User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Federal Trade Commission Bans Noncompete Agreements, Urges More Protections for Healthcare Workers
But business groups have vowed to challenge the decision in court.
The proposed final rule passed on a 3-2 vote, with the dissenting commissioners disputing the FTC’s authority to broadly ban noncompetes.
Tensions around noncompetes have been building for years. In 2021, President Biden issued an executive order supporting measures to improve economic competition, in which he urged the FTC to consider its rulemaking authority to address noncompete clauses that unfairly limit workers’ mobility. In January 2023, per that directive, the agency proposed ending the restrictive covenants.
While the FTC estimates that the final rule will reduce healthcare costs by up to $194 billion over the next decade and increase worker earnings by $300 million annually, the ruling faces legal hurdles.
US Chamber of Commerce president and CEO Suzanne P. Clark said in a statement that the move is a “blatant power grab” that will undermine competitive business practices, adding that the Chamber will sue to block the measure.
The FTC received more than 26,000 comments on noncompetes during the public feedback period, with about 25,000 supporting the measure, said Benjamin Cady, JD, an FTC attorney.
Mr. Cady called the feedback “compelling,” citing instances of workers who were forced to commute long distances, uproot their families, or risk expensive litigation for wanting to pursue job opportunities.
For example, a comment from a physician working in Appalachia highlights the potential real-life implications of the agreements. “With hospital systems merging, providers with aggressive noncompetes must abandon the community that they serve if they [choose] to leave their employer. Healthcare providers feel trapped in their current employment situation, leading to significant burnout that can shorten their [career] longevity.”
Commissioner Alvaro Bedoya said physicians have had their lives upended by cumbersome noncompetes, often having to move out of state to practice. “A pandemic killed a million people in this country, and there are doctors who cannot work because of a noncompete,” he said.
It’s unclear whether physicians and others who work for nonprofit healthcare groups or hospitals will be covered by the new ban. FTC Commissioner Rebecca Slaughter acknowledged that the agency’s jurisdictional limitations mean that employees of “certain nonprofit organizations” may not benefit from the rule.
“We want to be transparent about the limitation and recognize there are workers, especially healthcare workers, who are bound by anticompetitive and unfair noncompete clauses, that our rule will struggle to reach,” she said. To cover nonprofit healthcare employees, Ms. Slaughter urged Congress to pass legislation banning noncompetes, such as the Workforce Mobility Act of 2021 and the Freedom to Compete Act of 2023.
The FTC final rule will take effect 120 days after it is published in the federal register, and new noncompete agreements will be banned as of this date. However, existing contracts for senior executives will remain in effect because these individuals are less likely to experience “acute harm” due to their ability to negotiate accordingly, said Mr. Cady.
States, AMA Take Aim at Noncompetes
Before the federal ban, several states had already passed legislation limiting the reach of noncompetes. According to a recent article in the Journal of the American College of Cardiology, 12 states prohibit noncompete clauses for physicians: Alabama, California, Colorado, Delaware, Massachusetts, Montana, New Hampshire, New Mexico, North Dakota, Oklahoma, Rhode Island, and South Dakota.
The remaining states allow noncompetes in some form, often excluding them for employees earning below a certain threshold. For example, in Oregon, noncompete agreements may apply to employees earning more than $113,241. Most states have provisions to adjust the threshold annually. The District of Columbia permits 2-year noncompetes for “medical specialists” earning over $250,000 annually.
Indiana employers can no longer enter into noncompete agreements with primary care providers. Other specialties may be subject to the clauses, except when the physician terminates the contract for cause or when an employer terminates the contract without cause.
Rachel Marcus, MD, a cardiologist in Washington, DC, found out how limiting her employment contract’s noncompete clause was when she wanted to leave a former position. Due to the restrictions, she told this news organization that she couldn’t work locally for a competitor for 2 years. The closest location she could seek employment without violating the agreement was Baltimore, approximately 40 miles away.
Dr. Marcus ultimately moved to another position within the same organization because of the company’s reputation for being “aggressive” in their enforcement actions.
Although the American Medical Association (AMA) does not support a total ban, its House of Delegates adopted policies last year to support the prohibition of noncompete contracts for physicians employed by for-profit or nonprofit hospitals, hospital systems, or staffing companies.
Challenges Await
The American Hospital Association, which opposed the proposed rule, called it “bad policy.” The decision “will likely be short-lived, with courts almost certain to stop it before it can do damage to hospitals’ ability to care for their patients and communities,” the association said in a statement.
To ease the transition to the new rule, the FTC also released a model language for employers to use when discussing the changes with their employees. “All employers need to do to comply with the rule is to stop enforcing existing noncompetes with workers other than senior executives and provide notice to such workers,” he said.
Dr. Marcus hopes the ban improves doctors’ lives. “Your employer is going to have to treat you better because they know that you can easily go across town to a place that has a higher salary, and your patient can go with you.”
A version of this article appeared on Medscape.com.
But business groups have vowed to challenge the decision in court.
The proposed final rule passed on a 3-2 vote, with the dissenting commissioners disputing the FTC’s authority to broadly ban noncompetes.
Tensions around noncompetes have been building for years. In 2021, President Biden issued an executive order supporting measures to improve economic competition, in which he urged the FTC to consider its rulemaking authority to address noncompete clauses that unfairly limit workers’ mobility. In January 2023, per that directive, the agency proposed ending the restrictive covenants.
While the FTC estimates that the final rule will reduce healthcare costs by up to $194 billion over the next decade and increase worker earnings by $300 million annually, the ruling faces legal hurdles.
US Chamber of Commerce president and CEO Suzanne P. Clark said in a statement that the move is a “blatant power grab” that will undermine competitive business practices, adding that the Chamber will sue to block the measure.
The FTC received more than 26,000 comments on noncompetes during the public feedback period, with about 25,000 supporting the measure, said Benjamin Cady, JD, an FTC attorney.
Mr. Cady called the feedback “compelling,” citing instances of workers who were forced to commute long distances, uproot their families, or risk expensive litigation for wanting to pursue job opportunities.
For example, a comment from a physician working in Appalachia highlights the potential real-life implications of the agreements. “With hospital systems merging, providers with aggressive noncompetes must abandon the community that they serve if they [choose] to leave their employer. Healthcare providers feel trapped in their current employment situation, leading to significant burnout that can shorten their [career] longevity.”
Commissioner Alvaro Bedoya said physicians have had their lives upended by cumbersome noncompetes, often having to move out of state to practice. “A pandemic killed a million people in this country, and there are doctors who cannot work because of a noncompete,” he said.
It’s unclear whether physicians and others who work for nonprofit healthcare groups or hospitals will be covered by the new ban. FTC Commissioner Rebecca Slaughter acknowledged that the agency’s jurisdictional limitations mean that employees of “certain nonprofit organizations” may not benefit from the rule.
“We want to be transparent about the limitation and recognize there are workers, especially healthcare workers, who are bound by anticompetitive and unfair noncompete clauses, that our rule will struggle to reach,” she said. To cover nonprofit healthcare employees, Ms. Slaughter urged Congress to pass legislation banning noncompetes, such as the Workforce Mobility Act of 2021 and the Freedom to Compete Act of 2023.
The FTC final rule will take effect 120 days after it is published in the federal register, and new noncompete agreements will be banned as of this date. However, existing contracts for senior executives will remain in effect because these individuals are less likely to experience “acute harm” due to their ability to negotiate accordingly, said Mr. Cady.
States, AMA Take Aim at Noncompetes
Before the federal ban, several states had already passed legislation limiting the reach of noncompetes. According to a recent article in the Journal of the American College of Cardiology, 12 states prohibit noncompete clauses for physicians: Alabama, California, Colorado, Delaware, Massachusetts, Montana, New Hampshire, New Mexico, North Dakota, Oklahoma, Rhode Island, and South Dakota.
The remaining states allow noncompetes in some form, often excluding them for employees earning below a certain threshold. For example, in Oregon, noncompete agreements may apply to employees earning more than $113,241. Most states have provisions to adjust the threshold annually. The District of Columbia permits 2-year noncompetes for “medical specialists” earning over $250,000 annually.
Indiana employers can no longer enter into noncompete agreements with primary care providers. Other specialties may be subject to the clauses, except when the physician terminates the contract for cause or when an employer terminates the contract without cause.
Rachel Marcus, MD, a cardiologist in Washington, DC, found out how limiting her employment contract’s noncompete clause was when she wanted to leave a former position. Due to the restrictions, she told this news organization that she couldn’t work locally for a competitor for 2 years. The closest location she could seek employment without violating the agreement was Baltimore, approximately 40 miles away.
Dr. Marcus ultimately moved to another position within the same organization because of the company’s reputation for being “aggressive” in their enforcement actions.
Although the American Medical Association (AMA) does not support a total ban, its House of Delegates adopted policies last year to support the prohibition of noncompete contracts for physicians employed by for-profit or nonprofit hospitals, hospital systems, or staffing companies.
Challenges Await
The American Hospital Association, which opposed the proposed rule, called it “bad policy.” The decision “will likely be short-lived, with courts almost certain to stop it before it can do damage to hospitals’ ability to care for their patients and communities,” the association said in a statement.
To ease the transition to the new rule, the FTC also released a model language for employers to use when discussing the changes with their employees. “All employers need to do to comply with the rule is to stop enforcing existing noncompetes with workers other than senior executives and provide notice to such workers,” he said.
Dr. Marcus hopes the ban improves doctors’ lives. “Your employer is going to have to treat you better because they know that you can easily go across town to a place that has a higher salary, and your patient can go with you.”
A version of this article appeared on Medscape.com.
But business groups have vowed to challenge the decision in court.
The proposed final rule passed on a 3-2 vote, with the dissenting commissioners disputing the FTC’s authority to broadly ban noncompetes.
Tensions around noncompetes have been building for years. In 2021, President Biden issued an executive order supporting measures to improve economic competition, in which he urged the FTC to consider its rulemaking authority to address noncompete clauses that unfairly limit workers’ mobility. In January 2023, per that directive, the agency proposed ending the restrictive covenants.
While the FTC estimates that the final rule will reduce healthcare costs by up to $194 billion over the next decade and increase worker earnings by $300 million annually, the ruling faces legal hurdles.
US Chamber of Commerce president and CEO Suzanne P. Clark said in a statement that the move is a “blatant power grab” that will undermine competitive business practices, adding that the Chamber will sue to block the measure.
The FTC received more than 26,000 comments on noncompetes during the public feedback period, with about 25,000 supporting the measure, said Benjamin Cady, JD, an FTC attorney.
Mr. Cady called the feedback “compelling,” citing instances of workers who were forced to commute long distances, uproot their families, or risk expensive litigation for wanting to pursue job opportunities.
For example, a comment from a physician working in Appalachia highlights the potential real-life implications of the agreements. “With hospital systems merging, providers with aggressive noncompetes must abandon the community that they serve if they [choose] to leave their employer. Healthcare providers feel trapped in their current employment situation, leading to significant burnout that can shorten their [career] longevity.”
Commissioner Alvaro Bedoya said physicians have had their lives upended by cumbersome noncompetes, often having to move out of state to practice. “A pandemic killed a million people in this country, and there are doctors who cannot work because of a noncompete,” he said.
It’s unclear whether physicians and others who work for nonprofit healthcare groups or hospitals will be covered by the new ban. FTC Commissioner Rebecca Slaughter acknowledged that the agency’s jurisdictional limitations mean that employees of “certain nonprofit organizations” may not benefit from the rule.
“We want to be transparent about the limitation and recognize there are workers, especially healthcare workers, who are bound by anticompetitive and unfair noncompete clauses, that our rule will struggle to reach,” she said. To cover nonprofit healthcare employees, Ms. Slaughter urged Congress to pass legislation banning noncompetes, such as the Workforce Mobility Act of 2021 and the Freedom to Compete Act of 2023.
The FTC final rule will take effect 120 days after it is published in the federal register, and new noncompete agreements will be banned as of this date. However, existing contracts for senior executives will remain in effect because these individuals are less likely to experience “acute harm” due to their ability to negotiate accordingly, said Mr. Cady.
States, AMA Take Aim at Noncompetes
Before the federal ban, several states had already passed legislation limiting the reach of noncompetes. According to a recent article in the Journal of the American College of Cardiology, 12 states prohibit noncompete clauses for physicians: Alabama, California, Colorado, Delaware, Massachusetts, Montana, New Hampshire, New Mexico, North Dakota, Oklahoma, Rhode Island, and South Dakota.
The remaining states allow noncompetes in some form, often excluding them for employees earning below a certain threshold. For example, in Oregon, noncompete agreements may apply to employees earning more than $113,241. Most states have provisions to adjust the threshold annually. The District of Columbia permits 2-year noncompetes for “medical specialists” earning over $250,000 annually.
Indiana employers can no longer enter into noncompete agreements with primary care providers. Other specialties may be subject to the clauses, except when the physician terminates the contract for cause or when an employer terminates the contract without cause.
Rachel Marcus, MD, a cardiologist in Washington, DC, found out how limiting her employment contract’s noncompete clause was when she wanted to leave a former position. Due to the restrictions, she told this news organization that she couldn’t work locally for a competitor for 2 years. The closest location she could seek employment without violating the agreement was Baltimore, approximately 40 miles away.
Dr. Marcus ultimately moved to another position within the same organization because of the company’s reputation for being “aggressive” in their enforcement actions.
Although the American Medical Association (AMA) does not support a total ban, its House of Delegates adopted policies last year to support the prohibition of noncompete contracts for physicians employed by for-profit or nonprofit hospitals, hospital systems, or staffing companies.
Challenges Await
The American Hospital Association, which opposed the proposed rule, called it “bad policy.” The decision “will likely be short-lived, with courts almost certain to stop it before it can do damage to hospitals’ ability to care for their patients and communities,” the association said in a statement.
To ease the transition to the new rule, the FTC also released a model language for employers to use when discussing the changes with their employees. “All employers need to do to comply with the rule is to stop enforcing existing noncompetes with workers other than senior executives and provide notice to such workers,” he said.
Dr. Marcus hopes the ban improves doctors’ lives. “Your employer is going to have to treat you better because they know that you can easily go across town to a place that has a higher salary, and your patient can go with you.”
A version of this article appeared on Medscape.com.
Are Women Better Doctors Than Men?
This transcript has been edited for clarity.
It’s a battle of the sexes today as we dive into a paper that makes you say, “Wow, what an interesting study” and also “Boy, am I glad I didn’t do that study.” That’s because studies like this are always somewhat fraught; they say something about medicine but also something about society — and that makes this a bit precarious. But that’s never stopped us before. So, let’s go ahead and try to answer the question: Do women make better doctors than men?
On the surface, this question seems nearly impossible to answer. It’s too broad; what does it mean to be a “better” doctor? At first blush it seems that there are just too many variables to control for here: the type of doctor, the type of patient, the clinical scenario, and so on.
But this study, “Comparison of hospital mortality and readmission rates by physician and patient sex,” which appears in Annals of Internal Medicine, uses a fairly ingenious method to cut through all the bias by leveraging two simple facts: First, hospital medicine is largely conducted by hospitalists these days; second, due to the shift-based nature of hospitalist work, the hospitalist you get when you are admitted to the hospital is pretty much random.
In other words, if you are admitted to the hospital for an acute illness and get a hospitalist as your attending, you have no control over whether it is a man or a woman. Is this a randomized trial? No, but it’s not bad.
Researchers used Medicare claims data to identify adults over age 65 who had nonelective hospital admissions throughout the United States. The claims revealed the sex of the patient and the name of the attending physician. By linking to a medical provider database, they could determine the sex of the provider.
The goal was to look at outcomes across four dyads:
- Male patient – male doctor
- Male patient – female doctor
- Female patient – male doctor
- Female patient – female doctor
The primary outcome was 30-day mortality.
I told you that focusing on hospitalists produces some pseudorandomization, but let’s look at the data to be sure. Just under a million patients were treated by approximately 50,000 physicians, 30% of whom were female. And, though female patients and male patients differed, they did not differ with respect to the sex of their hospitalist. So, by physician sex, patients were similar in mean age, race, ethnicity, household income, eligibility for Medicaid, and comorbid conditions. The authors even created a “predicted mortality” score which was similar across the groups as well.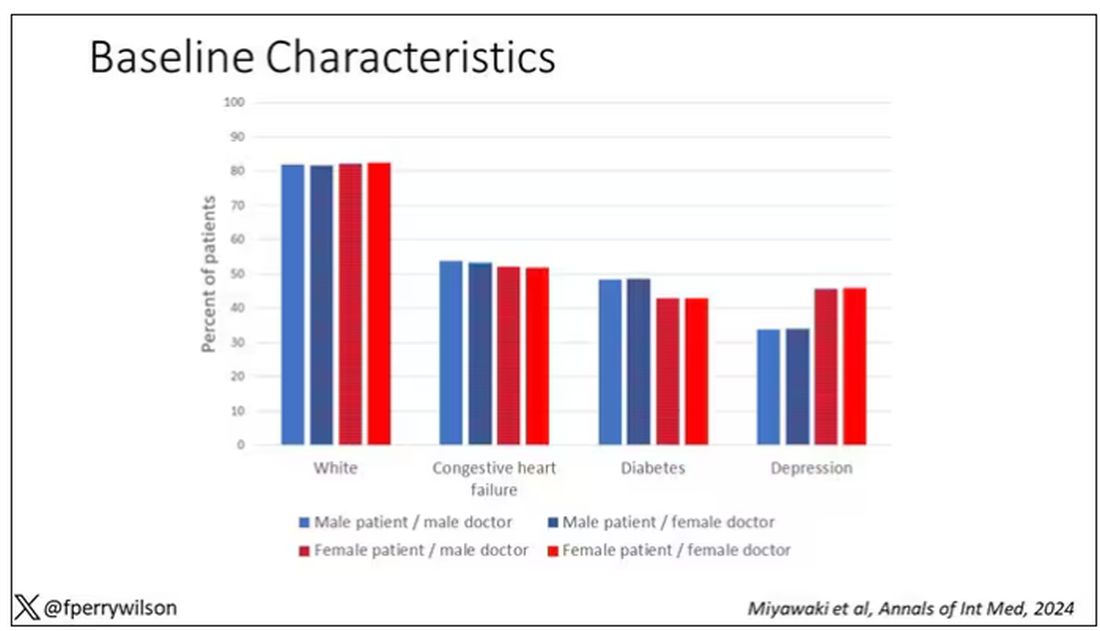
Now, the female physicians were a bit different from the male physicians. The female hospitalists were slightly more likely to have an osteopathic degree, had slightly fewer admissions per year, and were a bit younger.
So, we have broadly similar patients regardless of who their hospitalist was, but hospitalists differ by factors other than their sex. Fine.
I’ve graphed the results here. 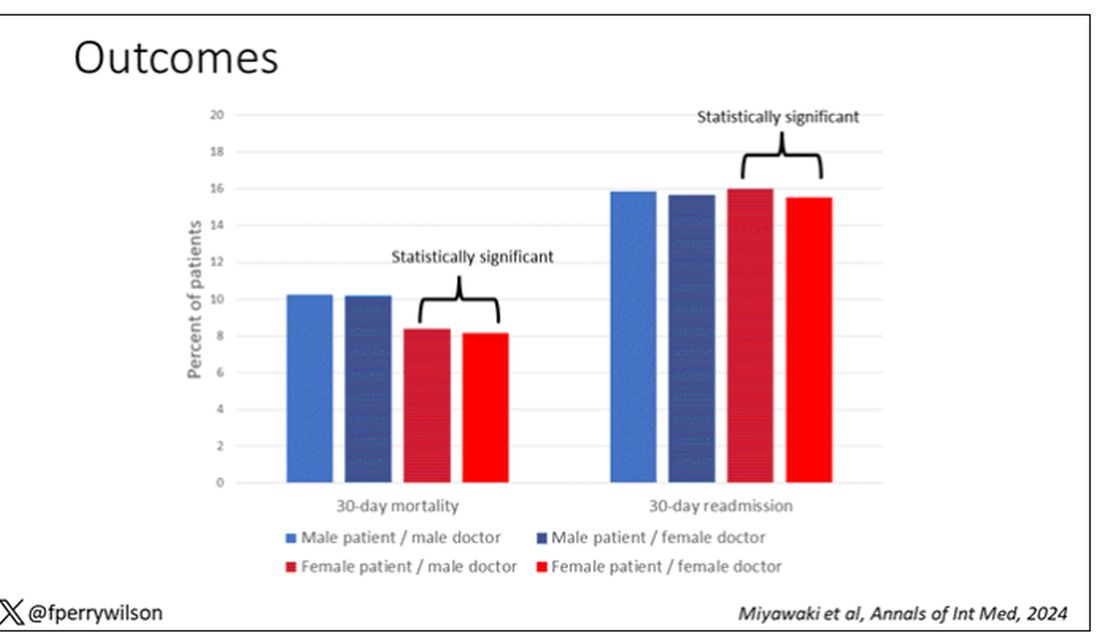
This is a relatively small effect, to be sure, but if you multiply it across the millions of hospitalist admissions per year, you can start to put up some real numbers.
So, what is going on here? I see four broad buckets of possibilities.
Let’s start with the obvious explanation: Women, on average, are better doctors than men. I am married to a woman doctor, and based on my personal experience, this explanation is undoubtedly true. But why would that be?
The authors cite data that suggest that female physicians are less likely than male physicians to dismiss patient concerns — and in particular, the concerns of female patients — perhaps leading to fewer missed diagnoses. But this is impossible to measure with administrative data, so this study can no more tell us whether these female hospitalists are more attentive than their male counterparts than it can suggest that the benefit is mediated by the shorter average height of female physicians. Perhaps the key is being closer to the patient?
The second possibility here is that this has nothing to do with the sex of the physician at all; it has to do with those other things that associate with the sex of the physician. We know, for example, that the female physicians saw fewer patients per year than the male physicians, but the study authors adjusted for this in the statistical models. Still, other unmeasured factors (confounders) could be present. By the way, confounders wouldn’t necessarily change the primary finding — you are better off being cared for by female physicians. It’s just not because they are female; it’s a convenient marker for some other quality, such as age.
The third possibility is that the study represents a phenomenon called collider bias. The idea here is that physicians only get into the study if they are hospitalists, and the quality of physicians who choose to become a hospitalist may differ by sex. When deciding on a specialty, a talented resident considering certain lifestyle issues may find hospital medicine particularly attractive — and that draw toward a more lifestyle-friendly specialty may differ by sex, as some prior studies have shown. If true, the pool of women hospitalists may be better than their male counterparts because male physicians of that caliber don’t become hospitalists.
Okay, don’t write in. I’m just trying to cite examples of how to think about collider bias. I can’t prove that this is the case, and in fact the authors do a sensitivity analysis of all physicians, not just hospitalists, and show the same thing. So this is probably not true, but epidemiology is fun, right?
And the fourth possibility: This is nothing but statistical noise. The effect size is incredibly small and just on the border of statistical significance. Especially when you’re working with very large datasets like this, you’ve got to be really careful about overinterpreting statistically significant findings that are nevertheless of small magnitude.
Regardless, it’s an interesting study, one that made me think and, of course, worry a bit about how I would present it. Forgive me if I’ve been indelicate in handling the complex issues of sex, gender, and society here. But I’m not sure what you expect; after all, I’m only a male doctor.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s a battle of the sexes today as we dive into a paper that makes you say, “Wow, what an interesting study” and also “Boy, am I glad I didn’t do that study.” That’s because studies like this are always somewhat fraught; they say something about medicine but also something about society — and that makes this a bit precarious. But that’s never stopped us before. So, let’s go ahead and try to answer the question: Do women make better doctors than men?
On the surface, this question seems nearly impossible to answer. It’s too broad; what does it mean to be a “better” doctor? At first blush it seems that there are just too many variables to control for here: the type of doctor, the type of patient, the clinical scenario, and so on.
But this study, “Comparison of hospital mortality and readmission rates by physician and patient sex,” which appears in Annals of Internal Medicine, uses a fairly ingenious method to cut through all the bias by leveraging two simple facts: First, hospital medicine is largely conducted by hospitalists these days; second, due to the shift-based nature of hospitalist work, the hospitalist you get when you are admitted to the hospital is pretty much random.
In other words, if you are admitted to the hospital for an acute illness and get a hospitalist as your attending, you have no control over whether it is a man or a woman. Is this a randomized trial? No, but it’s not bad.
Researchers used Medicare claims data to identify adults over age 65 who had nonelective hospital admissions throughout the United States. The claims revealed the sex of the patient and the name of the attending physician. By linking to a medical provider database, they could determine the sex of the provider.
The goal was to look at outcomes across four dyads:
- Male patient – male doctor
- Male patient – female doctor
- Female patient – male doctor
- Female patient – female doctor
The primary outcome was 30-day mortality.
I told you that focusing on hospitalists produces some pseudorandomization, but let’s look at the data to be sure. Just under a million patients were treated by approximately 50,000 physicians, 30% of whom were female. And, though female patients and male patients differed, they did not differ with respect to the sex of their hospitalist. So, by physician sex, patients were similar in mean age, race, ethnicity, household income, eligibility for Medicaid, and comorbid conditions. The authors even created a “predicted mortality” score which was similar across the groups as well.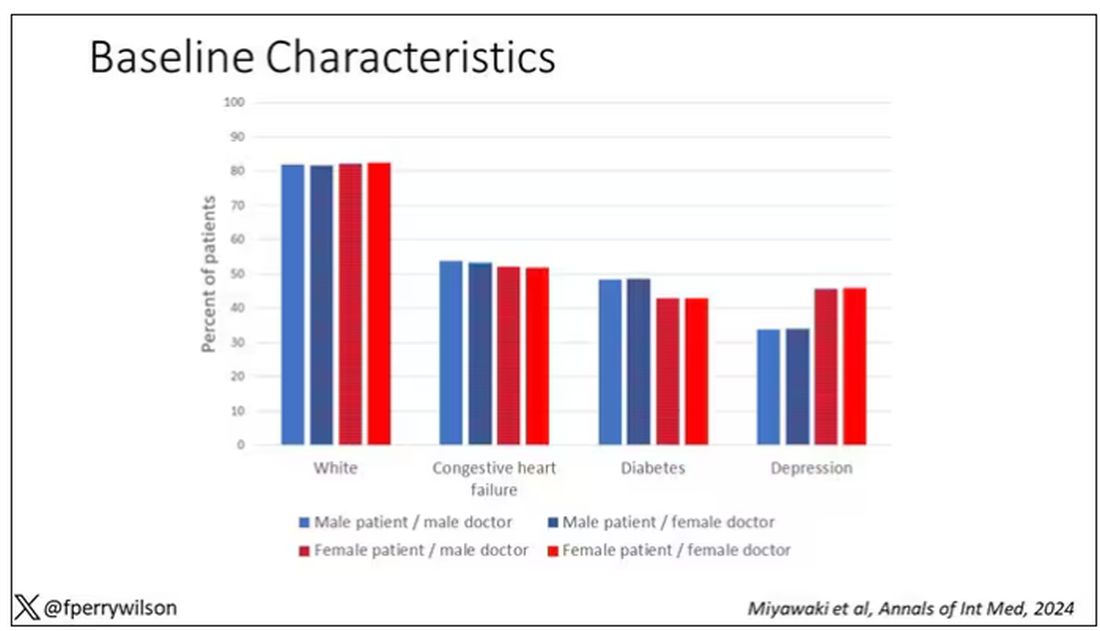
Now, the female physicians were a bit different from the male physicians. The female hospitalists were slightly more likely to have an osteopathic degree, had slightly fewer admissions per year, and were a bit younger.
So, we have broadly similar patients regardless of who their hospitalist was, but hospitalists differ by factors other than their sex. Fine.
I’ve graphed the results here. 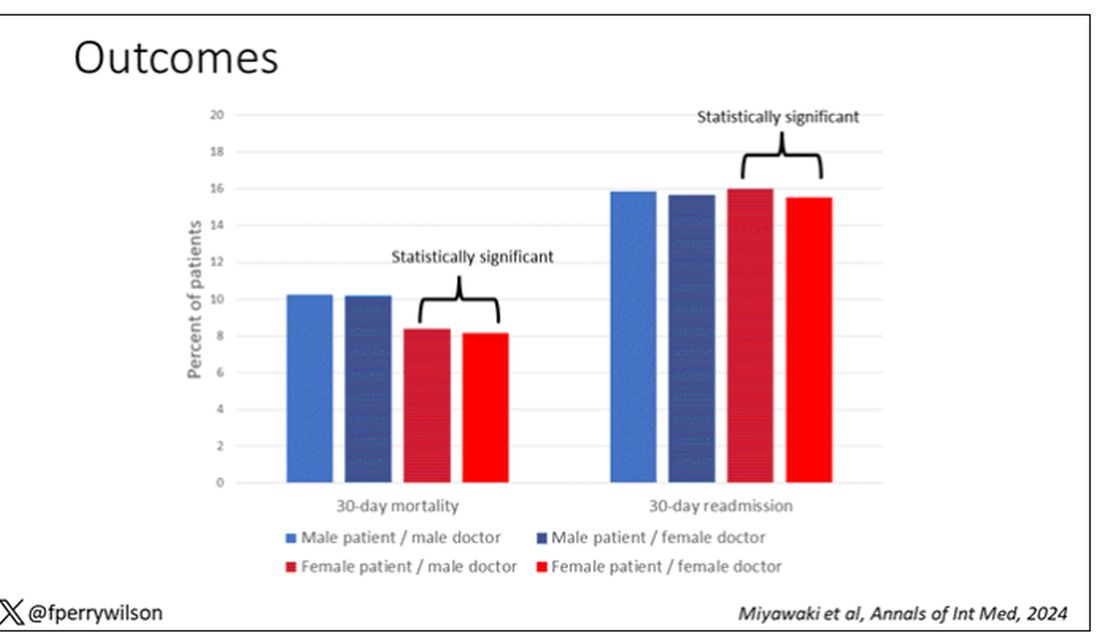
This is a relatively small effect, to be sure, but if you multiply it across the millions of hospitalist admissions per year, you can start to put up some real numbers.
So, what is going on here? I see four broad buckets of possibilities.
Let’s start with the obvious explanation: Women, on average, are better doctors than men. I am married to a woman doctor, and based on my personal experience, this explanation is undoubtedly true. But why would that be?
The authors cite data that suggest that female physicians are less likely than male physicians to dismiss patient concerns — and in particular, the concerns of female patients — perhaps leading to fewer missed diagnoses. But this is impossible to measure with administrative data, so this study can no more tell us whether these female hospitalists are more attentive than their male counterparts than it can suggest that the benefit is mediated by the shorter average height of female physicians. Perhaps the key is being closer to the patient?
The second possibility here is that this has nothing to do with the sex of the physician at all; it has to do with those other things that associate with the sex of the physician. We know, for example, that the female physicians saw fewer patients per year than the male physicians, but the study authors adjusted for this in the statistical models. Still, other unmeasured factors (confounders) could be present. By the way, confounders wouldn’t necessarily change the primary finding — you are better off being cared for by female physicians. It’s just not because they are female; it’s a convenient marker for some other quality, such as age.
The third possibility is that the study represents a phenomenon called collider bias. The idea here is that physicians only get into the study if they are hospitalists, and the quality of physicians who choose to become a hospitalist may differ by sex. When deciding on a specialty, a talented resident considering certain lifestyle issues may find hospital medicine particularly attractive — and that draw toward a more lifestyle-friendly specialty may differ by sex, as some prior studies have shown. If true, the pool of women hospitalists may be better than their male counterparts because male physicians of that caliber don’t become hospitalists.
Okay, don’t write in. I’m just trying to cite examples of how to think about collider bias. I can’t prove that this is the case, and in fact the authors do a sensitivity analysis of all physicians, not just hospitalists, and show the same thing. So this is probably not true, but epidemiology is fun, right?
And the fourth possibility: This is nothing but statistical noise. The effect size is incredibly small and just on the border of statistical significance. Especially when you’re working with very large datasets like this, you’ve got to be really careful about overinterpreting statistically significant findings that are nevertheless of small magnitude.
Regardless, it’s an interesting study, one that made me think and, of course, worry a bit about how I would present it. Forgive me if I’ve been indelicate in handling the complex issues of sex, gender, and society here. But I’m not sure what you expect; after all, I’m only a male doctor.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s a battle of the sexes today as we dive into a paper that makes you say, “Wow, what an interesting study” and also “Boy, am I glad I didn’t do that study.” That’s because studies like this are always somewhat fraught; they say something about medicine but also something about society — and that makes this a bit precarious. But that’s never stopped us before. So, let’s go ahead and try to answer the question: Do women make better doctors than men?
On the surface, this question seems nearly impossible to answer. It’s too broad; what does it mean to be a “better” doctor? At first blush it seems that there are just too many variables to control for here: the type of doctor, the type of patient, the clinical scenario, and so on.
But this study, “Comparison of hospital mortality and readmission rates by physician and patient sex,” which appears in Annals of Internal Medicine, uses a fairly ingenious method to cut through all the bias by leveraging two simple facts: First, hospital medicine is largely conducted by hospitalists these days; second, due to the shift-based nature of hospitalist work, the hospitalist you get when you are admitted to the hospital is pretty much random.
In other words, if you are admitted to the hospital for an acute illness and get a hospitalist as your attending, you have no control over whether it is a man or a woman. Is this a randomized trial? No, but it’s not bad.
Researchers used Medicare claims data to identify adults over age 65 who had nonelective hospital admissions throughout the United States. The claims revealed the sex of the patient and the name of the attending physician. By linking to a medical provider database, they could determine the sex of the provider.
The goal was to look at outcomes across four dyads:
- Male patient – male doctor
- Male patient – female doctor
- Female patient – male doctor
- Female patient – female doctor
The primary outcome was 30-day mortality.
I told you that focusing on hospitalists produces some pseudorandomization, but let’s look at the data to be sure. Just under a million patients were treated by approximately 50,000 physicians, 30% of whom were female. And, though female patients and male patients differed, they did not differ with respect to the sex of their hospitalist. So, by physician sex, patients were similar in mean age, race, ethnicity, household income, eligibility for Medicaid, and comorbid conditions. The authors even created a “predicted mortality” score which was similar across the groups as well.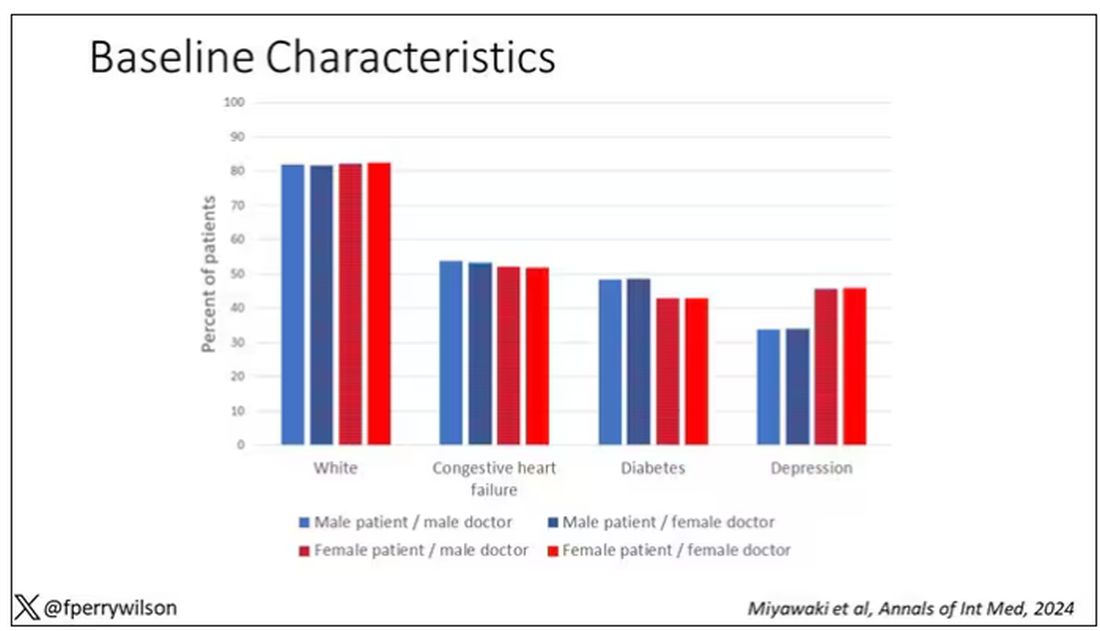
Now, the female physicians were a bit different from the male physicians. The female hospitalists were slightly more likely to have an osteopathic degree, had slightly fewer admissions per year, and were a bit younger.
So, we have broadly similar patients regardless of who their hospitalist was, but hospitalists differ by factors other than their sex. Fine.
I’ve graphed the results here. 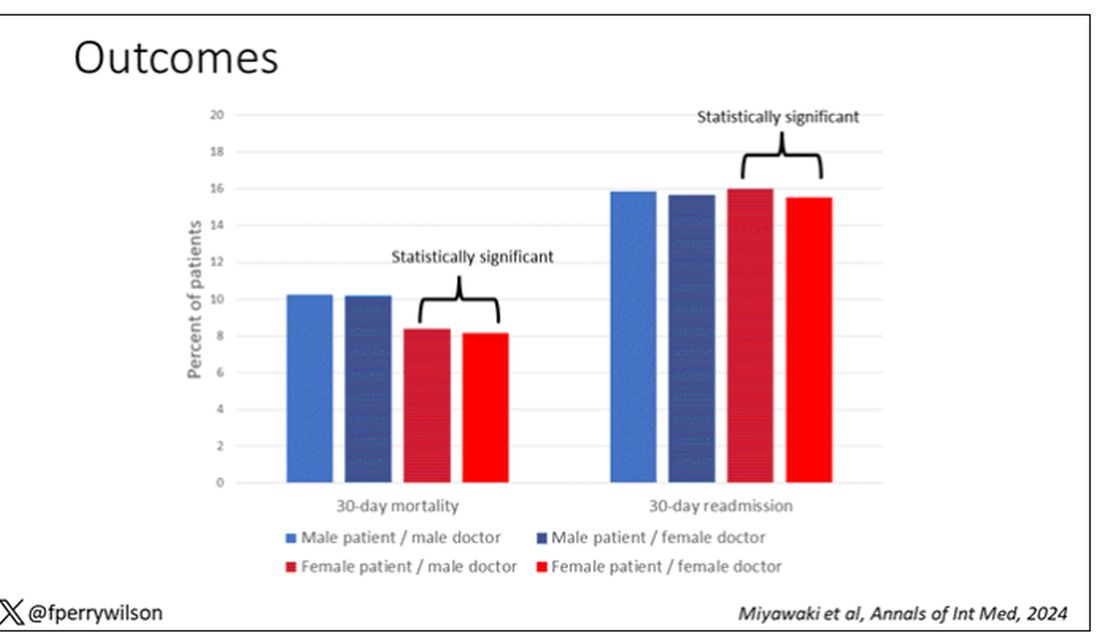
This is a relatively small effect, to be sure, but if you multiply it across the millions of hospitalist admissions per year, you can start to put up some real numbers.
So, what is going on here? I see four broad buckets of possibilities.
Let’s start with the obvious explanation: Women, on average, are better doctors than men. I am married to a woman doctor, and based on my personal experience, this explanation is undoubtedly true. But why would that be?
The authors cite data that suggest that female physicians are less likely than male physicians to dismiss patient concerns — and in particular, the concerns of female patients — perhaps leading to fewer missed diagnoses. But this is impossible to measure with administrative data, so this study can no more tell us whether these female hospitalists are more attentive than their male counterparts than it can suggest that the benefit is mediated by the shorter average height of female physicians. Perhaps the key is being closer to the patient?
The second possibility here is that this has nothing to do with the sex of the physician at all; it has to do with those other things that associate with the sex of the physician. We know, for example, that the female physicians saw fewer patients per year than the male physicians, but the study authors adjusted for this in the statistical models. Still, other unmeasured factors (confounders) could be present. By the way, confounders wouldn’t necessarily change the primary finding — you are better off being cared for by female physicians. It’s just not because they are female; it’s a convenient marker for some other quality, such as age.
The third possibility is that the study represents a phenomenon called collider bias. The idea here is that physicians only get into the study if they are hospitalists, and the quality of physicians who choose to become a hospitalist may differ by sex. When deciding on a specialty, a talented resident considering certain lifestyle issues may find hospital medicine particularly attractive — and that draw toward a more lifestyle-friendly specialty may differ by sex, as some prior studies have shown. If true, the pool of women hospitalists may be better than their male counterparts because male physicians of that caliber don’t become hospitalists.
Okay, don’t write in. I’m just trying to cite examples of how to think about collider bias. I can’t prove that this is the case, and in fact the authors do a sensitivity analysis of all physicians, not just hospitalists, and show the same thing. So this is probably not true, but epidemiology is fun, right?
And the fourth possibility: This is nothing but statistical noise. The effect size is incredibly small and just on the border of statistical significance. Especially when you’re working with very large datasets like this, you’ve got to be really careful about overinterpreting statistically significant findings that are nevertheless of small magnitude.
Regardless, it’s an interesting study, one that made me think and, of course, worry a bit about how I would present it. Forgive me if I’ve been indelicate in handling the complex issues of sex, gender, and society here. But I’m not sure what you expect; after all, I’m only a male doctor.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Weighing the Benefits of Integrating AI-based Clinical Notes Into Your Practice
Picture a healthcare system where physicians aren’t bogged down by excessive charting but are instead fully present with their patients, offering undivided attention and personalized care. In a recent X post, Stuart Blitz, COO and co-founder of Hone Health, sparked a thought-provoking conversation. “The problem with US healthcare is physicians are burned out since they spend way too much time charting, not enough with patients,” he wrote. “If you created a health system that did zero charting, you’d attract the best physicians and all patients would go there. Who is working on this?”
This resonates with many in the medical community, myself included, because the strain of extensive documentation detracts from patient care. Having worked in both large and small healthcare systems, I know the burden of extensive charting is a palpable challenge, often detracting from the time we can devote to our patients.
The first part of this two-part series examines the overarching benefits of artificial intelligence (AI)–based clinical documentation in modern healthcare, a field witnessing a paradigm shift thanks to advancements in AI.
Transformative Evolution of Clinical Documentation
The transition from manual documentation to AI-driven solutions marks a significant shift in the field, with a number of products in development including Nuance, Abridge, Ambience, ScribeAmerica, 3M, and DeepScribe. These tools use ambient clinical intelligence (ACI) to automate documentation, capturing patient conversations and translating them into structured clinical summaries. This innovation aligns with the vision of reducing charting burdens and enhancing patient-physician interactions.
How does it work? ACI refers to a sophisticated form of AI applied in healthcare settings, particularly focusing on enhancing the clinical documentation process without disrupting the natural flow of the consultation. Here’s a technical yet practical breakdown of ACI and the algorithms it typically employs:
Data capture and processing: ACI systems employ various sensors and processing units, typically integrated into clinical settings. These sensors, like microphones and cameras, gather diverse data such as audio from patient-doctor dialogues and visual cues. This information is then processed in real-time or near–real-time.
Natural language processing (NLP): A core component of ACI is advanced NLP algorithms. These algorithms analyze the captured audio data, transcribing spoken words into text. NLP goes beyond mere transcription; it involves understanding context, extracting relevant medical information (like symptoms, diagnoses, and treatment plans), and interpreting the nuances of human language.
Deep learning: Machine learning, particularly deep-learning techniques, are employed to improve the accuracy of ACI systems continually. These algorithms can learn from vast datasets of clinical interactions, enhancing their ability to transcribe and interpret future conversations accurately. As they learn, they become better at understanding different accents, complex medical terms, and variations in speech patterns.
Integration with electronic health records (EHRs): ACI systems are often designed to integrate seamlessly with existing EHR systems. They can automatically populate patient records with information from patient-clinician interactions, reducing manual entry and potential errors.
Customization and personalization: Many ACI systems offer customizable templates or allow clinicians to tailor documentation workflows. This flexibility ensures that the output aligns with the specific needs and preferences of healthcare providers.
Ethical and privacy considerations: ACI systems must navigate significant ethical and privacy concerns, especially related to patient consent and data security. These systems need to comply with healthcare privacy regulations such as HIPAA. They need to securely manage sensitive patient data and restrict access to authorized personnel only.
Broad-Spectrum Benefits of AI in Documentation
- Reducing clinician burnout: By automating the documentation process, AI tools like DAX Copilot alleviate a significant contributor to physician burnout, enabling clinicians to focus more on patient care.
- Enhanced patient care: With AI handling documentation, clinicians can engage more with their patients, leading to improved care quality and patient satisfaction.
- Data accuracy and quality: AI-driven documentation captures detailed patient encounters accurately, ensuring high-quality and comprehensive medical records.
- Response to the growing need for efficient healthcare: AI-based documentation is a direct response to the growing call for more efficient healthcare practices, where clinicians spend less time on paperwork and more with patients.
The shift toward AI-based clinical documentation represents a critical step in addressing the inefficiencies in healthcare systems. It’s a move towards a more patient-centered approach, where clinicians can focus more on patient care by reducing the time spent on excessive charting. Hopefully, we can integrate these solutions into our clinics at a large enough scale to make such an impact.
In the next column, we will explore in-depth insights from Kenneth Harper at Nuance on the technical implementation of these tools, with DAX as an example.
I would love to read your comments on AI in clinical trials as well as other AI-related topics. Write me at [email protected] or find me on X @DrBonillaOnc.
Dr. Loaiza-Bonilla is the co-founder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr Loaiza-Bonilla serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has served as a consultant for Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, and Guardant; served as a speaker or a member of a speakers bureau for Amgen, Guardant, Eisai, Ipsen, Natera, Merck, Bristol-Myers Squibb, and AstraZeneca. He holds a 5% or greater equity interest in Massive Bio.
A version of this article appeared on Medscape.com.
Picture a healthcare system where physicians aren’t bogged down by excessive charting but are instead fully present with their patients, offering undivided attention and personalized care. In a recent X post, Stuart Blitz, COO and co-founder of Hone Health, sparked a thought-provoking conversation. “The problem with US healthcare is physicians are burned out since they spend way too much time charting, not enough with patients,” he wrote. “If you created a health system that did zero charting, you’d attract the best physicians and all patients would go there. Who is working on this?”
This resonates with many in the medical community, myself included, because the strain of extensive documentation detracts from patient care. Having worked in both large and small healthcare systems, I know the burden of extensive charting is a palpable challenge, often detracting from the time we can devote to our patients.
The first part of this two-part series examines the overarching benefits of artificial intelligence (AI)–based clinical documentation in modern healthcare, a field witnessing a paradigm shift thanks to advancements in AI.
Transformative Evolution of Clinical Documentation
The transition from manual documentation to AI-driven solutions marks a significant shift in the field, with a number of products in development including Nuance, Abridge, Ambience, ScribeAmerica, 3M, and DeepScribe. These tools use ambient clinical intelligence (ACI) to automate documentation, capturing patient conversations and translating them into structured clinical summaries. This innovation aligns with the vision of reducing charting burdens and enhancing patient-physician interactions.
How does it work? ACI refers to a sophisticated form of AI applied in healthcare settings, particularly focusing on enhancing the clinical documentation process without disrupting the natural flow of the consultation. Here’s a technical yet practical breakdown of ACI and the algorithms it typically employs:
Data capture and processing: ACI systems employ various sensors and processing units, typically integrated into clinical settings. These sensors, like microphones and cameras, gather diverse data such as audio from patient-doctor dialogues and visual cues. This information is then processed in real-time or near–real-time.
Natural language processing (NLP): A core component of ACI is advanced NLP algorithms. These algorithms analyze the captured audio data, transcribing spoken words into text. NLP goes beyond mere transcription; it involves understanding context, extracting relevant medical information (like symptoms, diagnoses, and treatment plans), and interpreting the nuances of human language.
Deep learning: Machine learning, particularly deep-learning techniques, are employed to improve the accuracy of ACI systems continually. These algorithms can learn from vast datasets of clinical interactions, enhancing their ability to transcribe and interpret future conversations accurately. As they learn, they become better at understanding different accents, complex medical terms, and variations in speech patterns.
Integration with electronic health records (EHRs): ACI systems are often designed to integrate seamlessly with existing EHR systems. They can automatically populate patient records with information from patient-clinician interactions, reducing manual entry and potential errors.
Customization and personalization: Many ACI systems offer customizable templates or allow clinicians to tailor documentation workflows. This flexibility ensures that the output aligns with the specific needs and preferences of healthcare providers.
Ethical and privacy considerations: ACI systems must navigate significant ethical and privacy concerns, especially related to patient consent and data security. These systems need to comply with healthcare privacy regulations such as HIPAA. They need to securely manage sensitive patient data and restrict access to authorized personnel only.
Broad-Spectrum Benefits of AI in Documentation
- Reducing clinician burnout: By automating the documentation process, AI tools like DAX Copilot alleviate a significant contributor to physician burnout, enabling clinicians to focus more on patient care.
- Enhanced patient care: With AI handling documentation, clinicians can engage more with their patients, leading to improved care quality and patient satisfaction.
- Data accuracy and quality: AI-driven documentation captures detailed patient encounters accurately, ensuring high-quality and comprehensive medical records.
- Response to the growing need for efficient healthcare: AI-based documentation is a direct response to the growing call for more efficient healthcare practices, where clinicians spend less time on paperwork and more with patients.
The shift toward AI-based clinical documentation represents a critical step in addressing the inefficiencies in healthcare systems. It’s a move towards a more patient-centered approach, where clinicians can focus more on patient care by reducing the time spent on excessive charting. Hopefully, we can integrate these solutions into our clinics at a large enough scale to make such an impact.
In the next column, we will explore in-depth insights from Kenneth Harper at Nuance on the technical implementation of these tools, with DAX as an example.
I would love to read your comments on AI in clinical trials as well as other AI-related topics. Write me at [email protected] or find me on X @DrBonillaOnc.
Dr. Loaiza-Bonilla is the co-founder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr Loaiza-Bonilla serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has served as a consultant for Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, and Guardant; served as a speaker or a member of a speakers bureau for Amgen, Guardant, Eisai, Ipsen, Natera, Merck, Bristol-Myers Squibb, and AstraZeneca. He holds a 5% or greater equity interest in Massive Bio.
A version of this article appeared on Medscape.com.
Picture a healthcare system where physicians aren’t bogged down by excessive charting but are instead fully present with their patients, offering undivided attention and personalized care. In a recent X post, Stuart Blitz, COO and co-founder of Hone Health, sparked a thought-provoking conversation. “The problem with US healthcare is physicians are burned out since they spend way too much time charting, not enough with patients,” he wrote. “If you created a health system that did zero charting, you’d attract the best physicians and all patients would go there. Who is working on this?”
This resonates with many in the medical community, myself included, because the strain of extensive documentation detracts from patient care. Having worked in both large and small healthcare systems, I know the burden of extensive charting is a palpable challenge, often detracting from the time we can devote to our patients.
The first part of this two-part series examines the overarching benefits of artificial intelligence (AI)–based clinical documentation in modern healthcare, a field witnessing a paradigm shift thanks to advancements in AI.
Transformative Evolution of Clinical Documentation
The transition from manual documentation to AI-driven solutions marks a significant shift in the field, with a number of products in development including Nuance, Abridge, Ambience, ScribeAmerica, 3M, and DeepScribe. These tools use ambient clinical intelligence (ACI) to automate documentation, capturing patient conversations and translating them into structured clinical summaries. This innovation aligns with the vision of reducing charting burdens and enhancing patient-physician interactions.
How does it work? ACI refers to a sophisticated form of AI applied in healthcare settings, particularly focusing on enhancing the clinical documentation process without disrupting the natural flow of the consultation. Here’s a technical yet practical breakdown of ACI and the algorithms it typically employs:
Data capture and processing: ACI systems employ various sensors and processing units, typically integrated into clinical settings. These sensors, like microphones and cameras, gather diverse data such as audio from patient-doctor dialogues and visual cues. This information is then processed in real-time or near–real-time.
Natural language processing (NLP): A core component of ACI is advanced NLP algorithms. These algorithms analyze the captured audio data, transcribing spoken words into text. NLP goes beyond mere transcription; it involves understanding context, extracting relevant medical information (like symptoms, diagnoses, and treatment plans), and interpreting the nuances of human language.
Deep learning: Machine learning, particularly deep-learning techniques, are employed to improve the accuracy of ACI systems continually. These algorithms can learn from vast datasets of clinical interactions, enhancing their ability to transcribe and interpret future conversations accurately. As they learn, they become better at understanding different accents, complex medical terms, and variations in speech patterns.
Integration with electronic health records (EHRs): ACI systems are often designed to integrate seamlessly with existing EHR systems. They can automatically populate patient records with information from patient-clinician interactions, reducing manual entry and potential errors.
Customization and personalization: Many ACI systems offer customizable templates or allow clinicians to tailor documentation workflows. This flexibility ensures that the output aligns with the specific needs and preferences of healthcare providers.
Ethical and privacy considerations: ACI systems must navigate significant ethical and privacy concerns, especially related to patient consent and data security. These systems need to comply with healthcare privacy regulations such as HIPAA. They need to securely manage sensitive patient data and restrict access to authorized personnel only.
Broad-Spectrum Benefits of AI in Documentation
- Reducing clinician burnout: By automating the documentation process, AI tools like DAX Copilot alleviate a significant contributor to physician burnout, enabling clinicians to focus more on patient care.
- Enhanced patient care: With AI handling documentation, clinicians can engage more with their patients, leading to improved care quality and patient satisfaction.
- Data accuracy and quality: AI-driven documentation captures detailed patient encounters accurately, ensuring high-quality and comprehensive medical records.
- Response to the growing need for efficient healthcare: AI-based documentation is a direct response to the growing call for more efficient healthcare practices, where clinicians spend less time on paperwork and more with patients.
The shift toward AI-based clinical documentation represents a critical step in addressing the inefficiencies in healthcare systems. It’s a move towards a more patient-centered approach, where clinicians can focus more on patient care by reducing the time spent on excessive charting. Hopefully, we can integrate these solutions into our clinics at a large enough scale to make such an impact.
In the next column, we will explore in-depth insights from Kenneth Harper at Nuance on the technical implementation of these tools, with DAX as an example.
I would love to read your comments on AI in clinical trials as well as other AI-related topics. Write me at [email protected] or find me on X @DrBonillaOnc.
Dr. Loaiza-Bonilla is the co-founder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr Loaiza-Bonilla serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has served as a consultant for Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, and Guardant; served as a speaker or a member of a speakers bureau for Amgen, Guardant, Eisai, Ipsen, Natera, Merck, Bristol-Myers Squibb, and AstraZeneca. He holds a 5% or greater equity interest in Massive Bio.
A version of this article appeared on Medscape.com.
New Federal Rule Delivers Workplace Support, Time Off for Pregnant Docs
Pregnant physicians may receive more workplace accommodations and protection against discrimination thanks to an updated rule from the US Equal Employment Opportunity Commission (EEOC). The guidelines could prevent women from losing critical career momentum.
The Pregnant Workers Fairness Act (PWFA) aims to help workers balance professional demands with healthy pregnancies. It requires employers to provide reasonable accommodations for a “worker’s known limitations,” including physical or mental conditions associated with “pregnancy, childbirth, or related medical conditions.”
Reasonable accommodations vary but may involve time off to attend healthcare appointments or recover from childbirth, extra breaks during a shift, shorter work hours, or the ability to sit instead of stand. Private and public sector employers, including state and local governments, federal agencies, and employment agencies, must abide by the new guidelines unless they can provide evidence that doing so will cause undue hardship.
Female doctors have historically encountered significant barriers to family planning. Years of training cause them to delay having children, often leading to higher rates of infertility, miscarriage, and pregnancy complications than in the general population.
Some specialties, like surgeons, are particularly at risk, with 42% reporting at least one pregnancy loss. Most surgeons work their regular schedules until delivery despite desiring workload reductions, commonly citing unsupportive workplaces as a reason for not seeking accommodations.
Trauma surgeon Qaali Hussein, MD, became pregnant with her first child during her intern year in 2008. She told this news organization that her residency program didn’t even have a maternity policy at the time, and her male supervisor was certain that motherhood would end her surgical career.
She shared how “women usually waited until the end of their training to get pregnant. No one had ever gotten pregnant during the program and returned from maternity leave. I was the first to do so, so there wasn’t a policy or any program support to say, ‘What can we do to help?’ ”
Dr. Hussein used her vacation and sick time, returning to work 4 weeks after delivery. She had five more children, including twins her chief year and another baby during fellowship training in 2014.
Each subsequent pregnancy was met with the same response from program leadership, she recalled. “They’d say, ‘This is it. You may have been able to do the first and second child, but this one will be impossible.’ ”
After the PWFA regulations first became enforceable in June, the EEOC accepted public feedback. The guidelines received nearly 100,000 comments, spurred mainly by the inclusion of abortion care as a qualifying condition for which an employee could receive accommodations. About 54,000 comments called for abortion to be excluded from the final rule, and 40,000 supported keeping the clause.
The EEOC issued the final rule on April 15. It includes abortion care. However, the updated rule “does not require any employee to have — or not to have — an abortion, does not require taxpayers to pay for any abortions, and does not compel health care providers to provide any abortions,” the unpublished version of the final rule said. It is scheduled to take effect 60 days after its publication in the Federal Register on April 19.
Increasing Support for Doctor-Moms
The PWFA supplements other EEOC protections, such as pregnancy discrimination under Title VII of the Civil Rights Act of 1964 and access to reasonable accommodations under the Americans with Disabilities Act. In addition, it builds upon Department of Labor regulations, like the PUMP Act for breastfeeding employees and the Family and Medical Leave Act, which provides 12 weeks of unpaid, job-protected leave for the arrival of a child or certain medical conditions.
FMLA applies only to employees who have worked full-time for at least 12 months for an employer with 50 or more employees. Meanwhile, the unpaid, job-protected leave under the PWFA has no waiting period, lowers the required number of employees to 15, and permits accommodations for up to 40 weeks.
Employers are encouraged to honor “common and simple” requests, like using a closer parking space or pumping or nursing at work, without requiring a doctor’s note, the rule said.
Efforts to improve family leave policies for physicians and residents have been gaining traction. In 2021, the American Board of Medical Specialties began requiring its member boards with training programs lasting 2 or more years to allow at least 6 weeks off for parental, caregiver, and medical leave. This time can be taken without exhausting vacation or sick leave or requiring an extension in training. Over half of the 24 member boards permit leave beyond 6 weeks, including the American Boards of Allergy and Immunology, Emergency Medicine, Family Medicine, Radiology, and Surgery.
Estefania Oliveros, MD, MSc, cardiologist and assistant professor at the Lewis Katz School of Medicine at Temple University, Philadelphia, told this news organization that the Accreditation Council for Graduate Medical Education also requires that residents and fellows receive 6 weeks of paid leave.
“We add to that vacation time, so it gives them at least 8 weeks,” she said. The school has created spaces for nursing mothers — something neither she nor Dr. Hussein had access to when breastfeeding — and encourages the attendings to be proactive in excusing pregnant fellows for appointments.
This differs significantly from her fellowship training experience 6 years ago at another institution, where she worked without accommodations until the day before her cesarean delivery. Dr. Oliveros had to use all her vacation time for recovery, returning to the program after 4 weeks instead of the recommended 6.
“And that’s the story you hear all the time. Not because people are ill-intended; I just don’t think the system is designed to accommodate women, so we lose a lot of talent that way,” said Dr. Oliveros, whose 2019 survey in the Journal of the American College of Cardiology called for more support and protections for pregnant doctors.
Both doctors believe the PWFA will be beneficial but only if leadership in the field takes up the cause.
“The cultures of these institutions determine whether women feel safe or even confident enough to have children in medical school or residency,” said Dr. Hussein.
A version of this article appeared on Medscape.com.
Pregnant physicians may receive more workplace accommodations and protection against discrimination thanks to an updated rule from the US Equal Employment Opportunity Commission (EEOC). The guidelines could prevent women from losing critical career momentum.
The Pregnant Workers Fairness Act (PWFA) aims to help workers balance professional demands with healthy pregnancies. It requires employers to provide reasonable accommodations for a “worker’s known limitations,” including physical or mental conditions associated with “pregnancy, childbirth, or related medical conditions.”
Reasonable accommodations vary but may involve time off to attend healthcare appointments or recover from childbirth, extra breaks during a shift, shorter work hours, or the ability to sit instead of stand. Private and public sector employers, including state and local governments, federal agencies, and employment agencies, must abide by the new guidelines unless they can provide evidence that doing so will cause undue hardship.
Female doctors have historically encountered significant barriers to family planning. Years of training cause them to delay having children, often leading to higher rates of infertility, miscarriage, and pregnancy complications than in the general population.
Some specialties, like surgeons, are particularly at risk, with 42% reporting at least one pregnancy loss. Most surgeons work their regular schedules until delivery despite desiring workload reductions, commonly citing unsupportive workplaces as a reason for not seeking accommodations.
Trauma surgeon Qaali Hussein, MD, became pregnant with her first child during her intern year in 2008. She told this news organization that her residency program didn’t even have a maternity policy at the time, and her male supervisor was certain that motherhood would end her surgical career.
She shared how “women usually waited until the end of their training to get pregnant. No one had ever gotten pregnant during the program and returned from maternity leave. I was the first to do so, so there wasn’t a policy or any program support to say, ‘What can we do to help?’ ”
Dr. Hussein used her vacation and sick time, returning to work 4 weeks after delivery. She had five more children, including twins her chief year and another baby during fellowship training in 2014.
Each subsequent pregnancy was met with the same response from program leadership, she recalled. “They’d say, ‘This is it. You may have been able to do the first and second child, but this one will be impossible.’ ”
After the PWFA regulations first became enforceable in June, the EEOC accepted public feedback. The guidelines received nearly 100,000 comments, spurred mainly by the inclusion of abortion care as a qualifying condition for which an employee could receive accommodations. About 54,000 comments called for abortion to be excluded from the final rule, and 40,000 supported keeping the clause.
The EEOC issued the final rule on April 15. It includes abortion care. However, the updated rule “does not require any employee to have — or not to have — an abortion, does not require taxpayers to pay for any abortions, and does not compel health care providers to provide any abortions,” the unpublished version of the final rule said. It is scheduled to take effect 60 days after its publication in the Federal Register on April 19.
Increasing Support for Doctor-Moms
The PWFA supplements other EEOC protections, such as pregnancy discrimination under Title VII of the Civil Rights Act of 1964 and access to reasonable accommodations under the Americans with Disabilities Act. In addition, it builds upon Department of Labor regulations, like the PUMP Act for breastfeeding employees and the Family and Medical Leave Act, which provides 12 weeks of unpaid, job-protected leave for the arrival of a child or certain medical conditions.
FMLA applies only to employees who have worked full-time for at least 12 months for an employer with 50 or more employees. Meanwhile, the unpaid, job-protected leave under the PWFA has no waiting period, lowers the required number of employees to 15, and permits accommodations for up to 40 weeks.
Employers are encouraged to honor “common and simple” requests, like using a closer parking space or pumping or nursing at work, without requiring a doctor’s note, the rule said.
Efforts to improve family leave policies for physicians and residents have been gaining traction. In 2021, the American Board of Medical Specialties began requiring its member boards with training programs lasting 2 or more years to allow at least 6 weeks off for parental, caregiver, and medical leave. This time can be taken without exhausting vacation or sick leave or requiring an extension in training. Over half of the 24 member boards permit leave beyond 6 weeks, including the American Boards of Allergy and Immunology, Emergency Medicine, Family Medicine, Radiology, and Surgery.
Estefania Oliveros, MD, MSc, cardiologist and assistant professor at the Lewis Katz School of Medicine at Temple University, Philadelphia, told this news organization that the Accreditation Council for Graduate Medical Education also requires that residents and fellows receive 6 weeks of paid leave.
“We add to that vacation time, so it gives them at least 8 weeks,” she said. The school has created spaces for nursing mothers — something neither she nor Dr. Hussein had access to when breastfeeding — and encourages the attendings to be proactive in excusing pregnant fellows for appointments.
This differs significantly from her fellowship training experience 6 years ago at another institution, where she worked without accommodations until the day before her cesarean delivery. Dr. Oliveros had to use all her vacation time for recovery, returning to the program after 4 weeks instead of the recommended 6.
“And that’s the story you hear all the time. Not because people are ill-intended; I just don’t think the system is designed to accommodate women, so we lose a lot of talent that way,” said Dr. Oliveros, whose 2019 survey in the Journal of the American College of Cardiology called for more support and protections for pregnant doctors.
Both doctors believe the PWFA will be beneficial but only if leadership in the field takes up the cause.
“The cultures of these institutions determine whether women feel safe or even confident enough to have children in medical school or residency,” said Dr. Hussein.
A version of this article appeared on Medscape.com.
Pregnant physicians may receive more workplace accommodations and protection against discrimination thanks to an updated rule from the US Equal Employment Opportunity Commission (EEOC). The guidelines could prevent women from losing critical career momentum.
The Pregnant Workers Fairness Act (PWFA) aims to help workers balance professional demands with healthy pregnancies. It requires employers to provide reasonable accommodations for a “worker’s known limitations,” including physical or mental conditions associated with “pregnancy, childbirth, or related medical conditions.”
Reasonable accommodations vary but may involve time off to attend healthcare appointments or recover from childbirth, extra breaks during a shift, shorter work hours, or the ability to sit instead of stand. Private and public sector employers, including state and local governments, federal agencies, and employment agencies, must abide by the new guidelines unless they can provide evidence that doing so will cause undue hardship.
Female doctors have historically encountered significant barriers to family planning. Years of training cause them to delay having children, often leading to higher rates of infertility, miscarriage, and pregnancy complications than in the general population.
Some specialties, like surgeons, are particularly at risk, with 42% reporting at least one pregnancy loss. Most surgeons work their regular schedules until delivery despite desiring workload reductions, commonly citing unsupportive workplaces as a reason for not seeking accommodations.
Trauma surgeon Qaali Hussein, MD, became pregnant with her first child during her intern year in 2008. She told this news organization that her residency program didn’t even have a maternity policy at the time, and her male supervisor was certain that motherhood would end her surgical career.
She shared how “women usually waited until the end of their training to get pregnant. No one had ever gotten pregnant during the program and returned from maternity leave. I was the first to do so, so there wasn’t a policy or any program support to say, ‘What can we do to help?’ ”
Dr. Hussein used her vacation and sick time, returning to work 4 weeks after delivery. She had five more children, including twins her chief year and another baby during fellowship training in 2014.
Each subsequent pregnancy was met with the same response from program leadership, she recalled. “They’d say, ‘This is it. You may have been able to do the first and second child, but this one will be impossible.’ ”
After the PWFA regulations first became enforceable in June, the EEOC accepted public feedback. The guidelines received nearly 100,000 comments, spurred mainly by the inclusion of abortion care as a qualifying condition for which an employee could receive accommodations. About 54,000 comments called for abortion to be excluded from the final rule, and 40,000 supported keeping the clause.
The EEOC issued the final rule on April 15. It includes abortion care. However, the updated rule “does not require any employee to have — or not to have — an abortion, does not require taxpayers to pay for any abortions, and does not compel health care providers to provide any abortions,” the unpublished version of the final rule said. It is scheduled to take effect 60 days after its publication in the Federal Register on April 19.
Increasing Support for Doctor-Moms
The PWFA supplements other EEOC protections, such as pregnancy discrimination under Title VII of the Civil Rights Act of 1964 and access to reasonable accommodations under the Americans with Disabilities Act. In addition, it builds upon Department of Labor regulations, like the PUMP Act for breastfeeding employees and the Family and Medical Leave Act, which provides 12 weeks of unpaid, job-protected leave for the arrival of a child or certain medical conditions.
FMLA applies only to employees who have worked full-time for at least 12 months for an employer with 50 or more employees. Meanwhile, the unpaid, job-protected leave under the PWFA has no waiting period, lowers the required number of employees to 15, and permits accommodations for up to 40 weeks.
Employers are encouraged to honor “common and simple” requests, like using a closer parking space or pumping or nursing at work, without requiring a doctor’s note, the rule said.
Efforts to improve family leave policies for physicians and residents have been gaining traction. In 2021, the American Board of Medical Specialties began requiring its member boards with training programs lasting 2 or more years to allow at least 6 weeks off for parental, caregiver, and medical leave. This time can be taken without exhausting vacation or sick leave or requiring an extension in training. Over half of the 24 member boards permit leave beyond 6 weeks, including the American Boards of Allergy and Immunology, Emergency Medicine, Family Medicine, Radiology, and Surgery.
Estefania Oliveros, MD, MSc, cardiologist and assistant professor at the Lewis Katz School of Medicine at Temple University, Philadelphia, told this news organization that the Accreditation Council for Graduate Medical Education also requires that residents and fellows receive 6 weeks of paid leave.
“We add to that vacation time, so it gives them at least 8 weeks,” she said. The school has created spaces for nursing mothers — something neither she nor Dr. Hussein had access to when breastfeeding — and encourages the attendings to be proactive in excusing pregnant fellows for appointments.
This differs significantly from her fellowship training experience 6 years ago at another institution, where she worked without accommodations until the day before her cesarean delivery. Dr. Oliveros had to use all her vacation time for recovery, returning to the program after 4 weeks instead of the recommended 6.
“And that’s the story you hear all the time. Not because people are ill-intended; I just don’t think the system is designed to accommodate women, so we lose a lot of talent that way,” said Dr. Oliveros, whose 2019 survey in the Journal of the American College of Cardiology called for more support and protections for pregnant doctors.
Both doctors believe the PWFA will be beneficial but only if leadership in the field takes up the cause.
“The cultures of these institutions determine whether women feel safe or even confident enough to have children in medical school or residency,” said Dr. Hussein.
A version of this article appeared on Medscape.com.
AI Surpasses Harvard Docs on Clinical Reasoning Test
TOPLINE:
The AI had more instances of incorrect reasoning than the doctors did but scored better overall.
METHODOLOGY:
- The study involved 39 physicians from two academic medical centers in Boston and the generative AI model GPT-4.
- Participants were presented with 20 simulated clinical cases involving common problems such as pharyngitis, headache, abdominal pain, cough, and chest pain. Each case included sections describing the triage presentation, review of systems, physical examination, and diagnostic testing.
- The primary outcome was the Revised-IDEA (R-IDEA) score, a 10-point scale evaluating clinical reasoning documentation across four domains: Interpretive summary, differential diagnosis, explanation of the lead diagnosis, and alternative diagnoses.
TAKEAWAY:
- AI achieved a median R-IDEA score of 10, higher than attending physicians (median score, 9) and residents (8).
- The chatbot had a significantly higher estimated probability of achieving a high R-IDEA score of 8-10 (0.99) compared with attendings (0.76) and residents (0.56).
- AI provided more responses that contained instances of incorrect clinical reasoning (13.8%) than residents (2.8%) and attending physicians (12.5%). It performed similarly to physicians in diagnostic accuracy and inclusion of cannot-miss diagnoses.
IN PRACTICE:
“Future research should assess clinical reasoning of the LLM-physician interaction, as LLMs will more likely augment, not replace, the human reasoning process,” the authors of the study wrote.
SOURCE:
Adam Rodman, MD, MPH, with Beth Israel Deaconess Medical Center, Boston, was the corresponding author on the paper. The research was published online in JAMA Internal Medicine.
LIMITATIONS:
Simulated clinical cases may not replicate performance in real-world scenarios. Further training could enhance the performance of the AI, so the study may underestimate its capabilities, the researchers noted.
DISCLOSURES:
The study was supported by the Harvard Clinical and Translational Science Center and Harvard University. Authors disclosed financial ties to publishing companies and Solera Health. Dr. Rodman received funding from the Gordon and Betty Moore Foundation.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
The AI had more instances of incorrect reasoning than the doctors did but scored better overall.
METHODOLOGY:
- The study involved 39 physicians from two academic medical centers in Boston and the generative AI model GPT-4.
- Participants were presented with 20 simulated clinical cases involving common problems such as pharyngitis, headache, abdominal pain, cough, and chest pain. Each case included sections describing the triage presentation, review of systems, physical examination, and diagnostic testing.
- The primary outcome was the Revised-IDEA (R-IDEA) score, a 10-point scale evaluating clinical reasoning documentation across four domains: Interpretive summary, differential diagnosis, explanation of the lead diagnosis, and alternative diagnoses.
TAKEAWAY:
- AI achieved a median R-IDEA score of 10, higher than attending physicians (median score, 9) and residents (8).
- The chatbot had a significantly higher estimated probability of achieving a high R-IDEA score of 8-10 (0.99) compared with attendings (0.76) and residents (0.56).
- AI provided more responses that contained instances of incorrect clinical reasoning (13.8%) than residents (2.8%) and attending physicians (12.5%). It performed similarly to physicians in diagnostic accuracy and inclusion of cannot-miss diagnoses.
IN PRACTICE:
“Future research should assess clinical reasoning of the LLM-physician interaction, as LLMs will more likely augment, not replace, the human reasoning process,” the authors of the study wrote.
SOURCE:
Adam Rodman, MD, MPH, with Beth Israel Deaconess Medical Center, Boston, was the corresponding author on the paper. The research was published online in JAMA Internal Medicine.
LIMITATIONS:
Simulated clinical cases may not replicate performance in real-world scenarios. Further training could enhance the performance of the AI, so the study may underestimate its capabilities, the researchers noted.
DISCLOSURES:
The study was supported by the Harvard Clinical and Translational Science Center and Harvard University. Authors disclosed financial ties to publishing companies and Solera Health. Dr. Rodman received funding from the Gordon and Betty Moore Foundation.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
The AI had more instances of incorrect reasoning than the doctors did but scored better overall.
METHODOLOGY:
- The study involved 39 physicians from two academic medical centers in Boston and the generative AI model GPT-4.
- Participants were presented with 20 simulated clinical cases involving common problems such as pharyngitis, headache, abdominal pain, cough, and chest pain. Each case included sections describing the triage presentation, review of systems, physical examination, and diagnostic testing.
- The primary outcome was the Revised-IDEA (R-IDEA) score, a 10-point scale evaluating clinical reasoning documentation across four domains: Interpretive summary, differential diagnosis, explanation of the lead diagnosis, and alternative diagnoses.
TAKEAWAY:
- AI achieved a median R-IDEA score of 10, higher than attending physicians (median score, 9) and residents (8).
- The chatbot had a significantly higher estimated probability of achieving a high R-IDEA score of 8-10 (0.99) compared with attendings (0.76) and residents (0.56).
- AI provided more responses that contained instances of incorrect clinical reasoning (13.8%) than residents (2.8%) and attending physicians (12.5%). It performed similarly to physicians in diagnostic accuracy and inclusion of cannot-miss diagnoses.
IN PRACTICE:
“Future research should assess clinical reasoning of the LLM-physician interaction, as LLMs will more likely augment, not replace, the human reasoning process,” the authors of the study wrote.
SOURCE:
Adam Rodman, MD, MPH, with Beth Israel Deaconess Medical Center, Boston, was the corresponding author on the paper. The research was published online in JAMA Internal Medicine.
LIMITATIONS:
Simulated clinical cases may not replicate performance in real-world scenarios. Further training could enhance the performance of the AI, so the study may underestimate its capabilities, the researchers noted.
DISCLOSURES:
The study was supported by the Harvard Clinical and Translational Science Center and Harvard University. Authors disclosed financial ties to publishing companies and Solera Health. Dr. Rodman received funding from the Gordon and Betty Moore Foundation.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Diabetic Foot Ulcers: Life-Threatening Issue in Need of Help
The photo of the patient’s foot, sent from his campsite, included a cheeky note: “I remember you telling me that getting in trouble doing something was better than getting in trouble doing nothing. This lets me get out there and know that I have feedback.”
The “this” was the patient’s “foot selfie,” an approach that allows patients at a risk for diabetic foot ulcers (DFUs) to snap a picture and send it to their healthcare providers for evaluation.
This particular patient had an extensive history of previous wounds. Some had essentially kept him house-bound in the past, as he was afraid to get another one.
This time, however, he got an all-clear to keep on camping, “and we scheduled him in on the following Tuesday [for follow-up],” said the camper’s physician David G. Armstrong, DPM, MD, PhD, professor of surgery and neurological surgery, USC Keck School of Medicine, Los Angeles.
Dr. Armstrong is one of the researchers evaluating the concept of foot selfies. It’s a welcome advance, he and others said, and has been shown to help heal wounds and reverse pre-ulcer lesions. Research on foot selfies continues, but much more is needed to solve the issue of DFUs, diabetic foot infections (DFIs), and the high rates of reinfection, experts know.
Worldwide, about 18.6 million people have a DFU each year, including 1.6 million in the United States. About 50%-60% of ulcers become infected, with 20% of moderate to severe infections requiring amputation of the limb. The 5-year mortality rate for DFUs is 30%, but it climbs to 70% after amputation. While about 40% of ulcers heal within 12 weeks, 42% recur at the 1-year mark, setting up a vicious and costly cycle. Healthcare costs for patients with diabetes and DFUs are five times as high as costs for patients with diabetes but no DFUs. The per capita cost to treat a DFU in America is $17,500.
While the statistics paint a grim picture, progress is being made on several fronts:
- US Food and Drug Administration (FDA) guidance on the development of drugs for DFUs, under evaluation, is forthcoming.
- New treatments are under study.
- A multidisciplinary team approach is known to improve outcomes.
Anatomy of a DFU
When neuropathy develops in those with diabetes, they no longer have what Dr. Armstrong calls the “gift” of pain perception. “They can wear a hole in their foot like you and I wear a hole in our sock or shoe,” he said. “That hole is called a diabetic foot ulcer.”
A DFU is an open wound on the foot, often occurring when bleeding develops beneath a callus and then the callus wears away. Deeper tissues of the foot are then exposed.
About half of the DFUs get infected, hence the FDA guidance, said Dr. Armstrong, who is also founding president of the American Limb Preservation Society, which aims to eliminate preventable amputations within the next generation. Every 20 seconds, Dr. Armstrong said, someone in the world loses a leg due to diabetes.
FDA Guidance on Drug Development for DFIs
In October, the FDA issued draft guidance for industry to articulate the design of clinical trials for developing antibacterial drugs to treat DFIs without concomitant bone and joint involvement. Comments closed on December 18. Among the points in the guidance, which is nonbinding, are to include DFIs of varying depths and extent in phase 3 trials and ideally to include only those patients who have not had prior antibacterial treatment for the current DFI.
According to an FDA spokesperson, “The agency is working to finalize the guidance. However, a timeline for its release has not yet been established.”
The good news about the upcoming FDA guidance, Dr. Armstrong said, is that the agency has realized the importance of treating the infections. Fully one third of direct costs of care for diabetes are spent on the lower extremities, he said. Keeping patients out of the hospital, uninfected, and “keeping legs on bodies” are all important goals, he said.
Pharmaceutical firms need to understand that “you aren’t dealing with a normal ulcer,” said Andrew J.M. Boulton, MD, professor of medicine at the University of Manchester and physician consultant at the Manchester Royal Infirmary, Manchester, England, and a visiting professor at the University of Miami. For research, “the most important thing is to take account of off-loading the ulcers,” he said. “Most ulcers will heal if put in a boot.”
Dr. Boulton, like Dr. Armstrong, a long-time expert in the field, contended that pharma has not understood this concept and has wasted millions over the last three decades doing studies that were poorly designed and controlled.
Treatments: Current, Under Study
Currently, DFIs are treated with antimicrobial therapy, without or without debridement, along with a clinical assessment for ischemia. If ischemia is found, care progresses to wound care and off-loading devices, such as healing sandals. Clinicians then assess the likelihood of improved outcomes with revascularization based on operative risks and distribution of lower extremity artery disease and proceed depending on the likelihood. If osteomyelitis testing shows it is present, providers proceed to wound debridement, limb-sparing amputation, and prolonged antimicrobials, as needed.
More options are needed, Dr. Armstrong said.
Among the many approaches under study:
- DFUs can be accurately detected by applying artificial intelligence to the “foot selfie” images taken by patients on smartphones, research by Dr. and has found.
- After a phase 3 study of for DFUs originally intending to enroll 300 subjects was discontinued because of slow patient recruitment, an interim analysis was conducted on 44 participants. It showed a positive trend toward wound closure in the group receiving the injected gene therapy, VM202 (ENGENSIS), in their calf muscles. VM202 is a plasmid DNA-encoding human hepatocyte growth factor. While those in both the intervention and placebo groups showed wound-closing effects at month 6, in 23 patients with neuro-ischemic ulcers, the percentage of those reaching complete closure of the DFU was significantly higher in the treated group at months 3, 4, and 5 (P = .0391, .0391, and .0361, respectively). After excluding two outliers, the difference in months 3-6 became more significant (P = .03).
- An closed more DFUs than standard care after 12 weeks — 70% vs 34% (P = .00032). Of the 100 participants randomized, 50 per group, 42% of the treatment group and 56% of the control group experienced adverse events, with eight withdrawn due to serious adverse events (such as osteomyelitis).
- A closed more refractory DFUs over a 16-week study than standard sharp debridement, with 65% of water-treated ulcers healed but just 42% of the standard care group (P = .021, unadjusted).
- Researchers from UC Davis and VA Northern California Healthcare are evaluating timolol, a beta adrenergic receptor blocker already approved for topical administration for glaucoma, as a way to heal chronic DFUs faster. After demonstrating that the medication worked in animal models, researchers then launched a study to use it off-label for DFUs. While data are still being analyzed, researcher Roslyn (Rivkah) Isseroff, MD, of UC Davis and VA, said that data so far demonstrate that the timolol reduced transepidermal water loss in the healed wounds, and that is linked with a decrease in re-ulceration.
The Power of a Team
Multidisciplinary approaches to treatment are effective in reducing amputation, with one review of 33 studies finding the approach worked to decrease amputation in 94% of them. “The American Limb Preservation Society (ALPS) lists 30 programs,” said Dr. Armstrong, the founding president of the organization. “There may be as many as 100.”
Team compositions vary but usually include at least one medical specialty clinician, such as infectious disease, primary care, or endocrinology, and two or more specialty clinicians, such as vascular, podiatric, orthopedic, or plastic surgery. A shoe specialist is needed to prescribe and manage footwear. Other important team members include nutrition experts and behavioral health professionals to deal with associated depression.
Johns Hopkins’ Multidisciplinary Diabetic Foot and Wound Service launched in 2012 and includes vascular surgeons, surgical podiatrists, endocrinologists, wound care nurses, advanced practice staff, board-certified wound care specialists, orthopedic surgeons, infection disease experts, physical therapists, and certified orthotists.
“This interdisciplinary care model has been repeatedly validated by research as superior for limb salvage and wound healing,” said Nestoras Mathioudakis, MD, codirector of the service. “For instance, endocrinologists and diabetes educators are crucial for managing uncontrolled diabetes — a key factor in infection and delayed wound healing. Similarly, vascular surgeons play a vital role in addressing peripheral arterial disease to improve blood flow to the affected area.”
“Diabetic foot ulcers might require prolonged periods of specialized care, including meticulous wound management and off-loading, overseen by surgical podiatrists and wound care experts,” he said. “In cases where infection is present, particularly with multidrug resistant organisms or when standard antibiotics are contraindicated, the insight of an infectious disease specialist is invaluable.”
While the makeup of teams varies from location to location, he said “the hallmark of effective teams is their ability to comprehensively manage glycemic control, foot wounds, vascular disease, and infections.”
The power of teams, Dr. Armstrong said, is very much evident after his weekly “foot selfie rounds” conducted Mondays at 7 AM, with an “all feet on deck” approach. “Not a week goes by when we don’t stop a hospitalization,” he said of the team evaluating the photos, due to detecting issues early, while still in the manageable state.
Teams can trump technology, Dr. Armstrong said. A team of just a primary care doctor and a podiatrist can make a significant reduction in amputations, he said, just by a “Knock your socks off” approach. He reminds primary care doctors that observing the feet of their patients with diabetes can go a long way to reducing DFUs and the hospitalizations and amputations that can result.
Dr. Mathioudakis and Dr. Isseroff reported no disclosures. Dr. Boulton consults for Urgo Medical, Nevro Corporation, and AOT, Inc. Dr. Armstrong reported receiving consulting fees from Podimetrics; Molnlycke; Cardiovascular Systems, Inc.; Endo Pharmaceuticals; and Averitas Pharma (GRT US).
A version of this article first appeared on Medscape.com.
The photo of the patient’s foot, sent from his campsite, included a cheeky note: “I remember you telling me that getting in trouble doing something was better than getting in trouble doing nothing. This lets me get out there and know that I have feedback.”
The “this” was the patient’s “foot selfie,” an approach that allows patients at a risk for diabetic foot ulcers (DFUs) to snap a picture and send it to their healthcare providers for evaluation.
This particular patient had an extensive history of previous wounds. Some had essentially kept him house-bound in the past, as he was afraid to get another one.
This time, however, he got an all-clear to keep on camping, “and we scheduled him in on the following Tuesday [for follow-up],” said the camper’s physician David G. Armstrong, DPM, MD, PhD, professor of surgery and neurological surgery, USC Keck School of Medicine, Los Angeles.
Dr. Armstrong is one of the researchers evaluating the concept of foot selfies. It’s a welcome advance, he and others said, and has been shown to help heal wounds and reverse pre-ulcer lesions. Research on foot selfies continues, but much more is needed to solve the issue of DFUs, diabetic foot infections (DFIs), and the high rates of reinfection, experts know.
Worldwide, about 18.6 million people have a DFU each year, including 1.6 million in the United States. About 50%-60% of ulcers become infected, with 20% of moderate to severe infections requiring amputation of the limb. The 5-year mortality rate for DFUs is 30%, but it climbs to 70% after amputation. While about 40% of ulcers heal within 12 weeks, 42% recur at the 1-year mark, setting up a vicious and costly cycle. Healthcare costs for patients with diabetes and DFUs are five times as high as costs for patients with diabetes but no DFUs. The per capita cost to treat a DFU in America is $17,500.
While the statistics paint a grim picture, progress is being made on several fronts:
- US Food and Drug Administration (FDA) guidance on the development of drugs for DFUs, under evaluation, is forthcoming.
- New treatments are under study.
- A multidisciplinary team approach is known to improve outcomes.
Anatomy of a DFU
When neuropathy develops in those with diabetes, they no longer have what Dr. Armstrong calls the “gift” of pain perception. “They can wear a hole in their foot like you and I wear a hole in our sock or shoe,” he said. “That hole is called a diabetic foot ulcer.”
A DFU is an open wound on the foot, often occurring when bleeding develops beneath a callus and then the callus wears away. Deeper tissues of the foot are then exposed.
About half of the DFUs get infected, hence the FDA guidance, said Dr. Armstrong, who is also founding president of the American Limb Preservation Society, which aims to eliminate preventable amputations within the next generation. Every 20 seconds, Dr. Armstrong said, someone in the world loses a leg due to diabetes.
FDA Guidance on Drug Development for DFIs
In October, the FDA issued draft guidance for industry to articulate the design of clinical trials for developing antibacterial drugs to treat DFIs without concomitant bone and joint involvement. Comments closed on December 18. Among the points in the guidance, which is nonbinding, are to include DFIs of varying depths and extent in phase 3 trials and ideally to include only those patients who have not had prior antibacterial treatment for the current DFI.
According to an FDA spokesperson, “The agency is working to finalize the guidance. However, a timeline for its release has not yet been established.”
The good news about the upcoming FDA guidance, Dr. Armstrong said, is that the agency has realized the importance of treating the infections. Fully one third of direct costs of care for diabetes are spent on the lower extremities, he said. Keeping patients out of the hospital, uninfected, and “keeping legs on bodies” are all important goals, he said.
Pharmaceutical firms need to understand that “you aren’t dealing with a normal ulcer,” said Andrew J.M. Boulton, MD, professor of medicine at the University of Manchester and physician consultant at the Manchester Royal Infirmary, Manchester, England, and a visiting professor at the University of Miami. For research, “the most important thing is to take account of off-loading the ulcers,” he said. “Most ulcers will heal if put in a boot.”
Dr. Boulton, like Dr. Armstrong, a long-time expert in the field, contended that pharma has not understood this concept and has wasted millions over the last three decades doing studies that were poorly designed and controlled.
Treatments: Current, Under Study
Currently, DFIs are treated with antimicrobial therapy, without or without debridement, along with a clinical assessment for ischemia. If ischemia is found, care progresses to wound care and off-loading devices, such as healing sandals. Clinicians then assess the likelihood of improved outcomes with revascularization based on operative risks and distribution of lower extremity artery disease and proceed depending on the likelihood. If osteomyelitis testing shows it is present, providers proceed to wound debridement, limb-sparing amputation, and prolonged antimicrobials, as needed.
More options are needed, Dr. Armstrong said.
Among the many approaches under study:
- DFUs can be accurately detected by applying artificial intelligence to the “foot selfie” images taken by patients on smartphones, research by Dr. and has found.
- After a phase 3 study of for DFUs originally intending to enroll 300 subjects was discontinued because of slow patient recruitment, an interim analysis was conducted on 44 participants. It showed a positive trend toward wound closure in the group receiving the injected gene therapy, VM202 (ENGENSIS), in their calf muscles. VM202 is a plasmid DNA-encoding human hepatocyte growth factor. While those in both the intervention and placebo groups showed wound-closing effects at month 6, in 23 patients with neuro-ischemic ulcers, the percentage of those reaching complete closure of the DFU was significantly higher in the treated group at months 3, 4, and 5 (P = .0391, .0391, and .0361, respectively). After excluding two outliers, the difference in months 3-6 became more significant (P = .03).
- An closed more DFUs than standard care after 12 weeks — 70% vs 34% (P = .00032). Of the 100 participants randomized, 50 per group, 42% of the treatment group and 56% of the control group experienced adverse events, with eight withdrawn due to serious adverse events (such as osteomyelitis).
- A closed more refractory DFUs over a 16-week study than standard sharp debridement, with 65% of water-treated ulcers healed but just 42% of the standard care group (P = .021, unadjusted).
- Researchers from UC Davis and VA Northern California Healthcare are evaluating timolol, a beta adrenergic receptor blocker already approved for topical administration for glaucoma, as a way to heal chronic DFUs faster. After demonstrating that the medication worked in animal models, researchers then launched a study to use it off-label for DFUs. While data are still being analyzed, researcher Roslyn (Rivkah) Isseroff, MD, of UC Davis and VA, said that data so far demonstrate that the timolol reduced transepidermal water loss in the healed wounds, and that is linked with a decrease in re-ulceration.
The Power of a Team
Multidisciplinary approaches to treatment are effective in reducing amputation, with one review of 33 studies finding the approach worked to decrease amputation in 94% of them. “The American Limb Preservation Society (ALPS) lists 30 programs,” said Dr. Armstrong, the founding president of the organization. “There may be as many as 100.”
Team compositions vary but usually include at least one medical specialty clinician, such as infectious disease, primary care, or endocrinology, and two or more specialty clinicians, such as vascular, podiatric, orthopedic, or plastic surgery. A shoe specialist is needed to prescribe and manage footwear. Other important team members include nutrition experts and behavioral health professionals to deal with associated depression.
Johns Hopkins’ Multidisciplinary Diabetic Foot and Wound Service launched in 2012 and includes vascular surgeons, surgical podiatrists, endocrinologists, wound care nurses, advanced practice staff, board-certified wound care specialists, orthopedic surgeons, infection disease experts, physical therapists, and certified orthotists.
“This interdisciplinary care model has been repeatedly validated by research as superior for limb salvage and wound healing,” said Nestoras Mathioudakis, MD, codirector of the service. “For instance, endocrinologists and diabetes educators are crucial for managing uncontrolled diabetes — a key factor in infection and delayed wound healing. Similarly, vascular surgeons play a vital role in addressing peripheral arterial disease to improve blood flow to the affected area.”
“Diabetic foot ulcers might require prolonged periods of specialized care, including meticulous wound management and off-loading, overseen by surgical podiatrists and wound care experts,” he said. “In cases where infection is present, particularly with multidrug resistant organisms or when standard antibiotics are contraindicated, the insight of an infectious disease specialist is invaluable.”
While the makeup of teams varies from location to location, he said “the hallmark of effective teams is their ability to comprehensively manage glycemic control, foot wounds, vascular disease, and infections.”
The power of teams, Dr. Armstrong said, is very much evident after his weekly “foot selfie rounds” conducted Mondays at 7 AM, with an “all feet on deck” approach. “Not a week goes by when we don’t stop a hospitalization,” he said of the team evaluating the photos, due to detecting issues early, while still in the manageable state.
Teams can trump technology, Dr. Armstrong said. A team of just a primary care doctor and a podiatrist can make a significant reduction in amputations, he said, just by a “Knock your socks off” approach. He reminds primary care doctors that observing the feet of their patients with diabetes can go a long way to reducing DFUs and the hospitalizations and amputations that can result.
Dr. Mathioudakis and Dr. Isseroff reported no disclosures. Dr. Boulton consults for Urgo Medical, Nevro Corporation, and AOT, Inc. Dr. Armstrong reported receiving consulting fees from Podimetrics; Molnlycke; Cardiovascular Systems, Inc.; Endo Pharmaceuticals; and Averitas Pharma (GRT US).
A version of this article first appeared on Medscape.com.
The photo of the patient’s foot, sent from his campsite, included a cheeky note: “I remember you telling me that getting in trouble doing something was better than getting in trouble doing nothing. This lets me get out there and know that I have feedback.”
The “this” was the patient’s “foot selfie,” an approach that allows patients at a risk for diabetic foot ulcers (DFUs) to snap a picture and send it to their healthcare providers for evaluation.
This particular patient had an extensive history of previous wounds. Some had essentially kept him house-bound in the past, as he was afraid to get another one.
This time, however, he got an all-clear to keep on camping, “and we scheduled him in on the following Tuesday [for follow-up],” said the camper’s physician David G. Armstrong, DPM, MD, PhD, professor of surgery and neurological surgery, USC Keck School of Medicine, Los Angeles.
Dr. Armstrong is one of the researchers evaluating the concept of foot selfies. It’s a welcome advance, he and others said, and has been shown to help heal wounds and reverse pre-ulcer lesions. Research on foot selfies continues, but much more is needed to solve the issue of DFUs, diabetic foot infections (DFIs), and the high rates of reinfection, experts know.
Worldwide, about 18.6 million people have a DFU each year, including 1.6 million in the United States. About 50%-60% of ulcers become infected, with 20% of moderate to severe infections requiring amputation of the limb. The 5-year mortality rate for DFUs is 30%, but it climbs to 70% after amputation. While about 40% of ulcers heal within 12 weeks, 42% recur at the 1-year mark, setting up a vicious and costly cycle. Healthcare costs for patients with diabetes and DFUs are five times as high as costs for patients with diabetes but no DFUs. The per capita cost to treat a DFU in America is $17,500.
While the statistics paint a grim picture, progress is being made on several fronts:
- US Food and Drug Administration (FDA) guidance on the development of drugs for DFUs, under evaluation, is forthcoming.
- New treatments are under study.
- A multidisciplinary team approach is known to improve outcomes.
Anatomy of a DFU
When neuropathy develops in those with diabetes, they no longer have what Dr. Armstrong calls the “gift” of pain perception. “They can wear a hole in their foot like you and I wear a hole in our sock or shoe,” he said. “That hole is called a diabetic foot ulcer.”
A DFU is an open wound on the foot, often occurring when bleeding develops beneath a callus and then the callus wears away. Deeper tissues of the foot are then exposed.
About half of the DFUs get infected, hence the FDA guidance, said Dr. Armstrong, who is also founding president of the American Limb Preservation Society, which aims to eliminate preventable amputations within the next generation. Every 20 seconds, Dr. Armstrong said, someone in the world loses a leg due to diabetes.
FDA Guidance on Drug Development for DFIs
In October, the FDA issued draft guidance for industry to articulate the design of clinical trials for developing antibacterial drugs to treat DFIs without concomitant bone and joint involvement. Comments closed on December 18. Among the points in the guidance, which is nonbinding, are to include DFIs of varying depths and extent in phase 3 trials and ideally to include only those patients who have not had prior antibacterial treatment for the current DFI.
According to an FDA spokesperson, “The agency is working to finalize the guidance. However, a timeline for its release has not yet been established.”
The good news about the upcoming FDA guidance, Dr. Armstrong said, is that the agency has realized the importance of treating the infections. Fully one third of direct costs of care for diabetes are spent on the lower extremities, he said. Keeping patients out of the hospital, uninfected, and “keeping legs on bodies” are all important goals, he said.
Pharmaceutical firms need to understand that “you aren’t dealing with a normal ulcer,” said Andrew J.M. Boulton, MD, professor of medicine at the University of Manchester and physician consultant at the Manchester Royal Infirmary, Manchester, England, and a visiting professor at the University of Miami. For research, “the most important thing is to take account of off-loading the ulcers,” he said. “Most ulcers will heal if put in a boot.”
Dr. Boulton, like Dr. Armstrong, a long-time expert in the field, contended that pharma has not understood this concept and has wasted millions over the last three decades doing studies that were poorly designed and controlled.
Treatments: Current, Under Study
Currently, DFIs are treated with antimicrobial therapy, without or without debridement, along with a clinical assessment for ischemia. If ischemia is found, care progresses to wound care and off-loading devices, such as healing sandals. Clinicians then assess the likelihood of improved outcomes with revascularization based on operative risks and distribution of lower extremity artery disease and proceed depending on the likelihood. If osteomyelitis testing shows it is present, providers proceed to wound debridement, limb-sparing amputation, and prolonged antimicrobials, as needed.
More options are needed, Dr. Armstrong said.
Among the many approaches under study:
- DFUs can be accurately detected by applying artificial intelligence to the “foot selfie” images taken by patients on smartphones, research by Dr. and has found.
- After a phase 3 study of for DFUs originally intending to enroll 300 subjects was discontinued because of slow patient recruitment, an interim analysis was conducted on 44 participants. It showed a positive trend toward wound closure in the group receiving the injected gene therapy, VM202 (ENGENSIS), in their calf muscles. VM202 is a plasmid DNA-encoding human hepatocyte growth factor. While those in both the intervention and placebo groups showed wound-closing effects at month 6, in 23 patients with neuro-ischemic ulcers, the percentage of those reaching complete closure of the DFU was significantly higher in the treated group at months 3, 4, and 5 (P = .0391, .0391, and .0361, respectively). After excluding two outliers, the difference in months 3-6 became more significant (P = .03).
- An closed more DFUs than standard care after 12 weeks — 70% vs 34% (P = .00032). Of the 100 participants randomized, 50 per group, 42% of the treatment group and 56% of the control group experienced adverse events, with eight withdrawn due to serious adverse events (such as osteomyelitis).
- A closed more refractory DFUs over a 16-week study than standard sharp debridement, with 65% of water-treated ulcers healed but just 42% of the standard care group (P = .021, unadjusted).
- Researchers from UC Davis and VA Northern California Healthcare are evaluating timolol, a beta adrenergic receptor blocker already approved for topical administration for glaucoma, as a way to heal chronic DFUs faster. After demonstrating that the medication worked in animal models, researchers then launched a study to use it off-label for DFUs. While data are still being analyzed, researcher Roslyn (Rivkah) Isseroff, MD, of UC Davis and VA, said that data so far demonstrate that the timolol reduced transepidermal water loss in the healed wounds, and that is linked with a decrease in re-ulceration.
The Power of a Team
Multidisciplinary approaches to treatment are effective in reducing amputation, with one review of 33 studies finding the approach worked to decrease amputation in 94% of them. “The American Limb Preservation Society (ALPS) lists 30 programs,” said Dr. Armstrong, the founding president of the organization. “There may be as many as 100.”
Team compositions vary but usually include at least one medical specialty clinician, such as infectious disease, primary care, or endocrinology, and two or more specialty clinicians, such as vascular, podiatric, orthopedic, or plastic surgery. A shoe specialist is needed to prescribe and manage footwear. Other important team members include nutrition experts and behavioral health professionals to deal with associated depression.
Johns Hopkins’ Multidisciplinary Diabetic Foot and Wound Service launched in 2012 and includes vascular surgeons, surgical podiatrists, endocrinologists, wound care nurses, advanced practice staff, board-certified wound care specialists, orthopedic surgeons, infection disease experts, physical therapists, and certified orthotists.
“This interdisciplinary care model has been repeatedly validated by research as superior for limb salvage and wound healing,” said Nestoras Mathioudakis, MD, codirector of the service. “For instance, endocrinologists and diabetes educators are crucial for managing uncontrolled diabetes — a key factor in infection and delayed wound healing. Similarly, vascular surgeons play a vital role in addressing peripheral arterial disease to improve blood flow to the affected area.”
“Diabetic foot ulcers might require prolonged periods of specialized care, including meticulous wound management and off-loading, overseen by surgical podiatrists and wound care experts,” he said. “In cases where infection is present, particularly with multidrug resistant organisms or when standard antibiotics are contraindicated, the insight of an infectious disease specialist is invaluable.”
While the makeup of teams varies from location to location, he said “the hallmark of effective teams is their ability to comprehensively manage glycemic control, foot wounds, vascular disease, and infections.”
The power of teams, Dr. Armstrong said, is very much evident after his weekly “foot selfie rounds” conducted Mondays at 7 AM, with an “all feet on deck” approach. “Not a week goes by when we don’t stop a hospitalization,” he said of the team evaluating the photos, due to detecting issues early, while still in the manageable state.
Teams can trump technology, Dr. Armstrong said. A team of just a primary care doctor and a podiatrist can make a significant reduction in amputations, he said, just by a “Knock your socks off” approach. He reminds primary care doctors that observing the feet of their patients with diabetes can go a long way to reducing DFUs and the hospitalizations and amputations that can result.
Dr. Mathioudakis and Dr. Isseroff reported no disclosures. Dr. Boulton consults for Urgo Medical, Nevro Corporation, and AOT, Inc. Dr. Armstrong reported receiving consulting fees from Podimetrics; Molnlycke; Cardiovascular Systems, Inc.; Endo Pharmaceuticals; and Averitas Pharma (GRT US).
A version of this article first appeared on Medscape.com.
Physicians Own Less Than Half of US Practices; Federal Agencies Want Outside Input
Physician practice ownership by corporations, including health insurers, private equity firms, and large pharmacy chains, reached 30.1% as of January for the first time surpassing ownership by hospitals and health systems (28.4%), according to a new report.
As a result, about three in five physician practices are now owned by nonphysicians.
In early 2020, corporations owned just about 17% of US medical practices, while hospitals and health systems owned about 25%, according to the report released Thursday by nonprofit Physician Advocacy Institute (PAI). But corporate ownership of medical groups surged during the pandemic.
These trends raise questions about how best to protect patients and physicians in a changing employment landscape, said Kelly Kenney, PAI’s chief executive officer, in a statement.
“Corporate entities are assuming control of physician practices and changing the face of medicine in the United States with little to no scrutiny from regulators,” Ms. Kenney said.
The research, conducted by consulting group Avalere for PAI, used the IQVIA OneKey database that contains physician and practice location information on hospital and health system ownership.
By 2022-2023, there was a 7.3% increase in the percentage of practices owned by hospitals and 5.9% increase in the percentage of physicians employed by these organizations, PAI said. In the same time frame, there was an 11% increase in the percentage of practices owned by corporations and a 3.0% increase in the percentage of physicians employed by these entities.
“Physicians have an ethical responsibility to their patients’ health,” Ms. Kenney said. “Corporate entities have a fiduciary responsibility to their shareholders and are motivated to put profits first…these interests can conflict with providing the best medical care to patients.”
Federal Scrutiny Increases
However, both federal and state regulators are paying more attention to what happens to patients and physicians when corporations acquire practices.
“Given recent trends, we are concerned that some transactions may generate profits for those firms at the expense of patients’ health, workers’ safety, quality of care, and affordable healthcare for patients and taxpayers,” said the Federal Trade Commission (FTC) and the Justice (DOJ) and Health and Human Services (HHS) departments.
This statement appears in those agencies’ joint request for information (RFI) announced in March. An RFI is a tool that federal agencies can use to gauge the level of both support and opposition they would face if they were to try to change policies. Public comments are due May 6.
Corporations and advocacy groups often submit detailed comments outlining reasons why the federal government should or should not act on an issue. But individuals also can make their case in this forum.
The FTC, DOJ, and HHS are looking broadly at consolidation in healthcare, but they also spell out potential concerns related to acquisition of physician practices.
For example, they asked clinicians and support staff to provide feedback about whether acquisitions lead to changes in:
- Take-home pay
- Staffing levels
- Workplace safety
- Compensation model (eg, from fixed salary to volume based)
- Policies regarding patient referrals
- Mix of patients
- The volume of patients
- The way providers practice medicine (eg, incentives, prescribing decisions, forced protocols, restrictions on time spent with patients, or mandatory coding practices)
- Administrative or managerial organization (eg, transition to a management services organization).
A version of this article appeared on Medscape.com.
Physician practice ownership by corporations, including health insurers, private equity firms, and large pharmacy chains, reached 30.1% as of January for the first time surpassing ownership by hospitals and health systems (28.4%), according to a new report.
As a result, about three in five physician practices are now owned by nonphysicians.
In early 2020, corporations owned just about 17% of US medical practices, while hospitals and health systems owned about 25%, according to the report released Thursday by nonprofit Physician Advocacy Institute (PAI). But corporate ownership of medical groups surged during the pandemic.
These trends raise questions about how best to protect patients and physicians in a changing employment landscape, said Kelly Kenney, PAI’s chief executive officer, in a statement.
“Corporate entities are assuming control of physician practices and changing the face of medicine in the United States with little to no scrutiny from regulators,” Ms. Kenney said.
The research, conducted by consulting group Avalere for PAI, used the IQVIA OneKey database that contains physician and practice location information on hospital and health system ownership.
By 2022-2023, there was a 7.3% increase in the percentage of practices owned by hospitals and 5.9% increase in the percentage of physicians employed by these organizations, PAI said. In the same time frame, there was an 11% increase in the percentage of practices owned by corporations and a 3.0% increase in the percentage of physicians employed by these entities.
“Physicians have an ethical responsibility to their patients’ health,” Ms. Kenney said. “Corporate entities have a fiduciary responsibility to their shareholders and are motivated to put profits first…these interests can conflict with providing the best medical care to patients.”
Federal Scrutiny Increases
However, both federal and state regulators are paying more attention to what happens to patients and physicians when corporations acquire practices.
“Given recent trends, we are concerned that some transactions may generate profits for those firms at the expense of patients’ health, workers’ safety, quality of care, and affordable healthcare for patients and taxpayers,” said the Federal Trade Commission (FTC) and the Justice (DOJ) and Health and Human Services (HHS) departments.
This statement appears in those agencies’ joint request for information (RFI) announced in March. An RFI is a tool that federal agencies can use to gauge the level of both support and opposition they would face if they were to try to change policies. Public comments are due May 6.
Corporations and advocacy groups often submit detailed comments outlining reasons why the federal government should or should not act on an issue. But individuals also can make their case in this forum.
The FTC, DOJ, and HHS are looking broadly at consolidation in healthcare, but they also spell out potential concerns related to acquisition of physician practices.
For example, they asked clinicians and support staff to provide feedback about whether acquisitions lead to changes in:
- Take-home pay
- Staffing levels
- Workplace safety
- Compensation model (eg, from fixed salary to volume based)
- Policies regarding patient referrals
- Mix of patients
- The volume of patients
- The way providers practice medicine (eg, incentives, prescribing decisions, forced protocols, restrictions on time spent with patients, or mandatory coding practices)
- Administrative or managerial organization (eg, transition to a management services organization).
A version of this article appeared on Medscape.com.
Physician practice ownership by corporations, including health insurers, private equity firms, and large pharmacy chains, reached 30.1% as of January for the first time surpassing ownership by hospitals and health systems (28.4%), according to a new report.
As a result, about three in five physician practices are now owned by nonphysicians.
In early 2020, corporations owned just about 17% of US medical practices, while hospitals and health systems owned about 25%, according to the report released Thursday by nonprofit Physician Advocacy Institute (PAI). But corporate ownership of medical groups surged during the pandemic.
These trends raise questions about how best to protect patients and physicians in a changing employment landscape, said Kelly Kenney, PAI’s chief executive officer, in a statement.
“Corporate entities are assuming control of physician practices and changing the face of medicine in the United States with little to no scrutiny from regulators,” Ms. Kenney said.
The research, conducted by consulting group Avalere for PAI, used the IQVIA OneKey database that contains physician and practice location information on hospital and health system ownership.
By 2022-2023, there was a 7.3% increase in the percentage of practices owned by hospitals and 5.9% increase in the percentage of physicians employed by these organizations, PAI said. In the same time frame, there was an 11% increase in the percentage of practices owned by corporations and a 3.0% increase in the percentage of physicians employed by these entities.
“Physicians have an ethical responsibility to their patients’ health,” Ms. Kenney said. “Corporate entities have a fiduciary responsibility to their shareholders and are motivated to put profits first…these interests can conflict with providing the best medical care to patients.”
Federal Scrutiny Increases
However, both federal and state regulators are paying more attention to what happens to patients and physicians when corporations acquire practices.
“Given recent trends, we are concerned that some transactions may generate profits for those firms at the expense of patients’ health, workers’ safety, quality of care, and affordable healthcare for patients and taxpayers,” said the Federal Trade Commission (FTC) and the Justice (DOJ) and Health and Human Services (HHS) departments.
This statement appears in those agencies’ joint request for information (RFI) announced in March. An RFI is a tool that federal agencies can use to gauge the level of both support and opposition they would face if they were to try to change policies. Public comments are due May 6.
Corporations and advocacy groups often submit detailed comments outlining reasons why the federal government should or should not act on an issue. But individuals also can make their case in this forum.
The FTC, DOJ, and HHS are looking broadly at consolidation in healthcare, but they also spell out potential concerns related to acquisition of physician practices.
For example, they asked clinicians and support staff to provide feedback about whether acquisitions lead to changes in:
- Take-home pay
- Staffing levels
- Workplace safety
- Compensation model (eg, from fixed salary to volume based)
- Policies regarding patient referrals
- Mix of patients
- The volume of patients
- The way providers practice medicine (eg, incentives, prescribing decisions, forced protocols, restrictions on time spent with patients, or mandatory coding practices)
- Administrative or managerial organization (eg, transition to a management services organization).
A version of this article appeared on Medscape.com.
‘Difficult Patient’: Stigmatizing Words and Medical Error
This transcript has been edited for clarity.
When I was doing my nephrology training, I had an attending who would write notes that were, well, kind of funny. I remember one time we were seeing a patient whose first name was “Lucky.” He dryly opened his section of the consult note as follows: “This is a 56-year-old woman with an ironic name who presents with acute renal failure.”
As an exhausted renal fellow, I appreciated the bit of color amid the ongoing series of tragedies that was the consult service. But let’s be clear — writing like this in the medical record is not a good idea. It wasn’t a good idea then, when any record might end up disclosed during a malpractice suit, and it’s really not a good idea now, when patients have ready and automated access to all the notes we write about them.
And yet, worse language than that of my attending appears in hospital notes all the time; there is research about this. Specifically, I’m talking about language that does not have high clinical utility but telegraphs the biases of the person writing the note. This is known as “stigmatizing language” and it can be overt or subtle.
For example, a physician wrote “I listed several fictitious medication names and she reported she was taking them.”
This casts suspicions about the patient’s credibility, as does the more subtle statement, “he claims nicotine patches don’t work for him.” Stigmatizing language may cast the patient in a difficult light, like this note: “she persevered on the fact that ... ‘you wouldn’t understand.’ ”
Stay with me.
We are going to start by defining a very sick patient population: those admitted to the hospital and who, within 48 hours, have either been transferred to the intensive care unit or died. Because of the severity of illness in this population we’ve just defined, figuring out whether a diagnostic or other error was made would be extremely high yield; these can mean the difference between life and death.
In a letter appearing in JAMA Internal Medicine, researchers examined a group of more than 2300 patients just like this from 29 hospitals, scouring the medical records for evidence of these types of errors.
Nearly one in four (23.2%) had at least one diagnostic error, which could include a missed physical exam finding, failure to ask a key question on history taking, inadequate testing, and so on.
Understanding why we make these errors is clearly critical to improving care for these patients. The researchers hypothesized that stigmatizing language might lead to errors like this. For example, by demonstrating that you don’t find a patient credible, you may ignore statements that would help make a better diagnosis.
Just over 5% of these patients had evidence of stigmatizing language in their medical notes. Like earlier studies, this language was more common if the patient was Black or had unstable housing.
Critically, stigmatizing language was more likely to be found among those who had diagnostic errors — a rate of 8.2% vs 4.1%. After adjustment for factors like race, the presence of stigmatizing language was associated with roughly a doubling of the risk for diagnostic errors.
Now, I’m all for eliminating stigmatizing language from our medical notes. And, given the increased transparency of all medical notes these days, I expect that we’ll see less of this over time. But of course, the fact that a physician doesn’t write something that disparages the patient does not necessarily mean that they don’t retain that bias. That said, those comments have an effect on all the other team members who care for that patient as well; it sets a tone and can entrench an individual’s bias more broadly. We should strive to eliminate our biases when it comes to caring for patients. But perhaps the second best thing is to work to keep those biases to ourselves.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When I was doing my nephrology training, I had an attending who would write notes that were, well, kind of funny. I remember one time we were seeing a patient whose first name was “Lucky.” He dryly opened his section of the consult note as follows: “This is a 56-year-old woman with an ironic name who presents with acute renal failure.”
As an exhausted renal fellow, I appreciated the bit of color amid the ongoing series of tragedies that was the consult service. But let’s be clear — writing like this in the medical record is not a good idea. It wasn’t a good idea then, when any record might end up disclosed during a malpractice suit, and it’s really not a good idea now, when patients have ready and automated access to all the notes we write about them.
And yet, worse language than that of my attending appears in hospital notes all the time; there is research about this. Specifically, I’m talking about language that does not have high clinical utility but telegraphs the biases of the person writing the note. This is known as “stigmatizing language” and it can be overt or subtle.
For example, a physician wrote “I listed several fictitious medication names and she reported she was taking them.”
This casts suspicions about the patient’s credibility, as does the more subtle statement, “he claims nicotine patches don’t work for him.” Stigmatizing language may cast the patient in a difficult light, like this note: “she persevered on the fact that ... ‘you wouldn’t understand.’ ”
Stay with me.
We are going to start by defining a very sick patient population: those admitted to the hospital and who, within 48 hours, have either been transferred to the intensive care unit or died. Because of the severity of illness in this population we’ve just defined, figuring out whether a diagnostic or other error was made would be extremely high yield; these can mean the difference between life and death.
In a letter appearing in JAMA Internal Medicine, researchers examined a group of more than 2300 patients just like this from 29 hospitals, scouring the medical records for evidence of these types of errors.
Nearly one in four (23.2%) had at least one diagnostic error, which could include a missed physical exam finding, failure to ask a key question on history taking, inadequate testing, and so on.
Understanding why we make these errors is clearly critical to improving care for these patients. The researchers hypothesized that stigmatizing language might lead to errors like this. For example, by demonstrating that you don’t find a patient credible, you may ignore statements that would help make a better diagnosis.
Just over 5% of these patients had evidence of stigmatizing language in their medical notes. Like earlier studies, this language was more common if the patient was Black or had unstable housing.
Critically, stigmatizing language was more likely to be found among those who had diagnostic errors — a rate of 8.2% vs 4.1%. After adjustment for factors like race, the presence of stigmatizing language was associated with roughly a doubling of the risk for diagnostic errors.
Now, I’m all for eliminating stigmatizing language from our medical notes. And, given the increased transparency of all medical notes these days, I expect that we’ll see less of this over time. But of course, the fact that a physician doesn’t write something that disparages the patient does not necessarily mean that they don’t retain that bias. That said, those comments have an effect on all the other team members who care for that patient as well; it sets a tone and can entrench an individual’s bias more broadly. We should strive to eliminate our biases when it comes to caring for patients. But perhaps the second best thing is to work to keep those biases to ourselves.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When I was doing my nephrology training, I had an attending who would write notes that were, well, kind of funny. I remember one time we were seeing a patient whose first name was “Lucky.” He dryly opened his section of the consult note as follows: “This is a 56-year-old woman with an ironic name who presents with acute renal failure.”
As an exhausted renal fellow, I appreciated the bit of color amid the ongoing series of tragedies that was the consult service. But let’s be clear — writing like this in the medical record is not a good idea. It wasn’t a good idea then, when any record might end up disclosed during a malpractice suit, and it’s really not a good idea now, when patients have ready and automated access to all the notes we write about them.
And yet, worse language than that of my attending appears in hospital notes all the time; there is research about this. Specifically, I’m talking about language that does not have high clinical utility but telegraphs the biases of the person writing the note. This is known as “stigmatizing language” and it can be overt or subtle.
For example, a physician wrote “I listed several fictitious medication names and she reported she was taking them.”
This casts suspicions about the patient’s credibility, as does the more subtle statement, “he claims nicotine patches don’t work for him.” Stigmatizing language may cast the patient in a difficult light, like this note: “she persevered on the fact that ... ‘you wouldn’t understand.’ ”
Stay with me.
We are going to start by defining a very sick patient population: those admitted to the hospital and who, within 48 hours, have either been transferred to the intensive care unit or died. Because of the severity of illness in this population we’ve just defined, figuring out whether a diagnostic or other error was made would be extremely high yield; these can mean the difference between life and death.
In a letter appearing in JAMA Internal Medicine, researchers examined a group of more than 2300 patients just like this from 29 hospitals, scouring the medical records for evidence of these types of errors.
Nearly one in four (23.2%) had at least one diagnostic error, which could include a missed physical exam finding, failure to ask a key question on history taking, inadequate testing, and so on.
Understanding why we make these errors is clearly critical to improving care for these patients. The researchers hypothesized that stigmatizing language might lead to errors like this. For example, by demonstrating that you don’t find a patient credible, you may ignore statements that would help make a better diagnosis.
Just over 5% of these patients had evidence of stigmatizing language in their medical notes. Like earlier studies, this language was more common if the patient was Black or had unstable housing.
Critically, stigmatizing language was more likely to be found among those who had diagnostic errors — a rate of 8.2% vs 4.1%. After adjustment for factors like race, the presence of stigmatizing language was associated with roughly a doubling of the risk for diagnostic errors.
Now, I’m all for eliminating stigmatizing language from our medical notes. And, given the increased transparency of all medical notes these days, I expect that we’ll see less of this over time. But of course, the fact that a physician doesn’t write something that disparages the patient does not necessarily mean that they don’t retain that bias. That said, those comments have an effect on all the other team members who care for that patient as well; it sets a tone and can entrench an individual’s bias more broadly. We should strive to eliminate our biases when it comes to caring for patients. But perhaps the second best thing is to work to keep those biases to ourselves.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Working From Home: Doctors’ Options Are Not Limited to Classic Telemedicine
The appeal of working from home is undeniable. It comes with no daily commute, casual dress, and the ability to manage work-life balance more effectively.
Telemedicine is often the first thing that comes to mind when physicians think about remote medical practice. In its traditional sense, telemedicine entails live video consults, replicating the in-person experience as closely as possible, minus the hands-on component. However, this format is just one of many types of virtual care presenting opportunities to practice medicine from home.
The scope and volume of such opportunities are expanding due to technology, regulatory shifts at the state and federal levels favoring remote healthcare, and a wider move toward remote work. Virtual practice options for physicians range from full-time employment to flexible part-time positions that can be used to earn supplementary income.
Just a few of those virtual options are:
Remote Patient Monitoring
Remote patient monitoring uses technology for tracking patient health data, applicable in real-time or asynchronously, through devices ranging from specialized monitors to consumer wearables. Data are securely transmitted to healthcare providers, enabling them to guide or make treatment choices remotely. This method has proven particularly valuable in managing chronic diseases where continuous monitoring can significantly affect outcomes.
Like standard telemedicine, remote patient monitoring offers flexibility, autonomy, and the ability to work from home. It is picking up steam across the healthcare industry, especially in critical care, surgery, post-acute care, and primary care, so there are opportunities for physicians across a variety of specialties.
Online Medication Management and Text-Based Consults
Gathering necessary information for patient care decisions often doesn’t require a direct, face-to-face visit in person or by telemedicine. Clinical data can be efficiently collected through online forms, HIPAA-compliant messaging, medical record reviews, and information gathered by staff.
An approach that uses all these sources enables effective medication management for stable chronic conditions (such as hypertension), as well as straightforward but simple acute issues (such as urinary tract infections). It also is useful for quick follow-ups with patients after starting new treatments, to address questions between visits, and to give them educational material.
Some medical practices and virtual healthcare corporations have made online medication management and text-based consults the center of their business model. Part-time positions with platforms that offer this type of care let physicians fit consultations into their schedule as time permits, without committing to scheduled appointments.
eConsults
Electronic consultations, or eConsults, facilitate collaboration among healthcare professionals about complex cases without direct patient interaction.
These services operate via online platforms that support asynchronous communication and often bypass the need for a traditional referral. Typically, a primary care provider submits a query that is then assigned to a specialist. Next, the specialist reviews the information and offers recommendations for the patient’s care plan.
Major eConsult platforms such as AristaMD and RubiconMD contract with healthcare systems and medical practices. Physicians can easily join the specialist panels of these companies and complete assigned consultations from their homes or offices, paid on a per-consult basis. They should check their employment contracts to make sure such independent contract work is allowed.
Phone-Only On-Call Positions
On-call rotations for after-hour care bring with them challenges in staffing and scheduling vacations. These challenges have helped trigger as-needed or per diem on-call roles, in which a physician provides recommendations and orders over the phone without needing to visit an office or a hospital.
Examples of workplaces that employ phone-only on-call physicians include smaller jails, mental health facilities, dialysis centers, long-term care facilities, and sporting groups or events needing back-up for on-site nurses or emergency medical technicians.
While these positions can sometimes be challenging for a physician to find, they are out there. They can be a fantastic option to earn additional income through low-stress clinical work performed from home.
Supervision of Nurse Practitioners (NPs) and Physician Assistants (PAs)
In states that mandate such physician oversight, it often be conducted remotely — depending on that state’s rules, the practice type, and the scope of services being provided. This remote option introduces part-time opportunities for physicians to oversee NPs and PAs without being in the medical office. Essentially, the doctor needs to be available for phone or email consultations, complete chart reviews, and meet regularly with the provider.
Remote supervision roles are available across various types of healthcare organizations and medical practices. There also are opportunities with insurers, many of which have established NP-run, in-home member assessment programs that require remote supervision by a doctor.
Remote Medical Directorships
Medical directors are a key part of the clinician team in a wide variety of healthcare settings requiring clinical protocol oversight, regulatory compliance, and guidance for other clinicians making treatment decisions. Many directorships do not require direct patient contact and therefore are conducive to remote work, given technologies such as electronic health record and secure messaging systems.
Organizations such as emergency medical service agencies, hospice services, med spas, blood and plasma donation centers, home health agencies, and substance use disorder treatment programs increasingly rely on remote medical directorships to meet legal requirements and accreditation standards.
Although these positions are often viewed as “nonclinical,” they carry significant clinical responsibilities. Examples are developing and reviewing treatment protocols, ensuring adherence to healthcare regulations, and sometimes intervening in complex patient cases or when adverse outcomes occur.
Keeping a Role in Patient Welfare
Clearly, working from home as a physician doesn’t have to mean taking on a nonclinical job. Beyond the options already mentioned, there are numerous others — for example, working as a medical monitor for clinical trials, in utilization management for insurance companies, or in conducting independent medical exams for insurance claims. While these roles don’t involve direct patient treatment, they require similar skills and affect the quality of care.
If such remote opportunities aren’t currently available in your workplace, consider approaching your management about trying them.
Physicians who are experiencing burnout, seeking a career change, or interested in earning extra income should consider exploring more of the unconventional ways that they can practice medicine.
A version of this article appeared on Medscape.com.
The appeal of working from home is undeniable. It comes with no daily commute, casual dress, and the ability to manage work-life balance more effectively.
Telemedicine is often the first thing that comes to mind when physicians think about remote medical practice. In its traditional sense, telemedicine entails live video consults, replicating the in-person experience as closely as possible, minus the hands-on component. However, this format is just one of many types of virtual care presenting opportunities to practice medicine from home.
The scope and volume of such opportunities are expanding due to technology, regulatory shifts at the state and federal levels favoring remote healthcare, and a wider move toward remote work. Virtual practice options for physicians range from full-time employment to flexible part-time positions that can be used to earn supplementary income.
Just a few of those virtual options are:
Remote Patient Monitoring
Remote patient monitoring uses technology for tracking patient health data, applicable in real-time or asynchronously, through devices ranging from specialized monitors to consumer wearables. Data are securely transmitted to healthcare providers, enabling them to guide or make treatment choices remotely. This method has proven particularly valuable in managing chronic diseases where continuous monitoring can significantly affect outcomes.
Like standard telemedicine, remote patient monitoring offers flexibility, autonomy, and the ability to work from home. It is picking up steam across the healthcare industry, especially in critical care, surgery, post-acute care, and primary care, so there are opportunities for physicians across a variety of specialties.
Online Medication Management and Text-Based Consults
Gathering necessary information for patient care decisions often doesn’t require a direct, face-to-face visit in person or by telemedicine. Clinical data can be efficiently collected through online forms, HIPAA-compliant messaging, medical record reviews, and information gathered by staff.
An approach that uses all these sources enables effective medication management for stable chronic conditions (such as hypertension), as well as straightforward but simple acute issues (such as urinary tract infections). It also is useful for quick follow-ups with patients after starting new treatments, to address questions between visits, and to give them educational material.
Some medical practices and virtual healthcare corporations have made online medication management and text-based consults the center of their business model. Part-time positions with platforms that offer this type of care let physicians fit consultations into their schedule as time permits, without committing to scheduled appointments.
eConsults
Electronic consultations, or eConsults, facilitate collaboration among healthcare professionals about complex cases without direct patient interaction.
These services operate via online platforms that support asynchronous communication and often bypass the need for a traditional referral. Typically, a primary care provider submits a query that is then assigned to a specialist. Next, the specialist reviews the information and offers recommendations for the patient’s care plan.
Major eConsult platforms such as AristaMD and RubiconMD contract with healthcare systems and medical practices. Physicians can easily join the specialist panels of these companies and complete assigned consultations from their homes or offices, paid on a per-consult basis. They should check their employment contracts to make sure such independent contract work is allowed.
Phone-Only On-Call Positions
On-call rotations for after-hour care bring with them challenges in staffing and scheduling vacations. These challenges have helped trigger as-needed or per diem on-call roles, in which a physician provides recommendations and orders over the phone without needing to visit an office or a hospital.
Examples of workplaces that employ phone-only on-call physicians include smaller jails, mental health facilities, dialysis centers, long-term care facilities, and sporting groups or events needing back-up for on-site nurses or emergency medical technicians.
While these positions can sometimes be challenging for a physician to find, they are out there. They can be a fantastic option to earn additional income through low-stress clinical work performed from home.
Supervision of Nurse Practitioners (NPs) and Physician Assistants (PAs)
In states that mandate such physician oversight, it often be conducted remotely — depending on that state’s rules, the practice type, and the scope of services being provided. This remote option introduces part-time opportunities for physicians to oversee NPs and PAs without being in the medical office. Essentially, the doctor needs to be available for phone or email consultations, complete chart reviews, and meet regularly with the provider.
Remote supervision roles are available across various types of healthcare organizations and medical practices. There also are opportunities with insurers, many of which have established NP-run, in-home member assessment programs that require remote supervision by a doctor.
Remote Medical Directorships
Medical directors are a key part of the clinician team in a wide variety of healthcare settings requiring clinical protocol oversight, regulatory compliance, and guidance for other clinicians making treatment decisions. Many directorships do not require direct patient contact and therefore are conducive to remote work, given technologies such as electronic health record and secure messaging systems.
Organizations such as emergency medical service agencies, hospice services, med spas, blood and plasma donation centers, home health agencies, and substance use disorder treatment programs increasingly rely on remote medical directorships to meet legal requirements and accreditation standards.
Although these positions are often viewed as “nonclinical,” they carry significant clinical responsibilities. Examples are developing and reviewing treatment protocols, ensuring adherence to healthcare regulations, and sometimes intervening in complex patient cases or when adverse outcomes occur.
Keeping a Role in Patient Welfare
Clearly, working from home as a physician doesn’t have to mean taking on a nonclinical job. Beyond the options already mentioned, there are numerous others — for example, working as a medical monitor for clinical trials, in utilization management for insurance companies, or in conducting independent medical exams for insurance claims. While these roles don’t involve direct patient treatment, they require similar skills and affect the quality of care.
If such remote opportunities aren’t currently available in your workplace, consider approaching your management about trying them.
Physicians who are experiencing burnout, seeking a career change, or interested in earning extra income should consider exploring more of the unconventional ways that they can practice medicine.
A version of this article appeared on Medscape.com.
The appeal of working from home is undeniable. It comes with no daily commute, casual dress, and the ability to manage work-life balance more effectively.
Telemedicine is often the first thing that comes to mind when physicians think about remote medical practice. In its traditional sense, telemedicine entails live video consults, replicating the in-person experience as closely as possible, minus the hands-on component. However, this format is just one of many types of virtual care presenting opportunities to practice medicine from home.
The scope and volume of such opportunities are expanding due to technology, regulatory shifts at the state and federal levels favoring remote healthcare, and a wider move toward remote work. Virtual practice options for physicians range from full-time employment to flexible part-time positions that can be used to earn supplementary income.
Just a few of those virtual options are:
Remote Patient Monitoring
Remote patient monitoring uses technology for tracking patient health data, applicable in real-time or asynchronously, through devices ranging from specialized monitors to consumer wearables. Data are securely transmitted to healthcare providers, enabling them to guide or make treatment choices remotely. This method has proven particularly valuable in managing chronic diseases where continuous monitoring can significantly affect outcomes.
Like standard telemedicine, remote patient monitoring offers flexibility, autonomy, and the ability to work from home. It is picking up steam across the healthcare industry, especially in critical care, surgery, post-acute care, and primary care, so there are opportunities for physicians across a variety of specialties.
Online Medication Management and Text-Based Consults
Gathering necessary information for patient care decisions often doesn’t require a direct, face-to-face visit in person or by telemedicine. Clinical data can be efficiently collected through online forms, HIPAA-compliant messaging, medical record reviews, and information gathered by staff.
An approach that uses all these sources enables effective medication management for stable chronic conditions (such as hypertension), as well as straightforward but simple acute issues (such as urinary tract infections). It also is useful for quick follow-ups with patients after starting new treatments, to address questions between visits, and to give them educational material.
Some medical practices and virtual healthcare corporations have made online medication management and text-based consults the center of their business model. Part-time positions with platforms that offer this type of care let physicians fit consultations into their schedule as time permits, without committing to scheduled appointments.
eConsults
Electronic consultations, or eConsults, facilitate collaboration among healthcare professionals about complex cases without direct patient interaction.
These services operate via online platforms that support asynchronous communication and often bypass the need for a traditional referral. Typically, a primary care provider submits a query that is then assigned to a specialist. Next, the specialist reviews the information and offers recommendations for the patient’s care plan.
Major eConsult platforms such as AristaMD and RubiconMD contract with healthcare systems and medical practices. Physicians can easily join the specialist panels of these companies and complete assigned consultations from their homes or offices, paid on a per-consult basis. They should check their employment contracts to make sure such independent contract work is allowed.
Phone-Only On-Call Positions
On-call rotations for after-hour care bring with them challenges in staffing and scheduling vacations. These challenges have helped trigger as-needed or per diem on-call roles, in which a physician provides recommendations and orders over the phone without needing to visit an office or a hospital.
Examples of workplaces that employ phone-only on-call physicians include smaller jails, mental health facilities, dialysis centers, long-term care facilities, and sporting groups or events needing back-up for on-site nurses or emergency medical technicians.
While these positions can sometimes be challenging for a physician to find, they are out there. They can be a fantastic option to earn additional income through low-stress clinical work performed from home.
Supervision of Nurse Practitioners (NPs) and Physician Assistants (PAs)
In states that mandate such physician oversight, it often be conducted remotely — depending on that state’s rules, the practice type, and the scope of services being provided. This remote option introduces part-time opportunities for physicians to oversee NPs and PAs without being in the medical office. Essentially, the doctor needs to be available for phone or email consultations, complete chart reviews, and meet regularly with the provider.
Remote supervision roles are available across various types of healthcare organizations and medical practices. There also are opportunities with insurers, many of which have established NP-run, in-home member assessment programs that require remote supervision by a doctor.
Remote Medical Directorships
Medical directors are a key part of the clinician team in a wide variety of healthcare settings requiring clinical protocol oversight, regulatory compliance, and guidance for other clinicians making treatment decisions. Many directorships do not require direct patient contact and therefore are conducive to remote work, given technologies such as electronic health record and secure messaging systems.
Organizations such as emergency medical service agencies, hospice services, med spas, blood and plasma donation centers, home health agencies, and substance use disorder treatment programs increasingly rely on remote medical directorships to meet legal requirements and accreditation standards.
Although these positions are often viewed as “nonclinical,” they carry significant clinical responsibilities. Examples are developing and reviewing treatment protocols, ensuring adherence to healthcare regulations, and sometimes intervening in complex patient cases or when adverse outcomes occur.
Keeping a Role in Patient Welfare
Clearly, working from home as a physician doesn’t have to mean taking on a nonclinical job. Beyond the options already mentioned, there are numerous others — for example, working as a medical monitor for clinical trials, in utilization management for insurance companies, or in conducting independent medical exams for insurance claims. While these roles don’t involve direct patient treatment, they require similar skills and affect the quality of care.
If such remote opportunities aren’t currently available in your workplace, consider approaching your management about trying them.
Physicians who are experiencing burnout, seeking a career change, or interested in earning extra income should consider exploring more of the unconventional ways that they can practice medicine.
A version of this article appeared on Medscape.com.
Is Axillary Surgery in Early Breast Cancer on Its Way Out?
TOPLINE:
METHODOLOGY:
- A growing body of evidence has indicated that patients with one or two positive sentinel nodes undergoing breast-conserving surgery and radiation therapy can skip axillary lymph node dissection and achieve similar outcomes compared with patients receiving axillary dissection.
- However, these earlier studies had notable limitations, such as limited statistical power, uncertain nodal radiotherapy target volumes, and minimal data on relevant clinical subgroups.
- To fill the gaps in the literature, the researchers conducted a trial with a large, inclusive cohort of patients with node-negative stage T1-T3 breast cancer who had one or two sentinel-node macrometastases and had undergone a mastectomy or breast-conserving surgery.
- The trial randomized 2540 patients to either completion axillary lymph node dissection (n = 1205) or sentinel-node biopsy only (n = 1335). Nearly 90% of patients received adjuvant radiation therapy, and the majority also received systematic therapy.
- Earlier recurrence-free survival findings and patient-reported outcomes were reported last December. The researchers now reported overall survival findings as well as secondary endpoints of breast cancer-specific survival.
TAKEAWAY:
- The researchers reported 191 recurrences or deaths over a median follow-up of 46.8 months; 62 patients (4.6%) in the sentinel-node biopsy–only group died, and 69 patients (5.7%) in the dissection group died.
- The biopsy-only group had an estimated 5-year overall survival of 92.9% compared with 92.0% in the dissection group and an estimated 5-year breast cancer-specific survival of 97.1% vs 96.6% in the dissection group.
- The estimated 5-year recurrence-free survival was 89.7% in the biopsy-only group vs 88.7% in the dissection group (hazard ratio [HR], 0.89; 95% CI, 0.66-1.19).
- This non-inferior difference held across all prespecified patient subgroups, except in patients with estrogen receptor-positive, human epidermal growth factor receptor 2–positive disease, in which sentinel biopsy alone appeared to be better (HR, 0.26).
IN PRACTICE:
“This trial provides robust evidence that the omission of completion axillary-lymph-node dissection was safe in patients with clinically node-negative T1, T2, or T3 breast cancer and one or two sentinel-node macrometastases who received adjuvant systemic treatment and radiation therapy according to national guidelines,” the authors concluded.
“It is clear that the role of axillary dissection is rapidly disappearing,” Kandace P. McGuire, MD, of Virginia Commonwealth University, Richmond, wrote in an accompanying editorial. “However, axillary staging continues to be vital with regard to decisions about appropriate breast cancer therapy.”
SOURCE:
This work, led by Jana de Boniface, MD, PhD, from Karolinska Institute, Stockholm, was published online in The New England Journal of Medicine, alongside the accompanying editorial by Dr. McGuire.
LIMITATIONS:
The study limitations include unavailable radiation therapy details for comparison, low male recruitment hindering sex-based analysis, short follow-up for luminal subtype breast cancer, unmet enrollment targets, and higher withdrawal rates in the dissection group.
DISCLOSURES:
This study was supported by the Swedish Research Council, Swedish Cancer Society, Nordic Cancer Union, and Swedish Breast Cancer Association. One coauthor reported receiving consultancy fees from various pharmaceutical companies outside this work.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- A growing body of evidence has indicated that patients with one or two positive sentinel nodes undergoing breast-conserving surgery and radiation therapy can skip axillary lymph node dissection and achieve similar outcomes compared with patients receiving axillary dissection.
- However, these earlier studies had notable limitations, such as limited statistical power, uncertain nodal radiotherapy target volumes, and minimal data on relevant clinical subgroups.
- To fill the gaps in the literature, the researchers conducted a trial with a large, inclusive cohort of patients with node-negative stage T1-T3 breast cancer who had one or two sentinel-node macrometastases and had undergone a mastectomy or breast-conserving surgery.
- The trial randomized 2540 patients to either completion axillary lymph node dissection (n = 1205) or sentinel-node biopsy only (n = 1335). Nearly 90% of patients received adjuvant radiation therapy, and the majority also received systematic therapy.
- Earlier recurrence-free survival findings and patient-reported outcomes were reported last December. The researchers now reported overall survival findings as well as secondary endpoints of breast cancer-specific survival.
TAKEAWAY:
- The researchers reported 191 recurrences or deaths over a median follow-up of 46.8 months; 62 patients (4.6%) in the sentinel-node biopsy–only group died, and 69 patients (5.7%) in the dissection group died.
- The biopsy-only group had an estimated 5-year overall survival of 92.9% compared with 92.0% in the dissection group and an estimated 5-year breast cancer-specific survival of 97.1% vs 96.6% in the dissection group.
- The estimated 5-year recurrence-free survival was 89.7% in the biopsy-only group vs 88.7% in the dissection group (hazard ratio [HR], 0.89; 95% CI, 0.66-1.19).
- This non-inferior difference held across all prespecified patient subgroups, except in patients with estrogen receptor-positive, human epidermal growth factor receptor 2–positive disease, in which sentinel biopsy alone appeared to be better (HR, 0.26).
IN PRACTICE:
“This trial provides robust evidence that the omission of completion axillary-lymph-node dissection was safe in patients with clinically node-negative T1, T2, or T3 breast cancer and one or two sentinel-node macrometastases who received adjuvant systemic treatment and radiation therapy according to national guidelines,” the authors concluded.
“It is clear that the role of axillary dissection is rapidly disappearing,” Kandace P. McGuire, MD, of Virginia Commonwealth University, Richmond, wrote in an accompanying editorial. “However, axillary staging continues to be vital with regard to decisions about appropriate breast cancer therapy.”
SOURCE:
This work, led by Jana de Boniface, MD, PhD, from Karolinska Institute, Stockholm, was published online in The New England Journal of Medicine, alongside the accompanying editorial by Dr. McGuire.
LIMITATIONS:
The study limitations include unavailable radiation therapy details for comparison, low male recruitment hindering sex-based analysis, short follow-up for luminal subtype breast cancer, unmet enrollment targets, and higher withdrawal rates in the dissection group.
DISCLOSURES:
This study was supported by the Swedish Research Council, Swedish Cancer Society, Nordic Cancer Union, and Swedish Breast Cancer Association. One coauthor reported receiving consultancy fees from various pharmaceutical companies outside this work.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- A growing body of evidence has indicated that patients with one or two positive sentinel nodes undergoing breast-conserving surgery and radiation therapy can skip axillary lymph node dissection and achieve similar outcomes compared with patients receiving axillary dissection.
- However, these earlier studies had notable limitations, such as limited statistical power, uncertain nodal radiotherapy target volumes, and minimal data on relevant clinical subgroups.
- To fill the gaps in the literature, the researchers conducted a trial with a large, inclusive cohort of patients with node-negative stage T1-T3 breast cancer who had one or two sentinel-node macrometastases and had undergone a mastectomy or breast-conserving surgery.
- The trial randomized 2540 patients to either completion axillary lymph node dissection (n = 1205) or sentinel-node biopsy only (n = 1335). Nearly 90% of patients received adjuvant radiation therapy, and the majority also received systematic therapy.
- Earlier recurrence-free survival findings and patient-reported outcomes were reported last December. The researchers now reported overall survival findings as well as secondary endpoints of breast cancer-specific survival.
TAKEAWAY:
- The researchers reported 191 recurrences or deaths over a median follow-up of 46.8 months; 62 patients (4.6%) in the sentinel-node biopsy–only group died, and 69 patients (5.7%) in the dissection group died.
- The biopsy-only group had an estimated 5-year overall survival of 92.9% compared with 92.0% in the dissection group and an estimated 5-year breast cancer-specific survival of 97.1% vs 96.6% in the dissection group.
- The estimated 5-year recurrence-free survival was 89.7% in the biopsy-only group vs 88.7% in the dissection group (hazard ratio [HR], 0.89; 95% CI, 0.66-1.19).
- This non-inferior difference held across all prespecified patient subgroups, except in patients with estrogen receptor-positive, human epidermal growth factor receptor 2–positive disease, in which sentinel biopsy alone appeared to be better (HR, 0.26).
IN PRACTICE:
“This trial provides robust evidence that the omission of completion axillary-lymph-node dissection was safe in patients with clinically node-negative T1, T2, or T3 breast cancer and one or two sentinel-node macrometastases who received adjuvant systemic treatment and radiation therapy according to national guidelines,” the authors concluded.
“It is clear that the role of axillary dissection is rapidly disappearing,” Kandace P. McGuire, MD, of Virginia Commonwealth University, Richmond, wrote in an accompanying editorial. “However, axillary staging continues to be vital with regard to decisions about appropriate breast cancer therapy.”
SOURCE:
This work, led by Jana de Boniface, MD, PhD, from Karolinska Institute, Stockholm, was published online in The New England Journal of Medicine, alongside the accompanying editorial by Dr. McGuire.
LIMITATIONS:
The study limitations include unavailable radiation therapy details for comparison, low male recruitment hindering sex-based analysis, short follow-up for luminal subtype breast cancer, unmet enrollment targets, and higher withdrawal rates in the dissection group.
DISCLOSURES:
This study was supported by the Swedish Research Council, Swedish Cancer Society, Nordic Cancer Union, and Swedish Breast Cancer Association. One coauthor reported receiving consultancy fees from various pharmaceutical companies outside this work.
A version of this article appeared on Medscape.com.