pain relief possible, but your patient might be focused on practical issues such as increased mobility or ability to socialize. By talking openly, you can reach consensus and agree upon realistic treatment goals.
This approach can improve patients’ outcomes and satisfaction with treatment; it also has been shown to improve physician satisfaction when treating patients with chronic pain.21 In a recent qualitative study, older individuals varied in how much they wanted to participate in making decisions and being a “source of control” in their pain treatment. 22 Some patients—particularly those ages 80 and older—prefer to have their physicians make treatment decisions for them, whereas others embrace active participation. Regardless of how much older individuals wish to share in treatment decisions, they all value being listened to and understood by their physicians.21
Recommendations. The patient’s goals and expectations for treatment may or may not be the same as yours. Before starting a medication trial, address potential unrealistic expectations such as complete relief of pain or a belief that treatment is not likely to help. Come to a mutual decision as to what constitutes the most important outcomes, and you will then be able to monitor and assess treatment success.
Step 4. Identify barriers to initiating and adhering to therapy
Cognitive impairment is a strong risk factor for undertreatment of pain. It can lead to underreporting of pain by patients or difficulty for clinicians in assessing treatment response from those who are unable to communicate pain effectively. A study of nursing home residents found that only 56% of those with cognitive impairment received pain medications, compared with 80% of those with intact cognition.23 Older patients with cognitive deficits and memory loss also may take analgesic medications inappropriately or forget when/if they took them, increasing the risk of undertreatment or overdosing.
Fifty-six percent of nursing home residents with cognitive impairment received pain medications vs 80% of those with intact cognition.
Sensory impairment. Patients with visual deficits may have difficulty reading prescription bottle labels and information sheets. Those with auditory deficits may have trouble hearing, communicating, and understanding treatment instructions during a busy clinical encounter.
Sociodemographic factors. Many older adults live alone and have limited social support to encourage medication adherence.24 Some have significant caregiving responsibilities of their own (such as a spouse in poor health), which can lead to stress and inconsistent use of prescribed medications.25 Some older adults can’t afford the costs of certain pain medications and may take less than the prescribed amount.
Many older adults lack the necessary skills to read and process basic health care information, including understanding pill bottle instructions, information that appears in patient handouts, and clinicians’ instructions about possible adverse effects.26,27 Low health literacy can lead to problems with medication adherence (taking too much or too little of an analgesic medication) and associated complications.
Health beliefs. Many older adults believe chronic pain is a natural part of aging; in one study, this was true of 61% of approximately 700 primary care patients with osteoarthritis pain.28 Some older adults believe pain only gets worse over time,28 and others believe treatment for pain is not likely to provide any meaningful benefit.29,30 Beliefs such as these can lead to stoicism or acceptance of the status quo.31
Older adults also may endorse beliefs about pain medications that are likely to decrease their willingness to engage in, or adhere to, recommended pharmacologic interventions. Some use pain medicines sparingly because they fear addiction or dependence.32,33 Caregivers—often a spouse or adult child—also may express fears about the possibility of addiction.32 Finally, some older adults believe that using prescription analgesic medications invariably results in adverse effects;32 those who endorse this belief report minimizing medication use except when the pain is “very bad.”34
Recommendations. Elicit concerns patients may have about using analgesic medications and discuss them openly. Although not all barriers (such as economic issues) are modifiable, most (such as beliefs that pain medications are addictive) can be successfully addressed through patient education.
If other social support, such as a family member or caregiver in the home, could positively affect analgesic engagement/adherence, include these facilitators when discussing treatment decisions and in monitoring for medication effectiveness and adverse effects.
Step 5. Start low and go slow when initiating analgesia
Advancing age is associated with increased sensitivity to the anticholinergic effects of many commonly prescribed and OTC medications, including NSAIDs and opioids.35 Increasing the anticholinergic load can lead to cognitive impairments, including confusion, which can be particularly troublesome for older adults.1
Changes in pharmacokinetics (what the body does to the drug in terms of altering absorption, distribution, metabolism and excretion) and pharmacodynamics (what the drug does to the body in the form of adverse effects) occur as a function of advancing age. 1 Body fat increases by 20% to 40% on average, which increases the volume of distribution for fat-soluble medications.16 Hepatic and renal clearance decrease, leading to an increased half-life and decreased excretion of medications cleared by the liver or kidneys. Age-associated changes in gastrointestinal (GI) absorption and function include slower GI transit times and the possibility of increased opioid-related constipation from dysmotility problems.1
As a result of these physiologic changes, advancing age is associated with a greater incidence of drug-related adverse effects. Even so, individuals within the older population are highly heterogeneous, and no geriatric-specific dosing guidelines exist for prescribing pain medications to older adults.
Recommendations. We recommend the adage “start low and go slow” when initiating an analgesic trial for an older patient with chronic pain. This does not mean you should “start low and stay low,” which can contribute to undertreatment.36 If treatment goals are not being met and the patient is tolerating the therapy, advancing the dose is reasonable before moving on to another intervention.
We recommend that you “start low and go slow” but this does not mean that you should “start low and stay low.”
Step 6. Assess for effects and outcomes outside the office
Adverse effects are a primary reason older adults discontinue an analgesic trial.37 Make certain the patient (or caregiver, as appropriate) understands what adverse effects might occur, and create a plan to address them if they do.
Recommendations. Because many older people are reluctant to communicate with their physicians outside of an office visit, establish how often and when communication should occur. Telephone calls and/or e-mail are practical tools for patients to communicate questions or concerns to you, and you can enhance treatment outcomes with timely replies. In the near future, mobile health technologies may play a key role in monitoring for adverse effects and communicating positive treatment outcomes.
Sickle cell disease: Gaining control over the pain
Treating herpes zoster and postherpetic neuralgia: An evidence-based approach
Managing chronic pain in older adults: 6 steps to overcoming medication barriers
Dr. Reid is a consultant to sanofi aventis. Dr. Ayres and Mr. Warmington reported no potential conflict of interest relevant to this article.
Managing chronic pain in an older adult can be a complicated task, with risks for adverse effects, under- or overmedication, and nonadherence. Pain can be alleviated in many cases, however, if you address potential complications and barriers to effective treatment when prescribing analgesic medications.
Pain is a part of daily life for many older adults
As many as 50% of community-dwelling older adults experience a chronic pain disorder, defined as pain on most days for at least 3 consecutive months.1 Prevalence rates are typically higher (49%-84%) among residents of long-term care facilities.2 Untreated chronic pain can lead to health consequences such as depression, decreased ability to socialize, impaired ambulation, impaired sleep, increased falls, malnutrition, and decreased quality of life.1,3 Among older women, pain is the most common reported cause of impairment in activities of daily living.4
Arthritis and arthritis-related diseases (such as back pain) are common causes of chronic pain in older adults.5 Other causes include neuropathies, vertebral compression fractures, cancer and cancer treatments, and advanced chronic diseases such as end-stage heart, lung, and kidney disease.6-10
Substantial literature documents that chronic pain is underdetected and undertreated with advancing age11,12 and strongly supports efforts to improve pain care in later life. Treatment guidelines recommend a multimodal approach, including evidence-based nonpharmacologic treatments such as cognitive-behavioral therapy, exercise, and physical therapy.1 At the same time, pharmacotherapies remain the primary treatment used by physicians,13 and studies indicate that older people use analgesics frequently:
- When 551 older black and non-Hispanic white adults with osteoarthritis were interviewed, more than 80% of each group reported regular use of prescription and over-the-counter (OTC) analgesic medications.14
- In a cross-sectional study of 272 community-dwelling older adults with chronic pain from diverse causes, 59% reported routine use of an analgesic medication.15
The following 6 steps can improve the likelihood of a successful analgesic trial when managing chronic pain in people ages 65 and older. They take into account barriers you are likely to encounter, including polypharmacy, multimorbidity, cognitive and sensory impairment, sociodemographic factors, specific health beliefs about pain and pain treatments, and age-related physiologic changes.
TABLE
Refine your approach to chronic pain in older patients with these 6 steps
| 1. Conduct a comprehensive pain history | Assess pain location and intensity, and ask how pain limits activity. What treatments have been tried? What worked best? Any intolerable adverse effects? |
| 2. Review the problem list | Obtain a full medication list (OTC and supplements) to identify potential interactions. What chronic conditions (kidney or liver disease, movement disorders, neurologic problems) might worsen with analgesic medication or operate as a contraindication? Which drugs or comorbidities might affect treatment choices? |
| 3. Establish treatment goals | Address potential unrealistic expectations (eg, complete relief of pain or no benefit from treatment). The patient’s goals might differ from yours; come to a mutual decision about the most important outcomes. |
| 4. Identify barriers to therapy | Be aware of how cognitive or sensory impairment, sociodemographic factors, or health beliefs may limit medication adherence. Elicit the patient’s concerns about medications and discuss openly. Include the caregiver, as needed, when discussing treatments and monitoring outcomes. |
| 5. Start low and go slow when initiating analgesia | Avoid “start low and stay low,” which can contribute to undertreatment. If treatment goals are not met and the patient is tolerating therapy, advancing the dose is reasonable before trying another intervention. |
| 6. Assess for effects and outcomes | Make certain that the patient (or caregiver) understands what adverse effects might occur, and create a plan to address them. Establish how often and when communication should occur. Encourage telephone calls and/or e-mail to communicate questions or concerns. |
| OTC, over the counter | |
Step 1. Conduct a comprehensive pain history
The first step in pain management is to perform a comprehensive pain assessment. Without a proper pain assessment, it will be difficult to effectively treat and monitor response to treatment. Whichever pain scale you decide to use, it is important to use the same pain scale consistently each time a pain assessment takes place.3 The numeric rating scale and verbal descriptor scales (or pain thermometer) are widely used and have been shown to be preferred in the older adult population.3,16 The numeric rating scale asks a patient to rate his or her pain on a scale of 0 to 10, with 0 being no pain and 10 being the most severe pain imaginable. The verbal descriptor scale is a measure of pain intensity on a vertical scale (typically a thermometer) from “no pain” to “excruciating.”3
Recommendations. In addition to assessing the intensity of the pain using a pain assessment tool, it is important to determine certain characteristics of the pain. What is the location and quality of the pain? Ask patients how the pain limits them. What prior treatments have been tried and failed? What has worked the best? What treatment/coping strategies are they using now? Have they had any intolerable adverse effects from specific treatments? Reliable predictors of treatment response require further definition,17 but a successful trial of a given analgesic in the past is often a good indicator of what might work again.
Step 2. Review the patient’s problem list
Use of multiple medications. Polypharmacy—with 5 or more being a typical threshold criterion—is common in people ages 65 and older and frequently complicates the pharmacologic management of chronic pain.16,18 Complications most often occur as a result of drug-drug interactions.
Multiple coexisting chronic conditions. Multimorbidity is common in older adults with chronic pain. Consider co-occurring diabetes, hypertension, and osteoporosis when initiating any trial of a pain medication. Nonsteroidal anti-inflammatory drugs (NSAIDs) can be effective in treating pain syndromes, but their use can be hazardous in older individuals, particularly those with coexisting hypertension, cardiovascular disease, history of peptic ulcer disease or gastropathy, or impaired renal function. NSAID use has been implicated as a cause of approximately one-quarter of all hospitalizations related to drug adverse effects among adults over age 65.1
NSAIDs can be effective in treating pain syndromes, but their use can be hazardous in older patients with hypertension, peptic ulcer disease, or impaired renal function.
The geriatric syndrome of frailty is defined by deficits in physiologic reserve and decreased resistance to multiple stressors.19 Risk of fracture is a particular concern of clinicians, older patients, and their caregivers. Opioids are the analgesic medications most often associated with increased fracture risk. In a recent analysis of Medicare claims data, opioid users were found to have a significantly increased fracture risk compared with users of nonselective NSAIDs.20 Mechanisms underlying this association include opioid-associated cognitive dysfunction and worsening gait/balance function.
Recommendations. Obtain a full list of the patient’s medications, including all OTC and complementary preparations. Also consider chronic kidney problems, liver disease, movement disorders, and neurologic problems when selecting a pharmacologic agent. Consider what chronic conditions might be made worse by an analgesic trial or would operate as a contraindication to starting a specific pain medication. Establish which medications or comorbidities might modify your treatment choices.
Step 3. Establish the patient’s treatment goals
We recommend shared decision-making when planning treatment and monitoring outcomes for older adults with chronic pain. Use your patient’s reports of the experience of pain— including pain intensity and how pain affects daily functioning1 —and identify his or her treatment goals, which might differ from yours. You may be aiming for the best pain relief possible, but your patient might be focused on practical issues such as increased mobility or ability to socialize. By talking openly, you can reach consensus and agree upon realistic treatment goals.
This approach can improve patients’ outcomes and satisfaction with treatment; it also has been shown to improve physician satisfaction when treating patients with chronic pain.21 In a recent qualitative study, older individuals varied in how much they wanted to participate in making decisions and being a “source of control” in their pain treatment. 22 Some patients—particularly those ages 80 and older—prefer to have their physicians make treatment decisions for them, whereas others embrace active participation. Regardless of how much older individuals wish to share in treatment decisions, they all value being listened to and understood by their physicians.21
Recommendations. The patient’s goals and expectations for treatment may or may not be the same as yours. Before starting a medication trial, address potential unrealistic expectations such as complete relief of pain or a belief that treatment is not likely to help. Come to a mutual decision as to what constitutes the most important outcomes, and you will then be able to monitor and assess treatment success.
Step 4. Identify barriers to initiating and adhering to therapy
Cognitive impairment is a strong risk factor for undertreatment of pain. It can lead to underreporting of pain by patients or difficulty for clinicians in assessing treatment response from those who are unable to communicate pain effectively. A study of nursing home residents found that only 56% of those with cognitive impairment received pain medications, compared with 80% of those with intact cognition.23 Older patients with cognitive deficits and memory loss also may take analgesic medications inappropriately or forget when/if they took them, increasing the risk of undertreatment or overdosing.
Fifty-six percent of nursing home residents with cognitive impairment received pain medications vs 80% of those with intact cognition.
Sensory impairment. Patients with visual deficits may have difficulty reading prescription bottle labels and information sheets. Those with auditory deficits may have trouble hearing, communicating, and understanding treatment instructions during a busy clinical encounter.
Sociodemographic factors. Many older adults live alone and have limited social support to encourage medication adherence.24 Some have significant caregiving responsibilities of their own (such as a spouse in poor health), which can lead to stress and inconsistent use of prescribed medications.25 Some older adults can’t afford the costs of certain pain medications and may take less than the prescribed amount.
Many older adults lack the necessary skills to read and process basic health care information, including understanding pill bottle instructions, information that appears in patient handouts, and clinicians’ instructions about possible adverse effects.26,27 Low health literacy can lead to problems with medication adherence (taking too much or too little of an analgesic medication) and associated complications.
Health beliefs. Many older adults believe chronic pain is a natural part of aging; in one study, this was true of 61% of approximately 700 primary care patients with osteoarthritis pain.28 Some older adults believe pain only gets worse over time,28 and others believe treatment for pain is not likely to provide any meaningful benefit.29,30 Beliefs such as these can lead to stoicism or acceptance of the status quo.31
Older adults also may endorse beliefs about pain medications that are likely to decrease their willingness to engage in, or adhere to, recommended pharmacologic interventions. Some use pain medicines sparingly because they fear addiction or dependence.32,33 Caregivers—often a spouse or adult child—also may express fears about the possibility of addiction.32 Finally, some older adults believe that using prescription analgesic medications invariably results in adverse effects;32 those who endorse this belief report minimizing medication use except when the pain is “very bad.”34
Recommendations. Elicit concerns patients may have about using analgesic medications and discuss them openly. Although not all barriers (such as economic issues) are modifiable, most (such as beliefs that pain medications are addictive) can be successfully addressed through patient education.
If other social support, such as a family member or caregiver in the home, could positively affect analgesic engagement/adherence, include these facilitators when discussing treatment decisions and in monitoring for medication effectiveness and adverse effects.
Step 5. Start low and go slow when initiating analgesia
Advancing age is associated with increased sensitivity to the anticholinergic effects of many commonly prescribed and OTC medications, including NSAIDs and opioids.35 Increasing the anticholinergic load can lead to cognitive impairments, including confusion, which can be particularly troublesome for older adults.1
Changes in pharmacokinetics (what the body does to the drug in terms of altering absorption, distribution, metabolism and excretion) and pharmacodynamics (what the drug does to the body in the form of adverse effects) occur as a function of advancing age. 1 Body fat increases by 20% to 40% on average, which increases the volume of distribution for fat-soluble medications.16 Hepatic and renal clearance decrease, leading to an increased half-life and decreased excretion of medications cleared by the liver or kidneys. Age-associated changes in gastrointestinal (GI) absorption and function include slower GI transit times and the possibility of increased opioid-related constipation from dysmotility problems.1
As a result of these physiologic changes, advancing age is associated with a greater incidence of drug-related adverse effects. Even so, individuals within the older population are highly heterogeneous, and no geriatric-specific dosing guidelines exist for prescribing pain medications to older adults.
Recommendations. We recommend the adage “start low and go slow” when initiating an analgesic trial for an older patient with chronic pain. This does not mean you should “start low and stay low,” which can contribute to undertreatment.36 If treatment goals are not being met and the patient is tolerating the therapy, advancing the dose is reasonable before moving on to another intervention.
We recommend that you “start low and go slow” but this does not mean that you should “start low and stay low.”
Step 6. Assess for effects and outcomes outside the office
Adverse effects are a primary reason older adults discontinue an analgesic trial.37 Make certain the patient (or caregiver, as appropriate) understands what adverse effects might occur, and create a plan to address them if they do.
Recommendations. Because many older people are reluctant to communicate with their physicians outside of an office visit, establish how often and when communication should occur. Telephone calls and/or e-mail are practical tools for patients to communicate questions or concerns to you, and you can enhance treatment outcomes with timely replies. In the near future, mobile health technologies may play a key role in monitoring for adverse effects and communicating positive treatment outcomes.
1. American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57:1331-1346.
2. Won AB, Lapane KL, Vallow S, et al. Persistent nonmalignant pain and analgesic prescribing patterns in elderly nursing home residents. J Am Geriatr Soc. 2004;52:867-874.
3. Gagliese L, Melzack R. Chronic pain in elderly people. Pain. 1997;70:3-14.
4. Leveille SG, Fried L, Guralnik JM. Disabling symptoms: what do older women report? J Gen Intern Med. 2002;17:766-773.
5. Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778-799.
6. Schmader KE. Epidemiology and impact on quality of life of postherpetic neuralgia and painful diabetic neuropathy. Clin J Pain. 2002;18:350-354.
7. Rao A, Cohen HJ. Symptom management in the elderly cancer patient: fatigue, pain, and depression. J Natl Cancer Inst Monogr. 2004;32:150-157.
8. Potter J, Hami F, Bryan T, et al. Symptoms in 400 patients referred to palliative care services: prevalence and patterns. Palliat Med. 2003;17:310-314.
9. Walke LM, Byers AL, Tinetti ME, et al. Range and severity of symptoms over time among older adults with chronic obstructive pulmonary disease and heart failure. Arch Intern Med. 2007;167:2503-2508.
10. Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31:58-69.
11. Landi F, Onder G, Cesari M, et al. Pain management in frail, community-living elderly patients. Arch Intern Med. 2001;161:2721-2724.
12. Institute of Medicine of the National Academies. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. June 29, 2011. Available at: http://www.iom.edu/Reports/2011/Relieving-Pain-in-America-A-Blueprint-for-Transforming-Prevention-Care-Education-Research.aspx. Accessed June 27, 2012.
13. Sarzi-Puttini P, Cimmino MA, Scarpa R, et al. Do physicians treat symptomatic osteoarthritis patients properly? Results of the AMICA experience. Semin Arthritis Rheum. 2005;35(suppl 1):38-42.
14. Silverman M, Nutini J, Musa D, et al. Daily temporal self-care responses to osteoarthritis symptoms by older African Americans and whites. J Cross Cult Gerontol. 2008;23:319-337.
15. Barry LC, Gill TM, Kerns RD, et al. Identification of pain-reduction strategies used by community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 2005;60:1569-1575.
16. Fine PG. Treatment guidelines for the pharmacological management of pain in older persons. Pain Med. 2012;13(suppl 2):S57-S66.
17. Reid MC, Bennett DA, Chen WG, et al. Improving the pharmacologic management of pain in older adults: identifying the research gaps and methods to address them. Pain Med. 2011;12:1336-1357.
18. Slone Epidemiology Center at Boston University. Patterns of medication use in the United States 2006: a report from the Slone Survey. Available at: http://www.bu.edu/slone/SloneSurvey/AnnualRpt/SloneSurveyWebReport2006.pdf. Accessed June 27, 2012.
19. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146-M156.
20. Solomon DH, Rassen JA, Glynn RJ, et al. The comparative safety of analgesics in older adults with arthritis. Arch Intern Med. 2010;170:1968-1976.
21. Sullivan MD, Leigh J, Gaster B. Brief report: training internists in shared decision making about chronic opioid treatment for noncancer pain. J Gen Intern Med. 2006;21:360-362.
22. Teh CF, Karp JF, Kleinman A, et al. Older people’s experiences of patient-centered treatment for chronic pain: a qualitative study. Pain Med. 2009;10:521-530.
23. Reynolds KS, Hanson LC, DeVellis RF, et al. Disparities in pain management between cognitively intact and cognitively impaired nursing home residents. J Pain Symptom Manage. 2008;35:388-396.
24. Elliott RA. Poor adherence to medication in adults with rheumatoid arthritis: reasons and solutions. Dis Manage Health Outcomes. 2008;16:13-29.
25. Cardenas-Valladolid J, Martin-Madrazo C, Salinero-Fort MA, et al. Prevalence of adherence to treatment in homebound elderly people in primary health care: a descriptive cross-sectional, multicentre study. Drugs Aging. 2010;27:641-651.
26. Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475-482.
27. Gazmararian JA, Baker DW, Williams MV, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545-551.
28. Appelt CJ, Burant CJ, Siminoff LA, et al. Arthritis-specific health beliefs related to aging among older male patients with knee and/or hip osteoarthritis. J Gerontol A Biol Sci Med Sci. 2007;62:184-190.
29. Weiner DK, Rudy TE. Attitudinal barriers to effective treatment of persistent pain in nursing home residents. J Am Geriatr Soc. 2002;50:2035-2040.
30. Yates P, Dewar A, Fentiman B. Pain: the views of elderly people living in long-term residential care settings. J Adv Nurs. 1995;21:667-674.
31. Cornally N, McCarthy G. Chronic pain: the help-seeking behavior, attitudes, and beliefs of older adults living in the community. Pain Manage Nurs. 2011;12:206-217.
32. Spitz A, Moore AA, Papaleontiou M, et al. Primary care providers’ perspective on prescribing opioids to older adults with chronic non-cancer pain: a qualitative study. BMC Geriatrics. 2011;11:35.-
33. Chia LR, Schlenk EA, Dunbar-Jacob J. Effect of personal and cultural beliefs on medication adherence in the elderly. Drugs Aging. 2006;23:191-202.
34. Sale J, Gignac M, Hawker G. How “bad” does the pain have to be? A qualitative study examining adherence to pain medication in older adults with osteoarthritis. Arthritis Rheum. 2006;55:272-278.
35. Rudolph JL, Salow MJ, Angelini MC, et al. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008;168:508-513.
36. Hanlon JT, Backonja M, Weiner D, et al. Evolving pharmacological management of persistent pain in older persons. Pain Med. 2009;10:959-961.
37. Reid MC, Henderson CR, Jr, Papaleontiou M, et al. Characteristics of older adults receiving opioids in primary care: treatment duration and outcomes. Pain Med. 2010;11:1063-1071.
1. American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57:1331-1346.
2. Won AB, Lapane KL, Vallow S, et al. Persistent nonmalignant pain and analgesic prescribing patterns in elderly nursing home residents. J Am Geriatr Soc. 2004;52:867-874.
3. Gagliese L, Melzack R. Chronic pain in elderly people. Pain. 1997;70:3-14.
4. Leveille SG, Fried L, Guralnik JM. Disabling symptoms: what do older women report? J Gen Intern Med. 2002;17:766-773.
5. Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778-799.
6. Schmader KE. Epidemiology and impact on quality of life of postherpetic neuralgia and painful diabetic neuropathy. Clin J Pain. 2002;18:350-354.
7. Rao A, Cohen HJ. Symptom management in the elderly cancer patient: fatigue, pain, and depression. J Natl Cancer Inst Monogr. 2004;32:150-157.
8. Potter J, Hami F, Bryan T, et al. Symptoms in 400 patients referred to palliative care services: prevalence and patterns. Palliat Med. 2003;17:310-314.
9. Walke LM, Byers AL, Tinetti ME, et al. Range and severity of symptoms over time among older adults with chronic obstructive pulmonary disease and heart failure. Arch Intern Med. 2007;167:2503-2508.
10. Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31:58-69.
11. Landi F, Onder G, Cesari M, et al. Pain management in frail, community-living elderly patients. Arch Intern Med. 2001;161:2721-2724.
12. Institute of Medicine of the National Academies. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. June 29, 2011. Available at: http://www.iom.edu/Reports/2011/Relieving-Pain-in-America-A-Blueprint-for-Transforming-Prevention-Care-Education-Research.aspx. Accessed June 27, 2012.
13. Sarzi-Puttini P, Cimmino MA, Scarpa R, et al. Do physicians treat symptomatic osteoarthritis patients properly? Results of the AMICA experience. Semin Arthritis Rheum. 2005;35(suppl 1):38-42.
14. Silverman M, Nutini J, Musa D, et al. Daily temporal self-care responses to osteoarthritis symptoms by older African Americans and whites. J Cross Cult Gerontol. 2008;23:319-337.
15. Barry LC, Gill TM, Kerns RD, et al. Identification of pain-reduction strategies used by community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 2005;60:1569-1575.
16. Fine PG. Treatment guidelines for the pharmacological management of pain in older persons. Pain Med. 2012;13(suppl 2):S57-S66.
17. Reid MC, Bennett DA, Chen WG, et al. Improving the pharmacologic management of pain in older adults: identifying the research gaps and methods to address them. Pain Med. 2011;12:1336-1357.
18. Slone Epidemiology Center at Boston University. Patterns of medication use in the United States 2006: a report from the Slone Survey. Available at: http://www.bu.edu/slone/SloneSurvey/AnnualRpt/SloneSurveyWebReport2006.pdf. Accessed June 27, 2012.
19. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146-M156.
20. Solomon DH, Rassen JA, Glynn RJ, et al. The comparative safety of analgesics in older adults with arthritis. Arch Intern Med. 2010;170:1968-1976.
21. Sullivan MD, Leigh J, Gaster B. Brief report: training internists in shared decision making about chronic opioid treatment for noncancer pain. J Gen Intern Med. 2006;21:360-362.
22. Teh CF, Karp JF, Kleinman A, et al. Older people’s experiences of patient-centered treatment for chronic pain: a qualitative study. Pain Med. 2009;10:521-530.
23. Reynolds KS, Hanson LC, DeVellis RF, et al. Disparities in pain management between cognitively intact and cognitively impaired nursing home residents. J Pain Symptom Manage. 2008;35:388-396.
24. Elliott RA. Poor adherence to medication in adults with rheumatoid arthritis: reasons and solutions. Dis Manage Health Outcomes. 2008;16:13-29.
25. Cardenas-Valladolid J, Martin-Madrazo C, Salinero-Fort MA, et al. Prevalence of adherence to treatment in homebound elderly people in primary health care: a descriptive cross-sectional, multicentre study. Drugs Aging. 2010;27:641-651.
26. Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475-482.
27. Gazmararian JA, Baker DW, Williams MV, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545-551.
28. Appelt CJ, Burant CJ, Siminoff LA, et al. Arthritis-specific health beliefs related to aging among older male patients with knee and/or hip osteoarthritis. J Gerontol A Biol Sci Med Sci. 2007;62:184-190.
29. Weiner DK, Rudy TE. Attitudinal barriers to effective treatment of persistent pain in nursing home residents. J Am Geriatr Soc. 2002;50:2035-2040.
30. Yates P, Dewar A, Fentiman B. Pain: the views of elderly people living in long-term residential care settings. J Adv Nurs. 1995;21:667-674.
31. Cornally N, McCarthy G. Chronic pain: the help-seeking behavior, attitudes, and beliefs of older adults living in the community. Pain Manage Nurs. 2011;12:206-217.
32. Spitz A, Moore AA, Papaleontiou M, et al. Primary care providers’ perspective on prescribing opioids to older adults with chronic non-cancer pain: a qualitative study. BMC Geriatrics. 2011;11:35.-
33. Chia LR, Schlenk EA, Dunbar-Jacob J. Effect of personal and cultural beliefs on medication adherence in the elderly. Drugs Aging. 2006;23:191-202.
34. Sale J, Gignac M, Hawker G. How “bad” does the pain have to be? A qualitative study examining adherence to pain medication in older adults with osteoarthritis. Arthritis Rheum. 2006;55:272-278.
35. Rudolph JL, Salow MJ, Angelini MC, et al. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med. 2008;168:508-513.
36. Hanlon JT, Backonja M, Weiner D, et al. Evolving pharmacological management of persistent pain in older persons. Pain Med. 2009;10:959-961.
37. Reid MC, Henderson CR, Jr, Papaleontiou M, et al. Characteristics of older adults receiving opioids in primary care: treatment duration and outcomes. Pain Med. 2010;11:1063-1071.
The benefits of interdisciplinary pain management
The Institute of Medicine (IOM) published a consensus report in June 2011 on the “national challenge” of chronic pain.1 Below the heading “Underlying Principles,” the report states,
“Given chronic pain’s diverse effects, interdisciplinary assessment and treatment may produce the best results for people with the most severe and persistent pain problems.” 1
Yet much of the medical community tends to treat pain as a physical problem with pharmacologic solutions, effectively dismissing the value of interdisciplinary pain management and the biopsychosocial model underlying this approach, even though its interrelated factors are clearly linked to improved physical symptoms and decreased use of costly medical resources.2,3 However, over the past 2 decades an undeniable body of evidence favoring an interdisciplinary approach has been growing.
Rationale and research
Success with a multimodal approach to pain management has been demonstrated for a number of pain conditions, perhaps most clearly in studies of chronic low back pain (LBP). In one study, 108 patients (63% with LBP) underwent multiple sessions of individual cognitive behavioral therapy (CBT), physical therapy, aquatic physical therapy, occupational therapy, group education, and group relaxation.4 At program enrollment, program completion, and long-term follow-up, researchers gathered data on changes in pain severity, emotional stress, interference of pain on functioning, perceived control of pain, helpfulness of treatment, and hours resting. At 6 months and 1 year following completion of the study, all 6 measures showed statistically significant improvement over baseline, with 95% confidence intervals in 5 of the 6 showing no overlap between pre-program and follow-up measures. [TABLE 1]
TABLE 1: Variance of outcomes of a comprehensive pain management program with 1-year follow-up (n=46)
| Mean ± standard error (95% confidence interval) |
| Variables | Pretreatment | Posttreatment | 1-year follow-up |
| Pain severity | 8.8 ± .29 (8.21-9.40) | 6.59 ± .31 (5.96-7.21)* | 6.94 ± .45 (6.03-7.84)* |
| Interference | 10.43 ± .30 (9.83-11.04) | 8.04 ± .42 (7.19-8.90)* | 7.35 ± .56 (6.22-8.48)* |
| Distress | 7.07 ± .49 (6.08-8.05) | 3.91 ± .38 (3.15-4.67)* | 5.57 ± .45 (4.65-6.48) |
| Control | 5.91 ± .29 (5.10-6.72) | 8.8 ± .24 (8.16-9.45)* | 8.67 ± .29 (8.02-9.33)* |
| Helpfulness | 2.37 ± .22 (1.93-2.81) | 7.35 ± .29 (6.76-7.93)* | 7.13 ± .4 (6.34-7.93)* |
| Hours resting** | 5.45 ± .51 (4.42-6.48) | 2.63 ± .24 (2.14-3.12)* | 3.29 ± .44 (2.40-4.18)* |
* No overlap in confidence interval between pretreatment and either posttreatment or 1-year scores
**n=40
Source: Adapted with permission from Oslund S, et al. Long-term effectiveness of a comprehensive pain management program: strengthening the case for interdisciplinary care. Proc (Bayl Univ Med Cent). 2009;22(3)211-214.
In a systematic review of 10 randomized controlled trials encompassing 1964 patients with disabling LBP, researchers found strong evidence that intensive multidisciplinary biopsychosocial rehabilitation improves function when compared with inpatient or outpatient treatments. The review also found moderate evidence of pain reduction with multidisciplinary care compared with non-multidisciplinary care.5
Studies of musculoskeletal pain also have reported good results with interdisciplinary care. In a study of interdisciplinary pain management for chronic musculoskeletal pain, military personnel were to receive either interdisciplinary care with physical therapy, occupational therapy, and psychosocial intervention, or standard anesthesia treatment alone.6 At 6 months and 1 year, data collected on pain, disability, functional status, and fitness for return to duty showed that interdisciplinary care was far superior to standard care.
A systematic review of randomized controlled trials found strong evidence that multidisciplinary care is more effective for nonmalignant chronic pain diagnoses (chronic LBP, back pain, fibromyalgia, and mixed chronic pain) than standard medical treatment, and moderate evidence for its effectiveness compared with other nonmultidisciplinary treatments.7 According to the study authors, the data support, at minimum, offering a range of treatments—including individual exercising, training in relaxation techniques, group therapy with a clinical psychologist, patient education, physiotherapy, and medical training therapy—and providing neurophysiology information. They also point out that no particular combination or duration of therapy has proved superior to others in clinical outcomes.
Risks of interdisciplinary care versus standard care
Therapies employed in interdisciplinary pain management are relatively low-risk compared with other interventions, such as opioid use or surgery. A 2010 Cochrane review of opioid use for chronic non-cancer pain found that concerns about long-term use of opioids can present a potential barrier to treatment. Opioids often lead to adverse effects (gastrointestinal effects such as constipation and nausea; headache; fatigue; urinary complications) severe enough to warrant discontinuation.8 This review found the rate of opioid addiction in these study populations was extremely low, however, and concluded that potential iatrogenic opioid addiction should not be a barrier for well-selected and well-supervised patients. As this study indicates, patients who gain pain relief from prescribed opioids might become drug dependent, but will not become addicted.
Also, although opioids are widely used,their ability to control pain varies. A study from the Mayo Comprehensive Rehabilitation Center of 233 consecutively enrolled patients with chronic nonmalignant pain found 48% were using opioids daily at baseline, at a cost of $23.13 per day or $8326.90 per year (average wholesale price) per patient.9 Patients who completed a 3-week multidisciplinary intervention significantly reduced their medication use at 6-month follow-up, for an estimated annual savings of $2404.80 per patient.
Two studies comparing interdisciplinary care with spine fusion surgery for chronic back pain found interdisciplinary care to be a reasonable alternative for many patients. In a study of patients with chronic LBP who had previous surgery for disc herniation, spinal fusion showed no benefit over cognitive intervention and exercise after 1 year.10 [TABLE 2] A multicenter trial comparing surgical stabilization of the lumbar spine with an intensive rehabilitation program based on CBT found no clear evidence that spinal fusion provided greater benefit.11
TABLE 2 : Primary and secondary outcomes comparing spinal
fusion with CBT and exercise
| Outcome | Lumbar fusion (n=28) | CBT/exercises (n=29) |
| Oswestry* Baseline 1-year | 47 38.1 | 45.1 32.3 |
| Back pain** Baseline 1-year | 64.6 50.7 | 64.7 49.5 |
| Leg pain** Baseline 1-year | 52.7 45 | 55.3 47.7 |
| Working | 10% | 40% |
*Oswestry Disability Questionnaire in which the sum of response scores ranges from 0 to 100,where 100 represents the worst possible pain and disability.
**Based on a vertical visual analog scale ranging from 0 to 100, where 100 reflected the worst pain imaginable.
Source: Adapted from Brox JI, et al. Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic back pain after previous surgery for disc herniation: A prospective randomized controlled study. Pain. 2006;122(1):145-155. This table has been reproduced with permission of the International Association for the Study of Pain® (IASP®). The table
may not be reproduced for any other purpose without permission.
What interdisciplinary pain management looks like
Key disciplines of an interdisciplinary pain management program are medicine, psychology, and rehabilitation. However, programs vary in available services and professional disciplines, setting, and duration. A fully integrated pain treatment center offers a range of therapies that may include transcutaneous electrical nerve stimulation, CBT, biofeedback, physical therapy, psychoeducational group treatment, and medications such as nonnarcotic analgesics and nerve blocks. Additional disciplines may include outcome database managers, vocational specialists, nutrition, case management, nursing, chaplaincy, and other disciplines an individual patient may need.
Patients should be evaluated by a pain medicine specialist and a behavioral medicine specialist. Treatment recommendations should include a structured curriculum including education, CBT, and physical therapy to address fear avoidance behavior, medication use, disability, affective distress, health care overutilization, quality of life, activities of daily living, and other patient-centric goals of rehabilitation. The interdisciplinary treatment team should be housed in the same facility and meet at least once per week to discuss new and existing patients and monitor progress toward outcome goals.
At our clinic, the Eugene McDermott Center for Pain Management at the University of Texas Southwestern Medical Center in Dallas, each patient undergoes consecutive evaluations by a pain physician, psychologist, physical therapist, and perhaps a psychiatrist. A case manager helps patients navigate through the evaluation and treatment process. At weekly case conferences, the team meets to discuss new patients, review the progress of current patients, and reinforce or modify treatment plans.
Individualizing goals
“Among steps to improving care, health-care providers should increasingly aim at tailoring pain care to each person’s experience and self-management of pain should be promoted.”1
Pain influences and inhibits numerous areas of a patient’s life. For many chronic pain patients, duration of pain brings with it the belief that “hurt equals harm.” As a result, they decrease physical activities, become socially isolated, and often feel unable to effectively manage, control, and conquer their pain. The longer chronic pain endures, the more deleterious the psychosocial consequences, even if pain and dysfunction do not worsen.
Chronic pain causes patients to feel a domino effect of psychological and cognitive disturbances including anxiety, depression, anger, and sleep disturbance. Disability caused by pain may bring on economic and domestic difficulties. Relationships can suffer, in part because it is hard for others to understand the impact of pain, especially when there is no obvious pathology.
Part of the evaluation process is to assess these possibilities and to address them in a concerted way. We encourage patients to focus on making progress toward their treatment goals rather than hoping to find a definitive cure for a pain generator that may or may not be identifiable. Therefore, in addition to the standard outcomes we aim for with each patient (eg, improvement in physical and psychological function measures), we establish individual treatment goals based on the initial interviews and the patient’s desire to return to work, get into vocational retraining or education, or achieve other productivity or recreational outcomes.
Patients typically receive 8 to 10 sessions of CBT, with each session covering a topic such as sleep hygiene, assertiveness training, anger management, or controlling automatic thoughts that lead to catastrophization or fear of the pain getting worse.
At our center we spend an hour educating patients about pain medications, explaining how they work and why some pose risks. Patients undergo 6 to 8 sessions of physical therapy and graded exercise, starting slow and gradually building to a level that does not aggravate their pain. Teaching them correct posture and how to lift objects also is important.
Planning for long-term success
Pain management takes place on numerous levels that incorporate self care, primary care, specialty care, and the multimodal care of interdisciplinary pain centers. To avoid relapse after patients have been treated at an interdisciplinary pain center, it is important that they have a clear idea of how to proceed with their individualized programs in a self-directed manner. Those who do well in the program and return to work or the home environment may be vulnerable to stressors that can lead to relapse.
Patients who fear they cannot control the pain or that they may do something to worsen it are at risk of becoming depressed, dependent, or guarded in their activities.12 Our program is developing a system to monitor patients more closely after they finish their program to identify those who may be spiraling downward. Patients are invited to return at any time for “booster” sessions.
Primary care involvement can strengthen patient resolve
“Also, primary care physicians—who handle most front-line pain care—should collaborate with pain specialists in cases where pain persists.”1
The degree to which primary care physicians (PCPs) want to be involved with chronic pain management varies, of course. Interdisciplinary programs should explore the comfort level of individual providers and work with them accordingly—at the very least communicating with and including the PCP in the patient’s process so that he or she understands what the patient has encountered and achieved.13 This collaborative approach enables PCPs to motivate patients to continue the progress they’ve made, reinforce the biopsychosocial model for treating pain, and communicate with the interdisciplinary team about patients who may be relapsing.
Barriers to interdisciplinary care
“System and organizational barriers, many of them driven by current reimbursement policies, obstruct patient-centered care.”1
The IOM has estimated the direct and indirect costs of pain in America to be over a half a trillion dollars per year. The potential for interdisciplinary pain care to contribute to national deficit reduction is real and is not limited to chronic pain. In fact, the application of interdisciplinary evaluations and treatment to acute and subacute pain may be more important to reduce costs related to preventing high-risk patients from becoming chronic.
A cost-utility analysis of 994 patients in pain clinics with acute back pain at high risk of becoming chronic who were provided early intervention with an interdisciplinary approach resulted in fewer health care visits and fewer missed days of work compared with patients who received usual care.14
Additional cost savings could be realized by routinely applying the biopsychosocial model to acute and subacute pain. Through well-developed evaluation systems, we could identify patients at high risk of progressing to chronicity. Screening for risk stratification is key to reducing the large number of chronic pain patients who are overmedicated, disabled, and depressed. Just as it makes sense to reduce individuals’ cardiac risk factors and not wait until they are in heart failure to act, employing a comprehensive interdisciplinary program for acute pain would be less expensive than waiting to treat pain that has become chronic.
However, only some insurers cover use of interdisciplinary pain programs, often to a limited extent, and may employ carve outs for specific therapies. Medicare does not reimburse well for interdisciplinary treatment. Consequently, many programs are paid through worker’s compensation. It is therefore challenging for interdisciplinary programs to remain viable.
Further benefits to the wider community
Our current health care system in the United States is not financially sustainable. To help curtail overutilization of health care resources in this country, we have to acknowledge psychosocial issues and embrace interdisciplinary pain programs when treating patients with pain. But it will take time and a huge cultural change for this to happen.
The future may require a combination of interdisciplinary treatment with a strong component of analgesic treatments rather than an “all or none” approach in which patients receive either “behavioral” treatment or “medical” treatment only. By definition, interdisciplinary pain treatment requires medicine as a discipline to reduce pain using everything medicine has to offer to accomplish this end.
Helpful information for you and your patients
The American Academy of Pain Management (AAPM) offers professional credentialing in pain management and accredits pain management clinics in the United States. You may be able to locate a specialist or clinic in your area at the academy’s Web site: https://members.aapainmanage.org/aapmssa/censsacustlkup.query_page.
Disclosures
Carl Noe, MD, has served as a consultant to Palladian Partners, Inc., a health communications and services company.
Charles F. Williams has no conflicts of interest to disclose.
1. Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC; 2011. Available at: http://www.iom.edu/Reports/2011/Relieving-Pain-in-America-A-Blueprint-for-Transforming-Prevention-Care-Education-Research.aspx. Accessed March 15, 2012.
2. Robbins H, Gatchel RJ, Noe C, et al. A prospective one-year outcome study of interdisciplinary chronic pain management: compromising its efficacy by managed care policies. Anesth Analg. 2003;97:156-162.
3. Chou R, Loeser JD, Owens DK, et al. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain. Spine. 2009;34:1066-1077.
4. Oslund S, Robinson RC, Clark TC, et al. Long-term effectiveness of a comprehensive pain management program: strengthening the case for interdisciplinary care. Proc (Bayl Univ Med Cent). 2009;22:211-214.
5. Guzman J, Esmail R, Karjalainen K, et al. Multidisciplinary rehabilitation for chronic low back pain: a systematic review. BMJ. 2001;332:1511-1516.
6. Gatchel RJ, McGeary DD, Peterson A, et al. Preliminary findings of a randomized controlled trial of an interdisciplinary military pain program. Mil Med. 2009;174:270-277.
7. Scascighini L, Toma V, Dober-Spielmann S, et al. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology. 2008;47:670-678.
8. Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010;(1):CD006605.
9. Cunningham JL, Rome JD, Kerkvliet JL, et al. Reduction in medication costs for patients with chronic nonmalignant pain completing a pain rehabilitation program: a prospective analysis of admission, discharge, and 6-month follow-up medication costs. Pain Med. 2009;10:787-796.
10. Brox JI, Reikeras O, Nygaard O, et al. Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic pain after previous surgery for disc herniation: A prospective randomized controlled study. Pain. 2006;122:145-155.
11. Fairbank J, Frost H, Wilson-MacDonald J, et al. Randomized controlled trial to compare surgical stabilization with an intensive rehabilitation program for patients with chronic low back pain: the MRC spine stabilization trial. BMJ. 2005;330(7502):1233.
12. Jensen MP, Turner JA, Romano JM. Changes after multidisciplinary pain treatment in patient pain beliefs and coping are associated with concurrent changes in patient functioning. Pain. 2007;131:38-47.
13. Mitchinson AR, Kerr EA, Krein SL. Management of chronic noncancer pain by VA primary care providers: when is pain control a priority? Am J Managed Care. 2008;14:77-84.
14. Rogerson MD, Gatchel RJ, Bierner SM. A cost utility analysis of interdisciplinary early intervention versus treatment as usual for high-risk acute low back pain patients. Pain Pract. 2009;10:382-395.
The Institute of Medicine (IOM) published a consensus report in June 2011 on the “national challenge” of chronic pain.1 Below the heading “Underlying Principles,” the report states,
“Given chronic pain’s diverse effects, interdisciplinary assessment and treatment may produce the best results for people with the most severe and persistent pain problems.” 1
Yet much of the medical community tends to treat pain as a physical problem with pharmacologic solutions, effectively dismissing the value of interdisciplinary pain management and the biopsychosocial model underlying this approach, even though its interrelated factors are clearly linked to improved physical symptoms and decreased use of costly medical resources.2,3 However, over the past 2 decades an undeniable body of evidence favoring an interdisciplinary approach has been growing.
Rationale and research
Success with a multimodal approach to pain management has been demonstrated for a number of pain conditions, perhaps most clearly in studies of chronic low back pain (LBP). In one study, 108 patients (63% with LBP) underwent multiple sessions of individual cognitive behavioral therapy (CBT), physical therapy, aquatic physical therapy, occupational therapy, group education, and group relaxation.4 At program enrollment, program completion, and long-term follow-up, researchers gathered data on changes in pain severity, emotional stress, interference of pain on functioning, perceived control of pain, helpfulness of treatment, and hours resting. At 6 months and 1 year following completion of the study, all 6 measures showed statistically significant improvement over baseline, with 95% confidence intervals in 5 of the 6 showing no overlap between pre-program and follow-up measures. [TABLE 1]
TABLE 1: Variance of outcomes of a comprehensive pain management program with 1-year follow-up (n=46)
| Mean ± standard error (95% confidence interval) |
| Variables | Pretreatment | Posttreatment | 1-year follow-up |
| Pain severity | 8.8 ± .29 (8.21-9.40) | 6.59 ± .31 (5.96-7.21)* | 6.94 ± .45 (6.03-7.84)* |
| Interference | 10.43 ± .30 (9.83-11.04) | 8.04 ± .42 (7.19-8.90)* | 7.35 ± .56 (6.22-8.48)* |
| Distress | 7.07 ± .49 (6.08-8.05) | 3.91 ± .38 (3.15-4.67)* | 5.57 ± .45 (4.65-6.48) |
| Control | 5.91 ± .29 (5.10-6.72) | 8.8 ± .24 (8.16-9.45)* | 8.67 ± .29 (8.02-9.33)* |
| Helpfulness | 2.37 ± .22 (1.93-2.81) | 7.35 ± .29 (6.76-7.93)* | 7.13 ± .4 (6.34-7.93)* |
| Hours resting** | 5.45 ± .51 (4.42-6.48) | 2.63 ± .24 (2.14-3.12)* | 3.29 ± .44 (2.40-4.18)* |
* No overlap in confidence interval between pretreatment and either posttreatment or 1-year scores
**n=40
Source: Adapted with permission from Oslund S, et al. Long-term effectiveness of a comprehensive pain management program: strengthening the case for interdisciplinary care. Proc (Bayl Univ Med Cent). 2009;22(3)211-214.
In a systematic review of 10 randomized controlled trials encompassing 1964 patients with disabling LBP, researchers found strong evidence that intensive multidisciplinary biopsychosocial rehabilitation improves function when compared with inpatient or outpatient treatments. The review also found moderate evidence of pain reduction with multidisciplinary care compared with non-multidisciplinary care.5
Studies of musculoskeletal pain also have reported good results with interdisciplinary care. In a study of interdisciplinary pain management for chronic musculoskeletal pain, military personnel were to receive either interdisciplinary care with physical therapy, occupational therapy, and psychosocial intervention, or standard anesthesia treatment alone.6 At 6 months and 1 year, data collected on pain, disability, functional status, and fitness for return to duty showed that interdisciplinary care was far superior to standard care.
A systematic review of randomized controlled trials found strong evidence that multidisciplinary care is more effective for nonmalignant chronic pain diagnoses (chronic LBP, back pain, fibromyalgia, and mixed chronic pain) than standard medical treatment, and moderate evidence for its effectiveness compared with other nonmultidisciplinary treatments.7 According to the study authors, the data support, at minimum, offering a range of treatments—including individual exercising, training in relaxation techniques, group therapy with a clinical psychologist, patient education, physiotherapy, and medical training therapy—and providing neurophysiology information. They also point out that no particular combination or duration of therapy has proved superior to others in clinical outcomes.
Risks of interdisciplinary care versus standard care
Therapies employed in interdisciplinary pain management are relatively low-risk compared with other interventions, such as opioid use or surgery. A 2010 Cochrane review of opioid use for chronic non-cancer pain found that concerns about long-term use of opioids can present a potential barrier to treatment. Opioids often lead to adverse effects (gastrointestinal effects such as constipation and nausea; headache; fatigue; urinary complications) severe enough to warrant discontinuation.8 This review found the rate of opioid addiction in these study populations was extremely low, however, and concluded that potential iatrogenic opioid addiction should not be a barrier for well-selected and well-supervised patients. As this study indicates, patients who gain pain relief from prescribed opioids might become drug dependent, but will not become addicted.
Also, although opioids are widely used,their ability to control pain varies. A study from the Mayo Comprehensive Rehabilitation Center of 233 consecutively enrolled patients with chronic nonmalignant pain found 48% were using opioids daily at baseline, at a cost of $23.13 per day or $8326.90 per year (average wholesale price) per patient.9 Patients who completed a 3-week multidisciplinary intervention significantly reduced their medication use at 6-month follow-up, for an estimated annual savings of $2404.80 per patient.
Two studies comparing interdisciplinary care with spine fusion surgery for chronic back pain found interdisciplinary care to be a reasonable alternative for many patients. In a study of patients with chronic LBP who had previous surgery for disc herniation, spinal fusion showed no benefit over cognitive intervention and exercise after 1 year.10 [TABLE 2] A multicenter trial comparing surgical stabilization of the lumbar spine with an intensive rehabilitation program based on CBT found no clear evidence that spinal fusion provided greater benefit.11
TABLE 2 : Primary and secondary outcomes comparing spinal
fusion with CBT and exercise
| Outcome | Lumbar fusion (n=28) | CBT/exercises (n=29) |
| Oswestry* Baseline 1-year | 47 38.1 | 45.1 32.3 |
| Back pain** Baseline 1-year | 64.6 50.7 | 64.7 49.5 |
| Leg pain** Baseline 1-year | 52.7 45 | 55.3 47.7 |
| Working | 10% | 40% |
*Oswestry Disability Questionnaire in which the sum of response scores ranges from 0 to 100,where 100 represents the worst possible pain and disability.
**Based on a vertical visual analog scale ranging from 0 to 100, where 100 reflected the worst pain imaginable.
Source: Adapted from Brox JI, et al. Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic back pain after previous surgery for disc herniation: A prospective randomized controlled study. Pain. 2006;122(1):145-155. This table has been reproduced with permission of the International Association for the Study of Pain® (IASP®). The table
may not be reproduced for any other purpose without permission.
What interdisciplinary pain management looks like
Key disciplines of an interdisciplinary pain management program are medicine, psychology, and rehabilitation. However, programs vary in available services and professional disciplines, setting, and duration. A fully integrated pain treatment center offers a range of therapies that may include transcutaneous electrical nerve stimulation, CBT, biofeedback, physical therapy, psychoeducational group treatment, and medications such as nonnarcotic analgesics and nerve blocks. Additional disciplines may include outcome database managers, vocational specialists, nutrition, case management, nursing, chaplaincy, and other disciplines an individual patient may need.
Patients should be evaluated by a pain medicine specialist and a behavioral medicine specialist. Treatment recommendations should include a structured curriculum including education, CBT, and physical therapy to address fear avoidance behavior, medication use, disability, affective distress, health care overutilization, quality of life, activities of daily living, and other patient-centric goals of rehabilitation. The interdisciplinary treatment team should be housed in the same facility and meet at least once per week to discuss new and existing patients and monitor progress toward outcome goals.
At our clinic, the Eugene McDermott Center for Pain Management at the University of Texas Southwestern Medical Center in Dallas, each patient undergoes consecutive evaluations by a pain physician, psychologist, physical therapist, and perhaps a psychiatrist. A case manager helps patients navigate through the evaluation and treatment process. At weekly case conferences, the team meets to discuss new patients, review the progress of current patients, and reinforce or modify treatment plans.
Individualizing goals
“Among steps to improving care, health-care providers should increasingly aim at tailoring pain care to each person’s experience and self-management of pain should be promoted.”1
Pain influences and inhibits numerous areas of a patient’s life. For many chronic pain patients, duration of pain brings with it the belief that “hurt equals harm.” As a result, they decrease physical activities, become socially isolated, and often feel unable to effectively manage, control, and conquer their pain. The longer chronic pain endures, the more deleterious the psychosocial consequences, even if pain and dysfunction do not worsen.
Chronic pain causes patients to feel a domino effect of psychological and cognitive disturbances including anxiety, depression, anger, and sleep disturbance. Disability caused by pain may bring on economic and domestic difficulties. Relationships can suffer, in part because it is hard for others to understand the impact of pain, especially when there is no obvious pathology.
Part of the evaluation process is to assess these possibilities and to address them in a concerted way. We encourage patients to focus on making progress toward their treatment goals rather than hoping to find a definitive cure for a pain generator that may or may not be identifiable. Therefore, in addition to the standard outcomes we aim for with each patient (eg, improvement in physical and psychological function measures), we establish individual treatment goals based on the initial interviews and the patient’s desire to return to work, get into vocational retraining or education, or achieve other productivity or recreational outcomes.
Patients typically receive 8 to 10 sessions of CBT, with each session covering a topic such as sleep hygiene, assertiveness training, anger management, or controlling automatic thoughts that lead to catastrophization or fear of the pain getting worse.
At our center we spend an hour educating patients about pain medications, explaining how they work and why some pose risks. Patients undergo 6 to 8 sessions of physical therapy and graded exercise, starting slow and gradually building to a level that does not aggravate their pain. Teaching them correct posture and how to lift objects also is important.
Planning for long-term success
Pain management takes place on numerous levels that incorporate self care, primary care, specialty care, and the multimodal care of interdisciplinary pain centers. To avoid relapse after patients have been treated at an interdisciplinary pain center, it is important that they have a clear idea of how to proceed with their individualized programs in a self-directed manner. Those who do well in the program and return to work or the home environment may be vulnerable to stressors that can lead to relapse.
Patients who fear they cannot control the pain or that they may do something to worsen it are at risk of becoming depressed, dependent, or guarded in their activities.12 Our program is developing a system to monitor patients more closely after they finish their program to identify those who may be spiraling downward. Patients are invited to return at any time for “booster” sessions.
Primary care involvement can strengthen patient resolve
“Also, primary care physicians—who handle most front-line pain care—should collaborate with pain specialists in cases where pain persists.”1
The degree to which primary care physicians (PCPs) want to be involved with chronic pain management varies, of course. Interdisciplinary programs should explore the comfort level of individual providers and work with them accordingly—at the very least communicating with and including the PCP in the patient’s process so that he or she understands what the patient has encountered and achieved.13 This collaborative approach enables PCPs to motivate patients to continue the progress they’ve made, reinforce the biopsychosocial model for treating pain, and communicate with the interdisciplinary team about patients who may be relapsing.
Barriers to interdisciplinary care
“System and organizational barriers, many of them driven by current reimbursement policies, obstruct patient-centered care.”1
The IOM has estimated the direct and indirect costs of pain in America to be over a half a trillion dollars per year. The potential for interdisciplinary pain care to contribute to national deficit reduction is real and is not limited to chronic pain. In fact, the application of interdisciplinary evaluations and treatment to acute and subacute pain may be more important to reduce costs related to preventing high-risk patients from becoming chronic.
A cost-utility analysis of 994 patients in pain clinics with acute back pain at high risk of becoming chronic who were provided early intervention with an interdisciplinary approach resulted in fewer health care visits and fewer missed days of work compared with patients who received usual care.14
Additional cost savings could be realized by routinely applying the biopsychosocial model to acute and subacute pain. Through well-developed evaluation systems, we could identify patients at high risk of progressing to chronicity. Screening for risk stratification is key to reducing the large number of chronic pain patients who are overmedicated, disabled, and depressed. Just as it makes sense to reduce individuals’ cardiac risk factors and not wait until they are in heart failure to act, employing a comprehensive interdisciplinary program for acute pain would be less expensive than waiting to treat pain that has become chronic.
However, only some insurers cover use of interdisciplinary pain programs, often to a limited extent, and may employ carve outs for specific therapies. Medicare does not reimburse well for interdisciplinary treatment. Consequently, many programs are paid through worker’s compensation. It is therefore challenging for interdisciplinary programs to remain viable.
Further benefits to the wider community
Our current health care system in the United States is not financially sustainable. To help curtail overutilization of health care resources in this country, we have to acknowledge psychosocial issues and embrace interdisciplinary pain programs when treating patients with pain. But it will take time and a huge cultural change for this to happen.
The future may require a combination of interdisciplinary treatment with a strong component of analgesic treatments rather than an “all or none” approach in which patients receive either “behavioral” treatment or “medical” treatment only. By definition, interdisciplinary pain treatment requires medicine as a discipline to reduce pain using everything medicine has to offer to accomplish this end.
Helpful information for you and your patients
The American Academy of Pain Management (AAPM) offers professional credentialing in pain management and accredits pain management clinics in the United States. You may be able to locate a specialist or clinic in your area at the academy’s Web site: https://members.aapainmanage.org/aapmssa/censsacustlkup.query_page.
Disclosures
Carl Noe, MD, has served as a consultant to Palladian Partners, Inc., a health communications and services company.
Charles F. Williams has no conflicts of interest to disclose.
The Institute of Medicine (IOM) published a consensus report in June 2011 on the “national challenge” of chronic pain.1 Below the heading “Underlying Principles,” the report states,
“Given chronic pain’s diverse effects, interdisciplinary assessment and treatment may produce the best results for people with the most severe and persistent pain problems.” 1
Yet much of the medical community tends to treat pain as a physical problem with pharmacologic solutions, effectively dismissing the value of interdisciplinary pain management and the biopsychosocial model underlying this approach, even though its interrelated factors are clearly linked to improved physical symptoms and decreased use of costly medical resources.2,3 However, over the past 2 decades an undeniable body of evidence favoring an interdisciplinary approach has been growing.
Rationale and research
Success with a multimodal approach to pain management has been demonstrated for a number of pain conditions, perhaps most clearly in studies of chronic low back pain (LBP). In one study, 108 patients (63% with LBP) underwent multiple sessions of individual cognitive behavioral therapy (CBT), physical therapy, aquatic physical therapy, occupational therapy, group education, and group relaxation.4 At program enrollment, program completion, and long-term follow-up, researchers gathered data on changes in pain severity, emotional stress, interference of pain on functioning, perceived control of pain, helpfulness of treatment, and hours resting. At 6 months and 1 year following completion of the study, all 6 measures showed statistically significant improvement over baseline, with 95% confidence intervals in 5 of the 6 showing no overlap between pre-program and follow-up measures. [TABLE 1]
TABLE 1: Variance of outcomes of a comprehensive pain management program with 1-year follow-up (n=46)
| Mean ± standard error (95% confidence interval) |
| Variables | Pretreatment | Posttreatment | 1-year follow-up |
| Pain severity | 8.8 ± .29 (8.21-9.40) | 6.59 ± .31 (5.96-7.21)* | 6.94 ± .45 (6.03-7.84)* |
| Interference | 10.43 ± .30 (9.83-11.04) | 8.04 ± .42 (7.19-8.90)* | 7.35 ± .56 (6.22-8.48)* |
| Distress | 7.07 ± .49 (6.08-8.05) | 3.91 ± .38 (3.15-4.67)* | 5.57 ± .45 (4.65-6.48) |
| Control | 5.91 ± .29 (5.10-6.72) | 8.8 ± .24 (8.16-9.45)* | 8.67 ± .29 (8.02-9.33)* |
| Helpfulness | 2.37 ± .22 (1.93-2.81) | 7.35 ± .29 (6.76-7.93)* | 7.13 ± .4 (6.34-7.93)* |
| Hours resting** | 5.45 ± .51 (4.42-6.48) | 2.63 ± .24 (2.14-3.12)* | 3.29 ± .44 (2.40-4.18)* |
* No overlap in confidence interval between pretreatment and either posttreatment or 1-year scores
**n=40
Source: Adapted with permission from Oslund S, et al. Long-term effectiveness of a comprehensive pain management program: strengthening the case for interdisciplinary care. Proc (Bayl Univ Med Cent). 2009;22(3)211-214.
In a systematic review of 10 randomized controlled trials encompassing 1964 patients with disabling LBP, researchers found strong evidence that intensive multidisciplinary biopsychosocial rehabilitation improves function when compared with inpatient or outpatient treatments. The review also found moderate evidence of pain reduction with multidisciplinary care compared with non-multidisciplinary care.5
Studies of musculoskeletal pain also have reported good results with interdisciplinary care. In a study of interdisciplinary pain management for chronic musculoskeletal pain, military personnel were to receive either interdisciplinary care with physical therapy, occupational therapy, and psychosocial intervention, or standard anesthesia treatment alone.6 At 6 months and 1 year, data collected on pain, disability, functional status, and fitness for return to duty showed that interdisciplinary care was far superior to standard care.
A systematic review of randomized controlled trials found strong evidence that multidisciplinary care is more effective for nonmalignant chronic pain diagnoses (chronic LBP, back pain, fibromyalgia, and mixed chronic pain) than standard medical treatment, and moderate evidence for its effectiveness compared with other nonmultidisciplinary treatments.7 According to the study authors, the data support, at minimum, offering a range of treatments—including individual exercising, training in relaxation techniques, group therapy with a clinical psychologist, patient education, physiotherapy, and medical training therapy—and providing neurophysiology information. They also point out that no particular combination or duration of therapy has proved superior to others in clinical outcomes.
Risks of interdisciplinary care versus standard care
Therapies employed in interdisciplinary pain management are relatively low-risk compared with other interventions, such as opioid use or surgery. A 2010 Cochrane review of opioid use for chronic non-cancer pain found that concerns about long-term use of opioids can present a potential barrier to treatment. Opioids often lead to adverse effects (gastrointestinal effects such as constipation and nausea; headache; fatigue; urinary complications) severe enough to warrant discontinuation.8 This review found the rate of opioid addiction in these study populations was extremely low, however, and concluded that potential iatrogenic opioid addiction should not be a barrier for well-selected and well-supervised patients. As this study indicates, patients who gain pain relief from prescribed opioids might become drug dependent, but will not become addicted.
Also, although opioids are widely used,their ability to control pain varies. A study from the Mayo Comprehensive Rehabilitation Center of 233 consecutively enrolled patients with chronic nonmalignant pain found 48% were using opioids daily at baseline, at a cost of $23.13 per day or $8326.90 per year (average wholesale price) per patient.9 Patients who completed a 3-week multidisciplinary intervention significantly reduced their medication use at 6-month follow-up, for an estimated annual savings of $2404.80 per patient.
Two studies comparing interdisciplinary care with spine fusion surgery for chronic back pain found interdisciplinary care to be a reasonable alternative for many patients. In a study of patients with chronic LBP who had previous surgery for disc herniation, spinal fusion showed no benefit over cognitive intervention and exercise after 1 year.10 [TABLE 2] A multicenter trial comparing surgical stabilization of the lumbar spine with an intensive rehabilitation program based on CBT found no clear evidence that spinal fusion provided greater benefit.11
TABLE 2 : Primary and secondary outcomes comparing spinal
fusion with CBT and exercise
| Outcome | Lumbar fusion (n=28) | CBT/exercises (n=29) |
| Oswestry* Baseline 1-year | 47 38.1 | 45.1 32.3 |
| Back pain** Baseline 1-year | 64.6 50.7 | 64.7 49.5 |
| Leg pain** Baseline 1-year | 52.7 45 | 55.3 47.7 |
| Working | 10% | 40% |
*Oswestry Disability Questionnaire in which the sum of response scores ranges from 0 to 100,where 100 represents the worst possible pain and disability.
**Based on a vertical visual analog scale ranging from 0 to 100, where 100 reflected the worst pain imaginable.
Source: Adapted from Brox JI, et al. Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic back pain after previous surgery for disc herniation: A prospective randomized controlled study. Pain. 2006;122(1):145-155. This table has been reproduced with permission of the International Association for the Study of Pain® (IASP®). The table
may not be reproduced for any other purpose without permission.
What interdisciplinary pain management looks like
Key disciplines of an interdisciplinary pain management program are medicine, psychology, and rehabilitation. However, programs vary in available services and professional disciplines, setting, and duration. A fully integrated pain treatment center offers a range of therapies that may include transcutaneous electrical nerve stimulation, CBT, biofeedback, physical therapy, psychoeducational group treatment, and medications such as nonnarcotic analgesics and nerve blocks. Additional disciplines may include outcome database managers, vocational specialists, nutrition, case management, nursing, chaplaincy, and other disciplines an individual patient may need.
Patients should be evaluated by a pain medicine specialist and a behavioral medicine specialist. Treatment recommendations should include a structured curriculum including education, CBT, and physical therapy to address fear avoidance behavior, medication use, disability, affective distress, health care overutilization, quality of life, activities of daily living, and other patient-centric goals of rehabilitation. The interdisciplinary treatment team should be housed in the same facility and meet at least once per week to discuss new and existing patients and monitor progress toward outcome goals.
At our clinic, the Eugene McDermott Center for Pain Management at the University of Texas Southwestern Medical Center in Dallas, each patient undergoes consecutive evaluations by a pain physician, psychologist, physical therapist, and perhaps a psychiatrist. A case manager helps patients navigate through the evaluation and treatment process. At weekly case conferences, the team meets to discuss new patients, review the progress of current patients, and reinforce or modify treatment plans.
Individualizing goals
“Among steps to improving care, health-care providers should increasingly aim at tailoring pain care to each person’s experience and self-management of pain should be promoted.”1
Pain influences and inhibits numerous areas of a patient’s life. For many chronic pain patients, duration of pain brings with it the belief that “hurt equals harm.” As a result, they decrease physical activities, become socially isolated, and often feel unable to effectively manage, control, and conquer their pain. The longer chronic pain endures, the more deleterious the psychosocial consequences, even if pain and dysfunction do not worsen.
Chronic pain causes patients to feel a domino effect of psychological and cognitive disturbances including anxiety, depression, anger, and sleep disturbance. Disability caused by pain may bring on economic and domestic difficulties. Relationships can suffer, in part because it is hard for others to understand the impact of pain, especially when there is no obvious pathology.
Part of the evaluation process is to assess these possibilities and to address them in a concerted way. We encourage patients to focus on making progress toward their treatment goals rather than hoping to find a definitive cure for a pain generator that may or may not be identifiable. Therefore, in addition to the standard outcomes we aim for with each patient (eg, improvement in physical and psychological function measures), we establish individual treatment goals based on the initial interviews and the patient’s desire to return to work, get into vocational retraining or education, or achieve other productivity or recreational outcomes.
Patients typically receive 8 to 10 sessions of CBT, with each session covering a topic such as sleep hygiene, assertiveness training, anger management, or controlling automatic thoughts that lead to catastrophization or fear of the pain getting worse.
At our center we spend an hour educating patients about pain medications, explaining how they work and why some pose risks. Patients undergo 6 to 8 sessions of physical therapy and graded exercise, starting slow and gradually building to a level that does not aggravate their pain. Teaching them correct posture and how to lift objects also is important.
Planning for long-term success
Pain management takes place on numerous levels that incorporate self care, primary care, specialty care, and the multimodal care of interdisciplinary pain centers. To avoid relapse after patients have been treated at an interdisciplinary pain center, it is important that they have a clear idea of how to proceed with their individualized programs in a self-directed manner. Those who do well in the program and return to work or the home environment may be vulnerable to stressors that can lead to relapse.
Patients who fear they cannot control the pain or that they may do something to worsen it are at risk of becoming depressed, dependent, or guarded in their activities.12 Our program is developing a system to monitor patients more closely after they finish their program to identify those who may be spiraling downward. Patients are invited to return at any time for “booster” sessions.
Primary care involvement can strengthen patient resolve
“Also, primary care physicians—who handle most front-line pain care—should collaborate with pain specialists in cases where pain persists.”1
The degree to which primary care physicians (PCPs) want to be involved with chronic pain management varies, of course. Interdisciplinary programs should explore the comfort level of individual providers and work with them accordingly—at the very least communicating with and including the PCP in the patient’s process so that he or she understands what the patient has encountered and achieved.13 This collaborative approach enables PCPs to motivate patients to continue the progress they’ve made, reinforce the biopsychosocial model for treating pain, and communicate with the interdisciplinary team about patients who may be relapsing.
Barriers to interdisciplinary care
“System and organizational barriers, many of them driven by current reimbursement policies, obstruct patient-centered care.”1
The IOM has estimated the direct and indirect costs of pain in America to be over a half a trillion dollars per year. The potential for interdisciplinary pain care to contribute to national deficit reduction is real and is not limited to chronic pain. In fact, the application of interdisciplinary evaluations and treatment to acute and subacute pain may be more important to reduce costs related to preventing high-risk patients from becoming chronic.
A cost-utility analysis of 994 patients in pain clinics with acute back pain at high risk of becoming chronic who were provided early intervention with an interdisciplinary approach resulted in fewer health care visits and fewer missed days of work compared with patients who received usual care.14
Additional cost savings could be realized by routinely applying the biopsychosocial model to acute and subacute pain. Through well-developed evaluation systems, we could identify patients at high risk of progressing to chronicity. Screening for risk stratification is key to reducing the large number of chronic pain patients who are overmedicated, disabled, and depressed. Just as it makes sense to reduce individuals’ cardiac risk factors and not wait until they are in heart failure to act, employing a comprehensive interdisciplinary program for acute pain would be less expensive than waiting to treat pain that has become chronic.
However, only some insurers cover use of interdisciplinary pain programs, often to a limited extent, and may employ carve outs for specific therapies. Medicare does not reimburse well for interdisciplinary treatment. Consequently, many programs are paid through worker’s compensation. It is therefore challenging for interdisciplinary programs to remain viable.
Further benefits to the wider community
Our current health care system in the United States is not financially sustainable. To help curtail overutilization of health care resources in this country, we have to acknowledge psychosocial issues and embrace interdisciplinary pain programs when treating patients with pain. But it will take time and a huge cultural change for this to happen.
The future may require a combination of interdisciplinary treatment with a strong component of analgesic treatments rather than an “all or none” approach in which patients receive either “behavioral” treatment or “medical” treatment only. By definition, interdisciplinary pain treatment requires medicine as a discipline to reduce pain using everything medicine has to offer to accomplish this end.
Helpful information for you and your patients
The American Academy of Pain Management (AAPM) offers professional credentialing in pain management and accredits pain management clinics in the United States. You may be able to locate a specialist or clinic in your area at the academy’s Web site: https://members.aapainmanage.org/aapmssa/censsacustlkup.query_page.
Disclosures
Carl Noe, MD, has served as a consultant to Palladian Partners, Inc., a health communications and services company.
Charles F. Williams has no conflicts of interest to disclose.
1. Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC; 2011. Available at: http://www.iom.edu/Reports/2011/Relieving-Pain-in-America-A-Blueprint-for-Transforming-Prevention-Care-Education-Research.aspx. Accessed March 15, 2012.
2. Robbins H, Gatchel RJ, Noe C, et al. A prospective one-year outcome study of interdisciplinary chronic pain management: compromising its efficacy by managed care policies. Anesth Analg. 2003;97:156-162.
3. Chou R, Loeser JD, Owens DK, et al. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain. Spine. 2009;34:1066-1077.
4. Oslund S, Robinson RC, Clark TC, et al. Long-term effectiveness of a comprehensive pain management program: strengthening the case for interdisciplinary care. Proc (Bayl Univ Med Cent). 2009;22:211-214.
5. Guzman J, Esmail R, Karjalainen K, et al. Multidisciplinary rehabilitation for chronic low back pain: a systematic review. BMJ. 2001;332:1511-1516.
6. Gatchel RJ, McGeary DD, Peterson A, et al. Preliminary findings of a randomized controlled trial of an interdisciplinary military pain program. Mil Med. 2009;174:270-277.
7. Scascighini L, Toma V, Dober-Spielmann S, et al. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology. 2008;47:670-678.
8. Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010;(1):CD006605.
9. Cunningham JL, Rome JD, Kerkvliet JL, et al. Reduction in medication costs for patients with chronic nonmalignant pain completing a pain rehabilitation program: a prospective analysis of admission, discharge, and 6-month follow-up medication costs. Pain Med. 2009;10:787-796.
10. Brox JI, Reikeras O, Nygaard O, et al. Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic pain after previous surgery for disc herniation: A prospective randomized controlled study. Pain. 2006;122:145-155.
11. Fairbank J, Frost H, Wilson-MacDonald J, et al. Randomized controlled trial to compare surgical stabilization with an intensive rehabilitation program for patients with chronic low back pain: the MRC spine stabilization trial. BMJ. 2005;330(7502):1233.
12. Jensen MP, Turner JA, Romano JM. Changes after multidisciplinary pain treatment in patient pain beliefs and coping are associated with concurrent changes in patient functioning. Pain. 2007;131:38-47.
13. Mitchinson AR, Kerr EA, Krein SL. Management of chronic noncancer pain by VA primary care providers: when is pain control a priority? Am J Managed Care. 2008;14:77-84.
14. Rogerson MD, Gatchel RJ, Bierner SM. A cost utility analysis of interdisciplinary early intervention versus treatment as usual for high-risk acute low back pain patients. Pain Pract. 2009;10:382-395.
1. Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC; 2011. Available at: http://www.iom.edu/Reports/2011/Relieving-Pain-in-America-A-Blueprint-for-Transforming-Prevention-Care-Education-Research.aspx. Accessed March 15, 2012.
2. Robbins H, Gatchel RJ, Noe C, et al. A prospective one-year outcome study of interdisciplinary chronic pain management: compromising its efficacy by managed care policies. Anesth Analg. 2003;97:156-162.
3. Chou R, Loeser JD, Owens DK, et al. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain. Spine. 2009;34:1066-1077.
4. Oslund S, Robinson RC, Clark TC, et al. Long-term effectiveness of a comprehensive pain management program: strengthening the case for interdisciplinary care. Proc (Bayl Univ Med Cent). 2009;22:211-214.
5. Guzman J, Esmail R, Karjalainen K, et al. Multidisciplinary rehabilitation for chronic low back pain: a systematic review. BMJ. 2001;332:1511-1516.
6. Gatchel RJ, McGeary DD, Peterson A, et al. Preliminary findings of a randomized controlled trial of an interdisciplinary military pain program. Mil Med. 2009;174:270-277.
7. Scascighini L, Toma V, Dober-Spielmann S, et al. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology. 2008;47:670-678.
8. Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010;(1):CD006605.
9. Cunningham JL, Rome JD, Kerkvliet JL, et al. Reduction in medication costs for patients with chronic nonmalignant pain completing a pain rehabilitation program: a prospective analysis of admission, discharge, and 6-month follow-up medication costs. Pain Med. 2009;10:787-796.
10. Brox JI, Reikeras O, Nygaard O, et al. Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic pain after previous surgery for disc herniation: A prospective randomized controlled study. Pain. 2006;122:145-155.
11. Fairbank J, Frost H, Wilson-MacDonald J, et al. Randomized controlled trial to compare surgical stabilization with an intensive rehabilitation program for patients with chronic low back pain: the MRC spine stabilization trial. BMJ. 2005;330(7502):1233.
12. Jensen MP, Turner JA, Romano JM. Changes after multidisciplinary pain treatment in patient pain beliefs and coping are associated with concurrent changes in patient functioning. Pain. 2007;131:38-47.
13. Mitchinson AR, Kerr EA, Krein SL. Management of chronic noncancer pain by VA primary care providers: when is pain control a priority? Am J Managed Care. 2008;14:77-84.
14. Rogerson MD, Gatchel RJ, Bierner SM. A cost utility analysis of interdisciplinary early intervention versus treatment as usual for high-risk acute low back pain patients. Pain Pract. 2009;10:382-395.
BEST PRACTICES IN: Acne Management
Medical Education Library
A Best Practices Supplement to Skin & Allergy News®. This supplement was sponsored by Valeant Dermatology.
- Introduction
- CL/BPO 2.5%
- CL/BPO 2.5% In Clinical Practice
- Conclusion
Faculty/Faculty Disclosure
Julie Harper, MD
Physician/Speaker
The Dermatology and Skin Care Center of Birmingham, PC
Birmingham, AL
Dr Harper received an honorarium for writing this article.
Copyright © 2012 Elsevier Inc.
Medical Education Library
A Best Practices Supplement to Skin & Allergy News®. This supplement was sponsored by Valeant Dermatology.
- Introduction
- CL/BPO 2.5%
- CL/BPO 2.5% In Clinical Practice
- Conclusion
Faculty/Faculty Disclosure
Julie Harper, MD
Physician/Speaker
The Dermatology and Skin Care Center of Birmingham, PC
Birmingham, AL
Dr Harper received an honorarium for writing this article.
Copyright © 2012 Elsevier Inc.
Medical Education Library
A Best Practices Supplement to Skin & Allergy News®. This supplement was sponsored by Valeant Dermatology.
- Introduction
- CL/BPO 2.5%
- CL/BPO 2.5% In Clinical Practice
- Conclusion
Faculty/Faculty Disclosure
Julie Harper, MD
Physician/Speaker
The Dermatology and Skin Care Center of Birmingham, PC
Birmingham, AL
Dr Harper received an honorarium for writing this article.
Copyright © 2012 Elsevier Inc.
MODULE 4: Enhancing Adherence with Antihypertensives: The Role of Fixed-Dose Combinations and Home Blood Pressure Monitoring
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
MODULE 4: Enhancing Adherence with Antihypertensives: The Role of Fixed-Dose Combinations and Home Blood Pressure Monitoring
Dr Kuritzky is a paid consultant to Takeda Pharmaceuticals International, Inc.
Although an estimated 1 out of 3 people in the United States has been diagnosed with hypertension, data from the 2007-2008 National Health and Nutrition Examination Survey found that just 72% are currently being treated and, of those, just half have their blood pressure (BP) controlled with lifestyle changes and/or medication.1
The failure of so many people with hypertension to obtain BP control, despite the availability of numerous effective medications, is partially due to a lack of adherence to recommended treatments (eg, taking medication, following a diet, and executing lifestyle changes). Adherence is a significant problem in hypertension and evidence shows that just half of patients who initiate drug therapy are persistent with treatment after 1 year.2
Although few studies link nonadherence with long-term outcomes, 1 study found that patients who “forgot” to take their antihypertensive medication were nearly one-third more likely to experience a cardiovascular event or death (hazard ratio [HR], 1.28; 95% confidence interval [CI], 1.04-1.57).3 Adherence is important not only for the health of the patient, but also to provide overall cost savings from the reductions of hospitalizations for complications from an untreated disease.4
Barriers to adherence
A significant contributor to nonadherence is treatment complexity, which manifests in hypertension as pill burden. Up to 75% of patients will require more than 1 medication to control their BP; those with resistant hypertension will require 4 or more.5,6 These medications must often be taken at different times of the day, with varying frequency.6-9
Reducing the number of daily doses has been consistently found to enhance adherence, and should be considered routinely as a first-line strategy. Complex strategies (eg, group visits, designated office staff to assist hypertensive patients, pharmacist consultation and comanagement, exercise counseling, dietary counseling, multidisciplinary hypertension team care, specific interviewing techniques such as motivational interviewing) are promising, but individual clinicians may not have the resources to take advantage of such labor-intensive intervention. Further, when multimodal intervention is employed, it is often difficult to discern which component(s) of the intervention were most impactful, unless multifactorial study design is employed, which it rarely is. We await further randomized controlled trials in this regard.
A study of approximately 85,000 members of a large managed care organization found that the greater the number of antihypertensive medications prescribed, the lower the rate of patient adherence. Just 63% of those receiving 3-drug regimens and 55% of those receiving 4-drug regimens were completely adherent.10
In addition, many patients with hypertension, particularly older patients, have comorbid conditions (eg, dyslipidemia or diabetes) that also require treatment, leading to increased treatment complexity and pill burden.11,12
One option for reducing pill burden is the use of fixed-dose therapies ( TABLE ). Since 2000, many new fixed-dose combinations, including at least 3 triple therapies, have entered the market.13 In addition, a so-called “poly-pill” that combines aspirin, 3 antihypertensives, and a statin is under investigation and demonstrating good results in reducing BP and cholesterol levels.14
TABLE
Currently available combination therapies
| Fixed-Dose Combination | Brand Name | Dose Range, Total, mg/da |
|---|---|---|
| Angiotensin II Receptor Blocker + Thiazide Diuretic | ||
| Azilsartan/chlorthalidone | Edarbyclor | 40/12.5; 40/25 |
| Candesartan/HCTZ | Atacand HCT | 16/12.5; 32/12.5; 32/25 |
| Eprosartan/HCTZ | Teveten HCT | 600/12.5; 600/25 |
| Irbesartan/HCTZ | Avalide | 150/12.5; 300/25 |
| Losartan/HCTZ | Hyzaar | 50/12.5; 100/12.5; 100/25 |
| Olmesartan/HCTZ | Benicar HCT | 20/12.5; 30/12.5 |
| Telmisartan/HCTZ | Micardis HCT | 40/12.5; 80/12.5; 80/25 |
| Valsartan/HCTZ | Diovan HCT | 80/12.5; 160/12.5; 160/25; 320/12.5 |
| β-Blocker + Thiazide Diuretic | ||
| Atenolol/chlorthalidone | Tenoretic | 50/25; 100/25 |
| Bisoprolol/HCTZ | Ziac | 2.5/6.25; 5/6.25; 10/6.25 |
| Metoprolol tartrate/HCTZ | Lopressor HCT | 50/25; 100/25; 100/50 |
| Metoprolol succinate extended/release + HCTZ | Dutoprol | 25/12.5; 50/12.5; 100/12.5 |
| Nadolol + bendroflumethiazide | Corzide | 40/5; 80/5 |
| Propanolol + HCTZ | Inderide | 40/25; 80/25 |
| Calcium Channel Blocker + ACEI | ||
| Amlodipine/benazepril | Lotrel | 2.5/10; 5/10; 5/20; 5/40; 10/20; 10/40 |
| ACEI + Thiazide Diuretic | ||
| Benazepril/HCTZ | Lotensin HCT | 5/6.25; 10/12.5; 20/12.5; 20/25 |
| Captopril/HCTZ | Capozide | 25/15; 25/25; 50/15; 50/25 |
| Enalapril/HCTZ | Vaseretic | 10/25 (1-2) |
| Fosinopril/HCTZ | Monopril HCT | 10/12.5; 20/12.5 |
| Lisinopril/HCTZ | Prinzide Zestoretic | 10/12.5; 20/12.5 20/25 |
| Moexipril/HCTZ | Uniretic | 7.5/12.5; 15/12.5; 15/25 |
| Quinapril + HCTZ | Accuretic | 10/12.5; 20/12.5; 20/25 |
| ACEI + Calcium Channel Blocker | ||
| Trandolapril/verapamil | Tarka | 2/180; 2/240; 4/240 |
| Enalapril/felodipine | Lexxel | 5/5 |
| Angiotensin II Receptor Blocker + Calcium Channel Blocker | ||
| Telmisartan/amlodipine | Twynsta | 40/5; 40/10; 80/5; 80/10 |
| Angiotensin II Receptor Blocker + Calcium Channel Blocker + Thiazide Diuretic | ||
| Olmesartan/amlodipine/HCTZ | Tribenzor | 40/10/25 |
| Calcium Channel Blocker + Angiotensin II Receptor Blocker | ||
| Amlodipine/olmesartan | Azor | 5/20; 5/40; 10/20; 10/40 |
| Amlodipine/valsartan | Exforge | 5/160; 10/160; 5/320; 10/320 |
| Calcium Channel Blocker + Angiotensin II Receptor Blocker + Thiazide Diuretic | ||
| Amlodipine/valsartan/HCTZ | Exforge HCT | 5/160/12.5; 10/160/12.5; 5/160/25; 10/160/25; 10/320/25 |
| Central α-Agonist + Thiazide Diuretic | ||
| Methyldopa/HCTZ | Aldoril Aldoril D | 250/15; 250/25 500/30; 500/50 |
| Direct Renin Inhibitor + Angiotensin II Receptor Blocker | ||
| Aliskiren/valsartan | Valturna | 150/160; 300/320 |
| Direct Renin Inhibitor + Calcium Channel Blocker | ||
| Aliskiren + amlodipine | Tekamlo | 150/5; 150/10; 300/5; 300/10 |
| Direct Renin Inhibitor + Thiazide Diuretic | ||
| Aliskiren/HCTZ | Tekturna HCT | 150/12.5; 150/25; 300/12.5; 300/25 |
| Direct Renin Inhibitor + Calcium Channel Blocker + Thiazide Diuretic | ||
| Aliskiren/amlodipine/HCTZ | Amturnide | 150/5/12.5; 300/5/12.5; 300/5/25; 300/10/12.5; 300/10/25 |
| Diuretic Combination (K+ Sparing + Thiazide) | ||
| Amiloride/HCTZ | Several generics | 5/50 (1-2) |
| Spironolactone/HCTZ | Aldactazide | 25/25 (1/2-1) |
| Triamterene/HCTZ | Dyazide Maxide | 37.5/25 (1/2-1) 37.5/25; 75/50 |
| ACEI, angiotensin-converting enzyme inhibitor; HCTZ, hydrochlorothiazide. aAll 1 dose/d unless otherwise noted. Source: Available at: http://www.RxList.com; http://www.Drugs.com; http://www.empr.com/combination-treatments-for-hypertension-chart/article/191718/. Accessed June 27-28, 2012. | ||
Studies have found that patients receiving fixed-dose combination pills are more likely to reach their target BP, physicians are more satisfied with their ability to manage hypertension, and adverse effects are either similar or less with the fixed-dose therapies compared with monotherapies.15,16
Studies of adherence patterns among patients treated with fixed-dose combinations of antihypertensive agents vs separate antihypertensive agents demonstrate increased adherence among patients treated with fixed-dose combinations.17-21 In a clinical trial involving 4146 participants who were treated with a fixed dose of amlodipine and atorvastatin or separate pills, 33% of patients in the fixed-dose cohort had ceased treatment by 12 months compared with 59% of patients who were taking the 2-pill regimen (HR, 2.17; 95% CI, 2.05–2.13; P < .0001), resulting in a 117% higher rate of nonadherence in the 2-pill regimen. The median persistence time (ie, time to discontinuation with medication) was 8 months with the 2-pill regimen, but 37 months or longer with the fixed-dose combination.21
A meta-analysis of 9 studies found that fixed-dose combinations reduced the risk of nonadherence by 26% compared with single-pill combination therapy.22
One downside to fixed-dose therapy is cost. Out-of-pocket costs are a significant barrier to medication adherence and most fixed-dose options are branded drugs that generally require higher copayments or coinsurance vs generic single-pill drugs that may have copayments as low as $4.6
Other opportunities to improve adherence to antihypertensive medications
Other evidence-based opportunities to improve adherence to antihypertensive medications include improved relationships with, and communication from, health care providers, given that patients often do not understand their disease and recommended treatments.23,24
Interviews with 826 patients with hypertension found that although 90% knew that lowering their BP would improve their health and 91% reported that a health care provider had told them that they had hypertension or high BP, 41% did not know their BP level. In addition, just 34% of patients with hypertension identified systolic BP (SBP) as the “top” number of their reading and only 32% identified diastolic BP (DBP) as the “bottom” number. Finally, only one-third of patients were able to identify both SBP and DBP, and one-quarter of them did not know the optimal level for either.25
Other provider interventions that have resulted in improved adherence include changing medication to reduce or avoid adverse effects, simplifying dosing (as described earlier), and switching to less-expensive drugs if cost is an issue. Nurses and pharmacists are also important members of the team when it comes to improving adherence and reinforcing education.24
Home blood pressure monitoring
Another reason for nonadherence is that patients may not believe they need treatment since hypertension rarely manifests with symptoms. Furthermore, patients may not perceive that the medication they take has any effect because they did not have symptoms to begin with. Home BP monitoring (HBPM), or self BP monitoring, is one tool for improving adherence, possibly by providing immediate feedback to patients on how well their BP is controlled.26 Many major medical societies recommend HBPM as part of any hypertension management strategy.27-30
Patients who use HBPM can avoid many limitations associated with office BP monitoring (OBPM), including poor measurement techniques, infrequent measurement, white coat hypertension, and masked hypertension. Patients can also avoid reverse white coat hypertension, where OBPM is normal although out-of-office BP is high.28 Patients should take 3 readings at 1-minute intervals, usually in the morning and evening. The weekly average of these readings is their home BP (normotension is defined as an average BP <135/85 mm Hg).31 Typically, the HBPM monitoring is more accurate in identifying risk than OBPM when there are discrepancies between them.28 It is good practice to instruct patients utilizing HBPM to bring their home BP device to the office for a comparison.
There is some evidence that HBPM may contribute to improved adherence. A systematic review of 11 randomized controlled trials found that in 6 trials the use of HBPM resulted in improved medication adherence, although in 5 of those studies additional interventions were used. These interventions included patient counseling about adverse effects of the medication, timepiece caps that reminded patients to take their medication, tips to enhance adherence, and reinforcement of positive behavior by nurses, pharmacists, lay health workers, or a telephonic system.32 This illustrates an important point in adherence interventions: more is better, and it usually takes a combination of approaches to improve adherence.33,34
The only trial in the review that demonstrated that HBPM alone improved adherence randomized 628 patients to either HBPM or usual care for 6 weeks. The groups had similar compliance rates at baseline, and both demonstrated less adherence at the end of the 6-week trial. However, patients who measured their BP at home still demonstrated greater compliance than those receiving usual care (P < .05).35
A more recent trial in 57 patients, 38 of whom measured their BP at home and 19 of whom received usual care, found greater medication adherence in the HBPM group than in the control group (100% vs 88%, P < .031). The HBPM group also reached their treatment goals significantly faster than the control group (P = .02).36
Conclusion
Approximately 50% of individuals with hypertension who receive antihypertensive medication still do not reach their BP goal. One reason is nonadherence to medication, which is often related to treatment complexity, or pill burden. Given that most patients with hypertension will require more than 1 drug to manage their blood pressure, it is important that clinicians identify opportunities to simplify treatment. This may include fixed-dose combination therapy, which can improve adherence, as well as additional education regarding the efficacy and adverse effects of therapy.
The use of HBPM may also improve adherence by providing frequent feedback on treatment effectiveness.
It is important, however, that clinicians understand that no single approach to adherence will work for every patient. The greatest success comes with combining several approaches based on the barriers that affect each individual patient.
1. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043-2050.
2. Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336(7653):1114-1117.
3. Nelson MR, Reid CM, Ryan P, Willson K, Yelland L. Self-reported adherence with medication and cardiovascular disease outcomes in the Second Australian National Blood Pressure Study (ANBP2). Med J Aust. 2006;185(9):487-489.
4. Muszbek N, Brixner D, Benedict A, Keskinaslan A, Khan ZM. The economic consequences of noncompliance in cardiovascular disease and related conditions: a literature review. Int J Clin Pract. 2008;62(2):338-351.
5. Jamerson K, Bakris GL, Dahlöf B, et al; . ACCOMPLISH Investigators. Exceptional early blood pressure control rates: the ACCOMPLISH trial. Blood Press. 2007;16(2):80-86.
6. Gradman AH, Basile JN, Carter BL, et al. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(2):90-98.
7. World Health Organization. Adherence to long-term therapies: evidence for action. http://apps.who.int/medicinedocs/en/d/Js4883e/. Published 2003. Accessed March 21, 2012.
8. Chapman RH, Benner JS, Petrilla AA, et al. Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med. 2005;165(10):1147-1152.
9. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487-497.
10. Fung V, Huang J, Brand R, Newhouse JP, Hsu J. Hypertension treatment in a medicare population: adherence and systolic blood pressure control. Clin Ther. 2007;29(5):972-984.
11. Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002;287(3):337-344.
12. Sica DA. Rationale for fixed-dose combinations in the treatment of hypertension: the cycle repeats. Drugs. 2002;62(3):443-462.
13. Paulis L, Steckelings UM, Unger T. Key advances in antihypertensive treatment. Nat Rev Cardiol. 2012;9(5):276-285.
14. Wood S. TIPS 2: Full-dose polypill boosts efficacy, with no increased side effects. theHeart.org Web site. http://www.theheart.org/article/1387105.do?utm_campaign=newsletter&utm_medium=email&utm_source=20120419_EN_Heartwire. Published April 19, 2012. Accessed April 20, 2012.
15. Hilleman DE, Ryschon KL, Mohiuddin SM, Wurdeman RL. Fixed-dose combination vs monotherapy in hypertension: a meta-analysis evaluation. J Hum Hyper-tens. 1999;13(7):477-483.
16. Feldman RD, Zou GY, Vandervoort MK, Wong CJ, Nelson SA, Feagan BG. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension. 2009;53(4):646-653.
17. Dezii CM. A retrospective study of persistence with single-pill combination therapy vs. concurrent two-pill therapy in patients with hypertension. Manag Care. 2000;9(9 suppl):2-6.
18. Gerbino PP, Shoheiber O. Adherence patterns among patients treated with fixed-dose combination versus separate antihypertensive agents. Am J Health Syst Pharm. 2007;64(12):1279-1283.
19. Brixner DI, Jackson KC, II, Sheng X, Nelson RE, Keskinaslan A. Assessment of adherence, persistence, and costs among valsartan and hydrochlorothiazide retrospective cohorts in free-and fixed-dose combinations. Curr Med Res Opin. 2008;24(9):2597-2607.
20. Baser O, Andrews LM, Wang L, Xie L. Comparison of real-world adherence, healthcare resource utilization and costs for newly initiated valsartan/amlodi-pine single-pill combination versus angiotensin receptor blocker/calcium channel blocker free-combination therapy. J Med Econ. 2011;14(5):576-583.
21. Simons LA, Ortiz M, Calcino G. Persistence with a single pill versus two pills of amlodipine and atorvastatin: the Australian experience, 2006-2010. Med J Aust. 2011;195(3):134-137.
22. Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120(8):713-719.
23. Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80(8):991-994.
24. Harmon G, Lefante J, Krousel-Wood M. Overcoming barriers: the role of providers in improving patient adherence to antihypertensive medications. Curr Opin Cardiol. 2006;21(4):310-315.
25. Oliveria SA, Chen RS, McCarthy BD, Davis CC, Hill MN. Hypertension knowledge, awareness, and attitudes in a hypertensive population. J Gen Intern Med. 2005;20(3):219-225.
26. Abdullah A, Othman S. The influence of self-owned home blood pressure monitoring (HBPM) on primary care patients with hypertension: a qualitative study. BMC Fam Pract. 2011;12:143.-
27. Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment: A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-1419.
28. Pickering TG, White WB. American Society of Hypertension Writing Group. When and how to use self (home) and ambulatory blood pressure monitoring. J Am Soc Hypertens. 2008;2(3):119-124.
29. Institute for Clinical Systems Improvement. Health Care Guideline: Hypertension Diagnosis and Treatment. 13th ed. http://icsi.org/hypertension_4/hypertension_diagnosis_and_treatment_4.html. Published November 2010. Accessed March 26, 2012.
30. National Institute for Health and Clinical Evidence. Hypertension: Clinical management of primary hypertension in adults. http://guidance.nice.org.uk/CG127. Published August 2011. Accessed March 26, 2012.
31. Mengden T, Chamontin B, Phong Chau N, Luis Palma Gamiz J, Chanudet X. User procedure for self-measurement of blood pressure. First International Consensus Conference on Self Blood Pressure Measurement. Blood Press Monit. 2000;5(2):111-129.
32. Ogedegbe G, Schoenthaler A. A systematic review of the effects of home blood pressure monitoring on medication adherence. J Clin Hypertens (Greenwich). 2006;8(3):174-180.
33. McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review [published correction appears in JAMA. 2003;289(24):3242]. JAMA. 2002;288(22):2868-2879.
34. Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60(7):657-665.
35. Vrijens B, Goetghebeur E. Comparing compliance patterns between randomized treatments. Control Clin Trials. 1997;18(3):187-203.
36. Souza WK, Jardim PC, Brito LP, Araújo FA, Sousa AL. Self measurement of blood pressure for control of blood pressure levels and adherence to treatment. Arq Bras Cardiol. 2012;98(2):167-174.
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
MODULE 4: Enhancing Adherence with Antihypertensives: The Role of Fixed-Dose Combinations and Home Blood Pressure Monitoring
Dr Kuritzky is a paid consultant to Takeda Pharmaceuticals International, Inc.
Although an estimated 1 out of 3 people in the United States has been diagnosed with hypertension, data from the 2007-2008 National Health and Nutrition Examination Survey found that just 72% are currently being treated and, of those, just half have their blood pressure (BP) controlled with lifestyle changes and/or medication.1
The failure of so many people with hypertension to obtain BP control, despite the availability of numerous effective medications, is partially due to a lack of adherence to recommended treatments (eg, taking medication, following a diet, and executing lifestyle changes). Adherence is a significant problem in hypertension and evidence shows that just half of patients who initiate drug therapy are persistent with treatment after 1 year.2
Although few studies link nonadherence with long-term outcomes, 1 study found that patients who “forgot” to take their antihypertensive medication were nearly one-third more likely to experience a cardiovascular event or death (hazard ratio [HR], 1.28; 95% confidence interval [CI], 1.04-1.57).3 Adherence is important not only for the health of the patient, but also to provide overall cost savings from the reductions of hospitalizations for complications from an untreated disease.4
Barriers to adherence
A significant contributor to nonadherence is treatment complexity, which manifests in hypertension as pill burden. Up to 75% of patients will require more than 1 medication to control their BP; those with resistant hypertension will require 4 or more.5,6 These medications must often be taken at different times of the day, with varying frequency.6-9
Reducing the number of daily doses has been consistently found to enhance adherence, and should be considered routinely as a first-line strategy. Complex strategies (eg, group visits, designated office staff to assist hypertensive patients, pharmacist consultation and comanagement, exercise counseling, dietary counseling, multidisciplinary hypertension team care, specific interviewing techniques such as motivational interviewing) are promising, but individual clinicians may not have the resources to take advantage of such labor-intensive intervention. Further, when multimodal intervention is employed, it is often difficult to discern which component(s) of the intervention were most impactful, unless multifactorial study design is employed, which it rarely is. We await further randomized controlled trials in this regard.
A study of approximately 85,000 members of a large managed care organization found that the greater the number of antihypertensive medications prescribed, the lower the rate of patient adherence. Just 63% of those receiving 3-drug regimens and 55% of those receiving 4-drug regimens were completely adherent.10
In addition, many patients with hypertension, particularly older patients, have comorbid conditions (eg, dyslipidemia or diabetes) that also require treatment, leading to increased treatment complexity and pill burden.11,12
One option for reducing pill burden is the use of fixed-dose therapies ( TABLE ). Since 2000, many new fixed-dose combinations, including at least 3 triple therapies, have entered the market.13 In addition, a so-called “poly-pill” that combines aspirin, 3 antihypertensives, and a statin is under investigation and demonstrating good results in reducing BP and cholesterol levels.14
TABLE
Currently available combination therapies
| Fixed-Dose Combination | Brand Name | Dose Range, Total, mg/da |
|---|---|---|
| Angiotensin II Receptor Blocker + Thiazide Diuretic | ||
| Azilsartan/chlorthalidone | Edarbyclor | 40/12.5; 40/25 |
| Candesartan/HCTZ | Atacand HCT | 16/12.5; 32/12.5; 32/25 |
| Eprosartan/HCTZ | Teveten HCT | 600/12.5; 600/25 |
| Irbesartan/HCTZ | Avalide | 150/12.5; 300/25 |
| Losartan/HCTZ | Hyzaar | 50/12.5; 100/12.5; 100/25 |
| Olmesartan/HCTZ | Benicar HCT | 20/12.5; 30/12.5 |
| Telmisartan/HCTZ | Micardis HCT | 40/12.5; 80/12.5; 80/25 |
| Valsartan/HCTZ | Diovan HCT | 80/12.5; 160/12.5; 160/25; 320/12.5 |
| β-Blocker + Thiazide Diuretic | ||
| Atenolol/chlorthalidone | Tenoretic | 50/25; 100/25 |
| Bisoprolol/HCTZ | Ziac | 2.5/6.25; 5/6.25; 10/6.25 |
| Metoprolol tartrate/HCTZ | Lopressor HCT | 50/25; 100/25; 100/50 |
| Metoprolol succinate extended/release + HCTZ | Dutoprol | 25/12.5; 50/12.5; 100/12.5 |
| Nadolol + bendroflumethiazide | Corzide | 40/5; 80/5 |
| Propanolol + HCTZ | Inderide | 40/25; 80/25 |
| Calcium Channel Blocker + ACEI | ||
| Amlodipine/benazepril | Lotrel | 2.5/10; 5/10; 5/20; 5/40; 10/20; 10/40 |
| ACEI + Thiazide Diuretic | ||
| Benazepril/HCTZ | Lotensin HCT | 5/6.25; 10/12.5; 20/12.5; 20/25 |
| Captopril/HCTZ | Capozide | 25/15; 25/25; 50/15; 50/25 |
| Enalapril/HCTZ | Vaseretic | 10/25 (1-2) |
| Fosinopril/HCTZ | Monopril HCT | 10/12.5; 20/12.5 |
| Lisinopril/HCTZ | Prinzide Zestoretic | 10/12.5; 20/12.5 20/25 |
| Moexipril/HCTZ | Uniretic | 7.5/12.5; 15/12.5; 15/25 |
| Quinapril + HCTZ | Accuretic | 10/12.5; 20/12.5; 20/25 |
| ACEI + Calcium Channel Blocker | ||
| Trandolapril/verapamil | Tarka | 2/180; 2/240; 4/240 |
| Enalapril/felodipine | Lexxel | 5/5 |
| Angiotensin II Receptor Blocker + Calcium Channel Blocker | ||
| Telmisartan/amlodipine | Twynsta | 40/5; 40/10; 80/5; 80/10 |
| Angiotensin II Receptor Blocker + Calcium Channel Blocker + Thiazide Diuretic | ||
| Olmesartan/amlodipine/HCTZ | Tribenzor | 40/10/25 |
| Calcium Channel Blocker + Angiotensin II Receptor Blocker | ||
| Amlodipine/olmesartan | Azor | 5/20; 5/40; 10/20; 10/40 |
| Amlodipine/valsartan | Exforge | 5/160; 10/160; 5/320; 10/320 |
| Calcium Channel Blocker + Angiotensin II Receptor Blocker + Thiazide Diuretic | ||
| Amlodipine/valsartan/HCTZ | Exforge HCT | 5/160/12.5; 10/160/12.5; 5/160/25; 10/160/25; 10/320/25 |
| Central α-Agonist + Thiazide Diuretic | ||
| Methyldopa/HCTZ | Aldoril Aldoril D | 250/15; 250/25 500/30; 500/50 |
| Direct Renin Inhibitor + Angiotensin II Receptor Blocker | ||
| Aliskiren/valsartan | Valturna | 150/160; 300/320 |
| Direct Renin Inhibitor + Calcium Channel Blocker | ||
| Aliskiren + amlodipine | Tekamlo | 150/5; 150/10; 300/5; 300/10 |
| Direct Renin Inhibitor + Thiazide Diuretic | ||
| Aliskiren/HCTZ | Tekturna HCT | 150/12.5; 150/25; 300/12.5; 300/25 |
| Direct Renin Inhibitor + Calcium Channel Blocker + Thiazide Diuretic | ||
| Aliskiren/amlodipine/HCTZ | Amturnide | 150/5/12.5; 300/5/12.5; 300/5/25; 300/10/12.5; 300/10/25 |
| Diuretic Combination (K+ Sparing + Thiazide) | ||
| Amiloride/HCTZ | Several generics | 5/50 (1-2) |
| Spironolactone/HCTZ | Aldactazide | 25/25 (1/2-1) |
| Triamterene/HCTZ | Dyazide Maxide | 37.5/25 (1/2-1) 37.5/25; 75/50 |
| ACEI, angiotensin-converting enzyme inhibitor; HCTZ, hydrochlorothiazide. aAll 1 dose/d unless otherwise noted. Source: Available at: http://www.RxList.com; http://www.Drugs.com; http://www.empr.com/combination-treatments-for-hypertension-chart/article/191718/. Accessed June 27-28, 2012. | ||
Studies have found that patients receiving fixed-dose combination pills are more likely to reach their target BP, physicians are more satisfied with their ability to manage hypertension, and adverse effects are either similar or less with the fixed-dose therapies compared with monotherapies.15,16
Studies of adherence patterns among patients treated with fixed-dose combinations of antihypertensive agents vs separate antihypertensive agents demonstrate increased adherence among patients treated with fixed-dose combinations.17-21 In a clinical trial involving 4146 participants who were treated with a fixed dose of amlodipine and atorvastatin or separate pills, 33% of patients in the fixed-dose cohort had ceased treatment by 12 months compared with 59% of patients who were taking the 2-pill regimen (HR, 2.17; 95% CI, 2.05–2.13; P < .0001), resulting in a 117% higher rate of nonadherence in the 2-pill regimen. The median persistence time (ie, time to discontinuation with medication) was 8 months with the 2-pill regimen, but 37 months or longer with the fixed-dose combination.21
A meta-analysis of 9 studies found that fixed-dose combinations reduced the risk of nonadherence by 26% compared with single-pill combination therapy.22
One downside to fixed-dose therapy is cost. Out-of-pocket costs are a significant barrier to medication adherence and most fixed-dose options are branded drugs that generally require higher copayments or coinsurance vs generic single-pill drugs that may have copayments as low as $4.6
Other opportunities to improve adherence to antihypertensive medications
Other evidence-based opportunities to improve adherence to antihypertensive medications include improved relationships with, and communication from, health care providers, given that patients often do not understand their disease and recommended treatments.23,24
Interviews with 826 patients with hypertension found that although 90% knew that lowering their BP would improve their health and 91% reported that a health care provider had told them that they had hypertension or high BP, 41% did not know their BP level. In addition, just 34% of patients with hypertension identified systolic BP (SBP) as the “top” number of their reading and only 32% identified diastolic BP (DBP) as the “bottom” number. Finally, only one-third of patients were able to identify both SBP and DBP, and one-quarter of them did not know the optimal level for either.25
Other provider interventions that have resulted in improved adherence include changing medication to reduce or avoid adverse effects, simplifying dosing (as described earlier), and switching to less-expensive drugs if cost is an issue. Nurses and pharmacists are also important members of the team when it comes to improving adherence and reinforcing education.24
Home blood pressure monitoring
Another reason for nonadherence is that patients may not believe they need treatment since hypertension rarely manifests with symptoms. Furthermore, patients may not perceive that the medication they take has any effect because they did not have symptoms to begin with. Home BP monitoring (HBPM), or self BP monitoring, is one tool for improving adherence, possibly by providing immediate feedback to patients on how well their BP is controlled.26 Many major medical societies recommend HBPM as part of any hypertension management strategy.27-30
Patients who use HBPM can avoid many limitations associated with office BP monitoring (OBPM), including poor measurement techniques, infrequent measurement, white coat hypertension, and masked hypertension. Patients can also avoid reverse white coat hypertension, where OBPM is normal although out-of-office BP is high.28 Patients should take 3 readings at 1-minute intervals, usually in the morning and evening. The weekly average of these readings is their home BP (normotension is defined as an average BP <135/85 mm Hg).31 Typically, the HBPM monitoring is more accurate in identifying risk than OBPM when there are discrepancies between them.28 It is good practice to instruct patients utilizing HBPM to bring their home BP device to the office for a comparison.
There is some evidence that HBPM may contribute to improved adherence. A systematic review of 11 randomized controlled trials found that in 6 trials the use of HBPM resulted in improved medication adherence, although in 5 of those studies additional interventions were used. These interventions included patient counseling about adverse effects of the medication, timepiece caps that reminded patients to take their medication, tips to enhance adherence, and reinforcement of positive behavior by nurses, pharmacists, lay health workers, or a telephonic system.32 This illustrates an important point in adherence interventions: more is better, and it usually takes a combination of approaches to improve adherence.33,34
The only trial in the review that demonstrated that HBPM alone improved adherence randomized 628 patients to either HBPM or usual care for 6 weeks. The groups had similar compliance rates at baseline, and both demonstrated less adherence at the end of the 6-week trial. However, patients who measured their BP at home still demonstrated greater compliance than those receiving usual care (P < .05).35
A more recent trial in 57 patients, 38 of whom measured their BP at home and 19 of whom received usual care, found greater medication adherence in the HBPM group than in the control group (100% vs 88%, P < .031). The HBPM group also reached their treatment goals significantly faster than the control group (P = .02).36
Conclusion
Approximately 50% of individuals with hypertension who receive antihypertensive medication still do not reach their BP goal. One reason is nonadherence to medication, which is often related to treatment complexity, or pill burden. Given that most patients with hypertension will require more than 1 drug to manage their blood pressure, it is important that clinicians identify opportunities to simplify treatment. This may include fixed-dose combination therapy, which can improve adherence, as well as additional education regarding the efficacy and adverse effects of therapy.
The use of HBPM may also improve adherence by providing frequent feedback on treatment effectiveness.
It is important, however, that clinicians understand that no single approach to adherence will work for every patient. The greatest success comes with combining several approaches based on the barriers that affect each individual patient.
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
MODULE 4: Enhancing Adherence with Antihypertensives: The Role of Fixed-Dose Combinations and Home Blood Pressure Monitoring
Dr Kuritzky is a paid consultant to Takeda Pharmaceuticals International, Inc.
Although an estimated 1 out of 3 people in the United States has been diagnosed with hypertension, data from the 2007-2008 National Health and Nutrition Examination Survey found that just 72% are currently being treated and, of those, just half have their blood pressure (BP) controlled with lifestyle changes and/or medication.1
The failure of so many people with hypertension to obtain BP control, despite the availability of numerous effective medications, is partially due to a lack of adherence to recommended treatments (eg, taking medication, following a diet, and executing lifestyle changes). Adherence is a significant problem in hypertension and evidence shows that just half of patients who initiate drug therapy are persistent with treatment after 1 year.2
Although few studies link nonadherence with long-term outcomes, 1 study found that patients who “forgot” to take their antihypertensive medication were nearly one-third more likely to experience a cardiovascular event or death (hazard ratio [HR], 1.28; 95% confidence interval [CI], 1.04-1.57).3 Adherence is important not only for the health of the patient, but also to provide overall cost savings from the reductions of hospitalizations for complications from an untreated disease.4
Barriers to adherence
A significant contributor to nonadherence is treatment complexity, which manifests in hypertension as pill burden. Up to 75% of patients will require more than 1 medication to control their BP; those with resistant hypertension will require 4 or more.5,6 These medications must often be taken at different times of the day, with varying frequency.6-9
Reducing the number of daily doses has been consistently found to enhance adherence, and should be considered routinely as a first-line strategy. Complex strategies (eg, group visits, designated office staff to assist hypertensive patients, pharmacist consultation and comanagement, exercise counseling, dietary counseling, multidisciplinary hypertension team care, specific interviewing techniques such as motivational interviewing) are promising, but individual clinicians may not have the resources to take advantage of such labor-intensive intervention. Further, when multimodal intervention is employed, it is often difficult to discern which component(s) of the intervention were most impactful, unless multifactorial study design is employed, which it rarely is. We await further randomized controlled trials in this regard.
A study of approximately 85,000 members of a large managed care organization found that the greater the number of antihypertensive medications prescribed, the lower the rate of patient adherence. Just 63% of those receiving 3-drug regimens and 55% of those receiving 4-drug regimens were completely adherent.10
In addition, many patients with hypertension, particularly older patients, have comorbid conditions (eg, dyslipidemia or diabetes) that also require treatment, leading to increased treatment complexity and pill burden.11,12
One option for reducing pill burden is the use of fixed-dose therapies ( TABLE ). Since 2000, many new fixed-dose combinations, including at least 3 triple therapies, have entered the market.13 In addition, a so-called “poly-pill” that combines aspirin, 3 antihypertensives, and a statin is under investigation and demonstrating good results in reducing BP and cholesterol levels.14
TABLE
Currently available combination therapies
| Fixed-Dose Combination | Brand Name | Dose Range, Total, mg/da |
|---|---|---|
| Angiotensin II Receptor Blocker + Thiazide Diuretic | ||
| Azilsartan/chlorthalidone | Edarbyclor | 40/12.5; 40/25 |
| Candesartan/HCTZ | Atacand HCT | 16/12.5; 32/12.5; 32/25 |
| Eprosartan/HCTZ | Teveten HCT | 600/12.5; 600/25 |
| Irbesartan/HCTZ | Avalide | 150/12.5; 300/25 |
| Losartan/HCTZ | Hyzaar | 50/12.5; 100/12.5; 100/25 |
| Olmesartan/HCTZ | Benicar HCT | 20/12.5; 30/12.5 |
| Telmisartan/HCTZ | Micardis HCT | 40/12.5; 80/12.5; 80/25 |
| Valsartan/HCTZ | Diovan HCT | 80/12.5; 160/12.5; 160/25; 320/12.5 |
| β-Blocker + Thiazide Diuretic | ||
| Atenolol/chlorthalidone | Tenoretic | 50/25; 100/25 |
| Bisoprolol/HCTZ | Ziac | 2.5/6.25; 5/6.25; 10/6.25 |
| Metoprolol tartrate/HCTZ | Lopressor HCT | 50/25; 100/25; 100/50 |
| Metoprolol succinate extended/release + HCTZ | Dutoprol | 25/12.5; 50/12.5; 100/12.5 |
| Nadolol + bendroflumethiazide | Corzide | 40/5; 80/5 |
| Propanolol + HCTZ | Inderide | 40/25; 80/25 |
| Calcium Channel Blocker + ACEI | ||
| Amlodipine/benazepril | Lotrel | 2.5/10; 5/10; 5/20; 5/40; 10/20; 10/40 |
| ACEI + Thiazide Diuretic | ||
| Benazepril/HCTZ | Lotensin HCT | 5/6.25; 10/12.5; 20/12.5; 20/25 |
| Captopril/HCTZ | Capozide | 25/15; 25/25; 50/15; 50/25 |
| Enalapril/HCTZ | Vaseretic | 10/25 (1-2) |
| Fosinopril/HCTZ | Monopril HCT | 10/12.5; 20/12.5 |
| Lisinopril/HCTZ | Prinzide Zestoretic | 10/12.5; 20/12.5 20/25 |
| Moexipril/HCTZ | Uniretic | 7.5/12.5; 15/12.5; 15/25 |
| Quinapril + HCTZ | Accuretic | 10/12.5; 20/12.5; 20/25 |
| ACEI + Calcium Channel Blocker | ||
| Trandolapril/verapamil | Tarka | 2/180; 2/240; 4/240 |
| Enalapril/felodipine | Lexxel | 5/5 |
| Angiotensin II Receptor Blocker + Calcium Channel Blocker | ||
| Telmisartan/amlodipine | Twynsta | 40/5; 40/10; 80/5; 80/10 |
| Angiotensin II Receptor Blocker + Calcium Channel Blocker + Thiazide Diuretic | ||
| Olmesartan/amlodipine/HCTZ | Tribenzor | 40/10/25 |
| Calcium Channel Blocker + Angiotensin II Receptor Blocker | ||
| Amlodipine/olmesartan | Azor | 5/20; 5/40; 10/20; 10/40 |
| Amlodipine/valsartan | Exforge | 5/160; 10/160; 5/320; 10/320 |
| Calcium Channel Blocker + Angiotensin II Receptor Blocker + Thiazide Diuretic | ||
| Amlodipine/valsartan/HCTZ | Exforge HCT | 5/160/12.5; 10/160/12.5; 5/160/25; 10/160/25; 10/320/25 |
| Central α-Agonist + Thiazide Diuretic | ||
| Methyldopa/HCTZ | Aldoril Aldoril D | 250/15; 250/25 500/30; 500/50 |
| Direct Renin Inhibitor + Angiotensin II Receptor Blocker | ||
| Aliskiren/valsartan | Valturna | 150/160; 300/320 |
| Direct Renin Inhibitor + Calcium Channel Blocker | ||
| Aliskiren + amlodipine | Tekamlo | 150/5; 150/10; 300/5; 300/10 |
| Direct Renin Inhibitor + Thiazide Diuretic | ||
| Aliskiren/HCTZ | Tekturna HCT | 150/12.5; 150/25; 300/12.5; 300/25 |
| Direct Renin Inhibitor + Calcium Channel Blocker + Thiazide Diuretic | ||
| Aliskiren/amlodipine/HCTZ | Amturnide | 150/5/12.5; 300/5/12.5; 300/5/25; 300/10/12.5; 300/10/25 |
| Diuretic Combination (K+ Sparing + Thiazide) | ||
| Amiloride/HCTZ | Several generics | 5/50 (1-2) |
| Spironolactone/HCTZ | Aldactazide | 25/25 (1/2-1) |
| Triamterene/HCTZ | Dyazide Maxide | 37.5/25 (1/2-1) 37.5/25; 75/50 |
| ACEI, angiotensin-converting enzyme inhibitor; HCTZ, hydrochlorothiazide. aAll 1 dose/d unless otherwise noted. Source: Available at: http://www.RxList.com; http://www.Drugs.com; http://www.empr.com/combination-treatments-for-hypertension-chart/article/191718/. Accessed June 27-28, 2012. | ||
Studies have found that patients receiving fixed-dose combination pills are more likely to reach their target BP, physicians are more satisfied with their ability to manage hypertension, and adverse effects are either similar or less with the fixed-dose therapies compared with monotherapies.15,16
Studies of adherence patterns among patients treated with fixed-dose combinations of antihypertensive agents vs separate antihypertensive agents demonstrate increased adherence among patients treated with fixed-dose combinations.17-21 In a clinical trial involving 4146 participants who were treated with a fixed dose of amlodipine and atorvastatin or separate pills, 33% of patients in the fixed-dose cohort had ceased treatment by 12 months compared with 59% of patients who were taking the 2-pill regimen (HR, 2.17; 95% CI, 2.05–2.13; P < .0001), resulting in a 117% higher rate of nonadherence in the 2-pill regimen. The median persistence time (ie, time to discontinuation with medication) was 8 months with the 2-pill regimen, but 37 months or longer with the fixed-dose combination.21
A meta-analysis of 9 studies found that fixed-dose combinations reduced the risk of nonadherence by 26% compared with single-pill combination therapy.22
One downside to fixed-dose therapy is cost. Out-of-pocket costs are a significant barrier to medication adherence and most fixed-dose options are branded drugs that generally require higher copayments or coinsurance vs generic single-pill drugs that may have copayments as low as $4.6
Other opportunities to improve adherence to antihypertensive medications
Other evidence-based opportunities to improve adherence to antihypertensive medications include improved relationships with, and communication from, health care providers, given that patients often do not understand their disease and recommended treatments.23,24
Interviews with 826 patients with hypertension found that although 90% knew that lowering their BP would improve their health and 91% reported that a health care provider had told them that they had hypertension or high BP, 41% did not know their BP level. In addition, just 34% of patients with hypertension identified systolic BP (SBP) as the “top” number of their reading and only 32% identified diastolic BP (DBP) as the “bottom” number. Finally, only one-third of patients were able to identify both SBP and DBP, and one-quarter of them did not know the optimal level for either.25
Other provider interventions that have resulted in improved adherence include changing medication to reduce or avoid adverse effects, simplifying dosing (as described earlier), and switching to less-expensive drugs if cost is an issue. Nurses and pharmacists are also important members of the team when it comes to improving adherence and reinforcing education.24
Home blood pressure monitoring
Another reason for nonadherence is that patients may not believe they need treatment since hypertension rarely manifests with symptoms. Furthermore, patients may not perceive that the medication they take has any effect because they did not have symptoms to begin with. Home BP monitoring (HBPM), or self BP monitoring, is one tool for improving adherence, possibly by providing immediate feedback to patients on how well their BP is controlled.26 Many major medical societies recommend HBPM as part of any hypertension management strategy.27-30
Patients who use HBPM can avoid many limitations associated with office BP monitoring (OBPM), including poor measurement techniques, infrequent measurement, white coat hypertension, and masked hypertension. Patients can also avoid reverse white coat hypertension, where OBPM is normal although out-of-office BP is high.28 Patients should take 3 readings at 1-minute intervals, usually in the morning and evening. The weekly average of these readings is their home BP (normotension is defined as an average BP <135/85 mm Hg).31 Typically, the HBPM monitoring is more accurate in identifying risk than OBPM when there are discrepancies between them.28 It is good practice to instruct patients utilizing HBPM to bring their home BP device to the office for a comparison.
There is some evidence that HBPM may contribute to improved adherence. A systematic review of 11 randomized controlled trials found that in 6 trials the use of HBPM resulted in improved medication adherence, although in 5 of those studies additional interventions were used. These interventions included patient counseling about adverse effects of the medication, timepiece caps that reminded patients to take their medication, tips to enhance adherence, and reinforcement of positive behavior by nurses, pharmacists, lay health workers, or a telephonic system.32 This illustrates an important point in adherence interventions: more is better, and it usually takes a combination of approaches to improve adherence.33,34
The only trial in the review that demonstrated that HBPM alone improved adherence randomized 628 patients to either HBPM or usual care for 6 weeks. The groups had similar compliance rates at baseline, and both demonstrated less adherence at the end of the 6-week trial. However, patients who measured their BP at home still demonstrated greater compliance than those receiving usual care (P < .05).35
A more recent trial in 57 patients, 38 of whom measured their BP at home and 19 of whom received usual care, found greater medication adherence in the HBPM group than in the control group (100% vs 88%, P < .031). The HBPM group also reached their treatment goals significantly faster than the control group (P = .02).36
Conclusion
Approximately 50% of individuals with hypertension who receive antihypertensive medication still do not reach their BP goal. One reason is nonadherence to medication, which is often related to treatment complexity, or pill burden. Given that most patients with hypertension will require more than 1 drug to manage their blood pressure, it is important that clinicians identify opportunities to simplify treatment. This may include fixed-dose combination therapy, which can improve adherence, as well as additional education regarding the efficacy and adverse effects of therapy.
The use of HBPM may also improve adherence by providing frequent feedback on treatment effectiveness.
It is important, however, that clinicians understand that no single approach to adherence will work for every patient. The greatest success comes with combining several approaches based on the barriers that affect each individual patient.
1. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043-2050.
2. Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336(7653):1114-1117.
3. Nelson MR, Reid CM, Ryan P, Willson K, Yelland L. Self-reported adherence with medication and cardiovascular disease outcomes in the Second Australian National Blood Pressure Study (ANBP2). Med J Aust. 2006;185(9):487-489.
4. Muszbek N, Brixner D, Benedict A, Keskinaslan A, Khan ZM. The economic consequences of noncompliance in cardiovascular disease and related conditions: a literature review. Int J Clin Pract. 2008;62(2):338-351.
5. Jamerson K, Bakris GL, Dahlöf B, et al; . ACCOMPLISH Investigators. Exceptional early blood pressure control rates: the ACCOMPLISH trial. Blood Press. 2007;16(2):80-86.
6. Gradman AH, Basile JN, Carter BL, et al. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(2):90-98.
7. World Health Organization. Adherence to long-term therapies: evidence for action. http://apps.who.int/medicinedocs/en/d/Js4883e/. Published 2003. Accessed March 21, 2012.
8. Chapman RH, Benner JS, Petrilla AA, et al. Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med. 2005;165(10):1147-1152.
9. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487-497.
10. Fung V, Huang J, Brand R, Newhouse JP, Hsu J. Hypertension treatment in a medicare population: adherence and systolic blood pressure control. Clin Ther. 2007;29(5):972-984.
11. Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002;287(3):337-344.
12. Sica DA. Rationale for fixed-dose combinations in the treatment of hypertension: the cycle repeats. Drugs. 2002;62(3):443-462.
13. Paulis L, Steckelings UM, Unger T. Key advances in antihypertensive treatment. Nat Rev Cardiol. 2012;9(5):276-285.
14. Wood S. TIPS 2: Full-dose polypill boosts efficacy, with no increased side effects. theHeart.org Web site. http://www.theheart.org/article/1387105.do?utm_campaign=newsletter&utm_medium=email&utm_source=20120419_EN_Heartwire. Published April 19, 2012. Accessed April 20, 2012.
15. Hilleman DE, Ryschon KL, Mohiuddin SM, Wurdeman RL. Fixed-dose combination vs monotherapy in hypertension: a meta-analysis evaluation. J Hum Hyper-tens. 1999;13(7):477-483.
16. Feldman RD, Zou GY, Vandervoort MK, Wong CJ, Nelson SA, Feagan BG. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension. 2009;53(4):646-653.
17. Dezii CM. A retrospective study of persistence with single-pill combination therapy vs. concurrent two-pill therapy in patients with hypertension. Manag Care. 2000;9(9 suppl):2-6.
18. Gerbino PP, Shoheiber O. Adherence patterns among patients treated with fixed-dose combination versus separate antihypertensive agents. Am J Health Syst Pharm. 2007;64(12):1279-1283.
19. Brixner DI, Jackson KC, II, Sheng X, Nelson RE, Keskinaslan A. Assessment of adherence, persistence, and costs among valsartan and hydrochlorothiazide retrospective cohorts in free-and fixed-dose combinations. Curr Med Res Opin. 2008;24(9):2597-2607.
20. Baser O, Andrews LM, Wang L, Xie L. Comparison of real-world adherence, healthcare resource utilization and costs for newly initiated valsartan/amlodi-pine single-pill combination versus angiotensin receptor blocker/calcium channel blocker free-combination therapy. J Med Econ. 2011;14(5):576-583.
21. Simons LA, Ortiz M, Calcino G. Persistence with a single pill versus two pills of amlodipine and atorvastatin: the Australian experience, 2006-2010. Med J Aust. 2011;195(3):134-137.
22. Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120(8):713-719.
23. Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80(8):991-994.
24. Harmon G, Lefante J, Krousel-Wood M. Overcoming barriers: the role of providers in improving patient adherence to antihypertensive medications. Curr Opin Cardiol. 2006;21(4):310-315.
25. Oliveria SA, Chen RS, McCarthy BD, Davis CC, Hill MN. Hypertension knowledge, awareness, and attitudes in a hypertensive population. J Gen Intern Med. 2005;20(3):219-225.
26. Abdullah A, Othman S. The influence of self-owned home blood pressure monitoring (HBPM) on primary care patients with hypertension: a qualitative study. BMC Fam Pract. 2011;12:143.-
27. Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment: A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-1419.
28. Pickering TG, White WB. American Society of Hypertension Writing Group. When and how to use self (home) and ambulatory blood pressure monitoring. J Am Soc Hypertens. 2008;2(3):119-124.
29. Institute for Clinical Systems Improvement. Health Care Guideline: Hypertension Diagnosis and Treatment. 13th ed. http://icsi.org/hypertension_4/hypertension_diagnosis_and_treatment_4.html. Published November 2010. Accessed March 26, 2012.
30. National Institute for Health and Clinical Evidence. Hypertension: Clinical management of primary hypertension in adults. http://guidance.nice.org.uk/CG127. Published August 2011. Accessed March 26, 2012.
31. Mengden T, Chamontin B, Phong Chau N, Luis Palma Gamiz J, Chanudet X. User procedure for self-measurement of blood pressure. First International Consensus Conference on Self Blood Pressure Measurement. Blood Press Monit. 2000;5(2):111-129.
32. Ogedegbe G, Schoenthaler A. A systematic review of the effects of home blood pressure monitoring on medication adherence. J Clin Hypertens (Greenwich). 2006;8(3):174-180.
33. McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review [published correction appears in JAMA. 2003;289(24):3242]. JAMA. 2002;288(22):2868-2879.
34. Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60(7):657-665.
35. Vrijens B, Goetghebeur E. Comparing compliance patterns between randomized treatments. Control Clin Trials. 1997;18(3):187-203.
36. Souza WK, Jardim PC, Brito LP, Araújo FA, Sousa AL. Self measurement of blood pressure for control of blood pressure levels and adherence to treatment. Arq Bras Cardiol. 2012;98(2):167-174.
1. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043-2050.
2. Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336(7653):1114-1117.
3. Nelson MR, Reid CM, Ryan P, Willson K, Yelland L. Self-reported adherence with medication and cardiovascular disease outcomes in the Second Australian National Blood Pressure Study (ANBP2). Med J Aust. 2006;185(9):487-489.
4. Muszbek N, Brixner D, Benedict A, Keskinaslan A, Khan ZM. The economic consequences of noncompliance in cardiovascular disease and related conditions: a literature review. Int J Clin Pract. 2008;62(2):338-351.
5. Jamerson K, Bakris GL, Dahlöf B, et al; . ACCOMPLISH Investigators. Exceptional early blood pressure control rates: the ACCOMPLISH trial. Blood Press. 2007;16(2):80-86.
6. Gradman AH, Basile JN, Carter BL, et al. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(2):90-98.
7. World Health Organization. Adherence to long-term therapies: evidence for action. http://apps.who.int/medicinedocs/en/d/Js4883e/. Published 2003. Accessed March 21, 2012.
8. Chapman RH, Benner JS, Petrilla AA, et al. Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med. 2005;165(10):1147-1152.
9. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487-497.
10. Fung V, Huang J, Brand R, Newhouse JP, Hsu J. Hypertension treatment in a medicare population: adherence and systolic blood pressure control. Clin Ther. 2007;29(5):972-984.
11. Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002;287(3):337-344.
12. Sica DA. Rationale for fixed-dose combinations in the treatment of hypertension: the cycle repeats. Drugs. 2002;62(3):443-462.
13. Paulis L, Steckelings UM, Unger T. Key advances in antihypertensive treatment. Nat Rev Cardiol. 2012;9(5):276-285.
14. Wood S. TIPS 2: Full-dose polypill boosts efficacy, with no increased side effects. theHeart.org Web site. http://www.theheart.org/article/1387105.do?utm_campaign=newsletter&utm_medium=email&utm_source=20120419_EN_Heartwire. Published April 19, 2012. Accessed April 20, 2012.
15. Hilleman DE, Ryschon KL, Mohiuddin SM, Wurdeman RL. Fixed-dose combination vs monotherapy in hypertension: a meta-analysis evaluation. J Hum Hyper-tens. 1999;13(7):477-483.
16. Feldman RD, Zou GY, Vandervoort MK, Wong CJ, Nelson SA, Feagan BG. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension. 2009;53(4):646-653.
17. Dezii CM. A retrospective study of persistence with single-pill combination therapy vs. concurrent two-pill therapy in patients with hypertension. Manag Care. 2000;9(9 suppl):2-6.
18. Gerbino PP, Shoheiber O. Adherence patterns among patients treated with fixed-dose combination versus separate antihypertensive agents. Am J Health Syst Pharm. 2007;64(12):1279-1283.
19. Brixner DI, Jackson KC, II, Sheng X, Nelson RE, Keskinaslan A. Assessment of adherence, persistence, and costs among valsartan and hydrochlorothiazide retrospective cohorts in free-and fixed-dose combinations. Curr Med Res Opin. 2008;24(9):2597-2607.
20. Baser O, Andrews LM, Wang L, Xie L. Comparison of real-world adherence, healthcare resource utilization and costs for newly initiated valsartan/amlodi-pine single-pill combination versus angiotensin receptor blocker/calcium channel blocker free-combination therapy. J Med Econ. 2011;14(5):576-583.
21. Simons LA, Ortiz M, Calcino G. Persistence with a single pill versus two pills of amlodipine and atorvastatin: the Australian experience, 2006-2010. Med J Aust. 2011;195(3):134-137.
22. Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120(8):713-719.
23. Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80(8):991-994.
24. Harmon G, Lefante J, Krousel-Wood M. Overcoming barriers: the role of providers in improving patient adherence to antihypertensive medications. Curr Opin Cardiol. 2006;21(4):310-315.
25. Oliveria SA, Chen RS, McCarthy BD, Davis CC, Hill MN. Hypertension knowledge, awareness, and attitudes in a hypertensive population. J Gen Intern Med. 2005;20(3):219-225.
26. Abdullah A, Othman S. The influence of self-owned home blood pressure monitoring (HBPM) on primary care patients with hypertension: a qualitative study. BMC Fam Pract. 2011;12:143.-
27. Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment: A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51(6):1403-1419.
28. Pickering TG, White WB. American Society of Hypertension Writing Group. When and how to use self (home) and ambulatory blood pressure monitoring. J Am Soc Hypertens. 2008;2(3):119-124.
29. Institute for Clinical Systems Improvement. Health Care Guideline: Hypertension Diagnosis and Treatment. 13th ed. http://icsi.org/hypertension_4/hypertension_diagnosis_and_treatment_4.html. Published November 2010. Accessed March 26, 2012.
30. National Institute for Health and Clinical Evidence. Hypertension: Clinical management of primary hypertension in adults. http://guidance.nice.org.uk/CG127. Published August 2011. Accessed March 26, 2012.
31. Mengden T, Chamontin B, Phong Chau N, Luis Palma Gamiz J, Chanudet X. User procedure for self-measurement of blood pressure. First International Consensus Conference on Self Blood Pressure Measurement. Blood Press Monit. 2000;5(2):111-129.
32. Ogedegbe G, Schoenthaler A. A systematic review of the effects of home blood pressure monitoring on medication adherence. J Clin Hypertens (Greenwich). 2006;8(3):174-180.
33. McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review [published correction appears in JAMA. 2003;289(24):3242]. JAMA. 2002;288(22):2868-2879.
34. Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60(7):657-665.
35. Vrijens B, Goetghebeur E. Comparing compliance patterns between randomized treatments. Control Clin Trials. 1997;18(3):187-203.
36. Souza WK, Jardim PC, Brito LP, Araújo FA, Sousa AL. Self measurement of blood pressure for control of blood pressure levels and adherence to treatment. Arq Bras Cardiol. 2012;98(2):167-174.
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
Dr Wright is a paid consultant to The Medical Letter, Inc, and Takeda Pharmaceuticals International, Inc. He is on an advisory board of Medtronic, Inc.
Introduction
Hypertension and hypertensive target organ damage are more prevalent and more severe in certain minority populations, especially African Americans. Hypertension is more common, more severe, develops at an earlier age, and leads to greater morbidity and mortality in African Americans than in age-matched non-Hispanic whites.1 African Americans have among the highest rates of hypertension in the world (41% overall, 44% among black women) and develop the condition an average of 5 years earlier than whites.1
A recent report found that although treatment rates between whites and African Americans overall are similar, a smaller percentage of African Americans with hypertension are controlled to <140/90 mm Hg compared with whites.2 This may at least partly explain the 4 to 5 times higher hypertension-related mortality, 2 to 4 times increased risk of left ventricular hypertrophy (LVH), coronary heart disease (CHD), congestive heart failure, and stroke, and the 4 times higher rate of end-stage renal disease (ESRD) in African Americans compared with whites.1,3 The higher prevalence of diabetes mellitus, cigarette smoking, obesity, lipid disorders, and LVH in blacks exacerbates the existing risk posed by hypertension, making the need for aggressive blood pressure (BP) control even more critical.1
Antihypertensive treatment in African Americans
Lifestyle modification is recommended for all hypertensive patients but is especially important for African Americans. This population has a greater prevalence of obesity than whites, so weight loss is critical.4 Further, African Americans tend to have a greater sensitivity to salt because of a combination of obesity, abnormalities in renal salt handling, and a tendency to consume a high salt/low potassium diet.3 African Americans have been shown to benefit at least as much as other subgroups with hypertension from reductions in dietary salt and improvements in diet quality, such as the Dietary Approaches to Stop Hypertension (DASH) diet.5-7
Several studies have documented the efficacy of diuretics in lowering BP in African Americans.3,8-10 In the Antihypertensive and Lipid-Lowering to Prevent Heart Attack Trial (ALLHAT), treatment initiated with the thiazide-type diuretic (THZD) chlorthalidone (CTD) reduced systolic BP (SBP) by 4 mm Hg more than treatment based on the angiotensin-converting enzyme inhibitor (ACEI) lisinopril or the alpha-blocker doxazosin in black ALLHAT participants who were receiving similar background antihypertensive drug treatment.9,10 The greater BP lowering in the THZD arm was associated with a significantly reduced rate in 1 or more cardiovascular disease (CVD) outcomes. Other inhibitors of the renin-angiotensin system (eg, angiotensin-receptor blockers [ARBs], direct renin inhibitors, and beta-blockers) are similarly less effective in lowering BP in African Americans.3 In contrast, when the calcium channel blocker (CCB) amlodipine was compared with CTD in blacks or when CTD was compared with lisinopril or doxazosin in nonblacks, SBP reductions were only ~1 mm Hg.8,10
As a class, diuretics have been shown to decrease hypertension-related morbidity and mortality in both African Americans and whites.10-15 In fact, much of the evidence for the benefits of antihypertensive therapy in preventing hypertension-related morbidity and mortality was conducted with THZDs, with several of the relevant trials containing significant numbers of African American participants (TABLE).8,10,13-16
TABLE
Outcomes of major clinical trials of diuretics in African Americans
| Clinical trial | Relative risk reduction (RRR) or hazard ratio (HR) by endpoint | |||||
|---|---|---|---|---|---|---|
| Mortality | CVD | CHD | Stroke | HF | ESRD | |
| VA Cooperative: HCTZ + RES + HYD vs placebo (RRR)13 | 0.46 | |||||
| HDFP: stepped therapy with CTD vs usual care (HR)14 | 0.76a | |||||
| SHEP: CTD + atenolol vs placebo (HR)15 | 0.68a | |||||
| ALLHAT: All African Americans (RRR)8,10 | ||||||
| AML vs CTD | 0.97 | 1.06 | 1.03 | 0.93 | 1.46a | 1.15 |
| DOX vs CTD | N/A | 1.28a | 1.11 | 1.38a | 1.84a | 0.99 |
| LIS vs CTD | 1.06 | 1.19a | 1.15a | 1.40a | 1.30a | 1.29 |
| ALLHAT: African Americans with diabetes and metabolic syndrome (RRR)16 | ||||||
| AML vs CTD | 1.02 | 1.14a | 1.09 | 1.01 | 1.50 | 1.50 |
| DOX vs CTD | 1.18 | 1.37a | 1.15 | 1.49a | 1.88a | 1.17 |
| LIS vs CTD | 0.96 | 1.24a | 1.19a | 1.37a | 1.49a | 1.70a |
| ALLHAT, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial; AML, amlodipine; CHD, coronary heart disease; CTD, chlorthalidone; CVD, cardiovascular disease; DOX, doxazosin; ESRD, end-stage renal disease; HCTZ, hydrochlorothiazide; HDFP, Hypertension Detection and Follow-up Program; HF, heart failure; HYD, hydralazine; LIS, lisinopril; RES, reserpine; SHEP, Systolic Hypertension in the Elderly Program; VA, Veterans Administration aP ≤0.05 | ||||||
In the Veterans Administration (VA) Cooperative Trial, African American men comprised 42% of participants, all of whom were randomized to a combination of hydrochlorothiazide, reserpine, and hydralazine, or to placebo.13 In the Hypertension Detection and Follow-Up Program (HDFP) trial, 44% of participants were African American. All participants were randomized to stepped therapy with CTD, reserpine, methyldopa, and hydralazine, or to usual community care.14 Both of these pioneering trials documented the benefit of a THZD-based regimen in lowering BP and improving clinical outcomes in African Americans with hypertension. The Systolic Hypertension in the Elderly Program (SHEP) trial, in which 14% of participants were African American, extended earlier results from the VA Cooperative and HDFP trials by demonstrating that, compared with placebo, active treatment with CTD and the beta-blocker atenolol produced clinical outcome reductions in African Americans and whites with isolated systolic hypertension as well as in those with elevated diastolic BP.15
In comparative trials with newer classes of antihypertensives, THZDs have remained unsurpassed in preventing complications of hypertension, including in African Americans (TABLE). ALLHAT was the first outcome study to evaluate the relative benefit of antihypertensive treatment initiated with newer classes of antihypertensive agents vs treatment initiated with a THZD in blacks. ALLHAT included more than 15,000 African Americans and Afro-Caribbeans and confirmed the findings of studies in other populations that neither an ACEI, a CCB, or alpha-blocker–initiated therapy surpassed therapy initiated with a THZD (CTD) in lowering BP or in preventing CVD or renal outcomes.8,10 Overall, the THZD-based therapy was superior to the alpha-blocker, ACEI, and CCB-based therapies in preventing 1 or more major forms of CVD, including stroke and heart failure (HF). In blacks, THZD-based therapy was superior to alpha-blocker–based therapy in lowering BP and in preventing overall CVD (especially HF and stroke), and was superior to the ACEI-based regimen in preventing stroke, HF, and overall CVD (a composite of CHD, stroke, and HF endpoints). Compared with CCB-based therapy (ie, amlodipine), THZD (CTD)-based therapy was similar in overall CVD protection but superior in preventing HF.
These results in ALLHAT were even more impressive in blacks with diabetes or the metabolic syndrome (TABLE).16 In addition to the above-mentioned CVD outcomes in black hypertensive patients, neither the CCB-based nor the ACEI-based regimens were superior to the THZD-based regimen in preventing ESRD overall or when stratified by diabetes or baseline estimated glomerular filtration rate.10,16,17 In black ALLHAT participants with diabetes or the metabolic syndrome, CTD was associated with substantially reduced rates of ESRD compared with those randomized to doxazosin, amlodipine, or the ACEI lisinopril.16 It should also be noted that nearly all previous renal outcome trials with renin-angiotensin system inhibitors included background therapy with a diuretic.17
Recommendations
Most national and international guidelines recommend THZDs as first-line therapy in African Americans.18-21 Calcium channel blockers are a reasonable alternate first-line choice in African Americans who are unable to tolerate a diuretic.
In addition, the Joint National Committee (JNC-7) guidelines recommend the use of ACEIs and ARBs as first-line therapy in all patients with hypertension comorbid with chronic kidney disease (CKD) or HF, including African Americans.18 These drugs, along with alpha-blockers and all other agents in the antihypertensive armamentarium, should be used as add-on therapy, as needed, to achieve BP goals in African Americans already receiving a THZD or CCB.
Importantly, multiple drug therapy should be considered for initial treatment in all individuals whose BP is more than 20/10 mm Hg above target.18 In addition, multiple antihypertensive agents are usually required to achieve long-term control in most patients, particularly in African Americans who, as noted earlier, tend to have more-severe hypertension.19
Conclusion
Treatment of hypertension in African Americans should include both lifestyle modifications and pharmacologic intervention, usually with multiple agents. In the absence of compelling indications for alternative therapies, THZD-based regimens should be considered first-line treatment given significant evidence from large randomized studies that document their ability to reduce both BP and hypertensive complications in this population.
Monotherapy with ACEIs, ARBs, direct renin inhibitors, or beta-blockers is less effective in lowering BP in African Americans than in other populations. ACEIs and ARBs should be included in antihypertensive regimens prescribed for African Americans with concomitant CKD or HF. They can also be considered as add-on therapy to regimens containing a THZD or CCB in the absence of these conditions.
1. Roger VL, Go AS, Lloyd-Jones DM, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2-e220.
2. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043-2050.
3. Johnson EF, Wright JT. Management of hypertension in black populations. In: Oparil S, Weber MA, eds. Hypertension: A Companion to Brenner and Rector’s The Kidney. 2nd ed. Philadelphia, PA: Elsevier Saunders; 2005:587–595.
4. National Center for Health Statistics. Health, United States, 2009: With Special Feature on Medical Technology. Hyattsville, MD. 2010. Table 72.
5. Prather AA, Blumenthal JA, Hinderliter AL, Sherwood A. Ethnic differences in the effects of the DASH diet on nocturnal blood pressure dipping in individuals with high blood pressure. Am J Hypertens. 2011;24(12):1338-1344.
6. Svetkey LP, Simons-Morton D, Vollmer WM, et al. Effects of dietary patterns on blood pressure: subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159(3):285-293.
7. Appel LJ, Moore TJ, Obarzanek E, et al. DASH Collaborative Research Group. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336(16):1117-1124.
8. Wright JT, Jr, Dunn JK, Cutler JA, et al. ALLHAT Collaborative Research Group. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA. 2005;293(13):1595-1608.
9. Materson BJ, Reda DJ, Cushman WC, et al. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. N Engl J Med. 1993;328(13):914-921.
10. Wright JT, Jr, Probstfield JL, Cushman WC, et al. ALLHAT findings revisited in the context of subsequent analyses, other trials, and meta-analyses. Arch Intern Med. 2009;169(9):832-842.
11. Neal B, MacMahon S, Chapman N. Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Lancet. 2000;356(9246):1955-1964.
12. Turnbull F. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-1535.
13. Effects of treatment on morbidity in hypertension. II. Results in patients with diastolic blood pressure averaging 90 through 114 mm Hg. JAMA. 1970;213(7):1143-1152.
14. Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the Hypertension Detection and Follow-up Program: mortality by race-sex and blood pressure level. A further analysis. J Community Health. 1984;9(4):314-327.
15. The Systolic Hypertension in the Elderly Program Cooperative Research Group. Implications of the systolic hypertension in the elderly program. Hypertension. 1993;21(3):335-343.
16. Wright JT, Jr, Harris-Haywood S, Pressel S, et al. Clinical outcomes by race in hypertensive patients with and without the metabolic syndrome: Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2008;168(2):207-217.
17. Rahman M, Pressel S, Davis BR, et al. Renal outcomes in high-risk hypertensive patients treated with an angiotensin-converting enzyme inhibitor or a calcium channel blocker vs a diuretic: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2005;165(8):936-946.
18. Chobanian AV, Bakris GL, Black HR, et al. Joint National Committee on Prevention Detection Evaluation and Treatment of High Blood Pressure; National Heart, Lung, and Blood Insitute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-1252.
19. Flack JM, Sica DA, Bakris G, et al. International Society on Hypertension in Blacks. Management of high blood pressure in blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension. 2010;56(5):780-800.
20. Mancia G, Laurent S, Agabiti-Rosei E, et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. Blood Press. 2009;18(6):308-347.
21. Canadian Hypertension Education Program. The 2012 CHEP Recommendations. Hypertension Canada Web site. http://www.hypertension.ca/chep-recommendations. Published 2012. Accessed April 15, 2012.
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
Dr Wright is a paid consultant to The Medical Letter, Inc, and Takeda Pharmaceuticals International, Inc. He is on an advisory board of Medtronic, Inc.
Introduction
Hypertension and hypertensive target organ damage are more prevalent and more severe in certain minority populations, especially African Americans. Hypertension is more common, more severe, develops at an earlier age, and leads to greater morbidity and mortality in African Americans than in age-matched non-Hispanic whites.1 African Americans have among the highest rates of hypertension in the world (41% overall, 44% among black women) and develop the condition an average of 5 years earlier than whites.1
A recent report found that although treatment rates between whites and African Americans overall are similar, a smaller percentage of African Americans with hypertension are controlled to <140/90 mm Hg compared with whites.2 This may at least partly explain the 4 to 5 times higher hypertension-related mortality, 2 to 4 times increased risk of left ventricular hypertrophy (LVH), coronary heart disease (CHD), congestive heart failure, and stroke, and the 4 times higher rate of end-stage renal disease (ESRD) in African Americans compared with whites.1,3 The higher prevalence of diabetes mellitus, cigarette smoking, obesity, lipid disorders, and LVH in blacks exacerbates the existing risk posed by hypertension, making the need for aggressive blood pressure (BP) control even more critical.1
Antihypertensive treatment in African Americans
Lifestyle modification is recommended for all hypertensive patients but is especially important for African Americans. This population has a greater prevalence of obesity than whites, so weight loss is critical.4 Further, African Americans tend to have a greater sensitivity to salt because of a combination of obesity, abnormalities in renal salt handling, and a tendency to consume a high salt/low potassium diet.3 African Americans have been shown to benefit at least as much as other subgroups with hypertension from reductions in dietary salt and improvements in diet quality, such as the Dietary Approaches to Stop Hypertension (DASH) diet.5-7
Several studies have documented the efficacy of diuretics in lowering BP in African Americans.3,8-10 In the Antihypertensive and Lipid-Lowering to Prevent Heart Attack Trial (ALLHAT), treatment initiated with the thiazide-type diuretic (THZD) chlorthalidone (CTD) reduced systolic BP (SBP) by 4 mm Hg more than treatment based on the angiotensin-converting enzyme inhibitor (ACEI) lisinopril or the alpha-blocker doxazosin in black ALLHAT participants who were receiving similar background antihypertensive drug treatment.9,10 The greater BP lowering in the THZD arm was associated with a significantly reduced rate in 1 or more cardiovascular disease (CVD) outcomes. Other inhibitors of the renin-angiotensin system (eg, angiotensin-receptor blockers [ARBs], direct renin inhibitors, and beta-blockers) are similarly less effective in lowering BP in African Americans.3 In contrast, when the calcium channel blocker (CCB) amlodipine was compared with CTD in blacks or when CTD was compared with lisinopril or doxazosin in nonblacks, SBP reductions were only ~1 mm Hg.8,10
As a class, diuretics have been shown to decrease hypertension-related morbidity and mortality in both African Americans and whites.10-15 In fact, much of the evidence for the benefits of antihypertensive therapy in preventing hypertension-related morbidity and mortality was conducted with THZDs, with several of the relevant trials containing significant numbers of African American participants (TABLE).8,10,13-16
TABLE
Outcomes of major clinical trials of diuretics in African Americans
| Clinical trial | Relative risk reduction (RRR) or hazard ratio (HR) by endpoint | |||||
|---|---|---|---|---|---|---|
| Mortality | CVD | CHD | Stroke | HF | ESRD | |
| VA Cooperative: HCTZ + RES + HYD vs placebo (RRR)13 | 0.46 | |||||
| HDFP: stepped therapy with CTD vs usual care (HR)14 | 0.76a | |||||
| SHEP: CTD + atenolol vs placebo (HR)15 | 0.68a | |||||
| ALLHAT: All African Americans (RRR)8,10 | ||||||
| AML vs CTD | 0.97 | 1.06 | 1.03 | 0.93 | 1.46a | 1.15 |
| DOX vs CTD | N/A | 1.28a | 1.11 | 1.38a | 1.84a | 0.99 |
| LIS vs CTD | 1.06 | 1.19a | 1.15a | 1.40a | 1.30a | 1.29 |
| ALLHAT: African Americans with diabetes and metabolic syndrome (RRR)16 | ||||||
| AML vs CTD | 1.02 | 1.14a | 1.09 | 1.01 | 1.50 | 1.50 |
| DOX vs CTD | 1.18 | 1.37a | 1.15 | 1.49a | 1.88a | 1.17 |
| LIS vs CTD | 0.96 | 1.24a | 1.19a | 1.37a | 1.49a | 1.70a |
| ALLHAT, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial; AML, amlodipine; CHD, coronary heart disease; CTD, chlorthalidone; CVD, cardiovascular disease; DOX, doxazosin; ESRD, end-stage renal disease; HCTZ, hydrochlorothiazide; HDFP, Hypertension Detection and Follow-up Program; HF, heart failure; HYD, hydralazine; LIS, lisinopril; RES, reserpine; SHEP, Systolic Hypertension in the Elderly Program; VA, Veterans Administration aP ≤0.05 | ||||||
In the Veterans Administration (VA) Cooperative Trial, African American men comprised 42% of participants, all of whom were randomized to a combination of hydrochlorothiazide, reserpine, and hydralazine, or to placebo.13 In the Hypertension Detection and Follow-Up Program (HDFP) trial, 44% of participants were African American. All participants were randomized to stepped therapy with CTD, reserpine, methyldopa, and hydralazine, or to usual community care.14 Both of these pioneering trials documented the benefit of a THZD-based regimen in lowering BP and improving clinical outcomes in African Americans with hypertension. The Systolic Hypertension in the Elderly Program (SHEP) trial, in which 14% of participants were African American, extended earlier results from the VA Cooperative and HDFP trials by demonstrating that, compared with placebo, active treatment with CTD and the beta-blocker atenolol produced clinical outcome reductions in African Americans and whites with isolated systolic hypertension as well as in those with elevated diastolic BP.15
In comparative trials with newer classes of antihypertensives, THZDs have remained unsurpassed in preventing complications of hypertension, including in African Americans (TABLE). ALLHAT was the first outcome study to evaluate the relative benefit of antihypertensive treatment initiated with newer classes of antihypertensive agents vs treatment initiated with a THZD in blacks. ALLHAT included more than 15,000 African Americans and Afro-Caribbeans and confirmed the findings of studies in other populations that neither an ACEI, a CCB, or alpha-blocker–initiated therapy surpassed therapy initiated with a THZD (CTD) in lowering BP or in preventing CVD or renal outcomes.8,10 Overall, the THZD-based therapy was superior to the alpha-blocker, ACEI, and CCB-based therapies in preventing 1 or more major forms of CVD, including stroke and heart failure (HF). In blacks, THZD-based therapy was superior to alpha-blocker–based therapy in lowering BP and in preventing overall CVD (especially HF and stroke), and was superior to the ACEI-based regimen in preventing stroke, HF, and overall CVD (a composite of CHD, stroke, and HF endpoints). Compared with CCB-based therapy (ie, amlodipine), THZD (CTD)-based therapy was similar in overall CVD protection but superior in preventing HF.
These results in ALLHAT were even more impressive in blacks with diabetes or the metabolic syndrome (TABLE).16 In addition to the above-mentioned CVD outcomes in black hypertensive patients, neither the CCB-based nor the ACEI-based regimens were superior to the THZD-based regimen in preventing ESRD overall or when stratified by diabetes or baseline estimated glomerular filtration rate.10,16,17 In black ALLHAT participants with diabetes or the metabolic syndrome, CTD was associated with substantially reduced rates of ESRD compared with those randomized to doxazosin, amlodipine, or the ACEI lisinopril.16 It should also be noted that nearly all previous renal outcome trials with renin-angiotensin system inhibitors included background therapy with a diuretic.17
Recommendations
Most national and international guidelines recommend THZDs as first-line therapy in African Americans.18-21 Calcium channel blockers are a reasonable alternate first-line choice in African Americans who are unable to tolerate a diuretic.
In addition, the Joint National Committee (JNC-7) guidelines recommend the use of ACEIs and ARBs as first-line therapy in all patients with hypertension comorbid with chronic kidney disease (CKD) or HF, including African Americans.18 These drugs, along with alpha-blockers and all other agents in the antihypertensive armamentarium, should be used as add-on therapy, as needed, to achieve BP goals in African Americans already receiving a THZD or CCB.
Importantly, multiple drug therapy should be considered for initial treatment in all individuals whose BP is more than 20/10 mm Hg above target.18 In addition, multiple antihypertensive agents are usually required to achieve long-term control in most patients, particularly in African Americans who, as noted earlier, tend to have more-severe hypertension.19
Conclusion
Treatment of hypertension in African Americans should include both lifestyle modifications and pharmacologic intervention, usually with multiple agents. In the absence of compelling indications for alternative therapies, THZD-based regimens should be considered first-line treatment given significant evidence from large randomized studies that document their ability to reduce both BP and hypertensive complications in this population.
Monotherapy with ACEIs, ARBs, direct renin inhibitors, or beta-blockers is less effective in lowering BP in African Americans than in other populations. ACEIs and ARBs should be included in antihypertensive regimens prescribed for African Americans with concomitant CKD or HF. They can also be considered as add-on therapy to regimens containing a THZD or CCB in the absence of these conditions.
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
Dr Wright is a paid consultant to The Medical Letter, Inc, and Takeda Pharmaceuticals International, Inc. He is on an advisory board of Medtronic, Inc.
Introduction
Hypertension and hypertensive target organ damage are more prevalent and more severe in certain minority populations, especially African Americans. Hypertension is more common, more severe, develops at an earlier age, and leads to greater morbidity and mortality in African Americans than in age-matched non-Hispanic whites.1 African Americans have among the highest rates of hypertension in the world (41% overall, 44% among black women) and develop the condition an average of 5 years earlier than whites.1
A recent report found that although treatment rates between whites and African Americans overall are similar, a smaller percentage of African Americans with hypertension are controlled to <140/90 mm Hg compared with whites.2 This may at least partly explain the 4 to 5 times higher hypertension-related mortality, 2 to 4 times increased risk of left ventricular hypertrophy (LVH), coronary heart disease (CHD), congestive heart failure, and stroke, and the 4 times higher rate of end-stage renal disease (ESRD) in African Americans compared with whites.1,3 The higher prevalence of diabetes mellitus, cigarette smoking, obesity, lipid disorders, and LVH in blacks exacerbates the existing risk posed by hypertension, making the need for aggressive blood pressure (BP) control even more critical.1
Antihypertensive treatment in African Americans
Lifestyle modification is recommended for all hypertensive patients but is especially important for African Americans. This population has a greater prevalence of obesity than whites, so weight loss is critical.4 Further, African Americans tend to have a greater sensitivity to salt because of a combination of obesity, abnormalities in renal salt handling, and a tendency to consume a high salt/low potassium diet.3 African Americans have been shown to benefit at least as much as other subgroups with hypertension from reductions in dietary salt and improvements in diet quality, such as the Dietary Approaches to Stop Hypertension (DASH) diet.5-7
Several studies have documented the efficacy of diuretics in lowering BP in African Americans.3,8-10 In the Antihypertensive and Lipid-Lowering to Prevent Heart Attack Trial (ALLHAT), treatment initiated with the thiazide-type diuretic (THZD) chlorthalidone (CTD) reduced systolic BP (SBP) by 4 mm Hg more than treatment based on the angiotensin-converting enzyme inhibitor (ACEI) lisinopril or the alpha-blocker doxazosin in black ALLHAT participants who were receiving similar background antihypertensive drug treatment.9,10 The greater BP lowering in the THZD arm was associated with a significantly reduced rate in 1 or more cardiovascular disease (CVD) outcomes. Other inhibitors of the renin-angiotensin system (eg, angiotensin-receptor blockers [ARBs], direct renin inhibitors, and beta-blockers) are similarly less effective in lowering BP in African Americans.3 In contrast, when the calcium channel blocker (CCB) amlodipine was compared with CTD in blacks or when CTD was compared with lisinopril or doxazosin in nonblacks, SBP reductions were only ~1 mm Hg.8,10
As a class, diuretics have been shown to decrease hypertension-related morbidity and mortality in both African Americans and whites.10-15 In fact, much of the evidence for the benefits of antihypertensive therapy in preventing hypertension-related morbidity and mortality was conducted with THZDs, with several of the relevant trials containing significant numbers of African American participants (TABLE).8,10,13-16
TABLE
Outcomes of major clinical trials of diuretics in African Americans
| Clinical trial | Relative risk reduction (RRR) or hazard ratio (HR) by endpoint | |||||
|---|---|---|---|---|---|---|
| Mortality | CVD | CHD | Stroke | HF | ESRD | |
| VA Cooperative: HCTZ + RES + HYD vs placebo (RRR)13 | 0.46 | |||||
| HDFP: stepped therapy with CTD vs usual care (HR)14 | 0.76a | |||||
| SHEP: CTD + atenolol vs placebo (HR)15 | 0.68a | |||||
| ALLHAT: All African Americans (RRR)8,10 | ||||||
| AML vs CTD | 0.97 | 1.06 | 1.03 | 0.93 | 1.46a | 1.15 |
| DOX vs CTD | N/A | 1.28a | 1.11 | 1.38a | 1.84a | 0.99 |
| LIS vs CTD | 1.06 | 1.19a | 1.15a | 1.40a | 1.30a | 1.29 |
| ALLHAT: African Americans with diabetes and metabolic syndrome (RRR)16 | ||||||
| AML vs CTD | 1.02 | 1.14a | 1.09 | 1.01 | 1.50 | 1.50 |
| DOX vs CTD | 1.18 | 1.37a | 1.15 | 1.49a | 1.88a | 1.17 |
| LIS vs CTD | 0.96 | 1.24a | 1.19a | 1.37a | 1.49a | 1.70a |
| ALLHAT, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial; AML, amlodipine; CHD, coronary heart disease; CTD, chlorthalidone; CVD, cardiovascular disease; DOX, doxazosin; ESRD, end-stage renal disease; HCTZ, hydrochlorothiazide; HDFP, Hypertension Detection and Follow-up Program; HF, heart failure; HYD, hydralazine; LIS, lisinopril; RES, reserpine; SHEP, Systolic Hypertension in the Elderly Program; VA, Veterans Administration aP ≤0.05 | ||||||
In the Veterans Administration (VA) Cooperative Trial, African American men comprised 42% of participants, all of whom were randomized to a combination of hydrochlorothiazide, reserpine, and hydralazine, or to placebo.13 In the Hypertension Detection and Follow-Up Program (HDFP) trial, 44% of participants were African American. All participants were randomized to stepped therapy with CTD, reserpine, methyldopa, and hydralazine, or to usual community care.14 Both of these pioneering trials documented the benefit of a THZD-based regimen in lowering BP and improving clinical outcomes in African Americans with hypertension. The Systolic Hypertension in the Elderly Program (SHEP) trial, in which 14% of participants were African American, extended earlier results from the VA Cooperative and HDFP trials by demonstrating that, compared with placebo, active treatment with CTD and the beta-blocker atenolol produced clinical outcome reductions in African Americans and whites with isolated systolic hypertension as well as in those with elevated diastolic BP.15
In comparative trials with newer classes of antihypertensives, THZDs have remained unsurpassed in preventing complications of hypertension, including in African Americans (TABLE). ALLHAT was the first outcome study to evaluate the relative benefit of antihypertensive treatment initiated with newer classes of antihypertensive agents vs treatment initiated with a THZD in blacks. ALLHAT included more than 15,000 African Americans and Afro-Caribbeans and confirmed the findings of studies in other populations that neither an ACEI, a CCB, or alpha-blocker–initiated therapy surpassed therapy initiated with a THZD (CTD) in lowering BP or in preventing CVD or renal outcomes.8,10 Overall, the THZD-based therapy was superior to the alpha-blocker, ACEI, and CCB-based therapies in preventing 1 or more major forms of CVD, including stroke and heart failure (HF). In blacks, THZD-based therapy was superior to alpha-blocker–based therapy in lowering BP and in preventing overall CVD (especially HF and stroke), and was superior to the ACEI-based regimen in preventing stroke, HF, and overall CVD (a composite of CHD, stroke, and HF endpoints). Compared with CCB-based therapy (ie, amlodipine), THZD (CTD)-based therapy was similar in overall CVD protection but superior in preventing HF.
These results in ALLHAT were even more impressive in blacks with diabetes or the metabolic syndrome (TABLE).16 In addition to the above-mentioned CVD outcomes in black hypertensive patients, neither the CCB-based nor the ACEI-based regimens were superior to the THZD-based regimen in preventing ESRD overall or when stratified by diabetes or baseline estimated glomerular filtration rate.10,16,17 In black ALLHAT participants with diabetes or the metabolic syndrome, CTD was associated with substantially reduced rates of ESRD compared with those randomized to doxazosin, amlodipine, or the ACEI lisinopril.16 It should also be noted that nearly all previous renal outcome trials with renin-angiotensin system inhibitors included background therapy with a diuretic.17
Recommendations
Most national and international guidelines recommend THZDs as first-line therapy in African Americans.18-21 Calcium channel blockers are a reasonable alternate first-line choice in African Americans who are unable to tolerate a diuretic.
In addition, the Joint National Committee (JNC-7) guidelines recommend the use of ACEIs and ARBs as first-line therapy in all patients with hypertension comorbid with chronic kidney disease (CKD) or HF, including African Americans.18 These drugs, along with alpha-blockers and all other agents in the antihypertensive armamentarium, should be used as add-on therapy, as needed, to achieve BP goals in African Americans already receiving a THZD or CCB.
Importantly, multiple drug therapy should be considered for initial treatment in all individuals whose BP is more than 20/10 mm Hg above target.18 In addition, multiple antihypertensive agents are usually required to achieve long-term control in most patients, particularly in African Americans who, as noted earlier, tend to have more-severe hypertension.19
Conclusion
Treatment of hypertension in African Americans should include both lifestyle modifications and pharmacologic intervention, usually with multiple agents. In the absence of compelling indications for alternative therapies, THZD-based regimens should be considered first-line treatment given significant evidence from large randomized studies that document their ability to reduce both BP and hypertensive complications in this population.
Monotherapy with ACEIs, ARBs, direct renin inhibitors, or beta-blockers is less effective in lowering BP in African Americans than in other populations. ACEIs and ARBs should be included in antihypertensive regimens prescribed for African Americans with concomitant CKD or HF. They can also be considered as add-on therapy to regimens containing a THZD or CCB in the absence of these conditions.
1. Roger VL, Go AS, Lloyd-Jones DM, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2-e220.
2. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043-2050.
3. Johnson EF, Wright JT. Management of hypertension in black populations. In: Oparil S, Weber MA, eds. Hypertension: A Companion to Brenner and Rector’s The Kidney. 2nd ed. Philadelphia, PA: Elsevier Saunders; 2005:587–595.
4. National Center for Health Statistics. Health, United States, 2009: With Special Feature on Medical Technology. Hyattsville, MD. 2010. Table 72.
5. Prather AA, Blumenthal JA, Hinderliter AL, Sherwood A. Ethnic differences in the effects of the DASH diet on nocturnal blood pressure dipping in individuals with high blood pressure. Am J Hypertens. 2011;24(12):1338-1344.
6. Svetkey LP, Simons-Morton D, Vollmer WM, et al. Effects of dietary patterns on blood pressure: subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159(3):285-293.
7. Appel LJ, Moore TJ, Obarzanek E, et al. DASH Collaborative Research Group. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336(16):1117-1124.
8. Wright JT, Jr, Dunn JK, Cutler JA, et al. ALLHAT Collaborative Research Group. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA. 2005;293(13):1595-1608.
9. Materson BJ, Reda DJ, Cushman WC, et al. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. N Engl J Med. 1993;328(13):914-921.
10. Wright JT, Jr, Probstfield JL, Cushman WC, et al. ALLHAT findings revisited in the context of subsequent analyses, other trials, and meta-analyses. Arch Intern Med. 2009;169(9):832-842.
11. Neal B, MacMahon S, Chapman N. Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Lancet. 2000;356(9246):1955-1964.
12. Turnbull F. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-1535.
13. Effects of treatment on morbidity in hypertension. II. Results in patients with diastolic blood pressure averaging 90 through 114 mm Hg. JAMA. 1970;213(7):1143-1152.
14. Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the Hypertension Detection and Follow-up Program: mortality by race-sex and blood pressure level. A further analysis. J Community Health. 1984;9(4):314-327.
15. The Systolic Hypertension in the Elderly Program Cooperative Research Group. Implications of the systolic hypertension in the elderly program. Hypertension. 1993;21(3):335-343.
16. Wright JT, Jr, Harris-Haywood S, Pressel S, et al. Clinical outcomes by race in hypertensive patients with and without the metabolic syndrome: Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2008;168(2):207-217.
17. Rahman M, Pressel S, Davis BR, et al. Renal outcomes in high-risk hypertensive patients treated with an angiotensin-converting enzyme inhibitor or a calcium channel blocker vs a diuretic: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2005;165(8):936-946.
18. Chobanian AV, Bakris GL, Black HR, et al. Joint National Committee on Prevention Detection Evaluation and Treatment of High Blood Pressure; National Heart, Lung, and Blood Insitute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-1252.
19. Flack JM, Sica DA, Bakris G, et al. International Society on Hypertension in Blacks. Management of high blood pressure in blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension. 2010;56(5):780-800.
20. Mancia G, Laurent S, Agabiti-Rosei E, et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. Blood Press. 2009;18(6):308-347.
21. Canadian Hypertension Education Program. The 2012 CHEP Recommendations. Hypertension Canada Web site. http://www.hypertension.ca/chep-recommendations. Published 2012. Accessed April 15, 2012.
1. Roger VL, Go AS, Lloyd-Jones DM, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2-e220.
2. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043-2050.
3. Johnson EF, Wright JT. Management of hypertension in black populations. In: Oparil S, Weber MA, eds. Hypertension: A Companion to Brenner and Rector’s The Kidney. 2nd ed. Philadelphia, PA: Elsevier Saunders; 2005:587–595.
4. National Center for Health Statistics. Health, United States, 2009: With Special Feature on Medical Technology. Hyattsville, MD. 2010. Table 72.
5. Prather AA, Blumenthal JA, Hinderliter AL, Sherwood A. Ethnic differences in the effects of the DASH diet on nocturnal blood pressure dipping in individuals with high blood pressure. Am J Hypertens. 2011;24(12):1338-1344.
6. Svetkey LP, Simons-Morton D, Vollmer WM, et al. Effects of dietary patterns on blood pressure: subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159(3):285-293.
7. Appel LJ, Moore TJ, Obarzanek E, et al. DASH Collaborative Research Group. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336(16):1117-1124.
8. Wright JT, Jr, Dunn JK, Cutler JA, et al. ALLHAT Collaborative Research Group. Outcomes in hypertensive black and nonblack patients treated with chlorthalidone, amlodipine, and lisinopril. JAMA. 2005;293(13):1595-1608.
9. Materson BJ, Reda DJ, Cushman WC, et al. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. N Engl J Med. 1993;328(13):914-921.
10. Wright JT, Jr, Probstfield JL, Cushman WC, et al. ALLHAT findings revisited in the context of subsequent analyses, other trials, and meta-analyses. Arch Intern Med. 2009;169(9):832-842.
11. Neal B, MacMahon S, Chapman N. Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Lancet. 2000;356(9246):1955-1964.
12. Turnbull F. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-1535.
13. Effects of treatment on morbidity in hypertension. II. Results in patients with diastolic blood pressure averaging 90 through 114 mm Hg. JAMA. 1970;213(7):1143-1152.
14. Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the Hypertension Detection and Follow-up Program: mortality by race-sex and blood pressure level. A further analysis. J Community Health. 1984;9(4):314-327.
15. The Systolic Hypertension in the Elderly Program Cooperative Research Group. Implications of the systolic hypertension in the elderly program. Hypertension. 1993;21(3):335-343.
16. Wright JT, Jr, Harris-Haywood S, Pressel S, et al. Clinical outcomes by race in hypertensive patients with and without the metabolic syndrome: Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2008;168(2):207-217.
17. Rahman M, Pressel S, Davis BR, et al. Renal outcomes in high-risk hypertensive patients treated with an angiotensin-converting enzyme inhibitor or a calcium channel blocker vs a diuretic: a report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Arch Intern Med. 2005;165(8):936-946.
18. Chobanian AV, Bakris GL, Black HR, et al. Joint National Committee on Prevention Detection Evaluation and Treatment of High Blood Pressure; National Heart, Lung, and Blood Insitute; National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-1252.
19. Flack JM, Sica DA, Bakris G, et al. International Society on Hypertension in Blacks. Management of high blood pressure in blacks: an update of the International Society on Hypertension in Blacks consensus statement. Hypertension. 2010;56(5):780-800.
20. Mancia G, Laurent S, Agabiti-Rosei E, et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. Blood Press. 2009;18(6):308-347.
21. Canadian Hypertension Education Program. The 2012 CHEP Recommendations. Hypertension Canada Web site. http://www.hypertension.ca/chep-recommendations. Published 2012. Accessed April 15, 2012.
MODULE 2: Rethinking the Role of Thiazide-Type Diuretics in the Management of Hypertension: Which Diuretic Is Best?
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 2: Rethinking the Role of Thiazide-Type Diuretics in the Management of Hypertension: Which Diuretic Is Best?
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
Dr Cushman is a paid consultant to Daiichi-Sankyo, Inc; Merck & Co, Inc; Omron Healthcare, Inc; and Takeda Pharmaceuticals International, Inc. He has performed contracted research for Merck & Co, Inc.
Background
Despite the availability of 7 major classes of effective and safe antihypertensive medications and numerous combination drugs designed to reduce pill burden and improve adherence, just 50.1% of the estimated 76.4 million US adults with hypertension (33.5% of the population) have their condition under control.1
One of the greatest challenges for clinicians who manage patients with hypertension is choosing the most appropriate drug, whether as initial treatment or add-on therapy. Clinicians may be guided in this decision, however, by guidelines and algorithms that are provided for hypertension management. These algorithms are reviewed in the first article in this supplement by Dr William B. White.
National guidelines recommend thiazide-type diuretics as initial therapy for most patients with hypertension, regardless of the severity of the condition, either alone or in combination with 1 of the other classes of hypertension medications that have also been shown to reduce 1 or more hypertensive complications in randomized controlled outcome trials.2,3 These recommendations are based primarily on more than 50 years of data on the safety and efficacy of thiazide-type diuretics.
The first evidence of the benefits of thiazide-type diuretics came from publications of the VA (Veterans Administration) Cooperative Study in 1967 and 1970. It was the first trial to demonstrate reduced stroke, heart failure (HF), and progressive kidney damage in patients receiving antihypertensive treatment, including the then-newly released hydrochlorothiazide (HCTZ), a thiazide diuretic.4
Since then, hundreds of clinical trials have demonstrated the efficacy of thiazide-type diuretics. During that time, however, numerous other classes of antihypertensive medications were introduced, leading to the question of the appropriate place of thiazides within the antihypertensive arsenal. The seminal trial to answer this question was the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). This randomized, double-blind, multicenter, clinical trial was designed to determine whether the occurrence of fatal coronary heart disease (CHD) or nonfatal myocardial infarction (MI) was lower for high-risk hypertensive patients 55 years of age and older who were treated with the calcium channel blocker amlodipine, the angiotensin-converting enzyme inhibitor (ACEI) lisinopril, or the alpha-blocker doxazosin compared with the thiazide-type diuretic chlorthalidone (CTD).5 Investigators could add atenolol, clonidine, reserpine, and/or hydralazine as necessary to achieve blood pressure (BP) goal. The trial randomized 42,418 patients, 90% of whom had been previously treated.
At a mean follow-up of 4.9 years, there was no significant difference in the primary outcome or mortality between the 4 drugs.5 There was a 38% higher rate of HF with amlodipine, and a 10%, 15%, and 19% higher rate of cardiovascular disease (CVD), stroke, and HF, respectively, with lisinopril compared with CTD. For stroke, there was a statistically significant race-by-treatment interaction (40% higher stroke rate with lisinopril vs CTD in black participants). Participants in the doxazosin treatment group (n = 9061) were followed for a mean of 3.2 years. This arm was terminated early because of a 25% higher incidence of CVD events, including a nearly 2-fold higher risk of HF, accompanied by a low probability of reaching a statistically significant difference in the primary endpoint.5
Additional rationale for the use of diuretics in elderly populations came from the Systolic Hypertension in the Elderly Program (SHEP), a multicenter, randomized, double- blind, placebo-controlled trial of patients aged 60 years and older.6 Participants were randomized to either CTD 12.5 to 25 mg once daily±atenolol 25 to 50 mg once daily, or reserpine 0.05 mg once daily, or placebo. Treatment reduced the incidence of all fatal and nonfatal strokes by 36%, MI by 27%, all CHD by 27%, and all CVD by 32%.6
Underuse of diuretics
Despite trials such as SHEP and ALLHAT, and despite the long record of safety and efficacy in numerous patient populations, thiazide-type diuretics remain significantly under-used in clinical practice.7-10
Even intensive academic detailing designed to increase the use of thiazide-type diuretics found that the prescribing rates of 37.1% immediately before the intervention only increased to 39.6% overall after the intervention (46.5% in areas that received the most intensive intervention), reflecting what appears to be clinical resistance to this class of drugs (FIGURE 1).11 Even 4 years after the ALLHAT results were published, national use of thiazide-type drugs had not increased significantly.12
FIGURE 1
Proportion of visits by drug class among patients with drug-treated hypertension11
Data are from the IMS Health National Disease and Therapeutic Index, 2000 through 2008. “Other classes” indicates α-adrenergic receptor blockers, potassium-sparing diuretics, loop diuretics, and centrally acting agents.
Source: Archives of Internal Medicine by American Medical Association. Reproduced with permission of American Medical Association, in the format Journal via Copyright Clearance Center.
Hydrochlorothiazide and chlorthalidone: Similarities and differences
Underuse of thiazide-type diuretics is just 1 challenge. Others include which diuretic to use (HCTZ or CTD) and at what dosage.13-17 These 2 diuretics were approved at about the same time and, until recently, were considered equivalent and interchangeable despite differences in structure, pharmacokinetics, and pharmacodynamics.16,17
The publication of the VA Cooperative Morbidity Trial, the successful marketing and popularity of HCTZ and low-dose HCTZ/triamterene, the fear of hypokalemia (which was seen more often in the high doses of CTD initially used), and the subsequent inclusion of HCTZ as the primary diuretic in single-pill combination antihypertensives with ACEIs and angiotensin II receptor blockers (ARBs) led to HCTZ becoming the market leader for this class. Nonetheless, CTD was the diuretic chosen for many major randomized clinical trials, especially those sponsored by the National Heart, Lung, and Blood Institute (NHLBI).5,6,18-20
One reason for CTD’s relegation as a second-tier option to HCTZ could be the higher risk of hypokalemia observed at the higher dosages typically used in early studies.21-23 However, later studies found that substantially lower dosages of CTD could provide similar BP reductions with a significantly lower risk of hypokalemia.24 Materson et al,25 for instance, demonstrated that the 25-mg dosage of CTD was at least as effective for hypertension as the 50-mg and 75-mg dosages, while the 25-mg dosage was associated with less hypokalemia.
Increasingly, however, hypertension specialists, particularly those involved in research, have come to appreciate that CTD and HCTZ are, indeed, not interchangeable and do not have dosing equivalency. This understanding, together with the results of clinical trials like ALLHAT, has led to a resurgence of interest in the use of CTD.17,19,26
One assessment of outpatient prescription data from the VA from 2003 to 2008 found that although the proportion of patients receiving HCTZ during the period remained stable, the number of new users dropped 30% even as the proportion of thiazide users receiving CTD prescriptions doubled from 1.1% to 2.4% and the number of new prescriptions for CTD increased 40%.19
Chlorthalidone or hydrochlorothiazide: Study outcomes
The resurgence of interest in CTD has come with the publication of trials demonstrating its benefits in reducing CVD risk.5,6,27,28
The Multiple Risk Factor Intervention Trial (MRFIT) is the only large, long-term, randomized trial to directly compare HCTZ and CTD, although not in a randomized assignment. The primary endpoint was cardiovascular (CV) outcomes. The study launched in 1973 and enrolled 12,866 males aged 35 to 57 years who were in the upper 15% risk of death from chronic heart disease.29 Participants in the special care group were given HCTZ or CTD (investigator’s choice) at either 50 or 100 mg daily, depending on weight and sodium levels, and were given additional drugs as needed. The control group received usual care at that time from their health care provider. A 44% higher rate of CHD mortality in the HCTZ group observed towards the latter part of the trial led its Policy Advisory Board to change the option between the 2 diuretics and require CTD only. Following the change, the rate of CHD mortality decreased by 28% (P = .04 for comparison between the 2 time frames).29
A recent retrospective analysis of MRFIT found significantly lower CV event rates in participants who received either CTD or HCTZ than in those receiving neither (CTD: adjusted hazard ratio [aHR], 0.51; 95% confidence interval [CI], 0.43-0.61; P < .0001; HCTZ: aHR, 0.65; 95% CI, 0.55- 0.75; P < .0001), but rates of nonfatal CV events were significantly lower in participants who received CTD than those who received HCTZ (aHR, 0.79; 95% CI, 0.68-0.92; P < .0016).30 The results are depicted in FIGURE 2.30
FIGURE 2
Adjusted event-free probability of cardiovascular events30
CI, confidence interval; CTD, chlorthalidone; HCTZ, hydrochlorothiazide; HR, hazard ratio.
Source: Hypertension by American Heart Association; Council for High Blood Pressure Research (American Heart Association); InterAmerican Society of Hypertension. Reproduced with permission of Lippincott Williams & Wilkins in the format Journal via Copyright Clearance Center.A recent meta-analysis of 108 trials with HCTZ and 29 with CTD found that the 2 drugs did not provide equivalent reductions in systolic BP (SBP) within equivalent dosages. The study found that the median change in SBP with the median dose of HCTZ was –17 mm Hg, compared with -26 mm Hg for CTD. The slightly greater potassium loss observed with CTD was still nearly equivalent to that observed with HCTZ.31
Considerations for greater chlorthalidone efficacy
The differences between CTD and HCTZ, despite similar molecular structures, is a topic of much discussion.23 It is likely that these 2 drugs have different pharmacokinetic and pharmacodynamic properties, as shown in TABLE 1.17
TABLE 1
Pharmacokinetic/pharmacodynamic comparison of hydrochlorothiazide and chlorthalidone17
| Onset (h) | Peak (h) | Half-life (h) | Duration (h) | |
|---|---|---|---|---|
Hydrochlorothiazide | 2 | 4-6 | 6-9 (single dose) 8-15 (long-term dosing) | 12 (single dose) 16-24 (long-term dosing) |
Chlorthalidone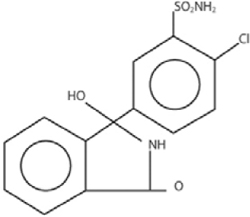 | 2-3 | 2-6 | 40 (single dose) 45-60 (long-term dosing) | 24-48 (single dose) 48-72 (long-term dosing) |
| Source: Hypertension by American Heart Association; Council for High Blood Pressure Research (American Heart Association); InterAmerican Society of Hypertension. Reproduced with permission of Lippincott Williams & Wilkins in the format Journal via Copyright Clearance Center | ||||
There is also evidence from an in vitro study that, compared with HCTZ, CTD has additional pleiotropic effects: reducing carbonic anhydrase activity, platelet aggregation, and vascular permeability while promoting angiogenesis.32
Another reason for the differences in efficacy between CTD and HCTZ could be the dosages of HCTZ used. Worldwide, nearly all prescriptions for HCTZ are for 12.5 to 25 mg/d, while most modern combination pills containing HCTZ incorporate these lower dosages.33 However, there is little evidence that such dosages lead to significantly improved outcomes.14,19,34-36
This was an issue in the Avoiding Cardiovascular Events Through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) trial. This study was designed to compare first-step therapy with benazepril/HCTZ 20/12.5 mg.37 Benazepril was force-titrated to 40 mg in each arm, whereas HCTZ and amlodipine were titrated to 25 mg and 10 mg, respectively, only if needed for BP control. The study was conducted in 11,506 high-risk patients 55 years of age and older. Other antihypertensive drugs could be added as needed for BP control. The study was stopped early after a mean follow-up of 36 months when the benazepril/amlodi-pine group demonstrated an HR of 0.8 (95% CI, 0.72-0.90) for the composite outcome of death from CV events, nonfatal MI or stroke, hospitalization for angina, resuscitation after sudden cardiac arrest, and coronary revascularization compared with the benazepril/HCTZ group.37
The ACCOMPLISH trial has been controversial for many reasons, with editorials suggesting that its design led to a “stacked deck” that favored amlodipine/benazepril over benazepril/HCTZ. Questions were raised as to why HCTZ was the diuretic of choice because CTD has been used in most thiazide-type trials. The dosages chosen were also questioned because outcome trials demonstrating reduced CV events with HCTZ used target doses of 50 mg/d or higher.14,21,22,38
Indeed, a meta-analysis published in 2011 found that despite the extensive use of HCTZ worldwide, the 12.5 to 25 mg dosage was inferior in reducing BP compared with standard doses of other antihypertensive agents (ACEIs, ARBs, beta blockers, and calcium channel blockers) in studies using 24-hour ambulatory BP monitoring.33 The efficacy of HCTZ closely mirrors that of the other drug classes at the 50-mg level, although that dose results in somewhat higher rates of hypokalemia. As the dose of HCTZ is increased to 100 mg, there is little or no further increase in antihypertensive efficacy, but hypokalemia becomes much more common.39
Thus, it can be clinically challenging to prescribe the optimum BP medication if practitioners prefer to use single-pill combinations that include HCTZ. Although the use of such single-pill combinations is warranted, particularly given the improved adherence with taking single-pill combinations compared with taking 2 or 3 pills, as noted in TABLE 1, most combinations include HCTZ dosages of 12.5 to 25 mg, which will often be less effective than full doses of 2 other medications.
Conclusion
Although thiazide-type diuretics are recommended as first-line therapy for most patients with hypertension, either alone or in combination with other classes of antihypertensives, they remain underused in clinical practice. In addition, HCTZ, which is the most commonly used diuretic (indeed, the most commonly prescribed antihypertensive) is prescribed at dosages too low to provide sufficient clinical efficacy in BP reduction and lower than what was proven to reduce CV events in clinical trials.
Chlorthalidone, a diuretic often considered a thiazide-type diuretic, has demonstrated superiority to HCTZ in reducing BP as evidenced in the MRFIT study and has been shown in numerous clinical trials to provide similar if not greater efficacy than other classes of antihypertensives in reducing BP, stroke, and CV events, with a good safety profile.
Clinicians need to manage patients with hypertension on an individual basis, selecting drugs and antihypertensive medication classes with the best outcomes in trials and then determining the most efficacious therapies with the lowest risk of adverse events for each patient. However, when prescribing a diuretic, they should also ensure that the drug used is prescribed at the appropriate therapeutic dosage level to enable patients to prevent the CV, thrombotic, and renal events that occur with long-term hypertension.
1. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043-2050.
2. Chobanian AV, Bakris GL, Black HR, et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-1252.
3. Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011;57(20):2037-2114.
4. Effects of treatment on morbidity in hypertension. II. Results in patients with diastolic blood pressure averaging 90 through 114 mm Hg. JAMA. 1970;213(7):1143-1152.
5. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) [published corrections appear in JAMA. 2003;289(2):178; JAMA. 2004;291(18):2196]. JAMA. 2002;288(23):2981-2997.
6. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265(24):3255-3264.
7. Petitti DB, Xie F, Barzilay JI. Prescribing patterns for thiazide diuretics in a large health maintenance organization: relationship to participation as an ALLHAT clinical center. Contemporary Clin Trials. 2006;27(5):397-403.
8. Dahlöf B, Devereux RB, Kjeldsen SE, et al. LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995-1003.
9. Psaty BM, Manolio TA, Smith NL, et al. Cardiovascular Health Study. Time trends in high blood pressure control and the use of antihypertensive medications in older adults: the Cardiovascular Health Study. Arch Intern Med. 2002;162(20):2325-2332.
10. Glasser SP, Basile JN, Lackland DT. Does prehypertension represent an increased risk for incident hypertension and adverse cardiovascular outcome? Hypertension. 2009;54(5):954-955.
11. Stafford RS, Bartholomew LK, Cushman WC, et al. ALLHAT Collaborative Research Group. Impact of the ALLHAT/JNC7 Dissemination Project on thiazide-type diuretic use. Arch Intern Med. 2010;170(10):851-858.
12. Furmaga EM, Cunningham FE, Cushman WC, et al. National utilization of antihypertensive medications from 2000 to 2006 in the Veterans Health Administration: focus on thiazide diuretics. J Clin Hypertens (Greenwich). 2008;10(10):770-778.
13. Pitt B. The role of chlorthalidone in patients with high-risk hypertension. J Clin Hypertens (Greenwich). 2009;11(9):460-461.
14. Ernst ME, Carter BL, Basile JN. All thiazide-like diuretics are not chlorthalidone: putting the ACCOMPLISH study into perspective. J Clin Hypertens (Greenwich). 2009;11(1):5-10.
15. Sica DA. Chlorthalidone—a renaissance in use? Expert Opin Pharmacother. 2009;10(13):2037-2039.
16. Kaplan NM. Chlorthalidone versus hydrochlorothiazide: a tale of tortoises and a hare. Hypertension. 2011;58(6):994-995.
17. Carter BL, Ernst ME, Cohen JD. Hydrochlorothiazide versus chlorthalidone: evidence supporting their interchangeability. Hypertension. 2004;43(1):4-9.
18. Carter BL, Malone DC, Ellis SL, Dombrowski RC. Antihypertensive drug utilization in hypertensive veterans with complex medication profiles. J Clin Hypertens (Greenwich). 2000;2(3):172-180.
19. Ernst ME, Lund BC. Renewed interest in chlorthalidone: evidence from the Veterans Health Administration. J Clin Hypertens (Greenwich). 2010;12(12):927-934.
20. Neaton JD, Grimm RH Jr, Prineas RJ, et al. Treatment of Mild Hypertension Study Research Group. Treatment of Mild Hypertension Study. Final results. JAMA. 1993;270(6):713-724.
21. Ford RV. Therapy of edema and hypertension, Comparative clinical effects of chlorothiazide and chlorthalidone. Tex State J Med. 1960;56:343-346.
22. Mach RS, Veyrat R. Clinical experiences with some of the newer diuretics, especially chlorthalidone. Ann N Y Acad Sci. 1960;88:841-863.
23. Dyrda I, Dufault C, Herbert JG, Tremblay G, Genest J. Studies on a new diuretic: chlorthalidone. Can Med Assoc J. 1962;86:475-482.
24. Kakaviatos N, Finnerty FA, Jr. Comparison of chlorthalidone, a long-acting antihypertensive and diuretic agent, with chlorothiazide. Analysis of one hundred twenty-three cases. Am J Cardiol. 1962;10:570-574.
25. Materson BJ, Oster JR, Michael UF, et al. Dose response to chlorthalidone in patients with mild hypertension. Efficacy of a lower dose. Clin Pharmacol Ther. 1978;24(2):192-198.
26. Ernst ME, Carter BL, Goerdt CJ, et al. Comparative antihypertensive effects of hydrochlorothiazide and chlorthalidone on ambulatory and office blood pressure. Hypertension. 2006;47(3):352-358.
27. Dunbar-Jacob J, Erlen JA, Schlenk EA, Ryan CM, Sereika SM, Doswell WM. Adherence in chronic disease. Annu Rev Nurs Res. 2000;18:48-90.
28. Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA. 1979;242(23):2562-2571.
29. Multiple Risk Factor Intervention Trial Research Group. Multiple risk factor intervention trial. Risk factor changes and mortality results. JAMA. 1982;248(12):1465-1477.
30. Dorsch MP, Gillespie BW, Erickson SR, Bleske BE, Weder AB. Chlorthalidone reduces cardiovascular events compared with hydrochlorothiazide: a retrospective cohort analysis. Hypertension. 2011;57(4):689-694.
31. Ernst ME, Carter BL, Zheng S, Grimm RH, Jr. Meta-analysis of dose-response characteristics of hydrochlorothiazide and chlorthalidone: effects on systolic blood pressure and potassium. Am J Hypertens. 2010;23(4):440-446.
32. Woodman R, Brown C, Lockette W. Chlorthalidone decreases platelet aggregation and vascular permeability and promotes angiogenesis. Hypertension. 2010;56(3):463-470.
33. Messerli FH, Makani H, Benjo A, Romero J, Alviar C, Bangalore S. Antihypertensive efficacy of hydrochlorothiazide as evaluated by ambulatory blood pressure monitoring: a meta-analysis of randomized trials. J Am Coll Cardiol. 2011;57(5):590-600.
34. Demirovic J, Prineas R, Rudolph M. Epidemiology of congestive heart failure in three ethnic groups. Congest Heart Fail. 2001;7(2):93-96.
35. Eide IK, Torjesen PA, Drolsum A, Babovic A, Lilledahl NP. Low-renin status in therapy-resistant hypertension: a clue to efficient treatment. J Hypertens. 2004;22(11):2217-2226.
36. Epstein M. Re-examining RAS-blocking treatment regimens for abrogating progression of chronic kidney disease. Nat Clin Pract Nephrol. 2008;5(1):12-13.
37. Jamerson K, Weber MA, Bakris GL, et al. ACCOMPLISH Trial Investigators. Ben-azepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359(23):2417-2428.
38. Parra D, Rosenstein R. Benazepril plus amlodipine or hydrochlorothiazide for hypertension. N Engl J Med. 2009;360(11):1147-1150.
39. Messerli FH, Bangalore S, Julius S. Risk/benefit assessment of beta-blockers and diuretics precludes their use for first-line therapy in hypertension. Circulation. 2008;117(20):2706-2715.
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 2: Rethinking the Role of Thiazide-Type Diuretics in the Management of Hypertension: Which Diuretic Is Best?
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
Dr Cushman is a paid consultant to Daiichi-Sankyo, Inc; Merck & Co, Inc; Omron Healthcare, Inc; and Takeda Pharmaceuticals International, Inc. He has performed contracted research for Merck & Co, Inc.
Background
Despite the availability of 7 major classes of effective and safe antihypertensive medications and numerous combination drugs designed to reduce pill burden and improve adherence, just 50.1% of the estimated 76.4 million US adults with hypertension (33.5% of the population) have their condition under control.1
One of the greatest challenges for clinicians who manage patients with hypertension is choosing the most appropriate drug, whether as initial treatment or add-on therapy. Clinicians may be guided in this decision, however, by guidelines and algorithms that are provided for hypertension management. These algorithms are reviewed in the first article in this supplement by Dr William B. White.
National guidelines recommend thiazide-type diuretics as initial therapy for most patients with hypertension, regardless of the severity of the condition, either alone or in combination with 1 of the other classes of hypertension medications that have also been shown to reduce 1 or more hypertensive complications in randomized controlled outcome trials.2,3 These recommendations are based primarily on more than 50 years of data on the safety and efficacy of thiazide-type diuretics.
The first evidence of the benefits of thiazide-type diuretics came from publications of the VA (Veterans Administration) Cooperative Study in 1967 and 1970. It was the first trial to demonstrate reduced stroke, heart failure (HF), and progressive kidney damage in patients receiving antihypertensive treatment, including the then-newly released hydrochlorothiazide (HCTZ), a thiazide diuretic.4
Since then, hundreds of clinical trials have demonstrated the efficacy of thiazide-type diuretics. During that time, however, numerous other classes of antihypertensive medications were introduced, leading to the question of the appropriate place of thiazides within the antihypertensive arsenal. The seminal trial to answer this question was the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). This randomized, double-blind, multicenter, clinical trial was designed to determine whether the occurrence of fatal coronary heart disease (CHD) or nonfatal myocardial infarction (MI) was lower for high-risk hypertensive patients 55 years of age and older who were treated with the calcium channel blocker amlodipine, the angiotensin-converting enzyme inhibitor (ACEI) lisinopril, or the alpha-blocker doxazosin compared with the thiazide-type diuretic chlorthalidone (CTD).5 Investigators could add atenolol, clonidine, reserpine, and/or hydralazine as necessary to achieve blood pressure (BP) goal. The trial randomized 42,418 patients, 90% of whom had been previously treated.
At a mean follow-up of 4.9 years, there was no significant difference in the primary outcome or mortality between the 4 drugs.5 There was a 38% higher rate of HF with amlodipine, and a 10%, 15%, and 19% higher rate of cardiovascular disease (CVD), stroke, and HF, respectively, with lisinopril compared with CTD. For stroke, there was a statistically significant race-by-treatment interaction (40% higher stroke rate with lisinopril vs CTD in black participants). Participants in the doxazosin treatment group (n = 9061) were followed for a mean of 3.2 years. This arm was terminated early because of a 25% higher incidence of CVD events, including a nearly 2-fold higher risk of HF, accompanied by a low probability of reaching a statistically significant difference in the primary endpoint.5
Additional rationale for the use of diuretics in elderly populations came from the Systolic Hypertension in the Elderly Program (SHEP), a multicenter, randomized, double- blind, placebo-controlled trial of patients aged 60 years and older.6 Participants were randomized to either CTD 12.5 to 25 mg once daily±atenolol 25 to 50 mg once daily, or reserpine 0.05 mg once daily, or placebo. Treatment reduced the incidence of all fatal and nonfatal strokes by 36%, MI by 27%, all CHD by 27%, and all CVD by 32%.6
Underuse of diuretics
Despite trials such as SHEP and ALLHAT, and despite the long record of safety and efficacy in numerous patient populations, thiazide-type diuretics remain significantly under-used in clinical practice.7-10
Even intensive academic detailing designed to increase the use of thiazide-type diuretics found that the prescribing rates of 37.1% immediately before the intervention only increased to 39.6% overall after the intervention (46.5% in areas that received the most intensive intervention), reflecting what appears to be clinical resistance to this class of drugs (FIGURE 1).11 Even 4 years after the ALLHAT results were published, national use of thiazide-type drugs had not increased significantly.12
FIGURE 1
Proportion of visits by drug class among patients with drug-treated hypertension11
Data are from the IMS Health National Disease and Therapeutic Index, 2000 through 2008. “Other classes” indicates α-adrenergic receptor blockers, potassium-sparing diuretics, loop diuretics, and centrally acting agents.
Source: Archives of Internal Medicine by American Medical Association. Reproduced with permission of American Medical Association, in the format Journal via Copyright Clearance Center.
Hydrochlorothiazide and chlorthalidone: Similarities and differences
Underuse of thiazide-type diuretics is just 1 challenge. Others include which diuretic to use (HCTZ or CTD) and at what dosage.13-17 These 2 diuretics were approved at about the same time and, until recently, were considered equivalent and interchangeable despite differences in structure, pharmacokinetics, and pharmacodynamics.16,17
The publication of the VA Cooperative Morbidity Trial, the successful marketing and popularity of HCTZ and low-dose HCTZ/triamterene, the fear of hypokalemia (which was seen more often in the high doses of CTD initially used), and the subsequent inclusion of HCTZ as the primary diuretic in single-pill combination antihypertensives with ACEIs and angiotensin II receptor blockers (ARBs) led to HCTZ becoming the market leader for this class. Nonetheless, CTD was the diuretic chosen for many major randomized clinical trials, especially those sponsored by the National Heart, Lung, and Blood Institute (NHLBI).5,6,18-20
One reason for CTD’s relegation as a second-tier option to HCTZ could be the higher risk of hypokalemia observed at the higher dosages typically used in early studies.21-23 However, later studies found that substantially lower dosages of CTD could provide similar BP reductions with a significantly lower risk of hypokalemia.24 Materson et al,25 for instance, demonstrated that the 25-mg dosage of CTD was at least as effective for hypertension as the 50-mg and 75-mg dosages, while the 25-mg dosage was associated with less hypokalemia.
Increasingly, however, hypertension specialists, particularly those involved in research, have come to appreciate that CTD and HCTZ are, indeed, not interchangeable and do not have dosing equivalency. This understanding, together with the results of clinical trials like ALLHAT, has led to a resurgence of interest in the use of CTD.17,19,26
One assessment of outpatient prescription data from the VA from 2003 to 2008 found that although the proportion of patients receiving HCTZ during the period remained stable, the number of new users dropped 30% even as the proportion of thiazide users receiving CTD prescriptions doubled from 1.1% to 2.4% and the number of new prescriptions for CTD increased 40%.19
Chlorthalidone or hydrochlorothiazide: Study outcomes
The resurgence of interest in CTD has come with the publication of trials demonstrating its benefits in reducing CVD risk.5,6,27,28
The Multiple Risk Factor Intervention Trial (MRFIT) is the only large, long-term, randomized trial to directly compare HCTZ and CTD, although not in a randomized assignment. The primary endpoint was cardiovascular (CV) outcomes. The study launched in 1973 and enrolled 12,866 males aged 35 to 57 years who were in the upper 15% risk of death from chronic heart disease.29 Participants in the special care group were given HCTZ or CTD (investigator’s choice) at either 50 or 100 mg daily, depending on weight and sodium levels, and were given additional drugs as needed. The control group received usual care at that time from their health care provider. A 44% higher rate of CHD mortality in the HCTZ group observed towards the latter part of the trial led its Policy Advisory Board to change the option between the 2 diuretics and require CTD only. Following the change, the rate of CHD mortality decreased by 28% (P = .04 for comparison between the 2 time frames).29
A recent retrospective analysis of MRFIT found significantly lower CV event rates in participants who received either CTD or HCTZ than in those receiving neither (CTD: adjusted hazard ratio [aHR], 0.51; 95% confidence interval [CI], 0.43-0.61; P < .0001; HCTZ: aHR, 0.65; 95% CI, 0.55- 0.75; P < .0001), but rates of nonfatal CV events were significantly lower in participants who received CTD than those who received HCTZ (aHR, 0.79; 95% CI, 0.68-0.92; P < .0016).30 The results are depicted in FIGURE 2.30
FIGURE 2
Adjusted event-free probability of cardiovascular events30
CI, confidence interval; CTD, chlorthalidone; HCTZ, hydrochlorothiazide; HR, hazard ratio.
Source: Hypertension by American Heart Association; Council for High Blood Pressure Research (American Heart Association); InterAmerican Society of Hypertension. Reproduced with permission of Lippincott Williams & Wilkins in the format Journal via Copyright Clearance Center.A recent meta-analysis of 108 trials with HCTZ and 29 with CTD found that the 2 drugs did not provide equivalent reductions in systolic BP (SBP) within equivalent dosages. The study found that the median change in SBP with the median dose of HCTZ was –17 mm Hg, compared with -26 mm Hg for CTD. The slightly greater potassium loss observed with CTD was still nearly equivalent to that observed with HCTZ.31
Considerations for greater chlorthalidone efficacy
The differences between CTD and HCTZ, despite similar molecular structures, is a topic of much discussion.23 It is likely that these 2 drugs have different pharmacokinetic and pharmacodynamic properties, as shown in TABLE 1.17
TABLE 1
Pharmacokinetic/pharmacodynamic comparison of hydrochlorothiazide and chlorthalidone17
| Onset (h) | Peak (h) | Half-life (h) | Duration (h) | |
|---|---|---|---|---|
Hydrochlorothiazide | 2 | 4-6 | 6-9 (single dose) 8-15 (long-term dosing) | 12 (single dose) 16-24 (long-term dosing) |
Chlorthalidone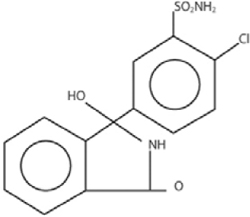 | 2-3 | 2-6 | 40 (single dose) 45-60 (long-term dosing) | 24-48 (single dose) 48-72 (long-term dosing) |
| Source: Hypertension by American Heart Association; Council for High Blood Pressure Research (American Heart Association); InterAmerican Society of Hypertension. Reproduced with permission of Lippincott Williams & Wilkins in the format Journal via Copyright Clearance Center | ||||
There is also evidence from an in vitro study that, compared with HCTZ, CTD has additional pleiotropic effects: reducing carbonic anhydrase activity, platelet aggregation, and vascular permeability while promoting angiogenesis.32
Another reason for the differences in efficacy between CTD and HCTZ could be the dosages of HCTZ used. Worldwide, nearly all prescriptions for HCTZ are for 12.5 to 25 mg/d, while most modern combination pills containing HCTZ incorporate these lower dosages.33 However, there is little evidence that such dosages lead to significantly improved outcomes.14,19,34-36
This was an issue in the Avoiding Cardiovascular Events Through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) trial. This study was designed to compare first-step therapy with benazepril/HCTZ 20/12.5 mg.37 Benazepril was force-titrated to 40 mg in each arm, whereas HCTZ and amlodipine were titrated to 25 mg and 10 mg, respectively, only if needed for BP control. The study was conducted in 11,506 high-risk patients 55 years of age and older. Other antihypertensive drugs could be added as needed for BP control. The study was stopped early after a mean follow-up of 36 months when the benazepril/amlodi-pine group demonstrated an HR of 0.8 (95% CI, 0.72-0.90) for the composite outcome of death from CV events, nonfatal MI or stroke, hospitalization for angina, resuscitation after sudden cardiac arrest, and coronary revascularization compared with the benazepril/HCTZ group.37
The ACCOMPLISH trial has been controversial for many reasons, with editorials suggesting that its design led to a “stacked deck” that favored amlodipine/benazepril over benazepril/HCTZ. Questions were raised as to why HCTZ was the diuretic of choice because CTD has been used in most thiazide-type trials. The dosages chosen were also questioned because outcome trials demonstrating reduced CV events with HCTZ used target doses of 50 mg/d or higher.14,21,22,38
Indeed, a meta-analysis published in 2011 found that despite the extensive use of HCTZ worldwide, the 12.5 to 25 mg dosage was inferior in reducing BP compared with standard doses of other antihypertensive agents (ACEIs, ARBs, beta blockers, and calcium channel blockers) in studies using 24-hour ambulatory BP monitoring.33 The efficacy of HCTZ closely mirrors that of the other drug classes at the 50-mg level, although that dose results in somewhat higher rates of hypokalemia. As the dose of HCTZ is increased to 100 mg, there is little or no further increase in antihypertensive efficacy, but hypokalemia becomes much more common.39
Thus, it can be clinically challenging to prescribe the optimum BP medication if practitioners prefer to use single-pill combinations that include HCTZ. Although the use of such single-pill combinations is warranted, particularly given the improved adherence with taking single-pill combinations compared with taking 2 or 3 pills, as noted in TABLE 1, most combinations include HCTZ dosages of 12.5 to 25 mg, which will often be less effective than full doses of 2 other medications.
Conclusion
Although thiazide-type diuretics are recommended as first-line therapy for most patients with hypertension, either alone or in combination with other classes of antihypertensives, they remain underused in clinical practice. In addition, HCTZ, which is the most commonly used diuretic (indeed, the most commonly prescribed antihypertensive) is prescribed at dosages too low to provide sufficient clinical efficacy in BP reduction and lower than what was proven to reduce CV events in clinical trials.
Chlorthalidone, a diuretic often considered a thiazide-type diuretic, has demonstrated superiority to HCTZ in reducing BP as evidenced in the MRFIT study and has been shown in numerous clinical trials to provide similar if not greater efficacy than other classes of antihypertensives in reducing BP, stroke, and CV events, with a good safety profile.
Clinicians need to manage patients with hypertension on an individual basis, selecting drugs and antihypertensive medication classes with the best outcomes in trials and then determining the most efficacious therapies with the lowest risk of adverse events for each patient. However, when prescribing a diuretic, they should also ensure that the drug used is prescribed at the appropriate therapeutic dosage level to enable patients to prevent the CV, thrombotic, and renal events that occur with long-term hypertension.
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 2: Rethinking the Role of Thiazide-Type Diuretics in the Management of Hypertension: Which Diuretic Is Best?
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
Dr Cushman is a paid consultant to Daiichi-Sankyo, Inc; Merck & Co, Inc; Omron Healthcare, Inc; and Takeda Pharmaceuticals International, Inc. He has performed contracted research for Merck & Co, Inc.
Background
Despite the availability of 7 major classes of effective and safe antihypertensive medications and numerous combination drugs designed to reduce pill burden and improve adherence, just 50.1% of the estimated 76.4 million US adults with hypertension (33.5% of the population) have their condition under control.1
One of the greatest challenges for clinicians who manage patients with hypertension is choosing the most appropriate drug, whether as initial treatment or add-on therapy. Clinicians may be guided in this decision, however, by guidelines and algorithms that are provided for hypertension management. These algorithms are reviewed in the first article in this supplement by Dr William B. White.
National guidelines recommend thiazide-type diuretics as initial therapy for most patients with hypertension, regardless of the severity of the condition, either alone or in combination with 1 of the other classes of hypertension medications that have also been shown to reduce 1 or more hypertensive complications in randomized controlled outcome trials.2,3 These recommendations are based primarily on more than 50 years of data on the safety and efficacy of thiazide-type diuretics.
The first evidence of the benefits of thiazide-type diuretics came from publications of the VA (Veterans Administration) Cooperative Study in 1967 and 1970. It was the first trial to demonstrate reduced stroke, heart failure (HF), and progressive kidney damage in patients receiving antihypertensive treatment, including the then-newly released hydrochlorothiazide (HCTZ), a thiazide diuretic.4
Since then, hundreds of clinical trials have demonstrated the efficacy of thiazide-type diuretics. During that time, however, numerous other classes of antihypertensive medications were introduced, leading to the question of the appropriate place of thiazides within the antihypertensive arsenal. The seminal trial to answer this question was the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). This randomized, double-blind, multicenter, clinical trial was designed to determine whether the occurrence of fatal coronary heart disease (CHD) or nonfatal myocardial infarction (MI) was lower for high-risk hypertensive patients 55 years of age and older who were treated with the calcium channel blocker amlodipine, the angiotensin-converting enzyme inhibitor (ACEI) lisinopril, or the alpha-blocker doxazosin compared with the thiazide-type diuretic chlorthalidone (CTD).5 Investigators could add atenolol, clonidine, reserpine, and/or hydralazine as necessary to achieve blood pressure (BP) goal. The trial randomized 42,418 patients, 90% of whom had been previously treated.
At a mean follow-up of 4.9 years, there was no significant difference in the primary outcome or mortality between the 4 drugs.5 There was a 38% higher rate of HF with amlodipine, and a 10%, 15%, and 19% higher rate of cardiovascular disease (CVD), stroke, and HF, respectively, with lisinopril compared with CTD. For stroke, there was a statistically significant race-by-treatment interaction (40% higher stroke rate with lisinopril vs CTD in black participants). Participants in the doxazosin treatment group (n = 9061) were followed for a mean of 3.2 years. This arm was terminated early because of a 25% higher incidence of CVD events, including a nearly 2-fold higher risk of HF, accompanied by a low probability of reaching a statistically significant difference in the primary endpoint.5
Additional rationale for the use of diuretics in elderly populations came from the Systolic Hypertension in the Elderly Program (SHEP), a multicenter, randomized, double- blind, placebo-controlled trial of patients aged 60 years and older.6 Participants were randomized to either CTD 12.5 to 25 mg once daily±atenolol 25 to 50 mg once daily, or reserpine 0.05 mg once daily, or placebo. Treatment reduced the incidence of all fatal and nonfatal strokes by 36%, MI by 27%, all CHD by 27%, and all CVD by 32%.6
Underuse of diuretics
Despite trials such as SHEP and ALLHAT, and despite the long record of safety and efficacy in numerous patient populations, thiazide-type diuretics remain significantly under-used in clinical practice.7-10
Even intensive academic detailing designed to increase the use of thiazide-type diuretics found that the prescribing rates of 37.1% immediately before the intervention only increased to 39.6% overall after the intervention (46.5% in areas that received the most intensive intervention), reflecting what appears to be clinical resistance to this class of drugs (FIGURE 1).11 Even 4 years after the ALLHAT results were published, national use of thiazide-type drugs had not increased significantly.12
FIGURE 1
Proportion of visits by drug class among patients with drug-treated hypertension11
Data are from the IMS Health National Disease and Therapeutic Index, 2000 through 2008. “Other classes” indicates α-adrenergic receptor blockers, potassium-sparing diuretics, loop diuretics, and centrally acting agents.
Source: Archives of Internal Medicine by American Medical Association. Reproduced with permission of American Medical Association, in the format Journal via Copyright Clearance Center.
Hydrochlorothiazide and chlorthalidone: Similarities and differences
Underuse of thiazide-type diuretics is just 1 challenge. Others include which diuretic to use (HCTZ or CTD) and at what dosage.13-17 These 2 diuretics were approved at about the same time and, until recently, were considered equivalent and interchangeable despite differences in structure, pharmacokinetics, and pharmacodynamics.16,17
The publication of the VA Cooperative Morbidity Trial, the successful marketing and popularity of HCTZ and low-dose HCTZ/triamterene, the fear of hypokalemia (which was seen more often in the high doses of CTD initially used), and the subsequent inclusion of HCTZ as the primary diuretic in single-pill combination antihypertensives with ACEIs and angiotensin II receptor blockers (ARBs) led to HCTZ becoming the market leader for this class. Nonetheless, CTD was the diuretic chosen for many major randomized clinical trials, especially those sponsored by the National Heart, Lung, and Blood Institute (NHLBI).5,6,18-20
One reason for CTD’s relegation as a second-tier option to HCTZ could be the higher risk of hypokalemia observed at the higher dosages typically used in early studies.21-23 However, later studies found that substantially lower dosages of CTD could provide similar BP reductions with a significantly lower risk of hypokalemia.24 Materson et al,25 for instance, demonstrated that the 25-mg dosage of CTD was at least as effective for hypertension as the 50-mg and 75-mg dosages, while the 25-mg dosage was associated with less hypokalemia.
Increasingly, however, hypertension specialists, particularly those involved in research, have come to appreciate that CTD and HCTZ are, indeed, not interchangeable and do not have dosing equivalency. This understanding, together with the results of clinical trials like ALLHAT, has led to a resurgence of interest in the use of CTD.17,19,26
One assessment of outpatient prescription data from the VA from 2003 to 2008 found that although the proportion of patients receiving HCTZ during the period remained stable, the number of new users dropped 30% even as the proportion of thiazide users receiving CTD prescriptions doubled from 1.1% to 2.4% and the number of new prescriptions for CTD increased 40%.19
Chlorthalidone or hydrochlorothiazide: Study outcomes
The resurgence of interest in CTD has come with the publication of trials demonstrating its benefits in reducing CVD risk.5,6,27,28
The Multiple Risk Factor Intervention Trial (MRFIT) is the only large, long-term, randomized trial to directly compare HCTZ and CTD, although not in a randomized assignment. The primary endpoint was cardiovascular (CV) outcomes. The study launched in 1973 and enrolled 12,866 males aged 35 to 57 years who were in the upper 15% risk of death from chronic heart disease.29 Participants in the special care group were given HCTZ or CTD (investigator’s choice) at either 50 or 100 mg daily, depending on weight and sodium levels, and were given additional drugs as needed. The control group received usual care at that time from their health care provider. A 44% higher rate of CHD mortality in the HCTZ group observed towards the latter part of the trial led its Policy Advisory Board to change the option between the 2 diuretics and require CTD only. Following the change, the rate of CHD mortality decreased by 28% (P = .04 for comparison between the 2 time frames).29
A recent retrospective analysis of MRFIT found significantly lower CV event rates in participants who received either CTD or HCTZ than in those receiving neither (CTD: adjusted hazard ratio [aHR], 0.51; 95% confidence interval [CI], 0.43-0.61; P < .0001; HCTZ: aHR, 0.65; 95% CI, 0.55- 0.75; P < .0001), but rates of nonfatal CV events were significantly lower in participants who received CTD than those who received HCTZ (aHR, 0.79; 95% CI, 0.68-0.92; P < .0016).30 The results are depicted in FIGURE 2.30
FIGURE 2
Adjusted event-free probability of cardiovascular events30
CI, confidence interval; CTD, chlorthalidone; HCTZ, hydrochlorothiazide; HR, hazard ratio.
Source: Hypertension by American Heart Association; Council for High Blood Pressure Research (American Heart Association); InterAmerican Society of Hypertension. Reproduced with permission of Lippincott Williams & Wilkins in the format Journal via Copyright Clearance Center.A recent meta-analysis of 108 trials with HCTZ and 29 with CTD found that the 2 drugs did not provide equivalent reductions in systolic BP (SBP) within equivalent dosages. The study found that the median change in SBP with the median dose of HCTZ was –17 mm Hg, compared with -26 mm Hg for CTD. The slightly greater potassium loss observed with CTD was still nearly equivalent to that observed with HCTZ.31
Considerations for greater chlorthalidone efficacy
The differences between CTD and HCTZ, despite similar molecular structures, is a topic of much discussion.23 It is likely that these 2 drugs have different pharmacokinetic and pharmacodynamic properties, as shown in TABLE 1.17
TABLE 1
Pharmacokinetic/pharmacodynamic comparison of hydrochlorothiazide and chlorthalidone17
| Onset (h) | Peak (h) | Half-life (h) | Duration (h) | |
|---|---|---|---|---|
Hydrochlorothiazide | 2 | 4-6 | 6-9 (single dose) 8-15 (long-term dosing) | 12 (single dose) 16-24 (long-term dosing) |
Chlorthalidone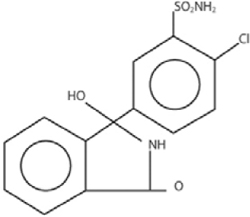 | 2-3 | 2-6 | 40 (single dose) 45-60 (long-term dosing) | 24-48 (single dose) 48-72 (long-term dosing) |
| Source: Hypertension by American Heart Association; Council for High Blood Pressure Research (American Heart Association); InterAmerican Society of Hypertension. Reproduced with permission of Lippincott Williams & Wilkins in the format Journal via Copyright Clearance Center | ||||
There is also evidence from an in vitro study that, compared with HCTZ, CTD has additional pleiotropic effects: reducing carbonic anhydrase activity, platelet aggregation, and vascular permeability while promoting angiogenesis.32
Another reason for the differences in efficacy between CTD and HCTZ could be the dosages of HCTZ used. Worldwide, nearly all prescriptions for HCTZ are for 12.5 to 25 mg/d, while most modern combination pills containing HCTZ incorporate these lower dosages.33 However, there is little evidence that such dosages lead to significantly improved outcomes.14,19,34-36
This was an issue in the Avoiding Cardiovascular Events Through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) trial. This study was designed to compare first-step therapy with benazepril/HCTZ 20/12.5 mg.37 Benazepril was force-titrated to 40 mg in each arm, whereas HCTZ and amlodipine were titrated to 25 mg and 10 mg, respectively, only if needed for BP control. The study was conducted in 11,506 high-risk patients 55 years of age and older. Other antihypertensive drugs could be added as needed for BP control. The study was stopped early after a mean follow-up of 36 months when the benazepril/amlodi-pine group demonstrated an HR of 0.8 (95% CI, 0.72-0.90) for the composite outcome of death from CV events, nonfatal MI or stroke, hospitalization for angina, resuscitation after sudden cardiac arrest, and coronary revascularization compared with the benazepril/HCTZ group.37
The ACCOMPLISH trial has been controversial for many reasons, with editorials suggesting that its design led to a “stacked deck” that favored amlodipine/benazepril over benazepril/HCTZ. Questions were raised as to why HCTZ was the diuretic of choice because CTD has been used in most thiazide-type trials. The dosages chosen were also questioned because outcome trials demonstrating reduced CV events with HCTZ used target doses of 50 mg/d or higher.14,21,22,38
Indeed, a meta-analysis published in 2011 found that despite the extensive use of HCTZ worldwide, the 12.5 to 25 mg dosage was inferior in reducing BP compared with standard doses of other antihypertensive agents (ACEIs, ARBs, beta blockers, and calcium channel blockers) in studies using 24-hour ambulatory BP monitoring.33 The efficacy of HCTZ closely mirrors that of the other drug classes at the 50-mg level, although that dose results in somewhat higher rates of hypokalemia. As the dose of HCTZ is increased to 100 mg, there is little or no further increase in antihypertensive efficacy, but hypokalemia becomes much more common.39
Thus, it can be clinically challenging to prescribe the optimum BP medication if practitioners prefer to use single-pill combinations that include HCTZ. Although the use of such single-pill combinations is warranted, particularly given the improved adherence with taking single-pill combinations compared with taking 2 or 3 pills, as noted in TABLE 1, most combinations include HCTZ dosages of 12.5 to 25 mg, which will often be less effective than full doses of 2 other medications.
Conclusion
Although thiazide-type diuretics are recommended as first-line therapy for most patients with hypertension, either alone or in combination with other classes of antihypertensives, they remain underused in clinical practice. In addition, HCTZ, which is the most commonly used diuretic (indeed, the most commonly prescribed antihypertensive) is prescribed at dosages too low to provide sufficient clinical efficacy in BP reduction and lower than what was proven to reduce CV events in clinical trials.
Chlorthalidone, a diuretic often considered a thiazide-type diuretic, has demonstrated superiority to HCTZ in reducing BP as evidenced in the MRFIT study and has been shown in numerous clinical trials to provide similar if not greater efficacy than other classes of antihypertensives in reducing BP, stroke, and CV events, with a good safety profile.
Clinicians need to manage patients with hypertension on an individual basis, selecting drugs and antihypertensive medication classes with the best outcomes in trials and then determining the most efficacious therapies with the lowest risk of adverse events for each patient. However, when prescribing a diuretic, they should also ensure that the drug used is prescribed at the appropriate therapeutic dosage level to enable patients to prevent the CV, thrombotic, and renal events that occur with long-term hypertension.
1. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043-2050.
2. Chobanian AV, Bakris GL, Black HR, et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-1252.
3. Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011;57(20):2037-2114.
4. Effects of treatment on morbidity in hypertension. II. Results in patients with diastolic blood pressure averaging 90 through 114 mm Hg. JAMA. 1970;213(7):1143-1152.
5. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) [published corrections appear in JAMA. 2003;289(2):178; JAMA. 2004;291(18):2196]. JAMA. 2002;288(23):2981-2997.
6. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265(24):3255-3264.
7. Petitti DB, Xie F, Barzilay JI. Prescribing patterns for thiazide diuretics in a large health maintenance organization: relationship to participation as an ALLHAT clinical center. Contemporary Clin Trials. 2006;27(5):397-403.
8. Dahlöf B, Devereux RB, Kjeldsen SE, et al. LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995-1003.
9. Psaty BM, Manolio TA, Smith NL, et al. Cardiovascular Health Study. Time trends in high blood pressure control and the use of antihypertensive medications in older adults: the Cardiovascular Health Study. Arch Intern Med. 2002;162(20):2325-2332.
10. Glasser SP, Basile JN, Lackland DT. Does prehypertension represent an increased risk for incident hypertension and adverse cardiovascular outcome? Hypertension. 2009;54(5):954-955.
11. Stafford RS, Bartholomew LK, Cushman WC, et al. ALLHAT Collaborative Research Group. Impact of the ALLHAT/JNC7 Dissemination Project on thiazide-type diuretic use. Arch Intern Med. 2010;170(10):851-858.
12. Furmaga EM, Cunningham FE, Cushman WC, et al. National utilization of antihypertensive medications from 2000 to 2006 in the Veterans Health Administration: focus on thiazide diuretics. J Clin Hypertens (Greenwich). 2008;10(10):770-778.
13. Pitt B. The role of chlorthalidone in patients with high-risk hypertension. J Clin Hypertens (Greenwich). 2009;11(9):460-461.
14. Ernst ME, Carter BL, Basile JN. All thiazide-like diuretics are not chlorthalidone: putting the ACCOMPLISH study into perspective. J Clin Hypertens (Greenwich). 2009;11(1):5-10.
15. Sica DA. Chlorthalidone—a renaissance in use? Expert Opin Pharmacother. 2009;10(13):2037-2039.
16. Kaplan NM. Chlorthalidone versus hydrochlorothiazide: a tale of tortoises and a hare. Hypertension. 2011;58(6):994-995.
17. Carter BL, Ernst ME, Cohen JD. Hydrochlorothiazide versus chlorthalidone: evidence supporting their interchangeability. Hypertension. 2004;43(1):4-9.
18. Carter BL, Malone DC, Ellis SL, Dombrowski RC. Antihypertensive drug utilization in hypertensive veterans with complex medication profiles. J Clin Hypertens (Greenwich). 2000;2(3):172-180.
19. Ernst ME, Lund BC. Renewed interest in chlorthalidone: evidence from the Veterans Health Administration. J Clin Hypertens (Greenwich). 2010;12(12):927-934.
20. Neaton JD, Grimm RH Jr, Prineas RJ, et al. Treatment of Mild Hypertension Study Research Group. Treatment of Mild Hypertension Study. Final results. JAMA. 1993;270(6):713-724.
21. Ford RV. Therapy of edema and hypertension, Comparative clinical effects of chlorothiazide and chlorthalidone. Tex State J Med. 1960;56:343-346.
22. Mach RS, Veyrat R. Clinical experiences with some of the newer diuretics, especially chlorthalidone. Ann N Y Acad Sci. 1960;88:841-863.
23. Dyrda I, Dufault C, Herbert JG, Tremblay G, Genest J. Studies on a new diuretic: chlorthalidone. Can Med Assoc J. 1962;86:475-482.
24. Kakaviatos N, Finnerty FA, Jr. Comparison of chlorthalidone, a long-acting antihypertensive and diuretic agent, with chlorothiazide. Analysis of one hundred twenty-three cases. Am J Cardiol. 1962;10:570-574.
25. Materson BJ, Oster JR, Michael UF, et al. Dose response to chlorthalidone in patients with mild hypertension. Efficacy of a lower dose. Clin Pharmacol Ther. 1978;24(2):192-198.
26. Ernst ME, Carter BL, Goerdt CJ, et al. Comparative antihypertensive effects of hydrochlorothiazide and chlorthalidone on ambulatory and office blood pressure. Hypertension. 2006;47(3):352-358.
27. Dunbar-Jacob J, Erlen JA, Schlenk EA, Ryan CM, Sereika SM, Doswell WM. Adherence in chronic disease. Annu Rev Nurs Res. 2000;18:48-90.
28. Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA. 1979;242(23):2562-2571.
29. Multiple Risk Factor Intervention Trial Research Group. Multiple risk factor intervention trial. Risk factor changes and mortality results. JAMA. 1982;248(12):1465-1477.
30. Dorsch MP, Gillespie BW, Erickson SR, Bleske BE, Weder AB. Chlorthalidone reduces cardiovascular events compared with hydrochlorothiazide: a retrospective cohort analysis. Hypertension. 2011;57(4):689-694.
31. Ernst ME, Carter BL, Zheng S, Grimm RH, Jr. Meta-analysis of dose-response characteristics of hydrochlorothiazide and chlorthalidone: effects on systolic blood pressure and potassium. Am J Hypertens. 2010;23(4):440-446.
32. Woodman R, Brown C, Lockette W. Chlorthalidone decreases platelet aggregation and vascular permeability and promotes angiogenesis. Hypertension. 2010;56(3):463-470.
33. Messerli FH, Makani H, Benjo A, Romero J, Alviar C, Bangalore S. Antihypertensive efficacy of hydrochlorothiazide as evaluated by ambulatory blood pressure monitoring: a meta-analysis of randomized trials. J Am Coll Cardiol. 2011;57(5):590-600.
34. Demirovic J, Prineas R, Rudolph M. Epidemiology of congestive heart failure in three ethnic groups. Congest Heart Fail. 2001;7(2):93-96.
35. Eide IK, Torjesen PA, Drolsum A, Babovic A, Lilledahl NP. Low-renin status in therapy-resistant hypertension: a clue to efficient treatment. J Hypertens. 2004;22(11):2217-2226.
36. Epstein M. Re-examining RAS-blocking treatment regimens for abrogating progression of chronic kidney disease. Nat Clin Pract Nephrol. 2008;5(1):12-13.
37. Jamerson K, Weber MA, Bakris GL, et al. ACCOMPLISH Trial Investigators. Ben-azepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359(23):2417-2428.
38. Parra D, Rosenstein R. Benazepril plus amlodipine or hydrochlorothiazide for hypertension. N Engl J Med. 2009;360(11):1147-1150.
39. Messerli FH, Bangalore S, Julius S. Risk/benefit assessment of beta-blockers and diuretics precludes their use for first-line therapy in hypertension. Circulation. 2008;117(20):2706-2715.
1. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043-2050.
2. Chobanian AV, Bakris GL, Black HR, et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206-1252.
3. Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011;57(20):2037-2114.
4. Effects of treatment on morbidity in hypertension. II. Results in patients with diastolic blood pressure averaging 90 through 114 mm Hg. JAMA. 1970;213(7):1143-1152.
5. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) [published corrections appear in JAMA. 2003;289(2):178; JAMA. 2004;291(18):2196]. JAMA. 2002;288(23):2981-2997.
6. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265(24):3255-3264.
7. Petitti DB, Xie F, Barzilay JI. Prescribing patterns for thiazide diuretics in a large health maintenance organization: relationship to participation as an ALLHAT clinical center. Contemporary Clin Trials. 2006;27(5):397-403.
8. Dahlöf B, Devereux RB, Kjeldsen SE, et al. LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995-1003.
9. Psaty BM, Manolio TA, Smith NL, et al. Cardiovascular Health Study. Time trends in high blood pressure control and the use of antihypertensive medications in older adults: the Cardiovascular Health Study. Arch Intern Med. 2002;162(20):2325-2332.
10. Glasser SP, Basile JN, Lackland DT. Does prehypertension represent an increased risk for incident hypertension and adverse cardiovascular outcome? Hypertension. 2009;54(5):954-955.
11. Stafford RS, Bartholomew LK, Cushman WC, et al. ALLHAT Collaborative Research Group. Impact of the ALLHAT/JNC7 Dissemination Project on thiazide-type diuretic use. Arch Intern Med. 2010;170(10):851-858.
12. Furmaga EM, Cunningham FE, Cushman WC, et al. National utilization of antihypertensive medications from 2000 to 2006 in the Veterans Health Administration: focus on thiazide diuretics. J Clin Hypertens (Greenwich). 2008;10(10):770-778.
13. Pitt B. The role of chlorthalidone in patients with high-risk hypertension. J Clin Hypertens (Greenwich). 2009;11(9):460-461.
14. Ernst ME, Carter BL, Basile JN. All thiazide-like diuretics are not chlorthalidone: putting the ACCOMPLISH study into perspective. J Clin Hypertens (Greenwich). 2009;11(1):5-10.
15. Sica DA. Chlorthalidone—a renaissance in use? Expert Opin Pharmacother. 2009;10(13):2037-2039.
16. Kaplan NM. Chlorthalidone versus hydrochlorothiazide: a tale of tortoises and a hare. Hypertension. 2011;58(6):994-995.
17. Carter BL, Ernst ME, Cohen JD. Hydrochlorothiazide versus chlorthalidone: evidence supporting their interchangeability. Hypertension. 2004;43(1):4-9.
18. Carter BL, Malone DC, Ellis SL, Dombrowski RC. Antihypertensive drug utilization in hypertensive veterans with complex medication profiles. J Clin Hypertens (Greenwich). 2000;2(3):172-180.
19. Ernst ME, Lund BC. Renewed interest in chlorthalidone: evidence from the Veterans Health Administration. J Clin Hypertens (Greenwich). 2010;12(12):927-934.
20. Neaton JD, Grimm RH Jr, Prineas RJ, et al. Treatment of Mild Hypertension Study Research Group. Treatment of Mild Hypertension Study. Final results. JAMA. 1993;270(6):713-724.
21. Ford RV. Therapy of edema and hypertension, Comparative clinical effects of chlorothiazide and chlorthalidone. Tex State J Med. 1960;56:343-346.
22. Mach RS, Veyrat R. Clinical experiences with some of the newer diuretics, especially chlorthalidone. Ann N Y Acad Sci. 1960;88:841-863.
23. Dyrda I, Dufault C, Herbert JG, Tremblay G, Genest J. Studies on a new diuretic: chlorthalidone. Can Med Assoc J. 1962;86:475-482.
24. Kakaviatos N, Finnerty FA, Jr. Comparison of chlorthalidone, a long-acting antihypertensive and diuretic agent, with chlorothiazide. Analysis of one hundred twenty-three cases. Am J Cardiol. 1962;10:570-574.
25. Materson BJ, Oster JR, Michael UF, et al. Dose response to chlorthalidone in patients with mild hypertension. Efficacy of a lower dose. Clin Pharmacol Ther. 1978;24(2):192-198.
26. Ernst ME, Carter BL, Goerdt CJ, et al. Comparative antihypertensive effects of hydrochlorothiazide and chlorthalidone on ambulatory and office blood pressure. Hypertension. 2006;47(3):352-358.
27. Dunbar-Jacob J, Erlen JA, Schlenk EA, Ryan CM, Sereika SM, Doswell WM. Adherence in chronic disease. Annu Rev Nurs Res. 2000;18:48-90.
28. Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA. 1979;242(23):2562-2571.
29. Multiple Risk Factor Intervention Trial Research Group. Multiple risk factor intervention trial. Risk factor changes and mortality results. JAMA. 1982;248(12):1465-1477.
30. Dorsch MP, Gillespie BW, Erickson SR, Bleske BE, Weder AB. Chlorthalidone reduces cardiovascular events compared with hydrochlorothiazide: a retrospective cohort analysis. Hypertension. 2011;57(4):689-694.
31. Ernst ME, Carter BL, Zheng S, Grimm RH, Jr. Meta-analysis of dose-response characteristics of hydrochlorothiazide and chlorthalidone: effects on systolic blood pressure and potassium. Am J Hypertens. 2010;23(4):440-446.
32. Woodman R, Brown C, Lockette W. Chlorthalidone decreases platelet aggregation and vascular permeability and promotes angiogenesis. Hypertension. 2010;56(3):463-470.
33. Messerli FH, Makani H, Benjo A, Romero J, Alviar C, Bangalore S. Antihypertensive efficacy of hydrochlorothiazide as evaluated by ambulatory blood pressure monitoring: a meta-analysis of randomized trials. J Am Coll Cardiol. 2011;57(5):590-600.
34. Demirovic J, Prineas R, Rudolph M. Epidemiology of congestive heart failure in three ethnic groups. Congest Heart Fail. 2001;7(2):93-96.
35. Eide IK, Torjesen PA, Drolsum A, Babovic A, Lilledahl NP. Low-renin status in therapy-resistant hypertension: a clue to efficient treatment. J Hypertens. 2004;22(11):2217-2226.
36. Epstein M. Re-examining RAS-blocking treatment regimens for abrogating progression of chronic kidney disease. Nat Clin Pract Nephrol. 2008;5(1):12-13.
37. Jamerson K, Weber MA, Bakris GL, et al. ACCOMPLISH Trial Investigators. Ben-azepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359(23):2417-2428.
38. Parra D, Rosenstein R. Benazepril plus amlodipine or hydrochlorothiazide for hypertension. N Engl J Med. 2009;360(11):1147-1150.
39. Messerli FH, Bangalore S, Julius S. Risk/benefit assessment of beta-blockers and diuretics precludes their use for first-line therapy in hypertension. Circulation. 2008;117(20):2706-2715.
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
Dr White is President of the American Society of Hypertension (voluntary unpaid position) and is a paid cardiovascular safety consultant to Abbott Immunology; Ardea Biosciences, Inc; AstraZeneca; BioSante Pharmaceuticals, Inc; Forest Research Institute, Inc; Novartis Corporation; Roche Laboratories, Inc; and Takeda Global Research & Development Center, Inc. He holds no stocks in pharmaceutical companies and is not a member of any speakers’ bureaus.
Introduction
Hypertension is a transformative condition in modern medicine due to the various numeric definitions of the disease, the decision of when to initiate therapy and to what level to treat, and the evolution of our understanding of the long-term complications of the hypertensive disease process. Hypertension is notable as 1 of the first conditions that only rarely manifested symptoms and whose eventual sequelae could take years, if not decades, to become known. In addition, hypertension was the first condition in which clinicians initiated therapy for patients who were otherwise healthy. Hypertension also led to 1 of the first screening programs for any disease as well as the first robust preventive effort for a chronic medical condition.1
Clinical trials have been performed for 5 decades to evaluate the potential benefits of lowering blood pressure (BP) in patients with hypertension and its comorbid conditions (FIGURE 1).2-37 The first clinical trial to identify the increased risk of cardiovascular (CV) mortality related to hypertension was published in the mid-1960s.2,38 In fact, the Veterans Administration (VA) Cooperative trial was the first randomized, placebo-controlled, double-blind, multi-institutional drug efficacy trial ever conducted in CV medicine.38 It involved 143 men who met the 1964 definition of hypertension (ie, diastolic BP [DBP] ≥115 mm Hg) and who were randomized to either triple therapy with low doses of hydrochlorothiazide (HCTZ), reserpine, and hydralazine, or to placebo. The trial was terminated early when, after 18 months of treatment, rates of morbidity and mortality were substantially lower in the treated group than in the placebo group.2 The trial was the first to confirm that antihypertensive treatment, even in patients with existing CV damage and significant hypertension, could dramatically reduce the incidence of stroke, congestive heart failure (CHF), and progressive kidney damage.38
FIGURE 1
Clinical trials in hypertension during the past 5 decades
ACCOMPLISH, Avoiding Cardiovascular Events Through Combination Therapy in Patients Living With Systolic Hypertension trial; ALLHAT, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial; ALTITUDE, Aliskiren Trial in Type 2 Diabetes Using Cardiovascular and Renal Disease Endpoints; ANBP1, Australian National Blood Pressure Study 1; ANBP2, Australian National Blood Pressure Study 2; ASCOT, Anglo-Scandinavian Cardiac Outcomes Trial; ATMOSPHERE, Efficacy and Safety of Aliskiren and Aliskiren/Enalapril Combination on Morbi-mortality in Patients With Chronic Heart Failure study; CAPPP, Captopril Prevention Project; CONVINCE, Controlled Onset Verapamil Investigation of Cardiovascular End Points trial; DBP, diastolic blood pressure; EWPHE, European Working Party on High Blood Pressure in the Elderly study; HAPPHY, Heart Attack Primary Prevention in Hypertension trial; HBP, high blood pressure; HDFP, Hypertension Detection and Follow-up Program; HOT, Hypertension Optimal Treatment study; INSIGHT, International Nifedipine GITS Study of Intervention as a Goal in Hypertension Treatment; I-PRESERVE, Irbesartan in Heart Failure with Preserved Systolic Function study; ISH, isolated systolic hypertension; LIFE, Losartan Intervention For Endpoint Reduction in Hypertension trial; MAPHY, Metoprolol Atherosclerosis Prevention in Hypertensives study; MRC-1, Medical Research Council trial of treatment of mild hypertension; MRC-2, Medical Research Council trial of treatment of hypertension in older adults; NORDIL, Nordic Diltiazem study; ONTARGET, Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial; SCOPE, Study on Cognition and Prognosis in the Elderly; SHEP, Systolic Hypertension in the Elderly Program; STOP-1, Swedish Trial in Old Patients with Hypertension-1; STOP-2, Swedish Trial in Old Patients with Hypertension-2; Syst-China, Systolic Hypertension in China trial; Syst-Eur, Systolic Hypertension in Europe trial; TOMHS, Treatment of Mild Hypertension Study; TROPHY, Trial of Preventing Hypertension; UKPDS, United Kingdom Prospective Diabetes Study; VA, Veterans Administration; VA MONORx, VA Monotherapy of Hypertension study; VALUE, Valsartan Antihypertensive Long-term Use Evaluation trial.Although the Framingham Study (www.framinghamheartstudy.org) was, of course, one of the seminal studies in the field of CV medicine, it was observational in nature, rather than interventional like most of the studies highlighted in this article.
The Medical Research Council trial of the treatment of mild hypertension (MRC-1) (ie, defined as DBP 90-109 mm Hg) demonstrated that a significant reduction in DBP among individuals receiving the diuretic bendroflumethiazide or the beta-blocker propranolol significantly reduced the rate of stroke compared with placebo, with a rate of 1.4 per 1000 patient-years of observation in the treatment group vs 2.6 per 1000 patient-years in the placebo group (P < .01).5 The treatment group also had significantly lower rates of all CV events than the placebo group, and this difference was statistically significant (P < .05). However, the treatment groups experienced significantly increased rates of adverse effects compared with placebo.5
Other early notable clinical trials that evaluated treatment options for hypertension in the general public include the Hypertension Detection and Follow-up Program (HDFP),3 the Hypertension Optimal Treatment (HOT) study,16 and the United Kingdom Prospective Diabetes Study/Hypertension in Diabetes (UKPDS/HDS).17,18 The key outcomes of these trials are shown in TABLE 1.3,4,11,12,16,20,22,25,39,40
TABLE 1
Findings from the early clinical trials in hypertension
| Clinical Trial | Intervention | Primary Outcome | Result |
|---|---|---|---|
| HDFP3,39 | Patients randomized to systemic antihypertensive treatment or community medical therapy (referral) | 5-year mortality | 5-year mortality reduced by 17% in treatment group (P < 0.01); after 12 years, BP still higher in treatment than in stepped-care treatment group |
| HOT16 | Patients all began on felodipine, with an ACEI or a BB added as necessary If BP goal was still not reached, HCTZ could be added Patients in each group also randomized to low-dose aspirin or placebo Subjects were randomly assigned to reach 1 of 3 DBP goals: ≤90 mm Hg; ≤85 mm Hg; or ≤80 mm Hg | Major CV events with 3 target DBPs reached during therapy and with low-dose aspirin therapy | Lowest incidence of major CV events achieved at mean BP of 138.5/82.6 mm Hg; lowest risk of CV mortality achieved at mean BP of 138.8/86.5 mm Hg Low-dose aspirin reduced major CV events by 15% and all MI by 36%, although nonfatal major bleeding was twice as common with low-dose aspirin than with placebo |
| UKPDS/HDS17,18 | Patients with T2DM randomized to atenolol or captopril, with additional antihypertensive agents (other than ACEIs or BBs) allowed | Effect of tight BP control on diabetes-related complications, morbidity, and mortality | Tight BP control (<150/85 mm Hg) with either atenolol or captopril significantly reduced the risk of all endpoints, including risk of diabetes-related death or complication, stroke, MI, and heart failure |
| EWPHPE4 | Patients ≥60 years of age randomized to HCTZ + triamterene + methyldopa or placebo | CV and MI mortality; nonfatal CV events | Significant reduction in CV and MI mortality (P < .05) but not nonfatal CV events in treatment group vs placebo Found U-shaped relationship between mortality and SBP in treated group vs mortality and DBP in placebo group |
| MRC-212 | Patients 65-74 years of age randomized to atenolol + HCTZ or amiloride | Reduction in mortality and morbidity due to stroke and CHD and reduction in mortality due to all causes | Only the HCTZ group demonstrated a significant reduction in stroke, coronary events, and all CV events (P=.4, P=.0009, and P=.0005, respectively) |
| STOP-222 | Patients 70-84 years of age randomized to atenolol + HCTZ or amiloride; or to metoprolol or prinodolol | Incidence of fatal stroke, MI, or other CVD mortality | Similar reductions in BP, mortality, and major events in all treatment groups |
| SCOPE25 | Patients 70-89 years of age randomized to candesartan or placebo (open-label antihypertensive therapy added as needed and extensively used in control group) | Major CV events; secondary measures included CV death, nonfatal and fatal stroke and MI, cognitive function | Greater BP decreases in candesartan group but no significant risk reduction in major CV events between the 2 groups Significant reduction in nonfatal stroke (P=.04) and all stroke (P=.06) in the treatment group No other significant differences between the groups, although a post-hoc analysis found less cognitive decline among those with only mild cognitive impairment at baseline in the candesartan-treated group (P=.04)40 |
| SHEP11 | Patients ≥60 years of age randomized to chlorthalidone with or without atenolol or reserpine, with nifedipine as third-line therapy, or to placebo | Stroke; nonfatal MI, coronary death, major CV events, death due to all causes | Significant reduction in 5-year incidence of total stroke in active treatment group (P=.0003) and significant reduction in all secondary endpoints |
| Syst-Eur19 | Patients >60 years of age randomized to nitrendipine with possible addition of enalapril, HCTZ, or both, or to placebo | Fatal and nonfatal stroke, fatal and nonfatal cardiac events including sudden death, all-cause mortality | Significant reductions in all endpoints except all-cause mortality in treatment group; study halted early because of the 42% total stroke reduction in treatment arm (P < .003) |
| Syst-China20 | Patients ≥60 years of age randomized to nitrendipine with captopril or HCTZ, or both if needed; or matching placebo | Nonfatal stroke; all-cause, CV, and stroke mortality; and all fatal and nonfatal CV events | Significant reductions in all endpoints |
| ACEI, angiotensin-converting enzyme inhibitor; BB, beta-blocker; BP, blood pressure; CV, cardiovascular; CHD, coronary heart disease; CVD, CV disease; DBP, diastolic BP; EWPHE, European Working Party on High Blood Pressure in the Elderly study; HDFP, Hypertension Detection and Follow-up Program; HCTZ, hydrochlorothiazide; HOT, Hypertension Optimal Treatment study; MI, myocardial infarction; MRC-2, Medical Research Council trial of treatment of hypertension in older adults; SBP, systolic BP; SCOPE, Study on Cognition and Prognosis in the Elderly; SHEP, Systolic Hypertension in the Elderly Program; STOP-2, Swedish Trial in Old Patients with Hypertension-2; Syst-Eur, Systolic Hypertension in Europe trial; Syst-China, Systolic Hypertension in China trial; T2DM, type 2 diabetes mellitus; UKPDS/HDS, United Kingdom Prospective Diabetes Study/Hypertension in Diabetes. | |||
Given that hypertension is far more common in older people who have increased rates of hypertensive target organ damage or CV disease (CVD), researchers have focused on the effects of antihypertensive therapy in this population for some time.41 Sentinel studies in this population include the European Working Party on High Blood Pressure in the Elderly (EWPHPE) study,4 the Medical Research Council trial of treatment of hypertension in older adults (MRC-2),12 the Swedish Trial in Old Patients with Hypertension-2 (STOP-2),22 the Study on Cognition and Prognosis in the Elderly (SCOPE),25 the Systolic Hypertension in the Elderly Program (SHEP) study,11 the Systolic Hypertension in Europe (Syst-Eur) study,19 and the Systolic Hypertension in China (Syst-China) study.20 The key outcomes of these trials are shown in TABLE 1. In general, these trials have shown that antihypertensive therapy has a marked benefit in a shorter period of time in older patients than in younger patients, particularly in terms of reduced stroke and CHF rates.
The Hypertension in the Very Elderly Trial (HYVET), which enrolled participants 80 years of age and older, demonstrated that reducing systolic BP (SBP) from 170 mm Hg to 145 mm Hg with indapamide sustained release 1.5 mg and perindopril 2 to 4 mg as needed reduced all-cause deaths 21% (P =.02), stroke-related deaths 39% (P =.05), and fatal and nonfatal heart failure (HF) 64% (P < .001), compared with placebo.42 The intervention group also experienced a 34% reduction in all CV events (P < .001) and a 30% reduction in stroke (P =.055).42 However, there is still no good evidence that reducing BP further in this population provides additional benefits over the concomitant risks.
In the 1980s, numerous trials were developed to address the question: “What is the best way to treat high BP?” These included the Heart Attack Primary Prevention in Hypertension (HAPPHY) trial,7 the Metoprolol Atherosclerosis Prevention in Hypertensives (MAPHY) study,8-10 the Treatment of Mild Hypertension Study (TOMHS),14 and the VA Cooperative Study on single drug therapy.15
Subsequently, several trials were conducted that focused on the safety of calcium antagonists for the primary or background treatment of hypertension. These included the International Nifedipine GITS Study of Intervention as a Goal in Hypertension Treatment (INSIGHT),23 the Nordic Diltiazem (NORDIL) study,24 the Australian National Blood Pressure Study 2 (ANBP2),28 the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) trial,26 the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial,29 and the Irbesartan in Heart Failure with Preserved Systolic Function (I-PRESERVE) study.37
These studies, conducted from the mid 1990s to the present, have shown that calcium antagonists, including amlodipine, diltiazem, nifedipine, and verapamil, are as effective as thiazide-type diuretics or beta-blockers in preventing CV events in patients with hypertension. Further, the LIFE trial demonstrated that the angiotensin II receptor blocker (ARB) losartan was more effective than the beta-blocker atenolol in reducing stroke events and that blockade of the renin- angiotensin system did not seem to affect CV outcomes in patients with HF with preserved systolic function, a common problem in patients with prolonged hypertension and left ventricular hypertrophy.29
The largest randomized, double-blind, antihypertensive trial performed to date is the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). It involved 33,357 participants 55 years of age and older with hypertension and at least 1 other coronary heart disease (CHD) risk factor.27 Participants were randomized to chlorthalidone, amlodipine, doxazosin, or lisinopril. The doxazosin arm was discontinued early because an increase in CV events was observed after 2 years, relative to the other treatment arms. At follow-up (mean, 4.9 years), there was no difference between the 3 groups in terms of the primary outcome (combined fatal CHD or nonfatal myocardial infarction [MI], analyzed by intent-to-treat) or all-cause mortality.27 Of note, 5-year SBP levels were higher in the amlodipine (0.8 mm Hg, P=.03) and lisinopril (2 mm Hg, P < .001) groups than in the chlorthalidone group, whereas the 5-year DBP levels were significantly lower in the amlodipine group (0.8 mm Hg, P < .001).27
Secondary analyses showed a higher 6-year rate of HF development in the amlodipine group than in the chlorthali-done group (10.2% vs 7.7%; relative risk [RR], 1.38; 95% con- fidence interval [CI], 1.25-1.52), whereas the lisinopril group had a higher 6-year rate of combined CVD (33.3% vs 30.9%; RR, 1.10; 95% CI, 1.05-1.16), stroke (6.3% vs 5.6%; RR, 1.15; 95% CI, 1.02-1.30), and HF (8.7% vs 7.7%; RR, 1.19; 95% CI, 1.07-1.31) than the chlorthalidone group. The design of ALLHAT led to worsened control of BP in African Americans relative to white patients who were receiving lisinopril, which may have been an important factor in the subsequent increased rate of stroke in African American patients who were receiving lisinopril rather than chlorthalidone.27
Subsequent to ALLHAT, the benefits and safety of calcium antagonists vs a thiazide diuretic combined with an angiotensin-converting enzyme inhibitor (ACEI) were ad-dressed by the Avoiding Cardiovascular Events Through Combination Therapy in Patients Living With Systolic Hypertension (ACCOMPLISH) trial.33 This study randomized 11,506 patients with a mean BP of 145/80 mm Hg to combination therapy with benazepril (40 mg/d) and amlodipine (5-10 mg/d) or benazepril and HCTZ (12.5-25 mg/d). Other antihypertensive medications could be added to reach a target BP <140/90 mm Hg (130/80 mm Hg in patients with diabetes or renal insufficiency).33 The study was stopped early at 3 years because the primary outcome of CV death, nonfatal MI or stroke, hospitalization for angina, resuscitation after sudden cardiac arrest, and coronary revascularization occurred in 552 patients in the benazepril-amlodipine group compared with 679 patients in the benazepril-HCTZ group (9.6% vs 11.8%; RR ratio, 19.6%; hazard ratio [HR], 0.80; P < .001). The mechanism for the benefit observed in the benazepril-amlodipine group may relate in part to improved coronary blood flow that occurs with a calcium antagonist (compared with a diuretic) since BP control was virtually the same in both groups.
Another major hypertension study during the same era was the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT).32 This study enrolled 19,257 patients in northern Europe with a mean age of 63 years, an untreated baseline BP ≥160/100 mm Hg or a treated mean BP ≥140/90 mm Hg, and 3 or more of 11 prespecified risk factors for CV. Patients were randomized to amlodipine, with or without perindopril, or atenolol, with or without a thiazide diuretic, and were titrated to reach a BP goal <140/90 mm Hg. The study was halted early after a mean follow up of 5.5 years. Although there was no statistically significant difference in the primary events of nonfatal MI plus fatal CHF between the 2 arms, fewer patients randomized to the amlodipine-based regimen experienced a fatal or nonfatal stroke (327 vs 422; HR, 0.77; 95% CI, 0.66-0.89; P=.0003) and total CV events and procedures were lower in patients taking the amlodipine-based regimen than in those taking the atenolol-based regimen (1362 vs 1602; HR, 0.84; 95% CI, 0.78-0.90; P < .0001).32 All-cause mortality was also lower in the amlodipine-based group (738 vs 820; HR, 0.89; 95% CI, 0.81-0.99; P=.025), and significantly fewer patients in this arm developed diabetes (567 vs 799; HR, 0.70; 95% CI, 0.63-0.78; P < .0001).32
Patients with diabetes in ASCOT who were titrated to achieve a target BP <130/80 mm Hg experienced significantly lower mortality and stroke when taking the amlodipine-based regimen than when taking the atenolol-based regimen (HR, 0.86; 95% CI, 0.76-0.98; P=.026).32 In the group taking the atenolol-based regimen, fatal and nonfatal strokes were reduced by 25% (P=.017), peripheral arterial disease by 48% (P=.004), and peripheral revascularization procedures by 57% (P < .001). There were no statistically significant differences in the endpoints of CHD deaths and nonfatal MI in the diabetes subgroup.
Combination therapy and guideline recommendations
By the 1970s, it became clear that combinations of antihypertensive drugs increased BP lowering efficacy through both additive and synergistic mechanisms. These combinations also reduced adverse events because lower doses of each drug could be used, whereas drugs from different classes might offset each other’s adverse effects. In addition, combining antihypertensive drugs could prolong duration of action, possibly providing additional target organ protection.43 Combining drugs from complementary classes has also been shown to increase the likelihood of BP lowering compared with increasing the dose of a single drug, thus reducing the time required to reach BP goal.31,44-46
The 2010 American Society of Hypertension (ASH) position statement on combination therapy in hypertension therapy notes that at least 75% of patients will require combination therapy to reach goal.47 In addition, a meta-analysis of 9 randomized clinical trials found that combination treatment using a thiazide or thiazide-like diuretic as one of the components could provide a significantly greater effect than monotherapy lacking the diuretic, with similar discontinuation rates.48
Government guidelines in the United States, now nearly 10 years old, do not recommend combination therapy as a first-line approach unless patients have stage 2 hypertension (SBP ≥160 mm Hg or DBP ≥100 mm Hg). At that point, the guidelines recommend combination therapy with a thiazide or thiazide-type diuretic plus either an ACEI, ARB, beta-blocker, or calcium antagonist.49 More-specific recommendations are provided for patients with compelling indications (eg, HF, ischemic heart disease, chronic kidney disease, recurrent stroke, diabetes, and high coronary disease risk), as shown in TABLE 2.41,49 New recommendations from the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 8) are expected later this year.
TABLE 2
Antihypertensive treatment in patients with compelling indications41,49
| Indication | Diuretic | BB | ACEI | ARB | Calcium antagonist | Aldosterone antagonist |
|---|---|---|---|---|---|---|
| Heart failure | ||||||
| Post MI | ||||||
| CVD or high CVD risk | ||||||
| Anginaa | ||||||
| Aortopathy/aortic aneurysma | ||||||
| Diabetes | ||||||
| Recurrent stroke prevention | ||||||
| CKDb | ||||||
| Early dementiaa | ||||||
ACCF, American College of Cardiology Foundation; ACEI, angiotensin-converting enzyme inhibitor; AHA, American Heart Association; ARB, angiotensin-receptor blocker; BB, beta-blocker; CVD, cardiovascular disease; CKD, chronic kidney disease; MI, myocardial infarction. aNot considered “compelling” indication in JNC-7 Express guidelines. bNot considered “compelling” recommendation in ACCF/AHA recommendations. Source: Journal of the American College of Cardiology by American College of Cardiology. Reproduced with permission of Elsevier Inc. in the format Journal via Copyright Clearance Center. | ||||||
Recent guidelines from ASH describe combination therapies of hypertension in categories of preferred, acceptable, and less effective, based on efficacy in lowering BP, safety and tolerability, and certain known outcomes from longer-term trials (TABLE 3).47
TABLE 3
Drug combinations in hypertension: Recommendations from the American Society of Hypertension47
| Preferred | Acceptable | Less Effective |
|---|---|---|
| ACEI + diuretica | BB + diuretica | ACEI + ARB |
| ARB + diuretica | Calcium antagonist + diuretic | ACEI + BB |
| ACEI + CCBa | Renin inhibitor + diuretic | ARB + BB |
| ARB + CCBa | Renin inhibitor + ARBa,b | CCB (non-dihydropyridine) + BB |
| Thiazide diuretic + potassium-sparing diuretica | Centrally acting agent + BB | |
| ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin-receptor blocker; BB, beta-blocker; CCB, calcium channel blocker. aAvailable as single-pill combination. bThis may be medically inappropriate in patients with diabetes and chronic diabetic nephropathy. Source: Journal of the American Society of Hypertension: JASH by American Society of Hypertension. Reproduced with permission of Elsevier Inc. in the format Journal via Copyright Clearance Center. | ||
In 2010, the American College of Cardiology Foundation (ACCF)/American Heart Association (AHA) published an expert consensus document on hypertension in the elderly. It recommends single therapy or combination therapy with an ACEI, ARB, calcium antagonist, or diuretic for patients 65 years of age and older with stage 1 hypertension and no “compelling” indications (eg, HF, post-MI, known coronary disease, angina, aortopathy/aortic aneurysm, diabetes, recurrent stroke prevention, chronic kidney disease, and early vascular dementia), but combination therapy for those with stage 2 hypertension and no compelling indications. For the former group, the panel notes that the combination of amlodipine with a renin-angiotensin aldosterone system blocker may be preferable to a diuretic combination, although either is acceptable.41
For patients with compelling indications, the ACCF/AHA panel recommends condition-based combination therapy with 2 or more of the therapies summarized in TABLE 2.41,49 The panel’s algorithm for the management of hypertension in the elderly is depicted in FIGURE 2.41
FIGURE 2
ACCF/AHA algorithm for the management of hypertension in the elderly41
ACCF, American College of Cardiology Foundation; ACEI, angiotensin-converting enzyme inhibitor; AHA, American Heart Association; ALDO ANT, aldosterone antagonist; ARB, angiotensin II receptor blocker; BB, beta-blocker; BP, blood pressure; CA, calcium antagonist; CAD, coronary artery disease; CVD, cardiovascular disease; DBP, diastolic BP; MI, myocardial infarction; RAS, renin-angiotensin system; SBP, systolic BP; THIAZ, thiazide diuretic.
aCombination therapy.
Source: Journal of the American College of Cardiology by American College of Cardiology. Reproduced with permission of Elsevier Inc. in the format Journal via Copyright Clearance Center.The National Institute for Health and Clinical Excellence (NICE), the United Kingdom-based clinical guideline development organization, recommends in its 2011 guidelines for the clinical management of primary hypertension in adults that patients less than 55 years of age, not of black African or Caribbean heritage, begin treatment with an ACEI or ARB.50 The guidelines do not recommend beta-blockers for initial therapy, noting that they should be considered only in younger patients with intolerance or contraindications to ACEIs and ARBs, reproductive-aged women, and those with clinical evidence of increased sympathetic drive.50
In contrast, patients 55 years and older, or blacks of African or Caribbean origin of any age, should begin treatment with a calcium channel blocker (CCB).50 If they cannot tolerate a CCB, or for those with HF (or at high risk of HF), the guidelines recommend beginning therapy with a diuretic (preferably chlorthalidone or in-dapamide unless the patient’s hypertension is already controlled with bendroflumethiazide or HCTZ).
If initial treatment fails to lower BP adequately, step 2 of the NICE guidelines for all populations is treatment with an ACEI or ARB in combination with a calcium antagonist.50 If further therapy is necessary (step 3), a thiazide diuretic (or thiazide-like) should be added to that combination. It is also recommended that patients with drug-resistant hypertension (ie, taking 3 agents at maximally tolerated doses, 1 of which should be a diuretic) should receive additional treatment with low-dose spironolactone (if their serum potassium level is ≤4.5 mmol/L) and higher-dose thiazide-type diuretics (if their serum potassium level is >4.5 mmol/L). If the diuretic is not tolerated or is ineffective, an alpha- or beta-blocker may be added. If patients continue to exhibit continued resistance, NICE recommends referral to a hypertension specialist. The NICE algorithm for the treatment of hypertension is shown in FIGURE 3.50
FIGURE 3
NICE algorithm for treatment of hypertension50
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; CCB, calcium channel blocker; NICE, National Institute for Health and Clinical Excellence.
aChoose a low-cost ARB.
bA CCB is preferred but consider a thiazide-like diuretic if a CCB is not tolerated or the person has edema, evidence of heart failure, or a high risk of heart failure.
cConsider a low dose of spironolactoned or higher doses of thiazide-like diuretic
dAt the time of publication (August 2011), spironolactone did not have a UK marketing authorization for this indication. Informed consent should be obtained and documented.
eConsider an alpha- or beta-blocker if further diuretic therapy is not tolerated or is contraindicated or ineffective.
Source: National Institute for Health and Clinical Excellence (2011) CG 127 Hypertension: clinical management of primary hypertension in adults. London: NICE. Available from www.nice.org.uk/guidance/CG127. Reproduced with permission. The NICE guidance that this algorithm relates to was prepared for the National Health Service in England and Wales. NICE guidance does not apply to the United States and NICE has not been involved in the development or adaptation of any guidance for use in the United States.The ACCF/AHA and NICE guidelines also recommend that clinicians monitor electrolyte levels of patients on ACEIs/ARBs, with The frequency depending on each patient’s medical condition.41,50
Conclusion
With 7 major classes of antihypertensive drugs and several drugs within each class, there are numerous combinations available to clinicians to manage hypertension. Existing clinical trials cannot possibly evaluate all possible combinations. Yet, as noted in the ASH statement on combination therapy, the importance of achieving goal BP in individual patients cannot be overemphasized because small differences in on-treatment BP translate into major differences in the rates of CV events.47 When considering appropriate and effective antihypertensive therapies, clinicians should assess the evidence presented in this article and from the various clinical guidelines cited. Each patient is unique and it is important for clinicians to identify the most-effective treatment regimen for each individual patient.
1. Hamdy RC. Hypertension: a turning point in the history of medicine…and mankind. South Med J. 2001;94(11):1045-1047.
2. Veterans Administration Cooperative Study Group on Antihypertensive Agents. Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA. 1967;202(11):1028-1034.
3. Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA. 1979;242(23):2562-2571.
4. Amery A, De Schaepdryver A. The European Working Party on High Blood Pressure in the Elderly. Am J Med. 1991;90(3A):1S-4S.
5. Medical Research Council Working Party. MRC trial of treatment of mild hypertension: principal results. Br Med J (Clin Res Ed). 1985;291(6488):97-104.
6. The Australian therapeutic trial in mild hypertension. Report by the Management Committee. Lancet. 1980;1(8181):1261-1267.
7. Wilhelmsen L, Berglund G, Elmfeldt D, et al. Beta-blockers versus diuretics in hypertensive men: main results from the HAPPHY trial. J Hypertens. 1987;5(5):561-572.
8. Wikstrand J, Berglund G, Tuomilehto J. Beta-blockade in the primary prevention of coronary heart disease in hypertensive patients. Review of present evidence. Circulation. 1991;84(6 Suppl):VI93-VI100.
9. Wikstrand J, Warnold I, Tuomilehto J, et al. Metoprolol versus thiazide diuretics in hypertension. Morbidity results from the MAPHY Study. Hypertension. 1991;17(4):579-588.
10. Olsson G, Tuomilehto J, Berglund G, et al. Primary prevention of sudden cardiovascular death in hypertensive patients. Mortality results from the MAPHY Study. Am J Hypertens. 1991;4(2 Pt 1):151-1511.
11. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265(24):3255-3264.
12. MRC Working Party. Medical Research Council trial of treatment of hypertension in older adults: principal results. BMJ. 1992;304(6824):405-412.
13. Dahlöf B, Lindholm LH, Hansson L, Scherstén B, Ekbom T, Wester PO. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension). Lancet. 1991;338(8778):1281-1285.
14. Neaton JD, Grimm RH, Jr, Prineas RJ, et al. Treatment of Mild Hypertension Study Research Group. Treatment of Mild Hypertension Study. Final results. JAMA. 1993;270(6):713-724.
15. Materson BJ, Reda DJ, Cushman WC, et al. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo [published correction appears in N Engl J Med. 1994;330(23):1689]. N Engl J Med. 1993;328(13):914-921.
16. Hansson L, Zanchetti A, Carruthers SG, et al. HOT Study Group. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998;351(9118):1755-1762.
17. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38 [published correction appears in BMJ. 1999;318(7175):29]. BMJ. 1998;317(7160):703-713.
18. UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. BMJ. 1998;317(7160):713-720.
19. Staessen JA, Fagard R, Thijs L, et al. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet. 1997;350(9080):757-764.
20. Liu L, Wang JG, Gong L, Liu G, Staessen JA. Systolic Hypertension in China (Syst-China) Collaborative Group. Comparison of active treatment and placebo in older Chinese patients with isolated systolic hypertension. J Hypertens. 1998;16(12 Pt 1):1823-1829.
21. Hansson L, Hedner T, Lindholm L, et al. The Captopril Prevention Project (CAPPP) in hypertension—baseline data and current status. Blood Press. 1997;6(6):365-367.
22. Hansson L, Lindholm LH, Ekbom T, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet. 1999;354(9192):1751-1756.
23. Brown MJ, Palmer CR, Castaigne A, et al. Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a Goal in Hypertension Treatment (INSIGHT) [published correction appears in Lancet. 2000;356(9228):514]. Lancet. 2000;356(9227):366-372.
24. Hansson L, Hedner T, Lund-Johansen P, et al. Randomised trial of effects of calcium antagonists compared with diuretics and beta-blockers on cardiovascular morbidity and mortality in hypertension: the Nordic Diltiazem (NORDIL) study. Lancet. 2000;356(9227):359-365.
25. Lithell H, Hansson L, Skoog I, et al. SCOPE Study Group. The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens. 2003;21(5):875-886.
26. Black HR, Elliott WJ, Grandits G, et al. CONVINCE Research Group. Principal results of the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) trial. JAMA. 2003;289(16):2073-2082.
27. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) [published corrections appear in JAMA. 2003;289(2):178; JAMA. 2004;291(18):2196]. JAMA. 2002;288(23):2981-2997.
28. Wing LM, Reid CM, Ryan P, et al. Second Australian National Blood Pressure Study Group. A comparison of outcomes with angiotensin-converting– enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med. 2003;348(7):583-592.
29. Dahlöf B, Devereux RB, Kjeldsen SE, et al. LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995-1003.
30. The ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358(15):1547-1559.
31. Weber MA, Julius S, Kjeldsen SE, et al. Blood pressure dependent and independent effects of antihypertensive treatment on clinical events in the VALUE Trial. Lancet. 2004;363(9426):2049-2051.
32. Dahlöf B, Sever PS, Poulter NR, et al. ASCOT Investigators. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895-906.
33. Jamerson K, Bakris GL, Dahlöf B, et al. ACCOMPLISH Investigators. Exceptional early blood pressure control rates: the ACCOMPLISH trial. Blood Press. 2007;16(2):80-86.
34. Julius S, Nesbitt SD, Egan BM, et al. Trial of Preventing Hypertension (TROPHY) Study Investigators. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med. 2006;354(16):1685-1697.
35. ATMOSPHERE study, [NCT00853658] ongoing trial. Trial-Results Center Web site. http://www.trialresultscenter.org/study9503-ATMOSPHERE.htm. Accessed March 28, 2012.
36. Parving HH, Brenner BM, McMurray JJ, et al. Aliskiren Trial in Type 2 Diabetes Using Cardio-Renal Endpoints (ALTITUDE): rationale and study design. Nephrol Dial Transplant. 2009;24(5):1663-1671.
37. Massie BM, Carson PE, McMurray JJ, et al. I-PRESERVE Investigators. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359(23):2456-2467.
38. US National Library of Medicine. The Edward D. Freis Papers: the VA Cooperative Study and the Beginning of Routine Hypertension Screening, 1964-1980. http://profiles.nlm.nih.gov/ps/retrieve/Narrative/XF/p-nid/172. Accessed March 26, 2012.
39. Comberg HU, Heyden S, Knowles M, et al. Long-term survey of 450 hypertensives of the HDFP. Munch Med Wochenschr. 1991;133:32-38.
40. Skoog I, Lithell H, Hansson L, et al. SCOPE Study Group. Effect of baseline cognitive function and antihypertensive treatment on cognitive and cardiovascular outcomes: Study on COgnition and Prognosis in the Elderly (SCOPE). Am J Hypertens. 2005;18(8):1052-1059.
41. Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011;57(20):2037-2114.
42. Beckett NS, Peters R, Fletcher AE, et al. HYVET Study Group. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887-1898.
43. Weber MA, Neutel JM, Frishman WH. Combination drug therapy. In: Frishman WH, Sonnenblick EH, Sica DA, eds. Cardiovascular Pharmacotherapeutics. 2nd ed. New York, NY: McGraw-Hill; 2003:355–368.
44. Pepine CJ, Handberg EM, Cooper-DeHoff RM, et al. INVEST Investigators. A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil- Trandolapril Study (INVEST): a randomized controlled trial. JAMA. 2003;290(21):2805-2816.
45. Mancia G, Messerli F, Bakris G, Zhou Q, Champion A, Pepine CJ. Blood pressure control and improved cardiovascular outcomes in the International Verapamil SR-Trandolapril Study. Hypertension. 2007;50(2):299-305.
46. Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290-300.
47. Gradman AH, Basile JN, Carter BL, et al. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(2):90-98.
48. Weir MR, Levy D, Crikelair N, Rocha R, Meng X, Glazer R. Time to achieve blood-pressure goal: influence of dose of valsartan monotherapy and valsartan and hydrochlorothiazide combination therapy. Am J Hypertens. 2007;20(7):807-815.
49. National Heart, . Lung, and Blood Institute. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. http://www.nhlbi.nih.gov/guidelines/hypertension/. Published 2003. Accessed March 27, 2012.
50. National Institute for Health and Clinical Excellence. Hypertension: Clinical management of primary hypertension in adults. http://www.nice.org.uk/nicemedia/live/13561/56008/56008.pdf. Published August 2011. Accessed March 27, 2012.
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
Dr White is President of the American Society of Hypertension (voluntary unpaid position) and is a paid cardiovascular safety consultant to Abbott Immunology; Ardea Biosciences, Inc; AstraZeneca; BioSante Pharmaceuticals, Inc; Forest Research Institute, Inc; Novartis Corporation; Roche Laboratories, Inc; and Takeda Global Research & Development Center, Inc. He holds no stocks in pharmaceutical companies and is not a member of any speakers’ bureaus.
Introduction
Hypertension is a transformative condition in modern medicine due to the various numeric definitions of the disease, the decision of when to initiate therapy and to what level to treat, and the evolution of our understanding of the long-term complications of the hypertensive disease process. Hypertension is notable as 1 of the first conditions that only rarely manifested symptoms and whose eventual sequelae could take years, if not decades, to become known. In addition, hypertension was the first condition in which clinicians initiated therapy for patients who were otherwise healthy. Hypertension also led to 1 of the first screening programs for any disease as well as the first robust preventive effort for a chronic medical condition.1
Clinical trials have been performed for 5 decades to evaluate the potential benefits of lowering blood pressure (BP) in patients with hypertension and its comorbid conditions (FIGURE 1).2-37 The first clinical trial to identify the increased risk of cardiovascular (CV) mortality related to hypertension was published in the mid-1960s.2,38 In fact, the Veterans Administration (VA) Cooperative trial was the first randomized, placebo-controlled, double-blind, multi-institutional drug efficacy trial ever conducted in CV medicine.38 It involved 143 men who met the 1964 definition of hypertension (ie, diastolic BP [DBP] ≥115 mm Hg) and who were randomized to either triple therapy with low doses of hydrochlorothiazide (HCTZ), reserpine, and hydralazine, or to placebo. The trial was terminated early when, after 18 months of treatment, rates of morbidity and mortality were substantially lower in the treated group than in the placebo group.2 The trial was the first to confirm that antihypertensive treatment, even in patients with existing CV damage and significant hypertension, could dramatically reduce the incidence of stroke, congestive heart failure (CHF), and progressive kidney damage.38
FIGURE 1
Clinical trials in hypertension during the past 5 decades
ACCOMPLISH, Avoiding Cardiovascular Events Through Combination Therapy in Patients Living With Systolic Hypertension trial; ALLHAT, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial; ALTITUDE, Aliskiren Trial in Type 2 Diabetes Using Cardiovascular and Renal Disease Endpoints; ANBP1, Australian National Blood Pressure Study 1; ANBP2, Australian National Blood Pressure Study 2; ASCOT, Anglo-Scandinavian Cardiac Outcomes Trial; ATMOSPHERE, Efficacy and Safety of Aliskiren and Aliskiren/Enalapril Combination on Morbi-mortality in Patients With Chronic Heart Failure study; CAPPP, Captopril Prevention Project; CONVINCE, Controlled Onset Verapamil Investigation of Cardiovascular End Points trial; DBP, diastolic blood pressure; EWPHE, European Working Party on High Blood Pressure in the Elderly study; HAPPHY, Heart Attack Primary Prevention in Hypertension trial; HBP, high blood pressure; HDFP, Hypertension Detection and Follow-up Program; HOT, Hypertension Optimal Treatment study; INSIGHT, International Nifedipine GITS Study of Intervention as a Goal in Hypertension Treatment; I-PRESERVE, Irbesartan in Heart Failure with Preserved Systolic Function study; ISH, isolated systolic hypertension; LIFE, Losartan Intervention For Endpoint Reduction in Hypertension trial; MAPHY, Metoprolol Atherosclerosis Prevention in Hypertensives study; MRC-1, Medical Research Council trial of treatment of mild hypertension; MRC-2, Medical Research Council trial of treatment of hypertension in older adults; NORDIL, Nordic Diltiazem study; ONTARGET, Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial; SCOPE, Study on Cognition and Prognosis in the Elderly; SHEP, Systolic Hypertension in the Elderly Program; STOP-1, Swedish Trial in Old Patients with Hypertension-1; STOP-2, Swedish Trial in Old Patients with Hypertension-2; Syst-China, Systolic Hypertension in China trial; Syst-Eur, Systolic Hypertension in Europe trial; TOMHS, Treatment of Mild Hypertension Study; TROPHY, Trial of Preventing Hypertension; UKPDS, United Kingdom Prospective Diabetes Study; VA, Veterans Administration; VA MONORx, VA Monotherapy of Hypertension study; VALUE, Valsartan Antihypertensive Long-term Use Evaluation trial.Although the Framingham Study (www.framinghamheartstudy.org) was, of course, one of the seminal studies in the field of CV medicine, it was observational in nature, rather than interventional like most of the studies highlighted in this article.
The Medical Research Council trial of the treatment of mild hypertension (MRC-1) (ie, defined as DBP 90-109 mm Hg) demonstrated that a significant reduction in DBP among individuals receiving the diuretic bendroflumethiazide or the beta-blocker propranolol significantly reduced the rate of stroke compared with placebo, with a rate of 1.4 per 1000 patient-years of observation in the treatment group vs 2.6 per 1000 patient-years in the placebo group (P < .01).5 The treatment group also had significantly lower rates of all CV events than the placebo group, and this difference was statistically significant (P < .05). However, the treatment groups experienced significantly increased rates of adverse effects compared with placebo.5
Other early notable clinical trials that evaluated treatment options for hypertension in the general public include the Hypertension Detection and Follow-up Program (HDFP),3 the Hypertension Optimal Treatment (HOT) study,16 and the United Kingdom Prospective Diabetes Study/Hypertension in Diabetes (UKPDS/HDS).17,18 The key outcomes of these trials are shown in TABLE 1.3,4,11,12,16,20,22,25,39,40
TABLE 1
Findings from the early clinical trials in hypertension
| Clinical Trial | Intervention | Primary Outcome | Result |
|---|---|---|---|
| HDFP3,39 | Patients randomized to systemic antihypertensive treatment or community medical therapy (referral) | 5-year mortality | 5-year mortality reduced by 17% in treatment group (P < 0.01); after 12 years, BP still higher in treatment than in stepped-care treatment group |
| HOT16 | Patients all began on felodipine, with an ACEI or a BB added as necessary If BP goal was still not reached, HCTZ could be added Patients in each group also randomized to low-dose aspirin or placebo Subjects were randomly assigned to reach 1 of 3 DBP goals: ≤90 mm Hg; ≤85 mm Hg; or ≤80 mm Hg | Major CV events with 3 target DBPs reached during therapy and with low-dose aspirin therapy | Lowest incidence of major CV events achieved at mean BP of 138.5/82.6 mm Hg; lowest risk of CV mortality achieved at mean BP of 138.8/86.5 mm Hg Low-dose aspirin reduced major CV events by 15% and all MI by 36%, although nonfatal major bleeding was twice as common with low-dose aspirin than with placebo |
| UKPDS/HDS17,18 | Patients with T2DM randomized to atenolol or captopril, with additional antihypertensive agents (other than ACEIs or BBs) allowed | Effect of tight BP control on diabetes-related complications, morbidity, and mortality | Tight BP control (<150/85 mm Hg) with either atenolol or captopril significantly reduced the risk of all endpoints, including risk of diabetes-related death or complication, stroke, MI, and heart failure |
| EWPHPE4 | Patients ≥60 years of age randomized to HCTZ + triamterene + methyldopa or placebo | CV and MI mortality; nonfatal CV events | Significant reduction in CV and MI mortality (P < .05) but not nonfatal CV events in treatment group vs placebo Found U-shaped relationship between mortality and SBP in treated group vs mortality and DBP in placebo group |
| MRC-212 | Patients 65-74 years of age randomized to atenolol + HCTZ or amiloride | Reduction in mortality and morbidity due to stroke and CHD and reduction in mortality due to all causes | Only the HCTZ group demonstrated a significant reduction in stroke, coronary events, and all CV events (P=.4, P=.0009, and P=.0005, respectively) |
| STOP-222 | Patients 70-84 years of age randomized to atenolol + HCTZ or amiloride; or to metoprolol or prinodolol | Incidence of fatal stroke, MI, or other CVD mortality | Similar reductions in BP, mortality, and major events in all treatment groups |
| SCOPE25 | Patients 70-89 years of age randomized to candesartan or placebo (open-label antihypertensive therapy added as needed and extensively used in control group) | Major CV events; secondary measures included CV death, nonfatal and fatal stroke and MI, cognitive function | Greater BP decreases in candesartan group but no significant risk reduction in major CV events between the 2 groups Significant reduction in nonfatal stroke (P=.04) and all stroke (P=.06) in the treatment group No other significant differences between the groups, although a post-hoc analysis found less cognitive decline among those with only mild cognitive impairment at baseline in the candesartan-treated group (P=.04)40 |
| SHEP11 | Patients ≥60 years of age randomized to chlorthalidone with or without atenolol or reserpine, with nifedipine as third-line therapy, or to placebo | Stroke; nonfatal MI, coronary death, major CV events, death due to all causes | Significant reduction in 5-year incidence of total stroke in active treatment group (P=.0003) and significant reduction in all secondary endpoints |
| Syst-Eur19 | Patients >60 years of age randomized to nitrendipine with possible addition of enalapril, HCTZ, or both, or to placebo | Fatal and nonfatal stroke, fatal and nonfatal cardiac events including sudden death, all-cause mortality | Significant reductions in all endpoints except all-cause mortality in treatment group; study halted early because of the 42% total stroke reduction in treatment arm (P < .003) |
| Syst-China20 | Patients ≥60 years of age randomized to nitrendipine with captopril or HCTZ, or both if needed; or matching placebo | Nonfatal stroke; all-cause, CV, and stroke mortality; and all fatal and nonfatal CV events | Significant reductions in all endpoints |
| ACEI, angiotensin-converting enzyme inhibitor; BB, beta-blocker; BP, blood pressure; CV, cardiovascular; CHD, coronary heart disease; CVD, CV disease; DBP, diastolic BP; EWPHE, European Working Party on High Blood Pressure in the Elderly study; HDFP, Hypertension Detection and Follow-up Program; HCTZ, hydrochlorothiazide; HOT, Hypertension Optimal Treatment study; MI, myocardial infarction; MRC-2, Medical Research Council trial of treatment of hypertension in older adults; SBP, systolic BP; SCOPE, Study on Cognition and Prognosis in the Elderly; SHEP, Systolic Hypertension in the Elderly Program; STOP-2, Swedish Trial in Old Patients with Hypertension-2; Syst-Eur, Systolic Hypertension in Europe trial; Syst-China, Systolic Hypertension in China trial; T2DM, type 2 diabetes mellitus; UKPDS/HDS, United Kingdom Prospective Diabetes Study/Hypertension in Diabetes. | |||
Given that hypertension is far more common in older people who have increased rates of hypertensive target organ damage or CV disease (CVD), researchers have focused on the effects of antihypertensive therapy in this population for some time.41 Sentinel studies in this population include the European Working Party on High Blood Pressure in the Elderly (EWPHPE) study,4 the Medical Research Council trial of treatment of hypertension in older adults (MRC-2),12 the Swedish Trial in Old Patients with Hypertension-2 (STOP-2),22 the Study on Cognition and Prognosis in the Elderly (SCOPE),25 the Systolic Hypertension in the Elderly Program (SHEP) study,11 the Systolic Hypertension in Europe (Syst-Eur) study,19 and the Systolic Hypertension in China (Syst-China) study.20 The key outcomes of these trials are shown in TABLE 1. In general, these trials have shown that antihypertensive therapy has a marked benefit in a shorter period of time in older patients than in younger patients, particularly in terms of reduced stroke and CHF rates.
The Hypertension in the Very Elderly Trial (HYVET), which enrolled participants 80 years of age and older, demonstrated that reducing systolic BP (SBP) from 170 mm Hg to 145 mm Hg with indapamide sustained release 1.5 mg and perindopril 2 to 4 mg as needed reduced all-cause deaths 21% (P =.02), stroke-related deaths 39% (P =.05), and fatal and nonfatal heart failure (HF) 64% (P < .001), compared with placebo.42 The intervention group also experienced a 34% reduction in all CV events (P < .001) and a 30% reduction in stroke (P =.055).42 However, there is still no good evidence that reducing BP further in this population provides additional benefits over the concomitant risks.
In the 1980s, numerous trials were developed to address the question: “What is the best way to treat high BP?” These included the Heart Attack Primary Prevention in Hypertension (HAPPHY) trial,7 the Metoprolol Atherosclerosis Prevention in Hypertensives (MAPHY) study,8-10 the Treatment of Mild Hypertension Study (TOMHS),14 and the VA Cooperative Study on single drug therapy.15
Subsequently, several trials were conducted that focused on the safety of calcium antagonists for the primary or background treatment of hypertension. These included the International Nifedipine GITS Study of Intervention as a Goal in Hypertension Treatment (INSIGHT),23 the Nordic Diltiazem (NORDIL) study,24 the Australian National Blood Pressure Study 2 (ANBP2),28 the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) trial,26 the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial,29 and the Irbesartan in Heart Failure with Preserved Systolic Function (I-PRESERVE) study.37
These studies, conducted from the mid 1990s to the present, have shown that calcium antagonists, including amlodipine, diltiazem, nifedipine, and verapamil, are as effective as thiazide-type diuretics or beta-blockers in preventing CV events in patients with hypertension. Further, the LIFE trial demonstrated that the angiotensin II receptor blocker (ARB) losartan was more effective than the beta-blocker atenolol in reducing stroke events and that blockade of the renin- angiotensin system did not seem to affect CV outcomes in patients with HF with preserved systolic function, a common problem in patients with prolonged hypertension and left ventricular hypertrophy.29
The largest randomized, double-blind, antihypertensive trial performed to date is the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). It involved 33,357 participants 55 years of age and older with hypertension and at least 1 other coronary heart disease (CHD) risk factor.27 Participants were randomized to chlorthalidone, amlodipine, doxazosin, or lisinopril. The doxazosin arm was discontinued early because an increase in CV events was observed after 2 years, relative to the other treatment arms. At follow-up (mean, 4.9 years), there was no difference between the 3 groups in terms of the primary outcome (combined fatal CHD or nonfatal myocardial infarction [MI], analyzed by intent-to-treat) or all-cause mortality.27 Of note, 5-year SBP levels were higher in the amlodipine (0.8 mm Hg, P=.03) and lisinopril (2 mm Hg, P < .001) groups than in the chlorthalidone group, whereas the 5-year DBP levels were significantly lower in the amlodipine group (0.8 mm Hg, P < .001).27
Secondary analyses showed a higher 6-year rate of HF development in the amlodipine group than in the chlorthali-done group (10.2% vs 7.7%; relative risk [RR], 1.38; 95% con- fidence interval [CI], 1.25-1.52), whereas the lisinopril group had a higher 6-year rate of combined CVD (33.3% vs 30.9%; RR, 1.10; 95% CI, 1.05-1.16), stroke (6.3% vs 5.6%; RR, 1.15; 95% CI, 1.02-1.30), and HF (8.7% vs 7.7%; RR, 1.19; 95% CI, 1.07-1.31) than the chlorthalidone group. The design of ALLHAT led to worsened control of BP in African Americans relative to white patients who were receiving lisinopril, which may have been an important factor in the subsequent increased rate of stroke in African American patients who were receiving lisinopril rather than chlorthalidone.27
Subsequent to ALLHAT, the benefits and safety of calcium antagonists vs a thiazide diuretic combined with an angiotensin-converting enzyme inhibitor (ACEI) were ad-dressed by the Avoiding Cardiovascular Events Through Combination Therapy in Patients Living With Systolic Hypertension (ACCOMPLISH) trial.33 This study randomized 11,506 patients with a mean BP of 145/80 mm Hg to combination therapy with benazepril (40 mg/d) and amlodipine (5-10 mg/d) or benazepril and HCTZ (12.5-25 mg/d). Other antihypertensive medications could be added to reach a target BP <140/90 mm Hg (130/80 mm Hg in patients with diabetes or renal insufficiency).33 The study was stopped early at 3 years because the primary outcome of CV death, nonfatal MI or stroke, hospitalization for angina, resuscitation after sudden cardiac arrest, and coronary revascularization occurred in 552 patients in the benazepril-amlodipine group compared with 679 patients in the benazepril-HCTZ group (9.6% vs 11.8%; RR ratio, 19.6%; hazard ratio [HR], 0.80; P < .001). The mechanism for the benefit observed in the benazepril-amlodipine group may relate in part to improved coronary blood flow that occurs with a calcium antagonist (compared with a diuretic) since BP control was virtually the same in both groups.
Another major hypertension study during the same era was the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT).32 This study enrolled 19,257 patients in northern Europe with a mean age of 63 years, an untreated baseline BP ≥160/100 mm Hg or a treated mean BP ≥140/90 mm Hg, and 3 or more of 11 prespecified risk factors for CV. Patients were randomized to amlodipine, with or without perindopril, or atenolol, with or without a thiazide diuretic, and were titrated to reach a BP goal <140/90 mm Hg. The study was halted early after a mean follow up of 5.5 years. Although there was no statistically significant difference in the primary events of nonfatal MI plus fatal CHF between the 2 arms, fewer patients randomized to the amlodipine-based regimen experienced a fatal or nonfatal stroke (327 vs 422; HR, 0.77; 95% CI, 0.66-0.89; P=.0003) and total CV events and procedures were lower in patients taking the amlodipine-based regimen than in those taking the atenolol-based regimen (1362 vs 1602; HR, 0.84; 95% CI, 0.78-0.90; P < .0001).32 All-cause mortality was also lower in the amlodipine-based group (738 vs 820; HR, 0.89; 95% CI, 0.81-0.99; P=.025), and significantly fewer patients in this arm developed diabetes (567 vs 799; HR, 0.70; 95% CI, 0.63-0.78; P < .0001).32
Patients with diabetes in ASCOT who were titrated to achieve a target BP <130/80 mm Hg experienced significantly lower mortality and stroke when taking the amlodipine-based regimen than when taking the atenolol-based regimen (HR, 0.86; 95% CI, 0.76-0.98; P=.026).32 In the group taking the atenolol-based regimen, fatal and nonfatal strokes were reduced by 25% (P=.017), peripheral arterial disease by 48% (P=.004), and peripheral revascularization procedures by 57% (P < .001). There were no statistically significant differences in the endpoints of CHD deaths and nonfatal MI in the diabetes subgroup.
Combination therapy and guideline recommendations
By the 1970s, it became clear that combinations of antihypertensive drugs increased BP lowering efficacy through both additive and synergistic mechanisms. These combinations also reduced adverse events because lower doses of each drug could be used, whereas drugs from different classes might offset each other’s adverse effects. In addition, combining antihypertensive drugs could prolong duration of action, possibly providing additional target organ protection.43 Combining drugs from complementary classes has also been shown to increase the likelihood of BP lowering compared with increasing the dose of a single drug, thus reducing the time required to reach BP goal.31,44-46
The 2010 American Society of Hypertension (ASH) position statement on combination therapy in hypertension therapy notes that at least 75% of patients will require combination therapy to reach goal.47 In addition, a meta-analysis of 9 randomized clinical trials found that combination treatment using a thiazide or thiazide-like diuretic as one of the components could provide a significantly greater effect than monotherapy lacking the diuretic, with similar discontinuation rates.48
Government guidelines in the United States, now nearly 10 years old, do not recommend combination therapy as a first-line approach unless patients have stage 2 hypertension (SBP ≥160 mm Hg or DBP ≥100 mm Hg). At that point, the guidelines recommend combination therapy with a thiazide or thiazide-type diuretic plus either an ACEI, ARB, beta-blocker, or calcium antagonist.49 More-specific recommendations are provided for patients with compelling indications (eg, HF, ischemic heart disease, chronic kidney disease, recurrent stroke, diabetes, and high coronary disease risk), as shown in TABLE 2.41,49 New recommendations from the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 8) are expected later this year.
TABLE 2
Antihypertensive treatment in patients with compelling indications41,49
| Indication | Diuretic | BB | ACEI | ARB | Calcium antagonist | Aldosterone antagonist |
|---|---|---|---|---|---|---|
| Heart failure | ||||||
| Post MI | ||||||
| CVD or high CVD risk | ||||||
| Anginaa | ||||||
| Aortopathy/aortic aneurysma | ||||||
| Diabetes | ||||||
| Recurrent stroke prevention | ||||||
| CKDb | ||||||
| Early dementiaa | ||||||
ACCF, American College of Cardiology Foundation; ACEI, angiotensin-converting enzyme inhibitor; AHA, American Heart Association; ARB, angiotensin-receptor blocker; BB, beta-blocker; CVD, cardiovascular disease; CKD, chronic kidney disease; MI, myocardial infarction. aNot considered “compelling” indication in JNC-7 Express guidelines. bNot considered “compelling” recommendation in ACCF/AHA recommendations. Source: Journal of the American College of Cardiology by American College of Cardiology. Reproduced with permission of Elsevier Inc. in the format Journal via Copyright Clearance Center. | ||||||
Recent guidelines from ASH describe combination therapies of hypertension in categories of preferred, acceptable, and less effective, based on efficacy in lowering BP, safety and tolerability, and certain known outcomes from longer-term trials (TABLE 3).47
TABLE 3
Drug combinations in hypertension: Recommendations from the American Society of Hypertension47
| Preferred | Acceptable | Less Effective |
|---|---|---|
| ACEI + diuretica | BB + diuretica | ACEI + ARB |
| ARB + diuretica | Calcium antagonist + diuretic | ACEI + BB |
| ACEI + CCBa | Renin inhibitor + diuretic | ARB + BB |
| ARB + CCBa | Renin inhibitor + ARBa,b | CCB (non-dihydropyridine) + BB |
| Thiazide diuretic + potassium-sparing diuretica | Centrally acting agent + BB | |
| ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin-receptor blocker; BB, beta-blocker; CCB, calcium channel blocker. aAvailable as single-pill combination. bThis may be medically inappropriate in patients with diabetes and chronic diabetic nephropathy. Source: Journal of the American Society of Hypertension: JASH by American Society of Hypertension. Reproduced with permission of Elsevier Inc. in the format Journal via Copyright Clearance Center. | ||
In 2010, the American College of Cardiology Foundation (ACCF)/American Heart Association (AHA) published an expert consensus document on hypertension in the elderly. It recommends single therapy or combination therapy with an ACEI, ARB, calcium antagonist, or diuretic for patients 65 years of age and older with stage 1 hypertension and no “compelling” indications (eg, HF, post-MI, known coronary disease, angina, aortopathy/aortic aneurysm, diabetes, recurrent stroke prevention, chronic kidney disease, and early vascular dementia), but combination therapy for those with stage 2 hypertension and no compelling indications. For the former group, the panel notes that the combination of amlodipine with a renin-angiotensin aldosterone system blocker may be preferable to a diuretic combination, although either is acceptable.41
For patients with compelling indications, the ACCF/AHA panel recommends condition-based combination therapy with 2 or more of the therapies summarized in TABLE 2.41,49 The panel’s algorithm for the management of hypertension in the elderly is depicted in FIGURE 2.41
FIGURE 2
ACCF/AHA algorithm for the management of hypertension in the elderly41
ACCF, American College of Cardiology Foundation; ACEI, angiotensin-converting enzyme inhibitor; AHA, American Heart Association; ALDO ANT, aldosterone antagonist; ARB, angiotensin II receptor blocker; BB, beta-blocker; BP, blood pressure; CA, calcium antagonist; CAD, coronary artery disease; CVD, cardiovascular disease; DBP, diastolic BP; MI, myocardial infarction; RAS, renin-angiotensin system; SBP, systolic BP; THIAZ, thiazide diuretic.
aCombination therapy.
Source: Journal of the American College of Cardiology by American College of Cardiology. Reproduced with permission of Elsevier Inc. in the format Journal via Copyright Clearance Center.The National Institute for Health and Clinical Excellence (NICE), the United Kingdom-based clinical guideline development organization, recommends in its 2011 guidelines for the clinical management of primary hypertension in adults that patients less than 55 years of age, not of black African or Caribbean heritage, begin treatment with an ACEI or ARB.50 The guidelines do not recommend beta-blockers for initial therapy, noting that they should be considered only in younger patients with intolerance or contraindications to ACEIs and ARBs, reproductive-aged women, and those with clinical evidence of increased sympathetic drive.50
In contrast, patients 55 years and older, or blacks of African or Caribbean origin of any age, should begin treatment with a calcium channel blocker (CCB).50 If they cannot tolerate a CCB, or for those with HF (or at high risk of HF), the guidelines recommend beginning therapy with a diuretic (preferably chlorthalidone or in-dapamide unless the patient’s hypertension is already controlled with bendroflumethiazide or HCTZ).
If initial treatment fails to lower BP adequately, step 2 of the NICE guidelines for all populations is treatment with an ACEI or ARB in combination with a calcium antagonist.50 If further therapy is necessary (step 3), a thiazide diuretic (or thiazide-like) should be added to that combination. It is also recommended that patients with drug-resistant hypertension (ie, taking 3 agents at maximally tolerated doses, 1 of which should be a diuretic) should receive additional treatment with low-dose spironolactone (if their serum potassium level is ≤4.5 mmol/L) and higher-dose thiazide-type diuretics (if their serum potassium level is >4.5 mmol/L). If the diuretic is not tolerated or is ineffective, an alpha- or beta-blocker may be added. If patients continue to exhibit continued resistance, NICE recommends referral to a hypertension specialist. The NICE algorithm for the treatment of hypertension is shown in FIGURE 3.50
FIGURE 3
NICE algorithm for treatment of hypertension50
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; CCB, calcium channel blocker; NICE, National Institute for Health and Clinical Excellence.
aChoose a low-cost ARB.
bA CCB is preferred but consider a thiazide-like diuretic if a CCB is not tolerated or the person has edema, evidence of heart failure, or a high risk of heart failure.
cConsider a low dose of spironolactoned or higher doses of thiazide-like diuretic
dAt the time of publication (August 2011), spironolactone did not have a UK marketing authorization for this indication. Informed consent should be obtained and documented.
eConsider an alpha- or beta-blocker if further diuretic therapy is not tolerated or is contraindicated or ineffective.
Source: National Institute for Health and Clinical Excellence (2011) CG 127 Hypertension: clinical management of primary hypertension in adults. London: NICE. Available from www.nice.org.uk/guidance/CG127. Reproduced with permission. The NICE guidance that this algorithm relates to was prepared for the National Health Service in England and Wales. NICE guidance does not apply to the United States and NICE has not been involved in the development or adaptation of any guidance for use in the United States.The ACCF/AHA and NICE guidelines also recommend that clinicians monitor electrolyte levels of patients on ACEIs/ARBs, with The frequency depending on each patient’s medical condition.41,50
Conclusion
With 7 major classes of antihypertensive drugs and several drugs within each class, there are numerous combinations available to clinicians to manage hypertension. Existing clinical trials cannot possibly evaluate all possible combinations. Yet, as noted in the ASH statement on combination therapy, the importance of achieving goal BP in individual patients cannot be overemphasized because small differences in on-treatment BP translate into major differences in the rates of CV events.47 When considering appropriate and effective antihypertensive therapies, clinicians should assess the evidence presented in this article and from the various clinical guidelines cited. Each patient is unique and it is important for clinicians to identify the most-effective treatment regimen for each individual patient.
MODULE 1: Historical Review of Evidence-Based Treatment of Hypertension
MODULE 3: Using Thiazide-Type Diuretics in African Americans with Hypertension
Dr White is President of the American Society of Hypertension (voluntary unpaid position) and is a paid cardiovascular safety consultant to Abbott Immunology; Ardea Biosciences, Inc; AstraZeneca; BioSante Pharmaceuticals, Inc; Forest Research Institute, Inc; Novartis Corporation; Roche Laboratories, Inc; and Takeda Global Research & Development Center, Inc. He holds no stocks in pharmaceutical companies and is not a member of any speakers’ bureaus.
Introduction
Hypertension is a transformative condition in modern medicine due to the various numeric definitions of the disease, the decision of when to initiate therapy and to what level to treat, and the evolution of our understanding of the long-term complications of the hypertensive disease process. Hypertension is notable as 1 of the first conditions that only rarely manifested symptoms and whose eventual sequelae could take years, if not decades, to become known. In addition, hypertension was the first condition in which clinicians initiated therapy for patients who were otherwise healthy. Hypertension also led to 1 of the first screening programs for any disease as well as the first robust preventive effort for a chronic medical condition.1
Clinical trials have been performed for 5 decades to evaluate the potential benefits of lowering blood pressure (BP) in patients with hypertension and its comorbid conditions (FIGURE 1).2-37 The first clinical trial to identify the increased risk of cardiovascular (CV) mortality related to hypertension was published in the mid-1960s.2,38 In fact, the Veterans Administration (VA) Cooperative trial was the first randomized, placebo-controlled, double-blind, multi-institutional drug efficacy trial ever conducted in CV medicine.38 It involved 143 men who met the 1964 definition of hypertension (ie, diastolic BP [DBP] ≥115 mm Hg) and who were randomized to either triple therapy with low doses of hydrochlorothiazide (HCTZ), reserpine, and hydralazine, or to placebo. The trial was terminated early when, after 18 months of treatment, rates of morbidity and mortality were substantially lower in the treated group than in the placebo group.2 The trial was the first to confirm that antihypertensive treatment, even in patients with existing CV damage and significant hypertension, could dramatically reduce the incidence of stroke, congestive heart failure (CHF), and progressive kidney damage.38
FIGURE 1
Clinical trials in hypertension during the past 5 decades
ACCOMPLISH, Avoiding Cardiovascular Events Through Combination Therapy in Patients Living With Systolic Hypertension trial; ALLHAT, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial; ALTITUDE, Aliskiren Trial in Type 2 Diabetes Using Cardiovascular and Renal Disease Endpoints; ANBP1, Australian National Blood Pressure Study 1; ANBP2, Australian National Blood Pressure Study 2; ASCOT, Anglo-Scandinavian Cardiac Outcomes Trial; ATMOSPHERE, Efficacy and Safety of Aliskiren and Aliskiren/Enalapril Combination on Morbi-mortality in Patients With Chronic Heart Failure study; CAPPP, Captopril Prevention Project; CONVINCE, Controlled Onset Verapamil Investigation of Cardiovascular End Points trial; DBP, diastolic blood pressure; EWPHE, European Working Party on High Blood Pressure in the Elderly study; HAPPHY, Heart Attack Primary Prevention in Hypertension trial; HBP, high blood pressure; HDFP, Hypertension Detection and Follow-up Program; HOT, Hypertension Optimal Treatment study; INSIGHT, International Nifedipine GITS Study of Intervention as a Goal in Hypertension Treatment; I-PRESERVE, Irbesartan in Heart Failure with Preserved Systolic Function study; ISH, isolated systolic hypertension; LIFE, Losartan Intervention For Endpoint Reduction in Hypertension trial; MAPHY, Metoprolol Atherosclerosis Prevention in Hypertensives study; MRC-1, Medical Research Council trial of treatment of mild hypertension; MRC-2, Medical Research Council trial of treatment of hypertension in older adults; NORDIL, Nordic Diltiazem study; ONTARGET, Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial; SCOPE, Study on Cognition and Prognosis in the Elderly; SHEP, Systolic Hypertension in the Elderly Program; STOP-1, Swedish Trial in Old Patients with Hypertension-1; STOP-2, Swedish Trial in Old Patients with Hypertension-2; Syst-China, Systolic Hypertension in China trial; Syst-Eur, Systolic Hypertension in Europe trial; TOMHS, Treatment of Mild Hypertension Study; TROPHY, Trial of Preventing Hypertension; UKPDS, United Kingdom Prospective Diabetes Study; VA, Veterans Administration; VA MONORx, VA Monotherapy of Hypertension study; VALUE, Valsartan Antihypertensive Long-term Use Evaluation trial.Although the Framingham Study (www.framinghamheartstudy.org) was, of course, one of the seminal studies in the field of CV medicine, it was observational in nature, rather than interventional like most of the studies highlighted in this article.
The Medical Research Council trial of the treatment of mild hypertension (MRC-1) (ie, defined as DBP 90-109 mm Hg) demonstrated that a significant reduction in DBP among individuals receiving the diuretic bendroflumethiazide or the beta-blocker propranolol significantly reduced the rate of stroke compared with placebo, with a rate of 1.4 per 1000 patient-years of observation in the treatment group vs 2.6 per 1000 patient-years in the placebo group (P < .01).5 The treatment group also had significantly lower rates of all CV events than the placebo group, and this difference was statistically significant (P < .05). However, the treatment groups experienced significantly increased rates of adverse effects compared with placebo.5
Other early notable clinical trials that evaluated treatment options for hypertension in the general public include the Hypertension Detection and Follow-up Program (HDFP),3 the Hypertension Optimal Treatment (HOT) study,16 and the United Kingdom Prospective Diabetes Study/Hypertension in Diabetes (UKPDS/HDS).17,18 The key outcomes of these trials are shown in TABLE 1.3,4,11,12,16,20,22,25,39,40
TABLE 1
Findings from the early clinical trials in hypertension
| Clinical Trial | Intervention | Primary Outcome | Result |
|---|---|---|---|
| HDFP3,39 | Patients randomized to systemic antihypertensive treatment or community medical therapy (referral) | 5-year mortality | 5-year mortality reduced by 17% in treatment group (P < 0.01); after 12 years, BP still higher in treatment than in stepped-care treatment group |
| HOT16 | Patients all began on felodipine, with an ACEI or a BB added as necessary If BP goal was still not reached, HCTZ could be added Patients in each group also randomized to low-dose aspirin or placebo Subjects were randomly assigned to reach 1 of 3 DBP goals: ≤90 mm Hg; ≤85 mm Hg; or ≤80 mm Hg | Major CV events with 3 target DBPs reached during therapy and with low-dose aspirin therapy | Lowest incidence of major CV events achieved at mean BP of 138.5/82.6 mm Hg; lowest risk of CV mortality achieved at mean BP of 138.8/86.5 mm Hg Low-dose aspirin reduced major CV events by 15% and all MI by 36%, although nonfatal major bleeding was twice as common with low-dose aspirin than with placebo |
| UKPDS/HDS17,18 | Patients with T2DM randomized to atenolol or captopril, with additional antihypertensive agents (other than ACEIs or BBs) allowed | Effect of tight BP control on diabetes-related complications, morbidity, and mortality | Tight BP control (<150/85 mm Hg) with either atenolol or captopril significantly reduced the risk of all endpoints, including risk of diabetes-related death or complication, stroke, MI, and heart failure |
| EWPHPE4 | Patients ≥60 years of age randomized to HCTZ + triamterene + methyldopa or placebo | CV and MI mortality; nonfatal CV events | Significant reduction in CV and MI mortality (P < .05) but not nonfatal CV events in treatment group vs placebo Found U-shaped relationship between mortality and SBP in treated group vs mortality and DBP in placebo group |
| MRC-212 | Patients 65-74 years of age randomized to atenolol + HCTZ or amiloride | Reduction in mortality and morbidity due to stroke and CHD and reduction in mortality due to all causes | Only the HCTZ group demonstrated a significant reduction in stroke, coronary events, and all CV events (P=.4, P=.0009, and P=.0005, respectively) |
| STOP-222 | Patients 70-84 years of age randomized to atenolol + HCTZ or amiloride; or to metoprolol or prinodolol | Incidence of fatal stroke, MI, or other CVD mortality | Similar reductions in BP, mortality, and major events in all treatment groups |
| SCOPE25 | Patients 70-89 years of age randomized to candesartan or placebo (open-label antihypertensive therapy added as needed and extensively used in control group) | Major CV events; secondary measures included CV death, nonfatal and fatal stroke and MI, cognitive function | Greater BP decreases in candesartan group but no significant risk reduction in major CV events between the 2 groups Significant reduction in nonfatal stroke (P=.04) and all stroke (P=.06) in the treatment group No other significant differences between the groups, although a post-hoc analysis found less cognitive decline among those with only mild cognitive impairment at baseline in the candesartan-treated group (P=.04)40 |
| SHEP11 | Patients ≥60 years of age randomized to chlorthalidone with or without atenolol or reserpine, with nifedipine as third-line therapy, or to placebo | Stroke; nonfatal MI, coronary death, major CV events, death due to all causes | Significant reduction in 5-year incidence of total stroke in active treatment group (P=.0003) and significant reduction in all secondary endpoints |
| Syst-Eur19 | Patients >60 years of age randomized to nitrendipine with possible addition of enalapril, HCTZ, or both, or to placebo | Fatal and nonfatal stroke, fatal and nonfatal cardiac events including sudden death, all-cause mortality | Significant reductions in all endpoints except all-cause mortality in treatment group; study halted early because of the 42% total stroke reduction in treatment arm (P < .003) |
| Syst-China20 | Patients ≥60 years of age randomized to nitrendipine with captopril or HCTZ, or both if needed; or matching placebo | Nonfatal stroke; all-cause, CV, and stroke mortality; and all fatal and nonfatal CV events | Significant reductions in all endpoints |
| ACEI, angiotensin-converting enzyme inhibitor; BB, beta-blocker; BP, blood pressure; CV, cardiovascular; CHD, coronary heart disease; CVD, CV disease; DBP, diastolic BP; EWPHE, European Working Party on High Blood Pressure in the Elderly study; HDFP, Hypertension Detection and Follow-up Program; HCTZ, hydrochlorothiazide; HOT, Hypertension Optimal Treatment study; MI, myocardial infarction; MRC-2, Medical Research Council trial of treatment of hypertension in older adults; SBP, systolic BP; SCOPE, Study on Cognition and Prognosis in the Elderly; SHEP, Systolic Hypertension in the Elderly Program; STOP-2, Swedish Trial in Old Patients with Hypertension-2; Syst-Eur, Systolic Hypertension in Europe trial; Syst-China, Systolic Hypertension in China trial; T2DM, type 2 diabetes mellitus; UKPDS/HDS, United Kingdom Prospective Diabetes Study/Hypertension in Diabetes. | |||
Given that hypertension is far more common in older people who have increased rates of hypertensive target organ damage or CV disease (CVD), researchers have focused on the effects of antihypertensive therapy in this population for some time.41 Sentinel studies in this population include the European Working Party on High Blood Pressure in the Elderly (EWPHPE) study,4 the Medical Research Council trial of treatment of hypertension in older adults (MRC-2),12 the Swedish Trial in Old Patients with Hypertension-2 (STOP-2),22 the Study on Cognition and Prognosis in the Elderly (SCOPE),25 the Systolic Hypertension in the Elderly Program (SHEP) study,11 the Systolic Hypertension in Europe (Syst-Eur) study,19 and the Systolic Hypertension in China (Syst-China) study.20 The key outcomes of these trials are shown in TABLE 1. In general, these trials have shown that antihypertensive therapy has a marked benefit in a shorter period of time in older patients than in younger patients, particularly in terms of reduced stroke and CHF rates.
The Hypertension in the Very Elderly Trial (HYVET), which enrolled participants 80 years of age and older, demonstrated that reducing systolic BP (SBP) from 170 mm Hg to 145 mm Hg with indapamide sustained release 1.5 mg and perindopril 2 to 4 mg as needed reduced all-cause deaths 21% (P =.02), stroke-related deaths 39% (P =.05), and fatal and nonfatal heart failure (HF) 64% (P < .001), compared with placebo.42 The intervention group also experienced a 34% reduction in all CV events (P < .001) and a 30% reduction in stroke (P =.055).42 However, there is still no good evidence that reducing BP further in this population provides additional benefits over the concomitant risks.
In the 1980s, numerous trials were developed to address the question: “What is the best way to treat high BP?” These included the Heart Attack Primary Prevention in Hypertension (HAPPHY) trial,7 the Metoprolol Atherosclerosis Prevention in Hypertensives (MAPHY) study,8-10 the Treatment of Mild Hypertension Study (TOMHS),14 and the VA Cooperative Study on single drug therapy.15
Subsequently, several trials were conducted that focused on the safety of calcium antagonists for the primary or background treatment of hypertension. These included the International Nifedipine GITS Study of Intervention as a Goal in Hypertension Treatment (INSIGHT),23 the Nordic Diltiazem (NORDIL) study,24 the Australian National Blood Pressure Study 2 (ANBP2),28 the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) trial,26 the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial,29 and the Irbesartan in Heart Failure with Preserved Systolic Function (I-PRESERVE) study.37
These studies, conducted from the mid 1990s to the present, have shown that calcium antagonists, including amlodipine, diltiazem, nifedipine, and verapamil, are as effective as thiazide-type diuretics or beta-blockers in preventing CV events in patients with hypertension. Further, the LIFE trial demonstrated that the angiotensin II receptor blocker (ARB) losartan was more effective than the beta-blocker atenolol in reducing stroke events and that blockade of the renin- angiotensin system did not seem to affect CV outcomes in patients with HF with preserved systolic function, a common problem in patients with prolonged hypertension and left ventricular hypertrophy.29
The largest randomized, double-blind, antihypertensive trial performed to date is the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). It involved 33,357 participants 55 years of age and older with hypertension and at least 1 other coronary heart disease (CHD) risk factor.27 Participants were randomized to chlorthalidone, amlodipine, doxazosin, or lisinopril. The doxazosin arm was discontinued early because an increase in CV events was observed after 2 years, relative to the other treatment arms. At follow-up (mean, 4.9 years), there was no difference between the 3 groups in terms of the primary outcome (combined fatal CHD or nonfatal myocardial infarction [MI], analyzed by intent-to-treat) or all-cause mortality.27 Of note, 5-year SBP levels were higher in the amlodipine (0.8 mm Hg, P=.03) and lisinopril (2 mm Hg, P < .001) groups than in the chlorthalidone group, whereas the 5-year DBP levels were significantly lower in the amlodipine group (0.8 mm Hg, P < .001).27
Secondary analyses showed a higher 6-year rate of HF development in the amlodipine group than in the chlorthali-done group (10.2% vs 7.7%; relative risk [RR], 1.38; 95% con- fidence interval [CI], 1.25-1.52), whereas the lisinopril group had a higher 6-year rate of combined CVD (33.3% vs 30.9%; RR, 1.10; 95% CI, 1.05-1.16), stroke (6.3% vs 5.6%; RR, 1.15; 95% CI, 1.02-1.30), and HF (8.7% vs 7.7%; RR, 1.19; 95% CI, 1.07-1.31) than the chlorthalidone group. The design of ALLHAT led to worsened control of BP in African Americans relative to white patients who were receiving lisinopril, which may have been an important factor in the subsequent increased rate of stroke in African American patients who were receiving lisinopril rather than chlorthalidone.27
Subsequent to ALLHAT, the benefits and safety of calcium antagonists vs a thiazide diuretic combined with an angiotensin-converting enzyme inhibitor (ACEI) were ad-dressed by the Avoiding Cardiovascular Events Through Combination Therapy in Patients Living With Systolic Hypertension (ACCOMPLISH) trial.33 This study randomized 11,506 patients with a mean BP of 145/80 mm Hg to combination therapy with benazepril (40 mg/d) and amlodipine (5-10 mg/d) or benazepril and HCTZ (12.5-25 mg/d). Other antihypertensive medications could be added to reach a target BP <140/90 mm Hg (130/80 mm Hg in patients with diabetes or renal insufficiency).33 The study was stopped early at 3 years because the primary outcome of CV death, nonfatal MI or stroke, hospitalization for angina, resuscitation after sudden cardiac arrest, and coronary revascularization occurred in 552 patients in the benazepril-amlodipine group compared with 679 patients in the benazepril-HCTZ group (9.6% vs 11.8%; RR ratio, 19.6%; hazard ratio [HR], 0.80; P < .001). The mechanism for the benefit observed in the benazepril-amlodipine group may relate in part to improved coronary blood flow that occurs with a calcium antagonist (compared with a diuretic) since BP control was virtually the same in both groups.
Another major hypertension study during the same era was the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT).32 This study enrolled 19,257 patients in northern Europe with a mean age of 63 years, an untreated baseline BP ≥160/100 mm Hg or a treated mean BP ≥140/90 mm Hg, and 3 or more of 11 prespecified risk factors for CV. Patients were randomized to amlodipine, with or without perindopril, or atenolol, with or without a thiazide diuretic, and were titrated to reach a BP goal <140/90 mm Hg. The study was halted early after a mean follow up of 5.5 years. Although there was no statistically significant difference in the primary events of nonfatal MI plus fatal CHF between the 2 arms, fewer patients randomized to the amlodipine-based regimen experienced a fatal or nonfatal stroke (327 vs 422; HR, 0.77; 95% CI, 0.66-0.89; P=.0003) and total CV events and procedures were lower in patients taking the amlodipine-based regimen than in those taking the atenolol-based regimen (1362 vs 1602; HR, 0.84; 95% CI, 0.78-0.90; P < .0001).32 All-cause mortality was also lower in the amlodipine-based group (738 vs 820; HR, 0.89; 95% CI, 0.81-0.99; P=.025), and significantly fewer patients in this arm developed diabetes (567 vs 799; HR, 0.70; 95% CI, 0.63-0.78; P < .0001).32
Patients with diabetes in ASCOT who were titrated to achieve a target BP <130/80 mm Hg experienced significantly lower mortality and stroke when taking the amlodipine-based regimen than when taking the atenolol-based regimen (HR, 0.86; 95% CI, 0.76-0.98; P=.026).32 In the group taking the atenolol-based regimen, fatal and nonfatal strokes were reduced by 25% (P=.017), peripheral arterial disease by 48% (P=.004), and peripheral revascularization procedures by 57% (P < .001). There were no statistically significant differences in the endpoints of CHD deaths and nonfatal MI in the diabetes subgroup.
Combination therapy and guideline recommendations
By the 1970s, it became clear that combinations of antihypertensive drugs increased BP lowering efficacy through both additive and synergistic mechanisms. These combinations also reduced adverse events because lower doses of each drug could be used, whereas drugs from different classes might offset each other’s adverse effects. In addition, combining antihypertensive drugs could prolong duration of action, possibly providing additional target organ protection.43 Combining drugs from complementary classes has also been shown to increase the likelihood of BP lowering compared with increasing the dose of a single drug, thus reducing the time required to reach BP goal.31,44-46
The 2010 American Society of Hypertension (ASH) position statement on combination therapy in hypertension therapy notes that at least 75% of patients will require combination therapy to reach goal.47 In addition, a meta-analysis of 9 randomized clinical trials found that combination treatment using a thiazide or thiazide-like diuretic as one of the components could provide a significantly greater effect than monotherapy lacking the diuretic, with similar discontinuation rates.48
Government guidelines in the United States, now nearly 10 years old, do not recommend combination therapy as a first-line approach unless patients have stage 2 hypertension (SBP ≥160 mm Hg or DBP ≥100 mm Hg). At that point, the guidelines recommend combination therapy with a thiazide or thiazide-type diuretic plus either an ACEI, ARB, beta-blocker, or calcium antagonist.49 More-specific recommendations are provided for patients with compelling indications (eg, HF, ischemic heart disease, chronic kidney disease, recurrent stroke, diabetes, and high coronary disease risk), as shown in TABLE 2.41,49 New recommendations from the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 8) are expected later this year.
TABLE 2
Antihypertensive treatment in patients with compelling indications41,49
| Indication | Diuretic | BB | ACEI | ARB | Calcium antagonist | Aldosterone antagonist |
|---|---|---|---|---|---|---|
| Heart failure | ||||||
| Post MI | ||||||
| CVD or high CVD risk | ||||||
| Anginaa | ||||||
| Aortopathy/aortic aneurysma | ||||||
| Diabetes | ||||||
| Recurrent stroke prevention | ||||||
| CKDb | ||||||
| Early dementiaa | ||||||
| = ACCF/AHA recommendation; ACCF, American College of Cardiology Foundation; ACEI, angiotensin-converting enzyme inhibitor; AHA, American Heart Association; ARB, angiotensin-receptor blocker; BB, beta-blocker; CVD, cardiovascular disease; CKD, chronic kidney disease; MI, myocardial infarction. aNot considered “compelling” indication in JNC-7 Express guidelines. bNot considered “compelling” recommendation in ACCF/AHA recommendations. Source: Journal of the American College of Cardiology by American College of Cardiology. Reproduced with permission of Elsevier Inc. in the format Journal via Copyright Clearance Center. | ||||||
Recent guidelines from ASH describe combination therapies of hypertension in categories of preferred, acceptable, and less effective, based on efficacy in lowering BP, safety and tolerability, and certain known outcomes from longer-term trials (TABLE 3).47
TABLE 3
Drug combinations in hypertension: Recommendations from the American Society of Hypertension47
| Preferred | Acceptable | Less Effective |
|---|---|---|
| ACEI + diuretica | BB + diuretica | ACEI + ARB |
| ARB + diuretica | Calcium antagonist + diuretic | ACEI + BB |
| ACEI + CCBa | Renin inhibitor + diuretic | ARB + BB |
| ARB + CCBa | Renin inhibitor + ARBa,b | CCB (non-dihydropyridine) + BB |
| Thiazide diuretic + potassium-sparing diuretica | Centrally acting agent + BB | |
| ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin-receptor blocker; BB, beta-blocker; CCB, calcium channel blocker. aAvailable as single-pill combination. bThis may be medically inappropriate in patients with diabetes and chronic diabetic nephropathy. Source: Journal of the American Society of Hypertension: JASH by American Society of Hypertension. Reproduced with permission of Elsevier Inc. in the format Journal via Copyright Clearance Center. | ||
In 2010, the American College of Cardiology Foundation (ACCF)/American Heart Association (AHA) published an expert consensus document on hypertension in the elderly. It recommends single therapy or combination therapy with an ACEI, ARB, calcium antagonist, or diuretic for patients 65 years of age and older with stage 1 hypertension and no “compelling” indications (eg, HF, post-MI, known coronary disease, angina, aortopathy/aortic aneurysm, diabetes, recurrent stroke prevention, chronic kidney disease, and early vascular dementia), but combination therapy for those with stage 2 hypertension and no compelling indications. For the former group, the panel notes that the combination of amlodipine with a renin-angiotensin aldosterone system blocker may be preferable to a diuretic combination, although either is acceptable.41
For patients with compelling indications, the ACCF/AHA panel recommends condition-based combination therapy with 2 or more of the therapies summarized in TABLE 2.41,49 The panel’s algorithm for the management of hypertension in the elderly is depicted in FIGURE 2.41
FIGURE 2
ACCF/AHA algorithm for the management of hypertension in the elderly41
ACCF, American College of Cardiology Foundation; ACEI, angiotensin-converting enzyme inhibitor; AHA, American Heart Association; ALDO ANT, aldosterone antagonist; ARB, angiotensin II receptor blocker; BB, beta-blocker; BP, blood pressure; CA, calcium antagonist; CAD, coronary artery disease; CVD, cardiovascular disease; DBP, diastolic BP; MI, myocardial infarction; RAS, renin-angiotensin system; SBP, systolic BP; THIAZ, thiazide diuretic.
aCombination therapy.
Source: Journal of the American College of Cardiology by American College of Cardiology. Reproduced with permission of Elsevier Inc. in the format Journal via Copyright Clearance Center.The National Institute for Health and Clinical Excellence (NICE), the United Kingdom-based clinical guideline development organization, recommends in its 2011 guidelines for the clinical management of primary hypertension in adults that patients less than 55 years of age, not of black African or Caribbean heritage, begin treatment with an ACEI or ARB.50 The guidelines do not recommend beta-blockers for initial therapy, noting that they should be considered only in younger patients with intolerance or contraindications to ACEIs and ARBs, reproductive-aged women, and those with clinical evidence of increased sympathetic drive.50
In contrast, patients 55 years and older, or blacks of African or Caribbean origin of any age, should begin treatment with a calcium channel blocker (CCB).50 If they cannot tolerate a CCB, or for those with HF (or at high risk of HF), the guidelines recommend beginning therapy with a diuretic (preferably chlorthalidone or in-dapamide unless the patient’s hypertension is already controlled with bendroflumethiazide or HCTZ).
If initial treatment fails to lower BP adequately, step 2 of the NICE guidelines for all populations is treatment with an ACEI or ARB in combination with a calcium antagonist.50 If further therapy is necessary (step 3), a thiazide diuretic (or thiazide-like) should be added to that combination. It is also recommended that patients with drug-resistant hypertension (ie, taking 3 agents at maximally tolerated doses, 1 of which should be a diuretic) should receive additional treatment with low-dose spironolactone (if their serum potassium level is ≤4.5 mmol/L) and higher-dose thiazide-type diuretics (if their serum potassium level is >4.5 mmol/L). If the diuretic is not tolerated or is ineffective, an alpha- or beta-blocker may be added. If patients continue to exhibit continued resistance, NICE recommends referral to a hypertension specialist. The NICE algorithm for the treatment of hypertension is shown in FIGURE 3.50
FIGURE 3
NICE algorithm for treatment of hypertension50
ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; CCB, calcium channel blocker; NICE, National Institute for Health and Clinical Excellence.
aChoose a low-cost ARB.
bA CCB is preferred but consider a thiazide-like diuretic if a CCB is not tolerated or the person has edema, evidence of heart failure, or a high risk of heart failure.
cConsider a low dose of spironolactoned or higher doses of thiazide-like diuretic
dAt the time of publication (August 2011), spironolactone did not have a UK marketing authorization for this indication. Informed consent should be obtained and documented.
eConsider an alpha- or beta-blocker if further diuretic therapy is not tolerated or is contraindicated or ineffective.
Source: National Institute for Health and Clinical Excellence (2011) CG 127 Hypertension: clinical management of primary hypertension in adults. London: NICE. Available from www.nice.org.uk/guidance/CG127. Reproduced with permission. The NICE guidance that this algorithm relates to was prepared for the National Health Service in England and Wales. NICE guidance does not apply to the United States and NICE has not been involved in the development or adaptation of any guidance for use in the United States.The ACCF/AHA and NICE guidelines also recommend that clinicians monitor electrolyte levels of patients on ACEIs/ARBs, with The frequency depending on each patient’s medical condition.41,50
Conclusion
With 7 major classes of antihypertensive drugs and several drugs within each class, there are numerous combinations available to clinicians to manage hypertension. Existing clinical trials cannot possibly evaluate all possible combinations. Yet, as noted in the ASH statement on combination therapy, the importance of achieving goal BP in individual patients cannot be overemphasized because small differences in on-treatment BP translate into major differences in the rates of CV events.47 When considering appropriate and effective antihypertensive therapies, clinicians should assess the evidence presented in this article and from the various clinical guidelines cited. Each patient is unique and it is important for clinicians to identify the most-effective treatment regimen for each individual patient.
1. Hamdy RC. Hypertension: a turning point in the history of medicine…and mankind. South Med J. 2001;94(11):1045-1047.
2. Veterans Administration Cooperative Study Group on Antihypertensive Agents. Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA. 1967;202(11):1028-1034.
3. Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA. 1979;242(23):2562-2571.
4. Amery A, De Schaepdryver A. The European Working Party on High Blood Pressure in the Elderly. Am J Med. 1991;90(3A):1S-4S.
5. Medical Research Council Working Party. MRC trial of treatment of mild hypertension: principal results. Br Med J (Clin Res Ed). 1985;291(6488):97-104.
6. The Australian therapeutic trial in mild hypertension. Report by the Management Committee. Lancet. 1980;1(8181):1261-1267.
7. Wilhelmsen L, Berglund G, Elmfeldt D, et al. Beta-blockers versus diuretics in hypertensive men: main results from the HAPPHY trial. J Hypertens. 1987;5(5):561-572.
8. Wikstrand J, Berglund G, Tuomilehto J. Beta-blockade in the primary prevention of coronary heart disease in hypertensive patients. Review of present evidence. Circulation. 1991;84(6 Suppl):VI93-VI100.
9. Wikstrand J, Warnold I, Tuomilehto J, et al. Metoprolol versus thiazide diuretics in hypertension. Morbidity results from the MAPHY Study. Hypertension. 1991;17(4):579-588.
10. Olsson G, Tuomilehto J, Berglund G, et al. Primary prevention of sudden cardiovascular death in hypertensive patients. Mortality results from the MAPHY Study. Am J Hypertens. 1991;4(2 Pt 1):151-1511.
11. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265(24):3255-3264.
12. MRC Working Party. Medical Research Council trial of treatment of hypertension in older adults: principal results. BMJ. 1992;304(6824):405-412.
13. Dahlöf B, Lindholm LH, Hansson L, Scherstén B, Ekbom T, Wester PO. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension). Lancet. 1991;338(8778):1281-1285.
14. Neaton JD, Grimm RH, Jr, Prineas RJ, et al. Treatment of Mild Hypertension Study Research Group. Treatment of Mild Hypertension Study. Final results. JAMA. 1993;270(6):713-724.
15. Materson BJ, Reda DJ, Cushman WC, et al. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo [published correction appears in N Engl J Med. 1994;330(23):1689]. N Engl J Med. 1993;328(13):914-921.
16. Hansson L, Zanchetti A, Carruthers SG, et al. HOT Study Group. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998;351(9118):1755-1762.
17. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38 [published correction appears in BMJ. 1999;318(7175):29]. BMJ. 1998;317(7160):703-713.
18. UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. BMJ. 1998;317(7160):713-720.
19. Staessen JA, Fagard R, Thijs L, et al. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet. 1997;350(9080):757-764.
20. Liu L, Wang JG, Gong L, Liu G, Staessen JA. Systolic Hypertension in China (Syst-China) Collaborative Group. Comparison of active treatment and placebo in older Chinese patients with isolated systolic hypertension. J Hypertens. 1998;16(12 Pt 1):1823-1829.
21. Hansson L, Hedner T, Lindholm L, et al. The Captopril Prevention Project (CAPPP) in hypertension—baseline data and current status. Blood Press. 1997;6(6):365-367.
22. Hansson L, Lindholm LH, Ekbom T, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet. 1999;354(9192):1751-1756.
23. Brown MJ, Palmer CR, Castaigne A, et al. Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a Goal in Hypertension Treatment (INSIGHT) [published correction appears in Lancet. 2000;356(9228):514]. Lancet. 2000;356(9227):366-372.
24. Hansson L, Hedner T, Lund-Johansen P, et al. Randomised trial of effects of calcium antagonists compared with diuretics and beta-blockers on cardiovascular morbidity and mortality in hypertension: the Nordic Diltiazem (NORDIL) study. Lancet. 2000;356(9227):359-365.
25. Lithell H, Hansson L, Skoog I, et al. SCOPE Study Group. The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens. 2003;21(5):875-886.
26. Black HR, Elliott WJ, Grandits G, et al. CONVINCE Research Group. Principal results of the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) trial. JAMA. 2003;289(16):2073-2082.
27. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) [published corrections appear in JAMA. 2003;289(2):178; JAMA. 2004;291(18):2196]. JAMA. 2002;288(23):2981-2997.
28. Wing LM, Reid CM, Ryan P, et al. Second Australian National Blood Pressure Study Group. A comparison of outcomes with angiotensin-converting– enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med. 2003;348(7):583-592.
29. Dahlöf B, Devereux RB, Kjeldsen SE, et al. LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995-1003.
30. The ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358(15):1547-1559.
31. Weber MA, Julius S, Kjeldsen SE, et al. Blood pressure dependent and independent effects of antihypertensive treatment on clinical events in the VALUE Trial. Lancet. 2004;363(9426):2049-2051.
32. Dahlöf B, Sever PS, Poulter NR, et al. ASCOT Investigators. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895-906.
33. Jamerson K, Bakris GL, Dahlöf B, et al. ACCOMPLISH Investigators. Exceptional early blood pressure control rates: the ACCOMPLISH trial. Blood Press. 2007;16(2):80-86.
34. Julius S, Nesbitt SD, Egan BM, et al. Trial of Preventing Hypertension (TROPHY) Study Investigators. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med. 2006;354(16):1685-1697.
35. ATMOSPHERE study, [NCT00853658] ongoing trial. Trial-Results Center Web site. http://www.trialresultscenter.org/study9503-ATMOSPHERE.htm. Accessed March 28, 2012.
36. Parving HH, Brenner BM, McMurray JJ, et al. Aliskiren Trial in Type 2 Diabetes Using Cardio-Renal Endpoints (ALTITUDE): rationale and study design. Nephrol Dial Transplant. 2009;24(5):1663-1671.
37. Massie BM, Carson PE, McMurray JJ, et al. I-PRESERVE Investigators. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359(23):2456-2467.
38. US National Library of Medicine. The Edward D. Freis Papers: the VA Cooperative Study and the Beginning of Routine Hypertension Screening, 1964-1980. http://profiles.nlm.nih.gov/ps/retrieve/Narrative/XF/p-nid/172. Accessed March 26, 2012.
39. Comberg HU, Heyden S, Knowles M, et al. Long-term survey of 450 hypertensives of the HDFP. Munch Med Wochenschr. 1991;133:32-38.
40. Skoog I, Lithell H, Hansson L, et al. SCOPE Study Group. Effect of baseline cognitive function and antihypertensive treatment on cognitive and cardiovascular outcomes: Study on COgnition and Prognosis in the Elderly (SCOPE). Am J Hypertens. 2005;18(8):1052-1059.
41. Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011;57(20):2037-2114.
42. Beckett NS, Peters R, Fletcher AE, et al. HYVET Study Group. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887-1898.
43. Weber MA, Neutel JM, Frishman WH. Combination drug therapy. In: Frishman WH, Sonnenblick EH, Sica DA, eds. Cardiovascular Pharmacotherapeutics. 2nd ed. New York, NY: McGraw-Hill; 2003:355–368.
44. Pepine CJ, Handberg EM, Cooper-DeHoff RM, et al. INVEST Investigators. A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil- Trandolapril Study (INVEST): a randomized controlled trial. JAMA. 2003;290(21):2805-2816.
45. Mancia G, Messerli F, Bakris G, Zhou Q, Champion A, Pepine CJ. Blood pressure control and improved cardiovascular outcomes in the International Verapamil SR-Trandolapril Study. Hypertension. 2007;50(2):299-305.
46. Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290-300.
47. Gradman AH, Basile JN, Carter BL, et al. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(2):90-98.
48. Weir MR, Levy D, Crikelair N, Rocha R, Meng X, Glazer R. Time to achieve blood-pressure goal: influence of dose of valsartan monotherapy and valsartan and hydrochlorothiazide combination therapy. Am J Hypertens. 2007;20(7):807-815.
49. National Heart, . Lung, and Blood Institute. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. http://www.nhlbi.nih.gov/guidelines/hypertension/. Published 2003. Accessed March 27, 2012.
50. National Institute for Health and Clinical Excellence. Hypertension: Clinical management of primary hypertension in adults. http://www.nice.org.uk/nicemedia/live/13561/56008/56008.pdf. Published August 2011. Accessed March 27, 2012.
1. Hamdy RC. Hypertension: a turning point in the history of medicine…and mankind. South Med J. 2001;94(11):1045-1047.
2. Veterans Administration Cooperative Study Group on Antihypertensive Agents. Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA. 1967;202(11):1028-1034.
3. Hypertension Detection and Follow-up Program Cooperative Group. Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA. 1979;242(23):2562-2571.
4. Amery A, De Schaepdryver A. The European Working Party on High Blood Pressure in the Elderly. Am J Med. 1991;90(3A):1S-4S.
5. Medical Research Council Working Party. MRC trial of treatment of mild hypertension: principal results. Br Med J (Clin Res Ed). 1985;291(6488):97-104.
6. The Australian therapeutic trial in mild hypertension. Report by the Management Committee. Lancet. 1980;1(8181):1261-1267.
7. Wilhelmsen L, Berglund G, Elmfeldt D, et al. Beta-blockers versus diuretics in hypertensive men: main results from the HAPPHY trial. J Hypertens. 1987;5(5):561-572.
8. Wikstrand J, Berglund G, Tuomilehto J. Beta-blockade in the primary prevention of coronary heart disease in hypertensive patients. Review of present evidence. Circulation. 1991;84(6 Suppl):VI93-VI100.
9. Wikstrand J, Warnold I, Tuomilehto J, et al. Metoprolol versus thiazide diuretics in hypertension. Morbidity results from the MAPHY Study. Hypertension. 1991;17(4):579-588.
10. Olsson G, Tuomilehto J, Berglund G, et al. Primary prevention of sudden cardiovascular death in hypertensive patients. Mortality results from the MAPHY Study. Am J Hypertens. 1991;4(2 Pt 1):151-1511.
11. SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265(24):3255-3264.
12. MRC Working Party. Medical Research Council trial of treatment of hypertension in older adults: principal results. BMJ. 1992;304(6824):405-412.
13. Dahlöf B, Lindholm LH, Hansson L, Scherstén B, Ekbom T, Wester PO. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension). Lancet. 1991;338(8778):1281-1285.
14. Neaton JD, Grimm RH, Jr, Prineas RJ, et al. Treatment of Mild Hypertension Study Research Group. Treatment of Mild Hypertension Study. Final results. JAMA. 1993;270(6):713-724.
15. Materson BJ, Reda DJ, Cushman WC, et al. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo [published correction appears in N Engl J Med. 1994;330(23):1689]. N Engl J Med. 1993;328(13):914-921.
16. Hansson L, Zanchetti A, Carruthers SG, et al. HOT Study Group. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998;351(9118):1755-1762.
17. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38 [published correction appears in BMJ. 1999;318(7175):29]. BMJ. 1998;317(7160):703-713.
18. UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. BMJ. 1998;317(7160):713-720.
19. Staessen JA, Fagard R, Thijs L, et al. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet. 1997;350(9080):757-764.
20. Liu L, Wang JG, Gong L, Liu G, Staessen JA. Systolic Hypertension in China (Syst-China) Collaborative Group. Comparison of active treatment and placebo in older Chinese patients with isolated systolic hypertension. J Hypertens. 1998;16(12 Pt 1):1823-1829.
21. Hansson L, Hedner T, Lindholm L, et al. The Captopril Prevention Project (CAPPP) in hypertension—baseline data and current status. Blood Press. 1997;6(6):365-367.
22. Hansson L, Lindholm LH, Ekbom T, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet. 1999;354(9192):1751-1756.
23. Brown MJ, Palmer CR, Castaigne A, et al. Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a Goal in Hypertension Treatment (INSIGHT) [published correction appears in Lancet. 2000;356(9228):514]. Lancet. 2000;356(9227):366-372.
24. Hansson L, Hedner T, Lund-Johansen P, et al. Randomised trial of effects of calcium antagonists compared with diuretics and beta-blockers on cardiovascular morbidity and mortality in hypertension: the Nordic Diltiazem (NORDIL) study. Lancet. 2000;356(9227):359-365.
25. Lithell H, Hansson L, Skoog I, et al. SCOPE Study Group. The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens. 2003;21(5):875-886.
26. Black HR, Elliott WJ, Grandits G, et al. CONVINCE Research Group. Principal results of the Controlled Onset Verapamil Investigation of Cardiovascular End Points (CONVINCE) trial. JAMA. 2003;289(16):2073-2082.
27. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) [published corrections appear in JAMA. 2003;289(2):178; JAMA. 2004;291(18):2196]. JAMA. 2002;288(23):2981-2997.
28. Wing LM, Reid CM, Ryan P, et al. Second Australian National Blood Pressure Study Group. A comparison of outcomes with angiotensin-converting– enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med. 2003;348(7):583-592.
29. Dahlöf B, Devereux RB, Kjeldsen SE, et al. LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995-1003.
30. The ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358(15):1547-1559.
31. Weber MA, Julius S, Kjeldsen SE, et al. Blood pressure dependent and independent effects of antihypertensive treatment on clinical events in the VALUE Trial. Lancet. 2004;363(9426):2049-2051.
32. Dahlöf B, Sever PS, Poulter NR, et al. ASCOT Investigators. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366(9489):895-906.
33. Jamerson K, Bakris GL, Dahlöf B, et al. ACCOMPLISH Investigators. Exceptional early blood pressure control rates: the ACCOMPLISH trial. Blood Press. 2007;16(2):80-86.
34. Julius S, Nesbitt SD, Egan BM, et al. Trial of Preventing Hypertension (TROPHY) Study Investigators. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N Engl J Med. 2006;354(16):1685-1697.
35. ATMOSPHERE study, [NCT00853658] ongoing trial. Trial-Results Center Web site. http://www.trialresultscenter.org/study9503-ATMOSPHERE.htm. Accessed March 28, 2012.
36. Parving HH, Brenner BM, McMurray JJ, et al. Aliskiren Trial in Type 2 Diabetes Using Cardio-Renal Endpoints (ALTITUDE): rationale and study design. Nephrol Dial Transplant. 2009;24(5):1663-1671.
37. Massie BM, Carson PE, McMurray JJ, et al. I-PRESERVE Investigators. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359(23):2456-2467.
38. US National Library of Medicine. The Edward D. Freis Papers: the VA Cooperative Study and the Beginning of Routine Hypertension Screening, 1964-1980. http://profiles.nlm.nih.gov/ps/retrieve/Narrative/XF/p-nid/172. Accessed March 26, 2012.
39. Comberg HU, Heyden S, Knowles M, et al. Long-term survey of 450 hypertensives of the HDFP. Munch Med Wochenschr. 1991;133:32-38.
40. Skoog I, Lithell H, Hansson L, et al. SCOPE Study Group. Effect of baseline cognitive function and antihypertensive treatment on cognitive and cardiovascular outcomes: Study on COgnition and Prognosis in the Elderly (SCOPE). Am J Hypertens. 2005;18(8):1052-1059.
41. Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Coll Cardiol. 2011;57(20):2037-2114.
42. Beckett NS, Peters R, Fletcher AE, et al. HYVET Study Group. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358(18):1887-1898.
43. Weber MA, Neutel JM, Frishman WH. Combination drug therapy. In: Frishman WH, Sonnenblick EH, Sica DA, eds. Cardiovascular Pharmacotherapeutics. 2nd ed. New York, NY: McGraw-Hill; 2003:355–368.
44. Pepine CJ, Handberg EM, Cooper-DeHoff RM, et al. INVEST Investigators. A calcium antagonist vs a non-calcium antagonist hypertension treatment strategy for patients with coronary artery disease. The International Verapamil- Trandolapril Study (INVEST): a randomized controlled trial. JAMA. 2003;290(21):2805-2816.
45. Mancia G, Messerli F, Bakris G, Zhou Q, Champion A, Pepine CJ. Blood pressure control and improved cardiovascular outcomes in the International Verapamil SR-Trandolapril Study. Hypertension. 2007;50(2):299-305.
46. Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122(3):290-300.
47. Gradman AH, Basile JN, Carter BL, et al. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4(2):90-98.
48. Weir MR, Levy D, Crikelair N, Rocha R, Meng X, Glazer R. Time to achieve blood-pressure goal: influence of dose of valsartan monotherapy and valsartan and hydrochlorothiazide combination therapy. Am J Hypertens. 2007;20(7):807-815.
49. National Heart, . Lung, and Blood Institute. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. http://www.nhlbi.nih.gov/guidelines/hypertension/. Published 2003. Accessed March 27, 2012.
50. National Institute for Health and Clinical Excellence. Hypertension: Clinical management of primary hypertension in adults. http://www.nice.org.uk/nicemedia/live/13561/56008/56008.pdf. Published August 2011. Accessed March 27, 2012.
CLINICAL UPDATE: The Treatment of Atopic Dermatitis
Click here to view the supplement
- Introduction
- Nonpharmacologic Management of AD
- Pharmacologic Management of AD
- Conclusions
Clinical Professor of Dermatology
University of Louisville, KY
Click here to view the supplement
- Introduction
- Nonpharmacologic Management of AD
- Pharmacologic Management of AD
- Conclusions
Clinical Professor of Dermatology
University of Louisville, KY
Click here to view the supplement
- Introduction
- Nonpharmacologic Management of AD
- Pharmacologic Management of AD
- Conclusions
Clinical Professor of Dermatology
University of Louisville, KY