User login
Surgical left atrial appendage closure slashes stroke risk
BARCELONA – Routine surgical closure of the left atrial appendage during open heart surgery provides long-term protection against cerebral ischemic events, according to the findings of the first-ever randomized controlled trial to address the issue.
“I think we can say, based on our study, that it would be advisable to routinely add surgical closure of the left atrial appendage to planned open heart surgery,” Jesper Park-Hansen, MD, said at the annual congress of the European Society of Cardiology.
In light of the demonstrated success of percutaneous closure of the LAA using the Watchman and other devices for stroke prevention in patients with atrial fibrillation, Dr. Park-Hansen and his coinvestigators at the University of Copenhagen organized LAACS (the Left Atrial Appendage Closure Study). The goal was to generate solid, randomized trial evidence as to whether preemptive routine surgical closure of the LAA at the time of cardiac surgery is of benefit. Some cardiac surgeons already do this routinely; many others don’t because of the lack of Level 1 supporting evidence.
LAACS included 141 patients randomized to surgical LAA closure or not at the point of first-time open heart surgery. The study population included patients with and without a history of atrial fibrillation. LAA closure was accomplished via a purse string closure with a silk string around the neck of the appendage backed up by an additional single running suture. Transesophageal echocardiography performed in 10 patients a mean of 520 days post closure showed no signs of leakage or incomplete closure.
The primary composite outcome was comprised of clinical stroke or transient ischemic attack diagnosed by a neurologist, or a silent cerebral infarct detected on MRI performed 2-4 weeks post discharge and again at least 6 months later. At a mean follow-up of 3.7 years and a maximum of 6 years, this outcome had occurred in 6.3% of the LAAC group, significantly lower than the 18.3% rate in controls. All but one patient with a cerebral ischemic event in the control group had atrial fibrillation. The risk of an event was unrelated to whether or not a patient had a history of atrial fibrillation prior to surgery or to CHA2DS2-VASc score.
Dr. Park-Hansen emphasized that he and his coinvestigators don’t consider LAACS to be the final word on routine prophylactic appendage closure.
“This is the first randomized study. We are eager to move on to another randomized study on a larger scale. That is the next step for us,” he said.
“The challenge now – and what we will be discussing with our surgeons – is to agree on a feasible safe and effective means of left atrial appendage closure. My personal opinion is the Lariat suture delivery device or some other easily reproducible method of closure could be a good way to go,” Dr. Park-Hansen added.
The research group’s cardiac surgeons already have ruled out excision and stapling because of concerns about bleeding risk and the additional cost imposed by stapling.
Discussant Volkmar Falk, MD, commented that LAACS was too small, probably severely underpowered, should have included a preoperative MRI so investigators could reliably capture perioperative silent cerebral infarcts, and the double suture purse string is “probably not the best method” to occlude the LAA.
“LAACS addresses an important question, but alas, it does not provide the answer,” declared Dr. Falk, professor and director of the department of cardiothoracic and vascular surgery at Charité Medical University in Berlin.
Dr. Park-Hansen and Dr. Falk reported having no financial conflicts of interest.
BARCELONA – Routine surgical closure of the left atrial appendage during open heart surgery provides long-term protection against cerebral ischemic events, according to the findings of the first-ever randomized controlled trial to address the issue.
“I think we can say, based on our study, that it would be advisable to routinely add surgical closure of the left atrial appendage to planned open heart surgery,” Jesper Park-Hansen, MD, said at the annual congress of the European Society of Cardiology.
In light of the demonstrated success of percutaneous closure of the LAA using the Watchman and other devices for stroke prevention in patients with atrial fibrillation, Dr. Park-Hansen and his coinvestigators at the University of Copenhagen organized LAACS (the Left Atrial Appendage Closure Study). The goal was to generate solid, randomized trial evidence as to whether preemptive routine surgical closure of the LAA at the time of cardiac surgery is of benefit. Some cardiac surgeons already do this routinely; many others don’t because of the lack of Level 1 supporting evidence.
LAACS included 141 patients randomized to surgical LAA closure or not at the point of first-time open heart surgery. The study population included patients with and without a history of atrial fibrillation. LAA closure was accomplished via a purse string closure with a silk string around the neck of the appendage backed up by an additional single running suture. Transesophageal echocardiography performed in 10 patients a mean of 520 days post closure showed no signs of leakage or incomplete closure.
The primary composite outcome was comprised of clinical stroke or transient ischemic attack diagnosed by a neurologist, or a silent cerebral infarct detected on MRI performed 2-4 weeks post discharge and again at least 6 months later. At a mean follow-up of 3.7 years and a maximum of 6 years, this outcome had occurred in 6.3% of the LAAC group, significantly lower than the 18.3% rate in controls. All but one patient with a cerebral ischemic event in the control group had atrial fibrillation. The risk of an event was unrelated to whether or not a patient had a history of atrial fibrillation prior to surgery or to CHA2DS2-VASc score.
Dr. Park-Hansen emphasized that he and his coinvestigators don’t consider LAACS to be the final word on routine prophylactic appendage closure.
“This is the first randomized study. We are eager to move on to another randomized study on a larger scale. That is the next step for us,” he said.
“The challenge now – and what we will be discussing with our surgeons – is to agree on a feasible safe and effective means of left atrial appendage closure. My personal opinion is the Lariat suture delivery device or some other easily reproducible method of closure could be a good way to go,” Dr. Park-Hansen added.
The research group’s cardiac surgeons already have ruled out excision and stapling because of concerns about bleeding risk and the additional cost imposed by stapling.
Discussant Volkmar Falk, MD, commented that LAACS was too small, probably severely underpowered, should have included a preoperative MRI so investigators could reliably capture perioperative silent cerebral infarcts, and the double suture purse string is “probably not the best method” to occlude the LAA.
“LAACS addresses an important question, but alas, it does not provide the answer,” declared Dr. Falk, professor and director of the department of cardiothoracic and vascular surgery at Charité Medical University in Berlin.
Dr. Park-Hansen and Dr. Falk reported having no financial conflicts of interest.
BARCELONA – Routine surgical closure of the left atrial appendage during open heart surgery provides long-term protection against cerebral ischemic events, according to the findings of the first-ever randomized controlled trial to address the issue.
“I think we can say, based on our study, that it would be advisable to routinely add surgical closure of the left atrial appendage to planned open heart surgery,” Jesper Park-Hansen, MD, said at the annual congress of the European Society of Cardiology.
In light of the demonstrated success of percutaneous closure of the LAA using the Watchman and other devices for stroke prevention in patients with atrial fibrillation, Dr. Park-Hansen and his coinvestigators at the University of Copenhagen organized LAACS (the Left Atrial Appendage Closure Study). The goal was to generate solid, randomized trial evidence as to whether preemptive routine surgical closure of the LAA at the time of cardiac surgery is of benefit. Some cardiac surgeons already do this routinely; many others don’t because of the lack of Level 1 supporting evidence.
LAACS included 141 patients randomized to surgical LAA closure or not at the point of first-time open heart surgery. The study population included patients with and without a history of atrial fibrillation. LAA closure was accomplished via a purse string closure with a silk string around the neck of the appendage backed up by an additional single running suture. Transesophageal echocardiography performed in 10 patients a mean of 520 days post closure showed no signs of leakage or incomplete closure.
The primary composite outcome was comprised of clinical stroke or transient ischemic attack diagnosed by a neurologist, or a silent cerebral infarct detected on MRI performed 2-4 weeks post discharge and again at least 6 months later. At a mean follow-up of 3.7 years and a maximum of 6 years, this outcome had occurred in 6.3% of the LAAC group, significantly lower than the 18.3% rate in controls. All but one patient with a cerebral ischemic event in the control group had atrial fibrillation. The risk of an event was unrelated to whether or not a patient had a history of atrial fibrillation prior to surgery or to CHA2DS2-VASc score.
Dr. Park-Hansen emphasized that he and his coinvestigators don’t consider LAACS to be the final word on routine prophylactic appendage closure.
“This is the first randomized study. We are eager to move on to another randomized study on a larger scale. That is the next step for us,” he said.
“The challenge now – and what we will be discussing with our surgeons – is to agree on a feasible safe and effective means of left atrial appendage closure. My personal opinion is the Lariat suture delivery device or some other easily reproducible method of closure could be a good way to go,” Dr. Park-Hansen added.
The research group’s cardiac surgeons already have ruled out excision and stapling because of concerns about bleeding risk and the additional cost imposed by stapling.
Discussant Volkmar Falk, MD, commented that LAACS was too small, probably severely underpowered, should have included a preoperative MRI so investigators could reliably capture perioperative silent cerebral infarcts, and the double suture purse string is “probably not the best method” to occlude the LAA.
“LAACS addresses an important question, but alas, it does not provide the answer,” declared Dr. Falk, professor and director of the department of cardiothoracic and vascular surgery at Charité Medical University in Berlin.
Dr. Park-Hansen and Dr. Falk reported having no financial conflicts of interest.
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: The composite rate of clinical stroke, TIA, or silent cerebral infarct in the years following open heart surgery was threefold higher in patients randomized to no prophylactic surgical closure of the left atrial appendage, compared with patients who got appendage closure during their surgery.
Data source: A randomized trial in which 141 patients undergoing first-time open heart surgery were assigned to prophylactic surgical closure of the left atrial appendage or not.
Disclosures: The study was conducted free of commercial support. The presenter reported having no financial conflicts of interest.
LDL levels below 10 mg/dL shown safe, effective
BARCELONA – The maxim that lower is better for LDL cholesterol continues to hold true, even at jaw-droppingly low levels of less than 10 mg/dL in a new analysis of data from the FOURIER trial.
The Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk (FOURIER) trial was the pivotal efficacy and safety study for the proprotein convertase subtilisin–kexin type 9 (PCSK9) inhibitor evolocumab (Repatha) and enrolled patients with atherosclerotic cardiovascular disease and LDL cholesterol levels of at least 70 mg/dL (N Engl J Med. 2017 May 4;376[18]:1713-22).
After a median follow-up of 26 months, the incidence of the study’s primary endpoint (cardiovascular death, MI, stroke, hospitalization for unstable angina, or coronary revascularization) dropped by a statistically significant 15% in patients with an achieved LDL cholesterol of 20-49 mg/dL, compared with patients whose 4-week LDL cholesterol was at or above 100 mg/dL (primarily patients randomized to the study’s control arm), by 24% in all patients with LDL cholesterol less than 20 mg/dL, and by 31% in the 2% of patients whose LDL cholesterol levels fell below 10 mg/dL.
These strikingly improved event rates at the lowest levels of LDL cholesterol occurred with no signal of excess adverse events, Robert P. Giugliano, MD, said at the annual congress of the European Society of Cardiology.
In contrast, the 13% of patents whose achieved LDL cholesterol was 50-69 mg/dL had an event rate just 6% below the referent group of 100 mg/dL or more, a nonsignificant difference. Existing cholesterol management guidelines that set LDL cholesterol targets for secondary prevention have used a level below 70 mg/dL as the target, such as the European Society of Cardiology’s 2016 guidelines (Eur Heart J. 2016 Oct 14;37[39]:2999-3058).
“The data suggest that we should target considerably lower LDL cholesterol than is currently recommended for our patients with atherosclerotic cardiovascular disease,” said Dr. Giugliano, a cardiologist at Brigham and Women’s Hospital in Boston.
“Lowest is best with LDL. You don’t need a lot of LDL in the serum for normal human function,” he noted during the discussion of his report.
While FOURIER’s event curve continued to drop as LDL cholesterol fell below 10 mg/dL, the study’s wide-ranging safety assessment showed no signal of harm at the lowest levels. This “gives us some reassurance it’s safe,” he said in an interview. “We saw benefit that continued down to the lowest LDL levels, so it’s hard to pick a LDL target. I no longer feel comfortable treating my patients to just less than 70 mg/dL. I’m not sure what is the optimal LDL target, but I think it needs to be lower than that.”
To achieve such ultralow LDL levels, most patients need treatment with a PCSK9 inhibitor plus at least one and perhaps two additional cholesterol-lowering drugs, a statin and ezetimibe, he noted.
The FOURIER analyses Dr. Giugliano reported included data on the incidence during the study of 10 specific types of adverse events: noncardiovascular death, serious adverse events, adverse events leading to study discontinuation, and new onset of diabetes, cancer, cataract, neurocognitive deficit, significant liver enzyme increase, significant creatine kinase increase, and hemorrhagic stroke. The incidence of each of these was similar among the patients in five study subgroups based on achieved levels of LDL cholesterol: less than 20 mg/dL, 20-49 mg/dL, 50-69 mg/dL, 70-99 mg/dL, and 100 mg/dL or higher. In addition, the rates of both serious adverse events and adverse events leading to study discontinuation was roughly the same in the subgroup of patients with an achieved LDL cholesterol of less than 10 mg/dL as in those with an achieved LDL of at least 100 mg/dL.
Concurrently with Dr. Giugliano’s report, the results also appeared in an online article (Lancet. 2017 Aug 28. doi: 10.1016/S0140-6736[17]32290-0).
FOURIER was funded by Amgen, the company that markets evolocumab (Repatha). Dr. Giugliano has been a consultant to and has received research funding from Amgen, and he has also been a consultant to Bristol-Myers Squibb, Daiichi Sankyo, GlaxoSmithKline, Merck, and Pfizer.
[email protected]
On Twitter @mitchelzoler
BARCELONA – The maxim that lower is better for LDL cholesterol continues to hold true, even at jaw-droppingly low levels of less than 10 mg/dL in a new analysis of data from the FOURIER trial.
The Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk (FOURIER) trial was the pivotal efficacy and safety study for the proprotein convertase subtilisin–kexin type 9 (PCSK9) inhibitor evolocumab (Repatha) and enrolled patients with atherosclerotic cardiovascular disease and LDL cholesterol levels of at least 70 mg/dL (N Engl J Med. 2017 May 4;376[18]:1713-22).
After a median follow-up of 26 months, the incidence of the study’s primary endpoint (cardiovascular death, MI, stroke, hospitalization for unstable angina, or coronary revascularization) dropped by a statistically significant 15% in patients with an achieved LDL cholesterol of 20-49 mg/dL, compared with patients whose 4-week LDL cholesterol was at or above 100 mg/dL (primarily patients randomized to the study’s control arm), by 24% in all patients with LDL cholesterol less than 20 mg/dL, and by 31% in the 2% of patients whose LDL cholesterol levels fell below 10 mg/dL.
These strikingly improved event rates at the lowest levels of LDL cholesterol occurred with no signal of excess adverse events, Robert P. Giugliano, MD, said at the annual congress of the European Society of Cardiology.
In contrast, the 13% of patents whose achieved LDL cholesterol was 50-69 mg/dL had an event rate just 6% below the referent group of 100 mg/dL or more, a nonsignificant difference. Existing cholesterol management guidelines that set LDL cholesterol targets for secondary prevention have used a level below 70 mg/dL as the target, such as the European Society of Cardiology’s 2016 guidelines (Eur Heart J. 2016 Oct 14;37[39]:2999-3058).
“The data suggest that we should target considerably lower LDL cholesterol than is currently recommended for our patients with atherosclerotic cardiovascular disease,” said Dr. Giugliano, a cardiologist at Brigham and Women’s Hospital in Boston.
“Lowest is best with LDL. You don’t need a lot of LDL in the serum for normal human function,” he noted during the discussion of his report.
While FOURIER’s event curve continued to drop as LDL cholesterol fell below 10 mg/dL, the study’s wide-ranging safety assessment showed no signal of harm at the lowest levels. This “gives us some reassurance it’s safe,” he said in an interview. “We saw benefit that continued down to the lowest LDL levels, so it’s hard to pick a LDL target. I no longer feel comfortable treating my patients to just less than 70 mg/dL. I’m not sure what is the optimal LDL target, but I think it needs to be lower than that.”
To achieve such ultralow LDL levels, most patients need treatment with a PCSK9 inhibitor plus at least one and perhaps two additional cholesterol-lowering drugs, a statin and ezetimibe, he noted.
The FOURIER analyses Dr. Giugliano reported included data on the incidence during the study of 10 specific types of adverse events: noncardiovascular death, serious adverse events, adverse events leading to study discontinuation, and new onset of diabetes, cancer, cataract, neurocognitive deficit, significant liver enzyme increase, significant creatine kinase increase, and hemorrhagic stroke. The incidence of each of these was similar among the patients in five study subgroups based on achieved levels of LDL cholesterol: less than 20 mg/dL, 20-49 mg/dL, 50-69 mg/dL, 70-99 mg/dL, and 100 mg/dL or higher. In addition, the rates of both serious adverse events and adverse events leading to study discontinuation was roughly the same in the subgroup of patients with an achieved LDL cholesterol of less than 10 mg/dL as in those with an achieved LDL of at least 100 mg/dL.
Concurrently with Dr. Giugliano’s report, the results also appeared in an online article (Lancet. 2017 Aug 28. doi: 10.1016/S0140-6736[17]32290-0).
FOURIER was funded by Amgen, the company that markets evolocumab (Repatha). Dr. Giugliano has been a consultant to and has received research funding from Amgen, and he has also been a consultant to Bristol-Myers Squibb, Daiichi Sankyo, GlaxoSmithKline, Merck, and Pfizer.
[email protected]
On Twitter @mitchelzoler
BARCELONA – The maxim that lower is better for LDL cholesterol continues to hold true, even at jaw-droppingly low levels of less than 10 mg/dL in a new analysis of data from the FOURIER trial.
The Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk (FOURIER) trial was the pivotal efficacy and safety study for the proprotein convertase subtilisin–kexin type 9 (PCSK9) inhibitor evolocumab (Repatha) and enrolled patients with atherosclerotic cardiovascular disease and LDL cholesterol levels of at least 70 mg/dL (N Engl J Med. 2017 May 4;376[18]:1713-22).
After a median follow-up of 26 months, the incidence of the study’s primary endpoint (cardiovascular death, MI, stroke, hospitalization for unstable angina, or coronary revascularization) dropped by a statistically significant 15% in patients with an achieved LDL cholesterol of 20-49 mg/dL, compared with patients whose 4-week LDL cholesterol was at or above 100 mg/dL (primarily patients randomized to the study’s control arm), by 24% in all patients with LDL cholesterol less than 20 mg/dL, and by 31% in the 2% of patients whose LDL cholesterol levels fell below 10 mg/dL.
These strikingly improved event rates at the lowest levels of LDL cholesterol occurred with no signal of excess adverse events, Robert P. Giugliano, MD, said at the annual congress of the European Society of Cardiology.
In contrast, the 13% of patents whose achieved LDL cholesterol was 50-69 mg/dL had an event rate just 6% below the referent group of 100 mg/dL or more, a nonsignificant difference. Existing cholesterol management guidelines that set LDL cholesterol targets for secondary prevention have used a level below 70 mg/dL as the target, such as the European Society of Cardiology’s 2016 guidelines (Eur Heart J. 2016 Oct 14;37[39]:2999-3058).
“The data suggest that we should target considerably lower LDL cholesterol than is currently recommended for our patients with atherosclerotic cardiovascular disease,” said Dr. Giugliano, a cardiologist at Brigham and Women’s Hospital in Boston.
“Lowest is best with LDL. You don’t need a lot of LDL in the serum for normal human function,” he noted during the discussion of his report.
While FOURIER’s event curve continued to drop as LDL cholesterol fell below 10 mg/dL, the study’s wide-ranging safety assessment showed no signal of harm at the lowest levels. This “gives us some reassurance it’s safe,” he said in an interview. “We saw benefit that continued down to the lowest LDL levels, so it’s hard to pick a LDL target. I no longer feel comfortable treating my patients to just less than 70 mg/dL. I’m not sure what is the optimal LDL target, but I think it needs to be lower than that.”
To achieve such ultralow LDL levels, most patients need treatment with a PCSK9 inhibitor plus at least one and perhaps two additional cholesterol-lowering drugs, a statin and ezetimibe, he noted.
The FOURIER analyses Dr. Giugliano reported included data on the incidence during the study of 10 specific types of adverse events: noncardiovascular death, serious adverse events, adverse events leading to study discontinuation, and new onset of diabetes, cancer, cataract, neurocognitive deficit, significant liver enzyme increase, significant creatine kinase increase, and hemorrhagic stroke. The incidence of each of these was similar among the patients in five study subgroups based on achieved levels of LDL cholesterol: less than 20 mg/dL, 20-49 mg/dL, 50-69 mg/dL, 70-99 mg/dL, and 100 mg/dL or higher. In addition, the rates of both serious adverse events and adverse events leading to study discontinuation was roughly the same in the subgroup of patients with an achieved LDL cholesterol of less than 10 mg/dL as in those with an achieved LDL of at least 100 mg/dL.
Concurrently with Dr. Giugliano’s report, the results also appeared in an online article (Lancet. 2017 Aug 28. doi: 10.1016/S0140-6736[17]32290-0).
FOURIER was funded by Amgen, the company that markets evolocumab (Repatha). Dr. Giugliano has been a consultant to and has received research funding from Amgen, and he has also been a consultant to Bristol-Myers Squibb, Daiichi Sankyo, GlaxoSmithKline, Merck, and Pfizer.
[email protected]
On Twitter @mitchelzoler
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: Patients with an achieved LDL of less than 10 mg/dL had an event rate 31% below patients with an LDL at or above 100 mg/dL.
Data source: FOURIER, an international multicenter trial with 27,564 patients.
Disclosures: FOURIER was funded by Amgen, the company that markets evolocumab (Repatha). Dr. Giugliano has been a consultant to and has received research funding from Amgen, and he has also been a consultant to Bristol-Myers Squibb, Daiichi Sankyo, GlaxoSmithKline, Merck, and Pfizer.
How to apply SPRINT findings to elderly patients
SAN FRANCISCO – The benefit of lowering blood pressure exceeded the potential for harm, even among the most frail elderly, in SPRINT, but it’s important to remember who was excluded from the trial when using the findings in the clinic, according to Mark Supiano, MD.
SPRINT (Systolic Blood Pressure Intervention Trial) excluded people with histories of stroke, diabetes, heart failure, and chronic kidney disease with a markedly reduced glomerular filtration rate. People living in nursing homes, assisted living centers, and those with prevalent dementia were also excluded, as were individuals with a standing systolic pressure below 110 mm Hg (N Engl J Med. 2015 Nov 26;373:2103-16).
Even with those exclusions, however, the 2,636 patients in SPRINT who were 75 years and older “were not a super healthy group of older people,” Dr. Supiano said at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
They were at high risk for cardiovascular disease (CVD), with a median 10-year Framingham risk score of almost 25%. More than a quarter had gait speeds below 0.8 m/sec, and almost a third were classified as frail. Many had mild cognitive impairment at baseline.
In the United States, Dr. Supiano and his colleagues estimate that there are almost 6 million similar people 75 years or older with hypertension who would likely achieve the same benefits from hypertension control as elderly subjects in the trial. “As a geriatrician, there are very few things that I can offer patients 75 years and older that will have a profound improvement in their overall mortality.” Blood pressure control is one of them, said Dr. Supiano, chief of geriatrics at the University of Utah, Salt Lake City, and a SPRINT investigator.
In SPRINT, intensive treatment to systolic pressure below 120 mm Hg showed greater benefit for patients 75 years and older than it did for younger patients, even among the frail, with a 34% reduction in fatal and nonfatal CVD events versus patients treated to below 140 mm Hg, and a 33% lower rate of death from any cause.
It should be no surprise that older patients had greater benefit from tighter control, because elderly patients have “a greater CVD risk. There’s more bang for the buck” with blood pressure lowering in an older population. “Overall, benefits exceed the potential for harm, even among the frailest older patients,” Dr. Supiano said.
“A systemic target of less than 140 mm Hg is, I believe, appropriate for most healthy people age 60 and older. A benefit-based systemic target of less than 120 mm Hg may be appropriate for those at higher CVD risk.” Among patients 60-75 years old, that would include those with a Framingham score above 15%. Among patients older than age 75 with an elevated CVD risk, treatment to below 120 mm Hg makes sense if it aligns with patient’s goals of care, Dr. Supiano said.
The 120–mm Hg target in SPRINT was associated with a greater incidence of some transient side effects in the elderly, including hypotension, syncope, acute kidney injury, and electrolyte imbalance, but not a higher risk of serious adverse events or injurious falls.
There were concerns raised at the joint sessions about the effect of blood pressure lowering on the cognitive function of older people. Dr. Supiano noted that the cognitive outcomes in SPRINT, as well as outcomes in patients with chronic kidney disease, have not yet been released, but are expected soon.
Dr. Supiano had no relevant disclosures.
SAN FRANCISCO – The benefit of lowering blood pressure exceeded the potential for harm, even among the most frail elderly, in SPRINT, but it’s important to remember who was excluded from the trial when using the findings in the clinic, according to Mark Supiano, MD.
SPRINT (Systolic Blood Pressure Intervention Trial) excluded people with histories of stroke, diabetes, heart failure, and chronic kidney disease with a markedly reduced glomerular filtration rate. People living in nursing homes, assisted living centers, and those with prevalent dementia were also excluded, as were individuals with a standing systolic pressure below 110 mm Hg (N Engl J Med. 2015 Nov 26;373:2103-16).
Even with those exclusions, however, the 2,636 patients in SPRINT who were 75 years and older “were not a super healthy group of older people,” Dr. Supiano said at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
They were at high risk for cardiovascular disease (CVD), with a median 10-year Framingham risk score of almost 25%. More than a quarter had gait speeds below 0.8 m/sec, and almost a third were classified as frail. Many had mild cognitive impairment at baseline.
In the United States, Dr. Supiano and his colleagues estimate that there are almost 6 million similar people 75 years or older with hypertension who would likely achieve the same benefits from hypertension control as elderly subjects in the trial. “As a geriatrician, there are very few things that I can offer patients 75 years and older that will have a profound improvement in their overall mortality.” Blood pressure control is one of them, said Dr. Supiano, chief of geriatrics at the University of Utah, Salt Lake City, and a SPRINT investigator.
In SPRINT, intensive treatment to systolic pressure below 120 mm Hg showed greater benefit for patients 75 years and older than it did for younger patients, even among the frail, with a 34% reduction in fatal and nonfatal CVD events versus patients treated to below 140 mm Hg, and a 33% lower rate of death from any cause.
It should be no surprise that older patients had greater benefit from tighter control, because elderly patients have “a greater CVD risk. There’s more bang for the buck” with blood pressure lowering in an older population. “Overall, benefits exceed the potential for harm, even among the frailest older patients,” Dr. Supiano said.
“A systemic target of less than 140 mm Hg is, I believe, appropriate for most healthy people age 60 and older. A benefit-based systemic target of less than 120 mm Hg may be appropriate for those at higher CVD risk.” Among patients 60-75 years old, that would include those with a Framingham score above 15%. Among patients older than age 75 with an elevated CVD risk, treatment to below 120 mm Hg makes sense if it aligns with patient’s goals of care, Dr. Supiano said.
The 120–mm Hg target in SPRINT was associated with a greater incidence of some transient side effects in the elderly, including hypotension, syncope, acute kidney injury, and electrolyte imbalance, but not a higher risk of serious adverse events or injurious falls.
There were concerns raised at the joint sessions about the effect of blood pressure lowering on the cognitive function of older people. Dr. Supiano noted that the cognitive outcomes in SPRINT, as well as outcomes in patients with chronic kidney disease, have not yet been released, but are expected soon.
Dr. Supiano had no relevant disclosures.
SAN FRANCISCO – The benefit of lowering blood pressure exceeded the potential for harm, even among the most frail elderly, in SPRINT, but it’s important to remember who was excluded from the trial when using the findings in the clinic, according to Mark Supiano, MD.
SPRINT (Systolic Blood Pressure Intervention Trial) excluded people with histories of stroke, diabetes, heart failure, and chronic kidney disease with a markedly reduced glomerular filtration rate. People living in nursing homes, assisted living centers, and those with prevalent dementia were also excluded, as were individuals with a standing systolic pressure below 110 mm Hg (N Engl J Med. 2015 Nov 26;373:2103-16).
Even with those exclusions, however, the 2,636 patients in SPRINT who were 75 years and older “were not a super healthy group of older people,” Dr. Supiano said at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
They were at high risk for cardiovascular disease (CVD), with a median 10-year Framingham risk score of almost 25%. More than a quarter had gait speeds below 0.8 m/sec, and almost a third were classified as frail. Many had mild cognitive impairment at baseline.
In the United States, Dr. Supiano and his colleagues estimate that there are almost 6 million similar people 75 years or older with hypertension who would likely achieve the same benefits from hypertension control as elderly subjects in the trial. “As a geriatrician, there are very few things that I can offer patients 75 years and older that will have a profound improvement in their overall mortality.” Blood pressure control is one of them, said Dr. Supiano, chief of geriatrics at the University of Utah, Salt Lake City, and a SPRINT investigator.
In SPRINT, intensive treatment to systolic pressure below 120 mm Hg showed greater benefit for patients 75 years and older than it did for younger patients, even among the frail, with a 34% reduction in fatal and nonfatal CVD events versus patients treated to below 140 mm Hg, and a 33% lower rate of death from any cause.
It should be no surprise that older patients had greater benefit from tighter control, because elderly patients have “a greater CVD risk. There’s more bang for the buck” with blood pressure lowering in an older population. “Overall, benefits exceed the potential for harm, even among the frailest older patients,” Dr. Supiano said.
“A systemic target of less than 140 mm Hg is, I believe, appropriate for most healthy people age 60 and older. A benefit-based systemic target of less than 120 mm Hg may be appropriate for those at higher CVD risk.” Among patients 60-75 years old, that would include those with a Framingham score above 15%. Among patients older than age 75 with an elevated CVD risk, treatment to below 120 mm Hg makes sense if it aligns with patient’s goals of care, Dr. Supiano said.
The 120–mm Hg target in SPRINT was associated with a greater incidence of some transient side effects in the elderly, including hypotension, syncope, acute kidney injury, and electrolyte imbalance, but not a higher risk of serious adverse events or injurious falls.
There were concerns raised at the joint sessions about the effect of blood pressure lowering on the cognitive function of older people. Dr. Supiano noted that the cognitive outcomes in SPRINT, as well as outcomes in patients with chronic kidney disease, have not yet been released, but are expected soon.
Dr. Supiano had no relevant disclosures.
EXPERT ANALYSIS FROM JOINT HYPERTENSION 2017
LVAD use soars in elderly Americans
DALLAS – The percentage of left ventricular assist devices placed in U.S. heart failure patients at least 75 years of age jumped sharply during 2003-2014, and concurrently the short-term survival of these patients improved dramatically, according to data collected by the National Inpatient Sample.
During the 12-year period examined, the percentage of left-ventricular assist devices (LVADs) placed in U.S. heart failure patients aged 75 years and older rose from 3% of all LVADs in 2003 to 11% in 2014, Aniket S. Rali, MD, said at the annual scientific meeting of the Heart Failure Society of America.
The U.S. national numbers also showed that throughout the period studied, elderly U.S. patients who received an LVAD were increasingly sicker, with steadily increasing numbers of patients with a Charlson Comorbidity Index score of four or greater. Despite this, in-hospital mortality rates of elderly patients receiving an LVAD plummeted, dropping from 61% of elderly LVAD recipients in 2003 to 18% in 2014. During the same time, the percentage of elderly patients with a Charlson Comorbidity Index score greater than four doubled from 33% in 2003 to 66% in 2014, said Dr. Rali, a cardiologist at the University of Kansas Medical Center in Kansas City.
“If the Charlson Comorbidity Index score is increasing but in-hospital mortality is decreasing, then increased LVAD use is not a bad trend,” Dr. Rali said in an interview. He hopes that future analysis of longitudinal data from patients could identify clinical factors that link with better patient survival and help target LVAD placement to the patients who stand to gain the most benefit.
“We may be able to give these elderly patients not just longer life but improved quality of life” by a more informed targeting of LVADs, he suggested. “I think these numbers will help convince people that all is not lost,” he noted, for elderly heart failure patients who receive an LVAD as destination therapy. Patients at least 75 years old are not eligible for heart transplantation, so when these patients receive an LVAD it is, by definition, destination therapy.
The data also showed a marked sex disparity in LVAD use, with LVAD placement in men at least 75 years old rising from 1.4/1,000 patients in 2003 to 2.78/1,000 patients in 2014. In contrast, among women these rates rose from 0.8/1,000 patients in 2003 to 1.36/1,000 patients in 2014.
The average age for elderly U.S. LVAD recipients for the entire 12-year period studied was 77.6 years among a total of 2,090 recipients. For all 21,323 U.S. LVAD recipients during 2003-2014 the average age was 51.5 years old.
[email protected]
On Twitter @mitchelzoler
DALLAS – The percentage of left ventricular assist devices placed in U.S. heart failure patients at least 75 years of age jumped sharply during 2003-2014, and concurrently the short-term survival of these patients improved dramatically, according to data collected by the National Inpatient Sample.
During the 12-year period examined, the percentage of left-ventricular assist devices (LVADs) placed in U.S. heart failure patients aged 75 years and older rose from 3% of all LVADs in 2003 to 11% in 2014, Aniket S. Rali, MD, said at the annual scientific meeting of the Heart Failure Society of America.
The U.S. national numbers also showed that throughout the period studied, elderly U.S. patients who received an LVAD were increasingly sicker, with steadily increasing numbers of patients with a Charlson Comorbidity Index score of four or greater. Despite this, in-hospital mortality rates of elderly patients receiving an LVAD plummeted, dropping from 61% of elderly LVAD recipients in 2003 to 18% in 2014. During the same time, the percentage of elderly patients with a Charlson Comorbidity Index score greater than four doubled from 33% in 2003 to 66% in 2014, said Dr. Rali, a cardiologist at the University of Kansas Medical Center in Kansas City.
“If the Charlson Comorbidity Index score is increasing but in-hospital mortality is decreasing, then increased LVAD use is not a bad trend,” Dr. Rali said in an interview. He hopes that future analysis of longitudinal data from patients could identify clinical factors that link with better patient survival and help target LVAD placement to the patients who stand to gain the most benefit.
“We may be able to give these elderly patients not just longer life but improved quality of life” by a more informed targeting of LVADs, he suggested. “I think these numbers will help convince people that all is not lost,” he noted, for elderly heart failure patients who receive an LVAD as destination therapy. Patients at least 75 years old are not eligible for heart transplantation, so when these patients receive an LVAD it is, by definition, destination therapy.
The data also showed a marked sex disparity in LVAD use, with LVAD placement in men at least 75 years old rising from 1.4/1,000 patients in 2003 to 2.78/1,000 patients in 2014. In contrast, among women these rates rose from 0.8/1,000 patients in 2003 to 1.36/1,000 patients in 2014.
The average age for elderly U.S. LVAD recipients for the entire 12-year period studied was 77.6 years among a total of 2,090 recipients. For all 21,323 U.S. LVAD recipients during 2003-2014 the average age was 51.5 years old.
[email protected]
On Twitter @mitchelzoler
DALLAS – The percentage of left ventricular assist devices placed in U.S. heart failure patients at least 75 years of age jumped sharply during 2003-2014, and concurrently the short-term survival of these patients improved dramatically, according to data collected by the National Inpatient Sample.
During the 12-year period examined, the percentage of left-ventricular assist devices (LVADs) placed in U.S. heart failure patients aged 75 years and older rose from 3% of all LVADs in 2003 to 11% in 2014, Aniket S. Rali, MD, said at the annual scientific meeting of the Heart Failure Society of America.
The U.S. national numbers also showed that throughout the period studied, elderly U.S. patients who received an LVAD were increasingly sicker, with steadily increasing numbers of patients with a Charlson Comorbidity Index score of four or greater. Despite this, in-hospital mortality rates of elderly patients receiving an LVAD plummeted, dropping from 61% of elderly LVAD recipients in 2003 to 18% in 2014. During the same time, the percentage of elderly patients with a Charlson Comorbidity Index score greater than four doubled from 33% in 2003 to 66% in 2014, said Dr. Rali, a cardiologist at the University of Kansas Medical Center in Kansas City.
“If the Charlson Comorbidity Index score is increasing but in-hospital mortality is decreasing, then increased LVAD use is not a bad trend,” Dr. Rali said in an interview. He hopes that future analysis of longitudinal data from patients could identify clinical factors that link with better patient survival and help target LVAD placement to the patients who stand to gain the most benefit.
“We may be able to give these elderly patients not just longer life but improved quality of life” by a more informed targeting of LVADs, he suggested. “I think these numbers will help convince people that all is not lost,” he noted, for elderly heart failure patients who receive an LVAD as destination therapy. Patients at least 75 years old are not eligible for heart transplantation, so when these patients receive an LVAD it is, by definition, destination therapy.
The data also showed a marked sex disparity in LVAD use, with LVAD placement in men at least 75 years old rising from 1.4/1,000 patients in 2003 to 2.78/1,000 patients in 2014. In contrast, among women these rates rose from 0.8/1,000 patients in 2003 to 1.36/1,000 patients in 2014.
The average age for elderly U.S. LVAD recipients for the entire 12-year period studied was 77.6 years among a total of 2,090 recipients. For all 21,323 U.S. LVAD recipients during 2003-2014 the average age was 51.5 years old.
[email protected]
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point:
Major finding: Elderly U.S. patients receiving an LVAD rose from 3% of all LVADs placed in 2003 to 11% in 2014.
Data source: The U.S. National Inpatient Survey during 2003-2014.
Disclosures: Dr. Rali had no disclosures.
Higher BP targets suggested for elderly, cognitively impaired
SAN FRANCISCO – Lowering blood pressure below 140/90 mm Hg might not be a good idea in the very elderly, especially if they have cognitive impairment, according to Philip Gorelick, MD.
“Lower blood pressure” in those patients “may be associated with worse cognitive outcomes,” he said at the joint scientific sessions of AHA Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The problem is that higher pressures may be needed to maintain cerebral perfusion. It’s possible the very elderly have impaired cerebral autoregulation, especially if there’s a history of hypertension. A little extra pressure is needed to overcome increased cerebral vascular resistance.
“Cautious blood pressure–lowering with a target of about 150 mm Hg systolic, may be prudent,” said Dr. Gorelick, professor of translational science and molecular medicine at Michigan State University in Grand Rapids. Meanwhile, “for those without cognitive impairment and who have intact cerebral autoregulation, lower blood pressure targets may be beneficial to preserve cognition.
It’s become clear in recent years that cognitive decline is not a strictly neurologic issue, but rather related to cardiovascular health, at least in some people. Good blood pressure control in midlife, in particular, seems to be important for prevention.
“The same risk factors for atherosclerotic disease [are] risks for Alzheimer’s disease. Vascular risks play a role in cognitive impairment, including Alzheimer’s,” he said.
But the evidence is not clear for blood pressure lowering after the age of 80. Several studies have suggested that angiotensin receptor blockers and other hypertension medications reduce pathologic and clinical changes associated with Alzheimer’s. “However, there’s certainly a downside” to using them in the elderly. “Everything that glistens is not gold,” Dr. Gorelick said.
“There have been studies in older persons with mild cognitive deficits who are placed on antihypertensives, and they actually have lower brain volumes: The brain is shrinking, possibly at a faster rate. Other studies have suggested that people around 80 years of age may have greater cognitive decline with lower blood pressure,” he said.
For those older than 80 and patients with cognitive impairment, the usefulness of blood pressure–lowering for prevention of dementia has not been established. Relaxing the blood pressure control targets might prevent harm, he said.
“There’s going to be a window of opportunity where were are going to see some benefit” in using, for instance, ARBs to slow cognitive decline, but “we have to be smart enough to find the right patients and the right window. We’re not there yet,” he said.
Dr. Gorelick is a consultant for Bayer, Novartis, and Amgen.
SAN FRANCISCO – Lowering blood pressure below 140/90 mm Hg might not be a good idea in the very elderly, especially if they have cognitive impairment, according to Philip Gorelick, MD.
“Lower blood pressure” in those patients “may be associated with worse cognitive outcomes,” he said at the joint scientific sessions of AHA Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The problem is that higher pressures may be needed to maintain cerebral perfusion. It’s possible the very elderly have impaired cerebral autoregulation, especially if there’s a history of hypertension. A little extra pressure is needed to overcome increased cerebral vascular resistance.
“Cautious blood pressure–lowering with a target of about 150 mm Hg systolic, may be prudent,” said Dr. Gorelick, professor of translational science and molecular medicine at Michigan State University in Grand Rapids. Meanwhile, “for those without cognitive impairment and who have intact cerebral autoregulation, lower blood pressure targets may be beneficial to preserve cognition.
It’s become clear in recent years that cognitive decline is not a strictly neurologic issue, but rather related to cardiovascular health, at least in some people. Good blood pressure control in midlife, in particular, seems to be important for prevention.
“The same risk factors for atherosclerotic disease [are] risks for Alzheimer’s disease. Vascular risks play a role in cognitive impairment, including Alzheimer’s,” he said.
But the evidence is not clear for blood pressure lowering after the age of 80. Several studies have suggested that angiotensin receptor blockers and other hypertension medications reduce pathologic and clinical changes associated with Alzheimer’s. “However, there’s certainly a downside” to using them in the elderly. “Everything that glistens is not gold,” Dr. Gorelick said.
“There have been studies in older persons with mild cognitive deficits who are placed on antihypertensives, and they actually have lower brain volumes: The brain is shrinking, possibly at a faster rate. Other studies have suggested that people around 80 years of age may have greater cognitive decline with lower blood pressure,” he said.
For those older than 80 and patients with cognitive impairment, the usefulness of blood pressure–lowering for prevention of dementia has not been established. Relaxing the blood pressure control targets might prevent harm, he said.
“There’s going to be a window of opportunity where were are going to see some benefit” in using, for instance, ARBs to slow cognitive decline, but “we have to be smart enough to find the right patients and the right window. We’re not there yet,” he said.
Dr. Gorelick is a consultant for Bayer, Novartis, and Amgen.
SAN FRANCISCO – Lowering blood pressure below 140/90 mm Hg might not be a good idea in the very elderly, especially if they have cognitive impairment, according to Philip Gorelick, MD.
“Lower blood pressure” in those patients “may be associated with worse cognitive outcomes,” he said at the joint scientific sessions of AHA Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The problem is that higher pressures may be needed to maintain cerebral perfusion. It’s possible the very elderly have impaired cerebral autoregulation, especially if there’s a history of hypertension. A little extra pressure is needed to overcome increased cerebral vascular resistance.
“Cautious blood pressure–lowering with a target of about 150 mm Hg systolic, may be prudent,” said Dr. Gorelick, professor of translational science and molecular medicine at Michigan State University in Grand Rapids. Meanwhile, “for those without cognitive impairment and who have intact cerebral autoregulation, lower blood pressure targets may be beneficial to preserve cognition.
It’s become clear in recent years that cognitive decline is not a strictly neurologic issue, but rather related to cardiovascular health, at least in some people. Good blood pressure control in midlife, in particular, seems to be important for prevention.
“The same risk factors for atherosclerotic disease [are] risks for Alzheimer’s disease. Vascular risks play a role in cognitive impairment, including Alzheimer’s,” he said.
But the evidence is not clear for blood pressure lowering after the age of 80. Several studies have suggested that angiotensin receptor blockers and other hypertension medications reduce pathologic and clinical changes associated with Alzheimer’s. “However, there’s certainly a downside” to using them in the elderly. “Everything that glistens is not gold,” Dr. Gorelick said.
“There have been studies in older persons with mild cognitive deficits who are placed on antihypertensives, and they actually have lower brain volumes: The brain is shrinking, possibly at a faster rate. Other studies have suggested that people around 80 years of age may have greater cognitive decline with lower blood pressure,” he said.
For those older than 80 and patients with cognitive impairment, the usefulness of blood pressure–lowering for prevention of dementia has not been established. Relaxing the blood pressure control targets might prevent harm, he said.
“There’s going to be a window of opportunity where were are going to see some benefit” in using, for instance, ARBs to slow cognitive decline, but “we have to be smart enough to find the right patients and the right window. We’re not there yet,” he said.
Dr. Gorelick is a consultant for Bayer, Novartis, and Amgen.
EXPERT ANALYSIS FROM Joint Hypertension 2017
Medtronic, others push forward with HTN renal artery denervation
SAN FRANCISCO – Hypertensive patients averaged about a 10-mm Hg drop in 24-hour ambulatory systolic blood pressure and about a 12-mm Hg drop in office systolic blood pressure, 2 years after treatment with Medtronic’s new Symplicity Spyral renal artery denervation catheter, according to a review of the company’s renal artery denervation registry.
No major safety issues were reported, but there was no reduction from baseline in the number of antihypertensive drugs that patients were prescribed, which averaged more than four.
The company withdrew the Flex catheter from development after a large, randomized U.S. trial found no benefit over a sham procedure for resistant hypertension (N Engl J Med. 2014 Apr 10;370[15]:1393-401). “In the future, everything will be built around the Spyral catheter,” said Michael Weber, MD, a Medtronic investigator and a professor of medicine at State University of New York, Brooklyn. He presented the registry findings at the joint scientific sessions of AHA Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The Spyral, he said, has two key advantages over the Flex. The Flex had just a single electrode, so operators had to rotate the tip into four quadrants to fully denervate renal arteries, “a tricky business at the best of times and very often not successfully achieved.” Inadequate ablation might have contributed to the trial failure, Dr. Weber said.
The Spyral catheter, on the other hand, has four electrodes placed radially around a spiral catheter, so all four quadrants can be ablated at once, without undue gymnastics. The Spyral can also enter the smaller branches of the main renal arteries, which might allow for more complete denervation, he said.
“We all anticipate better results with the Spyral, but let’s be cautious. We need more data and obviously data from controlled clinical trials. There’s a lot to be learned yet about this whole procedure,” Dr. Weber said.
Medtronic is planning a large trial of its new device following the recent publication of a successful proof-of-concept study that pitted the Spyral in 38 hypertensives against a sham procedure in 42. The Spyral group had a 5 mm Hg greater reduction in systolic ambulatory blood pressure at 3 months, among other findings. To avoid confounding, investigators took patients off their blood pressure medications during the study (Lancet. 2017 Aug 25. pii: S0140-6736(17)32281-X. doi: 10.1016/S0140-6736[17]32281-X).
Other companies are pushing forward with renal artery denervation, as well; Boston Scientific has its own four-quadrant ablation catheter – Vessix – in the pipeline.
In Medtronic’s denervation registry, office systolic blood pressure reductions were a bit larger at 2 years for the older Flex catheter than with the newer Spyral, 15.7 versus 12.0 mm Hg from a baseline of about 170 mm Hg in both groups. Spyral had a slight edge on 24-hour ambulatory systolic blood pressure at 2 years, with an average reduction of 10.4 versus 8.7 mm Hg from a mean baseline of about 155 mm Hg.
For both devices, “when you look at results patient-by-patient, they are dramatically all over the place, including a significant number of patients whose pressures actually increase. I have to assume that it’s patients” who stop taking their medications after the procedure. On the flip side, “I suspect some of our terrific results are because people finally get a touch of religion after the intervention and start taking their drugs for the first time,” Dr. Weber said.
So far, only a handful of Spyral patients have had ablations in renal artery branches. “It seems to have some benefit as judged by office pressure, but the numbers are small, so it’s premature to draw any conclusions,” he said.
Registry patients were in their early 60s, on average, at baseline, and there were more men than women. As with Spyral, Flex patients had no decrease in hypertension prescriptions over time and averaged more than four. “We have not seen many miracle cures in the sense of patients suddenly requiring no drugs at all,” Dr. Weber said.
The procedure seems safe, according to the registry. “There’s nothing to suggest the use of these catheters in the renal arteries causes any sort of acute or later-appearing major renal artery compromise.” With the Flex, less than 1% of patients required renal artery reintervention, which was possibly related to ablation trauma stenosis, “but it’s something to keep on our list of things to look for,” Dr. Weber said.
When asked if the registry fully captures adverse events, Dr. Weber said that “I suspect once [Spyral] goes to market, assuming it does go to market, there will be far more rigorous reporting requirements.”
He reported receiving travel funding, as well as consulting and lecture fees, from Medtronic and Boston Scientific, among other companies.
We need to see randomized trials. This technology looks encouraging, but there’s nothing definitive yet in terms of direct applicability. The initial proof of concept study suggested it does lower blood pressure – but not by a lot. I think it’s a long way from common clinical use, but it’s reasonable to keep looking at it.
We need to see randomized trials. This technology looks encouraging, but there’s nothing definitive yet in terms of direct applicability. The initial proof of concept study suggested it does lower blood pressure – but not by a lot. I think it’s a long way from common clinical use, but it’s reasonable to keep looking at it.
We need to see randomized trials. This technology looks encouraging, but there’s nothing definitive yet in terms of direct applicability. The initial proof of concept study suggested it does lower blood pressure – but not by a lot. I think it’s a long way from common clinical use, but it’s reasonable to keep looking at it.
SAN FRANCISCO – Hypertensive patients averaged about a 10-mm Hg drop in 24-hour ambulatory systolic blood pressure and about a 12-mm Hg drop in office systolic blood pressure, 2 years after treatment with Medtronic’s new Symplicity Spyral renal artery denervation catheter, according to a review of the company’s renal artery denervation registry.
No major safety issues were reported, but there was no reduction from baseline in the number of antihypertensive drugs that patients were prescribed, which averaged more than four.
The company withdrew the Flex catheter from development after a large, randomized U.S. trial found no benefit over a sham procedure for resistant hypertension (N Engl J Med. 2014 Apr 10;370[15]:1393-401). “In the future, everything will be built around the Spyral catheter,” said Michael Weber, MD, a Medtronic investigator and a professor of medicine at State University of New York, Brooklyn. He presented the registry findings at the joint scientific sessions of AHA Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The Spyral, he said, has two key advantages over the Flex. The Flex had just a single electrode, so operators had to rotate the tip into four quadrants to fully denervate renal arteries, “a tricky business at the best of times and very often not successfully achieved.” Inadequate ablation might have contributed to the trial failure, Dr. Weber said.
The Spyral catheter, on the other hand, has four electrodes placed radially around a spiral catheter, so all four quadrants can be ablated at once, without undue gymnastics. The Spyral can also enter the smaller branches of the main renal arteries, which might allow for more complete denervation, he said.
“We all anticipate better results with the Spyral, but let’s be cautious. We need more data and obviously data from controlled clinical trials. There’s a lot to be learned yet about this whole procedure,” Dr. Weber said.
Medtronic is planning a large trial of its new device following the recent publication of a successful proof-of-concept study that pitted the Spyral in 38 hypertensives against a sham procedure in 42. The Spyral group had a 5 mm Hg greater reduction in systolic ambulatory blood pressure at 3 months, among other findings. To avoid confounding, investigators took patients off their blood pressure medications during the study (Lancet. 2017 Aug 25. pii: S0140-6736(17)32281-X. doi: 10.1016/S0140-6736[17]32281-X).
Other companies are pushing forward with renal artery denervation, as well; Boston Scientific has its own four-quadrant ablation catheter – Vessix – in the pipeline.
In Medtronic’s denervation registry, office systolic blood pressure reductions were a bit larger at 2 years for the older Flex catheter than with the newer Spyral, 15.7 versus 12.0 mm Hg from a baseline of about 170 mm Hg in both groups. Spyral had a slight edge on 24-hour ambulatory systolic blood pressure at 2 years, with an average reduction of 10.4 versus 8.7 mm Hg from a mean baseline of about 155 mm Hg.
For both devices, “when you look at results patient-by-patient, they are dramatically all over the place, including a significant number of patients whose pressures actually increase. I have to assume that it’s patients” who stop taking their medications after the procedure. On the flip side, “I suspect some of our terrific results are because people finally get a touch of religion after the intervention and start taking their drugs for the first time,” Dr. Weber said.
So far, only a handful of Spyral patients have had ablations in renal artery branches. “It seems to have some benefit as judged by office pressure, but the numbers are small, so it’s premature to draw any conclusions,” he said.
Registry patients were in their early 60s, on average, at baseline, and there were more men than women. As with Spyral, Flex patients had no decrease in hypertension prescriptions over time and averaged more than four. “We have not seen many miracle cures in the sense of patients suddenly requiring no drugs at all,” Dr. Weber said.
The procedure seems safe, according to the registry. “There’s nothing to suggest the use of these catheters in the renal arteries causes any sort of acute or later-appearing major renal artery compromise.” With the Flex, less than 1% of patients required renal artery reintervention, which was possibly related to ablation trauma stenosis, “but it’s something to keep on our list of things to look for,” Dr. Weber said.
When asked if the registry fully captures adverse events, Dr. Weber said that “I suspect once [Spyral] goes to market, assuming it does go to market, there will be far more rigorous reporting requirements.”
He reported receiving travel funding, as well as consulting and lecture fees, from Medtronic and Boston Scientific, among other companies.
SAN FRANCISCO – Hypertensive patients averaged about a 10-mm Hg drop in 24-hour ambulatory systolic blood pressure and about a 12-mm Hg drop in office systolic blood pressure, 2 years after treatment with Medtronic’s new Symplicity Spyral renal artery denervation catheter, according to a review of the company’s renal artery denervation registry.
No major safety issues were reported, but there was no reduction from baseline in the number of antihypertensive drugs that patients were prescribed, which averaged more than four.
The company withdrew the Flex catheter from development after a large, randomized U.S. trial found no benefit over a sham procedure for resistant hypertension (N Engl J Med. 2014 Apr 10;370[15]:1393-401). “In the future, everything will be built around the Spyral catheter,” said Michael Weber, MD, a Medtronic investigator and a professor of medicine at State University of New York, Brooklyn. He presented the registry findings at the joint scientific sessions of AHA Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The Spyral, he said, has two key advantages over the Flex. The Flex had just a single electrode, so operators had to rotate the tip into four quadrants to fully denervate renal arteries, “a tricky business at the best of times and very often not successfully achieved.” Inadequate ablation might have contributed to the trial failure, Dr. Weber said.
The Spyral catheter, on the other hand, has four electrodes placed radially around a spiral catheter, so all four quadrants can be ablated at once, without undue gymnastics. The Spyral can also enter the smaller branches of the main renal arteries, which might allow for more complete denervation, he said.
“We all anticipate better results with the Spyral, but let’s be cautious. We need more data and obviously data from controlled clinical trials. There’s a lot to be learned yet about this whole procedure,” Dr. Weber said.
Medtronic is planning a large trial of its new device following the recent publication of a successful proof-of-concept study that pitted the Spyral in 38 hypertensives against a sham procedure in 42. The Spyral group had a 5 mm Hg greater reduction in systolic ambulatory blood pressure at 3 months, among other findings. To avoid confounding, investigators took patients off their blood pressure medications during the study (Lancet. 2017 Aug 25. pii: S0140-6736(17)32281-X. doi: 10.1016/S0140-6736[17]32281-X).
Other companies are pushing forward with renal artery denervation, as well; Boston Scientific has its own four-quadrant ablation catheter – Vessix – in the pipeline.
In Medtronic’s denervation registry, office systolic blood pressure reductions were a bit larger at 2 years for the older Flex catheter than with the newer Spyral, 15.7 versus 12.0 mm Hg from a baseline of about 170 mm Hg in both groups. Spyral had a slight edge on 24-hour ambulatory systolic blood pressure at 2 years, with an average reduction of 10.4 versus 8.7 mm Hg from a mean baseline of about 155 mm Hg.
For both devices, “when you look at results patient-by-patient, they are dramatically all over the place, including a significant number of patients whose pressures actually increase. I have to assume that it’s patients” who stop taking their medications after the procedure. On the flip side, “I suspect some of our terrific results are because people finally get a touch of religion after the intervention and start taking their drugs for the first time,” Dr. Weber said.
So far, only a handful of Spyral patients have had ablations in renal artery branches. “It seems to have some benefit as judged by office pressure, but the numbers are small, so it’s premature to draw any conclusions,” he said.
Registry patients were in their early 60s, on average, at baseline, and there were more men than women. As with Spyral, Flex patients had no decrease in hypertension prescriptions over time and averaged more than four. “We have not seen many miracle cures in the sense of patients suddenly requiring no drugs at all,” Dr. Weber said.
The procedure seems safe, according to the registry. “There’s nothing to suggest the use of these catheters in the renal arteries causes any sort of acute or later-appearing major renal artery compromise.” With the Flex, less than 1% of patients required renal artery reintervention, which was possibly related to ablation trauma stenosis, “but it’s something to keep on our list of things to look for,” Dr. Weber said.
When asked if the registry fully captures adverse events, Dr. Weber said that “I suspect once [Spyral] goes to market, assuming it does go to market, there will be far more rigorous reporting requirements.”
He reported receiving travel funding, as well as consulting and lecture fees, from Medtronic and Boston Scientific, among other companies.
AT JOINT HYPERTENSION 2017
Key clinical point:
Major finding: Two years after treatment with Medtronic’s new Symplicity Spyral renal artery denervation catheter, hypertensive patients averaged about a 10-mm Hg drop in 24-hour ambulatory systolic blood pressure and about a 12-mm Hg drop in office systolic blood pressure.
Data source: Review of Medtronic’s renal artery denervation registry
Disclosures: The presenter reported travel funding and consulting and lecture fees from Medtronic and Boston Scientific, among other companies.
While U.S. heart failure readmissions fall, deaths rise
DALLAS – U.S. hospitals have recently shown a consistent and disturbing disconnect between reductions in their heart failure hospital readmission rates and heart failure mortality. Readmissions have dropped while mortality has risen.
“Despite reductions in 30-day heart failure readmissions in 89% of U.S. hospitals” during 2009-2016, “30-day heart failure mortality rates increased at 73%* of these ‘successful’ hospitals” during the same period,” Ahmad A. Abdul-Aziz, MD, said at the annual scientific meeting of the Heart Failure Society of America.
These shifts in the outcomes of U.S. patients hospitalized for acute heart failure episodes are tied to the penalties that the Centers for Medicare & Medicaid Services began slapping on hospitals in 2013 for excess 30-day readmissions for heart failure patients and in 2014 for excess mortality. A problem with these two CMS programs is that the penalty on inferior readmissions performance is a lot stiffer than for excess mortality, Dr. Aziz noted: a 0.2% penalty on payments for high mortality, compared with a 3% penalty for excess readmissions, a disparity that can make hospitals focus more on the readmissions side, he suggested.
Dr. Aziz’s report isn’t the first to make this observation. Study results published earlier in 2017 used CMS Medicare data from 2008 to 2014 to show that during that period, heart failure 30-day mortality rates following hospital discharge rose by 1.3%, while 30-day readmissions fell by 2.1% (JAMA. 2017 July 18;318[3]:270-8). On the basis of these numbers, as many as 5,200 additional deaths to U.S. heart failure patients in 2014 “may be related to the Hospital Readmission Reduction Program” of CMS, Gregg C. Fonarow, MD, said during a separate talk at the meeting.
The analysis reported by Dr. Aziz included data from 3,265 U.S. hospitals for heart failure patients, and data from 1,621 hospitals that managed patients with acute MIs, another disease that the CMS has targeted for penalties based on 30-day readmissions and 30-day postdischarge mortality rates. During the 8-year period studied, heart failure 30-day readmissions fell by 2.2% while 30-day mortality rose by 1%. In contrast, among acute MI patients, readmissions fell by 3% and mortality also fell, by 2.2%, Dr. Abdul-Aziz reported.
Dr. Abdul-Aziz had no disclosures. Dr. Fonarow had been a consultant to Amgen, Janssen, Medtronic, Novartis, St. Jude, and ZS Pharma.
[email protected]
On Twitter @mitchelzoler
*This article was updated October 5, 2017
My colleagues and I have seen in results from recent trials a changing relationship between heart failure mortality and heart failure hospitalization. In the United States in particular, where penalties exist for high rates of hospital readmissions for heart failure, we are seeing more patients treated as outpatients and we see that these “outpatient” events are associated with the same risk for subsequent mortality as we had previously seen for heart failure hospitalization.
It may be that we are keeping patients out of the hospital to avoid a financial ding, but perhaps we are keeping out patients who really should be hospitalized.
What we have begun doing in trials is to look not just at hospitalizations but also consider the incidence of other heart failure events, such as patients treated for heart failure symptoms with an intravenous diuretic in the emergency department and patients who are kept in observation rooms and are not admitted. It’s not the same as a heart failure hospitalization, but some trials are now including these other heart failure events in their primary endpoint.
Scott D. Solomon, MD, professor of medicine at Harvard Medical School and director of noninvasive cardiology at Brigham and Women’s Hospital in Boston, made these comments as chair of the session where Dr. Aziz gave his report and in an interview. He has been a consultant to and/or received research support from Alnylam, Amgen, AstraZeneca, Bristol-Myers Squibb, Cytokinetics, GlaxoSmithKline, Ionis, Merck, Novartis, and Sanofi.
My colleagues and I have seen in results from recent trials a changing relationship between heart failure mortality and heart failure hospitalization. In the United States in particular, where penalties exist for high rates of hospital readmissions for heart failure, we are seeing more patients treated as outpatients and we see that these “outpatient” events are associated with the same risk for subsequent mortality as we had previously seen for heart failure hospitalization.
It may be that we are keeping patients out of the hospital to avoid a financial ding, but perhaps we are keeping out patients who really should be hospitalized.
What we have begun doing in trials is to look not just at hospitalizations but also consider the incidence of other heart failure events, such as patients treated for heart failure symptoms with an intravenous diuretic in the emergency department and patients who are kept in observation rooms and are not admitted. It’s not the same as a heart failure hospitalization, but some trials are now including these other heart failure events in their primary endpoint.
Scott D. Solomon, MD, professor of medicine at Harvard Medical School and director of noninvasive cardiology at Brigham and Women’s Hospital in Boston, made these comments as chair of the session where Dr. Aziz gave his report and in an interview. He has been a consultant to and/or received research support from Alnylam, Amgen, AstraZeneca, Bristol-Myers Squibb, Cytokinetics, GlaxoSmithKline, Ionis, Merck, Novartis, and Sanofi.
My colleagues and I have seen in results from recent trials a changing relationship between heart failure mortality and heart failure hospitalization. In the United States in particular, where penalties exist for high rates of hospital readmissions for heart failure, we are seeing more patients treated as outpatients and we see that these “outpatient” events are associated with the same risk for subsequent mortality as we had previously seen for heart failure hospitalization.
It may be that we are keeping patients out of the hospital to avoid a financial ding, but perhaps we are keeping out patients who really should be hospitalized.
What we have begun doing in trials is to look not just at hospitalizations but also consider the incidence of other heart failure events, such as patients treated for heart failure symptoms with an intravenous diuretic in the emergency department and patients who are kept in observation rooms and are not admitted. It’s not the same as a heart failure hospitalization, but some trials are now including these other heart failure events in their primary endpoint.
Scott D. Solomon, MD, professor of medicine at Harvard Medical School and director of noninvasive cardiology at Brigham and Women’s Hospital in Boston, made these comments as chair of the session where Dr. Aziz gave his report and in an interview. He has been a consultant to and/or received research support from Alnylam, Amgen, AstraZeneca, Bristol-Myers Squibb, Cytokinetics, GlaxoSmithKline, Ionis, Merck, Novartis, and Sanofi.
DALLAS – U.S. hospitals have recently shown a consistent and disturbing disconnect between reductions in their heart failure hospital readmission rates and heart failure mortality. Readmissions have dropped while mortality has risen.
“Despite reductions in 30-day heart failure readmissions in 89% of U.S. hospitals” during 2009-2016, “30-day heart failure mortality rates increased at 73%* of these ‘successful’ hospitals” during the same period,” Ahmad A. Abdul-Aziz, MD, said at the annual scientific meeting of the Heart Failure Society of America.
These shifts in the outcomes of U.S. patients hospitalized for acute heart failure episodes are tied to the penalties that the Centers for Medicare & Medicaid Services began slapping on hospitals in 2013 for excess 30-day readmissions for heart failure patients and in 2014 for excess mortality. A problem with these two CMS programs is that the penalty on inferior readmissions performance is a lot stiffer than for excess mortality, Dr. Aziz noted: a 0.2% penalty on payments for high mortality, compared with a 3% penalty for excess readmissions, a disparity that can make hospitals focus more on the readmissions side, he suggested.
Dr. Aziz’s report isn’t the first to make this observation. Study results published earlier in 2017 used CMS Medicare data from 2008 to 2014 to show that during that period, heart failure 30-day mortality rates following hospital discharge rose by 1.3%, while 30-day readmissions fell by 2.1% (JAMA. 2017 July 18;318[3]:270-8). On the basis of these numbers, as many as 5,200 additional deaths to U.S. heart failure patients in 2014 “may be related to the Hospital Readmission Reduction Program” of CMS, Gregg C. Fonarow, MD, said during a separate talk at the meeting.
The analysis reported by Dr. Aziz included data from 3,265 U.S. hospitals for heart failure patients, and data from 1,621 hospitals that managed patients with acute MIs, another disease that the CMS has targeted for penalties based on 30-day readmissions and 30-day postdischarge mortality rates. During the 8-year period studied, heart failure 30-day readmissions fell by 2.2% while 30-day mortality rose by 1%. In contrast, among acute MI patients, readmissions fell by 3% and mortality also fell, by 2.2%, Dr. Abdul-Aziz reported.
Dr. Abdul-Aziz had no disclosures. Dr. Fonarow had been a consultant to Amgen, Janssen, Medtronic, Novartis, St. Jude, and ZS Pharma.
[email protected]
On Twitter @mitchelzoler
*This article was updated October 5, 2017
DALLAS – U.S. hospitals have recently shown a consistent and disturbing disconnect between reductions in their heart failure hospital readmission rates and heart failure mortality. Readmissions have dropped while mortality has risen.
“Despite reductions in 30-day heart failure readmissions in 89% of U.S. hospitals” during 2009-2016, “30-day heart failure mortality rates increased at 73%* of these ‘successful’ hospitals” during the same period,” Ahmad A. Abdul-Aziz, MD, said at the annual scientific meeting of the Heart Failure Society of America.
These shifts in the outcomes of U.S. patients hospitalized for acute heart failure episodes are tied to the penalties that the Centers for Medicare & Medicaid Services began slapping on hospitals in 2013 for excess 30-day readmissions for heart failure patients and in 2014 for excess mortality. A problem with these two CMS programs is that the penalty on inferior readmissions performance is a lot stiffer than for excess mortality, Dr. Aziz noted: a 0.2% penalty on payments for high mortality, compared with a 3% penalty for excess readmissions, a disparity that can make hospitals focus more on the readmissions side, he suggested.
Dr. Aziz’s report isn’t the first to make this observation. Study results published earlier in 2017 used CMS Medicare data from 2008 to 2014 to show that during that period, heart failure 30-day mortality rates following hospital discharge rose by 1.3%, while 30-day readmissions fell by 2.1% (JAMA. 2017 July 18;318[3]:270-8). On the basis of these numbers, as many as 5,200 additional deaths to U.S. heart failure patients in 2014 “may be related to the Hospital Readmission Reduction Program” of CMS, Gregg C. Fonarow, MD, said during a separate talk at the meeting.
The analysis reported by Dr. Aziz included data from 3,265 U.S. hospitals for heart failure patients, and data from 1,621 hospitals that managed patients with acute MIs, another disease that the CMS has targeted for penalties based on 30-day readmissions and 30-day postdischarge mortality rates. During the 8-year period studied, heart failure 30-day readmissions fell by 2.2% while 30-day mortality rose by 1%. In contrast, among acute MI patients, readmissions fell by 3% and mortality also fell, by 2.2%, Dr. Abdul-Aziz reported.
Dr. Abdul-Aziz had no disclosures. Dr. Fonarow had been a consultant to Amgen, Janssen, Medtronic, Novartis, St. Jude, and ZS Pharma.
[email protected]
On Twitter @mitchelzoler
*This article was updated October 5, 2017
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point:
Major finding: From 2009 to 2016, U.S. 30-day heart failure readmissions fell by 2.2% while 30-day heart failure mortality rose by 1%.
Data source: Review of Medicare data for 3,265 U.S. hospitals managing heart failure patients.
Disclosures: Dr. Abdul-Aziz had no disclosures. Dr. Fonarow had been a consultant to Amgen, Janssen, Medtronic, Novartis, St. Jude, and ZS Pharma.
Hepatitis C falls as barrier to heart transplantation
DALLAS – The heart transplant team at Vanderbilt University has successfully placed hearts from deceased, hepatitis C virus–positive patients into recipients, and then eradicated the subsequent infection that appeared in most recipients using a standard regimen.
So far, five of nine heart transplant recipients who developed a posttransplant hepatitis C virus (HCV) infection had the infection eradicated using one of the highly effective HCV drug regimens, and an additional three patients from the series are nearing their 12th week without detectable virus following treatment that marks a sustained response, Kelly H. Schlendorf, MD, said at the annual scientific meeting of the Heart Failure Society of America. The ninth patient died after developing a pulmonary embolism during the 7th week on antiviral therapy.

The recipients have been patients in a marginal clinical state and facing a long projected wait on the heart-recipient queue of the United Network for Organ Sharing (UNOS), Dr. Schlendorf said in an interview.
These have been “patients with a morbidity and mortality risk from waiting that can be mitigated by expanding the donor pool.” She gave an example of a patient with a left ventricular assist device that required replacement by either a second device or transplant, “so getting the transplant quickly was a good thing,” said Dr. Schlendorf, a cardiologist at Vanderbilt in Nashville.
Based on her analysis of UNOS data, “upwards of 100” and perhaps as many as 300 additional donor hearts could be available annually for U.S. transplants if the organs weren’t excluded because of HCV infection.
The Vanderbilt team has so far approached 15 patients in their program wait-listed for hearts about the possibility of accepting an HCV-positive organ, and all 15 have given their consent, she said. “We spend a lot of time talking with patients and their caregivers about the risks and benefits and possible complications.”
The 13 recipients, starting in September 2016, included 12 patients who were HCV naive and 1 patient with a history of HCV exposure. All 13 received the program’s standard three-drug regimen for immunosuppression.
During close surveillance, 9 of the 13 developed an infection. Patients with genotype 1 HCV received 12 weeks of treatment with ledipasvir plus sofosbuvir. Those infected with genotype 3 received 12-24 weeks of treatment with sofosbuvir plus velpatasvir. Treatment with these direct-acting antivirals meant that patients had to adjust the time when they took their proton-pump inhibitors, and they needed to stop treatment with diltiazem and statins while on the antivirals.
“In the era of direct-acting antivirals, HCV-positive donors may provide a safe and effective way to expand the donor pool and reduce wait-list times,” Dr. Schlendorf said. She noted that in recent years an increased number of potential organ donors have been HCV positive. She also cautioned that so far follow-up has been relatively brief, with no patient yet followed as long as 1 year after transplant.
The direct-acting HCV antivirals are expensive, and some payers established clinical criteria that patients must meet to qualify for coverage of these regimens. “We have not encountered difficulties getting insurers to pay,” Dr. Schlendorf said. Despite the antivirals’ cost there are significant cost savings from fewer days in the ICU waiting for heart transplantation and a reduced need for mechanical support as a bridge to transplant, she noted.
[email protected]
On Twitter @mitchelzoler
DALLAS – The heart transplant team at Vanderbilt University has successfully placed hearts from deceased, hepatitis C virus–positive patients into recipients, and then eradicated the subsequent infection that appeared in most recipients using a standard regimen.
So far, five of nine heart transplant recipients who developed a posttransplant hepatitis C virus (HCV) infection had the infection eradicated using one of the highly effective HCV drug regimens, and an additional three patients from the series are nearing their 12th week without detectable virus following treatment that marks a sustained response, Kelly H. Schlendorf, MD, said at the annual scientific meeting of the Heart Failure Society of America. The ninth patient died after developing a pulmonary embolism during the 7th week on antiviral therapy.

The recipients have been patients in a marginal clinical state and facing a long projected wait on the heart-recipient queue of the United Network for Organ Sharing (UNOS), Dr. Schlendorf said in an interview.
These have been “patients with a morbidity and mortality risk from waiting that can be mitigated by expanding the donor pool.” She gave an example of a patient with a left ventricular assist device that required replacement by either a second device or transplant, “so getting the transplant quickly was a good thing,” said Dr. Schlendorf, a cardiologist at Vanderbilt in Nashville.
Based on her analysis of UNOS data, “upwards of 100” and perhaps as many as 300 additional donor hearts could be available annually for U.S. transplants if the organs weren’t excluded because of HCV infection.
The Vanderbilt team has so far approached 15 patients in their program wait-listed for hearts about the possibility of accepting an HCV-positive organ, and all 15 have given their consent, she said. “We spend a lot of time talking with patients and their caregivers about the risks and benefits and possible complications.”
The 13 recipients, starting in September 2016, included 12 patients who were HCV naive and 1 patient with a history of HCV exposure. All 13 received the program’s standard three-drug regimen for immunosuppression.
During close surveillance, 9 of the 13 developed an infection. Patients with genotype 1 HCV received 12 weeks of treatment with ledipasvir plus sofosbuvir. Those infected with genotype 3 received 12-24 weeks of treatment with sofosbuvir plus velpatasvir. Treatment with these direct-acting antivirals meant that patients had to adjust the time when they took their proton-pump inhibitors, and they needed to stop treatment with diltiazem and statins while on the antivirals.
“In the era of direct-acting antivirals, HCV-positive donors may provide a safe and effective way to expand the donor pool and reduce wait-list times,” Dr. Schlendorf said. She noted that in recent years an increased number of potential organ donors have been HCV positive. She also cautioned that so far follow-up has been relatively brief, with no patient yet followed as long as 1 year after transplant.
The direct-acting HCV antivirals are expensive, and some payers established clinical criteria that patients must meet to qualify for coverage of these regimens. “We have not encountered difficulties getting insurers to pay,” Dr. Schlendorf said. Despite the antivirals’ cost there are significant cost savings from fewer days in the ICU waiting for heart transplantation and a reduced need for mechanical support as a bridge to transplant, she noted.
[email protected]
On Twitter @mitchelzoler
DALLAS – The heart transplant team at Vanderbilt University has successfully placed hearts from deceased, hepatitis C virus–positive patients into recipients, and then eradicated the subsequent infection that appeared in most recipients using a standard regimen.
So far, five of nine heart transplant recipients who developed a posttransplant hepatitis C virus (HCV) infection had the infection eradicated using one of the highly effective HCV drug regimens, and an additional three patients from the series are nearing their 12th week without detectable virus following treatment that marks a sustained response, Kelly H. Schlendorf, MD, said at the annual scientific meeting of the Heart Failure Society of America. The ninth patient died after developing a pulmonary embolism during the 7th week on antiviral therapy.

The recipients have been patients in a marginal clinical state and facing a long projected wait on the heart-recipient queue of the United Network for Organ Sharing (UNOS), Dr. Schlendorf said in an interview.
These have been “patients with a morbidity and mortality risk from waiting that can be mitigated by expanding the donor pool.” She gave an example of a patient with a left ventricular assist device that required replacement by either a second device or transplant, “so getting the transplant quickly was a good thing,” said Dr. Schlendorf, a cardiologist at Vanderbilt in Nashville.
Based on her analysis of UNOS data, “upwards of 100” and perhaps as many as 300 additional donor hearts could be available annually for U.S. transplants if the organs weren’t excluded because of HCV infection.
The Vanderbilt team has so far approached 15 patients in their program wait-listed for hearts about the possibility of accepting an HCV-positive organ, and all 15 have given their consent, she said. “We spend a lot of time talking with patients and their caregivers about the risks and benefits and possible complications.”
The 13 recipients, starting in September 2016, included 12 patients who were HCV naive and 1 patient with a history of HCV exposure. All 13 received the program’s standard three-drug regimen for immunosuppression.
During close surveillance, 9 of the 13 developed an infection. Patients with genotype 1 HCV received 12 weeks of treatment with ledipasvir plus sofosbuvir. Those infected with genotype 3 received 12-24 weeks of treatment with sofosbuvir plus velpatasvir. Treatment with these direct-acting antivirals meant that patients had to adjust the time when they took their proton-pump inhibitors, and they needed to stop treatment with diltiazem and statins while on the antivirals.
“In the era of direct-acting antivirals, HCV-positive donors may provide a safe and effective way to expand the donor pool and reduce wait-list times,” Dr. Schlendorf said. She noted that in recent years an increased number of potential organ donors have been HCV positive. She also cautioned that so far follow-up has been relatively brief, with no patient yet followed as long as 1 year after transplant.
The direct-acting HCV antivirals are expensive, and some payers established clinical criteria that patients must meet to qualify for coverage of these regimens. “We have not encountered difficulties getting insurers to pay,” Dr. Schlendorf said. Despite the antivirals’ cost there are significant cost savings from fewer days in the ICU waiting for heart transplantation and a reduced need for mechanical support as a bridge to transplant, she noted.
[email protected]
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point:
Major finding: Eight of nine patients who developed HCV infection had it eradicated by a direct-acting antiviral regimen.
Data source: A series of 13 patients treated at one U.S. center.
Disclosures: Dr. Schlendorf had no disclosures.
New data prompt update to ACC guidance on nonstatin LDL lowering
The American College of Cardiology Task Force on Expert Consensus Decision Pathways has released a “focused update” for the 2016 ACC Expert Consensus Decision Pathway (ECDP) on the role of nonstatin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease (ASCVD) risk.
The update was deemed by the ECDP writing committee to be desirable given the additional evidence and perspectives that have emerged since the publication of the 2016 version, particularly with respect to the efficacy and safety of proprotein convertase subtilisin/kexin 9 (PCSK9) inhibitors for the secondary prevention of ASCVD, as well as the best use of ezetimibe in addition to statin therapy after acute coronary syndrome.
The ECDP algorithms endorse the four evidence-based statin benefit groups identified in the 2013 guidelines (adults aged 21 and older with clinical ASCVD, adults aged 21 and older with LDL-C of 190 mg/dL or greater, adults aged 40-75 years without ASCVD but with diabetes and with LDL-C of 70-189 mg/dL, and adults aged 40-75 without ASCVD or diabetes but with LDL-C of 70-189 mg/dL and an estimated 10-year risk for ASCVD of 7.5% or greater) and assume that the patient is currently taking or has attempted to take a statin, they noted.
Among the changes in the 2017 focused update are:
- Consideration of new randomized clinical trial data for the PCSK9 inhibitors evolocumab and bococizumab. Namely, they included results from the cardiovascular outcomes trials FOURIER (Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk) and SPIRE-1 and SPIRE-2 (Studies of PCSK9 Inhibition and the Reduction of Vascular Events), which were published in early 2017.
- An adjustment in the ECDP algorithms with respect to thresholds for consideration of net ASCVD risk reduction. The 2016 ECDP thresholds for risk reduction benefit were percent reduction in LDL-C with consideration of absolute LDL-C level in patients with clinical ASCVD, baseline LDL-C of 190 mg/dL or greater, and primary prevention. In patients with diabetes with or without clinical ASCVD, clinicians were allowed to consider absolute LDL-C and/or non-HDL-cholesterol levels. In the 2017 ECDP update, the thresholds are percent reduction in LDL-C with consideration of absolute LDL-C or non-HDL-C levels for patients in each of the four statin benefit groups. This change was based on the inclusion criteria of the FOURIER trial, the ongoing ODYSSEY Outcomes trial (Evaluation of Cardiovascular Outcomes after an Acute Coronary Syndrome During Treatment with Alirocumab), and the SPIRE-2 trial, all of which included non-HDL-C thresholds. “In alignment with these inclusion criteria, the 2017 Focused Update includes both LDL-C and non-HDL-C thresholds for evaluation of net ASCVD risk-reduction benefit when considering the addition of nonstatin therapies for patients in each of the four statin benefit groups” the update explained.
- An expansion of the threshold for consideration of net ASCVD risk-reduction benefit from a reduction of LDL C of at least 50%, as well as consideration of LDL-C less than 70 mg/dL or non-HDL-C less than 100 mg/dL for all patients (that is, both those with and those without comorbidities) who have clinical ASCVD and baseline LDL-C of 70-189 mg/dL. The 2016 ECDP had different thresholds for those with versus those without comorbidities. This change was based on findings from the FOURIER trial and the IMPROVE-IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial).“Based on consideration of all available evidence, the consensus of the writing committee members is that lower LDL-C levels are safe and optimal in patients with clinical ASCVD due to [their] increased risk of recurrent events,” they said.
- An expanded recommendation on the use of ezetimibe and PCSK9 inhibition. The 2016 ECDP stated that “if a decision is made to proceed with the addition of nonstatin therapy to maximally tolerated statin therapy, it is reasonable to consider the addition of ezetimibe as the initial agent and a PCSK9 inhibitor as the second agent.” However, based on the FOURIER findings, the ongoing ODYSSEY Outcomes trial, and the IMPROVE-IT trial, the 2017 Focused Update states that, if such a decision is made in patients with clinical ASCVD with comorbidities and baseline LDL-C of 70-189 mg/dL, it is reasonable to weigh the addition of either ezetimibe or a PCSK9 inhibitor in light of “considerations of the additional percent LDL-C reduction desired, patient preferences, costs, route of administration, and other factors.” The update also spells out considerations that may favor the initial choice of ezetimibe versus a PCSK9 inhibitor (such as requiring less than 25% additional lowering of LDL-C, an age of over 75 years, cost, and other patient factors and preferences) .
- Additional factors, based on the FOURIER trial results and inclusion criteria, that may be considered for the identification of higher-risk patients with clinical ASCVD. The 2016 ECDP included on this list diabetes, a recent ASCVD event, an ASCVD event while already taking a statin, poorly controlled other major ASCVD risk factors, elevated lipoprotein, chronic kidney disease, symptomatic heart failure, maintenance hemodialysis, and baseline LDL-C of at least 190 mg/dL not due to secondary causes. The 2017 update added being 65 years or older, prior MI or nonhemorrhagic stroke, current daily cigarette smoking, symptomatic peripheral artery disease with prior MI or stroke, history of non-MI related coronary revascularization, residual coronary artery disease with at least 40% stenosis in at least two large vessels, HDL-C less than 40 mg/dL for men and less than 50 mg/dL for women, high-sensitivity C-reactive protein greater than 2 mg/L, and metabolic syndrome.
The content of the full ECDP has been changed in accordance with these updates and now includes more extensive and detailed guidance for decision making – both in the text and in treatment algorithms.
Aspects that remain unchanged include the decision pathways and algorithms for the use of ezetimibe or PCSK9 inhibitors in primary prevention patients with LDL-C less than 190 mg/dL or in those without ASCVD and LDL-C of 190 mg/dL or greater unattributable to secondary causes.
In addition to other changes made for the purpose of clarification and consistency, recommendations regarding bile acid–sequestrant use were downgraded; these are now only recommended as optional secondary agents for consideration in patients who cannot tolerate ezetimibe.
“[These] recommendations attempt to provide practical guidance for clinicians and patients regarding the use of nonstatin therapies to further reduce ASCVD risk in situations not covered by the guideline until such time as the scientific evidence base expands and cardiovascular outcomes trials are completed with new agents for ASCVD risk reduction,” the committee concluded.
Dr. Lloyd-Jones reported having no disclosures.
The American College of Cardiology Task Force on Expert Consensus Decision Pathways has released a “focused update” for the 2016 ACC Expert Consensus Decision Pathway (ECDP) on the role of nonstatin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease (ASCVD) risk.
The update was deemed by the ECDP writing committee to be desirable given the additional evidence and perspectives that have emerged since the publication of the 2016 version, particularly with respect to the efficacy and safety of proprotein convertase subtilisin/kexin 9 (PCSK9) inhibitors for the secondary prevention of ASCVD, as well as the best use of ezetimibe in addition to statin therapy after acute coronary syndrome.
The ECDP algorithms endorse the four evidence-based statin benefit groups identified in the 2013 guidelines (adults aged 21 and older with clinical ASCVD, adults aged 21 and older with LDL-C of 190 mg/dL or greater, adults aged 40-75 years without ASCVD but with diabetes and with LDL-C of 70-189 mg/dL, and adults aged 40-75 without ASCVD or diabetes but with LDL-C of 70-189 mg/dL and an estimated 10-year risk for ASCVD of 7.5% or greater) and assume that the patient is currently taking or has attempted to take a statin, they noted.
Among the changes in the 2017 focused update are:
- Consideration of new randomized clinical trial data for the PCSK9 inhibitors evolocumab and bococizumab. Namely, they included results from the cardiovascular outcomes trials FOURIER (Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk) and SPIRE-1 and SPIRE-2 (Studies of PCSK9 Inhibition and the Reduction of Vascular Events), which were published in early 2017.
- An adjustment in the ECDP algorithms with respect to thresholds for consideration of net ASCVD risk reduction. The 2016 ECDP thresholds for risk reduction benefit were percent reduction in LDL-C with consideration of absolute LDL-C level in patients with clinical ASCVD, baseline LDL-C of 190 mg/dL or greater, and primary prevention. In patients with diabetes with or without clinical ASCVD, clinicians were allowed to consider absolute LDL-C and/or non-HDL-cholesterol levels. In the 2017 ECDP update, the thresholds are percent reduction in LDL-C with consideration of absolute LDL-C or non-HDL-C levels for patients in each of the four statin benefit groups. This change was based on the inclusion criteria of the FOURIER trial, the ongoing ODYSSEY Outcomes trial (Evaluation of Cardiovascular Outcomes after an Acute Coronary Syndrome During Treatment with Alirocumab), and the SPIRE-2 trial, all of which included non-HDL-C thresholds. “In alignment with these inclusion criteria, the 2017 Focused Update includes both LDL-C and non-HDL-C thresholds for evaluation of net ASCVD risk-reduction benefit when considering the addition of nonstatin therapies for patients in each of the four statin benefit groups” the update explained.
- An expansion of the threshold for consideration of net ASCVD risk-reduction benefit from a reduction of LDL C of at least 50%, as well as consideration of LDL-C less than 70 mg/dL or non-HDL-C less than 100 mg/dL for all patients (that is, both those with and those without comorbidities) who have clinical ASCVD and baseline LDL-C of 70-189 mg/dL. The 2016 ECDP had different thresholds for those with versus those without comorbidities. This change was based on findings from the FOURIER trial and the IMPROVE-IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial).“Based on consideration of all available evidence, the consensus of the writing committee members is that lower LDL-C levels are safe and optimal in patients with clinical ASCVD due to [their] increased risk of recurrent events,” they said.
- An expanded recommendation on the use of ezetimibe and PCSK9 inhibition. The 2016 ECDP stated that “if a decision is made to proceed with the addition of nonstatin therapy to maximally tolerated statin therapy, it is reasonable to consider the addition of ezetimibe as the initial agent and a PCSK9 inhibitor as the second agent.” However, based on the FOURIER findings, the ongoing ODYSSEY Outcomes trial, and the IMPROVE-IT trial, the 2017 Focused Update states that, if such a decision is made in patients with clinical ASCVD with comorbidities and baseline LDL-C of 70-189 mg/dL, it is reasonable to weigh the addition of either ezetimibe or a PCSK9 inhibitor in light of “considerations of the additional percent LDL-C reduction desired, patient preferences, costs, route of administration, and other factors.” The update also spells out considerations that may favor the initial choice of ezetimibe versus a PCSK9 inhibitor (such as requiring less than 25% additional lowering of LDL-C, an age of over 75 years, cost, and other patient factors and preferences) .
- Additional factors, based on the FOURIER trial results and inclusion criteria, that may be considered for the identification of higher-risk patients with clinical ASCVD. The 2016 ECDP included on this list diabetes, a recent ASCVD event, an ASCVD event while already taking a statin, poorly controlled other major ASCVD risk factors, elevated lipoprotein, chronic kidney disease, symptomatic heart failure, maintenance hemodialysis, and baseline LDL-C of at least 190 mg/dL not due to secondary causes. The 2017 update added being 65 years or older, prior MI or nonhemorrhagic stroke, current daily cigarette smoking, symptomatic peripheral artery disease with prior MI or stroke, history of non-MI related coronary revascularization, residual coronary artery disease with at least 40% stenosis in at least two large vessels, HDL-C less than 40 mg/dL for men and less than 50 mg/dL for women, high-sensitivity C-reactive protein greater than 2 mg/L, and metabolic syndrome.
The content of the full ECDP has been changed in accordance with these updates and now includes more extensive and detailed guidance for decision making – both in the text and in treatment algorithms.
Aspects that remain unchanged include the decision pathways and algorithms for the use of ezetimibe or PCSK9 inhibitors in primary prevention patients with LDL-C less than 190 mg/dL or in those without ASCVD and LDL-C of 190 mg/dL or greater unattributable to secondary causes.
In addition to other changes made for the purpose of clarification and consistency, recommendations regarding bile acid–sequestrant use were downgraded; these are now only recommended as optional secondary agents for consideration in patients who cannot tolerate ezetimibe.
“[These] recommendations attempt to provide practical guidance for clinicians and patients regarding the use of nonstatin therapies to further reduce ASCVD risk in situations not covered by the guideline until such time as the scientific evidence base expands and cardiovascular outcomes trials are completed with new agents for ASCVD risk reduction,” the committee concluded.
Dr. Lloyd-Jones reported having no disclosures.
The American College of Cardiology Task Force on Expert Consensus Decision Pathways has released a “focused update” for the 2016 ACC Expert Consensus Decision Pathway (ECDP) on the role of nonstatin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease (ASCVD) risk.
The update was deemed by the ECDP writing committee to be desirable given the additional evidence and perspectives that have emerged since the publication of the 2016 version, particularly with respect to the efficacy and safety of proprotein convertase subtilisin/kexin 9 (PCSK9) inhibitors for the secondary prevention of ASCVD, as well as the best use of ezetimibe in addition to statin therapy after acute coronary syndrome.
The ECDP algorithms endorse the four evidence-based statin benefit groups identified in the 2013 guidelines (adults aged 21 and older with clinical ASCVD, adults aged 21 and older with LDL-C of 190 mg/dL or greater, adults aged 40-75 years without ASCVD but with diabetes and with LDL-C of 70-189 mg/dL, and adults aged 40-75 without ASCVD or diabetes but with LDL-C of 70-189 mg/dL and an estimated 10-year risk for ASCVD of 7.5% or greater) and assume that the patient is currently taking or has attempted to take a statin, they noted.
Among the changes in the 2017 focused update are:
- Consideration of new randomized clinical trial data for the PCSK9 inhibitors evolocumab and bococizumab. Namely, they included results from the cardiovascular outcomes trials FOURIER (Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk) and SPIRE-1 and SPIRE-2 (Studies of PCSK9 Inhibition and the Reduction of Vascular Events), which were published in early 2017.
- An adjustment in the ECDP algorithms with respect to thresholds for consideration of net ASCVD risk reduction. The 2016 ECDP thresholds for risk reduction benefit were percent reduction in LDL-C with consideration of absolute LDL-C level in patients with clinical ASCVD, baseline LDL-C of 190 mg/dL or greater, and primary prevention. In patients with diabetes with or without clinical ASCVD, clinicians were allowed to consider absolute LDL-C and/or non-HDL-cholesterol levels. In the 2017 ECDP update, the thresholds are percent reduction in LDL-C with consideration of absolute LDL-C or non-HDL-C levels for patients in each of the four statin benefit groups. This change was based on the inclusion criteria of the FOURIER trial, the ongoing ODYSSEY Outcomes trial (Evaluation of Cardiovascular Outcomes after an Acute Coronary Syndrome During Treatment with Alirocumab), and the SPIRE-2 trial, all of which included non-HDL-C thresholds. “In alignment with these inclusion criteria, the 2017 Focused Update includes both LDL-C and non-HDL-C thresholds for evaluation of net ASCVD risk-reduction benefit when considering the addition of nonstatin therapies for patients in each of the four statin benefit groups” the update explained.
- An expansion of the threshold for consideration of net ASCVD risk-reduction benefit from a reduction of LDL C of at least 50%, as well as consideration of LDL-C less than 70 mg/dL or non-HDL-C less than 100 mg/dL for all patients (that is, both those with and those without comorbidities) who have clinical ASCVD and baseline LDL-C of 70-189 mg/dL. The 2016 ECDP had different thresholds for those with versus those without comorbidities. This change was based on findings from the FOURIER trial and the IMPROVE-IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial).“Based on consideration of all available evidence, the consensus of the writing committee members is that lower LDL-C levels are safe and optimal in patients with clinical ASCVD due to [their] increased risk of recurrent events,” they said.
- An expanded recommendation on the use of ezetimibe and PCSK9 inhibition. The 2016 ECDP stated that “if a decision is made to proceed with the addition of nonstatin therapy to maximally tolerated statin therapy, it is reasonable to consider the addition of ezetimibe as the initial agent and a PCSK9 inhibitor as the second agent.” However, based on the FOURIER findings, the ongoing ODYSSEY Outcomes trial, and the IMPROVE-IT trial, the 2017 Focused Update states that, if such a decision is made in patients with clinical ASCVD with comorbidities and baseline LDL-C of 70-189 mg/dL, it is reasonable to weigh the addition of either ezetimibe or a PCSK9 inhibitor in light of “considerations of the additional percent LDL-C reduction desired, patient preferences, costs, route of administration, and other factors.” The update also spells out considerations that may favor the initial choice of ezetimibe versus a PCSK9 inhibitor (such as requiring less than 25% additional lowering of LDL-C, an age of over 75 years, cost, and other patient factors and preferences) .
- Additional factors, based on the FOURIER trial results and inclusion criteria, that may be considered for the identification of higher-risk patients with clinical ASCVD. The 2016 ECDP included on this list diabetes, a recent ASCVD event, an ASCVD event while already taking a statin, poorly controlled other major ASCVD risk factors, elevated lipoprotein, chronic kidney disease, symptomatic heart failure, maintenance hemodialysis, and baseline LDL-C of at least 190 mg/dL not due to secondary causes. The 2017 update added being 65 years or older, prior MI or nonhemorrhagic stroke, current daily cigarette smoking, symptomatic peripheral artery disease with prior MI or stroke, history of non-MI related coronary revascularization, residual coronary artery disease with at least 40% stenosis in at least two large vessels, HDL-C less than 40 mg/dL for men and less than 50 mg/dL for women, high-sensitivity C-reactive protein greater than 2 mg/L, and metabolic syndrome.
The content of the full ECDP has been changed in accordance with these updates and now includes more extensive and detailed guidance for decision making – both in the text and in treatment algorithms.
Aspects that remain unchanged include the decision pathways and algorithms for the use of ezetimibe or PCSK9 inhibitors in primary prevention patients with LDL-C less than 190 mg/dL or in those without ASCVD and LDL-C of 190 mg/dL or greater unattributable to secondary causes.
In addition to other changes made for the purpose of clarification and consistency, recommendations regarding bile acid–sequestrant use were downgraded; these are now only recommended as optional secondary agents for consideration in patients who cannot tolerate ezetimibe.
“[These] recommendations attempt to provide practical guidance for clinicians and patients regarding the use of nonstatin therapies to further reduce ASCVD risk in situations not covered by the guideline until such time as the scientific evidence base expands and cardiovascular outcomes trials are completed with new agents for ASCVD risk reduction,” the committee concluded.
Dr. Lloyd-Jones reported having no disclosures.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
BIMA’s benefits extend to high-risk CABG patients
COLORADO SPRINGS – The survival advantage of bilateral internal over left internal mammary artery grafts persists even among multivessel CABG patients perceived to be at high surgical risk, Nishant Saran, MD, reported at the annual meeting of the Western Thoracic Surgical Association.
Many surgeons hesitate to perform bilateral internal mammary artery (BIMA) grafting in high-risk patients on the presumption that BIMA might not benefit them. It’s a concern that appears to be without merit, however, based on a retrospective analysis of the 6,468 multivessel CABG procedures performed at the Mayo Clinic during 2000-2015, said Dr. Saran of the Mayo Clinic in Rochester, Minn.
The BIMA patients were as a whole significantly younger, primarily men, and less likely to have diabetes or to be obese than the LIMA patients. Also, LIMA patients were fourfold more likely to have baseline heart failure, twice as likely to have a history of stroke, and had a twofold greater prevalence of chronic lung disease.
“The unmatched comparison shows the clear treatment selection bias we have: BIMA goes to the healthier patients,” Dr. Saran observed.
But is that bias justified? To find out, he and his coinvestigators performed extensive propensity score matching using several dozen baseline variables in order to identify 1,011 closely matched patient pairs. In this propensity score-matched analysis, 5- and 10-year survival rates were significantly better in the BIMA group. The gap between the two survival curves widened after about 7 years and continued to expand steadily through year 10. Incision time averaged 298 minutes in the BIMA group and 254 minutes in the propensity-matched LIMA group.
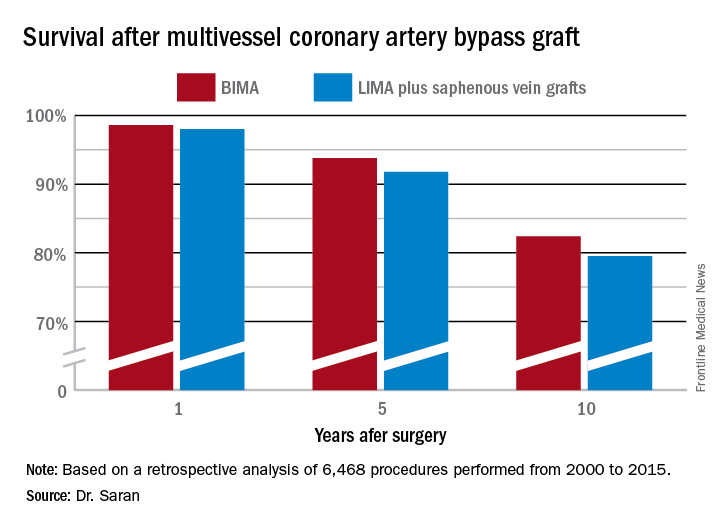
Discussant Eric J. Lehr, MD, a cardiac surgeon at Swedish Medical Center in Seattle, noted that the impressive survival benefit for BIMA in the retrospective Mayo Clinic study came at what he termed “a modest cost”: a doubled incidence of sternal site infections, from 1.4% in the LIMA group to 3% with BIMA. Importantly, though, there was no significant difference in the more serious deep sternal wound infections.
He agreed with Dr. Saran that BIMA is seriously underutilized, noting that only one cardiothoracic surgery program in the state of Washington uses BIMA more than 10% of the time in multivessel CABG.
Dr. Lehr then posed a provocative question: “Should BIMA grafting be considered a quality metric in coronary revascularization surgery, despite the small increase in sternal site infections, even though sternal wound infections have been declared a ‘never’ event and are tied to reimbursement?”
“I think BIMA should be a gold standard,” Dr. Saran replied. “The first thing that a cardiac surgeon should always think of when a patient is going to have CABG is ‘BIMA first,’ and only then look into reasons for not doing it. But I guess in current real-world practice, things are different.”
Howard K. Song, MD, commented, “I think a study like this doesn’t necessarily show that every surgeon should be using BIMA liberally, it shows that surgeons in your practice who do that have excellent outcomes.”
Dr. Song, professor of surgery and chief of the division of cardiothoracic surgery at Oregon Health and Science University, Portland, added that he believes extensive use of BIMA is actually a surrogate marker for a highly skilled subspecialist who would be expected to have very good outcomes as a matter of course.
“That may be one way of looking at it; however, I do think that even very skilled surgeons still have an inherent resistance to doing BIMA,” Dr. Saran responded.
“In the current era, the surgeon is pressured to achieve improved short-term outcomes and improved OR turnover times. An extra half hour for BIMA tends to push the surgeon away,” he added.
Dr. Saran reported having no financial conflicts of interest.
COLORADO SPRINGS – The survival advantage of bilateral internal over left internal mammary artery grafts persists even among multivessel CABG patients perceived to be at high surgical risk, Nishant Saran, MD, reported at the annual meeting of the Western Thoracic Surgical Association.
Many surgeons hesitate to perform bilateral internal mammary artery (BIMA) grafting in high-risk patients on the presumption that BIMA might not benefit them. It’s a concern that appears to be without merit, however, based on a retrospective analysis of the 6,468 multivessel CABG procedures performed at the Mayo Clinic during 2000-2015, said Dr. Saran of the Mayo Clinic in Rochester, Minn.
The BIMA patients were as a whole significantly younger, primarily men, and less likely to have diabetes or to be obese than the LIMA patients. Also, LIMA patients were fourfold more likely to have baseline heart failure, twice as likely to have a history of stroke, and had a twofold greater prevalence of chronic lung disease.
“The unmatched comparison shows the clear treatment selection bias we have: BIMA goes to the healthier patients,” Dr. Saran observed.
But is that bias justified? To find out, he and his coinvestigators performed extensive propensity score matching using several dozen baseline variables in order to identify 1,011 closely matched patient pairs. In this propensity score-matched analysis, 5- and 10-year survival rates were significantly better in the BIMA group. The gap between the two survival curves widened after about 7 years and continued to expand steadily through year 10. Incision time averaged 298 minutes in the BIMA group and 254 minutes in the propensity-matched LIMA group.
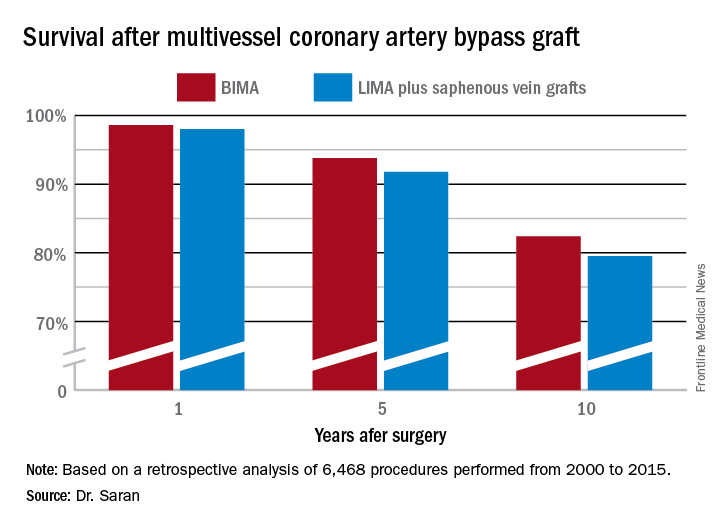
Discussant Eric J. Lehr, MD, a cardiac surgeon at Swedish Medical Center in Seattle, noted that the impressive survival benefit for BIMA in the retrospective Mayo Clinic study came at what he termed “a modest cost”: a doubled incidence of sternal site infections, from 1.4% in the LIMA group to 3% with BIMA. Importantly, though, there was no significant difference in the more serious deep sternal wound infections.
He agreed with Dr. Saran that BIMA is seriously underutilized, noting that only one cardiothoracic surgery program in the state of Washington uses BIMA more than 10% of the time in multivessel CABG.
Dr. Lehr then posed a provocative question: “Should BIMA grafting be considered a quality metric in coronary revascularization surgery, despite the small increase in sternal site infections, even though sternal wound infections have been declared a ‘never’ event and are tied to reimbursement?”
“I think BIMA should be a gold standard,” Dr. Saran replied. “The first thing that a cardiac surgeon should always think of when a patient is going to have CABG is ‘BIMA first,’ and only then look into reasons for not doing it. But I guess in current real-world practice, things are different.”
Howard K. Song, MD, commented, “I think a study like this doesn’t necessarily show that every surgeon should be using BIMA liberally, it shows that surgeons in your practice who do that have excellent outcomes.”
Dr. Song, professor of surgery and chief of the division of cardiothoracic surgery at Oregon Health and Science University, Portland, added that he believes extensive use of BIMA is actually a surrogate marker for a highly skilled subspecialist who would be expected to have very good outcomes as a matter of course.
“That may be one way of looking at it; however, I do think that even very skilled surgeons still have an inherent resistance to doing BIMA,” Dr. Saran responded.
“In the current era, the surgeon is pressured to achieve improved short-term outcomes and improved OR turnover times. An extra half hour for BIMA tends to push the surgeon away,” he added.
Dr. Saran reported having no financial conflicts of interest.
COLORADO SPRINGS – The survival advantage of bilateral internal over left internal mammary artery grafts persists even among multivessel CABG patients perceived to be at high surgical risk, Nishant Saran, MD, reported at the annual meeting of the Western Thoracic Surgical Association.
Many surgeons hesitate to perform bilateral internal mammary artery (BIMA) grafting in high-risk patients on the presumption that BIMA might not benefit them. It’s a concern that appears to be without merit, however, based on a retrospective analysis of the 6,468 multivessel CABG procedures performed at the Mayo Clinic during 2000-2015, said Dr. Saran of the Mayo Clinic in Rochester, Minn.
The BIMA patients were as a whole significantly younger, primarily men, and less likely to have diabetes or to be obese than the LIMA patients. Also, LIMA patients were fourfold more likely to have baseline heart failure, twice as likely to have a history of stroke, and had a twofold greater prevalence of chronic lung disease.
“The unmatched comparison shows the clear treatment selection bias we have: BIMA goes to the healthier patients,” Dr. Saran observed.
But is that bias justified? To find out, he and his coinvestigators performed extensive propensity score matching using several dozen baseline variables in order to identify 1,011 closely matched patient pairs. In this propensity score-matched analysis, 5- and 10-year survival rates were significantly better in the BIMA group. The gap between the two survival curves widened after about 7 years and continued to expand steadily through year 10. Incision time averaged 298 minutes in the BIMA group and 254 minutes in the propensity-matched LIMA group.
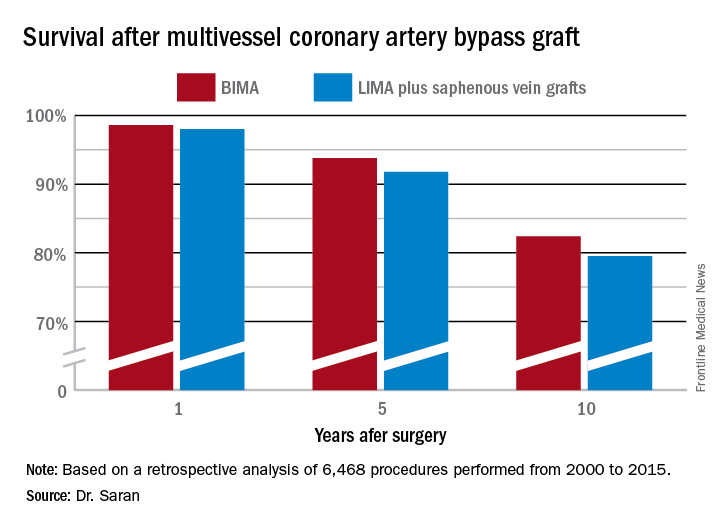
Discussant Eric J. Lehr, MD, a cardiac surgeon at Swedish Medical Center in Seattle, noted that the impressive survival benefit for BIMA in the retrospective Mayo Clinic study came at what he termed “a modest cost”: a doubled incidence of sternal site infections, from 1.4% in the LIMA group to 3% with BIMA. Importantly, though, there was no significant difference in the more serious deep sternal wound infections.
He agreed with Dr. Saran that BIMA is seriously underutilized, noting that only one cardiothoracic surgery program in the state of Washington uses BIMA more than 10% of the time in multivessel CABG.
Dr. Lehr then posed a provocative question: “Should BIMA grafting be considered a quality metric in coronary revascularization surgery, despite the small increase in sternal site infections, even though sternal wound infections have been declared a ‘never’ event and are tied to reimbursement?”
“I think BIMA should be a gold standard,” Dr. Saran replied. “The first thing that a cardiac surgeon should always think of when a patient is going to have CABG is ‘BIMA first,’ and only then look into reasons for not doing it. But I guess in current real-world practice, things are different.”
Howard K. Song, MD, commented, “I think a study like this doesn’t necessarily show that every surgeon should be using BIMA liberally, it shows that surgeons in your practice who do that have excellent outcomes.”
Dr. Song, professor of surgery and chief of the division of cardiothoracic surgery at Oregon Health and Science University, Portland, added that he believes extensive use of BIMA is actually a surrogate marker for a highly skilled subspecialist who would be expected to have very good outcomes as a matter of course.
“That may be one way of looking at it; however, I do think that even very skilled surgeons still have an inherent resistance to doing BIMA,” Dr. Saran responded.
“In the current era, the surgeon is pressured to achieve improved short-term outcomes and improved OR turnover times. An extra half hour for BIMA tends to push the surgeon away,” he added.
Dr. Saran reported having no financial conflicts of interest.
AT THE WTSA ANNUAL MEETING
Key clinical point:
Major finding: Ten-year survival following multivessel CABG using bilateral internal mammary artery grafting was 82.4%, significantly better than the 79.5% rate with left internal mammary artery grafting plus saphenous vein grafts.
Data source: This retrospective observational single-center included 6,468 patients who underwent multivessel CABG during 2000-2015.
Disclosures: Dr. Saran reported having no financial conflicts of interest.