User login
The Hospitalist only
Trio of awardees illustrate excellence in SHM chapters
2020 required resiliency, innovation
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
2020 required resiliency, innovation
2020 required resiliency, innovation
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
The Society of Hospital Medicine’s annual Chapter Excellence Exemplary Awards have additional meaning this year, in the wake of the persistent challenges faced by the medical profession as a result of the COVID-19 pandemic.

“The Chapter Excellence Award program is an annual rewards program to recognize outstanding work conducted by chapters to carry out the SHM mission locally,” Lisa Kroll, associate director of membership at SHM, said in an interview.
The Chapter Excellence Award program is composed of Status Awards (Platinum, Gold, Silver, and Bronze) and Exemplary Awards. “Chapters that receive these awards have demonstrated growth, sustenance, and innovation within their chapter activities,” Ms. Kroll said.
For 2020, the Houston Chapter received the Outstanding Chapter of the Year Award, the Hampton Roads (Va.) Chapter received the Resiliency Award, and Amith Skandhan, MD, SFHM, of the Wiregrass Chapter in Alabama, received the Most Engaged Chapter Leader Award.
“SHM members are assigned to a chapter based on their geographical location and are provided opportunities for education and networking through in-person and virtual events, volunteering in a chapter leadership position, and connecting with local hospitalists through the chapter’s community in HMX, SHM’s online engagement platform,” Ms. Kroll said.
The Houston Chapter received the Outstanding Chapter of the Year Award because it “exemplified high performance during 2020,” Ms. Kroll said. “During a particularly challenging year for everyone, the chapter was able to rethink how they could make the largest impact for members and expand their audience with the use of virtual meetings, provide incentives for participants, and expand their leadership team.”
“The Houston Chapter has been successful in establishing a Houston-wide Resident Interest Group to better involve and provide SHM resources to the residents within the four local internal medicine residency programs who are interested in hospital medicine,” Ms. Kroll said. “Additionally, the chapter created its first curriculum to assist residents in knowing more about hospital medicine and how to approach the job search. The Houston Chapter has provided sources of support, both emotionally and professionally, and incorporated comedians and musicians into their web meetings to provide a much-needed break from medical content.”
The Resiliency Award is a new SHM award category that goes to one chapter that has gone “above and beyond” to showcase their ability to withstand and rise above hardships, as well as to successfully adapt and position the chapter for long term sustainability and success, according to Ms. Kroll. “The Hampton Roads Chapter received this award for the 2020 year. Some of the chapter’s accomplishments included initiating a provider well-being series.”
Ms. Kroll noted that the Hampton Roads Chapter thrived by trying new approaches and ideas to bring hospitalists together across a wide region, such as by utilizing the virtual format to provide more specialized outreach to providers and recognize hospitalists’ contributions to the broader community.
The Most Engaged Chapter Leader Award was given to Alabama-based hospitalist Dr. Skandhan, who “has demonstrated how he goes above and beyond to grow and sustain the Wiregrass Chapter of SHM and continues to carry out the SHM mission,” Ms. Kroll said.
Dr. Skandhan’s accomplishments in 2020 include inviting four Alabama state representatives and three Alabama state senators to participate in a case discussion with Wiregrass Chapter leaders; creating and moderating a weekly check-in platform for the Alabama state hospital-medicine program directors’ forum through the Wiregrass Chapter – a project that enabled him to encourage the sharing of information between hospital medicine program directors; and working with the other Wiregrass Chapter leaders to launch a poster competition on Twitter with more than 80 posters presented.
Hampton Roads Chapter embraces virtual connections
“I believe chapters are one of the best answers to the question: ‘What’s the value of joining SHM?’” Thomas Miller, MD, FHM, leader of the Hampton Roads Chapter, said in an interview.
“Sharing ideas and experiences with other hospitalist teams in a region, coordinating efforts to improve care, and the personal connection with others in your field are very important for hospitalists,” he emphasized. “Chapters are uniquely positioned to do just that. Recognizing individual chapters is a great way to highlight these benefits and to promote new ideas – which other chapters can incorporate into their future plans.”
The Hampton Roads Chapter demonstrated its resilience in many ways during the challenging year of 2020, Dr. Miller said.
“We love our in-person meetings,” he emphasized. “When 2020 took that away from us, we tried to make the most of the situation by embracing the reduced overhead of the virtual format to offer more specialized outreach programs, such as ‘Cultural Context Matters: How Race and Culture Impact Health Outcomes’ and ‘Critical Care: Impact of Immigration Policy on U.S. Healthcare.’ ” The critical care and immigration program “was a great outreach to our many international physicians who have faced special struggles during COVID; it not only highlighted these issues to other hospitalists, but to the broader community, since it was a joint meeting with our local World Affairs Council,” he added.
Dr. Miller also was impressed with the resilience of other chapter members, “such as our vice president, Dr. Gwen Williams, who put together a provider well-being series, ‘Hospitalist Well Being & Support in Times of Crisis.’ ” He expressed further appreciation for the multiple chapter members who supported the chapter’s virtual resident abstract/poster competition.
“Despite the limitations imposed by 2020, we have used unique approaches that have held together a strong core group while broadening outreach to new providers in our region through programs like those described,” said Dr. Miller. “At the same time, we have promoted hospital medicine to the broader community through a joint program, increased social media presence, and achieved cover articles in Hampton Roads Physician about hospital medicine and a ‘Heroes of COVID’ story featuring chapter members. We also continued our effort to add value by providing ready access to the newly state-mandated CME with ‘Opiate Prescribing in the 21st Century.’
“In a time when even family and close friends struggled to maintain connection, we found ways to offer that to our hospitalist teams, at the same time experimenting with new tools that we can put to use long after COVID is gone,” Dr. Miller added.
Houston Chapter supports residents, provides levity
“As a medical community, we hope that the award recognition brings more attention to the issues for which our chapter advocates,” Jeffrey W. Chen, MD, of the Houston Chapter and a hospitalist at Memorial Hermann Hospital Texas Medical Center, said in an interview.
“We hope that it encourages more residents to pursue hospital medicine, and encourages early career hospitalists to get plugged in to the incredible opportunities our chapter offers,” he said. “We are so incredibly honored that the Society of Hospital Medicine has recognized the decade of work that has gone on to get to where we are now. We started with one officer, and we have worked so hard to grow and expand over the years so we can help support our fellow hospitalists across the city and state.
“We are excited about what our chapter has been able to achieve,” said Dr. Chen. “We united the four internal medicine residencies around Houston and created a Houston-wide Hospitalist Interest Group to support residents, providing them the resources they need to be successful in pursuing a career in hospital medicine. We also are proud of the support we provided this year to our early career hospitalists, helping them navigate the transitions and stay up to date in topics relevant to hospital medicine. We held our biggest abstract competition yet, and held a virtual research showcase to celebrate the incredible clinical advancements still happening during the midst of the pandemic.
“It was certainly a tough and challenging year for all chapters, but despite us not being able to hold the in-person dinners that our members love so much, we were proud that we were able to have such a big year,” said Dr. Chen. “We were thankful for the physicians who led our COVID-19 talks, which provided an opportunity for hospitalists across Houston to collaborate and share ideas on which treatments and therapies were working well for their patients. During such a difficult year, we also hosted our first wellness events, including a comedian and band to bring some light during tough times.”
Strong leader propels team efforts
“The Chapter Exemplary Awards Program is important because it encourages higher performance while increasing membership engagement and retaining talent,” said Dr. Skandhan, of Southeast Health Medical Center in Dothan, Ala., and winner of the Most Engaged Chapter Leader award. “Being recognized as the most engaged chapter leader is an honor, especially given the national and international presence of SHM.
“Success is achieved through the help and support of your peers and mentors, and I am fortunate to have found them through this organization,” said Dr. Skandhan. “This award brings attention to the fantastic work done by the engaged membership and leadership of the Wiregrass Chapter. This recognition makes me proud to be part of a team that prides itself on improving the quality health and wellbeing of the patients, providers, and public through innovation and collaboration; this is a testament to their work.”
Dr. Skandhan’s activities as a chapter leader included visiting health care facilities in the rural Southeastern United States. “I slowly began to learn how small towns and their economies tied into a health system, how invested the health care providers were towards their communities, and how health care disparities existed between the rural and urban populations,” he explained. “When the COVID-19 pandemic hit, I worried about these hospitals and their providers. COVID-19 was a new disease with limited understanding of the virus, treatment options, and prevention protocols.” To help smaller hospitals, the Wiregrass Chapter created a weekly check-in for hospital medicine program directors in the state of Alabama, he said.
“We would start the meeting with each participant reporting the total number of cases, ventilator usage, COVID-19 deaths, and one policy change they did that week to address a pressing issue,” Dr. Skandhan said. “Over time the meetings helped address common challenges and were a source of physician well-being.”
In addition, Dr. Skandhan and his chapter colleagues were concerned that academics were taking a back seat to the pandemic, so they rose to the challenge by designing a Twitter-based poster competition using judges from across the country. “This project was led by one of our chapter leaders, Dr. Arash Velayati of Southeast Health Medical Center,” said Dr. Skandhan. The contest included 82 posters, and the participants were able to showcase their work to a large, virtual audience.
Dr. Skandhan and colleagues also decided to partner with religious leaders in their community to help combat the spread of misinformation about COVID-19. “We teamed with the Southern Alabama Baptist Association and Interfaith Council to educate these religious leaders on the issues around COVID-19,” and addressed topics including masking and social distancing, and provided resources for religious leaders to tackle misinformation in their communities, he said.
“As chapter leaders, we need to learn to think outside the box,” Dr. Skandhan emphasized. “We can affect health care quality when we strive to solve more significant problems by bringing people together, brainstorming, and collaborating. SHM and chapter-level engagement provide us with that opportunity.“Hospitalists are often affected by the downstream effects of limited preventive care addressing chronic illnesses. Therefore, we have to strive to see the bigger picture. As we make changes at our local institutions and chapter levels, we will start seeing the improvement we hope to see in the care of our patients and our communities.”
PHM 2021: Achieving gender equity in medicine
PHM 2021 session
Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion
Presenter
Julie Silver, MD
Session summary
Gender inequity in medicine has been well documented and further highlighted by the tremendous impact of the COVID-19 pandemic on women in medicine. While more women than men are entering medical schools across the U.S., women still struggle to reach the highest levels of academic rank, achieve leadership positions of power and influence, receive fair equitable pay, attain leadership roles in national societies, and receive funding from national agencies. They also continue to face discrimination and implicit and explicit biases. Women of color or from other minority backgrounds face even greater barriers and biases. Despite being a specialty in which women represent almost 70% of the workforce, pediatrics is not immune to these disparities.
In her PHM21 plenary on Aug. 3, 2021, Dr. Julie Silver, a national expert in gender equity disparities, detailed the landscape for women in medicine and proposed some solutions to accelerate systemic change for gender equity. In order to understand and mitigate gender inequity, Dr. Silver encouraged the PHM community to identify influential “gatekeepers” of promotion, advancement, and salary compensation. In academic medicine medical schools, funding agencies, professional societies, and journals are the gatekeepers to advancement and compensation for women. Women are traditionally underrepresented as members and influential leaders of these gatekeeping organizations and in their recognition structures, therefore their advancement, compensation, and wellbeing are hindered.
Key takeaways
- Critical mass theory will not help alleviate gender inequity in medicine, as women make up a critical mass in pediatrics and are still experiencing stark inequities. Critical actor leaders are needed to highlight disparities and drive change even once a critical mass is reached.
- Our current diversity, equity, and inclusion (DEI) efforts are ineffective and are creating an “illusion of fairness that causes majority group members to become less sensitive to recognizing discrimination against minorities.” Many of the activities that are considered citizenship, including committees focused on DEI efforts, should be counted as scholarship, and appropriately compensated to ensure promotion of our women and minority colleagues.
- Male allies are critical to documenting, disseminating, and addressing gender inequality. Without the support of men in the field, we will see little progress.
- While there are numerous advocacy angles we can take when advocating for gender equity, the most effective will be the financial angle. Gender pay gaps at the start of a career can lead to roughly 2 million dollars of salary loss for a woman over the course of her career. In order to alleviate those salary pay gaps our institutions must not expect women to negotiate for fair pay, make salary benchmarks transparent, continue to monitor and conduct research on compensation disparities, and attempt to alleviate the weight of educational debt.
- COVID-19 is causing immense stress on women in medicine, and the impact could be disastrous. We must recognize and reward the “4th shift” women are working for COVID-19–related activities at home and at work, and put measures in place to #GiveHerAReasonToStay in health care.
- Men and other women leaders have a responsibility to sponsor the many and well-qualified women in medicine for awards, committees, and speaking engagements. These opportunities are key markers of success in academic medicine and are critical to advancement and salary compensation.
Dr. Casillas is the internal medicine-pediatric chief resident for the University of Cincinnati/Cincinnati Children’s Internal Medicine-Pediatric program. His career goal is to serve as a hospitalist for children and adults, and he is interested in health equity and Latinx health. Dr. O’Toole is a pediatric and adult hospitalist at Cincinnati Children’s Hospital Medical Center and University of Cincinnati Medical Center, and a professor of pediatrics and internal medicine at the University of Cincinnati College of Medicine. She serves as program director of Cincinnati’s Combined Internal Medicine and Pediatrics Residency Program.
PHM 2021 session
Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion
Presenter
Julie Silver, MD
Session summary
Gender inequity in medicine has been well documented and further highlighted by the tremendous impact of the COVID-19 pandemic on women in medicine. While more women than men are entering medical schools across the U.S., women still struggle to reach the highest levels of academic rank, achieve leadership positions of power and influence, receive fair equitable pay, attain leadership roles in national societies, and receive funding from national agencies. They also continue to face discrimination and implicit and explicit biases. Women of color or from other minority backgrounds face even greater barriers and biases. Despite being a specialty in which women represent almost 70% of the workforce, pediatrics is not immune to these disparities.
In her PHM21 plenary on Aug. 3, 2021, Dr. Julie Silver, a national expert in gender equity disparities, detailed the landscape for women in medicine and proposed some solutions to accelerate systemic change for gender equity. In order to understand and mitigate gender inequity, Dr. Silver encouraged the PHM community to identify influential “gatekeepers” of promotion, advancement, and salary compensation. In academic medicine medical schools, funding agencies, professional societies, and journals are the gatekeepers to advancement and compensation for women. Women are traditionally underrepresented as members and influential leaders of these gatekeeping organizations and in their recognition structures, therefore their advancement, compensation, and wellbeing are hindered.
Key takeaways
- Critical mass theory will not help alleviate gender inequity in medicine, as women make up a critical mass in pediatrics and are still experiencing stark inequities. Critical actor leaders are needed to highlight disparities and drive change even once a critical mass is reached.
- Our current diversity, equity, and inclusion (DEI) efforts are ineffective and are creating an “illusion of fairness that causes majority group members to become less sensitive to recognizing discrimination against minorities.” Many of the activities that are considered citizenship, including committees focused on DEI efforts, should be counted as scholarship, and appropriately compensated to ensure promotion of our women and minority colleagues.
- Male allies are critical to documenting, disseminating, and addressing gender inequality. Without the support of men in the field, we will see little progress.
- While there are numerous advocacy angles we can take when advocating for gender equity, the most effective will be the financial angle. Gender pay gaps at the start of a career can lead to roughly 2 million dollars of salary loss for a woman over the course of her career. In order to alleviate those salary pay gaps our institutions must not expect women to negotiate for fair pay, make salary benchmarks transparent, continue to monitor and conduct research on compensation disparities, and attempt to alleviate the weight of educational debt.
- COVID-19 is causing immense stress on women in medicine, and the impact could be disastrous. We must recognize and reward the “4th shift” women are working for COVID-19–related activities at home and at work, and put measures in place to #GiveHerAReasonToStay in health care.
- Men and other women leaders have a responsibility to sponsor the many and well-qualified women in medicine for awards, committees, and speaking engagements. These opportunities are key markers of success in academic medicine and are critical to advancement and salary compensation.
Dr. Casillas is the internal medicine-pediatric chief resident for the University of Cincinnati/Cincinnati Children’s Internal Medicine-Pediatric program. His career goal is to serve as a hospitalist for children and adults, and he is interested in health equity and Latinx health. Dr. O’Toole is a pediatric and adult hospitalist at Cincinnati Children’s Hospital Medical Center and University of Cincinnati Medical Center, and a professor of pediatrics and internal medicine at the University of Cincinnati College of Medicine. She serves as program director of Cincinnati’s Combined Internal Medicine and Pediatrics Residency Program.
PHM 2021 session
Accelerating Patient Care and Healthcare Workforce Diversity and Inclusion
Presenter
Julie Silver, MD
Session summary
Gender inequity in medicine has been well documented and further highlighted by the tremendous impact of the COVID-19 pandemic on women in medicine. While more women than men are entering medical schools across the U.S., women still struggle to reach the highest levels of academic rank, achieve leadership positions of power and influence, receive fair equitable pay, attain leadership roles in national societies, and receive funding from national agencies. They also continue to face discrimination and implicit and explicit biases. Women of color or from other minority backgrounds face even greater barriers and biases. Despite being a specialty in which women represent almost 70% of the workforce, pediatrics is not immune to these disparities.
In her PHM21 plenary on Aug. 3, 2021, Dr. Julie Silver, a national expert in gender equity disparities, detailed the landscape for women in medicine and proposed some solutions to accelerate systemic change for gender equity. In order to understand and mitigate gender inequity, Dr. Silver encouraged the PHM community to identify influential “gatekeepers” of promotion, advancement, and salary compensation. In academic medicine medical schools, funding agencies, professional societies, and journals are the gatekeepers to advancement and compensation for women. Women are traditionally underrepresented as members and influential leaders of these gatekeeping organizations and in their recognition structures, therefore their advancement, compensation, and wellbeing are hindered.
Key takeaways
- Critical mass theory will not help alleviate gender inequity in medicine, as women make up a critical mass in pediatrics and are still experiencing stark inequities. Critical actor leaders are needed to highlight disparities and drive change even once a critical mass is reached.
- Our current diversity, equity, and inclusion (DEI) efforts are ineffective and are creating an “illusion of fairness that causes majority group members to become less sensitive to recognizing discrimination against minorities.” Many of the activities that are considered citizenship, including committees focused on DEI efforts, should be counted as scholarship, and appropriately compensated to ensure promotion of our women and minority colleagues.
- Male allies are critical to documenting, disseminating, and addressing gender inequality. Without the support of men in the field, we will see little progress.
- While there are numerous advocacy angles we can take when advocating for gender equity, the most effective will be the financial angle. Gender pay gaps at the start of a career can lead to roughly 2 million dollars of salary loss for a woman over the course of her career. In order to alleviate those salary pay gaps our institutions must not expect women to negotiate for fair pay, make salary benchmarks transparent, continue to monitor and conduct research on compensation disparities, and attempt to alleviate the weight of educational debt.
- COVID-19 is causing immense stress on women in medicine, and the impact could be disastrous. We must recognize and reward the “4th shift” women are working for COVID-19–related activities at home and at work, and put measures in place to #GiveHerAReasonToStay in health care.
- Men and other women leaders have a responsibility to sponsor the many and well-qualified women in medicine for awards, committees, and speaking engagements. These opportunities are key markers of success in academic medicine and are critical to advancement and salary compensation.
Dr. Casillas is the internal medicine-pediatric chief resident for the University of Cincinnati/Cincinnati Children’s Internal Medicine-Pediatric program. His career goal is to serve as a hospitalist for children and adults, and he is interested in health equity and Latinx health. Dr. O’Toole is a pediatric and adult hospitalist at Cincinnati Children’s Hospital Medical Center and University of Cincinnati Medical Center, and a professor of pediatrics and internal medicine at the University of Cincinnati College of Medicine. She serves as program director of Cincinnati’s Combined Internal Medicine and Pediatrics Residency Program.
Health care workers eager for COVID booster shots
As COVID vaccine boosters move closer to reality, most physicians and nurses are ready and willing to get another shot in the arm, according to a new Medscape survey.
Altogether, 93% of physicians and 87% of nurses/advanced practice nurses (APNs) said they wanted to get a booster, although the timing of when they wanted the shots differed somewhat between the two groups surveyed Aug. 4-15.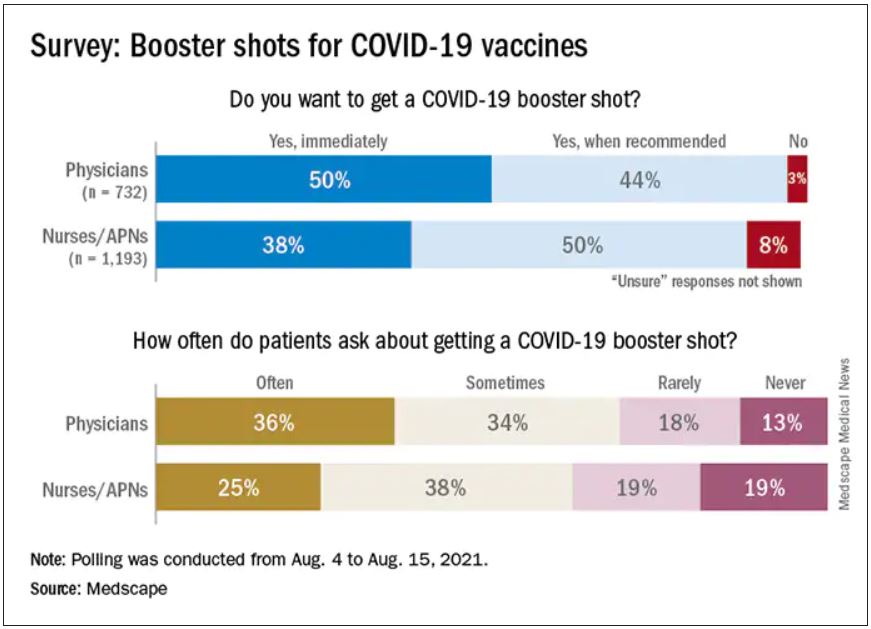
Among the 732 physicians polled, 50% wanted to get their shot immediately, compared with 38% of the 1,193 nurses/APNs who responded, while 44% of physicians and 50% of nurses/APNs said that they would wait until the vaccine booster was authorized and recommended.
At this point in time, almost all of the health care workers surveyed – 98% of physicians and 94% of nurses/APNs – have been fully vaccinated against COVID-19. A small proportion of each group, however, received the Johnson & Johnson vaccine (1% of physicians and 3% of nurses) and are not included in the current plan for booster shots.
The Medscape survey sample did include one group that is already eligible for a third dose: About 20% of physicians and 26% of nurses/ANPs said they have a condition or take a medication that compromises their immune system.
Respondents’ experiences with patient requests for boosters suggest a somewhat lower level of interest. About two-thirds of the health care workers (69% of physicians and 63% of nurses) said that patients frequently or sometimes asked about COVID boosters, compared with 13% (physicians) and 19% (nurses) who said their patients had never asked.
Interest lower among general population
In a separate survey conducted by WebMD, 82% of those who have been at least partially vaccinated said they want to get a COVID vaccine booster (14% immediately and 68% after authorization and recommendation). Of the remaining vaccinees, 7% said they do not want to get a booster and 11% were unsure.
The full sample of 592 respondents surveyed Aug. 5-10, however, included 19% who do not plan to get vaccinated and 6% who are planning to be vaccinated but have not yet done so.
The proportion of immunocompromised individuals in the two survey groups was similar, with about 25% of those in the WebMD survey reporting they have a condition or take a medication that compromises their immune system. Those respondents were more than twice as likely to want to get a booster immediately, compared to those with an uncompromised immune system (24% vs. 11%).
The distribution of vaccines received by brand was also comparable between the two groups surveyed. Of health care workers and readers, over half of each group received the Pfizer/BioNTech vaccine (59% vs. 54%), followed by Moderna (38% vs. 40%) and Johnson & Johnson (3% vs. 5%).
A version of this article first appeared on Medscape.com.
As COVID vaccine boosters move closer to reality, most physicians and nurses are ready and willing to get another shot in the arm, according to a new Medscape survey.
Altogether, 93% of physicians and 87% of nurses/advanced practice nurses (APNs) said they wanted to get a booster, although the timing of when they wanted the shots differed somewhat between the two groups surveyed Aug. 4-15.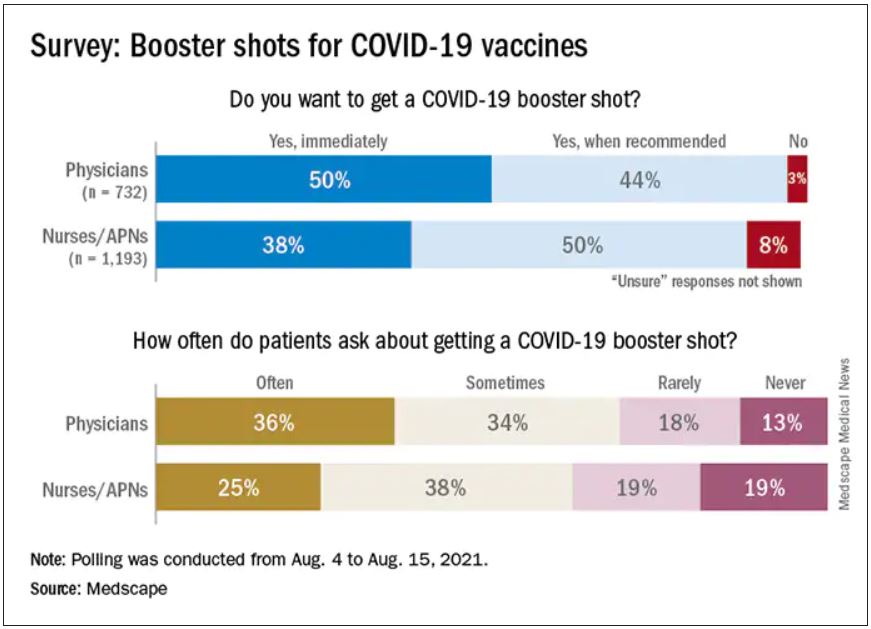
Among the 732 physicians polled, 50% wanted to get their shot immediately, compared with 38% of the 1,193 nurses/APNs who responded, while 44% of physicians and 50% of nurses/APNs said that they would wait until the vaccine booster was authorized and recommended.
At this point in time, almost all of the health care workers surveyed – 98% of physicians and 94% of nurses/APNs – have been fully vaccinated against COVID-19. A small proportion of each group, however, received the Johnson & Johnson vaccine (1% of physicians and 3% of nurses) and are not included in the current plan for booster shots.
The Medscape survey sample did include one group that is already eligible for a third dose: About 20% of physicians and 26% of nurses/ANPs said they have a condition or take a medication that compromises their immune system.
Respondents’ experiences with patient requests for boosters suggest a somewhat lower level of interest. About two-thirds of the health care workers (69% of physicians and 63% of nurses) said that patients frequently or sometimes asked about COVID boosters, compared with 13% (physicians) and 19% (nurses) who said their patients had never asked.
Interest lower among general population
In a separate survey conducted by WebMD, 82% of those who have been at least partially vaccinated said they want to get a COVID vaccine booster (14% immediately and 68% after authorization and recommendation). Of the remaining vaccinees, 7% said they do not want to get a booster and 11% were unsure.
The full sample of 592 respondents surveyed Aug. 5-10, however, included 19% who do not plan to get vaccinated and 6% who are planning to be vaccinated but have not yet done so.
The proportion of immunocompromised individuals in the two survey groups was similar, with about 25% of those in the WebMD survey reporting they have a condition or take a medication that compromises their immune system. Those respondents were more than twice as likely to want to get a booster immediately, compared to those with an uncompromised immune system (24% vs. 11%).
The distribution of vaccines received by brand was also comparable between the two groups surveyed. Of health care workers and readers, over half of each group received the Pfizer/BioNTech vaccine (59% vs. 54%), followed by Moderna (38% vs. 40%) and Johnson & Johnson (3% vs. 5%).
A version of this article first appeared on Medscape.com.
As COVID vaccine boosters move closer to reality, most physicians and nurses are ready and willing to get another shot in the arm, according to a new Medscape survey.
Altogether, 93% of physicians and 87% of nurses/advanced practice nurses (APNs) said they wanted to get a booster, although the timing of when they wanted the shots differed somewhat between the two groups surveyed Aug. 4-15.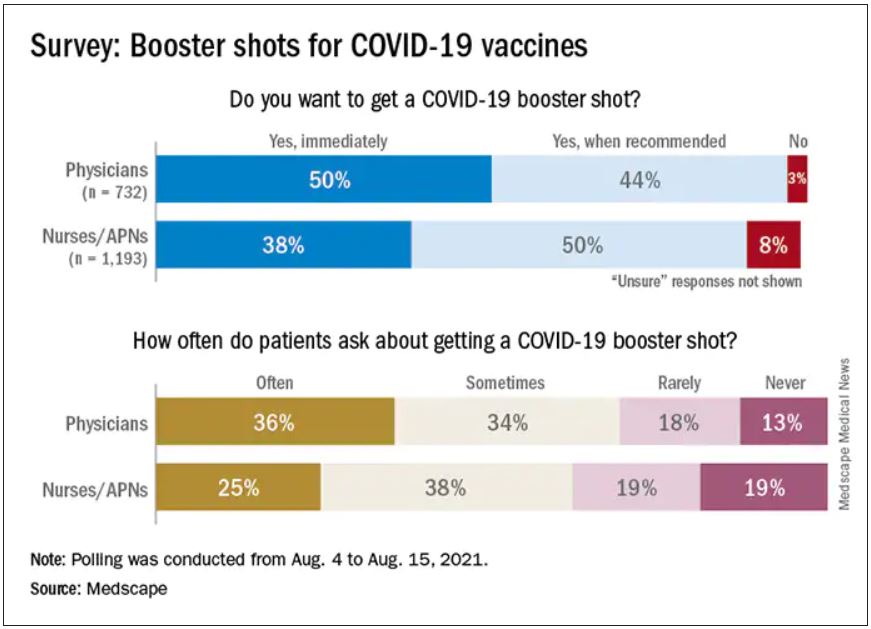
Among the 732 physicians polled, 50% wanted to get their shot immediately, compared with 38% of the 1,193 nurses/APNs who responded, while 44% of physicians and 50% of nurses/APNs said that they would wait until the vaccine booster was authorized and recommended.
At this point in time, almost all of the health care workers surveyed – 98% of physicians and 94% of nurses/APNs – have been fully vaccinated against COVID-19. A small proportion of each group, however, received the Johnson & Johnson vaccine (1% of physicians and 3% of nurses) and are not included in the current plan for booster shots.
The Medscape survey sample did include one group that is already eligible for a third dose: About 20% of physicians and 26% of nurses/ANPs said they have a condition or take a medication that compromises their immune system.
Respondents’ experiences with patient requests for boosters suggest a somewhat lower level of interest. About two-thirds of the health care workers (69% of physicians and 63% of nurses) said that patients frequently or sometimes asked about COVID boosters, compared with 13% (physicians) and 19% (nurses) who said their patients had never asked.
Interest lower among general population
In a separate survey conducted by WebMD, 82% of those who have been at least partially vaccinated said they want to get a COVID vaccine booster (14% immediately and 68% after authorization and recommendation). Of the remaining vaccinees, 7% said they do not want to get a booster and 11% were unsure.
The full sample of 592 respondents surveyed Aug. 5-10, however, included 19% who do not plan to get vaccinated and 6% who are planning to be vaccinated but have not yet done so.
The proportion of immunocompromised individuals in the two survey groups was similar, with about 25% of those in the WebMD survey reporting they have a condition or take a medication that compromises their immune system. Those respondents were more than twice as likely to want to get a booster immediately, compared to those with an uncompromised immune system (24% vs. 11%).
The distribution of vaccines received by brand was also comparable between the two groups surveyed. Of health care workers and readers, over half of each group received the Pfizer/BioNTech vaccine (59% vs. 54%), followed by Moderna (38% vs. 40%) and Johnson & Johnson (3% vs. 5%).
A version of this article first appeared on Medscape.com.
Weathering this storm and the next
Perspectives on disaster preparedness amid COVID-19
The COVID-19 pandemic has tested disaster preparedness in hospitals across the nation. The pandemic brought many unique disaster planning challenges not commonly seen with other emergencies disasters. These included an uncertain and prolonged time frame, the implementation of physical distancing, and the challenges of preserving the health care work force.
But how do we prepare for the next disaster when the health care system and staff are already stretched thin? Here, we discuss the concept of maintaining a state of preparedness through and beyond COVID-19, using a disaster preparedness cycle – including continuous assessments of vulnerabilities, dynamic staffing adjustments to support patient and hospital needs, and broadening of the pandemic response to incorporate planning for the next disaster.
Disaster preparedness and assessing ongoing needs
Disaster preparedness cycle and Hazard Vulnerability Assessment
The disaster preparedness cycle illustrates that disaster preparedness is continuous. Disaster preparedness is achieved with the non-stop cycle of planning, coordinating, and recognizing vulnerable areas.1-5 Hazard vulnerability analysis (HVA) can play a critical role in recognizing areas in which a hospital system has strengths and weaknesses for different disaster scenarios. There are several tools available, but the overarching goal is to provide an objective and systematic approach to evaluate the potential damage and impact a disaster could have on the health care system and surrounding community.
The HVA can also be utilized to reassess system or personnel vulnerabilities that may have been exposed or highlighted during the pandemic.6,7 These vulnerabilities must be addressed during preparations for the next disaster while concurrently “assuming the incident happens at the worst possible time.”7
Disaster preparedness staffing considerations
Management, communication, and staffing issues are critical to disaster response. Key leadership responses during COVID-19 included providing frequent and transparent communication, down-staffing for physical distancing during low census, and prioritizing staff well-being. These measures serve as a strong foundation moving into preparations for the next disaster.8
To ensure adequate staffing during an unexpected natural disaster, we recommend creating “ride-out” and “relief teams” as part of disaster staffing preparedness.9,10 The ride-out team provides the initial care and these providers are expected to stay in the hospital during the primary impact of the event. Once the initial threat of disaster is over and it is deemed safe to travel, the relief team is activated and offers reprieve to the ride-out team. Leaders and backup leaders within these teams should be identified in the event teams are activated. These assignments should be made at the start of the year and updated yearly or more frequently, if needed.
While the COVID-19 pandemic did not significantly affect children, our ride-out and relief teams would have played a significant role in case a surge of pediatric cases had occurred.
Other considerations for disaster staffing include expanding backup coverage and for multisite groups, identifying site leads to help field specific questions or concerns. Lastly, understanding the staffing needs of the hospital during a disaster is vital – bidirectional communication between physicians and hospital leadership optimizes preparedness plans. These measures will help staff feel supported before, during, and after a disaster.
Dynamic disaster response
Supporting patient and hospital needs
The next step in the disaster preparedness cycle is adjusting to changing needs during the disaster. The pediatric inpatient population was less affected initially by COVID-19, allowing hospitalists to support the unpredicted needs of the pandemic. A dynamic and flexible physician response is important to disaster preparedness.
As there has been a continued shift to telehealth during the pandemic, our group has engaged in telehealth calls related to COVID-19. Seizing these new opportunities not only provided additional services to our patients, but also strengthened community support, physician worth, and the hospital’s financial state. This is also an opportunity for higher-risk clinicians or quarantined faculty to offer patient care during the pandemic.
Cram et al. describe the importance of “unspecializing” during the COVID-19 pandemic.11 Starting discussions early with adult and pediatric critical care colleagues is vital. Hospitalists take care of a broad patient population, and therefore, can adapt to where the clinical need may be. Optimizing and expanding our skill sets can bring value to the hospital system during uncertain times.
Hospitalists are also instrumental for patient flow during the pandemic. To address this, our group partnered with hospital leadership from many different areas including administration, nursing, emergency medicine, critical care, and ancillary services. By collaborating as one cohesive hospital unit, we were able to efficiently develop, implement, and update best clinical care guidelines and algorithms for COVID-19–related topics such as testing indications, admission criteria, infection control, and proper personal protective equipment use. Lastly, working with specialists to consolidate teams during a pandemic presents an opportunity for hospitalists to highlight expertise while bringing value to the hospital.
Unique staffing situations related to COVID-19
Different from other disasters, the COVID-19 pandemic affected older or immunocompromised staff in a unique way. Beauhaus et al. note that 20% of the physician workforce in the United Sates is between 55 and 64 years of age, and 9% are 65 years and older.12 Hospitalist groups should focus on how to optimize and preserve their workforce, specifically those that are higher risk due to age or other health conditions.
We used a tiered guide to safely accommodate our physicians that were determined to be at higher-risk for complications of COVID-19; these recommendations included limiting exposure to patients with acute respiratory illnesses and shifting some providers to a different clinical environments with a lower exposure risk, such as telemedicine visits.
Other COVID-19 preparedness considerations that affected our group in particular include the changes in learner staffing. Similar to attending down-staffing to encourage physical distancing during low census, learners (residents, medical students, and physician assistant students) also experienced decreased hours or suspension of rotations. To maintain optimal patient care, adjusting to changing disaster needs may include assessing attendings’ capacity to assume responsibilities typically supported by learners.
Due to the ongoing nature of the pandemic, we have had to maintain a dynamic response while adjusting to changing and ongoing needs during recovery. Creating a measured and staggered approach helps facilitate a smooth transition back to nonemergent activities. The education of learners, academic and scholarly work, and administrative duties will resume, but likely in a different steady state. Also, awareness of physician burnout and fatigue is critical as an institution enters a phase of recovery.
Preparing for the next disaster during the pandemic
This brings us back to the beginning of the disaster preparedness cycle and the need to plan for the next disaster. Current disaster preparedness plans among physician groups and hospitals are likely focused on an individual disaster scenario, but adjusting current disaster plans to account for the uncertain time frame of an event like the COVID-19 pandemic is critical. Several articles in the national news posed similar questions, although these publications focused mainly on the Federal Emergency Management Agency and the governmental response to prepare for the next disaster when resources are already stretched.13-15
How do we adequately plan, maintain a dynamic response, and continue to efficiently move through the disaster staffing cycle during an event like the COVID-19 pandemic? Being aware of current vulnerabilities and addressing gaps at the department and hospital level are vital to disaster preparedness. For example, we reassessed disaster (ride-out/relief) teams and the minimum number of staff needed to maintain safe and quality care, and what in-house arrangements would be needed (food, supplies, sleeping arrangements) while having to maintain physical distance.
Newman et al. explain “in disaster planning, having as many physicians as possible on hand may seem like an advantage, but being overstaffed in tight quarters was almost as bad as being understaffed.”9 This has been particularly true during the COVID-19 pandemic. It is crucial to have backup plans for faculty that are unable to serve ride-out duties from unexpected issues – such as availability, illnesses/quarantines, childcare/dependents. Also, it is important to be aware that some supply chains are already strained because of the pandemic and how this may play a role in the availability of certain supplies. Being aware and proactive about specific constraints allows for a better level of preparedness. Continued collaboration and communication with other services to provide care should be ongoing throughout the disaster preparedness cycle.
Conclusion
Providing and maintaining optimal and safe patient care should be the overarching goal throughout disaster preparedness. Being aware of group and institutional vulnerabilities, collaboration with hospital leadership, and remaining flexible as hospitalists are critical components for successful preparedness amid disasters. A dynamic and responsive disaster plan has been vital amid COVID-19, and for the next disasters we will certainly encounter.
Dr. Hadvani is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Uremovich is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Quinonez is associate professor of pediatrics and chief of pediatric hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Lopez is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Mothner is associate professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital and is the pediatric hospital medicine medical director for the main campus.
References
1. Malilay J et al. The role of applied epidemiology methods in the disaster management cycle. Am J Public Health. 2014;104(11):2092-102. doi: 10.2105/AJPH.2014.302010.
2. Federal Emergency Management Agency. Developing and maintaining emergency operations plans. 2010 Nov.
3. Federal Emergency Management Agency. National preparedness system. 2020 Jul 31.
4. Federal Emergency Management Agency. National preparedness goal. 2011 Sep.
5. Environmental health in emergencies and disasters: A practical guide. World Health Organization, Geneva. 2002:9-24. Edited by B. Wisner and J. Adams.
6. U.S. Department of Health and Human Services. Topic collection: Hazard vulnerability/risk assessment.
7. Hospital Association of Southern California. Hazard and vulnerability analysis.
8. Meier K et al. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020 May;15(5):308-10. doi: 10.12788/jhm.3435.
9. Newman B and Gallion C. Hurricane Harvey: Firsthand preparedness in graduate medical education. Acad Med. 2019 Sep;94(9):1267-69. doi: 10.1097/ACM.0000000000002696.
10. Brevard S et al. Analysis of disaster response plans and the aftermath of Hurricane Katrina: Lessons learned from a level I trauma center. J Trauma. 2008 Nov;65(5):1126-32. doi: 10.1097/TA.0b013e318188d6e5.
11. Cram P et al. All hands on deck learning to “un-specialize” in the COVID-19 pandemic. J Hosp Med. 2020 May;15(5):314-5. doi: 10.12788/jhm.3426.
12. Buerhaus P et al. Older clinicians and the surge in novel coronavirus disease 2019 (COVID-19). JAMA. 2020 May 12;323(18):1777-8. doi: 10.1001/jama.2020.4978.
13. VOX Media. Imagine Hurricane Katrina during a pandemic. The US needs to prepare for that – now. 2020 May 27.
14. The Hill. Democratic lawmakers ask how FEMA is planning to balance natural disasters, COVID-19 response. 2020 Apr 20.
15. The Atlantic. What happens if a ‘big one’ strikes during the pandemic? 2020 May 9.
Perspectives on disaster preparedness amid COVID-19
Perspectives on disaster preparedness amid COVID-19
The COVID-19 pandemic has tested disaster preparedness in hospitals across the nation. The pandemic brought many unique disaster planning challenges not commonly seen with other emergencies disasters. These included an uncertain and prolonged time frame, the implementation of physical distancing, and the challenges of preserving the health care work force.
But how do we prepare for the next disaster when the health care system and staff are already stretched thin? Here, we discuss the concept of maintaining a state of preparedness through and beyond COVID-19, using a disaster preparedness cycle – including continuous assessments of vulnerabilities, dynamic staffing adjustments to support patient and hospital needs, and broadening of the pandemic response to incorporate planning for the next disaster.
Disaster preparedness and assessing ongoing needs
Disaster preparedness cycle and Hazard Vulnerability Assessment
The disaster preparedness cycle illustrates that disaster preparedness is continuous. Disaster preparedness is achieved with the non-stop cycle of planning, coordinating, and recognizing vulnerable areas.1-5 Hazard vulnerability analysis (HVA) can play a critical role in recognizing areas in which a hospital system has strengths and weaknesses for different disaster scenarios. There are several tools available, but the overarching goal is to provide an objective and systematic approach to evaluate the potential damage and impact a disaster could have on the health care system and surrounding community.
The HVA can also be utilized to reassess system or personnel vulnerabilities that may have been exposed or highlighted during the pandemic.6,7 These vulnerabilities must be addressed during preparations for the next disaster while concurrently “assuming the incident happens at the worst possible time.”7
Disaster preparedness staffing considerations
Management, communication, and staffing issues are critical to disaster response. Key leadership responses during COVID-19 included providing frequent and transparent communication, down-staffing for physical distancing during low census, and prioritizing staff well-being. These measures serve as a strong foundation moving into preparations for the next disaster.8
To ensure adequate staffing during an unexpected natural disaster, we recommend creating “ride-out” and “relief teams” as part of disaster staffing preparedness.9,10 The ride-out team provides the initial care and these providers are expected to stay in the hospital during the primary impact of the event. Once the initial threat of disaster is over and it is deemed safe to travel, the relief team is activated and offers reprieve to the ride-out team. Leaders and backup leaders within these teams should be identified in the event teams are activated. These assignments should be made at the start of the year and updated yearly or more frequently, if needed.
While the COVID-19 pandemic did not significantly affect children, our ride-out and relief teams would have played a significant role in case a surge of pediatric cases had occurred.
Other considerations for disaster staffing include expanding backup coverage and for multisite groups, identifying site leads to help field specific questions or concerns. Lastly, understanding the staffing needs of the hospital during a disaster is vital – bidirectional communication between physicians and hospital leadership optimizes preparedness plans. These measures will help staff feel supported before, during, and after a disaster.
Dynamic disaster response
Supporting patient and hospital needs
The next step in the disaster preparedness cycle is adjusting to changing needs during the disaster. The pediatric inpatient population was less affected initially by COVID-19, allowing hospitalists to support the unpredicted needs of the pandemic. A dynamic and flexible physician response is important to disaster preparedness.
As there has been a continued shift to telehealth during the pandemic, our group has engaged in telehealth calls related to COVID-19. Seizing these new opportunities not only provided additional services to our patients, but also strengthened community support, physician worth, and the hospital’s financial state. This is also an opportunity for higher-risk clinicians or quarantined faculty to offer patient care during the pandemic.
Cram et al. describe the importance of “unspecializing” during the COVID-19 pandemic.11 Starting discussions early with adult and pediatric critical care colleagues is vital. Hospitalists take care of a broad patient population, and therefore, can adapt to where the clinical need may be. Optimizing and expanding our skill sets can bring value to the hospital system during uncertain times.
Hospitalists are also instrumental for patient flow during the pandemic. To address this, our group partnered with hospital leadership from many different areas including administration, nursing, emergency medicine, critical care, and ancillary services. By collaborating as one cohesive hospital unit, we were able to efficiently develop, implement, and update best clinical care guidelines and algorithms for COVID-19–related topics such as testing indications, admission criteria, infection control, and proper personal protective equipment use. Lastly, working with specialists to consolidate teams during a pandemic presents an opportunity for hospitalists to highlight expertise while bringing value to the hospital.
Unique staffing situations related to COVID-19
Different from other disasters, the COVID-19 pandemic affected older or immunocompromised staff in a unique way. Beauhaus et al. note that 20% of the physician workforce in the United Sates is between 55 and 64 years of age, and 9% are 65 years and older.12 Hospitalist groups should focus on how to optimize and preserve their workforce, specifically those that are higher risk due to age or other health conditions.
We used a tiered guide to safely accommodate our physicians that were determined to be at higher-risk for complications of COVID-19; these recommendations included limiting exposure to patients with acute respiratory illnesses and shifting some providers to a different clinical environments with a lower exposure risk, such as telemedicine visits.
Other COVID-19 preparedness considerations that affected our group in particular include the changes in learner staffing. Similar to attending down-staffing to encourage physical distancing during low census, learners (residents, medical students, and physician assistant students) also experienced decreased hours or suspension of rotations. To maintain optimal patient care, adjusting to changing disaster needs may include assessing attendings’ capacity to assume responsibilities typically supported by learners.
Due to the ongoing nature of the pandemic, we have had to maintain a dynamic response while adjusting to changing and ongoing needs during recovery. Creating a measured and staggered approach helps facilitate a smooth transition back to nonemergent activities. The education of learners, academic and scholarly work, and administrative duties will resume, but likely in a different steady state. Also, awareness of physician burnout and fatigue is critical as an institution enters a phase of recovery.
Preparing for the next disaster during the pandemic
This brings us back to the beginning of the disaster preparedness cycle and the need to plan for the next disaster. Current disaster preparedness plans among physician groups and hospitals are likely focused on an individual disaster scenario, but adjusting current disaster plans to account for the uncertain time frame of an event like the COVID-19 pandemic is critical. Several articles in the national news posed similar questions, although these publications focused mainly on the Federal Emergency Management Agency and the governmental response to prepare for the next disaster when resources are already stretched.13-15
How do we adequately plan, maintain a dynamic response, and continue to efficiently move through the disaster staffing cycle during an event like the COVID-19 pandemic? Being aware of current vulnerabilities and addressing gaps at the department and hospital level are vital to disaster preparedness. For example, we reassessed disaster (ride-out/relief) teams and the minimum number of staff needed to maintain safe and quality care, and what in-house arrangements would be needed (food, supplies, sleeping arrangements) while having to maintain physical distance.
Newman et al. explain “in disaster planning, having as many physicians as possible on hand may seem like an advantage, but being overstaffed in tight quarters was almost as bad as being understaffed.”9 This has been particularly true during the COVID-19 pandemic. It is crucial to have backup plans for faculty that are unable to serve ride-out duties from unexpected issues – such as availability, illnesses/quarantines, childcare/dependents. Also, it is important to be aware that some supply chains are already strained because of the pandemic and how this may play a role in the availability of certain supplies. Being aware and proactive about specific constraints allows for a better level of preparedness. Continued collaboration and communication with other services to provide care should be ongoing throughout the disaster preparedness cycle.
Conclusion
Providing and maintaining optimal and safe patient care should be the overarching goal throughout disaster preparedness. Being aware of group and institutional vulnerabilities, collaboration with hospital leadership, and remaining flexible as hospitalists are critical components for successful preparedness amid disasters. A dynamic and responsive disaster plan has been vital amid COVID-19, and for the next disasters we will certainly encounter.
Dr. Hadvani is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Uremovich is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Quinonez is associate professor of pediatrics and chief of pediatric hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Lopez is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Mothner is associate professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital and is the pediatric hospital medicine medical director for the main campus.
References
1. Malilay J et al. The role of applied epidemiology methods in the disaster management cycle. Am J Public Health. 2014;104(11):2092-102. doi: 10.2105/AJPH.2014.302010.
2. Federal Emergency Management Agency. Developing and maintaining emergency operations plans. 2010 Nov.
3. Federal Emergency Management Agency. National preparedness system. 2020 Jul 31.
4. Federal Emergency Management Agency. National preparedness goal. 2011 Sep.
5. Environmental health in emergencies and disasters: A practical guide. World Health Organization, Geneva. 2002:9-24. Edited by B. Wisner and J. Adams.
6. U.S. Department of Health and Human Services. Topic collection: Hazard vulnerability/risk assessment.
7. Hospital Association of Southern California. Hazard and vulnerability analysis.
8. Meier K et al. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020 May;15(5):308-10. doi: 10.12788/jhm.3435.
9. Newman B and Gallion C. Hurricane Harvey: Firsthand preparedness in graduate medical education. Acad Med. 2019 Sep;94(9):1267-69. doi: 10.1097/ACM.0000000000002696.
10. Brevard S et al. Analysis of disaster response plans and the aftermath of Hurricane Katrina: Lessons learned from a level I trauma center. J Trauma. 2008 Nov;65(5):1126-32. doi: 10.1097/TA.0b013e318188d6e5.
11. Cram P et al. All hands on deck learning to “un-specialize” in the COVID-19 pandemic. J Hosp Med. 2020 May;15(5):314-5. doi: 10.12788/jhm.3426.
12. Buerhaus P et al. Older clinicians and the surge in novel coronavirus disease 2019 (COVID-19). JAMA. 2020 May 12;323(18):1777-8. doi: 10.1001/jama.2020.4978.
13. VOX Media. Imagine Hurricane Katrina during a pandemic. The US needs to prepare for that – now. 2020 May 27.
14. The Hill. Democratic lawmakers ask how FEMA is planning to balance natural disasters, COVID-19 response. 2020 Apr 20.
15. The Atlantic. What happens if a ‘big one’ strikes during the pandemic? 2020 May 9.
The COVID-19 pandemic has tested disaster preparedness in hospitals across the nation. The pandemic brought many unique disaster planning challenges not commonly seen with other emergencies disasters. These included an uncertain and prolonged time frame, the implementation of physical distancing, and the challenges of preserving the health care work force.
But how do we prepare for the next disaster when the health care system and staff are already stretched thin? Here, we discuss the concept of maintaining a state of preparedness through and beyond COVID-19, using a disaster preparedness cycle – including continuous assessments of vulnerabilities, dynamic staffing adjustments to support patient and hospital needs, and broadening of the pandemic response to incorporate planning for the next disaster.
Disaster preparedness and assessing ongoing needs
Disaster preparedness cycle and Hazard Vulnerability Assessment
The disaster preparedness cycle illustrates that disaster preparedness is continuous. Disaster preparedness is achieved with the non-stop cycle of planning, coordinating, and recognizing vulnerable areas.1-5 Hazard vulnerability analysis (HVA) can play a critical role in recognizing areas in which a hospital system has strengths and weaknesses for different disaster scenarios. There are several tools available, but the overarching goal is to provide an objective and systematic approach to evaluate the potential damage and impact a disaster could have on the health care system and surrounding community.
The HVA can also be utilized to reassess system or personnel vulnerabilities that may have been exposed or highlighted during the pandemic.6,7 These vulnerabilities must be addressed during preparations for the next disaster while concurrently “assuming the incident happens at the worst possible time.”7
Disaster preparedness staffing considerations
Management, communication, and staffing issues are critical to disaster response. Key leadership responses during COVID-19 included providing frequent and transparent communication, down-staffing for physical distancing during low census, and prioritizing staff well-being. These measures serve as a strong foundation moving into preparations for the next disaster.8
To ensure adequate staffing during an unexpected natural disaster, we recommend creating “ride-out” and “relief teams” as part of disaster staffing preparedness.9,10 The ride-out team provides the initial care and these providers are expected to stay in the hospital during the primary impact of the event. Once the initial threat of disaster is over and it is deemed safe to travel, the relief team is activated and offers reprieve to the ride-out team. Leaders and backup leaders within these teams should be identified in the event teams are activated. These assignments should be made at the start of the year and updated yearly or more frequently, if needed.
While the COVID-19 pandemic did not significantly affect children, our ride-out and relief teams would have played a significant role in case a surge of pediatric cases had occurred.
Other considerations for disaster staffing include expanding backup coverage and for multisite groups, identifying site leads to help field specific questions or concerns. Lastly, understanding the staffing needs of the hospital during a disaster is vital – bidirectional communication between physicians and hospital leadership optimizes preparedness plans. These measures will help staff feel supported before, during, and after a disaster.
Dynamic disaster response
Supporting patient and hospital needs
The next step in the disaster preparedness cycle is adjusting to changing needs during the disaster. The pediatric inpatient population was less affected initially by COVID-19, allowing hospitalists to support the unpredicted needs of the pandemic. A dynamic and flexible physician response is important to disaster preparedness.
As there has been a continued shift to telehealth during the pandemic, our group has engaged in telehealth calls related to COVID-19. Seizing these new opportunities not only provided additional services to our patients, but also strengthened community support, physician worth, and the hospital’s financial state. This is also an opportunity for higher-risk clinicians or quarantined faculty to offer patient care during the pandemic.
Cram et al. describe the importance of “unspecializing” during the COVID-19 pandemic.11 Starting discussions early with adult and pediatric critical care colleagues is vital. Hospitalists take care of a broad patient population, and therefore, can adapt to where the clinical need may be. Optimizing and expanding our skill sets can bring value to the hospital system during uncertain times.
Hospitalists are also instrumental for patient flow during the pandemic. To address this, our group partnered with hospital leadership from many different areas including administration, nursing, emergency medicine, critical care, and ancillary services. By collaborating as one cohesive hospital unit, we were able to efficiently develop, implement, and update best clinical care guidelines and algorithms for COVID-19–related topics such as testing indications, admission criteria, infection control, and proper personal protective equipment use. Lastly, working with specialists to consolidate teams during a pandemic presents an opportunity for hospitalists to highlight expertise while bringing value to the hospital.
Unique staffing situations related to COVID-19
Different from other disasters, the COVID-19 pandemic affected older or immunocompromised staff in a unique way. Beauhaus et al. note that 20% of the physician workforce in the United Sates is between 55 and 64 years of age, and 9% are 65 years and older.12 Hospitalist groups should focus on how to optimize and preserve their workforce, specifically those that are higher risk due to age or other health conditions.
We used a tiered guide to safely accommodate our physicians that were determined to be at higher-risk for complications of COVID-19; these recommendations included limiting exposure to patients with acute respiratory illnesses and shifting some providers to a different clinical environments with a lower exposure risk, such as telemedicine visits.
Other COVID-19 preparedness considerations that affected our group in particular include the changes in learner staffing. Similar to attending down-staffing to encourage physical distancing during low census, learners (residents, medical students, and physician assistant students) also experienced decreased hours or suspension of rotations. To maintain optimal patient care, adjusting to changing disaster needs may include assessing attendings’ capacity to assume responsibilities typically supported by learners.
Due to the ongoing nature of the pandemic, we have had to maintain a dynamic response while adjusting to changing and ongoing needs during recovery. Creating a measured and staggered approach helps facilitate a smooth transition back to nonemergent activities. The education of learners, academic and scholarly work, and administrative duties will resume, but likely in a different steady state. Also, awareness of physician burnout and fatigue is critical as an institution enters a phase of recovery.
Preparing for the next disaster during the pandemic
This brings us back to the beginning of the disaster preparedness cycle and the need to plan for the next disaster. Current disaster preparedness plans among physician groups and hospitals are likely focused on an individual disaster scenario, but adjusting current disaster plans to account for the uncertain time frame of an event like the COVID-19 pandemic is critical. Several articles in the national news posed similar questions, although these publications focused mainly on the Federal Emergency Management Agency and the governmental response to prepare for the next disaster when resources are already stretched.13-15
How do we adequately plan, maintain a dynamic response, and continue to efficiently move through the disaster staffing cycle during an event like the COVID-19 pandemic? Being aware of current vulnerabilities and addressing gaps at the department and hospital level are vital to disaster preparedness. For example, we reassessed disaster (ride-out/relief) teams and the minimum number of staff needed to maintain safe and quality care, and what in-house arrangements would be needed (food, supplies, sleeping arrangements) while having to maintain physical distance.
Newman et al. explain “in disaster planning, having as many physicians as possible on hand may seem like an advantage, but being overstaffed in tight quarters was almost as bad as being understaffed.”9 This has been particularly true during the COVID-19 pandemic. It is crucial to have backup plans for faculty that are unable to serve ride-out duties from unexpected issues – such as availability, illnesses/quarantines, childcare/dependents. Also, it is important to be aware that some supply chains are already strained because of the pandemic and how this may play a role in the availability of certain supplies. Being aware and proactive about specific constraints allows for a better level of preparedness. Continued collaboration and communication with other services to provide care should be ongoing throughout the disaster preparedness cycle.
Conclusion
Providing and maintaining optimal and safe patient care should be the overarching goal throughout disaster preparedness. Being aware of group and institutional vulnerabilities, collaboration with hospital leadership, and remaining flexible as hospitalists are critical components for successful preparedness amid disasters. A dynamic and responsive disaster plan has been vital amid COVID-19, and for the next disasters we will certainly encounter.
Dr. Hadvani is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Uremovich is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Quinonez is associate professor of pediatrics and chief of pediatric hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Lopez is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Mothner is associate professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital and is the pediatric hospital medicine medical director for the main campus.
References
1. Malilay J et al. The role of applied epidemiology methods in the disaster management cycle. Am J Public Health. 2014;104(11):2092-102. doi: 10.2105/AJPH.2014.302010.
2. Federal Emergency Management Agency. Developing and maintaining emergency operations plans. 2010 Nov.
3. Federal Emergency Management Agency. National preparedness system. 2020 Jul 31.
4. Federal Emergency Management Agency. National preparedness goal. 2011 Sep.
5. Environmental health in emergencies and disasters: A practical guide. World Health Organization, Geneva. 2002:9-24. Edited by B. Wisner and J. Adams.
6. U.S. Department of Health and Human Services. Topic collection: Hazard vulnerability/risk assessment.
7. Hospital Association of Southern California. Hazard and vulnerability analysis.
8. Meier K et al. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020 May;15(5):308-10. doi: 10.12788/jhm.3435.
9. Newman B and Gallion C. Hurricane Harvey: Firsthand preparedness in graduate medical education. Acad Med. 2019 Sep;94(9):1267-69. doi: 10.1097/ACM.0000000000002696.
10. Brevard S et al. Analysis of disaster response plans and the aftermath of Hurricane Katrina: Lessons learned from a level I trauma center. J Trauma. 2008 Nov;65(5):1126-32. doi: 10.1097/TA.0b013e318188d6e5.
11. Cram P et al. All hands on deck learning to “un-specialize” in the COVID-19 pandemic. J Hosp Med. 2020 May;15(5):314-5. doi: 10.12788/jhm.3426.
12. Buerhaus P et al. Older clinicians and the surge in novel coronavirus disease 2019 (COVID-19). JAMA. 2020 May 12;323(18):1777-8. doi: 10.1001/jama.2020.4978.
13. VOX Media. Imagine Hurricane Katrina during a pandemic. The US needs to prepare for that – now. 2020 May 27.
14. The Hill. Democratic lawmakers ask how FEMA is planning to balance natural disasters, COVID-19 response. 2020 Apr 20.
15. The Atlantic. What happens if a ‘big one’ strikes during the pandemic? 2020 May 9.
Open notes in health care: The good, the bad, and the ugly of the Cures Act
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
On April 5, 2021, a requirement of the 21st Century Cures Act went into effect: Patients must be able to access information in their EHRs “without delay.” (This requirement does not apply to paper records.) The Cures Act prohibition against information blocking, often referred to as an “open notes” provision, provides patients with transparency in the outcomes of their health care via convenient access to information in their EHR, which can positively or negatively impact the patient-doctor relationship.
Patient access to records is not new, and neither is the Cures Act, which dates to 2016. What is new is the requirement that patients have electronic records access that is fast and easy. This requirement is expected to result in more patients – still a small proportion overall, but more patients – accessing additional EHR information, including providers’ notes.
The requirement to provide patients with EHR access raises questions for health care practices. Some questions are logistical, and some are relational. Concerns include the potential for increased time for patient education, or patient requests for changes to their records that the clinician cannot support.
Health care providers should understand the good, bad, and ugly implications of the Cures Act open notes provisions so they can meet the requirements and reap their benefits, while avoiding the potential for fines or sanctions based on noncompliance, or other negative impacts.
Good news about open notes
Many patients feel better about their provider after reading a note. Positive effects on the patient-provider relationship may be most significant among vulnerable patients, such as those with fewer years of formal education.
Further, open notes have positive impacts on patient engagement and understanding. Patients report that reading notes is a way to better understand and feel more in control of their health care. They also say it builds trust with their provider. The nonprofit organization OpenNotes (not a part of the Cures Act) cites helping laypeople maintain trust in scientific medicine as one benefit of the transparency created by the Cures Act open notes provisions.
Bad news about open notes
Concerns about open notes mainly revolve around the potential for conflicts with patients and potential time conflicts.
Concerns include:
- Timing: The originally planned implementation date for the open notes provisions in the Cures Act was November 2020. Because of the COVID-19 pandemic, this was pushed back to April 2021. However, many providers and practices are still feeling the pandemic’s effects, leading to the question: “Will new demands never end?”
- Uncertainty about the documentation process: Most patients will not understand clinical shorthand, and providers may need added time for explanation. Providers are wondering: “How can I make my notes comprehensible to patients while still writing them quickly?”
- Technology: Some EHR vendors are still racing to provide services that allow practices to remain in compliance with the Cures Act. It may be necessary for a provider to call their EHR vendor and say: “What are you doing to ensure my interoperability compliance?” Meanwhile, secure drop box options for records requests provide a workaround.
Ugly news about open notes
Some patient requests for record amendment are legitimate and easily handled. Some patients, however, will request removal of material they find embarrassing, even though it is accurate.
More frequent requests for records changes from patients could increase already weighty administrative burdens on providers. Worse, some of these requests will be for changes providers cannot support, and making time for careful conversations with patients and providing written responses for requests that are rejected will be a challenge. Inevitably, some of these conversations will not go well, whether through the patient feeling the provider did not adequately respond to their concerns, or through the patient insisting on unreasonable demands. These negative relationship outcomes will add emotional stress on both the patient and the provider, as well as a reputational threat to providers from angry patients posting negative reviews online.
More tangibly, noncompliance with the open notes requirement carries the potential for fines, penalties, and/or sanctions from medical boards. The specifics of potential penalties are not yet known – there are more changes coming with the Cures Act.
Making changes in open notes
Patients will ask providers to amend their medical records. Be familiar with what the patient has the right to ask, what the provider can grant and/or refuse, and how to amend notes.
Here are some highlights:
- Patients have the right to request amendments to their medical records: HIPAA requires a signed, dated request from the patient regarding what they want changed and why.
- Providers have the right to determine whether the requested amendment will be made: The provider must respond, in writing, within 60 days of receipt of the patient’s request.
- Common reasons to deny a patient’s request include that the provider who received the request did not create the record entry, or that the medical record is accurate as is.
- The patient’s request and the provider’s response both become part of the patient’s medical record.
Strategies for success
When composing notes, certain simple strategies will raise the odds that notes will be well understood and well received. Beyond being clear and succinct, strategies for success include composing at least a portion of the note as instructions directly addressed to the patient – “Start taking lisinopril and check your blood pressure twice a week” versus “Initiated lisinopril and instructed her to check her blood pressure twice a week” – and providing a list of commonly used medical terms and abbreviations.
For an in-depth review of strategies for success when composing notes, see “12 Strategies for Success With Open Notes in Healthcare: The Cures Act.”
Exceptions
Unless an exception applies, clinical notes must not be blocked, but the Cures Act allows for a fairly long list of specific, well-delineated exceptions. For instance, a record can be blocked if a provider believes that viewing a note presents a substantial risk of harm to the physical safety of the patient or someone else. The Cures Act also recognizes exemptions that apply to certain caregiving situations, such as when parents attempt to access confidential parts of an adolescent child’s records.
For information regarding exceptions to open notes, please see “What Open Notes Exceptions Does the Cures Act Allow?”
Seeing open notes as part of high-touch, high-value care
While many physicians and other providers have anticipated open notes with dread, most outcomes so far have been positive. Patients have reacted well to clarity. They have used open notes as a tool to improve their own understanding of and adherence to care instructions. When patients have noted valid issues or miscommunications, they have appreciated being able to quickly clear them up. More than an administrative burden, open notes present an opportunity to improve documentation, patient-provider relationships, and patient safety. By improving patient adherence to treatment plans, open notes have the potential to improve provider satisfaction, as well.
Chad Anguilm, MBA, is vice president, in-practice technology services, Medical Advantage, part of TDC Group. Richard F. Cahill, JD, is vice president and associate general counsel, The Doctors Company, part of TDC Group. Kathleen Stillwell, MPA/HSA, RN, is senior patient safety risk manager, The Doctors Company, part of TDC Group.
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
On April 5, 2021, a requirement of the 21st Century Cures Act went into effect: Patients must be able to access information in their EHRs “without delay.” (This requirement does not apply to paper records.) The Cures Act prohibition against information blocking, often referred to as an “open notes” provision, provides patients with transparency in the outcomes of their health care via convenient access to information in their EHR, which can positively or negatively impact the patient-doctor relationship.
Patient access to records is not new, and neither is the Cures Act, which dates to 2016. What is new is the requirement that patients have electronic records access that is fast and easy. This requirement is expected to result in more patients – still a small proportion overall, but more patients – accessing additional EHR information, including providers’ notes.
The requirement to provide patients with EHR access raises questions for health care practices. Some questions are logistical, and some are relational. Concerns include the potential for increased time for patient education, or patient requests for changes to their records that the clinician cannot support.
Health care providers should understand the good, bad, and ugly implications of the Cures Act open notes provisions so they can meet the requirements and reap their benefits, while avoiding the potential for fines or sanctions based on noncompliance, or other negative impacts.
Good news about open notes
Many patients feel better about their provider after reading a note. Positive effects on the patient-provider relationship may be most significant among vulnerable patients, such as those with fewer years of formal education.
Further, open notes have positive impacts on patient engagement and understanding. Patients report that reading notes is a way to better understand and feel more in control of their health care. They also say it builds trust with their provider. The nonprofit organization OpenNotes (not a part of the Cures Act) cites helping laypeople maintain trust in scientific medicine as one benefit of the transparency created by the Cures Act open notes provisions.
Bad news about open notes
Concerns about open notes mainly revolve around the potential for conflicts with patients and potential time conflicts.
Concerns include:
- Timing: The originally planned implementation date for the open notes provisions in the Cures Act was November 2020. Because of the COVID-19 pandemic, this was pushed back to April 2021. However, many providers and practices are still feeling the pandemic’s effects, leading to the question: “Will new demands never end?”
- Uncertainty about the documentation process: Most patients will not understand clinical shorthand, and providers may need added time for explanation. Providers are wondering: “How can I make my notes comprehensible to patients while still writing them quickly?”
- Technology: Some EHR vendors are still racing to provide services that allow practices to remain in compliance with the Cures Act. It may be necessary for a provider to call their EHR vendor and say: “What are you doing to ensure my interoperability compliance?” Meanwhile, secure drop box options for records requests provide a workaround.
Ugly news about open notes
Some patient requests for record amendment are legitimate and easily handled. Some patients, however, will request removal of material they find embarrassing, even though it is accurate.
More frequent requests for records changes from patients could increase already weighty administrative burdens on providers. Worse, some of these requests will be for changes providers cannot support, and making time for careful conversations with patients and providing written responses for requests that are rejected will be a challenge. Inevitably, some of these conversations will not go well, whether through the patient feeling the provider did not adequately respond to their concerns, or through the patient insisting on unreasonable demands. These negative relationship outcomes will add emotional stress on both the patient and the provider, as well as a reputational threat to providers from angry patients posting negative reviews online.
More tangibly, noncompliance with the open notes requirement carries the potential for fines, penalties, and/or sanctions from medical boards. The specifics of potential penalties are not yet known – there are more changes coming with the Cures Act.
Making changes in open notes
Patients will ask providers to amend their medical records. Be familiar with what the patient has the right to ask, what the provider can grant and/or refuse, and how to amend notes.
Here are some highlights:
- Patients have the right to request amendments to their medical records: HIPAA requires a signed, dated request from the patient regarding what they want changed and why.
- Providers have the right to determine whether the requested amendment will be made: The provider must respond, in writing, within 60 days of receipt of the patient’s request.
- Common reasons to deny a patient’s request include that the provider who received the request did not create the record entry, or that the medical record is accurate as is.
- The patient’s request and the provider’s response both become part of the patient’s medical record.
Strategies for success
When composing notes, certain simple strategies will raise the odds that notes will be well understood and well received. Beyond being clear and succinct, strategies for success include composing at least a portion of the note as instructions directly addressed to the patient – “Start taking lisinopril and check your blood pressure twice a week” versus “Initiated lisinopril and instructed her to check her blood pressure twice a week” – and providing a list of commonly used medical terms and abbreviations.
For an in-depth review of strategies for success when composing notes, see “12 Strategies for Success With Open Notes in Healthcare: The Cures Act.”
Exceptions
Unless an exception applies, clinical notes must not be blocked, but the Cures Act allows for a fairly long list of specific, well-delineated exceptions. For instance, a record can be blocked if a provider believes that viewing a note presents a substantial risk of harm to the physical safety of the patient or someone else. The Cures Act also recognizes exemptions that apply to certain caregiving situations, such as when parents attempt to access confidential parts of an adolescent child’s records.
For information regarding exceptions to open notes, please see “What Open Notes Exceptions Does the Cures Act Allow?”
Seeing open notes as part of high-touch, high-value care
While many physicians and other providers have anticipated open notes with dread, most outcomes so far have been positive. Patients have reacted well to clarity. They have used open notes as a tool to improve their own understanding of and adherence to care instructions. When patients have noted valid issues or miscommunications, they have appreciated being able to quickly clear them up. More than an administrative burden, open notes present an opportunity to improve documentation, patient-provider relationships, and patient safety. By improving patient adherence to treatment plans, open notes have the potential to improve provider satisfaction, as well.
Chad Anguilm, MBA, is vice president, in-practice technology services, Medical Advantage, part of TDC Group. Richard F. Cahill, JD, is vice president and associate general counsel, The Doctors Company, part of TDC Group. Kathleen Stillwell, MPA/HSA, RN, is senior patient safety risk manager, The Doctors Company, part of TDC Group.
Editor’s note: This article has been provided by The Doctors Company, the exclusively endorsed medical malpractice carrier for the Society of Hospital Medicine.
On April 5, 2021, a requirement of the 21st Century Cures Act went into effect: Patients must be able to access information in their EHRs “without delay.” (This requirement does not apply to paper records.) The Cures Act prohibition against information blocking, often referred to as an “open notes” provision, provides patients with transparency in the outcomes of their health care via convenient access to information in their EHR, which can positively or negatively impact the patient-doctor relationship.
Patient access to records is not new, and neither is the Cures Act, which dates to 2016. What is new is the requirement that patients have electronic records access that is fast and easy. This requirement is expected to result in more patients – still a small proportion overall, but more patients – accessing additional EHR information, including providers’ notes.
The requirement to provide patients with EHR access raises questions for health care practices. Some questions are logistical, and some are relational. Concerns include the potential for increased time for patient education, or patient requests for changes to their records that the clinician cannot support.
Health care providers should understand the good, bad, and ugly implications of the Cures Act open notes provisions so they can meet the requirements and reap their benefits, while avoiding the potential for fines or sanctions based on noncompliance, or other negative impacts.
Good news about open notes
Many patients feel better about their provider after reading a note. Positive effects on the patient-provider relationship may be most significant among vulnerable patients, such as those with fewer years of formal education.
Further, open notes have positive impacts on patient engagement and understanding. Patients report that reading notes is a way to better understand and feel more in control of their health care. They also say it builds trust with their provider. The nonprofit organization OpenNotes (not a part of the Cures Act) cites helping laypeople maintain trust in scientific medicine as one benefit of the transparency created by the Cures Act open notes provisions.
Bad news about open notes
Concerns about open notes mainly revolve around the potential for conflicts with patients and potential time conflicts.
Concerns include:
- Timing: The originally planned implementation date for the open notes provisions in the Cures Act was November 2020. Because of the COVID-19 pandemic, this was pushed back to April 2021. However, many providers and practices are still feeling the pandemic’s effects, leading to the question: “Will new demands never end?”
- Uncertainty about the documentation process: Most patients will not understand clinical shorthand, and providers may need added time for explanation. Providers are wondering: “How can I make my notes comprehensible to patients while still writing them quickly?”
- Technology: Some EHR vendors are still racing to provide services that allow practices to remain in compliance with the Cures Act. It may be necessary for a provider to call their EHR vendor and say: “What are you doing to ensure my interoperability compliance?” Meanwhile, secure drop box options for records requests provide a workaround.
Ugly news about open notes
Some patient requests for record amendment are legitimate and easily handled. Some patients, however, will request removal of material they find embarrassing, even though it is accurate.
More frequent requests for records changes from patients could increase already weighty administrative burdens on providers. Worse, some of these requests will be for changes providers cannot support, and making time for careful conversations with patients and providing written responses for requests that are rejected will be a challenge. Inevitably, some of these conversations will not go well, whether through the patient feeling the provider did not adequately respond to their concerns, or through the patient insisting on unreasonable demands. These negative relationship outcomes will add emotional stress on both the patient and the provider, as well as a reputational threat to providers from angry patients posting negative reviews online.
More tangibly, noncompliance with the open notes requirement carries the potential for fines, penalties, and/or sanctions from medical boards. The specifics of potential penalties are not yet known – there are more changes coming with the Cures Act.
Making changes in open notes
Patients will ask providers to amend their medical records. Be familiar with what the patient has the right to ask, what the provider can grant and/or refuse, and how to amend notes.
Here are some highlights:
- Patients have the right to request amendments to their medical records: HIPAA requires a signed, dated request from the patient regarding what they want changed and why.
- Providers have the right to determine whether the requested amendment will be made: The provider must respond, in writing, within 60 days of receipt of the patient’s request.
- Common reasons to deny a patient’s request include that the provider who received the request did not create the record entry, or that the medical record is accurate as is.
- The patient’s request and the provider’s response both become part of the patient’s medical record.
Strategies for success
When composing notes, certain simple strategies will raise the odds that notes will be well understood and well received. Beyond being clear and succinct, strategies for success include composing at least a portion of the note as instructions directly addressed to the patient – “Start taking lisinopril and check your blood pressure twice a week” versus “Initiated lisinopril and instructed her to check her blood pressure twice a week” – and providing a list of commonly used medical terms and abbreviations.
For an in-depth review of strategies for success when composing notes, see “12 Strategies for Success With Open Notes in Healthcare: The Cures Act.”
Exceptions
Unless an exception applies, clinical notes must not be blocked, but the Cures Act allows for a fairly long list of specific, well-delineated exceptions. For instance, a record can be blocked if a provider believes that viewing a note presents a substantial risk of harm to the physical safety of the patient or someone else. The Cures Act also recognizes exemptions that apply to certain caregiving situations, such as when parents attempt to access confidential parts of an adolescent child’s records.
For information regarding exceptions to open notes, please see “What Open Notes Exceptions Does the Cures Act Allow?”
Seeing open notes as part of high-touch, high-value care
While many physicians and other providers have anticipated open notes with dread, most outcomes so far have been positive. Patients have reacted well to clarity. They have used open notes as a tool to improve their own understanding of and adherence to care instructions. When patients have noted valid issues or miscommunications, they have appreciated being able to quickly clear them up. More than an administrative burden, open notes present an opportunity to improve documentation, patient-provider relationships, and patient safety. By improving patient adherence to treatment plans, open notes have the potential to improve provider satisfaction, as well.
Chad Anguilm, MBA, is vice president, in-practice technology services, Medical Advantage, part of TDC Group. Richard F. Cahill, JD, is vice president and associate general counsel, The Doctors Company, part of TDC Group. Kathleen Stillwell, MPA/HSA, RN, is senior patient safety risk manager, The Doctors Company, part of TDC Group.
HM administrators plan for 2021 and beyond
COVID’s impact on practice management
The COVID-19 pandemic has given hospitalists a time to shine. Perhaps few people see – and value – this more than the hospital medicine administrators who work to support them behind the scenes.
“I’m very proud to have been given this opportunity to serve alongside these wonderful hospitalists,” said Elda Dede, FHM, hospital medicine division administrator at the University of Kentucky Healthcare in Lexington, Ky.
As with everything else in U.S. health care, the pandemic has affected hospital medicine administrators planning for 2021 and subsequent years in a big way. Despite all the challenges, some organizations are maintaining equilibrium, while others are even expanding. And intertwined through it all is a bright outlook and a distinct sense of team support.
Pandemic impacts on 2021 planning
Though the Texas Health Physicians Group (THPG) in Fort Worth is part of Texas Health Resources (THR), Ajay Kharbanda, MBA, SFHM, vice president of practice operations at THPG, said that each hospital within the THR system decides who that hospital will contract with for hospitalist services. Because the process is competitive and there’s no guarantee that THPG will get the contract each time, THPG has a large focus on the value they can bring to the hospitals they serve and the patients they care for.
“Having our physicians engaged with their hospital entity leaders was extremely important this year with planning around COVID because multiple hospitals had to create new COVID units,” said Mr. Kharbanda.
With the pressure of not enough volume early in the pandemic, other hospitalist groups were forced to cut back on staffing. “Within our health system, we made the cultural decision not to cancel any shifts or cut back on staffing because we didn’t want our hospitalists to be impacted negatively by things that were out of their control,” Mr. Kharbanda said.
This commitment to their hospitalists paid off when there was a surge of patients during the last quarter of 2020. “We were struggling to ensure there were adequate physicians available to take care of the patients in the hospital, but because we did the right thing by our physicians in the beginning, people did whatever it took to make sure there was enough staffing available for that increased patient volume,” Mr. Kharbanda said.
The first priority for University of Kentucky Healthcare is patient care, said Ms. Dede. Before the pandemic, the health system already had a two-layer jeopardy system in place to deal with scheduling needs in case a staff member couldn’t come in. “For the pandemic, we created six teams with an escalation and de-escalation pattern so that we could be ready to face whatever changes came in,” Ms. Dede said. Thankfully, the community wasn’t hit very hard by COVID-19, so the six new teams ended up being unnecessary, “but we were fully prepared, and everybody was ready to go.”
Making staffing plans amidst all the uncertainty surrounding the pandemic was a big challenge in planning for 2021, said Tiffani Panek, CLHM, SFHM, hospital medicine division administrator at Johns Hopkins School of Medicine, Johns Hopkins Bayview Medical Center, in Baltimore. “We don’t know what next week is going to look like, let alone what two or three months from now is going to look like, so we’ve really had to learn to be flexible,” she said. No longer is there just a Plan A that can be adjusted as needed; now there has to be a Plan B, C, and D as well.
Because the hospital medicine division’s budget is tied to the hospital, Ms. Panek said there hasn’t been a negative impact. “The hospital supports the program and continues to support the program, regardless of COVID,” she said. The health system as a whole did have to reduce benefits and freeze raises temporarily to ensure employees could keep their jobs. However, she said they have been fortunate in that their staff has been able to – and will continue to – stay in place.
As with others, volume fluctuation was an enormous hurdle in 2021 planning, said Larissa Smith, adult hospitalist and palliative care manager at The Salem Health Medical Group, Salem Health Hospitals and Clinics, in Salem, Ore. “It’s really highlighted the continued need for us to be agile in how we structure and operationalize our staffing,” Ms. Smith said. “Adapting to volume fluctuations has been our main focus.”
To prepare for both high and low patient volumes in 2021 and be able to adjust accordingly, The Salem Health Medical Group finalized in December 2020 what they call “team efficiency plans.” These plans consist of four primary areas: surge capacity, low census planning, right providers and right patient collaboration, and right team size.
Ms. Smith is working on the “right providers and right patient collaboration” component with the trauma and acute care, vascular, and general surgery teams to figure out the best ways to utilize hospitalists and specialists. “It’s been really great collaboration,” she said.
Administrative priorities during COVID-19
The pandemic hasn’t changed Ms. Panek’s administrative priorities, which include making sure her staff has whatever they need to do their jobs and that her providers have administrative support. “The work that’s had to be done to fulfill those priorities has changed in light of COVID though,” she said.
For example, she and her staff are all still off site, which she said has been challenging, especially given the lack of preparation they had. “In order to support my staff and to make sure they aren’t getting overwhelmed by being at home, that means my job looks a little bit different, but it doesn’t change my priorities,” said Ms. Panek.
By mid-summer, Ms. Dede said her main priority has been onboarding new team members, which she said is difficult with so many meetings being held virtually. “I’m not walking around the hallways with these people and having opportunities to get feedback about how their onboarding is going, so engaging so many new team members organically into the culture, the vision, the goals of our practice, is a challenge,” she said.
Taking advantage of opportunities for hospital medicine is another administrative priority for Ms. Dede. “For us to be able to take a seat at every possible table where decisions are being made, participate in shaping the strategic vision of the entire institution and be an active player in bringing that vision to life,” she said. “I feel like this is a crucial moment for hospitalists.”
Lean work, which includes the new team efficiency plans, is an administrative priority for Ms. Smith, as it is for the entire organization. “I would say that my biggest priority is just supporting our team,” Ms. Smith said. “We’ve been on a resiliency journey for a couple years.”
Their resiliency work involves periodic team training courtesy of Bryan Sexton, PhD, director of the Duke Center for Healthcare Safety and Quality. The goal of resiliency is to strengthen positive emotion, which enables a quicker recovery when difficulties occur. “I can’t imagine where we would be, this far into the pandemic, without that work,” said Ms. Smith. “I think it has really set us up to weather the storm, literally and figuratively.”
Ensuring the well-being of his provider group’s physicians is a high administrative priority for Mr. Kharbanda. Considering that the work they’ve always done is difficult, and the pandemic has been going on for such a long time, hospitalists are stretched thin. “We are bringing some additional resources to our providers that relate to taking care of themselves and helping them cope with the additional shifts,” Mr. Kharbanda said.
Going forward
The hospital medicine team at University of Kentucky Healthcare was already in the process of planning and adopting a new funds flow model, which increases the budget for HM, when the pandemic hit. “This is actually very good timing for us,” noted Ms. Dede. “We are currently working on building a new incentive model that maximizes engagement and academic productivity for our physicians, which in turn, will allow their careers to flourish and the involvement with enterprise leadership to increase.”
They had also planned to expand their teams and services before the pandemic, so in 2021, they’re hiring “an unprecedented number of hospitalists,” Ms. Dede said.
Mr. Kharbanda said that COVID has shown how much impact hospitalists can have on a hospital’s success, which has further highlighted their value. “Most of our programs are holding steady and we have some growth expected at some of our entities, so for those sites, we are hiring,” he said. Budget-wise, he expected to feel the pandemic’s impact for the first half of 2021, but for the second half, he hopes to return to normal.
Other than some low volumes in the spring, Salem Health has mostly maintained its typical capacities and funds. “Obviously, we don’t have control over external forces that impact health care, but we really try to home in on how we utilize our resources,” said Ms. Smith. “We’re a financially secure organization and I think our lean work really drives that.” The Salem Hospital is currently expanding a building tower to add another 150 beds, giving them more than 600 beds. “That will make us the largest hospital in Oregon,” Ms. Smith said.
Positive takeaways from the pandemic
Ms. Dede feels that hospital medicine has entered the health care spotlight with regard to hospitalists’ role in caring for patients during the pandemic. “Every challenge is an opportunity for growth and an opportunity to show that you know what you’re made of,” she said. “If there was ever doubt that the hospitalists are the beating heart of the hospital, this doubt is now gone. Hospitalists have, and will continue to, shoulder most of the care for COVID patients.”
The pandemic has also presented an opportunity at University of Kentucky Healthcare that helps accomplish both physician and hospital goals. “Hospital medicine is currently being asked to staff units and to participate in leadership committees, so this has been a great opportunity for growth for us,” Ms. Dede said.
The flexibility her team has shown has been a positive outcome for Ms. Panek. “You never really know what you’re going to be capable of doing until you have to do it,” she said. “I’m really proud of my group of administrative staff for how well that they’ve handled this considering it was supposed to be temporary. It’s really shown just how amazing the members of our team are and I think sometimes we take that for granted. COVID has made it so you don’t take things for granted anymore.”
Mr. Kharbanda sees how the pandemic has brought his hospitalist team together. Now, “it’s more like a family,” he said. “I think having the conversations around well-being and family safety were the real value as we learn to survive the pandemic. That was beautiful to see.”
The resiliency work her organization has done has helped Ms. Smith find plenty of positives in the face of the pandemic. “We are really resilient in health care and we can adapt quickly, but also safely,” she said.
Ms. Smith said the pandemic has also brought about changes for the better that will likely be permanent, like having time-saving virtual meetings and working from home. “We’ve put a lot of resources into physical structures and that takes away value from patients,” said Ms. Smith. “If we’re able to shift people in different roles to work from home, that just creates more future value for our community.”
Ms. Dede also sees the potential benefits that stem from people’s newfound comfort with video conferencing. “You can basically have grand rounds presenters from anywhere in the world,” she said. “You don’t have to fly them in, you don’t have to host them and have a whole program for a couple of days. They can talk to your people for an hour from the comfort of their home. I feel that we should take advantage of this too.”
Ms. Dede believes that expanding telehealth options and figuring out how hospitals can maximize that use is a priority right now. “Telehealth has been on the minds of so many hospital medicine practices, but there were still so many questions without answers about how to implement it,” she said. “During the pandemic, we were forced to find those solutions, but a lot of the barriers we are faced with have not been eliminated. I would recommend that groups keep their eyes open for new technological solutions that may empower your expansion into telehealth.”
COVID’s impact on practice management
COVID’s impact on practice management
The COVID-19 pandemic has given hospitalists a time to shine. Perhaps few people see – and value – this more than the hospital medicine administrators who work to support them behind the scenes.
“I’m very proud to have been given this opportunity to serve alongside these wonderful hospitalists,” said Elda Dede, FHM, hospital medicine division administrator at the University of Kentucky Healthcare in Lexington, Ky.
As with everything else in U.S. health care, the pandemic has affected hospital medicine administrators planning for 2021 and subsequent years in a big way. Despite all the challenges, some organizations are maintaining equilibrium, while others are even expanding. And intertwined through it all is a bright outlook and a distinct sense of team support.
Pandemic impacts on 2021 planning
Though the Texas Health Physicians Group (THPG) in Fort Worth is part of Texas Health Resources (THR), Ajay Kharbanda, MBA, SFHM, vice president of practice operations at THPG, said that each hospital within the THR system decides who that hospital will contract with for hospitalist services. Because the process is competitive and there’s no guarantee that THPG will get the contract each time, THPG has a large focus on the value they can bring to the hospitals they serve and the patients they care for.
“Having our physicians engaged with their hospital entity leaders was extremely important this year with planning around COVID because multiple hospitals had to create new COVID units,” said Mr. Kharbanda.
With the pressure of not enough volume early in the pandemic, other hospitalist groups were forced to cut back on staffing. “Within our health system, we made the cultural decision not to cancel any shifts or cut back on staffing because we didn’t want our hospitalists to be impacted negatively by things that were out of their control,” Mr. Kharbanda said.
This commitment to their hospitalists paid off when there was a surge of patients during the last quarter of 2020. “We were struggling to ensure there were adequate physicians available to take care of the patients in the hospital, but because we did the right thing by our physicians in the beginning, people did whatever it took to make sure there was enough staffing available for that increased patient volume,” Mr. Kharbanda said.
The first priority for University of Kentucky Healthcare is patient care, said Ms. Dede. Before the pandemic, the health system already had a two-layer jeopardy system in place to deal with scheduling needs in case a staff member couldn’t come in. “For the pandemic, we created six teams with an escalation and de-escalation pattern so that we could be ready to face whatever changes came in,” Ms. Dede said. Thankfully, the community wasn’t hit very hard by COVID-19, so the six new teams ended up being unnecessary, “but we were fully prepared, and everybody was ready to go.”
Making staffing plans amidst all the uncertainty surrounding the pandemic was a big challenge in planning for 2021, said Tiffani Panek, CLHM, SFHM, hospital medicine division administrator at Johns Hopkins School of Medicine, Johns Hopkins Bayview Medical Center, in Baltimore. “We don’t know what next week is going to look like, let alone what two or three months from now is going to look like, so we’ve really had to learn to be flexible,” she said. No longer is there just a Plan A that can be adjusted as needed; now there has to be a Plan B, C, and D as well.
Because the hospital medicine division’s budget is tied to the hospital, Ms. Panek said there hasn’t been a negative impact. “The hospital supports the program and continues to support the program, regardless of COVID,” she said. The health system as a whole did have to reduce benefits and freeze raises temporarily to ensure employees could keep their jobs. However, she said they have been fortunate in that their staff has been able to – and will continue to – stay in place.
As with others, volume fluctuation was an enormous hurdle in 2021 planning, said Larissa Smith, adult hospitalist and palliative care manager at The Salem Health Medical Group, Salem Health Hospitals and Clinics, in Salem, Ore. “It’s really highlighted the continued need for us to be agile in how we structure and operationalize our staffing,” Ms. Smith said. “Adapting to volume fluctuations has been our main focus.”
To prepare for both high and low patient volumes in 2021 and be able to adjust accordingly, The Salem Health Medical Group finalized in December 2020 what they call “team efficiency plans.” These plans consist of four primary areas: surge capacity, low census planning, right providers and right patient collaboration, and right team size.
Ms. Smith is working on the “right providers and right patient collaboration” component with the trauma and acute care, vascular, and general surgery teams to figure out the best ways to utilize hospitalists and specialists. “It’s been really great collaboration,” she said.
Administrative priorities during COVID-19
The pandemic hasn’t changed Ms. Panek’s administrative priorities, which include making sure her staff has whatever they need to do their jobs and that her providers have administrative support. “The work that’s had to be done to fulfill those priorities has changed in light of COVID though,” she said.
For example, she and her staff are all still off site, which she said has been challenging, especially given the lack of preparation they had. “In order to support my staff and to make sure they aren’t getting overwhelmed by being at home, that means my job looks a little bit different, but it doesn’t change my priorities,” said Ms. Panek.
By mid-summer, Ms. Dede said her main priority has been onboarding new team members, which she said is difficult with so many meetings being held virtually. “I’m not walking around the hallways with these people and having opportunities to get feedback about how their onboarding is going, so engaging so many new team members organically into the culture, the vision, the goals of our practice, is a challenge,” she said.
Taking advantage of opportunities for hospital medicine is another administrative priority for Ms. Dede. “For us to be able to take a seat at every possible table where decisions are being made, participate in shaping the strategic vision of the entire institution and be an active player in bringing that vision to life,” she said. “I feel like this is a crucial moment for hospitalists.”
Lean work, which includes the new team efficiency plans, is an administrative priority for Ms. Smith, as it is for the entire organization. “I would say that my biggest priority is just supporting our team,” Ms. Smith said. “We’ve been on a resiliency journey for a couple years.”
Their resiliency work involves periodic team training courtesy of Bryan Sexton, PhD, director of the Duke Center for Healthcare Safety and Quality. The goal of resiliency is to strengthen positive emotion, which enables a quicker recovery when difficulties occur. “I can’t imagine where we would be, this far into the pandemic, without that work,” said Ms. Smith. “I think it has really set us up to weather the storm, literally and figuratively.”
Ensuring the well-being of his provider group’s physicians is a high administrative priority for Mr. Kharbanda. Considering that the work they’ve always done is difficult, and the pandemic has been going on for such a long time, hospitalists are stretched thin. “We are bringing some additional resources to our providers that relate to taking care of themselves and helping them cope with the additional shifts,” Mr. Kharbanda said.
Going forward
The hospital medicine team at University of Kentucky Healthcare was already in the process of planning and adopting a new funds flow model, which increases the budget for HM, when the pandemic hit. “This is actually very good timing for us,” noted Ms. Dede. “We are currently working on building a new incentive model that maximizes engagement and academic productivity for our physicians, which in turn, will allow their careers to flourish and the involvement with enterprise leadership to increase.”
They had also planned to expand their teams and services before the pandemic, so in 2021, they’re hiring “an unprecedented number of hospitalists,” Ms. Dede said.
Mr. Kharbanda said that COVID has shown how much impact hospitalists can have on a hospital’s success, which has further highlighted their value. “Most of our programs are holding steady and we have some growth expected at some of our entities, so for those sites, we are hiring,” he said. Budget-wise, he expected to feel the pandemic’s impact for the first half of 2021, but for the second half, he hopes to return to normal.
Other than some low volumes in the spring, Salem Health has mostly maintained its typical capacities and funds. “Obviously, we don’t have control over external forces that impact health care, but we really try to home in on how we utilize our resources,” said Ms. Smith. “We’re a financially secure organization and I think our lean work really drives that.” The Salem Hospital is currently expanding a building tower to add another 150 beds, giving them more than 600 beds. “That will make us the largest hospital in Oregon,” Ms. Smith said.
Positive takeaways from the pandemic
Ms. Dede feels that hospital medicine has entered the health care spotlight with regard to hospitalists’ role in caring for patients during the pandemic. “Every challenge is an opportunity for growth and an opportunity to show that you know what you’re made of,” she said. “If there was ever doubt that the hospitalists are the beating heart of the hospital, this doubt is now gone. Hospitalists have, and will continue to, shoulder most of the care for COVID patients.”
The pandemic has also presented an opportunity at University of Kentucky Healthcare that helps accomplish both physician and hospital goals. “Hospital medicine is currently being asked to staff units and to participate in leadership committees, so this has been a great opportunity for growth for us,” Ms. Dede said.
The flexibility her team has shown has been a positive outcome for Ms. Panek. “You never really know what you’re going to be capable of doing until you have to do it,” she said. “I’m really proud of my group of administrative staff for how well that they’ve handled this considering it was supposed to be temporary. It’s really shown just how amazing the members of our team are and I think sometimes we take that for granted. COVID has made it so you don’t take things for granted anymore.”
Mr. Kharbanda sees how the pandemic has brought his hospitalist team together. Now, “it’s more like a family,” he said. “I think having the conversations around well-being and family safety were the real value as we learn to survive the pandemic. That was beautiful to see.”
The resiliency work her organization has done has helped Ms. Smith find plenty of positives in the face of the pandemic. “We are really resilient in health care and we can adapt quickly, but also safely,” she said.
Ms. Smith said the pandemic has also brought about changes for the better that will likely be permanent, like having time-saving virtual meetings and working from home. “We’ve put a lot of resources into physical structures and that takes away value from patients,” said Ms. Smith. “If we’re able to shift people in different roles to work from home, that just creates more future value for our community.”
Ms. Dede also sees the potential benefits that stem from people’s newfound comfort with video conferencing. “You can basically have grand rounds presenters from anywhere in the world,” she said. “You don’t have to fly them in, you don’t have to host them and have a whole program for a couple of days. They can talk to your people for an hour from the comfort of their home. I feel that we should take advantage of this too.”
Ms. Dede believes that expanding telehealth options and figuring out how hospitals can maximize that use is a priority right now. “Telehealth has been on the minds of so many hospital medicine practices, but there were still so many questions without answers about how to implement it,” she said. “During the pandemic, we were forced to find those solutions, but a lot of the barriers we are faced with have not been eliminated. I would recommend that groups keep their eyes open for new technological solutions that may empower your expansion into telehealth.”
The COVID-19 pandemic has given hospitalists a time to shine. Perhaps few people see – and value – this more than the hospital medicine administrators who work to support them behind the scenes.
“I’m very proud to have been given this opportunity to serve alongside these wonderful hospitalists,” said Elda Dede, FHM, hospital medicine division administrator at the University of Kentucky Healthcare in Lexington, Ky.
As with everything else in U.S. health care, the pandemic has affected hospital medicine administrators planning for 2021 and subsequent years in a big way. Despite all the challenges, some organizations are maintaining equilibrium, while others are even expanding. And intertwined through it all is a bright outlook and a distinct sense of team support.
Pandemic impacts on 2021 planning
Though the Texas Health Physicians Group (THPG) in Fort Worth is part of Texas Health Resources (THR), Ajay Kharbanda, MBA, SFHM, vice president of practice operations at THPG, said that each hospital within the THR system decides who that hospital will contract with for hospitalist services. Because the process is competitive and there’s no guarantee that THPG will get the contract each time, THPG has a large focus on the value they can bring to the hospitals they serve and the patients they care for.
“Having our physicians engaged with their hospital entity leaders was extremely important this year with planning around COVID because multiple hospitals had to create new COVID units,” said Mr. Kharbanda.
With the pressure of not enough volume early in the pandemic, other hospitalist groups were forced to cut back on staffing. “Within our health system, we made the cultural decision not to cancel any shifts or cut back on staffing because we didn’t want our hospitalists to be impacted negatively by things that were out of their control,” Mr. Kharbanda said.
This commitment to their hospitalists paid off when there was a surge of patients during the last quarter of 2020. “We were struggling to ensure there were adequate physicians available to take care of the patients in the hospital, but because we did the right thing by our physicians in the beginning, people did whatever it took to make sure there was enough staffing available for that increased patient volume,” Mr. Kharbanda said.
The first priority for University of Kentucky Healthcare is patient care, said Ms. Dede. Before the pandemic, the health system already had a two-layer jeopardy system in place to deal with scheduling needs in case a staff member couldn’t come in. “For the pandemic, we created six teams with an escalation and de-escalation pattern so that we could be ready to face whatever changes came in,” Ms. Dede said. Thankfully, the community wasn’t hit very hard by COVID-19, so the six new teams ended up being unnecessary, “but we were fully prepared, and everybody was ready to go.”
Making staffing plans amidst all the uncertainty surrounding the pandemic was a big challenge in planning for 2021, said Tiffani Panek, CLHM, SFHM, hospital medicine division administrator at Johns Hopkins School of Medicine, Johns Hopkins Bayview Medical Center, in Baltimore. “We don’t know what next week is going to look like, let alone what two or three months from now is going to look like, so we’ve really had to learn to be flexible,” she said. No longer is there just a Plan A that can be adjusted as needed; now there has to be a Plan B, C, and D as well.
Because the hospital medicine division’s budget is tied to the hospital, Ms. Panek said there hasn’t been a negative impact. “The hospital supports the program and continues to support the program, regardless of COVID,” she said. The health system as a whole did have to reduce benefits and freeze raises temporarily to ensure employees could keep their jobs. However, she said they have been fortunate in that their staff has been able to – and will continue to – stay in place.
As with others, volume fluctuation was an enormous hurdle in 2021 planning, said Larissa Smith, adult hospitalist and palliative care manager at The Salem Health Medical Group, Salem Health Hospitals and Clinics, in Salem, Ore. “It’s really highlighted the continued need for us to be agile in how we structure and operationalize our staffing,” Ms. Smith said. “Adapting to volume fluctuations has been our main focus.”
To prepare for both high and low patient volumes in 2021 and be able to adjust accordingly, The Salem Health Medical Group finalized in December 2020 what they call “team efficiency plans.” These plans consist of four primary areas: surge capacity, low census planning, right providers and right patient collaboration, and right team size.
Ms. Smith is working on the “right providers and right patient collaboration” component with the trauma and acute care, vascular, and general surgery teams to figure out the best ways to utilize hospitalists and specialists. “It’s been really great collaboration,” she said.
Administrative priorities during COVID-19
The pandemic hasn’t changed Ms. Panek’s administrative priorities, which include making sure her staff has whatever they need to do their jobs and that her providers have administrative support. “The work that’s had to be done to fulfill those priorities has changed in light of COVID though,” she said.
For example, she and her staff are all still off site, which she said has been challenging, especially given the lack of preparation they had. “In order to support my staff and to make sure they aren’t getting overwhelmed by being at home, that means my job looks a little bit different, but it doesn’t change my priorities,” said Ms. Panek.
By mid-summer, Ms. Dede said her main priority has been onboarding new team members, which she said is difficult with so many meetings being held virtually. “I’m not walking around the hallways with these people and having opportunities to get feedback about how their onboarding is going, so engaging so many new team members organically into the culture, the vision, the goals of our practice, is a challenge,” she said.
Taking advantage of opportunities for hospital medicine is another administrative priority for Ms. Dede. “For us to be able to take a seat at every possible table where decisions are being made, participate in shaping the strategic vision of the entire institution and be an active player in bringing that vision to life,” she said. “I feel like this is a crucial moment for hospitalists.”
Lean work, which includes the new team efficiency plans, is an administrative priority for Ms. Smith, as it is for the entire organization. “I would say that my biggest priority is just supporting our team,” Ms. Smith said. “We’ve been on a resiliency journey for a couple years.”
Their resiliency work involves periodic team training courtesy of Bryan Sexton, PhD, director of the Duke Center for Healthcare Safety and Quality. The goal of resiliency is to strengthen positive emotion, which enables a quicker recovery when difficulties occur. “I can’t imagine where we would be, this far into the pandemic, without that work,” said Ms. Smith. “I think it has really set us up to weather the storm, literally and figuratively.”
Ensuring the well-being of his provider group’s physicians is a high administrative priority for Mr. Kharbanda. Considering that the work they’ve always done is difficult, and the pandemic has been going on for such a long time, hospitalists are stretched thin. “We are bringing some additional resources to our providers that relate to taking care of themselves and helping them cope with the additional shifts,” Mr. Kharbanda said.
Going forward
The hospital medicine team at University of Kentucky Healthcare was already in the process of planning and adopting a new funds flow model, which increases the budget for HM, when the pandemic hit. “This is actually very good timing for us,” noted Ms. Dede. “We are currently working on building a new incentive model that maximizes engagement and academic productivity for our physicians, which in turn, will allow their careers to flourish and the involvement with enterprise leadership to increase.”
They had also planned to expand their teams and services before the pandemic, so in 2021, they’re hiring “an unprecedented number of hospitalists,” Ms. Dede said.
Mr. Kharbanda said that COVID has shown how much impact hospitalists can have on a hospital’s success, which has further highlighted their value. “Most of our programs are holding steady and we have some growth expected at some of our entities, so for those sites, we are hiring,” he said. Budget-wise, he expected to feel the pandemic’s impact for the first half of 2021, but for the second half, he hopes to return to normal.
Other than some low volumes in the spring, Salem Health has mostly maintained its typical capacities and funds. “Obviously, we don’t have control over external forces that impact health care, but we really try to home in on how we utilize our resources,” said Ms. Smith. “We’re a financially secure organization and I think our lean work really drives that.” The Salem Hospital is currently expanding a building tower to add another 150 beds, giving them more than 600 beds. “That will make us the largest hospital in Oregon,” Ms. Smith said.
Positive takeaways from the pandemic
Ms. Dede feels that hospital medicine has entered the health care spotlight with regard to hospitalists’ role in caring for patients during the pandemic. “Every challenge is an opportunity for growth and an opportunity to show that you know what you’re made of,” she said. “If there was ever doubt that the hospitalists are the beating heart of the hospital, this doubt is now gone. Hospitalists have, and will continue to, shoulder most of the care for COVID patients.”
The pandemic has also presented an opportunity at University of Kentucky Healthcare that helps accomplish both physician and hospital goals. “Hospital medicine is currently being asked to staff units and to participate in leadership committees, so this has been a great opportunity for growth for us,” Ms. Dede said.
The flexibility her team has shown has been a positive outcome for Ms. Panek. “You never really know what you’re going to be capable of doing until you have to do it,” she said. “I’m really proud of my group of administrative staff for how well that they’ve handled this considering it was supposed to be temporary. It’s really shown just how amazing the members of our team are and I think sometimes we take that for granted. COVID has made it so you don’t take things for granted anymore.”
Mr. Kharbanda sees how the pandemic has brought his hospitalist team together. Now, “it’s more like a family,” he said. “I think having the conversations around well-being and family safety were the real value as we learn to survive the pandemic. That was beautiful to see.”
The resiliency work her organization has done has helped Ms. Smith find plenty of positives in the face of the pandemic. “We are really resilient in health care and we can adapt quickly, but also safely,” she said.
Ms. Smith said the pandemic has also brought about changes for the better that will likely be permanent, like having time-saving virtual meetings and working from home. “We’ve put a lot of resources into physical structures and that takes away value from patients,” said Ms. Smith. “If we’re able to shift people in different roles to work from home, that just creates more future value for our community.”
Ms. Dede also sees the potential benefits that stem from people’s newfound comfort with video conferencing. “You can basically have grand rounds presenters from anywhere in the world,” she said. “You don’t have to fly them in, you don’t have to host them and have a whole program for a couple of days. They can talk to your people for an hour from the comfort of their home. I feel that we should take advantage of this too.”
Ms. Dede believes that expanding telehealth options and figuring out how hospitals can maximize that use is a priority right now. “Telehealth has been on the minds of so many hospital medicine practices, but there were still so many questions without answers about how to implement it,” she said. “During the pandemic, we were forced to find those solutions, but a lot of the barriers we are faced with have not been eliminated. I would recommend that groups keep their eyes open for new technological solutions that may empower your expansion into telehealth.”
Move from awareness to action to combat racism in medicine
Structural racism and implicit bias are connected, and both must be addressed to move from awareness of racism to action, said Nathan Chomilo, MD, of HealthPartners/Park Nicollet, Brooklyn Center, Minn., in a presentation at the virtual Pediatric Hospital Medicine annual conference.
“We need pediatricians with the courage to address racism head on,” he said.
One step in moving from awareness to action against structural and institutional racism in medicine is examining policies, Dr. Chomilo said. He cited the creation of Medicare and Medicaid in 1965 as examples of how policy changes can make a difference, illustrated by data from 1955-1975 that showed a significant decrease in infant deaths among Black infants in Mississippi after 1965.
Medicaid expansion has helped to narrow, but not eliminate, racial disparities in health care, Dr. Chomilo said. The impact of Medicare and Medicaid is evident in the current COVID-19 pandemic, as county level data show that areas where more than 25% of the population are uninsured have higher rates of COVID-19 infections, said Dr. Chomilo. Policies that impact access to care also impact their incidence of chronic diseases and risk for severe disease, he noted.
“If you don’t have ready access to a health care provider, you don’t have access to the vaccine, and you don’t have information that would inform your getting the vaccine,” he added.
Prioritizing the power of voting
“Voting is one of many ways we can impact structural racism in health care policy,” Dr. Chomilo emphasized.
However, voting inequity remains a challenge, Dr. Chomilo noted. Community level disparities lead to inequity in voting access and subsequent disparities in voter participation, he said. “Leaders are less responsive to nonvoting constituents,” which can result in policies that impact health inequitably, and loop back to community level health disparities, he explained.
Historically, physicians have had an 8%-9% lower voter turnout than the general public, although this may have changed in recent elections, Dr. Chomilo said. He encouraged all clinicians to set an example and vote, and to empower their patients to vote. Evidence shows that enfranchisement of Black voters is associated with reductions in education gaps for Blacks and Whites, and that enfranchisement of women is associated with increased spending on children and lower child mortality, he said. Dr. Chomilo encouraged pediatricians and all clinicians to take advantage of the resources on voting available from the American Academy of Pediatrics (aap.org/votekids).
“When we see more people in a community vote, leaders are more responsive to their needs,” he said.
Informing racial identity
“Racial identity is informed by racial socialization,” Dr. Chomilo said. “All of us are socialized along the lines of race; it happens in conversations with parents, family, peers, community.” Another point in moving from awareness to action in eliminating structural racism is recognizing that children are not too young to talk about race, Dr. Chomilo emphasized.
Children start to navigate racial identity and to take note of other differences at an early age. For example, a 3-year-old might ask, “why does that person talk funny, why is that person being pushed in a chair?” Dr. Chomilo said, and it is important for parents and as pediatricians to be prepared for these questions, which are part of normal development. As children get older, they start to reflect on what differences mean for them, which is not rooted in anything negative, he noted.
Children first develop racial identity at home, but children solidify their identities in child care and school settings, Dr. Chomilo said. The American Academy of Pediatrics has acknowledged the potential for racial bias in education and child care, and said in a statement that, “it is critical for pediatricians to recognize the institutional personally mediated, and internalized levels of racism that occur in the educational setting, because education is a critical social determinant of health for children.” In fact, data from children in preschool show that they use racial categories to identify themselves and others, to include or exclude children from activities, and to negotiate power in their social and play networks.
Early intervention matters in educating children about racism, Dr. Chomilo said. “If we were not taught to talk about race, it is on us to learn about it ourselves as well,” he said.
Ultimately, the goal is to create active antiracism among adults and children, said Dr. Chomilo. He encouraged pediatricians and parents not to shut down or discourage children when they raise questions of race, but to take the opportunity to teach. “There may be hurt feelings around what a child said, even if they didn’t mean to offend someone,” he noted. Take the topic seriously, and make racism conversations ongoing; teach children to safely oppose negative messages and behaviors in others, and replace them with something positive, he emphasized.
Addressing bias in clinical settings
Dr. Chomilo also encouraged hospitalists to consider internalized racism in clinical settings and take action to build confidence and cultural pride in all patients by ensuring that a pediatric hospital unit is welcoming and representative of the diversity in a given community, with appropriate options for books, movies, and toys. He also encouraged pediatric hospitalists to assess children for experiences of racism as part of a social assessment. Be aware of signs of posttraumatic stress, anxiety, depression, or grief that might have a racial component, he said.
Dr. Chomilo had no financial conflicts to disclose.
Structural racism and implicit bias are connected, and both must be addressed to move from awareness of racism to action, said Nathan Chomilo, MD, of HealthPartners/Park Nicollet, Brooklyn Center, Minn., in a presentation at the virtual Pediatric Hospital Medicine annual conference.
“We need pediatricians with the courage to address racism head on,” he said.
One step in moving from awareness to action against structural and institutional racism in medicine is examining policies, Dr. Chomilo said. He cited the creation of Medicare and Medicaid in 1965 as examples of how policy changes can make a difference, illustrated by data from 1955-1975 that showed a significant decrease in infant deaths among Black infants in Mississippi after 1965.
Medicaid expansion has helped to narrow, but not eliminate, racial disparities in health care, Dr. Chomilo said. The impact of Medicare and Medicaid is evident in the current COVID-19 pandemic, as county level data show that areas where more than 25% of the population are uninsured have higher rates of COVID-19 infections, said Dr. Chomilo. Policies that impact access to care also impact their incidence of chronic diseases and risk for severe disease, he noted.
“If you don’t have ready access to a health care provider, you don’t have access to the vaccine, and you don’t have information that would inform your getting the vaccine,” he added.
Prioritizing the power of voting
“Voting is one of many ways we can impact structural racism in health care policy,” Dr. Chomilo emphasized.
However, voting inequity remains a challenge, Dr. Chomilo noted. Community level disparities lead to inequity in voting access and subsequent disparities in voter participation, he said. “Leaders are less responsive to nonvoting constituents,” which can result in policies that impact health inequitably, and loop back to community level health disparities, he explained.
Historically, physicians have had an 8%-9% lower voter turnout than the general public, although this may have changed in recent elections, Dr. Chomilo said. He encouraged all clinicians to set an example and vote, and to empower their patients to vote. Evidence shows that enfranchisement of Black voters is associated with reductions in education gaps for Blacks and Whites, and that enfranchisement of women is associated with increased spending on children and lower child mortality, he said. Dr. Chomilo encouraged pediatricians and all clinicians to take advantage of the resources on voting available from the American Academy of Pediatrics (aap.org/votekids).
“When we see more people in a community vote, leaders are more responsive to their needs,” he said.
Informing racial identity
“Racial identity is informed by racial socialization,” Dr. Chomilo said. “All of us are socialized along the lines of race; it happens in conversations with parents, family, peers, community.” Another point in moving from awareness to action in eliminating structural racism is recognizing that children are not too young to talk about race, Dr. Chomilo emphasized.
Children start to navigate racial identity and to take note of other differences at an early age. For example, a 3-year-old might ask, “why does that person talk funny, why is that person being pushed in a chair?” Dr. Chomilo said, and it is important for parents and as pediatricians to be prepared for these questions, which are part of normal development. As children get older, they start to reflect on what differences mean for them, which is not rooted in anything negative, he noted.
Children first develop racial identity at home, but children solidify their identities in child care and school settings, Dr. Chomilo said. The American Academy of Pediatrics has acknowledged the potential for racial bias in education and child care, and said in a statement that, “it is critical for pediatricians to recognize the institutional personally mediated, and internalized levels of racism that occur in the educational setting, because education is a critical social determinant of health for children.” In fact, data from children in preschool show that they use racial categories to identify themselves and others, to include or exclude children from activities, and to negotiate power in their social and play networks.
Early intervention matters in educating children about racism, Dr. Chomilo said. “If we were not taught to talk about race, it is on us to learn about it ourselves as well,” he said.
Ultimately, the goal is to create active antiracism among adults and children, said Dr. Chomilo. He encouraged pediatricians and parents not to shut down or discourage children when they raise questions of race, but to take the opportunity to teach. “There may be hurt feelings around what a child said, even if they didn’t mean to offend someone,” he noted. Take the topic seriously, and make racism conversations ongoing; teach children to safely oppose negative messages and behaviors in others, and replace them with something positive, he emphasized.
Addressing bias in clinical settings
Dr. Chomilo also encouraged hospitalists to consider internalized racism in clinical settings and take action to build confidence and cultural pride in all patients by ensuring that a pediatric hospital unit is welcoming and representative of the diversity in a given community, with appropriate options for books, movies, and toys. He also encouraged pediatric hospitalists to assess children for experiences of racism as part of a social assessment. Be aware of signs of posttraumatic stress, anxiety, depression, or grief that might have a racial component, he said.
Dr. Chomilo had no financial conflicts to disclose.
Structural racism and implicit bias are connected, and both must be addressed to move from awareness of racism to action, said Nathan Chomilo, MD, of HealthPartners/Park Nicollet, Brooklyn Center, Minn., in a presentation at the virtual Pediatric Hospital Medicine annual conference.
“We need pediatricians with the courage to address racism head on,” he said.
One step in moving from awareness to action against structural and institutional racism in medicine is examining policies, Dr. Chomilo said. He cited the creation of Medicare and Medicaid in 1965 as examples of how policy changes can make a difference, illustrated by data from 1955-1975 that showed a significant decrease in infant deaths among Black infants in Mississippi after 1965.
Medicaid expansion has helped to narrow, but not eliminate, racial disparities in health care, Dr. Chomilo said. The impact of Medicare and Medicaid is evident in the current COVID-19 pandemic, as county level data show that areas where more than 25% of the population are uninsured have higher rates of COVID-19 infections, said Dr. Chomilo. Policies that impact access to care also impact their incidence of chronic diseases and risk for severe disease, he noted.
“If you don’t have ready access to a health care provider, you don’t have access to the vaccine, and you don’t have information that would inform your getting the vaccine,” he added.
Prioritizing the power of voting
“Voting is one of many ways we can impact structural racism in health care policy,” Dr. Chomilo emphasized.
However, voting inequity remains a challenge, Dr. Chomilo noted. Community level disparities lead to inequity in voting access and subsequent disparities in voter participation, he said. “Leaders are less responsive to nonvoting constituents,” which can result in policies that impact health inequitably, and loop back to community level health disparities, he explained.
Historically, physicians have had an 8%-9% lower voter turnout than the general public, although this may have changed in recent elections, Dr. Chomilo said. He encouraged all clinicians to set an example and vote, and to empower their patients to vote. Evidence shows that enfranchisement of Black voters is associated with reductions in education gaps for Blacks and Whites, and that enfranchisement of women is associated with increased spending on children and lower child mortality, he said. Dr. Chomilo encouraged pediatricians and all clinicians to take advantage of the resources on voting available from the American Academy of Pediatrics (aap.org/votekids).
“When we see more people in a community vote, leaders are more responsive to their needs,” he said.
Informing racial identity
“Racial identity is informed by racial socialization,” Dr. Chomilo said. “All of us are socialized along the lines of race; it happens in conversations with parents, family, peers, community.” Another point in moving from awareness to action in eliminating structural racism is recognizing that children are not too young to talk about race, Dr. Chomilo emphasized.
Children start to navigate racial identity and to take note of other differences at an early age. For example, a 3-year-old might ask, “why does that person talk funny, why is that person being pushed in a chair?” Dr. Chomilo said, and it is important for parents and as pediatricians to be prepared for these questions, which are part of normal development. As children get older, they start to reflect on what differences mean for them, which is not rooted in anything negative, he noted.
Children first develop racial identity at home, but children solidify their identities in child care and school settings, Dr. Chomilo said. The American Academy of Pediatrics has acknowledged the potential for racial bias in education and child care, and said in a statement that, “it is critical for pediatricians to recognize the institutional personally mediated, and internalized levels of racism that occur in the educational setting, because education is a critical social determinant of health for children.” In fact, data from children in preschool show that they use racial categories to identify themselves and others, to include or exclude children from activities, and to negotiate power in their social and play networks.
Early intervention matters in educating children about racism, Dr. Chomilo said. “If we were not taught to talk about race, it is on us to learn about it ourselves as well,” he said.
Ultimately, the goal is to create active antiracism among adults and children, said Dr. Chomilo. He encouraged pediatricians and parents not to shut down or discourage children when they raise questions of race, but to take the opportunity to teach. “There may be hurt feelings around what a child said, even if they didn’t mean to offend someone,” he noted. Take the topic seriously, and make racism conversations ongoing; teach children to safely oppose negative messages and behaviors in others, and replace them with something positive, he emphasized.
Addressing bias in clinical settings
Dr. Chomilo also encouraged hospitalists to consider internalized racism in clinical settings and take action to build confidence and cultural pride in all patients by ensuring that a pediatric hospital unit is welcoming and representative of the diversity in a given community, with appropriate options for books, movies, and toys. He also encouraged pediatric hospitalists to assess children for experiences of racism as part of a social assessment. Be aware of signs of posttraumatic stress, anxiety, depression, or grief that might have a racial component, he said.
Dr. Chomilo had no financial conflicts to disclose.
FROM PHM 2021
Pandemic demand for NPs soars, softens for primary care: Report
The COVID-19 pandemic has fueled a growing demand for nurse practitioners (NPs), while demand for primary care physicians has cooled, according to Merritt Hawkins’ annual review of physician and advanced practitioner recruiting trends.
according to the medical search firm. In the 27 prior years, physicians held the top spot. For the previous 14 years, the No. 1 position was held by family physicians.
“COVID-19 and other market forces are changing the dynamics of physician and advanced practitioner recruiting. NPs are coming into their own in a market that puts a premium on easy access to care and cost containment,” Tom Florence, president of Merritt Hawkins, said in a statement.
Primary care ‘recruiting frenzy’ over
Mr. Florence said primary care physicians remain a “vital part of team-based care and will be increasingly responsible for coordinating the care of older patients with multiple chronic conditions. But the recruiting frenzy in primary care is over.”
Merritt Hawkins says that overall COVID-19 has had a “severely inhibiting” effect on demand for physicians. The number of searches the company conducted dropped 25%, compared with 2020, and many hospitals and medical groups shut down or lost money during the pandemic.
But the drop-off in demand for physicians is likely to be temporary because the underlying dynamics driving physician supply and demand remain in place, according to the report. These include a growing and aging population, a limited supply of newly trained physicians, and an aging physician workforce.
COVID-19 will not permanently change these market conditions, and demand for physicians already is rebounding, the company said.
The 2021 review of physician and advanced practitioner recruiting is based on a representative sample of 2,458 permanent search engagements that Merritt Hawkins/AMN Healthcare’s physician staffing companies conducted or were in the process of conducting during the 12-month period from April 1, 2020, to March 31, 2021.
Among the key findings:
- 18% of Merritt Hawkins’ recruiting searches were for advanced practitioners, including NPs, physician assistants (PAs), and certified registered nurse anesthetists, up from 13% in the 2020 review. This represents the highest percentage in the 28 years the review has been conducted.
- About two-thirds (64%) of Merritt Hawkins’ search engagements were for physician specialists, including radiologists, psychiatrists, gastroenterologists, and others, “highlighting the robust demand for specialty physicians.”
- In 2021, 18% of Merritt Hawkins’ search engagements were for primary care physicians, down from 20% in 2020 and 22% in 2019, “signaling a relative decline in demand for primary care doctors.”
- Psychiatrists placed fourth on the list of most requested search engagements, a sign of continued strong demand for mental health professionals that is likely to accelerate because of COVID-19.
Starting salaries take a pandemic hit
Owing to the reduced demand for practitioners, starting salaries decreased for many types of health care professions, with the exception of NPs and PAs.
Average starting salaries for NPs showed strong growth, increasing 12% year over year, from $125,000 to $140,000. The average starting salaries for PAs also showed strong growth, increasing by 14% year over year, from $112,000 to $128,000.
Among physicians, interventional cardiologists were offered the highest average starting salaries, at $611,000, followed by orthopedic surgeons, at $546,000. Pediatricians were offered the lowest average starting salaries, at $236,000.
Merritt Hawkins said only 3% of their search engagements were for solo practice or partnership settings, “underscoring the decline of physician private practice.”
Roughly two-thirds (67%) of Merritt Hawkins’ search engagements were in communities of 100,000 people or more, indicating that demand for physicians and advanced practitioners is not limited to small or rural communities.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic has fueled a growing demand for nurse practitioners (NPs), while demand for primary care physicians has cooled, according to Merritt Hawkins’ annual review of physician and advanced practitioner recruiting trends.
according to the medical search firm. In the 27 prior years, physicians held the top spot. For the previous 14 years, the No. 1 position was held by family physicians.
“COVID-19 and other market forces are changing the dynamics of physician and advanced practitioner recruiting. NPs are coming into their own in a market that puts a premium on easy access to care and cost containment,” Tom Florence, president of Merritt Hawkins, said in a statement.
Primary care ‘recruiting frenzy’ over
Mr. Florence said primary care physicians remain a “vital part of team-based care and will be increasingly responsible for coordinating the care of older patients with multiple chronic conditions. But the recruiting frenzy in primary care is over.”
Merritt Hawkins says that overall COVID-19 has had a “severely inhibiting” effect on demand for physicians. The number of searches the company conducted dropped 25%, compared with 2020, and many hospitals and medical groups shut down or lost money during the pandemic.
But the drop-off in demand for physicians is likely to be temporary because the underlying dynamics driving physician supply and demand remain in place, according to the report. These include a growing and aging population, a limited supply of newly trained physicians, and an aging physician workforce.
COVID-19 will not permanently change these market conditions, and demand for physicians already is rebounding, the company said.
The 2021 review of physician and advanced practitioner recruiting is based on a representative sample of 2,458 permanent search engagements that Merritt Hawkins/AMN Healthcare’s physician staffing companies conducted or were in the process of conducting during the 12-month period from April 1, 2020, to March 31, 2021.
Among the key findings:
- 18% of Merritt Hawkins’ recruiting searches were for advanced practitioners, including NPs, physician assistants (PAs), and certified registered nurse anesthetists, up from 13% in the 2020 review. This represents the highest percentage in the 28 years the review has been conducted.
- About two-thirds (64%) of Merritt Hawkins’ search engagements were for physician specialists, including radiologists, psychiatrists, gastroenterologists, and others, “highlighting the robust demand for specialty physicians.”
- In 2021, 18% of Merritt Hawkins’ search engagements were for primary care physicians, down from 20% in 2020 and 22% in 2019, “signaling a relative decline in demand for primary care doctors.”
- Psychiatrists placed fourth on the list of most requested search engagements, a sign of continued strong demand for mental health professionals that is likely to accelerate because of COVID-19.
Starting salaries take a pandemic hit
Owing to the reduced demand for practitioners, starting salaries decreased for many types of health care professions, with the exception of NPs and PAs.
Average starting salaries for NPs showed strong growth, increasing 12% year over year, from $125,000 to $140,000. The average starting salaries for PAs also showed strong growth, increasing by 14% year over year, from $112,000 to $128,000.
Among physicians, interventional cardiologists were offered the highest average starting salaries, at $611,000, followed by orthopedic surgeons, at $546,000. Pediatricians were offered the lowest average starting salaries, at $236,000.
Merritt Hawkins said only 3% of their search engagements were for solo practice or partnership settings, “underscoring the decline of physician private practice.”
Roughly two-thirds (67%) of Merritt Hawkins’ search engagements were in communities of 100,000 people or more, indicating that demand for physicians and advanced practitioners is not limited to small or rural communities.
A version of this article first appeared on Medscape.com.
The COVID-19 pandemic has fueled a growing demand for nurse practitioners (NPs), while demand for primary care physicians has cooled, according to Merritt Hawkins’ annual review of physician and advanced practitioner recruiting trends.
according to the medical search firm. In the 27 prior years, physicians held the top spot. For the previous 14 years, the No. 1 position was held by family physicians.
“COVID-19 and other market forces are changing the dynamics of physician and advanced practitioner recruiting. NPs are coming into their own in a market that puts a premium on easy access to care and cost containment,” Tom Florence, president of Merritt Hawkins, said in a statement.
Primary care ‘recruiting frenzy’ over
Mr. Florence said primary care physicians remain a “vital part of team-based care and will be increasingly responsible for coordinating the care of older patients with multiple chronic conditions. But the recruiting frenzy in primary care is over.”
Merritt Hawkins says that overall COVID-19 has had a “severely inhibiting” effect on demand for physicians. The number of searches the company conducted dropped 25%, compared with 2020, and many hospitals and medical groups shut down or lost money during the pandemic.
But the drop-off in demand for physicians is likely to be temporary because the underlying dynamics driving physician supply and demand remain in place, according to the report. These include a growing and aging population, a limited supply of newly trained physicians, and an aging physician workforce.
COVID-19 will not permanently change these market conditions, and demand for physicians already is rebounding, the company said.
The 2021 review of physician and advanced practitioner recruiting is based on a representative sample of 2,458 permanent search engagements that Merritt Hawkins/AMN Healthcare’s physician staffing companies conducted or were in the process of conducting during the 12-month period from April 1, 2020, to March 31, 2021.
Among the key findings:
- 18% of Merritt Hawkins’ recruiting searches were for advanced practitioners, including NPs, physician assistants (PAs), and certified registered nurse anesthetists, up from 13% in the 2020 review. This represents the highest percentage in the 28 years the review has been conducted.
- About two-thirds (64%) of Merritt Hawkins’ search engagements were for physician specialists, including radiologists, psychiatrists, gastroenterologists, and others, “highlighting the robust demand for specialty physicians.”
- In 2021, 18% of Merritt Hawkins’ search engagements were for primary care physicians, down from 20% in 2020 and 22% in 2019, “signaling a relative decline in demand for primary care doctors.”
- Psychiatrists placed fourth on the list of most requested search engagements, a sign of continued strong demand for mental health professionals that is likely to accelerate because of COVID-19.
Starting salaries take a pandemic hit
Owing to the reduced demand for practitioners, starting salaries decreased for many types of health care professions, with the exception of NPs and PAs.
Average starting salaries for NPs showed strong growth, increasing 12% year over year, from $125,000 to $140,000. The average starting salaries for PAs also showed strong growth, increasing by 14% year over year, from $112,000 to $128,000.
Among physicians, interventional cardiologists were offered the highest average starting salaries, at $611,000, followed by orthopedic surgeons, at $546,000. Pediatricians were offered the lowest average starting salaries, at $236,000.
Merritt Hawkins said only 3% of their search engagements were for solo practice or partnership settings, “underscoring the decline of physician private practice.”
Roughly two-thirds (67%) of Merritt Hawkins’ search engagements were in communities of 100,000 people or more, indicating that demand for physicians and advanced practitioners is not limited to small or rural communities.
A version of this article first appeared on Medscape.com.
Microlearning during the pandemic
How to become a hospitalist
The vast amounts of information generated this past year related to the COVID-19 pandemic was a feat of wonder – recommendations and guidelines on the hospital level and on the national level came in a flurry, more often overwhelming and confusing than clarifying for the frontline provider. In addition, “routine” hospital care for non-infected patients and improvement processes had to continue as we all dealt with the whirlwind of increasing COVID cases, torrents of new guidelines, and educating our trainees.
Thus, the individual-level question: how does a clinician stay engaged and distill the relentless stream of new information?
In Spring 2020, when the first patients with COVID were admitted, our hospital medicine section was tasked to create a surge plan. This included organizing, orienting, and educating off-service providers on how to become hospitalists. Undoubtedly, the call to arms for our center was heard, and many responded. However, backgrounds were diverse in specialty – clinicians and trainees from psychiatry, general surgery, and various fellowships all answered. It was an exhausting and inefficient effort to produce the material, hold webinars, and schedule training, especially for those who were more removed from a hospital medicine experience. We knew we had to come up with an alternative plan moving forward.
Thus, the systems-level question: how does a health care system educate its clinicians, or any other health care providers, when reallocation of their talents and skills is both necessary, time-sensitive, and occuring during a period where new information is constantly being produced and changing?
To reach the most clinicians as possible, with the most succinct and distilled information, we had to come up with a method to do so. Ultimately, in considering the situation at hand, we had to understand who we were as the provider of the information, and who the recipient would be. We would like to share the initiatives and processes by which we constructed our solution to the two questions – microlearning through hospital podcasting.
Learning from our health care colleagues
With the initial webinars and training sessions for our staff, we assessed our learners’ motivations and background in managing in a hospital medicine capacity. Overall, we discovered that our trainees and clinicians have an innate drive to learn; all of them recognized the importance of keeping up with evidence-based information. However, the difficulty highlighted was the individual time available to dedicate to acquiring new information and awareness of new information being available to the health care sector during the chaotic times of the pandemic.
From our section’s perspective, we had a difficulty with coordinating among multiple professional development groups within our hospital, cost, and resources to execute training. These difficulties between providing knowledge and receiving knowledge have already been expertly analyzed.1
Parallel to this, the pedagogic paradigm shifts as we progress through our careers – the methods and skills we used in school contrast in many ways with those we use on a daily basis when it comes to learning. Instead of dedicating hours at a time to new challenges in our workflow or our interests, we watch videos, search retailers for product solutions, check our email correspondence, and peruse social media accounts several times a day. Information comes at us very quickly, but in small pieces.
One such innovation in pedagogy is the practice of microlearning. This refers to the use of small lesson modules and short-term activities intended to teach and reinforce concepts.2 It is the opposite of “macrolearning,” which is the principle of dedicating reading material, structured coursework, and traditional knowledge evaluation in the form of exams to reinforce learning. Certainly, microlearning has other names as well – “just-in-time,” “just-enough,” and “micro-courses” are a few synonyms seen in the current literature. Though a highly relevant concept for our situation, translating it to an endproduct for our trainees and clinicians required more thought.
From theory to application
Microlearning allows for faster delivery of information – fewer things to write means shorter course distribution times, allowing the learner to respond faster to changing educational goals and training demands. Microlearning is flexible – “micro-courses” can give a broad overview of a subject or cover complex topics broken down into simple parts. In addition, micro-learning promotes retention of key concepts – given the length of each lesson, repetition of the topic by the learner is possible at any point in time. The whole experience is similar to checking your favorite social media application on your smartphone.
Certainly, many examples of the application of microlearning are available in the health care sector – pharmaceutical and nursing training both have utilized the theory extensively.3-4 However, in many instances, individuals were still required to sit at a workstation to complete modules and lessons. We envisioned our application of microlearning to be “on-the-go,” without necessarily requiring a computer workstation or laptop to complete.
In thinking about how social media attracts and influences clinicians, many content creators on social media come to mind. In addition, most, if not all, have branched into various social media platforms – podcasting, blogging, YouTube, for example. In thinking about our colleagues and trainees, we wanted a platform that they could take on the go, without the need to focus their visual attention (such as while driving or running). Ultimately, we believe the podcast would be the best platform to disseminate our information.
Podcasting is not foreign to medicine. A variety of medical podcasts exist, whether produced by major medical journals or by various independent health care practitioners. Both, however, have their drawbacks – the podcasts created by major medical journals are typically a summary of the publication’s content and are less engaging. Alternatively, podcasts produced by independent creators are certainly engaging and entertaining, and have a wealth of information, but the line is often blurred between just that: education and entertainment. In both instances, there is no follow-up or feedback offered to the learner in the form of surveys, or other types of feedback, which is arguably an important piece in any form of pedagogy. Thus, we sought to strike a balance between the two forms for our purposes.
Process of two podcasts
Our section was aware of the two aims during the pandemic – (1) disseminate new information regarding COVID-19 to the rest of our staff members and trainees as quickly as possible, and (2) maintain and improve the current quality of care of our patients. Thus, we sought to apply the reach and efficiency of the podcasting medium to provide ongoing education and feedback with respect to these two aims.
“The Cure” podcast. We recognized the constant flow of new COVID-19 information and updates and we wanted to find a readily accessible platform to reach staff with timely updates. Our marketing & communications team later helped us realize that the content we wanted to share was relevant to our patients and the community, so we formatted the material to be practical and easily digestible- something that may help an individual make decisions at the bedside as well as have conversations at the dinner table. Most recently, we engaged with our human resources department to use our platform in orienting new hires with the goal of helping staff familiarize with the institutions policies, procedures, and job aids that keep staff and patients safe.
“Antibiotry” podcast. Prior to the COVID-19 pandemic, our antibiotic stewardship group noticed an increase in antibiotic use on our medical floors. This is monitored not only through internal metrics by our pharmacy department, but also via the SAAR (standardized antibiotic administration ratio). Both sources demonstrated an increase in antibiotic use, greater than expected. An initiative was formed between our hospital medicine and infectious disease sections, and our pharmacy department to raise awareness of this increase in use, provide education to our trainees, and to create systems solutions for clinicians.
Initially, we sought to hold in-person sessions once a month for our trainees. This was led by a senior resident at the time. Topics of discussion were geared towards clinical decision making regarding empiric antibiotic use on the hospital medicine service. At the same time, our team published empiric antibiotic use guidelines, accessible through our electronic medical record. In addition, the resident leader gave a voluntary survey at the end of the session to assess not only confidence of antibiotic use, but also baseline knowledge regarding antibiotics in various clinical scenarios. This survey was repeated at the end of the resident group’s month-long rotation. Altogether, each in-person session was no longer than 10 minutes.
Unfortunately, the initiative was just gaining momentum when the COVID-19 pandemic was declared. However, we sought to take this challenge and translate it into an opportunity.
We directed our focus towards stewardship during pandemic times. Initially, our resident leader sent out email primers, approximately 3-5 minute reads, as a substitute for the in-person sessions. Our primers’ uniqueness was in its incorporation of prescription pattern data that was developed by our resident leader and our initiative’s data analyst. In doing so, we provided professional feedback regarding our antibiotic use based on the clinical indication. This was a powerful tool to not only engage our learners and staff clinicians, but also as a benchmarking tool for continued quality improvement.
But email primers are not engaging, and despite the ubiquity of teleconferencing, it was difficult to ask our housestaff to break from their morning rounds for a 10 minute tele-meeting. Thus, we devised a podcast method of education – 5-10 minute audio clips with conversation regarding a topic of discussion. This way, our trainees and learners can access episodes of education on their own time throughout the pandemic without disrupting their workflow. Given the brevity of, but high-yield content in, each episode, it would not only be convenient for listeners to access and repeat, but also for the podcaster (our resident leader) to create, as recording of the audio portion takes anywhere between 10-20 minutes for each episode, with postprocessing similarly fast.
The interdisciplinary nature of continued medical education cannot be stressed enough. With the help of our professional development team and their educators, we were able to centralize our podcast and attach surveys and additional graphics for each episode, if appropriate. This additional detail allowed for feedback, engagement with our learners, and the chance to provide additional educational points, if the learner was interested. Given the integrated nature of this platform, quality metrics could easily be recorded in the form of “click” data and various other more conventional metrics, such as listener counts and the duration of each podcast played.
Future applications and initiatives
Thus far, we have had great success in the reception and use of both podcasts within our institution as an application of microlearning. “The Cure” has been widely listened to by all hospital staff from various services; it has caught the attention of state-wide radio programs, and plans to expand it into the community are being discussed.
As for “Antibiotry” podcast, the concept has been lauded by our medical educators. Given its centralization within our institution, we are able to publish institution-based data as a form of professional and educational feedback to our trainees and staff physicians. This is currently coupled with the development of a provider dashboard, visualizing antibiotic prescriptions and narrowing patterns of practice within our medicine department. We plan to expand “Antibiotry” to other services at the hospital.
For both podcasts, the steps it took to achieve the final product from the microlearning concept were possible through a combination of institutional need and a motivated team. We are fortunate to have highly energetic individuals, making the coordination and planning with our hospitalists, various sub-specialists, and professional development teams straightforward. As the team grows with more individuals interested in the initiatives, keen insight into interests, individual clinical expertise, presentation skills, and technical skills ought to be carefully weighed to sustain our podcasts most efficiently, and perhaps expand them through different social media platforms.
Our objective for sustainability is through the continued outreach to and recruitment of residents and medical students, who can play key roles in the development of future projects related to these educational innovations. Both microlearning podcasts were developed through the initial planning, trial and error, and execution by two resident leaders. Their initiative and motivation to educate our institution through these platforms were highly unique; their pathfinding set the foundation for sustainability and expansion to other services.
Of course, one of the key measures we would like to investigate is whether our microlearning platform translates to improved patient outcomes. Regarding “Antibiotry,” we hope to see a decrease in unnecessary broad-spectrum antibiotic use by drawing attention to clinician practice patterns. Quality and outcome metrics will continue to be developed and measured. In addition to patient care metrics, further investigation of pedagogical metrics will be conducted, especially in the evolving realm of graduate and continuing medical education.
Measuring educational quality is neither a new ethical nor philosophical debate – neither does it carry a definitive answer. Further help from education experts may be needed to assess the quality of the information provided and its impact on our learners.
Conclusion
Medicine is ever-changing – the guidelines and criteria for patient care and pathology that we learned in medical school have likely changed. There is no single “best” method of learning new information in medicine, simply due to the breadth and volume of such information generated on a daily basis. This poses both a challenge for present-day clinicians and trainees, and a stimulus for change in the methods of acquiring, absorbing, and applying new information to clinical decision making and practice.
We have found that podcasting is a well-received medium of information transfer that is convenient for both the learner and the content creator. Through the podcast format, we were able to distill non-engaging pieces of education and information and transform them into short-duration lessons that the learner can listen to at their own convenience. This proved to be especially handy during the chaos of the pandemic, not only for dissemination of information regarding the management of COVID-19, but also for sustaining quality improvement goals within our institution.
Further investigation on patient outcomes and information quality are the planned next steps. In addition, expansion of other microlearning media, such as group SMS texting, YouTube videos, and Twitter, ought to be considered. Though many publications discuss the theory, potential benefits, and predicted pitfalls of microlearning, few assess the real-world application of microlearning to the clinical setting for medical education.
So what did we learn? We should think of microlearning as moments when you turn to your smartphone or tablet in order to discover something, answer a question, or complete a task. These are moments when decisions are made and knowledge is reinforced. The goal is to capture these moments and fill them with essential pieces of information.
We offer these suggestions as a place to start. The microlearning platform allows for the collection of data on the interaction between user and course content. The data collected can be used for continuous quality improvement of the curriculum. Microlearning is a dynamic platform where creative ideas are encouraged and a multi-disciplinary approach is valuable to keeping an audience engaged. In the future, we hope to be able to correlate microlearning courses to provider performance and measurable patient outcomes.
Dr. Mercado is medical director at Alice Peck Day Memorial Hospital, and associate hospital epidemiologist, Dartmouth-Hitchcock Medical Center, both in Lebanon, N.H., and assistant professor at the Geisel School of Medicine at Dartmouth, Hanover, N.H. Dr. Feng is a Fellow in the Leadership/Preventive Medicine Program in the Department of Internal Medicine at Dartmouth-Hitchcock Medical Center.
References
1. Duggan F and Banwell L. Constructing a model of effective information dissemination in a crisis. Information Research. 2004;9(3). Paper 178 [Available at http://InformationR.net/ir/9-3/paper178.html].
2. Filipe HP, et al. Microlearning to improve CPD learning objectives. Clin Teach. 2020 Dec;17(6):695-699. doi: 10.1111/tct.13208.
3. Hegerius A, et al. E-Learning in Pharmacovigilance: An Evaluation of Microlearning-Based Modules Developed by Uppsala Monitoring Centre. Drug Saf. 2020 Nov;43(11):1171-1180. doi: 10.1007/s40264-020-00981-w.
4. Orwoll B, et al. Gamification and Microlearning for Engagement With Quality Improvement (GAMEQI): A Bundled Digital Intervention for the Prevention of Central Line-Associated Bloodstream Infection. Am J Med Qual. Jan/Feb 2018;33(1):21-29. doi: 10.1177/1062860617706542.
How to become a hospitalist
How to become a hospitalist
The vast amounts of information generated this past year related to the COVID-19 pandemic was a feat of wonder – recommendations and guidelines on the hospital level and on the national level came in a flurry, more often overwhelming and confusing than clarifying for the frontline provider. In addition, “routine” hospital care for non-infected patients and improvement processes had to continue as we all dealt with the whirlwind of increasing COVID cases, torrents of new guidelines, and educating our trainees.
Thus, the individual-level question: how does a clinician stay engaged and distill the relentless stream of new information?
In Spring 2020, when the first patients with COVID were admitted, our hospital medicine section was tasked to create a surge plan. This included organizing, orienting, and educating off-service providers on how to become hospitalists. Undoubtedly, the call to arms for our center was heard, and many responded. However, backgrounds were diverse in specialty – clinicians and trainees from psychiatry, general surgery, and various fellowships all answered. It was an exhausting and inefficient effort to produce the material, hold webinars, and schedule training, especially for those who were more removed from a hospital medicine experience. We knew we had to come up with an alternative plan moving forward.
Thus, the systems-level question: how does a health care system educate its clinicians, or any other health care providers, when reallocation of their talents and skills is both necessary, time-sensitive, and occuring during a period where new information is constantly being produced and changing?
To reach the most clinicians as possible, with the most succinct and distilled information, we had to come up with a method to do so. Ultimately, in considering the situation at hand, we had to understand who we were as the provider of the information, and who the recipient would be. We would like to share the initiatives and processes by which we constructed our solution to the two questions – microlearning through hospital podcasting.
Learning from our health care colleagues
With the initial webinars and training sessions for our staff, we assessed our learners’ motivations and background in managing in a hospital medicine capacity. Overall, we discovered that our trainees and clinicians have an innate drive to learn; all of them recognized the importance of keeping up with evidence-based information. However, the difficulty highlighted was the individual time available to dedicate to acquiring new information and awareness of new information being available to the health care sector during the chaotic times of the pandemic.
From our section’s perspective, we had a difficulty with coordinating among multiple professional development groups within our hospital, cost, and resources to execute training. These difficulties between providing knowledge and receiving knowledge have already been expertly analyzed.1
Parallel to this, the pedagogic paradigm shifts as we progress through our careers – the methods and skills we used in school contrast in many ways with those we use on a daily basis when it comes to learning. Instead of dedicating hours at a time to new challenges in our workflow or our interests, we watch videos, search retailers for product solutions, check our email correspondence, and peruse social media accounts several times a day. Information comes at us very quickly, but in small pieces.
One such innovation in pedagogy is the practice of microlearning. This refers to the use of small lesson modules and short-term activities intended to teach and reinforce concepts.2 It is the opposite of “macrolearning,” which is the principle of dedicating reading material, structured coursework, and traditional knowledge evaluation in the form of exams to reinforce learning. Certainly, microlearning has other names as well – “just-in-time,” “just-enough,” and “micro-courses” are a few synonyms seen in the current literature. Though a highly relevant concept for our situation, translating it to an endproduct for our trainees and clinicians required more thought.
From theory to application
Microlearning allows for faster delivery of information – fewer things to write means shorter course distribution times, allowing the learner to respond faster to changing educational goals and training demands. Microlearning is flexible – “micro-courses” can give a broad overview of a subject or cover complex topics broken down into simple parts. In addition, micro-learning promotes retention of key concepts – given the length of each lesson, repetition of the topic by the learner is possible at any point in time. The whole experience is similar to checking your favorite social media application on your smartphone.
Certainly, many examples of the application of microlearning are available in the health care sector – pharmaceutical and nursing training both have utilized the theory extensively.3-4 However, in many instances, individuals were still required to sit at a workstation to complete modules and lessons. We envisioned our application of microlearning to be “on-the-go,” without necessarily requiring a computer workstation or laptop to complete.
In thinking about how social media attracts and influences clinicians, many content creators on social media come to mind. In addition, most, if not all, have branched into various social media platforms – podcasting, blogging, YouTube, for example. In thinking about our colleagues and trainees, we wanted a platform that they could take on the go, without the need to focus their visual attention (such as while driving or running). Ultimately, we believe the podcast would be the best platform to disseminate our information.
Podcasting is not foreign to medicine. A variety of medical podcasts exist, whether produced by major medical journals or by various independent health care practitioners. Both, however, have their drawbacks – the podcasts created by major medical journals are typically a summary of the publication’s content and are less engaging. Alternatively, podcasts produced by independent creators are certainly engaging and entertaining, and have a wealth of information, but the line is often blurred between just that: education and entertainment. In both instances, there is no follow-up or feedback offered to the learner in the form of surveys, or other types of feedback, which is arguably an important piece in any form of pedagogy. Thus, we sought to strike a balance between the two forms for our purposes.
Process of two podcasts
Our section was aware of the two aims during the pandemic – (1) disseminate new information regarding COVID-19 to the rest of our staff members and trainees as quickly as possible, and (2) maintain and improve the current quality of care of our patients. Thus, we sought to apply the reach and efficiency of the podcasting medium to provide ongoing education and feedback with respect to these two aims.
“The Cure” podcast. We recognized the constant flow of new COVID-19 information and updates and we wanted to find a readily accessible platform to reach staff with timely updates. Our marketing & communications team later helped us realize that the content we wanted to share was relevant to our patients and the community, so we formatted the material to be practical and easily digestible- something that may help an individual make decisions at the bedside as well as have conversations at the dinner table. Most recently, we engaged with our human resources department to use our platform in orienting new hires with the goal of helping staff familiarize with the institutions policies, procedures, and job aids that keep staff and patients safe.
“Antibiotry” podcast. Prior to the COVID-19 pandemic, our antibiotic stewardship group noticed an increase in antibiotic use on our medical floors. This is monitored not only through internal metrics by our pharmacy department, but also via the SAAR (standardized antibiotic administration ratio). Both sources demonstrated an increase in antibiotic use, greater than expected. An initiative was formed between our hospital medicine and infectious disease sections, and our pharmacy department to raise awareness of this increase in use, provide education to our trainees, and to create systems solutions for clinicians.
Initially, we sought to hold in-person sessions once a month for our trainees. This was led by a senior resident at the time. Topics of discussion were geared towards clinical decision making regarding empiric antibiotic use on the hospital medicine service. At the same time, our team published empiric antibiotic use guidelines, accessible through our electronic medical record. In addition, the resident leader gave a voluntary survey at the end of the session to assess not only confidence of antibiotic use, but also baseline knowledge regarding antibiotics in various clinical scenarios. This survey was repeated at the end of the resident group’s month-long rotation. Altogether, each in-person session was no longer than 10 minutes.
Unfortunately, the initiative was just gaining momentum when the COVID-19 pandemic was declared. However, we sought to take this challenge and translate it into an opportunity.
We directed our focus towards stewardship during pandemic times. Initially, our resident leader sent out email primers, approximately 3-5 minute reads, as a substitute for the in-person sessions. Our primers’ uniqueness was in its incorporation of prescription pattern data that was developed by our resident leader and our initiative’s data analyst. In doing so, we provided professional feedback regarding our antibiotic use based on the clinical indication. This was a powerful tool to not only engage our learners and staff clinicians, but also as a benchmarking tool for continued quality improvement.
But email primers are not engaging, and despite the ubiquity of teleconferencing, it was difficult to ask our housestaff to break from their morning rounds for a 10 minute tele-meeting. Thus, we devised a podcast method of education – 5-10 minute audio clips with conversation regarding a topic of discussion. This way, our trainees and learners can access episodes of education on their own time throughout the pandemic without disrupting their workflow. Given the brevity of, but high-yield content in, each episode, it would not only be convenient for listeners to access and repeat, but also for the podcaster (our resident leader) to create, as recording of the audio portion takes anywhere between 10-20 minutes for each episode, with postprocessing similarly fast.
The interdisciplinary nature of continued medical education cannot be stressed enough. With the help of our professional development team and their educators, we were able to centralize our podcast and attach surveys and additional graphics for each episode, if appropriate. This additional detail allowed for feedback, engagement with our learners, and the chance to provide additional educational points, if the learner was interested. Given the integrated nature of this platform, quality metrics could easily be recorded in the form of “click” data and various other more conventional metrics, such as listener counts and the duration of each podcast played.
Future applications and initiatives
Thus far, we have had great success in the reception and use of both podcasts within our institution as an application of microlearning. “The Cure” has been widely listened to by all hospital staff from various services; it has caught the attention of state-wide radio programs, and plans to expand it into the community are being discussed.
As for “Antibiotry” podcast, the concept has been lauded by our medical educators. Given its centralization within our institution, we are able to publish institution-based data as a form of professional and educational feedback to our trainees and staff physicians. This is currently coupled with the development of a provider dashboard, visualizing antibiotic prescriptions and narrowing patterns of practice within our medicine department. We plan to expand “Antibiotry” to other services at the hospital.
For both podcasts, the steps it took to achieve the final product from the microlearning concept were possible through a combination of institutional need and a motivated team. We are fortunate to have highly energetic individuals, making the coordination and planning with our hospitalists, various sub-specialists, and professional development teams straightforward. As the team grows with more individuals interested in the initiatives, keen insight into interests, individual clinical expertise, presentation skills, and technical skills ought to be carefully weighed to sustain our podcasts most efficiently, and perhaps expand them through different social media platforms.
Our objective for sustainability is through the continued outreach to and recruitment of residents and medical students, who can play key roles in the development of future projects related to these educational innovations. Both microlearning podcasts were developed through the initial planning, trial and error, and execution by two resident leaders. Their initiative and motivation to educate our institution through these platforms were highly unique; their pathfinding set the foundation for sustainability and expansion to other services.
Of course, one of the key measures we would like to investigate is whether our microlearning platform translates to improved patient outcomes. Regarding “Antibiotry,” we hope to see a decrease in unnecessary broad-spectrum antibiotic use by drawing attention to clinician practice patterns. Quality and outcome metrics will continue to be developed and measured. In addition to patient care metrics, further investigation of pedagogical metrics will be conducted, especially in the evolving realm of graduate and continuing medical education.
Measuring educational quality is neither a new ethical nor philosophical debate – neither does it carry a definitive answer. Further help from education experts may be needed to assess the quality of the information provided and its impact on our learners.
Conclusion
Medicine is ever-changing – the guidelines and criteria for patient care and pathology that we learned in medical school have likely changed. There is no single “best” method of learning new information in medicine, simply due to the breadth and volume of such information generated on a daily basis. This poses both a challenge for present-day clinicians and trainees, and a stimulus for change in the methods of acquiring, absorbing, and applying new information to clinical decision making and practice.
We have found that podcasting is a well-received medium of information transfer that is convenient for both the learner and the content creator. Through the podcast format, we were able to distill non-engaging pieces of education and information and transform them into short-duration lessons that the learner can listen to at their own convenience. This proved to be especially handy during the chaos of the pandemic, not only for dissemination of information regarding the management of COVID-19, but also for sustaining quality improvement goals within our institution.
Further investigation on patient outcomes and information quality are the planned next steps. In addition, expansion of other microlearning media, such as group SMS texting, YouTube videos, and Twitter, ought to be considered. Though many publications discuss the theory, potential benefits, and predicted pitfalls of microlearning, few assess the real-world application of microlearning to the clinical setting for medical education.
So what did we learn? We should think of microlearning as moments when you turn to your smartphone or tablet in order to discover something, answer a question, or complete a task. These are moments when decisions are made and knowledge is reinforced. The goal is to capture these moments and fill them with essential pieces of information.
We offer these suggestions as a place to start. The microlearning platform allows for the collection of data on the interaction between user and course content. The data collected can be used for continuous quality improvement of the curriculum. Microlearning is a dynamic platform where creative ideas are encouraged and a multi-disciplinary approach is valuable to keeping an audience engaged. In the future, we hope to be able to correlate microlearning courses to provider performance and measurable patient outcomes.
Dr. Mercado is medical director at Alice Peck Day Memorial Hospital, and associate hospital epidemiologist, Dartmouth-Hitchcock Medical Center, both in Lebanon, N.H., and assistant professor at the Geisel School of Medicine at Dartmouth, Hanover, N.H. Dr. Feng is a Fellow in the Leadership/Preventive Medicine Program in the Department of Internal Medicine at Dartmouth-Hitchcock Medical Center.
References
1. Duggan F and Banwell L. Constructing a model of effective information dissemination in a crisis. Information Research. 2004;9(3). Paper 178 [Available at http://InformationR.net/ir/9-3/paper178.html].
2. Filipe HP, et al. Microlearning to improve CPD learning objectives. Clin Teach. 2020 Dec;17(6):695-699. doi: 10.1111/tct.13208.
3. Hegerius A, et al. E-Learning in Pharmacovigilance: An Evaluation of Microlearning-Based Modules Developed by Uppsala Monitoring Centre. Drug Saf. 2020 Nov;43(11):1171-1180. doi: 10.1007/s40264-020-00981-w.
4. Orwoll B, et al. Gamification and Microlearning for Engagement With Quality Improvement (GAMEQI): A Bundled Digital Intervention for the Prevention of Central Line-Associated Bloodstream Infection. Am J Med Qual. Jan/Feb 2018;33(1):21-29. doi: 10.1177/1062860617706542.
The vast amounts of information generated this past year related to the COVID-19 pandemic was a feat of wonder – recommendations and guidelines on the hospital level and on the national level came in a flurry, more often overwhelming and confusing than clarifying for the frontline provider. In addition, “routine” hospital care for non-infected patients and improvement processes had to continue as we all dealt with the whirlwind of increasing COVID cases, torrents of new guidelines, and educating our trainees.
Thus, the individual-level question: how does a clinician stay engaged and distill the relentless stream of new information?
In Spring 2020, when the first patients with COVID were admitted, our hospital medicine section was tasked to create a surge plan. This included organizing, orienting, and educating off-service providers on how to become hospitalists. Undoubtedly, the call to arms for our center was heard, and many responded. However, backgrounds were diverse in specialty – clinicians and trainees from psychiatry, general surgery, and various fellowships all answered. It was an exhausting and inefficient effort to produce the material, hold webinars, and schedule training, especially for those who were more removed from a hospital medicine experience. We knew we had to come up with an alternative plan moving forward.
Thus, the systems-level question: how does a health care system educate its clinicians, or any other health care providers, when reallocation of their talents and skills is both necessary, time-sensitive, and occuring during a period where new information is constantly being produced and changing?
To reach the most clinicians as possible, with the most succinct and distilled information, we had to come up with a method to do so. Ultimately, in considering the situation at hand, we had to understand who we were as the provider of the information, and who the recipient would be. We would like to share the initiatives and processes by which we constructed our solution to the two questions – microlearning through hospital podcasting.
Learning from our health care colleagues
With the initial webinars and training sessions for our staff, we assessed our learners’ motivations and background in managing in a hospital medicine capacity. Overall, we discovered that our trainees and clinicians have an innate drive to learn; all of them recognized the importance of keeping up with evidence-based information. However, the difficulty highlighted was the individual time available to dedicate to acquiring new information and awareness of new information being available to the health care sector during the chaotic times of the pandemic.
From our section’s perspective, we had a difficulty with coordinating among multiple professional development groups within our hospital, cost, and resources to execute training. These difficulties between providing knowledge and receiving knowledge have already been expertly analyzed.1
Parallel to this, the pedagogic paradigm shifts as we progress through our careers – the methods and skills we used in school contrast in many ways with those we use on a daily basis when it comes to learning. Instead of dedicating hours at a time to new challenges in our workflow or our interests, we watch videos, search retailers for product solutions, check our email correspondence, and peruse social media accounts several times a day. Information comes at us very quickly, but in small pieces.
One such innovation in pedagogy is the practice of microlearning. This refers to the use of small lesson modules and short-term activities intended to teach and reinforce concepts.2 It is the opposite of “macrolearning,” which is the principle of dedicating reading material, structured coursework, and traditional knowledge evaluation in the form of exams to reinforce learning. Certainly, microlearning has other names as well – “just-in-time,” “just-enough,” and “micro-courses” are a few synonyms seen in the current literature. Though a highly relevant concept for our situation, translating it to an endproduct for our trainees and clinicians required more thought.
From theory to application
Microlearning allows for faster delivery of information – fewer things to write means shorter course distribution times, allowing the learner to respond faster to changing educational goals and training demands. Microlearning is flexible – “micro-courses” can give a broad overview of a subject or cover complex topics broken down into simple parts. In addition, micro-learning promotes retention of key concepts – given the length of each lesson, repetition of the topic by the learner is possible at any point in time. The whole experience is similar to checking your favorite social media application on your smartphone.
Certainly, many examples of the application of microlearning are available in the health care sector – pharmaceutical and nursing training both have utilized the theory extensively.3-4 However, in many instances, individuals were still required to sit at a workstation to complete modules and lessons. We envisioned our application of microlearning to be “on-the-go,” without necessarily requiring a computer workstation or laptop to complete.
In thinking about how social media attracts and influences clinicians, many content creators on social media come to mind. In addition, most, if not all, have branched into various social media platforms – podcasting, blogging, YouTube, for example. In thinking about our colleagues and trainees, we wanted a platform that they could take on the go, without the need to focus their visual attention (such as while driving or running). Ultimately, we believe the podcast would be the best platform to disseminate our information.
Podcasting is not foreign to medicine. A variety of medical podcasts exist, whether produced by major medical journals or by various independent health care practitioners. Both, however, have their drawbacks – the podcasts created by major medical journals are typically a summary of the publication’s content and are less engaging. Alternatively, podcasts produced by independent creators are certainly engaging and entertaining, and have a wealth of information, but the line is often blurred between just that: education and entertainment. In both instances, there is no follow-up or feedback offered to the learner in the form of surveys, or other types of feedback, which is arguably an important piece in any form of pedagogy. Thus, we sought to strike a balance between the two forms for our purposes.
Process of two podcasts
Our section was aware of the two aims during the pandemic – (1) disseminate new information regarding COVID-19 to the rest of our staff members and trainees as quickly as possible, and (2) maintain and improve the current quality of care of our patients. Thus, we sought to apply the reach and efficiency of the podcasting medium to provide ongoing education and feedback with respect to these two aims.
“The Cure” podcast. We recognized the constant flow of new COVID-19 information and updates and we wanted to find a readily accessible platform to reach staff with timely updates. Our marketing & communications team later helped us realize that the content we wanted to share was relevant to our patients and the community, so we formatted the material to be practical and easily digestible- something that may help an individual make decisions at the bedside as well as have conversations at the dinner table. Most recently, we engaged with our human resources department to use our platform in orienting new hires with the goal of helping staff familiarize with the institutions policies, procedures, and job aids that keep staff and patients safe.
“Antibiotry” podcast. Prior to the COVID-19 pandemic, our antibiotic stewardship group noticed an increase in antibiotic use on our medical floors. This is monitored not only through internal metrics by our pharmacy department, but also via the SAAR (standardized antibiotic administration ratio). Both sources demonstrated an increase in antibiotic use, greater than expected. An initiative was formed between our hospital medicine and infectious disease sections, and our pharmacy department to raise awareness of this increase in use, provide education to our trainees, and to create systems solutions for clinicians.
Initially, we sought to hold in-person sessions once a month for our trainees. This was led by a senior resident at the time. Topics of discussion were geared towards clinical decision making regarding empiric antibiotic use on the hospital medicine service. At the same time, our team published empiric antibiotic use guidelines, accessible through our electronic medical record. In addition, the resident leader gave a voluntary survey at the end of the session to assess not only confidence of antibiotic use, but also baseline knowledge regarding antibiotics in various clinical scenarios. This survey was repeated at the end of the resident group’s month-long rotation. Altogether, each in-person session was no longer than 10 minutes.
Unfortunately, the initiative was just gaining momentum when the COVID-19 pandemic was declared. However, we sought to take this challenge and translate it into an opportunity.
We directed our focus towards stewardship during pandemic times. Initially, our resident leader sent out email primers, approximately 3-5 minute reads, as a substitute for the in-person sessions. Our primers’ uniqueness was in its incorporation of prescription pattern data that was developed by our resident leader and our initiative’s data analyst. In doing so, we provided professional feedback regarding our antibiotic use based on the clinical indication. This was a powerful tool to not only engage our learners and staff clinicians, but also as a benchmarking tool for continued quality improvement.
But email primers are not engaging, and despite the ubiquity of teleconferencing, it was difficult to ask our housestaff to break from their morning rounds for a 10 minute tele-meeting. Thus, we devised a podcast method of education – 5-10 minute audio clips with conversation regarding a topic of discussion. This way, our trainees and learners can access episodes of education on their own time throughout the pandemic without disrupting their workflow. Given the brevity of, but high-yield content in, each episode, it would not only be convenient for listeners to access and repeat, but also for the podcaster (our resident leader) to create, as recording of the audio portion takes anywhere between 10-20 minutes for each episode, with postprocessing similarly fast.
The interdisciplinary nature of continued medical education cannot be stressed enough. With the help of our professional development team and their educators, we were able to centralize our podcast and attach surveys and additional graphics for each episode, if appropriate. This additional detail allowed for feedback, engagement with our learners, and the chance to provide additional educational points, if the learner was interested. Given the integrated nature of this platform, quality metrics could easily be recorded in the form of “click” data and various other more conventional metrics, such as listener counts and the duration of each podcast played.
Future applications and initiatives
Thus far, we have had great success in the reception and use of both podcasts within our institution as an application of microlearning. “The Cure” has been widely listened to by all hospital staff from various services; it has caught the attention of state-wide radio programs, and plans to expand it into the community are being discussed.
As for “Antibiotry” podcast, the concept has been lauded by our medical educators. Given its centralization within our institution, we are able to publish institution-based data as a form of professional and educational feedback to our trainees and staff physicians. This is currently coupled with the development of a provider dashboard, visualizing antibiotic prescriptions and narrowing patterns of practice within our medicine department. We plan to expand “Antibiotry” to other services at the hospital.
For both podcasts, the steps it took to achieve the final product from the microlearning concept were possible through a combination of institutional need and a motivated team. We are fortunate to have highly energetic individuals, making the coordination and planning with our hospitalists, various sub-specialists, and professional development teams straightforward. As the team grows with more individuals interested in the initiatives, keen insight into interests, individual clinical expertise, presentation skills, and technical skills ought to be carefully weighed to sustain our podcasts most efficiently, and perhaps expand them through different social media platforms.
Our objective for sustainability is through the continued outreach to and recruitment of residents and medical students, who can play key roles in the development of future projects related to these educational innovations. Both microlearning podcasts were developed through the initial planning, trial and error, and execution by two resident leaders. Their initiative and motivation to educate our institution through these platforms were highly unique; their pathfinding set the foundation for sustainability and expansion to other services.
Of course, one of the key measures we would like to investigate is whether our microlearning platform translates to improved patient outcomes. Regarding “Antibiotry,” we hope to see a decrease in unnecessary broad-spectrum antibiotic use by drawing attention to clinician practice patterns. Quality and outcome metrics will continue to be developed and measured. In addition to patient care metrics, further investigation of pedagogical metrics will be conducted, especially in the evolving realm of graduate and continuing medical education.
Measuring educational quality is neither a new ethical nor philosophical debate – neither does it carry a definitive answer. Further help from education experts may be needed to assess the quality of the information provided and its impact on our learners.
Conclusion
Medicine is ever-changing – the guidelines and criteria for patient care and pathology that we learned in medical school have likely changed. There is no single “best” method of learning new information in medicine, simply due to the breadth and volume of such information generated on a daily basis. This poses both a challenge for present-day clinicians and trainees, and a stimulus for change in the methods of acquiring, absorbing, and applying new information to clinical decision making and practice.
We have found that podcasting is a well-received medium of information transfer that is convenient for both the learner and the content creator. Through the podcast format, we were able to distill non-engaging pieces of education and information and transform them into short-duration lessons that the learner can listen to at their own convenience. This proved to be especially handy during the chaos of the pandemic, not only for dissemination of information regarding the management of COVID-19, but also for sustaining quality improvement goals within our institution.
Further investigation on patient outcomes and information quality are the planned next steps. In addition, expansion of other microlearning media, such as group SMS texting, YouTube videos, and Twitter, ought to be considered. Though many publications discuss the theory, potential benefits, and predicted pitfalls of microlearning, few assess the real-world application of microlearning to the clinical setting for medical education.
So what did we learn? We should think of microlearning as moments when you turn to your smartphone or tablet in order to discover something, answer a question, or complete a task. These are moments when decisions are made and knowledge is reinforced. The goal is to capture these moments and fill them with essential pieces of information.
We offer these suggestions as a place to start. The microlearning platform allows for the collection of data on the interaction between user and course content. The data collected can be used for continuous quality improvement of the curriculum. Microlearning is a dynamic platform where creative ideas are encouraged and a multi-disciplinary approach is valuable to keeping an audience engaged. In the future, we hope to be able to correlate microlearning courses to provider performance and measurable patient outcomes.
Dr. Mercado is medical director at Alice Peck Day Memorial Hospital, and associate hospital epidemiologist, Dartmouth-Hitchcock Medical Center, both in Lebanon, N.H., and assistant professor at the Geisel School of Medicine at Dartmouth, Hanover, N.H. Dr. Feng is a Fellow in the Leadership/Preventive Medicine Program in the Department of Internal Medicine at Dartmouth-Hitchcock Medical Center.
References
1. Duggan F and Banwell L. Constructing a model of effective information dissemination in a crisis. Information Research. 2004;9(3). Paper 178 [Available at http://InformationR.net/ir/9-3/paper178.html].
2. Filipe HP, et al. Microlearning to improve CPD learning objectives. Clin Teach. 2020 Dec;17(6):695-699. doi: 10.1111/tct.13208.
3. Hegerius A, et al. E-Learning in Pharmacovigilance: An Evaluation of Microlearning-Based Modules Developed by Uppsala Monitoring Centre. Drug Saf. 2020 Nov;43(11):1171-1180. doi: 10.1007/s40264-020-00981-w.
4. Orwoll B, et al. Gamification and Microlearning for Engagement With Quality Improvement (GAMEQI): A Bundled Digital Intervention for the Prevention of Central Line-Associated Bloodstream Infection. Am J Med Qual. Jan/Feb 2018;33(1):21-29. doi: 10.1177/1062860617706542.