User login
Brown spots on face

The results of a 4-mm punch biopsy confirmed a diagnosis of actinic lichen planus. As the name implies, this form of lichen planus occurs in areas of sun exposure. Treatment is the same as for other forms of lichen planus, with the addition of avoiding the sun.
The FP counseled the patient about the use of sunscreen and avoiding sun exposure as much as possible. The FP then prescribed a mid-potency topical corticosteroid, 0.1% triamcinolone cream. (A low-potency steroid is unlikely to be beneficial.) In cases like this one, a short course of a mid-potency steroid should be safe on the face without causing atrophy.
At follow-up, there was a significant improvement in the appearance of the patient’s face and hands. The patient was pleased with these results and said she’d been more careful with sun exposure. The FP prescribed 2.5% hydrocortisone cream to be used on the face as needed, in conjunction with the continued use of triamcinolone on the hands as needed.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

The results of a 4-mm punch biopsy confirmed a diagnosis of actinic lichen planus. As the name implies, this form of lichen planus occurs in areas of sun exposure. Treatment is the same as for other forms of lichen planus, with the addition of avoiding the sun.
The FP counseled the patient about the use of sunscreen and avoiding sun exposure as much as possible. The FP then prescribed a mid-potency topical corticosteroid, 0.1% triamcinolone cream. (A low-potency steroid is unlikely to be beneficial.) In cases like this one, a short course of a mid-potency steroid should be safe on the face without causing atrophy.
At follow-up, there was a significant improvement in the appearance of the patient’s face and hands. The patient was pleased with these results and said she’d been more careful with sun exposure. The FP prescribed 2.5% hydrocortisone cream to be used on the face as needed, in conjunction with the continued use of triamcinolone on the hands as needed.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

The results of a 4-mm punch biopsy confirmed a diagnosis of actinic lichen planus. As the name implies, this form of lichen planus occurs in areas of sun exposure. Treatment is the same as for other forms of lichen planus, with the addition of avoiding the sun.
The FP counseled the patient about the use of sunscreen and avoiding sun exposure as much as possible. The FP then prescribed a mid-potency topical corticosteroid, 0.1% triamcinolone cream. (A low-potency steroid is unlikely to be beneficial.) In cases like this one, a short course of a mid-potency steroid should be safe on the face without causing atrophy.
At follow-up, there was a significant improvement in the appearance of the patient’s face and hands. The patient was pleased with these results and said she’d been more careful with sun exposure. The FP prescribed 2.5% hydrocortisone cream to be used on the face as needed, in conjunction with the continued use of triamcinolone on the hands as needed.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
Cheek pain

Based on the presence of bilateral Wickham striae, the FP diagnosed oral lichen planus in this patient. If the pattern were unilateral or the patient had a history of tobacco or alcohol use, the FP’s suspicion would have turned to a diagnosis of oral leukoplakia—a precursor to squamous cell carcinoma.
A mid-potency topical steroid is a good initial treatment for oral lichen planus. Triamcinolone can be prescribed in an oral base, but because it is very thick and sticky, it is better for local application to small areas around the teeth. Other treatment options include a gel or ointment, but these are not necessarily better inside the mouth. Most patients will find the cream easier to apply, even if it doesn’t taste good. If a mid-potency steroid doesn’t work, it is possible to use a high-potency steroid and change the vehicle according to the patient’s preference.
The FP in this case prescribed topical triamcinolone 0.1% cream to be applied twice daily to the buccal mucosa. At follow-up one month later, the patient’s cheeks no longer hurt, and the white Wickham striae were less visible. The FP instructed the patient to continue using the topical steroid twice daily as needed, and to return if her condition worsened.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

Based on the presence of bilateral Wickham striae, the FP diagnosed oral lichen planus in this patient. If the pattern were unilateral or the patient had a history of tobacco or alcohol use, the FP’s suspicion would have turned to a diagnosis of oral leukoplakia—a precursor to squamous cell carcinoma.
A mid-potency topical steroid is a good initial treatment for oral lichen planus. Triamcinolone can be prescribed in an oral base, but because it is very thick and sticky, it is better for local application to small areas around the teeth. Other treatment options include a gel or ointment, but these are not necessarily better inside the mouth. Most patients will find the cream easier to apply, even if it doesn’t taste good. If a mid-potency steroid doesn’t work, it is possible to use a high-potency steroid and change the vehicle according to the patient’s preference.
The FP in this case prescribed topical triamcinolone 0.1% cream to be applied twice daily to the buccal mucosa. At follow-up one month later, the patient’s cheeks no longer hurt, and the white Wickham striae were less visible. The FP instructed the patient to continue using the topical steroid twice daily as needed, and to return if her condition worsened.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

Based on the presence of bilateral Wickham striae, the FP diagnosed oral lichen planus in this patient. If the pattern were unilateral or the patient had a history of tobacco or alcohol use, the FP’s suspicion would have turned to a diagnosis of oral leukoplakia—a precursor to squamous cell carcinoma.
A mid-potency topical steroid is a good initial treatment for oral lichen planus. Triamcinolone can be prescribed in an oral base, but because it is very thick and sticky, it is better for local application to small areas around the teeth. Other treatment options include a gel or ointment, but these are not necessarily better inside the mouth. Most patients will find the cream easier to apply, even if it doesn’t taste good. If a mid-potency steroid doesn’t work, it is possible to use a high-potency steroid and change the vehicle according to the patient’s preference.
The FP in this case prescribed topical triamcinolone 0.1% cream to be applied twice daily to the buccal mucosa. At follow-up one month later, the patient’s cheeks no longer hurt, and the white Wickham striae were less visible. The FP instructed the patient to continue using the topical steroid twice daily as needed, and to return if her condition worsened.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
Red and brown lesions

Biopsy results revealed that this was a case of atrophic lichen planus, one of the rarer types of lichen planus that is defined by nonpalpable lesions. The FP examined areas of the patient where lichen planus is commonly found (including the wrist, ankles, and back) and discovered a few similar lesions around the patient’s ankles.
The FP explained the diagnosis to the patient and offered a mid-potency topical corticosteroid—0.1% triamcinolone cream. She advised the patient that if the lesions became more atrophic, they could try to get a topical vitamin D medication approved as an alternative. There is evidence that topical vitamin D may be beneficial, with no risk of skin atrophy. However, these are high-cost medications—despite the fact that some are now generic. A prior authorization for one of these vitamin D medications is more likely to be approved if there has been a failure, or adverse effects, from a first-line topical steroid.
Other treatment options for atrophic lichen planus include oral metronidazole and oral prednisone. The mechanism for the effectiveness of oral metronidazole is unknown, but it is a relatively safe option if topical treatments fail. Oral prednisone taken for 20 to 30 days is more likely to be effective, but is also more likely to cause adverse effects.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

Biopsy results revealed that this was a case of atrophic lichen planus, one of the rarer types of lichen planus that is defined by nonpalpable lesions. The FP examined areas of the patient where lichen planus is commonly found (including the wrist, ankles, and back) and discovered a few similar lesions around the patient’s ankles.
The FP explained the diagnosis to the patient and offered a mid-potency topical corticosteroid—0.1% triamcinolone cream. She advised the patient that if the lesions became more atrophic, they could try to get a topical vitamin D medication approved as an alternative. There is evidence that topical vitamin D may be beneficial, with no risk of skin atrophy. However, these are high-cost medications—despite the fact that some are now generic. A prior authorization for one of these vitamin D medications is more likely to be approved if there has been a failure, or adverse effects, from a first-line topical steroid.
Other treatment options for atrophic lichen planus include oral metronidazole and oral prednisone. The mechanism for the effectiveness of oral metronidazole is unknown, but it is a relatively safe option if topical treatments fail. Oral prednisone taken for 20 to 30 days is more likely to be effective, but is also more likely to cause adverse effects.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

Biopsy results revealed that this was a case of atrophic lichen planus, one of the rarer types of lichen planus that is defined by nonpalpable lesions. The FP examined areas of the patient where lichen planus is commonly found (including the wrist, ankles, and back) and discovered a few similar lesions around the patient’s ankles.
The FP explained the diagnosis to the patient and offered a mid-potency topical corticosteroid—0.1% triamcinolone cream. She advised the patient that if the lesions became more atrophic, they could try to get a topical vitamin D medication approved as an alternative. There is evidence that topical vitamin D may be beneficial, with no risk of skin atrophy. However, these are high-cost medications—despite the fact that some are now generic. A prior authorization for one of these vitamin D medications is more likely to be approved if there has been a failure, or adverse effects, from a first-line topical steroid.
Other treatment options for atrophic lichen planus include oral metronidazole and oral prednisone. The mechanism for the effectiveness of oral metronidazole is unknown, but it is a relatively safe option if topical treatments fail. Oral prednisone taken for 20 to 30 days is more likely to be effective, but is also more likely to cause adverse effects.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
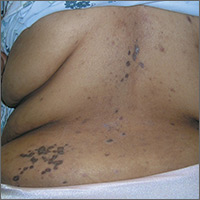
Rash on back and wrists

The FP was aware that HCTZ might precipitate lichen planus or create a lichenoid drug reaction, so he performed a 4-mm punch biopsy and asked the patient to stop taking her HCTZ while the biopsy results were pending. (The patient also had several of the 5 Ps of lichen planus: planar, polygonal, pruritic, papular, and purple lesions. She didn’t have any papular lesions and the lesions she did have were more brown than purple because of her dark skin color.)
The FP prescribed topical fluocinonide 0.05% ointment to be applied twice daily to the affected areas until the biopsy results were available. The FP also increased her lisinopril dose, hoping to keep her BP under control.
Biopsy results came back as probable lichen planus and possible lichenoid drug reaction. As treatment for each condition would be the same, it didn’t matter that the pathologist couldn’t be more specific.
On the patient’s second visit for suture removal and discussion of the biopsy results, she said she was feeling better. Her BP was still under control, so the FP decided to continue the treatment plan. At follow-up one month later, the pruritus had resolved completely and the skin lesions were no longer palpable. There was postinflammatory hyperpigmentation at the sites of the lesions, but the patient was not concerned about this because most of it was on her back.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

The FP was aware that HCTZ might precipitate lichen planus or create a lichenoid drug reaction, so he performed a 4-mm punch biopsy and asked the patient to stop taking her HCTZ while the biopsy results were pending. (The patient also had several of the 5 Ps of lichen planus: planar, polygonal, pruritic, papular, and purple lesions. She didn’t have any papular lesions and the lesions she did have were more brown than purple because of her dark skin color.)
The FP prescribed topical fluocinonide 0.05% ointment to be applied twice daily to the affected areas until the biopsy results were available. The FP also increased her lisinopril dose, hoping to keep her BP under control.
Biopsy results came back as probable lichen planus and possible lichenoid drug reaction. As treatment for each condition would be the same, it didn’t matter that the pathologist couldn’t be more specific.
On the patient’s second visit for suture removal and discussion of the biopsy results, she said she was feeling better. Her BP was still under control, so the FP decided to continue the treatment plan. At follow-up one month later, the pruritus had resolved completely and the skin lesions were no longer palpable. There was postinflammatory hyperpigmentation at the sites of the lesions, but the patient was not concerned about this because most of it was on her back.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

The FP was aware that HCTZ might precipitate lichen planus or create a lichenoid drug reaction, so he performed a 4-mm punch biopsy and asked the patient to stop taking her HCTZ while the biopsy results were pending. (The patient also had several of the 5 Ps of lichen planus: planar, polygonal, pruritic, papular, and purple lesions. She didn’t have any papular lesions and the lesions she did have were more brown than purple because of her dark skin color.)
The FP prescribed topical fluocinonide 0.05% ointment to be applied twice daily to the affected areas until the biopsy results were available. The FP also increased her lisinopril dose, hoping to keep her BP under control.
Biopsy results came back as probable lichen planus and possible lichenoid drug reaction. As treatment for each condition would be the same, it didn’t matter that the pathologist couldn’t be more specific.
On the patient’s second visit for suture removal and discussion of the biopsy results, she said she was feeling better. Her BP was still under control, so the FP decided to continue the treatment plan. At follow-up one month later, the pruritus had resolved completely and the skin lesions were no longer palpable. There was postinflammatory hyperpigmentation at the sites of the lesions, but the patient was not concerned about this because most of it was on her back.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Kraft RL, Usatine R. Lichen planus. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 901-909.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
Confusion recurs 2 weeks after fall
A 77-year-old woman presented to the emergency department complaining of a headache following a syncopal episode (while standing) earlier that day. She said that she’d lost consciousness for several minutes, and then experienced several minutes of mild confusion that resolved spontaneously.
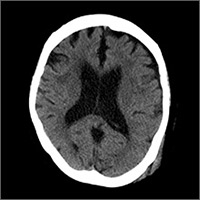
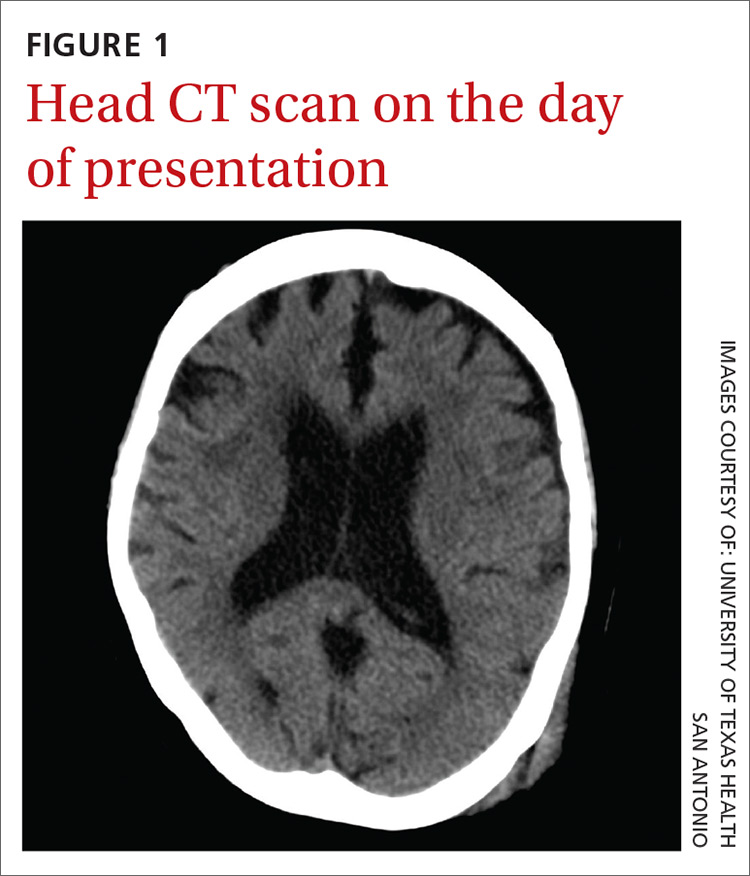
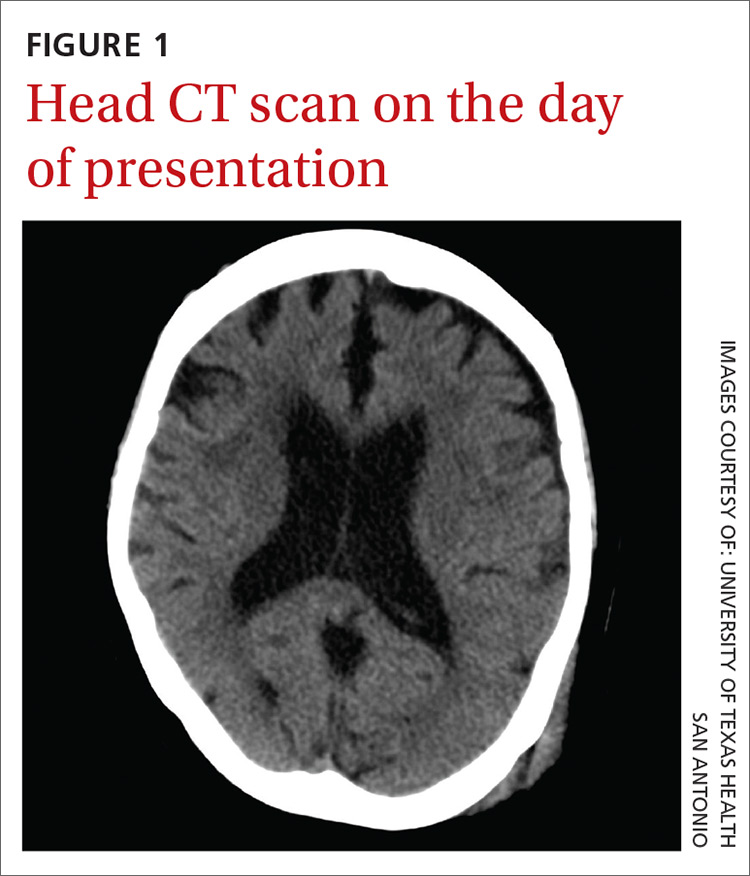
On physical exam, she was oriented to person and place, but not time. She had a contusion in her left occipitoparietal region without extensive bruising or deformity. The patient had normal cardiopulmonary, abdominal, and neurologic exams. Her past medical history included hypertension and normal pressure hydrocephalus, and her vital signs were within normal limits. She was taking aspirin once daily.The patient’s initial head and neck computerized tomography (CT) scans were normal (FIGURE 1), but she was hospitalized because of her confusion. During her hospitalization, the patient had mild episodic headaches that resolved with acetaminophen. The next day, her confusion resolved, and repeat CT scans were unchanged. She was discharged within 24 hours.
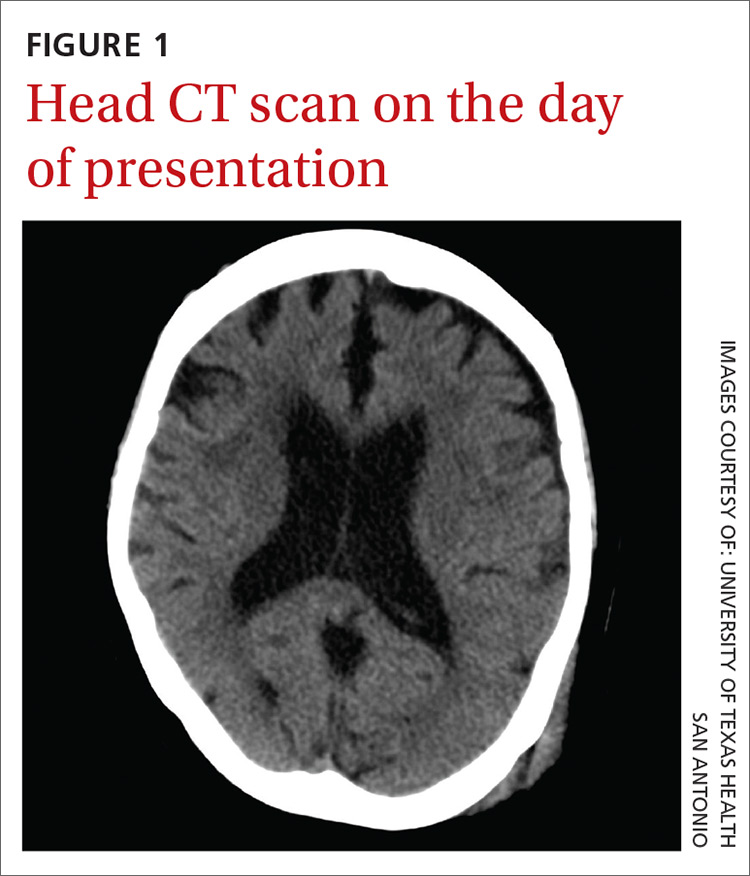
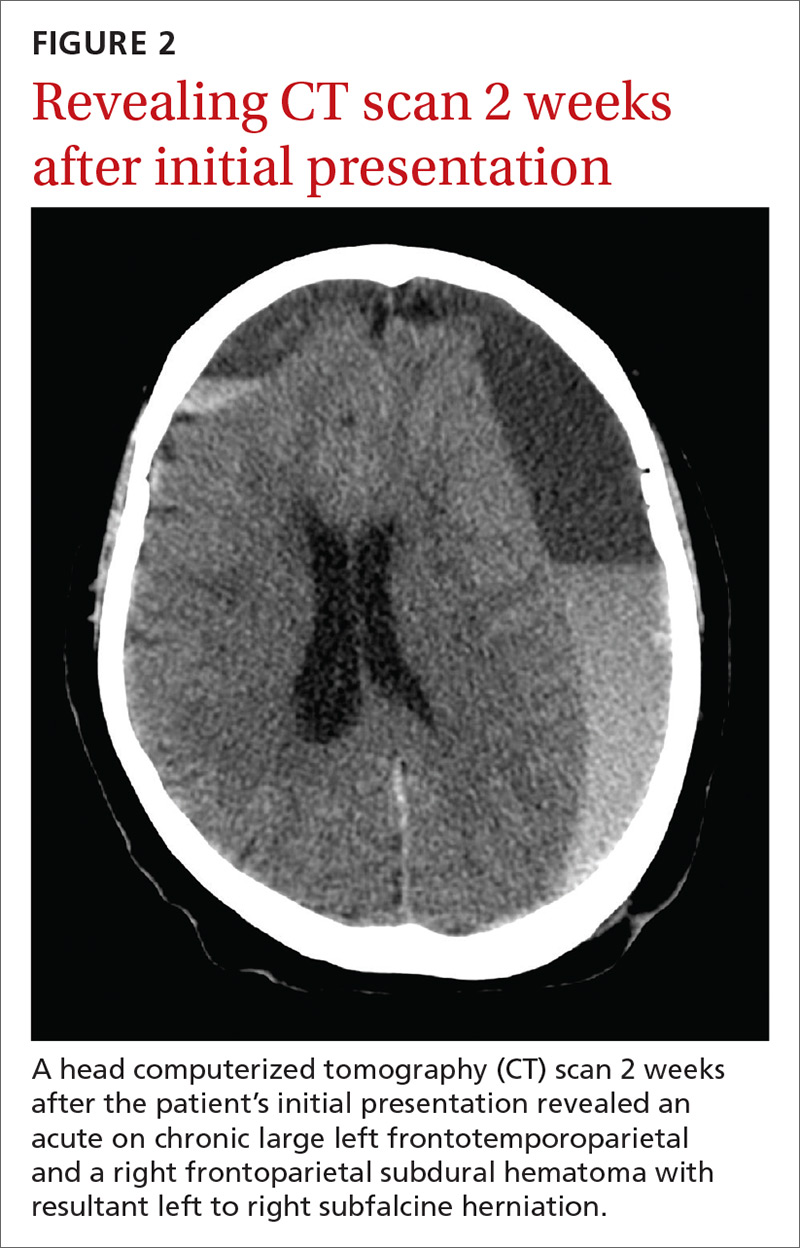
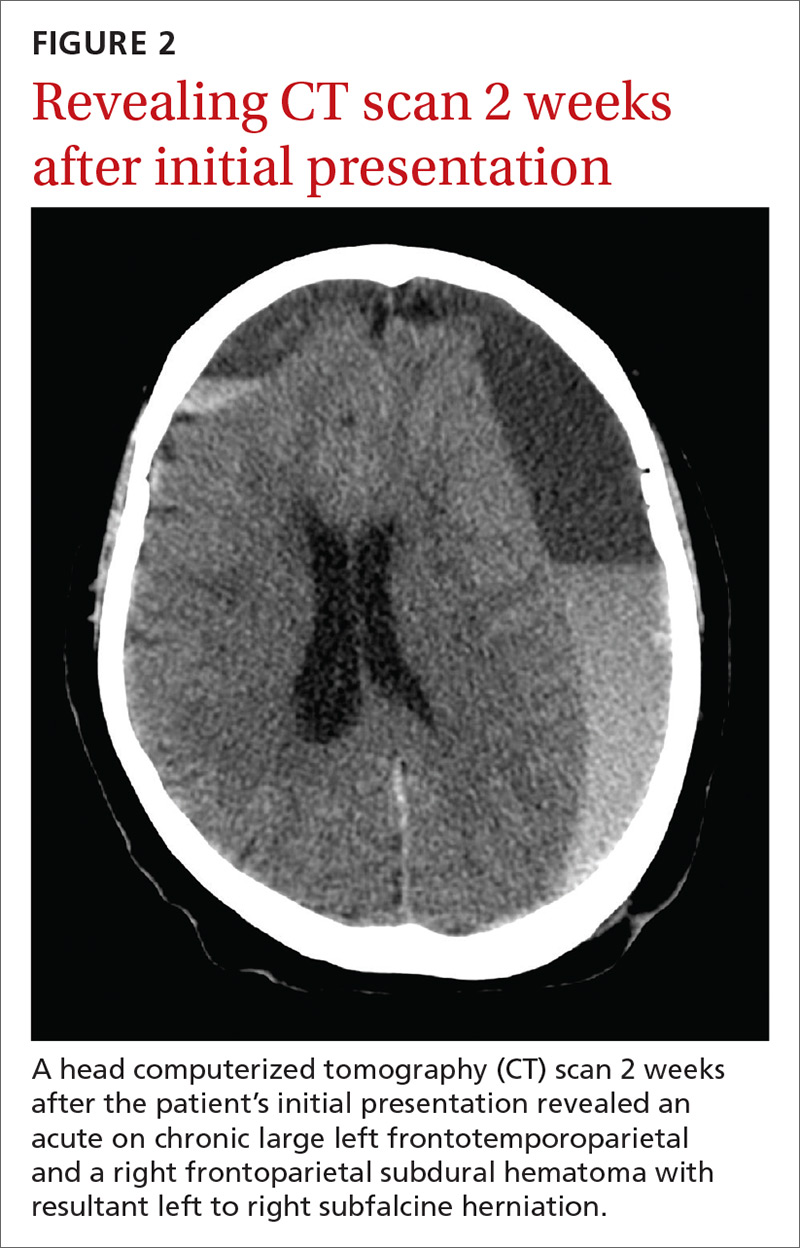
Two weeks later, the patient returned to the hospital after her daughter found her on the toilet, unable to stand up from the sitting position. She was confused and experienced a worsening of headache during transport to the hospital. No recurrent falls or additional episodes of trauma were reported. A CT scan was performed.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Delayed acute subdural hematoma
The CT scan (FIGURE 2) revealed an acute on chronic large left frontotemporoparietal and a right frontoparietal subdural hematoma (SDH) with resultant left to right subfalcine herniation. The patient was given a diagnosis of a delayed acute subdural hematoma (DASH)—an acute subdural hematoma that is not apparent on an initial CT scan, but is detected on follow-up CT imaging days or weeks after the injury.1 The incidence of DASH is approximately 0.5% among acute SDH patients who require operative treatment.1
Because DASH is rare, there is a lot of uncertainty surrounding its presentation, pathophysiology, and outcomes. In the few cases that have been described, patients have varied from those who were healthy, and had no coagulation abnormalities, to those who were elderly and taking anticoagulants.2,3 In addition, the period between the head injury and the development of SDH is variable.3
While not much is known about DASH, the mechanism of acute SDH has been widely studied and researched. Acute SDH, which typically follows a head trauma, results from the tearing of bridging veins that lack supporting structures and are most vulnerable to injury when crossing the subdural space.4 The potential pathophysiology for DASH is not completely understood, but is likely to involve subtle damage to the bridging veins of the brain that continue to leak over a matter of hours and days.1,5
Two risk factors to consider. Increasing age and use of oral anticoagulants can increase the risk of developing an intracranial lesion after head injury.3 Due to the infrequency of DASH, the same risk factors for SDH should be considered for DASH. These factors make it increasingly important to establish guidelines on how to approach mild traumatic brain injury (TBI) in both DASH and SDH, especially for those who are elderly or have been on anticoagulation therapy.
Differential Dx
The differential diagnosis for our patient’s decline and altered mentation weeks after the initial event included worsening normal pressure hydrocephalus, cerebrovascular accident, and seizure.
Normal pressure hydrocephalus typically has a more chronic onset than DASH. It manifests with the classic triad of dementia, incontinence, and magnetic or festinating gait (“wild, wet, and wobbly”).
Cerebrovascular accidents are most often associated with focal neurologic deficits, which can be ischemic or hemorrhagic. If hemorrhagic, the hemorrhage is typically parenchymal and not subdural.
Seizure, especially partial complex seizure, can arise after trauma and may not involve obvious motor movements. Symptoms generally abate over a few minutes to hours with treatment. Electroencephalogram and CT scan can differentiate seizure from a subdural hematoma.
Keep DASH on your radar screen
The American College of Emergency Physicians states that a non-contrast head CT scan is indicated in head trauma patients with loss of consciousness if one or more of the following is present: age >60 years, vomiting, headache, drug or alcohol intoxication, short-term memory deficits, posttraumatic seizure, Glasgow Coma Scale score of <15, focal neurologic deficits, and coagulopathy.6
Some have suggested that the initial head CT scan be delayed by up to 8 hours to prevent missing a slowly developing intracranial hemorrhage. Others suggest that the CT scan be repeated at 24 hours. Still others have suggested that patients with even mild TBI be admitted for a period of observation if any risk factors, such as age or history of anticoagulation therapy, are noted.
Because there is no evidence to support delaying the initial head CT scan, physicians should be thorough in their evaluation of head trauma patients with loss of consciousness and consider a repeat CT scan of the head if worsening of any symptoms occurs. Physicians should also consider a repeat CT scan of the head for patients at high risk, including the elderly and those who have taken anticoagulants.
In addition, patients with traumatic head injuries must be properly counseled to return if they experience repeated vomiting, worsening headache, memory loss, confusion, focal neurologic deficit, abnormal behavior, increased sleepiness, or seizures.6 An extra precaution for high-risk patients includes suggesting adequate follow-up with a primary care physician to help monitor recovery and prevent any occurrences of DASH from going unnoticed.
Our patient underwent a mini-craniotomy. Postoperatively, she was discharged to a skilled nursing facility and ultimately made a complete recovery.
CORRESPONDENCE
Andrew Muck, MD, Department of Emergency Medicine, University of Texas Health San Antonio, 7703 Floyd Curl Drive, MSC 7736, San Antonio, TX 78229; [email protected].
1. Cohen T, Gudeman S. In: Narayan RK, ed. Delayed Traumatic Intracranial Hematoma. Neurotrauma. New York, NY: McGraw-Hill;1995:689-701.
2. Matsuda W, Sugimoto K, Sato N, et al. Delayed onset of posttraumatic acute subdural hematoma after mild head injury with normal computed tomography: a case report and brief review. J Trauma. 2008;65:461-463.
3. Itshayek E, Rosenthal G, Fraifeld S, et al. Delayed posttraumatic acute subdural hematoma in elderly patients on anticoagulation. Neurosurgery. 2006;58:E851-E856.
4. Culotta VP, Sermentilli ME, Gerold K, et al. Clinicopathological heterogeneity in the classification of mild head injury. Neurosurgery. 1996;38:245-250.
5. Shabani S, Nguyen HS, Doan N, et al. Case Report and Review of Literature of Delayed Acute Subdural Hematoma. World Neurosurg. 2016;96:66-71.
6. Jagoda AS, Bazarian JJ, Bruns Jr JJ, et al. Clinical Policy: Neuroimaging and Decisionmaking in Adult Mild Traumatic Brain Injury in the Acute Setting. Ann Emerg Med. 2008;52:714-748.
A 77-year-old woman presented to the emergency department complaining of a headache following a syncopal episode (while standing) earlier that day. She said that she’d lost consciousness for several minutes, and then experienced several minutes of mild confusion that resolved spontaneously.
On physical exam, she was oriented to person and place, but not time. She had a contusion in her left occipitoparietal region without extensive bruising or deformity. The patient had normal cardiopulmonary, abdominal, and neurologic exams. Her past medical history included hypertension and normal pressure hydrocephalus, and her vital signs were within normal limits. She was taking aspirin once daily.The patient’s initial head and neck computerized tomography (CT) scans were normal (FIGURE 1), but she was hospitalized because of her confusion. During her hospitalization, the patient had mild episodic headaches that resolved with acetaminophen. The next day, her confusion resolved, and repeat CT scans were unchanged. She was discharged within 24 hours.
Two weeks later, the patient returned to the hospital after her daughter found her on the toilet, unable to stand up from the sitting position. She was confused and experienced a worsening of headache during transport to the hospital. No recurrent falls or additional episodes of trauma were reported. A CT scan was performed.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Delayed acute subdural hematoma
The CT scan (FIGURE 2) revealed an acute on chronic large left frontotemporoparietal and a right frontoparietal subdural hematoma (SDH) with resultant left to right subfalcine herniation. The patient was given a diagnosis of a delayed acute subdural hematoma (DASH)—an acute subdural hematoma that is not apparent on an initial CT scan, but is detected on follow-up CT imaging days or weeks after the injury.1 The incidence of DASH is approximately 0.5% among acute SDH patients who require operative treatment.1
Because DASH is rare, there is a lot of uncertainty surrounding its presentation, pathophysiology, and outcomes. In the few cases that have been described, patients have varied from those who were healthy, and had no coagulation abnormalities, to those who were elderly and taking anticoagulants.2,3 In addition, the period between the head injury and the development of SDH is variable.3
While not much is known about DASH, the mechanism of acute SDH has been widely studied and researched. Acute SDH, which typically follows a head trauma, results from the tearing of bridging veins that lack supporting structures and are most vulnerable to injury when crossing the subdural space.4 The potential pathophysiology for DASH is not completely understood, but is likely to involve subtle damage to the bridging veins of the brain that continue to leak over a matter of hours and days.1,5
Two risk factors to consider. Increasing age and use of oral anticoagulants can increase the risk of developing an intracranial lesion after head injury.3 Due to the infrequency of DASH, the same risk factors for SDH should be considered for DASH. These factors make it increasingly important to establish guidelines on how to approach mild traumatic brain injury (TBI) in both DASH and SDH, especially for those who are elderly or have been on anticoagulation therapy.
Differential Dx
The differential diagnosis for our patient’s decline and altered mentation weeks after the initial event included worsening normal pressure hydrocephalus, cerebrovascular accident, and seizure.
Normal pressure hydrocephalus typically has a more chronic onset than DASH. It manifests with the classic triad of dementia, incontinence, and magnetic or festinating gait (“wild, wet, and wobbly”).
Cerebrovascular accidents are most often associated with focal neurologic deficits, which can be ischemic or hemorrhagic. If hemorrhagic, the hemorrhage is typically parenchymal and not subdural.
Seizure, especially partial complex seizure, can arise after trauma and may not involve obvious motor movements. Symptoms generally abate over a few minutes to hours with treatment. Electroencephalogram and CT scan can differentiate seizure from a subdural hematoma.
Keep DASH on your radar screen
The American College of Emergency Physicians states that a non-contrast head CT scan is indicated in head trauma patients with loss of consciousness if one or more of the following is present: age >60 years, vomiting, headache, drug or alcohol intoxication, short-term memory deficits, posttraumatic seizure, Glasgow Coma Scale score of <15, focal neurologic deficits, and coagulopathy.6
Some have suggested that the initial head CT scan be delayed by up to 8 hours to prevent missing a slowly developing intracranial hemorrhage. Others suggest that the CT scan be repeated at 24 hours. Still others have suggested that patients with even mild TBI be admitted for a period of observation if any risk factors, such as age or history of anticoagulation therapy, are noted.
Because there is no evidence to support delaying the initial head CT scan, physicians should be thorough in their evaluation of head trauma patients with loss of consciousness and consider a repeat CT scan of the head if worsening of any symptoms occurs. Physicians should also consider a repeat CT scan of the head for patients at high risk, including the elderly and those who have taken anticoagulants.
In addition, patients with traumatic head injuries must be properly counseled to return if they experience repeated vomiting, worsening headache, memory loss, confusion, focal neurologic deficit, abnormal behavior, increased sleepiness, or seizures.6 An extra precaution for high-risk patients includes suggesting adequate follow-up with a primary care physician to help monitor recovery and prevent any occurrences of DASH from going unnoticed.
Our patient underwent a mini-craniotomy. Postoperatively, she was discharged to a skilled nursing facility and ultimately made a complete recovery.
CORRESPONDENCE
Andrew Muck, MD, Department of Emergency Medicine, University of Texas Health San Antonio, 7703 Floyd Curl Drive, MSC 7736, San Antonio, TX 78229; [email protected].
A 77-year-old woman presented to the emergency department complaining of a headache following a syncopal episode (while standing) earlier that day. She said that she’d lost consciousness for several minutes, and then experienced several minutes of mild confusion that resolved spontaneously.
On physical exam, she was oriented to person and place, but not time. She had a contusion in her left occipitoparietal region without extensive bruising or deformity. The patient had normal cardiopulmonary, abdominal, and neurologic exams. Her past medical history included hypertension and normal pressure hydrocephalus, and her vital signs were within normal limits. She was taking aspirin once daily.The patient’s initial head and neck computerized tomography (CT) scans were normal (FIGURE 1), but she was hospitalized because of her confusion. During her hospitalization, the patient had mild episodic headaches that resolved with acetaminophen. The next day, her confusion resolved, and repeat CT scans were unchanged. She was discharged within 24 hours.
Two weeks later, the patient returned to the hospital after her daughter found her on the toilet, unable to stand up from the sitting position. She was confused and experienced a worsening of headache during transport to the hospital. No recurrent falls or additional episodes of trauma were reported. A CT scan was performed.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Delayed acute subdural hematoma
The CT scan (FIGURE 2) revealed an acute on chronic large left frontotemporoparietal and a right frontoparietal subdural hematoma (SDH) with resultant left to right subfalcine herniation. The patient was given a diagnosis of a delayed acute subdural hematoma (DASH)—an acute subdural hematoma that is not apparent on an initial CT scan, but is detected on follow-up CT imaging days or weeks after the injury.1 The incidence of DASH is approximately 0.5% among acute SDH patients who require operative treatment.1
Because DASH is rare, there is a lot of uncertainty surrounding its presentation, pathophysiology, and outcomes. In the few cases that have been described, patients have varied from those who were healthy, and had no coagulation abnormalities, to those who were elderly and taking anticoagulants.2,3 In addition, the period between the head injury and the development of SDH is variable.3
While not much is known about DASH, the mechanism of acute SDH has been widely studied and researched. Acute SDH, which typically follows a head trauma, results from the tearing of bridging veins that lack supporting structures and are most vulnerable to injury when crossing the subdural space.4 The potential pathophysiology for DASH is not completely understood, but is likely to involve subtle damage to the bridging veins of the brain that continue to leak over a matter of hours and days.1,5
Two risk factors to consider. Increasing age and use of oral anticoagulants can increase the risk of developing an intracranial lesion after head injury.3 Due to the infrequency of DASH, the same risk factors for SDH should be considered for DASH. These factors make it increasingly important to establish guidelines on how to approach mild traumatic brain injury (TBI) in both DASH and SDH, especially for those who are elderly or have been on anticoagulation therapy.
Differential Dx
The differential diagnosis for our patient’s decline and altered mentation weeks after the initial event included worsening normal pressure hydrocephalus, cerebrovascular accident, and seizure.
Normal pressure hydrocephalus typically has a more chronic onset than DASH. It manifests with the classic triad of dementia, incontinence, and magnetic or festinating gait (“wild, wet, and wobbly”).
Cerebrovascular accidents are most often associated with focal neurologic deficits, which can be ischemic or hemorrhagic. If hemorrhagic, the hemorrhage is typically parenchymal and not subdural.
Seizure, especially partial complex seizure, can arise after trauma and may not involve obvious motor movements. Symptoms generally abate over a few minutes to hours with treatment. Electroencephalogram and CT scan can differentiate seizure from a subdural hematoma.
Keep DASH on your radar screen
The American College of Emergency Physicians states that a non-contrast head CT scan is indicated in head trauma patients with loss of consciousness if one or more of the following is present: age >60 years, vomiting, headache, drug or alcohol intoxication, short-term memory deficits, posttraumatic seizure, Glasgow Coma Scale score of <15, focal neurologic deficits, and coagulopathy.6
Some have suggested that the initial head CT scan be delayed by up to 8 hours to prevent missing a slowly developing intracranial hemorrhage. Others suggest that the CT scan be repeated at 24 hours. Still others have suggested that patients with even mild TBI be admitted for a period of observation if any risk factors, such as age or history of anticoagulation therapy, are noted.
Because there is no evidence to support delaying the initial head CT scan, physicians should be thorough in their evaluation of head trauma patients with loss of consciousness and consider a repeat CT scan of the head if worsening of any symptoms occurs. Physicians should also consider a repeat CT scan of the head for patients at high risk, including the elderly and those who have taken anticoagulants.
In addition, patients with traumatic head injuries must be properly counseled to return if they experience repeated vomiting, worsening headache, memory loss, confusion, focal neurologic deficit, abnormal behavior, increased sleepiness, or seizures.6 An extra precaution for high-risk patients includes suggesting adequate follow-up with a primary care physician to help monitor recovery and prevent any occurrences of DASH from going unnoticed.
Our patient underwent a mini-craniotomy. Postoperatively, she was discharged to a skilled nursing facility and ultimately made a complete recovery.
CORRESPONDENCE
Andrew Muck, MD, Department of Emergency Medicine, University of Texas Health San Antonio, 7703 Floyd Curl Drive, MSC 7736, San Antonio, TX 78229; [email protected].
1. Cohen T, Gudeman S. In: Narayan RK, ed. Delayed Traumatic Intracranial Hematoma. Neurotrauma. New York, NY: McGraw-Hill;1995:689-701.
2. Matsuda W, Sugimoto K, Sato N, et al. Delayed onset of posttraumatic acute subdural hematoma after mild head injury with normal computed tomography: a case report and brief review. J Trauma. 2008;65:461-463.
3. Itshayek E, Rosenthal G, Fraifeld S, et al. Delayed posttraumatic acute subdural hematoma in elderly patients on anticoagulation. Neurosurgery. 2006;58:E851-E856.
4. Culotta VP, Sermentilli ME, Gerold K, et al. Clinicopathological heterogeneity in the classification of mild head injury. Neurosurgery. 1996;38:245-250.
5. Shabani S, Nguyen HS, Doan N, et al. Case Report and Review of Literature of Delayed Acute Subdural Hematoma. World Neurosurg. 2016;96:66-71.
6. Jagoda AS, Bazarian JJ, Bruns Jr JJ, et al. Clinical Policy: Neuroimaging and Decisionmaking in Adult Mild Traumatic Brain Injury in the Acute Setting. Ann Emerg Med. 2008;52:714-748.
1. Cohen T, Gudeman S. In: Narayan RK, ed. Delayed Traumatic Intracranial Hematoma. Neurotrauma. New York, NY: McGraw-Hill;1995:689-701.
2. Matsuda W, Sugimoto K, Sato N, et al. Delayed onset of posttraumatic acute subdural hematoma after mild head injury with normal computed tomography: a case report and brief review. J Trauma. 2008;65:461-463.
3. Itshayek E, Rosenthal G, Fraifeld S, et al. Delayed posttraumatic acute subdural hematoma in elderly patients on anticoagulation. Neurosurgery. 2006;58:E851-E856.
4. Culotta VP, Sermentilli ME, Gerold K, et al. Clinicopathological heterogeneity in the classification of mild head injury. Neurosurgery. 1996;38:245-250.
5. Shabani S, Nguyen HS, Doan N, et al. Case Report and Review of Literature of Delayed Acute Subdural Hematoma. World Neurosurg. 2016;96:66-71.
6. Jagoda AS, Bazarian JJ, Bruns Jr JJ, et al. Clinical Policy: Neuroimaging and Decisionmaking in Adult Mild Traumatic Brain Injury in the Acute Setting. Ann Emerg Med. 2008;52:714-748.
Nonpruritic rash on arms

Based on the results of the punch biopsy and the slight scale seen on the periphery of the lesions (a collarette scale pattern), the FP made a diagnosis of pityriasis rosea.
The distribution of the lesions in this case was not typical for pityriasis rosea; lesions are typically found on the trunk (not the arms) and may start with a herald patch. Given the distribution of the lesions in this case, the more precise diagnosis was inverse pityriasis rosea.
The physician explained to the patient and her mother that the rash would resolve spontaneously and was unlikely to leave any scarring. Six months later, the FP saw the mother for an unrelated issue and she said her daughter’s rash had gotten better within a month of her daughter’s visit, and there had been no scarring.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Henderson D, Usatine R. Pityriasis rosea. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 896-900.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

Based on the results of the punch biopsy and the slight scale seen on the periphery of the lesions (a collarette scale pattern), the FP made a diagnosis of pityriasis rosea.
The distribution of the lesions in this case was not typical for pityriasis rosea; lesions are typically found on the trunk (not the arms) and may start with a herald patch. Given the distribution of the lesions in this case, the more precise diagnosis was inverse pityriasis rosea.
The physician explained to the patient and her mother that the rash would resolve spontaneously and was unlikely to leave any scarring. Six months later, the FP saw the mother for an unrelated issue and she said her daughter’s rash had gotten better within a month of her daughter’s visit, and there had been no scarring.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Henderson D, Usatine R. Pityriasis rosea. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 896-900.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

Based on the results of the punch biopsy and the slight scale seen on the periphery of the lesions (a collarette scale pattern), the FP made a diagnosis of pityriasis rosea.
The distribution of the lesions in this case was not typical for pityriasis rosea; lesions are typically found on the trunk (not the arms) and may start with a herald patch. Given the distribution of the lesions in this case, the more precise diagnosis was inverse pityriasis rosea.
The physician explained to the patient and her mother that the rash would resolve spontaneously and was unlikely to leave any scarring. Six months later, the FP saw the mother for an unrelated issue and she said her daughter’s rash had gotten better within a month of her daughter’s visit, and there had been no scarring.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Henderson D, Usatine R. Pityriasis rosea. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 896-900.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
Rash on arms and legs

Based on the negative RPR test and the results of a subsequent 4-mm punch biopsy, the FP made a diagnosis of pityriasis rosea. The trunk is typically more involved in this condition, making this case (involvement of arms and legs) a type of inverse pityriasis rosea.
Because secondary syphilis can also present as a papulosquamous eruption, it can be difficult to distinguish from pityriasis rosea on clinical grounds. Therefore, taking a sexual history is important when a diagnosis of pityriasis rosea is being considered. In patients with a history of sexually transmitted diseases (STDs) or high-risk sexual practices, an RPR test should be ordered.
The patient in this case was relieved to learn that he didn’t have an STD and said he’d be more careful in the future. The FP assured him that the condition would go away spontaneously and that no medications would be needed.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Henderson D, Usatine R. Pityriasis rosea. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 896-900.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

Based on the negative RPR test and the results of a subsequent 4-mm punch biopsy, the FP made a diagnosis of pityriasis rosea. The trunk is typically more involved in this condition, making this case (involvement of arms and legs) a type of inverse pityriasis rosea.
Because secondary syphilis can also present as a papulosquamous eruption, it can be difficult to distinguish from pityriasis rosea on clinical grounds. Therefore, taking a sexual history is important when a diagnosis of pityriasis rosea is being considered. In patients with a history of sexually transmitted diseases (STDs) or high-risk sexual practices, an RPR test should be ordered.
The patient in this case was relieved to learn that he didn’t have an STD and said he’d be more careful in the future. The FP assured him that the condition would go away spontaneously and that no medications would be needed.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Henderson D, Usatine R. Pityriasis rosea. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 896-900.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

Based on the negative RPR test and the results of a subsequent 4-mm punch biopsy, the FP made a diagnosis of pityriasis rosea. The trunk is typically more involved in this condition, making this case (involvement of arms and legs) a type of inverse pityriasis rosea.
Because secondary syphilis can also present as a papulosquamous eruption, it can be difficult to distinguish from pityriasis rosea on clinical grounds. Therefore, taking a sexual history is important when a diagnosis of pityriasis rosea is being considered. In patients with a history of sexually transmitted diseases (STDs) or high-risk sexual practices, an RPR test should be ordered.
The patient in this case was relieved to learn that he didn’t have an STD and said he’d be more careful in the future. The FP assured him that the condition would go away spontaneously and that no medications would be needed.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Henderson D, Usatine R. Pityriasis rosea. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 896-900.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com
Rash on trunk and upper arms

The FP recognized a “Christmas tree” pattern on the patient’s back, which led to a diagnosis of pityriasis rosea. Because there are no lab tests to confirm pityriasis rosea, it is usually a clinical diagnosis.
The Christmas tree pattern that signals pityriasis rosea is caused by the long axis of the plaques following the skin lines of the back. While it is a helpful indicator of pityriasis rosea when present, most cases do not show this pattern. In this case, a collarette scale pattern was also visible. This is seen when scaling is visibly raised on the edge of the plaques, like the collar of a shirt.
Pityriasis rosea can be difficult to distinguish from secondary syphilis, which can also present as a papulosquamous eruption. Therefore, taking a sexual history is important when a diagnosis of pityriasis rosea is being considered. In patients with a history of sexually transmitted diseases or high-risk sexual practices, a rapid plasma reagin test should be ordered.
The FP assured the patient and his mother that the pityriasis rosea rash was not contagious, would not cause scarring, and would resolve in one to 2 months without any treatment. The patient declined any medication for the pruritus. At a subsequent visit for a sports physical, the skin was found to be completely clear with no evidence of scarring.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Henderson D, Usatine R. Pityriasis rosea. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 896-900.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

The FP recognized a “Christmas tree” pattern on the patient’s back, which led to a diagnosis of pityriasis rosea. Because there are no lab tests to confirm pityriasis rosea, it is usually a clinical diagnosis.
The Christmas tree pattern that signals pityriasis rosea is caused by the long axis of the plaques following the skin lines of the back. While it is a helpful indicator of pityriasis rosea when present, most cases do not show this pattern. In this case, a collarette scale pattern was also visible. This is seen when scaling is visibly raised on the edge of the plaques, like the collar of a shirt.
Pityriasis rosea can be difficult to distinguish from secondary syphilis, which can also present as a papulosquamous eruption. Therefore, taking a sexual history is important when a diagnosis of pityriasis rosea is being considered. In patients with a history of sexually transmitted diseases or high-risk sexual practices, a rapid plasma reagin test should be ordered.
The FP assured the patient and his mother that the pityriasis rosea rash was not contagious, would not cause scarring, and would resolve in one to 2 months without any treatment. The patient declined any medication for the pruritus. At a subsequent visit for a sports physical, the skin was found to be completely clear with no evidence of scarring.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Henderson D, Usatine R. Pityriasis rosea. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 896-900.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com

The FP recognized a “Christmas tree” pattern on the patient’s back, which led to a diagnosis of pityriasis rosea. Because there are no lab tests to confirm pityriasis rosea, it is usually a clinical diagnosis.
The Christmas tree pattern that signals pityriasis rosea is caused by the long axis of the plaques following the skin lines of the back. While it is a helpful indicator of pityriasis rosea when present, most cases do not show this pattern. In this case, a collarette scale pattern was also visible. This is seen when scaling is visibly raised on the edge of the plaques, like the collar of a shirt.
Pityriasis rosea can be difficult to distinguish from secondary syphilis, which can also present as a papulosquamous eruption. Therefore, taking a sexual history is important when a diagnosis of pityriasis rosea is being considered. In patients with a history of sexually transmitted diseases or high-risk sexual practices, a rapid plasma reagin test should be ordered.
The FP assured the patient and his mother that the pityriasis rosea rash was not contagious, would not cause scarring, and would resolve in one to 2 months without any treatment. The patient declined any medication for the pruritus. At a subsequent visit for a sports physical, the skin was found to be completely clear with no evidence of scarring.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Henderson D, Usatine R. Pityriasis rosea. In: Usatine R, Smith M, Mayeaux EJ, et al, eds. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013: 896-900.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com