User login
AF patients receive unnecessary oral anticoagulants
About a quarter of U.S. atrial fibrillation patients under 60 years old and in otherwise good health received oral anticoagulants contrary to guidelines, according to a research letter from Dr. Jonathan Hsu of the University of California, San Diego, and his associates.
In patients in the National Cardiovascular Data Registry’s PINNACLE (Practice Innovation and Clinical Excellence) registry who had a CHADS2 and CHA2DS2-VASc score of zero, the average age of those who received oral anticoagulants was just under 51 years, compared with just over 46 years for those who did not receive oral anticoagulants. In addition to age, higher body mass index and having Medicare or no insurance vs. private insurance were associated with a higher prescription chance.
Patients treated in the South were significantly less likely to be prescribed anticoagulants than were those treated in the Northeast.
“Prescription of oral anticoagulants by cardiovascular specialists in a significant proportion of patients at the lowest thrombotic risk suggests that these health care professionals may not be fully aware of the potential risks associated with oral anticoagulation or the particularly low risk of stroke in this population,” the investigators concluded. Find the full research letter in JAMA Internal Medicine (doi:10.1001/jamainternmed.2015.0920).
About a quarter of U.S. atrial fibrillation patients under 60 years old and in otherwise good health received oral anticoagulants contrary to guidelines, according to a research letter from Dr. Jonathan Hsu of the University of California, San Diego, and his associates.
In patients in the National Cardiovascular Data Registry’s PINNACLE (Practice Innovation and Clinical Excellence) registry who had a CHADS2 and CHA2DS2-VASc score of zero, the average age of those who received oral anticoagulants was just under 51 years, compared with just over 46 years for those who did not receive oral anticoagulants. In addition to age, higher body mass index and having Medicare or no insurance vs. private insurance were associated with a higher prescription chance.
Patients treated in the South were significantly less likely to be prescribed anticoagulants than were those treated in the Northeast.
“Prescription of oral anticoagulants by cardiovascular specialists in a significant proportion of patients at the lowest thrombotic risk suggests that these health care professionals may not be fully aware of the potential risks associated with oral anticoagulation or the particularly low risk of stroke in this population,” the investigators concluded. Find the full research letter in JAMA Internal Medicine (doi:10.1001/jamainternmed.2015.0920).
About a quarter of U.S. atrial fibrillation patients under 60 years old and in otherwise good health received oral anticoagulants contrary to guidelines, according to a research letter from Dr. Jonathan Hsu of the University of California, San Diego, and his associates.
In patients in the National Cardiovascular Data Registry’s PINNACLE (Practice Innovation and Clinical Excellence) registry who had a CHADS2 and CHA2DS2-VASc score of zero, the average age of those who received oral anticoagulants was just under 51 years, compared with just over 46 years for those who did not receive oral anticoagulants. In addition to age, higher body mass index and having Medicare or no insurance vs. private insurance were associated with a higher prescription chance.
Patients treated in the South were significantly less likely to be prescribed anticoagulants than were those treated in the Northeast.
“Prescription of oral anticoagulants by cardiovascular specialists in a significant proportion of patients at the lowest thrombotic risk suggests that these health care professionals may not be fully aware of the potential risks associated with oral anticoagulation or the particularly low risk of stroke in this population,” the investigators concluded. Find the full research letter in JAMA Internal Medicine (doi:10.1001/jamainternmed.2015.0920).
Poor control of CVD risk factors raises morbidity, mortality risk in diabetes
Optimal control of glucose, blood pressure, LDL cholesterol, and smoking in adults with diabetes could result in substantial reductions of cardiovascular risk, according to results from a large cohort study of diabetes patients with and without underlying cardiovascular disease.
CV events and deaths associated with inadequate control of any of these four modifiable risk factors were about 11% and 3%, respectively, for subjects with baseline CVD, and 34% and 7%, respectively, for those without it.
Though risk was much higher for those with CVD, as expected, more attention to these traditional CVD risk factors in all diabetic patients – with or without CVD – would significantly reduce CVD-related morbidity and mortality, investigators concluded.
For their research, published online in Diabetes Care, epidemiologist Gabriela Vasquez-Benitez, Ph.D., of the Health Partners Institute for Education and Research in Minneapolis and her associates identified 859,617 patients with diabetes (31% with CVD) receiving treatment at a network of 11 U.S. health centers for 6 months or more, with mean follow-up of 5 years. About half of patients were female, and 45% were white. Risk factors were defined as LDL-C ≥100 mg/dL, glycosylated hemoglobin (HbA1c) ≥7%, blood pressure ≥140/90 mm Hg, or smoking.
Dr. Vasquez-Benitez and associates used a regression analysis to quantify the contributions each risk factor made to CVD risk and type of CV event in both patient groups.
In patients without CVD (n = 593,167), the vast majority had HbA1c, BP, and LDL-C not at goal or were current smokers. Inadequately controlled LDL cholesterol was associated with 19.6% of myocardial infarction or acute coronary syndrome (95% confidence interval, 18.7-20.5), and 13.7% of strokes. Smoking was associated with 3.8% of all CV events, while inadequately controlled blood pressure was associated with 11.6% of strokes. Dr. Vasquez-Benitez and colleagues found an increased CV risk for HbA1c above 9%, but no increased risk for HbA1c of 7%-7.9%, compared with 6.5%-6.9%. This finding supports current guidelines recommending HbA1c targets below 7% or 8% for patients with diabetes, according to the investigators (Diab. Care 2015 Feb. 20 [doi:10.2337/dc14-1877]).
In subjects with diabetes and CVD, 7% of stroke was found attributable to inadequate blood pressure control and 5.9% to poor glycemic control. Smoking was the only factor seen associated with an increase in all-cause mortality in this patient group, with 2.6% of deaths seen linked to smoking.
Dr. Vasquez-Benitez and her colleagues noted in their analysis that a substantial share of risk could not be attributed to the modifiable factors investigated in their study, raising the possibility that “unidentified genetic, metabolic, or psychosocial risk factors may affect risk.”
The investigators noted as limitations of their study the fact that risk factors and comorbidities were assessed at baseline and may have changed during follow-up, and that data were obtained from routine care settings with varying time intervals. Patients with type I diabetes may have been included in the cohort due to difficulties distinguishing diabetes types in patient records, they said.
The study was funded by the Agency for Healthcare Research & Quality. None of its authors reported conflicts of interest.
Optimal control of glucose, blood pressure, LDL cholesterol, and smoking in adults with diabetes could result in substantial reductions of cardiovascular risk, according to results from a large cohort study of diabetes patients with and without underlying cardiovascular disease.
CV events and deaths associated with inadequate control of any of these four modifiable risk factors were about 11% and 3%, respectively, for subjects with baseline CVD, and 34% and 7%, respectively, for those without it.
Though risk was much higher for those with CVD, as expected, more attention to these traditional CVD risk factors in all diabetic patients – with or without CVD – would significantly reduce CVD-related morbidity and mortality, investigators concluded.
For their research, published online in Diabetes Care, epidemiologist Gabriela Vasquez-Benitez, Ph.D., of the Health Partners Institute for Education and Research in Minneapolis and her associates identified 859,617 patients with diabetes (31% with CVD) receiving treatment at a network of 11 U.S. health centers for 6 months or more, with mean follow-up of 5 years. About half of patients were female, and 45% were white. Risk factors were defined as LDL-C ≥100 mg/dL, glycosylated hemoglobin (HbA1c) ≥7%, blood pressure ≥140/90 mm Hg, or smoking.
Dr. Vasquez-Benitez and associates used a regression analysis to quantify the contributions each risk factor made to CVD risk and type of CV event in both patient groups.
In patients without CVD (n = 593,167), the vast majority had HbA1c, BP, and LDL-C not at goal or were current smokers. Inadequately controlled LDL cholesterol was associated with 19.6% of myocardial infarction or acute coronary syndrome (95% confidence interval, 18.7-20.5), and 13.7% of strokes. Smoking was associated with 3.8% of all CV events, while inadequately controlled blood pressure was associated with 11.6% of strokes. Dr. Vasquez-Benitez and colleagues found an increased CV risk for HbA1c above 9%, but no increased risk for HbA1c of 7%-7.9%, compared with 6.5%-6.9%. This finding supports current guidelines recommending HbA1c targets below 7% or 8% for patients with diabetes, according to the investigators (Diab. Care 2015 Feb. 20 [doi:10.2337/dc14-1877]).
In subjects with diabetes and CVD, 7% of stroke was found attributable to inadequate blood pressure control and 5.9% to poor glycemic control. Smoking was the only factor seen associated with an increase in all-cause mortality in this patient group, with 2.6% of deaths seen linked to smoking.
Dr. Vasquez-Benitez and her colleagues noted in their analysis that a substantial share of risk could not be attributed to the modifiable factors investigated in their study, raising the possibility that “unidentified genetic, metabolic, or psychosocial risk factors may affect risk.”
The investigators noted as limitations of their study the fact that risk factors and comorbidities were assessed at baseline and may have changed during follow-up, and that data were obtained from routine care settings with varying time intervals. Patients with type I diabetes may have been included in the cohort due to difficulties distinguishing diabetes types in patient records, they said.
The study was funded by the Agency for Healthcare Research & Quality. None of its authors reported conflicts of interest.
Optimal control of glucose, blood pressure, LDL cholesterol, and smoking in adults with diabetes could result in substantial reductions of cardiovascular risk, according to results from a large cohort study of diabetes patients with and without underlying cardiovascular disease.
CV events and deaths associated with inadequate control of any of these four modifiable risk factors were about 11% and 3%, respectively, for subjects with baseline CVD, and 34% and 7%, respectively, for those without it.
Though risk was much higher for those with CVD, as expected, more attention to these traditional CVD risk factors in all diabetic patients – with or without CVD – would significantly reduce CVD-related morbidity and mortality, investigators concluded.
For their research, published online in Diabetes Care, epidemiologist Gabriela Vasquez-Benitez, Ph.D., of the Health Partners Institute for Education and Research in Minneapolis and her associates identified 859,617 patients with diabetes (31% with CVD) receiving treatment at a network of 11 U.S. health centers for 6 months or more, with mean follow-up of 5 years. About half of patients were female, and 45% were white. Risk factors were defined as LDL-C ≥100 mg/dL, glycosylated hemoglobin (HbA1c) ≥7%, blood pressure ≥140/90 mm Hg, or smoking.
Dr. Vasquez-Benitez and associates used a regression analysis to quantify the contributions each risk factor made to CVD risk and type of CV event in both patient groups.
In patients without CVD (n = 593,167), the vast majority had HbA1c, BP, and LDL-C not at goal or were current smokers. Inadequately controlled LDL cholesterol was associated with 19.6% of myocardial infarction or acute coronary syndrome (95% confidence interval, 18.7-20.5), and 13.7% of strokes. Smoking was associated with 3.8% of all CV events, while inadequately controlled blood pressure was associated with 11.6% of strokes. Dr. Vasquez-Benitez and colleagues found an increased CV risk for HbA1c above 9%, but no increased risk for HbA1c of 7%-7.9%, compared with 6.5%-6.9%. This finding supports current guidelines recommending HbA1c targets below 7% or 8% for patients with diabetes, according to the investigators (Diab. Care 2015 Feb. 20 [doi:10.2337/dc14-1877]).
In subjects with diabetes and CVD, 7% of stroke was found attributable to inadequate blood pressure control and 5.9% to poor glycemic control. Smoking was the only factor seen associated with an increase in all-cause mortality in this patient group, with 2.6% of deaths seen linked to smoking.
Dr. Vasquez-Benitez and her colleagues noted in their analysis that a substantial share of risk could not be attributed to the modifiable factors investigated in their study, raising the possibility that “unidentified genetic, metabolic, or psychosocial risk factors may affect risk.”
The investigators noted as limitations of their study the fact that risk factors and comorbidities were assessed at baseline and may have changed during follow-up, and that data were obtained from routine care settings with varying time intervals. Patients with type I diabetes may have been included in the cohort due to difficulties distinguishing diabetes types in patient records, they said.
The study was funded by the Agency for Healthcare Research & Quality. None of its authors reported conflicts of interest.
FROM DIABETES CARE
Key clinical point: Optimal control of cardiac risk factors in patients with diabetes can substantially lower their CV risks.
Major finding: Traditional cardiovascular risk factors contribute to more than one-third of CV morbidity in patients with diabetes without known underlying cardiovascular disease.
Data source: More than 850,000 patients with diabetes treated at 11 linked healthcare centers between 2005 and 2011, of whom nearly 600,000 had no CVD at baseline.
Disclosures: Dr. Vasquez-Benitez and her associates reported no relevant conflicts of interest.
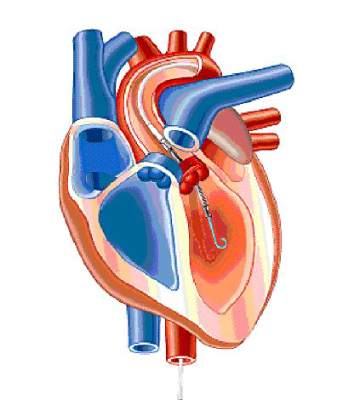
CoreValve receives first TAVR valve-in-valve indication
The U.S. Food and Drug Administration on March 30 expanded its approved use of the CoreValve transcatheter aortic-valve replacement (TAVR) system to include patients who already have undergone aortic valve replacement and need a second valve replacement done as a valve-in-valve placement.
With this action, CoreValve became the first TAVR system to receive U.S. approval for valve-in-valve use. The CoreValve System received FDA approval for TAVR performed on native aortic valves in January 2014 in patients at “extreme risk,” and in June 2014 for those at “high risk,” for surgical aortic valve replacement.* Valve-in-valve TAVR is only feasible in patients with a failing bioprosthetic aortic valve: It is not an option for patients with a failing mechanical aortic valve.
“The CoreValve System offers a less-invasive treatment option for a significant number of patients with failed tissue aortic valves whose medical teams determine that the risks associated with repeat open-heart surgery are high or extremely high,” Dr. William H. Maisel, deputy center director for science and chief scientist in the FDA’s Center for Devices and Radiological Health, said in a written statement. “The approval is an important expansion of the authorized use of the transcatheter aortic valve replacement technology.”
The CoreValve, which is designed to sit in a supra-annular location 12 mm above the aortic valve annulus, is well suited for valve-in-valve replacement because the only portion of the CoreValve that actually fills the annular space and the ring of the existing valve is the CoreValve’s sealer. This results in a tight seal that produces less paravalvular leak than when the sealer sits in a native annulus that is often deformed with calcium, noted Dr. Michael J. Reardon, professor of cardiothoracic surgery at Methodist Hospital in Houston.
In addition, because the sealer exerts pressure on the old valve ring in the annulus instead of on myocardium, placing the CoreValve as a valve-in-valve produces much less conduction disruption and results in fewer patients who need a pacemaker following TAVR, he said.
The CoreValve as a valve-in-valve “works quite well, and is not hard to position,” said Dr. Reardon, who added that he has now performed several valve-in-valve TAVRs using the CoreValve.
Similar TAVR procedures are usually not possible using the balloon-expandable SAPIEN System because the SAPIEN valve is designed to sit directly in the annulus and, in most patients, the existing valve ring does not provide enough space to accommodate a SAPIEN valve.
Dr. Reardon anticipates that many U.S. patients now in their 80s with a failing bioprosthetic aortic valve will be interested in nonsurgical TAVR replacement. These patients often do not want conventional open-heart surgery, he said in an interview.
To evaluate the safety and efficacy of the CoreValve System for aortic valve-in-valve replacement, the FDA reviewed clinical data collected from a U.S. clinical trial with 143 patients, an agency representative said in the statement. In the clinical trial, the estimated rate of 30-day survival without major stroke was 96%, and 89% after 6 months. “This compares well to the corresponding rates reported previously for trial participants who received the same device to replace their own, native diseased or damaged aortic valve,” the agency’s statement said.
According to the agency, aortic valve-in-valve use of the CoreValve System should be limited to patients who need replacement of a failed tissue aortic valve but are at extreme or high risk of death or serious complications from traditional open-heart surgery. A decision as to whether the product and procedure are appropriate for a patient “should involve careful evaluation by the patient’s heart medical team, including a cardiologist and a cardiac surgeon.”
The FDA said that the CoreValve System should not be used in patients who have any infection, have a mechanical aortic heart valve, cannot tolerate anticoagulant drugs, or have sensitivity to titanium, nickel, or contrast media.
Dr. Maisel had no disclosures. Dr. Reardon has served as an advisor to Medtronic, the company that markets the CoreValve.
On Twitter @mitchelzoler
*Correction, 4/1/2015: An earlier version of this article misstated the device’s approval history.
The U.S. Food and Drug Administration on March 30 expanded its approved use of the CoreValve transcatheter aortic-valve replacement (TAVR) system to include patients who already have undergone aortic valve replacement and need a second valve replacement done as a valve-in-valve placement.
With this action, CoreValve became the first TAVR system to receive U.S. approval for valve-in-valve use. The CoreValve System received FDA approval for TAVR performed on native aortic valves in January 2014 in patients at “extreme risk,” and in June 2014 for those at “high risk,” for surgical aortic valve replacement.* Valve-in-valve TAVR is only feasible in patients with a failing bioprosthetic aortic valve: It is not an option for patients with a failing mechanical aortic valve.
“The CoreValve System offers a less-invasive treatment option for a significant number of patients with failed tissue aortic valves whose medical teams determine that the risks associated with repeat open-heart surgery are high or extremely high,” Dr. William H. Maisel, deputy center director for science and chief scientist in the FDA’s Center for Devices and Radiological Health, said in a written statement. “The approval is an important expansion of the authorized use of the transcatheter aortic valve replacement technology.”
The CoreValve, which is designed to sit in a supra-annular location 12 mm above the aortic valve annulus, is well suited for valve-in-valve replacement because the only portion of the CoreValve that actually fills the annular space and the ring of the existing valve is the CoreValve’s sealer. This results in a tight seal that produces less paravalvular leak than when the sealer sits in a native annulus that is often deformed with calcium, noted Dr. Michael J. Reardon, professor of cardiothoracic surgery at Methodist Hospital in Houston.
In addition, because the sealer exerts pressure on the old valve ring in the annulus instead of on myocardium, placing the CoreValve as a valve-in-valve produces much less conduction disruption and results in fewer patients who need a pacemaker following TAVR, he said.
The CoreValve as a valve-in-valve “works quite well, and is not hard to position,” said Dr. Reardon, who added that he has now performed several valve-in-valve TAVRs using the CoreValve.
Similar TAVR procedures are usually not possible using the balloon-expandable SAPIEN System because the SAPIEN valve is designed to sit directly in the annulus and, in most patients, the existing valve ring does not provide enough space to accommodate a SAPIEN valve.
Dr. Reardon anticipates that many U.S. patients now in their 80s with a failing bioprosthetic aortic valve will be interested in nonsurgical TAVR replacement. These patients often do not want conventional open-heart surgery, he said in an interview.
To evaluate the safety and efficacy of the CoreValve System for aortic valve-in-valve replacement, the FDA reviewed clinical data collected from a U.S. clinical trial with 143 patients, an agency representative said in the statement. In the clinical trial, the estimated rate of 30-day survival without major stroke was 96%, and 89% after 6 months. “This compares well to the corresponding rates reported previously for trial participants who received the same device to replace their own, native diseased or damaged aortic valve,” the agency’s statement said.
According to the agency, aortic valve-in-valve use of the CoreValve System should be limited to patients who need replacement of a failed tissue aortic valve but are at extreme or high risk of death or serious complications from traditional open-heart surgery. A decision as to whether the product and procedure are appropriate for a patient “should involve careful evaluation by the patient’s heart medical team, including a cardiologist and a cardiac surgeon.”
The FDA said that the CoreValve System should not be used in patients who have any infection, have a mechanical aortic heart valve, cannot tolerate anticoagulant drugs, or have sensitivity to titanium, nickel, or contrast media.
Dr. Maisel had no disclosures. Dr. Reardon has served as an advisor to Medtronic, the company that markets the CoreValve.
On Twitter @mitchelzoler
*Correction, 4/1/2015: An earlier version of this article misstated the device’s approval history.
The U.S. Food and Drug Administration on March 30 expanded its approved use of the CoreValve transcatheter aortic-valve replacement (TAVR) system to include patients who already have undergone aortic valve replacement and need a second valve replacement done as a valve-in-valve placement.
With this action, CoreValve became the first TAVR system to receive U.S. approval for valve-in-valve use. The CoreValve System received FDA approval for TAVR performed on native aortic valves in January 2014 in patients at “extreme risk,” and in June 2014 for those at “high risk,” for surgical aortic valve replacement.* Valve-in-valve TAVR is only feasible in patients with a failing bioprosthetic aortic valve: It is not an option for patients with a failing mechanical aortic valve.
“The CoreValve System offers a less-invasive treatment option for a significant number of patients with failed tissue aortic valves whose medical teams determine that the risks associated with repeat open-heart surgery are high or extremely high,” Dr. William H. Maisel, deputy center director for science and chief scientist in the FDA’s Center for Devices and Radiological Health, said in a written statement. “The approval is an important expansion of the authorized use of the transcatheter aortic valve replacement technology.”
The CoreValve, which is designed to sit in a supra-annular location 12 mm above the aortic valve annulus, is well suited for valve-in-valve replacement because the only portion of the CoreValve that actually fills the annular space and the ring of the existing valve is the CoreValve’s sealer. This results in a tight seal that produces less paravalvular leak than when the sealer sits in a native annulus that is often deformed with calcium, noted Dr. Michael J. Reardon, professor of cardiothoracic surgery at Methodist Hospital in Houston.
In addition, because the sealer exerts pressure on the old valve ring in the annulus instead of on myocardium, placing the CoreValve as a valve-in-valve produces much less conduction disruption and results in fewer patients who need a pacemaker following TAVR, he said.
The CoreValve as a valve-in-valve “works quite well, and is not hard to position,” said Dr. Reardon, who added that he has now performed several valve-in-valve TAVRs using the CoreValve.
Similar TAVR procedures are usually not possible using the balloon-expandable SAPIEN System because the SAPIEN valve is designed to sit directly in the annulus and, in most patients, the existing valve ring does not provide enough space to accommodate a SAPIEN valve.
Dr. Reardon anticipates that many U.S. patients now in their 80s with a failing bioprosthetic aortic valve will be interested in nonsurgical TAVR replacement. These patients often do not want conventional open-heart surgery, he said in an interview.
To evaluate the safety and efficacy of the CoreValve System for aortic valve-in-valve replacement, the FDA reviewed clinical data collected from a U.S. clinical trial with 143 patients, an agency representative said in the statement. In the clinical trial, the estimated rate of 30-day survival without major stroke was 96%, and 89% after 6 months. “This compares well to the corresponding rates reported previously for trial participants who received the same device to replace their own, native diseased or damaged aortic valve,” the agency’s statement said.
According to the agency, aortic valve-in-valve use of the CoreValve System should be limited to patients who need replacement of a failed tissue aortic valve but are at extreme or high risk of death or serious complications from traditional open-heart surgery. A decision as to whether the product and procedure are appropriate for a patient “should involve careful evaluation by the patient’s heart medical team, including a cardiologist and a cardiac surgeon.”
The FDA said that the CoreValve System should not be used in patients who have any infection, have a mechanical aortic heart valve, cannot tolerate anticoagulant drugs, or have sensitivity to titanium, nickel, or contrast media.
Dr. Maisel had no disclosures. Dr. Reardon has served as an advisor to Medtronic, the company that markets the CoreValve.
On Twitter @mitchelzoler
*Correction, 4/1/2015: An earlier version of this article misstated the device’s approval history.
AHA/ACC updates hypertension guidelines for CAD patients
The first update to U.S. guidelines for managing hypertension in adult patients with coronary artery disease in 8 years reset the target blood pressure for most of these patients to less than 140/90 mm Hg, and highlighted beta-blockers, renin-angiotensin-aldosterone system blockers, and thiazide diuretics as the mainstays of drug treatment for these patients.
The main messages in the new scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension, released on March 31 in an article published online (Hypertension 2015 [doi:10.116/HYP.0000000000000018]) are the blood pressure targets set for patients with coronary artery disease (CAD) and the designations of the preferred drugs to use to achieve the blood pressure goals when lifestyle measures alone prove inadequate, said Dr. Clive Rosendorff, chair of the panel that wrote the new statement.
But the statement also highlighted that a blood pressure target of less than 130/80 mm Hg “could be considered” and was reasonable for selected CAD patients whom physicians judge capable of achieving this lower blood pressure level safely and who are at especially high risk for cerebrovascular events.
“We felt the best evidence [to prevent future cardiovascular events] was to reduce pressure below 140/90 mm Hg, but a goal pressure of less than 130/80 mm Hg may be appropriate in some cases; we left it to the discretion of physicians to decide which blood pressure target to choose,” said Dr. Rosendorff, professor of medicine at Mount Sinai Hospital in New York.
The default blood pressure goal of less than 140/90 for most CAD patients represented an increase from the less than 130/80 mm Hg goal set by the prior edition of this guideline, issued in 2007 (Circulation 2007;115:2761-88). Current evidence for the lower blood pressure target of less than 130/80 mm Hg “was not as strong,” Dr. Rosendorff said in an interview. He suggested that physicians consider using the lower target for patients who are younger, reasonably healthy, able to tolerate a regimen that brings them to a lower blood pressure without an increase in angina or other significant effects caused by the drugs themselves, do not experience compromised renal function with reduced blood pressure, and have an increased risk for cerebrovascular events.
“These guidelines are not rigid, and should involve a discussion with the patient of the benefits and risks,” he said.
The new statement targets a blood pressure goal of less than 150/90 mm Hg for CAD patients who are more than 80 years old.
The new target for CAD patients represents something of a response to the blood pressure target of less than 150/90 mm Hg for people at least 60 years old recommended last year in recommendations made by the panel originally assembled as the Eighth Joint National Committee (JNC 8) (JAMA 2014;311:507-20). Although the JNC 8 recommendations aimed at the general population in a primary prevention setting, as opposed to CAD patients for whom secondary prevention is the goal, the target of less than 150/90 mm Hg became “highly controversial” and was a factor in composing the new recommendation, Dr. Rosendorff said. He also stressed that the AHA, ACC, and ASH have assembled a group that is formulating new recommendations for diagnosing and managing hypertension for the general population in a primary prevention setting that will come out sometime in the future.
The new hypertension guideline for CAD patients and the 2014 statement from the JNC 8 panel should be seen as distinct recommendations because they targeted different patient populations and because they were based on different ground rules for evidence, said Dr. Suzanne Oparil, one of three people who served on both writing groups. The JNC 8 group focused exclusively on findings from randomized, controlled trials that used hard cardiovascular disease endpoints. The writing committee for the new guidelines targeted specifically at CAD patients also considered evidence from epidemiologic studies. In addition, the new guidelines is targeted at primarily a cardiologist audience, while the 2014 JNC 8 guidelines were written primarily for primary care physicians, she said in an interview.
“I do not believe that the new CAD guidelines will change practice. They reflect what most cardiologists already do,” said Dr. Oparil, professor of medicine and director of the vascular biology and hypertension program at the University of Alabama, Birmingham.
Regarding antihypertensive drug selection the new statement endorses a focus on treating hypertensive patients with established CAD with a beta-blocker, a renin-angiotensin-aldosterone system blocker such as an ACE inhibitor or angiotensin-receptor blocker, and a thiazide or thiazide-like diuretic. Hypertensive patients with CAD should immediately start on all three drug classes, Dr. Rosendorff said.
“For patients with established CAD, a treatment with a beta-blocker moves from the limbo they are in for treating uncomplicated hypertension to center stage,” he said. The statement gives more detailed guidance on which specific drugs from the beta-blocker class have the best evidence for efficacy in various types of patients with CAD.
Dr. Rosendorff had no disclosures. Dr. Oparil has been a consultant to Bayer, Daiichi Sankyo, and Pfizer, and has received research grants from Medtronic, Merck, Novartis, and Takeda.
On Twitter @mitchelzoler
The new statement on treating hypertension in patients with established coronary artery disease clears up what had been a confusing situation for U.S. physicians during the past year.
In early 2014, the panel that had originally been assembled as the Eighth Joint National Committee (JNC 8) issued a statement that called for a blood pressure target of less than 150/90 mm Hg for people 60 years or older (JAMA 2014;311:507-20). People were very confused about that, and may have erroneously believed that this recommendation applied to patients with CAD. I and many of my colleagues believe that having a recommendation to treat to just less than 150/90 mm Hg potentially put millions of CAD patients at risk, especially at risk for stroke. The new statement highlights the high risk faced by CAD patients who need special attention to their blood pressure.

|
| Mitchel L. Zoler/Fronbtline Medical News Dr. Elliott M. Antman |
The epidemiologic evidence clearly shows that increased blood pressure relates to an increased risk for cardiovascular events across a blood pressure range from 115/75 mm Hg to 185/115 mm Hg.
The new recommendations for CAD patients also say that a target blood pressure of less than 130/80 mm Hg may be preferred for selected patients, although the statement does not offer clear steps on how to identify these patients. Physicians must use their clinical judgment.
In my practice, I make sure not to drop a patient’s creatinine clearance to an unacceptably low level, and I would especially consider the lower target for patients with a history of heart failure or left ventricular dilatation or hypertrophy. I believe that in the past, physicians have been too conservative about blood pressure reduction in CAD patients, in part out of a concern about reducing perfusion pressure too much. I believe that if a CAD patient can tolerate a lower blood pressure and the treatment it takes to achieve it, then it is better to be more aggressive.
We also must always remember that the lifestyle modifications, including less dietary sodium, weight loss, and exercise, are the first steps to reducing blood pressure.
Dr. Elliott M. Antman is professor of medicine at Harvard University in Boston and president of the American Heart Association. He had no relevant disclosures. He made these comments in an interview.
The new statement on treating hypertension in patients with established coronary artery disease clears up what had been a confusing situation for U.S. physicians during the past year.
In early 2014, the panel that had originally been assembled as the Eighth Joint National Committee (JNC 8) issued a statement that called for a blood pressure target of less than 150/90 mm Hg for people 60 years or older (JAMA 2014;311:507-20). People were very confused about that, and may have erroneously believed that this recommendation applied to patients with CAD. I and many of my colleagues believe that having a recommendation to treat to just less than 150/90 mm Hg potentially put millions of CAD patients at risk, especially at risk for stroke. The new statement highlights the high risk faced by CAD patients who need special attention to their blood pressure.

|
| Mitchel L. Zoler/Fronbtline Medical News Dr. Elliott M. Antman |
The epidemiologic evidence clearly shows that increased blood pressure relates to an increased risk for cardiovascular events across a blood pressure range from 115/75 mm Hg to 185/115 mm Hg.
The new recommendations for CAD patients also say that a target blood pressure of less than 130/80 mm Hg may be preferred for selected patients, although the statement does not offer clear steps on how to identify these patients. Physicians must use their clinical judgment.
In my practice, I make sure not to drop a patient’s creatinine clearance to an unacceptably low level, and I would especially consider the lower target for patients with a history of heart failure or left ventricular dilatation or hypertrophy. I believe that in the past, physicians have been too conservative about blood pressure reduction in CAD patients, in part out of a concern about reducing perfusion pressure too much. I believe that if a CAD patient can tolerate a lower blood pressure and the treatment it takes to achieve it, then it is better to be more aggressive.
We also must always remember that the lifestyle modifications, including less dietary sodium, weight loss, and exercise, are the first steps to reducing blood pressure.
Dr. Elliott M. Antman is professor of medicine at Harvard University in Boston and president of the American Heart Association. He had no relevant disclosures. He made these comments in an interview.
The new statement on treating hypertension in patients with established coronary artery disease clears up what had been a confusing situation for U.S. physicians during the past year.
In early 2014, the panel that had originally been assembled as the Eighth Joint National Committee (JNC 8) issued a statement that called for a blood pressure target of less than 150/90 mm Hg for people 60 years or older (JAMA 2014;311:507-20). People were very confused about that, and may have erroneously believed that this recommendation applied to patients with CAD. I and many of my colleagues believe that having a recommendation to treat to just less than 150/90 mm Hg potentially put millions of CAD patients at risk, especially at risk for stroke. The new statement highlights the high risk faced by CAD patients who need special attention to their blood pressure.

|
| Mitchel L. Zoler/Fronbtline Medical News Dr. Elliott M. Antman |
The epidemiologic evidence clearly shows that increased blood pressure relates to an increased risk for cardiovascular events across a blood pressure range from 115/75 mm Hg to 185/115 mm Hg.
The new recommendations for CAD patients also say that a target blood pressure of less than 130/80 mm Hg may be preferred for selected patients, although the statement does not offer clear steps on how to identify these patients. Physicians must use their clinical judgment.
In my practice, I make sure not to drop a patient’s creatinine clearance to an unacceptably low level, and I would especially consider the lower target for patients with a history of heart failure or left ventricular dilatation or hypertrophy. I believe that in the past, physicians have been too conservative about blood pressure reduction in CAD patients, in part out of a concern about reducing perfusion pressure too much. I believe that if a CAD patient can tolerate a lower blood pressure and the treatment it takes to achieve it, then it is better to be more aggressive.
We also must always remember that the lifestyle modifications, including less dietary sodium, weight loss, and exercise, are the first steps to reducing blood pressure.
Dr. Elliott M. Antman is professor of medicine at Harvard University in Boston and president of the American Heart Association. He had no relevant disclosures. He made these comments in an interview.
The first update to U.S. guidelines for managing hypertension in adult patients with coronary artery disease in 8 years reset the target blood pressure for most of these patients to less than 140/90 mm Hg, and highlighted beta-blockers, renin-angiotensin-aldosterone system blockers, and thiazide diuretics as the mainstays of drug treatment for these patients.
The main messages in the new scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension, released on March 31 in an article published online (Hypertension 2015 [doi:10.116/HYP.0000000000000018]) are the blood pressure targets set for patients with coronary artery disease (CAD) and the designations of the preferred drugs to use to achieve the blood pressure goals when lifestyle measures alone prove inadequate, said Dr. Clive Rosendorff, chair of the panel that wrote the new statement.
But the statement also highlighted that a blood pressure target of less than 130/80 mm Hg “could be considered” and was reasonable for selected CAD patients whom physicians judge capable of achieving this lower blood pressure level safely and who are at especially high risk for cerebrovascular events.
“We felt the best evidence [to prevent future cardiovascular events] was to reduce pressure below 140/90 mm Hg, but a goal pressure of less than 130/80 mm Hg may be appropriate in some cases; we left it to the discretion of physicians to decide which blood pressure target to choose,” said Dr. Rosendorff, professor of medicine at Mount Sinai Hospital in New York.
The default blood pressure goal of less than 140/90 for most CAD patients represented an increase from the less than 130/80 mm Hg goal set by the prior edition of this guideline, issued in 2007 (Circulation 2007;115:2761-88). Current evidence for the lower blood pressure target of less than 130/80 mm Hg “was not as strong,” Dr. Rosendorff said in an interview. He suggested that physicians consider using the lower target for patients who are younger, reasonably healthy, able to tolerate a regimen that brings them to a lower blood pressure without an increase in angina or other significant effects caused by the drugs themselves, do not experience compromised renal function with reduced blood pressure, and have an increased risk for cerebrovascular events.
“These guidelines are not rigid, and should involve a discussion with the patient of the benefits and risks,” he said.
The new statement targets a blood pressure goal of less than 150/90 mm Hg for CAD patients who are more than 80 years old.
The new target for CAD patients represents something of a response to the blood pressure target of less than 150/90 mm Hg for people at least 60 years old recommended last year in recommendations made by the panel originally assembled as the Eighth Joint National Committee (JNC 8) (JAMA 2014;311:507-20). Although the JNC 8 recommendations aimed at the general population in a primary prevention setting, as opposed to CAD patients for whom secondary prevention is the goal, the target of less than 150/90 mm Hg became “highly controversial” and was a factor in composing the new recommendation, Dr. Rosendorff said. He also stressed that the AHA, ACC, and ASH have assembled a group that is formulating new recommendations for diagnosing and managing hypertension for the general population in a primary prevention setting that will come out sometime in the future.
The new hypertension guideline for CAD patients and the 2014 statement from the JNC 8 panel should be seen as distinct recommendations because they targeted different patient populations and because they were based on different ground rules for evidence, said Dr. Suzanne Oparil, one of three people who served on both writing groups. The JNC 8 group focused exclusively on findings from randomized, controlled trials that used hard cardiovascular disease endpoints. The writing committee for the new guidelines targeted specifically at CAD patients also considered evidence from epidemiologic studies. In addition, the new guidelines is targeted at primarily a cardiologist audience, while the 2014 JNC 8 guidelines were written primarily for primary care physicians, she said in an interview.
“I do not believe that the new CAD guidelines will change practice. They reflect what most cardiologists already do,” said Dr. Oparil, professor of medicine and director of the vascular biology and hypertension program at the University of Alabama, Birmingham.
Regarding antihypertensive drug selection the new statement endorses a focus on treating hypertensive patients with established CAD with a beta-blocker, a renin-angiotensin-aldosterone system blocker such as an ACE inhibitor or angiotensin-receptor blocker, and a thiazide or thiazide-like diuretic. Hypertensive patients with CAD should immediately start on all three drug classes, Dr. Rosendorff said.
“For patients with established CAD, a treatment with a beta-blocker moves from the limbo they are in for treating uncomplicated hypertension to center stage,” he said. The statement gives more detailed guidance on which specific drugs from the beta-blocker class have the best evidence for efficacy in various types of patients with CAD.
Dr. Rosendorff had no disclosures. Dr. Oparil has been a consultant to Bayer, Daiichi Sankyo, and Pfizer, and has received research grants from Medtronic, Merck, Novartis, and Takeda.
On Twitter @mitchelzoler
The first update to U.S. guidelines for managing hypertension in adult patients with coronary artery disease in 8 years reset the target blood pressure for most of these patients to less than 140/90 mm Hg, and highlighted beta-blockers, renin-angiotensin-aldosterone system blockers, and thiazide diuretics as the mainstays of drug treatment for these patients.
The main messages in the new scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension, released on March 31 in an article published online (Hypertension 2015 [doi:10.116/HYP.0000000000000018]) are the blood pressure targets set for patients with coronary artery disease (CAD) and the designations of the preferred drugs to use to achieve the blood pressure goals when lifestyle measures alone prove inadequate, said Dr. Clive Rosendorff, chair of the panel that wrote the new statement.
But the statement also highlighted that a blood pressure target of less than 130/80 mm Hg “could be considered” and was reasonable for selected CAD patients whom physicians judge capable of achieving this lower blood pressure level safely and who are at especially high risk for cerebrovascular events.
“We felt the best evidence [to prevent future cardiovascular events] was to reduce pressure below 140/90 mm Hg, but a goal pressure of less than 130/80 mm Hg may be appropriate in some cases; we left it to the discretion of physicians to decide which blood pressure target to choose,” said Dr. Rosendorff, professor of medicine at Mount Sinai Hospital in New York.
The default blood pressure goal of less than 140/90 for most CAD patients represented an increase from the less than 130/80 mm Hg goal set by the prior edition of this guideline, issued in 2007 (Circulation 2007;115:2761-88). Current evidence for the lower blood pressure target of less than 130/80 mm Hg “was not as strong,” Dr. Rosendorff said in an interview. He suggested that physicians consider using the lower target for patients who are younger, reasonably healthy, able to tolerate a regimen that brings them to a lower blood pressure without an increase in angina or other significant effects caused by the drugs themselves, do not experience compromised renal function with reduced blood pressure, and have an increased risk for cerebrovascular events.
“These guidelines are not rigid, and should involve a discussion with the patient of the benefits and risks,” he said.
The new statement targets a blood pressure goal of less than 150/90 mm Hg for CAD patients who are more than 80 years old.
The new target for CAD patients represents something of a response to the blood pressure target of less than 150/90 mm Hg for people at least 60 years old recommended last year in recommendations made by the panel originally assembled as the Eighth Joint National Committee (JNC 8) (JAMA 2014;311:507-20). Although the JNC 8 recommendations aimed at the general population in a primary prevention setting, as opposed to CAD patients for whom secondary prevention is the goal, the target of less than 150/90 mm Hg became “highly controversial” and was a factor in composing the new recommendation, Dr. Rosendorff said. He also stressed that the AHA, ACC, and ASH have assembled a group that is formulating new recommendations for diagnosing and managing hypertension for the general population in a primary prevention setting that will come out sometime in the future.
The new hypertension guideline for CAD patients and the 2014 statement from the JNC 8 panel should be seen as distinct recommendations because they targeted different patient populations and because they were based on different ground rules for evidence, said Dr. Suzanne Oparil, one of three people who served on both writing groups. The JNC 8 group focused exclusively on findings from randomized, controlled trials that used hard cardiovascular disease endpoints. The writing committee for the new guidelines targeted specifically at CAD patients also considered evidence from epidemiologic studies. In addition, the new guidelines is targeted at primarily a cardiologist audience, while the 2014 JNC 8 guidelines were written primarily for primary care physicians, she said in an interview.
“I do not believe that the new CAD guidelines will change practice. They reflect what most cardiologists already do,” said Dr. Oparil, professor of medicine and director of the vascular biology and hypertension program at the University of Alabama, Birmingham.
Regarding antihypertensive drug selection the new statement endorses a focus on treating hypertensive patients with established CAD with a beta-blocker, a renin-angiotensin-aldosterone system blocker such as an ACE inhibitor or angiotensin-receptor blocker, and a thiazide or thiazide-like diuretic. Hypertensive patients with CAD should immediately start on all three drug classes, Dr. Rosendorff said.
“For patients with established CAD, a treatment with a beta-blocker moves from the limbo they are in for treating uncomplicated hypertension to center stage,” he said. The statement gives more detailed guidance on which specific drugs from the beta-blocker class have the best evidence for efficacy in various types of patients with CAD.
Dr. Rosendorff had no disclosures. Dr. Oparil has been a consultant to Bayer, Daiichi Sankyo, and Pfizer, and has received research grants from Medtronic, Merck, Novartis, and Takeda.
On Twitter @mitchelzoler
FROM HYPERTENSION
Advanced age no barrier to aggressive heart attack treatment
SAN DIEGO – Patients aged 80 years and older benefit from more invasive early treatment after non-ST-elevation myocardial infarction or unstable angina, the After Eighty Trial showed.
After a median follow-up of 1.5 years, an invasive strategy that included coronary angiography significantly reduced the primary endpoint of myocardial infarction (MI), need for urgent revascularization, stroke, and death from 61% with optimal medical treatment to 41% (risk ratio, 0.48; P value < .00001).
That drop was driven primarily by significantly fewer MIs (17% vs. 30%; RR, 0.50; P = .0003) and urgent revascularizations (2% vs. 11%; RR, 0.19; P = .0001), lead author Dr. Nicolai Tegn reported at the American College of Cardiology/Cardiovascular Research Foundation Innovation in Intervention Summit.
There were no significant differences between the invasive and conservative strategy groups in rates of stroke (3% vs. 6%; RR, 0.61; P = .26) or all-cause death (25% vs. 27%; RR, 0.87; P = .53).
The composite of death and MI, however, significantly favored the invasive group (35% vs. 48%; RR, 0.54; P < .0001), he said during a latebreaking clinical trial session.
After Eighty randomly assigned 457 patients, aged 80 years or older, to either optimal medical therapy with no invasive treatments or coronary angiography at a percutaneous coronary intervention (PCI) center the day after inclusion, plus optimal medical therapy after about 4-5 hours if PCI was not performed or about 6-18 hours if it was. Of the 225 patients receiving angiography, 48% went on to balloon angioplasty and/or coronary stenting, and 3% had bypass surgery.
Patients 80 years or older account for roughly one-third of all patients with non-STEMI and unstable angina, but they are underrepresented in clinical trials. As a result, the role of an early invasive strategy, and even an invasive strategy at all, in those elderly patients is still a subject of debate, observed Dr. Tegn, a cardiologist from Rikshospitalet, Oslo University Hospital, Oslo.
The study demonstrated that an invasive strategy is superior to a conservative strategy in patients at least 80 years with NSTEMI or unstable angina, he concluded.
After Eighty is a welcome study because of the under-representation of the elderly in clinical trials, Dr. David Kandzari, director of interventional cardiology at the Piedmont Heart Center in Atlanta, said during a press briefing at the meeting. But it raises the challenge of identifying patients in clinical practice with the same qualifying characteristics, he added, given that the study population represents only 10% of the entire screened population,
There was also a fairly high prevalence of patients who angiographically did not have significant coronary artery disease, yet MI and stroke rates were quite considerable.
That said, “the study in other ways reminds us that the coronary anatomy does not know the age of the patient, meaning that the findings of a benefit of an early invasive strategy seem consistent with previous studies we know across the management of patients with acute coronary syndromes,” Dr. Kandzari said.
After Eighty investigators screened 4,187 elderly patients presenting at 17 community hospitals in Norway with non-STEMI or unstable angina, with or without ST-segment depression in ECG, and normal or elevated troponin T or I levels. Patients had to have no chest pain or other ischemic symptoms after medical treatment and mobilization.
In all, 3,730 patients were excluded for life expectancy less than 12 months because of a serious comorbidity; ongoing or recent bleeding; inability to comply with protocol; clinically unstable including ongoing ischemia; refusal to participate; logistic reasons; or other reasons.
The average age was 84.7 years in the invasive group (range 80-93 years) and 84.9 years in the conservative group (range 80-94 years).
Medical treatment during the index admission included 75 mg aspirin in 97% of both the invasive and conservative groups, clopidogrel (85% vs. 82%), ticagrelor (both 5%), angiotensin-converting enzyme (ACE) inhibitor/angiotensin receptor blockers (ARB) (43% vs. 50%), beta blocker (83% vs. 85%), statins (90% vs. 85%), loop or thiazide diuretics (41% vs. 33%), calcium channel blocker (20% vs. 21%), nitrates (45% vs. 55%), warfarin (17% vs. 9%), low molecular-weight heparin (both 76% ), and dabigatran in one patient in each group.
Medical therapy at discharge in the invasive and conservative groups was aspirin (both 93%), clopidogrel (both 72%), ticagrelor (both 4%), ACE inhibitor/ARB (52% vs. 54%), beta blockers (both 84%), statins (90% vs. 86%), diuretics (45% vs. 38%), calcium channel blocker (24% vs. 23%), nitrates (34% vs. 48%), warfarin (21% vs. 14%), rivaroxaban (three patients in both groups), and dabigatran (one patient vs. six patients).
There were no differences in bleeding rates between the two groups, Dr. Tegn said. Four major bleeding events were reported in both groups, while 23 patients in the invasive group and 16 patients in the conservative group had minor bleeds.
The Norwegian Health Association sponsored the study. Dr. Tegn reported nothing to disclose. Dr. Kandazari reported research and grant support from Abbott Vascular, Biotronic, Boston Scientific, and Medtronic, and minor consulting honoraria from Boston Scientific and Medtronic.
SAN DIEGO – Patients aged 80 years and older benefit from more invasive early treatment after non-ST-elevation myocardial infarction or unstable angina, the After Eighty Trial showed.
After a median follow-up of 1.5 years, an invasive strategy that included coronary angiography significantly reduced the primary endpoint of myocardial infarction (MI), need for urgent revascularization, stroke, and death from 61% with optimal medical treatment to 41% (risk ratio, 0.48; P value < .00001).
That drop was driven primarily by significantly fewer MIs (17% vs. 30%; RR, 0.50; P = .0003) and urgent revascularizations (2% vs. 11%; RR, 0.19; P = .0001), lead author Dr. Nicolai Tegn reported at the American College of Cardiology/Cardiovascular Research Foundation Innovation in Intervention Summit.
There were no significant differences between the invasive and conservative strategy groups in rates of stroke (3% vs. 6%; RR, 0.61; P = .26) or all-cause death (25% vs. 27%; RR, 0.87; P = .53).
The composite of death and MI, however, significantly favored the invasive group (35% vs. 48%; RR, 0.54; P < .0001), he said during a latebreaking clinical trial session.
After Eighty randomly assigned 457 patients, aged 80 years or older, to either optimal medical therapy with no invasive treatments or coronary angiography at a percutaneous coronary intervention (PCI) center the day after inclusion, plus optimal medical therapy after about 4-5 hours if PCI was not performed or about 6-18 hours if it was. Of the 225 patients receiving angiography, 48% went on to balloon angioplasty and/or coronary stenting, and 3% had bypass surgery.
Patients 80 years or older account for roughly one-third of all patients with non-STEMI and unstable angina, but they are underrepresented in clinical trials. As a result, the role of an early invasive strategy, and even an invasive strategy at all, in those elderly patients is still a subject of debate, observed Dr. Tegn, a cardiologist from Rikshospitalet, Oslo University Hospital, Oslo.
The study demonstrated that an invasive strategy is superior to a conservative strategy in patients at least 80 years with NSTEMI or unstable angina, he concluded.
After Eighty is a welcome study because of the under-representation of the elderly in clinical trials, Dr. David Kandzari, director of interventional cardiology at the Piedmont Heart Center in Atlanta, said during a press briefing at the meeting. But it raises the challenge of identifying patients in clinical practice with the same qualifying characteristics, he added, given that the study population represents only 10% of the entire screened population,
There was also a fairly high prevalence of patients who angiographically did not have significant coronary artery disease, yet MI and stroke rates were quite considerable.
That said, “the study in other ways reminds us that the coronary anatomy does not know the age of the patient, meaning that the findings of a benefit of an early invasive strategy seem consistent with previous studies we know across the management of patients with acute coronary syndromes,” Dr. Kandzari said.
After Eighty investigators screened 4,187 elderly patients presenting at 17 community hospitals in Norway with non-STEMI or unstable angina, with or without ST-segment depression in ECG, and normal or elevated troponin T or I levels. Patients had to have no chest pain or other ischemic symptoms after medical treatment and mobilization.
In all, 3,730 patients were excluded for life expectancy less than 12 months because of a serious comorbidity; ongoing or recent bleeding; inability to comply with protocol; clinically unstable including ongoing ischemia; refusal to participate; logistic reasons; or other reasons.
The average age was 84.7 years in the invasive group (range 80-93 years) and 84.9 years in the conservative group (range 80-94 years).
Medical treatment during the index admission included 75 mg aspirin in 97% of both the invasive and conservative groups, clopidogrel (85% vs. 82%), ticagrelor (both 5%), angiotensin-converting enzyme (ACE) inhibitor/angiotensin receptor blockers (ARB) (43% vs. 50%), beta blocker (83% vs. 85%), statins (90% vs. 85%), loop or thiazide diuretics (41% vs. 33%), calcium channel blocker (20% vs. 21%), nitrates (45% vs. 55%), warfarin (17% vs. 9%), low molecular-weight heparin (both 76% ), and dabigatran in one patient in each group.
Medical therapy at discharge in the invasive and conservative groups was aspirin (both 93%), clopidogrel (both 72%), ticagrelor (both 4%), ACE inhibitor/ARB (52% vs. 54%), beta blockers (both 84%), statins (90% vs. 86%), diuretics (45% vs. 38%), calcium channel blocker (24% vs. 23%), nitrates (34% vs. 48%), warfarin (21% vs. 14%), rivaroxaban (three patients in both groups), and dabigatran (one patient vs. six patients).
There were no differences in bleeding rates between the two groups, Dr. Tegn said. Four major bleeding events were reported in both groups, while 23 patients in the invasive group and 16 patients in the conservative group had minor bleeds.
The Norwegian Health Association sponsored the study. Dr. Tegn reported nothing to disclose. Dr. Kandazari reported research and grant support from Abbott Vascular, Biotronic, Boston Scientific, and Medtronic, and minor consulting honoraria from Boston Scientific and Medtronic.
SAN DIEGO – Patients aged 80 years and older benefit from more invasive early treatment after non-ST-elevation myocardial infarction or unstable angina, the After Eighty Trial showed.
After a median follow-up of 1.5 years, an invasive strategy that included coronary angiography significantly reduced the primary endpoint of myocardial infarction (MI), need for urgent revascularization, stroke, and death from 61% with optimal medical treatment to 41% (risk ratio, 0.48; P value < .00001).
That drop was driven primarily by significantly fewer MIs (17% vs. 30%; RR, 0.50; P = .0003) and urgent revascularizations (2% vs. 11%; RR, 0.19; P = .0001), lead author Dr. Nicolai Tegn reported at the American College of Cardiology/Cardiovascular Research Foundation Innovation in Intervention Summit.
There were no significant differences between the invasive and conservative strategy groups in rates of stroke (3% vs. 6%; RR, 0.61; P = .26) or all-cause death (25% vs. 27%; RR, 0.87; P = .53).
The composite of death and MI, however, significantly favored the invasive group (35% vs. 48%; RR, 0.54; P < .0001), he said during a latebreaking clinical trial session.
After Eighty randomly assigned 457 patients, aged 80 years or older, to either optimal medical therapy with no invasive treatments or coronary angiography at a percutaneous coronary intervention (PCI) center the day after inclusion, plus optimal medical therapy after about 4-5 hours if PCI was not performed or about 6-18 hours if it was. Of the 225 patients receiving angiography, 48% went on to balloon angioplasty and/or coronary stenting, and 3% had bypass surgery.
Patients 80 years or older account for roughly one-third of all patients with non-STEMI and unstable angina, but they are underrepresented in clinical trials. As a result, the role of an early invasive strategy, and even an invasive strategy at all, in those elderly patients is still a subject of debate, observed Dr. Tegn, a cardiologist from Rikshospitalet, Oslo University Hospital, Oslo.
The study demonstrated that an invasive strategy is superior to a conservative strategy in patients at least 80 years with NSTEMI or unstable angina, he concluded.
After Eighty is a welcome study because of the under-representation of the elderly in clinical trials, Dr. David Kandzari, director of interventional cardiology at the Piedmont Heart Center in Atlanta, said during a press briefing at the meeting. But it raises the challenge of identifying patients in clinical practice with the same qualifying characteristics, he added, given that the study population represents only 10% of the entire screened population,
There was also a fairly high prevalence of patients who angiographically did not have significant coronary artery disease, yet MI and stroke rates were quite considerable.
That said, “the study in other ways reminds us that the coronary anatomy does not know the age of the patient, meaning that the findings of a benefit of an early invasive strategy seem consistent with previous studies we know across the management of patients with acute coronary syndromes,” Dr. Kandzari said.
After Eighty investigators screened 4,187 elderly patients presenting at 17 community hospitals in Norway with non-STEMI or unstable angina, with or without ST-segment depression in ECG, and normal or elevated troponin T or I levels. Patients had to have no chest pain or other ischemic symptoms after medical treatment and mobilization.
In all, 3,730 patients were excluded for life expectancy less than 12 months because of a serious comorbidity; ongoing or recent bleeding; inability to comply with protocol; clinically unstable including ongoing ischemia; refusal to participate; logistic reasons; or other reasons.
The average age was 84.7 years in the invasive group (range 80-93 years) and 84.9 years in the conservative group (range 80-94 years).
Medical treatment during the index admission included 75 mg aspirin in 97% of both the invasive and conservative groups, clopidogrel (85% vs. 82%), ticagrelor (both 5%), angiotensin-converting enzyme (ACE) inhibitor/angiotensin receptor blockers (ARB) (43% vs. 50%), beta blocker (83% vs. 85%), statins (90% vs. 85%), loop or thiazide diuretics (41% vs. 33%), calcium channel blocker (20% vs. 21%), nitrates (45% vs. 55%), warfarin (17% vs. 9%), low molecular-weight heparin (both 76% ), and dabigatran in one patient in each group.
Medical therapy at discharge in the invasive and conservative groups was aspirin (both 93%), clopidogrel (both 72%), ticagrelor (both 4%), ACE inhibitor/ARB (52% vs. 54%), beta blockers (both 84%), statins (90% vs. 86%), diuretics (45% vs. 38%), calcium channel blocker (24% vs. 23%), nitrates (34% vs. 48%), warfarin (21% vs. 14%), rivaroxaban (three patients in both groups), and dabigatran (one patient vs. six patients).
There were no differences in bleeding rates between the two groups, Dr. Tegn said. Four major bleeding events were reported in both groups, while 23 patients in the invasive group and 16 patients in the conservative group had minor bleeds.
The Norwegian Health Association sponsored the study. Dr. Tegn reported nothing to disclose. Dr. Kandazari reported research and grant support from Abbott Vascular, Biotronic, Boston Scientific, and Medtronic, and minor consulting honoraria from Boston Scientific and Medtronic.
AT ACC/CRF i2 SUMMIT
Key clinical point: An early invasive treatment strategy improved most outcomes in patients aged 80 years and older with acute coronary syndromes.
Major finding: Myocardial infarction, need for urgent revascularization, stroke, and death were significantly lower with invasive vs. conservative care (41% vs. 61%; risk ratio, 0.48; P < .00001).
Data source: Randomized study in 457 patients aged 80 years or older with non-STEMI or unstable angina.
Disclosures: The Norwegian Health Association sponsored the study. Dr. Tegn reported nothing to disclose. Dr. Kandzari reported research and grant support from Abbott Vascular, Biotronic, Boston Scientific, and Medtronic, and minor consulting honoraria from Boston Scientific and Medtronic.
FDA approves miniature heart pump for use during high risk PCI
A miniature heart pump has been approved by the Food and Drug Administration to “help certain patients maintain stable heart function and circulation during certain high-risk percutaneous coronary intervention (HRPCI) procedures,” the agency has announced.
The Impella 2.5 System, manufactured by Abiomed, is “intended for temporary use by patients with severe symptomatic CAD [coronary artery disease] and diminished (but stable) heart function who are undergoing HRPCI but are not candidates for surgical coronary bypass treatment,” according to the FDA’s statement.
“Use of the Impella 2.5 System is intended to prevent episodes of unstable heart function, including unstable blood pressure and poor circulation, in patients who are at high risk for its occurrence,” Dr. William Maisel, acting director of the Office of Device Evaluation in the FDA’s Center for Devices and Radiological Health, said in the statement.
Approval was based on the PROTECT II study and observational data from the USpella Registry.
“The overall data provided evidence that, for patients with severe CAD and diminished heart function, the temporary circulatory support provided by the Impella 2.5 System during an HRPCI procedure may allow a longer and more thorough procedure by preventing episodes of hemodynamic instability ... due to temporary abnormalities in heart function,” the FDA statement said. In addition, “fewer later adverse events” such as the need for repeat HRPCI procedures, “may occur in patients undergoing HRPCI with the pump compared to patients undergoing HRPCI with an intra-aortic balloon pump,” according to the FDA.
The FDA statement also noted that the system can be used as an alternative to the intra-aortic balloon pump “without significantly increasing the safety risks of the HRPCI procedure.”
As a postmarketing requirement, the manufacturer will conduct a single arm study of the device in high-risk PCI patients, according to the company’s statement announcing approval.
The wording of the approved indication is as follows, according to Abiomed: “The Impella 2.5 is a temporary (less than or equal to 6 hours) ventricular support device indicated for use during high-risk PCI performed in elective or urgent hemodynamically stable patients with severe coronary artery disease and depressed left ventricular ejection fraction, when a heart team, including a cardiac surgeon, has determined high-risk PCI is the appropriate therapeutic option. Use of the Impella 2.5 in these patients may prevent hemodynamic instability that may occur during planned temporary coronary occlusions and may reduce peri- and postprocedural adverse events.”
A miniature heart pump has been approved by the Food and Drug Administration to “help certain patients maintain stable heart function and circulation during certain high-risk percutaneous coronary intervention (HRPCI) procedures,” the agency has announced.
The Impella 2.5 System, manufactured by Abiomed, is “intended for temporary use by patients with severe symptomatic CAD [coronary artery disease] and diminished (but stable) heart function who are undergoing HRPCI but are not candidates for surgical coronary bypass treatment,” according to the FDA’s statement.
“Use of the Impella 2.5 System is intended to prevent episodes of unstable heart function, including unstable blood pressure and poor circulation, in patients who are at high risk for its occurrence,” Dr. William Maisel, acting director of the Office of Device Evaluation in the FDA’s Center for Devices and Radiological Health, said in the statement.
Approval was based on the PROTECT II study and observational data from the USpella Registry.
“The overall data provided evidence that, for patients with severe CAD and diminished heart function, the temporary circulatory support provided by the Impella 2.5 System during an HRPCI procedure may allow a longer and more thorough procedure by preventing episodes of hemodynamic instability ... due to temporary abnormalities in heart function,” the FDA statement said. In addition, “fewer later adverse events” such as the need for repeat HRPCI procedures, “may occur in patients undergoing HRPCI with the pump compared to patients undergoing HRPCI with an intra-aortic balloon pump,” according to the FDA.
The FDA statement also noted that the system can be used as an alternative to the intra-aortic balloon pump “without significantly increasing the safety risks of the HRPCI procedure.”
As a postmarketing requirement, the manufacturer will conduct a single arm study of the device in high-risk PCI patients, according to the company’s statement announcing approval.
The wording of the approved indication is as follows, according to Abiomed: “The Impella 2.5 is a temporary (less than or equal to 6 hours) ventricular support device indicated for use during high-risk PCI performed in elective or urgent hemodynamically stable patients with severe coronary artery disease and depressed left ventricular ejection fraction, when a heart team, including a cardiac surgeon, has determined high-risk PCI is the appropriate therapeutic option. Use of the Impella 2.5 in these patients may prevent hemodynamic instability that may occur during planned temporary coronary occlusions and may reduce peri- and postprocedural adverse events.”
A miniature heart pump has been approved by the Food and Drug Administration to “help certain patients maintain stable heart function and circulation during certain high-risk percutaneous coronary intervention (HRPCI) procedures,” the agency has announced.
The Impella 2.5 System, manufactured by Abiomed, is “intended for temporary use by patients with severe symptomatic CAD [coronary artery disease] and diminished (but stable) heart function who are undergoing HRPCI but are not candidates for surgical coronary bypass treatment,” according to the FDA’s statement.
“Use of the Impella 2.5 System is intended to prevent episodes of unstable heart function, including unstable blood pressure and poor circulation, in patients who are at high risk for its occurrence,” Dr. William Maisel, acting director of the Office of Device Evaluation in the FDA’s Center for Devices and Radiological Health, said in the statement.
Approval was based on the PROTECT II study and observational data from the USpella Registry.
“The overall data provided evidence that, for patients with severe CAD and diminished heart function, the temporary circulatory support provided by the Impella 2.5 System during an HRPCI procedure may allow a longer and more thorough procedure by preventing episodes of hemodynamic instability ... due to temporary abnormalities in heart function,” the FDA statement said. In addition, “fewer later adverse events” such as the need for repeat HRPCI procedures, “may occur in patients undergoing HRPCI with the pump compared to patients undergoing HRPCI with an intra-aortic balloon pump,” according to the FDA.
The FDA statement also noted that the system can be used as an alternative to the intra-aortic balloon pump “without significantly increasing the safety risks of the HRPCI procedure.”
As a postmarketing requirement, the manufacturer will conduct a single arm study of the device in high-risk PCI patients, according to the company’s statement announcing approval.
The wording of the approved indication is as follows, according to Abiomed: “The Impella 2.5 is a temporary (less than or equal to 6 hours) ventricular support device indicated for use during high-risk PCI performed in elective or urgent hemodynamically stable patients with severe coronary artery disease and depressed left ventricular ejection fraction, when a heart team, including a cardiac surgeon, has determined high-risk PCI is the appropriate therapeutic option. Use of the Impella 2.5 in these patients may prevent hemodynamic instability that may occur during planned temporary coronary occlusions and may reduce peri- and postprocedural adverse events.”
Cost comparison favors minimally invasive over conventional AVR
Outcomes were similar, but hospital costs improved with use of mini-aortic valve replacement, compared with conventional AVR, according to the results of a Society of Thoracic Surgeons (STS) database study of 1,341 patients who underwent primary AVR at 17 hospitals.
A propensity match cohort analysis was done to compare patients who had conventional (67%) vs. mini-AVR (33%) performed using either partial sternotomy or right thoracotomy.
Mortality, stroke, renal failure, atrial fibrillation, reoperation for bleeding, and respiratory insufficiency were not statistically significantly different between the two groups. There was also no significant difference in ICU or hospital length of stay between the two groups. However, mini-AVR was associated with both significantly decreased ventilator time (5 vs. 6 hours) and blood product transfusion (25% vs. 32%), according to the report, which was published online and scheduled for the April issue of the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j/jtcvs.2015.01.014).
Total hospital cost was significantly lower in the mini-AVR group ($36,348) vs. the conventional repair group ($38,239, P = .02), wrote Dr. Ravi Kiran Ghanta of the University of Virginia, Charlottesville, and his colleagues.
The authors discussed the previously raised issue of longer cross-clamp and bypass times seen in earlier studies of mini-AVR. In their current study, such was not the case, with mini-AVR appearing equivalent with conventional operations. The authors suggested that surgeons have now adopted techniques to reduce bypass and cross-clamp times with mini-AVR.
Data were limited to in-hospital costs. Other costs, such as those of rehabilitation and lost productivity, were not included in the analysis. “Including these health-care costs may have increased overall savings with mini-AVR compared to conventional AVR,” the authors noted.
“Mini-AVR is associated with decreased ventilator time, blood product utilization, early discharge, and reduced total hospital cost. In contemporary clinical practice, mini-AVR is safe and cost-effective,” the researchers concluded.
The authors reported that they had no conflicts.
“Measurement of cost and outcome, the determinant of ‘value’ in health care, is assuming increasing importance in the evaluation of all medial interventions, especially those surgical procedures done frequently and at higher cost,” wrote Dr. Verdi J. DiSesa in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.049]).
Although applauding the timeliness and importance of analyzing the costs and outcomes in propensity-matched patients undergoing aortic valve replacement via full sternotomy of mini-AVR using a partial sternotomy or limited thoracotomy incision, he questioned some of the methodology. The cost-to-charge ratio used, which provides an estimate of the cost of services, is not uniform throughout departments in a single hospital, and differs from hospital to hospital, although the latter was accounted for. He suggested that “activity-based costing” would have been a better approach, although more labor intensive. In this approach, every encounter with a caregiver is assigned a unit cost and the cost of a patient encounter is calculated by estimating the number of units of service and multiplying by the unit cost for service.
“This method is demanding of resources but has the potential to become the most accurate and therefore the preferred way to determine the costs of medical services,” he wrote. In addition, the authors included but did not separately analyze patients having AVR via minithoracotomy.
“What might be the conclusions of this research were these patients excluded or analyzed separately?” he asked.
In terms of the propensity model, the matching procedure included only three clinical factors – STS Predicted Rate of Mortality (PROM) score, the operative year, and the surgeon who performed the procedure – resulting in 35% of patients remaining unmatched, which may have biased the results.
This analysis, Dr. DiSesa concluded, is “perhaps an early version of the kind of analyses, which increasingly will be required for the evaluation of the services provided by all health care providers, not only cardiac surgeons.”
Dr. DiSesa is professor of surgery at Temple University, Philadelphia.
“Measurement of cost and outcome, the determinant of ‘value’ in health care, is assuming increasing importance in the evaluation of all medial interventions, especially those surgical procedures done frequently and at higher cost,” wrote Dr. Verdi J. DiSesa in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.049]).
Although applauding the timeliness and importance of analyzing the costs and outcomes in propensity-matched patients undergoing aortic valve replacement via full sternotomy of mini-AVR using a partial sternotomy or limited thoracotomy incision, he questioned some of the methodology. The cost-to-charge ratio used, which provides an estimate of the cost of services, is not uniform throughout departments in a single hospital, and differs from hospital to hospital, although the latter was accounted for. He suggested that “activity-based costing” would have been a better approach, although more labor intensive. In this approach, every encounter with a caregiver is assigned a unit cost and the cost of a patient encounter is calculated by estimating the number of units of service and multiplying by the unit cost for service.
“This method is demanding of resources but has the potential to become the most accurate and therefore the preferred way to determine the costs of medical services,” he wrote. In addition, the authors included but did not separately analyze patients having AVR via minithoracotomy.
“What might be the conclusions of this research were these patients excluded or analyzed separately?” he asked.
In terms of the propensity model, the matching procedure included only three clinical factors – STS Predicted Rate of Mortality (PROM) score, the operative year, and the surgeon who performed the procedure – resulting in 35% of patients remaining unmatched, which may have biased the results.
This analysis, Dr. DiSesa concluded, is “perhaps an early version of the kind of analyses, which increasingly will be required for the evaluation of the services provided by all health care providers, not only cardiac surgeons.”
Dr. DiSesa is professor of surgery at Temple University, Philadelphia.
“Measurement of cost and outcome, the determinant of ‘value’ in health care, is assuming increasing importance in the evaluation of all medial interventions, especially those surgical procedures done frequently and at higher cost,” wrote Dr. Verdi J. DiSesa in his invited commentary (J. Thorac. Cardiovasc. Surg. 2015 [doi:10.1016/j.jtcvs.2015.01.049]).
Although applauding the timeliness and importance of analyzing the costs and outcomes in propensity-matched patients undergoing aortic valve replacement via full sternotomy of mini-AVR using a partial sternotomy or limited thoracotomy incision, he questioned some of the methodology. The cost-to-charge ratio used, which provides an estimate of the cost of services, is not uniform throughout departments in a single hospital, and differs from hospital to hospital, although the latter was accounted for. He suggested that “activity-based costing” would have been a better approach, although more labor intensive. In this approach, every encounter with a caregiver is assigned a unit cost and the cost of a patient encounter is calculated by estimating the number of units of service and multiplying by the unit cost for service.
“This method is demanding of resources but has the potential to become the most accurate and therefore the preferred way to determine the costs of medical services,” he wrote. In addition, the authors included but did not separately analyze patients having AVR via minithoracotomy.
“What might be the conclusions of this research were these patients excluded or analyzed separately?” he asked.
In terms of the propensity model, the matching procedure included only three clinical factors – STS Predicted Rate of Mortality (PROM) score, the operative year, and the surgeon who performed the procedure – resulting in 35% of patients remaining unmatched, which may have biased the results.
This analysis, Dr. DiSesa concluded, is “perhaps an early version of the kind of analyses, which increasingly will be required for the evaluation of the services provided by all health care providers, not only cardiac surgeons.”
Dr. DiSesa is professor of surgery at Temple University, Philadelphia.
Outcomes were similar, but hospital costs improved with use of mini-aortic valve replacement, compared with conventional AVR, according to the results of a Society of Thoracic Surgeons (STS) database study of 1,341 patients who underwent primary AVR at 17 hospitals.
A propensity match cohort analysis was done to compare patients who had conventional (67%) vs. mini-AVR (33%) performed using either partial sternotomy or right thoracotomy.
Mortality, stroke, renal failure, atrial fibrillation, reoperation for bleeding, and respiratory insufficiency were not statistically significantly different between the two groups. There was also no significant difference in ICU or hospital length of stay between the two groups. However, mini-AVR was associated with both significantly decreased ventilator time (5 vs. 6 hours) and blood product transfusion (25% vs. 32%), according to the report, which was published online and scheduled for the April issue of the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j/jtcvs.2015.01.014).
Total hospital cost was significantly lower in the mini-AVR group ($36,348) vs. the conventional repair group ($38,239, P = .02), wrote Dr. Ravi Kiran Ghanta of the University of Virginia, Charlottesville, and his colleagues.
The authors discussed the previously raised issue of longer cross-clamp and bypass times seen in earlier studies of mini-AVR. In their current study, such was not the case, with mini-AVR appearing equivalent with conventional operations. The authors suggested that surgeons have now adopted techniques to reduce bypass and cross-clamp times with mini-AVR.
Data were limited to in-hospital costs. Other costs, such as those of rehabilitation and lost productivity, were not included in the analysis. “Including these health-care costs may have increased overall savings with mini-AVR compared to conventional AVR,” the authors noted.
“Mini-AVR is associated with decreased ventilator time, blood product utilization, early discharge, and reduced total hospital cost. In contemporary clinical practice, mini-AVR is safe and cost-effective,” the researchers concluded.
The authors reported that they had no conflicts.
Outcomes were similar, but hospital costs improved with use of mini-aortic valve replacement, compared with conventional AVR, according to the results of a Society of Thoracic Surgeons (STS) database study of 1,341 patients who underwent primary AVR at 17 hospitals.
A propensity match cohort analysis was done to compare patients who had conventional (67%) vs. mini-AVR (33%) performed using either partial sternotomy or right thoracotomy.
Mortality, stroke, renal failure, atrial fibrillation, reoperation for bleeding, and respiratory insufficiency were not statistically significantly different between the two groups. There was also no significant difference in ICU or hospital length of stay between the two groups. However, mini-AVR was associated with both significantly decreased ventilator time (5 vs. 6 hours) and blood product transfusion (25% vs. 32%), according to the report, which was published online and scheduled for the April issue of the Journal of Thoracic and Cardiovascular Surgery (doi:10.1016/j/jtcvs.2015.01.014).
Total hospital cost was significantly lower in the mini-AVR group ($36,348) vs. the conventional repair group ($38,239, P = .02), wrote Dr. Ravi Kiran Ghanta of the University of Virginia, Charlottesville, and his colleagues.
The authors discussed the previously raised issue of longer cross-clamp and bypass times seen in earlier studies of mini-AVR. In their current study, such was not the case, with mini-AVR appearing equivalent with conventional operations. The authors suggested that surgeons have now adopted techniques to reduce bypass and cross-clamp times with mini-AVR.
Data were limited to in-hospital costs. Other costs, such as those of rehabilitation and lost productivity, were not included in the analysis. “Including these health-care costs may have increased overall savings with mini-AVR compared to conventional AVR,” the authors noted.
“Mini-AVR is associated with decreased ventilator time, blood product utilization, early discharge, and reduced total hospital cost. In contemporary clinical practice, mini-AVR is safe and cost-effective,” the researchers concluded.
The authors reported that they had no conflicts.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Mortality, stroke, renal failure, and other complications were not significantly different between mini-aortic valve replacement and conventional replacement.
Major finding: Total hospital costs were significantly lower with mini-AVR, compared with conventional replacement ($36,348 vs. $38,239).
Data source: A retrospective data analysis of patient records for isolated AVR repair, extracted from a regional, multi-institutional Society of Thoracic Surgeons database.
Disclosures: The authors reported that they had no relevant conflicts of interest.
Privacy issues transformed in the genomic era
Researchers are attempting to develop new models to deal with patient privacy issues, including profound levels of patient participation in the dissemination of personal data, in the new era of genomic medicine, according to an article in the January issue of Science written by Jennifer Couzin-Frankel, based on interviews with participants and investigators in the RUDY trial and other projects.
The RUDY rheumatology registry in London is an example of such a new approach. RUDY, a registry used for research into rare bone diseases and vasculitis, has an emphasis on patients’ self-reported outcomes. In order to alleviate patients’ fears of loss of privacy because of data sharing, the study offers patients various controls over dissemination, according to one of the study’s principal investigators, Dr. Kassim Javaid, a University of Oxford (England) rheumatologist, wrote Ms. Couzin-Frankel (Science 2015;347:501-3).
Patients in the study can determine whether their blood, scans, and medical histories can be shared with other researchers. In addition, they will have access to a clinical trial Web page where they can find out whether their tissues samples are being used by other research groups.
This model is thought to not only increase the sense of patient participation and authority in the study, but also to provide transparency and accountability as to how their information is being used. Dr. Javaid refers to this strategy as “dynamic consent,” because patients can choose which portions of the study to participate in and whether to restrict their data and samples to RUDY investigators or to allow others to study them.
The problem of maintaining privacy is profound, because DNA sequencing provides such a potent means of individual identification. Ms. Couzin-Frankel cites in particular a case published in Science (2013;339:321-4), in which a group working with Dr. Yaniv Erlich showed that a man could be uniquely identified based on a partial DNA sequence of his Y chromosome, age, and U.S. state of residence, which is the type of information commonly posted in DNA databases widely accessible to the research community. By combining this information with data he found for others in the same family on popular genealogy databases, where more than 100,000 people already have posted DNA markers, Dr. Erlich could not only identify the donors of the DNA but also could identify their family members as far as second cousins once removed.
Although such data can be encrypted, reported Ms. Couzin-Frankel, Dr. Erlich pointed out that this can render the information largely useless for research and doesn’t even always protect the donor.
In contrast, however, many participants in trials and databases, such as the database/Web group PatientsLikeMe, see patient altruism as key. PatientsLikeMe has recruited more 300,000 people with more than 2,300 different diseases, who are sharing their health data, how they’re faring in clinical trials, and acting as a support group to one another in order to help medical scientists and drug companies further research their conditions. Patients voluntarily agree to this free flow of information, even though it decreases their privacy.
In another example in which patients cite altruistic reasons for giving up their privacy, the Personal Genome Project at Harvard Medical School in Boston, founded by geneticist George M. Church, Ph.D., has nearly 4,000 participants sharing their DNA sequences and health histories online for anyone to view. The Personal Genome Project even has a “real name” option, which allows participants to post their identity, Ms. Couzin-Frankel reports.
The Science article author, Ms. Couzin-Frankel, is a science journalist with no relevant financial conflicts. The RUDY study is funded by the University of Oxford and the U.K. National Institute for Health Research.
The article in Science raises important ethical questions, re: the deidentification of data and obtaining [of] informed consent when data or tissue or DNA alone can actually be used to identify the patient.

|
Dr. Jennifer S. Lawton |
When we obtain informed consent for participation in clinical trials, we ask our patients to take a “leap of faith” and trust us to maintain their privacy. Our patients personally gain little or nothing for participation, yet they altruistically allow their data or tissue to be used to improve the lives of others. Just as we do not want our Social Security number, bank account information, and credit card numbers to be public knowledge, we also do not want our genetic information – with potential risks of developing or predispositions for life-threatening diseases – public knowledge (or accessible to employers and insurance companies). These questions will be the topic of many ethical discussions in the future, and will provide an opportunity for innovative and advanced technology and methods to protect personal information.
Dr. Jennifer S. Lawton is the Acquired Cardiovascular Disease section editor for Thoracic Surgery News.
The article in Science raises important ethical questions, re: the deidentification of data and obtaining [of] informed consent when data or tissue or DNA alone can actually be used to identify the patient.

|
Dr. Jennifer S. Lawton |
When we obtain informed consent for participation in clinical trials, we ask our patients to take a “leap of faith” and trust us to maintain their privacy. Our patients personally gain little or nothing for participation, yet they altruistically allow their data or tissue to be used to improve the lives of others. Just as we do not want our Social Security number, bank account information, and credit card numbers to be public knowledge, we also do not want our genetic information – with potential risks of developing or predispositions for life-threatening diseases – public knowledge (or accessible to employers and insurance companies). These questions will be the topic of many ethical discussions in the future, and will provide an opportunity for innovative and advanced technology and methods to protect personal information.
Dr. Jennifer S. Lawton is the Acquired Cardiovascular Disease section editor for Thoracic Surgery News.
The article in Science raises important ethical questions, re: the deidentification of data and obtaining [of] informed consent when data or tissue or DNA alone can actually be used to identify the patient.

|
Dr. Jennifer S. Lawton |
When we obtain informed consent for participation in clinical trials, we ask our patients to take a “leap of faith” and trust us to maintain their privacy. Our patients personally gain little or nothing for participation, yet they altruistically allow their data or tissue to be used to improve the lives of others. Just as we do not want our Social Security number, bank account information, and credit card numbers to be public knowledge, we also do not want our genetic information – with potential risks of developing or predispositions for life-threatening diseases – public knowledge (or accessible to employers and insurance companies). These questions will be the topic of many ethical discussions in the future, and will provide an opportunity for innovative and advanced technology and methods to protect personal information.
Dr. Jennifer S. Lawton is the Acquired Cardiovascular Disease section editor for Thoracic Surgery News.
Researchers are attempting to develop new models to deal with patient privacy issues, including profound levels of patient participation in the dissemination of personal data, in the new era of genomic medicine, according to an article in the January issue of Science written by Jennifer Couzin-Frankel, based on interviews with participants and investigators in the RUDY trial and other projects.
The RUDY rheumatology registry in London is an example of such a new approach. RUDY, a registry used for research into rare bone diseases and vasculitis, has an emphasis on patients’ self-reported outcomes. In order to alleviate patients’ fears of loss of privacy because of data sharing, the study offers patients various controls over dissemination, according to one of the study’s principal investigators, Dr. Kassim Javaid, a University of Oxford (England) rheumatologist, wrote Ms. Couzin-Frankel (Science 2015;347:501-3).
Patients in the study can determine whether their blood, scans, and medical histories can be shared with other researchers. In addition, they will have access to a clinical trial Web page where they can find out whether their tissues samples are being used by other research groups.
This model is thought to not only increase the sense of patient participation and authority in the study, but also to provide transparency and accountability as to how their information is being used. Dr. Javaid refers to this strategy as “dynamic consent,” because patients can choose which portions of the study to participate in and whether to restrict their data and samples to RUDY investigators or to allow others to study them.
The problem of maintaining privacy is profound, because DNA sequencing provides such a potent means of individual identification. Ms. Couzin-Frankel cites in particular a case published in Science (2013;339:321-4), in which a group working with Dr. Yaniv Erlich showed that a man could be uniquely identified based on a partial DNA sequence of his Y chromosome, age, and U.S. state of residence, which is the type of information commonly posted in DNA databases widely accessible to the research community. By combining this information with data he found for others in the same family on popular genealogy databases, where more than 100,000 people already have posted DNA markers, Dr. Erlich could not only identify the donors of the DNA but also could identify their family members as far as second cousins once removed.
Although such data can be encrypted, reported Ms. Couzin-Frankel, Dr. Erlich pointed out that this can render the information largely useless for research and doesn’t even always protect the donor.
In contrast, however, many participants in trials and databases, such as the database/Web group PatientsLikeMe, see patient altruism as key. PatientsLikeMe has recruited more 300,000 people with more than 2,300 different diseases, who are sharing their health data, how they’re faring in clinical trials, and acting as a support group to one another in order to help medical scientists and drug companies further research their conditions. Patients voluntarily agree to this free flow of information, even though it decreases their privacy.
In another example in which patients cite altruistic reasons for giving up their privacy, the Personal Genome Project at Harvard Medical School in Boston, founded by geneticist George M. Church, Ph.D., has nearly 4,000 participants sharing their DNA sequences and health histories online for anyone to view. The Personal Genome Project even has a “real name” option, which allows participants to post their identity, Ms. Couzin-Frankel reports.
The Science article author, Ms. Couzin-Frankel, is a science journalist with no relevant financial conflicts. The RUDY study is funded by the University of Oxford and the U.K. National Institute for Health Research.
Researchers are attempting to develop new models to deal with patient privacy issues, including profound levels of patient participation in the dissemination of personal data, in the new era of genomic medicine, according to an article in the January issue of Science written by Jennifer Couzin-Frankel, based on interviews with participants and investigators in the RUDY trial and other projects.
The RUDY rheumatology registry in London is an example of such a new approach. RUDY, a registry used for research into rare bone diseases and vasculitis, has an emphasis on patients’ self-reported outcomes. In order to alleviate patients’ fears of loss of privacy because of data sharing, the study offers patients various controls over dissemination, according to one of the study’s principal investigators, Dr. Kassim Javaid, a University of Oxford (England) rheumatologist, wrote Ms. Couzin-Frankel (Science 2015;347:501-3).
Patients in the study can determine whether their blood, scans, and medical histories can be shared with other researchers. In addition, they will have access to a clinical trial Web page where they can find out whether their tissues samples are being used by other research groups.
This model is thought to not only increase the sense of patient participation and authority in the study, but also to provide transparency and accountability as to how their information is being used. Dr. Javaid refers to this strategy as “dynamic consent,” because patients can choose which portions of the study to participate in and whether to restrict their data and samples to RUDY investigators or to allow others to study them.
The problem of maintaining privacy is profound, because DNA sequencing provides such a potent means of individual identification. Ms. Couzin-Frankel cites in particular a case published in Science (2013;339:321-4), in which a group working with Dr. Yaniv Erlich showed that a man could be uniquely identified based on a partial DNA sequence of his Y chromosome, age, and U.S. state of residence, which is the type of information commonly posted in DNA databases widely accessible to the research community. By combining this information with data he found for others in the same family on popular genealogy databases, where more than 100,000 people already have posted DNA markers, Dr. Erlich could not only identify the donors of the DNA but also could identify their family members as far as second cousins once removed.
Although such data can be encrypted, reported Ms. Couzin-Frankel, Dr. Erlich pointed out that this can render the information largely useless for research and doesn’t even always protect the donor.
In contrast, however, many participants in trials and databases, such as the database/Web group PatientsLikeMe, see patient altruism as key. PatientsLikeMe has recruited more 300,000 people with more than 2,300 different diseases, who are sharing their health data, how they’re faring in clinical trials, and acting as a support group to one another in order to help medical scientists and drug companies further research their conditions. Patients voluntarily agree to this free flow of information, even though it decreases their privacy.
In another example in which patients cite altruistic reasons for giving up their privacy, the Personal Genome Project at Harvard Medical School in Boston, founded by geneticist George M. Church, Ph.D., has nearly 4,000 participants sharing their DNA sequences and health histories online for anyone to view. The Personal Genome Project even has a “real name” option, which allows participants to post their identity, Ms. Couzin-Frankel reports.
The Science article author, Ms. Couzin-Frankel, is a science journalist with no relevant financial conflicts. The RUDY study is funded by the University of Oxford and the U.K. National Institute for Health Research.
FROM SCIENCE
Key clinical point: The RUDY rheumatology registry represents a new data-sharing model based on patient-researcher trust.
Major finding: Openness, full documentation, and reviews are the key to creating a community of trust that obviates the need for cryptographic protection of DNA sequences.
Data source: A review and interview-based summary of new modes of data-sharing in medical research, focusing on the RUDY trial.
Disclosures: Jennifer Couzin-Frankel, a science journalist, has no relevant financial conflicts. The RUDY study is funded by the University of Oxford (England) and the U.K. National Institute for Health Research.
Poor response to statins predicts growth in plaque
For about one in five patients with known atherosclerotic coronary artery disease, standard-dose therapy with statins did not result in significant lowering of LDL cholesterol.
Furthermore, the results of this large pooled data sample showed that for statin hyporesponders, statin therapy did not prevent progression of intravascular plaque volume as measured by grayscale intravascular ultrasound.
Patients exhibit a wide range of response to standard statin dosing, and the effect of minimal LDL-C lowering on atherosclerotic disease progression had not previously been determined, according to Dr. Yu Kataoka of the University of Adelaide, Australia, and his colleagues (Arterioscler. Thromb. Vasc. Biol. 2015 [doi:10.1161/ATVBAHA.114.304477]).
Investigators pooled data from seven clinical trials that examined 647 total patients with angiographically confirmed CAD who were initiated on statins and followed by serial intravascular ultrasound. The present study analyzed baseline characteristics, serial lipid profile, and atheroma burden for the group.
In all, 130 patients of the 647 (20%) had minimal LDL-C lowering with statin therapy, showing nonsignificant lowering or even an increase in LDL-C levels during the study period. This group of hyporesponders differed in being slightly younger, more obese, less likely to have hypertension and dyslipidemia, and less likely to be receiving beta-blockers than were the statin responders. Other patient characteristics were similar between the two groups. A variety of agents were used, including atorvastatin, rosuvastatin, simvastatin, and pravastatin. Concurrent administration of other antiatherosclerotic agents was permitted and was similar between the groups. Atheroma burden at baseline was also similar between the two groups.
Measuring serial changes in atheroma burden showed a significant difference between statin responders and hyporesponders. The adjusted change in atheroma volume was –0.21% for the responders, compared with +0.83% for the hyporesponders (P = .006). Lumen volume decreased 11.64 mm3 for the responders, while the reduction was 16.54 mm3 for the hyporesponders (P = .006). Of those who responded to lipid therapy with LDL-C lowering, 29.8% had substantial atheroma regression, while 25.9% had substantial plaque progression; among hyporesponders, however, just 13.8% experienced significant plaque regression, while 37.7% had significant atheroma progression, both significant differences.
Dr. Kataoka and his colleagues emphasized that the factors contributing to poor statin response are not well understood. They noted that for this study, the pooled trials all showed adherence rates over 90%, eliminating patient compliance as a variable. Rigorous statistical techniques were used to control for comorbidities and coadministered medications. There are known genetic polymorphisms and phenotypic variations in statin metabolism, though these were not reported here. Although the results were not statistically significant, C-reactive protein levels were higher for the hyporesponse group, suggesting that another factor may be individual response to the anti-inflammatory effect that is among the known pleiotropic effects of this drug class.
In an interview, lead author Stephen Nicholls noted that many clinicians are still reluctant to treat to full effect. Citing the concept of “clinical inertia,” Dr. Nicholls pointed out that “Even when statins are prescribed, they are often at lower doses than ideal. That translated to more plaque growth, which leads directly to more heart attacks and more revascularization procedures.”
Study limitations included the potential residual confounding effects of pooling data from seven discrete clinical trials, though mixed modeling techniques attempted to correct for this effect. The present study also reported atheroma burden, but not actual clinical events. The study authors noted, however, that they had previously reported a direct relationship between atheroma progression and the occurrence of cardiovascular events.
Dr. Nicholls has received speaking honoraria and research support from many pharmaceutical companies, and from Infraredx. Dr. Steven E. Nissen of the Cleveland Clinic was a coinvestigator and has received research support from and is a consultant/adviser to numerous pharmaceutical companies; all honoraria or consulting fees go directly to charity so that he receives neither income nor a tax deduction. The other authors report no conflicts.
For about one in five patients with known atherosclerotic coronary artery disease, standard-dose therapy with statins did not result in significant lowering of LDL cholesterol.
Furthermore, the results of this large pooled data sample showed that for statin hyporesponders, statin therapy did not prevent progression of intravascular plaque volume as measured by grayscale intravascular ultrasound.
Patients exhibit a wide range of response to standard statin dosing, and the effect of minimal LDL-C lowering on atherosclerotic disease progression had not previously been determined, according to Dr. Yu Kataoka of the University of Adelaide, Australia, and his colleagues (Arterioscler. Thromb. Vasc. Biol. 2015 [doi:10.1161/ATVBAHA.114.304477]).
Investigators pooled data from seven clinical trials that examined 647 total patients with angiographically confirmed CAD who were initiated on statins and followed by serial intravascular ultrasound. The present study analyzed baseline characteristics, serial lipid profile, and atheroma burden for the group.
In all, 130 patients of the 647 (20%) had minimal LDL-C lowering with statin therapy, showing nonsignificant lowering or even an increase in LDL-C levels during the study period. This group of hyporesponders differed in being slightly younger, more obese, less likely to have hypertension and dyslipidemia, and less likely to be receiving beta-blockers than were the statin responders. Other patient characteristics were similar between the two groups. A variety of agents were used, including atorvastatin, rosuvastatin, simvastatin, and pravastatin. Concurrent administration of other antiatherosclerotic agents was permitted and was similar between the groups. Atheroma burden at baseline was also similar between the two groups.
Measuring serial changes in atheroma burden showed a significant difference between statin responders and hyporesponders. The adjusted change in atheroma volume was –0.21% for the responders, compared with +0.83% for the hyporesponders (P = .006). Lumen volume decreased 11.64 mm3 for the responders, while the reduction was 16.54 mm3 for the hyporesponders (P = .006). Of those who responded to lipid therapy with LDL-C lowering, 29.8% had substantial atheroma regression, while 25.9% had substantial plaque progression; among hyporesponders, however, just 13.8% experienced significant plaque regression, while 37.7% had significant atheroma progression, both significant differences.
Dr. Kataoka and his colleagues emphasized that the factors contributing to poor statin response are not well understood. They noted that for this study, the pooled trials all showed adherence rates over 90%, eliminating patient compliance as a variable. Rigorous statistical techniques were used to control for comorbidities and coadministered medications. There are known genetic polymorphisms and phenotypic variations in statin metabolism, though these were not reported here. Although the results were not statistically significant, C-reactive protein levels were higher for the hyporesponse group, suggesting that another factor may be individual response to the anti-inflammatory effect that is among the known pleiotropic effects of this drug class.
In an interview, lead author Stephen Nicholls noted that many clinicians are still reluctant to treat to full effect. Citing the concept of “clinical inertia,” Dr. Nicholls pointed out that “Even when statins are prescribed, they are often at lower doses than ideal. That translated to more plaque growth, which leads directly to more heart attacks and more revascularization procedures.”
Study limitations included the potential residual confounding effects of pooling data from seven discrete clinical trials, though mixed modeling techniques attempted to correct for this effect. The present study also reported atheroma burden, but not actual clinical events. The study authors noted, however, that they had previously reported a direct relationship between atheroma progression and the occurrence of cardiovascular events.
Dr. Nicholls has received speaking honoraria and research support from many pharmaceutical companies, and from Infraredx. Dr. Steven E. Nissen of the Cleveland Clinic was a coinvestigator and has received research support from and is a consultant/adviser to numerous pharmaceutical companies; all honoraria or consulting fees go directly to charity so that he receives neither income nor a tax deduction. The other authors report no conflicts.
For about one in five patients with known atherosclerotic coronary artery disease, standard-dose therapy with statins did not result in significant lowering of LDL cholesterol.
Furthermore, the results of this large pooled data sample showed that for statin hyporesponders, statin therapy did not prevent progression of intravascular plaque volume as measured by grayscale intravascular ultrasound.
Patients exhibit a wide range of response to standard statin dosing, and the effect of minimal LDL-C lowering on atherosclerotic disease progression had not previously been determined, according to Dr. Yu Kataoka of the University of Adelaide, Australia, and his colleagues (Arterioscler. Thromb. Vasc. Biol. 2015 [doi:10.1161/ATVBAHA.114.304477]).
Investigators pooled data from seven clinical trials that examined 647 total patients with angiographically confirmed CAD who were initiated on statins and followed by serial intravascular ultrasound. The present study analyzed baseline characteristics, serial lipid profile, and atheroma burden for the group.
In all, 130 patients of the 647 (20%) had minimal LDL-C lowering with statin therapy, showing nonsignificant lowering or even an increase in LDL-C levels during the study period. This group of hyporesponders differed in being slightly younger, more obese, less likely to have hypertension and dyslipidemia, and less likely to be receiving beta-blockers than were the statin responders. Other patient characteristics were similar between the two groups. A variety of agents were used, including atorvastatin, rosuvastatin, simvastatin, and pravastatin. Concurrent administration of other antiatherosclerotic agents was permitted and was similar between the groups. Atheroma burden at baseline was also similar between the two groups.
Measuring serial changes in atheroma burden showed a significant difference between statin responders and hyporesponders. The adjusted change in atheroma volume was –0.21% for the responders, compared with +0.83% for the hyporesponders (P = .006). Lumen volume decreased 11.64 mm3 for the responders, while the reduction was 16.54 mm3 for the hyporesponders (P = .006). Of those who responded to lipid therapy with LDL-C lowering, 29.8% had substantial atheroma regression, while 25.9% had substantial plaque progression; among hyporesponders, however, just 13.8% experienced significant plaque regression, while 37.7% had significant atheroma progression, both significant differences.
Dr. Kataoka and his colleagues emphasized that the factors contributing to poor statin response are not well understood. They noted that for this study, the pooled trials all showed adherence rates over 90%, eliminating patient compliance as a variable. Rigorous statistical techniques were used to control for comorbidities and coadministered medications. There are known genetic polymorphisms and phenotypic variations in statin metabolism, though these were not reported here. Although the results were not statistically significant, C-reactive protein levels were higher for the hyporesponse group, suggesting that another factor may be individual response to the anti-inflammatory effect that is among the known pleiotropic effects of this drug class.
In an interview, lead author Stephen Nicholls noted that many clinicians are still reluctant to treat to full effect. Citing the concept of “clinical inertia,” Dr. Nicholls pointed out that “Even when statins are prescribed, they are often at lower doses than ideal. That translated to more plaque growth, which leads directly to more heart attacks and more revascularization procedures.”
Study limitations included the potential residual confounding effects of pooling data from seven discrete clinical trials, though mixed modeling techniques attempted to correct for this effect. The present study also reported atheroma burden, but not actual clinical events. The study authors noted, however, that they had previously reported a direct relationship between atheroma progression and the occurrence of cardiovascular events.
Dr. Nicholls has received speaking honoraria and research support from many pharmaceutical companies, and from Infraredx. Dr. Steven E. Nissen of the Cleveland Clinic was a coinvestigator and has received research support from and is a consultant/adviser to numerous pharmaceutical companies; all honoraria or consulting fees go directly to charity so that he receives neither income nor a tax deduction. The other authors report no conflicts.
FROM ARTERIOSCLEROSIS, THROMBOSIS, AND VASCULAR BIOLOGY
Key clinical point: Patients on statins who had minimal LDL-C lowering also showed increased atheroma progression.
Major finding: Of 647 patients with CAD, 20% were hyporesponders to statin therapy and experienced greater progression of atheroma volume than statin responders (adjusted +0.83% vs. –0.21%, P = .006).
Data source: Pooled data from seven clinical trials, yielding 647 patients with angiographically confirmed CAD who were initiated on standard lipid dosing and followed by baseline and serial grayscale intravascular ultrasounds.
Disclosures: Dr. Nicholls has received speaking honoraria and research support from many pharmaceutical companies, and from Infraredx. Dr. Steven E. Nissen of the Cleveland Clinic was a coinvestigator and has received research support from and is a consultant/adviser to numerous pharmaceutical companies; all honoraria or consulting fees go directly to charity so that he receives neither income nor a tax deduction. The other authors report no conflicts.
Device reduces coronary sinus, relieves refractory angina
A new endoluminal device that reduces the coronary sinus significantly improved refractory angina in patients with advanced coronary artery disease who weren’t candidates for revascularization in a small phase II clinical trial. The results were published online Feb. 5 in the New England Journal of Medicine.
The international, randomized, double-blind study, sponsored by Neovasc, maker of the Reducer device, involved 104 patients enrolled who had Canadian Cardiovascular Society (CCS) class III or IV angina despite maximal medical therapy, evidence of reversible myocardial ischemia, and a left ventricular ejection fraction over 25%. These participants (mean age 68 years; range, 35-87 years) underwent right heart catheterization with angiography of the coronary sinus to determine whether the anatomy was suitable for implantation. Then 52 underwent implantation (the treatment group) and 52 underwent a sham procedure (the control group), and all were followed for up to 3 years, said Dr. Stefan Verheye of Antwerp (Belgium) Cardiovascular Center and his associates.
The stainless steel device is balloon expandable and shaped like an hourglass. It creates a focal narrowing that increases pressure in the coronary sinus, which is thought to recruit coronary collateral blood flow, redistributing blood from the less-ischemic epicardium to the ischemic endocardium. The primary efficacy end point of the trial – the number of patients whose angina improved by two or more CCS classes within 6 months – was achieved by more than twice as many patients in the treatment group (18, or 35%) as in the control group (8, or 15%).
A total of 37 patients (71%) who received active treatment showed an improvement of at least one CCS class, compared with 22 (42%) of those who received the sham treatment. Quality of life, as measured by Seattle Angina Questionnaire score, improved by 17.6 out of a possible 100 points for active treatment, compared with 7.6 points for sham treatment. And exercise duration improved by 1 minute (13%) for active treatment, compared with 4 seconds (1%) for sham treatment, Dr. Verheye and his associates said (N. Engl. J. Med. 2015 Feb. 5 [doi:10.1056/NEJMoa1402556]). “Our study was not statistically powered to detect an improvement in ischemia by means of objective measures such as stress testing or wall-motion index. A larger trial would be necessary to show such a benefit,” they noted.
There were 76 adverse events in patients who received the implant and 93 in the control group; the numbers of serious adverse events in this high-risk cohort were 10 and 24, respectively. This included one periprocedural MI that occurred in a patient receiving active treatment. Among 36 of the patients who received the implant and later underwent CT angiography, none showed any evidence of device migration or occlusion, the investigators added.
This study was supported by Neovasc, manufacturer of the Reducer device. Dr. Verheye reported having no financial disclosures. His associates reported ties to Neovasc, Abbott, Boston Scientific, Novo Nordisk, Eli Lilly, and Zealand Pharma.

|
Dr. Bernard Gersh |
Even though this trial was of high quality and well performed, the total number of patients in both study groups who had a positive outcome is only 26, which is not sufficient for a reliable estimation of modest treatment effects.
The small sample size necessarily limits confidence about this new device’s effectiveness. But if these findings are confirmed in future studies, coronary-sinus–reducing therapy may become a welcome and necessary addition to our options to improve quality of life for patients with refractory angina.
Christopher B. Granger, M.D., is at Duke Clinical Research Institute, Durham N.C. He reported numerous ties to industry sources. Bernard J. Gersh, M.D., D.Phil., is in the department of cardiovascular diseases at the Mayo Clinic, Rochester Minn. He reported having no financial disclosures. Dr. Granger and Dr. Gersh made these remarks in an editorial accompanying Dr. Verheye’s report (N. Engl. J. Med. 2015 Feb. 5 [doi:10.1056/NEJMe1413941]).

|
Dr. Bernard Gersh |
Even though this trial was of high quality and well performed, the total number of patients in both study groups who had a positive outcome is only 26, which is not sufficient for a reliable estimation of modest treatment effects.
The small sample size necessarily limits confidence about this new device’s effectiveness. But if these findings are confirmed in future studies, coronary-sinus–reducing therapy may become a welcome and necessary addition to our options to improve quality of life for patients with refractory angina.
Christopher B. Granger, M.D., is at Duke Clinical Research Institute, Durham N.C. He reported numerous ties to industry sources. Bernard J. Gersh, M.D., D.Phil., is in the department of cardiovascular diseases at the Mayo Clinic, Rochester Minn. He reported having no financial disclosures. Dr. Granger and Dr. Gersh made these remarks in an editorial accompanying Dr. Verheye’s report (N. Engl. J. Med. 2015 Feb. 5 [doi:10.1056/NEJMe1413941]).

|
Dr. Bernard Gersh |
Even though this trial was of high quality and well performed, the total number of patients in both study groups who had a positive outcome is only 26, which is not sufficient for a reliable estimation of modest treatment effects.
The small sample size necessarily limits confidence about this new device’s effectiveness. But if these findings are confirmed in future studies, coronary-sinus–reducing therapy may become a welcome and necessary addition to our options to improve quality of life for patients with refractory angina.
Christopher B. Granger, M.D., is at Duke Clinical Research Institute, Durham N.C. He reported numerous ties to industry sources. Bernard J. Gersh, M.D., D.Phil., is in the department of cardiovascular diseases at the Mayo Clinic, Rochester Minn. He reported having no financial disclosures. Dr. Granger and Dr. Gersh made these remarks in an editorial accompanying Dr. Verheye’s report (N. Engl. J. Med. 2015 Feb. 5 [doi:10.1056/NEJMe1413941]).
A new endoluminal device that reduces the coronary sinus significantly improved refractory angina in patients with advanced coronary artery disease who weren’t candidates for revascularization in a small phase II clinical trial. The results were published online Feb. 5 in the New England Journal of Medicine.
The international, randomized, double-blind study, sponsored by Neovasc, maker of the Reducer device, involved 104 patients enrolled who had Canadian Cardiovascular Society (CCS) class III or IV angina despite maximal medical therapy, evidence of reversible myocardial ischemia, and a left ventricular ejection fraction over 25%. These participants (mean age 68 years; range, 35-87 years) underwent right heart catheterization with angiography of the coronary sinus to determine whether the anatomy was suitable for implantation. Then 52 underwent implantation (the treatment group) and 52 underwent a sham procedure (the control group), and all were followed for up to 3 years, said Dr. Stefan Verheye of Antwerp (Belgium) Cardiovascular Center and his associates.
The stainless steel device is balloon expandable and shaped like an hourglass. It creates a focal narrowing that increases pressure in the coronary sinus, which is thought to recruit coronary collateral blood flow, redistributing blood from the less-ischemic epicardium to the ischemic endocardium. The primary efficacy end point of the trial – the number of patients whose angina improved by two or more CCS classes within 6 months – was achieved by more than twice as many patients in the treatment group (18, or 35%) as in the control group (8, or 15%).
A total of 37 patients (71%) who received active treatment showed an improvement of at least one CCS class, compared with 22 (42%) of those who received the sham treatment. Quality of life, as measured by Seattle Angina Questionnaire score, improved by 17.6 out of a possible 100 points for active treatment, compared with 7.6 points for sham treatment. And exercise duration improved by 1 minute (13%) for active treatment, compared with 4 seconds (1%) for sham treatment, Dr. Verheye and his associates said (N. Engl. J. Med. 2015 Feb. 5 [doi:10.1056/NEJMoa1402556]). “Our study was not statistically powered to detect an improvement in ischemia by means of objective measures such as stress testing or wall-motion index. A larger trial would be necessary to show such a benefit,” they noted.
There were 76 adverse events in patients who received the implant and 93 in the control group; the numbers of serious adverse events in this high-risk cohort were 10 and 24, respectively. This included one periprocedural MI that occurred in a patient receiving active treatment. Among 36 of the patients who received the implant and later underwent CT angiography, none showed any evidence of device migration or occlusion, the investigators added.
This study was supported by Neovasc, manufacturer of the Reducer device. Dr. Verheye reported having no financial disclosures. His associates reported ties to Neovasc, Abbott, Boston Scientific, Novo Nordisk, Eli Lilly, and Zealand Pharma.
A new endoluminal device that reduces the coronary sinus significantly improved refractory angina in patients with advanced coronary artery disease who weren’t candidates for revascularization in a small phase II clinical trial. The results were published online Feb. 5 in the New England Journal of Medicine.
The international, randomized, double-blind study, sponsored by Neovasc, maker of the Reducer device, involved 104 patients enrolled who had Canadian Cardiovascular Society (CCS) class III or IV angina despite maximal medical therapy, evidence of reversible myocardial ischemia, and a left ventricular ejection fraction over 25%. These participants (mean age 68 years; range, 35-87 years) underwent right heart catheterization with angiography of the coronary sinus to determine whether the anatomy was suitable for implantation. Then 52 underwent implantation (the treatment group) and 52 underwent a sham procedure (the control group), and all were followed for up to 3 years, said Dr. Stefan Verheye of Antwerp (Belgium) Cardiovascular Center and his associates.
The stainless steel device is balloon expandable and shaped like an hourglass. It creates a focal narrowing that increases pressure in the coronary sinus, which is thought to recruit coronary collateral blood flow, redistributing blood from the less-ischemic epicardium to the ischemic endocardium. The primary efficacy end point of the trial – the number of patients whose angina improved by two or more CCS classes within 6 months – was achieved by more than twice as many patients in the treatment group (18, or 35%) as in the control group (8, or 15%).
A total of 37 patients (71%) who received active treatment showed an improvement of at least one CCS class, compared with 22 (42%) of those who received the sham treatment. Quality of life, as measured by Seattle Angina Questionnaire score, improved by 17.6 out of a possible 100 points for active treatment, compared with 7.6 points for sham treatment. And exercise duration improved by 1 minute (13%) for active treatment, compared with 4 seconds (1%) for sham treatment, Dr. Verheye and his associates said (N. Engl. J. Med. 2015 Feb. 5 [doi:10.1056/NEJMoa1402556]). “Our study was not statistically powered to detect an improvement in ischemia by means of objective measures such as stress testing or wall-motion index. A larger trial would be necessary to show such a benefit,” they noted.
There were 76 adverse events in patients who received the implant and 93 in the control group; the numbers of serious adverse events in this high-risk cohort were 10 and 24, respectively. This included one periprocedural MI that occurred in a patient receiving active treatment. Among 36 of the patients who received the implant and later underwent CT angiography, none showed any evidence of device migration or occlusion, the investigators added.
This study was supported by Neovasc, manufacturer of the Reducer device. Dr. Verheye reported having no financial disclosures. His associates reported ties to Neovasc, Abbott, Boston Scientific, Novo Nordisk, Eli Lilly, and Zealand Pharma.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: A new endoluminal device inserted into the coronary sinus creates focal pressure that relieves refractory angina in patients who can’t undergo revascularization.
Major finding: The number of patients whose angina improved by two or more CCS classes within 6 months was achieved by more than twice as many patients in the treatment group (18, or 35%) than in the control group (8, or 15%).
Data source: A small, multicenter, randomized, sham-controlled phase II clinical trial involving 104 patients with refractory, severe angina who were followed for 3 years.
Disclosures: This study was supported by Neovasc, manufacturer of the Reducer device. Dr. Verheye reported having no financial disclosures; his associates reported ties to Neovasc, Abbott, Boston Scientific, Novo Nordisk, Eli Lilly, and Zealand Pharma.