User login
Nigerian-Born Hospitalist Steers Career Down Path of Administrative Challenges
In some ways, Femi Adewunmi, MD, MBA, CPE, SFHM, seemed destined to become a physician. He grew up in a medical family—his mother is an orthodontist; his father is an obstetrician/gynecologist. As a child, he often spent holidays visiting patients at the hospital where his dad worked. He grew to appreciate medicine as a noble profession, and when he reached his teens, he never seriously considered another career path.
“There were times when I was in medical school, dreading having to study for the numerous tests and exams, when I wished I had someone I could have blamed my decision to go to medical school on,” says Dr. Adewunmi, a native of Nigeria who has practiced as a hospitalist in the U.S. since 2003. “But no one pushed me to do it. It was something I always looked forward to doing, and I’m very glad I stuck with it.”
Dr. Adewunmi has only become more passionate about his work since then. His experience as a front-line hospitalist laid the foundation for a series of leadership roles, first directing the HM program at Johnston Memorial Hospital in Smithfield, N.C., and now as regional chief medical officer for Sound Physicians, which provides inpatient services to more than 70 hospitals nationally.
“I really want to be a good physician executive,” he says. “It’s definitely a case of ‘The more you learn, the more you realize how little you know.’ I still have a lot to learn, but I’m looking forward to the challenge.”
When did you decide to go into HM?
During residency, I realized I loved taking care of patients in the hospital, both along the wards and in the ICU. I enjoyed my outpatient clinics but found myself looking for any reason I could to stay in the hospital caring for patients. I was interested in patient safety and I was doing a little bit of utilization review, so I also felt it would give me a great overall perspective of the healthcare system.
What about leading the hospitalist program at Johnston Memorial appealed to you?
I enjoyed clinical medicine, and I still do, but I was looking to do more. I wanted to make an impact at a systems level, and I knew, to do that, I eventually had to gain some leadership experience.
What is the most valuable lesson you learned in that role?
Understanding that change doesn’t happen instantaneously. For instance, as a clinician, you sometimes admit patients with congestive heart failure. You diagnose correctly, treat appropriately, and in a few days, the patients do better and go home. You get pretty swift gratification. Administration is much different. You put processes in place and it could take weeks or several quarters before you start to see the effects of the changes you implement.
What appealed to you about moving from a single-site leadership position at Johnston to a regional position with Sound?
I wanted to continue evolving. I wanted more of a challenge and was seeking opportunities where I would have operational responsibility—overseeing performance improvement in quality, satisfaction, and financial performance for several programs. In addition, I wanted to be accountable for physician development, recruiting, negotiations, and the whole gamut of business development. It was the next logical step in my career.
Why did you pursue an MBA?
I’d made that decision just before I got into medical school. I recall first thinking about it after a conversation I had with my father as a teenager. When I told him that I had made up my mind to study medicine, he said, “You should consider getting an MBA as well. Your generation is going to need to have business experience and expertise, and be better in that area than our generation was.” It’s been invaluable for me in terms of preparing me for handling the business side of medicine, including ways to make operations more efficient and to reduce costs without compromising the quality of care provided.
You have worked in both hospital-employed and privately contracted HM programs. Do you prefer one model?
In general, the larger organizations tend to have an advantage in that they have established protocols and processes that work and have been refined over time. Couple that with the economies of scale they enjoy, as we move into an era of value-based purchasing, it’s becoming harder for the smaller community-based hospital to do that as well. That said, I have seen local hospital-run programs that function really well and have administrative support, so there is definitely enough room for both models.
You were in the inaugural FHM class. What did that recognition mean to you?
I saw it as validation of how we were starting to mature as a specialty and as recognition of a commitment to being a hospitalist, not just an internist. I never practiced outpatient medicine. I went straight from residency to hospitalist medicine. That’s how I identify myself, and I was happy to see that physicians specializing in hospital medicine were starting to get recognized.
What is your biggest professional reward?
The satisfaction from knowing you’re making a difference—not just by the care you provide one-on-one to your patients, but also knowing you’re contributing at a systems level or a population level because you’re making decisions and trying to redefine processes that actually could impact a much larger cohort.
What is your biggest professional challenge?
Trying to find enough hours in the day to do all that needs to be done.
What is next for you professionally?
I enjoy having varied opportunities and being involved in many different aspects of operations. That’s what attracted me to a larger company such as Sound Physicians, and I see myself staying in that type of role. Down the road, I’d love to be able to take some of my knowledge to Nigeria and find a way to help develop and shape the healthcare sector back home.
Why would that mean so much to you?
It would be a chance to give back. We still have people dying from largely preventable diseases, and our healthcare system is not what it should be. We don’t have enough physicians for the population, and most of the physicians are in urban areas.
Close to half of the members of my graduating medical school class are either in the U.S., Europe, Asia, or South Africa.
That type of brain drain has a tremendous effect over several decades. That’s a lot of talent outside the country, and we need that back home.
Mark Leiser is a freelance writer in New Jersey.
In some ways, Femi Adewunmi, MD, MBA, CPE, SFHM, seemed destined to become a physician. He grew up in a medical family—his mother is an orthodontist; his father is an obstetrician/gynecologist. As a child, he often spent holidays visiting patients at the hospital where his dad worked. He grew to appreciate medicine as a noble profession, and when he reached his teens, he never seriously considered another career path.
“There were times when I was in medical school, dreading having to study for the numerous tests and exams, when I wished I had someone I could have blamed my decision to go to medical school on,” says Dr. Adewunmi, a native of Nigeria who has practiced as a hospitalist in the U.S. since 2003. “But no one pushed me to do it. It was something I always looked forward to doing, and I’m very glad I stuck with it.”
Dr. Adewunmi has only become more passionate about his work since then. His experience as a front-line hospitalist laid the foundation for a series of leadership roles, first directing the HM program at Johnston Memorial Hospital in Smithfield, N.C., and now as regional chief medical officer for Sound Physicians, which provides inpatient services to more than 70 hospitals nationally.
“I really want to be a good physician executive,” he says. “It’s definitely a case of ‘The more you learn, the more you realize how little you know.’ I still have a lot to learn, but I’m looking forward to the challenge.”
When did you decide to go into HM?
During residency, I realized I loved taking care of patients in the hospital, both along the wards and in the ICU. I enjoyed my outpatient clinics but found myself looking for any reason I could to stay in the hospital caring for patients. I was interested in patient safety and I was doing a little bit of utilization review, so I also felt it would give me a great overall perspective of the healthcare system.
What about leading the hospitalist program at Johnston Memorial appealed to you?
I enjoyed clinical medicine, and I still do, but I was looking to do more. I wanted to make an impact at a systems level, and I knew, to do that, I eventually had to gain some leadership experience.
What is the most valuable lesson you learned in that role?
Understanding that change doesn’t happen instantaneously. For instance, as a clinician, you sometimes admit patients with congestive heart failure. You diagnose correctly, treat appropriately, and in a few days, the patients do better and go home. You get pretty swift gratification. Administration is much different. You put processes in place and it could take weeks or several quarters before you start to see the effects of the changes you implement.
What appealed to you about moving from a single-site leadership position at Johnston to a regional position with Sound?
I wanted to continue evolving. I wanted more of a challenge and was seeking opportunities where I would have operational responsibility—overseeing performance improvement in quality, satisfaction, and financial performance for several programs. In addition, I wanted to be accountable for physician development, recruiting, negotiations, and the whole gamut of business development. It was the next logical step in my career.
Why did you pursue an MBA?
I’d made that decision just before I got into medical school. I recall first thinking about it after a conversation I had with my father as a teenager. When I told him that I had made up my mind to study medicine, he said, “You should consider getting an MBA as well. Your generation is going to need to have business experience and expertise, and be better in that area than our generation was.” It’s been invaluable for me in terms of preparing me for handling the business side of medicine, including ways to make operations more efficient and to reduce costs without compromising the quality of care provided.
You have worked in both hospital-employed and privately contracted HM programs. Do you prefer one model?
In general, the larger organizations tend to have an advantage in that they have established protocols and processes that work and have been refined over time. Couple that with the economies of scale they enjoy, as we move into an era of value-based purchasing, it’s becoming harder for the smaller community-based hospital to do that as well. That said, I have seen local hospital-run programs that function really well and have administrative support, so there is definitely enough room for both models.
You were in the inaugural FHM class. What did that recognition mean to you?
I saw it as validation of how we were starting to mature as a specialty and as recognition of a commitment to being a hospitalist, not just an internist. I never practiced outpatient medicine. I went straight from residency to hospitalist medicine. That’s how I identify myself, and I was happy to see that physicians specializing in hospital medicine were starting to get recognized.
What is your biggest professional reward?
The satisfaction from knowing you’re making a difference—not just by the care you provide one-on-one to your patients, but also knowing you’re contributing at a systems level or a population level because you’re making decisions and trying to redefine processes that actually could impact a much larger cohort.
What is your biggest professional challenge?
Trying to find enough hours in the day to do all that needs to be done.
What is next for you professionally?
I enjoy having varied opportunities and being involved in many different aspects of operations. That’s what attracted me to a larger company such as Sound Physicians, and I see myself staying in that type of role. Down the road, I’d love to be able to take some of my knowledge to Nigeria and find a way to help develop and shape the healthcare sector back home.
Why would that mean so much to you?
It would be a chance to give back. We still have people dying from largely preventable diseases, and our healthcare system is not what it should be. We don’t have enough physicians for the population, and most of the physicians are in urban areas.
Close to half of the members of my graduating medical school class are either in the U.S., Europe, Asia, or South Africa.
That type of brain drain has a tremendous effect over several decades. That’s a lot of talent outside the country, and we need that back home.
Mark Leiser is a freelance writer in New Jersey.
In some ways, Femi Adewunmi, MD, MBA, CPE, SFHM, seemed destined to become a physician. He grew up in a medical family—his mother is an orthodontist; his father is an obstetrician/gynecologist. As a child, he often spent holidays visiting patients at the hospital where his dad worked. He grew to appreciate medicine as a noble profession, and when he reached his teens, he never seriously considered another career path.
“There were times when I was in medical school, dreading having to study for the numerous tests and exams, when I wished I had someone I could have blamed my decision to go to medical school on,” says Dr. Adewunmi, a native of Nigeria who has practiced as a hospitalist in the U.S. since 2003. “But no one pushed me to do it. It was something I always looked forward to doing, and I’m very glad I stuck with it.”
Dr. Adewunmi has only become more passionate about his work since then. His experience as a front-line hospitalist laid the foundation for a series of leadership roles, first directing the HM program at Johnston Memorial Hospital in Smithfield, N.C., and now as regional chief medical officer for Sound Physicians, which provides inpatient services to more than 70 hospitals nationally.
“I really want to be a good physician executive,” he says. “It’s definitely a case of ‘The more you learn, the more you realize how little you know.’ I still have a lot to learn, but I’m looking forward to the challenge.”
When did you decide to go into HM?
During residency, I realized I loved taking care of patients in the hospital, both along the wards and in the ICU. I enjoyed my outpatient clinics but found myself looking for any reason I could to stay in the hospital caring for patients. I was interested in patient safety and I was doing a little bit of utilization review, so I also felt it would give me a great overall perspective of the healthcare system.
What about leading the hospitalist program at Johnston Memorial appealed to you?
I enjoyed clinical medicine, and I still do, but I was looking to do more. I wanted to make an impact at a systems level, and I knew, to do that, I eventually had to gain some leadership experience.
What is the most valuable lesson you learned in that role?
Understanding that change doesn’t happen instantaneously. For instance, as a clinician, you sometimes admit patients with congestive heart failure. You diagnose correctly, treat appropriately, and in a few days, the patients do better and go home. You get pretty swift gratification. Administration is much different. You put processes in place and it could take weeks or several quarters before you start to see the effects of the changes you implement.
What appealed to you about moving from a single-site leadership position at Johnston to a regional position with Sound?
I wanted to continue evolving. I wanted more of a challenge and was seeking opportunities where I would have operational responsibility—overseeing performance improvement in quality, satisfaction, and financial performance for several programs. In addition, I wanted to be accountable for physician development, recruiting, negotiations, and the whole gamut of business development. It was the next logical step in my career.
Why did you pursue an MBA?
I’d made that decision just before I got into medical school. I recall first thinking about it after a conversation I had with my father as a teenager. When I told him that I had made up my mind to study medicine, he said, “You should consider getting an MBA as well. Your generation is going to need to have business experience and expertise, and be better in that area than our generation was.” It’s been invaluable for me in terms of preparing me for handling the business side of medicine, including ways to make operations more efficient and to reduce costs without compromising the quality of care provided.
You have worked in both hospital-employed and privately contracted HM programs. Do you prefer one model?
In general, the larger organizations tend to have an advantage in that they have established protocols and processes that work and have been refined over time. Couple that with the economies of scale they enjoy, as we move into an era of value-based purchasing, it’s becoming harder for the smaller community-based hospital to do that as well. That said, I have seen local hospital-run programs that function really well and have administrative support, so there is definitely enough room for both models.
You were in the inaugural FHM class. What did that recognition mean to you?
I saw it as validation of how we were starting to mature as a specialty and as recognition of a commitment to being a hospitalist, not just an internist. I never practiced outpatient medicine. I went straight from residency to hospitalist medicine. That’s how I identify myself, and I was happy to see that physicians specializing in hospital medicine were starting to get recognized.
What is your biggest professional reward?
The satisfaction from knowing you’re making a difference—not just by the care you provide one-on-one to your patients, but also knowing you’re contributing at a systems level or a population level because you’re making decisions and trying to redefine processes that actually could impact a much larger cohort.
What is your biggest professional challenge?
Trying to find enough hours in the day to do all that needs to be done.
What is next for you professionally?
I enjoy having varied opportunities and being involved in many different aspects of operations. That’s what attracted me to a larger company such as Sound Physicians, and I see myself staying in that type of role. Down the road, I’d love to be able to take some of my knowledge to Nigeria and find a way to help develop and shape the healthcare sector back home.
Why would that mean so much to you?
It would be a chance to give back. We still have people dying from largely preventable diseases, and our healthcare system is not what it should be. We don’t have enough physicians for the population, and most of the physicians are in urban areas.
Close to half of the members of my graduating medical school class are either in the U.S., Europe, Asia, or South Africa.
That type of brain drain has a tremendous effect over several decades. That’s a lot of talent outside the country, and we need that back home.
Mark Leiser is a freelance writer in New Jersey.
Time-based billing allows hospitalists to avoid
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
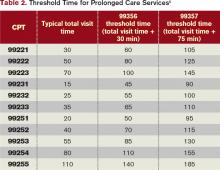
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
Providers typically rely on the “key components” (history, exam, medical decision-making) when documenting in the medical record. However, there are instances when the majority of the encounter constitutes counseling/coordination of care (C/CC). Physicians might only document a brief history and exam, or nothing at all. Utilizing time-based billing principles allows a physician to disregard the “key component” requirements and select a visit level reflective of this effort.
For example, a 64-year-old female is hospitalized with newly diagnosed diabetes and requires extensive counseling regarding disease management, lifestyle modification, and medication regime, as well as coordination of care for outpatient programs and services. The hospitalist reviews some of the pertinent information with the patient and leaves the room to coordinate the patient’s ongoing care (25 minutes). The hospitalist then asks a resident to assist with the remaining counseling efforts (20 minutes). Code 99232 (inpatient visit, 25 minutes total visit time) would be appropriate to report.
Counseling, Coordination of Care
Time may be used as the determining factor for the visit level, if more than 50% of the total visit time involves C/CC.1 Time is not used for visit-level selection if C/CC is minimal or absent from the patient encounter. Total visit time is acknowledged as the physician’s face-to-face (i.e. bedside) time combined with time spent on the unit/floor reviewing data, obtaining relevant patient information, and discussing the individual case with other involved healthcare providers.
Time associated with activities performed outside of the patient’s unit/floor is not considered when calculating total visit time. Time associated with teaching students/interns also is excluded; only the attending physician’s time counts.
When the requirements have been met, the physician selects the visit level that corresponds with the documented total visit time (see Table 1). In the scenario above, the visit level is chosen based on the attending physician’s documented time (25 minutes). The resident’s time cannot be included.
Documentation Requirements
Physicians must document the interaction during the patient encounter: history and exam, if updated or performed; discussion points; and patient response, if applicable. The medical record entry must contain both the C/CC time and the total visit time.2 “Total visit time=35 minutes; >50% spent counseling/coordinating care” or “20 of 35 minutes spent counseling/coordinating care.”
A payor may prefer one documentation style over another. It is always best to ask about the payor’s policy and review local documentation standards to ensure compliance.
Family Discussions
Physicians are always involved in family discussions. It is appropriate to count this as C/CC time. In the event that the family discussion takes place without the patient present, only count this as C/CC time if:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision-makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.4
The medical record should reflect these criteria. Do not consider the time if the discussion takes place in an area outside of the patient’s unit/floor, or if the time is spent counseling family members through their grieving process.
It is not uncommon for the family discussion to take place later in the day, after the physician has made earlier rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient evaluation (i.e. history update and physical) and management service (i.e. care plan review/revision), this second encounter might be regarded as a prolonged care service.
Prolonged Care
Prolonged care codes exist for both outpatient and inpatient services. A hospitalists’ focus involves the inpatient code series:
99356: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, first hour; and
99357: Prolonged service in the inpatient or observation setting, requiring unit/floor time beyond the usual service, each additional 30 minutes.
Code 99356 is reported during the first hour of prolonged services, after the initial 30 minutes is reached; code 99357 is reported for each additional 30 minutes of prolonged care beyond the first hour, after the first 15 minutes of each additional segment. Both are “add on” codes and cannot be reported alone on a claim form; a “primary” code must be reported. Similarly, 99357 cannot be reported without 99356, and 99356 must be reported with one of the following inpatient service (primary) codes: 99218-99220, 99221-99223, 99231-99233, 99251-99255, 99304-99310. Only one unit of 99356 may be reported per patient per physician group per day, whereas multiple units of 99357 may be reported in a single day.
The CPT definition of prolonged care varies from that of the Centers for Medicare & Medicaid Services (CMS). Since 2009, CPT recognizes the total duration spent by a physician on a given date, even if the time spent by the physician on that date is not continuous; the time involves both face-to-face time and unit/floor time.5 CMS only attributes direct face-to-face time between the physician and the patient toward prolonged care billing. Time spent reviewing charts or discussion of a patient with house medical staff, waiting for test results, waiting for changes in the patient’s condition, waiting for end of a therapy session, or waiting for use of facilities cannot be billed as prolonged services.5 This is in direct opposition to its policy for C/CC services, and makes prolonged care services inefficient.
Medicare also identifies “threshold” time (see Table 2). The total physician visit time must exceed the time requirements associated with the “primary” codes by a 30-minute threshold (e.g. 99221+99356=30 minutes+30 minutes=60 minutes threshold time). The physician must document the total face-to-face time spent in separate notes throughout the day or, more realistically, in one cumulative note.
When two providers from the same group and same specialty perform services on the same date (e.g. physician A saw the patient during morning rounds, and physician B spoke with the patient/family in the afternoon), only one physician can report the cumulative service.6 As always, query payors for coverage, because some non-Medicare insurers do not recognize these codes.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare National Coverage Determinations Manual: Chapter 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed Jan. 8, 2012.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.15.1C. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011:7-21.
- Centers for Medicare & Medicaid Services (CMS). Medicare Claims Processing Manual: Chapter 12, Section 30.6.5. Centers for Medicare & Medicaid Services website. Available at: www.cms.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2012.
Hospitalists Provide Leadership as Unit Medical Directors
A project to formalize “local leadership models”—partnering leadership teams comprising a hospitalist and a nurse manager on each participating unit—at the University of Michigan Health System helped to redefine the role of unit medical director and led to allocating sufficient time (15% to 20% of an FTE) for hospitalists to fill that role. The process also led to a joint role description for the physician and nurse leaders.
“In our organization, we had the medical director concept in place previously, but things were missing, with no direct accountability, no dedicated effort, and lack of clarity on reporting,” explains hospitalist Christopher Kim, MD, MBA, lead author of an article about the project published in the American Journal of Medical Quality.1 “We learned from other organizations, and one of the first things we learned was to make sure we hired the right person as medical director. We need an energetic, enthusiastic physician who can reach out to nurses and bridge gaps in communication and coordination of care.”
The clinical partnership model was piloted on five units—four adult and one pediatric—and has since been adopted by eight others. The physician/nurse leaders work on such issues as improving care transitions, reducing pressure ulcers and catheter-related urinary tract infections, developing multi-disciplinary rounding on the units, and sharing quality data with staff.
“Take UTIs or pressure ulcers; we’re all familiar with recommended practice, but how it gets played out on the units varies. If team leaders understand this, they can champion the processes and
create an educational push for them,” Dr. Kim says. “Those organizations that have done this well cite higher staff satisfaction as a result.”
Study results show that the initial five units were “among the highest-performing units in our facility on satisfaction,” he adds. “It’s an exciting opportunity to bring change processes necessary to build a local clinical care environment that will improve the overall experience of the patient.”
Reference
A project to formalize “local leadership models”—partnering leadership teams comprising a hospitalist and a nurse manager on each participating unit—at the University of Michigan Health System helped to redefine the role of unit medical director and led to allocating sufficient time (15% to 20% of an FTE) for hospitalists to fill that role. The process also led to a joint role description for the physician and nurse leaders.
“In our organization, we had the medical director concept in place previously, but things were missing, with no direct accountability, no dedicated effort, and lack of clarity on reporting,” explains hospitalist Christopher Kim, MD, MBA, lead author of an article about the project published in the American Journal of Medical Quality.1 “We learned from other organizations, and one of the first things we learned was to make sure we hired the right person as medical director. We need an energetic, enthusiastic physician who can reach out to nurses and bridge gaps in communication and coordination of care.”
The clinical partnership model was piloted on five units—four adult and one pediatric—and has since been adopted by eight others. The physician/nurse leaders work on such issues as improving care transitions, reducing pressure ulcers and catheter-related urinary tract infections, developing multi-disciplinary rounding on the units, and sharing quality data with staff.
“Take UTIs or pressure ulcers; we’re all familiar with recommended practice, but how it gets played out on the units varies. If team leaders understand this, they can champion the processes and
create an educational push for them,” Dr. Kim says. “Those organizations that have done this well cite higher staff satisfaction as a result.”
Study results show that the initial five units were “among the highest-performing units in our facility on satisfaction,” he adds. “It’s an exciting opportunity to bring change processes necessary to build a local clinical care environment that will improve the overall experience of the patient.”
Reference
A project to formalize “local leadership models”—partnering leadership teams comprising a hospitalist and a nurse manager on each participating unit—at the University of Michigan Health System helped to redefine the role of unit medical director and led to allocating sufficient time (15% to 20% of an FTE) for hospitalists to fill that role. The process also led to a joint role description for the physician and nurse leaders.
“In our organization, we had the medical director concept in place previously, but things were missing, with no direct accountability, no dedicated effort, and lack of clarity on reporting,” explains hospitalist Christopher Kim, MD, MBA, lead author of an article about the project published in the American Journal of Medical Quality.1 “We learned from other organizations, and one of the first things we learned was to make sure we hired the right person as medical director. We need an energetic, enthusiastic physician who can reach out to nurses and bridge gaps in communication and coordination of care.”
The clinical partnership model was piloted on five units—four adult and one pediatric—and has since been adopted by eight others. The physician/nurse leaders work on such issues as improving care transitions, reducing pressure ulcers and catheter-related urinary tract infections, developing multi-disciplinary rounding on the units, and sharing quality data with staff.
“Take UTIs or pressure ulcers; we’re all familiar with recommended practice, but how it gets played out on the units varies. If team leaders understand this, they can champion the processes and
create an educational push for them,” Dr. Kim says. “Those organizations that have done this well cite higher staff satisfaction as a result.”
Study results show that the initial five units were “among the highest-performing units in our facility on satisfaction,” he adds. “It’s an exciting opportunity to bring change processes necessary to build a local clinical care environment that will improve the overall experience of the patient.”
Reference
First Set of CMS Advisors Includes Hospitalists
In January, the Centers for Medicare & Medicaid Services (CMS) selected 73 professionals as the initial set of advisors for its Innovation Center (http://innovations.cms.gov/). The advisors include 37 physicians, as well as some nurses and health administrators. Each advisor will receive six months of intensive training in quality-improvement (QI) methods and health systems research in order to deepen skills that could help drive improvements in patient care across the system.
Each of the 920 applicants named a project they wanted to pursue at their home institution; many already are involved in quality activities, says Fran Griffin, the program coordinator. CMS hopes that advisors will become “change agents” and mentors to others within their organizations and communities, she adds. “But we are clear that we are not funding research. We want people to come and be educated, and we want to know if they are learning these skills and applying what they learn in real time,” Griffin says.
Advisors will participate in four in-person meetings, the first of which was held in January, as well as four conference calls or webinars each month. The Innovation Center aims to eventually bring 200 advisors on board, with a second cycle of applications and selections expected later this spring.Funded by the Affordable Care Act, the program provides a stipend of up to $20,000 to the advisor’s institution to free up 10 hours a week for training and to complete their projects. Of the initial set of advisors, at least two are hospitalists: Stephen Liu, MD, MPH, FACPM, of Dartmouth-Hitchcock Medical Center in Hanover, N.H., and Jason Stein, MD, SFHM, director of the clinical research program at Emory School of Medicine in Atlanta. Topics pursued by the advisors include unnecessary hospital readmissions, improving care transitions, chronic disease management, and the development of medical homes outside the hospital.
Dr. Liu’s proposed project is to re-engineer and improve geriatric inpatient stays to help preserve patients’ functional status. “Overall, I had a great experience at the first meeting of the advisors,” Dr. Liu says. “It was great to discuss the challenges and opportunities for improvement at each of the different settings represented, and to learn that many of the challenges are similar to those we face in the inpatient setting, such as communication with primary-care providers, transitions of care, and avoiding complications from hospitalizations.”
For more information or to receive email updates, visit www.innovations.cms.gov/initiatives.
In January, the Centers for Medicare & Medicaid Services (CMS) selected 73 professionals as the initial set of advisors for its Innovation Center (http://innovations.cms.gov/). The advisors include 37 physicians, as well as some nurses and health administrators. Each advisor will receive six months of intensive training in quality-improvement (QI) methods and health systems research in order to deepen skills that could help drive improvements in patient care across the system.
Each of the 920 applicants named a project they wanted to pursue at their home institution; many already are involved in quality activities, says Fran Griffin, the program coordinator. CMS hopes that advisors will become “change agents” and mentors to others within their organizations and communities, she adds. “But we are clear that we are not funding research. We want people to come and be educated, and we want to know if they are learning these skills and applying what they learn in real time,” Griffin says.
Advisors will participate in four in-person meetings, the first of which was held in January, as well as four conference calls or webinars each month. The Innovation Center aims to eventually bring 200 advisors on board, with a second cycle of applications and selections expected later this spring.Funded by the Affordable Care Act, the program provides a stipend of up to $20,000 to the advisor’s institution to free up 10 hours a week for training and to complete their projects. Of the initial set of advisors, at least two are hospitalists: Stephen Liu, MD, MPH, FACPM, of Dartmouth-Hitchcock Medical Center in Hanover, N.H., and Jason Stein, MD, SFHM, director of the clinical research program at Emory School of Medicine in Atlanta. Topics pursued by the advisors include unnecessary hospital readmissions, improving care transitions, chronic disease management, and the development of medical homes outside the hospital.
Dr. Liu’s proposed project is to re-engineer and improve geriatric inpatient stays to help preserve patients’ functional status. “Overall, I had a great experience at the first meeting of the advisors,” Dr. Liu says. “It was great to discuss the challenges and opportunities for improvement at each of the different settings represented, and to learn that many of the challenges are similar to those we face in the inpatient setting, such as communication with primary-care providers, transitions of care, and avoiding complications from hospitalizations.”
For more information or to receive email updates, visit www.innovations.cms.gov/initiatives.
In January, the Centers for Medicare & Medicaid Services (CMS) selected 73 professionals as the initial set of advisors for its Innovation Center (http://innovations.cms.gov/). The advisors include 37 physicians, as well as some nurses and health administrators. Each advisor will receive six months of intensive training in quality-improvement (QI) methods and health systems research in order to deepen skills that could help drive improvements in patient care across the system.
Each of the 920 applicants named a project they wanted to pursue at their home institution; many already are involved in quality activities, says Fran Griffin, the program coordinator. CMS hopes that advisors will become “change agents” and mentors to others within their organizations and communities, she adds. “But we are clear that we are not funding research. We want people to come and be educated, and we want to know if they are learning these skills and applying what they learn in real time,” Griffin says.
Advisors will participate in four in-person meetings, the first of which was held in January, as well as four conference calls or webinars each month. The Innovation Center aims to eventually bring 200 advisors on board, with a second cycle of applications and selections expected later this spring.Funded by the Affordable Care Act, the program provides a stipend of up to $20,000 to the advisor’s institution to free up 10 hours a week for training and to complete their projects. Of the initial set of advisors, at least two are hospitalists: Stephen Liu, MD, MPH, FACPM, of Dartmouth-Hitchcock Medical Center in Hanover, N.H., and Jason Stein, MD, SFHM, director of the clinical research program at Emory School of Medicine in Atlanta. Topics pursued by the advisors include unnecessary hospital readmissions, improving care transitions, chronic disease management, and the development of medical homes outside the hospital.
Dr. Liu’s proposed project is to re-engineer and improve geriatric inpatient stays to help preserve patients’ functional status. “Overall, I had a great experience at the first meeting of the advisors,” Dr. Liu says. “It was great to discuss the challenges and opportunities for improvement at each of the different settings represented, and to learn that many of the challenges are similar to those we face in the inpatient setting, such as communication with primary-care providers, transitions of care, and avoiding complications from hospitalizations.”
For more information or to receive email updates, visit www.innovations.cms.gov/initiatives.
Understanding Physicians’ Attitudes toward Safety Culture
Results from a survey to assess physicians’ and medical trainees’ perceptions and attitudes about the culture of patient safety at the University of California at San Francisco (UCSF) Medical Center were reported at HM11 in Dallas by Patrick Kneeland, MD, who has since moved to Providence Regional Medical Center’s Everett Clinic in Seattle, where he co-chairs the Medical Quality Review Committee.
“We were interested in perceptions about what most determines a safety culture within a hospital,” and about differences and similarities between faculty, fellows, and residents, Dr. Kneeland explains. A positive safety culture is essential to enhancing patient safety, and it requires support and commitment at multiple levels.
Dr. Kneeland and colleagues used an established, validated instrument, the federal Agency for Healthcare Research and Quality’s “Hospital Survey on Patient Safety Culture,” which is used by hospitals to assess their staffs’ attitudes toward safety. But the UCSF team
modified the instrument to include additional survey dimensions, such as trainee supervision, event disclosure to patients, and physician-to-physician handoffs.1 Of 290 physicians surveyed in UCSF’s Department of Medicine, 53% completed the survey.
“What was surprising from our survey was the overall high degree of agreement, but with some interesting differences,” Dr. Kneeland explains. In terms of the overall rating of safety culture, on a 1-to-5 scale with five being the highest, fellows rated the safety culture the highest, followed by faculty, and then residents. “Even though, across the board, 70 percent or more said adverse events should be disclosed to patients, only half of the trainees felt encouraged to do so, and half felt there is some danger in doing so,” he says.
Findings led to a major educational initiative around error disclosure, and to having the chief residents openly discuss overnight adverse patient events at morning rounds. The goal is to make event reporting part of customary practice. UCSF plans to repeat the survey in five years, using the initial results as a benchmark, Dr. Kneeland adds.
For more information or to request a copy of the modified survey, email Dr. Kneeland at [email protected].
Larry Beresford is a freelance writer in Oakland, Calif.
Reference
Results from a survey to assess physicians’ and medical trainees’ perceptions and attitudes about the culture of patient safety at the University of California at San Francisco (UCSF) Medical Center were reported at HM11 in Dallas by Patrick Kneeland, MD, who has since moved to Providence Regional Medical Center’s Everett Clinic in Seattle, where he co-chairs the Medical Quality Review Committee.
“We were interested in perceptions about what most determines a safety culture within a hospital,” and about differences and similarities between faculty, fellows, and residents, Dr. Kneeland explains. A positive safety culture is essential to enhancing patient safety, and it requires support and commitment at multiple levels.
Dr. Kneeland and colleagues used an established, validated instrument, the federal Agency for Healthcare Research and Quality’s “Hospital Survey on Patient Safety Culture,” which is used by hospitals to assess their staffs’ attitudes toward safety. But the UCSF team
modified the instrument to include additional survey dimensions, such as trainee supervision, event disclosure to patients, and physician-to-physician handoffs.1 Of 290 physicians surveyed in UCSF’s Department of Medicine, 53% completed the survey.
“What was surprising from our survey was the overall high degree of agreement, but with some interesting differences,” Dr. Kneeland explains. In terms of the overall rating of safety culture, on a 1-to-5 scale with five being the highest, fellows rated the safety culture the highest, followed by faculty, and then residents. “Even though, across the board, 70 percent or more said adverse events should be disclosed to patients, only half of the trainees felt encouraged to do so, and half felt there is some danger in doing so,” he says.
Findings led to a major educational initiative around error disclosure, and to having the chief residents openly discuss overnight adverse patient events at morning rounds. The goal is to make event reporting part of customary practice. UCSF plans to repeat the survey in five years, using the initial results as a benchmark, Dr. Kneeland adds.
For more information or to request a copy of the modified survey, email Dr. Kneeland at [email protected].
Larry Beresford is a freelance writer in Oakland, Calif.
Reference
Results from a survey to assess physicians’ and medical trainees’ perceptions and attitudes about the culture of patient safety at the University of California at San Francisco (UCSF) Medical Center were reported at HM11 in Dallas by Patrick Kneeland, MD, who has since moved to Providence Regional Medical Center’s Everett Clinic in Seattle, where he co-chairs the Medical Quality Review Committee.
“We were interested in perceptions about what most determines a safety culture within a hospital,” and about differences and similarities between faculty, fellows, and residents, Dr. Kneeland explains. A positive safety culture is essential to enhancing patient safety, and it requires support and commitment at multiple levels.
Dr. Kneeland and colleagues used an established, validated instrument, the federal Agency for Healthcare Research and Quality’s “Hospital Survey on Patient Safety Culture,” which is used by hospitals to assess their staffs’ attitudes toward safety. But the UCSF team
modified the instrument to include additional survey dimensions, such as trainee supervision, event disclosure to patients, and physician-to-physician handoffs.1 Of 290 physicians surveyed in UCSF’s Department of Medicine, 53% completed the survey.
“What was surprising from our survey was the overall high degree of agreement, but with some interesting differences,” Dr. Kneeland explains. In terms of the overall rating of safety culture, on a 1-to-5 scale with five being the highest, fellows rated the safety culture the highest, followed by faculty, and then residents. “Even though, across the board, 70 percent or more said adverse events should be disclosed to patients, only half of the trainees felt encouraged to do so, and half felt there is some danger in doing so,” he says.
Findings led to a major educational initiative around error disclosure, and to having the chief residents openly discuss overnight adverse patient events at morning rounds. The goal is to make event reporting part of customary practice. UCSF plans to repeat the survey in five years, using the initial results as a benchmark, Dr. Kneeland adds.
For more information or to request a copy of the modified survey, email Dr. Kneeland at [email protected].
Larry Beresford is a freelance writer in Oakland, Calif.
Reference
By the Numbers: 8.3%
8.3%1 in 12 adults ages 21 and older Discharged from the hospital to the community were readmitted within 30 days, according to the National Institute for Health Care Reform. One in 3 (32.9%) were readmitted within one year, suggesting that a significant number of patients remain at risk for readmission far beyond the typically measured 30-day window.
8.3%1 in 12 adults ages 21 and older Discharged from the hospital to the community were readmitted within 30 days, according to the National Institute for Health Care Reform. One in 3 (32.9%) were readmitted within one year, suggesting that a significant number of patients remain at risk for readmission far beyond the typically measured 30-day window.
8.3%1 in 12 adults ages 21 and older Discharged from the hospital to the community were readmitted within 30 days, according to the National Institute for Health Care Reform. One in 3 (32.9%) were readmitted within one year, suggesting that a significant number of patients remain at risk for readmission far beyond the typically measured 30-day window.
Presenting Complaint Overshadows More Serious Problem
Cases reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Presenting Complaint Overshadows More Serious Problem
A Florida woman who presented to a walk-in clinic for a respiratory condition had also sustained a puncture wound on her finger from an air-powered paint gun. The defendant physician prescribed an antibiotic but did not order an x-ray.
The patient returned to the clinic two days later with increased pain, swelling, and blackening of the finger. The defendant prescribed two pain medications but did not order an x-ray; nor did he mention follow-up treatment.
Later that day, the woman presented to a hospital emergency department (ED) and subsequently underwent amputation of the distal end of her index finger.
The plaintiff alleged negligence on the physician’s failure to send her to the ED or to provide proper care for her finger injury. The defendants claimed that the plaintiff presented to the clinic for evaluation of a respiratory condition and was prescribed an antibiotic. When the plaintiff had a problem with the first antibiotic, the defendant substituted another. The defendant denied that the plaintiff ever complained of a finger injury.
OUTCOME
According to a published account, a verdict of $241,275 was returned. This included $2,000 to be awarded to the plaintiff’s husband for loss of services.
COMMENT
High-pressure injection injuries are often underestimated, legally risky, and potentially devastating to the patient.
As expected, the hands are most likely to be involved, and grease and paint are the substances most commonly injected. The most common injury sites are the index finger or palm of the nondominant hand, which is injected when the user attempts to clean the gun’s nozzle or to steady the gun with a free hand.
These cases can be catastrophic. Outwardly, the injury appears to be an innocuous puncture wound, but the internal injury is severe. Clinicians unfamiliar with high-pressure injection injuries often treat them as a typical puncture wound, as was done in this case. High-pressure injection injuries require immediate surgical consultation and operative management. Even when competent, prompt surgical management takes place, amputation rates are high.
Jurors find the loss of a limb or a digit compelling and recognize the important life-long consequences of such an injury. Jurors expect clinicians to recognize that paint or grease that fills a finger under high pressure represents a threat to the limb, and they will expect the clinician to act swiftly in an effort to save the digit.
Moreover, such cases are easy for the plaintiff’s attorney to try. Unlike electrolyte disturbances or complicated metabolic derangements, high-pressure injection injuries are easy to understand and will keep the average juror’s attention. The plaintiff’s attorney will offer dramatic testimonial evidence of necrosis and inflammation as the paint is shown to move along the tendon sheath. Damaging intraoperative photographic evidence may be produced, and photographs of the resulting wound are almost certain.
High-pressure injection injuries are limb/digit-threatening. Move quickly to offer the patient the best possible result and minimize your malpractice risk. —DML
Mismanaged Infection in Man With Previous Splenectomy
In Ohio, a 27-year-old man presented to the ED with a temperature of 103°F and other signs and symptoms of infection. He had a history of idiopathic thrombocytopenic purpura (ITP), for which he had previously undergone removal of his spleen. At the ED, he was seen by the defendant emergency physician, Dr. A., who made a diagnosis of flu and obtained a culture.
Dr. A. also called Dr. B., the defendant oncologist/hematologist, for a consult. According to Dr. A., he asked Dr. B. whether antibiotics should be prescribed before the patient was released, and Dr. B. told him antibiotics were not necessary. The man was then discharged.
By the next morning, his symptoms had worsened. He presented to a second ED, where he died as a result of an overwhelming infection.
Plaintiff for the decedent claimed that antibiotics should have been prescribed due to his pre-existing ITP and history of splenectomy. Dr. A. claimed that he had appropriately consulted with Dr. B. and had followed the instructions he was given. Dr. B. acknowledged that he had been called and notified that the decedent was in the ED, but he maintained that he had not been asked for advice about whether to prescribe antibiotics.
OUTCOME
According to a published account, a $750,000 verdict was returned. Dr. B. was found 70% at fault, and Dr. A. was found 30% at fault.
COMMENT
This case involves failure to recognize and treat overwhelming postsplenectomy infection (OPSI). Given the patient’s young age and the lost possibility for a full recovery, the jury’s verdict is restrained and probably reflects a relatively conservative jury pool.
Asplenic patients are usually aware that they do not have a spleen, but they may not recognize their associated risk for serious infection. The fact of the matter is that asplenic patients are immunocompromised. When an asplenic patient presents with a febrile illness that is consistent with OPSI, this is a true medical emergency. These patients must undergo a vigorous workup and expeditious administration of antibiotics to offer the best chance for survival. Even with appropriate antibiotic treatment and supportive therapies, mortality associated with OPSI ranges between 50% and 80%.
In this case, the emergency physician obtained a hematology/oncology consultation. There is a dispute between the defendant physicians as to whether antibiotics were recommended or even discussed. It is unclear from the record whether or not the emergency physician’s clinical note includes such a discussion. The jury apportioned the majority of the liability to the hematologist but still found the emergency physician negligent.
Conflict between clinicians or departments can get testy in the clinical record; don’t let that happen. An otherwise defensible record of care can become a nightmare for defense counsel when an interpersonal or interdepartmental conflict is played out in the clinical record. As with personal conflict, defensive addendums to a patient’s record can be damaging. Jurors generally reward “finger pointing” between medical professionals with a verdict for the plaintiff, even when the care itself may be defensible. Regularly held peer review offers clinicians an opportunity to discuss difficult cases without fearing that those discussions will be used as evidence. A formal peer review committee is the exclusive and proper outlet to discuss challenging clinical cases.
Appropriate care for our patients is the ultimate necessity. It can be tricky for a clinician seeking a consultation to challenge the consultant’s recommendation. When confronted with a recommendation that leaves you (the referring clinician) with “heartburn,” it may be helpful for you to restate your misgivings affirmatively—for example, “My concern with that approach is ___,” then state the risks in the gravest terms the situation will allow. Make your preferred course of action apparent: “Honestly, I’d like to admit the patient because of ____.”
If you remain uneasy, seek another colleague’s opinion. Record the substance of the consultation, concerns, and responses fully, accurately but dispassionately, in the patient’s record.
Make sure to give the consultant all the clinical information available; and if you are the consultant, be sure you have received all available information. Treat the consultation formally and with your full attention. The jury will expect the consultant to be fully involved in caring for the patient.
Here, if the emergency physician did not agree with the hematologist, it would have been reasonable for him to obtain a second opinion or to admit the patient and begin empiric antibiotic treatment. —DML
Cases reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Presenting Complaint Overshadows More Serious Problem
A Florida woman who presented to a walk-in clinic for a respiratory condition had also sustained a puncture wound on her finger from an air-powered paint gun. The defendant physician prescribed an antibiotic but did not order an x-ray.
The patient returned to the clinic two days later with increased pain, swelling, and blackening of the finger. The defendant prescribed two pain medications but did not order an x-ray; nor did he mention follow-up treatment.
Later that day, the woman presented to a hospital emergency department (ED) and subsequently underwent amputation of the distal end of her index finger.
The plaintiff alleged negligence on the physician’s failure to send her to the ED or to provide proper care for her finger injury. The defendants claimed that the plaintiff presented to the clinic for evaluation of a respiratory condition and was prescribed an antibiotic. When the plaintiff had a problem with the first antibiotic, the defendant substituted another. The defendant denied that the plaintiff ever complained of a finger injury.
OUTCOME
According to a published account, a verdict of $241,275 was returned. This included $2,000 to be awarded to the plaintiff’s husband for loss of services.
COMMENT
High-pressure injection injuries are often underestimated, legally risky, and potentially devastating to the patient.
As expected, the hands are most likely to be involved, and grease and paint are the substances most commonly injected. The most common injury sites are the index finger or palm of the nondominant hand, which is injected when the user attempts to clean the gun’s nozzle or to steady the gun with a free hand.
These cases can be catastrophic. Outwardly, the injury appears to be an innocuous puncture wound, but the internal injury is severe. Clinicians unfamiliar with high-pressure injection injuries often treat them as a typical puncture wound, as was done in this case. High-pressure injection injuries require immediate surgical consultation and operative management. Even when competent, prompt surgical management takes place, amputation rates are high.
Jurors find the loss of a limb or a digit compelling and recognize the important life-long consequences of such an injury. Jurors expect clinicians to recognize that paint or grease that fills a finger under high pressure represents a threat to the limb, and they will expect the clinician to act swiftly in an effort to save the digit.
Moreover, such cases are easy for the plaintiff’s attorney to try. Unlike electrolyte disturbances or complicated metabolic derangements, high-pressure injection injuries are easy to understand and will keep the average juror’s attention. The plaintiff’s attorney will offer dramatic testimonial evidence of necrosis and inflammation as the paint is shown to move along the tendon sheath. Damaging intraoperative photographic evidence may be produced, and photographs of the resulting wound are almost certain.
High-pressure injection injuries are limb/digit-threatening. Move quickly to offer the patient the best possible result and minimize your malpractice risk. —DML
Mismanaged Infection in Man With Previous Splenectomy
In Ohio, a 27-year-old man presented to the ED with a temperature of 103°F and other signs and symptoms of infection. He had a history of idiopathic thrombocytopenic purpura (ITP), for which he had previously undergone removal of his spleen. At the ED, he was seen by the defendant emergency physician, Dr. A., who made a diagnosis of flu and obtained a culture.
Dr. A. also called Dr. B., the defendant oncologist/hematologist, for a consult. According to Dr. A., he asked Dr. B. whether antibiotics should be prescribed before the patient was released, and Dr. B. told him antibiotics were not necessary. The man was then discharged.
By the next morning, his symptoms had worsened. He presented to a second ED, where he died as a result of an overwhelming infection.
Plaintiff for the decedent claimed that antibiotics should have been prescribed due to his pre-existing ITP and history of splenectomy. Dr. A. claimed that he had appropriately consulted with Dr. B. and had followed the instructions he was given. Dr. B. acknowledged that he had been called and notified that the decedent was in the ED, but he maintained that he had not been asked for advice about whether to prescribe antibiotics.
OUTCOME
According to a published account, a $750,000 verdict was returned. Dr. B. was found 70% at fault, and Dr. A. was found 30% at fault.
COMMENT
This case involves failure to recognize and treat overwhelming postsplenectomy infection (OPSI). Given the patient’s young age and the lost possibility for a full recovery, the jury’s verdict is restrained and probably reflects a relatively conservative jury pool.
Asplenic patients are usually aware that they do not have a spleen, but they may not recognize their associated risk for serious infection. The fact of the matter is that asplenic patients are immunocompromised. When an asplenic patient presents with a febrile illness that is consistent with OPSI, this is a true medical emergency. These patients must undergo a vigorous workup and expeditious administration of antibiotics to offer the best chance for survival. Even with appropriate antibiotic treatment and supportive therapies, mortality associated with OPSI ranges between 50% and 80%.
In this case, the emergency physician obtained a hematology/oncology consultation. There is a dispute between the defendant physicians as to whether antibiotics were recommended or even discussed. It is unclear from the record whether or not the emergency physician’s clinical note includes such a discussion. The jury apportioned the majority of the liability to the hematologist but still found the emergency physician negligent.
Conflict between clinicians or departments can get testy in the clinical record; don’t let that happen. An otherwise defensible record of care can become a nightmare for defense counsel when an interpersonal or interdepartmental conflict is played out in the clinical record. As with personal conflict, defensive addendums to a patient’s record can be damaging. Jurors generally reward “finger pointing” between medical professionals with a verdict for the plaintiff, even when the care itself may be defensible. Regularly held peer review offers clinicians an opportunity to discuss difficult cases without fearing that those discussions will be used as evidence. A formal peer review committee is the exclusive and proper outlet to discuss challenging clinical cases.
Appropriate care for our patients is the ultimate necessity. It can be tricky for a clinician seeking a consultation to challenge the consultant’s recommendation. When confronted with a recommendation that leaves you (the referring clinician) with “heartburn,” it may be helpful for you to restate your misgivings affirmatively—for example, “My concern with that approach is ___,” then state the risks in the gravest terms the situation will allow. Make your preferred course of action apparent: “Honestly, I’d like to admit the patient because of ____.”
If you remain uneasy, seek another colleague’s opinion. Record the substance of the consultation, concerns, and responses fully, accurately but dispassionately, in the patient’s record.
Make sure to give the consultant all the clinical information available; and if you are the consultant, be sure you have received all available information. Treat the consultation formally and with your full attention. The jury will expect the consultant to be fully involved in caring for the patient.
Here, if the emergency physician did not agree with the hematologist, it would have been reasonable for him to obtain a second opinion or to admit the patient and begin empiric antibiotic treatment. —DML
Cases reprinted with permission from Medical Malpractice Verdicts, Settlements and Experts, Lewis Laska, Editor, (800) 298-6288.
Presenting Complaint Overshadows More Serious Problem
A Florida woman who presented to a walk-in clinic for a respiratory condition had also sustained a puncture wound on her finger from an air-powered paint gun. The defendant physician prescribed an antibiotic but did not order an x-ray.
The patient returned to the clinic two days later with increased pain, swelling, and blackening of the finger. The defendant prescribed two pain medications but did not order an x-ray; nor did he mention follow-up treatment.
Later that day, the woman presented to a hospital emergency department (ED) and subsequently underwent amputation of the distal end of her index finger.
The plaintiff alleged negligence on the physician’s failure to send her to the ED or to provide proper care for her finger injury. The defendants claimed that the plaintiff presented to the clinic for evaluation of a respiratory condition and was prescribed an antibiotic. When the plaintiff had a problem with the first antibiotic, the defendant substituted another. The defendant denied that the plaintiff ever complained of a finger injury.
OUTCOME
According to a published account, a verdict of $241,275 was returned. This included $2,000 to be awarded to the plaintiff’s husband for loss of services.
COMMENT
High-pressure injection injuries are often underestimated, legally risky, and potentially devastating to the patient.
As expected, the hands are most likely to be involved, and grease and paint are the substances most commonly injected. The most common injury sites are the index finger or palm of the nondominant hand, which is injected when the user attempts to clean the gun’s nozzle or to steady the gun with a free hand.
These cases can be catastrophic. Outwardly, the injury appears to be an innocuous puncture wound, but the internal injury is severe. Clinicians unfamiliar with high-pressure injection injuries often treat them as a typical puncture wound, as was done in this case. High-pressure injection injuries require immediate surgical consultation and operative management. Even when competent, prompt surgical management takes place, amputation rates are high.
Jurors find the loss of a limb or a digit compelling and recognize the important life-long consequences of such an injury. Jurors expect clinicians to recognize that paint or grease that fills a finger under high pressure represents a threat to the limb, and they will expect the clinician to act swiftly in an effort to save the digit.
Moreover, such cases are easy for the plaintiff’s attorney to try. Unlike electrolyte disturbances or complicated metabolic derangements, high-pressure injection injuries are easy to understand and will keep the average juror’s attention. The plaintiff’s attorney will offer dramatic testimonial evidence of necrosis and inflammation as the paint is shown to move along the tendon sheath. Damaging intraoperative photographic evidence may be produced, and photographs of the resulting wound are almost certain.
High-pressure injection injuries are limb/digit-threatening. Move quickly to offer the patient the best possible result and minimize your malpractice risk. —DML
Mismanaged Infection in Man With Previous Splenectomy
In Ohio, a 27-year-old man presented to the ED with a temperature of 103°F and other signs and symptoms of infection. He had a history of idiopathic thrombocytopenic purpura (ITP), for which he had previously undergone removal of his spleen. At the ED, he was seen by the defendant emergency physician, Dr. A., who made a diagnosis of flu and obtained a culture.
Dr. A. also called Dr. B., the defendant oncologist/hematologist, for a consult. According to Dr. A., he asked Dr. B. whether antibiotics should be prescribed before the patient was released, and Dr. B. told him antibiotics were not necessary. The man was then discharged.
By the next morning, his symptoms had worsened. He presented to a second ED, where he died as a result of an overwhelming infection.
Plaintiff for the decedent claimed that antibiotics should have been prescribed due to his pre-existing ITP and history of splenectomy. Dr. A. claimed that he had appropriately consulted with Dr. B. and had followed the instructions he was given. Dr. B. acknowledged that he had been called and notified that the decedent was in the ED, but he maintained that he had not been asked for advice about whether to prescribe antibiotics.
OUTCOME
According to a published account, a $750,000 verdict was returned. Dr. B. was found 70% at fault, and Dr. A. was found 30% at fault.
COMMENT
This case involves failure to recognize and treat overwhelming postsplenectomy infection (OPSI). Given the patient’s young age and the lost possibility for a full recovery, the jury’s verdict is restrained and probably reflects a relatively conservative jury pool.
Asplenic patients are usually aware that they do not have a spleen, but they may not recognize their associated risk for serious infection. The fact of the matter is that asplenic patients are immunocompromised. When an asplenic patient presents with a febrile illness that is consistent with OPSI, this is a true medical emergency. These patients must undergo a vigorous workup and expeditious administration of antibiotics to offer the best chance for survival. Even with appropriate antibiotic treatment and supportive therapies, mortality associated with OPSI ranges between 50% and 80%.
In this case, the emergency physician obtained a hematology/oncology consultation. There is a dispute between the defendant physicians as to whether antibiotics were recommended or even discussed. It is unclear from the record whether or not the emergency physician’s clinical note includes such a discussion. The jury apportioned the majority of the liability to the hematologist but still found the emergency physician negligent.
Conflict between clinicians or departments can get testy in the clinical record; don’t let that happen. An otherwise defensible record of care can become a nightmare for defense counsel when an interpersonal or interdepartmental conflict is played out in the clinical record. As with personal conflict, defensive addendums to a patient’s record can be damaging. Jurors generally reward “finger pointing” between medical professionals with a verdict for the plaintiff, even when the care itself may be defensible. Regularly held peer review offers clinicians an opportunity to discuss difficult cases without fearing that those discussions will be used as evidence. A formal peer review committee is the exclusive and proper outlet to discuss challenging clinical cases.
Appropriate care for our patients is the ultimate necessity. It can be tricky for a clinician seeking a consultation to challenge the consultant’s recommendation. When confronted with a recommendation that leaves you (the referring clinician) with “heartburn,” it may be helpful for you to restate your misgivings affirmatively—for example, “My concern with that approach is ___,” then state the risks in the gravest terms the situation will allow. Make your preferred course of action apparent: “Honestly, I’d like to admit the patient because of ____.”
If you remain uneasy, seek another colleague’s opinion. Record the substance of the consultation, concerns, and responses fully, accurately but dispassionately, in the patient’s record.
Make sure to give the consultant all the clinical information available; and if you are the consultant, be sure you have received all available information. Treat the consultation formally and with your full attention. The jury will expect the consultant to be fully involved in caring for the patient.
Here, if the emergency physician did not agree with the hematologist, it would have been reasonable for him to obtain a second opinion or to admit the patient and begin empiric antibiotic treatment. —DML
Do you want to prevail at trial? Here are 10 keys to effective testimony
“10 strategies for the hot seat: Giving a successful deposition”
Andrew K. Worek, Esq (February 2012)
Mr. Worek reports no financial relationships relevant to this article.
You survived the deposition: Your attorney advised you that it went well and that nothing you said was catastrophically harmful to the defense of your case. Now it’s time to move on to trial.
A date has been set, and you’re anticipating it with a fair dose of trepidation. You may find yourself pacing nervously along the marble corridors of the courthouse or staring with foreboding at the witness stand, with its solitary chair and microphone. Rest assured: There is much to be done to navigate your way through the trial process.
In this article—a follow-up to “Strategies for the hot seat: Giving a successful deposition” (February 2012)—I offer 10 tips for getting through a medical malpractice trial.

1 Preparation is critical
How do you get to Carnegie Hall? You’ve heard the joke.
Preparation is absolutely critical. You are going to have six to 14 jurors, a judge, defense counsel, opposing counsel, the plaintiff, and a small audience watching your every move and hanging on every word, but there’s no need to be nervous if you have prepared.
That said, be informed that hours upon hours of discussion and review of the care rendered with your attorney may be necessary to ensure that you understand medical and legal issues and can address both with confidence.
Any hesitation or poorly chosen phrase can have a detrimental effect on your case. Review every aspect of your testimony, the exhibits you plan to use, and the questions likely to be asked by your own attorney and opposing counsel—and do so repeatedly. You should expect to spend several days immediately before trial in your lawyer’s office going over every detail, so clear your schedule.
Don’t stop until you are familiar with every aspect of your testimony and the facts. Anything less may cause you to appear un-prepared, confused, or, worse—incompetent.
2 Put on your educator’s cap
Now is the time to teach.
During your deposition, you concentrated on simply answering the question that was posed in the manner in which it was asked, and you tried to avoid educating opposing counsel. A trial is different—you have a panel of jurors who are eager to hear your side of the story. These are the people who will decide your fate. Now is the time to teach.
I was once told—and I truly believe—that most jurors understand science and medicine at the high school level. Of course, some jurors will have greater understanding, and some less. Teach the jury the reasons behind your medical decisions and explain why they were correct. A teaching approach—as opposed to monotone answers—will help hold the jury’s attention and address its inquisitiveness.
Work with your attorney to develop appropriate explanations of medical terms, diagnoses, and treatments at issue in the case.
3 Face the jury
We typically look at the person to whom we are speaking. In the courtroom, this tendency translates into a focus on the lawyer who is doing the questioning rather than the jury. In the big picture, however, you are testifying to the jury, not the attorney—so look at the jurors when you speak.
Your attorney may position himself (or herself) near the jury so that your gaze encompasses both him and the panel. However, even if the attorney asking questions is not near the jury, turn toward the jury when you answer.
It may help to turn your chair to angle slightly toward the jury when you take the witness stand to make yourself more comfortable and avoid appearing as though your head is on a swivel. Doing so will also help you face the jury more squarely and directly.
Look into the faces and eyes of the jury when you answer questions. Speak to them, not at them.
4 Be yourself
When you are preparing for trial with your attorney, review the answers you expect to give to various questions. Work on delivering those responses in your own words, the way you would present them to a patient or a peer. A jury can detect sincerity and its opposite—glibness.
You and your counsel may agree on the information or points to be disclosed in response to a certain question, but on the witness stand, you will have to respond with your own voice and vocabulary.
5 Prepare to be cross-examined
Most jurisdictions permit opposing counsel to call a defendant physician to the witness stand, “as if on cross-examination.” This means that the opposing attorney can ask you leading questions in an attempt to box you into “Yes” or “No” responses with little or no opportunity to explain. This is customary. You must be prepared to face heated examination.
A trial is an adversarial process, based on the general premise that, through heated exchanges and questioning, the truth will emerge. Opposing counsel will attempt to get you to answer questions based on the plaintiff’s view of the case. Most physicians find having their answers constrained in this manner to be very frustrating.
Work with your attorney until you are ready to answer even the toughest and narrowest of “Yes” or “No” questions. If a question cannot be answered reliably with a “Yes” or “No,” be prepared to point that fact out to the questioning attorney or the judge. Also be prepared to provide an explanation beyond “Yes” or “No” when it may be appropriate. The judge will ultimately decide whether an explanation is warranted; many judges permit elaboration.
Your own attorney will later have the opportunity to question you, as well. If you are not permitted to give an explanation during questioning by opposing counsel, your own attorney can afford you that opportunity. An opposing attorney who insists that a physician not explain runs the risk of diverting the jury’s focus to the unstated explanation rather than to the actual “Yes” or “No” response. Indicate when you would like to explain an answer, and retain your composure if refused.
When opposing counsel has finished questioning you, your own skillful defense attorney can rise from his chair and ask, “Doctor, what is it that you wanted to explain to the ladies and gentlemen of the jury?” Then, like the late radio commentator Paul Harvey, you can provide “the rest of the story.”
As you did during your deposition, you have the right to ask for clarification of a confusing or unintelligible question. The same is true for a question in which a medical principle or condition is improperly characterized or defined. If a question doesn’t make sense, ask for clarification. If the question is inaccurate, advise the opposing attorney of the improper characterization, and ask that he rephrase the question. On occasion, it may be best to respond to a mischaracterization of a medical principle by answering: “That’s not how it works.” By declining to offer more information, you can create a moment of uncomfortable silence while opposing counsel collects his thoughts and regroups.
6 Emulate a weather forecaster
Work with your attorney to find aspects of your testimony that will permit you to get off the witness stand and present a chart or graph or other evidence from a standing position before the jury. Think of how much more interesting a weather forecaster is than an anchor who sits behind a desk reading news. Lengthy testimony from the witness stand is boring for the jury and can be tiring for the witness. Get off the stand once or twice to illustrate a point or demonstrate, for example, how the McRoberts maneuver is accomplished. It will keep the jury focused and interested.
When you stand before the jury to illustrate a point, make sure every juror can see your presentation. Your attorney may also request that a photograph or other exhibit be “published” to the jury so that the panel members can pass it among themselves and examine it with their own hands.
7 Be on your best behavior
Jurors are curious. They are being asked to, quite literally, pass judgment on you, despite knowing next to nothing about you. Jurors typically take their duties very seriously and will naturally be motivated to analyze non-verbal as well as verbal cues in an effort to learn more about you. Be prepared: They will watch your every move and mannerism in the courtroom, so be conscious of your clothing, mannerisms, and behavior. This holds true in the hallways of the courthouse and any location within two or three blocks. It is not uncommon to encounter a juror a block or two away from a courthouse in a major city, or to see a juror in a nearby coffee shop.
8 Control your reactions to testimony
It may be difficult to sit and listen as opposing counsel presents his opening argument to the jury. It may be a challenge to listen to the plaintiff’s case during the first 2 or 3 days of the trial. The plaintiff goes first; you have to wait your turn.
Overt facial reactions to testimony are best avoided. Although it may be helpful for you to make notes during testimony, try not to pass or slide them across the table to your attorney, except for rare occasions. There will be periodic breaks in the testimony, during which you can discuss your notes with your attorney. Frantically jotting down notes and sliding them over to your attorney may cause the jury to conclude that you are overly emotional or lack confidence in your attorney.
9 Test the gadgets
If you are going to present an exhibit, such as a chart or graph, make absolutely certain that it is accurate. Any error will be noted by opposing counsel and may impair your credibility. Also consider whether the chart or diagram could be reinterpreted to support your opponent’s case. If it could, don’t use it.
High-tech gizmos were once frowned upon by old-school defense attorneys. Now, we’re well past the MTV generation, and high-tech illustrations and animations are common in courtrooms. Be careful to avoid any high-tech malfunctions, however, which can distract the jury during presentation of your evidence.
If you are planning to use a demonstrative exhibit such as a heart-rate monitor or portable pulse oximetry device, make sure the batteries are charged and that it works. Practice any maneuver you plan to perform using the device or machine. You don’t want to appear clumsy or unfamiliar with the device. If any demonstration involves a sharp or needle, use an abundance of caution! In a birth injury case, baby mannequins are sometimes used. Make sure they work as intended and don’t permit anyone to “play” with them in the courtroom during breaks in the case. Trial is a serious matter; any levity observed by a juror could leave a detrimental impression.
Over my career, I have seen 1) an orthopedic surgery expert drop several “easy to assemble” metal components, creating a cacophony of pings and clangs as they bounced across the marble floor; 2) a surgeon staple his own palm with an “empty” laparoscopic staple gun; and 3) a medical expert miss a step getting off the witness stand, causing him to tumble into the jury box, strike his head and render himself nearly unconscious. This last incident led to the cancellation of the afternoon court session.
10 Take your time— and a little water
It’s helpful to visit the courtroom with your attorney some time before the trial date to dispel the jitters that can arise in an unfamiliar place. Also take a moment to sit in the witness stand so that you can have some level of comfort when testifying and understand how well, or poorly, the jury will be able to see you (and vice versa).
During the trial, take your time when answering questions. You may want to speak slightly more slowly than normal so that all the jurors can hear and appreciate what you’re saying. The tempo and volume of your testimony may also need to be adjusted, depending on the acoustics of the courtroom, which can vary widely, particularly in some of the more majestic and ornate venues.
Most courtrooms offer water pitchers and cups. Take a half-cup of water with you to the stand. A full cup is easy to spill—and creates a mess when it does. Courtrooms are not known for having an ample supply of paper towels.
Your confident presence can humanize the courtroom
The trial of a medical malpractice case is a difficult and emotional experience for any physician. Preparing to testify with confidence and precision is an important step toward a successful defense. The courtroom is an unfamiliar, uncomfortable, and adversarial environment. With appropriate preparation, however, the daunting specter of the witness stand can be conquered.
They’re available in the archive at obgmanagement.com
- Data on liability claims offer bright spots for ObGyns—and sobering statistics
Janelle Yates (January 2012) - Sound strategies to avoid malpractice hazards on labor and delivery (Part 1)
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD (December 2010) - More strategies to avoid malpractice hazards on labor and delivery (Part 2)
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD (January 2011) - Afraid of getting sued? A plaintiff attorney offers counsel (but no sympathy)
Janelle Yates (October 2009) - 10 keys to defending (or, better, keeping clear of) a shoulder dystocia suit
Andrew K. Worek, Esq (March 2008)
We want to hear from you! Tell us what you think.
“10 strategies for the hot seat: Giving a successful deposition”
Andrew K. Worek, Esq (February 2012)
Mr. Worek reports no financial relationships relevant to this article.
You survived the deposition: Your attorney advised you that it went well and that nothing you said was catastrophically harmful to the defense of your case. Now it’s time to move on to trial.
A date has been set, and you’re anticipating it with a fair dose of trepidation. You may find yourself pacing nervously along the marble corridors of the courthouse or staring with foreboding at the witness stand, with its solitary chair and microphone. Rest assured: There is much to be done to navigate your way through the trial process.
In this article—a follow-up to “Strategies for the hot seat: Giving a successful deposition” (February 2012)—I offer 10 tips for getting through a medical malpractice trial.

1 Preparation is critical
How do you get to Carnegie Hall? You’ve heard the joke.
Preparation is absolutely critical. You are going to have six to 14 jurors, a judge, defense counsel, opposing counsel, the plaintiff, and a small audience watching your every move and hanging on every word, but there’s no need to be nervous if you have prepared.
That said, be informed that hours upon hours of discussion and review of the care rendered with your attorney may be necessary to ensure that you understand medical and legal issues and can address both with confidence.
Any hesitation or poorly chosen phrase can have a detrimental effect on your case. Review every aspect of your testimony, the exhibits you plan to use, and the questions likely to be asked by your own attorney and opposing counsel—and do so repeatedly. You should expect to spend several days immediately before trial in your lawyer’s office going over every detail, so clear your schedule.
Don’t stop until you are familiar with every aspect of your testimony and the facts. Anything less may cause you to appear un-prepared, confused, or, worse—incompetent.
2 Put on your educator’s cap
Now is the time to teach.
During your deposition, you concentrated on simply answering the question that was posed in the manner in which it was asked, and you tried to avoid educating opposing counsel. A trial is different—you have a panel of jurors who are eager to hear your side of the story. These are the people who will decide your fate. Now is the time to teach.
I was once told—and I truly believe—that most jurors understand science and medicine at the high school level. Of course, some jurors will have greater understanding, and some less. Teach the jury the reasons behind your medical decisions and explain why they were correct. A teaching approach—as opposed to monotone answers—will help hold the jury’s attention and address its inquisitiveness.
Work with your attorney to develop appropriate explanations of medical terms, diagnoses, and treatments at issue in the case.
3 Face the jury
We typically look at the person to whom we are speaking. In the courtroom, this tendency translates into a focus on the lawyer who is doing the questioning rather than the jury. In the big picture, however, you are testifying to the jury, not the attorney—so look at the jurors when you speak.
Your attorney may position himself (or herself) near the jury so that your gaze encompasses both him and the panel. However, even if the attorney asking questions is not near the jury, turn toward the jury when you answer.
It may help to turn your chair to angle slightly toward the jury when you take the witness stand to make yourself more comfortable and avoid appearing as though your head is on a swivel. Doing so will also help you face the jury more squarely and directly.
Look into the faces and eyes of the jury when you answer questions. Speak to them, not at them.
4 Be yourself
When you are preparing for trial with your attorney, review the answers you expect to give to various questions. Work on delivering those responses in your own words, the way you would present them to a patient or a peer. A jury can detect sincerity and its opposite—glibness.
You and your counsel may agree on the information or points to be disclosed in response to a certain question, but on the witness stand, you will have to respond with your own voice and vocabulary.
5 Prepare to be cross-examined
Most jurisdictions permit opposing counsel to call a defendant physician to the witness stand, “as if on cross-examination.” This means that the opposing attorney can ask you leading questions in an attempt to box you into “Yes” or “No” responses with little or no opportunity to explain. This is customary. You must be prepared to face heated examination.
A trial is an adversarial process, based on the general premise that, through heated exchanges and questioning, the truth will emerge. Opposing counsel will attempt to get you to answer questions based on the plaintiff’s view of the case. Most physicians find having their answers constrained in this manner to be very frustrating.
Work with your attorney until you are ready to answer even the toughest and narrowest of “Yes” or “No” questions. If a question cannot be answered reliably with a “Yes” or “No,” be prepared to point that fact out to the questioning attorney or the judge. Also be prepared to provide an explanation beyond “Yes” or “No” when it may be appropriate. The judge will ultimately decide whether an explanation is warranted; many judges permit elaboration.
Your own attorney will later have the opportunity to question you, as well. If you are not permitted to give an explanation during questioning by opposing counsel, your own attorney can afford you that opportunity. An opposing attorney who insists that a physician not explain runs the risk of diverting the jury’s focus to the unstated explanation rather than to the actual “Yes” or “No” response. Indicate when you would like to explain an answer, and retain your composure if refused.
When opposing counsel has finished questioning you, your own skillful defense attorney can rise from his chair and ask, “Doctor, what is it that you wanted to explain to the ladies and gentlemen of the jury?” Then, like the late radio commentator Paul Harvey, you can provide “the rest of the story.”
As you did during your deposition, you have the right to ask for clarification of a confusing or unintelligible question. The same is true for a question in which a medical principle or condition is improperly characterized or defined. If a question doesn’t make sense, ask for clarification. If the question is inaccurate, advise the opposing attorney of the improper characterization, and ask that he rephrase the question. On occasion, it may be best to respond to a mischaracterization of a medical principle by answering: “That’s not how it works.” By declining to offer more information, you can create a moment of uncomfortable silence while opposing counsel collects his thoughts and regroups.
6 Emulate a weather forecaster
Work with your attorney to find aspects of your testimony that will permit you to get off the witness stand and present a chart or graph or other evidence from a standing position before the jury. Think of how much more interesting a weather forecaster is than an anchor who sits behind a desk reading news. Lengthy testimony from the witness stand is boring for the jury and can be tiring for the witness. Get off the stand once or twice to illustrate a point or demonstrate, for example, how the McRoberts maneuver is accomplished. It will keep the jury focused and interested.
When you stand before the jury to illustrate a point, make sure every juror can see your presentation. Your attorney may also request that a photograph or other exhibit be “published” to the jury so that the panel members can pass it among themselves and examine it with their own hands.
7 Be on your best behavior
Jurors are curious. They are being asked to, quite literally, pass judgment on you, despite knowing next to nothing about you. Jurors typically take their duties very seriously and will naturally be motivated to analyze non-verbal as well as verbal cues in an effort to learn more about you. Be prepared: They will watch your every move and mannerism in the courtroom, so be conscious of your clothing, mannerisms, and behavior. This holds true in the hallways of the courthouse and any location within two or three blocks. It is not uncommon to encounter a juror a block or two away from a courthouse in a major city, or to see a juror in a nearby coffee shop.
8 Control your reactions to testimony
It may be difficult to sit and listen as opposing counsel presents his opening argument to the jury. It may be a challenge to listen to the plaintiff’s case during the first 2 or 3 days of the trial. The plaintiff goes first; you have to wait your turn.
Overt facial reactions to testimony are best avoided. Although it may be helpful for you to make notes during testimony, try not to pass or slide them across the table to your attorney, except for rare occasions. There will be periodic breaks in the testimony, during which you can discuss your notes with your attorney. Frantically jotting down notes and sliding them over to your attorney may cause the jury to conclude that you are overly emotional or lack confidence in your attorney.
9 Test the gadgets
If you are going to present an exhibit, such as a chart or graph, make absolutely certain that it is accurate. Any error will be noted by opposing counsel and may impair your credibility. Also consider whether the chart or diagram could be reinterpreted to support your opponent’s case. If it could, don’t use it.
High-tech gizmos were once frowned upon by old-school defense attorneys. Now, we’re well past the MTV generation, and high-tech illustrations and animations are common in courtrooms. Be careful to avoid any high-tech malfunctions, however, which can distract the jury during presentation of your evidence.
If you are planning to use a demonstrative exhibit such as a heart-rate monitor or portable pulse oximetry device, make sure the batteries are charged and that it works. Practice any maneuver you plan to perform using the device or machine. You don’t want to appear clumsy or unfamiliar with the device. If any demonstration involves a sharp or needle, use an abundance of caution! In a birth injury case, baby mannequins are sometimes used. Make sure they work as intended and don’t permit anyone to “play” with them in the courtroom during breaks in the case. Trial is a serious matter; any levity observed by a juror could leave a detrimental impression.
Over my career, I have seen 1) an orthopedic surgery expert drop several “easy to assemble” metal components, creating a cacophony of pings and clangs as they bounced across the marble floor; 2) a surgeon staple his own palm with an “empty” laparoscopic staple gun; and 3) a medical expert miss a step getting off the witness stand, causing him to tumble into the jury box, strike his head and render himself nearly unconscious. This last incident led to the cancellation of the afternoon court session.
10 Take your time— and a little water
It’s helpful to visit the courtroom with your attorney some time before the trial date to dispel the jitters that can arise in an unfamiliar place. Also take a moment to sit in the witness stand so that you can have some level of comfort when testifying and understand how well, or poorly, the jury will be able to see you (and vice versa).
During the trial, take your time when answering questions. You may want to speak slightly more slowly than normal so that all the jurors can hear and appreciate what you’re saying. The tempo and volume of your testimony may also need to be adjusted, depending on the acoustics of the courtroom, which can vary widely, particularly in some of the more majestic and ornate venues.
Most courtrooms offer water pitchers and cups. Take a half-cup of water with you to the stand. A full cup is easy to spill—and creates a mess when it does. Courtrooms are not known for having an ample supply of paper towels.
Your confident presence can humanize the courtroom
The trial of a medical malpractice case is a difficult and emotional experience for any physician. Preparing to testify with confidence and precision is an important step toward a successful defense. The courtroom is an unfamiliar, uncomfortable, and adversarial environment. With appropriate preparation, however, the daunting specter of the witness stand can be conquered.
They’re available in the archive at obgmanagement.com
- Data on liability claims offer bright spots for ObGyns—and sobering statistics
Janelle Yates (January 2012) - Sound strategies to avoid malpractice hazards on labor and delivery (Part 1)
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD (December 2010) - More strategies to avoid malpractice hazards on labor and delivery (Part 2)
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD (January 2011) - Afraid of getting sued? A plaintiff attorney offers counsel (but no sympathy)
Janelle Yates (October 2009) - 10 keys to defending (or, better, keeping clear of) a shoulder dystocia suit
Andrew K. Worek, Esq (March 2008)
We want to hear from you! Tell us what you think.
“10 strategies for the hot seat: Giving a successful deposition”
Andrew K. Worek, Esq (February 2012)
Mr. Worek reports no financial relationships relevant to this article.
You survived the deposition: Your attorney advised you that it went well and that nothing you said was catastrophically harmful to the defense of your case. Now it’s time to move on to trial.
A date has been set, and you’re anticipating it with a fair dose of trepidation. You may find yourself pacing nervously along the marble corridors of the courthouse or staring with foreboding at the witness stand, with its solitary chair and microphone. Rest assured: There is much to be done to navigate your way through the trial process.
In this article—a follow-up to “Strategies for the hot seat: Giving a successful deposition” (February 2012)—I offer 10 tips for getting through a medical malpractice trial.

1 Preparation is critical
How do you get to Carnegie Hall? You’ve heard the joke.
Preparation is absolutely critical. You are going to have six to 14 jurors, a judge, defense counsel, opposing counsel, the plaintiff, and a small audience watching your every move and hanging on every word, but there’s no need to be nervous if you have prepared.
That said, be informed that hours upon hours of discussion and review of the care rendered with your attorney may be necessary to ensure that you understand medical and legal issues and can address both with confidence.
Any hesitation or poorly chosen phrase can have a detrimental effect on your case. Review every aspect of your testimony, the exhibits you plan to use, and the questions likely to be asked by your own attorney and opposing counsel—and do so repeatedly. You should expect to spend several days immediately before trial in your lawyer’s office going over every detail, so clear your schedule.
Don’t stop until you are familiar with every aspect of your testimony and the facts. Anything less may cause you to appear un-prepared, confused, or, worse—incompetent.
2 Put on your educator’s cap
Now is the time to teach.
During your deposition, you concentrated on simply answering the question that was posed in the manner in which it was asked, and you tried to avoid educating opposing counsel. A trial is different—you have a panel of jurors who are eager to hear your side of the story. These are the people who will decide your fate. Now is the time to teach.
I was once told—and I truly believe—that most jurors understand science and medicine at the high school level. Of course, some jurors will have greater understanding, and some less. Teach the jury the reasons behind your medical decisions and explain why they were correct. A teaching approach—as opposed to monotone answers—will help hold the jury’s attention and address its inquisitiveness.
Work with your attorney to develop appropriate explanations of medical terms, diagnoses, and treatments at issue in the case.
3 Face the jury
We typically look at the person to whom we are speaking. In the courtroom, this tendency translates into a focus on the lawyer who is doing the questioning rather than the jury. In the big picture, however, you are testifying to the jury, not the attorney—so look at the jurors when you speak.
Your attorney may position himself (or herself) near the jury so that your gaze encompasses both him and the panel. However, even if the attorney asking questions is not near the jury, turn toward the jury when you answer.
It may help to turn your chair to angle slightly toward the jury when you take the witness stand to make yourself more comfortable and avoid appearing as though your head is on a swivel. Doing so will also help you face the jury more squarely and directly.
Look into the faces and eyes of the jury when you answer questions. Speak to them, not at them.
4 Be yourself
When you are preparing for trial with your attorney, review the answers you expect to give to various questions. Work on delivering those responses in your own words, the way you would present them to a patient or a peer. A jury can detect sincerity and its opposite—glibness.
You and your counsel may agree on the information or points to be disclosed in response to a certain question, but on the witness stand, you will have to respond with your own voice and vocabulary.
5 Prepare to be cross-examined
Most jurisdictions permit opposing counsel to call a defendant physician to the witness stand, “as if on cross-examination.” This means that the opposing attorney can ask you leading questions in an attempt to box you into “Yes” or “No” responses with little or no opportunity to explain. This is customary. You must be prepared to face heated examination.
A trial is an adversarial process, based on the general premise that, through heated exchanges and questioning, the truth will emerge. Opposing counsel will attempt to get you to answer questions based on the plaintiff’s view of the case. Most physicians find having their answers constrained in this manner to be very frustrating.
Work with your attorney until you are ready to answer even the toughest and narrowest of “Yes” or “No” questions. If a question cannot be answered reliably with a “Yes” or “No,” be prepared to point that fact out to the questioning attorney or the judge. Also be prepared to provide an explanation beyond “Yes” or “No” when it may be appropriate. The judge will ultimately decide whether an explanation is warranted; many judges permit elaboration.
Your own attorney will later have the opportunity to question you, as well. If you are not permitted to give an explanation during questioning by opposing counsel, your own attorney can afford you that opportunity. An opposing attorney who insists that a physician not explain runs the risk of diverting the jury’s focus to the unstated explanation rather than to the actual “Yes” or “No” response. Indicate when you would like to explain an answer, and retain your composure if refused.
When opposing counsel has finished questioning you, your own skillful defense attorney can rise from his chair and ask, “Doctor, what is it that you wanted to explain to the ladies and gentlemen of the jury?” Then, like the late radio commentator Paul Harvey, you can provide “the rest of the story.”
As you did during your deposition, you have the right to ask for clarification of a confusing or unintelligible question. The same is true for a question in which a medical principle or condition is improperly characterized or defined. If a question doesn’t make sense, ask for clarification. If the question is inaccurate, advise the opposing attorney of the improper characterization, and ask that he rephrase the question. On occasion, it may be best to respond to a mischaracterization of a medical principle by answering: “That’s not how it works.” By declining to offer more information, you can create a moment of uncomfortable silence while opposing counsel collects his thoughts and regroups.
6 Emulate a weather forecaster
Work with your attorney to find aspects of your testimony that will permit you to get off the witness stand and present a chart or graph or other evidence from a standing position before the jury. Think of how much more interesting a weather forecaster is than an anchor who sits behind a desk reading news. Lengthy testimony from the witness stand is boring for the jury and can be tiring for the witness. Get off the stand once or twice to illustrate a point or demonstrate, for example, how the McRoberts maneuver is accomplished. It will keep the jury focused and interested.
When you stand before the jury to illustrate a point, make sure every juror can see your presentation. Your attorney may also request that a photograph or other exhibit be “published” to the jury so that the panel members can pass it among themselves and examine it with their own hands.
7 Be on your best behavior
Jurors are curious. They are being asked to, quite literally, pass judgment on you, despite knowing next to nothing about you. Jurors typically take their duties very seriously and will naturally be motivated to analyze non-verbal as well as verbal cues in an effort to learn more about you. Be prepared: They will watch your every move and mannerism in the courtroom, so be conscious of your clothing, mannerisms, and behavior. This holds true in the hallways of the courthouse and any location within two or three blocks. It is not uncommon to encounter a juror a block or two away from a courthouse in a major city, or to see a juror in a nearby coffee shop.
8 Control your reactions to testimony
It may be difficult to sit and listen as opposing counsel presents his opening argument to the jury. It may be a challenge to listen to the plaintiff’s case during the first 2 or 3 days of the trial. The plaintiff goes first; you have to wait your turn.
Overt facial reactions to testimony are best avoided. Although it may be helpful for you to make notes during testimony, try not to pass or slide them across the table to your attorney, except for rare occasions. There will be periodic breaks in the testimony, during which you can discuss your notes with your attorney. Frantically jotting down notes and sliding them over to your attorney may cause the jury to conclude that you are overly emotional or lack confidence in your attorney.
9 Test the gadgets
If you are going to present an exhibit, such as a chart or graph, make absolutely certain that it is accurate. Any error will be noted by opposing counsel and may impair your credibility. Also consider whether the chart or diagram could be reinterpreted to support your opponent’s case. If it could, don’t use it.
High-tech gizmos were once frowned upon by old-school defense attorneys. Now, we’re well past the MTV generation, and high-tech illustrations and animations are common in courtrooms. Be careful to avoid any high-tech malfunctions, however, which can distract the jury during presentation of your evidence.
If you are planning to use a demonstrative exhibit such as a heart-rate monitor or portable pulse oximetry device, make sure the batteries are charged and that it works. Practice any maneuver you plan to perform using the device or machine. You don’t want to appear clumsy or unfamiliar with the device. If any demonstration involves a sharp or needle, use an abundance of caution! In a birth injury case, baby mannequins are sometimes used. Make sure they work as intended and don’t permit anyone to “play” with them in the courtroom during breaks in the case. Trial is a serious matter; any levity observed by a juror could leave a detrimental impression.
Over my career, I have seen 1) an orthopedic surgery expert drop several “easy to assemble” metal components, creating a cacophony of pings and clangs as they bounced across the marble floor; 2) a surgeon staple his own palm with an “empty” laparoscopic staple gun; and 3) a medical expert miss a step getting off the witness stand, causing him to tumble into the jury box, strike his head and render himself nearly unconscious. This last incident led to the cancellation of the afternoon court session.
10 Take your time— and a little water
It’s helpful to visit the courtroom with your attorney some time before the trial date to dispel the jitters that can arise in an unfamiliar place. Also take a moment to sit in the witness stand so that you can have some level of comfort when testifying and understand how well, or poorly, the jury will be able to see you (and vice versa).
During the trial, take your time when answering questions. You may want to speak slightly more slowly than normal so that all the jurors can hear and appreciate what you’re saying. The tempo and volume of your testimony may also need to be adjusted, depending on the acoustics of the courtroom, which can vary widely, particularly in some of the more majestic and ornate venues.
Most courtrooms offer water pitchers and cups. Take a half-cup of water with you to the stand. A full cup is easy to spill—and creates a mess when it does. Courtrooms are not known for having an ample supply of paper towels.
Your confident presence can humanize the courtroom
The trial of a medical malpractice case is a difficult and emotional experience for any physician. Preparing to testify with confidence and precision is an important step toward a successful defense. The courtroom is an unfamiliar, uncomfortable, and adversarial environment. With appropriate preparation, however, the daunting specter of the witness stand can be conquered.
They’re available in the archive at obgmanagement.com
- Data on liability claims offer bright spots for ObGyns—and sobering statistics
Janelle Yates (January 2012) - Sound strategies to avoid malpractice hazards on labor and delivery (Part 1)
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD (December 2010) - More strategies to avoid malpractice hazards on labor and delivery (Part 2)
Martin L. Gimovsky, MD, and Alexis C. Gimovsky, MD (January 2011) - Afraid of getting sued? A plaintiff attorney offers counsel (but no sympathy)
Janelle Yates (October 2009) - 10 keys to defending (or, better, keeping clear of) a shoulder dystocia suit
Andrew K. Worek, Esq (March 2008)
We want to hear from you! Tell us what you think.
Fetal decapitation at 21 weeks … and more

CERCLAGE WAS PERFORMED on a woman who had a short cervix. A week later, Dr. A, her ObGyn, found the cerclage weak, and placed her on bed rest. Three days later, she passed blood clots, and was admitted to the hospital, where Dr. B assumed her care. When membranes ruptured at 21 weeks’ gestation, the fetal feet extended out of the vagina. The baby’s head was amputated during delivery; the child weighed <1 lb. Nursing staff reattached the head with sutures and permitted the mother to hold the child.
PATIENT’S CLAIM Dr. A should have confirmed cerclage placement by ultrasonography. When he found the cerclage unstable, he should have hospitalized the patient. Dr. B used excessive force during delivery. The nurses failed to properly monitor the mother. She claimed psychological injury in having witnessed the infant’s decapitation and being allowed to hold the corpse. Unreasonable death was claimed on behalf of the child’s estate; with proper treatment, the child had a chance of survival.
DEFENDANTS’ DEFENSE Cerclage was performed properly; Dr. A’s care was appropriate. Dr. B did not use excessive force; the fetus had extremely thin skin that tore easily. The nurses’ treatment was appropriate. The hospital was required to allow the mother to hold her baby when requested. A fetus is not viable at 21 weeks.
VERDICT A $1,362,499 Kentucky verdict was returned against the ObGyns; a defense verdict was returned for the hospital. The jury refused to address the claim of wrongful death because a fetus is not viable at 21 weeks.
Which breast was it? 1 error cascades
A WOMAN UNDERWENT RIGHT-BREAST biopsy in the 1970s. In 2002, an architectural distortion appeared in the left breast on mammogram. The radiologist concluded that the abnormality was related to the biopsy—but failed to note that the biopsy had been performed on the right, not the left, breast. Mammography films made in 2003 and again in 2004 were incorrectly read as normal.
In December 2005, a radiologist found no change in the left breast. In June 2007, a radiologist reported a large area of parenchymal distortion but concluded that it was related to the previous biopsy.
In May 2008, another radiologist read the films and recommended follow-up to determine which breast underwent biopsy. The patient was found to have stage III breast cancer in the left breast with a positive lymph node. She underwent double mastectomy followed by breast reconstruction surgery.
PATIENT’S CLAIM Her ObGyns never read the radiographs themselves and did not detect the left-right error after reading the reports. Errors cascaded because radiologists relied only on a previous record, not reviewing the entire chart, and confusing right and left films, even though the films were clearly marked. Had the cancer been found in 2002, treatment would have been substantially less extensive.
DEFENDANTS’ DEFENSE The cancer was difficult to diagnose because it never changed in size. A double mastectomy was not required to treat the cancer.
VERDICT The statute of limitations restricted which radiologists were allowed to be included as defendants. A confidential settlement was reached with the ObGyn group and two of the radiologists.
OB’s priorities tested; child has cerebral palsy
WHEN A WOMAN WENT to the hospital for induction of labor, her ObGyn ruptured the membranes. Shortly thereafter, the fetal heart rate dropped and fetal distress was noted. Emergency cesarean delivery was ordered.
The ObGyn left to attend to another patient while nurses prepared the patient and contacted the anesthesiologist. After delivering another child, the ObGyn returned and delivered the baby, who has cerebral palsy.
PATIENT’S CLAIM The ObGyn should have stayed with this mother instead of delivering the other child. The delay caused the child’s brain damage.
PHYSICIAN’S DEFENSE Both patients’ deliveries were being carefully monitored; proper action was taken.
VERDICT A Georgia defense verdict was returned.
Post-hysterectomy vesicovaginal fistulae
WHEN A 46-YEAR-OLD WOMAN reported irregular bleeding, her gynecologist performed dilation and curettage in February. The pathology report was negative for malignancy; abnormal bleeding ceased.
In July, after symptoms returned, she underwent abdominal hysterectomy. In September, she reported leakage of urine from her vagina; cystoscopy revealed four vesicovaginal fistulae that were repaired by a urologic surgeon. Another fistula developed and was repaired subsequently.
PATIENT’S CLAIM The gynecologist failed to provide information about less invasive options, including endometrial ablation and hormone treatment. The fistulae developed because the gynecologist did not adequately identify the bladder before suturing the vaginal cuff.
PHYSICIAN’S DEFENSE The patient was given sufficient information and requested a hysterectomy; other treatments were offered. A fistula is a known complication of the procedure.
VERDICT A California defense verdict was returned.
Placental abruption: Child has brain damage
WHEN A LABOR AND DELIVERY NURSE called, Dr. A decided a cesarean delivery was needed. The on-call anesthesiologist was at another cesarean delivery, so the procedure was delayed for longer than an hour. Dr. B delivered the child, who was born severely depressed, was resuscitated, and transferred to the NICU. The child suffered hypoxic encephalopathy, is quadriplegic, and has hypotonia.
PATIENT’S CLAIM The cesarean delivery was not performed in a timely manner. Fetal distress occurred because of placental abruption. The child would not have been injured if 1) the nursing staff had summoned a back-up anesthesiologist and 2) the procedure had started within 30 minutes of the decision.
DEFENDANTS’ DEFENSE The hospital reported that Dr. A arrived at the hospital quickly, but decided to wait for Dr. B. Placental abruption occurred prior to the mother’s arrival at the hospital.
VERDICT The ObGyns settled for an undisclosed amount before trial. A California defense verdict was returned for the hospital.
Necrotizing infection in abdominal hematoma
DYSMENORRHEA and abnormal uterine bleeding developed in a 40-year-old woman. Her gynecologist recommended abdominal hysterectomy because she had undergone two cesarean deliveries. During surgery, bladder injury was recognized and repaired.
After several days, the patient suffered complications and was referred to a urogynecologist, who found a 2-mm vaginal fistula. Three days later, she was found unresponsive at home. During exploratory surgery, the gynecologist found necrotizing infection related to an abdominal hematoma. The patient died 2 weeks later.
ESTATE’S CLAIM The gynecologist was negligent in failing to identify signs of infection at two postoperative visits.
PHYSICIAN’S DEFENSE The patient was properly monitored and referred in a timely manner to the urogynecologist. Death was due to the aggressive nature of the infection, which did not develop until after the last office visit.
VERDICT A Tennessee defense verdict was returned.
C diff infection after antibiotics for cough
AT 34 WEEKS’ GESTATION, an ObGyn prescribed amoxicillin-clavulanate (Augmentin) for a woman’s cough. She developed diarrhea that did not respond to antidiarrheal medication and a change in diet. Another ObGyn prescribed empiric sulfamethoxazole and trimethoprim (Septra), and referred her to an infectious-disease specialist. The specialist prescribed empiric cefpodoxime proxetil (Vantin) and ordered stool cultures.
Before culture results were received, the patient went into labor and delivered by cesarean section. Her illness progressed to fulminant Clostridium difficile pseudomembranous colitis that required total colectomy. Re-anastomosis was accomplished a year later. She continues to have difficulty controlling bowel movements, and reports abdominal pain, frequent dehydration, and weight loss.
PATIENT’S CLAIM Antibiotics should not have been prescribed without a culture-proven bacterial illness. C. difficile should have been suspected and treated when diarrhea first developed. Empiric antibiotic treatment during pregnancy is contraindicated. The group’s practice model of having patients rotate among OBs impeded continuity of care.
PHYSICIANS’ DEFENSE C. difficile infection was difficult to diagnose because it is not known to arise in young, healthy women outside a hospital. Use of antibiotics was proper. The group’s practice model is appropriate; continuity of care was maintained.
VERDICT A Florida defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.

CERCLAGE WAS PERFORMED on a woman who had a short cervix. A week later, Dr. A, her ObGyn, found the cerclage weak, and placed her on bed rest. Three days later, she passed blood clots, and was admitted to the hospital, where Dr. B assumed her care. When membranes ruptured at 21 weeks’ gestation, the fetal feet extended out of the vagina. The baby’s head was amputated during delivery; the child weighed <1 lb. Nursing staff reattached the head with sutures and permitted the mother to hold the child.
PATIENT’S CLAIM Dr. A should have confirmed cerclage placement by ultrasonography. When he found the cerclage unstable, he should have hospitalized the patient. Dr. B used excessive force during delivery. The nurses failed to properly monitor the mother. She claimed psychological injury in having witnessed the infant’s decapitation and being allowed to hold the corpse. Unreasonable death was claimed on behalf of the child’s estate; with proper treatment, the child had a chance of survival.
DEFENDANTS’ DEFENSE Cerclage was performed properly; Dr. A’s care was appropriate. Dr. B did not use excessive force; the fetus had extremely thin skin that tore easily. The nurses’ treatment was appropriate. The hospital was required to allow the mother to hold her baby when requested. A fetus is not viable at 21 weeks.
VERDICT A $1,362,499 Kentucky verdict was returned against the ObGyns; a defense verdict was returned for the hospital. The jury refused to address the claim of wrongful death because a fetus is not viable at 21 weeks.
Which breast was it? 1 error cascades
A WOMAN UNDERWENT RIGHT-BREAST biopsy in the 1970s. In 2002, an architectural distortion appeared in the left breast on mammogram. The radiologist concluded that the abnormality was related to the biopsy—but failed to note that the biopsy had been performed on the right, not the left, breast. Mammography films made in 2003 and again in 2004 were incorrectly read as normal.
In December 2005, a radiologist found no change in the left breast. In June 2007, a radiologist reported a large area of parenchymal distortion but concluded that it was related to the previous biopsy.
In May 2008, another radiologist read the films and recommended follow-up to determine which breast underwent biopsy. The patient was found to have stage III breast cancer in the left breast with a positive lymph node. She underwent double mastectomy followed by breast reconstruction surgery.
PATIENT’S CLAIM Her ObGyns never read the radiographs themselves and did not detect the left-right error after reading the reports. Errors cascaded because radiologists relied only on a previous record, not reviewing the entire chart, and confusing right and left films, even though the films were clearly marked. Had the cancer been found in 2002, treatment would have been substantially less extensive.
DEFENDANTS’ DEFENSE The cancer was difficult to diagnose because it never changed in size. A double mastectomy was not required to treat the cancer.
VERDICT The statute of limitations restricted which radiologists were allowed to be included as defendants. A confidential settlement was reached with the ObGyn group and two of the radiologists.
OB’s priorities tested; child has cerebral palsy
WHEN A WOMAN WENT to the hospital for induction of labor, her ObGyn ruptured the membranes. Shortly thereafter, the fetal heart rate dropped and fetal distress was noted. Emergency cesarean delivery was ordered.
The ObGyn left to attend to another patient while nurses prepared the patient and contacted the anesthesiologist. After delivering another child, the ObGyn returned and delivered the baby, who has cerebral palsy.
PATIENT’S CLAIM The ObGyn should have stayed with this mother instead of delivering the other child. The delay caused the child’s brain damage.
PHYSICIAN’S DEFENSE Both patients’ deliveries were being carefully monitored; proper action was taken.
VERDICT A Georgia defense verdict was returned.
Post-hysterectomy vesicovaginal fistulae
WHEN A 46-YEAR-OLD WOMAN reported irregular bleeding, her gynecologist performed dilation and curettage in February. The pathology report was negative for malignancy; abnormal bleeding ceased.
In July, after symptoms returned, she underwent abdominal hysterectomy. In September, she reported leakage of urine from her vagina; cystoscopy revealed four vesicovaginal fistulae that were repaired by a urologic surgeon. Another fistula developed and was repaired subsequently.
PATIENT’S CLAIM The gynecologist failed to provide information about less invasive options, including endometrial ablation and hormone treatment. The fistulae developed because the gynecologist did not adequately identify the bladder before suturing the vaginal cuff.
PHYSICIAN’S DEFENSE The patient was given sufficient information and requested a hysterectomy; other treatments were offered. A fistula is a known complication of the procedure.
VERDICT A California defense verdict was returned.
Placental abruption: Child has brain damage
WHEN A LABOR AND DELIVERY NURSE called, Dr. A decided a cesarean delivery was needed. The on-call anesthesiologist was at another cesarean delivery, so the procedure was delayed for longer than an hour. Dr. B delivered the child, who was born severely depressed, was resuscitated, and transferred to the NICU. The child suffered hypoxic encephalopathy, is quadriplegic, and has hypotonia.
PATIENT’S CLAIM The cesarean delivery was not performed in a timely manner. Fetal distress occurred because of placental abruption. The child would not have been injured if 1) the nursing staff had summoned a back-up anesthesiologist and 2) the procedure had started within 30 minutes of the decision.
DEFENDANTS’ DEFENSE The hospital reported that Dr. A arrived at the hospital quickly, but decided to wait for Dr. B. Placental abruption occurred prior to the mother’s arrival at the hospital.
VERDICT The ObGyns settled for an undisclosed amount before trial. A California defense verdict was returned for the hospital.
Necrotizing infection in abdominal hematoma
DYSMENORRHEA and abnormal uterine bleeding developed in a 40-year-old woman. Her gynecologist recommended abdominal hysterectomy because she had undergone two cesarean deliveries. During surgery, bladder injury was recognized and repaired.
After several days, the patient suffered complications and was referred to a urogynecologist, who found a 2-mm vaginal fistula. Three days later, she was found unresponsive at home. During exploratory surgery, the gynecologist found necrotizing infection related to an abdominal hematoma. The patient died 2 weeks later.
ESTATE’S CLAIM The gynecologist was negligent in failing to identify signs of infection at two postoperative visits.
PHYSICIAN’S DEFENSE The patient was properly monitored and referred in a timely manner to the urogynecologist. Death was due to the aggressive nature of the infection, which did not develop until after the last office visit.
VERDICT A Tennessee defense verdict was returned.
C diff infection after antibiotics for cough
AT 34 WEEKS’ GESTATION, an ObGyn prescribed amoxicillin-clavulanate (Augmentin) for a woman’s cough. She developed diarrhea that did not respond to antidiarrheal medication and a change in diet. Another ObGyn prescribed empiric sulfamethoxazole and trimethoprim (Septra), and referred her to an infectious-disease specialist. The specialist prescribed empiric cefpodoxime proxetil (Vantin) and ordered stool cultures.
Before culture results were received, the patient went into labor and delivered by cesarean section. Her illness progressed to fulminant Clostridium difficile pseudomembranous colitis that required total colectomy. Re-anastomosis was accomplished a year later. She continues to have difficulty controlling bowel movements, and reports abdominal pain, frequent dehydration, and weight loss.
PATIENT’S CLAIM Antibiotics should not have been prescribed without a culture-proven bacterial illness. C. difficile should have been suspected and treated when diarrhea first developed. Empiric antibiotic treatment during pregnancy is contraindicated. The group’s practice model of having patients rotate among OBs impeded continuity of care.
PHYSICIANS’ DEFENSE C. difficile infection was difficult to diagnose because it is not known to arise in young, healthy women outside a hospital. Use of antibiotics was proper. The group’s practice model is appropriate; continuity of care was maintained.
VERDICT A Florida defense verdict was returned.

CERCLAGE WAS PERFORMED on a woman who had a short cervix. A week later, Dr. A, her ObGyn, found the cerclage weak, and placed her on bed rest. Three days later, she passed blood clots, and was admitted to the hospital, where Dr. B assumed her care. When membranes ruptured at 21 weeks’ gestation, the fetal feet extended out of the vagina. The baby’s head was amputated during delivery; the child weighed <1 lb. Nursing staff reattached the head with sutures and permitted the mother to hold the child.
PATIENT’S CLAIM Dr. A should have confirmed cerclage placement by ultrasonography. When he found the cerclage unstable, he should have hospitalized the patient. Dr. B used excessive force during delivery. The nurses failed to properly monitor the mother. She claimed psychological injury in having witnessed the infant’s decapitation and being allowed to hold the corpse. Unreasonable death was claimed on behalf of the child’s estate; with proper treatment, the child had a chance of survival.
DEFENDANTS’ DEFENSE Cerclage was performed properly; Dr. A’s care was appropriate. Dr. B did not use excessive force; the fetus had extremely thin skin that tore easily. The nurses’ treatment was appropriate. The hospital was required to allow the mother to hold her baby when requested. A fetus is not viable at 21 weeks.
VERDICT A $1,362,499 Kentucky verdict was returned against the ObGyns; a defense verdict was returned for the hospital. The jury refused to address the claim of wrongful death because a fetus is not viable at 21 weeks.
Which breast was it? 1 error cascades
A WOMAN UNDERWENT RIGHT-BREAST biopsy in the 1970s. In 2002, an architectural distortion appeared in the left breast on mammogram. The radiologist concluded that the abnormality was related to the biopsy—but failed to note that the biopsy had been performed on the right, not the left, breast. Mammography films made in 2003 and again in 2004 were incorrectly read as normal.
In December 2005, a radiologist found no change in the left breast. In June 2007, a radiologist reported a large area of parenchymal distortion but concluded that it was related to the previous biopsy.
In May 2008, another radiologist read the films and recommended follow-up to determine which breast underwent biopsy. The patient was found to have stage III breast cancer in the left breast with a positive lymph node. She underwent double mastectomy followed by breast reconstruction surgery.
PATIENT’S CLAIM Her ObGyns never read the radiographs themselves and did not detect the left-right error after reading the reports. Errors cascaded because radiologists relied only on a previous record, not reviewing the entire chart, and confusing right and left films, even though the films were clearly marked. Had the cancer been found in 2002, treatment would have been substantially less extensive.
DEFENDANTS’ DEFENSE The cancer was difficult to diagnose because it never changed in size. A double mastectomy was not required to treat the cancer.
VERDICT The statute of limitations restricted which radiologists were allowed to be included as defendants. A confidential settlement was reached with the ObGyn group and two of the radiologists.
OB’s priorities tested; child has cerebral palsy
WHEN A WOMAN WENT to the hospital for induction of labor, her ObGyn ruptured the membranes. Shortly thereafter, the fetal heart rate dropped and fetal distress was noted. Emergency cesarean delivery was ordered.
The ObGyn left to attend to another patient while nurses prepared the patient and contacted the anesthesiologist. After delivering another child, the ObGyn returned and delivered the baby, who has cerebral palsy.
PATIENT’S CLAIM The ObGyn should have stayed with this mother instead of delivering the other child. The delay caused the child’s brain damage.
PHYSICIAN’S DEFENSE Both patients’ deliveries were being carefully monitored; proper action was taken.
VERDICT A Georgia defense verdict was returned.
Post-hysterectomy vesicovaginal fistulae
WHEN A 46-YEAR-OLD WOMAN reported irregular bleeding, her gynecologist performed dilation and curettage in February. The pathology report was negative for malignancy; abnormal bleeding ceased.
In July, after symptoms returned, she underwent abdominal hysterectomy. In September, she reported leakage of urine from her vagina; cystoscopy revealed four vesicovaginal fistulae that were repaired by a urologic surgeon. Another fistula developed and was repaired subsequently.
PATIENT’S CLAIM The gynecologist failed to provide information about less invasive options, including endometrial ablation and hormone treatment. The fistulae developed because the gynecologist did not adequately identify the bladder before suturing the vaginal cuff.
PHYSICIAN’S DEFENSE The patient was given sufficient information and requested a hysterectomy; other treatments were offered. A fistula is a known complication of the procedure.
VERDICT A California defense verdict was returned.
Placental abruption: Child has brain damage
WHEN A LABOR AND DELIVERY NURSE called, Dr. A decided a cesarean delivery was needed. The on-call anesthesiologist was at another cesarean delivery, so the procedure was delayed for longer than an hour. Dr. B delivered the child, who was born severely depressed, was resuscitated, and transferred to the NICU. The child suffered hypoxic encephalopathy, is quadriplegic, and has hypotonia.
PATIENT’S CLAIM The cesarean delivery was not performed in a timely manner. Fetal distress occurred because of placental abruption. The child would not have been injured if 1) the nursing staff had summoned a back-up anesthesiologist and 2) the procedure had started within 30 minutes of the decision.
DEFENDANTS’ DEFENSE The hospital reported that Dr. A arrived at the hospital quickly, but decided to wait for Dr. B. Placental abruption occurred prior to the mother’s arrival at the hospital.
VERDICT The ObGyns settled for an undisclosed amount before trial. A California defense verdict was returned for the hospital.
Necrotizing infection in abdominal hematoma
DYSMENORRHEA and abnormal uterine bleeding developed in a 40-year-old woman. Her gynecologist recommended abdominal hysterectomy because she had undergone two cesarean deliveries. During surgery, bladder injury was recognized and repaired.
After several days, the patient suffered complications and was referred to a urogynecologist, who found a 2-mm vaginal fistula. Three days later, she was found unresponsive at home. During exploratory surgery, the gynecologist found necrotizing infection related to an abdominal hematoma. The patient died 2 weeks later.
ESTATE’S CLAIM The gynecologist was negligent in failing to identify signs of infection at two postoperative visits.
PHYSICIAN’S DEFENSE The patient was properly monitored and referred in a timely manner to the urogynecologist. Death was due to the aggressive nature of the infection, which did not develop until after the last office visit.
VERDICT A Tennessee defense verdict was returned.
C diff infection after antibiotics for cough
AT 34 WEEKS’ GESTATION, an ObGyn prescribed amoxicillin-clavulanate (Augmentin) for a woman’s cough. She developed diarrhea that did not respond to antidiarrheal medication and a change in diet. Another ObGyn prescribed empiric sulfamethoxazole and trimethoprim (Septra), and referred her to an infectious-disease specialist. The specialist prescribed empiric cefpodoxime proxetil (Vantin) and ordered stool cultures.
Before culture results were received, the patient went into labor and delivered by cesarean section. Her illness progressed to fulminant Clostridium difficile pseudomembranous colitis that required total colectomy. Re-anastomosis was accomplished a year later. She continues to have difficulty controlling bowel movements, and reports abdominal pain, frequent dehydration, and weight loss.
PATIENT’S CLAIM Antibiotics should not have been prescribed without a culture-proven bacterial illness. C. difficile should have been suspected and treated when diarrhea first developed. Empiric antibiotic treatment during pregnancy is contraindicated. The group’s practice model of having patients rotate among OBs impeded continuity of care.
PHYSICIANS’ DEFENSE C. difficile infection was difficult to diagnose because it is not known to arise in young, healthy women outside a hospital. Use of antibiotics was proper. The group’s practice model is appropriate; continuity of care was maintained.
VERDICT A Florida defense verdict was returned.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
These cases were selected by the editors of OBG Management from Medical Malpractice Verdicts, Settlements & Experts, with permission of the editor, Lewis Laska (www.verdictslaska.com). The information available to the editors about the cases presented here is sometimes incomplete. Moreover, the cases may or may not have merit. Nevertheless, these cases represent the types of clinical situations that typically result in litigation and are meant to illustrate nationwide variation in jury verdicts and awards.
We want to hear from you! Tell us what you think.
Facebook: Social networking meets professional duty
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
A patient has invited me to “friend” her on Facebook. I’m uncomfortable with this request, but I don’t want her to feel rejected. How should I respond?—Submitted by “Dr. V”
Among the many cultural developments that characterize the Internet era, few have had the impact of the social networking Web site Facebook. Because of Facebook, “friend” has become a transitive verb, and “like,” “wall,” “poke,” and “post” have acquired meanings that reflect new modes of communication and interpersonal connection. As of early 2012, Facebook had >800 million users.1 If you’re like most medical students, residents, and junior faculty members,2 you have a Facebook page.
The ubiquity of Facebook has added new dimensions to defining, teaching, and modeling professionalism in medicine.3,4 Facebook can be used to rapidly disseminate medical information through status updates and medical support groups.5 Professionals can create profiles, post their curricula vitae, and “like” professional journals—including Current Psychiatry.
But social media such as Facebook also present clinicians with new ethical and professional challenges.6 If you use Facebook personally or professionally, you need to decide how you will separate your personal and professional identities in a forum that rapidly distributes information across the Web for all to see. Sound, responsible decisions about your online profile can let you and your employing institutions prosper from the many benefits that accrue to savvy Facebook users—while avoiding potential embarrassments and liability.
Before you create a profile or “post” your next “status update” on your “wall,” you should:
- understand potential boundary violations
- know how to activate your security and privacy settings
- remember that you represent not only yourself but your profession.
Boundary crossings, violations
Feelings of online closeness and informality make receiving “friend” requests from patients far from uncommon.7 The Internet lets individuals quickly check out people and learn personal information (eg, where they live and what their homes cost) that was hard to discover 15 years ago. But the information on a person’s Facebook page usually is much more personal than what Internet searches reveal—and often much less dignified.
A quick Internet search of the phrase “professional boundaries” will show that concern about maintaining proper relationships between professionals and service recipients is not restricted to psychiatry. Yet the special, intensely personal nature of mental health care—especially psychotherapy—traditionally has made psychiatrists place special constraints on their relationships with patients.
Because psychiatrists recognize that even brief comments about ourselves can affect how patients feel, we refrain from forms of self-disclosure that non-psychiatric colleagues view as innocent.8 Psychiatrists also do not freely socialize with patients or provide care to persons we know well. We avoid blurring therapeutic and other types of relationships because such “boundary crossings” can cause problems and because “crossings” can be precursors to serious “boundary violations”—eg, sexual contact with patients.
Most doctors decline “friend” requests from patients because friending them could adversely affect the treatment relationship and could lead to new relationships that might interfere with patient care.9 The American Medical Association’s social media guidelines do not forbid friending patients, but physicians are advised to “consider separating personal and professional content online” and “maintain appropriate boundaries” with patients.10 The British Medical Association simply tells physicians to “politely refuse” patients’ friend requests.11
Privacy problems
Psychiatrists who friend patients need to be aware of potential privacy breeches among Facebook users. Individuals whose presence among a psychiatrist’s friends becomes known (eg, via a wall post) are revealing their connection to the psychiatrist, and other friends may surmise that an individual is a patient.
Also, Facebook’s “find friends” feature ostensibly lets Facebook locate individuals who are common to pairs of people and who can then be suggested as potential friends to others, but “find friends” imports members’ entire e-mail address books. If doctors who are on Facebook have patients in their webmail address books and have allowed “find friends,” then Facebook will import e-mail addresses, potentially disclosing associations between patients and their doctors.12
Facebook has tools that let users block their profiles from public view, but these privacy settings can be difficult to access and understand. Although social networking among medical trainees and new graduates is common in the culture of emerging professionals, most Facebook users allow anyone to view their profile—the default privacy setting.2,13 Even if you don’t friend patients, failing to privatize your account leaves your Facebook information readily available to the public, including your patients.
Professionalism in cyberspace
Under some circumstances, medical advice given in casual, outside-the-office contexts can establish a doctor-patient relationship, with all its accompanying obligations and liability risks. This is true of Facebook communications. If you communicate medical information or advice to someone in a form specific enough to be relied upon, you may be establishing a doctor-patient relationship. If harm comes to a person who relied upon your information, a negligence lawsuit could result—even though you never saw or spoke to the “patient.”14
Medical training programs have found that medical students and residents have posted work-related comments on Facebook that directly referenced specific patient situations or other patient care matters. Such actions can breach the Health Insurance Portability and Accountability Act of 1996 and can jeopardize careers.15 Medical professionals also have posted uncouth, inappropriate, and embarrassing content—profanity, frankly discriminatory language, tales of intoxication, and sexually explicit information. In a recent survey of 78 medical schools, 60% responded that their students had posted unprofessional online content.16 In 45 cases, schools reported such incidents and responded to follow-up questions about disciplinary actions; 30 schools gave informal warnings, and 2 schools reported student dismissals.
Using Facebook
Should psychiatrists stay off Facebook? Of course not. Many prominent American psychiatrists are on Facebook because, like everyone else, they enjoy keeping in contact with friends and family.17 Thousands of professional groups (eg, the American Psychiatric Association) and physician practices have Facebook pages. Institutions, schools, and agencies use social media to promote their curricula, notify students and staff of course changes, or organize meetings. Professionals join groups or “like” groups associated with their specialty to affiliate with each other, and they use Facebook to promote their practices, disseminate information, and network with colleagues.
Psychiatrists need not shy away from establishing an account on Facebook,18 but they should do so with greater circumspection than most persons, including physicians in other specialties. Table 1 lists several examples of Facebook behavior that all physicians should avoid.2,13,16,19,20
What about using Facebook to learn about your patients? Medical reports about checking Facebook to resolve emergencies have appeared,20 and forensic psychiatrists can use Facebook and other Internet resources to learn about evaluees.21 But if doctors search for information about a patient’s out-of-office behavior or statements, it may be like “driving down a patient’s street to see what he or she is up to,” which, although legal, seems inappropriate in a professional relationship.22
Recent experience suggests that medical schools and residencies should include “e-professionalism” in their curricula, emphasizing instruction and guidance on where personal and professional identities may intersect and where they should be kept separate. Table 2 lists several responses to the new challenges to medical professionalism posed by Facebook and other social media.5,6
Table 1
Facebook errors: What to avoid
| Category | Pitfalls |
|---|---|
| Information | Relationships, religious views, home address, and telephone number all may be readily viewable to the general public and patients if privacy settings are not properly configured |
| Photos | Intoxication, sexually explicit material, risk-taking behavior |
| “Wall posts” | Blatant comments about patients, disgruntlement with institution or supervisors |
| Security settings | Lack of privacy restrictions |
| “Friends” | Friending patients and supervisors |
| “Like” | “Liking” groups that contain pornographic material or other controversial topics |
| Source: References 2,13,16,19,20 | |
Table 2
Promoting e-professionalism
| Understand and activate all relevant privacy and security settings on social networking sites |
| Recognize the need to teach e-professionalism in the curricula of medical schools and residency training programs |
| Combine instruction on professional use of Facebook with teaching about relevant legal regulations in medicine (eg, HIPAA) |
| Guidance in online professionalism should come from faculty supervisors or program directors |
| Faculty should model appropriate Facebook behaviors for employees, medical students, and residents |
| Users of social media are well-advised to conduct Web searches on themselves and modify their pages to conform with professional standards |
| Politely decline patients’ “friend” requests |
| Discussions of medical professionalism, involving students, faculty, and employers, can help identify issues and define responses |
| Institutions should establish and enforce guidelines for Facebook professionalism |
| HIPAA: Health Insurance Portability and Accountability Act of 1996 Source: References 5,6 |
Responding to Dr. V
Psychiatrists should not “friend” patients. If you receive a “friend” request, you should proceed in 1 of the following ways:17
- Simply ignore the request. If your patient asks why you didn’t respond, explain that you use Facebook only for personal matters
- Ignore the request, and at the patient’s next appointment, mention the request and politely explain that you do not “friend” patients
- Ignore the request, but ask the patient about it at your next meeting. This is especially important for a patient whose treatment examines the doctor-patient relationship (eg, psychodynamic therapy), but may be valuable even in medication-focused care.
- Facebook. www.facebook.com.
- Foreman J. Think before you click. Boston Globe. April 12, 2010.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Facebook. Statistics. http://www.facebook.com/press/info.php?statistics. Accessed January 30, 2012.
2. MacDonald J, Sohn S, Ellis P. Privacy professionalism and Facebook: a dilemma for young doctors. Med Educ. 2010;44(8):805-813.
3. Gorrindo T, Gorrindo PC, Groves JE. Intersection of online social networking with medical professionalism: can medicine police the Facebook boom? J Gen Intern Med. 2008;23(12):2155.-
4. Baer W, Schwartz AC. Teaching professionalism in the digital age on the psychiatric consultation-liaison service. Psychosomatics. 2011;52(4):303-309.
5. Landman MP, Shelton J, Kauffmann RM, et al. Guidelines for maintaining a professional compass in the era of social networking. J Surg Educ. 2010;67(6):381-386.
6. Guseh JS 2nd, Brendel RW, Brendel DH. Medical professionalism in the age of online social networking. J Med Ethics. 2009;35(9):584-586.
7. Devi S. Facebook friend request from a patient? Lancet. 2011;377(9772):1141-1142.
8. Gruenberg PB. Boundary violations. In: Wahl DS Polster DS, eds. Ethics primer. Arlington, VA: American Psychiatric Association; 2001. http://www.psych.org/Departments/EDU/residentmit/dl01.aspx. Accessed January 4, 2012.
9. Moubarak G, Guiot A, Benhamou Y, et al. Facebook activity of residents and fellows and its impact on the doctor-patient relationship. J Med Ethics. 2011;37(2):101-104.
10. American Medical Association. AMA policy: professionalism in the use of social media. http://www.ama-assn.org/ama/pub/meeting/professionalism-social-media.shtml. Accessed January 4 2012.
11. British Medical Association. Using social media: practical and ethical guidance for doctors and medical students. http://www.bma.org.uk/press_centre/video_social_media/socialmediaguidance2011.jsp. Accessed January 4 2012.
12. Wilson S. A bigger threat to patient privacy when doctors use Facebook. J Med Ethics. http://jme.bmj.com/content/37/2/101.abstract/reply#medethics_el_3625. Published December 20 2010. Accessed January 4, 2012.
13. Thompson LA, Dawson K, Ferdig R, et al. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23(7):954-957.
14. Reisman N. Avoid being too social when using social media. Plastic Surgery News. September 13 2011. http://www.psnextra.org/Columns/OLG-September-11.html. Accessed January 4, 2012.
15. Greysen SR, Kind T, Chretien KC. Online professionalism and the mirror of social media. J Gen Intern Med. 2010;25(11):1227-1229.
16. Chretien KC, Greysen SR, Chretien JP, et al. Online posting of unprofessional content by medical students. JAMA. 2009;302(12):1309-1315.
17. Arehart-Treichel J. Facebook can be useful–if you use common sense. Psychiatric News. 2011;46(22):5A.-
18. O’Hanlon S, Shannon B. Comments further to: privacy professionalism and Facebook: a dilemma for young doctors. Med Educ. 2011;45(2):209.-
19. Metzger AH, Finley KN, Ulbrich TR, et al. Pharmacy faculty members’ perspectives on the student/faculty relationship in online social networks. Am J Pharm Educ. 2010;74(10):188.-
20. Ben-Yakov M, Snider C. How Facebook saved our day! Acad Emerg Med. 2011;18(11):1217-1219.
21. Metzner JL, Ash P. Commentary: the mental status examination in the age of the internet—challenges and opportunities. J Am Acad Psychiatry Law. 2010;38(1):27-31.
22. Bosslet GT. Commentary: the good the bad, and the ugly of social media. Acad Emerg Med. 2011;18(11):1221-1222.
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
A patient has invited me to “friend” her on Facebook. I’m uncomfortable with this request, but I don’t want her to feel rejected. How should I respond?—Submitted by “Dr. V”
Among the many cultural developments that characterize the Internet era, few have had the impact of the social networking Web site Facebook. Because of Facebook, “friend” has become a transitive verb, and “like,” “wall,” “poke,” and “post” have acquired meanings that reflect new modes of communication and interpersonal connection. As of early 2012, Facebook had >800 million users.1 If you’re like most medical students, residents, and junior faculty members,2 you have a Facebook page.
The ubiquity of Facebook has added new dimensions to defining, teaching, and modeling professionalism in medicine.3,4 Facebook can be used to rapidly disseminate medical information through status updates and medical support groups.5 Professionals can create profiles, post their curricula vitae, and “like” professional journals—including Current Psychiatry.
But social media such as Facebook also present clinicians with new ethical and professional challenges.6 If you use Facebook personally or professionally, you need to decide how you will separate your personal and professional identities in a forum that rapidly distributes information across the Web for all to see. Sound, responsible decisions about your online profile can let you and your employing institutions prosper from the many benefits that accrue to savvy Facebook users—while avoiding potential embarrassments and liability.
Before you create a profile or “post” your next “status update” on your “wall,” you should:
- understand potential boundary violations
- know how to activate your security and privacy settings
- remember that you represent not only yourself but your profession.
Boundary crossings, violations
Feelings of online closeness and informality make receiving “friend” requests from patients far from uncommon.7 The Internet lets individuals quickly check out people and learn personal information (eg, where they live and what their homes cost) that was hard to discover 15 years ago. But the information on a person’s Facebook page usually is much more personal than what Internet searches reveal—and often much less dignified.
A quick Internet search of the phrase “professional boundaries” will show that concern about maintaining proper relationships between professionals and service recipients is not restricted to psychiatry. Yet the special, intensely personal nature of mental health care—especially psychotherapy—traditionally has made psychiatrists place special constraints on their relationships with patients.
Because psychiatrists recognize that even brief comments about ourselves can affect how patients feel, we refrain from forms of self-disclosure that non-psychiatric colleagues view as innocent.8 Psychiatrists also do not freely socialize with patients or provide care to persons we know well. We avoid blurring therapeutic and other types of relationships because such “boundary crossings” can cause problems and because “crossings” can be precursors to serious “boundary violations”—eg, sexual contact with patients.
Most doctors decline “friend” requests from patients because friending them could adversely affect the treatment relationship and could lead to new relationships that might interfere with patient care.9 The American Medical Association’s social media guidelines do not forbid friending patients, but physicians are advised to “consider separating personal and professional content online” and “maintain appropriate boundaries” with patients.10 The British Medical Association simply tells physicians to “politely refuse” patients’ friend requests.11
Privacy problems
Psychiatrists who friend patients need to be aware of potential privacy breeches among Facebook users. Individuals whose presence among a psychiatrist’s friends becomes known (eg, via a wall post) are revealing their connection to the psychiatrist, and other friends may surmise that an individual is a patient.
Also, Facebook’s “find friends” feature ostensibly lets Facebook locate individuals who are common to pairs of people and who can then be suggested as potential friends to others, but “find friends” imports members’ entire e-mail address books. If doctors who are on Facebook have patients in their webmail address books and have allowed “find friends,” then Facebook will import e-mail addresses, potentially disclosing associations between patients and their doctors.12
Facebook has tools that let users block their profiles from public view, but these privacy settings can be difficult to access and understand. Although social networking among medical trainees and new graduates is common in the culture of emerging professionals, most Facebook users allow anyone to view their profile—the default privacy setting.2,13 Even if you don’t friend patients, failing to privatize your account leaves your Facebook information readily available to the public, including your patients.
Professionalism in cyberspace
Under some circumstances, medical advice given in casual, outside-the-office contexts can establish a doctor-patient relationship, with all its accompanying obligations and liability risks. This is true of Facebook communications. If you communicate medical information or advice to someone in a form specific enough to be relied upon, you may be establishing a doctor-patient relationship. If harm comes to a person who relied upon your information, a negligence lawsuit could result—even though you never saw or spoke to the “patient.”14
Medical training programs have found that medical students and residents have posted work-related comments on Facebook that directly referenced specific patient situations or other patient care matters. Such actions can breach the Health Insurance Portability and Accountability Act of 1996 and can jeopardize careers.15 Medical professionals also have posted uncouth, inappropriate, and embarrassing content—profanity, frankly discriminatory language, tales of intoxication, and sexually explicit information. In a recent survey of 78 medical schools, 60% responded that their students had posted unprofessional online content.16 In 45 cases, schools reported such incidents and responded to follow-up questions about disciplinary actions; 30 schools gave informal warnings, and 2 schools reported student dismissals.
Using Facebook
Should psychiatrists stay off Facebook? Of course not. Many prominent American psychiatrists are on Facebook because, like everyone else, they enjoy keeping in contact with friends and family.17 Thousands of professional groups (eg, the American Psychiatric Association) and physician practices have Facebook pages. Institutions, schools, and agencies use social media to promote their curricula, notify students and staff of course changes, or organize meetings. Professionals join groups or “like” groups associated with their specialty to affiliate with each other, and they use Facebook to promote their practices, disseminate information, and network with colleagues.
Psychiatrists need not shy away from establishing an account on Facebook,18 but they should do so with greater circumspection than most persons, including physicians in other specialties. Table 1 lists several examples of Facebook behavior that all physicians should avoid.2,13,16,19,20
What about using Facebook to learn about your patients? Medical reports about checking Facebook to resolve emergencies have appeared,20 and forensic psychiatrists can use Facebook and other Internet resources to learn about evaluees.21 But if doctors search for information about a patient’s out-of-office behavior or statements, it may be like “driving down a patient’s street to see what he or she is up to,” which, although legal, seems inappropriate in a professional relationship.22
Recent experience suggests that medical schools and residencies should include “e-professionalism” in their curricula, emphasizing instruction and guidance on where personal and professional identities may intersect and where they should be kept separate. Table 2 lists several responses to the new challenges to medical professionalism posed by Facebook and other social media.5,6
Table 1
Facebook errors: What to avoid
| Category | Pitfalls |
|---|---|
| Information | Relationships, religious views, home address, and telephone number all may be readily viewable to the general public and patients if privacy settings are not properly configured |
| Photos | Intoxication, sexually explicit material, risk-taking behavior |
| “Wall posts” | Blatant comments about patients, disgruntlement with institution or supervisors |
| Security settings | Lack of privacy restrictions |
| “Friends” | Friending patients and supervisors |
| “Like” | “Liking” groups that contain pornographic material or other controversial topics |
| Source: References 2,13,16,19,20 | |
Table 2
Promoting e-professionalism
| Understand and activate all relevant privacy and security settings on social networking sites |
| Recognize the need to teach e-professionalism in the curricula of medical schools and residency training programs |
| Combine instruction on professional use of Facebook with teaching about relevant legal regulations in medicine (eg, HIPAA) |
| Guidance in online professionalism should come from faculty supervisors or program directors |
| Faculty should model appropriate Facebook behaviors for employees, medical students, and residents |
| Users of social media are well-advised to conduct Web searches on themselves and modify their pages to conform with professional standards |
| Politely decline patients’ “friend” requests |
| Discussions of medical professionalism, involving students, faculty, and employers, can help identify issues and define responses |
| Institutions should establish and enforce guidelines for Facebook professionalism |
| HIPAA: Health Insurance Portability and Accountability Act of 1996 Source: References 5,6 |
Responding to Dr. V
Psychiatrists should not “friend” patients. If you receive a “friend” request, you should proceed in 1 of the following ways:17
- Simply ignore the request. If your patient asks why you didn’t respond, explain that you use Facebook only for personal matters
- Ignore the request, and at the patient’s next appointment, mention the request and politely explain that you do not “friend” patients
- Ignore the request, but ask the patient about it at your next meeting. This is especially important for a patient whose treatment examines the doctor-patient relationship (eg, psychodynamic therapy), but may be valuable even in medication-focused care.
- Facebook. www.facebook.com.
- Foreman J. Think before you click. Boston Globe. April 12, 2010.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
A patient has invited me to “friend” her on Facebook. I’m uncomfortable with this request, but I don’t want her to feel rejected. How should I respond?—Submitted by “Dr. V”
Among the many cultural developments that characterize the Internet era, few have had the impact of the social networking Web site Facebook. Because of Facebook, “friend” has become a transitive verb, and “like,” “wall,” “poke,” and “post” have acquired meanings that reflect new modes of communication and interpersonal connection. As of early 2012, Facebook had >800 million users.1 If you’re like most medical students, residents, and junior faculty members,2 you have a Facebook page.
The ubiquity of Facebook has added new dimensions to defining, teaching, and modeling professionalism in medicine.3,4 Facebook can be used to rapidly disseminate medical information through status updates and medical support groups.5 Professionals can create profiles, post their curricula vitae, and “like” professional journals—including Current Psychiatry.
But social media such as Facebook also present clinicians with new ethical and professional challenges.6 If you use Facebook personally or professionally, you need to decide how you will separate your personal and professional identities in a forum that rapidly distributes information across the Web for all to see. Sound, responsible decisions about your online profile can let you and your employing institutions prosper from the many benefits that accrue to savvy Facebook users—while avoiding potential embarrassments and liability.
Before you create a profile or “post” your next “status update” on your “wall,” you should:
- understand potential boundary violations
- know how to activate your security and privacy settings
- remember that you represent not only yourself but your profession.
Boundary crossings, violations
Feelings of online closeness and informality make receiving “friend” requests from patients far from uncommon.7 The Internet lets individuals quickly check out people and learn personal information (eg, where they live and what their homes cost) that was hard to discover 15 years ago. But the information on a person’s Facebook page usually is much more personal than what Internet searches reveal—and often much less dignified.
A quick Internet search of the phrase “professional boundaries” will show that concern about maintaining proper relationships between professionals and service recipients is not restricted to psychiatry. Yet the special, intensely personal nature of mental health care—especially psychotherapy—traditionally has made psychiatrists place special constraints on their relationships with patients.
Because psychiatrists recognize that even brief comments about ourselves can affect how patients feel, we refrain from forms of self-disclosure that non-psychiatric colleagues view as innocent.8 Psychiatrists also do not freely socialize with patients or provide care to persons we know well. We avoid blurring therapeutic and other types of relationships because such “boundary crossings” can cause problems and because “crossings” can be precursors to serious “boundary violations”—eg, sexual contact with patients.
Most doctors decline “friend” requests from patients because friending them could adversely affect the treatment relationship and could lead to new relationships that might interfere with patient care.9 The American Medical Association’s social media guidelines do not forbid friending patients, but physicians are advised to “consider separating personal and professional content online” and “maintain appropriate boundaries” with patients.10 The British Medical Association simply tells physicians to “politely refuse” patients’ friend requests.11
Privacy problems
Psychiatrists who friend patients need to be aware of potential privacy breeches among Facebook users. Individuals whose presence among a psychiatrist’s friends becomes known (eg, via a wall post) are revealing their connection to the psychiatrist, and other friends may surmise that an individual is a patient.
Also, Facebook’s “find friends” feature ostensibly lets Facebook locate individuals who are common to pairs of people and who can then be suggested as potential friends to others, but “find friends” imports members’ entire e-mail address books. If doctors who are on Facebook have patients in their webmail address books and have allowed “find friends,” then Facebook will import e-mail addresses, potentially disclosing associations between patients and their doctors.12
Facebook has tools that let users block their profiles from public view, but these privacy settings can be difficult to access and understand. Although social networking among medical trainees and new graduates is common in the culture of emerging professionals, most Facebook users allow anyone to view their profile—the default privacy setting.2,13 Even if you don’t friend patients, failing to privatize your account leaves your Facebook information readily available to the public, including your patients.
Professionalism in cyberspace
Under some circumstances, medical advice given in casual, outside-the-office contexts can establish a doctor-patient relationship, with all its accompanying obligations and liability risks. This is true of Facebook communications. If you communicate medical information or advice to someone in a form specific enough to be relied upon, you may be establishing a doctor-patient relationship. If harm comes to a person who relied upon your information, a negligence lawsuit could result—even though you never saw or spoke to the “patient.”14
Medical training programs have found that medical students and residents have posted work-related comments on Facebook that directly referenced specific patient situations or other patient care matters. Such actions can breach the Health Insurance Portability and Accountability Act of 1996 and can jeopardize careers.15 Medical professionals also have posted uncouth, inappropriate, and embarrassing content—profanity, frankly discriminatory language, tales of intoxication, and sexually explicit information. In a recent survey of 78 medical schools, 60% responded that their students had posted unprofessional online content.16 In 45 cases, schools reported such incidents and responded to follow-up questions about disciplinary actions; 30 schools gave informal warnings, and 2 schools reported student dismissals.
Using Facebook
Should psychiatrists stay off Facebook? Of course not. Many prominent American psychiatrists are on Facebook because, like everyone else, they enjoy keeping in contact with friends and family.17 Thousands of professional groups (eg, the American Psychiatric Association) and physician practices have Facebook pages. Institutions, schools, and agencies use social media to promote their curricula, notify students and staff of course changes, or organize meetings. Professionals join groups or “like” groups associated with their specialty to affiliate with each other, and they use Facebook to promote their practices, disseminate information, and network with colleagues.
Psychiatrists need not shy away from establishing an account on Facebook,18 but they should do so with greater circumspection than most persons, including physicians in other specialties. Table 1 lists several examples of Facebook behavior that all physicians should avoid.2,13,16,19,20
What about using Facebook to learn about your patients? Medical reports about checking Facebook to resolve emergencies have appeared,20 and forensic psychiatrists can use Facebook and other Internet resources to learn about evaluees.21 But if doctors search for information about a patient’s out-of-office behavior or statements, it may be like “driving down a patient’s street to see what he or she is up to,” which, although legal, seems inappropriate in a professional relationship.22
Recent experience suggests that medical schools and residencies should include “e-professionalism” in their curricula, emphasizing instruction and guidance on where personal and professional identities may intersect and where they should be kept separate. Table 2 lists several responses to the new challenges to medical professionalism posed by Facebook and other social media.5,6
Table 1
Facebook errors: What to avoid
| Category | Pitfalls |
|---|---|
| Information | Relationships, religious views, home address, and telephone number all may be readily viewable to the general public and patients if privacy settings are not properly configured |
| Photos | Intoxication, sexually explicit material, risk-taking behavior |
| “Wall posts” | Blatant comments about patients, disgruntlement with institution or supervisors |
| Security settings | Lack of privacy restrictions |
| “Friends” | Friending patients and supervisors |
| “Like” | “Liking” groups that contain pornographic material or other controversial topics |
| Source: References 2,13,16,19,20 | |
Table 2
Promoting e-professionalism
| Understand and activate all relevant privacy and security settings on social networking sites |
| Recognize the need to teach e-professionalism in the curricula of medical schools and residency training programs |
| Combine instruction on professional use of Facebook with teaching about relevant legal regulations in medicine (eg, HIPAA) |
| Guidance in online professionalism should come from faculty supervisors or program directors |
| Faculty should model appropriate Facebook behaviors for employees, medical students, and residents |
| Users of social media are well-advised to conduct Web searches on themselves and modify their pages to conform with professional standards |
| Politely decline patients’ “friend” requests |
| Discussions of medical professionalism, involving students, faculty, and employers, can help identify issues and define responses |
| Institutions should establish and enforce guidelines for Facebook professionalism |
| HIPAA: Health Insurance Portability and Accountability Act of 1996 Source: References 5,6 |
Responding to Dr. V
Psychiatrists should not “friend” patients. If you receive a “friend” request, you should proceed in 1 of the following ways:17
- Simply ignore the request. If your patient asks why you didn’t respond, explain that you use Facebook only for personal matters
- Ignore the request, and at the patient’s next appointment, mention the request and politely explain that you do not “friend” patients
- Ignore the request, but ask the patient about it at your next meeting. This is especially important for a patient whose treatment examines the doctor-patient relationship (eg, psychodynamic therapy), but may be valuable even in medication-focused care.
- Facebook. www.facebook.com.
- Foreman J. Think before you click. Boston Globe. April 12, 2010.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Facebook. Statistics. http://www.facebook.com/press/info.php?statistics. Accessed January 30, 2012.
2. MacDonald J, Sohn S, Ellis P. Privacy professionalism and Facebook: a dilemma for young doctors. Med Educ. 2010;44(8):805-813.
3. Gorrindo T, Gorrindo PC, Groves JE. Intersection of online social networking with medical professionalism: can medicine police the Facebook boom? J Gen Intern Med. 2008;23(12):2155.-
4. Baer W, Schwartz AC. Teaching professionalism in the digital age on the psychiatric consultation-liaison service. Psychosomatics. 2011;52(4):303-309.
5. Landman MP, Shelton J, Kauffmann RM, et al. Guidelines for maintaining a professional compass in the era of social networking. J Surg Educ. 2010;67(6):381-386.
6. Guseh JS 2nd, Brendel RW, Brendel DH. Medical professionalism in the age of online social networking. J Med Ethics. 2009;35(9):584-586.
7. Devi S. Facebook friend request from a patient? Lancet. 2011;377(9772):1141-1142.
8. Gruenberg PB. Boundary violations. In: Wahl DS Polster DS, eds. Ethics primer. Arlington, VA: American Psychiatric Association; 2001. http://www.psych.org/Departments/EDU/residentmit/dl01.aspx. Accessed January 4, 2012.
9. Moubarak G, Guiot A, Benhamou Y, et al. Facebook activity of residents and fellows and its impact on the doctor-patient relationship. J Med Ethics. 2011;37(2):101-104.
10. American Medical Association. AMA policy: professionalism in the use of social media. http://www.ama-assn.org/ama/pub/meeting/professionalism-social-media.shtml. Accessed January 4 2012.
11. British Medical Association. Using social media: practical and ethical guidance for doctors and medical students. http://www.bma.org.uk/press_centre/video_social_media/socialmediaguidance2011.jsp. Accessed January 4 2012.
12. Wilson S. A bigger threat to patient privacy when doctors use Facebook. J Med Ethics. http://jme.bmj.com/content/37/2/101.abstract/reply#medethics_el_3625. Published December 20 2010. Accessed January 4, 2012.
13. Thompson LA, Dawson K, Ferdig R, et al. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23(7):954-957.
14. Reisman N. Avoid being too social when using social media. Plastic Surgery News. September 13 2011. http://www.psnextra.org/Columns/OLG-September-11.html. Accessed January 4, 2012.
15. Greysen SR, Kind T, Chretien KC. Online professionalism and the mirror of social media. J Gen Intern Med. 2010;25(11):1227-1229.
16. Chretien KC, Greysen SR, Chretien JP, et al. Online posting of unprofessional content by medical students. JAMA. 2009;302(12):1309-1315.
17. Arehart-Treichel J. Facebook can be useful–if you use common sense. Psychiatric News. 2011;46(22):5A.-
18. O’Hanlon S, Shannon B. Comments further to: privacy professionalism and Facebook: a dilemma for young doctors. Med Educ. 2011;45(2):209.-
19. Metzger AH, Finley KN, Ulbrich TR, et al. Pharmacy faculty members’ perspectives on the student/faculty relationship in online social networks. Am J Pharm Educ. 2010;74(10):188.-
20. Ben-Yakov M, Snider C. How Facebook saved our day! Acad Emerg Med. 2011;18(11):1217-1219.
21. Metzner JL, Ash P. Commentary: the mental status examination in the age of the internet—challenges and opportunities. J Am Acad Psychiatry Law. 2010;38(1):27-31.
22. Bosslet GT. Commentary: the good the bad, and the ugly of social media. Acad Emerg Med. 2011;18(11):1221-1222.
1. Facebook. Statistics. http://www.facebook.com/press/info.php?statistics. Accessed January 30, 2012.
2. MacDonald J, Sohn S, Ellis P. Privacy professionalism and Facebook: a dilemma for young doctors. Med Educ. 2010;44(8):805-813.
3. Gorrindo T, Gorrindo PC, Groves JE. Intersection of online social networking with medical professionalism: can medicine police the Facebook boom? J Gen Intern Med. 2008;23(12):2155.-
4. Baer W, Schwartz AC. Teaching professionalism in the digital age on the psychiatric consultation-liaison service. Psychosomatics. 2011;52(4):303-309.
5. Landman MP, Shelton J, Kauffmann RM, et al. Guidelines for maintaining a professional compass in the era of social networking. J Surg Educ. 2010;67(6):381-386.
6. Guseh JS 2nd, Brendel RW, Brendel DH. Medical professionalism in the age of online social networking. J Med Ethics. 2009;35(9):584-586.
7. Devi S. Facebook friend request from a patient? Lancet. 2011;377(9772):1141-1142.
8. Gruenberg PB. Boundary violations. In: Wahl DS Polster DS, eds. Ethics primer. Arlington, VA: American Psychiatric Association; 2001. http://www.psych.org/Departments/EDU/residentmit/dl01.aspx. Accessed January 4, 2012.
9. Moubarak G, Guiot A, Benhamou Y, et al. Facebook activity of residents and fellows and its impact on the doctor-patient relationship. J Med Ethics. 2011;37(2):101-104.
10. American Medical Association. AMA policy: professionalism in the use of social media. http://www.ama-assn.org/ama/pub/meeting/professionalism-social-media.shtml. Accessed January 4 2012.
11. British Medical Association. Using social media: practical and ethical guidance for doctors and medical students. http://www.bma.org.uk/press_centre/video_social_media/socialmediaguidance2011.jsp. Accessed January 4 2012.
12. Wilson S. A bigger threat to patient privacy when doctors use Facebook. J Med Ethics. http://jme.bmj.com/content/37/2/101.abstract/reply#medethics_el_3625. Published December 20 2010. Accessed January 4, 2012.
13. Thompson LA, Dawson K, Ferdig R, et al. The intersection of online social networking with medical professionalism. J Gen Intern Med. 2008;23(7):954-957.
14. Reisman N. Avoid being too social when using social media. Plastic Surgery News. September 13 2011. http://www.psnextra.org/Columns/OLG-September-11.html. Accessed January 4, 2012.
15. Greysen SR, Kind T, Chretien KC. Online professionalism and the mirror of social media. J Gen Intern Med. 2010;25(11):1227-1229.
16. Chretien KC, Greysen SR, Chretien JP, et al. Online posting of unprofessional content by medical students. JAMA. 2009;302(12):1309-1315.
17. Arehart-Treichel J. Facebook can be useful–if you use common sense. Psychiatric News. 2011;46(22):5A.-
18. O’Hanlon S, Shannon B. Comments further to: privacy professionalism and Facebook: a dilemma for young doctors. Med Educ. 2011;45(2):209.-
19. Metzger AH, Finley KN, Ulbrich TR, et al. Pharmacy faculty members’ perspectives on the student/faculty relationship in online social networks. Am J Pharm Educ. 2010;74(10):188.-
20. Ben-Yakov M, Snider C. How Facebook saved our day! Acad Emerg Med. 2011;18(11):1217-1219.
21. Metzner JL, Ash P. Commentary: the mental status examination in the age of the internet—challenges and opportunities. J Am Acad Psychiatry Law. 2010;38(1):27-31.
22. Bosslet GT. Commentary: the good the bad, and the ugly of social media. Acad Emerg Med. 2011;18(11):1221-1222.