User login
Expert advice
I once answered online skin questions. The most popular one was, “Is my penis supposed to look like that?”
Then the site was bought by an entrepreneur with a corporate sensibility. He opened two forums: for 15 bucks, you could access the Medical Forum and ask a doctor. For 10, you could join the Community Forum and ask anybody with an opinion. One guess about which forum was more popular.
Years later, a colleague referred a fellow who had run a poison ivy website for a decade and wanted to interview a doctor. He had never spoken with one before, “because it never occurred to me.” His site featured the usual folklore: that blister fluid spreads the poison, that you can catch it from your dog. His website had many pictures. Some were in focus, and a few actually showed poison ivy.
I checked a year later and found that he had never uploaded our interview to his website. When I emailed to ask how come, he said he’d been busy, and did I want him to? I told him I was OK.
What made me think of these old episodes was a phone chat I had the other day with an IT guy about my laptop.
After I told him my problem, he said, “Since you’re a doctor, could I ask you a medical question?”
“Sure.”
“Is the COVID vaccine safe?” he asked.
“I had two shots myself,” I said, “and I’m planning a third. Does that tell you what I think about how safe it is?”
He didn’t answer, and we got back to the laptop.
Five minutes later he said, “I just wonder whether we should mess with vaccines. Maybe we should let nature take its course.”
“How about polio and diphtheria?” I said. “Should we let nature take its course with them?”
He thought for a moment and said, “If you don’t get vaccinated, can you spread the virus to other people?”
“Yes, you can,” I said. “It’s not just that you can get sick, but you can make other people sick, and possibly die if they’re old or vulnerable.”
Again, no response. We finished up with the laptop.
“Thanks for your medical advice,” he said. “I get conflicting information from so many sources.”
Yes, he does. He and everybody else always have. When the issues are poison ivy and genital blotchiness, the stakes are not high enough for anyone to talk about. To a large extent, people have always made their minds up about things based on what their friends think and tell them.
If your friends all wear masks, they will stare at you if you don’t. If your friends don’t wear masks, they will stare at you if you do. Or more than that. Very few people like to be stared at. Or worse.
or another: social media disinformation, distrust of the establishment, personal freedom. When the stakes are low, no reasons are needed. Who cares why someone blames Fido for his poison ivy?
Addressing the reasons people give for their positions, or the reasons others assign to them, may sometimes help people reconsider. For all those other times, the old adage applies: You cannot reason someone out of what he never reasoned himself into.
When it comes to contact dermatitis or penile blotches, you can try to straighten people out, but it doesn’t matter much if you fail. When the people you are trying to convince are spreading disease, filling up ICUs, or dying, it matters a great deal, which does not necessarily increase your odds of succeeding.
There have always been “Medical Forums” – where you ask a professional with official credentials – and “Community Forums” – where you ask Jerry next door or Hortense on Instagram. There always will be. Most of the time this is a curiosity of little general interest. Though not always.
Of course I believe in expert advice. I spent my whole career dispensing it.
Still, modesty is proper. Knowledge may be evolving and tentative, and sensible advice often ignored.
As Hippocrates said a long time ago: Life is short, and art long, opportunity fleeting, experimentation perilous, and judgment difficult.
They all still are.
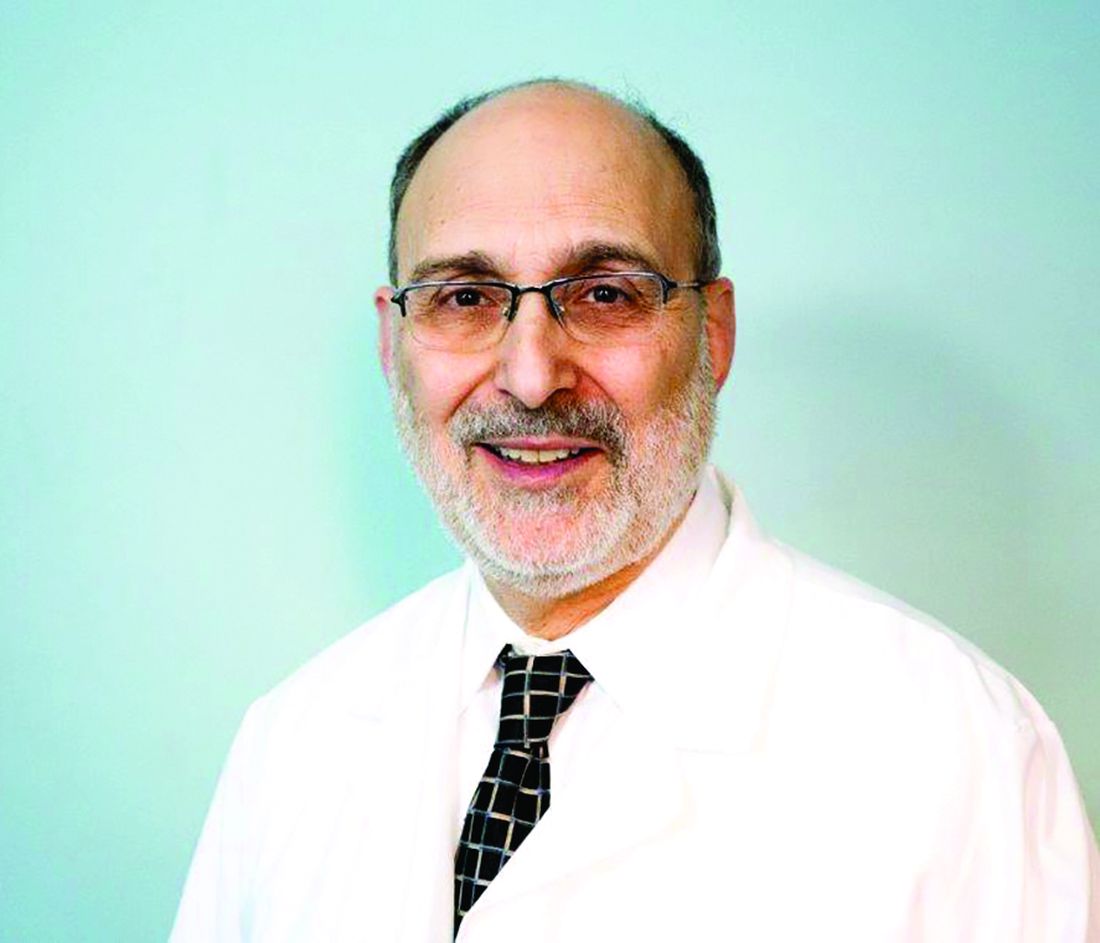
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now retired, after more than 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His latest book, “Doctoring from the Outside In,” was recently published. This is his last column for Dermatology News. Write to him at [email protected].
I once answered online skin questions. The most popular one was, “Is my penis supposed to look like that?”
Then the site was bought by an entrepreneur with a corporate sensibility. He opened two forums: for 15 bucks, you could access the Medical Forum and ask a doctor. For 10, you could join the Community Forum and ask anybody with an opinion. One guess about which forum was more popular.
Years later, a colleague referred a fellow who had run a poison ivy website for a decade and wanted to interview a doctor. He had never spoken with one before, “because it never occurred to me.” His site featured the usual folklore: that blister fluid spreads the poison, that you can catch it from your dog. His website had many pictures. Some were in focus, and a few actually showed poison ivy.
I checked a year later and found that he had never uploaded our interview to his website. When I emailed to ask how come, he said he’d been busy, and did I want him to? I told him I was OK.
What made me think of these old episodes was a phone chat I had the other day with an IT guy about my laptop.
After I told him my problem, he said, “Since you’re a doctor, could I ask you a medical question?”
“Sure.”
“Is the COVID vaccine safe?” he asked.
“I had two shots myself,” I said, “and I’m planning a third. Does that tell you what I think about how safe it is?”
He didn’t answer, and we got back to the laptop.
Five minutes later he said, “I just wonder whether we should mess with vaccines. Maybe we should let nature take its course.”
“How about polio and diphtheria?” I said. “Should we let nature take its course with them?”
He thought for a moment and said, “If you don’t get vaccinated, can you spread the virus to other people?”
“Yes, you can,” I said. “It’s not just that you can get sick, but you can make other people sick, and possibly die if they’re old or vulnerable.”
Again, no response. We finished up with the laptop.
“Thanks for your medical advice,” he said. “I get conflicting information from so many sources.”
Yes, he does. He and everybody else always have. When the issues are poison ivy and genital blotchiness, the stakes are not high enough for anyone to talk about. To a large extent, people have always made their minds up about things based on what their friends think and tell them.
If your friends all wear masks, they will stare at you if you don’t. If your friends don’t wear masks, they will stare at you if you do. Or more than that. Very few people like to be stared at. Or worse.
or another: social media disinformation, distrust of the establishment, personal freedom. When the stakes are low, no reasons are needed. Who cares why someone blames Fido for his poison ivy?
Addressing the reasons people give for their positions, or the reasons others assign to them, may sometimes help people reconsider. For all those other times, the old adage applies: You cannot reason someone out of what he never reasoned himself into.
When it comes to contact dermatitis or penile blotches, you can try to straighten people out, but it doesn’t matter much if you fail. When the people you are trying to convince are spreading disease, filling up ICUs, or dying, it matters a great deal, which does not necessarily increase your odds of succeeding.
There have always been “Medical Forums” – where you ask a professional with official credentials – and “Community Forums” – where you ask Jerry next door or Hortense on Instagram. There always will be. Most of the time this is a curiosity of little general interest. Though not always.
Of course I believe in expert advice. I spent my whole career dispensing it.
Still, modesty is proper. Knowledge may be evolving and tentative, and sensible advice often ignored.
As Hippocrates said a long time ago: Life is short, and art long, opportunity fleeting, experimentation perilous, and judgment difficult.
They all still are.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now retired, after more than 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His latest book, “Doctoring from the Outside In,” was recently published. This is his last column for Dermatology News. Write to him at [email protected].
I once answered online skin questions. The most popular one was, “Is my penis supposed to look like that?”
Then the site was bought by an entrepreneur with a corporate sensibility. He opened two forums: for 15 bucks, you could access the Medical Forum and ask a doctor. For 10, you could join the Community Forum and ask anybody with an opinion. One guess about which forum was more popular.
Years later, a colleague referred a fellow who had run a poison ivy website for a decade and wanted to interview a doctor. He had never spoken with one before, “because it never occurred to me.” His site featured the usual folklore: that blister fluid spreads the poison, that you can catch it from your dog. His website had many pictures. Some were in focus, and a few actually showed poison ivy.
I checked a year later and found that he had never uploaded our interview to his website. When I emailed to ask how come, he said he’d been busy, and did I want him to? I told him I was OK.
What made me think of these old episodes was a phone chat I had the other day with an IT guy about my laptop.
After I told him my problem, he said, “Since you’re a doctor, could I ask you a medical question?”
“Sure.”
“Is the COVID vaccine safe?” he asked.
“I had two shots myself,” I said, “and I’m planning a third. Does that tell you what I think about how safe it is?”
He didn’t answer, and we got back to the laptop.
Five minutes later he said, “I just wonder whether we should mess with vaccines. Maybe we should let nature take its course.”
“How about polio and diphtheria?” I said. “Should we let nature take its course with them?”
He thought for a moment and said, “If you don’t get vaccinated, can you spread the virus to other people?”
“Yes, you can,” I said. “It’s not just that you can get sick, but you can make other people sick, and possibly die if they’re old or vulnerable.”
Again, no response. We finished up with the laptop.
“Thanks for your medical advice,” he said. “I get conflicting information from so many sources.”
Yes, he does. He and everybody else always have. When the issues are poison ivy and genital blotchiness, the stakes are not high enough for anyone to talk about. To a large extent, people have always made their minds up about things based on what their friends think and tell them.
If your friends all wear masks, they will stare at you if you don’t. If your friends don’t wear masks, they will stare at you if you do. Or more than that. Very few people like to be stared at. Or worse.
or another: social media disinformation, distrust of the establishment, personal freedom. When the stakes are low, no reasons are needed. Who cares why someone blames Fido for his poison ivy?
Addressing the reasons people give for their positions, or the reasons others assign to them, may sometimes help people reconsider. For all those other times, the old adage applies: You cannot reason someone out of what he never reasoned himself into.
When it comes to contact dermatitis or penile blotches, you can try to straighten people out, but it doesn’t matter much if you fail. When the people you are trying to convince are spreading disease, filling up ICUs, or dying, it matters a great deal, which does not necessarily increase your odds of succeeding.
There have always been “Medical Forums” – where you ask a professional with official credentials – and “Community Forums” – where you ask Jerry next door or Hortense on Instagram. There always will be. Most of the time this is a curiosity of little general interest. Though not always.
Of course I believe in expert advice. I spent my whole career dispensing it.
Still, modesty is proper. Knowledge may be evolving and tentative, and sensible advice often ignored.
As Hippocrates said a long time ago: Life is short, and art long, opportunity fleeting, experimentation perilous, and judgment difficult.
They all still are.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now retired, after more than 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His latest book, “Doctoring from the Outside In,” was recently published. This is his last column for Dermatology News. Write to him at [email protected].
When can your hypochondria help patients?
Hypochondria has been useful to my patients. I mean my own hypochondria. It may not take one to know one, but we hypochondriacs understand each other.
Hypochondriacs worry that we are sick, worry that our fears are foolish and that we will be mocked for worrying about nothing, and worry even more that this time, we finally worried about something after all. Reassurance leaves us sheepish, then elated. Elation soon fades, and a new worry appears. Worry, rinse, repeat. . Some folks are just needy. Soothing the needs of the needy can feel like trying to drain the seven seas with a teaspoon. Those who work with people must either find ways to cope with the spectrum of neediness, or find another kind of work to do.
Some patient needs call for diagnosis and treatment. Other needs go beyond the strictly medical. Beyond knowing whether they are ill, patients have questions like, “Will this get worse?” “Will I be ashamed to go out in public?” “Can I visit my grandchildren, or will my daughter-in-law throw me out as contagious?” “Is this the beginning of the end?” or, worst of all, “Am I losing my hair?”
The list of possible patient needs is long, though not endless. Lining them up one after the other can make them sound melodramatic, even silly. (Other people’s worries often sound silly; your own never do.) Can a small growth or slight itch really cause existential agitation? Anyone who deals with complaints like these knows that the answer is yes.
Hypochondriacs with medical degrees cannot reassure themselves, but we can bring useful experience to help other members of the worry club. Doing so means paying attention not just to what doctors worry about but what patients do.
Sometimes a patient is terrified, the doctor not at all. Gentle sympathy may be enough. But the reverse can also be true: The doctor is concerned, but the patient thinks there is no problem. Sometimes I am worried enough to ask a patient to call or email an update. Patients who have already stopped worrying may not bother to answer the phone or shoot back an email. Failure to respond may mean they are fine, or in intensive care. Silence is hard to interpret.
Skin doctors have one advantageous disadvantage: Few tests help us beyond a skin scraping, the odd blood test, or a biopsy. Otherwise, most of the time all we can do is look, and perhaps apply “tincture of time,” watching the clinical course. We cannot send patients for the complex and expensive tests our colleagues use “just to be sure,” because we have no such tests to send them for.
Practice and experience help us recognize needs and worries that patients might not express. For instance, a man may show up with pimples on his back. His concerns seem intense. “What worries you?” we ask. The patient whispers, “It couldn’t be ... shingles, could it?” No, it couldn’t be shingles, because it is bilateral and for many other reasons.
The question is not whether he has shingles but why he thinks he does. Maybe his aunt suggested it. Or an article told him to watch out for it. Or his pharmacy is promoting zoster vaccination by showing huge, full-color photos of shingles cases worthy of horror movies. (Shingles the 13th!) Because he wants to visit his grandkids and his daughter is in her fourth month of pregnancy. In other words, along with the fear of cancer, fear of shingles is just out there. There are other such public concerns. Over time, we come to recognize them.
Anyone can worry, but anxiety paralyzes some to such an extent that referral to a mental health professional seems reasonable. The problem with advising it is that patients who somaticize may take exception to suggestions, however delicately put, that make us sound dismissive, locating their concern “all in the head.” Over the years, my attempts to make such referrals have met with limited success.
Dealing with needs – and neediness – can take up more of a doctor’s day than making specific diagnoses and prescribing helpful treatments. Besides, addressing needs and neediness demands skills not always stressed at school.
Practice at noting neediness makes you better at it, but no doctor nails the true wellsprings of worry all the time. We hypochondriacs can be devilishly inventive.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His latest book, “Doctoring from the Outside In,” was recently published. Write to him at [email protected].
Hypochondria has been useful to my patients. I mean my own hypochondria. It may not take one to know one, but we hypochondriacs understand each other.
Hypochondriacs worry that we are sick, worry that our fears are foolish and that we will be mocked for worrying about nothing, and worry even more that this time, we finally worried about something after all. Reassurance leaves us sheepish, then elated. Elation soon fades, and a new worry appears. Worry, rinse, repeat. . Some folks are just needy. Soothing the needs of the needy can feel like trying to drain the seven seas with a teaspoon. Those who work with people must either find ways to cope with the spectrum of neediness, or find another kind of work to do.
Some patient needs call for diagnosis and treatment. Other needs go beyond the strictly medical. Beyond knowing whether they are ill, patients have questions like, “Will this get worse?” “Will I be ashamed to go out in public?” “Can I visit my grandchildren, or will my daughter-in-law throw me out as contagious?” “Is this the beginning of the end?” or, worst of all, “Am I losing my hair?”
The list of possible patient needs is long, though not endless. Lining them up one after the other can make them sound melodramatic, even silly. (Other people’s worries often sound silly; your own never do.) Can a small growth or slight itch really cause existential agitation? Anyone who deals with complaints like these knows that the answer is yes.
Hypochondriacs with medical degrees cannot reassure themselves, but we can bring useful experience to help other members of the worry club. Doing so means paying attention not just to what doctors worry about but what patients do.
Sometimes a patient is terrified, the doctor not at all. Gentle sympathy may be enough. But the reverse can also be true: The doctor is concerned, but the patient thinks there is no problem. Sometimes I am worried enough to ask a patient to call or email an update. Patients who have already stopped worrying may not bother to answer the phone or shoot back an email. Failure to respond may mean they are fine, or in intensive care. Silence is hard to interpret.
Skin doctors have one advantageous disadvantage: Few tests help us beyond a skin scraping, the odd blood test, or a biopsy. Otherwise, most of the time all we can do is look, and perhaps apply “tincture of time,” watching the clinical course. We cannot send patients for the complex and expensive tests our colleagues use “just to be sure,” because we have no such tests to send them for.
Practice and experience help us recognize needs and worries that patients might not express. For instance, a man may show up with pimples on his back. His concerns seem intense. “What worries you?” we ask. The patient whispers, “It couldn’t be ... shingles, could it?” No, it couldn’t be shingles, because it is bilateral and for many other reasons.
The question is not whether he has shingles but why he thinks he does. Maybe his aunt suggested it. Or an article told him to watch out for it. Or his pharmacy is promoting zoster vaccination by showing huge, full-color photos of shingles cases worthy of horror movies. (Shingles the 13th!) Because he wants to visit his grandkids and his daughter is in her fourth month of pregnancy. In other words, along with the fear of cancer, fear of shingles is just out there. There are other such public concerns. Over time, we come to recognize them.
Anyone can worry, but anxiety paralyzes some to such an extent that referral to a mental health professional seems reasonable. The problem with advising it is that patients who somaticize may take exception to suggestions, however delicately put, that make us sound dismissive, locating their concern “all in the head.” Over the years, my attempts to make such referrals have met with limited success.
Dealing with needs – and neediness – can take up more of a doctor’s day than making specific diagnoses and prescribing helpful treatments. Besides, addressing needs and neediness demands skills not always stressed at school.
Practice at noting neediness makes you better at it, but no doctor nails the true wellsprings of worry all the time. We hypochondriacs can be devilishly inventive.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His latest book, “Doctoring from the Outside In,” was recently published. Write to him at [email protected].
Hypochondria has been useful to my patients. I mean my own hypochondria. It may not take one to know one, but we hypochondriacs understand each other.
Hypochondriacs worry that we are sick, worry that our fears are foolish and that we will be mocked for worrying about nothing, and worry even more that this time, we finally worried about something after all. Reassurance leaves us sheepish, then elated. Elation soon fades, and a new worry appears. Worry, rinse, repeat. . Some folks are just needy. Soothing the needs of the needy can feel like trying to drain the seven seas with a teaspoon. Those who work with people must either find ways to cope with the spectrum of neediness, or find another kind of work to do.
Some patient needs call for diagnosis and treatment. Other needs go beyond the strictly medical. Beyond knowing whether they are ill, patients have questions like, “Will this get worse?” “Will I be ashamed to go out in public?” “Can I visit my grandchildren, or will my daughter-in-law throw me out as contagious?” “Is this the beginning of the end?” or, worst of all, “Am I losing my hair?”
The list of possible patient needs is long, though not endless. Lining them up one after the other can make them sound melodramatic, even silly. (Other people’s worries often sound silly; your own never do.) Can a small growth or slight itch really cause existential agitation? Anyone who deals with complaints like these knows that the answer is yes.
Hypochondriacs with medical degrees cannot reassure themselves, but we can bring useful experience to help other members of the worry club. Doing so means paying attention not just to what doctors worry about but what patients do.
Sometimes a patient is terrified, the doctor not at all. Gentle sympathy may be enough. But the reverse can also be true: The doctor is concerned, but the patient thinks there is no problem. Sometimes I am worried enough to ask a patient to call or email an update. Patients who have already stopped worrying may not bother to answer the phone or shoot back an email. Failure to respond may mean they are fine, or in intensive care. Silence is hard to interpret.
Skin doctors have one advantageous disadvantage: Few tests help us beyond a skin scraping, the odd blood test, or a biopsy. Otherwise, most of the time all we can do is look, and perhaps apply “tincture of time,” watching the clinical course. We cannot send patients for the complex and expensive tests our colleagues use “just to be sure,” because we have no such tests to send them for.
Practice and experience help us recognize needs and worries that patients might not express. For instance, a man may show up with pimples on his back. His concerns seem intense. “What worries you?” we ask. The patient whispers, “It couldn’t be ... shingles, could it?” No, it couldn’t be shingles, because it is bilateral and for many other reasons.
The question is not whether he has shingles but why he thinks he does. Maybe his aunt suggested it. Or an article told him to watch out for it. Or his pharmacy is promoting zoster vaccination by showing huge, full-color photos of shingles cases worthy of horror movies. (Shingles the 13th!) Because he wants to visit his grandkids and his daughter is in her fourth month of pregnancy. In other words, along with the fear of cancer, fear of shingles is just out there. There are other such public concerns. Over time, we come to recognize them.
Anyone can worry, but anxiety paralyzes some to such an extent that referral to a mental health professional seems reasonable. The problem with advising it is that patients who somaticize may take exception to suggestions, however delicately put, that make us sound dismissive, locating their concern “all in the head.” Over the years, my attempts to make such referrals have met with limited success.
Dealing with needs – and neediness – can take up more of a doctor’s day than making specific diagnoses and prescribing helpful treatments. Besides, addressing needs and neediness demands skills not always stressed at school.
Practice at noting neediness makes you better at it, but no doctor nails the true wellsprings of worry all the time. We hypochondriacs can be devilishly inventive.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His latest book, “Doctoring from the Outside In,” was recently published. Write to him at [email protected].
I am the best. Sometimes.
The fifth and last time I was listed as Best of Boston was in 2019, when I shared honors with obstetrics, ice cream, interior design, and kitchenware.
My first time on that list was 10 years earlier, and came as a surprise. Though the magazine that runs the feature said that selections are “peer-generated,” I was never asked to evaluate any colleagues, so I don’t know who my admiring peers were or what they admired.
Three years later I was dropped from the list, for equally mysterious reasons. Maybe my acne patients did worse that year. Be that as it may, I was reinstated several years later. Perhaps my eczema outcomes surged.
How do you know when a doctor is good? I don’t need to remind you how many different ways we are evaluated. Hospitals and insurance companies monitor our prescribing practices and therapeutic outcomes. Many websites rate our performance. Read your own reviews, if you dare, penned by people who range from the totally disgruntled to the charmingly gruntled.
Often, their reasons are either beside the point or just wrong.
An example: (1 star out of 5): “Dr. Rockoff was terrible. He prescribed a very powerful regimen, and when I told him it was drying me out, he just insisted I keep using it.”
In fact – I was able to figure out who the patient was – my “powerful treatment” was over-the-counter benzoyl peroxide along with topical clindamycin. As for my insistence that she continue, she never came back for another visit. But she had called for refills.
You can surely come up with your own review tales.
But if patients don’t really understand how well we do, doctors are not necessarily much better at assessing colleagues. This came to mind recently when a close friend, increasingly hobbled by arthritis (you get more such friends as the years roll by) was looking into getting his knee replaced. He asked friends and family and got several names of orthopedists at respectable institutions. (I don’t know how many of them were Best of Boston, or even Best of Nashua, New Hampshire.)
The patients made these referrals because either they or people they knew had Dr. So-and-So replace their knee and had been pleased. That is nice to hear, but what does it prove? Even backup shortstops get on base sometimes.
So my friend called his rheumatologist, who recommended a knee specialist. My friend consulted that doctor, found her pleasant and personable, and liked what she had to say about the surgery and its expected aftermath.
My friend called back his rheumatologist to report his decision to go with his recommended doctor.
“I’m glad to hear that,” said the rheumatologist. “Three of my friends went to her and were very pleased.”
I am not in any way criticizing the rheumatologist. When people ask me for referrals – to internists, to plastic surgeons – I give them names of people I know or have sent patients to who had good experiences, or whom I just heard good things about. What can I really know about their diagnostic acumen or surgical dexterity?
A useful counterexample is what happened with my cousin who underwent back surgery a while back. He was considering several specialists when he had a discussion with a younger acquaintance who was chief resident in neurosurgery at a local medical center, and had actually operated with several of the surgeons under consideration. “Don’t go to Dr A,” said the young man. “It takes him 7 hours to do that procedure. Better go to Dr. B, who gets it done in under 3. The shorter operative time makes a big difference in speed of recovery.”
That is the kind of specialized and relevant knowledge that actually matters. How many referrals can you think of that you made or heard of about which the same can be said?
In the meantime, I will return to my own Bestness, which has been frequent, though intermittent. I like to think of myself as a vintage Chardonnay. Some years I am the best. Other years, not so much. Your best bet is to consult me in one of the former.
Preferably chilled.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
The fifth and last time I was listed as Best of Boston was in 2019, when I shared honors with obstetrics, ice cream, interior design, and kitchenware.
My first time on that list was 10 years earlier, and came as a surprise. Though the magazine that runs the feature said that selections are “peer-generated,” I was never asked to evaluate any colleagues, so I don’t know who my admiring peers were or what they admired.
Three years later I was dropped from the list, for equally mysterious reasons. Maybe my acne patients did worse that year. Be that as it may, I was reinstated several years later. Perhaps my eczema outcomes surged.
How do you know when a doctor is good? I don’t need to remind you how many different ways we are evaluated. Hospitals and insurance companies monitor our prescribing practices and therapeutic outcomes. Many websites rate our performance. Read your own reviews, if you dare, penned by people who range from the totally disgruntled to the charmingly gruntled.
Often, their reasons are either beside the point or just wrong.
An example: (1 star out of 5): “Dr. Rockoff was terrible. He prescribed a very powerful regimen, and when I told him it was drying me out, he just insisted I keep using it.”
In fact – I was able to figure out who the patient was – my “powerful treatment” was over-the-counter benzoyl peroxide along with topical clindamycin. As for my insistence that she continue, she never came back for another visit. But she had called for refills.
You can surely come up with your own review tales.
But if patients don’t really understand how well we do, doctors are not necessarily much better at assessing colleagues. This came to mind recently when a close friend, increasingly hobbled by arthritis (you get more such friends as the years roll by) was looking into getting his knee replaced. He asked friends and family and got several names of orthopedists at respectable institutions. (I don’t know how many of them were Best of Boston, or even Best of Nashua, New Hampshire.)
The patients made these referrals because either they or people they knew had Dr. So-and-So replace their knee and had been pleased. That is nice to hear, but what does it prove? Even backup shortstops get on base sometimes.
So my friend called his rheumatologist, who recommended a knee specialist. My friend consulted that doctor, found her pleasant and personable, and liked what she had to say about the surgery and its expected aftermath.
My friend called back his rheumatologist to report his decision to go with his recommended doctor.
“I’m glad to hear that,” said the rheumatologist. “Three of my friends went to her and were very pleased.”
I am not in any way criticizing the rheumatologist. When people ask me for referrals – to internists, to plastic surgeons – I give them names of people I know or have sent patients to who had good experiences, or whom I just heard good things about. What can I really know about their diagnostic acumen or surgical dexterity?
A useful counterexample is what happened with my cousin who underwent back surgery a while back. He was considering several specialists when he had a discussion with a younger acquaintance who was chief resident in neurosurgery at a local medical center, and had actually operated with several of the surgeons under consideration. “Don’t go to Dr A,” said the young man. “It takes him 7 hours to do that procedure. Better go to Dr. B, who gets it done in under 3. The shorter operative time makes a big difference in speed of recovery.”
That is the kind of specialized and relevant knowledge that actually matters. How many referrals can you think of that you made or heard of about which the same can be said?
In the meantime, I will return to my own Bestness, which has been frequent, though intermittent. I like to think of myself as a vintage Chardonnay. Some years I am the best. Other years, not so much. Your best bet is to consult me in one of the former.
Preferably chilled.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
The fifth and last time I was listed as Best of Boston was in 2019, when I shared honors with obstetrics, ice cream, interior design, and kitchenware.
My first time on that list was 10 years earlier, and came as a surprise. Though the magazine that runs the feature said that selections are “peer-generated,” I was never asked to evaluate any colleagues, so I don’t know who my admiring peers were or what they admired.
Three years later I was dropped from the list, for equally mysterious reasons. Maybe my acne patients did worse that year. Be that as it may, I was reinstated several years later. Perhaps my eczema outcomes surged.
How do you know when a doctor is good? I don’t need to remind you how many different ways we are evaluated. Hospitals and insurance companies monitor our prescribing practices and therapeutic outcomes. Many websites rate our performance. Read your own reviews, if you dare, penned by people who range from the totally disgruntled to the charmingly gruntled.
Often, their reasons are either beside the point or just wrong.
An example: (1 star out of 5): “Dr. Rockoff was terrible. He prescribed a very powerful regimen, and when I told him it was drying me out, he just insisted I keep using it.”
In fact – I was able to figure out who the patient was – my “powerful treatment” was over-the-counter benzoyl peroxide along with topical clindamycin. As for my insistence that she continue, she never came back for another visit. But she had called for refills.
You can surely come up with your own review tales.
But if patients don’t really understand how well we do, doctors are not necessarily much better at assessing colleagues. This came to mind recently when a close friend, increasingly hobbled by arthritis (you get more such friends as the years roll by) was looking into getting his knee replaced. He asked friends and family and got several names of orthopedists at respectable institutions. (I don’t know how many of them were Best of Boston, or even Best of Nashua, New Hampshire.)
The patients made these referrals because either they or people they knew had Dr. So-and-So replace their knee and had been pleased. That is nice to hear, but what does it prove? Even backup shortstops get on base sometimes.
So my friend called his rheumatologist, who recommended a knee specialist. My friend consulted that doctor, found her pleasant and personable, and liked what she had to say about the surgery and its expected aftermath.
My friend called back his rheumatologist to report his decision to go with his recommended doctor.
“I’m glad to hear that,” said the rheumatologist. “Three of my friends went to her and were very pleased.”
I am not in any way criticizing the rheumatologist. When people ask me for referrals – to internists, to plastic surgeons – I give them names of people I know or have sent patients to who had good experiences, or whom I just heard good things about. What can I really know about their diagnostic acumen or surgical dexterity?
A useful counterexample is what happened with my cousin who underwent back surgery a while back. He was considering several specialists when he had a discussion with a younger acquaintance who was chief resident in neurosurgery at a local medical center, and had actually operated with several of the surgeons under consideration. “Don’t go to Dr A,” said the young man. “It takes him 7 hours to do that procedure. Better go to Dr. B, who gets it done in under 3. The shorter operative time makes a big difference in speed of recovery.”
That is the kind of specialized and relevant knowledge that actually matters. How many referrals can you think of that you made or heard of about which the same can be said?
In the meantime, I will return to my own Bestness, which has been frequent, though intermittent. I like to think of myself as a vintage Chardonnay. Some years I am the best. Other years, not so much. Your best bet is to consult me in one of the former.
Preferably chilled.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Arguing with doctors
They think people should accept what experts advise. After all, experts work hard to learn accurate facts to promote the public’s best interests.
Those who disagree and justify their reluctance – to be vaccinated against COVID-19, for instance – are unrepentant. First of all, they are not so sure experts are public spirited. Perhaps doctors have something to gain from illness and approve vaccines for political reasons, or assign certain diagnoses to get higher reimbursement.
In this contentious climate, peculiar treatments and unproved “cures” are claimed to deserve more respect than so-called experts are willing to grant them: hydroxychloroquine, bleach, and so on.
From my perspective, what is notable about such public disputes with medical experts is not that they exist but that they are public. In private, people have always argued with doctors. Most of those arguments don’t reach public notice. They are not interesting enough.
For instance, as I think back over the years, I can recall:
- A man who preferred to treat his eczema using topical yogurt. And not just any yogurt: only low-fat, plain Market Basket. He had tried them all.
- The woman with perioral scarring. She had let an unlicensed practitioner apply a painful acid on her face – he never told her what the acid was, and she hadn’t asked – as she lay on a neighbor’s living room floor to have her “skin cancer” treated.
- The man with an obvious melanoma on his chest. He did not want to treat it, because his faith healer in Milwaukee, whom he had never met in person, assured him that “it’s all taken care of.”
I could go on.
I cite these examples only because they are striking. They are far from unique.
People argue with doctors for the same reason they argue with anybody – because they think they know better. They may have heard otherwise from a friend, a magazine article, a blog, a different kind of practitioner.
Many such disagreements are never spoken out loud, because people who expect to argue usually don’t show up at their doctors’ offices. They either stay home or see a different kind of healer. If they do visit a doctor whose point of view differs from their own, most keep disagreements to themselves, because few people relish in-person confrontation. Instead they go home and ignore medical advice there.
Even when overt disagreements do erupt at a medical visit, the doctor can often find a way to convince the patient to reconsider, or somehow deflect the clash. The physician has to at least try to convince a patient who thinks his melanoma has “been taken care of” to have it removed. Whereas if someone really prefers low-fat yogurt to topical steroids, there is no need to win the argument. If the patient decides at some point that his eczema is out of control, he can call and request a prescription. He usually won’t.
For dermatologists, medical arguments rarely involve stakes high enough to force the doctor to try changing patients’ minds or discharging them from the practice. Had I stayed in my original field of pediatrics, I would have confronted patients who refused to vaccinate their children. I would have had to negotiate a compromise – vaccinate “more slowly” – or else part ways with the family.
I always advised medical students, when they found themselves argued with, to separate patients’ needs from their own egos. Being challenged in a small room can be challenging. Still, what matters is how the patient fares, not how the doctor feels.
Public disputes with scientists during the COVID-19 pandemic strike me as being motivated by the same factors behind private disputes in physicians’ offices: skepticism, resentment, suspicion, and – often underlying all these – fear.
Public disputes carried out over social media allow for posturing and aggression. A tweet is a better medium behind which to cloak opinions in the mantle of a noble cause, such as personal freedom. It is also easier to express derision and hostility toward opponents, expert or otherwise, from behind the screen of a Twitter handle.
Fortunately, in everyday medical practice, in-your-face disputes don’t happen very often.
You do remember them, though.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at online. Write to him at [email protected].
They think people should accept what experts advise. After all, experts work hard to learn accurate facts to promote the public’s best interests.
Those who disagree and justify their reluctance – to be vaccinated against COVID-19, for instance – are unrepentant. First of all, they are not so sure experts are public spirited. Perhaps doctors have something to gain from illness and approve vaccines for political reasons, or assign certain diagnoses to get higher reimbursement.
In this contentious climate, peculiar treatments and unproved “cures” are claimed to deserve more respect than so-called experts are willing to grant them: hydroxychloroquine, bleach, and so on.
From my perspective, what is notable about such public disputes with medical experts is not that they exist but that they are public. In private, people have always argued with doctors. Most of those arguments don’t reach public notice. They are not interesting enough.
For instance, as I think back over the years, I can recall:
- A man who preferred to treat his eczema using topical yogurt. And not just any yogurt: only low-fat, plain Market Basket. He had tried them all.
- The woman with perioral scarring. She had let an unlicensed practitioner apply a painful acid on her face – he never told her what the acid was, and she hadn’t asked – as she lay on a neighbor’s living room floor to have her “skin cancer” treated.
- The man with an obvious melanoma on his chest. He did not want to treat it, because his faith healer in Milwaukee, whom he had never met in person, assured him that “it’s all taken care of.”
I could go on.
I cite these examples only because they are striking. They are far from unique.
People argue with doctors for the same reason they argue with anybody – because they think they know better. They may have heard otherwise from a friend, a magazine article, a blog, a different kind of practitioner.
Many such disagreements are never spoken out loud, because people who expect to argue usually don’t show up at their doctors’ offices. They either stay home or see a different kind of healer. If they do visit a doctor whose point of view differs from their own, most keep disagreements to themselves, because few people relish in-person confrontation. Instead they go home and ignore medical advice there.
Even when overt disagreements do erupt at a medical visit, the doctor can often find a way to convince the patient to reconsider, or somehow deflect the clash. The physician has to at least try to convince a patient who thinks his melanoma has “been taken care of” to have it removed. Whereas if someone really prefers low-fat yogurt to topical steroids, there is no need to win the argument. If the patient decides at some point that his eczema is out of control, he can call and request a prescription. He usually won’t.
For dermatologists, medical arguments rarely involve stakes high enough to force the doctor to try changing patients’ minds or discharging them from the practice. Had I stayed in my original field of pediatrics, I would have confronted patients who refused to vaccinate their children. I would have had to negotiate a compromise – vaccinate “more slowly” – or else part ways with the family.
I always advised medical students, when they found themselves argued with, to separate patients’ needs from their own egos. Being challenged in a small room can be challenging. Still, what matters is how the patient fares, not how the doctor feels.
Public disputes with scientists during the COVID-19 pandemic strike me as being motivated by the same factors behind private disputes in physicians’ offices: skepticism, resentment, suspicion, and – often underlying all these – fear.
Public disputes carried out over social media allow for posturing and aggression. A tweet is a better medium behind which to cloak opinions in the mantle of a noble cause, such as personal freedom. It is also easier to express derision and hostility toward opponents, expert or otherwise, from behind the screen of a Twitter handle.
Fortunately, in everyday medical practice, in-your-face disputes don’t happen very often.
You do remember them, though.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at online. Write to him at [email protected].
They think people should accept what experts advise. After all, experts work hard to learn accurate facts to promote the public’s best interests.
Those who disagree and justify their reluctance – to be vaccinated against COVID-19, for instance – are unrepentant. First of all, they are not so sure experts are public spirited. Perhaps doctors have something to gain from illness and approve vaccines for political reasons, or assign certain diagnoses to get higher reimbursement.
In this contentious climate, peculiar treatments and unproved “cures” are claimed to deserve more respect than so-called experts are willing to grant them: hydroxychloroquine, bleach, and so on.
From my perspective, what is notable about such public disputes with medical experts is not that they exist but that they are public. In private, people have always argued with doctors. Most of those arguments don’t reach public notice. They are not interesting enough.
For instance, as I think back over the years, I can recall:
- A man who preferred to treat his eczema using topical yogurt. And not just any yogurt: only low-fat, plain Market Basket. He had tried them all.
- The woman with perioral scarring. She had let an unlicensed practitioner apply a painful acid on her face – he never told her what the acid was, and she hadn’t asked – as she lay on a neighbor’s living room floor to have her “skin cancer” treated.
- The man with an obvious melanoma on his chest. He did not want to treat it, because his faith healer in Milwaukee, whom he had never met in person, assured him that “it’s all taken care of.”
I could go on.
I cite these examples only because they are striking. They are far from unique.
People argue with doctors for the same reason they argue with anybody – because they think they know better. They may have heard otherwise from a friend, a magazine article, a blog, a different kind of practitioner.
Many such disagreements are never spoken out loud, because people who expect to argue usually don’t show up at their doctors’ offices. They either stay home or see a different kind of healer. If they do visit a doctor whose point of view differs from their own, most keep disagreements to themselves, because few people relish in-person confrontation. Instead they go home and ignore medical advice there.
Even when overt disagreements do erupt at a medical visit, the doctor can often find a way to convince the patient to reconsider, or somehow deflect the clash. The physician has to at least try to convince a patient who thinks his melanoma has “been taken care of” to have it removed. Whereas if someone really prefers low-fat yogurt to topical steroids, there is no need to win the argument. If the patient decides at some point that his eczema is out of control, he can call and request a prescription. He usually won’t.
For dermatologists, medical arguments rarely involve stakes high enough to force the doctor to try changing patients’ minds or discharging them from the practice. Had I stayed in my original field of pediatrics, I would have confronted patients who refused to vaccinate their children. I would have had to negotiate a compromise – vaccinate “more slowly” – or else part ways with the family.
I always advised medical students, when they found themselves argued with, to separate patients’ needs from their own egos. Being challenged in a small room can be challenging. Still, what matters is how the patient fares, not how the doctor feels.
Public disputes with scientists during the COVID-19 pandemic strike me as being motivated by the same factors behind private disputes in physicians’ offices: skepticism, resentment, suspicion, and – often underlying all these – fear.
Public disputes carried out over social media allow for posturing and aggression. A tweet is a better medium behind which to cloak opinions in the mantle of a noble cause, such as personal freedom. It is also easier to express derision and hostility toward opponents, expert or otherwise, from behind the screen of a Twitter handle.
Fortunately, in everyday medical practice, in-your-face disputes don’t happen very often.
You do remember them, though.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at online. Write to him at [email protected].
Fenway data, the final frontier
Data, as we all know, have taken over the world. ”
Statistical objectivity is in, individuality is out. You may have taught for 30 years and gained a sense for which child has a problem that needs intervention and which one just needs patience and time to develop. You may have managed patients for decades and have a hunch about who needs immediate help and who can be watched. But “senses” and “hunches” can’t be measured and therefore do not exist, or better, don’t count. Numbers count!
Data-obsession reflects what Germans call the Zeitgeist, the spirit of the age. But the Germans will have to come up with a different word for our age, won’t they? Nobody can measure a “spirit.”
Still, you know the spirit’s there, when it knocks you over and stomps on you.
The one sphere of life that has resisted being reduced to numbers is sports. In sports, you don’t need complex analysis to know who’s No. 1 and who’s number everything else. No. 1 crosses the finish line first, wins the most games, knocks out the opponent. The one lying on the mat is No. 2.
Of course, sports always had lots of numbers. Baseball fans have always known about batting averages, runs batted in, earned run averages. But there were always those individual intangibles that goggle the eyes of small boys and keep sportswriters in business: this athlete’s “ferocious drive,” that one’s “will to win,” the way a third “always comes through in the clutch.” Pitchers who couldn’t throw fast anymore were “crafty.” Grizzled, tobacco-chewing scouts could sense which youngster “looked like a ballplayer.”
As if you didn’t already know, you can tell how old I am to talk this way. Bill James and his statistical acolytes put paid to that old kind of thinking a long time ago. Read Moneyball or see the movie. In sports too, it’s now all about the stats.
To generate flagging interest among the young for America’s now-stodgy pastime, Major League Baseball has brought out Statcast 2.0., which adds, according to a recent news story, “Doppler-based tracking of pitch velocity, exit velocity, launch angles, and spin rates, and defensive tracking of players.” Multicamera arrays produce “biomechanical imaging and skeletal models that can help pitchers with delivery issues or batters with swing path quandaries.”
And so we have lots of new data to ponder: exit velocity – how fast a hit ball leaves the bat; launch angle – what angle it leaves at; spin rate – how fast a thrown curveball spins; and defensive tracking – how many feet this shortstop can move left to snag a ground ball, or a right-fielder to catch a fly. And there are new, composite stats, like OPS (on-base plus slugging). I will not try to explain OPS, because it is a mathematical abstraction that I cannot grasp. It signifies a blend of on-base percentage and slugging percentage, which to me is like what you get when you blend a tomato with a broccoli. Or something.
And, stats aside, you do still have to win. Not long ago the Boston Red Sox had a relief pitcher whose spin rate was splendid, but he couldn’t get anybody out.
The real aim of the new broadcast innovations noted above comes at the end of the report:
In an effort to at least reach, if not grow, a younger fan base, MLB from now on will focus on video engagement, gaming, and augmented reality on Snapchat.
You got it: the goal is to reduce baseball to a video game, and its players to gaming characters, perhaps with big contracts and marketing deals. Hey, check out that dude’s OPS!
You can’t measure a Zeitgeist, but you certainly know when it’s sitting on your chest. Your respirations get depressed. Measurably.
Yeah, I sound like every cranky old man in history. But hey – I’m Emeritus! See this column’s title!
In addition, the article has one more detail:
Curiosity about whether a fly ball to deep right field at Fenway Park would be a home run at Yankee Stadium can be satisfied by overlaying the Yankee Stadium footprint on top of Fenway.
Maybe it would satisfy you, buddy, but anything that superimposes Yankee Stadium on top of Fenway Park dissatisfies me by a factor of 6.7!
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Data, as we all know, have taken over the world. ”
Statistical objectivity is in, individuality is out. You may have taught for 30 years and gained a sense for which child has a problem that needs intervention and which one just needs patience and time to develop. You may have managed patients for decades and have a hunch about who needs immediate help and who can be watched. But “senses” and “hunches” can’t be measured and therefore do not exist, or better, don’t count. Numbers count!
Data-obsession reflects what Germans call the Zeitgeist, the spirit of the age. But the Germans will have to come up with a different word for our age, won’t they? Nobody can measure a “spirit.”
Still, you know the spirit’s there, when it knocks you over and stomps on you.
The one sphere of life that has resisted being reduced to numbers is sports. In sports, you don’t need complex analysis to know who’s No. 1 and who’s number everything else. No. 1 crosses the finish line first, wins the most games, knocks out the opponent. The one lying on the mat is No. 2.
Of course, sports always had lots of numbers. Baseball fans have always known about batting averages, runs batted in, earned run averages. But there were always those individual intangibles that goggle the eyes of small boys and keep sportswriters in business: this athlete’s “ferocious drive,” that one’s “will to win,” the way a third “always comes through in the clutch.” Pitchers who couldn’t throw fast anymore were “crafty.” Grizzled, tobacco-chewing scouts could sense which youngster “looked like a ballplayer.”
As if you didn’t already know, you can tell how old I am to talk this way. Bill James and his statistical acolytes put paid to that old kind of thinking a long time ago. Read Moneyball or see the movie. In sports too, it’s now all about the stats.
To generate flagging interest among the young for America’s now-stodgy pastime, Major League Baseball has brought out Statcast 2.0., which adds, according to a recent news story, “Doppler-based tracking of pitch velocity, exit velocity, launch angles, and spin rates, and defensive tracking of players.” Multicamera arrays produce “biomechanical imaging and skeletal models that can help pitchers with delivery issues or batters with swing path quandaries.”
And so we have lots of new data to ponder: exit velocity – how fast a hit ball leaves the bat; launch angle – what angle it leaves at; spin rate – how fast a thrown curveball spins; and defensive tracking – how many feet this shortstop can move left to snag a ground ball, or a right-fielder to catch a fly. And there are new, composite stats, like OPS (on-base plus slugging). I will not try to explain OPS, because it is a mathematical abstraction that I cannot grasp. It signifies a blend of on-base percentage and slugging percentage, which to me is like what you get when you blend a tomato with a broccoli. Or something.
And, stats aside, you do still have to win. Not long ago the Boston Red Sox had a relief pitcher whose spin rate was splendid, but he couldn’t get anybody out.
The real aim of the new broadcast innovations noted above comes at the end of the report:
In an effort to at least reach, if not grow, a younger fan base, MLB from now on will focus on video engagement, gaming, and augmented reality on Snapchat.
You got it: the goal is to reduce baseball to a video game, and its players to gaming characters, perhaps with big contracts and marketing deals. Hey, check out that dude’s OPS!
You can’t measure a Zeitgeist, but you certainly know when it’s sitting on your chest. Your respirations get depressed. Measurably.
Yeah, I sound like every cranky old man in history. But hey – I’m Emeritus! See this column’s title!
In addition, the article has one more detail:
Curiosity about whether a fly ball to deep right field at Fenway Park would be a home run at Yankee Stadium can be satisfied by overlaying the Yankee Stadium footprint on top of Fenway.
Maybe it would satisfy you, buddy, but anything that superimposes Yankee Stadium on top of Fenway Park dissatisfies me by a factor of 6.7!
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Data, as we all know, have taken over the world. ”
Statistical objectivity is in, individuality is out. You may have taught for 30 years and gained a sense for which child has a problem that needs intervention and which one just needs patience and time to develop. You may have managed patients for decades and have a hunch about who needs immediate help and who can be watched. But “senses” and “hunches” can’t be measured and therefore do not exist, or better, don’t count. Numbers count!
Data-obsession reflects what Germans call the Zeitgeist, the spirit of the age. But the Germans will have to come up with a different word for our age, won’t they? Nobody can measure a “spirit.”
Still, you know the spirit’s there, when it knocks you over and stomps on you.
The one sphere of life that has resisted being reduced to numbers is sports. In sports, you don’t need complex analysis to know who’s No. 1 and who’s number everything else. No. 1 crosses the finish line first, wins the most games, knocks out the opponent. The one lying on the mat is No. 2.
Of course, sports always had lots of numbers. Baseball fans have always known about batting averages, runs batted in, earned run averages. But there were always those individual intangibles that goggle the eyes of small boys and keep sportswriters in business: this athlete’s “ferocious drive,” that one’s “will to win,” the way a third “always comes through in the clutch.” Pitchers who couldn’t throw fast anymore were “crafty.” Grizzled, tobacco-chewing scouts could sense which youngster “looked like a ballplayer.”
As if you didn’t already know, you can tell how old I am to talk this way. Bill James and his statistical acolytes put paid to that old kind of thinking a long time ago. Read Moneyball or see the movie. In sports too, it’s now all about the stats.
To generate flagging interest among the young for America’s now-stodgy pastime, Major League Baseball has brought out Statcast 2.0., which adds, according to a recent news story, “Doppler-based tracking of pitch velocity, exit velocity, launch angles, and spin rates, and defensive tracking of players.” Multicamera arrays produce “biomechanical imaging and skeletal models that can help pitchers with delivery issues or batters with swing path quandaries.”
And so we have lots of new data to ponder: exit velocity – how fast a hit ball leaves the bat; launch angle – what angle it leaves at; spin rate – how fast a thrown curveball spins; and defensive tracking – how many feet this shortstop can move left to snag a ground ball, or a right-fielder to catch a fly. And there are new, composite stats, like OPS (on-base plus slugging). I will not try to explain OPS, because it is a mathematical abstraction that I cannot grasp. It signifies a blend of on-base percentage and slugging percentage, which to me is like what you get when you blend a tomato with a broccoli. Or something.
And, stats aside, you do still have to win. Not long ago the Boston Red Sox had a relief pitcher whose spin rate was splendid, but he couldn’t get anybody out.
The real aim of the new broadcast innovations noted above comes at the end of the report:
In an effort to at least reach, if not grow, a younger fan base, MLB from now on will focus on video engagement, gaming, and augmented reality on Snapchat.
You got it: the goal is to reduce baseball to a video game, and its players to gaming characters, perhaps with big contracts and marketing deals. Hey, check out that dude’s OPS!
You can’t measure a Zeitgeist, but you certainly know when it’s sitting on your chest. Your respirations get depressed. Measurably.
Yeah, I sound like every cranky old man in history. But hey – I’m Emeritus! See this column’s title!
In addition, the article has one more detail:
Curiosity about whether a fly ball to deep right field at Fenway Park would be a home run at Yankee Stadium can be satisfied by overlaying the Yankee Stadium footprint on top of Fenway.
Maybe it would satisfy you, buddy, but anything that superimposes Yankee Stadium on top of Fenway Park dissatisfies me by a factor of 6.7!
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
The joys of telemedicine
Another great morning,
Here goes. I’ll invite Gretchen by text: 617-555-5555. “TOO LONG.” How can 10 digits be too long? Trying again: 617-555-5555. “TOO LONG!” What the heck, let me leave off the last digit: 617-555-555. “TOO SHORT.”
Never mind, I’ll invite her by email.
Five minutes have gone by. Better call to see if she got the invite.
“Hello, is this Gretchen? Don’t hang up, I’m not a telemarketer! This is Dr. Rockoff. I sent you an invitation for our computer visit.
“You got it, great. Yes, you have to click on it to sign in. I know, your appointment’s at 8:30. It’s now 8:28. Let’s start early, why not?
“Hi, there! I can see you. Can you hear me? You’re nodding and your lips are moving. I can’t hear you. Did you enable your microphone?
“Nope, still can’t hear. I’ll call your cell, and we’ll talk that way.
“Yes, it’s me, Dr. Rockoff. What’s that? You enabled the microphone along with your video when you logged on? Well, there we go. How can I help today?
“You want a refill on your tretinoin gel for age management? Not a problem. Let’s see, you’ve been using it since 1996. No, you look great! Not a day over 76, really! I’ll have the staff escribe it right over.
“Okay, take care. Three years should be about right. Happy 80th!”
Wonder what happened there. Maybe things will go better for the next patient. Okay, I’m emailing an invite to Rob.
There he is! “Hi. Can you see me? Hear me? Nope, can’t hear you. Let me just call your cell.”
Okay, 972-555-5555. Ringing ... oh no, right to voicemail. “You have reached 972-555-5555. The mailbox is full and cannot accept messages. Please try some other time.”
“Okay, I’m back with you on the screen, Rob. Nope, still can’t hear you. I tried your cell but it went to voicemail. Yes, I see you’re holding the phone in your hand. Let me try you again.
“972-555-5555. Right to voicemail. Doesn’t your phone ring? You never make voice calls, only send texts? Look, please call me: 781-555-5555, write it down.
“Excellent, we’re in business. You’re worried about a mole that’s changing. You sent a photo to the office. Great, I’ll look right now on your record ... nope, not uploaded. Can you email me the photo? Please write down my email address: alanrockoffmdskincarespecialistist@myfabuloustelemedicineportal.now. Got that? Okay, please send the picture ...
“Returned as undeliverable? Show me what you typed ... Oh, wait. It’s ‘telemedicine,’ not ‘TellaMedicine.’ ” Yeah, that should do it.
“Okay, got the picture. You do fabulous super-closeups! Is that your navel next to it? Your left nostril? Okay. You tried to razor off the hair growing out it? Yes, that could account for the bleeding. Tell you what, go easy on it for the next 2 weeks, and send me another picture. Same email address.
“You have another question? Sure. You want a refill of your clindamycin gel because the tube from 2013 ran out? Guess you haven’t grown out of your acne yet. Sure, happy to send it in for you. Same pharmacy we have on file? You’re bunking with your parents in Wichita? No problem. Just need the pharmacy name and street. Boston, Wichita, whatever.
“Sure, happy to help. Enjoy your stay with your parents. You’ve been there 4 months? Are you cleaning your room? Mostly? Good. Take care. I’ll respond to your email in 2 weeks. Meantime, you might empty out your full voicemail box ... Oh, right, your generation only texts ...”
Okay, one more. Here’s Henrietta. I emailed her an invitation ... Holy Cow, she’s checked in! Let’s see, click “Join.” I can see her!
“Henrietta, is that you? Can you hear me? You can? You can hear me! Henrietta can hear me! And I can hear her!
“Yes, Henrietta, I’m all right. Just doing cartwheels around my study. Between COVID and the 95-degree heat and 100% humidity, it’s all the exercise I get.
“How can I help you today?
“Henrietta? HENRIETTA! Where have you gone, Henrietta?”
THERE IS A PROBLEM WITH YOUR CALL. DISCONNECT YOUR ROUTER, WAIT 65 SECONDS, RECONNECT, THEN RESTART YOUR WIFI, AND LOG IN AGAIN.
Maybe it’s time to go back to the office. A face shield and HAZMAT suit are sounding better all the time.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Another great morning,
Here goes. I’ll invite Gretchen by text: 617-555-5555. “TOO LONG.” How can 10 digits be too long? Trying again: 617-555-5555. “TOO LONG!” What the heck, let me leave off the last digit: 617-555-555. “TOO SHORT.”
Never mind, I’ll invite her by email.
Five minutes have gone by. Better call to see if she got the invite.
“Hello, is this Gretchen? Don’t hang up, I’m not a telemarketer! This is Dr. Rockoff. I sent you an invitation for our computer visit.
“You got it, great. Yes, you have to click on it to sign in. I know, your appointment’s at 8:30. It’s now 8:28. Let’s start early, why not?
“Hi, there! I can see you. Can you hear me? You’re nodding and your lips are moving. I can’t hear you. Did you enable your microphone?
“Nope, still can’t hear. I’ll call your cell, and we’ll talk that way.
“Yes, it’s me, Dr. Rockoff. What’s that? You enabled the microphone along with your video when you logged on? Well, there we go. How can I help today?
“You want a refill on your tretinoin gel for age management? Not a problem. Let’s see, you’ve been using it since 1996. No, you look great! Not a day over 76, really! I’ll have the staff escribe it right over.
“Okay, take care. Three years should be about right. Happy 80th!”
Wonder what happened there. Maybe things will go better for the next patient. Okay, I’m emailing an invite to Rob.
There he is! “Hi. Can you see me? Hear me? Nope, can’t hear you. Let me just call your cell.”
Okay, 972-555-5555. Ringing ... oh no, right to voicemail. “You have reached 972-555-5555. The mailbox is full and cannot accept messages. Please try some other time.”
“Okay, I’m back with you on the screen, Rob. Nope, still can’t hear you. I tried your cell but it went to voicemail. Yes, I see you’re holding the phone in your hand. Let me try you again.
“972-555-5555. Right to voicemail. Doesn’t your phone ring? You never make voice calls, only send texts? Look, please call me: 781-555-5555, write it down.
“Excellent, we’re in business. You’re worried about a mole that’s changing. You sent a photo to the office. Great, I’ll look right now on your record ... nope, not uploaded. Can you email me the photo? Please write down my email address: alanrockoffmdskincarespecialistist@myfabuloustelemedicineportal.now. Got that? Okay, please send the picture ...
“Returned as undeliverable? Show me what you typed ... Oh, wait. It’s ‘telemedicine,’ not ‘TellaMedicine.’ ” Yeah, that should do it.
“Okay, got the picture. You do fabulous super-closeups! Is that your navel next to it? Your left nostril? Okay. You tried to razor off the hair growing out it? Yes, that could account for the bleeding. Tell you what, go easy on it for the next 2 weeks, and send me another picture. Same email address.
“You have another question? Sure. You want a refill of your clindamycin gel because the tube from 2013 ran out? Guess you haven’t grown out of your acne yet. Sure, happy to send it in for you. Same pharmacy we have on file? You’re bunking with your parents in Wichita? No problem. Just need the pharmacy name and street. Boston, Wichita, whatever.
“Sure, happy to help. Enjoy your stay with your parents. You’ve been there 4 months? Are you cleaning your room? Mostly? Good. Take care. I’ll respond to your email in 2 weeks. Meantime, you might empty out your full voicemail box ... Oh, right, your generation only texts ...”
Okay, one more. Here’s Henrietta. I emailed her an invitation ... Holy Cow, she’s checked in! Let’s see, click “Join.” I can see her!
“Henrietta, is that you? Can you hear me? You can? You can hear me! Henrietta can hear me! And I can hear her!
“Yes, Henrietta, I’m all right. Just doing cartwheels around my study. Between COVID and the 95-degree heat and 100% humidity, it’s all the exercise I get.
“How can I help you today?
“Henrietta? HENRIETTA! Where have you gone, Henrietta?”
THERE IS A PROBLEM WITH YOUR CALL. DISCONNECT YOUR ROUTER, WAIT 65 SECONDS, RECONNECT, THEN RESTART YOUR WIFI, AND LOG IN AGAIN.
Maybe it’s time to go back to the office. A face shield and HAZMAT suit are sounding better all the time.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Another great morning,
Here goes. I’ll invite Gretchen by text: 617-555-5555. “TOO LONG.” How can 10 digits be too long? Trying again: 617-555-5555. “TOO LONG!” What the heck, let me leave off the last digit: 617-555-555. “TOO SHORT.”
Never mind, I’ll invite her by email.
Five minutes have gone by. Better call to see if she got the invite.
“Hello, is this Gretchen? Don’t hang up, I’m not a telemarketer! This is Dr. Rockoff. I sent you an invitation for our computer visit.
“You got it, great. Yes, you have to click on it to sign in. I know, your appointment’s at 8:30. It’s now 8:28. Let’s start early, why not?
“Hi, there! I can see you. Can you hear me? You’re nodding and your lips are moving. I can’t hear you. Did you enable your microphone?
“Nope, still can’t hear. I’ll call your cell, and we’ll talk that way.
“Yes, it’s me, Dr. Rockoff. What’s that? You enabled the microphone along with your video when you logged on? Well, there we go. How can I help today?
“You want a refill on your tretinoin gel for age management? Not a problem. Let’s see, you’ve been using it since 1996. No, you look great! Not a day over 76, really! I’ll have the staff escribe it right over.
“Okay, take care. Three years should be about right. Happy 80th!”
Wonder what happened there. Maybe things will go better for the next patient. Okay, I’m emailing an invite to Rob.
There he is! “Hi. Can you see me? Hear me? Nope, can’t hear you. Let me just call your cell.”
Okay, 972-555-5555. Ringing ... oh no, right to voicemail. “You have reached 972-555-5555. The mailbox is full and cannot accept messages. Please try some other time.”
“Okay, I’m back with you on the screen, Rob. Nope, still can’t hear you. I tried your cell but it went to voicemail. Yes, I see you’re holding the phone in your hand. Let me try you again.
“972-555-5555. Right to voicemail. Doesn’t your phone ring? You never make voice calls, only send texts? Look, please call me: 781-555-5555, write it down.
“Excellent, we’re in business. You’re worried about a mole that’s changing. You sent a photo to the office. Great, I’ll look right now on your record ... nope, not uploaded. Can you email me the photo? Please write down my email address: alanrockoffmdskincarespecialistist@myfabuloustelemedicineportal.now. Got that? Okay, please send the picture ...
“Returned as undeliverable? Show me what you typed ... Oh, wait. It’s ‘telemedicine,’ not ‘TellaMedicine.’ ” Yeah, that should do it.
“Okay, got the picture. You do fabulous super-closeups! Is that your navel next to it? Your left nostril? Okay. You tried to razor off the hair growing out it? Yes, that could account for the bleeding. Tell you what, go easy on it for the next 2 weeks, and send me another picture. Same email address.
“You have another question? Sure. You want a refill of your clindamycin gel because the tube from 2013 ran out? Guess you haven’t grown out of your acne yet. Sure, happy to send it in for you. Same pharmacy we have on file? You’re bunking with your parents in Wichita? No problem. Just need the pharmacy name and street. Boston, Wichita, whatever.
“Sure, happy to help. Enjoy your stay with your parents. You’ve been there 4 months? Are you cleaning your room? Mostly? Good. Take care. I’ll respond to your email in 2 weeks. Meantime, you might empty out your full voicemail box ... Oh, right, your generation only texts ...”
Okay, one more. Here’s Henrietta. I emailed her an invitation ... Holy Cow, she’s checked in! Let’s see, click “Join.” I can see her!
“Henrietta, is that you? Can you hear me? You can? You can hear me! Henrietta can hear me! And I can hear her!
“Yes, Henrietta, I’m all right. Just doing cartwheels around my study. Between COVID and the 95-degree heat and 100% humidity, it’s all the exercise I get.
“How can I help you today?
“Henrietta? HENRIETTA! Where have you gone, Henrietta?”
THERE IS A PROBLEM WITH YOUR CALL. DISCONNECT YOUR ROUTER, WAIT 65 SECONDS, RECONNECT, THEN RESTART YOUR WIFI, AND LOG IN AGAIN.
Maybe it’s time to go back to the office. A face shield and HAZMAT suit are sounding better all the time.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
Practice During the Pandemic
The first installment of my new column was obsolete on arrival. It referred to walking abroad at midday, with no mention of masks and social distancing. The whole thing was so February 2020.
My last day in the office was in mid-March. Friday the 13th.
, using stored and forwarded images.
What I had in mind was visits by patients in nursing homes or too sick at home to come in. It always bothered me to see very aged and infirm patients brought to the office at great inconvenience and expense for what often turned out to be problems like xerosis or eczema that could have been managed quite well remotely.
The HMO never got back to me, though. There were too many hurdles, mostly bureaucratic rather than medical. Would insurance pay? What about consent? Malpractice? It has been interesting to watch the current crisis sweep away the inertia of such obstacles, including licensure considerations (seeing patients across state lines for cutaneous purposes). People get around to fixing the roof when it pours. Perhaps next time there will be tests, masks, respirators. Perhaps.
Seeing patients remotely has acquainted me with all the technical headaches everyone stuck at home talks and jokes about: Balky transmission (What did you say after, “and then the blood ...”?); patients who can’t figure out how to log on, or start the video, or unmute themselves, and on and on. Picture resolution is not great, as anyone knows from watching TV newscasters interview talking heads stuck in their homes.
I was never all that image-conscious, but my beard has grown fuller and my hair unkempter. Even though I sit at my desk, I do take care to keep my trousers on. Not taking any chances.
Everyone agonizes over what the “new normal” may be. Will people come back to doctors’ offices? Will practices survive economically if many patients don’t return to the office? Stay tuned. For a long time.
Mostly, though, remote visits seem to work. Helped if needed by additional, better-resolution emailed photos, it’s possible to make useful decisions, including which lesions can wait for in-person evaluation, until ...
... Until what? In an effort to keep this column up-to-the-nanosecond, I am writing it as many countries tentatively “open up.” Careful analysis of the knowledge behind this world-wide project shows ... not much. It seems to come down to some educated guesswork about what might work and what the risks might be, which leads to advice that differs widely from state to state and country to country. It’s as if people everywhere just decided that locking everyone down is a real drag, is financially ruinous, has a duration both uncertain and longer than most people and governments think they can handle, so let’s get out there and “be careful,” whatever that is said to mean.
And the risks? Well, more people will get sick and some will die. How many “extra” deaths are ethically acceptable? Thoughtful people are working on that. They’ll get back sometime to those who are still around.
I don’t blame anyone for our staggering ignorance about this terrifying new reality. But absorbing the ignorance in real time is not reassuring.
I have nothing but sympathy for those who are not emeritus, who have practices to sustain and families to feed. I didn’t ask to be born 73 years ago, and take no credit for having done so. So much of what happens to us depends on when and where we were born – two factors for which we deserve absolutely no credit – that it’s a wonder we take such pride in praising ourselves for what we think we accomplish. Having no better choice, we do the best we can.
Meantime, I am in a “high-risk” category. If I were obese, I could try to lose weight. But my risk factor is age, which tends not to decline. Risk-wise, there is just one way to exit my group.
So I don’t expect to get back to the office anytime soon. To paraphrase a comedian who shall remain nameless: I don’t want to live on in the hearts of men. I want to live on in my house.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
The first installment of my new column was obsolete on arrival. It referred to walking abroad at midday, with no mention of masks and social distancing. The whole thing was so February 2020.
My last day in the office was in mid-March. Friday the 13th.
, using stored and forwarded images.
What I had in mind was visits by patients in nursing homes or too sick at home to come in. It always bothered me to see very aged and infirm patients brought to the office at great inconvenience and expense for what often turned out to be problems like xerosis or eczema that could have been managed quite well remotely.
The HMO never got back to me, though. There were too many hurdles, mostly bureaucratic rather than medical. Would insurance pay? What about consent? Malpractice? It has been interesting to watch the current crisis sweep away the inertia of such obstacles, including licensure considerations (seeing patients across state lines for cutaneous purposes). People get around to fixing the roof when it pours. Perhaps next time there will be tests, masks, respirators. Perhaps.
Seeing patients remotely has acquainted me with all the technical headaches everyone stuck at home talks and jokes about: Balky transmission (What did you say after, “and then the blood ...”?); patients who can’t figure out how to log on, or start the video, or unmute themselves, and on and on. Picture resolution is not great, as anyone knows from watching TV newscasters interview talking heads stuck in their homes.
I was never all that image-conscious, but my beard has grown fuller and my hair unkempter. Even though I sit at my desk, I do take care to keep my trousers on. Not taking any chances.
Everyone agonizes over what the “new normal” may be. Will people come back to doctors’ offices? Will practices survive economically if many patients don’t return to the office? Stay tuned. For a long time.
Mostly, though, remote visits seem to work. Helped if needed by additional, better-resolution emailed photos, it’s possible to make useful decisions, including which lesions can wait for in-person evaluation, until ...
... Until what? In an effort to keep this column up-to-the-nanosecond, I am writing it as many countries tentatively “open up.” Careful analysis of the knowledge behind this world-wide project shows ... not much. It seems to come down to some educated guesswork about what might work and what the risks might be, which leads to advice that differs widely from state to state and country to country. It’s as if people everywhere just decided that locking everyone down is a real drag, is financially ruinous, has a duration both uncertain and longer than most people and governments think they can handle, so let’s get out there and “be careful,” whatever that is said to mean.
And the risks? Well, more people will get sick and some will die. How many “extra” deaths are ethically acceptable? Thoughtful people are working on that. They’ll get back sometime to those who are still around.
I don’t blame anyone for our staggering ignorance about this terrifying new reality. But absorbing the ignorance in real time is not reassuring.
I have nothing but sympathy for those who are not emeritus, who have practices to sustain and families to feed. I didn’t ask to be born 73 years ago, and take no credit for having done so. So much of what happens to us depends on when and where we were born – two factors for which we deserve absolutely no credit – that it’s a wonder we take such pride in praising ourselves for what we think we accomplish. Having no better choice, we do the best we can.
Meantime, I am in a “high-risk” category. If I were obese, I could try to lose weight. But my risk factor is age, which tends not to decline. Risk-wise, there is just one way to exit my group.
So I don’t expect to get back to the office anytime soon. To paraphrase a comedian who shall remain nameless: I don’t want to live on in the hearts of men. I want to live on in my house.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].
The first installment of my new column was obsolete on arrival. It referred to walking abroad at midday, with no mention of masks and social distancing. The whole thing was so February 2020.
My last day in the office was in mid-March. Friday the 13th.
, using stored and forwarded images.
What I had in mind was visits by patients in nursing homes or too sick at home to come in. It always bothered me to see very aged and infirm patients brought to the office at great inconvenience and expense for what often turned out to be problems like xerosis or eczema that could have been managed quite well remotely.
The HMO never got back to me, though. There were too many hurdles, mostly bureaucratic rather than medical. Would insurance pay? What about consent? Malpractice? It has been interesting to watch the current crisis sweep away the inertia of such obstacles, including licensure considerations (seeing patients across state lines for cutaneous purposes). People get around to fixing the roof when it pours. Perhaps next time there will be tests, masks, respirators. Perhaps.
Seeing patients remotely has acquainted me with all the technical headaches everyone stuck at home talks and jokes about: Balky transmission (What did you say after, “and then the blood ...”?); patients who can’t figure out how to log on, or start the video, or unmute themselves, and on and on. Picture resolution is not great, as anyone knows from watching TV newscasters interview talking heads stuck in their homes.
I was never all that image-conscious, but my beard has grown fuller and my hair unkempter. Even though I sit at my desk, I do take care to keep my trousers on. Not taking any chances.
Everyone agonizes over what the “new normal” may be. Will people come back to doctors’ offices? Will practices survive economically if many patients don’t return to the office? Stay tuned. For a long time.
Mostly, though, remote visits seem to work. Helped if needed by additional, better-resolution emailed photos, it’s possible to make useful decisions, including which lesions can wait for in-person evaluation, until ...
... Until what? In an effort to keep this column up-to-the-nanosecond, I am writing it as many countries tentatively “open up.” Careful analysis of the knowledge behind this world-wide project shows ... not much. It seems to come down to some educated guesswork about what might work and what the risks might be, which leads to advice that differs widely from state to state and country to country. It’s as if people everywhere just decided that locking everyone down is a real drag, is financially ruinous, has a duration both uncertain and longer than most people and governments think they can handle, so let’s get out there and “be careful,” whatever that is said to mean.
And the risks? Well, more people will get sick and some will die. How many “extra” deaths are ethically acceptable? Thoughtful people are working on that. They’ll get back sometime to those who are still around.
I don’t blame anyone for our staggering ignorance about this terrifying new reality. But absorbing the ignorance in real time is not reassuring.
I have nothing but sympathy for those who are not emeritus, who have practices to sustain and families to feed. I didn’t ask to be born 73 years ago, and take no credit for having done so. So much of what happens to us depends on when and where we were born – two factors for which we deserve absolutely no credit – that it’s a wonder we take such pride in praising ourselves for what we think we accomplish. Having no better choice, we do the best we can.
Meantime, I am in a “high-risk” category. If I were obese, I could try to lose weight. But my risk factor is age, which tends not to decline. Risk-wise, there is just one way to exit my group.
So I don’t expect to get back to the office anytime soon. To paraphrase a comedian who shall remain nameless: I don’t want to live on in the hearts of men. I want to live on in my house.
Dr. Rockoff, who wrote the Dermatology News column “Under My Skin,” is now semiretired, after 40 years of practice in Brookline, Mass. He served on the clinical faculty at Tufts University, Boston, and taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available online. Write to him at [email protected].